User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Thinking Outside the DRG Box
When choosing quality improvement activities, hospitalists have no shortage of choices. In this column, I offer a strategic guide for hospitalists as they assess where best to spend their energy as the shift to value-based care progresses. This includes the introduction of MACRA, the landmark new payment program for doctors and other clinicians (aka the Medicare Access and CHIP Reauthorization Act of 2015), with its incentives for participation in alternative payment models.
Since 1983, Medicare has reimbursed hospitals using a lump-sum payment known as a diagnosis-related group, or DRG. Since then, hospitals have focused a good deal of their energy on removing needless expenses from the hospitalization to improve their bottom line, recognizing the DRG payment they receive is relatively fixed. To this end, a major strategy has been to use hospitalists to decrease length of stay and “right size” the utilization of in-hospital tests and treatments.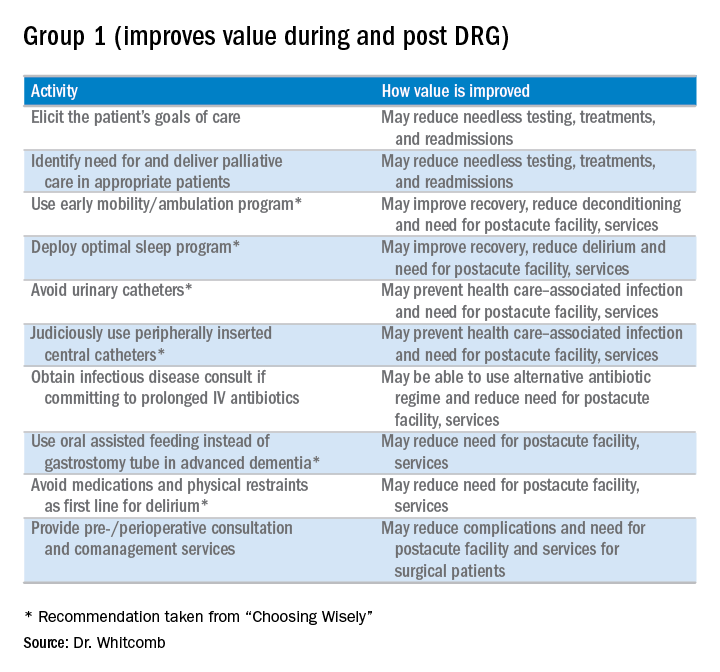
However, things are changing as we enter the era of alternative payment models such as accountable care organizations (ACOs) and bundled payments. The lens Medicare (and, to a great extent, commercial payors) peers through to assess inpatient hospital costs is the DRG payment amount. Beyond that, Medicare has little visibility into the actual costs hospitals incur. Since hospital spending equates to the payment amount for a DRG, it becomes apparent that the incremental opportunity for hospitalists to improve value (quality divided by cost) in alternative payment models stems from payments outside the DRG. Such payments include those related to the post-acute period such as nursing and rehabilitation facilities, readmissions, and part B activity (e.g., consultants and outpatient tests).
What does this mean for hospitalists? MACRA begins in 2019, but initial payments will be based on 2017 performance. The associated advantage of participating in an “advanced alternative payment model” where there is accountability for care beyond the hospitalization is that hospitalists will be rewarded for taking costs out of the post-acute time period.
To be clear, hospitalists should remain agents of in-hospital efficiency and quality. After all, that is how we add value to the hospitals in which we practice. All things being equal, however, hospitalists should focus on practices that will improve value beyond the four walls of the hospital.
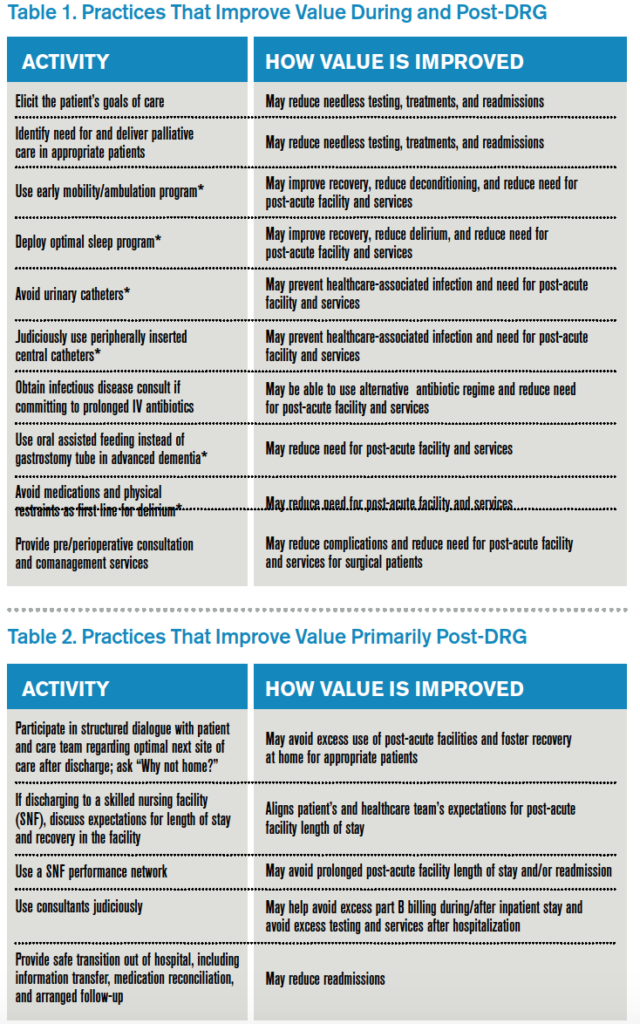
Here is my shortlist of these practices. While there is crossover between the categories, I divide the practices into those that improve value during the DRG period and also post-DRG and those that improve value primarily post-DRG (thanks to Choosing Wisely for contributing to the recommendations with an asterisk1):
Thinking outside the DRG box will require an adjustment to the approach taken by hospitalists because the current demands are often more than enough for a day’s work. Hospitalists will be called upon to innovate and fashion better approaches to care. This will require support by other members of the healthcare team so hospitalists can work smarter, not harder, to meet the requirements of a changing healthcare system. A prerequisite is better payment models that align financial incentives so that providing higher-value care is sustainable and appropriately rewarded.

Reference
Clinician lists. Choosing Wisely website. Accessed October 25, 2016.
When choosing quality improvement activities, hospitalists have no shortage of choices. In this column, I offer a strategic guide for hospitalists as they assess where best to spend their energy as the shift to value-based care progresses. This includes the introduction of MACRA, the landmark new payment program for doctors and other clinicians (aka the Medicare Access and CHIP Reauthorization Act of 2015), with its incentives for participation in alternative payment models.
Since 1983, Medicare has reimbursed hospitals using a lump-sum payment known as a diagnosis-related group, or DRG. Since then, hospitals have focused a good deal of their energy on removing needless expenses from the hospitalization to improve their bottom line, recognizing the DRG payment they receive is relatively fixed. To this end, a major strategy has been to use hospitalists to decrease length of stay and “right size” the utilization of in-hospital tests and treatments.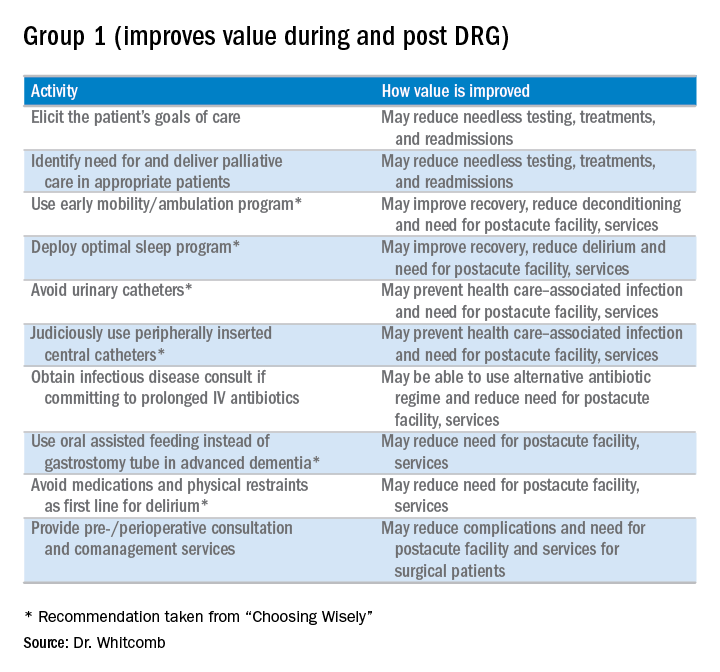
However, things are changing as we enter the era of alternative payment models such as accountable care organizations (ACOs) and bundled payments. The lens Medicare (and, to a great extent, commercial payors) peers through to assess inpatient hospital costs is the DRG payment amount. Beyond that, Medicare has little visibility into the actual costs hospitals incur. Since hospital spending equates to the payment amount for a DRG, it becomes apparent that the incremental opportunity for hospitalists to improve value (quality divided by cost) in alternative payment models stems from payments outside the DRG. Such payments include those related to the post-acute period such as nursing and rehabilitation facilities, readmissions, and part B activity (e.g., consultants and outpatient tests).
What does this mean for hospitalists? MACRA begins in 2019, but initial payments will be based on 2017 performance. The associated advantage of participating in an “advanced alternative payment model” where there is accountability for care beyond the hospitalization is that hospitalists will be rewarded for taking costs out of the post-acute time period.
To be clear, hospitalists should remain agents of in-hospital efficiency and quality. After all, that is how we add value to the hospitals in which we practice. All things being equal, however, hospitalists should focus on practices that will improve value beyond the four walls of the hospital.
Here is my shortlist of these practices. While there is crossover between the categories, I divide the practices into those that improve value during the DRG period and also post-DRG and those that improve value primarily post-DRG (thanks to Choosing Wisely for contributing to the recommendations with an asterisk1):
Thinking outside the DRG box will require an adjustment to the approach taken by hospitalists because the current demands are often more than enough for a day’s work. Hospitalists will be called upon to innovate and fashion better approaches to care. This will require support by other members of the healthcare team so hospitalists can work smarter, not harder, to meet the requirements of a changing healthcare system. A prerequisite is better payment models that align financial incentives so that providing higher-value care is sustainable and appropriately rewarded.

Reference
Clinician lists. Choosing Wisely website. Accessed October 25, 2016.
When choosing quality improvement activities, hospitalists have no shortage of choices. In this column, I offer a strategic guide for hospitalists as they assess where best to spend their energy as the shift to value-based care progresses. This includes the introduction of MACRA, the landmark new payment program for doctors and other clinicians (aka the Medicare Access and CHIP Reauthorization Act of 2015), with its incentives for participation in alternative payment models.
Since 1983, Medicare has reimbursed hospitals using a lump-sum payment known as a diagnosis-related group, or DRG. Since then, hospitals have focused a good deal of their energy on removing needless expenses from the hospitalization to improve their bottom line, recognizing the DRG payment they receive is relatively fixed. To this end, a major strategy has been to use hospitalists to decrease length of stay and “right size” the utilization of in-hospital tests and treatments.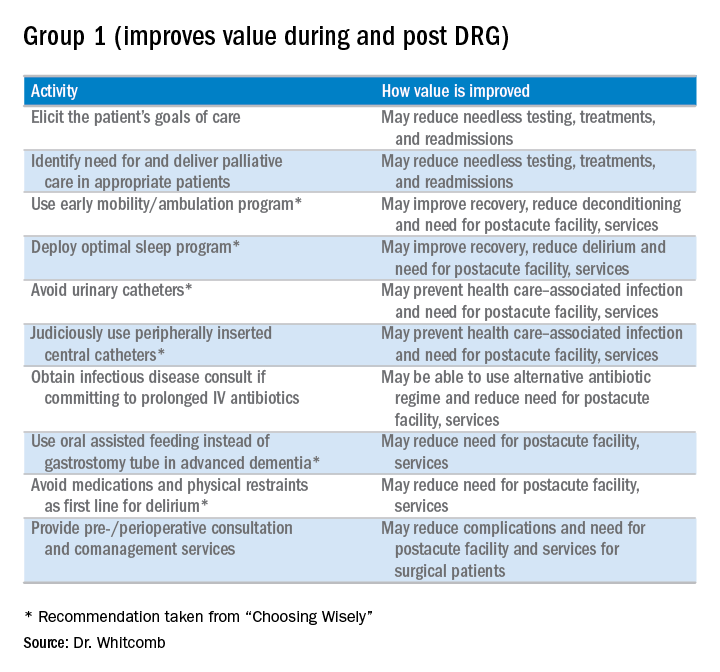
However, things are changing as we enter the era of alternative payment models such as accountable care organizations (ACOs) and bundled payments. The lens Medicare (and, to a great extent, commercial payors) peers through to assess inpatient hospital costs is the DRG payment amount. Beyond that, Medicare has little visibility into the actual costs hospitals incur. Since hospital spending equates to the payment amount for a DRG, it becomes apparent that the incremental opportunity for hospitalists to improve value (quality divided by cost) in alternative payment models stems from payments outside the DRG. Such payments include those related to the post-acute period such as nursing and rehabilitation facilities, readmissions, and part B activity (e.g., consultants and outpatient tests).
What does this mean for hospitalists? MACRA begins in 2019, but initial payments will be based on 2017 performance. The associated advantage of participating in an “advanced alternative payment model” where there is accountability for care beyond the hospitalization is that hospitalists will be rewarded for taking costs out of the post-acute time period.
To be clear, hospitalists should remain agents of in-hospital efficiency and quality. After all, that is how we add value to the hospitals in which we practice. All things being equal, however, hospitalists should focus on practices that will improve value beyond the four walls of the hospital.
Here is my shortlist of these practices. While there is crossover between the categories, I divide the practices into those that improve value during the DRG period and also post-DRG and those that improve value primarily post-DRG (thanks to Choosing Wisely for contributing to the recommendations with an asterisk1):
Thinking outside the DRG box will require an adjustment to the approach taken by hospitalists because the current demands are often more than enough for a day’s work. Hospitalists will be called upon to innovate and fashion better approaches to care. This will require support by other members of the healthcare team so hospitalists can work smarter, not harder, to meet the requirements of a changing healthcare system. A prerequisite is better payment models that align financial incentives so that providing higher-value care is sustainable and appropriately rewarded.

Reference
Clinician lists. Choosing Wisely website. Accessed October 25, 2016.
Tips for Working with Difficult Doctors
As a hospitalist, caring for critically ill or injured patients can be stressful and demanding. Working with difficult doctors, those who exhibit intimidating and disruptive behaviors such as verbal outbursts and physical threats as well as passive activities such as refusing to perform assigned tasks, can make the work environment even more challenging.1 Some docs are routinely reluctant—or refuse—to answer questions or return phone calls or pages. Some communicate in condescending language or voice intonation; some are brutally impatient.1
The most difficult doctors to work with are those who are not aligned with the hospital’s or treatment team’s goals and those who aren’t open to feedback and coaching, says Rob Zipper, MD, MMM, SFHM, regional chief medical officer of Sound Physicians, based in Tacoma, Wash.
“If physicians are aware of a practice’s guidelines and goals but simply won’t comply with them, it makes it harder on everyone else who is pulling the ship in the same direction,” he says.
Unruly physicians don’t just annoy their coworkers. According to a sentinel event alert from The Joint Commission, they can:
- foster medical errors;
- contribute to poor patient satisfaction;
- contribute to preventable adverse outcomes;
- increase the cost of care;
- undermine team effectiveness; and
- cause qualified clinicians, administrators, and managers to seek new positions in more professional environments.1
“These issues are all connected,” says Stephen R. Nichols, MD, chief of clinical operations performance at the Schumacher Group in Brownwood, Texas. “Disruptive behaviors create mitigated communications and dissatisfaction among staff, which bleeds over into other aspects that are involved secondarily.”
Stephen M. Paskoff, Esq., president and CEO of ELI in Atlanta, can attest to the most severe consequences of bad behavior on patient care.
At one institution, a surgeon’s disruptive behavior lead to a coworker forgetting to perform a procedure and a patient dying.2 In another incident, the emergency department stopped calling on a medical subspecialist who was predictably abusive. The subspecialist knew how to treat a specific patient with an unusual intervention. Since the specialist was not consulted initially, the patient ended up in the intensive care unit.2
One bad hospitalist can bring down the reputation of an entire team.
“Many programs are incentivized based on medical staff and primary-care physicians’ perceptions of their care, so there are direct and indirect consequences,” Dr. Zipper says.
The bottom line, says Felix Aguirre, MD, SFHM, vice president of medical affairs at IPC Healthcare in North Hollywood, Calif., is that it only takes one bad experience to tarnish a group, but it takes many positive experiences to erase the damage.
The Roots of Evil
Intimidating and disruptive behavior stems from both individual and systemic factors. Care providers who exhibit characteristics such as self-centeredness, immaturity, or defensiveness can be more prone to unprofessional behavior. They can lack interpersonal, coping, or conflict-management skills.1
Systemic factors are marked by pressures related to increased productivity demands, cost-containment requirements, embedded hierarchies, and fear of litigation in the healthcare environment. These pressures can be further exacerbated by changes to or differences in the authority, autonomy, empowerment, and roles or values of professionals on the healthcare team as well as by the continual daily changes in shifts, rotations, and interdepartmental support staff. This dynamic creates challenges for interprofessional communication and development of trust among team members.1
According to The Joint Commission, intimidating and disruptive behaviors are often manifested by healthcare professionals in positions of power.1 But other members of the care team can be problematic as well.
“In my experience, conflicts usually revolve around different perspectives and objectives, even if both parties are acting respectfully,” Dr. Zipper says. “Sometimes, however, providers or other care team members are tired or stressed and don’t behave professionally.”
Paskoff, who has more than 40 years of experience in healthcare-related workplace issues, including serving as an investigator for the U.S. Equal Employment Opportunity Commission, says some doctors learn bad behaviors from their mentors and that behaviors can be passed down through generations because they are tolerated.
“When I asked one physician who had outstanding training and an outstanding technical reputation how he became abusive, he said, ‘I learned from the best.’” Paskoff was actually able to track the doctor’s training to the late 1800s and physicians who were known for similar behaviors.
Confronting Those Who Misbehave
Dr. Zipper says physicians should confront behavioral issues directly.
“I will typically discuss a complaint with a doctor privately, and ask him or her what happened without being accusatory,” he says. “I try to provide as much concrete and objective information as I can. The doctor needs to know that you are trying to help him or her succeed. That said, if something is clearly bad behavior, feedback should be direct and include a statement such as, ‘This is not how we behave in this practice.’”
At times, it may not be possible to discuss an emergent matter, such as during a code blue.
“However, I will often ask if anyone on the code team has any ideas or concerns before ending the code,” Dr. Nichols says. “Then after the critical time has passed, it is important to debrief and reconnect with the team, especially the less-experienced members who may have lingering concerns.”
For many employees, however, it is difficult to report disruptive behaviors. This is due to a fear of retaliation and the stigma associated with “blowing the whistle” on a colleague as well as a general reluctance to confront an intimidator.1
If an employee cannot muster the courage to confront a disruptive coworker or if the issue isn’t resolved by talking with the difficult individual, an employee should be a good citizen and report bad behavior to the appropriate hospital authority in a timely manner, says A. Kevin Troutman, Esq., a partner at Fisher Phillips in Houston and a former healthcare human resources executive.
Hospitals accredited by The Joint Commission are required to create a code of conduct that defines disruptive and inappropriate behaviors. In addition, leaders must create and implement a process for managing these behaviors.1
Helping Difficult Doctors
After a physician or another employee has been called out for bad behavior, steps need to be taken to correct the problem. Robert Fuller, Esq., an attorney with Nelson Hardiman, LLP, in Los Angeles, has found a positive-oriented intervention called “the 3-Ds”—which stands for diagnose, design, and do—that has been a successful tool for achieving positive change. The strategy involves a supervisor and employee mutually developing a worksheet to diagnose the problem. Next, they design a remediation and improvement plan. Finally, they implement the plan and specify dates to achieve certain milestones. Coworkers should be informed of the plan and be urged to support it.
“Make it clear that the positive aspect of this plan turns to progressive discipline, including termination, if the employee doesn’t improve or abandons the plan of action,” Fuller says. In most cases, troublemakers will make a sincere effort to control disruptive tendencies.
Troutman suggests enlisting the assistance of a respected peer.
“Have a senior-level doctor help the noncompliant physician understand why his or her behavior creates problems for everyone, including the doctor himself,” he says. “Also, consider connecting compensation and other rewards to job performance, which encompasses good behavior and good citizenship within the organization. Make expectations and consequences clear.”
If an employee has a recent change in behavior, ask if there is a reason.
“It is my experience that sudden changes in behaviors are often the result of a personal or clinical issue, so it is important and humane to make certain that there is not some other cause for the change before assuming someone is simply being disruptive or difficult,” Dr. Nichols says.
Many healthcare institutions are now setting up centers of professionalism. Paskoff reports that The Center for Professionalism and Peer Support (CPPS) was created in 2008 at Brigham and Women’s Hospital in Boston to educate the hospital community regarding professionalism and manage unprofessional behavior.3 CPPS has established standards of behavior and a framework to deal with difficult behaviors.
“An employee is told what he or she is doing wrong, receives counseling, and is given resources to improve,” he explains. “If an employee doesn’t improve, he or she is told that the behavior won’t be tolerated.”
Dismissing Bad Employees
After addressing the specifics of unacceptable behavior and explaining the consequences of repeating it, leadership should monitor subsequent conduct and provide feedback.
“If the employee commits other violations or behaves badly, promptly address the misconduct again and make it clear that further such actions will not be tolerated,” Troutman says. “Expect immediate and sustained improvement and compliance. Be consistent, and if bad conduct continues after an opportunity to improve, do not prolong anyone’s suffering. Instead, terminate the disruptive employee. When you do, make the reasons clear.”
Karen Appold is a medical writer in Pennsylvania.
References
- Behaviors that undermine a culture of safety. The Joint Commission website. Accessed April 17, 2015.
- Whittemore AD, New England Society for Vascular Surgery. The impact of professionalism on safe surgical care. J Vasc Surg. 2007;45(2):415-419.
- Shapiro J, Whittemore A, Tsen LC. Instituting a culture of professionalism: the establishment of a center for professionalism and peer support. Jt Comm J Qual Patient Saf. 2014;40(4):168-177.
As a hospitalist, caring for critically ill or injured patients can be stressful and demanding. Working with difficult doctors, those who exhibit intimidating and disruptive behaviors such as verbal outbursts and physical threats as well as passive activities such as refusing to perform assigned tasks, can make the work environment even more challenging.1 Some docs are routinely reluctant—or refuse—to answer questions or return phone calls or pages. Some communicate in condescending language or voice intonation; some are brutally impatient.1
The most difficult doctors to work with are those who are not aligned with the hospital’s or treatment team’s goals and those who aren’t open to feedback and coaching, says Rob Zipper, MD, MMM, SFHM, regional chief medical officer of Sound Physicians, based in Tacoma, Wash.
“If physicians are aware of a practice’s guidelines and goals but simply won’t comply with them, it makes it harder on everyone else who is pulling the ship in the same direction,” he says.
Unruly physicians don’t just annoy their coworkers. According to a sentinel event alert from The Joint Commission, they can:
- foster medical errors;
- contribute to poor patient satisfaction;
- contribute to preventable adverse outcomes;
- increase the cost of care;
- undermine team effectiveness; and
- cause qualified clinicians, administrators, and managers to seek new positions in more professional environments.1
“These issues are all connected,” says Stephen R. Nichols, MD, chief of clinical operations performance at the Schumacher Group in Brownwood, Texas. “Disruptive behaviors create mitigated communications and dissatisfaction among staff, which bleeds over into other aspects that are involved secondarily.”
Stephen M. Paskoff, Esq., president and CEO of ELI in Atlanta, can attest to the most severe consequences of bad behavior on patient care.
At one institution, a surgeon’s disruptive behavior lead to a coworker forgetting to perform a procedure and a patient dying.2 In another incident, the emergency department stopped calling on a medical subspecialist who was predictably abusive. The subspecialist knew how to treat a specific patient with an unusual intervention. Since the specialist was not consulted initially, the patient ended up in the intensive care unit.2
One bad hospitalist can bring down the reputation of an entire team.
“Many programs are incentivized based on medical staff and primary-care physicians’ perceptions of their care, so there are direct and indirect consequences,” Dr. Zipper says.
The bottom line, says Felix Aguirre, MD, SFHM, vice president of medical affairs at IPC Healthcare in North Hollywood, Calif., is that it only takes one bad experience to tarnish a group, but it takes many positive experiences to erase the damage.
The Roots of Evil
Intimidating and disruptive behavior stems from both individual and systemic factors. Care providers who exhibit characteristics such as self-centeredness, immaturity, or defensiveness can be more prone to unprofessional behavior. They can lack interpersonal, coping, or conflict-management skills.1
Systemic factors are marked by pressures related to increased productivity demands, cost-containment requirements, embedded hierarchies, and fear of litigation in the healthcare environment. These pressures can be further exacerbated by changes to or differences in the authority, autonomy, empowerment, and roles or values of professionals on the healthcare team as well as by the continual daily changes in shifts, rotations, and interdepartmental support staff. This dynamic creates challenges for interprofessional communication and development of trust among team members.1
According to The Joint Commission, intimidating and disruptive behaviors are often manifested by healthcare professionals in positions of power.1 But other members of the care team can be problematic as well.
“In my experience, conflicts usually revolve around different perspectives and objectives, even if both parties are acting respectfully,” Dr. Zipper says. “Sometimes, however, providers or other care team members are tired or stressed and don’t behave professionally.”
Paskoff, who has more than 40 years of experience in healthcare-related workplace issues, including serving as an investigator for the U.S. Equal Employment Opportunity Commission, says some doctors learn bad behaviors from their mentors and that behaviors can be passed down through generations because they are tolerated.
“When I asked one physician who had outstanding training and an outstanding technical reputation how he became abusive, he said, ‘I learned from the best.’” Paskoff was actually able to track the doctor’s training to the late 1800s and physicians who were known for similar behaviors.
Confronting Those Who Misbehave
Dr. Zipper says physicians should confront behavioral issues directly.
“I will typically discuss a complaint with a doctor privately, and ask him or her what happened without being accusatory,” he says. “I try to provide as much concrete and objective information as I can. The doctor needs to know that you are trying to help him or her succeed. That said, if something is clearly bad behavior, feedback should be direct and include a statement such as, ‘This is not how we behave in this practice.’”
At times, it may not be possible to discuss an emergent matter, such as during a code blue.
“However, I will often ask if anyone on the code team has any ideas or concerns before ending the code,” Dr. Nichols says. “Then after the critical time has passed, it is important to debrief and reconnect with the team, especially the less-experienced members who may have lingering concerns.”
For many employees, however, it is difficult to report disruptive behaviors. This is due to a fear of retaliation and the stigma associated with “blowing the whistle” on a colleague as well as a general reluctance to confront an intimidator.1
If an employee cannot muster the courage to confront a disruptive coworker or if the issue isn’t resolved by talking with the difficult individual, an employee should be a good citizen and report bad behavior to the appropriate hospital authority in a timely manner, says A. Kevin Troutman, Esq., a partner at Fisher Phillips in Houston and a former healthcare human resources executive.
Hospitals accredited by The Joint Commission are required to create a code of conduct that defines disruptive and inappropriate behaviors. In addition, leaders must create and implement a process for managing these behaviors.1
Helping Difficult Doctors
After a physician or another employee has been called out for bad behavior, steps need to be taken to correct the problem. Robert Fuller, Esq., an attorney with Nelson Hardiman, LLP, in Los Angeles, has found a positive-oriented intervention called “the 3-Ds”—which stands for diagnose, design, and do—that has been a successful tool for achieving positive change. The strategy involves a supervisor and employee mutually developing a worksheet to diagnose the problem. Next, they design a remediation and improvement plan. Finally, they implement the plan and specify dates to achieve certain milestones. Coworkers should be informed of the plan and be urged to support it.
“Make it clear that the positive aspect of this plan turns to progressive discipline, including termination, if the employee doesn’t improve or abandons the plan of action,” Fuller says. In most cases, troublemakers will make a sincere effort to control disruptive tendencies.
Troutman suggests enlisting the assistance of a respected peer.
“Have a senior-level doctor help the noncompliant physician understand why his or her behavior creates problems for everyone, including the doctor himself,” he says. “Also, consider connecting compensation and other rewards to job performance, which encompasses good behavior and good citizenship within the organization. Make expectations and consequences clear.”
If an employee has a recent change in behavior, ask if there is a reason.
“It is my experience that sudden changes in behaviors are often the result of a personal or clinical issue, so it is important and humane to make certain that there is not some other cause for the change before assuming someone is simply being disruptive or difficult,” Dr. Nichols says.
Many healthcare institutions are now setting up centers of professionalism. Paskoff reports that The Center for Professionalism and Peer Support (CPPS) was created in 2008 at Brigham and Women’s Hospital in Boston to educate the hospital community regarding professionalism and manage unprofessional behavior.3 CPPS has established standards of behavior and a framework to deal with difficult behaviors.
“An employee is told what he or she is doing wrong, receives counseling, and is given resources to improve,” he explains. “If an employee doesn’t improve, he or she is told that the behavior won’t be tolerated.”
Dismissing Bad Employees
After addressing the specifics of unacceptable behavior and explaining the consequences of repeating it, leadership should monitor subsequent conduct and provide feedback.
“If the employee commits other violations or behaves badly, promptly address the misconduct again and make it clear that further such actions will not be tolerated,” Troutman says. “Expect immediate and sustained improvement and compliance. Be consistent, and if bad conduct continues after an opportunity to improve, do not prolong anyone’s suffering. Instead, terminate the disruptive employee. When you do, make the reasons clear.”
Karen Appold is a medical writer in Pennsylvania.
References
- Behaviors that undermine a culture of safety. The Joint Commission website. Accessed April 17, 2015.
- Whittemore AD, New England Society for Vascular Surgery. The impact of professionalism on safe surgical care. J Vasc Surg. 2007;45(2):415-419.
- Shapiro J, Whittemore A, Tsen LC. Instituting a culture of professionalism: the establishment of a center for professionalism and peer support. Jt Comm J Qual Patient Saf. 2014;40(4):168-177.
As a hospitalist, caring for critically ill or injured patients can be stressful and demanding. Working with difficult doctors, those who exhibit intimidating and disruptive behaviors such as verbal outbursts and physical threats as well as passive activities such as refusing to perform assigned tasks, can make the work environment even more challenging.1 Some docs are routinely reluctant—or refuse—to answer questions or return phone calls or pages. Some communicate in condescending language or voice intonation; some are brutally impatient.1
The most difficult doctors to work with are those who are not aligned with the hospital’s or treatment team’s goals and those who aren’t open to feedback and coaching, says Rob Zipper, MD, MMM, SFHM, regional chief medical officer of Sound Physicians, based in Tacoma, Wash.
“If physicians are aware of a practice’s guidelines and goals but simply won’t comply with them, it makes it harder on everyone else who is pulling the ship in the same direction,” he says.
Unruly physicians don’t just annoy their coworkers. According to a sentinel event alert from The Joint Commission, they can:
- foster medical errors;
- contribute to poor patient satisfaction;
- contribute to preventable adverse outcomes;
- increase the cost of care;
- undermine team effectiveness; and
- cause qualified clinicians, administrators, and managers to seek new positions in more professional environments.1
“These issues are all connected,” says Stephen R. Nichols, MD, chief of clinical operations performance at the Schumacher Group in Brownwood, Texas. “Disruptive behaviors create mitigated communications and dissatisfaction among staff, which bleeds over into other aspects that are involved secondarily.”
Stephen M. Paskoff, Esq., president and CEO of ELI in Atlanta, can attest to the most severe consequences of bad behavior on patient care.
At one institution, a surgeon’s disruptive behavior lead to a coworker forgetting to perform a procedure and a patient dying.2 In another incident, the emergency department stopped calling on a medical subspecialist who was predictably abusive. The subspecialist knew how to treat a specific patient with an unusual intervention. Since the specialist was not consulted initially, the patient ended up in the intensive care unit.2
One bad hospitalist can bring down the reputation of an entire team.
“Many programs are incentivized based on medical staff and primary-care physicians’ perceptions of their care, so there are direct and indirect consequences,” Dr. Zipper says.
The bottom line, says Felix Aguirre, MD, SFHM, vice president of medical affairs at IPC Healthcare in North Hollywood, Calif., is that it only takes one bad experience to tarnish a group, but it takes many positive experiences to erase the damage.
The Roots of Evil
Intimidating and disruptive behavior stems from both individual and systemic factors. Care providers who exhibit characteristics such as self-centeredness, immaturity, or defensiveness can be more prone to unprofessional behavior. They can lack interpersonal, coping, or conflict-management skills.1
Systemic factors are marked by pressures related to increased productivity demands, cost-containment requirements, embedded hierarchies, and fear of litigation in the healthcare environment. These pressures can be further exacerbated by changes to or differences in the authority, autonomy, empowerment, and roles or values of professionals on the healthcare team as well as by the continual daily changes in shifts, rotations, and interdepartmental support staff. This dynamic creates challenges for interprofessional communication and development of trust among team members.1
According to The Joint Commission, intimidating and disruptive behaviors are often manifested by healthcare professionals in positions of power.1 But other members of the care team can be problematic as well.
“In my experience, conflicts usually revolve around different perspectives and objectives, even if both parties are acting respectfully,” Dr. Zipper says. “Sometimes, however, providers or other care team members are tired or stressed and don’t behave professionally.”
Paskoff, who has more than 40 years of experience in healthcare-related workplace issues, including serving as an investigator for the U.S. Equal Employment Opportunity Commission, says some doctors learn bad behaviors from their mentors and that behaviors can be passed down through generations because they are tolerated.
“When I asked one physician who had outstanding training and an outstanding technical reputation how he became abusive, he said, ‘I learned from the best.’” Paskoff was actually able to track the doctor’s training to the late 1800s and physicians who were known for similar behaviors.
Confronting Those Who Misbehave
Dr. Zipper says physicians should confront behavioral issues directly.
“I will typically discuss a complaint with a doctor privately, and ask him or her what happened without being accusatory,” he says. “I try to provide as much concrete and objective information as I can. The doctor needs to know that you are trying to help him or her succeed. That said, if something is clearly bad behavior, feedback should be direct and include a statement such as, ‘This is not how we behave in this practice.’”
At times, it may not be possible to discuss an emergent matter, such as during a code blue.
“However, I will often ask if anyone on the code team has any ideas or concerns before ending the code,” Dr. Nichols says. “Then after the critical time has passed, it is important to debrief and reconnect with the team, especially the less-experienced members who may have lingering concerns.”
For many employees, however, it is difficult to report disruptive behaviors. This is due to a fear of retaliation and the stigma associated with “blowing the whistle” on a colleague as well as a general reluctance to confront an intimidator.1
If an employee cannot muster the courage to confront a disruptive coworker or if the issue isn’t resolved by talking with the difficult individual, an employee should be a good citizen and report bad behavior to the appropriate hospital authority in a timely manner, says A. Kevin Troutman, Esq., a partner at Fisher Phillips in Houston and a former healthcare human resources executive.
Hospitals accredited by The Joint Commission are required to create a code of conduct that defines disruptive and inappropriate behaviors. In addition, leaders must create and implement a process for managing these behaviors.1
Helping Difficult Doctors
After a physician or another employee has been called out for bad behavior, steps need to be taken to correct the problem. Robert Fuller, Esq., an attorney with Nelson Hardiman, LLP, in Los Angeles, has found a positive-oriented intervention called “the 3-Ds”—which stands for diagnose, design, and do—that has been a successful tool for achieving positive change. The strategy involves a supervisor and employee mutually developing a worksheet to diagnose the problem. Next, they design a remediation and improvement plan. Finally, they implement the plan and specify dates to achieve certain milestones. Coworkers should be informed of the plan and be urged to support it.
“Make it clear that the positive aspect of this plan turns to progressive discipline, including termination, if the employee doesn’t improve or abandons the plan of action,” Fuller says. In most cases, troublemakers will make a sincere effort to control disruptive tendencies.
Troutman suggests enlisting the assistance of a respected peer.
“Have a senior-level doctor help the noncompliant physician understand why his or her behavior creates problems for everyone, including the doctor himself,” he says. “Also, consider connecting compensation and other rewards to job performance, which encompasses good behavior and good citizenship within the organization. Make expectations and consequences clear.”
If an employee has a recent change in behavior, ask if there is a reason.
“It is my experience that sudden changes in behaviors are often the result of a personal or clinical issue, so it is important and humane to make certain that there is not some other cause for the change before assuming someone is simply being disruptive or difficult,” Dr. Nichols says.
Many healthcare institutions are now setting up centers of professionalism. Paskoff reports that The Center for Professionalism and Peer Support (CPPS) was created in 2008 at Brigham and Women’s Hospital in Boston to educate the hospital community regarding professionalism and manage unprofessional behavior.3 CPPS has established standards of behavior and a framework to deal with difficult behaviors.
“An employee is told what he or she is doing wrong, receives counseling, and is given resources to improve,” he explains. “If an employee doesn’t improve, he or she is told that the behavior won’t be tolerated.”
Dismissing Bad Employees
After addressing the specifics of unacceptable behavior and explaining the consequences of repeating it, leadership should monitor subsequent conduct and provide feedback.
“If the employee commits other violations or behaves badly, promptly address the misconduct again and make it clear that further such actions will not be tolerated,” Troutman says. “Expect immediate and sustained improvement and compliance. Be consistent, and if bad conduct continues after an opportunity to improve, do not prolong anyone’s suffering. Instead, terminate the disruptive employee. When you do, make the reasons clear.”
Karen Appold is a medical writer in Pennsylvania.
References
- Behaviors that undermine a culture of safety. The Joint Commission website. Accessed April 17, 2015.
- Whittemore AD, New England Society for Vascular Surgery. The impact of professionalism on safe surgical care. J Vasc Surg. 2007;45(2):415-419.
- Shapiro J, Whittemore A, Tsen LC. Instituting a culture of professionalism: the establishment of a center for professionalism and peer support. Jt Comm J Qual Patient Saf. 2014;40(4):168-177.
VIDEO: Tips & Strategies for the Hospital Medicine Job Search
Dr. Thomas Frederickson, Dr. Benjamin Frizner, and Dr. Darlene Tad-y are all experienced at hiring and mentoring hospitalists at all career stages. They offer tips and strategies for assessing opportunity and negotiating your ideal HM job.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Thomas Frederickson, Dr. Benjamin Frizner, and Dr. Darlene Tad-y are all experienced at hiring and mentoring hospitalists at all career stages. They offer tips and strategies for assessing opportunity and negotiating your ideal HM job.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Thomas Frederickson, Dr. Benjamin Frizner, and Dr. Darlene Tad-y are all experienced at hiring and mentoring hospitalists at all career stages. They offer tips and strategies for assessing opportunity and negotiating your ideal HM job.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
QUIZ: What is the Rate of Postoperative Atrial Fibrillation after Non-Cardiac Surgery?
[WpProQuiz 16]
[WpProQuiz_toplist 16]
[WpProQuiz 16]
[WpProQuiz_toplist 16]
[WpProQuiz 16]
[WpProQuiz_toplist 16]
Strategies for Preventing Patient Falls
Between 700,000 and 1 million people fall each year in U.S. hospitals, and about a third of those result in injuries that add an additional 6.3 days to hospital stays, according to a report from the Joint Commission Center for Transforming Healthcare. Some 11,000 falls are fatal. The Joint Commission Center for Transforming Healthcare has now issued a report on the subject called “Preventing Patient Falls: A Systematic Approach from the Joint Commission Center for Transforming Healthcare Project.”1
“We try to pick those topics that healthcare organizations just haven’t been able to fully tackle even though they’ve put a lot of time and resources into trying to fix them,” says Kelly Barnes, MS, a center project lead in the Center for Transforming Healthcare at The Joint Commission.
The Joint Commission project involved seven hospitals that used Robust Process Improvement, which incorporates tools from Lean Six Sigma and change management methodologies, to reduce falls with injury on inpatient pilot units within their organizations.
During the project, each organization identified the specific factors that led to falls with injury in their environment and developed solutions targeted to those factors. The organizations identified 30 root causes and developed 21 targeted solutions. Because the contributing factors were different at each organization, solution sets were unique to each. Afterward, the organizations saw an aggregate 35% reduction in falls and a 62% reduction in falls with injury.
“One of the takeaways is that you really need support across an organization to have success,” Barnes says. “The more engaged the entire organization is from top down all the way to the bottom, the more successful people are in solving the problems.”
The study resulted in a Targeted Solutions Tool (TST), free to all Joint Commission–accredited customers, to help hospitals.
“You can put your data right into the tool,” Barnes says. “It tells you what your top contributing factors are, and it gives you the solutions that have worked for those contributing factors at other organizations.”
Reference
Health Research & Educational Trust. Preventing patient falls: a systematic approach from the Joint Commission Center for Transforming Healthcare project. Hospitals in Pursuit of Excellence website.
Between 700,000 and 1 million people fall each year in U.S. hospitals, and about a third of those result in injuries that add an additional 6.3 days to hospital stays, according to a report from the Joint Commission Center for Transforming Healthcare. Some 11,000 falls are fatal. The Joint Commission Center for Transforming Healthcare has now issued a report on the subject called “Preventing Patient Falls: A Systematic Approach from the Joint Commission Center for Transforming Healthcare Project.”1
“We try to pick those topics that healthcare organizations just haven’t been able to fully tackle even though they’ve put a lot of time and resources into trying to fix them,” says Kelly Barnes, MS, a center project lead in the Center for Transforming Healthcare at The Joint Commission.
The Joint Commission project involved seven hospitals that used Robust Process Improvement, which incorporates tools from Lean Six Sigma and change management methodologies, to reduce falls with injury on inpatient pilot units within their organizations.
During the project, each organization identified the specific factors that led to falls with injury in their environment and developed solutions targeted to those factors. The organizations identified 30 root causes and developed 21 targeted solutions. Because the contributing factors were different at each organization, solution sets were unique to each. Afterward, the organizations saw an aggregate 35% reduction in falls and a 62% reduction in falls with injury.
“One of the takeaways is that you really need support across an organization to have success,” Barnes says. “The more engaged the entire organization is from top down all the way to the bottom, the more successful people are in solving the problems.”
The study resulted in a Targeted Solutions Tool (TST), free to all Joint Commission–accredited customers, to help hospitals.
“You can put your data right into the tool,” Barnes says. “It tells you what your top contributing factors are, and it gives you the solutions that have worked for those contributing factors at other organizations.”
Reference
Health Research & Educational Trust. Preventing patient falls: a systematic approach from the Joint Commission Center for Transforming Healthcare project. Hospitals in Pursuit of Excellence website.
Between 700,000 and 1 million people fall each year in U.S. hospitals, and about a third of those result in injuries that add an additional 6.3 days to hospital stays, according to a report from the Joint Commission Center for Transforming Healthcare. Some 11,000 falls are fatal. The Joint Commission Center for Transforming Healthcare has now issued a report on the subject called “Preventing Patient Falls: A Systematic Approach from the Joint Commission Center for Transforming Healthcare Project.”1
“We try to pick those topics that healthcare organizations just haven’t been able to fully tackle even though they’ve put a lot of time and resources into trying to fix them,” says Kelly Barnes, MS, a center project lead in the Center for Transforming Healthcare at The Joint Commission.
The Joint Commission project involved seven hospitals that used Robust Process Improvement, which incorporates tools from Lean Six Sigma and change management methodologies, to reduce falls with injury on inpatient pilot units within their organizations.
During the project, each organization identified the specific factors that led to falls with injury in their environment and developed solutions targeted to those factors. The organizations identified 30 root causes and developed 21 targeted solutions. Because the contributing factors were different at each organization, solution sets were unique to each. Afterward, the organizations saw an aggregate 35% reduction in falls and a 62% reduction in falls with injury.
“One of the takeaways is that you really need support across an organization to have success,” Barnes says. “The more engaged the entire organization is from top down all the way to the bottom, the more successful people are in solving the problems.”
The study resulted in a Targeted Solutions Tool (TST), free to all Joint Commission–accredited customers, to help hospitals.
“You can put your data right into the tool,” Barnes says. “It tells you what your top contributing factors are, and it gives you the solutions that have worked for those contributing factors at other organizations.”
Reference
Health Research & Educational Trust. Preventing patient falls: a systematic approach from the Joint Commission Center for Transforming Healthcare project. Hospitals in Pursuit of Excellence website.
Helping Patients Quit Smoking
Inpatient hospitalization can be a key time for patients to quit smoking, according to an abstract called “No More Butts: An Automated System for Inpatient Smoking Cessation Team Consults.”1
“Tobacco smoking continues to be one of the most important public health threats that we face,” says lead author Sujatha Sankaran, MD, assistant clinical professor in the division of hospital medicine and medical director of smoking cessation at the University of California, San Francisco. “Hospitalization is an extremely important moment and provides an excellent opportunity to counsel and provide cessation resources for people who are concerned about their health.”
Inpatients who receive smoking cessation counseling, nicotine replacement, and referral to outpatient resources have increased quit rates six weeks after hospital discharge, their research showed.
However, according to the abstract, in 2014:
- 34.5% of tobacco users admitted to one 600-bed academic hospital were documented as having received and accepted tobacco cessation counseling
- 45.7% of tobacco users received nicotine replacement therapy
- 1.35% of tobacco users received after-discharge consultations to outpatient smoking cessation resources
Researchers piloted a system in which a dedicated respiratory therapist–staffed smoking cessation consult service was trained to provide targeted tobacco cessation services to all inpatients who use tobacco. Of 1944 patients identified as using tobacco, 1545 received and accepted cessation counseling from a trained member of the Smoking Cessation Team, 1526 received nicotine replacement therapy, and 464 received an electronic referral to either a telephone or in-person quit line
“Hospitalists know firsthand the serious harm that tobacco use causes to patients but often are overwhelmed by the acute issues of patients and are unable to fully address tobacco use with hospitalized patients,” Dr. Sankaran says. “An automated cessation service can help lessen this burden by providing automatic cessation resources to all tobacco users.”
Reference
- Sankaran S, Burke R, O’Keefe S. No more butts: an automated system for inpatient smoking cessation team consults [abstract]. J Hosp Med. 2016;11(suppl 1). Accessed November 9, 2016.
Inpatient hospitalization can be a key time for patients to quit smoking, according to an abstract called “No More Butts: An Automated System for Inpatient Smoking Cessation Team Consults.”1
“Tobacco smoking continues to be one of the most important public health threats that we face,” says lead author Sujatha Sankaran, MD, assistant clinical professor in the division of hospital medicine and medical director of smoking cessation at the University of California, San Francisco. “Hospitalization is an extremely important moment and provides an excellent opportunity to counsel and provide cessation resources for people who are concerned about their health.”
Inpatients who receive smoking cessation counseling, nicotine replacement, and referral to outpatient resources have increased quit rates six weeks after hospital discharge, their research showed.
However, according to the abstract, in 2014:
- 34.5% of tobacco users admitted to one 600-bed academic hospital were documented as having received and accepted tobacco cessation counseling
- 45.7% of tobacco users received nicotine replacement therapy
- 1.35% of tobacco users received after-discharge consultations to outpatient smoking cessation resources
Researchers piloted a system in which a dedicated respiratory therapist–staffed smoking cessation consult service was trained to provide targeted tobacco cessation services to all inpatients who use tobacco. Of 1944 patients identified as using tobacco, 1545 received and accepted cessation counseling from a trained member of the Smoking Cessation Team, 1526 received nicotine replacement therapy, and 464 received an electronic referral to either a telephone or in-person quit line
“Hospitalists know firsthand the serious harm that tobacco use causes to patients but often are overwhelmed by the acute issues of patients and are unable to fully address tobacco use with hospitalized patients,” Dr. Sankaran says. “An automated cessation service can help lessen this burden by providing automatic cessation resources to all tobacco users.”
Reference
- Sankaran S, Burke R, O’Keefe S. No more butts: an automated system for inpatient smoking cessation team consults [abstract]. J Hosp Med. 2016;11(suppl 1). Accessed November 9, 2016.
Inpatient hospitalization can be a key time for patients to quit smoking, according to an abstract called “No More Butts: An Automated System for Inpatient Smoking Cessation Team Consults.”1
“Tobacco smoking continues to be one of the most important public health threats that we face,” says lead author Sujatha Sankaran, MD, assistant clinical professor in the division of hospital medicine and medical director of smoking cessation at the University of California, San Francisco. “Hospitalization is an extremely important moment and provides an excellent opportunity to counsel and provide cessation resources for people who are concerned about their health.”
Inpatients who receive smoking cessation counseling, nicotine replacement, and referral to outpatient resources have increased quit rates six weeks after hospital discharge, their research showed.
However, according to the abstract, in 2014:
- 34.5% of tobacco users admitted to one 600-bed academic hospital were documented as having received and accepted tobacco cessation counseling
- 45.7% of tobacco users received nicotine replacement therapy
- 1.35% of tobacco users received after-discharge consultations to outpatient smoking cessation resources
Researchers piloted a system in which a dedicated respiratory therapist–staffed smoking cessation consult service was trained to provide targeted tobacco cessation services to all inpatients who use tobacco. Of 1944 patients identified as using tobacco, 1545 received and accepted cessation counseling from a trained member of the Smoking Cessation Team, 1526 received nicotine replacement therapy, and 464 received an electronic referral to either a telephone or in-person quit line
“Hospitalists know firsthand the serious harm that tobacco use causes to patients but often are overwhelmed by the acute issues of patients and are unable to fully address tobacco use with hospitalized patients,” Dr. Sankaran says. “An automated cessation service can help lessen this burden by providing automatic cessation resources to all tobacco users.”
Reference
- Sankaran S, Burke R, O’Keefe S. No more butts: an automated system for inpatient smoking cessation team consults [abstract]. J Hosp Med. 2016;11(suppl 1). Accessed November 9, 2016.
Hospitalists See Benefit from Working with ‘Surgicalists’
Time was critical. He needed surgery right away to remove his gallbladder. But for that, he needed a surgeon.
“There was a surgeon on call, but the surgeon was not picking up the phone,” Dr. Singh says. “I’m scratching my head. Why is the surgeon not calling back? Where is the surgeon? Did the pager get lost? What if the patient has a bad outcome?”
Eventually, Dr. Singh had to give up on the on-call surgeon, and the patient was flown to a hospital 45 miles away in downtown Sacramento. His surgery had been delayed for almost 12 hours.
The man lived largely due to good luck, Dr. Singh says. The unresponsive surgeon had disciplinary proceedings started against his license but retired rather than face the consequences.
Today, hospitalists at Sutter Amador no longer have to anxiously wait for those responses to emergency pages. It’s one of many hospitals that have turned to a “surgicalist” model, with a surgeon always on hand at the hospital. Surgicalists perform both emergency procedures and procedures that are tied to a hospital admission, without which a patient can’t be discharged. Although it is growing in popularity, the model is still only seen in a small fraction of hospitals.
The model is widely supported by hospitalists because it brings several advantages, mainly a greater availability of the surgeon for consult.
“We don’t have to hunt them down, trying to call their office, trying to see if they’re available to call back,” says Dr. Singh, who is now also the chair of medical staff performance at Sutter Amador and adds that the change has helped with his job satisfaction.
A Clear Delineation
Arrangements between hospitalists and surgicalists vary depending on the hospital, but there typically are clearly delineated criteria on who cares for whom, with the more urgent surgical cases tending to fall under the surgicalists’ care and those with less urgent problems, even though surgery might be involved, tending to go to hospitalists.
When a surgery-related question or the need for actual surgery arises, the model calls for a quick response time from the surgicalist. Hospitalists and surgicalists collaborate on ways to reduce length of stay and prevent readmissions since they share the same institutional goals. Hospitalists are also more in tune with the needs of the surgeons, for instance, not feeding a patient who is going to need quick surgery and not administering blood thinners when a surgery is imminent unless there’s an overriding reason not to do so.
One advantage of this collaboration is that a hospitalist working alongside a surgicalist can get extra surgery-related guidance even when surgery probably isn’t needed, says John Nelson, MD, MHM, a hospitalist at Overlake Medical Center in Bellevue, Wash., a hospitalist management consultant, and a past president of SHM.
“Maybe the opinion of a general surgeon could be useful, but maybe I can get along without it because the general surgeons are busy. It’s going to be hard for them to find time to see this patient, and they’re not going to be very interested in it,” he says. “But if instead I have a surgical hospitalist who’s there all day, it’s much less of a bother for them to come by and take a look at my patient.”
Remaining Challenges
The model is not without its hurdles. When surgicalists are on a 24-hour shift, the patients will see a new one each day, sometimes prompting them to ask, “Who’s my doctor?” Also, complex cases can pose a challenge as they move from one surgicalist to another day to day.
John Maa, MD, who wrote a seminal paper on surgicalists in 2007 based on an early surgicalist model he started at San Mateo Medical Center in California,1 says he is now concerned that the principles he helped make popular—the absorption of surgeons into a system as they work hand in hand with other hospital staff all the time—might be eroding. Some small staffing companies are calling themselves surgicalists, promising fast response times, but are actually locum tenens surgeons under a surgicalist guise, he says.
Properly rolled out, surgicalist programs mean a much better working relationship between hospitalists and surgeons, says Lynette Scherer, MD, FACS, chief medical officer at Surgical Affiliates Management Group in Sacramento. The company, founded in 1996, employs about 200 surgeons, twice as many as three years ago, Dr. Scherer says, but the company declined to share what that amounts to in full-time equivalent positions.
“The hospitalists know all of our algorithms, and they know when to call us,” Dr. Scherer says. “We share the patients on the inpatient side as we need to. We keep the ones that are appropriate for us, and they keep the ones that are appropriate for them.”
The details depend on the hospital, she says.
“Whenever we go to a new site, we sit down with the hospitalist team and say, ‘What do you need here?’ And our admitting grids are different based on what the different needs of the hospitals are.”
To stay on top of complex cases with very sick patients, the medical director rounds with the team nearly every day to help guide that care, Dr. Scherer says.
At Sutter Amador, the arrival of the surgicalist model has helped shorten the length of stay by almost one day for surgery admissions, Dr. Singh says.
Reported outcomes, however, seem to be mixed.
In 2008, Sutter Medical Center in Sacramento switched from a nine-surgeon call panel to four surgeons who covered the acute-care surgery service in 24-hour shifts. Researchers looked at outcomes from 2007, before the new model was adopted, and from the four subsequent years. The results were published in 2014 in the Journal of the American College of Surgeons.2
The total number of operations rose significantly, with 497 performed in 2007 and 640 in 2011. The percentage of cases with complications also fell significantly, from 21% in 2007 to 12% in 2011, with a low of 11% in 2010.
But the mortality rate rose significantly, from 1.4% in 2007 to 2.2% in 2011, with a high of 4.1% in 2008. The study authors note that the mortality rate ultimately fell back to levels not statistically significantly higher than the rate before the service. They suggested the spike could have been due to a greater willingness by the service to treat severely ill patients and due to the “immaturity” of the service in its earlier years. The percentage of cases with a readmission fell from 6.4% in 2007 to 4.7% in 2011, with a low of 3% in 2009, but that change wasn’t quite statistically significant.
“The data’s really bearing out that emergency patients are different in terms of the care they demand,” Dr. Scherer says. “So the patient with alcoholic cirrhosis who presents with a hole in his colon is very different than somebody who presents for an elective colon resection. And you can really reduce complications when you have a team of educated people taking care of these patients.”
Dr. Nelson says adopting the model “just means you’re a smoother operator and you can provide better service to people.” He adds that for any hospital that is getting poor surgical coverage and is paying for it, “it might make sense to consider it.”
Thomas R. Collins is a freelance medical writer based in Florida.
References
- Maa J, Carter JT, Gosnell JE, Wachter R, Harris HW. The surgical hospitalist: a new model for emergency surgical care. J Am Coll Surg. 2007;205(5):704-711.
- O’Mara MS, Scherer L, Wisner D, Owens LJ. Sustainability and success of the acute care surgery model in the nontrauma setting. J Am Coll Surg. 2014;219(1):90-98.
Time was critical. He needed surgery right away to remove his gallbladder. But for that, he needed a surgeon.
“There was a surgeon on call, but the surgeon was not picking up the phone,” Dr. Singh says. “I’m scratching my head. Why is the surgeon not calling back? Where is the surgeon? Did the pager get lost? What if the patient has a bad outcome?”
Eventually, Dr. Singh had to give up on the on-call surgeon, and the patient was flown to a hospital 45 miles away in downtown Sacramento. His surgery had been delayed for almost 12 hours.
The man lived largely due to good luck, Dr. Singh says. The unresponsive surgeon had disciplinary proceedings started against his license but retired rather than face the consequences.
Today, hospitalists at Sutter Amador no longer have to anxiously wait for those responses to emergency pages. It’s one of many hospitals that have turned to a “surgicalist” model, with a surgeon always on hand at the hospital. Surgicalists perform both emergency procedures and procedures that are tied to a hospital admission, without which a patient can’t be discharged. Although it is growing in popularity, the model is still only seen in a small fraction of hospitals.
The model is widely supported by hospitalists because it brings several advantages, mainly a greater availability of the surgeon for consult.
“We don’t have to hunt them down, trying to call their office, trying to see if they’re available to call back,” says Dr. Singh, who is now also the chair of medical staff performance at Sutter Amador and adds that the change has helped with his job satisfaction.
A Clear Delineation
Arrangements between hospitalists and surgicalists vary depending on the hospital, but there typically are clearly delineated criteria on who cares for whom, with the more urgent surgical cases tending to fall under the surgicalists’ care and those with less urgent problems, even though surgery might be involved, tending to go to hospitalists.
When a surgery-related question or the need for actual surgery arises, the model calls for a quick response time from the surgicalist. Hospitalists and surgicalists collaborate on ways to reduce length of stay and prevent readmissions since they share the same institutional goals. Hospitalists are also more in tune with the needs of the surgeons, for instance, not feeding a patient who is going to need quick surgery and not administering blood thinners when a surgery is imminent unless there’s an overriding reason not to do so.
One advantage of this collaboration is that a hospitalist working alongside a surgicalist can get extra surgery-related guidance even when surgery probably isn’t needed, says John Nelson, MD, MHM, a hospitalist at Overlake Medical Center in Bellevue, Wash., a hospitalist management consultant, and a past president of SHM.
“Maybe the opinion of a general surgeon could be useful, but maybe I can get along without it because the general surgeons are busy. It’s going to be hard for them to find time to see this patient, and they’re not going to be very interested in it,” he says. “But if instead I have a surgical hospitalist who’s there all day, it’s much less of a bother for them to come by and take a look at my patient.”
Remaining Challenges
The model is not without its hurdles. When surgicalists are on a 24-hour shift, the patients will see a new one each day, sometimes prompting them to ask, “Who’s my doctor?” Also, complex cases can pose a challenge as they move from one surgicalist to another day to day.
John Maa, MD, who wrote a seminal paper on surgicalists in 2007 based on an early surgicalist model he started at San Mateo Medical Center in California,1 says he is now concerned that the principles he helped make popular—the absorption of surgeons into a system as they work hand in hand with other hospital staff all the time—might be eroding. Some small staffing companies are calling themselves surgicalists, promising fast response times, but are actually locum tenens surgeons under a surgicalist guise, he says.
Properly rolled out, surgicalist programs mean a much better working relationship between hospitalists and surgeons, says Lynette Scherer, MD, FACS, chief medical officer at Surgical Affiliates Management Group in Sacramento. The company, founded in 1996, employs about 200 surgeons, twice as many as three years ago, Dr. Scherer says, but the company declined to share what that amounts to in full-time equivalent positions.
“The hospitalists know all of our algorithms, and they know when to call us,” Dr. Scherer says. “We share the patients on the inpatient side as we need to. We keep the ones that are appropriate for us, and they keep the ones that are appropriate for them.”
The details depend on the hospital, she says.
“Whenever we go to a new site, we sit down with the hospitalist team and say, ‘What do you need here?’ And our admitting grids are different based on what the different needs of the hospitals are.”
To stay on top of complex cases with very sick patients, the medical director rounds with the team nearly every day to help guide that care, Dr. Scherer says.
At Sutter Amador, the arrival of the surgicalist model has helped shorten the length of stay by almost one day for surgery admissions, Dr. Singh says.
Reported outcomes, however, seem to be mixed.
In 2008, Sutter Medical Center in Sacramento switched from a nine-surgeon call panel to four surgeons who covered the acute-care surgery service in 24-hour shifts. Researchers looked at outcomes from 2007, before the new model was adopted, and from the four subsequent years. The results were published in 2014 in the Journal of the American College of Surgeons.2
The total number of operations rose significantly, with 497 performed in 2007 and 640 in 2011. The percentage of cases with complications also fell significantly, from 21% in 2007 to 12% in 2011, with a low of 11% in 2010.
But the mortality rate rose significantly, from 1.4% in 2007 to 2.2% in 2011, with a high of 4.1% in 2008. The study authors note that the mortality rate ultimately fell back to levels not statistically significantly higher than the rate before the service. They suggested the spike could have been due to a greater willingness by the service to treat severely ill patients and due to the “immaturity” of the service in its earlier years. The percentage of cases with a readmission fell from 6.4% in 2007 to 4.7% in 2011, with a low of 3% in 2009, but that change wasn’t quite statistically significant.
“The data’s really bearing out that emergency patients are different in terms of the care they demand,” Dr. Scherer says. “So the patient with alcoholic cirrhosis who presents with a hole in his colon is very different than somebody who presents for an elective colon resection. And you can really reduce complications when you have a team of educated people taking care of these patients.”
Dr. Nelson says adopting the model “just means you’re a smoother operator and you can provide better service to people.” He adds that for any hospital that is getting poor surgical coverage and is paying for it, “it might make sense to consider it.”
Thomas R. Collins is a freelance medical writer based in Florida.
References
- Maa J, Carter JT, Gosnell JE, Wachter R, Harris HW. The surgical hospitalist: a new model for emergency surgical care. J Am Coll Surg. 2007;205(5):704-711.
- O’Mara MS, Scherer L, Wisner D, Owens LJ. Sustainability and success of the acute care surgery model in the nontrauma setting. J Am Coll Surg. 2014;219(1):90-98.
Time was critical. He needed surgery right away to remove his gallbladder. But for that, he needed a surgeon.
“There was a surgeon on call, but the surgeon was not picking up the phone,” Dr. Singh says. “I’m scratching my head. Why is the surgeon not calling back? Where is the surgeon? Did the pager get lost? What if the patient has a bad outcome?”
Eventually, Dr. Singh had to give up on the on-call surgeon, and the patient was flown to a hospital 45 miles away in downtown Sacramento. His surgery had been delayed for almost 12 hours.
The man lived largely due to good luck, Dr. Singh says. The unresponsive surgeon had disciplinary proceedings started against his license but retired rather than face the consequences.
Today, hospitalists at Sutter Amador no longer have to anxiously wait for those responses to emergency pages. It’s one of many hospitals that have turned to a “surgicalist” model, with a surgeon always on hand at the hospital. Surgicalists perform both emergency procedures and procedures that are tied to a hospital admission, without which a patient can’t be discharged. Although it is growing in popularity, the model is still only seen in a small fraction of hospitals.
The model is widely supported by hospitalists because it brings several advantages, mainly a greater availability of the surgeon for consult.
“We don’t have to hunt them down, trying to call their office, trying to see if they’re available to call back,” says Dr. Singh, who is now also the chair of medical staff performance at Sutter Amador and adds that the change has helped with his job satisfaction.
A Clear Delineation
Arrangements between hospitalists and surgicalists vary depending on the hospital, but there typically are clearly delineated criteria on who cares for whom, with the more urgent surgical cases tending to fall under the surgicalists’ care and those with less urgent problems, even though surgery might be involved, tending to go to hospitalists.
When a surgery-related question or the need for actual surgery arises, the model calls for a quick response time from the surgicalist. Hospitalists and surgicalists collaborate on ways to reduce length of stay and prevent readmissions since they share the same institutional goals. Hospitalists are also more in tune with the needs of the surgeons, for instance, not feeding a patient who is going to need quick surgery and not administering blood thinners when a surgery is imminent unless there’s an overriding reason not to do so.
One advantage of this collaboration is that a hospitalist working alongside a surgicalist can get extra surgery-related guidance even when surgery probably isn’t needed, says John Nelson, MD, MHM, a hospitalist at Overlake Medical Center in Bellevue, Wash., a hospitalist management consultant, and a past president of SHM.
“Maybe the opinion of a general surgeon could be useful, but maybe I can get along without it because the general surgeons are busy. It’s going to be hard for them to find time to see this patient, and they’re not going to be very interested in it,” he says. “But if instead I have a surgical hospitalist who’s there all day, it’s much less of a bother for them to come by and take a look at my patient.”
Remaining Challenges
The model is not without its hurdles. When surgicalists are on a 24-hour shift, the patients will see a new one each day, sometimes prompting them to ask, “Who’s my doctor?” Also, complex cases can pose a challenge as they move from one surgicalist to another day to day.
John Maa, MD, who wrote a seminal paper on surgicalists in 2007 based on an early surgicalist model he started at San Mateo Medical Center in California,1 says he is now concerned that the principles he helped make popular—the absorption of surgeons into a system as they work hand in hand with other hospital staff all the time—might be eroding. Some small staffing companies are calling themselves surgicalists, promising fast response times, but are actually locum tenens surgeons under a surgicalist guise, he says.
Properly rolled out, surgicalist programs mean a much better working relationship between hospitalists and surgeons, says Lynette Scherer, MD, FACS, chief medical officer at Surgical Affiliates Management Group in Sacramento. The company, founded in 1996, employs about 200 surgeons, twice as many as three years ago, Dr. Scherer says, but the company declined to share what that amounts to in full-time equivalent positions.
“The hospitalists know all of our algorithms, and they know when to call us,” Dr. Scherer says. “We share the patients on the inpatient side as we need to. We keep the ones that are appropriate for us, and they keep the ones that are appropriate for them.”
The details depend on the hospital, she says.
“Whenever we go to a new site, we sit down with the hospitalist team and say, ‘What do you need here?’ And our admitting grids are different based on what the different needs of the hospitals are.”
To stay on top of complex cases with very sick patients, the medical director rounds with the team nearly every day to help guide that care, Dr. Scherer says.
At Sutter Amador, the arrival of the surgicalist model has helped shorten the length of stay by almost one day for surgery admissions, Dr. Singh says.
Reported outcomes, however, seem to be mixed.
In 2008, Sutter Medical Center in Sacramento switched from a nine-surgeon call panel to four surgeons who covered the acute-care surgery service in 24-hour shifts. Researchers looked at outcomes from 2007, before the new model was adopted, and from the four subsequent years. The results were published in 2014 in the Journal of the American College of Surgeons.2
The total number of operations rose significantly, with 497 performed in 2007 and 640 in 2011. The percentage of cases with complications also fell significantly, from 21% in 2007 to 12% in 2011, with a low of 11% in 2010.
But the mortality rate rose significantly, from 1.4% in 2007 to 2.2% in 2011, with a high of 4.1% in 2008. The study authors note that the mortality rate ultimately fell back to levels not statistically significantly higher than the rate before the service. They suggested the spike could have been due to a greater willingness by the service to treat severely ill patients and due to the “immaturity” of the service in its earlier years. The percentage of cases with a readmission fell from 6.4% in 2007 to 4.7% in 2011, with a low of 3% in 2009, but that change wasn’t quite statistically significant.
“The data’s really bearing out that emergency patients are different in terms of the care they demand,” Dr. Scherer says. “So the patient with alcoholic cirrhosis who presents with a hole in his colon is very different than somebody who presents for an elective colon resection. And you can really reduce complications when you have a team of educated people taking care of these patients.”
Dr. Nelson says adopting the model “just means you’re a smoother operator and you can provide better service to people.” He adds that for any hospital that is getting poor surgical coverage and is paying for it, “it might make sense to consider it.”
Thomas R. Collins is a freelance medical writer based in Florida.
References
- Maa J, Carter JT, Gosnell JE, Wachter R, Harris HW. The surgical hospitalist: a new model for emergency surgical care. J Am Coll Surg. 2007;205(5):704-711.
- O’Mara MS, Scherer L, Wisner D, Owens LJ. Sustainability and success of the acute care surgery model in the nontrauma setting. J Am Coll Surg. 2014;219(1):90-98.
Selected elderly trauma patients do well in non–ICU wards
CORONADO, CALIF. – When elderly patients are appropriately triaged, they can be selectively admitted to non–intensive care wards with acceptable outcomes, results from a single-center study showed.
“Trauma centers across the United States are caring for elderly trauma patients with greater frequency,” researchers led by Marc D. Trust, MD, wrote in an abstract presented during a poster session at the annual meeting of the Western Surgical Association.
“Previous literature showed improved outcomes in this population from aggressive care and invasive monitoring. This may have led to an increased utilization of intensive care resources for these patients,” they noted.
In an effort to assess the safety of admitting this population of patients to non–intensive care units, Dr. Trust, a surgery resident at the University of Texas at Austin, and his associates retrospectively reviewed the medical records of 3,682 trauma patients aged 65 and older who were admitted from 2006 to 2015. They compared demographic data and outcomes between patients admitted to the ICU and those admitted to the surgical ward. The primary endpoint was mortality, while secondary endpoints were transfer to higher level of care and hospital length of stay. Patients admitted only for comfort care and those with injuries thought to be terminal and irreversible were excluded from the analysis.
The mean age of the 3,682 patients was 76 years and 1,838 (50%) were admitted to the ICU, while the remaining 1,844 (50%) were admitted to the surgical ward. When the researchers compared patients admitted to the ICU with those admitted to the surgical ward, they observed significant differences in mortality (7% vs. 0.82%, respectively; P less than .001), as well as systolic blood pressure on admission (146 vs. 149 mm Hg, respectively; P = .0002), pulse (85 vs. 81 beats per minute; P less than .0001), Glasgow Coma Scale (14 vs. 15; P less than .001), Injury Severity Score (16 vs. 8; P less than .001), and hospital stay (a mean of 8 vs. 4 days; P less than .0001). In addition, fewer than 1% of patients admitted to the surgical ward required transfer to a higher level of care (P less than .0001).
Next, Dr. Trust and his associates conducted a subgroup analysis of 300 patients admitted to the ICU (28%) and 766 (72%) admitted to the surgical ward who had all-system Abbreviated Injury Scale scores of less than 3, no hypotension on admission, and a Glasgow Coma Scale of 14 or greater. Compared with those admitted to the surgical ward, those admitted to the ICU were older (77 vs. 76 years old, respectively; P = .003), more likely to be male (54% vs. 45%; P = .007), more tachycardic (HR 84 vs. 81; P = .004), more severely injured (ISS score of 5 vs. 4; P less than .0001), and more likely to have a longer hospital stay (a mean of 6 vs. 4 days; P less than .0001). Two patients admitted to the surgical ward died (0.26%; P = .0009) and none required transfer to a higher level of care.
The researchers reported having no financial disclosures.
CORONADO, CALIF. – When elderly patients are appropriately triaged, they can be selectively admitted to non–intensive care wards with acceptable outcomes, results from a single-center study showed.
“Trauma centers across the United States are caring for elderly trauma patients with greater frequency,” researchers led by Marc D. Trust, MD, wrote in an abstract presented during a poster session at the annual meeting of the Western Surgical Association.
“Previous literature showed improved outcomes in this population from aggressive care and invasive monitoring. This may have led to an increased utilization of intensive care resources for these patients,” they noted.
In an effort to assess the safety of admitting this population of patients to non–intensive care units, Dr. Trust, a surgery resident at the University of Texas at Austin, and his associates retrospectively reviewed the medical records of 3,682 trauma patients aged 65 and older who were admitted from 2006 to 2015. They compared demographic data and outcomes between patients admitted to the ICU and those admitted to the surgical ward. The primary endpoint was mortality, while secondary endpoints were transfer to higher level of care and hospital length of stay. Patients admitted only for comfort care and those with injuries thought to be terminal and irreversible were excluded from the analysis.
The mean age of the 3,682 patients was 76 years and 1,838 (50%) were admitted to the ICU, while the remaining 1,844 (50%) were admitted to the surgical ward. When the researchers compared patients admitted to the ICU with those admitted to the surgical ward, they observed significant differences in mortality (7% vs. 0.82%, respectively; P less than .001), as well as systolic blood pressure on admission (146 vs. 149 mm Hg, respectively; P = .0002), pulse (85 vs. 81 beats per minute; P less than .0001), Glasgow Coma Scale (14 vs. 15; P less than .001), Injury Severity Score (16 vs. 8; P less than .001), and hospital stay (a mean of 8 vs. 4 days; P less than .0001). In addition, fewer than 1% of patients admitted to the surgical ward required transfer to a higher level of care (P less than .0001).
Next, Dr. Trust and his associates conducted a subgroup analysis of 300 patients admitted to the ICU (28%) and 766 (72%) admitted to the surgical ward who had all-system Abbreviated Injury Scale scores of less than 3, no hypotension on admission, and a Glasgow Coma Scale of 14 or greater. Compared with those admitted to the surgical ward, those admitted to the ICU were older (77 vs. 76 years old, respectively; P = .003), more likely to be male (54% vs. 45%; P = .007), more tachycardic (HR 84 vs. 81; P = .004), more severely injured (ISS score of 5 vs. 4; P less than .0001), and more likely to have a longer hospital stay (a mean of 6 vs. 4 days; P less than .0001). Two patients admitted to the surgical ward died (0.26%; P = .0009) and none required transfer to a higher level of care.
The researchers reported having no financial disclosures.
CORONADO, CALIF. – When elderly patients are appropriately triaged, they can be selectively admitted to non–intensive care wards with acceptable outcomes, results from a single-center study showed.
“Trauma centers across the United States are caring for elderly trauma patients with greater frequency,” researchers led by Marc D. Trust, MD, wrote in an abstract presented during a poster session at the annual meeting of the Western Surgical Association.
“Previous literature showed improved outcomes in this population from aggressive care and invasive monitoring. This may have led to an increased utilization of intensive care resources for these patients,” they noted.
In an effort to assess the safety of admitting this population of patients to non–intensive care units, Dr. Trust, a surgery resident at the University of Texas at Austin, and his associates retrospectively reviewed the medical records of 3,682 trauma patients aged 65 and older who were admitted from 2006 to 2015. They compared demographic data and outcomes between patients admitted to the ICU and those admitted to the surgical ward. The primary endpoint was mortality, while secondary endpoints were transfer to higher level of care and hospital length of stay. Patients admitted only for comfort care and those with injuries thought to be terminal and irreversible were excluded from the analysis.
The mean age of the 3,682 patients was 76 years and 1,838 (50%) were admitted to the ICU, while the remaining 1,844 (50%) were admitted to the surgical ward. When the researchers compared patients admitted to the ICU with those admitted to the surgical ward, they observed significant differences in mortality (7% vs. 0.82%, respectively; P less than .001), as well as systolic blood pressure on admission (146 vs. 149 mm Hg, respectively; P = .0002), pulse (85 vs. 81 beats per minute; P less than .0001), Glasgow Coma Scale (14 vs. 15; P less than .001), Injury Severity Score (16 vs. 8; P less than .001), and hospital stay (a mean of 8 vs. 4 days; P less than .0001). In addition, fewer than 1% of patients admitted to the surgical ward required transfer to a higher level of care (P less than .0001).
Next, Dr. Trust and his associates conducted a subgroup analysis of 300 patients admitted to the ICU (28%) and 766 (72%) admitted to the surgical ward who had all-system Abbreviated Injury Scale scores of less than 3, no hypotension on admission, and a Glasgow Coma Scale of 14 or greater. Compared with those admitted to the surgical ward, those admitted to the ICU were older (77 vs. 76 years old, respectively; P = .003), more likely to be male (54% vs. 45%; P = .007), more tachycardic (HR 84 vs. 81; P = .004), more severely injured (ISS score of 5 vs. 4; P less than .0001), and more likely to have a longer hospital stay (a mean of 6 vs. 4 days; P less than .0001). Two patients admitted to the surgical ward died (0.26%; P = .0009) and none required transfer to a higher level of care.
The researchers reported having no financial disclosures.
AT WSA 2016
Key clinical point:
Major finding: Mortality rates were significantly higher among elderly trauma patients admitted to the ICU, compared with those admitted to the surgical ward (7% vs. 0.82%, respectively; P less than .001).
Data source: A retrospective review of 3,682 trauma patients aged 65 and older who were admitted from 2006 to 2015.
Disclosures: The researchers reported having no financial disclosures.
HM 2016: A Year in Review
From celebrating the 20th anniversary of hospital medicine’s arrival to rapid reimbursement reform to sought-after clarity for observation rules, the past 12 months have been eventful. The Hospitalist asked more than a dozen industry leaders what they thought were the biggest highlights of 2016. Here is what they said:
1. Happy Birthday, HM
August 15 marked the 20th anniversary of “The Emerging Role of ‘Hospitalists’ in the American Health Care System,”1 a New England Journal of Medicine paper authored by Lee Goldman, MD, and Robert Wachter, MD, MHM.2 It was the first time anyone defined what a hospitalist was, putting a sobriquet to an inpatient care model that had organically and independently started happening nationwide.
The paper laid the groundwork for a specialty that spread like a proverbial wildfire over the next 20 years. The model overcame early opposition from residents fearful they’d lose the ability to learn and critical-care specialists who wanted to maintain the caseloads they’d fought to build. The field has now swelled to an estimated 52,000 practitioners.
“I reflect back … and think today about what the hospitalist model brings to us,” James Merlino, MD, president and chief medical officer of Press Ganey’s strategic consulting division, told The Hospitalist. “It is an amazing transformation on how the hospitalist model really delivers.”1
2. Its Own Specialty Code
Hospitalist medicine received federal approval for its first dedicated specialty code3 in a decision hailed by many. The code, approved by the Centers for Medicare & Medicaid Services (CMS), should allow hospitalist-specific billing in 2017.
SHM leaders have long pushed for the code, particularly as healthcare transitions from fee-for-service (FFS) to quality-based payment models. Public Policy Committee Chair Ron Greeno, MD, MHM, says that a dedicated code is necessary to ensure that hospitalists are properly reimbursed for their work.
Historically, hospitalists have used codes more in line with the workload of general internal medicine, family medicine, and other specialties. But those codes don’t account for the complexity of what hospitalists deal with on a daily basis.
“We as hospitalists face unique challenges and work with patients from all demographics, often with severe illnesses, making it nearly impossible to rely on benchmarks used for these other specialties,” Dr. Greeno said.3
SHM pushed for the change and has said it is committed to educating members about how best to use it. Scott Sears, MD, FHM, CPE, MBA, chief clinical officer for Sound Physicians of Tacoma, Wash., said the move is great for HM but that more needs to be done to tailor billing and coding to the specialty’s actual workflow.
“A pediatric hospitalist may not want to be compared to an adult hospitalist. A critical-access hospitalist doesn’t want to be compared to a hospitalist in a tertiary academic medical center,” Dr. Sears said. “I don’t think it’s an end-all, be-all, but it’s a place to start.”3
3. Down with SGR, Long Live MACRA
While it’s unlikely hospitalists have that printed on bumper stickers, 2016 brought the end of the oft-maligned Sustainable Growth Rate (SGR) formula. This was the first year under the Medicare Access and CHIP Reauthorization Act of 2015, better known as MACRA.4
MACRA changes the ways hospitalists and other physicians are reimbursed by Medicare by continuing the broader trend of moving from volume-based reimbursements toward a value-based payment (VBP) system. Its two tracks for physicians to change how they get paid are the Merit-Based Incentive Payment System (MIPS) and the Alternative Payments Model (APM).
MIPS probably looks familiar because it is similar to the traditional FFS model. But to make value a more important factor in the reimbursement formula, MIPS will account for both volume and quality. APM allows physicians to opt out of MIPS by participating in other approved programs where providers take on “more than nominal” financial risk, report on their quality measures, and use certified electronic health record (EHR) technology.
4. The Surgeon General Is a Hospitalist
Any specialty’s annual meeting would be lucky to get the U.S. Surgeon General as a plenary speaker, but HM16 featured one of its own in hospitalist and U.S. Surgeon General Vivek Murthy, MD, MBA.
Dr. Murthy kicked off the confab in San Diego, and some 4,000 hospitalists listened to one of their own talk about ascending the highest perch a physician can attain in the federal government.7 Dr. Murthy, previously a hospitalist at Brigham and Women’s Hospital in Boston, was confirmed as the 19th Surgeon General in December 2014.
In an address titled “Bringing Health to America,” Dr. Murthy inspired with tales of hope and encouraged hospitalists to make the pursuit of healthy appealing while improving the safety of our communities. In particular, he suggested hospitalists look to leverage their leadership to improve systems and to be a powerful force of change both inside the walls of their institution and in their communities.
“In the end, the world gets better when people choose to come together to make it better,” he said.8
5. Nurse Practitioner Joins SHM Board of Directors
At HM16, Tracy Cardin, ACNP-BC, SFHM, was the first nurse practitioner (NP) or physician assistant (PA) given voting privileges on the society’s oversight panel.
“I can’t describe to you how passionately I believe that [NPs and PAs] have a huge role moving forward,” Cardin said. “I think our representation, our visibility, has sort of been flabby and kind of under the wire for a long time. We can really impact the design of care models at the bedside in a way that’s innovative and more efficient and in a way that’s really huge. I think there’s a transformation that’s going to be coming, and we’re going to be a huge part of it.”9
With Cardin’s ascension, it has added the voice of another constituency to its board. She was previously chair of SHM’s Nurse Practitioner/Physician Assistant Committee and in 2015 received the society’s Award in Excellence in Hospital Medicine for NPs and PAs. She has been at the University of Chicago for about 10 years.
“It does send a message to the rest of our membership that SHM values those other constituencies and that this is not a physician membership organization but rather a membership organization comprised of people who are interested in improving healthcare for our hospitalized patients,” immediate past president Robert Harrington Jr., MD, SFHM said.10
6. The State of Hospital Medicine Is Strong
According to the biennial 2016 State of Hospital Medicine Report6 from SHM and partially populated by data from the Medical Group Management Association (MGMA), median compensation for adult hospitalists rose 10% to $278,746 from 2013 to 2015. The double-digit increase continues the steady climb of hospitalist pay, which is up 30% since 2010. At the same time, productivity is flattening.
And nearly all HM groups (HMGs)—96%—are still getting financial support, mostly from their host hospitals, in addition to their professional fee revenue. However, that median support, $157,535 per full-time employee (FTE), increased just 1%.
The slowing growth in that contribution is a harbinger that the level of financial support can no longer grow unabated, said Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
“We’re pretty close to that breaking point,” she said. “When we go around the country and do consulting work, we are hearing many more hospital leaders telling us, ‘We’re concerned about how much money this program is costing us, and we are getting to the point where we can’t afford it.’”6
7. Pay Cut for ‘Two-Midnight’ Rule for Observations Is No More
CMS announced a proposed rule in April that would have Medicare stop imposing an inpatient payment cut to hospitals under the “two-midnight” rule, according to a report in Modern Healthcare.10 The final rule went into effect in October.
The rule, which continues to be a contentious issue for hospitalists even with the pay cut being eliminated, was put in place in October 2013 to define which Medicare beneficiary hospital stays are appropriate for Medicare Part A payment by stating that if the physician expected the patient to stay for fewer than two midnights, then the services should be billed as outpatient (Medicare Part B) and not inpatient.
For two years, the only exception to the pay withhold was for those diagnoses that CMS designated as “inpatient only.” An overhaul of the rule in October 2015 stated that exceptions could be determined by the physician (or other practitioner) on a “case-by-case basis.”
But a legal challenge and withering criticism from SHM and other professional organizations prompted CMS to undo the withheld payments associated rule.11–13 In fact, hospitals also will see a one-time increase of 0.6% in fiscal 2017, making up for the 0.2% reduction to the rates of the last three years. SHM has said it will continue to advocate for further changes to the rule.
8. Medicaid Expansion Takes Hold
Thirty-one states and the District of Columbia, under the auspices of the Affordable Care Act, have expanded Medicaid. One 2014 study in states including Minnesota, Kentucky, and Arizona showed a dramatic decrease in uninsured hospital stays and a significant increase in Medicaid stays. Meanwhile, in six states that did not expand, including Florida, Georgia, and Missouri, there was no significant change in payor mix.14
“What a lot of these early studies are saying is that when you expand Medicaid, people get on Medicaid, and that’s exactly what you hope will happen when you do a major public coverage expansion,” said Sayeh Nikpay, PhD, MPH, assistant professor of health policy at Vanderbilt University School of Medicine in Nashville, Tenn., and a lead author of the 2014 Health Affairs study. “Physicians are grappling with payment issues, and it should be quite a relief that people are coming in the door with some kind of insurance rather than uninsured.”15
While expansion from 2015 to 2016 was the main story for Medicaid, many observers are now watching to see what President-elect Donald Trump will do. As a candidate, he campaigned to repeal Obamacare, and that may have significant impacts on the expansion of Medicaid.
9. Antimicrobial Stewardship Rules Upgrade
In July, The Joint Commission announced a new Medication Management (MM) standard for hospitals, critical-access hospitals, and nursing care centers that goes into effect in 2017.16,17 Its stated purpose is to improve quality and patient safety. The Joint Commission move came a year after President Barack Obama made combatting antibiotic-resistant bacteria a national issue.
“If you review the scientific literature, it will indicate that we’re in crisis mode right now because of this,” said Kelly Podgorny, DNP, MS, CPHQ, RN, project director at The Joint Commission. 16
The standard encourages the prioritization of establishing antimicrobial stewardship programs. It suggests staff members at institutions receive training and education on dispensing, administering, and monitoring antimicrobial resistance and antimicrobial stewardship practice. And, in turn, those staffers should look to educate patients and caregivers on appropriate use of antimicrobial medications.
Lastly, when possible, an antimicrobial team should take a multidisciplinary approach and include an infectious disease physician, a pharmacist, and a practitioner.
10. Febrile-Infant Care Draws a Crowd
One of the most well-attended sessions at 2016 Pediatric Hospital Medicine in Chicago was an update on the anticipated American Academy of Pediatricians (AAP) guidelines for febrile infants.18
The guidelines, for infants 7–90 days old, are aimed at providing pediatric hospitalists and others evidence-based guidelines, not rules, from the most recent literature available. The PHM16 session, presented by Kenneth Roberts, MD, highlighted the need to separate individual components of serious bacterial infections such as urinary tract infections (UTIs), bacteremia, and meningitis. Dr. Roberts noted that the incidence and clinical course can vary greatly for the different diagnoses.
The new criteria would be for full-term infants (37–43 weeks’ gestation) who are well-appearing and present with a temperature of 38°C. Exclusion criteria would include perinatal/prenatal/neonatal maternal fever, infection, or antimicrobial treatment; the presence of any evident infection; being technology-dependent; and the presence of congenital anomalies.
In particular, the new guidelines will look to risk-stratify management by age groups of 7–28 days, 29–60 days, and 61–90 days. The criteria are expected to be released in the next year.
Richard Quinn is a freelance writer in New Jersey.
References
- Quinn R. HM turns 20: a look at the evolution of hospitalist medicine. The Hospitalist website. Accessed November 14, 2016.
- Wachter M, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514-517.
- Tyrrell KA. New hospitalist billing code should benefit hospitalists, patients. The Hospitalist website. Accessed November 14, 2016.
- Doctoroff L, Dutta S. MACRA provides new direction for U.S. healthcare. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. Everything you need to know about the Bundled Payments for Care Improvement Initiative. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. The state of hospital medicine is strong. The Hospitalist website. Accessed November 14, 2016.
- Scheurer D. U.S. surgeon general encourages hospitalists to remain hopeful, motivated. The Hospitalist website. Accessed November 14, 2016.
- Collins TR. HM16 speakers focus on public health, leadership, future of hospital medicine. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. SHM seats its first non-physician board member. The Hospitalist website. Accessed at November 14, 2016.
- Carris J. Centers for Medicare & Medicaid Services (CMS) eliminates two-midnight rule’s inpatient payment cuts: report. The Hospitalist website. Accessed November 14, 2016.
- Schencker L. Judge tells HHS to revisit two-midnight rule’s inpatient pay cut. Healh Affairs website. Accessed November 14, 2016.
- Tyrrell KA. Physicians critical of proposed changes to Medicare’s two-midnight rule. The Hospitalist website. Accessed November 14, 2016.
- Tyrrell KA. Ann Sheehy, MD, MS, FHM, outlines to lawmakers hospitalist concerns about two-midnight rule, Medicare policies. The Hospitalist website. Accessed November 14, 2016.
- Nikpay S, Buchmueller T, Levy HG. Affordable Care Act Medicaid expansion reduced uninsured hospital stays in 2014. Health Aff (Millwood). 2016;35(1):106-110.
- Tyrrell KA. Benefits of Medicaid expansion for hospitalists. The Hospitalist website. Accessed November 14, 2016.
- Bopp S. New standard announced for antimicrobial stewardship. The Hospitalist website. Accessed November 14, 2016.
- Prepublication standards – new antimicrobial stewardship standard. The Joint Commission website. Accessed November 14, 2016.
- 18. DeZure C. PHM16: the new AAP clinical practice guideline on evaluating, managing febrile infants. The Hospitalist website. Accessed November 14, 2016.
From celebrating the 20th anniversary of hospital medicine’s arrival to rapid reimbursement reform to sought-after clarity for observation rules, the past 12 months have been eventful. The Hospitalist asked more than a dozen industry leaders what they thought were the biggest highlights of 2016. Here is what they said:
1. Happy Birthday, HM
August 15 marked the 20th anniversary of “The Emerging Role of ‘Hospitalists’ in the American Health Care System,”1 a New England Journal of Medicine paper authored by Lee Goldman, MD, and Robert Wachter, MD, MHM.2 It was the first time anyone defined what a hospitalist was, putting a sobriquet to an inpatient care model that had organically and independently started happening nationwide.
The paper laid the groundwork for a specialty that spread like a proverbial wildfire over the next 20 years. The model overcame early opposition from residents fearful they’d lose the ability to learn and critical-care specialists who wanted to maintain the caseloads they’d fought to build. The field has now swelled to an estimated 52,000 practitioners.
“I reflect back … and think today about what the hospitalist model brings to us,” James Merlino, MD, president and chief medical officer of Press Ganey’s strategic consulting division, told The Hospitalist. “It is an amazing transformation on how the hospitalist model really delivers.”1
2. Its Own Specialty Code
Hospitalist medicine received federal approval for its first dedicated specialty code3 in a decision hailed by many. The code, approved by the Centers for Medicare & Medicaid Services (CMS), should allow hospitalist-specific billing in 2017.
SHM leaders have long pushed for the code, particularly as healthcare transitions from fee-for-service (FFS) to quality-based payment models. Public Policy Committee Chair Ron Greeno, MD, MHM, says that a dedicated code is necessary to ensure that hospitalists are properly reimbursed for their work.
Historically, hospitalists have used codes more in line with the workload of general internal medicine, family medicine, and other specialties. But those codes don’t account for the complexity of what hospitalists deal with on a daily basis.
“We as hospitalists face unique challenges and work with patients from all demographics, often with severe illnesses, making it nearly impossible to rely on benchmarks used for these other specialties,” Dr. Greeno said.3
SHM pushed for the change and has said it is committed to educating members about how best to use it. Scott Sears, MD, FHM, CPE, MBA, chief clinical officer for Sound Physicians of Tacoma, Wash., said the move is great for HM but that more needs to be done to tailor billing and coding to the specialty’s actual workflow.
“A pediatric hospitalist may not want to be compared to an adult hospitalist. A critical-access hospitalist doesn’t want to be compared to a hospitalist in a tertiary academic medical center,” Dr. Sears said. “I don’t think it’s an end-all, be-all, but it’s a place to start.”3
3. Down with SGR, Long Live MACRA
While it’s unlikely hospitalists have that printed on bumper stickers, 2016 brought the end of the oft-maligned Sustainable Growth Rate (SGR) formula. This was the first year under the Medicare Access and CHIP Reauthorization Act of 2015, better known as MACRA.4
MACRA changes the ways hospitalists and other physicians are reimbursed by Medicare by continuing the broader trend of moving from volume-based reimbursements toward a value-based payment (VBP) system. Its two tracks for physicians to change how they get paid are the Merit-Based Incentive Payment System (MIPS) and the Alternative Payments Model (APM).
MIPS probably looks familiar because it is similar to the traditional FFS model. But to make value a more important factor in the reimbursement formula, MIPS will account for both volume and quality. APM allows physicians to opt out of MIPS by participating in other approved programs where providers take on “more than nominal” financial risk, report on their quality measures, and use certified electronic health record (EHR) technology.
4. The Surgeon General Is a Hospitalist
Any specialty’s annual meeting would be lucky to get the U.S. Surgeon General as a plenary speaker, but HM16 featured one of its own in hospitalist and U.S. Surgeon General Vivek Murthy, MD, MBA.
Dr. Murthy kicked off the confab in San Diego, and some 4,000 hospitalists listened to one of their own talk about ascending the highest perch a physician can attain in the federal government.7 Dr. Murthy, previously a hospitalist at Brigham and Women’s Hospital in Boston, was confirmed as the 19th Surgeon General in December 2014.
In an address titled “Bringing Health to America,” Dr. Murthy inspired with tales of hope and encouraged hospitalists to make the pursuit of healthy appealing while improving the safety of our communities. In particular, he suggested hospitalists look to leverage their leadership to improve systems and to be a powerful force of change both inside the walls of their institution and in their communities.
“In the end, the world gets better when people choose to come together to make it better,” he said.8
5. Nurse Practitioner Joins SHM Board of Directors
At HM16, Tracy Cardin, ACNP-BC, SFHM, was the first nurse practitioner (NP) or physician assistant (PA) given voting privileges on the society’s oversight panel.
“I can’t describe to you how passionately I believe that [NPs and PAs] have a huge role moving forward,” Cardin said. “I think our representation, our visibility, has sort of been flabby and kind of under the wire for a long time. We can really impact the design of care models at the bedside in a way that’s innovative and more efficient and in a way that’s really huge. I think there’s a transformation that’s going to be coming, and we’re going to be a huge part of it.”9
With Cardin’s ascension, it has added the voice of another constituency to its board. She was previously chair of SHM’s Nurse Practitioner/Physician Assistant Committee and in 2015 received the society’s Award in Excellence in Hospital Medicine for NPs and PAs. She has been at the University of Chicago for about 10 years.
“It does send a message to the rest of our membership that SHM values those other constituencies and that this is not a physician membership organization but rather a membership organization comprised of people who are interested in improving healthcare for our hospitalized patients,” immediate past president Robert Harrington Jr., MD, SFHM said.10
6. The State of Hospital Medicine Is Strong
According to the biennial 2016 State of Hospital Medicine Report6 from SHM and partially populated by data from the Medical Group Management Association (MGMA), median compensation for adult hospitalists rose 10% to $278,746 from 2013 to 2015. The double-digit increase continues the steady climb of hospitalist pay, which is up 30% since 2010. At the same time, productivity is flattening.
And nearly all HM groups (HMGs)—96%—are still getting financial support, mostly from their host hospitals, in addition to their professional fee revenue. However, that median support, $157,535 per full-time employee (FTE), increased just 1%.
The slowing growth in that contribution is a harbinger that the level of financial support can no longer grow unabated, said Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
“We’re pretty close to that breaking point,” she said. “When we go around the country and do consulting work, we are hearing many more hospital leaders telling us, ‘We’re concerned about how much money this program is costing us, and we are getting to the point where we can’t afford it.’”6
7. Pay Cut for ‘Two-Midnight’ Rule for Observations Is No More
CMS announced a proposed rule in April that would have Medicare stop imposing an inpatient payment cut to hospitals under the “two-midnight” rule, according to a report in Modern Healthcare.10 The final rule went into effect in October.
The rule, which continues to be a contentious issue for hospitalists even with the pay cut being eliminated, was put in place in October 2013 to define which Medicare beneficiary hospital stays are appropriate for Medicare Part A payment by stating that if the physician expected the patient to stay for fewer than two midnights, then the services should be billed as outpatient (Medicare Part B) and not inpatient.
For two years, the only exception to the pay withhold was for those diagnoses that CMS designated as “inpatient only.” An overhaul of the rule in October 2015 stated that exceptions could be determined by the physician (or other practitioner) on a “case-by-case basis.”
But a legal challenge and withering criticism from SHM and other professional organizations prompted CMS to undo the withheld payments associated rule.11–13 In fact, hospitals also will see a one-time increase of 0.6% in fiscal 2017, making up for the 0.2% reduction to the rates of the last three years. SHM has said it will continue to advocate for further changes to the rule.
8. Medicaid Expansion Takes Hold
Thirty-one states and the District of Columbia, under the auspices of the Affordable Care Act, have expanded Medicaid. One 2014 study in states including Minnesota, Kentucky, and Arizona showed a dramatic decrease in uninsured hospital stays and a significant increase in Medicaid stays. Meanwhile, in six states that did not expand, including Florida, Georgia, and Missouri, there was no significant change in payor mix.14
“What a lot of these early studies are saying is that when you expand Medicaid, people get on Medicaid, and that’s exactly what you hope will happen when you do a major public coverage expansion,” said Sayeh Nikpay, PhD, MPH, assistant professor of health policy at Vanderbilt University School of Medicine in Nashville, Tenn., and a lead author of the 2014 Health Affairs study. “Physicians are grappling with payment issues, and it should be quite a relief that people are coming in the door with some kind of insurance rather than uninsured.”15
While expansion from 2015 to 2016 was the main story for Medicaid, many observers are now watching to see what President-elect Donald Trump will do. As a candidate, he campaigned to repeal Obamacare, and that may have significant impacts on the expansion of Medicaid.
9. Antimicrobial Stewardship Rules Upgrade
In July, The Joint Commission announced a new Medication Management (MM) standard for hospitals, critical-access hospitals, and nursing care centers that goes into effect in 2017.16,17 Its stated purpose is to improve quality and patient safety. The Joint Commission move came a year after President Barack Obama made combatting antibiotic-resistant bacteria a national issue.
“If you review the scientific literature, it will indicate that we’re in crisis mode right now because of this,” said Kelly Podgorny, DNP, MS, CPHQ, RN, project director at The Joint Commission. 16
The standard encourages the prioritization of establishing antimicrobial stewardship programs. It suggests staff members at institutions receive training and education on dispensing, administering, and monitoring antimicrobial resistance and antimicrobial stewardship practice. And, in turn, those staffers should look to educate patients and caregivers on appropriate use of antimicrobial medications.
Lastly, when possible, an antimicrobial team should take a multidisciplinary approach and include an infectious disease physician, a pharmacist, and a practitioner.
10. Febrile-Infant Care Draws a Crowd
One of the most well-attended sessions at 2016 Pediatric Hospital Medicine in Chicago was an update on the anticipated American Academy of Pediatricians (AAP) guidelines for febrile infants.18
The guidelines, for infants 7–90 days old, are aimed at providing pediatric hospitalists and others evidence-based guidelines, not rules, from the most recent literature available. The PHM16 session, presented by Kenneth Roberts, MD, highlighted the need to separate individual components of serious bacterial infections such as urinary tract infections (UTIs), bacteremia, and meningitis. Dr. Roberts noted that the incidence and clinical course can vary greatly for the different diagnoses.
The new criteria would be for full-term infants (37–43 weeks’ gestation) who are well-appearing and present with a temperature of 38°C. Exclusion criteria would include perinatal/prenatal/neonatal maternal fever, infection, or antimicrobial treatment; the presence of any evident infection; being technology-dependent; and the presence of congenital anomalies.
In particular, the new guidelines will look to risk-stratify management by age groups of 7–28 days, 29–60 days, and 61–90 days. The criteria are expected to be released in the next year.
Richard Quinn is a freelance writer in New Jersey.
References
- Quinn R. HM turns 20: a look at the evolution of hospitalist medicine. The Hospitalist website. Accessed November 14, 2016.
- Wachter M, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514-517.
- Tyrrell KA. New hospitalist billing code should benefit hospitalists, patients. The Hospitalist website. Accessed November 14, 2016.
- Doctoroff L, Dutta S. MACRA provides new direction for U.S. healthcare. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. Everything you need to know about the Bundled Payments for Care Improvement Initiative. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. The state of hospital medicine is strong. The Hospitalist website. Accessed November 14, 2016.
- Scheurer D. U.S. surgeon general encourages hospitalists to remain hopeful, motivated. The Hospitalist website. Accessed November 14, 2016.
- Collins TR. HM16 speakers focus on public health, leadership, future of hospital medicine. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. SHM seats its first non-physician board member. The Hospitalist website. Accessed at November 14, 2016.
- Carris J. Centers for Medicare & Medicaid Services (CMS) eliminates two-midnight rule’s inpatient payment cuts: report. The Hospitalist website. Accessed November 14, 2016.
- Schencker L. Judge tells HHS to revisit two-midnight rule’s inpatient pay cut. Healh Affairs website. Accessed November 14, 2016.
- Tyrrell KA. Physicians critical of proposed changes to Medicare’s two-midnight rule. The Hospitalist website. Accessed November 14, 2016.
- Tyrrell KA. Ann Sheehy, MD, MS, FHM, outlines to lawmakers hospitalist concerns about two-midnight rule, Medicare policies. The Hospitalist website. Accessed November 14, 2016.
- Nikpay S, Buchmueller T, Levy HG. Affordable Care Act Medicaid expansion reduced uninsured hospital stays in 2014. Health Aff (Millwood). 2016;35(1):106-110.
- Tyrrell KA. Benefits of Medicaid expansion for hospitalists. The Hospitalist website. Accessed November 14, 2016.
- Bopp S. New standard announced for antimicrobial stewardship. The Hospitalist website. Accessed November 14, 2016.
- Prepublication standards – new antimicrobial stewardship standard. The Joint Commission website. Accessed November 14, 2016.
- 18. DeZure C. PHM16: the new AAP clinical practice guideline on evaluating, managing febrile infants. The Hospitalist website. Accessed November 14, 2016.
From celebrating the 20th anniversary of hospital medicine’s arrival to rapid reimbursement reform to sought-after clarity for observation rules, the past 12 months have been eventful. The Hospitalist asked more than a dozen industry leaders what they thought were the biggest highlights of 2016. Here is what they said:
1. Happy Birthday, HM
August 15 marked the 20th anniversary of “The Emerging Role of ‘Hospitalists’ in the American Health Care System,”1 a New England Journal of Medicine paper authored by Lee Goldman, MD, and Robert Wachter, MD, MHM.2 It was the first time anyone defined what a hospitalist was, putting a sobriquet to an inpatient care model that had organically and independently started happening nationwide.
The paper laid the groundwork for a specialty that spread like a proverbial wildfire over the next 20 years. The model overcame early opposition from residents fearful they’d lose the ability to learn and critical-care specialists who wanted to maintain the caseloads they’d fought to build. The field has now swelled to an estimated 52,000 practitioners.
“I reflect back … and think today about what the hospitalist model brings to us,” James Merlino, MD, president and chief medical officer of Press Ganey’s strategic consulting division, told The Hospitalist. “It is an amazing transformation on how the hospitalist model really delivers.”1
2. Its Own Specialty Code
Hospitalist medicine received federal approval for its first dedicated specialty code3 in a decision hailed by many. The code, approved by the Centers for Medicare & Medicaid Services (CMS), should allow hospitalist-specific billing in 2017.
SHM leaders have long pushed for the code, particularly as healthcare transitions from fee-for-service (FFS) to quality-based payment models. Public Policy Committee Chair Ron Greeno, MD, MHM, says that a dedicated code is necessary to ensure that hospitalists are properly reimbursed for their work.
Historically, hospitalists have used codes more in line with the workload of general internal medicine, family medicine, and other specialties. But those codes don’t account for the complexity of what hospitalists deal with on a daily basis.
“We as hospitalists face unique challenges and work with patients from all demographics, often with severe illnesses, making it nearly impossible to rely on benchmarks used for these other specialties,” Dr. Greeno said.3
SHM pushed for the change and has said it is committed to educating members about how best to use it. Scott Sears, MD, FHM, CPE, MBA, chief clinical officer for Sound Physicians of Tacoma, Wash., said the move is great for HM but that more needs to be done to tailor billing and coding to the specialty’s actual workflow.
“A pediatric hospitalist may not want to be compared to an adult hospitalist. A critical-access hospitalist doesn’t want to be compared to a hospitalist in a tertiary academic medical center,” Dr. Sears said. “I don’t think it’s an end-all, be-all, but it’s a place to start.”3
3. Down with SGR, Long Live MACRA
While it’s unlikely hospitalists have that printed on bumper stickers, 2016 brought the end of the oft-maligned Sustainable Growth Rate (SGR) formula. This was the first year under the Medicare Access and CHIP Reauthorization Act of 2015, better known as MACRA.4
MACRA changes the ways hospitalists and other physicians are reimbursed by Medicare by continuing the broader trend of moving from volume-based reimbursements toward a value-based payment (VBP) system. Its two tracks for physicians to change how they get paid are the Merit-Based Incentive Payment System (MIPS) and the Alternative Payments Model (APM).
MIPS probably looks familiar because it is similar to the traditional FFS model. But to make value a more important factor in the reimbursement formula, MIPS will account for both volume and quality. APM allows physicians to opt out of MIPS by participating in other approved programs where providers take on “more than nominal” financial risk, report on their quality measures, and use certified electronic health record (EHR) technology.
4. The Surgeon General Is a Hospitalist
Any specialty’s annual meeting would be lucky to get the U.S. Surgeon General as a plenary speaker, but HM16 featured one of its own in hospitalist and U.S. Surgeon General Vivek Murthy, MD, MBA.
Dr. Murthy kicked off the confab in San Diego, and some 4,000 hospitalists listened to one of their own talk about ascending the highest perch a physician can attain in the federal government.7 Dr. Murthy, previously a hospitalist at Brigham and Women’s Hospital in Boston, was confirmed as the 19th Surgeon General in December 2014.
In an address titled “Bringing Health to America,” Dr. Murthy inspired with tales of hope and encouraged hospitalists to make the pursuit of healthy appealing while improving the safety of our communities. In particular, he suggested hospitalists look to leverage their leadership to improve systems and to be a powerful force of change both inside the walls of their institution and in their communities.
“In the end, the world gets better when people choose to come together to make it better,” he said.8
5. Nurse Practitioner Joins SHM Board of Directors
At HM16, Tracy Cardin, ACNP-BC, SFHM, was the first nurse practitioner (NP) or physician assistant (PA) given voting privileges on the society’s oversight panel.
“I can’t describe to you how passionately I believe that [NPs and PAs] have a huge role moving forward,” Cardin said. “I think our representation, our visibility, has sort of been flabby and kind of under the wire for a long time. We can really impact the design of care models at the bedside in a way that’s innovative and more efficient and in a way that’s really huge. I think there’s a transformation that’s going to be coming, and we’re going to be a huge part of it.”9
With Cardin’s ascension, it has added the voice of another constituency to its board. She was previously chair of SHM’s Nurse Practitioner/Physician Assistant Committee and in 2015 received the society’s Award in Excellence in Hospital Medicine for NPs and PAs. She has been at the University of Chicago for about 10 years.
“It does send a message to the rest of our membership that SHM values those other constituencies and that this is not a physician membership organization but rather a membership organization comprised of people who are interested in improving healthcare for our hospitalized patients,” immediate past president Robert Harrington Jr., MD, SFHM said.10
6. The State of Hospital Medicine Is Strong
According to the biennial 2016 State of Hospital Medicine Report6 from SHM and partially populated by data from the Medical Group Management Association (MGMA), median compensation for adult hospitalists rose 10% to $278,746 from 2013 to 2015. The double-digit increase continues the steady climb of hospitalist pay, which is up 30% since 2010. At the same time, productivity is flattening.
And nearly all HM groups (HMGs)—96%—are still getting financial support, mostly from their host hospitals, in addition to their professional fee revenue. However, that median support, $157,535 per full-time employee (FTE), increased just 1%.
The slowing growth in that contribution is a harbinger that the level of financial support can no longer grow unabated, said Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
“We’re pretty close to that breaking point,” she said. “When we go around the country and do consulting work, we are hearing many more hospital leaders telling us, ‘We’re concerned about how much money this program is costing us, and we are getting to the point where we can’t afford it.’”6
7. Pay Cut for ‘Two-Midnight’ Rule for Observations Is No More
CMS announced a proposed rule in April that would have Medicare stop imposing an inpatient payment cut to hospitals under the “two-midnight” rule, according to a report in Modern Healthcare.10 The final rule went into effect in October.
The rule, which continues to be a contentious issue for hospitalists even with the pay cut being eliminated, was put in place in October 2013 to define which Medicare beneficiary hospital stays are appropriate for Medicare Part A payment by stating that if the physician expected the patient to stay for fewer than two midnights, then the services should be billed as outpatient (Medicare Part B) and not inpatient.
For two years, the only exception to the pay withhold was for those diagnoses that CMS designated as “inpatient only.” An overhaul of the rule in October 2015 stated that exceptions could be determined by the physician (or other practitioner) on a “case-by-case basis.”
But a legal challenge and withering criticism from SHM and other professional organizations prompted CMS to undo the withheld payments associated rule.11–13 In fact, hospitals also will see a one-time increase of 0.6% in fiscal 2017, making up for the 0.2% reduction to the rates of the last three years. SHM has said it will continue to advocate for further changes to the rule.
8. Medicaid Expansion Takes Hold
Thirty-one states and the District of Columbia, under the auspices of the Affordable Care Act, have expanded Medicaid. One 2014 study in states including Minnesota, Kentucky, and Arizona showed a dramatic decrease in uninsured hospital stays and a significant increase in Medicaid stays. Meanwhile, in six states that did not expand, including Florida, Georgia, and Missouri, there was no significant change in payor mix.14
“What a lot of these early studies are saying is that when you expand Medicaid, people get on Medicaid, and that’s exactly what you hope will happen when you do a major public coverage expansion,” said Sayeh Nikpay, PhD, MPH, assistant professor of health policy at Vanderbilt University School of Medicine in Nashville, Tenn., and a lead author of the 2014 Health Affairs study. “Physicians are grappling with payment issues, and it should be quite a relief that people are coming in the door with some kind of insurance rather than uninsured.”15
While expansion from 2015 to 2016 was the main story for Medicaid, many observers are now watching to see what President-elect Donald Trump will do. As a candidate, he campaigned to repeal Obamacare, and that may have significant impacts on the expansion of Medicaid.
9. Antimicrobial Stewardship Rules Upgrade
In July, The Joint Commission announced a new Medication Management (MM) standard for hospitals, critical-access hospitals, and nursing care centers that goes into effect in 2017.16,17 Its stated purpose is to improve quality and patient safety. The Joint Commission move came a year after President Barack Obama made combatting antibiotic-resistant bacteria a national issue.
“If you review the scientific literature, it will indicate that we’re in crisis mode right now because of this,” said Kelly Podgorny, DNP, MS, CPHQ, RN, project director at The Joint Commission. 16
The standard encourages the prioritization of establishing antimicrobial stewardship programs. It suggests staff members at institutions receive training and education on dispensing, administering, and monitoring antimicrobial resistance and antimicrobial stewardship practice. And, in turn, those staffers should look to educate patients and caregivers on appropriate use of antimicrobial medications.
Lastly, when possible, an antimicrobial team should take a multidisciplinary approach and include an infectious disease physician, a pharmacist, and a practitioner.
10. Febrile-Infant Care Draws a Crowd
One of the most well-attended sessions at 2016 Pediatric Hospital Medicine in Chicago was an update on the anticipated American Academy of Pediatricians (AAP) guidelines for febrile infants.18
The guidelines, for infants 7–90 days old, are aimed at providing pediatric hospitalists and others evidence-based guidelines, not rules, from the most recent literature available. The PHM16 session, presented by Kenneth Roberts, MD, highlighted the need to separate individual components of serious bacterial infections such as urinary tract infections (UTIs), bacteremia, and meningitis. Dr. Roberts noted that the incidence and clinical course can vary greatly for the different diagnoses.
The new criteria would be for full-term infants (37–43 weeks’ gestation) who are well-appearing and present with a temperature of 38°C. Exclusion criteria would include perinatal/prenatal/neonatal maternal fever, infection, or antimicrobial treatment; the presence of any evident infection; being technology-dependent; and the presence of congenital anomalies.
In particular, the new guidelines will look to risk-stratify management by age groups of 7–28 days, 29–60 days, and 61–90 days. The criteria are expected to be released in the next year.
Richard Quinn is a freelance writer in New Jersey.
References
- Quinn R. HM turns 20: a look at the evolution of hospitalist medicine. The Hospitalist website. Accessed November 14, 2016.
- Wachter M, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514-517.
- Tyrrell KA. New hospitalist billing code should benefit hospitalists, patients. The Hospitalist website. Accessed November 14, 2016.
- Doctoroff L, Dutta S. MACRA provides new direction for U.S. healthcare. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. Everything you need to know about the Bundled Payments for Care Improvement Initiative. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. The state of hospital medicine is strong. The Hospitalist website. Accessed November 14, 2016.
- Scheurer D. U.S. surgeon general encourages hospitalists to remain hopeful, motivated. The Hospitalist website. Accessed November 14, 2016.
- Collins TR. HM16 speakers focus on public health, leadership, future of hospital medicine. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. SHM seats its first non-physician board member. The Hospitalist website. Accessed at November 14, 2016.
- Carris J. Centers for Medicare & Medicaid Services (CMS) eliminates two-midnight rule’s inpatient payment cuts: report. The Hospitalist website. Accessed November 14, 2016.
- Schencker L. Judge tells HHS to revisit two-midnight rule’s inpatient pay cut. Healh Affairs website. Accessed November 14, 2016.
- Tyrrell KA. Physicians critical of proposed changes to Medicare’s two-midnight rule. The Hospitalist website. Accessed November 14, 2016.
- Tyrrell KA. Ann Sheehy, MD, MS, FHM, outlines to lawmakers hospitalist concerns about two-midnight rule, Medicare policies. The Hospitalist website. Accessed November 14, 2016.
- Nikpay S, Buchmueller T, Levy HG. Affordable Care Act Medicaid expansion reduced uninsured hospital stays in 2014. Health Aff (Millwood). 2016;35(1):106-110.
- Tyrrell KA. Benefits of Medicaid expansion for hospitalists. The Hospitalist website. Accessed November 14, 2016.
- Bopp S. New standard announced for antimicrobial stewardship. The Hospitalist website. Accessed November 14, 2016.
- Prepublication standards – new antimicrobial stewardship standard. The Joint Commission website. Accessed November 14, 2016.
- 18. DeZure C. PHM16: the new AAP clinical practice guideline on evaluating, managing febrile infants. The Hospitalist website. Accessed November 14, 2016.
Keeping up with New Payment Models
While in medical school, I learned about what was then called GRID (gay-related immune deficiency) and we now know as HIV/AIDS. I thought this condition would become so central to practice in nearly any specialty that I decided to try to keep up with all of the literature on it. It wasn’t yet in textbooks, so I thought it would be very important to keep up with all the new research studies and review articles about it.
I kept in my apartment a growing file of articles photocopied and torn out of journals. But I had badly misjudged the enormity of the task, and within a few years, there were far too many articles for me to read or keep up with in any fashion. Before long, HIV medicine became its own specialty, and while it has always been something I, like any hospitalist, need to know something about, I’ve left it to others to be the real HIV experts.
I was naive to have embarked on the quest. What seemed manageable at first became overwhelming very quickly. The same could be said for trying to keep up with new payment models.
New Professional Fee Reimbursement Models
For decades, most physicians could understand the general concept of how their professional activities generated revenue. But it’s gotten a lot more complicated lately.
The growing prevalence of capitation and other managed-care reimbursement models in the ’80s and ’90s might have been when reimbursement complexity began to increase significantly. But while nearly every doctor in the country heard about managed care, for many, it was something happening elsewhere that never made its way to them.
But for hospitalists, I think the arrival of the Physician Quality Reporting System (PQRS, originally Physician Quality Reporting Initiative, or PQRI) marks the swerve in reimbursement complexity. Some years ago I wrote in these pages about the importance of hospitalists understanding PQRS and described key features of the program.
Like HIV/AIDS medicine literature, the breadth and complexity of reimbursement programs from the Centers for Medicare & Medicaid Services (and other payors) seem to have grown logarithmically since PQRS. The still relatively new bundled payment and MACRA-related models are far more complicated than PQRS. And they change often. Calendar milestones come and go with changes in relevant metrics and performance thresholds, etc. Even the terminology changes frequently. Did you know, for example, that under MIPSi “Advancing Care Information” is essentially a new name for EHR Meaningful Use?
Bundled payments and MACRA are only a small portion of new models implemented over the last few years. There are many others, and dedicated effort is required just to keep track of whether each model influences only physicians (and other providers), only hospitals, or both.
Clinicians’ Responsibility for Keeping Up
My thinking about most hospitalists, or doctors in any specialty, keeping up with all of these models has evolved the same way it did with HIV/AIDS. I think it’s pretty clear that it’s folly to expect most clinicians to know more than the broad outlines of these programs.
Payment models are important. Someone needs to know them in detail, but clinicians should reserve brain cells for clinical knowledge base and focus only on the big picture of payment models. Think how well you’ve done learning and keeping up with CPT coding, observation versus inpatient status determinations, and clinical documentation. You probably still aren’t an expert at these things, so is it wise to set about becoming an expert in new payment models?
Instead, most hospitalists should rely on others to keep up with the precise details of these programs. Most commonly that will mean our employer will appoint or hire one or more people, or engage an outside party, to do this.
Don’t Feel Guilty
It’s common to leave a presentation or doctor’s lounge conversation on payment models feeling like you need to study up on the details of this or that payment model since good performance under that model will be important for your paycheck and to remain a viable “player.” And speakers sometimes intentionally or unintentionally enhance your anxiety about this. Maybe they love to show off what they know, and it’s easy for them to think only about their topic and not keep in mind all of the other stuff you need to know.
It’s terrific if someone in your practice is particularly interested in payment models and chooses to stay on top of them. Just make sure that doesn’t come at the expense of keeping up with changes in clinical practice. Most groups won’t have such a person and should rely on others, including SHM, without feeling the smallest bit of guilt.
SHM is advocating on behalf of hospitalists and working diligently to distill the impact MACRA and its various alternative payment frameworks will have on hospital medicine. With webinars, Q&As, and additional online and print resources, SHM will continue to provide digestible updates for hospitalists and their practices.
The End of Small-Group Physician Practice?
While the intent of these programs is to encourage and reward improvements in clinical practice, keeping up with and managing them is a tax that takes resources away from clinical practice. This is an especially difficult burden for small private practices and may prove to be a significant factor in nearly extinguishing them. There are relatively few small private hospitalist groups,ii but all of them should carefully consider how they will keep up with new reimbursement models.
While in medical school, I learned about what was then called GRID (gay-related immune deficiency) and we now know as HIV/AIDS. I thought this condition would become so central to practice in nearly any specialty that I decided to try to keep up with all of the literature on it. It wasn’t yet in textbooks, so I thought it would be very important to keep up with all the new research studies and review articles about it.
I kept in my apartment a growing file of articles photocopied and torn out of journals. But I had badly misjudged the enormity of the task, and within a few years, there were far too many articles for me to read or keep up with in any fashion. Before long, HIV medicine became its own specialty, and while it has always been something I, like any hospitalist, need to know something about, I’ve left it to others to be the real HIV experts.
I was naive to have embarked on the quest. What seemed manageable at first became overwhelming very quickly. The same could be said for trying to keep up with new payment models.
New Professional Fee Reimbursement Models
For decades, most physicians could understand the general concept of how their professional activities generated revenue. But it’s gotten a lot more complicated lately.
The growing prevalence of capitation and other managed-care reimbursement models in the ’80s and ’90s might have been when reimbursement complexity began to increase significantly. But while nearly every doctor in the country heard about managed care, for many, it was something happening elsewhere that never made its way to them.
But for hospitalists, I think the arrival of the Physician Quality Reporting System (PQRS, originally Physician Quality Reporting Initiative, or PQRI) marks the swerve in reimbursement complexity. Some years ago I wrote in these pages about the importance of hospitalists understanding PQRS and described key features of the program.
Like HIV/AIDS medicine literature, the breadth and complexity of reimbursement programs from the Centers for Medicare & Medicaid Services (and other payors) seem to have grown logarithmically since PQRS. The still relatively new bundled payment and MACRA-related models are far more complicated than PQRS. And they change often. Calendar milestones come and go with changes in relevant metrics and performance thresholds, etc. Even the terminology changes frequently. Did you know, for example, that under MIPSi “Advancing Care Information” is essentially a new name for EHR Meaningful Use?
Bundled payments and MACRA are only a small portion of new models implemented over the last few years. There are many others, and dedicated effort is required just to keep track of whether each model influences only physicians (and other providers), only hospitals, or both.
Clinicians’ Responsibility for Keeping Up
My thinking about most hospitalists, or doctors in any specialty, keeping up with all of these models has evolved the same way it did with HIV/AIDS. I think it’s pretty clear that it’s folly to expect most clinicians to know more than the broad outlines of these programs.
Payment models are important. Someone needs to know them in detail, but clinicians should reserve brain cells for clinical knowledge base and focus only on the big picture of payment models. Think how well you’ve done learning and keeping up with CPT coding, observation versus inpatient status determinations, and clinical documentation. You probably still aren’t an expert at these things, so is it wise to set about becoming an expert in new payment models?
Instead, most hospitalists should rely on others to keep up with the precise details of these programs. Most commonly that will mean our employer will appoint or hire one or more people, or engage an outside party, to do this.
Don’t Feel Guilty
It’s common to leave a presentation or doctor’s lounge conversation on payment models feeling like you need to study up on the details of this or that payment model since good performance under that model will be important for your paycheck and to remain a viable “player.” And speakers sometimes intentionally or unintentionally enhance your anxiety about this. Maybe they love to show off what they know, and it’s easy for them to think only about their topic and not keep in mind all of the other stuff you need to know.
It’s terrific if someone in your practice is particularly interested in payment models and chooses to stay on top of them. Just make sure that doesn’t come at the expense of keeping up with changes in clinical practice. Most groups won’t have such a person and should rely on others, including SHM, without feeling the smallest bit of guilt.
SHM is advocating on behalf of hospitalists and working diligently to distill the impact MACRA and its various alternative payment frameworks will have on hospital medicine. With webinars, Q&As, and additional online and print resources, SHM will continue to provide digestible updates for hospitalists and their practices.
The End of Small-Group Physician Practice?
While the intent of these programs is to encourage and reward improvements in clinical practice, keeping up with and managing them is a tax that takes resources away from clinical practice. This is an especially difficult burden for small private practices and may prove to be a significant factor in nearly extinguishing them. There are relatively few small private hospitalist groups,ii but all of them should carefully consider how they will keep up with new reimbursement models.
While in medical school, I learned about what was then called GRID (gay-related immune deficiency) and we now know as HIV/AIDS. I thought this condition would become so central to practice in nearly any specialty that I decided to try to keep up with all of the literature on it. It wasn’t yet in textbooks, so I thought it would be very important to keep up with all the new research studies and review articles about it.
I kept in my apartment a growing file of articles photocopied and torn out of journals. But I had badly misjudged the enormity of the task, and within a few years, there were far too many articles for me to read or keep up with in any fashion. Before long, HIV medicine became its own specialty, and while it has always been something I, like any hospitalist, need to know something about, I’ve left it to others to be the real HIV experts.
I was naive to have embarked on the quest. What seemed manageable at first became overwhelming very quickly. The same could be said for trying to keep up with new payment models.
New Professional Fee Reimbursement Models
For decades, most physicians could understand the general concept of how their professional activities generated revenue. But it’s gotten a lot more complicated lately.
The growing prevalence of capitation and other managed-care reimbursement models in the ’80s and ’90s might have been when reimbursement complexity began to increase significantly. But while nearly every doctor in the country heard about managed care, for many, it was something happening elsewhere that never made its way to them.
But for hospitalists, I think the arrival of the Physician Quality Reporting System (PQRS, originally Physician Quality Reporting Initiative, or PQRI) marks the swerve in reimbursement complexity. Some years ago I wrote in these pages about the importance of hospitalists understanding PQRS and described key features of the program.
Like HIV/AIDS medicine literature, the breadth and complexity of reimbursement programs from the Centers for Medicare & Medicaid Services (and other payors) seem to have grown logarithmically since PQRS. The still relatively new bundled payment and MACRA-related models are far more complicated than PQRS. And they change often. Calendar milestones come and go with changes in relevant metrics and performance thresholds, etc. Even the terminology changes frequently. Did you know, for example, that under MIPSi “Advancing Care Information” is essentially a new name for EHR Meaningful Use?
Bundled payments and MACRA are only a small portion of new models implemented over the last few years. There are many others, and dedicated effort is required just to keep track of whether each model influences only physicians (and other providers), only hospitals, or both.
Clinicians’ Responsibility for Keeping Up
My thinking about most hospitalists, or doctors in any specialty, keeping up with all of these models has evolved the same way it did with HIV/AIDS. I think it’s pretty clear that it’s folly to expect most clinicians to know more than the broad outlines of these programs.
Payment models are important. Someone needs to know them in detail, but clinicians should reserve brain cells for clinical knowledge base and focus only on the big picture of payment models. Think how well you’ve done learning and keeping up with CPT coding, observation versus inpatient status determinations, and clinical documentation. You probably still aren’t an expert at these things, so is it wise to set about becoming an expert in new payment models?
Instead, most hospitalists should rely on others to keep up with the precise details of these programs. Most commonly that will mean our employer will appoint or hire one or more people, or engage an outside party, to do this.
Don’t Feel Guilty
It’s common to leave a presentation or doctor’s lounge conversation on payment models feeling like you need to study up on the details of this or that payment model since good performance under that model will be important for your paycheck and to remain a viable “player.” And speakers sometimes intentionally or unintentionally enhance your anxiety about this. Maybe they love to show off what they know, and it’s easy for them to think only about their topic and not keep in mind all of the other stuff you need to know.
It’s terrific if someone in your practice is particularly interested in payment models and chooses to stay on top of them. Just make sure that doesn’t come at the expense of keeping up with changes in clinical practice. Most groups won’t have such a person and should rely on others, including SHM, without feeling the smallest bit of guilt.
SHM is advocating on behalf of hospitalists and working diligently to distill the impact MACRA and its various alternative payment frameworks will have on hospital medicine. With webinars, Q&As, and additional online and print resources, SHM will continue to provide digestible updates for hospitalists and their practices.
The End of Small-Group Physician Practice?
While the intent of these programs is to encourage and reward improvements in clinical practice, keeping up with and managing them is a tax that takes resources away from clinical practice. This is an especially difficult burden for small private practices and may prove to be a significant factor in nearly extinguishing them. There are relatively few small private hospitalist groups,ii but all of them should carefully consider how they will keep up with new reimbursement models.