User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Higher rates of PTSD, BPD in transgender vs. cisgender psych patients
Although mood disorders, depression, and anxiety were the most common diagnoses in both TGD and cisgender patients, “when we compared the diagnostic profiles [of TGD patients] to those of cisgender patients, we found an increased prevalence of PTSD and BPD,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., told this news organization.
“What we concluded is that psychiatric programs that wish to treat TGD patients should either have or should develop expertise in treating PTSD and BPD, not just mood and anxiety disorders,” Dr. Zimmerman said.
The study was published online September 26 in the Journal of Clinical Psychiatry.
‘Piecemeal literature’
TGD individuals “experience high rates of various forms of psychopathology in general and when compared with cisgender persons,” the investigators note.
They point out that most empirical evidence has relied upon the use of brief, unstructured psychodiagnostic assessment measures and assessment of a “limited constellation of psychiatric symptoms domains,” resulting in a “piecemeal literature wherein each piece of research documents elevations in one – or a few – diagnostic domains.”
Studies pointing to broader psychosocial health variables have often relied upon self-reported measures. In addition, in studies that utilized a structured interview approach, none “used a formal interview procedure to assess psychiatric diagnoses” and most focused only on a “limited number of psychiatric conditions based on self-reports of past diagnosis.”
The goal of the current study was to use semistructured interviews administered by professionals to compare the diagnostic profiles of a samples of TGD and cisgender patients who presented for treatment at a single naturalistic, clinically acute setting – a partial hospital program.
Dr. Zimmerman said that there was an additional motive for conducting the study. “There has been discussion in the field as to whether or not transgender or gender-diverse individuals all have borderline personality disorder, but that hasn’t been our clinical impression.”
Rather, Dr. Zimmerman and colleagues believe TGD people “may have had more difficult childhoods and more difficult adjustments in society because of societal attitudes and have to deal with that stress, whether it be microaggressions or overt bullying and aggression.” The study was designed to investigate this issue.
In addition, studies conducted in primary care programs in individuals seeking gender-affirming surgery have “reported a limited number of psychiatric diagnoses, but we were wondering whether, amongst psychiatric patients specifically, there were differences in diagnostic profiles between transgender and gender-diverse patients and cisgender patients. If so, what might the implications be for providing care for this population?”
TGD not synonymous with borderline
To investigate, the researchers administered semistructured diagnostic interviews for DSM-IV disorders to 2,212 psychiatric patients (66% cisgender women, 30.8% cisgender men, 3.1% TGD; mean [standard deviation] age 36.7 [14.4] years) presenting to the Rhode Island Hospital Department of Psychiatry Partial Hospital Program between April 2014 and January 2021.
Patients also completed a demographic questionnaire including their assigned sex at birth and their current gender identity.
Most patients (44.9%) were single, followed by 23.5% who were married, 14.1% living in a relationship as if married, 12.0% divorced, 3.6% separated, and 1.9% widowed.
Almost three-quarters of participants (73.2%) identified as White, followed by Hispanic (10.7%), Black (6.7%), “other” or a combination of racial/ethnic backgrounds (6.6%), and Asian (2.7%).
There were no differences between cisgender and TGD groups in terms of race or education, but the TGD patients were significantly younger compared with their cisgender counterparts and were significantly more likely to have never been married.
The average number of psychiatric diagnoses in the sample was 3.05 (± 1.73), with TGD patients having a larger number of psychiatric diagnoses than did their cisgender peers (an average of 3.54 ± 1.88 vs. 3.04 ± 1.72, respectively; t = 2.37; P = .02).
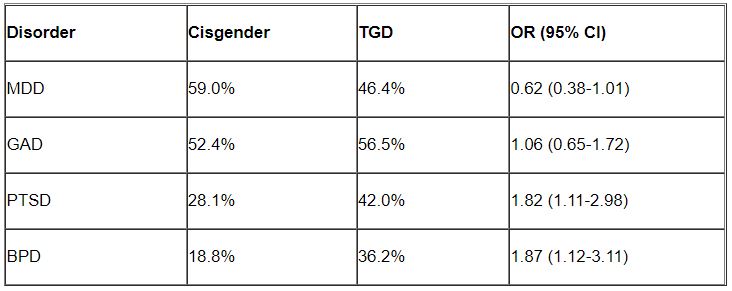
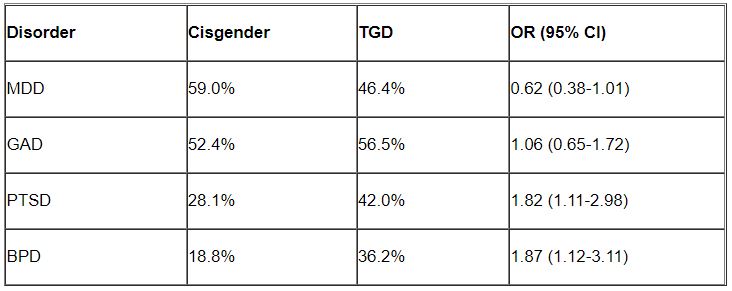
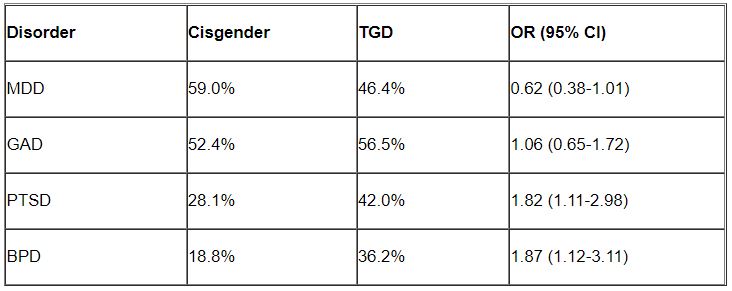
Major depressive disorder (MDD) and generalized anxiety disorder (GAD) were the most common disorders among both cisgender and TGD patients. However, after controlling for age, the researchers found that TGD patients were significantly more likely than were the cisgender patients to be diagnosed with PTSD and BPD (P < .05 for both).
“Of note, only about one-third of the TGD individuals were diagnosed with BPD, so it is important to realize that transgender or gender-diverse identity is not synonymous with BPD, as some have suggested,” noted Dr. Zimmerman, who is also the director of the outpatient division at the Partial Hospital Program, Rhode Island Hospital.
A representative sample?
Commenting on the study, Jack Drescher, MD, distinguished life fellow of the American Psychiatric Association and clinical professor of psychiatry, Columbia University, New York, called the findings “interesting” but noted that a limitation of the study is that it included “a patient population with likely more severe psychiatric illness, since they were all day hospital patients.”
The question is whether similar findings would be obtained in a less severely ill population, said Dr. Drescher, who is also a senior consulting analyst for sexuality and gender at Columbia University and was not involved with the study. “The patients in the study may not be representative of the general population, either cisgender or transgender.”
Dr. Drescher was “not surprised” by the finding regarding PTSD because the finding “is consistent with our understanding of the kinds of traumas that transgender people go through in day-to-day life.”
He noted that some people misunderstand the diagnostic criterion in BPD of identity confusion and think that because people with gender dysphoria may be confused about their identity, it means that all people who are transgender have borderline personality disorder, “but that’s not true.”
Dr. Zimmerman agreed. “The vast majority of individuals with BPD do not have a transgender or gender-diverse identity, and TGD should not be equated with BPD,” he said.
No source of study funding was disclosed. Dr. Zimmerman and coauthors and Dr. Drescher report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Although mood disorders, depression, and anxiety were the most common diagnoses in both TGD and cisgender patients, “when we compared the diagnostic profiles [of TGD patients] to those of cisgender patients, we found an increased prevalence of PTSD and BPD,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., told this news organization.
“What we concluded is that psychiatric programs that wish to treat TGD patients should either have or should develop expertise in treating PTSD and BPD, not just mood and anxiety disorders,” Dr. Zimmerman said.
The study was published online September 26 in the Journal of Clinical Psychiatry.
‘Piecemeal literature’
TGD individuals “experience high rates of various forms of psychopathology in general and when compared with cisgender persons,” the investigators note.
They point out that most empirical evidence has relied upon the use of brief, unstructured psychodiagnostic assessment measures and assessment of a “limited constellation of psychiatric symptoms domains,” resulting in a “piecemeal literature wherein each piece of research documents elevations in one – or a few – diagnostic domains.”
Studies pointing to broader psychosocial health variables have often relied upon self-reported measures. In addition, in studies that utilized a structured interview approach, none “used a formal interview procedure to assess psychiatric diagnoses” and most focused only on a “limited number of psychiatric conditions based on self-reports of past diagnosis.”
The goal of the current study was to use semistructured interviews administered by professionals to compare the diagnostic profiles of a samples of TGD and cisgender patients who presented for treatment at a single naturalistic, clinically acute setting – a partial hospital program.
Dr. Zimmerman said that there was an additional motive for conducting the study. “There has been discussion in the field as to whether or not transgender or gender-diverse individuals all have borderline personality disorder, but that hasn’t been our clinical impression.”
Rather, Dr. Zimmerman and colleagues believe TGD people “may have had more difficult childhoods and more difficult adjustments in society because of societal attitudes and have to deal with that stress, whether it be microaggressions or overt bullying and aggression.” The study was designed to investigate this issue.
In addition, studies conducted in primary care programs in individuals seeking gender-affirming surgery have “reported a limited number of psychiatric diagnoses, but we were wondering whether, amongst psychiatric patients specifically, there were differences in diagnostic profiles between transgender and gender-diverse patients and cisgender patients. If so, what might the implications be for providing care for this population?”
TGD not synonymous with borderline
To investigate, the researchers administered semistructured diagnostic interviews for DSM-IV disorders to 2,212 psychiatric patients (66% cisgender women, 30.8% cisgender men, 3.1% TGD; mean [standard deviation] age 36.7 [14.4] years) presenting to the Rhode Island Hospital Department of Psychiatry Partial Hospital Program between April 2014 and January 2021.
Patients also completed a demographic questionnaire including their assigned sex at birth and their current gender identity.
Most patients (44.9%) were single, followed by 23.5% who were married, 14.1% living in a relationship as if married, 12.0% divorced, 3.6% separated, and 1.9% widowed.
Almost three-quarters of participants (73.2%) identified as White, followed by Hispanic (10.7%), Black (6.7%), “other” or a combination of racial/ethnic backgrounds (6.6%), and Asian (2.7%).
There were no differences between cisgender and TGD groups in terms of race or education, but the TGD patients were significantly younger compared with their cisgender counterparts and were significantly more likely to have never been married.
The average number of psychiatric diagnoses in the sample was 3.05 (± 1.73), with TGD patients having a larger number of psychiatric diagnoses than did their cisgender peers (an average of 3.54 ± 1.88 vs. 3.04 ± 1.72, respectively; t = 2.37; P = .02).
Major depressive disorder (MDD) and generalized anxiety disorder (GAD) were the most common disorders among both cisgender and TGD patients. However, after controlling for age, the researchers found that TGD patients were significantly more likely than were the cisgender patients to be diagnosed with PTSD and BPD (P < .05 for both).
“Of note, only about one-third of the TGD individuals were diagnosed with BPD, so it is important to realize that transgender or gender-diverse identity is not synonymous with BPD, as some have suggested,” noted Dr. Zimmerman, who is also the director of the outpatient division at the Partial Hospital Program, Rhode Island Hospital.
A representative sample?
Commenting on the study, Jack Drescher, MD, distinguished life fellow of the American Psychiatric Association and clinical professor of psychiatry, Columbia University, New York, called the findings “interesting” but noted that a limitation of the study is that it included “a patient population with likely more severe psychiatric illness, since they were all day hospital patients.”
The question is whether similar findings would be obtained in a less severely ill population, said Dr. Drescher, who is also a senior consulting analyst for sexuality and gender at Columbia University and was not involved with the study. “The patients in the study may not be representative of the general population, either cisgender or transgender.”
Dr. Drescher was “not surprised” by the finding regarding PTSD because the finding “is consistent with our understanding of the kinds of traumas that transgender people go through in day-to-day life.”
He noted that some people misunderstand the diagnostic criterion in BPD of identity confusion and think that because people with gender dysphoria may be confused about their identity, it means that all people who are transgender have borderline personality disorder, “but that’s not true.”
Dr. Zimmerman agreed. “The vast majority of individuals with BPD do not have a transgender or gender-diverse identity, and TGD should not be equated with BPD,” he said.
No source of study funding was disclosed. Dr. Zimmerman and coauthors and Dr. Drescher report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Although mood disorders, depression, and anxiety were the most common diagnoses in both TGD and cisgender patients, “when we compared the diagnostic profiles [of TGD patients] to those of cisgender patients, we found an increased prevalence of PTSD and BPD,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., told this news organization.
“What we concluded is that psychiatric programs that wish to treat TGD patients should either have or should develop expertise in treating PTSD and BPD, not just mood and anxiety disorders,” Dr. Zimmerman said.
The study was published online September 26 in the Journal of Clinical Psychiatry.
‘Piecemeal literature’
TGD individuals “experience high rates of various forms of psychopathology in general and when compared with cisgender persons,” the investigators note.
They point out that most empirical evidence has relied upon the use of brief, unstructured psychodiagnostic assessment measures and assessment of a “limited constellation of psychiatric symptoms domains,” resulting in a “piecemeal literature wherein each piece of research documents elevations in one – or a few – diagnostic domains.”
Studies pointing to broader psychosocial health variables have often relied upon self-reported measures. In addition, in studies that utilized a structured interview approach, none “used a formal interview procedure to assess psychiatric diagnoses” and most focused only on a “limited number of psychiatric conditions based on self-reports of past diagnosis.”
The goal of the current study was to use semistructured interviews administered by professionals to compare the diagnostic profiles of a samples of TGD and cisgender patients who presented for treatment at a single naturalistic, clinically acute setting – a partial hospital program.
Dr. Zimmerman said that there was an additional motive for conducting the study. “There has been discussion in the field as to whether or not transgender or gender-diverse individuals all have borderline personality disorder, but that hasn’t been our clinical impression.”
Rather, Dr. Zimmerman and colleagues believe TGD people “may have had more difficult childhoods and more difficult adjustments in society because of societal attitudes and have to deal with that stress, whether it be microaggressions or overt bullying and aggression.” The study was designed to investigate this issue.
In addition, studies conducted in primary care programs in individuals seeking gender-affirming surgery have “reported a limited number of psychiatric diagnoses, but we were wondering whether, amongst psychiatric patients specifically, there were differences in diagnostic profiles between transgender and gender-diverse patients and cisgender patients. If so, what might the implications be for providing care for this population?”
TGD not synonymous with borderline
To investigate, the researchers administered semistructured diagnostic interviews for DSM-IV disorders to 2,212 psychiatric patients (66% cisgender women, 30.8% cisgender men, 3.1% TGD; mean [standard deviation] age 36.7 [14.4] years) presenting to the Rhode Island Hospital Department of Psychiatry Partial Hospital Program between April 2014 and January 2021.
Patients also completed a demographic questionnaire including their assigned sex at birth and their current gender identity.
Most patients (44.9%) were single, followed by 23.5% who were married, 14.1% living in a relationship as if married, 12.0% divorced, 3.6% separated, and 1.9% widowed.
Almost three-quarters of participants (73.2%) identified as White, followed by Hispanic (10.7%), Black (6.7%), “other” or a combination of racial/ethnic backgrounds (6.6%), and Asian (2.7%).
There were no differences between cisgender and TGD groups in terms of race or education, but the TGD patients were significantly younger compared with their cisgender counterparts and were significantly more likely to have never been married.
The average number of psychiatric diagnoses in the sample was 3.05 (± 1.73), with TGD patients having a larger number of psychiatric diagnoses than did their cisgender peers (an average of 3.54 ± 1.88 vs. 3.04 ± 1.72, respectively; t = 2.37; P = .02).
Major depressive disorder (MDD) and generalized anxiety disorder (GAD) were the most common disorders among both cisgender and TGD patients. However, after controlling for age, the researchers found that TGD patients were significantly more likely than were the cisgender patients to be diagnosed with PTSD and BPD (P < .05 for both).
“Of note, only about one-third of the TGD individuals were diagnosed with BPD, so it is important to realize that transgender or gender-diverse identity is not synonymous with BPD, as some have suggested,” noted Dr. Zimmerman, who is also the director of the outpatient division at the Partial Hospital Program, Rhode Island Hospital.
A representative sample?
Commenting on the study, Jack Drescher, MD, distinguished life fellow of the American Psychiatric Association and clinical professor of psychiatry, Columbia University, New York, called the findings “interesting” but noted that a limitation of the study is that it included “a patient population with likely more severe psychiatric illness, since they were all day hospital patients.”
The question is whether similar findings would be obtained in a less severely ill population, said Dr. Drescher, who is also a senior consulting analyst for sexuality and gender at Columbia University and was not involved with the study. “The patients in the study may not be representative of the general population, either cisgender or transgender.”
Dr. Drescher was “not surprised” by the finding regarding PTSD because the finding “is consistent with our understanding of the kinds of traumas that transgender people go through in day-to-day life.”
He noted that some people misunderstand the diagnostic criterion in BPD of identity confusion and think that because people with gender dysphoria may be confused about their identity, it means that all people who are transgender have borderline personality disorder, “but that’s not true.”
Dr. Zimmerman agreed. “The vast majority of individuals with BPD do not have a transgender or gender-diverse identity, and TGD should not be equated with BPD,” he said.
No source of study funding was disclosed. Dr. Zimmerman and coauthors and Dr. Drescher report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF CLINICAL PSYCHIATRY
Hormone therapy–depression link may depend on mode of administration
An analysis of more than 800,000 women in Denmark offers more insight into the murky links between female hormones and midlife mental illness in women: It hints that hormone therapy (HT) may boost the risk of depression, have no effect, or lower it – all depending on how it’s administered and when.
Women who took systemic HT had a higher risk of depression from age 48 to 50 (adjusted hazard ratio, 1.50; 95% confidence interval, 1.24-1.81), researchers reported in JAMA Network Open. However, there was no overall link between depression and locally administered HT (aHR, 1.15; 95% CI, 0.70-1.87) – except when HT was begun between ages 54 and 60, when there were signs of a protective effect (aHR, 0.80; 95% CI, 0.70-0.91).
“Women in menopause who initiate systemically administered HT should be aware of depression as a potential adverse effect,” epidemiologist and study corresponding author Merete Osler, MD, PhD, DMSc, of Bispebjerg and Frederiksberg (Denmark) Hospitals and the University of Copenhagen, said in an interview. ”Further, women and clinicians alike should be aware of any misinterpretation of symptoms of depression as menopausal disturbances.”
Dr. Osler said the researchers launched the study to better understand potential hormone-depression links in light of suspicions that lower levels of estrogen in menopause may contribute to depression.
Several randomized clinical trials and cohort and cross-sectional studies have explored whether systemic HT affects depression during menopause, Dr. Osler said, “but the results from these studies have been inconsistent, and few have explored the role of the route of administration.”
For the new registry-based study, researchers retrospectively tracked all women in Denmark who were aged 45 between 1995 and 2017 without prior oophorectomy, certain kinds of cancer, prior use of HT, or ongoing depression.
During follow-up to a mean age of 56, 23% of the women began HT (at a median age of 55), and 1.6% were hospitalized for depression. Of those on HT, 65.8% received locally administered HT.
Researchers adjusted hazard ratios for a long list of factors such as educational level, marital status, number of still births or live births, prior use of hormonal contraceptives, several medical conditions, and prior depression.
“We were surprised by our findings, which to some degree contradicted our prior hypothesis that systemic HT with estrogen would not be associated with first-time depression diagnosis in women aged 45 and above, while HT with progesterone would be associated with a slightly increased risk,” Dr. Osler said. “In our study, systemically administered HT was associated with an increased risk of depression with no difference between estrogen alone or in combination with progestin. As findings from previous studies have been inconsistent, our findings fit with some but not all previous studies.”
Why might the mode of administration make a difference? It’s possible that local administration may contribute less to the systemic circulation, Dr. Osler said, “or that menopausal symptoms including depression are more likely to be treated with systemic HT.”
As for age differences, Dr. Osler said “it is possible that women are more sensitive to the influence of HT on mood around menopause than at later ages. However, it should be noted that in the present study it was not possible to calculate precise risk estimates for use of systemic HT in menopausal women above age 54 because less than 1% initiated treatment with systemic HT after age 54 years.”
In an interview, psychiatrist Natalie Rasgon, MD, PhD, of Stanford (Calif.) University, who’s studied hormones and depression, said the study is “remarkably large and consistently executed.”
She cautioned, however, that the findings don’t prove any causality. “Saying that estrogen therapy or hormone therapy causes depression is patently incorrect.”
How can the findings be useful for medical professionals? “Women and physicians alike need to be very mindful of pre-existing mood disorders,” Dr. Rasgon said. “Women who in the past had anxiety disorders, mood swings, PTSD, or prior episodes of depression might have a differential response to hormone therapy in menopause.”
Also keep in mind, she said, that the transition from menopause to post menopause is “very volatile,” and depression may break through even in women undergoing treatment for the condition.
For her part, Dr. Osler said this study and others “emphasize the need for clinical guidelines to further consider the psychological side effects of systemic HT.”
Funding information was not provided. The study authors and Dr. Rasgon have no disclosures.
An analysis of more than 800,000 women in Denmark offers more insight into the murky links between female hormones and midlife mental illness in women: It hints that hormone therapy (HT) may boost the risk of depression, have no effect, or lower it – all depending on how it’s administered and when.
Women who took systemic HT had a higher risk of depression from age 48 to 50 (adjusted hazard ratio, 1.50; 95% confidence interval, 1.24-1.81), researchers reported in JAMA Network Open. However, there was no overall link between depression and locally administered HT (aHR, 1.15; 95% CI, 0.70-1.87) – except when HT was begun between ages 54 and 60, when there were signs of a protective effect (aHR, 0.80; 95% CI, 0.70-0.91).
“Women in menopause who initiate systemically administered HT should be aware of depression as a potential adverse effect,” epidemiologist and study corresponding author Merete Osler, MD, PhD, DMSc, of Bispebjerg and Frederiksberg (Denmark) Hospitals and the University of Copenhagen, said in an interview. ”Further, women and clinicians alike should be aware of any misinterpretation of symptoms of depression as menopausal disturbances.”
Dr. Osler said the researchers launched the study to better understand potential hormone-depression links in light of suspicions that lower levels of estrogen in menopause may contribute to depression.
Several randomized clinical trials and cohort and cross-sectional studies have explored whether systemic HT affects depression during menopause, Dr. Osler said, “but the results from these studies have been inconsistent, and few have explored the role of the route of administration.”
For the new registry-based study, researchers retrospectively tracked all women in Denmark who were aged 45 between 1995 and 2017 without prior oophorectomy, certain kinds of cancer, prior use of HT, or ongoing depression.
During follow-up to a mean age of 56, 23% of the women began HT (at a median age of 55), and 1.6% were hospitalized for depression. Of those on HT, 65.8% received locally administered HT.
Researchers adjusted hazard ratios for a long list of factors such as educational level, marital status, number of still births or live births, prior use of hormonal contraceptives, several medical conditions, and prior depression.
“We were surprised by our findings, which to some degree contradicted our prior hypothesis that systemic HT with estrogen would not be associated with first-time depression diagnosis in women aged 45 and above, while HT with progesterone would be associated with a slightly increased risk,” Dr. Osler said. “In our study, systemically administered HT was associated with an increased risk of depression with no difference between estrogen alone or in combination with progestin. As findings from previous studies have been inconsistent, our findings fit with some but not all previous studies.”
Why might the mode of administration make a difference? It’s possible that local administration may contribute less to the systemic circulation, Dr. Osler said, “or that menopausal symptoms including depression are more likely to be treated with systemic HT.”
As for age differences, Dr. Osler said “it is possible that women are more sensitive to the influence of HT on mood around menopause than at later ages. However, it should be noted that in the present study it was not possible to calculate precise risk estimates for use of systemic HT in menopausal women above age 54 because less than 1% initiated treatment with systemic HT after age 54 years.”
In an interview, psychiatrist Natalie Rasgon, MD, PhD, of Stanford (Calif.) University, who’s studied hormones and depression, said the study is “remarkably large and consistently executed.”
She cautioned, however, that the findings don’t prove any causality. “Saying that estrogen therapy or hormone therapy causes depression is patently incorrect.”
How can the findings be useful for medical professionals? “Women and physicians alike need to be very mindful of pre-existing mood disorders,” Dr. Rasgon said. “Women who in the past had anxiety disorders, mood swings, PTSD, or prior episodes of depression might have a differential response to hormone therapy in menopause.”
Also keep in mind, she said, that the transition from menopause to post menopause is “very volatile,” and depression may break through even in women undergoing treatment for the condition.
For her part, Dr. Osler said this study and others “emphasize the need for clinical guidelines to further consider the psychological side effects of systemic HT.”
Funding information was not provided. The study authors and Dr. Rasgon have no disclosures.
An analysis of more than 800,000 women in Denmark offers more insight into the murky links between female hormones and midlife mental illness in women: It hints that hormone therapy (HT) may boost the risk of depression, have no effect, or lower it – all depending on how it’s administered and when.
Women who took systemic HT had a higher risk of depression from age 48 to 50 (adjusted hazard ratio, 1.50; 95% confidence interval, 1.24-1.81), researchers reported in JAMA Network Open. However, there was no overall link between depression and locally administered HT (aHR, 1.15; 95% CI, 0.70-1.87) – except when HT was begun between ages 54 and 60, when there were signs of a protective effect (aHR, 0.80; 95% CI, 0.70-0.91).
“Women in menopause who initiate systemically administered HT should be aware of depression as a potential adverse effect,” epidemiologist and study corresponding author Merete Osler, MD, PhD, DMSc, of Bispebjerg and Frederiksberg (Denmark) Hospitals and the University of Copenhagen, said in an interview. ”Further, women and clinicians alike should be aware of any misinterpretation of symptoms of depression as menopausal disturbances.”
Dr. Osler said the researchers launched the study to better understand potential hormone-depression links in light of suspicions that lower levels of estrogen in menopause may contribute to depression.
Several randomized clinical trials and cohort and cross-sectional studies have explored whether systemic HT affects depression during menopause, Dr. Osler said, “but the results from these studies have been inconsistent, and few have explored the role of the route of administration.”
For the new registry-based study, researchers retrospectively tracked all women in Denmark who were aged 45 between 1995 and 2017 without prior oophorectomy, certain kinds of cancer, prior use of HT, or ongoing depression.
During follow-up to a mean age of 56, 23% of the women began HT (at a median age of 55), and 1.6% were hospitalized for depression. Of those on HT, 65.8% received locally administered HT.
Researchers adjusted hazard ratios for a long list of factors such as educational level, marital status, number of still births or live births, prior use of hormonal contraceptives, several medical conditions, and prior depression.
“We were surprised by our findings, which to some degree contradicted our prior hypothesis that systemic HT with estrogen would not be associated with first-time depression diagnosis in women aged 45 and above, while HT with progesterone would be associated with a slightly increased risk,” Dr. Osler said. “In our study, systemically administered HT was associated with an increased risk of depression with no difference between estrogen alone or in combination with progestin. As findings from previous studies have been inconsistent, our findings fit with some but not all previous studies.”
Why might the mode of administration make a difference? It’s possible that local administration may contribute less to the systemic circulation, Dr. Osler said, “or that menopausal symptoms including depression are more likely to be treated with systemic HT.”
As for age differences, Dr. Osler said “it is possible that women are more sensitive to the influence of HT on mood around menopause than at later ages. However, it should be noted that in the present study it was not possible to calculate precise risk estimates for use of systemic HT in menopausal women above age 54 because less than 1% initiated treatment with systemic HT after age 54 years.”
In an interview, psychiatrist Natalie Rasgon, MD, PhD, of Stanford (Calif.) University, who’s studied hormones and depression, said the study is “remarkably large and consistently executed.”
She cautioned, however, that the findings don’t prove any causality. “Saying that estrogen therapy or hormone therapy causes depression is patently incorrect.”
How can the findings be useful for medical professionals? “Women and physicians alike need to be very mindful of pre-existing mood disorders,” Dr. Rasgon said. “Women who in the past had anxiety disorders, mood swings, PTSD, or prior episodes of depression might have a differential response to hormone therapy in menopause.”
Also keep in mind, she said, that the transition from menopause to post menopause is “very volatile,” and depression may break through even in women undergoing treatment for the condition.
For her part, Dr. Osler said this study and others “emphasize the need for clinical guidelines to further consider the psychological side effects of systemic HT.”
Funding information was not provided. The study authors and Dr. Rasgon have no disclosures.
FROM JAMA NETWORK OPEN
Dementia prevalence study reveals inequities
based on new U.S. data from The Health and Retirement Study (HRS).
These inequities likely stem from structural racism and income inequality, necessitating a multifaceted response at an institutional level, according to lead author Jennifer J. Manly, PhD, a professor of neuropsychology in neurology at the Gertrude H. Sergievsky Center and the Taub Institute for Research in Aging and Alzheimer’s Disease at Columbia University, New York.
A more representative dataset
Between 2001 and 2003, a subset of HRS participants underwent extensive neuropsychological assessment in the Aging, Demographics, and Memory Study (ADAMS), providing data which have since been cited by hundreds of published studies, the investigators wrote in JAMA Neurology. Those data, however, failed to accurately represent the U.S. population at the time, and have not been updated since.
“The ADAMS substudy was small, and the limited inclusion of Black, Hispanic, and American Indian or Alaska Native participants contributed to lack of precision of estimates among minoritized racial and ethnic groups that have been shown to experience a higher burden of cognitive impairment and dementia,” Dr. Manly and colleagues wrote.
The present analysis used a more representative dataset from HRS participants who were 65 years or older in 2016. From June 2016 to October 2017, 3,496 of these individuals underwent comprehensive neuropsychological test battery and informant interview, with dementia and MCI classified based on standard diagnostic criteria.
In total, 393 people were classified with dementia (10%), while 804 had MCI (22%), both of which approximate estimates reported by previous studies, according to the investigators. In further alignment with past research, age was a clear risk factor; each 5-year increment added 17% and 95% increased risk of MCI and dementia, respectively.
Compared with college-educated participants, individuals who did not graduate from high school had a 60% increased risk for both dementia (odds ratio, 1.6; 95% confidence interval, 1.1-2.3) and MCI (OR, 1.6; 95% CI, 1.2-2.2). Other educational strata were not associated with significant differences in risk.
Compared with White participants, Black individuals had an 80% increased risk of dementia (OR, 1.8; 95% CI, 1.2-2.7), but no increased risk of MCI. Conversely, non-White Hispanic individuals had a 40% increased risk of MCI (OR, 1.4; 95% CI, 1.0-2.0), but no increased risk of dementia, compared with White participants.
“Older adults racialized as Black and Hispanic are more likely to develop cognitive impairment and dementia because of historical and current structural racism and income inequality that restrict access to brain-health benefits and increase exposure to harm,” Dr. Manly said in a written comment.
These inequities deserve a comprehensive response, she added.
“Actions and policies that decrease discriminatory and aggressive policing policies, invest in schools that serve children that are racialized as Black and Hispanic, repair housing and economic inequalities, and provide equitable access to mental and physical health, can help to narrow disparities in later life cognitive impairment,” Dr. Manly said. “Two other areas of focus for policy makers are the shortage in the workforce of dementia care specialists, and paid family leave for caregiving.”
Acknowledging the needs of the historically underrepresented
Lealani Mae Acosta, MD, MPH, associate professor of neurology at Vanderbilt University Medical Center, Nashville, Tenn., applauded the investigators for their “conscious effort to expand representation of historically underrepresented minorities.”
The findings themselves support what has been previously reported, Dr. Acosta said in an interview, including the disproportionate burden of cognitive disorders among people of color and those with less education.
Clinicians need to recognize that certain patient groups face increased risks of cognitive disorders, and should be screened accordingly, Dr. Acosta said, noting that all aging patients should undergo such screening. The push for screening should also occur on a community level, along with efforts to build trust between at-risk populations and health care providers.
While Dr. Acosta reiterated the importance of these new data from Black and Hispanic individuals, she noted that gaps in representation remain, and methods of characterizing populations deserve refinement.
“I’m a little bit biased because I’m an Asian physician,” Dr. Acosta said. “As much as I’m glad that they’re highlighting these different disparities, there weren’t enough [participants in] specific subgroups like American Indian or Alaska Native, Asian, Native Hawaiian or Pacific Islander, to be able to identify specific trends within [those groups] that are, again, historically underrepresented patient populations.”
Grouping all people of Asian descent may also be an oversimplification, she added, as differences may exist between individuals originating from different countries.
“We always have to be careful about lumping certain groups together in analyses,” Dr. Acosta said. “That’s just another reminder to us – as clinicians, as researchers – that we need to do better by our patients by expanding research opportunities, and really studying these historically underrepresented populations.”
The study was supported by the National Institute on Aging. The investigators disclosed additional relationships with the Alzheimer’s Association and the National Institutes of Health. Dr. Acosta reported no relevant competing interests.
based on new U.S. data from The Health and Retirement Study (HRS).
These inequities likely stem from structural racism and income inequality, necessitating a multifaceted response at an institutional level, according to lead author Jennifer J. Manly, PhD, a professor of neuropsychology in neurology at the Gertrude H. Sergievsky Center and the Taub Institute for Research in Aging and Alzheimer’s Disease at Columbia University, New York.
A more representative dataset
Between 2001 and 2003, a subset of HRS participants underwent extensive neuropsychological assessment in the Aging, Demographics, and Memory Study (ADAMS), providing data which have since been cited by hundreds of published studies, the investigators wrote in JAMA Neurology. Those data, however, failed to accurately represent the U.S. population at the time, and have not been updated since.
“The ADAMS substudy was small, and the limited inclusion of Black, Hispanic, and American Indian or Alaska Native participants contributed to lack of precision of estimates among minoritized racial and ethnic groups that have been shown to experience a higher burden of cognitive impairment and dementia,” Dr. Manly and colleagues wrote.
The present analysis used a more representative dataset from HRS participants who were 65 years or older in 2016. From June 2016 to October 2017, 3,496 of these individuals underwent comprehensive neuropsychological test battery and informant interview, with dementia and MCI classified based on standard diagnostic criteria.
In total, 393 people were classified with dementia (10%), while 804 had MCI (22%), both of which approximate estimates reported by previous studies, according to the investigators. In further alignment with past research, age was a clear risk factor; each 5-year increment added 17% and 95% increased risk of MCI and dementia, respectively.
Compared with college-educated participants, individuals who did not graduate from high school had a 60% increased risk for both dementia (odds ratio, 1.6; 95% confidence interval, 1.1-2.3) and MCI (OR, 1.6; 95% CI, 1.2-2.2). Other educational strata were not associated with significant differences in risk.
Compared with White participants, Black individuals had an 80% increased risk of dementia (OR, 1.8; 95% CI, 1.2-2.7), but no increased risk of MCI. Conversely, non-White Hispanic individuals had a 40% increased risk of MCI (OR, 1.4; 95% CI, 1.0-2.0), but no increased risk of dementia, compared with White participants.
“Older adults racialized as Black and Hispanic are more likely to develop cognitive impairment and dementia because of historical and current structural racism and income inequality that restrict access to brain-health benefits and increase exposure to harm,” Dr. Manly said in a written comment.
These inequities deserve a comprehensive response, she added.
“Actions and policies that decrease discriminatory and aggressive policing policies, invest in schools that serve children that are racialized as Black and Hispanic, repair housing and economic inequalities, and provide equitable access to mental and physical health, can help to narrow disparities in later life cognitive impairment,” Dr. Manly said. “Two other areas of focus for policy makers are the shortage in the workforce of dementia care specialists, and paid family leave for caregiving.”
Acknowledging the needs of the historically underrepresented
Lealani Mae Acosta, MD, MPH, associate professor of neurology at Vanderbilt University Medical Center, Nashville, Tenn., applauded the investigators for their “conscious effort to expand representation of historically underrepresented minorities.”
The findings themselves support what has been previously reported, Dr. Acosta said in an interview, including the disproportionate burden of cognitive disorders among people of color and those with less education.
Clinicians need to recognize that certain patient groups face increased risks of cognitive disorders, and should be screened accordingly, Dr. Acosta said, noting that all aging patients should undergo such screening. The push for screening should also occur on a community level, along with efforts to build trust between at-risk populations and health care providers.
While Dr. Acosta reiterated the importance of these new data from Black and Hispanic individuals, she noted that gaps in representation remain, and methods of characterizing populations deserve refinement.
“I’m a little bit biased because I’m an Asian physician,” Dr. Acosta said. “As much as I’m glad that they’re highlighting these different disparities, there weren’t enough [participants in] specific subgroups like American Indian or Alaska Native, Asian, Native Hawaiian or Pacific Islander, to be able to identify specific trends within [those groups] that are, again, historically underrepresented patient populations.”
Grouping all people of Asian descent may also be an oversimplification, she added, as differences may exist between individuals originating from different countries.
“We always have to be careful about lumping certain groups together in analyses,” Dr. Acosta said. “That’s just another reminder to us – as clinicians, as researchers – that we need to do better by our patients by expanding research opportunities, and really studying these historically underrepresented populations.”
The study was supported by the National Institute on Aging. The investigators disclosed additional relationships with the Alzheimer’s Association and the National Institutes of Health. Dr. Acosta reported no relevant competing interests.
based on new U.S. data from The Health and Retirement Study (HRS).
These inequities likely stem from structural racism and income inequality, necessitating a multifaceted response at an institutional level, according to lead author Jennifer J. Manly, PhD, a professor of neuropsychology in neurology at the Gertrude H. Sergievsky Center and the Taub Institute for Research in Aging and Alzheimer’s Disease at Columbia University, New York.
A more representative dataset
Between 2001 and 2003, a subset of HRS participants underwent extensive neuropsychological assessment in the Aging, Demographics, and Memory Study (ADAMS), providing data which have since been cited by hundreds of published studies, the investigators wrote in JAMA Neurology. Those data, however, failed to accurately represent the U.S. population at the time, and have not been updated since.
“The ADAMS substudy was small, and the limited inclusion of Black, Hispanic, and American Indian or Alaska Native participants contributed to lack of precision of estimates among minoritized racial and ethnic groups that have been shown to experience a higher burden of cognitive impairment and dementia,” Dr. Manly and colleagues wrote.
The present analysis used a more representative dataset from HRS participants who were 65 years or older in 2016. From June 2016 to October 2017, 3,496 of these individuals underwent comprehensive neuropsychological test battery and informant interview, with dementia and MCI classified based on standard diagnostic criteria.
In total, 393 people were classified with dementia (10%), while 804 had MCI (22%), both of which approximate estimates reported by previous studies, according to the investigators. In further alignment with past research, age was a clear risk factor; each 5-year increment added 17% and 95% increased risk of MCI and dementia, respectively.
Compared with college-educated participants, individuals who did not graduate from high school had a 60% increased risk for both dementia (odds ratio, 1.6; 95% confidence interval, 1.1-2.3) and MCI (OR, 1.6; 95% CI, 1.2-2.2). Other educational strata were not associated with significant differences in risk.
Compared with White participants, Black individuals had an 80% increased risk of dementia (OR, 1.8; 95% CI, 1.2-2.7), but no increased risk of MCI. Conversely, non-White Hispanic individuals had a 40% increased risk of MCI (OR, 1.4; 95% CI, 1.0-2.0), but no increased risk of dementia, compared with White participants.
“Older adults racialized as Black and Hispanic are more likely to develop cognitive impairment and dementia because of historical and current structural racism and income inequality that restrict access to brain-health benefits and increase exposure to harm,” Dr. Manly said in a written comment.
These inequities deserve a comprehensive response, she added.
“Actions and policies that decrease discriminatory and aggressive policing policies, invest in schools that serve children that are racialized as Black and Hispanic, repair housing and economic inequalities, and provide equitable access to mental and physical health, can help to narrow disparities in later life cognitive impairment,” Dr. Manly said. “Two other areas of focus for policy makers are the shortage in the workforce of dementia care specialists, and paid family leave for caregiving.”
Acknowledging the needs of the historically underrepresented
Lealani Mae Acosta, MD, MPH, associate professor of neurology at Vanderbilt University Medical Center, Nashville, Tenn., applauded the investigators for their “conscious effort to expand representation of historically underrepresented minorities.”
The findings themselves support what has been previously reported, Dr. Acosta said in an interview, including the disproportionate burden of cognitive disorders among people of color and those with less education.
Clinicians need to recognize that certain patient groups face increased risks of cognitive disorders, and should be screened accordingly, Dr. Acosta said, noting that all aging patients should undergo such screening. The push for screening should also occur on a community level, along with efforts to build trust between at-risk populations and health care providers.
While Dr. Acosta reiterated the importance of these new data from Black and Hispanic individuals, she noted that gaps in representation remain, and methods of characterizing populations deserve refinement.
“I’m a little bit biased because I’m an Asian physician,” Dr. Acosta said. “As much as I’m glad that they’re highlighting these different disparities, there weren’t enough [participants in] specific subgroups like American Indian or Alaska Native, Asian, Native Hawaiian or Pacific Islander, to be able to identify specific trends within [those groups] that are, again, historically underrepresented patient populations.”
Grouping all people of Asian descent may also be an oversimplification, she added, as differences may exist between individuals originating from different countries.
“We always have to be careful about lumping certain groups together in analyses,” Dr. Acosta said. “That’s just another reminder to us – as clinicians, as researchers – that we need to do better by our patients by expanding research opportunities, and really studying these historically underrepresented populations.”
The study was supported by the National Institute on Aging. The investigators disclosed additional relationships with the Alzheimer’s Association and the National Institutes of Health. Dr. Acosta reported no relevant competing interests.
FROM JAMA NEUROLOGY
Nicotine blocks estrogen production in women’s brains
VIENNA – The production of estrogen in the thalamus appears to be curtailed by just one dose of nicotine, equivalent to that in a cigarette, reveals a whole brain analysis of healthy women in the first study of its kind.
The findings were presented at the 35th European College of Neuropsychopharmacology (ECNP) Congress.
The researchers performed both MRI and positron emission tomography (PET) scans in 10 healthy women using a tracer that binds to aromatase, also known as estrogen synthase.
They found that, following an intranasal spray delivering 1 mg of nicotine, there was a significant reduction in estrogen synthase in both the right and left thalamus.
“For the first time, we can see that nicotine works to shut down the estrogen production mechanism in the brains of women,” said lead researcher Erika Comasco, PhD, department of neuroscience, Uppsala University, Sweden, in a release.
“We were surprised to see that this effect could be seen even with a single dose of nicotine, equivalent to just one cigarette, showing how powerful the effects of smoking are on a woman’s brain.”
Emphasizing the preliminary nature of the study and the need for a larger sample, she added: “We’re still not sure what the behavioral or cognitive outcomes are, only that nicotine acts on this area of the brain.
“However, we note that the affected brain system is a target for addictive drugs, such as nicotine.”
Previous research has revealed that women are less successful at quitting smoking than men, and appear to be more resistant to nicotine replacement therapy, and experience more relapses.
There is evidence to suggest that there is a complex interaction between sex and steroid hormones and the reward effect of nicotine, modulated by the dopaminergic system.
Moreover, women who smoke enter menopause earlier than nonsmokers, and have lower plasma estrogen levels, Dr. Camasco told this news organization.
Dr. Comasco explained that “besides its role in reproductive function and sexual behavior, estrogen has an impact on the brain wherever there are receptors, which is basically regions that are related to emotional regulation, cognitive function, and so on.”
Estrogen, she continued, has two main mechanisms of action, via dopaminergic and serotonergic signaling. However, levels of the hormone cannot be measured directly in the brain.
The researchers therefore turned to estrogen synthase, which regulates the synthesis of estrogen, and is highly expressed in the limbic system, a brain region associated with addiction.
Moreover, estrogen synthase levels can be measured in vivo, and previous animal studies have indicated that nicotine inhibits estrogen synthase.
To investigate its impact in humans, the researchers performed structural MRI and two 11C-cetrozole PET scans in 10 healthy women.
The assessments were performed before and after the nasal administration of 1 mg of nicotine, the dose contained in one cigarette, via two sprays of a nasal spray each containing 0.5 mg of nicotine.
A whole brain analysis was then used to determine changes in nondisplaceable binding potential of 11C-cetrozole to estrogen synthase between the two scans to indicate the availability of the enzyme at the two time points.
The results showed that, at baseline, high availability of estrogen synthase was observed in the thalamus, hypothalamus, and amygdala, with the highest levels in the right and left thalamus.
However, nicotine exposure was associated with a significant reduction in estrogen binding bilaterally in the thalamus when averaged across the participants (P < .01).
Region-of-interest analysis using within-individual voxel-wise comparison confirmed reduced estrogen synthase levels in both the right and left thalamus (P < .05), as well as in the subthalamic area.
Next, Dr. Comasco would like to test the impact of nicotine on estrogen synthase in men.
While men have lower levels of estrogen then women, “the reaction will take place anyway,” she said, although the “impact would be different.”
She would also like to look at the behavioral effects of reductions in estrogen synthase, and look at the effect of nicotine from a functional point of view.
Wim van den Brink, MD, PhD, professor of psychiatry and addiction at the Academic Medical Center, University of Amsterdam, commented that this is an “important first finding.”
“Smoking has many adverse effects in men and in women, but this particular effect of nicotine on the reduction of estrogen production in women was not known before,” he added in the release.
However, he underlined that tobacco addition is a “complex disorder” and it is “unlikely that this specific effect of nicotine on the thalamus explains all the observed differences in the development, treatment, and outcomes between male and female smokers.”
“It is still a long way from a nicotine-induced reduction in estrogen production to a reduced risk of nicotine addiction and negative effects of treatment and relapse in female cigarette smokers, but this work merits further investigation,” Dr. van den Brink said.
The study was funded by the Science for Life Laboratory/Uppsala University.
No relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
VIENNA – The production of estrogen in the thalamus appears to be curtailed by just one dose of nicotine, equivalent to that in a cigarette, reveals a whole brain analysis of healthy women in the first study of its kind.
The findings were presented at the 35th European College of Neuropsychopharmacology (ECNP) Congress.
The researchers performed both MRI and positron emission tomography (PET) scans in 10 healthy women using a tracer that binds to aromatase, also known as estrogen synthase.
They found that, following an intranasal spray delivering 1 mg of nicotine, there was a significant reduction in estrogen synthase in both the right and left thalamus.
“For the first time, we can see that nicotine works to shut down the estrogen production mechanism in the brains of women,” said lead researcher Erika Comasco, PhD, department of neuroscience, Uppsala University, Sweden, in a release.
“We were surprised to see that this effect could be seen even with a single dose of nicotine, equivalent to just one cigarette, showing how powerful the effects of smoking are on a woman’s brain.”
Emphasizing the preliminary nature of the study and the need for a larger sample, she added: “We’re still not sure what the behavioral or cognitive outcomes are, only that nicotine acts on this area of the brain.
“However, we note that the affected brain system is a target for addictive drugs, such as nicotine.”
Previous research has revealed that women are less successful at quitting smoking than men, and appear to be more resistant to nicotine replacement therapy, and experience more relapses.
There is evidence to suggest that there is a complex interaction between sex and steroid hormones and the reward effect of nicotine, modulated by the dopaminergic system.
Moreover, women who smoke enter menopause earlier than nonsmokers, and have lower plasma estrogen levels, Dr. Camasco told this news organization.
Dr. Comasco explained that “besides its role in reproductive function and sexual behavior, estrogen has an impact on the brain wherever there are receptors, which is basically regions that are related to emotional regulation, cognitive function, and so on.”
Estrogen, she continued, has two main mechanisms of action, via dopaminergic and serotonergic signaling. However, levels of the hormone cannot be measured directly in the brain.
The researchers therefore turned to estrogen synthase, which regulates the synthesis of estrogen, and is highly expressed in the limbic system, a brain region associated with addiction.
Moreover, estrogen synthase levels can be measured in vivo, and previous animal studies have indicated that nicotine inhibits estrogen synthase.
To investigate its impact in humans, the researchers performed structural MRI and two 11C-cetrozole PET scans in 10 healthy women.
The assessments were performed before and after the nasal administration of 1 mg of nicotine, the dose contained in one cigarette, via two sprays of a nasal spray each containing 0.5 mg of nicotine.
A whole brain analysis was then used to determine changes in nondisplaceable binding potential of 11C-cetrozole to estrogen synthase between the two scans to indicate the availability of the enzyme at the two time points.
The results showed that, at baseline, high availability of estrogen synthase was observed in the thalamus, hypothalamus, and amygdala, with the highest levels in the right and left thalamus.
However, nicotine exposure was associated with a significant reduction in estrogen binding bilaterally in the thalamus when averaged across the participants (P < .01).
Region-of-interest analysis using within-individual voxel-wise comparison confirmed reduced estrogen synthase levels in both the right and left thalamus (P < .05), as well as in the subthalamic area.
Next, Dr. Comasco would like to test the impact of nicotine on estrogen synthase in men.
While men have lower levels of estrogen then women, “the reaction will take place anyway,” she said, although the “impact would be different.”
She would also like to look at the behavioral effects of reductions in estrogen synthase, and look at the effect of nicotine from a functional point of view.
Wim van den Brink, MD, PhD, professor of psychiatry and addiction at the Academic Medical Center, University of Amsterdam, commented that this is an “important first finding.”
“Smoking has many adverse effects in men and in women, but this particular effect of nicotine on the reduction of estrogen production in women was not known before,” he added in the release.
However, he underlined that tobacco addition is a “complex disorder” and it is “unlikely that this specific effect of nicotine on the thalamus explains all the observed differences in the development, treatment, and outcomes between male and female smokers.”
“It is still a long way from a nicotine-induced reduction in estrogen production to a reduced risk of nicotine addiction and negative effects of treatment and relapse in female cigarette smokers, but this work merits further investigation,” Dr. van den Brink said.
The study was funded by the Science for Life Laboratory/Uppsala University.
No relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
VIENNA – The production of estrogen in the thalamus appears to be curtailed by just one dose of nicotine, equivalent to that in a cigarette, reveals a whole brain analysis of healthy women in the first study of its kind.
The findings were presented at the 35th European College of Neuropsychopharmacology (ECNP) Congress.
The researchers performed both MRI and positron emission tomography (PET) scans in 10 healthy women using a tracer that binds to aromatase, also known as estrogen synthase.
They found that, following an intranasal spray delivering 1 mg of nicotine, there was a significant reduction in estrogen synthase in both the right and left thalamus.
“For the first time, we can see that nicotine works to shut down the estrogen production mechanism in the brains of women,” said lead researcher Erika Comasco, PhD, department of neuroscience, Uppsala University, Sweden, in a release.
“We were surprised to see that this effect could be seen even with a single dose of nicotine, equivalent to just one cigarette, showing how powerful the effects of smoking are on a woman’s brain.”
Emphasizing the preliminary nature of the study and the need for a larger sample, she added: “We’re still not sure what the behavioral or cognitive outcomes are, only that nicotine acts on this area of the brain.
“However, we note that the affected brain system is a target for addictive drugs, such as nicotine.”
Previous research has revealed that women are less successful at quitting smoking than men, and appear to be more resistant to nicotine replacement therapy, and experience more relapses.
There is evidence to suggest that there is a complex interaction between sex and steroid hormones and the reward effect of nicotine, modulated by the dopaminergic system.
Moreover, women who smoke enter menopause earlier than nonsmokers, and have lower plasma estrogen levels, Dr. Camasco told this news organization.
Dr. Comasco explained that “besides its role in reproductive function and sexual behavior, estrogen has an impact on the brain wherever there are receptors, which is basically regions that are related to emotional regulation, cognitive function, and so on.”
Estrogen, she continued, has two main mechanisms of action, via dopaminergic and serotonergic signaling. However, levels of the hormone cannot be measured directly in the brain.
The researchers therefore turned to estrogen synthase, which regulates the synthesis of estrogen, and is highly expressed in the limbic system, a brain region associated with addiction.
Moreover, estrogen synthase levels can be measured in vivo, and previous animal studies have indicated that nicotine inhibits estrogen synthase.
To investigate its impact in humans, the researchers performed structural MRI and two 11C-cetrozole PET scans in 10 healthy women.
The assessments were performed before and after the nasal administration of 1 mg of nicotine, the dose contained in one cigarette, via two sprays of a nasal spray each containing 0.5 mg of nicotine.
A whole brain analysis was then used to determine changes in nondisplaceable binding potential of 11C-cetrozole to estrogen synthase between the two scans to indicate the availability of the enzyme at the two time points.
The results showed that, at baseline, high availability of estrogen synthase was observed in the thalamus, hypothalamus, and amygdala, with the highest levels in the right and left thalamus.
However, nicotine exposure was associated with a significant reduction in estrogen binding bilaterally in the thalamus when averaged across the participants (P < .01).
Region-of-interest analysis using within-individual voxel-wise comparison confirmed reduced estrogen synthase levels in both the right and left thalamus (P < .05), as well as in the subthalamic area.
Next, Dr. Comasco would like to test the impact of nicotine on estrogen synthase in men.
While men have lower levels of estrogen then women, “the reaction will take place anyway,” she said, although the “impact would be different.”
She would also like to look at the behavioral effects of reductions in estrogen synthase, and look at the effect of nicotine from a functional point of view.
Wim van den Brink, MD, PhD, professor of psychiatry and addiction at the Academic Medical Center, University of Amsterdam, commented that this is an “important first finding.”
“Smoking has many adverse effects in men and in women, but this particular effect of nicotine on the reduction of estrogen production in women was not known before,” he added in the release.
However, he underlined that tobacco addition is a “complex disorder” and it is “unlikely that this specific effect of nicotine on the thalamus explains all the observed differences in the development, treatment, and outcomes between male and female smokers.”
“It is still a long way from a nicotine-induced reduction in estrogen production to a reduced risk of nicotine addiction and negative effects of treatment and relapse in female cigarette smokers, but this work merits further investigation,” Dr. van den Brink said.
The study was funded by the Science for Life Laboratory/Uppsala University.
No relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
AT ECNP 2022
Sexual assault–related visits to the ED are on the rise
Data from the Federal Bureau of Investigation show an increase in reported rapes and sexual assaults (SAs) since 2006, and studies of victims show an increased risk of conditions such as suicidal ideation, PTSD, depression, substance use, and chronic conditions, write Emily L. Vogt of the University of Michigan, Ann Arbor, and colleagues.
However, trends and disparities in ED use by adults seeking care following SA have not been explored, they said.
For a study that was published in JAMA Network Open, researchers reviewed data from the Nationwide Emergency Department Sample (NEDS), a large, nationally representative database managed by the Agency for Healthcare Research and Quality. The dataset consisted of 120 million to 143 million weighted ED visits reported annually from 2006 through 2016. The study population included adults aged 18-65 years who had made an ED visit that was recorded in the NEDS and that was coded as an SA. SA was defined using ICD-9 codes until the fourth quarter of 2015, at which time ICD-10 codes came into use.
Overall, the number of SA-related ED visits increased by 1,533.0% during the study period, from 3,607 in 2006 to 55,296 in 2019. The average annual percentage change was 23.0% (P < .001). The greatest increase occurred from 2015 to 2016, when annual visits increased from 17,709 to 47,732. This increase likely reflected the updated ICD-10 codes, in which there are categories for suspected adult rape, confirmed adult rape, and adult forced sexual exploitation, the researchers note.
Patients presenting to the ED after an SA were mainly women (91.5%). Individuals aged 18-25 years accounted for nearly half of the presentations. Individuals in the lowest and second-lowest income quartiles also were overrepresented.
Despite the increased presentation to EDs, admission rates for SA decreased, from 12.6% to 4.3%, the researchers note. Patients who were older and were insured through Medicaid were more likely to be admitted than persons of other demographic groups.
The researchers also found that increases in ED presentations outpaced increases in SA reports to law enforcement. They compared the ED trends with FBI-reported rapes/SAs from 2015 to 2019 and found increases of 7% and 22% during the times of ICD-9 and ICD-10 codes, respectively. However, in 2019, the number of SA survivors who sought ED care remained below the number who reported to law enforcement (55,296 vs. 139,815, as determined on the basis of revised SA definitions).
“Although the association between increased coding specificity and documentation of SA is still unclear, ICD-10 likely contributed to increased ED documentation of SA,” but the data show steady increases that are independent of the coding change, the researchers write.
The study findings were limited by several factors, including the potential for multiple representations of patients, coding errors associated with the NEDS database, and the reliance on voluntary reports in the NEDS and FBI datasets, the researchers note. The results were strengthened by the large, diverse sample size and by the inclusion of hospital admissions and crime data for comparison, they say.
“As few as 21% of survivors seek medical care after SA, meaning that the survivors captured in this study represent a fraction of total SA-related care need,” the researchers write. “Our finding that most SA ED visits are by young, female, and low-income survivors can inform policy changes to better support these individuals,” which could include the development of outpatient and longitudinal care settings to better serve these populations, they conclude.
Better understanding not only of the trends underlying SA reporting but also of the demographics of survivors who seek treatment and evaluation after SA is vital, said Robert Glatter, MD, in an interview.
“Being able to better understand how social and societal movements affect a patient’s comfort in reporting an SA is vital in tracking the numbers of people who seek care in the ED,” said Dr. Glatter, an emergency medicine physician at Lenox Hill Hospital at Northwell Health, New York, and also of Hofstra University, Hempstead, N.Y.
Dr. Glatter said he was not surprised by the significant increase in sexual assault presentations, especially in light of increased awareness and the influence of the #MeToo movement and other social justice movements over the past decade.
“While I believe that victims of sexual violence may now feel more empowered to report an assault, the volume of SA that go unreported remains a serious public health issue and concern” in the United States and globally, he emphasized.
A key message from the current study is that there is a need for investment in “compassionate and comprehensive care for all survivors of SA,” Dr. Glatter said. “This includes recognition of the extensive mental health consequences of SA that can lead to not only depression, PTSD, and anxiety but also to suicidal ideation and suicide. The longer-term medical effects become life altering, permeating families and future generations,” he emphasized.
“As a society, we must also place a strong emphasis on caring for all SA survivors, but particularly those who come from economically or socially disadvantaged backgrounds who are uninsured or underinsured,” Dr. Glatter said. Issues of race, gender identity, and sexual identity among SA survivors also must be taken into consideration, he added.
“We need to better understand how our health care system can provide more nuanced follow-up care and reporting for survivors in outpatient settings. … Making access easier, while ensuring confidentiality, will allow more survivors of SA to seek treatment and care,” he said. “We also need to understand how using forensic nurses in this capacity, and beyond the ED, can better serve minority and racially diverse communities” and to increase the recruitment and training of such specialized nurses to care for SA victims, Dr. Glatter noted.
The study was supported by internal funding from the University of Michigan and the department of obstetrics and gynecology. Corresponding author Erica C. Marsh, MD, has received personal fees from Myovant Sciences and Pfizer unrelated to the current study. Dr. Glatter has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Data from the Federal Bureau of Investigation show an increase in reported rapes and sexual assaults (SAs) since 2006, and studies of victims show an increased risk of conditions such as suicidal ideation, PTSD, depression, substance use, and chronic conditions, write Emily L. Vogt of the University of Michigan, Ann Arbor, and colleagues.
However, trends and disparities in ED use by adults seeking care following SA have not been explored, they said.
For a study that was published in JAMA Network Open, researchers reviewed data from the Nationwide Emergency Department Sample (NEDS), a large, nationally representative database managed by the Agency for Healthcare Research and Quality. The dataset consisted of 120 million to 143 million weighted ED visits reported annually from 2006 through 2016. The study population included adults aged 18-65 years who had made an ED visit that was recorded in the NEDS and that was coded as an SA. SA was defined using ICD-9 codes until the fourth quarter of 2015, at which time ICD-10 codes came into use.
Overall, the number of SA-related ED visits increased by 1,533.0% during the study period, from 3,607 in 2006 to 55,296 in 2019. The average annual percentage change was 23.0% (P < .001). The greatest increase occurred from 2015 to 2016, when annual visits increased from 17,709 to 47,732. This increase likely reflected the updated ICD-10 codes, in which there are categories for suspected adult rape, confirmed adult rape, and adult forced sexual exploitation, the researchers note.
Patients presenting to the ED after an SA were mainly women (91.5%). Individuals aged 18-25 years accounted for nearly half of the presentations. Individuals in the lowest and second-lowest income quartiles also were overrepresented.
Despite the increased presentation to EDs, admission rates for SA decreased, from 12.6% to 4.3%, the researchers note. Patients who were older and were insured through Medicaid were more likely to be admitted than persons of other demographic groups.
The researchers also found that increases in ED presentations outpaced increases in SA reports to law enforcement. They compared the ED trends with FBI-reported rapes/SAs from 2015 to 2019 and found increases of 7% and 22% during the times of ICD-9 and ICD-10 codes, respectively. However, in 2019, the number of SA survivors who sought ED care remained below the number who reported to law enforcement (55,296 vs. 139,815, as determined on the basis of revised SA definitions).
“Although the association between increased coding specificity and documentation of SA is still unclear, ICD-10 likely contributed to increased ED documentation of SA,” but the data show steady increases that are independent of the coding change, the researchers write.
The study findings were limited by several factors, including the potential for multiple representations of patients, coding errors associated with the NEDS database, and the reliance on voluntary reports in the NEDS and FBI datasets, the researchers note. The results were strengthened by the large, diverse sample size and by the inclusion of hospital admissions and crime data for comparison, they say.
“As few as 21% of survivors seek medical care after SA, meaning that the survivors captured in this study represent a fraction of total SA-related care need,” the researchers write. “Our finding that most SA ED visits are by young, female, and low-income survivors can inform policy changes to better support these individuals,” which could include the development of outpatient and longitudinal care settings to better serve these populations, they conclude.
Better understanding not only of the trends underlying SA reporting but also of the demographics of survivors who seek treatment and evaluation after SA is vital, said Robert Glatter, MD, in an interview.
“Being able to better understand how social and societal movements affect a patient’s comfort in reporting an SA is vital in tracking the numbers of people who seek care in the ED,” said Dr. Glatter, an emergency medicine physician at Lenox Hill Hospital at Northwell Health, New York, and also of Hofstra University, Hempstead, N.Y.
Dr. Glatter said he was not surprised by the significant increase in sexual assault presentations, especially in light of increased awareness and the influence of the #MeToo movement and other social justice movements over the past decade.
“While I believe that victims of sexual violence may now feel more empowered to report an assault, the volume of SA that go unreported remains a serious public health issue and concern” in the United States and globally, he emphasized.
A key message from the current study is that there is a need for investment in “compassionate and comprehensive care for all survivors of SA,” Dr. Glatter said. “This includes recognition of the extensive mental health consequences of SA that can lead to not only depression, PTSD, and anxiety but also to suicidal ideation and suicide. The longer-term medical effects become life altering, permeating families and future generations,” he emphasized.
“As a society, we must also place a strong emphasis on caring for all SA survivors, but particularly those who come from economically or socially disadvantaged backgrounds who are uninsured or underinsured,” Dr. Glatter said. Issues of race, gender identity, and sexual identity among SA survivors also must be taken into consideration, he added.
“We need to better understand how our health care system can provide more nuanced follow-up care and reporting for survivors in outpatient settings. … Making access easier, while ensuring confidentiality, will allow more survivors of SA to seek treatment and care,” he said. “We also need to understand how using forensic nurses in this capacity, and beyond the ED, can better serve minority and racially diverse communities” and to increase the recruitment and training of such specialized nurses to care for SA victims, Dr. Glatter noted.
The study was supported by internal funding from the University of Michigan and the department of obstetrics and gynecology. Corresponding author Erica C. Marsh, MD, has received personal fees from Myovant Sciences and Pfizer unrelated to the current study. Dr. Glatter has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Data from the Federal Bureau of Investigation show an increase in reported rapes and sexual assaults (SAs) since 2006, and studies of victims show an increased risk of conditions such as suicidal ideation, PTSD, depression, substance use, and chronic conditions, write Emily L. Vogt of the University of Michigan, Ann Arbor, and colleagues.
However, trends and disparities in ED use by adults seeking care following SA have not been explored, they said.
For a study that was published in JAMA Network Open, researchers reviewed data from the Nationwide Emergency Department Sample (NEDS), a large, nationally representative database managed by the Agency for Healthcare Research and Quality. The dataset consisted of 120 million to 143 million weighted ED visits reported annually from 2006 through 2016. The study population included adults aged 18-65 years who had made an ED visit that was recorded in the NEDS and that was coded as an SA. SA was defined using ICD-9 codes until the fourth quarter of 2015, at which time ICD-10 codes came into use.
Overall, the number of SA-related ED visits increased by 1,533.0% during the study period, from 3,607 in 2006 to 55,296 in 2019. The average annual percentage change was 23.0% (P < .001). The greatest increase occurred from 2015 to 2016, when annual visits increased from 17,709 to 47,732. This increase likely reflected the updated ICD-10 codes, in which there are categories for suspected adult rape, confirmed adult rape, and adult forced sexual exploitation, the researchers note.
Patients presenting to the ED after an SA were mainly women (91.5%). Individuals aged 18-25 years accounted for nearly half of the presentations. Individuals in the lowest and second-lowest income quartiles also were overrepresented.
Despite the increased presentation to EDs, admission rates for SA decreased, from 12.6% to 4.3%, the researchers note. Patients who were older and were insured through Medicaid were more likely to be admitted than persons of other demographic groups.
The researchers also found that increases in ED presentations outpaced increases in SA reports to law enforcement. They compared the ED trends with FBI-reported rapes/SAs from 2015 to 2019 and found increases of 7% and 22% during the times of ICD-9 and ICD-10 codes, respectively. However, in 2019, the number of SA survivors who sought ED care remained below the number who reported to law enforcement (55,296 vs. 139,815, as determined on the basis of revised SA definitions).
“Although the association between increased coding specificity and documentation of SA is still unclear, ICD-10 likely contributed to increased ED documentation of SA,” but the data show steady increases that are independent of the coding change, the researchers write.
The study findings were limited by several factors, including the potential for multiple representations of patients, coding errors associated with the NEDS database, and the reliance on voluntary reports in the NEDS and FBI datasets, the researchers note. The results were strengthened by the large, diverse sample size and by the inclusion of hospital admissions and crime data for comparison, they say.
“As few as 21% of survivors seek medical care after SA, meaning that the survivors captured in this study represent a fraction of total SA-related care need,” the researchers write. “Our finding that most SA ED visits are by young, female, and low-income survivors can inform policy changes to better support these individuals,” which could include the development of outpatient and longitudinal care settings to better serve these populations, they conclude.
Better understanding not only of the trends underlying SA reporting but also of the demographics of survivors who seek treatment and evaluation after SA is vital, said Robert Glatter, MD, in an interview.
“Being able to better understand how social and societal movements affect a patient’s comfort in reporting an SA is vital in tracking the numbers of people who seek care in the ED,” said Dr. Glatter, an emergency medicine physician at Lenox Hill Hospital at Northwell Health, New York, and also of Hofstra University, Hempstead, N.Y.
Dr. Glatter said he was not surprised by the significant increase in sexual assault presentations, especially in light of increased awareness and the influence of the #MeToo movement and other social justice movements over the past decade.
“While I believe that victims of sexual violence may now feel more empowered to report an assault, the volume of SA that go unreported remains a serious public health issue and concern” in the United States and globally, he emphasized.
A key message from the current study is that there is a need for investment in “compassionate and comprehensive care for all survivors of SA,” Dr. Glatter said. “This includes recognition of the extensive mental health consequences of SA that can lead to not only depression, PTSD, and anxiety but also to suicidal ideation and suicide. The longer-term medical effects become life altering, permeating families and future generations,” he emphasized.
“As a society, we must also place a strong emphasis on caring for all SA survivors, but particularly those who come from economically or socially disadvantaged backgrounds who are uninsured or underinsured,” Dr. Glatter said. Issues of race, gender identity, and sexual identity among SA survivors also must be taken into consideration, he added.
“We need to better understand how our health care system can provide more nuanced follow-up care and reporting for survivors in outpatient settings. … Making access easier, while ensuring confidentiality, will allow more survivors of SA to seek treatment and care,” he said. “We also need to understand how using forensic nurses in this capacity, and beyond the ED, can better serve minority and racially diverse communities” and to increase the recruitment and training of such specialized nurses to care for SA victims, Dr. Glatter noted.
The study was supported by internal funding from the University of Michigan and the department of obstetrics and gynecology. Corresponding author Erica C. Marsh, MD, has received personal fees from Myovant Sciences and Pfizer unrelated to the current study. Dr. Glatter has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Patients with schizophrenia may be twice as likely to develop dementia
Results from a review and meta-analysis of almost 13 million total participants from nine countries showed that, across multiple different psychotic disorders, there was a 2.5-fold higher risk of developing dementia later in life compared with individuals who did not have a disorder. This was regardless of the age at which the patients first developed the mental illness.
Moreover, participants with a psychotic disorder tended to be younger than average when diagnosed with dementia. Two studies showed that those with psychotic disorders were more likely to be diagnosed with dementia as early as in their 60s.
“The findings add to a growing body of evidence linking psychiatric disorders with later cognitive decline and dementia,” senior investigator Jean Stafford, PhD, a research fellow at MRC Unit for Lifelong Health and Ageing, University College London, told this news organization.
Dr. Stafford noted that the results highlight the importance of being aware of and watchful for symptoms of cognitive decline in patients with psychotic disorders in mid- and late life.
“In addition, given that people with psychotic disorders are at higher risk of experiencing multiple health conditions, including dementia, managing overall physical and mental health in this group is crucial,” she said.
The findings were published online in Psychological Medicine.
Bringing the evidence together
There is increasing evidence that multiple psychiatric symptoms and diagnoses are associated with cognitive decline and dementia, with particularly strong evidence for late-life depression, Dr. Stafford said.
“However, the relationship between psychotic disorders and dementia is less well-established,” she added.
Last year, her team published a study showing a strong association between very late onset psychotic disorders, defined as first diagnosed after age 60 years, and increased risk for dementia in Swedish population register data.
“We also became aware of several other large studies on the topic published in the last few years and realized that an up-to-date systematic review and meta-analysis was needed to bring together the evidence, specifically focusing on longitudinal studies,” Dr. Stafford said.
The researchers searched four databases of prospective and retrospective longitudinal studies published through March 2022. Studies were required to focus on adults aged 18 years or older with a clinical diagnosis of a nonaffective psychotic disorder and a comparison group consisting of adults without a nonaffective psychotic disorder.
Of 9,496 papers, the investigators selected 11 published from 2003 to 2022 that met criteria for inclusion in their meta-analysis (12,997,101 participants), with follow-up periods ranging from 1.57 to 33 years.
The studies hailed from Denmark, Finland, Sweden, the United Kingdom, the United States, Australia, Taiwan, New Zealand, and Israel.
Random-effects meta-analyses were used to pool estimates across studies. The researchers assessed the risk of bias for each study. They also included two additional studies in the review, but not the meta-analysis, that focused specifically on late-onset acute and transient psychosis and late-onset delusional disorder.
The other studies focused on late-onset schizophrenia and/or very late onset schizophrenia-like psychoses, schizophrenia, psychotic disorders, and schizophrenia in older people.
Most studies investigated the incidence of all-cause dementia, although one study focused on the incidence of Alzheimer’s disease.
Potential mechanisms
The narrative review showed that most studies (n = 10) were of high methodological quality, although two were rated as fair and one as poor.
Almost all studies accounted for basic sociodemographic confounders. Several also adjusted for comorbidities, alcohol/substance use disorders, medications, smoking status, and income/education level.
Pooled estimates from the meta-analyzed studies showed that only one showed no significant association between psychotic disorders and dementia, whereas 10 reported increased risk (pooled risk ratio, 2.52; 95% confidence interval, 1.67-3.80; I2, 99.7%).
Subgroup analyses showed higher risk in participants with typical and late-onset psychotic disorders (pooled RR, 2.10; 95% CI, 2.33-4.14; I2, 77.5%; P = .004) vs. those with very late onset schizophrenia-like psychoses (pooled RR, 2.77; 95% CI, 1.74-4.40 I2, 98.9%; P < .001).
The effect was larger in studies with a follow-up of less than 10 years vs. those with a follow-up of 10 years or more, and it was also greater in studies conducted in non-European vs. European countries (all P < .001).
Studies with more female participants (≥ 60%) showed higher risk compared with those that had a lower percentage of female participants. Studies published during or after 2020 showed a stronger association than those published before 2020 (all P < .001).
There was also a higher risk for dementia in studies investigating broader nonaffective psychotic disorders compared with studies investigating only schizophrenia, in prospective vs. retrospective studies, and in studies with a minimum age of less than 60 years at baseline vs. a minimum age of 60 or older (all P < .001).
“Several possible mechanisms could underlie these findings, although we were not able to directly test these in our review,” Dr. Stafford said. She noted that psychotic disorders and other psychiatric diagnoses may cause dementia.
“People with psychotic disorders such as schizophrenia are also at higher risk of health conditions including cardiovascular disease and diabetes, which are known risk factors for dementia and could underpin these associations,” said Dr. Stafford.
It is also possible “that psychotic symptoms could be early markers of dementia for some people, rather than causes,” she added.
Neuroimaging evidence lacking
Commenting on the study, Dilip V. Jeste, MD, former senior associate dean for healthy aging and senior care and distinguished professor of psychiatry and neurosciences at the University of California, San Diego, complimented the investigators for “an excellent article on an important but difficult topic.”
Limitations “pertain not to the meta-analysis but to the original studies,” said Dr. Jeste, who was not involved with the review. Diagnosing dementia in individuals with psychotic disorders is “challenging because cognitive deficits and behavioral symptoms in psychotic disorders may be misdiagnosed as dementia in some individuals – and vice versa,” he added.
Moreover, the studies did not specify the type of dementia, such as Alzheimer’s disease, vascular, Lewy body, frontotemporal, or mixed. Together, “they account for 90% of the dementias, and most patients with these dementias have brain abnormalities that can clearly be seen on MRI,” Dr. Jeste said.
However, patients with schizophrenia who are diagnosed with dementia “rarely show severe brain atrophy, even in specific regions commonly observed in nonpsychotic people with these dementias,” Dr. Jeste noted.
Thus, objective neuroimaging-based evidence for dementia and its subtype “is lacking in most of the published studies of persons with psychotic disorders diagnosed as having dementia,” he said.
There is a “clear need for comprehensive studies of dementia in people with psychotic disorders to understand the significance of the results,” Dr. Jeste concluded.
The review did not receive any funding. Dr. Stafford was supported by an NIHR-UCLH BRC Postdoctoral Bridging Fellowship and the National Institute for Health Research Biomedical Research Centre at University College London Hospitals NHS Foundation Trust. Dr. Stafford was also the principal investigator in one of the studies meeting the inclusion criteria of the review. The other investigators and Dr. Jeste reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from a review and meta-analysis of almost 13 million total participants from nine countries showed that, across multiple different psychotic disorders, there was a 2.5-fold higher risk of developing dementia later in life compared with individuals who did not have a disorder. This was regardless of the age at which the patients first developed the mental illness.
Moreover, participants with a psychotic disorder tended to be younger than average when diagnosed with dementia. Two studies showed that those with psychotic disorders were more likely to be diagnosed with dementia as early as in their 60s.
“The findings add to a growing body of evidence linking psychiatric disorders with later cognitive decline and dementia,” senior investigator Jean Stafford, PhD, a research fellow at MRC Unit for Lifelong Health and Ageing, University College London, told this news organization.
Dr. Stafford noted that the results highlight the importance of being aware of and watchful for symptoms of cognitive decline in patients with psychotic disorders in mid- and late life.
“In addition, given that people with psychotic disorders are at higher risk of experiencing multiple health conditions, including dementia, managing overall physical and mental health in this group is crucial,” she said.
The findings were published online in Psychological Medicine.
Bringing the evidence together
There is increasing evidence that multiple psychiatric symptoms and diagnoses are associated with cognitive decline and dementia, with particularly strong evidence for late-life depression, Dr. Stafford said.
“However, the relationship between psychotic disorders and dementia is less well-established,” she added.
Last year, her team published a study showing a strong association between very late onset psychotic disorders, defined as first diagnosed after age 60 years, and increased risk for dementia in Swedish population register data.
“We also became aware of several other large studies on the topic published in the last few years and realized that an up-to-date systematic review and meta-analysis was needed to bring together the evidence, specifically focusing on longitudinal studies,” Dr. Stafford said.
The researchers searched four databases of prospective and retrospective longitudinal studies published through March 2022. Studies were required to focus on adults aged 18 years or older with a clinical diagnosis of a nonaffective psychotic disorder and a comparison group consisting of adults without a nonaffective psychotic disorder.
Of 9,496 papers, the investigators selected 11 published from 2003 to 2022 that met criteria for inclusion in their meta-analysis (12,997,101 participants), with follow-up periods ranging from 1.57 to 33 years.
The studies hailed from Denmark, Finland, Sweden, the United Kingdom, the United States, Australia, Taiwan, New Zealand, and Israel.
Random-effects meta-analyses were used to pool estimates across studies. The researchers assessed the risk of bias for each study. They also included two additional studies in the review, but not the meta-analysis, that focused specifically on late-onset acute and transient psychosis and late-onset delusional disorder.
The other studies focused on late-onset schizophrenia and/or very late onset schizophrenia-like psychoses, schizophrenia, psychotic disorders, and schizophrenia in older people.
Most studies investigated the incidence of all-cause dementia, although one study focused on the incidence of Alzheimer’s disease.
Potential mechanisms
The narrative review showed that most studies (n = 10) were of high methodological quality, although two were rated as fair and one as poor.
Almost all studies accounted for basic sociodemographic confounders. Several also adjusted for comorbidities, alcohol/substance use disorders, medications, smoking status, and income/education level.
Pooled estimates from the meta-analyzed studies showed that only one showed no significant association between psychotic disorders and dementia, whereas 10 reported increased risk (pooled risk ratio, 2.52; 95% confidence interval, 1.67-3.80; I2, 99.7%).
Subgroup analyses showed higher risk in participants with typical and late-onset psychotic disorders (pooled RR, 2.10; 95% CI, 2.33-4.14; I2, 77.5%; P = .004) vs. those with very late onset schizophrenia-like psychoses (pooled RR, 2.77; 95% CI, 1.74-4.40 I2, 98.9%; P < .001).
The effect was larger in studies with a follow-up of less than 10 years vs. those with a follow-up of 10 years or more, and it was also greater in studies conducted in non-European vs. European countries (all P < .001).
Studies with more female participants (≥ 60%) showed higher risk compared with those that had a lower percentage of female participants. Studies published during or after 2020 showed a stronger association than those published before 2020 (all P < .001).
There was also a higher risk for dementia in studies investigating broader nonaffective psychotic disorders compared with studies investigating only schizophrenia, in prospective vs. retrospective studies, and in studies with a minimum age of less than 60 years at baseline vs. a minimum age of 60 or older (all P < .001).
“Several possible mechanisms could underlie these findings, although we were not able to directly test these in our review,” Dr. Stafford said. She noted that psychotic disorders and other psychiatric diagnoses may cause dementia.
“People with psychotic disorders such as schizophrenia are also at higher risk of health conditions including cardiovascular disease and diabetes, which are known risk factors for dementia and could underpin these associations,” said Dr. Stafford.
It is also possible “that psychotic symptoms could be early markers of dementia for some people, rather than causes,” she added.
Neuroimaging evidence lacking
Commenting on the study, Dilip V. Jeste, MD, former senior associate dean for healthy aging and senior care and distinguished professor of psychiatry and neurosciences at the University of California, San Diego, complimented the investigators for “an excellent article on an important but difficult topic.”
Limitations “pertain not to the meta-analysis but to the original studies,” said Dr. Jeste, who was not involved with the review. Diagnosing dementia in individuals with psychotic disorders is “challenging because cognitive deficits and behavioral symptoms in psychotic disorders may be misdiagnosed as dementia in some individuals – and vice versa,” he added.
Moreover, the studies did not specify the type of dementia, such as Alzheimer’s disease, vascular, Lewy body, frontotemporal, or mixed. Together, “they account for 90% of the dementias, and most patients with these dementias have brain abnormalities that can clearly be seen on MRI,” Dr. Jeste said.
However, patients with schizophrenia who are diagnosed with dementia “rarely show severe brain atrophy, even in specific regions commonly observed in nonpsychotic people with these dementias,” Dr. Jeste noted.
Thus, objective neuroimaging-based evidence for dementia and its subtype “is lacking in most of the published studies of persons with psychotic disorders diagnosed as having dementia,” he said.
There is a “clear need for comprehensive studies of dementia in people with psychotic disorders to understand the significance of the results,” Dr. Jeste concluded.
The review did not receive any funding. Dr. Stafford was supported by an NIHR-UCLH BRC Postdoctoral Bridging Fellowship and the National Institute for Health Research Biomedical Research Centre at University College London Hospitals NHS Foundation Trust. Dr. Stafford was also the principal investigator in one of the studies meeting the inclusion criteria of the review. The other investigators and Dr. Jeste reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from a review and meta-analysis of almost 13 million total participants from nine countries showed that, across multiple different psychotic disorders, there was a 2.5-fold higher risk of developing dementia later in life compared with individuals who did not have a disorder. This was regardless of the age at which the patients first developed the mental illness.
Moreover, participants with a psychotic disorder tended to be younger than average when diagnosed with dementia. Two studies showed that those with psychotic disorders were more likely to be diagnosed with dementia as early as in their 60s.
“The findings add to a growing body of evidence linking psychiatric disorders with later cognitive decline and dementia,” senior investigator Jean Stafford, PhD, a research fellow at MRC Unit for Lifelong Health and Ageing, University College London, told this news organization.
Dr. Stafford noted that the results highlight the importance of being aware of and watchful for symptoms of cognitive decline in patients with psychotic disorders in mid- and late life.
“In addition, given that people with psychotic disorders are at higher risk of experiencing multiple health conditions, including dementia, managing overall physical and mental health in this group is crucial,” she said.
The findings were published online in Psychological Medicine.
Bringing the evidence together
There is increasing evidence that multiple psychiatric symptoms and diagnoses are associated with cognitive decline and dementia, with particularly strong evidence for late-life depression, Dr. Stafford said.
“However, the relationship between psychotic disorders and dementia is less well-established,” she added.
Last year, her team published a study showing a strong association between very late onset psychotic disorders, defined as first diagnosed after age 60 years, and increased risk for dementia in Swedish population register data.
“We also became aware of several other large studies on the topic published in the last few years and realized that an up-to-date systematic review and meta-analysis was needed to bring together the evidence, specifically focusing on longitudinal studies,” Dr. Stafford said.
The researchers searched four databases of prospective and retrospective longitudinal studies published through March 2022. Studies were required to focus on adults aged 18 years or older with a clinical diagnosis of a nonaffective psychotic disorder and a comparison group consisting of adults without a nonaffective psychotic disorder.
Of 9,496 papers, the investigators selected 11 published from 2003 to 2022 that met criteria for inclusion in their meta-analysis (12,997,101 participants), with follow-up periods ranging from 1.57 to 33 years.
The studies hailed from Denmark, Finland, Sweden, the United Kingdom, the United States, Australia, Taiwan, New Zealand, and Israel.
Random-effects meta-analyses were used to pool estimates across studies. The researchers assessed the risk of bias for each study. They also included two additional studies in the review, but not the meta-analysis, that focused specifically on late-onset acute and transient psychosis and late-onset delusional disorder.
The other studies focused on late-onset schizophrenia and/or very late onset schizophrenia-like psychoses, schizophrenia, psychotic disorders, and schizophrenia in older people.
Most studies investigated the incidence of all-cause dementia, although one study focused on the incidence of Alzheimer’s disease.
Potential mechanisms
The narrative review showed that most studies (n = 10) were of high methodological quality, although two were rated as fair and one as poor.
Almost all studies accounted for basic sociodemographic confounders. Several also adjusted for comorbidities, alcohol/substance use disorders, medications, smoking status, and income/education level.
Pooled estimates from the meta-analyzed studies showed that only one showed no significant association between psychotic disorders and dementia, whereas 10 reported increased risk (pooled risk ratio, 2.52; 95% confidence interval, 1.67-3.80; I2, 99.7%).
Subgroup analyses showed higher risk in participants with typical and late-onset psychotic disorders (pooled RR, 2.10; 95% CI, 2.33-4.14; I2, 77.5%; P = .004) vs. those with very late onset schizophrenia-like psychoses (pooled RR, 2.77; 95% CI, 1.74-4.40 I2, 98.9%; P < .001).
The effect was larger in studies with a follow-up of less than 10 years vs. those with a follow-up of 10 years or more, and it was also greater in studies conducted in non-European vs. European countries (all P < .001).
Studies with more female participants (≥ 60%) showed higher risk compared with those that had a lower percentage of female participants. Studies published during or after 2020 showed a stronger association than those published before 2020 (all P < .001).
There was also a higher risk for dementia in studies investigating broader nonaffective psychotic disorders compared with studies investigating only schizophrenia, in prospective vs. retrospective studies, and in studies with a minimum age of less than 60 years at baseline vs. a minimum age of 60 or older (all P < .001).
“Several possible mechanisms could underlie these findings, although we were not able to directly test these in our review,” Dr. Stafford said. She noted that psychotic disorders and other psychiatric diagnoses may cause dementia.
“People with psychotic disorders such as schizophrenia are also at higher risk of health conditions including cardiovascular disease and diabetes, which are known risk factors for dementia and could underpin these associations,” said Dr. Stafford.
It is also possible “that psychotic symptoms could be early markers of dementia for some people, rather than causes,” she added.
Neuroimaging evidence lacking
Commenting on the study, Dilip V. Jeste, MD, former senior associate dean for healthy aging and senior care and distinguished professor of psychiatry and neurosciences at the University of California, San Diego, complimented the investigators for “an excellent article on an important but difficult topic.”
Limitations “pertain not to the meta-analysis but to the original studies,” said Dr. Jeste, who was not involved with the review. Diagnosing dementia in individuals with psychotic disorders is “challenging because cognitive deficits and behavioral symptoms in psychotic disorders may be misdiagnosed as dementia in some individuals – and vice versa,” he added.
Moreover, the studies did not specify the type of dementia, such as Alzheimer’s disease, vascular, Lewy body, frontotemporal, or mixed. Together, “they account for 90% of the dementias, and most patients with these dementias have brain abnormalities that can clearly be seen on MRI,” Dr. Jeste said.
However, patients with schizophrenia who are diagnosed with dementia “rarely show severe brain atrophy, even in specific regions commonly observed in nonpsychotic people with these dementias,” Dr. Jeste noted.
Thus, objective neuroimaging-based evidence for dementia and its subtype “is lacking in most of the published studies of persons with psychotic disorders diagnosed as having dementia,” he said.
There is a “clear need for comprehensive studies of dementia in people with psychotic disorders to understand the significance of the results,” Dr. Jeste concluded.
The review did not receive any funding. Dr. Stafford was supported by an NIHR-UCLH BRC Postdoctoral Bridging Fellowship and the National Institute for Health Research Biomedical Research Centre at University College London Hospitals NHS Foundation Trust. Dr. Stafford was also the principal investigator in one of the studies meeting the inclusion criteria of the review. The other investigators and Dr. Jeste reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PSYCHOLOGICAL MEDICINE
Menopause an independent risk factor for schizophrenia relapse
Investigators studied a cohort of close to 62,000 people with SSDs, stratifying individuals by sex and age, and found that starting between the ages of 45 and 50 years – when the menopausal transition is underway – women were more frequently hospitalized for psychosis, compared with men and women younger than 45 years.
In addition, the protective effect of antipsychotic medication was highest in women younger than 45 years and lowest in women aged 45 years or older, even at higher doses.
“Women with schizophrenia who are older than 45 are a vulnerable group for relapse, and higher doses of antipsychotics are not the answer,” lead author Iris Sommer, MD, PhD, professor, department of neuroscience, University Medical Center of Groningen, the Netherlands, told this news organization.
The study was published online in Schizophrenia Bulletin.
Vulnerable period
There is an association between estrogen levels and disease severity throughout the life stages of women with SSDs, with lower estrogen levels associated with psychosis, for example, during low estrogenic phases of the menstrual cycle, the investigators note.
“After menopause, estrogen levels remain low, which is associated with a deterioration in the clinical course; therefore, women with SSD have sex-specific psychiatric needs that differ according to their life stage,” they add.
“Estrogens inhibit an important liver enzyme (cytochrome P-450 [CYP1A2]), which leads to higher blood levels of several antipsychotics like olanzapine and clozapine,” said Dr. Sommer. In addition, estrogens make the stomach less acidic, “leading to easier resorption of medication.”
As a clinician, Dr. Sommer said that she has “often witnessed a worsening of symptoms [of psychosis] after menopause.” As a researcher, she “knew that estrogens can have ameliorating effects on brain health, especially in schizophrenia.”
She and her colleagues were motivated to research the issue because there is a “remarkable paucity” of quantitative data on a “vulnerable period that all women with schizophrenia will experience.”
Detailed, quantitative data
The researchers sought to provide “detailed, quantitative data on life-stage dependent clinical changes occurring in women with SSD, using an intra-individual design to prevent confounding.”
They drew on data from a nationwide, register-based cohort study of all hospitalized patients with SSD between 1972 and 2014 in Finland (n = 61,889), with follow-up from Jan. 1, 1996, to Dec. 31, 2017.
People were stratified according to age (younger than 45 years and 45 years or older), with the same person contributing person-time to both age groups. The cohort was also subdivided into 5-year age groups, starting at age 20 years and ending at age 69 years.
The primary outcome measure was relapse (that is, inpatient hospitalization because of psychosis).
The researchers focused specifically on monotherapies, excluding time periods when two or more antipsychotics were used concomitantly. They also looked at antipsychotic nonuse periods.
Antipsychotic monotherapies were categorized into defined daily doses per day (DDDs/d):
- less than 0.4
- 0.4 to 0.6
- 0.6 to 0.9
- 0.9 to less than 1.1
- 1.1 to less than 1.4
- 1.4 to less than 1.6
- 1.6 or more
The researchers restricted the main analyses to the four most frequently used oral antipsychotic monotherapies: clozapine, olanzapine, quetiapine, and risperidone.
The turning tide
The cohort consisted of more men than women (31,104 vs. 30,785, respectively), with a mean (standard deviation) age of 49.8 (16.6) years in women vs. 43.6 (14.8) in men.
Among both sexes, olanzapine was the most prescribed antipsychotic (roughly one-quarter of patients). In women, the next most common antipsychotic was risperidone, followed by quetiapine and clozapine, whereas in men, the second most common antipsychotic was clozapine, followed by risperidone and quetiapine.
When the researchers compared men and women younger than 45 years, there were “few consistent differences” in proportions hospitalized for psychosis.
Starting at age 45 years and continuing through the oldest age group (65-69 years), higher proportions of women were hospitalized for psychosis, compared with their male peers (all Ps < .00001).
Women 45 or older had significantly higher risk for relapse associated with standard dose use, compared with the other groups.
When the researchers compared men and women older and younger than 45 years, women younger than 45 years showed lower adjusted hazard ratios (aHRs) at doses between of 0.6-0.9 DDDs/d, whereas for doses over 1.1 DDDs/d, women aged 45 years or older showed “remarkably higher” aHRs, compared with women younger than 45 years and men aged 45 years or older, with a difference that increased with increasing dose.
In women, the efficacy of the antipsychotics was decreased at these DDDs/d.
“We ... showed that antipsychotic monotherapy is most effective in preventing relapse in women below 45, as compared to women above that age, and also as compared to men of all ages,” the authors summarize. But after age 45 years, “the tide seems to turn for women,” compared with younger women and with men of the same age group.
One of several study limitations was the use of age as an estimation of menopausal status, they note.
Don’t just raise the dose
Commenting on the research, Mary Seeman, MD, professor emerita, department of psychiatry, University of Toronto, noted the study corroborates her group’s findings regarding the effect of menopause on antipsychotic response.
“When the efficacy of previously effective antipsychotic doses wanes at menopause, raising the dose is not the treatment of choice because it increases the risk of weight gain, cardiovascular, and cerebrovascular events,” said Dr. Seeman, who was not involved with the current research.
“Changing to an antipsychotic that is less affected by estrogen loss may work better,” she continued, noting that amisulpride and aripiprazole “work well post menopause.”
Additional interventions may include changing to a depot or skin-patch antipsychotic that “obviates first-pass metabolism,” adding hormone replacement or a selective estrogen receptor modulator or including phytoestrogens (bioidenticals) in the diet.
The study yields research recommendations, including comparing the effectiveness of different antipsychotics in postmenopausal women with SSDs, recruiting pre- and postmenopausal women in trials of antipsychotic drugs, and stratifying by hormonal status when analyzing results of antipsychotic trials, Dr. Seeman said.
This work was supported by the Finnish Ministry of Social Affairs and Health through the developmental fund for Niuvanniemi Hospital and the Academy of Finland. The Dutch Medical Research Association supported Dr. Sommer. Dr. Sommer declares no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. Seeman declares no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators studied a cohort of close to 62,000 people with SSDs, stratifying individuals by sex and age, and found that starting between the ages of 45 and 50 years – when the menopausal transition is underway – women were more frequently hospitalized for psychosis, compared with men and women younger than 45 years.
In addition, the protective effect of antipsychotic medication was highest in women younger than 45 years and lowest in women aged 45 years or older, even at higher doses.
“Women with schizophrenia who are older than 45 are a vulnerable group for relapse, and higher doses of antipsychotics are not the answer,” lead author Iris Sommer, MD, PhD, professor, department of neuroscience, University Medical Center of Groningen, the Netherlands, told this news organization.
The study was published online in Schizophrenia Bulletin.
Vulnerable period
There is an association between estrogen levels and disease severity throughout the life stages of women with SSDs, with lower estrogen levels associated with psychosis, for example, during low estrogenic phases of the menstrual cycle, the investigators note.
“After menopause, estrogen levels remain low, which is associated with a deterioration in the clinical course; therefore, women with SSD have sex-specific psychiatric needs that differ according to their life stage,” they add.
“Estrogens inhibit an important liver enzyme (cytochrome P-450 [CYP1A2]), which leads to higher blood levels of several antipsychotics like olanzapine and clozapine,” said Dr. Sommer. In addition, estrogens make the stomach less acidic, “leading to easier resorption of medication.”
As a clinician, Dr. Sommer said that she has “often witnessed a worsening of symptoms [of psychosis] after menopause.” As a researcher, she “knew that estrogens can have ameliorating effects on brain health, especially in schizophrenia.”
She and her colleagues were motivated to research the issue because there is a “remarkable paucity” of quantitative data on a “vulnerable period that all women with schizophrenia will experience.”
Detailed, quantitative data
The researchers sought to provide “detailed, quantitative data on life-stage dependent clinical changes occurring in women with SSD, using an intra-individual design to prevent confounding.”
They drew on data from a nationwide, register-based cohort study of all hospitalized patients with SSD between 1972 and 2014 in Finland (n = 61,889), with follow-up from Jan. 1, 1996, to Dec. 31, 2017.
People were stratified according to age (younger than 45 years and 45 years or older), with the same person contributing person-time to both age groups. The cohort was also subdivided into 5-year age groups, starting at age 20 years and ending at age 69 years.
The primary outcome measure was relapse (that is, inpatient hospitalization because of psychosis).
The researchers focused specifically on monotherapies, excluding time periods when two or more antipsychotics were used concomitantly. They also looked at antipsychotic nonuse periods.
Antipsychotic monotherapies were categorized into defined daily doses per day (DDDs/d):
- less than 0.4
- 0.4 to 0.6
- 0.6 to 0.9
- 0.9 to less than 1.1
- 1.1 to less than 1.4
- 1.4 to less than 1.6
- 1.6 or more
The researchers restricted the main analyses to the four most frequently used oral antipsychotic monotherapies: clozapine, olanzapine, quetiapine, and risperidone.
The turning tide
The cohort consisted of more men than women (31,104 vs. 30,785, respectively), with a mean (standard deviation) age of 49.8 (16.6) years in women vs. 43.6 (14.8) in men.
Among both sexes, olanzapine was the most prescribed antipsychotic (roughly one-quarter of patients). In women, the next most common antipsychotic was risperidone, followed by quetiapine and clozapine, whereas in men, the second most common antipsychotic was clozapine, followed by risperidone and quetiapine.
When the researchers compared men and women younger than 45 years, there were “few consistent differences” in proportions hospitalized for psychosis.
Starting at age 45 years and continuing through the oldest age group (65-69 years), higher proportions of women were hospitalized for psychosis, compared with their male peers (all Ps < .00001).
Women 45 or older had significantly higher risk for relapse associated with standard dose use, compared with the other groups.
When the researchers compared men and women older and younger than 45 years, women younger than 45 years showed lower adjusted hazard ratios (aHRs) at doses between of 0.6-0.9 DDDs/d, whereas for doses over 1.1 DDDs/d, women aged 45 years or older showed “remarkably higher” aHRs, compared with women younger than 45 years and men aged 45 years or older, with a difference that increased with increasing dose.
In women, the efficacy of the antipsychotics was decreased at these DDDs/d.
“We ... showed that antipsychotic monotherapy is most effective in preventing relapse in women below 45, as compared to women above that age, and also as compared to men of all ages,” the authors summarize. But after age 45 years, “the tide seems to turn for women,” compared with younger women and with men of the same age group.
One of several study limitations was the use of age as an estimation of menopausal status, they note.
Don’t just raise the dose
Commenting on the research, Mary Seeman, MD, professor emerita, department of psychiatry, University of Toronto, noted the study corroborates her group’s findings regarding the effect of menopause on antipsychotic response.
“When the efficacy of previously effective antipsychotic doses wanes at menopause, raising the dose is not the treatment of choice because it increases the risk of weight gain, cardiovascular, and cerebrovascular events,” said Dr. Seeman, who was not involved with the current research.
“Changing to an antipsychotic that is less affected by estrogen loss may work better,” she continued, noting that amisulpride and aripiprazole “work well post menopause.”
Additional interventions may include changing to a depot or skin-patch antipsychotic that “obviates first-pass metabolism,” adding hormone replacement or a selective estrogen receptor modulator or including phytoestrogens (bioidenticals) in the diet.
The study yields research recommendations, including comparing the effectiveness of different antipsychotics in postmenopausal women with SSDs, recruiting pre- and postmenopausal women in trials of antipsychotic drugs, and stratifying by hormonal status when analyzing results of antipsychotic trials, Dr. Seeman said.
This work was supported by the Finnish Ministry of Social Affairs and Health through the developmental fund for Niuvanniemi Hospital and the Academy of Finland. The Dutch Medical Research Association supported Dr. Sommer. Dr. Sommer declares no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. Seeman declares no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators studied a cohort of close to 62,000 people with SSDs, stratifying individuals by sex and age, and found that starting between the ages of 45 and 50 years – when the menopausal transition is underway – women were more frequently hospitalized for psychosis, compared with men and women younger than 45 years.
In addition, the protective effect of antipsychotic medication was highest in women younger than 45 years and lowest in women aged 45 years or older, even at higher doses.
“Women with schizophrenia who are older than 45 are a vulnerable group for relapse, and higher doses of antipsychotics are not the answer,” lead author Iris Sommer, MD, PhD, professor, department of neuroscience, University Medical Center of Groningen, the Netherlands, told this news organization.
The study was published online in Schizophrenia Bulletin.
Vulnerable period
There is an association between estrogen levels and disease severity throughout the life stages of women with SSDs, with lower estrogen levels associated with psychosis, for example, during low estrogenic phases of the menstrual cycle, the investigators note.
“After menopause, estrogen levels remain low, which is associated with a deterioration in the clinical course; therefore, women with SSD have sex-specific psychiatric needs that differ according to their life stage,” they add.
“Estrogens inhibit an important liver enzyme (cytochrome P-450 [CYP1A2]), which leads to higher blood levels of several antipsychotics like olanzapine and clozapine,” said Dr. Sommer. In addition, estrogens make the stomach less acidic, “leading to easier resorption of medication.”
As a clinician, Dr. Sommer said that she has “often witnessed a worsening of symptoms [of psychosis] after menopause.” As a researcher, she “knew that estrogens can have ameliorating effects on brain health, especially in schizophrenia.”
She and her colleagues were motivated to research the issue because there is a “remarkable paucity” of quantitative data on a “vulnerable period that all women with schizophrenia will experience.”
Detailed, quantitative data
The researchers sought to provide “detailed, quantitative data on life-stage dependent clinical changes occurring in women with SSD, using an intra-individual design to prevent confounding.”
They drew on data from a nationwide, register-based cohort study of all hospitalized patients with SSD between 1972 and 2014 in Finland (n = 61,889), with follow-up from Jan. 1, 1996, to Dec. 31, 2017.
People were stratified according to age (younger than 45 years and 45 years or older), with the same person contributing person-time to both age groups. The cohort was also subdivided into 5-year age groups, starting at age 20 years and ending at age 69 years.
The primary outcome measure was relapse (that is, inpatient hospitalization because of psychosis).
The researchers focused specifically on monotherapies, excluding time periods when two or more antipsychotics were used concomitantly. They also looked at antipsychotic nonuse periods.
Antipsychotic monotherapies were categorized into defined daily doses per day (DDDs/d):
- less than 0.4
- 0.4 to 0.6
- 0.6 to 0.9
- 0.9 to less than 1.1
- 1.1 to less than 1.4
- 1.4 to less than 1.6
- 1.6 or more
The researchers restricted the main analyses to the four most frequently used oral antipsychotic monotherapies: clozapine, olanzapine, quetiapine, and risperidone.
The turning tide
The cohort consisted of more men than women (31,104 vs. 30,785, respectively), with a mean (standard deviation) age of 49.8 (16.6) years in women vs. 43.6 (14.8) in men.
Among both sexes, olanzapine was the most prescribed antipsychotic (roughly one-quarter of patients). In women, the next most common antipsychotic was risperidone, followed by quetiapine and clozapine, whereas in men, the second most common antipsychotic was clozapine, followed by risperidone and quetiapine.
When the researchers compared men and women younger than 45 years, there were “few consistent differences” in proportions hospitalized for psychosis.
Starting at age 45 years and continuing through the oldest age group (65-69 years), higher proportions of women were hospitalized for psychosis, compared with their male peers (all Ps < .00001).
Women 45 or older had significantly higher risk for relapse associated with standard dose use, compared with the other groups.
When the researchers compared men and women older and younger than 45 years, women younger than 45 years showed lower adjusted hazard ratios (aHRs) at doses between of 0.6-0.9 DDDs/d, whereas for doses over 1.1 DDDs/d, women aged 45 years or older showed “remarkably higher” aHRs, compared with women younger than 45 years and men aged 45 years or older, with a difference that increased with increasing dose.
In women, the efficacy of the antipsychotics was decreased at these DDDs/d.
“We ... showed that antipsychotic monotherapy is most effective in preventing relapse in women below 45, as compared to women above that age, and also as compared to men of all ages,” the authors summarize. But after age 45 years, “the tide seems to turn for women,” compared with younger women and with men of the same age group.
One of several study limitations was the use of age as an estimation of menopausal status, they note.
Don’t just raise the dose
Commenting on the research, Mary Seeman, MD, professor emerita, department of psychiatry, University of Toronto, noted the study corroborates her group’s findings regarding the effect of menopause on antipsychotic response.
“When the efficacy of previously effective antipsychotic doses wanes at menopause, raising the dose is not the treatment of choice because it increases the risk of weight gain, cardiovascular, and cerebrovascular events,” said Dr. Seeman, who was not involved with the current research.
“Changing to an antipsychotic that is less affected by estrogen loss may work better,” she continued, noting that amisulpride and aripiprazole “work well post menopause.”
Additional interventions may include changing to a depot or skin-patch antipsychotic that “obviates first-pass metabolism,” adding hormone replacement or a selective estrogen receptor modulator or including phytoestrogens (bioidenticals) in the diet.
The study yields research recommendations, including comparing the effectiveness of different antipsychotics in postmenopausal women with SSDs, recruiting pre- and postmenopausal women in trials of antipsychotic drugs, and stratifying by hormonal status when analyzing results of antipsychotic trials, Dr. Seeman said.
This work was supported by the Finnish Ministry of Social Affairs and Health through the developmental fund for Niuvanniemi Hospital and the Academy of Finland. The Dutch Medical Research Association supported Dr. Sommer. Dr. Sommer declares no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. Seeman declares no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM SCHIZOPHRENIA BULLETIN
Younger doctors call for more attention to patients with disabilities
As an undergraduate student at Northeastern University in Boston, Meghan Chin spent her summers working for a day program in Rhode Island. Her charges were adults with various forms of intellectual and developmental disabilities (IDD).
“I was very much a caretaker,” Ms. Chin, now 29, said. “It was everything from helping them get dressed in the morning to getting them to medical appointments.”
During one such visit Ms. Chin got a lesson about how health care looks from the viewpoint of someone with an IDD.
The patient was a woman in her 60s and she was having gastrointestinal issues; symptoms she could have articulated, if asked. “She was perfectly capable of telling a clinician where it hurt, how long she had experienced the problem, and what she had done or not done to alleviate it,” Ms. Chin said.
And of comprehending a response. But she was not given the opportunity.
“She would explain what was going on to the clinician,” Ms. Chin recalled. “And the clinician would turn to me and answer. It was this weird three-way conversation – as if she wasn’t even there in the room with us.”
Ms. Chin was incensed at the rude and disrespectful way the patient had been treated. But her charge didn’t seem upset or surprised. Just resigned. “Sadly, she had become used to this,” Ms. Chin said.
For the young aide, however, the experience was searing. “It didn’t seem right to me,” Ms. Chin said. “That’s why, when I went to medical school, I knew I wanted to do better for this population.”
Serendipity led her to Georgetown University, Washington, where she met Kim Bullock, MD, one of the country’s leading advocates for improved health care delivery to those with IDDs.
Dr. Bullock, an associate professor of family medicine, seeks to create better training and educational opportunities for medical students who will likely encounter patients with these disabilities in their practices.
When Dr. Bullock heard Ms. Chin’s story about the patient being ignored, she was not surprised.
“This is not an unusual or unique situation,” said Dr. Bullock, who is also director of Georgetown’s community health division and a faculty member of the university’s Center for Excellence for Developmental Disabilities. “In fact, it’s quite common and is part of what spurred my own interest in educating pre-med and medical students about effective communication techniques, particularly when addressing neurodiverse patients.”
More than 13% of Americans, or roughly 44 million people, have some form of disability, according to the National Institute on Disability at the University of New Hampshire, a figure that does not include those who are institutionalized. The Centers for Disease Control and Prevention estimates that 17% of children aged 3-17 years have a developmental disability.
Even so, many physicians feel ill-prepared to care for disabled patients. A survey of physicians, published in the journal Health Affairs, found that some lacked the resources and training to properly care for patients with disabilities, or that they struggled to coordinate care for such individuals. Some said they did not know which types of accessible equipment, like adjustable tables and chair scales, were needed or how to use them. And some said they actively try to avoid treating patients with disabilities.
Don’t assume
The first step at correcting the problem, Dr. Bullock said, is to not assume that all IDD patients are incapable of communicating. By talking not to the patient but to their caregiver or spouse or child, as the clinician did with Ms. Chin years ago, “we are taking away their agency, their autonomy to speak for and about themselves.”
Change involves altering physicians’ attitudes and assumptions toward this population, through education. But how?
“The medical school curriculum is tight as it is,” Dr. Bullock acknowledged. “There’s a lot of things students have to learn. People wonder: where we will add this?”
Her suggestion: Incorporate IDD all along the way, through programs or experiences that will enable medical students to see such patients “not as something separate, but as people that have special needs just as other populations have.”
Case in point: Operation House Call, a program in Massachusetts designed to support young health care professionals, by building “confidence, interest, and sensitivity” toward individuals with IDD.
Eight medical and allied health schools, including those at Harvard Medical School and Yale School of Nursing, participate in the program, the centerpiece of which is time spent by teams of medical students in the homes of families with neurodiverse members. “It’s transformational,” said Susan Feeney, DNP, NP-C, director of adult gerontology and family nurse practitioner programs at the graduate school of nursing at the University of Massachusetts, Worcester. “They spend a few hours at the homes of these families, have this interaction with them, and journal about their experiences.”
Dr. Feeney described as “transformational” the experience of the students after getting to know these families. “They all come back profoundly changed,” she told this news organization. “As a medical or health care professional, you meet people in an artificial environment of the clinic and hospital. Here, they become human, like you. It takes the stigma away.”
One area of medicine in which this is an exception is pediatrics, where interaction with children with IDD and their families is common – and close. “They’re going to be much more attuned to this,” Dr. Feeney said. “The problem is primary care or internal medicine. Once these children get into their mid and later 20s, and they need a practitioner to talk to about adult concerns.”
And with adulthood come other medical needs, as the physical demands of age fall no less heavily on individuals with IDDs than those without. For example: “Neurodiverse people get pregnant,” Dr. Bullock said. They also can get heart disease as they age; or require the care of a rheumatologist, a neurologist, an orthopedic surgeon, or any other medical specialty.
Generation gap
Fortunately, the next generation of physicians may be more open to this more inclusionary approach toward a widely misunderstood population.
Like Ms. Chin, Sarah Bdeir had experience with this population prior to beginning her training in medicine. She had volunteered at a school for people with IDD.
“It was one of the best experiences I’ve ever had,” Ms. Bdeir, now 23 and a first-year medical student at Wayne State University, Detroit, said. She found that the neurodiverse individuals she worked with had as many abilities as disabilities. “They are capable of learning, but they do it differently,” she said. “You have to adjust to the way they learn. And you have to step out of your own box.”
Ms. Bdeir also heard about Dr. Bullock’s work and is assisting her in a research project on how to better improve nutritional education for people with IDDs. And although she said it may take time for curriculum boards at medical schools to integrate this kind of training into their programs, she believes they will, in part because the rising cohort of medical students today have an eagerness to engage with and learn more about IDD patients.
As does Ms. Chin.
“When I talk to my peers about this, they’re very receptive,” Ms. Chin said. “They want to learn how to better support the IDD population. And they will learn. I believe in my generation of future doctors.”
A version of this article first appeared on Medscape.com.
As an undergraduate student at Northeastern University in Boston, Meghan Chin spent her summers working for a day program in Rhode Island. Her charges were adults with various forms of intellectual and developmental disabilities (IDD).
“I was very much a caretaker,” Ms. Chin, now 29, said. “It was everything from helping them get dressed in the morning to getting them to medical appointments.”
During one such visit Ms. Chin got a lesson about how health care looks from the viewpoint of someone with an IDD.
The patient was a woman in her 60s and she was having gastrointestinal issues; symptoms she could have articulated, if asked. “She was perfectly capable of telling a clinician where it hurt, how long she had experienced the problem, and what she had done or not done to alleviate it,” Ms. Chin said.
And of comprehending a response. But she was not given the opportunity.
“She would explain what was going on to the clinician,” Ms. Chin recalled. “And the clinician would turn to me and answer. It was this weird three-way conversation – as if she wasn’t even there in the room with us.”
Ms. Chin was incensed at the rude and disrespectful way the patient had been treated. But her charge didn’t seem upset or surprised. Just resigned. “Sadly, she had become used to this,” Ms. Chin said.
For the young aide, however, the experience was searing. “It didn’t seem right to me,” Ms. Chin said. “That’s why, when I went to medical school, I knew I wanted to do better for this population.”
Serendipity led her to Georgetown University, Washington, where she met Kim Bullock, MD, one of the country’s leading advocates for improved health care delivery to those with IDDs.
Dr. Bullock, an associate professor of family medicine, seeks to create better training and educational opportunities for medical students who will likely encounter patients with these disabilities in their practices.
When Dr. Bullock heard Ms. Chin’s story about the patient being ignored, she was not surprised.
“This is not an unusual or unique situation,” said Dr. Bullock, who is also director of Georgetown’s community health division and a faculty member of the university’s Center for Excellence for Developmental Disabilities. “In fact, it’s quite common and is part of what spurred my own interest in educating pre-med and medical students about effective communication techniques, particularly when addressing neurodiverse patients.”
More than 13% of Americans, or roughly 44 million people, have some form of disability, according to the National Institute on Disability at the University of New Hampshire, a figure that does not include those who are institutionalized. The Centers for Disease Control and Prevention estimates that 17% of children aged 3-17 years have a developmental disability.
Even so, many physicians feel ill-prepared to care for disabled patients. A survey of physicians, published in the journal Health Affairs, found that some lacked the resources and training to properly care for patients with disabilities, or that they struggled to coordinate care for such individuals. Some said they did not know which types of accessible equipment, like adjustable tables and chair scales, were needed or how to use them. And some said they actively try to avoid treating patients with disabilities.
Don’t assume
The first step at correcting the problem, Dr. Bullock said, is to not assume that all IDD patients are incapable of communicating. By talking not to the patient but to their caregiver or spouse or child, as the clinician did with Ms. Chin years ago, “we are taking away their agency, their autonomy to speak for and about themselves.”
Change involves altering physicians’ attitudes and assumptions toward this population, through education. But how?
“The medical school curriculum is tight as it is,” Dr. Bullock acknowledged. “There’s a lot of things students have to learn. People wonder: where we will add this?”
Her suggestion: Incorporate IDD all along the way, through programs or experiences that will enable medical students to see such patients “not as something separate, but as people that have special needs just as other populations have.”
Case in point: Operation House Call, a program in Massachusetts designed to support young health care professionals, by building “confidence, interest, and sensitivity” toward individuals with IDD.
Eight medical and allied health schools, including those at Harvard Medical School and Yale School of Nursing, participate in the program, the centerpiece of which is time spent by teams of medical students in the homes of families with neurodiverse members. “It’s transformational,” said Susan Feeney, DNP, NP-C, director of adult gerontology and family nurse practitioner programs at the graduate school of nursing at the University of Massachusetts, Worcester. “They spend a few hours at the homes of these families, have this interaction with them, and journal about their experiences.”
Dr. Feeney described as “transformational” the experience of the students after getting to know these families. “They all come back profoundly changed,” she told this news organization. “As a medical or health care professional, you meet people in an artificial environment of the clinic and hospital. Here, they become human, like you. It takes the stigma away.”
One area of medicine in which this is an exception is pediatrics, where interaction with children with IDD and their families is common – and close. “They’re going to be much more attuned to this,” Dr. Feeney said. “The problem is primary care or internal medicine. Once these children get into their mid and later 20s, and they need a practitioner to talk to about adult concerns.”
And with adulthood come other medical needs, as the physical demands of age fall no less heavily on individuals with IDDs than those without. For example: “Neurodiverse people get pregnant,” Dr. Bullock said. They also can get heart disease as they age; or require the care of a rheumatologist, a neurologist, an orthopedic surgeon, or any other medical specialty.
Generation gap
Fortunately, the next generation of physicians may be more open to this more inclusionary approach toward a widely misunderstood population.
Like Ms. Chin, Sarah Bdeir had experience with this population prior to beginning her training in medicine. She had volunteered at a school for people with IDD.
“It was one of the best experiences I’ve ever had,” Ms. Bdeir, now 23 and a first-year medical student at Wayne State University, Detroit, said. She found that the neurodiverse individuals she worked with had as many abilities as disabilities. “They are capable of learning, but they do it differently,” she said. “You have to adjust to the way they learn. And you have to step out of your own box.”
Ms. Bdeir also heard about Dr. Bullock’s work and is assisting her in a research project on how to better improve nutritional education for people with IDDs. And although she said it may take time for curriculum boards at medical schools to integrate this kind of training into their programs, she believes they will, in part because the rising cohort of medical students today have an eagerness to engage with and learn more about IDD patients.
As does Ms. Chin.
“When I talk to my peers about this, they’re very receptive,” Ms. Chin said. “They want to learn how to better support the IDD population. And they will learn. I believe in my generation of future doctors.”
A version of this article first appeared on Medscape.com.
As an undergraduate student at Northeastern University in Boston, Meghan Chin spent her summers working for a day program in Rhode Island. Her charges were adults with various forms of intellectual and developmental disabilities (IDD).
“I was very much a caretaker,” Ms. Chin, now 29, said. “It was everything from helping them get dressed in the morning to getting them to medical appointments.”
During one such visit Ms. Chin got a lesson about how health care looks from the viewpoint of someone with an IDD.
The patient was a woman in her 60s and she was having gastrointestinal issues; symptoms she could have articulated, if asked. “She was perfectly capable of telling a clinician where it hurt, how long she had experienced the problem, and what she had done or not done to alleviate it,” Ms. Chin said.
And of comprehending a response. But she was not given the opportunity.
“She would explain what was going on to the clinician,” Ms. Chin recalled. “And the clinician would turn to me and answer. It was this weird three-way conversation – as if she wasn’t even there in the room with us.”
Ms. Chin was incensed at the rude and disrespectful way the patient had been treated. But her charge didn’t seem upset or surprised. Just resigned. “Sadly, she had become used to this,” Ms. Chin said.
For the young aide, however, the experience was searing. “It didn’t seem right to me,” Ms. Chin said. “That’s why, when I went to medical school, I knew I wanted to do better for this population.”
Serendipity led her to Georgetown University, Washington, where she met Kim Bullock, MD, one of the country’s leading advocates for improved health care delivery to those with IDDs.
Dr. Bullock, an associate professor of family medicine, seeks to create better training and educational opportunities for medical students who will likely encounter patients with these disabilities in their practices.
When Dr. Bullock heard Ms. Chin’s story about the patient being ignored, she was not surprised.
“This is not an unusual or unique situation,” said Dr. Bullock, who is also director of Georgetown’s community health division and a faculty member of the university’s Center for Excellence for Developmental Disabilities. “In fact, it’s quite common and is part of what spurred my own interest in educating pre-med and medical students about effective communication techniques, particularly when addressing neurodiverse patients.”
More than 13% of Americans, or roughly 44 million people, have some form of disability, according to the National Institute on Disability at the University of New Hampshire, a figure that does not include those who are institutionalized. The Centers for Disease Control and Prevention estimates that 17% of children aged 3-17 years have a developmental disability.
Even so, many physicians feel ill-prepared to care for disabled patients. A survey of physicians, published in the journal Health Affairs, found that some lacked the resources and training to properly care for patients with disabilities, or that they struggled to coordinate care for such individuals. Some said they did not know which types of accessible equipment, like adjustable tables and chair scales, were needed or how to use them. And some said they actively try to avoid treating patients with disabilities.
Don’t assume
The first step at correcting the problem, Dr. Bullock said, is to not assume that all IDD patients are incapable of communicating. By talking not to the patient but to their caregiver or spouse or child, as the clinician did with Ms. Chin years ago, “we are taking away their agency, their autonomy to speak for and about themselves.”
Change involves altering physicians’ attitudes and assumptions toward this population, through education. But how?
“The medical school curriculum is tight as it is,” Dr. Bullock acknowledged. “There’s a lot of things students have to learn. People wonder: where we will add this?”
Her suggestion: Incorporate IDD all along the way, through programs or experiences that will enable medical students to see such patients “not as something separate, but as people that have special needs just as other populations have.”
Case in point: Operation House Call, a program in Massachusetts designed to support young health care professionals, by building “confidence, interest, and sensitivity” toward individuals with IDD.
Eight medical and allied health schools, including those at Harvard Medical School and Yale School of Nursing, participate in the program, the centerpiece of which is time spent by teams of medical students in the homes of families with neurodiverse members. “It’s transformational,” said Susan Feeney, DNP, NP-C, director of adult gerontology and family nurse practitioner programs at the graduate school of nursing at the University of Massachusetts, Worcester. “They spend a few hours at the homes of these families, have this interaction with them, and journal about their experiences.”
Dr. Feeney described as “transformational” the experience of the students after getting to know these families. “They all come back profoundly changed,” she told this news organization. “As a medical or health care professional, you meet people in an artificial environment of the clinic and hospital. Here, they become human, like you. It takes the stigma away.”
One area of medicine in which this is an exception is pediatrics, where interaction with children with IDD and their families is common – and close. “They’re going to be much more attuned to this,” Dr. Feeney said. “The problem is primary care or internal medicine. Once these children get into their mid and later 20s, and they need a practitioner to talk to about adult concerns.”
And with adulthood come other medical needs, as the physical demands of age fall no less heavily on individuals with IDDs than those without. For example: “Neurodiverse people get pregnant,” Dr. Bullock said. They also can get heart disease as they age; or require the care of a rheumatologist, a neurologist, an orthopedic surgeon, or any other medical specialty.
Generation gap
Fortunately, the next generation of physicians may be more open to this more inclusionary approach toward a widely misunderstood population.
Like Ms. Chin, Sarah Bdeir had experience with this population prior to beginning her training in medicine. She had volunteered at a school for people with IDD.
“It was one of the best experiences I’ve ever had,” Ms. Bdeir, now 23 and a first-year medical student at Wayne State University, Detroit, said. She found that the neurodiverse individuals she worked with had as many abilities as disabilities. “They are capable of learning, but they do it differently,” she said. “You have to adjust to the way they learn. And you have to step out of your own box.”
Ms. Bdeir also heard about Dr. Bullock’s work and is assisting her in a research project on how to better improve nutritional education for people with IDDs. And although she said it may take time for curriculum boards at medical schools to integrate this kind of training into their programs, she believes they will, in part because the rising cohort of medical students today have an eagerness to engage with and learn more about IDD patients.
As does Ms. Chin.
“When I talk to my peers about this, they’re very receptive,” Ms. Chin said. “They want to learn how to better support the IDD population. And they will learn. I believe in my generation of future doctors.”
A version of this article first appeared on Medscape.com.
Viagra, Cialis, and Alzheimer’s risk: New data
The findings contradict results from a previous study that suggested that individuals who take sildenafil (Viagra) were significantly less likely to develop Alzheimer’s.
The new research, part of a larger effort to identify existing medications that could be repurposed to treat ADRD, employed a study design that reduced the risk for potential bias that may have influenced the earlier findings, the investigators note.
“That study came out last fall and was widely covered in the media, and we thought there were some methodological shortcomings that might have explained the results,” lead investigator Rishi Desai, PhD, assistant professor of medicine at Harvard Medical School and an associate epidemiologist at Brigham and Women’s Hospital, both in Boston, said in an interview.
The new study was published online in Brain Communications.
Not the final word?
Animal studies suggest that phosphodiesterase-5 (PDE5) inhibitors, a drug class that includes the ED drugs sildenafil and tadalafil (Cialis), improve memory and cognitive function and reduce amyloid burden. But studies in humans have yielded conflicting results.*
Although the new research and the work published last year both drew on Medicare data, they examined different patient populations.
The first study compared those who took sildenafil for any reason to those who did not take it. That design likely resulted in an analysis of a comparison of individuals with ED – the most common indication for sildenafil – to generally older individuals with diabetes or hypertension, Dr. Desai said.
In contrast, the current study included only those with pulmonary arterial hypertension (PAH), which is also an indication for PDE5 inhibitors. The researchers compared ADRD incidence in those who took PDE5 inhibitors with the incidence among those who took a different medication to treat their PAH. They used propensity matching to create two groups with similar characteristics and examined the data using four analytic strategies.
The investigators found no significant difference between groups in the incidence of ADRD, regardless of the strategy they used. Cell culture studies also revealed no protective effect from PDE5 inhibitors.
“No study of this kind should claim the final word,” Dr. Desai said. “It is extremely difficult to nail down causality from these types of data sources.”
Impressive study design
Commenting on the findings, David Knopman, MD, professor of neurology at Mayo Clinic, Rochester, Minn., described the study design as “impressive” for its efforts to minimize bias, a key limitation in the previous study.
“It was always the case that the claims about sildenafil needed further developmental work prior to testing the drug in randomized controlled trials,” Dr. Knopman said. “The evidence for the use of the drug was never sufficient for clinicians to use it in their patients.”
The study was funded by National Institute on Aging. Dr. Desai is an investigator who receives research grants from Bayer, Vertex, and Novartis that were given to the Brigham and Women’s Hospital for unrelated projects. Dr. Knopman has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Correction, 11/3/22: An earlier version of this article misstated the abbreviation for phosphodiesterase-5. It is PDE-5.
The findings contradict results from a previous study that suggested that individuals who take sildenafil (Viagra) were significantly less likely to develop Alzheimer’s.
The new research, part of a larger effort to identify existing medications that could be repurposed to treat ADRD, employed a study design that reduced the risk for potential bias that may have influenced the earlier findings, the investigators note.
“That study came out last fall and was widely covered in the media, and we thought there were some methodological shortcomings that might have explained the results,” lead investigator Rishi Desai, PhD, assistant professor of medicine at Harvard Medical School and an associate epidemiologist at Brigham and Women’s Hospital, both in Boston, said in an interview.
The new study was published online in Brain Communications.
Not the final word?
Animal studies suggest that phosphodiesterase-5 (PDE5) inhibitors, a drug class that includes the ED drugs sildenafil and tadalafil (Cialis), improve memory and cognitive function and reduce amyloid burden. But studies in humans have yielded conflicting results.*
Although the new research and the work published last year both drew on Medicare data, they examined different patient populations.
The first study compared those who took sildenafil for any reason to those who did not take it. That design likely resulted in an analysis of a comparison of individuals with ED – the most common indication for sildenafil – to generally older individuals with diabetes or hypertension, Dr. Desai said.
In contrast, the current study included only those with pulmonary arterial hypertension (PAH), which is also an indication for PDE5 inhibitors. The researchers compared ADRD incidence in those who took PDE5 inhibitors with the incidence among those who took a different medication to treat their PAH. They used propensity matching to create two groups with similar characteristics and examined the data using four analytic strategies.
The investigators found no significant difference between groups in the incidence of ADRD, regardless of the strategy they used. Cell culture studies also revealed no protective effect from PDE5 inhibitors.
“No study of this kind should claim the final word,” Dr. Desai said. “It is extremely difficult to nail down causality from these types of data sources.”
Impressive study design
Commenting on the findings, David Knopman, MD, professor of neurology at Mayo Clinic, Rochester, Minn., described the study design as “impressive” for its efforts to minimize bias, a key limitation in the previous study.
“It was always the case that the claims about sildenafil needed further developmental work prior to testing the drug in randomized controlled trials,” Dr. Knopman said. “The evidence for the use of the drug was never sufficient for clinicians to use it in their patients.”
The study was funded by National Institute on Aging. Dr. Desai is an investigator who receives research grants from Bayer, Vertex, and Novartis that were given to the Brigham and Women’s Hospital for unrelated projects. Dr. Knopman has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Correction, 11/3/22: An earlier version of this article misstated the abbreviation for phosphodiesterase-5. It is PDE-5.
The findings contradict results from a previous study that suggested that individuals who take sildenafil (Viagra) were significantly less likely to develop Alzheimer’s.
The new research, part of a larger effort to identify existing medications that could be repurposed to treat ADRD, employed a study design that reduced the risk for potential bias that may have influenced the earlier findings, the investigators note.
“That study came out last fall and was widely covered in the media, and we thought there were some methodological shortcomings that might have explained the results,” lead investigator Rishi Desai, PhD, assistant professor of medicine at Harvard Medical School and an associate epidemiologist at Brigham and Women’s Hospital, both in Boston, said in an interview.
The new study was published online in Brain Communications.
Not the final word?
Animal studies suggest that phosphodiesterase-5 (PDE5) inhibitors, a drug class that includes the ED drugs sildenafil and tadalafil (Cialis), improve memory and cognitive function and reduce amyloid burden. But studies in humans have yielded conflicting results.*
Although the new research and the work published last year both drew on Medicare data, they examined different patient populations.
The first study compared those who took sildenafil for any reason to those who did not take it. That design likely resulted in an analysis of a comparison of individuals with ED – the most common indication for sildenafil – to generally older individuals with diabetes or hypertension, Dr. Desai said.
In contrast, the current study included only those with pulmonary arterial hypertension (PAH), which is also an indication for PDE5 inhibitors. The researchers compared ADRD incidence in those who took PDE5 inhibitors with the incidence among those who took a different medication to treat their PAH. They used propensity matching to create two groups with similar characteristics and examined the data using four analytic strategies.
The investigators found no significant difference between groups in the incidence of ADRD, regardless of the strategy they used. Cell culture studies also revealed no protective effect from PDE5 inhibitors.
“No study of this kind should claim the final word,” Dr. Desai said. “It is extremely difficult to nail down causality from these types of data sources.”
Impressive study design
Commenting on the findings, David Knopman, MD, professor of neurology at Mayo Clinic, Rochester, Minn., described the study design as “impressive” for its efforts to minimize bias, a key limitation in the previous study.
“It was always the case that the claims about sildenafil needed further developmental work prior to testing the drug in randomized controlled trials,” Dr. Knopman said. “The evidence for the use of the drug was never sufficient for clinicians to use it in their patients.”
The study was funded by National Institute on Aging. Dr. Desai is an investigator who receives research grants from Bayer, Vertex, and Novartis that were given to the Brigham and Women’s Hospital for unrelated projects. Dr. Knopman has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Correction, 11/3/22: An earlier version of this article misstated the abbreviation for phosphodiesterase-5. It is PDE-5.
FROM BRAIN COMMUNICATIONS
Listen up: Birdsong may calm anxiety, paranoia
Investigators found that people who listened to recordings of birds singing experienced a significant reduction in anxiety and paranoia. In contrast, the researchers also found that recordings of traffic noises, including car engines, sirens, and construction, increased depressive states.
“The results suggest that it may be worthwhile to investigate the targeted use of natural sounds such as birdsong in a clinical setting – for example, in hospital waiting rooms or in psychiatric settings,” study investigator Emil Stobbe, MSc, a predoctoral fellow at the Max Planck Institute for Human Development, Berlin, said in an interview.
“If someone is seeking an easily accessible intervention to lower distress, listening to an audio clip of birds singing might be a great option,” he added.
The study was published online in Scientific Reports.
Nature’s calming effect
The aim of the research was “to investigate how the physical environment impact brain and mental health,” Mr. Stobbe said.
Mr. Stobbe said that there is significantly more research examining visual properties of the physical environment but that the auditory domain is not as well researched, although, he added, that the beneficial effects of interactions with nature are “well studied.”
He noted that anxiety and paranoia can be experienced by many individuals even though they may be unaware that they are experiencing these states.
“We wanted to investigate if the beneficial effects of nature can also exert their impact on these states. In theory, birds can be representational for natural and vital environment, which, in turn, transfer the positive effects of nature on birdsong listeners,” he said.
A previous study compared nature versus city soundscape conditions and showed that the nature soundscape improved participants’ cognitive performance but did not improve mood. The present study added diversity to the soundscapes and focused not only on cognition and general mood but also on state paranoia, “which can be measured in a change-sensitive manner” and “has been shown to increase in response to traffic noise.”
The researchers hypothesized that birdsong would have a greater beneficial effect on mood and paranoia and on cognitive performance compared with traffic noise. They also investigated whether greater versus lower diversity of bird species or noise sources within the soundscapes “would be a relevant factor modulating the effects.”
The researchers recruited participants (n = 295) from a crowdsourcing platform. Participants’ mean age was late 20s (standard deviations ranged from 6.30 to 7.72), with a greater proportion of male versus female participants.
To be included, participants were required to have no history of mental illness, hearing difficulties, substance/drug intake, or suicidal thoughts/tendencies.
The outcomes of interest (mood, paranoia, cognitive performance) were measured before and after soundscape exposure and each soundscape had a low- versus high-diversity version. This resulted in several analyses that compared two types of sounds (birdsongs vs. traffic noise) x two levels of diversity (low vs. high diversity) and two time points (pre- vs. post exposure).
The exposure to sounds lasted for 6 minutes, after which they were asked to report (on a 0-100 visual scale) how diverse/monotone, beautiful, and pleasant they perceived the soundscape to be.
Reduction in depressive symptoms
Participants were divided into four groups: low-diversity traffic noise soundscape (n = 83), high-diversity traffic noise soundscape (n = 60), low-diversity birdsong soundscape (n = 63), and high-diversity birdsong soundscape (n = 80)
In addition to listening to the sounds, participants completed questionnaires measuring mood (depression and anxiety) and paranoia as well as a test of digit span cognitive performance (both the forward and the backward versions).
The type, diversity, and type x diversity all revealed significant effect sizes (F[3, 276] = 78.6; P < .001; eta-squared = 0.461; F[3, 276] = 3.16; P = .025; eta-squared = 0.033; and F[3, 276] = 2.66; P = .028, respectively), “suggesting that all of these factors, as well as their interaction, had a significant impact on the perception of soundscapes (that is, ratings on monotony/diversity, beauty, and pleasantness).”
A post hoc examination showed that depressive symptoms significantly increased within the low- and high-diversity urban soundscapes but decreased significantly in the high-diversity birdsong soundscapes (T[1, 60] = –2.57; P = .012; d = –0.29).
For anxiety, the post hoc within-group analyses found no effects within low- and high-diversity traffic noise conditions (T[1, 82] = –1.37; P = .174; d = –0.15 and T[1, 68] = 0.49; P = .629; d = 0.06, respectively). By contrast, there were significant declines in both birdsong conditions (low diversity: T[1, 62] = –6.13; P < .001; d = –0.77; high diversity: T[1, 60] = –6.32; P < .001; d = –0.70).
Similarly, there were no changes in participants with paranoia when they listened to either low- or high-diversity traffic noises (T[1, 82] = –0.55; P = .583; d = –0.06 and T[1, 68] = 0.67; P = .507; d = 0.08, respectively). On the other hand, both birdsong conditions yielded reductions in paranoia (low diversity: T[1, 62] = –5.90; P < .001; d = –0.74; high diversity: T[1, 60] = –4.11; P < .001; d = –0.46).
None of the soundscapes had any effect on cognition.
“In theory, birds can be representational for natural and vital environments which, in turn, transfer the positive effects of nature on birdsong listeners,” said Mr. Stobbe.
“Taken together, the findings of the current study provide another facet of why interactions with nature can be beneficial for our mental health, and it is highly important to preserve nature,” he added.
Mr. Stobbe said that future research should focus on investigating mixed soundscapes including examining whether the presence of natural sounds in urban settings lower stressors such as traffic noise.
An understudied area
Commenting for this article, Ken Duckworth, MD, chief medical officer of the National Alliance on Mental Illness called the study “interesting but limited.”
Dr. Duckworth, who was not involved in the research said that the “benefits of nature are understudied” and agreed with the investigators that it is potentially important to study the use of birdsongs in psychiatric facilities. “Future studies could also correlate the role of birdsong with the mental health benefits/aspects of ‘being in nature,’ which has been found to have some effect.”
Open Access funding was enabled and organized by Projekt DEAL. The authors and Dr. Duckworth declared no competing interests.
A version of this article first appeared on Medscape.com.
Investigators found that people who listened to recordings of birds singing experienced a significant reduction in anxiety and paranoia. In contrast, the researchers also found that recordings of traffic noises, including car engines, sirens, and construction, increased depressive states.
“The results suggest that it may be worthwhile to investigate the targeted use of natural sounds such as birdsong in a clinical setting – for example, in hospital waiting rooms or in psychiatric settings,” study investigator Emil Stobbe, MSc, a predoctoral fellow at the Max Planck Institute for Human Development, Berlin, said in an interview.
“If someone is seeking an easily accessible intervention to lower distress, listening to an audio clip of birds singing might be a great option,” he added.
The study was published online in Scientific Reports.
Nature’s calming effect
The aim of the research was “to investigate how the physical environment impact brain and mental health,” Mr. Stobbe said.
Mr. Stobbe said that there is significantly more research examining visual properties of the physical environment but that the auditory domain is not as well researched, although, he added, that the beneficial effects of interactions with nature are “well studied.”
He noted that anxiety and paranoia can be experienced by many individuals even though they may be unaware that they are experiencing these states.
“We wanted to investigate if the beneficial effects of nature can also exert their impact on these states. In theory, birds can be representational for natural and vital environment, which, in turn, transfer the positive effects of nature on birdsong listeners,” he said.
A previous study compared nature versus city soundscape conditions and showed that the nature soundscape improved participants’ cognitive performance but did not improve mood. The present study added diversity to the soundscapes and focused not only on cognition and general mood but also on state paranoia, “which can be measured in a change-sensitive manner” and “has been shown to increase in response to traffic noise.”
The researchers hypothesized that birdsong would have a greater beneficial effect on mood and paranoia and on cognitive performance compared with traffic noise. They also investigated whether greater versus lower diversity of bird species or noise sources within the soundscapes “would be a relevant factor modulating the effects.”
The researchers recruited participants (n = 295) from a crowdsourcing platform. Participants’ mean age was late 20s (standard deviations ranged from 6.30 to 7.72), with a greater proportion of male versus female participants.
To be included, participants were required to have no history of mental illness, hearing difficulties, substance/drug intake, or suicidal thoughts/tendencies.
The outcomes of interest (mood, paranoia, cognitive performance) were measured before and after soundscape exposure and each soundscape had a low- versus high-diversity version. This resulted in several analyses that compared two types of sounds (birdsongs vs. traffic noise) x two levels of diversity (low vs. high diversity) and two time points (pre- vs. post exposure).
The exposure to sounds lasted for 6 minutes, after which they were asked to report (on a 0-100 visual scale) how diverse/monotone, beautiful, and pleasant they perceived the soundscape to be.
Reduction in depressive symptoms
Participants were divided into four groups: low-diversity traffic noise soundscape (n = 83), high-diversity traffic noise soundscape (n = 60), low-diversity birdsong soundscape (n = 63), and high-diversity birdsong soundscape (n = 80)
In addition to listening to the sounds, participants completed questionnaires measuring mood (depression and anxiety) and paranoia as well as a test of digit span cognitive performance (both the forward and the backward versions).
The type, diversity, and type x diversity all revealed significant effect sizes (F[3, 276] = 78.6; P < .001; eta-squared = 0.461; F[3, 276] = 3.16; P = .025; eta-squared = 0.033; and F[3, 276] = 2.66; P = .028, respectively), “suggesting that all of these factors, as well as their interaction, had a significant impact on the perception of soundscapes (that is, ratings on monotony/diversity, beauty, and pleasantness).”
A post hoc examination showed that depressive symptoms significantly increased within the low- and high-diversity urban soundscapes but decreased significantly in the high-diversity birdsong soundscapes (T[1, 60] = –2.57; P = .012; d = –0.29).
For anxiety, the post hoc within-group analyses found no effects within low- and high-diversity traffic noise conditions (T[1, 82] = –1.37; P = .174; d = –0.15 and T[1, 68] = 0.49; P = .629; d = 0.06, respectively). By contrast, there were significant declines in both birdsong conditions (low diversity: T[1, 62] = –6.13; P < .001; d = –0.77; high diversity: T[1, 60] = –6.32; P < .001; d = –0.70).
Similarly, there were no changes in participants with paranoia when they listened to either low- or high-diversity traffic noises (T[1, 82] = –0.55; P = .583; d = –0.06 and T[1, 68] = 0.67; P = .507; d = 0.08, respectively). On the other hand, both birdsong conditions yielded reductions in paranoia (low diversity: T[1, 62] = –5.90; P < .001; d = –0.74; high diversity: T[1, 60] = –4.11; P < .001; d = –0.46).
None of the soundscapes had any effect on cognition.
“In theory, birds can be representational for natural and vital environments which, in turn, transfer the positive effects of nature on birdsong listeners,” said Mr. Stobbe.
“Taken together, the findings of the current study provide another facet of why interactions with nature can be beneficial for our mental health, and it is highly important to preserve nature,” he added.
Mr. Stobbe said that future research should focus on investigating mixed soundscapes including examining whether the presence of natural sounds in urban settings lower stressors such as traffic noise.
An understudied area
Commenting for this article, Ken Duckworth, MD, chief medical officer of the National Alliance on Mental Illness called the study “interesting but limited.”
Dr. Duckworth, who was not involved in the research said that the “benefits of nature are understudied” and agreed with the investigators that it is potentially important to study the use of birdsongs in psychiatric facilities. “Future studies could also correlate the role of birdsong with the mental health benefits/aspects of ‘being in nature,’ which has been found to have some effect.”
Open Access funding was enabled and organized by Projekt DEAL. The authors and Dr. Duckworth declared no competing interests.
A version of this article first appeared on Medscape.com.
Investigators found that people who listened to recordings of birds singing experienced a significant reduction in anxiety and paranoia. In contrast, the researchers also found that recordings of traffic noises, including car engines, sirens, and construction, increased depressive states.
“The results suggest that it may be worthwhile to investigate the targeted use of natural sounds such as birdsong in a clinical setting – for example, in hospital waiting rooms or in psychiatric settings,” study investigator Emil Stobbe, MSc, a predoctoral fellow at the Max Planck Institute for Human Development, Berlin, said in an interview.
“If someone is seeking an easily accessible intervention to lower distress, listening to an audio clip of birds singing might be a great option,” he added.
The study was published online in Scientific Reports.
Nature’s calming effect
The aim of the research was “to investigate how the physical environment impact brain and mental health,” Mr. Stobbe said.
Mr. Stobbe said that there is significantly more research examining visual properties of the physical environment but that the auditory domain is not as well researched, although, he added, that the beneficial effects of interactions with nature are “well studied.”
He noted that anxiety and paranoia can be experienced by many individuals even though they may be unaware that they are experiencing these states.
“We wanted to investigate if the beneficial effects of nature can also exert their impact on these states. In theory, birds can be representational for natural and vital environment, which, in turn, transfer the positive effects of nature on birdsong listeners,” he said.
A previous study compared nature versus city soundscape conditions and showed that the nature soundscape improved participants’ cognitive performance but did not improve mood. The present study added diversity to the soundscapes and focused not only on cognition and general mood but also on state paranoia, “which can be measured in a change-sensitive manner” and “has been shown to increase in response to traffic noise.”
The researchers hypothesized that birdsong would have a greater beneficial effect on mood and paranoia and on cognitive performance compared with traffic noise. They also investigated whether greater versus lower diversity of bird species or noise sources within the soundscapes “would be a relevant factor modulating the effects.”
The researchers recruited participants (n = 295) from a crowdsourcing platform. Participants’ mean age was late 20s (standard deviations ranged from 6.30 to 7.72), with a greater proportion of male versus female participants.
To be included, participants were required to have no history of mental illness, hearing difficulties, substance/drug intake, or suicidal thoughts/tendencies.
The outcomes of interest (mood, paranoia, cognitive performance) were measured before and after soundscape exposure and each soundscape had a low- versus high-diversity version. This resulted in several analyses that compared two types of sounds (birdsongs vs. traffic noise) x two levels of diversity (low vs. high diversity) and two time points (pre- vs. post exposure).
The exposure to sounds lasted for 6 minutes, after which they were asked to report (on a 0-100 visual scale) how diverse/monotone, beautiful, and pleasant they perceived the soundscape to be.
Reduction in depressive symptoms
Participants were divided into four groups: low-diversity traffic noise soundscape (n = 83), high-diversity traffic noise soundscape (n = 60), low-diversity birdsong soundscape (n = 63), and high-diversity birdsong soundscape (n = 80)
In addition to listening to the sounds, participants completed questionnaires measuring mood (depression and anxiety) and paranoia as well as a test of digit span cognitive performance (both the forward and the backward versions).
The type, diversity, and type x diversity all revealed significant effect sizes (F[3, 276] = 78.6; P < .001; eta-squared = 0.461; F[3, 276] = 3.16; P = .025; eta-squared = 0.033; and F[3, 276] = 2.66; P = .028, respectively), “suggesting that all of these factors, as well as their interaction, had a significant impact on the perception of soundscapes (that is, ratings on monotony/diversity, beauty, and pleasantness).”
A post hoc examination showed that depressive symptoms significantly increased within the low- and high-diversity urban soundscapes but decreased significantly in the high-diversity birdsong soundscapes (T[1, 60] = –2.57; P = .012; d = –0.29).
For anxiety, the post hoc within-group analyses found no effects within low- and high-diversity traffic noise conditions (T[1, 82] = –1.37; P = .174; d = –0.15 and T[1, 68] = 0.49; P = .629; d = 0.06, respectively). By contrast, there were significant declines in both birdsong conditions (low diversity: T[1, 62] = –6.13; P < .001; d = –0.77; high diversity: T[1, 60] = –6.32; P < .001; d = –0.70).
Similarly, there were no changes in participants with paranoia when they listened to either low- or high-diversity traffic noises (T[1, 82] = –0.55; P = .583; d = –0.06 and T[1, 68] = 0.67; P = .507; d = 0.08, respectively). On the other hand, both birdsong conditions yielded reductions in paranoia (low diversity: T[1, 62] = –5.90; P < .001; d = –0.74; high diversity: T[1, 60] = –4.11; P < .001; d = –0.46).
None of the soundscapes had any effect on cognition.
“In theory, birds can be representational for natural and vital environments which, in turn, transfer the positive effects of nature on birdsong listeners,” said Mr. Stobbe.
“Taken together, the findings of the current study provide another facet of why interactions with nature can be beneficial for our mental health, and it is highly important to preserve nature,” he added.
Mr. Stobbe said that future research should focus on investigating mixed soundscapes including examining whether the presence of natural sounds in urban settings lower stressors such as traffic noise.
An understudied area
Commenting for this article, Ken Duckworth, MD, chief medical officer of the National Alliance on Mental Illness called the study “interesting but limited.”
Dr. Duckworth, who was not involved in the research said that the “benefits of nature are understudied” and agreed with the investigators that it is potentially important to study the use of birdsongs in psychiatric facilities. “Future studies could also correlate the role of birdsong with the mental health benefits/aspects of ‘being in nature,’ which has been found to have some effect.”
Open Access funding was enabled and organized by Projekt DEAL. The authors and Dr. Duckworth declared no competing interests.
A version of this article first appeared on Medscape.com.
FROM SCIENTIFIC REPORTS












