User login
In Case You Missed It: COVID
Why pregnant people were left behind while vaccines moved at ‘warp speed’ to help the masses
Kia Slade was 7 months pregnant, unvaccinated, and fighting for breath, her oxygen levels plummeting, when her son came into the world last May.
A severe case of COVID-19 pneumonia had left Ms. Slade delirious. When the intensive care team tried to place an oxygen mask on her face, she snatched it away, she recalled. Her baby’s heart rate began to drop.
Ms. Slade’s doctor performed an emergency cesarean section at her bedside in the intensive care unit, delivering baby Tristan 10 weeks early. He weighed just 2 pounds, 14 ounces, about half the size of small full-term baby.
But Ms. Slade wouldn’t meet him until July. She was on a ventilator in a medically-induced coma for 8 weeks, and she developed a serious infection and blood clot while unconscious. It was only after a perilous 2½ months in the hospital, during which her heart stopped twice, that Ms. Slade was vaccinated against COVID-19.
“I wish I had gotten the vaccine earlier,” said Ms. Slade, 42, who remains too sick to return to work as a special education teacher in Baltimore. Doctors “kept pushing me to get vaccinated, but there just wasn’t enough information out there for me to do it.”
A year ago, there was little to no vaccine safety data for pregnant people like Ms. Slade, because they had been excluded from clinical trials run by Pfizer, Moderna, and other vaccine makers.
Lacking data, health experts were unsure and divided about how to advise expectant parents. Although U.S. health officials permitted pregnant people to be vaccinated, the World Health Organization in January 2021 actually discouraged them from doing so; it later reversed that recommendation.
The uncertainty led many women to delay vaccination, and only about two-thirds of the pregnant people who have been tracked by the Centers for Disease Control and Prevention were fully vaccinated as of Feb. 5, 2022, leaving many expectant moms at a high risk of infection and life-threatening complications.
More than 29,000 pregnant people have been hospitalized with COVID-19 and 274 have died, according to the CDC.
“There were surely women who were hospitalized because there wasn’t information available to them,” said Paul A. Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia.
Vaccine developers say that pregnant people – who have special health needs and risks – were excluded from clinical trials to protect them from potential side effects of novel technologies, including the Pfizer and Moderna mRNA vaccines and formulations made with cold viruses, such as the Johnson & Johnson vaccine.
But a KHN analysis also shows that pregnant people were left behind because including them in vaccine studies would have complicated and potentially delayed the delivery of COVID-19 vaccines to the broader population.
A growing number of women’s health researchers and advocates say that excluding pregnant people – and the months-long delay in recommending that they be immunized – helped fuel widespread vaccine hesitancy in this vulnerable group.
“Women and their unborn fetuses are dying of COVID infection,” said Jane Van Dis, MD, an ob.gyn. at the University of Rochester (N.Y.) Medical Center who has treated many patients like Ms. Slade. “Our failure as a society to vaccinate women in pregnancy will be remembered by the children and families who lost their mothers to this disease.”
New technology, uncertain risks
At the time COVID-19 vaccines were being developed, scientists had very little experience using mRNA vaccines in pregnant women, said Jacqueline Miller, MD, a senior vice president involved in vaccine research at Moderna.
“When you study anything in pregnant women, you have two patients, the mom and the unborn child,” Dr. Miller said. “Until we had more safety data on the platform, it wasn’t something we wanted to undertake.”
But Dr. Offit noted that vaccines have a strong record of safety in pregnancy and he sees no reason to have excluded pregnant people. None of the vaccines currently in use – including the chickenpox and rubella vaccines, which contain live viruses – have been shown to harm fetuses, he said. Doctors routinely recommend that pregnant people receive pertussis and flu vaccinations.
Dr. Offit, the coinventor of a rotavirus vaccine, said that some concerns about vaccines stem from commercial, not medical, interests. Drug makers don’t want to risk that their product will be blamed for any problems occurring in pregnant people, even if coincidental, he said.
“These companies don’t want bad news,” Dr. Offit said.
In the United States, health officials typically would have told expectant mothers not to take a vaccine that was untested during pregnancy, said Dr. Offit, a member of a committee that advises the Food and Drug Administration on vaccines.
Due to the urgency of the pandemic, health agencies instead permitted pregnant people to make up their own minds about vaccines without recommending them.
Women’s medical associations were also hampered by the lack of data. Neither the American College of Obstetricians and Gynecologists nor the Society for Maternal-Fetal Medicine actively encouraged pregnant people to be vaccinated until July 30, 2021, after the first real-world vaccine studies had been published. The CDC followed suit in August of 2021.
“If we had had this data in the beginning, we would have been able to vaccinate more women,” said Kelli Burroughs, MD, the department chair of obstetrics and gynecology at Memorial Hermann Sugar Land Hospital near Houston.
Yet anti-vaccine groups wasted no time in scaring pregnant people, flooding social media with misinformation about impaired fertility and harm to the fetus.
In the first few months after the COVID-19 vaccines were approved, some doctors were ambivalent about recommending them, and some still advise pregnant patients against vaccination.
An estimated 67% of pregnant people today are fully vaccinated, compared with about 89% of people 65 and older, another high-risk group, and 65% of Americans overall. Vaccination rates are lower among minorities, with 65% of expectant Hispanic mothers and 53% of pregnant African Americans fully vaccinated, according to the CDC.
Vaccination is especially important during pregnancy, because of increased risks of hospitalization, ICU admission, and mechanical ventilation, Dr. Burroughs said. A study released in February from the National Institutes of Health found that pregnant people with a moderate to severe COVID-19 infection also were more likely to have a C-section, deliver preterm, or develop a postpartum hemorrhage.
Black moms such as Ms. Slade were already at higher risk of maternal and infant mortality before the pandemic, because of higher underlying risks, unequal access to health care, and other factors. COVID-19 has magnified those risks, said Dr. Burroughs, who has persuaded reluctant patients by revealing that she had a healthy pregnancy and child after being vaccinated.
Ms. Slade said she has never opposed vaccines and had no hesitation about receiving other vaccines while pregnant. But she said she “just wasn’t comfortable” with COVID-19 shots.
“If there had been data out there saying the COVID shot was safe, and that nothing would happen to my baby and there was no risk of birth defects, I would have taken it,” said Ms. Slade, who has had type 2 diabetes for 12 years.
Working at warp speed
Government scientists at the NIH were concerned about the risk of COVID-19 to pregnant people from the very beginning and knew that expectant moms needed vaccines as much or more than anyone else, said Larry Corey, MD, a leader of the COVID-19 Prevention Network, which coordinated COVID-19 vaccine trials for the federal government.
But including pregnant volunteers in the larger vaccine trials could have led to interruptions and delays, Dr. Corey said. Researchers would have had to enroll thousands of pregnant volunteers to achieve statistically robust results that weren’t due to chance, he said.
Pregnancy can bring on a wide range of complications: gestational diabetes, hypertension, anemia, bleeding, blood clots, or problems with the placenta, for example. Up to 20% of people who know they’re pregnant miscarry. Because researchers would have been obliged to investigate any medical problem to make sure it wasn’t caused by one of the COVID-19 vaccines, including pregnant people might have meant having to hit pause on those trials, Dr. Corey said.
With death tolls from the pandemic mounting, “we had a mission to do this as quickly and as thoroughly as possible,” Dr. Corey said. Making COVID-19 vaccines available within a year “saved hundreds of thousands of lives.”
The first data on COVID-19 vaccine safety in pregnancy was published in April of 2021 when the CDC released an analysis of nearly 36,000 vaccinated pregnant people who had enrolled in a registry called V-safe, which allows users to log the dates of their vaccinations and any subsequent symptoms.
Later research showed that COVID-19 vaccines weren’t associated with increased risk of miscarriage or premature delivery.
Brenna Hughes, MD, a maternal-fetal medicine specialist and member of the American College of Obstetricians and Gynecologists’ COVID-19 expert group, agrees that adding pregnant people to large-scale COVID-19 vaccine and drug trials may have been impractical. But researchers could have launched parallel trials of pregnant women, once early studies showed the vaccines were safe in humans, she said.
“Would it have been hard? Everything with COVID is hard,” Dr. Hughes said. “But it would have been feasible.”
The FDA requires that researchers perform additional animal studies – called developmental and reproductive toxicity studies – before testing vaccines in pregnant people. Although these studies are essential, they take 5-6 months, and weren’t completed until late 2020, around the time the first COVID-19 vaccines were authorized for adults, said Emily Erbelding, MD, director of microbiology and infectious diseases at the National Institute of Allergy and Infectious Diseases, part of the NIH.
Pregnancy studies “were an afterthought,” said Irina Burd, MD, director of Johns Hopkins’ Integrated Research Center for Fetal Medicine and a professor of gynecology and obstetrics. “They should have been done sooner.”
The NIH is conducting a study of pregnant and postpartum people who decided on their own to be vaccinated, Dr. Erbelding said. The study is due to be completed by July 2023.
Janssen and Moderna are also conducting studies in pregnant people, both due to be completed in 2024.
Pfizer scientists encountered problems when they initiated a clinical trial, which would have randomly assigned pregnant people to receive either a vaccine or placebo. Once vaccines were widely available, many patients weren’t willing to take a chance on being unvaccinated until after delivery.
Pfizer has stopped recruiting patients and has not said whether it will publicly report any data from the trial.
Dr. Hughes said vaccine developers need to include pregnant people from the very beginning.
“There is this notion of protecting pregnant people from research,” Dr. Hughes said. “But we should be protecting patients through research, not from research.”
Recovering physically and emotionally
Ms. Slade still regrets being deprived of time with her children while she fought the disease.
Being on a ventilator kept her from spending those early weeks with her newborn, or from seeing her 9-year-old daughter, Zoe.
Even when Ms. Slade was finally able to see her son, she wasn’t able to tell him she loved him or sing a lullaby, or even talk at all, because of a breathing tube in her throat.
Today, Ms. Slade is a strong advocate of COVID-19 vaccinations, urging her friends and family to get their shots to avoid suffering the way she has.
Ms. Slade had to relearn to walk after being bedridden for weeks. Her many weeks on a ventilator may have contributed to her stomach paralysis, which often causes intense pain, nausea, and even vomiting when she eats or drinks. Ms. Slade weighs 50 pounds less today than before she became pregnant and has resorted to going to the emergency department when the pain is unbearable. “Most days, I’m just miserable,” she said.
Her family suffered as well. Like many babies born prematurely, Tristan, now nearly 9 months old and crawling, receives physical therapy to strengthen his muscles. At 15 pounds, Tristan is largely healthy, although his doctor said he has symptoms of asthma.
Ms. Slade said she would like to attend family counseling with Zoe, who rarely complains and tends to keep her feelings to herself. Ms. Slade said she knows her illness must have been terrifying for her little girl.
“The other day she was talking to me,” Ms. Slade said, “and she said, ‘You know, I almost had to bury you.’ ”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Kia Slade was 7 months pregnant, unvaccinated, and fighting for breath, her oxygen levels plummeting, when her son came into the world last May.
A severe case of COVID-19 pneumonia had left Ms. Slade delirious. When the intensive care team tried to place an oxygen mask on her face, she snatched it away, she recalled. Her baby’s heart rate began to drop.
Ms. Slade’s doctor performed an emergency cesarean section at her bedside in the intensive care unit, delivering baby Tristan 10 weeks early. He weighed just 2 pounds, 14 ounces, about half the size of small full-term baby.
But Ms. Slade wouldn’t meet him until July. She was on a ventilator in a medically-induced coma for 8 weeks, and she developed a serious infection and blood clot while unconscious. It was only after a perilous 2½ months in the hospital, during which her heart stopped twice, that Ms. Slade was vaccinated against COVID-19.
“I wish I had gotten the vaccine earlier,” said Ms. Slade, 42, who remains too sick to return to work as a special education teacher in Baltimore. Doctors “kept pushing me to get vaccinated, but there just wasn’t enough information out there for me to do it.”
A year ago, there was little to no vaccine safety data for pregnant people like Ms. Slade, because they had been excluded from clinical trials run by Pfizer, Moderna, and other vaccine makers.
Lacking data, health experts were unsure and divided about how to advise expectant parents. Although U.S. health officials permitted pregnant people to be vaccinated, the World Health Organization in January 2021 actually discouraged them from doing so; it later reversed that recommendation.
The uncertainty led many women to delay vaccination, and only about two-thirds of the pregnant people who have been tracked by the Centers for Disease Control and Prevention were fully vaccinated as of Feb. 5, 2022, leaving many expectant moms at a high risk of infection and life-threatening complications.
More than 29,000 pregnant people have been hospitalized with COVID-19 and 274 have died, according to the CDC.
“There were surely women who were hospitalized because there wasn’t information available to them,” said Paul A. Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia.
Vaccine developers say that pregnant people – who have special health needs and risks – were excluded from clinical trials to protect them from potential side effects of novel technologies, including the Pfizer and Moderna mRNA vaccines and formulations made with cold viruses, such as the Johnson & Johnson vaccine.
But a KHN analysis also shows that pregnant people were left behind because including them in vaccine studies would have complicated and potentially delayed the delivery of COVID-19 vaccines to the broader population.
A growing number of women’s health researchers and advocates say that excluding pregnant people – and the months-long delay in recommending that they be immunized – helped fuel widespread vaccine hesitancy in this vulnerable group.
“Women and their unborn fetuses are dying of COVID infection,” said Jane Van Dis, MD, an ob.gyn. at the University of Rochester (N.Y.) Medical Center who has treated many patients like Ms. Slade. “Our failure as a society to vaccinate women in pregnancy will be remembered by the children and families who lost their mothers to this disease.”
New technology, uncertain risks
At the time COVID-19 vaccines were being developed, scientists had very little experience using mRNA vaccines in pregnant women, said Jacqueline Miller, MD, a senior vice president involved in vaccine research at Moderna.
“When you study anything in pregnant women, you have two patients, the mom and the unborn child,” Dr. Miller said. “Until we had more safety data on the platform, it wasn’t something we wanted to undertake.”
But Dr. Offit noted that vaccines have a strong record of safety in pregnancy and he sees no reason to have excluded pregnant people. None of the vaccines currently in use – including the chickenpox and rubella vaccines, which contain live viruses – have been shown to harm fetuses, he said. Doctors routinely recommend that pregnant people receive pertussis and flu vaccinations.
Dr. Offit, the coinventor of a rotavirus vaccine, said that some concerns about vaccines stem from commercial, not medical, interests. Drug makers don’t want to risk that their product will be blamed for any problems occurring in pregnant people, even if coincidental, he said.
“These companies don’t want bad news,” Dr. Offit said.
In the United States, health officials typically would have told expectant mothers not to take a vaccine that was untested during pregnancy, said Dr. Offit, a member of a committee that advises the Food and Drug Administration on vaccines.
Due to the urgency of the pandemic, health agencies instead permitted pregnant people to make up their own minds about vaccines without recommending them.
Women’s medical associations were also hampered by the lack of data. Neither the American College of Obstetricians and Gynecologists nor the Society for Maternal-Fetal Medicine actively encouraged pregnant people to be vaccinated until July 30, 2021, after the first real-world vaccine studies had been published. The CDC followed suit in August of 2021.
“If we had had this data in the beginning, we would have been able to vaccinate more women,” said Kelli Burroughs, MD, the department chair of obstetrics and gynecology at Memorial Hermann Sugar Land Hospital near Houston.
Yet anti-vaccine groups wasted no time in scaring pregnant people, flooding social media with misinformation about impaired fertility and harm to the fetus.
In the first few months after the COVID-19 vaccines were approved, some doctors were ambivalent about recommending them, and some still advise pregnant patients against vaccination.
An estimated 67% of pregnant people today are fully vaccinated, compared with about 89% of people 65 and older, another high-risk group, and 65% of Americans overall. Vaccination rates are lower among minorities, with 65% of expectant Hispanic mothers and 53% of pregnant African Americans fully vaccinated, according to the CDC.
Vaccination is especially important during pregnancy, because of increased risks of hospitalization, ICU admission, and mechanical ventilation, Dr. Burroughs said. A study released in February from the National Institutes of Health found that pregnant people with a moderate to severe COVID-19 infection also were more likely to have a C-section, deliver preterm, or develop a postpartum hemorrhage.
Black moms such as Ms. Slade were already at higher risk of maternal and infant mortality before the pandemic, because of higher underlying risks, unequal access to health care, and other factors. COVID-19 has magnified those risks, said Dr. Burroughs, who has persuaded reluctant patients by revealing that she had a healthy pregnancy and child after being vaccinated.
Ms. Slade said she has never opposed vaccines and had no hesitation about receiving other vaccines while pregnant. But she said she “just wasn’t comfortable” with COVID-19 shots.
“If there had been data out there saying the COVID shot was safe, and that nothing would happen to my baby and there was no risk of birth defects, I would have taken it,” said Ms. Slade, who has had type 2 diabetes for 12 years.
Working at warp speed
Government scientists at the NIH were concerned about the risk of COVID-19 to pregnant people from the very beginning and knew that expectant moms needed vaccines as much or more than anyone else, said Larry Corey, MD, a leader of the COVID-19 Prevention Network, which coordinated COVID-19 vaccine trials for the federal government.
But including pregnant volunteers in the larger vaccine trials could have led to interruptions and delays, Dr. Corey said. Researchers would have had to enroll thousands of pregnant volunteers to achieve statistically robust results that weren’t due to chance, he said.
Pregnancy can bring on a wide range of complications: gestational diabetes, hypertension, anemia, bleeding, blood clots, or problems with the placenta, for example. Up to 20% of people who know they’re pregnant miscarry. Because researchers would have been obliged to investigate any medical problem to make sure it wasn’t caused by one of the COVID-19 vaccines, including pregnant people might have meant having to hit pause on those trials, Dr. Corey said.
With death tolls from the pandemic mounting, “we had a mission to do this as quickly and as thoroughly as possible,” Dr. Corey said. Making COVID-19 vaccines available within a year “saved hundreds of thousands of lives.”
The first data on COVID-19 vaccine safety in pregnancy was published in April of 2021 when the CDC released an analysis of nearly 36,000 vaccinated pregnant people who had enrolled in a registry called V-safe, which allows users to log the dates of their vaccinations and any subsequent symptoms.
Later research showed that COVID-19 vaccines weren’t associated with increased risk of miscarriage or premature delivery.
Brenna Hughes, MD, a maternal-fetal medicine specialist and member of the American College of Obstetricians and Gynecologists’ COVID-19 expert group, agrees that adding pregnant people to large-scale COVID-19 vaccine and drug trials may have been impractical. But researchers could have launched parallel trials of pregnant women, once early studies showed the vaccines were safe in humans, she said.
“Would it have been hard? Everything with COVID is hard,” Dr. Hughes said. “But it would have been feasible.”
The FDA requires that researchers perform additional animal studies – called developmental and reproductive toxicity studies – before testing vaccines in pregnant people. Although these studies are essential, they take 5-6 months, and weren’t completed until late 2020, around the time the first COVID-19 vaccines were authorized for adults, said Emily Erbelding, MD, director of microbiology and infectious diseases at the National Institute of Allergy and Infectious Diseases, part of the NIH.
Pregnancy studies “were an afterthought,” said Irina Burd, MD, director of Johns Hopkins’ Integrated Research Center for Fetal Medicine and a professor of gynecology and obstetrics. “They should have been done sooner.”
The NIH is conducting a study of pregnant and postpartum people who decided on their own to be vaccinated, Dr. Erbelding said. The study is due to be completed by July 2023.
Janssen and Moderna are also conducting studies in pregnant people, both due to be completed in 2024.
Pfizer scientists encountered problems when they initiated a clinical trial, which would have randomly assigned pregnant people to receive either a vaccine or placebo. Once vaccines were widely available, many patients weren’t willing to take a chance on being unvaccinated until after delivery.
Pfizer has stopped recruiting patients and has not said whether it will publicly report any data from the trial.
Dr. Hughes said vaccine developers need to include pregnant people from the very beginning.
“There is this notion of protecting pregnant people from research,” Dr. Hughes said. “But we should be protecting patients through research, not from research.”
Recovering physically and emotionally
Ms. Slade still regrets being deprived of time with her children while she fought the disease.
Being on a ventilator kept her from spending those early weeks with her newborn, or from seeing her 9-year-old daughter, Zoe.
Even when Ms. Slade was finally able to see her son, she wasn’t able to tell him she loved him or sing a lullaby, or even talk at all, because of a breathing tube in her throat.
Today, Ms. Slade is a strong advocate of COVID-19 vaccinations, urging her friends and family to get their shots to avoid suffering the way she has.
Ms. Slade had to relearn to walk after being bedridden for weeks. Her many weeks on a ventilator may have contributed to her stomach paralysis, which often causes intense pain, nausea, and even vomiting when she eats or drinks. Ms. Slade weighs 50 pounds less today than before she became pregnant and has resorted to going to the emergency department when the pain is unbearable. “Most days, I’m just miserable,” she said.
Her family suffered as well. Like many babies born prematurely, Tristan, now nearly 9 months old and crawling, receives physical therapy to strengthen his muscles. At 15 pounds, Tristan is largely healthy, although his doctor said he has symptoms of asthma.
Ms. Slade said she would like to attend family counseling with Zoe, who rarely complains and tends to keep her feelings to herself. Ms. Slade said she knows her illness must have been terrifying for her little girl.
“The other day she was talking to me,” Ms. Slade said, “and she said, ‘You know, I almost had to bury you.’ ”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Kia Slade was 7 months pregnant, unvaccinated, and fighting for breath, her oxygen levels plummeting, when her son came into the world last May.
A severe case of COVID-19 pneumonia had left Ms. Slade delirious. When the intensive care team tried to place an oxygen mask on her face, she snatched it away, she recalled. Her baby’s heart rate began to drop.
Ms. Slade’s doctor performed an emergency cesarean section at her bedside in the intensive care unit, delivering baby Tristan 10 weeks early. He weighed just 2 pounds, 14 ounces, about half the size of small full-term baby.
But Ms. Slade wouldn’t meet him until July. She was on a ventilator in a medically-induced coma for 8 weeks, and she developed a serious infection and blood clot while unconscious. It was only after a perilous 2½ months in the hospital, during which her heart stopped twice, that Ms. Slade was vaccinated against COVID-19.
“I wish I had gotten the vaccine earlier,” said Ms. Slade, 42, who remains too sick to return to work as a special education teacher in Baltimore. Doctors “kept pushing me to get vaccinated, but there just wasn’t enough information out there for me to do it.”
A year ago, there was little to no vaccine safety data for pregnant people like Ms. Slade, because they had been excluded from clinical trials run by Pfizer, Moderna, and other vaccine makers.
Lacking data, health experts were unsure and divided about how to advise expectant parents. Although U.S. health officials permitted pregnant people to be vaccinated, the World Health Organization in January 2021 actually discouraged them from doing so; it later reversed that recommendation.
The uncertainty led many women to delay vaccination, and only about two-thirds of the pregnant people who have been tracked by the Centers for Disease Control and Prevention were fully vaccinated as of Feb. 5, 2022, leaving many expectant moms at a high risk of infection and life-threatening complications.
More than 29,000 pregnant people have been hospitalized with COVID-19 and 274 have died, according to the CDC.
“There were surely women who were hospitalized because there wasn’t information available to them,” said Paul A. Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia.
Vaccine developers say that pregnant people – who have special health needs and risks – were excluded from clinical trials to protect them from potential side effects of novel technologies, including the Pfizer and Moderna mRNA vaccines and formulations made with cold viruses, such as the Johnson & Johnson vaccine.
But a KHN analysis also shows that pregnant people were left behind because including them in vaccine studies would have complicated and potentially delayed the delivery of COVID-19 vaccines to the broader population.
A growing number of women’s health researchers and advocates say that excluding pregnant people – and the months-long delay in recommending that they be immunized – helped fuel widespread vaccine hesitancy in this vulnerable group.
“Women and their unborn fetuses are dying of COVID infection,” said Jane Van Dis, MD, an ob.gyn. at the University of Rochester (N.Y.) Medical Center who has treated many patients like Ms. Slade. “Our failure as a society to vaccinate women in pregnancy will be remembered by the children and families who lost their mothers to this disease.”
New technology, uncertain risks
At the time COVID-19 vaccines were being developed, scientists had very little experience using mRNA vaccines in pregnant women, said Jacqueline Miller, MD, a senior vice president involved in vaccine research at Moderna.
“When you study anything in pregnant women, you have two patients, the mom and the unborn child,” Dr. Miller said. “Until we had more safety data on the platform, it wasn’t something we wanted to undertake.”
But Dr. Offit noted that vaccines have a strong record of safety in pregnancy and he sees no reason to have excluded pregnant people. None of the vaccines currently in use – including the chickenpox and rubella vaccines, which contain live viruses – have been shown to harm fetuses, he said. Doctors routinely recommend that pregnant people receive pertussis and flu vaccinations.
Dr. Offit, the coinventor of a rotavirus vaccine, said that some concerns about vaccines stem from commercial, not medical, interests. Drug makers don’t want to risk that their product will be blamed for any problems occurring in pregnant people, even if coincidental, he said.
“These companies don’t want bad news,” Dr. Offit said.
In the United States, health officials typically would have told expectant mothers not to take a vaccine that was untested during pregnancy, said Dr. Offit, a member of a committee that advises the Food and Drug Administration on vaccines.
Due to the urgency of the pandemic, health agencies instead permitted pregnant people to make up their own minds about vaccines without recommending them.
Women’s medical associations were also hampered by the lack of data. Neither the American College of Obstetricians and Gynecologists nor the Society for Maternal-Fetal Medicine actively encouraged pregnant people to be vaccinated until July 30, 2021, after the first real-world vaccine studies had been published. The CDC followed suit in August of 2021.
“If we had had this data in the beginning, we would have been able to vaccinate more women,” said Kelli Burroughs, MD, the department chair of obstetrics and gynecology at Memorial Hermann Sugar Land Hospital near Houston.
Yet anti-vaccine groups wasted no time in scaring pregnant people, flooding social media with misinformation about impaired fertility and harm to the fetus.
In the first few months after the COVID-19 vaccines were approved, some doctors were ambivalent about recommending them, and some still advise pregnant patients against vaccination.
An estimated 67% of pregnant people today are fully vaccinated, compared with about 89% of people 65 and older, another high-risk group, and 65% of Americans overall. Vaccination rates are lower among minorities, with 65% of expectant Hispanic mothers and 53% of pregnant African Americans fully vaccinated, according to the CDC.
Vaccination is especially important during pregnancy, because of increased risks of hospitalization, ICU admission, and mechanical ventilation, Dr. Burroughs said. A study released in February from the National Institutes of Health found that pregnant people with a moderate to severe COVID-19 infection also were more likely to have a C-section, deliver preterm, or develop a postpartum hemorrhage.
Black moms such as Ms. Slade were already at higher risk of maternal and infant mortality before the pandemic, because of higher underlying risks, unequal access to health care, and other factors. COVID-19 has magnified those risks, said Dr. Burroughs, who has persuaded reluctant patients by revealing that she had a healthy pregnancy and child after being vaccinated.
Ms. Slade said she has never opposed vaccines and had no hesitation about receiving other vaccines while pregnant. But she said she “just wasn’t comfortable” with COVID-19 shots.
“If there had been data out there saying the COVID shot was safe, and that nothing would happen to my baby and there was no risk of birth defects, I would have taken it,” said Ms. Slade, who has had type 2 diabetes for 12 years.
Working at warp speed
Government scientists at the NIH were concerned about the risk of COVID-19 to pregnant people from the very beginning and knew that expectant moms needed vaccines as much or more than anyone else, said Larry Corey, MD, a leader of the COVID-19 Prevention Network, which coordinated COVID-19 vaccine trials for the federal government.
But including pregnant volunteers in the larger vaccine trials could have led to interruptions and delays, Dr. Corey said. Researchers would have had to enroll thousands of pregnant volunteers to achieve statistically robust results that weren’t due to chance, he said.
Pregnancy can bring on a wide range of complications: gestational diabetes, hypertension, anemia, bleeding, blood clots, or problems with the placenta, for example. Up to 20% of people who know they’re pregnant miscarry. Because researchers would have been obliged to investigate any medical problem to make sure it wasn’t caused by one of the COVID-19 vaccines, including pregnant people might have meant having to hit pause on those trials, Dr. Corey said.
With death tolls from the pandemic mounting, “we had a mission to do this as quickly and as thoroughly as possible,” Dr. Corey said. Making COVID-19 vaccines available within a year “saved hundreds of thousands of lives.”
The first data on COVID-19 vaccine safety in pregnancy was published in April of 2021 when the CDC released an analysis of nearly 36,000 vaccinated pregnant people who had enrolled in a registry called V-safe, which allows users to log the dates of their vaccinations and any subsequent symptoms.
Later research showed that COVID-19 vaccines weren’t associated with increased risk of miscarriage or premature delivery.
Brenna Hughes, MD, a maternal-fetal medicine specialist and member of the American College of Obstetricians and Gynecologists’ COVID-19 expert group, agrees that adding pregnant people to large-scale COVID-19 vaccine and drug trials may have been impractical. But researchers could have launched parallel trials of pregnant women, once early studies showed the vaccines were safe in humans, she said.
“Would it have been hard? Everything with COVID is hard,” Dr. Hughes said. “But it would have been feasible.”
The FDA requires that researchers perform additional animal studies – called developmental and reproductive toxicity studies – before testing vaccines in pregnant people. Although these studies are essential, they take 5-6 months, and weren’t completed until late 2020, around the time the first COVID-19 vaccines were authorized for adults, said Emily Erbelding, MD, director of microbiology and infectious diseases at the National Institute of Allergy and Infectious Diseases, part of the NIH.
Pregnancy studies “were an afterthought,” said Irina Burd, MD, director of Johns Hopkins’ Integrated Research Center for Fetal Medicine and a professor of gynecology and obstetrics. “They should have been done sooner.”
The NIH is conducting a study of pregnant and postpartum people who decided on their own to be vaccinated, Dr. Erbelding said. The study is due to be completed by July 2023.
Janssen and Moderna are also conducting studies in pregnant people, both due to be completed in 2024.
Pfizer scientists encountered problems when they initiated a clinical trial, which would have randomly assigned pregnant people to receive either a vaccine or placebo. Once vaccines were widely available, many patients weren’t willing to take a chance on being unvaccinated until after delivery.
Pfizer has stopped recruiting patients and has not said whether it will publicly report any data from the trial.
Dr. Hughes said vaccine developers need to include pregnant people from the very beginning.
“There is this notion of protecting pregnant people from research,” Dr. Hughes said. “But we should be protecting patients through research, not from research.”
Recovering physically and emotionally
Ms. Slade still regrets being deprived of time with her children while she fought the disease.
Being on a ventilator kept her from spending those early weeks with her newborn, or from seeing her 9-year-old daughter, Zoe.
Even when Ms. Slade was finally able to see her son, she wasn’t able to tell him she loved him or sing a lullaby, or even talk at all, because of a breathing tube in her throat.
Today, Ms. Slade is a strong advocate of COVID-19 vaccinations, urging her friends and family to get their shots to avoid suffering the way she has.
Ms. Slade had to relearn to walk after being bedridden for weeks. Her many weeks on a ventilator may have contributed to her stomach paralysis, which often causes intense pain, nausea, and even vomiting when she eats or drinks. Ms. Slade weighs 50 pounds less today than before she became pregnant and has resorted to going to the emergency department when the pain is unbearable. “Most days, I’m just miserable,” she said.
Her family suffered as well. Like many babies born prematurely, Tristan, now nearly 9 months old and crawling, receives physical therapy to strengthen his muscles. At 15 pounds, Tristan is largely healthy, although his doctor said he has symptoms of asthma.
Ms. Slade said she would like to attend family counseling with Zoe, who rarely complains and tends to keep her feelings to herself. Ms. Slade said she knows her illness must have been terrifying for her little girl.
“The other day she was talking to me,” Ms. Slade said, “and she said, ‘You know, I almost had to bury you.’ ”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Five million children have lost a caregiver to COVID-19
As the COVID-19 pandemic enters its third year, the death toll continues to rise and with it, the number of children who may be left without anyone to care for them.
By Oct. 31, 2021, more than 5 million people worldwide had died from COVID-19, and about 5.2 million children had lost a parent or caregiver, according to new research published in the Lancet Child and Adolescent Health.
Of particular note, wrote the authors, was how the number of affected children surged during the latter part of their study period. During the first 14 months of the pandemic (March 1, 2020, to April 30, 2021), 2,737,300 children were affected by COVID-19-related caregiver death. But that number jumped by 90% during the next 6 months, from April 30 to Oct. 31, 2021, to 5,209,000. Essentially, the number of children who were affected nearly doubled, compared with those observed during that first year.
To put these numbers into perspective, study author Charles Nelson, PhD, professor of pediatrics and neuroscience and professor of psychology in the department of psychiatry at Harvard Medical School, Boston, compared it to the HIV/AIDS pandemic. “The current worldwide estimate is now approaching 6 million,” he said. “For HIV, it took 10 years before the number of orphans hit 5 million but for COVID it took 2 years. This should provide some perspective.”
Dr. Nelson pointed out that there are many other differences between the two pandemics. “There was no vaccine for HIV/AIDS, in contrast to the last year or so for COVID, when illness and death could largely be prevented,” he explained. “The politics surrounding HIV-related deaths seemed ‘relatively’ apolitical compared to COVID.”
Another major difference is that children whose parents had HIV were allowed to visit their parents, but for COVID-19, isolation was in place so many children could not see their parents before they died.
There is also more misinformation versus lack of information about COVID-19, compared to HIV/AIDS. “As an example, one young girl who lost her father to COVID was told by her classmates that her father hadn’t really died, he just abandoned the family,” Dr. Nelson said.
Minority communities face heaviest loss
A “companion study” was conducted by the Centers for Disease Control and Prevention, which looked at parental/caregiver death just within the United States. During the period between April 1, 2020, through June 30, 2021, the researchers found that more than 140,000 children under the age of 18 years had lost a parent, custodial grandparent, or grandparent caregiver because of COVID-19. In addition, there were significant racial, ethnic, and geographic disparities in COVID-19–associated death of caregivers, and the highest burden of death was observed in the Southern states along the U.S.-Mexican border for Hispanic children, Southeastern states for Black children, and in states with tribal areas for American Indian/Alaska Native populations. Overall, almost two-thirds (65%) of the children who lost a primary caregiver belonged to a racial or ethnic minority.
But as with the international data, the number of affected children has continued to rise since the end of the original study period. “Seth Flaxman, at Imperial College London, has updated the figures as of end of December for the U.S.,” said Dr. Nelson. The 140,000 has increased to 222,718 who lost a primary or secondary caregiver.
In addition, 192,449 lost a primary caregiver, 175,151 lost a parent, and 30,269 lost a secondary caregiver.
The rate, unfortunately, remains disproportionate to minorities. These data do reflect the inequities that have been observed since the beginning of the pandemic, as COVID-19 unequally affected many racial and ethnic minority groups and put them at a higher risk of severe illness and death. “Native Americans are four times more likely than Whites to be orphaned, and Black and Hispanic children 2.5 times more likely,” said Dr. Nelson.
The COVID Collaborative, a diverse group of leading experts from a wide range of disciplines including health, education, and economics, is working to develop consensus recommendations on pandemic-related issues such as vaccination of children who have lost caregivers. In December 2021, they released Hidden Pain: Children Who Lost a Parent or Caretaker to COVID-19 and What the Nation Can Do to Help Them, a report providing estimates of the number of children who lost a caregiver and concrete recommendations to support them.
“The death of an adult caregiver is life-altering for any child regardless of the circumstances or cause,” said Dan Treglia, PhD, associate professor of practice at the University of Pennsylvania, Philadelphia, and a contributor to Hidden Pain. “Traumatic grief is more common in sudden deaths like accidents where support systems are unable to mobilize in anticipation of the death and COVID-19 patients who die are typically in the hospital for barely a week before they pass.”
This suggests that responses to COVID-19 deaths may be more typical of sudden deaths than those of chronic illness such as cancer, he noted, adding that the pandemic has hindered the systems that children and their caregivers would normally rely on for support.
“Social distancing, for example, has limited informal community relationships critical for emotional health and in the current National Emergency in Children’s Mental Health, as noted by the American Academy of Pediatrics, among others, formal community-based and clinical services are overwhelmed,” said Dr. Treglia.
The authors of Hidden Pain note that the children most likely to lose a parent or other caregiver are generally the most likely to have faced “significant previous adversities that hinder their ability to successfully adapt to new experiences of adversity or trauma.” Studies have now revealed the magnitude of COVID-19–associated parent and caregiver death, and Dr. Treglia pointed out that action is needed from federal, state, and local policymakers to help children who have lost a caregiver to COVID-19.
Solutions needed now
“Their whole world has collapsed around them, as they have lost a provider of love, affection, developmental support, and in many cases a provider of critical financial support,” he said. “The federal government has an unparalleled ability to direct resources and attention and shape policy at lower levels of government, and its leadership is critical if we want to ensure care for COVID-bereaved children in all corners of the country.”
At least one state thus far is moving toward legislation to help this population. In California, a state with a high number of children who have lost a caregiver, the Hope, Opportunity, Perseverance, and Empowerment (HOPE) for Children Act has been introduced into the state legislature. If passed into law, children who lost a parent or caregiver to COVID-19 and are in the state’s foster care system or a low-income household would be eligible for a state-funded trust fund.
But while this is a start, the consequences of caregiver loss go far beyond the economics, and can include depression, PTSD, substance use disorder, lower levels of educational attainment, and subsequent lower levels of employment. However, most children (90%-95%) will experience a normative course of grief, according to the COVID Collaboration, which can be managed through family and social support systems. Community-based interventions, such as grief camps, peer support groups, or a mentoring program can also be very helpful.
Camp Erin, for example, is a bereavement camp for children aged 6-17 years. It is run by Eluna, a national nonprofit that supports children and families impacted by grief or addiction. “Camp Erin is the largest national bereavement program for children who are grieving the loss of a family member or caregiver, or other significant person in their lives,” said Mary FitzGerald, CEO of Eluna. “Many families needed help with these new dynamics of loss due to COVID.”
Led by bereavement professionals and volunteers, Camp Erin is a weekend experience that combines grief education and emotional support with traditional and fun activities. “It’s a safe environment for children to explore grief, and be with other children who are also grieving,” said Ms. FitzGerald. “There are 33 locations and it’s free of charge.”
Dr. Treglia emphasized the necessity of providing immediate financial assistance through well-established funding streams. “For example, Temporary Assistance to Needy Families, Supplemental Nutritional Assistance Program, and Social Security Survivor’s Benefits are a good start to reinforce their economic stability and keep financial disaster from piling onto their personal tragedy,” he said. “We also need to buttress community-based organizations and schools to ensure they have the resources and grief competence to identify bereaved children and can either provide services directly or refer them to organizations that can.”
He added that the infrastructure and knowledge already exist and “it’s a matter of making strategic investments at the necessary scale.”
As the COVID-19 pandemic enters its third year, the death toll continues to rise and with it, the number of children who may be left without anyone to care for them.
By Oct. 31, 2021, more than 5 million people worldwide had died from COVID-19, and about 5.2 million children had lost a parent or caregiver, according to new research published in the Lancet Child and Adolescent Health.
Of particular note, wrote the authors, was how the number of affected children surged during the latter part of their study period. During the first 14 months of the pandemic (March 1, 2020, to April 30, 2021), 2,737,300 children were affected by COVID-19-related caregiver death. But that number jumped by 90% during the next 6 months, from April 30 to Oct. 31, 2021, to 5,209,000. Essentially, the number of children who were affected nearly doubled, compared with those observed during that first year.
To put these numbers into perspective, study author Charles Nelson, PhD, professor of pediatrics and neuroscience and professor of psychology in the department of psychiatry at Harvard Medical School, Boston, compared it to the HIV/AIDS pandemic. “The current worldwide estimate is now approaching 6 million,” he said. “For HIV, it took 10 years before the number of orphans hit 5 million but for COVID it took 2 years. This should provide some perspective.”
Dr. Nelson pointed out that there are many other differences between the two pandemics. “There was no vaccine for HIV/AIDS, in contrast to the last year or so for COVID, when illness and death could largely be prevented,” he explained. “The politics surrounding HIV-related deaths seemed ‘relatively’ apolitical compared to COVID.”
Another major difference is that children whose parents had HIV were allowed to visit their parents, but for COVID-19, isolation was in place so many children could not see their parents before they died.
There is also more misinformation versus lack of information about COVID-19, compared to HIV/AIDS. “As an example, one young girl who lost her father to COVID was told by her classmates that her father hadn’t really died, he just abandoned the family,” Dr. Nelson said.
Minority communities face heaviest loss
A “companion study” was conducted by the Centers for Disease Control and Prevention, which looked at parental/caregiver death just within the United States. During the period between April 1, 2020, through June 30, 2021, the researchers found that more than 140,000 children under the age of 18 years had lost a parent, custodial grandparent, or grandparent caregiver because of COVID-19. In addition, there were significant racial, ethnic, and geographic disparities in COVID-19–associated death of caregivers, and the highest burden of death was observed in the Southern states along the U.S.-Mexican border for Hispanic children, Southeastern states for Black children, and in states with tribal areas for American Indian/Alaska Native populations. Overall, almost two-thirds (65%) of the children who lost a primary caregiver belonged to a racial or ethnic minority.
But as with the international data, the number of affected children has continued to rise since the end of the original study period. “Seth Flaxman, at Imperial College London, has updated the figures as of end of December for the U.S.,” said Dr. Nelson. The 140,000 has increased to 222,718 who lost a primary or secondary caregiver.
In addition, 192,449 lost a primary caregiver, 175,151 lost a parent, and 30,269 lost a secondary caregiver.
The rate, unfortunately, remains disproportionate to minorities. These data do reflect the inequities that have been observed since the beginning of the pandemic, as COVID-19 unequally affected many racial and ethnic minority groups and put them at a higher risk of severe illness and death. “Native Americans are four times more likely than Whites to be orphaned, and Black and Hispanic children 2.5 times more likely,” said Dr. Nelson.
The COVID Collaborative, a diverse group of leading experts from a wide range of disciplines including health, education, and economics, is working to develop consensus recommendations on pandemic-related issues such as vaccination of children who have lost caregivers. In December 2021, they released Hidden Pain: Children Who Lost a Parent or Caretaker to COVID-19 and What the Nation Can Do to Help Them, a report providing estimates of the number of children who lost a caregiver and concrete recommendations to support them.
“The death of an adult caregiver is life-altering for any child regardless of the circumstances or cause,” said Dan Treglia, PhD, associate professor of practice at the University of Pennsylvania, Philadelphia, and a contributor to Hidden Pain. “Traumatic grief is more common in sudden deaths like accidents where support systems are unable to mobilize in anticipation of the death and COVID-19 patients who die are typically in the hospital for barely a week before they pass.”
This suggests that responses to COVID-19 deaths may be more typical of sudden deaths than those of chronic illness such as cancer, he noted, adding that the pandemic has hindered the systems that children and their caregivers would normally rely on for support.
“Social distancing, for example, has limited informal community relationships critical for emotional health and in the current National Emergency in Children’s Mental Health, as noted by the American Academy of Pediatrics, among others, formal community-based and clinical services are overwhelmed,” said Dr. Treglia.
The authors of Hidden Pain note that the children most likely to lose a parent or other caregiver are generally the most likely to have faced “significant previous adversities that hinder their ability to successfully adapt to new experiences of adversity or trauma.” Studies have now revealed the magnitude of COVID-19–associated parent and caregiver death, and Dr. Treglia pointed out that action is needed from federal, state, and local policymakers to help children who have lost a caregiver to COVID-19.
Solutions needed now
“Their whole world has collapsed around them, as they have lost a provider of love, affection, developmental support, and in many cases a provider of critical financial support,” he said. “The federal government has an unparalleled ability to direct resources and attention and shape policy at lower levels of government, and its leadership is critical if we want to ensure care for COVID-bereaved children in all corners of the country.”
At least one state thus far is moving toward legislation to help this population. In California, a state with a high number of children who have lost a caregiver, the Hope, Opportunity, Perseverance, and Empowerment (HOPE) for Children Act has been introduced into the state legislature. If passed into law, children who lost a parent or caregiver to COVID-19 and are in the state’s foster care system or a low-income household would be eligible for a state-funded trust fund.
But while this is a start, the consequences of caregiver loss go far beyond the economics, and can include depression, PTSD, substance use disorder, lower levels of educational attainment, and subsequent lower levels of employment. However, most children (90%-95%) will experience a normative course of grief, according to the COVID Collaboration, which can be managed through family and social support systems. Community-based interventions, such as grief camps, peer support groups, or a mentoring program can also be very helpful.
Camp Erin, for example, is a bereavement camp for children aged 6-17 years. It is run by Eluna, a national nonprofit that supports children and families impacted by grief or addiction. “Camp Erin is the largest national bereavement program for children who are grieving the loss of a family member or caregiver, or other significant person in their lives,” said Mary FitzGerald, CEO of Eluna. “Many families needed help with these new dynamics of loss due to COVID.”
Led by bereavement professionals and volunteers, Camp Erin is a weekend experience that combines grief education and emotional support with traditional and fun activities. “It’s a safe environment for children to explore grief, and be with other children who are also grieving,” said Ms. FitzGerald. “There are 33 locations and it’s free of charge.”
Dr. Treglia emphasized the necessity of providing immediate financial assistance through well-established funding streams. “For example, Temporary Assistance to Needy Families, Supplemental Nutritional Assistance Program, and Social Security Survivor’s Benefits are a good start to reinforce their economic stability and keep financial disaster from piling onto their personal tragedy,” he said. “We also need to buttress community-based organizations and schools to ensure they have the resources and grief competence to identify bereaved children and can either provide services directly or refer them to organizations that can.”
He added that the infrastructure and knowledge already exist and “it’s a matter of making strategic investments at the necessary scale.”
As the COVID-19 pandemic enters its third year, the death toll continues to rise and with it, the number of children who may be left without anyone to care for them.
By Oct. 31, 2021, more than 5 million people worldwide had died from COVID-19, and about 5.2 million children had lost a parent or caregiver, according to new research published in the Lancet Child and Adolescent Health.
Of particular note, wrote the authors, was how the number of affected children surged during the latter part of their study period. During the first 14 months of the pandemic (March 1, 2020, to April 30, 2021), 2,737,300 children were affected by COVID-19-related caregiver death. But that number jumped by 90% during the next 6 months, from April 30 to Oct. 31, 2021, to 5,209,000. Essentially, the number of children who were affected nearly doubled, compared with those observed during that first year.
To put these numbers into perspective, study author Charles Nelson, PhD, professor of pediatrics and neuroscience and professor of psychology in the department of psychiatry at Harvard Medical School, Boston, compared it to the HIV/AIDS pandemic. “The current worldwide estimate is now approaching 6 million,” he said. “For HIV, it took 10 years before the number of orphans hit 5 million but for COVID it took 2 years. This should provide some perspective.”
Dr. Nelson pointed out that there are many other differences between the two pandemics. “There was no vaccine for HIV/AIDS, in contrast to the last year or so for COVID, when illness and death could largely be prevented,” he explained. “The politics surrounding HIV-related deaths seemed ‘relatively’ apolitical compared to COVID.”
Another major difference is that children whose parents had HIV were allowed to visit their parents, but for COVID-19, isolation was in place so many children could not see their parents before they died.
There is also more misinformation versus lack of information about COVID-19, compared to HIV/AIDS. “As an example, one young girl who lost her father to COVID was told by her classmates that her father hadn’t really died, he just abandoned the family,” Dr. Nelson said.
Minority communities face heaviest loss
A “companion study” was conducted by the Centers for Disease Control and Prevention, which looked at parental/caregiver death just within the United States. During the period between April 1, 2020, through June 30, 2021, the researchers found that more than 140,000 children under the age of 18 years had lost a parent, custodial grandparent, or grandparent caregiver because of COVID-19. In addition, there were significant racial, ethnic, and geographic disparities in COVID-19–associated death of caregivers, and the highest burden of death was observed in the Southern states along the U.S.-Mexican border for Hispanic children, Southeastern states for Black children, and in states with tribal areas for American Indian/Alaska Native populations. Overall, almost two-thirds (65%) of the children who lost a primary caregiver belonged to a racial or ethnic minority.
But as with the international data, the number of affected children has continued to rise since the end of the original study period. “Seth Flaxman, at Imperial College London, has updated the figures as of end of December for the U.S.,” said Dr. Nelson. The 140,000 has increased to 222,718 who lost a primary or secondary caregiver.
In addition, 192,449 lost a primary caregiver, 175,151 lost a parent, and 30,269 lost a secondary caregiver.
The rate, unfortunately, remains disproportionate to minorities. These data do reflect the inequities that have been observed since the beginning of the pandemic, as COVID-19 unequally affected many racial and ethnic minority groups and put them at a higher risk of severe illness and death. “Native Americans are four times more likely than Whites to be orphaned, and Black and Hispanic children 2.5 times more likely,” said Dr. Nelson.
The COVID Collaborative, a diverse group of leading experts from a wide range of disciplines including health, education, and economics, is working to develop consensus recommendations on pandemic-related issues such as vaccination of children who have lost caregivers. In December 2021, they released Hidden Pain: Children Who Lost a Parent or Caretaker to COVID-19 and What the Nation Can Do to Help Them, a report providing estimates of the number of children who lost a caregiver and concrete recommendations to support them.
“The death of an adult caregiver is life-altering for any child regardless of the circumstances or cause,” said Dan Treglia, PhD, associate professor of practice at the University of Pennsylvania, Philadelphia, and a contributor to Hidden Pain. “Traumatic grief is more common in sudden deaths like accidents where support systems are unable to mobilize in anticipation of the death and COVID-19 patients who die are typically in the hospital for barely a week before they pass.”
This suggests that responses to COVID-19 deaths may be more typical of sudden deaths than those of chronic illness such as cancer, he noted, adding that the pandemic has hindered the systems that children and their caregivers would normally rely on for support.
“Social distancing, for example, has limited informal community relationships critical for emotional health and in the current National Emergency in Children’s Mental Health, as noted by the American Academy of Pediatrics, among others, formal community-based and clinical services are overwhelmed,” said Dr. Treglia.
The authors of Hidden Pain note that the children most likely to lose a parent or other caregiver are generally the most likely to have faced “significant previous adversities that hinder their ability to successfully adapt to new experiences of adversity or trauma.” Studies have now revealed the magnitude of COVID-19–associated parent and caregiver death, and Dr. Treglia pointed out that action is needed from federal, state, and local policymakers to help children who have lost a caregiver to COVID-19.
Solutions needed now
“Their whole world has collapsed around them, as they have lost a provider of love, affection, developmental support, and in many cases a provider of critical financial support,” he said. “The federal government has an unparalleled ability to direct resources and attention and shape policy at lower levels of government, and its leadership is critical if we want to ensure care for COVID-bereaved children in all corners of the country.”
At least one state thus far is moving toward legislation to help this population. In California, a state with a high number of children who have lost a caregiver, the Hope, Opportunity, Perseverance, and Empowerment (HOPE) for Children Act has been introduced into the state legislature. If passed into law, children who lost a parent or caregiver to COVID-19 and are in the state’s foster care system or a low-income household would be eligible for a state-funded trust fund.
But while this is a start, the consequences of caregiver loss go far beyond the economics, and can include depression, PTSD, substance use disorder, lower levels of educational attainment, and subsequent lower levels of employment. However, most children (90%-95%) will experience a normative course of grief, according to the COVID Collaboration, which can be managed through family and social support systems. Community-based interventions, such as grief camps, peer support groups, or a mentoring program can also be very helpful.
Camp Erin, for example, is a bereavement camp for children aged 6-17 years. It is run by Eluna, a national nonprofit that supports children and families impacted by grief or addiction. “Camp Erin is the largest national bereavement program for children who are grieving the loss of a family member or caregiver, or other significant person in their lives,” said Mary FitzGerald, CEO of Eluna. “Many families needed help with these new dynamics of loss due to COVID.”
Led by bereavement professionals and volunteers, Camp Erin is a weekend experience that combines grief education and emotional support with traditional and fun activities. “It’s a safe environment for children to explore grief, and be with other children who are also grieving,” said Ms. FitzGerald. “There are 33 locations and it’s free of charge.”
Dr. Treglia emphasized the necessity of providing immediate financial assistance through well-established funding streams. “For example, Temporary Assistance to Needy Families, Supplemental Nutritional Assistance Program, and Social Security Survivor’s Benefits are a good start to reinforce their economic stability and keep financial disaster from piling onto their personal tragedy,” he said. “We also need to buttress community-based organizations and schools to ensure they have the resources and grief competence to identify bereaved children and can either provide services directly or refer them to organizations that can.”
He added that the infrastructure and knowledge already exist and “it’s a matter of making strategic investments at the necessary scale.”
FROM THE LANCET CHILD AND ADOLESCENT HEALTH
PTSD symptoms common in families of COVID-19 patients
The pandemic has significantly affected the mental health of family members of patients with COVID-19, including high rates of posttraumatic stress disorder (PTSD), anxiety, and depression, new research suggests.
They also had a higher prevalence of depression and anxiety symptoms.
The results illustrate how the mental health of families has been adversely affected by strict isolation measures instituted at the height of the COVID pandemic, lead author Elie Azoulay, MD, PhD, professor of medicine at Diderot University and director of the Medical Intensive Care Unit, Saint Louis Hospital, Paris, told this news organization.
Such restrictions were unnecessary, Dr. Azoulay noted, adding that everyone, including health care professionals, benefits when families are allowed to interact with their loved ones in the ICU.
He added the study findings also emphasize the importance of social supports.
“We need to develop and really increase what we can do for family members” of patients staying in the ICU, said Dr. Azoulay.
The findings were published online Feb. 18 in JAMA.
Twenty-three ICUs in France
The study included adult family members of patients admitted with ARDS to 23 ICUs in France from January to October 2020.
Patients had a partial pressure of arterial oxygen to fraction of inspired oxygen ratio (PaO2/FiO2) of less than 300, and bilateral opacities on chest radiography not fully explained by cardiac failure or fluid overload.
Two trained clinical psychologists interviewed family members and patients by telephone a median of 112 days after ICU discharge. During this interview, participants completed the Impact of Event Scale Revised (IES-R) and the Hospital Anxiety and Depression Scale (HADS).
The IES-R score ranges from 0 (best) to 88 (worst) with a score of more than 22 indicating presence of PTSD-related symptoms of clinical concern. The HADS has separate subscales for anxiety and depression, with a score of 7 or greater on a 21-point scale indicating symptoms of anxiety or depression.
Family members also rated social supports on a scale from 0 (extremely limited) to 10 (extremely effective). Dr. Azoulay noted that social support is the subjective perception of the extent to which friends, mental health specialists, and others are available and helpful.
Investigators divided patients into two groups depending on whether or not the cause of ARDS was COVID-19. Causes other than COVID-19 mainly included community-acquired pneumonia and influenza.
The primary outcome was the prevalence of PTSD-related symptoms among family members. Secondary outcomes were the prevalence of anxiety and depression in family members.
The analysis included 303 family members of patients with COVID-19 ARDS and 214 family members of patients with non–COVID-19 ARDS. Almost half of the family members were spouses.
Those with family members with COVID-19 were younger than the non-COVID group (median age, 50 vs. 55 years). They were less frequently allowed to visit the ICU (35% vs. 88%) and more commonly received patient information by phone (84% vs. 20%).
Better strategies needed
Results showed PTSD symptoms were significantly more common in family members of patients with than without COVID-10 (35% vs. 19%; difference of 16%; 95% confidence interval, 8%-24%; P < .001).
Anxiety symptoms were significantly more common in the COVID-19 group (41% vs. 34%; difference of 8%; 95% CI, 0%-16%; P = .05), as were depression symptoms (31% vs. 18%; difference of 13%; 95% CI, 6%-21%; P < .001).
About 26% of the hospitalized relatives died. PTSD symptoms were more common among bereaved family members of patients who died from COVID-19 than of patients without COVID-19 (63% vs. 39%; difference of 24%; 95% CI, 7%-40%; P = .008).
In the COVID-19 group, significantly fewer family members reported having attended the funeral (77% vs. 91%, P = .04). This could be because of concerns over transmitting the virus, the investigators noted.
After adjustment for age, sex, and level of social support in a multivariable analysis, COVID-19 ARDS was significantly associated with increased risk for PTSD-related symptoms in family members (odds ratio, 2.05; 95% CI, 1.30-3.23; P =.002).
Other factors independently associated with PTSD symptoms were age, level of social support, and being male.
Factors associated with anxiety included having COVID-19 ARDS, age, being male, and level of social support. COVID-19 ARDS and level of social support were independently associated with depression.
Although isolation measures were implemented to prevent viral transmission during the pandemic, severely restricting family members from interacting with their sick loved ones in the ICU is “very destructive [and] deeply distressing,” said Dr. Azoulay. “It’s almost cruel.”
Fear may be at the heart of the “psycho-trauma” experienced by family members, he said.
“I would say one of the main sources is fear of getting infected, fear of abandoning family members, fear of leaving the kids alone without any support, and fear of infecting others,” he added.
Health care providers should develop strategies to better communicate with family members, who also feel a lot of guilt when they’re unable to be with their sick loved ones, said Dr. Azoulay.
‘Element of fear’
Commenting on the findings for this news organization, O. Joseph Bienvenu, MD, PhD, professor of psychiatry and behavioral sciences at Johns Hopkins Medicine, Baltimore, called the study “solid” and noted the lead author is “a well-recognized clinical researcher.”
It was “remarkable” that investigators were able to include a control group of family members of patients with ARDS not due to COVID-19, added Dr. Bienvenu, who was not involved with the research.
“It sounds like the bottom line is COVID adds an additional element of fear in loved ones,” he said.
Dr. Bienvenu added this fits with his own clinical experience – and noted that some COVID-19 follow-up clinics now include family members in their assessments and care.
“I think this study nicely illustrates the utility of this,” he concluded.
The study received funding from the French Ministry of Health. Dr. Azoulay reported receipt of personal fees from lectures from Pfizer, Gilead, Baxter, and Alexion, and institutional research grants from Merck Sharp and Dohme, Pfizer, Baxter, and Alexion. Dr. Bienvenu has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The pandemic has significantly affected the mental health of family members of patients with COVID-19, including high rates of posttraumatic stress disorder (PTSD), anxiety, and depression, new research suggests.
They also had a higher prevalence of depression and anxiety symptoms.
The results illustrate how the mental health of families has been adversely affected by strict isolation measures instituted at the height of the COVID pandemic, lead author Elie Azoulay, MD, PhD, professor of medicine at Diderot University and director of the Medical Intensive Care Unit, Saint Louis Hospital, Paris, told this news organization.
Such restrictions were unnecessary, Dr. Azoulay noted, adding that everyone, including health care professionals, benefits when families are allowed to interact with their loved ones in the ICU.
He added the study findings also emphasize the importance of social supports.
“We need to develop and really increase what we can do for family members” of patients staying in the ICU, said Dr. Azoulay.
The findings were published online Feb. 18 in JAMA.
Twenty-three ICUs in France
The study included adult family members of patients admitted with ARDS to 23 ICUs in France from January to October 2020.
Patients had a partial pressure of arterial oxygen to fraction of inspired oxygen ratio (PaO2/FiO2) of less than 300, and bilateral opacities on chest radiography not fully explained by cardiac failure or fluid overload.
Two trained clinical psychologists interviewed family members and patients by telephone a median of 112 days after ICU discharge. During this interview, participants completed the Impact of Event Scale Revised (IES-R) and the Hospital Anxiety and Depression Scale (HADS).
The IES-R score ranges from 0 (best) to 88 (worst) with a score of more than 22 indicating presence of PTSD-related symptoms of clinical concern. The HADS has separate subscales for anxiety and depression, with a score of 7 or greater on a 21-point scale indicating symptoms of anxiety or depression.
Family members also rated social supports on a scale from 0 (extremely limited) to 10 (extremely effective). Dr. Azoulay noted that social support is the subjective perception of the extent to which friends, mental health specialists, and others are available and helpful.
Investigators divided patients into two groups depending on whether or not the cause of ARDS was COVID-19. Causes other than COVID-19 mainly included community-acquired pneumonia and influenza.
The primary outcome was the prevalence of PTSD-related symptoms among family members. Secondary outcomes were the prevalence of anxiety and depression in family members.
The analysis included 303 family members of patients with COVID-19 ARDS and 214 family members of patients with non–COVID-19 ARDS. Almost half of the family members were spouses.
Those with family members with COVID-19 were younger than the non-COVID group (median age, 50 vs. 55 years). They were less frequently allowed to visit the ICU (35% vs. 88%) and more commonly received patient information by phone (84% vs. 20%).
Better strategies needed
Results showed PTSD symptoms were significantly more common in family members of patients with than without COVID-10 (35% vs. 19%; difference of 16%; 95% confidence interval, 8%-24%; P < .001).
Anxiety symptoms were significantly more common in the COVID-19 group (41% vs. 34%; difference of 8%; 95% CI, 0%-16%; P = .05), as were depression symptoms (31% vs. 18%; difference of 13%; 95% CI, 6%-21%; P < .001).
About 26% of the hospitalized relatives died. PTSD symptoms were more common among bereaved family members of patients who died from COVID-19 than of patients without COVID-19 (63% vs. 39%; difference of 24%; 95% CI, 7%-40%; P = .008).
In the COVID-19 group, significantly fewer family members reported having attended the funeral (77% vs. 91%, P = .04). This could be because of concerns over transmitting the virus, the investigators noted.
After adjustment for age, sex, and level of social support in a multivariable analysis, COVID-19 ARDS was significantly associated with increased risk for PTSD-related symptoms in family members (odds ratio, 2.05; 95% CI, 1.30-3.23; P =.002).
Other factors independently associated with PTSD symptoms were age, level of social support, and being male.
Factors associated with anxiety included having COVID-19 ARDS, age, being male, and level of social support. COVID-19 ARDS and level of social support were independently associated with depression.
Although isolation measures were implemented to prevent viral transmission during the pandemic, severely restricting family members from interacting with their sick loved ones in the ICU is “very destructive [and] deeply distressing,” said Dr. Azoulay. “It’s almost cruel.”
Fear may be at the heart of the “psycho-trauma” experienced by family members, he said.
“I would say one of the main sources is fear of getting infected, fear of abandoning family members, fear of leaving the kids alone without any support, and fear of infecting others,” he added.
Health care providers should develop strategies to better communicate with family members, who also feel a lot of guilt when they’re unable to be with their sick loved ones, said Dr. Azoulay.
‘Element of fear’
Commenting on the findings for this news organization, O. Joseph Bienvenu, MD, PhD, professor of psychiatry and behavioral sciences at Johns Hopkins Medicine, Baltimore, called the study “solid” and noted the lead author is “a well-recognized clinical researcher.”
It was “remarkable” that investigators were able to include a control group of family members of patients with ARDS not due to COVID-19, added Dr. Bienvenu, who was not involved with the research.
“It sounds like the bottom line is COVID adds an additional element of fear in loved ones,” he said.
Dr. Bienvenu added this fits with his own clinical experience – and noted that some COVID-19 follow-up clinics now include family members in their assessments and care.
“I think this study nicely illustrates the utility of this,” he concluded.
The study received funding from the French Ministry of Health. Dr. Azoulay reported receipt of personal fees from lectures from Pfizer, Gilead, Baxter, and Alexion, and institutional research grants from Merck Sharp and Dohme, Pfizer, Baxter, and Alexion. Dr. Bienvenu has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The pandemic has significantly affected the mental health of family members of patients with COVID-19, including high rates of posttraumatic stress disorder (PTSD), anxiety, and depression, new research suggests.
They also had a higher prevalence of depression and anxiety symptoms.
The results illustrate how the mental health of families has been adversely affected by strict isolation measures instituted at the height of the COVID pandemic, lead author Elie Azoulay, MD, PhD, professor of medicine at Diderot University and director of the Medical Intensive Care Unit, Saint Louis Hospital, Paris, told this news organization.
Such restrictions were unnecessary, Dr. Azoulay noted, adding that everyone, including health care professionals, benefits when families are allowed to interact with their loved ones in the ICU.
He added the study findings also emphasize the importance of social supports.
“We need to develop and really increase what we can do for family members” of patients staying in the ICU, said Dr. Azoulay.
The findings were published online Feb. 18 in JAMA.
Twenty-three ICUs in France
The study included adult family members of patients admitted with ARDS to 23 ICUs in France from January to October 2020.
Patients had a partial pressure of arterial oxygen to fraction of inspired oxygen ratio (PaO2/FiO2) of less than 300, and bilateral opacities on chest radiography not fully explained by cardiac failure or fluid overload.
Two trained clinical psychologists interviewed family members and patients by telephone a median of 112 days after ICU discharge. During this interview, participants completed the Impact of Event Scale Revised (IES-R) and the Hospital Anxiety and Depression Scale (HADS).
The IES-R score ranges from 0 (best) to 88 (worst) with a score of more than 22 indicating presence of PTSD-related symptoms of clinical concern. The HADS has separate subscales for anxiety and depression, with a score of 7 or greater on a 21-point scale indicating symptoms of anxiety or depression.
Family members also rated social supports on a scale from 0 (extremely limited) to 10 (extremely effective). Dr. Azoulay noted that social support is the subjective perception of the extent to which friends, mental health specialists, and others are available and helpful.
Investigators divided patients into two groups depending on whether or not the cause of ARDS was COVID-19. Causes other than COVID-19 mainly included community-acquired pneumonia and influenza.
The primary outcome was the prevalence of PTSD-related symptoms among family members. Secondary outcomes were the prevalence of anxiety and depression in family members.
The analysis included 303 family members of patients with COVID-19 ARDS and 214 family members of patients with non–COVID-19 ARDS. Almost half of the family members were spouses.
Those with family members with COVID-19 were younger than the non-COVID group (median age, 50 vs. 55 years). They were less frequently allowed to visit the ICU (35% vs. 88%) and more commonly received patient information by phone (84% vs. 20%).
Better strategies needed
Results showed PTSD symptoms were significantly more common in family members of patients with than without COVID-10 (35% vs. 19%; difference of 16%; 95% confidence interval, 8%-24%; P < .001).
Anxiety symptoms were significantly more common in the COVID-19 group (41% vs. 34%; difference of 8%; 95% CI, 0%-16%; P = .05), as were depression symptoms (31% vs. 18%; difference of 13%; 95% CI, 6%-21%; P < .001).
About 26% of the hospitalized relatives died. PTSD symptoms were more common among bereaved family members of patients who died from COVID-19 than of patients without COVID-19 (63% vs. 39%; difference of 24%; 95% CI, 7%-40%; P = .008).
In the COVID-19 group, significantly fewer family members reported having attended the funeral (77% vs. 91%, P = .04). This could be because of concerns over transmitting the virus, the investigators noted.
After adjustment for age, sex, and level of social support in a multivariable analysis, COVID-19 ARDS was significantly associated with increased risk for PTSD-related symptoms in family members (odds ratio, 2.05; 95% CI, 1.30-3.23; P =.002).
Other factors independently associated with PTSD symptoms were age, level of social support, and being male.
Factors associated with anxiety included having COVID-19 ARDS, age, being male, and level of social support. COVID-19 ARDS and level of social support were independently associated with depression.
Although isolation measures were implemented to prevent viral transmission during the pandemic, severely restricting family members from interacting with their sick loved ones in the ICU is “very destructive [and] deeply distressing,” said Dr. Azoulay. “It’s almost cruel.”
Fear may be at the heart of the “psycho-trauma” experienced by family members, he said.
“I would say one of the main sources is fear of getting infected, fear of abandoning family members, fear of leaving the kids alone without any support, and fear of infecting others,” he added.
Health care providers should develop strategies to better communicate with family members, who also feel a lot of guilt when they’re unable to be with their sick loved ones, said Dr. Azoulay.
‘Element of fear’
Commenting on the findings for this news organization, O. Joseph Bienvenu, MD, PhD, professor of psychiatry and behavioral sciences at Johns Hopkins Medicine, Baltimore, called the study “solid” and noted the lead author is “a well-recognized clinical researcher.”
It was “remarkable” that investigators were able to include a control group of family members of patients with ARDS not due to COVID-19, added Dr. Bienvenu, who was not involved with the research.
“It sounds like the bottom line is COVID adds an additional element of fear in loved ones,” he said.
Dr. Bienvenu added this fits with his own clinical experience – and noted that some COVID-19 follow-up clinics now include family members in their assessments and care.
“I think this study nicely illustrates the utility of this,” he concluded.
The study received funding from the French Ministry of Health. Dr. Azoulay reported receipt of personal fees from lectures from Pfizer, Gilead, Baxter, and Alexion, and institutional research grants from Merck Sharp and Dohme, Pfizer, Baxter, and Alexion. Dr. Bienvenu has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA
Mask mandates ending in all but one state
As COVID-19 cases and hospitalizations continue to decline across the United States,
Retailers and cruises are following along, with Apple and Target stores lifting their own mask mandates this week. Cruise lines such as Norwegian and Royal Caribbean International have said mask requirements will be relaxed for vaccinated passengers, according to the Washington Post.
But guidance from the Centers for Disease Control and Prevention hasn’t changed even as the Omicron variant recedes across the country. Vaccinated people should wear masks when indoors in areas of “substantial or high transmission,” which still covers more than 95% of the country, according to a CDC map.
As daily cases continue to fall, the CDC is reviewing its recommendations, Rochelle Walensky, MD, the CDC director, said during a briefing last week.
“We want to give people a break from things like mask-wearing, when these metrics are better, and then have the ability to reach for them again should things worsen,” she said.
As states relax mask rules, county and city officials are now deciding what to do in their jurisdictions. Vaccinated residents in Los Angeles County may soon be able to go maskless in indoor settings that check for proof of vaccination, according to the Los Angeles Times.
Chicago will also end its mask and COVID-19 vaccine mandates for public places such as restaurants Feb. 28, according to the Chicago Tribune. Illinois will end a statewide indoor mask mandate on the same day. Masks will still be required in health care settings and public transmit.
State and local school boards are debating their mask policies as well. The Maryland State Board of Education voted Feb. 22 to allow local school districts to decide whether students must wear face coverings in school, according to the Associated Press. The update will take effect on March 1 if approved by a Maryland General Assembly committee that oversees the rule.
In New York, state officials have begun lifting mask rules. At the same time, 58% of New York voters want to see early March data before school mask mandates are ended, according to a new poll, released Feb. 22 by the Siena College Research Institute. About 45% of those polled said the state’s indoor public mask mandate should also still be in place.
The debate about wearing masks in schools will likely continue, especially as districts get caught between health authorities and parents, according to the Wall Street Journal. District officials in several states are receiving hundreds of emails daily from both sides, with parents calling for mask rules to end or saying that requirements should remain in place for now to keep kids safe.
A version of this article first appeared on WebMD.com.
As COVID-19 cases and hospitalizations continue to decline across the United States,
Retailers and cruises are following along, with Apple and Target stores lifting their own mask mandates this week. Cruise lines such as Norwegian and Royal Caribbean International have said mask requirements will be relaxed for vaccinated passengers, according to the Washington Post.
But guidance from the Centers for Disease Control and Prevention hasn’t changed even as the Omicron variant recedes across the country. Vaccinated people should wear masks when indoors in areas of “substantial or high transmission,” which still covers more than 95% of the country, according to a CDC map.
As daily cases continue to fall, the CDC is reviewing its recommendations, Rochelle Walensky, MD, the CDC director, said during a briefing last week.
“We want to give people a break from things like mask-wearing, when these metrics are better, and then have the ability to reach for them again should things worsen,” she said.
As states relax mask rules, county and city officials are now deciding what to do in their jurisdictions. Vaccinated residents in Los Angeles County may soon be able to go maskless in indoor settings that check for proof of vaccination, according to the Los Angeles Times.
Chicago will also end its mask and COVID-19 vaccine mandates for public places such as restaurants Feb. 28, according to the Chicago Tribune. Illinois will end a statewide indoor mask mandate on the same day. Masks will still be required in health care settings and public transmit.
State and local school boards are debating their mask policies as well. The Maryland State Board of Education voted Feb. 22 to allow local school districts to decide whether students must wear face coverings in school, according to the Associated Press. The update will take effect on March 1 if approved by a Maryland General Assembly committee that oversees the rule.
In New York, state officials have begun lifting mask rules. At the same time, 58% of New York voters want to see early March data before school mask mandates are ended, according to a new poll, released Feb. 22 by the Siena College Research Institute. About 45% of those polled said the state’s indoor public mask mandate should also still be in place.
The debate about wearing masks in schools will likely continue, especially as districts get caught between health authorities and parents, according to the Wall Street Journal. District officials in several states are receiving hundreds of emails daily from both sides, with parents calling for mask rules to end or saying that requirements should remain in place for now to keep kids safe.
A version of this article first appeared on WebMD.com.
As COVID-19 cases and hospitalizations continue to decline across the United States,
Retailers and cruises are following along, with Apple and Target stores lifting their own mask mandates this week. Cruise lines such as Norwegian and Royal Caribbean International have said mask requirements will be relaxed for vaccinated passengers, according to the Washington Post.
But guidance from the Centers for Disease Control and Prevention hasn’t changed even as the Omicron variant recedes across the country. Vaccinated people should wear masks when indoors in areas of “substantial or high transmission,” which still covers more than 95% of the country, according to a CDC map.
As daily cases continue to fall, the CDC is reviewing its recommendations, Rochelle Walensky, MD, the CDC director, said during a briefing last week.
“We want to give people a break from things like mask-wearing, when these metrics are better, and then have the ability to reach for them again should things worsen,” she said.
As states relax mask rules, county and city officials are now deciding what to do in their jurisdictions. Vaccinated residents in Los Angeles County may soon be able to go maskless in indoor settings that check for proof of vaccination, according to the Los Angeles Times.
Chicago will also end its mask and COVID-19 vaccine mandates for public places such as restaurants Feb. 28, according to the Chicago Tribune. Illinois will end a statewide indoor mask mandate on the same day. Masks will still be required in health care settings and public transmit.
State and local school boards are debating their mask policies as well. The Maryland State Board of Education voted Feb. 22 to allow local school districts to decide whether students must wear face coverings in school, according to the Associated Press. The update will take effect on March 1 if approved by a Maryland General Assembly committee that oversees the rule.
In New York, state officials have begun lifting mask rules. At the same time, 58% of New York voters want to see early March data before school mask mandates are ended, according to a new poll, released Feb. 22 by the Siena College Research Institute. About 45% of those polled said the state’s indoor public mask mandate should also still be in place.
The debate about wearing masks in schools will likely continue, especially as districts get caught between health authorities and parents, according to the Wall Street Journal. District officials in several states are receiving hundreds of emails daily from both sides, with parents calling for mask rules to end or saying that requirements should remain in place for now to keep kids safe.
A version of this article first appeared on WebMD.com.
Twenty-three percent of health care workers likely to leave industry soon: Poll
according to a new poll.
About half of the respondents to the poll from USA Today/Ipsos reported feeling “burned out,” 43% said they were “anxious,” and 21% said they were “angry” about politics and abuse from patients and families.
“We’re trying to help people here, and we are getting verbally and physically abused for it,” Sarah Fried, a nurse in California who responded to the survey, told USA Today in a follow-up interview.
“Early in this pandemic, people were clapping for us and calling us heroes,” she said. “And what happened to that? What happened to them appreciating what nurses are doing?”
The poll was done Feb. 9-16 among 1,170 adults in the U.S. health care industry, including doctors, nurses, paramedics, therapists, home health aides, dentists, and other medical professionals.
A large majority of workers still reported being satisfied with their jobs, although that optimism has declined somewhat since early 2021 when the COVID-19 vaccine rollout was underway. About 80% of those in the recent poll said they were somewhat or very satisfied with their current job, which is down from 89% in an April 2021 poll from Kaiser Family Foundation/the Washington Post.
Most health care workers reported feeling “hopeful” (59%), “motivated” (59%), or “optimistic” (56%) about going to work. But “hopeful” is down from 76% and “optimistic” is down from 67%, compared with last year.
If they could pick a career over again, about 16% disagreed with the statement, “I would still decide to go into health care,” and 18% said they didn’t know how they felt about it.
“The pandemic has actually made me realize how important this career is and how I really do make a difference. I still love it,” Christina Rosa, a mental health counselor in Massachusetts, told USA Today.
During the pandemic, about 66% of those polled said they had treated a COVID-19 patient, which increased to 84% among nurses and 86% among hospital workers. Among those, 47% reported having a patient who died from COVID-19, including 53% of nurses and 55% of hospital workers.
What’s more, 81% of those who treated COVID-19 patients have cared for unvaccinated patients. Among those, 67% said their patients continued to express skepticism toward COVID-19 vaccines, and 38% said some patients expressed regret for not getting a vaccine. Beyond that, 26% said unvaccinated patients asked for unproven treatments, and 30% said the patient or family criticized the care they received.
Regarding coronavirus-related policy, most Americans working in health care expressed skepticism or criticism of the nation’s handling of the pandemic. About 39% agreed that the American health care system is “on the verge of collapse.”
Only 21% said the pandemic is mostly or completely under control. About 61% don’t think Americans are taking enough precautions to prevent the spread of the coronavirus.
Health care workers were slightly positive when it comes to the Centers for Disease Control and Prevention (54% approve, 34% disapprove), divided on the Biden administration (41% approve, 40% disapprove), and critical of the news media (20% approve, 61% disapprove) and the American public (18% approve, 68% disapprove).
Broadly, though, health care workers support public health efforts. About 85% back measures that provide N95 masks, and 83% back measures that provide COVID-19 tests.
A version of this article first appeared on WebMD.com.
according to a new poll.
About half of the respondents to the poll from USA Today/Ipsos reported feeling “burned out,” 43% said they were “anxious,” and 21% said they were “angry” about politics and abuse from patients and families.
“We’re trying to help people here, and we are getting verbally and physically abused for it,” Sarah Fried, a nurse in California who responded to the survey, told USA Today in a follow-up interview.
“Early in this pandemic, people were clapping for us and calling us heroes,” she said. “And what happened to that? What happened to them appreciating what nurses are doing?”
The poll was done Feb. 9-16 among 1,170 adults in the U.S. health care industry, including doctors, nurses, paramedics, therapists, home health aides, dentists, and other medical professionals.
A large majority of workers still reported being satisfied with their jobs, although that optimism has declined somewhat since early 2021 when the COVID-19 vaccine rollout was underway. About 80% of those in the recent poll said they were somewhat or very satisfied with their current job, which is down from 89% in an April 2021 poll from Kaiser Family Foundation/the Washington Post.
Most health care workers reported feeling “hopeful” (59%), “motivated” (59%), or “optimistic” (56%) about going to work. But “hopeful” is down from 76% and “optimistic” is down from 67%, compared with last year.
If they could pick a career over again, about 16% disagreed with the statement, “I would still decide to go into health care,” and 18% said they didn’t know how they felt about it.
“The pandemic has actually made me realize how important this career is and how I really do make a difference. I still love it,” Christina Rosa, a mental health counselor in Massachusetts, told USA Today.
During the pandemic, about 66% of those polled said they had treated a COVID-19 patient, which increased to 84% among nurses and 86% among hospital workers. Among those, 47% reported having a patient who died from COVID-19, including 53% of nurses and 55% of hospital workers.
What’s more, 81% of those who treated COVID-19 patients have cared for unvaccinated patients. Among those, 67% said their patients continued to express skepticism toward COVID-19 vaccines, and 38% said some patients expressed regret for not getting a vaccine. Beyond that, 26% said unvaccinated patients asked for unproven treatments, and 30% said the patient or family criticized the care they received.
Regarding coronavirus-related policy, most Americans working in health care expressed skepticism or criticism of the nation’s handling of the pandemic. About 39% agreed that the American health care system is “on the verge of collapse.”
Only 21% said the pandemic is mostly or completely under control. About 61% don’t think Americans are taking enough precautions to prevent the spread of the coronavirus.
Health care workers were slightly positive when it comes to the Centers for Disease Control and Prevention (54% approve, 34% disapprove), divided on the Biden administration (41% approve, 40% disapprove), and critical of the news media (20% approve, 61% disapprove) and the American public (18% approve, 68% disapprove).
Broadly, though, health care workers support public health efforts. About 85% back measures that provide N95 masks, and 83% back measures that provide COVID-19 tests.
A version of this article first appeared on WebMD.com.
according to a new poll.
About half of the respondents to the poll from USA Today/Ipsos reported feeling “burned out,” 43% said they were “anxious,” and 21% said they were “angry” about politics and abuse from patients and families.
“We’re trying to help people here, and we are getting verbally and physically abused for it,” Sarah Fried, a nurse in California who responded to the survey, told USA Today in a follow-up interview.
“Early in this pandemic, people were clapping for us and calling us heroes,” she said. “And what happened to that? What happened to them appreciating what nurses are doing?”
The poll was done Feb. 9-16 among 1,170 adults in the U.S. health care industry, including doctors, nurses, paramedics, therapists, home health aides, dentists, and other medical professionals.
A large majority of workers still reported being satisfied with their jobs, although that optimism has declined somewhat since early 2021 when the COVID-19 vaccine rollout was underway. About 80% of those in the recent poll said they were somewhat or very satisfied with their current job, which is down from 89% in an April 2021 poll from Kaiser Family Foundation/the Washington Post.
Most health care workers reported feeling “hopeful” (59%), “motivated” (59%), or “optimistic” (56%) about going to work. But “hopeful” is down from 76% and “optimistic” is down from 67%, compared with last year.
If they could pick a career over again, about 16% disagreed with the statement, “I would still decide to go into health care,” and 18% said they didn’t know how they felt about it.
“The pandemic has actually made me realize how important this career is and how I really do make a difference. I still love it,” Christina Rosa, a mental health counselor in Massachusetts, told USA Today.
During the pandemic, about 66% of those polled said they had treated a COVID-19 patient, which increased to 84% among nurses and 86% among hospital workers. Among those, 47% reported having a patient who died from COVID-19, including 53% of nurses and 55% of hospital workers.
What’s more, 81% of those who treated COVID-19 patients have cared for unvaccinated patients. Among those, 67% said their patients continued to express skepticism toward COVID-19 vaccines, and 38% said some patients expressed regret for not getting a vaccine. Beyond that, 26% said unvaccinated patients asked for unproven treatments, and 30% said the patient or family criticized the care they received.
Regarding coronavirus-related policy, most Americans working in health care expressed skepticism or criticism of the nation’s handling of the pandemic. About 39% agreed that the American health care system is “on the verge of collapse.”
Only 21% said the pandemic is mostly or completely under control. About 61% don’t think Americans are taking enough precautions to prevent the spread of the coronavirus.
Health care workers were slightly positive when it comes to the Centers for Disease Control and Prevention (54% approve, 34% disapprove), divided on the Biden administration (41% approve, 40% disapprove), and critical of the news media (20% approve, 61% disapprove) and the American public (18% approve, 68% disapprove).
Broadly, though, health care workers support public health efforts. About 85% back measures that provide N95 masks, and 83% back measures that provide COVID-19 tests.
A version of this article first appeared on WebMD.com.
Exploring the relationship of COVID-19 vaccines and fertility
Introduction
Amidst an aggressive vaccination campaign for COVID-19, misinformation has spread over the Internet, affecting public perception and making some people hesitant to participate in ongoing immunization campaigns. Of chief concern are issues pertaining to fertility or viability of sperm – information circulating on social networks posits that the coronavirus vaccine may influence infertility in men, which, according to physicians, is not grounded in reality. From the perspective of evidence-based medicine, there is a dearth of information suggesting an untoward effect of the vaccine on male fertility. The risk of adverse reactions arising from approved vaccines is negligible, with mild, albeit controllable, side effects demonstrated by patients in clinical trials. Therefore, there is no plausible reason for the general public to avoid vaccinations.1
Infertility following vaccination
The source of confusion can be traced back to a study conducted by researchers at the University of Miami Miller School of Medicine; the general public has conflated a side effect of the virus, namely, infertility and erectile dysfunction, with that of the vaccine.2 According to Ranjith Ramasamy, MD, director of the urology program at Miller, “We were the first to demonstrate that the COVID virus, itself, can affect male fertility and be a potential cause for erectile dysfunction. We are now the first to examine if there is any impact of the COVID vaccine on male fertility potential, which we did not find.”3
Coronavirus can indeed cause significant damage to the testicular tissue of infected men by means of mediating ACE2 expression on Leydig and Sertoli cells of the testis. It should be noted that COVID-19 may potentially attack any type of cell in the body that expresses the enzyme ACE2. However, it is particularly harmful to cells with high levels of expression of this enzyme, such as testicular cells. The spermatogenesis process can be affected, thereby posing a risk to male fertility.4
Expanding on the theme of fertility during the pandemic, a number of false claims5-7 about the vaccine and its overall effect on the placenta and fertility have also emerged as a contentious topic for debate on social media; doctors continue to explain why the theories are not reasonable or a cause for concern. The World Health Organization (WHO) provides recommendations on COVID-19 vaccinations for pregnant and/or lactating women and encourages a shared decision process involving risk/benefit assessment with the prescribing physician.5 Pregnant women, especially those with underlying comorbid conditions, are susceptible to developing severe symptom manifestations of COVID-19 with the disease also being associated with an increased likelihood of premature birth. As far as lactating women are concerned, the evidence thus far has indicated that the risk of side effects of the vaccine is very low, suggesting that these women could be vaccinated.5
The vaccine is the best option
While more studies are needed to ascertain the relationship between COVID-19 and male infertility, the vaccine is currently the best option for those who are concerned about their fertility from exposure to the coronavirus. Because of delayed wholesale acceptance of vaccines by the general population, clinicians should continue to emphasize the importance of preventive care with respect to disease exposure.6
In addition, those who are concerned with fertility can opt for ways to preserve their reproductive capacity, such as the removal of semen for freezing sperm, albeit with adherence to sperm-washing procedures to preclude cross-contamination from viruses.8,9 For the preservation of sperm, the noninvasive method is often performed, preferably collected in several samples. Then, the semen is cryopreserved.8 In some instances, the sperm can also be removed directly from the testicles with a simple needle or by means of a minor surgical procedure.
A wait and try approach is advocated by clinicians for individuals who have already experienced COVID-19 symptoms and are therefore concerned about the prospect of childbearing.10 If the couple is unable to conceive after a year of trying, it is recommended that they consult a reproductive specialist; the clinician can carry out a comprehensive evaluation and order a series of tests to identify the source of the problem, indicating whether there are alternative methods for helping the couple to start a family (addressing the underlying factors involved in infertility, or treating via assisted reproduction procedures, such as in vitro fertilization).11
Dr. Aman is faculty member at the biology department of City Colleges of Chicago, and a postdoctoral researcher at the International Maternal and Child Health Foundation (IMCHF). She disclosed no relevant financial relationships. Dr. Islam is a medical writer for the IMCHF, Montreal, is based in New York, and disclosed no relevant financial relationships. Mr. Choudhry is a research assistant at the IMCHF and he has no disclosures. Dr. Zia Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF. He has no disclosures.
References
1. Berry SD et al. J Am Geriatr Soc. 2021 May;69(5):1140-6.
2. Achua JK et al. World J Men’s Health. 2021 Jan;39(1):65-74.
3. Broderick JM. Urology Times. 2021 June.
4. Huang C et al. Andrology. 2021 Jan;9(1):80-7.
5. Sajjadi NB et al. J Osteopath Med. 2021 Apr 12;121(6):583-7.
6. Sallam M et al. Vaccines. 2021 Jan;9(1):42.
7. Islam MS et al. PloS One. 2021 May 12;16(5):e0251605.
8. Tesarik J. J Fertil Preserv. 2021;2:art246111.
9. Adiga SK et al. Reprod BioMed Online. 2020 Dec;41(6):991-7.
10. FAQs related to COVID-19. Q: If I get sick or test positive for COVID-19, when is it safe to become pregnant? American Society for Reproductive Medicine.
11. Cross C. Wellness and Prevention: Why can’t I get pregnant? John Hopkins Medicine.
Introduction
Amidst an aggressive vaccination campaign for COVID-19, misinformation has spread over the Internet, affecting public perception and making some people hesitant to participate in ongoing immunization campaigns. Of chief concern are issues pertaining to fertility or viability of sperm – information circulating on social networks posits that the coronavirus vaccine may influence infertility in men, which, according to physicians, is not grounded in reality. From the perspective of evidence-based medicine, there is a dearth of information suggesting an untoward effect of the vaccine on male fertility. The risk of adverse reactions arising from approved vaccines is negligible, with mild, albeit controllable, side effects demonstrated by patients in clinical trials. Therefore, there is no plausible reason for the general public to avoid vaccinations.1
Infertility following vaccination
The source of confusion can be traced back to a study conducted by researchers at the University of Miami Miller School of Medicine; the general public has conflated a side effect of the virus, namely, infertility and erectile dysfunction, with that of the vaccine.2 According to Ranjith Ramasamy, MD, director of the urology program at Miller, “We were the first to demonstrate that the COVID virus, itself, can affect male fertility and be a potential cause for erectile dysfunction. We are now the first to examine if there is any impact of the COVID vaccine on male fertility potential, which we did not find.”3
Coronavirus can indeed cause significant damage to the testicular tissue of infected men by means of mediating ACE2 expression on Leydig and Sertoli cells of the testis. It should be noted that COVID-19 may potentially attack any type of cell in the body that expresses the enzyme ACE2. However, it is particularly harmful to cells with high levels of expression of this enzyme, such as testicular cells. The spermatogenesis process can be affected, thereby posing a risk to male fertility.4
Expanding on the theme of fertility during the pandemic, a number of false claims5-7 about the vaccine and its overall effect on the placenta and fertility have also emerged as a contentious topic for debate on social media; doctors continue to explain why the theories are not reasonable or a cause for concern. The World Health Organization (WHO) provides recommendations on COVID-19 vaccinations for pregnant and/or lactating women and encourages a shared decision process involving risk/benefit assessment with the prescribing physician.5 Pregnant women, especially those with underlying comorbid conditions, are susceptible to developing severe symptom manifestations of COVID-19 with the disease also being associated with an increased likelihood of premature birth. As far as lactating women are concerned, the evidence thus far has indicated that the risk of side effects of the vaccine is very low, suggesting that these women could be vaccinated.5
The vaccine is the best option
While more studies are needed to ascertain the relationship between COVID-19 and male infertility, the vaccine is currently the best option for those who are concerned about their fertility from exposure to the coronavirus. Because of delayed wholesale acceptance of vaccines by the general population, clinicians should continue to emphasize the importance of preventive care with respect to disease exposure.6
In addition, those who are concerned with fertility can opt for ways to preserve their reproductive capacity, such as the removal of semen for freezing sperm, albeit with adherence to sperm-washing procedures to preclude cross-contamination from viruses.8,9 For the preservation of sperm, the noninvasive method is often performed, preferably collected in several samples. Then, the semen is cryopreserved.8 In some instances, the sperm can also be removed directly from the testicles with a simple needle or by means of a minor surgical procedure.
A wait and try approach is advocated by clinicians for individuals who have already experienced COVID-19 symptoms and are therefore concerned about the prospect of childbearing.10 If the couple is unable to conceive after a year of trying, it is recommended that they consult a reproductive specialist; the clinician can carry out a comprehensive evaluation and order a series of tests to identify the source of the problem, indicating whether there are alternative methods for helping the couple to start a family (addressing the underlying factors involved in infertility, or treating via assisted reproduction procedures, such as in vitro fertilization).11
Dr. Aman is faculty member at the biology department of City Colleges of Chicago, and a postdoctoral researcher at the International Maternal and Child Health Foundation (IMCHF). She disclosed no relevant financial relationships. Dr. Islam is a medical writer for the IMCHF, Montreal, is based in New York, and disclosed no relevant financial relationships. Mr. Choudhry is a research assistant at the IMCHF and he has no disclosures. Dr. Zia Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF. He has no disclosures.
References
1. Berry SD et al. J Am Geriatr Soc. 2021 May;69(5):1140-6.
2. Achua JK et al. World J Men’s Health. 2021 Jan;39(1):65-74.
3. Broderick JM. Urology Times. 2021 June.
4. Huang C et al. Andrology. 2021 Jan;9(1):80-7.
5. Sajjadi NB et al. J Osteopath Med. 2021 Apr 12;121(6):583-7.
6. Sallam M et al. Vaccines. 2021 Jan;9(1):42.
7. Islam MS et al. PloS One. 2021 May 12;16(5):e0251605.
8. Tesarik J. J Fertil Preserv. 2021;2:art246111.
9. Adiga SK et al. Reprod BioMed Online. 2020 Dec;41(6):991-7.
10. FAQs related to COVID-19. Q: If I get sick or test positive for COVID-19, when is it safe to become pregnant? American Society for Reproductive Medicine.
11. Cross C. Wellness and Prevention: Why can’t I get pregnant? John Hopkins Medicine.
Introduction
Amidst an aggressive vaccination campaign for COVID-19, misinformation has spread over the Internet, affecting public perception and making some people hesitant to participate in ongoing immunization campaigns. Of chief concern are issues pertaining to fertility or viability of sperm – information circulating on social networks posits that the coronavirus vaccine may influence infertility in men, which, according to physicians, is not grounded in reality. From the perspective of evidence-based medicine, there is a dearth of information suggesting an untoward effect of the vaccine on male fertility. The risk of adverse reactions arising from approved vaccines is negligible, with mild, albeit controllable, side effects demonstrated by patients in clinical trials. Therefore, there is no plausible reason for the general public to avoid vaccinations.1
Infertility following vaccination
The source of confusion can be traced back to a study conducted by researchers at the University of Miami Miller School of Medicine; the general public has conflated a side effect of the virus, namely, infertility and erectile dysfunction, with that of the vaccine.2 According to Ranjith Ramasamy, MD, director of the urology program at Miller, “We were the first to demonstrate that the COVID virus, itself, can affect male fertility and be a potential cause for erectile dysfunction. We are now the first to examine if there is any impact of the COVID vaccine on male fertility potential, which we did not find.”3
Coronavirus can indeed cause significant damage to the testicular tissue of infected men by means of mediating ACE2 expression on Leydig and Sertoli cells of the testis. It should be noted that COVID-19 may potentially attack any type of cell in the body that expresses the enzyme ACE2. However, it is particularly harmful to cells with high levels of expression of this enzyme, such as testicular cells. The spermatogenesis process can be affected, thereby posing a risk to male fertility.4
Expanding on the theme of fertility during the pandemic, a number of false claims5-7 about the vaccine and its overall effect on the placenta and fertility have also emerged as a contentious topic for debate on social media; doctors continue to explain why the theories are not reasonable or a cause for concern. The World Health Organization (WHO) provides recommendations on COVID-19 vaccinations for pregnant and/or lactating women and encourages a shared decision process involving risk/benefit assessment with the prescribing physician.5 Pregnant women, especially those with underlying comorbid conditions, are susceptible to developing severe symptom manifestations of COVID-19 with the disease also being associated with an increased likelihood of premature birth. As far as lactating women are concerned, the evidence thus far has indicated that the risk of side effects of the vaccine is very low, suggesting that these women could be vaccinated.5
The vaccine is the best option
While more studies are needed to ascertain the relationship between COVID-19 and male infertility, the vaccine is currently the best option for those who are concerned about their fertility from exposure to the coronavirus. Because of delayed wholesale acceptance of vaccines by the general population, clinicians should continue to emphasize the importance of preventive care with respect to disease exposure.6
In addition, those who are concerned with fertility can opt for ways to preserve their reproductive capacity, such as the removal of semen for freezing sperm, albeit with adherence to sperm-washing procedures to preclude cross-contamination from viruses.8,9 For the preservation of sperm, the noninvasive method is often performed, preferably collected in several samples. Then, the semen is cryopreserved.8 In some instances, the sperm can also be removed directly from the testicles with a simple needle or by means of a minor surgical procedure.
A wait and try approach is advocated by clinicians for individuals who have already experienced COVID-19 symptoms and are therefore concerned about the prospect of childbearing.10 If the couple is unable to conceive after a year of trying, it is recommended that they consult a reproductive specialist; the clinician can carry out a comprehensive evaluation and order a series of tests to identify the source of the problem, indicating whether there are alternative methods for helping the couple to start a family (addressing the underlying factors involved in infertility, or treating via assisted reproduction procedures, such as in vitro fertilization).11
Dr. Aman is faculty member at the biology department of City Colleges of Chicago, and a postdoctoral researcher at the International Maternal and Child Health Foundation (IMCHF). She disclosed no relevant financial relationships. Dr. Islam is a medical writer for the IMCHF, Montreal, is based in New York, and disclosed no relevant financial relationships. Mr. Choudhry is a research assistant at the IMCHF and he has no disclosures. Dr. Zia Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF. He has no disclosures.
References
1. Berry SD et al. J Am Geriatr Soc. 2021 May;69(5):1140-6.
2. Achua JK et al. World J Men’s Health. 2021 Jan;39(1):65-74.
3. Broderick JM. Urology Times. 2021 June.
4. Huang C et al. Andrology. 2021 Jan;9(1):80-7.
5. Sajjadi NB et al. J Osteopath Med. 2021 Apr 12;121(6):583-7.
6. Sallam M et al. Vaccines. 2021 Jan;9(1):42.
7. Islam MS et al. PloS One. 2021 May 12;16(5):e0251605.
8. Tesarik J. J Fertil Preserv. 2021;2:art246111.
9. Adiga SK et al. Reprod BioMed Online. 2020 Dec;41(6):991-7.
10. FAQs related to COVID-19. Q: If I get sick or test positive for COVID-19, when is it safe to become pregnant? American Society for Reproductive Medicine.
11. Cross C. Wellness and Prevention: Why can’t I get pregnant? John Hopkins Medicine.
Children and COVID: The Omicron surge has become a retreat
The Omicron decline continued for a fourth consecutive week as new cases of COVID-19 in children fell by 42% from the week before, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
That 42% represents a drop from the 299,000 new cases reported for Feb. 4-10 down to 174,000 for the most recent week, Feb. 11-17. 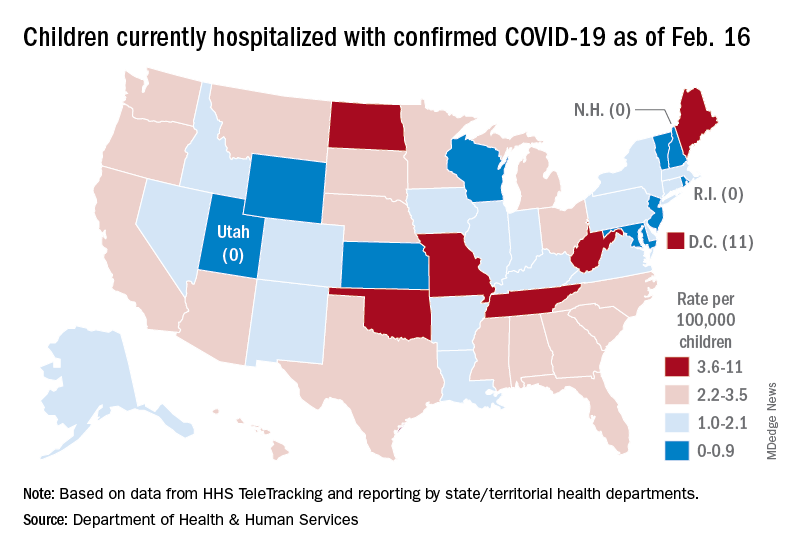
The overall count of COVID-19 cases in children is 12.5 million over the course of the pandemic, and that represents 19% of cases reported among all ages, the AAP and CHA said based on data collected from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
Hospital admissions also continued to fall, with the rate for children aged 0-17 at 0.43 per 100,000 population as of Feb. 20, down by almost 66% from the peak of 1.25 per 100,000 reached on Jan. 16, the Centers for Disease Control and Prevention reported.
A snapshot of the hospitalization situation shows that 1,687 children were occupying inpatient beds on Feb. 16, compared with 4,070 on Jan. 19, which appears to be the peak of the Omicron surge, according to data from the Department of Health & Human Services.
The state with the highest rate – 5.6 per 100,000 children – on Feb. 16 was North Dakota, although the District of Columbia came in at 11.0 per 100,000. They were followed by Oklahoma (5.3), Missouri (5.2), and West Virginia (4.1). There were three states – New Hampshire, Rhode Island, and Utah – with no children in the hospital on that date, the HHS said.
New vaccinations in children aged 5-11 years, which declined in mid- and late January, even as Omicron surged, continued to decline, as did vaccine completions. Vaccinations also fell among children aged 12-17 for the latest reporting week, Feb. 10-16, the AAP said in a separate report.
As more states and school districts drop mask mandates, data from the CDC indicate that 32.5% of 5- to 11-year olds and 67.4% of 12- to 17-year-olds have gotten at least one dose of the COVID-19 vaccine and that 25.1% and 57.3%, respectively, are fully vaccinated. Meanwhile, 20.5% of those fully vaccinated 12- to 17-year-olds have gotten a booster dose, the CDC said.
The Omicron decline continued for a fourth consecutive week as new cases of COVID-19 in children fell by 42% from the week before, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
That 42% represents a drop from the 299,000 new cases reported for Feb. 4-10 down to 174,000 for the most recent week, Feb. 11-17. 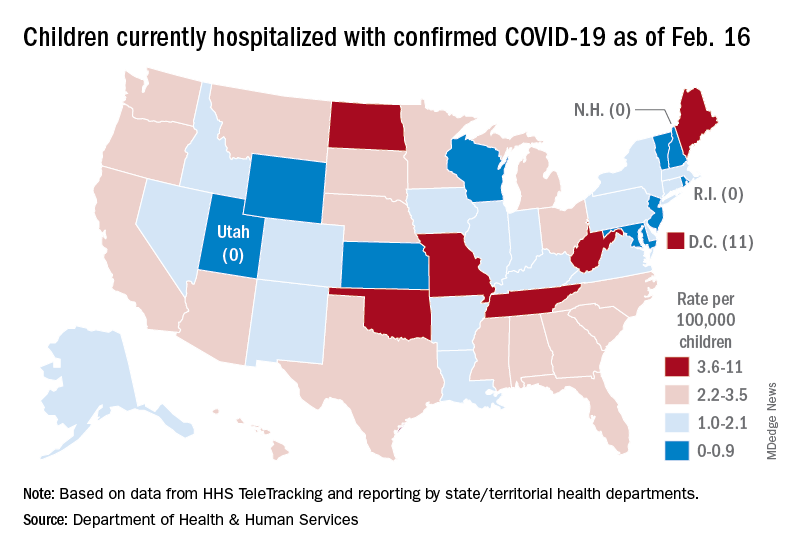
The overall count of COVID-19 cases in children is 12.5 million over the course of the pandemic, and that represents 19% of cases reported among all ages, the AAP and CHA said based on data collected from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
Hospital admissions also continued to fall, with the rate for children aged 0-17 at 0.43 per 100,000 population as of Feb. 20, down by almost 66% from the peak of 1.25 per 100,000 reached on Jan. 16, the Centers for Disease Control and Prevention reported.
A snapshot of the hospitalization situation shows that 1,687 children were occupying inpatient beds on Feb. 16, compared with 4,070 on Jan. 19, which appears to be the peak of the Omicron surge, according to data from the Department of Health & Human Services.
The state with the highest rate – 5.6 per 100,000 children – on Feb. 16 was North Dakota, although the District of Columbia came in at 11.0 per 100,000. They were followed by Oklahoma (5.3), Missouri (5.2), and West Virginia (4.1). There were three states – New Hampshire, Rhode Island, and Utah – with no children in the hospital on that date, the HHS said.
New vaccinations in children aged 5-11 years, which declined in mid- and late January, even as Omicron surged, continued to decline, as did vaccine completions. Vaccinations also fell among children aged 12-17 for the latest reporting week, Feb. 10-16, the AAP said in a separate report.
As more states and school districts drop mask mandates, data from the CDC indicate that 32.5% of 5- to 11-year olds and 67.4% of 12- to 17-year-olds have gotten at least one dose of the COVID-19 vaccine and that 25.1% and 57.3%, respectively, are fully vaccinated. Meanwhile, 20.5% of those fully vaccinated 12- to 17-year-olds have gotten a booster dose, the CDC said.
The Omicron decline continued for a fourth consecutive week as new cases of COVID-19 in children fell by 42% from the week before, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
That 42% represents a drop from the 299,000 new cases reported for Feb. 4-10 down to 174,000 for the most recent week, Feb. 11-17. 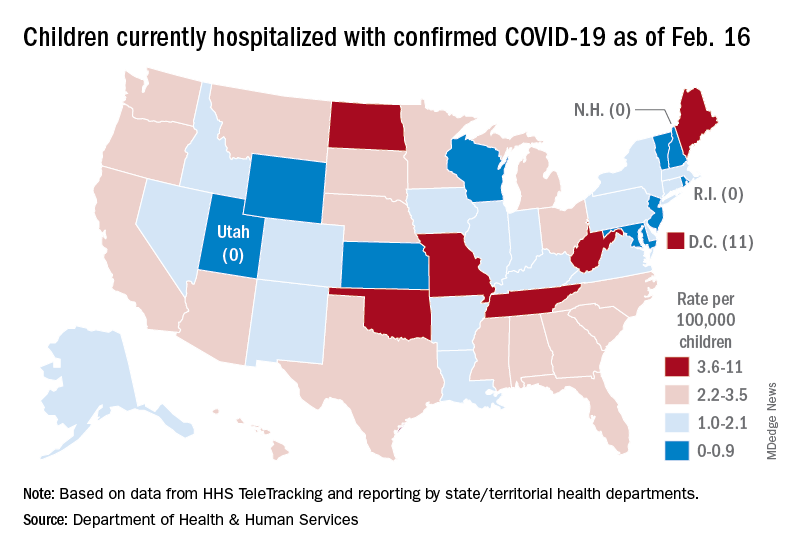
The overall count of COVID-19 cases in children is 12.5 million over the course of the pandemic, and that represents 19% of cases reported among all ages, the AAP and CHA said based on data collected from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
Hospital admissions also continued to fall, with the rate for children aged 0-17 at 0.43 per 100,000 population as of Feb. 20, down by almost 66% from the peak of 1.25 per 100,000 reached on Jan. 16, the Centers for Disease Control and Prevention reported.
A snapshot of the hospitalization situation shows that 1,687 children were occupying inpatient beds on Feb. 16, compared with 4,070 on Jan. 19, which appears to be the peak of the Omicron surge, according to data from the Department of Health & Human Services.
The state with the highest rate – 5.6 per 100,000 children – on Feb. 16 was North Dakota, although the District of Columbia came in at 11.0 per 100,000. They were followed by Oklahoma (5.3), Missouri (5.2), and West Virginia (4.1). There were three states – New Hampshire, Rhode Island, and Utah – with no children in the hospital on that date, the HHS said.
New vaccinations in children aged 5-11 years, which declined in mid- and late January, even as Omicron surged, continued to decline, as did vaccine completions. Vaccinations also fell among children aged 12-17 for the latest reporting week, Feb. 10-16, the AAP said in a separate report.
As more states and school districts drop mask mandates, data from the CDC indicate that 32.5% of 5- to 11-year olds and 67.4% of 12- to 17-year-olds have gotten at least one dose of the COVID-19 vaccine and that 25.1% and 57.3%, respectively, are fully vaccinated. Meanwhile, 20.5% of those fully vaccinated 12- to 17-year-olds have gotten a booster dose, the CDC said.
New MIS-C guidance addresses diagnostic challenges, cardiac care
Updated guidance for health care providers on multisystem inflammatory syndrome in children (MIS-C) recognizes the evolving nature of the disease and offers strategies for pediatric rheumatologists, who also may be asked to recommend treatment for hyperinflammation in children with acute COVID-19.
Guidance is needed for many reasons, including the variable case definitions for MIS-C, the presence of MIS-C features in other infections and childhood rheumatic diseases, the extrapolation of treatment strategies from other conditions with similar presentations, and the issue of myocardial dysfunction, wrote Lauren A. Henderson, MD, MMSC, of Boston Children’s Hospital, and members of the American College of Rheumatology MIS-C and COVID-19–Related Hyperinflammation Task Force.
However, “modifications to treatment plans, particularly in patients with complex conditions, are highly disease, patient, geography, and time specific, and therefore must be individualized as part of a shared decision-making process,” the authors said. The updated guidance was published in Arthritis & Rheumatology.
Update needed in wake of Omicron
“We continue to see cases of MIS-C across the United States due to the spike in SARS-CoV-2 infections from the Omicron variant,” and therefore updated guidance is important at this time, Dr. Henderson told this news organization.
“MIS-C remains a serious complication of COVID-19 in children and the ACR wanted to continue to provide pediatricians with up-to-date recommendations for the management of MIS-C,” she said.
“Children began to present with MIS-C in April 2020. At that time, little was known about this entity. Most of the recommendations in the first version of the MIS-C guidance were based on expert opinion,” she explained. However, “over the last 2 years, pediatricians have worked very hard to conduct high-quality research studies to better understand MIS-C, so we now have more scientific evidence to guide our recommendations.
“In version three of the MIS-C guidance, there are new recommendations on treatment. Previously, it was unclear what medications should be used for first-line treatment in patients with MIS-C. Some children were given intravenous immunoglobulin while others were given IVIg and steroids together. Several new studies show that children with MIS-C who are treated with a combination of IVIg and steroids have better outcomes. Accordingly, the MIS-C guidance now recommends dual therapy with IVIg and steroids in children with MIS-C.”
Diagnostic evaluation
The guidance calls for maintaining a broad differential diagnosis of MIS-C, given that the condition remains rare, and that most children with COVID-19 present with mild symptoms and have excellent outcomes, the authors noted. The range of clinical features associated with MIS-C include fever, mucocutaneous findings, myocardial dysfunction, cardiac conduction abnormalities, shock, gastrointestinal symptoms, and lymphadenopathy.
Some patients also experience neurologic involvement in the form of severe headache, altered mental status, seizures, cranial nerve palsies, meningismus, cerebral edema, and ischemic or hemorrhagic stroke. Given the nonspecific nature of these symptoms, “it is imperative that a diagnostic evaluation for MIS-C include investigation for other possible causes, as deemed appropriate by the treating provider,” the authors emphasized. Other diagnostic considerations include the prevalence and chronology of COVID-19 in the community, which may change over time.
MIS-C and Kawasaki disease phenotypes
Earlier in the pandemic, when MIS-C first emerged, it was compared with Kawasaki disease (KD). “However, a closer examination of the literature shows that only about one-quarter to half of patients with a reported diagnosis of MIS-C meet the full diagnostic criteria for KD,” the authors wrote. Key features that separate MIS-C from KD include the greater incidence of KD among children in Japan and East Asia versus the higher incidence of MIS-C among non-Hispanic Black children. In addition, children with MIS-C have shown a wider age range, more prominent gastrointestinal and neurologic symptoms, and more frequent cardiac dysfunction, compared with those with KD.
Cardiac management
Close follow-up with cardiology is essential for children with MIS-C, according to the authors. The recommendations call for repeat echocardiograms for all children with MIS-C at a minimum of 7-14 days, then again at 4-6 weeks after the initial presentation. The authors also recommended additional echocardiograms for children with left ventricular dysfunction and cardiac aortic aneurysms.
MIS-C treatment
Current treatment recommendations emphasize that patients under investigation for MIS-C with life-threatening manifestations may need immunomodulatory therapy before a full diagnostic evaluation is complete, the authors said. However, patients without life-threatening manifestations should be evaluated before starting immunomodulatory treatment to avoid potentially harmful therapies for pediatric patients who don’t need them.
When MIS-C is refractory to initial immunomodulatory treatment, a second dose of IVIg is not recommended, but intensification therapy is advised with either high-dose (10-30 mg/kg per day) glucocorticoids, anakinra, or infliximab. However, there is little evidence available for selecting a specific agent for intensification therapy.
The task force also advises giving low-dose aspirin (3-5 mg/kg per day, up to 81 mg once daily) to all MIS-C patients without active bleeding or significant bleeding risk until normalization of the platelet count and confirmed normal coronary arteries at least 4 weeks after diagnosis.
COVID-19 and hyperinflammation
The task force also noted a distinction between MIS-C and severe COVID-19 in children. Although many children with MIS-C are previously healthy, most children who develop severe COVID-19 during an initial infection have complex conditions or comorbidities such as developmental delay or genetic anomaly, or chronic conditions such as congenital heart disease, type 1 diabetes, or asthma, the authors said. They recommend that “hospitalized children with COVID-19 requiring supplemental oxygen or respiratory support should be considered for immunomodulatory therapy in addition to supportive care and antiviral medications.”
The authors acknowledged the limitations and evolving nature of the recommendations, which will continue to change and do not replace clinical judgment for the management of individual patients. In the meantime, the ACR will support the task force in reviewing new evidence and providing revised versions of the current document.
Many questions about MIS-C remain, Dr. Henderson said in an interview. “It can be very hard to diagnose children with MIS-C because many of the symptoms are similar to those seen in other febrile illness of childhood. We need to identify better biomarkers to help us make the diagnosis of MIS-C. In addition, we need studies to provide information about what treatments should be used if children fail to respond to IVIg and steroids. Finally, it appears that vaccination [against SARS-CoV-2] protects against severe forms of MIS-C, and studies are needed to see how vaccination protects children from MIS-C.”
The development of the guidance was supported by the American College of Rheumatology. Dr. Henderson disclosed relationships with companies including Sobi, Pfizer, and Adaptive Biotechnologies (less than $10,000) and research support from the Childhood Arthritis and Rheumatology Research Alliance and research grant support from Bristol-Myers Squibb.
A version of this article first appeared on Medscape.com.
Updated guidance for health care providers on multisystem inflammatory syndrome in children (MIS-C) recognizes the evolving nature of the disease and offers strategies for pediatric rheumatologists, who also may be asked to recommend treatment for hyperinflammation in children with acute COVID-19.
Guidance is needed for many reasons, including the variable case definitions for MIS-C, the presence of MIS-C features in other infections and childhood rheumatic diseases, the extrapolation of treatment strategies from other conditions with similar presentations, and the issue of myocardial dysfunction, wrote Lauren A. Henderson, MD, MMSC, of Boston Children’s Hospital, and members of the American College of Rheumatology MIS-C and COVID-19–Related Hyperinflammation Task Force.
However, “modifications to treatment plans, particularly in patients with complex conditions, are highly disease, patient, geography, and time specific, and therefore must be individualized as part of a shared decision-making process,” the authors said. The updated guidance was published in Arthritis & Rheumatology.
Update needed in wake of Omicron
“We continue to see cases of MIS-C across the United States due to the spike in SARS-CoV-2 infections from the Omicron variant,” and therefore updated guidance is important at this time, Dr. Henderson told this news organization.
“MIS-C remains a serious complication of COVID-19 in children and the ACR wanted to continue to provide pediatricians with up-to-date recommendations for the management of MIS-C,” she said.
“Children began to present with MIS-C in April 2020. At that time, little was known about this entity. Most of the recommendations in the first version of the MIS-C guidance were based on expert opinion,” she explained. However, “over the last 2 years, pediatricians have worked very hard to conduct high-quality research studies to better understand MIS-C, so we now have more scientific evidence to guide our recommendations.
“In version three of the MIS-C guidance, there are new recommendations on treatment. Previously, it was unclear what medications should be used for first-line treatment in patients with MIS-C. Some children were given intravenous immunoglobulin while others were given IVIg and steroids together. Several new studies show that children with MIS-C who are treated with a combination of IVIg and steroids have better outcomes. Accordingly, the MIS-C guidance now recommends dual therapy with IVIg and steroids in children with MIS-C.”
Diagnostic evaluation
The guidance calls for maintaining a broad differential diagnosis of MIS-C, given that the condition remains rare, and that most children with COVID-19 present with mild symptoms and have excellent outcomes, the authors noted. The range of clinical features associated with MIS-C include fever, mucocutaneous findings, myocardial dysfunction, cardiac conduction abnormalities, shock, gastrointestinal symptoms, and lymphadenopathy.
Some patients also experience neurologic involvement in the form of severe headache, altered mental status, seizures, cranial nerve palsies, meningismus, cerebral edema, and ischemic or hemorrhagic stroke. Given the nonspecific nature of these symptoms, “it is imperative that a diagnostic evaluation for MIS-C include investigation for other possible causes, as deemed appropriate by the treating provider,” the authors emphasized. Other diagnostic considerations include the prevalence and chronology of COVID-19 in the community, which may change over time.
MIS-C and Kawasaki disease phenotypes
Earlier in the pandemic, when MIS-C first emerged, it was compared with Kawasaki disease (KD). “However, a closer examination of the literature shows that only about one-quarter to half of patients with a reported diagnosis of MIS-C meet the full diagnostic criteria for KD,” the authors wrote. Key features that separate MIS-C from KD include the greater incidence of KD among children in Japan and East Asia versus the higher incidence of MIS-C among non-Hispanic Black children. In addition, children with MIS-C have shown a wider age range, more prominent gastrointestinal and neurologic symptoms, and more frequent cardiac dysfunction, compared with those with KD.
Cardiac management
Close follow-up with cardiology is essential for children with MIS-C, according to the authors. The recommendations call for repeat echocardiograms for all children with MIS-C at a minimum of 7-14 days, then again at 4-6 weeks after the initial presentation. The authors also recommended additional echocardiograms for children with left ventricular dysfunction and cardiac aortic aneurysms.
MIS-C treatment
Current treatment recommendations emphasize that patients under investigation for MIS-C with life-threatening manifestations may need immunomodulatory therapy before a full diagnostic evaluation is complete, the authors said. However, patients without life-threatening manifestations should be evaluated before starting immunomodulatory treatment to avoid potentially harmful therapies for pediatric patients who don’t need them.
When MIS-C is refractory to initial immunomodulatory treatment, a second dose of IVIg is not recommended, but intensification therapy is advised with either high-dose (10-30 mg/kg per day) glucocorticoids, anakinra, or infliximab. However, there is little evidence available for selecting a specific agent for intensification therapy.
The task force also advises giving low-dose aspirin (3-5 mg/kg per day, up to 81 mg once daily) to all MIS-C patients without active bleeding or significant bleeding risk until normalization of the platelet count and confirmed normal coronary arteries at least 4 weeks after diagnosis.
COVID-19 and hyperinflammation
The task force also noted a distinction between MIS-C and severe COVID-19 in children. Although many children with MIS-C are previously healthy, most children who develop severe COVID-19 during an initial infection have complex conditions or comorbidities such as developmental delay or genetic anomaly, or chronic conditions such as congenital heart disease, type 1 diabetes, or asthma, the authors said. They recommend that “hospitalized children with COVID-19 requiring supplemental oxygen or respiratory support should be considered for immunomodulatory therapy in addition to supportive care and antiviral medications.”
The authors acknowledged the limitations and evolving nature of the recommendations, which will continue to change and do not replace clinical judgment for the management of individual patients. In the meantime, the ACR will support the task force in reviewing new evidence and providing revised versions of the current document.
Many questions about MIS-C remain, Dr. Henderson said in an interview. “It can be very hard to diagnose children with MIS-C because many of the symptoms are similar to those seen in other febrile illness of childhood. We need to identify better biomarkers to help us make the diagnosis of MIS-C. In addition, we need studies to provide information about what treatments should be used if children fail to respond to IVIg and steroids. Finally, it appears that vaccination [against SARS-CoV-2] protects against severe forms of MIS-C, and studies are needed to see how vaccination protects children from MIS-C.”
The development of the guidance was supported by the American College of Rheumatology. Dr. Henderson disclosed relationships with companies including Sobi, Pfizer, and Adaptive Biotechnologies (less than $10,000) and research support from the Childhood Arthritis and Rheumatology Research Alliance and research grant support from Bristol-Myers Squibb.
A version of this article first appeared on Medscape.com.
Updated guidance for health care providers on multisystem inflammatory syndrome in children (MIS-C) recognizes the evolving nature of the disease and offers strategies for pediatric rheumatologists, who also may be asked to recommend treatment for hyperinflammation in children with acute COVID-19.
Guidance is needed for many reasons, including the variable case definitions for MIS-C, the presence of MIS-C features in other infections and childhood rheumatic diseases, the extrapolation of treatment strategies from other conditions with similar presentations, and the issue of myocardial dysfunction, wrote Lauren A. Henderson, MD, MMSC, of Boston Children’s Hospital, and members of the American College of Rheumatology MIS-C and COVID-19–Related Hyperinflammation Task Force.
However, “modifications to treatment plans, particularly in patients with complex conditions, are highly disease, patient, geography, and time specific, and therefore must be individualized as part of a shared decision-making process,” the authors said. The updated guidance was published in Arthritis & Rheumatology.
Update needed in wake of Omicron
“We continue to see cases of MIS-C across the United States due to the spike in SARS-CoV-2 infections from the Omicron variant,” and therefore updated guidance is important at this time, Dr. Henderson told this news organization.
“MIS-C remains a serious complication of COVID-19 in children and the ACR wanted to continue to provide pediatricians with up-to-date recommendations for the management of MIS-C,” she said.
“Children began to present with MIS-C in April 2020. At that time, little was known about this entity. Most of the recommendations in the first version of the MIS-C guidance were based on expert opinion,” she explained. However, “over the last 2 years, pediatricians have worked very hard to conduct high-quality research studies to better understand MIS-C, so we now have more scientific evidence to guide our recommendations.
“In version three of the MIS-C guidance, there are new recommendations on treatment. Previously, it was unclear what medications should be used for first-line treatment in patients with MIS-C. Some children were given intravenous immunoglobulin while others were given IVIg and steroids together. Several new studies show that children with MIS-C who are treated with a combination of IVIg and steroids have better outcomes. Accordingly, the MIS-C guidance now recommends dual therapy with IVIg and steroids in children with MIS-C.”
Diagnostic evaluation
The guidance calls for maintaining a broad differential diagnosis of MIS-C, given that the condition remains rare, and that most children with COVID-19 present with mild symptoms and have excellent outcomes, the authors noted. The range of clinical features associated with MIS-C include fever, mucocutaneous findings, myocardial dysfunction, cardiac conduction abnormalities, shock, gastrointestinal symptoms, and lymphadenopathy.
Some patients also experience neurologic involvement in the form of severe headache, altered mental status, seizures, cranial nerve palsies, meningismus, cerebral edema, and ischemic or hemorrhagic stroke. Given the nonspecific nature of these symptoms, “it is imperative that a diagnostic evaluation for MIS-C include investigation for other possible causes, as deemed appropriate by the treating provider,” the authors emphasized. Other diagnostic considerations include the prevalence and chronology of COVID-19 in the community, which may change over time.
MIS-C and Kawasaki disease phenotypes
Earlier in the pandemic, when MIS-C first emerged, it was compared with Kawasaki disease (KD). “However, a closer examination of the literature shows that only about one-quarter to half of patients with a reported diagnosis of MIS-C meet the full diagnostic criteria for KD,” the authors wrote. Key features that separate MIS-C from KD include the greater incidence of KD among children in Japan and East Asia versus the higher incidence of MIS-C among non-Hispanic Black children. In addition, children with MIS-C have shown a wider age range, more prominent gastrointestinal and neurologic symptoms, and more frequent cardiac dysfunction, compared with those with KD.
Cardiac management
Close follow-up with cardiology is essential for children with MIS-C, according to the authors. The recommendations call for repeat echocardiograms for all children with MIS-C at a minimum of 7-14 days, then again at 4-6 weeks after the initial presentation. The authors also recommended additional echocardiograms for children with left ventricular dysfunction and cardiac aortic aneurysms.
MIS-C treatment
Current treatment recommendations emphasize that patients under investigation for MIS-C with life-threatening manifestations may need immunomodulatory therapy before a full diagnostic evaluation is complete, the authors said. However, patients without life-threatening manifestations should be evaluated before starting immunomodulatory treatment to avoid potentially harmful therapies for pediatric patients who don’t need them.
When MIS-C is refractory to initial immunomodulatory treatment, a second dose of IVIg is not recommended, but intensification therapy is advised with either high-dose (10-30 mg/kg per day) glucocorticoids, anakinra, or infliximab. However, there is little evidence available for selecting a specific agent for intensification therapy.
The task force also advises giving low-dose aspirin (3-5 mg/kg per day, up to 81 mg once daily) to all MIS-C patients without active bleeding or significant bleeding risk until normalization of the platelet count and confirmed normal coronary arteries at least 4 weeks after diagnosis.
COVID-19 and hyperinflammation
The task force also noted a distinction between MIS-C and severe COVID-19 in children. Although many children with MIS-C are previously healthy, most children who develop severe COVID-19 during an initial infection have complex conditions or comorbidities such as developmental delay or genetic anomaly, or chronic conditions such as congenital heart disease, type 1 diabetes, or asthma, the authors said. They recommend that “hospitalized children with COVID-19 requiring supplemental oxygen or respiratory support should be considered for immunomodulatory therapy in addition to supportive care and antiviral medications.”
The authors acknowledged the limitations and evolving nature of the recommendations, which will continue to change and do not replace clinical judgment for the management of individual patients. In the meantime, the ACR will support the task force in reviewing new evidence and providing revised versions of the current document.
Many questions about MIS-C remain, Dr. Henderson said in an interview. “It can be very hard to diagnose children with MIS-C because many of the symptoms are similar to those seen in other febrile illness of childhood. We need to identify better biomarkers to help us make the diagnosis of MIS-C. In addition, we need studies to provide information about what treatments should be used if children fail to respond to IVIg and steroids. Finally, it appears that vaccination [against SARS-CoV-2] protects against severe forms of MIS-C, and studies are needed to see how vaccination protects children from MIS-C.”
The development of the guidance was supported by the American College of Rheumatology. Dr. Henderson disclosed relationships with companies including Sobi, Pfizer, and Adaptive Biotechnologies (less than $10,000) and research support from the Childhood Arthritis and Rheumatology Research Alliance and research grant support from Bristol-Myers Squibb.
A version of this article first appeared on Medscape.com.
FROM ARTHRITIS AND RHEUMATOLOGY
Subvariant may be more dangerous than original Omicron strain
, a lab study from Japan says.
“Our multiscale investigations suggest that the risk of BA.2 for global health is potentially higher than that of BA.1,” the researchers said in the study published on the preprint server bioRxiv. The study has not been peer-reviewed.
The researchers infected hamsters with BA.1 and BA.2. The hamsters infected with BA.2 got sicker, with more lung damage and loss of body weight. Results were similar when mice were infected with BA.1 and BA.2.
“Infection experiments using hamsters show that BA.2 is more pathogenic than BA.1,” the study said.
BA.1 and BA.2 both appear to evade immunity created by COVID-19 vaccines, the study said. But a booster shot makes illness after infection 74% less likely, CNN said.
What’s more, therapeutic monoclonal antibodies used to treat people infected with COVID didn’t have much effect on BA.2.
BA.2 was “almost completely resistant” to casirivimab and imdevimab and was 35 times more resistant to sotrovimab, compared to the original B.1.1 virus, the researchers wrote.
“In summary, our data suggest the possibility that BA.2 would be the most concerned variant to global health,” the researchers wrote. “Currently, both BA.2 and BA.1 are recognised together as Omicron and these are almost undistinguishable. Based on our findings, we propose that BA.2 should be recognised as a unique variant of concern, and this SARS-CoV-2 variant should be monitored in depth.”
If the World Health Organization recognized BA.2 as a “unique variant of concern,” it would be given its own Greek letter.
But some scientists noted that findings in the lab don’t always reflect what’s happening in the real world of people.
“I think it’s always hard to translate differences in animal and cell culture models to what’s going on with regards to human disease,” Jeremy Kamil, PhD, an associate professor of microbiology and immunology at Louisiana State University Health Shreveport, told Newsweek. “That said, the differences do look real.”
“It might be, from a human’s perspective, a worse virus than BA.1 and might be able to transmit better and cause worse disease,” Daniel Rhoads, MD, section head of microbiology at the Cleveland Clinic in Ohio, told CNN. He reviewed the Japanese study but was not involved in it.
Another scientist who reviewed the study but was not involved in the research noted that human immune systems are evolving along with the COVID variants.
“One of the caveats that we have to think about, as we get new variants that might seem more dangerous, is the fact that there’s two sides to the story,” Deborah Fuller, PhD, a virologist at the University of Washington School of Medicine, told CNN. “Our immune system is evolving as well. And so that’s pushing back on things.”
Scientists have already established that BA.2 is more transmissible than BA.1. The Omicron subvariant has been detected in 74 countries and 47 U.S. states, according to CNN. About 4% of Americans with COVID were infected with BA.2, the outlet reported, citing the CDC, but it’s now the dominant strain in other nations.
It’s not clear yet if BA.2 causes more severe illness in people. While BA.2 spreads faster than BA.1, there’s no evidence the subvariant makes people any sicker, an official with the World Health Organization said, according to CNBC.
A version of this article first appeared on WebMD.com.
, a lab study from Japan says.
“Our multiscale investigations suggest that the risk of BA.2 for global health is potentially higher than that of BA.1,” the researchers said in the study published on the preprint server bioRxiv. The study has not been peer-reviewed.
The researchers infected hamsters with BA.1 and BA.2. The hamsters infected with BA.2 got sicker, with more lung damage and loss of body weight. Results were similar when mice were infected with BA.1 and BA.2.
“Infection experiments using hamsters show that BA.2 is more pathogenic than BA.1,” the study said.
BA.1 and BA.2 both appear to evade immunity created by COVID-19 vaccines, the study said. But a booster shot makes illness after infection 74% less likely, CNN said.
What’s more, therapeutic monoclonal antibodies used to treat people infected with COVID didn’t have much effect on BA.2.
BA.2 was “almost completely resistant” to casirivimab and imdevimab and was 35 times more resistant to sotrovimab, compared to the original B.1.1 virus, the researchers wrote.
“In summary, our data suggest the possibility that BA.2 would be the most concerned variant to global health,” the researchers wrote. “Currently, both BA.2 and BA.1 are recognised together as Omicron and these are almost undistinguishable. Based on our findings, we propose that BA.2 should be recognised as a unique variant of concern, and this SARS-CoV-2 variant should be monitored in depth.”
If the World Health Organization recognized BA.2 as a “unique variant of concern,” it would be given its own Greek letter.
But some scientists noted that findings in the lab don’t always reflect what’s happening in the real world of people.
“I think it’s always hard to translate differences in animal and cell culture models to what’s going on with regards to human disease,” Jeremy Kamil, PhD, an associate professor of microbiology and immunology at Louisiana State University Health Shreveport, told Newsweek. “That said, the differences do look real.”
“It might be, from a human’s perspective, a worse virus than BA.1 and might be able to transmit better and cause worse disease,” Daniel Rhoads, MD, section head of microbiology at the Cleveland Clinic in Ohio, told CNN. He reviewed the Japanese study but was not involved in it.
Another scientist who reviewed the study but was not involved in the research noted that human immune systems are evolving along with the COVID variants.
“One of the caveats that we have to think about, as we get new variants that might seem more dangerous, is the fact that there’s two sides to the story,” Deborah Fuller, PhD, a virologist at the University of Washington School of Medicine, told CNN. “Our immune system is evolving as well. And so that’s pushing back on things.”
Scientists have already established that BA.2 is more transmissible than BA.1. The Omicron subvariant has been detected in 74 countries and 47 U.S. states, according to CNN. About 4% of Americans with COVID were infected with BA.2, the outlet reported, citing the CDC, but it’s now the dominant strain in other nations.
It’s not clear yet if BA.2 causes more severe illness in people. While BA.2 spreads faster than BA.1, there’s no evidence the subvariant makes people any sicker, an official with the World Health Organization said, according to CNBC.
A version of this article first appeared on WebMD.com.
, a lab study from Japan says.
“Our multiscale investigations suggest that the risk of BA.2 for global health is potentially higher than that of BA.1,” the researchers said in the study published on the preprint server bioRxiv. The study has not been peer-reviewed.
The researchers infected hamsters with BA.1 and BA.2. The hamsters infected with BA.2 got sicker, with more lung damage and loss of body weight. Results were similar when mice were infected with BA.1 and BA.2.
“Infection experiments using hamsters show that BA.2 is more pathogenic than BA.1,” the study said.
BA.1 and BA.2 both appear to evade immunity created by COVID-19 vaccines, the study said. But a booster shot makes illness after infection 74% less likely, CNN said.
What’s more, therapeutic monoclonal antibodies used to treat people infected with COVID didn’t have much effect on BA.2.
BA.2 was “almost completely resistant” to casirivimab and imdevimab and was 35 times more resistant to sotrovimab, compared to the original B.1.1 virus, the researchers wrote.
“In summary, our data suggest the possibility that BA.2 would be the most concerned variant to global health,” the researchers wrote. “Currently, both BA.2 and BA.1 are recognised together as Omicron and these are almost undistinguishable. Based on our findings, we propose that BA.2 should be recognised as a unique variant of concern, and this SARS-CoV-2 variant should be monitored in depth.”
If the World Health Organization recognized BA.2 as a “unique variant of concern,” it would be given its own Greek letter.
But some scientists noted that findings in the lab don’t always reflect what’s happening in the real world of people.
“I think it’s always hard to translate differences in animal and cell culture models to what’s going on with regards to human disease,” Jeremy Kamil, PhD, an associate professor of microbiology and immunology at Louisiana State University Health Shreveport, told Newsweek. “That said, the differences do look real.”
“It might be, from a human’s perspective, a worse virus than BA.1 and might be able to transmit better and cause worse disease,” Daniel Rhoads, MD, section head of microbiology at the Cleveland Clinic in Ohio, told CNN. He reviewed the Japanese study but was not involved in it.
Another scientist who reviewed the study but was not involved in the research noted that human immune systems are evolving along with the COVID variants.
“One of the caveats that we have to think about, as we get new variants that might seem more dangerous, is the fact that there’s two sides to the story,” Deborah Fuller, PhD, a virologist at the University of Washington School of Medicine, told CNN. “Our immune system is evolving as well. And so that’s pushing back on things.”
Scientists have already established that BA.2 is more transmissible than BA.1. The Omicron subvariant has been detected in 74 countries and 47 U.S. states, according to CNN. About 4% of Americans with COVID were infected with BA.2, the outlet reported, citing the CDC, but it’s now the dominant strain in other nations.
It’s not clear yet if BA.2 causes more severe illness in people. While BA.2 spreads faster than BA.1, there’s no evidence the subvariant makes people any sicker, an official with the World Health Organization said, according to CNBC.
A version of this article first appeared on WebMD.com.
Two factors linked to higher risk of long COVID in IBD
Two features are significantly associated with a higher risk for developing long COVID symptoms among people with inflammatory bowel disease (IBD), according to a large Danish population study.
People with Crohn’s disease (CD) who experienced adverse acute COVID-19, defined as requiring hospitalization, were nearly three times more likely to report persistent symptoms 12 weeks after acute infection.
“Long-term, persisting symptoms following COVID-19 is a frequently occurring problem, which is probably underappreciated. IBD specialists should therefore be aware of any of these symptoms and actively ask patients whether they have these problems,” lead author Mohamed Attauabi, MD, PhD, said in an interview.
Dr. Attauabi and colleagues also found that people with ulcerative colitis (UC) who discontinued immunosuppressive agents because of COVID-19 were 1.5 times more likely to experience long COVID symptoms, a result that surprised the researchers.
“This has not been shown before and remains to be confirmed,” said Dr. Attauabi, a fellow in the department of gastroenterology at Herlev Hospital at the University of Copenhagen.
Attauabi presented the results as a digital oral presentation at the 17th congress of the European Crohn’s and Colitis Organisation.
A closer look at IBD and COVID-19
Large, hospital-based studies of symptoms consistent with long COVID reveal a high prevalence of fatigue, sleep difficulties, and anxiety at 12 weeks or more post acute infection. However, these were not specific to people with CD or UC, Dr. Attauabi said.
“In patients with IBD, the risk of long-term sequelae of COVID-19 remains to be investigated,” he said.
Dr. Attauabi and colleagues studied 197 people with CD and 319 with UC, all of whom had polymerase chain reaction–confirmed COVID-19. Participants were prospectively enrolled in the population-based Danish IBD-COVID registry from January 28, 2020 to April 1, 2021. At a median of 5.1 months, a subset of 85 people with CD and 137 with UC agreed to report any post-COVID symptoms.
Older age, smoking, IBD disease activity, and presence of comorbidities were not associated with a significantly elevated risk of long COVID.
In a multivariate analysis, hospitalization for COVID-19 among people with CD was significantly associated with long COVID (odds ratio, 2.76; 95% confidence interval, 1.05-3.90; P = .04).
Furthermore, people with UC who stopped taking immunosuppressive agents also had a significantly higher risk (OR, 1.50; 95% CI, 1.07-10.22; P = .01).
“However, IBD medications such as systemic steroids were not associated with this outcome,” Dr. Attauabi said.
Fatigue most common long COVID symptom
Fatigue was the most common long COVID symptom, reported by 37% of patients with CD and 36% with UC.
Anosmia and ageusia were also common, reported by 29% and 28% of patients with CD, and 27% and 19% of those with UC, respectively.
“In our cohort of patients with UC or CD who developed COVID-19, the long-term health effects of COVID-19 did not appear to differ among patients with UC or CD nor according to IBD medications,” Dr. Attauabi said.
That is a “great study,” said session cochair Torsten Kucharzik, MD, PhD, head of internal medicine and gastroenterology at Lueneburg (Germany) Hospital.
When Dr. Kucharzik asked about smoking, Dr. Attauabi responded that they collected information on current and previous smoking, but they chose not to include the data because it was not statistically significant.
Dr. Attauabi has reported no relevant financial relationships. Dr. Kucharzik has reported receiving grants from Takeda and personal fees from companies including MSD/Essex, AbbVie, Falk Foundation, Biogen, Bristol-Myers Squibb, Arena, Celgene, Celltrion, Ferring, Janssen, Galapagos, Olympus, Mundipharma, Takeda, Amgen, Pfizer, Roche, and Vifor Pharma.
A version of this article first appeared on Medscape.com.
Two features are significantly associated with a higher risk for developing long COVID symptoms among people with inflammatory bowel disease (IBD), according to a large Danish population study.
People with Crohn’s disease (CD) who experienced adverse acute COVID-19, defined as requiring hospitalization, were nearly three times more likely to report persistent symptoms 12 weeks after acute infection.
“Long-term, persisting symptoms following COVID-19 is a frequently occurring problem, which is probably underappreciated. IBD specialists should therefore be aware of any of these symptoms and actively ask patients whether they have these problems,” lead author Mohamed Attauabi, MD, PhD, said in an interview.
Dr. Attauabi and colleagues also found that people with ulcerative colitis (UC) who discontinued immunosuppressive agents because of COVID-19 were 1.5 times more likely to experience long COVID symptoms, a result that surprised the researchers.
“This has not been shown before and remains to be confirmed,” said Dr. Attauabi, a fellow in the department of gastroenterology at Herlev Hospital at the University of Copenhagen.
Attauabi presented the results as a digital oral presentation at the 17th congress of the European Crohn’s and Colitis Organisation.
A closer look at IBD and COVID-19
Large, hospital-based studies of symptoms consistent with long COVID reveal a high prevalence of fatigue, sleep difficulties, and anxiety at 12 weeks or more post acute infection. However, these were not specific to people with CD or UC, Dr. Attauabi said.
“In patients with IBD, the risk of long-term sequelae of COVID-19 remains to be investigated,” he said.
Dr. Attauabi and colleagues studied 197 people with CD and 319 with UC, all of whom had polymerase chain reaction–confirmed COVID-19. Participants were prospectively enrolled in the population-based Danish IBD-COVID registry from January 28, 2020 to April 1, 2021. At a median of 5.1 months, a subset of 85 people with CD and 137 with UC agreed to report any post-COVID symptoms.
Older age, smoking, IBD disease activity, and presence of comorbidities were not associated with a significantly elevated risk of long COVID.
In a multivariate analysis, hospitalization for COVID-19 among people with CD was significantly associated with long COVID (odds ratio, 2.76; 95% confidence interval, 1.05-3.90; P = .04).
Furthermore, people with UC who stopped taking immunosuppressive agents also had a significantly higher risk (OR, 1.50; 95% CI, 1.07-10.22; P = .01).
“However, IBD medications such as systemic steroids were not associated with this outcome,” Dr. Attauabi said.
Fatigue most common long COVID symptom
Fatigue was the most common long COVID symptom, reported by 37% of patients with CD and 36% with UC.
Anosmia and ageusia were also common, reported by 29% and 28% of patients with CD, and 27% and 19% of those with UC, respectively.
“In our cohort of patients with UC or CD who developed COVID-19, the long-term health effects of COVID-19 did not appear to differ among patients with UC or CD nor according to IBD medications,” Dr. Attauabi said.
That is a “great study,” said session cochair Torsten Kucharzik, MD, PhD, head of internal medicine and gastroenterology at Lueneburg (Germany) Hospital.
When Dr. Kucharzik asked about smoking, Dr. Attauabi responded that they collected information on current and previous smoking, but they chose not to include the data because it was not statistically significant.
Dr. Attauabi has reported no relevant financial relationships. Dr. Kucharzik has reported receiving grants from Takeda and personal fees from companies including MSD/Essex, AbbVie, Falk Foundation, Biogen, Bristol-Myers Squibb, Arena, Celgene, Celltrion, Ferring, Janssen, Galapagos, Olympus, Mundipharma, Takeda, Amgen, Pfizer, Roche, and Vifor Pharma.
A version of this article first appeared on Medscape.com.
Two features are significantly associated with a higher risk for developing long COVID symptoms among people with inflammatory bowel disease (IBD), according to a large Danish population study.
People with Crohn’s disease (CD) who experienced adverse acute COVID-19, defined as requiring hospitalization, were nearly three times more likely to report persistent symptoms 12 weeks after acute infection.
“Long-term, persisting symptoms following COVID-19 is a frequently occurring problem, which is probably underappreciated. IBD specialists should therefore be aware of any of these symptoms and actively ask patients whether they have these problems,” lead author Mohamed Attauabi, MD, PhD, said in an interview.
Dr. Attauabi and colleagues also found that people with ulcerative colitis (UC) who discontinued immunosuppressive agents because of COVID-19 were 1.5 times more likely to experience long COVID symptoms, a result that surprised the researchers.
“This has not been shown before and remains to be confirmed,” said Dr. Attauabi, a fellow in the department of gastroenterology at Herlev Hospital at the University of Copenhagen.
Attauabi presented the results as a digital oral presentation at the 17th congress of the European Crohn’s and Colitis Organisation.
A closer look at IBD and COVID-19
Large, hospital-based studies of symptoms consistent with long COVID reveal a high prevalence of fatigue, sleep difficulties, and anxiety at 12 weeks or more post acute infection. However, these were not specific to people with CD or UC, Dr. Attauabi said.
“In patients with IBD, the risk of long-term sequelae of COVID-19 remains to be investigated,” he said.
Dr. Attauabi and colleagues studied 197 people with CD and 319 with UC, all of whom had polymerase chain reaction–confirmed COVID-19. Participants were prospectively enrolled in the population-based Danish IBD-COVID registry from January 28, 2020 to April 1, 2021. At a median of 5.1 months, a subset of 85 people with CD and 137 with UC agreed to report any post-COVID symptoms.
Older age, smoking, IBD disease activity, and presence of comorbidities were not associated with a significantly elevated risk of long COVID.
In a multivariate analysis, hospitalization for COVID-19 among people with CD was significantly associated with long COVID (odds ratio, 2.76; 95% confidence interval, 1.05-3.90; P = .04).
Furthermore, people with UC who stopped taking immunosuppressive agents also had a significantly higher risk (OR, 1.50; 95% CI, 1.07-10.22; P = .01).
“However, IBD medications such as systemic steroids were not associated with this outcome,” Dr. Attauabi said.
Fatigue most common long COVID symptom
Fatigue was the most common long COVID symptom, reported by 37% of patients with CD and 36% with UC.
Anosmia and ageusia were also common, reported by 29% and 28% of patients with CD, and 27% and 19% of those with UC, respectively.
“In our cohort of patients with UC or CD who developed COVID-19, the long-term health effects of COVID-19 did not appear to differ among patients with UC or CD nor according to IBD medications,” Dr. Attauabi said.
That is a “great study,” said session cochair Torsten Kucharzik, MD, PhD, head of internal medicine and gastroenterology at Lueneburg (Germany) Hospital.
When Dr. Kucharzik asked about smoking, Dr. Attauabi responded that they collected information on current and previous smoking, but they chose not to include the data because it was not statistically significant.
Dr. Attauabi has reported no relevant financial relationships. Dr. Kucharzik has reported receiving grants from Takeda and personal fees from companies including MSD/Essex, AbbVie, Falk Foundation, Biogen, Bristol-Myers Squibb, Arena, Celgene, Celltrion, Ferring, Janssen, Galapagos, Olympus, Mundipharma, Takeda, Amgen, Pfizer, Roche, and Vifor Pharma.
A version of this article first appeared on Medscape.com.
FROM ECCO 2022