User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
FDA Approves AI Diagnostic Tool for Early Sepsis Detection
The US Food and Drug Administration (FDA) has approved a medical device named the Sepsis ImmunoScore, which is an artificial intelligence/machine learning software, to guide rapid diagnosis and prediction of sepsis. The authorization was granted through the FDA’s De Novo pathway.
Sepsis is a complex condition, so diagnosing it early is difficult and has been a decades-long challenge for the US healthcare system.
Using both biomarkers and clinical data with the assistance of AI, the Sepsis ImmunoScore helps assess the risk for the presence of or progression to sepsis within 24 hours of patient evaluation in the emergency department or hospital. By considering 22 diverse parameters, the AI-powered tool provides a comprehensive evaluation of the patient’s biological condition, resulting in a risk score and categorization into four distinct risk levels.
It’s important to note that this system is not an alert mechanism. These risk categories are correlated with the risk for patient deterioration, including length of hospital stay, in-hospital mortality, and the need for escalated care within 24 hours (such as intensive care unit admission, mechanical ventilation, or vasopressor use). The diagnostic software is integrated directly into hospital electronic medical records.
This is the first AI diagnostic tool for sepsis to receive marketing authorization from the FDA.
A version of this article appeared on Medscape.com.
The US Food and Drug Administration (FDA) has approved a medical device named the Sepsis ImmunoScore, which is an artificial intelligence/machine learning software, to guide rapid diagnosis and prediction of sepsis. The authorization was granted through the FDA’s De Novo pathway.
Sepsis is a complex condition, so diagnosing it early is difficult and has been a decades-long challenge for the US healthcare system.
Using both biomarkers and clinical data with the assistance of AI, the Sepsis ImmunoScore helps assess the risk for the presence of or progression to sepsis within 24 hours of patient evaluation in the emergency department or hospital. By considering 22 diverse parameters, the AI-powered tool provides a comprehensive evaluation of the patient’s biological condition, resulting in a risk score and categorization into four distinct risk levels.
It’s important to note that this system is not an alert mechanism. These risk categories are correlated with the risk for patient deterioration, including length of hospital stay, in-hospital mortality, and the need for escalated care within 24 hours (such as intensive care unit admission, mechanical ventilation, or vasopressor use). The diagnostic software is integrated directly into hospital electronic medical records.
This is the first AI diagnostic tool for sepsis to receive marketing authorization from the FDA.
A version of this article appeared on Medscape.com.
The US Food and Drug Administration (FDA) has approved a medical device named the Sepsis ImmunoScore, which is an artificial intelligence/machine learning software, to guide rapid diagnosis and prediction of sepsis. The authorization was granted through the FDA’s De Novo pathway.
Sepsis is a complex condition, so diagnosing it early is difficult and has been a decades-long challenge for the US healthcare system.
Using both biomarkers and clinical data with the assistance of AI, the Sepsis ImmunoScore helps assess the risk for the presence of or progression to sepsis within 24 hours of patient evaluation in the emergency department or hospital. By considering 22 diverse parameters, the AI-powered tool provides a comprehensive evaluation of the patient’s biological condition, resulting in a risk score and categorization into four distinct risk levels.
It’s important to note that this system is not an alert mechanism. These risk categories are correlated with the risk for patient deterioration, including length of hospital stay, in-hospital mortality, and the need for escalated care within 24 hours (such as intensive care unit admission, mechanical ventilation, or vasopressor use). The diagnostic software is integrated directly into hospital electronic medical records.
This is the first AI diagnostic tool for sepsis to receive marketing authorization from the FDA.
A version of this article appeared on Medscape.com.
COVID Vaccinations Less Prevalent in Marginalized Patients
Primary care physicians who served marginalized communities had the highest proportion of patients who were unvaccinated against COVID-19, Canadian data suggested.
A study of more than 9000 family physicians in Ontario also found that the physicians with the largest proportion of unvaccinated patients were more likely to be male, to have trained outside Canada, to be older, and to work in an enhanced fee-for-service model than their counterparts who had lower proportions of unvaccinated patients.
“The family physicians with the most unvaccinated patients were also more likely to be solo practitioners and less likely to practice in team-based models, meaning they may have fewer support staff in their clinics,” lead author Jennifer Shuldiner, PhD, a scientist at Women’s College Hospital in Toronto, Ontario, Canada, told this news organization.
The findings were published in CMAJ.
Need vs Resources
Dr. Shuldiner and her team had been working on a project to provide additional support to family physicians with large numbers of patients who had not received their COVID-19 vaccinations. Their goal was to encourage family physicians to support these patients in getting vaccinated.
“As we were designing this project, we wondered how these physicians and their patients might differ. What characteristics might they have that would enable us to design and implement an intervention with high uptake and impact?” she said.
The researchers conducted a cross-sectional, population-based cohort study using linked administrative datasets in Ontario. They calculated the percentage of patients unvaccinated against SARS-CoV-2 who were enrolled with each comprehensive care family physician, ranked physicians according to the proportion of unvaccinated patients, and identified 906 physicians in the top 10% of unvaccinated patients. These physicians were compared with the remaining 90% of family physicians.
The physicians with the highest proportion of unvaccinated patients cared for 259,130 unvaccinated patients as of November 1, 2021. The proportion of patients who received two or more doses of the SARS-CoV-2 vaccine in this group was 74.2%. In comparison, the proportion of patients who received two or more doses of the vaccine was 87.0% in the remaining 90% of physicians.
Physicians with the largest proportion of unvaccinated patients were more likely to be male (64.6% vs 48.1%), to have trained outside Canada (46.9% vs 29.3%), to be older (mean age, 56 years vs 49 years), and to work in an enhanced fee-for-service model (49% vs 28%).
The study also found that patients enrolled with physicians in the most unvaccinated group tended to live in places with more ethnic diversity, higher material deprivation, and lower incomes. The proportion of recent immigrants was higher in this group.
“Clinics or practices with a large number of unvaccinated patients could be viable targets for efforts to coordinate public health and primary care,” said Dr. Shuldiner.
The findings indicate “the ongoing inverse relationship between the need for care and its accessibility and utilization. In other words, the practices with the highest need receive the fewest resources,” she noted.
“We know that relationships with trusted family physicians can positively influence patients’ decisions. Our study highlights the need to create equitable systems and processes that create opportunities for primary care teams to play a crucial role in influencing general and COVID-19-specific vaccine-related decision-making.”
Helping Primary Care Physicians
Commenting on the study for this news organization, Sabrina Wong, RN, PhD, professor of nursing at the University of British Columbia in Vancouver, British Columbia, Canada, said, “They did quite a nice analysis to show this using administrative data, and I think the information they’ve uncovered will be helpful in trying to fill the gaps and provide these practitioners with more support.”
Dr. Wong did not participate in the study. “The information they provide will be useful in helping us to move forward working with underserved, underresourced communities and also hopefully provide the clinicians, family physicians, and nurse practitioners working in these areas with more resources,” she said.
“The authors also point out that there needs to be more collaboration between public health and primary care to support these communities in their efforts to get the vaccines to the people in these communities who need them.”
The study was supported by a Canadian Institutes of Health Research grant. Dr. Shuldiner and Dr. Wong reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Primary care physicians who served marginalized communities had the highest proportion of patients who were unvaccinated against COVID-19, Canadian data suggested.
A study of more than 9000 family physicians in Ontario also found that the physicians with the largest proportion of unvaccinated patients were more likely to be male, to have trained outside Canada, to be older, and to work in an enhanced fee-for-service model than their counterparts who had lower proportions of unvaccinated patients.
“The family physicians with the most unvaccinated patients were also more likely to be solo practitioners and less likely to practice in team-based models, meaning they may have fewer support staff in their clinics,” lead author Jennifer Shuldiner, PhD, a scientist at Women’s College Hospital in Toronto, Ontario, Canada, told this news organization.
The findings were published in CMAJ.
Need vs Resources
Dr. Shuldiner and her team had been working on a project to provide additional support to family physicians with large numbers of patients who had not received their COVID-19 vaccinations. Their goal was to encourage family physicians to support these patients in getting vaccinated.
“As we were designing this project, we wondered how these physicians and their patients might differ. What characteristics might they have that would enable us to design and implement an intervention with high uptake and impact?” she said.
The researchers conducted a cross-sectional, population-based cohort study using linked administrative datasets in Ontario. They calculated the percentage of patients unvaccinated against SARS-CoV-2 who were enrolled with each comprehensive care family physician, ranked physicians according to the proportion of unvaccinated patients, and identified 906 physicians in the top 10% of unvaccinated patients. These physicians were compared with the remaining 90% of family physicians.
The physicians with the highest proportion of unvaccinated patients cared for 259,130 unvaccinated patients as of November 1, 2021. The proportion of patients who received two or more doses of the SARS-CoV-2 vaccine in this group was 74.2%. In comparison, the proportion of patients who received two or more doses of the vaccine was 87.0% in the remaining 90% of physicians.
Physicians with the largest proportion of unvaccinated patients were more likely to be male (64.6% vs 48.1%), to have trained outside Canada (46.9% vs 29.3%), to be older (mean age, 56 years vs 49 years), and to work in an enhanced fee-for-service model (49% vs 28%).
The study also found that patients enrolled with physicians in the most unvaccinated group tended to live in places with more ethnic diversity, higher material deprivation, and lower incomes. The proportion of recent immigrants was higher in this group.
“Clinics or practices with a large number of unvaccinated patients could be viable targets for efforts to coordinate public health and primary care,” said Dr. Shuldiner.
The findings indicate “the ongoing inverse relationship between the need for care and its accessibility and utilization. In other words, the practices with the highest need receive the fewest resources,” she noted.
“We know that relationships with trusted family physicians can positively influence patients’ decisions. Our study highlights the need to create equitable systems and processes that create opportunities for primary care teams to play a crucial role in influencing general and COVID-19-specific vaccine-related decision-making.”
Helping Primary Care Physicians
Commenting on the study for this news organization, Sabrina Wong, RN, PhD, professor of nursing at the University of British Columbia in Vancouver, British Columbia, Canada, said, “They did quite a nice analysis to show this using administrative data, and I think the information they’ve uncovered will be helpful in trying to fill the gaps and provide these practitioners with more support.”
Dr. Wong did not participate in the study. “The information they provide will be useful in helping us to move forward working with underserved, underresourced communities and also hopefully provide the clinicians, family physicians, and nurse practitioners working in these areas with more resources,” she said.
“The authors also point out that there needs to be more collaboration between public health and primary care to support these communities in their efforts to get the vaccines to the people in these communities who need them.”
The study was supported by a Canadian Institutes of Health Research grant. Dr. Shuldiner and Dr. Wong reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Primary care physicians who served marginalized communities had the highest proportion of patients who were unvaccinated against COVID-19, Canadian data suggested.
A study of more than 9000 family physicians in Ontario also found that the physicians with the largest proportion of unvaccinated patients were more likely to be male, to have trained outside Canada, to be older, and to work in an enhanced fee-for-service model than their counterparts who had lower proportions of unvaccinated patients.
“The family physicians with the most unvaccinated patients were also more likely to be solo practitioners and less likely to practice in team-based models, meaning they may have fewer support staff in their clinics,” lead author Jennifer Shuldiner, PhD, a scientist at Women’s College Hospital in Toronto, Ontario, Canada, told this news organization.
The findings were published in CMAJ.
Need vs Resources
Dr. Shuldiner and her team had been working on a project to provide additional support to family physicians with large numbers of patients who had not received their COVID-19 vaccinations. Their goal was to encourage family physicians to support these patients in getting vaccinated.
“As we were designing this project, we wondered how these physicians and their patients might differ. What characteristics might they have that would enable us to design and implement an intervention with high uptake and impact?” she said.
The researchers conducted a cross-sectional, population-based cohort study using linked administrative datasets in Ontario. They calculated the percentage of patients unvaccinated against SARS-CoV-2 who were enrolled with each comprehensive care family physician, ranked physicians according to the proportion of unvaccinated patients, and identified 906 physicians in the top 10% of unvaccinated patients. These physicians were compared with the remaining 90% of family physicians.
The physicians with the highest proportion of unvaccinated patients cared for 259,130 unvaccinated patients as of November 1, 2021. The proportion of patients who received two or more doses of the SARS-CoV-2 vaccine in this group was 74.2%. In comparison, the proportion of patients who received two or more doses of the vaccine was 87.0% in the remaining 90% of physicians.
Physicians with the largest proportion of unvaccinated patients were more likely to be male (64.6% vs 48.1%), to have trained outside Canada (46.9% vs 29.3%), to be older (mean age, 56 years vs 49 years), and to work in an enhanced fee-for-service model (49% vs 28%).
The study also found that patients enrolled with physicians in the most unvaccinated group tended to live in places with more ethnic diversity, higher material deprivation, and lower incomes. The proportion of recent immigrants was higher in this group.
“Clinics or practices with a large number of unvaccinated patients could be viable targets for efforts to coordinate public health and primary care,” said Dr. Shuldiner.
The findings indicate “the ongoing inverse relationship between the need for care and its accessibility and utilization. In other words, the practices with the highest need receive the fewest resources,” she noted.
“We know that relationships with trusted family physicians can positively influence patients’ decisions. Our study highlights the need to create equitable systems and processes that create opportunities for primary care teams to play a crucial role in influencing general and COVID-19-specific vaccine-related decision-making.”
Helping Primary Care Physicians
Commenting on the study for this news organization, Sabrina Wong, RN, PhD, professor of nursing at the University of British Columbia in Vancouver, British Columbia, Canada, said, “They did quite a nice analysis to show this using administrative data, and I think the information they’ve uncovered will be helpful in trying to fill the gaps and provide these practitioners with more support.”
Dr. Wong did not participate in the study. “The information they provide will be useful in helping us to move forward working with underserved, underresourced communities and also hopefully provide the clinicians, family physicians, and nurse practitioners working in these areas with more resources,” she said.
“The authors also point out that there needs to be more collaboration between public health and primary care to support these communities in their efforts to get the vaccines to the people in these communities who need them.”
The study was supported by a Canadian Institutes of Health Research grant. Dr. Shuldiner and Dr. Wong reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CMAJ
4 Years In, a Sobering Look at Long COVID Progress
Four years ago in the spring of 2020, physicians and patients coined the term “long COVID” to describe a form of the viral infection from which recovery seemed impossible. (And the old nickname “long-haulers” seems so quaint now.)
What started as a pandemic that killed nearly 3 million people globally in 2020 alone would turn into a chronic disease causing a long list of symptoms — from extreme fatigue, to brain fog, tremors, nausea, headaches, rapid heartbeat, and more.
Today, 6.4% of Americans report symptoms of long COVID, and many have never recovered.
Still, we’ve come a long way, although there’s much we don’t understand about the condition. At the very least, physicians have a greater understanding that long COVID exists and can cause serious long-term symptoms.
While physicians may not have a blanket diagnostic tool that works for all patients with long COVID, they have refined existing tests for more accurate results, said Nisha Viswanathan, MD, director of the University of California Los Angeles Long COVID Program at UCLA Health.
Also, a range of new treatments, now undergoing clinical trials, have emerged that have proved effective in managing long COVID symptoms.
Catecholamine testing, for example, is now commonly used to diagnose long COVID, particularly in those who have dysautonomia, a condition caused by dysfunction of the autonomic nervous system and marked by dizziness, low blood pressure, nausea, and brain fog.
Very high levels of the neurotransmitter, for example, were shown to indicate long COVID in a January 2021 study published in the journal Clinical Medicine.
Certain biomarkers have also been shown indicative of the condition, including low serotonin levels. A study published this year in Cell found lower serotonin levels in patients with long COVID driven by low levels of circulating SARS-CoV-2, the virus that causes the condition.
Still, said Dr. Viswanathan, long COVID is a disease diagnosed by figuring out what a patient does not have — by ruling out other causes — rather than what they do. “It’s still a moving target,” she said, meaning that the disease is always changing based on the variant of acute COVID.
Promising Treatments Have Emerged
Dysautonomia, and especially the associated brain fog, fatigue, and dizziness, are now common conditions. As a result, physicians have gotten better at treating them. The vagus nerve is the main nerve of the parasympathetic nervous system that controls everything from digestion to mental health. A February 2022 pilot study suggested a link between vagus nerve dysfunction and some long COVID symptoms.
Vagus nerve stimulation is one form of treatment which involves using a device to stimulate the vagus nerve with electrical impulses. Dr. Viswanathan has been using the treatment in patients with fatigue, brain fog, anxiety, and depression — results, she contends, have been positive.
“This is something tangible that we can offer to patients,” she said.
Curative treatments for long COVID remain elusive, but doctors have many more tools for symptom management than before, said Ziyad Al-Aly, MD, a global expert on long COVID and chief of research and development at the Veterans Affairs St. Louis Health Care System.
For example, physicians are using beta-blockers to treat postural tachycardia syndrome (POTS), a symptom of long COVID that happens when the heart rate increases rapidly after someone stands up or lies down. Beta-blockers, such as the off-label medication ivabradine, have been used clinically to control heart rate, according to a March 2022 study published in the journal HeartRhythm Case Reports.
“It’s not a cure, but beta-blockers can help patients manage their symptoms,” said Dr. Al-Aly.
Additionally, some patients respond well to low-dose naltrexone for the treatment of extreme fatigue associated with long COVID. A January 2024 article in the journal Clinical Therapeutics found that fatigue symptoms improved in patients taking the medication.
Dr. Al-Aly said doctors treating patients with long COVID are getting better at pinpointing the phenotype or manifestation of the condition and diagnosing a treatment accordingly. Treating long COVID fatigue is not the same as treating POTS or symptoms of headache and joint pain.
It’s still all about the management of symptoms and doctors lack any US Food and Drug Administration–approved medications specifically for the condition.
Clinical Trials Exploring New Therapies
Still, a number of large clinical trials currently underway may change that, said David F. Putrino, PhD, who runs the long COVID clinic at Mount Sinai Health System in New York City.
Two clinical trials headed by Dr. Putrino’s lab are looking into repurposing two HIV antivirals to see whether they affect the levels of circulating SARS-CoV-2 virus in the body that may cause long COVID. The hope is that the antivirals Truvada and maraviroc can reduce the «reactivation of latent virus» that, said Dr. Putrino, causes lingering long COVID symptoms.
Ongoing trials are looking into the promise of SARS-CoV-2 monoclonal antibodies, produced from cells made by cloning a unique white blood cell, as a treatment option. The trials are investigating whether these antibodies may similarly target viral reservoirs that are causing persistence of symptoms in some patients.
Other trials are underway through the National Institutes of Health (NIH) RECOVER initiative in which more than 17,000 patients are enrolled, the largest study of its kind, said Grace McComsey, MD.
Dr. McComsey, who leads the study at University Hospitals Health System in Cleveland, said that after following patients for up to 4 years researchers have gathered “a massive repository of information” they hope will help scientists crack the code of this very complex disease.
She and other RECOVER researchers have recently published studies on a variety of findings, reporting in February, for example, that COVID infections may trigger other autoimmune diseases such as rheumatoid arthritis and type 2 diabetes. Another recent finding showed that people with HIV are at a higher risk for complications due to acute COVID-19.
Lack of Urgency Holds Back Progress
Still, others like Dr. Al-Aly and Dr. Putrino felt that the initiative isn’t moving fast enough. Dr. Al-Aly said that the NIH needs to “get its act together” and do more for long COVID. In the future, he said that we need to double down on our efforts to expand funding and increase urgency to better understand the mechanism of disease, risk factors, and treatments, as well as societal and economic implications.
“We did trials for COVID-19 vaccines at warp speed, but we’re doing trials for long COVID at a snail’s pace,” he said.
Dr. Al-Aly is concerned about the chronic nature of the disease and how it affects patients down the line. His large-scale study published last month in the journal Science looked specifically at chronic fatigue syndrome triggered by the infection and its long-term impact on patients.
He’s concerned about the practical implications for people who are weighted down with symptoms for multiple years.
“Being fatigued and ill for a few months is one thing, but being at home for 5 years is a totally different ballgame.”
A version of this article first appeared on Medscape.com.
Four years ago in the spring of 2020, physicians and patients coined the term “long COVID” to describe a form of the viral infection from which recovery seemed impossible. (And the old nickname “long-haulers” seems so quaint now.)
What started as a pandemic that killed nearly 3 million people globally in 2020 alone would turn into a chronic disease causing a long list of symptoms — from extreme fatigue, to brain fog, tremors, nausea, headaches, rapid heartbeat, and more.
Today, 6.4% of Americans report symptoms of long COVID, and many have never recovered.
Still, we’ve come a long way, although there’s much we don’t understand about the condition. At the very least, physicians have a greater understanding that long COVID exists and can cause serious long-term symptoms.
While physicians may not have a blanket diagnostic tool that works for all patients with long COVID, they have refined existing tests for more accurate results, said Nisha Viswanathan, MD, director of the University of California Los Angeles Long COVID Program at UCLA Health.
Also, a range of new treatments, now undergoing clinical trials, have emerged that have proved effective in managing long COVID symptoms.
Catecholamine testing, for example, is now commonly used to diagnose long COVID, particularly in those who have dysautonomia, a condition caused by dysfunction of the autonomic nervous system and marked by dizziness, low blood pressure, nausea, and brain fog.
Very high levels of the neurotransmitter, for example, were shown to indicate long COVID in a January 2021 study published in the journal Clinical Medicine.
Certain biomarkers have also been shown indicative of the condition, including low serotonin levels. A study published this year in Cell found lower serotonin levels in patients with long COVID driven by low levels of circulating SARS-CoV-2, the virus that causes the condition.
Still, said Dr. Viswanathan, long COVID is a disease diagnosed by figuring out what a patient does not have — by ruling out other causes — rather than what they do. “It’s still a moving target,” she said, meaning that the disease is always changing based on the variant of acute COVID.
Promising Treatments Have Emerged
Dysautonomia, and especially the associated brain fog, fatigue, and dizziness, are now common conditions. As a result, physicians have gotten better at treating them. The vagus nerve is the main nerve of the parasympathetic nervous system that controls everything from digestion to mental health. A February 2022 pilot study suggested a link between vagus nerve dysfunction and some long COVID symptoms.
Vagus nerve stimulation is one form of treatment which involves using a device to stimulate the vagus nerve with electrical impulses. Dr. Viswanathan has been using the treatment in patients with fatigue, brain fog, anxiety, and depression — results, she contends, have been positive.
“This is something tangible that we can offer to patients,” she said.
Curative treatments for long COVID remain elusive, but doctors have many more tools for symptom management than before, said Ziyad Al-Aly, MD, a global expert on long COVID and chief of research and development at the Veterans Affairs St. Louis Health Care System.
For example, physicians are using beta-blockers to treat postural tachycardia syndrome (POTS), a symptom of long COVID that happens when the heart rate increases rapidly after someone stands up or lies down. Beta-blockers, such as the off-label medication ivabradine, have been used clinically to control heart rate, according to a March 2022 study published in the journal HeartRhythm Case Reports.
“It’s not a cure, but beta-blockers can help patients manage their symptoms,” said Dr. Al-Aly.
Additionally, some patients respond well to low-dose naltrexone for the treatment of extreme fatigue associated with long COVID. A January 2024 article in the journal Clinical Therapeutics found that fatigue symptoms improved in patients taking the medication.
Dr. Al-Aly said doctors treating patients with long COVID are getting better at pinpointing the phenotype or manifestation of the condition and diagnosing a treatment accordingly. Treating long COVID fatigue is not the same as treating POTS or symptoms of headache and joint pain.
It’s still all about the management of symptoms and doctors lack any US Food and Drug Administration–approved medications specifically for the condition.
Clinical Trials Exploring New Therapies
Still, a number of large clinical trials currently underway may change that, said David F. Putrino, PhD, who runs the long COVID clinic at Mount Sinai Health System in New York City.
Two clinical trials headed by Dr. Putrino’s lab are looking into repurposing two HIV antivirals to see whether they affect the levels of circulating SARS-CoV-2 virus in the body that may cause long COVID. The hope is that the antivirals Truvada and maraviroc can reduce the «reactivation of latent virus» that, said Dr. Putrino, causes lingering long COVID symptoms.
Ongoing trials are looking into the promise of SARS-CoV-2 monoclonal antibodies, produced from cells made by cloning a unique white blood cell, as a treatment option. The trials are investigating whether these antibodies may similarly target viral reservoirs that are causing persistence of symptoms in some patients.
Other trials are underway through the National Institutes of Health (NIH) RECOVER initiative in which more than 17,000 patients are enrolled, the largest study of its kind, said Grace McComsey, MD.
Dr. McComsey, who leads the study at University Hospitals Health System in Cleveland, said that after following patients for up to 4 years researchers have gathered “a massive repository of information” they hope will help scientists crack the code of this very complex disease.
She and other RECOVER researchers have recently published studies on a variety of findings, reporting in February, for example, that COVID infections may trigger other autoimmune diseases such as rheumatoid arthritis and type 2 diabetes. Another recent finding showed that people with HIV are at a higher risk for complications due to acute COVID-19.
Lack of Urgency Holds Back Progress
Still, others like Dr. Al-Aly and Dr. Putrino felt that the initiative isn’t moving fast enough. Dr. Al-Aly said that the NIH needs to “get its act together” and do more for long COVID. In the future, he said that we need to double down on our efforts to expand funding and increase urgency to better understand the mechanism of disease, risk factors, and treatments, as well as societal and economic implications.
“We did trials for COVID-19 vaccines at warp speed, but we’re doing trials for long COVID at a snail’s pace,” he said.
Dr. Al-Aly is concerned about the chronic nature of the disease and how it affects patients down the line. His large-scale study published last month in the journal Science looked specifically at chronic fatigue syndrome triggered by the infection and its long-term impact on patients.
He’s concerned about the practical implications for people who are weighted down with symptoms for multiple years.
“Being fatigued and ill for a few months is one thing, but being at home for 5 years is a totally different ballgame.”
A version of this article first appeared on Medscape.com.
Four years ago in the spring of 2020, physicians and patients coined the term “long COVID” to describe a form of the viral infection from which recovery seemed impossible. (And the old nickname “long-haulers” seems so quaint now.)
What started as a pandemic that killed nearly 3 million people globally in 2020 alone would turn into a chronic disease causing a long list of symptoms — from extreme fatigue, to brain fog, tremors, nausea, headaches, rapid heartbeat, and more.
Today, 6.4% of Americans report symptoms of long COVID, and many have never recovered.
Still, we’ve come a long way, although there’s much we don’t understand about the condition. At the very least, physicians have a greater understanding that long COVID exists and can cause serious long-term symptoms.
While physicians may not have a blanket diagnostic tool that works for all patients with long COVID, they have refined existing tests for more accurate results, said Nisha Viswanathan, MD, director of the University of California Los Angeles Long COVID Program at UCLA Health.
Also, a range of new treatments, now undergoing clinical trials, have emerged that have proved effective in managing long COVID symptoms.
Catecholamine testing, for example, is now commonly used to diagnose long COVID, particularly in those who have dysautonomia, a condition caused by dysfunction of the autonomic nervous system and marked by dizziness, low blood pressure, nausea, and brain fog.
Very high levels of the neurotransmitter, for example, were shown to indicate long COVID in a January 2021 study published in the journal Clinical Medicine.
Certain biomarkers have also been shown indicative of the condition, including low serotonin levels. A study published this year in Cell found lower serotonin levels in patients with long COVID driven by low levels of circulating SARS-CoV-2, the virus that causes the condition.
Still, said Dr. Viswanathan, long COVID is a disease diagnosed by figuring out what a patient does not have — by ruling out other causes — rather than what they do. “It’s still a moving target,” she said, meaning that the disease is always changing based on the variant of acute COVID.
Promising Treatments Have Emerged
Dysautonomia, and especially the associated brain fog, fatigue, and dizziness, are now common conditions. As a result, physicians have gotten better at treating them. The vagus nerve is the main nerve of the parasympathetic nervous system that controls everything from digestion to mental health. A February 2022 pilot study suggested a link between vagus nerve dysfunction and some long COVID symptoms.
Vagus nerve stimulation is one form of treatment which involves using a device to stimulate the vagus nerve with electrical impulses. Dr. Viswanathan has been using the treatment in patients with fatigue, brain fog, anxiety, and depression — results, she contends, have been positive.
“This is something tangible that we can offer to patients,” she said.
Curative treatments for long COVID remain elusive, but doctors have many more tools for symptom management than before, said Ziyad Al-Aly, MD, a global expert on long COVID and chief of research and development at the Veterans Affairs St. Louis Health Care System.
For example, physicians are using beta-blockers to treat postural tachycardia syndrome (POTS), a symptom of long COVID that happens when the heart rate increases rapidly after someone stands up or lies down. Beta-blockers, such as the off-label medication ivabradine, have been used clinically to control heart rate, according to a March 2022 study published in the journal HeartRhythm Case Reports.
“It’s not a cure, but beta-blockers can help patients manage their symptoms,” said Dr. Al-Aly.
Additionally, some patients respond well to low-dose naltrexone for the treatment of extreme fatigue associated with long COVID. A January 2024 article in the journal Clinical Therapeutics found that fatigue symptoms improved in patients taking the medication.
Dr. Al-Aly said doctors treating patients with long COVID are getting better at pinpointing the phenotype or manifestation of the condition and diagnosing a treatment accordingly. Treating long COVID fatigue is not the same as treating POTS or symptoms of headache and joint pain.
It’s still all about the management of symptoms and doctors lack any US Food and Drug Administration–approved medications specifically for the condition.
Clinical Trials Exploring New Therapies
Still, a number of large clinical trials currently underway may change that, said David F. Putrino, PhD, who runs the long COVID clinic at Mount Sinai Health System in New York City.
Two clinical trials headed by Dr. Putrino’s lab are looking into repurposing two HIV antivirals to see whether they affect the levels of circulating SARS-CoV-2 virus in the body that may cause long COVID. The hope is that the antivirals Truvada and maraviroc can reduce the «reactivation of latent virus» that, said Dr. Putrino, causes lingering long COVID symptoms.
Ongoing trials are looking into the promise of SARS-CoV-2 monoclonal antibodies, produced from cells made by cloning a unique white blood cell, as a treatment option. The trials are investigating whether these antibodies may similarly target viral reservoirs that are causing persistence of symptoms in some patients.
Other trials are underway through the National Institutes of Health (NIH) RECOVER initiative in which more than 17,000 patients are enrolled, the largest study of its kind, said Grace McComsey, MD.
Dr. McComsey, who leads the study at University Hospitals Health System in Cleveland, said that after following patients for up to 4 years researchers have gathered “a massive repository of information” they hope will help scientists crack the code of this very complex disease.
She and other RECOVER researchers have recently published studies on a variety of findings, reporting in February, for example, that COVID infections may trigger other autoimmune diseases such as rheumatoid arthritis and type 2 diabetes. Another recent finding showed that people with HIV are at a higher risk for complications due to acute COVID-19.
Lack of Urgency Holds Back Progress
Still, others like Dr. Al-Aly and Dr. Putrino felt that the initiative isn’t moving fast enough. Dr. Al-Aly said that the NIH needs to “get its act together” and do more for long COVID. In the future, he said that we need to double down on our efforts to expand funding and increase urgency to better understand the mechanism of disease, risk factors, and treatments, as well as societal and economic implications.
“We did trials for COVID-19 vaccines at warp speed, but we’re doing trials for long COVID at a snail’s pace,” he said.
Dr. Al-Aly is concerned about the chronic nature of the disease and how it affects patients down the line. His large-scale study published last month in the journal Science looked specifically at chronic fatigue syndrome triggered by the infection and its long-term impact on patients.
He’s concerned about the practical implications for people who are weighted down with symptoms for multiple years.
“Being fatigued and ill for a few months is one thing, but being at home for 5 years is a totally different ballgame.”
A version of this article first appeared on Medscape.com.
Physicians Own Less Than Half of US Practices; Federal Agencies Want Outside Input
Physician practice ownership by corporations, including health insurers, private equity firms, and large pharmacy chains, reached 30.1% as of January for the first time surpassing ownership by hospitals and health systems (28.4%), according to a new report.
As a result, about three in five physician practices are now owned by nonphysicians.
In early 2020, corporations owned just about 17% of US medical practices, while hospitals and health systems owned about 25%, according to the report released Thursday by nonprofit Physician Advocacy Institute (PAI). But corporate ownership of medical groups surged during the pandemic.
These trends raise questions about how best to protect patients and physicians in a changing employment landscape, said Kelly Kenney, PAI’s chief executive officer, in a statement.
“Corporate entities are assuming control of physician practices and changing the face of medicine in the United States with little to no scrutiny from regulators,” Ms. Kenney said.
The research, conducted by consulting group Avalere for PAI, used the IQVIA OneKey database that contains physician and practice location information on hospital and health system ownership.
By 2022-2023, there was a 7.3% increase in the percentage of practices owned by hospitals and 5.9% increase in the percentage of physicians employed by these organizations, PAI said. In the same time frame, there was an 11% increase in the percentage of practices owned by corporations and a 3.0% increase in the percentage of physicians employed by these entities.
“Physicians have an ethical responsibility to their patients’ health,” Ms. Kenney said. “Corporate entities have a fiduciary responsibility to their shareholders and are motivated to put profits first…these interests can conflict with providing the best medical care to patients.”
Federal Scrutiny Increases
However, both federal and state regulators are paying more attention to what happens to patients and physicians when corporations acquire practices.
“Given recent trends, we are concerned that some transactions may generate profits for those firms at the expense of patients’ health, workers’ safety, quality of care, and affordable healthcare for patients and taxpayers,” said the Federal Trade Commission (FTC) and the Justice (DOJ) and Health and Human Services (HHS) departments.
This statement appears in those agencies’ joint request for information (RFI) announced in March. An RFI is a tool that federal agencies can use to gauge the level of both support and opposition they would face if they were to try to change policies. Public comments are due May 6.
Corporations and advocacy groups often submit detailed comments outlining reasons why the federal government should or should not act on an issue. But individuals also can make their case in this forum.
The FTC, DOJ, and HHS are looking broadly at consolidation in healthcare, but they also spell out potential concerns related to acquisition of physician practices.
For example, they asked clinicians and support staff to provide feedback about whether acquisitions lead to changes in:
- Take-home pay
- Staffing levels
- Workplace safety
- Compensation model (eg, from fixed salary to volume based)
- Policies regarding patient referrals
- Mix of patients
- The volume of patients
- The way providers practice medicine (eg, incentives, prescribing decisions, forced protocols, restrictions on time spent with patients, or mandatory coding practices)
- Administrative or managerial organization (eg, transition to a management services organization).
A version of this article appeared on Medscape.com.
Physician practice ownership by corporations, including health insurers, private equity firms, and large pharmacy chains, reached 30.1% as of January for the first time surpassing ownership by hospitals and health systems (28.4%), according to a new report.
As a result, about three in five physician practices are now owned by nonphysicians.
In early 2020, corporations owned just about 17% of US medical practices, while hospitals and health systems owned about 25%, according to the report released Thursday by nonprofit Physician Advocacy Institute (PAI). But corporate ownership of medical groups surged during the pandemic.
These trends raise questions about how best to protect patients and physicians in a changing employment landscape, said Kelly Kenney, PAI’s chief executive officer, in a statement.
“Corporate entities are assuming control of physician practices and changing the face of medicine in the United States with little to no scrutiny from regulators,” Ms. Kenney said.
The research, conducted by consulting group Avalere for PAI, used the IQVIA OneKey database that contains physician and practice location information on hospital and health system ownership.
By 2022-2023, there was a 7.3% increase in the percentage of practices owned by hospitals and 5.9% increase in the percentage of physicians employed by these organizations, PAI said. In the same time frame, there was an 11% increase in the percentage of practices owned by corporations and a 3.0% increase in the percentage of physicians employed by these entities.
“Physicians have an ethical responsibility to their patients’ health,” Ms. Kenney said. “Corporate entities have a fiduciary responsibility to their shareholders and are motivated to put profits first…these interests can conflict with providing the best medical care to patients.”
Federal Scrutiny Increases
However, both federal and state regulators are paying more attention to what happens to patients and physicians when corporations acquire practices.
“Given recent trends, we are concerned that some transactions may generate profits for those firms at the expense of patients’ health, workers’ safety, quality of care, and affordable healthcare for patients and taxpayers,” said the Federal Trade Commission (FTC) and the Justice (DOJ) and Health and Human Services (HHS) departments.
This statement appears in those agencies’ joint request for information (RFI) announced in March. An RFI is a tool that federal agencies can use to gauge the level of both support and opposition they would face if they were to try to change policies. Public comments are due May 6.
Corporations and advocacy groups often submit detailed comments outlining reasons why the federal government should or should not act on an issue. But individuals also can make their case in this forum.
The FTC, DOJ, and HHS are looking broadly at consolidation in healthcare, but they also spell out potential concerns related to acquisition of physician practices.
For example, they asked clinicians and support staff to provide feedback about whether acquisitions lead to changes in:
- Take-home pay
- Staffing levels
- Workplace safety
- Compensation model (eg, from fixed salary to volume based)
- Policies regarding patient referrals
- Mix of patients
- The volume of patients
- The way providers practice medicine (eg, incentives, prescribing decisions, forced protocols, restrictions on time spent with patients, or mandatory coding practices)
- Administrative or managerial organization (eg, transition to a management services organization).
A version of this article appeared on Medscape.com.
Physician practice ownership by corporations, including health insurers, private equity firms, and large pharmacy chains, reached 30.1% as of January for the first time surpassing ownership by hospitals and health systems (28.4%), according to a new report.
As a result, about three in five physician practices are now owned by nonphysicians.
In early 2020, corporations owned just about 17% of US medical practices, while hospitals and health systems owned about 25%, according to the report released Thursday by nonprofit Physician Advocacy Institute (PAI). But corporate ownership of medical groups surged during the pandemic.
These trends raise questions about how best to protect patients and physicians in a changing employment landscape, said Kelly Kenney, PAI’s chief executive officer, in a statement.
“Corporate entities are assuming control of physician practices and changing the face of medicine in the United States with little to no scrutiny from regulators,” Ms. Kenney said.
The research, conducted by consulting group Avalere for PAI, used the IQVIA OneKey database that contains physician and practice location information on hospital and health system ownership.
By 2022-2023, there was a 7.3% increase in the percentage of practices owned by hospitals and 5.9% increase in the percentage of physicians employed by these organizations, PAI said. In the same time frame, there was an 11% increase in the percentage of practices owned by corporations and a 3.0% increase in the percentage of physicians employed by these entities.
“Physicians have an ethical responsibility to their patients’ health,” Ms. Kenney said. “Corporate entities have a fiduciary responsibility to their shareholders and are motivated to put profits first…these interests can conflict with providing the best medical care to patients.”
Federal Scrutiny Increases
However, both federal and state regulators are paying more attention to what happens to patients and physicians when corporations acquire practices.
“Given recent trends, we are concerned that some transactions may generate profits for those firms at the expense of patients’ health, workers’ safety, quality of care, and affordable healthcare for patients and taxpayers,” said the Federal Trade Commission (FTC) and the Justice (DOJ) and Health and Human Services (HHS) departments.
This statement appears in those agencies’ joint request for information (RFI) announced in March. An RFI is a tool that federal agencies can use to gauge the level of both support and opposition they would face if they were to try to change policies. Public comments are due May 6.
Corporations and advocacy groups often submit detailed comments outlining reasons why the federal government should or should not act on an issue. But individuals also can make their case in this forum.
The FTC, DOJ, and HHS are looking broadly at consolidation in healthcare, but they also spell out potential concerns related to acquisition of physician practices.
For example, they asked clinicians and support staff to provide feedback about whether acquisitions lead to changes in:
- Take-home pay
- Staffing levels
- Workplace safety
- Compensation model (eg, from fixed salary to volume based)
- Policies regarding patient referrals
- Mix of patients
- The volume of patients
- The way providers practice medicine (eg, incentives, prescribing decisions, forced protocols, restrictions on time spent with patients, or mandatory coding practices)
- Administrative or managerial organization (eg, transition to a management services organization).
A version of this article appeared on Medscape.com.
‘Difficult Patient’: Stigmatizing Words and Medical Error
This transcript has been edited for clarity.
When I was doing my nephrology training, I had an attending who would write notes that were, well, kind of funny. I remember one time we were seeing a patient whose first name was “Lucky.” He dryly opened his section of the consult note as follows: “This is a 56-year-old woman with an ironic name who presents with acute renal failure.”
As an exhausted renal fellow, I appreciated the bit of color amid the ongoing series of tragedies that was the consult service. But let’s be clear — writing like this in the medical record is not a good idea. It wasn’t a good idea then, when any record might end up disclosed during a malpractice suit, and it’s really not a good idea now, when patients have ready and automated access to all the notes we write about them.
And yet, worse language than that of my attending appears in hospital notes all the time; there is research about this. Specifically, I’m talking about language that does not have high clinical utility but telegraphs the biases of the person writing the note. This is known as “stigmatizing language” and it can be overt or subtle.
For example, a physician wrote “I listed several fictitious medication names and she reported she was taking them.”
This casts suspicions about the patient’s credibility, as does the more subtle statement, “he claims nicotine patches don’t work for him.” Stigmatizing language may cast the patient in a difficult light, like this note: “she persevered on the fact that ... ‘you wouldn’t understand.’ ”
Stay with me.
We are going to start by defining a very sick patient population: those admitted to the hospital and who, within 48 hours, have either been transferred to the intensive care unit or died. Because of the severity of illness in this population we’ve just defined, figuring out whether a diagnostic or other error was made would be extremely high yield; these can mean the difference between life and death.
In a letter appearing in JAMA Internal Medicine, researchers examined a group of more than 2300 patients just like this from 29 hospitals, scouring the medical records for evidence of these types of errors.
Nearly one in four (23.2%) had at least one diagnostic error, which could include a missed physical exam finding, failure to ask a key question on history taking, inadequate testing, and so on.
Understanding why we make these errors is clearly critical to improving care for these patients. The researchers hypothesized that stigmatizing language might lead to errors like this. For example, by demonstrating that you don’t find a patient credible, you may ignore statements that would help make a better diagnosis.
Just over 5% of these patients had evidence of stigmatizing language in their medical notes. Like earlier studies, this language was more common if the patient was Black or had unstable housing.
Critically, stigmatizing language was more likely to be found among those who had diagnostic errors — a rate of 8.2% vs 4.1%. After adjustment for factors like race, the presence of stigmatizing language was associated with roughly a doubling of the risk for diagnostic errors.
Now, I’m all for eliminating stigmatizing language from our medical notes. And, given the increased transparency of all medical notes these days, I expect that we’ll see less of this over time. But of course, the fact that a physician doesn’t write something that disparages the patient does not necessarily mean that they don’t retain that bias. That said, those comments have an effect on all the other team members who care for that patient as well; it sets a tone and can entrench an individual’s bias more broadly. We should strive to eliminate our biases when it comes to caring for patients. But perhaps the second best thing is to work to keep those biases to ourselves.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
When I was doing my nephrology training, I had an attending who would write notes that were, well, kind of funny. I remember one time we were seeing a patient whose first name was “Lucky.” He dryly opened his section of the consult note as follows: “This is a 56-year-old woman with an ironic name who presents with acute renal failure.”
As an exhausted renal fellow, I appreciated the bit of color amid the ongoing series of tragedies that was the consult service. But let’s be clear — writing like this in the medical record is not a good idea. It wasn’t a good idea then, when any record might end up disclosed during a malpractice suit, and it’s really not a good idea now, when patients have ready and automated access to all the notes we write about them.
And yet, worse language than that of my attending appears in hospital notes all the time; there is research about this. Specifically, I’m talking about language that does not have high clinical utility but telegraphs the biases of the person writing the note. This is known as “stigmatizing language” and it can be overt or subtle.
For example, a physician wrote “I listed several fictitious medication names and she reported she was taking them.”
This casts suspicions about the patient’s credibility, as does the more subtle statement, “he claims nicotine patches don’t work for him.” Stigmatizing language may cast the patient in a difficult light, like this note: “she persevered on the fact that ... ‘you wouldn’t understand.’ ”
Stay with me.
We are going to start by defining a very sick patient population: those admitted to the hospital and who, within 48 hours, have either been transferred to the intensive care unit or died. Because of the severity of illness in this population we’ve just defined, figuring out whether a diagnostic or other error was made would be extremely high yield; these can mean the difference between life and death.
In a letter appearing in JAMA Internal Medicine, researchers examined a group of more than 2300 patients just like this from 29 hospitals, scouring the medical records for evidence of these types of errors.
Nearly one in four (23.2%) had at least one diagnostic error, which could include a missed physical exam finding, failure to ask a key question on history taking, inadequate testing, and so on.
Understanding why we make these errors is clearly critical to improving care for these patients. The researchers hypothesized that stigmatizing language might lead to errors like this. For example, by demonstrating that you don’t find a patient credible, you may ignore statements that would help make a better diagnosis.
Just over 5% of these patients had evidence of stigmatizing language in their medical notes. Like earlier studies, this language was more common if the patient was Black or had unstable housing.
Critically, stigmatizing language was more likely to be found among those who had diagnostic errors — a rate of 8.2% vs 4.1%. After adjustment for factors like race, the presence of stigmatizing language was associated with roughly a doubling of the risk for diagnostic errors.
Now, I’m all for eliminating stigmatizing language from our medical notes. And, given the increased transparency of all medical notes these days, I expect that we’ll see less of this over time. But of course, the fact that a physician doesn’t write something that disparages the patient does not necessarily mean that they don’t retain that bias. That said, those comments have an effect on all the other team members who care for that patient as well; it sets a tone and can entrench an individual’s bias more broadly. We should strive to eliminate our biases when it comes to caring for patients. But perhaps the second best thing is to work to keep those biases to ourselves.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
When I was doing my nephrology training, I had an attending who would write notes that were, well, kind of funny. I remember one time we were seeing a patient whose first name was “Lucky.” He dryly opened his section of the consult note as follows: “This is a 56-year-old woman with an ironic name who presents with acute renal failure.”
As an exhausted renal fellow, I appreciated the bit of color amid the ongoing series of tragedies that was the consult service. But let’s be clear — writing like this in the medical record is not a good idea. It wasn’t a good idea then, when any record might end up disclosed during a malpractice suit, and it’s really not a good idea now, when patients have ready and automated access to all the notes we write about them.
And yet, worse language than that of my attending appears in hospital notes all the time; there is research about this. Specifically, I’m talking about language that does not have high clinical utility but telegraphs the biases of the person writing the note. This is known as “stigmatizing language” and it can be overt or subtle.
For example, a physician wrote “I listed several fictitious medication names and she reported she was taking them.”
This casts suspicions about the patient’s credibility, as does the more subtle statement, “he claims nicotine patches don’t work for him.” Stigmatizing language may cast the patient in a difficult light, like this note: “she persevered on the fact that ... ‘you wouldn’t understand.’ ”
Stay with me.
We are going to start by defining a very sick patient population: those admitted to the hospital and who, within 48 hours, have either been transferred to the intensive care unit or died. Because of the severity of illness in this population we’ve just defined, figuring out whether a diagnostic or other error was made would be extremely high yield; these can mean the difference between life and death.
In a letter appearing in JAMA Internal Medicine, researchers examined a group of more than 2300 patients just like this from 29 hospitals, scouring the medical records for evidence of these types of errors.
Nearly one in four (23.2%) had at least one diagnostic error, which could include a missed physical exam finding, failure to ask a key question on history taking, inadequate testing, and so on.
Understanding why we make these errors is clearly critical to improving care for these patients. The researchers hypothesized that stigmatizing language might lead to errors like this. For example, by demonstrating that you don’t find a patient credible, you may ignore statements that would help make a better diagnosis.
Just over 5% of these patients had evidence of stigmatizing language in their medical notes. Like earlier studies, this language was more common if the patient was Black or had unstable housing.
Critically, stigmatizing language was more likely to be found among those who had diagnostic errors — a rate of 8.2% vs 4.1%. After adjustment for factors like race, the presence of stigmatizing language was associated with roughly a doubling of the risk for diagnostic errors.
Now, I’m all for eliminating stigmatizing language from our medical notes. And, given the increased transparency of all medical notes these days, I expect that we’ll see less of this over time. But of course, the fact that a physician doesn’t write something that disparages the patient does not necessarily mean that they don’t retain that bias. That said, those comments have an effect on all the other team members who care for that patient as well; it sets a tone and can entrench an individual’s bias more broadly. We should strive to eliminate our biases when it comes to caring for patients. But perhaps the second best thing is to work to keep those biases to ourselves.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Recently Immunized Febrile Infants Have Low Infection Risk
TOPLINE:
METHODOLOGY:
- Researchers evaluated 508 infants aged 6-12 weeks who presented with a fever of 38 °C or greater at two US military academic emergency departments (EDs) over a span of 4 years.
- The infants were categorized as “recently immunized” if they had received immunizations within 72 hours before ED presentation and “not recently immunized” if they had not. Among the 508 infants, 114 were immunized recently.
- The primary outcome was the prevalence of a serious bacterial infection (SBI), categorized into IBI and non-IBI on the basis of culture and radiography findings.
TAKEAWAY:
- The prevalence of SBI was 3.5% in the recently immunized febrile infants and 13.7% in not recently immunized febrile infants.
- Among the recently immunized infants, the prevalence of SBI was lower in those immunized within the first 24 hours than those immunized more than 24 hours before ED presentation (2% vs 14.3%, respectively).
- Almost all identified SBI cases were of urinary tract infection (UTI), with the only non-UTI case being pneumonia in an infant who exhibited respiratory symptoms within 24 hours of receiving immunization.
IN PRACTICE:
Physicians should discuss the possibilities of a less invasive approach for evaluating recently immunized febrile infants. The study findings support the general recommendation to obtain a urinalysis for all recently immunized infants over 60 days presenting with fever, including those presenting less than 24 hours post immunization.
SOURCE:
This study, led by Kyla Casey, MD, Department of Emergency Medicine, Naval Medical Center San Diego, was published online in The American Journal of Emergency Medicine.
LIMITATIONS:
The small sample size and retrospective design might have resulted in an overestimation of outcomes like IBIs within 24 hours after immunization. As the study was conducted in a specific clinical setting with febrile infants from military medical centers, the findings may have limited generalizability. Moreover, the inclusion of premature infants without age correction for prematurity could have impacted the prevalence of IBIs. Factors like missing vaccination history, healthcare referral patterns, and immunization practices in the military system may have introduced bias.
DISCLOSURE:
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors. The authors had no conflicts of interest to disclose.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers evaluated 508 infants aged 6-12 weeks who presented with a fever of 38 °C or greater at two US military academic emergency departments (EDs) over a span of 4 years.
- The infants were categorized as “recently immunized” if they had received immunizations within 72 hours before ED presentation and “not recently immunized” if they had not. Among the 508 infants, 114 were immunized recently.
- The primary outcome was the prevalence of a serious bacterial infection (SBI), categorized into IBI and non-IBI on the basis of culture and radiography findings.
TAKEAWAY:
- The prevalence of SBI was 3.5% in the recently immunized febrile infants and 13.7% in not recently immunized febrile infants.
- Among the recently immunized infants, the prevalence of SBI was lower in those immunized within the first 24 hours than those immunized more than 24 hours before ED presentation (2% vs 14.3%, respectively).
- Almost all identified SBI cases were of urinary tract infection (UTI), with the only non-UTI case being pneumonia in an infant who exhibited respiratory symptoms within 24 hours of receiving immunization.
IN PRACTICE:
Physicians should discuss the possibilities of a less invasive approach for evaluating recently immunized febrile infants. The study findings support the general recommendation to obtain a urinalysis for all recently immunized infants over 60 days presenting with fever, including those presenting less than 24 hours post immunization.
SOURCE:
This study, led by Kyla Casey, MD, Department of Emergency Medicine, Naval Medical Center San Diego, was published online in The American Journal of Emergency Medicine.
LIMITATIONS:
The small sample size and retrospective design might have resulted in an overestimation of outcomes like IBIs within 24 hours after immunization. As the study was conducted in a specific clinical setting with febrile infants from military medical centers, the findings may have limited generalizability. Moreover, the inclusion of premature infants without age correction for prematurity could have impacted the prevalence of IBIs. Factors like missing vaccination history, healthcare referral patterns, and immunization practices in the military system may have introduced bias.
DISCLOSURE:
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors. The authors had no conflicts of interest to disclose.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers evaluated 508 infants aged 6-12 weeks who presented with a fever of 38 °C or greater at two US military academic emergency departments (EDs) over a span of 4 years.
- The infants were categorized as “recently immunized” if they had received immunizations within 72 hours before ED presentation and “not recently immunized” if they had not. Among the 508 infants, 114 were immunized recently.
- The primary outcome was the prevalence of a serious bacterial infection (SBI), categorized into IBI and non-IBI on the basis of culture and radiography findings.
TAKEAWAY:
- The prevalence of SBI was 3.5% in the recently immunized febrile infants and 13.7% in not recently immunized febrile infants.
- Among the recently immunized infants, the prevalence of SBI was lower in those immunized within the first 24 hours than those immunized more than 24 hours before ED presentation (2% vs 14.3%, respectively).
- Almost all identified SBI cases were of urinary tract infection (UTI), with the only non-UTI case being pneumonia in an infant who exhibited respiratory symptoms within 24 hours of receiving immunization.
IN PRACTICE:
Physicians should discuss the possibilities of a less invasive approach for evaluating recently immunized febrile infants. The study findings support the general recommendation to obtain a urinalysis for all recently immunized infants over 60 days presenting with fever, including those presenting less than 24 hours post immunization.
SOURCE:
This study, led by Kyla Casey, MD, Department of Emergency Medicine, Naval Medical Center San Diego, was published online in The American Journal of Emergency Medicine.
LIMITATIONS:
The small sample size and retrospective design might have resulted in an overestimation of outcomes like IBIs within 24 hours after immunization. As the study was conducted in a specific clinical setting with febrile infants from military medical centers, the findings may have limited generalizability. Moreover, the inclusion of premature infants without age correction for prematurity could have impacted the prevalence of IBIs. Factors like missing vaccination history, healthcare referral patterns, and immunization practices in the military system may have introduced bias.
DISCLOSURE:
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors. The authors had no conflicts of interest to disclose.
A version of this article appeared on Medscape.com.
D-Mannose as UTI Treatment Offers No Benefit
TOPLINE:
A natural sugar used to treat recurring urinary tract infections (rUTIs) did not reduce future episodes, outpatient visits, the use of antibiotics, or symptoms compared with a placebo, according to a new study.
METHODOLOGY:
- D-Mannose is recommended as a natural alternative to antibiotics and sold as a dietary supplement; research showing the efficacy of D-mannose in treating UTIs is mixed.
- The double-blind, randomized controlled trial followed 598 women older than 18 years (median age, 61.3; range 18.2-93.5 years) with a history of rUTIs over 6 months from nearly 100 primary care clinics in the United Kingdom.
- Patients took 2 g of D-mannose or placebo powder daily and recorded their symptoms using a daily diary or through responses to health surveys, weekly questionnaires, and phone calls.
- Researchers checked medical records for urine culture results, antibiotic prescriptions, hospitalizations, and outpatient visits for UTIs.
TAKEAWAY:
- Approximately 51% of participants who took D-mannose and 55.7% of those who took a placebo contacted a healthcare professional reporting a UTI (relative risk, 0.92; 95% CI, 0.80-1.05; P = .22).
- Women in both groups reported similar durations of “moderately bad” or “worse” symptoms, and the number of antibiotic courses, instances of clinically suspected UTIs, and hospital admissions were similar between the two groups.
- Some studies have reported that synthetic mannosides are promising alternatives to D-mannose.
IN PRACTICE:
“D-Mannose should not be recommended to prevent future episodes of medically attended UTI in women with recurrent UTI in primary care,” the study authors wrote.
SOURCE:
The study was led by Gail Hayward, DPhil, associate professor at the Nuffield Department of Primary Care Health Sciences at the University of Oxford in England, and was published online in JAMA Internal Medicine.
LIMITATIONS:
Some participants may have taken less than 2 mg/d or skipped days. Because researchers used powder rather than capsules, dosing could have been inconsistent. Researchers did not obtain a microbiologic confirmation for each rUTI. A small percentage of women were taking antibiotics.
DISCLOSURES:
The study was funded by the National Institute for Health and Care Research (NIHR) School for Primary Care Research and the NIHR Oxford Biomedical Research Centre. Various authors reported receiving support from the NIHR Health Protection Research Unit on Healthcare-Associated Infections and Antimicrobial Resistance and were NIHR investigators.
A version of this article first appeared on Medscape.com.
TOPLINE:
A natural sugar used to treat recurring urinary tract infections (rUTIs) did not reduce future episodes, outpatient visits, the use of antibiotics, or symptoms compared with a placebo, according to a new study.
METHODOLOGY:
- D-Mannose is recommended as a natural alternative to antibiotics and sold as a dietary supplement; research showing the efficacy of D-mannose in treating UTIs is mixed.
- The double-blind, randomized controlled trial followed 598 women older than 18 years (median age, 61.3; range 18.2-93.5 years) with a history of rUTIs over 6 months from nearly 100 primary care clinics in the United Kingdom.
- Patients took 2 g of D-mannose or placebo powder daily and recorded their symptoms using a daily diary or through responses to health surveys, weekly questionnaires, and phone calls.
- Researchers checked medical records for urine culture results, antibiotic prescriptions, hospitalizations, and outpatient visits for UTIs.
TAKEAWAY:
- Approximately 51% of participants who took D-mannose and 55.7% of those who took a placebo contacted a healthcare professional reporting a UTI (relative risk, 0.92; 95% CI, 0.80-1.05; P = .22).
- Women in both groups reported similar durations of “moderately bad” or “worse” symptoms, and the number of antibiotic courses, instances of clinically suspected UTIs, and hospital admissions were similar between the two groups.
- Some studies have reported that synthetic mannosides are promising alternatives to D-mannose.
IN PRACTICE:
“D-Mannose should not be recommended to prevent future episodes of medically attended UTI in women with recurrent UTI in primary care,” the study authors wrote.
SOURCE:
The study was led by Gail Hayward, DPhil, associate professor at the Nuffield Department of Primary Care Health Sciences at the University of Oxford in England, and was published online in JAMA Internal Medicine.
LIMITATIONS:
Some participants may have taken less than 2 mg/d or skipped days. Because researchers used powder rather than capsules, dosing could have been inconsistent. Researchers did not obtain a microbiologic confirmation for each rUTI. A small percentage of women were taking antibiotics.
DISCLOSURES:
The study was funded by the National Institute for Health and Care Research (NIHR) School for Primary Care Research and the NIHR Oxford Biomedical Research Centre. Various authors reported receiving support from the NIHR Health Protection Research Unit on Healthcare-Associated Infections and Antimicrobial Resistance and were NIHR investigators.
A version of this article first appeared on Medscape.com.
TOPLINE:
A natural sugar used to treat recurring urinary tract infections (rUTIs) did not reduce future episodes, outpatient visits, the use of antibiotics, or symptoms compared with a placebo, according to a new study.
METHODOLOGY:
- D-Mannose is recommended as a natural alternative to antibiotics and sold as a dietary supplement; research showing the efficacy of D-mannose in treating UTIs is mixed.
- The double-blind, randomized controlled trial followed 598 women older than 18 years (median age, 61.3; range 18.2-93.5 years) with a history of rUTIs over 6 months from nearly 100 primary care clinics in the United Kingdom.
- Patients took 2 g of D-mannose or placebo powder daily and recorded their symptoms using a daily diary or through responses to health surveys, weekly questionnaires, and phone calls.
- Researchers checked medical records for urine culture results, antibiotic prescriptions, hospitalizations, and outpatient visits for UTIs.
TAKEAWAY:
- Approximately 51% of participants who took D-mannose and 55.7% of those who took a placebo contacted a healthcare professional reporting a UTI (relative risk, 0.92; 95% CI, 0.80-1.05; P = .22).
- Women in both groups reported similar durations of “moderately bad” or “worse” symptoms, and the number of antibiotic courses, instances of clinically suspected UTIs, and hospital admissions were similar between the two groups.
- Some studies have reported that synthetic mannosides are promising alternatives to D-mannose.
IN PRACTICE:
“D-Mannose should not be recommended to prevent future episodes of medically attended UTI in women with recurrent UTI in primary care,” the study authors wrote.
SOURCE:
The study was led by Gail Hayward, DPhil, associate professor at the Nuffield Department of Primary Care Health Sciences at the University of Oxford in England, and was published online in JAMA Internal Medicine.
LIMITATIONS:
Some participants may have taken less than 2 mg/d or skipped days. Because researchers used powder rather than capsules, dosing could have been inconsistent. Researchers did not obtain a microbiologic confirmation for each rUTI. A small percentage of women were taking antibiotics.
DISCLOSURES:
The study was funded by the National Institute for Health and Care Research (NIHR) School for Primary Care Research and the NIHR Oxford Biomedical Research Centre. Various authors reported receiving support from the NIHR Health Protection Research Unit on Healthcare-Associated Infections and Antimicrobial Resistance and were NIHR investigators.
A version of this article first appeared on Medscape.com.
Worldwide Uptick in Invasive Group A Streptococcus Disease Post Pandemic — What Should We Know?
Invasive group A streptococcus (iGAS) infections are rare (4-9 cases/100,000 US population annually) but potentially devastating (approximately 2,300 deaths annually in US), and affect all ages. Cases increase in winter-spring, paralleling the “season” of increased noninvasive GAS, e.g., pharyngitis and scarlet fever. iGAS case rates are lower in children than adults. That said, one well-known pediatric iGAS scenario has been deep cellulitis and necrotizing fasciitis during the healing phase of varicella. Other forms of iGAS include bacteremia, pneumonia (particularly when empyema is present), lymphangitis, erysipelas, and toxic shock syndrome. iGAS can occur with/after influenza but has also occurred concurrently with other viral respiratory infections.
Persons with underlying conditions (cancer or immune compromised status; chronic diseases of the heart, kidney or lung; diabetes mellitus) are at higher risk. Other subpopulations at risk for iGAS are illicit drug users, the elderly, homeless persons, nursing home residents, American Indian persons, and Alaska Native persons. Most experts feel that highly toxigenic strains of GAS are responsible for most iGAS. Indeed, most iGAS isolates produce (sometimes hyper-produce) superantigens that cause exaggerated innate immune responses, higher levels of inflammation, and often times tissue destruction, e.g., “flesh eating bacteria.” And who can forget that Jim Henson, creator of the Muppets, died of iGAS?
But why discuss iGAS in 2024? The pattern for iGAS has fluctuated more than usual in the last decade. So much so that the recent upsurge has caught the collective eye of the lay press. So, patients and friends may have questions about why and how iGAS is increasing lately. The bottom line is that no one knows for sure. However, the most recent 2 years of uptick may reflect GAS circulating at relatively high levels even when taking into account that GAS season occurs in winter-spring most years. Yet it seems likely that additional factors may have played a role in the fluctuations noted this past decade, e.g., temporary changes in societal behavior, a new GAS strain with over two dozen mutations, and possibly rapid waning of protection against GAS exotoxins.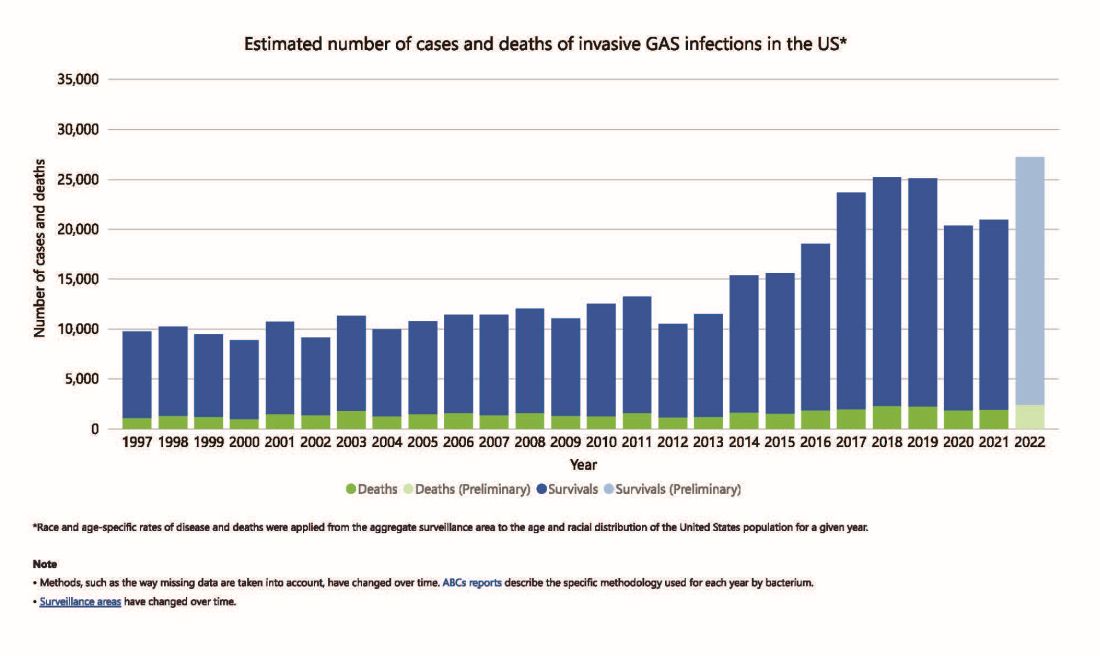
Social Behavior Factor
The SARS-CoV-2 pandemic brought extremes of disease and death to the world and dramatic changes in social behavior. A byproduct was dramatic decreases in nearly all infectious diseases, with numerous reports of near absence of many respiratory and gastrointestinal viruses in the 2020-2021 seasons. Interestingly, we did not see a drop in human rhinovirus infections, justifying its nickname as the cockroach of viruses. Reports also emerged about drops in bacterial diseases during 2020-2021 (although not so much for STIs), including noninvasive and invasive GAS disease, and also GAS-associated deaths (lowest since 2016).1 The drop in iGAS during social restrictions makes sense because GAS is spread by direct contact with infected persons or their secretions, and social contact had dramatically decreased particularly in the first 6 months of the pandemic.
However, since 2022 and the return to “normal” social behaviors, both viral diseases (e.g., RSV, influenza, and Norovirus), and some bacterial diseases have rebounded. That said, something else must be contributing, because iGAS rates had increased 4-5 years pre pandemic. In fact, the fluctuating pattern included “normal” annual rates in the early 2000s rising in ~2015 followed by the explainable pandemic drop (by nearly 25%), and not-too-unexpected 2-year postpandemic rise. But interestingly enough, the rebound is higher than might be expected for iGAS and children were overrepresented in first year’s rise (2022 rate for pediatric iGAS was the highest since 1997) while those older than 65 were overrepresented in second year (2023).1
Emergence of M1UK
One potential factor for the prepandemic rise in iGAS infections worldwide is the emergence and worldwide spread of a new GAS emm type variant designated M1UK.2 GAS isolates can be typed into categories designated as emm types based on DNA sequence. There are more than 240 emm types, with 6 being most common — M1, M3, and M28 (each up to 20% of GAS isolates) and M12, M82, and M89 (each up to 10%). M1, M3 and M28 have also been particularly associated with invasive disease. While emm types vary year to year and region by region, the overall emm type distribution among iGAS isolates in the United States had not been unusual since the turn of the century and the US M1 strain was the same as that which had been predominant worldwide (designated M1GLOBAL). This new M1UK sublineage had emerged around 2010 and had been increasing pre pandemic. The M1UK sequence contained a specific set of 27 SNPs (single nucleoside polymorphisms, i.e., single base mutations) and was associated with an uptick in scarlet fever in the United Kingdom starting around 2010. Its prevalence increased up to around 2015 while spreading internationally. It also had enhanced expression of SpeA, a phage-encoded superantigen. Some of the M1UK mutations also appear to alter GAS metabolic processes to allow better survival (better “fitness”) compared with other GAS. So, a more virulent hardier GAS had arisen and seems a reasonable candidate for contributing to the increased iGAS rates.
Waning Antibody to GAS As Potential Factor in Rebound
No consensus exists on correlates of protection from iGAS. However, adults seem to have less noninvasive GAS than children. One potential reason is that frequent GAS re-exposure, regardless of whether disease results, likely boosts anti-GAS antibodies. Pandemic social restrictions temporarily prevented such boosts. In children with developing antibody repertoires, anti-GAS antibodies may have waned below protective levels faster during a year without frequent boosting. Thus, children were iGAS susceptible soon after pandemic restrictions were dropped (2022). Increased iGAS rates in the elderly in 2023 may have occurred because of diminished GAS exposures accelerating immune senescence with anti-GAS antibodies dropping, but less quickly than in children. These speculations are simply hypotheses until future studies can test them.
All that said, how do we use information on increased iGAS in our daily practices? In addition to standard preventive strategies for viral coinfections (e.g., varicella and influenza vaccine), reminding families about rigorous attention to wound care is the one high-risk scenario we have not yet discussed. During 2024, a time of expected increased prevalence of iGAS, early wound care needs to be fastidious. Further, share warning signs with families (e.g., rapidly expanding painful erythema), “streaks” ascending from extremity wounds, fever and a highly painful wound, darkening almost purple color within cellulitis or soft tissue infection, or loss of sensation in the middle of an otherwise painful soft tissue infection. These presentations require immediate medical attention.
If such a patient presents, the Centers for Disease Control and Prevention (CDC) recommends admission along with blood and, where possible, wound cultures. If in the context of pneumonia with pleural effusion, culturing pleural fluid is also important. Remember, leading edge cultures are not often positive for GAS, seemingly because GAS exotoxins are found at erythema’s leading edge, not the bacteria. The bacteria are somewhere more central in the inflammatory process. Despite not being prominent among recent iGAS cases, another scenario that could sneak up on you is the infected surgical wound as nascent iGAS.
Finally, remember that nationally increasing numbers of iGAS isolates are resistant to erythromycin and clindamycin, the latter usually recommended to reduce tissue damage in iGAS.3 So, it is important to be aware of susceptibility patterns in your locale and consider an ID consultation. My hope is that you do not see an iGAS case this year, but we all need to remain alert. With a high index of suspicion and rapid diagnosis, you can minimize long-term sequelae and potential fatalities.
While it is too early to tell how the rest of 2024 will turn out, preliminary indications are that GAS is circulating at higher than usual levels (30%-35% GAS positive throat swabs in early April 2024 in Kansas City area) and iGAS rates will likely also be relatively high, particularly if Ontario, Canada, data are any indication.4 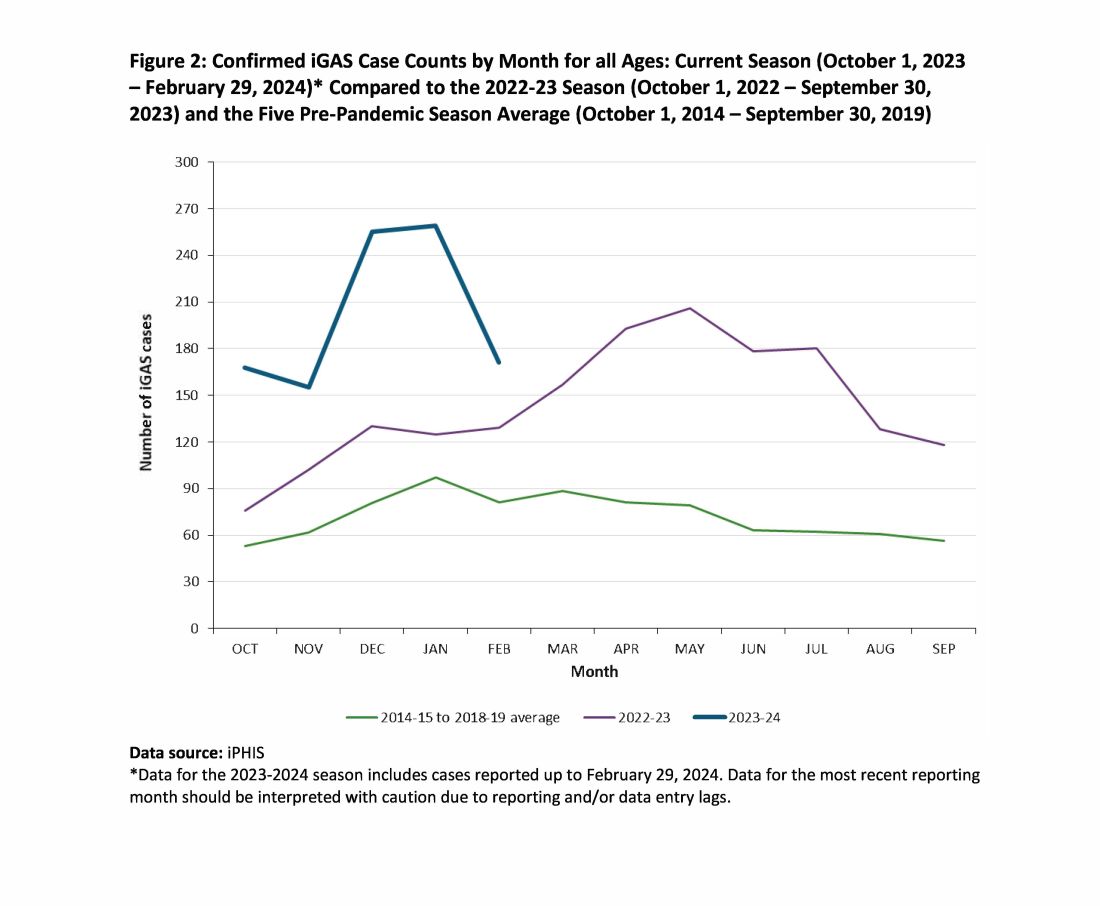
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. Current Group A Strep Activity, Centers for Disease Control and Prevention. April 2024. CDC webpage on current invasive GAS disease. April 2024.
2. Li Y et al. Expansion of Invasive Group A Streptococcus M1UK Lineage in Active Bacterial Core Surveillance, United States, 2019-2021 Emerg Infect Dis. 2023;29(10):2116-2120. doi: 10.3201/eid2910.230675.
3. Andreoni F et al. Clindamycin Affects Group A Streptococcus Virulence Factors and Improves Clinical Outcome. J Infect Dis. 2017 Jan 15;215(2):269-277. doi: 10.1093/infdis/jiw229.
4. Group A Streptococcal Disease, Invasive (iGAS), Public Health Ontario.
Invasive group A streptococcus (iGAS) infections are rare (4-9 cases/100,000 US population annually) but potentially devastating (approximately 2,300 deaths annually in US), and affect all ages. Cases increase in winter-spring, paralleling the “season” of increased noninvasive GAS, e.g., pharyngitis and scarlet fever. iGAS case rates are lower in children than adults. That said, one well-known pediatric iGAS scenario has been deep cellulitis and necrotizing fasciitis during the healing phase of varicella. Other forms of iGAS include bacteremia, pneumonia (particularly when empyema is present), lymphangitis, erysipelas, and toxic shock syndrome. iGAS can occur with/after influenza but has also occurred concurrently with other viral respiratory infections.
Persons with underlying conditions (cancer or immune compromised status; chronic diseases of the heart, kidney or lung; diabetes mellitus) are at higher risk. Other subpopulations at risk for iGAS are illicit drug users, the elderly, homeless persons, nursing home residents, American Indian persons, and Alaska Native persons. Most experts feel that highly toxigenic strains of GAS are responsible for most iGAS. Indeed, most iGAS isolates produce (sometimes hyper-produce) superantigens that cause exaggerated innate immune responses, higher levels of inflammation, and often times tissue destruction, e.g., “flesh eating bacteria.” And who can forget that Jim Henson, creator of the Muppets, died of iGAS?
But why discuss iGAS in 2024? The pattern for iGAS has fluctuated more than usual in the last decade. So much so that the recent upsurge has caught the collective eye of the lay press. So, patients and friends may have questions about why and how iGAS is increasing lately. The bottom line is that no one knows for sure. However, the most recent 2 years of uptick may reflect GAS circulating at relatively high levels even when taking into account that GAS season occurs in winter-spring most years. Yet it seems likely that additional factors may have played a role in the fluctuations noted this past decade, e.g., temporary changes in societal behavior, a new GAS strain with over two dozen mutations, and possibly rapid waning of protection against GAS exotoxins.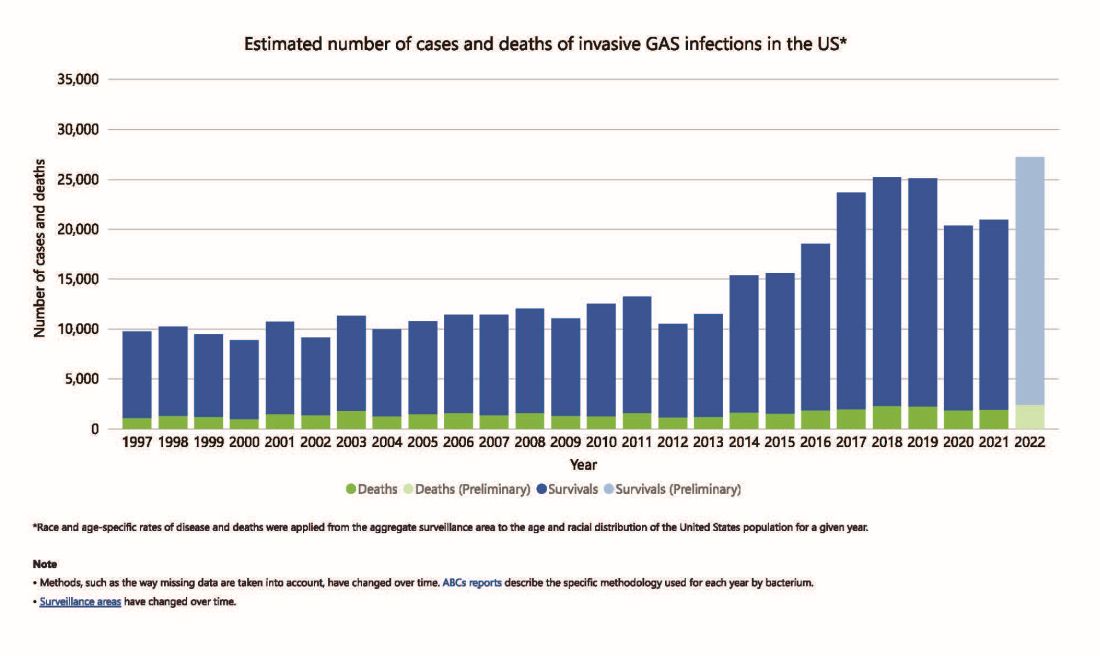
Social Behavior Factor
The SARS-CoV-2 pandemic brought extremes of disease and death to the world and dramatic changes in social behavior. A byproduct was dramatic decreases in nearly all infectious diseases, with numerous reports of near absence of many respiratory and gastrointestinal viruses in the 2020-2021 seasons. Interestingly, we did not see a drop in human rhinovirus infections, justifying its nickname as the cockroach of viruses. Reports also emerged about drops in bacterial diseases during 2020-2021 (although not so much for STIs), including noninvasive and invasive GAS disease, and also GAS-associated deaths (lowest since 2016).1 The drop in iGAS during social restrictions makes sense because GAS is spread by direct contact with infected persons or their secretions, and social contact had dramatically decreased particularly in the first 6 months of the pandemic.
However, since 2022 and the return to “normal” social behaviors, both viral diseases (e.g., RSV, influenza, and Norovirus), and some bacterial diseases have rebounded. That said, something else must be contributing, because iGAS rates had increased 4-5 years pre pandemic. In fact, the fluctuating pattern included “normal” annual rates in the early 2000s rising in ~2015 followed by the explainable pandemic drop (by nearly 25%), and not-too-unexpected 2-year postpandemic rise. But interestingly enough, the rebound is higher than might be expected for iGAS and children were overrepresented in first year’s rise (2022 rate for pediatric iGAS was the highest since 1997) while those older than 65 were overrepresented in second year (2023).1
Emergence of M1UK
One potential factor for the prepandemic rise in iGAS infections worldwide is the emergence and worldwide spread of a new GAS emm type variant designated M1UK.2 GAS isolates can be typed into categories designated as emm types based on DNA sequence. There are more than 240 emm types, with 6 being most common — M1, M3, and M28 (each up to 20% of GAS isolates) and M12, M82, and M89 (each up to 10%). M1, M3 and M28 have also been particularly associated with invasive disease. While emm types vary year to year and region by region, the overall emm type distribution among iGAS isolates in the United States had not been unusual since the turn of the century and the US M1 strain was the same as that which had been predominant worldwide (designated M1GLOBAL). This new M1UK sublineage had emerged around 2010 and had been increasing pre pandemic. The M1UK sequence contained a specific set of 27 SNPs (single nucleoside polymorphisms, i.e., single base mutations) and was associated with an uptick in scarlet fever in the United Kingdom starting around 2010. Its prevalence increased up to around 2015 while spreading internationally. It also had enhanced expression of SpeA, a phage-encoded superantigen. Some of the M1UK mutations also appear to alter GAS metabolic processes to allow better survival (better “fitness”) compared with other GAS. So, a more virulent hardier GAS had arisen and seems a reasonable candidate for contributing to the increased iGAS rates.
Waning Antibody to GAS As Potential Factor in Rebound
No consensus exists on correlates of protection from iGAS. However, adults seem to have less noninvasive GAS than children. One potential reason is that frequent GAS re-exposure, regardless of whether disease results, likely boosts anti-GAS antibodies. Pandemic social restrictions temporarily prevented such boosts. In children with developing antibody repertoires, anti-GAS antibodies may have waned below protective levels faster during a year without frequent boosting. Thus, children were iGAS susceptible soon after pandemic restrictions were dropped (2022). Increased iGAS rates in the elderly in 2023 may have occurred because of diminished GAS exposures accelerating immune senescence with anti-GAS antibodies dropping, but less quickly than in children. These speculations are simply hypotheses until future studies can test them.
All that said, how do we use information on increased iGAS in our daily practices? In addition to standard preventive strategies for viral coinfections (e.g., varicella and influenza vaccine), reminding families about rigorous attention to wound care is the one high-risk scenario we have not yet discussed. During 2024, a time of expected increased prevalence of iGAS, early wound care needs to be fastidious. Further, share warning signs with families (e.g., rapidly expanding painful erythema), “streaks” ascending from extremity wounds, fever and a highly painful wound, darkening almost purple color within cellulitis or soft tissue infection, or loss of sensation in the middle of an otherwise painful soft tissue infection. These presentations require immediate medical attention.
If such a patient presents, the Centers for Disease Control and Prevention (CDC) recommends admission along with blood and, where possible, wound cultures. If in the context of pneumonia with pleural effusion, culturing pleural fluid is also important. Remember, leading edge cultures are not often positive for GAS, seemingly because GAS exotoxins are found at erythema’s leading edge, not the bacteria. The bacteria are somewhere more central in the inflammatory process. Despite not being prominent among recent iGAS cases, another scenario that could sneak up on you is the infected surgical wound as nascent iGAS.
Finally, remember that nationally increasing numbers of iGAS isolates are resistant to erythromycin and clindamycin, the latter usually recommended to reduce tissue damage in iGAS.3 So, it is important to be aware of susceptibility patterns in your locale and consider an ID consultation. My hope is that you do not see an iGAS case this year, but we all need to remain alert. With a high index of suspicion and rapid diagnosis, you can minimize long-term sequelae and potential fatalities.
While it is too early to tell how the rest of 2024 will turn out, preliminary indications are that GAS is circulating at higher than usual levels (30%-35% GAS positive throat swabs in early April 2024 in Kansas City area) and iGAS rates will likely also be relatively high, particularly if Ontario, Canada, data are any indication.4 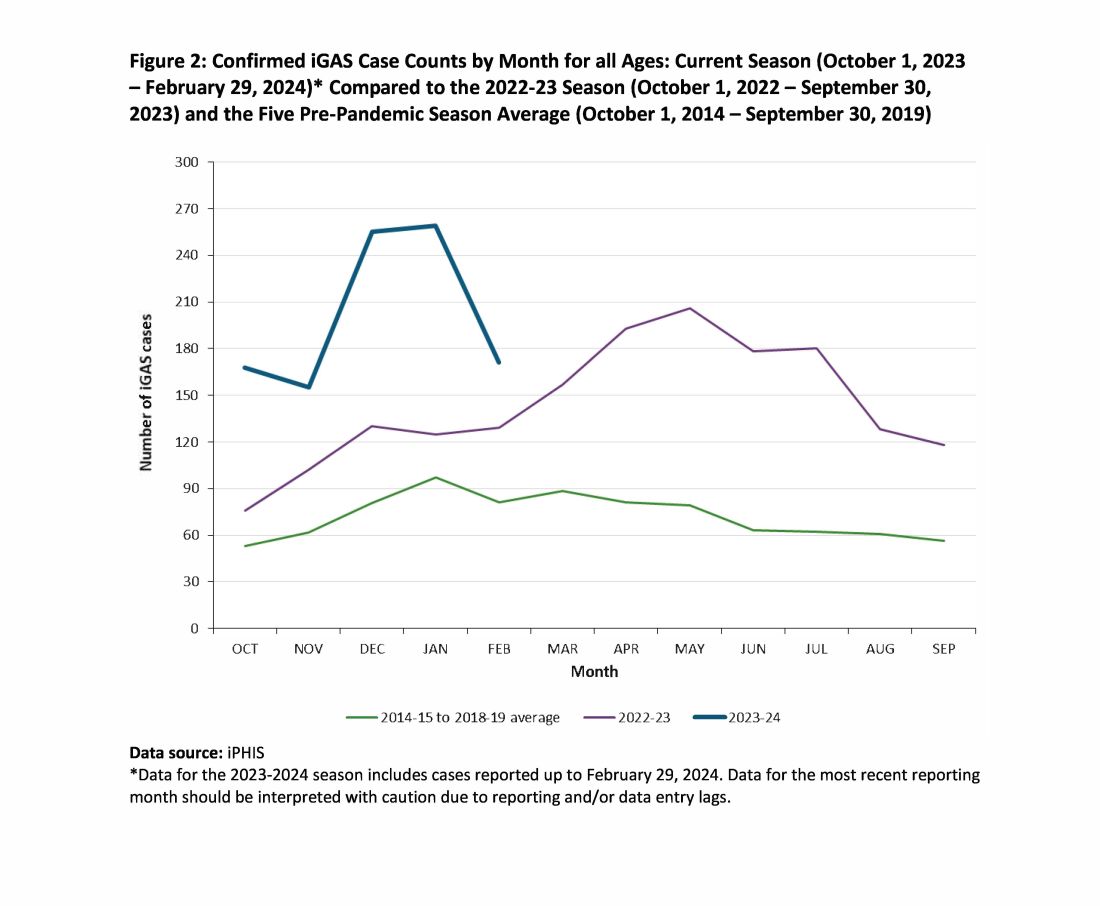
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. Current Group A Strep Activity, Centers for Disease Control and Prevention. April 2024. CDC webpage on current invasive GAS disease. April 2024.
2. Li Y et al. Expansion of Invasive Group A Streptococcus M1UK Lineage in Active Bacterial Core Surveillance, United States, 2019-2021 Emerg Infect Dis. 2023;29(10):2116-2120. doi: 10.3201/eid2910.230675.
3. Andreoni F et al. Clindamycin Affects Group A Streptococcus Virulence Factors and Improves Clinical Outcome. J Infect Dis. 2017 Jan 15;215(2):269-277. doi: 10.1093/infdis/jiw229.
4. Group A Streptococcal Disease, Invasive (iGAS), Public Health Ontario.
Invasive group A streptococcus (iGAS) infections are rare (4-9 cases/100,000 US population annually) but potentially devastating (approximately 2,300 deaths annually in US), and affect all ages. Cases increase in winter-spring, paralleling the “season” of increased noninvasive GAS, e.g., pharyngitis and scarlet fever. iGAS case rates are lower in children than adults. That said, one well-known pediatric iGAS scenario has been deep cellulitis and necrotizing fasciitis during the healing phase of varicella. Other forms of iGAS include bacteremia, pneumonia (particularly when empyema is present), lymphangitis, erysipelas, and toxic shock syndrome. iGAS can occur with/after influenza but has also occurred concurrently with other viral respiratory infections.
Persons with underlying conditions (cancer or immune compromised status; chronic diseases of the heart, kidney or lung; diabetes mellitus) are at higher risk. Other subpopulations at risk for iGAS are illicit drug users, the elderly, homeless persons, nursing home residents, American Indian persons, and Alaska Native persons. Most experts feel that highly toxigenic strains of GAS are responsible for most iGAS. Indeed, most iGAS isolates produce (sometimes hyper-produce) superantigens that cause exaggerated innate immune responses, higher levels of inflammation, and often times tissue destruction, e.g., “flesh eating bacteria.” And who can forget that Jim Henson, creator of the Muppets, died of iGAS?
But why discuss iGAS in 2024? The pattern for iGAS has fluctuated more than usual in the last decade. So much so that the recent upsurge has caught the collective eye of the lay press. So, patients and friends may have questions about why and how iGAS is increasing lately. The bottom line is that no one knows for sure. However, the most recent 2 years of uptick may reflect GAS circulating at relatively high levels even when taking into account that GAS season occurs in winter-spring most years. Yet it seems likely that additional factors may have played a role in the fluctuations noted this past decade, e.g., temporary changes in societal behavior, a new GAS strain with over two dozen mutations, and possibly rapid waning of protection against GAS exotoxins.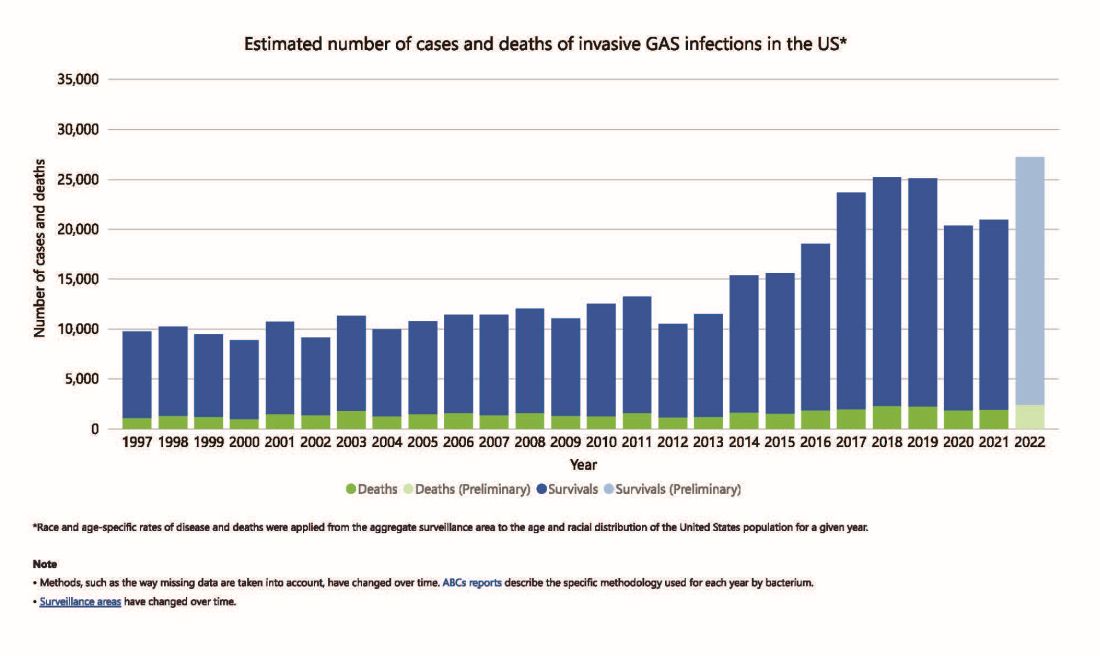
Social Behavior Factor
The SARS-CoV-2 pandemic brought extremes of disease and death to the world and dramatic changes in social behavior. A byproduct was dramatic decreases in nearly all infectious diseases, with numerous reports of near absence of many respiratory and gastrointestinal viruses in the 2020-2021 seasons. Interestingly, we did not see a drop in human rhinovirus infections, justifying its nickname as the cockroach of viruses. Reports also emerged about drops in bacterial diseases during 2020-2021 (although not so much for STIs), including noninvasive and invasive GAS disease, and also GAS-associated deaths (lowest since 2016).1 The drop in iGAS during social restrictions makes sense because GAS is spread by direct contact with infected persons or their secretions, and social contact had dramatically decreased particularly in the first 6 months of the pandemic.
However, since 2022 and the return to “normal” social behaviors, both viral diseases (e.g., RSV, influenza, and Norovirus), and some bacterial diseases have rebounded. That said, something else must be contributing, because iGAS rates had increased 4-5 years pre pandemic. In fact, the fluctuating pattern included “normal” annual rates in the early 2000s rising in ~2015 followed by the explainable pandemic drop (by nearly 25%), and not-too-unexpected 2-year postpandemic rise. But interestingly enough, the rebound is higher than might be expected for iGAS and children were overrepresented in first year’s rise (2022 rate for pediatric iGAS was the highest since 1997) while those older than 65 were overrepresented in second year (2023).1
Emergence of M1UK
One potential factor for the prepandemic rise in iGAS infections worldwide is the emergence and worldwide spread of a new GAS emm type variant designated M1UK.2 GAS isolates can be typed into categories designated as emm types based on DNA sequence. There are more than 240 emm types, with 6 being most common — M1, M3, and M28 (each up to 20% of GAS isolates) and M12, M82, and M89 (each up to 10%). M1, M3 and M28 have also been particularly associated with invasive disease. While emm types vary year to year and region by region, the overall emm type distribution among iGAS isolates in the United States had not been unusual since the turn of the century and the US M1 strain was the same as that which had been predominant worldwide (designated M1GLOBAL). This new M1UK sublineage had emerged around 2010 and had been increasing pre pandemic. The M1UK sequence contained a specific set of 27 SNPs (single nucleoside polymorphisms, i.e., single base mutations) and was associated with an uptick in scarlet fever in the United Kingdom starting around 2010. Its prevalence increased up to around 2015 while spreading internationally. It also had enhanced expression of SpeA, a phage-encoded superantigen. Some of the M1UK mutations also appear to alter GAS metabolic processes to allow better survival (better “fitness”) compared with other GAS. So, a more virulent hardier GAS had arisen and seems a reasonable candidate for contributing to the increased iGAS rates.
Waning Antibody to GAS As Potential Factor in Rebound
No consensus exists on correlates of protection from iGAS. However, adults seem to have less noninvasive GAS than children. One potential reason is that frequent GAS re-exposure, regardless of whether disease results, likely boosts anti-GAS antibodies. Pandemic social restrictions temporarily prevented such boosts. In children with developing antibody repertoires, anti-GAS antibodies may have waned below protective levels faster during a year without frequent boosting. Thus, children were iGAS susceptible soon after pandemic restrictions were dropped (2022). Increased iGAS rates in the elderly in 2023 may have occurred because of diminished GAS exposures accelerating immune senescence with anti-GAS antibodies dropping, but less quickly than in children. These speculations are simply hypotheses until future studies can test them.
All that said, how do we use information on increased iGAS in our daily practices? In addition to standard preventive strategies for viral coinfections (e.g., varicella and influenza vaccine), reminding families about rigorous attention to wound care is the one high-risk scenario we have not yet discussed. During 2024, a time of expected increased prevalence of iGAS, early wound care needs to be fastidious. Further, share warning signs with families (e.g., rapidly expanding painful erythema), “streaks” ascending from extremity wounds, fever and a highly painful wound, darkening almost purple color within cellulitis or soft tissue infection, or loss of sensation in the middle of an otherwise painful soft tissue infection. These presentations require immediate medical attention.
If such a patient presents, the Centers for Disease Control and Prevention (CDC) recommends admission along with blood and, where possible, wound cultures. If in the context of pneumonia with pleural effusion, culturing pleural fluid is also important. Remember, leading edge cultures are not often positive for GAS, seemingly because GAS exotoxins are found at erythema’s leading edge, not the bacteria. The bacteria are somewhere more central in the inflammatory process. Despite not being prominent among recent iGAS cases, another scenario that could sneak up on you is the infected surgical wound as nascent iGAS.
Finally, remember that nationally increasing numbers of iGAS isolates are resistant to erythromycin and clindamycin, the latter usually recommended to reduce tissue damage in iGAS.3 So, it is important to be aware of susceptibility patterns in your locale and consider an ID consultation. My hope is that you do not see an iGAS case this year, but we all need to remain alert. With a high index of suspicion and rapid diagnosis, you can minimize long-term sequelae and potential fatalities.
While it is too early to tell how the rest of 2024 will turn out, preliminary indications are that GAS is circulating at higher than usual levels (30%-35% GAS positive throat swabs in early April 2024 in Kansas City area) and iGAS rates will likely also be relatively high, particularly if Ontario, Canada, data are any indication.4 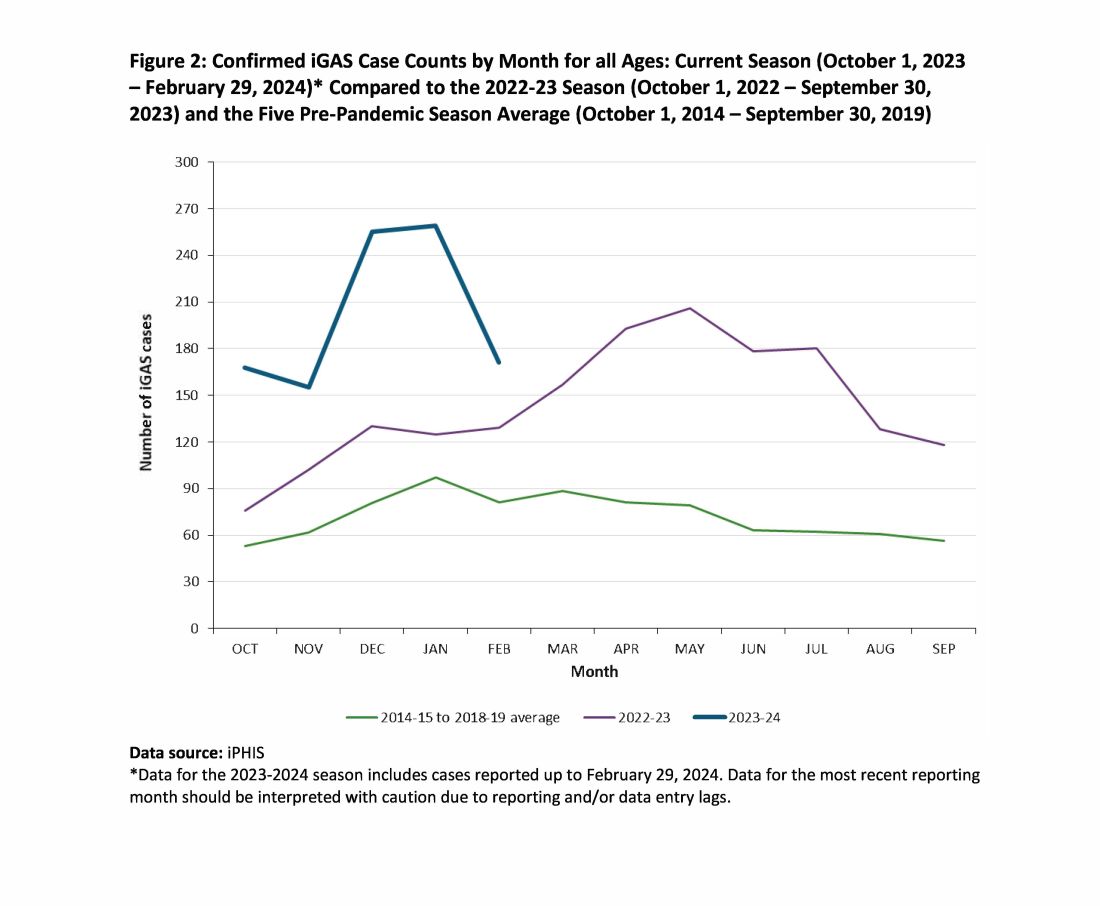
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. Current Group A Strep Activity, Centers for Disease Control and Prevention. April 2024. CDC webpage on current invasive GAS disease. April 2024.
2. Li Y et al. Expansion of Invasive Group A Streptococcus M1UK Lineage in Active Bacterial Core Surveillance, United States, 2019-2021 Emerg Infect Dis. 2023;29(10):2116-2120. doi: 10.3201/eid2910.230675.
3. Andreoni F et al. Clindamycin Affects Group A Streptococcus Virulence Factors and Improves Clinical Outcome. J Infect Dis. 2017 Jan 15;215(2):269-277. doi: 10.1093/infdis/jiw229.
4. Group A Streptococcal Disease, Invasive (iGAS), Public Health Ontario.
Working From Home: Doctors’ Options Are Not Limited to Classic Telemedicine
The appeal of working from home is undeniable. It comes with no daily commute, casual dress, and the ability to manage work-life balance more effectively.
Telemedicine is often the first thing that comes to mind when physicians think about remote medical practice. In its traditional sense, telemedicine entails live video consults, replicating the in-person experience as closely as possible, minus the hands-on component. However, this format is just one of many types of virtual care presenting opportunities to practice medicine from home.
The scope and volume of such opportunities are expanding due to technology, regulatory shifts at the state and federal levels favoring remote healthcare, and a wider move toward remote work. Virtual practice options for physicians range from full-time employment to flexible part-time positions that can be used to earn supplementary income.
Just a few of those virtual options are:
Remote Patient Monitoring
Remote patient monitoring uses technology for tracking patient health data, applicable in real-time or asynchronously, through devices ranging from specialized monitors to consumer wearables. Data are securely transmitted to healthcare providers, enabling them to guide or make treatment choices remotely. This method has proven particularly valuable in managing chronic diseases where continuous monitoring can significantly affect outcomes.
Like standard telemedicine, remote patient monitoring offers flexibility, autonomy, and the ability to work from home. It is picking up steam across the healthcare industry, especially in critical care, surgery, post-acute care, and primary care, so there are opportunities for physicians across a variety of specialties.
Online Medication Management and Text-Based Consults
Gathering necessary information for patient care decisions often doesn’t require a direct, face-to-face visit in person or by telemedicine. Clinical data can be efficiently collected through online forms, HIPAA-compliant messaging, medical record reviews, and information gathered by staff.
An approach that uses all these sources enables effective medication management for stable chronic conditions (such as hypertension), as well as straightforward but simple acute issues (such as urinary tract infections). It also is useful for quick follow-ups with patients after starting new treatments, to address questions between visits, and to give them educational material.
Some medical practices and virtual healthcare corporations have made online medication management and text-based consults the center of their business model. Part-time positions with platforms that offer this type of care let physicians fit consultations into their schedule as time permits, without committing to scheduled appointments.
eConsults
Electronic consultations, or eConsults, facilitate collaboration among healthcare professionals about complex cases without direct patient interaction.
These services operate via online platforms that support asynchronous communication and often bypass the need for a traditional referral. Typically, a primary care provider submits a query that is then assigned to a specialist. Next, the specialist reviews the information and offers recommendations for the patient’s care plan.
Major eConsult platforms such as AristaMD and RubiconMD contract with healthcare systems and medical practices. Physicians can easily join the specialist panels of these companies and complete assigned consultations from their homes or offices, paid on a per-consult basis. They should check their employment contracts to make sure such independent contract work is allowed.
Phone-Only On-Call Positions
On-call rotations for after-hour care bring with them challenges in staffing and scheduling vacations. These challenges have helped trigger as-needed or per diem on-call roles, in which a physician provides recommendations and orders over the phone without needing to visit an office or a hospital.
Examples of workplaces that employ phone-only on-call physicians include smaller jails, mental health facilities, dialysis centers, long-term care facilities, and sporting groups or events needing back-up for on-site nurses or emergency medical technicians.
While these positions can sometimes be challenging for a physician to find, they are out there. They can be a fantastic option to earn additional income through low-stress clinical work performed from home.
Supervision of Nurse Practitioners (NPs) and Physician Assistants (PAs)
In states that mandate such physician oversight, it often be conducted remotely — depending on that state’s rules, the practice type, and the scope of services being provided. This remote option introduces part-time opportunities for physicians to oversee NPs and PAs without being in the medical office. Essentially, the doctor needs to be available for phone or email consultations, complete chart reviews, and meet regularly with the provider.
Remote supervision roles are available across various types of healthcare organizations and medical practices. There also are opportunities with insurers, many of which have established NP-run, in-home member assessment programs that require remote supervision by a doctor.
Remote Medical Directorships
Medical directors are a key part of the clinician team in a wide variety of healthcare settings requiring clinical protocol oversight, regulatory compliance, and guidance for other clinicians making treatment decisions. Many directorships do not require direct patient contact and therefore are conducive to remote work, given technologies such as electronic health record and secure messaging systems.
Organizations such as emergency medical service agencies, hospice services, med spas, blood and plasma donation centers, home health agencies, and substance use disorder treatment programs increasingly rely on remote medical directorships to meet legal requirements and accreditation standards.
Although these positions are often viewed as “nonclinical,” they carry significant clinical responsibilities. Examples are developing and reviewing treatment protocols, ensuring adherence to healthcare regulations, and sometimes intervening in complex patient cases or when adverse outcomes occur.
Keeping a Role in Patient Welfare
Clearly, working from home as a physician doesn’t have to mean taking on a nonclinical job. Beyond the options already mentioned, there are numerous others — for example, working as a medical monitor for clinical trials, in utilization management for insurance companies, or in conducting independent medical exams for insurance claims. While these roles don’t involve direct patient treatment, they require similar skills and affect the quality of care.
If such remote opportunities aren’t currently available in your workplace, consider approaching your management about trying them.
Physicians who are experiencing burnout, seeking a career change, or interested in earning extra income should consider exploring more of the unconventional ways that they can practice medicine.
A version of this article appeared on Medscape.com.
The appeal of working from home is undeniable. It comes with no daily commute, casual dress, and the ability to manage work-life balance more effectively.
Telemedicine is often the first thing that comes to mind when physicians think about remote medical practice. In its traditional sense, telemedicine entails live video consults, replicating the in-person experience as closely as possible, minus the hands-on component. However, this format is just one of many types of virtual care presenting opportunities to practice medicine from home.
The scope and volume of such opportunities are expanding due to technology, regulatory shifts at the state and federal levels favoring remote healthcare, and a wider move toward remote work. Virtual practice options for physicians range from full-time employment to flexible part-time positions that can be used to earn supplementary income.
Just a few of those virtual options are:
Remote Patient Monitoring
Remote patient monitoring uses technology for tracking patient health data, applicable in real-time or asynchronously, through devices ranging from specialized monitors to consumer wearables. Data are securely transmitted to healthcare providers, enabling them to guide or make treatment choices remotely. This method has proven particularly valuable in managing chronic diseases where continuous monitoring can significantly affect outcomes.
Like standard telemedicine, remote patient monitoring offers flexibility, autonomy, and the ability to work from home. It is picking up steam across the healthcare industry, especially in critical care, surgery, post-acute care, and primary care, so there are opportunities for physicians across a variety of specialties.
Online Medication Management and Text-Based Consults
Gathering necessary information for patient care decisions often doesn’t require a direct, face-to-face visit in person or by telemedicine. Clinical data can be efficiently collected through online forms, HIPAA-compliant messaging, medical record reviews, and information gathered by staff.
An approach that uses all these sources enables effective medication management for stable chronic conditions (such as hypertension), as well as straightforward but simple acute issues (such as urinary tract infections). It also is useful for quick follow-ups with patients after starting new treatments, to address questions between visits, and to give them educational material.
Some medical practices and virtual healthcare corporations have made online medication management and text-based consults the center of their business model. Part-time positions with platforms that offer this type of care let physicians fit consultations into their schedule as time permits, without committing to scheduled appointments.
eConsults
Electronic consultations, or eConsults, facilitate collaboration among healthcare professionals about complex cases without direct patient interaction.
These services operate via online platforms that support asynchronous communication and often bypass the need for a traditional referral. Typically, a primary care provider submits a query that is then assigned to a specialist. Next, the specialist reviews the information and offers recommendations for the patient’s care plan.
Major eConsult platforms such as AristaMD and RubiconMD contract with healthcare systems and medical practices. Physicians can easily join the specialist panels of these companies and complete assigned consultations from their homes or offices, paid on a per-consult basis. They should check their employment contracts to make sure such independent contract work is allowed.
Phone-Only On-Call Positions
On-call rotations for after-hour care bring with them challenges in staffing and scheduling vacations. These challenges have helped trigger as-needed or per diem on-call roles, in which a physician provides recommendations and orders over the phone without needing to visit an office or a hospital.
Examples of workplaces that employ phone-only on-call physicians include smaller jails, mental health facilities, dialysis centers, long-term care facilities, and sporting groups or events needing back-up for on-site nurses or emergency medical technicians.
While these positions can sometimes be challenging for a physician to find, they are out there. They can be a fantastic option to earn additional income through low-stress clinical work performed from home.
Supervision of Nurse Practitioners (NPs) and Physician Assistants (PAs)
In states that mandate such physician oversight, it often be conducted remotely — depending on that state’s rules, the practice type, and the scope of services being provided. This remote option introduces part-time opportunities for physicians to oversee NPs and PAs without being in the medical office. Essentially, the doctor needs to be available for phone or email consultations, complete chart reviews, and meet regularly with the provider.
Remote supervision roles are available across various types of healthcare organizations and medical practices. There also are opportunities with insurers, many of which have established NP-run, in-home member assessment programs that require remote supervision by a doctor.
Remote Medical Directorships
Medical directors are a key part of the clinician team in a wide variety of healthcare settings requiring clinical protocol oversight, regulatory compliance, and guidance for other clinicians making treatment decisions. Many directorships do not require direct patient contact and therefore are conducive to remote work, given technologies such as electronic health record and secure messaging systems.
Organizations such as emergency medical service agencies, hospice services, med spas, blood and plasma donation centers, home health agencies, and substance use disorder treatment programs increasingly rely on remote medical directorships to meet legal requirements and accreditation standards.
Although these positions are often viewed as “nonclinical,” they carry significant clinical responsibilities. Examples are developing and reviewing treatment protocols, ensuring adherence to healthcare regulations, and sometimes intervening in complex patient cases or when adverse outcomes occur.
Keeping a Role in Patient Welfare
Clearly, working from home as a physician doesn’t have to mean taking on a nonclinical job. Beyond the options already mentioned, there are numerous others — for example, working as a medical monitor for clinical trials, in utilization management for insurance companies, or in conducting independent medical exams for insurance claims. While these roles don’t involve direct patient treatment, they require similar skills and affect the quality of care.
If such remote opportunities aren’t currently available in your workplace, consider approaching your management about trying them.
Physicians who are experiencing burnout, seeking a career change, or interested in earning extra income should consider exploring more of the unconventional ways that they can practice medicine.
A version of this article appeared on Medscape.com.
The appeal of working from home is undeniable. It comes with no daily commute, casual dress, and the ability to manage work-life balance more effectively.
Telemedicine is often the first thing that comes to mind when physicians think about remote medical practice. In its traditional sense, telemedicine entails live video consults, replicating the in-person experience as closely as possible, minus the hands-on component. However, this format is just one of many types of virtual care presenting opportunities to practice medicine from home.
The scope and volume of such opportunities are expanding due to technology, regulatory shifts at the state and federal levels favoring remote healthcare, and a wider move toward remote work. Virtual practice options for physicians range from full-time employment to flexible part-time positions that can be used to earn supplementary income.
Just a few of those virtual options are:
Remote Patient Monitoring
Remote patient monitoring uses technology for tracking patient health data, applicable in real-time or asynchronously, through devices ranging from specialized monitors to consumer wearables. Data are securely transmitted to healthcare providers, enabling them to guide or make treatment choices remotely. This method has proven particularly valuable in managing chronic diseases where continuous monitoring can significantly affect outcomes.
Like standard telemedicine, remote patient monitoring offers flexibility, autonomy, and the ability to work from home. It is picking up steam across the healthcare industry, especially in critical care, surgery, post-acute care, and primary care, so there are opportunities for physicians across a variety of specialties.
Online Medication Management and Text-Based Consults
Gathering necessary information for patient care decisions often doesn’t require a direct, face-to-face visit in person or by telemedicine. Clinical data can be efficiently collected through online forms, HIPAA-compliant messaging, medical record reviews, and information gathered by staff.
An approach that uses all these sources enables effective medication management for stable chronic conditions (such as hypertension), as well as straightforward but simple acute issues (such as urinary tract infections). It also is useful for quick follow-ups with patients after starting new treatments, to address questions between visits, and to give them educational material.
Some medical practices and virtual healthcare corporations have made online medication management and text-based consults the center of their business model. Part-time positions with platforms that offer this type of care let physicians fit consultations into their schedule as time permits, without committing to scheduled appointments.
eConsults
Electronic consultations, or eConsults, facilitate collaboration among healthcare professionals about complex cases without direct patient interaction.
These services operate via online platforms that support asynchronous communication and often bypass the need for a traditional referral. Typically, a primary care provider submits a query that is then assigned to a specialist. Next, the specialist reviews the information and offers recommendations for the patient’s care plan.
Major eConsult platforms such as AristaMD and RubiconMD contract with healthcare systems and medical practices. Physicians can easily join the specialist panels of these companies and complete assigned consultations from their homes or offices, paid on a per-consult basis. They should check their employment contracts to make sure such independent contract work is allowed.
Phone-Only On-Call Positions
On-call rotations for after-hour care bring with them challenges in staffing and scheduling vacations. These challenges have helped trigger as-needed or per diem on-call roles, in which a physician provides recommendations and orders over the phone without needing to visit an office or a hospital.
Examples of workplaces that employ phone-only on-call physicians include smaller jails, mental health facilities, dialysis centers, long-term care facilities, and sporting groups or events needing back-up for on-site nurses or emergency medical technicians.
While these positions can sometimes be challenging for a physician to find, they are out there. They can be a fantastic option to earn additional income through low-stress clinical work performed from home.
Supervision of Nurse Practitioners (NPs) and Physician Assistants (PAs)
In states that mandate such physician oversight, it often be conducted remotely — depending on that state’s rules, the practice type, and the scope of services being provided. This remote option introduces part-time opportunities for physicians to oversee NPs and PAs without being in the medical office. Essentially, the doctor needs to be available for phone or email consultations, complete chart reviews, and meet regularly with the provider.
Remote supervision roles are available across various types of healthcare organizations and medical practices. There also are opportunities with insurers, many of which have established NP-run, in-home member assessment programs that require remote supervision by a doctor.
Remote Medical Directorships
Medical directors are a key part of the clinician team in a wide variety of healthcare settings requiring clinical protocol oversight, regulatory compliance, and guidance for other clinicians making treatment decisions. Many directorships do not require direct patient contact and therefore are conducive to remote work, given technologies such as electronic health record and secure messaging systems.
Organizations such as emergency medical service agencies, hospice services, med spas, blood and plasma donation centers, home health agencies, and substance use disorder treatment programs increasingly rely on remote medical directorships to meet legal requirements and accreditation standards.
Although these positions are often viewed as “nonclinical,” they carry significant clinical responsibilities. Examples are developing and reviewing treatment protocols, ensuring adherence to healthcare regulations, and sometimes intervening in complex patient cases or when adverse outcomes occur.
Keeping a Role in Patient Welfare
Clearly, working from home as a physician doesn’t have to mean taking on a nonclinical job. Beyond the options already mentioned, there are numerous others — for example, working as a medical monitor for clinical trials, in utilization management for insurance companies, or in conducting independent medical exams for insurance claims. While these roles don’t involve direct patient treatment, they require similar skills and affect the quality of care.
If such remote opportunities aren’t currently available in your workplace, consider approaching your management about trying them.
Physicians who are experiencing burnout, seeking a career change, or interested in earning extra income should consider exploring more of the unconventional ways that they can practice medicine.
A version of this article appeared on Medscape.com.
Antibiotics of Little Benefit in Lower Respiratory Tract Infection
Antibiotics had no measurable effect on the severity or duration of coughs due to acute lower respiratory tract infection (LRTI, or acute bronchitis), a large prospective study found.
In fact, those receiving an antibiotic in the primary- and urgent-care setting had a small but significant increase in overall length of illness (17.5 vs 15.9 days; P = .05) — largely because patients with longer illness before the index visit were more likely to receive these drugs. The study adds further support for reducing the prescription of antibiotics for LRTIs.
“Importantly, the pathogen data demonstrated that the length of time until illness resolution for those with bacterial infection was the same as for those not receiving an antibiotic versus those receiving one (17.3 vs 17.4 days),” researchers led by Daniel J. Merenstein, MD, a professor and director of research programs, family medicine, at Georgetown University Medical Center in Washington, wrote in the Journal of General Internal Medicine (doi: 10.1007/s11606-024-08758-y).
Patients believed an antibiotic would shorten their illness by an average of about 4 days, from 13.4 days to 9.7 days, whereas the average duration of all coughs was more than 2 weeks regardless of pathogen type or receipt of an antibiotic.
“Patients had unrealistic expectations regarding the duration of LRTI and the effect of antibiotics, which should be the target of antibiotic stewardship efforts,” the group wrote.
LRTIs can, however, be dangerous, with 3%-5% progressing to pneumonia, “but not everyone has easy access at an initial visit to an x-ray, which may be the reason clinicians still give antibiotics without any other evidence of a bacterial infection,” Dr. Merenstein said in a news release. “Patients have come to expect antibiotics for a cough, even if it doesn’t help. Basic symptom-relieving medications plus time bring a resolution to most people’s infections.”
The authors noted that cough is the most common reason for an ambulatory care visit, accounting for 2.7 million outpatient visits and more than 4 million emergency department visits annually.
Risks
Overuse of antibiotics can result in dizziness, nausea, diarrhea, and rash, along with a roughly 4% chance of serious adverse effects including anaphylaxis; Stevens-Johnson syndrome, a serious skin and mucous membrane disorder; and Clostridioides difficile-associated diarrhea.
An estimated half of all antibiotic prescriptions for acute respiratory conditions are unnecessary. Before the COVID-19 pandemic, antibiotics were prescribed about 70% of the time for a diagnosis of uncomplicated cough and LRTI. The viral pandemic did not change this practice according to a meta-analysis of 130 studies showing that 78% of COVID-19 patients were prescribed an antibiotic.
The study
The study looked at a cohort of 718 patients, with a mean age of 38.9 years, 65.3% female, of whom 207 received an antibiotic and 511 did not. Of those with baseline data, 29% had an antibiotic prescribed at baseline, the most common (in 85%) being amoxicillin-clavulanate, azithromycin, doxycycline, and amoxicillin. Antibiotics had no effect on the duration or overall severity of cough in viral, bacterial, or mixed infections. Receipt of an antibiotic did, however, reduce the likelihood of a follow-up visit: 14.1% vs 8.2% (adjusted odds ratio, 0.47; 95% confidence interval, 0.26-0.84) — perhaps because it removed the motivation for seeking another consultation. Antibiotic recipients were more likely to receive a systemic corticosteroid (31.9% vs 4.5%, P <.001) and were also more likely to receive an albuterol inhaler (22.7% vs 7.6%, P <.001).
Jeffrey A. Linder, MD, MPH, a primary care physician and chief of internal medicine and geriatrics at Northwestern University Feinberg School of Medicine in Chicago, agrees that in the vast majority of LRTIs — usually acute bronchitis — antibiotics do not speed the healing process. “Forty years of research show that antibiotics do not make acute bronchitis go away any faster,” Dr. Linder, who was not involved in the current study, said in an interview. “There’s even growing evidence that a lot of pneumonia is viral as well, and 10 or 20 years from now we may often not be giving antibiotics for pneumonia because we’ll be able to see better if it’s caused by a virus.”
A large 2018 review by Dr. Linder and associates reported that 46% of antibiotics were prescribed without any infection-related diagnosis code and 20% without an office visit.
Dr. Linder routinely informs patients requesting an antibiotic about the risks of putting an ineffective chemical into their body. “I stress that it can cause rash and other allergic reactions, and even promote C diff infection,” he said. “And I also say it messes with the good bacteria in the microbiome, and they usually come around.”
Patients need to know, Dr. Linder added, that the normal course of healing the respiratory tract after acute bronchitis takes weeks. While a wet cough with sputum or phlegm will last a few days, it’s replaced with a dry annoying cough that persists for up to 3 weeks. “As long as they’re feeling generally better, that cough is normal,” he said. “A virus has run roughshod over their airways and they need a long time to heal and the cough is part of the healing process. Think how long it takes to heal a cut on a finger.”
In an era of escalating antimicrobial resistance fueled by antibiotic overuse, it’s become increasingly important to reserve antibiotics for necessary cases. According to a recent World Health Organization call to action, “Uncontrolled antimicrobial resistance is expected to lower life expectancy and lead to unprecedented health expenditure and economic losses.”
That said, there is important clinical work to be done to determine if there is a limited role for antibiotics in patients with cough, perhaps based on age and baseline severity. “Serious cough symptoms and how to treat them properly needs to be studied more, perhaps in a randomized clinical trial as this study was observational and there haven’t been any randomized trials looking at this issue since about 2012,” Dr. Merenstein said.
This research was funded by the Agency for Healthcare Research and Quality. The authors have no conflicts of interest to declare. Dr. Linder reported stock ownership in pharmaceutical companies but none that make antibiotics or other infectious disease drugs.
Antibiotics had no measurable effect on the severity or duration of coughs due to acute lower respiratory tract infection (LRTI, or acute bronchitis), a large prospective study found.
In fact, those receiving an antibiotic in the primary- and urgent-care setting had a small but significant increase in overall length of illness (17.5 vs 15.9 days; P = .05) — largely because patients with longer illness before the index visit were more likely to receive these drugs. The study adds further support for reducing the prescription of antibiotics for LRTIs.
“Importantly, the pathogen data demonstrated that the length of time until illness resolution for those with bacterial infection was the same as for those not receiving an antibiotic versus those receiving one (17.3 vs 17.4 days),” researchers led by Daniel J. Merenstein, MD, a professor and director of research programs, family medicine, at Georgetown University Medical Center in Washington, wrote in the Journal of General Internal Medicine (doi: 10.1007/s11606-024-08758-y).
Patients believed an antibiotic would shorten their illness by an average of about 4 days, from 13.4 days to 9.7 days, whereas the average duration of all coughs was more than 2 weeks regardless of pathogen type or receipt of an antibiotic.
“Patients had unrealistic expectations regarding the duration of LRTI and the effect of antibiotics, which should be the target of antibiotic stewardship efforts,” the group wrote.
LRTIs can, however, be dangerous, with 3%-5% progressing to pneumonia, “but not everyone has easy access at an initial visit to an x-ray, which may be the reason clinicians still give antibiotics without any other evidence of a bacterial infection,” Dr. Merenstein said in a news release. “Patients have come to expect antibiotics for a cough, even if it doesn’t help. Basic symptom-relieving medications plus time bring a resolution to most people’s infections.”
The authors noted that cough is the most common reason for an ambulatory care visit, accounting for 2.7 million outpatient visits and more than 4 million emergency department visits annually.
Risks
Overuse of antibiotics can result in dizziness, nausea, diarrhea, and rash, along with a roughly 4% chance of serious adverse effects including anaphylaxis; Stevens-Johnson syndrome, a serious skin and mucous membrane disorder; and Clostridioides difficile-associated diarrhea.
An estimated half of all antibiotic prescriptions for acute respiratory conditions are unnecessary. Before the COVID-19 pandemic, antibiotics were prescribed about 70% of the time for a diagnosis of uncomplicated cough and LRTI. The viral pandemic did not change this practice according to a meta-analysis of 130 studies showing that 78% of COVID-19 patients were prescribed an antibiotic.
The study
The study looked at a cohort of 718 patients, with a mean age of 38.9 years, 65.3% female, of whom 207 received an antibiotic and 511 did not. Of those with baseline data, 29% had an antibiotic prescribed at baseline, the most common (in 85%) being amoxicillin-clavulanate, azithromycin, doxycycline, and amoxicillin. Antibiotics had no effect on the duration or overall severity of cough in viral, bacterial, or mixed infections. Receipt of an antibiotic did, however, reduce the likelihood of a follow-up visit: 14.1% vs 8.2% (adjusted odds ratio, 0.47; 95% confidence interval, 0.26-0.84) — perhaps because it removed the motivation for seeking another consultation. Antibiotic recipients were more likely to receive a systemic corticosteroid (31.9% vs 4.5%, P <.001) and were also more likely to receive an albuterol inhaler (22.7% vs 7.6%, P <.001).
Jeffrey A. Linder, MD, MPH, a primary care physician and chief of internal medicine and geriatrics at Northwestern University Feinberg School of Medicine in Chicago, agrees that in the vast majority of LRTIs — usually acute bronchitis — antibiotics do not speed the healing process. “Forty years of research show that antibiotics do not make acute bronchitis go away any faster,” Dr. Linder, who was not involved in the current study, said in an interview. “There’s even growing evidence that a lot of pneumonia is viral as well, and 10 or 20 years from now we may often not be giving antibiotics for pneumonia because we’ll be able to see better if it’s caused by a virus.”
A large 2018 review by Dr. Linder and associates reported that 46% of antibiotics were prescribed without any infection-related diagnosis code and 20% without an office visit.
Dr. Linder routinely informs patients requesting an antibiotic about the risks of putting an ineffective chemical into their body. “I stress that it can cause rash and other allergic reactions, and even promote C diff infection,” he said. “And I also say it messes with the good bacteria in the microbiome, and they usually come around.”
Patients need to know, Dr. Linder added, that the normal course of healing the respiratory tract after acute bronchitis takes weeks. While a wet cough with sputum or phlegm will last a few days, it’s replaced with a dry annoying cough that persists for up to 3 weeks. “As long as they’re feeling generally better, that cough is normal,” he said. “A virus has run roughshod over their airways and they need a long time to heal and the cough is part of the healing process. Think how long it takes to heal a cut on a finger.”
In an era of escalating antimicrobial resistance fueled by antibiotic overuse, it’s become increasingly important to reserve antibiotics for necessary cases. According to a recent World Health Organization call to action, “Uncontrolled antimicrobial resistance is expected to lower life expectancy and lead to unprecedented health expenditure and economic losses.”
That said, there is important clinical work to be done to determine if there is a limited role for antibiotics in patients with cough, perhaps based on age and baseline severity. “Serious cough symptoms and how to treat them properly needs to be studied more, perhaps in a randomized clinical trial as this study was observational and there haven’t been any randomized trials looking at this issue since about 2012,” Dr. Merenstein said.
This research was funded by the Agency for Healthcare Research and Quality. The authors have no conflicts of interest to declare. Dr. Linder reported stock ownership in pharmaceutical companies but none that make antibiotics or other infectious disease drugs.
Antibiotics had no measurable effect on the severity or duration of coughs due to acute lower respiratory tract infection (LRTI, or acute bronchitis), a large prospective study found.
In fact, those receiving an antibiotic in the primary- and urgent-care setting had a small but significant increase in overall length of illness (17.5 vs 15.9 days; P = .05) — largely because patients with longer illness before the index visit were more likely to receive these drugs. The study adds further support for reducing the prescription of antibiotics for LRTIs.
“Importantly, the pathogen data demonstrated that the length of time until illness resolution for those with bacterial infection was the same as for those not receiving an antibiotic versus those receiving one (17.3 vs 17.4 days),” researchers led by Daniel J. Merenstein, MD, a professor and director of research programs, family medicine, at Georgetown University Medical Center in Washington, wrote in the Journal of General Internal Medicine (doi: 10.1007/s11606-024-08758-y).
Patients believed an antibiotic would shorten their illness by an average of about 4 days, from 13.4 days to 9.7 days, whereas the average duration of all coughs was more than 2 weeks regardless of pathogen type or receipt of an antibiotic.
“Patients had unrealistic expectations regarding the duration of LRTI and the effect of antibiotics, which should be the target of antibiotic stewardship efforts,” the group wrote.
LRTIs can, however, be dangerous, with 3%-5% progressing to pneumonia, “but not everyone has easy access at an initial visit to an x-ray, which may be the reason clinicians still give antibiotics without any other evidence of a bacterial infection,” Dr. Merenstein said in a news release. “Patients have come to expect antibiotics for a cough, even if it doesn’t help. Basic symptom-relieving medications plus time bring a resolution to most people’s infections.”
The authors noted that cough is the most common reason for an ambulatory care visit, accounting for 2.7 million outpatient visits and more than 4 million emergency department visits annually.
Risks
Overuse of antibiotics can result in dizziness, nausea, diarrhea, and rash, along with a roughly 4% chance of serious adverse effects including anaphylaxis; Stevens-Johnson syndrome, a serious skin and mucous membrane disorder; and Clostridioides difficile-associated diarrhea.
An estimated half of all antibiotic prescriptions for acute respiratory conditions are unnecessary. Before the COVID-19 pandemic, antibiotics were prescribed about 70% of the time for a diagnosis of uncomplicated cough and LRTI. The viral pandemic did not change this practice according to a meta-analysis of 130 studies showing that 78% of COVID-19 patients were prescribed an antibiotic.
The study
The study looked at a cohort of 718 patients, with a mean age of 38.9 years, 65.3% female, of whom 207 received an antibiotic and 511 did not. Of those with baseline data, 29% had an antibiotic prescribed at baseline, the most common (in 85%) being amoxicillin-clavulanate, azithromycin, doxycycline, and amoxicillin. Antibiotics had no effect on the duration or overall severity of cough in viral, bacterial, or mixed infections. Receipt of an antibiotic did, however, reduce the likelihood of a follow-up visit: 14.1% vs 8.2% (adjusted odds ratio, 0.47; 95% confidence interval, 0.26-0.84) — perhaps because it removed the motivation for seeking another consultation. Antibiotic recipients were more likely to receive a systemic corticosteroid (31.9% vs 4.5%, P <.001) and were also more likely to receive an albuterol inhaler (22.7% vs 7.6%, P <.001).
Jeffrey A. Linder, MD, MPH, a primary care physician and chief of internal medicine and geriatrics at Northwestern University Feinberg School of Medicine in Chicago, agrees that in the vast majority of LRTIs — usually acute bronchitis — antibiotics do not speed the healing process. “Forty years of research show that antibiotics do not make acute bronchitis go away any faster,” Dr. Linder, who was not involved in the current study, said in an interview. “There’s even growing evidence that a lot of pneumonia is viral as well, and 10 or 20 years from now we may often not be giving antibiotics for pneumonia because we’ll be able to see better if it’s caused by a virus.”
A large 2018 review by Dr. Linder and associates reported that 46% of antibiotics were prescribed without any infection-related diagnosis code and 20% without an office visit.
Dr. Linder routinely informs patients requesting an antibiotic about the risks of putting an ineffective chemical into their body. “I stress that it can cause rash and other allergic reactions, and even promote C diff infection,” he said. “And I also say it messes with the good bacteria in the microbiome, and they usually come around.”
Patients need to know, Dr. Linder added, that the normal course of healing the respiratory tract after acute bronchitis takes weeks. While a wet cough with sputum or phlegm will last a few days, it’s replaced with a dry annoying cough that persists for up to 3 weeks. “As long as they’re feeling generally better, that cough is normal,” he said. “A virus has run roughshod over their airways and they need a long time to heal and the cough is part of the healing process. Think how long it takes to heal a cut on a finger.”
In an era of escalating antimicrobial resistance fueled by antibiotic overuse, it’s become increasingly important to reserve antibiotics for necessary cases. According to a recent World Health Organization call to action, “Uncontrolled antimicrobial resistance is expected to lower life expectancy and lead to unprecedented health expenditure and economic losses.”
That said, there is important clinical work to be done to determine if there is a limited role for antibiotics in patients with cough, perhaps based on age and baseline severity. “Serious cough symptoms and how to treat them properly needs to be studied more, perhaps in a randomized clinical trial as this study was observational and there haven’t been any randomized trials looking at this issue since about 2012,” Dr. Merenstein said.
This research was funded by the Agency for Healthcare Research and Quality. The authors have no conflicts of interest to declare. Dr. Linder reported stock ownership in pharmaceutical companies but none that make antibiotics or other infectious disease drugs.
FROM JOURNAL OF GENERAL INTERNAL MEDICINE



