User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Stepdown to oral ciprofloxacin looks safe in gram-negative bloodstream infections
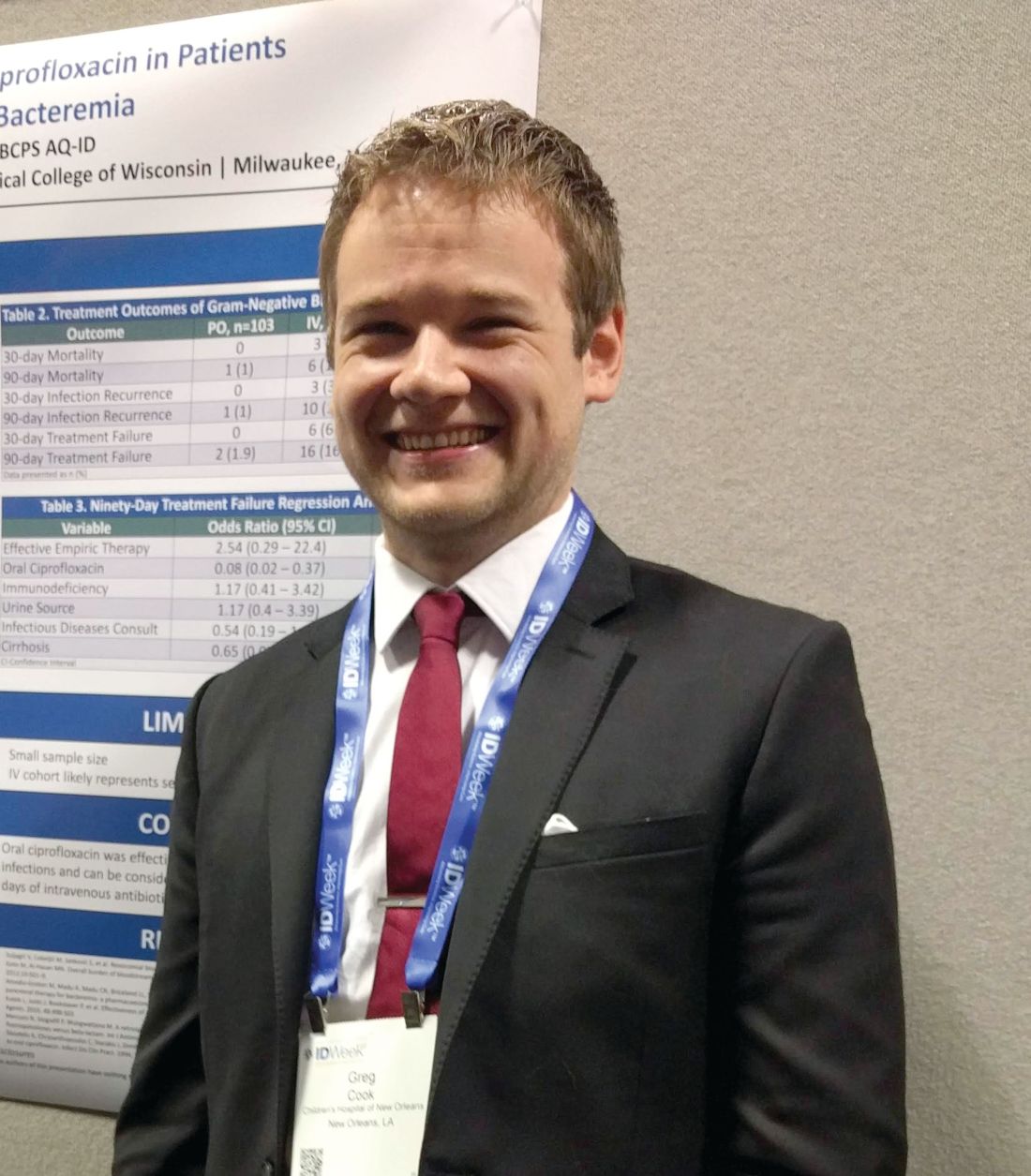
SAN FRANCISCO – In gram-negative bloodstream infections, in patients who are stable at 48 hours, are no longer feverish, and whose infections aren’t invasive, it may be safe to step down from IV antibiotics to oral ciprofloxacin (PO). That is the tentative conclusion from a new single-center, retrospective chart review.
The study adds to growing suspicion among practitioners that stepping down may be safe in gram-negative patients, as well as mounting evidence that shorter treatment durations may also be safe, according to Gregory Cook, PharmD, who presented the study at a poster session at an annual scientific meeting on infectious diseases. “We’re getting more aggressive” in backing off IV treatment, he said in an interview.
Oral medications are associated with shorter hospital stays and decreased costs.
Froedtert & the Medical College of Wisconsin, where the study was performed, switched some years ago from levofloxacin to ciprofloxacin for cost reasons. But ciprofloxacin has a lower bioavailability, and a recent study showed levofloxacin had less treatment failure at 90 days than ciprofloxacin. Levofloxacin is restricted at the institution and requires antibiotic stewardship approval for use, whereas ciprofloxacin can be used without approval.
But the researchers were concerned about bioavailability. “We like to think of ciprofloxacin as having excellent bioavailability, and it does, it has 80% bioavailability, but it’s still not exactly the same as levofloxacin. We wanted to look into this and see if we were doing our patients a disservice or not (by stepping down to ciprofloxacin),” said Dr. Cook, who is now the antimicrobial stewardship pharmacist at Children’s Hospital New Orleans. The results were reassuring. “Ultimately we were trying to see how our patients were doing on oral ciprofloxacin, and after 2-3 days of IV therapy, most of them did extremely well,” he said.
The researchers analyzed the records of 198 patients who presented with a monomicrobial, gram-negative bloodstream infection between January 2015 and January 2018, and who survived at least 5 days past blood culture collection. One hundred and three switched to PO within 5 days, while 95 remained on intravenous antibiotics for longer than 5 days. On average, patients in the PO group received IV antibiotics for 2 days, while the IV group averaged 15 days. Oral ciprofloxacin treatment length averaged 12 days.
The primary endpoint of treatment failure at 90 days, defined as recurrent infection or all-cause mortality, favored the PO group (1.9% versus 16.8%, P less than .01). This was likely because of patient selection, as those in the IV group tended to be more ill, according to Dr. Cook. More were immunosuppressed (41% IV versus 22% in PO group, P less than .01). There were more nonurinary sources of infection (41% in IV group, P less than .01; 65% urinary source in PO group). Thirty-four percent of the PO group had an infectious disease consult, compared with 60% of the IV group.
SOURCE: Gregory Cook et al. ID Week 2018. Abstract 39.
SAN FRANCISCO – In gram-negative bloodstream infections, in patients who are stable at 48 hours, are no longer feverish, and whose infections aren’t invasive, it may be safe to step down from IV antibiotics to oral ciprofloxacin (PO). That is the tentative conclusion from a new single-center, retrospective chart review.
The study adds to growing suspicion among practitioners that stepping down may be safe in gram-negative patients, as well as mounting evidence that shorter treatment durations may also be safe, according to Gregory Cook, PharmD, who presented the study at a poster session at an annual scientific meeting on infectious diseases. “We’re getting more aggressive” in backing off IV treatment, he said in an interview.
Oral medications are associated with shorter hospital stays and decreased costs.
Froedtert & the Medical College of Wisconsin, where the study was performed, switched some years ago from levofloxacin to ciprofloxacin for cost reasons. But ciprofloxacin has a lower bioavailability, and a recent study showed levofloxacin had less treatment failure at 90 days than ciprofloxacin. Levofloxacin is restricted at the institution and requires antibiotic stewardship approval for use, whereas ciprofloxacin can be used without approval.
But the researchers were concerned about bioavailability. “We like to think of ciprofloxacin as having excellent bioavailability, and it does, it has 80% bioavailability, but it’s still not exactly the same as levofloxacin. We wanted to look into this and see if we were doing our patients a disservice or not (by stepping down to ciprofloxacin),” said Dr. Cook, who is now the antimicrobial stewardship pharmacist at Children’s Hospital New Orleans. The results were reassuring. “Ultimately we were trying to see how our patients were doing on oral ciprofloxacin, and after 2-3 days of IV therapy, most of them did extremely well,” he said.
The researchers analyzed the records of 198 patients who presented with a monomicrobial, gram-negative bloodstream infection between January 2015 and January 2018, and who survived at least 5 days past blood culture collection. One hundred and three switched to PO within 5 days, while 95 remained on intravenous antibiotics for longer than 5 days. On average, patients in the PO group received IV antibiotics for 2 days, while the IV group averaged 15 days. Oral ciprofloxacin treatment length averaged 12 days.
The primary endpoint of treatment failure at 90 days, defined as recurrent infection or all-cause mortality, favored the PO group (1.9% versus 16.8%, P less than .01). This was likely because of patient selection, as those in the IV group tended to be more ill, according to Dr. Cook. More were immunosuppressed (41% IV versus 22% in PO group, P less than .01). There were more nonurinary sources of infection (41% in IV group, P less than .01; 65% urinary source in PO group). Thirty-four percent of the PO group had an infectious disease consult, compared with 60% of the IV group.
SOURCE: Gregory Cook et al. ID Week 2018. Abstract 39.
SAN FRANCISCO – In gram-negative bloodstream infections, in patients who are stable at 48 hours, are no longer feverish, and whose infections aren’t invasive, it may be safe to step down from IV antibiotics to oral ciprofloxacin (PO). That is the tentative conclusion from a new single-center, retrospective chart review.
The study adds to growing suspicion among practitioners that stepping down may be safe in gram-negative patients, as well as mounting evidence that shorter treatment durations may also be safe, according to Gregory Cook, PharmD, who presented the study at a poster session at an annual scientific meeting on infectious diseases. “We’re getting more aggressive” in backing off IV treatment, he said in an interview.
Oral medications are associated with shorter hospital stays and decreased costs.
Froedtert & the Medical College of Wisconsin, where the study was performed, switched some years ago from levofloxacin to ciprofloxacin for cost reasons. But ciprofloxacin has a lower bioavailability, and a recent study showed levofloxacin had less treatment failure at 90 days than ciprofloxacin. Levofloxacin is restricted at the institution and requires antibiotic stewardship approval for use, whereas ciprofloxacin can be used without approval.
But the researchers were concerned about bioavailability. “We like to think of ciprofloxacin as having excellent bioavailability, and it does, it has 80% bioavailability, but it’s still not exactly the same as levofloxacin. We wanted to look into this and see if we were doing our patients a disservice or not (by stepping down to ciprofloxacin),” said Dr. Cook, who is now the antimicrobial stewardship pharmacist at Children’s Hospital New Orleans. The results were reassuring. “Ultimately we were trying to see how our patients were doing on oral ciprofloxacin, and after 2-3 days of IV therapy, most of them did extremely well,” he said.
The researchers analyzed the records of 198 patients who presented with a monomicrobial, gram-negative bloodstream infection between January 2015 and January 2018, and who survived at least 5 days past blood culture collection. One hundred and three switched to PO within 5 days, while 95 remained on intravenous antibiotics for longer than 5 days. On average, patients in the PO group received IV antibiotics for 2 days, while the IV group averaged 15 days. Oral ciprofloxacin treatment length averaged 12 days.
The primary endpoint of treatment failure at 90 days, defined as recurrent infection or all-cause mortality, favored the PO group (1.9% versus 16.8%, P less than .01). This was likely because of patient selection, as those in the IV group tended to be more ill, according to Dr. Cook. More were immunosuppressed (41% IV versus 22% in PO group, P less than .01). There were more nonurinary sources of infection (41% in IV group, P less than .01; 65% urinary source in PO group). Thirty-four percent of the PO group had an infectious disease consult, compared with 60% of the IV group.
SOURCE: Gregory Cook et al. ID Week 2018. Abstract 39.
REPORTING FROM IDWEEK 2018
Key clinical point: Stepping down to oral ciprofloxacin at 48 hours is likely safe in stable patients.
Major finding: The 90-day treatment failure rate was 1.9% in patients switched to oral ciprofloxacin.
Study details: Retrospective analysis of 193 cases.
Disclosures: The study was not funded. Dr. Cook declared no financial conflicts of interest.
Source: ID Week 2018. Abstract 39.
In C. difficile, metronidazole may not benefit ICU patients on vancomycin
SAN FRANCISCO – , according to a review of 101 cases at the University of Maryland.
Adding metronidazole is a common move in ICUs when patients start circling the drain with C. difficile, in part because delivery to the gut doesn’t depend on gut motility. “At that point, you are throwing the kitchen sink at them, but it’s” based, like much in C. difficile management, on expert opinion, not evidence, said study lead Ana Vega, PharmD, a former resident at the university’s school of pharmacy in Baltimore, and now an infectious disease pharmacist at Jackson Memorial Hospital, Miami. The investigators wanted to plug the evidence gap. Forty-seven of the 101 patients in their review – all with signs of C. difficile sepsis – had IV metronidazole added to their vancomycin regimens. Thirty-day mortality was 14.9% in the combination group versus 7.4% in the monotherapy arm, and not significantly different (P = .338). There were also no significant differences in resolution rates or normalization of white blood cell counts and temperature.
“Our data question the utility of” of adding IV metronidazole to oral vancomycin in patients with severe disease. “It’s definitely something to think twice about because metronidazole isn’t benign. It makes people feel crummy; you can induce resistance; and it increases the risk of vancomycin-resistant Enterococci colonization,” already a risk with vancomycin, Dr. Vega said at an annual scientific meeting on infectious diseases.
“When you get to the point that you are trying combination therapy based on expert opinion, I think fecal transplants are something to consider” because the success rates are so high. “That would be my suggestion,” she said, even though “it’s much easier to write an order for a drug than to get a fecal transplant.”
The issue is far from resolved, and debate will continue. A similar review of ICU patients at Wake Forest University in Winston-Salem, N.C., did find a significant mortality benefit with combination therapy, regardless of C. difficile severity (Clin Infect Dis. 2015 Sep 15. doi: 10.1093/cid/civ409).
The Maryland investigators excluded patients with toxic megacolon and other life-threatening intra-abdominal complications requiring surgery, because combination therapy is more strongly recommended in fulminant disease. They were interested in people who were not quite ready for the operating room, when what to do is more in doubt.
Subjects were admitted to the ICU from April 2016 to April 2018 with positive C. difficile nucleic acid testing and an order for oral vancomycin. The only statistically significant baseline differences were that patients who got IV metronidazole had higher median white blood cell counts (18,400 versus 13,900 cells/mL; P = .035) and were more likely to receive higher than 500-mg doses of vancomycin (36.2% versus 7.4%; P less than .0001).
The Mean Acute Physiology and Chronic Health Evaluation II (APACHE II) score in the combination group was 23 versus 19 in the monotherapy arm (P = .247). There was no difference in the probability of receiving metronidazole based on the score.
The study again found no significant 30-day mortality differences among 76 patients matched by their APACHE II scores (15.8% in the combination arm versus 9.7%; P = .480).
Severe C. difficile infection was defined as either a white cell count above 15,000 or below 4,000 cells/mL, or a serum creatinine at least 1.5 times above baseline, plus at least one other sign of severe sepsis, such as a mean arterial pressure at or below 60 mm Hg. Metronidazole was started within 72 hours of the first vancomycin dose, and subjects on combination therapy were on both for at least 72 hours.
The mean age in the study was about 60 years old, and just over half of the subjects were men.
Dr. Vega said the investigators hope to expand their sample size and see if patients with more virulent strains of C. difficile do better on combination therapy.
There was no industry funding for the work, and the investigators didn’t have any relevant disclosures.
SOURCE: Vega AD et al. ID Week 2018, Abstract 488.
SAN FRANCISCO – , according to a review of 101 cases at the University of Maryland.
Adding metronidazole is a common move in ICUs when patients start circling the drain with C. difficile, in part because delivery to the gut doesn’t depend on gut motility. “At that point, you are throwing the kitchen sink at them, but it’s” based, like much in C. difficile management, on expert opinion, not evidence, said study lead Ana Vega, PharmD, a former resident at the university’s school of pharmacy in Baltimore, and now an infectious disease pharmacist at Jackson Memorial Hospital, Miami. The investigators wanted to plug the evidence gap. Forty-seven of the 101 patients in their review – all with signs of C. difficile sepsis – had IV metronidazole added to their vancomycin regimens. Thirty-day mortality was 14.9% in the combination group versus 7.4% in the monotherapy arm, and not significantly different (P = .338). There were also no significant differences in resolution rates or normalization of white blood cell counts and temperature.
“Our data question the utility of” of adding IV metronidazole to oral vancomycin in patients with severe disease. “It’s definitely something to think twice about because metronidazole isn’t benign. It makes people feel crummy; you can induce resistance; and it increases the risk of vancomycin-resistant Enterococci colonization,” already a risk with vancomycin, Dr. Vega said at an annual scientific meeting on infectious diseases.
“When you get to the point that you are trying combination therapy based on expert opinion, I think fecal transplants are something to consider” because the success rates are so high. “That would be my suggestion,” she said, even though “it’s much easier to write an order for a drug than to get a fecal transplant.”
The issue is far from resolved, and debate will continue. A similar review of ICU patients at Wake Forest University in Winston-Salem, N.C., did find a significant mortality benefit with combination therapy, regardless of C. difficile severity (Clin Infect Dis. 2015 Sep 15. doi: 10.1093/cid/civ409).
The Maryland investigators excluded patients with toxic megacolon and other life-threatening intra-abdominal complications requiring surgery, because combination therapy is more strongly recommended in fulminant disease. They were interested in people who were not quite ready for the operating room, when what to do is more in doubt.
Subjects were admitted to the ICU from April 2016 to April 2018 with positive C. difficile nucleic acid testing and an order for oral vancomycin. The only statistically significant baseline differences were that patients who got IV metronidazole had higher median white blood cell counts (18,400 versus 13,900 cells/mL; P = .035) and were more likely to receive higher than 500-mg doses of vancomycin (36.2% versus 7.4%; P less than .0001).
The Mean Acute Physiology and Chronic Health Evaluation II (APACHE II) score in the combination group was 23 versus 19 in the monotherapy arm (P = .247). There was no difference in the probability of receiving metronidazole based on the score.
The study again found no significant 30-day mortality differences among 76 patients matched by their APACHE II scores (15.8% in the combination arm versus 9.7%; P = .480).
Severe C. difficile infection was defined as either a white cell count above 15,000 or below 4,000 cells/mL, or a serum creatinine at least 1.5 times above baseline, plus at least one other sign of severe sepsis, such as a mean arterial pressure at or below 60 mm Hg. Metronidazole was started within 72 hours of the first vancomycin dose, and subjects on combination therapy were on both for at least 72 hours.
The mean age in the study was about 60 years old, and just over half of the subjects were men.
Dr. Vega said the investigators hope to expand their sample size and see if patients with more virulent strains of C. difficile do better on combination therapy.
There was no industry funding for the work, and the investigators didn’t have any relevant disclosures.
SOURCE: Vega AD et al. ID Week 2018, Abstract 488.
SAN FRANCISCO – , according to a review of 101 cases at the University of Maryland.
Adding metronidazole is a common move in ICUs when patients start circling the drain with C. difficile, in part because delivery to the gut doesn’t depend on gut motility. “At that point, you are throwing the kitchen sink at them, but it’s” based, like much in C. difficile management, on expert opinion, not evidence, said study lead Ana Vega, PharmD, a former resident at the university’s school of pharmacy in Baltimore, and now an infectious disease pharmacist at Jackson Memorial Hospital, Miami. The investigators wanted to plug the evidence gap. Forty-seven of the 101 patients in their review – all with signs of C. difficile sepsis – had IV metronidazole added to their vancomycin regimens. Thirty-day mortality was 14.9% in the combination group versus 7.4% in the monotherapy arm, and not significantly different (P = .338). There were also no significant differences in resolution rates or normalization of white blood cell counts and temperature.
“Our data question the utility of” of adding IV metronidazole to oral vancomycin in patients with severe disease. “It’s definitely something to think twice about because metronidazole isn’t benign. It makes people feel crummy; you can induce resistance; and it increases the risk of vancomycin-resistant Enterococci colonization,” already a risk with vancomycin, Dr. Vega said at an annual scientific meeting on infectious diseases.
“When you get to the point that you are trying combination therapy based on expert opinion, I think fecal transplants are something to consider” because the success rates are so high. “That would be my suggestion,” she said, even though “it’s much easier to write an order for a drug than to get a fecal transplant.”
The issue is far from resolved, and debate will continue. A similar review of ICU patients at Wake Forest University in Winston-Salem, N.C., did find a significant mortality benefit with combination therapy, regardless of C. difficile severity (Clin Infect Dis. 2015 Sep 15. doi: 10.1093/cid/civ409).
The Maryland investigators excluded patients with toxic megacolon and other life-threatening intra-abdominal complications requiring surgery, because combination therapy is more strongly recommended in fulminant disease. They were interested in people who were not quite ready for the operating room, when what to do is more in doubt.
Subjects were admitted to the ICU from April 2016 to April 2018 with positive C. difficile nucleic acid testing and an order for oral vancomycin. The only statistically significant baseline differences were that patients who got IV metronidazole had higher median white blood cell counts (18,400 versus 13,900 cells/mL; P = .035) and were more likely to receive higher than 500-mg doses of vancomycin (36.2% versus 7.4%; P less than .0001).
The Mean Acute Physiology and Chronic Health Evaluation II (APACHE II) score in the combination group was 23 versus 19 in the monotherapy arm (P = .247). There was no difference in the probability of receiving metronidazole based on the score.
The study again found no significant 30-day mortality differences among 76 patients matched by their APACHE II scores (15.8% in the combination arm versus 9.7%; P = .480).
Severe C. difficile infection was defined as either a white cell count above 15,000 or below 4,000 cells/mL, or a serum creatinine at least 1.5 times above baseline, plus at least one other sign of severe sepsis, such as a mean arterial pressure at or below 60 mm Hg. Metronidazole was started within 72 hours of the first vancomycin dose, and subjects on combination therapy were on both for at least 72 hours.
The mean age in the study was about 60 years old, and just over half of the subjects were men.
Dr. Vega said the investigators hope to expand their sample size and see if patients with more virulent strains of C. difficile do better on combination therapy.
There was no industry funding for the work, and the investigators didn’t have any relevant disclosures.
SOURCE: Vega AD et al. ID Week 2018, Abstract 488.
REPORTING FROM ID WEEK 2018
Key clinical point: The jury is still out on whether adding IV metronidazole helps C. difficile patients already on oral vancomycin in the ICU. Consider fecal transplant.
Major finding: Thirty-day mortality was 14.9% in the combination group versus 7.4% in the monotherapy arm (P = .338).
Study details: Review of 101 ICU patients with severe C. difficile infections
Disclosures: There was no industry funding for the work, and the investigators didn’t have any disclosures.
Source: Vega AD. ID Week 2018, Abstract 488.
Need blood STAT? Call for a drone
BOSTON – While Amazon and other retailers are experimenting with drones to deliver toasters and toilet seats to your doorstep, drone-delivered platelets and fresh frozen plasma may be coming soon to a hospital near you, experts said at AABB 2018, the annual meeting of the group formerly known as the American Association of Blood Banks.
Using a system of completely autonomous delivery drones launched from a central location, U.S.-based Zipline International delivers blood products to treat postpartum hemorrhage, trauma, malaria, and other life-threatening conditions to patients in rural Rwanda, according to company spokesman Chris Kenney.
“In less than 2 years in Rwanda, we’ve made almost 10,000 deliveries – that’s almost 20,000 units of blood,” he said.
One-third of all deliveries are needed for urgent, life-saving interventions, he said.
The system, which delivers 30% of all blood products used in Rwanda outside the capital Kigali, has resulted in 100% availability of blood products when needed, a 98% reduction in waste (i.e., when unused blood products are discarded because of age), and a 175% increase in the use of platelets and fresh frozen plasma, Mr. Kenney said.
Setting up an airborne delivery network in the largely unregulated and uncrowded Rwandan airspace was a relatively simple process, however, compared with the myriad challenges of establishing a similar system for deliveries to urban medical centers in Boston, Chicago, New York, or Los Angeles, said Paul Eastvold, MD, chief medical officer at Vitalant, a nonprofit network of community blood banks headquartered in Spokane, Wash.
Dr. Eastvold, who is also a private pilot, described the regulatory hurdles that will need to be surmounted before blood-delivery drones are as common a sight as traffic helicopters are currently. He added, however, “I can guarantee you that in the future this is going to be an applicable technology to our industry in one way, shape, or another.”
Fast and cheap
Speed and cost are two of the most compelling arguments for blood banks to use drones. Mr. Kenney described the case of a 24-year-old Rwandan woman who had uncontrolled bleeding from complications following a cesarean section. The clinicians treating her opted to give her an immediate red blood cell transfusion, but she continued to bleed, and the hospital ran out of red blood cells in about 15 minutes.
They placed an order for more blood products – ordering can be done by text message or via WhatsApp, a free, cross-platform messaging and voiceover IP calling service – and over the course of 90 minutes Zipline was able to deliver, using multiple drone launches, 7 units of red blood cells, 4 units of plasma, and 2 units of platelets, all of which were transfused into the patient and allowed her condition to stabilize.
Deliveries that would take a minimum of 3 hours by road can be accomplished in about 15-25 minutes by air, Mr. Kenney said.
The drones – more formally known as “unmanned aerial vehicles” (UAVs) – fly a loop starting at the distribution center, find their target, descend to a height of about 10 meters and drop the package, which has a parachute attached. Packages can be delivered within a drop zone the size of two parking spaces, even in gale-force winds, Mr. Kenney said.
“The whole process is 100% autonomous. The aircraft knows where it’s going, it knows what conditions [are], it knows what its payload characteristics are and flies to the delivery point and drops its package,” he explained.
As drones return to the distribution center, they are snared from the air with a wire that catches a small tail hook on the fuselage.
Airborne deliveries are also significantly cheaper than ground-based services for local delivery, Dr. Eastvold noted. He cited a study showing that the cost of ground shipping from a local warehouse by carriers such as UPS or FedEx could be $6 or more, drones could be as cheap as 5 cents per mile with delivery within about 30 minutes, he said.
The fly in the ointment
Dr. Eastvold outlined the significant barriers to adoption of drone-based delivery systems in the United States, ranging from differences in state laws about when, where, and how drones can be used and who can operate them, to Federal Aviation Administration airspace restrictions and regulations.
For example, the FAA currently requires “line-of-sight” operation only for most drone operators, meaning that the operator must have visual contact with the drone at all times. The FAA will, however, grant waivers to individual operators for specified flying conditions on a case-by-case basis, if compelling need or extenuating circumstances can be satisfactorily explained.
In addition, federal regulations require commercial drone pilots to be 16 years old or older, be fluent in English, be in a physical and mental condition that would not interfere with safe operation of a drone, pass an aeronautical knowledge exam at an FAA-approved testing center, and undergo a Transportation Safety Administration background security screening.
Despite these challenges, at least one U.S. medical center, Johns Hopkins University, is testing the use of drones for blood delivery. In 2017, they demonstrated that a drone could successfully deliver human blood samples in temperature-controlled conditions across 161 miles of Arizona desert, in a flight lasting 3 hours.
Mr. Kenney said that his company is developing a second distribution center in Rwanda that will expand coverage to the entire country and is also working with the FAA, federal regulators, and the state of North Carolina to develop a drone-based blood delivery system in the United States.
BOSTON – While Amazon and other retailers are experimenting with drones to deliver toasters and toilet seats to your doorstep, drone-delivered platelets and fresh frozen plasma may be coming soon to a hospital near you, experts said at AABB 2018, the annual meeting of the group formerly known as the American Association of Blood Banks.
Using a system of completely autonomous delivery drones launched from a central location, U.S.-based Zipline International delivers blood products to treat postpartum hemorrhage, trauma, malaria, and other life-threatening conditions to patients in rural Rwanda, according to company spokesman Chris Kenney.
“In less than 2 years in Rwanda, we’ve made almost 10,000 deliveries – that’s almost 20,000 units of blood,” he said.
One-third of all deliveries are needed for urgent, life-saving interventions, he said.
The system, which delivers 30% of all blood products used in Rwanda outside the capital Kigali, has resulted in 100% availability of blood products when needed, a 98% reduction in waste (i.e., when unused blood products are discarded because of age), and a 175% increase in the use of platelets and fresh frozen plasma, Mr. Kenney said.
Setting up an airborne delivery network in the largely unregulated and uncrowded Rwandan airspace was a relatively simple process, however, compared with the myriad challenges of establishing a similar system for deliveries to urban medical centers in Boston, Chicago, New York, or Los Angeles, said Paul Eastvold, MD, chief medical officer at Vitalant, a nonprofit network of community blood banks headquartered in Spokane, Wash.
Dr. Eastvold, who is also a private pilot, described the regulatory hurdles that will need to be surmounted before blood-delivery drones are as common a sight as traffic helicopters are currently. He added, however, “I can guarantee you that in the future this is going to be an applicable technology to our industry in one way, shape, or another.”
Fast and cheap
Speed and cost are two of the most compelling arguments for blood banks to use drones. Mr. Kenney described the case of a 24-year-old Rwandan woman who had uncontrolled bleeding from complications following a cesarean section. The clinicians treating her opted to give her an immediate red blood cell transfusion, but she continued to bleed, and the hospital ran out of red blood cells in about 15 minutes.
They placed an order for more blood products – ordering can be done by text message or via WhatsApp, a free, cross-platform messaging and voiceover IP calling service – and over the course of 90 minutes Zipline was able to deliver, using multiple drone launches, 7 units of red blood cells, 4 units of plasma, and 2 units of platelets, all of which were transfused into the patient and allowed her condition to stabilize.
Deliveries that would take a minimum of 3 hours by road can be accomplished in about 15-25 minutes by air, Mr. Kenney said.
The drones – more formally known as “unmanned aerial vehicles” (UAVs) – fly a loop starting at the distribution center, find their target, descend to a height of about 10 meters and drop the package, which has a parachute attached. Packages can be delivered within a drop zone the size of two parking spaces, even in gale-force winds, Mr. Kenney said.
“The whole process is 100% autonomous. The aircraft knows where it’s going, it knows what conditions [are], it knows what its payload characteristics are and flies to the delivery point and drops its package,” he explained.
As drones return to the distribution center, they are snared from the air with a wire that catches a small tail hook on the fuselage.
Airborne deliveries are also significantly cheaper than ground-based services for local delivery, Dr. Eastvold noted. He cited a study showing that the cost of ground shipping from a local warehouse by carriers such as UPS or FedEx could be $6 or more, drones could be as cheap as 5 cents per mile with delivery within about 30 minutes, he said.
The fly in the ointment
Dr. Eastvold outlined the significant barriers to adoption of drone-based delivery systems in the United States, ranging from differences in state laws about when, where, and how drones can be used and who can operate them, to Federal Aviation Administration airspace restrictions and regulations.
For example, the FAA currently requires “line-of-sight” operation only for most drone operators, meaning that the operator must have visual contact with the drone at all times. The FAA will, however, grant waivers to individual operators for specified flying conditions on a case-by-case basis, if compelling need or extenuating circumstances can be satisfactorily explained.
In addition, federal regulations require commercial drone pilots to be 16 years old or older, be fluent in English, be in a physical and mental condition that would not interfere with safe operation of a drone, pass an aeronautical knowledge exam at an FAA-approved testing center, and undergo a Transportation Safety Administration background security screening.
Despite these challenges, at least one U.S. medical center, Johns Hopkins University, is testing the use of drones for blood delivery. In 2017, they demonstrated that a drone could successfully deliver human blood samples in temperature-controlled conditions across 161 miles of Arizona desert, in a flight lasting 3 hours.
Mr. Kenney said that his company is developing a second distribution center in Rwanda that will expand coverage to the entire country and is also working with the FAA, federal regulators, and the state of North Carolina to develop a drone-based blood delivery system in the United States.
BOSTON – While Amazon and other retailers are experimenting with drones to deliver toasters and toilet seats to your doorstep, drone-delivered platelets and fresh frozen plasma may be coming soon to a hospital near you, experts said at AABB 2018, the annual meeting of the group formerly known as the American Association of Blood Banks.
Using a system of completely autonomous delivery drones launched from a central location, U.S.-based Zipline International delivers blood products to treat postpartum hemorrhage, trauma, malaria, and other life-threatening conditions to patients in rural Rwanda, according to company spokesman Chris Kenney.
“In less than 2 years in Rwanda, we’ve made almost 10,000 deliveries – that’s almost 20,000 units of blood,” he said.
One-third of all deliveries are needed for urgent, life-saving interventions, he said.
The system, which delivers 30% of all blood products used in Rwanda outside the capital Kigali, has resulted in 100% availability of blood products when needed, a 98% reduction in waste (i.e., when unused blood products are discarded because of age), and a 175% increase in the use of platelets and fresh frozen plasma, Mr. Kenney said.
Setting up an airborne delivery network in the largely unregulated and uncrowded Rwandan airspace was a relatively simple process, however, compared with the myriad challenges of establishing a similar system for deliveries to urban medical centers in Boston, Chicago, New York, or Los Angeles, said Paul Eastvold, MD, chief medical officer at Vitalant, a nonprofit network of community blood banks headquartered in Spokane, Wash.
Dr. Eastvold, who is also a private pilot, described the regulatory hurdles that will need to be surmounted before blood-delivery drones are as common a sight as traffic helicopters are currently. He added, however, “I can guarantee you that in the future this is going to be an applicable technology to our industry in one way, shape, or another.”
Fast and cheap
Speed and cost are two of the most compelling arguments for blood banks to use drones. Mr. Kenney described the case of a 24-year-old Rwandan woman who had uncontrolled bleeding from complications following a cesarean section. The clinicians treating her opted to give her an immediate red blood cell transfusion, but she continued to bleed, and the hospital ran out of red blood cells in about 15 minutes.
They placed an order for more blood products – ordering can be done by text message or via WhatsApp, a free, cross-platform messaging and voiceover IP calling service – and over the course of 90 minutes Zipline was able to deliver, using multiple drone launches, 7 units of red blood cells, 4 units of plasma, and 2 units of platelets, all of which were transfused into the patient and allowed her condition to stabilize.
Deliveries that would take a minimum of 3 hours by road can be accomplished in about 15-25 minutes by air, Mr. Kenney said.
The drones – more formally known as “unmanned aerial vehicles” (UAVs) – fly a loop starting at the distribution center, find their target, descend to a height of about 10 meters and drop the package, which has a parachute attached. Packages can be delivered within a drop zone the size of two parking spaces, even in gale-force winds, Mr. Kenney said.
“The whole process is 100% autonomous. The aircraft knows where it’s going, it knows what conditions [are], it knows what its payload characteristics are and flies to the delivery point and drops its package,” he explained.
As drones return to the distribution center, they are snared from the air with a wire that catches a small tail hook on the fuselage.
Airborne deliveries are also significantly cheaper than ground-based services for local delivery, Dr. Eastvold noted. He cited a study showing that the cost of ground shipping from a local warehouse by carriers such as UPS or FedEx could be $6 or more, drones could be as cheap as 5 cents per mile with delivery within about 30 minutes, he said.
The fly in the ointment
Dr. Eastvold outlined the significant barriers to adoption of drone-based delivery systems in the United States, ranging from differences in state laws about when, where, and how drones can be used and who can operate them, to Federal Aviation Administration airspace restrictions and regulations.
For example, the FAA currently requires “line-of-sight” operation only for most drone operators, meaning that the operator must have visual contact with the drone at all times. The FAA will, however, grant waivers to individual operators for specified flying conditions on a case-by-case basis, if compelling need or extenuating circumstances can be satisfactorily explained.
In addition, federal regulations require commercial drone pilots to be 16 years old or older, be fluent in English, be in a physical and mental condition that would not interfere with safe operation of a drone, pass an aeronautical knowledge exam at an FAA-approved testing center, and undergo a Transportation Safety Administration background security screening.
Despite these challenges, at least one U.S. medical center, Johns Hopkins University, is testing the use of drones for blood delivery. In 2017, they demonstrated that a drone could successfully deliver human blood samples in temperature-controlled conditions across 161 miles of Arizona desert, in a flight lasting 3 hours.
Mr. Kenney said that his company is developing a second distribution center in Rwanda that will expand coverage to the entire country and is also working with the FAA, federal regulators, and the state of North Carolina to develop a drone-based blood delivery system in the United States.
AT AABB 2018
Paradigm shifts in palliative care
Better engagement with patients essential
A 57-year-old man is admitted to the hospital with new back pain, which has been getting worse over the past 6 days. He had been diagnosed with stage 4 lung cancer in mid-2017 and underwent treatment with a platinum-based double therapy.
The man also has a history of heroin use – as recently as two years earlier – and he was divorced not long ago. He has been using an old prescription for Vicodin to treat himself, taking as many as 10-12 tablets a day.
This man is an example of the kind of complicated patient hospitalists are called on to treat – complex pain in an era when opioid abuse is considered a public scourge. How is a hospitalist to handle a case like this?
Pain cases are far from the only types of increasingly complex, often palliative cases in which hospitalists are being asked to provide help. Care for the elderly is also becoming increasingly difficult as the U.S. population ages and as hospitalists step in to provide care in the absence of geriatricians. .
Pain management in the opioid era and the need for new approaches in elderly care were highlighted at the Hospital Medicine 2018 annual conference, with experts drawing attention to subtleties that are often overlooked in these sometimes desperate cases.
James Risser, MD, medical director of palliative care at Regions Hospital in Minneapolis, said the complex problems of the 57-year-old man with back pain amounted to an example of “pain’s greatest hits.”
That particular case underscores the need to identify individual types of pain, he said, because they all need to be handled differently. If hospitalists don’t consider all the different aspects of pain, a patient might endure more suffering than necessary.
“All of this pain is swirling around in a very complicated patient,” Dr. Risser said, noting that it is important to “tease out the individual parts” of a complex patient’s history.
“Pain is a very complicated construct, from the physical to the neurological to the emotional,” Dr. Risser said. “Pain is a subjective experience, and the way people interact with their pain really depends not just on physical pain but also their psychological state, their social state, and even their spiritual state.”
Understanding this array of causes has led Dr. Risser to approach the problem of pain from different angles – including perspectives that might not be traditional, he said.
“One of the things that I’ve gotten better at is taking a spiritual history,” he said. “I don’t know if that’s part of everybody’s armamentarium. But if you’re dealing with people who are very, very sick, sometimes that’s the fundamental fabric of how they live and how they die. If there are unresolved issues along those lines, it’s possible they could be experiencing their pain in a different or more severe way.”
Varieties of pain
Treatment depends on the pain type, Dr. Risser said. Somatic pain often responds to nonsteroidal anti-inflammatories or steroids.
Neuropathic pain usually responds poorly to anti-inflammatories and to opioids. There is some research suggesting methadone could be helpful, but the data are not very strong. The most common medications prescribed are antiseizure medications and antidepressants, such as gabapentin and serotonin, and norepinephrine reuptake inhibitors.
The question of cancer pain versus noncancer pain can be tricky, Dr. Risser said. If a person’s life expectancy is limited, there can be a reason, or even a requirement, to use higher-risk medications. But, he said, that doesn’t mean the patient still won’t have problems with overuse of pain medication.
“We have a lot of patients now living post cancer who have been put on methadone or have been put on Oxycontin, and now we’re trying to figure out what to do with them,” he said. “I don’t think it’s that clear anymore that there’s a massive difference between cancer and noncancer pain, especially for those survivors.”
Clinicians, he said, should “fix what can be fixed” – and with the right tools. “If you have a patient who’s got severe lower abdominal pain because they have a bladder full or urine, really the treatment would probably not be … opioids. It probably would be a Foley catheter,” he said.
Hospitalists should treat patients based on sound principles of pain management, Dr. Risser said, but “while you try to create a diagnostic framework, know that people continually defy the boxes we put them in.”
Indeed, in an era of pain-medication addiction, it might be a good idea to worry about prescribing opioids, but clinicians have to remember that their goal is to help patients get relief – and that they themselves bring biases to the table, said Amy Davis, DO, MS, of Drexel University, Philadelphia.
In a presentation at HM18, Dr. Davis displayed images of a variety of patients on a large screen – different races and genders, some in business attire, some rougher around the edges.
“Would pain decisions change based on what people look like?” she asked. “Can you really spot who the drug traffickers are? We need to remember that our biases play a huge role not only in the treatment of our patients but in their outcomes. I’m challenging everybody to start thinking about these folks not as drug-seekers but as comfort-seekers.”
When it comes right down to it, she said, patients want a better life, not their drug of choice.
“That is the nature of the disease. [The illegal drug] is not what they’re looking for in reality because that does not provide a good quality of life,” Dr. Davis said. “The [practice of medicine] is supposed to be about helping people live their lives, not just checking off boxes.”
People with an opioid use disorder are physically different, she said. The processing of pain stimuli by their brain and spinal cord is physically altered – they have an increased perception of pain and lower pain tolerance.
“This is not a character flaw,” Dr. Davis affirmed. The increased sensitivity to pain does not resolve with opioid cessation; it can last for decades. Clinicians may need to spend more time interacting with certain patients to get a sense of the physical and nonphysical pain from which they suffer.
“Consistent, open, nonjudgmental communication improves not only the information we gather from patients and families, but it actually changes the adherence,” Dr. Davis said. “Ultimately the treatment outcomes are what all of this is about.”
Paradigm shift
Another palliative care role that hospitalists often find themselves in is “comforter” of elderly patients.

Ryan Greysen, MD, MHS, chief of hospital medicine at the University of Pennsylvania, Philadelphia, said hospitals must respond to a shift in the paradigm of elderly care. To explain the nature of this change, he referenced the “paradigm shift” model devised by the philosopher of science Thomas Kuhn, PhD. According to Kuhn, science proceeds in a settled pattern for many years, but on the rare occasions, when there is a fundamental drift in thinking, new problems present themselves and put the old model in a crisis mode, which prompts an intellectual revolution and a shift in the paradigm itself.
“This is a way of thinking about changes in scientific paradigms, but I think it works in clinical practice as well,” Dr. Greysen said.
The need for a paradigm shift in the care of elderly inpatients has largely to do with demographics. By 2050, the number of people aged 65 years and older is expected to be about 80 million, roughly double what it was in 2000. The number of people aged 85 years and up is expected to be about 20 million, or about four times the total in 2000.
In 2010, 40% of the hospitalized population was over 65 years. In 2030, that will flip: Only 40% of inpatients will be under 65 years. This will mean that hospitalists must care for more patients who are older, and the patients themselves will have more complicated medical issues.
“To be ready for the aging century, we must be better able to adapt and address those things that affect seniors,” Dr. Greysen said. With the number of geriatricians falling, much more of this care will fall to hospitalists, he said.
More attention must be paid to the potential harms of hospital-based care to older patients: decreased muscle strength and aerobic capacity, vasomotor instability, lower bone density, poor ventilation, altered thirst and nutrition, and fragile skin, among others, Dr. Greysen said.
In a study published in 2015, Dr. Greysen assessed outcomes for elderly patients who were assessed before hospitalization for functional impairment. The more impaired they were, the more likely they were to be readmitted within 30 days of discharge – from a 13.5% readmission rate for those with no impairment up to 18.2% for those considered to have “dependency” in three or more activities of daily living.1
In another analysis, severe functional impairment – dependency in at least two activities of daily living – was associated with more post-acute care Medicare costs than neurological disorders or renal failure.2
Acute care for the elderly (ACE) programs, which have care specifically tailored to the needs of older patients, have been found to be associated with less functional decline, shorter lengths of stay, fewer adverse events, and lower costs and readmission rates, Dr. Greysen said.
These programs are becoming more common, but they are not spreading as quickly as perhaps they should, he said. In part, this is because of the “know-do” gap, in which practical steps that have been shown to work are not actually implemented because of assumptions that they are already in place or the mistaken belief that simple steps could not possibly make a difference.
Part of the paradigm shift that’s needed, Dr. Greysen said, is an appreciation of the concept of “posthospitalization syndrome,” which is composed of several domains: sleep, function, nutrition, symptom burden such as pain and discomfort, cognition, level of engagement, psychosocial status including emotional stress, and treatment burden including the adverse effects of medications.
Better patient engagement in discharge planning – including asking patients about whether they’ve had help reading hospital discharge–related documents, their level of education, and how often they are getting out of bed – is one necessary step toward change. Surveys of satisfaction using tablets and patient portals is another option, Dr. Greysen said.
The patients of the future will likely prompt their own change, he said, quoting from a 2013 publication.
“Possibly the most promising predictor for change in delivery of care is change in the patients themselves,” the authors wrote. “Baby boomers have redefined the norms at every stage of their lives. ... They will expect providers to engage them in shared decision making, elicit their health care goals and treatment preferences, communicate with providers across sites, and provide needed social supports.”3
References
1. Greysen SR et al. Functional impairment and hospital readmission in medicare seniors. JAMA Intern Med. 2015 Apr;175(4):559-65.
2. Greysen SR et al. Functional impairment: An unmeasured marker of medicare costs for postacute care of older adults. J Am Geriatr Soc. 2017 Sep;65(9):1996-2002.
3. Laura A. Levit, Erin P. Balogh, Sharyl J. Nass, and Patricia A. Ganz, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. (Washington (DC): National Academies Press (US), 2013 Dec 27).
Better engagement with patients essential
Better engagement with patients essential
A 57-year-old man is admitted to the hospital with new back pain, which has been getting worse over the past 6 days. He had been diagnosed with stage 4 lung cancer in mid-2017 and underwent treatment with a platinum-based double therapy.
The man also has a history of heroin use – as recently as two years earlier – and he was divorced not long ago. He has been using an old prescription for Vicodin to treat himself, taking as many as 10-12 tablets a day.
This man is an example of the kind of complicated patient hospitalists are called on to treat – complex pain in an era when opioid abuse is considered a public scourge. How is a hospitalist to handle a case like this?
Pain cases are far from the only types of increasingly complex, often palliative cases in which hospitalists are being asked to provide help. Care for the elderly is also becoming increasingly difficult as the U.S. population ages and as hospitalists step in to provide care in the absence of geriatricians. .
Pain management in the opioid era and the need for new approaches in elderly care were highlighted at the Hospital Medicine 2018 annual conference, with experts drawing attention to subtleties that are often overlooked in these sometimes desperate cases.
James Risser, MD, medical director of palliative care at Regions Hospital in Minneapolis, said the complex problems of the 57-year-old man with back pain amounted to an example of “pain’s greatest hits.”
That particular case underscores the need to identify individual types of pain, he said, because they all need to be handled differently. If hospitalists don’t consider all the different aspects of pain, a patient might endure more suffering than necessary.
“All of this pain is swirling around in a very complicated patient,” Dr. Risser said, noting that it is important to “tease out the individual parts” of a complex patient’s history.
“Pain is a very complicated construct, from the physical to the neurological to the emotional,” Dr. Risser said. “Pain is a subjective experience, and the way people interact with their pain really depends not just on physical pain but also their psychological state, their social state, and even their spiritual state.”
Understanding this array of causes has led Dr. Risser to approach the problem of pain from different angles – including perspectives that might not be traditional, he said.
“One of the things that I’ve gotten better at is taking a spiritual history,” he said. “I don’t know if that’s part of everybody’s armamentarium. But if you’re dealing with people who are very, very sick, sometimes that’s the fundamental fabric of how they live and how they die. If there are unresolved issues along those lines, it’s possible they could be experiencing their pain in a different or more severe way.”
Varieties of pain
Treatment depends on the pain type, Dr. Risser said. Somatic pain often responds to nonsteroidal anti-inflammatories or steroids.
Neuropathic pain usually responds poorly to anti-inflammatories and to opioids. There is some research suggesting methadone could be helpful, but the data are not very strong. The most common medications prescribed are antiseizure medications and antidepressants, such as gabapentin and serotonin, and norepinephrine reuptake inhibitors.
The question of cancer pain versus noncancer pain can be tricky, Dr. Risser said. If a person’s life expectancy is limited, there can be a reason, or even a requirement, to use higher-risk medications. But, he said, that doesn’t mean the patient still won’t have problems with overuse of pain medication.
“We have a lot of patients now living post cancer who have been put on methadone or have been put on Oxycontin, and now we’re trying to figure out what to do with them,” he said. “I don’t think it’s that clear anymore that there’s a massive difference between cancer and noncancer pain, especially for those survivors.”
Clinicians, he said, should “fix what can be fixed” – and with the right tools. “If you have a patient who’s got severe lower abdominal pain because they have a bladder full or urine, really the treatment would probably not be … opioids. It probably would be a Foley catheter,” he said.
Hospitalists should treat patients based on sound principles of pain management, Dr. Risser said, but “while you try to create a diagnostic framework, know that people continually defy the boxes we put them in.”
Indeed, in an era of pain-medication addiction, it might be a good idea to worry about prescribing opioids, but clinicians have to remember that their goal is to help patients get relief – and that they themselves bring biases to the table, said Amy Davis, DO, MS, of Drexel University, Philadelphia.
In a presentation at HM18, Dr. Davis displayed images of a variety of patients on a large screen – different races and genders, some in business attire, some rougher around the edges.
“Would pain decisions change based on what people look like?” she asked. “Can you really spot who the drug traffickers are? We need to remember that our biases play a huge role not only in the treatment of our patients but in their outcomes. I’m challenging everybody to start thinking about these folks not as drug-seekers but as comfort-seekers.”
When it comes right down to it, she said, patients want a better life, not their drug of choice.
“That is the nature of the disease. [The illegal drug] is not what they’re looking for in reality because that does not provide a good quality of life,” Dr. Davis said. “The [practice of medicine] is supposed to be about helping people live their lives, not just checking off boxes.”
People with an opioid use disorder are physically different, she said. The processing of pain stimuli by their brain and spinal cord is physically altered – they have an increased perception of pain and lower pain tolerance.
“This is not a character flaw,” Dr. Davis affirmed. The increased sensitivity to pain does not resolve with opioid cessation; it can last for decades. Clinicians may need to spend more time interacting with certain patients to get a sense of the physical and nonphysical pain from which they suffer.
“Consistent, open, nonjudgmental communication improves not only the information we gather from patients and families, but it actually changes the adherence,” Dr. Davis said. “Ultimately the treatment outcomes are what all of this is about.”
Paradigm shift
Another palliative care role that hospitalists often find themselves in is “comforter” of elderly patients.

Ryan Greysen, MD, MHS, chief of hospital medicine at the University of Pennsylvania, Philadelphia, said hospitals must respond to a shift in the paradigm of elderly care. To explain the nature of this change, he referenced the “paradigm shift” model devised by the philosopher of science Thomas Kuhn, PhD. According to Kuhn, science proceeds in a settled pattern for many years, but on the rare occasions, when there is a fundamental drift in thinking, new problems present themselves and put the old model in a crisis mode, which prompts an intellectual revolution and a shift in the paradigm itself.
“This is a way of thinking about changes in scientific paradigms, but I think it works in clinical practice as well,” Dr. Greysen said.
The need for a paradigm shift in the care of elderly inpatients has largely to do with demographics. By 2050, the number of people aged 65 years and older is expected to be about 80 million, roughly double what it was in 2000. The number of people aged 85 years and up is expected to be about 20 million, or about four times the total in 2000.
In 2010, 40% of the hospitalized population was over 65 years. In 2030, that will flip: Only 40% of inpatients will be under 65 years. This will mean that hospitalists must care for more patients who are older, and the patients themselves will have more complicated medical issues.
“To be ready for the aging century, we must be better able to adapt and address those things that affect seniors,” Dr. Greysen said. With the number of geriatricians falling, much more of this care will fall to hospitalists, he said.
More attention must be paid to the potential harms of hospital-based care to older patients: decreased muscle strength and aerobic capacity, vasomotor instability, lower bone density, poor ventilation, altered thirst and nutrition, and fragile skin, among others, Dr. Greysen said.
In a study published in 2015, Dr. Greysen assessed outcomes for elderly patients who were assessed before hospitalization for functional impairment. The more impaired they were, the more likely they were to be readmitted within 30 days of discharge – from a 13.5% readmission rate for those with no impairment up to 18.2% for those considered to have “dependency” in three or more activities of daily living.1
In another analysis, severe functional impairment – dependency in at least two activities of daily living – was associated with more post-acute care Medicare costs than neurological disorders or renal failure.2
Acute care for the elderly (ACE) programs, which have care specifically tailored to the needs of older patients, have been found to be associated with less functional decline, shorter lengths of stay, fewer adverse events, and lower costs and readmission rates, Dr. Greysen said.
These programs are becoming more common, but they are not spreading as quickly as perhaps they should, he said. In part, this is because of the “know-do” gap, in which practical steps that have been shown to work are not actually implemented because of assumptions that they are already in place or the mistaken belief that simple steps could not possibly make a difference.
Part of the paradigm shift that’s needed, Dr. Greysen said, is an appreciation of the concept of “posthospitalization syndrome,” which is composed of several domains: sleep, function, nutrition, symptom burden such as pain and discomfort, cognition, level of engagement, psychosocial status including emotional stress, and treatment burden including the adverse effects of medications.
Better patient engagement in discharge planning – including asking patients about whether they’ve had help reading hospital discharge–related documents, their level of education, and how often they are getting out of bed – is one necessary step toward change. Surveys of satisfaction using tablets and patient portals is another option, Dr. Greysen said.
The patients of the future will likely prompt their own change, he said, quoting from a 2013 publication.
“Possibly the most promising predictor for change in delivery of care is change in the patients themselves,” the authors wrote. “Baby boomers have redefined the norms at every stage of their lives. ... They will expect providers to engage them in shared decision making, elicit their health care goals and treatment preferences, communicate with providers across sites, and provide needed social supports.”3
References
1. Greysen SR et al. Functional impairment and hospital readmission in medicare seniors. JAMA Intern Med. 2015 Apr;175(4):559-65.
2. Greysen SR et al. Functional impairment: An unmeasured marker of medicare costs for postacute care of older adults. J Am Geriatr Soc. 2017 Sep;65(9):1996-2002.
3. Laura A. Levit, Erin P. Balogh, Sharyl J. Nass, and Patricia A. Ganz, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. (Washington (DC): National Academies Press (US), 2013 Dec 27).
A 57-year-old man is admitted to the hospital with new back pain, which has been getting worse over the past 6 days. He had been diagnosed with stage 4 lung cancer in mid-2017 and underwent treatment with a platinum-based double therapy.
The man also has a history of heroin use – as recently as two years earlier – and he was divorced not long ago. He has been using an old prescription for Vicodin to treat himself, taking as many as 10-12 tablets a day.
This man is an example of the kind of complicated patient hospitalists are called on to treat – complex pain in an era when opioid abuse is considered a public scourge. How is a hospitalist to handle a case like this?
Pain cases are far from the only types of increasingly complex, often palliative cases in which hospitalists are being asked to provide help. Care for the elderly is also becoming increasingly difficult as the U.S. population ages and as hospitalists step in to provide care in the absence of geriatricians. .
Pain management in the opioid era and the need for new approaches in elderly care were highlighted at the Hospital Medicine 2018 annual conference, with experts drawing attention to subtleties that are often overlooked in these sometimes desperate cases.
James Risser, MD, medical director of palliative care at Regions Hospital in Minneapolis, said the complex problems of the 57-year-old man with back pain amounted to an example of “pain’s greatest hits.”
That particular case underscores the need to identify individual types of pain, he said, because they all need to be handled differently. If hospitalists don’t consider all the different aspects of pain, a patient might endure more suffering than necessary.
“All of this pain is swirling around in a very complicated patient,” Dr. Risser said, noting that it is important to “tease out the individual parts” of a complex patient’s history.
“Pain is a very complicated construct, from the physical to the neurological to the emotional,” Dr. Risser said. “Pain is a subjective experience, and the way people interact with their pain really depends not just on physical pain but also their psychological state, their social state, and even their spiritual state.”
Understanding this array of causes has led Dr. Risser to approach the problem of pain from different angles – including perspectives that might not be traditional, he said.
“One of the things that I’ve gotten better at is taking a spiritual history,” he said. “I don’t know if that’s part of everybody’s armamentarium. But if you’re dealing with people who are very, very sick, sometimes that’s the fundamental fabric of how they live and how they die. If there are unresolved issues along those lines, it’s possible they could be experiencing their pain in a different or more severe way.”
Varieties of pain
Treatment depends on the pain type, Dr. Risser said. Somatic pain often responds to nonsteroidal anti-inflammatories or steroids.
Neuropathic pain usually responds poorly to anti-inflammatories and to opioids. There is some research suggesting methadone could be helpful, but the data are not very strong. The most common medications prescribed are antiseizure medications and antidepressants, such as gabapentin and serotonin, and norepinephrine reuptake inhibitors.
The question of cancer pain versus noncancer pain can be tricky, Dr. Risser said. If a person’s life expectancy is limited, there can be a reason, or even a requirement, to use higher-risk medications. But, he said, that doesn’t mean the patient still won’t have problems with overuse of pain medication.
“We have a lot of patients now living post cancer who have been put on methadone or have been put on Oxycontin, and now we’re trying to figure out what to do with them,” he said. “I don’t think it’s that clear anymore that there’s a massive difference between cancer and noncancer pain, especially for those survivors.”
Clinicians, he said, should “fix what can be fixed” – and with the right tools. “If you have a patient who’s got severe lower abdominal pain because they have a bladder full or urine, really the treatment would probably not be … opioids. It probably would be a Foley catheter,” he said.
Hospitalists should treat patients based on sound principles of pain management, Dr. Risser said, but “while you try to create a diagnostic framework, know that people continually defy the boxes we put them in.”
Indeed, in an era of pain-medication addiction, it might be a good idea to worry about prescribing opioids, but clinicians have to remember that their goal is to help patients get relief – and that they themselves bring biases to the table, said Amy Davis, DO, MS, of Drexel University, Philadelphia.
In a presentation at HM18, Dr. Davis displayed images of a variety of patients on a large screen – different races and genders, some in business attire, some rougher around the edges.
“Would pain decisions change based on what people look like?” she asked. “Can you really spot who the drug traffickers are? We need to remember that our biases play a huge role not only in the treatment of our patients but in their outcomes. I’m challenging everybody to start thinking about these folks not as drug-seekers but as comfort-seekers.”
When it comes right down to it, she said, patients want a better life, not their drug of choice.
“That is the nature of the disease. [The illegal drug] is not what they’re looking for in reality because that does not provide a good quality of life,” Dr. Davis said. “The [practice of medicine] is supposed to be about helping people live their lives, not just checking off boxes.”
People with an opioid use disorder are physically different, she said. The processing of pain stimuli by their brain and spinal cord is physically altered – they have an increased perception of pain and lower pain tolerance.
“This is not a character flaw,” Dr. Davis affirmed. The increased sensitivity to pain does not resolve with opioid cessation; it can last for decades. Clinicians may need to spend more time interacting with certain patients to get a sense of the physical and nonphysical pain from which they suffer.
“Consistent, open, nonjudgmental communication improves not only the information we gather from patients and families, but it actually changes the adherence,” Dr. Davis said. “Ultimately the treatment outcomes are what all of this is about.”
Paradigm shift
Another palliative care role that hospitalists often find themselves in is “comforter” of elderly patients.

Ryan Greysen, MD, MHS, chief of hospital medicine at the University of Pennsylvania, Philadelphia, said hospitals must respond to a shift in the paradigm of elderly care. To explain the nature of this change, he referenced the “paradigm shift” model devised by the philosopher of science Thomas Kuhn, PhD. According to Kuhn, science proceeds in a settled pattern for many years, but on the rare occasions, when there is a fundamental drift in thinking, new problems present themselves and put the old model in a crisis mode, which prompts an intellectual revolution and a shift in the paradigm itself.
“This is a way of thinking about changes in scientific paradigms, but I think it works in clinical practice as well,” Dr. Greysen said.
The need for a paradigm shift in the care of elderly inpatients has largely to do with demographics. By 2050, the number of people aged 65 years and older is expected to be about 80 million, roughly double what it was in 2000. The number of people aged 85 years and up is expected to be about 20 million, or about four times the total in 2000.
In 2010, 40% of the hospitalized population was over 65 years. In 2030, that will flip: Only 40% of inpatients will be under 65 years. This will mean that hospitalists must care for more patients who are older, and the patients themselves will have more complicated medical issues.
“To be ready for the aging century, we must be better able to adapt and address those things that affect seniors,” Dr. Greysen said. With the number of geriatricians falling, much more of this care will fall to hospitalists, he said.
More attention must be paid to the potential harms of hospital-based care to older patients: decreased muscle strength and aerobic capacity, vasomotor instability, lower bone density, poor ventilation, altered thirst and nutrition, and fragile skin, among others, Dr. Greysen said.
In a study published in 2015, Dr. Greysen assessed outcomes for elderly patients who were assessed before hospitalization for functional impairment. The more impaired they were, the more likely they were to be readmitted within 30 days of discharge – from a 13.5% readmission rate for those with no impairment up to 18.2% for those considered to have “dependency” in three or more activities of daily living.1
In another analysis, severe functional impairment – dependency in at least two activities of daily living – was associated with more post-acute care Medicare costs than neurological disorders or renal failure.2
Acute care for the elderly (ACE) programs, which have care specifically tailored to the needs of older patients, have been found to be associated with less functional decline, shorter lengths of stay, fewer adverse events, and lower costs and readmission rates, Dr. Greysen said.
These programs are becoming more common, but they are not spreading as quickly as perhaps they should, he said. In part, this is because of the “know-do” gap, in which practical steps that have been shown to work are not actually implemented because of assumptions that they are already in place or the mistaken belief that simple steps could not possibly make a difference.
Part of the paradigm shift that’s needed, Dr. Greysen said, is an appreciation of the concept of “posthospitalization syndrome,” which is composed of several domains: sleep, function, nutrition, symptom burden such as pain and discomfort, cognition, level of engagement, psychosocial status including emotional stress, and treatment burden including the adverse effects of medications.
Better patient engagement in discharge planning – including asking patients about whether they’ve had help reading hospital discharge–related documents, their level of education, and how often they are getting out of bed – is one necessary step toward change. Surveys of satisfaction using tablets and patient portals is another option, Dr. Greysen said.
The patients of the future will likely prompt their own change, he said, quoting from a 2013 publication.
“Possibly the most promising predictor for change in delivery of care is change in the patients themselves,” the authors wrote. “Baby boomers have redefined the norms at every stage of their lives. ... They will expect providers to engage them in shared decision making, elicit their health care goals and treatment preferences, communicate with providers across sites, and provide needed social supports.”3
References
1. Greysen SR et al. Functional impairment and hospital readmission in medicare seniors. JAMA Intern Med. 2015 Apr;175(4):559-65.
2. Greysen SR et al. Functional impairment: An unmeasured marker of medicare costs for postacute care of older adults. J Am Geriatr Soc. 2017 Sep;65(9):1996-2002.
3. Laura A. Levit, Erin P. Balogh, Sharyl J. Nass, and Patricia A. Ganz, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. (Washington (DC): National Academies Press (US), 2013 Dec 27).
Be proactive with prophylaxis to tame VTE
Venous thromboembolism (VTE) is the No. 1 cause of preventable deaths in hospitals, and 60% of all VTE cases occur during or following hospitalization, according to Jeffrey I. Weitz, MD, of McMaster University in Hamilton, Ont.
, he said in a webinar to promote World Thrombosis Day.
“To prevent VTE, people need to be aware of the problem,” he said. Hospitalization for any reason increases the risk of VTE, but thromboprophylaxis may be underused in medical patients, compared with surgical patients, because most surgical patients are automatically considered at risk.
Prevention of VTE involves understanding the risk factors, Dr. Weitz said. He pointed to a triad of conditions that promote clotting: slow blood flow, injury to the vessel wall, and increased clotability of the blood.
In a study of VTE risk factors, recent surgery with hospitalization and trauma topped the list, but hospitalization without recent surgery was associated with a nearly 8-fold increase in risk (Arch Intern Med. 2000;160[6]:809-15).
Evidence supports the value of anticoagulant prophylaxis, Dr. Weitz said. In a 2007 meta-analysis, use of anticoagulants reduced the risk of VTE by approximately 60% (Ann Intern Med. 2007 Feb 20;146[4]:278-88), and a 2011 update showed a reduction in risk of approximately 30% (Ann Intern Med. 2011 Nov 1;155[9]:602-15).
While risk assessment remains a challenge, several models can help, said Dr. Weitz.
Current guidelines from the American College of Chest Physicians suggest a shift toward individualized assessment of VTE risk, and the Centers for Medicare & Medicaid Services mandates VTE risk assessment, Dr. Weitz said.
He offered seven steps to improve prophylaxis in the hospital:
1. Obtain commitment from hospital leadership, including formation of a committee.
2. Have a written hospital policy on thromboprophylaxis.
3. Keep the policy simple and standard in terms of who gets prophylaxis and when.
4. Use order sets, computer order entry, and decision support.
5. Make the prophylaxis decision mandatory.
6. Involve of all the members of the care team and patients.
7. Use audits to measure improvement.
Several risk assessment models for VTE in hospitalized medical patients have been studied, including the Padua and IMPROVE models, Dr. Weitz said. For any model, factoring in the D-dimer can provide more information. “If D-dimer is increased more than twice the upper limit of normal, it is a risk factor for VTE,” he said.
Another consideration in thromboprophylaxis involves extending the duration of prophylaxis beyond the hospital stay, which is becoming a larger issue because of the pressure to move patients out of the hospital as quickly as possible, Dr. Weitz said. However, trials of extended thromboprophylaxis have yielded mixed results. Extended doses of medications, including rivaroxaban, enoxaparin, apixaban, and betrixaban can reduce the risk of VTE, but can also increase the risk of major bleeding.
“I think at this point we are not yet there at identifying patients who should have thromboprophylaxis beyond the hospital stay,” Dr. Weitz said.
But VTE risk should be assessed in all hospitalized patients, and “appropriate thromboprophylaxis is essential for reducing the burden of hospital-associated VTE,” he said.
Dr. Weitz encouraged clinicians to explore more resources for managing VTE risk at worldthrombosisday.org.
Dr. Weitz reported relationships with companies including Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, Daiichi-Sankyo, Pfizer, Portola, Ionis Pharmaceuticals, Janssen, Merck, Novartis, and Servier. He also reported research support from the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, and the Canadian Fund for Innovation.
Venous thromboembolism (VTE) is the No. 1 cause of preventable deaths in hospitals, and 60% of all VTE cases occur during or following hospitalization, according to Jeffrey I. Weitz, MD, of McMaster University in Hamilton, Ont.
, he said in a webinar to promote World Thrombosis Day.
“To prevent VTE, people need to be aware of the problem,” he said. Hospitalization for any reason increases the risk of VTE, but thromboprophylaxis may be underused in medical patients, compared with surgical patients, because most surgical patients are automatically considered at risk.
Prevention of VTE involves understanding the risk factors, Dr. Weitz said. He pointed to a triad of conditions that promote clotting: slow blood flow, injury to the vessel wall, and increased clotability of the blood.
In a study of VTE risk factors, recent surgery with hospitalization and trauma topped the list, but hospitalization without recent surgery was associated with a nearly 8-fold increase in risk (Arch Intern Med. 2000;160[6]:809-15).
Evidence supports the value of anticoagulant prophylaxis, Dr. Weitz said. In a 2007 meta-analysis, use of anticoagulants reduced the risk of VTE by approximately 60% (Ann Intern Med. 2007 Feb 20;146[4]:278-88), and a 2011 update showed a reduction in risk of approximately 30% (Ann Intern Med. 2011 Nov 1;155[9]:602-15).
While risk assessment remains a challenge, several models can help, said Dr. Weitz.
Current guidelines from the American College of Chest Physicians suggest a shift toward individualized assessment of VTE risk, and the Centers for Medicare & Medicaid Services mandates VTE risk assessment, Dr. Weitz said.
He offered seven steps to improve prophylaxis in the hospital:
1. Obtain commitment from hospital leadership, including formation of a committee.
2. Have a written hospital policy on thromboprophylaxis.
3. Keep the policy simple and standard in terms of who gets prophylaxis and when.
4. Use order sets, computer order entry, and decision support.
5. Make the prophylaxis decision mandatory.
6. Involve of all the members of the care team and patients.
7. Use audits to measure improvement.
Several risk assessment models for VTE in hospitalized medical patients have been studied, including the Padua and IMPROVE models, Dr. Weitz said. For any model, factoring in the D-dimer can provide more information. “If D-dimer is increased more than twice the upper limit of normal, it is a risk factor for VTE,” he said.
Another consideration in thromboprophylaxis involves extending the duration of prophylaxis beyond the hospital stay, which is becoming a larger issue because of the pressure to move patients out of the hospital as quickly as possible, Dr. Weitz said. However, trials of extended thromboprophylaxis have yielded mixed results. Extended doses of medications, including rivaroxaban, enoxaparin, apixaban, and betrixaban can reduce the risk of VTE, but can also increase the risk of major bleeding.
“I think at this point we are not yet there at identifying patients who should have thromboprophylaxis beyond the hospital stay,” Dr. Weitz said.
But VTE risk should be assessed in all hospitalized patients, and “appropriate thromboprophylaxis is essential for reducing the burden of hospital-associated VTE,” he said.
Dr. Weitz encouraged clinicians to explore more resources for managing VTE risk at worldthrombosisday.org.
Dr. Weitz reported relationships with companies including Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, Daiichi-Sankyo, Pfizer, Portola, Ionis Pharmaceuticals, Janssen, Merck, Novartis, and Servier. He also reported research support from the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, and the Canadian Fund for Innovation.
Venous thromboembolism (VTE) is the No. 1 cause of preventable deaths in hospitals, and 60% of all VTE cases occur during or following hospitalization, according to Jeffrey I. Weitz, MD, of McMaster University in Hamilton, Ont.
, he said in a webinar to promote World Thrombosis Day.
“To prevent VTE, people need to be aware of the problem,” he said. Hospitalization for any reason increases the risk of VTE, but thromboprophylaxis may be underused in medical patients, compared with surgical patients, because most surgical patients are automatically considered at risk.
Prevention of VTE involves understanding the risk factors, Dr. Weitz said. He pointed to a triad of conditions that promote clotting: slow blood flow, injury to the vessel wall, and increased clotability of the blood.
In a study of VTE risk factors, recent surgery with hospitalization and trauma topped the list, but hospitalization without recent surgery was associated with a nearly 8-fold increase in risk (Arch Intern Med. 2000;160[6]:809-15).
Evidence supports the value of anticoagulant prophylaxis, Dr. Weitz said. In a 2007 meta-analysis, use of anticoagulants reduced the risk of VTE by approximately 60% (Ann Intern Med. 2007 Feb 20;146[4]:278-88), and a 2011 update showed a reduction in risk of approximately 30% (Ann Intern Med. 2011 Nov 1;155[9]:602-15).
While risk assessment remains a challenge, several models can help, said Dr. Weitz.
Current guidelines from the American College of Chest Physicians suggest a shift toward individualized assessment of VTE risk, and the Centers for Medicare & Medicaid Services mandates VTE risk assessment, Dr. Weitz said.
He offered seven steps to improve prophylaxis in the hospital:
1. Obtain commitment from hospital leadership, including formation of a committee.
2. Have a written hospital policy on thromboprophylaxis.
3. Keep the policy simple and standard in terms of who gets prophylaxis and when.
4. Use order sets, computer order entry, and decision support.
5. Make the prophylaxis decision mandatory.
6. Involve of all the members of the care team and patients.
7. Use audits to measure improvement.
Several risk assessment models for VTE in hospitalized medical patients have been studied, including the Padua and IMPROVE models, Dr. Weitz said. For any model, factoring in the D-dimer can provide more information. “If D-dimer is increased more than twice the upper limit of normal, it is a risk factor for VTE,” he said.
Another consideration in thromboprophylaxis involves extending the duration of prophylaxis beyond the hospital stay, which is becoming a larger issue because of the pressure to move patients out of the hospital as quickly as possible, Dr. Weitz said. However, trials of extended thromboprophylaxis have yielded mixed results. Extended doses of medications, including rivaroxaban, enoxaparin, apixaban, and betrixaban can reduce the risk of VTE, but can also increase the risk of major bleeding.
“I think at this point we are not yet there at identifying patients who should have thromboprophylaxis beyond the hospital stay,” Dr. Weitz said.
But VTE risk should be assessed in all hospitalized patients, and “appropriate thromboprophylaxis is essential for reducing the burden of hospital-associated VTE,” he said.
Dr. Weitz encouraged clinicians to explore more resources for managing VTE risk at worldthrombosisday.org.
Dr. Weitz reported relationships with companies including Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, Daiichi-Sankyo, Pfizer, Portola, Ionis Pharmaceuticals, Janssen, Merck, Novartis, and Servier. He also reported research support from the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, and the Canadian Fund for Innovation.
FROM WORLD THROMBOSIS DAY 2018 WEBINAR
Bias in the clinical setting can impact patient care
SAN ANTONIO – Physicians and other health care providers may harbor implicit, or unconscious, biases that contribute to health care disparities, patient communication researcher Stacey Passalacqua, PhD, said here at the annual meeting of the American College of Chest Physicians.
Implicit biases are beliefs or attitudes, for example, about certain social groups, that exist outside of a health care provider’s conscious awareness, said Dr. Passalacqua of the department of communication at the University of Texas, San Antonio. If bias is implicit, it can be difficult self-assess.
among other social, ethnic, and racial groups, Dr. Passalacqua told attendees in workshops at the meeting.
“If a health care provider has negative biases toward a particular patient – maybe they think that these patients doesn’t care that much about their health or that they really have no interest in participating – then obviously that health care provider is far less likely to engage that patient in shared decision making,” she said in a video interview.
Diagnosis and treatment are subject to influence by the bias that physicians have toward certain patient groups, according to Dr. Passalacqua. For example, she said women with heart disease are less likely to be accurately diagnosed.
The bias in the medical setting might be mitigated by the presence of more individuals from the at-risk groups in the health care workforce, she added. In one recent retrospective study, investigators found that after an MI, a woman treated by a male physician was associated with higher mortality, while women and men had similar outcomes when treated by female physicians.
“That is one of the reasons why it is so important to have a diverse workforce, to have health care providers of different ethnicities, of different genders, or different backgrounds, because they are less subject to some of these implicit biases that we know are highly problematic in health care,” she said in the interview.
Dr. Passalacqua had no disclosures related to her presentation.
SAN ANTONIO – Physicians and other health care providers may harbor implicit, or unconscious, biases that contribute to health care disparities, patient communication researcher Stacey Passalacqua, PhD, said here at the annual meeting of the American College of Chest Physicians.
Implicit biases are beliefs or attitudes, for example, about certain social groups, that exist outside of a health care provider’s conscious awareness, said Dr. Passalacqua of the department of communication at the University of Texas, San Antonio. If bias is implicit, it can be difficult self-assess.
among other social, ethnic, and racial groups, Dr. Passalacqua told attendees in workshops at the meeting.
“If a health care provider has negative biases toward a particular patient – maybe they think that these patients doesn’t care that much about their health or that they really have no interest in participating – then obviously that health care provider is far less likely to engage that patient in shared decision making,” she said in a video interview.
Diagnosis and treatment are subject to influence by the bias that physicians have toward certain patient groups, according to Dr. Passalacqua. For example, she said women with heart disease are less likely to be accurately diagnosed.
The bias in the medical setting might be mitigated by the presence of more individuals from the at-risk groups in the health care workforce, she added. In one recent retrospective study, investigators found that after an MI, a woman treated by a male physician was associated with higher mortality, while women and men had similar outcomes when treated by female physicians.
“That is one of the reasons why it is so important to have a diverse workforce, to have health care providers of different ethnicities, of different genders, or different backgrounds, because they are less subject to some of these implicit biases that we know are highly problematic in health care,” she said in the interview.
Dr. Passalacqua had no disclosures related to her presentation.
SAN ANTONIO – Physicians and other health care providers may harbor implicit, or unconscious, biases that contribute to health care disparities, patient communication researcher Stacey Passalacqua, PhD, said here at the annual meeting of the American College of Chest Physicians.
Implicit biases are beliefs or attitudes, for example, about certain social groups, that exist outside of a health care provider’s conscious awareness, said Dr. Passalacqua of the department of communication at the University of Texas, San Antonio. If bias is implicit, it can be difficult self-assess.
among other social, ethnic, and racial groups, Dr. Passalacqua told attendees in workshops at the meeting.
“If a health care provider has negative biases toward a particular patient – maybe they think that these patients doesn’t care that much about their health or that they really have no interest in participating – then obviously that health care provider is far less likely to engage that patient in shared decision making,” she said in a video interview.
Diagnosis and treatment are subject to influence by the bias that physicians have toward certain patient groups, according to Dr. Passalacqua. For example, she said women with heart disease are less likely to be accurately diagnosed.
The bias in the medical setting might be mitigated by the presence of more individuals from the at-risk groups in the health care workforce, she added. In one recent retrospective study, investigators found that after an MI, a woman treated by a male physician was associated with higher mortality, while women and men had similar outcomes when treated by female physicians.
“That is one of the reasons why it is so important to have a diverse workforce, to have health care providers of different ethnicities, of different genders, or different backgrounds, because they are less subject to some of these implicit biases that we know are highly problematic in health care,” she said in the interview.
Dr. Passalacqua had no disclosures related to her presentation.
REPORTING FROM CHEST 2018
CT for evaluating pulmonary embolism overused
SAN ANTONIO – The recommended approach to evaluating suspected pulmonary embolism is “greatly underutilized” in the Veterans Health Administration system, Nancy Hsu, MD, said at the annual meeting of the American College of Chest Physicians.
Most Veterans Affairs sites did not require incorporation of a clinical decision rule (CDR) and highly sensitive D-dimer prior to ordering CT pulmonary angiography (CTPA) for suspected pulmonary embolism (PE), according to results of a survey by Dr. Hsu and her coinvestigator, Guy Soo Hoo, MD.
While CTPA has become the imaging modality of choice for evaluating suspected PE, it is overused and potentially avoidable in one-third of cases, said Dr. Hsu, who is with the VA Greater Los Angeles Healthcare System.
“In the 10 years following the advent of CTPA use, there was a 14-fold increase in usage, but there was no change in mortality,” Dr. Hsu said. “This is consistent with overdiagnosis.”
Dr. Hsu said.
Dr. Hsu and Dr. Soo Hoo surveyed 606 individuals at 18 Veterans Integrated Service Networks (VISNs) and 143 medical centers. A total of 120 fully completed questionnaires were analyzed.
Most respondents (63%) were chiefs, and 80% had 11+ years of experience, Dr. Hsu reported.
Almost all respondents (85%) said CDR with or without D-dimer was not required before ordering a CTPA, survey results show, while only about 7% required both.
“A very small minority of [Veterans Integrated Service Networks], or geographic regions, contained even one hospital that adhered to the guidelines,” Dr. Hsu added.
Though further analysis was limited by sample size, the average CTPA yield for PE appeared to be higher when both components were used in the evaluation, according to Dr. Hsu, who noted an 11.9% yield for CDR plus D-dimer.
Use of CTPA appeared lower at sites with CDR and D-dimer testing, Dr. Hsu added.
These results suggest a need for further research to compare CTPA use and yield in sites that have the algorithm in place, Dr. Hsu told attendees at the meeting.
Adherence to the CDR plus D-dimer diagnostic strategy is “modest at best” despite being a Top 5 Choosing Wisely recommendation in pulmonary medicine, Dr. Hsu told attendees.
The biggest barrier to optimal practice may be the fear of having a patient who “falls through the cracks” based on false-negative CDR and D-dimer data, according to Dr. Hsu.
On the other hand, judicious use of CTPA likely avoids negative sequelae related to radiation, contrast exposure, and treatment-related bleeding, Dr. Hsu said.
“It’s all about balancing risks and benefits,” she said from the podium in a discussion of the study results.
Dr. Hsu and Dr. Soo Hoo disclosed that they had no relationships relevant to their research.
SOURCE: Hsu N et al. CHEST. 2018 Oct. doi: 10.1016/j.chest.2018.08.937
SAN ANTONIO – The recommended approach to evaluating suspected pulmonary embolism is “greatly underutilized” in the Veterans Health Administration system, Nancy Hsu, MD, said at the annual meeting of the American College of Chest Physicians.
Most Veterans Affairs sites did not require incorporation of a clinical decision rule (CDR) and highly sensitive D-dimer prior to ordering CT pulmonary angiography (CTPA) for suspected pulmonary embolism (PE), according to results of a survey by Dr. Hsu and her coinvestigator, Guy Soo Hoo, MD.
While CTPA has become the imaging modality of choice for evaluating suspected PE, it is overused and potentially avoidable in one-third of cases, said Dr. Hsu, who is with the VA Greater Los Angeles Healthcare System.
“In the 10 years following the advent of CTPA use, there was a 14-fold increase in usage, but there was no change in mortality,” Dr. Hsu said. “This is consistent with overdiagnosis.”
Dr. Hsu said.
Dr. Hsu and Dr. Soo Hoo surveyed 606 individuals at 18 Veterans Integrated Service Networks (VISNs) and 143 medical centers. A total of 120 fully completed questionnaires were analyzed.
Most respondents (63%) were chiefs, and 80% had 11+ years of experience, Dr. Hsu reported.
Almost all respondents (85%) said CDR with or without D-dimer was not required before ordering a CTPA, survey results show, while only about 7% required both.
“A very small minority of [Veterans Integrated Service Networks], or geographic regions, contained even one hospital that adhered to the guidelines,” Dr. Hsu added.
Though further analysis was limited by sample size, the average CTPA yield for PE appeared to be higher when both components were used in the evaluation, according to Dr. Hsu, who noted an 11.9% yield for CDR plus D-dimer.
Use of CTPA appeared lower at sites with CDR and D-dimer testing, Dr. Hsu added.
These results suggest a need for further research to compare CTPA use and yield in sites that have the algorithm in place, Dr. Hsu told attendees at the meeting.
Adherence to the CDR plus D-dimer diagnostic strategy is “modest at best” despite being a Top 5 Choosing Wisely recommendation in pulmonary medicine, Dr. Hsu told attendees.
The biggest barrier to optimal practice may be the fear of having a patient who “falls through the cracks” based on false-negative CDR and D-dimer data, according to Dr. Hsu.
On the other hand, judicious use of CTPA likely avoids negative sequelae related to radiation, contrast exposure, and treatment-related bleeding, Dr. Hsu said.
“It’s all about balancing risks and benefits,” she said from the podium in a discussion of the study results.
Dr. Hsu and Dr. Soo Hoo disclosed that they had no relationships relevant to their research.
SOURCE: Hsu N et al. CHEST. 2018 Oct. doi: 10.1016/j.chest.2018.08.937
SAN ANTONIO – The recommended approach to evaluating suspected pulmonary embolism is “greatly underutilized” in the Veterans Health Administration system, Nancy Hsu, MD, said at the annual meeting of the American College of Chest Physicians.
Most Veterans Affairs sites did not require incorporation of a clinical decision rule (CDR) and highly sensitive D-dimer prior to ordering CT pulmonary angiography (CTPA) for suspected pulmonary embolism (PE), according to results of a survey by Dr. Hsu and her coinvestigator, Guy Soo Hoo, MD.
While CTPA has become the imaging modality of choice for evaluating suspected PE, it is overused and potentially avoidable in one-third of cases, said Dr. Hsu, who is with the VA Greater Los Angeles Healthcare System.
“In the 10 years following the advent of CTPA use, there was a 14-fold increase in usage, but there was no change in mortality,” Dr. Hsu said. “This is consistent with overdiagnosis.”
Dr. Hsu said.
Dr. Hsu and Dr. Soo Hoo surveyed 606 individuals at 18 Veterans Integrated Service Networks (VISNs) and 143 medical centers. A total of 120 fully completed questionnaires were analyzed.
Most respondents (63%) were chiefs, and 80% had 11+ years of experience, Dr. Hsu reported.
Almost all respondents (85%) said CDR with or without D-dimer was not required before ordering a CTPA, survey results show, while only about 7% required both.
“A very small minority of [Veterans Integrated Service Networks], or geographic regions, contained even one hospital that adhered to the guidelines,” Dr. Hsu added.
Though further analysis was limited by sample size, the average CTPA yield for PE appeared to be higher when both components were used in the evaluation, according to Dr. Hsu, who noted an 11.9% yield for CDR plus D-dimer.
Use of CTPA appeared lower at sites with CDR and D-dimer testing, Dr. Hsu added.
These results suggest a need for further research to compare CTPA use and yield in sites that have the algorithm in place, Dr. Hsu told attendees at the meeting.
Adherence to the CDR plus D-dimer diagnostic strategy is “modest at best” despite being a Top 5 Choosing Wisely recommendation in pulmonary medicine, Dr. Hsu told attendees.
The biggest barrier to optimal practice may be the fear of having a patient who “falls through the cracks” based on false-negative CDR and D-dimer data, according to Dr. Hsu.
On the other hand, judicious use of CTPA likely avoids negative sequelae related to radiation, contrast exposure, and treatment-related bleeding, Dr. Hsu said.
“It’s all about balancing risks and benefits,” she said from the podium in a discussion of the study results.
Dr. Hsu and Dr. Soo Hoo disclosed that they had no relationships relevant to their research.
SOURCE: Hsu N et al. CHEST. 2018 Oct. doi: 10.1016/j.chest.2018.08.937
REPORTING FROM CHEST 2018
Key clinical point: The recommended approach to evaluating suspected pulmonary embolism was underutilized in VA facilities.
Major finding: 85% of respondents said incorporation of a clinical decision rule plus highly sensitive D-dimer was not required prior to CTPA.
Study details: Analysis of 120 survey questionnaires completed by individuals working in Veterans Integrated Service Networks and medical centers.
Disclosures: Study authors reported no conflicts of interest.
Source: Hsu N et al. CHEST 2018 Oct. doi: 10/1016/j.chest.2018.08.937.
ICU infections: Chlorhexidine wipes tame MRSA, CRE
according to a report presented at ID Week 2018.
The move prevented an estimated eight methicillin-resistant Staphylococcus aureus (MRSA) and three carbapenem-resistant Enterobacteriaceae (CRE) infections and saved the medical center more than $150,000 in the year following the November 2016 switch.
The goal was to address the rate of MRSA bacteremia, which was higher than national ICU averages. Contact precautions began to make less sense as MRSA became more common in the surrounding community, and “we just wanted to get rid of contact precautions,” said study lead Jason Moss, DO, an infectious disease fellow at the university.
Contact precautions are expensive, make patients feel isolated, and according to some studies, lead to worse outcomes, he said at the annual scientific meeting on infectious diseases.
Decolonization is not routine in most ICUs, but it’s gaining traction. Guidelines recommend chlorhexidine bathing with wipes to stop CRE transmission, and chlorhexidine is used to prevent central line–associated bloodstream infections (CLABSI).
A recent analysis of 17 trials found marked decreases in MRSA and CLABSI with decolonization and concluded that chlorhexidine bathing “appears to be of the most clinical benefit when infection rates are high for a given ICU population,” as was the case in Kentucky (Crit Care. 2016 Nov 23;20[1]:379).
When researchers compared the year before the change to the year after, “we were pretty surprised at how much the rates of infection and colonization decreased. There have been some people that have been doing this in the ICU, but probably not to our extent. If you want to get rid of contact precautions, this is a great process to do it with,” Dr. Moss said.
Rates of colonization with MRSA or CRE fell from about 14 isolates per 10,000 patient-days to fewer than 6 (P = .026). Infection rates fell from 3.9 isolates per 10,000 patient-days to 2 (P = .083). Combined rates of infections and colonizations fell from almost 18 isolates per 10,000 patient-days to fewer than 8 (P = .010).
Decolonization is now standard practice at the university. Every ICU patient gets a one-time povidone iodine nasal swab at admission, then daily baths with 2% chlorhexidine gluconate applied by impregnated wipe. It usually takes four or five wipes to do the entire body.
Spending on gowns fell from about $153,000 per year to just under $60,000, but spending on wipes went up from about $2,700 to $275,000, and spending on povidone iodine nasal swabs went up to more than $100,000.
When balanced against the money not spent on those 11 prevented infections, however, the program saved the medical center about $152,000 in its first year, according to Dr. Moss and his team.
There was no funding for the work, and the investigators had no disclosures.
SOURCE: Moss J et al. ID Week 2018, Abstract 32.
according to a report presented at ID Week 2018.
The move prevented an estimated eight methicillin-resistant Staphylococcus aureus (MRSA) and three carbapenem-resistant Enterobacteriaceae (CRE) infections and saved the medical center more than $150,000 in the year following the November 2016 switch.
The goal was to address the rate of MRSA bacteremia, which was higher than national ICU averages. Contact precautions began to make less sense as MRSA became more common in the surrounding community, and “we just wanted to get rid of contact precautions,” said study lead Jason Moss, DO, an infectious disease fellow at the university.
Contact precautions are expensive, make patients feel isolated, and according to some studies, lead to worse outcomes, he said at the annual scientific meeting on infectious diseases.
Decolonization is not routine in most ICUs, but it’s gaining traction. Guidelines recommend chlorhexidine bathing with wipes to stop CRE transmission, and chlorhexidine is used to prevent central line–associated bloodstream infections (CLABSI).
A recent analysis of 17 trials found marked decreases in MRSA and CLABSI with decolonization and concluded that chlorhexidine bathing “appears to be of the most clinical benefit when infection rates are high for a given ICU population,” as was the case in Kentucky (Crit Care. 2016 Nov 23;20[1]:379).
When researchers compared the year before the change to the year after, “we were pretty surprised at how much the rates of infection and colonization decreased. There have been some people that have been doing this in the ICU, but probably not to our extent. If you want to get rid of contact precautions, this is a great process to do it with,” Dr. Moss said.
Rates of colonization with MRSA or CRE fell from about 14 isolates per 10,000 patient-days to fewer than 6 (P = .026). Infection rates fell from 3.9 isolates per 10,000 patient-days to 2 (P = .083). Combined rates of infections and colonizations fell from almost 18 isolates per 10,000 patient-days to fewer than 8 (P = .010).
Decolonization is now standard practice at the university. Every ICU patient gets a one-time povidone iodine nasal swab at admission, then daily baths with 2% chlorhexidine gluconate applied by impregnated wipe. It usually takes four or five wipes to do the entire body.
Spending on gowns fell from about $153,000 per year to just under $60,000, but spending on wipes went up from about $2,700 to $275,000, and spending on povidone iodine nasal swabs went up to more than $100,000.
When balanced against the money not spent on those 11 prevented infections, however, the program saved the medical center about $152,000 in its first year, according to Dr. Moss and his team.
There was no funding for the work, and the investigators had no disclosures.
SOURCE: Moss J et al. ID Week 2018, Abstract 32.
according to a report presented at ID Week 2018.
The move prevented an estimated eight methicillin-resistant Staphylococcus aureus (MRSA) and three carbapenem-resistant Enterobacteriaceae (CRE) infections and saved the medical center more than $150,000 in the year following the November 2016 switch.
The goal was to address the rate of MRSA bacteremia, which was higher than national ICU averages. Contact precautions began to make less sense as MRSA became more common in the surrounding community, and “we just wanted to get rid of contact precautions,” said study lead Jason Moss, DO, an infectious disease fellow at the university.
Contact precautions are expensive, make patients feel isolated, and according to some studies, lead to worse outcomes, he said at the annual scientific meeting on infectious diseases.
Decolonization is not routine in most ICUs, but it’s gaining traction. Guidelines recommend chlorhexidine bathing with wipes to stop CRE transmission, and chlorhexidine is used to prevent central line–associated bloodstream infections (CLABSI).
A recent analysis of 17 trials found marked decreases in MRSA and CLABSI with decolonization and concluded that chlorhexidine bathing “appears to be of the most clinical benefit when infection rates are high for a given ICU population,” as was the case in Kentucky (Crit Care. 2016 Nov 23;20[1]:379).
When researchers compared the year before the change to the year after, “we were pretty surprised at how much the rates of infection and colonization decreased. There have been some people that have been doing this in the ICU, but probably not to our extent. If you want to get rid of contact precautions, this is a great process to do it with,” Dr. Moss said.
Rates of colonization with MRSA or CRE fell from about 14 isolates per 10,000 patient-days to fewer than 6 (P = .026). Infection rates fell from 3.9 isolates per 10,000 patient-days to 2 (P = .083). Combined rates of infections and colonizations fell from almost 18 isolates per 10,000 patient-days to fewer than 8 (P = .010).
Decolonization is now standard practice at the university. Every ICU patient gets a one-time povidone iodine nasal swab at admission, then daily baths with 2% chlorhexidine gluconate applied by impregnated wipe. It usually takes four or five wipes to do the entire body.
Spending on gowns fell from about $153,000 per year to just under $60,000, but spending on wipes went up from about $2,700 to $275,000, and spending on povidone iodine nasal swabs went up to more than $100,000.
When balanced against the money not spent on those 11 prevented infections, however, the program saved the medical center about $152,000 in its first year, according to Dr. Moss and his team.
There was no funding for the work, and the investigators had no disclosures.
SOURCE: Moss J et al. ID Week 2018, Abstract 32.
REPORTING FROM ID WEEK 2018
Key clinical point: For high rates of MRSA and CRE in the ICU, consider decolonization instead of contact precautions.
Major finding: Rates of colonization with MRSA or CRE fell from about 14 isolates per 10,000 patient-days to fewer than 6; infection rates fell from 3.9 isolates to 2 per 10,000 patient-days.
Study details: Review of ICU quality improvement initiative
Disclosures: There was no funding for the work, and the investigators had no disclosures.
Source: Moss J et al. ID Week 2018, Abstract 32.
Readmissions after GI bleeds
Clinical question: What is the rate of hospital readmission within 30 days of nonvariceal upper GI hemorrhage, and what are its effects on mortality, morbidity, and health care use in the United States?
Background: Nonvariceal upper GI hemorrhage is the most common GI emergency that leads to hospital admission (approximately 300,000 admissions/year in the United States). Because of the advances in endoscopic therapy and overall medical care, associated in-hospital mortality has been steadily decreasing. As a result of Medicare and Medicaid shifts toward an alternative payment model, quantifying hospital readmission rate after an episode of nonvariceal upper GI hemorrhage and measuring its effects on patient outcomes and resource use have become a key step in both improving treatment outcomes and health care reimbursement.
Study design: Retrospective study.
Setting: The Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project Nationwide Readmission Database for the year 2014.
Synopsis: The study collected data on hospital readmissions for 203,220 adults who were hospitalized for urgent nonvariceal upper gastrointestinal hemorrhage and discharged. The primary outcome was rate of all-cause readmission within 30 days of discharge. Secondary outcomes were reasons for readmission, readmission mortality rate, morbidity (shock and prolonged mechanical ventilation), and resource use (length of stay and total hospitalization costs and charges).
The rate of readmission was determined to be 13%, with only 18% caused by recurrent nonvariceal upper gastrointestinal bleeding. The rate of death among readmissions was higher than that among index admissions, and a higher proportion of readmitted patients had morbidities requiring prolonged mechanical ventilation. The total economic in-hospital burden was $30.3 million in costs and $108 million in charges over the span of readmission-associated 133,368 hospital days. Independent predictors of readmission were having Medicaid insurance, having a higher comorbidity score, having a lower income, residence in a metropolitan area, hemorrhagic shock, and longer stays in the hospital.
Bottom line: Readmissions within 30 days of discharge for upper GI hemorrhage are associated with higher morbidity and mortality and lead to higher resource use.
Citation: Abougergi M et al. Thirty-day readmission among patients with nonvariceal upper gastrointestinal hemorrhage and effects on outcomes. Gastroenterology. 2018 Jul;155(1):38-46.
Dr. White is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Clinical question: What is the rate of hospital readmission within 30 days of nonvariceal upper GI hemorrhage, and what are its effects on mortality, morbidity, and health care use in the United States?
Background: Nonvariceal upper GI hemorrhage is the most common GI emergency that leads to hospital admission (approximately 300,000 admissions/year in the United States). Because of the advances in endoscopic therapy and overall medical care, associated in-hospital mortality has been steadily decreasing. As a result of Medicare and Medicaid shifts toward an alternative payment model, quantifying hospital readmission rate after an episode of nonvariceal upper GI hemorrhage and measuring its effects on patient outcomes and resource use have become a key step in both improving treatment outcomes and health care reimbursement.
Study design: Retrospective study.
Setting: The Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project Nationwide Readmission Database for the year 2014.
Synopsis: The study collected data on hospital readmissions for 203,220 adults who were hospitalized for urgent nonvariceal upper gastrointestinal hemorrhage and discharged. The primary outcome was rate of all-cause readmission within 30 days of discharge. Secondary outcomes were reasons for readmission, readmission mortality rate, morbidity (shock and prolonged mechanical ventilation), and resource use (length of stay and total hospitalization costs and charges).
The rate of readmission was determined to be 13%, with only 18% caused by recurrent nonvariceal upper gastrointestinal bleeding. The rate of death among readmissions was higher than that among index admissions, and a higher proportion of readmitted patients had morbidities requiring prolonged mechanical ventilation. The total economic in-hospital burden was $30.3 million in costs and $108 million in charges over the span of readmission-associated 133,368 hospital days. Independent predictors of readmission were having Medicaid insurance, having a higher comorbidity score, having a lower income, residence in a metropolitan area, hemorrhagic shock, and longer stays in the hospital.
Bottom line: Readmissions within 30 days of discharge for upper GI hemorrhage are associated with higher morbidity and mortality and lead to higher resource use.
Citation: Abougergi M et al. Thirty-day readmission among patients with nonvariceal upper gastrointestinal hemorrhage and effects on outcomes. Gastroenterology. 2018 Jul;155(1):38-46.
Dr. White is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Clinical question: What is the rate of hospital readmission within 30 days of nonvariceal upper GI hemorrhage, and what are its effects on mortality, morbidity, and health care use in the United States?
Background: Nonvariceal upper GI hemorrhage is the most common GI emergency that leads to hospital admission (approximately 300,000 admissions/year in the United States). Because of the advances in endoscopic therapy and overall medical care, associated in-hospital mortality has been steadily decreasing. As a result of Medicare and Medicaid shifts toward an alternative payment model, quantifying hospital readmission rate after an episode of nonvariceal upper GI hemorrhage and measuring its effects on patient outcomes and resource use have become a key step in both improving treatment outcomes and health care reimbursement.
Study design: Retrospective study.
Setting: The Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project Nationwide Readmission Database for the year 2014.
Synopsis: The study collected data on hospital readmissions for 203,220 adults who were hospitalized for urgent nonvariceal upper gastrointestinal hemorrhage and discharged. The primary outcome was rate of all-cause readmission within 30 days of discharge. Secondary outcomes were reasons for readmission, readmission mortality rate, morbidity (shock and prolonged mechanical ventilation), and resource use (length of stay and total hospitalization costs and charges).
The rate of readmission was determined to be 13%, with only 18% caused by recurrent nonvariceal upper gastrointestinal bleeding. The rate of death among readmissions was higher than that among index admissions, and a higher proportion of readmitted patients had morbidities requiring prolonged mechanical ventilation. The total economic in-hospital burden was $30.3 million in costs and $108 million in charges over the span of readmission-associated 133,368 hospital days. Independent predictors of readmission were having Medicaid insurance, having a higher comorbidity score, having a lower income, residence in a metropolitan area, hemorrhagic shock, and longer stays in the hospital.
Bottom line: Readmissions within 30 days of discharge for upper GI hemorrhage are associated with higher morbidity and mortality and lead to higher resource use.
Citation: Abougergi M et al. Thirty-day readmission among patients with nonvariceal upper gastrointestinal hemorrhage and effects on outcomes. Gastroenterology. 2018 Jul;155(1):38-46.
Dr. White is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
GARFIELD-AF registry: DOACs cut mortality 19%
MUNICH – Treatment of real-world patients newly diagnosed with atrial fibrillation using a direct oral anticoagulant led to benefits that tracked the advantages previously seen in randomized, controlled trials of these drugs, based on findings from more than 26,000 patients enrolled in a global registry.
Atrial fibrillation patients enrolled in the GARFIELD-AF(Global Anticoagulant Registry in the Field) study who started treatment with a direct oral anticoagulant (DOAC) had a 19% relative risk reduction in all-cause mortality during 2 years of follow-up, compared with patients on an oral vitamin K antagonist (VKA) regimen (such as warfarin), a statistically significant difference after adjustment for 30 demographic, clinical, and registry variables, A. John Camm, MD, said at the annual congress of the European Society of Cardiology. The analysis also showed trends toward lower rates of stroke or systemic thrombosis as well as major bleeding events when patients received a DOAC, compared with those on VKA, but these differences were not statistically significant, reported Dr. Camm, a professor of clinical cardiology at St. George’s University of London.
The analyses run by Dr. Camm and his associates also confirmed the superiority of oral anticoagulation. There was an adjusted 17% relative risk reduction in all-cause mortality during 2-year follow-up in patients on any form of oral anticoagulation, compared with patients who did not receive anticoagulation, a statistically significant difference. The comparison of patients on any oral anticoagulant with those not on treatment also showed a significant lowering of stroke or systemic embolism, as well as a 36% relative increase in the risk for a major bleeding episode that was close to statistical significance.
These findings in a registry of patients undergoing routine care “suggest that the effectiveness of oral anticoagulants in randomized clinical trials can be translated to the broad cross section of patients treated in everyday practice,” Dr. Camm said. However, he highlighted two important qualifications to the findings.
First, the analysis focused on the type of anticoagulation patients received at the time they entered the GARFIELD-AF registry and did not account for possible changes in treatment after that. Second, the analysis did not adjust for additional potential confounding variables, which Dr. Camm was certain existed and affected the findings.
“I’m concerned that a confounder we have not been able to account for is the quality of medical care that patients received,” he noted. “The substantial reduction in mortality [using a DOAC, compared with a VKA] is not simply due to reductions in stroke or major bleeding. We must look at other explanations, such as differences in quality of care and access to care.”
The analyses have also not yet looked at outcomes based on the specific DOAC a patient received – apixaban, dabigatran, edoxaban, or rivaroxaban – something that Dr. Camm said is in the works.
GARFIELD-AF enrolled nearly 35,000 patients with newly diagnosed atrial fibrillation and at least one stroke risk factor in 35 countries from April 2013 to September 2016. The analysis winnowed this down to 26,742 patients who also had a CHA2DS2-VASc score of at least 2 (which identifies patients with a high thrombotic risk) and had complete enrollment and follow-up data.
GARFIELD-AF was funded in part by Bayer. Dr. Camm reported being an adviser to Bayer, Boehringer Ingelheim, Daiichi Sankyo, and Pfizer/Bristol-Myers Squibb.
MUNICH – Treatment of real-world patients newly diagnosed with atrial fibrillation using a direct oral anticoagulant led to benefits that tracked the advantages previously seen in randomized, controlled trials of these drugs, based on findings from more than 26,000 patients enrolled in a global registry.
Atrial fibrillation patients enrolled in the GARFIELD-AF(Global Anticoagulant Registry in the Field) study who started treatment with a direct oral anticoagulant (DOAC) had a 19% relative risk reduction in all-cause mortality during 2 years of follow-up, compared with patients on an oral vitamin K antagonist (VKA) regimen (such as warfarin), a statistically significant difference after adjustment for 30 demographic, clinical, and registry variables, A. John Camm, MD, said at the annual congress of the European Society of Cardiology. The analysis also showed trends toward lower rates of stroke or systemic thrombosis as well as major bleeding events when patients received a DOAC, compared with those on VKA, but these differences were not statistically significant, reported Dr. Camm, a professor of clinical cardiology at St. George’s University of London.
The analyses run by Dr. Camm and his associates also confirmed the superiority of oral anticoagulation. There was an adjusted 17% relative risk reduction in all-cause mortality during 2-year follow-up in patients on any form of oral anticoagulation, compared with patients who did not receive anticoagulation, a statistically significant difference. The comparison of patients on any oral anticoagulant with those not on treatment also showed a significant lowering of stroke or systemic embolism, as well as a 36% relative increase in the risk for a major bleeding episode that was close to statistical significance.
These findings in a registry of patients undergoing routine care “suggest that the effectiveness of oral anticoagulants in randomized clinical trials can be translated to the broad cross section of patients treated in everyday practice,” Dr. Camm said. However, he highlighted two important qualifications to the findings.
First, the analysis focused on the type of anticoagulation patients received at the time they entered the GARFIELD-AF registry and did not account for possible changes in treatment after that. Second, the analysis did not adjust for additional potential confounding variables, which Dr. Camm was certain existed and affected the findings.
“I’m concerned that a confounder we have not been able to account for is the quality of medical care that patients received,” he noted. “The substantial reduction in mortality [using a DOAC, compared with a VKA] is not simply due to reductions in stroke or major bleeding. We must look at other explanations, such as differences in quality of care and access to care.”
The analyses have also not yet looked at outcomes based on the specific DOAC a patient received – apixaban, dabigatran, edoxaban, or rivaroxaban – something that Dr. Camm said is in the works.
GARFIELD-AF enrolled nearly 35,000 patients with newly diagnosed atrial fibrillation and at least one stroke risk factor in 35 countries from April 2013 to September 2016. The analysis winnowed this down to 26,742 patients who also had a CHA2DS2-VASc score of at least 2 (which identifies patients with a high thrombotic risk) and had complete enrollment and follow-up data.
GARFIELD-AF was funded in part by Bayer. Dr. Camm reported being an adviser to Bayer, Boehringer Ingelheim, Daiichi Sankyo, and Pfizer/Bristol-Myers Squibb.
MUNICH – Treatment of real-world patients newly diagnosed with atrial fibrillation using a direct oral anticoagulant led to benefits that tracked the advantages previously seen in randomized, controlled trials of these drugs, based on findings from more than 26,000 patients enrolled in a global registry.
Atrial fibrillation patients enrolled in the GARFIELD-AF(Global Anticoagulant Registry in the Field) study who started treatment with a direct oral anticoagulant (DOAC) had a 19% relative risk reduction in all-cause mortality during 2 years of follow-up, compared with patients on an oral vitamin K antagonist (VKA) regimen (such as warfarin), a statistically significant difference after adjustment for 30 demographic, clinical, and registry variables, A. John Camm, MD, said at the annual congress of the European Society of Cardiology. The analysis also showed trends toward lower rates of stroke or systemic thrombosis as well as major bleeding events when patients received a DOAC, compared with those on VKA, but these differences were not statistically significant, reported Dr. Camm, a professor of clinical cardiology at St. George’s University of London.
The analyses run by Dr. Camm and his associates also confirmed the superiority of oral anticoagulation. There was an adjusted 17% relative risk reduction in all-cause mortality during 2-year follow-up in patients on any form of oral anticoagulation, compared with patients who did not receive anticoagulation, a statistically significant difference. The comparison of patients on any oral anticoagulant with those not on treatment also showed a significant lowering of stroke or systemic embolism, as well as a 36% relative increase in the risk for a major bleeding episode that was close to statistical significance.
These findings in a registry of patients undergoing routine care “suggest that the effectiveness of oral anticoagulants in randomized clinical trials can be translated to the broad cross section of patients treated in everyday practice,” Dr. Camm said. However, he highlighted two important qualifications to the findings.
First, the analysis focused on the type of anticoagulation patients received at the time they entered the GARFIELD-AF registry and did not account for possible changes in treatment after that. Second, the analysis did not adjust for additional potential confounding variables, which Dr. Camm was certain existed and affected the findings.
“I’m concerned that a confounder we have not been able to account for is the quality of medical care that patients received,” he noted. “The substantial reduction in mortality [using a DOAC, compared with a VKA] is not simply due to reductions in stroke or major bleeding. We must look at other explanations, such as differences in quality of care and access to care.”
The analyses have also not yet looked at outcomes based on the specific DOAC a patient received – apixaban, dabigatran, edoxaban, or rivaroxaban – something that Dr. Camm said is in the works.
GARFIELD-AF enrolled nearly 35,000 patients with newly diagnosed atrial fibrillation and at least one stroke risk factor in 35 countries from April 2013 to September 2016. The analysis winnowed this down to 26,742 patients who also had a CHA2DS2-VASc score of at least 2 (which identifies patients with a high thrombotic risk) and had complete enrollment and follow-up data.
GARFIELD-AF was funded in part by Bayer. Dr. Camm reported being an adviser to Bayer, Boehringer Ingelheim, Daiichi Sankyo, and Pfizer/Bristol-Myers Squibb.
REPORTING FROM THE ESC CONGRESS 2018
Key clinical point:
Major finding: Direct oral anticoagulant–treated patients had a 19% relative reduction in all-cause death, compared with patients on a vitamin K antagonist.
Study details: The GARFIELD-AF registry, which included 26,742 patients with newly diagnosed atrial fibrillation.
Disclosures: GARFIELD-AF was funded in part by Bayer. Dr. Camm has been an adviser to Bayer, Boehringer Ingelheim, Daiichi Sankyo, and Pfizer/Bristol-Myers Squibb.