User login
Diabetes Hub contains news and clinical review articles for physicians seeking the most up-to-date information on the rapidly evolving options for treating and preventing Type 2 Diabetes in at-risk patients. The Diabetes Hub is powered by Frontline Medical Communications.
STAMPEDE: Metabolic surgery bests medical therapy long term
CHICAGO – The superiority of metabolic surgery over intensive medical therapy for achieving glycemic control in patients with type 2 diabetes was largely maintained at the final 5-year follow-up evaluation in the randomized, controlled STAMPEDE trial.
The 150 subjects, who had “fairly severe diabetes” with an average disease duration of 8 years, were randomized to receive intensive medical therapy alone, or intensive medical therapy with Roux-en-Y gastric bypass surgery or sleeve gastrectomy surgery. The primary endpoint of hemoglobin A1c less than 6% was achieved in 5%, 29%, and 23% of patients in the groups, respectively. The difference was statistically significant in favor of both types of surgery, Dr. Philip Raymond Schauer reported at the annual meeting of the American College of Cardiology.
Furthermore, patients in the surgery groups fared better than those in the intensive medical therapy group on several other measures, including disease remission (defied as HbA1c less than 6% without diabetes medication), HbA1c less than 7% (the American Diabetes Association target for therapy), change in fasting plasma glucose from baseline, and changes in high- and low-density lipoprotein cholesterol levels, said Dr. Schauer, director of the Cleveland Clinic Bariatric and Metabolic Institute.
Patients in the surgery groups also experienced a significantly greater reduction in the use of antihypertensive medications and lipid-lowering agents, he added.
The “very dramatic drop” in HbA1c seen early on in the surgical patients was, for the most part, sustained out to 5 years, he said.
The results for both surgeries were significantly better than those for intensive medical therapy, but the results with gastric bypass were more effective at 5 years than were those for sleeve gastrectomy, he added, noting that the surgery patients had better quality of life, compared with the intensive medical therapy patients.
As for adverse events in the surgery groups, no perioperative deaths occurred, and while there were some surgical complications, none resulted in long-term disability, Dr. Schauer said.
Anemia was more common in the surgery patients, but was fairly mild. The most common complication was weight gain in 20% of patients, and the overall reoperation rate was 7%.
Of note, patients in the study had body mass index ranging from 27 to 43 kg/m2, and those with BMI less than 35 had similar benefits as those with more severe obesity. This is important, as many insurance companies won’t cover metabolic surgery for patients with BMI less than 35, he explained.
These findings represent the longest follow-up to date comparing the efficacy of the two most common metabolic surgery procedures with medical treatment of type 2 diabetes for maintaining glycemic control or reducing end-organ complications. Three-year outcomes of STAMPEDE (Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently) were reported in 2014 (N Engl J Med. 2014;370:2002-13).
The participants ranged in age from 20 to 60 years. The average HbA1c was about 9%, the average BMI was 36, and most were on at least three antidiabetic medications at baseline. Half were on insulin.
The findings are important, because of the roughly 25 million Americans with type 2 diabetes, only about half have good glycemic control on their current medical treatment strategies, Dr. Schauer said.
Though limited by the single-center study design, the STAMPEDE findings show that metabolic surgery is more effective long term than intensive medical therapy in patients with uncontrolled type 2 diabetes and should be considered a treatment option in this population, he concluded, adding that multicenter studies would be helpful for determining the generalizability of the findings.
Dr. Schauer reported receiving consulting fees/honoraria from Ethicon Endosurgery and The Medicines Company, and having ownership interest in Surgical Excellence.
CHICAGO – The superiority of metabolic surgery over intensive medical therapy for achieving glycemic control in patients with type 2 diabetes was largely maintained at the final 5-year follow-up evaluation in the randomized, controlled STAMPEDE trial.
The 150 subjects, who had “fairly severe diabetes” with an average disease duration of 8 years, were randomized to receive intensive medical therapy alone, or intensive medical therapy with Roux-en-Y gastric bypass surgery or sleeve gastrectomy surgery. The primary endpoint of hemoglobin A1c less than 6% was achieved in 5%, 29%, and 23% of patients in the groups, respectively. The difference was statistically significant in favor of both types of surgery, Dr. Philip Raymond Schauer reported at the annual meeting of the American College of Cardiology.
Furthermore, patients in the surgery groups fared better than those in the intensive medical therapy group on several other measures, including disease remission (defied as HbA1c less than 6% without diabetes medication), HbA1c less than 7% (the American Diabetes Association target for therapy), change in fasting plasma glucose from baseline, and changes in high- and low-density lipoprotein cholesterol levels, said Dr. Schauer, director of the Cleveland Clinic Bariatric and Metabolic Institute.
Patients in the surgery groups also experienced a significantly greater reduction in the use of antihypertensive medications and lipid-lowering agents, he added.
The “very dramatic drop” in HbA1c seen early on in the surgical patients was, for the most part, sustained out to 5 years, he said.
The results for both surgeries were significantly better than those for intensive medical therapy, but the results with gastric bypass were more effective at 5 years than were those for sleeve gastrectomy, he added, noting that the surgery patients had better quality of life, compared with the intensive medical therapy patients.
As for adverse events in the surgery groups, no perioperative deaths occurred, and while there were some surgical complications, none resulted in long-term disability, Dr. Schauer said.
Anemia was more common in the surgery patients, but was fairly mild. The most common complication was weight gain in 20% of patients, and the overall reoperation rate was 7%.
Of note, patients in the study had body mass index ranging from 27 to 43 kg/m2, and those with BMI less than 35 had similar benefits as those with more severe obesity. This is important, as many insurance companies won’t cover metabolic surgery for patients with BMI less than 35, he explained.
These findings represent the longest follow-up to date comparing the efficacy of the two most common metabolic surgery procedures with medical treatment of type 2 diabetes for maintaining glycemic control or reducing end-organ complications. Three-year outcomes of STAMPEDE (Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently) were reported in 2014 (N Engl J Med. 2014;370:2002-13).
The participants ranged in age from 20 to 60 years. The average HbA1c was about 9%, the average BMI was 36, and most were on at least three antidiabetic medications at baseline. Half were on insulin.
The findings are important, because of the roughly 25 million Americans with type 2 diabetes, only about half have good glycemic control on their current medical treatment strategies, Dr. Schauer said.
Though limited by the single-center study design, the STAMPEDE findings show that metabolic surgery is more effective long term than intensive medical therapy in patients with uncontrolled type 2 diabetes and should be considered a treatment option in this population, he concluded, adding that multicenter studies would be helpful for determining the generalizability of the findings.
Dr. Schauer reported receiving consulting fees/honoraria from Ethicon Endosurgery and The Medicines Company, and having ownership interest in Surgical Excellence.
CHICAGO – The superiority of metabolic surgery over intensive medical therapy for achieving glycemic control in patients with type 2 diabetes was largely maintained at the final 5-year follow-up evaluation in the randomized, controlled STAMPEDE trial.
The 150 subjects, who had “fairly severe diabetes” with an average disease duration of 8 years, were randomized to receive intensive medical therapy alone, or intensive medical therapy with Roux-en-Y gastric bypass surgery or sleeve gastrectomy surgery. The primary endpoint of hemoglobin A1c less than 6% was achieved in 5%, 29%, and 23% of patients in the groups, respectively. The difference was statistically significant in favor of both types of surgery, Dr. Philip Raymond Schauer reported at the annual meeting of the American College of Cardiology.
Furthermore, patients in the surgery groups fared better than those in the intensive medical therapy group on several other measures, including disease remission (defied as HbA1c less than 6% without diabetes medication), HbA1c less than 7% (the American Diabetes Association target for therapy), change in fasting plasma glucose from baseline, and changes in high- and low-density lipoprotein cholesterol levels, said Dr. Schauer, director of the Cleveland Clinic Bariatric and Metabolic Institute.
Patients in the surgery groups also experienced a significantly greater reduction in the use of antihypertensive medications and lipid-lowering agents, he added.
The “very dramatic drop” in HbA1c seen early on in the surgical patients was, for the most part, sustained out to 5 years, he said.
The results for both surgeries were significantly better than those for intensive medical therapy, but the results with gastric bypass were more effective at 5 years than were those for sleeve gastrectomy, he added, noting that the surgery patients had better quality of life, compared with the intensive medical therapy patients.
As for adverse events in the surgery groups, no perioperative deaths occurred, and while there were some surgical complications, none resulted in long-term disability, Dr. Schauer said.
Anemia was more common in the surgery patients, but was fairly mild. The most common complication was weight gain in 20% of patients, and the overall reoperation rate was 7%.
Of note, patients in the study had body mass index ranging from 27 to 43 kg/m2, and those with BMI less than 35 had similar benefits as those with more severe obesity. This is important, as many insurance companies won’t cover metabolic surgery for patients with BMI less than 35, he explained.
These findings represent the longest follow-up to date comparing the efficacy of the two most common metabolic surgery procedures with medical treatment of type 2 diabetes for maintaining glycemic control or reducing end-organ complications. Three-year outcomes of STAMPEDE (Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently) were reported in 2014 (N Engl J Med. 2014;370:2002-13).
The participants ranged in age from 20 to 60 years. The average HbA1c was about 9%, the average BMI was 36, and most were on at least three antidiabetic medications at baseline. Half were on insulin.
The findings are important, because of the roughly 25 million Americans with type 2 diabetes, only about half have good glycemic control on their current medical treatment strategies, Dr. Schauer said.
Though limited by the single-center study design, the STAMPEDE findings show that metabolic surgery is more effective long term than intensive medical therapy in patients with uncontrolled type 2 diabetes and should be considered a treatment option in this population, he concluded, adding that multicenter studies would be helpful for determining the generalizability of the findings.
Dr. Schauer reported receiving consulting fees/honoraria from Ethicon Endosurgery and The Medicines Company, and having ownership interest in Surgical Excellence.
AT ACC 16
Key clinical point: The superiority of metabolic surgery over intensive medical therapy for achieving glycemic control among patients with type 2 diabetes in the randomized, controlled STAMPEDE persisted at the final 5-year follow-up evaluation.
Major finding: The primary endpoint of HbA1c less than 6% was achieved in 5%, 29%, and 23% of patients in the medication and medication plus Roux-en-Y or sleeve gastrectomy groups, respectively.
Data source: The randomized, controlled STAMPEDE trial in 150 subjects.
Disclosures: Dr. Schauer reported receiving consulting fees/honoraria from Ethicon Endosurgery and The Medicines Company, and having ownership interest in Surgical Excellence.
Earlier bariatric surgery may improve cardiovascular outcomes
CHICAGO – Sooner may be better than later when it comes to the timing of bariatric surgery in patients with morbid obesity.
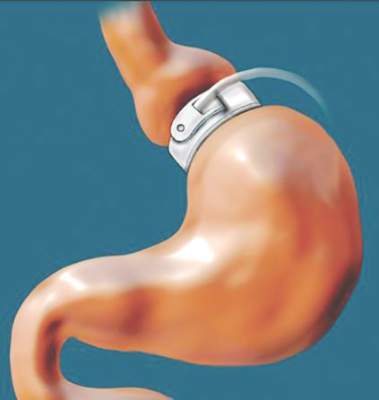
Of 828 patients with body mass index of at least 35 kg/m2 who underwent laparoscopic adjustable gastric banding performed by a single surgeon and were followed for up to 11 years (mean of 10 years), 423 were aged 45 years or younger, and 405 were over age 45 years at the time of surgery. A comparison of outcomes between the two age groups showed that older age at the time of surgery was an independent predictor of cardiovascular events (hazard ratio, 1.8), Maharaj Singh, Ph.D., a biostatistician at the Aurora Research Institute, Milwaukee, reported in a poster at the annual meeting of the American College of Cardiology.
Despite a similar reduction in body weight after gastric banding surgery, the older patients experienced more cardiovascular events: myocardial infarction occurred in 0.2% and 1.7% of patients in the younger and older age groups, respectively, pulmonary embolism occurred in 0.7% and 4.3%, congestive heart failure occurred in 2.8% and 7.8%, and stroke occurred in 3.7% and 7.6%, Dr. Singh said.
“Although the older group had more comorbidities, these were accounted for by multivariate analysis and age over 45 years remained an independent predictor of poor cardiovascular outcomes,” senior coauthor Dr. Arshad Jahangir, professor of medicine at the University of Wisconsin–Madison, said in an interview.
Other independent predictors of adverse cardiovascular outcomes in the study were sleep apnea (hazard ratio, 4), history of hypertension (HR, 1.9), and depression, (HR, 1.8), Dr. Jahangir said.
“Gender, race, and diabetes mellitus did not independently predict cardiovascular events,” he said.
Weight loss after bariatric surgery has been shown to reduce the risk of adverse cardiovascular events, but it has remained unclear whether the reduction in risk varies based on age at the time of surgery, he said.
The current findings suggest that the effects of laparoscopic adjustable gastric banding–induced weight loss on cardiovascular outcomes are greater in patients who undergo the surgery at a younger age, he said, adding that the findings also “raise important questions about whether better control of sleep apnea, hypertension, and depression could help further reduce cardiovascular events in morbidly obese individuals undergoing bariatric surgery and should be addressed in a prospective study of these patients.”
The authors reported having no disclosures.
CHICAGO – Sooner may be better than later when it comes to the timing of bariatric surgery in patients with morbid obesity.
Of 828 patients with body mass index of at least 35 kg/m2 who underwent laparoscopic adjustable gastric banding performed by a single surgeon and were followed for up to 11 years (mean of 10 years), 423 were aged 45 years or younger, and 405 were over age 45 years at the time of surgery. A comparison of outcomes between the two age groups showed that older age at the time of surgery was an independent predictor of cardiovascular events (hazard ratio, 1.8), Maharaj Singh, Ph.D., a biostatistician at the Aurora Research Institute, Milwaukee, reported in a poster at the annual meeting of the American College of Cardiology.
Despite a similar reduction in body weight after gastric banding surgery, the older patients experienced more cardiovascular events: myocardial infarction occurred in 0.2% and 1.7% of patients in the younger and older age groups, respectively, pulmonary embolism occurred in 0.7% and 4.3%, congestive heart failure occurred in 2.8% and 7.8%, and stroke occurred in 3.7% and 7.6%, Dr. Singh said.
“Although the older group had more comorbidities, these were accounted for by multivariate analysis and age over 45 years remained an independent predictor of poor cardiovascular outcomes,” senior coauthor Dr. Arshad Jahangir, professor of medicine at the University of Wisconsin–Madison, said in an interview.
Other independent predictors of adverse cardiovascular outcomes in the study were sleep apnea (hazard ratio, 4), history of hypertension (HR, 1.9), and depression, (HR, 1.8), Dr. Jahangir said.
“Gender, race, and diabetes mellitus did not independently predict cardiovascular events,” he said.
Weight loss after bariatric surgery has been shown to reduce the risk of adverse cardiovascular events, but it has remained unclear whether the reduction in risk varies based on age at the time of surgery, he said.
The current findings suggest that the effects of laparoscopic adjustable gastric banding–induced weight loss on cardiovascular outcomes are greater in patients who undergo the surgery at a younger age, he said, adding that the findings also “raise important questions about whether better control of sleep apnea, hypertension, and depression could help further reduce cardiovascular events in morbidly obese individuals undergoing bariatric surgery and should be addressed in a prospective study of these patients.”
The authors reported having no disclosures.
CHICAGO – Sooner may be better than later when it comes to the timing of bariatric surgery in patients with morbid obesity.
Of 828 patients with body mass index of at least 35 kg/m2 who underwent laparoscopic adjustable gastric banding performed by a single surgeon and were followed for up to 11 years (mean of 10 years), 423 were aged 45 years or younger, and 405 were over age 45 years at the time of surgery. A comparison of outcomes between the two age groups showed that older age at the time of surgery was an independent predictor of cardiovascular events (hazard ratio, 1.8), Maharaj Singh, Ph.D., a biostatistician at the Aurora Research Institute, Milwaukee, reported in a poster at the annual meeting of the American College of Cardiology.
Despite a similar reduction in body weight after gastric banding surgery, the older patients experienced more cardiovascular events: myocardial infarction occurred in 0.2% and 1.7% of patients in the younger and older age groups, respectively, pulmonary embolism occurred in 0.7% and 4.3%, congestive heart failure occurred in 2.8% and 7.8%, and stroke occurred in 3.7% and 7.6%, Dr. Singh said.
“Although the older group had more comorbidities, these were accounted for by multivariate analysis and age over 45 years remained an independent predictor of poor cardiovascular outcomes,” senior coauthor Dr. Arshad Jahangir, professor of medicine at the University of Wisconsin–Madison, said in an interview.
Other independent predictors of adverse cardiovascular outcomes in the study were sleep apnea (hazard ratio, 4), history of hypertension (HR, 1.9), and depression, (HR, 1.8), Dr. Jahangir said.
“Gender, race, and diabetes mellitus did not independently predict cardiovascular events,” he said.
Weight loss after bariatric surgery has been shown to reduce the risk of adverse cardiovascular events, but it has remained unclear whether the reduction in risk varies based on age at the time of surgery, he said.
The current findings suggest that the effects of laparoscopic adjustable gastric banding–induced weight loss on cardiovascular outcomes are greater in patients who undergo the surgery at a younger age, he said, adding that the findings also “raise important questions about whether better control of sleep apnea, hypertension, and depression could help further reduce cardiovascular events in morbidly obese individuals undergoing bariatric surgery and should be addressed in a prospective study of these patients.”
The authors reported having no disclosures.
AT ACC 16
Key clinical point: Morbidly obese patients who underwent bariatric surgery before age 45 years had a reduced risk of adverse cardiovascular outcomes vs. those aged 45 or older at the time of surgery, despite similar weight loss.
Major finding: Older vs. younger age at the time of surgery was an independent predictor of cardiovascular events (hazard ratio, 1.8).
Data source: A review of outcomes in 828 laparoscopic adjustable gastric banding patients.
Disclosures: The authors reported having no disclosures.
New analysis bolsters metformin as first line in type 2 diabetes
Patients with type 2 diabetes treated with metformin as a monotherapy are at a decreased risk for cardiovascular mortality when compared with those on sulfonylurea monotherapy, according to a report in the Annals of Internal Medicine.
Dr. Nisa M. Maruthur and her associates conducted an update of a previous systematic literature review and meta-analysis to assess the comparative effectiveness and safety of metformin monotherapy and combination therapies including metformin with nonmetformin monotherapies in patients with type 2 diabetes. They focused on original, adult human experimental, and observational studies (Ann Intern Med. 2016 Apr 19. doi: 10.7326/M15-2650).
Dr. Maruthur and colleagues identified a total of 19,423 articles, of which 234 were found to meet the study inclusion criteria. The majority of the included studies were randomized, controlled trials, with 98 assessing all-cause mortality and macro- and microvascular outcomes.
On the basis of consistent findings from two randomized, controlled trials including 3,199 total participants (ADOPT and SPREAD-DIMCAD), a lower risk for cardiovascular mortality was found for metformin monotherapy versus sulfonylurea monotherapy. For those on metformin monotherapy, 2 of the 1,454 patients had a fatal MI and 7 of 156 patients died from cardiovascular disease. Three of 1,441 patients on monotherapy with a sulfonylurea had a fatal MI and 11 of 148 patients died from cardiovascular disease.
The evidence from this systematic review supports current type 2 diabetes guidelines that recommend metformin as the first-line agent to treat adults, based on its beneficial effects on hemoglobin A1c, weight, and cardiovascular mortality versus sulfonylureas, as well as its relative safety profile, Dr. Maruthur of the department of medicine and epidemiology at Johns Hopkins University, Baltimore, and her coinvestigators said.
The study was funded by Agency for Healthcare Research and Quality. Several of the coauthors disclosed contracts with the funding source during the conduct of the study. The remaining coauthors disclosed no conflicts of interest.
Patients with type 2 diabetes treated with metformin as a monotherapy are at a decreased risk for cardiovascular mortality when compared with those on sulfonylurea monotherapy, according to a report in the Annals of Internal Medicine.
Dr. Nisa M. Maruthur and her associates conducted an update of a previous systematic literature review and meta-analysis to assess the comparative effectiveness and safety of metformin monotherapy and combination therapies including metformin with nonmetformin monotherapies in patients with type 2 diabetes. They focused on original, adult human experimental, and observational studies (Ann Intern Med. 2016 Apr 19. doi: 10.7326/M15-2650).
Dr. Maruthur and colleagues identified a total of 19,423 articles, of which 234 were found to meet the study inclusion criteria. The majority of the included studies were randomized, controlled trials, with 98 assessing all-cause mortality and macro- and microvascular outcomes.
On the basis of consistent findings from two randomized, controlled trials including 3,199 total participants (ADOPT and SPREAD-DIMCAD), a lower risk for cardiovascular mortality was found for metformin monotherapy versus sulfonylurea monotherapy. For those on metformin monotherapy, 2 of the 1,454 patients had a fatal MI and 7 of 156 patients died from cardiovascular disease. Three of 1,441 patients on monotherapy with a sulfonylurea had a fatal MI and 11 of 148 patients died from cardiovascular disease.
The evidence from this systematic review supports current type 2 diabetes guidelines that recommend metformin as the first-line agent to treat adults, based on its beneficial effects on hemoglobin A1c, weight, and cardiovascular mortality versus sulfonylureas, as well as its relative safety profile, Dr. Maruthur of the department of medicine and epidemiology at Johns Hopkins University, Baltimore, and her coinvestigators said.
The study was funded by Agency for Healthcare Research and Quality. Several of the coauthors disclosed contracts with the funding source during the conduct of the study. The remaining coauthors disclosed no conflicts of interest.
Patients with type 2 diabetes treated with metformin as a monotherapy are at a decreased risk for cardiovascular mortality when compared with those on sulfonylurea monotherapy, according to a report in the Annals of Internal Medicine.
Dr. Nisa M. Maruthur and her associates conducted an update of a previous systematic literature review and meta-analysis to assess the comparative effectiveness and safety of metformin monotherapy and combination therapies including metformin with nonmetformin monotherapies in patients with type 2 diabetes. They focused on original, adult human experimental, and observational studies (Ann Intern Med. 2016 Apr 19. doi: 10.7326/M15-2650).
Dr. Maruthur and colleagues identified a total of 19,423 articles, of which 234 were found to meet the study inclusion criteria. The majority of the included studies were randomized, controlled trials, with 98 assessing all-cause mortality and macro- and microvascular outcomes.
On the basis of consistent findings from two randomized, controlled trials including 3,199 total participants (ADOPT and SPREAD-DIMCAD), a lower risk for cardiovascular mortality was found for metformin monotherapy versus sulfonylurea monotherapy. For those on metformin monotherapy, 2 of the 1,454 patients had a fatal MI and 7 of 156 patients died from cardiovascular disease. Three of 1,441 patients on monotherapy with a sulfonylurea had a fatal MI and 11 of 148 patients died from cardiovascular disease.
The evidence from this systematic review supports current type 2 diabetes guidelines that recommend metformin as the first-line agent to treat adults, based on its beneficial effects on hemoglobin A1c, weight, and cardiovascular mortality versus sulfonylureas, as well as its relative safety profile, Dr. Maruthur of the department of medicine and epidemiology at Johns Hopkins University, Baltimore, and her coinvestigators said.
The study was funded by Agency for Healthcare Research and Quality. Several of the coauthors disclosed contracts with the funding source during the conduct of the study. The remaining coauthors disclosed no conflicts of interest.
Key clinical point: Clinical trial data support the use of metformin monotherapy, as opposed to sulfonylurea monotherapy, as a first-line therapy for type 2 diabetes.
Major finding: Two randomized, controlled trials showed a lower risk for cardiovascular mortality with metformin versus a sulfonylurea.
Data sources: Literature review and meta-analysis involving 204 studies, two of which were randomized, controlled trials comparing the effects of metformin and sulfonylurea monotherapy on cardiovascular mortality among patients with type 2 diabetes.
Disclosures: The study was funded by Agency for Healthcare Research and Quality. Several of the coauthors disclosed contracts with the funding source during the conduct of the study. The remaining coauthors disclosed no conflicts of interest.
Ticagrelor cuts post-MI events in diabetes patients
CHICAGO – The benefit from dual-antiplatelet therapy in high-risk patients following a myocardial infarction was especially apparent in post-MI patients with diabetes in a prespecified secondary analysis from a multicenter trial of ticagrelor with more than 21,000 patients.
Among post-MI patients with diabetes, treatment with ticagrelor plus aspirin led to an absolute 1.5% reduction in the rate of cardiovascular death, MI, or stroke during a median 33-month follow-up, compared with an absolute 1.1% cut in patients without diabetes, Dr. Deepak L. Bhatt said at the annual meeting of the American College of Cardiology. The relative risk reduction, compared with placebo was 16% in both the diabetes and no diabetes subgroups, statistically significant differences in both subgroups.
“Long-term treatment with ticagrelor reduced the composite of cardiovascular death, MI, or stroke in diabetic patients with a greater absolute risk reduction than in nondiabetic patients,” said Dr. Bhatt, professor of medicine at Harvard Medical School and executive director of Interventional Cardiovascular Programs at Brigham and Women’s Hospital in Boston. Treatment with ticagrelor plus aspirin in post-MI patients with diabetes also led to an increased number of major bleeding episodes, compared with patients on aspirin alone, but no excess of intracerebral hemorrhages or fatal bleeds, he noted.
This finding of a significant benefit from ticagrelor in post-MI patients with diabetes confirms similar, prior findings with other antiplatelet drugs (including clopidogrel, prasugrel, and vorapaxar) and prior findings with ticagrelor, Dr. Bhatt noted.
The new analysis used data collected in the Prevention of Cardiovascular Events in Patients With Prior Heart Attack Using Ticagrelor Compared to Placebo on a Background of Aspirin–Thrombolysis in Myocardial Infarction 54 (PEGASUS-TIMI 54) trial. The primary results from PEGASUS-TIMI 54 had shown that adding ticagrelor to aspirin treatment of high-risk post-MI patients, including those who both had or did not have diabetes, significantly cut the composite rate of cardiovascular death, MI, and stroke, compared with aspirin alone (N Engl J Med. 2015 May 7;372[19]:1791-800). The study group included 6,806 patients with diabetes (type 2 diabetes in 99% of these patients), and 14,355 without diabetes. All patients had their MI 1-3 years before entering the study.
Dr. Bhatt and his associates examined the incidence of the various clinical endpoints measured in the study among only the patients with diabetes divided into those who received any dosage of ticagrelor (60 mg b.i.d. or 90 mg b.i.d.) or placebo, and also among the patients without diabetes. In addition to the primary endpoint, the new analysis showed that the rate of cardiovascular death during follow-up was 3.9% in the diabetes patients on dual therapy and 5.0% among the diabetes patients on aspirin only, a 22% relative risk reduction with ticagrelor added that was statistically significant. In contrast, among patients without diabetes the rates of cardiovascular death between those on and not on ticagrelor only differed by 0.2%, a 9% relative risk reduction that was not statistically significant. The same pattern occurred for the endpoint of death from coronary artery disease.
Concurrent with Dr. Bhatt’s report, the results appeared in an article published online (J Am Coll Cardiol. 2016 Apr; doi: 10.1016/S0735-1097[16]30023-7).
A new study, THEMIS, is examining the safety and efficacy of combined ticagrelor and aspirin treatment in a lower-risk group of patients with diabetes, those with coronary artery disease who have not had a prior MI. Those results may be available in 2018.
PEGASUS-TIMI 54 was sponsored by AstraZeneca, the company that markets ticagrelor (Brilinta). Dr. Bhatt has been an advisor to Cardax and Regado Biosciences and has received research support from AstraZeneca and several other companies.
On Twitter @mitchelzoler
CHICAGO – The benefit from dual-antiplatelet therapy in high-risk patients following a myocardial infarction was especially apparent in post-MI patients with diabetes in a prespecified secondary analysis from a multicenter trial of ticagrelor with more than 21,000 patients.
Among post-MI patients with diabetes, treatment with ticagrelor plus aspirin led to an absolute 1.5% reduction in the rate of cardiovascular death, MI, or stroke during a median 33-month follow-up, compared with an absolute 1.1% cut in patients without diabetes, Dr. Deepak L. Bhatt said at the annual meeting of the American College of Cardiology. The relative risk reduction, compared with placebo was 16% in both the diabetes and no diabetes subgroups, statistically significant differences in both subgroups.
“Long-term treatment with ticagrelor reduced the composite of cardiovascular death, MI, or stroke in diabetic patients with a greater absolute risk reduction than in nondiabetic patients,” said Dr. Bhatt, professor of medicine at Harvard Medical School and executive director of Interventional Cardiovascular Programs at Brigham and Women’s Hospital in Boston. Treatment with ticagrelor plus aspirin in post-MI patients with diabetes also led to an increased number of major bleeding episodes, compared with patients on aspirin alone, but no excess of intracerebral hemorrhages or fatal bleeds, he noted.
This finding of a significant benefit from ticagrelor in post-MI patients with diabetes confirms similar, prior findings with other antiplatelet drugs (including clopidogrel, prasugrel, and vorapaxar) and prior findings with ticagrelor, Dr. Bhatt noted.
The new analysis used data collected in the Prevention of Cardiovascular Events in Patients With Prior Heart Attack Using Ticagrelor Compared to Placebo on a Background of Aspirin–Thrombolysis in Myocardial Infarction 54 (PEGASUS-TIMI 54) trial. The primary results from PEGASUS-TIMI 54 had shown that adding ticagrelor to aspirin treatment of high-risk post-MI patients, including those who both had or did not have diabetes, significantly cut the composite rate of cardiovascular death, MI, and stroke, compared with aspirin alone (N Engl J Med. 2015 May 7;372[19]:1791-800). The study group included 6,806 patients with diabetes (type 2 diabetes in 99% of these patients), and 14,355 without diabetes. All patients had their MI 1-3 years before entering the study.
Dr. Bhatt and his associates examined the incidence of the various clinical endpoints measured in the study among only the patients with diabetes divided into those who received any dosage of ticagrelor (60 mg b.i.d. or 90 mg b.i.d.) or placebo, and also among the patients without diabetes. In addition to the primary endpoint, the new analysis showed that the rate of cardiovascular death during follow-up was 3.9% in the diabetes patients on dual therapy and 5.0% among the diabetes patients on aspirin only, a 22% relative risk reduction with ticagrelor added that was statistically significant. In contrast, among patients without diabetes the rates of cardiovascular death between those on and not on ticagrelor only differed by 0.2%, a 9% relative risk reduction that was not statistically significant. The same pattern occurred for the endpoint of death from coronary artery disease.
Concurrent with Dr. Bhatt’s report, the results appeared in an article published online (J Am Coll Cardiol. 2016 Apr; doi: 10.1016/S0735-1097[16]30023-7).
A new study, THEMIS, is examining the safety and efficacy of combined ticagrelor and aspirin treatment in a lower-risk group of patients with diabetes, those with coronary artery disease who have not had a prior MI. Those results may be available in 2018.
PEGASUS-TIMI 54 was sponsored by AstraZeneca, the company that markets ticagrelor (Brilinta). Dr. Bhatt has been an advisor to Cardax and Regado Biosciences and has received research support from AstraZeneca and several other companies.
On Twitter @mitchelzoler
CHICAGO – The benefit from dual-antiplatelet therapy in high-risk patients following a myocardial infarction was especially apparent in post-MI patients with diabetes in a prespecified secondary analysis from a multicenter trial of ticagrelor with more than 21,000 patients.
Among post-MI patients with diabetes, treatment with ticagrelor plus aspirin led to an absolute 1.5% reduction in the rate of cardiovascular death, MI, or stroke during a median 33-month follow-up, compared with an absolute 1.1% cut in patients without diabetes, Dr. Deepak L. Bhatt said at the annual meeting of the American College of Cardiology. The relative risk reduction, compared with placebo was 16% in both the diabetes and no diabetes subgroups, statistically significant differences in both subgroups.
“Long-term treatment with ticagrelor reduced the composite of cardiovascular death, MI, or stroke in diabetic patients with a greater absolute risk reduction than in nondiabetic patients,” said Dr. Bhatt, professor of medicine at Harvard Medical School and executive director of Interventional Cardiovascular Programs at Brigham and Women’s Hospital in Boston. Treatment with ticagrelor plus aspirin in post-MI patients with diabetes also led to an increased number of major bleeding episodes, compared with patients on aspirin alone, but no excess of intracerebral hemorrhages or fatal bleeds, he noted.
This finding of a significant benefit from ticagrelor in post-MI patients with diabetes confirms similar, prior findings with other antiplatelet drugs (including clopidogrel, prasugrel, and vorapaxar) and prior findings with ticagrelor, Dr. Bhatt noted.
The new analysis used data collected in the Prevention of Cardiovascular Events in Patients With Prior Heart Attack Using Ticagrelor Compared to Placebo on a Background of Aspirin–Thrombolysis in Myocardial Infarction 54 (PEGASUS-TIMI 54) trial. The primary results from PEGASUS-TIMI 54 had shown that adding ticagrelor to aspirin treatment of high-risk post-MI patients, including those who both had or did not have diabetes, significantly cut the composite rate of cardiovascular death, MI, and stroke, compared with aspirin alone (N Engl J Med. 2015 May 7;372[19]:1791-800). The study group included 6,806 patients with diabetes (type 2 diabetes in 99% of these patients), and 14,355 without diabetes. All patients had their MI 1-3 years before entering the study.
Dr. Bhatt and his associates examined the incidence of the various clinical endpoints measured in the study among only the patients with diabetes divided into those who received any dosage of ticagrelor (60 mg b.i.d. or 90 mg b.i.d.) or placebo, and also among the patients without diabetes. In addition to the primary endpoint, the new analysis showed that the rate of cardiovascular death during follow-up was 3.9% in the diabetes patients on dual therapy and 5.0% among the diabetes patients on aspirin only, a 22% relative risk reduction with ticagrelor added that was statistically significant. In contrast, among patients without diabetes the rates of cardiovascular death between those on and not on ticagrelor only differed by 0.2%, a 9% relative risk reduction that was not statistically significant. The same pattern occurred for the endpoint of death from coronary artery disease.
Concurrent with Dr. Bhatt’s report, the results appeared in an article published online (J Am Coll Cardiol. 2016 Apr; doi: 10.1016/S0735-1097[16]30023-7).
A new study, THEMIS, is examining the safety and efficacy of combined ticagrelor and aspirin treatment in a lower-risk group of patients with diabetes, those with coronary artery disease who have not had a prior MI. Those results may be available in 2018.
PEGASUS-TIMI 54 was sponsored by AstraZeneca, the company that markets ticagrelor (Brilinta). Dr. Bhatt has been an advisor to Cardax and Regado Biosciences and has received research support from AstraZeneca and several other companies.
On Twitter @mitchelzoler
AT ACC 2016
Key clinical point: Among post-MI patients with diabetes, dual-antiplatelet therapy with aspirin and ticagrelor produced a significant drop in the rate of cardiovascular death and other ischemic events.
Major finding: Post-MI patients with diabetes had a 10.1% combined endpoint rate on ticagrelor and a 11.6% rate on placebo.
Data source: Prespecified secondary analysis of data from PEGASUS-TIMI 54, a multicenter randomized trial with 21,162 patients.
Disclosures: PEGASUS-TIMI 54 was sponsored by AstraZeneca, the company that markets ticagrelor (Brilinta). Dr. Bhatt has been an advisor to Cardax and Regado Biosciences and has received research support from AstraZeneca and several other companies.
VIDEO: Weight cycling common following weight loss in obese individuals
BOSTON – Examination of weight-loss patterns in over 177,000 people has revealed that, regardless of the initial 6-month weight loss, after 2 years the majority of patients become “cyclers,” with periods of weight gain and loss rather than maintenance of the initial weight loss.
“One-third of American adults are obese. In 2010, the cost of obesity and obesity-related comorbidities in the United States was estimated to be $315.8 billion. Achieving and maintaining weight loss has proven to be difficult,” said Joanna Huang, PharmD, senior manager of health economics and outcomes research at Novo Nordisk, Plainsboro, N.J., and lead investigator of the study presented at the annual meeting of the Endocrine Society.
The study examined the electronic records of about 178,000 obese patients whose weight loss had been by deliberate intent and not due to illness. The subjects were allocated into four groups based on the extent of weight loss in terms of body mass index (BMI) over 6 months: Those who remained stable and lost less than 5% (n = 151,902), those who lost 5%-10% (modest loss; n = 16,637), those who lost 10%-15% (moderate loss; n = 4,035), and those who lost in excess of 15% (high loss; n = 5,945).
The subjects who were at least 18 years of age at baseline (mean age 54-58 years), had at least one BMI measurement that was indicative of obesity (greater than or equal to 30 kg/m2), with at least four BMI determinations done over at least 5 years. Subjects were mostly white (about 66% in all four groups) and mostly from the southern United States.
Regardless of the amount that the participants lost in the first 6 months, regain of 50% of more of body weight was common in the modest weight-loss group (40%) and moderate weight-loss group (36%), while only 19% of those in the high weight-loss group cycled back up in weight, reported study presenter Maral DerSarkissian, PhD, of the Analysis Group in Boston.
More than 73% and about 70% of those in the moderate and modest weight-loss group, respectively, experienced weight cycling within 2 years. In the stable and high weight-loss groups, the situation was somewhat more optimistic, with about 60% of participants cycling in weight within 2 years. Total regain of lost weight occurred in about 23%, 16%, and 7% of the modest, moderate, and high weight-loss group, respectively.
“Weight loss maintenance, even in the moderate and high weight-loss groups, is very difficult to achieve,” said Dr. Huang.
Interventions that seek to maintain the weight conventionally are directed at dietary changes. But, according to Dr. DerSarkissian, “these modifications alone might not be enough to achieve and maintain weight loss.”
Pharmacotherapy is another weight-loss option. The data indicated that only 2% of the participants were receiving weight-loss pharmacotherapy. Whether this figure is accurate is an open question, according to Dr. Huang, since a lot of the data were compiled from physicians’ notes. Since clinicians may not record weight-loss advice offered to their patients, the data base may well not reflect lifestyle interventions, including pharmacotherapy.
In addition, since the data captured only primary outpatient care, whether or not a patient ever had bariatric surgery was unknown. Other unrecorded factors that can influence weight over time included comorbidities, use of medications, diet changes, and changes in physical activity.
The data points to a multifactor approach to weight loss that includes counseling, positive reinforcement, dietary advice, pharmacotherapy where appropriate, and, in some cases, bariatric surgery.
“Successful and sustained clinically meaningful weight loss requires chronic and effective weight management strategies,” said Dr. Huang.
Dr. Huang is an employee of Novo Nordisk and Dr. DerSarkissian is a researcher for Novo Nordisk.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Examination of weight-loss patterns in over 177,000 people has revealed that, regardless of the initial 6-month weight loss, after 2 years the majority of patients become “cyclers,” with periods of weight gain and loss rather than maintenance of the initial weight loss.
“One-third of American adults are obese. In 2010, the cost of obesity and obesity-related comorbidities in the United States was estimated to be $315.8 billion. Achieving and maintaining weight loss has proven to be difficult,” said Joanna Huang, PharmD, senior manager of health economics and outcomes research at Novo Nordisk, Plainsboro, N.J., and lead investigator of the study presented at the annual meeting of the Endocrine Society.
The study examined the electronic records of about 178,000 obese patients whose weight loss had been by deliberate intent and not due to illness. The subjects were allocated into four groups based on the extent of weight loss in terms of body mass index (BMI) over 6 months: Those who remained stable and lost less than 5% (n = 151,902), those who lost 5%-10% (modest loss; n = 16,637), those who lost 10%-15% (moderate loss; n = 4,035), and those who lost in excess of 15% (high loss; n = 5,945).
The subjects who were at least 18 years of age at baseline (mean age 54-58 years), had at least one BMI measurement that was indicative of obesity (greater than or equal to 30 kg/m2), with at least four BMI determinations done over at least 5 years. Subjects were mostly white (about 66% in all four groups) and mostly from the southern United States.
Regardless of the amount that the participants lost in the first 6 months, regain of 50% of more of body weight was common in the modest weight-loss group (40%) and moderate weight-loss group (36%), while only 19% of those in the high weight-loss group cycled back up in weight, reported study presenter Maral DerSarkissian, PhD, of the Analysis Group in Boston.
More than 73% and about 70% of those in the moderate and modest weight-loss group, respectively, experienced weight cycling within 2 years. In the stable and high weight-loss groups, the situation was somewhat more optimistic, with about 60% of participants cycling in weight within 2 years. Total regain of lost weight occurred in about 23%, 16%, and 7% of the modest, moderate, and high weight-loss group, respectively.
“Weight loss maintenance, even in the moderate and high weight-loss groups, is very difficult to achieve,” said Dr. Huang.
Interventions that seek to maintain the weight conventionally are directed at dietary changes. But, according to Dr. DerSarkissian, “these modifications alone might not be enough to achieve and maintain weight loss.”
Pharmacotherapy is another weight-loss option. The data indicated that only 2% of the participants were receiving weight-loss pharmacotherapy. Whether this figure is accurate is an open question, according to Dr. Huang, since a lot of the data were compiled from physicians’ notes. Since clinicians may not record weight-loss advice offered to their patients, the data base may well not reflect lifestyle interventions, including pharmacotherapy.
In addition, since the data captured only primary outpatient care, whether or not a patient ever had bariatric surgery was unknown. Other unrecorded factors that can influence weight over time included comorbidities, use of medications, diet changes, and changes in physical activity.
The data points to a multifactor approach to weight loss that includes counseling, positive reinforcement, dietary advice, pharmacotherapy where appropriate, and, in some cases, bariatric surgery.
“Successful and sustained clinically meaningful weight loss requires chronic and effective weight management strategies,” said Dr. Huang.
Dr. Huang is an employee of Novo Nordisk and Dr. DerSarkissian is a researcher for Novo Nordisk.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Examination of weight-loss patterns in over 177,000 people has revealed that, regardless of the initial 6-month weight loss, after 2 years the majority of patients become “cyclers,” with periods of weight gain and loss rather than maintenance of the initial weight loss.
“One-third of American adults are obese. In 2010, the cost of obesity and obesity-related comorbidities in the United States was estimated to be $315.8 billion. Achieving and maintaining weight loss has proven to be difficult,” said Joanna Huang, PharmD, senior manager of health economics and outcomes research at Novo Nordisk, Plainsboro, N.J., and lead investigator of the study presented at the annual meeting of the Endocrine Society.
The study examined the electronic records of about 178,000 obese patients whose weight loss had been by deliberate intent and not due to illness. The subjects were allocated into four groups based on the extent of weight loss in terms of body mass index (BMI) over 6 months: Those who remained stable and lost less than 5% (n = 151,902), those who lost 5%-10% (modest loss; n = 16,637), those who lost 10%-15% (moderate loss; n = 4,035), and those who lost in excess of 15% (high loss; n = 5,945).
The subjects who were at least 18 years of age at baseline (mean age 54-58 years), had at least one BMI measurement that was indicative of obesity (greater than or equal to 30 kg/m2), with at least four BMI determinations done over at least 5 years. Subjects were mostly white (about 66% in all four groups) and mostly from the southern United States.
Regardless of the amount that the participants lost in the first 6 months, regain of 50% of more of body weight was common in the modest weight-loss group (40%) and moderate weight-loss group (36%), while only 19% of those in the high weight-loss group cycled back up in weight, reported study presenter Maral DerSarkissian, PhD, of the Analysis Group in Boston.
More than 73% and about 70% of those in the moderate and modest weight-loss group, respectively, experienced weight cycling within 2 years. In the stable and high weight-loss groups, the situation was somewhat more optimistic, with about 60% of participants cycling in weight within 2 years. Total regain of lost weight occurred in about 23%, 16%, and 7% of the modest, moderate, and high weight-loss group, respectively.
“Weight loss maintenance, even in the moderate and high weight-loss groups, is very difficult to achieve,” said Dr. Huang.
Interventions that seek to maintain the weight conventionally are directed at dietary changes. But, according to Dr. DerSarkissian, “these modifications alone might not be enough to achieve and maintain weight loss.”
Pharmacotherapy is another weight-loss option. The data indicated that only 2% of the participants were receiving weight-loss pharmacotherapy. Whether this figure is accurate is an open question, according to Dr. Huang, since a lot of the data were compiled from physicians’ notes. Since clinicians may not record weight-loss advice offered to their patients, the data base may well not reflect lifestyle interventions, including pharmacotherapy.
In addition, since the data captured only primary outpatient care, whether or not a patient ever had bariatric surgery was unknown. Other unrecorded factors that can influence weight over time included comorbidities, use of medications, diet changes, and changes in physical activity.
The data points to a multifactor approach to weight loss that includes counseling, positive reinforcement, dietary advice, pharmacotherapy where appropriate, and, in some cases, bariatric surgery.
“Successful and sustained clinically meaningful weight loss requires chronic and effective weight management strategies,” said Dr. Huang.
Dr. Huang is an employee of Novo Nordisk and Dr. DerSarkissian is a researcher for Novo Nordisk.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ENDO 2016
Key clinical point: Most patients who lose modest or moderate amounts of weight experience periods of both gain and loss within 2 years.
Major finding: More than 73% and about 70% of those in the moderate and modest weight-loss group, respectively, experienced weight cycling within 2 years. Total regain of lost weight occurred in about 23%, 16%, and 7% of the modest, moderate, and high weight-loss group, respectively.
Data source: Electronic records of 177,743 obese patients whose weight loss had been by deliberate intent and not due to illness.
Disclosures: Dr. Huang is an employee of Novo Nordisk and Dr. DerSarkissian is a researcher for Novo Nordisk.
VIDEO: Childhood obesity predicted by infant BMI
BOSTON – Infants above the 85th percentile for body mass index at 6 months are up to nine times more likely to be severely obese by the age of 6, according to a Cincinnati Children’s Hospital investigation.
The finding means that pediatricians should routinely plot and follow body mass index (BMI) from an early age, just like height, weight, and head circumference, said investigator Dr. Allison Smego, an endocrinology fellow.
She and her colleagues reviewed the charts from birth to age 6 of 783 lean children and 480 children above the 99th BMI percentile. BMI started differentiating when children were as young as 4 months old, about a year and half before the onset of clinical obesity. The predictive value of the 85th percentile threshold held at 6, 12, and 18 months. The finding was subsequently validated in over 2,600 children.
In an interview at the annual meeting of the Endocrine Society, Dr. Smego explained how to use the findings.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Infants above the 85th percentile for body mass index at 6 months are up to nine times more likely to be severely obese by the age of 6, according to a Cincinnati Children’s Hospital investigation.
The finding means that pediatricians should routinely plot and follow body mass index (BMI) from an early age, just like height, weight, and head circumference, said investigator Dr. Allison Smego, an endocrinology fellow.
She and her colleagues reviewed the charts from birth to age 6 of 783 lean children and 480 children above the 99th BMI percentile. BMI started differentiating when children were as young as 4 months old, about a year and half before the onset of clinical obesity. The predictive value of the 85th percentile threshold held at 6, 12, and 18 months. The finding was subsequently validated in over 2,600 children.
In an interview at the annual meeting of the Endocrine Society, Dr. Smego explained how to use the findings.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Infants above the 85th percentile for body mass index at 6 months are up to nine times more likely to be severely obese by the age of 6, according to a Cincinnati Children’s Hospital investigation.
The finding means that pediatricians should routinely plot and follow body mass index (BMI) from an early age, just like height, weight, and head circumference, said investigator Dr. Allison Smego, an endocrinology fellow.
She and her colleagues reviewed the charts from birth to age 6 of 783 lean children and 480 children above the 99th BMI percentile. BMI started differentiating when children were as young as 4 months old, about a year and half before the onset of clinical obesity. The predictive value of the 85th percentile threshold held at 6, 12, and 18 months. The finding was subsequently validated in over 2,600 children.
In an interview at the annual meeting of the Endocrine Society, Dr. Smego explained how to use the findings.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ENDO 2016
VIDEO: HOPE-3 bolsters primary prevention in intermediate-risk patients
CHICAGO – Results from the HOPE-3 trial confirm what guidelines have already recommended: patients with intermediate risk for cardiovascular disease should be treated for primary prevention of coronary event, Dr. Prakash Deedwania said in an interview at the annual meeting of the American College of Cardiology.
In the Heart Outcomes Prevention Evaluation (HOPE)-3 trial, nearly 13,000 intermediate-risk men and women with no baseline cardiovascular disease were randomized to either lipid lowering with rosuvastatin at 10 mg/day or placebo, dual-antihypertensive therapy with candesartan plus chlorothiazide or placebo regardless of baseline blood pressure, or all three drugs or placebo. After a median of 5.6 years, the combined-therapy group had a 29% reduction in the composite of cardiovascular death or nonfatal MI or stroke, compared with placebo-treated controls, regardless of baseline LDL-cholesterol level. However, only subjects with a baseline pressure of greater than 143.5 mm Hg benefited from the dual-antihypertensive therapy.
In a video interview, Dr. Deedwania, professor of medicine at the University of California, San Francisco, Fresno, gave three takeaways from the HOPE-3 trial regarding primary prevention of cardiovascular events in patients at intermediate risk, how the results of the dual-antihypertensive treatment arm match up to guidelines, and whether there’s a future for the polypill.
Dr. Deedwania has received consultant fees and/or honoraria from Amgen, Pfizer, and Sanofi.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Results from the HOPE-3 trial confirm what guidelines have already recommended: patients with intermediate risk for cardiovascular disease should be treated for primary prevention of coronary event, Dr. Prakash Deedwania said in an interview at the annual meeting of the American College of Cardiology.
In the Heart Outcomes Prevention Evaluation (HOPE)-3 trial, nearly 13,000 intermediate-risk men and women with no baseline cardiovascular disease were randomized to either lipid lowering with rosuvastatin at 10 mg/day or placebo, dual-antihypertensive therapy with candesartan plus chlorothiazide or placebo regardless of baseline blood pressure, or all three drugs or placebo. After a median of 5.6 years, the combined-therapy group had a 29% reduction in the composite of cardiovascular death or nonfatal MI or stroke, compared with placebo-treated controls, regardless of baseline LDL-cholesterol level. However, only subjects with a baseline pressure of greater than 143.5 mm Hg benefited from the dual-antihypertensive therapy.
In a video interview, Dr. Deedwania, professor of medicine at the University of California, San Francisco, Fresno, gave three takeaways from the HOPE-3 trial regarding primary prevention of cardiovascular events in patients at intermediate risk, how the results of the dual-antihypertensive treatment arm match up to guidelines, and whether there’s a future for the polypill.
Dr. Deedwania has received consultant fees and/or honoraria from Amgen, Pfizer, and Sanofi.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Results from the HOPE-3 trial confirm what guidelines have already recommended: patients with intermediate risk for cardiovascular disease should be treated for primary prevention of coronary event, Dr. Prakash Deedwania said in an interview at the annual meeting of the American College of Cardiology.
In the Heart Outcomes Prevention Evaluation (HOPE)-3 trial, nearly 13,000 intermediate-risk men and women with no baseline cardiovascular disease were randomized to either lipid lowering with rosuvastatin at 10 mg/day or placebo, dual-antihypertensive therapy with candesartan plus chlorothiazide or placebo regardless of baseline blood pressure, or all three drugs or placebo. After a median of 5.6 years, the combined-therapy group had a 29% reduction in the composite of cardiovascular death or nonfatal MI or stroke, compared with placebo-treated controls, regardless of baseline LDL-cholesterol level. However, only subjects with a baseline pressure of greater than 143.5 mm Hg benefited from the dual-antihypertensive therapy.
In a video interview, Dr. Deedwania, professor of medicine at the University of California, San Francisco, Fresno, gave three takeaways from the HOPE-3 trial regarding primary prevention of cardiovascular events in patients at intermediate risk, how the results of the dual-antihypertensive treatment arm match up to guidelines, and whether there’s a future for the polypill.
Dr. Deedwania has received consultant fees and/or honoraria from Amgen, Pfizer, and Sanofi.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ACC 16
T2D patients on combination therapy benefit in switch from sitagliptin to liraglutide
BOSTON – Switching from sitagliptin to liraglutide, in combination with metformin, improved control of hypoglycemia and resulted in greater weight loss in patients with type 2 diabetes, reported Dr. Maximo Maislos at the annual meeting of the Endocrine Society.
Results of a randomized, double-blind, double-dummy, active-controlled 26-week trial have indicated that liraglutide can be used as an add-on to metformin for patients with type 2 diabetes who have remained hyperglycemic.
“Switching from sitagliptin to liraglutide resulted in superior [glycated hemoglobin] and body weight reductions, compared with continued sitagliptin treatment,” said Dr. Maximo Maislos of Ben-Gurion University, Beer-Sheva, Israel.
The LIRA-SWITCH trial (Efficacy and Safety of Switching From Sitagliptin to Liraglutide in Subjects With Type 2 Diabetes Not Achieving Adequate Glycaemic Control on Sitagliptin and Metformin) involved 407 patients. The majority (60%) were male; mean age was 56 years and mean body mass index was 32 kg/m2. The subjects had all been treated with sitagliptin (100 mg/day) and metformin (greater than or equal to 1,500 mg/day or a maximum tolerated dose greater than or equal to 1,000 mg/day) for at least 90 days. Hyperglycemia had not been well controlled, with a mean hemoglobin A1C (HbAIC) level of 8.3% (67 mmol/mol). The mean duration of type 2 diabetes was 8 years.
Subjects were randomized to continued sitagliptin along with metformin (n = 204) or liraglutide (1.8 mg daily) along with metformin (n = 203).
After 26 weeks of treatment, reduction in HbAIC was significantly greater in the liraglutide arm than in the sitagliptin arm (1.14% vs. 0.54%; estimated treatment difference [ETD], –0.61%; 95% confidence interval, –0.82 to –0.40; P less than .0001). Those receiving liraglutide had statistically significantly greater weight loss, compared with those who continued on sitagliptin.
The less than 7% and less than or equal to 6.5% target levels of HbAIC were achieved by 50.6% and 29.5%, respectively, of patients in the liraglutide arm. These percentages were significantly higher than the respective 26.9% and 9.9% of patients in the sitagliptin arm (P less than .0001 for both). Fasting plasma glucose levels were significantly reduced with liraglutide treatment while decreases in systolic and diastolic blood pressure were similar in the two study arms.
Adverse events (AEs) occurred more often in the liraglutide group than in the sitagliptin group (68.8% vs. 56.9%). Thirteen patients receiving liraglutide discontinued treatment, compared with five in the sitagliptin arm. The most common AEs in the liraglutide group were gastrointestinal disorders, principally nausea (21.8% with liraglutide vs. 7.8% with sitagliptin) and diarrhea (16.3% with liraglutide vs. 9.3% with sitagliptin), followed by decreased appetite (8.9% vs. 3.4%, respectively). These AEs tended to subside within the first few weeks of treatment.
Serious AEs occurred in eight patients in both arms. Rescue medication was needed for 30 patients receiving sitagliptin and 11 patients receiving liraglutide. No cases of pancreatitis were reported. In the sitagliptin group, one subject each developed bladder cancer and squamous cell carcinoma. Nocturnal hypoglycemia did not develop in either trial arm.
Funding was provided by liraglutide maker Novo Nordisk. Dr. Maislos had no disclosures.
BOSTON – Switching from sitagliptin to liraglutide, in combination with metformin, improved control of hypoglycemia and resulted in greater weight loss in patients with type 2 diabetes, reported Dr. Maximo Maislos at the annual meeting of the Endocrine Society.
Results of a randomized, double-blind, double-dummy, active-controlled 26-week trial have indicated that liraglutide can be used as an add-on to metformin for patients with type 2 diabetes who have remained hyperglycemic.
“Switching from sitagliptin to liraglutide resulted in superior [glycated hemoglobin] and body weight reductions, compared with continued sitagliptin treatment,” said Dr. Maximo Maislos of Ben-Gurion University, Beer-Sheva, Israel.
The LIRA-SWITCH trial (Efficacy and Safety of Switching From Sitagliptin to Liraglutide in Subjects With Type 2 Diabetes Not Achieving Adequate Glycaemic Control on Sitagliptin and Metformin) involved 407 patients. The majority (60%) were male; mean age was 56 years and mean body mass index was 32 kg/m2. The subjects had all been treated with sitagliptin (100 mg/day) and metformin (greater than or equal to 1,500 mg/day or a maximum tolerated dose greater than or equal to 1,000 mg/day) for at least 90 days. Hyperglycemia had not been well controlled, with a mean hemoglobin A1C (HbAIC) level of 8.3% (67 mmol/mol). The mean duration of type 2 diabetes was 8 years.
Subjects were randomized to continued sitagliptin along with metformin (n = 204) or liraglutide (1.8 mg daily) along with metformin (n = 203).
After 26 weeks of treatment, reduction in HbAIC was significantly greater in the liraglutide arm than in the sitagliptin arm (1.14% vs. 0.54%; estimated treatment difference [ETD], –0.61%; 95% confidence interval, –0.82 to –0.40; P less than .0001). Those receiving liraglutide had statistically significantly greater weight loss, compared with those who continued on sitagliptin.
The less than 7% and less than or equal to 6.5% target levels of HbAIC were achieved by 50.6% and 29.5%, respectively, of patients in the liraglutide arm. These percentages were significantly higher than the respective 26.9% and 9.9% of patients in the sitagliptin arm (P less than .0001 for both). Fasting plasma glucose levels were significantly reduced with liraglutide treatment while decreases in systolic and diastolic blood pressure were similar in the two study arms.
Adverse events (AEs) occurred more often in the liraglutide group than in the sitagliptin group (68.8% vs. 56.9%). Thirteen patients receiving liraglutide discontinued treatment, compared with five in the sitagliptin arm. The most common AEs in the liraglutide group were gastrointestinal disorders, principally nausea (21.8% with liraglutide vs. 7.8% with sitagliptin) and diarrhea (16.3% with liraglutide vs. 9.3% with sitagliptin), followed by decreased appetite (8.9% vs. 3.4%, respectively). These AEs tended to subside within the first few weeks of treatment.
Serious AEs occurred in eight patients in both arms. Rescue medication was needed for 30 patients receiving sitagliptin and 11 patients receiving liraglutide. No cases of pancreatitis were reported. In the sitagliptin group, one subject each developed bladder cancer and squamous cell carcinoma. Nocturnal hypoglycemia did not develop in either trial arm.
Funding was provided by liraglutide maker Novo Nordisk. Dr. Maislos had no disclosures.
BOSTON – Switching from sitagliptin to liraglutide, in combination with metformin, improved control of hypoglycemia and resulted in greater weight loss in patients with type 2 diabetes, reported Dr. Maximo Maislos at the annual meeting of the Endocrine Society.
Results of a randomized, double-blind, double-dummy, active-controlled 26-week trial have indicated that liraglutide can be used as an add-on to metformin for patients with type 2 diabetes who have remained hyperglycemic.
“Switching from sitagliptin to liraglutide resulted in superior [glycated hemoglobin] and body weight reductions, compared with continued sitagliptin treatment,” said Dr. Maximo Maislos of Ben-Gurion University, Beer-Sheva, Israel.
The LIRA-SWITCH trial (Efficacy and Safety of Switching From Sitagliptin to Liraglutide in Subjects With Type 2 Diabetes Not Achieving Adequate Glycaemic Control on Sitagliptin and Metformin) involved 407 patients. The majority (60%) were male; mean age was 56 years and mean body mass index was 32 kg/m2. The subjects had all been treated with sitagliptin (100 mg/day) and metformin (greater than or equal to 1,500 mg/day or a maximum tolerated dose greater than or equal to 1,000 mg/day) for at least 90 days. Hyperglycemia had not been well controlled, with a mean hemoglobin A1C (HbAIC) level of 8.3% (67 mmol/mol). The mean duration of type 2 diabetes was 8 years.
Subjects were randomized to continued sitagliptin along with metformin (n = 204) or liraglutide (1.8 mg daily) along with metformin (n = 203).
After 26 weeks of treatment, reduction in HbAIC was significantly greater in the liraglutide arm than in the sitagliptin arm (1.14% vs. 0.54%; estimated treatment difference [ETD], –0.61%; 95% confidence interval, –0.82 to –0.40; P less than .0001). Those receiving liraglutide had statistically significantly greater weight loss, compared with those who continued on sitagliptin.
The less than 7% and less than or equal to 6.5% target levels of HbAIC were achieved by 50.6% and 29.5%, respectively, of patients in the liraglutide arm. These percentages were significantly higher than the respective 26.9% and 9.9% of patients in the sitagliptin arm (P less than .0001 for both). Fasting plasma glucose levels were significantly reduced with liraglutide treatment while decreases in systolic and diastolic blood pressure were similar in the two study arms.
Adverse events (AEs) occurred more often in the liraglutide group than in the sitagliptin group (68.8% vs. 56.9%). Thirteen patients receiving liraglutide discontinued treatment, compared with five in the sitagliptin arm. The most common AEs in the liraglutide group were gastrointestinal disorders, principally nausea (21.8% with liraglutide vs. 7.8% with sitagliptin) and diarrhea (16.3% with liraglutide vs. 9.3% with sitagliptin), followed by decreased appetite (8.9% vs. 3.4%, respectively). These AEs tended to subside within the first few weeks of treatment.
Serious AEs occurred in eight patients in both arms. Rescue medication was needed for 30 patients receiving sitagliptin and 11 patients receiving liraglutide. No cases of pancreatitis were reported. In the sitagliptin group, one subject each developed bladder cancer and squamous cell carcinoma. Nocturnal hypoglycemia did not develop in either trial arm.
Funding was provided by liraglutide maker Novo Nordisk. Dr. Maislos had no disclosures.
AT ENDO 2016
Key clinical point: A switch from sitagliptin to liraglutide provides an option, in combination with metformin, to improve the management of type 2 diabetes, allowing patients to remain on dual therapy.
Major finding: After 26 weeks of treatment, reduction in HbAIC was significantly greater in the liraglutide arm than in the sitagliptin arm (–1.14% vs. –0.54%. Those receiving liraglutide had statistically significantly greater weight loss, compared with those who continued on sitagliptin.
Data source: 407 patients with type 2 diabetes enrolled in a randomized, double-blind, double-dummy, active-controlled 26-week trial.
Disclosures: Dr. Maislos had no disclosures.
FDA requires labeling changes to metformin-containing drugs
Metformin can be used safely in patients with mild impairment in kidney function and in some patients with moderate impairment in kidney function, according to the FDA’s recent review of several medical studies.
These findings have prompted the FDA to require manufacturers to change the labeling for metformin-containing drugs. These drugs’ labels now must include the results of the medical studies and new measures of kidney function for determining if a patient can use metformin, says a written statement from the FDA.
Metformin’s current labeling strongly recommends against its use in some patients with kidneys that do not work normally. The FDA is specifically requiring that new labels include the recommendation that the measure of kidney function used to determine whether a patient can receive metformin be changed from one based on a single laboratory parameter (blood creatinine concentration) to one that provides a better estimate of renal function (that is, the glomerular filtration rate estimating equation, eGFR).
The full labeling recommendations are available in the FDA’s written statement.
Additional information including a data summary and a list of metformin-containing drugs is available in the FDA Drug Safety Communication.
The FDA asks that healthcare professionals and patients report adverse events or side effects related to the use of metformin-containing drugs to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program.
Metformin can be used safely in patients with mild impairment in kidney function and in some patients with moderate impairment in kidney function, according to the FDA’s recent review of several medical studies.
These findings have prompted the FDA to require manufacturers to change the labeling for metformin-containing drugs. These drugs’ labels now must include the results of the medical studies and new measures of kidney function for determining if a patient can use metformin, says a written statement from the FDA.
Metformin’s current labeling strongly recommends against its use in some patients with kidneys that do not work normally. The FDA is specifically requiring that new labels include the recommendation that the measure of kidney function used to determine whether a patient can receive metformin be changed from one based on a single laboratory parameter (blood creatinine concentration) to one that provides a better estimate of renal function (that is, the glomerular filtration rate estimating equation, eGFR).
The full labeling recommendations are available in the FDA’s written statement.
Additional information including a data summary and a list of metformin-containing drugs is available in the FDA Drug Safety Communication.
The FDA asks that healthcare professionals and patients report adverse events or side effects related to the use of metformin-containing drugs to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program.
Metformin can be used safely in patients with mild impairment in kidney function and in some patients with moderate impairment in kidney function, according to the FDA’s recent review of several medical studies.
These findings have prompted the FDA to require manufacturers to change the labeling for metformin-containing drugs. These drugs’ labels now must include the results of the medical studies and new measures of kidney function for determining if a patient can use metformin, says a written statement from the FDA.
Metformin’s current labeling strongly recommends against its use in some patients with kidneys that do not work normally. The FDA is specifically requiring that new labels include the recommendation that the measure of kidney function used to determine whether a patient can receive metformin be changed from one based on a single laboratory parameter (blood creatinine concentration) to one that provides a better estimate of renal function (that is, the glomerular filtration rate estimating equation, eGFR).
The full labeling recommendations are available in the FDA’s written statement.
Additional information including a data summary and a list of metformin-containing drugs is available in the FDA Drug Safety Communication.
The FDA asks that healthcare professionals and patients report adverse events or side effects related to the use of metformin-containing drugs to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program.
VIDEO: New ACC consensus guidance addresses nonstatin therapies
CHICAGO – A new American College of Cardiology expert consensus decision pathway for the use of nonstatin therapies to lower cholesterol in high-risk patients addresses situations not covered by an evidence-based 2013 guideline on managing atherosclerotic cardiovascular disease risk.
Like the 2013 guideline (the 2013 American College of Cardiology/American Heart Association Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Disease Risk in Adults), the new guidance emphasizes the importance of a healthy lifestyle, but also addresses the use of two monoclonal antibodies–proprotein convertase subtilisin/kexon 9 (PCSK9) inhibitors–approved for certain patient groups since the 2013 guideline was released, as well as other nonstatin therapies, including ezetimibe and bile acid sequestrants.
“At the time [the 2013 guideline was published] the only really good outcomes data ... were for statin medication and there were no data from clinical trials that showed additional benefit of medications over and above being on the maximally tolerated dose of a statin,” according to Dr. Donald M. Lloyd-Jones, a professor at Northwestern University, Chicago and chair of the writing committee for the new guidance. “However, since 2013, a number of trials have been published that actually move the field forward in our understanding of which patients might benefit from adding non statin therapy on top of effective statin therapy.”
The guidance was developed to address gaps in care until the guidelines can be updated, which will likely take a few years.
Based on findings from recent studies, including the IMPROVE IT trial, which examined ezetimibe as statin add-on therapy after acute coronary syndromes, the HPS2-THRIVE study, which examined use of niacin in high-risk patients, and short-term outcomes studies of PCSK9 inhibitors, which have been shown to dramatically reduce low-density lipoprotein cholesterol levels beyond the lowering provided by statin therapy, the committee developed algorithms for the four main high-risk statin benefit patient groups:
•Adults aged 21 years and older with clinical atherosclerotic cardiovascular disease (ASCVD), on statin for secondary prevention.
•Adults aged 21 years and older with LDL-C greater than or equal to 190 mg/dL not due to secondary modifiable causes, on statin for primary prevention.
•Adults aged 40-75 years without ASCVD but with diabetes and LDL-C of 70-189 mg/dL, on statin for primary prevention.
•Adults aged 40-75 years without clinical ASCVD or diabetes, with LDL-C of 70-189 mg/dL and an estimated 10-year risk for ASCVD of at least 7.5%, on statin for primary prevention.
The guidance suggests a number of steps to take with patients who fail to achieve treatment goals (such as addressing treatment adherence, intensifying lifestyle modifications, using a high-intensity stain, and evaluating for statin intolerance), and lists “clinician-patient discussion factors” to consider for each of a number of patient scenarios (including the potential benefits and risks associated with nonstatin therapies, as well as patient preferences).
Included for each of the patient scenarios is an algorithm for which nonstatin therapies to use in which order, building on the “rock-solid confidence” that for the four statin benefit groups, statins remain the starting point, Dr. Lloyd-Jones said. He discussed the guidance in a video interview.
In general, ezetimibe for those patients who are not achieving the types of reduction in LDL or the amount of risk reduction desired, “should probably be the first choice,” he said.
Bile acid sequestrants can be considered in those who are ezetimibe intolerant and who have triglycerides less than 300 mg/dL.
PCSK9 inhibitors are suggested for consideration only in very high-risk patients with ASCVD or with the familial hypercholesterolemia phenotype who are still not achieving the goal (ideally, a 50% reduction in LDL cholesterol), he said.
The committee did not recommend use of niacin, stating that there is no clear indication for the routine use of niacin preparations as additional nonstatin therapies due to an unfavorable risk-benefit profile.
Additionally, PCSK9 inhibitors are not recommended in any primary prevention scenarios, he noted.
Dr. Neil J. Stone, chair of the 2013 guideline writing committee, said the new guidance provides a useful tool for clinicians, extending, in a practical way, the current guideline as the field awaits the long-term outcomes data for PCSK9 inhibitors.
Despite some backlash in the wake of the 2013 guideline, which marked a move away from specific cholesterol treatment targets to a cardiovascular disease risk-based approach, the cardiovascular risk calculation formula introduced in that guideline has been shown to be useful and accurate, said Dr. Stone, also of Northwestern University.
“[The new guidance] is simply an amplification and extension of the guideline,” he said, adding that “it’s about a risk discussion, not automatic treatment.”
Dr. Lloyd-Jones and Dr. Stone each reported having no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – A new American College of Cardiology expert consensus decision pathway for the use of nonstatin therapies to lower cholesterol in high-risk patients addresses situations not covered by an evidence-based 2013 guideline on managing atherosclerotic cardiovascular disease risk.
Like the 2013 guideline (the 2013 American College of Cardiology/American Heart Association Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Disease Risk in Adults), the new guidance emphasizes the importance of a healthy lifestyle, but also addresses the use of two monoclonal antibodies–proprotein convertase subtilisin/kexon 9 (PCSK9) inhibitors–approved for certain patient groups since the 2013 guideline was released, as well as other nonstatin therapies, including ezetimibe and bile acid sequestrants.
“At the time [the 2013 guideline was published] the only really good outcomes data ... were for statin medication and there were no data from clinical trials that showed additional benefit of medications over and above being on the maximally tolerated dose of a statin,” according to Dr. Donald M. Lloyd-Jones, a professor at Northwestern University, Chicago and chair of the writing committee for the new guidance. “However, since 2013, a number of trials have been published that actually move the field forward in our understanding of which patients might benefit from adding non statin therapy on top of effective statin therapy.”
The guidance was developed to address gaps in care until the guidelines can be updated, which will likely take a few years.
Based on findings from recent studies, including the IMPROVE IT trial, which examined ezetimibe as statin add-on therapy after acute coronary syndromes, the HPS2-THRIVE study, which examined use of niacin in high-risk patients, and short-term outcomes studies of PCSK9 inhibitors, which have been shown to dramatically reduce low-density lipoprotein cholesterol levels beyond the lowering provided by statin therapy, the committee developed algorithms for the four main high-risk statin benefit patient groups:
•Adults aged 21 years and older with clinical atherosclerotic cardiovascular disease (ASCVD), on statin for secondary prevention.
•Adults aged 21 years and older with LDL-C greater than or equal to 190 mg/dL not due to secondary modifiable causes, on statin for primary prevention.
•Adults aged 40-75 years without ASCVD but with diabetes and LDL-C of 70-189 mg/dL, on statin for primary prevention.
•Adults aged 40-75 years without clinical ASCVD or diabetes, with LDL-C of 70-189 mg/dL and an estimated 10-year risk for ASCVD of at least 7.5%, on statin for primary prevention.
The guidance suggests a number of steps to take with patients who fail to achieve treatment goals (such as addressing treatment adherence, intensifying lifestyle modifications, using a high-intensity stain, and evaluating for statin intolerance), and lists “clinician-patient discussion factors” to consider for each of a number of patient scenarios (including the potential benefits and risks associated with nonstatin therapies, as well as patient preferences).
Included for each of the patient scenarios is an algorithm for which nonstatin therapies to use in which order, building on the “rock-solid confidence” that for the four statin benefit groups, statins remain the starting point, Dr. Lloyd-Jones said. He discussed the guidance in a video interview.
In general, ezetimibe for those patients who are not achieving the types of reduction in LDL or the amount of risk reduction desired, “should probably be the first choice,” he said.
Bile acid sequestrants can be considered in those who are ezetimibe intolerant and who have triglycerides less than 300 mg/dL.
PCSK9 inhibitors are suggested for consideration only in very high-risk patients with ASCVD or with the familial hypercholesterolemia phenotype who are still not achieving the goal (ideally, a 50% reduction in LDL cholesterol), he said.
The committee did not recommend use of niacin, stating that there is no clear indication for the routine use of niacin preparations as additional nonstatin therapies due to an unfavorable risk-benefit profile.
Additionally, PCSK9 inhibitors are not recommended in any primary prevention scenarios, he noted.
Dr. Neil J. Stone, chair of the 2013 guideline writing committee, said the new guidance provides a useful tool for clinicians, extending, in a practical way, the current guideline as the field awaits the long-term outcomes data for PCSK9 inhibitors.
Despite some backlash in the wake of the 2013 guideline, which marked a move away from specific cholesterol treatment targets to a cardiovascular disease risk-based approach, the cardiovascular risk calculation formula introduced in that guideline has been shown to be useful and accurate, said Dr. Stone, also of Northwestern University.
“[The new guidance] is simply an amplification and extension of the guideline,” he said, adding that “it’s about a risk discussion, not automatic treatment.”
Dr. Lloyd-Jones and Dr. Stone each reported having no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – A new American College of Cardiology expert consensus decision pathway for the use of nonstatin therapies to lower cholesterol in high-risk patients addresses situations not covered by an evidence-based 2013 guideline on managing atherosclerotic cardiovascular disease risk.
Like the 2013 guideline (the 2013 American College of Cardiology/American Heart Association Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Disease Risk in Adults), the new guidance emphasizes the importance of a healthy lifestyle, but also addresses the use of two monoclonal antibodies–proprotein convertase subtilisin/kexon 9 (PCSK9) inhibitors–approved for certain patient groups since the 2013 guideline was released, as well as other nonstatin therapies, including ezetimibe and bile acid sequestrants.
“At the time [the 2013 guideline was published] the only really good outcomes data ... were for statin medication and there were no data from clinical trials that showed additional benefit of medications over and above being on the maximally tolerated dose of a statin,” according to Dr. Donald M. Lloyd-Jones, a professor at Northwestern University, Chicago and chair of the writing committee for the new guidance. “However, since 2013, a number of trials have been published that actually move the field forward in our understanding of which patients might benefit from adding non statin therapy on top of effective statin therapy.”
The guidance was developed to address gaps in care until the guidelines can be updated, which will likely take a few years.
Based on findings from recent studies, including the IMPROVE IT trial, which examined ezetimibe as statin add-on therapy after acute coronary syndromes, the HPS2-THRIVE study, which examined use of niacin in high-risk patients, and short-term outcomes studies of PCSK9 inhibitors, which have been shown to dramatically reduce low-density lipoprotein cholesterol levels beyond the lowering provided by statin therapy, the committee developed algorithms for the four main high-risk statin benefit patient groups:
•Adults aged 21 years and older with clinical atherosclerotic cardiovascular disease (ASCVD), on statin for secondary prevention.
•Adults aged 21 years and older with LDL-C greater than or equal to 190 mg/dL not due to secondary modifiable causes, on statin for primary prevention.
•Adults aged 40-75 years without ASCVD but with diabetes and LDL-C of 70-189 mg/dL, on statin for primary prevention.
•Adults aged 40-75 years without clinical ASCVD or diabetes, with LDL-C of 70-189 mg/dL and an estimated 10-year risk for ASCVD of at least 7.5%, on statin for primary prevention.
The guidance suggests a number of steps to take with patients who fail to achieve treatment goals (such as addressing treatment adherence, intensifying lifestyle modifications, using a high-intensity stain, and evaluating for statin intolerance), and lists “clinician-patient discussion factors” to consider for each of a number of patient scenarios (including the potential benefits and risks associated with nonstatin therapies, as well as patient preferences).
Included for each of the patient scenarios is an algorithm for which nonstatin therapies to use in which order, building on the “rock-solid confidence” that for the four statin benefit groups, statins remain the starting point, Dr. Lloyd-Jones said. He discussed the guidance in a video interview.
In general, ezetimibe for those patients who are not achieving the types of reduction in LDL or the amount of risk reduction desired, “should probably be the first choice,” he said.
Bile acid sequestrants can be considered in those who are ezetimibe intolerant and who have triglycerides less than 300 mg/dL.
PCSK9 inhibitors are suggested for consideration only in very high-risk patients with ASCVD or with the familial hypercholesterolemia phenotype who are still not achieving the goal (ideally, a 50% reduction in LDL cholesterol), he said.
The committee did not recommend use of niacin, stating that there is no clear indication for the routine use of niacin preparations as additional nonstatin therapies due to an unfavorable risk-benefit profile.
Additionally, PCSK9 inhibitors are not recommended in any primary prevention scenarios, he noted.
Dr. Neil J. Stone, chair of the 2013 guideline writing committee, said the new guidance provides a useful tool for clinicians, extending, in a practical way, the current guideline as the field awaits the long-term outcomes data for PCSK9 inhibitors.
Despite some backlash in the wake of the 2013 guideline, which marked a move away from specific cholesterol treatment targets to a cardiovascular disease risk-based approach, the cardiovascular risk calculation formula introduced in that guideline has been shown to be useful and accurate, said Dr. Stone, also of Northwestern University.
“[The new guidance] is simply an amplification and extension of the guideline,” he said, adding that “it’s about a risk discussion, not automatic treatment.”
Dr. Lloyd-Jones and Dr. Stone each reported having no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ACC 16