User login
News and Views that Matter to Physicians
Cerebral protection in TAVI reduces ischemic brain lesions
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
These findings are compelling and encouraging, even though we don’t yet know whether the reduction in the number and volume of ischemic brain lesions translates into clinical benefit.
The results also confirm what previous research has suggested: that emboli to the brain are extremely common and do cause small infarctions detectable on MRI. In this trial, virtually every patient demonstrated such acute lesions, though the vast majority were quite small.
Steven R. Messe, MD, is in the department of neurology at the Hospital of the University of Pennsylvania, Philadelphia. Michael J. Mack, MD, is in the department of cardiac surgery at The Heart Hospital Baylor Plano in Plano, Tex. Dr. Messe reported ties to GlaxoSmithKline; Dr. Mack reported having no relevant financial disclosures. Dr. Messe and Dr. Mack made these remarks in an editorial accompanying Dr. Haussig’s report (JAMA 2016;316[6]:587-8).
These findings are compelling and encouraging, even though we don’t yet know whether the reduction in the number and volume of ischemic brain lesions translates into clinical benefit.
The results also confirm what previous research has suggested: that emboli to the brain are extremely common and do cause small infarctions detectable on MRI. In this trial, virtually every patient demonstrated such acute lesions, though the vast majority were quite small.
Steven R. Messe, MD, is in the department of neurology at the Hospital of the University of Pennsylvania, Philadelphia. Michael J. Mack, MD, is in the department of cardiac surgery at The Heart Hospital Baylor Plano in Plano, Tex. Dr. Messe reported ties to GlaxoSmithKline; Dr. Mack reported having no relevant financial disclosures. Dr. Messe and Dr. Mack made these remarks in an editorial accompanying Dr. Haussig’s report (JAMA 2016;316[6]:587-8).
These findings are compelling and encouraging, even though we don’t yet know whether the reduction in the number and volume of ischemic brain lesions translates into clinical benefit.
The results also confirm what previous research has suggested: that emboli to the brain are extremely common and do cause small infarctions detectable on MRI. In this trial, virtually every patient demonstrated such acute lesions, though the vast majority were quite small.
Steven R. Messe, MD, is in the department of neurology at the Hospital of the University of Pennsylvania, Philadelphia. Michael J. Mack, MD, is in the department of cardiac surgery at The Heart Hospital Baylor Plano in Plano, Tex. Dr. Messe reported ties to GlaxoSmithKline; Dr. Mack reported having no relevant financial disclosures. Dr. Messe and Dr. Mack made these remarks in an editorial accompanying Dr. Haussig’s report (JAMA 2016;316[6]:587-8).
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Key clinical point: In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions.
Major finding: At 2 days, the number of new brain lesions was markedly lower in the filter group than in the control group (8 vs. 16), as was the lesion volume (466 mm vs. 800 mm).
Data source: A prospective single-center randomized clinical trial involving 100 patients undergoing TAVI for severe aortic stenosis.
Disclosures: This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Sarcopenia an effective measure of frailty in elderly patients
WAIKOLOA, HAWAII – Sarcopenia is an independent predictor of 1-year mortality in elderly patients undergoing emergency abdominal surgery, results from a single-center study demonstrated.
“Setting expectations about operative outcomes is an important part of the preoperative counseling process, Erika L. Rangel, MD, FACS, said at the annual meeting of the American Association for the Surgery of Trauma. In a previous study that she and her associates conducted at Brigham and Women’s Hospital, Boston, the risk for mortality was found to continue long after hospital discharge in older patients who undergo emergency surgery: 16% at 30 days, 22% at 3 months, 28% at 6 months, and 32% 1 year after surgery (J Trauma and Acute Care Surg. 2015 Sep;79[3]:349-58).
Traditionally, surgeons use subjective opinion or basic scoring systems such as the American Society of Anesthesiologists (ASA) classification to stratify risk for surgery in elderly patients. “However, the ASA score can be subjective, and there’s inconsistency between evaluators,” Dr. Rangel said. “The Charlson Comorbidity [Index] rates a patient based on the presence or absence of 19 comorbidities, but it doesn’t tell the surgeon anything about the patient’s functional status.” Frailty is a good measure of an elderly patient’s physiologic reserve to withstand an operation, she continued, but is difficult to measure in the acute care setting. One solution is to measure sarcopenia, which predicts postoperative complications, disability, and mortality in elderly elective surgery patients. “The problem is that very few studies have looked at the impact of sarcopenia in the emergency surgery populations, and the ones that exist only look at short-term outcomes, which don’t completely capture the mortality risk,” she said.
In an effort to better understand how sarcopenia affects long-term outcomes after emergency surgery in the elderly, the researchers retrospectively reviewed patients aged 70 years or older who underwent urgent or emergent abdominal surgery at Brigham and Women’s between 2006 and 2011. Patients were stratified by operative severity using the POSSUM (Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity) score. Operations considered major included any laparotomy, open cholecystectomy, and bowel resection, while those considered moderate were laparoscopic cholecystectomy, appendectomy, and hernia repairs without bowel compromise. To measure sarcopenia, the researchers used preoperative CT images to calculate the average bilateral psoas muscle cross-sectional area at the L3 level, normalized for height. Primary outcome was 1-year mortality. Secondary outcomes were mortality at 30 days, 90 days, and 180 days.
Dr. Rangel reported results from 297 patients that were evaluated: 222 with no sarcopenia and 75 with sarcopenia. Their mean age was 78 years, 57% were female, and 84% were white. Compared with nonsarcopenic patients, sarcopenic patients did not differ in terms of age, sex, or race. Comorbidities were high in both groups, with 75% of patients having an ASA score of 3 or greater and 31% having a Charlson score of 4 or greater. More than 40% had some sort of underlying malignancy, yet there were no significant differences between the two groups in terms of ASA scores, Charlson scores, or the prevalence of malignancy.
Compared with nonsarcopenic patients, sarcopenic patients had longer hospital length of stay (14 vs. 11 days, respectively; P = .012), were more likely to require ICU care (67% vs. 50%; P = .012), and had higher in-hospital mortality (27% vs. 9%; P less than .01). In addition, sarcopenic patients had higher hazard ratios of mortality, compared with their nonsarcopenic counterparts, at 30 days (hazard ratio, 3.5; P = .01), 90 days (HR, 3.5; P less than .001), 180 days (HR, 2.6; P = .001), and at 1 year (HR, 2.5; P = .001).
“The measurement of sarcopenia is a practical tool that can be used at the bedside,” Dr. Rangel concluded. “It just takes 3 or 4 minutes using a single axial slice of a preoperative CT scan. Since it uses CT imaging that’s obtained for initial diagnostic purposes, it incurs no additional cost. The identification of sarcopenia has immediate applications for care of the geriatric patient. It should trigger the surgeon to set realistic goals of care and frame expectations about survival [and] should prompt processes of care that improve patient outcomes. High-risk patients might benefit from geriatric consultation or specialized geriatric pathways, early palliative care evaluation, and advance care planning.” She reported having no financial disclosures.
WAIKOLOA, HAWAII – Sarcopenia is an independent predictor of 1-year mortality in elderly patients undergoing emergency abdominal surgery, results from a single-center study demonstrated.
“Setting expectations about operative outcomes is an important part of the preoperative counseling process, Erika L. Rangel, MD, FACS, said at the annual meeting of the American Association for the Surgery of Trauma. In a previous study that she and her associates conducted at Brigham and Women’s Hospital, Boston, the risk for mortality was found to continue long after hospital discharge in older patients who undergo emergency surgery: 16% at 30 days, 22% at 3 months, 28% at 6 months, and 32% 1 year after surgery (J Trauma and Acute Care Surg. 2015 Sep;79[3]:349-58).
Traditionally, surgeons use subjective opinion or basic scoring systems such as the American Society of Anesthesiologists (ASA) classification to stratify risk for surgery in elderly patients. “However, the ASA score can be subjective, and there’s inconsistency between evaluators,” Dr. Rangel said. “The Charlson Comorbidity [Index] rates a patient based on the presence or absence of 19 comorbidities, but it doesn’t tell the surgeon anything about the patient’s functional status.” Frailty is a good measure of an elderly patient’s physiologic reserve to withstand an operation, she continued, but is difficult to measure in the acute care setting. One solution is to measure sarcopenia, which predicts postoperative complications, disability, and mortality in elderly elective surgery patients. “The problem is that very few studies have looked at the impact of sarcopenia in the emergency surgery populations, and the ones that exist only look at short-term outcomes, which don’t completely capture the mortality risk,” she said.
In an effort to better understand how sarcopenia affects long-term outcomes after emergency surgery in the elderly, the researchers retrospectively reviewed patients aged 70 years or older who underwent urgent or emergent abdominal surgery at Brigham and Women’s between 2006 and 2011. Patients were stratified by operative severity using the POSSUM (Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity) score. Operations considered major included any laparotomy, open cholecystectomy, and bowel resection, while those considered moderate were laparoscopic cholecystectomy, appendectomy, and hernia repairs without bowel compromise. To measure sarcopenia, the researchers used preoperative CT images to calculate the average bilateral psoas muscle cross-sectional area at the L3 level, normalized for height. Primary outcome was 1-year mortality. Secondary outcomes were mortality at 30 days, 90 days, and 180 days.
Dr. Rangel reported results from 297 patients that were evaluated: 222 with no sarcopenia and 75 with sarcopenia. Their mean age was 78 years, 57% were female, and 84% were white. Compared with nonsarcopenic patients, sarcopenic patients did not differ in terms of age, sex, or race. Comorbidities were high in both groups, with 75% of patients having an ASA score of 3 or greater and 31% having a Charlson score of 4 or greater. More than 40% had some sort of underlying malignancy, yet there were no significant differences between the two groups in terms of ASA scores, Charlson scores, or the prevalence of malignancy.
Compared with nonsarcopenic patients, sarcopenic patients had longer hospital length of stay (14 vs. 11 days, respectively; P = .012), were more likely to require ICU care (67% vs. 50%; P = .012), and had higher in-hospital mortality (27% vs. 9%; P less than .01). In addition, sarcopenic patients had higher hazard ratios of mortality, compared with their nonsarcopenic counterparts, at 30 days (hazard ratio, 3.5; P = .01), 90 days (HR, 3.5; P less than .001), 180 days (HR, 2.6; P = .001), and at 1 year (HR, 2.5; P = .001).
“The measurement of sarcopenia is a practical tool that can be used at the bedside,” Dr. Rangel concluded. “It just takes 3 or 4 minutes using a single axial slice of a preoperative CT scan. Since it uses CT imaging that’s obtained for initial diagnostic purposes, it incurs no additional cost. The identification of sarcopenia has immediate applications for care of the geriatric patient. It should trigger the surgeon to set realistic goals of care and frame expectations about survival [and] should prompt processes of care that improve patient outcomes. High-risk patients might benefit from geriatric consultation or specialized geriatric pathways, early palliative care evaluation, and advance care planning.” She reported having no financial disclosures.
WAIKOLOA, HAWAII – Sarcopenia is an independent predictor of 1-year mortality in elderly patients undergoing emergency abdominal surgery, results from a single-center study demonstrated.
“Setting expectations about operative outcomes is an important part of the preoperative counseling process, Erika L. Rangel, MD, FACS, said at the annual meeting of the American Association for the Surgery of Trauma. In a previous study that she and her associates conducted at Brigham and Women’s Hospital, Boston, the risk for mortality was found to continue long after hospital discharge in older patients who undergo emergency surgery: 16% at 30 days, 22% at 3 months, 28% at 6 months, and 32% 1 year after surgery (J Trauma and Acute Care Surg. 2015 Sep;79[3]:349-58).
Traditionally, surgeons use subjective opinion or basic scoring systems such as the American Society of Anesthesiologists (ASA) classification to stratify risk for surgery in elderly patients. “However, the ASA score can be subjective, and there’s inconsistency between evaluators,” Dr. Rangel said. “The Charlson Comorbidity [Index] rates a patient based on the presence or absence of 19 comorbidities, but it doesn’t tell the surgeon anything about the patient’s functional status.” Frailty is a good measure of an elderly patient’s physiologic reserve to withstand an operation, she continued, but is difficult to measure in the acute care setting. One solution is to measure sarcopenia, which predicts postoperative complications, disability, and mortality in elderly elective surgery patients. “The problem is that very few studies have looked at the impact of sarcopenia in the emergency surgery populations, and the ones that exist only look at short-term outcomes, which don’t completely capture the mortality risk,” she said.
In an effort to better understand how sarcopenia affects long-term outcomes after emergency surgery in the elderly, the researchers retrospectively reviewed patients aged 70 years or older who underwent urgent or emergent abdominal surgery at Brigham and Women’s between 2006 and 2011. Patients were stratified by operative severity using the POSSUM (Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity) score. Operations considered major included any laparotomy, open cholecystectomy, and bowel resection, while those considered moderate were laparoscopic cholecystectomy, appendectomy, and hernia repairs without bowel compromise. To measure sarcopenia, the researchers used preoperative CT images to calculate the average bilateral psoas muscle cross-sectional area at the L3 level, normalized for height. Primary outcome was 1-year mortality. Secondary outcomes were mortality at 30 days, 90 days, and 180 days.
Dr. Rangel reported results from 297 patients that were evaluated: 222 with no sarcopenia and 75 with sarcopenia. Their mean age was 78 years, 57% were female, and 84% were white. Compared with nonsarcopenic patients, sarcopenic patients did not differ in terms of age, sex, or race. Comorbidities were high in both groups, with 75% of patients having an ASA score of 3 or greater and 31% having a Charlson score of 4 or greater. More than 40% had some sort of underlying malignancy, yet there were no significant differences between the two groups in terms of ASA scores, Charlson scores, or the prevalence of malignancy.
Compared with nonsarcopenic patients, sarcopenic patients had longer hospital length of stay (14 vs. 11 days, respectively; P = .012), were more likely to require ICU care (67% vs. 50%; P = .012), and had higher in-hospital mortality (27% vs. 9%; P less than .01). In addition, sarcopenic patients had higher hazard ratios of mortality, compared with their nonsarcopenic counterparts, at 30 days (hazard ratio, 3.5; P = .01), 90 days (HR, 3.5; P less than .001), 180 days (HR, 2.6; P = .001), and at 1 year (HR, 2.5; P = .001).
“The measurement of sarcopenia is a practical tool that can be used at the bedside,” Dr. Rangel concluded. “It just takes 3 or 4 minutes using a single axial slice of a preoperative CT scan. Since it uses CT imaging that’s obtained for initial diagnostic purposes, it incurs no additional cost. The identification of sarcopenia has immediate applications for care of the geriatric patient. It should trigger the surgeon to set realistic goals of care and frame expectations about survival [and] should prompt processes of care that improve patient outcomes. High-risk patients might benefit from geriatric consultation or specialized geriatric pathways, early palliative care evaluation, and advance care planning.” She reported having no financial disclosures.
Key clinical point:
Major finding: Sarcopenic patients had higher hazard ratios of mortality, compared with their nonsarcopenic counterparts, at 30 days (HR, 3.5), 90 days (HR, 3.5), 180 days (HR, 2.6), and at 1 year (HR, 2.5).
Data source: A retrospective review of 297 patients aged 70 years or older who underwent urgent or emergent abdominal surgery at Brigham and Women’s between 2006 and 2011.
Disclosures: Dr. Rangel reported having no financial disclosures.
ACS should make firearm injury prevention a priority, COT member survey says
WAIKOLOA, HAWAII – Nearly 90% of American College of Surgeons Committee on Trauma members believe that the ACS should give the highest or a high priority to reducing firearm-related injuries, according to results from a national survey.
“In the United States, we value personal liberty and personal safety highly,” Deborah A. Kuhls, MD, FACS, said at the annual meeting of the American Association for the Surgery of Trauma. “However, that sometimes leads to a polarized view on firearms. Some view it as a freedom in personal safety. Others view it as a limitation of freedom and [as promotion of] violence.”
In an effort to evaluate ACS COT member attitudes about firearm ownership, freedom, responsibility, physician/patient freedom and policy, with the objective of using survey results to inform firearm injury prevention policy development, Dr. Kuhls and the COT Injury Prevention and Control Committee developed a 32-item anonymous survey that was sent to 254 COT members between December 2015 and February 2016. Results were extracted by ACS staff.
Of 254 COT members who received the survey, 237 completed the survey, for a response rate of 93%. Their mean age was 52 years, and 88% were male, 88% were married, 85% were white, and 58% had children in the home. More than one-quarter (29%) had military experience, 88% practiced acute care, trauma, general surgery, or pediatric surgery; 43% had firearms in the home, and 33% had personal experience with a family or friend injured or killed from firearm injury. A significantly higher proportion of respondents with military experience had firearms in the home, compared with those who had no military experience (56% vs. 37%, respectively; P less than .01). By Centers for Disease Control and Prevention demographic region, the percentage of members who have firearms in their home was lowest in the Northeast (14%), followed by the West (38%), the Midwest (48%), and the South (56%).
Dr. Kuhls also reported that 88% of respondents indicated that they think the ACS should give a high or the highest level of priority to firearm injury prevention. When asked about private ownership of firearms, about 53% thought that gun ownership is generally beneficial/an important personal liberty, while 30% believed that gun ownership is generally harmful and limits personal liberty. The remaining 17% had no opinion on the issue.
The majority of respondents (95%) said that health care professionals should be allowed to counsel patients (or parents of patients) about how to prevent gun-related injuries, while 96% felt that the CDC and other federal agencies should fund research on the epidemiology and prevention of gun-related injuries.
Survey respondents were then asked to rate their opinion on the ACS initiating efforts to advocate for or support legislation on 15 possible initiatives to prevent firearm violence, ranging from “improve mental health screening and treatment to reduce suicides and gun violence” to increase penalties when guns [are] provided to others illegally including dealers” to “require safety features, including child-proof locks and ‘smart gun’ technology,” and “identify and implement evidence-based injury prevention programs.”
The greatest consensus was reached in the advocacy area titled “improve mental health screening and treatment to reduce suicides and gun violence” (ranging from 89% to 93%), while the least consensus was in the advocacy area titled “require firearms owners to be 21 years of age or older” (ranging from 41% to 71%).
The most common themes that emerged on qualitative analysis were concern that the topic is too political, as well as calls to improve existing data “to understand what role we can play in injury prevention,” and that “surgeons should be involved in solving the problem,” Dr. Kuhls said. “There were also a lot of comments on responsible ownership.” She noted that more than 90% of respondents support 7 out of 15 proposed initiatives, 80%-90% support an additional 3 initiatives, and 70%-80% support an additional 4 proposed initiatives.
The invited discussant, Ernest E. Moore, MD, FACS, a surgeon in Denver, described the effort to develop firearm injury prevention policy as laudable. However, “this process carries a risk of merely supporting the bandwagons already in motion,” Dr. Moore said. “In that light I would like to focus on the conspicuous areas of disagreement, specifically civilian access to assault rifles. The fundamental issue is the magazine capacity of rifles – housing 30 or more bullets, enabling rapid shooting. Mass shootings, defined as greater than or equal to five victims, are currently an epidemic in our country. The volatile issues are eliminating assault rifles to reduce mass shootings [and] the interpretation of the Second Amendment to keep and bear arms. I do not believe a randomized prospective trial is necessary to establish the fact that mass shootings are only feasible because irresponsible individuals have access to these weapons. The urgency in this issue is heightened by the reality that mass shootings are increasingly inspired by terrorist activity, beyond individuals traditionally considered mentally ill.”
Dr. Kuhls described the current survey as “the initial step” in an effort to develop firearm injury prevention policy. “We are just about to receive results from a survey of the Board of Governors for the ACS,” she said. “We plan to develop short- and long-term plans to address this public health challenge that leverages survey consensus findings in four ACS pillars: advocacy, quality, systems, and education. We need to continue this conversation.” She expressed gratitude to the COT Executive Committee and liaison members from the ACS Board of Regents in addition to members of the COT Injury Prevention and Control Committee. She reported having no financial disclosures.
WAIKOLOA, HAWAII – Nearly 90% of American College of Surgeons Committee on Trauma members believe that the ACS should give the highest or a high priority to reducing firearm-related injuries, according to results from a national survey.
“In the United States, we value personal liberty and personal safety highly,” Deborah A. Kuhls, MD, FACS, said at the annual meeting of the American Association for the Surgery of Trauma. “However, that sometimes leads to a polarized view on firearms. Some view it as a freedom in personal safety. Others view it as a limitation of freedom and [as promotion of] violence.”
In an effort to evaluate ACS COT member attitudes about firearm ownership, freedom, responsibility, physician/patient freedom and policy, with the objective of using survey results to inform firearm injury prevention policy development, Dr. Kuhls and the COT Injury Prevention and Control Committee developed a 32-item anonymous survey that was sent to 254 COT members between December 2015 and February 2016. Results were extracted by ACS staff.
Of 254 COT members who received the survey, 237 completed the survey, for a response rate of 93%. Their mean age was 52 years, and 88% were male, 88% were married, 85% were white, and 58% had children in the home. More than one-quarter (29%) had military experience, 88% practiced acute care, trauma, general surgery, or pediatric surgery; 43% had firearms in the home, and 33% had personal experience with a family or friend injured or killed from firearm injury. A significantly higher proportion of respondents with military experience had firearms in the home, compared with those who had no military experience (56% vs. 37%, respectively; P less than .01). By Centers for Disease Control and Prevention demographic region, the percentage of members who have firearms in their home was lowest in the Northeast (14%), followed by the West (38%), the Midwest (48%), and the South (56%).
Dr. Kuhls also reported that 88% of respondents indicated that they think the ACS should give a high or the highest level of priority to firearm injury prevention. When asked about private ownership of firearms, about 53% thought that gun ownership is generally beneficial/an important personal liberty, while 30% believed that gun ownership is generally harmful and limits personal liberty. The remaining 17% had no opinion on the issue.
The majority of respondents (95%) said that health care professionals should be allowed to counsel patients (or parents of patients) about how to prevent gun-related injuries, while 96% felt that the CDC and other federal agencies should fund research on the epidemiology and prevention of gun-related injuries.
Survey respondents were then asked to rate their opinion on the ACS initiating efforts to advocate for or support legislation on 15 possible initiatives to prevent firearm violence, ranging from “improve mental health screening and treatment to reduce suicides and gun violence” to increase penalties when guns [are] provided to others illegally including dealers” to “require safety features, including child-proof locks and ‘smart gun’ technology,” and “identify and implement evidence-based injury prevention programs.”
The greatest consensus was reached in the advocacy area titled “improve mental health screening and treatment to reduce suicides and gun violence” (ranging from 89% to 93%), while the least consensus was in the advocacy area titled “require firearms owners to be 21 years of age or older” (ranging from 41% to 71%).
The most common themes that emerged on qualitative analysis were concern that the topic is too political, as well as calls to improve existing data “to understand what role we can play in injury prevention,” and that “surgeons should be involved in solving the problem,” Dr. Kuhls said. “There were also a lot of comments on responsible ownership.” She noted that more than 90% of respondents support 7 out of 15 proposed initiatives, 80%-90% support an additional 3 initiatives, and 70%-80% support an additional 4 proposed initiatives.
The invited discussant, Ernest E. Moore, MD, FACS, a surgeon in Denver, described the effort to develop firearm injury prevention policy as laudable. However, “this process carries a risk of merely supporting the bandwagons already in motion,” Dr. Moore said. “In that light I would like to focus on the conspicuous areas of disagreement, specifically civilian access to assault rifles. The fundamental issue is the magazine capacity of rifles – housing 30 or more bullets, enabling rapid shooting. Mass shootings, defined as greater than or equal to five victims, are currently an epidemic in our country. The volatile issues are eliminating assault rifles to reduce mass shootings [and] the interpretation of the Second Amendment to keep and bear arms. I do not believe a randomized prospective trial is necessary to establish the fact that mass shootings are only feasible because irresponsible individuals have access to these weapons. The urgency in this issue is heightened by the reality that mass shootings are increasingly inspired by terrorist activity, beyond individuals traditionally considered mentally ill.”
Dr. Kuhls described the current survey as “the initial step” in an effort to develop firearm injury prevention policy. “We are just about to receive results from a survey of the Board of Governors for the ACS,” she said. “We plan to develop short- and long-term plans to address this public health challenge that leverages survey consensus findings in four ACS pillars: advocacy, quality, systems, and education. We need to continue this conversation.” She expressed gratitude to the COT Executive Committee and liaison members from the ACS Board of Regents in addition to members of the COT Injury Prevention and Control Committee. She reported having no financial disclosures.
WAIKOLOA, HAWAII – Nearly 90% of American College of Surgeons Committee on Trauma members believe that the ACS should give the highest or a high priority to reducing firearm-related injuries, according to results from a national survey.
“In the United States, we value personal liberty and personal safety highly,” Deborah A. Kuhls, MD, FACS, said at the annual meeting of the American Association for the Surgery of Trauma. “However, that sometimes leads to a polarized view on firearms. Some view it as a freedom in personal safety. Others view it as a limitation of freedom and [as promotion of] violence.”
In an effort to evaluate ACS COT member attitudes about firearm ownership, freedom, responsibility, physician/patient freedom and policy, with the objective of using survey results to inform firearm injury prevention policy development, Dr. Kuhls and the COT Injury Prevention and Control Committee developed a 32-item anonymous survey that was sent to 254 COT members between December 2015 and February 2016. Results were extracted by ACS staff.
Of 254 COT members who received the survey, 237 completed the survey, for a response rate of 93%. Their mean age was 52 years, and 88% were male, 88% were married, 85% were white, and 58% had children in the home. More than one-quarter (29%) had military experience, 88% practiced acute care, trauma, general surgery, or pediatric surgery; 43% had firearms in the home, and 33% had personal experience with a family or friend injured or killed from firearm injury. A significantly higher proportion of respondents with military experience had firearms in the home, compared with those who had no military experience (56% vs. 37%, respectively; P less than .01). By Centers for Disease Control and Prevention demographic region, the percentage of members who have firearms in their home was lowest in the Northeast (14%), followed by the West (38%), the Midwest (48%), and the South (56%).
Dr. Kuhls also reported that 88% of respondents indicated that they think the ACS should give a high or the highest level of priority to firearm injury prevention. When asked about private ownership of firearms, about 53% thought that gun ownership is generally beneficial/an important personal liberty, while 30% believed that gun ownership is generally harmful and limits personal liberty. The remaining 17% had no opinion on the issue.
The majority of respondents (95%) said that health care professionals should be allowed to counsel patients (or parents of patients) about how to prevent gun-related injuries, while 96% felt that the CDC and other federal agencies should fund research on the epidemiology and prevention of gun-related injuries.
Survey respondents were then asked to rate their opinion on the ACS initiating efforts to advocate for or support legislation on 15 possible initiatives to prevent firearm violence, ranging from “improve mental health screening and treatment to reduce suicides and gun violence” to increase penalties when guns [are] provided to others illegally including dealers” to “require safety features, including child-proof locks and ‘smart gun’ technology,” and “identify and implement evidence-based injury prevention programs.”
The greatest consensus was reached in the advocacy area titled “improve mental health screening and treatment to reduce suicides and gun violence” (ranging from 89% to 93%), while the least consensus was in the advocacy area titled “require firearms owners to be 21 years of age or older” (ranging from 41% to 71%).
The most common themes that emerged on qualitative analysis were concern that the topic is too political, as well as calls to improve existing data “to understand what role we can play in injury prevention,” and that “surgeons should be involved in solving the problem,” Dr. Kuhls said. “There were also a lot of comments on responsible ownership.” She noted that more than 90% of respondents support 7 out of 15 proposed initiatives, 80%-90% support an additional 3 initiatives, and 70%-80% support an additional 4 proposed initiatives.
The invited discussant, Ernest E. Moore, MD, FACS, a surgeon in Denver, described the effort to develop firearm injury prevention policy as laudable. However, “this process carries a risk of merely supporting the bandwagons already in motion,” Dr. Moore said. “In that light I would like to focus on the conspicuous areas of disagreement, specifically civilian access to assault rifles. The fundamental issue is the magazine capacity of rifles – housing 30 or more bullets, enabling rapid shooting. Mass shootings, defined as greater than or equal to five victims, are currently an epidemic in our country. The volatile issues are eliminating assault rifles to reduce mass shootings [and] the interpretation of the Second Amendment to keep and bear arms. I do not believe a randomized prospective trial is necessary to establish the fact that mass shootings are only feasible because irresponsible individuals have access to these weapons. The urgency in this issue is heightened by the reality that mass shootings are increasingly inspired by terrorist activity, beyond individuals traditionally considered mentally ill.”
Dr. Kuhls described the current survey as “the initial step” in an effort to develop firearm injury prevention policy. “We are just about to receive results from a survey of the Board of Governors for the ACS,” she said. “We plan to develop short- and long-term plans to address this public health challenge that leverages survey consensus findings in four ACS pillars: advocacy, quality, systems, and education. We need to continue this conversation.” She expressed gratitude to the COT Executive Committee and liaison members from the ACS Board of Regents in addition to members of the COT Injury Prevention and Control Committee. She reported having no financial disclosures.
Key clinical point:
Major finding: A majority of respondents (88%) indicated that they think the ACS should give a high or the highest level of priority to firearm injury prevention.
Data source: Responses to 32-item anonymous survey that was completed by 237 members of the ACS COT between December 2015 and February 2016.
Disclosures: Dr. Kuhls reported having no financial disclosures.
No increase in CV events with long-acting bronchodilators in COPD
Long-acting bronchodilators, including tiotropium, do not appear to increase the risk of cardiovascular events in the first year of use, according to a study in patients with chronic obstructive pulmonary disease.
Long-acting bronchodilators are recommended as first-line maintenance therapy for chronic obstructive pulmonary disease (COPD), but they can cause cardiac complications, wrote Samy Suissa, PhD, and his colleagues at the Centre for Clinical Epidemiology, Lady Davis Institute, Montreal.
“Indeed, long-acting anticholinergics are believed to suppress parasympathetic control, while LABAs [long-acting beta2-agonists] stimulate sympathetic tone, possibly leading to tachyarrhythmia and coronary insufficiency,” the authors wrote (Chest. 2016 Aug 20. doi: 10.1016/j.chest.2016.08.001). “Furthermore, these pharmacologic effects would be expected to occur immediately at initiation of therapy.”
However, the observational studies and randomized trials comparing the safety of LABAs and the long-acting anticholinergic tiotropium have shown inconclusive results, possibly because of insufficient numbers, short follow-ups or “treatment-experienced” patients.
Dr. Suissa and his colleagues analyzed data from 26,442 new tiotropium users and 26,442 LABA initiators from a U.K. primary care database. Participants in each arm were matched on high-dimensional propensity scores and prior inhaled corticosteroid use, and followed for 1 year for occurrence of acute myocardial infarction, stroke, heart failure, arrhythmia, and pneumonia.
The researchers saw no significant difference between tiotropium and LABA users in the risk of acute myocardial infarction (hazard ratio, 1.10; 95% CI, 0.88-1.38), stroke (HR, 1.02; 95% CI, 0.78-1.34), arrhythmia (HR, 0.81; 95% CI, 0.60-1.09), or heart failure (HR, 0.90; 95% CI, 0.79-1.02). This was the case even when the current exposure time window was varied from 60-day periods to 30- or 90-day periods.
There was a significantly lower incidence of pneumonia in individuals treated with tiotropium (HR, 0.81; 95% CI, 0.72-0.92), which the authors suggested was likely due to the presence of inhaled corticosteroids in many LABAs.
“In our study, 78% of the LABA users were receiving a combined inhaler that included an inhaled corticosteroid, two-thirds of which were for fluticasone, which has been associated with an up to twofold increase in the risk of pneumonia,” they reported.
The authors acknowledged that the presence of an inhaled corticosteroid in combination with many of the LABAs could attract criticism that the study was therefore not a strict comparison between tiotropium and a LABA. However, they noted that the study aimed to represent the real-world experience of clinical practice.
“In this real-world–setting study of the treatment of COPD, the initiation of maintenance treatment with tiotropium compared with a LABA does not increase cardiovascular risk, but reduces significantly the risk of pneumonia, albeit a likely adverse effect of the inhaled corticosteroid component present in many LABA inhalers,” the authors wrote.
“This differential risk that appears to confer a safety advantage to tiotropium as the initial long-acting bronchodilator in COPD should be considered against the comparative effectiveness of these two treatments at initiation,” they noted.
The Canadian Institutes of Health Research, the Canadian Foundation for Innovation, and Boehringer Ingelheim supported the study. One author disclosed ties with Boehringer Ingelheim, AstraZeneca, Novartis, and Pfizer. No other conflicts of interest were declared.
Long-acting bronchodilators, including tiotropium, do not appear to increase the risk of cardiovascular events in the first year of use, according to a study in patients with chronic obstructive pulmonary disease.
Long-acting bronchodilators are recommended as first-line maintenance therapy for chronic obstructive pulmonary disease (COPD), but they can cause cardiac complications, wrote Samy Suissa, PhD, and his colleagues at the Centre for Clinical Epidemiology, Lady Davis Institute, Montreal.
“Indeed, long-acting anticholinergics are believed to suppress parasympathetic control, while LABAs [long-acting beta2-agonists] stimulate sympathetic tone, possibly leading to tachyarrhythmia and coronary insufficiency,” the authors wrote (Chest. 2016 Aug 20. doi: 10.1016/j.chest.2016.08.001). “Furthermore, these pharmacologic effects would be expected to occur immediately at initiation of therapy.”
However, the observational studies and randomized trials comparing the safety of LABAs and the long-acting anticholinergic tiotropium have shown inconclusive results, possibly because of insufficient numbers, short follow-ups or “treatment-experienced” patients.
Dr. Suissa and his colleagues analyzed data from 26,442 new tiotropium users and 26,442 LABA initiators from a U.K. primary care database. Participants in each arm were matched on high-dimensional propensity scores and prior inhaled corticosteroid use, and followed for 1 year for occurrence of acute myocardial infarction, stroke, heart failure, arrhythmia, and pneumonia.
The researchers saw no significant difference between tiotropium and LABA users in the risk of acute myocardial infarction (hazard ratio, 1.10; 95% CI, 0.88-1.38), stroke (HR, 1.02; 95% CI, 0.78-1.34), arrhythmia (HR, 0.81; 95% CI, 0.60-1.09), or heart failure (HR, 0.90; 95% CI, 0.79-1.02). This was the case even when the current exposure time window was varied from 60-day periods to 30- or 90-day periods.
There was a significantly lower incidence of pneumonia in individuals treated with tiotropium (HR, 0.81; 95% CI, 0.72-0.92), which the authors suggested was likely due to the presence of inhaled corticosteroids in many LABAs.
“In our study, 78% of the LABA users were receiving a combined inhaler that included an inhaled corticosteroid, two-thirds of which were for fluticasone, which has been associated with an up to twofold increase in the risk of pneumonia,” they reported.
The authors acknowledged that the presence of an inhaled corticosteroid in combination with many of the LABAs could attract criticism that the study was therefore not a strict comparison between tiotropium and a LABA. However, they noted that the study aimed to represent the real-world experience of clinical practice.
“In this real-world–setting study of the treatment of COPD, the initiation of maintenance treatment with tiotropium compared with a LABA does not increase cardiovascular risk, but reduces significantly the risk of pneumonia, albeit a likely adverse effect of the inhaled corticosteroid component present in many LABA inhalers,” the authors wrote.
“This differential risk that appears to confer a safety advantage to tiotropium as the initial long-acting bronchodilator in COPD should be considered against the comparative effectiveness of these two treatments at initiation,” they noted.
The Canadian Institutes of Health Research, the Canadian Foundation for Innovation, and Boehringer Ingelheim supported the study. One author disclosed ties with Boehringer Ingelheim, AstraZeneca, Novartis, and Pfizer. No other conflicts of interest were declared.
Long-acting bronchodilators, including tiotropium, do not appear to increase the risk of cardiovascular events in the first year of use, according to a study in patients with chronic obstructive pulmonary disease.
Long-acting bronchodilators are recommended as first-line maintenance therapy for chronic obstructive pulmonary disease (COPD), but they can cause cardiac complications, wrote Samy Suissa, PhD, and his colleagues at the Centre for Clinical Epidemiology, Lady Davis Institute, Montreal.
“Indeed, long-acting anticholinergics are believed to suppress parasympathetic control, while LABAs [long-acting beta2-agonists] stimulate sympathetic tone, possibly leading to tachyarrhythmia and coronary insufficiency,” the authors wrote (Chest. 2016 Aug 20. doi: 10.1016/j.chest.2016.08.001). “Furthermore, these pharmacologic effects would be expected to occur immediately at initiation of therapy.”
However, the observational studies and randomized trials comparing the safety of LABAs and the long-acting anticholinergic tiotropium have shown inconclusive results, possibly because of insufficient numbers, short follow-ups or “treatment-experienced” patients.
Dr. Suissa and his colleagues analyzed data from 26,442 new tiotropium users and 26,442 LABA initiators from a U.K. primary care database. Participants in each arm were matched on high-dimensional propensity scores and prior inhaled corticosteroid use, and followed for 1 year for occurrence of acute myocardial infarction, stroke, heart failure, arrhythmia, and pneumonia.
The researchers saw no significant difference between tiotropium and LABA users in the risk of acute myocardial infarction (hazard ratio, 1.10; 95% CI, 0.88-1.38), stroke (HR, 1.02; 95% CI, 0.78-1.34), arrhythmia (HR, 0.81; 95% CI, 0.60-1.09), or heart failure (HR, 0.90; 95% CI, 0.79-1.02). This was the case even when the current exposure time window was varied from 60-day periods to 30- or 90-day periods.
There was a significantly lower incidence of pneumonia in individuals treated with tiotropium (HR, 0.81; 95% CI, 0.72-0.92), which the authors suggested was likely due to the presence of inhaled corticosteroids in many LABAs.
“In our study, 78% of the LABA users were receiving a combined inhaler that included an inhaled corticosteroid, two-thirds of which were for fluticasone, which has been associated with an up to twofold increase in the risk of pneumonia,” they reported.
The authors acknowledged that the presence of an inhaled corticosteroid in combination with many of the LABAs could attract criticism that the study was therefore not a strict comparison between tiotropium and a LABA. However, they noted that the study aimed to represent the real-world experience of clinical practice.
“In this real-world–setting study of the treatment of COPD, the initiation of maintenance treatment with tiotropium compared with a LABA does not increase cardiovascular risk, but reduces significantly the risk of pneumonia, albeit a likely adverse effect of the inhaled corticosteroid component present in many LABA inhalers,” the authors wrote.
“This differential risk that appears to confer a safety advantage to tiotropium as the initial long-acting bronchodilator in COPD should be considered against the comparative effectiveness of these two treatments at initiation,” they noted.
The Canadian Institutes of Health Research, the Canadian Foundation for Innovation, and Boehringer Ingelheim supported the study. One author disclosed ties with Boehringer Ingelheim, AstraZeneca, Novartis, and Pfizer. No other conflicts of interest were declared.
Key clinical point: Long-acting bronchodilators do not appear to increase the risk of cardiovascular events in the first year of use in individuals with chronic obstructive pulmonary disease.
Major finding: Tiotropium and long-acting beta2-agonists were not associated with any significant increases in the risk of acute myocardial infarction, stroke, heart failure, or arrhythmia in the first year of use.
Data source: Population-based cohort study of 26,442 new tiotropium users and 26,442 LABA initiators.
Disclosures: The Canadian Institutes of Health Research, the Canadian Foundation for Innovation, and Boehringer Ingelheim supported the study. One author disclosed ties with Boehringer Ingelheim, AstraZeneca, Novartis, and Pfizer. No other conflicts of interest were declared.
Trauma operative training declining for general surgery residents
WAIKOLOA, HAWAII – Trauma training for general surgery residents has significantly declined in recent years, results from an analysis of the Accreditation Council for Graduate Medical Education data registry on surgical education showed.
Aaron Strumwasser, MD, an attending trauma surgeon and surgical intensivist at the Los Angeles County/University of Southern California Medical Center, characterized the decline in trauma training as “sobering.” In an effort to test their hypothesis that trauma training for general surgery residents is on the decline since the inception of the 80-hour workweek, Dr. Strumwasser and his associates set out to compare the operative caseloads before and after the inception of the 80-hour workweek; to note trends in specific operative domains and determine if deficiencies exist and to determine whether subspecialty training (specifically, vascular fellowship and integrated vascular surgery residency) has altered general surgery resident operative volume. They extracted data from the ACGME database on resident trauma volume for trauma cases by category and by resident training year for the years 1999-2015. Only those cases logged as primary surgery were included. The researchers subdivided trauma cases into five domains: head and neck, thoracic, abdomen, solid organ, and extremity. Resident trauma experience (operative caseload) was compared, based on before the inception of the 80-hour workweek (1999-2002) and after (2003-present).
Solutions to the current situation seem to fall into one of three categories, Dr. Strumwasser said: advanced simulation training such as Advanced Surgical Skills Exposure in Trauma and Advanced Trauma Operative Management; extending or changing the structure of general surgery training and promoting trauma and Acute Care Surgery fellowships.
“Subspecialization has clearly narrowed the scope of general surgery and trauma surgery practice. As a result, we now treat many complex injuries with a team-based approach. So unless societal trends reverse, it is highly unlikely that we will do more open operations in the future, since many nonoperative and noninvasive options work just as well or even better, said Dr. Malangoni. “It’s easy to blame these changes on duty hours requirements and the corresponding reduction in call, and decreasing exposure to trauma and emergent conditions. However, it’s important to recognize that there are 10% more residencies as well as 15% more resident graduates in 2015, compared to 15 years ago, which further magnifies the effect of the overall decline in trauma operative volume. So how do we meet the challenge of teaching residents to perform operations uncommonly done not only during but also after residency, while maintaining quality care for our patients? This is a challenge shared by nearly every surgical specialty due to a general decline in open operations overall.”
Dr. Strumwasser reported having no financial disclosures.
WAIKOLOA, HAWAII – Trauma training for general surgery residents has significantly declined in recent years, results from an analysis of the Accreditation Council for Graduate Medical Education data registry on surgical education showed.
Aaron Strumwasser, MD, an attending trauma surgeon and surgical intensivist at the Los Angeles County/University of Southern California Medical Center, characterized the decline in trauma training as “sobering.” In an effort to test their hypothesis that trauma training for general surgery residents is on the decline since the inception of the 80-hour workweek, Dr. Strumwasser and his associates set out to compare the operative caseloads before and after the inception of the 80-hour workweek; to note trends in specific operative domains and determine if deficiencies exist and to determine whether subspecialty training (specifically, vascular fellowship and integrated vascular surgery residency) has altered general surgery resident operative volume. They extracted data from the ACGME database on resident trauma volume for trauma cases by category and by resident training year for the years 1999-2015. Only those cases logged as primary surgery were included. The researchers subdivided trauma cases into five domains: head and neck, thoracic, abdomen, solid organ, and extremity. Resident trauma experience (operative caseload) was compared, based on before the inception of the 80-hour workweek (1999-2002) and after (2003-present).
Solutions to the current situation seem to fall into one of three categories, Dr. Strumwasser said: advanced simulation training such as Advanced Surgical Skills Exposure in Trauma and Advanced Trauma Operative Management; extending or changing the structure of general surgery training and promoting trauma and Acute Care Surgery fellowships.
“Subspecialization has clearly narrowed the scope of general surgery and trauma surgery practice. As a result, we now treat many complex injuries with a team-based approach. So unless societal trends reverse, it is highly unlikely that we will do more open operations in the future, since many nonoperative and noninvasive options work just as well or even better, said Dr. Malangoni. “It’s easy to blame these changes on duty hours requirements and the corresponding reduction in call, and decreasing exposure to trauma and emergent conditions. However, it’s important to recognize that there are 10% more residencies as well as 15% more resident graduates in 2015, compared to 15 years ago, which further magnifies the effect of the overall decline in trauma operative volume. So how do we meet the challenge of teaching residents to perform operations uncommonly done not only during but also after residency, while maintaining quality care for our patients? This is a challenge shared by nearly every surgical specialty due to a general decline in open operations overall.”
Dr. Strumwasser reported having no financial disclosures.
WAIKOLOA, HAWAII – Trauma training for general surgery residents has significantly declined in recent years, results from an analysis of the Accreditation Council for Graduate Medical Education data registry on surgical education showed.
Aaron Strumwasser, MD, an attending trauma surgeon and surgical intensivist at the Los Angeles County/University of Southern California Medical Center, characterized the decline in trauma training as “sobering.” In an effort to test their hypothesis that trauma training for general surgery residents is on the decline since the inception of the 80-hour workweek, Dr. Strumwasser and his associates set out to compare the operative caseloads before and after the inception of the 80-hour workweek; to note trends in specific operative domains and determine if deficiencies exist and to determine whether subspecialty training (specifically, vascular fellowship and integrated vascular surgery residency) has altered general surgery resident operative volume. They extracted data from the ACGME database on resident trauma volume for trauma cases by category and by resident training year for the years 1999-2015. Only those cases logged as primary surgery were included. The researchers subdivided trauma cases into five domains: head and neck, thoracic, abdomen, solid organ, and extremity. Resident trauma experience (operative caseload) was compared, based on before the inception of the 80-hour workweek (1999-2002) and after (2003-present).
Solutions to the current situation seem to fall into one of three categories, Dr. Strumwasser said: advanced simulation training such as Advanced Surgical Skills Exposure in Trauma and Advanced Trauma Operative Management; extending or changing the structure of general surgery training and promoting trauma and Acute Care Surgery fellowships.
“Subspecialization has clearly narrowed the scope of general surgery and trauma surgery practice. As a result, we now treat many complex injuries with a team-based approach. So unless societal trends reverse, it is highly unlikely that we will do more open operations in the future, since many nonoperative and noninvasive options work just as well or even better, said Dr. Malangoni. “It’s easy to blame these changes on duty hours requirements and the corresponding reduction in call, and decreasing exposure to trauma and emergent conditions. However, it’s important to recognize that there are 10% more residencies as well as 15% more resident graduates in 2015, compared to 15 years ago, which further magnifies the effect of the overall decline in trauma operative volume. So how do we meet the challenge of teaching residents to perform operations uncommonly done not only during but also after residency, while maintaining quality care for our patients? This is a challenge shared by nearly every surgical specialty due to a general decline in open operations overall.”
Dr. Strumwasser reported having no financial disclosures.
Key clinical point:
Major finding: A trend toward decreased operative trauma for general surgery residents was observed in the time periods before and after implementation of the 80-hour workweek (a mean of 39,252 vs. 36,065 cases, respectively; P = .07).
Data source: An analysis of data from the ACGME database on resident trauma volume for trauma cases by category and by resident training year for the years 1999-2015.
Disclosures: Dr. Strumwasser reported having no financial disclosures.
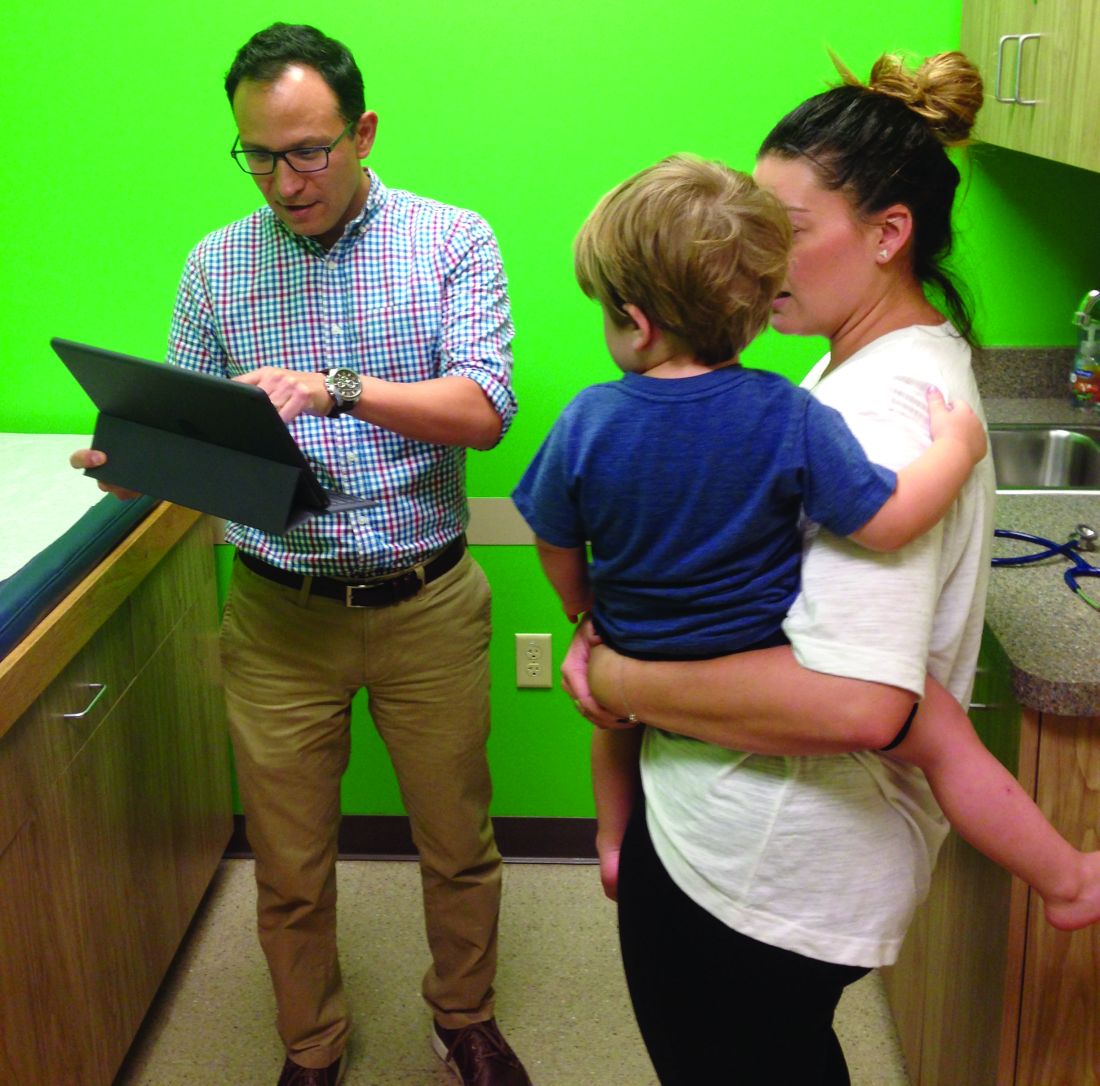
Pediatricians partner with hospitals for value-based models
When Jason Vargas, MD, first moved to the Phoenix area 13 years ago, he found an atmosphere of distant relationships between general pediatricians like him, subspecialists, and hospitals. Getting patients a referral to a subspecialist could take months, and communication among providers was often weak, Dr. Vargas said.
Today, things are vastly different thanks in large part to the clinically integrated network of which Dr. Vargas and 950 area providers are a part.
Phoenix Children’s Care Network (PCCN), established in 2014, coordinates health care across multiple providers and settings in the Phoenix area, including half of all general pediatricians and 80% of pediatric subspecialists practicing in Maricopa County. The network is a value- and risk-based system that provides financial incentives to participating providers and health systems that meet established quality metrics. Patients have access to 950 providers within the network, including primary and specialty care sites of service, urgent care locations, surgery centers, and Phoenix Children’s Hospital.
Meanwhile, 2,000 miles away, another unique payment model is changing the way pediatric care is delivered in the Columbus, Ohio area. Partners For Kids (PFK) is a pediatric accountable care organization (ACO) that coordinates care between Nationwide Children’s Hospital and more than 1,000 doctors. Through its 20-year evolution, PFK has successfully assumed full financial and clinical risk for children under age 19 enrolled in Medicaid managed care. This means PFK is responsible for paying for the costs of all patient care, no matter how much or where that care occurs.
The two models illustrate how pediatricians are affiliating with value-centric networks while keeping their independence, said Timothy Johnson, senior vice president of pediatrics at Valence Health, a consulting firm that helps health providers transition to value-based care.
With MACRA (the Medicare Access and CHIP Reauthorization Act of 2015) “it’s going to be difficult for individual pediatricians to do what is required in a value-based medical system because they just don’t have the resources,” Mr. Johnson said in an interview. “That doesn’t mean they can’t be independent. It means they are going to have to band together in some way, whether with a health system, with other practices. It is extremely important for pediatricians to start thinking about how to do that.”
Going from splintered to unified
Like most communities, care delivery in the Phoenix area was relatively fractured prior to 2014. To bring everyone together, Phoenix Children’s started with community outreach and education.
Along with building trust among providers, project leaders had to overcome operational hurdles. This included creating a process for 110 practices to collectively negotiate contracts, operate under a new structure, and adhere to quality metrics, he said.
“Operationally, you have to take 110 different ways of doing things and try merge them into one common way as you develop these new contractual risk-based models,” he said. “At the same time, we had to transition people away from what they were used to as a purely fee-for-service model. It was a very big operational transition.”
To bolster engagement by community pediatricians, PCCN developed a physician-governance approach, assigning participating providers leadership responsibilities. Participating physicians then worked to create the benchmarks by which doctors are measured against. To date, provider performance is tracked against 14 primary care and 34 specialist metrics encompassing engagement, safety, quality, and transparency.
PCCN leaders also had to ensure that participating in such a network was beneficial for busy doctors, said Dr. Vargas, who is chair of the PCCN Network and Utilization committee and a member of the network’s board of managers.
Asking physicians to change their framework, track patient data, and meet metrics, all while potentially losing money if they fail to hit benchmarks is not the most popular proposition, he said. So PCCN created advantages for member doctors, such as nighttime pediatric triage, a negotiated discount for professional services, IT support, streamlined access to specialists, and more avenues to communicate with subspecialists.
“With so many schedules, professional, and academic pressures on our daily professional lives, we have wanted to make sure that there were practical value added benefits to members,” he said. “I think right now that the benefits outweigh the administrative burdens.”
A changing payer relationship
As a network, PCCN works with payers to assume the risk that insurers have historically taken. Payers continue to handle the administrative and billing side of the equation, while the network controls the medical management and care coordination of the patient population, Mr. Johnson said.
“We feel we can do it much more efficiently, much more effectively, and we feel it’s better care for the patient when we’re the one controlling that,” he said. “The insurance companies don’t disagree.”
The network partners with Medicaid and commercial payers and has a direct-to-employer agreement with a major employer in conjunction with an adult partner system/network. Early performance efforts by the PCCN have been rewarded by shared savings disbursements from two payers, according to PCCN officials. The network has also met or exceeded state Medicaid pediatric quality targets and consistently contained medical expenses below expected medical cost trends for its managed pediatric populations.
Building a population health model
For more than 2 decades, PFK in Ohio has taken a novel care delivery approach that has focused on value and community partnerships.
Back in 1994, Nationwide Children’s Hospital partnered with community pediatricians to create PFK, a physician/hospital organization with governance shared equally. Today, PFK has assumed full financial and clinical risk for pediatric managed Medicaid enrollees, and is the largest and oldest known pediatric ACO.
A key hurdle was collecting timely, complete, and accurate data for the patient population, Dr. Gleeson said, adding that working with data and understanding changing trends is an everyday challenge. Interacting with busy physicians and securing their time and cooperation also has been an obstacle.
“The lessons learned for us is that we really need to approach them understanding that there is a limited amount of time that practices can invest in infrastructure or invest in the processes of care,” he said. “We have to approach things knowing that [doctors] are going to struggle with the amount of time necessary to engage in large projects, so it needs to be chopped up into bite-sized pieces that they can consume on the run, so they can keep their practices running well.”
PFK efforts have paid off in terms of lowering costs and improving care. Between 2008 and 2013, PFK achieved lower cost growth than Medicaid fee-for-service programs and managed care plans in the Columbus, Ohio, area (Pediatrics. 2015 Mar;135[3];e582-9).
Fundamentally, the model has remained the same over the years, Dr. Gleeson said, but in 2005, PFK made the decision to expand and take responsibility for all the Medicaid-enrolled children in the region.
“It really gives a much broader field of view and perspective on patients in the region,” he said. “We know that they are all our responsibility so we take more of a population health type of approach, working with any physician who is caring for those children.”
Guidance for other practices
Dr. Gleeson encouraged other pediatricians interested in transitioning to value-based care to start by evaluating their data. Take a hard look at the quality of care you provide and begin to measure it, he said. For smaller practices, consider joining a larger group or network that will allow pediatricians to engage in collaborative work, he added.
Dr. Vargas stressed that change is coming whether pediatricians are prepared or not. Aligning with the right partners will be the difference between sinking or staying afloat in the value-based landscape.
“Payers are moving toward value-based models and it is not practical for the general pediatrician to be able to provide the infrastructure and professional resources necessary,” he said. “To maintain our professional livelihood as independent pediatricians, and to continue to provide the individually crafted, quality care our families are accustomed to, we will have to align ourselves with organizations that value the experience and insight of the independent pediatrician to deliver that care.”
[email protected]
On Twitter @legal_med
When Jason Vargas, MD, first moved to the Phoenix area 13 years ago, he found an atmosphere of distant relationships between general pediatricians like him, subspecialists, and hospitals. Getting patients a referral to a subspecialist could take months, and communication among providers was often weak, Dr. Vargas said.
Today, things are vastly different thanks in large part to the clinically integrated network of which Dr. Vargas and 950 area providers are a part.
Phoenix Children’s Care Network (PCCN), established in 2014, coordinates health care across multiple providers and settings in the Phoenix area, including half of all general pediatricians and 80% of pediatric subspecialists practicing in Maricopa County. The network is a value- and risk-based system that provides financial incentives to participating providers and health systems that meet established quality metrics. Patients have access to 950 providers within the network, including primary and specialty care sites of service, urgent care locations, surgery centers, and Phoenix Children’s Hospital.
Meanwhile, 2,000 miles away, another unique payment model is changing the way pediatric care is delivered in the Columbus, Ohio area. Partners For Kids (PFK) is a pediatric accountable care organization (ACO) that coordinates care between Nationwide Children’s Hospital and more than 1,000 doctors. Through its 20-year evolution, PFK has successfully assumed full financial and clinical risk for children under age 19 enrolled in Medicaid managed care. This means PFK is responsible for paying for the costs of all patient care, no matter how much or where that care occurs.
The two models illustrate how pediatricians are affiliating with value-centric networks while keeping their independence, said Timothy Johnson, senior vice president of pediatrics at Valence Health, a consulting firm that helps health providers transition to value-based care.
With MACRA (the Medicare Access and CHIP Reauthorization Act of 2015) “it’s going to be difficult for individual pediatricians to do what is required in a value-based medical system because they just don’t have the resources,” Mr. Johnson said in an interview. “That doesn’t mean they can’t be independent. It means they are going to have to band together in some way, whether with a health system, with other practices. It is extremely important for pediatricians to start thinking about how to do that.”
Going from splintered to unified
Like most communities, care delivery in the Phoenix area was relatively fractured prior to 2014. To bring everyone together, Phoenix Children’s started with community outreach and education.
Along with building trust among providers, project leaders had to overcome operational hurdles. This included creating a process for 110 practices to collectively negotiate contracts, operate under a new structure, and adhere to quality metrics, he said.
“Operationally, you have to take 110 different ways of doing things and try merge them into one common way as you develop these new contractual risk-based models,” he said. “At the same time, we had to transition people away from what they were used to as a purely fee-for-service model. It was a very big operational transition.”
To bolster engagement by community pediatricians, PCCN developed a physician-governance approach, assigning participating providers leadership responsibilities. Participating physicians then worked to create the benchmarks by which doctors are measured against. To date, provider performance is tracked against 14 primary care and 34 specialist metrics encompassing engagement, safety, quality, and transparency.
PCCN leaders also had to ensure that participating in such a network was beneficial for busy doctors, said Dr. Vargas, who is chair of the PCCN Network and Utilization committee and a member of the network’s board of managers.
Asking physicians to change their framework, track patient data, and meet metrics, all while potentially losing money if they fail to hit benchmarks is not the most popular proposition, he said. So PCCN created advantages for member doctors, such as nighttime pediatric triage, a negotiated discount for professional services, IT support, streamlined access to specialists, and more avenues to communicate with subspecialists.
“With so many schedules, professional, and academic pressures on our daily professional lives, we have wanted to make sure that there were practical value added benefits to members,” he said. “I think right now that the benefits outweigh the administrative burdens.”
A changing payer relationship
As a network, PCCN works with payers to assume the risk that insurers have historically taken. Payers continue to handle the administrative and billing side of the equation, while the network controls the medical management and care coordination of the patient population, Mr. Johnson said.
“We feel we can do it much more efficiently, much more effectively, and we feel it’s better care for the patient when we’re the one controlling that,” he said. “The insurance companies don’t disagree.”
The network partners with Medicaid and commercial payers and has a direct-to-employer agreement with a major employer in conjunction with an adult partner system/network. Early performance efforts by the PCCN have been rewarded by shared savings disbursements from two payers, according to PCCN officials. The network has also met or exceeded state Medicaid pediatric quality targets and consistently contained medical expenses below expected medical cost trends for its managed pediatric populations.
Building a population health model
For more than 2 decades, PFK in Ohio has taken a novel care delivery approach that has focused on value and community partnerships.
Back in 1994, Nationwide Children’s Hospital partnered with community pediatricians to create PFK, a physician/hospital organization with governance shared equally. Today, PFK has assumed full financial and clinical risk for pediatric managed Medicaid enrollees, and is the largest and oldest known pediatric ACO.
A key hurdle was collecting timely, complete, and accurate data for the patient population, Dr. Gleeson said, adding that working with data and understanding changing trends is an everyday challenge. Interacting with busy physicians and securing their time and cooperation also has been an obstacle.
“The lessons learned for us is that we really need to approach them understanding that there is a limited amount of time that practices can invest in infrastructure or invest in the processes of care,” he said. “We have to approach things knowing that [doctors] are going to struggle with the amount of time necessary to engage in large projects, so it needs to be chopped up into bite-sized pieces that they can consume on the run, so they can keep their practices running well.”
PFK efforts have paid off in terms of lowering costs and improving care. Between 2008 and 2013, PFK achieved lower cost growth than Medicaid fee-for-service programs and managed care plans in the Columbus, Ohio, area (Pediatrics. 2015 Mar;135[3];e582-9).
Fundamentally, the model has remained the same over the years, Dr. Gleeson said, but in 2005, PFK made the decision to expand and take responsibility for all the Medicaid-enrolled children in the region.
“It really gives a much broader field of view and perspective on patients in the region,” he said. “We know that they are all our responsibility so we take more of a population health type of approach, working with any physician who is caring for those children.”
Guidance for other practices
Dr. Gleeson encouraged other pediatricians interested in transitioning to value-based care to start by evaluating their data. Take a hard look at the quality of care you provide and begin to measure it, he said. For smaller practices, consider joining a larger group or network that will allow pediatricians to engage in collaborative work, he added.
Dr. Vargas stressed that change is coming whether pediatricians are prepared or not. Aligning with the right partners will be the difference between sinking or staying afloat in the value-based landscape.
“Payers are moving toward value-based models and it is not practical for the general pediatrician to be able to provide the infrastructure and professional resources necessary,” he said. “To maintain our professional livelihood as independent pediatricians, and to continue to provide the individually crafted, quality care our families are accustomed to, we will have to align ourselves with organizations that value the experience and insight of the independent pediatrician to deliver that care.”
[email protected]
On Twitter @legal_med
When Jason Vargas, MD, first moved to the Phoenix area 13 years ago, he found an atmosphere of distant relationships between general pediatricians like him, subspecialists, and hospitals. Getting patients a referral to a subspecialist could take months, and communication among providers was often weak, Dr. Vargas said.
Today, things are vastly different thanks in large part to the clinically integrated network of which Dr. Vargas and 950 area providers are a part.
Phoenix Children’s Care Network (PCCN), established in 2014, coordinates health care across multiple providers and settings in the Phoenix area, including half of all general pediatricians and 80% of pediatric subspecialists practicing in Maricopa County. The network is a value- and risk-based system that provides financial incentives to participating providers and health systems that meet established quality metrics. Patients have access to 950 providers within the network, including primary and specialty care sites of service, urgent care locations, surgery centers, and Phoenix Children’s Hospital.
Meanwhile, 2,000 miles away, another unique payment model is changing the way pediatric care is delivered in the Columbus, Ohio area. Partners For Kids (PFK) is a pediatric accountable care organization (ACO) that coordinates care between Nationwide Children’s Hospital and more than 1,000 doctors. Through its 20-year evolution, PFK has successfully assumed full financial and clinical risk for children under age 19 enrolled in Medicaid managed care. This means PFK is responsible for paying for the costs of all patient care, no matter how much or where that care occurs.
The two models illustrate how pediatricians are affiliating with value-centric networks while keeping their independence, said Timothy Johnson, senior vice president of pediatrics at Valence Health, a consulting firm that helps health providers transition to value-based care.
With MACRA (the Medicare Access and CHIP Reauthorization Act of 2015) “it’s going to be difficult for individual pediatricians to do what is required in a value-based medical system because they just don’t have the resources,” Mr. Johnson said in an interview. “That doesn’t mean they can’t be independent. It means they are going to have to band together in some way, whether with a health system, with other practices. It is extremely important for pediatricians to start thinking about how to do that.”
Going from splintered to unified
Like most communities, care delivery in the Phoenix area was relatively fractured prior to 2014. To bring everyone together, Phoenix Children’s started with community outreach and education.
Along with building trust among providers, project leaders had to overcome operational hurdles. This included creating a process for 110 practices to collectively negotiate contracts, operate under a new structure, and adhere to quality metrics, he said.
“Operationally, you have to take 110 different ways of doing things and try merge them into one common way as you develop these new contractual risk-based models,” he said. “At the same time, we had to transition people away from what they were used to as a purely fee-for-service model. It was a very big operational transition.”
To bolster engagement by community pediatricians, PCCN developed a physician-governance approach, assigning participating providers leadership responsibilities. Participating physicians then worked to create the benchmarks by which doctors are measured against. To date, provider performance is tracked against 14 primary care and 34 specialist metrics encompassing engagement, safety, quality, and transparency.
PCCN leaders also had to ensure that participating in such a network was beneficial for busy doctors, said Dr. Vargas, who is chair of the PCCN Network and Utilization committee and a member of the network’s board of managers.
Asking physicians to change their framework, track patient data, and meet metrics, all while potentially losing money if they fail to hit benchmarks is not the most popular proposition, he said. So PCCN created advantages for member doctors, such as nighttime pediatric triage, a negotiated discount for professional services, IT support, streamlined access to specialists, and more avenues to communicate with subspecialists.
“With so many schedules, professional, and academic pressures on our daily professional lives, we have wanted to make sure that there were practical value added benefits to members,” he said. “I think right now that the benefits outweigh the administrative burdens.”
A changing payer relationship
As a network, PCCN works with payers to assume the risk that insurers have historically taken. Payers continue to handle the administrative and billing side of the equation, while the network controls the medical management and care coordination of the patient population, Mr. Johnson said.
“We feel we can do it much more efficiently, much more effectively, and we feel it’s better care for the patient when we’re the one controlling that,” he said. “The insurance companies don’t disagree.”
The network partners with Medicaid and commercial payers and has a direct-to-employer agreement with a major employer in conjunction with an adult partner system/network. Early performance efforts by the PCCN have been rewarded by shared savings disbursements from two payers, according to PCCN officials. The network has also met or exceeded state Medicaid pediatric quality targets and consistently contained medical expenses below expected medical cost trends for its managed pediatric populations.
Building a population health model
For more than 2 decades, PFK in Ohio has taken a novel care delivery approach that has focused on value and community partnerships.
Back in 1994, Nationwide Children’s Hospital partnered with community pediatricians to create PFK, a physician/hospital organization with governance shared equally. Today, PFK has assumed full financial and clinical risk for pediatric managed Medicaid enrollees, and is the largest and oldest known pediatric ACO.
A key hurdle was collecting timely, complete, and accurate data for the patient population, Dr. Gleeson said, adding that working with data and understanding changing trends is an everyday challenge. Interacting with busy physicians and securing their time and cooperation also has been an obstacle.
“The lessons learned for us is that we really need to approach them understanding that there is a limited amount of time that practices can invest in infrastructure or invest in the processes of care,” he said. “We have to approach things knowing that [doctors] are going to struggle with the amount of time necessary to engage in large projects, so it needs to be chopped up into bite-sized pieces that they can consume on the run, so they can keep their practices running well.”
PFK efforts have paid off in terms of lowering costs and improving care. Between 2008 and 2013, PFK achieved lower cost growth than Medicaid fee-for-service programs and managed care plans in the Columbus, Ohio, area (Pediatrics. 2015 Mar;135[3];e582-9).
Fundamentally, the model has remained the same over the years, Dr. Gleeson said, but in 2005, PFK made the decision to expand and take responsibility for all the Medicaid-enrolled children in the region.
“It really gives a much broader field of view and perspective on patients in the region,” he said. “We know that they are all our responsibility so we take more of a population health type of approach, working with any physician who is caring for those children.”
Guidance for other practices
Dr. Gleeson encouraged other pediatricians interested in transitioning to value-based care to start by evaluating their data. Take a hard look at the quality of care you provide and begin to measure it, he said. For smaller practices, consider joining a larger group or network that will allow pediatricians to engage in collaborative work, he added.
Dr. Vargas stressed that change is coming whether pediatricians are prepared or not. Aligning with the right partners will be the difference between sinking or staying afloat in the value-based landscape.
“Payers are moving toward value-based models and it is not practical for the general pediatrician to be able to provide the infrastructure and professional resources necessary,” he said. “To maintain our professional livelihood as independent pediatricians, and to continue to provide the individually crafted, quality care our families are accustomed to, we will have to align ourselves with organizations that value the experience and insight of the independent pediatrician to deliver that care.”
[email protected]
On Twitter @legal_med
Algorithm for suspected pulmonary embolism safely cut CT rate
ROME – A newly validated, simplified algorithm for the management of patients with suspected acute pulmonary embolism enables physicians to safely exclude the disorder in roughly half of patients without resorting to CT pulmonary angiography, Tom van der Hulle, MD, reported at the annual congress of the European Society of Cardiology.
“This is the largest study ever performed in the diagnostic management of suspected pulmonary embolism. Based on our results, I think the YEARS algorithm is ready to be used in daily clinical practice,” declared Dr. van der Hulle of the department of thrombosis and hemostasis at Leiden (the Netherlands) University Medical Center.
Using the YEARS algorithm, PE was reliably ruled out without need for CT pulmonary angiography – considered the standard in the diagnosis of PE – in 48% of patients. In contrast, adherence to the Wells rule would have meant that 62% of patients would have gotten a CT scan to rule out PE with a comparably high degree of accuracy.
But that 62% figure underestimates the actual CT rate in clinical practice. The reality is that although the guideline-recommended Wells rule and revised Geneva score have been shown to be safe and accurate, they are so complex, cumbersome, and out of sync with the flow of routine clinical practice that many physicians skip the algorithms and go straight to CT, Dr. van der Hulle said. This approach results in many unnecessary CTs, needlessly exposing patients to the risks of radiation and intravenous contrast material while driving up health care costs, he added.
Using the Wells rule or revised Geneva score, the patient evaluation begins with an assessment of the clinical probability of PE based upon a risk score involving seven or eight factors. Only patients with a low or intermediate clinical probability of PE get a D-dimer test; those with a high clinical probability go straight to CT.
The YEARS algorithm is much simpler than that, Dr. van der Hulle explained. Everyone who presents with suspected acute PE gets a D-dimer test while the physician simultaneously applies a brief, three-item clinical prediction rule. These three items were selected by the Dutch investigators because they were the three strongest predictors of PE out of the original seven in the Wells rule. They are hemoptysis, clinical signs of deep vein thrombosis such as leg swelling or hyperpigmentation, and the clinician’s global impression of PE as being the most likely diagnosis.
In the YEARS algorithm, the threshold for a positive D-dimer test warranting CT pulmonary angiography depends upon whether any of the three clinical predictors is present. If none is present, the threshold is 1,000 ng/mL or above; if one or more is present, the threshold for a positive D-dimer test drops to 500 ng/mL.
Using these criteria, PE was excluded without resort to CT in 1,306 patients with none of the three YEARS items and a D-dimer test result below 1,000 ng/mL, as well as in another 327 patients with one or more YEARS items present but a D-dimer below 500 ng/mL. Those two groups were left untreated and followed prospectively for 3 months.
The 964 patients with one or more YEARS predictors present and a D-dimer score of at least 500 ng/mL underwent CT imaging, as did the 352 with no YEARS items and a D-dimer of at least 1,000 ng/mL.
The prevalence of CT-confirmed PE in the study was 13.2%. Affected patients were treated with anticoagulants.
The primary study endpoint was the total rate of deep vein thrombosis during 3 months of follow-up after PE had been excluded. The rate was 0.61%, including a fatal PE rate of 0.20%. The rate in patients managed without CT was 0.43%, including a 0.12% rate of fatal PE. In patients managed with diagnostic CT, the deep vein thrombosis rate was 0.84%, with a fatal PE rate of 0.30%.
“I think these results are completely comparable to those in previous studies using the standard algorithms,” Dr. van der Hulle commented.
The study’s main limitation is that it wasn’t a randomized, controlled trial. But given the tiny event rates, detecting any small differences between management strategies would require an unrealistically huge sample size, he added.
Asked if he thinks physicians will actually use the new tool, Dr. van der Hulle replied that some physicians feel driven to be 100% sure that a patient doesn’t have PE, and they will probably keep overordering CT scans. But others will embrace the YEARS algorithm because it reduces wasted resources and minimizes radiation exposure, a particularly compelling consideration in young female patients.
Discussant Marion Delcroix, MD, had reservations. She said she appreciated the appeal of a simple algorithm, but she asked, “Couldn’t we do better with a bit more sophistication, perhaps by adjusting the D-dimer cutoff for age and also adding some other items, like oxygen saturation and estrogen use?
“My concern is about the applicability. The age of the study cohort is relatively young, at a mean of 53 years. The peak age of PE in a very large contemporary German database is 70-80 years. We don’t know if the YEARS score is any good in this older population,” asserted Dr. Delcroix, professor of medicine and respiratory physiology and head of the center for pulmonary vascular diseases at University Hospital in Leuven, Belgium.
“If the aim is to decrease the number of CT pulmonary angiograms for safety reasons, why not reintroduce compression ultrasound of the lower limbs in the diagnostic algorithm?” she continued. “It has been shown to effectively reduce the need for further imaging.”
Dr. Delcroix predicted that the YEARS algorithm study will prove “too optimistic” regarding the number of CT scans avoided, particularly in elderly patients.
The YEARS study was funded by the trial’s 12 participating Dutch hospitals. Dr. van der Hulle reported having no financial conflicts of interest.
ROME – A newly validated, simplified algorithm for the management of patients with suspected acute pulmonary embolism enables physicians to safely exclude the disorder in roughly half of patients without resorting to CT pulmonary angiography, Tom van der Hulle, MD, reported at the annual congress of the European Society of Cardiology.
“This is the largest study ever performed in the diagnostic management of suspected pulmonary embolism. Based on our results, I think the YEARS algorithm is ready to be used in daily clinical practice,” declared Dr. van der Hulle of the department of thrombosis and hemostasis at Leiden (the Netherlands) University Medical Center.
Using the YEARS algorithm, PE was reliably ruled out without need for CT pulmonary angiography – considered the standard in the diagnosis of PE – in 48% of patients. In contrast, adherence to the Wells rule would have meant that 62% of patients would have gotten a CT scan to rule out PE with a comparably high degree of accuracy.
But that 62% figure underestimates the actual CT rate in clinical practice. The reality is that although the guideline-recommended Wells rule and revised Geneva score have been shown to be safe and accurate, they are so complex, cumbersome, and out of sync with the flow of routine clinical practice that many physicians skip the algorithms and go straight to CT, Dr. van der Hulle said. This approach results in many unnecessary CTs, needlessly exposing patients to the risks of radiation and intravenous contrast material while driving up health care costs, he added.
Using the Wells rule or revised Geneva score, the patient evaluation begins with an assessment of the clinical probability of PE based upon a risk score involving seven or eight factors. Only patients with a low or intermediate clinical probability of PE get a D-dimer test; those with a high clinical probability go straight to CT.
The YEARS algorithm is much simpler than that, Dr. van der Hulle explained. Everyone who presents with suspected acute PE gets a D-dimer test while the physician simultaneously applies a brief, three-item clinical prediction rule. These three items were selected by the Dutch investigators because they were the three strongest predictors of PE out of the original seven in the Wells rule. They are hemoptysis, clinical signs of deep vein thrombosis such as leg swelling or hyperpigmentation, and the clinician’s global impression of PE as being the most likely diagnosis.
In the YEARS algorithm, the threshold for a positive D-dimer test warranting CT pulmonary angiography depends upon whether any of the three clinical predictors is present. If none is present, the threshold is 1,000 ng/mL or above; if one or more is present, the threshold for a positive D-dimer test drops to 500 ng/mL.
Using these criteria, PE was excluded without resort to CT in 1,306 patients with none of the three YEARS items and a D-dimer test result below 1,000 ng/mL, as well as in another 327 patients with one or more YEARS items present but a D-dimer below 500 ng/mL. Those two groups were left untreated and followed prospectively for 3 months.
The 964 patients with one or more YEARS predictors present and a D-dimer score of at least 500 ng/mL underwent CT imaging, as did the 352 with no YEARS items and a D-dimer of at least 1,000 ng/mL.
The prevalence of CT-confirmed PE in the study was 13.2%. Affected patients were treated with anticoagulants.
The primary study endpoint was the total rate of deep vein thrombosis during 3 months of follow-up after PE had been excluded. The rate was 0.61%, including a fatal PE rate of 0.20%. The rate in patients managed without CT was 0.43%, including a 0.12% rate of fatal PE. In patients managed with diagnostic CT, the deep vein thrombosis rate was 0.84%, with a fatal PE rate of 0.30%.
“I think these results are completely comparable to those in previous studies using the standard algorithms,” Dr. van der Hulle commented.
The study’s main limitation is that it wasn’t a randomized, controlled trial. But given the tiny event rates, detecting any small differences between management strategies would require an unrealistically huge sample size, he added.
Asked if he thinks physicians will actually use the new tool, Dr. van der Hulle replied that some physicians feel driven to be 100% sure that a patient doesn’t have PE, and they will probably keep overordering CT scans. But others will embrace the YEARS algorithm because it reduces wasted resources and minimizes radiation exposure, a particularly compelling consideration in young female patients.
Discussant Marion Delcroix, MD, had reservations. She said she appreciated the appeal of a simple algorithm, but she asked, “Couldn’t we do better with a bit more sophistication, perhaps by adjusting the D-dimer cutoff for age and also adding some other items, like oxygen saturation and estrogen use?
“My concern is about the applicability. The age of the study cohort is relatively young, at a mean of 53 years. The peak age of PE in a very large contemporary German database is 70-80 years. We don’t know if the YEARS score is any good in this older population,” asserted Dr. Delcroix, professor of medicine and respiratory physiology and head of the center for pulmonary vascular diseases at University Hospital in Leuven, Belgium.
“If the aim is to decrease the number of CT pulmonary angiograms for safety reasons, why not reintroduce compression ultrasound of the lower limbs in the diagnostic algorithm?” she continued. “It has been shown to effectively reduce the need for further imaging.”
Dr. Delcroix predicted that the YEARS algorithm study will prove “too optimistic” regarding the number of CT scans avoided, particularly in elderly patients.
The YEARS study was funded by the trial’s 12 participating Dutch hospitals. Dr. van der Hulle reported having no financial conflicts of interest.
ROME – A newly validated, simplified algorithm for the management of patients with suspected acute pulmonary embolism enables physicians to safely exclude the disorder in roughly half of patients without resorting to CT pulmonary angiography, Tom van der Hulle, MD, reported at the annual congress of the European Society of Cardiology.
“This is the largest study ever performed in the diagnostic management of suspected pulmonary embolism. Based on our results, I think the YEARS algorithm is ready to be used in daily clinical practice,” declared Dr. van der Hulle of the department of thrombosis and hemostasis at Leiden (the Netherlands) University Medical Center.
Using the YEARS algorithm, PE was reliably ruled out without need for CT pulmonary angiography – considered the standard in the diagnosis of PE – in 48% of patients. In contrast, adherence to the Wells rule would have meant that 62% of patients would have gotten a CT scan to rule out PE with a comparably high degree of accuracy.
But that 62% figure underestimates the actual CT rate in clinical practice. The reality is that although the guideline-recommended Wells rule and revised Geneva score have been shown to be safe and accurate, they are so complex, cumbersome, and out of sync with the flow of routine clinical practice that many physicians skip the algorithms and go straight to CT, Dr. van der Hulle said. This approach results in many unnecessary CTs, needlessly exposing patients to the risks of radiation and intravenous contrast material while driving up health care costs, he added.
Using the Wells rule or revised Geneva score, the patient evaluation begins with an assessment of the clinical probability of PE based upon a risk score involving seven or eight factors. Only patients with a low or intermediate clinical probability of PE get a D-dimer test; those with a high clinical probability go straight to CT.
The YEARS algorithm is much simpler than that, Dr. van der Hulle explained. Everyone who presents with suspected acute PE gets a D-dimer test while the physician simultaneously applies a brief, three-item clinical prediction rule. These three items were selected by the Dutch investigators because they were the three strongest predictors of PE out of the original seven in the Wells rule. They are hemoptysis, clinical signs of deep vein thrombosis such as leg swelling or hyperpigmentation, and the clinician’s global impression of PE as being the most likely diagnosis.
In the YEARS algorithm, the threshold for a positive D-dimer test warranting CT pulmonary angiography depends upon whether any of the three clinical predictors is present. If none is present, the threshold is 1,000 ng/mL or above; if one or more is present, the threshold for a positive D-dimer test drops to 500 ng/mL.
Using these criteria, PE was excluded without resort to CT in 1,306 patients with none of the three YEARS items and a D-dimer test result below 1,000 ng/mL, as well as in another 327 patients with one or more YEARS items present but a D-dimer below 500 ng/mL. Those two groups were left untreated and followed prospectively for 3 months.
The 964 patients with one or more YEARS predictors present and a D-dimer score of at least 500 ng/mL underwent CT imaging, as did the 352 with no YEARS items and a D-dimer of at least 1,000 ng/mL.
The prevalence of CT-confirmed PE in the study was 13.2%. Affected patients were treated with anticoagulants.
The primary study endpoint was the total rate of deep vein thrombosis during 3 months of follow-up after PE had been excluded. The rate was 0.61%, including a fatal PE rate of 0.20%. The rate in patients managed without CT was 0.43%, including a 0.12% rate of fatal PE. In patients managed with diagnostic CT, the deep vein thrombosis rate was 0.84%, with a fatal PE rate of 0.30%.
“I think these results are completely comparable to those in previous studies using the standard algorithms,” Dr. van der Hulle commented.
The study’s main limitation is that it wasn’t a randomized, controlled trial. But given the tiny event rates, detecting any small differences between management strategies would require an unrealistically huge sample size, he added.
Asked if he thinks physicians will actually use the new tool, Dr. van der Hulle replied that some physicians feel driven to be 100% sure that a patient doesn’t have PE, and they will probably keep overordering CT scans. But others will embrace the YEARS algorithm because it reduces wasted resources and minimizes radiation exposure, a particularly compelling consideration in young female patients.
Discussant Marion Delcroix, MD, had reservations. She said she appreciated the appeal of a simple algorithm, but she asked, “Couldn’t we do better with a bit more sophistication, perhaps by adjusting the D-dimer cutoff for age and also adding some other items, like oxygen saturation and estrogen use?
“My concern is about the applicability. The age of the study cohort is relatively young, at a mean of 53 years. The peak age of PE in a very large contemporary German database is 70-80 years. We don’t know if the YEARS score is any good in this older population,” asserted Dr. Delcroix, professor of medicine and respiratory physiology and head of the center for pulmonary vascular diseases at University Hospital in Leuven, Belgium.
“If the aim is to decrease the number of CT pulmonary angiograms for safety reasons, why not reintroduce compression ultrasound of the lower limbs in the diagnostic algorithm?” she continued. “It has been shown to effectively reduce the need for further imaging.”
Dr. Delcroix predicted that the YEARS algorithm study will prove “too optimistic” regarding the number of CT scans avoided, particularly in elderly patients.
The YEARS study was funded by the trial’s 12 participating Dutch hospitals. Dr. van der Hulle reported having no financial conflicts of interest.
Key clinical point:
Major finding: Applying the YEARS algorithm to a large population of patients with suspected PE, the 3-month incidence of deep vein thrombosis after PE had been excluded was 0.61%.
Data source: This was a prospective study of clinical outcomes in nearly 3,000 consecutive Dutch patients who presented with suspected acute PE and were managed in accord with the YEARS algorithm.
Disclosures: The YEARS algorithm validation study was funded by the trial’s 12 participating Dutch hospitals. The study presenter reported having no financial conflicts of interest.
‘Bionic pancreas’ employs glucagon and insulin to stabilize blood sugar
MUNICH – A “bionic pancreas” that delivers glucagon as well as insulin fared well against conventional insulin pump therapy, significantly reducing mean glucose levels and minimizing time spent in hypoglycemia.
The iLet bionic pancreas is being developed by Beta Bionics in conjunction with Eli Lilly and with support from the National Institutes of Health. Beta Bionics bills itself as a public benefit corporation – “a for-profit entity also dedicated to social responsibility and a public benefit mission,” according to an article published by Boston University.
Glucagon is the key that takes the bionic pancreas above and beyond what current insulin pump systems can do, said Dr. Russell, an endocrinologist at Massachusetts General Hospital, Boston.
“Even the pancreas, which has all the advantages of releasing insulin right into the portal vein and directly sensing glucose in the blood, uses the countering hormone, glucagon, to prevent hypoglycemia, particularly during exercise and in the late postprandial phase,” he said. “We are trying to mimic that capability. Glucagon gives us an additional tool to further reduce the risk of hypoglycemia.”
The algorithm is almost completely independent of user input – another key benefit, Dr. Russell said. It initializes with input about the patient’s weight and adapts its insulin delivery by essentially learning each user. There is no need to count carbohydrates, for example. The system “learns” over time its user’s typical meal patterns and can be programmed to deliver insulin accordingly.
“The user can enter, for example, ‘typical lunch,’ and the system will dispense some insulin before the meal and the rest later, in automatic delivery mode.”
The iLet has been studied in several settings and populations including, most recently, a successful crossover trial in 19 children at a diabetes camp (Lancet Diabetes Endocrinol. 2016; 4[3]:233-43).
The device was similarly successful in both teens and adults.
The study Dr. Russell reported at EASD 2016 comprised 39 patients with type 1 diabetes who were using an insulin pump. The mean age of the patients was 33 years, and mean disease duration was 17 years. The mean daily insulin dose was 0.6 U/kg. The mean baseline hemoglobin A1c was 7.7% and mean blood glucose, 176 mg/dL.
The crossover trial randomized patients to 11 days of treatment with their existing Medtronic insulin pump or the iLet system. The primary outcomes were the mean glucose level and time spent in hypoglycemic range (less than 60 mg/dL).
Under the usual care arm, “We saw a wide range of glucose values, which became much tighter when patients were using the bionic pancreas,” Dr. Russell said.
The overall average glucose level was 9 mmol/L in the usual care arm vs. 7.8 mmol/L in the bionic pancreas arm. Time in hypoglycemia was significantly reduced (27 minutes/24 hours vs. 9 minutes/24 hours).
“The standard deviation of the mean glucose was also larger in usual care, which is consistent with the automatic adaptive function of the bionic pancreas. If the mean glucose gets too high, it treats more aggressively; and if glucose is too low, it becomes less aggressive.”
The average amount of insulin used per day was similar (0.62 U/kg vs. 0.66 U/kg) and the average amount of glucagon used was 0.5 mg/day in each group.
During the night, the bionic pancreas kept mean blood glucose lower (134 mg/dL vs. 165 mg/dL) and more stable, reducing time in hypoglycemia (1.4 minutes/night vs. 4.8 minutes/night).
There was one incident of severe hypoglycemia in the usual-care arm, and none in the bionic-pancreas arm. There was a statistically significant increase in nausea associated with the glucagon, Dr. Russell noted, but the impact was still quite small. On a 0-10 rating scale, nausea in the bionic pancreas group was rated a 0.5 compared to a 0.05 in the usual care arm.
There were no changes in blood pressure, weight, or any lab test.
The ongoing studies continue to show “that automated bihormonal control of glycemia in the home-use setting is feasible,” Dr. Russell said. “Micro-dose glucagon was well tolerated and the bihormonal pancreas reduced both mean glucose and hypoglycemia relative to the patients’ usual care devices.”
The iLet continues to undergo modifications that are making it more user friendly, he added.
Dr. Stevens disclosed that he has a patent pending on “certain aspects” of the device, and that he is an unpaid scientific consultant for Beta Bionics. He also disclosed financial relationships with several pharmaceutical and device companies, including Eli Lilly and Medtronic.
MUNICH – A “bionic pancreas” that delivers glucagon as well as insulin fared well against conventional insulin pump therapy, significantly reducing mean glucose levels and minimizing time spent in hypoglycemia.
The iLet bionic pancreas is being developed by Beta Bionics in conjunction with Eli Lilly and with support from the National Institutes of Health. Beta Bionics bills itself as a public benefit corporation – “a for-profit entity also dedicated to social responsibility and a public benefit mission,” according to an article published by Boston University.
Glucagon is the key that takes the bionic pancreas above and beyond what current insulin pump systems can do, said Dr. Russell, an endocrinologist at Massachusetts General Hospital, Boston.
“Even the pancreas, which has all the advantages of releasing insulin right into the portal vein and directly sensing glucose in the blood, uses the countering hormone, glucagon, to prevent hypoglycemia, particularly during exercise and in the late postprandial phase,” he said. “We are trying to mimic that capability. Glucagon gives us an additional tool to further reduce the risk of hypoglycemia.”
The algorithm is almost completely independent of user input – another key benefit, Dr. Russell said. It initializes with input about the patient’s weight and adapts its insulin delivery by essentially learning each user. There is no need to count carbohydrates, for example. The system “learns” over time its user’s typical meal patterns and can be programmed to deliver insulin accordingly.
“The user can enter, for example, ‘typical lunch,’ and the system will dispense some insulin before the meal and the rest later, in automatic delivery mode.”
The iLet has been studied in several settings and populations including, most recently, a successful crossover trial in 19 children at a diabetes camp (Lancet Diabetes Endocrinol. 2016; 4[3]:233-43).
The device was similarly successful in both teens and adults.
The study Dr. Russell reported at EASD 2016 comprised 39 patients with type 1 diabetes who were using an insulin pump. The mean age of the patients was 33 years, and mean disease duration was 17 years. The mean daily insulin dose was 0.6 U/kg. The mean baseline hemoglobin A1c was 7.7% and mean blood glucose, 176 mg/dL.
The crossover trial randomized patients to 11 days of treatment with their existing Medtronic insulin pump or the iLet system. The primary outcomes were the mean glucose level and time spent in hypoglycemic range (less than 60 mg/dL).
Under the usual care arm, “We saw a wide range of glucose values, which became much tighter when patients were using the bionic pancreas,” Dr. Russell said.
The overall average glucose level was 9 mmol/L in the usual care arm vs. 7.8 mmol/L in the bionic pancreas arm. Time in hypoglycemia was significantly reduced (27 minutes/24 hours vs. 9 minutes/24 hours).
“The standard deviation of the mean glucose was also larger in usual care, which is consistent with the automatic adaptive function of the bionic pancreas. If the mean glucose gets too high, it treats more aggressively; and if glucose is too low, it becomes less aggressive.”
The average amount of insulin used per day was similar (0.62 U/kg vs. 0.66 U/kg) and the average amount of glucagon used was 0.5 mg/day in each group.
During the night, the bionic pancreas kept mean blood glucose lower (134 mg/dL vs. 165 mg/dL) and more stable, reducing time in hypoglycemia (1.4 minutes/night vs. 4.8 minutes/night).
There was one incident of severe hypoglycemia in the usual-care arm, and none in the bionic-pancreas arm. There was a statistically significant increase in nausea associated with the glucagon, Dr. Russell noted, but the impact was still quite small. On a 0-10 rating scale, nausea in the bionic pancreas group was rated a 0.5 compared to a 0.05 in the usual care arm.
There were no changes in blood pressure, weight, or any lab test.
The ongoing studies continue to show “that automated bihormonal control of glycemia in the home-use setting is feasible,” Dr. Russell said. “Micro-dose glucagon was well tolerated and the bihormonal pancreas reduced both mean glucose and hypoglycemia relative to the patients’ usual care devices.”
The iLet continues to undergo modifications that are making it more user friendly, he added.
Dr. Stevens disclosed that he has a patent pending on “certain aspects” of the device, and that he is an unpaid scientific consultant for Beta Bionics. He also disclosed financial relationships with several pharmaceutical and device companies, including Eli Lilly and Medtronic.
MUNICH – A “bionic pancreas” that delivers glucagon as well as insulin fared well against conventional insulin pump therapy, significantly reducing mean glucose levels and minimizing time spent in hypoglycemia.
The iLet bionic pancreas is being developed by Beta Bionics in conjunction with Eli Lilly and with support from the National Institutes of Health. Beta Bionics bills itself as a public benefit corporation – “a for-profit entity also dedicated to social responsibility and a public benefit mission,” according to an article published by Boston University.
Glucagon is the key that takes the bionic pancreas above and beyond what current insulin pump systems can do, said Dr. Russell, an endocrinologist at Massachusetts General Hospital, Boston.
“Even the pancreas, which has all the advantages of releasing insulin right into the portal vein and directly sensing glucose in the blood, uses the countering hormone, glucagon, to prevent hypoglycemia, particularly during exercise and in the late postprandial phase,” he said. “We are trying to mimic that capability. Glucagon gives us an additional tool to further reduce the risk of hypoglycemia.”
The algorithm is almost completely independent of user input – another key benefit, Dr. Russell said. It initializes with input about the patient’s weight and adapts its insulin delivery by essentially learning each user. There is no need to count carbohydrates, for example. The system “learns” over time its user’s typical meal patterns and can be programmed to deliver insulin accordingly.
“The user can enter, for example, ‘typical lunch,’ and the system will dispense some insulin before the meal and the rest later, in automatic delivery mode.”
The iLet has been studied in several settings and populations including, most recently, a successful crossover trial in 19 children at a diabetes camp (Lancet Diabetes Endocrinol. 2016; 4[3]:233-43).
The device was similarly successful in both teens and adults.
The study Dr. Russell reported at EASD 2016 comprised 39 patients with type 1 diabetes who were using an insulin pump. The mean age of the patients was 33 years, and mean disease duration was 17 years. The mean daily insulin dose was 0.6 U/kg. The mean baseline hemoglobin A1c was 7.7% and mean blood glucose, 176 mg/dL.
The crossover trial randomized patients to 11 days of treatment with their existing Medtronic insulin pump or the iLet system. The primary outcomes were the mean glucose level and time spent in hypoglycemic range (less than 60 mg/dL).
Under the usual care arm, “We saw a wide range of glucose values, which became much tighter when patients were using the bionic pancreas,” Dr. Russell said.
The overall average glucose level was 9 mmol/L in the usual care arm vs. 7.8 mmol/L in the bionic pancreas arm. Time in hypoglycemia was significantly reduced (27 minutes/24 hours vs. 9 minutes/24 hours).
“The standard deviation of the mean glucose was also larger in usual care, which is consistent with the automatic adaptive function of the bionic pancreas. If the mean glucose gets too high, it treats more aggressively; and if glucose is too low, it becomes less aggressive.”
The average amount of insulin used per day was similar (0.62 U/kg vs. 0.66 U/kg) and the average amount of glucagon used was 0.5 mg/day in each group.
During the night, the bionic pancreas kept mean blood glucose lower (134 mg/dL vs. 165 mg/dL) and more stable, reducing time in hypoglycemia (1.4 minutes/night vs. 4.8 minutes/night).
There was one incident of severe hypoglycemia in the usual-care arm, and none in the bionic-pancreas arm. There was a statistically significant increase in nausea associated with the glucagon, Dr. Russell noted, but the impact was still quite small. On a 0-10 rating scale, nausea in the bionic pancreas group was rated a 0.5 compared to a 0.05 in the usual care arm.
There were no changes in blood pressure, weight, or any lab test.
The ongoing studies continue to show “that automated bihormonal control of glycemia in the home-use setting is feasible,” Dr. Russell said. “Micro-dose glucagon was well tolerated and the bihormonal pancreas reduced both mean glucose and hypoglycemia relative to the patients’ usual care devices.”
The iLet continues to undergo modifications that are making it more user friendly, he added.
Dr. Stevens disclosed that he has a patent pending on “certain aspects” of the device, and that he is an unpaid scientific consultant for Beta Bionics. He also disclosed financial relationships with several pharmaceutical and device companies, including Eli Lilly and Medtronic.
Key clinical point:
Major finding: The overall average glucose level was 9 mmol/L in the usual care arm vs. 7.8 mmol/L in the bionic pancreas arm.
Data source: The randomized crossover trial comprised 39 patients with type 1 diabetes.
Disclosures: Dr. Stevens disclosed that he has a patent pending on “certain aspects” of the device and that he is an unpaid scientific consultant for Beta Bionics. He disclosed financial relationships with several pharmaceutical and device companies, including Eli Lilly and Medtronic.
Seven days of antibiotics sufficient for most hospital-acquired pneumonia
A 1-week course of antibiotics is sufficient for most hospital-acquired and ventilator-associated pneumonia, regardless of the microbial etiology of the infection, according to an updated Clinical Practice Guidelines for managing adults with these disorders.
In addition, every hospital should develop its own antibiogram to align clinicians’ choice of treatments with the local distribution of likely pathogens and their antimicrobial susceptibilities. Both of these recommendations, as well as others that are also new to the updated guidelines, are intended to minimize patient exposure to unnecessary antibiotics and reduce antibiotic resistance, said Andre C. Kalil, MD, and Mark L. Metersky, MD, cochairs of the guidelines panel of 18 experts in infectious diseases, pulmonary medicine, critical care medicine, laboratory medicine, microbiology, pharmacology, and guideline methodology.
The guidelines, an update of the last version issued in 2005 and developed jointly by representatives of the Infectious Disease Society of America (including Dr. Kalil) and the American Thoracic Society (including Dr. Metersky), are intended for use by all clinicians who care for patients at risk for hospital-acquired pneumonia (HAP) or ventilator-associated pneumonia (VAP), including surgeons, anesthesiologists, and hospitalists as well as specialists in infectious diseases, pulmonary diseases, and critical care. The guidelines no longer use the concept of health care–associated pneumonia (HCAP), chiefly because new evidence shows that designation is too general: HCAP patients are not at high risk for multidrug-resistant organisms simply because of their contact with the health care system, the guidelines panel wrote (Clin Infect Dis. 2016 Sep 1;63[5]:e61-e111).
The IDSA/ATS Guidelines strongly recommend short-course (1-week) antibiotic therapy instead of longer courses for both HAP and VAP and assert that antibiotic doses should be de-escalated rather than fixed. It advises that serum procalcitonin level plus clinical criteria, not just clinical criteria alone, should be used to guide antibiotic discontinuation, and suggests that the Clinical Pulmonary Infection Score not be used to guide discontinuation.
The guidelines also address empiric treatments when MRSA is suspected and give detailed guidance for selecting antibiotics once the causative organism is identified, including Pseudomonas aeruginosa, extended-spectrum beta-lactamase–producing gram-negative bacilli, Acinetobacter species, and pathogens resistant to carbapenem.
The guidelines include numerous other recommendations concerning the diagnosis of HAP and VAP, the optimal initial treatments, the pharmacokinetic and pharmacodynamic optimization of antibiotic therapies, and the use of inhaled antibiotics. All the recommendations “are a compromise between the competing goals of providing early appropriate antibiotic coverage and avoiding superfluous treatment that may lead to adverse drug effects, Clostridium difficile infections, antibiotic resistance, and increased costs,” the guidelines panel noted.
The full-text guidelines, including details about the panel’s methodology in reviewing the current literature and the summaries of evidence that support each recommendation, is available free on the Clinical Infectious Diseases website.
The Infectious Diseases Society of America and the American Thoracic Society provided financial and administrative support to develop the guidelines. No industry funding was permitted. Dr. Kalil reported having no potential conflicts of interest; Dr. Metersky reported ties to Aradigm, Gilead, Pfizer, Bayer, and their associates reported ties to numerous industry sources.
A 1-week course of antibiotics is sufficient for most hospital-acquired and ventilator-associated pneumonia, regardless of the microbial etiology of the infection, according to an updated Clinical Practice Guidelines for managing adults with these disorders.
In addition, every hospital should develop its own antibiogram to align clinicians’ choice of treatments with the local distribution of likely pathogens and their antimicrobial susceptibilities. Both of these recommendations, as well as others that are also new to the updated guidelines, are intended to minimize patient exposure to unnecessary antibiotics and reduce antibiotic resistance, said Andre C. Kalil, MD, and Mark L. Metersky, MD, cochairs of the guidelines panel of 18 experts in infectious diseases, pulmonary medicine, critical care medicine, laboratory medicine, microbiology, pharmacology, and guideline methodology.
The guidelines, an update of the last version issued in 2005 and developed jointly by representatives of the Infectious Disease Society of America (including Dr. Kalil) and the American Thoracic Society (including Dr. Metersky), are intended for use by all clinicians who care for patients at risk for hospital-acquired pneumonia (HAP) or ventilator-associated pneumonia (VAP), including surgeons, anesthesiologists, and hospitalists as well as specialists in infectious diseases, pulmonary diseases, and critical care. The guidelines no longer use the concept of health care–associated pneumonia (HCAP), chiefly because new evidence shows that designation is too general: HCAP patients are not at high risk for multidrug-resistant organisms simply because of their contact with the health care system, the guidelines panel wrote (Clin Infect Dis. 2016 Sep 1;63[5]:e61-e111).
The IDSA/ATS Guidelines strongly recommend short-course (1-week) antibiotic therapy instead of longer courses for both HAP and VAP and assert that antibiotic doses should be de-escalated rather than fixed. It advises that serum procalcitonin level plus clinical criteria, not just clinical criteria alone, should be used to guide antibiotic discontinuation, and suggests that the Clinical Pulmonary Infection Score not be used to guide discontinuation.
The guidelines also address empiric treatments when MRSA is suspected and give detailed guidance for selecting antibiotics once the causative organism is identified, including Pseudomonas aeruginosa, extended-spectrum beta-lactamase–producing gram-negative bacilli, Acinetobacter species, and pathogens resistant to carbapenem.
The guidelines include numerous other recommendations concerning the diagnosis of HAP and VAP, the optimal initial treatments, the pharmacokinetic and pharmacodynamic optimization of antibiotic therapies, and the use of inhaled antibiotics. All the recommendations “are a compromise between the competing goals of providing early appropriate antibiotic coverage and avoiding superfluous treatment that may lead to adverse drug effects, Clostridium difficile infections, antibiotic resistance, and increased costs,” the guidelines panel noted.
The full-text guidelines, including details about the panel’s methodology in reviewing the current literature and the summaries of evidence that support each recommendation, is available free on the Clinical Infectious Diseases website.
The Infectious Diseases Society of America and the American Thoracic Society provided financial and administrative support to develop the guidelines. No industry funding was permitted. Dr. Kalil reported having no potential conflicts of interest; Dr. Metersky reported ties to Aradigm, Gilead, Pfizer, Bayer, and their associates reported ties to numerous industry sources.
A 1-week course of antibiotics is sufficient for most hospital-acquired and ventilator-associated pneumonia, regardless of the microbial etiology of the infection, according to an updated Clinical Practice Guidelines for managing adults with these disorders.
In addition, every hospital should develop its own antibiogram to align clinicians’ choice of treatments with the local distribution of likely pathogens and their antimicrobial susceptibilities. Both of these recommendations, as well as others that are also new to the updated guidelines, are intended to minimize patient exposure to unnecessary antibiotics and reduce antibiotic resistance, said Andre C. Kalil, MD, and Mark L. Metersky, MD, cochairs of the guidelines panel of 18 experts in infectious diseases, pulmonary medicine, critical care medicine, laboratory medicine, microbiology, pharmacology, and guideline methodology.
The guidelines, an update of the last version issued in 2005 and developed jointly by representatives of the Infectious Disease Society of America (including Dr. Kalil) and the American Thoracic Society (including Dr. Metersky), are intended for use by all clinicians who care for patients at risk for hospital-acquired pneumonia (HAP) or ventilator-associated pneumonia (VAP), including surgeons, anesthesiologists, and hospitalists as well as specialists in infectious diseases, pulmonary diseases, and critical care. The guidelines no longer use the concept of health care–associated pneumonia (HCAP), chiefly because new evidence shows that designation is too general: HCAP patients are not at high risk for multidrug-resistant organisms simply because of their contact with the health care system, the guidelines panel wrote (Clin Infect Dis. 2016 Sep 1;63[5]:e61-e111).
The IDSA/ATS Guidelines strongly recommend short-course (1-week) antibiotic therapy instead of longer courses for both HAP and VAP and assert that antibiotic doses should be de-escalated rather than fixed. It advises that serum procalcitonin level plus clinical criteria, not just clinical criteria alone, should be used to guide antibiotic discontinuation, and suggests that the Clinical Pulmonary Infection Score not be used to guide discontinuation.
The guidelines also address empiric treatments when MRSA is suspected and give detailed guidance for selecting antibiotics once the causative organism is identified, including Pseudomonas aeruginosa, extended-spectrum beta-lactamase–producing gram-negative bacilli, Acinetobacter species, and pathogens resistant to carbapenem.
The guidelines include numerous other recommendations concerning the diagnosis of HAP and VAP, the optimal initial treatments, the pharmacokinetic and pharmacodynamic optimization of antibiotic therapies, and the use of inhaled antibiotics. All the recommendations “are a compromise between the competing goals of providing early appropriate antibiotic coverage and avoiding superfluous treatment that may lead to adverse drug effects, Clostridium difficile infections, antibiotic resistance, and increased costs,” the guidelines panel noted.
The full-text guidelines, including details about the panel’s methodology in reviewing the current literature and the summaries of evidence that support each recommendation, is available free on the Clinical Infectious Diseases website.
The Infectious Diseases Society of America and the American Thoracic Society provided financial and administrative support to develop the guidelines. No industry funding was permitted. Dr. Kalil reported having no potential conflicts of interest; Dr. Metersky reported ties to Aradigm, Gilead, Pfizer, Bayer, and their associates reported ties to numerous industry sources.
Key clinical point: A 1-week course of antibiotics is sufficient for most hospital-acquired and ventilator-associated pneumonia, regardless of the microbial etiology.
Major finding: The joint IDSA/ATS Guidelines include 25 recommendations regarding diagnosis, empiric therapy, and pathogen-targeted antibiotics for HAP and VAP.
Data source: An update to the 2005 Clinical Practice Guidelines for managing adults with HAP or VAP.
Disclosures: The Infectious Diseases Society of America and the American Thoracic Society provided financial and administrative support to develop the guidelines. No industry funding was permitted. Dr. Kalil reported having no potential conflicts of interest; Dr. Metersky reported ties to Aradigm, Gilead, Pfizer, Bayer, and their associates reported ties to numerous industry sources.
Continuous glucose monitoring recommended over finger sticks for type 1 diabetes
“Studies have found that people with type 1 diabetes who use CGMs [continuous glucose monitors] are able to maintain better control of their blood sugar without increasing episodes of hypoglycemia when blood sugar drops to dangerous levels, compared to those who self-monitor blood glucose with periodic finger sticks,” the chair of the guideline task force, Anne Peters, MD, a professor of medicine at the University of Southern California, Los Angeles, said in a Sept. 26 statement.
The group recommended CGMs for well-controlled type 1 patients as well as those above hemoglobin A1c (HbA1c) targets, so long as they want and understand how to use the devices. It also suggested short-term, intermittent CGM use to help type 2 patients meet HbA1cgoals. Insulin pumps were recommended over multiple daily injections for type 1 patients above target HbA1clevels, as well as those who meet their target but continue to have severe hypoglycemia or high glucose variability. For patients with type 2 disease, pumps were suggested for cases of poor glycemic control despite intensive insulin therapy, oral agents, and other measures.
The Endocrine Society and others have been pushing Medicare to cover CGMs for a while; the new guideline seems to support the effort. Although the devices are used by type 1 patients and covered by some insurance plans, they are only indicated as finger-stick adjuncts, not replacements. For Medicare coverage, they would “need to serve a primary medical purpose and not be used adjunctively,” according to a recent review by Dexcom, a company seeking a primary monitoring indication for its CGM.
The Endocrine Society noted in its evidence-based guideline that standard capillary blood glucose measurements “offer only a limited perspective on the constant daily changes in blood glucose levels,” and, unlike continuous monitoring, “do not provide alarms that indicate when blood glucose levels are above or below various thresholds, and do not indicate trends in blood glucose levels.”
The society commissioned a pooled analysis of 11 randomized trials that showed a 0.3% reduction in HbA1c with real-time glucose monitoring, mostly in patients 15 years or older. Other studies cited by the group also showed better HbA1c control than with finger sticks, without an increased risk of hypoglycemia.
The guideline also suggested insulin pumps for type 1 patients who want greater flexibility and convenience and that insulin pump therapy should continue during hospitalizations. It also suggested encouraging patients to use the embedded bolus calculators in their pumps so long as they “have appropriate education regarding their use and limitations.”
The Endocrine Society funded the work, with cosponsorship from the American Association for Clinical Chemistry, the American Association of Diabetes Educators, and the European Society of Endocrinology. Several of the authors have industry ties to companies that make CGMs or insulin pumps. Dr. Peters is an advisor for Abbott, Becton Dickinson, AstraZeneca, Biodel, Medtronic, and other companies, as well as a speaker, investigator, and advisor for Janssen.
“Studies have found that people with type 1 diabetes who use CGMs [continuous glucose monitors] are able to maintain better control of their blood sugar without increasing episodes of hypoglycemia when blood sugar drops to dangerous levels, compared to those who self-monitor blood glucose with periodic finger sticks,” the chair of the guideline task force, Anne Peters, MD, a professor of medicine at the University of Southern California, Los Angeles, said in a Sept. 26 statement.
The group recommended CGMs for well-controlled type 1 patients as well as those above hemoglobin A1c (HbA1c) targets, so long as they want and understand how to use the devices. It also suggested short-term, intermittent CGM use to help type 2 patients meet HbA1cgoals. Insulin pumps were recommended over multiple daily injections for type 1 patients above target HbA1clevels, as well as those who meet their target but continue to have severe hypoglycemia or high glucose variability. For patients with type 2 disease, pumps were suggested for cases of poor glycemic control despite intensive insulin therapy, oral agents, and other measures.
The Endocrine Society and others have been pushing Medicare to cover CGMs for a while; the new guideline seems to support the effort. Although the devices are used by type 1 patients and covered by some insurance plans, they are only indicated as finger-stick adjuncts, not replacements. For Medicare coverage, they would “need to serve a primary medical purpose and not be used adjunctively,” according to a recent review by Dexcom, a company seeking a primary monitoring indication for its CGM.
The Endocrine Society noted in its evidence-based guideline that standard capillary blood glucose measurements “offer only a limited perspective on the constant daily changes in blood glucose levels,” and, unlike continuous monitoring, “do not provide alarms that indicate when blood glucose levels are above or below various thresholds, and do not indicate trends in blood glucose levels.”
The society commissioned a pooled analysis of 11 randomized trials that showed a 0.3% reduction in HbA1c with real-time glucose monitoring, mostly in patients 15 years or older. Other studies cited by the group also showed better HbA1c control than with finger sticks, without an increased risk of hypoglycemia.
The guideline also suggested insulin pumps for type 1 patients who want greater flexibility and convenience and that insulin pump therapy should continue during hospitalizations. It also suggested encouraging patients to use the embedded bolus calculators in their pumps so long as they “have appropriate education regarding their use and limitations.”
The Endocrine Society funded the work, with cosponsorship from the American Association for Clinical Chemistry, the American Association of Diabetes Educators, and the European Society of Endocrinology. Several of the authors have industry ties to companies that make CGMs or insulin pumps. Dr. Peters is an advisor for Abbott, Becton Dickinson, AstraZeneca, Biodel, Medtronic, and other companies, as well as a speaker, investigator, and advisor for Janssen.
“Studies have found that people with type 1 diabetes who use CGMs [continuous glucose monitors] are able to maintain better control of their blood sugar without increasing episodes of hypoglycemia when blood sugar drops to dangerous levels, compared to those who self-monitor blood glucose with periodic finger sticks,” the chair of the guideline task force, Anne Peters, MD, a professor of medicine at the University of Southern California, Los Angeles, said in a Sept. 26 statement.
The group recommended CGMs for well-controlled type 1 patients as well as those above hemoglobin A1c (HbA1c) targets, so long as they want and understand how to use the devices. It also suggested short-term, intermittent CGM use to help type 2 patients meet HbA1cgoals. Insulin pumps were recommended over multiple daily injections for type 1 patients above target HbA1clevels, as well as those who meet their target but continue to have severe hypoglycemia or high glucose variability. For patients with type 2 disease, pumps were suggested for cases of poor glycemic control despite intensive insulin therapy, oral agents, and other measures.
The Endocrine Society and others have been pushing Medicare to cover CGMs for a while; the new guideline seems to support the effort. Although the devices are used by type 1 patients and covered by some insurance plans, they are only indicated as finger-stick adjuncts, not replacements. For Medicare coverage, they would “need to serve a primary medical purpose and not be used adjunctively,” according to a recent review by Dexcom, a company seeking a primary monitoring indication for its CGM.
The Endocrine Society noted in its evidence-based guideline that standard capillary blood glucose measurements “offer only a limited perspective on the constant daily changes in blood glucose levels,” and, unlike continuous monitoring, “do not provide alarms that indicate when blood glucose levels are above or below various thresholds, and do not indicate trends in blood glucose levels.”
The society commissioned a pooled analysis of 11 randomized trials that showed a 0.3% reduction in HbA1c with real-time glucose monitoring, mostly in patients 15 years or older. Other studies cited by the group also showed better HbA1c control than with finger sticks, without an increased risk of hypoglycemia.
The guideline also suggested insulin pumps for type 1 patients who want greater flexibility and convenience and that insulin pump therapy should continue during hospitalizations. It also suggested encouraging patients to use the embedded bolus calculators in their pumps so long as they “have appropriate education regarding their use and limitations.”
The Endocrine Society funded the work, with cosponsorship from the American Association for Clinical Chemistry, the American Association of Diabetes Educators, and the European Society of Endocrinology. Several of the authors have industry ties to companies that make CGMs or insulin pumps. Dr. Peters is an advisor for Abbott, Becton Dickinson, AstraZeneca, Biodel, Medtronic, and other companies, as well as a speaker, investigator, and advisor for Janssen.