User login
In Case You Missed It: COVID
Fired for good judgment a sign of physicians’ lost respect
What happened to Hasan Gokal, MD, should stick painfully in the craws of all physicians. It should serve as a call to action, because Dr. Gokal is sitting at home today without a job and under threat of further legal action while we continue about our day.
Dr. Gokal’s “crime” is that he vaccinated 10 strangers and acquaintances with soon-to-expire doses of the Moderna COVID-19 vaccine. He drove to the homes of some in the dark of night and injected others on his Sugar Land, Texas, lawn. He spent hours in a frantic search for willing recipients to beat the expiration clock. With minutes to spare, he gave the last dose to his at-risk wife, who has symptomatic pulmonary sarcoidosis, but whose age meant she did not fall into a vaccine priority tier.
According to the New York Times, Dr. Gokal’s wife was hesitant, afraid he might get into trouble. But why would she be hesitant? He wasn’t doing anything immoral. Perhaps she knew how far physicians have fallen and how bitterly they both could suffer.
In Barren County, Ky., where I live, a state of emergency was declared by our judge executive because of inclement weather. This directive allows our emergency management to “waive procedures and formalities otherwise required by the law.” It’s too bad that the same courtesy was not afforded to Dr. Gokal in Texas. It’s a shame that ice and snow didn’t drive his actions. Perhaps that would have protected him against the harsh criticism. Rather, it was his oath to patients and dedication to his fellow humans that motivated him, and for that, he was made to suffer.
Dr. Gokal was right to think that pouring the last 10 vaccine doses down the toilet would be an egregious act. But he was wrong in thinking his decision to find takers for the vaccine would be viewed as expedient. Instead, he was accused of graft and even nepotism. And there is the rub. That he was fired and charged with the theft of $137 worth of vaccines says everything about how physicians are treated in the year 2021. Dr. Gokal’s lawyer says the charge carried a maximum penalty of 1 year in prison and a fine of nearly $4,000.
Thank God a sage judge threw out the case and “rebuked” the office of District Attorney Kim Ogg. That hasn’t stopped her from threatening to bring the case to a grand jury. That threat invites anyone faced with the same scenario to flush the extra vaccine doses into the septic system. It encourages us to choose the toilet handle to avoid a mug shot.
And we can’t ignore the racial slant to this story. The Times reported that Dr. Gokal asked the officials, “Are you suggesting that there were too many Indian names in this group?”
“Exactly” was the answer. Let that sink in.
None of this would have happened 20 years ago. Back then, no one would have questioned the wisdom a physician gains from all our years of training and residency. In an age when anyone who conducts an office visit is now called “doctor,” respect for the letters “MD” has been leveled. We physicians have lost our autonomy and been cowed into submission.
But whatever his profession, Hasan Gokal was fired for being a good human. Today, the sun rose on 10 individuals who now enjoy better protection against a deadly pandemic. They include a bed-bound nonagenarian. A woman in her 80s with dementia. A mother with a child who uses a ventilator. All now have antibodies against SARS-CoV2 because of the tireless actions of Dr. Gokal.
Yet Dr. Gokal’s future is uncertain. Will we help him, or will we leave him to the wolves? In an email exchange with his lawyer’s office, I learned that Dr. Gokal has received offers of employment but is unable to entertain them because the actions by the Harris County District Attorney triggered an automatic review by the Texas Medical Board. A GoFundMe page was launched, but an appreciative Dr. Gokal stated publicly that he’d rather the money go to a needy charity.
In the last paragraph of the Times article, Dr. Gokal asks, “How can I take it back?” referencing stories about “the Pakistani doctor in Houston who stole all those vaccines.”
Let’s help him take back his story. In helping him, perhaps we can take back a little control. We could start with letters of support that could be mailed to his lawyer, Paul Doyle, Esq., of Houston, or tweet, respectfully of course, to the district attorney @Kimoggforda.
We can also let the Harris County Public Health Department in Houston know what we think of their actions.
On Martin Luther King Day, Kim Ogg, the district attorney who charged Dr. Gokal, tweeted MLK’s famous quote: “Injustice anywhere is a threat to justice everywhere.”
Let that motivate us to action.
Melissa Walton-Shirley, MD, is a native Kentuckian who retired from full-time invasive cardiology. She enjoys locums work in Montana and is a champion of physician rights and patient safety. In addition to opinion writing, she enjoys spending time with her husband, daughters and parents, and sidelines as a backing vocalist for local rock bands. A version of this article first appeared on Medscape.com.
What happened to Hasan Gokal, MD, should stick painfully in the craws of all physicians. It should serve as a call to action, because Dr. Gokal is sitting at home today without a job and under threat of further legal action while we continue about our day.
Dr. Gokal’s “crime” is that he vaccinated 10 strangers and acquaintances with soon-to-expire doses of the Moderna COVID-19 vaccine. He drove to the homes of some in the dark of night and injected others on his Sugar Land, Texas, lawn. He spent hours in a frantic search for willing recipients to beat the expiration clock. With minutes to spare, he gave the last dose to his at-risk wife, who has symptomatic pulmonary sarcoidosis, but whose age meant she did not fall into a vaccine priority tier.
According to the New York Times, Dr. Gokal’s wife was hesitant, afraid he might get into trouble. But why would she be hesitant? He wasn’t doing anything immoral. Perhaps she knew how far physicians have fallen and how bitterly they both could suffer.
In Barren County, Ky., where I live, a state of emergency was declared by our judge executive because of inclement weather. This directive allows our emergency management to “waive procedures and formalities otherwise required by the law.” It’s too bad that the same courtesy was not afforded to Dr. Gokal in Texas. It’s a shame that ice and snow didn’t drive his actions. Perhaps that would have protected him against the harsh criticism. Rather, it was his oath to patients and dedication to his fellow humans that motivated him, and for that, he was made to suffer.
Dr. Gokal was right to think that pouring the last 10 vaccine doses down the toilet would be an egregious act. But he was wrong in thinking his decision to find takers for the vaccine would be viewed as expedient. Instead, he was accused of graft and even nepotism. And there is the rub. That he was fired and charged with the theft of $137 worth of vaccines says everything about how physicians are treated in the year 2021. Dr. Gokal’s lawyer says the charge carried a maximum penalty of 1 year in prison and a fine of nearly $4,000.
Thank God a sage judge threw out the case and “rebuked” the office of District Attorney Kim Ogg. That hasn’t stopped her from threatening to bring the case to a grand jury. That threat invites anyone faced with the same scenario to flush the extra vaccine doses into the septic system. It encourages us to choose the toilet handle to avoid a mug shot.
And we can’t ignore the racial slant to this story. The Times reported that Dr. Gokal asked the officials, “Are you suggesting that there were too many Indian names in this group?”
“Exactly” was the answer. Let that sink in.
None of this would have happened 20 years ago. Back then, no one would have questioned the wisdom a physician gains from all our years of training and residency. In an age when anyone who conducts an office visit is now called “doctor,” respect for the letters “MD” has been leveled. We physicians have lost our autonomy and been cowed into submission.
But whatever his profession, Hasan Gokal was fired for being a good human. Today, the sun rose on 10 individuals who now enjoy better protection against a deadly pandemic. They include a bed-bound nonagenarian. A woman in her 80s with dementia. A mother with a child who uses a ventilator. All now have antibodies against SARS-CoV2 because of the tireless actions of Dr. Gokal.
Yet Dr. Gokal’s future is uncertain. Will we help him, or will we leave him to the wolves? In an email exchange with his lawyer’s office, I learned that Dr. Gokal has received offers of employment but is unable to entertain them because the actions by the Harris County District Attorney triggered an automatic review by the Texas Medical Board. A GoFundMe page was launched, but an appreciative Dr. Gokal stated publicly that he’d rather the money go to a needy charity.
In the last paragraph of the Times article, Dr. Gokal asks, “How can I take it back?” referencing stories about “the Pakistani doctor in Houston who stole all those vaccines.”
Let’s help him take back his story. In helping him, perhaps we can take back a little control. We could start with letters of support that could be mailed to his lawyer, Paul Doyle, Esq., of Houston, or tweet, respectfully of course, to the district attorney @Kimoggforda.
We can also let the Harris County Public Health Department in Houston know what we think of their actions.
On Martin Luther King Day, Kim Ogg, the district attorney who charged Dr. Gokal, tweeted MLK’s famous quote: “Injustice anywhere is a threat to justice everywhere.”
Let that motivate us to action.
Melissa Walton-Shirley, MD, is a native Kentuckian who retired from full-time invasive cardiology. She enjoys locums work in Montana and is a champion of physician rights and patient safety. In addition to opinion writing, she enjoys spending time with her husband, daughters and parents, and sidelines as a backing vocalist for local rock bands. A version of this article first appeared on Medscape.com.
What happened to Hasan Gokal, MD, should stick painfully in the craws of all physicians. It should serve as a call to action, because Dr. Gokal is sitting at home today without a job and under threat of further legal action while we continue about our day.
Dr. Gokal’s “crime” is that he vaccinated 10 strangers and acquaintances with soon-to-expire doses of the Moderna COVID-19 vaccine. He drove to the homes of some in the dark of night and injected others on his Sugar Land, Texas, lawn. He spent hours in a frantic search for willing recipients to beat the expiration clock. With minutes to spare, he gave the last dose to his at-risk wife, who has symptomatic pulmonary sarcoidosis, but whose age meant she did not fall into a vaccine priority tier.
According to the New York Times, Dr. Gokal’s wife was hesitant, afraid he might get into trouble. But why would she be hesitant? He wasn’t doing anything immoral. Perhaps she knew how far physicians have fallen and how bitterly they both could suffer.
In Barren County, Ky., where I live, a state of emergency was declared by our judge executive because of inclement weather. This directive allows our emergency management to “waive procedures and formalities otherwise required by the law.” It’s too bad that the same courtesy was not afforded to Dr. Gokal in Texas. It’s a shame that ice and snow didn’t drive his actions. Perhaps that would have protected him against the harsh criticism. Rather, it was his oath to patients and dedication to his fellow humans that motivated him, and for that, he was made to suffer.
Dr. Gokal was right to think that pouring the last 10 vaccine doses down the toilet would be an egregious act. But he was wrong in thinking his decision to find takers for the vaccine would be viewed as expedient. Instead, he was accused of graft and even nepotism. And there is the rub. That he was fired and charged with the theft of $137 worth of vaccines says everything about how physicians are treated in the year 2021. Dr. Gokal’s lawyer says the charge carried a maximum penalty of 1 year in prison and a fine of nearly $4,000.
Thank God a sage judge threw out the case and “rebuked” the office of District Attorney Kim Ogg. That hasn’t stopped her from threatening to bring the case to a grand jury. That threat invites anyone faced with the same scenario to flush the extra vaccine doses into the septic system. It encourages us to choose the toilet handle to avoid a mug shot.
And we can’t ignore the racial slant to this story. The Times reported that Dr. Gokal asked the officials, “Are you suggesting that there were too many Indian names in this group?”
“Exactly” was the answer. Let that sink in.
None of this would have happened 20 years ago. Back then, no one would have questioned the wisdom a physician gains from all our years of training and residency. In an age when anyone who conducts an office visit is now called “doctor,” respect for the letters “MD” has been leveled. We physicians have lost our autonomy and been cowed into submission.
But whatever his profession, Hasan Gokal was fired for being a good human. Today, the sun rose on 10 individuals who now enjoy better protection against a deadly pandemic. They include a bed-bound nonagenarian. A woman in her 80s with dementia. A mother with a child who uses a ventilator. All now have antibodies against SARS-CoV2 because of the tireless actions of Dr. Gokal.
Yet Dr. Gokal’s future is uncertain. Will we help him, or will we leave him to the wolves? In an email exchange with his lawyer’s office, I learned that Dr. Gokal has received offers of employment but is unable to entertain them because the actions by the Harris County District Attorney triggered an automatic review by the Texas Medical Board. A GoFundMe page was launched, but an appreciative Dr. Gokal stated publicly that he’d rather the money go to a needy charity.
In the last paragraph of the Times article, Dr. Gokal asks, “How can I take it back?” referencing stories about “the Pakistani doctor in Houston who stole all those vaccines.”
Let’s help him take back his story. In helping him, perhaps we can take back a little control. We could start with letters of support that could be mailed to his lawyer, Paul Doyle, Esq., of Houston, or tweet, respectfully of course, to the district attorney @Kimoggforda.
We can also let the Harris County Public Health Department in Houston know what we think of their actions.
On Martin Luther King Day, Kim Ogg, the district attorney who charged Dr. Gokal, tweeted MLK’s famous quote: “Injustice anywhere is a threat to justice everywhere.”
Let that motivate us to action.
Melissa Walton-Shirley, MD, is a native Kentuckian who retired from full-time invasive cardiology. She enjoys locums work in Montana and is a champion of physician rights and patient safety. In addition to opinion writing, she enjoys spending time with her husband, daughters and parents, and sidelines as a backing vocalist for local rock bands. A version of this article first appeared on Medscape.com.
Mindfulness can help patients manage ‘good’ change – and relief
Two themes have emerged recently in my psychotherapy practice, and in the mirror: relief and exhaustion. Some peace in the public discourse, or at least a pause in the ominous discord, has had the effect of a lightening, an unburdening. Some release from a contracted sense of tension around the specifics of violence and a broader sense of civil fracture has been palpable like a big, deep breath, exhaled. No sensible person would mistake this for being out of the metaphoric woods. A virus menaces and mutates, economic woes follow, and lots of us don’t get along. But, yes, there is some relief, some good change.
But even good change, even a downshift into relief, can pose some challenges to look for and overcome.
Consider for a moment the notion that every change represents a loss, a metaphoric “death” of the prior state of things. This is true of big, painful losses, like the death of a loved one, and small ones, like finding an empty cookie jar. It’s also true in changes we associate with benefit or relief: a refund check, a job promotion, a resolving migraine, or the breaking out of some civility.
In changes of all sorts, the world outside of one’s mind has shifted – at odds, momentarily, with our inner, now obsolete understanding of that changed world. The inside of the head does not match the outside. How we make that adjustment, so “inside = outside,” is a clinically familiar process: it’s grieving, with a sequence famously elaborated upon by Elisabeth Kübler-Ross, MD,1 and others.
We all likely know the steps: shock/denial, anger, “bargaining,” depression, and acceptance. A quick review: Our initial anxious/threat reaction leads to grievous judgment, to rationalizing “woulda/coulda/shoulda’s,” then to truly landing in the disappointment of a loss or change, and the accepting of a new steady state. Inside proceeds to match outside.
So, what then of relief? How do we process “good” change? I think we still must move from “in ≠ out” to “in = out,” navigating some pitfalls along the way.
Initial threat often remains; apprehension of the “new” still can generate energy, and even a sense of threat, regardless of a kiss or a shove. Our brainstems run roughshod over this first phase.
Step two is about judgment. We can move past the threat to, “How do I feel about it?” Here’s where grievous feeling gets swapped out for something more peak-positive – joy, or relief if the change represents an ending of a state of suffering, tension, or uncertainty.
The “bargaining” step still happens, but often around a kind of testing regimen: Is this too good to be true? Is it really different? We run scenarios.
The thud of disappointment also gets a makeover. It’s a settling into the beneficial change and its associations: gratitude, a sense of energy shifting.
The bookend “OK” seems anodyne here – why would anyone not accept relief, some good change?2 But it can nevertheless represent a challenge for many. The receding tension of the last year could open into a burst of energy, but I’m finding that exhaustion is just as or more common. That’s not illness, but a weary exhaling from the longest of held breaths.
One other twist: What happens when one of those steps is an individual obstacle, trigger, or hard-to-hold state? Especially for those with deep experience in disappointment or even trauma, buying into acceptance of a new normal can feel like a fool’s game. This is an especially complex spot for individuals who won’t quite allow for joyful acceptance to break out, lest it reveals itself as a humiliating trick or a too-brief respite from the “usual.”
Mindfulness practices, such as meditation, are helpful in managing this process. Committed time and optimal conditions to witness and adapt to the various inner states that ebb and flow generate a clear therapeutic benefit. Patients improve their identification of somatic manifestations, emotional reactions, and cycling ruminations of thought. What generates distraction and loss of mindful attention becomes better recognized. Contemplative work in between sessions becomes more productive.
What else do I advise?3 Patience, and some compassion for ourselves in this unusual time. Grief, and relief, are complex but truly human processes that generate not just one state of experience, but a cascade of them. While that cascade can hurt, it’s actually normal, not illness. But it can be exhausting.
Dr. Sazima is a Northern California psychiatrist, educator, and author. He is senior behavioral faculty at the Stanford-O’Connor Family Medicine Residency Program in San José, Calif. His latest book is “Practical Mindfulness: A Physician’s No-Nonsense Guide to Meditation for Beginners,” Miami: Mango Publishing, 2021. Dr. Sazima disclosed no relevant financial relationships.
References
1. Kübler-Ross E. “On Death And Dying,” New York: Simon & Schuster, 1969.
2. Selye H. “Stress Without Distress,” New York: Lippincott, Williams & Wilkins, 1974.
3. Sazima G. “Practical Mindfulness: A Physician’s No-Nonsense Guide to Meditation for Beginners,” Miami: Mango Publishing, 2021.
Two themes have emerged recently in my psychotherapy practice, and in the mirror: relief and exhaustion. Some peace in the public discourse, or at least a pause in the ominous discord, has had the effect of a lightening, an unburdening. Some release from a contracted sense of tension around the specifics of violence and a broader sense of civil fracture has been palpable like a big, deep breath, exhaled. No sensible person would mistake this for being out of the metaphoric woods. A virus menaces and mutates, economic woes follow, and lots of us don’t get along. But, yes, there is some relief, some good change.
But even good change, even a downshift into relief, can pose some challenges to look for and overcome.
Consider for a moment the notion that every change represents a loss, a metaphoric “death” of the prior state of things. This is true of big, painful losses, like the death of a loved one, and small ones, like finding an empty cookie jar. It’s also true in changes we associate with benefit or relief: a refund check, a job promotion, a resolving migraine, or the breaking out of some civility.
In changes of all sorts, the world outside of one’s mind has shifted – at odds, momentarily, with our inner, now obsolete understanding of that changed world. The inside of the head does not match the outside. How we make that adjustment, so “inside = outside,” is a clinically familiar process: it’s grieving, with a sequence famously elaborated upon by Elisabeth Kübler-Ross, MD,1 and others.
We all likely know the steps: shock/denial, anger, “bargaining,” depression, and acceptance. A quick review: Our initial anxious/threat reaction leads to grievous judgment, to rationalizing “woulda/coulda/shoulda’s,” then to truly landing in the disappointment of a loss or change, and the accepting of a new steady state. Inside proceeds to match outside.
So, what then of relief? How do we process “good” change? I think we still must move from “in ≠ out” to “in = out,” navigating some pitfalls along the way.
Initial threat often remains; apprehension of the “new” still can generate energy, and even a sense of threat, regardless of a kiss or a shove. Our brainstems run roughshod over this first phase.
Step two is about judgment. We can move past the threat to, “How do I feel about it?” Here’s where grievous feeling gets swapped out for something more peak-positive – joy, or relief if the change represents an ending of a state of suffering, tension, or uncertainty.
The “bargaining” step still happens, but often around a kind of testing regimen: Is this too good to be true? Is it really different? We run scenarios.
The thud of disappointment also gets a makeover. It’s a settling into the beneficial change and its associations: gratitude, a sense of energy shifting.
The bookend “OK” seems anodyne here – why would anyone not accept relief, some good change?2 But it can nevertheless represent a challenge for many. The receding tension of the last year could open into a burst of energy, but I’m finding that exhaustion is just as or more common. That’s not illness, but a weary exhaling from the longest of held breaths.
One other twist: What happens when one of those steps is an individual obstacle, trigger, or hard-to-hold state? Especially for those with deep experience in disappointment or even trauma, buying into acceptance of a new normal can feel like a fool’s game. This is an especially complex spot for individuals who won’t quite allow for joyful acceptance to break out, lest it reveals itself as a humiliating trick or a too-brief respite from the “usual.”
Mindfulness practices, such as meditation, are helpful in managing this process. Committed time and optimal conditions to witness and adapt to the various inner states that ebb and flow generate a clear therapeutic benefit. Patients improve their identification of somatic manifestations, emotional reactions, and cycling ruminations of thought. What generates distraction and loss of mindful attention becomes better recognized. Contemplative work in between sessions becomes more productive.
What else do I advise?3 Patience, and some compassion for ourselves in this unusual time. Grief, and relief, are complex but truly human processes that generate not just one state of experience, but a cascade of them. While that cascade can hurt, it’s actually normal, not illness. But it can be exhausting.
Dr. Sazima is a Northern California psychiatrist, educator, and author. He is senior behavioral faculty at the Stanford-O’Connor Family Medicine Residency Program in San José, Calif. His latest book is “Practical Mindfulness: A Physician’s No-Nonsense Guide to Meditation for Beginners,” Miami: Mango Publishing, 2021. Dr. Sazima disclosed no relevant financial relationships.
References
1. Kübler-Ross E. “On Death And Dying,” New York: Simon & Schuster, 1969.
2. Selye H. “Stress Without Distress,” New York: Lippincott, Williams & Wilkins, 1974.
3. Sazima G. “Practical Mindfulness: A Physician’s No-Nonsense Guide to Meditation for Beginners,” Miami: Mango Publishing, 2021.
Two themes have emerged recently in my psychotherapy practice, and in the mirror: relief and exhaustion. Some peace in the public discourse, or at least a pause in the ominous discord, has had the effect of a lightening, an unburdening. Some release from a contracted sense of tension around the specifics of violence and a broader sense of civil fracture has been palpable like a big, deep breath, exhaled. No sensible person would mistake this for being out of the metaphoric woods. A virus menaces and mutates, economic woes follow, and lots of us don’t get along. But, yes, there is some relief, some good change.
But even good change, even a downshift into relief, can pose some challenges to look for and overcome.
Consider for a moment the notion that every change represents a loss, a metaphoric “death” of the prior state of things. This is true of big, painful losses, like the death of a loved one, and small ones, like finding an empty cookie jar. It’s also true in changes we associate with benefit or relief: a refund check, a job promotion, a resolving migraine, or the breaking out of some civility.
In changes of all sorts, the world outside of one’s mind has shifted – at odds, momentarily, with our inner, now obsolete understanding of that changed world. The inside of the head does not match the outside. How we make that adjustment, so “inside = outside,” is a clinically familiar process: it’s grieving, with a sequence famously elaborated upon by Elisabeth Kübler-Ross, MD,1 and others.
We all likely know the steps: shock/denial, anger, “bargaining,” depression, and acceptance. A quick review: Our initial anxious/threat reaction leads to grievous judgment, to rationalizing “woulda/coulda/shoulda’s,” then to truly landing in the disappointment of a loss or change, and the accepting of a new steady state. Inside proceeds to match outside.
So, what then of relief? How do we process “good” change? I think we still must move from “in ≠ out” to “in = out,” navigating some pitfalls along the way.
Initial threat often remains; apprehension of the “new” still can generate energy, and even a sense of threat, regardless of a kiss or a shove. Our brainstems run roughshod over this first phase.
Step two is about judgment. We can move past the threat to, “How do I feel about it?” Here’s where grievous feeling gets swapped out for something more peak-positive – joy, or relief if the change represents an ending of a state of suffering, tension, or uncertainty.
The “bargaining” step still happens, but often around a kind of testing regimen: Is this too good to be true? Is it really different? We run scenarios.
The thud of disappointment also gets a makeover. It’s a settling into the beneficial change and its associations: gratitude, a sense of energy shifting.
The bookend “OK” seems anodyne here – why would anyone not accept relief, some good change?2 But it can nevertheless represent a challenge for many. The receding tension of the last year could open into a burst of energy, but I’m finding that exhaustion is just as or more common. That’s not illness, but a weary exhaling from the longest of held breaths.
One other twist: What happens when one of those steps is an individual obstacle, trigger, or hard-to-hold state? Especially for those with deep experience in disappointment or even trauma, buying into acceptance of a new normal can feel like a fool’s game. This is an especially complex spot for individuals who won’t quite allow for joyful acceptance to break out, lest it reveals itself as a humiliating trick or a too-brief respite from the “usual.”
Mindfulness practices, such as meditation, are helpful in managing this process. Committed time and optimal conditions to witness and adapt to the various inner states that ebb and flow generate a clear therapeutic benefit. Patients improve their identification of somatic manifestations, emotional reactions, and cycling ruminations of thought. What generates distraction and loss of mindful attention becomes better recognized. Contemplative work in between sessions becomes more productive.
What else do I advise?3 Patience, and some compassion for ourselves in this unusual time. Grief, and relief, are complex but truly human processes that generate not just one state of experience, but a cascade of them. While that cascade can hurt, it’s actually normal, not illness. But it can be exhausting.
Dr. Sazima is a Northern California psychiatrist, educator, and author. He is senior behavioral faculty at the Stanford-O’Connor Family Medicine Residency Program in San José, Calif. His latest book is “Practical Mindfulness: A Physician’s No-Nonsense Guide to Meditation for Beginners,” Miami: Mango Publishing, 2021. Dr. Sazima disclosed no relevant financial relationships.
References
1. Kübler-Ross E. “On Death And Dying,” New York: Simon & Schuster, 1969.
2. Selye H. “Stress Without Distress,” New York: Lippincott, Williams & Wilkins, 1974.
3. Sazima G. “Practical Mindfulness: A Physician’s No-Nonsense Guide to Meditation for Beginners,” Miami: Mango Publishing, 2021.
COVID-19 vaccination linked to less mechanical ventilation
new evidence reveals.
Compared with residents younger than 50 – so far vaccinated at lower rates than those of the higher-risk older people – Israelis 70 and older were 67% less likely to require mechanical ventilation for SARS-CoV-2 infection in February 2021 compared with October-December 2020.
“This study provides preliminary evidence at the population level for the reduction in risk for severe COVID-19, as manifested by need for mechanical ventilation, after vaccination with the Pfizer-BioNTech COVID-19 vaccine,” wrote lead author Ehud Rinott, department of public health, faculty of health sciences, Ben-Gurion University of the Negev in Beer-Sheva, Israel, and colleagues.
The study was published online Feb. 26, 2021, in Morbidity and Mortality Weekly Report.
The progress of COVID-19 vaccination across Israel presents researchers with a unique opportunity to study effectiveness on a population level. In this study, 84% of residents 70 and older received two-dose vaccinations. In contrast, only 10% of people in Israel younger than 50 received the same vaccine coverage.
Along with senior author Yair Lewis, MD, PhD, and coauthor Ilan Youngster, MD, Mr. Rinott compared mechanical ventilation rates between Oct. 2, 2020, and Feb. 9, 2021. They found that the ratio of people 70 and older compared with those younger than 50 requiring mechanical ventilation changed from 5.8:1 to 1.9:1 between these periods. This translates to the 67% decrease.
The study offers a “real-world” look at vaccination effectiveness, adding to more controlled evidence from clinical trials. “Achieving high vaccination coverage through intensive vaccination campaigns has the potential to substantially reduce COVID-19-associated morbidity and mortality,” the researchers wrote.
Israel started a national vaccination program on Dec. 20, 2020, targeting high-risk residents including people 60 and older, health care workers, and those with relevant comorbidities. At the same time, in addition to immunization, Israel has used strategies like stay-at-home orders, school closures, mask mandates, and more.
Potential limitations include a limited ability to account for the effect of the stay-at-home orders, spread of virus variants, and other concomitant factors; a potential for a delayed reporting of cases; and variability in mitigation measures by age group.
Dr. Youngster reported receipt of consulting fees from MyBiotix Ltd.
A version of this article first appeared on Medscape.com.
new evidence reveals.
Compared with residents younger than 50 – so far vaccinated at lower rates than those of the higher-risk older people – Israelis 70 and older were 67% less likely to require mechanical ventilation for SARS-CoV-2 infection in February 2021 compared with October-December 2020.
“This study provides preliminary evidence at the population level for the reduction in risk for severe COVID-19, as manifested by need for mechanical ventilation, after vaccination with the Pfizer-BioNTech COVID-19 vaccine,” wrote lead author Ehud Rinott, department of public health, faculty of health sciences, Ben-Gurion University of the Negev in Beer-Sheva, Israel, and colleagues.
The study was published online Feb. 26, 2021, in Morbidity and Mortality Weekly Report.
The progress of COVID-19 vaccination across Israel presents researchers with a unique opportunity to study effectiveness on a population level. In this study, 84% of residents 70 and older received two-dose vaccinations. In contrast, only 10% of people in Israel younger than 50 received the same vaccine coverage.
Along with senior author Yair Lewis, MD, PhD, and coauthor Ilan Youngster, MD, Mr. Rinott compared mechanical ventilation rates between Oct. 2, 2020, and Feb. 9, 2021. They found that the ratio of people 70 and older compared with those younger than 50 requiring mechanical ventilation changed from 5.8:1 to 1.9:1 between these periods. This translates to the 67% decrease.
The study offers a “real-world” look at vaccination effectiveness, adding to more controlled evidence from clinical trials. “Achieving high vaccination coverage through intensive vaccination campaigns has the potential to substantially reduce COVID-19-associated morbidity and mortality,” the researchers wrote.
Israel started a national vaccination program on Dec. 20, 2020, targeting high-risk residents including people 60 and older, health care workers, and those with relevant comorbidities. At the same time, in addition to immunization, Israel has used strategies like stay-at-home orders, school closures, mask mandates, and more.
Potential limitations include a limited ability to account for the effect of the stay-at-home orders, spread of virus variants, and other concomitant factors; a potential for a delayed reporting of cases; and variability in mitigation measures by age group.
Dr. Youngster reported receipt of consulting fees from MyBiotix Ltd.
A version of this article first appeared on Medscape.com.
new evidence reveals.
Compared with residents younger than 50 – so far vaccinated at lower rates than those of the higher-risk older people – Israelis 70 and older were 67% less likely to require mechanical ventilation for SARS-CoV-2 infection in February 2021 compared with October-December 2020.
“This study provides preliminary evidence at the population level for the reduction in risk for severe COVID-19, as manifested by need for mechanical ventilation, after vaccination with the Pfizer-BioNTech COVID-19 vaccine,” wrote lead author Ehud Rinott, department of public health, faculty of health sciences, Ben-Gurion University of the Negev in Beer-Sheva, Israel, and colleagues.
The study was published online Feb. 26, 2021, in Morbidity and Mortality Weekly Report.
The progress of COVID-19 vaccination across Israel presents researchers with a unique opportunity to study effectiveness on a population level. In this study, 84% of residents 70 and older received two-dose vaccinations. In contrast, only 10% of people in Israel younger than 50 received the same vaccine coverage.
Along with senior author Yair Lewis, MD, PhD, and coauthor Ilan Youngster, MD, Mr. Rinott compared mechanical ventilation rates between Oct. 2, 2020, and Feb. 9, 2021. They found that the ratio of people 70 and older compared with those younger than 50 requiring mechanical ventilation changed from 5.8:1 to 1.9:1 between these periods. This translates to the 67% decrease.
The study offers a “real-world” look at vaccination effectiveness, adding to more controlled evidence from clinical trials. “Achieving high vaccination coverage through intensive vaccination campaigns has the potential to substantially reduce COVID-19-associated morbidity and mortality,” the researchers wrote.
Israel started a national vaccination program on Dec. 20, 2020, targeting high-risk residents including people 60 and older, health care workers, and those with relevant comorbidities. At the same time, in addition to immunization, Israel has used strategies like stay-at-home orders, school closures, mask mandates, and more.
Potential limitations include a limited ability to account for the effect of the stay-at-home orders, spread of virus variants, and other concomitant factors; a potential for a delayed reporting of cases; and variability in mitigation measures by age group.
Dr. Youngster reported receipt of consulting fees from MyBiotix Ltd.
A version of this article first appeared on Medscape.com.
Pulmonary and critical care session highlights new advances and research
An overview of five important advances in pulmonary and critical care medicine are on the agenda for the “Update in Pulmonary and Critical Care” session on Tuesday, May 4, at the virtual 2021 SHM Converge conference.
“I hope this session gives attendees a nice, broad look at advances both in the intensive care unit and in general pulmonary medicine,” said James Walter, MD, of Northwestern Medicine in Chicago, who serves as director of the session.
On the critical care medicine side, Dr. Walter will review the latest research on the efficacy of ascorbic acid in treating patients with severe sepsis and septic shock. “There was a lot of excitement and some skepticism about early results promising a really large treatment effect in giving critically ill patients with sepsis large doses of vitamin C,” Dr. Walter said. The last year has produced some high-quality randomized trials that have contributed to a better understanding of the potential effects ascorbic acid in sepsis can have, he noted.
Dr. Walter, who is also medical director of the Northwestern Lung Rescue Program, intends to discuss what he believes is a definitive trial regarding the benefit of preemptively starting critically ill patients with acute kidney injury on renal replacement therapy instead of waiting until there are specific clinical signs. “This has been another area of uncertainty in critical care and I think we finally have a very definitive answer with this high quality, randomized, controlled trial that I plan to review,” he said.
Though he said there have been a number of important advances in pulmonary medicine over the past year, Dr. Walter will highlight just two.
Up until recently, the antifibrotics nintedanib and pirfenidone have mostly been used in patients with idiopathic pulmonary fibrosis. However, recent research suggests there may be a potential benefit to using these drugs in patients with fibrotic lung disease outside of idiopathic pulmonary fibrosis. “I think this is an important advance for hospital medicine providers to be aware of,” said Dr. Walter.
He will also go over some large randomized controlled trials of the use of triple therapy – a combination of a long-acting beta agonist (LABA), a long-acting muscarinic antagonist (LAMA), and an inhaled corticosteroid in one inhaler – in chronic obstructive pulmonary disease. The trials looked at whether triple inhaler therapy was beneficial compared to the typical therapies used for COPD.
The session wouldn’t be complete without a nod to COVID-19, which Dr. Walter said has significantly changed the landscape for hospital medicine providers. He plans to discuss what he considers the most impactful study – the RECOVERY trial. This study looked at the role of dexamethasone in patients with more severe manifestations of SARS-CoV-2.
“From the incredible amount of data that’s come out in the last year about COVID, I think this is probably the trial that’s changed practice the most and shown the largest therapeutic benefit of all the pharmacotherapies,” Dr. Walter said. “It’s an important one for providers to be aware of in terms of what the trial shows and how it informs which patients are most likely to benefit from dexamethasone therapy.”
Dr. Walter hopes clinicians who participate in the session will leave with these takeaways:
- Be able to summarize recent trials of ascorbic acid in sepsis and think about how to incorporate – or not – the use of vitamin C in critically ill sepsis patients.
- A thorough understanding of when renal replacement therapy should be offered to critically ill patients with acute kidney dysfunction.
- Be able to discuss the impact of antifibrotic therapy in interstitial lung diseases outside of idiopathic pulmonary fibrosis.
- An understanding of the role of triple inhaler combinations in COPD.
- Be able to explain when dexamethasone is most likely to benefit hypoxemic patients with COVID-19.
An overview of five important advances in pulmonary and critical care medicine are on the agenda for the “Update in Pulmonary and Critical Care” session on Tuesday, May 4, at the virtual 2021 SHM Converge conference.
“I hope this session gives attendees a nice, broad look at advances both in the intensive care unit and in general pulmonary medicine,” said James Walter, MD, of Northwestern Medicine in Chicago, who serves as director of the session.
On the critical care medicine side, Dr. Walter will review the latest research on the efficacy of ascorbic acid in treating patients with severe sepsis and septic shock. “There was a lot of excitement and some skepticism about early results promising a really large treatment effect in giving critically ill patients with sepsis large doses of vitamin C,” Dr. Walter said. The last year has produced some high-quality randomized trials that have contributed to a better understanding of the potential effects ascorbic acid in sepsis can have, he noted.
Dr. Walter, who is also medical director of the Northwestern Lung Rescue Program, intends to discuss what he believes is a definitive trial regarding the benefit of preemptively starting critically ill patients with acute kidney injury on renal replacement therapy instead of waiting until there are specific clinical signs. “This has been another area of uncertainty in critical care and I think we finally have a very definitive answer with this high quality, randomized, controlled trial that I plan to review,” he said.
Though he said there have been a number of important advances in pulmonary medicine over the past year, Dr. Walter will highlight just two.
Up until recently, the antifibrotics nintedanib and pirfenidone have mostly been used in patients with idiopathic pulmonary fibrosis. However, recent research suggests there may be a potential benefit to using these drugs in patients with fibrotic lung disease outside of idiopathic pulmonary fibrosis. “I think this is an important advance for hospital medicine providers to be aware of,” said Dr. Walter.
He will also go over some large randomized controlled trials of the use of triple therapy – a combination of a long-acting beta agonist (LABA), a long-acting muscarinic antagonist (LAMA), and an inhaled corticosteroid in one inhaler – in chronic obstructive pulmonary disease. The trials looked at whether triple inhaler therapy was beneficial compared to the typical therapies used for COPD.
The session wouldn’t be complete without a nod to COVID-19, which Dr. Walter said has significantly changed the landscape for hospital medicine providers. He plans to discuss what he considers the most impactful study – the RECOVERY trial. This study looked at the role of dexamethasone in patients with more severe manifestations of SARS-CoV-2.
“From the incredible amount of data that’s come out in the last year about COVID, I think this is probably the trial that’s changed practice the most and shown the largest therapeutic benefit of all the pharmacotherapies,” Dr. Walter said. “It’s an important one for providers to be aware of in terms of what the trial shows and how it informs which patients are most likely to benefit from dexamethasone therapy.”
Dr. Walter hopes clinicians who participate in the session will leave with these takeaways:
- Be able to summarize recent trials of ascorbic acid in sepsis and think about how to incorporate – or not – the use of vitamin C in critically ill sepsis patients.
- A thorough understanding of when renal replacement therapy should be offered to critically ill patients with acute kidney dysfunction.
- Be able to discuss the impact of antifibrotic therapy in interstitial lung diseases outside of idiopathic pulmonary fibrosis.
- An understanding of the role of triple inhaler combinations in COPD.
- Be able to explain when dexamethasone is most likely to benefit hypoxemic patients with COVID-19.
An overview of five important advances in pulmonary and critical care medicine are on the agenda for the “Update in Pulmonary and Critical Care” session on Tuesday, May 4, at the virtual 2021 SHM Converge conference.
“I hope this session gives attendees a nice, broad look at advances both in the intensive care unit and in general pulmonary medicine,” said James Walter, MD, of Northwestern Medicine in Chicago, who serves as director of the session.
On the critical care medicine side, Dr. Walter will review the latest research on the efficacy of ascorbic acid in treating patients with severe sepsis and septic shock. “There was a lot of excitement and some skepticism about early results promising a really large treatment effect in giving critically ill patients with sepsis large doses of vitamin C,” Dr. Walter said. The last year has produced some high-quality randomized trials that have contributed to a better understanding of the potential effects ascorbic acid in sepsis can have, he noted.
Dr. Walter, who is also medical director of the Northwestern Lung Rescue Program, intends to discuss what he believes is a definitive trial regarding the benefit of preemptively starting critically ill patients with acute kidney injury on renal replacement therapy instead of waiting until there are specific clinical signs. “This has been another area of uncertainty in critical care and I think we finally have a very definitive answer with this high quality, randomized, controlled trial that I plan to review,” he said.
Though he said there have been a number of important advances in pulmonary medicine over the past year, Dr. Walter will highlight just two.
Up until recently, the antifibrotics nintedanib and pirfenidone have mostly been used in patients with idiopathic pulmonary fibrosis. However, recent research suggests there may be a potential benefit to using these drugs in patients with fibrotic lung disease outside of idiopathic pulmonary fibrosis. “I think this is an important advance for hospital medicine providers to be aware of,” said Dr. Walter.
He will also go over some large randomized controlled trials of the use of triple therapy – a combination of a long-acting beta agonist (LABA), a long-acting muscarinic antagonist (LAMA), and an inhaled corticosteroid in one inhaler – in chronic obstructive pulmonary disease. The trials looked at whether triple inhaler therapy was beneficial compared to the typical therapies used for COPD.
The session wouldn’t be complete without a nod to COVID-19, which Dr. Walter said has significantly changed the landscape for hospital medicine providers. He plans to discuss what he considers the most impactful study – the RECOVERY trial. This study looked at the role of dexamethasone in patients with more severe manifestations of SARS-CoV-2.
“From the incredible amount of data that’s come out in the last year about COVID, I think this is probably the trial that’s changed practice the most and shown the largest therapeutic benefit of all the pharmacotherapies,” Dr. Walter said. “It’s an important one for providers to be aware of in terms of what the trial shows and how it informs which patients are most likely to benefit from dexamethasone therapy.”
Dr. Walter hopes clinicians who participate in the session will leave with these takeaways:
- Be able to summarize recent trials of ascorbic acid in sepsis and think about how to incorporate – or not – the use of vitamin C in critically ill sepsis patients.
- A thorough understanding of when renal replacement therapy should be offered to critically ill patients with acute kidney dysfunction.
- Be able to discuss the impact of antifibrotic therapy in interstitial lung diseases outside of idiopathic pulmonary fibrosis.
- An understanding of the role of triple inhaler combinations in COPD.
- Be able to explain when dexamethasone is most likely to benefit hypoxemic patients with COVID-19.
The ABCs of successful vaccinations: A role for psychiatry
While the implementation of mass vaccinations is a public health task, individual clinicians are critical for the success of any vaccination campaign. Psychiatrists may be well positioned to help increase vaccine uptake among psychiatric patients. They see their patients more frequently than primary care physicians do, which allows for patient engagement over time regarding vaccinations. Also, as physicians, psychiatrists are a trusted source of medical information, and they are well-versed in using the tools of nudging and motivational interviewing to manage ambivalence about receiving a vaccine (vaccine hesitancy).1
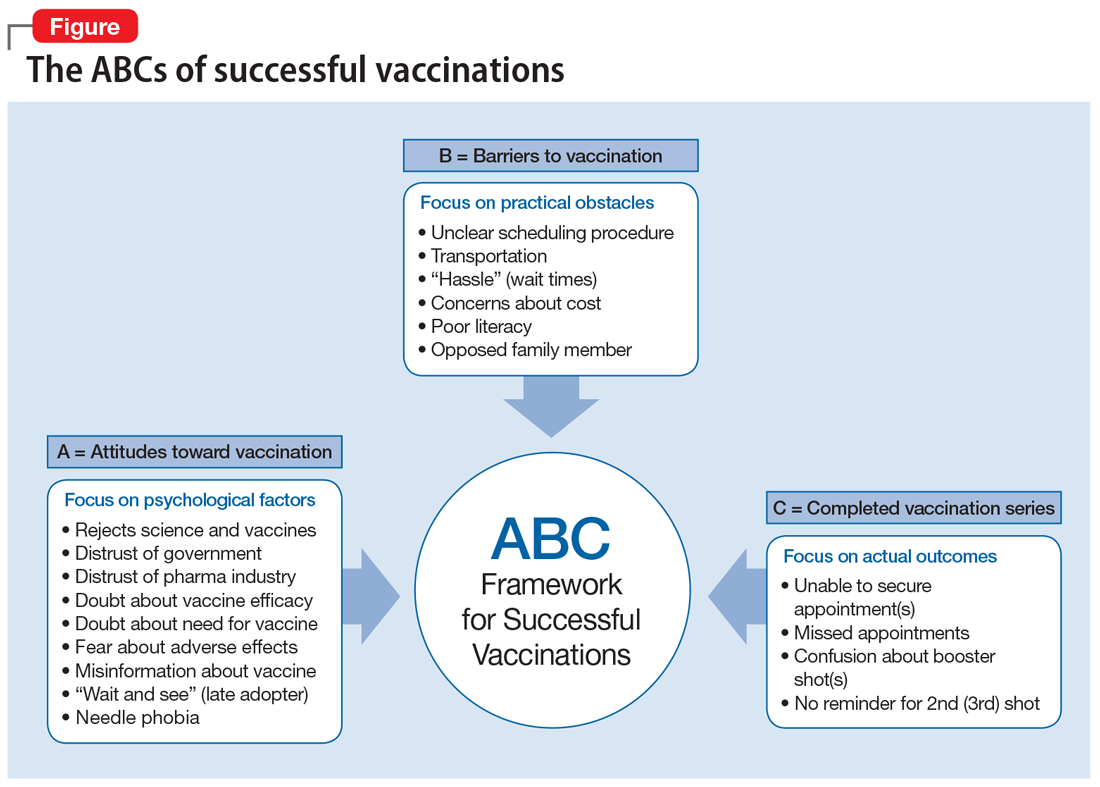
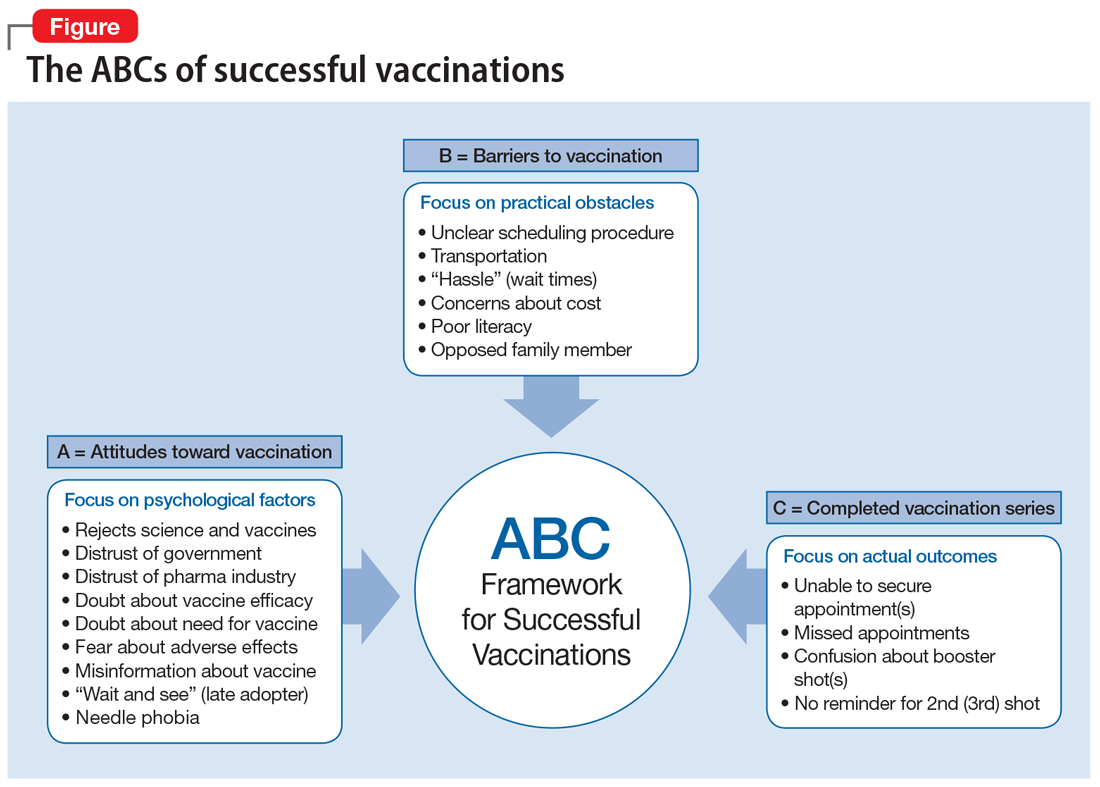
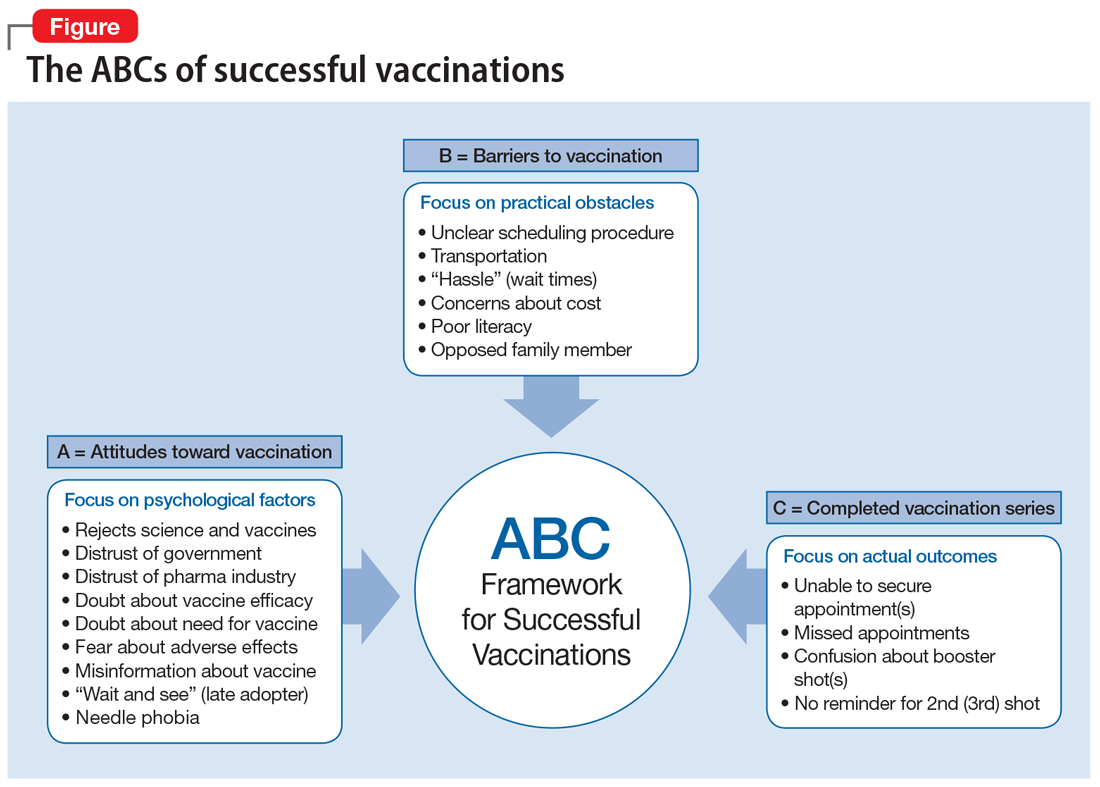
The “ABCs of successful vaccinations” (Figure) provide a framework that psychiatrists can use when speaking with their patients about vaccinations. The ABCs assess psychological factors that hinder acceptance of vaccination (A = Attitudes toward vaccination), practical challenges in vaccine access for patients who are willing to get vaccinated (B = Barriers to vaccination), and the actual outcome of “shot in the arm” (C = Completed vaccination series). The Figure provides examples of each area of focus.
How to talk to patients about vaccines
“Attitudes toward vaccination” is an area in which psychiatrists can potentially move patients from hesitancy to vaccine confidence and acceptance. First, express confidence in the vaccine (ie, make a clear statement: “You are an excellent candidate for this vaccine.”). Then, begin a discussion using presumptive language: “You must be ready to receive the vaccine.” In individuals who hesitate, elicit their concern: “What would make vaccination more acceptable?” In those who agree in principle about the benefits of vaccinations, ask about any impediments: “What would get in the way of getting vaccinated?” While some patients may require more information about the vaccine, others may need more time or mostly concrete help, such as assistance with scheduling a vaccine appointment. Do not to forget to follow up to see if a planned and complete vaccination series has taken place. The CDC offers an excellent online toolkit to help clinicians discuss vaccinations with their patients.2
Psychiatric patients, particularly those from disadvantaged and marginalized populations, have much to gain if psychiatrists are involved in preventive health care, including the coronavirus vaccination drive or the annual flu vaccination campaign.
1. McClure CC, Cataldi JR, O’Leary ST. Vaccine hesitancy: where we are and where we are going. Clin Ther. 2017;39(8):1550-1562.
2. Centers for Disease Control and Prevention. COVID-19 vaccination toolkits. Accessed February 8, 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/toolkits.html
While the implementation of mass vaccinations is a public health task, individual clinicians are critical for the success of any vaccination campaign. Psychiatrists may be well positioned to help increase vaccine uptake among psychiatric patients. They see their patients more frequently than primary care physicians do, which allows for patient engagement over time regarding vaccinations. Also, as physicians, psychiatrists are a trusted source of medical information, and they are well-versed in using the tools of nudging and motivational interviewing to manage ambivalence about receiving a vaccine (vaccine hesitancy).1
The “ABCs of successful vaccinations” (Figure) provide a framework that psychiatrists can use when speaking with their patients about vaccinations. The ABCs assess psychological factors that hinder acceptance of vaccination (A = Attitudes toward vaccination), practical challenges in vaccine access for patients who are willing to get vaccinated (B = Barriers to vaccination), and the actual outcome of “shot in the arm” (C = Completed vaccination series). The Figure provides examples of each area of focus.
How to talk to patients about vaccines
“Attitudes toward vaccination” is an area in which psychiatrists can potentially move patients from hesitancy to vaccine confidence and acceptance. First, express confidence in the vaccine (ie, make a clear statement: “You are an excellent candidate for this vaccine.”). Then, begin a discussion using presumptive language: “You must be ready to receive the vaccine.” In individuals who hesitate, elicit their concern: “What would make vaccination more acceptable?” In those who agree in principle about the benefits of vaccinations, ask about any impediments: “What would get in the way of getting vaccinated?” While some patients may require more information about the vaccine, others may need more time or mostly concrete help, such as assistance with scheduling a vaccine appointment. Do not to forget to follow up to see if a planned and complete vaccination series has taken place. The CDC offers an excellent online toolkit to help clinicians discuss vaccinations with their patients.2
Psychiatric patients, particularly those from disadvantaged and marginalized populations, have much to gain if psychiatrists are involved in preventive health care, including the coronavirus vaccination drive or the annual flu vaccination campaign.
While the implementation of mass vaccinations is a public health task, individual clinicians are critical for the success of any vaccination campaign. Psychiatrists may be well positioned to help increase vaccine uptake among psychiatric patients. They see their patients more frequently than primary care physicians do, which allows for patient engagement over time regarding vaccinations. Also, as physicians, psychiatrists are a trusted source of medical information, and they are well-versed in using the tools of nudging and motivational interviewing to manage ambivalence about receiving a vaccine (vaccine hesitancy).1
The “ABCs of successful vaccinations” (Figure) provide a framework that psychiatrists can use when speaking with their patients about vaccinations. The ABCs assess psychological factors that hinder acceptance of vaccination (A = Attitudes toward vaccination), practical challenges in vaccine access for patients who are willing to get vaccinated (B = Barriers to vaccination), and the actual outcome of “shot in the arm” (C = Completed vaccination series). The Figure provides examples of each area of focus.
How to talk to patients about vaccines
“Attitudes toward vaccination” is an area in which psychiatrists can potentially move patients from hesitancy to vaccine confidence and acceptance. First, express confidence in the vaccine (ie, make a clear statement: “You are an excellent candidate for this vaccine.”). Then, begin a discussion using presumptive language: “You must be ready to receive the vaccine.” In individuals who hesitate, elicit their concern: “What would make vaccination more acceptable?” In those who agree in principle about the benefits of vaccinations, ask about any impediments: “What would get in the way of getting vaccinated?” While some patients may require more information about the vaccine, others may need more time or mostly concrete help, such as assistance with scheduling a vaccine appointment. Do not to forget to follow up to see if a planned and complete vaccination series has taken place. The CDC offers an excellent online toolkit to help clinicians discuss vaccinations with their patients.2
Psychiatric patients, particularly those from disadvantaged and marginalized populations, have much to gain if psychiatrists are involved in preventive health care, including the coronavirus vaccination drive or the annual flu vaccination campaign.
1. McClure CC, Cataldi JR, O’Leary ST. Vaccine hesitancy: where we are and where we are going. Clin Ther. 2017;39(8):1550-1562.
2. Centers for Disease Control and Prevention. COVID-19 vaccination toolkits. Accessed February 8, 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/toolkits.html
1. McClure CC, Cataldi JR, O’Leary ST. Vaccine hesitancy: where we are and where we are going. Clin Ther. 2017;39(8):1550-1562.
2. Centers for Disease Control and Prevention. COVID-19 vaccination toolkits. Accessed February 8, 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/toolkits.html
Asthma not an independent risk factor for severe COVID-19, hospitalization
Asthma is not an independent risk factor for more severe disease or hospitalization due to COVID-19, according to recent research presented at the annual meeting of the American Academy of Allergy, Asthma, and Immunology, held virtually this year.
“In our cohort of patients tested for SARS-CoV-2 at Stanford between March and September, asthma was not an independent risk factor in and of itself for hospitalization or more severe disease from COVID,” Lauren E. Eggert, MD, of the Sean N. Parker Center for Allergy and Asthma Research at Stanford (Calif.) University, said in a poster presentation at the meeting. “What’s more, allergic asthma actually decreased the risk of hospitalization by nearly half.”
Dr. Eggert noted that there have been conflicting data on whether comorbid asthma is or is not a risk factor for more severe COVID-19. “The general thought at the beginning of the pandemic was that because COVID-19 is predominantly a viral respiratory illness, and viral illnesses are known to cause asthma exacerbations, that patients with asthma may be at higher risk if they got COVID infection,” she explained. “But some of the data also showed that Th2 inflammation downregulates ACE2 receptor [expression], which has been shown to be the port of entry for the SARS-CoV-2 virus, so maybe allergy might have a protective effect.”
The researchers at Stanford University identified 168,190 patients at Stanford Health Care who had a positive real-time reverse transcriptase polymerase chain reaction (RT-PCR) test for SARS-CoV-2 between March and September 2020 and collected data from their electronic medical records on their history of asthma, if they were hospitalized, comorbid conditions, and laboratory values. Patients who had no other data available except for a positive SARS-CoV-2 result, or were younger than 28 days, were excluded from the study. Dr. Eggert and colleagues used COVID-19 treatment guidelines from the National Institutes of Health to assess disease severity, which grades COVID-19 severity as asymptomatic or presymptomatic infection, mild illness, moderate illness, severe illness, and critical illness.
In total, the researchers analyzed 5,596 patients who were SARS-CoV-2 positive, with 605 patients (10.8%) hospitalized within 14 days of receiving a positive test. Of these, 100 patients (16.5%) were patients with asthma. There were no significant differences between groups hospitalized and not hospitalized due to COVID-19 in patients with asthma and with no asthma.
Among patients with asthma and COVID-19, 28.0% had asymptomatic illness, 19.0% had moderate disease, 33.0% had severe disease, and 20.0% had critical COVID-19, compared with 36.0% of patients without asthma who had asymptomatic illness, 12.0% with moderate disease, 30.0% with severe disease, and 21.0% with critical COVID-19. Dr. Eggert and colleagues performed a univariate analysis, which showed a significant association between asthma and COVID-19 related hospitalization (odds ratio, 1.53; 95% confidence interval, 1.2-1.93; P < .001), but when adjusting for factors such as diabetes, obesity coronary heart disease, and hypertension, they found there was not a significant association between asthma and hospitalization due to COVID-19 (OR, 1.12; 95% CI, 0.86-1.45; P < .40).
In a univariate analysis, asthma was associated with more severe disease in patients hospitalized for COVID-19, but the results were not significant (OR, 1.21; 95% CI, 0.8-1.85; P = .37). When analyzing allergic asthma alone in a univariate analysis, the researchers found a significant association between allergic asthma and lower hospitalization risk, compared with patients who had nonallergic asthma (OR, 0.55; 95% CI, 0.31-0.92; P = .029), and this association remained after they performed a multivariate analysis as well.
“When we stratified by allergic asthma versus nonallergic asthma, we found that having a diagnosis of allergic asthma actually conferred a protective effect, and there was almost half the risk of hospitalization in asthmatics with allergic asthma as compared to others, which we thought was very interesting,” Dr. Eggert said.
“Eosinophil levels during hospitalization, even when adjusted for systemic steroid use – and we followed patients out through September, when dexamethasone was standard of care – also correlated with better outcomes,” she explained. “This is independent of asthmatic status.”
The researchers noted that confirmation of these results are needed through large, multicenter cohort studies, particularly with regard to how allergic asthma might have a protective effect against SARS-CoV-2 infection. “I think going forward, these findings are very interesting and need to be looked at further to explain the mechanism behind them better,” Dr. Eggert said.
“I think there is also a lot of interest in how this might affect our patients on biologics, which deplete the eosinophils and get rid of that allergic phenotype,” she added. “Does that have any effect on disease severity? Unfortunately, the number of patents on biologics was very small in our cohort, but I do think this is an interesting area for exploration.”
This study was funded in part by the Sean N. Parker Center for Allergy & Asthma Research, Stanford University, Sunshine Foundation, Crown Foundation, and the Parker Foundation.
Asthma is not an independent risk factor for more severe disease or hospitalization due to COVID-19, according to recent research presented at the annual meeting of the American Academy of Allergy, Asthma, and Immunology, held virtually this year.
“In our cohort of patients tested for SARS-CoV-2 at Stanford between March and September, asthma was not an independent risk factor in and of itself for hospitalization or more severe disease from COVID,” Lauren E. Eggert, MD, of the Sean N. Parker Center for Allergy and Asthma Research at Stanford (Calif.) University, said in a poster presentation at the meeting. “What’s more, allergic asthma actually decreased the risk of hospitalization by nearly half.”
Dr. Eggert noted that there have been conflicting data on whether comorbid asthma is or is not a risk factor for more severe COVID-19. “The general thought at the beginning of the pandemic was that because COVID-19 is predominantly a viral respiratory illness, and viral illnesses are known to cause asthma exacerbations, that patients with asthma may be at higher risk if they got COVID infection,” she explained. “But some of the data also showed that Th2 inflammation downregulates ACE2 receptor [expression], which has been shown to be the port of entry for the SARS-CoV-2 virus, so maybe allergy might have a protective effect.”
The researchers at Stanford University identified 168,190 patients at Stanford Health Care who had a positive real-time reverse transcriptase polymerase chain reaction (RT-PCR) test for SARS-CoV-2 between March and September 2020 and collected data from their electronic medical records on their history of asthma, if they were hospitalized, comorbid conditions, and laboratory values. Patients who had no other data available except for a positive SARS-CoV-2 result, or were younger than 28 days, were excluded from the study. Dr. Eggert and colleagues used COVID-19 treatment guidelines from the National Institutes of Health to assess disease severity, which grades COVID-19 severity as asymptomatic or presymptomatic infection, mild illness, moderate illness, severe illness, and critical illness.
In total, the researchers analyzed 5,596 patients who were SARS-CoV-2 positive, with 605 patients (10.8%) hospitalized within 14 days of receiving a positive test. Of these, 100 patients (16.5%) were patients with asthma. There were no significant differences between groups hospitalized and not hospitalized due to COVID-19 in patients with asthma and with no asthma.
Among patients with asthma and COVID-19, 28.0% had asymptomatic illness, 19.0% had moderate disease, 33.0% had severe disease, and 20.0% had critical COVID-19, compared with 36.0% of patients without asthma who had asymptomatic illness, 12.0% with moderate disease, 30.0% with severe disease, and 21.0% with critical COVID-19. Dr. Eggert and colleagues performed a univariate analysis, which showed a significant association between asthma and COVID-19 related hospitalization (odds ratio, 1.53; 95% confidence interval, 1.2-1.93; P < .001), but when adjusting for factors such as diabetes, obesity coronary heart disease, and hypertension, they found there was not a significant association between asthma and hospitalization due to COVID-19 (OR, 1.12; 95% CI, 0.86-1.45; P < .40).
In a univariate analysis, asthma was associated with more severe disease in patients hospitalized for COVID-19, but the results were not significant (OR, 1.21; 95% CI, 0.8-1.85; P = .37). When analyzing allergic asthma alone in a univariate analysis, the researchers found a significant association between allergic asthma and lower hospitalization risk, compared with patients who had nonallergic asthma (OR, 0.55; 95% CI, 0.31-0.92; P = .029), and this association remained after they performed a multivariate analysis as well.
“When we stratified by allergic asthma versus nonallergic asthma, we found that having a diagnosis of allergic asthma actually conferred a protective effect, and there was almost half the risk of hospitalization in asthmatics with allergic asthma as compared to others, which we thought was very interesting,” Dr. Eggert said.
“Eosinophil levels during hospitalization, even when adjusted for systemic steroid use – and we followed patients out through September, when dexamethasone was standard of care – also correlated with better outcomes,” she explained. “This is independent of asthmatic status.”
The researchers noted that confirmation of these results are needed through large, multicenter cohort studies, particularly with regard to how allergic asthma might have a protective effect against SARS-CoV-2 infection. “I think going forward, these findings are very interesting and need to be looked at further to explain the mechanism behind them better,” Dr. Eggert said.
“I think there is also a lot of interest in how this might affect our patients on biologics, which deplete the eosinophils and get rid of that allergic phenotype,” she added. “Does that have any effect on disease severity? Unfortunately, the number of patents on biologics was very small in our cohort, but I do think this is an interesting area for exploration.”
This study was funded in part by the Sean N. Parker Center for Allergy & Asthma Research, Stanford University, Sunshine Foundation, Crown Foundation, and the Parker Foundation.
Asthma is not an independent risk factor for more severe disease or hospitalization due to COVID-19, according to recent research presented at the annual meeting of the American Academy of Allergy, Asthma, and Immunology, held virtually this year.
“In our cohort of patients tested for SARS-CoV-2 at Stanford between March and September, asthma was not an independent risk factor in and of itself for hospitalization or more severe disease from COVID,” Lauren E. Eggert, MD, of the Sean N. Parker Center for Allergy and Asthma Research at Stanford (Calif.) University, said in a poster presentation at the meeting. “What’s more, allergic asthma actually decreased the risk of hospitalization by nearly half.”
Dr. Eggert noted that there have been conflicting data on whether comorbid asthma is or is not a risk factor for more severe COVID-19. “The general thought at the beginning of the pandemic was that because COVID-19 is predominantly a viral respiratory illness, and viral illnesses are known to cause asthma exacerbations, that patients with asthma may be at higher risk if they got COVID infection,” she explained. “But some of the data also showed that Th2 inflammation downregulates ACE2 receptor [expression], which has been shown to be the port of entry for the SARS-CoV-2 virus, so maybe allergy might have a protective effect.”
The researchers at Stanford University identified 168,190 patients at Stanford Health Care who had a positive real-time reverse transcriptase polymerase chain reaction (RT-PCR) test for SARS-CoV-2 between March and September 2020 and collected data from their electronic medical records on their history of asthma, if they were hospitalized, comorbid conditions, and laboratory values. Patients who had no other data available except for a positive SARS-CoV-2 result, or were younger than 28 days, were excluded from the study. Dr. Eggert and colleagues used COVID-19 treatment guidelines from the National Institutes of Health to assess disease severity, which grades COVID-19 severity as asymptomatic or presymptomatic infection, mild illness, moderate illness, severe illness, and critical illness.
In total, the researchers analyzed 5,596 patients who were SARS-CoV-2 positive, with 605 patients (10.8%) hospitalized within 14 days of receiving a positive test. Of these, 100 patients (16.5%) were patients with asthma. There were no significant differences between groups hospitalized and not hospitalized due to COVID-19 in patients with asthma and with no asthma.
Among patients with asthma and COVID-19, 28.0% had asymptomatic illness, 19.0% had moderate disease, 33.0% had severe disease, and 20.0% had critical COVID-19, compared with 36.0% of patients without asthma who had asymptomatic illness, 12.0% with moderate disease, 30.0% with severe disease, and 21.0% with critical COVID-19. Dr. Eggert and colleagues performed a univariate analysis, which showed a significant association between asthma and COVID-19 related hospitalization (odds ratio, 1.53; 95% confidence interval, 1.2-1.93; P < .001), but when adjusting for factors such as diabetes, obesity coronary heart disease, and hypertension, they found there was not a significant association between asthma and hospitalization due to COVID-19 (OR, 1.12; 95% CI, 0.86-1.45; P < .40).
In a univariate analysis, asthma was associated with more severe disease in patients hospitalized for COVID-19, but the results were not significant (OR, 1.21; 95% CI, 0.8-1.85; P = .37). When analyzing allergic asthma alone in a univariate analysis, the researchers found a significant association between allergic asthma and lower hospitalization risk, compared with patients who had nonallergic asthma (OR, 0.55; 95% CI, 0.31-0.92; P = .029), and this association remained after they performed a multivariate analysis as well.
“When we stratified by allergic asthma versus nonallergic asthma, we found that having a diagnosis of allergic asthma actually conferred a protective effect, and there was almost half the risk of hospitalization in asthmatics with allergic asthma as compared to others, which we thought was very interesting,” Dr. Eggert said.
“Eosinophil levels during hospitalization, even when adjusted for systemic steroid use – and we followed patients out through September, when dexamethasone was standard of care – also correlated with better outcomes,” she explained. “This is independent of asthmatic status.”
The researchers noted that confirmation of these results are needed through large, multicenter cohort studies, particularly with regard to how allergic asthma might have a protective effect against SARS-CoV-2 infection. “I think going forward, these findings are very interesting and need to be looked at further to explain the mechanism behind them better,” Dr. Eggert said.
“I think there is also a lot of interest in how this might affect our patients on biologics, which deplete the eosinophils and get rid of that allergic phenotype,” she added. “Does that have any effect on disease severity? Unfortunately, the number of patents on biologics was very small in our cohort, but I do think this is an interesting area for exploration.”
This study was funded in part by the Sean N. Parker Center for Allergy & Asthma Research, Stanford University, Sunshine Foundation, Crown Foundation, and the Parker Foundation.
FROM AAAAI
Masks don’t affect oxygen saturation in people with asthma
Wearing a mask to protect against transmission of COVID-19 does not decrease oxygen saturation, according to a new study.
Oxygen saturation did not decline in more than 200 mask-wearing individuals attending an asthma and allergy clinic, regardless of the type of mask they were wearing and how long they had been wearing the mask.
The study was presented in a late breaking poster session by Marisa Hodges, MD, University of Michigan, Ann Arbor, at the virtual annual meeting of the American Academy of Allergy, Asthma, and Immunology.
“In patients with or without asthma, wearing a mask does not decrease your oxygen level,” coauthor Alan P. Baptist, MD, MPH, director of the University of Michigan Comprehensive Asthma Program, said in an interview.
“Some of my asthma patients had called me requesting an exemption from wearing a mask because they feared that their oxygen intake may be affected, and that got me thinking,” said Malika Gupta, MD, assistant professor, division of allergy and immunology, University of Michigan, Ann Arbor, and the study’s lead investigator.
“We say masks are safe, but I couldn’t find any data to support that statement, and we wanted to provide them with evidence, so they could feel comfortable about wearing their masks,” Dr. Gupta added.
The study collected 223 surveys from adult and pediatric patients presenting to the University of Michigan Medicine Allergy Clinic between Sept. 10 and Oct. 23, 2020.
The patients were asked whether they had a diagnosis of asthma, their degree of perceived control if they did have asthma, the type of mask they were wearing, and how long they had been wearing it.
Investigators obtained resting pulse oximetry readings to measure oxygen saturation (SpO2) from all study participants.
Forty percent of the participants were male, 46% reported having asthma, and 27% were age 19 years or younger.
Overall, the mean SpO2 was 98% (range, 93%-100%) in both asthma and nonasthma groups.
The study also looked at SpO2 with 3 different types of masks: fabric, surgical, and N95.
The mean SpO2 for a fabric mask was 98% (119 patients), for a surgical mask it was also 98% (83 patients), and for the N95 mask it was 99% (3 patients).
Similar results were found with duration of mask use, with the mean SpO2 98% in those wearing a mask for 1 hour or less and 99% in those wearing a mask for 1 hour or longer.
People with asthma who reported they were well controlled showed similar mean SpO2 levels (98%) compared with those who reported they were not well controlled (96.5%)
“No effect on oxygen saturation was noted in any patients, whether they had asthma or not, whether it was well controlled or not, and this was also true regardless of what masks they wore and how long they wore the masks for. So our data reinforce that wearing a mask, whether it be a surgical mask, cloth mask, or N95, is completely safe,” Dr. Baptist said.
“We know wearing a mask is an essential step we can all take to reduce the spread of COVID-19, and we hope these data will give peace of mind to individuals who fear that wearing a mask will adversely affect their oxygen levels,” Dr. Gupta added.
Leonard B. Bacharier, MD, professor of pediatrics and director of the Center for Pediatric Asthma, Monroe Carell Jr. Children’s Hospital at Vanderbilt University Medical Center, Nashville, Tenn., agreed with the investigators’ conclusions.
“The authors found no differences in oxygen saturations between asthmatic and nonasthmatic patients, nor was there a difference based upon mask use or type,” Dr. Bacharier, who was not part of the study, said in an interview.
“These findings provide reassurance that patients, including those with stable asthma, do not experience impaired oxygenation while wearing a mask.”
Dr. Hodges, Dr. Baptist, and Dr. Bacharier have disclosed no relevant financial relationships.
This article was updated 3/11/21.
A version of this article first appeared on Medscape.com.
Wearing a mask to protect against transmission of COVID-19 does not decrease oxygen saturation, according to a new study.
Oxygen saturation did not decline in more than 200 mask-wearing individuals attending an asthma and allergy clinic, regardless of the type of mask they were wearing and how long they had been wearing the mask.
The study was presented in a late breaking poster session by Marisa Hodges, MD, University of Michigan, Ann Arbor, at the virtual annual meeting of the American Academy of Allergy, Asthma, and Immunology.
“In patients with or without asthma, wearing a mask does not decrease your oxygen level,” coauthor Alan P. Baptist, MD, MPH, director of the University of Michigan Comprehensive Asthma Program, said in an interview.
“Some of my asthma patients had called me requesting an exemption from wearing a mask because they feared that their oxygen intake may be affected, and that got me thinking,” said Malika Gupta, MD, assistant professor, division of allergy and immunology, University of Michigan, Ann Arbor, and the study’s lead investigator.
“We say masks are safe, but I couldn’t find any data to support that statement, and we wanted to provide them with evidence, so they could feel comfortable about wearing their masks,” Dr. Gupta added.
The study collected 223 surveys from adult and pediatric patients presenting to the University of Michigan Medicine Allergy Clinic between Sept. 10 and Oct. 23, 2020.
The patients were asked whether they had a diagnosis of asthma, their degree of perceived control if they did have asthma, the type of mask they were wearing, and how long they had been wearing it.
Investigators obtained resting pulse oximetry readings to measure oxygen saturation (SpO2) from all study participants.
Forty percent of the participants were male, 46% reported having asthma, and 27% were age 19 years or younger.
Overall, the mean SpO2 was 98% (range, 93%-100%) in both asthma and nonasthma groups.
The study also looked at SpO2 with 3 different types of masks: fabric, surgical, and N95.
The mean SpO2 for a fabric mask was 98% (119 patients), for a surgical mask it was also 98% (83 patients), and for the N95 mask it was 99% (3 patients).
Similar results were found with duration of mask use, with the mean SpO2 98% in those wearing a mask for 1 hour or less and 99% in those wearing a mask for 1 hour or longer.
People with asthma who reported they were well controlled showed similar mean SpO2 levels (98%) compared with those who reported they were not well controlled (96.5%)
“No effect on oxygen saturation was noted in any patients, whether they had asthma or not, whether it was well controlled or not, and this was also true regardless of what masks they wore and how long they wore the masks for. So our data reinforce that wearing a mask, whether it be a surgical mask, cloth mask, or N95, is completely safe,” Dr. Baptist said.
“We know wearing a mask is an essential step we can all take to reduce the spread of COVID-19, and we hope these data will give peace of mind to individuals who fear that wearing a mask will adversely affect their oxygen levels,” Dr. Gupta added.
Leonard B. Bacharier, MD, professor of pediatrics and director of the Center for Pediatric Asthma, Monroe Carell Jr. Children’s Hospital at Vanderbilt University Medical Center, Nashville, Tenn., agreed with the investigators’ conclusions.
“The authors found no differences in oxygen saturations between asthmatic and nonasthmatic patients, nor was there a difference based upon mask use or type,” Dr. Bacharier, who was not part of the study, said in an interview.
“These findings provide reassurance that patients, including those with stable asthma, do not experience impaired oxygenation while wearing a mask.”
Dr. Hodges, Dr. Baptist, and Dr. Bacharier have disclosed no relevant financial relationships.
This article was updated 3/11/21.
A version of this article first appeared on Medscape.com.
Wearing a mask to protect against transmission of COVID-19 does not decrease oxygen saturation, according to a new study.
Oxygen saturation did not decline in more than 200 mask-wearing individuals attending an asthma and allergy clinic, regardless of the type of mask they were wearing and how long they had been wearing the mask.
The study was presented in a late breaking poster session by Marisa Hodges, MD, University of Michigan, Ann Arbor, at the virtual annual meeting of the American Academy of Allergy, Asthma, and Immunology.
“In patients with or without asthma, wearing a mask does not decrease your oxygen level,” coauthor Alan P. Baptist, MD, MPH, director of the University of Michigan Comprehensive Asthma Program, said in an interview.
“Some of my asthma patients had called me requesting an exemption from wearing a mask because they feared that their oxygen intake may be affected, and that got me thinking,” said Malika Gupta, MD, assistant professor, division of allergy and immunology, University of Michigan, Ann Arbor, and the study’s lead investigator.
“We say masks are safe, but I couldn’t find any data to support that statement, and we wanted to provide them with evidence, so they could feel comfortable about wearing their masks,” Dr. Gupta added.
The study collected 223 surveys from adult and pediatric patients presenting to the University of Michigan Medicine Allergy Clinic between Sept. 10 and Oct. 23, 2020.
The patients were asked whether they had a diagnosis of asthma, their degree of perceived control if they did have asthma, the type of mask they were wearing, and how long they had been wearing it.
Investigators obtained resting pulse oximetry readings to measure oxygen saturation (SpO2) from all study participants.
Forty percent of the participants were male, 46% reported having asthma, and 27% were age 19 years or younger.
Overall, the mean SpO2 was 98% (range, 93%-100%) in both asthma and nonasthma groups.
The study also looked at SpO2 with 3 different types of masks: fabric, surgical, and N95.
The mean SpO2 for a fabric mask was 98% (119 patients), for a surgical mask it was also 98% (83 patients), and for the N95 mask it was 99% (3 patients).
Similar results were found with duration of mask use, with the mean SpO2 98% in those wearing a mask for 1 hour or less and 99% in those wearing a mask for 1 hour or longer.
People with asthma who reported they were well controlled showed similar mean SpO2 levels (98%) compared with those who reported they were not well controlled (96.5%)
“No effect on oxygen saturation was noted in any patients, whether they had asthma or not, whether it was well controlled or not, and this was also true regardless of what masks they wore and how long they wore the masks for. So our data reinforce that wearing a mask, whether it be a surgical mask, cloth mask, or N95, is completely safe,” Dr. Baptist said.
“We know wearing a mask is an essential step we can all take to reduce the spread of COVID-19, and we hope these data will give peace of mind to individuals who fear that wearing a mask will adversely affect their oxygen levels,” Dr. Gupta added.
Leonard B. Bacharier, MD, professor of pediatrics and director of the Center for Pediatric Asthma, Monroe Carell Jr. Children’s Hospital at Vanderbilt University Medical Center, Nashville, Tenn., agreed with the investigators’ conclusions.
“The authors found no differences in oxygen saturations between asthmatic and nonasthmatic patients, nor was there a difference based upon mask use or type,” Dr. Bacharier, who was not part of the study, said in an interview.
“These findings provide reassurance that patients, including those with stable asthma, do not experience impaired oxygenation while wearing a mask.”
Dr. Hodges, Dr. Baptist, and Dr. Bacharier have disclosed no relevant financial relationships.
This article was updated 3/11/21.
A version of this article first appeared on Medscape.com.
FROM AAAAI
FDA grants emergency use authorization to Johnson & Johnson COVID-19 vaccine
And then there were three.
More vaccine availability at a time of high demand and limited supply could help officials vaccinate more Americans, more quickly. In addition, the J&J vaccine offers one-dose convenience and storage at conventional refrigeration temperatures.
Initial reactions to the EUA for the J&J vaccine have been positive.
“The advantages of having a third vaccine, especially one that is a single shot and can be stored without special refrigeration requirements, will be a major contribution in getting the general public vaccinated sooner, both in the U.S. and around the world,” Phyllis Tien, MD, professor of medicine in the division of infectious diseases at the University of California, San Francisco, told Medscape Medical News.
“It’s great news. We have yet a third vaccine that is highly effective at preventing COVID, and even more effective at preventing severe COVID,” said Paul Goepfert, MD. It’s a “tremendous boon for our country and other countries as well.”
“This vaccine has also been shown to be effective against the B.1.351 strain that was first described in South Africa,” added Dr. Goepfert, director of the Alabama Vaccine Research Clinic and infectious disease specialist at the University of Alabama at Birmingham.
The EUA “is indeed exciting news,” Colleen Kraft, MD, associate chief medical officer at Emory University Hospital and associate professor at Emory University School of Medicine in Atlanta, said during a February 25 media briefing.
One recent concern centers on people aged 60 years and older. Documents the FDA released earlier this week suggest a lower efficacy, 42%, for the J&J immunization among people in this age group with certain relevant comorbidities. In contrast, without underlying conditions like heart disease or diabetes, efficacy in this cohort was 72%.
The more the merrier
The scope and urgency of the COVID-19 pandemic necessitates as many protective measures as possible, said Raj Shah, MD, geriatrician, and associate professor of family medicine and codirector of the Center for Community Health Equity at Rush University in Chicago.
“Trying to vaccinate as many individuals living in the United States to prevent the spread of COVID is such a big project that no one company or one vaccine was going to be able to ramp up fast enough on its own,” Dr. Shah told Medscape Medical News.“This has been the hope for us,” he added, “to get to multiple vaccines with slightly different properties that will provide more options.”
Experience with the J&J vaccine so far suggests reactions are less severe. “The nice thing about the Johnson and Johnson [vaccine] is that it definitely has less side effects,” Dr. Kraft said.
On the other hand, low-grade fever, chills, or fatigue after vaccination can be considered a positive because they can reflect how well the immune system is responding, she added.
One and done?
Single-dose administration could be more than a convenience — it could also help clinicians vaccinate members of underserved communities and rural locations, where returning for a second dose could be more difficult for some people.
“In a controlled setting, in a clinical trial, we do a lot to make sure people get all the treatment they need,” Dr. Shah said. “We’re not seeing it right now, but we’re always worried when we have more than one dose that has to be administered, that some people will drop off and not come back for the second vaccine.”
This group could include the needle-phobic, he added. “For them, having it done once alleviates a lot of the anxiety.”
Looking beyond the numbers
The phase 3 ENSEMBLE study of the J&J vaccine revealed a 72% efficacy for preventing moderate-to-severe COVID-19 among U.S. participants. In contrast, researchers reported 94% to 95% efficacy for the Pfizer/BioNTech and Moderna vaccines.
However, experts agreed that focusing solely on these numbers can miss more important points. For example, no participants who received the J&J vaccine in the phase 3 trial died from COVID-19-related illness. There were five such deaths in the placebo cohort.
“One of the things that these vaccines do very well is they minimize severe disease,” Dr. Kraft said. “As somebody that has spent an inordinate time in the hospital taking care of patients with severe disease from COVID, this is very much a welcome addition to our armamentarium to fight this virus.”
“If you can give something that prevents people from dying, that is a true path to normalcy,” Dr. Goepfert added.
More work to do
“The demand is strong from all groups right now. We just have to work on getting more vaccines out there,” Dr. Shah said.
“We are at a point in this country where we are getting better with the distribution of the vaccine,” he added, “but we are nowhere close to achieving that distribution of vaccines to get to everybody.”
Dr. Goepfert, Dr. Shah, and Dr. Kraft disclosed no relevant financial relationships. Dr. Tien received support from Johnson & Johnson to conduct the J&J COVID-19 vaccine trial in the San Francisco VA Health Care System.
A version of this article first appeared on Medscape.com.
And then there were three.
More vaccine availability at a time of high demand and limited supply could help officials vaccinate more Americans, more quickly. In addition, the J&J vaccine offers one-dose convenience and storage at conventional refrigeration temperatures.
Initial reactions to the EUA for the J&J vaccine have been positive.
“The advantages of having a third vaccine, especially one that is a single shot and can be stored without special refrigeration requirements, will be a major contribution in getting the general public vaccinated sooner, both in the U.S. and around the world,” Phyllis Tien, MD, professor of medicine in the division of infectious diseases at the University of California, San Francisco, told Medscape Medical News.
“It’s great news. We have yet a third vaccine that is highly effective at preventing COVID, and even more effective at preventing severe COVID,” said Paul Goepfert, MD. It’s a “tremendous boon for our country and other countries as well.”
“This vaccine has also been shown to be effective against the B.1.351 strain that was first described in South Africa,” added Dr. Goepfert, director of the Alabama Vaccine Research Clinic and infectious disease specialist at the University of Alabama at Birmingham.
The EUA “is indeed exciting news,” Colleen Kraft, MD, associate chief medical officer at Emory University Hospital and associate professor at Emory University School of Medicine in Atlanta, said during a February 25 media briefing.
One recent concern centers on people aged 60 years and older. Documents the FDA released earlier this week suggest a lower efficacy, 42%, for the J&J immunization among people in this age group with certain relevant comorbidities. In contrast, without underlying conditions like heart disease or diabetes, efficacy in this cohort was 72%.
The more the merrier
The scope and urgency of the COVID-19 pandemic necessitates as many protective measures as possible, said Raj Shah, MD, geriatrician, and associate professor of family medicine and codirector of the Center for Community Health Equity at Rush University in Chicago.
“Trying to vaccinate as many individuals living in the United States to prevent the spread of COVID is such a big project that no one company or one vaccine was going to be able to ramp up fast enough on its own,” Dr. Shah told Medscape Medical News.“This has been the hope for us,” he added, “to get to multiple vaccines with slightly different properties that will provide more options.”
Experience with the J&J vaccine so far suggests reactions are less severe. “The nice thing about the Johnson and Johnson [vaccine] is that it definitely has less side effects,” Dr. Kraft said.
On the other hand, low-grade fever, chills, or fatigue after vaccination can be considered a positive because they can reflect how well the immune system is responding, she added.
One and done?
Single-dose administration could be more than a convenience — it could also help clinicians vaccinate members of underserved communities and rural locations, where returning for a second dose could be more difficult for some people.
“In a controlled setting, in a clinical trial, we do a lot to make sure people get all the treatment they need,” Dr. Shah said. “We’re not seeing it right now, but we’re always worried when we have more than one dose that has to be administered, that some people will drop off and not come back for the second vaccine.”
This group could include the needle-phobic, he added. “For them, having it done once alleviates a lot of the anxiety.”
Looking beyond the numbers
The phase 3 ENSEMBLE study of the J&J vaccine revealed a 72% efficacy for preventing moderate-to-severe COVID-19 among U.S. participants. In contrast, researchers reported 94% to 95% efficacy for the Pfizer/BioNTech and Moderna vaccines.
However, experts agreed that focusing solely on these numbers can miss more important points. For example, no participants who received the J&J vaccine in the phase 3 trial died from COVID-19-related illness. There were five such deaths in the placebo cohort.
“One of the things that these vaccines do very well is they minimize severe disease,” Dr. Kraft said. “As somebody that has spent an inordinate time in the hospital taking care of patients with severe disease from COVID, this is very much a welcome addition to our armamentarium to fight this virus.”
“If you can give something that prevents people from dying, that is a true path to normalcy,” Dr. Goepfert added.
More work to do
“The demand is strong from all groups right now. We just have to work on getting more vaccines out there,” Dr. Shah said.
“We are at a point in this country where we are getting better with the distribution of the vaccine,” he added, “but we are nowhere close to achieving that distribution of vaccines to get to everybody.”
Dr. Goepfert, Dr. Shah, and Dr. Kraft disclosed no relevant financial relationships. Dr. Tien received support from Johnson & Johnson to conduct the J&J COVID-19 vaccine trial in the San Francisco VA Health Care System.
A version of this article first appeared on Medscape.com.
And then there were three.
More vaccine availability at a time of high demand and limited supply could help officials vaccinate more Americans, more quickly. In addition, the J&J vaccine offers one-dose convenience and storage at conventional refrigeration temperatures.
Initial reactions to the EUA for the J&J vaccine have been positive.
“The advantages of having a third vaccine, especially one that is a single shot and can be stored without special refrigeration requirements, will be a major contribution in getting the general public vaccinated sooner, both in the U.S. and around the world,” Phyllis Tien, MD, professor of medicine in the division of infectious diseases at the University of California, San Francisco, told Medscape Medical News.
“It’s great news. We have yet a third vaccine that is highly effective at preventing COVID, and even more effective at preventing severe COVID,” said Paul Goepfert, MD. It’s a “tremendous boon for our country and other countries as well.”
“This vaccine has also been shown to be effective against the B.1.351 strain that was first described in South Africa,” added Dr. Goepfert, director of the Alabama Vaccine Research Clinic and infectious disease specialist at the University of Alabama at Birmingham.
The EUA “is indeed exciting news,” Colleen Kraft, MD, associate chief medical officer at Emory University Hospital and associate professor at Emory University School of Medicine in Atlanta, said during a February 25 media briefing.
One recent concern centers on people aged 60 years and older. Documents the FDA released earlier this week suggest a lower efficacy, 42%, for the J&J immunization among people in this age group with certain relevant comorbidities. In contrast, without underlying conditions like heart disease or diabetes, efficacy in this cohort was 72%.
The more the merrier
The scope and urgency of the COVID-19 pandemic necessitates as many protective measures as possible, said Raj Shah, MD, geriatrician, and associate professor of family medicine and codirector of the Center for Community Health Equity at Rush University in Chicago.
“Trying to vaccinate as many individuals living in the United States to prevent the spread of COVID is such a big project that no one company or one vaccine was going to be able to ramp up fast enough on its own,” Dr. Shah told Medscape Medical News.“This has been the hope for us,” he added, “to get to multiple vaccines with slightly different properties that will provide more options.”
Experience with the J&J vaccine so far suggests reactions are less severe. “The nice thing about the Johnson and Johnson [vaccine] is that it definitely has less side effects,” Dr. Kraft said.
On the other hand, low-grade fever, chills, or fatigue after vaccination can be considered a positive because they can reflect how well the immune system is responding, she added.
One and done?
Single-dose administration could be more than a convenience — it could also help clinicians vaccinate members of underserved communities and rural locations, where returning for a second dose could be more difficult for some people.
“In a controlled setting, in a clinical trial, we do a lot to make sure people get all the treatment they need,” Dr. Shah said. “We’re not seeing it right now, but we’re always worried when we have more than one dose that has to be administered, that some people will drop off and not come back for the second vaccine.”
This group could include the needle-phobic, he added. “For them, having it done once alleviates a lot of the anxiety.”
Looking beyond the numbers
The phase 3 ENSEMBLE study of the J&J vaccine revealed a 72% efficacy for preventing moderate-to-severe COVID-19 among U.S. participants. In contrast, researchers reported 94% to 95% efficacy for the Pfizer/BioNTech and Moderna vaccines.
However, experts agreed that focusing solely on these numbers can miss more important points. For example, no participants who received the J&J vaccine in the phase 3 trial died from COVID-19-related illness. There were five such deaths in the placebo cohort.
“One of the things that these vaccines do very well is they minimize severe disease,” Dr. Kraft said. “As somebody that has spent an inordinate time in the hospital taking care of patients with severe disease from COVID, this is very much a welcome addition to our armamentarium to fight this virus.”
“If you can give something that prevents people from dying, that is a true path to normalcy,” Dr. Goepfert added.
More work to do
“The demand is strong from all groups right now. We just have to work on getting more vaccines out there,” Dr. Shah said.
“We are at a point in this country where we are getting better with the distribution of the vaccine,” he added, “but we are nowhere close to achieving that distribution of vaccines to get to everybody.”
Dr. Goepfert, Dr. Shah, and Dr. Kraft disclosed no relevant financial relationships. Dr. Tien received support from Johnson & Johnson to conduct the J&J COVID-19 vaccine trial in the San Francisco VA Health Care System.
A version of this article first appeared on Medscape.com.
J&J COVID-19 vaccine wins unanimous backing of FDA panel
The Food and Drug Administration (FDA) is expected to quickly provide an emergency use authorization (EUA) for the vaccine following the recommendation by the panel. The FDA’s Vaccines and Related Biological Products Advisory Committee voted 22-0 on this question: Based on the totality of scientific evidence available, do the benefits of the Johnson & Johnson COVID-19 Vaccine outweigh its risks for use in individuals 18 years of age and older?
The Johnson & Johnson vaccine is expected to offer more convenient dosing and be easier to distribute than the two rival products already available in the United States. Janssen’s vaccine is intended to be given in a single dose. In December, the FDA granted EUAs for the Pfizer/BioNTech and Moderna COVID-19 vaccines, which are each two-dose regimens.
Johnson & Johnson’s vaccine can be stored for at least 3 months at normal refrigerator temperatures of 2°C to 8°C (36°F to 46°F). Its shipping and storage fits into the existing medical supply infrastructure, the company said in its briefing materials for the FDA advisory committee meeting. In contrast, Pfizer’s vaccine is stored in ultracold freezers at temperatures between -80°C and -60°C (-112°F and -76°F), according to the Centers for Disease Control and Prevention. Moderna’s vaccine may be stored in a freezer between -25°C and -15°C (-13°F and 5°F).
But FDA advisers focused more in their deliberations on concerns about Janssen’s vaccine, including emerging reports of allergic reactions.
The advisers also discussed how patients might respond to the widely reported gap between Johnson & Johnson’s topline efficacy rates compared with rivals. The company’s initial unveiling last month of key results for its vaccine caused an initial wave of disappointment, with its overall efficacy against moderate-to-severe COVID-19 28 days postvaccination first reported at about 66% globally. By contrast, results for the Pfizer and Moderna vaccines suggest they have efficacy rates of 95% and 94%.
But in concluding, the advisers spoke of the Janssen vaccine as a much-needed tool to address the COVID-19 pandemic. The death toll in the United States attributed to the virus has reached 501,414, according to the World Health Organization.
“Despite the concerns that were raised during the discussion. I think what we have to keep in mind is that we’re still in the midst of this deadly pandemic,” said FDA adviser Archana Chatterjee, MD, PhD, from Rosalind Franklin University. “There is a shortage of vaccines that are currently authorized, and I think authorization of this vaccine will help meet the needs at the moment.”
The FDA is not bound to accept the recommendations of its advisers, but it often does so.
Anaphylaxis case
FDA advisers raised only a few questions for Johnson & Johnson and FDA staff ahead of their vote. The committee’s deliberations were less contentious and heated than had been during its December reviews of the Pfizer and Moderna vaccines. In those meetings, the panel voted 17-4, with one abstention, in favor of Pfizer’s vaccine and 20-0, with one abstention, on the Moderna vaccine.
“We are very comfortable now with the procedure, as well as the vaccines,” said Arnold Monto, MD, after the Feb. 26 vote on the Janssen vaccine. Dr. Monto, from the University of Michigan School of Public Health in Ann Arbor, has served as the chairman of the FDA panel through its review of all three COVID-19 vaccines.
Among the issues noted in the deliberations was the emergence of a concern about anaphylaxis with the vaccine.
This serious allergic reaction has been seen in people who have taken the Pfizer and Moderna vaccines. Before the week of the panel meeting, though, there had not been reports of anaphylaxis with the Johnson & Johnson vaccine, said Macaya Douoguih, MD, MPH, head of clinical development and medical affairs for Janssen/ Johnson & Johnson’s vaccines division.
However, on February 24, Johnson & Johnson received preliminary reports about two cases of severe allergic reaction from an open-label study in South Africa, with one of these being anaphylaxis, Dr. Douoguih said. The company will continue to closely monitor for these events as outlined in their pharmacovigilance plan, Dr. Douoguih said.
Federal health officials have sought to make clinicians aware of the rare risk for anaphylaxis with COVID vaccines, while reminding the public that this reaction can be managed.
The FDA had Tom Shimabukuro, MD, MPH, MBA, from the CDC, give an update on postmarketing surveillance for the Pfizer and Moderna vaccines as part of the review of the Johnson & Johnson application. Dr. Shimabukuro and CDC colleagues published a report in JAMA on February 14 that looked at an anaphylaxis case reported connected with COVID vaccines between December 14, 2020, and January 18, 2021.
The CDC identified 66 case reports received that met Brighton Collaboration case definition criteria for anaphylaxis (levels 1, 2, or 3): 47 following Pfizer/BioNTech vaccine, for a reporting rate of 4.7 cases/million doses administered, and 19 following Moderna vaccine, for a reporting rate of 2.5 cases/million doses administered, Dr. Shimabukuro and CDC colleagues wrote.
The CDC has published materials to help clinicians prepare for the possibility of this rare event, Dr. Shimabukuro told the FDA advisers.
“The take-home message here is that these are rare events and anaphylaxis, although clinically serious, is treatable,” Dr. Shimabukuro said.
At the conclusion of the meeting, FDA panelist Patrick Moore, MD, MPH, from the University of Pittsburgh in Pennsylvania, stressed the need to convey to the public that the COVID vaccines appear so far to be safe. Many people earlier had doubts about how the FDA could both safely and quickly review the applications for EUAs for these products.
“As of February 26, things are looking good. That could change tomorrow,” Dr. Moore said. But “this whole EUA process does seem to have worked, despite my own personal concerns about it.”
No second-class vaccines
The Johnson & Johnson vaccine, known as Ad26.COV2.S, is composed of a recombinant, replication-incompetent human adenovirus type 26 (Ad26) vector. It’s intended to encode a stabilized form of SARS-CoV-2 spike (S) protein. The Pfizer and Moderna vaccines use a different mechanism. They rely on mRNA.
The FDA advisers also discussed how patients might respond to the widely reported gap between Janssen’s topline efficacy rates compared with rivals. They urged against people parsing study details too finely and seeking to pick and choose their shots.
“It’s important that people do not think that one vaccine is better than another,” said FDA adviser H. Cody Meissner, MD, from Tufts University School of Medicine in Boston.
Dr. Monto agreed, noting that many people in the United States are still waiting for their turn to get COVID vaccines because of the limited early supply.
Trying to game the system to get one vaccine instead of another would not be wise. “In this environment, whatever you can get, get,” Dr. Monto said.
During an open public hearing, Sarah Christopherson, policy advocacy director of the National Women’s Health Network, said that press reports are fueling a damaging impression in the public that there are “first and second-class” vaccines.
“That has the potential to exacerbate existing mistrust” in vaccines, she said. “Public health authorities must address these perceptions head on.”
She urged against attempts to compare the Janssen vaccine to others, noting the potential effects of emerging variants of the virus.
“It’s difficult to make an apples-to-apples comparison between vaccines,” she said.
Johnson & Johnson’s efficacy results, which are lower than those of the mRNA vaccines, may be a reflection of the ways in which SARS-Co-V-2 is mutating and thus becoming more of a threat, according to the company. A key study of the new vaccine, involving about 44,000 people, coincided with the emergence of new SARS-CoV-2 variants, which were emerging in some of the countries where the pivotal COV3001 study was being conducted, the company said.
At least 14 days after vaccination, the Johnson & Johnson COVID vaccine efficacy (95% confidence interval) was 72.0% (58.2, 81.7) in the United States, 68.1% (48.8, 80.7) in Brazil, and 64.0% (41.2, 78.7) in South Africa.
Weakened standards?
Several researchers called on the FDA to maintain a critical attitude when assessing Johnson & Johnson’s application for the EUA, warning of a potential for a permanent erosion of agency rules due to hasty action on COVID vaccines.
They raised concerns about the FDA demanding too little in terms of follow-up studies on COVID vaccines and with persisting murkiness resulting in attempts to determine how well these treatments work beyond the initial study period.
“I worry about FDA lowering its approval standards,” said Peter Doshi, PhD, from The BMJ and a faculty member at the University of Maryland School of Medicine in Baltimore, during an open public hearing at the meeting.
“There’s a real urgency to stand back right now and look at the forest here, as well as the trees, and I urge the committee to consider the effects FDA decisions may have on the entire regulatory approval process,” Dr. Doshi said.
Dr. Doshi asked why Johnson & Johnson did not seek a standard full approval — a biologics license application (BLA) — instead of aiming for the lower bar of an EUA. The FDA already has allowed wide distribution of the Pfizer/BioNTech and Moderna vaccines through EUAs. That removes the sense of urgency that FDA faced last year in his view.
The FDA’s June 2020 guidance on the development of COVID vaccines had asked drugmakers to plan on following participants in COVID vaccine trials for “ideally at least one to two years.” Yet people who got placebo in Moderna and Pfizer trials already are being vaccinated, Dr. Doshi said. And Johnson & Johnson said in its presentation to the FDA that if the Ad26.COV2.S vaccine were granted an EUA, the COV3001 study design would be amended to “facilitate cross-over of placebo participants in all participating countries to receive one dose of active study vaccine as fast as operationally feasible.”
“I’m nervous about the prospect of there never being a COVID vaccine that meets the FDA’s approval standard” for a BLA instead of the more limited EUA, Dr. Doshi said.
Diana Zuckerman, PhD, president of the nonprofit National Center for Health Research, noted that the FDA’s subsequent guidance tailored for EUAs for COVID vaccines “drastically shortened” the follow-up time to a median of 2 months. Dr. Zuckerman said that a crossover design would be “a reasonable compromise, but only if the placebo group has at least 6 months of data.” Dr. Zuckerman opened her remarks in the open public hearing by saying she had inherited Johnson & Johnson stock, so was speaking at the meeting against her own financial interest.
“As soon as a vaccine is authorized, we start losing the placebo group. If FDA lets that happen, that’s a huge loss for public health and a huge loss of information about how we can all stay safe,” Dr. Zuckerman said.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration (FDA) is expected to quickly provide an emergency use authorization (EUA) for the vaccine following the recommendation by the panel. The FDA’s Vaccines and Related Biological Products Advisory Committee voted 22-0 on this question: Based on the totality of scientific evidence available, do the benefits of the Johnson & Johnson COVID-19 Vaccine outweigh its risks for use in individuals 18 years of age and older?
The Johnson & Johnson vaccine is expected to offer more convenient dosing and be easier to distribute than the two rival products already available in the United States. Janssen’s vaccine is intended to be given in a single dose. In December, the FDA granted EUAs for the Pfizer/BioNTech and Moderna COVID-19 vaccines, which are each two-dose regimens.
Johnson & Johnson’s vaccine can be stored for at least 3 months at normal refrigerator temperatures of 2°C to 8°C (36°F to 46°F). Its shipping and storage fits into the existing medical supply infrastructure, the company said in its briefing materials for the FDA advisory committee meeting. In contrast, Pfizer’s vaccine is stored in ultracold freezers at temperatures between -80°C and -60°C (-112°F and -76°F), according to the Centers for Disease Control and Prevention. Moderna’s vaccine may be stored in a freezer between -25°C and -15°C (-13°F and 5°F).
But FDA advisers focused more in their deliberations on concerns about Janssen’s vaccine, including emerging reports of allergic reactions.
The advisers also discussed how patients might respond to the widely reported gap between Johnson & Johnson’s topline efficacy rates compared with rivals. The company’s initial unveiling last month of key results for its vaccine caused an initial wave of disappointment, with its overall efficacy against moderate-to-severe COVID-19 28 days postvaccination first reported at about 66% globally. By contrast, results for the Pfizer and Moderna vaccines suggest they have efficacy rates of 95% and 94%.
But in concluding, the advisers spoke of the Janssen vaccine as a much-needed tool to address the COVID-19 pandemic. The death toll in the United States attributed to the virus has reached 501,414, according to the World Health Organization.
“Despite the concerns that were raised during the discussion. I think what we have to keep in mind is that we’re still in the midst of this deadly pandemic,” said FDA adviser Archana Chatterjee, MD, PhD, from Rosalind Franklin University. “There is a shortage of vaccines that are currently authorized, and I think authorization of this vaccine will help meet the needs at the moment.”
The FDA is not bound to accept the recommendations of its advisers, but it often does so.
Anaphylaxis case
FDA advisers raised only a few questions for Johnson & Johnson and FDA staff ahead of their vote. The committee’s deliberations were less contentious and heated than had been during its December reviews of the Pfizer and Moderna vaccines. In those meetings, the panel voted 17-4, with one abstention, in favor of Pfizer’s vaccine and 20-0, with one abstention, on the Moderna vaccine.
“We are very comfortable now with the procedure, as well as the vaccines,” said Arnold Monto, MD, after the Feb. 26 vote on the Janssen vaccine. Dr. Monto, from the University of Michigan School of Public Health in Ann Arbor, has served as the chairman of the FDA panel through its review of all three COVID-19 vaccines.
Among the issues noted in the deliberations was the emergence of a concern about anaphylaxis with the vaccine.
This serious allergic reaction has been seen in people who have taken the Pfizer and Moderna vaccines. Before the week of the panel meeting, though, there had not been reports of anaphylaxis with the Johnson & Johnson vaccine, said Macaya Douoguih, MD, MPH, head of clinical development and medical affairs for Janssen/ Johnson & Johnson’s vaccines division.
However, on February 24, Johnson & Johnson received preliminary reports about two cases of severe allergic reaction from an open-label study in South Africa, with one of these being anaphylaxis, Dr. Douoguih said. The company will continue to closely monitor for these events as outlined in their pharmacovigilance plan, Dr. Douoguih said.
Federal health officials have sought to make clinicians aware of the rare risk for anaphylaxis with COVID vaccines, while reminding the public that this reaction can be managed.
The FDA had Tom Shimabukuro, MD, MPH, MBA, from the CDC, give an update on postmarketing surveillance for the Pfizer and Moderna vaccines as part of the review of the Johnson & Johnson application. Dr. Shimabukuro and CDC colleagues published a report in JAMA on February 14 that looked at an anaphylaxis case reported connected with COVID vaccines between December 14, 2020, and January 18, 2021.
The CDC identified 66 case reports received that met Brighton Collaboration case definition criteria for anaphylaxis (levels 1, 2, or 3): 47 following Pfizer/BioNTech vaccine, for a reporting rate of 4.7 cases/million doses administered, and 19 following Moderna vaccine, for a reporting rate of 2.5 cases/million doses administered, Dr. Shimabukuro and CDC colleagues wrote.
The CDC has published materials to help clinicians prepare for the possibility of this rare event, Dr. Shimabukuro told the FDA advisers.
“The take-home message here is that these are rare events and anaphylaxis, although clinically serious, is treatable,” Dr. Shimabukuro said.
At the conclusion of the meeting, FDA panelist Patrick Moore, MD, MPH, from the University of Pittsburgh in Pennsylvania, stressed the need to convey to the public that the COVID vaccines appear so far to be safe. Many people earlier had doubts about how the FDA could both safely and quickly review the applications for EUAs for these products.
“As of February 26, things are looking good. That could change tomorrow,” Dr. Moore said. But “this whole EUA process does seem to have worked, despite my own personal concerns about it.”
No second-class vaccines
The Johnson & Johnson vaccine, known as Ad26.COV2.S, is composed of a recombinant, replication-incompetent human adenovirus type 26 (Ad26) vector. It’s intended to encode a stabilized form of SARS-CoV-2 spike (S) protein. The Pfizer and Moderna vaccines use a different mechanism. They rely on mRNA.
The FDA advisers also discussed how patients might respond to the widely reported gap between Janssen’s topline efficacy rates compared with rivals. They urged against people parsing study details too finely and seeking to pick and choose their shots.
“It’s important that people do not think that one vaccine is better than another,” said FDA adviser H. Cody Meissner, MD, from Tufts University School of Medicine in Boston.
Dr. Monto agreed, noting that many people in the United States are still waiting for their turn to get COVID vaccines because of the limited early supply.
Trying to game the system to get one vaccine instead of another would not be wise. “In this environment, whatever you can get, get,” Dr. Monto said.
During an open public hearing, Sarah Christopherson, policy advocacy director of the National Women’s Health Network, said that press reports are fueling a damaging impression in the public that there are “first and second-class” vaccines.
“That has the potential to exacerbate existing mistrust” in vaccines, she said. “Public health authorities must address these perceptions head on.”
She urged against attempts to compare the Janssen vaccine to others, noting the potential effects of emerging variants of the virus.
“It’s difficult to make an apples-to-apples comparison between vaccines,” she said.
Johnson & Johnson’s efficacy results, which are lower than those of the mRNA vaccines, may be a reflection of the ways in which SARS-Co-V-2 is mutating and thus becoming more of a threat, according to the company. A key study of the new vaccine, involving about 44,000 people, coincided with the emergence of new SARS-CoV-2 variants, which were emerging in some of the countries where the pivotal COV3001 study was being conducted, the company said.
At least 14 days after vaccination, the Johnson & Johnson COVID vaccine efficacy (95% confidence interval) was 72.0% (58.2, 81.7) in the United States, 68.1% (48.8, 80.7) in Brazil, and 64.0% (41.2, 78.7) in South Africa.
Weakened standards?
Several researchers called on the FDA to maintain a critical attitude when assessing Johnson & Johnson’s application for the EUA, warning of a potential for a permanent erosion of agency rules due to hasty action on COVID vaccines.
They raised concerns about the FDA demanding too little in terms of follow-up studies on COVID vaccines and with persisting murkiness resulting in attempts to determine how well these treatments work beyond the initial study period.
“I worry about FDA lowering its approval standards,” said Peter Doshi, PhD, from The BMJ and a faculty member at the University of Maryland School of Medicine in Baltimore, during an open public hearing at the meeting.
“There’s a real urgency to stand back right now and look at the forest here, as well as the trees, and I urge the committee to consider the effects FDA decisions may have on the entire regulatory approval process,” Dr. Doshi said.
Dr. Doshi asked why Johnson & Johnson did not seek a standard full approval — a biologics license application (BLA) — instead of aiming for the lower bar of an EUA. The FDA already has allowed wide distribution of the Pfizer/BioNTech and Moderna vaccines through EUAs. That removes the sense of urgency that FDA faced last year in his view.
The FDA’s June 2020 guidance on the development of COVID vaccines had asked drugmakers to plan on following participants in COVID vaccine trials for “ideally at least one to two years.” Yet people who got placebo in Moderna and Pfizer trials already are being vaccinated, Dr. Doshi said. And Johnson & Johnson said in its presentation to the FDA that if the Ad26.COV2.S vaccine were granted an EUA, the COV3001 study design would be amended to “facilitate cross-over of placebo participants in all participating countries to receive one dose of active study vaccine as fast as operationally feasible.”
“I’m nervous about the prospect of there never being a COVID vaccine that meets the FDA’s approval standard” for a BLA instead of the more limited EUA, Dr. Doshi said.
Diana Zuckerman, PhD, president of the nonprofit National Center for Health Research, noted that the FDA’s subsequent guidance tailored for EUAs for COVID vaccines “drastically shortened” the follow-up time to a median of 2 months. Dr. Zuckerman said that a crossover design would be “a reasonable compromise, but only if the placebo group has at least 6 months of data.” Dr. Zuckerman opened her remarks in the open public hearing by saying she had inherited Johnson & Johnson stock, so was speaking at the meeting against her own financial interest.
“As soon as a vaccine is authorized, we start losing the placebo group. If FDA lets that happen, that’s a huge loss for public health and a huge loss of information about how we can all stay safe,” Dr. Zuckerman said.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration (FDA) is expected to quickly provide an emergency use authorization (EUA) for the vaccine following the recommendation by the panel. The FDA’s Vaccines and Related Biological Products Advisory Committee voted 22-0 on this question: Based on the totality of scientific evidence available, do the benefits of the Johnson & Johnson COVID-19 Vaccine outweigh its risks for use in individuals 18 years of age and older?
The Johnson & Johnson vaccine is expected to offer more convenient dosing and be easier to distribute than the two rival products already available in the United States. Janssen’s vaccine is intended to be given in a single dose. In December, the FDA granted EUAs for the Pfizer/BioNTech and Moderna COVID-19 vaccines, which are each two-dose regimens.
Johnson & Johnson’s vaccine can be stored for at least 3 months at normal refrigerator temperatures of 2°C to 8°C (36°F to 46°F). Its shipping and storage fits into the existing medical supply infrastructure, the company said in its briefing materials for the FDA advisory committee meeting. In contrast, Pfizer’s vaccine is stored in ultracold freezers at temperatures between -80°C and -60°C (-112°F and -76°F), according to the Centers for Disease Control and Prevention. Moderna’s vaccine may be stored in a freezer between -25°C and -15°C (-13°F and 5°F).
But FDA advisers focused more in their deliberations on concerns about Janssen’s vaccine, including emerging reports of allergic reactions.
The advisers also discussed how patients might respond to the widely reported gap between Johnson & Johnson’s topline efficacy rates compared with rivals. The company’s initial unveiling last month of key results for its vaccine caused an initial wave of disappointment, with its overall efficacy against moderate-to-severe COVID-19 28 days postvaccination first reported at about 66% globally. By contrast, results for the Pfizer and Moderna vaccines suggest they have efficacy rates of 95% and 94%.
But in concluding, the advisers spoke of the Janssen vaccine as a much-needed tool to address the COVID-19 pandemic. The death toll in the United States attributed to the virus has reached 501,414, according to the World Health Organization.
“Despite the concerns that were raised during the discussion. I think what we have to keep in mind is that we’re still in the midst of this deadly pandemic,” said FDA adviser Archana Chatterjee, MD, PhD, from Rosalind Franklin University. “There is a shortage of vaccines that are currently authorized, and I think authorization of this vaccine will help meet the needs at the moment.”
The FDA is not bound to accept the recommendations of its advisers, but it often does so.
Anaphylaxis case
FDA advisers raised only a few questions for Johnson & Johnson and FDA staff ahead of their vote. The committee’s deliberations were less contentious and heated than had been during its December reviews of the Pfizer and Moderna vaccines. In those meetings, the panel voted 17-4, with one abstention, in favor of Pfizer’s vaccine and 20-0, with one abstention, on the Moderna vaccine.
“We are very comfortable now with the procedure, as well as the vaccines,” said Arnold Monto, MD, after the Feb. 26 vote on the Janssen vaccine. Dr. Monto, from the University of Michigan School of Public Health in Ann Arbor, has served as the chairman of the FDA panel through its review of all three COVID-19 vaccines.
Among the issues noted in the deliberations was the emergence of a concern about anaphylaxis with the vaccine.
This serious allergic reaction has been seen in people who have taken the Pfizer and Moderna vaccines. Before the week of the panel meeting, though, there had not been reports of anaphylaxis with the Johnson & Johnson vaccine, said Macaya Douoguih, MD, MPH, head of clinical development and medical affairs for Janssen/ Johnson & Johnson’s vaccines division.
However, on February 24, Johnson & Johnson received preliminary reports about two cases of severe allergic reaction from an open-label study in South Africa, with one of these being anaphylaxis, Dr. Douoguih said. The company will continue to closely monitor for these events as outlined in their pharmacovigilance plan, Dr. Douoguih said.
Federal health officials have sought to make clinicians aware of the rare risk for anaphylaxis with COVID vaccines, while reminding the public that this reaction can be managed.
The FDA had Tom Shimabukuro, MD, MPH, MBA, from the CDC, give an update on postmarketing surveillance for the Pfizer and Moderna vaccines as part of the review of the Johnson & Johnson application. Dr. Shimabukuro and CDC colleagues published a report in JAMA on February 14 that looked at an anaphylaxis case reported connected with COVID vaccines between December 14, 2020, and January 18, 2021.
The CDC identified 66 case reports received that met Brighton Collaboration case definition criteria for anaphylaxis (levels 1, 2, or 3): 47 following Pfizer/BioNTech vaccine, for a reporting rate of 4.7 cases/million doses administered, and 19 following Moderna vaccine, for a reporting rate of 2.5 cases/million doses administered, Dr. Shimabukuro and CDC colleagues wrote.
The CDC has published materials to help clinicians prepare for the possibility of this rare event, Dr. Shimabukuro told the FDA advisers.
“The take-home message here is that these are rare events and anaphylaxis, although clinically serious, is treatable,” Dr. Shimabukuro said.
At the conclusion of the meeting, FDA panelist Patrick Moore, MD, MPH, from the University of Pittsburgh in Pennsylvania, stressed the need to convey to the public that the COVID vaccines appear so far to be safe. Many people earlier had doubts about how the FDA could both safely and quickly review the applications for EUAs for these products.
“As of February 26, things are looking good. That could change tomorrow,” Dr. Moore said. But “this whole EUA process does seem to have worked, despite my own personal concerns about it.”
No second-class vaccines
The Johnson & Johnson vaccine, known as Ad26.COV2.S, is composed of a recombinant, replication-incompetent human adenovirus type 26 (Ad26) vector. It’s intended to encode a stabilized form of SARS-CoV-2 spike (S) protein. The Pfizer and Moderna vaccines use a different mechanism. They rely on mRNA.
The FDA advisers also discussed how patients might respond to the widely reported gap between Janssen’s topline efficacy rates compared with rivals. They urged against people parsing study details too finely and seeking to pick and choose their shots.
“It’s important that people do not think that one vaccine is better than another,” said FDA adviser H. Cody Meissner, MD, from Tufts University School of Medicine in Boston.
Dr. Monto agreed, noting that many people in the United States are still waiting for their turn to get COVID vaccines because of the limited early supply.
Trying to game the system to get one vaccine instead of another would not be wise. “In this environment, whatever you can get, get,” Dr. Monto said.
During an open public hearing, Sarah Christopherson, policy advocacy director of the National Women’s Health Network, said that press reports are fueling a damaging impression in the public that there are “first and second-class” vaccines.
“That has the potential to exacerbate existing mistrust” in vaccines, she said. “Public health authorities must address these perceptions head on.”
She urged against attempts to compare the Janssen vaccine to others, noting the potential effects of emerging variants of the virus.
“It’s difficult to make an apples-to-apples comparison between vaccines,” she said.
Johnson & Johnson’s efficacy results, which are lower than those of the mRNA vaccines, may be a reflection of the ways in which SARS-Co-V-2 is mutating and thus becoming more of a threat, according to the company. A key study of the new vaccine, involving about 44,000 people, coincided with the emergence of new SARS-CoV-2 variants, which were emerging in some of the countries where the pivotal COV3001 study was being conducted, the company said.
At least 14 days after vaccination, the Johnson & Johnson COVID vaccine efficacy (95% confidence interval) was 72.0% (58.2, 81.7) in the United States, 68.1% (48.8, 80.7) in Brazil, and 64.0% (41.2, 78.7) in South Africa.
Weakened standards?
Several researchers called on the FDA to maintain a critical attitude when assessing Johnson & Johnson’s application for the EUA, warning of a potential for a permanent erosion of agency rules due to hasty action on COVID vaccines.
They raised concerns about the FDA demanding too little in terms of follow-up studies on COVID vaccines and with persisting murkiness resulting in attempts to determine how well these treatments work beyond the initial study period.
“I worry about FDA lowering its approval standards,” said Peter Doshi, PhD, from The BMJ and a faculty member at the University of Maryland School of Medicine in Baltimore, during an open public hearing at the meeting.
“There’s a real urgency to stand back right now and look at the forest here, as well as the trees, and I urge the committee to consider the effects FDA decisions may have on the entire regulatory approval process,” Dr. Doshi said.
Dr. Doshi asked why Johnson & Johnson did not seek a standard full approval — a biologics license application (BLA) — instead of aiming for the lower bar of an EUA. The FDA already has allowed wide distribution of the Pfizer/BioNTech and Moderna vaccines through EUAs. That removes the sense of urgency that FDA faced last year in his view.
The FDA’s June 2020 guidance on the development of COVID vaccines had asked drugmakers to plan on following participants in COVID vaccine trials for “ideally at least one to two years.” Yet people who got placebo in Moderna and Pfizer trials already are being vaccinated, Dr. Doshi said. And Johnson & Johnson said in its presentation to the FDA that if the Ad26.COV2.S vaccine were granted an EUA, the COV3001 study design would be amended to “facilitate cross-over of placebo participants in all participating countries to receive one dose of active study vaccine as fast as operationally feasible.”
“I’m nervous about the prospect of there never being a COVID vaccine that meets the FDA’s approval standard” for a BLA instead of the more limited EUA, Dr. Doshi said.
Diana Zuckerman, PhD, president of the nonprofit National Center for Health Research, noted that the FDA’s subsequent guidance tailored for EUAs for COVID vaccines “drastically shortened” the follow-up time to a median of 2 months. Dr. Zuckerman said that a crossover design would be “a reasonable compromise, but only if the placebo group has at least 6 months of data.” Dr. Zuckerman opened her remarks in the open public hearing by saying she had inherited Johnson & Johnson stock, so was speaking at the meeting against her own financial interest.
“As soon as a vaccine is authorized, we start losing the placebo group. If FDA lets that happen, that’s a huge loss for public health and a huge loss of information about how we can all stay safe,” Dr. Zuckerman said.
A version of this article first appeared on Medscape.com.
PTSD prevalent in survivors of severe COVID-19
Posttraumatic stress disorder may occur in up to a third of patients who recover from severe COVID-19 infection, new research suggests.
A study of more than 300 patients who presented to the emergency department with the virus showed a 30.2% prevalence for PTSD 30-120 days after COVID recovery.
or having persistent medical symptoms after hospitalization.
Additional diagnoses, such as depressive and hypomanic episodes and generalized anxiety disorder (GAD), were also present in some of the survivors.
“Previous coronavirus epidemics were associated with PTSD diagnoses in postillness stages, with meta-analytic findings indicating a prevalence of 32.2%,” write the investigators, led by Delfina Janiri, MD, department of psychiatry, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome.
However, data focused specifically on COVID-19 have been “piecemeal,” they add.
The findings were published online Feb. 18 in a research letter in JAMA Psychiatry.
A traumatic event
From April to October 2020, the researchers assessed 381 consecutive patients (100% white; 56.4% men; mean age, 55.3 years) who presented to the ED and subsequently participated in a health check at the Fondazione Policlinico Universitario Agostino Gemelli.
The mean length of stay for the 309 patients hospitalized with severe COVID-19 was 18.4 days.
Results showed that 115 participants (30.2%) had PTSD, based on DSM-5 criteria, and 55.7% of the women had the disorder. Additional diagnoses found in the full patient population included:
- Depressive episodes (17.3%).
- GAD (7%).
- Hypomanic episodes (0.7%).
- Psychotic disorders (0.2%).
Patients with PTSD had higher rates than those without PTSD of a previous history of psychiatric disorders (34.8% vs. 20.7%; P = .003) and of delirium or agitation during hospitalization, as assessed with the Confusion Assessment Method (16.5% vs. 6.4%; P = .002).
In addition, 62.6% of those with PTSD had three or more persistent COVID-19 symptoms vs. 37.2% of their counterparts without PTSD (P < .001).
After logistic regression analyses, significant factors associated with a PTSD diagnosis were persistent medical symptoms (P = .002), delirium or agitation (P = .02), and being female (P = .02).
The investigators note that their results are “in line” with findings reported in research examining other traumatic events. This includes about 30% of Hurricane Katrina survivors who experienced PTSD, as did around 25% of survivors of the 2011 “Great Japan Earthquake and Tsunami.”
Study limitations cited include the “relatively small” size of the patient population, that it focused on only one participating center, and that it didn’t include a control group of non-COVID patients who reported to the ED.
“Further longitudinal studies are needed to tailor therapeutic interventions and prevention strategies,” the researchers write.
Dr. Janiri and four of the five other authors have disclosed no relevant financial relationships. The other author, Gabriele Sani, MD, reported having received personal fees from Angelini Spa, Janssen, and Lundbeck outside the submitted work.
A version of this article first appeared on Medscape.com.
Posttraumatic stress disorder may occur in up to a third of patients who recover from severe COVID-19 infection, new research suggests.
A study of more than 300 patients who presented to the emergency department with the virus showed a 30.2% prevalence for PTSD 30-120 days after COVID recovery.
or having persistent medical symptoms after hospitalization.
Additional diagnoses, such as depressive and hypomanic episodes and generalized anxiety disorder (GAD), were also present in some of the survivors.
“Previous coronavirus epidemics were associated with PTSD diagnoses in postillness stages, with meta-analytic findings indicating a prevalence of 32.2%,” write the investigators, led by Delfina Janiri, MD, department of psychiatry, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome.
However, data focused specifically on COVID-19 have been “piecemeal,” they add.
The findings were published online Feb. 18 in a research letter in JAMA Psychiatry.
A traumatic event
From April to October 2020, the researchers assessed 381 consecutive patients (100% white; 56.4% men; mean age, 55.3 years) who presented to the ED and subsequently participated in a health check at the Fondazione Policlinico Universitario Agostino Gemelli.
The mean length of stay for the 309 patients hospitalized with severe COVID-19 was 18.4 days.
Results showed that 115 participants (30.2%) had PTSD, based on DSM-5 criteria, and 55.7% of the women had the disorder. Additional diagnoses found in the full patient population included:
- Depressive episodes (17.3%).
- GAD (7%).
- Hypomanic episodes (0.7%).
- Psychotic disorders (0.2%).
Patients with PTSD had higher rates than those without PTSD of a previous history of psychiatric disorders (34.8% vs. 20.7%; P = .003) and of delirium or agitation during hospitalization, as assessed with the Confusion Assessment Method (16.5% vs. 6.4%; P = .002).
In addition, 62.6% of those with PTSD had three or more persistent COVID-19 symptoms vs. 37.2% of their counterparts without PTSD (P < .001).
After logistic regression analyses, significant factors associated with a PTSD diagnosis were persistent medical symptoms (P = .002), delirium or agitation (P = .02), and being female (P = .02).
The investigators note that their results are “in line” with findings reported in research examining other traumatic events. This includes about 30% of Hurricane Katrina survivors who experienced PTSD, as did around 25% of survivors of the 2011 “Great Japan Earthquake and Tsunami.”
Study limitations cited include the “relatively small” size of the patient population, that it focused on only one participating center, and that it didn’t include a control group of non-COVID patients who reported to the ED.
“Further longitudinal studies are needed to tailor therapeutic interventions and prevention strategies,” the researchers write.
Dr. Janiri and four of the five other authors have disclosed no relevant financial relationships. The other author, Gabriele Sani, MD, reported having received personal fees from Angelini Spa, Janssen, and Lundbeck outside the submitted work.
A version of this article first appeared on Medscape.com.
Posttraumatic stress disorder may occur in up to a third of patients who recover from severe COVID-19 infection, new research suggests.
A study of more than 300 patients who presented to the emergency department with the virus showed a 30.2% prevalence for PTSD 30-120 days after COVID recovery.
or having persistent medical symptoms after hospitalization.
Additional diagnoses, such as depressive and hypomanic episodes and generalized anxiety disorder (GAD), were also present in some of the survivors.
“Previous coronavirus epidemics were associated with PTSD diagnoses in postillness stages, with meta-analytic findings indicating a prevalence of 32.2%,” write the investigators, led by Delfina Janiri, MD, department of psychiatry, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome.
However, data focused specifically on COVID-19 have been “piecemeal,” they add.
The findings were published online Feb. 18 in a research letter in JAMA Psychiatry.
A traumatic event
From April to October 2020, the researchers assessed 381 consecutive patients (100% white; 56.4% men; mean age, 55.3 years) who presented to the ED and subsequently participated in a health check at the Fondazione Policlinico Universitario Agostino Gemelli.
The mean length of stay for the 309 patients hospitalized with severe COVID-19 was 18.4 days.
Results showed that 115 participants (30.2%) had PTSD, based on DSM-5 criteria, and 55.7% of the women had the disorder. Additional diagnoses found in the full patient population included:
- Depressive episodes (17.3%).
- GAD (7%).
- Hypomanic episodes (0.7%).
- Psychotic disorders (0.2%).
Patients with PTSD had higher rates than those without PTSD of a previous history of psychiatric disorders (34.8% vs. 20.7%; P = .003) and of delirium or agitation during hospitalization, as assessed with the Confusion Assessment Method (16.5% vs. 6.4%; P = .002).
In addition, 62.6% of those with PTSD had three or more persistent COVID-19 symptoms vs. 37.2% of their counterparts without PTSD (P < .001).
After logistic regression analyses, significant factors associated with a PTSD diagnosis were persistent medical symptoms (P = .002), delirium or agitation (P = .02), and being female (P = .02).
The investigators note that their results are “in line” with findings reported in research examining other traumatic events. This includes about 30% of Hurricane Katrina survivors who experienced PTSD, as did around 25% of survivors of the 2011 “Great Japan Earthquake and Tsunami.”
Study limitations cited include the “relatively small” size of the patient population, that it focused on only one participating center, and that it didn’t include a control group of non-COVID patients who reported to the ED.
“Further longitudinal studies are needed to tailor therapeutic interventions and prevention strategies,” the researchers write.
Dr. Janiri and four of the five other authors have disclosed no relevant financial relationships. The other author, Gabriele Sani, MD, reported having received personal fees from Angelini Spa, Janssen, and Lundbeck outside the submitted work.
A version of this article first appeared on Medscape.com.






