User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Pfizer COVID vaccine is 100% effective in adolescents: Study
Pfizer announced on Nov. 22 that its COVID-19 vaccine provided long-term protection against the virus in a late-stage clinical trial among adolescents ages 12-15.
A two-dose series was 100% effective against COVID-19, which was measured between 7 days and 4 months after the second dose.
“As the global health community works to increase the number of vaccinated people around the world, these additional data provide further confidence in our vaccine safety and effectiveness profile in adolescents,” Albert Bourla, PhD, chairman and CEO of Pfizer, said in a statement.
The clinical trial researchers found no serious safety concerns while following patients for 6 months. The adverse events were consistent with other clinical safety data for the vaccine, the company said.
Pfizer will incorporate the data into its submissions for full regulatory approval of the vaccine for ages 12-15 in the United States and worldwide.
The company will request clearance for a 30-mcg dose of the vaccines for ages 12 and older. The shot received FDA emergency use authorization for ages 12-15 in May and full approval for ages 16 and older in August.
The study included 2,228 clinical trial participants who were monitored between November 2020 and September 2021. There were 30 confirmed symptomatic cases of COVID-19 in the placebo group that didn’t receive the vaccine and 0 COVID-19 cases among the vaccinated group.
The efficacy was consistently high across gender, race, ethnicity, and health conditions, the company said.
“This is especially important as we see rates of COVID-19 climbing in this age group in some regions, while vaccine uptake has slowed,” Mr. Bourla said. “We look forward to sharing these data with the FDA and other regulators.”
A version of this article first appeared on WebMD.com.
Pfizer announced on Nov. 22 that its COVID-19 vaccine provided long-term protection against the virus in a late-stage clinical trial among adolescents ages 12-15.
A two-dose series was 100% effective against COVID-19, which was measured between 7 days and 4 months after the second dose.
“As the global health community works to increase the number of vaccinated people around the world, these additional data provide further confidence in our vaccine safety and effectiveness profile in adolescents,” Albert Bourla, PhD, chairman and CEO of Pfizer, said in a statement.
The clinical trial researchers found no serious safety concerns while following patients for 6 months. The adverse events were consistent with other clinical safety data for the vaccine, the company said.
Pfizer will incorporate the data into its submissions for full regulatory approval of the vaccine for ages 12-15 in the United States and worldwide.
The company will request clearance for a 30-mcg dose of the vaccines for ages 12 and older. The shot received FDA emergency use authorization for ages 12-15 in May and full approval for ages 16 and older in August.
The study included 2,228 clinical trial participants who were monitored between November 2020 and September 2021. There were 30 confirmed symptomatic cases of COVID-19 in the placebo group that didn’t receive the vaccine and 0 COVID-19 cases among the vaccinated group.
The efficacy was consistently high across gender, race, ethnicity, and health conditions, the company said.
“This is especially important as we see rates of COVID-19 climbing in this age group in some regions, while vaccine uptake has slowed,” Mr. Bourla said. “We look forward to sharing these data with the FDA and other regulators.”
A version of this article first appeared on WebMD.com.
Pfizer announced on Nov. 22 that its COVID-19 vaccine provided long-term protection against the virus in a late-stage clinical trial among adolescents ages 12-15.
A two-dose series was 100% effective against COVID-19, which was measured between 7 days and 4 months after the second dose.
“As the global health community works to increase the number of vaccinated people around the world, these additional data provide further confidence in our vaccine safety and effectiveness profile in adolescents,” Albert Bourla, PhD, chairman and CEO of Pfizer, said in a statement.
The clinical trial researchers found no serious safety concerns while following patients for 6 months. The adverse events were consistent with other clinical safety data for the vaccine, the company said.
Pfizer will incorporate the data into its submissions for full regulatory approval of the vaccine for ages 12-15 in the United States and worldwide.
The company will request clearance for a 30-mcg dose of the vaccines for ages 12 and older. The shot received FDA emergency use authorization for ages 12-15 in May and full approval for ages 16 and older in August.
The study included 2,228 clinical trial participants who were monitored between November 2020 and September 2021. There were 30 confirmed symptomatic cases of COVID-19 in the placebo group that didn’t receive the vaccine and 0 COVID-19 cases among the vaccinated group.
The efficacy was consistently high across gender, race, ethnicity, and health conditions, the company said.
“This is especially important as we see rates of COVID-19 climbing in this age group in some regions, while vaccine uptake has slowed,” Mr. Bourla said. “We look forward to sharing these data with the FDA and other regulators.”
A version of this article first appeared on WebMD.com.
Fueling an ‘already raging fire’: Fifth COVID surge approaches
“A significant rise in cases just before Thanksgiving is not what we want to be seeing,” said Stephen Kissler, PhD, a postdoctoral researcher and data modeler at the Harvard TH Chan School of Public Health in Boston.
Dr. Kissler said he’d rather see increases in daily cases coming 2 weeks after busy travel periods, as that would mean they could come back down as people returned to their routines.
Seeing big increases in cases ahead of the holidays, he said, “is sort of like adding fuel to an already raging fire.”
Last winter, vaccines hadn’t been rolled out as the nation prepared for Thanksgiving. COVID-19 was burning through family gatherings.
But now that two-thirds of Americans over age 5 are fully vaccinated and booster doses are approved for all adults, will a rise in cases translate, once again, into a strain on our still thinly stretched healthcare system?
Experts say the vaccines are keeping people out of the hospital, which will help. And new antiviral pills are coming that seem to be able to cut a COVID-19 infection off at the knees, at least according to early data. A U.S. Food and Drug Administration panel meets next week to discuss the first application for a pill by Merck.
But experts caution that the coming surge will almost certainly tax hospitals again, especially in areas with lower vaccination rates.
And even states where blood testing shows that significant numbers of people have antibodies after a COVID-19 infection aren’t out of the woods, in part because we still don’t know how long the immunity generated by infection may last.
“Erosion of immunity”
“It’s hard to know how much risk is out there,” said Jeffrey Shaman, PhD, professor of environmental health sciences at Columbia University’s Mailman School of Public Health in New York City, who has been modeling the trajectory of the pandemic.
“We’re estimating, unfortunately, and we have for many weeks now, that there is an erosion of immunity,” Dr. Shaman said. “I think it could get bad. How bad? I’m not sure.”
Ali Mokdad, PhD, a professor of health metrics sciences at the University of Washington’s Institute for Health Metrics and Evaluation in Seattle, agrees.
Because there are so few studies on how long immunity from natural infection lasts, Dr. Mokdad and his colleagues are assuming that waning immunity after infection happens at least as quickly as it does after vaccination.
Their model is predicting that the average number of daily cases will peak at around 100,000, with another 100,000 going undetected, and will stay at that level until the end of January, as some states recover from their surges and others pick up steam.
While the number of daily deaths won’t climb to the heights seen during the summer surge, Dr. Mokdad said their model is predicting that daily deaths will climb again to about 1,200 a day.
“We are almost there right now, and it will be with us for a while,” he said. “We are predicting 881,000 deaths by March 1.”
The United States has currently recorded 773,000 COVID-19 deaths, so Dr. Mokdad is predicting about 120,000 more deaths between now and then.
He said his model shows that more than half of those deaths could be prevented if 95% of Americans wore their masks while in close proximity to strangers.
Currently, only about 36% of Americans are consistently wearing masks, according to surveys. While people are moving around more now, mobility is at prepandemic levels in some states.
“The rise that you are seeing right now is high mobility and low mask wearing in the United States,” Dr. Mokdad said.
The solution, he said, is for all adults to get another dose of vaccine — he doesn’t like calling it a booster.
“Because they’re vaccinated and they have two doses they have a false sense of security that they are protected. We needed to come ahead of it immediately and say you need a third dose, and we were late to do so,” Dr. Mokdad said.
A version of this article first appeared on Medscape.com.
“A significant rise in cases just before Thanksgiving is not what we want to be seeing,” said Stephen Kissler, PhD, a postdoctoral researcher and data modeler at the Harvard TH Chan School of Public Health in Boston.
Dr. Kissler said he’d rather see increases in daily cases coming 2 weeks after busy travel periods, as that would mean they could come back down as people returned to their routines.
Seeing big increases in cases ahead of the holidays, he said, “is sort of like adding fuel to an already raging fire.”
Last winter, vaccines hadn’t been rolled out as the nation prepared for Thanksgiving. COVID-19 was burning through family gatherings.
But now that two-thirds of Americans over age 5 are fully vaccinated and booster doses are approved for all adults, will a rise in cases translate, once again, into a strain on our still thinly stretched healthcare system?
Experts say the vaccines are keeping people out of the hospital, which will help. And new antiviral pills are coming that seem to be able to cut a COVID-19 infection off at the knees, at least according to early data. A U.S. Food and Drug Administration panel meets next week to discuss the first application for a pill by Merck.
But experts caution that the coming surge will almost certainly tax hospitals again, especially in areas with lower vaccination rates.
And even states where blood testing shows that significant numbers of people have antibodies after a COVID-19 infection aren’t out of the woods, in part because we still don’t know how long the immunity generated by infection may last.
“Erosion of immunity”
“It’s hard to know how much risk is out there,” said Jeffrey Shaman, PhD, professor of environmental health sciences at Columbia University’s Mailman School of Public Health in New York City, who has been modeling the trajectory of the pandemic.
“We’re estimating, unfortunately, and we have for many weeks now, that there is an erosion of immunity,” Dr. Shaman said. “I think it could get bad. How bad? I’m not sure.”
Ali Mokdad, PhD, a professor of health metrics sciences at the University of Washington’s Institute for Health Metrics and Evaluation in Seattle, agrees.
Because there are so few studies on how long immunity from natural infection lasts, Dr. Mokdad and his colleagues are assuming that waning immunity after infection happens at least as quickly as it does after vaccination.
Their model is predicting that the average number of daily cases will peak at around 100,000, with another 100,000 going undetected, and will stay at that level until the end of January, as some states recover from their surges and others pick up steam.
While the number of daily deaths won’t climb to the heights seen during the summer surge, Dr. Mokdad said their model is predicting that daily deaths will climb again to about 1,200 a day.
“We are almost there right now, and it will be with us for a while,” he said. “We are predicting 881,000 deaths by March 1.”
The United States has currently recorded 773,000 COVID-19 deaths, so Dr. Mokdad is predicting about 120,000 more deaths between now and then.
He said his model shows that more than half of those deaths could be prevented if 95% of Americans wore their masks while in close proximity to strangers.
Currently, only about 36% of Americans are consistently wearing masks, according to surveys. While people are moving around more now, mobility is at prepandemic levels in some states.
“The rise that you are seeing right now is high mobility and low mask wearing in the United States,” Dr. Mokdad said.
The solution, he said, is for all adults to get another dose of vaccine — he doesn’t like calling it a booster.
“Because they’re vaccinated and they have two doses they have a false sense of security that they are protected. We needed to come ahead of it immediately and say you need a third dose, and we were late to do so,” Dr. Mokdad said.
A version of this article first appeared on Medscape.com.
“A significant rise in cases just before Thanksgiving is not what we want to be seeing,” said Stephen Kissler, PhD, a postdoctoral researcher and data modeler at the Harvard TH Chan School of Public Health in Boston.
Dr. Kissler said he’d rather see increases in daily cases coming 2 weeks after busy travel periods, as that would mean they could come back down as people returned to their routines.
Seeing big increases in cases ahead of the holidays, he said, “is sort of like adding fuel to an already raging fire.”
Last winter, vaccines hadn’t been rolled out as the nation prepared for Thanksgiving. COVID-19 was burning through family gatherings.
But now that two-thirds of Americans over age 5 are fully vaccinated and booster doses are approved for all adults, will a rise in cases translate, once again, into a strain on our still thinly stretched healthcare system?
Experts say the vaccines are keeping people out of the hospital, which will help. And new antiviral pills are coming that seem to be able to cut a COVID-19 infection off at the knees, at least according to early data. A U.S. Food and Drug Administration panel meets next week to discuss the first application for a pill by Merck.
But experts caution that the coming surge will almost certainly tax hospitals again, especially in areas with lower vaccination rates.
And even states where blood testing shows that significant numbers of people have antibodies after a COVID-19 infection aren’t out of the woods, in part because we still don’t know how long the immunity generated by infection may last.
“Erosion of immunity”
“It’s hard to know how much risk is out there,” said Jeffrey Shaman, PhD, professor of environmental health sciences at Columbia University’s Mailman School of Public Health in New York City, who has been modeling the trajectory of the pandemic.
“We’re estimating, unfortunately, and we have for many weeks now, that there is an erosion of immunity,” Dr. Shaman said. “I think it could get bad. How bad? I’m not sure.”
Ali Mokdad, PhD, a professor of health metrics sciences at the University of Washington’s Institute for Health Metrics and Evaluation in Seattle, agrees.
Because there are so few studies on how long immunity from natural infection lasts, Dr. Mokdad and his colleagues are assuming that waning immunity after infection happens at least as quickly as it does after vaccination.
Their model is predicting that the average number of daily cases will peak at around 100,000, with another 100,000 going undetected, and will stay at that level until the end of January, as some states recover from their surges and others pick up steam.
While the number of daily deaths won’t climb to the heights seen during the summer surge, Dr. Mokdad said their model is predicting that daily deaths will climb again to about 1,200 a day.
“We are almost there right now, and it will be with us for a while,” he said. “We are predicting 881,000 deaths by March 1.”
The United States has currently recorded 773,000 COVID-19 deaths, so Dr. Mokdad is predicting about 120,000 more deaths between now and then.
He said his model shows that more than half of those deaths could be prevented if 95% of Americans wore their masks while in close proximity to strangers.
Currently, only about 36% of Americans are consistently wearing masks, according to surveys. While people are moving around more now, mobility is at prepandemic levels in some states.
“The rise that you are seeing right now is high mobility and low mask wearing in the United States,” Dr. Mokdad said.
The solution, he said, is for all adults to get another dose of vaccine — he doesn’t like calling it a booster.
“Because they’re vaccinated and they have two doses they have a false sense of security that they are protected. We needed to come ahead of it immediately and say you need a third dose, and we were late to do so,” Dr. Mokdad said.
A version of this article first appeared on Medscape.com.
Headache is a common post–COVID-19 complaint
The Centers for Disease Control and Prevention has identified it as a sentinel symptom of COVID-19 disease. “A lot of the recommendations surrounding post-COVID headache is that if you identify a patient who has headaches associated with fever, and myalgia, and other systemic symptoms, the specificity of a COVID-19 diagnosis goes up. So [COVID-19] is a really important feature to look out for in patients with headache,” Deena Kuruvilla, MD, said during a presentation on post–COVID-19 headache at the 2021 Scottsdale Headache Symposium.
Estimates of the prevalence of headache in COVID-19 range widely, from 6.5% to 71%, but Dr. Kuruvilla has plenty of personal experience with it. “During my stint on the inpatient neurology service during the peak of COVID, I saw patients with headache being one of the most frequent complaints, [along with] dizziness, stroke, and seizure among many other neurological manifestations,” said Dr. Kuruvilla, director of the Westport (Conn.) Headache Institute.
One meta-analysis showed that 47% of patients with COVID-19 complain of headache within 30 days of diagnosis, and this drops to around 10% at 60-90 days, and around 8% at 180 days.
A survey of 3,458 patients, published in the Journal of Headache Pain, found that migraine is the most common type of post–COVID-19 headache phenotype, and patients reporting anosmia-ageusia were more likely to have post–COVID-19 headache (odds ratio [OR], 5.39; 95% confidence interval, 1.66-17.45).
A case-control study of post–COVID-19 headache patients with and without a history of migraine found that those with a history of migraine were more likely to have post–COVID-19 symptoms (OR, 1.70; P < .001) and fatigue (OR, 2.89; P = .008). “Interestingly, they found no difference in headache as post-COVID symptoms in people who had a history of migraine compared with people without a history of migraine,” said Dr. Kuruvilla.
Headache and COVID-19: What is the connection?
Several mechanisms have been proposed for direct invasion of the central nervous system, either via infection through the angiotensin-converting enzyme 2 (ACE-2) receptor, which is expressed in brain regions including the motor cortex, the posterior cingulate cortex, and the olfactory bulb, among other locations. Another potential mechanism is direct entry through the olfactory nerve and the associated olfactory epithelium. There are various potential mechanisms for spread among the peripheral nervous system, and the blood-brain barrier can be compromised by infection of vascular endothelial cells. According to the literature, neuronal damage seems to occur directly from viral damage rather than from the immune response, said Dr. Kuruvilla.
The virus may also gain entry to the CNS indirectly, as a result of hypoxia and metabolic disturbances, as well as dehydration and systematic inflammation. The cytokine storm associated with COVID-19 infection can activate C-reactive protein and calcitonin gene-related peptide (CGRP), which plays a key role in migraine pathology. The CGRP receptor antagonist vazegepant is being studied in a phase 2 clinical trial for the treatment of COVID-19–related lung inflammation.
Testing and treatment
“If I see patients with new headache, worsening headache from their baseline, or headache with systemic symptoms, I often consider screening them for COVID. If that screening is positive, I proceed with PCR testing. I also consider an MRI of the brain with and without gadolinium just to rule out any secondary causes for headache,” said Dr. Kuruvilla, noting that she has diagnosed patients with venous sinus thrombosis, ischemic stroke, and meningitis following COVID-19.
The existing literature suggests that lumbar puncture in patients with SARS-CoV-2 typically returns normal results, but Dr. Kuruvilla proceeds with it anyway with viral, bacterial, fungal, and autoimmune studies to rule out potential secondary causes for headache.
There are few studies on how to treat post–COVID-19 headache, and the general recommendation is that headache phenotype should drive treatment decisions.
In a case series, three patients with persistent headache following mild COVID-19 infection were treated with onabotulinumtoxinA and amitriptyline. They had daily headaches, along with post–COVID-19 symptoms including fatigue and insomnia. After treatment, each patient converted to episodic headaches.
One retrospective study of 37 patients found that a 5-day course of indomethacin 50 mg twice per day and pantoprazole 40 mg once per day was associated with a 50% or greater improvement in headache on the third day in 36 of the 37 patients. Five patients were free of pain by day 5.
A common problem
Neurologists have been involved in the treatment of COVID-19 since the beginning, and post–COVID-19 headache has added another layer. “It’s been a remarkably common clinical problem. And the fact that it’s actually reached the level of headache specialist actually shows that in some cases, it’s really quite a significant problem, in both its severity and persistence. So I think it’s a very, very significant issue,” said Andrew Charles, MD, professor of neurology at the University of California, Los Angeles, and director of the UCLA Goldberg Migraine Program.
Dr. Kuruvilla also discussed the question of whether neurological damage is due to direct damage from the virus, or indirect damage from an immune response. This was debated during the Q&A session following Dr. Kuruvilla’s talk, and it was pointed out that headache is a frequent side effect of the Pfizer and Moderna vaccines.
“It’s a huge open question about how much is direct invasion or damage or not even damage, but just change in function with the viral infection, as opposed to inflammation. The fact that very often the response to the vaccine is similar to what you see with COVID suggests that at least some component of it is inflammation. I wouldn’t commit to one mechanism or the other, but I’d say that it’s possible that it’s really both,” said Dr. Charles.
Dr. Kuruvilla has consulted for Cefaly, Neurolief, Theranica, Now What Media, and KX advisors. She has been on the speakers bureau for Abbvie/Allergan, Amgen/Novartis, and Lilly. She has been on advisory boards for Abbvie/Allergan, Lilly, Theranica, and Amgen/Novartis. Dr. Charles has no relevant financial disclosures.
The Centers for Disease Control and Prevention has identified it as a sentinel symptom of COVID-19 disease. “A lot of the recommendations surrounding post-COVID headache is that if you identify a patient who has headaches associated with fever, and myalgia, and other systemic symptoms, the specificity of a COVID-19 diagnosis goes up. So [COVID-19] is a really important feature to look out for in patients with headache,” Deena Kuruvilla, MD, said during a presentation on post–COVID-19 headache at the 2021 Scottsdale Headache Symposium.
Estimates of the prevalence of headache in COVID-19 range widely, from 6.5% to 71%, but Dr. Kuruvilla has plenty of personal experience with it. “During my stint on the inpatient neurology service during the peak of COVID, I saw patients with headache being one of the most frequent complaints, [along with] dizziness, stroke, and seizure among many other neurological manifestations,” said Dr. Kuruvilla, director of the Westport (Conn.) Headache Institute.
One meta-analysis showed that 47% of patients with COVID-19 complain of headache within 30 days of diagnosis, and this drops to around 10% at 60-90 days, and around 8% at 180 days.
A survey of 3,458 patients, published in the Journal of Headache Pain, found that migraine is the most common type of post–COVID-19 headache phenotype, and patients reporting anosmia-ageusia were more likely to have post–COVID-19 headache (odds ratio [OR], 5.39; 95% confidence interval, 1.66-17.45).
A case-control study of post–COVID-19 headache patients with and without a history of migraine found that those with a history of migraine were more likely to have post–COVID-19 symptoms (OR, 1.70; P < .001) and fatigue (OR, 2.89; P = .008). “Interestingly, they found no difference in headache as post-COVID symptoms in people who had a history of migraine compared with people without a history of migraine,” said Dr. Kuruvilla.
Headache and COVID-19: What is the connection?
Several mechanisms have been proposed for direct invasion of the central nervous system, either via infection through the angiotensin-converting enzyme 2 (ACE-2) receptor, which is expressed in brain regions including the motor cortex, the posterior cingulate cortex, and the olfactory bulb, among other locations. Another potential mechanism is direct entry through the olfactory nerve and the associated olfactory epithelium. There are various potential mechanisms for spread among the peripheral nervous system, and the blood-brain barrier can be compromised by infection of vascular endothelial cells. According to the literature, neuronal damage seems to occur directly from viral damage rather than from the immune response, said Dr. Kuruvilla.
The virus may also gain entry to the CNS indirectly, as a result of hypoxia and metabolic disturbances, as well as dehydration and systematic inflammation. The cytokine storm associated with COVID-19 infection can activate C-reactive protein and calcitonin gene-related peptide (CGRP), which plays a key role in migraine pathology. The CGRP receptor antagonist vazegepant is being studied in a phase 2 clinical trial for the treatment of COVID-19–related lung inflammation.
Testing and treatment
“If I see patients with new headache, worsening headache from their baseline, or headache with systemic symptoms, I often consider screening them for COVID. If that screening is positive, I proceed with PCR testing. I also consider an MRI of the brain with and without gadolinium just to rule out any secondary causes for headache,” said Dr. Kuruvilla, noting that she has diagnosed patients with venous sinus thrombosis, ischemic stroke, and meningitis following COVID-19.
The existing literature suggests that lumbar puncture in patients with SARS-CoV-2 typically returns normal results, but Dr. Kuruvilla proceeds with it anyway with viral, bacterial, fungal, and autoimmune studies to rule out potential secondary causes for headache.
There are few studies on how to treat post–COVID-19 headache, and the general recommendation is that headache phenotype should drive treatment decisions.
In a case series, three patients with persistent headache following mild COVID-19 infection were treated with onabotulinumtoxinA and amitriptyline. They had daily headaches, along with post–COVID-19 symptoms including fatigue and insomnia. After treatment, each patient converted to episodic headaches.
One retrospective study of 37 patients found that a 5-day course of indomethacin 50 mg twice per day and pantoprazole 40 mg once per day was associated with a 50% or greater improvement in headache on the third day in 36 of the 37 patients. Five patients were free of pain by day 5.
A common problem
Neurologists have been involved in the treatment of COVID-19 since the beginning, and post–COVID-19 headache has added another layer. “It’s been a remarkably common clinical problem. And the fact that it’s actually reached the level of headache specialist actually shows that in some cases, it’s really quite a significant problem, in both its severity and persistence. So I think it’s a very, very significant issue,” said Andrew Charles, MD, professor of neurology at the University of California, Los Angeles, and director of the UCLA Goldberg Migraine Program.
Dr. Kuruvilla also discussed the question of whether neurological damage is due to direct damage from the virus, or indirect damage from an immune response. This was debated during the Q&A session following Dr. Kuruvilla’s talk, and it was pointed out that headache is a frequent side effect of the Pfizer and Moderna vaccines.
“It’s a huge open question about how much is direct invasion or damage or not even damage, but just change in function with the viral infection, as opposed to inflammation. The fact that very often the response to the vaccine is similar to what you see with COVID suggests that at least some component of it is inflammation. I wouldn’t commit to one mechanism or the other, but I’d say that it’s possible that it’s really both,” said Dr. Charles.
Dr. Kuruvilla has consulted for Cefaly, Neurolief, Theranica, Now What Media, and KX advisors. She has been on the speakers bureau for Abbvie/Allergan, Amgen/Novartis, and Lilly. She has been on advisory boards for Abbvie/Allergan, Lilly, Theranica, and Amgen/Novartis. Dr. Charles has no relevant financial disclosures.
The Centers for Disease Control and Prevention has identified it as a sentinel symptom of COVID-19 disease. “A lot of the recommendations surrounding post-COVID headache is that if you identify a patient who has headaches associated with fever, and myalgia, and other systemic symptoms, the specificity of a COVID-19 diagnosis goes up. So [COVID-19] is a really important feature to look out for in patients with headache,” Deena Kuruvilla, MD, said during a presentation on post–COVID-19 headache at the 2021 Scottsdale Headache Symposium.
Estimates of the prevalence of headache in COVID-19 range widely, from 6.5% to 71%, but Dr. Kuruvilla has plenty of personal experience with it. “During my stint on the inpatient neurology service during the peak of COVID, I saw patients with headache being one of the most frequent complaints, [along with] dizziness, stroke, and seizure among many other neurological manifestations,” said Dr. Kuruvilla, director of the Westport (Conn.) Headache Institute.
One meta-analysis showed that 47% of patients with COVID-19 complain of headache within 30 days of diagnosis, and this drops to around 10% at 60-90 days, and around 8% at 180 days.
A survey of 3,458 patients, published in the Journal of Headache Pain, found that migraine is the most common type of post–COVID-19 headache phenotype, and patients reporting anosmia-ageusia were more likely to have post–COVID-19 headache (odds ratio [OR], 5.39; 95% confidence interval, 1.66-17.45).
A case-control study of post–COVID-19 headache patients with and without a history of migraine found that those with a history of migraine were more likely to have post–COVID-19 symptoms (OR, 1.70; P < .001) and fatigue (OR, 2.89; P = .008). “Interestingly, they found no difference in headache as post-COVID symptoms in people who had a history of migraine compared with people without a history of migraine,” said Dr. Kuruvilla.
Headache and COVID-19: What is the connection?
Several mechanisms have been proposed for direct invasion of the central nervous system, either via infection through the angiotensin-converting enzyme 2 (ACE-2) receptor, which is expressed in brain regions including the motor cortex, the posterior cingulate cortex, and the olfactory bulb, among other locations. Another potential mechanism is direct entry through the olfactory nerve and the associated olfactory epithelium. There are various potential mechanisms for spread among the peripheral nervous system, and the blood-brain barrier can be compromised by infection of vascular endothelial cells. According to the literature, neuronal damage seems to occur directly from viral damage rather than from the immune response, said Dr. Kuruvilla.
The virus may also gain entry to the CNS indirectly, as a result of hypoxia and metabolic disturbances, as well as dehydration and systematic inflammation. The cytokine storm associated with COVID-19 infection can activate C-reactive protein and calcitonin gene-related peptide (CGRP), which plays a key role in migraine pathology. The CGRP receptor antagonist vazegepant is being studied in a phase 2 clinical trial for the treatment of COVID-19–related lung inflammation.
Testing and treatment
“If I see patients with new headache, worsening headache from their baseline, or headache with systemic symptoms, I often consider screening them for COVID. If that screening is positive, I proceed with PCR testing. I also consider an MRI of the brain with and without gadolinium just to rule out any secondary causes for headache,” said Dr. Kuruvilla, noting that she has diagnosed patients with venous sinus thrombosis, ischemic stroke, and meningitis following COVID-19.
The existing literature suggests that lumbar puncture in patients with SARS-CoV-2 typically returns normal results, but Dr. Kuruvilla proceeds with it anyway with viral, bacterial, fungal, and autoimmune studies to rule out potential secondary causes for headache.
There are few studies on how to treat post–COVID-19 headache, and the general recommendation is that headache phenotype should drive treatment decisions.
In a case series, three patients with persistent headache following mild COVID-19 infection were treated with onabotulinumtoxinA and amitriptyline. They had daily headaches, along with post–COVID-19 symptoms including fatigue and insomnia. After treatment, each patient converted to episodic headaches.
One retrospective study of 37 patients found that a 5-day course of indomethacin 50 mg twice per day and pantoprazole 40 mg once per day was associated with a 50% or greater improvement in headache on the third day in 36 of the 37 patients. Five patients were free of pain by day 5.
A common problem
Neurologists have been involved in the treatment of COVID-19 since the beginning, and post–COVID-19 headache has added another layer. “It’s been a remarkably common clinical problem. And the fact that it’s actually reached the level of headache specialist actually shows that in some cases, it’s really quite a significant problem, in both its severity and persistence. So I think it’s a very, very significant issue,” said Andrew Charles, MD, professor of neurology at the University of California, Los Angeles, and director of the UCLA Goldberg Migraine Program.
Dr. Kuruvilla also discussed the question of whether neurological damage is due to direct damage from the virus, or indirect damage from an immune response. This was debated during the Q&A session following Dr. Kuruvilla’s talk, and it was pointed out that headache is a frequent side effect of the Pfizer and Moderna vaccines.
“It’s a huge open question about how much is direct invasion or damage or not even damage, but just change in function with the viral infection, as opposed to inflammation. The fact that very often the response to the vaccine is similar to what you see with COVID suggests that at least some component of it is inflammation. I wouldn’t commit to one mechanism or the other, but I’d say that it’s possible that it’s really both,” said Dr. Charles.
Dr. Kuruvilla has consulted for Cefaly, Neurolief, Theranica, Now What Media, and KX advisors. She has been on the speakers bureau for Abbvie/Allergan, Amgen/Novartis, and Lilly. She has been on advisory boards for Abbvie/Allergan, Lilly, Theranica, and Amgen/Novartis. Dr. Charles has no relevant financial disclosures.
FROM 2021 SCOTTSDALE HEADACHE SYMPOSIUM
Children and COVID: New cases increase for third straight week
There were almost 142,000 new cases reported during the week of Nov. 12-18, marking an increase of 16% over the previous week and the 15th straight week with a weekly total over 100,000, the American Academy of Pediatrics and the Children’s Hospital Association said.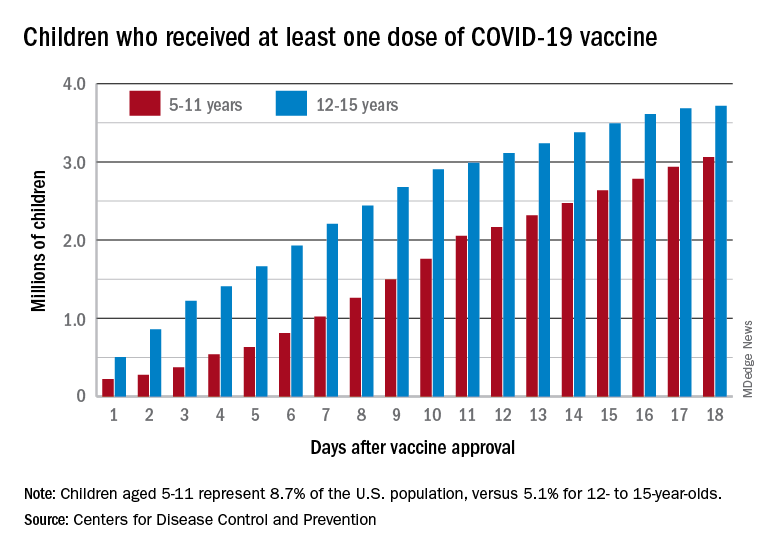
Regional data show that the Midwest has experienced the largest share of this latest surge, followed by the Northeast. Cases increased in the South during the week of Nov. 12-18 after holding steady over the previous 2 weeks, while new cases in the West dropped in the last week. At the state level, Maine, New Hampshire, and Vermont again reported the largest percent increases, with Michigan, Minnesota, and New Mexico also above average, the AAP and CHA said in their weekly COVID report.
Data from the Centers for Disease Control and Prevention show similar trends for both emergency department visits and hospital admissions, as both have risen in November after declines that began in late August and early September.
The cumulative number of pediatric cases is 6.77 million since the pandemic began, based on the AAP/CHA accounting of state cases, although Alabama, Nebraska, and Texas stopped reporting over the summer, suggesting the actual number is higher. The CDC puts the total number of COVID cases in children at 5.96 million, but there are age discrepancies between the CDC and the AAP/CHA’s state-based data.
The vaccine gap is closing
Vaccinations among the recently eligible 5- to 11-year-olds have steadily increased following a somewhat slow start. The initial pace was behind that of the 12- to 15-years-olds through the first postapproval week but has since closed the gap, based on data from the CDC’s COVID Data Tracker.
The tally of children who received at least one dose of the COVID vaccine among the 5- to 11-year-olds was behind the older group by almost 1.2 million on day 7 after the CDC’s Nov. 2 approval, but by day 18 the deficit was down to about 650,000, the CDC reported.
Altogether, just over 3 million children aged 5-11 have received at least one dose, which is 10.7% of that age group’s total population. Among children aged 12-17, the proportions are 60.7% with at least one dose and 51.1% at full vaccination. Children aged 5-11, who make up 8.7% of the total U.S. population, represented 42.8% of all vaccinations initiated over the 2 weeks ending Nov. 21, compared with 4.2% for those aged 12-17, the CDC said.
There were almost 142,000 new cases reported during the week of Nov. 12-18, marking an increase of 16% over the previous week and the 15th straight week with a weekly total over 100,000, the American Academy of Pediatrics and the Children’s Hospital Association said.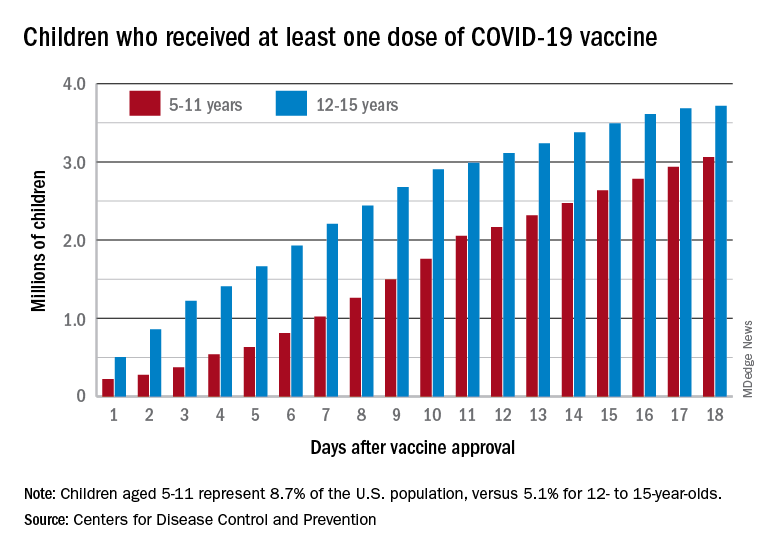
Regional data show that the Midwest has experienced the largest share of this latest surge, followed by the Northeast. Cases increased in the South during the week of Nov. 12-18 after holding steady over the previous 2 weeks, while new cases in the West dropped in the last week. At the state level, Maine, New Hampshire, and Vermont again reported the largest percent increases, with Michigan, Minnesota, and New Mexico also above average, the AAP and CHA said in their weekly COVID report.
Data from the Centers for Disease Control and Prevention show similar trends for both emergency department visits and hospital admissions, as both have risen in November after declines that began in late August and early September.
The cumulative number of pediatric cases is 6.77 million since the pandemic began, based on the AAP/CHA accounting of state cases, although Alabama, Nebraska, and Texas stopped reporting over the summer, suggesting the actual number is higher. The CDC puts the total number of COVID cases in children at 5.96 million, but there are age discrepancies between the CDC and the AAP/CHA’s state-based data.
The vaccine gap is closing
Vaccinations among the recently eligible 5- to 11-year-olds have steadily increased following a somewhat slow start. The initial pace was behind that of the 12- to 15-years-olds through the first postapproval week but has since closed the gap, based on data from the CDC’s COVID Data Tracker.
The tally of children who received at least one dose of the COVID vaccine among the 5- to 11-year-olds was behind the older group by almost 1.2 million on day 7 after the CDC’s Nov. 2 approval, but by day 18 the deficit was down to about 650,000, the CDC reported.
Altogether, just over 3 million children aged 5-11 have received at least one dose, which is 10.7% of that age group’s total population. Among children aged 12-17, the proportions are 60.7% with at least one dose and 51.1% at full vaccination. Children aged 5-11, who make up 8.7% of the total U.S. population, represented 42.8% of all vaccinations initiated over the 2 weeks ending Nov. 21, compared with 4.2% for those aged 12-17, the CDC said.
There were almost 142,000 new cases reported during the week of Nov. 12-18, marking an increase of 16% over the previous week and the 15th straight week with a weekly total over 100,000, the American Academy of Pediatrics and the Children’s Hospital Association said.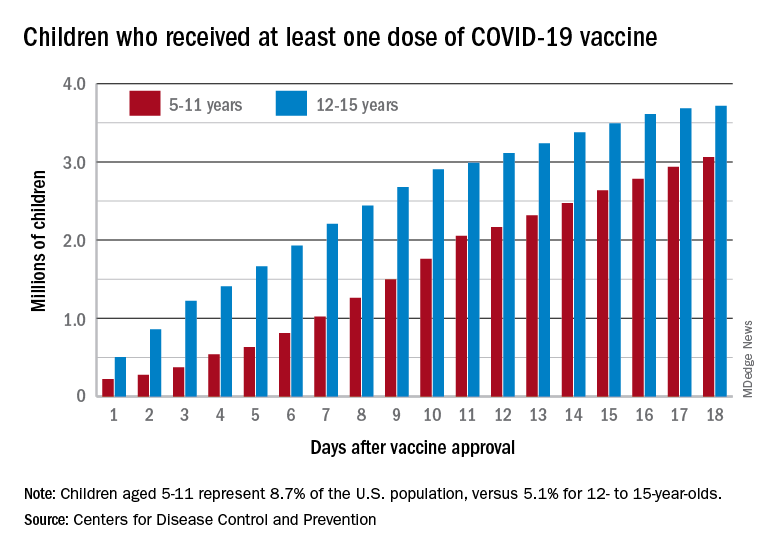
Regional data show that the Midwest has experienced the largest share of this latest surge, followed by the Northeast. Cases increased in the South during the week of Nov. 12-18 after holding steady over the previous 2 weeks, while new cases in the West dropped in the last week. At the state level, Maine, New Hampshire, and Vermont again reported the largest percent increases, with Michigan, Minnesota, and New Mexico also above average, the AAP and CHA said in their weekly COVID report.
Data from the Centers for Disease Control and Prevention show similar trends for both emergency department visits and hospital admissions, as both have risen in November after declines that began in late August and early September.
The cumulative number of pediatric cases is 6.77 million since the pandemic began, based on the AAP/CHA accounting of state cases, although Alabama, Nebraska, and Texas stopped reporting over the summer, suggesting the actual number is higher. The CDC puts the total number of COVID cases in children at 5.96 million, but there are age discrepancies between the CDC and the AAP/CHA’s state-based data.
The vaccine gap is closing
Vaccinations among the recently eligible 5- to 11-year-olds have steadily increased following a somewhat slow start. The initial pace was behind that of the 12- to 15-years-olds through the first postapproval week but has since closed the gap, based on data from the CDC’s COVID Data Tracker.
The tally of children who received at least one dose of the COVID vaccine among the 5- to 11-year-olds was behind the older group by almost 1.2 million on day 7 after the CDC’s Nov. 2 approval, but by day 18 the deficit was down to about 650,000, the CDC reported.
Altogether, just over 3 million children aged 5-11 have received at least one dose, which is 10.7% of that age group’s total population. Among children aged 12-17, the proportions are 60.7% with at least one dose and 51.1% at full vaccination. Children aged 5-11, who make up 8.7% of the total U.S. population, represented 42.8% of all vaccinations initiated over the 2 weeks ending Nov. 21, compared with 4.2% for those aged 12-17, the CDC said.
Inexplicably drunk: A case of an underdiagnosed condition?
A 46-year-old North Carolina man, who was pulled over on suspicion of drunk driving, vehemently denied consuming alcohol. When he refused to take a breathalyzer test, he was hospitalized and doctors confirmed what police suspected – his blood alcohol level was 0.20, two-and-a-half times the state’s legal limit – and he was charged with driving while intoxicated (DWI).
For an entire year after his arrest, the cause of his “intoxication” remained a mystery. It wasn’t until his aunt learned about a similar case that had been successfully treated at an Ohio clinic that he understood what was happening to him – he had auto brewery syndrome (ABS).
and suffer all the medical and social implications of alcoholism.
“ABS occurs when ingested carbohydrates are converted to alcohol by fungi in the gastrointestinal tract,” Fahad Malik, MD, who reported the case in BMJ Open Gastroenterology while a resident at Richmond University Medical Center in New York, told this news organization.
At the urging of his aunt, the patient attended the Ohio clinic where he underwent a complete blood count, comprehensive metabolic panel, immunology panel and urinalysis, all of which were normal.
However, stool testing revealed the presence of two strains of yeast – Saccharomyces cerevisiae, commonly used in winemaking, baking, and beer brewing, and Saccharomyces boulardii.
To confirm the ABS diagnosis, the patient received a carbohydrate meal and clinicians monitored his blood alcohol level, which, after 8 hours, reached 57 mg/dL. He was treated with antifungals for the Saccharomyces fungi in his stool and discharged on a strict carbohydrate-free diet along with special supplements, including multivitamins and probiotics, but no further antifungal therapy.
Probiotics, said Dr. Malik, competitively inhibit bad bacteria and fungi, but currently there is evidence to show they are useful for ABS.
Although the patient adhered to his prescribed treatment regimen, after a few weeks of no symptoms, intermittent “flares” returned. In one instance of inebriation, he fell and hit his head, resulting in intracranial bleeding that resulted in a transfer to a neurosurgical center. During his hospital stay, his blood alcohol levels ranged from 50 to 400 mg/dL.
Antibiotics the culprit?
Disheartened by the continuation of his symptoms, the patient sought support from an online forum. It was there he read about Dr. Malik and gastroenterologist Prasanna Wickremesinghe, MD (a colleague of Dr. Malik’s at Richmond MC), who had treated a complicated, very similar case of ABS. The patient made contact with the two physicians and they assessed him.
“We went from A to Z with the patient, because we were trying to look for similar things in the history – we wanted to know the exact point at which it started and understand when he started experiencing mental fog,” said Dr. Malik.
After speaking to the patient, Dr. Malik and Dr. Wickremesinghe traced his initial symptoms to a 2011 course of antibiotics (cephalexin 250 mg oral three times a day for 3 weeks) prescribed for a complicated traumatic thumb injury.
About a week after he finished the antibiotics, he experienced noticeable behavioral changes, including depression, brain fog, and aggressive outbursts, all of which were very uncharacteristic.
He visited his primary care physician in 2014 for treatment, which resulted in a referral to a psychiatrist, who treated him with lorazepam and fluoxetine. The patient noted that he was previously healthy, with no significant medical or psychiatric history.
Dr. Malik believes the antibiotics prescribed all those years ago is the culprit. “We were postulating that the antibiotics had changed the microbiome of his gut and allowed the fungi to develop,” he said.
Since there are no established diagnostic criteria or treatment regimen for ABS, Dr. Malik and Dr. Wickremesinghe developed their own.
Diagnosis consisted of a standardized carbohydrate challenge test vs. a carbohydrate meal, where they gave the patient 200 g of glucose by mouth after an overnight fast and drew blood at timed intervals of 0, 0.5, 1, 2, 4, 8, 16, and 24 hours to test for glucose and blood alcohol levels.
“After that we needed to isolate the fungi by examining the gut secretions through an upper and lower endoscopy,” said Dr. Wickremesinghe. Fungal cultures from the upper small gut and cecal secretions grew Candida albicans and C. parapsilosis.
Both fungi were sensitive to azoles and the physicians prescribed oral itraconazole 150 mg per day as an initial therapy. After 10 days, his symptoms did not improve so the dose was increased to 200 mg/day and the patient became “completely asymptomatic.”
“We had nothing to follow. We didn’t know how long to treat the patient, it was really just a process of trial and error,” said Dr. Malik. The physicians asked the patient to monitor his breath alcohol levels twice a day during treatment and immediately report any increases. Over time, he also received treatment with various probiotics to help normalize his gut flora.
Underdiagnosed condition?
At the time of the case study’s publication in the summer of 2019, the patient had been asymptomatic for 18 months and had been able to resume a normal diet, but still checks his breath alcohol levels from time to time.
“Before this patient’s case, I went all through the literature and found only a few cases of ABS,” said Dr. Malik.
However, he added, after this case study was published 10 other patients contacted him with a similar history of antibiotic use and the same symptoms. This, said Dr. Malik, is “significant” and suggests ABS is much more common than previously thought.
The clinicians also note that to the best of their knowledge this is the first report of antibiotic exposure initiating ABS.
“What we tried to do was set up a protocol by which to identify these patients, confirm a diagnosis, and treat them for a sufficient amount of time,” said Dr. Wickremesinghe. “We also wanted to inform other physicians that this may function as a standardized way of treating these patients, and may promote further study,” added Dr. Malik, who emphasized that the role of probiotics in ABS still needs to be studied.
Dr. Malik and Dr. Wickremesinghe note that physicians should be aware that mood changes, brain fog, and delirium in patients who deny alcohol ingestion may be the first symptoms of ABS.
Dr. Wickremesinghe said since the case study was published he and Dr. Malik have received queries from all over the world. “It’s unbelievable the amount of interest we have had in the paper, so if we have made the medical community and the general population aware of this condition and how to treat it, we have done a major thing for medicine,” he said.
A version of this article first appeared on Medscape.com.
A 46-year-old North Carolina man, who was pulled over on suspicion of drunk driving, vehemently denied consuming alcohol. When he refused to take a breathalyzer test, he was hospitalized and doctors confirmed what police suspected – his blood alcohol level was 0.20, two-and-a-half times the state’s legal limit – and he was charged with driving while intoxicated (DWI).
For an entire year after his arrest, the cause of his “intoxication” remained a mystery. It wasn’t until his aunt learned about a similar case that had been successfully treated at an Ohio clinic that he understood what was happening to him – he had auto brewery syndrome (ABS).
and suffer all the medical and social implications of alcoholism.
“ABS occurs when ingested carbohydrates are converted to alcohol by fungi in the gastrointestinal tract,” Fahad Malik, MD, who reported the case in BMJ Open Gastroenterology while a resident at Richmond University Medical Center in New York, told this news organization.
At the urging of his aunt, the patient attended the Ohio clinic where he underwent a complete blood count, comprehensive metabolic panel, immunology panel and urinalysis, all of which were normal.
However, stool testing revealed the presence of two strains of yeast – Saccharomyces cerevisiae, commonly used in winemaking, baking, and beer brewing, and Saccharomyces boulardii.
To confirm the ABS diagnosis, the patient received a carbohydrate meal and clinicians monitored his blood alcohol level, which, after 8 hours, reached 57 mg/dL. He was treated with antifungals for the Saccharomyces fungi in his stool and discharged on a strict carbohydrate-free diet along with special supplements, including multivitamins and probiotics, but no further antifungal therapy.
Probiotics, said Dr. Malik, competitively inhibit bad bacteria and fungi, but currently there is evidence to show they are useful for ABS.
Although the patient adhered to his prescribed treatment regimen, after a few weeks of no symptoms, intermittent “flares” returned. In one instance of inebriation, he fell and hit his head, resulting in intracranial bleeding that resulted in a transfer to a neurosurgical center. During his hospital stay, his blood alcohol levels ranged from 50 to 400 mg/dL.
Antibiotics the culprit?
Disheartened by the continuation of his symptoms, the patient sought support from an online forum. It was there he read about Dr. Malik and gastroenterologist Prasanna Wickremesinghe, MD (a colleague of Dr. Malik’s at Richmond MC), who had treated a complicated, very similar case of ABS. The patient made contact with the two physicians and they assessed him.
“We went from A to Z with the patient, because we were trying to look for similar things in the history – we wanted to know the exact point at which it started and understand when he started experiencing mental fog,” said Dr. Malik.
After speaking to the patient, Dr. Malik and Dr. Wickremesinghe traced his initial symptoms to a 2011 course of antibiotics (cephalexin 250 mg oral three times a day for 3 weeks) prescribed for a complicated traumatic thumb injury.
About a week after he finished the antibiotics, he experienced noticeable behavioral changes, including depression, brain fog, and aggressive outbursts, all of which were very uncharacteristic.
He visited his primary care physician in 2014 for treatment, which resulted in a referral to a psychiatrist, who treated him with lorazepam and fluoxetine. The patient noted that he was previously healthy, with no significant medical or psychiatric history.
Dr. Malik believes the antibiotics prescribed all those years ago is the culprit. “We were postulating that the antibiotics had changed the microbiome of his gut and allowed the fungi to develop,” he said.
Since there are no established diagnostic criteria or treatment regimen for ABS, Dr. Malik and Dr. Wickremesinghe developed their own.
Diagnosis consisted of a standardized carbohydrate challenge test vs. a carbohydrate meal, where they gave the patient 200 g of glucose by mouth after an overnight fast and drew blood at timed intervals of 0, 0.5, 1, 2, 4, 8, 16, and 24 hours to test for glucose and blood alcohol levels.
“After that we needed to isolate the fungi by examining the gut secretions through an upper and lower endoscopy,” said Dr. Wickremesinghe. Fungal cultures from the upper small gut and cecal secretions grew Candida albicans and C. parapsilosis.
Both fungi were sensitive to azoles and the physicians prescribed oral itraconazole 150 mg per day as an initial therapy. After 10 days, his symptoms did not improve so the dose was increased to 200 mg/day and the patient became “completely asymptomatic.”
“We had nothing to follow. We didn’t know how long to treat the patient, it was really just a process of trial and error,” said Dr. Malik. The physicians asked the patient to monitor his breath alcohol levels twice a day during treatment and immediately report any increases. Over time, he also received treatment with various probiotics to help normalize his gut flora.
Underdiagnosed condition?
At the time of the case study’s publication in the summer of 2019, the patient had been asymptomatic for 18 months and had been able to resume a normal diet, but still checks his breath alcohol levels from time to time.
“Before this patient’s case, I went all through the literature and found only a few cases of ABS,” said Dr. Malik.
However, he added, after this case study was published 10 other patients contacted him with a similar history of antibiotic use and the same symptoms. This, said Dr. Malik, is “significant” and suggests ABS is much more common than previously thought.
The clinicians also note that to the best of their knowledge this is the first report of antibiotic exposure initiating ABS.
“What we tried to do was set up a protocol by which to identify these patients, confirm a diagnosis, and treat them for a sufficient amount of time,” said Dr. Wickremesinghe. “We also wanted to inform other physicians that this may function as a standardized way of treating these patients, and may promote further study,” added Dr. Malik, who emphasized that the role of probiotics in ABS still needs to be studied.
Dr. Malik and Dr. Wickremesinghe note that physicians should be aware that mood changes, brain fog, and delirium in patients who deny alcohol ingestion may be the first symptoms of ABS.
Dr. Wickremesinghe said since the case study was published he and Dr. Malik have received queries from all over the world. “It’s unbelievable the amount of interest we have had in the paper, so if we have made the medical community and the general population aware of this condition and how to treat it, we have done a major thing for medicine,” he said.
A version of this article first appeared on Medscape.com.
A 46-year-old North Carolina man, who was pulled over on suspicion of drunk driving, vehemently denied consuming alcohol. When he refused to take a breathalyzer test, he was hospitalized and doctors confirmed what police suspected – his blood alcohol level was 0.20, two-and-a-half times the state’s legal limit – and he was charged with driving while intoxicated (DWI).
For an entire year after his arrest, the cause of his “intoxication” remained a mystery. It wasn’t until his aunt learned about a similar case that had been successfully treated at an Ohio clinic that he understood what was happening to him – he had auto brewery syndrome (ABS).
and suffer all the medical and social implications of alcoholism.
“ABS occurs when ingested carbohydrates are converted to alcohol by fungi in the gastrointestinal tract,” Fahad Malik, MD, who reported the case in BMJ Open Gastroenterology while a resident at Richmond University Medical Center in New York, told this news organization.
At the urging of his aunt, the patient attended the Ohio clinic where he underwent a complete blood count, comprehensive metabolic panel, immunology panel and urinalysis, all of which were normal.
However, stool testing revealed the presence of two strains of yeast – Saccharomyces cerevisiae, commonly used in winemaking, baking, and beer brewing, and Saccharomyces boulardii.
To confirm the ABS diagnosis, the patient received a carbohydrate meal and clinicians monitored his blood alcohol level, which, after 8 hours, reached 57 mg/dL. He was treated with antifungals for the Saccharomyces fungi in his stool and discharged on a strict carbohydrate-free diet along with special supplements, including multivitamins and probiotics, but no further antifungal therapy.
Probiotics, said Dr. Malik, competitively inhibit bad bacteria and fungi, but currently there is evidence to show they are useful for ABS.
Although the patient adhered to his prescribed treatment regimen, after a few weeks of no symptoms, intermittent “flares” returned. In one instance of inebriation, he fell and hit his head, resulting in intracranial bleeding that resulted in a transfer to a neurosurgical center. During his hospital stay, his blood alcohol levels ranged from 50 to 400 mg/dL.
Antibiotics the culprit?
Disheartened by the continuation of his symptoms, the patient sought support from an online forum. It was there he read about Dr. Malik and gastroenterologist Prasanna Wickremesinghe, MD (a colleague of Dr. Malik’s at Richmond MC), who had treated a complicated, very similar case of ABS. The patient made contact with the two physicians and they assessed him.
“We went from A to Z with the patient, because we were trying to look for similar things in the history – we wanted to know the exact point at which it started and understand when he started experiencing mental fog,” said Dr. Malik.
After speaking to the patient, Dr. Malik and Dr. Wickremesinghe traced his initial symptoms to a 2011 course of antibiotics (cephalexin 250 mg oral three times a day for 3 weeks) prescribed for a complicated traumatic thumb injury.
About a week after he finished the antibiotics, he experienced noticeable behavioral changes, including depression, brain fog, and aggressive outbursts, all of which were very uncharacteristic.
He visited his primary care physician in 2014 for treatment, which resulted in a referral to a psychiatrist, who treated him with lorazepam and fluoxetine. The patient noted that he was previously healthy, with no significant medical or psychiatric history.
Dr. Malik believes the antibiotics prescribed all those years ago is the culprit. “We were postulating that the antibiotics had changed the microbiome of his gut and allowed the fungi to develop,” he said.
Since there are no established diagnostic criteria or treatment regimen for ABS, Dr. Malik and Dr. Wickremesinghe developed their own.
Diagnosis consisted of a standardized carbohydrate challenge test vs. a carbohydrate meal, where they gave the patient 200 g of glucose by mouth after an overnight fast and drew blood at timed intervals of 0, 0.5, 1, 2, 4, 8, 16, and 24 hours to test for glucose and blood alcohol levels.
“After that we needed to isolate the fungi by examining the gut secretions through an upper and lower endoscopy,” said Dr. Wickremesinghe. Fungal cultures from the upper small gut and cecal secretions grew Candida albicans and C. parapsilosis.
Both fungi were sensitive to azoles and the physicians prescribed oral itraconazole 150 mg per day as an initial therapy. After 10 days, his symptoms did not improve so the dose was increased to 200 mg/day and the patient became “completely asymptomatic.”
“We had nothing to follow. We didn’t know how long to treat the patient, it was really just a process of trial and error,” said Dr. Malik. The physicians asked the patient to monitor his breath alcohol levels twice a day during treatment and immediately report any increases. Over time, he also received treatment with various probiotics to help normalize his gut flora.
Underdiagnosed condition?
At the time of the case study’s publication in the summer of 2019, the patient had been asymptomatic for 18 months and had been able to resume a normal diet, but still checks his breath alcohol levels from time to time.
“Before this patient’s case, I went all through the literature and found only a few cases of ABS,” said Dr. Malik.
However, he added, after this case study was published 10 other patients contacted him with a similar history of antibiotic use and the same symptoms. This, said Dr. Malik, is “significant” and suggests ABS is much more common than previously thought.
The clinicians also note that to the best of their knowledge this is the first report of antibiotic exposure initiating ABS.
“What we tried to do was set up a protocol by which to identify these patients, confirm a diagnosis, and treat them for a sufficient amount of time,” said Dr. Wickremesinghe. “We also wanted to inform other physicians that this may function as a standardized way of treating these patients, and may promote further study,” added Dr. Malik, who emphasized that the role of probiotics in ABS still needs to be studied.
Dr. Malik and Dr. Wickremesinghe note that physicians should be aware that mood changes, brain fog, and delirium in patients who deny alcohol ingestion may be the first symptoms of ABS.
Dr. Wickremesinghe said since the case study was published he and Dr. Malik have received queries from all over the world. “It’s unbelievable the amount of interest we have had in the paper, so if we have made the medical community and the general population aware of this condition and how to treat it, we have done a major thing for medicine,” he said.
A version of this article first appeared on Medscape.com.
‘Misleading’ results in colchicine COVID-19 trials meta-analysis
A new meta-analysis appears to show that colchicine has no benefit as a treatment for COVID-19, but its inclusion of trials studying differing patient populations and testing different outcomes led to “misleading” results, says a researcher involved in one of the trials.
The meta-analysis, which includes data from the recent Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial, was published Nov. 22 in RMD Open.
Kedar Gautambhai Mehta, MBBS, MD, of the GMERS Medical College Gotri in Vadodara, India, and colleagues included outcomes from six studies of 16,148 patients with COVID-19 who received colchicine or supportive care. They evaluated the efficacy outcomes of mortality, need for ventilation, intensive care unit admission, and length of stay in hospital, as well as safety outcomes of adverse events, serious adverse events, and diarrhea.
The studies in the meta-analysis included a randomized, controlled trial (RCT) of 105 patients hospitalized with COVID-19 in Greece, the international, open-label RECOVERY RCT of 11,340 patients hospitalized with COVID-19, an RCT of 72 hospitalized patients with moderate or severe COVID-19 in Brazil, an RCT of 100 patients hospitalized with COVID-19 in Iran, the international COLCORONA trial of 4,488 patients with COVID-19 who were treated with colchicine or placebo on an outpatient basis, and the randomized COLORIT trial of 43 patients hospitalized with COVID-19 in Russia.
Studies “asked very different questions” about colchicine
Commenting on the meta-analysis, Michael H. Pillinger, MD, a rheumatologist and professor of medicine, biochemistry, and molecular pharmacology with New York University, said the authors combined studies “that are not comparable and that asked very different questions.” Two of the studies in the meta-analysis are very large, and four are very small, which skews the results, he explained.
“The larger studies therefore drive the outcome, and while the small studies are potentially insight providing, the large studies are the only ones worth giving our attention to in the context of the meta-analysis,” he said. The two largest studies – RECOVERY and COLCORONA – taken together show no benefit for colchicine as a treatment, even though the former demonstrated no benefit and the latter did show a benefit, explained Dr. Pillinger, a co–principal investigator for the COLCORONA trial in the United States.
The studies were designed differently and should not have been included in the same analysis, Dr. Pillinger argued. In the case of COLCORONA, early treatment with colchicine was the intervention, whereas RECOVERY focused on hospitalized patients.
“In designing [COLCORONA], the author group (of whom I was a member) expressly rejected the idea that colchicine might be useful for the sicker hospitalized patients, based on the long experience with colchicine of some of us as rheumatologists,” Dr. Pillinger said.
“In short, COLCORONA proved a benefit of colchicine in outpatient COVID-19, and its authors presumed there would be no inpatient benefit; RECOVERY went ahead and proved a lack of inpatient benefit, at least when high-dose steroids were also given,” he said. “While there is no conflict between these results, the combination of the two studies in this meta-analysis suggests there might be no benefit for colchicine overall, which is misleading and can lead physicians to reject the potential of outpatient colchicine, even for future studies.”
Dr. Pillinger said he still believes colchicine has potential value as a COVID-19 treatment option for patients with mild disease, “especially for low–vaccine rate, resource-starved countries.
“It would be unfortunate if meta-analyses such as this one would put a stop to colchicine’s use, or at least its further investigation,” he said.
Study details
The authors of the study assessed heterogeneity of the trials’ data across the outcomes using an I2 test. They evaluated the quality of the evidence for the outcomes using the Grades of Recommendation, Assessment, Development and Evaluation (GRADE).
The results of their meta-analysis showed that colchicine offered no significant improvement in mortality in six studies (risk difference, –0.0; 95% confidence interval, –0.01 to 0.01; I2 = 15%). It showed no benefit with respect to requiring ventilatory support in five studies of 15,519 patients (risk ratio, 0.67; 95% CI, 0.38-1.21; I2 = 47%); being admitted to the ICU in three studies with 220 patients (RR, 0.49; 95% CI, 0.19-1.25; I2 = 34%); and length of stay while in the hospital in four studies of 11,560 patients (mean difference, –1.17; 95% CI, –3.02 to 0.67; I2 = 77%).
There was no difference in serious adverse events in three studies with 4,665 patients (RD, –0.01; 95% CI, –0.02 to 0.00; I2 = 28%) for patients who received colchicine, compared with supportive care alone. Patients who received colchicine were more likely to have a higher rate of adverse events (RR, 1.58; 95% CI, 1.07-2.33; I2 = 81%) and to experience diarrhea (RR, 1.93; 95% CI, 1.62-2.29; I2 = 0%) than were patients who received supportive care alone. The researchers note that for most outcomes, the GRADE quality of evidence was moderate.
“Our findings on colchicine should be interpreted cautiously due to the inclusion of open-labeled, randomized clinical trials,” Dr. Mehta and colleagues write. “The analysis of efficacy and safety outcomes are based on a small number of RCTs in control interventions.”
The authors reported no relevant financial relationships. Dr. Pillinger is co–principal investigator of the U.S. component of the COLCORONA trial; he reported no other relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
A new meta-analysis appears to show that colchicine has no benefit as a treatment for COVID-19, but its inclusion of trials studying differing patient populations and testing different outcomes led to “misleading” results, says a researcher involved in one of the trials.
The meta-analysis, which includes data from the recent Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial, was published Nov. 22 in RMD Open.
Kedar Gautambhai Mehta, MBBS, MD, of the GMERS Medical College Gotri in Vadodara, India, and colleagues included outcomes from six studies of 16,148 patients with COVID-19 who received colchicine or supportive care. They evaluated the efficacy outcomes of mortality, need for ventilation, intensive care unit admission, and length of stay in hospital, as well as safety outcomes of adverse events, serious adverse events, and diarrhea.
The studies in the meta-analysis included a randomized, controlled trial (RCT) of 105 patients hospitalized with COVID-19 in Greece, the international, open-label RECOVERY RCT of 11,340 patients hospitalized with COVID-19, an RCT of 72 hospitalized patients with moderate or severe COVID-19 in Brazil, an RCT of 100 patients hospitalized with COVID-19 in Iran, the international COLCORONA trial of 4,488 patients with COVID-19 who were treated with colchicine or placebo on an outpatient basis, and the randomized COLORIT trial of 43 patients hospitalized with COVID-19 in Russia.
Studies “asked very different questions” about colchicine
Commenting on the meta-analysis, Michael H. Pillinger, MD, a rheumatologist and professor of medicine, biochemistry, and molecular pharmacology with New York University, said the authors combined studies “that are not comparable and that asked very different questions.” Two of the studies in the meta-analysis are very large, and four are very small, which skews the results, he explained.
“The larger studies therefore drive the outcome, and while the small studies are potentially insight providing, the large studies are the only ones worth giving our attention to in the context of the meta-analysis,” he said. The two largest studies – RECOVERY and COLCORONA – taken together show no benefit for colchicine as a treatment, even though the former demonstrated no benefit and the latter did show a benefit, explained Dr. Pillinger, a co–principal investigator for the COLCORONA trial in the United States.
The studies were designed differently and should not have been included in the same analysis, Dr. Pillinger argued. In the case of COLCORONA, early treatment with colchicine was the intervention, whereas RECOVERY focused on hospitalized patients.
“In designing [COLCORONA], the author group (of whom I was a member) expressly rejected the idea that colchicine might be useful for the sicker hospitalized patients, based on the long experience with colchicine of some of us as rheumatologists,” Dr. Pillinger said.
“In short, COLCORONA proved a benefit of colchicine in outpatient COVID-19, and its authors presumed there would be no inpatient benefit; RECOVERY went ahead and proved a lack of inpatient benefit, at least when high-dose steroids were also given,” he said. “While there is no conflict between these results, the combination of the two studies in this meta-analysis suggests there might be no benefit for colchicine overall, which is misleading and can lead physicians to reject the potential of outpatient colchicine, even for future studies.”
Dr. Pillinger said he still believes colchicine has potential value as a COVID-19 treatment option for patients with mild disease, “especially for low–vaccine rate, resource-starved countries.
“It would be unfortunate if meta-analyses such as this one would put a stop to colchicine’s use, or at least its further investigation,” he said.
Study details
The authors of the study assessed heterogeneity of the trials’ data across the outcomes using an I2 test. They evaluated the quality of the evidence for the outcomes using the Grades of Recommendation, Assessment, Development and Evaluation (GRADE).
The results of their meta-analysis showed that colchicine offered no significant improvement in mortality in six studies (risk difference, –0.0; 95% confidence interval, –0.01 to 0.01; I2 = 15%). It showed no benefit with respect to requiring ventilatory support in five studies of 15,519 patients (risk ratio, 0.67; 95% CI, 0.38-1.21; I2 = 47%); being admitted to the ICU in three studies with 220 patients (RR, 0.49; 95% CI, 0.19-1.25; I2 = 34%); and length of stay while in the hospital in four studies of 11,560 patients (mean difference, –1.17; 95% CI, –3.02 to 0.67; I2 = 77%).
There was no difference in serious adverse events in three studies with 4,665 patients (RD, –0.01; 95% CI, –0.02 to 0.00; I2 = 28%) for patients who received colchicine, compared with supportive care alone. Patients who received colchicine were more likely to have a higher rate of adverse events (RR, 1.58; 95% CI, 1.07-2.33; I2 = 81%) and to experience diarrhea (RR, 1.93; 95% CI, 1.62-2.29; I2 = 0%) than were patients who received supportive care alone. The researchers note that for most outcomes, the GRADE quality of evidence was moderate.
“Our findings on colchicine should be interpreted cautiously due to the inclusion of open-labeled, randomized clinical trials,” Dr. Mehta and colleagues write. “The analysis of efficacy and safety outcomes are based on a small number of RCTs in control interventions.”
The authors reported no relevant financial relationships. Dr. Pillinger is co–principal investigator of the U.S. component of the COLCORONA trial; he reported no other relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
A new meta-analysis appears to show that colchicine has no benefit as a treatment for COVID-19, but its inclusion of trials studying differing patient populations and testing different outcomes led to “misleading” results, says a researcher involved in one of the trials.
The meta-analysis, which includes data from the recent Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial, was published Nov. 22 in RMD Open.
Kedar Gautambhai Mehta, MBBS, MD, of the GMERS Medical College Gotri in Vadodara, India, and colleagues included outcomes from six studies of 16,148 patients with COVID-19 who received colchicine or supportive care. They evaluated the efficacy outcomes of mortality, need for ventilation, intensive care unit admission, and length of stay in hospital, as well as safety outcomes of adverse events, serious adverse events, and diarrhea.
The studies in the meta-analysis included a randomized, controlled trial (RCT) of 105 patients hospitalized with COVID-19 in Greece, the international, open-label RECOVERY RCT of 11,340 patients hospitalized with COVID-19, an RCT of 72 hospitalized patients with moderate or severe COVID-19 in Brazil, an RCT of 100 patients hospitalized with COVID-19 in Iran, the international COLCORONA trial of 4,488 patients with COVID-19 who were treated with colchicine or placebo on an outpatient basis, and the randomized COLORIT trial of 43 patients hospitalized with COVID-19 in Russia.
Studies “asked very different questions” about colchicine
Commenting on the meta-analysis, Michael H. Pillinger, MD, a rheumatologist and professor of medicine, biochemistry, and molecular pharmacology with New York University, said the authors combined studies “that are not comparable and that asked very different questions.” Two of the studies in the meta-analysis are very large, and four are very small, which skews the results, he explained.
“The larger studies therefore drive the outcome, and while the small studies are potentially insight providing, the large studies are the only ones worth giving our attention to in the context of the meta-analysis,” he said. The two largest studies – RECOVERY and COLCORONA – taken together show no benefit for colchicine as a treatment, even though the former demonstrated no benefit and the latter did show a benefit, explained Dr. Pillinger, a co–principal investigator for the COLCORONA trial in the United States.
The studies were designed differently and should not have been included in the same analysis, Dr. Pillinger argued. In the case of COLCORONA, early treatment with colchicine was the intervention, whereas RECOVERY focused on hospitalized patients.
“In designing [COLCORONA], the author group (of whom I was a member) expressly rejected the idea that colchicine might be useful for the sicker hospitalized patients, based on the long experience with colchicine of some of us as rheumatologists,” Dr. Pillinger said.
“In short, COLCORONA proved a benefit of colchicine in outpatient COVID-19, and its authors presumed there would be no inpatient benefit; RECOVERY went ahead and proved a lack of inpatient benefit, at least when high-dose steroids were also given,” he said. “While there is no conflict between these results, the combination of the two studies in this meta-analysis suggests there might be no benefit for colchicine overall, which is misleading and can lead physicians to reject the potential of outpatient colchicine, even for future studies.”
Dr. Pillinger said he still believes colchicine has potential value as a COVID-19 treatment option for patients with mild disease, “especially for low–vaccine rate, resource-starved countries.
“It would be unfortunate if meta-analyses such as this one would put a stop to colchicine’s use, or at least its further investigation,” he said.
Study details
The authors of the study assessed heterogeneity of the trials’ data across the outcomes using an I2 test. They evaluated the quality of the evidence for the outcomes using the Grades of Recommendation, Assessment, Development and Evaluation (GRADE).
The results of their meta-analysis showed that colchicine offered no significant improvement in mortality in six studies (risk difference, –0.0; 95% confidence interval, –0.01 to 0.01; I2 = 15%). It showed no benefit with respect to requiring ventilatory support in five studies of 15,519 patients (risk ratio, 0.67; 95% CI, 0.38-1.21; I2 = 47%); being admitted to the ICU in three studies with 220 patients (RR, 0.49; 95% CI, 0.19-1.25; I2 = 34%); and length of stay while in the hospital in four studies of 11,560 patients (mean difference, –1.17; 95% CI, –3.02 to 0.67; I2 = 77%).
There was no difference in serious adverse events in three studies with 4,665 patients (RD, –0.01; 95% CI, –0.02 to 0.00; I2 = 28%) for patients who received colchicine, compared with supportive care alone. Patients who received colchicine were more likely to have a higher rate of adverse events (RR, 1.58; 95% CI, 1.07-2.33; I2 = 81%) and to experience diarrhea (RR, 1.93; 95% CI, 1.62-2.29; I2 = 0%) than were patients who received supportive care alone. The researchers note that for most outcomes, the GRADE quality of evidence was moderate.
“Our findings on colchicine should be interpreted cautiously due to the inclusion of open-labeled, randomized clinical trials,” Dr. Mehta and colleagues write. “The analysis of efficacy and safety outcomes are based on a small number of RCTs in control interventions.”
The authors reported no relevant financial relationships. Dr. Pillinger is co–principal investigator of the U.S. component of the COLCORONA trial; he reported no other relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
COVID surge in Europe: A preview of what’s ahead for the U.S.?
Health experts are warning the United States could be headed for another COVID-19 surge just as we enter the holiday season, following a massive new wave of infections in Europe – a troubling pattern seen throughout the pandemic.
Eighteen months into the global health crisis that has killed 5.1 million people worldwide including more than 767,000 Americans, Europe has become the epicenter of the global health crisis once again.
And some infectious disease specialists say the United States may be next.
“It’s déjà vu, yet again,” says Eric Topol, M.D., founder and director of the Scripps Research Translational Institute. In a new analysis published in The Guardian, the professor of molecular medicine argues that it’s “wishful thinking” for U.S. authorities to believe the nation is “immune” to what’s happening in Europe.
Dr. Topol is also editor-in-chief of Medscape, MDedge’s sister site for medical professionals.
Three times over the past 18 months coronavirus surges in the United States followed similar spikes in Europe, where COVID-19 deaths grew by 10% this month.
Dr. Topol argues another wave may be in store for the states, as European countries implement new lockdowns. COVID-19 spikes are hitting some regions of the continent hard, including areas with high vaccination rates and strict control measures.
Eastern Europe and Russia, where vaccination rates are low, have experienced the worst of it. But even western countries, such as Germany, Austria and the United Kingdom, are reporting some of the highest daily infection figures in the world today.
Countries are responding in increasingly drastic ways.
In Russia, President Vladimir Putin ordered tens of thousands of workers to stay home earlier this month.
In the Dutch city of Utrecht, traditional Christmas celebrations have been canceled as the country is headed for a partial lockdown.
Austria announced a 20-day lockdown beginning Nov. 22 and on Nov. 19 leaders there announced that all 9 million residents will be required to be vaccinated by February. Leaders there are telling unvaccinated individuals to stay at home and out of restaurants, cafes, and other shops in hard-hit regions of the country.
And in Germany, where daily new-infection rates now stand at 50,000, officials have introduced stricter mask mandates and made proof of vaccination or past infection mandatory for entry to many venues. Berlin is also eyeing proposals to shut down the city’s traditional Christmas markets while authorities in Cologne have already called off holiday celebrations, after the ceremonial head of festivities tested positive for COVID-19. Bavaria canceled its popular Christmas markets and will order lockdowns in particularly vulnerable districts, while unvaccinated people will face serious restrictions on where they can go.
Former FDA Commissioner Scott Gottlieb, MD, says what’s happening across the European continent is troubling.
But he also believes it’s possible the United States may be better prepared to head off a similar surge this time around, with increased testing, vaccination and new therapies such as monoclonal antibodies, and antiviral therapeutics.
“Germany’s challenges are [a] caution to [the] world, the COVID pandemic isn’t over globally, won’t be for long time,” he says. “But [the] U.S. is further along than many other countries, in part because we already suffered more spread, in part because we’re making progress on vaccines, therapeutics, testing.”
Other experts agree the United States may not be as vulnerable to another wave of COVID-19 in coming weeks but have stopped short of suggesting we’re out of the woods.
“I don’t think that what we’re seeing in Europe necessarily means that we’re in for a huge surge of serious illness and death the way that we saw last year here in the states,” says David Dowdy, MD, PhD, an associate professor of epidemiology at the Johns Hopkins Bloomberg School of Public Health and a general internist with Baltimore Medical Services.
“But I think anyone who says that they can predict the course of the pandemic for the next few months or few years has been proven wrong in the past and will probably be proven wrong in the future,” Dr. Dowdy says. “None of us knows the future of this pandemic, but I do think that we are in for an increase of cases, not necessarily of deaths and serious illness.”
Looking back, and forward
What’s happening in Europe today mirrors past COVID-19 spikes that presaged big upticks in cases, hospitalizations, and deaths in the United States.
When the pandemic first hit Europe in March 2020, then-President Donald Trump downplayed the threat of the virus despite the warnings of his own advisors and independent public health experts who said COVID-19 could have dire impacts without an aggressive federal action plan.
By late spring the United States had become the epicenter of the pandemic, when case totals eclipsed those of other countries and New York City became a hot zone, according to data compiled by the Johns Hopkins Coronavirus Resource Center. Over the summer, spread of the disease slowed in New York, after tough control measures were instituted, but steadily increased in other states.
Then, later in the year, the Alpha variant of the virus took hold in the United Kingdom and the United States was again unprepared. By winter, the number of cases accelerated in every state in a major second surge that kept millions of Americans from traveling and gathering for the winter holidays.
With the rollout of COVID vaccines last December, cases in the United States – and in many parts of the world – began to fall. Some experts even suggested we’d turned a corner on the pandemic.
But then, last spring and summer, the Delta variant popped up in India and spread to the United Kingdom in a third major wave of COVID. Once again, the United States was unprepared, with 4 in 10 Americans refusing the vaccine and even some vaccinated individuals succumbing to breakthrough Delta infections.
The resulting Delta surge swept the country, preventing many businesses and schools from fully reopening and stressing hospitals in some areas of the country – particularly southern states – with new influxes of COVID-19 patients.
Now, Europe is facing another rise in COVID, with about 350 cases per 100,000 people and many countries hitting new record highs.
What’s driving the European resurgence?
So, what’s behind the new COVID-19 wave in Europe and what might it mean for the United States?
Shaun Truelove, PhD, an infectious disease epidemiologist and faculty member of the Johns Hopkins School of Public Health, says experts are examining several likely factors:
Waning immunity from the vaccines. Data from Johns Hopkins shows infections rising in nations with lower vaccination rates.
The impact of the Delta variant, which is three times more transmissible than the original virus and can even sicken some vaccinated individuals.
The spread of COVID-19 among teens and children; the easing of precautions (such as masking and social distancing); differences in the types of vaccines used in European nations and the United States.
“These are all possibilities,” says Dr. Truelove. “There are so many factors and so it’s difficult to pinpoint exactly what’s driving it and what effect each of those things might be having.”
As a result, it’s difficult to predict and prepare for what might lie ahead for the United States, he says.
“There’s a ton of uncertainty and we’re trying to understand what’s going to happen here over the next 6 months,” he says.
Even so, Dr. Truelove adds that what’s happening overseas might not be “super predictive” of a new wave of COVID in the United States.
For one thing, he says, the Pfizer and Moderna vaccines, the two mRNA vaccines used predominantly in the United States, are far more effective – 94-95% – than the Oxford/AstraZeneca COVID shot (63%) widely administered across Europe.
Secondly, European countries have imposed much stronger and stricter control measures throughout the pandemic than the United States. That might actually be driving the new surges because fewer unvaccinated people have been exposed to the virus, which means they have lower “natural immunity” from prior COVID infection.
Dr. Truelove explains: “Stronger and stricter control measures … have the consequence of leaving a lot more susceptible individuals in the population, [because] the stronger the controls, the fewer people get infected. And so, you have more individuals remaining in the population who are more susceptible and at risk of getting infected in the future.”
By contrast, he notes, a “large chunk” of the United States has not put strict lockdowns in place.
“So, what we’ve seen over the past couple months with the Delta wave is that in a lot of those states with lower vaccination coverage and lower controls this virus has really burned through a lot of the susceptible population. As a result, we’re seeing the curves coming down and what really looks like a lot of the built-up immunity in these states, especially southern states.”
But whether these differences will be enough for the United States to dodge another COVID-19 bullet this winter is uncertain.
“I don’t want to say that the [Europe] surge is NOT a predictor of what might come in the U.S., because I think that it very well could be,” Dr. Truelove says. “And so, people need to be aware of that, and be cautious and be sure get their vaccines and everything else.
“But I’m hopeful that because of some of the differences that maybe we’ll have a little bit of a different situation.”
The takeaway: How best to prepare?
Dr. Dowdy agrees that Europe’s current troubles might not necessarily mean a major new winter surge in the United States.
But he also points out that cases are beginning to head up again in New England, the Midwest, and other regions of the country that are just experiencing the first chill of winter.
“After reaching a low point about 3 weeks ago, cases due to COVID-19 have started to rise again in the United States,” he says. “Cases were falling consistently until mid-October, but over the last 3 weeks, cases have started to rise again in most states.
“Cases in Eastern and Central Europe have more than doubled during that time, meaning that the possibility of a winter surge here is very real.”
Even so, Dr. Dowdy believes the rising rates of vaccination could limit the number of Americans who will be hospitalized with severe disease or die this winter.
Still, he warns against being too optimistic, as Americans travel and get together for the winter holidays.
None of us knows the future of this pandemic, but I do think that we are in for an increase of cases, not necessarily of deaths and serious illness, Dr. Dowdy says.”
The upshot?
“People need to realize that it’s not quite over,” Dr. Truelove says. “We still have a substantial amount of infection in our country. We’re still above 200 cases per million [and] 500,000 incident cases per week or so. That’s a lot of death and a lot of hospitalizations. So, we still have to be concerned and do our best to reduce transmission … by wearing masks, getting vaccinated, getting a booster shot, and getting your children vaccinated.”
Johns Hopkins social and behavioral scientist Rupali Limaye, PhD, MPH, adds that while COVID vaccines have been a “game changer” in the pandemic, more than a third of Americans have yet to receive one.
“That’s really what we need to be messaging around -- that people can still get COVID, there can still be breakthrough infections,” says Dr. Limaye, a health communications scholar. “But the great news is if you have been vaccinated, you are very much less likely, I think it’s 12 times, to be hospitalized or have severe COVID compared to those that are un-vaccinated.”
Dr. Topol agrees, adding: “Now is the time for the U.S. to heed the European signal for the first time, to pull out all the stops. Promote primary vaccination and boosters like there’s no tomorrow. Aggressively counter the pervasive misinformation and disinformation. Accelerate and expand the vaccine mandates ...
“Instead of succumbing to yet another major rise in cases and their sequelae, this is a chance for America to finally rise to the occasion, showing an ability to lead and execute.”
A version of this article first appeared on WebMD.com.
Health experts are warning the United States could be headed for another COVID-19 surge just as we enter the holiday season, following a massive new wave of infections in Europe – a troubling pattern seen throughout the pandemic.
Eighteen months into the global health crisis that has killed 5.1 million people worldwide including more than 767,000 Americans, Europe has become the epicenter of the global health crisis once again.
And some infectious disease specialists say the United States may be next.
“It’s déjà vu, yet again,” says Eric Topol, M.D., founder and director of the Scripps Research Translational Institute. In a new analysis published in The Guardian, the professor of molecular medicine argues that it’s “wishful thinking” for U.S. authorities to believe the nation is “immune” to what’s happening in Europe.
Dr. Topol is also editor-in-chief of Medscape, MDedge’s sister site for medical professionals.
Three times over the past 18 months coronavirus surges in the United States followed similar spikes in Europe, where COVID-19 deaths grew by 10% this month.
Dr. Topol argues another wave may be in store for the states, as European countries implement new lockdowns. COVID-19 spikes are hitting some regions of the continent hard, including areas with high vaccination rates and strict control measures.
Eastern Europe and Russia, where vaccination rates are low, have experienced the worst of it. But even western countries, such as Germany, Austria and the United Kingdom, are reporting some of the highest daily infection figures in the world today.
Countries are responding in increasingly drastic ways.
In Russia, President Vladimir Putin ordered tens of thousands of workers to stay home earlier this month.
In the Dutch city of Utrecht, traditional Christmas celebrations have been canceled as the country is headed for a partial lockdown.
Austria announced a 20-day lockdown beginning Nov. 22 and on Nov. 19 leaders there announced that all 9 million residents will be required to be vaccinated by February. Leaders there are telling unvaccinated individuals to stay at home and out of restaurants, cafes, and other shops in hard-hit regions of the country.
And in Germany, where daily new-infection rates now stand at 50,000, officials have introduced stricter mask mandates and made proof of vaccination or past infection mandatory for entry to many venues. Berlin is also eyeing proposals to shut down the city’s traditional Christmas markets while authorities in Cologne have already called off holiday celebrations, after the ceremonial head of festivities tested positive for COVID-19. Bavaria canceled its popular Christmas markets and will order lockdowns in particularly vulnerable districts, while unvaccinated people will face serious restrictions on where they can go.
Former FDA Commissioner Scott Gottlieb, MD, says what’s happening across the European continent is troubling.
But he also believes it’s possible the United States may be better prepared to head off a similar surge this time around, with increased testing, vaccination and new therapies such as monoclonal antibodies, and antiviral therapeutics.
“Germany’s challenges are [a] caution to [the] world, the COVID pandemic isn’t over globally, won’t be for long time,” he says. “But [the] U.S. is further along than many other countries, in part because we already suffered more spread, in part because we’re making progress on vaccines, therapeutics, testing.”
Other experts agree the United States may not be as vulnerable to another wave of COVID-19 in coming weeks but have stopped short of suggesting we’re out of the woods.
“I don’t think that what we’re seeing in Europe necessarily means that we’re in for a huge surge of serious illness and death the way that we saw last year here in the states,” says David Dowdy, MD, PhD, an associate professor of epidemiology at the Johns Hopkins Bloomberg School of Public Health and a general internist with Baltimore Medical Services.
“But I think anyone who says that they can predict the course of the pandemic for the next few months or few years has been proven wrong in the past and will probably be proven wrong in the future,” Dr. Dowdy says. “None of us knows the future of this pandemic, but I do think that we are in for an increase of cases, not necessarily of deaths and serious illness.”
Looking back, and forward
What’s happening in Europe today mirrors past COVID-19 spikes that presaged big upticks in cases, hospitalizations, and deaths in the United States.
When the pandemic first hit Europe in March 2020, then-President Donald Trump downplayed the threat of the virus despite the warnings of his own advisors and independent public health experts who said COVID-19 could have dire impacts without an aggressive federal action plan.
By late spring the United States had become the epicenter of the pandemic, when case totals eclipsed those of other countries and New York City became a hot zone, according to data compiled by the Johns Hopkins Coronavirus Resource Center. Over the summer, spread of the disease slowed in New York, after tough control measures were instituted, but steadily increased in other states.
Then, later in the year, the Alpha variant of the virus took hold in the United Kingdom and the United States was again unprepared. By winter, the number of cases accelerated in every state in a major second surge that kept millions of Americans from traveling and gathering for the winter holidays.
With the rollout of COVID vaccines last December, cases in the United States – and in many parts of the world – began to fall. Some experts even suggested we’d turned a corner on the pandemic.
But then, last spring and summer, the Delta variant popped up in India and spread to the United Kingdom in a third major wave of COVID. Once again, the United States was unprepared, with 4 in 10 Americans refusing the vaccine and even some vaccinated individuals succumbing to breakthrough Delta infections.
The resulting Delta surge swept the country, preventing many businesses and schools from fully reopening and stressing hospitals in some areas of the country – particularly southern states – with new influxes of COVID-19 patients.
Now, Europe is facing another rise in COVID, with about 350 cases per 100,000 people and many countries hitting new record highs.
What’s driving the European resurgence?
So, what’s behind the new COVID-19 wave in Europe and what might it mean for the United States?
Shaun Truelove, PhD, an infectious disease epidemiologist and faculty member of the Johns Hopkins School of Public Health, says experts are examining several likely factors:
Waning immunity from the vaccines. Data from Johns Hopkins shows infections rising in nations with lower vaccination rates.
The impact of the Delta variant, which is three times more transmissible than the original virus and can even sicken some vaccinated individuals.
The spread of COVID-19 among teens and children; the easing of precautions (such as masking and social distancing); differences in the types of vaccines used in European nations and the United States.
“These are all possibilities,” says Dr. Truelove. “There are so many factors and so it’s difficult to pinpoint exactly what’s driving it and what effect each of those things might be having.”
As a result, it’s difficult to predict and prepare for what might lie ahead for the United States, he says.
“There’s a ton of uncertainty and we’re trying to understand what’s going to happen here over the next 6 months,” he says.
Even so, Dr. Truelove adds that what’s happening overseas might not be “super predictive” of a new wave of COVID in the United States.
For one thing, he says, the Pfizer and Moderna vaccines, the two mRNA vaccines used predominantly in the United States, are far more effective – 94-95% – than the Oxford/AstraZeneca COVID shot (63%) widely administered across Europe.
Secondly, European countries have imposed much stronger and stricter control measures throughout the pandemic than the United States. That might actually be driving the new surges because fewer unvaccinated people have been exposed to the virus, which means they have lower “natural immunity” from prior COVID infection.
Dr. Truelove explains: “Stronger and stricter control measures … have the consequence of leaving a lot more susceptible individuals in the population, [because] the stronger the controls, the fewer people get infected. And so, you have more individuals remaining in the population who are more susceptible and at risk of getting infected in the future.”
By contrast, he notes, a “large chunk” of the United States has not put strict lockdowns in place.
“So, what we’ve seen over the past couple months with the Delta wave is that in a lot of those states with lower vaccination coverage and lower controls this virus has really burned through a lot of the susceptible population. As a result, we’re seeing the curves coming down and what really looks like a lot of the built-up immunity in these states, especially southern states.”
But whether these differences will be enough for the United States to dodge another COVID-19 bullet this winter is uncertain.
“I don’t want to say that the [Europe] surge is NOT a predictor of what might come in the U.S., because I think that it very well could be,” Dr. Truelove says. “And so, people need to be aware of that, and be cautious and be sure get their vaccines and everything else.
“But I’m hopeful that because of some of the differences that maybe we’ll have a little bit of a different situation.”
The takeaway: How best to prepare?
Dr. Dowdy agrees that Europe’s current troubles might not necessarily mean a major new winter surge in the United States.
But he also points out that cases are beginning to head up again in New England, the Midwest, and other regions of the country that are just experiencing the first chill of winter.
“After reaching a low point about 3 weeks ago, cases due to COVID-19 have started to rise again in the United States,” he says. “Cases were falling consistently until mid-October, but over the last 3 weeks, cases have started to rise again in most states.
“Cases in Eastern and Central Europe have more than doubled during that time, meaning that the possibility of a winter surge here is very real.”
Even so, Dr. Dowdy believes the rising rates of vaccination could limit the number of Americans who will be hospitalized with severe disease or die this winter.
Still, he warns against being too optimistic, as Americans travel and get together for the winter holidays.
None of us knows the future of this pandemic, but I do think that we are in for an increase of cases, not necessarily of deaths and serious illness, Dr. Dowdy says.”
The upshot?
“People need to realize that it’s not quite over,” Dr. Truelove says. “We still have a substantial amount of infection in our country. We’re still above 200 cases per million [and] 500,000 incident cases per week or so. That’s a lot of death and a lot of hospitalizations. So, we still have to be concerned and do our best to reduce transmission … by wearing masks, getting vaccinated, getting a booster shot, and getting your children vaccinated.”
Johns Hopkins social and behavioral scientist Rupali Limaye, PhD, MPH, adds that while COVID vaccines have been a “game changer” in the pandemic, more than a third of Americans have yet to receive one.
“That’s really what we need to be messaging around -- that people can still get COVID, there can still be breakthrough infections,” says Dr. Limaye, a health communications scholar. “But the great news is if you have been vaccinated, you are very much less likely, I think it’s 12 times, to be hospitalized or have severe COVID compared to those that are un-vaccinated.”
Dr. Topol agrees, adding: “Now is the time for the U.S. to heed the European signal for the first time, to pull out all the stops. Promote primary vaccination and boosters like there’s no tomorrow. Aggressively counter the pervasive misinformation and disinformation. Accelerate and expand the vaccine mandates ...
“Instead of succumbing to yet another major rise in cases and their sequelae, this is a chance for America to finally rise to the occasion, showing an ability to lead and execute.”
A version of this article first appeared on WebMD.com.
Health experts are warning the United States could be headed for another COVID-19 surge just as we enter the holiday season, following a massive new wave of infections in Europe – a troubling pattern seen throughout the pandemic.
Eighteen months into the global health crisis that has killed 5.1 million people worldwide including more than 767,000 Americans, Europe has become the epicenter of the global health crisis once again.
And some infectious disease specialists say the United States may be next.
“It’s déjà vu, yet again,” says Eric Topol, M.D., founder and director of the Scripps Research Translational Institute. In a new analysis published in The Guardian, the professor of molecular medicine argues that it’s “wishful thinking” for U.S. authorities to believe the nation is “immune” to what’s happening in Europe.
Dr. Topol is also editor-in-chief of Medscape, MDedge’s sister site for medical professionals.
Three times over the past 18 months coronavirus surges in the United States followed similar spikes in Europe, where COVID-19 deaths grew by 10% this month.
Dr. Topol argues another wave may be in store for the states, as European countries implement new lockdowns. COVID-19 spikes are hitting some regions of the continent hard, including areas with high vaccination rates and strict control measures.
Eastern Europe and Russia, where vaccination rates are low, have experienced the worst of it. But even western countries, such as Germany, Austria and the United Kingdom, are reporting some of the highest daily infection figures in the world today.
Countries are responding in increasingly drastic ways.
In Russia, President Vladimir Putin ordered tens of thousands of workers to stay home earlier this month.
In the Dutch city of Utrecht, traditional Christmas celebrations have been canceled as the country is headed for a partial lockdown.
Austria announced a 20-day lockdown beginning Nov. 22 and on Nov. 19 leaders there announced that all 9 million residents will be required to be vaccinated by February. Leaders there are telling unvaccinated individuals to stay at home and out of restaurants, cafes, and other shops in hard-hit regions of the country.
And in Germany, where daily new-infection rates now stand at 50,000, officials have introduced stricter mask mandates and made proof of vaccination or past infection mandatory for entry to many venues. Berlin is also eyeing proposals to shut down the city’s traditional Christmas markets while authorities in Cologne have already called off holiday celebrations, after the ceremonial head of festivities tested positive for COVID-19. Bavaria canceled its popular Christmas markets and will order lockdowns in particularly vulnerable districts, while unvaccinated people will face serious restrictions on where they can go.
Former FDA Commissioner Scott Gottlieb, MD, says what’s happening across the European continent is troubling.
But he also believes it’s possible the United States may be better prepared to head off a similar surge this time around, with increased testing, vaccination and new therapies such as monoclonal antibodies, and antiviral therapeutics.
“Germany’s challenges are [a] caution to [the] world, the COVID pandemic isn’t over globally, won’t be for long time,” he says. “But [the] U.S. is further along than many other countries, in part because we already suffered more spread, in part because we’re making progress on vaccines, therapeutics, testing.”
Other experts agree the United States may not be as vulnerable to another wave of COVID-19 in coming weeks but have stopped short of suggesting we’re out of the woods.
“I don’t think that what we’re seeing in Europe necessarily means that we’re in for a huge surge of serious illness and death the way that we saw last year here in the states,” says David Dowdy, MD, PhD, an associate professor of epidemiology at the Johns Hopkins Bloomberg School of Public Health and a general internist with Baltimore Medical Services.
“But I think anyone who says that they can predict the course of the pandemic for the next few months or few years has been proven wrong in the past and will probably be proven wrong in the future,” Dr. Dowdy says. “None of us knows the future of this pandemic, but I do think that we are in for an increase of cases, not necessarily of deaths and serious illness.”
Looking back, and forward
What’s happening in Europe today mirrors past COVID-19 spikes that presaged big upticks in cases, hospitalizations, and deaths in the United States.
When the pandemic first hit Europe in March 2020, then-President Donald Trump downplayed the threat of the virus despite the warnings of his own advisors and independent public health experts who said COVID-19 could have dire impacts without an aggressive federal action plan.
By late spring the United States had become the epicenter of the pandemic, when case totals eclipsed those of other countries and New York City became a hot zone, according to data compiled by the Johns Hopkins Coronavirus Resource Center. Over the summer, spread of the disease slowed in New York, after tough control measures were instituted, but steadily increased in other states.
Then, later in the year, the Alpha variant of the virus took hold in the United Kingdom and the United States was again unprepared. By winter, the number of cases accelerated in every state in a major second surge that kept millions of Americans from traveling and gathering for the winter holidays.
With the rollout of COVID vaccines last December, cases in the United States – and in many parts of the world – began to fall. Some experts even suggested we’d turned a corner on the pandemic.
But then, last spring and summer, the Delta variant popped up in India and spread to the United Kingdom in a third major wave of COVID. Once again, the United States was unprepared, with 4 in 10 Americans refusing the vaccine and even some vaccinated individuals succumbing to breakthrough Delta infections.
The resulting Delta surge swept the country, preventing many businesses and schools from fully reopening and stressing hospitals in some areas of the country – particularly southern states – with new influxes of COVID-19 patients.
Now, Europe is facing another rise in COVID, with about 350 cases per 100,000 people and many countries hitting new record highs.
What’s driving the European resurgence?
So, what’s behind the new COVID-19 wave in Europe and what might it mean for the United States?
Shaun Truelove, PhD, an infectious disease epidemiologist and faculty member of the Johns Hopkins School of Public Health, says experts are examining several likely factors:
Waning immunity from the vaccines. Data from Johns Hopkins shows infections rising in nations with lower vaccination rates.
The impact of the Delta variant, which is three times more transmissible than the original virus and can even sicken some vaccinated individuals.
The spread of COVID-19 among teens and children; the easing of precautions (such as masking and social distancing); differences in the types of vaccines used in European nations and the United States.
“These are all possibilities,” says Dr. Truelove. “There are so many factors and so it’s difficult to pinpoint exactly what’s driving it and what effect each of those things might be having.”
As a result, it’s difficult to predict and prepare for what might lie ahead for the United States, he says.
“There’s a ton of uncertainty and we’re trying to understand what’s going to happen here over the next 6 months,” he says.
Even so, Dr. Truelove adds that what’s happening overseas might not be “super predictive” of a new wave of COVID in the United States.
For one thing, he says, the Pfizer and Moderna vaccines, the two mRNA vaccines used predominantly in the United States, are far more effective – 94-95% – than the Oxford/AstraZeneca COVID shot (63%) widely administered across Europe.
Secondly, European countries have imposed much stronger and stricter control measures throughout the pandemic than the United States. That might actually be driving the new surges because fewer unvaccinated people have been exposed to the virus, which means they have lower “natural immunity” from prior COVID infection.
Dr. Truelove explains: “Stronger and stricter control measures … have the consequence of leaving a lot more susceptible individuals in the population, [because] the stronger the controls, the fewer people get infected. And so, you have more individuals remaining in the population who are more susceptible and at risk of getting infected in the future.”
By contrast, he notes, a “large chunk” of the United States has not put strict lockdowns in place.
“So, what we’ve seen over the past couple months with the Delta wave is that in a lot of those states with lower vaccination coverage and lower controls this virus has really burned through a lot of the susceptible population. As a result, we’re seeing the curves coming down and what really looks like a lot of the built-up immunity in these states, especially southern states.”
But whether these differences will be enough for the United States to dodge another COVID-19 bullet this winter is uncertain.
“I don’t want to say that the [Europe] surge is NOT a predictor of what might come in the U.S., because I think that it very well could be,” Dr. Truelove says. “And so, people need to be aware of that, and be cautious and be sure get their vaccines and everything else.
“But I’m hopeful that because of some of the differences that maybe we’ll have a little bit of a different situation.”
The takeaway: How best to prepare?
Dr. Dowdy agrees that Europe’s current troubles might not necessarily mean a major new winter surge in the United States.
But he also points out that cases are beginning to head up again in New England, the Midwest, and other regions of the country that are just experiencing the first chill of winter.
“After reaching a low point about 3 weeks ago, cases due to COVID-19 have started to rise again in the United States,” he says. “Cases were falling consistently until mid-October, but over the last 3 weeks, cases have started to rise again in most states.
“Cases in Eastern and Central Europe have more than doubled during that time, meaning that the possibility of a winter surge here is very real.”
Even so, Dr. Dowdy believes the rising rates of vaccination could limit the number of Americans who will be hospitalized with severe disease or die this winter.
Still, he warns against being too optimistic, as Americans travel and get together for the winter holidays.
None of us knows the future of this pandemic, but I do think that we are in for an increase of cases, not necessarily of deaths and serious illness, Dr. Dowdy says.”
The upshot?
“People need to realize that it’s not quite over,” Dr. Truelove says. “We still have a substantial amount of infection in our country. We’re still above 200 cases per million [and] 500,000 incident cases per week or so. That’s a lot of death and a lot of hospitalizations. So, we still have to be concerned and do our best to reduce transmission … by wearing masks, getting vaccinated, getting a booster shot, and getting your children vaccinated.”
Johns Hopkins social and behavioral scientist Rupali Limaye, PhD, MPH, adds that while COVID vaccines have been a “game changer” in the pandemic, more than a third of Americans have yet to receive one.
“That’s really what we need to be messaging around -- that people can still get COVID, there can still be breakthrough infections,” says Dr. Limaye, a health communications scholar. “But the great news is if you have been vaccinated, you are very much less likely, I think it’s 12 times, to be hospitalized or have severe COVID compared to those that are un-vaccinated.”
Dr. Topol agrees, adding: “Now is the time for the U.S. to heed the European signal for the first time, to pull out all the stops. Promote primary vaccination and boosters like there’s no tomorrow. Aggressively counter the pervasive misinformation and disinformation. Accelerate and expand the vaccine mandates ...
“Instead of succumbing to yet another major rise in cases and their sequelae, this is a chance for America to finally rise to the occasion, showing an ability to lead and execute.”
A version of this article first appeared on WebMD.com.
HIV services are bouncing back from COVID-19 disruptions, data suggest, but recovery is ‘precarious’
Over the past 2 years, the COVID-19 pandemic has caused numerous disruptions in health care, including in global HIV/AIDS services. But new data presented at the Association of Nurses in AIDS Care (ANAC) 2021 Annual Meeting suggest that practitioners quickly adapted to challenges posed by the pandemic, and care and prevention services around the world have begun to return to prepandemic levels.
These rebounding numbers “show how resilient the HIV system can be,” Jennifer Kates, PhD, senior vice president and director of global health and HIV policy at the Kaiser Family Foundation (KFF), said in an interview. She presented the data during her ANAC plenary talk on Nov. 11. Dr. Kates noted that continued recovery relies on improving global access to and delivery of COVID-19 vaccines. “If we do not have control of COVID, we are going to see endless cycles of impact,” she said during her talk.
COVID-19 and HIV services
Although there was concern that the pandemic could disrupt access to antiretrovirals, the Global Fund previously reported a nearly 9% increase in people receiving antiretroviral therapy (ART) from 2019 to 2020. HIV prevention and testing did take a hit: There was a 22% decrease in testing for HIV and an 11% decline in the number of people receiving HIV prevention services over that period.
New data from the President’s Emergency Plan for AIDS Relief (PEPFAR) showed similar trends. Consistent with the Global Fund’s findings, a KFF analysis of PEPFAR data found that the number of people receiving ART grew in 2020, climbing from 16.0 million in the first quarter (Q1) of 2020 to 17.4 million by the end of the year. The most recent data from PEPFAR suggest that the number had climbed to 18.4 million by September 2021.
However, there was a 24% decrease in the number of newly enrolled individuals receiving ART from Q2 to Q3 in 2020. It dipped from 669,436 to 509,509. There was a similar decrease in the number of people being tested for HIV, dropping 25% from an estimated 16,700 to 12,500 from Q2 to Q3. But by the end of the year, both measurements had rebounded: New enrollments in ART grew 31%, and HIV testing grew nearly 41% compared to Q3.
The DREAMS (Determined, Resilient, Empowered, AIDS-free, Mentored, and Safe) program, which is focused on adolescent girls and young women, saw a dip in preexposure prophylaxis (PrEP) and other preventive services in Q4 2020, but numbers surpassed prepandemic levels by June 2021.
PEPFAR helped speed recovery, Dr. Kates said, by providing guidance on COVID-19 protocols to the field and implementing innovations, such as accelerated 3- and 6-month medication dispensing, virtual platforms, and decentralized drug delivery. In addition, the U.S. Congress allocated $3.8 billion in emergency funding in fiscal year 2021 to help mitigate the effects of COVID-19 on HIV and AIDS care.
Longer-term outcomes still unclear
Although these numbers are encouraging, some of the effects of COVID-19 on the HIV epidemic are still unknown – in particular, whether these documented dips in preventive services will translate to an increase in new infections. This will not be clear until a year or 2 from now, Dr. Kates noted. Increased use of ART as well as an increase in some behaviors associated with the pandemic, such as decreased social contact, are factors that mitigate an increase in the rate of infections, she said, but “how that all is going to play out we don’t know for sure.”
Other conference attendees expressed anxiety about the possibility of an increase in the rate of infections. “I’m waiting for the other shoe to drop, as it were,” Barb Cardell, training and technical assistance director at Positive Women’s Network–USA, in Oakland, Calif., said in an interview. The Positive Women’s Network is a national organization of women living with HIV. “Starting late in 2019, we have been cautioning public health officials in states and federally that there will likely be an uptick in HIV diagnosis as we return to whatever ‘normal’ looks like these days,” Ms. Cardell noted, adding, “We have all heard stories of folks that had an exposure and weren’t able to access PrEP during the pandemic and hence seroconverted.”
Kara McGee, associate clinical professor at Duke University School of Nursing, Durham, N.C., shared similar sentiments. “Many people at risk of acquiring HIV had trouble accessing testing and prevention prior to the pandemic, and service interruptions due to the COVID-19 pandemic have only worsened access – especially in rural areas,” she told this news organization.
Need for equitable vaccine access
For HIV services to continue to rebound, COVID-19 vaccination needs to be made a priority globally, Dr. Kates said. But data suggest lower-income countries are being left behind. In high-income countries, 65% of the population has been fully vaccinated, compared to 2% of people in the lowest-income countries. A KFF analysis projected that at the current rates of vaccination, these disparities will widen over time. COVID-19 testing rates in lower-income countries also lag. In high-income countries, 740 tests per 100,000 individuals are conducted daily; in low-income countries, that rate is 13 daily tests per 100,000 people. Until we can achieve more equitable access globally, the documented recovery of HIV is “precarious,” Dr. Kates said.
Ms. McGee agreed with Dr. Kates and was surprised by the extent of global inequities in the COVID-19 response. She said these issues should be a focus for the HIV health care community moving forward. “I think there are lot of us who have worked in the HIV field for many years – both domestically and internationally – who did not fully grasp the global disparities and need to consider how we can advocate for more equal access and distribution,” she said.
A version of this article first appeared on Medscape.com.
Over the past 2 years, the COVID-19 pandemic has caused numerous disruptions in health care, including in global HIV/AIDS services. But new data presented at the Association of Nurses in AIDS Care (ANAC) 2021 Annual Meeting suggest that practitioners quickly adapted to challenges posed by the pandemic, and care and prevention services around the world have begun to return to prepandemic levels.
These rebounding numbers “show how resilient the HIV system can be,” Jennifer Kates, PhD, senior vice president and director of global health and HIV policy at the Kaiser Family Foundation (KFF), said in an interview. She presented the data during her ANAC plenary talk on Nov. 11. Dr. Kates noted that continued recovery relies on improving global access to and delivery of COVID-19 vaccines. “If we do not have control of COVID, we are going to see endless cycles of impact,” she said during her talk.
COVID-19 and HIV services
Although there was concern that the pandemic could disrupt access to antiretrovirals, the Global Fund previously reported a nearly 9% increase in people receiving antiretroviral therapy (ART) from 2019 to 2020. HIV prevention and testing did take a hit: There was a 22% decrease in testing for HIV and an 11% decline in the number of people receiving HIV prevention services over that period.
New data from the President’s Emergency Plan for AIDS Relief (PEPFAR) showed similar trends. Consistent with the Global Fund’s findings, a KFF analysis of PEPFAR data found that the number of people receiving ART grew in 2020, climbing from 16.0 million in the first quarter (Q1) of 2020 to 17.4 million by the end of the year. The most recent data from PEPFAR suggest that the number had climbed to 18.4 million by September 2021.
However, there was a 24% decrease in the number of newly enrolled individuals receiving ART from Q2 to Q3 in 2020. It dipped from 669,436 to 509,509. There was a similar decrease in the number of people being tested for HIV, dropping 25% from an estimated 16,700 to 12,500 from Q2 to Q3. But by the end of the year, both measurements had rebounded: New enrollments in ART grew 31%, and HIV testing grew nearly 41% compared to Q3.
The DREAMS (Determined, Resilient, Empowered, AIDS-free, Mentored, and Safe) program, which is focused on adolescent girls and young women, saw a dip in preexposure prophylaxis (PrEP) and other preventive services in Q4 2020, but numbers surpassed prepandemic levels by June 2021.
PEPFAR helped speed recovery, Dr. Kates said, by providing guidance on COVID-19 protocols to the field and implementing innovations, such as accelerated 3- and 6-month medication dispensing, virtual platforms, and decentralized drug delivery. In addition, the U.S. Congress allocated $3.8 billion in emergency funding in fiscal year 2021 to help mitigate the effects of COVID-19 on HIV and AIDS care.
Longer-term outcomes still unclear
Although these numbers are encouraging, some of the effects of COVID-19 on the HIV epidemic are still unknown – in particular, whether these documented dips in preventive services will translate to an increase in new infections. This will not be clear until a year or 2 from now, Dr. Kates noted. Increased use of ART as well as an increase in some behaviors associated with the pandemic, such as decreased social contact, are factors that mitigate an increase in the rate of infections, she said, but “how that all is going to play out we don’t know for sure.”
Other conference attendees expressed anxiety about the possibility of an increase in the rate of infections. “I’m waiting for the other shoe to drop, as it were,” Barb Cardell, training and technical assistance director at Positive Women’s Network–USA, in Oakland, Calif., said in an interview. The Positive Women’s Network is a national organization of women living with HIV. “Starting late in 2019, we have been cautioning public health officials in states and federally that there will likely be an uptick in HIV diagnosis as we return to whatever ‘normal’ looks like these days,” Ms. Cardell noted, adding, “We have all heard stories of folks that had an exposure and weren’t able to access PrEP during the pandemic and hence seroconverted.”
Kara McGee, associate clinical professor at Duke University School of Nursing, Durham, N.C., shared similar sentiments. “Many people at risk of acquiring HIV had trouble accessing testing and prevention prior to the pandemic, and service interruptions due to the COVID-19 pandemic have only worsened access – especially in rural areas,” she told this news organization.
Need for equitable vaccine access
For HIV services to continue to rebound, COVID-19 vaccination needs to be made a priority globally, Dr. Kates said. But data suggest lower-income countries are being left behind. In high-income countries, 65% of the population has been fully vaccinated, compared to 2% of people in the lowest-income countries. A KFF analysis projected that at the current rates of vaccination, these disparities will widen over time. COVID-19 testing rates in lower-income countries also lag. In high-income countries, 740 tests per 100,000 individuals are conducted daily; in low-income countries, that rate is 13 daily tests per 100,000 people. Until we can achieve more equitable access globally, the documented recovery of HIV is “precarious,” Dr. Kates said.
Ms. McGee agreed with Dr. Kates and was surprised by the extent of global inequities in the COVID-19 response. She said these issues should be a focus for the HIV health care community moving forward. “I think there are lot of us who have worked in the HIV field for many years – both domestically and internationally – who did not fully grasp the global disparities and need to consider how we can advocate for more equal access and distribution,” she said.
A version of this article first appeared on Medscape.com.
Over the past 2 years, the COVID-19 pandemic has caused numerous disruptions in health care, including in global HIV/AIDS services. But new data presented at the Association of Nurses in AIDS Care (ANAC) 2021 Annual Meeting suggest that practitioners quickly adapted to challenges posed by the pandemic, and care and prevention services around the world have begun to return to prepandemic levels.
These rebounding numbers “show how resilient the HIV system can be,” Jennifer Kates, PhD, senior vice president and director of global health and HIV policy at the Kaiser Family Foundation (KFF), said in an interview. She presented the data during her ANAC plenary talk on Nov. 11. Dr. Kates noted that continued recovery relies on improving global access to and delivery of COVID-19 vaccines. “If we do not have control of COVID, we are going to see endless cycles of impact,” she said during her talk.
COVID-19 and HIV services
Although there was concern that the pandemic could disrupt access to antiretrovirals, the Global Fund previously reported a nearly 9% increase in people receiving antiretroviral therapy (ART) from 2019 to 2020. HIV prevention and testing did take a hit: There was a 22% decrease in testing for HIV and an 11% decline in the number of people receiving HIV prevention services over that period.
New data from the President’s Emergency Plan for AIDS Relief (PEPFAR) showed similar trends. Consistent with the Global Fund’s findings, a KFF analysis of PEPFAR data found that the number of people receiving ART grew in 2020, climbing from 16.0 million in the first quarter (Q1) of 2020 to 17.4 million by the end of the year. The most recent data from PEPFAR suggest that the number had climbed to 18.4 million by September 2021.
However, there was a 24% decrease in the number of newly enrolled individuals receiving ART from Q2 to Q3 in 2020. It dipped from 669,436 to 509,509. There was a similar decrease in the number of people being tested for HIV, dropping 25% from an estimated 16,700 to 12,500 from Q2 to Q3. But by the end of the year, both measurements had rebounded: New enrollments in ART grew 31%, and HIV testing grew nearly 41% compared to Q3.
The DREAMS (Determined, Resilient, Empowered, AIDS-free, Mentored, and Safe) program, which is focused on adolescent girls and young women, saw a dip in preexposure prophylaxis (PrEP) and other preventive services in Q4 2020, but numbers surpassed prepandemic levels by June 2021.
PEPFAR helped speed recovery, Dr. Kates said, by providing guidance on COVID-19 protocols to the field and implementing innovations, such as accelerated 3- and 6-month medication dispensing, virtual platforms, and decentralized drug delivery. In addition, the U.S. Congress allocated $3.8 billion in emergency funding in fiscal year 2021 to help mitigate the effects of COVID-19 on HIV and AIDS care.
Longer-term outcomes still unclear
Although these numbers are encouraging, some of the effects of COVID-19 on the HIV epidemic are still unknown – in particular, whether these documented dips in preventive services will translate to an increase in new infections. This will not be clear until a year or 2 from now, Dr. Kates noted. Increased use of ART as well as an increase in some behaviors associated with the pandemic, such as decreased social contact, are factors that mitigate an increase in the rate of infections, she said, but “how that all is going to play out we don’t know for sure.”
Other conference attendees expressed anxiety about the possibility of an increase in the rate of infections. “I’m waiting for the other shoe to drop, as it were,” Barb Cardell, training and technical assistance director at Positive Women’s Network–USA, in Oakland, Calif., said in an interview. The Positive Women’s Network is a national organization of women living with HIV. “Starting late in 2019, we have been cautioning public health officials in states and federally that there will likely be an uptick in HIV diagnosis as we return to whatever ‘normal’ looks like these days,” Ms. Cardell noted, adding, “We have all heard stories of folks that had an exposure and weren’t able to access PrEP during the pandemic and hence seroconverted.”
Kara McGee, associate clinical professor at Duke University School of Nursing, Durham, N.C., shared similar sentiments. “Many people at risk of acquiring HIV had trouble accessing testing and prevention prior to the pandemic, and service interruptions due to the COVID-19 pandemic have only worsened access – especially in rural areas,” she told this news organization.
Need for equitable vaccine access
For HIV services to continue to rebound, COVID-19 vaccination needs to be made a priority globally, Dr. Kates said. But data suggest lower-income countries are being left behind. In high-income countries, 65% of the population has been fully vaccinated, compared to 2% of people in the lowest-income countries. A KFF analysis projected that at the current rates of vaccination, these disparities will widen over time. COVID-19 testing rates in lower-income countries also lag. In high-income countries, 740 tests per 100,000 individuals are conducted daily; in low-income countries, that rate is 13 daily tests per 100,000 people. Until we can achieve more equitable access globally, the documented recovery of HIV is “precarious,” Dr. Kates said.
Ms. McGee agreed with Dr. Kates and was surprised by the extent of global inequities in the COVID-19 response. She said these issues should be a focus for the HIV health care community moving forward. “I think there are lot of us who have worked in the HIV field for many years – both domestically and internationally – who did not fully grasp the global disparities and need to consider how we can advocate for more equal access and distribution,” she said.
A version of this article first appeared on Medscape.com.
CDC unveils mental health protection plan for health care workers
Federal health officials have outlined a five-part plan to improve and protect the mental health and well-being of America’s health care workers (HCWs) and create sustainable change for the next generation of HCWs.
“It’s long past time for us to care for the people who care for all of us and address burnout in our health care workers,” U.S. Surgeon General Vivek H. Murthy, MD, MBA, said during a webinar hosted by the National Institute for Occupational Safety and Health, part of the U.S. Centers for Disease Control and Prevention.
“My hope is that, going forward, we will be able to embark on this journey together to create a health care system, a health care environment, a country where we can not only provide extraordinary care to all those who need it, but where we can take good care of those who have sacrificed so much and make sure that they are well,” Dr. Murthy said.
Burnout is not selective
There are 20 million HCWs in the United States, and no one is immune from burnout, said NIOSH Director John Howard, MD.
He noted that from June through Sept. of 2020 – the height of the COVID-19 pandemic – 93% of HCWs experienced some degree of stress, with 22% reporting moderate depression and post-traumatic stress disorder.
Looking at subsets of HCWs, a recent survey showed that one in five nurses contemplated leaving the profession because of insufficient staffing, intensity of workload, emotional and physical toll of the job, and lack of support, Dr. Howard noted.
Physician burnout was a significant issue even before the pandemic, with about 79% of physicians reporting burnout. , Dr. Howard said.
Women in health care jobs are especially vulnerable to burnout; 76% of health care jobs are held by women and 64% of physicians that feel burned-out are women, according to federal data.
“We have significant work to do in shoring up the safety and health of women in health care,” Dr. Howard said.
Mental health is also suffering among local and state public health workers. In a recent CDC survey of 26,000 of these workers, 53% reported symptoms of at least one mental health condition in the past 2 weeks.
“That is really an alarming proportion of public health workers who are as vital and essential as nurses and doctors are in our health care system,” Dr. Howard said.
Primary prevention approach
To tackle the burnout crisis, NIOSH plans to:
- Take a deep dive into understanding the personal, social, and economic burdens HCWs face on a daily basis.
- Assimilate the evidence and create a repository of best practices, resources, and interventions.
- Partner with key stakeholders, including the American Hospital Association, the American Nurses Association, National Nurses United, the Joint Commission.
- Identify and adapt tools for the health care workplace that emphasize stress reduction.
NIOSH also plans to “generate awareness through a national, multidimensional social marketing campaign to get the word out about stress so health care workers don’t feel so alone,” Dr. Howard said.
This five-part plan takes a primary prevention approach to identifying and eliminating risk factors for burnout and stress, he added.
Secondary prevention, “when damage has already been done and you’re trying to save a health care worker who is suffering from a mental health issue, that’s a lot harder than taking a good look at what you can do to organizational practices that lead to health care workers’ stress and burnout,” Dr. Howard said.
A version of this article first appeared on Medscape.com.
Federal health officials have outlined a five-part plan to improve and protect the mental health and well-being of America’s health care workers (HCWs) and create sustainable change for the next generation of HCWs.
“It’s long past time for us to care for the people who care for all of us and address burnout in our health care workers,” U.S. Surgeon General Vivek H. Murthy, MD, MBA, said during a webinar hosted by the National Institute for Occupational Safety and Health, part of the U.S. Centers for Disease Control and Prevention.
“My hope is that, going forward, we will be able to embark on this journey together to create a health care system, a health care environment, a country where we can not only provide extraordinary care to all those who need it, but where we can take good care of those who have sacrificed so much and make sure that they are well,” Dr. Murthy said.
Burnout is not selective
There are 20 million HCWs in the United States, and no one is immune from burnout, said NIOSH Director John Howard, MD.
He noted that from June through Sept. of 2020 – the height of the COVID-19 pandemic – 93% of HCWs experienced some degree of stress, with 22% reporting moderate depression and post-traumatic stress disorder.
Looking at subsets of HCWs, a recent survey showed that one in five nurses contemplated leaving the profession because of insufficient staffing, intensity of workload, emotional and physical toll of the job, and lack of support, Dr. Howard noted.
Physician burnout was a significant issue even before the pandemic, with about 79% of physicians reporting burnout. , Dr. Howard said.
Women in health care jobs are especially vulnerable to burnout; 76% of health care jobs are held by women and 64% of physicians that feel burned-out are women, according to federal data.
“We have significant work to do in shoring up the safety and health of women in health care,” Dr. Howard said.
Mental health is also suffering among local and state public health workers. In a recent CDC survey of 26,000 of these workers, 53% reported symptoms of at least one mental health condition in the past 2 weeks.
“That is really an alarming proportion of public health workers who are as vital and essential as nurses and doctors are in our health care system,” Dr. Howard said.
Primary prevention approach
To tackle the burnout crisis, NIOSH plans to:
- Take a deep dive into understanding the personal, social, and economic burdens HCWs face on a daily basis.
- Assimilate the evidence and create a repository of best practices, resources, and interventions.
- Partner with key stakeholders, including the American Hospital Association, the American Nurses Association, National Nurses United, the Joint Commission.
- Identify and adapt tools for the health care workplace that emphasize stress reduction.
NIOSH also plans to “generate awareness through a national, multidimensional social marketing campaign to get the word out about stress so health care workers don’t feel so alone,” Dr. Howard said.
This five-part plan takes a primary prevention approach to identifying and eliminating risk factors for burnout and stress, he added.
Secondary prevention, “when damage has already been done and you’re trying to save a health care worker who is suffering from a mental health issue, that’s a lot harder than taking a good look at what you can do to organizational practices that lead to health care workers’ stress and burnout,” Dr. Howard said.
A version of this article first appeared on Medscape.com.
Federal health officials have outlined a five-part plan to improve and protect the mental health and well-being of America’s health care workers (HCWs) and create sustainable change for the next generation of HCWs.
“It’s long past time for us to care for the people who care for all of us and address burnout in our health care workers,” U.S. Surgeon General Vivek H. Murthy, MD, MBA, said during a webinar hosted by the National Institute for Occupational Safety and Health, part of the U.S. Centers for Disease Control and Prevention.
“My hope is that, going forward, we will be able to embark on this journey together to create a health care system, a health care environment, a country where we can not only provide extraordinary care to all those who need it, but where we can take good care of those who have sacrificed so much and make sure that they are well,” Dr. Murthy said.
Burnout is not selective
There are 20 million HCWs in the United States, and no one is immune from burnout, said NIOSH Director John Howard, MD.
He noted that from June through Sept. of 2020 – the height of the COVID-19 pandemic – 93% of HCWs experienced some degree of stress, with 22% reporting moderate depression and post-traumatic stress disorder.
Looking at subsets of HCWs, a recent survey showed that one in five nurses contemplated leaving the profession because of insufficient staffing, intensity of workload, emotional and physical toll of the job, and lack of support, Dr. Howard noted.
Physician burnout was a significant issue even before the pandemic, with about 79% of physicians reporting burnout. , Dr. Howard said.
Women in health care jobs are especially vulnerable to burnout; 76% of health care jobs are held by women and 64% of physicians that feel burned-out are women, according to federal data.
“We have significant work to do in shoring up the safety and health of women in health care,” Dr. Howard said.
Mental health is also suffering among local and state public health workers. In a recent CDC survey of 26,000 of these workers, 53% reported symptoms of at least one mental health condition in the past 2 weeks.
“That is really an alarming proportion of public health workers who are as vital and essential as nurses and doctors are in our health care system,” Dr. Howard said.
Primary prevention approach
To tackle the burnout crisis, NIOSH plans to:
- Take a deep dive into understanding the personal, social, and economic burdens HCWs face on a daily basis.
- Assimilate the evidence and create a repository of best practices, resources, and interventions.
- Partner with key stakeholders, including the American Hospital Association, the American Nurses Association, National Nurses United, the Joint Commission.
- Identify and adapt tools for the health care workplace that emphasize stress reduction.
NIOSH also plans to “generate awareness through a national, multidimensional social marketing campaign to get the word out about stress so health care workers don’t feel so alone,” Dr. Howard said.
This five-part plan takes a primary prevention approach to identifying and eliminating risk factors for burnout and stress, he added.
Secondary prevention, “when damage has already been done and you’re trying to save a health care worker who is suffering from a mental health issue, that’s a lot harder than taking a good look at what you can do to organizational practices that lead to health care workers’ stress and burnout,” Dr. Howard said.
A version of this article first appeared on Medscape.com.
CDC: All adults should be eligible for Pfizer, Moderna boosters
on its vaccine recommendations.
The Advisory Committee on Immunization Practices, or ACIP, recommended that all adults be eligible for a third dose of a Pfizer or Moderna mRNA vaccine, at least 6 months after their second dose.
They also strengthened a recommendation that everyone over the age of 50 should get a third dose, whether or not they have an underlying health condition that may increase their risk from a COVID-19 infection.
The committee voted 11 to 0 in favor of both policies.
CDC Director Rochelle Walensky, MD, must now sign off on both policies, which she is expected to do.
More than 70 million adults are now eligible for booster shots in the United States, but only about 31 million people have received one. About half of those who have been boosted are over the age of 65.
In a recent survey, the Kaiser Family Foundation found that about 4 in 10 younger adults said they were unsure if they qualified for a booster.
Under the current policy, boosters are recommended for everyone age 65 and older. But people who are younger than age 65 are eligible for boosters if they have an underlying health condition or live or work in a high-risk situation—something individuals have to determine on their own. Experts said that shading of the policy had created confusion that was holding people back.
Nirav Shah, MD, JD, president of the Association of State and Territorial Health Officials, noted that public health officials have been swamped with calls from people who are trying to figure out if they are eligible to get a booster dose.
He said that in a call the evening of Nov. 18 with state health departments, “There was not a single state that voiced opposition to this move,” he told the ACIP.
Dr. Shah said that the current guidelines were well intentioned, but “in pursuit of precision, they create confusion.”
“Our concern is that eligible individuals are not receiving boosters right now as a result of this confusion,” he said.
The committee based its decision on the results of a new study of boosters in Pfizer vaccine recipients, as well as reassuring safety information that’s being collected through the CDC and FDA’s monitoring systems.
Pfizer presented the early results from a study of 10,000 people who had all received two doses of its vaccine. Half of the study participants received a third shot, or booster. The other half got a placebo.
The study is ongoing, but so far, six of the people in the booster group have gotten a COVID-19 infection with symptoms compared to 123 people who got COVID-19 in the placebo group, making boosters 95% effective at keeping people from getting sick. Most people in the study had gotten their original doses about 10 months earlier. They’ve been followed for about 10 weeks since their booster. Importantly, there were no study participants hospitalized for COVID-19 infections in either the placebo or booster group, indicating that the first two doses were still very effective at preventing severe outcomes from infection.
The majority of side effects after a third Pfizer dose were mild and temporary. Side effects like sore arms, swelling, fever, headache, and fatigue were more common in the booster group — affecting about 1 in 4 people who got a third shot. Vaccination side effects were less common after boosters than have been seen after the second dose of the vaccine.
Some cases of myocarditis and pericarditis have been reported after people received vaccine boosters, but the risk for this heart inflammation appears to be extremely low, about two cases for every million doses given. There were 54 cases of myocarditis reported so far to the Vaccine Adverse Event Reporting System, or VAERS. So far, only 12 have met the case definition and are considered related to vaccination. Most of the reported cases are still being studied.
on its vaccine recommendations.
The Advisory Committee on Immunization Practices, or ACIP, recommended that all adults be eligible for a third dose of a Pfizer or Moderna mRNA vaccine, at least 6 months after their second dose.
They also strengthened a recommendation that everyone over the age of 50 should get a third dose, whether or not they have an underlying health condition that may increase their risk from a COVID-19 infection.
The committee voted 11 to 0 in favor of both policies.
CDC Director Rochelle Walensky, MD, must now sign off on both policies, which she is expected to do.
More than 70 million adults are now eligible for booster shots in the United States, but only about 31 million people have received one. About half of those who have been boosted are over the age of 65.
In a recent survey, the Kaiser Family Foundation found that about 4 in 10 younger adults said they were unsure if they qualified for a booster.
Under the current policy, boosters are recommended for everyone age 65 and older. But people who are younger than age 65 are eligible for boosters if they have an underlying health condition or live or work in a high-risk situation—something individuals have to determine on their own. Experts said that shading of the policy had created confusion that was holding people back.
Nirav Shah, MD, JD, president of the Association of State and Territorial Health Officials, noted that public health officials have been swamped with calls from people who are trying to figure out if they are eligible to get a booster dose.
He said that in a call the evening of Nov. 18 with state health departments, “There was not a single state that voiced opposition to this move,” he told the ACIP.
Dr. Shah said that the current guidelines were well intentioned, but “in pursuit of precision, they create confusion.”
“Our concern is that eligible individuals are not receiving boosters right now as a result of this confusion,” he said.
The committee based its decision on the results of a new study of boosters in Pfizer vaccine recipients, as well as reassuring safety information that’s being collected through the CDC and FDA’s monitoring systems.
Pfizer presented the early results from a study of 10,000 people who had all received two doses of its vaccine. Half of the study participants received a third shot, or booster. The other half got a placebo.
The study is ongoing, but so far, six of the people in the booster group have gotten a COVID-19 infection with symptoms compared to 123 people who got COVID-19 in the placebo group, making boosters 95% effective at keeping people from getting sick. Most people in the study had gotten their original doses about 10 months earlier. They’ve been followed for about 10 weeks since their booster. Importantly, there were no study participants hospitalized for COVID-19 infections in either the placebo or booster group, indicating that the first two doses were still very effective at preventing severe outcomes from infection.
The majority of side effects after a third Pfizer dose were mild and temporary. Side effects like sore arms, swelling, fever, headache, and fatigue were more common in the booster group — affecting about 1 in 4 people who got a third shot. Vaccination side effects were less common after boosters than have been seen after the second dose of the vaccine.
Some cases of myocarditis and pericarditis have been reported after people received vaccine boosters, but the risk for this heart inflammation appears to be extremely low, about two cases for every million doses given. There were 54 cases of myocarditis reported so far to the Vaccine Adverse Event Reporting System, or VAERS. So far, only 12 have met the case definition and are considered related to vaccination. Most of the reported cases are still being studied.
on its vaccine recommendations.
The Advisory Committee on Immunization Practices, or ACIP, recommended that all adults be eligible for a third dose of a Pfizer or Moderna mRNA vaccine, at least 6 months after their second dose.
They also strengthened a recommendation that everyone over the age of 50 should get a third dose, whether or not they have an underlying health condition that may increase their risk from a COVID-19 infection.
The committee voted 11 to 0 in favor of both policies.
CDC Director Rochelle Walensky, MD, must now sign off on both policies, which she is expected to do.
More than 70 million adults are now eligible for booster shots in the United States, but only about 31 million people have received one. About half of those who have been boosted are over the age of 65.
In a recent survey, the Kaiser Family Foundation found that about 4 in 10 younger adults said they were unsure if they qualified for a booster.
Under the current policy, boosters are recommended for everyone age 65 and older. But people who are younger than age 65 are eligible for boosters if they have an underlying health condition or live or work in a high-risk situation—something individuals have to determine on their own. Experts said that shading of the policy had created confusion that was holding people back.
Nirav Shah, MD, JD, president of the Association of State and Territorial Health Officials, noted that public health officials have been swamped with calls from people who are trying to figure out if they are eligible to get a booster dose.
He said that in a call the evening of Nov. 18 with state health departments, “There was not a single state that voiced opposition to this move,” he told the ACIP.
Dr. Shah said that the current guidelines were well intentioned, but “in pursuit of precision, they create confusion.”
“Our concern is that eligible individuals are not receiving boosters right now as a result of this confusion,” he said.
The committee based its decision on the results of a new study of boosters in Pfizer vaccine recipients, as well as reassuring safety information that’s being collected through the CDC and FDA’s monitoring systems.
Pfizer presented the early results from a study of 10,000 people who had all received two doses of its vaccine. Half of the study participants received a third shot, or booster. The other half got a placebo.
The study is ongoing, but so far, six of the people in the booster group have gotten a COVID-19 infection with symptoms compared to 123 people who got COVID-19 in the placebo group, making boosters 95% effective at keeping people from getting sick. Most people in the study had gotten their original doses about 10 months earlier. They’ve been followed for about 10 weeks since their booster. Importantly, there were no study participants hospitalized for COVID-19 infections in either the placebo or booster group, indicating that the first two doses were still very effective at preventing severe outcomes from infection.
The majority of side effects after a third Pfizer dose were mild and temporary. Side effects like sore arms, swelling, fever, headache, and fatigue were more common in the booster group — affecting about 1 in 4 people who got a third shot. Vaccination side effects were less common after boosters than have been seen after the second dose of the vaccine.
Some cases of myocarditis and pericarditis have been reported after people received vaccine boosters, but the risk for this heart inflammation appears to be extremely low, about two cases for every million doses given. There were 54 cases of myocarditis reported so far to the Vaccine Adverse Event Reporting System, or VAERS. So far, only 12 have met the case definition and are considered related to vaccination. Most of the reported cases are still being studied.



