User login
Comprehensive diabetic retinopathy screening challenging
NEW ORLEANS – Fewer than one-third of patients with diabetes being cared for by a public hospital system underwent screening for retinopathy within the past year, judging from the results from a survey of administrative data.
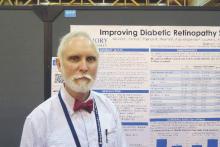
“Diabetic retinopathy is a major cause of vision loss in the United States,” researchers led by Dr. David C. Ziemer wrote in an abstract presented during a poster session at the annual scientific sessions of the American Diabetes Association.
“In 2011, the age-adjusted percentage of adults with diagnosed diabetes reporting visual impairment was 17.6%. This is a pressing issue as the number of Americans with diabetic retinopathy is expected to double from 7.7 million in 2010 to 15.6 million in 2050.”
In an effort to plan for better diabetic retinopathy screening, Dr. Ziemer and his associates analyzed 2014 administrative data from 19,361 patients with diabetes who attended one of several clinics operated by the Atlanta-based Grady Health System. Diabetic retinopathy was considered complete if ophthalmology clinic, optometry, or retinal photograph visit was attended. The researchers also surveyed a convenience sample of 80 patients about their diabetic retinopathy screening in the past year.
The mean age of patients was 57 years, their mean hemoglobin A1c level was 7.8%, 59% were female, and 83% were African-American. Of the 19,361 patients, 5,595 (29%) underwent diabetic retinopathy screening and 13,766 (71%) did not. The unscreened had a mean of 1 clinic visit for diabetes care, compared with a mean of 3.1 for those who underwent screening (P less than .0005). In the analysis of administrative data, Dr. Ziemer, of the division of endocrinology at Emory University, Atlanta, reported that 29% of patients underwent diabetic retinopathy screening in the past year, with variation by care site that ranged from 5% to 66%, and 5,000 had no diabetes continuity care visit.
Factors associated with increased diabetic retinopathy screening were treatment in a diabetes clinic (odds ratio, 2.8), treatment in a primary care clinic (OR, 2.1), and being older (OR, 1.03/year; P less than .001 for all associations), according to a multivariable analysis. Factors associated with decreased diabetic retinopathy screening were Hispanic ethnicity (OR, 0.7) and having a mental health diagnosis (OR, .8; P less than .001 for both associations). The researchers also found that having an in-clinic eye screening doubled the proportion of diabetic retinopathy screenings (48% vs. 22%) and decreased the number of screenings done in an outside clinic (45% vs. 95%).
Of the 80 patients who completed the survey, 68% reported that they underwent diabetic retinopathy screening within the past year, which was in contrast to the 29% reported by administrative data. In addition, 50% of survey respondents who did not undergo diabetic retinopathy screening reported that they received a referral, yet more than 40% failed to honor eye appointments. “The first barrier to address is people who don’t keep appointments,” Dr. Ziemer said in an interview. “Getting people in care is one issue. Having the capacity is another. That’s a real problem.”
The study was supported by the American Diabetes Association. Dr. Ziemer reported having no financial disclosures.
NEW ORLEANS – Fewer than one-third of patients with diabetes being cared for by a public hospital system underwent screening for retinopathy within the past year, judging from the results from a survey of administrative data.
“Diabetic retinopathy is a major cause of vision loss in the United States,” researchers led by Dr. David C. Ziemer wrote in an abstract presented during a poster session at the annual scientific sessions of the American Diabetes Association.
“In 2011, the age-adjusted percentage of adults with diagnosed diabetes reporting visual impairment was 17.6%. This is a pressing issue as the number of Americans with diabetic retinopathy is expected to double from 7.7 million in 2010 to 15.6 million in 2050.”
In an effort to plan for better diabetic retinopathy screening, Dr. Ziemer and his associates analyzed 2014 administrative data from 19,361 patients with diabetes who attended one of several clinics operated by the Atlanta-based Grady Health System. Diabetic retinopathy was considered complete if ophthalmology clinic, optometry, or retinal photograph visit was attended. The researchers also surveyed a convenience sample of 80 patients about their diabetic retinopathy screening in the past year.
The mean age of patients was 57 years, their mean hemoglobin A1c level was 7.8%, 59% were female, and 83% were African-American. Of the 19,361 patients, 5,595 (29%) underwent diabetic retinopathy screening and 13,766 (71%) did not. The unscreened had a mean of 1 clinic visit for diabetes care, compared with a mean of 3.1 for those who underwent screening (P less than .0005). In the analysis of administrative data, Dr. Ziemer, of the division of endocrinology at Emory University, Atlanta, reported that 29% of patients underwent diabetic retinopathy screening in the past year, with variation by care site that ranged from 5% to 66%, and 5,000 had no diabetes continuity care visit.
Factors associated with increased diabetic retinopathy screening were treatment in a diabetes clinic (odds ratio, 2.8), treatment in a primary care clinic (OR, 2.1), and being older (OR, 1.03/year; P less than .001 for all associations), according to a multivariable analysis. Factors associated with decreased diabetic retinopathy screening were Hispanic ethnicity (OR, 0.7) and having a mental health diagnosis (OR, .8; P less than .001 for both associations). The researchers also found that having an in-clinic eye screening doubled the proportion of diabetic retinopathy screenings (48% vs. 22%) and decreased the number of screenings done in an outside clinic (45% vs. 95%).
Of the 80 patients who completed the survey, 68% reported that they underwent diabetic retinopathy screening within the past year, which was in contrast to the 29% reported by administrative data. In addition, 50% of survey respondents who did not undergo diabetic retinopathy screening reported that they received a referral, yet more than 40% failed to honor eye appointments. “The first barrier to address is people who don’t keep appointments,” Dr. Ziemer said in an interview. “Getting people in care is one issue. Having the capacity is another. That’s a real problem.”
The study was supported by the American Diabetes Association. Dr. Ziemer reported having no financial disclosures.
NEW ORLEANS – Fewer than one-third of patients with diabetes being cared for by a public hospital system underwent screening for retinopathy within the past year, judging from the results from a survey of administrative data.
“Diabetic retinopathy is a major cause of vision loss in the United States,” researchers led by Dr. David C. Ziemer wrote in an abstract presented during a poster session at the annual scientific sessions of the American Diabetes Association.
“In 2011, the age-adjusted percentage of adults with diagnosed diabetes reporting visual impairment was 17.6%. This is a pressing issue as the number of Americans with diabetic retinopathy is expected to double from 7.7 million in 2010 to 15.6 million in 2050.”
In an effort to plan for better diabetic retinopathy screening, Dr. Ziemer and his associates analyzed 2014 administrative data from 19,361 patients with diabetes who attended one of several clinics operated by the Atlanta-based Grady Health System. Diabetic retinopathy was considered complete if ophthalmology clinic, optometry, or retinal photograph visit was attended. The researchers also surveyed a convenience sample of 80 patients about their diabetic retinopathy screening in the past year.
The mean age of patients was 57 years, their mean hemoglobin A1c level was 7.8%, 59% were female, and 83% were African-American. Of the 19,361 patients, 5,595 (29%) underwent diabetic retinopathy screening and 13,766 (71%) did not. The unscreened had a mean of 1 clinic visit for diabetes care, compared with a mean of 3.1 for those who underwent screening (P less than .0005). In the analysis of administrative data, Dr. Ziemer, of the division of endocrinology at Emory University, Atlanta, reported that 29% of patients underwent diabetic retinopathy screening in the past year, with variation by care site that ranged from 5% to 66%, and 5,000 had no diabetes continuity care visit.
Factors associated with increased diabetic retinopathy screening were treatment in a diabetes clinic (odds ratio, 2.8), treatment in a primary care clinic (OR, 2.1), and being older (OR, 1.03/year; P less than .001 for all associations), according to a multivariable analysis. Factors associated with decreased diabetic retinopathy screening were Hispanic ethnicity (OR, 0.7) and having a mental health diagnosis (OR, .8; P less than .001 for both associations). The researchers also found that having an in-clinic eye screening doubled the proportion of diabetic retinopathy screenings (48% vs. 22%) and decreased the number of screenings done in an outside clinic (45% vs. 95%).
Of the 80 patients who completed the survey, 68% reported that they underwent diabetic retinopathy screening within the past year, which was in contrast to the 29% reported by administrative data. In addition, 50% of survey respondents who did not undergo diabetic retinopathy screening reported that they received a referral, yet more than 40% failed to honor eye appointments. “The first barrier to address is people who don’t keep appointments,” Dr. Ziemer said in an interview. “Getting people in care is one issue. Having the capacity is another. That’s a real problem.”
The study was supported by the American Diabetes Association. Dr. Ziemer reported having no financial disclosures.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: Some 71% of diabetes patients did not undergo screening for diabetic retinopathy.
Major finding: Only 29% of patients underwent diabetic retinopathy screening in the past year, with variation by care site that ranged from 5% to 66%.
Data source: An analysis of administrative data from 19,361 patients with diabetes who attended one of several clinics operated by the Atlanta-based Grady Health System in 2014.
Disclosures: The study was supported by the American Diabetes Association. Dr. Ziemer reported having no financial disclosures.
VIDEO: ASD doesn’t appear any more prevalent in children with type 1 diabetes
NEW ORLEANS – The prevalence of autism spectrum disorder in children and adolescents with type 1 diabetes appears to be similar to that in the general pediatric population, according to a study conducted in Colorado.
“There is no known literature on management of patients with autism spectrum disorder and type 1 diabetes to assess if management is different in this population,” Dr. Shideh Majidi said in an interview at the annual scientific sessions of the American Diabetes Association.
In what she said is the first study of its kind conducted in the United States, Dr. Majidi and her associates investigated the prevalence of autism spectrum disorder (ASD) in a large diabetes center to better understand the diabetes characteristics and management of those with both type 1 diabetes and ASD. The researchers evaluated 2,360 patients aged 18 months to 18 years cared for at the Barbara Davis Center for Childhood Diabetes at the University of Colorado, Aurora. Of the 2,360 patients, 30 (28 males and 2 females) had ASD, for a prevalence of 1 in 87 (1.15%). This was similar to the prevalence of ASD in the general Colorado population, which is estimated to be 1 in 85 (1.18%).
Patients with type 1 diabetes and ASD had a mean age of 12.9 years and had the disease for a mean of 5 years. There were fewer females with type 1 diabetes and ASD, compared with those who had type 1 diabetes only (7% vs. 48%, respectively; P less than .001).
Compared with patients who had type 1 diabetes, those with type 1 diabetes and ASD had similar hemoglobin A1c levels (a median of 8.2% vs. 8.8%, P = .17) and number of blood glucose tests per day (a median of 5.1 vs. 4.9, P = .32), but were less likely to be on an insulin pump (43.3% vs. 57%, P = .14).
The overall findings suggest that management in patients with ASD and type 1 diabetes does not necessarily need to differ from those without ASD. “For instance, it is possible for ASD patients to do well on an insulin pump,” said Dr. Majidi, who is a pediatric endocrinologist at the Barbara Davis Center for Childhood Diabetes. “Also, A1c and blood sugar checks are similar between those with and without ASD, and thus similar intensive management can be recommended for this group. So just like in patients without ASD, diabetes should be managed on an individual basis, looking at individual needs, but having a diagnosis of ASD does not have to limit our views as providers of what types of management we can offer for ideal diabetes management.”
She acknowledged certain limitations of the study, including its single-center design and relatively small sample size. “It would be beneficial to obtain larger numbers of patients with ASD and type 1 diabetes via multicenter studies in order to get a larger group of patients with both diagnoses, in order to see if our results remain when looking on a larger scale.”
In a video interview at the meeting, Dr. Majidi and Dr. Kelly Stanek of the Barbara Davis Center for Childhood Diabetes discussed the study's findings and the next steps for research, including a closer examination of the challenges parents face in caring for children with type 1 diabetes and ASD.
Dr. Majidi and Dr. Stanek reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – The prevalence of autism spectrum disorder in children and adolescents with type 1 diabetes appears to be similar to that in the general pediatric population, according to a study conducted in Colorado.
“There is no known literature on management of patients with autism spectrum disorder and type 1 diabetes to assess if management is different in this population,” Dr. Shideh Majidi said in an interview at the annual scientific sessions of the American Diabetes Association.
In what she said is the first study of its kind conducted in the United States, Dr. Majidi and her associates investigated the prevalence of autism spectrum disorder (ASD) in a large diabetes center to better understand the diabetes characteristics and management of those with both type 1 diabetes and ASD. The researchers evaluated 2,360 patients aged 18 months to 18 years cared for at the Barbara Davis Center for Childhood Diabetes at the University of Colorado, Aurora. Of the 2,360 patients, 30 (28 males and 2 females) had ASD, for a prevalence of 1 in 87 (1.15%). This was similar to the prevalence of ASD in the general Colorado population, which is estimated to be 1 in 85 (1.18%).
Patients with type 1 diabetes and ASD had a mean age of 12.9 years and had the disease for a mean of 5 years. There were fewer females with type 1 diabetes and ASD, compared with those who had type 1 diabetes only (7% vs. 48%, respectively; P less than .001).
Compared with patients who had type 1 diabetes, those with type 1 diabetes and ASD had similar hemoglobin A1c levels (a median of 8.2% vs. 8.8%, P = .17) and number of blood glucose tests per day (a median of 5.1 vs. 4.9, P = .32), but were less likely to be on an insulin pump (43.3% vs. 57%, P = .14).
The overall findings suggest that management in patients with ASD and type 1 diabetes does not necessarily need to differ from those without ASD. “For instance, it is possible for ASD patients to do well on an insulin pump,” said Dr. Majidi, who is a pediatric endocrinologist at the Barbara Davis Center for Childhood Diabetes. “Also, A1c and blood sugar checks are similar between those with and without ASD, and thus similar intensive management can be recommended for this group. So just like in patients without ASD, diabetes should be managed on an individual basis, looking at individual needs, but having a diagnosis of ASD does not have to limit our views as providers of what types of management we can offer for ideal diabetes management.”
She acknowledged certain limitations of the study, including its single-center design and relatively small sample size. “It would be beneficial to obtain larger numbers of patients with ASD and type 1 diabetes via multicenter studies in order to get a larger group of patients with both diagnoses, in order to see if our results remain when looking on a larger scale.”
In a video interview at the meeting, Dr. Majidi and Dr. Kelly Stanek of the Barbara Davis Center for Childhood Diabetes discussed the study's findings and the next steps for research, including a closer examination of the challenges parents face in caring for children with type 1 diabetes and ASD.
Dr. Majidi and Dr. Stanek reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – The prevalence of autism spectrum disorder in children and adolescents with type 1 diabetes appears to be similar to that in the general pediatric population, according to a study conducted in Colorado.
“There is no known literature on management of patients with autism spectrum disorder and type 1 diabetes to assess if management is different in this population,” Dr. Shideh Majidi said in an interview at the annual scientific sessions of the American Diabetes Association.
In what she said is the first study of its kind conducted in the United States, Dr. Majidi and her associates investigated the prevalence of autism spectrum disorder (ASD) in a large diabetes center to better understand the diabetes characteristics and management of those with both type 1 diabetes and ASD. The researchers evaluated 2,360 patients aged 18 months to 18 years cared for at the Barbara Davis Center for Childhood Diabetes at the University of Colorado, Aurora. Of the 2,360 patients, 30 (28 males and 2 females) had ASD, for a prevalence of 1 in 87 (1.15%). This was similar to the prevalence of ASD in the general Colorado population, which is estimated to be 1 in 85 (1.18%).
Patients with type 1 diabetes and ASD had a mean age of 12.9 years and had the disease for a mean of 5 years. There were fewer females with type 1 diabetes and ASD, compared with those who had type 1 diabetes only (7% vs. 48%, respectively; P less than .001).
Compared with patients who had type 1 diabetes, those with type 1 diabetes and ASD had similar hemoglobin A1c levels (a median of 8.2% vs. 8.8%, P = .17) and number of blood glucose tests per day (a median of 5.1 vs. 4.9, P = .32), but were less likely to be on an insulin pump (43.3% vs. 57%, P = .14).
The overall findings suggest that management in patients with ASD and type 1 diabetes does not necessarily need to differ from those without ASD. “For instance, it is possible for ASD patients to do well on an insulin pump,” said Dr. Majidi, who is a pediatric endocrinologist at the Barbara Davis Center for Childhood Diabetes. “Also, A1c and blood sugar checks are similar between those with and without ASD, and thus similar intensive management can be recommended for this group. So just like in patients without ASD, diabetes should be managed on an individual basis, looking at individual needs, but having a diagnosis of ASD does not have to limit our views as providers of what types of management we can offer for ideal diabetes management.”
She acknowledged certain limitations of the study, including its single-center design and relatively small sample size. “It would be beneficial to obtain larger numbers of patients with ASD and type 1 diabetes via multicenter studies in order to get a larger group of patients with both diagnoses, in order to see if our results remain when looking on a larger scale.”
In a video interview at the meeting, Dr. Majidi and Dr. Kelly Stanek of the Barbara Davis Center for Childhood Diabetes discussed the study's findings and the next steps for research, including a closer examination of the challenges parents face in caring for children with type 1 diabetes and ASD.
Dr. Majidi and Dr. Stanek reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ADA SCIENTIFIC SESSIONS
Key clinical point: Overall, the prevalence of autism spectrum disorder among Colorado youth with type 1 diabetes is similar to the prevalence of ASD in the general Colorado pediatric population.
Major finding: The prevalence of pediatric patients in Colorado with type 1 diabetes and ASD was 1 in 87 (1.15%), which was similar to the prevalence of ASD in the general Colorado pediatric population, 1 in 85 (1.18%).
Data source: An analysis of 2,360 patients with type 1 diabetes aged 18 months to 18 years old who were cared for at a single center in Colorado.
Disclosures: Dr. Majidi and Dr. Stanek reported having no relevant financial disclosures.
Subdermal mini-pump with exenatide superior to sitagliptin in reducing HbA1c
NEW ORLEANS – The second trial involving a sub-dermal matchstick-size osmotic mini-pump that releases exenatide over 6 months in people who have poorly controlled type 2 diabetes achieved superior blood glucose levels and weight loss after a year, compared with sitagliptin alone, Dr. Julio Rosenstock reported at the annual scientific sessions of the American Diabetes Association.
Dr. Rosenstock, director of the Dallas Diabetes and Endocrine Center, reported on the findings of the study, known as FREEDOM-2. The study randomized 535 adults with poorly controlled type 2 diabetes to either the mini-pump, known as the ITCA 650, that releases 60 μg of exenatide a day, or 100 mg of daily sitagliptin. This is a follow-on trial to FREEDOM-1 that compared the ICTA 650 mini-pump to twice-daily exenatide in people with type 2 diabetes who were taking metformin (Diabetes Care. 2013 Sep;36[9]:2559-65). All participants in FREEDOM-2 had been on metformin greater than or equal to 1,500 mg daily and had HbA1c greater than or equal to 7.5%.
“The continuous subcutaneous delivery of exenatide with ICTA 650 is a novel approach to improve glycemic control, ensuring adherence and consistent delivery of therapy for 6-12 months for people with type 2 diabetes,” Dr. Rosenstock said. The ICTA recipients first received a dose of 20 μg of exenatide daily for the first 12 weeks, then had that increased to 60 μg for the remainder of the study.
After 1 year, average reduction in HbA1c was 1.5% with ITCA 650 vs. 0.8% with sitagliptin, Dr. Rosenstock said. Sixty-one percent of those in the ITCA 650 group achieved greater than 0.5% reductions in HbA1c and more than 2 kg loss in body weight after a year, compared with 28% of the sitagliptin group.
Overall, the patients who receive the ITCA 650 achieved an average body weight reduction of 4 kg vs. 1.3 kg for the sitagliptin patients. Again, 61% of the ITCA patients achieved target HbA1c of less than 7% vs. 42% of the sitagliptin group. Rescue therapy was required in 15% with ITCA 650 and 35% with sitagliptin, and minor hypoglycemia occurred in 4.2% with ITCA 650 vs. 1.9% with sitagliptin.
The ICTA 650 group did have a higher incidence of adverse events, Dr. Rosenstock said, 82% vs. 74%. These included side effects at the application site like hematoma, bleeding, infection, or pain, as well as gastrointestinal (GI) problems such as nausea and vomiting. “The GI adverse events were similar to what we have seen with other GLP-1 receptor agonists,” Dr. Rosenstock said. “The incidence of nausea spiked at the initial insertion and then when we increased the dose from 20 μg to 60 μg, but the second time the ICTA 650 was replaced for 60 μg dosing, the nausea rates did not spike.” The ICTA 650 group had a discontinuation rate of 1%.
Each mini-pump inserted in the FREEDOM-2 trial had a duration of 6 months, but Dr. Rosenstock said the goal is to achieve extended-release dosing with a single mini-pump for 2 years.
Dr. Rosenstock disclosed he serves on the advisory panels of Boehringer Ingelheim Pharmaceuticals, Daiichi-Sankyo Co., Eli Lilly and Company, GlaxoSmithKline, Intarcia Therapeutics, Janssen Pharmaceuticals, Lexicon Pharmaceuticals, MannKind Corporation, Merck & Co., Novartis, Novo Nordisk, Sanofi U.S., and Takeda Pharmaceutical Company; and that he has received research support from Amylin Pharmaceuticals, AstraZeneca, Boehringer Ingelheim, Daiichi-Sankyo, Eli Lilly, GlaxoSmithKline, Intarcia Therapeutics, Janssen Pharmaceuticals, Lexicon Pharmaceuticals, MannKind Corporation, Merck & Co., Novartis, Novo Nordisk, Pfizer, Roche Pharmaceuticals, Sanofi U.S. and Takeda.
NEW ORLEANS – The second trial involving a sub-dermal matchstick-size osmotic mini-pump that releases exenatide over 6 months in people who have poorly controlled type 2 diabetes achieved superior blood glucose levels and weight loss after a year, compared with sitagliptin alone, Dr. Julio Rosenstock reported at the annual scientific sessions of the American Diabetes Association.
Dr. Rosenstock, director of the Dallas Diabetes and Endocrine Center, reported on the findings of the study, known as FREEDOM-2. The study randomized 535 adults with poorly controlled type 2 diabetes to either the mini-pump, known as the ITCA 650, that releases 60 μg of exenatide a day, or 100 mg of daily sitagliptin. This is a follow-on trial to FREEDOM-1 that compared the ICTA 650 mini-pump to twice-daily exenatide in people with type 2 diabetes who were taking metformin (Diabetes Care. 2013 Sep;36[9]:2559-65). All participants in FREEDOM-2 had been on metformin greater than or equal to 1,500 mg daily and had HbA1c greater than or equal to 7.5%.
“The continuous subcutaneous delivery of exenatide with ICTA 650 is a novel approach to improve glycemic control, ensuring adherence and consistent delivery of therapy for 6-12 months for people with type 2 diabetes,” Dr. Rosenstock said. The ICTA recipients first received a dose of 20 μg of exenatide daily for the first 12 weeks, then had that increased to 60 μg for the remainder of the study.
After 1 year, average reduction in HbA1c was 1.5% with ITCA 650 vs. 0.8% with sitagliptin, Dr. Rosenstock said. Sixty-one percent of those in the ITCA 650 group achieved greater than 0.5% reductions in HbA1c and more than 2 kg loss in body weight after a year, compared with 28% of the sitagliptin group.
Overall, the patients who receive the ITCA 650 achieved an average body weight reduction of 4 kg vs. 1.3 kg for the sitagliptin patients. Again, 61% of the ITCA patients achieved target HbA1c of less than 7% vs. 42% of the sitagliptin group. Rescue therapy was required in 15% with ITCA 650 and 35% with sitagliptin, and minor hypoglycemia occurred in 4.2% with ITCA 650 vs. 1.9% with sitagliptin.
The ICTA 650 group did have a higher incidence of adverse events, Dr. Rosenstock said, 82% vs. 74%. These included side effects at the application site like hematoma, bleeding, infection, or pain, as well as gastrointestinal (GI) problems such as nausea and vomiting. “The GI adverse events were similar to what we have seen with other GLP-1 receptor agonists,” Dr. Rosenstock said. “The incidence of nausea spiked at the initial insertion and then when we increased the dose from 20 μg to 60 μg, but the second time the ICTA 650 was replaced for 60 μg dosing, the nausea rates did not spike.” The ICTA 650 group had a discontinuation rate of 1%.
Each mini-pump inserted in the FREEDOM-2 trial had a duration of 6 months, but Dr. Rosenstock said the goal is to achieve extended-release dosing with a single mini-pump for 2 years.
Dr. Rosenstock disclosed he serves on the advisory panels of Boehringer Ingelheim Pharmaceuticals, Daiichi-Sankyo Co., Eli Lilly and Company, GlaxoSmithKline, Intarcia Therapeutics, Janssen Pharmaceuticals, Lexicon Pharmaceuticals, MannKind Corporation, Merck & Co., Novartis, Novo Nordisk, Sanofi U.S., and Takeda Pharmaceutical Company; and that he has received research support from Amylin Pharmaceuticals, AstraZeneca, Boehringer Ingelheim, Daiichi-Sankyo, Eli Lilly, GlaxoSmithKline, Intarcia Therapeutics, Janssen Pharmaceuticals, Lexicon Pharmaceuticals, MannKind Corporation, Merck & Co., Novartis, Novo Nordisk, Pfizer, Roche Pharmaceuticals, Sanofi U.S. and Takeda.
NEW ORLEANS – The second trial involving a sub-dermal matchstick-size osmotic mini-pump that releases exenatide over 6 months in people who have poorly controlled type 2 diabetes achieved superior blood glucose levels and weight loss after a year, compared with sitagliptin alone, Dr. Julio Rosenstock reported at the annual scientific sessions of the American Diabetes Association.
Dr. Rosenstock, director of the Dallas Diabetes and Endocrine Center, reported on the findings of the study, known as FREEDOM-2. The study randomized 535 adults with poorly controlled type 2 diabetes to either the mini-pump, known as the ITCA 650, that releases 60 μg of exenatide a day, or 100 mg of daily sitagliptin. This is a follow-on trial to FREEDOM-1 that compared the ICTA 650 mini-pump to twice-daily exenatide in people with type 2 diabetes who were taking metformin (Diabetes Care. 2013 Sep;36[9]:2559-65). All participants in FREEDOM-2 had been on metformin greater than or equal to 1,500 mg daily and had HbA1c greater than or equal to 7.5%.
“The continuous subcutaneous delivery of exenatide with ICTA 650 is a novel approach to improve glycemic control, ensuring adherence and consistent delivery of therapy for 6-12 months for people with type 2 diabetes,” Dr. Rosenstock said. The ICTA recipients first received a dose of 20 μg of exenatide daily for the first 12 weeks, then had that increased to 60 μg for the remainder of the study.
After 1 year, average reduction in HbA1c was 1.5% with ITCA 650 vs. 0.8% with sitagliptin, Dr. Rosenstock said. Sixty-one percent of those in the ITCA 650 group achieved greater than 0.5% reductions in HbA1c and more than 2 kg loss in body weight after a year, compared with 28% of the sitagliptin group.
Overall, the patients who receive the ITCA 650 achieved an average body weight reduction of 4 kg vs. 1.3 kg for the sitagliptin patients. Again, 61% of the ITCA patients achieved target HbA1c of less than 7% vs. 42% of the sitagliptin group. Rescue therapy was required in 15% with ITCA 650 and 35% with sitagliptin, and minor hypoglycemia occurred in 4.2% with ITCA 650 vs. 1.9% with sitagliptin.
The ICTA 650 group did have a higher incidence of adverse events, Dr. Rosenstock said, 82% vs. 74%. These included side effects at the application site like hematoma, bleeding, infection, or pain, as well as gastrointestinal (GI) problems such as nausea and vomiting. “The GI adverse events were similar to what we have seen with other GLP-1 receptor agonists,” Dr. Rosenstock said. “The incidence of nausea spiked at the initial insertion and then when we increased the dose from 20 μg to 60 μg, but the second time the ICTA 650 was replaced for 60 μg dosing, the nausea rates did not spike.” The ICTA 650 group had a discontinuation rate of 1%.
Each mini-pump inserted in the FREEDOM-2 trial had a duration of 6 months, but Dr. Rosenstock said the goal is to achieve extended-release dosing with a single mini-pump for 2 years.
Dr. Rosenstock disclosed he serves on the advisory panels of Boehringer Ingelheim Pharmaceuticals, Daiichi-Sankyo Co., Eli Lilly and Company, GlaxoSmithKline, Intarcia Therapeutics, Janssen Pharmaceuticals, Lexicon Pharmaceuticals, MannKind Corporation, Merck & Co., Novartis, Novo Nordisk, Sanofi U.S., and Takeda Pharmaceutical Company; and that he has received research support from Amylin Pharmaceuticals, AstraZeneca, Boehringer Ingelheim, Daiichi-Sankyo, Eli Lilly, GlaxoSmithKline, Intarcia Therapeutics, Janssen Pharmaceuticals, Lexicon Pharmaceuticals, MannKind Corporation, Merck & Co., Novartis, Novo Nordisk, Pfizer, Roche Pharmaceuticals, Sanofi U.S. and Takeda.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: An osmotic mini-pump that releases exenatide over 6 months achieves superior blood glucose levels and weight loss after 1 year, compared with daily sitagliptin therapy.
Major finding: After 1 year, average reduction in HbA1c was 1.5% with the ITCA 650 mini-pump vs. 0.8% with sitagliptin.
Data source: Randomized trial of 535 patients with type 2 diabetes assigned to receive ICTA 650 mini-pump or sitagliptin greater than or equal to 1,500 mg daily.
Disclosures: Dr. Rosenstock disclosed he serves on the advisory panels of Boehringer Ingelheim Pharmaceuticals, Daiichi-Sankyo Co., Eli Lilly and Company, GlaxoSmithKline, Intarcia Therapeutics, Janssen Pharmaceuticals, Lexicon Pharmaceuticals, MannKind Corporation, Merck & Co., Novartis, Novo Nordisk, Sanofi U.S., and Takeda Pharmaceutical Company; and that he has received research support from Amylin Pharmaceuticals, AstraZeneca, Boehringer Ingelheim, Daiichi-Sankyo, Eli Lilly, GlaxoSmithKline, Intarcia Therapeutics, Janssen Pharmaceuticals, Lexicon Pharmaceuticals, MannKind Corporation, Merck & Co., Novartis, Novo Nordisk, Pfizer, Roche Pharmaceuticals, Sanofi U.S., and Takeda.
VIDEO: Bionic pancreas configurations may help control type 1 diabetes
NEW ORLEANS — The bionic pancreas, otherwise known as the closed-loop system, can effectively control blood glucose levels and hypoglycemia in adults with type 1 diabetes, according to three different early-stage studies presented at the annual scientific sessions of the American Diabetes Association.
Edward R. Damiano, Ph.D., professor of biomedical engineering at Boston University and co-developer of an iPhone-based bionic pancreas that releases both glucagon and insulin, reported results from the first study of the fully automated device.
Dr. Damiano described this bionic pancreas as a “cobbling together of components” – an iPhone with an app that uses algorithms to control continuous glucose monitor and a couple of pumps that use an unstable form of glucagon that has to be reconstituted every day. Since the study, he and his colleagues have created a company, Beta Bionics, to develop a fully integrated device that replaces the iPhone with a self-contained unit called the iLet that runs on two AA batteries.
The first study of the bionic pancreas was a randomized, cross-over study of 39 adults with type 1 diabetes who used the bionic pancreas for 11 consecutive days and then their own insulin pump for 11 days, or vice versa, while continuing their normal activity.
“What we found with the multi-center study relative to insulin pump therapy, the bionic pancreas is associated with a reduction in both the blood sugar level in the 20 mg/dL mean glucose range as well as the simultaneous reduction in hypoglycemia,” Dr. Damiano said. He added that the bionic pancreas also resulted in less variability in blood glucose levels in individual participants, with a standard deviation of ±10 mg/dL vs. ±30 mg/dL for the insulin pump.
“Our goal is to bring this into clinical trials later this year and start the final pivotal trial in the first half of next year,” Dr. Damiano said, with commercial availability expected by 2018.
Another study of a bionic pancreas investigated automated glucagon-only delivery to reduce the severity and frequency of hypoglycemia. Courtney Balliro of Massachusetts General Hospital, Boston, explained that the double-blind, randomized, placebo-controlled crossover trial involved 22 patients with type 1 diabetes who use an insulin pump or daily insulin injections, but had reduced awareness of hypoglycemia.
The patients wore an experimental closed-loop device to deliver glucagon or a placebo device. “Our study found that using automatic glucagon delivery reduced hypoglycemia by 75% during the day and 91% at night,” the registered nurse reported. The goal is to develop a device that delivers both insulin and glucagon for type 1 diabetics, but a glucagon-only version could be an option for people with type 1 diabetes who are already comfortable with an insulin regimen, either by pump or self-administration, and people with type 2 diabetes or those who have had bariatric surgery.
The third study compared the effectiveness of a bihormonal bionic pancreas – one that delivers both insulin and glucagon – with a system that uses the same insulin algorithm as the bihormonal system to deliver insulin only. Dr. Laya Ekhlaspour of MassGeneral Hospital for Children, Boston, explained the system was configured with a higher glucose target than the 100 mg/dL used in previous bionic pancreas trials to determine if the insulin-only version could both effectively control blood glucose levels and maintain low rates of hypoglycemia.
This random-order, crossover study, involved two insulin-only configurations of the bionic pancreas (at glucose targets of 130 mg/dL and 145 mg/dL), comparing them with three bihormonal configurations (glucose target of 130 mg/dL, 115 mg/dL, and 100 mg/dL) and to usual care (patient-managed, conventional insulin pump therapy) over 3 days. Twenty subjects completed the study.
Raising the blood glucose target to 130 mg/dL increased the mean glucose the bihormonal bionic pancreas achieved (156 mg/dL in the 130-mg/dL configuration vs. 146 mg/dL in the 115-mg/dL target configuration vs. 136 mg/dl in the 100-mg/dL configuration, P less than or equal to .016 for each comparison). But the target glucose of 130 mg/dl yielded no significant difference between the mean glucose achieved in the insulin-only configuration and the bihormonal configuration of the bionic pancreas (161 mg/dL vs.156 mg/dL, P greater than 0.28, respectively), and no difference in hypoglycemia between the two bionic pancreas configurations (0.8% vs. 0.6%, P greater than .28). Likewise, both bionic pancreas configurations at the 130-mg/dl target had similar mean glucose and hypoglycemia vs. the usual care arm.
Dr. Ekhlaspour explained that the goal now is to complete two more arms of the study with a blood glucose target of 110 mg/dL. “We’re hoping we can release the results in the next couple of months, and these results will inform us of what glucose target we can use in a much larger pivotal study with the insulin-only version of the bionic pancreas in 2017,” Dr. Ekhlaspour said.
Vincent Crabtree, Ph.D., director of research business development for the Juvenile Diabetes Research Foundation, said he is encouraged by the studies. “They reinforce everyone’s belief that artificial pancreas/bionic pancreas systems can make a tremendous difference in the lives of people with type 1 diabetes by both reducing the day-to-day unrelenting burden of managing the disease and simultaneously improving the long term outcomes.”
The iLet development team included Steven J. Russell, M.D., Ph.D., assistant professor of medicine at the Diabetes Research Center at Massachusetts General Hospital, Boston. In a video interview at the meeting, Dr. Russell discussed the iLet device and the results of the 39-patient study.
Besides Dr. Damiano’s commercial interest in Beta Bionics, he also disclosed relationships with Dexcom, Eli Lily, Tandem Diabetes Care, NOVA Biomedical, and Sweetspot Diabetes. Dr. Russell disclosed relationships with Abbott Diabetes Care, Beta Bionics, Companion Medical, Dexcom, Eli Lilly, Insulet, International Biomedical, Medtronic MiniMed, Sanofi U.S., and Tandem Diabetes Care. The other study authors had no financial relationships to disclose.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS — The bionic pancreas, otherwise known as the closed-loop system, can effectively control blood glucose levels and hypoglycemia in adults with type 1 diabetes, according to three different early-stage studies presented at the annual scientific sessions of the American Diabetes Association.
Edward R. Damiano, Ph.D., professor of biomedical engineering at Boston University and co-developer of an iPhone-based bionic pancreas that releases both glucagon and insulin, reported results from the first study of the fully automated device.
Dr. Damiano described this bionic pancreas as a “cobbling together of components” – an iPhone with an app that uses algorithms to control continuous glucose monitor and a couple of pumps that use an unstable form of glucagon that has to be reconstituted every day. Since the study, he and his colleagues have created a company, Beta Bionics, to develop a fully integrated device that replaces the iPhone with a self-contained unit called the iLet that runs on two AA batteries.
The first study of the bionic pancreas was a randomized, cross-over study of 39 adults with type 1 diabetes who used the bionic pancreas for 11 consecutive days and then their own insulin pump for 11 days, or vice versa, while continuing their normal activity.
“What we found with the multi-center study relative to insulin pump therapy, the bionic pancreas is associated with a reduction in both the blood sugar level in the 20 mg/dL mean glucose range as well as the simultaneous reduction in hypoglycemia,” Dr. Damiano said. He added that the bionic pancreas also resulted in less variability in blood glucose levels in individual participants, with a standard deviation of ±10 mg/dL vs. ±30 mg/dL for the insulin pump.
“Our goal is to bring this into clinical trials later this year and start the final pivotal trial in the first half of next year,” Dr. Damiano said, with commercial availability expected by 2018.
Another study of a bionic pancreas investigated automated glucagon-only delivery to reduce the severity and frequency of hypoglycemia. Courtney Balliro of Massachusetts General Hospital, Boston, explained that the double-blind, randomized, placebo-controlled crossover trial involved 22 patients with type 1 diabetes who use an insulin pump or daily insulin injections, but had reduced awareness of hypoglycemia.
The patients wore an experimental closed-loop device to deliver glucagon or a placebo device. “Our study found that using automatic glucagon delivery reduced hypoglycemia by 75% during the day and 91% at night,” the registered nurse reported. The goal is to develop a device that delivers both insulin and glucagon for type 1 diabetics, but a glucagon-only version could be an option for people with type 1 diabetes who are already comfortable with an insulin regimen, either by pump or self-administration, and people with type 2 diabetes or those who have had bariatric surgery.
The third study compared the effectiveness of a bihormonal bionic pancreas – one that delivers both insulin and glucagon – with a system that uses the same insulin algorithm as the bihormonal system to deliver insulin only. Dr. Laya Ekhlaspour of MassGeneral Hospital for Children, Boston, explained the system was configured with a higher glucose target than the 100 mg/dL used in previous bionic pancreas trials to determine if the insulin-only version could both effectively control blood glucose levels and maintain low rates of hypoglycemia.
This random-order, crossover study, involved two insulin-only configurations of the bionic pancreas (at glucose targets of 130 mg/dL and 145 mg/dL), comparing them with three bihormonal configurations (glucose target of 130 mg/dL, 115 mg/dL, and 100 mg/dL) and to usual care (patient-managed, conventional insulin pump therapy) over 3 days. Twenty subjects completed the study.
Raising the blood glucose target to 130 mg/dL increased the mean glucose the bihormonal bionic pancreas achieved (156 mg/dL in the 130-mg/dL configuration vs. 146 mg/dL in the 115-mg/dL target configuration vs. 136 mg/dl in the 100-mg/dL configuration, P less than or equal to .016 for each comparison). But the target glucose of 130 mg/dl yielded no significant difference between the mean glucose achieved in the insulin-only configuration and the bihormonal configuration of the bionic pancreas (161 mg/dL vs.156 mg/dL, P greater than 0.28, respectively), and no difference in hypoglycemia between the two bionic pancreas configurations (0.8% vs. 0.6%, P greater than .28). Likewise, both bionic pancreas configurations at the 130-mg/dl target had similar mean glucose and hypoglycemia vs. the usual care arm.
Dr. Ekhlaspour explained that the goal now is to complete two more arms of the study with a blood glucose target of 110 mg/dL. “We’re hoping we can release the results in the next couple of months, and these results will inform us of what glucose target we can use in a much larger pivotal study with the insulin-only version of the bionic pancreas in 2017,” Dr. Ekhlaspour said.
Vincent Crabtree, Ph.D., director of research business development for the Juvenile Diabetes Research Foundation, said he is encouraged by the studies. “They reinforce everyone’s belief that artificial pancreas/bionic pancreas systems can make a tremendous difference in the lives of people with type 1 diabetes by both reducing the day-to-day unrelenting burden of managing the disease and simultaneously improving the long term outcomes.”
The iLet development team included Steven J. Russell, M.D., Ph.D., assistant professor of medicine at the Diabetes Research Center at Massachusetts General Hospital, Boston. In a video interview at the meeting, Dr. Russell discussed the iLet device and the results of the 39-patient study.
Besides Dr. Damiano’s commercial interest in Beta Bionics, he also disclosed relationships with Dexcom, Eli Lily, Tandem Diabetes Care, NOVA Biomedical, and Sweetspot Diabetes. Dr. Russell disclosed relationships with Abbott Diabetes Care, Beta Bionics, Companion Medical, Dexcom, Eli Lilly, Insulet, International Biomedical, Medtronic MiniMed, Sanofi U.S., and Tandem Diabetes Care. The other study authors had no financial relationships to disclose.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS — The bionic pancreas, otherwise known as the closed-loop system, can effectively control blood glucose levels and hypoglycemia in adults with type 1 diabetes, according to three different early-stage studies presented at the annual scientific sessions of the American Diabetes Association.
Edward R. Damiano, Ph.D., professor of biomedical engineering at Boston University and co-developer of an iPhone-based bionic pancreas that releases both glucagon and insulin, reported results from the first study of the fully automated device.
Dr. Damiano described this bionic pancreas as a “cobbling together of components” – an iPhone with an app that uses algorithms to control continuous glucose monitor and a couple of pumps that use an unstable form of glucagon that has to be reconstituted every day. Since the study, he and his colleagues have created a company, Beta Bionics, to develop a fully integrated device that replaces the iPhone with a self-contained unit called the iLet that runs on two AA batteries.
The first study of the bionic pancreas was a randomized, cross-over study of 39 adults with type 1 diabetes who used the bionic pancreas for 11 consecutive days and then their own insulin pump for 11 days, or vice versa, while continuing their normal activity.
“What we found with the multi-center study relative to insulin pump therapy, the bionic pancreas is associated with a reduction in both the blood sugar level in the 20 mg/dL mean glucose range as well as the simultaneous reduction in hypoglycemia,” Dr. Damiano said. He added that the bionic pancreas also resulted in less variability in blood glucose levels in individual participants, with a standard deviation of ±10 mg/dL vs. ±30 mg/dL for the insulin pump.
“Our goal is to bring this into clinical trials later this year and start the final pivotal trial in the first half of next year,” Dr. Damiano said, with commercial availability expected by 2018.
Another study of a bionic pancreas investigated automated glucagon-only delivery to reduce the severity and frequency of hypoglycemia. Courtney Balliro of Massachusetts General Hospital, Boston, explained that the double-blind, randomized, placebo-controlled crossover trial involved 22 patients with type 1 diabetes who use an insulin pump or daily insulin injections, but had reduced awareness of hypoglycemia.
The patients wore an experimental closed-loop device to deliver glucagon or a placebo device. “Our study found that using automatic glucagon delivery reduced hypoglycemia by 75% during the day and 91% at night,” the registered nurse reported. The goal is to develop a device that delivers both insulin and glucagon for type 1 diabetics, but a glucagon-only version could be an option for people with type 1 diabetes who are already comfortable with an insulin regimen, either by pump or self-administration, and people with type 2 diabetes or those who have had bariatric surgery.
The third study compared the effectiveness of a bihormonal bionic pancreas – one that delivers both insulin and glucagon – with a system that uses the same insulin algorithm as the bihormonal system to deliver insulin only. Dr. Laya Ekhlaspour of MassGeneral Hospital for Children, Boston, explained the system was configured with a higher glucose target than the 100 mg/dL used in previous bionic pancreas trials to determine if the insulin-only version could both effectively control blood glucose levels and maintain low rates of hypoglycemia.
This random-order, crossover study, involved two insulin-only configurations of the bionic pancreas (at glucose targets of 130 mg/dL and 145 mg/dL), comparing them with three bihormonal configurations (glucose target of 130 mg/dL, 115 mg/dL, and 100 mg/dL) and to usual care (patient-managed, conventional insulin pump therapy) over 3 days. Twenty subjects completed the study.
Raising the blood glucose target to 130 mg/dL increased the mean glucose the bihormonal bionic pancreas achieved (156 mg/dL in the 130-mg/dL configuration vs. 146 mg/dL in the 115-mg/dL target configuration vs. 136 mg/dl in the 100-mg/dL configuration, P less than or equal to .016 for each comparison). But the target glucose of 130 mg/dl yielded no significant difference between the mean glucose achieved in the insulin-only configuration and the bihormonal configuration of the bionic pancreas (161 mg/dL vs.156 mg/dL, P greater than 0.28, respectively), and no difference in hypoglycemia between the two bionic pancreas configurations (0.8% vs. 0.6%, P greater than .28). Likewise, both bionic pancreas configurations at the 130-mg/dl target had similar mean glucose and hypoglycemia vs. the usual care arm.
Dr. Ekhlaspour explained that the goal now is to complete two more arms of the study with a blood glucose target of 110 mg/dL. “We’re hoping we can release the results in the next couple of months, and these results will inform us of what glucose target we can use in a much larger pivotal study with the insulin-only version of the bionic pancreas in 2017,” Dr. Ekhlaspour said.
Vincent Crabtree, Ph.D., director of research business development for the Juvenile Diabetes Research Foundation, said he is encouraged by the studies. “They reinforce everyone’s belief that artificial pancreas/bionic pancreas systems can make a tremendous difference in the lives of people with type 1 diabetes by both reducing the day-to-day unrelenting burden of managing the disease and simultaneously improving the long term outcomes.”
The iLet development team included Steven J. Russell, M.D., Ph.D., assistant professor of medicine at the Diabetes Research Center at Massachusetts General Hospital, Boston. In a video interview at the meeting, Dr. Russell discussed the iLet device and the results of the 39-patient study.
Besides Dr. Damiano’s commercial interest in Beta Bionics, he also disclosed relationships with Dexcom, Eli Lily, Tandem Diabetes Care, NOVA Biomedical, and Sweetspot Diabetes. Dr. Russell disclosed relationships with Abbott Diabetes Care, Beta Bionics, Companion Medical, Dexcom, Eli Lilly, Insulet, International Biomedical, Medtronic MiniMed, Sanofi U.S., and Tandem Diabetes Care. The other study authors had no financial relationships to disclose.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: Three studies have validated the safety and efficacy of different configurations of the bionic pancreas, also known as the closed-loop system, to control blood glucose levels and hypoglycemia in type 1 diabetes.
Major finding: Varied configurations of the bionic pancreas were found to reduce blood sugar around 20 mg/dL, and to reduce hypoglycemia by 75% during the day and 91% at night; the bihormonal bionic pancreas achieved results equivalent to traditional treatment.
Data source: Three early stage studies involving 81 adults with type 1 diabetes.
Disclosures: Dr. Damiano disclosed a commercial interest in Beta Bionics, and also disclosed relationships with Dexcom, Eli Lily, Tandem Diabetes Care, NOVA Biomedical, and Sweetspot Diabetes. Dr. Russell disclosed relationships with Abbott Diabetes Care, Beta Bionics, Companion Medical, Dexcom, Eli Lilly, Insulet, International Biomedical, Medtronic MiniMed, Sanofi U.S., and Tandem Diabetes Care. The other study authors had no financial relationships to disclose.
Smart Insole System Helped Reduce Reulceration Risk
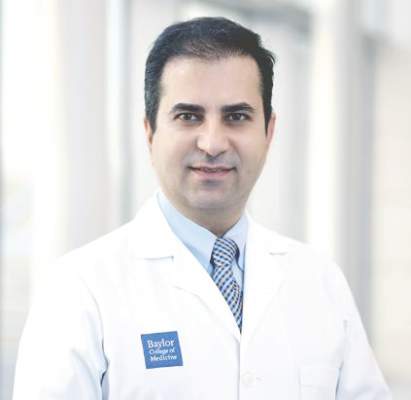
NEW ORLEANS – Patients with diabetes and peripheral neuropathy who used a smart watch and specially designed smart insoles equipped with an alert system minimized their reulceration risk, results from a proof-of-concept study demonstrated.
The findings suggest that mobile health “could be an effective method to educate patients to change their harmful activity behavior, could enhance adherence to regularly inspect their feet and seek for care in a timely manner, and ultimately may assist in prevention of recurrence of ulcers,” lead author Bijan Najafi, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association.
Dr. Najafi, professor of surgery at Baylor College of Medicine, Houston, said that in 2015, approximately one-third of all diabetes-related costs in the United States were spent on diabetic foot ulcers (DFUs). “Unfortunately, many DFUs end up in amputation, which could devastate patients and their families,” he said. “On the same note, persons within the lowest income brackets are estimated to have 38% higher amputation rate, compared with those in the highest income bracket. All these highlight an important gap in effective management of DFUs, in particular among poor working-class people.”
He also noted that DFU recurrence rates are 30%-40% in the first year, compared with 7.5% annual incidence for patients with peripheral neuropathy and no ulcer history. “The good news is that 75% of recurrent foot ulcers are preventable,” said Dr. Najafi, who is also director of clinical research in Baylor’s division of vascular surgery and endovascular therapy and director of the Interdisciplinary Consortium on Advanced Motion Performance. “An effective method is empowering patients to take care of their own health via regular self-inspection of their feet as well as providing timely and personalized foot care. The big challenge is adherence to prevention and regular foot inspection.”
In a study supported in part by Orpyx Medical Technologies, the investigators used a smart watch and smart insoles to enhance adherence to footwear and effective offloading by providing real-time feedback to 19 patients at high risk of DFUs about a harmful plantar pressure event. The patients wore the insole system for 3 months and were alerted through a smart watch if their plantar pressure exceeded 50 mm Hg over 95% of a moving 15-minute window. A successful response to an alert was recorded when offloading occurred within 20 minutes.
Dr. Najafi reported that by the third month, patients who received a higher number of alerts were more likely to use devices and technique to offload weight from their foot, compared with those who received a lower number of alerts (55% vs. 17%, respectively; P less than .01). In addition, patients whose wear time increased during the study tended to have more alerts, compared with other participants (a mean of .82 vs. .36 alerts per hour; P = .09). The best results occurred when patients received at least one alert every 2 hours. “We found that those who frequently received alerts about harmful plantar pressure events improved their adherence to the prescribed footwear and were more responsive to alerts,” he said. At the same time, those patients who received fewer alerts per day, “started to neglect alerts and adherence to footwear over time, despite having initially good adherence at the first month.”
Going forward, Dr. Najafi said, a key challenge is to continue engaging patients to use such technologies on a daily basis. “This could be addressable by providing frequent and comprehensive alerts which not only address harmful plantar pressure during walking but also any harmful foot-loading conditions, including prolonged harmful foot-loading pressure during standing as well as sitting,” he said.
In a video interview at the meeting, Dr. Najafi discussed the study and the challenges of encouraging treatment adherence.
Orpyx Medical Technologies provided partial funding support for the study. Dr. Najafi reported having no financial disclosures. The other authors of this study are Eyal Ron, Ana Enriquez, Ivan Marin, Jacqueline Lee-Eng, Javad Razjouyan, Ph.D., and Dr. David Armstrong. All subjects were recruited at the University of Arizona, College of Medicine, Tucson.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – Patients with diabetes and peripheral neuropathy who used a smart watch and specially designed smart insoles equipped with an alert system minimized their reulceration risk, results from a proof-of-concept study demonstrated.
The findings suggest that mobile health “could be an effective method to educate patients to change their harmful activity behavior, could enhance adherence to regularly inspect their feet and seek for care in a timely manner, and ultimately may assist in prevention of recurrence of ulcers,” lead author Bijan Najafi, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association.
Dr. Najafi, professor of surgery at Baylor College of Medicine, Houston, said that in 2015, approximately one-third of all diabetes-related costs in the United States were spent on diabetic foot ulcers (DFUs). “Unfortunately, many DFUs end up in amputation, which could devastate patients and their families,” he said. “On the same note, persons within the lowest income brackets are estimated to have 38% higher amputation rate, compared with those in the highest income bracket. All these highlight an important gap in effective management of DFUs, in particular among poor working-class people.”
He also noted that DFU recurrence rates are 30%-40% in the first year, compared with 7.5% annual incidence for patients with peripheral neuropathy and no ulcer history. “The good news is that 75% of recurrent foot ulcers are preventable,” said Dr. Najafi, who is also director of clinical research in Baylor’s division of vascular surgery and endovascular therapy and director of the Interdisciplinary Consortium on Advanced Motion Performance. “An effective method is empowering patients to take care of their own health via regular self-inspection of their feet as well as providing timely and personalized foot care. The big challenge is adherence to prevention and regular foot inspection.”
In a study supported in part by Orpyx Medical Technologies, the investigators used a smart watch and smart insoles to enhance adherence to footwear and effective offloading by providing real-time feedback to 19 patients at high risk of DFUs about a harmful plantar pressure event. The patients wore the insole system for 3 months and were alerted through a smart watch if their plantar pressure exceeded 50 mm Hg over 95% of a moving 15-minute window. A successful response to an alert was recorded when offloading occurred within 20 minutes.
Dr. Najafi reported that by the third month, patients who received a higher number of alerts were more likely to use devices and technique to offload weight from their foot, compared with those who received a lower number of alerts (55% vs. 17%, respectively; P less than .01). In addition, patients whose wear time increased during the study tended to have more alerts, compared with other participants (a mean of .82 vs. .36 alerts per hour; P = .09). The best results occurred when patients received at least one alert every 2 hours. “We found that those who frequently received alerts about harmful plantar pressure events improved their adherence to the prescribed footwear and were more responsive to alerts,” he said. At the same time, those patients who received fewer alerts per day, “started to neglect alerts and adherence to footwear over time, despite having initially good adherence at the first month.”
Going forward, Dr. Najafi said, a key challenge is to continue engaging patients to use such technologies on a daily basis. “This could be addressable by providing frequent and comprehensive alerts which not only address harmful plantar pressure during walking but also any harmful foot-loading conditions, including prolonged harmful foot-loading pressure during standing as well as sitting,” he said.
In a video interview at the meeting, Dr. Najafi discussed the study and the challenges of encouraging treatment adherence.
Orpyx Medical Technologies provided partial funding support for the study. Dr. Najafi reported having no financial disclosures. The other authors of this study are Eyal Ron, Ana Enriquez, Ivan Marin, Jacqueline Lee-Eng, Javad Razjouyan, Ph.D., and Dr. David Armstrong. All subjects were recruited at the University of Arizona, College of Medicine, Tucson.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – Patients with diabetes and peripheral neuropathy who used a smart watch and specially designed smart insoles equipped with an alert system minimized their reulceration risk, results from a proof-of-concept study demonstrated.
The findings suggest that mobile health “could be an effective method to educate patients to change their harmful activity behavior, could enhance adherence to regularly inspect their feet and seek for care in a timely manner, and ultimately may assist in prevention of recurrence of ulcers,” lead author Bijan Najafi, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association.
Dr. Najafi, professor of surgery at Baylor College of Medicine, Houston, said that in 2015, approximately one-third of all diabetes-related costs in the United States were spent on diabetic foot ulcers (DFUs). “Unfortunately, many DFUs end up in amputation, which could devastate patients and their families,” he said. “On the same note, persons within the lowest income brackets are estimated to have 38% higher amputation rate, compared with those in the highest income bracket. All these highlight an important gap in effective management of DFUs, in particular among poor working-class people.”
He also noted that DFU recurrence rates are 30%-40% in the first year, compared with 7.5% annual incidence for patients with peripheral neuropathy and no ulcer history. “The good news is that 75% of recurrent foot ulcers are preventable,” said Dr. Najafi, who is also director of clinical research in Baylor’s division of vascular surgery and endovascular therapy and director of the Interdisciplinary Consortium on Advanced Motion Performance. “An effective method is empowering patients to take care of their own health via regular self-inspection of their feet as well as providing timely and personalized foot care. The big challenge is adherence to prevention and regular foot inspection.”
In a study supported in part by Orpyx Medical Technologies, the investigators used a smart watch and smart insoles to enhance adherence to footwear and effective offloading by providing real-time feedback to 19 patients at high risk of DFUs about a harmful plantar pressure event. The patients wore the insole system for 3 months and were alerted through a smart watch if their plantar pressure exceeded 50 mm Hg over 95% of a moving 15-minute window. A successful response to an alert was recorded when offloading occurred within 20 minutes.
Dr. Najafi reported that by the third month, patients who received a higher number of alerts were more likely to use devices and technique to offload weight from their foot, compared with those who received a lower number of alerts (55% vs. 17%, respectively; P less than .01). In addition, patients whose wear time increased during the study tended to have more alerts, compared with other participants (a mean of .82 vs. .36 alerts per hour; P = .09). The best results occurred when patients received at least one alert every 2 hours. “We found that those who frequently received alerts about harmful plantar pressure events improved their adherence to the prescribed footwear and were more responsive to alerts,” he said. At the same time, those patients who received fewer alerts per day, “started to neglect alerts and adherence to footwear over time, despite having initially good adherence at the first month.”
Going forward, Dr. Najafi said, a key challenge is to continue engaging patients to use such technologies on a daily basis. “This could be addressable by providing frequent and comprehensive alerts which not only address harmful plantar pressure during walking but also any harmful foot-loading conditions, including prolonged harmful foot-loading pressure during standing as well as sitting,” he said.
In a video interview at the meeting, Dr. Najafi discussed the study and the challenges of encouraging treatment adherence.
Orpyx Medical Technologies provided partial funding support for the study. Dr. Najafi reported having no financial disclosures. The other authors of this study are Eyal Ron, Ana Enriquez, Ivan Marin, Jacqueline Lee-Eng, Javad Razjouyan, Ph.D., and Dr. David Armstrong. All subjects were recruited at the University of Arizona, College of Medicine, Tucson.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
VIDEO: Smart insole system helped reduce reulceration risk
NEW ORLEANS – Patients with diabetes and peripheral neuropathy who used a smart watch and specially designed smart insoles equipped with an alert system minimized their reulceration risk, results from a proof-of-concept study demonstrated.
The findings suggest that mobile health “could be an effective method to educate patients to change their harmful activity behavior, could enhance adherence to regularly inspect their feet and seek for care in a timely manner, and ultimately may assist in prevention of recurrence of ulcers,” lead author Bijan Najafi, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association.
Dr. Najafi, professor of surgery at Baylor College of Medicine, Houston, said that in 2015, approximately one-third of all diabetes-related costs in the United States were spent on diabetic foot ulcers (DFUs). “Unfortunately, many DFUs end up in amputation, which could devastate patients and their families,” he said. “On the same note, persons within the lowest income brackets are estimated to have 38% higher amputation rate, compared with those in the highest income bracket. All these highlight an important gap in effective management of DFUs, in particular among poor working-class people.”
He also noted that DFU recurrence rates are 30%-40% in the first year, compared with 7.5% annual incidence for patients with peripheral neuropathy and no ulcer history. “The good news is that 75% of recurrent foot ulcers are preventable,” said Dr. Najafi, who is also director of clinical research in Baylor’s division of vascular surgery and endovascular therapy and director of the Interdisciplinary Consortium on Advanced Motion Performance. “An effective method is empowering patients to take care of their own health via regular self-inspection of their feet as well as providing timely and personalized foot care. The big challenge is adherence to prevention and regular foot inspection.”
In a study supported in part by Orpyx Medical Technologies, the investigators used a smart watch and smart insoles to enhance adherence to footwear and effective offloading by providing real-time feedback to 19 patients at high risk of DFUs about a harmful plantar pressure event. The patients wore the insole system for 3 months and were alerted through a smart watch if their plantar pressure exceeded 50 mm Hg over 95% of a moving 15-minute window. A successful response to an alert was recorded when offloading occurred within 20 minutes.
Dr. Najafi reported that by the third month, patients who received a higher number of alerts were more likely to use devices and technique to offload weight from their foot, compared with those who received a lower number of alerts (55% vs. 17%, respectively; P less than .01). In addition, patients whose wear time increased during the study tended to have more alerts, compared with other participants (a mean of .82 vs. .36 alerts per hour; P = .09). The best results occurred when patients received at least one alert every 2 hours. “We found that those who frequently received alerts about harmful plantar pressure events improved their adherence to the prescribed footwear and were more responsive to alerts,” he said. At the same time, those patients who received fewer alerts per day, “started to neglect alerts and adherence to footwear over time, despite having initially good adherence at the first month.”
Going forward, Dr. Najafi said, a key challenge is to continue engaging patients to use such technologies on a daily basis. “This could be addressable by providing frequent and comprehensive alerts which not only address harmful plantar pressure during walking but also any harmful foot-loading conditions, including prolonged harmful foot-loading pressure during standing as well as sitting,” he said.
In a video interview at the meeting, Dr. Najafi discussed the study and the challenges of encouraging treatment adherence.
Orpyx Medical Technologies provided partial funding support for the study. Dr. Najafi reported having no financial disclosures. The other authors of this study are Eyal Ron, Ana Enriquez, Ivan Marin, Jacqueline Lee-Eng, Javad Razjouyan, Ph.D., and Dr. David Armstrong. All subjects were recruited at the University of Arizona, College of Medicine, Tucson.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – Patients with diabetes and peripheral neuropathy who used a smart watch and specially designed smart insoles equipped with an alert system minimized their reulceration risk, results from a proof-of-concept study demonstrated.
The findings suggest that mobile health “could be an effective method to educate patients to change their harmful activity behavior, could enhance adherence to regularly inspect their feet and seek for care in a timely manner, and ultimately may assist in prevention of recurrence of ulcers,” lead author Bijan Najafi, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association.
Dr. Najafi, professor of surgery at Baylor College of Medicine, Houston, said that in 2015, approximately one-third of all diabetes-related costs in the United States were spent on diabetic foot ulcers (DFUs). “Unfortunately, many DFUs end up in amputation, which could devastate patients and their families,” he said. “On the same note, persons within the lowest income brackets are estimated to have 38% higher amputation rate, compared with those in the highest income bracket. All these highlight an important gap in effective management of DFUs, in particular among poor working-class people.”
He also noted that DFU recurrence rates are 30%-40% in the first year, compared with 7.5% annual incidence for patients with peripheral neuropathy and no ulcer history. “The good news is that 75% of recurrent foot ulcers are preventable,” said Dr. Najafi, who is also director of clinical research in Baylor’s division of vascular surgery and endovascular therapy and director of the Interdisciplinary Consortium on Advanced Motion Performance. “An effective method is empowering patients to take care of their own health via regular self-inspection of their feet as well as providing timely and personalized foot care. The big challenge is adherence to prevention and regular foot inspection.”
In a study supported in part by Orpyx Medical Technologies, the investigators used a smart watch and smart insoles to enhance adherence to footwear and effective offloading by providing real-time feedback to 19 patients at high risk of DFUs about a harmful plantar pressure event. The patients wore the insole system for 3 months and were alerted through a smart watch if their plantar pressure exceeded 50 mm Hg over 95% of a moving 15-minute window. A successful response to an alert was recorded when offloading occurred within 20 minutes.
Dr. Najafi reported that by the third month, patients who received a higher number of alerts were more likely to use devices and technique to offload weight from their foot, compared with those who received a lower number of alerts (55% vs. 17%, respectively; P less than .01). In addition, patients whose wear time increased during the study tended to have more alerts, compared with other participants (a mean of .82 vs. .36 alerts per hour; P = .09). The best results occurred when patients received at least one alert every 2 hours. “We found that those who frequently received alerts about harmful plantar pressure events improved their adherence to the prescribed footwear and were more responsive to alerts,” he said. At the same time, those patients who received fewer alerts per day, “started to neglect alerts and adherence to footwear over time, despite having initially good adherence at the first month.”
Going forward, Dr. Najafi said, a key challenge is to continue engaging patients to use such technologies on a daily basis. “This could be addressable by providing frequent and comprehensive alerts which not only address harmful plantar pressure during walking but also any harmful foot-loading conditions, including prolonged harmful foot-loading pressure during standing as well as sitting,” he said.
In a video interview at the meeting, Dr. Najafi discussed the study and the challenges of encouraging treatment adherence.
Orpyx Medical Technologies provided partial funding support for the study. Dr. Najafi reported having no financial disclosures. The other authors of this study are Eyal Ron, Ana Enriquez, Ivan Marin, Jacqueline Lee-Eng, Javad Razjouyan, Ph.D., and Dr. David Armstrong. All subjects were recruited at the University of Arizona, College of Medicine, Tucson.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – Patients with diabetes and peripheral neuropathy who used a smart watch and specially designed smart insoles equipped with an alert system minimized their reulceration risk, results from a proof-of-concept study demonstrated.
The findings suggest that mobile health “could be an effective method to educate patients to change their harmful activity behavior, could enhance adherence to regularly inspect their feet and seek for care in a timely manner, and ultimately may assist in prevention of recurrence of ulcers,” lead author Bijan Najafi, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association.
Dr. Najafi, professor of surgery at Baylor College of Medicine, Houston, said that in 2015, approximately one-third of all diabetes-related costs in the United States were spent on diabetic foot ulcers (DFUs). “Unfortunately, many DFUs end up in amputation, which could devastate patients and their families,” he said. “On the same note, persons within the lowest income brackets are estimated to have 38% higher amputation rate, compared with those in the highest income bracket. All these highlight an important gap in effective management of DFUs, in particular among poor working-class people.”
He also noted that DFU recurrence rates are 30%-40% in the first year, compared with 7.5% annual incidence for patients with peripheral neuropathy and no ulcer history. “The good news is that 75% of recurrent foot ulcers are preventable,” said Dr. Najafi, who is also director of clinical research in Baylor’s division of vascular surgery and endovascular therapy and director of the Interdisciplinary Consortium on Advanced Motion Performance. “An effective method is empowering patients to take care of their own health via regular self-inspection of their feet as well as providing timely and personalized foot care. The big challenge is adherence to prevention and regular foot inspection.”
In a study supported in part by Orpyx Medical Technologies, the investigators used a smart watch and smart insoles to enhance adherence to footwear and effective offloading by providing real-time feedback to 19 patients at high risk of DFUs about a harmful plantar pressure event. The patients wore the insole system for 3 months and were alerted through a smart watch if their plantar pressure exceeded 50 mm Hg over 95% of a moving 15-minute window. A successful response to an alert was recorded when offloading occurred within 20 minutes.
Dr. Najafi reported that by the third month, patients who received a higher number of alerts were more likely to use devices and technique to offload weight from their foot, compared with those who received a lower number of alerts (55% vs. 17%, respectively; P less than .01). In addition, patients whose wear time increased during the study tended to have more alerts, compared with other participants (a mean of .82 vs. .36 alerts per hour; P = .09). The best results occurred when patients received at least one alert every 2 hours. “We found that those who frequently received alerts about harmful plantar pressure events improved their adherence to the prescribed footwear and were more responsive to alerts,” he said. At the same time, those patients who received fewer alerts per day, “started to neglect alerts and adherence to footwear over time, despite having initially good adherence at the first month.”
Going forward, Dr. Najafi said, a key challenge is to continue engaging patients to use such technologies on a daily basis. “This could be addressable by providing frequent and comprehensive alerts which not only address harmful plantar pressure during walking but also any harmful foot-loading conditions, including prolonged harmful foot-loading pressure during standing as well as sitting,” he said.
In a video interview at the meeting, Dr. Najafi discussed the study and the challenges of encouraging treatment adherence.
Orpyx Medical Technologies provided partial funding support for the study. Dr. Najafi reported having no financial disclosures. The other authors of this study are Eyal Ron, Ana Enriquez, Ivan Marin, Jacqueline Lee-Eng, Javad Razjouyan, Ph.D., and Dr. David Armstrong. All subjects were recruited at the University of Arizona, College of Medicine, Tucson.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: A smart insole system helped to minimize reulceration risk among patients with diabetes and peripheral neuropathy.
Major finding: By the third month, patients who received a higher number of alerts were more likely to use devices to reduce pressure on the foot, compared with those who received a lower number of alerts (55% vs. 17%, respectively; P less than .01).
Data source: A proof-of-concept study conducted with 19 patients at high risk of diabetic foot ulcers that used a smart watch and smart insole device.
Disclosures: Orpyx Medical Technologies provided partial funding support for the study. Dr. Najafi reported having no financial disclosures.
Potential new ways to supply islet cells to diabetes patients
NEW ORLEANS — Two researchers shared innovative ideas at the annual scientific sessions of the American Diabetes Association for tapping virtually unlimited supplies of islet cells with less risk of an immune reaction.
Transplanting pancreatic islet stem cells from deceased donors into patients with type 1 diabetes has long been known to be an effective way of improve blood-glucose levels and temporarily eliminate the need for insulin injections, but getting an adequate supply of islet cells to treat the 1 million-2 million Americans with Type 1 diabetes, not to mention the risk of rejection and the need for long-term immunosuppressive therapy, makes this approach challenging.
At the University of Pittsburgh, investigators have developed a way to harvest islet cells from genetically engineered pigs and implant them into monkeys, while at the Harvard Stem Cell Institute in Boston, researchers have used gene editing to grow islet cells from blood cells.
“Human islet cells are in very scarce supply and will never solve the problem of diabetes,” said Dr. David K.C. Cooper, professor at the Thomas E. Starzi Transplantation Institute at the University of Pittsburgh. But growing evidence has shown that islet cells harvested from pigs could provide a viable source.
The challenge with stem cells from deceased human donors is that they require long term immunosuppression therapy to prevent the host body from rejecting them. When Dr. Cooper and his team injected islet cells from genetically engineered pigs into the stomachs of monkeys, they found the monkeys were able to maintain blood glucose control for about a year while on “fairly basic immunosuppressive therapy.” Dr. Cooper explained that the immunosuppressive regimen is a nonthrombogenic, monoclonal antibody not yet approved by the Food and Drug Administration. He noted that work at the Seoul National University in Korea has found similar results in monkeys out to 2 years.
The concept involves raising genetically engineered pigs in a biosecure facility, of which there are “two or three” in the United States, to ensure the cells are infection free. “The pig will be the answer to our problems,” Dr. Cooper said.
At Harvard, meanwhile, researchers are developing a way to produce pluripotent stem cells using an individual’s own blood cells that function like embryonic stem cells, but can multiply in a virtually unlimited fashion, Chad Cowan, PhD, reported. The challenge with using stem cells produced from an individual’s own cells has been the “immune barrier” – that is, the person’s immune system would attack the new cells.
However, Dr. Cowan and his team have found a way around this so-called “immune barrier” by producing “universal donor” pluripotent stem cell lines.
“You have an unlimited supply of cells,” Dr. Cowan said. “The key, though, is to teach these cells to do something, and because they come from a very early stage in development, they have the ability to become any of the adult cells in the human body. Our mission has been to teach them to become insulin-producing beta cells.”
The idea is to grow an “off-the-shelf, quality-controlled” product that can be produced in large numbers. By editing the genes, the researchers aim to reduce the immunogenicity of these cells and induce tolerance.
The work is some time away from human trials. “Once created, the next step would be to test these universal donor pluripotent stem cell lines in a humanized mouse model of type 1 diabetes,” Dr. Cowan said.
This type of gene editing also could have implications beyond diabetes, Dr. Cowan said. “If successful, our proposed work could have an enormous impact on regenerative medicine,” he said. “It could lead the way to rigorously tested universal donor stem cells that could be grown and differentiated into very large numbers of cells, made widely available to all medical institutions and used on demand to treat patients suffering from type 1 diabetes and a variety of degenerative illnesses,” including Parkinson’s disease.
Dr. Cowan and Dr. Cooper reported having no financial disclosures.
NEW ORLEANS — Two researchers shared innovative ideas at the annual scientific sessions of the American Diabetes Association for tapping virtually unlimited supplies of islet cells with less risk of an immune reaction.
Transplanting pancreatic islet stem cells from deceased donors into patients with type 1 diabetes has long been known to be an effective way of improve blood-glucose levels and temporarily eliminate the need for insulin injections, but getting an adequate supply of islet cells to treat the 1 million-2 million Americans with Type 1 diabetes, not to mention the risk of rejection and the need for long-term immunosuppressive therapy, makes this approach challenging.
At the University of Pittsburgh, investigators have developed a way to harvest islet cells from genetically engineered pigs and implant them into monkeys, while at the Harvard Stem Cell Institute in Boston, researchers have used gene editing to grow islet cells from blood cells.
“Human islet cells are in very scarce supply and will never solve the problem of diabetes,” said Dr. David K.C. Cooper, professor at the Thomas E. Starzi Transplantation Institute at the University of Pittsburgh. But growing evidence has shown that islet cells harvested from pigs could provide a viable source.
The challenge with stem cells from deceased human donors is that they require long term immunosuppression therapy to prevent the host body from rejecting them. When Dr. Cooper and his team injected islet cells from genetically engineered pigs into the stomachs of monkeys, they found the monkeys were able to maintain blood glucose control for about a year while on “fairly basic immunosuppressive therapy.” Dr. Cooper explained that the immunosuppressive regimen is a nonthrombogenic, monoclonal antibody not yet approved by the Food and Drug Administration. He noted that work at the Seoul National University in Korea has found similar results in monkeys out to 2 years.
The concept involves raising genetically engineered pigs in a biosecure facility, of which there are “two or three” in the United States, to ensure the cells are infection free. “The pig will be the answer to our problems,” Dr. Cooper said.
At Harvard, meanwhile, researchers are developing a way to produce pluripotent stem cells using an individual’s own blood cells that function like embryonic stem cells, but can multiply in a virtually unlimited fashion, Chad Cowan, PhD, reported. The challenge with using stem cells produced from an individual’s own cells has been the “immune barrier” – that is, the person’s immune system would attack the new cells.
However, Dr. Cowan and his team have found a way around this so-called “immune barrier” by producing “universal donor” pluripotent stem cell lines.
“You have an unlimited supply of cells,” Dr. Cowan said. “The key, though, is to teach these cells to do something, and because they come from a very early stage in development, they have the ability to become any of the adult cells in the human body. Our mission has been to teach them to become insulin-producing beta cells.”
The idea is to grow an “off-the-shelf, quality-controlled” product that can be produced in large numbers. By editing the genes, the researchers aim to reduce the immunogenicity of these cells and induce tolerance.
The work is some time away from human trials. “Once created, the next step would be to test these universal donor pluripotent stem cell lines in a humanized mouse model of type 1 diabetes,” Dr. Cowan said.
This type of gene editing also could have implications beyond diabetes, Dr. Cowan said. “If successful, our proposed work could have an enormous impact on regenerative medicine,” he said. “It could lead the way to rigorously tested universal donor stem cells that could be grown and differentiated into very large numbers of cells, made widely available to all medical institutions and used on demand to treat patients suffering from type 1 diabetes and a variety of degenerative illnesses,” including Parkinson’s disease.
Dr. Cowan and Dr. Cooper reported having no financial disclosures.
NEW ORLEANS — Two researchers shared innovative ideas at the annual scientific sessions of the American Diabetes Association for tapping virtually unlimited supplies of islet cells with less risk of an immune reaction.
Transplanting pancreatic islet stem cells from deceased donors into patients with type 1 diabetes has long been known to be an effective way of improve blood-glucose levels and temporarily eliminate the need for insulin injections, but getting an adequate supply of islet cells to treat the 1 million-2 million Americans with Type 1 diabetes, not to mention the risk of rejection and the need for long-term immunosuppressive therapy, makes this approach challenging.
At the University of Pittsburgh, investigators have developed a way to harvest islet cells from genetically engineered pigs and implant them into monkeys, while at the Harvard Stem Cell Institute in Boston, researchers have used gene editing to grow islet cells from blood cells.
“Human islet cells are in very scarce supply and will never solve the problem of diabetes,” said Dr. David K.C. Cooper, professor at the Thomas E. Starzi Transplantation Institute at the University of Pittsburgh. But growing evidence has shown that islet cells harvested from pigs could provide a viable source.
The challenge with stem cells from deceased human donors is that they require long term immunosuppression therapy to prevent the host body from rejecting them. When Dr. Cooper and his team injected islet cells from genetically engineered pigs into the stomachs of monkeys, they found the monkeys were able to maintain blood glucose control for about a year while on “fairly basic immunosuppressive therapy.” Dr. Cooper explained that the immunosuppressive regimen is a nonthrombogenic, monoclonal antibody not yet approved by the Food and Drug Administration. He noted that work at the Seoul National University in Korea has found similar results in monkeys out to 2 years.
The concept involves raising genetically engineered pigs in a biosecure facility, of which there are “two or three” in the United States, to ensure the cells are infection free. “The pig will be the answer to our problems,” Dr. Cooper said.
At Harvard, meanwhile, researchers are developing a way to produce pluripotent stem cells using an individual’s own blood cells that function like embryonic stem cells, but can multiply in a virtually unlimited fashion, Chad Cowan, PhD, reported. The challenge with using stem cells produced from an individual’s own cells has been the “immune barrier” – that is, the person’s immune system would attack the new cells.
However, Dr. Cowan and his team have found a way around this so-called “immune barrier” by producing “universal donor” pluripotent stem cell lines.
“You have an unlimited supply of cells,” Dr. Cowan said. “The key, though, is to teach these cells to do something, and because they come from a very early stage in development, they have the ability to become any of the adult cells in the human body. Our mission has been to teach them to become insulin-producing beta cells.”
The idea is to grow an “off-the-shelf, quality-controlled” product that can be produced in large numbers. By editing the genes, the researchers aim to reduce the immunogenicity of these cells and induce tolerance.
The work is some time away from human trials. “Once created, the next step would be to test these universal donor pluripotent stem cell lines in a humanized mouse model of type 1 diabetes,” Dr. Cowan said.
This type of gene editing also could have implications beyond diabetes, Dr. Cowan said. “If successful, our proposed work could have an enormous impact on regenerative medicine,” he said. “It could lead the way to rigorously tested universal donor stem cells that could be grown and differentiated into very large numbers of cells, made widely available to all medical institutions and used on demand to treat patients suffering from type 1 diabetes and a variety of degenerative illnesses,” including Parkinson’s disease.
Dr. Cowan and Dr. Cooper reported having no financial disclosures.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: Islet cells from pigs and “universal donor” cells offer potential to control blood-glucose in humans.
Major finding: Transplanted pig islet cells achieved blood glucose control in recipient monkeys for up to 2 years, and gene editing may enable researchers to create stem cells that may avoid the body’s natural immune response.
Data source: Animal studies of pig islet cell transplants and concept studies of universal donor stem cells.
Disclosures: Dr. Cowan and Dr. Cooper reported having no financial disclosures.
Recurrent DKA episodes found to trigger cognitive changes
NEW ORLEANS – Recurrent episodes of diabetic ketoacidosis (DKA) resulted in altered brain metabolite concentration, as well as differences in mental processing speed, compared with healthy controls, judging from the results from a small pilot study.
While previous work examining the relationship of DKA to cognition and neural structure has focused upon children and adolescents, researchers at Emory University and the Georgia Institute of Technology, both in Atlanta, set out of evaluate for the first time acute neuroanatomical and cognitive changes in adult patients with first and recurrent episodes of DKA. In an interview in advance of the annual scientific sessions of the American Diabetes Association, one of the researchers, Gilda E. Ennis, Ph.D., said that DKA is the most serious diabetic emergency in patients with type 1 and 2 diabetes and results in an estimated health care cost of $2.4 billion annually. “While we know that one of the major precipitating causes of DKA in adult patients is poor adherence to insulin therapy, we do not understand why patients are noncompliant,” said Dr. Ennis, who is a postdoctoral fellow in the Georgia Institute of Technology’s school of psychology.
She and her associates conducted a pilot study examining advanced MRI metrics and cognitive measures 72 hours after resolution of DKA in 10 patients with a first episode of DKA and 11 patients with three or more episodes of DKA. The same MRI and cognitive measures were collected from 10 healthy controls and 10 patients with type 1 diabetes and no history of DKA.
MRI spectroscopy revealed reduced N-acetylaspartate concentrations in diabetes patients with multiple episodes of DKA, compared with healthy controls, but no significant differences were seen between diabetes patients with and without DKA. Cognitive testing revealed that patients with recurrent DKA had significantly worse processing speed, compared with healthy controls (P = .02), while processing speed deficits in patients with a single DKA and those with diabetes and no DKA was intermediate between healthy controls and those with recurrent DKA.
“We were surprised to find significant cognitive and neural deficits in the recurrent DKA group relative to healthy controls in such a small sample,” Dr. Ennis said. “This suggests that statistical differences in cognition and neural structure between patients with recurrent DKA and healthy controls may be large. We found that recurrent DKA was associated with significant deficits in processing speed and memory, decreases in right putamen volume, regionally decreased white matter integrity, and altered brain metabolite concentrations, suggestive of CNS inflammatory changes and neuronal injury.”
The findings may explain the high rates of medication noncompliance commonly seen in this patient population. “If this proposition is true, conventional education and standard care approaches to the treatment of type 1 diabetes, especially in patients with a history of DKA, may need to change,” she said. “Strategies to improve insulin adherence may require a special insulin compliance intervention that includes persistent medication adherence reminders, such as text messaging and nurse-telephone follow-up.”
Dr. Ennis acknowledged that the findings require replication in a prospective longitudinal study with a larger sample size. “It will be important to determine if acute neuroanatomical and cognitive deficits in patients with recurrent DKA persist over time,” she said. “Duration of type 1 diabetes could produce similar findings and would need to be controlled in future research.” She reported having no financial disclosures.
NEW ORLEANS – Recurrent episodes of diabetic ketoacidosis (DKA) resulted in altered brain metabolite concentration, as well as differences in mental processing speed, compared with healthy controls, judging from the results from a small pilot study.
While previous work examining the relationship of DKA to cognition and neural structure has focused upon children and adolescents, researchers at Emory University and the Georgia Institute of Technology, both in Atlanta, set out of evaluate for the first time acute neuroanatomical and cognitive changes in adult patients with first and recurrent episodes of DKA. In an interview in advance of the annual scientific sessions of the American Diabetes Association, one of the researchers, Gilda E. Ennis, Ph.D., said that DKA is the most serious diabetic emergency in patients with type 1 and 2 diabetes and results in an estimated health care cost of $2.4 billion annually. “While we know that one of the major precipitating causes of DKA in adult patients is poor adherence to insulin therapy, we do not understand why patients are noncompliant,” said Dr. Ennis, who is a postdoctoral fellow in the Georgia Institute of Technology’s school of psychology.
She and her associates conducted a pilot study examining advanced MRI metrics and cognitive measures 72 hours after resolution of DKA in 10 patients with a first episode of DKA and 11 patients with three or more episodes of DKA. The same MRI and cognitive measures were collected from 10 healthy controls and 10 patients with type 1 diabetes and no history of DKA.
MRI spectroscopy revealed reduced N-acetylaspartate concentrations in diabetes patients with multiple episodes of DKA, compared with healthy controls, but no significant differences were seen between diabetes patients with and without DKA. Cognitive testing revealed that patients with recurrent DKA had significantly worse processing speed, compared with healthy controls (P = .02), while processing speed deficits in patients with a single DKA and those with diabetes and no DKA was intermediate between healthy controls and those with recurrent DKA.
“We were surprised to find significant cognitive and neural deficits in the recurrent DKA group relative to healthy controls in such a small sample,” Dr. Ennis said. “This suggests that statistical differences in cognition and neural structure between patients with recurrent DKA and healthy controls may be large. We found that recurrent DKA was associated with significant deficits in processing speed and memory, decreases in right putamen volume, regionally decreased white matter integrity, and altered brain metabolite concentrations, suggestive of CNS inflammatory changes and neuronal injury.”
The findings may explain the high rates of medication noncompliance commonly seen in this patient population. “If this proposition is true, conventional education and standard care approaches to the treatment of type 1 diabetes, especially in patients with a history of DKA, may need to change,” she said. “Strategies to improve insulin adherence may require a special insulin compliance intervention that includes persistent medication adherence reminders, such as text messaging and nurse-telephone follow-up.”
Dr. Ennis acknowledged that the findings require replication in a prospective longitudinal study with a larger sample size. “It will be important to determine if acute neuroanatomical and cognitive deficits in patients with recurrent DKA persist over time,” she said. “Duration of type 1 diabetes could produce similar findings and would need to be controlled in future research.” She reported having no financial disclosures.
NEW ORLEANS – Recurrent episodes of diabetic ketoacidosis (DKA) resulted in altered brain metabolite concentration, as well as differences in mental processing speed, compared with healthy controls, judging from the results from a small pilot study.
While previous work examining the relationship of DKA to cognition and neural structure has focused upon children and adolescents, researchers at Emory University and the Georgia Institute of Technology, both in Atlanta, set out of evaluate for the first time acute neuroanatomical and cognitive changes in adult patients with first and recurrent episodes of DKA. In an interview in advance of the annual scientific sessions of the American Diabetes Association, one of the researchers, Gilda E. Ennis, Ph.D., said that DKA is the most serious diabetic emergency in patients with type 1 and 2 diabetes and results in an estimated health care cost of $2.4 billion annually. “While we know that one of the major precipitating causes of DKA in adult patients is poor adherence to insulin therapy, we do not understand why patients are noncompliant,” said Dr. Ennis, who is a postdoctoral fellow in the Georgia Institute of Technology’s school of psychology.
She and her associates conducted a pilot study examining advanced MRI metrics and cognitive measures 72 hours after resolution of DKA in 10 patients with a first episode of DKA and 11 patients with three or more episodes of DKA. The same MRI and cognitive measures were collected from 10 healthy controls and 10 patients with type 1 diabetes and no history of DKA.
MRI spectroscopy revealed reduced N-acetylaspartate concentrations in diabetes patients with multiple episodes of DKA, compared with healthy controls, but no significant differences were seen between diabetes patients with and without DKA. Cognitive testing revealed that patients with recurrent DKA had significantly worse processing speed, compared with healthy controls (P = .02), while processing speed deficits in patients with a single DKA and those with diabetes and no DKA was intermediate between healthy controls and those with recurrent DKA.
“We were surprised to find significant cognitive and neural deficits in the recurrent DKA group relative to healthy controls in such a small sample,” Dr. Ennis said. “This suggests that statistical differences in cognition and neural structure between patients with recurrent DKA and healthy controls may be large. We found that recurrent DKA was associated with significant deficits in processing speed and memory, decreases in right putamen volume, regionally decreased white matter integrity, and altered brain metabolite concentrations, suggestive of CNS inflammatory changes and neuronal injury.”
The findings may explain the high rates of medication noncompliance commonly seen in this patient population. “If this proposition is true, conventional education and standard care approaches to the treatment of type 1 diabetes, especially in patients with a history of DKA, may need to change,” she said. “Strategies to improve insulin adherence may require a special insulin compliance intervention that includes persistent medication adherence reminders, such as text messaging and nurse-telephone follow-up.”
Dr. Ennis acknowledged that the findings require replication in a prospective longitudinal study with a larger sample size. “It will be important to determine if acute neuroanatomical and cognitive deficits in patients with recurrent DKA persist over time,” she said. “Duration of type 1 diabetes could produce similar findings and would need to be controlled in future research.” She reported having no financial disclosures.
AT THE ADA SCIENTIFIC SESSIONS
Key clinical point: Recurrent episodes of diabetic ketoacidosis were found to cause certain cognitive changes in adults with type 1 diabetes.
Major finding: Cognitive testing revealed that patients with recurrent DKA had significantly worse processing speed, compared with healthy controls (P = .02), while processing speed deficits in patients with a single DKA and those with diabetes and no DKA was intermediate between healthy controls and those with recurrent DKA.
Data source: A pilot study examining advanced MRI metrics and cognitive measures 72 hours after resolution of DKA in 10 patients with a first episode of DKA and 11 patients with three or more episodes of DKA. The same measures were collected from 10 healthy controls and 10 patients with type 1 diabetes and no history of DKA.
Disclosures: Dr. Ennis reported having no financial disclosures.
VIDEO: Using dogs to detect hypoglycemia remains an imperfect science
NEW ORLEANS – In the first known controlled study of its kind, researchers demonstrated the reliability of trained dogs to alert hypoglycemia in human companions with type 1 diabetes, but at the cost of a high false-positive rate, compared with continuous glucose monitoring.
“The use of trained dogs to alert to changes in blood glucose in human companions with diabetes is increasing yet we don’t know how effective they are,” lead author Dr. Evan Los said in an interview in advance of the annual scientific sessions of the American Diabetes Association. “Enthusiastic anecdotal reports and limited in vitro studies are promising but rigorous studies have not been done. Clinicians are unable to provide informed advice when patients ask, ‘What do you think about diabetes alert dogs?’”
Dr. Los, a pediatric endocrinology fellow at Oregon Health and Science University, Portland, and his associates set out to conduct a controlled study of the reliability of diabetes alert dogs to detect hypoglycemia in their human companions with type 1 diabetes under real-life conditions. Capillary blood glucose (CBG) and continuous glucose monitoring (CGM) were used as comparators, and the study participants consisted of eight dog-human pairs. The human subjects ranged in age from 4 to 48 years old. Hypoglycemia was defined as CBG and/or CGM below 70 mg/dL and the human subjects answered survey questions regarding their impressions of the dog’s reliability and reasons for obtaining a diabetes alert dog. A timely alert was defined as occurring within 10 minutes before to 30 minutes after onset of hypoglycemia.
On a 10-point Likert scale, the dog users reported being “very satisfied” and “largely confident” in their dog’s ability to detect hypoglycemia (scores of 8.9 and 7.9, respectively), and they universally cited detection of hypoglycemia as the chief reason for obtaining a trained service dog. The researchers found that spontaneous dog alerts occurred 3.2 times more often than the rate of alerts during euglycemia, which was defined as 70-180 mg/dL, but the positive predictive value of dog alerts for hypoglycemia was only 12%. When Dr. Los and his associates reviewed event diaries and blinded CGM data, they observed that trained dogs provided a timely alert in 36% of all 45 hypoglycemia events. In the 30 events when both the dog-alerted and the blinded-CGM reached the hypoglycemia threshold, CGM would have alerted prior to the dog in 73% of events, which translated into a median difference of 22 minutes sooner.
“Trained dogs often alert a human companion to otherwise unknown hypoglycemia,” Dr. Los said. “However, due to high false-positive rates, a dog alert alone is unlikely to be helpful in differentiating hypo-/hyper-/euglycemia. CGM often detects hypoglycemia before a trained dog by a clinically significant margin.”
He acknowledged the study’s small sample size as a limitation. “Dog breeds and training methods were not universal, so there are likely to be variation in the reliability between dogs,” Dr. Los added. “This is not the final word on whether trained dogs might be helpful for patients with diabetes and there may be other benefits not assessed by this study such as having a positive partner in the daily management of a chronic disease.” He reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – In the first known controlled study of its kind, researchers demonstrated the reliability of trained dogs to alert hypoglycemia in human companions with type 1 diabetes, but at the cost of a high false-positive rate, compared with continuous glucose monitoring.
“The use of trained dogs to alert to changes in blood glucose in human companions with diabetes is increasing yet we don’t know how effective they are,” lead author Dr. Evan Los said in an interview in advance of the annual scientific sessions of the American Diabetes Association. “Enthusiastic anecdotal reports and limited in vitro studies are promising but rigorous studies have not been done. Clinicians are unable to provide informed advice when patients ask, ‘What do you think about diabetes alert dogs?’”
Dr. Los, a pediatric endocrinology fellow at Oregon Health and Science University, Portland, and his associates set out to conduct a controlled study of the reliability of diabetes alert dogs to detect hypoglycemia in their human companions with type 1 diabetes under real-life conditions. Capillary blood glucose (CBG) and continuous glucose monitoring (CGM) were used as comparators, and the study participants consisted of eight dog-human pairs. The human subjects ranged in age from 4 to 48 years old. Hypoglycemia was defined as CBG and/or CGM below 70 mg/dL and the human subjects answered survey questions regarding their impressions of the dog’s reliability and reasons for obtaining a diabetes alert dog. A timely alert was defined as occurring within 10 minutes before to 30 minutes after onset of hypoglycemia.
On a 10-point Likert scale, the dog users reported being “very satisfied” and “largely confident” in their dog’s ability to detect hypoglycemia (scores of 8.9 and 7.9, respectively), and they universally cited detection of hypoglycemia as the chief reason for obtaining a trained service dog. The researchers found that spontaneous dog alerts occurred 3.2 times more often than the rate of alerts during euglycemia, which was defined as 70-180 mg/dL, but the positive predictive value of dog alerts for hypoglycemia was only 12%. When Dr. Los and his associates reviewed event diaries and blinded CGM data, they observed that trained dogs provided a timely alert in 36% of all 45 hypoglycemia events. In the 30 events when both the dog-alerted and the blinded-CGM reached the hypoglycemia threshold, CGM would have alerted prior to the dog in 73% of events, which translated into a median difference of 22 minutes sooner.
“Trained dogs often alert a human companion to otherwise unknown hypoglycemia,” Dr. Los said. “However, due to high false-positive rates, a dog alert alone is unlikely to be helpful in differentiating hypo-/hyper-/euglycemia. CGM often detects hypoglycemia before a trained dog by a clinically significant margin.”
He acknowledged the study’s small sample size as a limitation. “Dog breeds and training methods were not universal, so there are likely to be variation in the reliability between dogs,” Dr. Los added. “This is not the final word on whether trained dogs might be helpful for patients with diabetes and there may be other benefits not assessed by this study such as having a positive partner in the daily management of a chronic disease.” He reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – In the first known controlled study of its kind, researchers demonstrated the reliability of trained dogs to alert hypoglycemia in human companions with type 1 diabetes, but at the cost of a high false-positive rate, compared with continuous glucose monitoring.
“The use of trained dogs to alert to changes in blood glucose in human companions with diabetes is increasing yet we don’t know how effective they are,” lead author Dr. Evan Los said in an interview in advance of the annual scientific sessions of the American Diabetes Association. “Enthusiastic anecdotal reports and limited in vitro studies are promising but rigorous studies have not been done. Clinicians are unable to provide informed advice when patients ask, ‘What do you think about diabetes alert dogs?’”
Dr. Los, a pediatric endocrinology fellow at Oregon Health and Science University, Portland, and his associates set out to conduct a controlled study of the reliability of diabetes alert dogs to detect hypoglycemia in their human companions with type 1 diabetes under real-life conditions. Capillary blood glucose (CBG) and continuous glucose monitoring (CGM) were used as comparators, and the study participants consisted of eight dog-human pairs. The human subjects ranged in age from 4 to 48 years old. Hypoglycemia was defined as CBG and/or CGM below 70 mg/dL and the human subjects answered survey questions regarding their impressions of the dog’s reliability and reasons for obtaining a diabetes alert dog. A timely alert was defined as occurring within 10 minutes before to 30 minutes after onset of hypoglycemia.
On a 10-point Likert scale, the dog users reported being “very satisfied” and “largely confident” in their dog’s ability to detect hypoglycemia (scores of 8.9 and 7.9, respectively), and they universally cited detection of hypoglycemia as the chief reason for obtaining a trained service dog. The researchers found that spontaneous dog alerts occurred 3.2 times more often than the rate of alerts during euglycemia, which was defined as 70-180 mg/dL, but the positive predictive value of dog alerts for hypoglycemia was only 12%. When Dr. Los and his associates reviewed event diaries and blinded CGM data, they observed that trained dogs provided a timely alert in 36% of all 45 hypoglycemia events. In the 30 events when both the dog-alerted and the blinded-CGM reached the hypoglycemia threshold, CGM would have alerted prior to the dog in 73% of events, which translated into a median difference of 22 minutes sooner.
“Trained dogs often alert a human companion to otherwise unknown hypoglycemia,” Dr. Los said. “However, due to high false-positive rates, a dog alert alone is unlikely to be helpful in differentiating hypo-/hyper-/euglycemia. CGM often detects hypoglycemia before a trained dog by a clinically significant margin.”
He acknowledged the study’s small sample size as a limitation. “Dog breeds and training methods were not universal, so there are likely to be variation in the reliability between dogs,” Dr. Los added. “This is not the final word on whether trained dogs might be helpful for patients with diabetes and there may be other benefits not assessed by this study such as having a positive partner in the daily management of a chronic disease.” He reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
FROM THE ADA SCIENTIFIC SESSIONS
Key clinical point: Trained dogs often alert a human companion to otherwise unknown hypoglycemia.
Major finding: During hypoglycemia, spontaneous dog alerts occurred 3.2 times more often than the rate of alerts during euglycemia, but the positive predictive value of dog alerts for hypoglycemia was only 12%.
Data source: An exploratory study to evaluate the reliability of eight trained service dogs in alerting to hypoglycemia in their eight human companions with type 1 diabetes, with capillary blood glucose and continuous glucose monitoring as comparators.
Disclosures: Dr. Los reported having no financial disclosures.