User login
In Case You Missed It: COVID
Headache is a common post–COVID-19 complaint
The Centers for Disease Control and Prevention has identified it as a sentinel symptom of COVID-19 disease. “A lot of the recommendations surrounding post-COVID headache is that if you identify a patient who has headaches associated with fever, and myalgia, and other systemic symptoms, the specificity of a COVID-19 diagnosis goes up. So [COVID-19] is a really important feature to look out for in patients with headache,” Deena Kuruvilla, MD, said during a presentation on post–COVID-19 headache at the 2021 Scottsdale Headache Symposium.
Estimates of the prevalence of headache in COVID-19 range widely, from 6.5% to 71%, but Dr. Kuruvilla has plenty of personal experience with it. “During my stint on the inpatient neurology service during the peak of COVID, I saw patients with headache being one of the most frequent complaints, [along with] dizziness, stroke, and seizure among many other neurological manifestations,” said Dr. Kuruvilla, director of the Westport (Conn.) Headache Institute.
One meta-analysis showed that 47% of patients with COVID-19 complain of headache within 30 days of diagnosis, and this drops to around 10% at 60-90 days, and around 8% at 180 days.
A survey of 3,458 patients, published in the Journal of Headache Pain, found that migraine is the most common type of post–COVID-19 headache phenotype, and patients reporting anosmia-ageusia were more likely to have post–COVID-19 headache (odds ratio [OR], 5.39; 95% confidence interval, 1.66-17.45).
A case-control study of post–COVID-19 headache patients with and without a history of migraine found that those with a history of migraine were more likely to have post–COVID-19 symptoms (OR, 1.70; P < .001) and fatigue (OR, 2.89; P = .008). “Interestingly, they found no difference in headache as post-COVID symptoms in people who had a history of migraine compared with people without a history of migraine,” said Dr. Kuruvilla.
Headache and COVID-19: What is the connection?
Several mechanisms have been proposed for direct invasion of the central nervous system, either via infection through the angiotensin-converting enzyme 2 (ACE-2) receptor, which is expressed in brain regions including the motor cortex, the posterior cingulate cortex, and the olfactory bulb, among other locations. Another potential mechanism is direct entry through the olfactory nerve and the associated olfactory epithelium. There are various potential mechanisms for spread among the peripheral nervous system, and the blood-brain barrier can be compromised by infection of vascular endothelial cells. According to the literature, neuronal damage seems to occur directly from viral damage rather than from the immune response, said Dr. Kuruvilla.
The virus may also gain entry to the CNS indirectly, as a result of hypoxia and metabolic disturbances, as well as dehydration and systematic inflammation. The cytokine storm associated with COVID-19 infection can activate C-reactive protein and calcitonin gene-related peptide (CGRP), which plays a key role in migraine pathology. The CGRP receptor antagonist vazegepant is being studied in a phase 2 clinical trial for the treatment of COVID-19–related lung inflammation.
Testing and treatment
“If I see patients with new headache, worsening headache from their baseline, or headache with systemic symptoms, I often consider screening them for COVID. If that screening is positive, I proceed with PCR testing. I also consider an MRI of the brain with and without gadolinium just to rule out any secondary causes for headache,” said Dr. Kuruvilla, noting that she has diagnosed patients with venous sinus thrombosis, ischemic stroke, and meningitis following COVID-19.
The existing literature suggests that lumbar puncture in patients with SARS-CoV-2 typically returns normal results, but Dr. Kuruvilla proceeds with it anyway with viral, bacterial, fungal, and autoimmune studies to rule out potential secondary causes for headache.
There are few studies on how to treat post–COVID-19 headache, and the general recommendation is that headache phenotype should drive treatment decisions.
In a case series, three patients with persistent headache following mild COVID-19 infection were treated with onabotulinumtoxinA and amitriptyline. They had daily headaches, along with post–COVID-19 symptoms including fatigue and insomnia. After treatment, each patient converted to episodic headaches.
One retrospective study of 37 patients found that a 5-day course of indomethacin 50 mg twice per day and pantoprazole 40 mg once per day was associated with a 50% or greater improvement in headache on the third day in 36 of the 37 patients. Five patients were free of pain by day 5.
A common problem
Neurologists have been involved in the treatment of COVID-19 since the beginning, and post–COVID-19 headache has added another layer. “It’s been a remarkably common clinical problem. And the fact that it’s actually reached the level of headache specialist actually shows that in some cases, it’s really quite a significant problem, in both its severity and persistence. So I think it’s a very, very significant issue,” said Andrew Charles, MD, professor of neurology at the University of California, Los Angeles, and director of the UCLA Goldberg Migraine Program.
Dr. Kuruvilla also discussed the question of whether neurological damage is due to direct damage from the virus, or indirect damage from an immune response. This was debated during the Q&A session following Dr. Kuruvilla’s talk, and it was pointed out that headache is a frequent side effect of the Pfizer and Moderna vaccines.
“It’s a huge open question about how much is direct invasion or damage or not even damage, but just change in function with the viral infection, as opposed to inflammation. The fact that very often the response to the vaccine is similar to what you see with COVID suggests that at least some component of it is inflammation. I wouldn’t commit to one mechanism or the other, but I’d say that it’s possible that it’s really both,” said Dr. Charles.
Dr. Kuruvilla has consulted for Cefaly, Neurolief, Theranica, Now What Media, and KX advisors. She has been on the speakers bureau for Abbvie/Allergan, Amgen/Novartis, and Lilly. She has been on advisory boards for Abbvie/Allergan, Lilly, Theranica, and Amgen/Novartis. Dr. Charles has no relevant financial disclosures.
The Centers for Disease Control and Prevention has identified it as a sentinel symptom of COVID-19 disease. “A lot of the recommendations surrounding post-COVID headache is that if you identify a patient who has headaches associated with fever, and myalgia, and other systemic symptoms, the specificity of a COVID-19 diagnosis goes up. So [COVID-19] is a really important feature to look out for in patients with headache,” Deena Kuruvilla, MD, said during a presentation on post–COVID-19 headache at the 2021 Scottsdale Headache Symposium.
Estimates of the prevalence of headache in COVID-19 range widely, from 6.5% to 71%, but Dr. Kuruvilla has plenty of personal experience with it. “During my stint on the inpatient neurology service during the peak of COVID, I saw patients with headache being one of the most frequent complaints, [along with] dizziness, stroke, and seizure among many other neurological manifestations,” said Dr. Kuruvilla, director of the Westport (Conn.) Headache Institute.
One meta-analysis showed that 47% of patients with COVID-19 complain of headache within 30 days of diagnosis, and this drops to around 10% at 60-90 days, and around 8% at 180 days.
A survey of 3,458 patients, published in the Journal of Headache Pain, found that migraine is the most common type of post–COVID-19 headache phenotype, and patients reporting anosmia-ageusia were more likely to have post–COVID-19 headache (odds ratio [OR], 5.39; 95% confidence interval, 1.66-17.45).
A case-control study of post–COVID-19 headache patients with and without a history of migraine found that those with a history of migraine were more likely to have post–COVID-19 symptoms (OR, 1.70; P < .001) and fatigue (OR, 2.89; P = .008). “Interestingly, they found no difference in headache as post-COVID symptoms in people who had a history of migraine compared with people without a history of migraine,” said Dr. Kuruvilla.
Headache and COVID-19: What is the connection?
Several mechanisms have been proposed for direct invasion of the central nervous system, either via infection through the angiotensin-converting enzyme 2 (ACE-2) receptor, which is expressed in brain regions including the motor cortex, the posterior cingulate cortex, and the olfactory bulb, among other locations. Another potential mechanism is direct entry through the olfactory nerve and the associated olfactory epithelium. There are various potential mechanisms for spread among the peripheral nervous system, and the blood-brain barrier can be compromised by infection of vascular endothelial cells. According to the literature, neuronal damage seems to occur directly from viral damage rather than from the immune response, said Dr. Kuruvilla.
The virus may also gain entry to the CNS indirectly, as a result of hypoxia and metabolic disturbances, as well as dehydration and systematic inflammation. The cytokine storm associated with COVID-19 infection can activate C-reactive protein and calcitonin gene-related peptide (CGRP), which plays a key role in migraine pathology. The CGRP receptor antagonist vazegepant is being studied in a phase 2 clinical trial for the treatment of COVID-19–related lung inflammation.
Testing and treatment
“If I see patients with new headache, worsening headache from their baseline, or headache with systemic symptoms, I often consider screening them for COVID. If that screening is positive, I proceed with PCR testing. I also consider an MRI of the brain with and without gadolinium just to rule out any secondary causes for headache,” said Dr. Kuruvilla, noting that she has diagnosed patients with venous sinus thrombosis, ischemic stroke, and meningitis following COVID-19.
The existing literature suggests that lumbar puncture in patients with SARS-CoV-2 typically returns normal results, but Dr. Kuruvilla proceeds with it anyway with viral, bacterial, fungal, and autoimmune studies to rule out potential secondary causes for headache.
There are few studies on how to treat post–COVID-19 headache, and the general recommendation is that headache phenotype should drive treatment decisions.
In a case series, three patients with persistent headache following mild COVID-19 infection were treated with onabotulinumtoxinA and amitriptyline. They had daily headaches, along with post–COVID-19 symptoms including fatigue and insomnia. After treatment, each patient converted to episodic headaches.
One retrospective study of 37 patients found that a 5-day course of indomethacin 50 mg twice per day and pantoprazole 40 mg once per day was associated with a 50% or greater improvement in headache on the third day in 36 of the 37 patients. Five patients were free of pain by day 5.
A common problem
Neurologists have been involved in the treatment of COVID-19 since the beginning, and post–COVID-19 headache has added another layer. “It’s been a remarkably common clinical problem. And the fact that it’s actually reached the level of headache specialist actually shows that in some cases, it’s really quite a significant problem, in both its severity and persistence. So I think it’s a very, very significant issue,” said Andrew Charles, MD, professor of neurology at the University of California, Los Angeles, and director of the UCLA Goldberg Migraine Program.
Dr. Kuruvilla also discussed the question of whether neurological damage is due to direct damage from the virus, or indirect damage from an immune response. This was debated during the Q&A session following Dr. Kuruvilla’s talk, and it was pointed out that headache is a frequent side effect of the Pfizer and Moderna vaccines.
“It’s a huge open question about how much is direct invasion or damage or not even damage, but just change in function with the viral infection, as opposed to inflammation. The fact that very often the response to the vaccine is similar to what you see with COVID suggests that at least some component of it is inflammation. I wouldn’t commit to one mechanism or the other, but I’d say that it’s possible that it’s really both,” said Dr. Charles.
Dr. Kuruvilla has consulted for Cefaly, Neurolief, Theranica, Now What Media, and KX advisors. She has been on the speakers bureau for Abbvie/Allergan, Amgen/Novartis, and Lilly. She has been on advisory boards for Abbvie/Allergan, Lilly, Theranica, and Amgen/Novartis. Dr. Charles has no relevant financial disclosures.
The Centers for Disease Control and Prevention has identified it as a sentinel symptom of COVID-19 disease. “A lot of the recommendations surrounding post-COVID headache is that if you identify a patient who has headaches associated with fever, and myalgia, and other systemic symptoms, the specificity of a COVID-19 diagnosis goes up. So [COVID-19] is a really important feature to look out for in patients with headache,” Deena Kuruvilla, MD, said during a presentation on post–COVID-19 headache at the 2021 Scottsdale Headache Symposium.
Estimates of the prevalence of headache in COVID-19 range widely, from 6.5% to 71%, but Dr. Kuruvilla has plenty of personal experience with it. “During my stint on the inpatient neurology service during the peak of COVID, I saw patients with headache being one of the most frequent complaints, [along with] dizziness, stroke, and seizure among many other neurological manifestations,” said Dr. Kuruvilla, director of the Westport (Conn.) Headache Institute.
One meta-analysis showed that 47% of patients with COVID-19 complain of headache within 30 days of diagnosis, and this drops to around 10% at 60-90 days, and around 8% at 180 days.
A survey of 3,458 patients, published in the Journal of Headache Pain, found that migraine is the most common type of post–COVID-19 headache phenotype, and patients reporting anosmia-ageusia were more likely to have post–COVID-19 headache (odds ratio [OR], 5.39; 95% confidence interval, 1.66-17.45).
A case-control study of post–COVID-19 headache patients with and without a history of migraine found that those with a history of migraine were more likely to have post–COVID-19 symptoms (OR, 1.70; P < .001) and fatigue (OR, 2.89; P = .008). “Interestingly, they found no difference in headache as post-COVID symptoms in people who had a history of migraine compared with people without a history of migraine,” said Dr. Kuruvilla.
Headache and COVID-19: What is the connection?
Several mechanisms have been proposed for direct invasion of the central nervous system, either via infection through the angiotensin-converting enzyme 2 (ACE-2) receptor, which is expressed in brain regions including the motor cortex, the posterior cingulate cortex, and the olfactory bulb, among other locations. Another potential mechanism is direct entry through the olfactory nerve and the associated olfactory epithelium. There are various potential mechanisms for spread among the peripheral nervous system, and the blood-brain barrier can be compromised by infection of vascular endothelial cells. According to the literature, neuronal damage seems to occur directly from viral damage rather than from the immune response, said Dr. Kuruvilla.
The virus may also gain entry to the CNS indirectly, as a result of hypoxia and metabolic disturbances, as well as dehydration and systematic inflammation. The cytokine storm associated with COVID-19 infection can activate C-reactive protein and calcitonin gene-related peptide (CGRP), which plays a key role in migraine pathology. The CGRP receptor antagonist vazegepant is being studied in a phase 2 clinical trial for the treatment of COVID-19–related lung inflammation.
Testing and treatment
“If I see patients with new headache, worsening headache from their baseline, or headache with systemic symptoms, I often consider screening them for COVID. If that screening is positive, I proceed with PCR testing. I also consider an MRI of the brain with and without gadolinium just to rule out any secondary causes for headache,” said Dr. Kuruvilla, noting that she has diagnosed patients with venous sinus thrombosis, ischemic stroke, and meningitis following COVID-19.
The existing literature suggests that lumbar puncture in patients with SARS-CoV-2 typically returns normal results, but Dr. Kuruvilla proceeds with it anyway with viral, bacterial, fungal, and autoimmune studies to rule out potential secondary causes for headache.
There are few studies on how to treat post–COVID-19 headache, and the general recommendation is that headache phenotype should drive treatment decisions.
In a case series, three patients with persistent headache following mild COVID-19 infection were treated with onabotulinumtoxinA and amitriptyline. They had daily headaches, along with post–COVID-19 symptoms including fatigue and insomnia. After treatment, each patient converted to episodic headaches.
One retrospective study of 37 patients found that a 5-day course of indomethacin 50 mg twice per day and pantoprazole 40 mg once per day was associated with a 50% or greater improvement in headache on the third day in 36 of the 37 patients. Five patients were free of pain by day 5.
A common problem
Neurologists have been involved in the treatment of COVID-19 since the beginning, and post–COVID-19 headache has added another layer. “It’s been a remarkably common clinical problem. And the fact that it’s actually reached the level of headache specialist actually shows that in some cases, it’s really quite a significant problem, in both its severity and persistence. So I think it’s a very, very significant issue,” said Andrew Charles, MD, professor of neurology at the University of California, Los Angeles, and director of the UCLA Goldberg Migraine Program.
Dr. Kuruvilla also discussed the question of whether neurological damage is due to direct damage from the virus, or indirect damage from an immune response. This was debated during the Q&A session following Dr. Kuruvilla’s talk, and it was pointed out that headache is a frequent side effect of the Pfizer and Moderna vaccines.
“It’s a huge open question about how much is direct invasion or damage or not even damage, but just change in function with the viral infection, as opposed to inflammation. The fact that very often the response to the vaccine is similar to what you see with COVID suggests that at least some component of it is inflammation. I wouldn’t commit to one mechanism or the other, but I’d say that it’s possible that it’s really both,” said Dr. Charles.
Dr. Kuruvilla has consulted for Cefaly, Neurolief, Theranica, Now What Media, and KX advisors. She has been on the speakers bureau for Abbvie/Allergan, Amgen/Novartis, and Lilly. She has been on advisory boards for Abbvie/Allergan, Lilly, Theranica, and Amgen/Novartis. Dr. Charles has no relevant financial disclosures.
FROM 2021 SCOTTSDALE HEADACHE SYMPOSIUM
Children and COVID: New cases increase for third straight week
There were almost 142,000 new cases reported during the week of Nov. 12-18, marking an increase of 16% over the previous week and the 15th straight week with a weekly total over 100,000, the American Academy of Pediatrics and the Children’s Hospital Association said.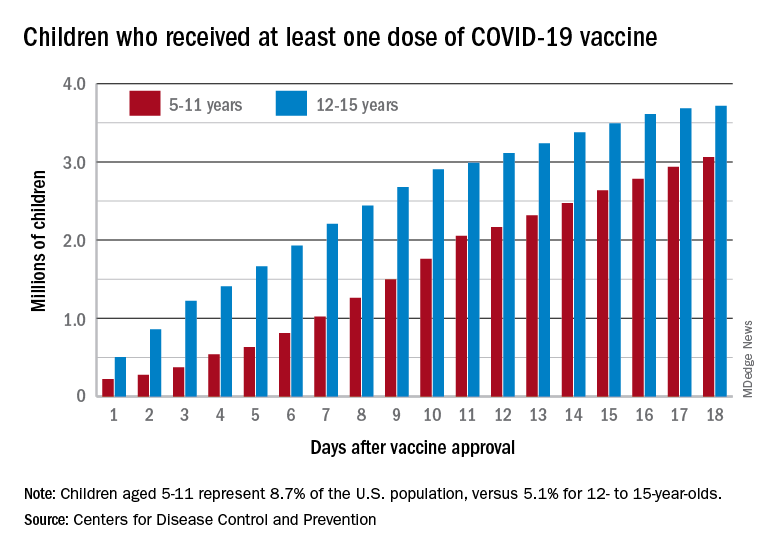
Regional data show that the Midwest has experienced the largest share of this latest surge, followed by the Northeast. Cases increased in the South during the week of Nov. 12-18 after holding steady over the previous 2 weeks, while new cases in the West dropped in the last week. At the state level, Maine, New Hampshire, and Vermont again reported the largest percent increases, with Michigan, Minnesota, and New Mexico also above average, the AAP and CHA said in their weekly COVID report.
Data from the Centers for Disease Control and Prevention show similar trends for both emergency department visits and hospital admissions, as both have risen in November after declines that began in late August and early September.
The cumulative number of pediatric cases is 6.77 million since the pandemic began, based on the AAP/CHA accounting of state cases, although Alabama, Nebraska, and Texas stopped reporting over the summer, suggesting the actual number is higher. The CDC puts the total number of COVID cases in children at 5.96 million, but there are age discrepancies between the CDC and the AAP/CHA’s state-based data.
The vaccine gap is closing
Vaccinations among the recently eligible 5- to 11-year-olds have steadily increased following a somewhat slow start. The initial pace was behind that of the 12- to 15-years-olds through the first postapproval week but has since closed the gap, based on data from the CDC’s COVID Data Tracker.
The tally of children who received at least one dose of the COVID vaccine among the 5- to 11-year-olds was behind the older group by almost 1.2 million on day 7 after the CDC’s Nov. 2 approval, but by day 18 the deficit was down to about 650,000, the CDC reported.
Altogether, just over 3 million children aged 5-11 have received at least one dose, which is 10.7% of that age group’s total population. Among children aged 12-17, the proportions are 60.7% with at least one dose and 51.1% at full vaccination. Children aged 5-11, who make up 8.7% of the total U.S. population, represented 42.8% of all vaccinations initiated over the 2 weeks ending Nov. 21, compared with 4.2% for those aged 12-17, the CDC said.
There were almost 142,000 new cases reported during the week of Nov. 12-18, marking an increase of 16% over the previous week and the 15th straight week with a weekly total over 100,000, the American Academy of Pediatrics and the Children’s Hospital Association said.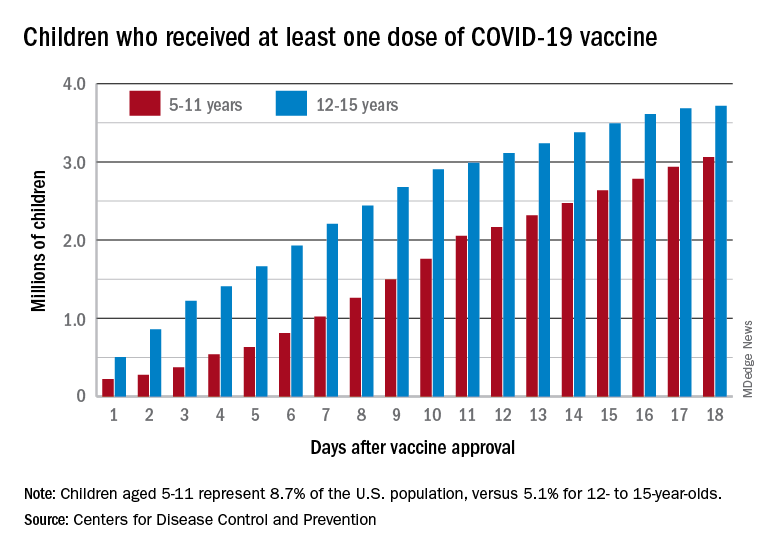
Regional data show that the Midwest has experienced the largest share of this latest surge, followed by the Northeast. Cases increased in the South during the week of Nov. 12-18 after holding steady over the previous 2 weeks, while new cases in the West dropped in the last week. At the state level, Maine, New Hampshire, and Vermont again reported the largest percent increases, with Michigan, Minnesota, and New Mexico also above average, the AAP and CHA said in their weekly COVID report.
Data from the Centers for Disease Control and Prevention show similar trends for both emergency department visits and hospital admissions, as both have risen in November after declines that began in late August and early September.
The cumulative number of pediatric cases is 6.77 million since the pandemic began, based on the AAP/CHA accounting of state cases, although Alabama, Nebraska, and Texas stopped reporting over the summer, suggesting the actual number is higher. The CDC puts the total number of COVID cases in children at 5.96 million, but there are age discrepancies between the CDC and the AAP/CHA’s state-based data.
The vaccine gap is closing
Vaccinations among the recently eligible 5- to 11-year-olds have steadily increased following a somewhat slow start. The initial pace was behind that of the 12- to 15-years-olds through the first postapproval week but has since closed the gap, based on data from the CDC’s COVID Data Tracker.
The tally of children who received at least one dose of the COVID vaccine among the 5- to 11-year-olds was behind the older group by almost 1.2 million on day 7 after the CDC’s Nov. 2 approval, but by day 18 the deficit was down to about 650,000, the CDC reported.
Altogether, just over 3 million children aged 5-11 have received at least one dose, which is 10.7% of that age group’s total population. Among children aged 12-17, the proportions are 60.7% with at least one dose and 51.1% at full vaccination. Children aged 5-11, who make up 8.7% of the total U.S. population, represented 42.8% of all vaccinations initiated over the 2 weeks ending Nov. 21, compared with 4.2% for those aged 12-17, the CDC said.
There were almost 142,000 new cases reported during the week of Nov. 12-18, marking an increase of 16% over the previous week and the 15th straight week with a weekly total over 100,000, the American Academy of Pediatrics and the Children’s Hospital Association said.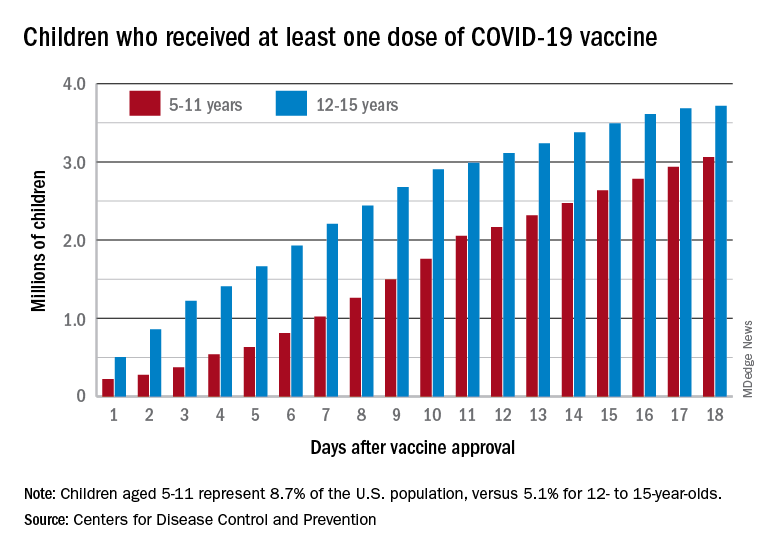
Regional data show that the Midwest has experienced the largest share of this latest surge, followed by the Northeast. Cases increased in the South during the week of Nov. 12-18 after holding steady over the previous 2 weeks, while new cases in the West dropped in the last week. At the state level, Maine, New Hampshire, and Vermont again reported the largest percent increases, with Michigan, Minnesota, and New Mexico also above average, the AAP and CHA said in their weekly COVID report.
Data from the Centers for Disease Control and Prevention show similar trends for both emergency department visits and hospital admissions, as both have risen in November after declines that began in late August and early September.
The cumulative number of pediatric cases is 6.77 million since the pandemic began, based on the AAP/CHA accounting of state cases, although Alabama, Nebraska, and Texas stopped reporting over the summer, suggesting the actual number is higher. The CDC puts the total number of COVID cases in children at 5.96 million, but there are age discrepancies between the CDC and the AAP/CHA’s state-based data.
The vaccine gap is closing
Vaccinations among the recently eligible 5- to 11-year-olds have steadily increased following a somewhat slow start. The initial pace was behind that of the 12- to 15-years-olds through the first postapproval week but has since closed the gap, based on data from the CDC’s COVID Data Tracker.
The tally of children who received at least one dose of the COVID vaccine among the 5- to 11-year-olds was behind the older group by almost 1.2 million on day 7 after the CDC’s Nov. 2 approval, but by day 18 the deficit was down to about 650,000, the CDC reported.
Altogether, just over 3 million children aged 5-11 have received at least one dose, which is 10.7% of that age group’s total population. Among children aged 12-17, the proportions are 60.7% with at least one dose and 51.1% at full vaccination. Children aged 5-11, who make up 8.7% of the total U.S. population, represented 42.8% of all vaccinations initiated over the 2 weeks ending Nov. 21, compared with 4.2% for those aged 12-17, the CDC said.
‘Misleading’ results in colchicine COVID-19 trials meta-analysis
A new meta-analysis appears to show that colchicine has no benefit as a treatment for COVID-19, but its inclusion of trials studying differing patient populations and testing different outcomes led to “misleading” results, says a researcher involved in one of the trials.
The meta-analysis, which includes data from the recent Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial, was published Nov. 22 in RMD Open.
Kedar Gautambhai Mehta, MBBS, MD, of the GMERS Medical College Gotri in Vadodara, India, and colleagues included outcomes from six studies of 16,148 patients with COVID-19 who received colchicine or supportive care. They evaluated the efficacy outcomes of mortality, need for ventilation, intensive care unit admission, and length of stay in hospital, as well as safety outcomes of adverse events, serious adverse events, and diarrhea.
The studies in the meta-analysis included a randomized, controlled trial (RCT) of 105 patients hospitalized with COVID-19 in Greece, the international, open-label RECOVERY RCT of 11,340 patients hospitalized with COVID-19, an RCT of 72 hospitalized patients with moderate or severe COVID-19 in Brazil, an RCT of 100 patients hospitalized with COVID-19 in Iran, the international COLCORONA trial of 4,488 patients with COVID-19 who were treated with colchicine or placebo on an outpatient basis, and the randomized COLORIT trial of 43 patients hospitalized with COVID-19 in Russia.
Studies “asked very different questions” about colchicine
Commenting on the meta-analysis, Michael H. Pillinger, MD, a rheumatologist and professor of medicine, biochemistry, and molecular pharmacology with New York University, said the authors combined studies “that are not comparable and that asked very different questions.” Two of the studies in the meta-analysis are very large, and four are very small, which skews the results, he explained.
“The larger studies therefore drive the outcome, and while the small studies are potentially insight providing, the large studies are the only ones worth giving our attention to in the context of the meta-analysis,” he said. The two largest studies – RECOVERY and COLCORONA – taken together show no benefit for colchicine as a treatment, even though the former demonstrated no benefit and the latter did show a benefit, explained Dr. Pillinger, a co–principal investigator for the COLCORONA trial in the United States.
The studies were designed differently and should not have been included in the same analysis, Dr. Pillinger argued. In the case of COLCORONA, early treatment with colchicine was the intervention, whereas RECOVERY focused on hospitalized patients.
“In designing [COLCORONA], the author group (of whom I was a member) expressly rejected the idea that colchicine might be useful for the sicker hospitalized patients, based on the long experience with colchicine of some of us as rheumatologists,” Dr. Pillinger said.
“In short, COLCORONA proved a benefit of colchicine in outpatient COVID-19, and its authors presumed there would be no inpatient benefit; RECOVERY went ahead and proved a lack of inpatient benefit, at least when high-dose steroids were also given,” he said. “While there is no conflict between these results, the combination of the two studies in this meta-analysis suggests there might be no benefit for colchicine overall, which is misleading and can lead physicians to reject the potential of outpatient colchicine, even for future studies.”
Dr. Pillinger said he still believes colchicine has potential value as a COVID-19 treatment option for patients with mild disease, “especially for low–vaccine rate, resource-starved countries.
“It would be unfortunate if meta-analyses such as this one would put a stop to colchicine’s use, or at least its further investigation,” he said.
Study details
The authors of the study assessed heterogeneity of the trials’ data across the outcomes using an I2 test. They evaluated the quality of the evidence for the outcomes using the Grades of Recommendation, Assessment, Development and Evaluation (GRADE).
The results of their meta-analysis showed that colchicine offered no significant improvement in mortality in six studies (risk difference, –0.0; 95% confidence interval, –0.01 to 0.01; I2 = 15%). It showed no benefit with respect to requiring ventilatory support in five studies of 15,519 patients (risk ratio, 0.67; 95% CI, 0.38-1.21; I2 = 47%); being admitted to the ICU in three studies with 220 patients (RR, 0.49; 95% CI, 0.19-1.25; I2 = 34%); and length of stay while in the hospital in four studies of 11,560 patients (mean difference, –1.17; 95% CI, –3.02 to 0.67; I2 = 77%).
There was no difference in serious adverse events in three studies with 4,665 patients (RD, –0.01; 95% CI, –0.02 to 0.00; I2 = 28%) for patients who received colchicine, compared with supportive care alone. Patients who received colchicine were more likely to have a higher rate of adverse events (RR, 1.58; 95% CI, 1.07-2.33; I2 = 81%) and to experience diarrhea (RR, 1.93; 95% CI, 1.62-2.29; I2 = 0%) than were patients who received supportive care alone. The researchers note that for most outcomes, the GRADE quality of evidence was moderate.
“Our findings on colchicine should be interpreted cautiously due to the inclusion of open-labeled, randomized clinical trials,” Dr. Mehta and colleagues write. “The analysis of efficacy and safety outcomes are based on a small number of RCTs in control interventions.”
The authors reported no relevant financial relationships. Dr. Pillinger is co–principal investigator of the U.S. component of the COLCORONA trial; he reported no other relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
A new meta-analysis appears to show that colchicine has no benefit as a treatment for COVID-19, but its inclusion of trials studying differing patient populations and testing different outcomes led to “misleading” results, says a researcher involved in one of the trials.
The meta-analysis, which includes data from the recent Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial, was published Nov. 22 in RMD Open.
Kedar Gautambhai Mehta, MBBS, MD, of the GMERS Medical College Gotri in Vadodara, India, and colleagues included outcomes from six studies of 16,148 patients with COVID-19 who received colchicine or supportive care. They evaluated the efficacy outcomes of mortality, need for ventilation, intensive care unit admission, and length of stay in hospital, as well as safety outcomes of adverse events, serious adverse events, and diarrhea.
The studies in the meta-analysis included a randomized, controlled trial (RCT) of 105 patients hospitalized with COVID-19 in Greece, the international, open-label RECOVERY RCT of 11,340 patients hospitalized with COVID-19, an RCT of 72 hospitalized patients with moderate or severe COVID-19 in Brazil, an RCT of 100 patients hospitalized with COVID-19 in Iran, the international COLCORONA trial of 4,488 patients with COVID-19 who were treated with colchicine or placebo on an outpatient basis, and the randomized COLORIT trial of 43 patients hospitalized with COVID-19 in Russia.
Studies “asked very different questions” about colchicine
Commenting on the meta-analysis, Michael H. Pillinger, MD, a rheumatologist and professor of medicine, biochemistry, and molecular pharmacology with New York University, said the authors combined studies “that are not comparable and that asked very different questions.” Two of the studies in the meta-analysis are very large, and four are very small, which skews the results, he explained.
“The larger studies therefore drive the outcome, and while the small studies are potentially insight providing, the large studies are the only ones worth giving our attention to in the context of the meta-analysis,” he said. The two largest studies – RECOVERY and COLCORONA – taken together show no benefit for colchicine as a treatment, even though the former demonstrated no benefit and the latter did show a benefit, explained Dr. Pillinger, a co–principal investigator for the COLCORONA trial in the United States.
The studies were designed differently and should not have been included in the same analysis, Dr. Pillinger argued. In the case of COLCORONA, early treatment with colchicine was the intervention, whereas RECOVERY focused on hospitalized patients.
“In designing [COLCORONA], the author group (of whom I was a member) expressly rejected the idea that colchicine might be useful for the sicker hospitalized patients, based on the long experience with colchicine of some of us as rheumatologists,” Dr. Pillinger said.
“In short, COLCORONA proved a benefit of colchicine in outpatient COVID-19, and its authors presumed there would be no inpatient benefit; RECOVERY went ahead and proved a lack of inpatient benefit, at least when high-dose steroids were also given,” he said. “While there is no conflict between these results, the combination of the two studies in this meta-analysis suggests there might be no benefit for colchicine overall, which is misleading and can lead physicians to reject the potential of outpatient colchicine, even for future studies.”
Dr. Pillinger said he still believes colchicine has potential value as a COVID-19 treatment option for patients with mild disease, “especially for low–vaccine rate, resource-starved countries.
“It would be unfortunate if meta-analyses such as this one would put a stop to colchicine’s use, or at least its further investigation,” he said.
Study details
The authors of the study assessed heterogeneity of the trials’ data across the outcomes using an I2 test. They evaluated the quality of the evidence for the outcomes using the Grades of Recommendation, Assessment, Development and Evaluation (GRADE).
The results of their meta-analysis showed that colchicine offered no significant improvement in mortality in six studies (risk difference, –0.0; 95% confidence interval, –0.01 to 0.01; I2 = 15%). It showed no benefit with respect to requiring ventilatory support in five studies of 15,519 patients (risk ratio, 0.67; 95% CI, 0.38-1.21; I2 = 47%); being admitted to the ICU in three studies with 220 patients (RR, 0.49; 95% CI, 0.19-1.25; I2 = 34%); and length of stay while in the hospital in four studies of 11,560 patients (mean difference, –1.17; 95% CI, –3.02 to 0.67; I2 = 77%).
There was no difference in serious adverse events in three studies with 4,665 patients (RD, –0.01; 95% CI, –0.02 to 0.00; I2 = 28%) for patients who received colchicine, compared with supportive care alone. Patients who received colchicine were more likely to have a higher rate of adverse events (RR, 1.58; 95% CI, 1.07-2.33; I2 = 81%) and to experience diarrhea (RR, 1.93; 95% CI, 1.62-2.29; I2 = 0%) than were patients who received supportive care alone. The researchers note that for most outcomes, the GRADE quality of evidence was moderate.
“Our findings on colchicine should be interpreted cautiously due to the inclusion of open-labeled, randomized clinical trials,” Dr. Mehta and colleagues write. “The analysis of efficacy and safety outcomes are based on a small number of RCTs in control interventions.”
The authors reported no relevant financial relationships. Dr. Pillinger is co–principal investigator of the U.S. component of the COLCORONA trial; he reported no other relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
A new meta-analysis appears to show that colchicine has no benefit as a treatment for COVID-19, but its inclusion of trials studying differing patient populations and testing different outcomes led to “misleading” results, says a researcher involved in one of the trials.
The meta-analysis, which includes data from the recent Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial, was published Nov. 22 in RMD Open.
Kedar Gautambhai Mehta, MBBS, MD, of the GMERS Medical College Gotri in Vadodara, India, and colleagues included outcomes from six studies of 16,148 patients with COVID-19 who received colchicine or supportive care. They evaluated the efficacy outcomes of mortality, need for ventilation, intensive care unit admission, and length of stay in hospital, as well as safety outcomes of adverse events, serious adverse events, and diarrhea.
The studies in the meta-analysis included a randomized, controlled trial (RCT) of 105 patients hospitalized with COVID-19 in Greece, the international, open-label RECOVERY RCT of 11,340 patients hospitalized with COVID-19, an RCT of 72 hospitalized patients with moderate or severe COVID-19 in Brazil, an RCT of 100 patients hospitalized with COVID-19 in Iran, the international COLCORONA trial of 4,488 patients with COVID-19 who were treated with colchicine or placebo on an outpatient basis, and the randomized COLORIT trial of 43 patients hospitalized with COVID-19 in Russia.
Studies “asked very different questions” about colchicine
Commenting on the meta-analysis, Michael H. Pillinger, MD, a rheumatologist and professor of medicine, biochemistry, and molecular pharmacology with New York University, said the authors combined studies “that are not comparable and that asked very different questions.” Two of the studies in the meta-analysis are very large, and four are very small, which skews the results, he explained.
“The larger studies therefore drive the outcome, and while the small studies are potentially insight providing, the large studies are the only ones worth giving our attention to in the context of the meta-analysis,” he said. The two largest studies – RECOVERY and COLCORONA – taken together show no benefit for colchicine as a treatment, even though the former demonstrated no benefit and the latter did show a benefit, explained Dr. Pillinger, a co–principal investigator for the COLCORONA trial in the United States.
The studies were designed differently and should not have been included in the same analysis, Dr. Pillinger argued. In the case of COLCORONA, early treatment with colchicine was the intervention, whereas RECOVERY focused on hospitalized patients.
“In designing [COLCORONA], the author group (of whom I was a member) expressly rejected the idea that colchicine might be useful for the sicker hospitalized patients, based on the long experience with colchicine of some of us as rheumatologists,” Dr. Pillinger said.
“In short, COLCORONA proved a benefit of colchicine in outpatient COVID-19, and its authors presumed there would be no inpatient benefit; RECOVERY went ahead and proved a lack of inpatient benefit, at least when high-dose steroids were also given,” he said. “While there is no conflict between these results, the combination of the two studies in this meta-analysis suggests there might be no benefit for colchicine overall, which is misleading and can lead physicians to reject the potential of outpatient colchicine, even for future studies.”
Dr. Pillinger said he still believes colchicine has potential value as a COVID-19 treatment option for patients with mild disease, “especially for low–vaccine rate, resource-starved countries.
“It would be unfortunate if meta-analyses such as this one would put a stop to colchicine’s use, or at least its further investigation,” he said.
Study details
The authors of the study assessed heterogeneity of the trials’ data across the outcomes using an I2 test. They evaluated the quality of the evidence for the outcomes using the Grades of Recommendation, Assessment, Development and Evaluation (GRADE).
The results of their meta-analysis showed that colchicine offered no significant improvement in mortality in six studies (risk difference, –0.0; 95% confidence interval, –0.01 to 0.01; I2 = 15%). It showed no benefit with respect to requiring ventilatory support in five studies of 15,519 patients (risk ratio, 0.67; 95% CI, 0.38-1.21; I2 = 47%); being admitted to the ICU in three studies with 220 patients (RR, 0.49; 95% CI, 0.19-1.25; I2 = 34%); and length of stay while in the hospital in four studies of 11,560 patients (mean difference, –1.17; 95% CI, –3.02 to 0.67; I2 = 77%).
There was no difference in serious adverse events in three studies with 4,665 patients (RD, –0.01; 95% CI, –0.02 to 0.00; I2 = 28%) for patients who received colchicine, compared with supportive care alone. Patients who received colchicine were more likely to have a higher rate of adverse events (RR, 1.58; 95% CI, 1.07-2.33; I2 = 81%) and to experience diarrhea (RR, 1.93; 95% CI, 1.62-2.29; I2 = 0%) than were patients who received supportive care alone. The researchers note that for most outcomes, the GRADE quality of evidence was moderate.
“Our findings on colchicine should be interpreted cautiously due to the inclusion of open-labeled, randomized clinical trials,” Dr. Mehta and colleagues write. “The analysis of efficacy and safety outcomes are based on a small number of RCTs in control interventions.”
The authors reported no relevant financial relationships. Dr. Pillinger is co–principal investigator of the U.S. component of the COLCORONA trial; he reported no other relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Social media use associated with depression in adults
Use of social media has been linked to increased anxiety and depression, as well as reduced well-being in adolescents and young adults, but similar associations in older adults have not been well studied, and longitudinal data are lacking, Ron H. Perlis, MD, of Massachusetts General Hospital, Boston, and colleagues wrote in their paper, which was published in JAMA Network Open.
To examine the association between social media use and depressive symptoms in older adults, the researchers reviewed data from 13 waves of an internet survey conducted each month between May 2020 and May 2021. The survey respondents included individuals aged 18 years and older, with a mean age of 56 years.
In the study the researchers analyzed responses from 5,395 individuals aged 18 years and older, with a mean age of 56 years. The study participants had minimal or no depressive symptoms at baseline, according to scores on the nine-item Patient Health Questionnaire (PHQ-9).
Overall, 8.9% of the respondents reported a worsening of 5 points or more on the PHQ-9 score on a follow-up survey, which was the primary outcome. Participants who reported using social media platforms Snapchat, Facebook, or TikTok were significantly more likely to report increased depressive symptoms, compared with those who did not report use of social media. The fully adjusted odds ratio was largest for Snapchat (aOR, 1.53), followed by Facebook (aOR, 1.42), and TikTok (aOR, 1.39).
Incorporating recent television and internet news terms, such as COVID-19, changed the association for Snapchat, for which the aOR decreased from 1.53 to 1.12 when news source terms were included in the survey. TikTok and Facebook associations remained similar.
When the results were further stratified by age, use of TikTok and Snapchat was associated with depressive symptoms in those aged 35 years and older, but not in those younger than 35 years. However, the opposite pattern emerged for Facebook; use was associated with depressive symptoms for individuals younger than 35 years, but not in those aged 35 years and older (aOR, 2.60 vs. aOR, 1.12).
The association between increased self-reported depressive symptoms and use of certain social media platforms was not impacted by baseline social support or face-to-face interactions, the researchers noted.
Family physician was surprised results weren’t more significant
In the current study, “I was honestly surprised the results weren’t more significant,” Mary Ann Dakkak, MD, of Boston University said in an interview. “That said, social media uses during the COVID pandemic may have been a necessary social outlet and form of connection for many people who were otherwise isolated.”
To still see a significant increase in depression when social media could have been a positive force may suggest a heavier impact during “normal” times, she added.
“It is not surprising that what we see in youth is shown among adults,” noted Dr. Dakkak, who was not involved with this study. “I always tell my patients that what is good for their children is good for the adults too, and vice versa.
“We expect to see outcomes of this on youth and adults who have been more isolated, who have used more screen time for learning, work, connection and boredom, in the near future,” she said. “The complex nature of why social media may have been used more heavily for connection during a time when in-person meetings were not possible may be a heavy confounder as the typical profile of heavy social media users may have differed during the COVID shutdowns.”
Psychiatrist: Balance benefits of social media with mental health risks
The current study was likely conducted before the recent news on “hidden” Facebook data and the implications that Facebook knew it was contributing to worsened mental health in teens, particularly around self-esteem, Jessica “Jessi” Gold, MD, a psychiatrist at Washington University, St. Louis, said in an interview.
“If you look more specifically at other studies, however, the data around social media and mental health is constantly varied, with some showing benefits and some showing negatives, and none conclusively suggesting either way,” said Dr. Gold, who also was not involved with the new research. “More data are needed, especially longitudinally and on a broader age group, to understand social media’s impact on mental health over time.
“It is also even more important in the wake of COVID-19, as so many people have turned to social media as a primary source of social support and connection, and are using it even more than before,” she emphasized.
In the current study, “I think the most interesting information is that, for TikTok and Snapchat, the effects seemed to be more pronounced in those older than 35 years who used social media,” said Dr. Gold.
What this study leaves unanswered is “whether people who might develop depression are simply more prone to use social media in the first place, such as to seek out social support,” Dr. Gold said. “Also, we don’t know anything about how long they are using social media or what they are using it for, which to me is important for understanding more about the nuance of the relationship with mental health and social media.”
Experts advise clinicians to discuss social media with patients
This new research suggests that clinicians should be talking to their patients about how social media impacts their emotional reactions, as well as their sleep, Dr. Gold said.
“Patients should be asking themselves how they are feeling when they are on social media and not using it before sleep. They should also be considering time limits and how to effectively use social media while taking care of their mental health,” she said. This conversation between clinician and patient should be had with any patient of any age, who uses social media, not only with teenagers.
“This is also a conversation about moderation, and knowing that individuals may feel they benefit from social media, that they should balance these benefits with potential mental health risks,” she said.
“Studies such as this one shed light onto why social media consumption should be at least a point of discussion with our patients,” said Dr. Dakkak.
She advised clinicians to ask and listen to patients and their families when it comes to screen time habits. “Whenever I see a patient with mood symptoms, I ask about their habits – eating, sleeping, socializing, screen time – including phone time. I ask about the family dynamics around screen time.
“I’ve added screen time to my adolescent assessment. Discussing safe use of cell phones and social media can have a significant impact on adolescent behavior and wellbeing, and parents are very thankful for the help,” she said. “This study encourages us to add screen time to the assessments we do at all adult ages, especially if mood symptoms exist,” Dr. Dakkak emphasized.
Suggestions for future research
Dr. Dakkak added that more areas for research include the differences in the impact of social media use on content creators versus content consumers. Also, “I would like to see research using the real data of use, the times of use, interruptions in sleep and use, possible confounding variables to include exercise, presence of intimate relationship and school/job performance.”
Given the many confounding variables, more controlled studies are needed to examine mental health outcomes in use, how long people use social media, and the impact of interventions such as time limits, Dr. Gold said.
“We can’t ignore the benefits of social media, such as helping those with social anxiety, finding peer support, and normalizing mental health, and those factors need to be studied and measured more effectively as well, she said.
Take-home message
It is important to recognize that the current study represents a correlation, not causality, said Dr. Gold. In addressing the issues of how social media impact mental health, “as always, the hardest thing is that many people get their news from social media, and often get social support from social media, so there has to be a balance of not removing social media completely, but of helping people see how it affects their mental health and how to find balance.”
The study findings were limited by several factors, including the inability to control for all potential confounders, the inability to assess the nature of social media use, and the lack of dose-response data, the researchers noted. Although the surveys in the current study were not specific to COVID-19, the effects of social media on depression may be specific to the content, and the findings may not generalize beyond the COVID-19 pandemic period.
Approximately two-thirds (66%) of the study participants identified as female, and 76% as White; 11% as Black; 6% as Asian; 5% as Hispanic; and 2% as American Indian or Alaska Native, Pacific Islander or Native Hawaiian, or other.
The National Institute of Mental Health provided a grant for the study to Dr. Pelis, who disclosed consulting fees from various companies and equity in Psy Therapeutics. The study’s lead author also serves as associate editor for JAMA Network Open, but was not involved in the decision process for publication of this study. Dr. Gold disclosed conducting a conference for Johnson & Johnson about social media and health care workers, and was on the advisory council.
Use of social media has been linked to increased anxiety and depression, as well as reduced well-being in adolescents and young adults, but similar associations in older adults have not been well studied, and longitudinal data are lacking, Ron H. Perlis, MD, of Massachusetts General Hospital, Boston, and colleagues wrote in their paper, which was published in JAMA Network Open.
To examine the association between social media use and depressive symptoms in older adults, the researchers reviewed data from 13 waves of an internet survey conducted each month between May 2020 and May 2021. The survey respondents included individuals aged 18 years and older, with a mean age of 56 years.
In the study the researchers analyzed responses from 5,395 individuals aged 18 years and older, with a mean age of 56 years. The study participants had minimal or no depressive symptoms at baseline, according to scores on the nine-item Patient Health Questionnaire (PHQ-9).
Overall, 8.9% of the respondents reported a worsening of 5 points or more on the PHQ-9 score on a follow-up survey, which was the primary outcome. Participants who reported using social media platforms Snapchat, Facebook, or TikTok were significantly more likely to report increased depressive symptoms, compared with those who did not report use of social media. The fully adjusted odds ratio was largest for Snapchat (aOR, 1.53), followed by Facebook (aOR, 1.42), and TikTok (aOR, 1.39).
Incorporating recent television and internet news terms, such as COVID-19, changed the association for Snapchat, for which the aOR decreased from 1.53 to 1.12 when news source terms were included in the survey. TikTok and Facebook associations remained similar.
When the results were further stratified by age, use of TikTok and Snapchat was associated with depressive symptoms in those aged 35 years and older, but not in those younger than 35 years. However, the opposite pattern emerged for Facebook; use was associated with depressive symptoms for individuals younger than 35 years, but not in those aged 35 years and older (aOR, 2.60 vs. aOR, 1.12).
The association between increased self-reported depressive symptoms and use of certain social media platforms was not impacted by baseline social support or face-to-face interactions, the researchers noted.
Family physician was surprised results weren’t more significant
In the current study, “I was honestly surprised the results weren’t more significant,” Mary Ann Dakkak, MD, of Boston University said in an interview. “That said, social media uses during the COVID pandemic may have been a necessary social outlet and form of connection for many people who were otherwise isolated.”
To still see a significant increase in depression when social media could have been a positive force may suggest a heavier impact during “normal” times, she added.
“It is not surprising that what we see in youth is shown among adults,” noted Dr. Dakkak, who was not involved with this study. “I always tell my patients that what is good for their children is good for the adults too, and vice versa.
“We expect to see outcomes of this on youth and adults who have been more isolated, who have used more screen time for learning, work, connection and boredom, in the near future,” she said. “The complex nature of why social media may have been used more heavily for connection during a time when in-person meetings were not possible may be a heavy confounder as the typical profile of heavy social media users may have differed during the COVID shutdowns.”
Psychiatrist: Balance benefits of social media with mental health risks
The current study was likely conducted before the recent news on “hidden” Facebook data and the implications that Facebook knew it was contributing to worsened mental health in teens, particularly around self-esteem, Jessica “Jessi” Gold, MD, a psychiatrist at Washington University, St. Louis, said in an interview.
“If you look more specifically at other studies, however, the data around social media and mental health is constantly varied, with some showing benefits and some showing negatives, and none conclusively suggesting either way,” said Dr. Gold, who also was not involved with the new research. “More data are needed, especially longitudinally and on a broader age group, to understand social media’s impact on mental health over time.
“It is also even more important in the wake of COVID-19, as so many people have turned to social media as a primary source of social support and connection, and are using it even more than before,” she emphasized.
In the current study, “I think the most interesting information is that, for TikTok and Snapchat, the effects seemed to be more pronounced in those older than 35 years who used social media,” said Dr. Gold.
What this study leaves unanswered is “whether people who might develop depression are simply more prone to use social media in the first place, such as to seek out social support,” Dr. Gold said. “Also, we don’t know anything about how long they are using social media or what they are using it for, which to me is important for understanding more about the nuance of the relationship with mental health and social media.”
Experts advise clinicians to discuss social media with patients
This new research suggests that clinicians should be talking to their patients about how social media impacts their emotional reactions, as well as their sleep, Dr. Gold said.
“Patients should be asking themselves how they are feeling when they are on social media and not using it before sleep. They should also be considering time limits and how to effectively use social media while taking care of their mental health,” she said. This conversation between clinician and patient should be had with any patient of any age, who uses social media, not only with teenagers.
“This is also a conversation about moderation, and knowing that individuals may feel they benefit from social media, that they should balance these benefits with potential mental health risks,” she said.
“Studies such as this one shed light onto why social media consumption should be at least a point of discussion with our patients,” said Dr. Dakkak.
She advised clinicians to ask and listen to patients and their families when it comes to screen time habits. “Whenever I see a patient with mood symptoms, I ask about their habits – eating, sleeping, socializing, screen time – including phone time. I ask about the family dynamics around screen time.
“I’ve added screen time to my adolescent assessment. Discussing safe use of cell phones and social media can have a significant impact on adolescent behavior and wellbeing, and parents are very thankful for the help,” she said. “This study encourages us to add screen time to the assessments we do at all adult ages, especially if mood symptoms exist,” Dr. Dakkak emphasized.
Suggestions for future research
Dr. Dakkak added that more areas for research include the differences in the impact of social media use on content creators versus content consumers. Also, “I would like to see research using the real data of use, the times of use, interruptions in sleep and use, possible confounding variables to include exercise, presence of intimate relationship and school/job performance.”
Given the many confounding variables, more controlled studies are needed to examine mental health outcomes in use, how long people use social media, and the impact of interventions such as time limits, Dr. Gold said.
“We can’t ignore the benefits of social media, such as helping those with social anxiety, finding peer support, and normalizing mental health, and those factors need to be studied and measured more effectively as well, she said.
Take-home message
It is important to recognize that the current study represents a correlation, not causality, said Dr. Gold. In addressing the issues of how social media impact mental health, “as always, the hardest thing is that many people get their news from social media, and often get social support from social media, so there has to be a balance of not removing social media completely, but of helping people see how it affects their mental health and how to find balance.”
The study findings were limited by several factors, including the inability to control for all potential confounders, the inability to assess the nature of social media use, and the lack of dose-response data, the researchers noted. Although the surveys in the current study were not specific to COVID-19, the effects of social media on depression may be specific to the content, and the findings may not generalize beyond the COVID-19 pandemic period.
Approximately two-thirds (66%) of the study participants identified as female, and 76% as White; 11% as Black; 6% as Asian; 5% as Hispanic; and 2% as American Indian or Alaska Native, Pacific Islander or Native Hawaiian, or other.
The National Institute of Mental Health provided a grant for the study to Dr. Pelis, who disclosed consulting fees from various companies and equity in Psy Therapeutics. The study’s lead author also serves as associate editor for JAMA Network Open, but was not involved in the decision process for publication of this study. Dr. Gold disclosed conducting a conference for Johnson & Johnson about social media and health care workers, and was on the advisory council.
Use of social media has been linked to increased anxiety and depression, as well as reduced well-being in adolescents and young adults, but similar associations in older adults have not been well studied, and longitudinal data are lacking, Ron H. Perlis, MD, of Massachusetts General Hospital, Boston, and colleagues wrote in their paper, which was published in JAMA Network Open.
To examine the association between social media use and depressive symptoms in older adults, the researchers reviewed data from 13 waves of an internet survey conducted each month between May 2020 and May 2021. The survey respondents included individuals aged 18 years and older, with a mean age of 56 years.
In the study the researchers analyzed responses from 5,395 individuals aged 18 years and older, with a mean age of 56 years. The study participants had minimal or no depressive symptoms at baseline, according to scores on the nine-item Patient Health Questionnaire (PHQ-9).
Overall, 8.9% of the respondents reported a worsening of 5 points or more on the PHQ-9 score on a follow-up survey, which was the primary outcome. Participants who reported using social media platforms Snapchat, Facebook, or TikTok were significantly more likely to report increased depressive symptoms, compared with those who did not report use of social media. The fully adjusted odds ratio was largest for Snapchat (aOR, 1.53), followed by Facebook (aOR, 1.42), and TikTok (aOR, 1.39).
Incorporating recent television and internet news terms, such as COVID-19, changed the association for Snapchat, for which the aOR decreased from 1.53 to 1.12 when news source terms were included in the survey. TikTok and Facebook associations remained similar.
When the results were further stratified by age, use of TikTok and Snapchat was associated with depressive symptoms in those aged 35 years and older, but not in those younger than 35 years. However, the opposite pattern emerged for Facebook; use was associated with depressive symptoms for individuals younger than 35 years, but not in those aged 35 years and older (aOR, 2.60 vs. aOR, 1.12).
The association between increased self-reported depressive symptoms and use of certain social media platforms was not impacted by baseline social support or face-to-face interactions, the researchers noted.
Family physician was surprised results weren’t more significant
In the current study, “I was honestly surprised the results weren’t more significant,” Mary Ann Dakkak, MD, of Boston University said in an interview. “That said, social media uses during the COVID pandemic may have been a necessary social outlet and form of connection for many people who were otherwise isolated.”
To still see a significant increase in depression when social media could have been a positive force may suggest a heavier impact during “normal” times, she added.
“It is not surprising that what we see in youth is shown among adults,” noted Dr. Dakkak, who was not involved with this study. “I always tell my patients that what is good for their children is good for the adults too, and vice versa.
“We expect to see outcomes of this on youth and adults who have been more isolated, who have used more screen time for learning, work, connection and boredom, in the near future,” she said. “The complex nature of why social media may have been used more heavily for connection during a time when in-person meetings were not possible may be a heavy confounder as the typical profile of heavy social media users may have differed during the COVID shutdowns.”
Psychiatrist: Balance benefits of social media with mental health risks
The current study was likely conducted before the recent news on “hidden” Facebook data and the implications that Facebook knew it was contributing to worsened mental health in teens, particularly around self-esteem, Jessica “Jessi” Gold, MD, a psychiatrist at Washington University, St. Louis, said in an interview.
“If you look more specifically at other studies, however, the data around social media and mental health is constantly varied, with some showing benefits and some showing negatives, and none conclusively suggesting either way,” said Dr. Gold, who also was not involved with the new research. “More data are needed, especially longitudinally and on a broader age group, to understand social media’s impact on mental health over time.
“It is also even more important in the wake of COVID-19, as so many people have turned to social media as a primary source of social support and connection, and are using it even more than before,” she emphasized.
In the current study, “I think the most interesting information is that, for TikTok and Snapchat, the effects seemed to be more pronounced in those older than 35 years who used social media,” said Dr. Gold.
What this study leaves unanswered is “whether people who might develop depression are simply more prone to use social media in the first place, such as to seek out social support,” Dr. Gold said. “Also, we don’t know anything about how long they are using social media or what they are using it for, which to me is important for understanding more about the nuance of the relationship with mental health and social media.”
Experts advise clinicians to discuss social media with patients
This new research suggests that clinicians should be talking to their patients about how social media impacts their emotional reactions, as well as their sleep, Dr. Gold said.
“Patients should be asking themselves how they are feeling when they are on social media and not using it before sleep. They should also be considering time limits and how to effectively use social media while taking care of their mental health,” she said. This conversation between clinician and patient should be had with any patient of any age, who uses social media, not only with teenagers.
“This is also a conversation about moderation, and knowing that individuals may feel they benefit from social media, that they should balance these benefits with potential mental health risks,” she said.
“Studies such as this one shed light onto why social media consumption should be at least a point of discussion with our patients,” said Dr. Dakkak.
She advised clinicians to ask and listen to patients and their families when it comes to screen time habits. “Whenever I see a patient with mood symptoms, I ask about their habits – eating, sleeping, socializing, screen time – including phone time. I ask about the family dynamics around screen time.
“I’ve added screen time to my adolescent assessment. Discussing safe use of cell phones and social media can have a significant impact on adolescent behavior and wellbeing, and parents are very thankful for the help,” she said. “This study encourages us to add screen time to the assessments we do at all adult ages, especially if mood symptoms exist,” Dr. Dakkak emphasized.
Suggestions for future research
Dr. Dakkak added that more areas for research include the differences in the impact of social media use on content creators versus content consumers. Also, “I would like to see research using the real data of use, the times of use, interruptions in sleep and use, possible confounding variables to include exercise, presence of intimate relationship and school/job performance.”
Given the many confounding variables, more controlled studies are needed to examine mental health outcomes in use, how long people use social media, and the impact of interventions such as time limits, Dr. Gold said.
“We can’t ignore the benefits of social media, such as helping those with social anxiety, finding peer support, and normalizing mental health, and those factors need to be studied and measured more effectively as well, she said.
Take-home message
It is important to recognize that the current study represents a correlation, not causality, said Dr. Gold. In addressing the issues of how social media impact mental health, “as always, the hardest thing is that many people get their news from social media, and often get social support from social media, so there has to be a balance of not removing social media completely, but of helping people see how it affects their mental health and how to find balance.”
The study findings were limited by several factors, including the inability to control for all potential confounders, the inability to assess the nature of social media use, and the lack of dose-response data, the researchers noted. Although the surveys in the current study were not specific to COVID-19, the effects of social media on depression may be specific to the content, and the findings may not generalize beyond the COVID-19 pandemic period.
Approximately two-thirds (66%) of the study participants identified as female, and 76% as White; 11% as Black; 6% as Asian; 5% as Hispanic; and 2% as American Indian or Alaska Native, Pacific Islander or Native Hawaiian, or other.
The National Institute of Mental Health provided a grant for the study to Dr. Pelis, who disclosed consulting fees from various companies and equity in Psy Therapeutics. The study’s lead author also serves as associate editor for JAMA Network Open, but was not involved in the decision process for publication of this study. Dr. Gold disclosed conducting a conference for Johnson & Johnson about social media and health care workers, and was on the advisory council.
FROM JAMA NETWORK OPEN
COVID surge in Europe: A preview of what’s ahead for the U.S.?
Health experts are warning the United States could be headed for another COVID-19 surge just as we enter the holiday season, following a massive new wave of infections in Europe – a troubling pattern seen throughout the pandemic.
Eighteen months into the global health crisis that has killed 5.1 million people worldwide including more than 767,000 Americans, Europe has become the epicenter of the global health crisis once again.
And some infectious disease specialists say the United States may be next.
“It’s déjà vu, yet again,” says Eric Topol, M.D., founder and director of the Scripps Research Translational Institute. In a new analysis published in The Guardian, the professor of molecular medicine argues that it’s “wishful thinking” for U.S. authorities to believe the nation is “immune” to what’s happening in Europe.
Dr. Topol is also editor-in-chief of Medscape, MDedge’s sister site for medical professionals.
Three times over the past 18 months coronavirus surges in the United States followed similar spikes in Europe, where COVID-19 deaths grew by 10% this month.
Dr. Topol argues another wave may be in store for the states, as European countries implement new lockdowns. COVID-19 spikes are hitting some regions of the continent hard, including areas with high vaccination rates and strict control measures.
Eastern Europe and Russia, where vaccination rates are low, have experienced the worst of it. But even western countries, such as Germany, Austria and the United Kingdom, are reporting some of the highest daily infection figures in the world today.
Countries are responding in increasingly drastic ways.
In Russia, President Vladimir Putin ordered tens of thousands of workers to stay home earlier this month.
In the Dutch city of Utrecht, traditional Christmas celebrations have been canceled as the country is headed for a partial lockdown.
Austria announced a 20-day lockdown beginning Nov. 22 and on Nov. 19 leaders there announced that all 9 million residents will be required to be vaccinated by February. Leaders there are telling unvaccinated individuals to stay at home and out of restaurants, cafes, and other shops in hard-hit regions of the country.
And in Germany, where daily new-infection rates now stand at 50,000, officials have introduced stricter mask mandates and made proof of vaccination or past infection mandatory for entry to many venues. Berlin is also eyeing proposals to shut down the city’s traditional Christmas markets while authorities in Cologne have already called off holiday celebrations, after the ceremonial head of festivities tested positive for COVID-19. Bavaria canceled its popular Christmas markets and will order lockdowns in particularly vulnerable districts, while unvaccinated people will face serious restrictions on where they can go.
Former FDA Commissioner Scott Gottlieb, MD, says what’s happening across the European continent is troubling.
But he also believes it’s possible the United States may be better prepared to head off a similar surge this time around, with increased testing, vaccination and new therapies such as monoclonal antibodies, and antiviral therapeutics.
“Germany’s challenges are [a] caution to [the] world, the COVID pandemic isn’t over globally, won’t be for long time,” he says. “But [the] U.S. is further along than many other countries, in part because we already suffered more spread, in part because we’re making progress on vaccines, therapeutics, testing.”
Other experts agree the United States may not be as vulnerable to another wave of COVID-19 in coming weeks but have stopped short of suggesting we’re out of the woods.
“I don’t think that what we’re seeing in Europe necessarily means that we’re in for a huge surge of serious illness and death the way that we saw last year here in the states,” says David Dowdy, MD, PhD, an associate professor of epidemiology at the Johns Hopkins Bloomberg School of Public Health and a general internist with Baltimore Medical Services.
“But I think anyone who says that they can predict the course of the pandemic for the next few months or few years has been proven wrong in the past and will probably be proven wrong in the future,” Dr. Dowdy says. “None of us knows the future of this pandemic, but I do think that we are in for an increase of cases, not necessarily of deaths and serious illness.”
Looking back, and forward
What’s happening in Europe today mirrors past COVID-19 spikes that presaged big upticks in cases, hospitalizations, and deaths in the United States.
When the pandemic first hit Europe in March 2020, then-President Donald Trump downplayed the threat of the virus despite the warnings of his own advisors and independent public health experts who said COVID-19 could have dire impacts without an aggressive federal action plan.
By late spring the United States had become the epicenter of the pandemic, when case totals eclipsed those of other countries and New York City became a hot zone, according to data compiled by the Johns Hopkins Coronavirus Resource Center. Over the summer, spread of the disease slowed in New York, after tough control measures were instituted, but steadily increased in other states.
Then, later in the year, the Alpha variant of the virus took hold in the United Kingdom and the United States was again unprepared. By winter, the number of cases accelerated in every state in a major second surge that kept millions of Americans from traveling and gathering for the winter holidays.
With the rollout of COVID vaccines last December, cases in the United States – and in many parts of the world – began to fall. Some experts even suggested we’d turned a corner on the pandemic.
But then, last spring and summer, the Delta variant popped up in India and spread to the United Kingdom in a third major wave of COVID. Once again, the United States was unprepared, with 4 in 10 Americans refusing the vaccine and even some vaccinated individuals succumbing to breakthrough Delta infections.
The resulting Delta surge swept the country, preventing many businesses and schools from fully reopening and stressing hospitals in some areas of the country – particularly southern states – with new influxes of COVID-19 patients.
Now, Europe is facing another rise in COVID, with about 350 cases per 100,000 people and many countries hitting new record highs.
What’s driving the European resurgence?
So, what’s behind the new COVID-19 wave in Europe and what might it mean for the United States?
Shaun Truelove, PhD, an infectious disease epidemiologist and faculty member of the Johns Hopkins School of Public Health, says experts are examining several likely factors:
Waning immunity from the vaccines. Data from Johns Hopkins shows infections rising in nations with lower vaccination rates.
The impact of the Delta variant, which is three times more transmissible than the original virus and can even sicken some vaccinated individuals.
The spread of COVID-19 among teens and children; the easing of precautions (such as masking and social distancing); differences in the types of vaccines used in European nations and the United States.
“These are all possibilities,” says Dr. Truelove. “There are so many factors and so it’s difficult to pinpoint exactly what’s driving it and what effect each of those things might be having.”
As a result, it’s difficult to predict and prepare for what might lie ahead for the United States, he says.
“There’s a ton of uncertainty and we’re trying to understand what’s going to happen here over the next 6 months,” he says.
Even so, Dr. Truelove adds that what’s happening overseas might not be “super predictive” of a new wave of COVID in the United States.
For one thing, he says, the Pfizer and Moderna vaccines, the two mRNA vaccines used predominantly in the United States, are far more effective – 94-95% – than the Oxford/AstraZeneca COVID shot (63%) widely administered across Europe.
Secondly, European countries have imposed much stronger and stricter control measures throughout the pandemic than the United States. That might actually be driving the new surges because fewer unvaccinated people have been exposed to the virus, which means they have lower “natural immunity” from prior COVID infection.
Dr. Truelove explains: “Stronger and stricter control measures … have the consequence of leaving a lot more susceptible individuals in the population, [because] the stronger the controls, the fewer people get infected. And so, you have more individuals remaining in the population who are more susceptible and at risk of getting infected in the future.”
By contrast, he notes, a “large chunk” of the United States has not put strict lockdowns in place.
“So, what we’ve seen over the past couple months with the Delta wave is that in a lot of those states with lower vaccination coverage and lower controls this virus has really burned through a lot of the susceptible population. As a result, we’re seeing the curves coming down and what really looks like a lot of the built-up immunity in these states, especially southern states.”
But whether these differences will be enough for the United States to dodge another COVID-19 bullet this winter is uncertain.
“I don’t want to say that the [Europe] surge is NOT a predictor of what might come in the U.S., because I think that it very well could be,” Dr. Truelove says. “And so, people need to be aware of that, and be cautious and be sure get their vaccines and everything else.
“But I’m hopeful that because of some of the differences that maybe we’ll have a little bit of a different situation.”
The takeaway: How best to prepare?
Dr. Dowdy agrees that Europe’s current troubles might not necessarily mean a major new winter surge in the United States.
But he also points out that cases are beginning to head up again in New England, the Midwest, and other regions of the country that are just experiencing the first chill of winter.
“After reaching a low point about 3 weeks ago, cases due to COVID-19 have started to rise again in the United States,” he says. “Cases were falling consistently until mid-October, but over the last 3 weeks, cases have started to rise again in most states.
“Cases in Eastern and Central Europe have more than doubled during that time, meaning that the possibility of a winter surge here is very real.”
Even so, Dr. Dowdy believes the rising rates of vaccination could limit the number of Americans who will be hospitalized with severe disease or die this winter.
Still, he warns against being too optimistic, as Americans travel and get together for the winter holidays.
None of us knows the future of this pandemic, but I do think that we are in for an increase of cases, not necessarily of deaths and serious illness, Dr. Dowdy says.”
The upshot?
“People need to realize that it’s not quite over,” Dr. Truelove says. “We still have a substantial amount of infection in our country. We’re still above 200 cases per million [and] 500,000 incident cases per week or so. That’s a lot of death and a lot of hospitalizations. So, we still have to be concerned and do our best to reduce transmission … by wearing masks, getting vaccinated, getting a booster shot, and getting your children vaccinated.”
Johns Hopkins social and behavioral scientist Rupali Limaye, PhD, MPH, adds that while COVID vaccines have been a “game changer” in the pandemic, more than a third of Americans have yet to receive one.
“That’s really what we need to be messaging around -- that people can still get COVID, there can still be breakthrough infections,” says Dr. Limaye, a health communications scholar. “But the great news is if you have been vaccinated, you are very much less likely, I think it’s 12 times, to be hospitalized or have severe COVID compared to those that are un-vaccinated.”
Dr. Topol agrees, adding: “Now is the time for the U.S. to heed the European signal for the first time, to pull out all the stops. Promote primary vaccination and boosters like there’s no tomorrow. Aggressively counter the pervasive misinformation and disinformation. Accelerate and expand the vaccine mandates ...
“Instead of succumbing to yet another major rise in cases and their sequelae, this is a chance for America to finally rise to the occasion, showing an ability to lead and execute.”
A version of this article first appeared on WebMD.com.
Health experts are warning the United States could be headed for another COVID-19 surge just as we enter the holiday season, following a massive new wave of infections in Europe – a troubling pattern seen throughout the pandemic.
Eighteen months into the global health crisis that has killed 5.1 million people worldwide including more than 767,000 Americans, Europe has become the epicenter of the global health crisis once again.
And some infectious disease specialists say the United States may be next.
“It’s déjà vu, yet again,” says Eric Topol, M.D., founder and director of the Scripps Research Translational Institute. In a new analysis published in The Guardian, the professor of molecular medicine argues that it’s “wishful thinking” for U.S. authorities to believe the nation is “immune” to what’s happening in Europe.
Dr. Topol is also editor-in-chief of Medscape, MDedge’s sister site for medical professionals.
Three times over the past 18 months coronavirus surges in the United States followed similar spikes in Europe, where COVID-19 deaths grew by 10% this month.
Dr. Topol argues another wave may be in store for the states, as European countries implement new lockdowns. COVID-19 spikes are hitting some regions of the continent hard, including areas with high vaccination rates and strict control measures.
Eastern Europe and Russia, where vaccination rates are low, have experienced the worst of it. But even western countries, such as Germany, Austria and the United Kingdom, are reporting some of the highest daily infection figures in the world today.
Countries are responding in increasingly drastic ways.
In Russia, President Vladimir Putin ordered tens of thousands of workers to stay home earlier this month.
In the Dutch city of Utrecht, traditional Christmas celebrations have been canceled as the country is headed for a partial lockdown.
Austria announced a 20-day lockdown beginning Nov. 22 and on Nov. 19 leaders there announced that all 9 million residents will be required to be vaccinated by February. Leaders there are telling unvaccinated individuals to stay at home and out of restaurants, cafes, and other shops in hard-hit regions of the country.
And in Germany, where daily new-infection rates now stand at 50,000, officials have introduced stricter mask mandates and made proof of vaccination or past infection mandatory for entry to many venues. Berlin is also eyeing proposals to shut down the city’s traditional Christmas markets while authorities in Cologne have already called off holiday celebrations, after the ceremonial head of festivities tested positive for COVID-19. Bavaria canceled its popular Christmas markets and will order lockdowns in particularly vulnerable districts, while unvaccinated people will face serious restrictions on where they can go.
Former FDA Commissioner Scott Gottlieb, MD, says what’s happening across the European continent is troubling.
But he also believes it’s possible the United States may be better prepared to head off a similar surge this time around, with increased testing, vaccination and new therapies such as monoclonal antibodies, and antiviral therapeutics.
“Germany’s challenges are [a] caution to [the] world, the COVID pandemic isn’t over globally, won’t be for long time,” he says. “But [the] U.S. is further along than many other countries, in part because we already suffered more spread, in part because we’re making progress on vaccines, therapeutics, testing.”
Other experts agree the United States may not be as vulnerable to another wave of COVID-19 in coming weeks but have stopped short of suggesting we’re out of the woods.
“I don’t think that what we’re seeing in Europe necessarily means that we’re in for a huge surge of serious illness and death the way that we saw last year here in the states,” says David Dowdy, MD, PhD, an associate professor of epidemiology at the Johns Hopkins Bloomberg School of Public Health and a general internist with Baltimore Medical Services.
“But I think anyone who says that they can predict the course of the pandemic for the next few months or few years has been proven wrong in the past and will probably be proven wrong in the future,” Dr. Dowdy says. “None of us knows the future of this pandemic, but I do think that we are in for an increase of cases, not necessarily of deaths and serious illness.”
Looking back, and forward
What’s happening in Europe today mirrors past COVID-19 spikes that presaged big upticks in cases, hospitalizations, and deaths in the United States.
When the pandemic first hit Europe in March 2020, then-President Donald Trump downplayed the threat of the virus despite the warnings of his own advisors and independent public health experts who said COVID-19 could have dire impacts without an aggressive federal action plan.
By late spring the United States had become the epicenter of the pandemic, when case totals eclipsed those of other countries and New York City became a hot zone, according to data compiled by the Johns Hopkins Coronavirus Resource Center. Over the summer, spread of the disease slowed in New York, after tough control measures were instituted, but steadily increased in other states.
Then, later in the year, the Alpha variant of the virus took hold in the United Kingdom and the United States was again unprepared. By winter, the number of cases accelerated in every state in a major second surge that kept millions of Americans from traveling and gathering for the winter holidays.
With the rollout of COVID vaccines last December, cases in the United States – and in many parts of the world – began to fall. Some experts even suggested we’d turned a corner on the pandemic.
But then, last spring and summer, the Delta variant popped up in India and spread to the United Kingdom in a third major wave of COVID. Once again, the United States was unprepared, with 4 in 10 Americans refusing the vaccine and even some vaccinated individuals succumbing to breakthrough Delta infections.
The resulting Delta surge swept the country, preventing many businesses and schools from fully reopening and stressing hospitals in some areas of the country – particularly southern states – with new influxes of COVID-19 patients.
Now, Europe is facing another rise in COVID, with about 350 cases per 100,000 people and many countries hitting new record highs.
What’s driving the European resurgence?
So, what’s behind the new COVID-19 wave in Europe and what might it mean for the United States?
Shaun Truelove, PhD, an infectious disease epidemiologist and faculty member of the Johns Hopkins School of Public Health, says experts are examining several likely factors:
Waning immunity from the vaccines. Data from Johns Hopkins shows infections rising in nations with lower vaccination rates.
The impact of the Delta variant, which is three times more transmissible than the original virus and can even sicken some vaccinated individuals.
The spread of COVID-19 among teens and children; the easing of precautions (such as masking and social distancing); differences in the types of vaccines used in European nations and the United States.
“These are all possibilities,” says Dr. Truelove. “There are so many factors and so it’s difficult to pinpoint exactly what’s driving it and what effect each of those things might be having.”
As a result, it’s difficult to predict and prepare for what might lie ahead for the United States, he says.
“There’s a ton of uncertainty and we’re trying to understand what’s going to happen here over the next 6 months,” he says.
Even so, Dr. Truelove adds that what’s happening overseas might not be “super predictive” of a new wave of COVID in the United States.
For one thing, he says, the Pfizer and Moderna vaccines, the two mRNA vaccines used predominantly in the United States, are far more effective – 94-95% – than the Oxford/AstraZeneca COVID shot (63%) widely administered across Europe.
Secondly, European countries have imposed much stronger and stricter control measures throughout the pandemic than the United States. That might actually be driving the new surges because fewer unvaccinated people have been exposed to the virus, which means they have lower “natural immunity” from prior COVID infection.
Dr. Truelove explains: “Stronger and stricter control measures … have the consequence of leaving a lot more susceptible individuals in the population, [because] the stronger the controls, the fewer people get infected. And so, you have more individuals remaining in the population who are more susceptible and at risk of getting infected in the future.”
By contrast, he notes, a “large chunk” of the United States has not put strict lockdowns in place.
“So, what we’ve seen over the past couple months with the Delta wave is that in a lot of those states with lower vaccination coverage and lower controls this virus has really burned through a lot of the susceptible population. As a result, we’re seeing the curves coming down and what really looks like a lot of the built-up immunity in these states, especially southern states.”
But whether these differences will be enough for the United States to dodge another COVID-19 bullet this winter is uncertain.
“I don’t want to say that the [Europe] surge is NOT a predictor of what might come in the U.S., because I think that it very well could be,” Dr. Truelove says. “And so, people need to be aware of that, and be cautious and be sure get their vaccines and everything else.
“But I’m hopeful that because of some of the differences that maybe we’ll have a little bit of a different situation.”
The takeaway: How best to prepare?
Dr. Dowdy agrees that Europe’s current troubles might not necessarily mean a major new winter surge in the United States.
But he also points out that cases are beginning to head up again in New England, the Midwest, and other regions of the country that are just experiencing the first chill of winter.
“After reaching a low point about 3 weeks ago, cases due to COVID-19 have started to rise again in the United States,” he says. “Cases were falling consistently until mid-October, but over the last 3 weeks, cases have started to rise again in most states.
“Cases in Eastern and Central Europe have more than doubled during that time, meaning that the possibility of a winter surge here is very real.”
Even so, Dr. Dowdy believes the rising rates of vaccination could limit the number of Americans who will be hospitalized with severe disease or die this winter.
Still, he warns against being too optimistic, as Americans travel and get together for the winter holidays.
None of us knows the future of this pandemic, but I do think that we are in for an increase of cases, not necessarily of deaths and serious illness, Dr. Dowdy says.”
The upshot?
“People need to realize that it’s not quite over,” Dr. Truelove says. “We still have a substantial amount of infection in our country. We’re still above 200 cases per million [and] 500,000 incident cases per week or so. That’s a lot of death and a lot of hospitalizations. So, we still have to be concerned and do our best to reduce transmission … by wearing masks, getting vaccinated, getting a booster shot, and getting your children vaccinated.”
Johns Hopkins social and behavioral scientist Rupali Limaye, PhD, MPH, adds that while COVID vaccines have been a “game changer” in the pandemic, more than a third of Americans have yet to receive one.
“That’s really what we need to be messaging around -- that people can still get COVID, there can still be breakthrough infections,” says Dr. Limaye, a health communications scholar. “But the great news is if you have been vaccinated, you are very much less likely, I think it’s 12 times, to be hospitalized or have severe COVID compared to those that are un-vaccinated.”
Dr. Topol agrees, adding: “Now is the time for the U.S. to heed the European signal for the first time, to pull out all the stops. Promote primary vaccination and boosters like there’s no tomorrow. Aggressively counter the pervasive misinformation and disinformation. Accelerate and expand the vaccine mandates ...
“Instead of succumbing to yet another major rise in cases and their sequelae, this is a chance for America to finally rise to the occasion, showing an ability to lead and execute.”
A version of this article first appeared on WebMD.com.
Health experts are warning the United States could be headed for another COVID-19 surge just as we enter the holiday season, following a massive new wave of infections in Europe – a troubling pattern seen throughout the pandemic.
Eighteen months into the global health crisis that has killed 5.1 million people worldwide including more than 767,000 Americans, Europe has become the epicenter of the global health crisis once again.
And some infectious disease specialists say the United States may be next.
“It’s déjà vu, yet again,” says Eric Topol, M.D., founder and director of the Scripps Research Translational Institute. In a new analysis published in The Guardian, the professor of molecular medicine argues that it’s “wishful thinking” for U.S. authorities to believe the nation is “immune” to what’s happening in Europe.
Dr. Topol is also editor-in-chief of Medscape, MDedge’s sister site for medical professionals.
Three times over the past 18 months coronavirus surges in the United States followed similar spikes in Europe, where COVID-19 deaths grew by 10% this month.
Dr. Topol argues another wave may be in store for the states, as European countries implement new lockdowns. COVID-19 spikes are hitting some regions of the continent hard, including areas with high vaccination rates and strict control measures.
Eastern Europe and Russia, where vaccination rates are low, have experienced the worst of it. But even western countries, such as Germany, Austria and the United Kingdom, are reporting some of the highest daily infection figures in the world today.
Countries are responding in increasingly drastic ways.
In Russia, President Vladimir Putin ordered tens of thousands of workers to stay home earlier this month.
In the Dutch city of Utrecht, traditional Christmas celebrations have been canceled as the country is headed for a partial lockdown.
Austria announced a 20-day lockdown beginning Nov. 22 and on Nov. 19 leaders there announced that all 9 million residents will be required to be vaccinated by February. Leaders there are telling unvaccinated individuals to stay at home and out of restaurants, cafes, and other shops in hard-hit regions of the country.
And in Germany, where daily new-infection rates now stand at 50,000, officials have introduced stricter mask mandates and made proof of vaccination or past infection mandatory for entry to many venues. Berlin is also eyeing proposals to shut down the city’s traditional Christmas markets while authorities in Cologne have already called off holiday celebrations, after the ceremonial head of festivities tested positive for COVID-19. Bavaria canceled its popular Christmas markets and will order lockdowns in particularly vulnerable districts, while unvaccinated people will face serious restrictions on where they can go.
Former FDA Commissioner Scott Gottlieb, MD, says what’s happening across the European continent is troubling.
But he also believes it’s possible the United States may be better prepared to head off a similar surge this time around, with increased testing, vaccination and new therapies such as monoclonal antibodies, and antiviral therapeutics.
“Germany’s challenges are [a] caution to [the] world, the COVID pandemic isn’t over globally, won’t be for long time,” he says. “But [the] U.S. is further along than many other countries, in part because we already suffered more spread, in part because we’re making progress on vaccines, therapeutics, testing.”
Other experts agree the United States may not be as vulnerable to another wave of COVID-19 in coming weeks but have stopped short of suggesting we’re out of the woods.
“I don’t think that what we’re seeing in Europe necessarily means that we’re in for a huge surge of serious illness and death the way that we saw last year here in the states,” says David Dowdy, MD, PhD, an associate professor of epidemiology at the Johns Hopkins Bloomberg School of Public Health and a general internist with Baltimore Medical Services.
“But I think anyone who says that they can predict the course of the pandemic for the next few months or few years has been proven wrong in the past and will probably be proven wrong in the future,” Dr. Dowdy says. “None of us knows the future of this pandemic, but I do think that we are in for an increase of cases, not necessarily of deaths and serious illness.”
Looking back, and forward
What’s happening in Europe today mirrors past COVID-19 spikes that presaged big upticks in cases, hospitalizations, and deaths in the United States.
When the pandemic first hit Europe in March 2020, then-President Donald Trump downplayed the threat of the virus despite the warnings of his own advisors and independent public health experts who said COVID-19 could have dire impacts without an aggressive federal action plan.
By late spring the United States had become the epicenter of the pandemic, when case totals eclipsed those of other countries and New York City became a hot zone, according to data compiled by the Johns Hopkins Coronavirus Resource Center. Over the summer, spread of the disease slowed in New York, after tough control measures were instituted, but steadily increased in other states.
Then, later in the year, the Alpha variant of the virus took hold in the United Kingdom and the United States was again unprepared. By winter, the number of cases accelerated in every state in a major second surge that kept millions of Americans from traveling and gathering for the winter holidays.
With the rollout of COVID vaccines last December, cases in the United States – and in many parts of the world – began to fall. Some experts even suggested we’d turned a corner on the pandemic.
But then, last spring and summer, the Delta variant popped up in India and spread to the United Kingdom in a third major wave of COVID. Once again, the United States was unprepared, with 4 in 10 Americans refusing the vaccine and even some vaccinated individuals succumbing to breakthrough Delta infections.
The resulting Delta surge swept the country, preventing many businesses and schools from fully reopening and stressing hospitals in some areas of the country – particularly southern states – with new influxes of COVID-19 patients.
Now, Europe is facing another rise in COVID, with about 350 cases per 100,000 people and many countries hitting new record highs.
What’s driving the European resurgence?
So, what’s behind the new COVID-19 wave in Europe and what might it mean for the United States?
Shaun Truelove, PhD, an infectious disease epidemiologist and faculty member of the Johns Hopkins School of Public Health, says experts are examining several likely factors:
Waning immunity from the vaccines. Data from Johns Hopkins shows infections rising in nations with lower vaccination rates.
The impact of the Delta variant, which is three times more transmissible than the original virus and can even sicken some vaccinated individuals.
The spread of COVID-19 among teens and children; the easing of precautions (such as masking and social distancing); differences in the types of vaccines used in European nations and the United States.
“These are all possibilities,” says Dr. Truelove. “There are so many factors and so it’s difficult to pinpoint exactly what’s driving it and what effect each of those things might be having.”
As a result, it’s difficult to predict and prepare for what might lie ahead for the United States, he says.
“There’s a ton of uncertainty and we’re trying to understand what’s going to happen here over the next 6 months,” he says.
Even so, Dr. Truelove adds that what’s happening overseas might not be “super predictive” of a new wave of COVID in the United States.
For one thing, he says, the Pfizer and Moderna vaccines, the two mRNA vaccines used predominantly in the United States, are far more effective – 94-95% – than the Oxford/AstraZeneca COVID shot (63%) widely administered across Europe.
Secondly, European countries have imposed much stronger and stricter control measures throughout the pandemic than the United States. That might actually be driving the new surges because fewer unvaccinated people have been exposed to the virus, which means they have lower “natural immunity” from prior COVID infection.
Dr. Truelove explains: “Stronger and stricter control measures … have the consequence of leaving a lot more susceptible individuals in the population, [because] the stronger the controls, the fewer people get infected. And so, you have more individuals remaining in the population who are more susceptible and at risk of getting infected in the future.”
By contrast, he notes, a “large chunk” of the United States has not put strict lockdowns in place.
“So, what we’ve seen over the past couple months with the Delta wave is that in a lot of those states with lower vaccination coverage and lower controls this virus has really burned through a lot of the susceptible population. As a result, we’re seeing the curves coming down and what really looks like a lot of the built-up immunity in these states, especially southern states.”
But whether these differences will be enough for the United States to dodge another COVID-19 bullet this winter is uncertain.
“I don’t want to say that the [Europe] surge is NOT a predictor of what might come in the U.S., because I think that it very well could be,” Dr. Truelove says. “And so, people need to be aware of that, and be cautious and be sure get their vaccines and everything else.
“But I’m hopeful that because of some of the differences that maybe we’ll have a little bit of a different situation.”
The takeaway: How best to prepare?
Dr. Dowdy agrees that Europe’s current troubles might not necessarily mean a major new winter surge in the United States.
But he also points out that cases are beginning to head up again in New England, the Midwest, and other regions of the country that are just experiencing the first chill of winter.
“After reaching a low point about 3 weeks ago, cases due to COVID-19 have started to rise again in the United States,” he says. “Cases were falling consistently until mid-October, but over the last 3 weeks, cases have started to rise again in most states.
“Cases in Eastern and Central Europe have more than doubled during that time, meaning that the possibility of a winter surge here is very real.”
Even so, Dr. Dowdy believes the rising rates of vaccination could limit the number of Americans who will be hospitalized with severe disease or die this winter.
Still, he warns against being too optimistic, as Americans travel and get together for the winter holidays.
None of us knows the future of this pandemic, but I do think that we are in for an increase of cases, not necessarily of deaths and serious illness, Dr. Dowdy says.”
The upshot?
“People need to realize that it’s not quite over,” Dr. Truelove says. “We still have a substantial amount of infection in our country. We’re still above 200 cases per million [and] 500,000 incident cases per week or so. That’s a lot of death and a lot of hospitalizations. So, we still have to be concerned and do our best to reduce transmission … by wearing masks, getting vaccinated, getting a booster shot, and getting your children vaccinated.”
Johns Hopkins social and behavioral scientist Rupali Limaye, PhD, MPH, adds that while COVID vaccines have been a “game changer” in the pandemic, more than a third of Americans have yet to receive one.
“That’s really what we need to be messaging around -- that people can still get COVID, there can still be breakthrough infections,” says Dr. Limaye, a health communications scholar. “But the great news is if you have been vaccinated, you are very much less likely, I think it’s 12 times, to be hospitalized or have severe COVID compared to those that are un-vaccinated.”
Dr. Topol agrees, adding: “Now is the time for the U.S. to heed the European signal for the first time, to pull out all the stops. Promote primary vaccination and boosters like there’s no tomorrow. Aggressively counter the pervasive misinformation and disinformation. Accelerate and expand the vaccine mandates ...
“Instead of succumbing to yet another major rise in cases and their sequelae, this is a chance for America to finally rise to the occasion, showing an ability to lead and execute.”
A version of this article first appeared on WebMD.com.
HIV services are bouncing back from COVID-19 disruptions, data suggest, but recovery is ‘precarious’
Over the past 2 years, the COVID-19 pandemic has caused numerous disruptions in health care, including in global HIV/AIDS services. But new data presented at the Association of Nurses in AIDS Care (ANAC) 2021 Annual Meeting suggest that practitioners quickly adapted to challenges posed by the pandemic, and care and prevention services around the world have begun to return to prepandemic levels.
These rebounding numbers “show how resilient the HIV system can be,” Jennifer Kates, PhD, senior vice president and director of global health and HIV policy at the Kaiser Family Foundation (KFF), said in an interview. She presented the data during her ANAC plenary talk on Nov. 11. Dr. Kates noted that continued recovery relies on improving global access to and delivery of COVID-19 vaccines. “If we do not have control of COVID, we are going to see endless cycles of impact,” she said during her talk.
COVID-19 and HIV services
Although there was concern that the pandemic could disrupt access to antiretrovirals, the Global Fund previously reported a nearly 9% increase in people receiving antiretroviral therapy (ART) from 2019 to 2020. HIV prevention and testing did take a hit: There was a 22% decrease in testing for HIV and an 11% decline in the number of people receiving HIV prevention services over that period.
New data from the President’s Emergency Plan for AIDS Relief (PEPFAR) showed similar trends. Consistent with the Global Fund’s findings, a KFF analysis of PEPFAR data found that the number of people receiving ART grew in 2020, climbing from 16.0 million in the first quarter (Q1) of 2020 to 17.4 million by the end of the year. The most recent data from PEPFAR suggest that the number had climbed to 18.4 million by September 2021.
However, there was a 24% decrease in the number of newly enrolled individuals receiving ART from Q2 to Q3 in 2020. It dipped from 669,436 to 509,509. There was a similar decrease in the number of people being tested for HIV, dropping 25% from an estimated 16,700 to 12,500 from Q2 to Q3. But by the end of the year, both measurements had rebounded: New enrollments in ART grew 31%, and HIV testing grew nearly 41% compared to Q3.
The DREAMS (Determined, Resilient, Empowered, AIDS-free, Mentored, and Safe) program, which is focused on adolescent girls and young women, saw a dip in preexposure prophylaxis (PrEP) and other preventive services in Q4 2020, but numbers surpassed prepandemic levels by June 2021.
PEPFAR helped speed recovery, Dr. Kates said, by providing guidance on COVID-19 protocols to the field and implementing innovations, such as accelerated 3- and 6-month medication dispensing, virtual platforms, and decentralized drug delivery. In addition, the U.S. Congress allocated $3.8 billion in emergency funding in fiscal year 2021 to help mitigate the effects of COVID-19 on HIV and AIDS care.
Longer-term outcomes still unclear
Although these numbers are encouraging, some of the effects of COVID-19 on the HIV epidemic are still unknown – in particular, whether these documented dips in preventive services will translate to an increase in new infections. This will not be clear until a year or 2 from now, Dr. Kates noted. Increased use of ART as well as an increase in some behaviors associated with the pandemic, such as decreased social contact, are factors that mitigate an increase in the rate of infections, she said, but “how that all is going to play out we don’t know for sure.”
Other conference attendees expressed anxiety about the possibility of an increase in the rate of infections. “I’m waiting for the other shoe to drop, as it were,” Barb Cardell, training and technical assistance director at Positive Women’s Network–USA, in Oakland, Calif., said in an interview. The Positive Women’s Network is a national organization of women living with HIV. “Starting late in 2019, we have been cautioning public health officials in states and federally that there will likely be an uptick in HIV diagnosis as we return to whatever ‘normal’ looks like these days,” Ms. Cardell noted, adding, “We have all heard stories of folks that had an exposure and weren’t able to access PrEP during the pandemic and hence seroconverted.”
Kara McGee, associate clinical professor at Duke University School of Nursing, Durham, N.C., shared similar sentiments. “Many people at risk of acquiring HIV had trouble accessing testing and prevention prior to the pandemic, and service interruptions due to the COVID-19 pandemic have only worsened access – especially in rural areas,” she told this news organization.
Need for equitable vaccine access
For HIV services to continue to rebound, COVID-19 vaccination needs to be made a priority globally, Dr. Kates said. But data suggest lower-income countries are being left behind. In high-income countries, 65% of the population has been fully vaccinated, compared to 2% of people in the lowest-income countries. A KFF analysis projected that at the current rates of vaccination, these disparities will widen over time. COVID-19 testing rates in lower-income countries also lag. In high-income countries, 740 tests per 100,000 individuals are conducted daily; in low-income countries, that rate is 13 daily tests per 100,000 people. Until we can achieve more equitable access globally, the documented recovery of HIV is “precarious,” Dr. Kates said.
Ms. McGee agreed with Dr. Kates and was surprised by the extent of global inequities in the COVID-19 response. She said these issues should be a focus for the HIV health care community moving forward. “I think there are lot of us who have worked in the HIV field for many years – both domestically and internationally – who did not fully grasp the global disparities and need to consider how we can advocate for more equal access and distribution,” she said.
A version of this article first appeared on Medscape.com.
Over the past 2 years, the COVID-19 pandemic has caused numerous disruptions in health care, including in global HIV/AIDS services. But new data presented at the Association of Nurses in AIDS Care (ANAC) 2021 Annual Meeting suggest that practitioners quickly adapted to challenges posed by the pandemic, and care and prevention services around the world have begun to return to prepandemic levels.
These rebounding numbers “show how resilient the HIV system can be,” Jennifer Kates, PhD, senior vice president and director of global health and HIV policy at the Kaiser Family Foundation (KFF), said in an interview. She presented the data during her ANAC plenary talk on Nov. 11. Dr. Kates noted that continued recovery relies on improving global access to and delivery of COVID-19 vaccines. “If we do not have control of COVID, we are going to see endless cycles of impact,” she said during her talk.
COVID-19 and HIV services
Although there was concern that the pandemic could disrupt access to antiretrovirals, the Global Fund previously reported a nearly 9% increase in people receiving antiretroviral therapy (ART) from 2019 to 2020. HIV prevention and testing did take a hit: There was a 22% decrease in testing for HIV and an 11% decline in the number of people receiving HIV prevention services over that period.
New data from the President’s Emergency Plan for AIDS Relief (PEPFAR) showed similar trends. Consistent with the Global Fund’s findings, a KFF analysis of PEPFAR data found that the number of people receiving ART grew in 2020, climbing from 16.0 million in the first quarter (Q1) of 2020 to 17.4 million by the end of the year. The most recent data from PEPFAR suggest that the number had climbed to 18.4 million by September 2021.
However, there was a 24% decrease in the number of newly enrolled individuals receiving ART from Q2 to Q3 in 2020. It dipped from 669,436 to 509,509. There was a similar decrease in the number of people being tested for HIV, dropping 25% from an estimated 16,700 to 12,500 from Q2 to Q3. But by the end of the year, both measurements had rebounded: New enrollments in ART grew 31%, and HIV testing grew nearly 41% compared to Q3.
The DREAMS (Determined, Resilient, Empowered, AIDS-free, Mentored, and Safe) program, which is focused on adolescent girls and young women, saw a dip in preexposure prophylaxis (PrEP) and other preventive services in Q4 2020, but numbers surpassed prepandemic levels by June 2021.
PEPFAR helped speed recovery, Dr. Kates said, by providing guidance on COVID-19 protocols to the field and implementing innovations, such as accelerated 3- and 6-month medication dispensing, virtual platforms, and decentralized drug delivery. In addition, the U.S. Congress allocated $3.8 billion in emergency funding in fiscal year 2021 to help mitigate the effects of COVID-19 on HIV and AIDS care.
Longer-term outcomes still unclear
Although these numbers are encouraging, some of the effects of COVID-19 on the HIV epidemic are still unknown – in particular, whether these documented dips in preventive services will translate to an increase in new infections. This will not be clear until a year or 2 from now, Dr. Kates noted. Increased use of ART as well as an increase in some behaviors associated with the pandemic, such as decreased social contact, are factors that mitigate an increase in the rate of infections, she said, but “how that all is going to play out we don’t know for sure.”
Other conference attendees expressed anxiety about the possibility of an increase in the rate of infections. “I’m waiting for the other shoe to drop, as it were,” Barb Cardell, training and technical assistance director at Positive Women’s Network–USA, in Oakland, Calif., said in an interview. The Positive Women’s Network is a national organization of women living with HIV. “Starting late in 2019, we have been cautioning public health officials in states and federally that there will likely be an uptick in HIV diagnosis as we return to whatever ‘normal’ looks like these days,” Ms. Cardell noted, adding, “We have all heard stories of folks that had an exposure and weren’t able to access PrEP during the pandemic and hence seroconverted.”
Kara McGee, associate clinical professor at Duke University School of Nursing, Durham, N.C., shared similar sentiments. “Many people at risk of acquiring HIV had trouble accessing testing and prevention prior to the pandemic, and service interruptions due to the COVID-19 pandemic have only worsened access – especially in rural areas,” she told this news organization.
Need for equitable vaccine access
For HIV services to continue to rebound, COVID-19 vaccination needs to be made a priority globally, Dr. Kates said. But data suggest lower-income countries are being left behind. In high-income countries, 65% of the population has been fully vaccinated, compared to 2% of people in the lowest-income countries. A KFF analysis projected that at the current rates of vaccination, these disparities will widen over time. COVID-19 testing rates in lower-income countries also lag. In high-income countries, 740 tests per 100,000 individuals are conducted daily; in low-income countries, that rate is 13 daily tests per 100,000 people. Until we can achieve more equitable access globally, the documented recovery of HIV is “precarious,” Dr. Kates said.
Ms. McGee agreed with Dr. Kates and was surprised by the extent of global inequities in the COVID-19 response. She said these issues should be a focus for the HIV health care community moving forward. “I think there are lot of us who have worked in the HIV field for many years – both domestically and internationally – who did not fully grasp the global disparities and need to consider how we can advocate for more equal access and distribution,” she said.
A version of this article first appeared on Medscape.com.
Over the past 2 years, the COVID-19 pandemic has caused numerous disruptions in health care, including in global HIV/AIDS services. But new data presented at the Association of Nurses in AIDS Care (ANAC) 2021 Annual Meeting suggest that practitioners quickly adapted to challenges posed by the pandemic, and care and prevention services around the world have begun to return to prepandemic levels.
These rebounding numbers “show how resilient the HIV system can be,” Jennifer Kates, PhD, senior vice president and director of global health and HIV policy at the Kaiser Family Foundation (KFF), said in an interview. She presented the data during her ANAC plenary talk on Nov. 11. Dr. Kates noted that continued recovery relies on improving global access to and delivery of COVID-19 vaccines. “If we do not have control of COVID, we are going to see endless cycles of impact,” she said during her talk.
COVID-19 and HIV services
Although there was concern that the pandemic could disrupt access to antiretrovirals, the Global Fund previously reported a nearly 9% increase in people receiving antiretroviral therapy (ART) from 2019 to 2020. HIV prevention and testing did take a hit: There was a 22% decrease in testing for HIV and an 11% decline in the number of people receiving HIV prevention services over that period.
New data from the President’s Emergency Plan for AIDS Relief (PEPFAR) showed similar trends. Consistent with the Global Fund’s findings, a KFF analysis of PEPFAR data found that the number of people receiving ART grew in 2020, climbing from 16.0 million in the first quarter (Q1) of 2020 to 17.4 million by the end of the year. The most recent data from PEPFAR suggest that the number had climbed to 18.4 million by September 2021.
However, there was a 24% decrease in the number of newly enrolled individuals receiving ART from Q2 to Q3 in 2020. It dipped from 669,436 to 509,509. There was a similar decrease in the number of people being tested for HIV, dropping 25% from an estimated 16,700 to 12,500 from Q2 to Q3. But by the end of the year, both measurements had rebounded: New enrollments in ART grew 31%, and HIV testing grew nearly 41% compared to Q3.
The DREAMS (Determined, Resilient, Empowered, AIDS-free, Mentored, and Safe) program, which is focused on adolescent girls and young women, saw a dip in preexposure prophylaxis (PrEP) and other preventive services in Q4 2020, but numbers surpassed prepandemic levels by June 2021.
PEPFAR helped speed recovery, Dr. Kates said, by providing guidance on COVID-19 protocols to the field and implementing innovations, such as accelerated 3- and 6-month medication dispensing, virtual platforms, and decentralized drug delivery. In addition, the U.S. Congress allocated $3.8 billion in emergency funding in fiscal year 2021 to help mitigate the effects of COVID-19 on HIV and AIDS care.
Longer-term outcomes still unclear
Although these numbers are encouraging, some of the effects of COVID-19 on the HIV epidemic are still unknown – in particular, whether these documented dips in preventive services will translate to an increase in new infections. This will not be clear until a year or 2 from now, Dr. Kates noted. Increased use of ART as well as an increase in some behaviors associated with the pandemic, such as decreased social contact, are factors that mitigate an increase in the rate of infections, she said, but “how that all is going to play out we don’t know for sure.”
Other conference attendees expressed anxiety about the possibility of an increase in the rate of infections. “I’m waiting for the other shoe to drop, as it were,” Barb Cardell, training and technical assistance director at Positive Women’s Network–USA, in Oakland, Calif., said in an interview. The Positive Women’s Network is a national organization of women living with HIV. “Starting late in 2019, we have been cautioning public health officials in states and federally that there will likely be an uptick in HIV diagnosis as we return to whatever ‘normal’ looks like these days,” Ms. Cardell noted, adding, “We have all heard stories of folks that had an exposure and weren’t able to access PrEP during the pandemic and hence seroconverted.”
Kara McGee, associate clinical professor at Duke University School of Nursing, Durham, N.C., shared similar sentiments. “Many people at risk of acquiring HIV had trouble accessing testing and prevention prior to the pandemic, and service interruptions due to the COVID-19 pandemic have only worsened access – especially in rural areas,” she told this news organization.
Need for equitable vaccine access
For HIV services to continue to rebound, COVID-19 vaccination needs to be made a priority globally, Dr. Kates said. But data suggest lower-income countries are being left behind. In high-income countries, 65% of the population has been fully vaccinated, compared to 2% of people in the lowest-income countries. A KFF analysis projected that at the current rates of vaccination, these disparities will widen over time. COVID-19 testing rates in lower-income countries also lag. In high-income countries, 740 tests per 100,000 individuals are conducted daily; in low-income countries, that rate is 13 daily tests per 100,000 people. Until we can achieve more equitable access globally, the documented recovery of HIV is “precarious,” Dr. Kates said.
Ms. McGee agreed with Dr. Kates and was surprised by the extent of global inequities in the COVID-19 response. She said these issues should be a focus for the HIV health care community moving forward. “I think there are lot of us who have worked in the HIV field for many years – both domestically and internationally – who did not fully grasp the global disparities and need to consider how we can advocate for more equal access and distribution,” she said.
A version of this article first appeared on Medscape.com.
CDC unveils mental health protection plan for health care workers
Federal health officials have outlined a five-part plan to improve and protect the mental health and well-being of America’s health care workers (HCWs) and create sustainable change for the next generation of HCWs.
“It’s long past time for us to care for the people who care for all of us and address burnout in our health care workers,” U.S. Surgeon General Vivek H. Murthy, MD, MBA, said during a webinar hosted by the National Institute for Occupational Safety and Health, part of the U.S. Centers for Disease Control and Prevention.
“My hope is that, going forward, we will be able to embark on this journey together to create a health care system, a health care environment, a country where we can not only provide extraordinary care to all those who need it, but where we can take good care of those who have sacrificed so much and make sure that they are well,” Dr. Murthy said.
Burnout is not selective
There are 20 million HCWs in the United States, and no one is immune from burnout, said NIOSH Director John Howard, MD.
He noted that from June through Sept. of 2020 – the height of the COVID-19 pandemic – 93% of HCWs experienced some degree of stress, with 22% reporting moderate depression and post-traumatic stress disorder.
Looking at subsets of HCWs, a recent survey showed that one in five nurses contemplated leaving the profession because of insufficient staffing, intensity of workload, emotional and physical toll of the job, and lack of support, Dr. Howard noted.
Physician burnout was a significant issue even before the pandemic, with about 79% of physicians reporting burnout. , Dr. Howard said.
Women in health care jobs are especially vulnerable to burnout; 76% of health care jobs are held by women and 64% of physicians that feel burned-out are women, according to federal data.
“We have significant work to do in shoring up the safety and health of women in health care,” Dr. Howard said.
Mental health is also suffering among local and state public health workers. In a recent CDC survey of 26,000 of these workers, 53% reported symptoms of at least one mental health condition in the past 2 weeks.
“That is really an alarming proportion of public health workers who are as vital and essential as nurses and doctors are in our health care system,” Dr. Howard said.
Primary prevention approach
To tackle the burnout crisis, NIOSH plans to:
- Take a deep dive into understanding the personal, social, and economic burdens HCWs face on a daily basis.
- Assimilate the evidence and create a repository of best practices, resources, and interventions.
- Partner with key stakeholders, including the American Hospital Association, the American Nurses Association, National Nurses United, the Joint Commission.
- Identify and adapt tools for the health care workplace that emphasize stress reduction.
NIOSH also plans to “generate awareness through a national, multidimensional social marketing campaign to get the word out about stress so health care workers don’t feel so alone,” Dr. Howard said.
This five-part plan takes a primary prevention approach to identifying and eliminating risk factors for burnout and stress, he added.
Secondary prevention, “when damage has already been done and you’re trying to save a health care worker who is suffering from a mental health issue, that’s a lot harder than taking a good look at what you can do to organizational practices that lead to health care workers’ stress and burnout,” Dr. Howard said.
A version of this article first appeared on Medscape.com.
Federal health officials have outlined a five-part plan to improve and protect the mental health and well-being of America’s health care workers (HCWs) and create sustainable change for the next generation of HCWs.
“It’s long past time for us to care for the people who care for all of us and address burnout in our health care workers,” U.S. Surgeon General Vivek H. Murthy, MD, MBA, said during a webinar hosted by the National Institute for Occupational Safety and Health, part of the U.S. Centers for Disease Control and Prevention.
“My hope is that, going forward, we will be able to embark on this journey together to create a health care system, a health care environment, a country where we can not only provide extraordinary care to all those who need it, but where we can take good care of those who have sacrificed so much and make sure that they are well,” Dr. Murthy said.
Burnout is not selective
There are 20 million HCWs in the United States, and no one is immune from burnout, said NIOSH Director John Howard, MD.
He noted that from June through Sept. of 2020 – the height of the COVID-19 pandemic – 93% of HCWs experienced some degree of stress, with 22% reporting moderate depression and post-traumatic stress disorder.
Looking at subsets of HCWs, a recent survey showed that one in five nurses contemplated leaving the profession because of insufficient staffing, intensity of workload, emotional and physical toll of the job, and lack of support, Dr. Howard noted.
Physician burnout was a significant issue even before the pandemic, with about 79% of physicians reporting burnout. , Dr. Howard said.
Women in health care jobs are especially vulnerable to burnout; 76% of health care jobs are held by women and 64% of physicians that feel burned-out are women, according to federal data.
“We have significant work to do in shoring up the safety and health of women in health care,” Dr. Howard said.
Mental health is also suffering among local and state public health workers. In a recent CDC survey of 26,000 of these workers, 53% reported symptoms of at least one mental health condition in the past 2 weeks.
“That is really an alarming proportion of public health workers who are as vital and essential as nurses and doctors are in our health care system,” Dr. Howard said.
Primary prevention approach
To tackle the burnout crisis, NIOSH plans to:
- Take a deep dive into understanding the personal, social, and economic burdens HCWs face on a daily basis.
- Assimilate the evidence and create a repository of best practices, resources, and interventions.
- Partner with key stakeholders, including the American Hospital Association, the American Nurses Association, National Nurses United, the Joint Commission.
- Identify and adapt tools for the health care workplace that emphasize stress reduction.
NIOSH also plans to “generate awareness through a national, multidimensional social marketing campaign to get the word out about stress so health care workers don’t feel so alone,” Dr. Howard said.
This five-part plan takes a primary prevention approach to identifying and eliminating risk factors for burnout and stress, he added.
Secondary prevention, “when damage has already been done and you’re trying to save a health care worker who is suffering from a mental health issue, that’s a lot harder than taking a good look at what you can do to organizational practices that lead to health care workers’ stress and burnout,” Dr. Howard said.
A version of this article first appeared on Medscape.com.
Federal health officials have outlined a five-part plan to improve and protect the mental health and well-being of America’s health care workers (HCWs) and create sustainable change for the next generation of HCWs.
“It’s long past time for us to care for the people who care for all of us and address burnout in our health care workers,” U.S. Surgeon General Vivek H. Murthy, MD, MBA, said during a webinar hosted by the National Institute for Occupational Safety and Health, part of the U.S. Centers for Disease Control and Prevention.
“My hope is that, going forward, we will be able to embark on this journey together to create a health care system, a health care environment, a country where we can not only provide extraordinary care to all those who need it, but where we can take good care of those who have sacrificed so much and make sure that they are well,” Dr. Murthy said.
Burnout is not selective
There are 20 million HCWs in the United States, and no one is immune from burnout, said NIOSH Director John Howard, MD.
He noted that from June through Sept. of 2020 – the height of the COVID-19 pandemic – 93% of HCWs experienced some degree of stress, with 22% reporting moderate depression and post-traumatic stress disorder.
Looking at subsets of HCWs, a recent survey showed that one in five nurses contemplated leaving the profession because of insufficient staffing, intensity of workload, emotional and physical toll of the job, and lack of support, Dr. Howard noted.
Physician burnout was a significant issue even before the pandemic, with about 79% of physicians reporting burnout. , Dr. Howard said.
Women in health care jobs are especially vulnerable to burnout; 76% of health care jobs are held by women and 64% of physicians that feel burned-out are women, according to federal data.
“We have significant work to do in shoring up the safety and health of women in health care,” Dr. Howard said.
Mental health is also suffering among local and state public health workers. In a recent CDC survey of 26,000 of these workers, 53% reported symptoms of at least one mental health condition in the past 2 weeks.
“That is really an alarming proportion of public health workers who are as vital and essential as nurses and doctors are in our health care system,” Dr. Howard said.
Primary prevention approach
To tackle the burnout crisis, NIOSH plans to:
- Take a deep dive into understanding the personal, social, and economic burdens HCWs face on a daily basis.
- Assimilate the evidence and create a repository of best practices, resources, and interventions.
- Partner with key stakeholders, including the American Hospital Association, the American Nurses Association, National Nurses United, the Joint Commission.
- Identify and adapt tools for the health care workplace that emphasize stress reduction.
NIOSH also plans to “generate awareness through a national, multidimensional social marketing campaign to get the word out about stress so health care workers don’t feel so alone,” Dr. Howard said.
This five-part plan takes a primary prevention approach to identifying and eliminating risk factors for burnout and stress, he added.
Secondary prevention, “when damage has already been done and you’re trying to save a health care worker who is suffering from a mental health issue, that’s a lot harder than taking a good look at what you can do to organizational practices that lead to health care workers’ stress and burnout,” Dr. Howard said.
A version of this article first appeared on Medscape.com.
CDC: All adults should be eligible for Pfizer, Moderna boosters
on its vaccine recommendations.
The Advisory Committee on Immunization Practices, or ACIP, recommended that all adults be eligible for a third dose of a Pfizer or Moderna mRNA vaccine, at least 6 months after their second dose.
They also strengthened a recommendation that everyone over the age of 50 should get a third dose, whether or not they have an underlying health condition that may increase their risk from a COVID-19 infection.
The committee voted 11 to 0 in favor of both policies.
CDC Director Rochelle Walensky, MD, must now sign off on both policies, which she is expected to do.
More than 70 million adults are now eligible for booster shots in the United States, but only about 31 million people have received one. About half of those who have been boosted are over the age of 65.
In a recent survey, the Kaiser Family Foundation found that about 4 in 10 younger adults said they were unsure if they qualified for a booster.
Under the current policy, boosters are recommended for everyone age 65 and older. But people who are younger than age 65 are eligible for boosters if they have an underlying health condition or live or work in a high-risk situation—something individuals have to determine on their own. Experts said that shading of the policy had created confusion that was holding people back.
Nirav Shah, MD, JD, president of the Association of State and Territorial Health Officials, noted that public health officials have been swamped with calls from people who are trying to figure out if they are eligible to get a booster dose.
He said that in a call the evening of Nov. 18 with state health departments, “There was not a single state that voiced opposition to this move,” he told the ACIP.
Dr. Shah said that the current guidelines were well intentioned, but “in pursuit of precision, they create confusion.”
“Our concern is that eligible individuals are not receiving boosters right now as a result of this confusion,” he said.
The committee based its decision on the results of a new study of boosters in Pfizer vaccine recipients, as well as reassuring safety information that’s being collected through the CDC and FDA’s monitoring systems.
Pfizer presented the early results from a study of 10,000 people who had all received two doses of its vaccine. Half of the study participants received a third shot, or booster. The other half got a placebo.
The study is ongoing, but so far, six of the people in the booster group have gotten a COVID-19 infection with symptoms compared to 123 people who got COVID-19 in the placebo group, making boosters 95% effective at keeping people from getting sick. Most people in the study had gotten their original doses about 10 months earlier. They’ve been followed for about 10 weeks since their booster. Importantly, there were no study participants hospitalized for COVID-19 infections in either the placebo or booster group, indicating that the first two doses were still very effective at preventing severe outcomes from infection.
The majority of side effects after a third Pfizer dose were mild and temporary. Side effects like sore arms, swelling, fever, headache, and fatigue were more common in the booster group — affecting about 1 in 4 people who got a third shot. Vaccination side effects were less common after boosters than have been seen after the second dose of the vaccine.
Some cases of myocarditis and pericarditis have been reported after people received vaccine boosters, but the risk for this heart inflammation appears to be extremely low, about two cases for every million doses given. There were 54 cases of myocarditis reported so far to the Vaccine Adverse Event Reporting System, or VAERS. So far, only 12 have met the case definition and are considered related to vaccination. Most of the reported cases are still being studied.
on its vaccine recommendations.
The Advisory Committee on Immunization Practices, or ACIP, recommended that all adults be eligible for a third dose of a Pfizer or Moderna mRNA vaccine, at least 6 months after their second dose.
They also strengthened a recommendation that everyone over the age of 50 should get a third dose, whether or not they have an underlying health condition that may increase their risk from a COVID-19 infection.
The committee voted 11 to 0 in favor of both policies.
CDC Director Rochelle Walensky, MD, must now sign off on both policies, which she is expected to do.
More than 70 million adults are now eligible for booster shots in the United States, but only about 31 million people have received one. About half of those who have been boosted are over the age of 65.
In a recent survey, the Kaiser Family Foundation found that about 4 in 10 younger adults said they were unsure if they qualified for a booster.
Under the current policy, boosters are recommended for everyone age 65 and older. But people who are younger than age 65 are eligible for boosters if they have an underlying health condition or live or work in a high-risk situation—something individuals have to determine on their own. Experts said that shading of the policy had created confusion that was holding people back.
Nirav Shah, MD, JD, president of the Association of State and Territorial Health Officials, noted that public health officials have been swamped with calls from people who are trying to figure out if they are eligible to get a booster dose.
He said that in a call the evening of Nov. 18 with state health departments, “There was not a single state that voiced opposition to this move,” he told the ACIP.
Dr. Shah said that the current guidelines were well intentioned, but “in pursuit of precision, they create confusion.”
“Our concern is that eligible individuals are not receiving boosters right now as a result of this confusion,” he said.
The committee based its decision on the results of a new study of boosters in Pfizer vaccine recipients, as well as reassuring safety information that’s being collected through the CDC and FDA’s monitoring systems.
Pfizer presented the early results from a study of 10,000 people who had all received two doses of its vaccine. Half of the study participants received a third shot, or booster. The other half got a placebo.
The study is ongoing, but so far, six of the people in the booster group have gotten a COVID-19 infection with symptoms compared to 123 people who got COVID-19 in the placebo group, making boosters 95% effective at keeping people from getting sick. Most people in the study had gotten their original doses about 10 months earlier. They’ve been followed for about 10 weeks since their booster. Importantly, there were no study participants hospitalized for COVID-19 infections in either the placebo or booster group, indicating that the first two doses were still very effective at preventing severe outcomes from infection.
The majority of side effects after a third Pfizer dose were mild and temporary. Side effects like sore arms, swelling, fever, headache, and fatigue were more common in the booster group — affecting about 1 in 4 people who got a third shot. Vaccination side effects were less common after boosters than have been seen after the second dose of the vaccine.
Some cases of myocarditis and pericarditis have been reported after people received vaccine boosters, but the risk for this heart inflammation appears to be extremely low, about two cases for every million doses given. There were 54 cases of myocarditis reported so far to the Vaccine Adverse Event Reporting System, or VAERS. So far, only 12 have met the case definition and are considered related to vaccination. Most of the reported cases are still being studied.
on its vaccine recommendations.
The Advisory Committee on Immunization Practices, or ACIP, recommended that all adults be eligible for a third dose of a Pfizer or Moderna mRNA vaccine, at least 6 months after their second dose.
They also strengthened a recommendation that everyone over the age of 50 should get a third dose, whether or not they have an underlying health condition that may increase their risk from a COVID-19 infection.
The committee voted 11 to 0 in favor of both policies.
CDC Director Rochelle Walensky, MD, must now sign off on both policies, which she is expected to do.
More than 70 million adults are now eligible for booster shots in the United States, but only about 31 million people have received one. About half of those who have been boosted are over the age of 65.
In a recent survey, the Kaiser Family Foundation found that about 4 in 10 younger adults said they were unsure if they qualified for a booster.
Under the current policy, boosters are recommended for everyone age 65 and older. But people who are younger than age 65 are eligible for boosters if they have an underlying health condition or live or work in a high-risk situation—something individuals have to determine on their own. Experts said that shading of the policy had created confusion that was holding people back.
Nirav Shah, MD, JD, president of the Association of State and Territorial Health Officials, noted that public health officials have been swamped with calls from people who are trying to figure out if they are eligible to get a booster dose.
He said that in a call the evening of Nov. 18 with state health departments, “There was not a single state that voiced opposition to this move,” he told the ACIP.
Dr. Shah said that the current guidelines were well intentioned, but “in pursuit of precision, they create confusion.”
“Our concern is that eligible individuals are not receiving boosters right now as a result of this confusion,” he said.
The committee based its decision on the results of a new study of boosters in Pfizer vaccine recipients, as well as reassuring safety information that’s being collected through the CDC and FDA’s monitoring systems.
Pfizer presented the early results from a study of 10,000 people who had all received two doses of its vaccine. Half of the study participants received a third shot, or booster. The other half got a placebo.
The study is ongoing, but so far, six of the people in the booster group have gotten a COVID-19 infection with symptoms compared to 123 people who got COVID-19 in the placebo group, making boosters 95% effective at keeping people from getting sick. Most people in the study had gotten their original doses about 10 months earlier. They’ve been followed for about 10 weeks since their booster. Importantly, there were no study participants hospitalized for COVID-19 infections in either the placebo or booster group, indicating that the first two doses were still very effective at preventing severe outcomes from infection.
The majority of side effects after a third Pfizer dose were mild and temporary. Side effects like sore arms, swelling, fever, headache, and fatigue were more common in the booster group — affecting about 1 in 4 people who got a third shot. Vaccination side effects were less common after boosters than have been seen after the second dose of the vaccine.
Some cases of myocarditis and pericarditis have been reported after people received vaccine boosters, but the risk for this heart inflammation appears to be extremely low, about two cases for every million doses given. There were 54 cases of myocarditis reported so far to the Vaccine Adverse Event Reporting System, or VAERS. So far, only 12 have met the case definition and are considered related to vaccination. Most of the reported cases are still being studied.
CDC: Thirty percent of hospital workers in U.S. still unvaccinated
, according to a new survey by the Centers for Disease Control and Prevention.
The snapshot in time – Jan. 20, 2021 to Sept. 15, 2021 – is based on voluntary weekly reports from hospitals. Only about 48% of the 5,085 hospitals in the U.S. Health and Human Services department’s Unified Hospital Data Surveillance System reported data on vaccination coverage during the period, and, after validation checks, the study included reports from 2,086 facilities, or just 41% of all hospitals, covering 3.35 million workers.
Overall, the number who were fully vaccinated rose from 36.1% in Jan. 2021 to 60.2% in April 2021, and then crept slowly up to 70% by Sept. 15, the CDC researchers reported in the American Journal of Infection Control.
The slowdown among hospital workers seems to mirror the same decline as in the general population.
Arjun Srinivasan, MD, associate director for health care–associated infection prevention programs at the CDC, said the decline in part may be the result of misinformation.
Health care personnel “are not fully immune from vaccine misinformation,” he said, adding that such misinformation “is contributing to decreased vaccine uptake among non–health care personnel.”
“The take-home message is that there is a lot of work to do in health care settings in order to get all of our health care personnel vaccinated,” Dr. Srinivasan told this news organization. “We need them to be vaccinated to protect themselves. It is also really important that we as health care personnel get vaccinated to protect our patients.”
Vaccine mandates
The analysis shows that workers were more likely to be vaccinated if they worked at a children’s hospital (77%), lived in metropolitan counties (71%), or worked in a hospital with lower cumulative admissions of COVID-19 patients, or lower cumulative COVID-19 cases.
The odds of being fully vaccinated were lower if the surrounding community had lower vaccination coverage. Workers in non-metropolitan counties (63.3%) and in rural counties (65.1%) were also less likely to be fully vaccinated, as well as those who were in critical access hospitals (64%) or long-term acute care hospitals (68.8%).
Surveys have shown that health care personnel who are vaccine-hesitant cited concerns they had about vaccine efficacy, adverse effects, the speed of vaccine development, and lack of full Food and Drug Administration approval, the study authors noted. In addition, many reported low trust in the government.
A Medscape survey this past April found that 25% of health care workers said they did not plan to be fully vaccinated. Some 40% of the 9,349 workers who responded said that employers should never require a COVID-19 vaccine for clinicians.
But the Centers for Medicare & Medicaid Services is attempting to require all health care facilities that receive Medicare or Medicaid payment to vaccinate workers. All eligible staff must receive the first dose of a two-dose COVID-19 vaccine or a one-dose vaccine by Dec. 6, and a second dose by Jan. 4, 2022. The policy allows exemptions based on recognized medical conditions or religious beliefs.
Some hospitals and health systems and various states and cities have already begun implementing vaccine mandates. Northwell Health in New York, for instance, lost 1,400 workers (evenly split between clinical and nonclinical staff), or 2% of its 77,000 employees, as a result of the state’s mandate.
Northwell’s workforce is now considered 100% vaccinated, a hospital spokesman said in an interview. In addition, “we have allowed for team members who changed their minds and presented proof of vaccination to return,” said the spokesman, adding that “a couple of hundred employees have done just that.”
Ten states sued the Biden administration recently, aiming to stop the health care worker vaccine mandate. Other challenges to vaccine mandates have generally been unsuccessful. The U.S. Supreme Court, for example, in October declined to hear a challenge to Maine’s mandate for health care workers, even though it did not allow religious exemptions, according to the Washington Post.
“The courts seem to agree that health care personnel are different, and could be subject to these mandates,” said Dr. Srinivasan.
A version of this article first appeared on Medscape.com.
, according to a new survey by the Centers for Disease Control and Prevention.
The snapshot in time – Jan. 20, 2021 to Sept. 15, 2021 – is based on voluntary weekly reports from hospitals. Only about 48% of the 5,085 hospitals in the U.S. Health and Human Services department’s Unified Hospital Data Surveillance System reported data on vaccination coverage during the period, and, after validation checks, the study included reports from 2,086 facilities, or just 41% of all hospitals, covering 3.35 million workers.
Overall, the number who were fully vaccinated rose from 36.1% in Jan. 2021 to 60.2% in April 2021, and then crept slowly up to 70% by Sept. 15, the CDC researchers reported in the American Journal of Infection Control.
The slowdown among hospital workers seems to mirror the same decline as in the general population.
Arjun Srinivasan, MD, associate director for health care–associated infection prevention programs at the CDC, said the decline in part may be the result of misinformation.
Health care personnel “are not fully immune from vaccine misinformation,” he said, adding that such misinformation “is contributing to decreased vaccine uptake among non–health care personnel.”
“The take-home message is that there is a lot of work to do in health care settings in order to get all of our health care personnel vaccinated,” Dr. Srinivasan told this news organization. “We need them to be vaccinated to protect themselves. It is also really important that we as health care personnel get vaccinated to protect our patients.”
Vaccine mandates
The analysis shows that workers were more likely to be vaccinated if they worked at a children’s hospital (77%), lived in metropolitan counties (71%), or worked in a hospital with lower cumulative admissions of COVID-19 patients, or lower cumulative COVID-19 cases.
The odds of being fully vaccinated were lower if the surrounding community had lower vaccination coverage. Workers in non-metropolitan counties (63.3%) and in rural counties (65.1%) were also less likely to be fully vaccinated, as well as those who were in critical access hospitals (64%) or long-term acute care hospitals (68.8%).
Surveys have shown that health care personnel who are vaccine-hesitant cited concerns they had about vaccine efficacy, adverse effects, the speed of vaccine development, and lack of full Food and Drug Administration approval, the study authors noted. In addition, many reported low trust in the government.
A Medscape survey this past April found that 25% of health care workers said they did not plan to be fully vaccinated. Some 40% of the 9,349 workers who responded said that employers should never require a COVID-19 vaccine for clinicians.
But the Centers for Medicare & Medicaid Services is attempting to require all health care facilities that receive Medicare or Medicaid payment to vaccinate workers. All eligible staff must receive the first dose of a two-dose COVID-19 vaccine or a one-dose vaccine by Dec. 6, and a second dose by Jan. 4, 2022. The policy allows exemptions based on recognized medical conditions or religious beliefs.
Some hospitals and health systems and various states and cities have already begun implementing vaccine mandates. Northwell Health in New York, for instance, lost 1,400 workers (evenly split between clinical and nonclinical staff), or 2% of its 77,000 employees, as a result of the state’s mandate.
Northwell’s workforce is now considered 100% vaccinated, a hospital spokesman said in an interview. In addition, “we have allowed for team members who changed their minds and presented proof of vaccination to return,” said the spokesman, adding that “a couple of hundred employees have done just that.”
Ten states sued the Biden administration recently, aiming to stop the health care worker vaccine mandate. Other challenges to vaccine mandates have generally been unsuccessful. The U.S. Supreme Court, for example, in October declined to hear a challenge to Maine’s mandate for health care workers, even though it did not allow religious exemptions, according to the Washington Post.
“The courts seem to agree that health care personnel are different, and could be subject to these mandates,” said Dr. Srinivasan.
A version of this article first appeared on Medscape.com.
, according to a new survey by the Centers for Disease Control and Prevention.
The snapshot in time – Jan. 20, 2021 to Sept. 15, 2021 – is based on voluntary weekly reports from hospitals. Only about 48% of the 5,085 hospitals in the U.S. Health and Human Services department’s Unified Hospital Data Surveillance System reported data on vaccination coverage during the period, and, after validation checks, the study included reports from 2,086 facilities, or just 41% of all hospitals, covering 3.35 million workers.
Overall, the number who were fully vaccinated rose from 36.1% in Jan. 2021 to 60.2% in April 2021, and then crept slowly up to 70% by Sept. 15, the CDC researchers reported in the American Journal of Infection Control.
The slowdown among hospital workers seems to mirror the same decline as in the general population.
Arjun Srinivasan, MD, associate director for health care–associated infection prevention programs at the CDC, said the decline in part may be the result of misinformation.
Health care personnel “are not fully immune from vaccine misinformation,” he said, adding that such misinformation “is contributing to decreased vaccine uptake among non–health care personnel.”
“The take-home message is that there is a lot of work to do in health care settings in order to get all of our health care personnel vaccinated,” Dr. Srinivasan told this news organization. “We need them to be vaccinated to protect themselves. It is also really important that we as health care personnel get vaccinated to protect our patients.”
Vaccine mandates
The analysis shows that workers were more likely to be vaccinated if they worked at a children’s hospital (77%), lived in metropolitan counties (71%), or worked in a hospital with lower cumulative admissions of COVID-19 patients, or lower cumulative COVID-19 cases.
The odds of being fully vaccinated were lower if the surrounding community had lower vaccination coverage. Workers in non-metropolitan counties (63.3%) and in rural counties (65.1%) were also less likely to be fully vaccinated, as well as those who were in critical access hospitals (64%) or long-term acute care hospitals (68.8%).
Surveys have shown that health care personnel who are vaccine-hesitant cited concerns they had about vaccine efficacy, adverse effects, the speed of vaccine development, and lack of full Food and Drug Administration approval, the study authors noted. In addition, many reported low trust in the government.
A Medscape survey this past April found that 25% of health care workers said they did not plan to be fully vaccinated. Some 40% of the 9,349 workers who responded said that employers should never require a COVID-19 vaccine for clinicians.
But the Centers for Medicare & Medicaid Services is attempting to require all health care facilities that receive Medicare or Medicaid payment to vaccinate workers. All eligible staff must receive the first dose of a two-dose COVID-19 vaccine or a one-dose vaccine by Dec. 6, and a second dose by Jan. 4, 2022. The policy allows exemptions based on recognized medical conditions or religious beliefs.
Some hospitals and health systems and various states and cities have already begun implementing vaccine mandates. Northwell Health in New York, for instance, lost 1,400 workers (evenly split between clinical and nonclinical staff), or 2% of its 77,000 employees, as a result of the state’s mandate.
Northwell’s workforce is now considered 100% vaccinated, a hospital spokesman said in an interview. In addition, “we have allowed for team members who changed their minds and presented proof of vaccination to return,” said the spokesman, adding that “a couple of hundred employees have done just that.”
Ten states sued the Biden administration recently, aiming to stop the health care worker vaccine mandate. Other challenges to vaccine mandates have generally been unsuccessful. The U.S. Supreme Court, for example, in October declined to hear a challenge to Maine’s mandate for health care workers, even though it did not allow religious exemptions, according to the Washington Post.
“The courts seem to agree that health care personnel are different, and could be subject to these mandates,” said Dr. Srinivasan.
A version of this article first appeared on Medscape.com.
FDA authorizes COVID boosters for all U.S. adults
“Authorizing the use of a single booster dose of either the Moderna or Pfizer-BioNTech COVID-19 vaccine for individuals 18 years of age and older helps to provide continued protection against COVID-19, including the serious consequences that can occur, such as hospitalization and death,” said acting FDA Commissioner Janet Woodcock, MD, in an FDA press statement.
The Center for Disease Control and Prevention’s Advisory Committee on Immunization Practices will meet on Nov. 19 to review the science supporting a more widespread need for booster doses, and is expected to vote on official recommendations for their use in the United States. The CDC director must then sign off on the panel’s recommendations.
“As soon as the FDA reviews those data and provides an authorization, we at CDC will act swiftly,” Rochelle P. Walensky, MD, MPH, said at a recent White House briefing.
Several states – including Louisiana, Maine, and Colorado – have already authorized boosters for all adults as cases rise in Europe and across the Western and Northeastern regions of the United States.
FDA officials said they hoped that widening eligibility for boosters would cut down on confusion for people and hopefully speed uptake of the shots.
“Streamlining the eligibility criteria and making booster doses available to all individuals 18 years of age and older will also help to eliminate confusion about who may receive a booster dose and ensure booster doses are available to all who may need one,” said Peter Marks, MD, PhD, who heads the FDA’s Center for Biologics Evaluation and Research.
A version of this article first appeared on WebMD.com.
“Authorizing the use of a single booster dose of either the Moderna or Pfizer-BioNTech COVID-19 vaccine for individuals 18 years of age and older helps to provide continued protection against COVID-19, including the serious consequences that can occur, such as hospitalization and death,” said acting FDA Commissioner Janet Woodcock, MD, in an FDA press statement.
The Center for Disease Control and Prevention’s Advisory Committee on Immunization Practices will meet on Nov. 19 to review the science supporting a more widespread need for booster doses, and is expected to vote on official recommendations for their use in the United States. The CDC director must then sign off on the panel’s recommendations.
“As soon as the FDA reviews those data and provides an authorization, we at CDC will act swiftly,” Rochelle P. Walensky, MD, MPH, said at a recent White House briefing.
Several states – including Louisiana, Maine, and Colorado – have already authorized boosters for all adults as cases rise in Europe and across the Western and Northeastern regions of the United States.
FDA officials said they hoped that widening eligibility for boosters would cut down on confusion for people and hopefully speed uptake of the shots.
“Streamlining the eligibility criteria and making booster doses available to all individuals 18 years of age and older will also help to eliminate confusion about who may receive a booster dose and ensure booster doses are available to all who may need one,” said Peter Marks, MD, PhD, who heads the FDA’s Center for Biologics Evaluation and Research.
A version of this article first appeared on WebMD.com.
“Authorizing the use of a single booster dose of either the Moderna or Pfizer-BioNTech COVID-19 vaccine for individuals 18 years of age and older helps to provide continued protection against COVID-19, including the serious consequences that can occur, such as hospitalization and death,” said acting FDA Commissioner Janet Woodcock, MD, in an FDA press statement.
The Center for Disease Control and Prevention’s Advisory Committee on Immunization Practices will meet on Nov. 19 to review the science supporting a more widespread need for booster doses, and is expected to vote on official recommendations for their use in the United States. The CDC director must then sign off on the panel’s recommendations.
“As soon as the FDA reviews those data and provides an authorization, we at CDC will act swiftly,” Rochelle P. Walensky, MD, MPH, said at a recent White House briefing.
Several states – including Louisiana, Maine, and Colorado – have already authorized boosters for all adults as cases rise in Europe and across the Western and Northeastern regions of the United States.
FDA officials said they hoped that widening eligibility for boosters would cut down on confusion for people and hopefully speed uptake of the shots.
“Streamlining the eligibility criteria and making booster doses available to all individuals 18 years of age and older will also help to eliminate confusion about who may receive a booster dose and ensure booster doses are available to all who may need one,” said Peter Marks, MD, PhD, who heads the FDA’s Center for Biologics Evaluation and Research.
A version of this article first appeared on WebMD.com.



