User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Surgeries account for almost half of hospital costs
according to the Agency for Healthcare Research and Quality (AHRQ).
Of the 35.4 million inpatient stays in 2014 – the last full year of ICD-9-CM coding – 10.1 million (28.6%) involved at least one any-listed surgical procedure, and 25.2 million (71.4%) did not. The total cost of all admissions was $386.2 billion, of which $187.1 billion (48.4%) went for stays with surgeries and $199.1 billion (51.6%) went for nonsurgical stays, the AHRQ reported in a statistical brief.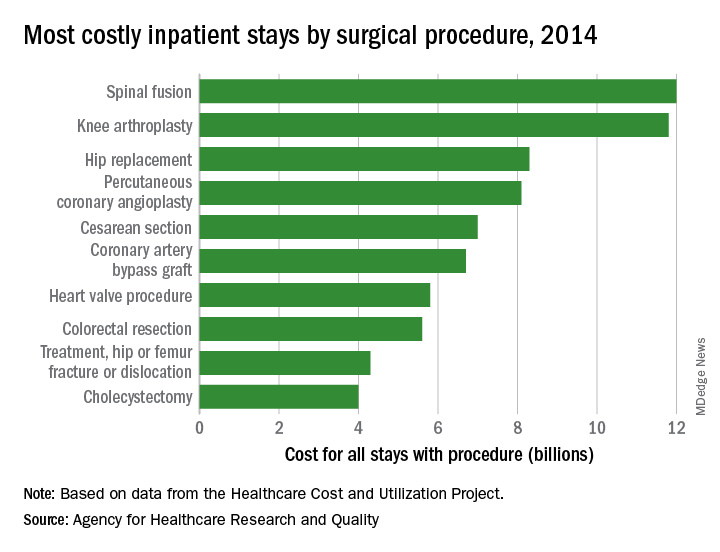
There were five other musculoskeletal procedures among the 20 most costly surgery-related admissions: knee arthroplasty was second at $11.8 billion, hip replacement was third at $8.3 billion, treatment of hip and femur fracture/dislocation was ninth at $4.3 billion, amputation of lower extremity was 13th at $2.5 billion, and treatment of lower extremity (other than hip or femur) fracture/dislocation was 14th at $2.4 billion. Those six procedures combined were $41.2 billion in hospital costs, which was a quarter of the total for all stays with a first-listed OR procedure, the AHRQ said.
The nonmusculoskeletal procedures in the top five were percutaneous coronary angioplasty in fourth, with an aggregate cost of $8.1 billion, and cesarean section in fifth at an even $7 billion. Coronary artery bypass graft, the most expensive procedure per stay ($52,000) among the top 20 procedures, was sixth in aggregate cost at $6.7 billion, according to the AHRQ researchers.
according to the Agency for Healthcare Research and Quality (AHRQ).
Of the 35.4 million inpatient stays in 2014 – the last full year of ICD-9-CM coding – 10.1 million (28.6%) involved at least one any-listed surgical procedure, and 25.2 million (71.4%) did not. The total cost of all admissions was $386.2 billion, of which $187.1 billion (48.4%) went for stays with surgeries and $199.1 billion (51.6%) went for nonsurgical stays, the AHRQ reported in a statistical brief.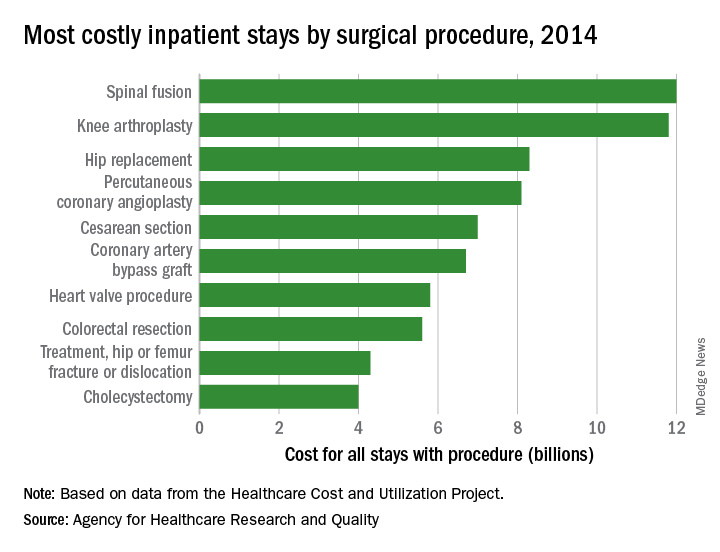
There were five other musculoskeletal procedures among the 20 most costly surgery-related admissions: knee arthroplasty was second at $11.8 billion, hip replacement was third at $8.3 billion, treatment of hip and femur fracture/dislocation was ninth at $4.3 billion, amputation of lower extremity was 13th at $2.5 billion, and treatment of lower extremity (other than hip or femur) fracture/dislocation was 14th at $2.4 billion. Those six procedures combined were $41.2 billion in hospital costs, which was a quarter of the total for all stays with a first-listed OR procedure, the AHRQ said.
The nonmusculoskeletal procedures in the top five were percutaneous coronary angioplasty in fourth, with an aggregate cost of $8.1 billion, and cesarean section in fifth at an even $7 billion. Coronary artery bypass graft, the most expensive procedure per stay ($52,000) among the top 20 procedures, was sixth in aggregate cost at $6.7 billion, according to the AHRQ researchers.
according to the Agency for Healthcare Research and Quality (AHRQ).
Of the 35.4 million inpatient stays in 2014 – the last full year of ICD-9-CM coding – 10.1 million (28.6%) involved at least one any-listed surgical procedure, and 25.2 million (71.4%) did not. The total cost of all admissions was $386.2 billion, of which $187.1 billion (48.4%) went for stays with surgeries and $199.1 billion (51.6%) went for nonsurgical stays, the AHRQ reported in a statistical brief.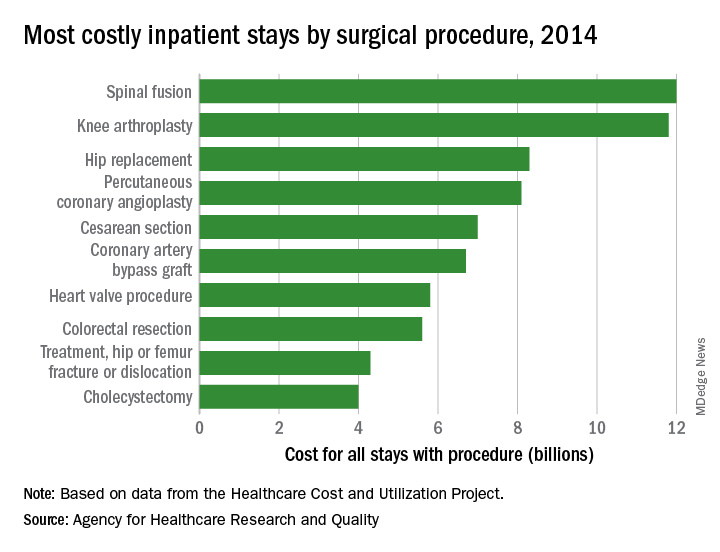
There were five other musculoskeletal procedures among the 20 most costly surgery-related admissions: knee arthroplasty was second at $11.8 billion, hip replacement was third at $8.3 billion, treatment of hip and femur fracture/dislocation was ninth at $4.3 billion, amputation of lower extremity was 13th at $2.5 billion, and treatment of lower extremity (other than hip or femur) fracture/dislocation was 14th at $2.4 billion. Those six procedures combined were $41.2 billion in hospital costs, which was a quarter of the total for all stays with a first-listed OR procedure, the AHRQ said.
The nonmusculoskeletal procedures in the top five were percutaneous coronary angioplasty in fourth, with an aggregate cost of $8.1 billion, and cesarean section in fifth at an even $7 billion. Coronary artery bypass graft, the most expensive procedure per stay ($52,000) among the top 20 procedures, was sixth in aggregate cost at $6.7 billion, according to the AHRQ researchers.
24-hour ambulatory BP measurements strongly predict mortality
Ambulatory measurements of blood pressure more strongly predicted all-cause and cardiovascular mortality than did BP measured in the clinic, according to analysis of a large patient registry in Spain.
The results also showed an increased risk of death associated with white coat hypertension and an even stronger association between death and masked hypertension. They were published in the New England Journal of Medicine.
Previous investigations had found that 24-hour ambulatory BP measurements were better predictors of patient outcomes than those obtained in the clinic or at home, but those investigations were small or population based.“In these studies, the number of clinical outcomes was limited, which reduced the ability to assess the predictive value of clinic blood pressure data as compared with ambulatory data,” reported José R. Banegas, MD, of the department of preventive medicine and public health at the Autonomous University of Madrid and his colleagues.
To better define the prognostic value of 24-hour ambulatory blood pressure measurement, Dr. Banegas and his colleagues looked at data on a large cohort of primary care patients in the Spanish Ambulatory Blood Pressure Registry. Their analysis included 63,910 adults recruited to the registry during 2004-2014.
Patients had blood pressure measurements taken in the clinic according to standard procedures. Afterward, they had ambulatory blood pressure monitoring that used an automated device programmed to record BP every 20 minutes during the day and every 30 minutes at night.
They found that overall clinic and ambulatory blood pressure measurements had a relatively similar magnitude of association with all-cause and cardiovascular mortality.
However, clinic systolic pressure lost its predictive power for all-cause mortality after adjustment for 24-hour ambulatory systolic pressure. The hazard ratio for all-cause mortality dropped from 1.54 before the adjustment to 1.02 after the adjustment, Dr. Banegas and his colleagues reported.
By contrast, ambulatory systolic pressure kept its predictive value after accounting for clinical systolic pressure, with a hazard ratio for all-cause mortality of 1.58 before and after the adjustment, they said in the report.
The strongest association with all-cause mortality was found in patients with masked hypertension – normal clinic readings but elevated ambulatory readings. The hazard ratio for all-cause mortality in that group was 2.83 when adjusted for clinic blood pressure, with similar findings reported for cardiovascular mortality.
White coat hypertension was also associated with increased risk of mortality. The finding of elevated clinic BP and normal 24-hour ambulatory BP had a hazard ratio of 1.79 for all-cause mortality after adjustment for clinic BP, results showed.
“In our study, white coat hypertension was not benign, which may be due in part to the higher mean blood pressure over 24 hours in these patients (119.9/71.9 mm Hg vs. 116.6/70.6 mm Hg in normotensive patients; P less than .001) or to their metabolic phenotype,” the investigators wrote.
Lacer Laboratories, the Spanish Society of Hypertension, and some European government agencies supported the study. Dr. Banegas reported grants from Fondo de Investigación Sanitaria and personal fees from Lacer. Coauthors reported disclosures related to Vascular Dynamics USA, Relypsa USA, Novartis Pharma USA, Daiichi Sankyo, Boehringer Ingelheim, Pfizer, Lacer Laboratories Spain, and others.
SOURCE: Banegas JR et al. N Engl J Med. 2018;378:1509-20.
The investigation by Dr. Banegas and colleagues confirms that ambulatory blood pressure monitoring is useful for assessing blood pressure, the most important and treatable factor contributing to death and disability.
The registry study addresses several clinically relevant issues. In particular, ambulatory blood pressure measures more strongly predicted all-cause and cardiovascular mortality as compared with blood pressure measured in the clinic.
Moreover, the highest hazard ratio of death was seen in patients with masked hypertension, or those with normal clinic-measured blood pressure but elevated ambulatory measurements.
Finally, patients with white coat hypertension (elevated clinic but normal ambulatory blood pressure) had a risk of cardiovascular death twice as high as patients with normal clinic and ambulatory values.
The ominous effect of white coat hypertension has been noted by others, and it is probably related to the increasing magnitude (that is, the difference between clinic blood pressure and ambulatory blood pressure) to white coat hypertension with age.
Ambulatory blood pressure monitoring equipment has evolved and is much lighter than in the past, making it more acceptable to patients.
With more patients undergoing ambulatory blood pressure monitoring, several countries established ambulatory monitoring registries, such as the Spanish registry evaluated in this study.
Ultimately, one hopes the results of this registry study would serve as one more spur to providers and device manufacturers to initiate a registry in the United States.
Raymond R. Townsend, MD, is from the University of Pennsylvania, Philadelphia. These comments are based on his editorial that appeared in the New England Journal of Medicine . Dr. Townsend reported disclosures related to Medtronic, AXIO, and CLARUS Therapeutics, among others.
The investigation by Dr. Banegas and colleagues confirms that ambulatory blood pressure monitoring is useful for assessing blood pressure, the most important and treatable factor contributing to death and disability.
The registry study addresses several clinically relevant issues. In particular, ambulatory blood pressure measures more strongly predicted all-cause and cardiovascular mortality as compared with blood pressure measured in the clinic.
Moreover, the highest hazard ratio of death was seen in patients with masked hypertension, or those with normal clinic-measured blood pressure but elevated ambulatory measurements.
Finally, patients with white coat hypertension (elevated clinic but normal ambulatory blood pressure) had a risk of cardiovascular death twice as high as patients with normal clinic and ambulatory values.
The ominous effect of white coat hypertension has been noted by others, and it is probably related to the increasing magnitude (that is, the difference between clinic blood pressure and ambulatory blood pressure) to white coat hypertension with age.
Ambulatory blood pressure monitoring equipment has evolved and is much lighter than in the past, making it more acceptable to patients.
With more patients undergoing ambulatory blood pressure monitoring, several countries established ambulatory monitoring registries, such as the Spanish registry evaluated in this study.
Ultimately, one hopes the results of this registry study would serve as one more spur to providers and device manufacturers to initiate a registry in the United States.
Raymond R. Townsend, MD, is from the University of Pennsylvania, Philadelphia. These comments are based on his editorial that appeared in the New England Journal of Medicine . Dr. Townsend reported disclosures related to Medtronic, AXIO, and CLARUS Therapeutics, among others.
The investigation by Dr. Banegas and colleagues confirms that ambulatory blood pressure monitoring is useful for assessing blood pressure, the most important and treatable factor contributing to death and disability.
The registry study addresses several clinically relevant issues. In particular, ambulatory blood pressure measures more strongly predicted all-cause and cardiovascular mortality as compared with blood pressure measured in the clinic.
Moreover, the highest hazard ratio of death was seen in patients with masked hypertension, or those with normal clinic-measured blood pressure but elevated ambulatory measurements.
Finally, patients with white coat hypertension (elevated clinic but normal ambulatory blood pressure) had a risk of cardiovascular death twice as high as patients with normal clinic and ambulatory values.
The ominous effect of white coat hypertension has been noted by others, and it is probably related to the increasing magnitude (that is, the difference between clinic blood pressure and ambulatory blood pressure) to white coat hypertension with age.
Ambulatory blood pressure monitoring equipment has evolved and is much lighter than in the past, making it more acceptable to patients.
With more patients undergoing ambulatory blood pressure monitoring, several countries established ambulatory monitoring registries, such as the Spanish registry evaluated in this study.
Ultimately, one hopes the results of this registry study would serve as one more spur to providers and device manufacturers to initiate a registry in the United States.
Raymond R. Townsend, MD, is from the University of Pennsylvania, Philadelphia. These comments are based on his editorial that appeared in the New England Journal of Medicine . Dr. Townsend reported disclosures related to Medtronic, AXIO, and CLARUS Therapeutics, among others.
Ambulatory measurements of blood pressure more strongly predicted all-cause and cardiovascular mortality than did BP measured in the clinic, according to analysis of a large patient registry in Spain.
The results also showed an increased risk of death associated with white coat hypertension and an even stronger association between death and masked hypertension. They were published in the New England Journal of Medicine.
Previous investigations had found that 24-hour ambulatory BP measurements were better predictors of patient outcomes than those obtained in the clinic or at home, but those investigations were small or population based.“In these studies, the number of clinical outcomes was limited, which reduced the ability to assess the predictive value of clinic blood pressure data as compared with ambulatory data,” reported José R. Banegas, MD, of the department of preventive medicine and public health at the Autonomous University of Madrid and his colleagues.
To better define the prognostic value of 24-hour ambulatory blood pressure measurement, Dr. Banegas and his colleagues looked at data on a large cohort of primary care patients in the Spanish Ambulatory Blood Pressure Registry. Their analysis included 63,910 adults recruited to the registry during 2004-2014.
Patients had blood pressure measurements taken in the clinic according to standard procedures. Afterward, they had ambulatory blood pressure monitoring that used an automated device programmed to record BP every 20 minutes during the day and every 30 minutes at night.
They found that overall clinic and ambulatory blood pressure measurements had a relatively similar magnitude of association with all-cause and cardiovascular mortality.
However, clinic systolic pressure lost its predictive power for all-cause mortality after adjustment for 24-hour ambulatory systolic pressure. The hazard ratio for all-cause mortality dropped from 1.54 before the adjustment to 1.02 after the adjustment, Dr. Banegas and his colleagues reported.
By contrast, ambulatory systolic pressure kept its predictive value after accounting for clinical systolic pressure, with a hazard ratio for all-cause mortality of 1.58 before and after the adjustment, they said in the report.
The strongest association with all-cause mortality was found in patients with masked hypertension – normal clinic readings but elevated ambulatory readings. The hazard ratio for all-cause mortality in that group was 2.83 when adjusted for clinic blood pressure, with similar findings reported for cardiovascular mortality.
White coat hypertension was also associated with increased risk of mortality. The finding of elevated clinic BP and normal 24-hour ambulatory BP had a hazard ratio of 1.79 for all-cause mortality after adjustment for clinic BP, results showed.
“In our study, white coat hypertension was not benign, which may be due in part to the higher mean blood pressure over 24 hours in these patients (119.9/71.9 mm Hg vs. 116.6/70.6 mm Hg in normotensive patients; P less than .001) or to their metabolic phenotype,” the investigators wrote.
Lacer Laboratories, the Spanish Society of Hypertension, and some European government agencies supported the study. Dr. Banegas reported grants from Fondo de Investigación Sanitaria and personal fees from Lacer. Coauthors reported disclosures related to Vascular Dynamics USA, Relypsa USA, Novartis Pharma USA, Daiichi Sankyo, Boehringer Ingelheim, Pfizer, Lacer Laboratories Spain, and others.
SOURCE: Banegas JR et al. N Engl J Med. 2018;378:1509-20.
Ambulatory measurements of blood pressure more strongly predicted all-cause and cardiovascular mortality than did BP measured in the clinic, according to analysis of a large patient registry in Spain.
The results also showed an increased risk of death associated with white coat hypertension and an even stronger association between death and masked hypertension. They were published in the New England Journal of Medicine.
Previous investigations had found that 24-hour ambulatory BP measurements were better predictors of patient outcomes than those obtained in the clinic or at home, but those investigations were small or population based.“In these studies, the number of clinical outcomes was limited, which reduced the ability to assess the predictive value of clinic blood pressure data as compared with ambulatory data,” reported José R. Banegas, MD, of the department of preventive medicine and public health at the Autonomous University of Madrid and his colleagues.
To better define the prognostic value of 24-hour ambulatory blood pressure measurement, Dr. Banegas and his colleagues looked at data on a large cohort of primary care patients in the Spanish Ambulatory Blood Pressure Registry. Their analysis included 63,910 adults recruited to the registry during 2004-2014.
Patients had blood pressure measurements taken in the clinic according to standard procedures. Afterward, they had ambulatory blood pressure monitoring that used an automated device programmed to record BP every 20 minutes during the day and every 30 minutes at night.
They found that overall clinic and ambulatory blood pressure measurements had a relatively similar magnitude of association with all-cause and cardiovascular mortality.
However, clinic systolic pressure lost its predictive power for all-cause mortality after adjustment for 24-hour ambulatory systolic pressure. The hazard ratio for all-cause mortality dropped from 1.54 before the adjustment to 1.02 after the adjustment, Dr. Banegas and his colleagues reported.
By contrast, ambulatory systolic pressure kept its predictive value after accounting for clinical systolic pressure, with a hazard ratio for all-cause mortality of 1.58 before and after the adjustment, they said in the report.
The strongest association with all-cause mortality was found in patients with masked hypertension – normal clinic readings but elevated ambulatory readings. The hazard ratio for all-cause mortality in that group was 2.83 when adjusted for clinic blood pressure, with similar findings reported for cardiovascular mortality.
White coat hypertension was also associated with increased risk of mortality. The finding of elevated clinic BP and normal 24-hour ambulatory BP had a hazard ratio of 1.79 for all-cause mortality after adjustment for clinic BP, results showed.
“In our study, white coat hypertension was not benign, which may be due in part to the higher mean blood pressure over 24 hours in these patients (119.9/71.9 mm Hg vs. 116.6/70.6 mm Hg in normotensive patients; P less than .001) or to their metabolic phenotype,” the investigators wrote.
Lacer Laboratories, the Spanish Society of Hypertension, and some European government agencies supported the study. Dr. Banegas reported grants from Fondo de Investigación Sanitaria and personal fees from Lacer. Coauthors reported disclosures related to Vascular Dynamics USA, Relypsa USA, Novartis Pharma USA, Daiichi Sankyo, Boehringer Ingelheim, Pfizer, Lacer Laboratories Spain, and others.
SOURCE: Banegas JR et al. N Engl J Med. 2018;378:1509-20.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: Modeling showed a stronger association between ambulatory systolic pressure and all-cause mortality (adjusted HR, 1.58 per 1-SD pressure increase) than between clinic systolic pressure and all-cause mortality (adjusted HR, 1.02).
Study details: Retrospective analysis of mortality from a cohort of 63,910 adults recruited to a registry in Spain during 2004-2014.
Disclosures: Lacer Laboratories, the Spanish Society of Hypertension, and some European government agencies supported the study. Dr. Banegas reported grants from Fondo de Investigación Sanitaria and personal fees from Lacer. Coauthors reported disclosures related to Vascular Dynamics USA, Relypsa USA, Novartis Pharma USA, Daiichi Sankyo, Boehringer Ingelheim, Pfizer, Lacer Laboratories Spain, and others.
Source: Banegas JR et al. N Engl J Med 2018;378:1509-20.
High 5-year mortality in patients admitted with heart failure regardless of ejection fraction
Background: Heart failure with preserved EF is a common cause of inpatient admission and previously was thought to carry a better prognosis than heart failure with reduced EF. Recent analysis using data from Get With the Guidelines–Heart Failure (GWTG-HF) registry has shown similarly poor survival rates at 30 days and 1 year when compared with heart failure with reduced EF.
Study design: Multicenter retrospective cohort study.
Setting: 276 hospitals in the GWTG-HF registry during 2005-2009, with 5 years of follow-up through 2014.
Synopsis: A total 39,982 patients who were admitted for heart failure during 2005-2009 were included in the study with stratification into three groups based on ejection fraction; 18,398 (46%) with heart failure with reduced EF; 2,385 (8.2%) with heart failure with borderline EF; and 18,299 (46%) with heart failure with preserved EF. The 5-year mortality rate for the entire cohort was 75.4% with similar mortality rates for patient with preserved EF (75.3%), compared with those with reduced EF (75.7%).
Bottom line: Among patients hospitalized with heart failure, irrespective of their ejection fraction, the 5-year survival rates were equally dismal. Hospitalists may wish to use this information in goals of care discussions.
Citation: Shah KS et al. Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes. J Am Coll Cardiol. 2017 Oct 31. doi: 10.1016/j.jacc.2017.08.074.
Dr. Gomez-Sanchez is a hospitalist at the University of Virginia Medical Center.
Background: Heart failure with preserved EF is a common cause of inpatient admission and previously was thought to carry a better prognosis than heart failure with reduced EF. Recent analysis using data from Get With the Guidelines–Heart Failure (GWTG-HF) registry has shown similarly poor survival rates at 30 days and 1 year when compared with heart failure with reduced EF.
Study design: Multicenter retrospective cohort study.
Setting: 276 hospitals in the GWTG-HF registry during 2005-2009, with 5 years of follow-up through 2014.
Synopsis: A total 39,982 patients who were admitted for heart failure during 2005-2009 were included in the study with stratification into three groups based on ejection fraction; 18,398 (46%) with heart failure with reduced EF; 2,385 (8.2%) with heart failure with borderline EF; and 18,299 (46%) with heart failure with preserved EF. The 5-year mortality rate for the entire cohort was 75.4% with similar mortality rates for patient with preserved EF (75.3%), compared with those with reduced EF (75.7%).
Bottom line: Among patients hospitalized with heart failure, irrespective of their ejection fraction, the 5-year survival rates were equally dismal. Hospitalists may wish to use this information in goals of care discussions.
Citation: Shah KS et al. Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes. J Am Coll Cardiol. 2017 Oct 31. doi: 10.1016/j.jacc.2017.08.074.
Dr. Gomez-Sanchez is a hospitalist at the University of Virginia Medical Center.
Background: Heart failure with preserved EF is a common cause of inpatient admission and previously was thought to carry a better prognosis than heart failure with reduced EF. Recent analysis using data from Get With the Guidelines–Heart Failure (GWTG-HF) registry has shown similarly poor survival rates at 30 days and 1 year when compared with heart failure with reduced EF.
Study design: Multicenter retrospective cohort study.
Setting: 276 hospitals in the GWTG-HF registry during 2005-2009, with 5 years of follow-up through 2014.
Synopsis: A total 39,982 patients who were admitted for heart failure during 2005-2009 were included in the study with stratification into three groups based on ejection fraction; 18,398 (46%) with heart failure with reduced EF; 2,385 (8.2%) with heart failure with borderline EF; and 18,299 (46%) with heart failure with preserved EF. The 5-year mortality rate for the entire cohort was 75.4% with similar mortality rates for patient with preserved EF (75.3%), compared with those with reduced EF (75.7%).
Bottom line: Among patients hospitalized with heart failure, irrespective of their ejection fraction, the 5-year survival rates were equally dismal. Hospitalists may wish to use this information in goals of care discussions.
Citation: Shah KS et al. Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes. J Am Coll Cardiol. 2017 Oct 31. doi: 10.1016/j.jacc.2017.08.074.
Dr. Gomez-Sanchez is a hospitalist at the University of Virginia Medical Center.
Do hospitalists improve inpatient outcomes?
Long continues the debate on what impact hospitalists have on inpatient outcomes. This issue has been playing out in the medical literature for 20 years, since the coining of the term in 1997. In a recent iteration of the debate, a study was published in JAMA Internal Medicine entitled “Comparison of Hospital Resource Use and Outcomes Among Hospitalists, Primary Care Physicians, and Other Generalists.”
The study retrospectively evaluated health care resources and outcomes from over a half-million Medicare beneficiaries hospitalized in 2013 for 20 common diagnosis-related groups, by type of physician provider (hospitalist, their primary care physician, or other generalist). The study found that nonhospitalists used more consultations and had longer lengths of stays, compared with hospitalists. In addition, relative to hospitalists, PCPs were more likely to discharge patients to home, had similar readmission rates, and lower 30-day mortality rates, but generalists were less likely to discharge patients home, had higher readmission rates, and higher mortality rates.
As hospitalists, we need to understand and acknowledge that most of our patients are “brand new” to us, and it is paramount that we use all available resources to gain a deep understanding of the patient in as short a time as possible. For example, ensuring all medical records available are reviewed, at least as much as possible, including a medical list (including a medication reconciliation). Interviewing family members or caregivers is also obviously a “best practice.” As well, having the insight of the PCP in these patients’ care is unquestionably good for us, for the PCP, and for the patient.
With good communication processes and an eye for excellence in care transitions, hospitalists can and should achieve the best outcomes for all of their patients. I look forward to more research in this arena, including a better understanding of the mechanisms by which we can all reliably produce excellent outcomes for the patients we serve.
Read the full post at hospitalleader.org.
Also on The Hospital Leader …
• Locums vs. F/T Hospitalists: Do Temps Stack Up? by Brad Flansbaum, DO, MPH, MHM
• Rounds: Are We Spinning Our Wheels? by Vineet Arora, MD, MPP, MHM
• Up Your Game in APP Integration by Tracy Cardin, ACNP-BC, SFHM
Long continues the debate on what impact hospitalists have on inpatient outcomes. This issue has been playing out in the medical literature for 20 years, since the coining of the term in 1997. In a recent iteration of the debate, a study was published in JAMA Internal Medicine entitled “Comparison of Hospital Resource Use and Outcomes Among Hospitalists, Primary Care Physicians, and Other Generalists.”
The study retrospectively evaluated health care resources and outcomes from over a half-million Medicare beneficiaries hospitalized in 2013 for 20 common diagnosis-related groups, by type of physician provider (hospitalist, their primary care physician, or other generalist). The study found that nonhospitalists used more consultations and had longer lengths of stays, compared with hospitalists. In addition, relative to hospitalists, PCPs were more likely to discharge patients to home, had similar readmission rates, and lower 30-day mortality rates, but generalists were less likely to discharge patients home, had higher readmission rates, and higher mortality rates.
As hospitalists, we need to understand and acknowledge that most of our patients are “brand new” to us, and it is paramount that we use all available resources to gain a deep understanding of the patient in as short a time as possible. For example, ensuring all medical records available are reviewed, at least as much as possible, including a medical list (including a medication reconciliation). Interviewing family members or caregivers is also obviously a “best practice.” As well, having the insight of the PCP in these patients’ care is unquestionably good for us, for the PCP, and for the patient.
With good communication processes and an eye for excellence in care transitions, hospitalists can and should achieve the best outcomes for all of their patients. I look forward to more research in this arena, including a better understanding of the mechanisms by which we can all reliably produce excellent outcomes for the patients we serve.
Read the full post at hospitalleader.org.
Also on The Hospital Leader …
• Locums vs. F/T Hospitalists: Do Temps Stack Up? by Brad Flansbaum, DO, MPH, MHM
• Rounds: Are We Spinning Our Wheels? by Vineet Arora, MD, MPP, MHM
• Up Your Game in APP Integration by Tracy Cardin, ACNP-BC, SFHM
Long continues the debate on what impact hospitalists have on inpatient outcomes. This issue has been playing out in the medical literature for 20 years, since the coining of the term in 1997. In a recent iteration of the debate, a study was published in JAMA Internal Medicine entitled “Comparison of Hospital Resource Use and Outcomes Among Hospitalists, Primary Care Physicians, and Other Generalists.”
The study retrospectively evaluated health care resources and outcomes from over a half-million Medicare beneficiaries hospitalized in 2013 for 20 common diagnosis-related groups, by type of physician provider (hospitalist, their primary care physician, or other generalist). The study found that nonhospitalists used more consultations and had longer lengths of stays, compared with hospitalists. In addition, relative to hospitalists, PCPs were more likely to discharge patients to home, had similar readmission rates, and lower 30-day mortality rates, but generalists were less likely to discharge patients home, had higher readmission rates, and higher mortality rates.
As hospitalists, we need to understand and acknowledge that most of our patients are “brand new” to us, and it is paramount that we use all available resources to gain a deep understanding of the patient in as short a time as possible. For example, ensuring all medical records available are reviewed, at least as much as possible, including a medical list (including a medication reconciliation). Interviewing family members or caregivers is also obviously a “best practice.” As well, having the insight of the PCP in these patients’ care is unquestionably good for us, for the PCP, and for the patient.
With good communication processes and an eye for excellence in care transitions, hospitalists can and should achieve the best outcomes for all of their patients. I look forward to more research in this arena, including a better understanding of the mechanisms by which we can all reliably produce excellent outcomes for the patients we serve.
Read the full post at hospitalleader.org.
Also on The Hospital Leader …
• Locums vs. F/T Hospitalists: Do Temps Stack Up? by Brad Flansbaum, DO, MPH, MHM
• Rounds: Are We Spinning Our Wheels? by Vineet Arora, MD, MPP, MHM
• Up Your Game in APP Integration by Tracy Cardin, ACNP-BC, SFHM
Short Takes
Giving iron supplements every other day may be superior to daily divided doses
Serum hepcidin levels and iron absorption were compared in women given daily dosing of ferrous sulfate, women given alternate-day dosing, and women given two divided doses daily. Women on the alternate-day regimen and the single-day regimens had higher iron absorption and lower hepcidin levels than did the women on the split-dosing regimen; these findings need to be confirmed in patients with iron-deficiency anemia.
Immediate percutaneous coronary intervention (PCI) of the culprit lesion only in patients presenting with acute myocardial infarction and cardiogenic shock may lead to better outcomes, even in those with multivessel disease
A total of 706 patients with multivessel coronary artery disease who presented with acute MI and cardiogenic shock were randomized to either PCI of the culprit lesion only (followed by optional staged revascularization of nonculprit lesions) or to immediate multivessel PCI. Patients who received PCI of the culprit lesion only had a lower 30-day risk of death or severe renal failure leading to renal-replacement therapy than did those who underwent immediate multivessel PCI.
Citation: Thiele H et al. PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N Engl J Med. 2017 Oct. doi: 10.1056/NEJMoa1710261 (epub ahead of print).
Giving iron supplements every other day may be superior to daily divided doses
Serum hepcidin levels and iron absorption were compared in women given daily dosing of ferrous sulfate, women given alternate-day dosing, and women given two divided doses daily. Women on the alternate-day regimen and the single-day regimens had higher iron absorption and lower hepcidin levels than did the women on the split-dosing regimen; these findings need to be confirmed in patients with iron-deficiency anemia.
Immediate percutaneous coronary intervention (PCI) of the culprit lesion only in patients presenting with acute myocardial infarction and cardiogenic shock may lead to better outcomes, even in those with multivessel disease
A total of 706 patients with multivessel coronary artery disease who presented with acute MI and cardiogenic shock were randomized to either PCI of the culprit lesion only (followed by optional staged revascularization of nonculprit lesions) or to immediate multivessel PCI. Patients who received PCI of the culprit lesion only had a lower 30-day risk of death or severe renal failure leading to renal-replacement therapy than did those who underwent immediate multivessel PCI.
Citation: Thiele H et al. PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N Engl J Med. 2017 Oct. doi: 10.1056/NEJMoa1710261 (epub ahead of print).
Giving iron supplements every other day may be superior to daily divided doses
Serum hepcidin levels and iron absorption were compared in women given daily dosing of ferrous sulfate, women given alternate-day dosing, and women given two divided doses daily. Women on the alternate-day regimen and the single-day regimens had higher iron absorption and lower hepcidin levels than did the women on the split-dosing regimen; these findings need to be confirmed in patients with iron-deficiency anemia.
Immediate percutaneous coronary intervention (PCI) of the culprit lesion only in patients presenting with acute myocardial infarction and cardiogenic shock may lead to better outcomes, even in those with multivessel disease
A total of 706 patients with multivessel coronary artery disease who presented with acute MI and cardiogenic shock were randomized to either PCI of the culprit lesion only (followed by optional staged revascularization of nonculprit lesions) or to immediate multivessel PCI. Patients who received PCI of the culprit lesion only had a lower 30-day risk of death or severe renal failure leading to renal-replacement therapy than did those who underwent immediate multivessel PCI.
Citation: Thiele H et al. PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N Engl J Med. 2017 Oct. doi: 10.1056/NEJMoa1710261 (epub ahead of print).
Common infections are potent risk factor for MI, stroke
ORLANDO – , according to a “big data” registry study from the United Kingdom.
“Our data show infection was just as much a risk factor or more compared with the traditional atherosclerotic cardiovascular disease risk factors,” Paul Carter, MD, said at the annual meeting of the American College of Cardiology.
Dr. Carter of Aston Medical School in Birmingham, England, presented a retrospective analysis from the ACALM (Algorithm for Comorbidities Associated with Length of stay and Mortality) study of administrative data on all of the more than 1.22 million patients admitted to seven U.K. hospitals in 2000-2013. His analysis included all 34,027 adults aged 40 years or older admitted with a urinary tract or respiratory infection on their index hospitalization who had no history of ischemic heart disease or ischemic stroke.
These patients, with a mean age of 73 years, 59% of whom were women, were compared with an equal number of age- and gender-matched adults whose index hospitalization was for reasons other than ischemic heart disease, stroke, urinary tract infection (UTI), or respiratory infection – the two most common infections resulting in hospitalization in the United Kingdom.
Patients with a respiratory infection or UTI had a 9.9% incidence of new-onset ischemic heart disease and a 4.1% rate of ischemic stroke during follow-up starting upon discharge from their index hospitalization, significantly higher than the 5.9% and 1.5% rates in controls. In a multivariate logistic regression analysis adjusted for demographics, standard cardiovascular risk factors, and the top 10 causes of mortality in the United Kingdom, patients with respiratory infection or UTI as their admitting diagnosis had a 1.36-fold increased likelihood of developing ischemic heart disease post discharge and a 2.5-fold greater risk of ischemic stroke than matched controls.
Moreover, mortality following diagnosis of ischemic heart disease was 75.2% in patients whose index hospitalization was for infection, compared with 51.1% in controls who developed ischemic heart disease without a history of hospitalization for infection, for an adjusted 2.98-fold increased likelihood of death. Similarly, mortality after an ischemic stroke was 59.8% in patients with a prior severe infection, compared with 30.8% in controls, which translated to an adjusted 3.1-fold increased risk of death post stroke in patients with a prior hospitalization for infection.
In the multivariate analysis, hospitalization for infection was a stronger risk factor for subsequent ischemic stroke than was atrial fibrillation, heart failure, type 1 or type 2 diabetes, hypertension, or hyperlipidemia. The risk of ischemic heart disease in patients with an infectious disease hospitalization was similar to the risks associated with most of those recognized risk factors.
Two possible mechanisms by which infection might predispose to subsequent ischemic heart disease and stroke are via a direct effect whereby pathogens such as Chlamydia pneumoniae are taken up into arterial plaques, where they cause a local inflammatory response, or an indirect effect in which systemic inflammation primes the atherosclerotic plaque through distribution of inflammatory cytokines, according to Dr. Carter.
He said the ACALM findings are particularly intriguing when considered in the context of the 2017 results of the landmark CANTOS trial, in which canakinumab (Ilaris), a targeted anti-inflammatory agent that inhibits the interleukin-1 beta innate immunity pathway, reduced recurrent ischemic events in post-MI patients who had high systemic inflammation as evidenced by their elevated C-reactive protein level but a normal-range LDL cholesterol (N Engl J Med. 2017 Aug 27. doi: 10.1056/NEJMoa1707914).
“If atherosclerosis is an inflammatory condition, this begs the question of whether other inflammatory conditions, like infection, which induces a large systemic inflammatory response, might drive atherosclerosis,” Dr. Carter commented.
“It’s now very well understood that inflammatory mediators, cells, and processes are involved in every step from the initial endothelial dysfunction that leads to uptake of LDL, inflammatory cells, and monocytes all the way through to plaque progression and rupture, where Th1 cytokines have been implicated in causing that rupture, and ultimately in patient presentation at the hospital,” he added.
He sees the ACALM findings as hypothesis generating, serving to help lay the groundwork for future clinical trials of vaccine or anti-inflammatory antibiotic therapies.
Dr. Carter reported having no financial conflicts related to his presentation.
SOURCE: Carter P. ACC 2018, Abstract 1325M-0.
ORLANDO – , according to a “big data” registry study from the United Kingdom.
“Our data show infection was just as much a risk factor or more compared with the traditional atherosclerotic cardiovascular disease risk factors,” Paul Carter, MD, said at the annual meeting of the American College of Cardiology.
Dr. Carter of Aston Medical School in Birmingham, England, presented a retrospective analysis from the ACALM (Algorithm for Comorbidities Associated with Length of stay and Mortality) study of administrative data on all of the more than 1.22 million patients admitted to seven U.K. hospitals in 2000-2013. His analysis included all 34,027 adults aged 40 years or older admitted with a urinary tract or respiratory infection on their index hospitalization who had no history of ischemic heart disease or ischemic stroke.
These patients, with a mean age of 73 years, 59% of whom were women, were compared with an equal number of age- and gender-matched adults whose index hospitalization was for reasons other than ischemic heart disease, stroke, urinary tract infection (UTI), or respiratory infection – the two most common infections resulting in hospitalization in the United Kingdom.
Patients with a respiratory infection or UTI had a 9.9% incidence of new-onset ischemic heart disease and a 4.1% rate of ischemic stroke during follow-up starting upon discharge from their index hospitalization, significantly higher than the 5.9% and 1.5% rates in controls. In a multivariate logistic regression analysis adjusted for demographics, standard cardiovascular risk factors, and the top 10 causes of mortality in the United Kingdom, patients with respiratory infection or UTI as their admitting diagnosis had a 1.36-fold increased likelihood of developing ischemic heart disease post discharge and a 2.5-fold greater risk of ischemic stroke than matched controls.
Moreover, mortality following diagnosis of ischemic heart disease was 75.2% in patients whose index hospitalization was for infection, compared with 51.1% in controls who developed ischemic heart disease without a history of hospitalization for infection, for an adjusted 2.98-fold increased likelihood of death. Similarly, mortality after an ischemic stroke was 59.8% in patients with a prior severe infection, compared with 30.8% in controls, which translated to an adjusted 3.1-fold increased risk of death post stroke in patients with a prior hospitalization for infection.
In the multivariate analysis, hospitalization for infection was a stronger risk factor for subsequent ischemic stroke than was atrial fibrillation, heart failure, type 1 or type 2 diabetes, hypertension, or hyperlipidemia. The risk of ischemic heart disease in patients with an infectious disease hospitalization was similar to the risks associated with most of those recognized risk factors.
Two possible mechanisms by which infection might predispose to subsequent ischemic heart disease and stroke are via a direct effect whereby pathogens such as Chlamydia pneumoniae are taken up into arterial plaques, where they cause a local inflammatory response, or an indirect effect in which systemic inflammation primes the atherosclerotic plaque through distribution of inflammatory cytokines, according to Dr. Carter.
He said the ACALM findings are particularly intriguing when considered in the context of the 2017 results of the landmark CANTOS trial, in which canakinumab (Ilaris), a targeted anti-inflammatory agent that inhibits the interleukin-1 beta innate immunity pathway, reduced recurrent ischemic events in post-MI patients who had high systemic inflammation as evidenced by their elevated C-reactive protein level but a normal-range LDL cholesterol (N Engl J Med. 2017 Aug 27. doi: 10.1056/NEJMoa1707914).
“If atherosclerosis is an inflammatory condition, this begs the question of whether other inflammatory conditions, like infection, which induces a large systemic inflammatory response, might drive atherosclerosis,” Dr. Carter commented.
“It’s now very well understood that inflammatory mediators, cells, and processes are involved in every step from the initial endothelial dysfunction that leads to uptake of LDL, inflammatory cells, and monocytes all the way through to plaque progression and rupture, where Th1 cytokines have been implicated in causing that rupture, and ultimately in patient presentation at the hospital,” he added.
He sees the ACALM findings as hypothesis generating, serving to help lay the groundwork for future clinical trials of vaccine or anti-inflammatory antibiotic therapies.
Dr. Carter reported having no financial conflicts related to his presentation.
SOURCE: Carter P. ACC 2018, Abstract 1325M-0.
ORLANDO – , according to a “big data” registry study from the United Kingdom.
“Our data show infection was just as much a risk factor or more compared with the traditional atherosclerotic cardiovascular disease risk factors,” Paul Carter, MD, said at the annual meeting of the American College of Cardiology.
Dr. Carter of Aston Medical School in Birmingham, England, presented a retrospective analysis from the ACALM (Algorithm for Comorbidities Associated with Length of stay and Mortality) study of administrative data on all of the more than 1.22 million patients admitted to seven U.K. hospitals in 2000-2013. His analysis included all 34,027 adults aged 40 years or older admitted with a urinary tract or respiratory infection on their index hospitalization who had no history of ischemic heart disease or ischemic stroke.
These patients, with a mean age of 73 years, 59% of whom were women, were compared with an equal number of age- and gender-matched adults whose index hospitalization was for reasons other than ischemic heart disease, stroke, urinary tract infection (UTI), or respiratory infection – the two most common infections resulting in hospitalization in the United Kingdom.
Patients with a respiratory infection or UTI had a 9.9% incidence of new-onset ischemic heart disease and a 4.1% rate of ischemic stroke during follow-up starting upon discharge from their index hospitalization, significantly higher than the 5.9% and 1.5% rates in controls. In a multivariate logistic regression analysis adjusted for demographics, standard cardiovascular risk factors, and the top 10 causes of mortality in the United Kingdom, patients with respiratory infection or UTI as their admitting diagnosis had a 1.36-fold increased likelihood of developing ischemic heart disease post discharge and a 2.5-fold greater risk of ischemic stroke than matched controls.
Moreover, mortality following diagnosis of ischemic heart disease was 75.2% in patients whose index hospitalization was for infection, compared with 51.1% in controls who developed ischemic heart disease without a history of hospitalization for infection, for an adjusted 2.98-fold increased likelihood of death. Similarly, mortality after an ischemic stroke was 59.8% in patients with a prior severe infection, compared with 30.8% in controls, which translated to an adjusted 3.1-fold increased risk of death post stroke in patients with a prior hospitalization for infection.
In the multivariate analysis, hospitalization for infection was a stronger risk factor for subsequent ischemic stroke than was atrial fibrillation, heart failure, type 1 or type 2 diabetes, hypertension, or hyperlipidemia. The risk of ischemic heart disease in patients with an infectious disease hospitalization was similar to the risks associated with most of those recognized risk factors.
Two possible mechanisms by which infection might predispose to subsequent ischemic heart disease and stroke are via a direct effect whereby pathogens such as Chlamydia pneumoniae are taken up into arterial plaques, where they cause a local inflammatory response, or an indirect effect in which systemic inflammation primes the atherosclerotic plaque through distribution of inflammatory cytokines, according to Dr. Carter.
He said the ACALM findings are particularly intriguing when considered in the context of the 2017 results of the landmark CANTOS trial, in which canakinumab (Ilaris), a targeted anti-inflammatory agent that inhibits the interleukin-1 beta innate immunity pathway, reduced recurrent ischemic events in post-MI patients who had high systemic inflammation as evidenced by their elevated C-reactive protein level but a normal-range LDL cholesterol (N Engl J Med. 2017 Aug 27. doi: 10.1056/NEJMoa1707914).
“If atherosclerosis is an inflammatory condition, this begs the question of whether other inflammatory conditions, like infection, which induces a large systemic inflammatory response, might drive atherosclerosis,” Dr. Carter commented.
“It’s now very well understood that inflammatory mediators, cells, and processes are involved in every step from the initial endothelial dysfunction that leads to uptake of LDL, inflammatory cells, and monocytes all the way through to plaque progression and rupture, where Th1 cytokines have been implicated in causing that rupture, and ultimately in patient presentation at the hospital,” he added.
He sees the ACALM findings as hypothesis generating, serving to help lay the groundwork for future clinical trials of vaccine or anti-inflammatory antibiotic therapies.
Dr. Carter reported having no financial conflicts related to his presentation.
SOURCE: Carter P. ACC 2018, Abstract 1325M-0.
REPORTING FROM ACC 2018
Key clinical point: Once patients have been hospitalized for a respiratory infection or UTI, their postdischarge risk of ischemic stroke is 2.5-fold greater than in those without such a history.
Major finding: Patients with a history of hospitalization for UTI or a respiratory infection who later develop ischemic heart disease or stroke have a threefold higher mortality risk than those without such a hospitalization.
Study details: This was a retrospective study of more than 68,000 subjects in the U.K. ACALM registry study.
Disclosures: The study presenter reported having no financial conflicts of interest.
Source: Carter P. ACC 2018, Abstract 1325M-0.
From #MeToo to troponins: Updates in hospital medicine
How do you summarize a year’s worth of hospitalist-relevant research in an hour? If you’re Cynthia Cooper, MD, and Barbara Slawski, MD, MS, SFHM, you do it with teamwork, rigor, and style.
When the two physicians signed on for the 2018 “Update in Hospital Medicine” talk, they knew the bar was high. The updates talk is a perennial crowd favorite at the Society of Hospital Medicine annual conferences, and this year’s talk, which touched on topics from #MeToo to kidney injury, didn’t disappoint.
“One of the things that made the news a lot this last year is gender bias, so we thought we’d start out with that,” said Dr. Slawski, chief of the section of perioperative medicine at the Medical College of Wisconsin in Milwaukee.
In a retrospective observational study, the investigators looked at archived grand rounds video to see how often speakers with doctoral degrees were introduced by title, rather than by first name. Mixed-gender evaluators found that females were much more likely than were males to introduce either females or males by title (P less than .001).
“Have any of you ever had this experience? Me, too,” said Dr. Slawski, to wide and prolonged applause.
Females introducing males were almost twice as likely to use the speaker’s title as when males introduced females (95% vs. 49%; P less than .001). These revelations, said Dr. Slawski, present an “opportunity for improving professional interactions in an environment of mutual respect,” a comment that the room again greeted with a round of applause.
The inpatient syncope evaluation was made a little easier with another top study presented by Dr. Slawski. Using a large multinational database, investigators looked at a subgroup of patients with syncope who were admitted to the hospital. They found that fewer than 2% of patients with syncope were diagnosed with pulmonary embolus (PE) or deep venous thrombosis within 90 days of the index admission. For Dr. Slawski, this means clinicians may be able to relax their worry about thromboembolic events just a bit: “Although this diagnosis should be considered, not all patients need evaluation,” she said.
Dr. Slawski did point out that this observational, retrospective trial differed in many ways from the earlier-published PESIT trial that found a rate of 17% for PE among patients hospitalized for syncope.
Another common clinical dilemma – how to rule out MI in low-risk patients – was addressed in a meta-analysis looking at high-sensitivity troponin T levels in patients with negative ECGs.
In patients coming to the emergency department with a suspicion of acute coronary syndrome, investigators found just a 0.49% incidence of cardiac events in patients who had no ECG evidence of new ischemia and very-low high-sensitivity troponin T. The study looked at two proposed lower limits – less than .0005 mcg/L and less than .003 mcg/L.
Between these two levels, “Sensitivity and negative predictive values were about the same; no patients had mortality within 30 days if they met the criteria,” said Dr. Slawski. However, “You have to remember that sensitivity was below the preset consensus of 99%,” she said; the pooled sensitivity was 98.7%, with fairly high heterogeneity between studies. Also, she said, “If you’re going to use this strategy as your hospital, you have to remember that these values are specific to the assay” at your particular institution.
Dr. Cooper, a nephrologist who practices hospital medicine at Massachusetts General Hospital, Boston, ran through several kidney-related studies. Among these was a retrospective study of the use of IV contrast for computerized tomography (CT), examining the risk of acute kidney injury when patients who received IV contrast were compared both with those who had a CT without contrast and with those who did not have CT. Nearly 17,000 patients were included, with propensity matching used to limit confounding.
Both in this study and in a later meta-analysis, no significant differences were seen in acute kidney injury, the need for renal replacement therapy, or mortality after CT with contrast. However, Dr. Cooper said that as a nephrologist, “This doesn’t make physiological sense to me, so I’m not convinced,” she said. “Ultimately, we need to have a randomized, controlled trial, though it’s hard to imagine” just how such a study could be structured and conducted, she said.
“Influenza H3N2 has dominated outbreaks in the United States over the last few years,” and this fact contributed significantly to the severity of the past year’s influenza season, said Dr. Cooper. Not only does this strain “seem to have greater variability in how often it mutates,” but “it’s also less likely to grow in egg media – so it’s less likely to appear in the vaccine,” she said.
Antivirals are effective only if instituted promptly, meaning that many patients who are admitted to the hospital with influenza and pulmonary infiltrates are beyond this window. Building on what was known about the theoretical efficacy of both macrolides and NSAID medications, a group of researchers in Hong Kong conducted a randomized placebo-controlled trial to compare outcomes when 500 mg of clarithromycin and 200 mg of naproxen were added on days 1 and 2 of hospitalization.
When these two interventions were added to the usual regime of amoxicillin clavulanate, oseltamivir, and esomeprazole, hospital stay was 1 day shorter. Importantly, said Dr. Cooper, 30-day and 90-day mortality rates were shorter and there was a significant reduction in viral titer. This is a strategy Dr. Cooper plans to implement. “My expectation is just like this past year, next year will likely be a bad year for influenza,” she said.
How do you summarize a year’s worth of hospitalist-relevant research in an hour? If you’re Cynthia Cooper, MD, and Barbara Slawski, MD, MS, SFHM, you do it with teamwork, rigor, and style.
When the two physicians signed on for the 2018 “Update in Hospital Medicine” talk, they knew the bar was high. The updates talk is a perennial crowd favorite at the Society of Hospital Medicine annual conferences, and this year’s talk, which touched on topics from #MeToo to kidney injury, didn’t disappoint.
“One of the things that made the news a lot this last year is gender bias, so we thought we’d start out with that,” said Dr. Slawski, chief of the section of perioperative medicine at the Medical College of Wisconsin in Milwaukee.
In a retrospective observational study, the investigators looked at archived grand rounds video to see how often speakers with doctoral degrees were introduced by title, rather than by first name. Mixed-gender evaluators found that females were much more likely than were males to introduce either females or males by title (P less than .001).
“Have any of you ever had this experience? Me, too,” said Dr. Slawski, to wide and prolonged applause.
Females introducing males were almost twice as likely to use the speaker’s title as when males introduced females (95% vs. 49%; P less than .001). These revelations, said Dr. Slawski, present an “opportunity for improving professional interactions in an environment of mutual respect,” a comment that the room again greeted with a round of applause.
The inpatient syncope evaluation was made a little easier with another top study presented by Dr. Slawski. Using a large multinational database, investigators looked at a subgroup of patients with syncope who were admitted to the hospital. They found that fewer than 2% of patients with syncope were diagnosed with pulmonary embolus (PE) or deep venous thrombosis within 90 days of the index admission. For Dr. Slawski, this means clinicians may be able to relax their worry about thromboembolic events just a bit: “Although this diagnosis should be considered, not all patients need evaluation,” she said.
Dr. Slawski did point out that this observational, retrospective trial differed in many ways from the earlier-published PESIT trial that found a rate of 17% for PE among patients hospitalized for syncope.
Another common clinical dilemma – how to rule out MI in low-risk patients – was addressed in a meta-analysis looking at high-sensitivity troponin T levels in patients with negative ECGs.
In patients coming to the emergency department with a suspicion of acute coronary syndrome, investigators found just a 0.49% incidence of cardiac events in patients who had no ECG evidence of new ischemia and very-low high-sensitivity troponin T. The study looked at two proposed lower limits – less than .0005 mcg/L and less than .003 mcg/L.
Between these two levels, “Sensitivity and negative predictive values were about the same; no patients had mortality within 30 days if they met the criteria,” said Dr. Slawski. However, “You have to remember that sensitivity was below the preset consensus of 99%,” she said; the pooled sensitivity was 98.7%, with fairly high heterogeneity between studies. Also, she said, “If you’re going to use this strategy as your hospital, you have to remember that these values are specific to the assay” at your particular institution.
Dr. Cooper, a nephrologist who practices hospital medicine at Massachusetts General Hospital, Boston, ran through several kidney-related studies. Among these was a retrospective study of the use of IV contrast for computerized tomography (CT), examining the risk of acute kidney injury when patients who received IV contrast were compared both with those who had a CT without contrast and with those who did not have CT. Nearly 17,000 patients were included, with propensity matching used to limit confounding.
Both in this study and in a later meta-analysis, no significant differences were seen in acute kidney injury, the need for renal replacement therapy, or mortality after CT with contrast. However, Dr. Cooper said that as a nephrologist, “This doesn’t make physiological sense to me, so I’m not convinced,” she said. “Ultimately, we need to have a randomized, controlled trial, though it’s hard to imagine” just how such a study could be structured and conducted, she said.
“Influenza H3N2 has dominated outbreaks in the United States over the last few years,” and this fact contributed significantly to the severity of the past year’s influenza season, said Dr. Cooper. Not only does this strain “seem to have greater variability in how often it mutates,” but “it’s also less likely to grow in egg media – so it’s less likely to appear in the vaccine,” she said.
Antivirals are effective only if instituted promptly, meaning that many patients who are admitted to the hospital with influenza and pulmonary infiltrates are beyond this window. Building on what was known about the theoretical efficacy of both macrolides and NSAID medications, a group of researchers in Hong Kong conducted a randomized placebo-controlled trial to compare outcomes when 500 mg of clarithromycin and 200 mg of naproxen were added on days 1 and 2 of hospitalization.
When these two interventions were added to the usual regime of amoxicillin clavulanate, oseltamivir, and esomeprazole, hospital stay was 1 day shorter. Importantly, said Dr. Cooper, 30-day and 90-day mortality rates were shorter and there was a significant reduction in viral titer. This is a strategy Dr. Cooper plans to implement. “My expectation is just like this past year, next year will likely be a bad year for influenza,” she said.
How do you summarize a year’s worth of hospitalist-relevant research in an hour? If you’re Cynthia Cooper, MD, and Barbara Slawski, MD, MS, SFHM, you do it with teamwork, rigor, and style.
When the two physicians signed on for the 2018 “Update in Hospital Medicine” talk, they knew the bar was high. The updates talk is a perennial crowd favorite at the Society of Hospital Medicine annual conferences, and this year’s talk, which touched on topics from #MeToo to kidney injury, didn’t disappoint.
“One of the things that made the news a lot this last year is gender bias, so we thought we’d start out with that,” said Dr. Slawski, chief of the section of perioperative medicine at the Medical College of Wisconsin in Milwaukee.
In a retrospective observational study, the investigators looked at archived grand rounds video to see how often speakers with doctoral degrees were introduced by title, rather than by first name. Mixed-gender evaluators found that females were much more likely than were males to introduce either females or males by title (P less than .001).
“Have any of you ever had this experience? Me, too,” said Dr. Slawski, to wide and prolonged applause.
Females introducing males were almost twice as likely to use the speaker’s title as when males introduced females (95% vs. 49%; P less than .001). These revelations, said Dr. Slawski, present an “opportunity for improving professional interactions in an environment of mutual respect,” a comment that the room again greeted with a round of applause.
The inpatient syncope evaluation was made a little easier with another top study presented by Dr. Slawski. Using a large multinational database, investigators looked at a subgroup of patients with syncope who were admitted to the hospital. They found that fewer than 2% of patients with syncope were diagnosed with pulmonary embolus (PE) or deep venous thrombosis within 90 days of the index admission. For Dr. Slawski, this means clinicians may be able to relax their worry about thromboembolic events just a bit: “Although this diagnosis should be considered, not all patients need evaluation,” she said.
Dr. Slawski did point out that this observational, retrospective trial differed in many ways from the earlier-published PESIT trial that found a rate of 17% for PE among patients hospitalized for syncope.
Another common clinical dilemma – how to rule out MI in low-risk patients – was addressed in a meta-analysis looking at high-sensitivity troponin T levels in patients with negative ECGs.
In patients coming to the emergency department with a suspicion of acute coronary syndrome, investigators found just a 0.49% incidence of cardiac events in patients who had no ECG evidence of new ischemia and very-low high-sensitivity troponin T. The study looked at two proposed lower limits – less than .0005 mcg/L and less than .003 mcg/L.
Between these two levels, “Sensitivity and negative predictive values were about the same; no patients had mortality within 30 days if they met the criteria,” said Dr. Slawski. However, “You have to remember that sensitivity was below the preset consensus of 99%,” she said; the pooled sensitivity was 98.7%, with fairly high heterogeneity between studies. Also, she said, “If you’re going to use this strategy as your hospital, you have to remember that these values are specific to the assay” at your particular institution.
Dr. Cooper, a nephrologist who practices hospital medicine at Massachusetts General Hospital, Boston, ran through several kidney-related studies. Among these was a retrospective study of the use of IV contrast for computerized tomography (CT), examining the risk of acute kidney injury when patients who received IV contrast were compared both with those who had a CT without contrast and with those who did not have CT. Nearly 17,000 patients were included, with propensity matching used to limit confounding.
Both in this study and in a later meta-analysis, no significant differences were seen in acute kidney injury, the need for renal replacement therapy, or mortality after CT with contrast. However, Dr. Cooper said that as a nephrologist, “This doesn’t make physiological sense to me, so I’m not convinced,” she said. “Ultimately, we need to have a randomized, controlled trial, though it’s hard to imagine” just how such a study could be structured and conducted, she said.
“Influenza H3N2 has dominated outbreaks in the United States over the last few years,” and this fact contributed significantly to the severity of the past year’s influenza season, said Dr. Cooper. Not only does this strain “seem to have greater variability in how often it mutates,” but “it’s also less likely to grow in egg media – so it’s less likely to appear in the vaccine,” she said.
Antivirals are effective only if instituted promptly, meaning that many patients who are admitted to the hospital with influenza and pulmonary infiltrates are beyond this window. Building on what was known about the theoretical efficacy of both macrolides and NSAID medications, a group of researchers in Hong Kong conducted a randomized placebo-controlled trial to compare outcomes when 500 mg of clarithromycin and 200 mg of naproxen were added on days 1 and 2 of hospitalization.
When these two interventions were added to the usual regime of amoxicillin clavulanate, oseltamivir, and esomeprazole, hospital stay was 1 day shorter. Importantly, said Dr. Cooper, 30-day and 90-day mortality rates were shorter and there was a significant reduction in viral titer. This is a strategy Dr. Cooper plans to implement. “My expectation is just like this past year, next year will likely be a bad year for influenza,” she said.
Use procalcitonin-guided algorithms to guide antibiotic therapy for acute respiratory infections to improve patient outcomes
Clinical question: How does using procalcitonin levels for adults with acute respiratory infections (ARIs) affect patient outcomes?
Background: While the ARI diagnosis encompasses bacterial, viral, and inflammatory etiologies, as many as 75% of ARIs are treated with antibiotics. Procalcitonin is a biomarker released by tissues in response to bacterial infections. Its production is also inhibited by interferon-gamma, a cytokine released in response to viral infections, therefore, making procalcitonin a biomarker of particular interest to support the use of antibiotic therapy in the treatment of ARIs.
Study design: Cochrane Review.
Setting: Medical wards, intensive care units, primary care clinics, and emergency departments across 12 countries.
Synopsis: The review included 26 randomized control trials of 6,708 immunocompetent adults with ARIs who received antibiotics either based on procalcitonin-guided antibiotic therapy or routine care. Primary endpoints evaluated included all-cause mortality and treatment failure at 30 days. Secondary endpoints were antibiotic use, antibiotic-related side effects, and length of hospital stay. There were significantly fewer deaths in the procalcitonin-guided group than in the control group (286/8.6% vs. 336/10%; adjusted odds ratio, 0.83; 95% confidence interval, 0.70-0.99; P = .037). Treatment failure was not statistically different between the procalcitonin-guided participants and the controls. Of the secondary endpoints, antibiotic use and antibiotic-related side effects were lower in the procalcitonin-guided group (5.7 days vs. 8.1 days; P less than .001; and 16.3% vs. 22.1%; P less than .001). Each of the RCTs had varying algorithms for the use of procalcitonin-guided therapy, so no specific treatment guidelines can be gleaned from this review.
Bottom line: Procalcitonin-guided algorithms are associated with lower mortality, lower antibiotic exposure, and lower antibiotic-related side effects. However, more research is needed to determine best practice algorithms for using procalcitonin levels to guide treatment decisions.
Citation: Schuetz P et al. Procalcitonin to initiate or discontinue antibiotics in acute respiratory tract infections. Cochrane Database Syst Rev. 2017 Oct 12. doi: 10.1002/14651858.cd007498.pub3.
Dr. Sundar is assistant professor of medicine in the division of hospital medicine, Emory University, Atlanta.
Clinical question: How does using procalcitonin levels for adults with acute respiratory infections (ARIs) affect patient outcomes?
Background: While the ARI diagnosis encompasses bacterial, viral, and inflammatory etiologies, as many as 75% of ARIs are treated with antibiotics. Procalcitonin is a biomarker released by tissues in response to bacterial infections. Its production is also inhibited by interferon-gamma, a cytokine released in response to viral infections, therefore, making procalcitonin a biomarker of particular interest to support the use of antibiotic therapy in the treatment of ARIs.
Study design: Cochrane Review.
Setting: Medical wards, intensive care units, primary care clinics, and emergency departments across 12 countries.
Synopsis: The review included 26 randomized control trials of 6,708 immunocompetent adults with ARIs who received antibiotics either based on procalcitonin-guided antibiotic therapy or routine care. Primary endpoints evaluated included all-cause mortality and treatment failure at 30 days. Secondary endpoints were antibiotic use, antibiotic-related side effects, and length of hospital stay. There were significantly fewer deaths in the procalcitonin-guided group than in the control group (286/8.6% vs. 336/10%; adjusted odds ratio, 0.83; 95% confidence interval, 0.70-0.99; P = .037). Treatment failure was not statistically different between the procalcitonin-guided participants and the controls. Of the secondary endpoints, antibiotic use and antibiotic-related side effects were lower in the procalcitonin-guided group (5.7 days vs. 8.1 days; P less than .001; and 16.3% vs. 22.1%; P less than .001). Each of the RCTs had varying algorithms for the use of procalcitonin-guided therapy, so no specific treatment guidelines can be gleaned from this review.
Bottom line: Procalcitonin-guided algorithms are associated with lower mortality, lower antibiotic exposure, and lower antibiotic-related side effects. However, more research is needed to determine best practice algorithms for using procalcitonin levels to guide treatment decisions.
Citation: Schuetz P et al. Procalcitonin to initiate or discontinue antibiotics in acute respiratory tract infections. Cochrane Database Syst Rev. 2017 Oct 12. doi: 10.1002/14651858.cd007498.pub3.
Dr. Sundar is assistant professor of medicine in the division of hospital medicine, Emory University, Atlanta.
Clinical question: How does using procalcitonin levels for adults with acute respiratory infections (ARIs) affect patient outcomes?
Background: While the ARI diagnosis encompasses bacterial, viral, and inflammatory etiologies, as many as 75% of ARIs are treated with antibiotics. Procalcitonin is a biomarker released by tissues in response to bacterial infections. Its production is also inhibited by interferon-gamma, a cytokine released in response to viral infections, therefore, making procalcitonin a biomarker of particular interest to support the use of antibiotic therapy in the treatment of ARIs.
Study design: Cochrane Review.
Setting: Medical wards, intensive care units, primary care clinics, and emergency departments across 12 countries.
Synopsis: The review included 26 randomized control trials of 6,708 immunocompetent adults with ARIs who received antibiotics either based on procalcitonin-guided antibiotic therapy or routine care. Primary endpoints evaluated included all-cause mortality and treatment failure at 30 days. Secondary endpoints were antibiotic use, antibiotic-related side effects, and length of hospital stay. There were significantly fewer deaths in the procalcitonin-guided group than in the control group (286/8.6% vs. 336/10%; adjusted odds ratio, 0.83; 95% confidence interval, 0.70-0.99; P = .037). Treatment failure was not statistically different between the procalcitonin-guided participants and the controls. Of the secondary endpoints, antibiotic use and antibiotic-related side effects were lower in the procalcitonin-guided group (5.7 days vs. 8.1 days; P less than .001; and 16.3% vs. 22.1%; P less than .001). Each of the RCTs had varying algorithms for the use of procalcitonin-guided therapy, so no specific treatment guidelines can be gleaned from this review.
Bottom line: Procalcitonin-guided algorithms are associated with lower mortality, lower antibiotic exposure, and lower antibiotic-related side effects. However, more research is needed to determine best practice algorithms for using procalcitonin levels to guide treatment decisions.
Citation: Schuetz P et al. Procalcitonin to initiate or discontinue antibiotics in acute respiratory tract infections. Cochrane Database Syst Rev. 2017 Oct 12. doi: 10.1002/14651858.cd007498.pub3.
Dr. Sundar is assistant professor of medicine in the division of hospital medicine, Emory University, Atlanta.
Launching into the future
Hospital Medicine: 10 years ago
My first Society of Hospital Medicine Annual Conference was HM08, and it changed the course of my professional career.
I was a first-year hospitalist from an academic program of fewer than 10 physicians. My knowledge about my field did not extend much beyond the clinical practice of hospital medicine. I remember sitting at the airport on my way to HM08 and excitedly looking over the schedule for the meeting. I diligently circled the sessions that I was looking forward to attending, the majority of which focused on the clinical tracks. But by the end of the meeting, in additional to valuable medical knowledge, I walked away with novel insights that launched me into my future.
New ideas in HM: In 2008, comanagement was still a new concept. As I attended sessions and spoke with hospitalists from across the country, it became clear that this was a collaboration that would be core to our specialty. Within a couple of months of returning home from the annual conference, I was approached by the chair of neurosurgery at my institution with a proposal to develop a quality program for his group. While at that time I was considering other competing interests, my experience at HM08 helped me recognize that this was a unique opportunity to build bridges across specialties and to collaborate. I subsequently became the executive director of quality for neurosurgery and over the years was able to create a strong relationship between our departments that led to building a nationally recognized program with exceptional performance in hospital-based quality.
Side note: If you’re interested in resources on comanagement, please check out SHM’s Resources for Effective Co-Management of Hospitalized Patients at https://www.hospitalmedicine.org/comanagement .
Emerging themes and trends in health care: While the quality movement had launched about a decade before HM08, many institutions still did not have robust programs. As I attended sessions during the annual meeting and spoke with thought leaders, one message became clear: Hospitalists would have to lead the quality movement at their institutions. When I returned home, I began learning about quality improvement and started to lead various initiatives. These efforts led to my appointment as associate chief medical officer for the health system. This position enabled me to leverage my knowledge of hospital-based care and collaborate across various specialties to reduce our mortality and readmission rates in the organization.
Side note: If you’re interested in learning more about quality improvement educational and mentorship opportunities, please visit https://www.hospitalmedicine.org/qi and look at the resources for each specific topic.
And, most importantly, friendships: By far the most important thing I took away from HM08 was the friendships that started at that meeting and have developed over the years since. A decade later, I continue to rely on, grow from, and be challenged by the same people I met at that meeting. They are the colleagues I call when I find myself in a tough spot at work and need advice, the collaborators I work with on grants and projects, and the friends I text when I travel to a new town and want to grab a bite to eat.
Side note: If you’re interested in connecting with colleagues who share similar interests, please visit https://www.hospitalmedicine.org/sigs and review SHM’s Special Interest Groups to find ones that are right for you. To connect on a more local level, find an SHM Chapter near you at https://www.hospitalmedicine.org/chapters.
I’ve shared these stories with you because for me my journey with our society has been a deeply personal one. And I feel indebted to SHM and the incredible people who drawn to it for helping me develop and enjoy a rich and rewarding career thus far. So, as I look forward to the next decade, I wanted to share my thoughts on HM and emerging themes in health care with you.
Hospital medicine: The next decade
New ideas in HM: Population health management
Building on our strong culture of collaboration as we move forward into this next decade, we have to define how we deliver value in the context of population health management. As hospitalists, we have to push the boundaries of the hospital and provide high-value care beyond our four walls.
How can we do that? I think technology will play a critical role in extending our reach beyond the hospital. As we move toward delivering greater value to our patients, lower acuity patients will receive care in their homes. Telehealth will enable us to monitor and manage these patients remotely while transferring our bedside management to patients’ bedrooms in their own homes. Virtual hospitals will further enable us to evaluate, triage, monitor, and manage patients remotely. Our active engagement in these efforts is critical to ensure the continued growth and value we bring to our patients, our organizations, and our society.
Emerging themes and trends in health care: Transitioning from quality to value
In the next decade, value will prevail. This is not a novel concept – much like how quality was not a new idea in 2008.
Value has been around for a while: There are some robust programs nationally, there is research around the topic, and there are policies with implications for reimbursements. However, the full potential of value has not yet been realized by health care – it exists in individual programs, not in everything we do. The unprecedented number of mergers and acquisitions in health care in 2018 support the fact that the future will belong to those institutions that can deliver the highest quality of care at the most appropriate cost throughout the entire continuum of care.
What are some of the tools that will help us get there? Artificial intelligence and machine learning will improve the predictive value for the care we deliver to individual patients; some preliminary work in this area has already revealed that factors that we previously associated with higher risk of readmissions are not truly predictive. Another emerging technology is blockchain: By creating a single source of truth for our patients’ medical information, it enables us to have dynamic, high-integrity records regardless of which health systems and EHRs have cared for those patients.
I wish you an energizing journey as you launch your future into the next dynamic decade of health care, and I look forward to connecting with you as we continue to build a society that prepares us for the challenges and opportunities ahead.
Dr. Afsar is the president of the Society of Hospital Medicine and the chief ambulatory officer and chief medical officer for the accountable care organizations at UC Irvine Health.
Hospital Medicine: 10 years ago
My first Society of Hospital Medicine Annual Conference was HM08, and it changed the course of my professional career.
I was a first-year hospitalist from an academic program of fewer than 10 physicians. My knowledge about my field did not extend much beyond the clinical practice of hospital medicine. I remember sitting at the airport on my way to HM08 and excitedly looking over the schedule for the meeting. I diligently circled the sessions that I was looking forward to attending, the majority of which focused on the clinical tracks. But by the end of the meeting, in additional to valuable medical knowledge, I walked away with novel insights that launched me into my future.
New ideas in HM: In 2008, comanagement was still a new concept. As I attended sessions and spoke with hospitalists from across the country, it became clear that this was a collaboration that would be core to our specialty. Within a couple of months of returning home from the annual conference, I was approached by the chair of neurosurgery at my institution with a proposal to develop a quality program for his group. While at that time I was considering other competing interests, my experience at HM08 helped me recognize that this was a unique opportunity to build bridges across specialties and to collaborate. I subsequently became the executive director of quality for neurosurgery and over the years was able to create a strong relationship between our departments that led to building a nationally recognized program with exceptional performance in hospital-based quality.
Side note: If you’re interested in resources on comanagement, please check out SHM’s Resources for Effective Co-Management of Hospitalized Patients at https://www.hospitalmedicine.org/comanagement .
Emerging themes and trends in health care: While the quality movement had launched about a decade before HM08, many institutions still did not have robust programs. As I attended sessions during the annual meeting and spoke with thought leaders, one message became clear: Hospitalists would have to lead the quality movement at their institutions. When I returned home, I began learning about quality improvement and started to lead various initiatives. These efforts led to my appointment as associate chief medical officer for the health system. This position enabled me to leverage my knowledge of hospital-based care and collaborate across various specialties to reduce our mortality and readmission rates in the organization.
Side note: If you’re interested in learning more about quality improvement educational and mentorship opportunities, please visit https://www.hospitalmedicine.org/qi and look at the resources for each specific topic.
And, most importantly, friendships: By far the most important thing I took away from HM08 was the friendships that started at that meeting and have developed over the years since. A decade later, I continue to rely on, grow from, and be challenged by the same people I met at that meeting. They are the colleagues I call when I find myself in a tough spot at work and need advice, the collaborators I work with on grants and projects, and the friends I text when I travel to a new town and want to grab a bite to eat.
Side note: If you’re interested in connecting with colleagues who share similar interests, please visit https://www.hospitalmedicine.org/sigs and review SHM’s Special Interest Groups to find ones that are right for you. To connect on a more local level, find an SHM Chapter near you at https://www.hospitalmedicine.org/chapters.
I’ve shared these stories with you because for me my journey with our society has been a deeply personal one. And I feel indebted to SHM and the incredible people who drawn to it for helping me develop and enjoy a rich and rewarding career thus far. So, as I look forward to the next decade, I wanted to share my thoughts on HM and emerging themes in health care with you.
Hospital medicine: The next decade
New ideas in HM: Population health management
Building on our strong culture of collaboration as we move forward into this next decade, we have to define how we deliver value in the context of population health management. As hospitalists, we have to push the boundaries of the hospital and provide high-value care beyond our four walls.
How can we do that? I think technology will play a critical role in extending our reach beyond the hospital. As we move toward delivering greater value to our patients, lower acuity patients will receive care in their homes. Telehealth will enable us to monitor and manage these patients remotely while transferring our bedside management to patients’ bedrooms in their own homes. Virtual hospitals will further enable us to evaluate, triage, monitor, and manage patients remotely. Our active engagement in these efforts is critical to ensure the continued growth and value we bring to our patients, our organizations, and our society.
Emerging themes and trends in health care: Transitioning from quality to value
In the next decade, value will prevail. This is not a novel concept – much like how quality was not a new idea in 2008.
Value has been around for a while: There are some robust programs nationally, there is research around the topic, and there are policies with implications for reimbursements. However, the full potential of value has not yet been realized by health care – it exists in individual programs, not in everything we do. The unprecedented number of mergers and acquisitions in health care in 2018 support the fact that the future will belong to those institutions that can deliver the highest quality of care at the most appropriate cost throughout the entire continuum of care.
What are some of the tools that will help us get there? Artificial intelligence and machine learning will improve the predictive value for the care we deliver to individual patients; some preliminary work in this area has already revealed that factors that we previously associated with higher risk of readmissions are not truly predictive. Another emerging technology is blockchain: By creating a single source of truth for our patients’ medical information, it enables us to have dynamic, high-integrity records regardless of which health systems and EHRs have cared for those patients.
I wish you an energizing journey as you launch your future into the next dynamic decade of health care, and I look forward to connecting with you as we continue to build a society that prepares us for the challenges and opportunities ahead.
Dr. Afsar is the president of the Society of Hospital Medicine and the chief ambulatory officer and chief medical officer for the accountable care organizations at UC Irvine Health.
Hospital Medicine: 10 years ago
My first Society of Hospital Medicine Annual Conference was HM08, and it changed the course of my professional career.
I was a first-year hospitalist from an academic program of fewer than 10 physicians. My knowledge about my field did not extend much beyond the clinical practice of hospital medicine. I remember sitting at the airport on my way to HM08 and excitedly looking over the schedule for the meeting. I diligently circled the sessions that I was looking forward to attending, the majority of which focused on the clinical tracks. But by the end of the meeting, in additional to valuable medical knowledge, I walked away with novel insights that launched me into my future.
New ideas in HM: In 2008, comanagement was still a new concept. As I attended sessions and spoke with hospitalists from across the country, it became clear that this was a collaboration that would be core to our specialty. Within a couple of months of returning home from the annual conference, I was approached by the chair of neurosurgery at my institution with a proposal to develop a quality program for his group. While at that time I was considering other competing interests, my experience at HM08 helped me recognize that this was a unique opportunity to build bridges across specialties and to collaborate. I subsequently became the executive director of quality for neurosurgery and over the years was able to create a strong relationship between our departments that led to building a nationally recognized program with exceptional performance in hospital-based quality.
Side note: If you’re interested in resources on comanagement, please check out SHM’s Resources for Effective Co-Management of Hospitalized Patients at https://www.hospitalmedicine.org/comanagement .
Emerging themes and trends in health care: While the quality movement had launched about a decade before HM08, many institutions still did not have robust programs. As I attended sessions during the annual meeting and spoke with thought leaders, one message became clear: Hospitalists would have to lead the quality movement at their institutions. When I returned home, I began learning about quality improvement and started to lead various initiatives. These efforts led to my appointment as associate chief medical officer for the health system. This position enabled me to leverage my knowledge of hospital-based care and collaborate across various specialties to reduce our mortality and readmission rates in the organization.
Side note: If you’re interested in learning more about quality improvement educational and mentorship opportunities, please visit https://www.hospitalmedicine.org/qi and look at the resources for each specific topic.
And, most importantly, friendships: By far the most important thing I took away from HM08 was the friendships that started at that meeting and have developed over the years since. A decade later, I continue to rely on, grow from, and be challenged by the same people I met at that meeting. They are the colleagues I call when I find myself in a tough spot at work and need advice, the collaborators I work with on grants and projects, and the friends I text when I travel to a new town and want to grab a bite to eat.
Side note: If you’re interested in connecting with colleagues who share similar interests, please visit https://www.hospitalmedicine.org/sigs and review SHM’s Special Interest Groups to find ones that are right for you. To connect on a more local level, find an SHM Chapter near you at https://www.hospitalmedicine.org/chapters.
I’ve shared these stories with you because for me my journey with our society has been a deeply personal one. And I feel indebted to SHM and the incredible people who drawn to it for helping me develop and enjoy a rich and rewarding career thus far. So, as I look forward to the next decade, I wanted to share my thoughts on HM and emerging themes in health care with you.
Hospital medicine: The next decade
New ideas in HM: Population health management
Building on our strong culture of collaboration as we move forward into this next decade, we have to define how we deliver value in the context of population health management. As hospitalists, we have to push the boundaries of the hospital and provide high-value care beyond our four walls.
How can we do that? I think technology will play a critical role in extending our reach beyond the hospital. As we move toward delivering greater value to our patients, lower acuity patients will receive care in their homes. Telehealth will enable us to monitor and manage these patients remotely while transferring our bedside management to patients’ bedrooms in their own homes. Virtual hospitals will further enable us to evaluate, triage, monitor, and manage patients remotely. Our active engagement in these efforts is critical to ensure the continued growth and value we bring to our patients, our organizations, and our society.
Emerging themes and trends in health care: Transitioning from quality to value
In the next decade, value will prevail. This is not a novel concept – much like how quality was not a new idea in 2008.
Value has been around for a while: There are some robust programs nationally, there is research around the topic, and there are policies with implications for reimbursements. However, the full potential of value has not yet been realized by health care – it exists in individual programs, not in everything we do. The unprecedented number of mergers and acquisitions in health care in 2018 support the fact that the future will belong to those institutions that can deliver the highest quality of care at the most appropriate cost throughout the entire continuum of care.
What are some of the tools that will help us get there? Artificial intelligence and machine learning will improve the predictive value for the care we deliver to individual patients; some preliminary work in this area has already revealed that factors that we previously associated with higher risk of readmissions are not truly predictive. Another emerging technology is blockchain: By creating a single source of truth for our patients’ medical information, it enables us to have dynamic, high-integrity records regardless of which health systems and EHRs have cared for those patients.
I wish you an energizing journey as you launch your future into the next dynamic decade of health care, and I look forward to connecting with you as we continue to build a society that prepares us for the challenges and opportunities ahead.
Dr. Afsar is the president of the Society of Hospital Medicine and the chief ambulatory officer and chief medical officer for the accountable care organizations at UC Irvine Health.
Closing the gender gap
It wasn’t something she planned to have happen but about 2 years ago, Vineet Arora, MD, MAPP, MHM, became what she calls an “accidental advocate” for gender parity in medicine.
“I was asked to review a paper around gender pay,” the University of Chicago Medical Center hospitalist said. “It was stunning to me just how different salaries were – between male and female physicians – even when the authors were attempting to control for various factors.”
That paper was published in the Journal of the American Medical Association (JAMA) in September 2016 by researchers at Harvard Medical School and Massachusetts General Hospital (MGH). It found that even after adjustment for age, experience, specialty, faculty rank, research productivity, and clinical revenue, female physicians at 24 public medical schools in 12 states earned nearly $20,000 less per year than their male colleagues.1
Dr. Arora wrote an editorial to accompany that 2016 paper in JAMA, and in September 2017, she and her colleague at the University of Chicago, Jeanne Farnan, MD, MHPE, coauthored another piece in Annals of Internal Medicine titled, “Inpatient Notes: Gender Equality in Hospital Medicine – Are We There Yet?”2
In the 2017 paper, Dr. Arora and Dr. Farnan assessed recent studies documenting inequity in regard to compensation, discrimination around child-rearing, and gender disparities in medical leadership. They also discussed strategies that might improve the future outlook for female physicians.
“As I approach mid-career, I see these issues affecting my career and my colleagues’ careers and I decided we need to be doing more work in this space,” said Dr. Arora.
Fueling the conversation
When asked whether he thinks his research inspired the current conversation around gender inequity in medicine, Anupam Bapu Jena, MD, PhD – lead author of the September 2016 gender pay paper – said that while he did not initiate it, his work “has fueled the conversation.”
“This is an issue that has been going on in the scientific literature for at least 25-30 years,” said Dr. Jena, the Ruth L. Newhouse Associate Professor of Health Care Policy at Harvard Medical School and a physician in the department of medicine at MGH. “I am sure women in medicine have been feeling this since women entered medicine.”
Many female hospitalists hoped that, as a relatively new field, hospital medicine would avoid some of the time-worn challenges women in other specialties faced.
“The birth of hospital medicine held the promise that, as a new field, it would be immune to the ‘old boys’ club mentality that plagues established specialties,” Dr. Farnan and Dr. Arora wrote in their September 2017 Annals article. And yet, they continued, “gender disparities developed in the areas of leadership and academic productivity.”
A 2015 study in the Journal of Hospital Medicine found that just 16% of university hospital medicine divisions were led by women, and women made up just 28% of those physicians leading general internal medicine divisions. Meanwhile, female hospitalists gave just 26% of presentations at national meetings, were first authors on only 33% of publications, and were senior authors on only 21% of manuscripts.3
In addition, Dr. Farnan and Dr. Arora wrote in their review, another recent survey of female physicians – primarily internists – found that 36% reported discrimination based on pregnancy, maternity leave, or breastfeeding. This was – at least in part, Dr. Farnan said – because “physician-mothers were not present at the table when discussions were held about scheduling.”
And while hospitalists have relatively flexible schedules, they can be unforgiving when it comes to traditional child care arrangements, Dr. Arora said.
But, there is hope, particularly within the Society of Hospital Medicine, Dr. Arora and Dr. Farnan wrote. The organization has seen an increase in female leadership – including its president-elect Nasim Afsar, MD, MBA, SFHM – and a board of directors that is split evenly between men and women. Mentorship of junior women is also on the rise, which allows opportunities for senior female physicians to teach younger women how to better negotiate and advocate for themselves.
“I think it has to come from both sides. Leadership does need to recognize that women may be less aggressive in their negotiating skills,” said Dr. Farnan. “But I think there also needs to be some recognition by women that it is okay to ask for more money.”
But it isn’t all about money, she said. “It can be negotiating for anything important in career development, career opportunities, research opportunities.” This also extends to schedule flexibility, training and more.
Leadership in hospitalist groups can help, Dr. Arora and Dr. Farnan wrote in their Annals article, by providing schedule flexibility, support for training, and structured on-boarding for new faculty. Citing efforts in other specialties such as cardiology and general surgery, female hospitalists may benefit from negotiation skills training, structured mentorship, and education around personal and professional development.
However, both physicians recognize the challenges of implicit bias and stereotype threat that may confront many women. For example, women who exert more stereotypically “male” traits such as assertiveness and confidence may face a “harsh likability penalty because they are going against gender norms,” said Dr. Arora.
Being taken seriously
Expectations around gender norms may also affect relationships female doctors have with their patients. In a June 2017 Washington Post editorial, Faye Reiff-Pasarew, MD, describes being objectified as “cute” and “adorable” and not being taken seriously by her patients.4
“I’d had a number of interactions with patients that upset me,” said Dr. Reiff-Pasarew, assistant professor of hospital medicine, director of the humanism in medicine program, and unit medical director at Icahn School of Medicine at Mount Sinai in New York City. “Later, I reflected upon them and realized that bias was a systemic problem. There needs to be a conversation amongst the broader medical community about the effect that these biases have on our patients and our practice.”
In her editorial, Dr. Reiff-Pasarew explained that when a female physician is written off as too young or is not recognized as a physician, it can delay necessary care. She also touches on the challenge of earning the trust of hospitalized patients.
“There’s a lot of evidence that the success of medical therapy is influenced by the context in which it is given, beyond mere adherence to a regimen or medication,” Dr. Reiff-Pasarew said, noting that it is a result of “the very powerful placebo effect.
“If patients don’t trust the care they are given, it can impact outcomes,” she added. “There is a lot to being a hospitalist that is diagnostic, such as finding the correct diagnosis and implementing the appropriate treatment. However, beyond that, a huge part of this role is to be a knowledgeable caregiver, someone who guides a patient through the experience of being ill in a complex medical system. This requires immense trust.”
Dr. Reiff-Pasarew also believes better mentoring and feedback opportunities would benefit female physicians and trainees. “I often see that equally knowledgeable female trainees and medical students are much more self-deprecating when presenting research,” she said. “They give disclaimers that they don’t know enough, while their male peers are more confident.”
She is quick, however, not to blame women, largely because the same social pressures that Dr. Arora and Dr. Farnan acknowledged may have molded their behaviors. “I meet with residents to talk explicitly about situations where they are treated inappropriately by patients or other staff,” Dr. Reiff-Pasarew said. “We discuss how they might react in those situations in the future and how they can process these challenges.”
Modern American culture equips men and women with “different essential skill sets,” Dr. Reiff-Pasarew noted, but she suggested men and women can learn from one another. “We should be teaching men to be more empathetic listeners, a skill that is generally taught to girls. Similarly, we need to teach women confidence, a skill predominantly taught to boys.”
Just as important, male clinicians should believe in and trust the experiences that women report having, Dr. Reiff-Pasarew said. “It’s very difficult to understand the subtleties of how people are treated differently in patient interactions if you’ve never been in that situation.”
Equal compensation for equal work
Ultimately, it is in the best interest of all physicians, their employers, and their patients to ensure female physicians are satisfied and fulfilled in their professions, said Dr. Jena, and that includes recognizing and rewarding their value.
“What I am trying to argue in my work is for equal pay – equal compensation for equal work,” Dr. Jena said. “Man or woman, it’s a good idea.”
Dr. Jena, who is also a faculty research fellow at the National Bureau of Economic Research, said that when the contributions of a group of people are systematically undervalued, “you run the risk of having those individuals invest less in their career.” In health care, he said, “if fewer women want to go into academic medicine because they know they are underpaid, what impact does it have on new ideas when you eliminate highly successful, intelligent people from a field?”
Dr. Jena and his colleagues authored a February 2017 study in JAMA Internal Medicine that showed hospitalized Medicare patients treated by female internists have lower 30-day mortality and readmissions rates compared with those treated by male internists, including hospitalists. This included millions of hospitalizations and accounted for myriad confounders.5
“Here is evidence that women may be doing a modestly better job than men in terms of outcomes,” Dr. Jena said. “If we are in the business of underpaying and underrewarding females, we are disincentivizing female physicians from entering the field, and in certain specialties female physicians see better patient outcomes.”
Dr. Arora and Dr. Farnan are optimistic that as more studies like those by Dr. Jena and colleagues are published – utilizing large data sets never before available, which account for many of the factors that have been used to justify pay and leadership disparities in the past – times will change for the better.
“There comes a time when everyone realizes a group has been wronged and it’s time to right it. I think now is the time for women. It’s tragic it’s come so late but I’m glad it’s here,” Dr. Arora said. “A lot of work is being done on the ground and in institutions to promote women leaders, to include women in search committees, and improve pay. These are always difficult discussions but now we can have transparency in salaries and we can we discuss them.”
However, Dr. Arora is also concerned about blowback, particularly as issues of sexual harassment of women in the workplace finally emerge from the shadows. “The blowback may be that more people tiptoe around women and are more cautious around them,” she said. “This could end up hurting women in the workplace. Something so deeply cemented like this doesn’t die easily and I think it requires culture change. I do think we’re on that journey and starting to see things change.”
But the real measure of that, said Dr. Farnan, is when these conversations are no longer taking place.
“We will know we’ve achieved what we want to achieve when we don’t have to discuss this anymore,” she said. “We will know we’ve achieved parity when we stop talking about it.”
References
1. Jena AB, Olenski AR, Blumenthal DM. Sex differences in physician salary in US public medical schools. JAMA Intern Med. 2016;176(9):1294-1304. doi: 10.1001/jamainternmed.2016.3284.
2. Farnan JM and Arora VM. Gender equality in hospital medicine – are we there yet? Ann Intern Med. 2017;167(6):HO2-HO3. doi: 10.7326/M17-2119.
3. Burden M, Frank MG, Keniston A, et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med 2015;8;481-5. doi: 10.1002/jhm.2340.
4. Reiff-Pasarew F. I’m a young, female doctor. Calling me ‘sweetie’ won’t help me save your life. Washington Post. Published June 29, 2017. Accessed Dec. 4, 2017.
5. Tsugawa Y, Jena AB, Figueroa JF, et al. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs female physicians. JAMA Intern Med. 2017;177(2):206-13. doi: 10.1001/jamainternmed.2016.7875.
It wasn’t something she planned to have happen but about 2 years ago, Vineet Arora, MD, MAPP, MHM, became what she calls an “accidental advocate” for gender parity in medicine.
“I was asked to review a paper around gender pay,” the University of Chicago Medical Center hospitalist said. “It was stunning to me just how different salaries were – between male and female physicians – even when the authors were attempting to control for various factors.”
That paper was published in the Journal of the American Medical Association (JAMA) in September 2016 by researchers at Harvard Medical School and Massachusetts General Hospital (MGH). It found that even after adjustment for age, experience, specialty, faculty rank, research productivity, and clinical revenue, female physicians at 24 public medical schools in 12 states earned nearly $20,000 less per year than their male colleagues.1
Dr. Arora wrote an editorial to accompany that 2016 paper in JAMA, and in September 2017, she and her colleague at the University of Chicago, Jeanne Farnan, MD, MHPE, coauthored another piece in Annals of Internal Medicine titled, “Inpatient Notes: Gender Equality in Hospital Medicine – Are We There Yet?”2
In the 2017 paper, Dr. Arora and Dr. Farnan assessed recent studies documenting inequity in regard to compensation, discrimination around child-rearing, and gender disparities in medical leadership. They also discussed strategies that might improve the future outlook for female physicians.
“As I approach mid-career, I see these issues affecting my career and my colleagues’ careers and I decided we need to be doing more work in this space,” said Dr. Arora.
Fueling the conversation
When asked whether he thinks his research inspired the current conversation around gender inequity in medicine, Anupam Bapu Jena, MD, PhD – lead author of the September 2016 gender pay paper – said that while he did not initiate it, his work “has fueled the conversation.”
“This is an issue that has been going on in the scientific literature for at least 25-30 years,” said Dr. Jena, the Ruth L. Newhouse Associate Professor of Health Care Policy at Harvard Medical School and a physician in the department of medicine at MGH. “I am sure women in medicine have been feeling this since women entered medicine.”
Many female hospitalists hoped that, as a relatively new field, hospital medicine would avoid some of the time-worn challenges women in other specialties faced.
“The birth of hospital medicine held the promise that, as a new field, it would be immune to the ‘old boys’ club mentality that plagues established specialties,” Dr. Farnan and Dr. Arora wrote in their September 2017 Annals article. And yet, they continued, “gender disparities developed in the areas of leadership and academic productivity.”
A 2015 study in the Journal of Hospital Medicine found that just 16% of university hospital medicine divisions were led by women, and women made up just 28% of those physicians leading general internal medicine divisions. Meanwhile, female hospitalists gave just 26% of presentations at national meetings, were first authors on only 33% of publications, and were senior authors on only 21% of manuscripts.3
In addition, Dr. Farnan and Dr. Arora wrote in their review, another recent survey of female physicians – primarily internists – found that 36% reported discrimination based on pregnancy, maternity leave, or breastfeeding. This was – at least in part, Dr. Farnan said – because “physician-mothers were not present at the table when discussions were held about scheduling.”
And while hospitalists have relatively flexible schedules, they can be unforgiving when it comes to traditional child care arrangements, Dr. Arora said.
But, there is hope, particularly within the Society of Hospital Medicine, Dr. Arora and Dr. Farnan wrote. The organization has seen an increase in female leadership – including its president-elect Nasim Afsar, MD, MBA, SFHM – and a board of directors that is split evenly between men and women. Mentorship of junior women is also on the rise, which allows opportunities for senior female physicians to teach younger women how to better negotiate and advocate for themselves.
“I think it has to come from both sides. Leadership does need to recognize that women may be less aggressive in their negotiating skills,” said Dr. Farnan. “But I think there also needs to be some recognition by women that it is okay to ask for more money.”
But it isn’t all about money, she said. “It can be negotiating for anything important in career development, career opportunities, research opportunities.” This also extends to schedule flexibility, training and more.
Leadership in hospitalist groups can help, Dr. Arora and Dr. Farnan wrote in their Annals article, by providing schedule flexibility, support for training, and structured on-boarding for new faculty. Citing efforts in other specialties such as cardiology and general surgery, female hospitalists may benefit from negotiation skills training, structured mentorship, and education around personal and professional development.
However, both physicians recognize the challenges of implicit bias and stereotype threat that may confront many women. For example, women who exert more stereotypically “male” traits such as assertiveness and confidence may face a “harsh likability penalty because they are going against gender norms,” said Dr. Arora.
Being taken seriously
Expectations around gender norms may also affect relationships female doctors have with their patients. In a June 2017 Washington Post editorial, Faye Reiff-Pasarew, MD, describes being objectified as “cute” and “adorable” and not being taken seriously by her patients.4
“I’d had a number of interactions with patients that upset me,” said Dr. Reiff-Pasarew, assistant professor of hospital medicine, director of the humanism in medicine program, and unit medical director at Icahn School of Medicine at Mount Sinai in New York City. “Later, I reflected upon them and realized that bias was a systemic problem. There needs to be a conversation amongst the broader medical community about the effect that these biases have on our patients and our practice.”
In her editorial, Dr. Reiff-Pasarew explained that when a female physician is written off as too young or is not recognized as a physician, it can delay necessary care. She also touches on the challenge of earning the trust of hospitalized patients.
“There’s a lot of evidence that the success of medical therapy is influenced by the context in which it is given, beyond mere adherence to a regimen or medication,” Dr. Reiff-Pasarew said, noting that it is a result of “the very powerful placebo effect.
“If patients don’t trust the care they are given, it can impact outcomes,” she added. “There is a lot to being a hospitalist that is diagnostic, such as finding the correct diagnosis and implementing the appropriate treatment. However, beyond that, a huge part of this role is to be a knowledgeable caregiver, someone who guides a patient through the experience of being ill in a complex medical system. This requires immense trust.”
Dr. Reiff-Pasarew also believes better mentoring and feedback opportunities would benefit female physicians and trainees. “I often see that equally knowledgeable female trainees and medical students are much more self-deprecating when presenting research,” she said. “They give disclaimers that they don’t know enough, while their male peers are more confident.”
She is quick, however, not to blame women, largely because the same social pressures that Dr. Arora and Dr. Farnan acknowledged may have molded their behaviors. “I meet with residents to talk explicitly about situations where they are treated inappropriately by patients or other staff,” Dr. Reiff-Pasarew said. “We discuss how they might react in those situations in the future and how they can process these challenges.”
Modern American culture equips men and women with “different essential skill sets,” Dr. Reiff-Pasarew noted, but she suggested men and women can learn from one another. “We should be teaching men to be more empathetic listeners, a skill that is generally taught to girls. Similarly, we need to teach women confidence, a skill predominantly taught to boys.”
Just as important, male clinicians should believe in and trust the experiences that women report having, Dr. Reiff-Pasarew said. “It’s very difficult to understand the subtleties of how people are treated differently in patient interactions if you’ve never been in that situation.”
Equal compensation for equal work
Ultimately, it is in the best interest of all physicians, their employers, and their patients to ensure female physicians are satisfied and fulfilled in their professions, said Dr. Jena, and that includes recognizing and rewarding their value.
“What I am trying to argue in my work is for equal pay – equal compensation for equal work,” Dr. Jena said. “Man or woman, it’s a good idea.”
Dr. Jena, who is also a faculty research fellow at the National Bureau of Economic Research, said that when the contributions of a group of people are systematically undervalued, “you run the risk of having those individuals invest less in their career.” In health care, he said, “if fewer women want to go into academic medicine because they know they are underpaid, what impact does it have on new ideas when you eliminate highly successful, intelligent people from a field?”
Dr. Jena and his colleagues authored a February 2017 study in JAMA Internal Medicine that showed hospitalized Medicare patients treated by female internists have lower 30-day mortality and readmissions rates compared with those treated by male internists, including hospitalists. This included millions of hospitalizations and accounted for myriad confounders.5
“Here is evidence that women may be doing a modestly better job than men in terms of outcomes,” Dr. Jena said. “If we are in the business of underpaying and underrewarding females, we are disincentivizing female physicians from entering the field, and in certain specialties female physicians see better patient outcomes.”
Dr. Arora and Dr. Farnan are optimistic that as more studies like those by Dr. Jena and colleagues are published – utilizing large data sets never before available, which account for many of the factors that have been used to justify pay and leadership disparities in the past – times will change for the better.
“There comes a time when everyone realizes a group has been wronged and it’s time to right it. I think now is the time for women. It’s tragic it’s come so late but I’m glad it’s here,” Dr. Arora said. “A lot of work is being done on the ground and in institutions to promote women leaders, to include women in search committees, and improve pay. These are always difficult discussions but now we can have transparency in salaries and we can we discuss them.”
However, Dr. Arora is also concerned about blowback, particularly as issues of sexual harassment of women in the workplace finally emerge from the shadows. “The blowback may be that more people tiptoe around women and are more cautious around them,” she said. “This could end up hurting women in the workplace. Something so deeply cemented like this doesn’t die easily and I think it requires culture change. I do think we’re on that journey and starting to see things change.”
But the real measure of that, said Dr. Farnan, is when these conversations are no longer taking place.
“We will know we’ve achieved what we want to achieve when we don’t have to discuss this anymore,” she said. “We will know we’ve achieved parity when we stop talking about it.”
References
1. Jena AB, Olenski AR, Blumenthal DM. Sex differences in physician salary in US public medical schools. JAMA Intern Med. 2016;176(9):1294-1304. doi: 10.1001/jamainternmed.2016.3284.
2. Farnan JM and Arora VM. Gender equality in hospital medicine – are we there yet? Ann Intern Med. 2017;167(6):HO2-HO3. doi: 10.7326/M17-2119.
3. Burden M, Frank MG, Keniston A, et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med 2015;8;481-5. doi: 10.1002/jhm.2340.
4. Reiff-Pasarew F. I’m a young, female doctor. Calling me ‘sweetie’ won’t help me save your life. Washington Post. Published June 29, 2017. Accessed Dec. 4, 2017.
5. Tsugawa Y, Jena AB, Figueroa JF, et al. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs female physicians. JAMA Intern Med. 2017;177(2):206-13. doi: 10.1001/jamainternmed.2016.7875.
It wasn’t something she planned to have happen but about 2 years ago, Vineet Arora, MD, MAPP, MHM, became what she calls an “accidental advocate” for gender parity in medicine.
“I was asked to review a paper around gender pay,” the University of Chicago Medical Center hospitalist said. “It was stunning to me just how different salaries were – between male and female physicians – even when the authors were attempting to control for various factors.”
That paper was published in the Journal of the American Medical Association (JAMA) in September 2016 by researchers at Harvard Medical School and Massachusetts General Hospital (MGH). It found that even after adjustment for age, experience, specialty, faculty rank, research productivity, and clinical revenue, female physicians at 24 public medical schools in 12 states earned nearly $20,000 less per year than their male colleagues.1
Dr. Arora wrote an editorial to accompany that 2016 paper in JAMA, and in September 2017, she and her colleague at the University of Chicago, Jeanne Farnan, MD, MHPE, coauthored another piece in Annals of Internal Medicine titled, “Inpatient Notes: Gender Equality in Hospital Medicine – Are We There Yet?”2
In the 2017 paper, Dr. Arora and Dr. Farnan assessed recent studies documenting inequity in regard to compensation, discrimination around child-rearing, and gender disparities in medical leadership. They also discussed strategies that might improve the future outlook for female physicians.
“As I approach mid-career, I see these issues affecting my career and my colleagues’ careers and I decided we need to be doing more work in this space,” said Dr. Arora.
Fueling the conversation
When asked whether he thinks his research inspired the current conversation around gender inequity in medicine, Anupam Bapu Jena, MD, PhD – lead author of the September 2016 gender pay paper – said that while he did not initiate it, his work “has fueled the conversation.”
“This is an issue that has been going on in the scientific literature for at least 25-30 years,” said Dr. Jena, the Ruth L. Newhouse Associate Professor of Health Care Policy at Harvard Medical School and a physician in the department of medicine at MGH. “I am sure women in medicine have been feeling this since women entered medicine.”
Many female hospitalists hoped that, as a relatively new field, hospital medicine would avoid some of the time-worn challenges women in other specialties faced.
“The birth of hospital medicine held the promise that, as a new field, it would be immune to the ‘old boys’ club mentality that plagues established specialties,” Dr. Farnan and Dr. Arora wrote in their September 2017 Annals article. And yet, they continued, “gender disparities developed in the areas of leadership and academic productivity.”
A 2015 study in the Journal of Hospital Medicine found that just 16% of university hospital medicine divisions were led by women, and women made up just 28% of those physicians leading general internal medicine divisions. Meanwhile, female hospitalists gave just 26% of presentations at national meetings, were first authors on only 33% of publications, and were senior authors on only 21% of manuscripts.3
In addition, Dr. Farnan and Dr. Arora wrote in their review, another recent survey of female physicians – primarily internists – found that 36% reported discrimination based on pregnancy, maternity leave, or breastfeeding. This was – at least in part, Dr. Farnan said – because “physician-mothers were not present at the table when discussions were held about scheduling.”
And while hospitalists have relatively flexible schedules, they can be unforgiving when it comes to traditional child care arrangements, Dr. Arora said.
But, there is hope, particularly within the Society of Hospital Medicine, Dr. Arora and Dr. Farnan wrote. The organization has seen an increase in female leadership – including its president-elect Nasim Afsar, MD, MBA, SFHM – and a board of directors that is split evenly between men and women. Mentorship of junior women is also on the rise, which allows opportunities for senior female physicians to teach younger women how to better negotiate and advocate for themselves.
“I think it has to come from both sides. Leadership does need to recognize that women may be less aggressive in their negotiating skills,” said Dr. Farnan. “But I think there also needs to be some recognition by women that it is okay to ask for more money.”
But it isn’t all about money, she said. “It can be negotiating for anything important in career development, career opportunities, research opportunities.” This also extends to schedule flexibility, training and more.
Leadership in hospitalist groups can help, Dr. Arora and Dr. Farnan wrote in their Annals article, by providing schedule flexibility, support for training, and structured on-boarding for new faculty. Citing efforts in other specialties such as cardiology and general surgery, female hospitalists may benefit from negotiation skills training, structured mentorship, and education around personal and professional development.
However, both physicians recognize the challenges of implicit bias and stereotype threat that may confront many women. For example, women who exert more stereotypically “male” traits such as assertiveness and confidence may face a “harsh likability penalty because they are going against gender norms,” said Dr. Arora.
Being taken seriously
Expectations around gender norms may also affect relationships female doctors have with their patients. In a June 2017 Washington Post editorial, Faye Reiff-Pasarew, MD, describes being objectified as “cute” and “adorable” and not being taken seriously by her patients.4
“I’d had a number of interactions with patients that upset me,” said Dr. Reiff-Pasarew, assistant professor of hospital medicine, director of the humanism in medicine program, and unit medical director at Icahn School of Medicine at Mount Sinai in New York City. “Later, I reflected upon them and realized that bias was a systemic problem. There needs to be a conversation amongst the broader medical community about the effect that these biases have on our patients and our practice.”
In her editorial, Dr. Reiff-Pasarew explained that when a female physician is written off as too young or is not recognized as a physician, it can delay necessary care. She also touches on the challenge of earning the trust of hospitalized patients.
“There’s a lot of evidence that the success of medical therapy is influenced by the context in which it is given, beyond mere adherence to a regimen or medication,” Dr. Reiff-Pasarew said, noting that it is a result of “the very powerful placebo effect.
“If patients don’t trust the care they are given, it can impact outcomes,” she added. “There is a lot to being a hospitalist that is diagnostic, such as finding the correct diagnosis and implementing the appropriate treatment. However, beyond that, a huge part of this role is to be a knowledgeable caregiver, someone who guides a patient through the experience of being ill in a complex medical system. This requires immense trust.”
Dr. Reiff-Pasarew also believes better mentoring and feedback opportunities would benefit female physicians and trainees. “I often see that equally knowledgeable female trainees and medical students are much more self-deprecating when presenting research,” she said. “They give disclaimers that they don’t know enough, while their male peers are more confident.”
She is quick, however, not to blame women, largely because the same social pressures that Dr. Arora and Dr. Farnan acknowledged may have molded their behaviors. “I meet with residents to talk explicitly about situations where they are treated inappropriately by patients or other staff,” Dr. Reiff-Pasarew said. “We discuss how they might react in those situations in the future and how they can process these challenges.”
Modern American culture equips men and women with “different essential skill sets,” Dr. Reiff-Pasarew noted, but she suggested men and women can learn from one another. “We should be teaching men to be more empathetic listeners, a skill that is generally taught to girls. Similarly, we need to teach women confidence, a skill predominantly taught to boys.”
Just as important, male clinicians should believe in and trust the experiences that women report having, Dr. Reiff-Pasarew said. “It’s very difficult to understand the subtleties of how people are treated differently in patient interactions if you’ve never been in that situation.”
Equal compensation for equal work
Ultimately, it is in the best interest of all physicians, their employers, and their patients to ensure female physicians are satisfied and fulfilled in their professions, said Dr. Jena, and that includes recognizing and rewarding their value.
“What I am trying to argue in my work is for equal pay – equal compensation for equal work,” Dr. Jena said. “Man or woman, it’s a good idea.”
Dr. Jena, who is also a faculty research fellow at the National Bureau of Economic Research, said that when the contributions of a group of people are systematically undervalued, “you run the risk of having those individuals invest less in their career.” In health care, he said, “if fewer women want to go into academic medicine because they know they are underpaid, what impact does it have on new ideas when you eliminate highly successful, intelligent people from a field?”
Dr. Jena and his colleagues authored a February 2017 study in JAMA Internal Medicine that showed hospitalized Medicare patients treated by female internists have lower 30-day mortality and readmissions rates compared with those treated by male internists, including hospitalists. This included millions of hospitalizations and accounted for myriad confounders.5
“Here is evidence that women may be doing a modestly better job than men in terms of outcomes,” Dr. Jena said. “If we are in the business of underpaying and underrewarding females, we are disincentivizing female physicians from entering the field, and in certain specialties female physicians see better patient outcomes.”
Dr. Arora and Dr. Farnan are optimistic that as more studies like those by Dr. Jena and colleagues are published – utilizing large data sets never before available, which account for many of the factors that have been used to justify pay and leadership disparities in the past – times will change for the better.
“There comes a time when everyone realizes a group has been wronged and it’s time to right it. I think now is the time for women. It’s tragic it’s come so late but I’m glad it’s here,” Dr. Arora said. “A lot of work is being done on the ground and in institutions to promote women leaders, to include women in search committees, and improve pay. These are always difficult discussions but now we can have transparency in salaries and we can we discuss them.”
However, Dr. Arora is also concerned about blowback, particularly as issues of sexual harassment of women in the workplace finally emerge from the shadows. “The blowback may be that more people tiptoe around women and are more cautious around them,” she said. “This could end up hurting women in the workplace. Something so deeply cemented like this doesn’t die easily and I think it requires culture change. I do think we’re on that journey and starting to see things change.”
But the real measure of that, said Dr. Farnan, is when these conversations are no longer taking place.
“We will know we’ve achieved what we want to achieve when we don’t have to discuss this anymore,” she said. “We will know we’ve achieved parity when we stop talking about it.”
References
1. Jena AB, Olenski AR, Blumenthal DM. Sex differences in physician salary in US public medical schools. JAMA Intern Med. 2016;176(9):1294-1304. doi: 10.1001/jamainternmed.2016.3284.
2. Farnan JM and Arora VM. Gender equality in hospital medicine – are we there yet? Ann Intern Med. 2017;167(6):HO2-HO3. doi: 10.7326/M17-2119.
3. Burden M, Frank MG, Keniston A, et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med 2015;8;481-5. doi: 10.1002/jhm.2340.
4. Reiff-Pasarew F. I’m a young, female doctor. Calling me ‘sweetie’ won’t help me save your life. Washington Post. Published June 29, 2017. Accessed Dec. 4, 2017.
5. Tsugawa Y, Jena AB, Figueroa JF, et al. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs female physicians. JAMA Intern Med. 2017;177(2):206-13. doi: 10.1001/jamainternmed.2016.7875.