User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
How These Young MDs Impressed the Hell Out of Their Bosses
Safe to say that anyone undertaking the physician journey does so with intense motivation and book smarts. Still, it can be incredibly hard to stand out. Everyone’s a go-getter, but what’s the X factor?
Here’s what they said ...
Lesson #1: Never Be Scared to Ask
Brien Barnewolt, MD, chairman and chief of the Department of Emergency Medicine at Tufts Medical Center, was very much surprised when a resident named Scott G. Weiner did something unexpected: Go after a job in the fall of his junior year residency instead of following the typical senior year trajectory.
“It’s very unusual for a trainee to apply for a job virtually a year ahead of schedule. But he knew what he wanted,” said Dr. Barnewolt. “I’d never had anybody come to me in that same scenario, and I’ve been doing this a long time.”
Under normal circumstances it would’ve been easy for Dr. Barnewolt to say no. But the unexpected request made him and his colleagues take a closer look, and they were impressed with Dr. Weiner’s skills. That, paired with his ambition and demeanor, compelled them to offer him an early job. But there’s more.
As the next year approached, Dr. Weiner explained he had an opportunity to work in emergency medicine in Tuscany and asked if he could take a 1-year delayed start for the position he applied a year early for.
The department held his position, and upon his return, Dr. Weiner made a lasting impact at Tufts before eventually moving on. “He outgrew us, which is nice to see,” Dr. Barnewolt said. (Dr. Weiner is currently McGraw Distinguished Chair in Emergency Medicine at Brigham and Women’s Hospital and associate professor at Harvard Medical School.)
Bottom line: Why did Dr. Barnewolt and his colleagues do so much to accommodate a young candidate? Yes, Dr. Weiner was talented, but he was also up-front about his ambitions from the get-go. Dr. Barnewolt said that kind of initiative can only be looked at positively.
“My advice would be, if you see an opportunity or a potential place where you might want to work, put out those feelers, start those conversations,” he said. “It’s not too early, especially in certain specialties, where the job market is very tight. Then, when circumstances change, be open about it and have that conversation. The worst that somebody can say is no, so it never hurts to be honest and open about where you want to go and what you want to be.”
Lesson #2: Chase Your Passion ‘Relentlessly’
Vance G. Fowler, MD, MHS, an infectious disease specialist at Duke University School of Medicine, runs a laboratory that researches methicillin-resistant Staphylococcus aureus (MRSA). Over the years, he’s mentored many doctors but understands the ambitions of young trainees don’t always align with the little free time that they have. “Many of them drop away when you give them a [side] project,” he said.
So when Tori Kinamon asked him to work on an MRSA project — in her first year — he gave her one that focused on researching vertebral osteomyelitis, a bone infection that can coincide with S aureus. What Dr. Fowler didn’t know: Kinamon (now MD) had been a competitive gymnast at Brown and battled her own life-threatening infection with MRSA.
“To my absolute astonishment, not only did she stick to it, but she was able to compile a presentation on the science and gave an oral presentation within a year of walking in the door,” said Dr. Fowler.
She went on to lead an initiative between the National Institutes of Health and US Food and Drug Administration to create endpoints for clinical drug trials, all of which occurred before starting her residency, which she’s about to embark upon.
Dr. Kinamon’s a good example, he said, of what happens when you add genuine passion to book smarts. Those who do always stand out because you can’t fake that. “Find your passion, and then chase it down relentlessly,” he said. “Once you’ve found your passion, things get easy because it stops being work and it starts being something else.”
If you haven’t identified a focus area, Dr. Fowler said to “be agnostic and observant. Keep your eyes open and your options open because you may surprise yourself. It may turn out that you end up liking something a whole lot more than you thought you did.”
Lesson #3: When You Say You’ve Always Wanted to Do Something, Do Something
As the chief of pulmonary and critical care medicine at the Northwestern Medicine Canning Thoracic Institute, Scott Budinger, MD, often hears lip service from doctors who want to put their skills to use in their local communities. One of his students actually did it.
Justin Fiala, MD, a pulmonary, critical care, and sleep specialist at Northwestern Medicine, joined Northwestern as a pulmonary fellow with a big interest in addressing health equity issues.
Dr. Fiala began volunteering with CommunityHealth during his fellowship and saw that many patients of the free Chicago-area clinic needed help with sleep disorders. He launched the organization’s first sleep clinic and its Patient-Centered Apnea Protocols Initiative.
“He developed a plan with some of the partners of the sleep apnea equipment to do home sleep testing for these patients that’s free of cost,” said Dr. Budinger.
Dr. Fiala goes in on Saturdays and runs a free clinic conducting sleep studies for patients and outfits them with devices that they need to improve their conditions, said Dr. Budinger.
“And these patients are the severest of the severe patients,” he said. “These are people that have severe sleep apnea that are driving around the roads, oftentimes don’t have insurance because they’re also precluded from having auto insurance. So, this is really something that not just benefits these patients but benefits our whole community.”
The fact that Dr. Fiala followed through on something that all doctors aspire to do — and in the middle of a very busy training program — is something that Dr. Budinger said makes him stand out in a big way.
“If you talk to any of our trainees or young faculty, everybody’s interested in addressing the issue of health disparities,” said Dr. Budinger. “Justin looked at that and said, ‘Well, you know, I’m not interested in talking about it. What can I do about this problem? And how can I actually get boots on the ground and help?’ That requires a big activation energy that many people don’t have.”
Lesson #4: Be a People-Person and a Patient-Person
When hiring employees at American Family Care in Portland, Oregon, Andrew Miller, MD, director of provider training, is always on the lookout for young MDs with emotional intelligence and a good bedside manner. He has been recently blown away, however, by a young physician’s assistant named Joseph Van Bindsbergen, PA-C, who was described as “all-around wonderful” during his reference check.
“Having less than 6 months of experience out of school, he is our highest ranked provider, whether it’s a nurse practitioner, PA, or doctor, in terms of patient satisfaction,” said Dr. Miller. The young PA has an “unprecedented perfect score” on his NPS rating.
Why? Patients said they’ve never felt as heard as they felt with Van Bindsbergen.
“That’s the thing I think that the up-and-coming providers should be focusing on is making your patients feel heard,” explained Dr. Miller. Van Bindsbergen is great at building rapport with a patient, whether they are 6 or 96. “He doesn’t just ask about sore throat symptoms. He asks, ‘what is the impact on your life of the sore throat? How does it affect your family or your work? What do you think this could be besides just strep? What are your concerns?’ ”
Dr. Miller said the magic of Van Bindsbergen is that he has an innate ability to look at patients “not just as a diagnosis but as a person, which they love.”
Lesson #5: Remember to Make That Difference With Each Patient
Doctors are used to swooping in and seeing a patient, ordering further testing if needed, and then moving on to the next patient. But one young intern at the start of his medical career broke this mold by giving a very anxious patient some much-needed support.
“There was a resident who was working overnight, and this poor young woman came in who had a new diagnosis of an advanced illness and a lot of anxiety around her condition, the newness of it, and the impact this is going to have on her family and her life,” said Elizabeth Horn Prsic, MD, assistant professor at Yale School of Medicine and firm chief for medical oncology and the director of Adult Inpatient Palliative Care.
Dr. Prsic found out the next morning that this trainee accompanied the patient to the MRI and held her hand as much as he was allowed to throughout the entire experience. “I was like, ‘wait you went down with her to radiology?’ And he’s like, ‘Yes, I was there the whole time,’ ” she recalled.
This gesture not only helped the patient feel calmer after receiving a potentially life-altering diagnosis but also helped ensure the test results were as clear as possible.
“If the study is not done well and a patient is moving or uncomfortable, it has to be stopped early or paused,” said Dr. Prsic. “Then the study is not very useful. In situations like these, medical decisions may be made based on imperfect data. The fact that we had this full complete good quality scan helped us get the care that she needed in a much timelier manner to help her and to move along the care that she that was medically appropriate for her.”
Dr. Prsic got emotional reflecting on the experience. Working at Yale, she saw a ton of intelligent doctors come through the ranks. But this gesture, she said, should serve as a reminder that “you don’t need to be the smartest person in the room to just be there for a patient. It was pure empathic presence and human connection. It gave me hope in the next generation of physicians.”
A version of this article appeared on Medscape.com.
Safe to say that anyone undertaking the physician journey does so with intense motivation and book smarts. Still, it can be incredibly hard to stand out. Everyone’s a go-getter, but what’s the X factor?
Here’s what they said ...
Lesson #1: Never Be Scared to Ask
Brien Barnewolt, MD, chairman and chief of the Department of Emergency Medicine at Tufts Medical Center, was very much surprised when a resident named Scott G. Weiner did something unexpected: Go after a job in the fall of his junior year residency instead of following the typical senior year trajectory.
“It’s very unusual for a trainee to apply for a job virtually a year ahead of schedule. But he knew what he wanted,” said Dr. Barnewolt. “I’d never had anybody come to me in that same scenario, and I’ve been doing this a long time.”
Under normal circumstances it would’ve been easy for Dr. Barnewolt to say no. But the unexpected request made him and his colleagues take a closer look, and they were impressed with Dr. Weiner’s skills. That, paired with his ambition and demeanor, compelled them to offer him an early job. But there’s more.
As the next year approached, Dr. Weiner explained he had an opportunity to work in emergency medicine in Tuscany and asked if he could take a 1-year delayed start for the position he applied a year early for.
The department held his position, and upon his return, Dr. Weiner made a lasting impact at Tufts before eventually moving on. “He outgrew us, which is nice to see,” Dr. Barnewolt said. (Dr. Weiner is currently McGraw Distinguished Chair in Emergency Medicine at Brigham and Women’s Hospital and associate professor at Harvard Medical School.)
Bottom line: Why did Dr. Barnewolt and his colleagues do so much to accommodate a young candidate? Yes, Dr. Weiner was talented, but he was also up-front about his ambitions from the get-go. Dr. Barnewolt said that kind of initiative can only be looked at positively.
“My advice would be, if you see an opportunity or a potential place where you might want to work, put out those feelers, start those conversations,” he said. “It’s not too early, especially in certain specialties, where the job market is very tight. Then, when circumstances change, be open about it and have that conversation. The worst that somebody can say is no, so it never hurts to be honest and open about where you want to go and what you want to be.”
Lesson #2: Chase Your Passion ‘Relentlessly’
Vance G. Fowler, MD, MHS, an infectious disease specialist at Duke University School of Medicine, runs a laboratory that researches methicillin-resistant Staphylococcus aureus (MRSA). Over the years, he’s mentored many doctors but understands the ambitions of young trainees don’t always align with the little free time that they have. “Many of them drop away when you give them a [side] project,” he said.
So when Tori Kinamon asked him to work on an MRSA project — in her first year — he gave her one that focused on researching vertebral osteomyelitis, a bone infection that can coincide with S aureus. What Dr. Fowler didn’t know: Kinamon (now MD) had been a competitive gymnast at Brown and battled her own life-threatening infection with MRSA.
“To my absolute astonishment, not only did she stick to it, but she was able to compile a presentation on the science and gave an oral presentation within a year of walking in the door,” said Dr. Fowler.
She went on to lead an initiative between the National Institutes of Health and US Food and Drug Administration to create endpoints for clinical drug trials, all of which occurred before starting her residency, which she’s about to embark upon.
Dr. Kinamon’s a good example, he said, of what happens when you add genuine passion to book smarts. Those who do always stand out because you can’t fake that. “Find your passion, and then chase it down relentlessly,” he said. “Once you’ve found your passion, things get easy because it stops being work and it starts being something else.”
If you haven’t identified a focus area, Dr. Fowler said to “be agnostic and observant. Keep your eyes open and your options open because you may surprise yourself. It may turn out that you end up liking something a whole lot more than you thought you did.”
Lesson #3: When You Say You’ve Always Wanted to Do Something, Do Something
As the chief of pulmonary and critical care medicine at the Northwestern Medicine Canning Thoracic Institute, Scott Budinger, MD, often hears lip service from doctors who want to put their skills to use in their local communities. One of his students actually did it.
Justin Fiala, MD, a pulmonary, critical care, and sleep specialist at Northwestern Medicine, joined Northwestern as a pulmonary fellow with a big interest in addressing health equity issues.
Dr. Fiala began volunteering with CommunityHealth during his fellowship and saw that many patients of the free Chicago-area clinic needed help with sleep disorders. He launched the organization’s first sleep clinic and its Patient-Centered Apnea Protocols Initiative.
“He developed a plan with some of the partners of the sleep apnea equipment to do home sleep testing for these patients that’s free of cost,” said Dr. Budinger.
Dr. Fiala goes in on Saturdays and runs a free clinic conducting sleep studies for patients and outfits them with devices that they need to improve their conditions, said Dr. Budinger.
“And these patients are the severest of the severe patients,” he said. “These are people that have severe sleep apnea that are driving around the roads, oftentimes don’t have insurance because they’re also precluded from having auto insurance. So, this is really something that not just benefits these patients but benefits our whole community.”
The fact that Dr. Fiala followed through on something that all doctors aspire to do — and in the middle of a very busy training program — is something that Dr. Budinger said makes him stand out in a big way.
“If you talk to any of our trainees or young faculty, everybody’s interested in addressing the issue of health disparities,” said Dr. Budinger. “Justin looked at that and said, ‘Well, you know, I’m not interested in talking about it. What can I do about this problem? And how can I actually get boots on the ground and help?’ That requires a big activation energy that many people don’t have.”
Lesson #4: Be a People-Person and a Patient-Person
When hiring employees at American Family Care in Portland, Oregon, Andrew Miller, MD, director of provider training, is always on the lookout for young MDs with emotional intelligence and a good bedside manner. He has been recently blown away, however, by a young physician’s assistant named Joseph Van Bindsbergen, PA-C, who was described as “all-around wonderful” during his reference check.
“Having less than 6 months of experience out of school, he is our highest ranked provider, whether it’s a nurse practitioner, PA, or doctor, in terms of patient satisfaction,” said Dr. Miller. The young PA has an “unprecedented perfect score” on his NPS rating.
Why? Patients said they’ve never felt as heard as they felt with Van Bindsbergen.
“That’s the thing I think that the up-and-coming providers should be focusing on is making your patients feel heard,” explained Dr. Miller. Van Bindsbergen is great at building rapport with a patient, whether they are 6 or 96. “He doesn’t just ask about sore throat symptoms. He asks, ‘what is the impact on your life of the sore throat? How does it affect your family or your work? What do you think this could be besides just strep? What are your concerns?’ ”
Dr. Miller said the magic of Van Bindsbergen is that he has an innate ability to look at patients “not just as a diagnosis but as a person, which they love.”
Lesson #5: Remember to Make That Difference With Each Patient
Doctors are used to swooping in and seeing a patient, ordering further testing if needed, and then moving on to the next patient. But one young intern at the start of his medical career broke this mold by giving a very anxious patient some much-needed support.
“There was a resident who was working overnight, and this poor young woman came in who had a new diagnosis of an advanced illness and a lot of anxiety around her condition, the newness of it, and the impact this is going to have on her family and her life,” said Elizabeth Horn Prsic, MD, assistant professor at Yale School of Medicine and firm chief for medical oncology and the director of Adult Inpatient Palliative Care.
Dr. Prsic found out the next morning that this trainee accompanied the patient to the MRI and held her hand as much as he was allowed to throughout the entire experience. “I was like, ‘wait you went down with her to radiology?’ And he’s like, ‘Yes, I was there the whole time,’ ” she recalled.
This gesture not only helped the patient feel calmer after receiving a potentially life-altering diagnosis but also helped ensure the test results were as clear as possible.
“If the study is not done well and a patient is moving or uncomfortable, it has to be stopped early or paused,” said Dr. Prsic. “Then the study is not very useful. In situations like these, medical decisions may be made based on imperfect data. The fact that we had this full complete good quality scan helped us get the care that she needed in a much timelier manner to help her and to move along the care that she that was medically appropriate for her.”
Dr. Prsic got emotional reflecting on the experience. Working at Yale, she saw a ton of intelligent doctors come through the ranks. But this gesture, she said, should serve as a reminder that “you don’t need to be the smartest person in the room to just be there for a patient. It was pure empathic presence and human connection. It gave me hope in the next generation of physicians.”
A version of this article appeared on Medscape.com.
Safe to say that anyone undertaking the physician journey does so with intense motivation and book smarts. Still, it can be incredibly hard to stand out. Everyone’s a go-getter, but what’s the X factor?
Here’s what they said ...
Lesson #1: Never Be Scared to Ask
Brien Barnewolt, MD, chairman and chief of the Department of Emergency Medicine at Tufts Medical Center, was very much surprised when a resident named Scott G. Weiner did something unexpected: Go after a job in the fall of his junior year residency instead of following the typical senior year trajectory.
“It’s very unusual for a trainee to apply for a job virtually a year ahead of schedule. But he knew what he wanted,” said Dr. Barnewolt. “I’d never had anybody come to me in that same scenario, and I’ve been doing this a long time.”
Under normal circumstances it would’ve been easy for Dr. Barnewolt to say no. But the unexpected request made him and his colleagues take a closer look, and they were impressed with Dr. Weiner’s skills. That, paired with his ambition and demeanor, compelled them to offer him an early job. But there’s more.
As the next year approached, Dr. Weiner explained he had an opportunity to work in emergency medicine in Tuscany and asked if he could take a 1-year delayed start for the position he applied a year early for.
The department held his position, and upon his return, Dr. Weiner made a lasting impact at Tufts before eventually moving on. “He outgrew us, which is nice to see,” Dr. Barnewolt said. (Dr. Weiner is currently McGraw Distinguished Chair in Emergency Medicine at Brigham and Women’s Hospital and associate professor at Harvard Medical School.)
Bottom line: Why did Dr. Barnewolt and his colleagues do so much to accommodate a young candidate? Yes, Dr. Weiner was talented, but he was also up-front about his ambitions from the get-go. Dr. Barnewolt said that kind of initiative can only be looked at positively.
“My advice would be, if you see an opportunity or a potential place where you might want to work, put out those feelers, start those conversations,” he said. “It’s not too early, especially in certain specialties, where the job market is very tight. Then, when circumstances change, be open about it and have that conversation. The worst that somebody can say is no, so it never hurts to be honest and open about where you want to go and what you want to be.”
Lesson #2: Chase Your Passion ‘Relentlessly’
Vance G. Fowler, MD, MHS, an infectious disease specialist at Duke University School of Medicine, runs a laboratory that researches methicillin-resistant Staphylococcus aureus (MRSA). Over the years, he’s mentored many doctors but understands the ambitions of young trainees don’t always align with the little free time that they have. “Many of them drop away when you give them a [side] project,” he said.
So when Tori Kinamon asked him to work on an MRSA project — in her first year — he gave her one that focused on researching vertebral osteomyelitis, a bone infection that can coincide with S aureus. What Dr. Fowler didn’t know: Kinamon (now MD) had been a competitive gymnast at Brown and battled her own life-threatening infection with MRSA.
“To my absolute astonishment, not only did she stick to it, but she was able to compile a presentation on the science and gave an oral presentation within a year of walking in the door,” said Dr. Fowler.
She went on to lead an initiative between the National Institutes of Health and US Food and Drug Administration to create endpoints for clinical drug trials, all of which occurred before starting her residency, which she’s about to embark upon.
Dr. Kinamon’s a good example, he said, of what happens when you add genuine passion to book smarts. Those who do always stand out because you can’t fake that. “Find your passion, and then chase it down relentlessly,” he said. “Once you’ve found your passion, things get easy because it stops being work and it starts being something else.”
If you haven’t identified a focus area, Dr. Fowler said to “be agnostic and observant. Keep your eyes open and your options open because you may surprise yourself. It may turn out that you end up liking something a whole lot more than you thought you did.”
Lesson #3: When You Say You’ve Always Wanted to Do Something, Do Something
As the chief of pulmonary and critical care medicine at the Northwestern Medicine Canning Thoracic Institute, Scott Budinger, MD, often hears lip service from doctors who want to put their skills to use in their local communities. One of his students actually did it.
Justin Fiala, MD, a pulmonary, critical care, and sleep specialist at Northwestern Medicine, joined Northwestern as a pulmonary fellow with a big interest in addressing health equity issues.
Dr. Fiala began volunteering with CommunityHealth during his fellowship and saw that many patients of the free Chicago-area clinic needed help with sleep disorders. He launched the organization’s first sleep clinic and its Patient-Centered Apnea Protocols Initiative.
“He developed a plan with some of the partners of the sleep apnea equipment to do home sleep testing for these patients that’s free of cost,” said Dr. Budinger.
Dr. Fiala goes in on Saturdays and runs a free clinic conducting sleep studies for patients and outfits them with devices that they need to improve their conditions, said Dr. Budinger.
“And these patients are the severest of the severe patients,” he said. “These are people that have severe sleep apnea that are driving around the roads, oftentimes don’t have insurance because they’re also precluded from having auto insurance. So, this is really something that not just benefits these patients but benefits our whole community.”
The fact that Dr. Fiala followed through on something that all doctors aspire to do — and in the middle of a very busy training program — is something that Dr. Budinger said makes him stand out in a big way.
“If you talk to any of our trainees or young faculty, everybody’s interested in addressing the issue of health disparities,” said Dr. Budinger. “Justin looked at that and said, ‘Well, you know, I’m not interested in talking about it. What can I do about this problem? And how can I actually get boots on the ground and help?’ That requires a big activation energy that many people don’t have.”
Lesson #4: Be a People-Person and a Patient-Person
When hiring employees at American Family Care in Portland, Oregon, Andrew Miller, MD, director of provider training, is always on the lookout for young MDs with emotional intelligence and a good bedside manner. He has been recently blown away, however, by a young physician’s assistant named Joseph Van Bindsbergen, PA-C, who was described as “all-around wonderful” during his reference check.
“Having less than 6 months of experience out of school, he is our highest ranked provider, whether it’s a nurse practitioner, PA, or doctor, in terms of patient satisfaction,” said Dr. Miller. The young PA has an “unprecedented perfect score” on his NPS rating.
Why? Patients said they’ve never felt as heard as they felt with Van Bindsbergen.
“That’s the thing I think that the up-and-coming providers should be focusing on is making your patients feel heard,” explained Dr. Miller. Van Bindsbergen is great at building rapport with a patient, whether they are 6 or 96. “He doesn’t just ask about sore throat symptoms. He asks, ‘what is the impact on your life of the sore throat? How does it affect your family or your work? What do you think this could be besides just strep? What are your concerns?’ ”
Dr. Miller said the magic of Van Bindsbergen is that he has an innate ability to look at patients “not just as a diagnosis but as a person, which they love.”
Lesson #5: Remember to Make That Difference With Each Patient
Doctors are used to swooping in and seeing a patient, ordering further testing if needed, and then moving on to the next patient. But one young intern at the start of his medical career broke this mold by giving a very anxious patient some much-needed support.
“There was a resident who was working overnight, and this poor young woman came in who had a new diagnosis of an advanced illness and a lot of anxiety around her condition, the newness of it, and the impact this is going to have on her family and her life,” said Elizabeth Horn Prsic, MD, assistant professor at Yale School of Medicine and firm chief for medical oncology and the director of Adult Inpatient Palliative Care.
Dr. Prsic found out the next morning that this trainee accompanied the patient to the MRI and held her hand as much as he was allowed to throughout the entire experience. “I was like, ‘wait you went down with her to radiology?’ And he’s like, ‘Yes, I was there the whole time,’ ” she recalled.
This gesture not only helped the patient feel calmer after receiving a potentially life-altering diagnosis but also helped ensure the test results were as clear as possible.
“If the study is not done well and a patient is moving or uncomfortable, it has to be stopped early or paused,” said Dr. Prsic. “Then the study is not very useful. In situations like these, medical decisions may be made based on imperfect data. The fact that we had this full complete good quality scan helped us get the care that she needed in a much timelier manner to help her and to move along the care that she that was medically appropriate for her.”
Dr. Prsic got emotional reflecting on the experience. Working at Yale, she saw a ton of intelligent doctors come through the ranks. But this gesture, she said, should serve as a reminder that “you don’t need to be the smartest person in the room to just be there for a patient. It was pure empathic presence and human connection. It gave me hope in the next generation of physicians.”
A version of this article appeared on Medscape.com.
Syphilis Treatment Falls Short for Pregnant Patients
Approximately one third of pregnant individuals with syphilis were inadequately treated or not treated for syphilis despite receiving timely prenatal care, based on data from nearly 1500 patients.
Although congenital syphilis is preventable with treatment before or early in pregnancy, data from the Centers for Disease Control and Prevention (CDC) show a doubling of syphilis rates in the United States between 2018 and 2021 wrote Ayzsa Tannis, MPH, of the Centers for Disease Control and Prevention, Atlanta, and colleagues.
To better understand factors contributing to inadequate syphilis treatment during pregnancy, the researchers examined data from 1476 individuals with syphilis during pregnancy. The study population came from six jurisdictions that participated in the Surveillance for Emerging Threats to Pregnant People and Infants Network, and sources included case investigations, medical records, and links between laboratory data and vital records.
The researchers characterized the status of syphilis during pregnancy as adequate, inadequate, or not treated based on the CDC’s Sexually Transmitted Infections Treatment Guidelines, 2021. Prenatal care was defined as timely (at least 30 days prior to pregnancy outcome), nontimely (less than 30 days before pregnancy outcome), and no prenatal care. The findings were published in Obstetrics & Gynecology.
Of the 1476 individuals studied, 855 (57.9%) were adequately treated for syphilis and 621 (42.1%) were inadequately or not treated.
Overall, 82% of the study population received timely prenatal care. However, 32.1% of those who received timely prenatal care were inadequately treated, including 14.8% who received no syphilis treatment. Individuals with nontimely or no prenatal care were significantly more likely to receive inadequate or no treatment for syphilis than those who received timely care (risk ratio, 2.50 and 2.73, respectively).
The findings were consistent with previous studies of missed opportunities for prevention and treatment, the researchers noted. Factors behind nontimely treatment (less than 30 days before pregnancy outcome) may include intermittent shortages of benzathine penicillin G, the standard treatment for syphilis, as well as the lack of time and administrative support for clinicians to communicate with patients and health departments, and to expedite treatment, the researchers wrote.
The results were limited by several factors including the use of data from six US jurisdictions that may not generalize to other areas, the variations in reporting years for the different jurisdictions, and variation in mandates for syphilis screening during pregnancy, the researchers noted.
More research is needed to improve syphilis testing itself, and to develop more treatment options, the researchers concluded. Partnerships among public health, patient advocacy groups, prenatal care clinicians, and other clinicians outside the prenatal care setting also are needed for effective intervention in pregnant individuals with syphilis, they said.
The study was carried out as part of the regular work of the CDC, supported by the Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases Cooperative Agreement and through contractual mechanisms including the Local Health Department Initiative to Chickasaw Health Consulting. The researchers had no financial conflicts to disclose.
Approximately one third of pregnant individuals with syphilis were inadequately treated or not treated for syphilis despite receiving timely prenatal care, based on data from nearly 1500 patients.
Although congenital syphilis is preventable with treatment before or early in pregnancy, data from the Centers for Disease Control and Prevention (CDC) show a doubling of syphilis rates in the United States between 2018 and 2021 wrote Ayzsa Tannis, MPH, of the Centers for Disease Control and Prevention, Atlanta, and colleagues.
To better understand factors contributing to inadequate syphilis treatment during pregnancy, the researchers examined data from 1476 individuals with syphilis during pregnancy. The study population came from six jurisdictions that participated in the Surveillance for Emerging Threats to Pregnant People and Infants Network, and sources included case investigations, medical records, and links between laboratory data and vital records.
The researchers characterized the status of syphilis during pregnancy as adequate, inadequate, or not treated based on the CDC’s Sexually Transmitted Infections Treatment Guidelines, 2021. Prenatal care was defined as timely (at least 30 days prior to pregnancy outcome), nontimely (less than 30 days before pregnancy outcome), and no prenatal care. The findings were published in Obstetrics & Gynecology.
Of the 1476 individuals studied, 855 (57.9%) were adequately treated for syphilis and 621 (42.1%) were inadequately or not treated.
Overall, 82% of the study population received timely prenatal care. However, 32.1% of those who received timely prenatal care were inadequately treated, including 14.8% who received no syphilis treatment. Individuals with nontimely or no prenatal care were significantly more likely to receive inadequate or no treatment for syphilis than those who received timely care (risk ratio, 2.50 and 2.73, respectively).
The findings were consistent with previous studies of missed opportunities for prevention and treatment, the researchers noted. Factors behind nontimely treatment (less than 30 days before pregnancy outcome) may include intermittent shortages of benzathine penicillin G, the standard treatment for syphilis, as well as the lack of time and administrative support for clinicians to communicate with patients and health departments, and to expedite treatment, the researchers wrote.
The results were limited by several factors including the use of data from six US jurisdictions that may not generalize to other areas, the variations in reporting years for the different jurisdictions, and variation in mandates for syphilis screening during pregnancy, the researchers noted.
More research is needed to improve syphilis testing itself, and to develop more treatment options, the researchers concluded. Partnerships among public health, patient advocacy groups, prenatal care clinicians, and other clinicians outside the prenatal care setting also are needed for effective intervention in pregnant individuals with syphilis, they said.
The study was carried out as part of the regular work of the CDC, supported by the Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases Cooperative Agreement and through contractual mechanisms including the Local Health Department Initiative to Chickasaw Health Consulting. The researchers had no financial conflicts to disclose.
Approximately one third of pregnant individuals with syphilis were inadequately treated or not treated for syphilis despite receiving timely prenatal care, based on data from nearly 1500 patients.
Although congenital syphilis is preventable with treatment before or early in pregnancy, data from the Centers for Disease Control and Prevention (CDC) show a doubling of syphilis rates in the United States between 2018 and 2021 wrote Ayzsa Tannis, MPH, of the Centers for Disease Control and Prevention, Atlanta, and colleagues.
To better understand factors contributing to inadequate syphilis treatment during pregnancy, the researchers examined data from 1476 individuals with syphilis during pregnancy. The study population came from six jurisdictions that participated in the Surveillance for Emerging Threats to Pregnant People and Infants Network, and sources included case investigations, medical records, and links between laboratory data and vital records.
The researchers characterized the status of syphilis during pregnancy as adequate, inadequate, or not treated based on the CDC’s Sexually Transmitted Infections Treatment Guidelines, 2021. Prenatal care was defined as timely (at least 30 days prior to pregnancy outcome), nontimely (less than 30 days before pregnancy outcome), and no prenatal care. The findings were published in Obstetrics & Gynecology.
Of the 1476 individuals studied, 855 (57.9%) were adequately treated for syphilis and 621 (42.1%) were inadequately or not treated.
Overall, 82% of the study population received timely prenatal care. However, 32.1% of those who received timely prenatal care were inadequately treated, including 14.8% who received no syphilis treatment. Individuals with nontimely or no prenatal care were significantly more likely to receive inadequate or no treatment for syphilis than those who received timely care (risk ratio, 2.50 and 2.73, respectively).
The findings were consistent with previous studies of missed opportunities for prevention and treatment, the researchers noted. Factors behind nontimely treatment (less than 30 days before pregnancy outcome) may include intermittent shortages of benzathine penicillin G, the standard treatment for syphilis, as well as the lack of time and administrative support for clinicians to communicate with patients and health departments, and to expedite treatment, the researchers wrote.
The results were limited by several factors including the use of data from six US jurisdictions that may not generalize to other areas, the variations in reporting years for the different jurisdictions, and variation in mandates for syphilis screening during pregnancy, the researchers noted.
More research is needed to improve syphilis testing itself, and to develop more treatment options, the researchers concluded. Partnerships among public health, patient advocacy groups, prenatal care clinicians, and other clinicians outside the prenatal care setting also are needed for effective intervention in pregnant individuals with syphilis, they said.
The study was carried out as part of the regular work of the CDC, supported by the Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases Cooperative Agreement and through contractual mechanisms including the Local Health Department Initiative to Chickasaw Health Consulting. The researchers had no financial conflicts to disclose.
FROM OBSTETRICS & GYNECOLOGY
Federal Trade Commission Bans Noncompete Agreements, Urges More Protections for Healthcare Workers
But business groups have vowed to challenge the decision in court.
The proposed final rule passed on a 3-2 vote, with the dissenting commissioners disputing the FTC’s authority to broadly ban noncompetes.
Tensions around noncompetes have been building for years. In 2021, President Biden issued an executive order supporting measures to improve economic competition, in which he urged the FTC to consider its rulemaking authority to address noncompete clauses that unfairly limit workers’ mobility. In January 2023, per that directive, the agency proposed ending the restrictive covenants.
While the FTC estimates that the final rule will reduce healthcare costs by up to $194 billion over the next decade and increase worker earnings by $300 million annually, the ruling faces legal hurdles.
US Chamber of Commerce president and CEO Suzanne P. Clark said in a statement that the move is a “blatant power grab” that will undermine competitive business practices, adding that the Chamber will sue to block the measure.
The FTC received more than 26,000 comments on noncompetes during the public feedback period, with about 25,000 supporting the measure, said Benjamin Cady, JD, an FTC attorney.
Mr. Cady called the feedback “compelling,” citing instances of workers who were forced to commute long distances, uproot their families, or risk expensive litigation for wanting to pursue job opportunities.
For example, a comment from a physician working in Appalachia highlights the potential real-life implications of the agreements. “With hospital systems merging, providers with aggressive noncompetes must abandon the community that they serve if they [choose] to leave their employer. Healthcare providers feel trapped in their current employment situation, leading to significant burnout that can shorten their [career] longevity.”
Commissioner Alvaro Bedoya said physicians have had their lives upended by cumbersome noncompetes, often having to move out of state to practice. “A pandemic killed a million people in this country, and there are doctors who cannot work because of a noncompete,” he said.
It’s unclear whether physicians and others who work for nonprofit healthcare groups or hospitals will be covered by the new ban. FTC Commissioner Rebecca Slaughter acknowledged that the agency’s jurisdictional limitations mean that employees of “certain nonprofit organizations” may not benefit from the rule.
“We want to be transparent about the limitation and recognize there are workers, especially healthcare workers, who are bound by anticompetitive and unfair noncompete clauses, that our rule will struggle to reach,” she said. To cover nonprofit healthcare employees, Ms. Slaughter urged Congress to pass legislation banning noncompetes, such as the Workforce Mobility Act of 2021 and the Freedom to Compete Act of 2023.
The FTC final rule will take effect 120 days after it is published in the federal register, and new noncompete agreements will be banned as of this date. However, existing contracts for senior executives will remain in effect because these individuals are less likely to experience “acute harm” due to their ability to negotiate accordingly, said Mr. Cady.
States, AMA Take Aim at Noncompetes
Before the federal ban, several states had already passed legislation limiting the reach of noncompetes. According to a recent article in the Journal of the American College of Cardiology, 12 states prohibit noncompete clauses for physicians: Alabama, California, Colorado, Delaware, Massachusetts, Montana, New Hampshire, New Mexico, North Dakota, Oklahoma, Rhode Island, and South Dakota.
The remaining states allow noncompetes in some form, often excluding them for employees earning below a certain threshold. For example, in Oregon, noncompete agreements may apply to employees earning more than $113,241. Most states have provisions to adjust the threshold annually. The District of Columbia permits 2-year noncompetes for “medical specialists” earning over $250,000 annually.
Indiana employers can no longer enter into noncompete agreements with primary care providers. Other specialties may be subject to the clauses, except when the physician terminates the contract for cause or when an employer terminates the contract without cause.
Rachel Marcus, MD, a cardiologist in Washington, DC, found out how limiting her employment contract’s noncompete clause was when she wanted to leave a former position. Due to the restrictions, she told this news organization that she couldn’t work locally for a competitor for 2 years. The closest location she could seek employment without violating the agreement was Baltimore, approximately 40 miles away.
Dr. Marcus ultimately moved to another position within the same organization because of the company’s reputation for being “aggressive” in their enforcement actions.
Although the American Medical Association (AMA) does not support a total ban, its House of Delegates adopted policies last year to support the prohibition of noncompete contracts for physicians employed by for-profit or nonprofit hospitals, hospital systems, or staffing companies.
Challenges Await
The American Hospital Association, which opposed the proposed rule, called it “bad policy.” The decision “will likely be short-lived, with courts almost certain to stop it before it can do damage to hospitals’ ability to care for their patients and communities,” the association said in a statement.
To ease the transition to the new rule, the FTC also released a model language for employers to use when discussing the changes with their employees. “All employers need to do to comply with the rule is to stop enforcing existing noncompetes with workers other than senior executives and provide notice to such workers,” he said.
Dr. Marcus hopes the ban improves doctors’ lives. “Your employer is going to have to treat you better because they know that you can easily go across town to a place that has a higher salary, and your patient can go with you.”
A version of this article appeared on Medscape.com.
But business groups have vowed to challenge the decision in court.
The proposed final rule passed on a 3-2 vote, with the dissenting commissioners disputing the FTC’s authority to broadly ban noncompetes.
Tensions around noncompetes have been building for years. In 2021, President Biden issued an executive order supporting measures to improve economic competition, in which he urged the FTC to consider its rulemaking authority to address noncompete clauses that unfairly limit workers’ mobility. In January 2023, per that directive, the agency proposed ending the restrictive covenants.
While the FTC estimates that the final rule will reduce healthcare costs by up to $194 billion over the next decade and increase worker earnings by $300 million annually, the ruling faces legal hurdles.
US Chamber of Commerce president and CEO Suzanne P. Clark said in a statement that the move is a “blatant power grab” that will undermine competitive business practices, adding that the Chamber will sue to block the measure.
The FTC received more than 26,000 comments on noncompetes during the public feedback period, with about 25,000 supporting the measure, said Benjamin Cady, JD, an FTC attorney.
Mr. Cady called the feedback “compelling,” citing instances of workers who were forced to commute long distances, uproot their families, or risk expensive litigation for wanting to pursue job opportunities.
For example, a comment from a physician working in Appalachia highlights the potential real-life implications of the agreements. “With hospital systems merging, providers with aggressive noncompetes must abandon the community that they serve if they [choose] to leave their employer. Healthcare providers feel trapped in their current employment situation, leading to significant burnout that can shorten their [career] longevity.”
Commissioner Alvaro Bedoya said physicians have had their lives upended by cumbersome noncompetes, often having to move out of state to practice. “A pandemic killed a million people in this country, and there are doctors who cannot work because of a noncompete,” he said.
It’s unclear whether physicians and others who work for nonprofit healthcare groups or hospitals will be covered by the new ban. FTC Commissioner Rebecca Slaughter acknowledged that the agency’s jurisdictional limitations mean that employees of “certain nonprofit organizations” may not benefit from the rule.
“We want to be transparent about the limitation and recognize there are workers, especially healthcare workers, who are bound by anticompetitive and unfair noncompete clauses, that our rule will struggle to reach,” she said. To cover nonprofit healthcare employees, Ms. Slaughter urged Congress to pass legislation banning noncompetes, such as the Workforce Mobility Act of 2021 and the Freedom to Compete Act of 2023.
The FTC final rule will take effect 120 days after it is published in the federal register, and new noncompete agreements will be banned as of this date. However, existing contracts for senior executives will remain in effect because these individuals are less likely to experience “acute harm” due to their ability to negotiate accordingly, said Mr. Cady.
States, AMA Take Aim at Noncompetes
Before the federal ban, several states had already passed legislation limiting the reach of noncompetes. According to a recent article in the Journal of the American College of Cardiology, 12 states prohibit noncompete clauses for physicians: Alabama, California, Colorado, Delaware, Massachusetts, Montana, New Hampshire, New Mexico, North Dakota, Oklahoma, Rhode Island, and South Dakota.
The remaining states allow noncompetes in some form, often excluding them for employees earning below a certain threshold. For example, in Oregon, noncompete agreements may apply to employees earning more than $113,241. Most states have provisions to adjust the threshold annually. The District of Columbia permits 2-year noncompetes for “medical specialists” earning over $250,000 annually.
Indiana employers can no longer enter into noncompete agreements with primary care providers. Other specialties may be subject to the clauses, except when the physician terminates the contract for cause or when an employer terminates the contract without cause.
Rachel Marcus, MD, a cardiologist in Washington, DC, found out how limiting her employment contract’s noncompete clause was when she wanted to leave a former position. Due to the restrictions, she told this news organization that she couldn’t work locally for a competitor for 2 years. The closest location she could seek employment without violating the agreement was Baltimore, approximately 40 miles away.
Dr. Marcus ultimately moved to another position within the same organization because of the company’s reputation for being “aggressive” in their enforcement actions.
Although the American Medical Association (AMA) does not support a total ban, its House of Delegates adopted policies last year to support the prohibition of noncompete contracts for physicians employed by for-profit or nonprofit hospitals, hospital systems, or staffing companies.
Challenges Await
The American Hospital Association, which opposed the proposed rule, called it “bad policy.” The decision “will likely be short-lived, with courts almost certain to stop it before it can do damage to hospitals’ ability to care for their patients and communities,” the association said in a statement.
To ease the transition to the new rule, the FTC also released a model language for employers to use when discussing the changes with their employees. “All employers need to do to comply with the rule is to stop enforcing existing noncompetes with workers other than senior executives and provide notice to such workers,” he said.
Dr. Marcus hopes the ban improves doctors’ lives. “Your employer is going to have to treat you better because they know that you can easily go across town to a place that has a higher salary, and your patient can go with you.”
A version of this article appeared on Medscape.com.
But business groups have vowed to challenge the decision in court.
The proposed final rule passed on a 3-2 vote, with the dissenting commissioners disputing the FTC’s authority to broadly ban noncompetes.
Tensions around noncompetes have been building for years. In 2021, President Biden issued an executive order supporting measures to improve economic competition, in which he urged the FTC to consider its rulemaking authority to address noncompete clauses that unfairly limit workers’ mobility. In January 2023, per that directive, the agency proposed ending the restrictive covenants.
While the FTC estimates that the final rule will reduce healthcare costs by up to $194 billion over the next decade and increase worker earnings by $300 million annually, the ruling faces legal hurdles.
US Chamber of Commerce president and CEO Suzanne P. Clark said in a statement that the move is a “blatant power grab” that will undermine competitive business practices, adding that the Chamber will sue to block the measure.
The FTC received more than 26,000 comments on noncompetes during the public feedback period, with about 25,000 supporting the measure, said Benjamin Cady, JD, an FTC attorney.
Mr. Cady called the feedback “compelling,” citing instances of workers who were forced to commute long distances, uproot their families, or risk expensive litigation for wanting to pursue job opportunities.
For example, a comment from a physician working in Appalachia highlights the potential real-life implications of the agreements. “With hospital systems merging, providers with aggressive noncompetes must abandon the community that they serve if they [choose] to leave their employer. Healthcare providers feel trapped in their current employment situation, leading to significant burnout that can shorten their [career] longevity.”
Commissioner Alvaro Bedoya said physicians have had their lives upended by cumbersome noncompetes, often having to move out of state to practice. “A pandemic killed a million people in this country, and there are doctors who cannot work because of a noncompete,” he said.
It’s unclear whether physicians and others who work for nonprofit healthcare groups or hospitals will be covered by the new ban. FTC Commissioner Rebecca Slaughter acknowledged that the agency’s jurisdictional limitations mean that employees of “certain nonprofit organizations” may not benefit from the rule.
“We want to be transparent about the limitation and recognize there are workers, especially healthcare workers, who are bound by anticompetitive and unfair noncompete clauses, that our rule will struggle to reach,” she said. To cover nonprofit healthcare employees, Ms. Slaughter urged Congress to pass legislation banning noncompetes, such as the Workforce Mobility Act of 2021 and the Freedom to Compete Act of 2023.
The FTC final rule will take effect 120 days after it is published in the federal register, and new noncompete agreements will be banned as of this date. However, existing contracts for senior executives will remain in effect because these individuals are less likely to experience “acute harm” due to their ability to negotiate accordingly, said Mr. Cady.
States, AMA Take Aim at Noncompetes
Before the federal ban, several states had already passed legislation limiting the reach of noncompetes. According to a recent article in the Journal of the American College of Cardiology, 12 states prohibit noncompete clauses for physicians: Alabama, California, Colorado, Delaware, Massachusetts, Montana, New Hampshire, New Mexico, North Dakota, Oklahoma, Rhode Island, and South Dakota.
The remaining states allow noncompetes in some form, often excluding them for employees earning below a certain threshold. For example, in Oregon, noncompete agreements may apply to employees earning more than $113,241. Most states have provisions to adjust the threshold annually. The District of Columbia permits 2-year noncompetes for “medical specialists” earning over $250,000 annually.
Indiana employers can no longer enter into noncompete agreements with primary care providers. Other specialties may be subject to the clauses, except when the physician terminates the contract for cause or when an employer terminates the contract without cause.
Rachel Marcus, MD, a cardiologist in Washington, DC, found out how limiting her employment contract’s noncompete clause was when she wanted to leave a former position. Due to the restrictions, she told this news organization that she couldn’t work locally for a competitor for 2 years. The closest location she could seek employment without violating the agreement was Baltimore, approximately 40 miles away.
Dr. Marcus ultimately moved to another position within the same organization because of the company’s reputation for being “aggressive” in their enforcement actions.
Although the American Medical Association (AMA) does not support a total ban, its House of Delegates adopted policies last year to support the prohibition of noncompete contracts for physicians employed by for-profit or nonprofit hospitals, hospital systems, or staffing companies.
Challenges Await
The American Hospital Association, which opposed the proposed rule, called it “bad policy.” The decision “will likely be short-lived, with courts almost certain to stop it before it can do damage to hospitals’ ability to care for their patients and communities,” the association said in a statement.
To ease the transition to the new rule, the FTC also released a model language for employers to use when discussing the changes with their employees. “All employers need to do to comply with the rule is to stop enforcing existing noncompetes with workers other than senior executives and provide notice to such workers,” he said.
Dr. Marcus hopes the ban improves doctors’ lives. “Your employer is going to have to treat you better because they know that you can easily go across town to a place that has a higher salary, and your patient can go with you.”
A version of this article appeared on Medscape.com.
Are Women Better Doctors Than Men?
This transcript has been edited for clarity.
It’s a battle of the sexes today as we dive into a paper that makes you say, “Wow, what an interesting study” and also “Boy, am I glad I didn’t do that study.” That’s because studies like this are always somewhat fraught; they say something about medicine but also something about society — and that makes this a bit precarious. But that’s never stopped us before. So, let’s go ahead and try to answer the question: Do women make better doctors than men?
On the surface, this question seems nearly impossible to answer. It’s too broad; what does it mean to be a “better” doctor? At first blush it seems that there are just too many variables to control for here: the type of doctor, the type of patient, the clinical scenario, and so on.
But this study, “Comparison of hospital mortality and readmission rates by physician and patient sex,” which appears in Annals of Internal Medicine, uses a fairly ingenious method to cut through all the bias by leveraging two simple facts: First, hospital medicine is largely conducted by hospitalists these days; second, due to the shift-based nature of hospitalist work, the hospitalist you get when you are admitted to the hospital is pretty much random.
In other words, if you are admitted to the hospital for an acute illness and get a hospitalist as your attending, you have no control over whether it is a man or a woman. Is this a randomized trial? No, but it’s not bad.
Researchers used Medicare claims data to identify adults over age 65 who had nonelective hospital admissions throughout the United States. The claims revealed the sex of the patient and the name of the attending physician. By linking to a medical provider database, they could determine the sex of the provider.
The goal was to look at outcomes across four dyads:
- Male patient – male doctor
- Male patient – female doctor
- Female patient – male doctor
- Female patient – female doctor
The primary outcome was 30-day mortality.
I told you that focusing on hospitalists produces some pseudorandomization, but let’s look at the data to be sure. Just under a million patients were treated by approximately 50,000 physicians, 30% of whom were female. And, though female patients and male patients differed, they did not differ with respect to the sex of their hospitalist. So, by physician sex, patients were similar in mean age, race, ethnicity, household income, eligibility for Medicaid, and comorbid conditions. The authors even created a “predicted mortality” score which was similar across the groups as well.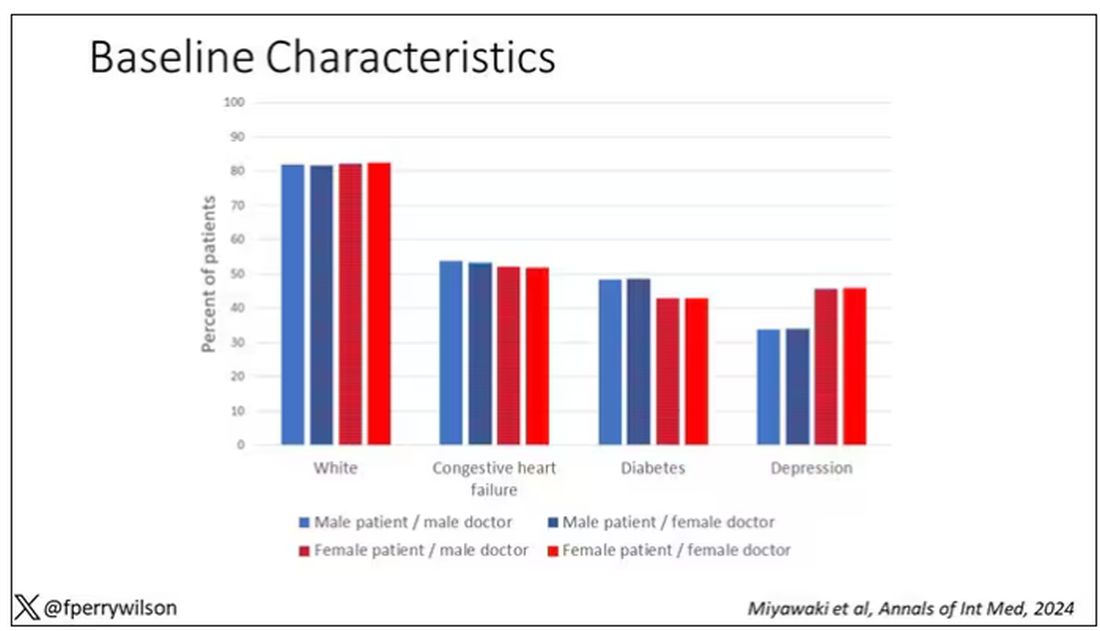
Now, the female physicians were a bit different from the male physicians. The female hospitalists were slightly more likely to have an osteopathic degree, had slightly fewer admissions per year, and were a bit younger.
So, we have broadly similar patients regardless of who their hospitalist was, but hospitalists differ by factors other than their sex. Fine.
I’ve graphed the results here. 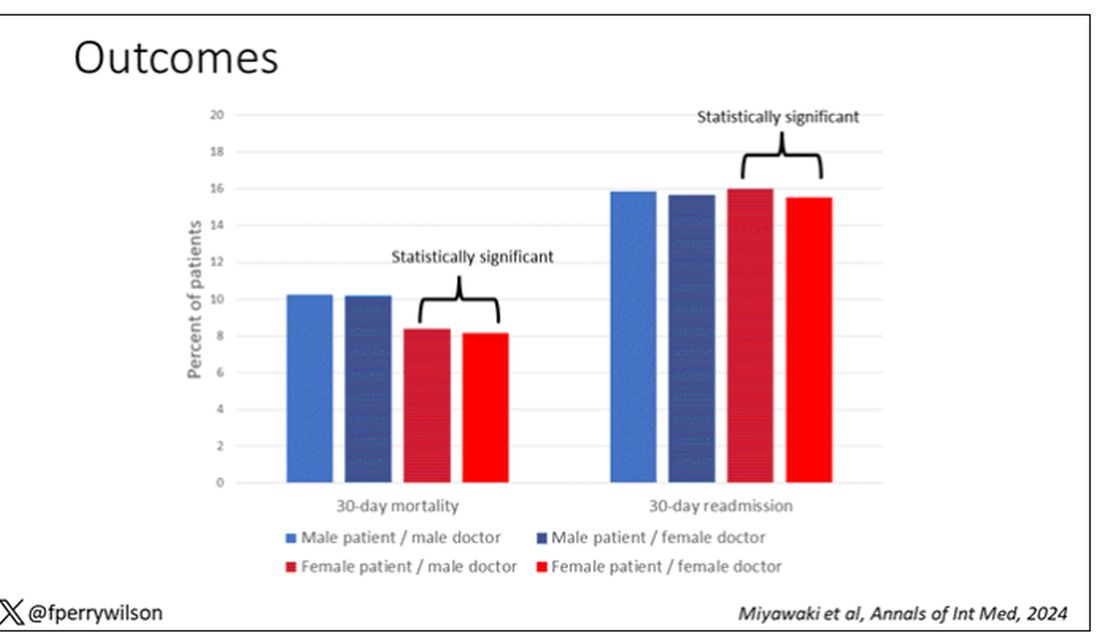
This is a relatively small effect, to be sure, but if you multiply it across the millions of hospitalist admissions per year, you can start to put up some real numbers.
So, what is going on here? I see four broad buckets of possibilities.
Let’s start with the obvious explanation: Women, on average, are better doctors than men. I am married to a woman doctor, and based on my personal experience, this explanation is undoubtedly true. But why would that be?
The authors cite data that suggest that female physicians are less likely than male physicians to dismiss patient concerns — and in particular, the concerns of female patients — perhaps leading to fewer missed diagnoses. But this is impossible to measure with administrative data, so this study can no more tell us whether these female hospitalists are more attentive than their male counterparts than it can suggest that the benefit is mediated by the shorter average height of female physicians. Perhaps the key is being closer to the patient?
The second possibility here is that this has nothing to do with the sex of the physician at all; it has to do with those other things that associate with the sex of the physician. We know, for example, that the female physicians saw fewer patients per year than the male physicians, but the study authors adjusted for this in the statistical models. Still, other unmeasured factors (confounders) could be present. By the way, confounders wouldn’t necessarily change the primary finding — you are better off being cared for by female physicians. It’s just not because they are female; it’s a convenient marker for some other quality, such as age.
The third possibility is that the study represents a phenomenon called collider bias. The idea here is that physicians only get into the study if they are hospitalists, and the quality of physicians who choose to become a hospitalist may differ by sex. When deciding on a specialty, a talented resident considering certain lifestyle issues may find hospital medicine particularly attractive — and that draw toward a more lifestyle-friendly specialty may differ by sex, as some prior studies have shown. If true, the pool of women hospitalists may be better than their male counterparts because male physicians of that caliber don’t become hospitalists.
Okay, don’t write in. I’m just trying to cite examples of how to think about collider bias. I can’t prove that this is the case, and in fact the authors do a sensitivity analysis of all physicians, not just hospitalists, and show the same thing. So this is probably not true, but epidemiology is fun, right?
And the fourth possibility: This is nothing but statistical noise. The effect size is incredibly small and just on the border of statistical significance. Especially when you’re working with very large datasets like this, you’ve got to be really careful about overinterpreting statistically significant findings that are nevertheless of small magnitude.
Regardless, it’s an interesting study, one that made me think and, of course, worry a bit about how I would present it. Forgive me if I’ve been indelicate in handling the complex issues of sex, gender, and society here. But I’m not sure what you expect; after all, I’m only a male doctor.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It’s a battle of the sexes today as we dive into a paper that makes you say, “Wow, what an interesting study” and also “Boy, am I glad I didn’t do that study.” That’s because studies like this are always somewhat fraught; they say something about medicine but also something about society — and that makes this a bit precarious. But that’s never stopped us before. So, let’s go ahead and try to answer the question: Do women make better doctors than men?
On the surface, this question seems nearly impossible to answer. It’s too broad; what does it mean to be a “better” doctor? At first blush it seems that there are just too many variables to control for here: the type of doctor, the type of patient, the clinical scenario, and so on.
But this study, “Comparison of hospital mortality and readmission rates by physician and patient sex,” which appears in Annals of Internal Medicine, uses a fairly ingenious method to cut through all the bias by leveraging two simple facts: First, hospital medicine is largely conducted by hospitalists these days; second, due to the shift-based nature of hospitalist work, the hospitalist you get when you are admitted to the hospital is pretty much random.
In other words, if you are admitted to the hospital for an acute illness and get a hospitalist as your attending, you have no control over whether it is a man or a woman. Is this a randomized trial? No, but it’s not bad.
Researchers used Medicare claims data to identify adults over age 65 who had nonelective hospital admissions throughout the United States. The claims revealed the sex of the patient and the name of the attending physician. By linking to a medical provider database, they could determine the sex of the provider.
The goal was to look at outcomes across four dyads:
- Male patient – male doctor
- Male patient – female doctor
- Female patient – male doctor
- Female patient – female doctor
The primary outcome was 30-day mortality.
I told you that focusing on hospitalists produces some pseudorandomization, but let’s look at the data to be sure. Just under a million patients were treated by approximately 50,000 physicians, 30% of whom were female. And, though female patients and male patients differed, they did not differ with respect to the sex of their hospitalist. So, by physician sex, patients were similar in mean age, race, ethnicity, household income, eligibility for Medicaid, and comorbid conditions. The authors even created a “predicted mortality” score which was similar across the groups as well.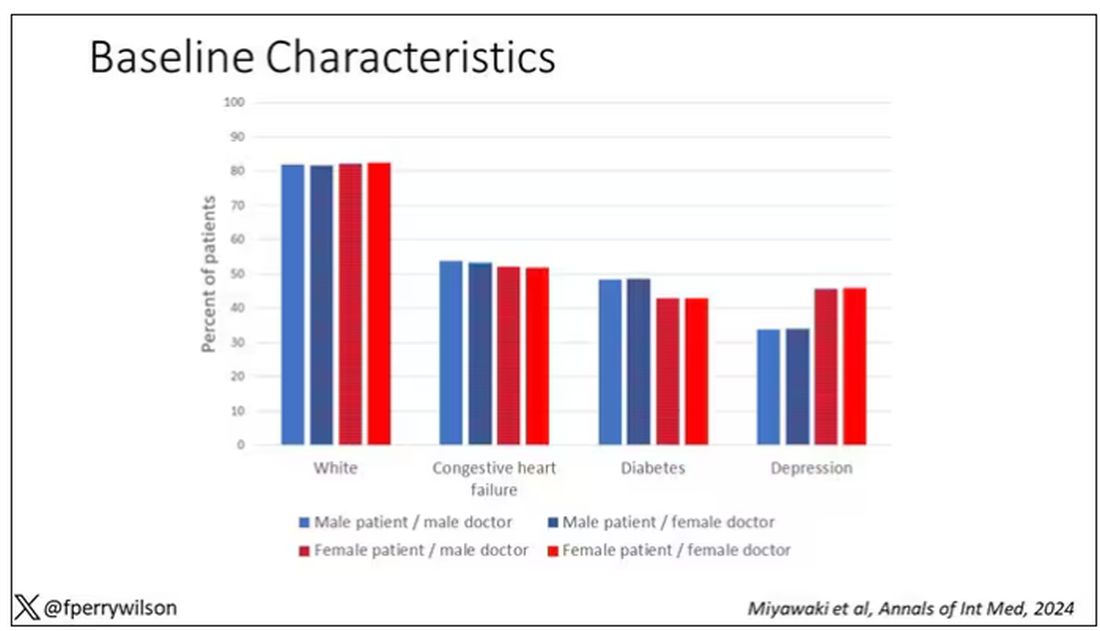
Now, the female physicians were a bit different from the male physicians. The female hospitalists were slightly more likely to have an osteopathic degree, had slightly fewer admissions per year, and were a bit younger.
So, we have broadly similar patients regardless of who their hospitalist was, but hospitalists differ by factors other than their sex. Fine.
I’ve graphed the results here. 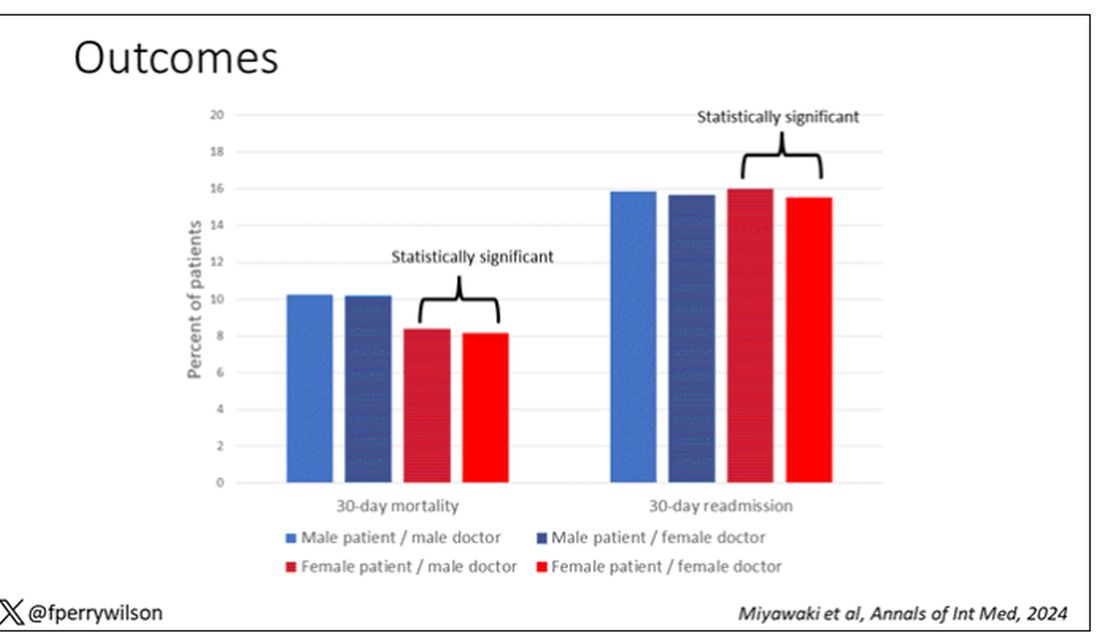
This is a relatively small effect, to be sure, but if you multiply it across the millions of hospitalist admissions per year, you can start to put up some real numbers.
So, what is going on here? I see four broad buckets of possibilities.
Let’s start with the obvious explanation: Women, on average, are better doctors than men. I am married to a woman doctor, and based on my personal experience, this explanation is undoubtedly true. But why would that be?
The authors cite data that suggest that female physicians are less likely than male physicians to dismiss patient concerns — and in particular, the concerns of female patients — perhaps leading to fewer missed diagnoses. But this is impossible to measure with administrative data, so this study can no more tell us whether these female hospitalists are more attentive than their male counterparts than it can suggest that the benefit is mediated by the shorter average height of female physicians. Perhaps the key is being closer to the patient?
The second possibility here is that this has nothing to do with the sex of the physician at all; it has to do with those other things that associate with the sex of the physician. We know, for example, that the female physicians saw fewer patients per year than the male physicians, but the study authors adjusted for this in the statistical models. Still, other unmeasured factors (confounders) could be present. By the way, confounders wouldn’t necessarily change the primary finding — you are better off being cared for by female physicians. It’s just not because they are female; it’s a convenient marker for some other quality, such as age.
The third possibility is that the study represents a phenomenon called collider bias. The idea here is that physicians only get into the study if they are hospitalists, and the quality of physicians who choose to become a hospitalist may differ by sex. When deciding on a specialty, a talented resident considering certain lifestyle issues may find hospital medicine particularly attractive — and that draw toward a more lifestyle-friendly specialty may differ by sex, as some prior studies have shown. If true, the pool of women hospitalists may be better than their male counterparts because male physicians of that caliber don’t become hospitalists.
Okay, don’t write in. I’m just trying to cite examples of how to think about collider bias. I can’t prove that this is the case, and in fact the authors do a sensitivity analysis of all physicians, not just hospitalists, and show the same thing. So this is probably not true, but epidemiology is fun, right?
And the fourth possibility: This is nothing but statistical noise. The effect size is incredibly small and just on the border of statistical significance. Especially when you’re working with very large datasets like this, you’ve got to be really careful about overinterpreting statistically significant findings that are nevertheless of small magnitude.
Regardless, it’s an interesting study, one that made me think and, of course, worry a bit about how I would present it. Forgive me if I’ve been indelicate in handling the complex issues of sex, gender, and society here. But I’m not sure what you expect; after all, I’m only a male doctor.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It’s a battle of the sexes today as we dive into a paper that makes you say, “Wow, what an interesting study” and also “Boy, am I glad I didn’t do that study.” That’s because studies like this are always somewhat fraught; they say something about medicine but also something about society — and that makes this a bit precarious. But that’s never stopped us before. So, let’s go ahead and try to answer the question: Do women make better doctors than men?
On the surface, this question seems nearly impossible to answer. It’s too broad; what does it mean to be a “better” doctor? At first blush it seems that there are just too many variables to control for here: the type of doctor, the type of patient, the clinical scenario, and so on.
But this study, “Comparison of hospital mortality and readmission rates by physician and patient sex,” which appears in Annals of Internal Medicine, uses a fairly ingenious method to cut through all the bias by leveraging two simple facts: First, hospital medicine is largely conducted by hospitalists these days; second, due to the shift-based nature of hospitalist work, the hospitalist you get when you are admitted to the hospital is pretty much random.
In other words, if you are admitted to the hospital for an acute illness and get a hospitalist as your attending, you have no control over whether it is a man or a woman. Is this a randomized trial? No, but it’s not bad.
Researchers used Medicare claims data to identify adults over age 65 who had nonelective hospital admissions throughout the United States. The claims revealed the sex of the patient and the name of the attending physician. By linking to a medical provider database, they could determine the sex of the provider.
The goal was to look at outcomes across four dyads:
- Male patient – male doctor
- Male patient – female doctor
- Female patient – male doctor
- Female patient – female doctor
The primary outcome was 30-day mortality.
I told you that focusing on hospitalists produces some pseudorandomization, but let’s look at the data to be sure. Just under a million patients were treated by approximately 50,000 physicians, 30% of whom were female. And, though female patients and male patients differed, they did not differ with respect to the sex of their hospitalist. So, by physician sex, patients were similar in mean age, race, ethnicity, household income, eligibility for Medicaid, and comorbid conditions. The authors even created a “predicted mortality” score which was similar across the groups as well.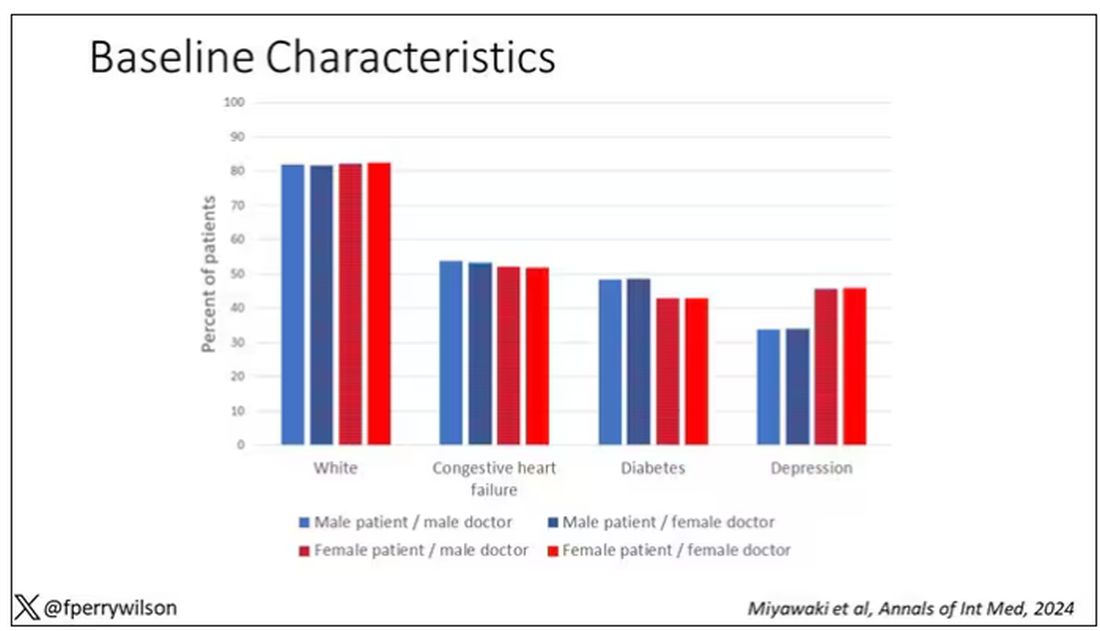
Now, the female physicians were a bit different from the male physicians. The female hospitalists were slightly more likely to have an osteopathic degree, had slightly fewer admissions per year, and were a bit younger.
So, we have broadly similar patients regardless of who their hospitalist was, but hospitalists differ by factors other than their sex. Fine.
I’ve graphed the results here. 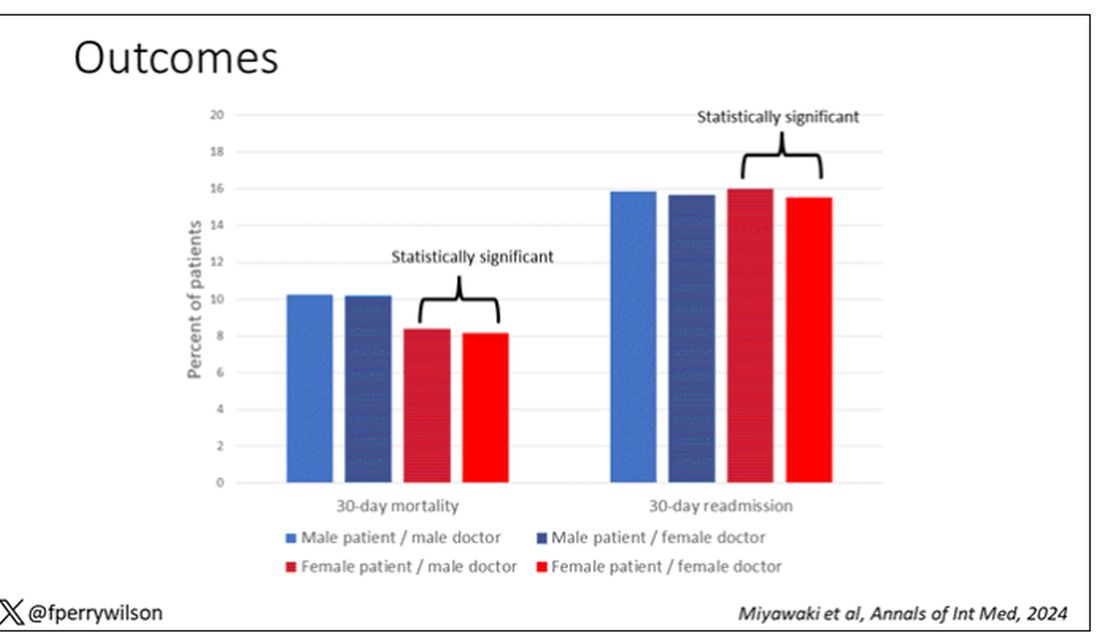
This is a relatively small effect, to be sure, but if you multiply it across the millions of hospitalist admissions per year, you can start to put up some real numbers.
So, what is going on here? I see four broad buckets of possibilities.
Let’s start with the obvious explanation: Women, on average, are better doctors than men. I am married to a woman doctor, and based on my personal experience, this explanation is undoubtedly true. But why would that be?
The authors cite data that suggest that female physicians are less likely than male physicians to dismiss patient concerns — and in particular, the concerns of female patients — perhaps leading to fewer missed diagnoses. But this is impossible to measure with administrative data, so this study can no more tell us whether these female hospitalists are more attentive than their male counterparts than it can suggest that the benefit is mediated by the shorter average height of female physicians. Perhaps the key is being closer to the patient?
The second possibility here is that this has nothing to do with the sex of the physician at all; it has to do with those other things that associate with the sex of the physician. We know, for example, that the female physicians saw fewer patients per year than the male physicians, but the study authors adjusted for this in the statistical models. Still, other unmeasured factors (confounders) could be present. By the way, confounders wouldn’t necessarily change the primary finding — you are better off being cared for by female physicians. It’s just not because they are female; it’s a convenient marker for some other quality, such as age.
The third possibility is that the study represents a phenomenon called collider bias. The idea here is that physicians only get into the study if they are hospitalists, and the quality of physicians who choose to become a hospitalist may differ by sex. When deciding on a specialty, a talented resident considering certain lifestyle issues may find hospital medicine particularly attractive — and that draw toward a more lifestyle-friendly specialty may differ by sex, as some prior studies have shown. If true, the pool of women hospitalists may be better than their male counterparts because male physicians of that caliber don’t become hospitalists.
Okay, don’t write in. I’m just trying to cite examples of how to think about collider bias. I can’t prove that this is the case, and in fact the authors do a sensitivity analysis of all physicians, not just hospitalists, and show the same thing. So this is probably not true, but epidemiology is fun, right?
And the fourth possibility: This is nothing but statistical noise. The effect size is incredibly small and just on the border of statistical significance. Especially when you’re working with very large datasets like this, you’ve got to be really careful about overinterpreting statistically significant findings that are nevertheless of small magnitude.
Regardless, it’s an interesting study, one that made me think and, of course, worry a bit about how I would present it. Forgive me if I’ve been indelicate in handling the complex issues of sex, gender, and society here. But I’m not sure what you expect; after all, I’m only a male doctor.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Menopause, RSV, and More: 4 New Meds to Know
BOSTON — The US Food and Drug Administration (FDA) approved 55 new medications in 2023 and 11 more in 2024 to date.
A New First-Line for GERD?
Vonoprazan, an oral potassium-competitive acid blocker — which received FDA approval in November 2023 — may be a good alternative for patients whose symptoms continue to linger despite taking medications designated to treat gastroesophageal reflux disease (GERD).
GERD is the most common gastrointestinal symptom encountered by primary care physicians. Proton-pump inhibitors (PPIs) are the first-line treatment for the condition but can have long-term side effects such as Clostridioides difficile infection and kidney lesions.
“We know that not all patients are going to have symptom relief with H2 blockers and PPIs, so there’s an opportunity for patients who don’t get full symptom relief,” Dr. Smetana told attendees.
Vonoprazan blocks potassium binding to ATPase proton pumps and inhibits the secretion of gastric acid.
The approval of vonoprazan for erosive GERD was based on results from the phase 3 PHALCON-EE study, a randomized, double-blind, multicenter study that found the drug to be more effective than lansoprazole in treating erosive esophagitis.
Vonoprazan “has more rapid absorption than PPIs [and a] longer half-life and is more potent than PPIs, so theoretically it could be more effective in certain settings,” Dr. Smetana said.
Vonoprazan is FDA approved for only 6 months of use. Despite its efficacy, cost may be a barrier to many patients. H2 blockers generally cost patients less than $10 for 1 month’s supply, whereas vonoprazan can cost up to $650.
Nonhormonal Drug for Menopause
Fezolinetant, the first neurokinin receptor antagonist to receive approval from the FDA to treat vasomotor symptoms, may be an option for women concerned about hormone-based therapy for menopausal hot flashes.
“[Fezolinetant] specifically works in the area of the brain that’s involved in body temperature regulation and sweating,” Dr. Smetana said.
Results from the SKYLIGHT 1 randomized controlled trial of fezolinetant found the medication reduced the frequency and severity of hot flashes. Some of the side effects include abdominal pain, diarrhea, and insomnia.
Other nonestrogen treatments, including selective serotonin reuptake inhibitors (SSRIs), gabapentin, cognitive-behavioral therapy, and hypnosis, are modestly effective, according to the North American Menopause Society.
“[Fezolinetant] offers a different option that physicians may be more comfortable prescribing,” Dr. Smetana said. “And I think this will be an important addition to nonhormonal therapy.”
RSV Vaccine for Everyone
Once considered an illness that is more prevalent in young children, respiratory syncytial virus (RSV) has become more prevalent and severe among older adults. Between 60,000 and 120,000 older adults are hospitalized and 6000-10,000 die of RSV infection each year, according to the US Centers for Disease Control and Prevention.
The FDA has approved two RSV vaccines approved for older adults, but clinicians may find it challenging to get older patients vaccinated for this and other preventable illnesses.
Patients who received the RSV vaccine had an 83% relative risk reduction for the illness, according to a recent study, and an overall lower risk for hospitalization.
Moderna is developing an mRNA vaccine for RSV that is similar to many COVID-19 vaccines. A study published in 2023 in The New England Journal of Medicine found no cases of neuroinflammatory disorders among patients who received the mRNA RSV vaccine, with a median follow-up of 112 days.
“This is important given ongoing concerns of neurological safety,” among older adults who receive the RSV vaccine, Dr. Smetana said.
As of March 2024, the CDC recommends shared decision-making for adults older than 60 years and for healthcare providers to “consider” rather than “recommend” the vaccine for their patients. The agency’s Adult RSV Work Group plans to meet at June 2024 to reconsider whether shared clinical decision-making remains the preferred policy option.
New Antidepressants
A medication thrice rejected by the FDA is now heading a new class of drugs to treat major depressive disorder.
Gepirone, a 5-HT1A receptor agonist, has a different mechanism of action from that of SSRIs, which are currently considered the first-line treatment for depression.
Gepirone was rejected by the FDA in 2002, 2004, and 2007, with concerns that the efficacy studies were too small. In 2015, an FDA advisory committee agreed that the evidence to date did not support approval of an extended-release form of the drug. But the agency decided to approve the medication in September 2023.
“So why is this medication worth discussing now?” Dr. Smetana said. “It’s because the side effect profile is different from existing antidepressants.”
Many patients may stop using SSRIs because of side effects such as insomnia and loss of libido, Dr. Smetana said. Gepirone has the potential to avoid activation of other 5-HT receptors that mediate side effects, he said.
Studies suggest that gepirone reduces both anxiety and depression scores on the Hamilton Depression Rating Scale in patients who have both conditions and decreases rates of depression relapse compared with placebo through at least 48 weeks. The drug also may be less likely than SSRIs to cause sexual dysfunction in men, Dr. Smetana said.
Gepirone will be available to prescribe to patients in fall 2024.
Dr. Smetana reported no relevant financial conflicts of interest.
A version of this article appeared on Medscape.com.
BOSTON — The US Food and Drug Administration (FDA) approved 55 new medications in 2023 and 11 more in 2024 to date.
A New First-Line for GERD?
Vonoprazan, an oral potassium-competitive acid blocker — which received FDA approval in November 2023 — may be a good alternative for patients whose symptoms continue to linger despite taking medications designated to treat gastroesophageal reflux disease (GERD).
GERD is the most common gastrointestinal symptom encountered by primary care physicians. Proton-pump inhibitors (PPIs) are the first-line treatment for the condition but can have long-term side effects such as Clostridioides difficile infection and kidney lesions.
“We know that not all patients are going to have symptom relief with H2 blockers and PPIs, so there’s an opportunity for patients who don’t get full symptom relief,” Dr. Smetana told attendees.
Vonoprazan blocks potassium binding to ATPase proton pumps and inhibits the secretion of gastric acid.
The approval of vonoprazan for erosive GERD was based on results from the phase 3 PHALCON-EE study, a randomized, double-blind, multicenter study that found the drug to be more effective than lansoprazole in treating erosive esophagitis.
Vonoprazan “has more rapid absorption than PPIs [and a] longer half-life and is more potent than PPIs, so theoretically it could be more effective in certain settings,” Dr. Smetana said.
Vonoprazan is FDA approved for only 6 months of use. Despite its efficacy, cost may be a barrier to many patients. H2 blockers generally cost patients less than $10 for 1 month’s supply, whereas vonoprazan can cost up to $650.
Nonhormonal Drug for Menopause
Fezolinetant, the first neurokinin receptor antagonist to receive approval from the FDA to treat vasomotor symptoms, may be an option for women concerned about hormone-based therapy for menopausal hot flashes.
“[Fezolinetant] specifically works in the area of the brain that’s involved in body temperature regulation and sweating,” Dr. Smetana said.
Results from the SKYLIGHT 1 randomized controlled trial of fezolinetant found the medication reduced the frequency and severity of hot flashes. Some of the side effects include abdominal pain, diarrhea, and insomnia.
Other nonestrogen treatments, including selective serotonin reuptake inhibitors (SSRIs), gabapentin, cognitive-behavioral therapy, and hypnosis, are modestly effective, according to the North American Menopause Society.
“[Fezolinetant] offers a different option that physicians may be more comfortable prescribing,” Dr. Smetana said. “And I think this will be an important addition to nonhormonal therapy.”
RSV Vaccine for Everyone
Once considered an illness that is more prevalent in young children, respiratory syncytial virus (RSV) has become more prevalent and severe among older adults. Between 60,000 and 120,000 older adults are hospitalized and 6000-10,000 die of RSV infection each year, according to the US Centers for Disease Control and Prevention.
The FDA has approved two RSV vaccines approved for older adults, but clinicians may find it challenging to get older patients vaccinated for this and other preventable illnesses.
Patients who received the RSV vaccine had an 83% relative risk reduction for the illness, according to a recent study, and an overall lower risk for hospitalization.
Moderna is developing an mRNA vaccine for RSV that is similar to many COVID-19 vaccines. A study published in 2023 in The New England Journal of Medicine found no cases of neuroinflammatory disorders among patients who received the mRNA RSV vaccine, with a median follow-up of 112 days.
“This is important given ongoing concerns of neurological safety,” among older adults who receive the RSV vaccine, Dr. Smetana said.
As of March 2024, the CDC recommends shared decision-making for adults older than 60 years and for healthcare providers to “consider” rather than “recommend” the vaccine for their patients. The agency’s Adult RSV Work Group plans to meet at June 2024 to reconsider whether shared clinical decision-making remains the preferred policy option.
New Antidepressants
A medication thrice rejected by the FDA is now heading a new class of drugs to treat major depressive disorder.
Gepirone, a 5-HT1A receptor agonist, has a different mechanism of action from that of SSRIs, which are currently considered the first-line treatment for depression.
Gepirone was rejected by the FDA in 2002, 2004, and 2007, with concerns that the efficacy studies were too small. In 2015, an FDA advisory committee agreed that the evidence to date did not support approval of an extended-release form of the drug. But the agency decided to approve the medication in September 2023.
“So why is this medication worth discussing now?” Dr. Smetana said. “It’s because the side effect profile is different from existing antidepressants.”
Many patients may stop using SSRIs because of side effects such as insomnia and loss of libido, Dr. Smetana said. Gepirone has the potential to avoid activation of other 5-HT receptors that mediate side effects, he said.
Studies suggest that gepirone reduces both anxiety and depression scores on the Hamilton Depression Rating Scale in patients who have both conditions and decreases rates of depression relapse compared with placebo through at least 48 weeks. The drug also may be less likely than SSRIs to cause sexual dysfunction in men, Dr. Smetana said.
Gepirone will be available to prescribe to patients in fall 2024.
Dr. Smetana reported no relevant financial conflicts of interest.
A version of this article appeared on Medscape.com.
BOSTON — The US Food and Drug Administration (FDA) approved 55 new medications in 2023 and 11 more in 2024 to date.
A New First-Line for GERD?
Vonoprazan, an oral potassium-competitive acid blocker — which received FDA approval in November 2023 — may be a good alternative for patients whose symptoms continue to linger despite taking medications designated to treat gastroesophageal reflux disease (GERD).
GERD is the most common gastrointestinal symptom encountered by primary care physicians. Proton-pump inhibitors (PPIs) are the first-line treatment for the condition but can have long-term side effects such as Clostridioides difficile infection and kidney lesions.
“We know that not all patients are going to have symptom relief with H2 blockers and PPIs, so there’s an opportunity for patients who don’t get full symptom relief,” Dr. Smetana told attendees.
Vonoprazan blocks potassium binding to ATPase proton pumps and inhibits the secretion of gastric acid.
The approval of vonoprazan for erosive GERD was based on results from the phase 3 PHALCON-EE study, a randomized, double-blind, multicenter study that found the drug to be more effective than lansoprazole in treating erosive esophagitis.
Vonoprazan “has more rapid absorption than PPIs [and a] longer half-life and is more potent than PPIs, so theoretically it could be more effective in certain settings,” Dr. Smetana said.
Vonoprazan is FDA approved for only 6 months of use. Despite its efficacy, cost may be a barrier to many patients. H2 blockers generally cost patients less than $10 for 1 month’s supply, whereas vonoprazan can cost up to $650.
Nonhormonal Drug for Menopause
Fezolinetant, the first neurokinin receptor antagonist to receive approval from the FDA to treat vasomotor symptoms, may be an option for women concerned about hormone-based therapy for menopausal hot flashes.
“[Fezolinetant] specifically works in the area of the brain that’s involved in body temperature regulation and sweating,” Dr. Smetana said.
Results from the SKYLIGHT 1 randomized controlled trial of fezolinetant found the medication reduced the frequency and severity of hot flashes. Some of the side effects include abdominal pain, diarrhea, and insomnia.
Other nonestrogen treatments, including selective serotonin reuptake inhibitors (SSRIs), gabapentin, cognitive-behavioral therapy, and hypnosis, are modestly effective, according to the North American Menopause Society.
“[Fezolinetant] offers a different option that physicians may be more comfortable prescribing,” Dr. Smetana said. “And I think this will be an important addition to nonhormonal therapy.”
RSV Vaccine for Everyone
Once considered an illness that is more prevalent in young children, respiratory syncytial virus (RSV) has become more prevalent and severe among older adults. Between 60,000 and 120,000 older adults are hospitalized and 6000-10,000 die of RSV infection each year, according to the US Centers for Disease Control and Prevention.
The FDA has approved two RSV vaccines approved for older adults, but clinicians may find it challenging to get older patients vaccinated for this and other preventable illnesses.
Patients who received the RSV vaccine had an 83% relative risk reduction for the illness, according to a recent study, and an overall lower risk for hospitalization.
Moderna is developing an mRNA vaccine for RSV that is similar to many COVID-19 vaccines. A study published in 2023 in The New England Journal of Medicine found no cases of neuroinflammatory disorders among patients who received the mRNA RSV vaccine, with a median follow-up of 112 days.
“This is important given ongoing concerns of neurological safety,” among older adults who receive the RSV vaccine, Dr. Smetana said.
As of March 2024, the CDC recommends shared decision-making for adults older than 60 years and for healthcare providers to “consider” rather than “recommend” the vaccine for their patients. The agency’s Adult RSV Work Group plans to meet at June 2024 to reconsider whether shared clinical decision-making remains the preferred policy option.
New Antidepressants
A medication thrice rejected by the FDA is now heading a new class of drugs to treat major depressive disorder.
Gepirone, a 5-HT1A receptor agonist, has a different mechanism of action from that of SSRIs, which are currently considered the first-line treatment for depression.
Gepirone was rejected by the FDA in 2002, 2004, and 2007, with concerns that the efficacy studies were too small. In 2015, an FDA advisory committee agreed that the evidence to date did not support approval of an extended-release form of the drug. But the agency decided to approve the medication in September 2023.
“So why is this medication worth discussing now?” Dr. Smetana said. “It’s because the side effect profile is different from existing antidepressants.”
Many patients may stop using SSRIs because of side effects such as insomnia and loss of libido, Dr. Smetana said. Gepirone has the potential to avoid activation of other 5-HT receptors that mediate side effects, he said.
Studies suggest that gepirone reduces both anxiety and depression scores on the Hamilton Depression Rating Scale in patients who have both conditions and decreases rates of depression relapse compared with placebo through at least 48 weeks. The drug also may be less likely than SSRIs to cause sexual dysfunction in men, Dr. Smetana said.
Gepirone will be available to prescribe to patients in fall 2024.
Dr. Smetana reported no relevant financial conflicts of interest.
A version of this article appeared on Medscape.com.
Weighing the Benefits of Integrating AI-based Clinical Notes Into Your Practice
Picture a healthcare system where physicians aren’t bogged down by excessive charting but are instead fully present with their patients, offering undivided attention and personalized care. In a recent X post, Stuart Blitz, COO and co-founder of Hone Health, sparked a thought-provoking conversation. “The problem with US healthcare is physicians are burned out since they spend way too much time charting, not enough with patients,” he wrote. “If you created a health system that did zero charting, you’d attract the best physicians and all patients would go there. Who is working on this?”
This resonates with many in the medical community, myself included, because the strain of extensive documentation detracts from patient care. Having worked in both large and small healthcare systems, I know the burden of extensive charting is a palpable challenge, often detracting from the time we can devote to our patients.
The first part of this two-part series examines the overarching benefits of artificial intelligence (AI)–based clinical documentation in modern healthcare, a field witnessing a paradigm shift thanks to advancements in AI.
Transformative Evolution of Clinical Documentation
The transition from manual documentation to AI-driven solutions marks a significant shift in the field, with a number of products in development including Nuance, Abridge, Ambience, ScribeAmerica, 3M, and DeepScribe. These tools use ambient clinical intelligence (ACI) to automate documentation, capturing patient conversations and translating them into structured clinical summaries. This innovation aligns with the vision of reducing charting burdens and enhancing patient-physician interactions.
How does it work? ACI refers to a sophisticated form of AI applied in healthcare settings, particularly focusing on enhancing the clinical documentation process without disrupting the natural flow of the consultation. Here’s a technical yet practical breakdown of ACI and the algorithms it typically employs:
Data capture and processing: ACI systems employ various sensors and processing units, typically integrated into clinical settings. These sensors, like microphones and cameras, gather diverse data such as audio from patient-doctor dialogues and visual cues. This information is then processed in real-time or near–real-time.
Natural language processing (NLP): A core component of ACI is advanced NLP algorithms. These algorithms analyze the captured audio data, transcribing spoken words into text. NLP goes beyond mere transcription; it involves understanding context, extracting relevant medical information (like symptoms, diagnoses, and treatment plans), and interpreting the nuances of human language.
Deep learning: Machine learning, particularly deep-learning techniques, are employed to improve the accuracy of ACI systems continually. These algorithms can learn from vast datasets of clinical interactions, enhancing their ability to transcribe and interpret future conversations accurately. As they learn, they become better at understanding different accents, complex medical terms, and variations in speech patterns.
Integration with electronic health records (EHRs): ACI systems are often designed to integrate seamlessly with existing EHR systems. They can automatically populate patient records with information from patient-clinician interactions, reducing manual entry and potential errors.
Customization and personalization: Many ACI systems offer customizable templates or allow clinicians to tailor documentation workflows. This flexibility ensures that the output aligns with the specific needs and preferences of healthcare providers.
Ethical and privacy considerations: ACI systems must navigate significant ethical and privacy concerns, especially related to patient consent and data security. These systems need to comply with healthcare privacy regulations such as HIPAA. They need to securely manage sensitive patient data and restrict access to authorized personnel only.
Broad-Spectrum Benefits of AI in Documentation
- Reducing clinician burnout: By automating the documentation process, AI tools like DAX Copilot alleviate a significant contributor to physician burnout, enabling clinicians to focus more on patient care.
- Enhanced patient care: With AI handling documentation, clinicians can engage more with their patients, leading to improved care quality and patient satisfaction.
- Data accuracy and quality: AI-driven documentation captures detailed patient encounters accurately, ensuring high-quality and comprehensive medical records.
- Response to the growing need for efficient healthcare: AI-based documentation is a direct response to the growing call for more efficient healthcare practices, where clinicians spend less time on paperwork and more with patients.
The shift toward AI-based clinical documentation represents a critical step in addressing the inefficiencies in healthcare systems. It’s a move towards a more patient-centered approach, where clinicians can focus more on patient care by reducing the time spent on excessive charting. Hopefully, we can integrate these solutions into our clinics at a large enough scale to make such an impact.
In the next column, we will explore in-depth insights from Kenneth Harper at Nuance on the technical implementation of these tools, with DAX as an example.
I would love to read your comments on AI in clinical trials as well as other AI-related topics. Write me at [email protected] or find me on X @DrBonillaOnc.
Dr. Loaiza-Bonilla is the co-founder and chief medical officer at Massive Bio, a company connecting patients to clinical trials using artificial intelligence. His research and professional interests focus on precision medicine, clinical trial design, digital health, entrepreneurship, and patient advocacy. Dr Loaiza-Bonilla serves as medical director of oncology research at Capital Health in New Jersey, where he maintains a connection to patient care by attending to patients 2 days a week. He has served as a consultant for Verify, PSI CRO, Bayer, AstraZeneca, Cardinal Health, BrightInsight, The Lynx Group, Fresenius, Pfizer, Ipsen, and Guardant; served as a speaker or a member of a speakers bureau for Amgen, Guardant, Eisai, Ipsen, Natera, Merck, Bristol-Myers Squibb, and AstraZeneca. He holds a 5% or greater equity interest in Massive Bio.
A version of this article appeared on Medscape.com.
Picture a healthcare system where physicians aren’t bogged down by excessive charting but are instead fully present with their patients, offering undivided attention and personalized care. In a recent X post, Stuart Blitz, COO and co-founder of Hone Health, sparked a thought-provoking conversation. “The problem with US healthcare is physicians are burned out since they spend way too much time charting, not enough with patients,” he wrote. “If you created a health system that did zero charting, you’d attract the best physicians and all patients would go there. Who is working on this?”
This resonates with many in the medical community, myself included, because the strain of extensive documentation detracts from patient care. Having worked in both large and small healthcare systems, I know the burden of extensive charting is a palpable challenge, often detracting from the time we can devote to our patients.
The first part of this two-part series examines the overarching benefits of artificial intelligence (AI)–based clinical documentation in modern healthcare, a field witnessing a paradigm shift thanks to advancements in AI.
Transformative Evolution of Clinical Documentation
The transition from manual documentation to AI-driven solutions marks a significant shift in the field, with a number of products in development including Nuance, Abridge, Ambience, ScribeAmerica, 3M, and DeepScribe. These tools use ambient clinical intelligence (ACI) to automate documentation, capturing patient conversations and translating them into structured clinical summaries. This innovation aligns with the vision of reducing charting burdens and enhancing patient-physician interactions.
How does it work? ACI refers to a sophisticated form of AI applied in healthcare settings, particularly focusing on enhancing the clinical documentation process without disrupting the natural flow of the consultation. Here’s a technical yet practical breakdown of ACI and the algorithms it typically employs:
Data capture and processing: ACI systems employ various sensors and processing units, typically integrated into clinical settings. These sensors, like microphones and cameras, gather diverse data such as audio from patient-doctor dialogues and visual cues. This information is then processed in real-time or near–real-time.
Natural language processing (NLP): A core component of ACI is advanced NLP algorithms. These algorithms analyze the captured audio data, transcribing spoken words into text. NLP goes beyond mere transcription; it involves understanding context, extracting relevant medical information (like symptoms, diagnoses, and treatment plans), and interpreting the nuances of human language.
Deep learning: Machine learning, particularly deep-learning techniques, are employed to improve the accuracy of ACI systems continually. These algorithms can learn from vast datasets of clinical interactions, enhancing their ability to transcribe and interpret future conversations accurately. As they learn, they become better at understanding different accents, complex medical terms, and variations in speech patterns.
Integration with electronic health records (EHRs): ACI systems are often designed to integrate seamlessly with existing EHR systems. They can automatically populate patient records with information from patient-clinician interactions, reducing manual entry and potential errors.
Customization and personalization: Many ACI systems offer customizable templates or allow clinicians to tailor documentation workflows. This flexibility ensures that the output aligns with the specific needs and preferences of healthcare providers.
Ethical and privacy considerations: ACI systems must navigate significant ethical and privacy concerns, especially related to patient consent and data security. These systems need to comply with healthcare privacy regulations such as HIPAA. They need to securely manage sensitive patient data and restrict access to authorized personnel only.
Broad-Spectrum Benefits of AI in Documentation
- Reducing clinician burnout: By automating the documentation process, AI tools like DAX Copilot alleviate a significant contributor to physician burnout, enabling clinicians to focus more on patient care.
- Enhanced patient care: With AI handling documentation, clinicians can engage more with their patients, leading to improved care quality and patient satisfaction.
- Data accuracy and quality: AI-driven documentation captures detailed patient encounters accurately, ensuring high-quality and comprehensive medical records.
- Response to the growing need for efficient healthcare: AI-based documentation is a direct response to the growing call for more efficient healthcare practices, where clinicians spend less time on paperwork and more with patients.
The shift toward AI-based clinical documentation represents a critical step in addressing the inefficiencies in healthcare systems. It’s a move towards a more patient-centered approach, where clinicians can focus more on patient care by reducing the time spent on excessive charting. Hopefully, we can integrate these solutions into our clinics at a large enough scale to make such an impact.
In the next column, we will explore in-depth insights from Kenneth Harper at Nuance on the technical implementation of these tools, with DAX as an example.
I would love to read your comments on AI in clinical trials as well as other AI-related topics. Write me at [email protected] or find me on X @DrBonillaOnc.
Dr. Loaiza-Bonilla is the co-founder and chief medical officer at Massive Bio, a company connecting patients to clinical trials using artificial intelligence. His research and professional interests focus on precision medicine, clinical trial design, digital health, entrepreneurship, and patient advocacy. Dr Loaiza-Bonilla serves as medical director of oncology research at Capital Health in New Jersey, where he maintains a connection to patient care by attending to patients 2 days a week. He has served as a consultant for Verify, PSI CRO, Bayer, AstraZeneca, Cardinal Health, BrightInsight, The Lynx Group, Fresenius, Pfizer, Ipsen, and Guardant; served as a speaker or a member of a speakers bureau for Amgen, Guardant, Eisai, Ipsen, Natera, Merck, Bristol-Myers Squibb, and AstraZeneca. He holds a 5% or greater equity interest in Massive Bio.
A version of this article appeared on Medscape.com.
Picture a healthcare system where physicians aren’t bogged down by excessive charting but are instead fully present with their patients, offering undivided attention and personalized care. In a recent X post, Stuart Blitz, COO and co-founder of Hone Health, sparked a thought-provoking conversation. “The problem with US healthcare is physicians are burned out since they spend way too much time charting, not enough with patients,” he wrote. “If you created a health system that did zero charting, you’d attract the best physicians and all patients would go there. Who is working on this?”
This resonates with many in the medical community, myself included, because the strain of extensive documentation detracts from patient care. Having worked in both large and small healthcare systems, I know the burden of extensive charting is a palpable challenge, often detracting from the time we can devote to our patients.
The first part of this two-part series examines the overarching benefits of artificial intelligence (AI)–based clinical documentation in modern healthcare, a field witnessing a paradigm shift thanks to advancements in AI.
Transformative Evolution of Clinical Documentation
The transition from manual documentation to AI-driven solutions marks a significant shift in the field, with a number of products in development including Nuance, Abridge, Ambience, ScribeAmerica, 3M, and DeepScribe. These tools use ambient clinical intelligence (ACI) to automate documentation, capturing patient conversations and translating them into structured clinical summaries. This innovation aligns with the vision of reducing charting burdens and enhancing patient-physician interactions.
How does it work? ACI refers to a sophisticated form of AI applied in healthcare settings, particularly focusing on enhancing the clinical documentation process without disrupting the natural flow of the consultation. Here’s a technical yet practical breakdown of ACI and the algorithms it typically employs:
Data capture and processing: ACI systems employ various sensors and processing units, typically integrated into clinical settings. These sensors, like microphones and cameras, gather diverse data such as audio from patient-doctor dialogues and visual cues. This information is then processed in real-time or near–real-time.
Natural language processing (NLP): A core component of ACI is advanced NLP algorithms. These algorithms analyze the captured audio data, transcribing spoken words into text. NLP goes beyond mere transcription; it involves understanding context, extracting relevant medical information (like symptoms, diagnoses, and treatment plans), and interpreting the nuances of human language.
Deep learning: Machine learning, particularly deep-learning techniques, are employed to improve the accuracy of ACI systems continually. These algorithms can learn from vast datasets of clinical interactions, enhancing their ability to transcribe and interpret future conversations accurately. As they learn, they become better at understanding different accents, complex medical terms, and variations in speech patterns.
Integration with electronic health records (EHRs): ACI systems are often designed to integrate seamlessly with existing EHR systems. They can automatically populate patient records with information from patient-clinician interactions, reducing manual entry and potential errors.
Customization and personalization: Many ACI systems offer customizable templates or allow clinicians to tailor documentation workflows. This flexibility ensures that the output aligns with the specific needs and preferences of healthcare providers.
Ethical and privacy considerations: ACI systems must navigate significant ethical and privacy concerns, especially related to patient consent and data security. These systems need to comply with healthcare privacy regulations such as HIPAA. They need to securely manage sensitive patient data and restrict access to authorized personnel only.
Broad-Spectrum Benefits of AI in Documentation
- Reducing clinician burnout: By automating the documentation process, AI tools like DAX Copilot alleviate a significant contributor to physician burnout, enabling clinicians to focus more on patient care.
- Enhanced patient care: With AI handling documentation, clinicians can engage more with their patients, leading to improved care quality and patient satisfaction.
- Data accuracy and quality: AI-driven documentation captures detailed patient encounters accurately, ensuring high-quality and comprehensive medical records.
- Response to the growing need for efficient healthcare: AI-based documentation is a direct response to the growing call for more efficient healthcare practices, where clinicians spend less time on paperwork and more with patients.
The shift toward AI-based clinical documentation represents a critical step in addressing the inefficiencies in healthcare systems. It’s a move towards a more patient-centered approach, where clinicians can focus more on patient care by reducing the time spent on excessive charting. Hopefully, we can integrate these solutions into our clinics at a large enough scale to make such an impact.
In the next column, we will explore in-depth insights from Kenneth Harper at Nuance on the technical implementation of these tools, with DAX as an example.
I would love to read your comments on AI in clinical trials as well as other AI-related topics. Write me at [email protected] or find me on X @DrBonillaOnc.
Dr. Loaiza-Bonilla is the co-founder and chief medical officer at Massive Bio, a company connecting patients to clinical trials using artificial intelligence. His research and professional interests focus on precision medicine, clinical trial design, digital health, entrepreneurship, and patient advocacy. Dr Loaiza-Bonilla serves as medical director of oncology research at Capital Health in New Jersey, where he maintains a connection to patient care by attending to patients 2 days a week. He has served as a consultant for Verify, PSI CRO, Bayer, AstraZeneca, Cardinal Health, BrightInsight, The Lynx Group, Fresenius, Pfizer, Ipsen, and Guardant; served as a speaker or a member of a speakers bureau for Amgen, Guardant, Eisai, Ipsen, Natera, Merck, Bristol-Myers Squibb, and AstraZeneca. He holds a 5% or greater equity interest in Massive Bio.
A version of this article appeared on Medscape.com.
New Federal Rule Delivers Workplace Support, Time Off for Pregnant Docs
Pregnant physicians may receive more workplace accommodations and protection against discrimination thanks to an updated rule from the US Equal Employment Opportunity Commission (EEOC). The guidelines could prevent women from losing critical career momentum.
The Pregnant Workers Fairness Act (PWFA) aims to help workers balance professional demands with healthy pregnancies. It requires employers to provide reasonable accommodations for a “worker’s known limitations,” including physical or mental conditions associated with “pregnancy, childbirth, or related medical conditions.”
Reasonable accommodations vary but may involve time off to attend healthcare appointments or recover from childbirth, extra breaks during a shift, shorter work hours, or the ability to sit instead of stand. Private and public sector employers, including state and local governments, federal agencies, and employment agencies, must abide by the new guidelines unless they can provide evidence that doing so will cause undue hardship.
Female doctors have historically encountered significant barriers to family planning. Years of training cause them to delay having children, often leading to higher rates of infertility, miscarriage, and pregnancy complications than in the general population.
Some specialties, like surgeons, are particularly at risk, with 42% reporting at least one pregnancy loss. Most surgeons work their regular schedules until delivery despite desiring workload reductions, commonly citing unsupportive workplaces as a reason for not seeking accommodations.
Trauma surgeon Qaali Hussein, MD, became pregnant with her first child during her intern year in 2008. She told this news organization that her residency program didn’t even have a maternity policy at the time, and her male supervisor was certain that motherhood would end her surgical career.
She shared how “women usually waited until the end of their training to get pregnant. No one had ever gotten pregnant during the program and returned from maternity leave. I was the first to do so, so there wasn’t a policy or any program support to say, ‘What can we do to help?’ ”
Dr. Hussein used her vacation and sick time, returning to work 4 weeks after delivery. She had five more children, including twins her chief year and another baby during fellowship training in 2014.
Each subsequent pregnancy was met with the same response from program leadership, she recalled. “They’d say, ‘This is it. You may have been able to do the first and second child, but this one will be impossible.’ ”
After the PWFA regulations first became enforceable in June, the EEOC accepted public feedback. The guidelines received nearly 100,000 comments, spurred mainly by the inclusion of abortion care as a qualifying condition for which an employee could receive accommodations. About 54,000 comments called for abortion to be excluded from the final rule, and 40,000 supported keeping the clause.
The EEOC issued the final rule on April 15. It includes abortion care. However, the updated rule “does not require any employee to have — or not to have — an abortion, does not require taxpayers to pay for any abortions, and does not compel health care providers to provide any abortions,” the unpublished version of the final rule said. It is scheduled to take effect 60 days after its publication in the Federal Register on April 19.
Increasing Support for Doctor-Moms
The PWFA supplements other EEOC protections, such as pregnancy discrimination under Title VII of the Civil Rights Act of 1964 and access to reasonable accommodations under the Americans with Disabilities Act. In addition, it builds upon Department of Labor regulations, like the PUMP Act for breastfeeding employees and the Family and Medical Leave Act, which provides 12 weeks of unpaid, job-protected leave for the arrival of a child or certain medical conditions.
FMLA applies only to employees who have worked full-time for at least 12 months for an employer with 50 or more employees. Meanwhile, the unpaid, job-protected leave under the PWFA has no waiting period, lowers the required number of employees to 15, and permits accommodations for up to 40 weeks.
Employers are encouraged to honor “common and simple” requests, like using a closer parking space or pumping or nursing at work, without requiring a doctor’s note, the rule said.
Efforts to improve family leave policies for physicians and residents have been gaining traction. In 2021, the American Board of Medical Specialties began requiring its member boards with training programs lasting 2 or more years to allow at least 6 weeks off for parental, caregiver, and medical leave. This time can be taken without exhausting vacation or sick leave or requiring an extension in training. Over half of the 24 member boards permit leave beyond 6 weeks, including the American Boards of Allergy and Immunology, Emergency Medicine, Family Medicine, Radiology, and Surgery.
Estefania Oliveros, MD, MSc, cardiologist and assistant professor at the Lewis Katz School of Medicine at Temple University, Philadelphia, told this news organization that the Accreditation Council for Graduate Medical Education also requires that residents and fellows receive 6 weeks of paid leave.
“We add to that vacation time, so it gives them at least 8 weeks,” she said. The school has created spaces for nursing mothers — something neither she nor Dr. Hussein had access to when breastfeeding — and encourages the attendings to be proactive in excusing pregnant fellows for appointments.
This differs significantly from her fellowship training experience 6 years ago at another institution, where she worked without accommodations until the day before her cesarean delivery. Dr. Oliveros had to use all her vacation time for recovery, returning to the program after 4 weeks instead of the recommended 6.
“And that’s the story you hear all the time. Not because people are ill-intended; I just don’t think the system is designed to accommodate women, so we lose a lot of talent that way,” said Dr. Oliveros, whose 2019 survey in the Journal of the American College of Cardiology called for more support and protections for pregnant doctors.
Both doctors believe the PWFA will be beneficial but only if leadership in the field takes up the cause.
“The cultures of these institutions determine whether women feel safe or even confident enough to have children in medical school or residency,” said Dr. Hussein.
A version of this article appeared on Medscape.com.
Pregnant physicians may receive more workplace accommodations and protection against discrimination thanks to an updated rule from the US Equal Employment Opportunity Commission (EEOC). The guidelines could prevent women from losing critical career momentum.
The Pregnant Workers Fairness Act (PWFA) aims to help workers balance professional demands with healthy pregnancies. It requires employers to provide reasonable accommodations for a “worker’s known limitations,” including physical or mental conditions associated with “pregnancy, childbirth, or related medical conditions.”
Reasonable accommodations vary but may involve time off to attend healthcare appointments or recover from childbirth, extra breaks during a shift, shorter work hours, or the ability to sit instead of stand. Private and public sector employers, including state and local governments, federal agencies, and employment agencies, must abide by the new guidelines unless they can provide evidence that doing so will cause undue hardship.
Female doctors have historically encountered significant barriers to family planning. Years of training cause them to delay having children, often leading to higher rates of infertility, miscarriage, and pregnancy complications than in the general population.
Some specialties, like surgeons, are particularly at risk, with 42% reporting at least one pregnancy loss. Most surgeons work their regular schedules until delivery despite desiring workload reductions, commonly citing unsupportive workplaces as a reason for not seeking accommodations.
Trauma surgeon Qaali Hussein, MD, became pregnant with her first child during her intern year in 2008. She told this news organization that her residency program didn’t even have a maternity policy at the time, and her male supervisor was certain that motherhood would end her surgical career.
She shared how “women usually waited until the end of their training to get pregnant. No one had ever gotten pregnant during the program and returned from maternity leave. I was the first to do so, so there wasn’t a policy or any program support to say, ‘What can we do to help?’ ”
Dr. Hussein used her vacation and sick time, returning to work 4 weeks after delivery. She had five more children, including twins her chief year and another baby during fellowship training in 2014.
Each subsequent pregnancy was met with the same response from program leadership, she recalled. “They’d say, ‘This is it. You may have been able to do the first and second child, but this one will be impossible.’ ”
After the PWFA regulations first became enforceable in June, the EEOC accepted public feedback. The guidelines received nearly 100,000 comments, spurred mainly by the inclusion of abortion care as a qualifying condition for which an employee could receive accommodations. About 54,000 comments called for abortion to be excluded from the final rule, and 40,000 supported keeping the clause.
The EEOC issued the final rule on April 15. It includes abortion care. However, the updated rule “does not require any employee to have — or not to have — an abortion, does not require taxpayers to pay for any abortions, and does not compel health care providers to provide any abortions,” the unpublished version of the final rule said. It is scheduled to take effect 60 days after its publication in the Federal Register on April 19.
Increasing Support for Doctor-Moms
The PWFA supplements other EEOC protections, such as pregnancy discrimination under Title VII of the Civil Rights Act of 1964 and access to reasonable accommodations under the Americans with Disabilities Act. In addition, it builds upon Department of Labor regulations, like the PUMP Act for breastfeeding employees and the Family and Medical Leave Act, which provides 12 weeks of unpaid, job-protected leave for the arrival of a child or certain medical conditions.
FMLA applies only to employees who have worked full-time for at least 12 months for an employer with 50 or more employees. Meanwhile, the unpaid, job-protected leave under the PWFA has no waiting period, lowers the required number of employees to 15, and permits accommodations for up to 40 weeks.
Employers are encouraged to honor “common and simple” requests, like using a closer parking space or pumping or nursing at work, without requiring a doctor’s note, the rule said.
Efforts to improve family leave policies for physicians and residents have been gaining traction. In 2021, the American Board of Medical Specialties began requiring its member boards with training programs lasting 2 or more years to allow at least 6 weeks off for parental, caregiver, and medical leave. This time can be taken without exhausting vacation or sick leave or requiring an extension in training. Over half of the 24 member boards permit leave beyond 6 weeks, including the American Boards of Allergy and Immunology, Emergency Medicine, Family Medicine, Radiology, and Surgery.
Estefania Oliveros, MD, MSc, cardiologist and assistant professor at the Lewis Katz School of Medicine at Temple University, Philadelphia, told this news organization that the Accreditation Council for Graduate Medical Education also requires that residents and fellows receive 6 weeks of paid leave.
“We add to that vacation time, so it gives them at least 8 weeks,” she said. The school has created spaces for nursing mothers — something neither she nor Dr. Hussein had access to when breastfeeding — and encourages the attendings to be proactive in excusing pregnant fellows for appointments.
This differs significantly from her fellowship training experience 6 years ago at another institution, where she worked without accommodations until the day before her cesarean delivery. Dr. Oliveros had to use all her vacation time for recovery, returning to the program after 4 weeks instead of the recommended 6.
“And that’s the story you hear all the time. Not because people are ill-intended; I just don’t think the system is designed to accommodate women, so we lose a lot of talent that way,” said Dr. Oliveros, whose 2019 survey in the Journal of the American College of Cardiology called for more support and protections for pregnant doctors.
Both doctors believe the PWFA will be beneficial but only if leadership in the field takes up the cause.
“The cultures of these institutions determine whether women feel safe or even confident enough to have children in medical school or residency,” said Dr. Hussein.
A version of this article appeared on Medscape.com.
Pregnant physicians may receive more workplace accommodations and protection against discrimination thanks to an updated rule from the US Equal Employment Opportunity Commission (EEOC). The guidelines could prevent women from losing critical career momentum.
The Pregnant Workers Fairness Act (PWFA) aims to help workers balance professional demands with healthy pregnancies. It requires employers to provide reasonable accommodations for a “worker’s known limitations,” including physical or mental conditions associated with “pregnancy, childbirth, or related medical conditions.”
Reasonable accommodations vary but may involve time off to attend healthcare appointments or recover from childbirth, extra breaks during a shift, shorter work hours, or the ability to sit instead of stand. Private and public sector employers, including state and local governments, federal agencies, and employment agencies, must abide by the new guidelines unless they can provide evidence that doing so will cause undue hardship.
Female doctors have historically encountered significant barriers to family planning. Years of training cause them to delay having children, often leading to higher rates of infertility, miscarriage, and pregnancy complications than in the general population.
Some specialties, like surgeons, are particularly at risk, with 42% reporting at least one pregnancy loss. Most surgeons work their regular schedules until delivery despite desiring workload reductions, commonly citing unsupportive workplaces as a reason for not seeking accommodations.
Trauma surgeon Qaali Hussein, MD, became pregnant with her first child during her intern year in 2008. She told this news organization that her residency program didn’t even have a maternity policy at the time, and her male supervisor was certain that motherhood would end her surgical career.
She shared how “women usually waited until the end of their training to get pregnant. No one had ever gotten pregnant during the program and returned from maternity leave. I was the first to do so, so there wasn’t a policy or any program support to say, ‘What can we do to help?’ ”
Dr. Hussein used her vacation and sick time, returning to work 4 weeks after delivery. She had five more children, including twins her chief year and another baby during fellowship training in 2014.
Each subsequent pregnancy was met with the same response from program leadership, she recalled. “They’d say, ‘This is it. You may have been able to do the first and second child, but this one will be impossible.’ ”
After the PWFA regulations first became enforceable in June, the EEOC accepted public feedback. The guidelines received nearly 100,000 comments, spurred mainly by the inclusion of abortion care as a qualifying condition for which an employee could receive accommodations. About 54,000 comments called for abortion to be excluded from the final rule, and 40,000 supported keeping the clause.
The EEOC issued the final rule on April 15. It includes abortion care. However, the updated rule “does not require any employee to have — or not to have — an abortion, does not require taxpayers to pay for any abortions, and does not compel health care providers to provide any abortions,” the unpublished version of the final rule said. It is scheduled to take effect 60 days after its publication in the Federal Register on April 19.
Increasing Support for Doctor-Moms
The PWFA supplements other EEOC protections, such as pregnancy discrimination under Title VII of the Civil Rights Act of 1964 and access to reasonable accommodations under the Americans with Disabilities Act. In addition, it builds upon Department of Labor regulations, like the PUMP Act for breastfeeding employees and the Family and Medical Leave Act, which provides 12 weeks of unpaid, job-protected leave for the arrival of a child or certain medical conditions.
FMLA applies only to employees who have worked full-time for at least 12 months for an employer with 50 or more employees. Meanwhile, the unpaid, job-protected leave under the PWFA has no waiting period, lowers the required number of employees to 15, and permits accommodations for up to 40 weeks.
Employers are encouraged to honor “common and simple” requests, like using a closer parking space or pumping or nursing at work, without requiring a doctor’s note, the rule said.
Efforts to improve family leave policies for physicians and residents have been gaining traction. In 2021, the American Board of Medical Specialties began requiring its member boards with training programs lasting 2 or more years to allow at least 6 weeks off for parental, caregiver, and medical leave. This time can be taken without exhausting vacation or sick leave or requiring an extension in training. Over half of the 24 member boards permit leave beyond 6 weeks, including the American Boards of Allergy and Immunology, Emergency Medicine, Family Medicine, Radiology, and Surgery.
Estefania Oliveros, MD, MSc, cardiologist and assistant professor at the Lewis Katz School of Medicine at Temple University, Philadelphia, told this news organization that the Accreditation Council for Graduate Medical Education also requires that residents and fellows receive 6 weeks of paid leave.
“We add to that vacation time, so it gives them at least 8 weeks,” she said. The school has created spaces for nursing mothers — something neither she nor Dr. Hussein had access to when breastfeeding — and encourages the attendings to be proactive in excusing pregnant fellows for appointments.
This differs significantly from her fellowship training experience 6 years ago at another institution, where she worked without accommodations until the day before her cesarean delivery. Dr. Oliveros had to use all her vacation time for recovery, returning to the program after 4 weeks instead of the recommended 6.
“And that’s the story you hear all the time. Not because people are ill-intended; I just don’t think the system is designed to accommodate women, so we lose a lot of talent that way,” said Dr. Oliveros, whose 2019 survey in the Journal of the American College of Cardiology called for more support and protections for pregnant doctors.
Both doctors believe the PWFA will be beneficial but only if leadership in the field takes up the cause.
“The cultures of these institutions determine whether women feel safe or even confident enough to have children in medical school or residency,” said Dr. Hussein.
A version of this article appeared on Medscape.com.
AI Surpasses Harvard Docs on Clinical Reasoning Test
TOPLINE:
The AI had more instances of incorrect reasoning than the doctors did but scored better overall.
METHODOLOGY:
- The study involved 39 physicians from two academic medical centers in Boston and the generative AI model GPT-4.
- Participants were presented with 20 simulated clinical cases involving common problems such as pharyngitis, headache, abdominal pain, cough, and chest pain. Each case included sections describing the triage presentation, review of systems, physical examination, and diagnostic testing.
- The primary outcome was the Revised-IDEA (R-IDEA) score, a 10-point scale evaluating clinical reasoning documentation across four domains: Interpretive summary, differential diagnosis, explanation of the lead diagnosis, and alternative diagnoses.
TAKEAWAY:
- AI achieved a median R-IDEA score of 10, higher than attending physicians (median score, 9) and residents (8).
- The chatbot had a significantly higher estimated probability of achieving a high R-IDEA score of 8-10 (0.99) compared with attendings (0.76) and residents (0.56).
- AI provided more responses that contained instances of incorrect clinical reasoning (13.8%) than residents (2.8%) and attending physicians (12.5%). It performed similarly to physicians in diagnostic accuracy and inclusion of cannot-miss diagnoses.
IN PRACTICE:
“Future research should assess clinical reasoning of the LLM-physician interaction, as LLMs will more likely augment, not replace, the human reasoning process,” the authors of the study wrote.
SOURCE:
Adam Rodman, MD, MPH, with Beth Israel Deaconess Medical Center, Boston, was the corresponding author on the paper. The research was published online in JAMA Internal Medicine.
LIMITATIONS:
Simulated clinical cases may not replicate performance in real-world scenarios. Further training could enhance the performance of the AI, so the study may underestimate its capabilities, the researchers noted.
DISCLOSURES:
The study was supported by the Harvard Clinical and Translational Science Center and Harvard University. Authors disclosed financial ties to publishing companies and Solera Health. Dr. Rodman received funding from the Gordon and Betty Moore Foundation.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
The AI had more instances of incorrect reasoning than the doctors did but scored better overall.
METHODOLOGY:
- The study involved 39 physicians from two academic medical centers in Boston and the generative AI model GPT-4.
- Participants were presented with 20 simulated clinical cases involving common problems such as pharyngitis, headache, abdominal pain, cough, and chest pain. Each case included sections describing the triage presentation, review of systems, physical examination, and diagnostic testing.
- The primary outcome was the Revised-IDEA (R-IDEA) score, a 10-point scale evaluating clinical reasoning documentation across four domains: Interpretive summary, differential diagnosis, explanation of the lead diagnosis, and alternative diagnoses.
TAKEAWAY:
- AI achieved a median R-IDEA score of 10, higher than attending physicians (median score, 9) and residents (8).
- The chatbot had a significantly higher estimated probability of achieving a high R-IDEA score of 8-10 (0.99) compared with attendings (0.76) and residents (0.56).
- AI provided more responses that contained instances of incorrect clinical reasoning (13.8%) than residents (2.8%) and attending physicians (12.5%). It performed similarly to physicians in diagnostic accuracy and inclusion of cannot-miss diagnoses.
IN PRACTICE:
“Future research should assess clinical reasoning of the LLM-physician interaction, as LLMs will more likely augment, not replace, the human reasoning process,” the authors of the study wrote.
SOURCE:
Adam Rodman, MD, MPH, with Beth Israel Deaconess Medical Center, Boston, was the corresponding author on the paper. The research was published online in JAMA Internal Medicine.
LIMITATIONS:
Simulated clinical cases may not replicate performance in real-world scenarios. Further training could enhance the performance of the AI, so the study may underestimate its capabilities, the researchers noted.
DISCLOSURES:
The study was supported by the Harvard Clinical and Translational Science Center and Harvard University. Authors disclosed financial ties to publishing companies and Solera Health. Dr. Rodman received funding from the Gordon and Betty Moore Foundation.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
The AI had more instances of incorrect reasoning than the doctors did but scored better overall.
METHODOLOGY:
- The study involved 39 physicians from two academic medical centers in Boston and the generative AI model GPT-4.
- Participants were presented with 20 simulated clinical cases involving common problems such as pharyngitis, headache, abdominal pain, cough, and chest pain. Each case included sections describing the triage presentation, review of systems, physical examination, and diagnostic testing.
- The primary outcome was the Revised-IDEA (R-IDEA) score, a 10-point scale evaluating clinical reasoning documentation across four domains: Interpretive summary, differential diagnosis, explanation of the lead diagnosis, and alternative diagnoses.
TAKEAWAY:
- AI achieved a median R-IDEA score of 10, higher than attending physicians (median score, 9) and residents (8).
- The chatbot had a significantly higher estimated probability of achieving a high R-IDEA score of 8-10 (0.99) compared with attendings (0.76) and residents (0.56).
- AI provided more responses that contained instances of incorrect clinical reasoning (13.8%) than residents (2.8%) and attending physicians (12.5%). It performed similarly to physicians in diagnostic accuracy and inclusion of cannot-miss diagnoses.
IN PRACTICE:
“Future research should assess clinical reasoning of the LLM-physician interaction, as LLMs will more likely augment, not replace, the human reasoning process,” the authors of the study wrote.
SOURCE:
Adam Rodman, MD, MPH, with Beth Israel Deaconess Medical Center, Boston, was the corresponding author on the paper. The research was published online in JAMA Internal Medicine.
LIMITATIONS:
Simulated clinical cases may not replicate performance in real-world scenarios. Further training could enhance the performance of the AI, so the study may underestimate its capabilities, the researchers noted.
DISCLOSURES:
The study was supported by the Harvard Clinical and Translational Science Center and Harvard University. Authors disclosed financial ties to publishing companies and Solera Health. Dr. Rodman received funding from the Gordon and Betty Moore Foundation.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Integrating Telemedicine for HCV With Opioid Use Disorder Treatment Works
People with opioid use disorder (OUD) who have hepatitis C virus (HCV) were twice as likely to be treated and cured of HCV if they received facilitated telemedicine treatment within their opioid treatment program than if they were referred for off-site treatment, the results of a new study showed.
In addition, among cured patients, illicit drug use fell significantly, and there were few reinfections, reported the researchers, led by Andrew Talal, MD, MPH, with the University at Buffalo, State University of New York, Buffalo.
The study was published online in JAMA.
HCV is a major public health concern, especially among people with OUD. Geographic and logistical barriers often prevent this underserved population from accessing treatment; however, telemedicine has the potential to overcome these obstacles.
In a prospective cluster randomized clinical trial, Dr. Talal and colleagues assessed the impact of embedding facilitated telemedicine for HCV care into 12 opioid treatment programs in New York State.
They studied 602 HCV-infected adults (61% male; 51% White) with OUD. Of these, 290 (mean age, 47.1 years) were enrolled in facilitated telemedicine programs onsite, and 312 (mean age, 48.9 years) received an off-site referral (usual care).
Telemedicine participants had an initial telemedicine encounter facilitated by study case managers onsite who also administered a blood test. The telemedicine clinician subsequently evaluated participants and ordered direct-acting antiviral (DAA) medication that was delivered to the opioid treatment program monthly (as refills required) and dispensed along with methadone.
In the telemedicine group, 268 of 290 individuals (92.4%) initiated HCV treatment compared with 126 of 312 (40.4%) in the referral group.
Participants in the telemedicine group were also seen sooner and started treatment faster.
The interval between screening and initial appointments was 14 days with telemedicine vs 18 days with a referral (P = .04). The time between the initial visit and DAA initiation was 49.9 days with telemedicine vs 123.5 days with a referral (P < .001).
Intention-to-treat analysis showed significantly higher HCV cure rates with telemedicine than with referral (90.3% vs 39.4%, respectively). Similarly, the observed cure rates were also higher in the telemedicine group (84.8% vs 34.0%).
Sustained virologic response was durable, with only 13 reinfections (incidence, 2.5 per 100 person-years) occurring during the 2-year follow-up period, the researchers reported.
In addition, illicit drug use decreased significantly among cured patients in both the telemedicine group (P < .001) and the referral group (P = .001). Adults in both groups rated healthcare delivery satisfaction as high or very high.
“Our study demonstrates how telemedicine successfully integrates medical and behavioral treatment,” Dr. Talal said in a statement.
The intervention “builds patient-clinician trust across the screen, and significant decreases in substance use were observed in cured participants with minimal HCV reinfections,” the study team wrote.
Support for this research was provided by the Patient-Centered Outcomes Research Institute and by the Troup Fund of the Kaleida Health Foundation.
A version of this article appeared on Medscape.com .
People with opioid use disorder (OUD) who have hepatitis C virus (HCV) were twice as likely to be treated and cured of HCV if they received facilitated telemedicine treatment within their opioid treatment program than if they were referred for off-site treatment, the results of a new study showed.
In addition, among cured patients, illicit drug use fell significantly, and there were few reinfections, reported the researchers, led by Andrew Talal, MD, MPH, with the University at Buffalo, State University of New York, Buffalo.
The study was published online in JAMA.
HCV is a major public health concern, especially among people with OUD. Geographic and logistical barriers often prevent this underserved population from accessing treatment; however, telemedicine has the potential to overcome these obstacles.
In a prospective cluster randomized clinical trial, Dr. Talal and colleagues assessed the impact of embedding facilitated telemedicine for HCV care into 12 opioid treatment programs in New York State.
They studied 602 HCV-infected adults (61% male; 51% White) with OUD. Of these, 290 (mean age, 47.1 years) were enrolled in facilitated telemedicine programs onsite, and 312 (mean age, 48.9 years) received an off-site referral (usual care).
Telemedicine participants had an initial telemedicine encounter facilitated by study case managers onsite who also administered a blood test. The telemedicine clinician subsequently evaluated participants and ordered direct-acting antiviral (DAA) medication that was delivered to the opioid treatment program monthly (as refills required) and dispensed along with methadone.
In the telemedicine group, 268 of 290 individuals (92.4%) initiated HCV treatment compared with 126 of 312 (40.4%) in the referral group.
Participants in the telemedicine group were also seen sooner and started treatment faster.
The interval between screening and initial appointments was 14 days with telemedicine vs 18 days with a referral (P = .04). The time between the initial visit and DAA initiation was 49.9 days with telemedicine vs 123.5 days with a referral (P < .001).
Intention-to-treat analysis showed significantly higher HCV cure rates with telemedicine than with referral (90.3% vs 39.4%, respectively). Similarly, the observed cure rates were also higher in the telemedicine group (84.8% vs 34.0%).
Sustained virologic response was durable, with only 13 reinfections (incidence, 2.5 per 100 person-years) occurring during the 2-year follow-up period, the researchers reported.
In addition, illicit drug use decreased significantly among cured patients in both the telemedicine group (P < .001) and the referral group (P = .001). Adults in both groups rated healthcare delivery satisfaction as high or very high.
“Our study demonstrates how telemedicine successfully integrates medical and behavioral treatment,” Dr. Talal said in a statement.
The intervention “builds patient-clinician trust across the screen, and significant decreases in substance use were observed in cured participants with minimal HCV reinfections,” the study team wrote.
Support for this research was provided by the Patient-Centered Outcomes Research Institute and by the Troup Fund of the Kaleida Health Foundation.
A version of this article appeared on Medscape.com .
People with opioid use disorder (OUD) who have hepatitis C virus (HCV) were twice as likely to be treated and cured of HCV if they received facilitated telemedicine treatment within their opioid treatment program than if they were referred for off-site treatment, the results of a new study showed.
In addition, among cured patients, illicit drug use fell significantly, and there were few reinfections, reported the researchers, led by Andrew Talal, MD, MPH, with the University at Buffalo, State University of New York, Buffalo.
The study was published online in JAMA.
HCV is a major public health concern, especially among people with OUD. Geographic and logistical barriers often prevent this underserved population from accessing treatment; however, telemedicine has the potential to overcome these obstacles.
In a prospective cluster randomized clinical trial, Dr. Talal and colleagues assessed the impact of embedding facilitated telemedicine for HCV care into 12 opioid treatment programs in New York State.
They studied 602 HCV-infected adults (61% male; 51% White) with OUD. Of these, 290 (mean age, 47.1 years) were enrolled in facilitated telemedicine programs onsite, and 312 (mean age, 48.9 years) received an off-site referral (usual care).
Telemedicine participants had an initial telemedicine encounter facilitated by study case managers onsite who also administered a blood test. The telemedicine clinician subsequently evaluated participants and ordered direct-acting antiviral (DAA) medication that was delivered to the opioid treatment program monthly (as refills required) and dispensed along with methadone.
In the telemedicine group, 268 of 290 individuals (92.4%) initiated HCV treatment compared with 126 of 312 (40.4%) in the referral group.
Participants in the telemedicine group were also seen sooner and started treatment faster.
The interval between screening and initial appointments was 14 days with telemedicine vs 18 days with a referral (P = .04). The time between the initial visit and DAA initiation was 49.9 days with telemedicine vs 123.5 days with a referral (P < .001).
Intention-to-treat analysis showed significantly higher HCV cure rates with telemedicine than with referral (90.3% vs 39.4%, respectively). Similarly, the observed cure rates were also higher in the telemedicine group (84.8% vs 34.0%).
Sustained virologic response was durable, with only 13 reinfections (incidence, 2.5 per 100 person-years) occurring during the 2-year follow-up period, the researchers reported.
In addition, illicit drug use decreased significantly among cured patients in both the telemedicine group (P < .001) and the referral group (P = .001). Adults in both groups rated healthcare delivery satisfaction as high or very high.
“Our study demonstrates how telemedicine successfully integrates medical and behavioral treatment,” Dr. Talal said in a statement.
The intervention “builds patient-clinician trust across the screen, and significant decreases in substance use were observed in cured participants with minimal HCV reinfections,” the study team wrote.
Support for this research was provided by the Patient-Centered Outcomes Research Institute and by the Troup Fund of the Kaleida Health Foundation.
A version of this article appeared on Medscape.com .
FROM JAMA
Vaccine ‘Will Not Curb’ Dengue Epidemic, Says PAHO
The current tetravalent dengue vaccine TAK-003, from the Japanese laboratory Takeda, is not likely to control the ongoing epidemic, according to the Pan American Health Organization (PAHO). The organization emphasized the need to better understand the vaccine’s effectiveness against different serotypes and its safety under real-world clinical conditions.
The Americas are experiencing a record increase in dengue cases. Three times as many cases have been identified during 2024 (3.5 million) than were reported for the same period in 2023.
“The vaccine we have available will not curb the dengue epidemic; it should be used complementarily with other actions. The most important actions are field operations, vector control, prevention, and education,” said Daniel Salas, MD, executive manager of the PAHO Comprehensive Immunization Program, during a press conference on March 28.
“The vaccines we currently have are not the best response to reduce transmission and prevent deaths,” added Jarbas Barbosa, MD, PhD, PAHO’s director. The fatality rate remains below 0.05%, but this figure could be hard to maintain if the situation becomes more uncontrolled.
The TAK-003 regimen consists of two doses with a 3-month interval between applications, so “it is not a tool to control transmission at this moment. Studies have shown that only 8 years of [population-level] vaccination would have a significant impact on dengue transmission,” said Dr. Barbosa.
A new vaccine developed in Brazil in partnership with the company MSD, Butantan-DV, is in phase 3 trials and has the advantage of being a single-dose application, which could facilitate its use in situations with accelerated transmission. “But this vaccine will likely only be available in 2025,” said Dr. Barbosa.
PAHO officials also highlighted the need to better characterize the vaccine’s effectiveness and safety in the real world. They observed, for example, that when TAK-003 was investigated, the circulation of dengue serotype 3 was almost nonexistent, so the efficacy data against that serotype “are very limited.”
“The producer, Takeda, has very limited production capacity. Brazil is the country that uses this vaccine the most, followed by Argentina. Given that these countries have a good epidemiological surveillance system and adverse effect registration, they can conduct studies on how the vaccine performs in real life, which will greatly increase our knowledge about it. For example, we will see its effectiveness against serotype 3,” said Dr. Barbosa.
The PAHO Technical Advisory Group (TAG) on vaccine-preventable diseases recommended that any country using these vaccines have surveillance systems in place because it is important to promptly report and investigate any adverse events, said Dr. Salas. The organization also suggested that vaccination should ideally be administered in a “more controlled environment,” a phase 4 study, “to complete the safety and efficacy profile, especially in those who have not had dengue before and for dengue 3 and 4,” said Dr. Salas in response to a question from this news organization.
“People cannot expect that just because they were vaccinated, they will not get dengue. The vaccine has limited reach,” he emphasized.
Other research strategies for vector control, such as the use of the Wolbachia bacteria and mosquito sterilization, are future strategies and “not tools to control this outbreak,” noted Sylvain Aldighieri, MD, director of the Department of Prevention, Control, and Elimination of Transmissible Diseases at PAHO.
In his opening remarks, Dr. Barbosa urged the intensification of efforts with tools that are already available. These approaches include eliminating mosquito breeding sites (“80% are in or near homes”) and protecting against mosquito bites, preparing health services for early diagnosis and timely clinical management, and educating the population about dengue symptoms so they seek medical attention immediately.
Although dengue is increasing throughout Latin America and the Caribbean, the most affected countries are Brazil (83%), Paraguay (5.3%), and Argentina (3.7%), which account for 92% of the cases and 87% of the deaths, PAHO reported.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com .
The current tetravalent dengue vaccine TAK-003, from the Japanese laboratory Takeda, is not likely to control the ongoing epidemic, according to the Pan American Health Organization (PAHO). The organization emphasized the need to better understand the vaccine’s effectiveness against different serotypes and its safety under real-world clinical conditions.
The Americas are experiencing a record increase in dengue cases. Three times as many cases have been identified during 2024 (3.5 million) than were reported for the same period in 2023.
“The vaccine we have available will not curb the dengue epidemic; it should be used complementarily with other actions. The most important actions are field operations, vector control, prevention, and education,” said Daniel Salas, MD, executive manager of the PAHO Comprehensive Immunization Program, during a press conference on March 28.
“The vaccines we currently have are not the best response to reduce transmission and prevent deaths,” added Jarbas Barbosa, MD, PhD, PAHO’s director. The fatality rate remains below 0.05%, but this figure could be hard to maintain if the situation becomes more uncontrolled.
The TAK-003 regimen consists of two doses with a 3-month interval between applications, so “it is not a tool to control transmission at this moment. Studies have shown that only 8 years of [population-level] vaccination would have a significant impact on dengue transmission,” said Dr. Barbosa.
A new vaccine developed in Brazil in partnership with the company MSD, Butantan-DV, is in phase 3 trials and has the advantage of being a single-dose application, which could facilitate its use in situations with accelerated transmission. “But this vaccine will likely only be available in 2025,” said Dr. Barbosa.
PAHO officials also highlighted the need to better characterize the vaccine’s effectiveness and safety in the real world. They observed, for example, that when TAK-003 was investigated, the circulation of dengue serotype 3 was almost nonexistent, so the efficacy data against that serotype “are very limited.”
“The producer, Takeda, has very limited production capacity. Brazil is the country that uses this vaccine the most, followed by Argentina. Given that these countries have a good epidemiological surveillance system and adverse effect registration, they can conduct studies on how the vaccine performs in real life, which will greatly increase our knowledge about it. For example, we will see its effectiveness against serotype 3,” said Dr. Barbosa.
The PAHO Technical Advisory Group (TAG) on vaccine-preventable diseases recommended that any country using these vaccines have surveillance systems in place because it is important to promptly report and investigate any adverse events, said Dr. Salas. The organization also suggested that vaccination should ideally be administered in a “more controlled environment,” a phase 4 study, “to complete the safety and efficacy profile, especially in those who have not had dengue before and for dengue 3 and 4,” said Dr. Salas in response to a question from this news organization.
“People cannot expect that just because they were vaccinated, they will not get dengue. The vaccine has limited reach,” he emphasized.
Other research strategies for vector control, such as the use of the Wolbachia bacteria and mosquito sterilization, are future strategies and “not tools to control this outbreak,” noted Sylvain Aldighieri, MD, director of the Department of Prevention, Control, and Elimination of Transmissible Diseases at PAHO.
In his opening remarks, Dr. Barbosa urged the intensification of efforts with tools that are already available. These approaches include eliminating mosquito breeding sites (“80% are in or near homes”) and protecting against mosquito bites, preparing health services for early diagnosis and timely clinical management, and educating the population about dengue symptoms so they seek medical attention immediately.
Although dengue is increasing throughout Latin America and the Caribbean, the most affected countries are Brazil (83%), Paraguay (5.3%), and Argentina (3.7%), which account for 92% of the cases and 87% of the deaths, PAHO reported.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com .
The current tetravalent dengue vaccine TAK-003, from the Japanese laboratory Takeda, is not likely to control the ongoing epidemic, according to the Pan American Health Organization (PAHO). The organization emphasized the need to better understand the vaccine’s effectiveness against different serotypes and its safety under real-world clinical conditions.
The Americas are experiencing a record increase in dengue cases. Three times as many cases have been identified during 2024 (3.5 million) than were reported for the same period in 2023.
“The vaccine we have available will not curb the dengue epidemic; it should be used complementarily with other actions. The most important actions are field operations, vector control, prevention, and education,” said Daniel Salas, MD, executive manager of the PAHO Comprehensive Immunization Program, during a press conference on March 28.
“The vaccines we currently have are not the best response to reduce transmission and prevent deaths,” added Jarbas Barbosa, MD, PhD, PAHO’s director. The fatality rate remains below 0.05%, but this figure could be hard to maintain if the situation becomes more uncontrolled.
The TAK-003 regimen consists of two doses with a 3-month interval between applications, so “it is not a tool to control transmission at this moment. Studies have shown that only 8 years of [population-level] vaccination would have a significant impact on dengue transmission,” said Dr. Barbosa.
A new vaccine developed in Brazil in partnership with the company MSD, Butantan-DV, is in phase 3 trials and has the advantage of being a single-dose application, which could facilitate its use in situations with accelerated transmission. “But this vaccine will likely only be available in 2025,” said Dr. Barbosa.
PAHO officials also highlighted the need to better characterize the vaccine’s effectiveness and safety in the real world. They observed, for example, that when TAK-003 was investigated, the circulation of dengue serotype 3 was almost nonexistent, so the efficacy data against that serotype “are very limited.”
“The producer, Takeda, has very limited production capacity. Brazil is the country that uses this vaccine the most, followed by Argentina. Given that these countries have a good epidemiological surveillance system and adverse effect registration, they can conduct studies on how the vaccine performs in real life, which will greatly increase our knowledge about it. For example, we will see its effectiveness against serotype 3,” said Dr. Barbosa.
The PAHO Technical Advisory Group (TAG) on vaccine-preventable diseases recommended that any country using these vaccines have surveillance systems in place because it is important to promptly report and investigate any adverse events, said Dr. Salas. The organization also suggested that vaccination should ideally be administered in a “more controlled environment,” a phase 4 study, “to complete the safety and efficacy profile, especially in those who have not had dengue before and for dengue 3 and 4,” said Dr. Salas in response to a question from this news organization.
“People cannot expect that just because they were vaccinated, they will not get dengue. The vaccine has limited reach,” he emphasized.
Other research strategies for vector control, such as the use of the Wolbachia bacteria and mosquito sterilization, are future strategies and “not tools to control this outbreak,” noted Sylvain Aldighieri, MD, director of the Department of Prevention, Control, and Elimination of Transmissible Diseases at PAHO.
In his opening remarks, Dr. Barbosa urged the intensification of efforts with tools that are already available. These approaches include eliminating mosquito breeding sites (“80% are in or near homes”) and protecting against mosquito bites, preparing health services for early diagnosis and timely clinical management, and educating the population about dengue symptoms so they seek medical attention immediately.
Although dengue is increasing throughout Latin America and the Caribbean, the most affected countries are Brazil (83%), Paraguay (5.3%), and Argentina (3.7%), which account for 92% of the cases and 87% of the deaths, PAHO reported.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com .