User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Evidence suggests fondaparinux is more effective than LMWH in prevention of VTE and total DVT in the postoperative setting
Clinical question: How do pentasaccharides compare to other anticoagulants in postoperative venous thromboembolism prevention?
Background: Venous thromboembolism (VTE) remains a leading cause of preventable hospital related death. Pentasaccharides selectively inhibit factor Xa to inhibit clotting and exhibit a lower risk of heparin induced thrombocytopenia (HIT) compared to low molecular weight heparin (LMWH) and unfractionated heparin. We lack a formal recommendation regarding the pentasaccharides superiority or inferiority, relative to other anticoagulants, in the perioperative setting.
Study design: Cochrane review.
Setting: Hospital and outpatient.
Synopsis: Authors searched randomized controlled trials involving pentasaccharides versus other VTE prophylaxis to obtain 25 studies totaling 21,004 subjects undergoing orthopedic, abdominal, cardiac bypass, thoracic, and bariatric surgery; hospitalized patients, immobilized patients, and those with superficial venous thrombosis. Selected studies pertained to fondaparinux and VTE prevention. Fondaparinux was superior to placebo in prevention of DVT and VTE. Compared to LMWH, fondaparinux reduced total VTE (RR, 0.55, 95% CI, 0.42-0.73) and DVT (RR, 0.54, 95% CI, 0.40-0.71), but carried a higher rate of major bleeding compared to placebo (RR, 2.56, 95% CI, 1.48-4.44) and LMWH (RR, 1.38, 95% CI, 1.09-1.75). The all cause death and major adverse events for fondaparinux versus placebo and LMWH were not statistically significant. Limitations of this review include the predominance of orthopedic patients, variable duration of treatment, and low-moderate quality data.
Bottom line: Fondaparinux demonstrates better perioperative total VTE and DVT reduction compared to LMWH, but it increases the incidence of major bleeding.
Reference: Dong K, Song Y, Li X, Ding J, Gao Z, Lu D, Zhu Y. Pentasaccharides for the prevention of venous thromboembolism. Cochrane Database Syst Rev. 2016 Oct 31;10:CD005134.
Dr. Coleman is an assistant professor of clinical medicine at Cooper Medical School at Rowan University. She works as a hospitalist at Cooper University Hospital in Camden, N.J.
Clinical question: How do pentasaccharides compare to other anticoagulants in postoperative venous thromboembolism prevention?
Background: Venous thromboembolism (VTE) remains a leading cause of preventable hospital related death. Pentasaccharides selectively inhibit factor Xa to inhibit clotting and exhibit a lower risk of heparin induced thrombocytopenia (HIT) compared to low molecular weight heparin (LMWH) and unfractionated heparin. We lack a formal recommendation regarding the pentasaccharides superiority or inferiority, relative to other anticoagulants, in the perioperative setting.
Study design: Cochrane review.
Setting: Hospital and outpatient.
Synopsis: Authors searched randomized controlled trials involving pentasaccharides versus other VTE prophylaxis to obtain 25 studies totaling 21,004 subjects undergoing orthopedic, abdominal, cardiac bypass, thoracic, and bariatric surgery; hospitalized patients, immobilized patients, and those with superficial venous thrombosis. Selected studies pertained to fondaparinux and VTE prevention. Fondaparinux was superior to placebo in prevention of DVT and VTE. Compared to LMWH, fondaparinux reduced total VTE (RR, 0.55, 95% CI, 0.42-0.73) and DVT (RR, 0.54, 95% CI, 0.40-0.71), but carried a higher rate of major bleeding compared to placebo (RR, 2.56, 95% CI, 1.48-4.44) and LMWH (RR, 1.38, 95% CI, 1.09-1.75). The all cause death and major adverse events for fondaparinux versus placebo and LMWH were not statistically significant. Limitations of this review include the predominance of orthopedic patients, variable duration of treatment, and low-moderate quality data.
Bottom line: Fondaparinux demonstrates better perioperative total VTE and DVT reduction compared to LMWH, but it increases the incidence of major bleeding.
Reference: Dong K, Song Y, Li X, Ding J, Gao Z, Lu D, Zhu Y. Pentasaccharides for the prevention of venous thromboembolism. Cochrane Database Syst Rev. 2016 Oct 31;10:CD005134.
Dr. Coleman is an assistant professor of clinical medicine at Cooper Medical School at Rowan University. She works as a hospitalist at Cooper University Hospital in Camden, N.J.
Clinical question: How do pentasaccharides compare to other anticoagulants in postoperative venous thromboembolism prevention?
Background: Venous thromboembolism (VTE) remains a leading cause of preventable hospital related death. Pentasaccharides selectively inhibit factor Xa to inhibit clotting and exhibit a lower risk of heparin induced thrombocytopenia (HIT) compared to low molecular weight heparin (LMWH) and unfractionated heparin. We lack a formal recommendation regarding the pentasaccharides superiority or inferiority, relative to other anticoagulants, in the perioperative setting.
Study design: Cochrane review.
Setting: Hospital and outpatient.
Synopsis: Authors searched randomized controlled trials involving pentasaccharides versus other VTE prophylaxis to obtain 25 studies totaling 21,004 subjects undergoing orthopedic, abdominal, cardiac bypass, thoracic, and bariatric surgery; hospitalized patients, immobilized patients, and those with superficial venous thrombosis. Selected studies pertained to fondaparinux and VTE prevention. Fondaparinux was superior to placebo in prevention of DVT and VTE. Compared to LMWH, fondaparinux reduced total VTE (RR, 0.55, 95% CI, 0.42-0.73) and DVT (RR, 0.54, 95% CI, 0.40-0.71), but carried a higher rate of major bleeding compared to placebo (RR, 2.56, 95% CI, 1.48-4.44) and LMWH (RR, 1.38, 95% CI, 1.09-1.75). The all cause death and major adverse events for fondaparinux versus placebo and LMWH were not statistically significant. Limitations of this review include the predominance of orthopedic patients, variable duration of treatment, and low-moderate quality data.
Bottom line: Fondaparinux demonstrates better perioperative total VTE and DVT reduction compared to LMWH, but it increases the incidence of major bleeding.
Reference: Dong K, Song Y, Li X, Ding J, Gao Z, Lu D, Zhu Y. Pentasaccharides for the prevention of venous thromboembolism. Cochrane Database Syst Rev. 2016 Oct 31;10:CD005134.
Dr. Coleman is an assistant professor of clinical medicine at Cooper Medical School at Rowan University. She works as a hospitalist at Cooper University Hospital in Camden, N.J.
Trending at SHM
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
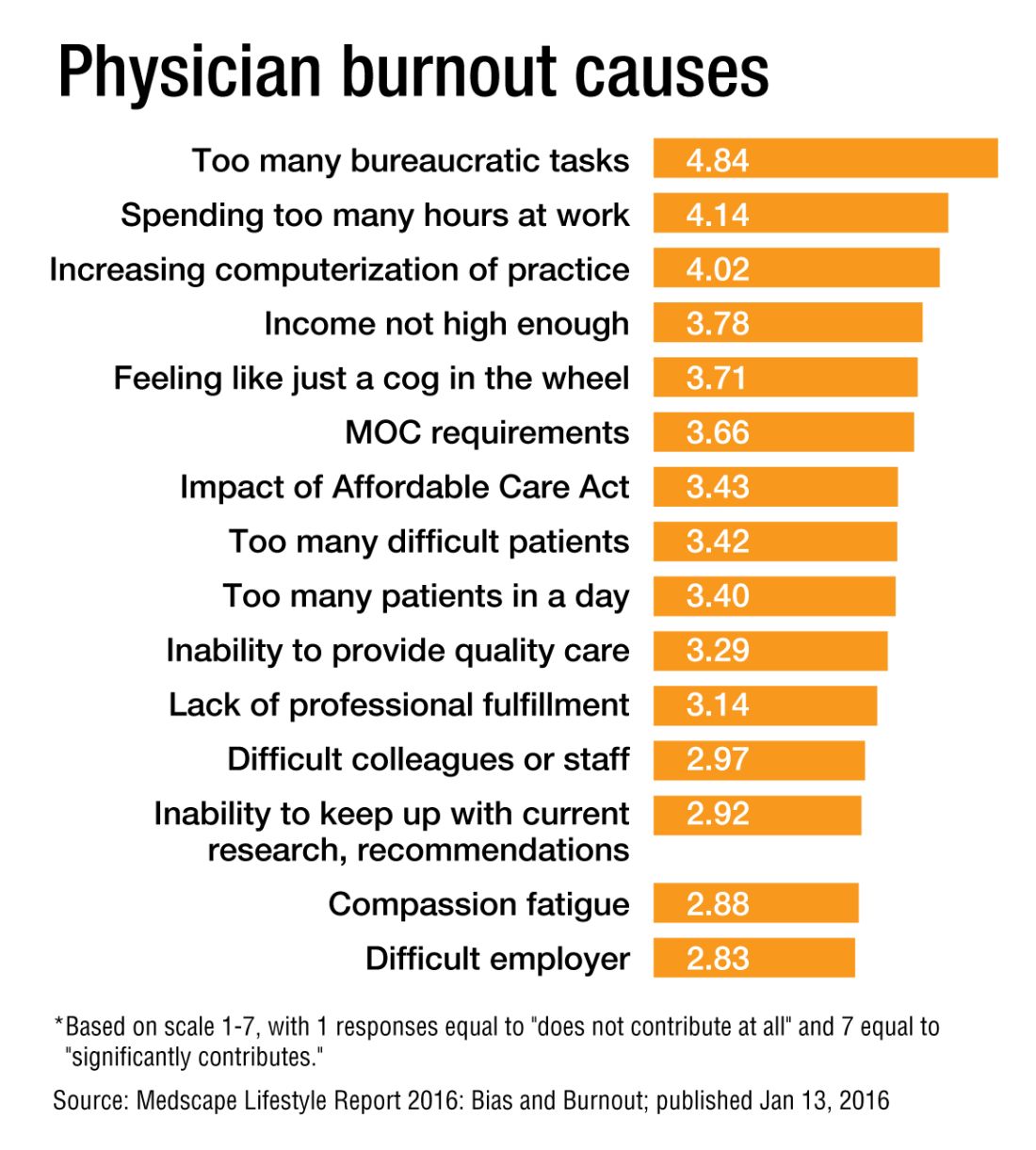
Don’t assume work is sole burnout determinant
Physician burnout is almost always linked to issues at work. Blame is placed on added duties piled onto a to-do list that barely makes enough time for prolonged patient interaction in the first place. Fault is laid upon the hours and hours per week – or even per day – wasted on cumbersome data entry into bulky electronic health record (EHR) systems.
But Dike Drummond, MD, a family physician and burnout coach/consultant, says burnout should not be viewed as job specific. “To say that burnout is always about work is absolutely an error,” said Dr. Drummond, whose website is www.thehappymd.com. “You can have people flame out spectacularly at work and nothing has changed about work at all. It’s because something’s going on at home that’s made it impossible to recharge on their time off. And, that list of recharge-blocking issues is huge.”
Money problems, marital problems, family problems: Dr. Drummond says any and all of those issues can eliminate the doctor’s ability to recharge at home.
“The strain of your practice continues, but now without the ability to balance your energy with some recovery when you’re away from the hospital, burnout can come on very rapidly,” he said. “So when you see a colleague flaming out at work, one of the questions you must ask is, “How is it going at home?” You may be the first to learn their spouse left them 2 weeks ago.”
Dr. Drummond’s advice is: Don’t always blame the stresses of work. Build your recharge strategy (rest, hobbies, date nights) and make sure you maintain your recharge capabilities.
“Ideally, with a hospitalist-type schedule, when you’re on you’re on and when you’re off you’re off,” he said. “It should be easier to create that boundary for hospitalists than other specialists who chart from home or are on call.
The “off switch” on your doctor programming is called a boundary ritual. Pick some activity you do on the way home from work, saying to yourself ‘with this action, I am coming all the way home.’ It can be as simple as a deep releasing breath as you step out of your car at home. Make sure you take that breath and let it all go before you walk into the house after each shift.”
Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout, refers to this phenomenon as “work-home interference.” On the bright side for hospitalists, he says, is that aspects of HM work schedules may help mitigate burnout; some work can be left at the hospital when shifts end, rather than following physicians into their home lives.
But Dr. West acknowledged that the rigors of the traditional 7-on/7-off schedule come with their own unique burnout challenges for hospitalists as well.
“A hospitalist can say ‘Well, jeez, I’m on nights for the next week, and that means during the day I’m sleeping and recovering,’” Dr. West explained. “Well, how do you maintain a family life for that period of time when you’re basically off-cycle with your family? There are those kinds of stressors. It’s a mixed bag for hospitalists there.”
Richard Quinn is a freelance writer in New Jersey.
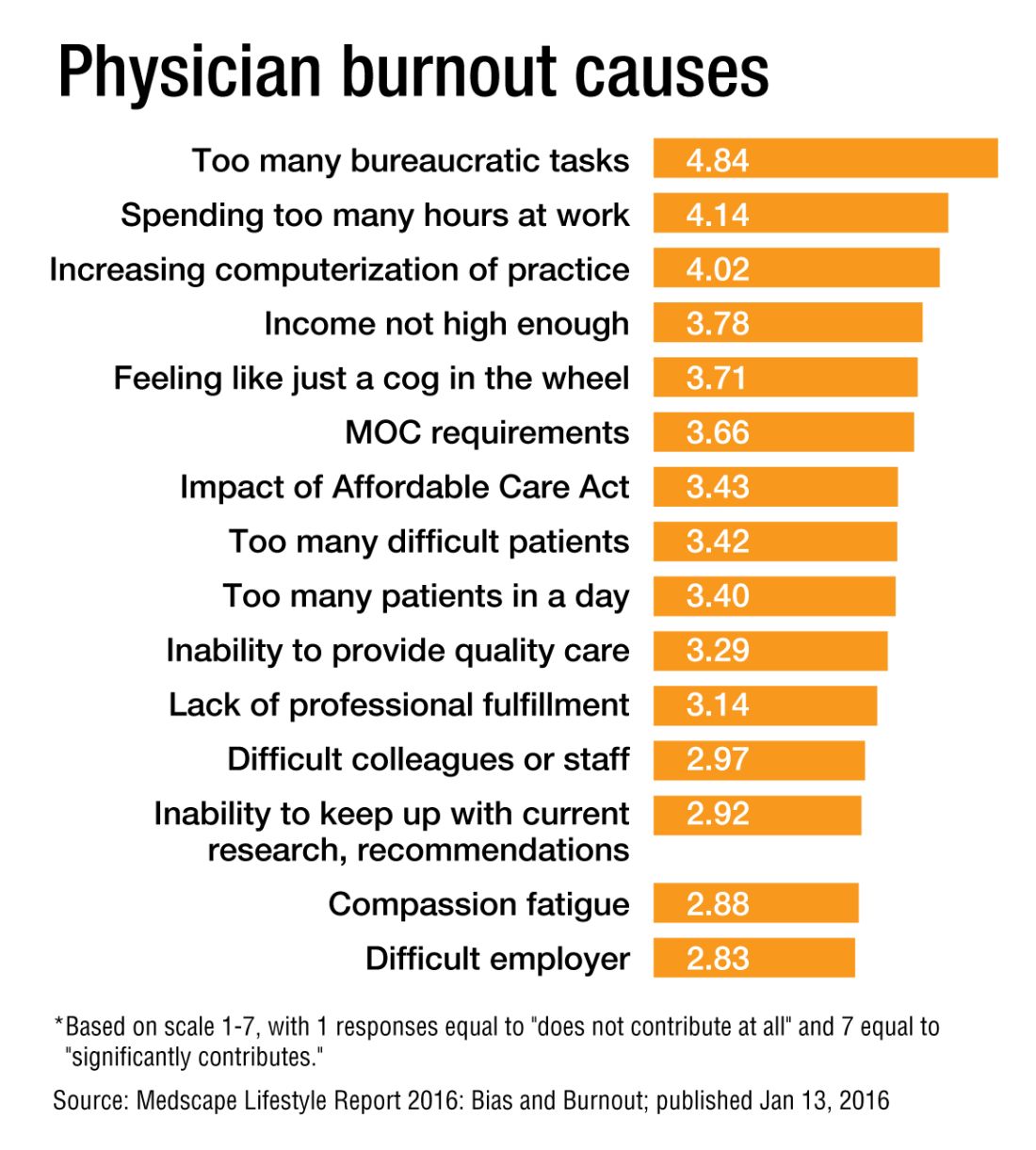
Physician burnout is almost always linked to issues at work. Blame is placed on added duties piled onto a to-do list that barely makes enough time for prolonged patient interaction in the first place. Fault is laid upon the hours and hours per week – or even per day – wasted on cumbersome data entry into bulky electronic health record (EHR) systems.
But Dike Drummond, MD, a family physician and burnout coach/consultant, says burnout should not be viewed as job specific. “To say that burnout is always about work is absolutely an error,” said Dr. Drummond, whose website is www.thehappymd.com. “You can have people flame out spectacularly at work and nothing has changed about work at all. It’s because something’s going on at home that’s made it impossible to recharge on their time off. And, that list of recharge-blocking issues is huge.”
Money problems, marital problems, family problems: Dr. Drummond says any and all of those issues can eliminate the doctor’s ability to recharge at home.
“The strain of your practice continues, but now without the ability to balance your energy with some recovery when you’re away from the hospital, burnout can come on very rapidly,” he said. “So when you see a colleague flaming out at work, one of the questions you must ask is, “How is it going at home?” You may be the first to learn their spouse left them 2 weeks ago.”
Dr. Drummond’s advice is: Don’t always blame the stresses of work. Build your recharge strategy (rest, hobbies, date nights) and make sure you maintain your recharge capabilities.
“Ideally, with a hospitalist-type schedule, when you’re on you’re on and when you’re off you’re off,” he said. “It should be easier to create that boundary for hospitalists than other specialists who chart from home or are on call.
The “off switch” on your doctor programming is called a boundary ritual. Pick some activity you do on the way home from work, saying to yourself ‘with this action, I am coming all the way home.’ It can be as simple as a deep releasing breath as you step out of your car at home. Make sure you take that breath and let it all go before you walk into the house after each shift.”
Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout, refers to this phenomenon as “work-home interference.” On the bright side for hospitalists, he says, is that aspects of HM work schedules may help mitigate burnout; some work can be left at the hospital when shifts end, rather than following physicians into their home lives.
But Dr. West acknowledged that the rigors of the traditional 7-on/7-off schedule come with their own unique burnout challenges for hospitalists as well.
“A hospitalist can say ‘Well, jeez, I’m on nights for the next week, and that means during the day I’m sleeping and recovering,’” Dr. West explained. “Well, how do you maintain a family life for that period of time when you’re basically off-cycle with your family? There are those kinds of stressors. It’s a mixed bag for hospitalists there.”
Richard Quinn is a freelance writer in New Jersey.
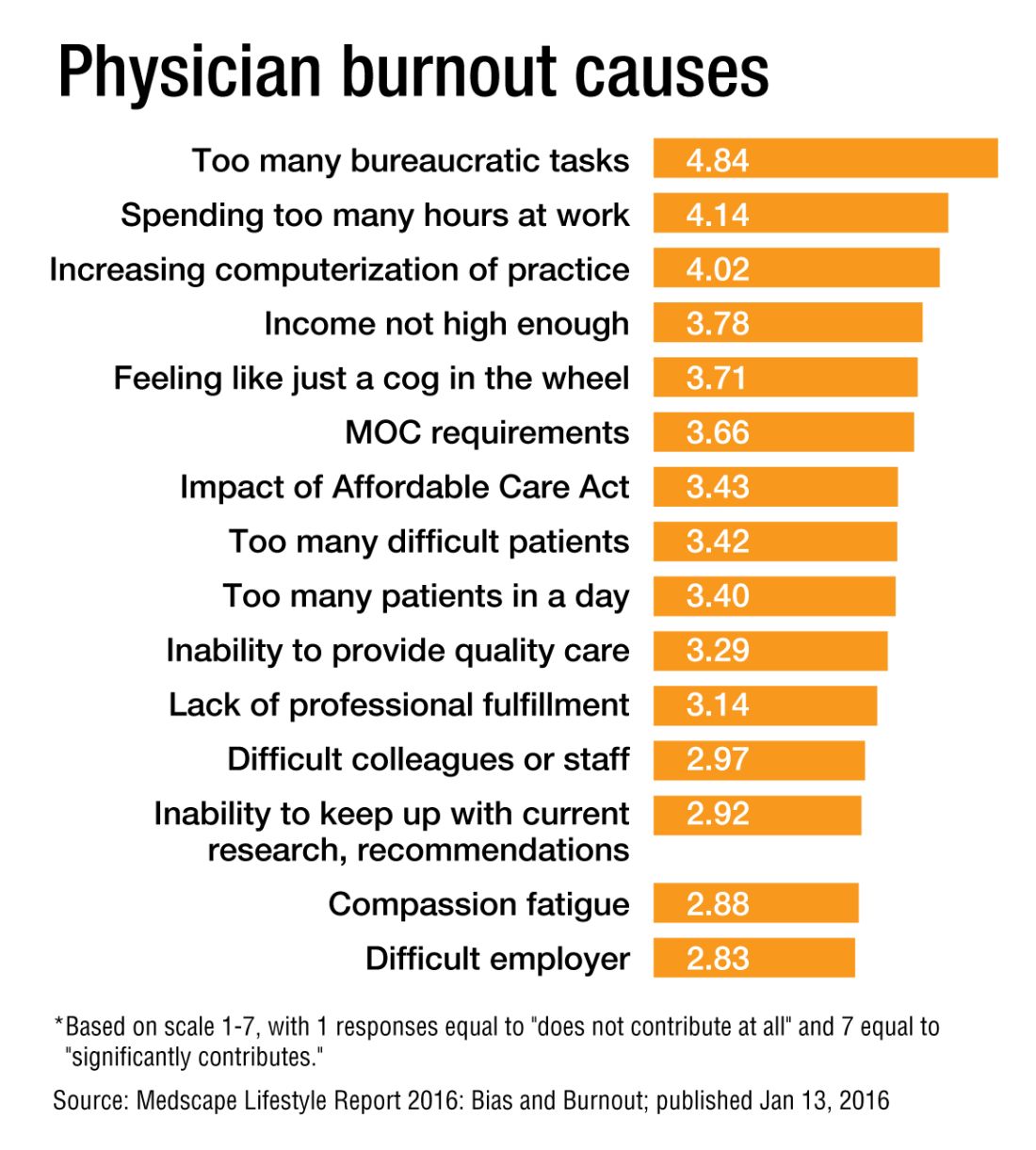
Physician burnout is almost always linked to issues at work. Blame is placed on added duties piled onto a to-do list that barely makes enough time for prolonged patient interaction in the first place. Fault is laid upon the hours and hours per week – or even per day – wasted on cumbersome data entry into bulky electronic health record (EHR) systems.
But Dike Drummond, MD, a family physician and burnout coach/consultant, says burnout should not be viewed as job specific. “To say that burnout is always about work is absolutely an error,” said Dr. Drummond, whose website is www.thehappymd.com. “You can have people flame out spectacularly at work and nothing has changed about work at all. It’s because something’s going on at home that’s made it impossible to recharge on their time off. And, that list of recharge-blocking issues is huge.”
Money problems, marital problems, family problems: Dr. Drummond says any and all of those issues can eliminate the doctor’s ability to recharge at home.
“The strain of your practice continues, but now without the ability to balance your energy with some recovery when you’re away from the hospital, burnout can come on very rapidly,” he said. “So when you see a colleague flaming out at work, one of the questions you must ask is, “How is it going at home?” You may be the first to learn their spouse left them 2 weeks ago.”
Dr. Drummond’s advice is: Don’t always blame the stresses of work. Build your recharge strategy (rest, hobbies, date nights) and make sure you maintain your recharge capabilities.
“Ideally, with a hospitalist-type schedule, when you’re on you’re on and when you’re off you’re off,” he said. “It should be easier to create that boundary for hospitalists than other specialists who chart from home or are on call.
The “off switch” on your doctor programming is called a boundary ritual. Pick some activity you do on the way home from work, saying to yourself ‘with this action, I am coming all the way home.’ It can be as simple as a deep releasing breath as you step out of your car at home. Make sure you take that breath and let it all go before you walk into the house after each shift.”
Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout, refers to this phenomenon as “work-home interference.” On the bright side for hospitalists, he says, is that aspects of HM work schedules may help mitigate burnout; some work can be left at the hospital when shifts end, rather than following physicians into their home lives.
But Dr. West acknowledged that the rigors of the traditional 7-on/7-off schedule come with their own unique burnout challenges for hospitalists as well.
“A hospitalist can say ‘Well, jeez, I’m on nights for the next week, and that means during the day I’m sleeping and recovering,’” Dr. West explained. “Well, how do you maintain a family life for that period of time when you’re basically off-cycle with your family? There are those kinds of stressors. It’s a mixed bag for hospitalists there.”
Richard Quinn is a freelance writer in New Jersey.
Hot-button issue: physician burnout
Some 15 years ago, when Daniel Roberts, MD, FHM, decided at the end of his medical residency that his career path was going to be that of a hospitalist, he heard the same thing. A lot.
“Geesh, don’t you think you’re going to burn out?”
The reasons for such a response are well known in HM circles: the 7-on, 7-off shift structure; the constant rounding; the push-pull between clinical, administrative, and – what many would term – clerical work.
“The truth is somewhere between,” Dr. Roberts said.
Burnout is a hot topic among hospitalists and all of health care these days, as the increasing burdens of a system in seemingly constant change have fostered pressures inside and out of hospitals. Increasingly, researchers are studying and publishing about how to recognize burnout, ways to deal with, or even proactively address the issues. Some MDs – experts in physician burnout – make a living by touring the country and talking about the issue.
But what causes burnout, specifically and exactly?
“The simplistic answer is that burnout is what happens when resources do not meet demand,” said Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout. “The more complicated answer, which, at this point, is fairly solidly evidence based actually, is that there are five broad categories of drivers of physician distress and burnout.”
Dr. West’s hierarchy of stressors encompasses:
• Work effort.
• Work efficiency.
• Work-home interference.
• A sense of meaning.
• “Flexibility, control, and autonomy.”
Basically, the five drivers lead to this: Physicians who work too much and too inefficiently, with too little control and sense of purpose, end up flaming out more so than do doctors who work fewer hours, with fewer obstacles – all the while feeling satisfied with their autonomy and value.
Academic hospitalist John Yoon, MD, assistant professor of medicine at the University of Chicago, says that health care has to work harder to promote its benefits as being more important than a highly paid profession. Instead, health care should focus on giving meaning to its practitioners.
“I think it is time for leaders of HM groups to honestly discuss the intrinsic meaning and essential ‘calling’ of what it means to be a good hospitalist,” Dr. Yoon wrote in an email interview with The Hospitalist. “What can we do to make the hospitalist vocation a meaningful, long-term career, so that they do not feel like simply revenue-generating ‘pawns’ in a medical-bureaucratic system?”
A ‘meaningful’ career
The modern discussion of burnout as a phenomenon traces back to the Maslach Burnout Inventory, a three-pronged test that measures emotional exhaustion, depersonalization, and personal accomplishment.1 But why does burnout hit physicians – hospitalists, in particular – so intensely? In part, it’s because – like their predecessors in emergency medicine – hospitalists are responsible for managing the care of patients other specialties consult with, operate on, or for whom they run tests.
“Once the patients come up from the emergency room or get admitted to the hospital from the outside, the hospitalist is the one who is largely running that show,” said Dr. West, whose researchshows that HM doctors suffer burnout more than the average across medical specialties.2 “So they’re the front line of inpatient medicine.”
Another factor contributing to burnout’s impact on hospitalists is that the specialty’s rank and file (by definition) work within the walls of institutions that have a lot of contentious and complicated issues that – while outside the purview of HM – can directly or indirectly affect the field. Dr. West calls it the hassle factor.
“You want to get a test in the hospital and, even though you’re the attending on the service, you end up going through three layers of bureaucracy with an insurance company to be able to finally get what you know that patient needs,” he said. “Anything like that contributes to the burnout problem because it pulls the physician away from what they want to be doing, what is purposeful, what is meaningful for them.”
For Dr. Yoon, the exhaustion and cynicism borne out by the work of Maslach and Dr. West’s team are measures indicative of a field where physicians struggle more and more to “make sense of why their practice is worthwhile.
“In the contemporary medical literature, we have been encouraged to adopt the concepts and practices of industrial engineering and quality improvement,” Dr. Yoon added. “In other words, it seems that to the extent physicians’ aspirations to practice good medicine are confined to the narrow and unimaginative constraints of mere scientific technique (more data, higher ‘quality,’ better outcomes) physicians will struggle to recognize and respond to their practice as meaningful. There is no intrinsic meaning to simply being a ‘cog’ in a medical-industrial process or an ‘independent variable’ in an economic equation.”
Finding meaning in one’s job, of course, is less empirical an endpoint than using a reversal agent for a GI bleed. Therein lies the challenge of battling burnout, whose causes and interventions can be as varied as the people who suffer the syndrome.
Local, customized solutions
Once a group leader identifies the symptoms of burnout, the obvious question is how to address it.
Dr. West and his colleagues have identified two broad categories of interventions: individual-focused approaches and organizational solutions. Physician-centered efforts include such tacks as mindfulness, stress reduction, resilience training and small-group communication. Institutional-level changes are, typically, much harder to implement and make successful.
“It doesn’t make sense to ... simply send physicians to stress-management training so that they’re better equipped to deal with a system that is not working to improve itself,” Dr. West said. “The system and the leadership in that system needs to take responsibility from an organizational standpoint.”
Health care as a whole has worked to address the systems-level issue. Duty-hour regulations have been reined in for trainees to be proactive in addressing both fatigue and its inevitable endpoint: burnout.
In a report, “Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-Analysis,”3 published online Dec. 5 in JAMA Internal Medicine, researchers concluded that interventions associated with small benefits “may be boosted by adoption of organization-directed approaches.
“This finding provides support for the view that burnout is a problem of the whole health care organization, rather than individuals,” they wrote.
But the issue typically remains a local one, as group leaders need to realize that what could cause or contribute to burnout in one employee might be enjoyable to another.
“The prospect of doing that was daunting,” Dr. Roberts recalled. “I didn’t know much about EHRs and it was going to be a lot of meetings ... and [it] was going to take me away from patient care. It really ended up being rewarding, despite all the time and frustration, because I got to help represent the interests of my hospitalist colleagues, the physician assistants, and nurses that I work with in trying to avoid some real problems that could have arisen in the EHR.”
Doing that work appealed to Dr. Roberts, so he embraced it. That approach is one championed by Thom Mayer, MD, FACEP, FAAP, executive vice president of EmCare, founder and CEO of BestPractices Inc., medical director for the NFL Players Association, and clinical professor of emergency medicine at George Washington University, Washington, and University of Virginia, Charlottesville. Dr. Mayer travels the country talking about burnout and suggests a three-pronged approach.
First, find what you like about your job and maximize those duties.
Second, label those tasks that are tolerable and don’t allow them to become issues leading to burnout.
Third, and perhaps most difficult, “take the things [you] hate and eliminate them to the best extent possible from [your] job.”
“I’ll give you an example,” he said. “What I hear from emergency physicians and hospitalists is: ‘What do I hate? Well, I hate chronic pain patients.’ Well, does that mean you’re going to be able to eliminate the fact that there are chronic pain patients? No. But, what you can do is ... really drill down on it, and say ‘Why do you hate that?’ The answer is, “Well, I don’t have a strategy for it.” No one likes doing things when they don’t know what they’re doing.
“Now you take the chronic pain patient and the problem is, most of us just haven’t really thought that out. Most of us haven’t sat down with our colleagues and said, “What are you doing that’s working? How are you handling these people? What are the scripts that I can use, the evidence-based language that I can use? What alternatives can I give them?” Instead of just assuming that the only answer to the problem of chronic pain is opioids.”
The silent epidemic
So if there are measurements for burnout, and even best practices on how to address it, why is the issue one that Dr. Mayer calls a silent epidemic? One word: stigma.
“We as physicians can’t afford to propagate that stigma any further,” Dr. Roberts said. “People who have even tougher jobs than we have, involving combat and hostage negotiation and things like that, have found a way to have honest conversations about the impact of their work on their lives. There is no reason physicians shouldn’t be able to slowly change the culture of medicine to be able to do that, so that there isn’t a stigma around saying, ‘I need some time away before this begins to impact the safety of our patients.’ ”
Dr. West said that when data show that as many as half of all physicians show symptoms of burnout, there is no need to stigmatize a group that large.
Dike Drummond, MD, a family physician, coach, and consultant on burnout prevention, said that the No. 1 mistake physicians and leaders make about burnout is labeling it a “problem.”
“Burnout does not have a single solution because it is not a problem to begin with,” he added. “Burnout is a classic dilemma – a never-ending balancing act. Think of the balancing act of burnout as a teeter-totter, like the one you see in a children’s playground. On one side is the energy you put into your practice and larger life … and on the other side your ability to recharge your energy levels.
“To prevent burnout you must keep your energy expenditure and your recharge activities in balance to keep this teeter-totter in a relatively horizontal position. And the way you address the dilemma is with a strategy: three to five individual tools you use to lower your stress levels or recharge your energy balance.”
And a strategy is a long-term approach to a long-term problem, he said.
“Burnout is not necessarily a terminal condition,” Dr. Roberts said. “If we can structure their work and the balance in their life in such a way that they don’t experience it, or that when they do experience it, they can recognize it and make the changes they need to avoid it getting worse, I think we’d be better off as a profession.”
Richard Quinn is a freelance writer in New Jersey.
References
1. Maslach C, Jackson S. The measurement of experienced burnout. J Occup Behavior. 1981;2:99-113
2. Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and outpatient general internists. J Hosp Med. 2014;9(3):176-81.
3. Panagioti M, Panagopoulou E, Brower P. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis [published online Dec. 5, 2016 ahead of print]. JAMA Intern Med. doi: 10.1001/jamainternmed.2016.7674.
Some 15 years ago, when Daniel Roberts, MD, FHM, decided at the end of his medical residency that his career path was going to be that of a hospitalist, he heard the same thing. A lot.
“Geesh, don’t you think you’re going to burn out?”
The reasons for such a response are well known in HM circles: the 7-on, 7-off shift structure; the constant rounding; the push-pull between clinical, administrative, and – what many would term – clerical work.
“The truth is somewhere between,” Dr. Roberts said.
Burnout is a hot topic among hospitalists and all of health care these days, as the increasing burdens of a system in seemingly constant change have fostered pressures inside and out of hospitals. Increasingly, researchers are studying and publishing about how to recognize burnout, ways to deal with, or even proactively address the issues. Some MDs – experts in physician burnout – make a living by touring the country and talking about the issue.
But what causes burnout, specifically and exactly?
“The simplistic answer is that burnout is what happens when resources do not meet demand,” said Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout. “The more complicated answer, which, at this point, is fairly solidly evidence based actually, is that there are five broad categories of drivers of physician distress and burnout.”
Dr. West’s hierarchy of stressors encompasses:
• Work effort.
• Work efficiency.
• Work-home interference.
• A sense of meaning.
• “Flexibility, control, and autonomy.”
Basically, the five drivers lead to this: Physicians who work too much and too inefficiently, with too little control and sense of purpose, end up flaming out more so than do doctors who work fewer hours, with fewer obstacles – all the while feeling satisfied with their autonomy and value.
Academic hospitalist John Yoon, MD, assistant professor of medicine at the University of Chicago, says that health care has to work harder to promote its benefits as being more important than a highly paid profession. Instead, health care should focus on giving meaning to its practitioners.
“I think it is time for leaders of HM groups to honestly discuss the intrinsic meaning and essential ‘calling’ of what it means to be a good hospitalist,” Dr. Yoon wrote in an email interview with The Hospitalist. “What can we do to make the hospitalist vocation a meaningful, long-term career, so that they do not feel like simply revenue-generating ‘pawns’ in a medical-bureaucratic system?”
A ‘meaningful’ career
The modern discussion of burnout as a phenomenon traces back to the Maslach Burnout Inventory, a three-pronged test that measures emotional exhaustion, depersonalization, and personal accomplishment.1 But why does burnout hit physicians – hospitalists, in particular – so intensely? In part, it’s because – like their predecessors in emergency medicine – hospitalists are responsible for managing the care of patients other specialties consult with, operate on, or for whom they run tests.
“Once the patients come up from the emergency room or get admitted to the hospital from the outside, the hospitalist is the one who is largely running that show,” said Dr. West, whose researchshows that HM doctors suffer burnout more than the average across medical specialties.2 “So they’re the front line of inpatient medicine.”
Another factor contributing to burnout’s impact on hospitalists is that the specialty’s rank and file (by definition) work within the walls of institutions that have a lot of contentious and complicated issues that – while outside the purview of HM – can directly or indirectly affect the field. Dr. West calls it the hassle factor.
“You want to get a test in the hospital and, even though you’re the attending on the service, you end up going through three layers of bureaucracy with an insurance company to be able to finally get what you know that patient needs,” he said. “Anything like that contributes to the burnout problem because it pulls the physician away from what they want to be doing, what is purposeful, what is meaningful for them.”
For Dr. Yoon, the exhaustion and cynicism borne out by the work of Maslach and Dr. West’s team are measures indicative of a field where physicians struggle more and more to “make sense of why their practice is worthwhile.
“In the contemporary medical literature, we have been encouraged to adopt the concepts and practices of industrial engineering and quality improvement,” Dr. Yoon added. “In other words, it seems that to the extent physicians’ aspirations to practice good medicine are confined to the narrow and unimaginative constraints of mere scientific technique (more data, higher ‘quality,’ better outcomes) physicians will struggle to recognize and respond to their practice as meaningful. There is no intrinsic meaning to simply being a ‘cog’ in a medical-industrial process or an ‘independent variable’ in an economic equation.”
Finding meaning in one’s job, of course, is less empirical an endpoint than using a reversal agent for a GI bleed. Therein lies the challenge of battling burnout, whose causes and interventions can be as varied as the people who suffer the syndrome.
Local, customized solutions
Once a group leader identifies the symptoms of burnout, the obvious question is how to address it.
Dr. West and his colleagues have identified two broad categories of interventions: individual-focused approaches and organizational solutions. Physician-centered efforts include such tacks as mindfulness, stress reduction, resilience training and small-group communication. Institutional-level changes are, typically, much harder to implement and make successful.
“It doesn’t make sense to ... simply send physicians to stress-management training so that they’re better equipped to deal with a system that is not working to improve itself,” Dr. West said. “The system and the leadership in that system needs to take responsibility from an organizational standpoint.”
Health care as a whole has worked to address the systems-level issue. Duty-hour regulations have been reined in for trainees to be proactive in addressing both fatigue and its inevitable endpoint: burnout.
In a report, “Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-Analysis,”3 published online Dec. 5 in JAMA Internal Medicine, researchers concluded that interventions associated with small benefits “may be boosted by adoption of organization-directed approaches.
“This finding provides support for the view that burnout is a problem of the whole health care organization, rather than individuals,” they wrote.
But the issue typically remains a local one, as group leaders need to realize that what could cause or contribute to burnout in one employee might be enjoyable to another.
“The prospect of doing that was daunting,” Dr. Roberts recalled. “I didn’t know much about EHRs and it was going to be a lot of meetings ... and [it] was going to take me away from patient care. It really ended up being rewarding, despite all the time and frustration, because I got to help represent the interests of my hospitalist colleagues, the physician assistants, and nurses that I work with in trying to avoid some real problems that could have arisen in the EHR.”
Doing that work appealed to Dr. Roberts, so he embraced it. That approach is one championed by Thom Mayer, MD, FACEP, FAAP, executive vice president of EmCare, founder and CEO of BestPractices Inc., medical director for the NFL Players Association, and clinical professor of emergency medicine at George Washington University, Washington, and University of Virginia, Charlottesville. Dr. Mayer travels the country talking about burnout and suggests a three-pronged approach.
First, find what you like about your job and maximize those duties.
Second, label those tasks that are tolerable and don’t allow them to become issues leading to burnout.
Third, and perhaps most difficult, “take the things [you] hate and eliminate them to the best extent possible from [your] job.”
“I’ll give you an example,” he said. “What I hear from emergency physicians and hospitalists is: ‘What do I hate? Well, I hate chronic pain patients.’ Well, does that mean you’re going to be able to eliminate the fact that there are chronic pain patients? No. But, what you can do is ... really drill down on it, and say ‘Why do you hate that?’ The answer is, “Well, I don’t have a strategy for it.” No one likes doing things when they don’t know what they’re doing.
“Now you take the chronic pain patient and the problem is, most of us just haven’t really thought that out. Most of us haven’t sat down with our colleagues and said, “What are you doing that’s working? How are you handling these people? What are the scripts that I can use, the evidence-based language that I can use? What alternatives can I give them?” Instead of just assuming that the only answer to the problem of chronic pain is opioids.”
The silent epidemic
So if there are measurements for burnout, and even best practices on how to address it, why is the issue one that Dr. Mayer calls a silent epidemic? One word: stigma.
“We as physicians can’t afford to propagate that stigma any further,” Dr. Roberts said. “People who have even tougher jobs than we have, involving combat and hostage negotiation and things like that, have found a way to have honest conversations about the impact of their work on their lives. There is no reason physicians shouldn’t be able to slowly change the culture of medicine to be able to do that, so that there isn’t a stigma around saying, ‘I need some time away before this begins to impact the safety of our patients.’ ”
Dr. West said that when data show that as many as half of all physicians show symptoms of burnout, there is no need to stigmatize a group that large.
Dike Drummond, MD, a family physician, coach, and consultant on burnout prevention, said that the No. 1 mistake physicians and leaders make about burnout is labeling it a “problem.”
“Burnout does not have a single solution because it is not a problem to begin with,” he added. “Burnout is a classic dilemma – a never-ending balancing act. Think of the balancing act of burnout as a teeter-totter, like the one you see in a children’s playground. On one side is the energy you put into your practice and larger life … and on the other side your ability to recharge your energy levels.
“To prevent burnout you must keep your energy expenditure and your recharge activities in balance to keep this teeter-totter in a relatively horizontal position. And the way you address the dilemma is with a strategy: three to five individual tools you use to lower your stress levels or recharge your energy balance.”
And a strategy is a long-term approach to a long-term problem, he said.
“Burnout is not necessarily a terminal condition,” Dr. Roberts said. “If we can structure their work and the balance in their life in such a way that they don’t experience it, or that when they do experience it, they can recognize it and make the changes they need to avoid it getting worse, I think we’d be better off as a profession.”
Richard Quinn is a freelance writer in New Jersey.
References
1. Maslach C, Jackson S. The measurement of experienced burnout. J Occup Behavior. 1981;2:99-113
2. Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and outpatient general internists. J Hosp Med. 2014;9(3):176-81.
3. Panagioti M, Panagopoulou E, Brower P. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis [published online Dec. 5, 2016 ahead of print]. JAMA Intern Med. doi: 10.1001/jamainternmed.2016.7674.
Some 15 years ago, when Daniel Roberts, MD, FHM, decided at the end of his medical residency that his career path was going to be that of a hospitalist, he heard the same thing. A lot.
“Geesh, don’t you think you’re going to burn out?”
The reasons for such a response are well known in HM circles: the 7-on, 7-off shift structure; the constant rounding; the push-pull between clinical, administrative, and – what many would term – clerical work.
“The truth is somewhere between,” Dr. Roberts said.
Burnout is a hot topic among hospitalists and all of health care these days, as the increasing burdens of a system in seemingly constant change have fostered pressures inside and out of hospitals. Increasingly, researchers are studying and publishing about how to recognize burnout, ways to deal with, or even proactively address the issues. Some MDs – experts in physician burnout – make a living by touring the country and talking about the issue.
But what causes burnout, specifically and exactly?
“The simplistic answer is that burnout is what happens when resources do not meet demand,” said Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout. “The more complicated answer, which, at this point, is fairly solidly evidence based actually, is that there are five broad categories of drivers of physician distress and burnout.”
Dr. West’s hierarchy of stressors encompasses:
• Work effort.
• Work efficiency.
• Work-home interference.
• A sense of meaning.
• “Flexibility, control, and autonomy.”
Basically, the five drivers lead to this: Physicians who work too much and too inefficiently, with too little control and sense of purpose, end up flaming out more so than do doctors who work fewer hours, with fewer obstacles – all the while feeling satisfied with their autonomy and value.
Academic hospitalist John Yoon, MD, assistant professor of medicine at the University of Chicago, says that health care has to work harder to promote its benefits as being more important than a highly paid profession. Instead, health care should focus on giving meaning to its practitioners.
“I think it is time for leaders of HM groups to honestly discuss the intrinsic meaning and essential ‘calling’ of what it means to be a good hospitalist,” Dr. Yoon wrote in an email interview with The Hospitalist. “What can we do to make the hospitalist vocation a meaningful, long-term career, so that they do not feel like simply revenue-generating ‘pawns’ in a medical-bureaucratic system?”
A ‘meaningful’ career
The modern discussion of burnout as a phenomenon traces back to the Maslach Burnout Inventory, a three-pronged test that measures emotional exhaustion, depersonalization, and personal accomplishment.1 But why does burnout hit physicians – hospitalists, in particular – so intensely? In part, it’s because – like their predecessors in emergency medicine – hospitalists are responsible for managing the care of patients other specialties consult with, operate on, or for whom they run tests.
“Once the patients come up from the emergency room or get admitted to the hospital from the outside, the hospitalist is the one who is largely running that show,” said Dr. West, whose researchshows that HM doctors suffer burnout more than the average across medical specialties.2 “So they’re the front line of inpatient medicine.”
Another factor contributing to burnout’s impact on hospitalists is that the specialty’s rank and file (by definition) work within the walls of institutions that have a lot of contentious and complicated issues that – while outside the purview of HM – can directly or indirectly affect the field. Dr. West calls it the hassle factor.
“You want to get a test in the hospital and, even though you’re the attending on the service, you end up going through three layers of bureaucracy with an insurance company to be able to finally get what you know that patient needs,” he said. “Anything like that contributes to the burnout problem because it pulls the physician away from what they want to be doing, what is purposeful, what is meaningful for them.”
For Dr. Yoon, the exhaustion and cynicism borne out by the work of Maslach and Dr. West’s team are measures indicative of a field where physicians struggle more and more to “make sense of why their practice is worthwhile.
“In the contemporary medical literature, we have been encouraged to adopt the concepts and practices of industrial engineering and quality improvement,” Dr. Yoon added. “In other words, it seems that to the extent physicians’ aspirations to practice good medicine are confined to the narrow and unimaginative constraints of mere scientific technique (more data, higher ‘quality,’ better outcomes) physicians will struggle to recognize and respond to their practice as meaningful. There is no intrinsic meaning to simply being a ‘cog’ in a medical-industrial process or an ‘independent variable’ in an economic equation.”
Finding meaning in one’s job, of course, is less empirical an endpoint than using a reversal agent for a GI bleed. Therein lies the challenge of battling burnout, whose causes and interventions can be as varied as the people who suffer the syndrome.
Local, customized solutions
Once a group leader identifies the symptoms of burnout, the obvious question is how to address it.
Dr. West and his colleagues have identified two broad categories of interventions: individual-focused approaches and organizational solutions. Physician-centered efforts include such tacks as mindfulness, stress reduction, resilience training and small-group communication. Institutional-level changes are, typically, much harder to implement and make successful.
“It doesn’t make sense to ... simply send physicians to stress-management training so that they’re better equipped to deal with a system that is not working to improve itself,” Dr. West said. “The system and the leadership in that system needs to take responsibility from an organizational standpoint.”
Health care as a whole has worked to address the systems-level issue. Duty-hour regulations have been reined in for trainees to be proactive in addressing both fatigue and its inevitable endpoint: burnout.
In a report, “Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-Analysis,”3 published online Dec. 5 in JAMA Internal Medicine, researchers concluded that interventions associated with small benefits “may be boosted by adoption of organization-directed approaches.
“This finding provides support for the view that burnout is a problem of the whole health care organization, rather than individuals,” they wrote.
But the issue typically remains a local one, as group leaders need to realize that what could cause or contribute to burnout in one employee might be enjoyable to another.
“The prospect of doing that was daunting,” Dr. Roberts recalled. “I didn’t know much about EHRs and it was going to be a lot of meetings ... and [it] was going to take me away from patient care. It really ended up being rewarding, despite all the time and frustration, because I got to help represent the interests of my hospitalist colleagues, the physician assistants, and nurses that I work with in trying to avoid some real problems that could have arisen in the EHR.”
Doing that work appealed to Dr. Roberts, so he embraced it. That approach is one championed by Thom Mayer, MD, FACEP, FAAP, executive vice president of EmCare, founder and CEO of BestPractices Inc., medical director for the NFL Players Association, and clinical professor of emergency medicine at George Washington University, Washington, and University of Virginia, Charlottesville. Dr. Mayer travels the country talking about burnout and suggests a three-pronged approach.
First, find what you like about your job and maximize those duties.
Second, label those tasks that are tolerable and don’t allow them to become issues leading to burnout.
Third, and perhaps most difficult, “take the things [you] hate and eliminate them to the best extent possible from [your] job.”
“I’ll give you an example,” he said. “What I hear from emergency physicians and hospitalists is: ‘What do I hate? Well, I hate chronic pain patients.’ Well, does that mean you’re going to be able to eliminate the fact that there are chronic pain patients? No. But, what you can do is ... really drill down on it, and say ‘Why do you hate that?’ The answer is, “Well, I don’t have a strategy for it.” No one likes doing things when they don’t know what they’re doing.
“Now you take the chronic pain patient and the problem is, most of us just haven’t really thought that out. Most of us haven’t sat down with our colleagues and said, “What are you doing that’s working? How are you handling these people? What are the scripts that I can use, the evidence-based language that I can use? What alternatives can I give them?” Instead of just assuming that the only answer to the problem of chronic pain is opioids.”
The silent epidemic
So if there are measurements for burnout, and even best practices on how to address it, why is the issue one that Dr. Mayer calls a silent epidemic? One word: stigma.
“We as physicians can’t afford to propagate that stigma any further,” Dr. Roberts said. “People who have even tougher jobs than we have, involving combat and hostage negotiation and things like that, have found a way to have honest conversations about the impact of their work on their lives. There is no reason physicians shouldn’t be able to slowly change the culture of medicine to be able to do that, so that there isn’t a stigma around saying, ‘I need some time away before this begins to impact the safety of our patients.’ ”
Dr. West said that when data show that as many as half of all physicians show symptoms of burnout, there is no need to stigmatize a group that large.
Dike Drummond, MD, a family physician, coach, and consultant on burnout prevention, said that the No. 1 mistake physicians and leaders make about burnout is labeling it a “problem.”
“Burnout does not have a single solution because it is not a problem to begin with,” he added. “Burnout is a classic dilemma – a never-ending balancing act. Think of the balancing act of burnout as a teeter-totter, like the one you see in a children’s playground. On one side is the energy you put into your practice and larger life … and on the other side your ability to recharge your energy levels.
“To prevent burnout you must keep your energy expenditure and your recharge activities in balance to keep this teeter-totter in a relatively horizontal position. And the way you address the dilemma is with a strategy: three to five individual tools you use to lower your stress levels or recharge your energy balance.”
And a strategy is a long-term approach to a long-term problem, he said.
“Burnout is not necessarily a terminal condition,” Dr. Roberts said. “If we can structure their work and the balance in their life in such a way that they don’t experience it, or that when they do experience it, they can recognize it and make the changes they need to avoid it getting worse, I think we’d be better off as a profession.”
Richard Quinn is a freelance writer in New Jersey.
References
1. Maslach C, Jackson S. The measurement of experienced burnout. J Occup Behavior. 1981;2:99-113
2. Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and outpatient general internists. J Hosp Med. 2014;9(3):176-81.
3. Panagioti M, Panagopoulou E, Brower P. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis [published online Dec. 5, 2016 ahead of print]. JAMA Intern Med. doi: 10.1001/jamainternmed.2016.7674.
Turnover rate for hospitalist groups trending downward
According to the 2016 State of Hospital Medicine Report based on 2015 data, the median physician turnover rate for hospital medicine groups (HMGs) serving adults only is 6.9%, lower compared with results from prior surveys. Particularly, turnover in 2010 was more than double the current rate (see Figure 1). This steady decline over the years is intriguing, yet encouraging, since hospital medicine is well known for its high turnover compared to other specialties.
Similarly, results from State of Hospital Medicine surveys also reveal a consistent trend for groups with no turnover. As expected, lower turnover rate usually parallels with higher percentage of groups with no turnover. This year, 40.2% of hospitalist groups reported no physician turnover at all, continuing the upward trend from 2014 (38.1%) and 2012 (36%). It is speculating that these groups are not just simply fortunate, but rather work zealously to build a strong internal culture within the group and proactively create a shared vision, values, accountability, and career goals. 
Sources in search of why providers leave a practice and advice on specific strategies to retain them are abundant. To secure retention, at a minimum, employers, leaders, or administrators should pay close attention to such basic factors as work schedules, workload, and compensation – and even consider using national and regional data from the State of Hospital Medicine Report for benchmarking to remain attractive and competitive in the market. Low or no turnover rate indicates workforce stability and program credibility, and allows cost saving as the overall estimated cost of turnover (losing a provider and hiring another one) ranges from $400,000 to $600,000 per provider.1
The turnover data further delineates differences based on academic status, Medicare Indirect Medical Education (IME) program status, and geographic region. For instance, the academic groups consistently report a higher turnover rate, compared with the nonacademic groups. The latter mirrors the overall decreasing trend of physician turnover. Non-teaching hospitals also score significantly higher on the number of groups with no turnover (42% as opposed to 24%-27% for teaching hospitals). Geographically, HMGs in the South and Midwest regions of the United States are the winners this year, with more than 50% of the groups reporting no turnover at all.
Specific information regarding turnover for nurse practitioners and physician assistants (NPs/PAs) can also be found in the report. This rate has been increasing slightly compared with the past, with a subsequent drop in the percentage of groups reporting no turnover. Yet, the overall percentage with no turnover for NPs/PAs remains impressively high at 62%.
The turnover rates for HMGs serving both adults and children, and groups serving children only, appear somewhat similar to those of groups serving adults only, though we cannot reliably analyze the data, elucidate significant differences, or detect any meaningful trends from these two groups because of insufficient numbers of responders.
The downward trend of hospitalist turnover found in SHM’s 2016 State of Hospital Medicine Report is reassuring, indicative of a higher retention rate and an extended stability for many programs. Although some hospitalists continue to shop around, most leaders and employers of HMGs work endlessly to strengthen their programs in hope to minimize turnover. The promising data likely reflect such effort. Hopefully, this trend will continue when the next State of Hospital Medicine report comes out.
Dr. Vuong is a hospitalist at HealthPartners Medical Group in St Paul, Minn., and an assistant professor of medicine at the University of Minnesota. He is a member of SHM’s Practice Analysis Committee.
Reference
1. Frenz, D (2016). The staggering costs of physician turnover. Today’s Hospitalist.
According to the 2016 State of Hospital Medicine Report based on 2015 data, the median physician turnover rate for hospital medicine groups (HMGs) serving adults only is 6.9%, lower compared with results from prior surveys. Particularly, turnover in 2010 was more than double the current rate (see Figure 1). This steady decline over the years is intriguing, yet encouraging, since hospital medicine is well known for its high turnover compared to other specialties.
Similarly, results from State of Hospital Medicine surveys also reveal a consistent trend for groups with no turnover. As expected, lower turnover rate usually parallels with higher percentage of groups with no turnover. This year, 40.2% of hospitalist groups reported no physician turnover at all, continuing the upward trend from 2014 (38.1%) and 2012 (36%). It is speculating that these groups are not just simply fortunate, but rather work zealously to build a strong internal culture within the group and proactively create a shared vision, values, accountability, and career goals. 
Sources in search of why providers leave a practice and advice on specific strategies to retain them are abundant. To secure retention, at a minimum, employers, leaders, or administrators should pay close attention to such basic factors as work schedules, workload, and compensation – and even consider using national and regional data from the State of Hospital Medicine Report for benchmarking to remain attractive and competitive in the market. Low or no turnover rate indicates workforce stability and program credibility, and allows cost saving as the overall estimated cost of turnover (losing a provider and hiring another one) ranges from $400,000 to $600,000 per provider.1
The turnover data further delineates differences based on academic status, Medicare Indirect Medical Education (IME) program status, and geographic region. For instance, the academic groups consistently report a higher turnover rate, compared with the nonacademic groups. The latter mirrors the overall decreasing trend of physician turnover. Non-teaching hospitals also score significantly higher on the number of groups with no turnover (42% as opposed to 24%-27% for teaching hospitals). Geographically, HMGs in the South and Midwest regions of the United States are the winners this year, with more than 50% of the groups reporting no turnover at all.
Specific information regarding turnover for nurse practitioners and physician assistants (NPs/PAs) can also be found in the report. This rate has been increasing slightly compared with the past, with a subsequent drop in the percentage of groups reporting no turnover. Yet, the overall percentage with no turnover for NPs/PAs remains impressively high at 62%.
The turnover rates for HMGs serving both adults and children, and groups serving children only, appear somewhat similar to those of groups serving adults only, though we cannot reliably analyze the data, elucidate significant differences, or detect any meaningful trends from these two groups because of insufficient numbers of responders.
The downward trend of hospitalist turnover found in SHM’s 2016 State of Hospital Medicine Report is reassuring, indicative of a higher retention rate and an extended stability for many programs. Although some hospitalists continue to shop around, most leaders and employers of HMGs work endlessly to strengthen their programs in hope to minimize turnover. The promising data likely reflect such effort. Hopefully, this trend will continue when the next State of Hospital Medicine report comes out.
Dr. Vuong is a hospitalist at HealthPartners Medical Group in St Paul, Minn., and an assistant professor of medicine at the University of Minnesota. He is a member of SHM’s Practice Analysis Committee.
Reference
1. Frenz, D (2016). The staggering costs of physician turnover. Today’s Hospitalist.
According to the 2016 State of Hospital Medicine Report based on 2015 data, the median physician turnover rate for hospital medicine groups (HMGs) serving adults only is 6.9%, lower compared with results from prior surveys. Particularly, turnover in 2010 was more than double the current rate (see Figure 1). This steady decline over the years is intriguing, yet encouraging, since hospital medicine is well known for its high turnover compared to other specialties.
Similarly, results from State of Hospital Medicine surveys also reveal a consistent trend for groups with no turnover. As expected, lower turnover rate usually parallels with higher percentage of groups with no turnover. This year, 40.2% of hospitalist groups reported no physician turnover at all, continuing the upward trend from 2014 (38.1%) and 2012 (36%). It is speculating that these groups are not just simply fortunate, but rather work zealously to build a strong internal culture within the group and proactively create a shared vision, values, accountability, and career goals. 
Sources in search of why providers leave a practice and advice on specific strategies to retain them are abundant. To secure retention, at a minimum, employers, leaders, or administrators should pay close attention to such basic factors as work schedules, workload, and compensation – and even consider using national and regional data from the State of Hospital Medicine Report for benchmarking to remain attractive and competitive in the market. Low or no turnover rate indicates workforce stability and program credibility, and allows cost saving as the overall estimated cost of turnover (losing a provider and hiring another one) ranges from $400,000 to $600,000 per provider.1
The turnover data further delineates differences based on academic status, Medicare Indirect Medical Education (IME) program status, and geographic region. For instance, the academic groups consistently report a higher turnover rate, compared with the nonacademic groups. The latter mirrors the overall decreasing trend of physician turnover. Non-teaching hospitals also score significantly higher on the number of groups with no turnover (42% as opposed to 24%-27% for teaching hospitals). Geographically, HMGs in the South and Midwest regions of the United States are the winners this year, with more than 50% of the groups reporting no turnover at all.
Specific information regarding turnover for nurse practitioners and physician assistants (NPs/PAs) can also be found in the report. This rate has been increasing slightly compared with the past, with a subsequent drop in the percentage of groups reporting no turnover. Yet, the overall percentage with no turnover for NPs/PAs remains impressively high at 62%.
The turnover rates for HMGs serving both adults and children, and groups serving children only, appear somewhat similar to those of groups serving adults only, though we cannot reliably analyze the data, elucidate significant differences, or detect any meaningful trends from these two groups because of insufficient numbers of responders.
The downward trend of hospitalist turnover found in SHM’s 2016 State of Hospital Medicine Report is reassuring, indicative of a higher retention rate and an extended stability for many programs. Although some hospitalists continue to shop around, most leaders and employers of HMGs work endlessly to strengthen their programs in hope to minimize turnover. The promising data likely reflect such effort. Hopefully, this trend will continue when the next State of Hospital Medicine report comes out.
Dr. Vuong is a hospitalist at HealthPartners Medical Group in St Paul, Minn., and an assistant professor of medicine at the University of Minnesota. He is a member of SHM’s Practice Analysis Committee.
Reference
1. Frenz, D (2016). The staggering costs of physician turnover. Today’s Hospitalist.
Taking the hammer to sickle pain crises
Clinical question: Are any novel medicines designed to interrupt the pathophysiology of vaso-occlusion available to reduce the frequency and severity of pain crises in sickle cell anemia?
Background: Hypoxemia-dependent HbS polymerization is just the initiating step in a complex cascade of events leading to sickle pain crises. Animal studies have suggested that blockade of P-selectin, an adhesion molecule expressed by endothelium, blunts the aggregation of sickled erythrocytes, leukocytes and activated platelets and may reduce progression to vaso-occlusive crises.
Study Design: Multicenter, double-blinded, randomized placebo-controlled trial.
Setting: International (60 study sites in 3 countries) from August 2013 to January 2015.
Synopsis: Crizanlizumab is a humanized monoclonal antibody directed against P-selectin. A total of 198 patients aged 16-65 with HbSS, HbSC, HbSbeta+ and select other genotypes experiencing 2-10 pain crises in the 12 months prior to trial were block randomized to receive high-dose crizanlizumab, low-dose crizanlizumab, or placebo. Roughly 62% of enrolled patients in all three arms were already taking hydroxyurea – for which dose changes during trial period were forbidden. Patients not already on hydroxyurea could not initiate treatment during the trial period. The primary outcome was annualized rate of sickle pain crises (defined as pain without other demonstrable cause requiring medical facility visit and treatment with oral or parenteral narcotics or NSAIDs), including acute chest, hepatic or splenic sequestration crises and priapism. Secondary outcomes were annualized rates of hospital days, rates of uncomplicated crises, time to first and second crises, rates of acute chest syndrome and Brief Pain Inventory questionnaire. Primary outcome data were processed via intention-to-treat analysis.
For high-dose crizanlizumab, there were a median 1.63 crises per year compared to 2.98 in the placebo group, representing a 45.3% lower rate (P = .01). The protective effect of crizanlizumab was more pronounced in the per-protocol analysis (1.04 crises per year for the high dose group). In the subgroup of patients on concomitant hydroxyurea, the median annualized crisis rate among high dose versus placebo was 2.43 compared to 3.58, representing a 32.1% lower rate. In the non-hydroxyurea subgroup, the median annualized crisis rate for high dose versus placebo was 1.0 vs. 2.0, representing a 50% lower rate. Secondary endpoints similarly trended in favor of crizanlizumab in a dose-dependent fashion, although statistical significance was mixed.
Bottom line: Crizanlizumab, a humanized monoclonal antibody that blocks the action of the endothelial adhesion molecule P-selectin, is promising as a novel medication to reduce frequency of vaso-occlusive crises in patients with HbS-related disease.
Citation: Ataga KI, Kutler A, Kanter J, et al. Crizanlizumab for prevention of pain crises in sickle cell disease. N Engl J Med. 2016 Dec. 3. doi: 10.1056/NEJMoa1611770.
Clinical question: Are any novel medicines designed to interrupt the pathophysiology of vaso-occlusion available to reduce the frequency and severity of pain crises in sickle cell anemia?
Background: Hypoxemia-dependent HbS polymerization is just the initiating step in a complex cascade of events leading to sickle pain crises. Animal studies have suggested that blockade of P-selectin, an adhesion molecule expressed by endothelium, blunts the aggregation of sickled erythrocytes, leukocytes and activated platelets and may reduce progression to vaso-occlusive crises.
Study Design: Multicenter, double-blinded, randomized placebo-controlled trial.
Setting: International (60 study sites in 3 countries) from August 2013 to January 2015.
Synopsis: Crizanlizumab is a humanized monoclonal antibody directed against P-selectin. A total of 198 patients aged 16-65 with HbSS, HbSC, HbSbeta+ and select other genotypes experiencing 2-10 pain crises in the 12 months prior to trial were block randomized to receive high-dose crizanlizumab, low-dose crizanlizumab, or placebo. Roughly 62% of enrolled patients in all three arms were already taking hydroxyurea – for which dose changes during trial period were forbidden. Patients not already on hydroxyurea could not initiate treatment during the trial period. The primary outcome was annualized rate of sickle pain crises (defined as pain without other demonstrable cause requiring medical facility visit and treatment with oral or parenteral narcotics or NSAIDs), including acute chest, hepatic or splenic sequestration crises and priapism. Secondary outcomes were annualized rates of hospital days, rates of uncomplicated crises, time to first and second crises, rates of acute chest syndrome and Brief Pain Inventory questionnaire. Primary outcome data were processed via intention-to-treat analysis.
For high-dose crizanlizumab, there were a median 1.63 crises per year compared to 2.98 in the placebo group, representing a 45.3% lower rate (P = .01). The protective effect of crizanlizumab was more pronounced in the per-protocol analysis (1.04 crises per year for the high dose group). In the subgroup of patients on concomitant hydroxyurea, the median annualized crisis rate among high dose versus placebo was 2.43 compared to 3.58, representing a 32.1% lower rate. In the non-hydroxyurea subgroup, the median annualized crisis rate for high dose versus placebo was 1.0 vs. 2.0, representing a 50% lower rate. Secondary endpoints similarly trended in favor of crizanlizumab in a dose-dependent fashion, although statistical significance was mixed.
Bottom line: Crizanlizumab, a humanized monoclonal antibody that blocks the action of the endothelial adhesion molecule P-selectin, is promising as a novel medication to reduce frequency of vaso-occlusive crises in patients with HbS-related disease.
Citation: Ataga KI, Kutler A, Kanter J, et al. Crizanlizumab for prevention of pain crises in sickle cell disease. N Engl J Med. 2016 Dec. 3. doi: 10.1056/NEJMoa1611770.
Clinical question: Are any novel medicines designed to interrupt the pathophysiology of vaso-occlusion available to reduce the frequency and severity of pain crises in sickle cell anemia?
Background: Hypoxemia-dependent HbS polymerization is just the initiating step in a complex cascade of events leading to sickle pain crises. Animal studies have suggested that blockade of P-selectin, an adhesion molecule expressed by endothelium, blunts the aggregation of sickled erythrocytes, leukocytes and activated platelets and may reduce progression to vaso-occlusive crises.
Study Design: Multicenter, double-blinded, randomized placebo-controlled trial.
Setting: International (60 study sites in 3 countries) from August 2013 to January 2015.
Synopsis: Crizanlizumab is a humanized monoclonal antibody directed against P-selectin. A total of 198 patients aged 16-65 with HbSS, HbSC, HbSbeta+ and select other genotypes experiencing 2-10 pain crises in the 12 months prior to trial were block randomized to receive high-dose crizanlizumab, low-dose crizanlizumab, or placebo. Roughly 62% of enrolled patients in all three arms were already taking hydroxyurea – for which dose changes during trial period were forbidden. Patients not already on hydroxyurea could not initiate treatment during the trial period. The primary outcome was annualized rate of sickle pain crises (defined as pain without other demonstrable cause requiring medical facility visit and treatment with oral or parenteral narcotics or NSAIDs), including acute chest, hepatic or splenic sequestration crises and priapism. Secondary outcomes were annualized rates of hospital days, rates of uncomplicated crises, time to first and second crises, rates of acute chest syndrome and Brief Pain Inventory questionnaire. Primary outcome data were processed via intention-to-treat analysis.
For high-dose crizanlizumab, there were a median 1.63 crises per year compared to 2.98 in the placebo group, representing a 45.3% lower rate (P = .01). The protective effect of crizanlizumab was more pronounced in the per-protocol analysis (1.04 crises per year for the high dose group). In the subgroup of patients on concomitant hydroxyurea, the median annualized crisis rate among high dose versus placebo was 2.43 compared to 3.58, representing a 32.1% lower rate. In the non-hydroxyurea subgroup, the median annualized crisis rate for high dose versus placebo was 1.0 vs. 2.0, representing a 50% lower rate. Secondary endpoints similarly trended in favor of crizanlizumab in a dose-dependent fashion, although statistical significance was mixed.
Bottom line: Crizanlizumab, a humanized monoclonal antibody that blocks the action of the endothelial adhesion molecule P-selectin, is promising as a novel medication to reduce frequency of vaso-occlusive crises in patients with HbS-related disease.
Citation: Ataga KI, Kutler A, Kanter J, et al. Crizanlizumab for prevention of pain crises in sickle cell disease. N Engl J Med. 2016 Dec. 3. doi: 10.1056/NEJMoa1611770.
DVT prophylaxis not needed after casting
Clinical question: Is DVT prophylaxis necessary with lower leg casting or after knee arthroscopy?
Background: Patients who undergo immobilization from casting or knee arthroscopic surgery are thought to be at increased risk for venous thromboembolism (VTE). Most patients who undergo orthopedic procedures receive thromboprophylaxis but controversy exists surrounding its use in low limb casting or knee arthroscopic surgery. Prior studies did not establish consensus because of methodologic weaknesses.
Study design: Two parallel randomized-controlled, open-label trials with blinded outcome (POD-KAST for knee arthroscopy and POD-CAST for casting lower leg.
Setting: International (32 pediatric intensive care units across Asia, Australia, Europe, and North America).
Synopsis: Patients were randomly assigned to receive either a prophylactic dose of low-molecular-weight heparin (either for the 8 days after arthroscopy or for the duration of casting-related immobilization) or no anticoagulant therapy. The primary outcomes were the cumulative incidences of symptomatic venous thromboembolism (VTE) and major bleeding within 3 months after the procedure. For the 1,543 patients undergoing knee arthroscopy, VTE occurred in 0.7% of the treatment group and 0.4% of the control group (relative risk, 1.6; 95% confidence interval [CI], 0.4-6.8; absolute difference in risk, 0.3 percentage points; 95% CI, −0.6 to 1.2) and major bleeding was seen in 0.1% of both groups.
For the 1,519 patients undergoing knee arthroscopy, VTE occurred in 1.4% of the treatment group and 1.8% of the control group (relative risk, 0.8; 95% CI, 0.3-1.7; absolute difference in risk, −0.4 percentage points; 95% CI, −1.8 to 1.0) and no episodes of major bleeding were reported in either group.
Bottom line: VTE prophylaxis either after arthroscopy or during immobilization from casting did not prevent DVT.
Citations: Van Adrichem RA, Nemeth B, Algra A, et al. Thromboprophylaxis after knee arthroscopy and low-leg casting. N Engl J Med. 2016 Dec 3. doi: 10.1056/NEJMoa1613303.
Dr. Cerceo is assistant professor in the division of hospital medicine, and associate director of the internal medicine residency program at Cooper Medical School of Rowan University, Camden, N.J.
Clinical question: Is DVT prophylaxis necessary with lower leg casting or after knee arthroscopy?
Background: Patients who undergo immobilization from casting or knee arthroscopic surgery are thought to be at increased risk for venous thromboembolism (VTE). Most patients who undergo orthopedic procedures receive thromboprophylaxis but controversy exists surrounding its use in low limb casting or knee arthroscopic surgery. Prior studies did not establish consensus because of methodologic weaknesses.
Study design: Two parallel randomized-controlled, open-label trials with blinded outcome (POD-KAST for knee arthroscopy and POD-CAST for casting lower leg.
Setting: International (32 pediatric intensive care units across Asia, Australia, Europe, and North America).
Synopsis: Patients were randomly assigned to receive either a prophylactic dose of low-molecular-weight heparin (either for the 8 days after arthroscopy or for the duration of casting-related immobilization) or no anticoagulant therapy. The primary outcomes were the cumulative incidences of symptomatic venous thromboembolism (VTE) and major bleeding within 3 months after the procedure. For the 1,543 patients undergoing knee arthroscopy, VTE occurred in 0.7% of the treatment group and 0.4% of the control group (relative risk, 1.6; 95% confidence interval [CI], 0.4-6.8; absolute difference in risk, 0.3 percentage points; 95% CI, −0.6 to 1.2) and major bleeding was seen in 0.1% of both groups.
For the 1,519 patients undergoing knee arthroscopy, VTE occurred in 1.4% of the treatment group and 1.8% of the control group (relative risk, 0.8; 95% CI, 0.3-1.7; absolute difference in risk, −0.4 percentage points; 95% CI, −1.8 to 1.0) and no episodes of major bleeding were reported in either group.
Bottom line: VTE prophylaxis either after arthroscopy or during immobilization from casting did not prevent DVT.
Citations: Van Adrichem RA, Nemeth B, Algra A, et al. Thromboprophylaxis after knee arthroscopy and low-leg casting. N Engl J Med. 2016 Dec 3. doi: 10.1056/NEJMoa1613303.
Dr. Cerceo is assistant professor in the division of hospital medicine, and associate director of the internal medicine residency program at Cooper Medical School of Rowan University, Camden, N.J.
Clinical question: Is DVT prophylaxis necessary with lower leg casting or after knee arthroscopy?
Background: Patients who undergo immobilization from casting or knee arthroscopic surgery are thought to be at increased risk for venous thromboembolism (VTE). Most patients who undergo orthopedic procedures receive thromboprophylaxis but controversy exists surrounding its use in low limb casting or knee arthroscopic surgery. Prior studies did not establish consensus because of methodologic weaknesses.
Study design: Two parallel randomized-controlled, open-label trials with blinded outcome (POD-KAST for knee arthroscopy and POD-CAST for casting lower leg.
Setting: International (32 pediatric intensive care units across Asia, Australia, Europe, and North America).
Synopsis: Patients were randomly assigned to receive either a prophylactic dose of low-molecular-weight heparin (either for the 8 days after arthroscopy or for the duration of casting-related immobilization) or no anticoagulant therapy. The primary outcomes were the cumulative incidences of symptomatic venous thromboembolism (VTE) and major bleeding within 3 months after the procedure. For the 1,543 patients undergoing knee arthroscopy, VTE occurred in 0.7% of the treatment group and 0.4% of the control group (relative risk, 1.6; 95% confidence interval [CI], 0.4-6.8; absolute difference in risk, 0.3 percentage points; 95% CI, −0.6 to 1.2) and major bleeding was seen in 0.1% of both groups.
For the 1,519 patients undergoing knee arthroscopy, VTE occurred in 1.4% of the treatment group and 1.8% of the control group (relative risk, 0.8; 95% CI, 0.3-1.7; absolute difference in risk, −0.4 percentage points; 95% CI, −1.8 to 1.0) and no episodes of major bleeding were reported in either group.
Bottom line: VTE prophylaxis either after arthroscopy or during immobilization from casting did not prevent DVT.
Citations: Van Adrichem RA, Nemeth B, Algra A, et al. Thromboprophylaxis after knee arthroscopy and low-leg casting. N Engl J Med. 2016 Dec 3. doi: 10.1056/NEJMoa1613303.
Dr. Cerceo is assistant professor in the division of hospital medicine, and associate director of the internal medicine residency program at Cooper Medical School of Rowan University, Camden, N.J.
Do 30-day readmissions mean anything?
Hospitalists have been paying close attention to 30-day readmission figures since public reporting and payment programs embraced that number as an indicator of the quality of hospital care. But there is limited evidence to demonstrate 30-day readmission is really a meaningful interval of time, according to a recent study, “Rethinking Thirty-Day Hospital Readmissions: Shorter Intervals Might Be Better Indicators of Quality of Care.”
“I began to dig through the literature to find some sort of evidence to support this figure – I couldn’t find anything. In talking with quality experts, they all, more or less, believe that things that happen outside of 7 or 10 days are really out of the control of the clinician,” says lead author David L. Chin, PhD, of the Center for Healthcare Policy and Research at the University of California, Davis.
Dr. Chin and his team examined the 30-day risk of unplanned inpatient readmission at the hospital level for Medicare patients aged 65 and older in four states and for three conditions: acute myocardial infarction, heart failure, and pneumonia. Across states and diagnoses, the hospital-level quality signal captured in readmission risk was highest on the first day after discharge, and it declined quickly to its lowest level at day 7.
“The rapid decay in the quality signal suggests that most readmissions after the seventh-day postdischarge were explained by community- and household-level factors beyond hospitals’ control,” the authors concluded.
Dr. Chin said the study results show the 30-day measure is “a blunt instrument.”
“It isn’t really measuring anything that we’re supposed to be measuring,” he explains. “Essentially, 97% of the reasons a person comes back to the hospital is due to some other, non-hospital thing.”
He does not advocate for 7 days as the new standard, however.
“This is more intended to be a message that this is really not the right way of approaching [readmissions] to begin with,” he says. “I think we convincingly showed that it shouldn’t be 30 days, but we don’t really have a very good picture of what is driving readmission. Hospitals are getting dinged on these things that have happened that, really, they don’t have direct influence on.”
Reference
1. Chin DL, Bang H, Manickam RN, Romano PS. Rethinking thirty-day hospital readmissions: shorter intervals might be better indicators of quality of care. Health Aff (Millwood). 2016;35(10):1867-75.
Quality Improvement: Overuse as medical error
Hospitalists may recognize a culture of overuse at their hospitals, but how can they address it? That’s the question behind an HM16 abstract, “Occam’s Conference: Overuse as a Medical Error.”
“We wanted to change the culture of overuse here among the hospitalists and the house staff,” said lead author Hyung Cho, MD, director of quality and patient safety at the Icahn School of Medicine at Mount Sinai in New York City. “We wanted to frame it in a way that people can recognize and feel free to talk about and also give it the weight that it deserves. It’s a common thing that we all do: the chest x-ray or the EKG before a surgery, things like that.”
Seeing overuse as a medical error is a place to start.
“A framework in which overuse is considered a medical error would facilitate understanding of the drivers of overuse and systems factors that lead to it,” the authors wrote.
Dr. Cho and colleagues chose a monthly inpatient conference format, with all the relevant players gathered together.
“We also wanted to use the formula that Brandon Combs had with the ‘Do No Harm’ project, which is taking cases of overuse that actually lead to harm or a near miss. I think people respond to that as opposed to just talking about the cost, which people have a hard time actually figuring out,” Dr. Cho said.
The resulting Occam’s Conference provides a process to identify and discuss overuse as a medical error. It uses a fish-bone diagram to help analyze each case.
“That conversation needs to happen,” Dr. Cho said. “You realize that people are all on the same page, and if they’re not, they need to get on the same page and have an open dialogue.”
Reference
1. Cho HJ, Lutz C, Truong TTN, et al. Occam’s Conference: overuse as a medical error [abstract]. J Hosp Med. 2016;11(suppl1).
Practice Management: There’s an app for … end-of-life communications
Hospitalists wanting to help patients navigate end-of-life decisions or assist bereaved families in dealing with the death of a loved one have some new tools, according to The New York Times article, “Start-Ups for the End of Life.”
A start-up called Grace is intended to help its users deal with the myriad issues family members face after a death; it connects users with estate lawyers, financial planners, funeral homes, and caterers. Grace customers receive a list of tasks to complete before and after a death, and it includes relevant paperwork. The app also has staff ready to assist customers.
Currently, there’s little guidance available in this area, Alex Kruger, Grace’s cofounder and chief executive, and a licensed funeral director, told the New York Times: “At Grace we say, ‘Here are the 17 things you need to do this week’ and you can check them off as you do them. Here’s what you do the week before someone dies, when they die and then two weeks later.”
Another start-up mentioned in the article that could be relevant to hospitalists and their patients is called Parting. It provides an online directory of funeral homes searchable by ZIP code so users can quickly compare prices, services, and locations.
Reference
1. Zimmerman E. “Start-ups for the end of life,” New York Times, Nov. 22, 2016.
Quality Improvement: How to create a high-value culture
Hospitalists today are overseeing the health system’s movement toward an emphasis on value over volume.
“As leaders begin to strategize the best ways to spur transformation, our team realized that checklists and algorithms alone would likely not be enough to create sustained change in divisions and practices across the country,” said Reshma Gupta, MD, MSHPM, of the Robert Wood Johnson Clinical Scholars Program in the department of medicine at the University of California, Los Angeles. She’s the lead author of the recent study, “Development of a High-Value Care Culture Survey: A Modified Delphi Process and Psychometric Evaluation.”“Patient safety culture surveys have previously been used to drive care improvements, but no comparable survey of high-value care culture currently exists,” the authors wrote. “We aimed to develop a High-Value Care Culture Survey (HVCCS) for use by health care leaders and training programs to target future improvements in value-based care.”
Researchers conducted a two-phase, national modified Delphi process among 28 physicians and nurse experts with diverse backgrounds. They then administered a cross-sectional survey at two large academic medical centers among 162 internal medicine residents and 91 hospitalists for psychometric evaluation.
Four factors emerged with strong reliability:
• Leadership and health system messaging.
• Data transparency and access.
• Comfort with cost conversations.
• Blame-free environment.
The HVCCS can assist hospitalists and administrators in identifying tangible areas to target, Dr. Gupta said. The instrument was found to have good reliability and appears to correlate with an important patient outcome metric: the Centers for Medicare & Medicaid Services value-based purchasing score that has determined hospital reimbursement in recent years.
Now that this instrument has been created, the next step is for hospitals to begin using it. Dr. Gupta recognizes hospital medicine already has been a national leader in efforts to promote value-based care.
“With hospitalists leading many operational or research efforts in this area,” she says, “it will be vital to measure and address culture change. We believe this tool can aid them in their efforts to shape the story of value promotion at their institutions.”
Reference
Gupta R, Moriates C, Harrison JD, et al. Development of a high-value care culture survey: a modified Delphi process and psychometric evaluation [published online ahead of print Oct. 26, 2016]. BMJ Qual Saf. doi: 10.1136/bmjqs-2016-005612.
Quick Byte: Cleaning robotic surgical instruments
Robotic surgical instruments can retain some contamination even after cleaning, a new study suggests. Over 21 months, the researchers assessed protein residue on robotic and standard surgical instruments that were cleaned according to manufacturers’ instructions. The cleanings were 99.1% effective on the standard instruments but 97.6% effective on the robotic instruments, suggesting complete eradication of surface contaminants from robotic surgical instruments may not be possible with the current cleaning procedures.
Reference
1. Preidt R. “Robotic surgical tools tough to keep clean,” HealthDay News, Nov. 1, 2016.
Suzanne Bopp is a freelance writer in New Jersey.
Hospitalists have been paying close attention to 30-day readmission figures since public reporting and payment programs embraced that number as an indicator of the quality of hospital care. But there is limited evidence to demonstrate 30-day readmission is really a meaningful interval of time, according to a recent study, “Rethinking Thirty-Day Hospital Readmissions: Shorter Intervals Might Be Better Indicators of Quality of Care.”
“I began to dig through the literature to find some sort of evidence to support this figure – I couldn’t find anything. In talking with quality experts, they all, more or less, believe that things that happen outside of 7 or 10 days are really out of the control of the clinician,” says lead author David L. Chin, PhD, of the Center for Healthcare Policy and Research at the University of California, Davis.
Dr. Chin and his team examined the 30-day risk of unplanned inpatient readmission at the hospital level for Medicare patients aged 65 and older in four states and for three conditions: acute myocardial infarction, heart failure, and pneumonia. Across states and diagnoses, the hospital-level quality signal captured in readmission risk was highest on the first day after discharge, and it declined quickly to its lowest level at day 7.
“The rapid decay in the quality signal suggests that most readmissions after the seventh-day postdischarge were explained by community- and household-level factors beyond hospitals’ control,” the authors concluded.
Dr. Chin said the study results show the 30-day measure is “a blunt instrument.”
“It isn’t really measuring anything that we’re supposed to be measuring,” he explains. “Essentially, 97% of the reasons a person comes back to the hospital is due to some other, non-hospital thing.”
He does not advocate for 7 days as the new standard, however.
“This is more intended to be a message that this is really not the right way of approaching [readmissions] to begin with,” he says. “I think we convincingly showed that it shouldn’t be 30 days, but we don’t really have a very good picture of what is driving readmission. Hospitals are getting dinged on these things that have happened that, really, they don’t have direct influence on.”
Reference
1. Chin DL, Bang H, Manickam RN, Romano PS. Rethinking thirty-day hospital readmissions: shorter intervals might be better indicators of quality of care. Health Aff (Millwood). 2016;35(10):1867-75.
Quality Improvement: Overuse as medical error
Hospitalists may recognize a culture of overuse at their hospitals, but how can they address it? That’s the question behind an HM16 abstract, “Occam’s Conference: Overuse as a Medical Error.”
“We wanted to change the culture of overuse here among the hospitalists and the house staff,” said lead author Hyung Cho, MD, director of quality and patient safety at the Icahn School of Medicine at Mount Sinai in New York City. “We wanted to frame it in a way that people can recognize and feel free to talk about and also give it the weight that it deserves. It’s a common thing that we all do: the chest x-ray or the EKG before a surgery, things like that.”
Seeing overuse as a medical error is a place to start.
“A framework in which overuse is considered a medical error would facilitate understanding of the drivers of overuse and systems factors that lead to it,” the authors wrote.
Dr. Cho and colleagues chose a monthly inpatient conference format, with all the relevant players gathered together.
“We also wanted to use the formula that Brandon Combs had with the ‘Do No Harm’ project, which is taking cases of overuse that actually lead to harm or a near miss. I think people respond to that as opposed to just talking about the cost, which people have a hard time actually figuring out,” Dr. Cho said.
The resulting Occam’s Conference provides a process to identify and discuss overuse as a medical error. It uses a fish-bone diagram to help analyze each case.
“That conversation needs to happen,” Dr. Cho said. “You realize that people are all on the same page, and if they’re not, they need to get on the same page and have an open dialogue.”
Reference
1. Cho HJ, Lutz C, Truong TTN, et al. Occam’s Conference: overuse as a medical error [abstract]. J Hosp Med. 2016;11(suppl1).
Practice Management: There’s an app for … end-of-life communications
Hospitalists wanting to help patients navigate end-of-life decisions or assist bereaved families in dealing with the death of a loved one have some new tools, according to The New York Times article, “Start-Ups for the End of Life.”
A start-up called Grace is intended to help its users deal with the myriad issues family members face after a death; it connects users with estate lawyers, financial planners, funeral homes, and caterers. Grace customers receive a list of tasks to complete before and after a death, and it includes relevant paperwork. The app also has staff ready to assist customers.
Currently, there’s little guidance available in this area, Alex Kruger, Grace’s cofounder and chief executive, and a licensed funeral director, told the New York Times: “At Grace we say, ‘Here are the 17 things you need to do this week’ and you can check them off as you do them. Here’s what you do the week before someone dies, when they die and then two weeks later.”
Another start-up mentioned in the article that could be relevant to hospitalists and their patients is called Parting. It provides an online directory of funeral homes searchable by ZIP code so users can quickly compare prices, services, and locations.
Reference
1. Zimmerman E. “Start-ups for the end of life,” New York Times, Nov. 22, 2016.
Quality Improvement: How to create a high-value culture
Hospitalists today are overseeing the health system’s movement toward an emphasis on value over volume.
“As leaders begin to strategize the best ways to spur transformation, our team realized that checklists and algorithms alone would likely not be enough to create sustained change in divisions and practices across the country,” said Reshma Gupta, MD, MSHPM, of the Robert Wood Johnson Clinical Scholars Program in the department of medicine at the University of California, Los Angeles. She’s the lead author of the recent study, “Development of a High-Value Care Culture Survey: A Modified Delphi Process and Psychometric Evaluation.”“Patient safety culture surveys have previously been used to drive care improvements, but no comparable survey of high-value care culture currently exists,” the authors wrote. “We aimed to develop a High-Value Care Culture Survey (HVCCS) for use by health care leaders and training programs to target future improvements in value-based care.”
Researchers conducted a two-phase, national modified Delphi process among 28 physicians and nurse experts with diverse backgrounds. They then administered a cross-sectional survey at two large academic medical centers among 162 internal medicine residents and 91 hospitalists for psychometric evaluation.
Four factors emerged with strong reliability:
• Leadership and health system messaging.
• Data transparency and access.
• Comfort with cost conversations.
• Blame-free environment.
The HVCCS can assist hospitalists and administrators in identifying tangible areas to target, Dr. Gupta said. The instrument was found to have good reliability and appears to correlate with an important patient outcome metric: the Centers for Medicare & Medicaid Services value-based purchasing score that has determined hospital reimbursement in recent years.
Now that this instrument has been created, the next step is for hospitals to begin using it. Dr. Gupta recognizes hospital medicine already has been a national leader in efforts to promote value-based care.
“With hospitalists leading many operational or research efforts in this area,” she says, “it will be vital to measure and address culture change. We believe this tool can aid them in their efforts to shape the story of value promotion at their institutions.”
Reference
Gupta R, Moriates C, Harrison JD, et al. Development of a high-value care culture survey: a modified Delphi process and psychometric evaluation [published online ahead of print Oct. 26, 2016]. BMJ Qual Saf. doi: 10.1136/bmjqs-2016-005612.
Quick Byte: Cleaning robotic surgical instruments
Robotic surgical instruments can retain some contamination even after cleaning, a new study suggests. Over 21 months, the researchers assessed protein residue on robotic and standard surgical instruments that were cleaned according to manufacturers’ instructions. The cleanings were 99.1% effective on the standard instruments but 97.6% effective on the robotic instruments, suggesting complete eradication of surface contaminants from robotic surgical instruments may not be possible with the current cleaning procedures.
Reference
1. Preidt R. “Robotic surgical tools tough to keep clean,” HealthDay News, Nov. 1, 2016.
Suzanne Bopp is a freelance writer in New Jersey.
Hospitalists have been paying close attention to 30-day readmission figures since public reporting and payment programs embraced that number as an indicator of the quality of hospital care. But there is limited evidence to demonstrate 30-day readmission is really a meaningful interval of time, according to a recent study, “Rethinking Thirty-Day Hospital Readmissions: Shorter Intervals Might Be Better Indicators of Quality of Care.”
“I began to dig through the literature to find some sort of evidence to support this figure – I couldn’t find anything. In talking with quality experts, they all, more or less, believe that things that happen outside of 7 or 10 days are really out of the control of the clinician,” says lead author David L. Chin, PhD, of the Center for Healthcare Policy and Research at the University of California, Davis.
Dr. Chin and his team examined the 30-day risk of unplanned inpatient readmission at the hospital level for Medicare patients aged 65 and older in four states and for three conditions: acute myocardial infarction, heart failure, and pneumonia. Across states and diagnoses, the hospital-level quality signal captured in readmission risk was highest on the first day after discharge, and it declined quickly to its lowest level at day 7.
“The rapid decay in the quality signal suggests that most readmissions after the seventh-day postdischarge were explained by community- and household-level factors beyond hospitals’ control,” the authors concluded.
Dr. Chin said the study results show the 30-day measure is “a blunt instrument.”
“It isn’t really measuring anything that we’re supposed to be measuring,” he explains. “Essentially, 97% of the reasons a person comes back to the hospital is due to some other, non-hospital thing.”
He does not advocate for 7 days as the new standard, however.
“This is more intended to be a message that this is really not the right way of approaching [readmissions] to begin with,” he says. “I think we convincingly showed that it shouldn’t be 30 days, but we don’t really have a very good picture of what is driving readmission. Hospitals are getting dinged on these things that have happened that, really, they don’t have direct influence on.”
Reference
1. Chin DL, Bang H, Manickam RN, Romano PS. Rethinking thirty-day hospital readmissions: shorter intervals might be better indicators of quality of care. Health Aff (Millwood). 2016;35(10):1867-75.
Quality Improvement: Overuse as medical error
Hospitalists may recognize a culture of overuse at their hospitals, but how can they address it? That’s the question behind an HM16 abstract, “Occam’s Conference: Overuse as a Medical Error.”
“We wanted to change the culture of overuse here among the hospitalists and the house staff,” said lead author Hyung Cho, MD, director of quality and patient safety at the Icahn School of Medicine at Mount Sinai in New York City. “We wanted to frame it in a way that people can recognize and feel free to talk about and also give it the weight that it deserves. It’s a common thing that we all do: the chest x-ray or the EKG before a surgery, things like that.”
Seeing overuse as a medical error is a place to start.
“A framework in which overuse is considered a medical error would facilitate understanding of the drivers of overuse and systems factors that lead to it,” the authors wrote.
Dr. Cho and colleagues chose a monthly inpatient conference format, with all the relevant players gathered together.
“We also wanted to use the formula that Brandon Combs had with the ‘Do No Harm’ project, which is taking cases of overuse that actually lead to harm or a near miss. I think people respond to that as opposed to just talking about the cost, which people have a hard time actually figuring out,” Dr. Cho said.
The resulting Occam’s Conference provides a process to identify and discuss overuse as a medical error. It uses a fish-bone diagram to help analyze each case.
“That conversation needs to happen,” Dr. Cho said. “You realize that people are all on the same page, and if they’re not, they need to get on the same page and have an open dialogue.”
Reference
1. Cho HJ, Lutz C, Truong TTN, et al. Occam’s Conference: overuse as a medical error [abstract]. J Hosp Med. 2016;11(suppl1).
Practice Management: There’s an app for … end-of-life communications
Hospitalists wanting to help patients navigate end-of-life decisions or assist bereaved families in dealing with the death of a loved one have some new tools, according to The New York Times article, “Start-Ups for the End of Life.”
A start-up called Grace is intended to help its users deal with the myriad issues family members face after a death; it connects users with estate lawyers, financial planners, funeral homes, and caterers. Grace customers receive a list of tasks to complete before and after a death, and it includes relevant paperwork. The app also has staff ready to assist customers.
Currently, there’s little guidance available in this area, Alex Kruger, Grace’s cofounder and chief executive, and a licensed funeral director, told the New York Times: “At Grace we say, ‘Here are the 17 things you need to do this week’ and you can check them off as you do them. Here’s what you do the week before someone dies, when they die and then two weeks later.”
Another start-up mentioned in the article that could be relevant to hospitalists and their patients is called Parting. It provides an online directory of funeral homes searchable by ZIP code so users can quickly compare prices, services, and locations.
Reference
1. Zimmerman E. “Start-ups for the end of life,” New York Times, Nov. 22, 2016.
Quality Improvement: How to create a high-value culture
Hospitalists today are overseeing the health system’s movement toward an emphasis on value over volume.
“As leaders begin to strategize the best ways to spur transformation, our team realized that checklists and algorithms alone would likely not be enough to create sustained change in divisions and practices across the country,” said Reshma Gupta, MD, MSHPM, of the Robert Wood Johnson Clinical Scholars Program in the department of medicine at the University of California, Los Angeles. She’s the lead author of the recent study, “Development of a High-Value Care Culture Survey: A Modified Delphi Process and Psychometric Evaluation.”“Patient safety culture surveys have previously been used to drive care improvements, but no comparable survey of high-value care culture currently exists,” the authors wrote. “We aimed to develop a High-Value Care Culture Survey (HVCCS) for use by health care leaders and training programs to target future improvements in value-based care.”
Researchers conducted a two-phase, national modified Delphi process among 28 physicians and nurse experts with diverse backgrounds. They then administered a cross-sectional survey at two large academic medical centers among 162 internal medicine residents and 91 hospitalists for psychometric evaluation.
Four factors emerged with strong reliability:
• Leadership and health system messaging.
• Data transparency and access.
• Comfort with cost conversations.
• Blame-free environment.
The HVCCS can assist hospitalists and administrators in identifying tangible areas to target, Dr. Gupta said. The instrument was found to have good reliability and appears to correlate with an important patient outcome metric: the Centers for Medicare & Medicaid Services value-based purchasing score that has determined hospital reimbursement in recent years.
Now that this instrument has been created, the next step is for hospitals to begin using it. Dr. Gupta recognizes hospital medicine already has been a national leader in efforts to promote value-based care.
“With hospitalists leading many operational or research efforts in this area,” she says, “it will be vital to measure and address culture change. We believe this tool can aid them in their efforts to shape the story of value promotion at their institutions.”
Reference
Gupta R, Moriates C, Harrison JD, et al. Development of a high-value care culture survey: a modified Delphi process and psychometric evaluation [published online ahead of print Oct. 26, 2016]. BMJ Qual Saf. doi: 10.1136/bmjqs-2016-005612.
Quick Byte: Cleaning robotic surgical instruments
Robotic surgical instruments can retain some contamination even after cleaning, a new study suggests. Over 21 months, the researchers assessed protein residue on robotic and standard surgical instruments that were cleaned according to manufacturers’ instructions. The cleanings were 99.1% effective on the standard instruments but 97.6% effective on the robotic instruments, suggesting complete eradication of surface contaminants from robotic surgical instruments may not be possible with the current cleaning procedures.
Reference
1. Preidt R. “Robotic surgical tools tough to keep clean,” HealthDay News, Nov. 1, 2016.
Suzanne Bopp is a freelance writer in New Jersey.
Sneak Peek: The Hospital Leader blog
Editor’s note: First published on The Hospital Leader blog under the title, “How I Realized QI Could Be a Dirty Word.”
With the recent election, there has been a new recognition of the various “bubbles” we all seem to be living in. It reminds me of the parable I like to often mention, popularized by the late great writer David Foster Wallace: Two fish were swimming along when an older fish swam by, nodded his head at them and said, “Mornin’ boys, how’s the water?” The two young fish nod back and swim for a bit, then one turns to the other and says, “What the hell is water?”
Imagine the hard reality that hit me when I read this quote from a resident: “Truly, the first thing I think of when I hear [QI] is going to make more work for residents.”
Wait – is QI actually a dirty word for other residents and physicians?
The quote comes from an Academic Medicine study titled “ ‘It Feels Like a Lot of Extra Work’: Resident Attitudes About Quality Improvement and Implications for an Effective Learning Health Care System.” I read on, and it got worse.
“This hasn’t really made any difference to the patients. Like this checklist we do on rounds, like I don’t know. Maybe it has.”
And, by far, most concerning: “There’s like the central line protocols … If you suspect that anybody has any type of bacteremia, you don’t do a blood culture; you just do a urine culture and pull the lines … we just don’t even test for it because the quality improvement then like marks you off.”
Wow.
That is some harsh truth about unintended consequences right there. (Also, apparently us kids of the 1990s still say “like” a lot, which is, like, not very professional and also like kinda grating.)
The residents in this study were from the University of Utah, Salt Lake City – an institution I frequently– and publicly – admire for their incredible progress on systematically introducing value improvement into their practice.
What can we do?
Read the full post at hospitalleader.org.
Also on The Hospital Leader…
- THIS Is What Teamwork Looks Like, by Danielle Scheurer, MD, MSCR, SFHM
- The Medicaid Overhaul and How Hospitals and Their Providers Could Be Hardest Hit, by Brad Flansbaum, DO, MPH, MHM
- Count Me – and My Intuition – In, by Tracy Cardin, ACNP-BC, SFHM
Editor’s note: First published on The Hospital Leader blog under the title, “How I Realized QI Could Be a Dirty Word.”
With the recent election, there has been a new recognition of the various “bubbles” we all seem to be living in. It reminds me of the parable I like to often mention, popularized by the late great writer David Foster Wallace: Two fish were swimming along when an older fish swam by, nodded his head at them and said, “Mornin’ boys, how’s the water?” The two young fish nod back and swim for a bit, then one turns to the other and says, “What the hell is water?”
Imagine the hard reality that hit me when I read this quote from a resident: “Truly, the first thing I think of when I hear [QI] is going to make more work for residents.”
Wait – is QI actually a dirty word for other residents and physicians?
The quote comes from an Academic Medicine study titled “ ‘It Feels Like a Lot of Extra Work’: Resident Attitudes About Quality Improvement and Implications for an Effective Learning Health Care System.” I read on, and it got worse.
“This hasn’t really made any difference to the patients. Like this checklist we do on rounds, like I don’t know. Maybe it has.”
And, by far, most concerning: “There’s like the central line protocols … If you suspect that anybody has any type of bacteremia, you don’t do a blood culture; you just do a urine culture and pull the lines … we just don’t even test for it because the quality improvement then like marks you off.”
Wow.
That is some harsh truth about unintended consequences right there. (Also, apparently us kids of the 1990s still say “like” a lot, which is, like, not very professional and also like kinda grating.)
The residents in this study were from the University of Utah, Salt Lake City – an institution I frequently– and publicly – admire for their incredible progress on systematically introducing value improvement into their practice.
What can we do?
Read the full post at hospitalleader.org.
Also on The Hospital Leader…
- THIS Is What Teamwork Looks Like, by Danielle Scheurer, MD, MSCR, SFHM
- The Medicaid Overhaul and How Hospitals and Their Providers Could Be Hardest Hit, by Brad Flansbaum, DO, MPH, MHM
- Count Me – and My Intuition – In, by Tracy Cardin, ACNP-BC, SFHM
Editor’s note: First published on The Hospital Leader blog under the title, “How I Realized QI Could Be a Dirty Word.”
With the recent election, there has been a new recognition of the various “bubbles” we all seem to be living in. It reminds me of the parable I like to often mention, popularized by the late great writer David Foster Wallace: Two fish were swimming along when an older fish swam by, nodded his head at them and said, “Mornin’ boys, how’s the water?” The two young fish nod back and swim for a bit, then one turns to the other and says, “What the hell is water?”
Imagine the hard reality that hit me when I read this quote from a resident: “Truly, the first thing I think of when I hear [QI] is going to make more work for residents.”
Wait – is QI actually a dirty word for other residents and physicians?
The quote comes from an Academic Medicine study titled “ ‘It Feels Like a Lot of Extra Work’: Resident Attitudes About Quality Improvement and Implications for an Effective Learning Health Care System.” I read on, and it got worse.
“This hasn’t really made any difference to the patients. Like this checklist we do on rounds, like I don’t know. Maybe it has.”
And, by far, most concerning: “There’s like the central line protocols … If you suspect that anybody has any type of bacteremia, you don’t do a blood culture; you just do a urine culture and pull the lines … we just don’t even test for it because the quality improvement then like marks you off.”
Wow.
That is some harsh truth about unintended consequences right there. (Also, apparently us kids of the 1990s still say “like” a lot, which is, like, not very professional and also like kinda grating.)
The residents in this study were from the University of Utah, Salt Lake City – an institution I frequently– and publicly – admire for their incredible progress on systematically introducing value improvement into their practice.
What can we do?
Read the full post at hospitalleader.org.
Also on The Hospital Leader…
- THIS Is What Teamwork Looks Like, by Danielle Scheurer, MD, MSCR, SFHM
- The Medicaid Overhaul and How Hospitals and Their Providers Could Be Hardest Hit, by Brad Flansbaum, DO, MPH, MHM
- Count Me – and My Intuition – In, by Tracy Cardin, ACNP-BC, SFHM
‘I can handle it’– The state of hospitalist group backup systems
It took my hospital medicine group (HMG) 20 years to implement a formal backup system. Of all the reasons we resisted creating a backup system, foremost was that we did not want to mandate additional work. Because our compensation model did not have a mechanism to financially reward hospitalists for unexpectedly having to come in on unscheduled work days (other than the work relative value units generated by seeing patients), there was not enough motivational energy to get a system started.
It turns out our group is not unlike many other HMGs across the nation. According to the 2016 State of Hospital Medicine report (SoHM), 58.3% of adult-only HMGs, 72.2% of pediatric-only HMGs, and 52.6% of HMGs serving both adults and children did not have staffing backup systems. Interestingly, the report also showed that for groups serving adults only, academic HMGs were more likely to have formal backup systems in place (62.6%, compared with 37.3% in nonacademic HMGs).
The reason most HMGs create backup systems is to have a consistent and fair approach for dealing with unanticipated absences and/or high-volume census. In addition to creating a safety net, implementing a backup system addresses the common problem of the same hospitalists disproportionately filling in during times of crisis.
Although our group created a formal backup system starting January 2015, it is not comprehensive and deals only with high patient volumes occurring during the late evening and night hours. Hospitalists rotate through a schedule, taking a week of backup call for which no additional compensation is offered. Then, if they are actually called to come in, an hourly stipend is paid in addition to work RVUs generated. Implementing a backup system was not necessarily a popular idea. Nevertheless, the system has successfully remained in place. Triggering the system infrequently, having a clear set of criteria for when to activate backup, and providing additional compensation for the additional work are key factors in our system’s success.

When data from the 2016 SoHM report are compared with the 2014 SoHM report, the proportion of groups with formal backup systems actually decreases for both adults-only HMGs and HMGs serving both adults and children. For adult-only HMGs, there was a decline to 41.8% from 57.6%. For adult/pediatric HMGs, there was a decline to 47.4% from 58.8%. It also is notable that pediatric HMGs in particular are much less likely to have formal backup systems, only 27.8%, which has changed little since the last survey (28.8 % in 2014).
All in all, the reasons for the decline in backup systems are unclear. Possibly, the decrease is because of issues surrounding compensation, as approximately one-third of survey respondents with backup systems received no additional compensation. But in my view, it’s more likely that the reason for the decreased percentage of groups with backup systems has to do with differences in the particular set of HMGs that responded to the survey this year.
Dr. Stephan is a hospitalist at Abbott Northwestern Hospital in Minneapolis and a member of SHM’s Practice Analysis Committee.
It took my hospital medicine group (HMG) 20 years to implement a formal backup system. Of all the reasons we resisted creating a backup system, foremost was that we did not want to mandate additional work. Because our compensation model did not have a mechanism to financially reward hospitalists for unexpectedly having to come in on unscheduled work days (other than the work relative value units generated by seeing patients), there was not enough motivational energy to get a system started.
It turns out our group is not unlike many other HMGs across the nation. According to the 2016 State of Hospital Medicine report (SoHM), 58.3% of adult-only HMGs, 72.2% of pediatric-only HMGs, and 52.6% of HMGs serving both adults and children did not have staffing backup systems. Interestingly, the report also showed that for groups serving adults only, academic HMGs were more likely to have formal backup systems in place (62.6%, compared with 37.3% in nonacademic HMGs).
The reason most HMGs create backup systems is to have a consistent and fair approach for dealing with unanticipated absences and/or high-volume census. In addition to creating a safety net, implementing a backup system addresses the common problem of the same hospitalists disproportionately filling in during times of crisis.
Although our group created a formal backup system starting January 2015, it is not comprehensive and deals only with high patient volumes occurring during the late evening and night hours. Hospitalists rotate through a schedule, taking a week of backup call for which no additional compensation is offered. Then, if they are actually called to come in, an hourly stipend is paid in addition to work RVUs generated. Implementing a backup system was not necessarily a popular idea. Nevertheless, the system has successfully remained in place. Triggering the system infrequently, having a clear set of criteria for when to activate backup, and providing additional compensation for the additional work are key factors in our system’s success.

When data from the 2016 SoHM report are compared with the 2014 SoHM report, the proportion of groups with formal backup systems actually decreases for both adults-only HMGs and HMGs serving both adults and children. For adult-only HMGs, there was a decline to 41.8% from 57.6%. For adult/pediatric HMGs, there was a decline to 47.4% from 58.8%. It also is notable that pediatric HMGs in particular are much less likely to have formal backup systems, only 27.8%, which has changed little since the last survey (28.8 % in 2014).
All in all, the reasons for the decline in backup systems are unclear. Possibly, the decrease is because of issues surrounding compensation, as approximately one-third of survey respondents with backup systems received no additional compensation. But in my view, it’s more likely that the reason for the decreased percentage of groups with backup systems has to do with differences in the particular set of HMGs that responded to the survey this year.
Dr. Stephan is a hospitalist at Abbott Northwestern Hospital in Minneapolis and a member of SHM’s Practice Analysis Committee.
It took my hospital medicine group (HMG) 20 years to implement a formal backup system. Of all the reasons we resisted creating a backup system, foremost was that we did not want to mandate additional work. Because our compensation model did not have a mechanism to financially reward hospitalists for unexpectedly having to come in on unscheduled work days (other than the work relative value units generated by seeing patients), there was not enough motivational energy to get a system started.
It turns out our group is not unlike many other HMGs across the nation. According to the 2016 State of Hospital Medicine report (SoHM), 58.3% of adult-only HMGs, 72.2% of pediatric-only HMGs, and 52.6% of HMGs serving both adults and children did not have staffing backup systems. Interestingly, the report also showed that for groups serving adults only, academic HMGs were more likely to have formal backup systems in place (62.6%, compared with 37.3% in nonacademic HMGs).
The reason most HMGs create backup systems is to have a consistent and fair approach for dealing with unanticipated absences and/or high-volume census. In addition to creating a safety net, implementing a backup system addresses the common problem of the same hospitalists disproportionately filling in during times of crisis.
Although our group created a formal backup system starting January 2015, it is not comprehensive and deals only with high patient volumes occurring during the late evening and night hours. Hospitalists rotate through a schedule, taking a week of backup call for which no additional compensation is offered. Then, if they are actually called to come in, an hourly stipend is paid in addition to work RVUs generated. Implementing a backup system was not necessarily a popular idea. Nevertheless, the system has successfully remained in place. Triggering the system infrequently, having a clear set of criteria for when to activate backup, and providing additional compensation for the additional work are key factors in our system’s success.

When data from the 2016 SoHM report are compared with the 2014 SoHM report, the proportion of groups with formal backup systems actually decreases for both adults-only HMGs and HMGs serving both adults and children. For adult-only HMGs, there was a decline to 41.8% from 57.6%. For adult/pediatric HMGs, there was a decline to 47.4% from 58.8%. It also is notable that pediatric HMGs in particular are much less likely to have formal backup systems, only 27.8%, which has changed little since the last survey (28.8 % in 2014).
All in all, the reasons for the decline in backup systems are unclear. Possibly, the decrease is because of issues surrounding compensation, as approximately one-third of survey respondents with backup systems received no additional compensation. But in my view, it’s more likely that the reason for the decreased percentage of groups with backup systems has to do with differences in the particular set of HMGs that responded to the survey this year.
Dr. Stephan is a hospitalist at Abbott Northwestern Hospital in Minneapolis and a member of SHM’s Practice Analysis Committee.










