User login
In Case You Missed It: COVID
Most people with Omicron don’t know they’re infected
Most people with Omicron likely don’t know it.
That’s according to a study in JAMA Network Open, which says 56% of people who have the Omicron variant of the coronavirus are unaware of their infection.
And it has an upside and a downside, depending on how you look at it, according to Time magazine.
“It’s good news, in some ways, since ) in vaccinated people,” Time says. “The downside is that many people are likely spreading the virus unintentionally.”
The study looked at 210 hospital patients and employees in the Los Angeles area. More than half who tested positive didn’t know it – because they had no symptoms, or they assumed they merely had a cold or allergies.
“The findings support early data from around the world suggesting that throughout the pandemic, anywhere from 25% to 40% of SARS-CoV-2 infections have been asymptomatic, which presents challenges for public health officials trying to control the spread of the virus,” Time reports.
The study found that awareness of infection rose after at-home tests became available this year. About three-quarters of people in January and February didn’t know their status, for example.
“Findings of this study suggest that low rates of Omicron variant infection awareness may be a key contributor to rapid transmission of the virus within communities,” the authors wrote. “Given that unawareness of active infection precludes self-initiated interventions, such as testing and self-isolation, even modest levels of undiagnosed infection can contribute to substantial population-level transmission.”
A version of this article first appeared on WebMD.com.
Most people with Omicron likely don’t know it.
That’s according to a study in JAMA Network Open, which says 56% of people who have the Omicron variant of the coronavirus are unaware of their infection.
And it has an upside and a downside, depending on how you look at it, according to Time magazine.
“It’s good news, in some ways, since ) in vaccinated people,” Time says. “The downside is that many people are likely spreading the virus unintentionally.”
The study looked at 210 hospital patients and employees in the Los Angeles area. More than half who tested positive didn’t know it – because they had no symptoms, or they assumed they merely had a cold or allergies.
“The findings support early data from around the world suggesting that throughout the pandemic, anywhere from 25% to 40% of SARS-CoV-2 infections have been asymptomatic, which presents challenges for public health officials trying to control the spread of the virus,” Time reports.
The study found that awareness of infection rose after at-home tests became available this year. About three-quarters of people in January and February didn’t know their status, for example.
“Findings of this study suggest that low rates of Omicron variant infection awareness may be a key contributor to rapid transmission of the virus within communities,” the authors wrote. “Given that unawareness of active infection precludes self-initiated interventions, such as testing and self-isolation, even modest levels of undiagnosed infection can contribute to substantial population-level transmission.”
A version of this article first appeared on WebMD.com.
Most people with Omicron likely don’t know it.
That’s according to a study in JAMA Network Open, which says 56% of people who have the Omicron variant of the coronavirus are unaware of their infection.
And it has an upside and a downside, depending on how you look at it, according to Time magazine.
“It’s good news, in some ways, since ) in vaccinated people,” Time says. “The downside is that many people are likely spreading the virus unintentionally.”
The study looked at 210 hospital patients and employees in the Los Angeles area. More than half who tested positive didn’t know it – because they had no symptoms, or they assumed they merely had a cold or allergies.
“The findings support early data from around the world suggesting that throughout the pandemic, anywhere from 25% to 40% of SARS-CoV-2 infections have been asymptomatic, which presents challenges for public health officials trying to control the spread of the virus,” Time reports.
The study found that awareness of infection rose after at-home tests became available this year. About three-quarters of people in January and February didn’t know their status, for example.
“Findings of this study suggest that low rates of Omicron variant infection awareness may be a key contributor to rapid transmission of the virus within communities,” the authors wrote. “Given that unawareness of active infection precludes self-initiated interventions, such as testing and self-isolation, even modest levels of undiagnosed infection can contribute to substantial population-level transmission.”
A version of this article first appeared on WebMD.com.
FROM JAMA NETWORK OPEN
‘Medical Methuselahs’: Treating the growing population of centenarians
For about the past year, Priya Goel, MD, can be seen cruising around the island of Manhattan as she makes her way between visits to some of New York City’s most treasured residents: a small but essential group of patients born before the Empire State Building scraped the sky and the old Yankee Stadium had become the House That Ruth Built.
– the oldest is a 108-year-old man – whom she visits monthly.
The gray wave
Dr. Goel’s charges are among America’s latest baby boom – babies born a century ago, that is.
Between 1980 and 2019, the share of American centenarians, those aged 100 and up, grew faster than the total population. In 2019, 100,322 persons in the United States were at least 100 years old – more than triple the 1980 figure of 32,194, according to the U.S. Administration on Aging. By 2060, experts predict, the U.S. centenarian population will reach nearly 600,000.
Although some of the ultra-aged live in nursing homes, many continue to live independently. They require both routine and acute medical care. So, what does it take to be a physician for a centenarian?
Dr. Goel, who is in her mid-30s and could well be the great-granddaughter of some of her patients, urged her colleagues not to stereotype patients on the basis of age.
“You have to consider their functional and cognitive abilities, their ability to understand disease processes and make decisions for themselves,” Dr. Goel said. “Age is just one factor in the grand scheme of things.”
Visiting patients in their homes provides her with insights into how well they’re doing, including the safety of their environments and the depth of their social networks.
New York City has its peculiar demands. Heal provides Dr. Goel with a driver who chauffeurs her to her patient visits. She takes notes between stops.
“The idea is to have these patients remain in an environment where they’re comfortable, in surroundings where they’ve grown up or lived for many years,” she said. “A lot of them are in elevator buildings and they are wheelchair-bound or bed-bound and they physically can’t leave.”
She said she gets a far different view of the patient than does an office-based physician.
“When you go into their home, it’s very personal. You’re seeing what their daily environment is like, what their diet is like. You can see their food on the counter. You can see the level of hygiene,” Dr. Goel said. “You get to see their social support. Are their kids involved? Are they hoarding? Stuff that they wouldn’t just necessarily disclose but on a visit you get to see going into the home. It’s an extra layer of understanding that patient.”
Dr. Goel contrasted home care from care in a nursing home, where the patients are seen daily. On the basis of her observations, she decides whether to see her patients every month or every 3 months.
She applies this strategy to everyone from age 60 to over 100.
Tracking a growing group
Since 1995, geriatrician Thomas Perls, MD, has directed the New England Centenarian Study at Boston University. The study, largely funded by the National Institute on Aging, has enrolled 2,599 centenarian persons and 700 of their offspring. At any given time in the study, about 10% of the centenarians are alive. The study has a high mortality rate.
The people in Dr. Perls’s study range in age, but they top out at 119, the third oldest person ever in the world. Most centenarians are women.
“When we first began the study in 1995, the prevalence of centenarians in the United States was about 1 per 10,000 in the population,” Perls told this news organization. “And now, that prevalence has doubled to 1 per 5,000.”
Even if no one has achieved the record of Methuselah, the Biblical patriarch who was purported to have lived to the age of 969, some people always have lived into their 90s and beyond. Dr. Perls attributed the increase in longevity to control at the turn of the 20th century of typhoid fever, diphtheria, and other infectious diseases with effective public health measures, including the availability of clean water and improvement in socioeconomic conditions.
“Infant mortality just plummeted. So, come around 1915, 1920, we were no longer losing a quarter of our population to these diseases. That meant a quarter more of the population could age into adulthood and middle age,” he said. “A certain component of that group was, therefore, able to continue to age to a very, very old age.”
Other advances, such as antibiotics and vaccinations in the 1960s; the availability in the 1970s of much better detection and effective treatment of high blood pressure; the recognition of the harms of smoking; and much more effective treatment of cardiovascular disease and cancer have allowed many people who would have otherwise died in their 70s and 80s to live much longer. “I think what this means is that there is a substantial proportion of the population that has the biology to get to 100,” Dr. Perls said.
Perls said the Latino population and Blacks have a better track record than Whites in reaching the 100-year milestone. “The average life expectancy might be lower in these populations because of socioeconomic factors, but if they are able to get to around their early 80s, compared to Whites, their ability to get to 100 is actually better,” he said.
Asians fare best when it comes to longevity. While around 1% of White women in the United States live to 100, 10% of Asian women in Hong Kong hit that mark.
“I think some of that is better environment and health habits in Hong Kong than in the United States,” Dr. Perls said. “I think another piece may be a genetic advantage in East Asians. We’re looking into that.”
Dr. Perls said he agreed with Dr. Goel that health care providers and the lay public should not make assumptions on the basis of age alone as to how a person is doing. “People can age so very differently from one another,” he said.
Up to about age 90, the vast majority of those differences are determined by our health behaviors, such as smoking, alcohol use, exercise, sleep, the effect of our diets on weight, and access to good health care, including regular screening for problems such as high blood pressure, diabetes, and cancer. “People who are able to do everything right generally add healthy years to their lives, while those who do not have shorter life expectancies and longer periods of chronic diseases,” Dr. Perls said.
Paying diligent attention to these behaviors over the long run can have a huge payoff.
Dr. Perls’s team has found that to live beyond age 90 and on into the early 100s, protective genes can play a strong role. These genes help slow aging and decrease one’s risk for aging-related diseases. Centenarians usually have a history of aging very slowly and greatly delaying aging-related diseases and disability toward the ends of their lives.
Centenarians are the antithesis of the misguided belief that the older you get, the sicker you get. Quite the opposite occurs. For Dr. Perls, “the older you get, the healthier you’ve been.”
MD bias against the elderly?
Care of elderly patients is becoming essential in the practice of primary care physicians – but not all of them enjoy the work.
To be effective, physicians who treat centenarians must get a better idea of the individual patient’s functional status and comorbidities. “You absolutely cannot make assumptions on age alone,” Dr. Perls said.
The so-called “normal” temperature, 98.6° F, can spell trouble for centenarians and other very old patients, warned Natalie Baker, DNP, CRNP, an associate professor of nursing at the University of Alabama, Birmingham, and president of the 3,000-member Gerontological Advanced Practice Nurses Association.
“We have to be very cognizant of what we call a typical presentation of disease or illness and that a very subtle change in an older adult can signal a serious infection or illness,” Dr. Baker said. “If your patient has a high fever, that is a potential problem.”
The average temperature of an older adult is lower than the accepted 98.6° F, and their body’s response to an infection is slow to exhibit an increase in temperature, Dr. Baker said. “When treating centenarians, clinicians must be cognizant of other subtle signs of infection, such as decreased appetite or change in mentation,” she cautioned.
A decline in appetite or insomnia may be a subtle sign that these patients need to be evaluated, she added.
COVID-19 and centenarians
Three-quarters of the 1 million U.S. deaths from COVID-19 occurred in people aged 65 and older. However, Dr. Perls said centenarians may be a special subpopulation when it comes to COVID.
The Japanese Health Ministry, which follows the large centenarian population in that country, noted a marked jump in the number of centenarians during the pandemic – although the reasons for the increase aren’t clear.
Centenarians may be a bit different. Dr. Perls said some evidence suggests that the over-100 crowd may have better immune systems than younger people. “Part of the trick of getting to 100 is having a pretty good immune system,” he said.
Don’t mess with success
“There is no need at that point for us to try to alter their diet to what we think it might be,” Dr. Baker said. “There’s no need to start with diabetic education. They may tell you their secret is a shot of vodka every day. Why should we stop it at that age? Accept their lifestyles, because they’ve done something right to get to that age.”
Opinions differ on how to approach screening for centenarians.
Dr. Goel said guidelines for routine screening, such as colonoscopies, mammograms, and PAP smears, drop off for patients starting at 75. Dr. Perls said this strategy stems from the belief that people will die from other things first, so screening is no longer needed. Dr. Perls said he disagrees with this approach.
“Again, we can’t base our screening and health care decisions on age alone. If I have an independently functioning and robust 95-year-old man in my office, you can be sure I am going to continue recommending regular screening for colon cancer and other screenings that are normal for people who are 30 years younger,” he said.
Justin Zaghi, MD, chief medical officer at Heal, said screening patients in their late 90s and 100s for cancer generally doesn’t make sense except in some rare circumstances in which the cancer would be unlikely to be a cause of death. “However, if we are talking about screening for fall risks, hearing difficulties, poor vision, pain, and malnutrition, those screenings still absolutely make sense for patients in their late 90s and 100s,” Dr. Zaghi said.
One high-functioning 104-year-old patient of Dr. Perls underwent a total hip replacement for a hip fracture and is faring well. “Obviously, if she had end-stage dementia, we’d do everything to keep the person comfortable, or if they had medical problems that made surgery too high risk, then you don’t do it,” he said. “But if they’re otherwise, I would proceed.”
Avoid the ED
Dr. Goel said doctors should avoid sending patients to the emergency department, an often chaotic place that is especially unfriendly to centenarians and the very old. “Sometimes I’ve seen older patients who are being rushed to the ER, and I ask, What are the goals of care?” she said.
Clinicians caring for seniors should keep in mind that infections can cause seniors to appear confused – and this may lead the clinician to think the patient has dementia. Or, Dr. Goel said, a patient with dementia may suddenly experience much worse dementia.
“In either case, you want to make sure you’re not dealing with any underlying infection, like urinary tract infection, or pneumonia brewing, or skin infections,” she said. “Their skin is so much frailer. You want to make sure there are no bedsores.”
She has had patients whose children report that their usually placid centenarian parents are suddenly acting out. “We’ll do a urinary test and it definitely shows a urinary tract infection. You want to make sure you’re not missing out on something else before you attribute it to dementia,” she said.
Environmental changes, such as moving a patient to a new room in a hospital setting, can trigger an acute mental status change, such as delirium, she added. Helping older patients feel in control as much as possible is important.
“You want to make sure you’re orienting them to the time of day. Make sure they get up at the same time, go to bed at the same time, have clocks and calendars present – just making sure that they feel like they’re still in control of their body and their day,” she said.
Physicians should be aware of potential depression in these patients, whose experience of loss – an unavoidable consequence of outliving family and friends – can result in problems with sleep and diet, as well as a sense of social isolation.
Neal Flomenbaum, MD, professor and emergency physician-in-chief emeritus, New York–Presbyterian/Weill Cornell Medical Center in New York, said sometimes the best thing for these very elderly patients is to “get them in and out of ED as quickly as possible, and do what you can diagnostically.”
He noted that EDs have been making accommodations to serve the elderly, such as using LEDs that replicate outdoor lighting conditions, as well as providing seniors with separate rooms with glass doors to protect them from noise, separate air handlers to prevent infections, and adequate space for visitors.
These patients often are subject to trauma from falls.
“The bones don’t heal as well as in younger people, and treating their comorbidities is essential. Once they have trouble with one area and they’re lying in bed and can’t move much, they can get bedsores,” Dr. Flomenbaum said. “In the hospital, they are vulnerable to infections. So, you’re thinking of all of these things at the same time and how to treat them appropriately and then get them out of the hospital as soon as possible with whatever care that they need in their own homes if at all possible.”
“I always err on the side of less is more,” Dr. Goel said. “Obviously, if there is something – if they have a cough, they need an x-ray. That’s very basic. We want to take care of that. Give them the antibiotic if they need that. But rushing them in and out of the hospital doesn’t add to their quality of life.”
Dr. Flomenbaum, a pioneer in geriatric emergency medicine, says physicians need to be aware that centenarians and other very old patients don’t present the same way as younger adults.
He began to notice more than 20 years ago that every night, patients would turn up in his ED who were in their late 90s into their 100s. Some would come in with what their children identified as sudden-onset dementia – they didn’t know their own names and couldn’t identify their kids. They didn’t know the time or day. Dr. Flomenbaum said the children often asked whether their parents should enter a nursing home.
“And I’d say, ‘Not so fast. Well, let’s take a look at this.’ You don’t develop that kind of dementia overnight. It usually takes a while,” he said.
He said he ordered complete blood cell counts and oxygen saturation tests that frequently turned out to be abnormal. They didn’t have a fever, and infiltrates initially weren’t seen on chest x-rays.
With rehydration and supplemental oxygen, their symptoms started to improve, and it became obvious that the symptoms were not of dementia but of pneumonia, and that they required antibiotics, Dr. Flomenbaum said.
Dementia dilemma
Too often, on the basis of age, doctors assume patients have dementia or other cognitive impairments.
“What a shock and a surprise when doctors actually talk to folks and do a neurocognitive screen and find they’re just fine,” Dr. Perls said.
The decline in hearing and vision can lead to a misdiagnosis of cognitive impairment because the patients are not able to hear what you’re asking them. “It’s really important that the person can hear you – whether you use an amplifying device or they have hearing aids, that’s critical,” he said. “You just have to be a good doctor.”
Often the physical toll of aging exacerbates social difficulties. Poor hearing, for example, can accelerate cognitive impairment and cause people to interact less often, and less meaningfully, with their environment. For some, wearing hearing aids seems demeaning – until they hear what they’ve been missing.
“I get them to wear their hearing aids and, lo and behold, they’re a whole new person because they’re now able to take in their environment and interact with others,” Dr. Perls said.
Dr. Flomenbaum said alcohol abuse and drug reactions can cause delirium, which, unlike dementia, is potentially reversible. Yet many physicians cannot reliably differentiate between dementia and delirium, he added.
The geriatric specialists talk about the lessons they’ve learned and the gratification they get from caring for centenarians.
“I have come to realize the importance of family, of having a close circle, whether that’s through friends or neighbors,” Dr. Goel said. “This work is very rewarding because, if it wasn’t for homebound organizations, how would these people get care or get access to care?”
For Dr. Baker, a joy of the job is hearing centenarians share their life stories.
“I love to hear their stories about how they’ve overcome adversity, living through the depression and living through different wars,” she said. “I love talking to veterans, and I think that oftentimes, we do not value our older adults in our society as we should. Sometimes they are dismissed because they move slowly or are hard to communicate with due to hearing deficits. But they are, I think, a very important part of our lives.”
‘They’ve already won’
Most centenarians readily offer the secrets to their longevity. Aline Jacobsohn, of Boca Raton, Fla., is no different.
Ms. Jacobsohn, who will be 101 in October, thinks a diet of small portions of fish, vegetables, and fruit, which she has followed since her husband Leo died in 1982, has helped keep her healthy. She eats lots of salmon and herring and is a fan of spinach sautéed with olive oil. “The only thing I don’t eat is meat,” the trim and active Ms. Jacobsohn said in a recent interview over Zoom.
Her other secret: “Doctors. I like to stay away from them as much as possible.”
Shari Rosenbaum, MD, Jacobsohn’s internist, doesn’t dismiss that approach. She uses a version of it when managing her three centenarian patients, the oldest of whom is 103.
“Let them smoke! Let them drink! They’re happy. It’s not causing harm. Let them eat cake! They’ve already won,” said Dr. Rosenbaum, who is affiliated with Boca Raton–based MDVIP, a national membership-based network of 1,100 primary care physicians serving 368,000 patients. Of those, nearly 460 are centenarians.
“You’re not preventing those problems in this population,” she said. “They’re here to enjoy every moment that they have, and they might as well.”
Dr. Rosenbaum sees a divergence in her patients – those who will reach very old age, and those who won’t – starting in their 60s.
“The centenarians don’t have medical problems,” she said. “They don’t get cancer. They don’t get diabetes. Some of them take good care of themselves. Some don’t take such good care of themselves. But they are all optimists. They all see the glass half full. They all participate in life. They all have excellent support systems. They have good genes, a positive attitude toward life, and a strong social network.”
Ms. Jacobsohn – whose surname at the time was Bakst – grew up in Frankfurt am Main, Germany, during the rise of the Nazi regime. The family fled to Columbia in 1938, where she met and eventually married her husband, Leo, who ran a business importing clocks and watches in Cali.
In 1989, the Jacobsohns and their three children moved to south Florida to escape the dangers of kidnappings and ransoms posed by the drug cartels.
Ms. Jacobsohn agreed that she appears to have longevity genes – “good stock,” she calls it. “My mother died 23 days before she was 100. My grandmother lived till 99, almost 100,” she said.
Two years ago, she donated her car to a charity and stopped driving in the interest of her own safety and that of other drivers and pedestrians.
Ms. Jacobsohn has a strong support system. Two of her children live nearby and visit her nearly every day. A live-in companion helps her with the activities of daily life, including preparing meals.
Ms. Jacobsohn plays bridge regularly, and well. “I’m sorry to say that I’m a very good bridge player,” she said, frankly. “How is it possible that I’ve played bridge so well and then I don’t remember what I had for lunch yesterday?”
She reads, mainly a diet of history but occasionally novels, too. “They have to be engaging,” she said.
The loss of loved ones is an inevitable part of very old age. Her husband of 47 years died of emphysema, and one of her sons died in his 70s of prostate cancer.
She knows well the fate that awaits us all and accepts it philosophically.
“It’s a very normal thing that people die. You don’t live forever. So, whenever it comes, it’s okay. Enough is enough. Dayenu,” she said, using the Hebrew word for, “It would have been enough” – a favorite in the Passover Seder celebrating the ancient Jews’ liberation from slavery in Egypt.
Ms. Jacobsohn sang the song and then took a reporter on a Zoom tour of her tidy home and her large flower garden featuring Cattleya orchids from Colombia.
A version of this article first appeared on Medscape.com.
For about the past year, Priya Goel, MD, can be seen cruising around the island of Manhattan as she makes her way between visits to some of New York City’s most treasured residents: a small but essential group of patients born before the Empire State Building scraped the sky and the old Yankee Stadium had become the House That Ruth Built.
– the oldest is a 108-year-old man – whom she visits monthly.
The gray wave
Dr. Goel’s charges are among America’s latest baby boom – babies born a century ago, that is.
Between 1980 and 2019, the share of American centenarians, those aged 100 and up, grew faster than the total population. In 2019, 100,322 persons in the United States were at least 100 years old – more than triple the 1980 figure of 32,194, according to the U.S. Administration on Aging. By 2060, experts predict, the U.S. centenarian population will reach nearly 600,000.
Although some of the ultra-aged live in nursing homes, many continue to live independently. They require both routine and acute medical care. So, what does it take to be a physician for a centenarian?
Dr. Goel, who is in her mid-30s and could well be the great-granddaughter of some of her patients, urged her colleagues not to stereotype patients on the basis of age.
“You have to consider their functional and cognitive abilities, their ability to understand disease processes and make decisions for themselves,” Dr. Goel said. “Age is just one factor in the grand scheme of things.”
Visiting patients in their homes provides her with insights into how well they’re doing, including the safety of their environments and the depth of their social networks.
New York City has its peculiar demands. Heal provides Dr. Goel with a driver who chauffeurs her to her patient visits. She takes notes between stops.
“The idea is to have these patients remain in an environment where they’re comfortable, in surroundings where they’ve grown up or lived for many years,” she said. “A lot of them are in elevator buildings and they are wheelchair-bound or bed-bound and they physically can’t leave.”
She said she gets a far different view of the patient than does an office-based physician.
“When you go into their home, it’s very personal. You’re seeing what their daily environment is like, what their diet is like. You can see their food on the counter. You can see the level of hygiene,” Dr. Goel said. “You get to see their social support. Are their kids involved? Are they hoarding? Stuff that they wouldn’t just necessarily disclose but on a visit you get to see going into the home. It’s an extra layer of understanding that patient.”
Dr. Goel contrasted home care from care in a nursing home, where the patients are seen daily. On the basis of her observations, she decides whether to see her patients every month or every 3 months.
She applies this strategy to everyone from age 60 to over 100.
Tracking a growing group
Since 1995, geriatrician Thomas Perls, MD, has directed the New England Centenarian Study at Boston University. The study, largely funded by the National Institute on Aging, has enrolled 2,599 centenarian persons and 700 of their offspring. At any given time in the study, about 10% of the centenarians are alive. The study has a high mortality rate.
The people in Dr. Perls’s study range in age, but they top out at 119, the third oldest person ever in the world. Most centenarians are women.
“When we first began the study in 1995, the prevalence of centenarians in the United States was about 1 per 10,000 in the population,” Perls told this news organization. “And now, that prevalence has doubled to 1 per 5,000.”
Even if no one has achieved the record of Methuselah, the Biblical patriarch who was purported to have lived to the age of 969, some people always have lived into their 90s and beyond. Dr. Perls attributed the increase in longevity to control at the turn of the 20th century of typhoid fever, diphtheria, and other infectious diseases with effective public health measures, including the availability of clean water and improvement in socioeconomic conditions.
“Infant mortality just plummeted. So, come around 1915, 1920, we were no longer losing a quarter of our population to these diseases. That meant a quarter more of the population could age into adulthood and middle age,” he said. “A certain component of that group was, therefore, able to continue to age to a very, very old age.”
Other advances, such as antibiotics and vaccinations in the 1960s; the availability in the 1970s of much better detection and effective treatment of high blood pressure; the recognition of the harms of smoking; and much more effective treatment of cardiovascular disease and cancer have allowed many people who would have otherwise died in their 70s and 80s to live much longer. “I think what this means is that there is a substantial proportion of the population that has the biology to get to 100,” Dr. Perls said.
Perls said the Latino population and Blacks have a better track record than Whites in reaching the 100-year milestone. “The average life expectancy might be lower in these populations because of socioeconomic factors, but if they are able to get to around their early 80s, compared to Whites, their ability to get to 100 is actually better,” he said.
Asians fare best when it comes to longevity. While around 1% of White women in the United States live to 100, 10% of Asian women in Hong Kong hit that mark.
“I think some of that is better environment and health habits in Hong Kong than in the United States,” Dr. Perls said. “I think another piece may be a genetic advantage in East Asians. We’re looking into that.”
Dr. Perls said he agreed with Dr. Goel that health care providers and the lay public should not make assumptions on the basis of age alone as to how a person is doing. “People can age so very differently from one another,” he said.
Up to about age 90, the vast majority of those differences are determined by our health behaviors, such as smoking, alcohol use, exercise, sleep, the effect of our diets on weight, and access to good health care, including regular screening for problems such as high blood pressure, diabetes, and cancer. “People who are able to do everything right generally add healthy years to their lives, while those who do not have shorter life expectancies and longer periods of chronic diseases,” Dr. Perls said.
Paying diligent attention to these behaviors over the long run can have a huge payoff.
Dr. Perls’s team has found that to live beyond age 90 and on into the early 100s, protective genes can play a strong role. These genes help slow aging and decrease one’s risk for aging-related diseases. Centenarians usually have a history of aging very slowly and greatly delaying aging-related diseases and disability toward the ends of their lives.
Centenarians are the antithesis of the misguided belief that the older you get, the sicker you get. Quite the opposite occurs. For Dr. Perls, “the older you get, the healthier you’ve been.”
MD bias against the elderly?
Care of elderly patients is becoming essential in the practice of primary care physicians – but not all of them enjoy the work.
To be effective, physicians who treat centenarians must get a better idea of the individual patient’s functional status and comorbidities. “You absolutely cannot make assumptions on age alone,” Dr. Perls said.
The so-called “normal” temperature, 98.6° F, can spell trouble for centenarians and other very old patients, warned Natalie Baker, DNP, CRNP, an associate professor of nursing at the University of Alabama, Birmingham, and president of the 3,000-member Gerontological Advanced Practice Nurses Association.
“We have to be very cognizant of what we call a typical presentation of disease or illness and that a very subtle change in an older adult can signal a serious infection or illness,” Dr. Baker said. “If your patient has a high fever, that is a potential problem.”
The average temperature of an older adult is lower than the accepted 98.6° F, and their body’s response to an infection is slow to exhibit an increase in temperature, Dr. Baker said. “When treating centenarians, clinicians must be cognizant of other subtle signs of infection, such as decreased appetite or change in mentation,” she cautioned.
A decline in appetite or insomnia may be a subtle sign that these patients need to be evaluated, she added.
COVID-19 and centenarians
Three-quarters of the 1 million U.S. deaths from COVID-19 occurred in people aged 65 and older. However, Dr. Perls said centenarians may be a special subpopulation when it comes to COVID.
The Japanese Health Ministry, which follows the large centenarian population in that country, noted a marked jump in the number of centenarians during the pandemic – although the reasons for the increase aren’t clear.
Centenarians may be a bit different. Dr. Perls said some evidence suggests that the over-100 crowd may have better immune systems than younger people. “Part of the trick of getting to 100 is having a pretty good immune system,” he said.
Don’t mess with success
“There is no need at that point for us to try to alter their diet to what we think it might be,” Dr. Baker said. “There’s no need to start with diabetic education. They may tell you their secret is a shot of vodka every day. Why should we stop it at that age? Accept their lifestyles, because they’ve done something right to get to that age.”
Opinions differ on how to approach screening for centenarians.
Dr. Goel said guidelines for routine screening, such as colonoscopies, mammograms, and PAP smears, drop off for patients starting at 75. Dr. Perls said this strategy stems from the belief that people will die from other things first, so screening is no longer needed. Dr. Perls said he disagrees with this approach.
“Again, we can’t base our screening and health care decisions on age alone. If I have an independently functioning and robust 95-year-old man in my office, you can be sure I am going to continue recommending regular screening for colon cancer and other screenings that are normal for people who are 30 years younger,” he said.
Justin Zaghi, MD, chief medical officer at Heal, said screening patients in their late 90s and 100s for cancer generally doesn’t make sense except in some rare circumstances in which the cancer would be unlikely to be a cause of death. “However, if we are talking about screening for fall risks, hearing difficulties, poor vision, pain, and malnutrition, those screenings still absolutely make sense for patients in their late 90s and 100s,” Dr. Zaghi said.
One high-functioning 104-year-old patient of Dr. Perls underwent a total hip replacement for a hip fracture and is faring well. “Obviously, if she had end-stage dementia, we’d do everything to keep the person comfortable, or if they had medical problems that made surgery too high risk, then you don’t do it,” he said. “But if they’re otherwise, I would proceed.”
Avoid the ED
Dr. Goel said doctors should avoid sending patients to the emergency department, an often chaotic place that is especially unfriendly to centenarians and the very old. “Sometimes I’ve seen older patients who are being rushed to the ER, and I ask, What are the goals of care?” she said.
Clinicians caring for seniors should keep in mind that infections can cause seniors to appear confused – and this may lead the clinician to think the patient has dementia. Or, Dr. Goel said, a patient with dementia may suddenly experience much worse dementia.
“In either case, you want to make sure you’re not dealing with any underlying infection, like urinary tract infection, or pneumonia brewing, or skin infections,” she said. “Their skin is so much frailer. You want to make sure there are no bedsores.”
She has had patients whose children report that their usually placid centenarian parents are suddenly acting out. “We’ll do a urinary test and it definitely shows a urinary tract infection. You want to make sure you’re not missing out on something else before you attribute it to dementia,” she said.
Environmental changes, such as moving a patient to a new room in a hospital setting, can trigger an acute mental status change, such as delirium, she added. Helping older patients feel in control as much as possible is important.
“You want to make sure you’re orienting them to the time of day. Make sure they get up at the same time, go to bed at the same time, have clocks and calendars present – just making sure that they feel like they’re still in control of their body and their day,” she said.
Physicians should be aware of potential depression in these patients, whose experience of loss – an unavoidable consequence of outliving family and friends – can result in problems with sleep and diet, as well as a sense of social isolation.
Neal Flomenbaum, MD, professor and emergency physician-in-chief emeritus, New York–Presbyterian/Weill Cornell Medical Center in New York, said sometimes the best thing for these very elderly patients is to “get them in and out of ED as quickly as possible, and do what you can diagnostically.”
He noted that EDs have been making accommodations to serve the elderly, such as using LEDs that replicate outdoor lighting conditions, as well as providing seniors with separate rooms with glass doors to protect them from noise, separate air handlers to prevent infections, and adequate space for visitors.
These patients often are subject to trauma from falls.
“The bones don’t heal as well as in younger people, and treating their comorbidities is essential. Once they have trouble with one area and they’re lying in bed and can’t move much, they can get bedsores,” Dr. Flomenbaum said. “In the hospital, they are vulnerable to infections. So, you’re thinking of all of these things at the same time and how to treat them appropriately and then get them out of the hospital as soon as possible with whatever care that they need in their own homes if at all possible.”
“I always err on the side of less is more,” Dr. Goel said. “Obviously, if there is something – if they have a cough, they need an x-ray. That’s very basic. We want to take care of that. Give them the antibiotic if they need that. But rushing them in and out of the hospital doesn’t add to their quality of life.”
Dr. Flomenbaum, a pioneer in geriatric emergency medicine, says physicians need to be aware that centenarians and other very old patients don’t present the same way as younger adults.
He began to notice more than 20 years ago that every night, patients would turn up in his ED who were in their late 90s into their 100s. Some would come in with what their children identified as sudden-onset dementia – they didn’t know their own names and couldn’t identify their kids. They didn’t know the time or day. Dr. Flomenbaum said the children often asked whether their parents should enter a nursing home.
“And I’d say, ‘Not so fast. Well, let’s take a look at this.’ You don’t develop that kind of dementia overnight. It usually takes a while,” he said.
He said he ordered complete blood cell counts and oxygen saturation tests that frequently turned out to be abnormal. They didn’t have a fever, and infiltrates initially weren’t seen on chest x-rays.
With rehydration and supplemental oxygen, their symptoms started to improve, and it became obvious that the symptoms were not of dementia but of pneumonia, and that they required antibiotics, Dr. Flomenbaum said.
Dementia dilemma
Too often, on the basis of age, doctors assume patients have dementia or other cognitive impairments.
“What a shock and a surprise when doctors actually talk to folks and do a neurocognitive screen and find they’re just fine,” Dr. Perls said.
The decline in hearing and vision can lead to a misdiagnosis of cognitive impairment because the patients are not able to hear what you’re asking them. “It’s really important that the person can hear you – whether you use an amplifying device or they have hearing aids, that’s critical,” he said. “You just have to be a good doctor.”
Often the physical toll of aging exacerbates social difficulties. Poor hearing, for example, can accelerate cognitive impairment and cause people to interact less often, and less meaningfully, with their environment. For some, wearing hearing aids seems demeaning – until they hear what they’ve been missing.
“I get them to wear their hearing aids and, lo and behold, they’re a whole new person because they’re now able to take in their environment and interact with others,” Dr. Perls said.
Dr. Flomenbaum said alcohol abuse and drug reactions can cause delirium, which, unlike dementia, is potentially reversible. Yet many physicians cannot reliably differentiate between dementia and delirium, he added.
The geriatric specialists talk about the lessons they’ve learned and the gratification they get from caring for centenarians.
“I have come to realize the importance of family, of having a close circle, whether that’s through friends or neighbors,” Dr. Goel said. “This work is very rewarding because, if it wasn’t for homebound organizations, how would these people get care or get access to care?”
For Dr. Baker, a joy of the job is hearing centenarians share their life stories.
“I love to hear their stories about how they’ve overcome adversity, living through the depression and living through different wars,” she said. “I love talking to veterans, and I think that oftentimes, we do not value our older adults in our society as we should. Sometimes they are dismissed because they move slowly or are hard to communicate with due to hearing deficits. But they are, I think, a very important part of our lives.”
‘They’ve already won’
Most centenarians readily offer the secrets to their longevity. Aline Jacobsohn, of Boca Raton, Fla., is no different.
Ms. Jacobsohn, who will be 101 in October, thinks a diet of small portions of fish, vegetables, and fruit, which she has followed since her husband Leo died in 1982, has helped keep her healthy. She eats lots of salmon and herring and is a fan of spinach sautéed with olive oil. “The only thing I don’t eat is meat,” the trim and active Ms. Jacobsohn said in a recent interview over Zoom.
Her other secret: “Doctors. I like to stay away from them as much as possible.”
Shari Rosenbaum, MD, Jacobsohn’s internist, doesn’t dismiss that approach. She uses a version of it when managing her three centenarian patients, the oldest of whom is 103.
“Let them smoke! Let them drink! They’re happy. It’s not causing harm. Let them eat cake! They’ve already won,” said Dr. Rosenbaum, who is affiliated with Boca Raton–based MDVIP, a national membership-based network of 1,100 primary care physicians serving 368,000 patients. Of those, nearly 460 are centenarians.
“You’re not preventing those problems in this population,” she said. “They’re here to enjoy every moment that they have, and they might as well.”
Dr. Rosenbaum sees a divergence in her patients – those who will reach very old age, and those who won’t – starting in their 60s.
“The centenarians don’t have medical problems,” she said. “They don’t get cancer. They don’t get diabetes. Some of them take good care of themselves. Some don’t take such good care of themselves. But they are all optimists. They all see the glass half full. They all participate in life. They all have excellent support systems. They have good genes, a positive attitude toward life, and a strong social network.”
Ms. Jacobsohn – whose surname at the time was Bakst – grew up in Frankfurt am Main, Germany, during the rise of the Nazi regime. The family fled to Columbia in 1938, where she met and eventually married her husband, Leo, who ran a business importing clocks and watches in Cali.
In 1989, the Jacobsohns and their three children moved to south Florida to escape the dangers of kidnappings and ransoms posed by the drug cartels.
Ms. Jacobsohn agreed that she appears to have longevity genes – “good stock,” she calls it. “My mother died 23 days before she was 100. My grandmother lived till 99, almost 100,” she said.
Two years ago, she donated her car to a charity and stopped driving in the interest of her own safety and that of other drivers and pedestrians.
Ms. Jacobsohn has a strong support system. Two of her children live nearby and visit her nearly every day. A live-in companion helps her with the activities of daily life, including preparing meals.
Ms. Jacobsohn plays bridge regularly, and well. “I’m sorry to say that I’m a very good bridge player,” she said, frankly. “How is it possible that I’ve played bridge so well and then I don’t remember what I had for lunch yesterday?”
She reads, mainly a diet of history but occasionally novels, too. “They have to be engaging,” she said.
The loss of loved ones is an inevitable part of very old age. Her husband of 47 years died of emphysema, and one of her sons died in his 70s of prostate cancer.
She knows well the fate that awaits us all and accepts it philosophically.
“It’s a very normal thing that people die. You don’t live forever. So, whenever it comes, it’s okay. Enough is enough. Dayenu,” she said, using the Hebrew word for, “It would have been enough” – a favorite in the Passover Seder celebrating the ancient Jews’ liberation from slavery in Egypt.
Ms. Jacobsohn sang the song and then took a reporter on a Zoom tour of her tidy home and her large flower garden featuring Cattleya orchids from Colombia.
A version of this article first appeared on Medscape.com.
For about the past year, Priya Goel, MD, can be seen cruising around the island of Manhattan as she makes her way between visits to some of New York City’s most treasured residents: a small but essential group of patients born before the Empire State Building scraped the sky and the old Yankee Stadium had become the House That Ruth Built.
– the oldest is a 108-year-old man – whom she visits monthly.
The gray wave
Dr. Goel’s charges are among America’s latest baby boom – babies born a century ago, that is.
Between 1980 and 2019, the share of American centenarians, those aged 100 and up, grew faster than the total population. In 2019, 100,322 persons in the United States were at least 100 years old – more than triple the 1980 figure of 32,194, according to the U.S. Administration on Aging. By 2060, experts predict, the U.S. centenarian population will reach nearly 600,000.
Although some of the ultra-aged live in nursing homes, many continue to live independently. They require both routine and acute medical care. So, what does it take to be a physician for a centenarian?
Dr. Goel, who is in her mid-30s and could well be the great-granddaughter of some of her patients, urged her colleagues not to stereotype patients on the basis of age.
“You have to consider their functional and cognitive abilities, their ability to understand disease processes and make decisions for themselves,” Dr. Goel said. “Age is just one factor in the grand scheme of things.”
Visiting patients in their homes provides her with insights into how well they’re doing, including the safety of their environments and the depth of their social networks.
New York City has its peculiar demands. Heal provides Dr. Goel with a driver who chauffeurs her to her patient visits. She takes notes between stops.
“The idea is to have these patients remain in an environment where they’re comfortable, in surroundings where they’ve grown up or lived for many years,” she said. “A lot of them are in elevator buildings and they are wheelchair-bound or bed-bound and they physically can’t leave.”
She said she gets a far different view of the patient than does an office-based physician.
“When you go into their home, it’s very personal. You’re seeing what their daily environment is like, what their diet is like. You can see their food on the counter. You can see the level of hygiene,” Dr. Goel said. “You get to see their social support. Are their kids involved? Are they hoarding? Stuff that they wouldn’t just necessarily disclose but on a visit you get to see going into the home. It’s an extra layer of understanding that patient.”
Dr. Goel contrasted home care from care in a nursing home, where the patients are seen daily. On the basis of her observations, she decides whether to see her patients every month or every 3 months.
She applies this strategy to everyone from age 60 to over 100.
Tracking a growing group
Since 1995, geriatrician Thomas Perls, MD, has directed the New England Centenarian Study at Boston University. The study, largely funded by the National Institute on Aging, has enrolled 2,599 centenarian persons and 700 of their offspring. At any given time in the study, about 10% of the centenarians are alive. The study has a high mortality rate.
The people in Dr. Perls’s study range in age, but they top out at 119, the third oldest person ever in the world. Most centenarians are women.
“When we first began the study in 1995, the prevalence of centenarians in the United States was about 1 per 10,000 in the population,” Perls told this news organization. “And now, that prevalence has doubled to 1 per 5,000.”
Even if no one has achieved the record of Methuselah, the Biblical patriarch who was purported to have lived to the age of 969, some people always have lived into their 90s and beyond. Dr. Perls attributed the increase in longevity to control at the turn of the 20th century of typhoid fever, diphtheria, and other infectious diseases with effective public health measures, including the availability of clean water and improvement in socioeconomic conditions.
“Infant mortality just plummeted. So, come around 1915, 1920, we were no longer losing a quarter of our population to these diseases. That meant a quarter more of the population could age into adulthood and middle age,” he said. “A certain component of that group was, therefore, able to continue to age to a very, very old age.”
Other advances, such as antibiotics and vaccinations in the 1960s; the availability in the 1970s of much better detection and effective treatment of high blood pressure; the recognition of the harms of smoking; and much more effective treatment of cardiovascular disease and cancer have allowed many people who would have otherwise died in their 70s and 80s to live much longer. “I think what this means is that there is a substantial proportion of the population that has the biology to get to 100,” Dr. Perls said.
Perls said the Latino population and Blacks have a better track record than Whites in reaching the 100-year milestone. “The average life expectancy might be lower in these populations because of socioeconomic factors, but if they are able to get to around their early 80s, compared to Whites, their ability to get to 100 is actually better,” he said.
Asians fare best when it comes to longevity. While around 1% of White women in the United States live to 100, 10% of Asian women in Hong Kong hit that mark.
“I think some of that is better environment and health habits in Hong Kong than in the United States,” Dr. Perls said. “I think another piece may be a genetic advantage in East Asians. We’re looking into that.”
Dr. Perls said he agreed with Dr. Goel that health care providers and the lay public should not make assumptions on the basis of age alone as to how a person is doing. “People can age so very differently from one another,” he said.
Up to about age 90, the vast majority of those differences are determined by our health behaviors, such as smoking, alcohol use, exercise, sleep, the effect of our diets on weight, and access to good health care, including regular screening for problems such as high blood pressure, diabetes, and cancer. “People who are able to do everything right generally add healthy years to their lives, while those who do not have shorter life expectancies and longer periods of chronic diseases,” Dr. Perls said.
Paying diligent attention to these behaviors over the long run can have a huge payoff.
Dr. Perls’s team has found that to live beyond age 90 and on into the early 100s, protective genes can play a strong role. These genes help slow aging and decrease one’s risk for aging-related diseases. Centenarians usually have a history of aging very slowly and greatly delaying aging-related diseases and disability toward the ends of their lives.
Centenarians are the antithesis of the misguided belief that the older you get, the sicker you get. Quite the opposite occurs. For Dr. Perls, “the older you get, the healthier you’ve been.”
MD bias against the elderly?
Care of elderly patients is becoming essential in the practice of primary care physicians – but not all of them enjoy the work.
To be effective, physicians who treat centenarians must get a better idea of the individual patient’s functional status and comorbidities. “You absolutely cannot make assumptions on age alone,” Dr. Perls said.
The so-called “normal” temperature, 98.6° F, can spell trouble for centenarians and other very old patients, warned Natalie Baker, DNP, CRNP, an associate professor of nursing at the University of Alabama, Birmingham, and president of the 3,000-member Gerontological Advanced Practice Nurses Association.
“We have to be very cognizant of what we call a typical presentation of disease or illness and that a very subtle change in an older adult can signal a serious infection or illness,” Dr. Baker said. “If your patient has a high fever, that is a potential problem.”
The average temperature of an older adult is lower than the accepted 98.6° F, and their body’s response to an infection is slow to exhibit an increase in temperature, Dr. Baker said. “When treating centenarians, clinicians must be cognizant of other subtle signs of infection, such as decreased appetite or change in mentation,” she cautioned.
A decline in appetite or insomnia may be a subtle sign that these patients need to be evaluated, she added.
COVID-19 and centenarians
Three-quarters of the 1 million U.S. deaths from COVID-19 occurred in people aged 65 and older. However, Dr. Perls said centenarians may be a special subpopulation when it comes to COVID.
The Japanese Health Ministry, which follows the large centenarian population in that country, noted a marked jump in the number of centenarians during the pandemic – although the reasons for the increase aren’t clear.
Centenarians may be a bit different. Dr. Perls said some evidence suggests that the over-100 crowd may have better immune systems than younger people. “Part of the trick of getting to 100 is having a pretty good immune system,” he said.
Don’t mess with success
“There is no need at that point for us to try to alter their diet to what we think it might be,” Dr. Baker said. “There’s no need to start with diabetic education. They may tell you their secret is a shot of vodka every day. Why should we stop it at that age? Accept their lifestyles, because they’ve done something right to get to that age.”
Opinions differ on how to approach screening for centenarians.
Dr. Goel said guidelines for routine screening, such as colonoscopies, mammograms, and PAP smears, drop off for patients starting at 75. Dr. Perls said this strategy stems from the belief that people will die from other things first, so screening is no longer needed. Dr. Perls said he disagrees with this approach.
“Again, we can’t base our screening and health care decisions on age alone. If I have an independently functioning and robust 95-year-old man in my office, you can be sure I am going to continue recommending regular screening for colon cancer and other screenings that are normal for people who are 30 years younger,” he said.
Justin Zaghi, MD, chief medical officer at Heal, said screening patients in their late 90s and 100s for cancer generally doesn’t make sense except in some rare circumstances in which the cancer would be unlikely to be a cause of death. “However, if we are talking about screening for fall risks, hearing difficulties, poor vision, pain, and malnutrition, those screenings still absolutely make sense for patients in their late 90s and 100s,” Dr. Zaghi said.
One high-functioning 104-year-old patient of Dr. Perls underwent a total hip replacement for a hip fracture and is faring well. “Obviously, if she had end-stage dementia, we’d do everything to keep the person comfortable, or if they had medical problems that made surgery too high risk, then you don’t do it,” he said. “But if they’re otherwise, I would proceed.”
Avoid the ED
Dr. Goel said doctors should avoid sending patients to the emergency department, an often chaotic place that is especially unfriendly to centenarians and the very old. “Sometimes I’ve seen older patients who are being rushed to the ER, and I ask, What are the goals of care?” she said.
Clinicians caring for seniors should keep in mind that infections can cause seniors to appear confused – and this may lead the clinician to think the patient has dementia. Or, Dr. Goel said, a patient with dementia may suddenly experience much worse dementia.
“In either case, you want to make sure you’re not dealing with any underlying infection, like urinary tract infection, or pneumonia brewing, or skin infections,” she said. “Their skin is so much frailer. You want to make sure there are no bedsores.”
She has had patients whose children report that their usually placid centenarian parents are suddenly acting out. “We’ll do a urinary test and it definitely shows a urinary tract infection. You want to make sure you’re not missing out on something else before you attribute it to dementia,” she said.
Environmental changes, such as moving a patient to a new room in a hospital setting, can trigger an acute mental status change, such as delirium, she added. Helping older patients feel in control as much as possible is important.
“You want to make sure you’re orienting them to the time of day. Make sure they get up at the same time, go to bed at the same time, have clocks and calendars present – just making sure that they feel like they’re still in control of their body and their day,” she said.
Physicians should be aware of potential depression in these patients, whose experience of loss – an unavoidable consequence of outliving family and friends – can result in problems with sleep and diet, as well as a sense of social isolation.
Neal Flomenbaum, MD, professor and emergency physician-in-chief emeritus, New York–Presbyterian/Weill Cornell Medical Center in New York, said sometimes the best thing for these very elderly patients is to “get them in and out of ED as quickly as possible, and do what you can diagnostically.”
He noted that EDs have been making accommodations to serve the elderly, such as using LEDs that replicate outdoor lighting conditions, as well as providing seniors with separate rooms with glass doors to protect them from noise, separate air handlers to prevent infections, and adequate space for visitors.
These patients often are subject to trauma from falls.
“The bones don’t heal as well as in younger people, and treating their comorbidities is essential. Once they have trouble with one area and they’re lying in bed and can’t move much, they can get bedsores,” Dr. Flomenbaum said. “In the hospital, they are vulnerable to infections. So, you’re thinking of all of these things at the same time and how to treat them appropriately and then get them out of the hospital as soon as possible with whatever care that they need in their own homes if at all possible.”
“I always err on the side of less is more,” Dr. Goel said. “Obviously, if there is something – if they have a cough, they need an x-ray. That’s very basic. We want to take care of that. Give them the antibiotic if they need that. But rushing them in and out of the hospital doesn’t add to their quality of life.”
Dr. Flomenbaum, a pioneer in geriatric emergency medicine, says physicians need to be aware that centenarians and other very old patients don’t present the same way as younger adults.
He began to notice more than 20 years ago that every night, patients would turn up in his ED who were in their late 90s into their 100s. Some would come in with what their children identified as sudden-onset dementia – they didn’t know their own names and couldn’t identify their kids. They didn’t know the time or day. Dr. Flomenbaum said the children often asked whether their parents should enter a nursing home.
“And I’d say, ‘Not so fast. Well, let’s take a look at this.’ You don’t develop that kind of dementia overnight. It usually takes a while,” he said.
He said he ordered complete blood cell counts and oxygen saturation tests that frequently turned out to be abnormal. They didn’t have a fever, and infiltrates initially weren’t seen on chest x-rays.
With rehydration and supplemental oxygen, their symptoms started to improve, and it became obvious that the symptoms were not of dementia but of pneumonia, and that they required antibiotics, Dr. Flomenbaum said.
Dementia dilemma
Too often, on the basis of age, doctors assume patients have dementia or other cognitive impairments.
“What a shock and a surprise when doctors actually talk to folks and do a neurocognitive screen and find they’re just fine,” Dr. Perls said.
The decline in hearing and vision can lead to a misdiagnosis of cognitive impairment because the patients are not able to hear what you’re asking them. “It’s really important that the person can hear you – whether you use an amplifying device or they have hearing aids, that’s critical,” he said. “You just have to be a good doctor.”
Often the physical toll of aging exacerbates social difficulties. Poor hearing, for example, can accelerate cognitive impairment and cause people to interact less often, and less meaningfully, with their environment. For some, wearing hearing aids seems demeaning – until they hear what they’ve been missing.
“I get them to wear their hearing aids and, lo and behold, they’re a whole new person because they’re now able to take in their environment and interact with others,” Dr. Perls said.
Dr. Flomenbaum said alcohol abuse and drug reactions can cause delirium, which, unlike dementia, is potentially reversible. Yet many physicians cannot reliably differentiate between dementia and delirium, he added.
The geriatric specialists talk about the lessons they’ve learned and the gratification they get from caring for centenarians.
“I have come to realize the importance of family, of having a close circle, whether that’s through friends or neighbors,” Dr. Goel said. “This work is very rewarding because, if it wasn’t for homebound organizations, how would these people get care or get access to care?”
For Dr. Baker, a joy of the job is hearing centenarians share their life stories.
“I love to hear their stories about how they’ve overcome adversity, living through the depression and living through different wars,” she said. “I love talking to veterans, and I think that oftentimes, we do not value our older adults in our society as we should. Sometimes they are dismissed because they move slowly or are hard to communicate with due to hearing deficits. But they are, I think, a very important part of our lives.”
‘They’ve already won’
Most centenarians readily offer the secrets to their longevity. Aline Jacobsohn, of Boca Raton, Fla., is no different.
Ms. Jacobsohn, who will be 101 in October, thinks a diet of small portions of fish, vegetables, and fruit, which she has followed since her husband Leo died in 1982, has helped keep her healthy. She eats lots of salmon and herring and is a fan of spinach sautéed with olive oil. “The only thing I don’t eat is meat,” the trim and active Ms. Jacobsohn said in a recent interview over Zoom.
Her other secret: “Doctors. I like to stay away from them as much as possible.”
Shari Rosenbaum, MD, Jacobsohn’s internist, doesn’t dismiss that approach. She uses a version of it when managing her three centenarian patients, the oldest of whom is 103.
“Let them smoke! Let them drink! They’re happy. It’s not causing harm. Let them eat cake! They’ve already won,” said Dr. Rosenbaum, who is affiliated with Boca Raton–based MDVIP, a national membership-based network of 1,100 primary care physicians serving 368,000 patients. Of those, nearly 460 are centenarians.
“You’re not preventing those problems in this population,” she said. “They’re here to enjoy every moment that they have, and they might as well.”
Dr. Rosenbaum sees a divergence in her patients – those who will reach very old age, and those who won’t – starting in their 60s.
“The centenarians don’t have medical problems,” she said. “They don’t get cancer. They don’t get diabetes. Some of them take good care of themselves. Some don’t take such good care of themselves. But they are all optimists. They all see the glass half full. They all participate in life. They all have excellent support systems. They have good genes, a positive attitude toward life, and a strong social network.”
Ms. Jacobsohn – whose surname at the time was Bakst – grew up in Frankfurt am Main, Germany, during the rise of the Nazi regime. The family fled to Columbia in 1938, where she met and eventually married her husband, Leo, who ran a business importing clocks and watches in Cali.
In 1989, the Jacobsohns and their three children moved to south Florida to escape the dangers of kidnappings and ransoms posed by the drug cartels.
Ms. Jacobsohn agreed that she appears to have longevity genes – “good stock,” she calls it. “My mother died 23 days before she was 100. My grandmother lived till 99, almost 100,” she said.
Two years ago, she donated her car to a charity and stopped driving in the interest of her own safety and that of other drivers and pedestrians.
Ms. Jacobsohn has a strong support system. Two of her children live nearby and visit her nearly every day. A live-in companion helps her with the activities of daily life, including preparing meals.
Ms. Jacobsohn plays bridge regularly, and well. “I’m sorry to say that I’m a very good bridge player,” she said, frankly. “How is it possible that I’ve played bridge so well and then I don’t remember what I had for lunch yesterday?”
She reads, mainly a diet of history but occasionally novels, too. “They have to be engaging,” she said.
The loss of loved ones is an inevitable part of very old age. Her husband of 47 years died of emphysema, and one of her sons died in his 70s of prostate cancer.
She knows well the fate that awaits us all and accepts it philosophically.
“It’s a very normal thing that people die. You don’t live forever. So, whenever it comes, it’s okay. Enough is enough. Dayenu,” she said, using the Hebrew word for, “It would have been enough” – a favorite in the Passover Seder celebrating the ancient Jews’ liberation from slavery in Egypt.
Ms. Jacobsohn sang the song and then took a reporter on a Zoom tour of her tidy home and her large flower garden featuring Cattleya orchids from Colombia.
A version of this article first appeared on Medscape.com.
COVID-19 may trigger irritable bowel syndrome
Gastrointestinal symptoms are common with long COVID, also known as post-acute COVID-19 syndrome, according to Walter Chan, MD, MPH, and Madhusudan Grover, MBBS.
Dr. Chan, an assistant professor at Harvard Medical School, Boston, and Dr. Grover, an associate professor of medicine and physiology at Mayo Clinic, Rochester, Minn., conducted a review of the literature on COVID-19’s long-term gastrointestinal effects. Their review was published in Clinical Gastroenterology and Hepatology.
Estimates of the prevalence of gastrointestinal symptoms with COVID-19 have ranged as high as 60%, Dr. Chan and Dr. Grover report, and the symptoms may be present in patients with long COVID, a syndrome that continues 4 weeks or longer.
In one survey of 749 COVID-19 survivors, 29% reported at least one new chronic gastrointestinal symptom. The most common were heartburn, constipation, diarrhea, and abdominal pain. Of those with abdominal pain, 39% had symptoms that met Rome IV criteria for irritable bowel syndrome.
People who have gastrointestinal symptoms after their initial SARS-CoV-2 infection are more likely to have them with long COVID. Psychiatric diagnoses, hospitalization, and the loss of smell and taste are predictors of gastrointestinal symptoms.
Infectious gastroenteritis can increase the risk for disorders of gut-brain interaction, especially postinfection IBS, Dr. Chan and Dr. Grover write.
COVID-19 likely causes gastrointestinal symptoms through multiple mechanisms. It may suppress angiotensin-converting enzyme 2, which protects intestinal cells. It can alter the microbiome. It can cause or worsen weight gain and diabetes. It may disrupt the immune system and trigger an autoimmune reaction. It can cause depression and anxiety, and it can alter dietary habits.
No specific treatments for gastrointestinal symptoms associated with long COVID have emerged, so clinicians should make use of established therapies for disorders of gut-brain interaction, Dr. Chan and Dr. Grover recommend.
Beyond adequate sleep and exercise, these may include high-fiber, low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), gluten-free, low-carbohydrate, or elimination diets.
For diarrhea, they list loperamide, ondansetron, alosetron, eluxadoline, antispasmodics, rifaximin, and bile acid sequestrants.
For constipation, they mention fiber supplements, polyethylene glycol, linaclotide, plecanatide, lubiprostone, tenapanor, tegaserod, and prucalopride.
For modulating intestinal permeability, they recommend glutamine.
Neuromodulation may be achieved with tricyclic antidepressants, selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, azaperones, and delta ligands, they write.
For psychological therapy, they recommend cognitive-behavioral therapy and gut-directed hypnotherapy.
A handful of studies have suggested benefits from Lactiplantibacillus plantarum and Pediococcus acidilactici as probiotic therapies. Additionally, one study showed positive results with a high-fiber formula, perhaps by nourishing short-chain fatty acid-producing bacteria, Dr. Chan and Dr. Grover write.
Dr. Chan reported financial relationships with Ironwood, Takeda, and Phathom Pharmaceuticals. Dr. Grover reported financial relationships with Takeda, Donga, Alexza Pharmaceuticals, and Alfasigma.
A version of this article first appeared on Medscape.com.
Gastrointestinal symptoms are common with long COVID, also known as post-acute COVID-19 syndrome, according to Walter Chan, MD, MPH, and Madhusudan Grover, MBBS.
Dr. Chan, an assistant professor at Harvard Medical School, Boston, and Dr. Grover, an associate professor of medicine and physiology at Mayo Clinic, Rochester, Minn., conducted a review of the literature on COVID-19’s long-term gastrointestinal effects. Their review was published in Clinical Gastroenterology and Hepatology.
Estimates of the prevalence of gastrointestinal symptoms with COVID-19 have ranged as high as 60%, Dr. Chan and Dr. Grover report, and the symptoms may be present in patients with long COVID, a syndrome that continues 4 weeks or longer.
In one survey of 749 COVID-19 survivors, 29% reported at least one new chronic gastrointestinal symptom. The most common were heartburn, constipation, diarrhea, and abdominal pain. Of those with abdominal pain, 39% had symptoms that met Rome IV criteria for irritable bowel syndrome.
People who have gastrointestinal symptoms after their initial SARS-CoV-2 infection are more likely to have them with long COVID. Psychiatric diagnoses, hospitalization, and the loss of smell and taste are predictors of gastrointestinal symptoms.
Infectious gastroenteritis can increase the risk for disorders of gut-brain interaction, especially postinfection IBS, Dr. Chan and Dr. Grover write.
COVID-19 likely causes gastrointestinal symptoms through multiple mechanisms. It may suppress angiotensin-converting enzyme 2, which protects intestinal cells. It can alter the microbiome. It can cause or worsen weight gain and diabetes. It may disrupt the immune system and trigger an autoimmune reaction. It can cause depression and anxiety, and it can alter dietary habits.
No specific treatments for gastrointestinal symptoms associated with long COVID have emerged, so clinicians should make use of established therapies for disorders of gut-brain interaction, Dr. Chan and Dr. Grover recommend.
Beyond adequate sleep and exercise, these may include high-fiber, low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), gluten-free, low-carbohydrate, or elimination diets.
For diarrhea, they list loperamide, ondansetron, alosetron, eluxadoline, antispasmodics, rifaximin, and bile acid sequestrants.
For constipation, they mention fiber supplements, polyethylene glycol, linaclotide, plecanatide, lubiprostone, tenapanor, tegaserod, and prucalopride.
For modulating intestinal permeability, they recommend glutamine.
Neuromodulation may be achieved with tricyclic antidepressants, selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, azaperones, and delta ligands, they write.
For psychological therapy, they recommend cognitive-behavioral therapy and gut-directed hypnotherapy.
A handful of studies have suggested benefits from Lactiplantibacillus plantarum and Pediococcus acidilactici as probiotic therapies. Additionally, one study showed positive results with a high-fiber formula, perhaps by nourishing short-chain fatty acid-producing bacteria, Dr. Chan and Dr. Grover write.
Dr. Chan reported financial relationships with Ironwood, Takeda, and Phathom Pharmaceuticals. Dr. Grover reported financial relationships with Takeda, Donga, Alexza Pharmaceuticals, and Alfasigma.
A version of this article first appeared on Medscape.com.
Gastrointestinal symptoms are common with long COVID, also known as post-acute COVID-19 syndrome, according to Walter Chan, MD, MPH, and Madhusudan Grover, MBBS.
Dr. Chan, an assistant professor at Harvard Medical School, Boston, and Dr. Grover, an associate professor of medicine and physiology at Mayo Clinic, Rochester, Minn., conducted a review of the literature on COVID-19’s long-term gastrointestinal effects. Their review was published in Clinical Gastroenterology and Hepatology.
Estimates of the prevalence of gastrointestinal symptoms with COVID-19 have ranged as high as 60%, Dr. Chan and Dr. Grover report, and the symptoms may be present in patients with long COVID, a syndrome that continues 4 weeks or longer.
In one survey of 749 COVID-19 survivors, 29% reported at least one new chronic gastrointestinal symptom. The most common were heartburn, constipation, diarrhea, and abdominal pain. Of those with abdominal pain, 39% had symptoms that met Rome IV criteria for irritable bowel syndrome.
People who have gastrointestinal symptoms after their initial SARS-CoV-2 infection are more likely to have them with long COVID. Psychiatric diagnoses, hospitalization, and the loss of smell and taste are predictors of gastrointestinal symptoms.
Infectious gastroenteritis can increase the risk for disorders of gut-brain interaction, especially postinfection IBS, Dr. Chan and Dr. Grover write.
COVID-19 likely causes gastrointestinal symptoms through multiple mechanisms. It may suppress angiotensin-converting enzyme 2, which protects intestinal cells. It can alter the microbiome. It can cause or worsen weight gain and diabetes. It may disrupt the immune system and trigger an autoimmune reaction. It can cause depression and anxiety, and it can alter dietary habits.
No specific treatments for gastrointestinal symptoms associated with long COVID have emerged, so clinicians should make use of established therapies for disorders of gut-brain interaction, Dr. Chan and Dr. Grover recommend.
Beyond adequate sleep and exercise, these may include high-fiber, low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), gluten-free, low-carbohydrate, or elimination diets.
For diarrhea, they list loperamide, ondansetron, alosetron, eluxadoline, antispasmodics, rifaximin, and bile acid sequestrants.
For constipation, they mention fiber supplements, polyethylene glycol, linaclotide, plecanatide, lubiprostone, tenapanor, tegaserod, and prucalopride.
For modulating intestinal permeability, they recommend glutamine.
Neuromodulation may be achieved with tricyclic antidepressants, selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, azaperones, and delta ligands, they write.
For psychological therapy, they recommend cognitive-behavioral therapy and gut-directed hypnotherapy.
A handful of studies have suggested benefits from Lactiplantibacillus plantarum and Pediococcus acidilactici as probiotic therapies. Additionally, one study showed positive results with a high-fiber formula, perhaps by nourishing short-chain fatty acid-producing bacteria, Dr. Chan and Dr. Grover write.
Dr. Chan reported financial relationships with Ironwood, Takeda, and Phathom Pharmaceuticals. Dr. Grover reported financial relationships with Takeda, Donga, Alexza Pharmaceuticals, and Alfasigma.
A version of this article first appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Long COVID case study: persistent hormone deficiencies
A case study of a 65-year-old man in Japan with long COVID describes how he recovered from certain impaired hormone deficiencies that persisted for more than a year.
Days after the patient recovered from respiratory failure and came off a ventilator, he had a sudden drop in blood pressure, which responded to hydrocortisone.
The patient was found to have low levels of growth hormone and adrenocorticotropic hormone (ACTH), hypopituitarism, that persisted for more than a year. He also had low levels of testosterone that remained low at 15 months (the study end).
“An important finding in the present case is the eventual recovery from hypopituitarism over time but not from hypogonadism,” the researchers write in their study published in Endocrine Journal.
, which was confirmed using an insulin tolerance test, Kai Yoshimura, Kakogawa Medical Center, Japan, and colleagues report.
The findings show that “pituitary insufficiency should be considered in patients with prolonged symptoms of COVID-19,” they report, since it can be treated with hormone supplements that markedly improve symptoms and quality of life.
“It might be worthwhile to screen for endocrine dysfunction in patients with such persistent symptoms after their recovery from the acute disease,” the researchers conclude.
Case study timeline
The patient in this study was healthy without obesity, previous endocrine disease, or steroid use. He was admitted to hospital because he had dyspnea and fever for 8 days and a reverse transcription-polymerase chain reaction (RT-PCR) test that was positive for COVID-19.
He received ciclesonide 200 mcg/day for 2 days. Then he was put on a ventilator and the drug was discontinued and “favipiravir, ritonavir, and lopinavir, a standard regimen during the early phase of the COVID-19 pandemic, were initiated;” the researchers explain.
On day 25 of his hospital stay the patient had recovered from respiratory failure and was extubated.
On day 31, he had a negative PCR test for COVID-19.
On day 36, the patient’s blood pressure suddenly dropped from 120/80 mmHg to 80/50 mmHg. His plasma ACTH and serum cortisol levels were low, suggesting secondary adrenal insufficiency. The low blood pressure responded to hydrocortisone 100 mg, which was gradually tapered.
At day 96, the patient was discharged from hospital with a dose of 15 mg/day hydrocortisone.
At 3 months after discharge, an insulin tolerance test revealed that the patient’s ACTH and cortisol responses were blunted, suggestive of adrenal insufficiency. The patient also had moderate growth hormone deficiency and symptoms of hypogonadism.
At 6 months after discharge, the patient started testosterone therapy because his dysspermatism had worsened.
At 12 months after discharge, a repeat insulin tolerance test showed that both ACTH and cortisol responses were low but improved. The patient was no longer deficient in growth hormone.
At 15 months after discharge, early morning levels of ACTH and cortisol were now in the normal range. The patient discontinued testosterone treatment, but the symptoms returned, so he resumed it.
Long COVID symptoms, possible biological mechanism
The present case shows how certain COVID-19–associated conditions develop after the onset of, or the recovery from, respiratory disorders, the authors note.
Symptoms of long COVID-19 include fatigue, weakness, hair loss, diarrhea, arthralgia, and depression, and these symptoms are associated with pituitary insufficiency, especially secondary adrenocortical insufficiency.
In addition, an estimated 25% of sexually active men who recover from COVID have semen disorders such as azoospermia and oligospermia.
The underlying mechanism by which COVID-19 might trigger pituitary insufficiency is unknown, but other viral infections such as influenza-A and herpes simplex are also associated with transient hypopituitarism. An exaggerated immune response triggered by SARS-CoV-2 may explain the dysfunction of multiple endocrine organs, the researchers write.
The researchers have declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
A case study of a 65-year-old man in Japan with long COVID describes how he recovered from certain impaired hormone deficiencies that persisted for more than a year.
Days after the patient recovered from respiratory failure and came off a ventilator, he had a sudden drop in blood pressure, which responded to hydrocortisone.
The patient was found to have low levels of growth hormone and adrenocorticotropic hormone (ACTH), hypopituitarism, that persisted for more than a year. He also had low levels of testosterone that remained low at 15 months (the study end).
“An important finding in the present case is the eventual recovery from hypopituitarism over time but not from hypogonadism,” the researchers write in their study published in Endocrine Journal.
, which was confirmed using an insulin tolerance test, Kai Yoshimura, Kakogawa Medical Center, Japan, and colleagues report.
The findings show that “pituitary insufficiency should be considered in patients with prolonged symptoms of COVID-19,” they report, since it can be treated with hormone supplements that markedly improve symptoms and quality of life.
“It might be worthwhile to screen for endocrine dysfunction in patients with such persistent symptoms after their recovery from the acute disease,” the researchers conclude.
Case study timeline
The patient in this study was healthy without obesity, previous endocrine disease, or steroid use. He was admitted to hospital because he had dyspnea and fever for 8 days and a reverse transcription-polymerase chain reaction (RT-PCR) test that was positive for COVID-19.
He received ciclesonide 200 mcg/day for 2 days. Then he was put on a ventilator and the drug was discontinued and “favipiravir, ritonavir, and lopinavir, a standard regimen during the early phase of the COVID-19 pandemic, were initiated;” the researchers explain.
On day 25 of his hospital stay the patient had recovered from respiratory failure and was extubated.
On day 31, he had a negative PCR test for COVID-19.
On day 36, the patient’s blood pressure suddenly dropped from 120/80 mmHg to 80/50 mmHg. His plasma ACTH and serum cortisol levels were low, suggesting secondary adrenal insufficiency. The low blood pressure responded to hydrocortisone 100 mg, which was gradually tapered.
At day 96, the patient was discharged from hospital with a dose of 15 mg/day hydrocortisone.
At 3 months after discharge, an insulin tolerance test revealed that the patient’s ACTH and cortisol responses were blunted, suggestive of adrenal insufficiency. The patient also had moderate growth hormone deficiency and symptoms of hypogonadism.
At 6 months after discharge, the patient started testosterone therapy because his dysspermatism had worsened.
At 12 months after discharge, a repeat insulin tolerance test showed that both ACTH and cortisol responses were low but improved. The patient was no longer deficient in growth hormone.
At 15 months after discharge, early morning levels of ACTH and cortisol were now in the normal range. The patient discontinued testosterone treatment, but the symptoms returned, so he resumed it.
Long COVID symptoms, possible biological mechanism
The present case shows how certain COVID-19–associated conditions develop after the onset of, or the recovery from, respiratory disorders, the authors note.
Symptoms of long COVID-19 include fatigue, weakness, hair loss, diarrhea, arthralgia, and depression, and these symptoms are associated with pituitary insufficiency, especially secondary adrenocortical insufficiency.
In addition, an estimated 25% of sexually active men who recover from COVID have semen disorders such as azoospermia and oligospermia.
The underlying mechanism by which COVID-19 might trigger pituitary insufficiency is unknown, but other viral infections such as influenza-A and herpes simplex are also associated with transient hypopituitarism. An exaggerated immune response triggered by SARS-CoV-2 may explain the dysfunction of multiple endocrine organs, the researchers write.
The researchers have declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
A case study of a 65-year-old man in Japan with long COVID describes how he recovered from certain impaired hormone deficiencies that persisted for more than a year.
Days after the patient recovered from respiratory failure and came off a ventilator, he had a sudden drop in blood pressure, which responded to hydrocortisone.
The patient was found to have low levels of growth hormone and adrenocorticotropic hormone (ACTH), hypopituitarism, that persisted for more than a year. He also had low levels of testosterone that remained low at 15 months (the study end).
“An important finding in the present case is the eventual recovery from hypopituitarism over time but not from hypogonadism,” the researchers write in their study published in Endocrine Journal.
, which was confirmed using an insulin tolerance test, Kai Yoshimura, Kakogawa Medical Center, Japan, and colleagues report.
The findings show that “pituitary insufficiency should be considered in patients with prolonged symptoms of COVID-19,” they report, since it can be treated with hormone supplements that markedly improve symptoms and quality of life.
“It might be worthwhile to screen for endocrine dysfunction in patients with such persistent symptoms after their recovery from the acute disease,” the researchers conclude.
Case study timeline
The patient in this study was healthy without obesity, previous endocrine disease, or steroid use. He was admitted to hospital because he had dyspnea and fever for 8 days and a reverse transcription-polymerase chain reaction (RT-PCR) test that was positive for COVID-19.
He received ciclesonide 200 mcg/day for 2 days. Then he was put on a ventilator and the drug was discontinued and “favipiravir, ritonavir, and lopinavir, a standard regimen during the early phase of the COVID-19 pandemic, were initiated;” the researchers explain.
On day 25 of his hospital stay the patient had recovered from respiratory failure and was extubated.
On day 31, he had a negative PCR test for COVID-19.
On day 36, the patient’s blood pressure suddenly dropped from 120/80 mmHg to 80/50 mmHg. His plasma ACTH and serum cortisol levels were low, suggesting secondary adrenal insufficiency. The low blood pressure responded to hydrocortisone 100 mg, which was gradually tapered.
At day 96, the patient was discharged from hospital with a dose of 15 mg/day hydrocortisone.
At 3 months after discharge, an insulin tolerance test revealed that the patient’s ACTH and cortisol responses were blunted, suggestive of adrenal insufficiency. The patient also had moderate growth hormone deficiency and symptoms of hypogonadism.
At 6 months after discharge, the patient started testosterone therapy because his dysspermatism had worsened.
At 12 months after discharge, a repeat insulin tolerance test showed that both ACTH and cortisol responses were low but improved. The patient was no longer deficient in growth hormone.
At 15 months after discharge, early morning levels of ACTH and cortisol were now in the normal range. The patient discontinued testosterone treatment, but the symptoms returned, so he resumed it.
Long COVID symptoms, possible biological mechanism
The present case shows how certain COVID-19–associated conditions develop after the onset of, or the recovery from, respiratory disorders, the authors note.
Symptoms of long COVID-19 include fatigue, weakness, hair loss, diarrhea, arthralgia, and depression, and these symptoms are associated with pituitary insufficiency, especially secondary adrenocortical insufficiency.
In addition, an estimated 25% of sexually active men who recover from COVID have semen disorders such as azoospermia and oligospermia.
The underlying mechanism by which COVID-19 might trigger pituitary insufficiency is unknown, but other viral infections such as influenza-A and herpes simplex are also associated with transient hypopituitarism. An exaggerated immune response triggered by SARS-CoV-2 may explain the dysfunction of multiple endocrine organs, the researchers write.
The researchers have declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
Large study amplifies evidence of COVID vaccine safety in pregnancy
The research team wrote in the BMJ that their reassuring findings – drawn from a registry of all births in Ontario over an 8-month period – “can inform evidence-based decision-making” about COVID vaccination during pregnancy.
Previous research has found that pregnant patients are at higher risk of severe complications and death if they become infected with COVID and that vaccination before or during pregnancy prevents such outcomes and reduces the risk of newborn infection, noted Jeffrey Ecker, chief of obstetrics and gynecology at Massachusetts General Hospital, Boston.
This new study “adds to a growing body of information arguing clearly and reassuringly that vaccination during pregnancy is not associated with complications during pregnancy,” said Dr. Ecker, who was not involved in the new study.
He added that it “should help obstetric providers further reassure those who are hesitant that vaccination is safe and best both for the pregnant patient and their pregnancy.”
Methods and results
For the new study, researchers tapped a provincial registry of all live and stillborn infants with a gestational age of at least 20 weeks or birth weight of at least 500 g. Unique health card numbers were used to link birth records to a database of COVID vaccinations.
Of 85,162 infants born from May through December of 2021, 43,099 (50.6%) were born to individuals who received at least one vaccine dose during pregnancy. Among those, 99.7% received an mRNA vaccine such as Pfizer-BioNTech or Moderna.
Vaccination during pregnancy was not associated with greater risk of overall preterm birth (6.5% among vaccinated individuals versus 6.9% among unvaccinated; hazard ratio, 1.02; 95% confidence interval, 0.96-1.08), spontaneous preterm birth (3.7% versus 4.4%; hazard ratio, 0.96; 95% CI, 0.90-1.03) or very preterm birth (0.59% versus 0.89%; hazard ratio, 0.80; 95% CI, 0.67-0.95).
Likewise, no increase was observed in the risk of an infant being small for gestational age at birth (9.1% versus 9.2%; hazard ratio, 0.98; 95% CI, 0.93-1.03).
The researchers observed a reduction in the risk of stillbirth, even after adjusting for potential confounders. Stillbirths occurred in 0.25% of vaccinated individuals, compared with 0.44% of unvaccinated individuals (hazard ratio, 0.65; 95% CI, 0.51-0.84).
A reduced risk of stillbirth – albeit to a smaller degree – was also found in a Scandinavian registry study that included 28,506 babies born to individuals who were vaccinated during pregnancy.
“Collectively, the findings from these two studies are reassuring and are consistent with no increased risk of stillbirth after COVID-19 vaccination during pregnancy. In contrast, COVID-19 disease during pregnancy has been associated with an increased risk of stillbirth,” the researchers wrote.
Findings did not vary by which mRNA vaccine a mother received, the number of doses she received, or the trimester in which a vaccine was given, the researchers reported.
Stillbirth findings will be ‘very reassuring’ for patients
The lead investigator, Deshayne Fell, PhD, said in an interview, the fact that the study comprised the entire population of pregnant people in Ontario during the study period “increases our confidence” about the validity and relevance of the findings for other geographic settings.
Dr. Fell, an associate professor in epidemiology and public health at the University of Ottawa and a scientist at the Children’s Hospital of Eastern Ontario Research Institute, Ottawa, said the evaluation of stillbirth in particular, “a rare but devastating outcome,” will be “very reassuring and useful for clinical counseling.”
A limitation cited by the research team included a lack of data on vaccination prior to pregnancy.
In the new study, Dr, Ecker said, “Though the investigators were able to adjust for many variables they cannot be certain that some unmeasured variable that, accordingly, was not adjusted for does not hide a small risk. This seems very unlikely, however.”
The Canadian research team said similar studies of non-mRNA COVID vaccines “should be a research priority.” However, such studies are not underway in Canada, where only mRNA vaccines are used in pregnancy, Dr. Fell said.
This study was supported by the Public Health Agency of Canada.
Dr. Fell and Dr. Ecker reported no competing financial interests.
The research team wrote in the BMJ that their reassuring findings – drawn from a registry of all births in Ontario over an 8-month period – “can inform evidence-based decision-making” about COVID vaccination during pregnancy.
Previous research has found that pregnant patients are at higher risk of severe complications and death if they become infected with COVID and that vaccination before or during pregnancy prevents such outcomes and reduces the risk of newborn infection, noted Jeffrey Ecker, chief of obstetrics and gynecology at Massachusetts General Hospital, Boston.
This new study “adds to a growing body of information arguing clearly and reassuringly that vaccination during pregnancy is not associated with complications during pregnancy,” said Dr. Ecker, who was not involved in the new study.
He added that it “should help obstetric providers further reassure those who are hesitant that vaccination is safe and best both for the pregnant patient and their pregnancy.”
Methods and results
For the new study, researchers tapped a provincial registry of all live and stillborn infants with a gestational age of at least 20 weeks or birth weight of at least 500 g. Unique health card numbers were used to link birth records to a database of COVID vaccinations.
Of 85,162 infants born from May through December of 2021, 43,099 (50.6%) were born to individuals who received at least one vaccine dose during pregnancy. Among those, 99.7% received an mRNA vaccine such as Pfizer-BioNTech or Moderna.
Vaccination during pregnancy was not associated with greater risk of overall preterm birth (6.5% among vaccinated individuals versus 6.9% among unvaccinated; hazard ratio, 1.02; 95% confidence interval, 0.96-1.08), spontaneous preterm birth (3.7% versus 4.4%; hazard ratio, 0.96; 95% CI, 0.90-1.03) or very preterm birth (0.59% versus 0.89%; hazard ratio, 0.80; 95% CI, 0.67-0.95).
Likewise, no increase was observed in the risk of an infant being small for gestational age at birth (9.1% versus 9.2%; hazard ratio, 0.98; 95% CI, 0.93-1.03).
The researchers observed a reduction in the risk of stillbirth, even after adjusting for potential confounders. Stillbirths occurred in 0.25% of vaccinated individuals, compared with 0.44% of unvaccinated individuals (hazard ratio, 0.65; 95% CI, 0.51-0.84).
A reduced risk of stillbirth – albeit to a smaller degree – was also found in a Scandinavian registry study that included 28,506 babies born to individuals who were vaccinated during pregnancy.
“Collectively, the findings from these two studies are reassuring and are consistent with no increased risk of stillbirth after COVID-19 vaccination during pregnancy. In contrast, COVID-19 disease during pregnancy has been associated with an increased risk of stillbirth,” the researchers wrote.
Findings did not vary by which mRNA vaccine a mother received, the number of doses she received, or the trimester in which a vaccine was given, the researchers reported.
Stillbirth findings will be ‘very reassuring’ for patients
The lead investigator, Deshayne Fell, PhD, said in an interview, the fact that the study comprised the entire population of pregnant people in Ontario during the study period “increases our confidence” about the validity and relevance of the findings for other geographic settings.
Dr. Fell, an associate professor in epidemiology and public health at the University of Ottawa and a scientist at the Children’s Hospital of Eastern Ontario Research Institute, Ottawa, said the evaluation of stillbirth in particular, “a rare but devastating outcome,” will be “very reassuring and useful for clinical counseling.”
A limitation cited by the research team included a lack of data on vaccination prior to pregnancy.
In the new study, Dr, Ecker said, “Though the investigators were able to adjust for many variables they cannot be certain that some unmeasured variable that, accordingly, was not adjusted for does not hide a small risk. This seems very unlikely, however.”
The Canadian research team said similar studies of non-mRNA COVID vaccines “should be a research priority.” However, such studies are not underway in Canada, where only mRNA vaccines are used in pregnancy, Dr. Fell said.
This study was supported by the Public Health Agency of Canada.
Dr. Fell and Dr. Ecker reported no competing financial interests.
The research team wrote in the BMJ that their reassuring findings – drawn from a registry of all births in Ontario over an 8-month period – “can inform evidence-based decision-making” about COVID vaccination during pregnancy.
Previous research has found that pregnant patients are at higher risk of severe complications and death if they become infected with COVID and that vaccination before or during pregnancy prevents such outcomes and reduces the risk of newborn infection, noted Jeffrey Ecker, chief of obstetrics and gynecology at Massachusetts General Hospital, Boston.
This new study “adds to a growing body of information arguing clearly and reassuringly that vaccination during pregnancy is not associated with complications during pregnancy,” said Dr. Ecker, who was not involved in the new study.
He added that it “should help obstetric providers further reassure those who are hesitant that vaccination is safe and best both for the pregnant patient and their pregnancy.”
Methods and results
For the new study, researchers tapped a provincial registry of all live and stillborn infants with a gestational age of at least 20 weeks or birth weight of at least 500 g. Unique health card numbers were used to link birth records to a database of COVID vaccinations.
Of 85,162 infants born from May through December of 2021, 43,099 (50.6%) were born to individuals who received at least one vaccine dose during pregnancy. Among those, 99.7% received an mRNA vaccine such as Pfizer-BioNTech or Moderna.
Vaccination during pregnancy was not associated with greater risk of overall preterm birth (6.5% among vaccinated individuals versus 6.9% among unvaccinated; hazard ratio, 1.02; 95% confidence interval, 0.96-1.08), spontaneous preterm birth (3.7% versus 4.4%; hazard ratio, 0.96; 95% CI, 0.90-1.03) or very preterm birth (0.59% versus 0.89%; hazard ratio, 0.80; 95% CI, 0.67-0.95).
Likewise, no increase was observed in the risk of an infant being small for gestational age at birth (9.1% versus 9.2%; hazard ratio, 0.98; 95% CI, 0.93-1.03).
The researchers observed a reduction in the risk of stillbirth, even after adjusting for potential confounders. Stillbirths occurred in 0.25% of vaccinated individuals, compared with 0.44% of unvaccinated individuals (hazard ratio, 0.65; 95% CI, 0.51-0.84).
A reduced risk of stillbirth – albeit to a smaller degree – was also found in a Scandinavian registry study that included 28,506 babies born to individuals who were vaccinated during pregnancy.
“Collectively, the findings from these two studies are reassuring and are consistent with no increased risk of stillbirth after COVID-19 vaccination during pregnancy. In contrast, COVID-19 disease during pregnancy has been associated with an increased risk of stillbirth,” the researchers wrote.
Findings did not vary by which mRNA vaccine a mother received, the number of doses she received, or the trimester in which a vaccine was given, the researchers reported.
Stillbirth findings will be ‘very reassuring’ for patients
The lead investigator, Deshayne Fell, PhD, said in an interview, the fact that the study comprised the entire population of pregnant people in Ontario during the study period “increases our confidence” about the validity and relevance of the findings for other geographic settings.
Dr. Fell, an associate professor in epidemiology and public health at the University of Ottawa and a scientist at the Children’s Hospital of Eastern Ontario Research Institute, Ottawa, said the evaluation of stillbirth in particular, “a rare but devastating outcome,” will be “very reassuring and useful for clinical counseling.”
A limitation cited by the research team included a lack of data on vaccination prior to pregnancy.
In the new study, Dr, Ecker said, “Though the investigators were able to adjust for many variables they cannot be certain that some unmeasured variable that, accordingly, was not adjusted for does not hide a small risk. This seems very unlikely, however.”
The Canadian research team said similar studies of non-mRNA COVID vaccines “should be a research priority.” However, such studies are not underway in Canada, where only mRNA vaccines are used in pregnancy, Dr. Fell said.
This study was supported by the Public Health Agency of Canada.
Dr. Fell and Dr. Ecker reported no competing financial interests.
FROM BMJ
Children and COVID: ED visits and new admissions change course
New child cases of COVID-19 made at least a temporary transition from slow increase to decrease, and emergency department visits and new admissions seem to be following a downward trend.
, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association. For some historical perspective, the latest weekly count falls below last year’s Delta surge figure of 121,000 (Aug. 6-12) but above the summer 2020 total of 26,000 (Aug. 7-13).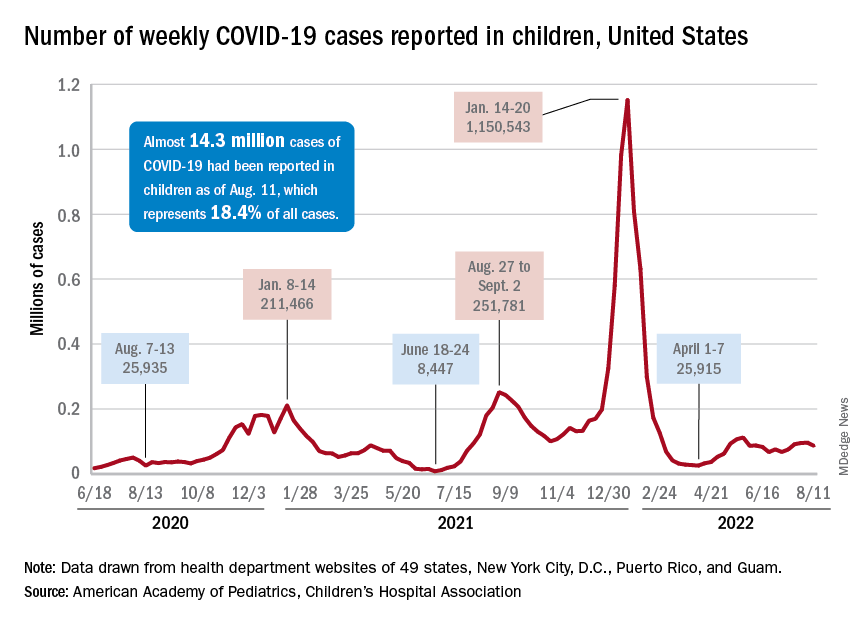
Measures of serious illness finally head downward
The prolonged rise in ED visits and new admissions over the last 5 months, which continued even through late spring when cases were declining, seems to have peaked, CDC data suggest.
That upward trend, driven largely by continued increases among younger children, peaked in late July, when 6.7% of all ED visits for children aged 0-11 years involved diagnosed COVID-19. The corresponding peaks for older children occurred around the same time but were only about half as high: 3.4% for 12- to 15-year-olds and 3.6% for those aged 16-17, the CDC reported.
The data for new admissions present a similar scenario: an increase starting in mid-April that continued unabated into late July despite the decline in new cases. By the time admissions among children aged 0-17 years peaked at 0.46 per 100,000 population in late July, they had reached the same level seen during the Delta surge. By Aug. 7, the rate of new hospitalizations was down to 0.42 per 100,000, the CDC said on its COVID Data Tracker.
The vaccine is ready for all students, but …
As children all over the country start or get ready to start a new school year, the only large-scale student vaccine mandate belongs to the District of Columbia. California has a mandate pending, but it will not go into effect until after July 1, 2023. There are, however, 20 states that have banned vaccine mandates for students, according to the National Academy for State Health Policy.
Nonmandated vaccination of the youngest children against COVID-19 continues to be slow. In the approximately 7 weeks (June 19 to Aug. 9) since the vaccine was approved for use in children younger than 5 years, just 4.4% of that age group has received at least one dose and 0.7% are fully vaccinated. Among those aged 5-11 years, who have been vaccine-eligible since early November of last year, 37.6% have received at least one dose and 30.2% are fully vaccinated, the CDC said.
New child cases of COVID-19 made at least a temporary transition from slow increase to decrease, and emergency department visits and new admissions seem to be following a downward trend.
, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association. For some historical perspective, the latest weekly count falls below last year’s Delta surge figure of 121,000 (Aug. 6-12) but above the summer 2020 total of 26,000 (Aug. 7-13).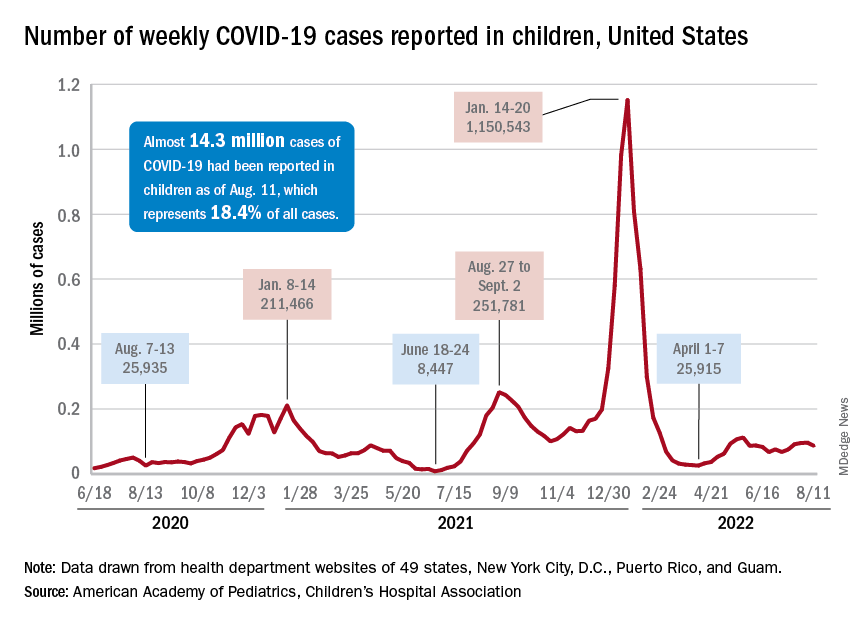
Measures of serious illness finally head downward
The prolonged rise in ED visits and new admissions over the last 5 months, which continued even through late spring when cases were declining, seems to have peaked, CDC data suggest.
That upward trend, driven largely by continued increases among younger children, peaked in late July, when 6.7% of all ED visits for children aged 0-11 years involved diagnosed COVID-19. The corresponding peaks for older children occurred around the same time but were only about half as high: 3.4% for 12- to 15-year-olds and 3.6% for those aged 16-17, the CDC reported.
The data for new admissions present a similar scenario: an increase starting in mid-April that continued unabated into late July despite the decline in new cases. By the time admissions among children aged 0-17 years peaked at 0.46 per 100,000 population in late July, they had reached the same level seen during the Delta surge. By Aug. 7, the rate of new hospitalizations was down to 0.42 per 100,000, the CDC said on its COVID Data Tracker.
The vaccine is ready for all students, but …
As children all over the country start or get ready to start a new school year, the only large-scale student vaccine mandate belongs to the District of Columbia. California has a mandate pending, but it will not go into effect until after July 1, 2023. There are, however, 20 states that have banned vaccine mandates for students, according to the National Academy for State Health Policy.
Nonmandated vaccination of the youngest children against COVID-19 continues to be slow. In the approximately 7 weeks (June 19 to Aug. 9) since the vaccine was approved for use in children younger than 5 years, just 4.4% of that age group has received at least one dose and 0.7% are fully vaccinated. Among those aged 5-11 years, who have been vaccine-eligible since early November of last year, 37.6% have received at least one dose and 30.2% are fully vaccinated, the CDC said.
New child cases of COVID-19 made at least a temporary transition from slow increase to decrease, and emergency department visits and new admissions seem to be following a downward trend.
, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association. For some historical perspective, the latest weekly count falls below last year’s Delta surge figure of 121,000 (Aug. 6-12) but above the summer 2020 total of 26,000 (Aug. 7-13).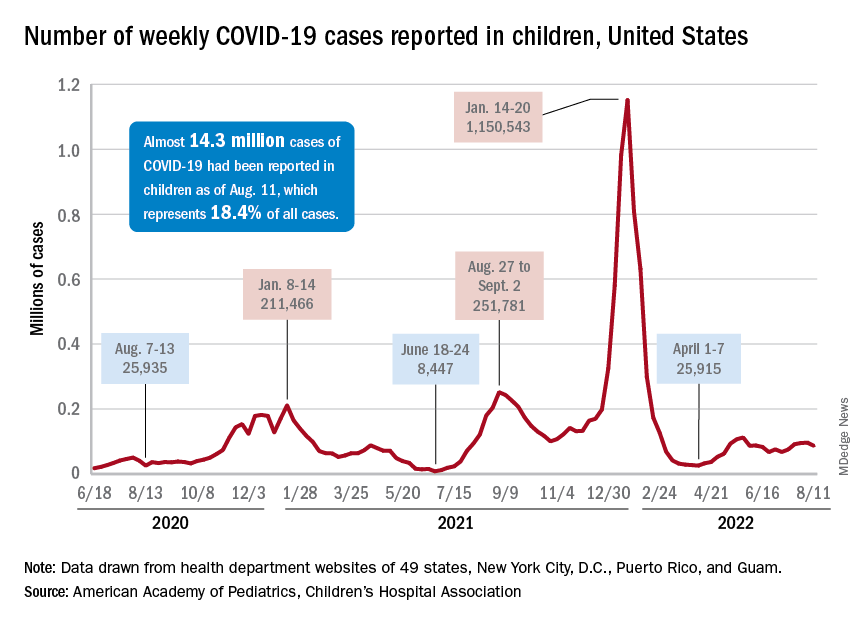
Measures of serious illness finally head downward
The prolonged rise in ED visits and new admissions over the last 5 months, which continued even through late spring when cases were declining, seems to have peaked, CDC data suggest.
That upward trend, driven largely by continued increases among younger children, peaked in late July, when 6.7% of all ED visits for children aged 0-11 years involved diagnosed COVID-19. The corresponding peaks for older children occurred around the same time but were only about half as high: 3.4% for 12- to 15-year-olds and 3.6% for those aged 16-17, the CDC reported.
The data for new admissions present a similar scenario: an increase starting in mid-April that continued unabated into late July despite the decline in new cases. By the time admissions among children aged 0-17 years peaked at 0.46 per 100,000 population in late July, they had reached the same level seen during the Delta surge. By Aug. 7, the rate of new hospitalizations was down to 0.42 per 100,000, the CDC said on its COVID Data Tracker.
The vaccine is ready for all students, but …
As children all over the country start or get ready to start a new school year, the only large-scale student vaccine mandate belongs to the District of Columbia. California has a mandate pending, but it will not go into effect until after July 1, 2023. There are, however, 20 states that have banned vaccine mandates for students, according to the National Academy for State Health Policy.
Nonmandated vaccination of the youngest children against COVID-19 continues to be slow. In the approximately 7 weeks (June 19 to Aug. 9) since the vaccine was approved for use in children younger than 5 years, just 4.4% of that age group has received at least one dose and 0.7% are fully vaccinated. Among those aged 5-11 years, who have been vaccine-eligible since early November of last year, 37.6% have received at least one dose and 30.2% are fully vaccinated, the CDC said.
Diagnosing children with long COVID can be tricky: Experts
When Spencer Siedlecki got COVID-19 in March 2021, he was sick for weeks with extreme fatigue, fevers, a sore throat, bad headaches, nausea, and eventually, pneumonia.
That was scary enough for the then-13-year-old and his parents, who live in Ohio. More than a year later, Spencer still had many of the symptoms and, more alarming, the once-healthy teen had postural orthostatic tachycardia syndrome, a condition that has caused dizziness, a racing heart when he stands, and fainting. Spencer missed most of the last few months of eighth grade because of long COVID.
“He gets sick very easily,” said his mother, Melissa Siedlecki, who works in technology sales. “The common cold that he would shake off in a few days takes weeks for him to feel better.”
The transformation from regular teen life to someone with a chronic illness “sucked,” said Spencer, who will turn 15 in August. “I felt like I was never going to get better.” Fortunately, after some therapy at a specialized clinic, Spencer is back to playing baseball and golf.
Spencer’s journey to better health was difficult; his regular pediatrician told the family at first that there were no treatments to help him – a reaction that is not uncommon. “I still get a lot of parents who heard of me through the grapevine,” said Amy Edwards, MD, director of the pediatric COVID clinic at University Hospitals Rainbow Babies & Children’s and an assistant professor of pediatrics at Case Western Reserve University, both in Cleveland. “The pediatricians either are unsure of what is wrong, or worse, tell children ‘there is nothing wrong with you. Stop faking it.’ ” Dr. Edwards treated Spencer after his mother found the clinic through an internet search.
Alexandra Yonts, MD, a pediatric infectious diseases doctor and director of the post-COVID program clinic at Children’s National Medical Center in Washington, has seen this too. she said.
But those who do get attention tend to be White and affluent, something Dr. Yonts said “doesn’t jibe with the epidemiologic data of who COVID has affected the most.” Black, Latino, and American Indian and Alaska Native children are more likely to be infected with COVID than White children, and have higher rates of hospitalization and death than White children.
It’s not clear whether these children have a particular risk factor, or if they are just the ones who have the resources to get to the clinics. But Dr. Yonts and Dr. Edwards believe many children are not getting the help they need. High-performing kids are coming in “because they are the ones whose symptoms are most obvious,” said Dr. Edwards. “I think there are kids out there who are getting missed because they’re already struggling because of socioeconomic reasons.”
Spencer is one of 14 million children who have tested positive for SARS-CoV-2 since the start of the pandemic. Many pediatricians are still grappling with how to address cases like Spencer’s. The American Academy of Pediatrics has issued only brief guidance on long COVID in children, in part because there have been so few studies to use as a basis for guidance.
The federal government is aiming to change that with a newly launched National Research Action Plan on Long COVID that includes speeding up research on how the condition affects children and youths, including their ability to learn and thrive.
A CDC study found children with COVID were significantly more likely to have smell and taste disturbances, circulatory system problems, fatigue and malaise, and pain. Those who had been infected had higher rates of acute blockage of a lung artery, myocarditis and weakening of the heart, kidney failure, and type 1 diabetes.
Difficult to diagnose
Even with increased media attention and more published studies on pediatric long COVID, it’s still hard for a busy primary care doctor “to sort through what could just be a cold or what could be a series of colds and trying to look at the bigger picture of what’s been going on in a 1- to 3-month period with a kid,” Dr. Yonts said.
Most children with potential or definite long COVID are still being seen by individual pediatricians, not in a specialized clinic with easy access to an army of specialists. It’s not clear how many of those pediatric clinics exist. Survivor Corps, an advocacy group for people with long COVID, has posted a map of locations providing care, but few are specialized or focus on pediatric long COVID.
Long COVID is different from multisystem inflammatory syndrome in children (MIS-C), which occurs within a month or so of infection, triggers high fevers and severe symptoms in the gut, and often results in hospitalization. MIS-C “is not subtle,” said Dr. Edwards.
The long COVID clinic doctors said most of their patients were not very sick at first. “Anecdotally, of the 83 kids that we’ve seen, most have had mild, very mild, or even asymptomatic infections initially,” and then went on to have long COVID, said Dr. Yonts.
“We see it even in children who have very mild disease or even are asymptomatic,” agreed Allison Eckard, MD, director of pediatric infectious diseases at the Medical University of South Carolina, Charleston.
Fatigue, mood problems
Dr. Yonts said 90% of her patients have fatigue, and many also have severe symptoms in their gut. Those and other long COVID symptoms will be looked at more closely in a 3-year study the Children’s National Medical Center is doing along with the National Institute of Allergy and Infectious Diseases.
There are no treatments for long COVID itself.
“Management is probably more the correct term for what we do in our clinic at this point,” said Dr. Yonts. That means dealing with fatigue and managing headache and digestive symptoms with medications or coping strategies. Guidelines from the American Academy of Physical Medicine and Rehabilitation help inform how to help kids safely resume exercise.
At the Children’s National Medical Center clinic, children will typically meet with a team of specialists including infectious diseases doctors on the same day, said Dr. Yonts. Psychologists help children with coping skills. Dr. Yonts is careful not to imply that long COVID is a psychological illness. Parents “will just shut down, because for so long, they’ve been told this is all a mental thing.”
In about a third of children, symptoms get better on their own, and most kids get better over time. But many still struggle. “We don’t talk about cure, because we don’t know what cure looks like,” said Dr. Edwards.
Vaccination may be best protection
Vaccination seems to help reduce the risk of long COVID, perhaps by as much as half. But parents have been slow to vaccinate children, especially the very young. The AAP reported that, as of Aug. 3, just 5% of children under age 5, 37% of those ages 5-11, and 69% of 12- to 17-year-olds have received at least one dose of a COVID-19 vaccine.
“We have tried to really push vaccine as one of the ways to help prevent some of these long COVID syndromes,” said Dr. Eckard. But that advice is not always welcome. Dr. Eckard told the story of a mother who refused to have her autistic son vaccinated, even as she tearfully pleaded for help with his long COVID symptoms, which had also worsened his autism. The woman told Dr. Eckard: “Nothing you can say will convince me to get him vaccinated.” She thought a vaccine could make his symptoms even worse.
The best prevention is to avoid being infected in the first place.
“The more times you get COVID, the more you increase your risk of getting long COVID,” said Dr. Yonts. “The more times you roll the dice, eventually your number could come up.
A version of this article first appeared on WebMD.com.
When Spencer Siedlecki got COVID-19 in March 2021, he was sick for weeks with extreme fatigue, fevers, a sore throat, bad headaches, nausea, and eventually, pneumonia.
That was scary enough for the then-13-year-old and his parents, who live in Ohio. More than a year later, Spencer still had many of the symptoms and, more alarming, the once-healthy teen had postural orthostatic tachycardia syndrome, a condition that has caused dizziness, a racing heart when he stands, and fainting. Spencer missed most of the last few months of eighth grade because of long COVID.
“He gets sick very easily,” said his mother, Melissa Siedlecki, who works in technology sales. “The common cold that he would shake off in a few days takes weeks for him to feel better.”
The transformation from regular teen life to someone with a chronic illness “sucked,” said Spencer, who will turn 15 in August. “I felt like I was never going to get better.” Fortunately, after some therapy at a specialized clinic, Spencer is back to playing baseball and golf.
Spencer’s journey to better health was difficult; his regular pediatrician told the family at first that there were no treatments to help him – a reaction that is not uncommon. “I still get a lot of parents who heard of me through the grapevine,” said Amy Edwards, MD, director of the pediatric COVID clinic at University Hospitals Rainbow Babies & Children’s and an assistant professor of pediatrics at Case Western Reserve University, both in Cleveland. “The pediatricians either are unsure of what is wrong, or worse, tell children ‘there is nothing wrong with you. Stop faking it.’ ” Dr. Edwards treated Spencer after his mother found the clinic through an internet search.
Alexandra Yonts, MD, a pediatric infectious diseases doctor and director of the post-COVID program clinic at Children’s National Medical Center in Washington, has seen this too. she said.
But those who do get attention tend to be White and affluent, something Dr. Yonts said “doesn’t jibe with the epidemiologic data of who COVID has affected the most.” Black, Latino, and American Indian and Alaska Native children are more likely to be infected with COVID than White children, and have higher rates of hospitalization and death than White children.
It’s not clear whether these children have a particular risk factor, or if they are just the ones who have the resources to get to the clinics. But Dr. Yonts and Dr. Edwards believe many children are not getting the help they need. High-performing kids are coming in “because they are the ones whose symptoms are most obvious,” said Dr. Edwards. “I think there are kids out there who are getting missed because they’re already struggling because of socioeconomic reasons.”
Spencer is one of 14 million children who have tested positive for SARS-CoV-2 since the start of the pandemic. Many pediatricians are still grappling with how to address cases like Spencer’s. The American Academy of Pediatrics has issued only brief guidance on long COVID in children, in part because there have been so few studies to use as a basis for guidance.
The federal government is aiming to change that with a newly launched National Research Action Plan on Long COVID that includes speeding up research on how the condition affects children and youths, including their ability to learn and thrive.
A CDC study found children with COVID were significantly more likely to have smell and taste disturbances, circulatory system problems, fatigue and malaise, and pain. Those who had been infected had higher rates of acute blockage of a lung artery, myocarditis and weakening of the heart, kidney failure, and type 1 diabetes.
Difficult to diagnose
Even with increased media attention and more published studies on pediatric long COVID, it’s still hard for a busy primary care doctor “to sort through what could just be a cold or what could be a series of colds and trying to look at the bigger picture of what’s been going on in a 1- to 3-month period with a kid,” Dr. Yonts said.
Most children with potential or definite long COVID are still being seen by individual pediatricians, not in a specialized clinic with easy access to an army of specialists. It’s not clear how many of those pediatric clinics exist. Survivor Corps, an advocacy group for people with long COVID, has posted a map of locations providing care, but few are specialized or focus on pediatric long COVID.
Long COVID is different from multisystem inflammatory syndrome in children (MIS-C), which occurs within a month or so of infection, triggers high fevers and severe symptoms in the gut, and often results in hospitalization. MIS-C “is not subtle,” said Dr. Edwards.
The long COVID clinic doctors said most of their patients were not very sick at first. “Anecdotally, of the 83 kids that we’ve seen, most have had mild, very mild, or even asymptomatic infections initially,” and then went on to have long COVID, said Dr. Yonts.
“We see it even in children who have very mild disease or even are asymptomatic,” agreed Allison Eckard, MD, director of pediatric infectious diseases at the Medical University of South Carolina, Charleston.
Fatigue, mood problems
Dr. Yonts said 90% of her patients have fatigue, and many also have severe symptoms in their gut. Those and other long COVID symptoms will be looked at more closely in a 3-year study the Children’s National Medical Center is doing along with the National Institute of Allergy and Infectious Diseases.
There are no treatments for long COVID itself.
“Management is probably more the correct term for what we do in our clinic at this point,” said Dr. Yonts. That means dealing with fatigue and managing headache and digestive symptoms with medications or coping strategies. Guidelines from the American Academy of Physical Medicine and Rehabilitation help inform how to help kids safely resume exercise.
At the Children’s National Medical Center clinic, children will typically meet with a team of specialists including infectious diseases doctors on the same day, said Dr. Yonts. Psychologists help children with coping skills. Dr. Yonts is careful not to imply that long COVID is a psychological illness. Parents “will just shut down, because for so long, they’ve been told this is all a mental thing.”
In about a third of children, symptoms get better on their own, and most kids get better over time. But many still struggle. “We don’t talk about cure, because we don’t know what cure looks like,” said Dr. Edwards.
Vaccination may be best protection
Vaccination seems to help reduce the risk of long COVID, perhaps by as much as half. But parents have been slow to vaccinate children, especially the very young. The AAP reported that, as of Aug. 3, just 5% of children under age 5, 37% of those ages 5-11, and 69% of 12- to 17-year-olds have received at least one dose of a COVID-19 vaccine.
“We have tried to really push vaccine as one of the ways to help prevent some of these long COVID syndromes,” said Dr. Eckard. But that advice is not always welcome. Dr. Eckard told the story of a mother who refused to have her autistic son vaccinated, even as she tearfully pleaded for help with his long COVID symptoms, which had also worsened his autism. The woman told Dr. Eckard: “Nothing you can say will convince me to get him vaccinated.” She thought a vaccine could make his symptoms even worse.
The best prevention is to avoid being infected in the first place.
“The more times you get COVID, the more you increase your risk of getting long COVID,” said Dr. Yonts. “The more times you roll the dice, eventually your number could come up.
A version of this article first appeared on WebMD.com.
When Spencer Siedlecki got COVID-19 in March 2021, he was sick for weeks with extreme fatigue, fevers, a sore throat, bad headaches, nausea, and eventually, pneumonia.
That was scary enough for the then-13-year-old and his parents, who live in Ohio. More than a year later, Spencer still had many of the symptoms and, more alarming, the once-healthy teen had postural orthostatic tachycardia syndrome, a condition that has caused dizziness, a racing heart when he stands, and fainting. Spencer missed most of the last few months of eighth grade because of long COVID.
“He gets sick very easily,” said his mother, Melissa Siedlecki, who works in technology sales. “The common cold that he would shake off in a few days takes weeks for him to feel better.”
The transformation from regular teen life to someone with a chronic illness “sucked,” said Spencer, who will turn 15 in August. “I felt like I was never going to get better.” Fortunately, after some therapy at a specialized clinic, Spencer is back to playing baseball and golf.
Spencer’s journey to better health was difficult; his regular pediatrician told the family at first that there were no treatments to help him – a reaction that is not uncommon. “I still get a lot of parents who heard of me through the grapevine,” said Amy Edwards, MD, director of the pediatric COVID clinic at University Hospitals Rainbow Babies & Children’s and an assistant professor of pediatrics at Case Western Reserve University, both in Cleveland. “The pediatricians either are unsure of what is wrong, or worse, tell children ‘there is nothing wrong with you. Stop faking it.’ ” Dr. Edwards treated Spencer after his mother found the clinic through an internet search.
Alexandra Yonts, MD, a pediatric infectious diseases doctor and director of the post-COVID program clinic at Children’s National Medical Center in Washington, has seen this too. she said.
But those who do get attention tend to be White and affluent, something Dr. Yonts said “doesn’t jibe with the epidemiologic data of who COVID has affected the most.” Black, Latino, and American Indian and Alaska Native children are more likely to be infected with COVID than White children, and have higher rates of hospitalization and death than White children.
It’s not clear whether these children have a particular risk factor, or if they are just the ones who have the resources to get to the clinics. But Dr. Yonts and Dr. Edwards believe many children are not getting the help they need. High-performing kids are coming in “because they are the ones whose symptoms are most obvious,” said Dr. Edwards. “I think there are kids out there who are getting missed because they’re already struggling because of socioeconomic reasons.”
Spencer is one of 14 million children who have tested positive for SARS-CoV-2 since the start of the pandemic. Many pediatricians are still grappling with how to address cases like Spencer’s. The American Academy of Pediatrics has issued only brief guidance on long COVID in children, in part because there have been so few studies to use as a basis for guidance.
The federal government is aiming to change that with a newly launched National Research Action Plan on Long COVID that includes speeding up research on how the condition affects children and youths, including their ability to learn and thrive.
A CDC study found children with COVID were significantly more likely to have smell and taste disturbances, circulatory system problems, fatigue and malaise, and pain. Those who had been infected had higher rates of acute blockage of a lung artery, myocarditis and weakening of the heart, kidney failure, and type 1 diabetes.
Difficult to diagnose
Even with increased media attention and more published studies on pediatric long COVID, it’s still hard for a busy primary care doctor “to sort through what could just be a cold or what could be a series of colds and trying to look at the bigger picture of what’s been going on in a 1- to 3-month period with a kid,” Dr. Yonts said.
Most children with potential or definite long COVID are still being seen by individual pediatricians, not in a specialized clinic with easy access to an army of specialists. It’s not clear how many of those pediatric clinics exist. Survivor Corps, an advocacy group for people with long COVID, has posted a map of locations providing care, but few are specialized or focus on pediatric long COVID.
Long COVID is different from multisystem inflammatory syndrome in children (MIS-C), which occurs within a month or so of infection, triggers high fevers and severe symptoms in the gut, and often results in hospitalization. MIS-C “is not subtle,” said Dr. Edwards.
The long COVID clinic doctors said most of their patients were not very sick at first. “Anecdotally, of the 83 kids that we’ve seen, most have had mild, very mild, or even asymptomatic infections initially,” and then went on to have long COVID, said Dr. Yonts.
“We see it even in children who have very mild disease or even are asymptomatic,” agreed Allison Eckard, MD, director of pediatric infectious diseases at the Medical University of South Carolina, Charleston.
Fatigue, mood problems
Dr. Yonts said 90% of her patients have fatigue, and many also have severe symptoms in their gut. Those and other long COVID symptoms will be looked at more closely in a 3-year study the Children’s National Medical Center is doing along with the National Institute of Allergy and Infectious Diseases.
There are no treatments for long COVID itself.
“Management is probably more the correct term for what we do in our clinic at this point,” said Dr. Yonts. That means dealing with fatigue and managing headache and digestive symptoms with medications or coping strategies. Guidelines from the American Academy of Physical Medicine and Rehabilitation help inform how to help kids safely resume exercise.
At the Children’s National Medical Center clinic, children will typically meet with a team of specialists including infectious diseases doctors on the same day, said Dr. Yonts. Psychologists help children with coping skills. Dr. Yonts is careful not to imply that long COVID is a psychological illness. Parents “will just shut down, because for so long, they’ve been told this is all a mental thing.”
In about a third of children, symptoms get better on their own, and most kids get better over time. But many still struggle. “We don’t talk about cure, because we don’t know what cure looks like,” said Dr. Edwards.
Vaccination may be best protection
Vaccination seems to help reduce the risk of long COVID, perhaps by as much as half. But parents have been slow to vaccinate children, especially the very young. The AAP reported that, as of Aug. 3, just 5% of children under age 5, 37% of those ages 5-11, and 69% of 12- to 17-year-olds have received at least one dose of a COVID-19 vaccine.
“We have tried to really push vaccine as one of the ways to help prevent some of these long COVID syndromes,” said Dr. Eckard. But that advice is not always welcome. Dr. Eckard told the story of a mother who refused to have her autistic son vaccinated, even as she tearfully pleaded for help with his long COVID symptoms, which had also worsened his autism. The woman told Dr. Eckard: “Nothing you can say will convince me to get him vaccinated.” She thought a vaccine could make his symptoms even worse.
The best prevention is to avoid being infected in the first place.
“The more times you get COVID, the more you increase your risk of getting long COVID,” said Dr. Yonts. “The more times you roll the dice, eventually your number could come up.
A version of this article first appeared on WebMD.com.
Guidelines: Convalescent plasma not recommended for most hospitalized with COVID
In summarizing the practice statement, the authors write, “CCP is most effective when transfused with high neutralizing titers early after symptom onset.”
The five guidelines, were published in Annals of Internal Medicine. The guidelines and strength of recommendations are:
- Nonhospitalized patients at high risk for disease progression should have CCP transfusion in addition to usual standard of care. (weak)
- CCP transfusion should not be done for unselected hospitalized patients with moderate or severe disease. This does not apply to immunosuppressed patients or those who lack antibodies against SARS-CoV-2. (strong)
- CCP transfusion is suggested in addition to the usual standard of care for hospitalized patients with COVID-19 who do not have SARS-CoV-2 antibodies at admission. (weak)
- Prophylactic CCP transfusion is not recommended for uninfected people with close contact exposure to someone with COVID-19. (weak)
- The AABB suggests CCP transfusion along with standard of care for hospitalized patients with COVID-19 and preexisting immunosuppression. (weak)
Multiple guidelines for use of CCP are similar
In an accompanying editorial, Jason V. Baker, MD, MS, and H. Clifford Lane, MD, who are part of the National Institutes of Health Treatment Guidelines Panel, say guidelines from that organization around CCP generally align with those of the AABB and the Infectious Diseases Society of America.
They all note CCP’s potential for helping immunocompromised patients and they recommend against CCP in unselected, hospitalized patients.
The main difference is that the AABB also “suggests” using CCP in combination with other standard treatments for outpatients at high risk for disease progression, regardless of their immune status, write Dr. Baker, who is with Hennepin Healthcare and the department of medicine at the University of Minnesota in Minneapolis, and Dr. Lane, who is with the National Institutes of Health.
The precise circumstance for recommending CCP remains unclear, Dr. Baker and Dr. Lane write. That’s because most available evidence has come in the absence of vaccines and antiviral agents, including nirmatrelvir–ritonavir (Paxlovid), they explain.
“At this point in the pandemic, it seems that the patient most likely to benefit from passive antibody therapy is the immunocompromised host with COVID-19 who cannot mount their own antibody response to vaccine or prior infection,” they write.
“In that setting, and in the absence of other antiviral treatments or progression despite receipt of standard treatments, high-titer CCP from a recently recovered donor is a reasonable approach,” they conclude.
Eileen Barrett, MD, MPH, an assistant professor in the division of hospital medicine at the University of New Mexico in Albuquerque, said in an interview that “clinical guidelines like this really help practicing physicians as we navigate the explosion of research findings since the start of the pandemic.”
One strong recommendation
Dr. Barrett pointed out that four of the five recommendations are rated “weak.”
“The weak recommendations for convalescent plasma in most situations is very humbling,” she said, “particularly as we recall the earliest days of the pandemic when many hospitalized patients received this treatment when little was known about what could help.”
She highlighted the paper’s only strong recommendation, which was against convalescent plasma use for the vast majority of hospitalized patients with COVID.
“That clinical bottom line is what most clinicians will look for,” she said.
“Similarly,” she said, “the accompanying editorial is so helpful in reminding the reader that, despite some possible benefit to convalescent plasma in a smaller subgroup of patients, variant-appropriate monoclonal antibodies and antivirals are better options.”
The disclosures for lead author of the guidelines, Lise J. Estcourt, MB BChir, DPhil, with the National Health Service Blood and Transplant Department and Radcliffe department of medicine at the University of Oxford (England) and her colleagues are available at https://rmed.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M22-1079. The editorialists and Dr. Barrett declare no relevant financial relationships.
In summarizing the practice statement, the authors write, “CCP is most effective when transfused with high neutralizing titers early after symptom onset.”
The five guidelines, were published in Annals of Internal Medicine. The guidelines and strength of recommendations are:
- Nonhospitalized patients at high risk for disease progression should have CCP transfusion in addition to usual standard of care. (weak)
- CCP transfusion should not be done for unselected hospitalized patients with moderate or severe disease. This does not apply to immunosuppressed patients or those who lack antibodies against SARS-CoV-2. (strong)
- CCP transfusion is suggested in addition to the usual standard of care for hospitalized patients with COVID-19 who do not have SARS-CoV-2 antibodies at admission. (weak)
- Prophylactic CCP transfusion is not recommended for uninfected people with close contact exposure to someone with COVID-19. (weak)
- The AABB suggests CCP transfusion along with standard of care for hospitalized patients with COVID-19 and preexisting immunosuppression. (weak)
Multiple guidelines for use of CCP are similar
In an accompanying editorial, Jason V. Baker, MD, MS, and H. Clifford Lane, MD, who are part of the National Institutes of Health Treatment Guidelines Panel, say guidelines from that organization around CCP generally align with those of the AABB and the Infectious Diseases Society of America.
They all note CCP’s potential for helping immunocompromised patients and they recommend against CCP in unselected, hospitalized patients.
The main difference is that the AABB also “suggests” using CCP in combination with other standard treatments for outpatients at high risk for disease progression, regardless of their immune status, write Dr. Baker, who is with Hennepin Healthcare and the department of medicine at the University of Minnesota in Minneapolis, and Dr. Lane, who is with the National Institutes of Health.
The precise circumstance for recommending CCP remains unclear, Dr. Baker and Dr. Lane write. That’s because most available evidence has come in the absence of vaccines and antiviral agents, including nirmatrelvir–ritonavir (Paxlovid), they explain.
“At this point in the pandemic, it seems that the patient most likely to benefit from passive antibody therapy is the immunocompromised host with COVID-19 who cannot mount their own antibody response to vaccine or prior infection,” they write.
“In that setting, and in the absence of other antiviral treatments or progression despite receipt of standard treatments, high-titer CCP from a recently recovered donor is a reasonable approach,” they conclude.
Eileen Barrett, MD, MPH, an assistant professor in the division of hospital medicine at the University of New Mexico in Albuquerque, said in an interview that “clinical guidelines like this really help practicing physicians as we navigate the explosion of research findings since the start of the pandemic.”
One strong recommendation
Dr. Barrett pointed out that four of the five recommendations are rated “weak.”
“The weak recommendations for convalescent plasma in most situations is very humbling,” she said, “particularly as we recall the earliest days of the pandemic when many hospitalized patients received this treatment when little was known about what could help.”
She highlighted the paper’s only strong recommendation, which was against convalescent plasma use for the vast majority of hospitalized patients with COVID.
“That clinical bottom line is what most clinicians will look for,” she said.
“Similarly,” she said, “the accompanying editorial is so helpful in reminding the reader that, despite some possible benefit to convalescent plasma in a smaller subgroup of patients, variant-appropriate monoclonal antibodies and antivirals are better options.”
The disclosures for lead author of the guidelines, Lise J. Estcourt, MB BChir, DPhil, with the National Health Service Blood and Transplant Department and Radcliffe department of medicine at the University of Oxford (England) and her colleagues are available at https://rmed.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M22-1079. The editorialists and Dr. Barrett declare no relevant financial relationships.
In summarizing the practice statement, the authors write, “CCP is most effective when transfused with high neutralizing titers early after symptom onset.”
The five guidelines, were published in Annals of Internal Medicine. The guidelines and strength of recommendations are:
- Nonhospitalized patients at high risk for disease progression should have CCP transfusion in addition to usual standard of care. (weak)
- CCP transfusion should not be done for unselected hospitalized patients with moderate or severe disease. This does not apply to immunosuppressed patients or those who lack antibodies against SARS-CoV-2. (strong)
- CCP transfusion is suggested in addition to the usual standard of care for hospitalized patients with COVID-19 who do not have SARS-CoV-2 antibodies at admission. (weak)
- Prophylactic CCP transfusion is not recommended for uninfected people with close contact exposure to someone with COVID-19. (weak)
- The AABB suggests CCP transfusion along with standard of care for hospitalized patients with COVID-19 and preexisting immunosuppression. (weak)
Multiple guidelines for use of CCP are similar
In an accompanying editorial, Jason V. Baker, MD, MS, and H. Clifford Lane, MD, who are part of the National Institutes of Health Treatment Guidelines Panel, say guidelines from that organization around CCP generally align with those of the AABB and the Infectious Diseases Society of America.
They all note CCP’s potential for helping immunocompromised patients and they recommend against CCP in unselected, hospitalized patients.
The main difference is that the AABB also “suggests” using CCP in combination with other standard treatments for outpatients at high risk for disease progression, regardless of their immune status, write Dr. Baker, who is with Hennepin Healthcare and the department of medicine at the University of Minnesota in Minneapolis, and Dr. Lane, who is with the National Institutes of Health.
The precise circumstance for recommending CCP remains unclear, Dr. Baker and Dr. Lane write. That’s because most available evidence has come in the absence of vaccines and antiviral agents, including nirmatrelvir–ritonavir (Paxlovid), they explain.
“At this point in the pandemic, it seems that the patient most likely to benefit from passive antibody therapy is the immunocompromised host with COVID-19 who cannot mount their own antibody response to vaccine or prior infection,” they write.
“In that setting, and in the absence of other antiviral treatments or progression despite receipt of standard treatments, high-titer CCP from a recently recovered donor is a reasonable approach,” they conclude.
Eileen Barrett, MD, MPH, an assistant professor in the division of hospital medicine at the University of New Mexico in Albuquerque, said in an interview that “clinical guidelines like this really help practicing physicians as we navigate the explosion of research findings since the start of the pandemic.”
One strong recommendation
Dr. Barrett pointed out that four of the five recommendations are rated “weak.”
“The weak recommendations for convalescent plasma in most situations is very humbling,” she said, “particularly as we recall the earliest days of the pandemic when many hospitalized patients received this treatment when little was known about what could help.”
She highlighted the paper’s only strong recommendation, which was against convalescent plasma use for the vast majority of hospitalized patients with COVID.
“That clinical bottom line is what most clinicians will look for,” she said.
“Similarly,” she said, “the accompanying editorial is so helpful in reminding the reader that, despite some possible benefit to convalescent plasma in a smaller subgroup of patients, variant-appropriate monoclonal antibodies and antivirals are better options.”
The disclosures for lead author of the guidelines, Lise J. Estcourt, MB BChir, DPhil, with the National Health Service Blood and Transplant Department and Radcliffe department of medicine at the University of Oxford (England) and her colleagues are available at https://rmed.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M22-1079. The editorialists and Dr. Barrett declare no relevant financial relationships.
FROM ANNALS OF INTERNAL MEDICINE
NYC switching children’s COVID vaccine sites to monkeypox
The city health department said demand for children’s COVID vaccines had been on the downswing at the clinics, which opened in late June. Meanwhile, monkeypox cases have increased, with the city declaring it a public health emergency July 30.
“We always planned to transition vaccination for very young children to providers,” the city’s health department said in a statement, according to Spectrum News NY1. “Due to the ongoing monkeypox emergency, we transitioned some of these sites to administer monkeypox vaccine.”
All the COVID vaccine sites for children will close by Aug. 14, Spectrum News NY1 said. It’s unclear if the other sites will transition to monkeypox vaccine.
No appointments for children’s COVID vaccinations had to be canceled, the city said. The plan is that children now needing the COVID vaccine can go to doctors, pharmacies, or the health department clinics.
Manhattan City Councilwoman Gale Brewer urged the health department to keep the kids’ COVID vaccine sites open through the fall.
“I strongly urge you to maintain these family-friendly sites, at least until mid-September so that children who are going to day care and school can get vaccinated,” Brewer wrote. City schools open Sept. 8
Ms. Brewer noted that the city-run sites administered the Moderna vaccines, while many doctors and neighborhood health clinics use the Pfizer vaccine. That could be a problem for a child that had not finished the Moderna regimen or for families that prefer Moderna.
According to the city health department, 2,130 people in New York City had tested positive for monkeypox as of Aug. 12.
On Friday, the city announced 9,000 additional monkeypox vaccines would be made available the morning of Aug. 13.
A version of this article first appeared on WebMD.com.
The city health department said demand for children’s COVID vaccines had been on the downswing at the clinics, which opened in late June. Meanwhile, monkeypox cases have increased, with the city declaring it a public health emergency July 30.
“We always planned to transition vaccination for very young children to providers,” the city’s health department said in a statement, according to Spectrum News NY1. “Due to the ongoing monkeypox emergency, we transitioned some of these sites to administer monkeypox vaccine.”
All the COVID vaccine sites for children will close by Aug. 14, Spectrum News NY1 said. It’s unclear if the other sites will transition to monkeypox vaccine.
No appointments for children’s COVID vaccinations had to be canceled, the city said. The plan is that children now needing the COVID vaccine can go to doctors, pharmacies, or the health department clinics.
Manhattan City Councilwoman Gale Brewer urged the health department to keep the kids’ COVID vaccine sites open through the fall.
“I strongly urge you to maintain these family-friendly sites, at least until mid-September so that children who are going to day care and school can get vaccinated,” Brewer wrote. City schools open Sept. 8
Ms. Brewer noted that the city-run sites administered the Moderna vaccines, while many doctors and neighborhood health clinics use the Pfizer vaccine. That could be a problem for a child that had not finished the Moderna regimen or for families that prefer Moderna.
According to the city health department, 2,130 people in New York City had tested positive for monkeypox as of Aug. 12.
On Friday, the city announced 9,000 additional monkeypox vaccines would be made available the morning of Aug. 13.
A version of this article first appeared on WebMD.com.
The city health department said demand for children’s COVID vaccines had been on the downswing at the clinics, which opened in late June. Meanwhile, monkeypox cases have increased, with the city declaring it a public health emergency July 30.
“We always planned to transition vaccination for very young children to providers,” the city’s health department said in a statement, according to Spectrum News NY1. “Due to the ongoing monkeypox emergency, we transitioned some of these sites to administer monkeypox vaccine.”
All the COVID vaccine sites for children will close by Aug. 14, Spectrum News NY1 said. It’s unclear if the other sites will transition to monkeypox vaccine.
No appointments for children’s COVID vaccinations had to be canceled, the city said. The plan is that children now needing the COVID vaccine can go to doctors, pharmacies, or the health department clinics.
Manhattan City Councilwoman Gale Brewer urged the health department to keep the kids’ COVID vaccine sites open through the fall.
“I strongly urge you to maintain these family-friendly sites, at least until mid-September so that children who are going to day care and school can get vaccinated,” Brewer wrote. City schools open Sept. 8
Ms. Brewer noted that the city-run sites administered the Moderna vaccines, while many doctors and neighborhood health clinics use the Pfizer vaccine. That could be a problem for a child that had not finished the Moderna regimen or for families that prefer Moderna.
According to the city health department, 2,130 people in New York City had tested positive for monkeypox as of Aug. 12.
On Friday, the city announced 9,000 additional monkeypox vaccines would be made available the morning of Aug. 13.
A version of this article first appeared on WebMD.com.
Seniors intend to receive variant-specific COVID booster in coming months
of 2022.
That finding comes from a new poll by researchers at the University of Michigan, Ann Arbor, who also report that when it comes to the shots, people appear to be putting more trust in their health care professionals than in public health authorities.
“When you are a doctor, you are a trusted source of medical information,” said Preeti Malani, MD, MSJ, an infectious disease specialist at the University of Michigan. “Use the ongoing conversation with your patient as an opportunity to answer their questions and counter any confusion.”
The vaccination campaign appears to be having a rub-off effect, too. More people say they’re likely to receive vaccines and boosters for other infections, such as flu, if they have already been vaccinated and boosted against COVID-19.
Inside the poll
Dr. Malani and her colleagues, who published their findings on the National Poll on Healthy Aging’s website, asked 1,024 adults older than 50 about their attitudes on COVID-19 vaccinations and their history of receiving the injections. The questions covered topics including whether the individual had contracted COVID, COVID vaccine doses, and the prevalence of a health care clinician’s opinion on vaccines and boosters. The poll was conducted July 21-26.
The researchers chose the age range of 50-65 years because this group is an important population for new booster shots that target specific variants of the SARS-CoV-2 virus that causes COVID-19.
Only 19% of people aged 50-64 and 44% of those older than 65 said they had received both their first and second COVID-19 booster shots. What’s more, 17% of people said they had not received any doses of a COVID-19 vaccine.
The vast majority (77%) of respondents said their clinician’s recommendations were “very important” or “somewhat important” in their decision to receive the vaccine.
Dr. Malani said that in her practice, patients have expressed hesitation about COVID-19 vaccines because of concerns about the potential side effects of the shots.
Monica Gandhi, MD, MPH, professor of medicine at the University of California, San Francisco, noted that Americans now appear to trust their physicians more than public health authorities such as the U.S. Centers for Disease Control and Prevention when it comes to COVID-19.
“More people are trusting their providers’ opinions [more] than the CDC or other public health agencies. That speaks volumes to me,” Dr. Gandhi said.
Among the more surprising findings of the poll, according to the researchers, was the number of people who said they had yet to contract COVID-19: 50% of those aged 50-64, and 69% of those older than 65. (Another 12% of those aged 50-64 said they were unsure if they’d ever had the infection.)
Dr. Malani said she hoped future studies would explore in depth the people who remain uninfected with COVID-19.
“We focus a lot on the science of COVID,” she said. “But we need to turn our attention to the behavioral aspects and how to address them.”
A version of this article first appeared on Medscape.com.
of 2022.
That finding comes from a new poll by researchers at the University of Michigan, Ann Arbor, who also report that when it comes to the shots, people appear to be putting more trust in their health care professionals than in public health authorities.
“When you are a doctor, you are a trusted source of medical information,” said Preeti Malani, MD, MSJ, an infectious disease specialist at the University of Michigan. “Use the ongoing conversation with your patient as an opportunity to answer their questions and counter any confusion.”
The vaccination campaign appears to be having a rub-off effect, too. More people say they’re likely to receive vaccines and boosters for other infections, such as flu, if they have already been vaccinated and boosted against COVID-19.
Inside the poll
Dr. Malani and her colleagues, who published their findings on the National Poll on Healthy Aging’s website, asked 1,024 adults older than 50 about their attitudes on COVID-19 vaccinations and their history of receiving the injections. The questions covered topics including whether the individual had contracted COVID, COVID vaccine doses, and the prevalence of a health care clinician’s opinion on vaccines and boosters. The poll was conducted July 21-26.
The researchers chose the age range of 50-65 years because this group is an important population for new booster shots that target specific variants of the SARS-CoV-2 virus that causes COVID-19.
Only 19% of people aged 50-64 and 44% of those older than 65 said they had received both their first and second COVID-19 booster shots. What’s more, 17% of people said they had not received any doses of a COVID-19 vaccine.
The vast majority (77%) of respondents said their clinician’s recommendations were “very important” or “somewhat important” in their decision to receive the vaccine.
Dr. Malani said that in her practice, patients have expressed hesitation about COVID-19 vaccines because of concerns about the potential side effects of the shots.
Monica Gandhi, MD, MPH, professor of medicine at the University of California, San Francisco, noted that Americans now appear to trust their physicians more than public health authorities such as the U.S. Centers for Disease Control and Prevention when it comes to COVID-19.
“More people are trusting their providers’ opinions [more] than the CDC or other public health agencies. That speaks volumes to me,” Dr. Gandhi said.
Among the more surprising findings of the poll, according to the researchers, was the number of people who said they had yet to contract COVID-19: 50% of those aged 50-64, and 69% of those older than 65. (Another 12% of those aged 50-64 said they were unsure if they’d ever had the infection.)
Dr. Malani said she hoped future studies would explore in depth the people who remain uninfected with COVID-19.
“We focus a lot on the science of COVID,” she said. “But we need to turn our attention to the behavioral aspects and how to address them.”
A version of this article first appeared on Medscape.com.
of 2022.
That finding comes from a new poll by researchers at the University of Michigan, Ann Arbor, who also report that when it comes to the shots, people appear to be putting more trust in their health care professionals than in public health authorities.
“When you are a doctor, you are a trusted source of medical information,” said Preeti Malani, MD, MSJ, an infectious disease specialist at the University of Michigan. “Use the ongoing conversation with your patient as an opportunity to answer their questions and counter any confusion.”
The vaccination campaign appears to be having a rub-off effect, too. More people say they’re likely to receive vaccines and boosters for other infections, such as flu, if they have already been vaccinated and boosted against COVID-19.
Inside the poll
Dr. Malani and her colleagues, who published their findings on the National Poll on Healthy Aging’s website, asked 1,024 adults older than 50 about their attitudes on COVID-19 vaccinations and their history of receiving the injections. The questions covered topics including whether the individual had contracted COVID, COVID vaccine doses, and the prevalence of a health care clinician’s opinion on vaccines and boosters. The poll was conducted July 21-26.
The researchers chose the age range of 50-65 years because this group is an important population for new booster shots that target specific variants of the SARS-CoV-2 virus that causes COVID-19.
Only 19% of people aged 50-64 and 44% of those older than 65 said they had received both their first and second COVID-19 booster shots. What’s more, 17% of people said they had not received any doses of a COVID-19 vaccine.
The vast majority (77%) of respondents said their clinician’s recommendations were “very important” or “somewhat important” in their decision to receive the vaccine.
Dr. Malani said that in her practice, patients have expressed hesitation about COVID-19 vaccines because of concerns about the potential side effects of the shots.
Monica Gandhi, MD, MPH, professor of medicine at the University of California, San Francisco, noted that Americans now appear to trust their physicians more than public health authorities such as the U.S. Centers for Disease Control and Prevention when it comes to COVID-19.
“More people are trusting their providers’ opinions [more] than the CDC or other public health agencies. That speaks volumes to me,” Dr. Gandhi said.
Among the more surprising findings of the poll, according to the researchers, was the number of people who said they had yet to contract COVID-19: 50% of those aged 50-64, and 69% of those older than 65. (Another 12% of those aged 50-64 said they were unsure if they’d ever had the infection.)
Dr. Malani said she hoped future studies would explore in depth the people who remain uninfected with COVID-19.
“We focus a lot on the science of COVID,” she said. “But we need to turn our attention to the behavioral aspects and how to address them.”
A version of this article first appeared on Medscape.com.