User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Scholar grants help future hospitalists explore career pathways
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
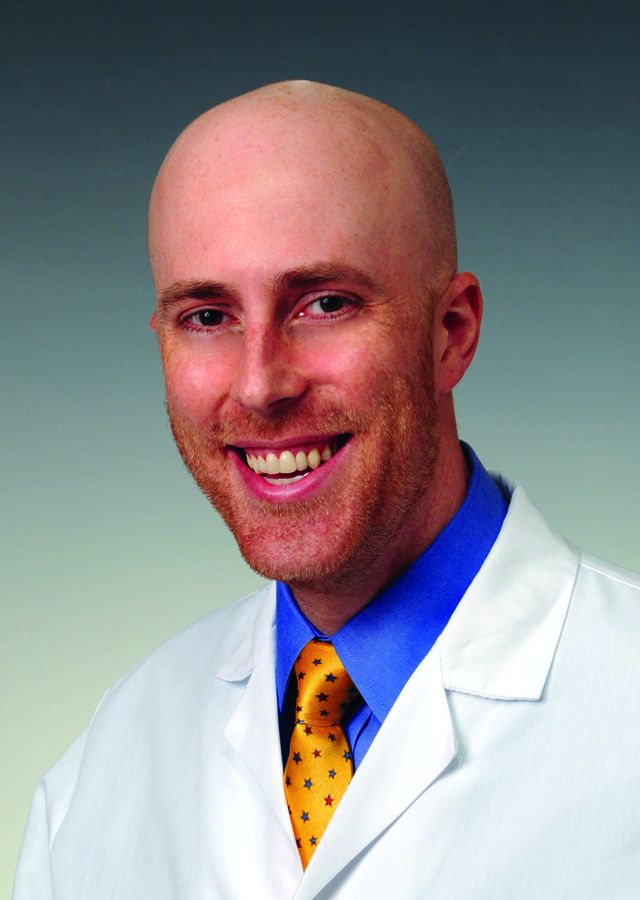
This month, The Hospitalist spotlights Ernie L. Esquivel, MD, FACP, FHM, the clerkship director, medicine, and assistant professor of clinical medicine in the Division of General Internal Medicine at the Weill Cornell Medical College in New York City. Dr. Esquivel is involved with SHM’s Physicians in Training Committee, and has spearheaded the creation of the Student Hospitalist Scholar Grant program.
What inspired you to become a hospitalist?
I became a hospitalist serendipitously. At a critical juncture in my life about 8 years ago (when a change in career direction became necessary), I chanced upon a locum tenens position in a small community hospital in Lansdale, Pa., as a hospitalist. Having been a primary care track resident who subsequently chose to specialize in nephrology, I rediscovered my generalist inclinations during this job. I fell in love with the fast pace of the hospitalist’s work, the complexity of delivering care and the diversity of diseases, and of personal life stories on the general medicine wards and the ICU.
Subsequently, I worked as an intensivist in Philadelphia for a year before joining the Academic Hospital Medicine Division at Weill Cornell in New York City. At Cornell, I have managed to cultivate my passion for medical education, especially for working with and mentoring students and residents, while continuing to care for patients on the general medicine wards. As the medicine clerkship director, I have had the privilege of creating an innovative curriculum that I hope prepares medical students for the challenges in, and the richness of, encounters in the practice of inpatient medicine.
How and why did you become a member of SHM and the Physicians in Training Committee (PIT)?
I joined SHM 6 years ago as I started to explore my career options more deeply. In 2010, I attended the Academic Hospitalist Academy, and that really offered me a closer look at the different ways in which SHM could help me advance. I went to my first SHM annual meeting 5 years ago; it motivated me to become involved in committee work. Because of my interest in medical education, I volunteered for the PIT Committee and it has given me the opportunity to work closely with other hospitalists around the country, and develop programming specifically targeted toward future hospitalists.
What is the PIT Committee working on?
The committee has continued to find ways for increased engagement of residents and students in SHM. Dr. Brian Kwan, an academic hospitalist at UC San Diego, and I have been developing a travel grant program for resident trainees and hospital medicine fellows to attend the annual meeting. By offering them a stipend to defray the costs of travel if their quality improvement innovation or research project is accepted, we hope that the annual meeting can become a venue for them to highlight their work, while becoming exposed to the many activities and opportunities offered by our society. In addition, it could be a way for them to network with other future hospitalists and established future mentors.
What prompted you to lead the creation of the Student Hospitalist Scholar Grant summer program?
Before I became a hospitalist, I spent about 7 years in research, studying renal genetics. I have always been fascinated by science and asked how I can help to advance our knowledge. As a hospitalist, it became clear to me early on that there are many questions that one can pose about the clinical work we do, the way we practice medicine, or ways to innovate education, and that there are many academic hospitalists who engage in advancing the field. I spearheaded this program because I would like students to see the field of hospital medicine as one in which they can develop a future career in academic medicine, not only by caring for patients, but also by involving themselves in research questions or QI projects.
Do you have any specific advice for students and residents interested in hospital medicine? In what ways can early-career hospitalists utilize SHM resources to leverage their careers?
The decision to pursue a career as a hospitalist will open up many more questions in the future, because there are so many opportunities available. I would suggest that trainees ask in which ways they see themselves growing in the future – clinical research, medical education, QI/patient safety, operations, and hospital leadership are the main avenues. When I interview future faculty, I always pose the same question to each of them: “Every year you are allocated X amount of money that you can use for CME, etc. How are you going to use this money to improve your skills in any particular area?” The ability of candidates to answer this question reflects for me their preparedness to develop themselves as career hospitalists and their willingness to contribute to their group or division in an innovative manner.
The reality is that as one gets older, most will find it difficult to sustain a 26-week/year schedule. So find ways for your energies, in whichever area, to be noticed and developed toward a position of leadership in the hospital or medical school.
As you take care of patients in the hospital or consider your education and training, identify ways in which things can be done better. Invariably, someone in the Society of Hospital Medicine is interested in the same issue(s). Explore your ideas, share them at the meeting, talk to people, go to the SHM website and identify what resources are already available.
If SHM will be your future academic home, volunteer to engage in activities at the chapter or national levels. Our society is really dedicated to identifying ways to welcome you into our exciting and continually evolving field.
Felicia Steele is SHM’s communications coordinator.
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Ernie L. Esquivel, MD, FACP, FHM, the clerkship director, medicine, and assistant professor of clinical medicine in the Division of General Internal Medicine at the Weill Cornell Medical College in New York City. Dr. Esquivel is involved with SHM’s Physicians in Training Committee, and has spearheaded the creation of the Student Hospitalist Scholar Grant program.
What inspired you to become a hospitalist?
I became a hospitalist serendipitously. At a critical juncture in my life about 8 years ago (when a change in career direction became necessary), I chanced upon a locum tenens position in a small community hospital in Lansdale, Pa., as a hospitalist. Having been a primary care track resident who subsequently chose to specialize in nephrology, I rediscovered my generalist inclinations during this job. I fell in love with the fast pace of the hospitalist’s work, the complexity of delivering care and the diversity of diseases, and of personal life stories on the general medicine wards and the ICU.
Subsequently, I worked as an intensivist in Philadelphia for a year before joining the Academic Hospital Medicine Division at Weill Cornell in New York City. At Cornell, I have managed to cultivate my passion for medical education, especially for working with and mentoring students and residents, while continuing to care for patients on the general medicine wards. As the medicine clerkship director, I have had the privilege of creating an innovative curriculum that I hope prepares medical students for the challenges in, and the richness of, encounters in the practice of inpatient medicine.
How and why did you become a member of SHM and the Physicians in Training Committee (PIT)?
I joined SHM 6 years ago as I started to explore my career options more deeply. In 2010, I attended the Academic Hospitalist Academy, and that really offered me a closer look at the different ways in which SHM could help me advance. I went to my first SHM annual meeting 5 years ago; it motivated me to become involved in committee work. Because of my interest in medical education, I volunteered for the PIT Committee and it has given me the opportunity to work closely with other hospitalists around the country, and develop programming specifically targeted toward future hospitalists.
What is the PIT Committee working on?
The committee has continued to find ways for increased engagement of residents and students in SHM. Dr. Brian Kwan, an academic hospitalist at UC San Diego, and I have been developing a travel grant program for resident trainees and hospital medicine fellows to attend the annual meeting. By offering them a stipend to defray the costs of travel if their quality improvement innovation or research project is accepted, we hope that the annual meeting can become a venue for them to highlight their work, while becoming exposed to the many activities and opportunities offered by our society. In addition, it could be a way for them to network with other future hospitalists and established future mentors.
What prompted you to lead the creation of the Student Hospitalist Scholar Grant summer program?
Before I became a hospitalist, I spent about 7 years in research, studying renal genetics. I have always been fascinated by science and asked how I can help to advance our knowledge. As a hospitalist, it became clear to me early on that there are many questions that one can pose about the clinical work we do, the way we practice medicine, or ways to innovate education, and that there are many academic hospitalists who engage in advancing the field. I spearheaded this program because I would like students to see the field of hospital medicine as one in which they can develop a future career in academic medicine, not only by caring for patients, but also by involving themselves in research questions or QI projects.
Do you have any specific advice for students and residents interested in hospital medicine? In what ways can early-career hospitalists utilize SHM resources to leverage their careers?
The decision to pursue a career as a hospitalist will open up many more questions in the future, because there are so many opportunities available. I would suggest that trainees ask in which ways they see themselves growing in the future – clinical research, medical education, QI/patient safety, operations, and hospital leadership are the main avenues. When I interview future faculty, I always pose the same question to each of them: “Every year you are allocated X amount of money that you can use for CME, etc. How are you going to use this money to improve your skills in any particular area?” The ability of candidates to answer this question reflects for me their preparedness to develop themselves as career hospitalists and their willingness to contribute to their group or division in an innovative manner.
The reality is that as one gets older, most will find it difficult to sustain a 26-week/year schedule. So find ways for your energies, in whichever area, to be noticed and developed toward a position of leadership in the hospital or medical school.
As you take care of patients in the hospital or consider your education and training, identify ways in which things can be done better. Invariably, someone in the Society of Hospital Medicine is interested in the same issue(s). Explore your ideas, share them at the meeting, talk to people, go to the SHM website and identify what resources are already available.
If SHM will be your future academic home, volunteer to engage in activities at the chapter or national levels. Our society is really dedicated to identifying ways to welcome you into our exciting and continually evolving field.
Felicia Steele is SHM’s communications coordinator.
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Ernie L. Esquivel, MD, FACP, FHM, the clerkship director, medicine, and assistant professor of clinical medicine in the Division of General Internal Medicine at the Weill Cornell Medical College in New York City. Dr. Esquivel is involved with SHM’s Physicians in Training Committee, and has spearheaded the creation of the Student Hospitalist Scholar Grant program.
What inspired you to become a hospitalist?
I became a hospitalist serendipitously. At a critical juncture in my life about 8 years ago (when a change in career direction became necessary), I chanced upon a locum tenens position in a small community hospital in Lansdale, Pa., as a hospitalist. Having been a primary care track resident who subsequently chose to specialize in nephrology, I rediscovered my generalist inclinations during this job. I fell in love with the fast pace of the hospitalist’s work, the complexity of delivering care and the diversity of diseases, and of personal life stories on the general medicine wards and the ICU.
Subsequently, I worked as an intensivist in Philadelphia for a year before joining the Academic Hospital Medicine Division at Weill Cornell in New York City. At Cornell, I have managed to cultivate my passion for medical education, especially for working with and mentoring students and residents, while continuing to care for patients on the general medicine wards. As the medicine clerkship director, I have had the privilege of creating an innovative curriculum that I hope prepares medical students for the challenges in, and the richness of, encounters in the practice of inpatient medicine.
How and why did you become a member of SHM and the Physicians in Training Committee (PIT)?
I joined SHM 6 years ago as I started to explore my career options more deeply. In 2010, I attended the Academic Hospitalist Academy, and that really offered me a closer look at the different ways in which SHM could help me advance. I went to my first SHM annual meeting 5 years ago; it motivated me to become involved in committee work. Because of my interest in medical education, I volunteered for the PIT Committee and it has given me the opportunity to work closely with other hospitalists around the country, and develop programming specifically targeted toward future hospitalists.
What is the PIT Committee working on?
The committee has continued to find ways for increased engagement of residents and students in SHM. Dr. Brian Kwan, an academic hospitalist at UC San Diego, and I have been developing a travel grant program for resident trainees and hospital medicine fellows to attend the annual meeting. By offering them a stipend to defray the costs of travel if their quality improvement innovation or research project is accepted, we hope that the annual meeting can become a venue for them to highlight their work, while becoming exposed to the many activities and opportunities offered by our society. In addition, it could be a way for them to network with other future hospitalists and established future mentors.
What prompted you to lead the creation of the Student Hospitalist Scholar Grant summer program?
Before I became a hospitalist, I spent about 7 years in research, studying renal genetics. I have always been fascinated by science and asked how I can help to advance our knowledge. As a hospitalist, it became clear to me early on that there are many questions that one can pose about the clinical work we do, the way we practice medicine, or ways to innovate education, and that there are many academic hospitalists who engage in advancing the field. I spearheaded this program because I would like students to see the field of hospital medicine as one in which they can develop a future career in academic medicine, not only by caring for patients, but also by involving themselves in research questions or QI projects.
Do you have any specific advice for students and residents interested in hospital medicine? In what ways can early-career hospitalists utilize SHM resources to leverage their careers?
The decision to pursue a career as a hospitalist will open up many more questions in the future, because there are so many opportunities available. I would suggest that trainees ask in which ways they see themselves growing in the future – clinical research, medical education, QI/patient safety, operations, and hospital leadership are the main avenues. When I interview future faculty, I always pose the same question to each of them: “Every year you are allocated X amount of money that you can use for CME, etc. How are you going to use this money to improve your skills in any particular area?” The ability of candidates to answer this question reflects for me their preparedness to develop themselves as career hospitalists and their willingness to contribute to their group or division in an innovative manner.
The reality is that as one gets older, most will find it difficult to sustain a 26-week/year schedule. So find ways for your energies, in whichever area, to be noticed and developed toward a position of leadership in the hospital or medical school.
As you take care of patients in the hospital or consider your education and training, identify ways in which things can be done better. Invariably, someone in the Society of Hospital Medicine is interested in the same issue(s). Explore your ideas, share them at the meeting, talk to people, go to the SHM website and identify what resources are already available.
If SHM will be your future academic home, volunteer to engage in activities at the chapter or national levels. Our society is really dedicated to identifying ways to welcome you into our exciting and continually evolving field.
Felicia Steele is SHM’s communications coordinator.
Postdischarge antibiotics for complicated pneumonia
Clinical question: Are oral antibiotics as effective as intravenous (IV) antibiotics in the treatment of complicated pneumonia after discharge to home?
Background: Pneumonia is the most common illness among hospitalized children and adolescents (excluding neonates). Among children admitted with community acquired pneumonia, 15% may develop a complicated pneumonia (one with a pleural effusion or empyema). Treatment for these complicated pneumonias may include a variety of invasive procedures, such as video-assisted thorascopic surgery or chest tube placement.
Typically, a long course of antibiotics is prescribed on discharge, which may be oral or parenterally administered via a peripherally inserted central catheter (PICC). Previous studies have shown that oral antibiotics are equivalent to parenteral antibiotics for outpatient treatment of osteomyelitis. However, little evidence exists comparing the effectiveness of the two routes in treating complicated pneumonia.
The rate of PICC complications in complicated pneumonia also has not been well studied.
Study design: Retrospective cohort study.
Setting: Thirty-eight children’s hospitals affiliated with the Children’s Hospital Association.
Synopsis: Over 4 years, 7,820 encounters were identified with 2,123 patients ultimately being included in the cohort. Inclusion criteria were age 2 months to 18 years, and discharge diagnoses of pneumonia and pleural effusion. The authors excluded patients with chronic medical conditions, length of stay (LOS) less than 4 and more than 14 days, patients transferred to or from other institutions, and patients receiving no antibiotics on hospital day 1. The final criteria attempted to avoid inclusion of patients with nosocomial pneumonia. After application of these criteria, individual patient records were reviewed.
Patients were categorized as PICC or oral antibiotics based upon antibiotic route at their initial discharge. Treatment failure was defined as an ED revisit or rehospitalization that led to a change in antibiotic, lengthening of antibiotic course, or pleural drainage. Records were searched for evidence of PICC complications, adverse drug reactions, and other illness-related revisits. Patients in the PICC arm and oral arm were matched by age, race, insurance, LOS, positive vs. negative blood culture, ICU admission, and timing and type of pleural drainage.
Fifty-seven patients had treatment failure (2.7%). In matched analysis, there was no difference in treatment failure between PICC and oral routes (PICC treatment failure OR, 1.26 95% CI, 0.54-2.94). PICC complications were found in 7.1% of patients. Patients with PICC had significantly higher rates of adverse drug reactions (OR, 19.1 95% CI, 4.2-87.3) and illness-related revisits (OR 3.27 95% CI, 1.65-6.48), and all revisits (OR, 4.71 95% CI, 2.97-7.46).
PICC use varied markedly across geographic regions and institutions, with rates varying from less than 10% of cases to approximately 70%. Of geographic regions, the Mid-Atlantic used PICCs least often while the East North Central used them the most.
Bottom line: Treatment failure with both oral and PICC treatment of complicated pneumonia occur at the same rate, and are uncommon. Patients with PICCs had an increased rate of complications, including adverse drug reactions and revisits.
Citation: Shah SS, Srivastava R, Wu S, et al. Intravenous versus oral antibiotics for postdischarge treatment of complicated pneumonia. Pediatrics. 2016;138(6):e20161692. doi: 10.1542/peds.2016-1692.
Dr. Stubblefield is a pediatric hospitalist at Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del., and clinical assistant professor of pediatrics at Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia.
Clinical question: Are oral antibiotics as effective as intravenous (IV) antibiotics in the treatment of complicated pneumonia after discharge to home?
Background: Pneumonia is the most common illness among hospitalized children and adolescents (excluding neonates). Among children admitted with community acquired pneumonia, 15% may develop a complicated pneumonia (one with a pleural effusion or empyema). Treatment for these complicated pneumonias may include a variety of invasive procedures, such as video-assisted thorascopic surgery or chest tube placement.
Typically, a long course of antibiotics is prescribed on discharge, which may be oral or parenterally administered via a peripherally inserted central catheter (PICC). Previous studies have shown that oral antibiotics are equivalent to parenteral antibiotics for outpatient treatment of osteomyelitis. However, little evidence exists comparing the effectiveness of the two routes in treating complicated pneumonia.
The rate of PICC complications in complicated pneumonia also has not been well studied.
Study design: Retrospective cohort study.
Setting: Thirty-eight children’s hospitals affiliated with the Children’s Hospital Association.
Synopsis: Over 4 years, 7,820 encounters were identified with 2,123 patients ultimately being included in the cohort. Inclusion criteria were age 2 months to 18 years, and discharge diagnoses of pneumonia and pleural effusion. The authors excluded patients with chronic medical conditions, length of stay (LOS) less than 4 and more than 14 days, patients transferred to or from other institutions, and patients receiving no antibiotics on hospital day 1. The final criteria attempted to avoid inclusion of patients with nosocomial pneumonia. After application of these criteria, individual patient records were reviewed.
Patients were categorized as PICC or oral antibiotics based upon antibiotic route at their initial discharge. Treatment failure was defined as an ED revisit or rehospitalization that led to a change in antibiotic, lengthening of antibiotic course, or pleural drainage. Records were searched for evidence of PICC complications, adverse drug reactions, and other illness-related revisits. Patients in the PICC arm and oral arm were matched by age, race, insurance, LOS, positive vs. negative blood culture, ICU admission, and timing and type of pleural drainage.
Fifty-seven patients had treatment failure (2.7%). In matched analysis, there was no difference in treatment failure between PICC and oral routes (PICC treatment failure OR, 1.26 95% CI, 0.54-2.94). PICC complications were found in 7.1% of patients. Patients with PICC had significantly higher rates of adverse drug reactions (OR, 19.1 95% CI, 4.2-87.3) and illness-related revisits (OR 3.27 95% CI, 1.65-6.48), and all revisits (OR, 4.71 95% CI, 2.97-7.46).
PICC use varied markedly across geographic regions and institutions, with rates varying from less than 10% of cases to approximately 70%. Of geographic regions, the Mid-Atlantic used PICCs least often while the East North Central used them the most.
Bottom line: Treatment failure with both oral and PICC treatment of complicated pneumonia occur at the same rate, and are uncommon. Patients with PICCs had an increased rate of complications, including adverse drug reactions and revisits.
Citation: Shah SS, Srivastava R, Wu S, et al. Intravenous versus oral antibiotics for postdischarge treatment of complicated pneumonia. Pediatrics. 2016;138(6):e20161692. doi: 10.1542/peds.2016-1692.
Dr. Stubblefield is a pediatric hospitalist at Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del., and clinical assistant professor of pediatrics at Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia.
Clinical question: Are oral antibiotics as effective as intravenous (IV) antibiotics in the treatment of complicated pneumonia after discharge to home?
Background: Pneumonia is the most common illness among hospitalized children and adolescents (excluding neonates). Among children admitted with community acquired pneumonia, 15% may develop a complicated pneumonia (one with a pleural effusion or empyema). Treatment for these complicated pneumonias may include a variety of invasive procedures, such as video-assisted thorascopic surgery or chest tube placement.
Typically, a long course of antibiotics is prescribed on discharge, which may be oral or parenterally administered via a peripherally inserted central catheter (PICC). Previous studies have shown that oral antibiotics are equivalent to parenteral antibiotics for outpatient treatment of osteomyelitis. However, little evidence exists comparing the effectiveness of the two routes in treating complicated pneumonia.
The rate of PICC complications in complicated pneumonia also has not been well studied.
Study design: Retrospective cohort study.
Setting: Thirty-eight children’s hospitals affiliated with the Children’s Hospital Association.
Synopsis: Over 4 years, 7,820 encounters were identified with 2,123 patients ultimately being included in the cohort. Inclusion criteria were age 2 months to 18 years, and discharge diagnoses of pneumonia and pleural effusion. The authors excluded patients with chronic medical conditions, length of stay (LOS) less than 4 and more than 14 days, patients transferred to or from other institutions, and patients receiving no antibiotics on hospital day 1. The final criteria attempted to avoid inclusion of patients with nosocomial pneumonia. After application of these criteria, individual patient records were reviewed.
Patients were categorized as PICC or oral antibiotics based upon antibiotic route at their initial discharge. Treatment failure was defined as an ED revisit or rehospitalization that led to a change in antibiotic, lengthening of antibiotic course, or pleural drainage. Records were searched for evidence of PICC complications, adverse drug reactions, and other illness-related revisits. Patients in the PICC arm and oral arm were matched by age, race, insurance, LOS, positive vs. negative blood culture, ICU admission, and timing and type of pleural drainage.
Fifty-seven patients had treatment failure (2.7%). In matched analysis, there was no difference in treatment failure between PICC and oral routes (PICC treatment failure OR, 1.26 95% CI, 0.54-2.94). PICC complications were found in 7.1% of patients. Patients with PICC had significantly higher rates of adverse drug reactions (OR, 19.1 95% CI, 4.2-87.3) and illness-related revisits (OR 3.27 95% CI, 1.65-6.48), and all revisits (OR, 4.71 95% CI, 2.97-7.46).
PICC use varied markedly across geographic regions and institutions, with rates varying from less than 10% of cases to approximately 70%. Of geographic regions, the Mid-Atlantic used PICCs least often while the East North Central used them the most.
Bottom line: Treatment failure with both oral and PICC treatment of complicated pneumonia occur at the same rate, and are uncommon. Patients with PICCs had an increased rate of complications, including adverse drug reactions and revisits.
Citation: Shah SS, Srivastava R, Wu S, et al. Intravenous versus oral antibiotics for postdischarge treatment of complicated pneumonia. Pediatrics. 2016;138(6):e20161692. doi: 10.1542/peds.2016-1692.
Dr. Stubblefield is a pediatric hospitalist at Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del., and clinical assistant professor of pediatrics at Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia.
Perioperative infliximab does not increase serious infection risk
Administration of infliximab within 4 weeks of elective knee or hip arthroplasty did not have any significant effect on patients’ risk of serious infection after surgery, whereas the use of glucocorticoids increased that risk, in an analysis of a Medicare claims database.
“This increased risk with glucocorticoids has been suggested by previous studies [and] although this risk may be related in part to increased disease severity among glucocorticoid treated patients, a direct medication effect is likely. [These data suggest] that prolonged interruptions in infliximab therapy prior to surgery may be counterproductive if higher dose glucocorticoid therapy is used in substitution,” wrote the authors of the new study, led by Michael D. George, MD, of the University of Pennsylvania in Philadelphia.
Dr. George and his colleagues examined data from the U.S. Medicare claims system on 4,288 elective knee or hip arthroplasties in individuals with rheumatoid arthritis, inflammatory bowel disease, psoriasis, psoriatic arthritis, or ankylosing spondylitis who received infliximab within 6 months prior to the operation during 2007-2013 (Arthritis Care Res. 2017 Jan 27. doi: 10.1002/acr.23209).
The patients had to have received infliximab at least three times within a year of their procedure to establish that they were receiving stable therapy over a long-term period. The investigators also looked at oral prednisone, prednisolone, and methylprednisolone prescriptions and used data on average dosing to determine how much was administered to each subject.
“Although previous studies have treated TNF stopping vs. not stopping as a dichotomous exposure based on an arbitrary (and variable) stopping definition, in this study the primary analysis evaluated stop timing as a more general categorical exposure using 4-week intervals (half the standard rheumatoid arthritis dosing interval) to allow better assessment of the optimal stop timing,” the authors explained.
Stopping infliximab within 4 weeks of the operation did not significantly influence the rate of serious infection within 30 days (adjusted odds ratio, 0.90; 95% CI, 0.60-1.34) and neither did stopping within 4-8 weeks (OR, 0.95; 95% CI, 0.62-1.36) when compared against stopping 8-12 weeks before surgery. Of the 4,288 arthroplasties, 270 serious infections (6.3%) occurred within 30 days of the operation.
There also was no significant difference between stopping within 4 weeks and 8-12 weeks in the rate of prosthetic joint infection within 1 year of the operation (hazard ratio, 0.98; 95% CI, 0.52-1.87). Overall, prosthetic joint infection occurred 2.9 times per 100 person-years.
However, glucocorticoid doses of more than 10 mg per day were risky. The odds for a serious infection within 30 days after surgery more than doubled with that level of use (OR, 2.11; 95% CI, 1.30-3.40), while the risk for a prosthetic joint infection within 1 year of the surgery also rose significantly (HR, 2.70; 95% CI, 1.30-5.60).
“This is a very well done paper that adds important observational data to our understanding of perioperative medication risk,” Dr. Goodman said.
But the study results will not, at least initially, bring about any changes to the proposed guidelines for perioperative management of patients taking antirheumatic drugs that were described at the 2016 annual meeting of the American College of Rheumatology, she said.
“We were aware of the abstract, which was also presented at the ACR last fall at the time the current perioperative medication management guidelines were presented, and it won’t change guidelines at this point,” said Dr. Goodman, who is one of the lead authors of the proposed guidelines. “[But] I think [the study] could provide important background information to use in a randomized clinical trial to compare infection on [and] not on TNF inhibitors.”
The proposed guidelines conditionally recommend that all biologics should be withheld prior to surgery in patients with inflammatory arthritis, that surgery should be planned for the end of the dosing cycle, and that current daily doses of glucocorticoids, rather than supraphysiologic doses, should be continued in adults with rheumatoid arthritis, lupus, or inflammatory arthritis.
The National Institutes of Health, the Rheumatology Research Foundation, and the Department of Veterans Affairs funded the study. Dr. George did not report any relevant financial disclosures. Two coauthors disclosed receiving research grants or consulting fees from pharmaceutical companies for unrelated work.
Administration of infliximab within 4 weeks of elective knee or hip arthroplasty did not have any significant effect on patients’ risk of serious infection after surgery, whereas the use of glucocorticoids increased that risk, in an analysis of a Medicare claims database.
“This increased risk with glucocorticoids has been suggested by previous studies [and] although this risk may be related in part to increased disease severity among glucocorticoid treated patients, a direct medication effect is likely. [These data suggest] that prolonged interruptions in infliximab therapy prior to surgery may be counterproductive if higher dose glucocorticoid therapy is used in substitution,” wrote the authors of the new study, led by Michael D. George, MD, of the University of Pennsylvania in Philadelphia.
Dr. George and his colleagues examined data from the U.S. Medicare claims system on 4,288 elective knee or hip arthroplasties in individuals with rheumatoid arthritis, inflammatory bowel disease, psoriasis, psoriatic arthritis, or ankylosing spondylitis who received infliximab within 6 months prior to the operation during 2007-2013 (Arthritis Care Res. 2017 Jan 27. doi: 10.1002/acr.23209).
The patients had to have received infliximab at least three times within a year of their procedure to establish that they were receiving stable therapy over a long-term period. The investigators also looked at oral prednisone, prednisolone, and methylprednisolone prescriptions and used data on average dosing to determine how much was administered to each subject.
“Although previous studies have treated TNF stopping vs. not stopping as a dichotomous exposure based on an arbitrary (and variable) stopping definition, in this study the primary analysis evaluated stop timing as a more general categorical exposure using 4-week intervals (half the standard rheumatoid arthritis dosing interval) to allow better assessment of the optimal stop timing,” the authors explained.
Stopping infliximab within 4 weeks of the operation did not significantly influence the rate of serious infection within 30 days (adjusted odds ratio, 0.90; 95% CI, 0.60-1.34) and neither did stopping within 4-8 weeks (OR, 0.95; 95% CI, 0.62-1.36) when compared against stopping 8-12 weeks before surgery. Of the 4,288 arthroplasties, 270 serious infections (6.3%) occurred within 30 days of the operation.
There also was no significant difference between stopping within 4 weeks and 8-12 weeks in the rate of prosthetic joint infection within 1 year of the operation (hazard ratio, 0.98; 95% CI, 0.52-1.87). Overall, prosthetic joint infection occurred 2.9 times per 100 person-years.
However, glucocorticoid doses of more than 10 mg per day were risky. The odds for a serious infection within 30 days after surgery more than doubled with that level of use (OR, 2.11; 95% CI, 1.30-3.40), while the risk for a prosthetic joint infection within 1 year of the surgery also rose significantly (HR, 2.70; 95% CI, 1.30-5.60).
“This is a very well done paper that adds important observational data to our understanding of perioperative medication risk,” Dr. Goodman said.
But the study results will not, at least initially, bring about any changes to the proposed guidelines for perioperative management of patients taking antirheumatic drugs that were described at the 2016 annual meeting of the American College of Rheumatology, she said.
“We were aware of the abstract, which was also presented at the ACR last fall at the time the current perioperative medication management guidelines were presented, and it won’t change guidelines at this point,” said Dr. Goodman, who is one of the lead authors of the proposed guidelines. “[But] I think [the study] could provide important background information to use in a randomized clinical trial to compare infection on [and] not on TNF inhibitors.”
The proposed guidelines conditionally recommend that all biologics should be withheld prior to surgery in patients with inflammatory arthritis, that surgery should be planned for the end of the dosing cycle, and that current daily doses of glucocorticoids, rather than supraphysiologic doses, should be continued in adults with rheumatoid arthritis, lupus, or inflammatory arthritis.
The National Institutes of Health, the Rheumatology Research Foundation, and the Department of Veterans Affairs funded the study. Dr. George did not report any relevant financial disclosures. Two coauthors disclosed receiving research grants or consulting fees from pharmaceutical companies for unrelated work.
Administration of infliximab within 4 weeks of elective knee or hip arthroplasty did not have any significant effect on patients’ risk of serious infection after surgery, whereas the use of glucocorticoids increased that risk, in an analysis of a Medicare claims database.
“This increased risk with glucocorticoids has been suggested by previous studies [and] although this risk may be related in part to increased disease severity among glucocorticoid treated patients, a direct medication effect is likely. [These data suggest] that prolonged interruptions in infliximab therapy prior to surgery may be counterproductive if higher dose glucocorticoid therapy is used in substitution,” wrote the authors of the new study, led by Michael D. George, MD, of the University of Pennsylvania in Philadelphia.
Dr. George and his colleagues examined data from the U.S. Medicare claims system on 4,288 elective knee or hip arthroplasties in individuals with rheumatoid arthritis, inflammatory bowel disease, psoriasis, psoriatic arthritis, or ankylosing spondylitis who received infliximab within 6 months prior to the operation during 2007-2013 (Arthritis Care Res. 2017 Jan 27. doi: 10.1002/acr.23209).
The patients had to have received infliximab at least three times within a year of their procedure to establish that they were receiving stable therapy over a long-term period. The investigators also looked at oral prednisone, prednisolone, and methylprednisolone prescriptions and used data on average dosing to determine how much was administered to each subject.
“Although previous studies have treated TNF stopping vs. not stopping as a dichotomous exposure based on an arbitrary (and variable) stopping definition, in this study the primary analysis evaluated stop timing as a more general categorical exposure using 4-week intervals (half the standard rheumatoid arthritis dosing interval) to allow better assessment of the optimal stop timing,” the authors explained.
Stopping infliximab within 4 weeks of the operation did not significantly influence the rate of serious infection within 30 days (adjusted odds ratio, 0.90; 95% CI, 0.60-1.34) and neither did stopping within 4-8 weeks (OR, 0.95; 95% CI, 0.62-1.36) when compared against stopping 8-12 weeks before surgery. Of the 4,288 arthroplasties, 270 serious infections (6.3%) occurred within 30 days of the operation.
There also was no significant difference between stopping within 4 weeks and 8-12 weeks in the rate of prosthetic joint infection within 1 year of the operation (hazard ratio, 0.98; 95% CI, 0.52-1.87). Overall, prosthetic joint infection occurred 2.9 times per 100 person-years.
However, glucocorticoid doses of more than 10 mg per day were risky. The odds for a serious infection within 30 days after surgery more than doubled with that level of use (OR, 2.11; 95% CI, 1.30-3.40), while the risk for a prosthetic joint infection within 1 year of the surgery also rose significantly (HR, 2.70; 95% CI, 1.30-5.60).
“This is a very well done paper that adds important observational data to our understanding of perioperative medication risk,” Dr. Goodman said.
But the study results will not, at least initially, bring about any changes to the proposed guidelines for perioperative management of patients taking antirheumatic drugs that were described at the 2016 annual meeting of the American College of Rheumatology, she said.
“We were aware of the abstract, which was also presented at the ACR last fall at the time the current perioperative medication management guidelines were presented, and it won’t change guidelines at this point,” said Dr. Goodman, who is one of the lead authors of the proposed guidelines. “[But] I think [the study] could provide important background information to use in a randomized clinical trial to compare infection on [and] not on TNF inhibitors.”
The proposed guidelines conditionally recommend that all biologics should be withheld prior to surgery in patients with inflammatory arthritis, that surgery should be planned for the end of the dosing cycle, and that current daily doses of glucocorticoids, rather than supraphysiologic doses, should be continued in adults with rheumatoid arthritis, lupus, or inflammatory arthritis.
The National Institutes of Health, the Rheumatology Research Foundation, and the Department of Veterans Affairs funded the study. Dr. George did not report any relevant financial disclosures. Two coauthors disclosed receiving research grants or consulting fees from pharmaceutical companies for unrelated work.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point:
Major finding: Subjects on glucocorticoids had an OR of 2.11 (95% CI 1.30-3.40) for serious infection within 30 days and an HR of 2.70 (95% CI 1.30-5.60) for prosthetic joint infection within 1 year.
Data source: Retrospective cohort study of 4,288 elective knee and hip arthroplasties in Medicare patients with rheumatoid arthritis, inflammatory bowel disease, psoriasis, psoriatic arthritis, or ankylosing spondylitis during 2007-2013.
Disclosures: The National Institutes of Health, the Rheumatology Research Foundation, and the Department of Veterans Affairs funded the study. Dr. George did not report any relevant financial disclosures. Two coauthors disclosed receiving research grants or consulting fees from pharmaceutical companies for unrelated work.
Lower C. difficile mortality with vancomycin than metronidazole
Treating Clostridium difficile infection with vancomycin achieves the same recurrence rates as does treatment with metronidazole, but with a significantly lower 30-day mortality, new research suggests.
A retrospective, propensity-matched cohort study examined U.S. Department of Veterans Affairs health care system data from 47,471 patients with C. difficile infection who were treated with either vancomycin or metronidazole, according to a report published online Feb. 6 in JAMA Internal Medicine.
“Current guidelines recommend metronidazole hydrochloride as initial therapy for most cases of mild to moderate CDI [Clostridium difficile infection],” wrote Vanessa W. Stevens, PhD, of Veterans Affairs Salt Lake City Health Care System, and her coauthors. “Although an early clinical trial found no difference in cure rates between vancomycin hydrochloride and metronidazole, subsequent observational data and clinical trials suggest that metronidazole is inferior to vancomycin for primary clinical cure, especially in severe cases.”
Their study found patients treated with vancomycin had a similar risk of recurrence compared with those treated with metronidazole (relative risk, 0.98; 95% confidence interval, 0.87 to 1.10), with an overall recurrence rate of 16%.
However, patients treated with vancomycin had a 14% reduction in 30-day mortality compared to the metronidazole-treated group. This was after adjustment for factors such as comorbidity scores, hospitalization history, receipt of chemotherapy, receipt of immunosuppressive medication or proton pump inhibitor therapy in the prior 30-days, or antibiotic use on the day of diagnosis.
The 30-day mortality was not significantly different among patients with mild to moderate CDI, but there was a significant 21% reduction among patients with severe infection. The number needed to treat to prevent one death among patients with severe infection was 25 (JAMA Intern Med. 2017 Feb 6. doi: 10.1001/jamainternmed.2016.9045).
“This is the largest study to date to compare vancomycin and metronidazole in a real-world setting and one of the few studies focused on downstream outcomes of CDI,” researchers reported.
The authors noted that despite strong evidence and guidelines supporting the use of vancomycin for severe CDI – and the fact that 42% of episodes in the study were classified as severe – only 4%-6% of patients were prescribed vancomycin.
“Although the excess treatment costs of vancomycin relative to metronidazole and the concern for vancomycin-resistant Enterococcus will likely remain barriers, improved clinical cure and mortality rates may warrant reconsideration of current prescribing practices,” they wrote. “One approach to minimizing the effects of increasing vancomycin use is to target vancomycin treatment to patients with severe disease.”
The study was supported by researcher grants from the U.S. Department of Veterans Affairs. No conflicts of interest were declared.
Treating Clostridium difficile infection with vancomycin achieves the same recurrence rates as does treatment with metronidazole, but with a significantly lower 30-day mortality, new research suggests.
A retrospective, propensity-matched cohort study examined U.S. Department of Veterans Affairs health care system data from 47,471 patients with C. difficile infection who were treated with either vancomycin or metronidazole, according to a report published online Feb. 6 in JAMA Internal Medicine.
“Current guidelines recommend metronidazole hydrochloride as initial therapy for most cases of mild to moderate CDI [Clostridium difficile infection],” wrote Vanessa W. Stevens, PhD, of Veterans Affairs Salt Lake City Health Care System, and her coauthors. “Although an early clinical trial found no difference in cure rates between vancomycin hydrochloride and metronidazole, subsequent observational data and clinical trials suggest that metronidazole is inferior to vancomycin for primary clinical cure, especially in severe cases.”
Their study found patients treated with vancomycin had a similar risk of recurrence compared with those treated with metronidazole (relative risk, 0.98; 95% confidence interval, 0.87 to 1.10), with an overall recurrence rate of 16%.
However, patients treated with vancomycin had a 14% reduction in 30-day mortality compared to the metronidazole-treated group. This was after adjustment for factors such as comorbidity scores, hospitalization history, receipt of chemotherapy, receipt of immunosuppressive medication or proton pump inhibitor therapy in the prior 30-days, or antibiotic use on the day of diagnosis.
The 30-day mortality was not significantly different among patients with mild to moderate CDI, but there was a significant 21% reduction among patients with severe infection. The number needed to treat to prevent one death among patients with severe infection was 25 (JAMA Intern Med. 2017 Feb 6. doi: 10.1001/jamainternmed.2016.9045).
“This is the largest study to date to compare vancomycin and metronidazole in a real-world setting and one of the few studies focused on downstream outcomes of CDI,” researchers reported.
The authors noted that despite strong evidence and guidelines supporting the use of vancomycin for severe CDI – and the fact that 42% of episodes in the study were classified as severe – only 4%-6% of patients were prescribed vancomycin.
“Although the excess treatment costs of vancomycin relative to metronidazole and the concern for vancomycin-resistant Enterococcus will likely remain barriers, improved clinical cure and mortality rates may warrant reconsideration of current prescribing practices,” they wrote. “One approach to minimizing the effects of increasing vancomycin use is to target vancomycin treatment to patients with severe disease.”
The study was supported by researcher grants from the U.S. Department of Veterans Affairs. No conflicts of interest were declared.
Treating Clostridium difficile infection with vancomycin achieves the same recurrence rates as does treatment with metronidazole, but with a significantly lower 30-day mortality, new research suggests.
A retrospective, propensity-matched cohort study examined U.S. Department of Veterans Affairs health care system data from 47,471 patients with C. difficile infection who were treated with either vancomycin or metronidazole, according to a report published online Feb. 6 in JAMA Internal Medicine.
“Current guidelines recommend metronidazole hydrochloride as initial therapy for most cases of mild to moderate CDI [Clostridium difficile infection],” wrote Vanessa W. Stevens, PhD, of Veterans Affairs Salt Lake City Health Care System, and her coauthors. “Although an early clinical trial found no difference in cure rates between vancomycin hydrochloride and metronidazole, subsequent observational data and clinical trials suggest that metronidazole is inferior to vancomycin for primary clinical cure, especially in severe cases.”
Their study found patients treated with vancomycin had a similar risk of recurrence compared with those treated with metronidazole (relative risk, 0.98; 95% confidence interval, 0.87 to 1.10), with an overall recurrence rate of 16%.
However, patients treated with vancomycin had a 14% reduction in 30-day mortality compared to the metronidazole-treated group. This was after adjustment for factors such as comorbidity scores, hospitalization history, receipt of chemotherapy, receipt of immunosuppressive medication or proton pump inhibitor therapy in the prior 30-days, or antibiotic use on the day of diagnosis.
The 30-day mortality was not significantly different among patients with mild to moderate CDI, but there was a significant 21% reduction among patients with severe infection. The number needed to treat to prevent one death among patients with severe infection was 25 (JAMA Intern Med. 2017 Feb 6. doi: 10.1001/jamainternmed.2016.9045).
“This is the largest study to date to compare vancomycin and metronidazole in a real-world setting and one of the few studies focused on downstream outcomes of CDI,” researchers reported.
The authors noted that despite strong evidence and guidelines supporting the use of vancomycin for severe CDI – and the fact that 42% of episodes in the study were classified as severe – only 4%-6% of patients were prescribed vancomycin.
“Although the excess treatment costs of vancomycin relative to metronidazole and the concern for vancomycin-resistant Enterococcus will likely remain barriers, improved clinical cure and mortality rates may warrant reconsideration of current prescribing practices,” they wrote. “One approach to minimizing the effects of increasing vancomycin use is to target vancomycin treatment to patients with severe disease.”
The study was supported by researcher grants from the U.S. Department of Veterans Affairs. No conflicts of interest were declared.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Vancomycin therapy is associated with significantly lower 30-day mortality from severe Clostridium difficile infection compared to metronidazole.
Major finding: Treatment with vancomycin prevented one death per 25 patients with severe C. difficile infection.
Data source: A retrospective, propensity-matched cohort study of 47,471 patients with C. difficile infection.
Disclosures: The study was supported by researcher grants from the U.S. Department of Veterans Affairs. No conflicts of interest were declared.
Everything We Say and Do: Use familiar terminology to allay patients’ fears
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM ’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I clearly explain diagnoses and treatment plans in plain terms.
Why I do it
We hear repeatedly from patients and families that a major source of their fear comes from “not knowing.” Fear of the unknown. If our patients and their families do not understand the message we are trying to communicate, these fears will be realized. It is our responsibility to explain their medical situation(s) to them in plain terms that they can comprehend, so as to allay those fears and enable them to become active, informed participants in their care.
How I do it
I start by reminding myself that I want to treat each patient as I would want a member of my own family to be treated. No one else in my family is in the medical field, so this means I must avoid medical terminology and use more familiar, everyday phrases. For example, I say “heart doctor” or “lung doctor” instead of “cardiologist” or “pulmonologist.” I also prefer “sonogram” to “ultrasound” because most people have heard that term in relation to a pregnancy. Even “EEG” and “EKG” need more plain descriptions.
I also try to use common, relatable analogies when explaining diseases. My favorite is to describe COPD (or any restrictive lung disease) like an old, hard sponge as compared with normal lungs, which are like a new, soft sponge.
I use the Teach-Back Method (which has already been well-discussed in this column by Dr. Trina Dorrah) to check for comprehension. If there are still issues with my message not being received as I had hoped, then I try again to find the terminology or an analogy that will connect with that patient.
Hopefully, using familiar, relatable language in this manner gives my patients and their families a better understanding of their diagnoses and care plans, quells their fears, and enhances their experience.
Dr. Sharp is a chief hospitalist with Sound Physicians at UF Health in Jacksonville, Fla., and a member of SHM's Patient Experience Committee.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM ’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I clearly explain diagnoses and treatment plans in plain terms.
Why I do it
We hear repeatedly from patients and families that a major source of their fear comes from “not knowing.” Fear of the unknown. If our patients and their families do not understand the message we are trying to communicate, these fears will be realized. It is our responsibility to explain their medical situation(s) to them in plain terms that they can comprehend, so as to allay those fears and enable them to become active, informed participants in their care.
How I do it
I start by reminding myself that I want to treat each patient as I would want a member of my own family to be treated. No one else in my family is in the medical field, so this means I must avoid medical terminology and use more familiar, everyday phrases. For example, I say “heart doctor” or “lung doctor” instead of “cardiologist” or “pulmonologist.” I also prefer “sonogram” to “ultrasound” because most people have heard that term in relation to a pregnancy. Even “EEG” and “EKG” need more plain descriptions.
I also try to use common, relatable analogies when explaining diseases. My favorite is to describe COPD (or any restrictive lung disease) like an old, hard sponge as compared with normal lungs, which are like a new, soft sponge.
I use the Teach-Back Method (which has already been well-discussed in this column by Dr. Trina Dorrah) to check for comprehension. If there are still issues with my message not being received as I had hoped, then I try again to find the terminology or an analogy that will connect with that patient.
Hopefully, using familiar, relatable language in this manner gives my patients and their families a better understanding of their diagnoses and care plans, quells their fears, and enhances their experience.
Dr. Sharp is a chief hospitalist with Sound Physicians at UF Health in Jacksonville, Fla., and a member of SHM's Patient Experience Committee.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM ’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I clearly explain diagnoses and treatment plans in plain terms.
Why I do it
We hear repeatedly from patients and families that a major source of their fear comes from “not knowing.” Fear of the unknown. If our patients and their families do not understand the message we are trying to communicate, these fears will be realized. It is our responsibility to explain their medical situation(s) to them in plain terms that they can comprehend, so as to allay those fears and enable them to become active, informed participants in their care.
How I do it
I start by reminding myself that I want to treat each patient as I would want a member of my own family to be treated. No one else in my family is in the medical field, so this means I must avoid medical terminology and use more familiar, everyday phrases. For example, I say “heart doctor” or “lung doctor” instead of “cardiologist” or “pulmonologist.” I also prefer “sonogram” to “ultrasound” because most people have heard that term in relation to a pregnancy. Even “EEG” and “EKG” need more plain descriptions.
I also try to use common, relatable analogies when explaining diseases. My favorite is to describe COPD (or any restrictive lung disease) like an old, hard sponge as compared with normal lungs, which are like a new, soft sponge.
I use the Teach-Back Method (which has already been well-discussed in this column by Dr. Trina Dorrah) to check for comprehension. If there are still issues with my message not being received as I had hoped, then I try again to find the terminology or an analogy that will connect with that patient.
Hopefully, using familiar, relatable language in this manner gives my patients and their families a better understanding of their diagnoses and care plans, quells their fears, and enhances their experience.
Dr. Sharp is a chief hospitalist with Sound Physicians at UF Health in Jacksonville, Fla., and a member of SHM's Patient Experience Committee.
Ventilator use in patients with advanced dementia
Clinical question: Does the increasing number of ICU beds in the U.S. affect the use of mechanical ventilation in nursing home patients with advanced dementia?
Background: Some physicians are concerned that increases in ICU beds in the U.S. will translate to increased treatment of advanced dementia in the ICU, which might not line up with their preferences, nor improve mortality.
Study design: Retrospective cohort study.
Setting: Hospitals that completed the American Hospital Association (AHA) annual survey.
Synopsis: From 2000 to 2013, there were 635,008 hospitalizations of 380,060 Medicare patients with advanced dementia who had been in a nursing home in the 120 days prior to hospital admission. ICU admissions increased to 38.5% from 16.9% during the same period. The rate of mechanical ventilation per 1,000 hospital admissions increased to 78 from 39, and 1-year mortality for ventilation was unchanged.
For each increase in 10 ICU beds within a hospital, the adjusted odds ratio for receiving mechanical ventilation was 1.06 (95% CI, 1.05-1.07).
Limitations of the study include that only hospitals completing the AHA annual survey were studied, and also lacked information on individual patients.
Bottom line: The use of mechanical ventilation increased in hospitalized nursing home patients with advanced dementia, correlating with increased ICU bed capacity, yet with no changes in survival.
Citation: Teno JM, Gozalo P, Khandelwal N, et al. Association of increasing use of mechanical ventilation among nursing home residents with advanced dementia and intensive care unit beds [published online ahead of print, Oct. 10, 2016]. JAMA Int Med. 2016;176(12):1809-16.
Dr. Balch is a clinical instructor at the University of Utah School of Medicine and an academic hospitalist at the University of Utah Hospital.
Clinical question: Does the increasing number of ICU beds in the U.S. affect the use of mechanical ventilation in nursing home patients with advanced dementia?
Background: Some physicians are concerned that increases in ICU beds in the U.S. will translate to increased treatment of advanced dementia in the ICU, which might not line up with their preferences, nor improve mortality.
Study design: Retrospective cohort study.
Setting: Hospitals that completed the American Hospital Association (AHA) annual survey.
Synopsis: From 2000 to 2013, there were 635,008 hospitalizations of 380,060 Medicare patients with advanced dementia who had been in a nursing home in the 120 days prior to hospital admission. ICU admissions increased to 38.5% from 16.9% during the same period. The rate of mechanical ventilation per 1,000 hospital admissions increased to 78 from 39, and 1-year mortality for ventilation was unchanged.
For each increase in 10 ICU beds within a hospital, the adjusted odds ratio for receiving mechanical ventilation was 1.06 (95% CI, 1.05-1.07).
Limitations of the study include that only hospitals completing the AHA annual survey were studied, and also lacked information on individual patients.
Bottom line: The use of mechanical ventilation increased in hospitalized nursing home patients with advanced dementia, correlating with increased ICU bed capacity, yet with no changes in survival.
Citation: Teno JM, Gozalo P, Khandelwal N, et al. Association of increasing use of mechanical ventilation among nursing home residents with advanced dementia and intensive care unit beds [published online ahead of print, Oct. 10, 2016]. JAMA Int Med. 2016;176(12):1809-16.
Dr. Balch is a clinical instructor at the University of Utah School of Medicine and an academic hospitalist at the University of Utah Hospital.
Clinical question: Does the increasing number of ICU beds in the U.S. affect the use of mechanical ventilation in nursing home patients with advanced dementia?
Background: Some physicians are concerned that increases in ICU beds in the U.S. will translate to increased treatment of advanced dementia in the ICU, which might not line up with their preferences, nor improve mortality.
Study design: Retrospective cohort study.
Setting: Hospitals that completed the American Hospital Association (AHA) annual survey.
Synopsis: From 2000 to 2013, there were 635,008 hospitalizations of 380,060 Medicare patients with advanced dementia who had been in a nursing home in the 120 days prior to hospital admission. ICU admissions increased to 38.5% from 16.9% during the same period. The rate of mechanical ventilation per 1,000 hospital admissions increased to 78 from 39, and 1-year mortality for ventilation was unchanged.
For each increase in 10 ICU beds within a hospital, the adjusted odds ratio for receiving mechanical ventilation was 1.06 (95% CI, 1.05-1.07).
Limitations of the study include that only hospitals completing the AHA annual survey were studied, and also lacked information on individual patients.
Bottom line: The use of mechanical ventilation increased in hospitalized nursing home patients with advanced dementia, correlating with increased ICU bed capacity, yet with no changes in survival.
Citation: Teno JM, Gozalo P, Khandelwal N, et al. Association of increasing use of mechanical ventilation among nursing home residents with advanced dementia and intensive care unit beds [published online ahead of print, Oct. 10, 2016]. JAMA Int Med. 2016;176(12):1809-16.
Dr. Balch is a clinical instructor at the University of Utah School of Medicine and an academic hospitalist at the University of Utah Hospital.
Consensus guidelines for calcium channel blocker poisoning
Clinical question: What is the best management approach for adults who are admitted to the hospital with a calcium channel blocker (CCB) overdose?
Background: There is significant morbidity and mortality from cardiac drug poisoning. Overall, the level of evidence in the literature on the treatment of CCB toxicity is very low. Prior to the current publication there were no guidelines for treating patients admitted to the hospital with a CCB overdose.
Setting: Panel members participated in online votes, telephone meetings, and two face-to-face meetings to develop the guidelines.
Synopsis: In symptomatic CCB poisoning, the following first-line measures are strongly recommended: IV calcium, with norepinephrine or epinephrine in the presence of shock, and high-dose IV insulin (with other first-line treatments) if there is myocardial dysfunction.
Further lower-strength suggestions were made: insulin therapy as monotherapy if cardiac dysfunction present, or in combination with other therapies if there is no cardiac dysfunction; atropine in the setting of symptomatic bradycardia; and dobutamine or epinephrine in the presence of cardiogenic shock.
For refractory CCB, toxicity suggestions included incremental doses of high-dose insulin (if myocardial dysfunction is present, or even if it is not present in periarrest situations), IV lipid emulsion therapy, and pacemaker for unstable bradycardia (if there is no evidence of cardiac dysfunction). If the patient is in refractory shock or periarrest, the panel suggests the use of venoarterial extracorporeal membrane oxygenation (VA-ECMO).
Limitations included the limited availability of evidence.
Bottom line: Management of CCB toxicity should include IV calcium and high-dose IV insulin, with vasopressors for shock, and other additional therapies for refractory cases.
Citation: St-Onge M, Anseeuw K, Cantrell FL, et al. Experts’ consensus recommendations for the management of calcium channel blocker poisoning in adults [published online ahead of print, Oct. 3, 2016]. Crit Care Med. doi: 10.1097/CCM.0000000000002087.
Dr. Balch is a clinical instructor at the University of Utah School of Medicine and an academic hospitalist at the University of Utah Hospital.
Clinical question: What is the best management approach for adults who are admitted to the hospital with a calcium channel blocker (CCB) overdose?
Background: There is significant morbidity and mortality from cardiac drug poisoning. Overall, the level of evidence in the literature on the treatment of CCB toxicity is very low. Prior to the current publication there were no guidelines for treating patients admitted to the hospital with a CCB overdose.
Setting: Panel members participated in online votes, telephone meetings, and two face-to-face meetings to develop the guidelines.
Synopsis: In symptomatic CCB poisoning, the following first-line measures are strongly recommended: IV calcium, with norepinephrine or epinephrine in the presence of shock, and high-dose IV insulin (with other first-line treatments) if there is myocardial dysfunction.
Further lower-strength suggestions were made: insulin therapy as monotherapy if cardiac dysfunction present, or in combination with other therapies if there is no cardiac dysfunction; atropine in the setting of symptomatic bradycardia; and dobutamine or epinephrine in the presence of cardiogenic shock.
For refractory CCB, toxicity suggestions included incremental doses of high-dose insulin (if myocardial dysfunction is present, or even if it is not present in periarrest situations), IV lipid emulsion therapy, and pacemaker for unstable bradycardia (if there is no evidence of cardiac dysfunction). If the patient is in refractory shock or periarrest, the panel suggests the use of venoarterial extracorporeal membrane oxygenation (VA-ECMO).
Limitations included the limited availability of evidence.
Bottom line: Management of CCB toxicity should include IV calcium and high-dose IV insulin, with vasopressors for shock, and other additional therapies for refractory cases.
Citation: St-Onge M, Anseeuw K, Cantrell FL, et al. Experts’ consensus recommendations for the management of calcium channel blocker poisoning in adults [published online ahead of print, Oct. 3, 2016]. Crit Care Med. doi: 10.1097/CCM.0000000000002087.
Dr. Balch is a clinical instructor at the University of Utah School of Medicine and an academic hospitalist at the University of Utah Hospital.
Clinical question: What is the best management approach for adults who are admitted to the hospital with a calcium channel blocker (CCB) overdose?
Background: There is significant morbidity and mortality from cardiac drug poisoning. Overall, the level of evidence in the literature on the treatment of CCB toxicity is very low. Prior to the current publication there were no guidelines for treating patients admitted to the hospital with a CCB overdose.
Setting: Panel members participated in online votes, telephone meetings, and two face-to-face meetings to develop the guidelines.
Synopsis: In symptomatic CCB poisoning, the following first-line measures are strongly recommended: IV calcium, with norepinephrine or epinephrine in the presence of shock, and high-dose IV insulin (with other first-line treatments) if there is myocardial dysfunction.
Further lower-strength suggestions were made: insulin therapy as monotherapy if cardiac dysfunction present, or in combination with other therapies if there is no cardiac dysfunction; atropine in the setting of symptomatic bradycardia; and dobutamine or epinephrine in the presence of cardiogenic shock.
For refractory CCB, toxicity suggestions included incremental doses of high-dose insulin (if myocardial dysfunction is present, or even if it is not present in periarrest situations), IV lipid emulsion therapy, and pacemaker for unstable bradycardia (if there is no evidence of cardiac dysfunction). If the patient is in refractory shock or periarrest, the panel suggests the use of venoarterial extracorporeal membrane oxygenation (VA-ECMO).
Limitations included the limited availability of evidence.
Bottom line: Management of CCB toxicity should include IV calcium and high-dose IV insulin, with vasopressors for shock, and other additional therapies for refractory cases.
Citation: St-Onge M, Anseeuw K, Cantrell FL, et al. Experts’ consensus recommendations for the management of calcium channel blocker poisoning in adults [published online ahead of print, Oct. 3, 2016]. Crit Care Med. doi: 10.1097/CCM.0000000000002087.
Dr. Balch is a clinical instructor at the University of Utah School of Medicine and an academic hospitalist at the University of Utah Hospital.
Burnout: No laughing matter
Much has been written about burnout in U.S. physicians over the course of many years. Burnout is a syndrome that is exemplified by emotional exhaustion, depersonalization, and a low sense of personal accomplishment. It appears that hospitalists are particularly prone to burnout, being at the very front line of patient care. In addition, the prevalence of burnout appears to be getting worse. According to a survey from the American Medical Association, the prevalence of burnout in 2011 was 45%. Three years later in 2014 the prevalence was up to 55%.1,2
Although triggers for the onset and intensity of burnout likely vary by specialty, a recent Medscape Lifestyle Report found the most common causes of burnout among physicians included (see graphic):3
• Bureaucratic tasks.
• Work hours.
• Computerization.
• Compensation.

• Lower work satisfaction.
• Disrupted personal relationships.
• Substance misuse.
• Depression.
• Suicide.
Burnout also leads to lower productivity, higher job turnover, and early retirement. In addition, from a systems perspective, burnout is associated with higher medical errors, reduced quality of patient care, and lower patient satisfaction. And, at its most extreme, burnout is deadly: Sadly, every year, 300-400 physicians in the United States commit suicide. Female physicians are 2.3 times more likely to commit suicide than are female nonphysicians; for males, the risk is 1.4 times higher among physicians compared to the general population.1
Proactive approaches
Despite all these sobering statistics on the prevalence and outcomes of burnout among physicians, the ongoing question is, what can we do about it? Although awareness and recognition of burnout has grown substantially over time, successful interventions to prevent or mitigate burnout have not. Many potential interventions and ideas have surfaced and have been published, but none have had impressive impacts or have been adopted widely within or across institutions. According to a Modern Healthcare survey of approximately 100 health care CEOs, only about one-third reported that their organization had programs to address physician burnout, although about another one-third reported attempts to develop such programs.1
The good news is that at least there is a lot of activity around trying new interventions to reduce burnout, including in medical schools and graduate training programs. The thought is that if you can employ healthy resilience tactics during training, these can be carried throughout a career to diminish the risk and/or severity of burnout, despite any challenges that arise along the way.
Some of these interventions are aimed at individuals (to enhance personal resilience and coping skills) while others are aimed at the level of organizations (to reduce organizational stress and/or workload). A recent Modern Healthcare article found several good examples:1
• New York’s Albert Einstein College of Medicine’s WellMed program has been designed to help students develop healthy and balanced habits and attitudes, and to enhance their personal resilience, for the short and the long term.
• Baystate Health in Massachusetts hosts a physician leadership academy that offers training in communication, unconscious bias, strategy, and other management skills, to enhance individual resilience and organizational engagement.
• HealthPartners, a not-for-profit, Minnesota-based health care organization, has specific programs to engage physicians and allow them to have organizational impact, as well as programs to simplify technology use.
Organization efforts are key to prevent, treat
The key to reducing burnout does seem to be employing a combination of self-directed and organization-directed interventions, each of which enhances resilience and reduces workplace stressors (i.e., administrative tasks and workload). Specific to hospitalists, Leslie Flores, MBA, recently wrote about burnout at The Hospital Leader blog. Her list included several specific examples to reduce the top causes of burnout among busy hospitalists:4
• Modifying the skill mix in hospital medicine groups so that less costly support staff are doing much of the work not requiring a physician’s expertise, freeing up hospitalists to provide better care to more patients.
• Reducing unnecessary interruptions and the stress they cause, via both technology and process improvement.
• Paying deliberate attention to hospitalist personal and professional well-being.
• Adjusting hospitalist schedules and work flow so that hospitalists can be more efficient (that is, do less low-value work and re-work) and have better work-life balance.
• Ensuring that hospitalists have the training, clinical competencies, and support to comfortably perform in expanded clinical roles.
Many of these systemic solutions were recently validated as likely able to have an impact on burnout (and seem to be more effective than interventions focused on individual resilience).5 A recent meta-analysis found that physician-directed interventions were associated with small but significant reductions in burnout; these were primarily mindfulness-based stress reduction techniques, educational interventions targeting physicians self-confidence and communication skills, exercise, or a combination of these features. More impactful were organization-directed interventions, which were associated with more significant reductions in burnout; these were primarily aimed at reducing workload and enhancing teamwork and leadership.
In sum
It is important for all of us hospitalists to understand and try to mitigate burnout within our teams. Although individual-focused interventions can have some effect, most efforts should primarily be focused on system-based interventions, to reduce administrative burdens and workload. Through such system design and redesign, we can likely reduce burnout amongst our teams, and therefore improve the sustainability of our specialty.
References
1.http://www.modernhealthcare.com/article/20161029/MAGAZINE/310299983
2. http://www.mayoclinicproceedings.org/article/S0025-6196(15)00716-8/abstract
3.http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview#page=5
4. http://blogs.hospitalmedicine.org/Blog/making-hospital-medicine-a-sustainable-specialty/
5.http://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2588814
Much has been written about burnout in U.S. physicians over the course of many years. Burnout is a syndrome that is exemplified by emotional exhaustion, depersonalization, and a low sense of personal accomplishment. It appears that hospitalists are particularly prone to burnout, being at the very front line of patient care. In addition, the prevalence of burnout appears to be getting worse. According to a survey from the American Medical Association, the prevalence of burnout in 2011 was 45%. Three years later in 2014 the prevalence was up to 55%.1,2
Although triggers for the onset and intensity of burnout likely vary by specialty, a recent Medscape Lifestyle Report found the most common causes of burnout among physicians included (see graphic):3
• Bureaucratic tasks.
• Work hours.
• Computerization.
• Compensation.

• Lower work satisfaction.
• Disrupted personal relationships.
• Substance misuse.
• Depression.
• Suicide.
Burnout also leads to lower productivity, higher job turnover, and early retirement. In addition, from a systems perspective, burnout is associated with higher medical errors, reduced quality of patient care, and lower patient satisfaction. And, at its most extreme, burnout is deadly: Sadly, every year, 300-400 physicians in the United States commit suicide. Female physicians are 2.3 times more likely to commit suicide than are female nonphysicians; for males, the risk is 1.4 times higher among physicians compared to the general population.1
Proactive approaches
Despite all these sobering statistics on the prevalence and outcomes of burnout among physicians, the ongoing question is, what can we do about it? Although awareness and recognition of burnout has grown substantially over time, successful interventions to prevent or mitigate burnout have not. Many potential interventions and ideas have surfaced and have been published, but none have had impressive impacts or have been adopted widely within or across institutions. According to a Modern Healthcare survey of approximately 100 health care CEOs, only about one-third reported that their organization had programs to address physician burnout, although about another one-third reported attempts to develop such programs.1
The good news is that at least there is a lot of activity around trying new interventions to reduce burnout, including in medical schools and graduate training programs. The thought is that if you can employ healthy resilience tactics during training, these can be carried throughout a career to diminish the risk and/or severity of burnout, despite any challenges that arise along the way.
Some of these interventions are aimed at individuals (to enhance personal resilience and coping skills) while others are aimed at the level of organizations (to reduce organizational stress and/or workload). A recent Modern Healthcare article found several good examples:1
• New York’s Albert Einstein College of Medicine’s WellMed program has been designed to help students develop healthy and balanced habits and attitudes, and to enhance their personal resilience, for the short and the long term.
• Baystate Health in Massachusetts hosts a physician leadership academy that offers training in communication, unconscious bias, strategy, and other management skills, to enhance individual resilience and organizational engagement.
• HealthPartners, a not-for-profit, Minnesota-based health care organization, has specific programs to engage physicians and allow them to have organizational impact, as well as programs to simplify technology use.
Organization efforts are key to prevent, treat
The key to reducing burnout does seem to be employing a combination of self-directed and organization-directed interventions, each of which enhances resilience and reduces workplace stressors (i.e., administrative tasks and workload). Specific to hospitalists, Leslie Flores, MBA, recently wrote about burnout at The Hospital Leader blog. Her list included several specific examples to reduce the top causes of burnout among busy hospitalists:4
• Modifying the skill mix in hospital medicine groups so that less costly support staff are doing much of the work not requiring a physician’s expertise, freeing up hospitalists to provide better care to more patients.
• Reducing unnecessary interruptions and the stress they cause, via both technology and process improvement.
• Paying deliberate attention to hospitalist personal and professional well-being.
• Adjusting hospitalist schedules and work flow so that hospitalists can be more efficient (that is, do less low-value work and re-work) and have better work-life balance.
• Ensuring that hospitalists have the training, clinical competencies, and support to comfortably perform in expanded clinical roles.
Many of these systemic solutions were recently validated as likely able to have an impact on burnout (and seem to be more effective than interventions focused on individual resilience).5 A recent meta-analysis found that physician-directed interventions were associated with small but significant reductions in burnout; these were primarily mindfulness-based stress reduction techniques, educational interventions targeting physicians self-confidence and communication skills, exercise, or a combination of these features. More impactful were organization-directed interventions, which were associated with more significant reductions in burnout; these were primarily aimed at reducing workload and enhancing teamwork and leadership.
In sum
It is important for all of us hospitalists to understand and try to mitigate burnout within our teams. Although individual-focused interventions can have some effect, most efforts should primarily be focused on system-based interventions, to reduce administrative burdens and workload. Through such system design and redesign, we can likely reduce burnout amongst our teams, and therefore improve the sustainability of our specialty.
References
1.http://www.modernhealthcare.com/article/20161029/MAGAZINE/310299983
2. http://www.mayoclinicproceedings.org/article/S0025-6196(15)00716-8/abstract
3.http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview#page=5
4. http://blogs.hospitalmedicine.org/Blog/making-hospital-medicine-a-sustainable-specialty/
5.http://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2588814
Much has been written about burnout in U.S. physicians over the course of many years. Burnout is a syndrome that is exemplified by emotional exhaustion, depersonalization, and a low sense of personal accomplishment. It appears that hospitalists are particularly prone to burnout, being at the very front line of patient care. In addition, the prevalence of burnout appears to be getting worse. According to a survey from the American Medical Association, the prevalence of burnout in 2011 was 45%. Three years later in 2014 the prevalence was up to 55%.1,2
Although triggers for the onset and intensity of burnout likely vary by specialty, a recent Medscape Lifestyle Report found the most common causes of burnout among physicians included (see graphic):3
• Bureaucratic tasks.
• Work hours.
• Computerization.
• Compensation.

• Lower work satisfaction.
• Disrupted personal relationships.
• Substance misuse.
• Depression.
• Suicide.
Burnout also leads to lower productivity, higher job turnover, and early retirement. In addition, from a systems perspective, burnout is associated with higher medical errors, reduced quality of patient care, and lower patient satisfaction. And, at its most extreme, burnout is deadly: Sadly, every year, 300-400 physicians in the United States commit suicide. Female physicians are 2.3 times more likely to commit suicide than are female nonphysicians; for males, the risk is 1.4 times higher among physicians compared to the general population.1
Proactive approaches
Despite all these sobering statistics on the prevalence and outcomes of burnout among physicians, the ongoing question is, what can we do about it? Although awareness and recognition of burnout has grown substantially over time, successful interventions to prevent or mitigate burnout have not. Many potential interventions and ideas have surfaced and have been published, but none have had impressive impacts or have been adopted widely within or across institutions. According to a Modern Healthcare survey of approximately 100 health care CEOs, only about one-third reported that their organization had programs to address physician burnout, although about another one-third reported attempts to develop such programs.1
The good news is that at least there is a lot of activity around trying new interventions to reduce burnout, including in medical schools and graduate training programs. The thought is that if you can employ healthy resilience tactics during training, these can be carried throughout a career to diminish the risk and/or severity of burnout, despite any challenges that arise along the way.
Some of these interventions are aimed at individuals (to enhance personal resilience and coping skills) while others are aimed at the level of organizations (to reduce organizational stress and/or workload). A recent Modern Healthcare article found several good examples:1
• New York’s Albert Einstein College of Medicine’s WellMed program has been designed to help students develop healthy and balanced habits and attitudes, and to enhance their personal resilience, for the short and the long term.
• Baystate Health in Massachusetts hosts a physician leadership academy that offers training in communication, unconscious bias, strategy, and other management skills, to enhance individual resilience and organizational engagement.
• HealthPartners, a not-for-profit, Minnesota-based health care organization, has specific programs to engage physicians and allow them to have organizational impact, as well as programs to simplify technology use.
Organization efforts are key to prevent, treat
The key to reducing burnout does seem to be employing a combination of self-directed and organization-directed interventions, each of which enhances resilience and reduces workplace stressors (i.e., administrative tasks and workload). Specific to hospitalists, Leslie Flores, MBA, recently wrote about burnout at The Hospital Leader blog. Her list included several specific examples to reduce the top causes of burnout among busy hospitalists:4
• Modifying the skill mix in hospital medicine groups so that less costly support staff are doing much of the work not requiring a physician’s expertise, freeing up hospitalists to provide better care to more patients.
• Reducing unnecessary interruptions and the stress they cause, via both technology and process improvement.
• Paying deliberate attention to hospitalist personal and professional well-being.
• Adjusting hospitalist schedules and work flow so that hospitalists can be more efficient (that is, do less low-value work and re-work) and have better work-life balance.
• Ensuring that hospitalists have the training, clinical competencies, and support to comfortably perform in expanded clinical roles.
Many of these systemic solutions were recently validated as likely able to have an impact on burnout (and seem to be more effective than interventions focused on individual resilience).5 A recent meta-analysis found that physician-directed interventions were associated with small but significant reductions in burnout; these were primarily mindfulness-based stress reduction techniques, educational interventions targeting physicians self-confidence and communication skills, exercise, or a combination of these features. More impactful were organization-directed interventions, which were associated with more significant reductions in burnout; these were primarily aimed at reducing workload and enhancing teamwork and leadership.
In sum
It is important for all of us hospitalists to understand and try to mitigate burnout within our teams. Although individual-focused interventions can have some effect, most efforts should primarily be focused on system-based interventions, to reduce administrative burdens and workload. Through such system design and redesign, we can likely reduce burnout amongst our teams, and therefore improve the sustainability of our specialty.
References
1.http://www.modernhealthcare.com/article/20161029/MAGAZINE/310299983
2. http://www.mayoclinicproceedings.org/article/S0025-6196(15)00716-8/abstract
3.http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview#page=5
4. http://blogs.hospitalmedicine.org/Blog/making-hospital-medicine-a-sustainable-specialty/
5.http://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2588814
Conservative oxygen therapy in critically ill patients
Clinical question: Does a conservative oxygenation strategy improve clinical outcomes, compared with standard clinical practice among critically ill patients?
Background: Supraphysiologic levels of oxygen have been linked to direct cellular injury through generation of reactive oxygen species. Hyperoxia is known to cause airway injury, including diffuse alveolar damage and tracheobronchitis; it also is linked to worse clinical outcomes in various cardiac and surgical patients. ICU patients have not been studied.
Setting: Single-center, academic hospital in Italy.
Synopsis: Investigators randomized 480 adults admitted to the ICU for at least 72 hours to either standard practice (allowing PaO2 up to 150 mmHg, SpO2 97%-100%) or the conservative protocol (PaO2 70-100 mmHg or SpO2 94%-98%). Patients who were pregnant, readmitted, immunosuppressed, neutropenic, with decompensated COPD or acute respiratory distress syndrome were excluded. Outcomes included ICU mortality, hospital mortality, new-onset organ failure, or new infection.
Enrollment was slow, the authors noted, partially due to an earthquake that damaged the facility, and the trial was stopped short of the planned 660 patient sample size.
In an intent-to-treat analysis, there was a statistically significant decrease in ICU and hospital mortality, shock, liver failure, and bacteremia among the conservative group.
Limitations included possible confounding from higher illness severity in the standard practice group, as well as the single-center focus that terminated early due to enrollment challenges.
Bottom line: A conservative oxygen strategy had a statistically significant decrease in ICU and hospital mortality, shock, liver failure, and bacteremia.
Citation: Girardis M, Busani S, Damiani E, et al. Effect of conservative vs conventional oxygen therapy on mortality among patients in an intensive care unit. JAMA. 2016;316(15):1583-9.
Dr. Marr is a clinical instructor at the University of Utah School of Medicine and an academic hospitalist at the University of Utah Hospital.
Clinical question: Does a conservative oxygenation strategy improve clinical outcomes, compared with standard clinical practice among critically ill patients?
Background: Supraphysiologic levels of oxygen have been linked to direct cellular injury through generation of reactive oxygen species. Hyperoxia is known to cause airway injury, including diffuse alveolar damage and tracheobronchitis; it also is linked to worse clinical outcomes in various cardiac and surgical patients. ICU patients have not been studied.
Setting: Single-center, academic hospital in Italy.
Synopsis: Investigators randomized 480 adults admitted to the ICU for at least 72 hours to either standard practice (allowing PaO2 up to 150 mmHg, SpO2 97%-100%) or the conservative protocol (PaO2 70-100 mmHg or SpO2 94%-98%). Patients who were pregnant, readmitted, immunosuppressed, neutropenic, with decompensated COPD or acute respiratory distress syndrome were excluded. Outcomes included ICU mortality, hospital mortality, new-onset organ failure, or new infection.
Enrollment was slow, the authors noted, partially due to an earthquake that damaged the facility, and the trial was stopped short of the planned 660 patient sample size.
In an intent-to-treat analysis, there was a statistically significant decrease in ICU and hospital mortality, shock, liver failure, and bacteremia among the conservative group.
Limitations included possible confounding from higher illness severity in the standard practice group, as well as the single-center focus that terminated early due to enrollment challenges.
Bottom line: A conservative oxygen strategy had a statistically significant decrease in ICU and hospital mortality, shock, liver failure, and bacteremia.
Citation: Girardis M, Busani S, Damiani E, et al. Effect of conservative vs conventional oxygen therapy on mortality among patients in an intensive care unit. JAMA. 2016;316(15):1583-9.
Dr. Marr is a clinical instructor at the University of Utah School of Medicine and an academic hospitalist at the University of Utah Hospital.
Clinical question: Does a conservative oxygenation strategy improve clinical outcomes, compared with standard clinical practice among critically ill patients?
Background: Supraphysiologic levels of oxygen have been linked to direct cellular injury through generation of reactive oxygen species. Hyperoxia is known to cause airway injury, including diffuse alveolar damage and tracheobronchitis; it also is linked to worse clinical outcomes in various cardiac and surgical patients. ICU patients have not been studied.
Setting: Single-center, academic hospital in Italy.
Synopsis: Investigators randomized 480 adults admitted to the ICU for at least 72 hours to either standard practice (allowing PaO2 up to 150 mmHg, SpO2 97%-100%) or the conservative protocol (PaO2 70-100 mmHg or SpO2 94%-98%). Patients who were pregnant, readmitted, immunosuppressed, neutropenic, with decompensated COPD or acute respiratory distress syndrome were excluded. Outcomes included ICU mortality, hospital mortality, new-onset organ failure, or new infection.
Enrollment was slow, the authors noted, partially due to an earthquake that damaged the facility, and the trial was stopped short of the planned 660 patient sample size.
In an intent-to-treat analysis, there was a statistically significant decrease in ICU and hospital mortality, shock, liver failure, and bacteremia among the conservative group.
Limitations included possible confounding from higher illness severity in the standard practice group, as well as the single-center focus that terminated early due to enrollment challenges.
Bottom line: A conservative oxygen strategy had a statistically significant decrease in ICU and hospital mortality, shock, liver failure, and bacteremia.
Citation: Girardis M, Busani S, Damiani E, et al. Effect of conservative vs conventional oxygen therapy on mortality among patients in an intensive care unit. JAMA. 2016;316(15):1583-9.
Dr. Marr is a clinical instructor at the University of Utah School of Medicine and an academic hospitalist at the University of Utah Hospital.
Prevalence of pulmonary embolism among syncope patients
Clinical question: What is the prevalence of acute pulmonary emboli (PE) in patients admitted for syncope?
Background: An acute pulmonary embolism is a differential consideration among patients admitted with syncope. However, current guidelines do not guide evaluation.
Study design: Cross-sectional study.
Setting: Two academic and nine non-academic hospitals in Italy.
Synopsis: Five hundred-sixty patients admitted with a first episode of syncope were evaluated for a PE. Patients with atrial fibrillation, treatment with anticoagulation, recurrent syncope, or who were pregnant were excluded. The simplified Wells score was used to stratify patients into low and high-risk groups, while low-risk groups received D-dimer testing; 230 patients had a positive D-dimer or a high-risk Wells score and received either CT pulmonary angiography or VQ scans.
Ninety-seven of the 230 patients were found to have a PE (42.2%), leading to a prevalence of 17.3% among the entire cohort. The study did not include the 1,867 patients who were discharged from the ED without admission, potentially leading to bias and overestimating the prevalence of pulmonary emboli (PE).
Bottom line: The prevalence of PE in patients with syncope is higher than previously thought, highlighting the importance of considering acute PE in patients hospitalized with syncope.
Citation: Prandoni P, Lensing AWA, Prins MH, et al. Prevalence of pulmonary embolism among patients hospitalized for syncope. N Engl J Med. 2016;375(16):1524-31.
Dr. Marr is a clinical instructor at the University of Utah School of Medicine and an academic hospitalist at the University of Utah Hospital.
Clinical question: What is the prevalence of acute pulmonary emboli (PE) in patients admitted for syncope?
Background: An acute pulmonary embolism is a differential consideration among patients admitted with syncope. However, current guidelines do not guide evaluation.
Study design: Cross-sectional study.
Setting: Two academic and nine non-academic hospitals in Italy.
Synopsis: Five hundred-sixty patients admitted with a first episode of syncope were evaluated for a PE. Patients with atrial fibrillation, treatment with anticoagulation, recurrent syncope, or who were pregnant were excluded. The simplified Wells score was used to stratify patients into low and high-risk groups, while low-risk groups received D-dimer testing; 230 patients had a positive D-dimer or a high-risk Wells score and received either CT pulmonary angiography or VQ scans.
Ninety-seven of the 230 patients were found to have a PE (42.2%), leading to a prevalence of 17.3% among the entire cohort. The study did not include the 1,867 patients who were discharged from the ED without admission, potentially leading to bias and overestimating the prevalence of pulmonary emboli (PE).
Bottom line: The prevalence of PE in patients with syncope is higher than previously thought, highlighting the importance of considering acute PE in patients hospitalized with syncope.
Citation: Prandoni P, Lensing AWA, Prins MH, et al. Prevalence of pulmonary embolism among patients hospitalized for syncope. N Engl J Med. 2016;375(16):1524-31.
Dr. Marr is a clinical instructor at the University of Utah School of Medicine and an academic hospitalist at the University of Utah Hospital.
Clinical question: What is the prevalence of acute pulmonary emboli (PE) in patients admitted for syncope?
Background: An acute pulmonary embolism is a differential consideration among patients admitted with syncope. However, current guidelines do not guide evaluation.
Study design: Cross-sectional study.
Setting: Two academic and nine non-academic hospitals in Italy.
Synopsis: Five hundred-sixty patients admitted with a first episode of syncope were evaluated for a PE. Patients with atrial fibrillation, treatment with anticoagulation, recurrent syncope, or who were pregnant were excluded. The simplified Wells score was used to stratify patients into low and high-risk groups, while low-risk groups received D-dimer testing; 230 patients had a positive D-dimer or a high-risk Wells score and received either CT pulmonary angiography or VQ scans.
Ninety-seven of the 230 patients were found to have a PE (42.2%), leading to a prevalence of 17.3% among the entire cohort. The study did not include the 1,867 patients who were discharged from the ED without admission, potentially leading to bias and overestimating the prevalence of pulmonary emboli (PE).
Bottom line: The prevalence of PE in patients with syncope is higher than previously thought, highlighting the importance of considering acute PE in patients hospitalized with syncope.
Citation: Prandoni P, Lensing AWA, Prins MH, et al. Prevalence of pulmonary embolism among patients hospitalized for syncope. N Engl J Med. 2016;375(16):1524-31.
Dr. Marr is a clinical instructor at the University of Utah School of Medicine and an academic hospitalist at the University of Utah Hospital.