User login
ID Practitioner is an independent news source that provides infectious disease specialists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the infectious disease specialist’s practice. Specialty focus topics include antimicrobial resistance, emerging infections, global ID, hepatitis, HIV, hospital-acquired infections, immunizations and vaccines, influenza, mycoses, pediatric infections, and STIs. Infectious Diseases News is owned by Frontline Medical Communications.
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
section[contains(@class, 'footer-nav-section-wrapper')]
div[contains(@class, 'pane-pub-article-idp')]
div[contains(@class, 'pane-medstat-latest-articles-articles-section')]
div[contains(@class, 'pane-pub-home-idp')]
div[contains(@class, 'pane-pub-topic-idp')]
More postpartum weight gain with dolutegravir-based ART
Women with HIV on dolutegravir-based antiretroviral therapy (ART) protocols had higher weights through 18 months of the postpartum period than women on efavirenz-based therapy, according to a recent study. However, women taking dolutegravir had similar postpartum weights to women who did not have HIV infection.
The results were shared by Jennifer Jao, MD, MPH, of Northwestern University, Chicago, in a video presentation of the research during the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
Dr. Jao, an internal medicine physician and pediatrician, and colleagues looked at the association between dolutegravir and postpartum weight for women with HIV, compared with women with HIV who were taking efavirenz-based ART and women who did not have HIV infection.
Though there was no significant difference among the three groups for body mass index at 4 weeks post partum (all were between 24 and 26 kg/m2), postpartum weight for the dolutegravir group was significantly higher.
Using a mixed models statistical approach that adjusted for potentially confounding variables, Dr. Jao and associates found that women on a dolutegravir-based regiment weighed an average of 5 kg more postpartum than women on an efavirenz-based regiment. (P less than .01).
Further adjustment that included CD4 count, viral load, and ART status at conception didn’t change the results from the original approach that included such variables as age, breastfeeding duration , gestational diabetes status, and second and third trimester weight gain (P = .04).
The study was a secondary analysis of the Tshilo Dikotla study conducted in Botswana. Dr. Jao said that the study addressed the known association of dolutegravir-based ART with higher weight gain than other ART regimens. Seeing how postpartum weight varies by regimen is important because “postpartum weight retention impacts cardiometabolic risk,” added Dr. Jao.
Of a total of 406 women, 170 were on dolutegravir-based therapy, 114 were on efavirenz-based therapy, and 122 weren’t HIV infected. Overall, the women on efavirenz-based therapy were older, with a median age of 33 years, compared with 28.5 and 25 years for the dolutegravir group and those without HIV, respectively. This and all other between-group differences were statistically significant at P less than .01.
Women without HIV had lower gravidity, with a median one pregnancy, compared with three in the other two groups. Other significant differences included a higher rate of weight gain in the second and third trimesters for the non–HIV-infected group, who gained at a rate of 0.3 kg/week, compared with 0.1 and 0.2 kg/week for the efavirenz and dolutegravir groups, respectively. Breastfeeding duration was longer in the non–HIV-infected group as well.
Finally, 86% of women on efavirenz-based therapy were on ART at the time of conception, compared with just 35.3% of women on dolutegravir-based treatment.
“Further studies to assess mechanisms of postpartum weight retention are needed,” said Dr. Jao.
The study was supported by the National Institutes of Health. Dr. Jao reported no relevant conflicts of interest.
SOURCE: Jao J et al. CROI 2020, Poster 00772.
Women with HIV on dolutegravir-based antiretroviral therapy (ART) protocols had higher weights through 18 months of the postpartum period than women on efavirenz-based therapy, according to a recent study. However, women taking dolutegravir had similar postpartum weights to women who did not have HIV infection.
The results were shared by Jennifer Jao, MD, MPH, of Northwestern University, Chicago, in a video presentation of the research during the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
Dr. Jao, an internal medicine physician and pediatrician, and colleagues looked at the association between dolutegravir and postpartum weight for women with HIV, compared with women with HIV who were taking efavirenz-based ART and women who did not have HIV infection.
Though there was no significant difference among the three groups for body mass index at 4 weeks post partum (all were between 24 and 26 kg/m2), postpartum weight for the dolutegravir group was significantly higher.
Using a mixed models statistical approach that adjusted for potentially confounding variables, Dr. Jao and associates found that women on a dolutegravir-based regiment weighed an average of 5 kg more postpartum than women on an efavirenz-based regiment. (P less than .01).
Further adjustment that included CD4 count, viral load, and ART status at conception didn’t change the results from the original approach that included such variables as age, breastfeeding duration , gestational diabetes status, and second and third trimester weight gain (P = .04).
The study was a secondary analysis of the Tshilo Dikotla study conducted in Botswana. Dr. Jao said that the study addressed the known association of dolutegravir-based ART with higher weight gain than other ART regimens. Seeing how postpartum weight varies by regimen is important because “postpartum weight retention impacts cardiometabolic risk,” added Dr. Jao.
Of a total of 406 women, 170 were on dolutegravir-based therapy, 114 were on efavirenz-based therapy, and 122 weren’t HIV infected. Overall, the women on efavirenz-based therapy were older, with a median age of 33 years, compared with 28.5 and 25 years for the dolutegravir group and those without HIV, respectively. This and all other between-group differences were statistically significant at P less than .01.
Women without HIV had lower gravidity, with a median one pregnancy, compared with three in the other two groups. Other significant differences included a higher rate of weight gain in the second and third trimesters for the non–HIV-infected group, who gained at a rate of 0.3 kg/week, compared with 0.1 and 0.2 kg/week for the efavirenz and dolutegravir groups, respectively. Breastfeeding duration was longer in the non–HIV-infected group as well.
Finally, 86% of women on efavirenz-based therapy were on ART at the time of conception, compared with just 35.3% of women on dolutegravir-based treatment.
“Further studies to assess mechanisms of postpartum weight retention are needed,” said Dr. Jao.
The study was supported by the National Institutes of Health. Dr. Jao reported no relevant conflicts of interest.
SOURCE: Jao J et al. CROI 2020, Poster 00772.
Women with HIV on dolutegravir-based antiretroviral therapy (ART) protocols had higher weights through 18 months of the postpartum period than women on efavirenz-based therapy, according to a recent study. However, women taking dolutegravir had similar postpartum weights to women who did not have HIV infection.
The results were shared by Jennifer Jao, MD, MPH, of Northwestern University, Chicago, in a video presentation of the research during the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
Dr. Jao, an internal medicine physician and pediatrician, and colleagues looked at the association between dolutegravir and postpartum weight for women with HIV, compared with women with HIV who were taking efavirenz-based ART and women who did not have HIV infection.
Though there was no significant difference among the three groups for body mass index at 4 weeks post partum (all were between 24 and 26 kg/m2), postpartum weight for the dolutegravir group was significantly higher.
Using a mixed models statistical approach that adjusted for potentially confounding variables, Dr. Jao and associates found that women on a dolutegravir-based regiment weighed an average of 5 kg more postpartum than women on an efavirenz-based regiment. (P less than .01).
Further adjustment that included CD4 count, viral load, and ART status at conception didn’t change the results from the original approach that included such variables as age, breastfeeding duration , gestational diabetes status, and second and third trimester weight gain (P = .04).
The study was a secondary analysis of the Tshilo Dikotla study conducted in Botswana. Dr. Jao said that the study addressed the known association of dolutegravir-based ART with higher weight gain than other ART regimens. Seeing how postpartum weight varies by regimen is important because “postpartum weight retention impacts cardiometabolic risk,” added Dr. Jao.
Of a total of 406 women, 170 were on dolutegravir-based therapy, 114 were on efavirenz-based therapy, and 122 weren’t HIV infected. Overall, the women on efavirenz-based therapy were older, with a median age of 33 years, compared with 28.5 and 25 years for the dolutegravir group and those without HIV, respectively. This and all other between-group differences were statistically significant at P less than .01.
Women without HIV had lower gravidity, with a median one pregnancy, compared with three in the other two groups. Other significant differences included a higher rate of weight gain in the second and third trimesters for the non–HIV-infected group, who gained at a rate of 0.3 kg/week, compared with 0.1 and 0.2 kg/week for the efavirenz and dolutegravir groups, respectively. Breastfeeding duration was longer in the non–HIV-infected group as well.
Finally, 86% of women on efavirenz-based therapy were on ART at the time of conception, compared with just 35.3% of women on dolutegravir-based treatment.
“Further studies to assess mechanisms of postpartum weight retention are needed,” said Dr. Jao.
The study was supported by the National Institutes of Health. Dr. Jao reported no relevant conflicts of interest.
SOURCE: Jao J et al. CROI 2020, Poster 00772.
FROM CROI 2020
HIV free 30 months after stem cell transplant, is the London patient cured?
A patient with HIV remission induced by stem cell transplantation continues to be disease free at the 30-month mark.
The individual, referred to as the London patient, received allogeneic hematopoietic stem cell transplantation (allo-HSCT) for stage IVB Hodgkin lymphoma. The transplant donor was homozygous for the CCR5 delta-32 mutation, which confers immunity to HIV because there’s no point of entry for the virus into immune cells.
After extensive sampling of various tissues, including gut, lymph node, blood, semen, and cerebrospinal fluid (CSF), Ravindra Kumar Gupta, MD, PhD, and colleagues found no detectable virus that was competent to replicate. However, they reported that the testing did detect some “fossilized” remnants of HIV DNA persisting in certain tissues.
The results were shared in a video presentation of the research during the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
The London patient’s HIV status had been reported the previous year at CROI 2019, but only blood samples were used in that analysis.
In a commentary accompanying the simultaneously published study in the Lancet, Jennifer Zerbato, PhD, and Sharon Lewin, FRACP, PHD, FAAHMS, asked: “A key question now for the area of HIV cure is how soon can one know if someone has been cured of HIV?
“We will need more than a handful of patients cured of HIV to really understand the duration of follow-up needed and the likelihood of an unexpected late rebound in virus replication,” continued Dr. Zerbato, of the University of Melbourne, and Dr. Lewin, of the Royal Melbourne Hospital and Monash University, also in Melbourne.
In their ongoing analysis of data from the London patient, Dr. Gupta, a virologist at the University of Cambridge (England), and associates constructed a mathematical model that maps the probability for lifetime remission or cure of HIV against several factors, including the degree of chimerism achieved with the stem cell transplant.
In this model, when chimerism reaches 80% in total HIV target cells, the probability of remission for life is 98%; when donor chimerism reaches 90%, the probability of lifetime remission is greater than 99%. Peripheral T-cell chimerism in the London patient has held steady at 99%.
Dr. Gupta and associates obtained some testing opportunistically: A PET-CT scan revealed an axillary lymph node that was biopsied after it was found to have avid radiotracer uptake. Similarly, the CSF sample was obtained in the course of a work-up for some neurologic symptoms that the London patient was having.
In contrast to the first patient who achieved ongoing HIV remission from a pair of stem cell transplants received over 13 years ago – the Berlin patient – the London patient did not receive whole-body radiation, but rather underwent a reduced-intensity conditioning regimen. The London patient experienced a bout of gut graft-versus-host disease (GVHD) about 2 months after his transplant, but has been free of GVHD in the interval. He hasn’t taken cytotoxic agents or any GVHD prophylaxis since 6 months post transplant.
Though there’s no sign of HIV that’s competent to replicate, “the London patient has shown somewhat slow CD4 reconstitution,” said Dr. Gupta and coauthors in discussing the results.
The patient had a reactivation of Epstein-Barr virus (EBV) about 21 months after analytic treatment interruption (ATI) of antiretroviral therapy that was managed without any specific treatment, but he hasn’t experienced any opportunistic infections. However, his CD4 count didn’t rebound to pretransplant levels until 28 months after ATI. At that point, his CD4 count was 430 cells per mcL, or 23.5% of total T cells. The CD4:CD8 ratio was 0.86; normal range is 1.5-2.5.
The researchers used quantitative real-time polymerase chain reaction (rt-PCR) to look for packaging site and envelope (env) DNA fragments, and droplet digital PCR to quantify HIV-1 DNA.
The patient’s HIV-1 plasma load measured at 30 months post ATI on an ultrasensitive assay was below the lower limit of detection (less than 1 copy per mL). Semen viremia measured at 21 months was also below the lower limit of detection, as was CSF measured at 25 months.
Samples were taken from the patient’s rectum, cecum, sigmoid colon, and terminal ileum during a colonoscopy conducted 22 months post ATI; all tested negative for HIV DNA via droplet digital PCR.
The lymph node had large numbers of EBV-positive cells and was positive for HIV-1 env and long-terminal repeat by double-drop PCR, but no integrase DNA was detected. Additionally, no intact proviral DNA was found on assay.
Dr. Gupta and associates speculated that “EBV reactivation could have triggered EBV-specific CD4 and CD8 T-cell responses and proliferation, potentially including CD4 T cells containing HIV-1 DNA.” Supporting this hypothesis, EBV-specific CD8 T-cell responses in peripheral blood were “robust,” and the researchers also saw some CD4 response.
“Similar to the Berlin patient, highly sensitive tests showed very low levels of so-called fossilized HIV-1 DNA in some tissue samples from the London patient. Residual HIV-1 DNA and axillary lymph node tissue could represent a defective clone that expanded during hyperplasia within the lymph note sampled,” noted Dr. Gupta and coauthors.
Responses of CD4 and CD8 T cells to HIV have also remained below the limit of detection, though cytomegalovirus-specific responses persist in the London patient.
As with the Berlin patient, standard enzyme-linked immunosorbent assay (ELISA) testing has remained positive in the London patient. “Standard ELISA testing, therefore, cannot be used as a marker for cure, although more work needs to be done to assess the role of detuned low-avidity antibody assays in defining cure,” noted Dr. Gupta and associates.
The ongoing follow-up plan for the London patient is to obtain viral load testing twice yearly up to 5 years post ATI, and then obtain yearly tests for a total of 10 years. Ongoing testing will confirm the investigators’ belief that “these findings probably represent the second recorded HIV-1 cure after CCR5 delta-32/delta-32 allo-HSCT, with evidence of residual low-level HIV-1 DNA.”
Dr. Zerbato and Dr. Lewin advised cautious optimism and ongoing surveillance: “In view of the many cells sampled in this case, and the absence of any intact virus, is the London patient truly cured? The additional data provided in this follow-up case report is certainly exciting and encouraging but, in the end, only time will tell.”
Dr. Gupta reported being a consultant for ViiV Healthcare and Gilead Sciences; several coauthors also reported financial relationships with pharmaceutical companies. The work was funded by amfAR, the American Foundation for AIDS Research, and the Wellcome Trust. Dr. Lewin reported grants from the National Health and Medical Research Council of Australia, the National Institutes of Health, the American Foundation for AIDS Research, Gilead Sciences, Merck, ViiV Healthcare, Leidos, the Wellcome Trust, the Australian Centre for HIV and Hepatitis Virology Research, and the Melbourne HIV Cure Consortium. Dr. Zerbato reported grants from the Melbourne HIV Cure Consortium,
SOURCE: Gupta R et al. Lancet. 2020 Mar 10. doi: 10.1016/ S2352-3018(20)30069-2.
A patient with HIV remission induced by stem cell transplantation continues to be disease free at the 30-month mark.
The individual, referred to as the London patient, received allogeneic hematopoietic stem cell transplantation (allo-HSCT) for stage IVB Hodgkin lymphoma. The transplant donor was homozygous for the CCR5 delta-32 mutation, which confers immunity to HIV because there’s no point of entry for the virus into immune cells.
After extensive sampling of various tissues, including gut, lymph node, blood, semen, and cerebrospinal fluid (CSF), Ravindra Kumar Gupta, MD, PhD, and colleagues found no detectable virus that was competent to replicate. However, they reported that the testing did detect some “fossilized” remnants of HIV DNA persisting in certain tissues.
The results were shared in a video presentation of the research during the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
The London patient’s HIV status had been reported the previous year at CROI 2019, but only blood samples were used in that analysis.
In a commentary accompanying the simultaneously published study in the Lancet, Jennifer Zerbato, PhD, and Sharon Lewin, FRACP, PHD, FAAHMS, asked: “A key question now for the area of HIV cure is how soon can one know if someone has been cured of HIV?
“We will need more than a handful of patients cured of HIV to really understand the duration of follow-up needed and the likelihood of an unexpected late rebound in virus replication,” continued Dr. Zerbato, of the University of Melbourne, and Dr. Lewin, of the Royal Melbourne Hospital and Monash University, also in Melbourne.
In their ongoing analysis of data from the London patient, Dr. Gupta, a virologist at the University of Cambridge (England), and associates constructed a mathematical model that maps the probability for lifetime remission or cure of HIV against several factors, including the degree of chimerism achieved with the stem cell transplant.
In this model, when chimerism reaches 80% in total HIV target cells, the probability of remission for life is 98%; when donor chimerism reaches 90%, the probability of lifetime remission is greater than 99%. Peripheral T-cell chimerism in the London patient has held steady at 99%.
Dr. Gupta and associates obtained some testing opportunistically: A PET-CT scan revealed an axillary lymph node that was biopsied after it was found to have avid radiotracer uptake. Similarly, the CSF sample was obtained in the course of a work-up for some neurologic symptoms that the London patient was having.
In contrast to the first patient who achieved ongoing HIV remission from a pair of stem cell transplants received over 13 years ago – the Berlin patient – the London patient did not receive whole-body radiation, but rather underwent a reduced-intensity conditioning regimen. The London patient experienced a bout of gut graft-versus-host disease (GVHD) about 2 months after his transplant, but has been free of GVHD in the interval. He hasn’t taken cytotoxic agents or any GVHD prophylaxis since 6 months post transplant.
Though there’s no sign of HIV that’s competent to replicate, “the London patient has shown somewhat slow CD4 reconstitution,” said Dr. Gupta and coauthors in discussing the results.
The patient had a reactivation of Epstein-Barr virus (EBV) about 21 months after analytic treatment interruption (ATI) of antiretroviral therapy that was managed without any specific treatment, but he hasn’t experienced any opportunistic infections. However, his CD4 count didn’t rebound to pretransplant levels until 28 months after ATI. At that point, his CD4 count was 430 cells per mcL, or 23.5% of total T cells. The CD4:CD8 ratio was 0.86; normal range is 1.5-2.5.
The researchers used quantitative real-time polymerase chain reaction (rt-PCR) to look for packaging site and envelope (env) DNA fragments, and droplet digital PCR to quantify HIV-1 DNA.
The patient’s HIV-1 plasma load measured at 30 months post ATI on an ultrasensitive assay was below the lower limit of detection (less than 1 copy per mL). Semen viremia measured at 21 months was also below the lower limit of detection, as was CSF measured at 25 months.
Samples were taken from the patient’s rectum, cecum, sigmoid colon, and terminal ileum during a colonoscopy conducted 22 months post ATI; all tested negative for HIV DNA via droplet digital PCR.
The lymph node had large numbers of EBV-positive cells and was positive for HIV-1 env and long-terminal repeat by double-drop PCR, but no integrase DNA was detected. Additionally, no intact proviral DNA was found on assay.
Dr. Gupta and associates speculated that “EBV reactivation could have triggered EBV-specific CD4 and CD8 T-cell responses and proliferation, potentially including CD4 T cells containing HIV-1 DNA.” Supporting this hypothesis, EBV-specific CD8 T-cell responses in peripheral blood were “robust,” and the researchers also saw some CD4 response.
“Similar to the Berlin patient, highly sensitive tests showed very low levels of so-called fossilized HIV-1 DNA in some tissue samples from the London patient. Residual HIV-1 DNA and axillary lymph node tissue could represent a defective clone that expanded during hyperplasia within the lymph note sampled,” noted Dr. Gupta and coauthors.
Responses of CD4 and CD8 T cells to HIV have also remained below the limit of detection, though cytomegalovirus-specific responses persist in the London patient.
As with the Berlin patient, standard enzyme-linked immunosorbent assay (ELISA) testing has remained positive in the London patient. “Standard ELISA testing, therefore, cannot be used as a marker for cure, although more work needs to be done to assess the role of detuned low-avidity antibody assays in defining cure,” noted Dr. Gupta and associates.
The ongoing follow-up plan for the London patient is to obtain viral load testing twice yearly up to 5 years post ATI, and then obtain yearly tests for a total of 10 years. Ongoing testing will confirm the investigators’ belief that “these findings probably represent the second recorded HIV-1 cure after CCR5 delta-32/delta-32 allo-HSCT, with evidence of residual low-level HIV-1 DNA.”
Dr. Zerbato and Dr. Lewin advised cautious optimism and ongoing surveillance: “In view of the many cells sampled in this case, and the absence of any intact virus, is the London patient truly cured? The additional data provided in this follow-up case report is certainly exciting and encouraging but, in the end, only time will tell.”
Dr. Gupta reported being a consultant for ViiV Healthcare and Gilead Sciences; several coauthors also reported financial relationships with pharmaceutical companies. The work was funded by amfAR, the American Foundation for AIDS Research, and the Wellcome Trust. Dr. Lewin reported grants from the National Health and Medical Research Council of Australia, the National Institutes of Health, the American Foundation for AIDS Research, Gilead Sciences, Merck, ViiV Healthcare, Leidos, the Wellcome Trust, the Australian Centre for HIV and Hepatitis Virology Research, and the Melbourne HIV Cure Consortium. Dr. Zerbato reported grants from the Melbourne HIV Cure Consortium,
SOURCE: Gupta R et al. Lancet. 2020 Mar 10. doi: 10.1016/ S2352-3018(20)30069-2.
A patient with HIV remission induced by stem cell transplantation continues to be disease free at the 30-month mark.
The individual, referred to as the London patient, received allogeneic hematopoietic stem cell transplantation (allo-HSCT) for stage IVB Hodgkin lymphoma. The transplant donor was homozygous for the CCR5 delta-32 mutation, which confers immunity to HIV because there’s no point of entry for the virus into immune cells.
After extensive sampling of various tissues, including gut, lymph node, blood, semen, and cerebrospinal fluid (CSF), Ravindra Kumar Gupta, MD, PhD, and colleagues found no detectable virus that was competent to replicate. However, they reported that the testing did detect some “fossilized” remnants of HIV DNA persisting in certain tissues.
The results were shared in a video presentation of the research during the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
The London patient’s HIV status had been reported the previous year at CROI 2019, but only blood samples were used in that analysis.
In a commentary accompanying the simultaneously published study in the Lancet, Jennifer Zerbato, PhD, and Sharon Lewin, FRACP, PHD, FAAHMS, asked: “A key question now for the area of HIV cure is how soon can one know if someone has been cured of HIV?
“We will need more than a handful of patients cured of HIV to really understand the duration of follow-up needed and the likelihood of an unexpected late rebound in virus replication,” continued Dr. Zerbato, of the University of Melbourne, and Dr. Lewin, of the Royal Melbourne Hospital and Monash University, also in Melbourne.
In their ongoing analysis of data from the London patient, Dr. Gupta, a virologist at the University of Cambridge (England), and associates constructed a mathematical model that maps the probability for lifetime remission or cure of HIV against several factors, including the degree of chimerism achieved with the stem cell transplant.
In this model, when chimerism reaches 80% in total HIV target cells, the probability of remission for life is 98%; when donor chimerism reaches 90%, the probability of lifetime remission is greater than 99%. Peripheral T-cell chimerism in the London patient has held steady at 99%.
Dr. Gupta and associates obtained some testing opportunistically: A PET-CT scan revealed an axillary lymph node that was biopsied after it was found to have avid radiotracer uptake. Similarly, the CSF sample was obtained in the course of a work-up for some neurologic symptoms that the London patient was having.
In contrast to the first patient who achieved ongoing HIV remission from a pair of stem cell transplants received over 13 years ago – the Berlin patient – the London patient did not receive whole-body radiation, but rather underwent a reduced-intensity conditioning regimen. The London patient experienced a bout of gut graft-versus-host disease (GVHD) about 2 months after his transplant, but has been free of GVHD in the interval. He hasn’t taken cytotoxic agents or any GVHD prophylaxis since 6 months post transplant.
Though there’s no sign of HIV that’s competent to replicate, “the London patient has shown somewhat slow CD4 reconstitution,” said Dr. Gupta and coauthors in discussing the results.
The patient had a reactivation of Epstein-Barr virus (EBV) about 21 months after analytic treatment interruption (ATI) of antiretroviral therapy that was managed without any specific treatment, but he hasn’t experienced any opportunistic infections. However, his CD4 count didn’t rebound to pretransplant levels until 28 months after ATI. At that point, his CD4 count was 430 cells per mcL, or 23.5% of total T cells. The CD4:CD8 ratio was 0.86; normal range is 1.5-2.5.
The researchers used quantitative real-time polymerase chain reaction (rt-PCR) to look for packaging site and envelope (env) DNA fragments, and droplet digital PCR to quantify HIV-1 DNA.
The patient’s HIV-1 plasma load measured at 30 months post ATI on an ultrasensitive assay was below the lower limit of detection (less than 1 copy per mL). Semen viremia measured at 21 months was also below the lower limit of detection, as was CSF measured at 25 months.
Samples were taken from the patient’s rectum, cecum, sigmoid colon, and terminal ileum during a colonoscopy conducted 22 months post ATI; all tested negative for HIV DNA via droplet digital PCR.
The lymph node had large numbers of EBV-positive cells and was positive for HIV-1 env and long-terminal repeat by double-drop PCR, but no integrase DNA was detected. Additionally, no intact proviral DNA was found on assay.
Dr. Gupta and associates speculated that “EBV reactivation could have triggered EBV-specific CD4 and CD8 T-cell responses and proliferation, potentially including CD4 T cells containing HIV-1 DNA.” Supporting this hypothesis, EBV-specific CD8 T-cell responses in peripheral blood were “robust,” and the researchers also saw some CD4 response.
“Similar to the Berlin patient, highly sensitive tests showed very low levels of so-called fossilized HIV-1 DNA in some tissue samples from the London patient. Residual HIV-1 DNA and axillary lymph node tissue could represent a defective clone that expanded during hyperplasia within the lymph note sampled,” noted Dr. Gupta and coauthors.
Responses of CD4 and CD8 T cells to HIV have also remained below the limit of detection, though cytomegalovirus-specific responses persist in the London patient.
As with the Berlin patient, standard enzyme-linked immunosorbent assay (ELISA) testing has remained positive in the London patient. “Standard ELISA testing, therefore, cannot be used as a marker for cure, although more work needs to be done to assess the role of detuned low-avidity antibody assays in defining cure,” noted Dr. Gupta and associates.
The ongoing follow-up plan for the London patient is to obtain viral load testing twice yearly up to 5 years post ATI, and then obtain yearly tests for a total of 10 years. Ongoing testing will confirm the investigators’ belief that “these findings probably represent the second recorded HIV-1 cure after CCR5 delta-32/delta-32 allo-HSCT, with evidence of residual low-level HIV-1 DNA.”
Dr. Zerbato and Dr. Lewin advised cautious optimism and ongoing surveillance: “In view of the many cells sampled in this case, and the absence of any intact virus, is the London patient truly cured? The additional data provided in this follow-up case report is certainly exciting and encouraging but, in the end, only time will tell.”
Dr. Gupta reported being a consultant for ViiV Healthcare and Gilead Sciences; several coauthors also reported financial relationships with pharmaceutical companies. The work was funded by amfAR, the American Foundation for AIDS Research, and the Wellcome Trust. Dr. Lewin reported grants from the National Health and Medical Research Council of Australia, the National Institutes of Health, the American Foundation for AIDS Research, Gilead Sciences, Merck, ViiV Healthcare, Leidos, the Wellcome Trust, the Australian Centre for HIV and Hepatitis Virology Research, and the Melbourne HIV Cure Consortium. Dr. Zerbato reported grants from the Melbourne HIV Cure Consortium,
SOURCE: Gupta R et al. Lancet. 2020 Mar 10. doi: 10.1016/ S2352-3018(20)30069-2.
FROM CROI 2020
Testosterone therapy linked to CV risk in men with HIV
Men with HIV are likely prone to the same cardiovascular risks from testosterone therapy as other men, according to new research.
There’s no reason to think they weren’t, but it hadn’t been demonstrated until now, and men with HIV are already at increased risk for cardiovascular disease. The take-home message is that “it would be prudent for clinicians to monitor closely for cardiovascular risk factors and recommend intervention to lower cardiovascular risk among men with HIV on or considering testosterone therapy,” lead investigator Sabina Haberlen, PhD, an assistant scientist in the infectious disease epidemiology division of Johns Hopkins University, Baltimore, said in a poster that was presented as part of the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers chose to hold a virtual meeting because concerns about the spread of COVID-19.
Testosterone therapy is common among middle-aged and older men with HIV to counter the hypogonadism associated with infection. The investigators turned to the Multicenter AIDS Cohort Study – a 30-year, four-city study of HIV-1 infection in men who have sex with men – to gauge its effect.
The 300 men in the study had a baseline coronary CT angiogram in 2010-2013 and a repeat study a mean of 4.5 years later. They had no history of coronary interventions or kidney dysfunction at baseline and were aged 40-70 years, with a median age of 51 years. About 70% reported never using testosterone, 8% were former users before entering the study, 7% started using testosterone between the two CTs, and 15% entered the study on testosterone and stayed on it.
Adjusting for age, race, cardiovascular risk factors, baseline serum testosterone levels, and other potential confounders, the risk of significant coronary artery calcium (CAC) progression was 2 times greater among continuous users (P = .03) and 2.4 times greater among new users (P = .01), compared with former users, who the investigators used as a control group because, at some point, they too had indications for testosterone replacement and so were more medically similar than never users.
The risk of noncalcified plaque volume progression was also more than twice as high among ongoing users, and elevated, although not significantly so, among ongoing users.
In short, “our findings are similar to those on subclinical atherosclerotic progression” in trials of older men in the general population on testosterone replacement, Dr. Haberlen said.
About half the subjects were white, 41% were at high risk for cardiovascular disease, 91% were on antiretroviral therapy, and 81% had undetectable HIV viral loads. Median total testosterone was 606 ng/dL. CAC progression was defined by incident CAC, at least a 10 Agatston unit/year increase if the baseline CAC score was 1-100, and a 10% or more annual increase if the baseline score was above 100.
Lower baseline serum testosterone was also associated with an increased risk of CAC progression, although not progression of noncalcified plaques.
The work was funded by the National Institutes of Health. Dr. Haberlen didn’t report any relevant disclosures.
SOURCE: Haberlen S et al. CROI 2020, Abstract 662.
Men with HIV are likely prone to the same cardiovascular risks from testosterone therapy as other men, according to new research.
There’s no reason to think they weren’t, but it hadn’t been demonstrated until now, and men with HIV are already at increased risk for cardiovascular disease. The take-home message is that “it would be prudent for clinicians to monitor closely for cardiovascular risk factors and recommend intervention to lower cardiovascular risk among men with HIV on or considering testosterone therapy,” lead investigator Sabina Haberlen, PhD, an assistant scientist in the infectious disease epidemiology division of Johns Hopkins University, Baltimore, said in a poster that was presented as part of the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers chose to hold a virtual meeting because concerns about the spread of COVID-19.
Testosterone therapy is common among middle-aged and older men with HIV to counter the hypogonadism associated with infection. The investigators turned to the Multicenter AIDS Cohort Study – a 30-year, four-city study of HIV-1 infection in men who have sex with men – to gauge its effect.
The 300 men in the study had a baseline coronary CT angiogram in 2010-2013 and a repeat study a mean of 4.5 years later. They had no history of coronary interventions or kidney dysfunction at baseline and were aged 40-70 years, with a median age of 51 years. About 70% reported never using testosterone, 8% were former users before entering the study, 7% started using testosterone between the two CTs, and 15% entered the study on testosterone and stayed on it.
Adjusting for age, race, cardiovascular risk factors, baseline serum testosterone levels, and other potential confounders, the risk of significant coronary artery calcium (CAC) progression was 2 times greater among continuous users (P = .03) and 2.4 times greater among new users (P = .01), compared with former users, who the investigators used as a control group because, at some point, they too had indications for testosterone replacement and so were more medically similar than never users.
The risk of noncalcified plaque volume progression was also more than twice as high among ongoing users, and elevated, although not significantly so, among ongoing users.
In short, “our findings are similar to those on subclinical atherosclerotic progression” in trials of older men in the general population on testosterone replacement, Dr. Haberlen said.
About half the subjects were white, 41% were at high risk for cardiovascular disease, 91% were on antiretroviral therapy, and 81% had undetectable HIV viral loads. Median total testosterone was 606 ng/dL. CAC progression was defined by incident CAC, at least a 10 Agatston unit/year increase if the baseline CAC score was 1-100, and a 10% or more annual increase if the baseline score was above 100.
Lower baseline serum testosterone was also associated with an increased risk of CAC progression, although not progression of noncalcified plaques.
The work was funded by the National Institutes of Health. Dr. Haberlen didn’t report any relevant disclosures.
SOURCE: Haberlen S et al. CROI 2020, Abstract 662.
Men with HIV are likely prone to the same cardiovascular risks from testosterone therapy as other men, according to new research.
There’s no reason to think they weren’t, but it hadn’t been demonstrated until now, and men with HIV are already at increased risk for cardiovascular disease. The take-home message is that “it would be prudent for clinicians to monitor closely for cardiovascular risk factors and recommend intervention to lower cardiovascular risk among men with HIV on or considering testosterone therapy,” lead investigator Sabina Haberlen, PhD, an assistant scientist in the infectious disease epidemiology division of Johns Hopkins University, Baltimore, said in a poster that was presented as part of the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers chose to hold a virtual meeting because concerns about the spread of COVID-19.
Testosterone therapy is common among middle-aged and older men with HIV to counter the hypogonadism associated with infection. The investigators turned to the Multicenter AIDS Cohort Study – a 30-year, four-city study of HIV-1 infection in men who have sex with men – to gauge its effect.
The 300 men in the study had a baseline coronary CT angiogram in 2010-2013 and a repeat study a mean of 4.5 years later. They had no history of coronary interventions or kidney dysfunction at baseline and were aged 40-70 years, with a median age of 51 years. About 70% reported never using testosterone, 8% were former users before entering the study, 7% started using testosterone between the two CTs, and 15% entered the study on testosterone and stayed on it.
Adjusting for age, race, cardiovascular risk factors, baseline serum testosterone levels, and other potential confounders, the risk of significant coronary artery calcium (CAC) progression was 2 times greater among continuous users (P = .03) and 2.4 times greater among new users (P = .01), compared with former users, who the investigators used as a control group because, at some point, they too had indications for testosterone replacement and so were more medically similar than never users.
The risk of noncalcified plaque volume progression was also more than twice as high among ongoing users, and elevated, although not significantly so, among ongoing users.
In short, “our findings are similar to those on subclinical atherosclerotic progression” in trials of older men in the general population on testosterone replacement, Dr. Haberlen said.
About half the subjects were white, 41% were at high risk for cardiovascular disease, 91% were on antiretroviral therapy, and 81% had undetectable HIV viral loads. Median total testosterone was 606 ng/dL. CAC progression was defined by incident CAC, at least a 10 Agatston unit/year increase if the baseline CAC score was 1-100, and a 10% or more annual increase if the baseline score was above 100.
Lower baseline serum testosterone was also associated with an increased risk of CAC progression, although not progression of noncalcified plaques.
The work was funded by the National Institutes of Health. Dr. Haberlen didn’t report any relevant disclosures.
SOURCE: Haberlen S et al. CROI 2020, Abstract 662.
FROM CROI 2020
Descovy safety no match for cost savings with generic Truvada, study says
Economically, the modest safety benefit of tenofovir alafenamide-emtricitabine (Descovy) for HIV preexposure prophylaxis won’t justify paying thousands of dollars more for it when tenofovir disoproxil fumarate-emtricitabine (Truvada) becomes available as a generic in a year or so, according to a population level cost-effectiveness analysis presented at the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers held a virtual meeting because of concerns about the spread of COVID-19.
Those benefits will translate to a health savings worth only a few hundred dollars over the likely generic price, said investigators led by Rochelle Walensky, MD, and infectious disease physician and professor of medicine at Harvard Medical School, Boston.
In a press statement, Gilead, which makes both medications, said it “strongly believes that the analysis ... is flawed, leading to inaccurate conclusions that severely underestimate the value of Descovy. The method and validation of the models, incomplete clinical data analyzed and the assumptions around potential pricing associated with a generic alternative to Truvada ... are inadequate to enable a sufficiently robust analysis.”
The company did not go into details about what exactly might have been off about the analysis.
Approved in Oct. 2019, tenofovir alafenamide-emtricitabine (also known as F/TAF) is the first new option for HIV preexposure prophylaxis (PrEP) since tenofovir disoproxil fumarate-emtricitabine (F/TDF) was approved in 2012; F/TDF is going off patent soon.
Amid a robust marketing campaign, the new medication has already captured 25% of the PrEP market, and Gilead expects up to 45% of patients to switch to F/TAF before generic F/TDF becomes available.
That worries the investigators. “At the current FSS [Federal Supply Schedule] price of $16,600 per year,” a nationwide PrEP program that uses F/TAF “would consume the entire $900.8 million federal budget for HIV prevention several times over ... If branded F/TAF drives out generic F/TDF,” rates of PrEP coverage “could decrease, and F/TAF could end up causing more avoidable HIV transmissions” than it prevents. “Given the very small, albeit statistically significant, differences in surrogate [safety] markers, without evidence of clinical significance, there is no urgency and no reason to switch PrEP regimens now,” they said. Both medications were equally effective in preventing HIV transmission in Gilead’s head-to-head phase 3 trial, but there was an a mean of about a 4 mL/min difference in estimated glomerular filtration rate at week 48 and about a 2% difference in hip and spine density at week 96, both favoring F/TAF. Marketing highlights those differences.
The investigators wanted to see how much they are worth, so they estimated savings from a possibly lower rate of bone fractures and renal failure with F/TAF and juxtaposed it with its cost and the anticipated cost of generic F/TDF at half-price, $8,300/patient-year.
They gave F/TAF the benefit of the doubt, skewing their model toward maximal harm and cost from F/TDF toxicity, and omitting the cost of increased lipid levels, weight gain, and other possible F/TAF adverse events.
In the end, they concluded that “the improved safety of F/TAF is worth no more than an additional $370 per person per year” over generic F/TDF based on toxicity differences. “
The team calculated that F/TAF would prevent a maximum of 2,101 fractures and 25 cases of end-stage renal disease among 123,610 U.S. men who have sex with men treated for 5 years. That translated to an incremental cost-effectiveness ratio of more than $7 million per quality-adjusted life-year, far above the $100,000 threshold considered acceptable in the United States.
“In the presence of a generic alternative, the current price of F/TAF would have to be reduced by over $7,900/year for F/TAF to satisfy generally accepted standards of societal value. If F/TDF can achieve the 75% price reduction that is commonly observed when generic competition ensues (that is, a cost of $4,150/year), the F/TAF price would need to be no higher than $4,520 to demonstrate value on the basis of cost-effectiveness,” the investigators said.
For older patients at unusually high risk for renal disease or bone-related adverse events, the switch from F/TDF to F/TAF would have greater clinical effect and benefit. Even in this population, however, it would be difficult to defend a price greater than $800 over the cost of the generic alternative,” they said.
“The message seems clear that the current cost of F/TAF does not justify wholesale conversion to F/TAF as the first-line agent for all PrEP-eligible patients,” said Carlos del Rio, MD, and Wendy Armstrong, MD, infectious disease professors at Emory University, Atlanta, in an editorial. “For PrEP-eligible persons at low risk for fracture and renal disease, it is very hard to justify use of F/TAF knowing that F/TDF will soon be generic” (Ann Intern Med. 2020 Mar 10. doi: 10.7326/M20-0799).
“Successful PrEP scale-up in other countries was made possible by drug costs that are less than $100/month in most countries. In the United States, without drastic reductions in the cost of PrEP, which may be achievable with generic F/TDF ... we will fail to avert otherwise preventable new HIV transmissions,” they said.
The study was simultaneously published online (Ann Intern Med. 2020 Mar 10. doi: 10.7326/M19-3478).
The work was funded by the National Institutes of Health and Massachusetts General Hospital. The investigators and editorialists didn’t have any industry disclosures.
SOURCE: Walensky RP et al. Ann Intern Med. 2020 Mar 10. doi: 10.7326/M19-3478.
Economically, the modest safety benefit of tenofovir alafenamide-emtricitabine (Descovy) for HIV preexposure prophylaxis won’t justify paying thousands of dollars more for it when tenofovir disoproxil fumarate-emtricitabine (Truvada) becomes available as a generic in a year or so, according to a population level cost-effectiveness analysis presented at the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers held a virtual meeting because of concerns about the spread of COVID-19.
Those benefits will translate to a health savings worth only a few hundred dollars over the likely generic price, said investigators led by Rochelle Walensky, MD, and infectious disease physician and professor of medicine at Harvard Medical School, Boston.
In a press statement, Gilead, which makes both medications, said it “strongly believes that the analysis ... is flawed, leading to inaccurate conclusions that severely underestimate the value of Descovy. The method and validation of the models, incomplete clinical data analyzed and the assumptions around potential pricing associated with a generic alternative to Truvada ... are inadequate to enable a sufficiently robust analysis.”
The company did not go into details about what exactly might have been off about the analysis.
Approved in Oct. 2019, tenofovir alafenamide-emtricitabine (also known as F/TAF) is the first new option for HIV preexposure prophylaxis (PrEP) since tenofovir disoproxil fumarate-emtricitabine (F/TDF) was approved in 2012; F/TDF is going off patent soon.
Amid a robust marketing campaign, the new medication has already captured 25% of the PrEP market, and Gilead expects up to 45% of patients to switch to F/TAF before generic F/TDF becomes available.
That worries the investigators. “At the current FSS [Federal Supply Schedule] price of $16,600 per year,” a nationwide PrEP program that uses F/TAF “would consume the entire $900.8 million federal budget for HIV prevention several times over ... If branded F/TAF drives out generic F/TDF,” rates of PrEP coverage “could decrease, and F/TAF could end up causing more avoidable HIV transmissions” than it prevents. “Given the very small, albeit statistically significant, differences in surrogate [safety] markers, without evidence of clinical significance, there is no urgency and no reason to switch PrEP regimens now,” they said. Both medications were equally effective in preventing HIV transmission in Gilead’s head-to-head phase 3 trial, but there was an a mean of about a 4 mL/min difference in estimated glomerular filtration rate at week 48 and about a 2% difference in hip and spine density at week 96, both favoring F/TAF. Marketing highlights those differences.
The investigators wanted to see how much they are worth, so they estimated savings from a possibly lower rate of bone fractures and renal failure with F/TAF and juxtaposed it with its cost and the anticipated cost of generic F/TDF at half-price, $8,300/patient-year.
They gave F/TAF the benefit of the doubt, skewing their model toward maximal harm and cost from F/TDF toxicity, and omitting the cost of increased lipid levels, weight gain, and other possible F/TAF adverse events.
In the end, they concluded that “the improved safety of F/TAF is worth no more than an additional $370 per person per year” over generic F/TDF based on toxicity differences. “
The team calculated that F/TAF would prevent a maximum of 2,101 fractures and 25 cases of end-stage renal disease among 123,610 U.S. men who have sex with men treated for 5 years. That translated to an incremental cost-effectiveness ratio of more than $7 million per quality-adjusted life-year, far above the $100,000 threshold considered acceptable in the United States.
“In the presence of a generic alternative, the current price of F/TAF would have to be reduced by over $7,900/year for F/TAF to satisfy generally accepted standards of societal value. If F/TDF can achieve the 75% price reduction that is commonly observed when generic competition ensues (that is, a cost of $4,150/year), the F/TAF price would need to be no higher than $4,520 to demonstrate value on the basis of cost-effectiveness,” the investigators said.
For older patients at unusually high risk for renal disease or bone-related adverse events, the switch from F/TDF to F/TAF would have greater clinical effect and benefit. Even in this population, however, it would be difficult to defend a price greater than $800 over the cost of the generic alternative,” they said.
“The message seems clear that the current cost of F/TAF does not justify wholesale conversion to F/TAF as the first-line agent for all PrEP-eligible patients,” said Carlos del Rio, MD, and Wendy Armstrong, MD, infectious disease professors at Emory University, Atlanta, in an editorial. “For PrEP-eligible persons at low risk for fracture and renal disease, it is very hard to justify use of F/TAF knowing that F/TDF will soon be generic” (Ann Intern Med. 2020 Mar 10. doi: 10.7326/M20-0799).
“Successful PrEP scale-up in other countries was made possible by drug costs that are less than $100/month in most countries. In the United States, without drastic reductions in the cost of PrEP, which may be achievable with generic F/TDF ... we will fail to avert otherwise preventable new HIV transmissions,” they said.
The study was simultaneously published online (Ann Intern Med. 2020 Mar 10. doi: 10.7326/M19-3478).
The work was funded by the National Institutes of Health and Massachusetts General Hospital. The investigators and editorialists didn’t have any industry disclosures.
SOURCE: Walensky RP et al. Ann Intern Med. 2020 Mar 10. doi: 10.7326/M19-3478.
Economically, the modest safety benefit of tenofovir alafenamide-emtricitabine (Descovy) for HIV preexposure prophylaxis won’t justify paying thousands of dollars more for it when tenofovir disoproxil fumarate-emtricitabine (Truvada) becomes available as a generic in a year or so, according to a population level cost-effectiveness analysis presented at the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers held a virtual meeting because of concerns about the spread of COVID-19.
Those benefits will translate to a health savings worth only a few hundred dollars over the likely generic price, said investigators led by Rochelle Walensky, MD, and infectious disease physician and professor of medicine at Harvard Medical School, Boston.
In a press statement, Gilead, which makes both medications, said it “strongly believes that the analysis ... is flawed, leading to inaccurate conclusions that severely underestimate the value of Descovy. The method and validation of the models, incomplete clinical data analyzed and the assumptions around potential pricing associated with a generic alternative to Truvada ... are inadequate to enable a sufficiently robust analysis.”
The company did not go into details about what exactly might have been off about the analysis.
Approved in Oct. 2019, tenofovir alafenamide-emtricitabine (also known as F/TAF) is the first new option for HIV preexposure prophylaxis (PrEP) since tenofovir disoproxil fumarate-emtricitabine (F/TDF) was approved in 2012; F/TDF is going off patent soon.
Amid a robust marketing campaign, the new medication has already captured 25% of the PrEP market, and Gilead expects up to 45% of patients to switch to F/TAF before generic F/TDF becomes available.
That worries the investigators. “At the current FSS [Federal Supply Schedule] price of $16,600 per year,” a nationwide PrEP program that uses F/TAF “would consume the entire $900.8 million federal budget for HIV prevention several times over ... If branded F/TAF drives out generic F/TDF,” rates of PrEP coverage “could decrease, and F/TAF could end up causing more avoidable HIV transmissions” than it prevents. “Given the very small, albeit statistically significant, differences in surrogate [safety] markers, without evidence of clinical significance, there is no urgency and no reason to switch PrEP regimens now,” they said. Both medications were equally effective in preventing HIV transmission in Gilead’s head-to-head phase 3 trial, but there was an a mean of about a 4 mL/min difference in estimated glomerular filtration rate at week 48 and about a 2% difference in hip and spine density at week 96, both favoring F/TAF. Marketing highlights those differences.
The investigators wanted to see how much they are worth, so they estimated savings from a possibly lower rate of bone fractures and renal failure with F/TAF and juxtaposed it with its cost and the anticipated cost of generic F/TDF at half-price, $8,300/patient-year.
They gave F/TAF the benefit of the doubt, skewing their model toward maximal harm and cost from F/TDF toxicity, and omitting the cost of increased lipid levels, weight gain, and other possible F/TAF adverse events.
In the end, they concluded that “the improved safety of F/TAF is worth no more than an additional $370 per person per year” over generic F/TDF based on toxicity differences. “
The team calculated that F/TAF would prevent a maximum of 2,101 fractures and 25 cases of end-stage renal disease among 123,610 U.S. men who have sex with men treated for 5 years. That translated to an incremental cost-effectiveness ratio of more than $7 million per quality-adjusted life-year, far above the $100,000 threshold considered acceptable in the United States.
“In the presence of a generic alternative, the current price of F/TAF would have to be reduced by over $7,900/year for F/TAF to satisfy generally accepted standards of societal value. If F/TDF can achieve the 75% price reduction that is commonly observed when generic competition ensues (that is, a cost of $4,150/year), the F/TAF price would need to be no higher than $4,520 to demonstrate value on the basis of cost-effectiveness,” the investigators said.
For older patients at unusually high risk for renal disease or bone-related adverse events, the switch from F/TDF to F/TAF would have greater clinical effect and benefit. Even in this population, however, it would be difficult to defend a price greater than $800 over the cost of the generic alternative,” they said.
“The message seems clear that the current cost of F/TAF does not justify wholesale conversion to F/TAF as the first-line agent for all PrEP-eligible patients,” said Carlos del Rio, MD, and Wendy Armstrong, MD, infectious disease professors at Emory University, Atlanta, in an editorial. “For PrEP-eligible persons at low risk for fracture and renal disease, it is very hard to justify use of F/TAF knowing that F/TDF will soon be generic” (Ann Intern Med. 2020 Mar 10. doi: 10.7326/M20-0799).
“Successful PrEP scale-up in other countries was made possible by drug costs that are less than $100/month in most countries. In the United States, without drastic reductions in the cost of PrEP, which may be achievable with generic F/TDF ... we will fail to avert otherwise preventable new HIV transmissions,” they said.
The study was simultaneously published online (Ann Intern Med. 2020 Mar 10. doi: 10.7326/M19-3478).
The work was funded by the National Institutes of Health and Massachusetts General Hospital. The investigators and editorialists didn’t have any industry disclosures.
SOURCE: Walensky RP et al. Ann Intern Med. 2020 Mar 10. doi: 10.7326/M19-3478.
FROM CROI 2020
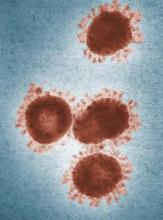
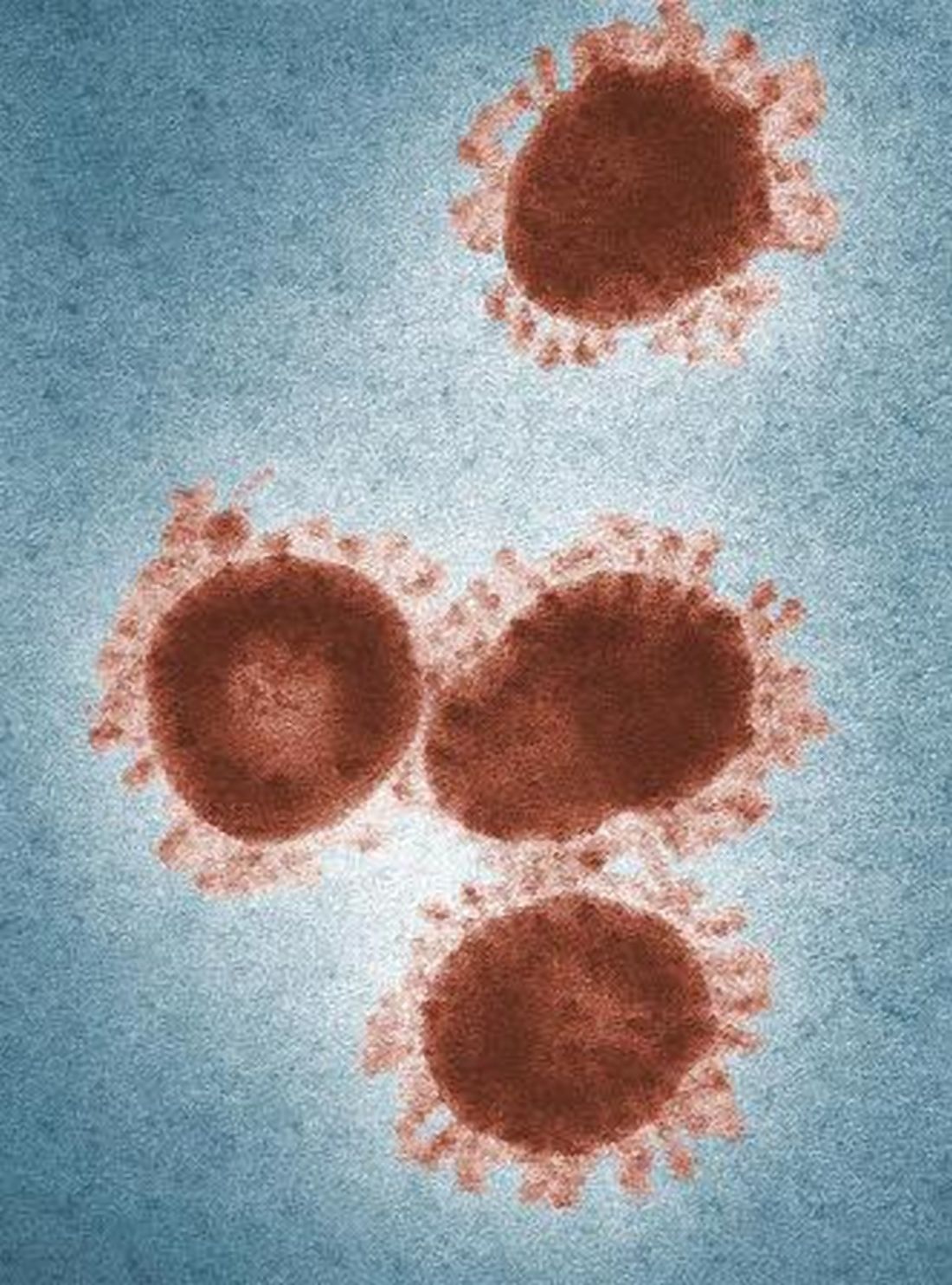
Some infected patients could show COVID-19 symptoms after quarantine
Although a 14-day quarantine after exposure to novel coronavirus is “well supported” by evidence, some infected individuals will not become symptomatic until after that period, according to authors of a recent analysis published in Annals of Internal Medicine.
Most individuals infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) will develop symptoms by day 12 of the infection, which is within the 14-day period of active monitoring currently recommended by the Centers for Disease Control and Prevention, the authors wrote.
However, an estimated 101 out of 10,000 cases could become symptomatic after the end of that 14-day monitoring period, they cautioned.
“Our analyses do not preclude that estimate from being higher,” said the investigators, led by Stephen A. Lauer, PhD, MD, of Johns Hopkins Bloomberg School of Public Health, Baltimore.
The analysis, based on 181 confirmed cases of coronavirus disease 2019 (COVID-19) that were documented outside of the outbreak epicenter, Wuhan, China, makes “more conservative assumptions” about the window of symptom onset and potential for continued exposure, compared with analyses in previous studies, the researchers wrote.
The estimated incubation period for SARS-CoV-2 in the 181-patient study was a median of 5.1 days, which is comparable with previous estimates based on COVID-19 cases outside of Wuhan and consistent with other known human coronavirus diseases, such as SARS, which had a reported mean incubation period of 5 days, Dr. Lauer and colleagues noted.
Symptoms developed within 11.5 days for 97.5% of patients in the study.
Whether it’s acceptable to have 101 out of 10,000 cases becoming symptomatic beyond the recommended quarantine window depends on two factors, according to the authors. The first is the expected infection risk in the population that is being monitored, and the second is “judgment about the cost of missing cases,” wrote the authors.
In an interview, Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau, Oceanside, N.Y., said that in practical terms, the results suggest that the majority of patients with COVID-19 will be identified within 14 days, with an “outside chance” of an infected individual leaving quarantine and transmitting virus for a short period of time before becoming symptomatic.
“I think the proper message to give those patients [who are asymptomatic upon leaving quarantine] is, ‘after 14 days, we’re pretty sure you’re out of the woods, but should you get any symptoms, immediately requarantine yourself and seek medical care,” he said.
Study coauthor Kyra H. Grantz, a doctoral graduate student at the Johns Hopkins Bloomberg School of Public Health, said that extending a quarantine beyond 14 days might be considered in the highest-risk scenarios, though the benefits of doing so would have to be weighed against the costs to public health and to the individuals under quarantine.
“Our estimate of the incubation period definitely supports the 14-day recommendation that the CDC has been using,” she said in an interview.
Dr. Grantz emphasized that the estimate of 101 out of 10,000 cases developing symptoms after day 14 of active monitoring – representing the 99th percentile of cases – assumes the “most conservative, worst-case scenario” in a population that is fully infected.
“If you’re looking at a following a cohort of 1,000 people whom you think may have been exposed, only a certain percentage will be infected, and only a certain percentage of those will even develop symptoms – before we get to this idea of how many people would we miss,” she said.
The study was supported by the Centers for Disease Control and Prevention, the National Institute of Allergy and Infectious Diseases, the National Institute of General Medical Sciences, and the Alexander von Humboldt Foundation. Four authors reported disclosures related to those entities, and the remaining five reported no conflicts of interest.
SOURCE: Lauer SA et al. Ann Intern Med. 2020 Mar 9. doi:10.1101/2020.02.02.20020016.
Although a 14-day quarantine after exposure to novel coronavirus is “well supported” by evidence, some infected individuals will not become symptomatic until after that period, according to authors of a recent analysis published in Annals of Internal Medicine.
Most individuals infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) will develop symptoms by day 12 of the infection, which is within the 14-day period of active monitoring currently recommended by the Centers for Disease Control and Prevention, the authors wrote.
However, an estimated 101 out of 10,000 cases could become symptomatic after the end of that 14-day monitoring period, they cautioned.
“Our analyses do not preclude that estimate from being higher,” said the investigators, led by Stephen A. Lauer, PhD, MD, of Johns Hopkins Bloomberg School of Public Health, Baltimore.
The analysis, based on 181 confirmed cases of coronavirus disease 2019 (COVID-19) that were documented outside of the outbreak epicenter, Wuhan, China, makes “more conservative assumptions” about the window of symptom onset and potential for continued exposure, compared with analyses in previous studies, the researchers wrote.
The estimated incubation period for SARS-CoV-2 in the 181-patient study was a median of 5.1 days, which is comparable with previous estimates based on COVID-19 cases outside of Wuhan and consistent with other known human coronavirus diseases, such as SARS, which had a reported mean incubation period of 5 days, Dr. Lauer and colleagues noted.
Symptoms developed within 11.5 days for 97.5% of patients in the study.
Whether it’s acceptable to have 101 out of 10,000 cases becoming symptomatic beyond the recommended quarantine window depends on two factors, according to the authors. The first is the expected infection risk in the population that is being monitored, and the second is “judgment about the cost of missing cases,” wrote the authors.
In an interview, Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau, Oceanside, N.Y., said that in practical terms, the results suggest that the majority of patients with COVID-19 will be identified within 14 days, with an “outside chance” of an infected individual leaving quarantine and transmitting virus for a short period of time before becoming symptomatic.
“I think the proper message to give those patients [who are asymptomatic upon leaving quarantine] is, ‘after 14 days, we’re pretty sure you’re out of the woods, but should you get any symptoms, immediately requarantine yourself and seek medical care,” he said.
Study coauthor Kyra H. Grantz, a doctoral graduate student at the Johns Hopkins Bloomberg School of Public Health, said that extending a quarantine beyond 14 days might be considered in the highest-risk scenarios, though the benefits of doing so would have to be weighed against the costs to public health and to the individuals under quarantine.
“Our estimate of the incubation period definitely supports the 14-day recommendation that the CDC has been using,” she said in an interview.
Dr. Grantz emphasized that the estimate of 101 out of 10,000 cases developing symptoms after day 14 of active monitoring – representing the 99th percentile of cases – assumes the “most conservative, worst-case scenario” in a population that is fully infected.
“If you’re looking at a following a cohort of 1,000 people whom you think may have been exposed, only a certain percentage will be infected, and only a certain percentage of those will even develop symptoms – before we get to this idea of how many people would we miss,” she said.
The study was supported by the Centers for Disease Control and Prevention, the National Institute of Allergy and Infectious Diseases, the National Institute of General Medical Sciences, and the Alexander von Humboldt Foundation. Four authors reported disclosures related to those entities, and the remaining five reported no conflicts of interest.
SOURCE: Lauer SA et al. Ann Intern Med. 2020 Mar 9. doi:10.1101/2020.02.02.20020016.
Although a 14-day quarantine after exposure to novel coronavirus is “well supported” by evidence, some infected individuals will not become symptomatic until after that period, according to authors of a recent analysis published in Annals of Internal Medicine.
Most individuals infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) will develop symptoms by day 12 of the infection, which is within the 14-day period of active monitoring currently recommended by the Centers for Disease Control and Prevention, the authors wrote.
However, an estimated 101 out of 10,000 cases could become symptomatic after the end of that 14-day monitoring period, they cautioned.
“Our analyses do not preclude that estimate from being higher,” said the investigators, led by Stephen A. Lauer, PhD, MD, of Johns Hopkins Bloomberg School of Public Health, Baltimore.
The analysis, based on 181 confirmed cases of coronavirus disease 2019 (COVID-19) that were documented outside of the outbreak epicenter, Wuhan, China, makes “more conservative assumptions” about the window of symptom onset and potential for continued exposure, compared with analyses in previous studies, the researchers wrote.
The estimated incubation period for SARS-CoV-2 in the 181-patient study was a median of 5.1 days, which is comparable with previous estimates based on COVID-19 cases outside of Wuhan and consistent with other known human coronavirus diseases, such as SARS, which had a reported mean incubation period of 5 days, Dr. Lauer and colleagues noted.
Symptoms developed within 11.5 days for 97.5% of patients in the study.
Whether it’s acceptable to have 101 out of 10,000 cases becoming symptomatic beyond the recommended quarantine window depends on two factors, according to the authors. The first is the expected infection risk in the population that is being monitored, and the second is “judgment about the cost of missing cases,” wrote the authors.
In an interview, Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau, Oceanside, N.Y., said that in practical terms, the results suggest that the majority of patients with COVID-19 will be identified within 14 days, with an “outside chance” of an infected individual leaving quarantine and transmitting virus for a short period of time before becoming symptomatic.
“I think the proper message to give those patients [who are asymptomatic upon leaving quarantine] is, ‘after 14 days, we’re pretty sure you’re out of the woods, but should you get any symptoms, immediately requarantine yourself and seek medical care,” he said.
Study coauthor Kyra H. Grantz, a doctoral graduate student at the Johns Hopkins Bloomberg School of Public Health, said that extending a quarantine beyond 14 days might be considered in the highest-risk scenarios, though the benefits of doing so would have to be weighed against the costs to public health and to the individuals under quarantine.
“Our estimate of the incubation period definitely supports the 14-day recommendation that the CDC has been using,” she said in an interview.
Dr. Grantz emphasized that the estimate of 101 out of 10,000 cases developing symptoms after day 14 of active monitoring – representing the 99th percentile of cases – assumes the “most conservative, worst-case scenario” in a population that is fully infected.
“If you’re looking at a following a cohort of 1,000 people whom you think may have been exposed, only a certain percentage will be infected, and only a certain percentage of those will even develop symptoms – before we get to this idea of how many people would we miss,” she said.
The study was supported by the Centers for Disease Control and Prevention, the National Institute of Allergy and Infectious Diseases, the National Institute of General Medical Sciences, and the Alexander von Humboldt Foundation. Four authors reported disclosures related to those entities, and the remaining five reported no conflicts of interest.
SOURCE: Lauer SA et al. Ann Intern Med. 2020 Mar 9. doi:10.1101/2020.02.02.20020016.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Some individuals who are infected with the novel coronavirus could become symptomatic after the active 14-day quarantine period.
Major finding: The median incubation period was 5.1 days, with 97.5% of patients developing symptoms within 11.5 days, implying that 101 of every 10,000 cases (99th percentile) would develop symptoms beyond the quarantine period.
Study details: Analysis of 181 confirmed COVID-19 cases identified outside of the outbreak epicenter, Wuhan, China.
Disclosures: The study was supported by the U.S. Centers for Disease Control and Prevention, the National Institute of Allergy and Infectious Diseases, the National Institute of General Medical Sciences, and the Alexander von Humboldt Foundation. Four authors reported disclosures related to those entities, and the remaining five reported no conflicts of interest.
Source: Lauer SA et al. Ann Intern Med. 2020 Mar 9. doi: 10.1101/2020.02.02.20020016.
Is there empathy erosion?
You learned a lot of things in medical school. But there must have been some things that you unlearned on the way to your degree. For instance, you unlearned that you could catch a cold by playing outside on a cold damp day without your jacket. You unlearned that handling a toad would give you warts.
The authors of a recent study suggest that over your 4 years in medical school you also unlearned how to be empathetic (“Does Empathy Decline in the Clinical Phase of Medical Education? A Nationwide, Multi-institutional, Cross-Sectional Study of Students at DO-Granting Medical Schools,” Acad Med. 2020 Jan 21. doi: 10.1097/ACM.0000000000003175). The researchers surveyed more than 10,000 medical students at nearly 50 DO-granting medical schools using standardized questionnaire called the Jefferson Scale of Empathy. They discovered that the students in the clinical phase (years 3 and 4) had lower “empathy scores” than the students in the preclinical phase of their education (years 1 and 2). This decline was statistically significant but “negligible” in magnitude. One wonders why they even chose to publish their results, particularly when the number of respondents to the web-based survey declined with each successive year in medical school. Having looked at the a sample of some of the questions being asked, I can understand why third- and fourth-year students couldn’t be bothered to respond. They were too busy to answer a few dozen “lame” questions.
There may be a decline in empathy over the course our medical training, but I’m not sure that this study can speak to it. An older study found that although medical students scores on a self-administered scale declined between the second and third year, the observed empathetic behavior actually increased. If I had to choose, I would lean more heavily on the results of the behavioral observations.
Certainly, we all changed over the course of our medical education. Including postgraduate training, it may have lasted a decade or more. We saw hundreds of patients, observed life and death on a scale and with an intensity that most of us previously had never experienced. Our perspective changed from being a naive observer to playing the role of an active participant. Did that change include a decline in our capacity for empathy?
Something had to change. We found quickly that we didn’t have the time or emotional energy to learn as much about the person hiding behind every complaint as we once thought we should. We had to cut corners. Sometimes we cut too many. On the other hand, as we saw more patients we may have learned more efficient ways of discovering what we needed to know about them to become an effective and caring physician. If we found ourselves in a specialty in which patients have a high mortality, we were forced to learn ways of protecting ourselves from the emotional damage.
What would you call this process? Was it empathy erosion? Was it a hardening or toughening? Or was it simply maturation? Whatever term you use, it was an obligatory process if we hoped to survive. However, not all of us have done it well. Some of us have narrowed our focus to see only the complaint and the diagnosis, and we too often fail to see the human hiding in plain sight.
For those of us who completed our training with our empathy intact, was this the result of a genetic gift or the atmosphere our parents had created at home? I suspect that in most cases our capacity for empathy as physicians was nurtured and enhanced by the role models we encountered during our training. The mentors we most revered were those who had already been through the annealing process of medical school and specialty training and become even more skilled at caring than when they left college. It is an intangible that can’t be taught. Sadly, there is no way of guaranteeing that everyone who enters medical school will be exposed to or benefit from even one of these master physicians.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
You learned a lot of things in medical school. But there must have been some things that you unlearned on the way to your degree. For instance, you unlearned that you could catch a cold by playing outside on a cold damp day without your jacket. You unlearned that handling a toad would give you warts.
The authors of a recent study suggest that over your 4 years in medical school you also unlearned how to be empathetic (“Does Empathy Decline in the Clinical Phase of Medical Education? A Nationwide, Multi-institutional, Cross-Sectional Study of Students at DO-Granting Medical Schools,” Acad Med. 2020 Jan 21. doi: 10.1097/ACM.0000000000003175). The researchers surveyed more than 10,000 medical students at nearly 50 DO-granting medical schools using standardized questionnaire called the Jefferson Scale of Empathy. They discovered that the students in the clinical phase (years 3 and 4) had lower “empathy scores” than the students in the preclinical phase of their education (years 1 and 2). This decline was statistically significant but “negligible” in magnitude. One wonders why they even chose to publish their results, particularly when the number of respondents to the web-based survey declined with each successive year in medical school. Having looked at the a sample of some of the questions being asked, I can understand why third- and fourth-year students couldn’t be bothered to respond. They were too busy to answer a few dozen “lame” questions.
There may be a decline in empathy over the course our medical training, but I’m not sure that this study can speak to it. An older study found that although medical students scores on a self-administered scale declined between the second and third year, the observed empathetic behavior actually increased. If I had to choose, I would lean more heavily on the results of the behavioral observations.
Certainly, we all changed over the course of our medical education. Including postgraduate training, it may have lasted a decade or more. We saw hundreds of patients, observed life and death on a scale and with an intensity that most of us previously had never experienced. Our perspective changed from being a naive observer to playing the role of an active participant. Did that change include a decline in our capacity for empathy?
Something had to change. We found quickly that we didn’t have the time or emotional energy to learn as much about the person hiding behind every complaint as we once thought we should. We had to cut corners. Sometimes we cut too many. On the other hand, as we saw more patients we may have learned more efficient ways of discovering what we needed to know about them to become an effective and caring physician. If we found ourselves in a specialty in which patients have a high mortality, we were forced to learn ways of protecting ourselves from the emotional damage.
What would you call this process? Was it empathy erosion? Was it a hardening or toughening? Or was it simply maturation? Whatever term you use, it was an obligatory process if we hoped to survive. However, not all of us have done it well. Some of us have narrowed our focus to see only the complaint and the diagnosis, and we too often fail to see the human hiding in plain sight.
For those of us who completed our training with our empathy intact, was this the result of a genetic gift or the atmosphere our parents had created at home? I suspect that in most cases our capacity for empathy as physicians was nurtured and enhanced by the role models we encountered during our training. The mentors we most revered were those who had already been through the annealing process of medical school and specialty training and become even more skilled at caring than when they left college. It is an intangible that can’t be taught. Sadly, there is no way of guaranteeing that everyone who enters medical school will be exposed to or benefit from even one of these master physicians.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
You learned a lot of things in medical school. But there must have been some things that you unlearned on the way to your degree. For instance, you unlearned that you could catch a cold by playing outside on a cold damp day without your jacket. You unlearned that handling a toad would give you warts.
The authors of a recent study suggest that over your 4 years in medical school you also unlearned how to be empathetic (“Does Empathy Decline in the Clinical Phase of Medical Education? A Nationwide, Multi-institutional, Cross-Sectional Study of Students at DO-Granting Medical Schools,” Acad Med. 2020 Jan 21. doi: 10.1097/ACM.0000000000003175). The researchers surveyed more than 10,000 medical students at nearly 50 DO-granting medical schools using standardized questionnaire called the Jefferson Scale of Empathy. They discovered that the students in the clinical phase (years 3 and 4) had lower “empathy scores” than the students in the preclinical phase of their education (years 1 and 2). This decline was statistically significant but “negligible” in magnitude. One wonders why they even chose to publish their results, particularly when the number of respondents to the web-based survey declined with each successive year in medical school. Having looked at the a sample of some of the questions being asked, I can understand why third- and fourth-year students couldn’t be bothered to respond. They were too busy to answer a few dozen “lame” questions.
There may be a decline in empathy over the course our medical training, but I’m not sure that this study can speak to it. An older study found that although medical students scores on a self-administered scale declined between the second and third year, the observed empathetic behavior actually increased. If I had to choose, I would lean more heavily on the results of the behavioral observations.
Certainly, we all changed over the course of our medical education. Including postgraduate training, it may have lasted a decade or more. We saw hundreds of patients, observed life and death on a scale and with an intensity that most of us previously had never experienced. Our perspective changed from being a naive observer to playing the role of an active participant. Did that change include a decline in our capacity for empathy?
Something had to change. We found quickly that we didn’t have the time or emotional energy to learn as much about the person hiding behind every complaint as we once thought we should. We had to cut corners. Sometimes we cut too many. On the other hand, as we saw more patients we may have learned more efficient ways of discovering what we needed to know about them to become an effective and caring physician. If we found ourselves in a specialty in which patients have a high mortality, we were forced to learn ways of protecting ourselves from the emotional damage.
What would you call this process? Was it empathy erosion? Was it a hardening or toughening? Or was it simply maturation? Whatever term you use, it was an obligatory process if we hoped to survive. However, not all of us have done it well. Some of us have narrowed our focus to see only the complaint and the diagnosis, and we too often fail to see the human hiding in plain sight.
For those of us who completed our training with our empathy intact, was this the result of a genetic gift or the atmosphere our parents had created at home? I suspect that in most cases our capacity for empathy as physicians was nurtured and enhanced by the role models we encountered during our training. The mentors we most revered were those who had already been through the annealing process of medical school and specialty training and become even more skilled at caring than when they left college. It is an intangible that can’t be taught. Sadly, there is no way of guaranteeing that everyone who enters medical school will be exposed to or benefit from even one of these master physicians.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Flu activity declines again but remains high

Outpatient visits to health care providers for influenza-like illness dropped from 5.5% the previous week to 5.3% of all visits for the week ending Feb. 29, the Centers for Disease Control and Prevention said on March 6.
The national baseline rate of 2.4% was first reached during the week of Nov. 9, 2019 – marking the start of flu season – and has remained at or above that level for 17 consecutive weeks. Last year’s season, which also was the longest in a decade, lasted 21 consecutive weeks but started 2 weeks later than the current season and had a lower outpatient-visit rate (4.5%) for the last week of February, CDC data show.
This season’s earlier start could mean that even a somewhat steep decline in visits to below the baseline rate – marking the end of the season – might take 5 or 6 weeks and would make 2019-2020 even longer than 2018-2019.
The activity situation on the state level reflects the small national decline. For the week ending Feb. 29, there were 33 states at level 10 on the CDC’s 1-10 activity scale, compared with 37 the week before, and a total of 40 in the “high” range of 8-10, compared with 43 the week before, the CDC’s influenza division reported.
The other main measure of influenza activity, percentage of respiratory specimens testing positive, also declined for the third week in a row and is now at 24.3% after reaching a high of 30.3% during the week of Feb. 2-8, the influenza division said.
The overall cumulative hospitalization rate continues to remain at a fairly typical 57.9 per 100,000 population, but rates for school-aged children (84.9 per 100,000) and young adults (31.2 per 100,000) are among the highest ever recorded at this point in the season. Mortality among children – now at 136 for 2019-2020 – is higher than for any season since reporting began in 2004, with the exception of the 2009 pandemic, the CDC said.

Outpatient visits to health care providers for influenza-like illness dropped from 5.5% the previous week to 5.3% of all visits for the week ending Feb. 29, the Centers for Disease Control and Prevention said on March 6.
The national baseline rate of 2.4% was first reached during the week of Nov. 9, 2019 – marking the start of flu season – and has remained at or above that level for 17 consecutive weeks. Last year’s season, which also was the longest in a decade, lasted 21 consecutive weeks but started 2 weeks later than the current season and had a lower outpatient-visit rate (4.5%) for the last week of February, CDC data show.
This season’s earlier start could mean that even a somewhat steep decline in visits to below the baseline rate – marking the end of the season – might take 5 or 6 weeks and would make 2019-2020 even longer than 2018-2019.
The activity situation on the state level reflects the small national decline. For the week ending Feb. 29, there were 33 states at level 10 on the CDC’s 1-10 activity scale, compared with 37 the week before, and a total of 40 in the “high” range of 8-10, compared with 43 the week before, the CDC’s influenza division reported.
The other main measure of influenza activity, percentage of respiratory specimens testing positive, also declined for the third week in a row and is now at 24.3% after reaching a high of 30.3% during the week of Feb. 2-8, the influenza division said.
The overall cumulative hospitalization rate continues to remain at a fairly typical 57.9 per 100,000 population, but rates for school-aged children (84.9 per 100,000) and young adults (31.2 per 100,000) are among the highest ever recorded at this point in the season. Mortality among children – now at 136 for 2019-2020 – is higher than for any season since reporting began in 2004, with the exception of the 2009 pandemic, the CDC said.

Outpatient visits to health care providers for influenza-like illness dropped from 5.5% the previous week to 5.3% of all visits for the week ending Feb. 29, the Centers for Disease Control and Prevention said on March 6.
The national baseline rate of 2.4% was first reached during the week of Nov. 9, 2019 – marking the start of flu season – and has remained at or above that level for 17 consecutive weeks. Last year’s season, which also was the longest in a decade, lasted 21 consecutive weeks but started 2 weeks later than the current season and had a lower outpatient-visit rate (4.5%) for the last week of February, CDC data show.
This season’s earlier start could mean that even a somewhat steep decline in visits to below the baseline rate – marking the end of the season – might take 5 or 6 weeks and would make 2019-2020 even longer than 2018-2019.
The activity situation on the state level reflects the small national decline. For the week ending Feb. 29, there were 33 states at level 10 on the CDC’s 1-10 activity scale, compared with 37 the week before, and a total of 40 in the “high” range of 8-10, compared with 43 the week before, the CDC’s influenza division reported.
The other main measure of influenza activity, percentage of respiratory specimens testing positive, also declined for the third week in a row and is now at 24.3% after reaching a high of 30.3% during the week of Feb. 2-8, the influenza division said.
The overall cumulative hospitalization rate continues to remain at a fairly typical 57.9 per 100,000 population, but rates for school-aged children (84.9 per 100,000) and young adults (31.2 per 100,000) are among the highest ever recorded at this point in the season. Mortality among children – now at 136 for 2019-2020 – is higher than for any season since reporting began in 2004, with the exception of the 2009 pandemic, the CDC said.
Novel coronavirus may cause environmental contamination through fecal shedding
The toilet bowl, sink, and bathroom door handle of an isolation room housing a patient with the novel coronavirus tested positive for the virus, raising the possibility that viral shedding in the stool could represent another route of transmission, investigators reported.
Air outlet fans and other room sites also tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), though an anteroom, a corridor, and most personal protective equipment (PPE) worn by health care providers tested negative, according to the researchers, led by Sean Wei Xiang Ong, MBBS, of the National Centre for Infectious Diseases, Singapore.
Taken together, these findings suggest a “need for strict adherence to environmental and hand hygiene” to combat significant environmental contamination through respiratory droplets and fecal shedding, Dr. Ong and colleagues wrote in JAMA.
Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau in New York, said these results demonstrate that SARS-CoV-2 is “clearly capable” of contaminating bathroom sinks and toilets.
“That wouldn’t have been the first place I would have thought of, before this study,” he said in an interview. “You need to pay attention to cleaning the bathrooms, which we obviously do, but that’s an important reminder.”
The report by Dr. Ong and coauthors included a total of three patients housed in airborne infection isolation rooms in a dedicated SARS-CoV-2 outbreak center in Singapore. For each patient, surface samples were taken from 26 sites in the isolation room, an anteroom, and a bathroom. Samples were also taken from PPE on physicians as they left the patient rooms.
Samples for the first patient, taken right after routine cleaning, were all negative, according to researchers. That room was sampled twice, on days 4 and 10 of the illness, while the patient was still symptomatic. Likewise, for the second patient, postcleaning samples were negative; those samples were taken 2 days after cleaning.
However, for the third patient, samples were taken before routine cleaning. In this case, Dr. Ong and colleagues said 13 of 15 room sites (87%) were positive, including air outlet fans, while 3 of 5 toilet sites (60%) were positive as well, though no contamination was found in the anteroom, corridor, or in air samples.
That patient had two stool samples that were positive for SARS-CoV-2, but no diarrhea, authors said, and had upper respiratory tract involvement without pneumonia.
The fact that swabs of the air exhaust outlets tested positive suggests that virus-laden droplets could be “displaced by airflows” and end up on vents or other equipment, Dr. Ong and coauthors reported.
All PPE samples tested negative, except for the front of one shoe.
“The risk of transmission from contaminated footwear is likely low, as evidenced by negative results in the anteroom and corridor,” they wrote.
While this study included only a small number of patients, Dr. Glatt said the findings represent an important and useful contribution to the literature on coronavirus disease 2019 (COVID-19).
“Every day we’re getting more information, and each little piece of the puzzle helps us in the overall management of individuals with COVID-19,” he said in the interview. “They’re adding to our ability to manage, control, and mitigate further spread of the disease.”
Funding for the study came from the National Medical Research Council in Singapore and DSO National Laboratories. Dr. Ong and colleagues reported no conflicts of interest.
SOURCE: Ong SWX et al. JAMA. 2020 Mar 4. doi: 10.1001/jama.2020.3227.
The toilet bowl, sink, and bathroom door handle of an isolation room housing a patient with the novel coronavirus tested positive for the virus, raising the possibility that viral shedding in the stool could represent another route of transmission, investigators reported.
Air outlet fans and other room sites also tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), though an anteroom, a corridor, and most personal protective equipment (PPE) worn by health care providers tested negative, according to the researchers, led by Sean Wei Xiang Ong, MBBS, of the National Centre for Infectious Diseases, Singapore.
Taken together, these findings suggest a “need for strict adherence to environmental and hand hygiene” to combat significant environmental contamination through respiratory droplets and fecal shedding, Dr. Ong and colleagues wrote in JAMA.
Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau in New York, said these results demonstrate that SARS-CoV-2 is “clearly capable” of contaminating bathroom sinks and toilets.
“That wouldn’t have been the first place I would have thought of, before this study,” he said in an interview. “You need to pay attention to cleaning the bathrooms, which we obviously do, but that’s an important reminder.”
The report by Dr. Ong and coauthors included a total of three patients housed in airborne infection isolation rooms in a dedicated SARS-CoV-2 outbreak center in Singapore. For each patient, surface samples were taken from 26 sites in the isolation room, an anteroom, and a bathroom. Samples were also taken from PPE on physicians as they left the patient rooms.
Samples for the first patient, taken right after routine cleaning, were all negative, according to researchers. That room was sampled twice, on days 4 and 10 of the illness, while the patient was still symptomatic. Likewise, for the second patient, postcleaning samples were negative; those samples were taken 2 days after cleaning.
However, for the third patient, samples were taken before routine cleaning. In this case, Dr. Ong and colleagues said 13 of 15 room sites (87%) were positive, including air outlet fans, while 3 of 5 toilet sites (60%) were positive as well, though no contamination was found in the anteroom, corridor, or in air samples.
That patient had two stool samples that were positive for SARS-CoV-2, but no diarrhea, authors said, and had upper respiratory tract involvement without pneumonia.
The fact that swabs of the air exhaust outlets tested positive suggests that virus-laden droplets could be “displaced by airflows” and end up on vents or other equipment, Dr. Ong and coauthors reported.
All PPE samples tested negative, except for the front of one shoe.
“The risk of transmission from contaminated footwear is likely low, as evidenced by negative results in the anteroom and corridor,” they wrote.
While this study included only a small number of patients, Dr. Glatt said the findings represent an important and useful contribution to the literature on coronavirus disease 2019 (COVID-19).
“Every day we’re getting more information, and each little piece of the puzzle helps us in the overall management of individuals with COVID-19,” he said in the interview. “They’re adding to our ability to manage, control, and mitigate further spread of the disease.”
Funding for the study came from the National Medical Research Council in Singapore and DSO National Laboratories. Dr. Ong and colleagues reported no conflicts of interest.
SOURCE: Ong SWX et al. JAMA. 2020 Mar 4. doi: 10.1001/jama.2020.3227.
The toilet bowl, sink, and bathroom door handle of an isolation room housing a patient with the novel coronavirus tested positive for the virus, raising the possibility that viral shedding in the stool could represent another route of transmission, investigators reported.
Air outlet fans and other room sites also tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), though an anteroom, a corridor, and most personal protective equipment (PPE) worn by health care providers tested negative, according to the researchers, led by Sean Wei Xiang Ong, MBBS, of the National Centre for Infectious Diseases, Singapore.
Taken together, these findings suggest a “need for strict adherence to environmental and hand hygiene” to combat significant environmental contamination through respiratory droplets and fecal shedding, Dr. Ong and colleagues wrote in JAMA.
Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau in New York, said these results demonstrate that SARS-CoV-2 is “clearly capable” of contaminating bathroom sinks and toilets.
“That wouldn’t have been the first place I would have thought of, before this study,” he said in an interview. “You need to pay attention to cleaning the bathrooms, which we obviously do, but that’s an important reminder.”
The report by Dr. Ong and coauthors included a total of three patients housed in airborne infection isolation rooms in a dedicated SARS-CoV-2 outbreak center in Singapore. For each patient, surface samples were taken from 26 sites in the isolation room, an anteroom, and a bathroom. Samples were also taken from PPE on physicians as they left the patient rooms.
Samples for the first patient, taken right after routine cleaning, were all negative, according to researchers. That room was sampled twice, on days 4 and 10 of the illness, while the patient was still symptomatic. Likewise, for the second patient, postcleaning samples were negative; those samples were taken 2 days after cleaning.
However, for the third patient, samples were taken before routine cleaning. In this case, Dr. Ong and colleagues said 13 of 15 room sites (87%) were positive, including air outlet fans, while 3 of 5 toilet sites (60%) were positive as well, though no contamination was found in the anteroom, corridor, or in air samples.
That patient had two stool samples that were positive for SARS-CoV-2, but no diarrhea, authors said, and had upper respiratory tract involvement without pneumonia.
The fact that swabs of the air exhaust outlets tested positive suggests that virus-laden droplets could be “displaced by airflows” and end up on vents or other equipment, Dr. Ong and coauthors reported.
All PPE samples tested negative, except for the front of one shoe.
“The risk of transmission from contaminated footwear is likely low, as evidenced by negative results in the anteroom and corridor,” they wrote.
While this study included only a small number of patients, Dr. Glatt said the findings represent an important and useful contribution to the literature on coronavirus disease 2019 (COVID-19).
“Every day we’re getting more information, and each little piece of the puzzle helps us in the overall management of individuals with COVID-19,” he said in the interview. “They’re adding to our ability to manage, control, and mitigate further spread of the disease.”
Funding for the study came from the National Medical Research Council in Singapore and DSO National Laboratories. Dr. Ong and colleagues reported no conflicts of interest.
SOURCE: Ong SWX et al. JAMA. 2020 Mar 4. doi: 10.1001/jama.2020.3227.
FROM JAMA
Telehealth seen as a key tool to help fight COVID-19
Telehealth is increasingly being viewed as a key way to help fight the COVID-19 outbreak in the United States. Recognizing the potential of this technology to slow the spread of the disease, the House of Representatives included a provision in an $8.3 billion emergency response bill it approved today that would temporarily lift restrictions on Medicare telehealth coverage to assist in the efforts to contain the virus.
Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention (CDC), said that hospitals should be prepared to use telehealth as one of their tools in fighting the outbreak, according to a recent news release from the American Hospital Association (AHA).
Congress is responding to that need by including the service in the new coronavirus legislation now headed to the Senate, after the funding bill was approved in a 415-2 vote by the House.
The bill empowers the Secretary of Health and Human Services (HHS) to “waive or modify application of certain Medicare requirements with respect to telehealth services furnished during certain emergency periods.”
While the measure adds telehealth to the waiver authority that the HHS secretary currently has during national emergencies, it’s only for the coronavirus crisis in this case, Krista Drobac, executive director of the Alliance for Connected Care, told Medscape Medical News.
The waiver would apply to originating sites of telehealth visits, she noted. Thus Medicare coverage of telemedicine would be expanded beyond rural areas.
In addition, the waiver would allow coverage of virtual visits conducted on smartphones with audio and video capabilities. A “qualified provider,” as defined by the legislation, would be a practitioner who has an established relationship with the patient or who is in the same practice as the provider who has that relationship.
An advantage of telehealth, proponents say, is that it can enable people who believe they have COVID-19 to be seen at home rather than visit offices or emergency departments (EDs) where they might spread the disease or be in proximity to others who have it.
In an editorial published March 2 in Modern Healthcare, medical directors from Stanford Medicine, MedStar Health, and Intermountain Healthcare also noted that telehealth can give patients 24/7 access to care, allow surveillance of patients at risk while keeping them at home, ensure that treatment in hospitals is reserved for high-need patients, and enable providers to triage and screen more patients than can be handled in brick-and-mortar care settings.
However, telehealth screening would allow physicians only to judge whether a patient’s symptoms might be indicative of COVID-19, the Alliance for Connected Care, a telehealth advocacy group, noted in a letter to Congressional leaders. Patients would still have to be seen in person to be tested for the disease.
The group, which represents technology companies, health insurers, pharmacies, and other healthcare players, has been lobbying Congress to include telehealth in federal funds to combat the outbreak.
The American Telemedicine Association (ATA) also supports this goal, ATA President Joseph Kvedar, MD, told Medscape Medical News. And the authors of the Modern Healthcare editorial also advocated for this legislative solution. Because the fatality rate for COVID-19 is significantly higher for older people than for other age groups, they noted, telehealth should be an economically viable option for all seniors.
The Centers for Medicare and Medicaid Services (CMS) long covered telemedicine only in rural areas and only when initiated in healthcare settings. Recently, however, CMS loosened its approach to some extent. Virtual “check-in visits” can now be initiated from any location, including home, to determine whether a Medicare patient needs to be seen in the office. In addition, CMS allows Medicare Advantage plans to offer telemedicine as a core benefit.
Are healthcare systems prepared?
Some large healthcare systems such as Stanford, MedStar, and Intermountain are already using telehealth to diagnose and treat patients who have traditional influenza. Telehealth providers at Stanford estimate that almost 50% of these patients are being prescribed the antiviral drug Tamiflu.
It’s unclear whether other healthcare systems are this well prepared to offer telehealth on a large scale. But, according to an AHA survey, Kvedar noted, three quarters of AHA members are engaged in some form of telehealth.
Drobac said “it wouldn’t require too much effort” to ramp up a wide-scale telehealth program that could help reduce the impact of the outbreak. “The technology is there,” she noted. “You need a HIPAA-compliant telehealth platform, but there are so many out there.”
Kvedar agreed. To begin with, he said, hospitals might sequester patients who visit the ED with COVID-19 symptoms in a video-equipped “isolation room.” Staff members could then do the patient intake from a different location in the hospital.
He admitted that this approach would be infeasible if a lot of patients arrived in EDs with coronavirus symptoms. However, Kvedar noted, “All the tools are in place to go well beyond that. American Well, Teladoc, and others are all offering ways to get out in front of this. There are plenty of vendors out there, and most people have a connected cell phone that you can do a video call on.”
Hospital leaders would have to decide whether to embrace telehealth, which would mean less use of services in their institutions, he said. “But it would be for the greater good of the public.”
Kvedar recalled that there was some use of telehealth in the New York area after 9/11. Telehealth was also used in the aftermath of Hurricane Katrina in 2005. But the ATA president, who is also vice president of connected health at Partners HealthCare in Boston, noted that the COVID-19 outbreak is the first public health emergency to occur in the era of Skype and smartphones.
If Congress does ultimately authorize CMS to cover telehealth across the board during this emergency, might that lead to a permanent change in Medicare coverage policy? Kvedar wouldn’t venture an opinion. “However, the current CMS leadership has been incredibly telehealth friendly,” he said. “So it’s possible they would [embrace a lifting of restrictions]. As patients get a sense of this modality of care and how convenient it is for them, they’ll start asking for more.”
Meanwhile, he said, the telehealth opportunity goes beyond video visits with doctors to mitigate the outbreak. Telehealth data could also be used to track disease spread, similar to how researchers have studied Google searches to predict the spread of the flu, he noted.
Teladoc, a major telehealth vendor, recently told stock analysts it’s already working with the CDC on disease surveillance, according to a report in FierceHealthcare.
This article first appeared on Medscape.com.
Telehealth is increasingly being viewed as a key way to help fight the COVID-19 outbreak in the United States. Recognizing the potential of this technology to slow the spread of the disease, the House of Representatives included a provision in an $8.3 billion emergency response bill it approved today that would temporarily lift restrictions on Medicare telehealth coverage to assist in the efforts to contain the virus.
Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention (CDC), said that hospitals should be prepared to use telehealth as one of their tools in fighting the outbreak, according to a recent news release from the American Hospital Association (AHA).
Congress is responding to that need by including the service in the new coronavirus legislation now headed to the Senate, after the funding bill was approved in a 415-2 vote by the House.
The bill empowers the Secretary of Health and Human Services (HHS) to “waive or modify application of certain Medicare requirements with respect to telehealth services furnished during certain emergency periods.”
While the measure adds telehealth to the waiver authority that the HHS secretary currently has during national emergencies, it’s only for the coronavirus crisis in this case, Krista Drobac, executive director of the Alliance for Connected Care, told Medscape Medical News.
The waiver would apply to originating sites of telehealth visits, she noted. Thus Medicare coverage of telemedicine would be expanded beyond rural areas.
In addition, the waiver would allow coverage of virtual visits conducted on smartphones with audio and video capabilities. A “qualified provider,” as defined by the legislation, would be a practitioner who has an established relationship with the patient or who is in the same practice as the provider who has that relationship.
An advantage of telehealth, proponents say, is that it can enable people who believe they have COVID-19 to be seen at home rather than visit offices or emergency departments (EDs) where they might spread the disease or be in proximity to others who have it.
In an editorial published March 2 in Modern Healthcare, medical directors from Stanford Medicine, MedStar Health, and Intermountain Healthcare also noted that telehealth can give patients 24/7 access to care, allow surveillance of patients at risk while keeping them at home, ensure that treatment in hospitals is reserved for high-need patients, and enable providers to triage and screen more patients than can be handled in brick-and-mortar care settings.
However, telehealth screening would allow physicians only to judge whether a patient’s symptoms might be indicative of COVID-19, the Alliance for Connected Care, a telehealth advocacy group, noted in a letter to Congressional leaders. Patients would still have to be seen in person to be tested for the disease.
The group, which represents technology companies, health insurers, pharmacies, and other healthcare players, has been lobbying Congress to include telehealth in federal funds to combat the outbreak.
The American Telemedicine Association (ATA) also supports this goal, ATA President Joseph Kvedar, MD, told Medscape Medical News. And the authors of the Modern Healthcare editorial also advocated for this legislative solution. Because the fatality rate for COVID-19 is significantly higher for older people than for other age groups, they noted, telehealth should be an economically viable option for all seniors.
The Centers for Medicare and Medicaid Services (CMS) long covered telemedicine only in rural areas and only when initiated in healthcare settings. Recently, however, CMS loosened its approach to some extent. Virtual “check-in visits” can now be initiated from any location, including home, to determine whether a Medicare patient needs to be seen in the office. In addition, CMS allows Medicare Advantage plans to offer telemedicine as a core benefit.
Are healthcare systems prepared?
Some large healthcare systems such as Stanford, MedStar, and Intermountain are already using telehealth to diagnose and treat patients who have traditional influenza. Telehealth providers at Stanford estimate that almost 50% of these patients are being prescribed the antiviral drug Tamiflu.
It’s unclear whether other healthcare systems are this well prepared to offer telehealth on a large scale. But, according to an AHA survey, Kvedar noted, three quarters of AHA members are engaged in some form of telehealth.
Drobac said “it wouldn’t require too much effort” to ramp up a wide-scale telehealth program that could help reduce the impact of the outbreak. “The technology is there,” she noted. “You need a HIPAA-compliant telehealth platform, but there are so many out there.”
Kvedar agreed. To begin with, he said, hospitals might sequester patients who visit the ED with COVID-19 symptoms in a video-equipped “isolation room.” Staff members could then do the patient intake from a different location in the hospital.
He admitted that this approach would be infeasible if a lot of patients arrived in EDs with coronavirus symptoms. However, Kvedar noted, “All the tools are in place to go well beyond that. American Well, Teladoc, and others are all offering ways to get out in front of this. There are plenty of vendors out there, and most people have a connected cell phone that you can do a video call on.”
Hospital leaders would have to decide whether to embrace telehealth, which would mean less use of services in their institutions, he said. “But it would be for the greater good of the public.”
Kvedar recalled that there was some use of telehealth in the New York area after 9/11. Telehealth was also used in the aftermath of Hurricane Katrina in 2005. But the ATA president, who is also vice president of connected health at Partners HealthCare in Boston, noted that the COVID-19 outbreak is the first public health emergency to occur in the era of Skype and smartphones.
If Congress does ultimately authorize CMS to cover telehealth across the board during this emergency, might that lead to a permanent change in Medicare coverage policy? Kvedar wouldn’t venture an opinion. “However, the current CMS leadership has been incredibly telehealth friendly,” he said. “So it’s possible they would [embrace a lifting of restrictions]. As patients get a sense of this modality of care and how convenient it is for them, they’ll start asking for more.”
Meanwhile, he said, the telehealth opportunity goes beyond video visits with doctors to mitigate the outbreak. Telehealth data could also be used to track disease spread, similar to how researchers have studied Google searches to predict the spread of the flu, he noted.
Teladoc, a major telehealth vendor, recently told stock analysts it’s already working with the CDC on disease surveillance, according to a report in FierceHealthcare.
This article first appeared on Medscape.com.
Telehealth is increasingly being viewed as a key way to help fight the COVID-19 outbreak in the United States. Recognizing the potential of this technology to slow the spread of the disease, the House of Representatives included a provision in an $8.3 billion emergency response bill it approved today that would temporarily lift restrictions on Medicare telehealth coverage to assist in the efforts to contain the virus.
Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention (CDC), said that hospitals should be prepared to use telehealth as one of their tools in fighting the outbreak, according to a recent news release from the American Hospital Association (AHA).
Congress is responding to that need by including the service in the new coronavirus legislation now headed to the Senate, after the funding bill was approved in a 415-2 vote by the House.
The bill empowers the Secretary of Health and Human Services (HHS) to “waive or modify application of certain Medicare requirements with respect to telehealth services furnished during certain emergency periods.”
While the measure adds telehealth to the waiver authority that the HHS secretary currently has during national emergencies, it’s only for the coronavirus crisis in this case, Krista Drobac, executive director of the Alliance for Connected Care, told Medscape Medical News.
The waiver would apply to originating sites of telehealth visits, she noted. Thus Medicare coverage of telemedicine would be expanded beyond rural areas.
In addition, the waiver would allow coverage of virtual visits conducted on smartphones with audio and video capabilities. A “qualified provider,” as defined by the legislation, would be a practitioner who has an established relationship with the patient or who is in the same practice as the provider who has that relationship.
An advantage of telehealth, proponents say, is that it can enable people who believe they have COVID-19 to be seen at home rather than visit offices or emergency departments (EDs) where they might spread the disease or be in proximity to others who have it.
In an editorial published March 2 in Modern Healthcare, medical directors from Stanford Medicine, MedStar Health, and Intermountain Healthcare also noted that telehealth can give patients 24/7 access to care, allow surveillance of patients at risk while keeping them at home, ensure that treatment in hospitals is reserved for high-need patients, and enable providers to triage and screen more patients than can be handled in brick-and-mortar care settings.
However, telehealth screening would allow physicians only to judge whether a patient’s symptoms might be indicative of COVID-19, the Alliance for Connected Care, a telehealth advocacy group, noted in a letter to Congressional leaders. Patients would still have to be seen in person to be tested for the disease.
The group, which represents technology companies, health insurers, pharmacies, and other healthcare players, has been lobbying Congress to include telehealth in federal funds to combat the outbreak.
The American Telemedicine Association (ATA) also supports this goal, ATA President Joseph Kvedar, MD, told Medscape Medical News. And the authors of the Modern Healthcare editorial also advocated for this legislative solution. Because the fatality rate for COVID-19 is significantly higher for older people than for other age groups, they noted, telehealth should be an economically viable option for all seniors.
The Centers for Medicare and Medicaid Services (CMS) long covered telemedicine only in rural areas and only when initiated in healthcare settings. Recently, however, CMS loosened its approach to some extent. Virtual “check-in visits” can now be initiated from any location, including home, to determine whether a Medicare patient needs to be seen in the office. In addition, CMS allows Medicare Advantage plans to offer telemedicine as a core benefit.
Are healthcare systems prepared?
Some large healthcare systems such as Stanford, MedStar, and Intermountain are already using telehealth to diagnose and treat patients who have traditional influenza. Telehealth providers at Stanford estimate that almost 50% of these patients are being prescribed the antiviral drug Tamiflu.
It’s unclear whether other healthcare systems are this well prepared to offer telehealth on a large scale. But, according to an AHA survey, Kvedar noted, three quarters of AHA members are engaged in some form of telehealth.
Drobac said “it wouldn’t require too much effort” to ramp up a wide-scale telehealth program that could help reduce the impact of the outbreak. “The technology is there,” she noted. “You need a HIPAA-compliant telehealth platform, but there are so many out there.”
Kvedar agreed. To begin with, he said, hospitals might sequester patients who visit the ED with COVID-19 symptoms in a video-equipped “isolation room.” Staff members could then do the patient intake from a different location in the hospital.
He admitted that this approach would be infeasible if a lot of patients arrived in EDs with coronavirus symptoms. However, Kvedar noted, “All the tools are in place to go well beyond that. American Well, Teladoc, and others are all offering ways to get out in front of this. There are plenty of vendors out there, and most people have a connected cell phone that you can do a video call on.”
Hospital leaders would have to decide whether to embrace telehealth, which would mean less use of services in their institutions, he said. “But it would be for the greater good of the public.”
Kvedar recalled that there was some use of telehealth in the New York area after 9/11. Telehealth was also used in the aftermath of Hurricane Katrina in 2005. But the ATA president, who is also vice president of connected health at Partners HealthCare in Boston, noted that the COVID-19 outbreak is the first public health emergency to occur in the era of Skype and smartphones.
If Congress does ultimately authorize CMS to cover telehealth across the board during this emergency, might that lead to a permanent change in Medicare coverage policy? Kvedar wouldn’t venture an opinion. “However, the current CMS leadership has been incredibly telehealth friendly,” he said. “So it’s possible they would [embrace a lifting of restrictions]. As patients get a sense of this modality of care and how convenient it is for them, they’ll start asking for more.”
Meanwhile, he said, the telehealth opportunity goes beyond video visits with doctors to mitigate the outbreak. Telehealth data could also be used to track disease spread, similar to how researchers have studied Google searches to predict the spread of the flu, he noted.
Teladoc, a major telehealth vendor, recently told stock analysts it’s already working with the CDC on disease surveillance, according to a report in FierceHealthcare.
This article first appeared on Medscape.com.
Infection control protects hospital staff from COVID-19, study shows
Hospital-related infections have been widely reported during the ongoing coronavirus outbreak, with healthcare professionals bearing a disproportionate risk. However, a proactive response in Hong Kong’s public hospital system appears to have bucked this trend and successfully protected both patients and staff from SARS-CoV-2, according to a study published online today in Infection Control & Hospital Epidemiology.
During the first 42 days of the outbreak, the 43 hospitals in the network tested 1275 suspected cases and treated 42 patients with confirmed COVID-19, the disease caused by SARS-CoV-2 infection. Yet, there were no nosocomial infections or infections among healthcare personnel, report Vincent C.C. Cheng, MD, FRCPath, the hospital’s infection control officer, and colleagues.
Cheng and colleagues note that 11 out of 413 healthcare workers who treat patients with confirmed infections had unprotected exposure and were in quarantine for 14 days, but none became ill.
In comparison, they note, the 2003 SARS outbreak saw almost 60% of nosocomial cases occurring in healthcare workers.
Proactive bundle
The Hong Kong success story may be due to a stepped-up proactive bundle of measures that included enhanced laboratory surveillance, early airborne infection isolation, and rapid-turnaround molecular diagnostics. Other strategies included staff forums and one-on-one discussions about infection control, employee training in protective equipment use, hand-hygiene compliance enforcement, and contact tracing for workers with unprotected exposure.
In addition, surgical masks were provided for all healthcare workers, patients, and visitors to clinical areas, a practice previously associated with reduced in-hospital transmission during influenza outbreaks, the authors note.
Hospitals also mandated use of personal protective equipment (PPE) for aerosol-generating procedures (AGPs), such as endotracheal intubation, open suctioning, and high-flow oxygen use, as AGPs had been linked to nosocomial transmission to healthcare workers during the 2003 SARS outbreak.
The infection control measures, which were part of a preparedness plan developed after the SARS outbreak, were initiated on December 31, when the first reports of a cluster of infections came from Wuhan, China.
As the outbreak evolved, the Hong Kong hospitals quickly widened the epidemiologic criteria for screening, from initially including only those who had been to a wet market in Wuhan within 14 days of symptom onset, to eventually including anyone who had been to Hubei province, been in a medical facility in mainland China, or in contact with a known case.
All suspected cases were sent to an airborne-infection isolation room (AIIR) or a ward with at least a meter of space between patients.
“Appropriate hospital infection control measures could prevent nosocomial transmission of SARS-CoV-2,” the authors write. “Vigilance in hand hygiene practice, wearing of surgical mask in the hospital, and appropriate use of PPE in patient care, especially [when] performing AGPs, are the key infection control measures to prevent nosocomial transmission of SARS-CoV-2 even before the availability of effective antiviral agents and vaccine.”
Asked for his perspective on the report, Aaron E. Glatt, MD, chairman of the department of medicine and chief of infectious diseases at Mount Sinai South Nassau in Oceanside, New York, said that apart from the widespread issuing of surgical masks to workers, patients, and visitors, the measures taken in Hong Kong are not different from standard infection-control practices in American hospitals. Glatt, who is also a hospital epidemiologist, said it was unclear how much impact the masks would have.
“Although the infection control was impressive, I don’t see any evidence of a difference in care,” he told Medscape Medical News.
Could zero infection transmission be achieved in the more far-flung and variable settings of hospitals across the United States? “The ability to get zero transmission is only possible if people adhere to the strictest infection-control guidelines,” Glatt said. “That is clearly the goal, and it will take time to see if our existing strict guidelines are sufficient to maintain zero or close to zero contamination and transmission rates in our hospitals.”
Rather than looking to change US practices, he stressed adherence to widely established tenets of care. “It’s critically important to keep paying close attention to the basics, to the simple blocking and tackling, and to identify which patients are at risk, and therefore, when workers need protective equipment,” he said.
“Follow the recommended standards,” continued Glatt, who is also a spokesperson for the Infectious Diseases Society of America and did not participate in this study.
In a finding from an ancillary pilot experiment, the Hong Kong researchers found exhaled air from a patient with a moderate coronavirus load showed no evidence of the virus, whether the patient was breathing normally or heavily, speaking, or coughing. And spot tests around the room detected the virus in just one location.
“We may not be able to make a definite conclusion based on the analysis of a single patient,” the authors write. “However, it may help to reassure our staff that the exhaled air may be rapidly diluted inside the AIIR with 12 air changes per hour, or probably the SARS-CoV-2 may not be predominantly transmitted by [the] airborne route.”
However, a recent Singapore study showed widespread environmental contamination by SARS-CoV-2 through respiratory droplets and fecal shedding, underlining the need for strict adherence to environmental and hand hygiene. Post-cleaning samples tested negative, suggesting that standard decontamination practices are effective.
This work was partly supported by the Consultancy Service for Enhancing Laboratory Surveillance of Emerging Infectious Diseases of the Department of Health, Hong Kong Special Administrative Region; and the Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, Ministry of Education of China. The authors and Glatt have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Hospital-related infections have been widely reported during the ongoing coronavirus outbreak, with healthcare professionals bearing a disproportionate risk. However, a proactive response in Hong Kong’s public hospital system appears to have bucked this trend and successfully protected both patients and staff from SARS-CoV-2, according to a study published online today in Infection Control & Hospital Epidemiology.
During the first 42 days of the outbreak, the 43 hospitals in the network tested 1275 suspected cases and treated 42 patients with confirmed COVID-19, the disease caused by SARS-CoV-2 infection. Yet, there were no nosocomial infections or infections among healthcare personnel, report Vincent C.C. Cheng, MD, FRCPath, the hospital’s infection control officer, and colleagues.
Cheng and colleagues note that 11 out of 413 healthcare workers who treat patients with confirmed infections had unprotected exposure and were in quarantine for 14 days, but none became ill.
In comparison, they note, the 2003 SARS outbreak saw almost 60% of nosocomial cases occurring in healthcare workers.
Proactive bundle
The Hong Kong success story may be due to a stepped-up proactive bundle of measures that included enhanced laboratory surveillance, early airborne infection isolation, and rapid-turnaround molecular diagnostics. Other strategies included staff forums and one-on-one discussions about infection control, employee training in protective equipment use, hand-hygiene compliance enforcement, and contact tracing for workers with unprotected exposure.
In addition, surgical masks were provided for all healthcare workers, patients, and visitors to clinical areas, a practice previously associated with reduced in-hospital transmission during influenza outbreaks, the authors note.
Hospitals also mandated use of personal protective equipment (PPE) for aerosol-generating procedures (AGPs), such as endotracheal intubation, open suctioning, and high-flow oxygen use, as AGPs had been linked to nosocomial transmission to healthcare workers during the 2003 SARS outbreak.
The infection control measures, which were part of a preparedness plan developed after the SARS outbreak, were initiated on December 31, when the first reports of a cluster of infections came from Wuhan, China.
As the outbreak evolved, the Hong Kong hospitals quickly widened the epidemiologic criteria for screening, from initially including only those who had been to a wet market in Wuhan within 14 days of symptom onset, to eventually including anyone who had been to Hubei province, been in a medical facility in mainland China, or in contact with a known case.
All suspected cases were sent to an airborne-infection isolation room (AIIR) or a ward with at least a meter of space between patients.
“Appropriate hospital infection control measures could prevent nosocomial transmission of SARS-CoV-2,” the authors write. “Vigilance in hand hygiene practice, wearing of surgical mask in the hospital, and appropriate use of PPE in patient care, especially [when] performing AGPs, are the key infection control measures to prevent nosocomial transmission of SARS-CoV-2 even before the availability of effective antiviral agents and vaccine.”
Asked for his perspective on the report, Aaron E. Glatt, MD, chairman of the department of medicine and chief of infectious diseases at Mount Sinai South Nassau in Oceanside, New York, said that apart from the widespread issuing of surgical masks to workers, patients, and visitors, the measures taken in Hong Kong are not different from standard infection-control practices in American hospitals. Glatt, who is also a hospital epidemiologist, said it was unclear how much impact the masks would have.
“Although the infection control was impressive, I don’t see any evidence of a difference in care,” he told Medscape Medical News.
Could zero infection transmission be achieved in the more far-flung and variable settings of hospitals across the United States? “The ability to get zero transmission is only possible if people adhere to the strictest infection-control guidelines,” Glatt said. “That is clearly the goal, and it will take time to see if our existing strict guidelines are sufficient to maintain zero or close to zero contamination and transmission rates in our hospitals.”
Rather than looking to change US practices, he stressed adherence to widely established tenets of care. “It’s critically important to keep paying close attention to the basics, to the simple blocking and tackling, and to identify which patients are at risk, and therefore, when workers need protective equipment,” he said.
“Follow the recommended standards,” continued Glatt, who is also a spokesperson for the Infectious Diseases Society of America and did not participate in this study.
In a finding from an ancillary pilot experiment, the Hong Kong researchers found exhaled air from a patient with a moderate coronavirus load showed no evidence of the virus, whether the patient was breathing normally or heavily, speaking, or coughing. And spot tests around the room detected the virus in just one location.
“We may not be able to make a definite conclusion based on the analysis of a single patient,” the authors write. “However, it may help to reassure our staff that the exhaled air may be rapidly diluted inside the AIIR with 12 air changes per hour, or probably the SARS-CoV-2 may not be predominantly transmitted by [the] airborne route.”
However, a recent Singapore study showed widespread environmental contamination by SARS-CoV-2 through respiratory droplets and fecal shedding, underlining the need for strict adherence to environmental and hand hygiene. Post-cleaning samples tested negative, suggesting that standard decontamination practices are effective.
This work was partly supported by the Consultancy Service for Enhancing Laboratory Surveillance of Emerging Infectious Diseases of the Department of Health, Hong Kong Special Administrative Region; and the Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, Ministry of Education of China. The authors and Glatt have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Hospital-related infections have been widely reported during the ongoing coronavirus outbreak, with healthcare professionals bearing a disproportionate risk. However, a proactive response in Hong Kong’s public hospital system appears to have bucked this trend and successfully protected both patients and staff from SARS-CoV-2, according to a study published online today in Infection Control & Hospital Epidemiology.
During the first 42 days of the outbreak, the 43 hospitals in the network tested 1275 suspected cases and treated 42 patients with confirmed COVID-19, the disease caused by SARS-CoV-2 infection. Yet, there were no nosocomial infections or infections among healthcare personnel, report Vincent C.C. Cheng, MD, FRCPath, the hospital’s infection control officer, and colleagues.
Cheng and colleagues note that 11 out of 413 healthcare workers who treat patients with confirmed infections had unprotected exposure and were in quarantine for 14 days, but none became ill.
In comparison, they note, the 2003 SARS outbreak saw almost 60% of nosocomial cases occurring in healthcare workers.
Proactive bundle
The Hong Kong success story may be due to a stepped-up proactive bundle of measures that included enhanced laboratory surveillance, early airborne infection isolation, and rapid-turnaround molecular diagnostics. Other strategies included staff forums and one-on-one discussions about infection control, employee training in protective equipment use, hand-hygiene compliance enforcement, and contact tracing for workers with unprotected exposure.
In addition, surgical masks were provided for all healthcare workers, patients, and visitors to clinical areas, a practice previously associated with reduced in-hospital transmission during influenza outbreaks, the authors note.
Hospitals also mandated use of personal protective equipment (PPE) for aerosol-generating procedures (AGPs), such as endotracheal intubation, open suctioning, and high-flow oxygen use, as AGPs had been linked to nosocomial transmission to healthcare workers during the 2003 SARS outbreak.
The infection control measures, which were part of a preparedness plan developed after the SARS outbreak, were initiated on December 31, when the first reports of a cluster of infections came from Wuhan, China.
As the outbreak evolved, the Hong Kong hospitals quickly widened the epidemiologic criteria for screening, from initially including only those who had been to a wet market in Wuhan within 14 days of symptom onset, to eventually including anyone who had been to Hubei province, been in a medical facility in mainland China, or in contact with a known case.
All suspected cases were sent to an airborne-infection isolation room (AIIR) or a ward with at least a meter of space between patients.
“Appropriate hospital infection control measures could prevent nosocomial transmission of SARS-CoV-2,” the authors write. “Vigilance in hand hygiene practice, wearing of surgical mask in the hospital, and appropriate use of PPE in patient care, especially [when] performing AGPs, are the key infection control measures to prevent nosocomial transmission of SARS-CoV-2 even before the availability of effective antiviral agents and vaccine.”
Asked for his perspective on the report, Aaron E. Glatt, MD, chairman of the department of medicine and chief of infectious diseases at Mount Sinai South Nassau in Oceanside, New York, said that apart from the widespread issuing of surgical masks to workers, patients, and visitors, the measures taken in Hong Kong are not different from standard infection-control practices in American hospitals. Glatt, who is also a hospital epidemiologist, said it was unclear how much impact the masks would have.
“Although the infection control was impressive, I don’t see any evidence of a difference in care,” he told Medscape Medical News.
Could zero infection transmission be achieved in the more far-flung and variable settings of hospitals across the United States? “The ability to get zero transmission is only possible if people adhere to the strictest infection-control guidelines,” Glatt said. “That is clearly the goal, and it will take time to see if our existing strict guidelines are sufficient to maintain zero or close to zero contamination and transmission rates in our hospitals.”
Rather than looking to change US practices, he stressed adherence to widely established tenets of care. “It’s critically important to keep paying close attention to the basics, to the simple blocking and tackling, and to identify which patients are at risk, and therefore, when workers need protective equipment,” he said.
“Follow the recommended standards,” continued Glatt, who is also a spokesperson for the Infectious Diseases Society of America and did not participate in this study.
In a finding from an ancillary pilot experiment, the Hong Kong researchers found exhaled air from a patient with a moderate coronavirus load showed no evidence of the virus, whether the patient was breathing normally or heavily, speaking, or coughing. And spot tests around the room detected the virus in just one location.
“We may not be able to make a definite conclusion based on the analysis of a single patient,” the authors write. “However, it may help to reassure our staff that the exhaled air may be rapidly diluted inside the AIIR with 12 air changes per hour, or probably the SARS-CoV-2 may not be predominantly transmitted by [the] airborne route.”
However, a recent Singapore study showed widespread environmental contamination by SARS-CoV-2 through respiratory droplets and fecal shedding, underlining the need for strict adherence to environmental and hand hygiene. Post-cleaning samples tested negative, suggesting that standard decontamination practices are effective.
This work was partly supported by the Consultancy Service for Enhancing Laboratory Surveillance of Emerging Infectious Diseases of the Department of Health, Hong Kong Special Administrative Region; and the Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, Ministry of Education of China. The authors and Glatt have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.