User login
European Society of Cardiology (ESC): Annual Congress
Every 10° C temperature drop increases STEMI risk by 7%
LONDON – For every 10° C drop in the highest daily air temperature, the risk for ST-elevation myocardial infraction was found to increase by 7% in a Canadian study.
Researchers at the University of Manitoba in Winnipeg performed a retrospective study of all STEMI cases that had occurred in the city during 2009-2014 and linked them to daily air temperatures collected from Environment Canada.
“There is a clear correlation between cold weather and heart attacks,” said Dr. Shuangbo Liu, who presented the findings at the annual congress of the European Society of Cardiology. Previous studies have shown that the incidence of, hospitalization for, and death as a result of, MI are all increased as the weather gets colder. But until now, it wasn’t known what the specific relationship between temperature drops and the rate of STEMI was, she explained.
STEMIs typically occur as a result of acute rupture of an atherosclerotic plaque, but although the risk factors for the development for the plaques have been widely studied, the risk factors for rupture are not so well defined. There is some suggestion that colder weather is linked to factors that might predispose to plaque rupture, such as an increased cardiac workload, higher blood pressure, and an increased procoagulant state.
Winnipeg is one of the coldest large cities in the world in winter, but has more temperate fall and spring seasons with hot and dry summers, and so provided the ideal place to study the effect of environmental temperature on the risk of STEMI, Dr. Liu said.
Over the 6-year retrospective audit period, 1,817 STEMIs were recorded. Only STEMIs that were reported within 12 hours of admission were included in the analyses, with almost all (95%) patients undergoing primary percutaneous coronary intervention.
The highest daily temperature reached was 20° C on 31% of the study days, 0°-20° on 38% of the study days, and less than 0° on 32% of the study days.
The cold – but not warm – weather was associated with the risk of STEMI, with the daily high temperature being the strongest predictor of having a heart attack. On the study days where the highest temperature reached was less than 0°, the STEMI event rate was 0.94 per day. This rate was significantly higher than that when the daily high temperature was above 0°, at a rate of 0.79 per day overall (P less than .001)
STEMI rates on days that were 0°-10°, 10°-20°, 20°-30°, and 30° and above were 0.89, 0.81, 0.74, and 0.61 per day, respectively.
Although any snowfall in the last 2 days was predictive of STEMI on univariate analysis, upping the risk by 20%, it did not remain so after adjustment for temperature.
The daily high temperatures on the 1-2 days preceding STEMI were found to be predictive in univariate analyses, increasing the relative risk by 19%-20% (P less than .001).
Dr. Liu acknowledged the limitations of using retrospective administrative data and that further prospective validation of the results would be needed. However, these data are “thought provoking,” she said, and suggest that increasing public awareness is needed and perhaps health care resources need to be reallocated to help prevent the seasonal surge in STEMI observed in the study.
Dr. Liu reported having no relevant financial disclosures.
LONDON – For every 10° C drop in the highest daily air temperature, the risk for ST-elevation myocardial infraction was found to increase by 7% in a Canadian study.
Researchers at the University of Manitoba in Winnipeg performed a retrospective study of all STEMI cases that had occurred in the city during 2009-2014 and linked them to daily air temperatures collected from Environment Canada.
“There is a clear correlation between cold weather and heart attacks,” said Dr. Shuangbo Liu, who presented the findings at the annual congress of the European Society of Cardiology. Previous studies have shown that the incidence of, hospitalization for, and death as a result of, MI are all increased as the weather gets colder. But until now, it wasn’t known what the specific relationship between temperature drops and the rate of STEMI was, she explained.
STEMIs typically occur as a result of acute rupture of an atherosclerotic plaque, but although the risk factors for the development for the plaques have been widely studied, the risk factors for rupture are not so well defined. There is some suggestion that colder weather is linked to factors that might predispose to plaque rupture, such as an increased cardiac workload, higher blood pressure, and an increased procoagulant state.
Winnipeg is one of the coldest large cities in the world in winter, but has more temperate fall and spring seasons with hot and dry summers, and so provided the ideal place to study the effect of environmental temperature on the risk of STEMI, Dr. Liu said.
Over the 6-year retrospective audit period, 1,817 STEMIs were recorded. Only STEMIs that were reported within 12 hours of admission were included in the analyses, with almost all (95%) patients undergoing primary percutaneous coronary intervention.
The highest daily temperature reached was 20° C on 31% of the study days, 0°-20° on 38% of the study days, and less than 0° on 32% of the study days.
The cold – but not warm – weather was associated with the risk of STEMI, with the daily high temperature being the strongest predictor of having a heart attack. On the study days where the highest temperature reached was less than 0°, the STEMI event rate was 0.94 per day. This rate was significantly higher than that when the daily high temperature was above 0°, at a rate of 0.79 per day overall (P less than .001)
STEMI rates on days that were 0°-10°, 10°-20°, 20°-30°, and 30° and above were 0.89, 0.81, 0.74, and 0.61 per day, respectively.
Although any snowfall in the last 2 days was predictive of STEMI on univariate analysis, upping the risk by 20%, it did not remain so after adjustment for temperature.
The daily high temperatures on the 1-2 days preceding STEMI were found to be predictive in univariate analyses, increasing the relative risk by 19%-20% (P less than .001).
Dr. Liu acknowledged the limitations of using retrospective administrative data and that further prospective validation of the results would be needed. However, these data are “thought provoking,” she said, and suggest that increasing public awareness is needed and perhaps health care resources need to be reallocated to help prevent the seasonal surge in STEMI observed in the study.
Dr. Liu reported having no relevant financial disclosures.
LONDON – For every 10° C drop in the highest daily air temperature, the risk for ST-elevation myocardial infraction was found to increase by 7% in a Canadian study.
Researchers at the University of Manitoba in Winnipeg performed a retrospective study of all STEMI cases that had occurred in the city during 2009-2014 and linked them to daily air temperatures collected from Environment Canada.
“There is a clear correlation between cold weather and heart attacks,” said Dr. Shuangbo Liu, who presented the findings at the annual congress of the European Society of Cardiology. Previous studies have shown that the incidence of, hospitalization for, and death as a result of, MI are all increased as the weather gets colder. But until now, it wasn’t known what the specific relationship between temperature drops and the rate of STEMI was, she explained.
STEMIs typically occur as a result of acute rupture of an atherosclerotic plaque, but although the risk factors for the development for the plaques have been widely studied, the risk factors for rupture are not so well defined. There is some suggestion that colder weather is linked to factors that might predispose to plaque rupture, such as an increased cardiac workload, higher blood pressure, and an increased procoagulant state.
Winnipeg is one of the coldest large cities in the world in winter, but has more temperate fall and spring seasons with hot and dry summers, and so provided the ideal place to study the effect of environmental temperature on the risk of STEMI, Dr. Liu said.
Over the 6-year retrospective audit period, 1,817 STEMIs were recorded. Only STEMIs that were reported within 12 hours of admission were included in the analyses, with almost all (95%) patients undergoing primary percutaneous coronary intervention.
The highest daily temperature reached was 20° C on 31% of the study days, 0°-20° on 38% of the study days, and less than 0° on 32% of the study days.
The cold – but not warm – weather was associated with the risk of STEMI, with the daily high temperature being the strongest predictor of having a heart attack. On the study days where the highest temperature reached was less than 0°, the STEMI event rate was 0.94 per day. This rate was significantly higher than that when the daily high temperature was above 0°, at a rate of 0.79 per day overall (P less than .001)
STEMI rates on days that were 0°-10°, 10°-20°, 20°-30°, and 30° and above were 0.89, 0.81, 0.74, and 0.61 per day, respectively.
Although any snowfall in the last 2 days was predictive of STEMI on univariate analysis, upping the risk by 20%, it did not remain so after adjustment for temperature.
The daily high temperatures on the 1-2 days preceding STEMI were found to be predictive in univariate analyses, increasing the relative risk by 19%-20% (P less than .001).
Dr. Liu acknowledged the limitations of using retrospective administrative data and that further prospective validation of the results would be needed. However, these data are “thought provoking,” she said, and suggest that increasing public awareness is needed and perhaps health care resources need to be reallocated to help prevent the seasonal surge in STEMI observed in the study.
Dr. Liu reported having no relevant financial disclosures.
Key clinical point: As the air temperature gets progressively lower, the STEMI risk increases.
Major finding: The STEMI event rate was 0.94 per day when the daily high temperature was below 0° C vs. 0.79 per day when it was above 0° C (P less than .001).
Data source: A retrospective audit of all 1,817 cases of STEMI occurring in Winnipeg between 2009 and 2014.
Disclosures: Dr. Liu reported having no relevant financial disclosures.
Depression, hypertension combo compounds cardiovascular risk
LONDON – The combination of depression and very high systolic blood pressure increased the risk for a major cardiovascular event by 83%, compared with normal blood pressure and no depression, in patients with existing heart disease, diabetes, or stroke.
In a large family practice–based study, the hazard ratio for first hospital admission due to myocardial infarction, stroke or heart failure, or cardiovascular death in patients with high (at least 160 mm Hg) systolic blood pressure who were also depressed was 1.83, a highly significant difference compared with individuals with normal BP and no depression.
The presence of depression also significantly increased the risk for these cardiovascular events by 36% in patients with lower systolic BPs, compared with those with normal BP and no depression.
“Patients with existing heart disease, diabetes, or stroke are more likely to have another heart attack or another stroke or die from heart problems than the general population,” Dr. Bhautesh Jani of the Institute of Health and Wellbeing, University of Glasgow (Scotland), said at the annual congress of the European Society of Cardiology.
“In particular, those who have extremes of blood pressure or those who have depressive symptoms are at higher risk, which has been shown by previous evidence. What is relatively unknown is the combined effect of having extremes of blood pressure and depressive symptoms together, and our study tried to address that problem,” Dr. Jani explained.
The study involved more than 35,500 individuals with existing heart disease, diabetes, or stroke living in Scotland, of whom 3,939 (11%) had at least one major cardiovascular event that needed hospital admission during a 4-year period. Patients had been divided into groups based on their systolic BP, and depressive symptoms were assessed using the Hospital Anxiety and Depression Scale (HADS) during 2008-2009. A HADS score of more than 7 was considered indicative of depression.
Dr. Jani noted that all the results were adjusted for multiple confounding factors, including age, gender, socioeconomic status, number of comorbid conditions, total cholesterol values, body mass index, and the initiation of antidepressant medication.
“The key implications I would suggest are for secondary prevention and to perhaps focus our resources on monitoring blood pressure and providing treatment in patients with associated depressive symptoms,” Dr. Jani proposed.
Dr. Christi Deaton, professor of clinical nursing research at the University of Cambridge (England), who commented on the study findings, noted that it highlighted the importance of raising awareness among both clinicians and patients of the potential risk associated with a combination of hypertension and depression, particularly among patients with a high level of other risk factors for further cardiovascular events.
“Screening patients for depression is very simple to do and you can start with a couple of questions asking about whether or not the patient felt sad or had low mood, and then go on to use other screening tools,” she observed. “All providers should be screening patients and thinking about the synergy of these two risk factors,” she said.
Other research presented at the ESC Congress by cardiologist Dr. Salim Hayek of Emory University in Atlanta also highlighted the importance of screening for depression, this time in patients with angina. In a study of 5,202 adults enrolled in the university’s biobank between 2004 and 2013 and who underwent left heart catheterization, patients with frequent chest pain were found to have more depressive symptoms than those without angina. Depressive symptoms in this study were assessed using the Patient Health Questionnaire (PHQ-9).
“Chest pain was more frequent in patients with mild depression with and without coronary artery disease, regardless of sex or history of myocardial infarction,” Dr. Hayek said. After multivariate analysis, depression was the most important predictor of frequent chest pain, he added. Other factors independently associated with chest pain frequency were female sex, coronary artery disease severity, history of MI, body mass index, and high blood lipid levels.
“At follow-up, a decrease in depressive symptoms was associated with improvement in chest pain,” Dr. Hayek said, but patients with depression who were revascularized did not show an improvement in chest pain.
The findings suggest that the association between chest pain and depression was independent of the underlying arterial disease and further studies are needed to look at the effect of revascularization and angina relief on depressive symptoms, and conversely if antidepressant medications could help alleviate chest pain.
The study Dr. Jani presented was funded by the Scottish Government. Dr. Jani and Dr. Hayek both reported having no disclosures.
This article was updated February 3, 2016.
LONDON – The combination of depression and very high systolic blood pressure increased the risk for a major cardiovascular event by 83%, compared with normal blood pressure and no depression, in patients with existing heart disease, diabetes, or stroke.
In a large family practice–based study, the hazard ratio for first hospital admission due to myocardial infarction, stroke or heart failure, or cardiovascular death in patients with high (at least 160 mm Hg) systolic blood pressure who were also depressed was 1.83, a highly significant difference compared with individuals with normal BP and no depression.
The presence of depression also significantly increased the risk for these cardiovascular events by 36% in patients with lower systolic BPs, compared with those with normal BP and no depression.
“Patients with existing heart disease, diabetes, or stroke are more likely to have another heart attack or another stroke or die from heart problems than the general population,” Dr. Bhautesh Jani of the Institute of Health and Wellbeing, University of Glasgow (Scotland), said at the annual congress of the European Society of Cardiology.
“In particular, those who have extremes of blood pressure or those who have depressive symptoms are at higher risk, which has been shown by previous evidence. What is relatively unknown is the combined effect of having extremes of blood pressure and depressive symptoms together, and our study tried to address that problem,” Dr. Jani explained.
The study involved more than 35,500 individuals with existing heart disease, diabetes, or stroke living in Scotland, of whom 3,939 (11%) had at least one major cardiovascular event that needed hospital admission during a 4-year period. Patients had been divided into groups based on their systolic BP, and depressive symptoms were assessed using the Hospital Anxiety and Depression Scale (HADS) during 2008-2009. A HADS score of more than 7 was considered indicative of depression.
Dr. Jani noted that all the results were adjusted for multiple confounding factors, including age, gender, socioeconomic status, number of comorbid conditions, total cholesterol values, body mass index, and the initiation of antidepressant medication.
“The key implications I would suggest are for secondary prevention and to perhaps focus our resources on monitoring blood pressure and providing treatment in patients with associated depressive symptoms,” Dr. Jani proposed.
Dr. Christi Deaton, professor of clinical nursing research at the University of Cambridge (England), who commented on the study findings, noted that it highlighted the importance of raising awareness among both clinicians and patients of the potential risk associated with a combination of hypertension and depression, particularly among patients with a high level of other risk factors for further cardiovascular events.
“Screening patients for depression is very simple to do and you can start with a couple of questions asking about whether or not the patient felt sad or had low mood, and then go on to use other screening tools,” she observed. “All providers should be screening patients and thinking about the synergy of these two risk factors,” she said.
Other research presented at the ESC Congress by cardiologist Dr. Salim Hayek of Emory University in Atlanta also highlighted the importance of screening for depression, this time in patients with angina. In a study of 5,202 adults enrolled in the university’s biobank between 2004 and 2013 and who underwent left heart catheterization, patients with frequent chest pain were found to have more depressive symptoms than those without angina. Depressive symptoms in this study were assessed using the Patient Health Questionnaire (PHQ-9).
“Chest pain was more frequent in patients with mild depression with and without coronary artery disease, regardless of sex or history of myocardial infarction,” Dr. Hayek said. After multivariate analysis, depression was the most important predictor of frequent chest pain, he added. Other factors independently associated with chest pain frequency were female sex, coronary artery disease severity, history of MI, body mass index, and high blood lipid levels.
“At follow-up, a decrease in depressive symptoms was associated with improvement in chest pain,” Dr. Hayek said, but patients with depression who were revascularized did not show an improvement in chest pain.
The findings suggest that the association between chest pain and depression was independent of the underlying arterial disease and further studies are needed to look at the effect of revascularization and angina relief on depressive symptoms, and conversely if antidepressant medications could help alleviate chest pain.
The study Dr. Jani presented was funded by the Scottish Government. Dr. Jani and Dr. Hayek both reported having no disclosures.
This article was updated February 3, 2016.
LONDON – The combination of depression and very high systolic blood pressure increased the risk for a major cardiovascular event by 83%, compared with normal blood pressure and no depression, in patients with existing heart disease, diabetes, or stroke.
In a large family practice–based study, the hazard ratio for first hospital admission due to myocardial infarction, stroke or heart failure, or cardiovascular death in patients with high (at least 160 mm Hg) systolic blood pressure who were also depressed was 1.83, a highly significant difference compared with individuals with normal BP and no depression.
The presence of depression also significantly increased the risk for these cardiovascular events by 36% in patients with lower systolic BPs, compared with those with normal BP and no depression.
“Patients with existing heart disease, diabetes, or stroke are more likely to have another heart attack or another stroke or die from heart problems than the general population,” Dr. Bhautesh Jani of the Institute of Health and Wellbeing, University of Glasgow (Scotland), said at the annual congress of the European Society of Cardiology.
“In particular, those who have extremes of blood pressure or those who have depressive symptoms are at higher risk, which has been shown by previous evidence. What is relatively unknown is the combined effect of having extremes of blood pressure and depressive symptoms together, and our study tried to address that problem,” Dr. Jani explained.
The study involved more than 35,500 individuals with existing heart disease, diabetes, or stroke living in Scotland, of whom 3,939 (11%) had at least one major cardiovascular event that needed hospital admission during a 4-year period. Patients had been divided into groups based on their systolic BP, and depressive symptoms were assessed using the Hospital Anxiety and Depression Scale (HADS) during 2008-2009. A HADS score of more than 7 was considered indicative of depression.
Dr. Jani noted that all the results were adjusted for multiple confounding factors, including age, gender, socioeconomic status, number of comorbid conditions, total cholesterol values, body mass index, and the initiation of antidepressant medication.
“The key implications I would suggest are for secondary prevention and to perhaps focus our resources on monitoring blood pressure and providing treatment in patients with associated depressive symptoms,” Dr. Jani proposed.
Dr. Christi Deaton, professor of clinical nursing research at the University of Cambridge (England), who commented on the study findings, noted that it highlighted the importance of raising awareness among both clinicians and patients of the potential risk associated with a combination of hypertension and depression, particularly among patients with a high level of other risk factors for further cardiovascular events.
“Screening patients for depression is very simple to do and you can start with a couple of questions asking about whether or not the patient felt sad or had low mood, and then go on to use other screening tools,” she observed. “All providers should be screening patients and thinking about the synergy of these two risk factors,” she said.
Other research presented at the ESC Congress by cardiologist Dr. Salim Hayek of Emory University in Atlanta also highlighted the importance of screening for depression, this time in patients with angina. In a study of 5,202 adults enrolled in the university’s biobank between 2004 and 2013 and who underwent left heart catheterization, patients with frequent chest pain were found to have more depressive symptoms than those without angina. Depressive symptoms in this study were assessed using the Patient Health Questionnaire (PHQ-9).
“Chest pain was more frequent in patients with mild depression with and without coronary artery disease, regardless of sex or history of myocardial infarction,” Dr. Hayek said. After multivariate analysis, depression was the most important predictor of frequent chest pain, he added. Other factors independently associated with chest pain frequency were female sex, coronary artery disease severity, history of MI, body mass index, and high blood lipid levels.
“At follow-up, a decrease in depressive symptoms was associated with improvement in chest pain,” Dr. Hayek said, but patients with depression who were revascularized did not show an improvement in chest pain.
The findings suggest that the association between chest pain and depression was independent of the underlying arterial disease and further studies are needed to look at the effect of revascularization and angina relief on depressive symptoms, and conversely if antidepressant medications could help alleviate chest pain.
The study Dr. Jani presented was funded by the Scottish Government. Dr. Jani and Dr. Hayek both reported having no disclosures.
This article was updated February 3, 2016.
AT THE ESC CONGRESS 2015
Key clinical point: Better monitoring and management of both hypertension and depression could help reduce further cardiovascular morbidity and mortality.
Major finding: The rate of major cardiovascular events was 83% higher in depressed patients with very high (at least 160 mm Hg) systolic BP, compared with individuals with normal pressure and no depression.
Data source: Large family practice study of 35,537 patients with existing coronary heart disease, diabetes, or stroke followed up for 4 years.
Disclosures: The study Dr. Jani presented was funded by the Scottish Government. Dr. Jani had no disclosures.
ESC: Air quality level linked to STEMI risk in men
LONDON – The risk for ST-elevation myocardial infarction (STEMI) increased in men when air quality dipped below acceptable levels as designated by the World Health Organization (WHO), based on the results of an observational study in Belgian.
The relative risk for a STEMI increased by 2.8% (1.026; 95% confidence interval, 1.005-1.048) for every 10 mcg/cm3 rise in fine particulate air pollution and by 5.1% (RR, 1.051; 95% CI, 1.018-1.084) for a comparable rise in nitric oxide air pollution. Ozone level was not associated with the risk for STEMI. Air pollution levels did not affect in-hospital mortality due to STEMI and had no clear effect on patients with coronary artery disease, diabetes or hypertension.
“Of course, it is very interesting that the results are only observed in men. This may be due to a statistical issue, because in our study population, the female group represents less than 25% of the population,” Dr. Jean-François Argacha, a study investigator, said during a press briefing at the annual congress of the European Society of Cardiology.
Subgroup analysis suggested that patients who were aged 75 years and older were more likely to develop STEMI in relation to exposure to particulate matter (RR, 1.046; 95% CI, 1.002-1.092, P = .041). Those aged 54 years and younger seemed more susceptible to nitric oxide levels (RR, 1.071; 95% CI, 1.010-1.136; P = .021).“The detrimental impact of nitric oxide exceeded that of fine particles and may be of particular concern in the younger population,” said Dr. Argacha, a cardiologist at University Hospital Brussels.
Previous research had shown that particulate matter is associated with an increased risk for acute myocardial infarction, but there had been no specific assessments on air pollution’s potential effects on STEMI, according to Dr. Argacha.
The study considered information on 11,428 patients in the Belgian Interdisciplinary Working Group on Acute Cardiology STEMI Registry between 2009 and 2013. Data on national air pollution parameters – particulate matter with an aerodynamic diameter of less than 10 (PM10) or 2.5 (PM2.5) mcm, nitric oxide and ozone – and air temperature were obtained from the Belgian Environment Agency database and adjusted for population density.
A case crossover analysis of STEMI risk was then performed, with risk being adjusted for ambient temperature, day of the week, and the season. The study’s case crossover design ensured that the effects were limited to air pollution and excluded other confounders including respiratory disease and air temperature.
Worldwide, WHO has estimated that poor urban air quality is responsible for around 1.3 million deaths per year, Dr. Argacha observed, noting that air pollution consists of fine (PM2.5) and larger (PM10) particles, nitric oxide, and ozone as well as sulfur dioxide and carbon monoxide.
During the observation period, the mean air pollution levels over the course of 1 year in Belgium were 23.9 mcg/cm3 for PM10, 16.1 mcg/cm3 for PM2.5, and 23.7 mcg/cm3 for nitric oxide. WHO guidelines set a daily limit of 25 mcg/cm3 for PM2.5. Dr. Argacha noted that this limit was exceeded in Belgium on 17.5% of days in the study.
Dr. Oscar Franco, professor of preventative medicine at the Erasmus University Medical Center in Rotterdam, the Netherlands, who cochaired the press conference noted that the European Society of Cardiology recently published a position paper on air pollution on cardiovascular disease (Eur Heart J. 2015;36:83-93) and has launched a major campaign to raise awareness of the detrimental effects that the environment can have on the heart.
The campaign notes that air and noise pollution are modifiable risk factors for the prevention and control of cardiovascular diseases, and advocated for acceptable limits that reflect WHO levels. Individuals “need to take action,” Dr. Franco urged. The decisions that people make every day – how they get to work for example – could have a potentially huge impact on the environment and health.
Dr. Argacha and Dr. Franco had no disclosures to report.
LONDON – The risk for ST-elevation myocardial infarction (STEMI) increased in men when air quality dipped below acceptable levels as designated by the World Health Organization (WHO), based on the results of an observational study in Belgian.
The relative risk for a STEMI increased by 2.8% (1.026; 95% confidence interval, 1.005-1.048) for every 10 mcg/cm3 rise in fine particulate air pollution and by 5.1% (RR, 1.051; 95% CI, 1.018-1.084) for a comparable rise in nitric oxide air pollution. Ozone level was not associated with the risk for STEMI. Air pollution levels did not affect in-hospital mortality due to STEMI and had no clear effect on patients with coronary artery disease, diabetes or hypertension.
“Of course, it is very interesting that the results are only observed in men. This may be due to a statistical issue, because in our study population, the female group represents less than 25% of the population,” Dr. Jean-François Argacha, a study investigator, said during a press briefing at the annual congress of the European Society of Cardiology.
Subgroup analysis suggested that patients who were aged 75 years and older were more likely to develop STEMI in relation to exposure to particulate matter (RR, 1.046; 95% CI, 1.002-1.092, P = .041). Those aged 54 years and younger seemed more susceptible to nitric oxide levels (RR, 1.071; 95% CI, 1.010-1.136; P = .021).“The detrimental impact of nitric oxide exceeded that of fine particles and may be of particular concern in the younger population,” said Dr. Argacha, a cardiologist at University Hospital Brussels.
Previous research had shown that particulate matter is associated with an increased risk for acute myocardial infarction, but there had been no specific assessments on air pollution’s potential effects on STEMI, according to Dr. Argacha.
The study considered information on 11,428 patients in the Belgian Interdisciplinary Working Group on Acute Cardiology STEMI Registry between 2009 and 2013. Data on national air pollution parameters – particulate matter with an aerodynamic diameter of less than 10 (PM10) or 2.5 (PM2.5) mcm, nitric oxide and ozone – and air temperature were obtained from the Belgian Environment Agency database and adjusted for population density.
A case crossover analysis of STEMI risk was then performed, with risk being adjusted for ambient temperature, day of the week, and the season. The study’s case crossover design ensured that the effects were limited to air pollution and excluded other confounders including respiratory disease and air temperature.
Worldwide, WHO has estimated that poor urban air quality is responsible for around 1.3 million deaths per year, Dr. Argacha observed, noting that air pollution consists of fine (PM2.5) and larger (PM10) particles, nitric oxide, and ozone as well as sulfur dioxide and carbon monoxide.
During the observation period, the mean air pollution levels over the course of 1 year in Belgium were 23.9 mcg/cm3 for PM10, 16.1 mcg/cm3 for PM2.5, and 23.7 mcg/cm3 for nitric oxide. WHO guidelines set a daily limit of 25 mcg/cm3 for PM2.5. Dr. Argacha noted that this limit was exceeded in Belgium on 17.5% of days in the study.
Dr. Oscar Franco, professor of preventative medicine at the Erasmus University Medical Center in Rotterdam, the Netherlands, who cochaired the press conference noted that the European Society of Cardiology recently published a position paper on air pollution on cardiovascular disease (Eur Heart J. 2015;36:83-93) and has launched a major campaign to raise awareness of the detrimental effects that the environment can have on the heart.
The campaign notes that air and noise pollution are modifiable risk factors for the prevention and control of cardiovascular diseases, and advocated for acceptable limits that reflect WHO levels. Individuals “need to take action,” Dr. Franco urged. The decisions that people make every day – how they get to work for example – could have a potentially huge impact on the environment and health.
Dr. Argacha and Dr. Franco had no disclosures to report.
LONDON – The risk for ST-elevation myocardial infarction (STEMI) increased in men when air quality dipped below acceptable levels as designated by the World Health Organization (WHO), based on the results of an observational study in Belgian.
The relative risk for a STEMI increased by 2.8% (1.026; 95% confidence interval, 1.005-1.048) for every 10 mcg/cm3 rise in fine particulate air pollution and by 5.1% (RR, 1.051; 95% CI, 1.018-1.084) for a comparable rise in nitric oxide air pollution. Ozone level was not associated with the risk for STEMI. Air pollution levels did not affect in-hospital mortality due to STEMI and had no clear effect on patients with coronary artery disease, diabetes or hypertension.
“Of course, it is very interesting that the results are only observed in men. This may be due to a statistical issue, because in our study population, the female group represents less than 25% of the population,” Dr. Jean-François Argacha, a study investigator, said during a press briefing at the annual congress of the European Society of Cardiology.
Subgroup analysis suggested that patients who were aged 75 years and older were more likely to develop STEMI in relation to exposure to particulate matter (RR, 1.046; 95% CI, 1.002-1.092, P = .041). Those aged 54 years and younger seemed more susceptible to nitric oxide levels (RR, 1.071; 95% CI, 1.010-1.136; P = .021).“The detrimental impact of nitric oxide exceeded that of fine particles and may be of particular concern in the younger population,” said Dr. Argacha, a cardiologist at University Hospital Brussels.
Previous research had shown that particulate matter is associated with an increased risk for acute myocardial infarction, but there had been no specific assessments on air pollution’s potential effects on STEMI, according to Dr. Argacha.
The study considered information on 11,428 patients in the Belgian Interdisciplinary Working Group on Acute Cardiology STEMI Registry between 2009 and 2013. Data on national air pollution parameters – particulate matter with an aerodynamic diameter of less than 10 (PM10) or 2.5 (PM2.5) mcm, nitric oxide and ozone – and air temperature were obtained from the Belgian Environment Agency database and adjusted for population density.
A case crossover analysis of STEMI risk was then performed, with risk being adjusted for ambient temperature, day of the week, and the season. The study’s case crossover design ensured that the effects were limited to air pollution and excluded other confounders including respiratory disease and air temperature.
Worldwide, WHO has estimated that poor urban air quality is responsible for around 1.3 million deaths per year, Dr. Argacha observed, noting that air pollution consists of fine (PM2.5) and larger (PM10) particles, nitric oxide, and ozone as well as sulfur dioxide and carbon monoxide.
During the observation period, the mean air pollution levels over the course of 1 year in Belgium were 23.9 mcg/cm3 for PM10, 16.1 mcg/cm3 for PM2.5, and 23.7 mcg/cm3 for nitric oxide. WHO guidelines set a daily limit of 25 mcg/cm3 for PM2.5. Dr. Argacha noted that this limit was exceeded in Belgium on 17.5% of days in the study.
Dr. Oscar Franco, professor of preventative medicine at the Erasmus University Medical Center in Rotterdam, the Netherlands, who cochaired the press conference noted that the European Society of Cardiology recently published a position paper on air pollution on cardiovascular disease (Eur Heart J. 2015;36:83-93) and has launched a major campaign to raise awareness of the detrimental effects that the environment can have on the heart.
The campaign notes that air and noise pollution are modifiable risk factors for the prevention and control of cardiovascular diseases, and advocated for acceptable limits that reflect WHO levels. Individuals “need to take action,” Dr. Franco urged. The decisions that people make every day – how they get to work for example – could have a potentially huge impact on the environment and health.
Dr. Argacha and Dr. Franco had no disclosures to report.
AT THE ESC CONGRESS 2015
Key clinical point: Air pollution may be a potentially modifiable risk factor for STEMI in men.
Major finding: The relative risk for a STEMI increased by 2.8% for a 10 mcg/cm3 rise in fine particulate air pollution and by 5.1% for a comparable rise in nitric oxide air pollution.
Data source: 11,428 patients logged in the Belgian Interdisciplinary Working Group on Acute Cardiology STEMI Registry between 2009 and 2013.
Disclosures: Dr. Argacha and Dr. Franco had no disclosures to report.
ESC: What’s the hottest recent advance in cardiology? And the winner is …
LONDON – What was the top development in all of cardiology during the past year, the advance that holds the most far-reaching implications for clinical practice?
At the annual congress of the European Society of Cardiology, six experts each made a case for the biggest game changer in their discipline – risk prevention, electrophysiology, imaging, heart failure, percutaneous coronary intervention, and acute cardiac care. And when the audience of perhaps 400-strong had cast their votes, the winner was … the novel angiotensin receptor neprilysin inhibitor (ARNI) known as LCZ696 or valsartan/sacubitril. In the landmark PARADIGM-HF trial, the drug reduced the risk of cardiovascular death by 20% and heart failure hospitalization by 21% over and above what’s achieved with enalapril plus the other current guideline-recommended heart failure medications. “I’m a device person, but I’ve decided a device is not the most important recent innovation in heart failure,” Dr. Cecilia Linde said in her winning argument.
“This ARNI is the first new drug in years with a very clear impact on morbidity and mortality. This is why I believe PARADIGM-HF is the most important study result of the last year in heart failure. It will directly impact treatment and will change the ESC guidelines for heart failure therapy. The PARADIGM-HF results suggest that the ARNI should be given as first-line therapy instead of an ACE inhibitor or angiotensin receptor blocker,” said Dr. Linde, professor and head of cardiology at the Karolinska Institute, Stockholm.
In the double-blind, randomized 8,399-patient PARADIGM-HF trial (N Engl J Med. 2014 Sep 11;371[11]:993-1004), the number needed to treat with LCZ696 instead of enalapril for 27 months in order to avoid one cardiovascular death or heart failure hospitalization was 21. The number needed to treat to avoid one cardiovascular death was 32.
Electrophysiology
The big news here is the concept of the autonomic nervous system as the master controller of atrial fibrillation, governing both the firing of arrhythmic triggers and the change in the arrhythmogenic substrate over time, according to Dr. Sabine Ernst of the National Heart and Lung Institute at Imperial College, London.
“There is a new recognition of how the sympathetic and parasympathetic nervous systems interact to initiate and maintain arrhythmias. This will change the electrophysiology world forever,” she predicted.
Indeed, the future of antiarrhythmic therapy lies in neuromodulation of the autonomic nervous system, and it’s a lot closer than most cardiologists realize, according to the electrophysiologist.
She pointed to a recent study in which investigators at the University of Oklahoma Heart Rhythm Institute randomized 40 patients with paroxysmal atrial fibrillation to noninvasive low-level electrical stimulation of the vagus nerve or to sham treatment. The stimulation at 20 Hz suppressed atrial fibrillation and reduced levels of inflammatory cytokines (J Am Coll Cardiol. 2015 Mar 10;65[9]:867-75).
Vagus nerve stimulation was accomplished using a pair of clips attached to the external ear in order to access the tragus nerve. At just 20 Hz, participants felt no discomfort.
“This is just the very first step. It’s probably not the right frequency or intensity yet. But maybe – and I just want you to start to dream about this – just maybe this could be easily implanted in something we put in our ears. How nice it would be if we could add it to a hearing aid for a patient with atrial fibrillation; we would not need to bother with rate control anymore. Or to prevent atrial fibrillation, [we could put] a low-level vagus stimulator in the headphones for a smartphone,” Dr. Ernst said.
The noninvasiveness of this novel approach is what she finds most appealing.
“I want to stop putting catheters in other people’s hearts. I want to use a method I can ideally apply in the outpatient setting. I think we’ve got to move away from just destroying myocardium in patients with arrhythmias,” she said.
Cardiovascular prevention
Dr. Joep Perk nominated as the most important development of the past year in this field a new set of refined ECG screening criteria for asymptomatic hypertrophic cardiomyopathy (HCM) in athletes. Previous criteria – both the 2010 ESC criteria and the recently published Seattle criteria developed by an international collaborative group (Br J Sports Med. 2013 Feb;47[3]:122-4) – have unacceptably high false-positive rates, which lead to further testing, particularly in black athletes.
“In my personal experience, these young athletes start to think there is something wrong with their heart. They’ll be worried and might be erroneously disqualified. So even though we mean well, it does a lot of psychological harm,” said Dr. Perk, head of the department of internal medicine at Oskarshamn (Sweden) Hospital.
The so-called refined criteria (Circulation. 2014 Apr 22;129[16]:1637-49) were designed to improve upon the specificity of the ESC and Seattle criteria by excluding several isolated ECG patterns that have been shown not relevant in black athletes.
When the developers of the refined criteria applied all three sets of criteria to a large population of black and white athletes, including 103 young athletes with HCM, all three showed 98% sensitivity for the detection of HCM. However, the false-positive ECG rate in black athletes improved from 40.4% using the ESC criteria, to 18.4% with the Seattle criteria, to 11.5% using the refined criteria. Among white athletes, the false-positive rates using the three sets of criteria were 16.2%, 7.1%, and 5.3%.
“These new refined criteria should be incorporated into guidelines for the screening of athletes. They provide a 71% reduction in positive ECGs in black athletes, compared with the ESC recommendations,” Dr. Perk said.
Cardiac imaging
“I really think 3-D printing is going to revolutionize every aspect of medicine,” asserted Dr. Luigi Badano of the University of Padua (Italy).
At the ESC congress, his research group presented a study in which they used custom software to create an exact model of a real patient’s tricuspid valve out of liquid resin based on transthoracic echo images. It took 90 minutes.
“This technology allows us to hold the physical structure of the heart in our hands,” he noted. “We can use it to teach anatomy to medical students without a corpse, plan surgical interventions, and communicate with patients, showing them exact structures and revolutionizing the concept of informed consent.”
And that’s just scratching the surface. He noted that investigators at Wake Forest Baptist Medical Center Institute for Regenerative Medicine in North Carolina recently utilized 3-D printing with bio-ink and bio-paper to print 3-D beating cardiac cells clustered into “organoids.” It’s the first step toward creating a prototype beating heart.
“Can you dream about that? The donor heart shortage could in the future be solved by printing a beating heart for insertion into the patient. The investigators predict they’ll have a functional beating heart within 20 years,” Dr. Badano said.
Acute cardiac care
Dr. Maddalena Lettino and her fellow leaders of the European Acute Cardiac Care Association agreed that the breakthrough of the year in their field was validation of a novel 1-hour rule-in/rule-out algorithm using high-sensitivity cardiac troponin T to accelerate management of patients who present to the emergency department with chest pain. According to studies totaling more than 3,000 patients with more than 600 MIs in which the assay and algorithm were tested, roughly 75% of patients can safely and accurately have acute MI ruled out or ruled in within 1 hour.
Given that close to 10% of all emergency department visits are for chest pain, adoption of this algorithm will reduce ED overcrowding, speed physician workflow, save health care systems money, and spare patients and families the anxiety that comes with a delayed diagnosis, said Dr. Lettino, director of the clinical cardiology unit at Humanitas Research Hospital in Milan.
Coronary intervention
The 15%-20% of coronary stent recipients who are at high bleeding risk constitute “the forgotten patient population,” said Dr. Philippe Garot of the Paris South Cardiovascular Institute.
He noted that the key question of whether such patients can be managed safely with a mere 1-month course of dual antiplatelet therapy will finally be answered this fall with the release of the LEADERS FREE trial results. This large, randomized double-blind trial compares safety and efficacy outcomes in patients assigned to a bare metal stent or the novel drug-eluting BioFreedom stent.
Stay tuned, because LEADERS FREE could be a game changer in interventional cardiology, he said.
The six presenters indicated they had no relevant financial conflicts.
LONDON – What was the top development in all of cardiology during the past year, the advance that holds the most far-reaching implications for clinical practice?
At the annual congress of the European Society of Cardiology, six experts each made a case for the biggest game changer in their discipline – risk prevention, electrophysiology, imaging, heart failure, percutaneous coronary intervention, and acute cardiac care. And when the audience of perhaps 400-strong had cast their votes, the winner was … the novel angiotensin receptor neprilysin inhibitor (ARNI) known as LCZ696 or valsartan/sacubitril. In the landmark PARADIGM-HF trial, the drug reduced the risk of cardiovascular death by 20% and heart failure hospitalization by 21% over and above what’s achieved with enalapril plus the other current guideline-recommended heart failure medications. “I’m a device person, but I’ve decided a device is not the most important recent innovation in heart failure,” Dr. Cecilia Linde said in her winning argument.
“This ARNI is the first new drug in years with a very clear impact on morbidity and mortality. This is why I believe PARADIGM-HF is the most important study result of the last year in heart failure. It will directly impact treatment and will change the ESC guidelines for heart failure therapy. The PARADIGM-HF results suggest that the ARNI should be given as first-line therapy instead of an ACE inhibitor or angiotensin receptor blocker,” said Dr. Linde, professor and head of cardiology at the Karolinska Institute, Stockholm.
In the double-blind, randomized 8,399-patient PARADIGM-HF trial (N Engl J Med. 2014 Sep 11;371[11]:993-1004), the number needed to treat with LCZ696 instead of enalapril for 27 months in order to avoid one cardiovascular death or heart failure hospitalization was 21. The number needed to treat to avoid one cardiovascular death was 32.
Electrophysiology
The big news here is the concept of the autonomic nervous system as the master controller of atrial fibrillation, governing both the firing of arrhythmic triggers and the change in the arrhythmogenic substrate over time, according to Dr. Sabine Ernst of the National Heart and Lung Institute at Imperial College, London.
“There is a new recognition of how the sympathetic and parasympathetic nervous systems interact to initiate and maintain arrhythmias. This will change the electrophysiology world forever,” she predicted.
Indeed, the future of antiarrhythmic therapy lies in neuromodulation of the autonomic nervous system, and it’s a lot closer than most cardiologists realize, according to the electrophysiologist.
She pointed to a recent study in which investigators at the University of Oklahoma Heart Rhythm Institute randomized 40 patients with paroxysmal atrial fibrillation to noninvasive low-level electrical stimulation of the vagus nerve or to sham treatment. The stimulation at 20 Hz suppressed atrial fibrillation and reduced levels of inflammatory cytokines (J Am Coll Cardiol. 2015 Mar 10;65[9]:867-75).
Vagus nerve stimulation was accomplished using a pair of clips attached to the external ear in order to access the tragus nerve. At just 20 Hz, participants felt no discomfort.
“This is just the very first step. It’s probably not the right frequency or intensity yet. But maybe – and I just want you to start to dream about this – just maybe this could be easily implanted in something we put in our ears. How nice it would be if we could add it to a hearing aid for a patient with atrial fibrillation; we would not need to bother with rate control anymore. Or to prevent atrial fibrillation, [we could put] a low-level vagus stimulator in the headphones for a smartphone,” Dr. Ernst said.
The noninvasiveness of this novel approach is what she finds most appealing.
“I want to stop putting catheters in other people’s hearts. I want to use a method I can ideally apply in the outpatient setting. I think we’ve got to move away from just destroying myocardium in patients with arrhythmias,” she said.
Cardiovascular prevention
Dr. Joep Perk nominated as the most important development of the past year in this field a new set of refined ECG screening criteria for asymptomatic hypertrophic cardiomyopathy (HCM) in athletes. Previous criteria – both the 2010 ESC criteria and the recently published Seattle criteria developed by an international collaborative group (Br J Sports Med. 2013 Feb;47[3]:122-4) – have unacceptably high false-positive rates, which lead to further testing, particularly in black athletes.
“In my personal experience, these young athletes start to think there is something wrong with their heart. They’ll be worried and might be erroneously disqualified. So even though we mean well, it does a lot of psychological harm,” said Dr. Perk, head of the department of internal medicine at Oskarshamn (Sweden) Hospital.
The so-called refined criteria (Circulation. 2014 Apr 22;129[16]:1637-49) were designed to improve upon the specificity of the ESC and Seattle criteria by excluding several isolated ECG patterns that have been shown not relevant in black athletes.
When the developers of the refined criteria applied all three sets of criteria to a large population of black and white athletes, including 103 young athletes with HCM, all three showed 98% sensitivity for the detection of HCM. However, the false-positive ECG rate in black athletes improved from 40.4% using the ESC criteria, to 18.4% with the Seattle criteria, to 11.5% using the refined criteria. Among white athletes, the false-positive rates using the three sets of criteria were 16.2%, 7.1%, and 5.3%.
“These new refined criteria should be incorporated into guidelines for the screening of athletes. They provide a 71% reduction in positive ECGs in black athletes, compared with the ESC recommendations,” Dr. Perk said.
Cardiac imaging
“I really think 3-D printing is going to revolutionize every aspect of medicine,” asserted Dr. Luigi Badano of the University of Padua (Italy).
At the ESC congress, his research group presented a study in which they used custom software to create an exact model of a real patient’s tricuspid valve out of liquid resin based on transthoracic echo images. It took 90 minutes.
“This technology allows us to hold the physical structure of the heart in our hands,” he noted. “We can use it to teach anatomy to medical students without a corpse, plan surgical interventions, and communicate with patients, showing them exact structures and revolutionizing the concept of informed consent.”
And that’s just scratching the surface. He noted that investigators at Wake Forest Baptist Medical Center Institute for Regenerative Medicine in North Carolina recently utilized 3-D printing with bio-ink and bio-paper to print 3-D beating cardiac cells clustered into “organoids.” It’s the first step toward creating a prototype beating heart.
“Can you dream about that? The donor heart shortage could in the future be solved by printing a beating heart for insertion into the patient. The investigators predict they’ll have a functional beating heart within 20 years,” Dr. Badano said.
Acute cardiac care
Dr. Maddalena Lettino and her fellow leaders of the European Acute Cardiac Care Association agreed that the breakthrough of the year in their field was validation of a novel 1-hour rule-in/rule-out algorithm using high-sensitivity cardiac troponin T to accelerate management of patients who present to the emergency department with chest pain. According to studies totaling more than 3,000 patients with more than 600 MIs in which the assay and algorithm were tested, roughly 75% of patients can safely and accurately have acute MI ruled out or ruled in within 1 hour.
Given that close to 10% of all emergency department visits are for chest pain, adoption of this algorithm will reduce ED overcrowding, speed physician workflow, save health care systems money, and spare patients and families the anxiety that comes with a delayed diagnosis, said Dr. Lettino, director of the clinical cardiology unit at Humanitas Research Hospital in Milan.
Coronary intervention
The 15%-20% of coronary stent recipients who are at high bleeding risk constitute “the forgotten patient population,” said Dr. Philippe Garot of the Paris South Cardiovascular Institute.
He noted that the key question of whether such patients can be managed safely with a mere 1-month course of dual antiplatelet therapy will finally be answered this fall with the release of the LEADERS FREE trial results. This large, randomized double-blind trial compares safety and efficacy outcomes in patients assigned to a bare metal stent or the novel drug-eluting BioFreedom stent.
Stay tuned, because LEADERS FREE could be a game changer in interventional cardiology, he said.
The six presenters indicated they had no relevant financial conflicts.
LONDON – What was the top development in all of cardiology during the past year, the advance that holds the most far-reaching implications for clinical practice?
At the annual congress of the European Society of Cardiology, six experts each made a case for the biggest game changer in their discipline – risk prevention, electrophysiology, imaging, heart failure, percutaneous coronary intervention, and acute cardiac care. And when the audience of perhaps 400-strong had cast their votes, the winner was … the novel angiotensin receptor neprilysin inhibitor (ARNI) known as LCZ696 or valsartan/sacubitril. In the landmark PARADIGM-HF trial, the drug reduced the risk of cardiovascular death by 20% and heart failure hospitalization by 21% over and above what’s achieved with enalapril plus the other current guideline-recommended heart failure medications. “I’m a device person, but I’ve decided a device is not the most important recent innovation in heart failure,” Dr. Cecilia Linde said in her winning argument.
“This ARNI is the first new drug in years with a very clear impact on morbidity and mortality. This is why I believe PARADIGM-HF is the most important study result of the last year in heart failure. It will directly impact treatment and will change the ESC guidelines for heart failure therapy. The PARADIGM-HF results suggest that the ARNI should be given as first-line therapy instead of an ACE inhibitor or angiotensin receptor blocker,” said Dr. Linde, professor and head of cardiology at the Karolinska Institute, Stockholm.
In the double-blind, randomized 8,399-patient PARADIGM-HF trial (N Engl J Med. 2014 Sep 11;371[11]:993-1004), the number needed to treat with LCZ696 instead of enalapril for 27 months in order to avoid one cardiovascular death or heart failure hospitalization was 21. The number needed to treat to avoid one cardiovascular death was 32.
Electrophysiology
The big news here is the concept of the autonomic nervous system as the master controller of atrial fibrillation, governing both the firing of arrhythmic triggers and the change in the arrhythmogenic substrate over time, according to Dr. Sabine Ernst of the National Heart and Lung Institute at Imperial College, London.
“There is a new recognition of how the sympathetic and parasympathetic nervous systems interact to initiate and maintain arrhythmias. This will change the electrophysiology world forever,” she predicted.
Indeed, the future of antiarrhythmic therapy lies in neuromodulation of the autonomic nervous system, and it’s a lot closer than most cardiologists realize, according to the electrophysiologist.
She pointed to a recent study in which investigators at the University of Oklahoma Heart Rhythm Institute randomized 40 patients with paroxysmal atrial fibrillation to noninvasive low-level electrical stimulation of the vagus nerve or to sham treatment. The stimulation at 20 Hz suppressed atrial fibrillation and reduced levels of inflammatory cytokines (J Am Coll Cardiol. 2015 Mar 10;65[9]:867-75).
Vagus nerve stimulation was accomplished using a pair of clips attached to the external ear in order to access the tragus nerve. At just 20 Hz, participants felt no discomfort.
“This is just the very first step. It’s probably not the right frequency or intensity yet. But maybe – and I just want you to start to dream about this – just maybe this could be easily implanted in something we put in our ears. How nice it would be if we could add it to a hearing aid for a patient with atrial fibrillation; we would not need to bother with rate control anymore. Or to prevent atrial fibrillation, [we could put] a low-level vagus stimulator in the headphones for a smartphone,” Dr. Ernst said.
The noninvasiveness of this novel approach is what she finds most appealing.
“I want to stop putting catheters in other people’s hearts. I want to use a method I can ideally apply in the outpatient setting. I think we’ve got to move away from just destroying myocardium in patients with arrhythmias,” she said.
Cardiovascular prevention
Dr. Joep Perk nominated as the most important development of the past year in this field a new set of refined ECG screening criteria for asymptomatic hypertrophic cardiomyopathy (HCM) in athletes. Previous criteria – both the 2010 ESC criteria and the recently published Seattle criteria developed by an international collaborative group (Br J Sports Med. 2013 Feb;47[3]:122-4) – have unacceptably high false-positive rates, which lead to further testing, particularly in black athletes.
“In my personal experience, these young athletes start to think there is something wrong with their heart. They’ll be worried and might be erroneously disqualified. So even though we mean well, it does a lot of psychological harm,” said Dr. Perk, head of the department of internal medicine at Oskarshamn (Sweden) Hospital.
The so-called refined criteria (Circulation. 2014 Apr 22;129[16]:1637-49) were designed to improve upon the specificity of the ESC and Seattle criteria by excluding several isolated ECG patterns that have been shown not relevant in black athletes.
When the developers of the refined criteria applied all three sets of criteria to a large population of black and white athletes, including 103 young athletes with HCM, all three showed 98% sensitivity for the detection of HCM. However, the false-positive ECG rate in black athletes improved from 40.4% using the ESC criteria, to 18.4% with the Seattle criteria, to 11.5% using the refined criteria. Among white athletes, the false-positive rates using the three sets of criteria were 16.2%, 7.1%, and 5.3%.
“These new refined criteria should be incorporated into guidelines for the screening of athletes. They provide a 71% reduction in positive ECGs in black athletes, compared with the ESC recommendations,” Dr. Perk said.
Cardiac imaging
“I really think 3-D printing is going to revolutionize every aspect of medicine,” asserted Dr. Luigi Badano of the University of Padua (Italy).
At the ESC congress, his research group presented a study in which they used custom software to create an exact model of a real patient’s tricuspid valve out of liquid resin based on transthoracic echo images. It took 90 minutes.
“This technology allows us to hold the physical structure of the heart in our hands,” he noted. “We can use it to teach anatomy to medical students without a corpse, plan surgical interventions, and communicate with patients, showing them exact structures and revolutionizing the concept of informed consent.”
And that’s just scratching the surface. He noted that investigators at Wake Forest Baptist Medical Center Institute for Regenerative Medicine in North Carolina recently utilized 3-D printing with bio-ink and bio-paper to print 3-D beating cardiac cells clustered into “organoids.” It’s the first step toward creating a prototype beating heart.
“Can you dream about that? The donor heart shortage could in the future be solved by printing a beating heart for insertion into the patient. The investigators predict they’ll have a functional beating heart within 20 years,” Dr. Badano said.
Acute cardiac care
Dr. Maddalena Lettino and her fellow leaders of the European Acute Cardiac Care Association agreed that the breakthrough of the year in their field was validation of a novel 1-hour rule-in/rule-out algorithm using high-sensitivity cardiac troponin T to accelerate management of patients who present to the emergency department with chest pain. According to studies totaling more than 3,000 patients with more than 600 MIs in which the assay and algorithm were tested, roughly 75% of patients can safely and accurately have acute MI ruled out or ruled in within 1 hour.
Given that close to 10% of all emergency department visits are for chest pain, adoption of this algorithm will reduce ED overcrowding, speed physician workflow, save health care systems money, and spare patients and families the anxiety that comes with a delayed diagnosis, said Dr. Lettino, director of the clinical cardiology unit at Humanitas Research Hospital in Milan.
Coronary intervention
The 15%-20% of coronary stent recipients who are at high bleeding risk constitute “the forgotten patient population,” said Dr. Philippe Garot of the Paris South Cardiovascular Institute.
He noted that the key question of whether such patients can be managed safely with a mere 1-month course of dual antiplatelet therapy will finally be answered this fall with the release of the LEADERS FREE trial results. This large, randomized double-blind trial compares safety and efficacy outcomes in patients assigned to a bare metal stent or the novel drug-eluting BioFreedom stent.
Stay tuned, because LEADERS FREE could be a game changer in interventional cardiology, he said.
The six presenters indicated they had no relevant financial conflicts.
EXPERT ANALYSIS FROM THE ESC CONGRESS 2015
ESC: Strong coffee raises hypertension and prediabetes risk
LONDON – Drinking three or more cups of caffeinated espresso per day predicted increasing blood pressure and rising blood glucose, according to the results of the Hypertension and Ambulatory Recording Venetia Study (HARVEST), a multicenter, observational study that began in Italy in 1990 and recruited more than 1,000 patients aged 18-45 years who had stage I hypertension and did not have diabetes.
Further, the risk of a cardiovascular event was increased by 50% in these study participants based on a total of 60 events during a mean of 12.5 years of follow-up.
“Controversy still exists about the long-term cardiovascular and metabolic effects of coffee consumption in hypertension,” Dr. Lucio Mos of Hospital San Daniele del Friuli in Udine, Italy, said during a press conference at the annual congress of the European Society of Cardiology.
Stage 1 hypertension was defined as a diastolic blood pressure of 90-99 mm Hg and a systolic blood pressure of 140-159 mm Hg and diagnosed on the basis of six office-based readings obtained on two separate visits. Enrolled participants underwent ambulatory blood pressure monitoring and three office-based measurements were repeated at 1, 2, 3 and 6 months, and at 6-month intervals thereafter. The endpoint was hypertension requiring any antihypertensive treatment according to international guidelines.
During the study, 24-hour urine samples were collected to assess catecholamine levels. Lifestyle factors such as body weight, physical activity, smoking status, and blood glucose were measured. Patients underwent echocardiography.
They were divided into three groups according to their caffeinated coffee intake: 316 (26%) were designated as abstainers because they did not drink coffee; 767 (64%) drank 1-2 cups a day and were categorized as moderate drinkers; and 119 (10%) drank three or more cups of coffee a day and were defined as heavy drinkers.
“I want to underline that, in this part of Italy, we have a population that drinks mainly espresso coffee and drinking American-style coffee is not usual,” Dr. Mos said.
Around 70% of the study population was male, with similar baseline blood pressures and heart rates among the groups. Heavy coffee drinkers tended to be older (37 years) than those who were more moderate drinkers (34 years) or those who abstained (31 years). They had significantly higher body weights (P less than .001), with a body mass index of 26.1 kg/m2 vs. 25.7 kg/m2 and 24.6 kg/m2, respectively.
Dr. Mos reported that in multivariate analysis, coffee consumption was a significant predictor for developing hypertension that required antihypertensive therapy, with a hazard ratio (HR) of 1.5 (95% confidence interval [CI], 1.1-1.19) for heavy drinkers and 1.1 (95% confidence interval, 1.1-1.19) for moderate drinkers, compared to abstainers. The difference was significant (P = .004) only for heavy coffee consumption.
“Coffee consumption was also a predictor of future prediabetes,” Dr. Mos reported. Indeed, the incidence of prediabetes was highest in the heavy coffee drinkers, and significantly predicted the risk of developing prediabetes compared to abstainers (HR, 2, 95% CI, 1.3-3.1. P = .0017). There was a nonsignificant trend for moderate drinkers also to be at risk for prediabetes when compared to nondrinkers (HR, 1.3, 95% CI 0.9-1.7).
Looking at the risk for prediabetes in relation to caffeine metabolism by analyzing patients by their CYP1A2 genotype, it was found that heavy coffee drinkers who were slow metabolizers of caffeine were at highest risk, with a HR of 2.78 (95% CI, 1.32-5.88). Furthermore, individuals were particularly at risk if they were also overweight or obese.
There was a significant (P = .0017) linear relationship found after multivariate adjustment between coffee intake and cardiovascular events such as heart attacks, with the risk increasing with higher coffee intake. Even moderate coffee intake, defined as one to three cups per day, could up the risk of a cardiovascular event when compared to that of non–coffee drinkers.
“The coffee story was very topical a couple of years ago so it is interesting to see it revisited,” said Dr. Ian Graham of Trinity College Dublin and one of the experts who chaired the press briefing on the study results. “We need a randomized controlled trial,” Dr. Graham suggested, noting that there were several prior studies that suggested there were beneficial effects of coffee.
Cochair Dr. José Gonzalez-Juanatey of Hospital Clínico Universitario de Santiago de Compostela in Spain observed: “The recommendation could be that if you are a young or middle-aged, stage 1 hypertensive patient probably you have to reduce your coffee intake. This is the take-home message based on the results of an observational study well performed and well conducted.”
LONDON – Drinking three or more cups of caffeinated espresso per day predicted increasing blood pressure and rising blood glucose, according to the results of the Hypertension and Ambulatory Recording Venetia Study (HARVEST), a multicenter, observational study that began in Italy in 1990 and recruited more than 1,000 patients aged 18-45 years who had stage I hypertension and did not have diabetes.
Further, the risk of a cardiovascular event was increased by 50% in these study participants based on a total of 60 events during a mean of 12.5 years of follow-up.
“Controversy still exists about the long-term cardiovascular and metabolic effects of coffee consumption in hypertension,” Dr. Lucio Mos of Hospital San Daniele del Friuli in Udine, Italy, said during a press conference at the annual congress of the European Society of Cardiology.
Stage 1 hypertension was defined as a diastolic blood pressure of 90-99 mm Hg and a systolic blood pressure of 140-159 mm Hg and diagnosed on the basis of six office-based readings obtained on two separate visits. Enrolled participants underwent ambulatory blood pressure monitoring and three office-based measurements were repeated at 1, 2, 3 and 6 months, and at 6-month intervals thereafter. The endpoint was hypertension requiring any antihypertensive treatment according to international guidelines.
During the study, 24-hour urine samples were collected to assess catecholamine levels. Lifestyle factors such as body weight, physical activity, smoking status, and blood glucose were measured. Patients underwent echocardiography.
They were divided into three groups according to their caffeinated coffee intake: 316 (26%) were designated as abstainers because they did not drink coffee; 767 (64%) drank 1-2 cups a day and were categorized as moderate drinkers; and 119 (10%) drank three or more cups of coffee a day and were defined as heavy drinkers.
“I want to underline that, in this part of Italy, we have a population that drinks mainly espresso coffee and drinking American-style coffee is not usual,” Dr. Mos said.
Around 70% of the study population was male, with similar baseline blood pressures and heart rates among the groups. Heavy coffee drinkers tended to be older (37 years) than those who were more moderate drinkers (34 years) or those who abstained (31 years). They had significantly higher body weights (P less than .001), with a body mass index of 26.1 kg/m2 vs. 25.7 kg/m2 and 24.6 kg/m2, respectively.
Dr. Mos reported that in multivariate analysis, coffee consumption was a significant predictor for developing hypertension that required antihypertensive therapy, with a hazard ratio (HR) of 1.5 (95% confidence interval [CI], 1.1-1.19) for heavy drinkers and 1.1 (95% confidence interval, 1.1-1.19) for moderate drinkers, compared to abstainers. The difference was significant (P = .004) only for heavy coffee consumption.
“Coffee consumption was also a predictor of future prediabetes,” Dr. Mos reported. Indeed, the incidence of prediabetes was highest in the heavy coffee drinkers, and significantly predicted the risk of developing prediabetes compared to abstainers (HR, 2, 95% CI, 1.3-3.1. P = .0017). There was a nonsignificant trend for moderate drinkers also to be at risk for prediabetes when compared to nondrinkers (HR, 1.3, 95% CI 0.9-1.7).
Looking at the risk for prediabetes in relation to caffeine metabolism by analyzing patients by their CYP1A2 genotype, it was found that heavy coffee drinkers who were slow metabolizers of caffeine were at highest risk, with a HR of 2.78 (95% CI, 1.32-5.88). Furthermore, individuals were particularly at risk if they were also overweight or obese.
There was a significant (P = .0017) linear relationship found after multivariate adjustment between coffee intake and cardiovascular events such as heart attacks, with the risk increasing with higher coffee intake. Even moderate coffee intake, defined as one to three cups per day, could up the risk of a cardiovascular event when compared to that of non–coffee drinkers.
“The coffee story was very topical a couple of years ago so it is interesting to see it revisited,” said Dr. Ian Graham of Trinity College Dublin and one of the experts who chaired the press briefing on the study results. “We need a randomized controlled trial,” Dr. Graham suggested, noting that there were several prior studies that suggested there were beneficial effects of coffee.
Cochair Dr. José Gonzalez-Juanatey of Hospital Clínico Universitario de Santiago de Compostela in Spain observed: “The recommendation could be that if you are a young or middle-aged, stage 1 hypertensive patient probably you have to reduce your coffee intake. This is the take-home message based on the results of an observational study well performed and well conducted.”
LONDON – Drinking three or more cups of caffeinated espresso per day predicted increasing blood pressure and rising blood glucose, according to the results of the Hypertension and Ambulatory Recording Venetia Study (HARVEST), a multicenter, observational study that began in Italy in 1990 and recruited more than 1,000 patients aged 18-45 years who had stage I hypertension and did not have diabetes.
Further, the risk of a cardiovascular event was increased by 50% in these study participants based on a total of 60 events during a mean of 12.5 years of follow-up.
“Controversy still exists about the long-term cardiovascular and metabolic effects of coffee consumption in hypertension,” Dr. Lucio Mos of Hospital San Daniele del Friuli in Udine, Italy, said during a press conference at the annual congress of the European Society of Cardiology.
Stage 1 hypertension was defined as a diastolic blood pressure of 90-99 mm Hg and a systolic blood pressure of 140-159 mm Hg and diagnosed on the basis of six office-based readings obtained on two separate visits. Enrolled participants underwent ambulatory blood pressure monitoring and three office-based measurements were repeated at 1, 2, 3 and 6 months, and at 6-month intervals thereafter. The endpoint was hypertension requiring any antihypertensive treatment according to international guidelines.
During the study, 24-hour urine samples were collected to assess catecholamine levels. Lifestyle factors such as body weight, physical activity, smoking status, and blood glucose were measured. Patients underwent echocardiography.
They were divided into three groups according to their caffeinated coffee intake: 316 (26%) were designated as abstainers because they did not drink coffee; 767 (64%) drank 1-2 cups a day and were categorized as moderate drinkers; and 119 (10%) drank three or more cups of coffee a day and were defined as heavy drinkers.
“I want to underline that, in this part of Italy, we have a population that drinks mainly espresso coffee and drinking American-style coffee is not usual,” Dr. Mos said.
Around 70% of the study population was male, with similar baseline blood pressures and heart rates among the groups. Heavy coffee drinkers tended to be older (37 years) than those who were more moderate drinkers (34 years) or those who abstained (31 years). They had significantly higher body weights (P less than .001), with a body mass index of 26.1 kg/m2 vs. 25.7 kg/m2 and 24.6 kg/m2, respectively.
Dr. Mos reported that in multivariate analysis, coffee consumption was a significant predictor for developing hypertension that required antihypertensive therapy, with a hazard ratio (HR) of 1.5 (95% confidence interval [CI], 1.1-1.19) for heavy drinkers and 1.1 (95% confidence interval, 1.1-1.19) for moderate drinkers, compared to abstainers. The difference was significant (P = .004) only for heavy coffee consumption.
“Coffee consumption was also a predictor of future prediabetes,” Dr. Mos reported. Indeed, the incidence of prediabetes was highest in the heavy coffee drinkers, and significantly predicted the risk of developing prediabetes compared to abstainers (HR, 2, 95% CI, 1.3-3.1. P = .0017). There was a nonsignificant trend for moderate drinkers also to be at risk for prediabetes when compared to nondrinkers (HR, 1.3, 95% CI 0.9-1.7).
Looking at the risk for prediabetes in relation to caffeine metabolism by analyzing patients by their CYP1A2 genotype, it was found that heavy coffee drinkers who were slow metabolizers of caffeine were at highest risk, with a HR of 2.78 (95% CI, 1.32-5.88). Furthermore, individuals were particularly at risk if they were also overweight or obese.
There was a significant (P = .0017) linear relationship found after multivariate adjustment between coffee intake and cardiovascular events such as heart attacks, with the risk increasing with higher coffee intake. Even moderate coffee intake, defined as one to three cups per day, could up the risk of a cardiovascular event when compared to that of non–coffee drinkers.
“The coffee story was very topical a couple of years ago so it is interesting to see it revisited,” said Dr. Ian Graham of Trinity College Dublin and one of the experts who chaired the press briefing on the study results. “We need a randomized controlled trial,” Dr. Graham suggested, noting that there were several prior studies that suggested there were beneficial effects of coffee.
Cochair Dr. José Gonzalez-Juanatey of Hospital Clínico Universitario de Santiago de Compostela in Spain observed: “The recommendation could be that if you are a young or middle-aged, stage 1 hypertensive patient probably you have to reduce your coffee intake. This is the take-home message based on the results of an observational study well performed and well conducted.”
AT THE ESC CONGRESS 2015
Key clinical point: There is a potential a risk for hypertension and prediabetes in relation to high caffeine consumption among adults with mild hypertension.
Major finding: Drinking more than three cups of caffeinated espresso per day increased the relative risk of a cardiovascular event by 50%, based on 60 events in 1,212 adults during a mean 12.5 years of follow-up.
Data source: Prospective, observational study of adults (mostly men) aged 18-45 years with stage 1, untreated hypertension.
Disclosures: Dr. Mos reported he had no disclosures.
ESC: LV response to exercise differs in women
LONDON – Left ventricular adaptation to intensive exercise is gender specific, and this novel observation could be useful in identifying female athletes who harbor a serious cardiac condition such as hypertrophic cardiomyopathy, Dr. Sanjay Sharma said at the annual congress of the European Society of Cardiology.
“Although the presence of concentric remodeling or hypertrophy in male athletes engaged in dynamic sports is a common phenotype, it should raise suspicion of underlying cardiomyopathy in female athletes,” declared Dr. Sharma, professor of inherited cardiac diseases in sports cardiology at St. George’s University of London and medical director of the London Marathon.
He drew this conclusion from a study he and his coinvestigators conducted in 1,082 white elite athletes, including 439 females, all of whom had an ECG and underwent echocardiography. The athletes were placed into one of three groups based upon the nature of the exercise entailed in their sport: dynamic exercise, as in endurance events such as distance running or bicycle racing; static exercise, such as weight lifting and wrestling; and sports involving a mix of both.
Normal left ventricular geometry was seen in 70% of male and female athletes. However, important gender-based differences in LV geometry were noted in the athletes participating in dynamic sports. The male athletes were far more likely to exhibit concentric hypertrophy or remodeling, which takes the form of increased LV wall thickness with little or no increase in LV mass, compared with norms. Indeed, 15% of male athletes specializing in dynamic sports had echocardiographic evidence of concentric hypertrophy or remodeling, compared with a mere 4% of female athletes in dynamic sports. In contrast, female athletes were far more likely to exhibit eccentric hypertrophy, featuring a normal LV relative wall thickness with an increased LV cavity size – although not to an extreme degree – when scaled for body surface area.
“In our study, a relative wall thickness greater than 0.5 or an LV mass greater than 145 g/m2 was not detected in any female. These data could be very important in differentiating between physiology and pathology in female athletes presenting potential cardiac symptoms,” according to Dr. Sharma.
He noted that people who exercise intensively for about 4 hours per week or more develop a constellation of structural and functional changes in the heart that allow generation of the large stroke volumes required to deliver sustained high cardiac output. Age and the type of sport play a large role in the magnitude of these changes. And it now appears that gender influences the form these changes will take.
Why do gender differences exist in remodeling in response to exercise? Dr. Sharma speculated that male athletes’ much higher levels of testosterone – an anabolic hormone – might explain their proclivity for LV wall thickening. Also, males are known to have a higher blood pressure response to exercise, which might promote wall thickening.
“An important point I want to make is that death in sport amongst females is extremely rare. The male to female ratio for death in competitive sports is 10:1, and among recreational athletes it’s 20:1,” the cardiologist said.
To help put that in perspective, he noted that among the 1 million runners of the London Marathon during the last 35 years there have been 14 cardiac deaths among male participants and none among females.
LONDON – Left ventricular adaptation to intensive exercise is gender specific, and this novel observation could be useful in identifying female athletes who harbor a serious cardiac condition such as hypertrophic cardiomyopathy, Dr. Sanjay Sharma said at the annual congress of the European Society of Cardiology.
“Although the presence of concentric remodeling or hypertrophy in male athletes engaged in dynamic sports is a common phenotype, it should raise suspicion of underlying cardiomyopathy in female athletes,” declared Dr. Sharma, professor of inherited cardiac diseases in sports cardiology at St. George’s University of London and medical director of the London Marathon.
He drew this conclusion from a study he and his coinvestigators conducted in 1,082 white elite athletes, including 439 females, all of whom had an ECG and underwent echocardiography. The athletes were placed into one of three groups based upon the nature of the exercise entailed in their sport: dynamic exercise, as in endurance events such as distance running or bicycle racing; static exercise, such as weight lifting and wrestling; and sports involving a mix of both.
Normal left ventricular geometry was seen in 70% of male and female athletes. However, important gender-based differences in LV geometry were noted in the athletes participating in dynamic sports. The male athletes were far more likely to exhibit concentric hypertrophy or remodeling, which takes the form of increased LV wall thickness with little or no increase in LV mass, compared with norms. Indeed, 15% of male athletes specializing in dynamic sports had echocardiographic evidence of concentric hypertrophy or remodeling, compared with a mere 4% of female athletes in dynamic sports. In contrast, female athletes were far more likely to exhibit eccentric hypertrophy, featuring a normal LV relative wall thickness with an increased LV cavity size – although not to an extreme degree – when scaled for body surface area.
“In our study, a relative wall thickness greater than 0.5 or an LV mass greater than 145 g/m2 was not detected in any female. These data could be very important in differentiating between physiology and pathology in female athletes presenting potential cardiac symptoms,” according to Dr. Sharma.
He noted that people who exercise intensively for about 4 hours per week or more develop a constellation of structural and functional changes in the heart that allow generation of the large stroke volumes required to deliver sustained high cardiac output. Age and the type of sport play a large role in the magnitude of these changes. And it now appears that gender influences the form these changes will take.
Why do gender differences exist in remodeling in response to exercise? Dr. Sharma speculated that male athletes’ much higher levels of testosterone – an anabolic hormone – might explain their proclivity for LV wall thickening. Also, males are known to have a higher blood pressure response to exercise, which might promote wall thickening.
“An important point I want to make is that death in sport amongst females is extremely rare. The male to female ratio for death in competitive sports is 10:1, and among recreational athletes it’s 20:1,” the cardiologist said.
To help put that in perspective, he noted that among the 1 million runners of the London Marathon during the last 35 years there have been 14 cardiac deaths among male participants and none among females.
LONDON – Left ventricular adaptation to intensive exercise is gender specific, and this novel observation could be useful in identifying female athletes who harbor a serious cardiac condition such as hypertrophic cardiomyopathy, Dr. Sanjay Sharma said at the annual congress of the European Society of Cardiology.
“Although the presence of concentric remodeling or hypertrophy in male athletes engaged in dynamic sports is a common phenotype, it should raise suspicion of underlying cardiomyopathy in female athletes,” declared Dr. Sharma, professor of inherited cardiac diseases in sports cardiology at St. George’s University of London and medical director of the London Marathon.
He drew this conclusion from a study he and his coinvestigators conducted in 1,082 white elite athletes, including 439 females, all of whom had an ECG and underwent echocardiography. The athletes were placed into one of three groups based upon the nature of the exercise entailed in their sport: dynamic exercise, as in endurance events such as distance running or bicycle racing; static exercise, such as weight lifting and wrestling; and sports involving a mix of both.
Normal left ventricular geometry was seen in 70% of male and female athletes. However, important gender-based differences in LV geometry were noted in the athletes participating in dynamic sports. The male athletes were far more likely to exhibit concentric hypertrophy or remodeling, which takes the form of increased LV wall thickness with little or no increase in LV mass, compared with norms. Indeed, 15% of male athletes specializing in dynamic sports had echocardiographic evidence of concentric hypertrophy or remodeling, compared with a mere 4% of female athletes in dynamic sports. In contrast, female athletes were far more likely to exhibit eccentric hypertrophy, featuring a normal LV relative wall thickness with an increased LV cavity size – although not to an extreme degree – when scaled for body surface area.
“In our study, a relative wall thickness greater than 0.5 or an LV mass greater than 145 g/m2 was not detected in any female. These data could be very important in differentiating between physiology and pathology in female athletes presenting potential cardiac symptoms,” according to Dr. Sharma.
He noted that people who exercise intensively for about 4 hours per week or more develop a constellation of structural and functional changes in the heart that allow generation of the large stroke volumes required to deliver sustained high cardiac output. Age and the type of sport play a large role in the magnitude of these changes. And it now appears that gender influences the form these changes will take.
Why do gender differences exist in remodeling in response to exercise? Dr. Sharma speculated that male athletes’ much higher levels of testosterone – an anabolic hormone – might explain their proclivity for LV wall thickening. Also, males are known to have a higher blood pressure response to exercise, which might promote wall thickening.
“An important point I want to make is that death in sport amongst females is extremely rare. The male to female ratio for death in competitive sports is 10:1, and among recreational athletes it’s 20:1,” the cardiologist said.
To help put that in perspective, he noted that among the 1 million runners of the London Marathon during the last 35 years there have been 14 cardiac deaths among male participants and none among females.
AT THE ESC CONGRESS 2015
Key clinical point: Cardiac adaptation to exercise differs by gender, a finding that may help in identifying female athletes with occult cardiomyopathy.
Major finding: The prevalence of left ventricular concentric hypertrophy or remodeling among female elite endurance-sport athletes was just 4%, compared with 15% among their male counterparts.
Data source: This study compared left ventricular geometry in 644 male and 439 female elite athletes.
Disclosures: The presenter reported having no financial conflicts regarding this study.
ESC: A novel ‘win-win’ combo for hypertension
LONDON – The combination of two old diuretics – amiloride and hydrochlorothiazide – at half-doses provides synergistic blood pressure lowering beyond the full doses of either drug alone while neutralizing the thiazide diuretic’s blood glucose– and uric acid–raising side effects, according to the results of the PATHWAY-3 trial.
“We think this combination of amiloride and hydrochlorothiazide at equipotent doses is a ‘win win,’ ” Dr. Morris J. Brown said in presenting the study findings at the annual congress of the European Society of Cardiology.
“Since unlocking the data, we’ve scarcely been able to contain our excitement at the results. I believe these results will return potassium-sparing diuretics to prominence,” said Dr. Brown, professor of clinical pharmacology at the University of Cambridge (England).
The thiazide diuretics as a group have fallen out of favor because of their adverse metabolic effects, including increased risks of diabetes and gout. But the PATHWAY-3 trial demonstrates that, with the half-dose combination approach, amiloride cancels those side effects, while hydrochlorothiazide (HCTZ) neutralizes amiloride’s tendency to boost serum potassium, he explained.
PATHWAY-3 was a 13-center, 24-week randomized trial involving 399 hypertensive patients with at least one additional component of the metabolic syndrome. They were assigned to 12 weeks of amiloride at 10 mg/day, HCTZ at 25 mg/day, or the combination at half-doses, followed by another 12 weeks at twice the dose in all three groups.
The primary outcome was a safety endpoint: the change from baseline in 2-hour oral glucose tolerance tests conducted at 12 and 24 weeks. Blood glucose levels rose in patients on HCTZ and fell significantly in patients on amiloride or the combination. At 24 weeks, the 2-hour blood glucose level was 0.71 mmol/L lower in the amiloride group and 0.58 mmol/L lower in the combination group than in the HCTZ group.
A key secondary endpoint was change in home systolic blood pressure levels. Averaged over 24 weeks, systolic blood pressure was reduced from baseline by 14.7 mm Hg with amiloride monotherapy, by 14.0 mm Hg with HCTZ, and by 17.5 mm Hg with half-dose combination therapy.
Serum potassium levels rose over time with amiloride, fell with HCTZ, and remained unchanged with combination therapy. But full-dose amiloride monotherapy was well tolerated, with no instances of hyperkalemia as defined by a level above 5.8 mmol/L, even though virtually all patients were on background therapy with an ACE inhibitor or angiotensin receptor blocker, Dr. Brown reported.
He noted that the amiloride-HCTZ combination is the only diuretic that has demonstrated superiority in terms of morbidity and mortality in long-term clinical trials versus a calcium channel blocker in the INSIGHT trial (Lancet. 2000 Jul 29;356[9227]:366-72) and versus beta blocker therapy in the MRC-Elderly trial (BMJ. 1992 Feb 15;304:405-12).
PATHWAY-3 is part of an ongoing program developed by the British Heart Foundation to reexamine old, inexpensive drugs that have been pushed aside by newer and far costlier alternatives.
“The continuing famine of new small molecules makes reappraisal and repurposing of old drugs even more important,” Dr. Brown noted.
Discussant Dr. Antonio Coca found the PATHWAY-3 results compelling.
“On the basis of PATHWAY-3, the combination of amiloride and hydrochlorothiazide in equivalent doses becomes the preferred choice for diuretic treatment in patients with insulin resistance, such as obese hypertensives or those with elevated fasting plasma glucose. These findings together with previous morbidity and mortality data from INSIGHT and MRC-Elderly support its first-line use in patients requiring diuretic therapy for hypertension, alone or in combination with other antihypertensive drugs,” said Dr. Coca of the University of Barcelona.
In an interview, Dr. Elliott M. Antmann, immediate past president of the American Heart Association, said he found the PATHWAY-3 study “very impressive.”
“I personally am going to be prescribing more amiloride, which I haven’t prescribed in years,” said Dr. Antmann of Harvard Medical School, Boston.
Dr. Brown reported no financial conflicts regarding the PATHWAY-3 trial, funded by the British Heart Foundation and the National Institute for Health Research.
LONDON – The combination of two old diuretics – amiloride and hydrochlorothiazide – at half-doses provides synergistic blood pressure lowering beyond the full doses of either drug alone while neutralizing the thiazide diuretic’s blood glucose– and uric acid–raising side effects, according to the results of the PATHWAY-3 trial.
“We think this combination of amiloride and hydrochlorothiazide at equipotent doses is a ‘win win,’ ” Dr. Morris J. Brown said in presenting the study findings at the annual congress of the European Society of Cardiology.
“Since unlocking the data, we’ve scarcely been able to contain our excitement at the results. I believe these results will return potassium-sparing diuretics to prominence,” said Dr. Brown, professor of clinical pharmacology at the University of Cambridge (England).
The thiazide diuretics as a group have fallen out of favor because of their adverse metabolic effects, including increased risks of diabetes and gout. But the PATHWAY-3 trial demonstrates that, with the half-dose combination approach, amiloride cancels those side effects, while hydrochlorothiazide (HCTZ) neutralizes amiloride’s tendency to boost serum potassium, he explained.
PATHWAY-3 was a 13-center, 24-week randomized trial involving 399 hypertensive patients with at least one additional component of the metabolic syndrome. They were assigned to 12 weeks of amiloride at 10 mg/day, HCTZ at 25 mg/day, or the combination at half-doses, followed by another 12 weeks at twice the dose in all three groups.
The primary outcome was a safety endpoint: the change from baseline in 2-hour oral glucose tolerance tests conducted at 12 and 24 weeks. Blood glucose levels rose in patients on HCTZ and fell significantly in patients on amiloride or the combination. At 24 weeks, the 2-hour blood glucose level was 0.71 mmol/L lower in the amiloride group and 0.58 mmol/L lower in the combination group than in the HCTZ group.
A key secondary endpoint was change in home systolic blood pressure levels. Averaged over 24 weeks, systolic blood pressure was reduced from baseline by 14.7 mm Hg with amiloride monotherapy, by 14.0 mm Hg with HCTZ, and by 17.5 mm Hg with half-dose combination therapy.
Serum potassium levels rose over time with amiloride, fell with HCTZ, and remained unchanged with combination therapy. But full-dose amiloride monotherapy was well tolerated, with no instances of hyperkalemia as defined by a level above 5.8 mmol/L, even though virtually all patients were on background therapy with an ACE inhibitor or angiotensin receptor blocker, Dr. Brown reported.
He noted that the amiloride-HCTZ combination is the only diuretic that has demonstrated superiority in terms of morbidity and mortality in long-term clinical trials versus a calcium channel blocker in the INSIGHT trial (Lancet. 2000 Jul 29;356[9227]:366-72) and versus beta blocker therapy in the MRC-Elderly trial (BMJ. 1992 Feb 15;304:405-12).
PATHWAY-3 is part of an ongoing program developed by the British Heart Foundation to reexamine old, inexpensive drugs that have been pushed aside by newer and far costlier alternatives.
“The continuing famine of new small molecules makes reappraisal and repurposing of old drugs even more important,” Dr. Brown noted.
Discussant Dr. Antonio Coca found the PATHWAY-3 results compelling.
“On the basis of PATHWAY-3, the combination of amiloride and hydrochlorothiazide in equivalent doses becomes the preferred choice for diuretic treatment in patients with insulin resistance, such as obese hypertensives or those with elevated fasting plasma glucose. These findings together with previous morbidity and mortality data from INSIGHT and MRC-Elderly support its first-line use in patients requiring diuretic therapy for hypertension, alone or in combination with other antihypertensive drugs,” said Dr. Coca of the University of Barcelona.
In an interview, Dr. Elliott M. Antmann, immediate past president of the American Heart Association, said he found the PATHWAY-3 study “very impressive.”
“I personally am going to be prescribing more amiloride, which I haven’t prescribed in years,” said Dr. Antmann of Harvard Medical School, Boston.
Dr. Brown reported no financial conflicts regarding the PATHWAY-3 trial, funded by the British Heart Foundation and the National Institute for Health Research.
LONDON – The combination of two old diuretics – amiloride and hydrochlorothiazide – at half-doses provides synergistic blood pressure lowering beyond the full doses of either drug alone while neutralizing the thiazide diuretic’s blood glucose– and uric acid–raising side effects, according to the results of the PATHWAY-3 trial.
“We think this combination of amiloride and hydrochlorothiazide at equipotent doses is a ‘win win,’ ” Dr. Morris J. Brown said in presenting the study findings at the annual congress of the European Society of Cardiology.
“Since unlocking the data, we’ve scarcely been able to contain our excitement at the results. I believe these results will return potassium-sparing diuretics to prominence,” said Dr. Brown, professor of clinical pharmacology at the University of Cambridge (England).
The thiazide diuretics as a group have fallen out of favor because of their adverse metabolic effects, including increased risks of diabetes and gout. But the PATHWAY-3 trial demonstrates that, with the half-dose combination approach, amiloride cancels those side effects, while hydrochlorothiazide (HCTZ) neutralizes amiloride’s tendency to boost serum potassium, he explained.
PATHWAY-3 was a 13-center, 24-week randomized trial involving 399 hypertensive patients with at least one additional component of the metabolic syndrome. They were assigned to 12 weeks of amiloride at 10 mg/day, HCTZ at 25 mg/day, or the combination at half-doses, followed by another 12 weeks at twice the dose in all three groups.
The primary outcome was a safety endpoint: the change from baseline in 2-hour oral glucose tolerance tests conducted at 12 and 24 weeks. Blood glucose levels rose in patients on HCTZ and fell significantly in patients on amiloride or the combination. At 24 weeks, the 2-hour blood glucose level was 0.71 mmol/L lower in the amiloride group and 0.58 mmol/L lower in the combination group than in the HCTZ group.
A key secondary endpoint was change in home systolic blood pressure levels. Averaged over 24 weeks, systolic blood pressure was reduced from baseline by 14.7 mm Hg with amiloride monotherapy, by 14.0 mm Hg with HCTZ, and by 17.5 mm Hg with half-dose combination therapy.
Serum potassium levels rose over time with amiloride, fell with HCTZ, and remained unchanged with combination therapy. But full-dose amiloride monotherapy was well tolerated, with no instances of hyperkalemia as defined by a level above 5.8 mmol/L, even though virtually all patients were on background therapy with an ACE inhibitor or angiotensin receptor blocker, Dr. Brown reported.
He noted that the amiloride-HCTZ combination is the only diuretic that has demonstrated superiority in terms of morbidity and mortality in long-term clinical trials versus a calcium channel blocker in the INSIGHT trial (Lancet. 2000 Jul 29;356[9227]:366-72) and versus beta blocker therapy in the MRC-Elderly trial (BMJ. 1992 Feb 15;304:405-12).
PATHWAY-3 is part of an ongoing program developed by the British Heart Foundation to reexamine old, inexpensive drugs that have been pushed aside by newer and far costlier alternatives.
“The continuing famine of new small molecules makes reappraisal and repurposing of old drugs even more important,” Dr. Brown noted.
Discussant Dr. Antonio Coca found the PATHWAY-3 results compelling.
“On the basis of PATHWAY-3, the combination of amiloride and hydrochlorothiazide in equivalent doses becomes the preferred choice for diuretic treatment in patients with insulin resistance, such as obese hypertensives or those with elevated fasting plasma glucose. These findings together with previous morbidity and mortality data from INSIGHT and MRC-Elderly support its first-line use in patients requiring diuretic therapy for hypertension, alone or in combination with other antihypertensive drugs,” said Dr. Coca of the University of Barcelona.
In an interview, Dr. Elliott M. Antmann, immediate past president of the American Heart Association, said he found the PATHWAY-3 study “very impressive.”
“I personally am going to be prescribing more amiloride, which I haven’t prescribed in years,” said Dr. Antmann of Harvard Medical School, Boston.
Dr. Brown reported no financial conflicts regarding the PATHWAY-3 trial, funded by the British Heart Foundation and the National Institute for Health Research.
AT THE ESC CONGRESS 2015
Key clinical point: Half-doses of the diuretics amiloride and hydrochlorothiazide given in combination had a synergistic effect on blood pressure lowering and were associated with fewer metabolic side effects than were full doses.
Major finding: The combination of amiloride and hydrochlorothiazide reduced systolic blood pressure by 17.5 mm Hg while leaving blood glucose, uric acid, and serum potassium levels unchanged.
Data source: A multicenter, prospective randomized trial involving 399 patients with hypertension and at least one other component of the metabolic syndrome.
Disclosures: The PATHWAY-3 trial was funded by the British Heart Foundation and the National Institute for Health Research. The presenter reported having no relevant financial conflicts.
ESC: Coronary artery calcium score gets an upgrade
LONDON – Coronary artery calcium as assessed by CT scan, widely considered the best marker of cardiovascular risk, just got significantly better.
The standard measure of coronary artery calcium (CAC) has been the Agatson score, which evaluates plaque calcium volume. But new evidence from the large, multicenter, prospective, observational Multi-Ethnic Study of Atherosclerosis (MESA) demonstrates that plaque calcium density is independently and inversely associated with both CHD and stroke risk. In other words, greater calcium density is protective against cardiovascular disease and counteracts the increased risk associated with greater calcium volume, Dr. Michael H. Criqui said at the annual congress of the European Society of Cardiology.
“We no longer believe in the Agatson score. We took a look at it and found out that at any given level of plaque calcium volume, a higher density score is protective. So when we look at our scans now, we no longer use the Agatson. We take the volume, then measure density separately, and we calculate a score that’s based on both,” explained Dr. Criqui, professor and chief of the division of preventive medicine at the University of California, San Diego.
Session moderator Dr. Sidney C. Smith Jr., was favorably impressed by the new analysis.
“Somehow we need to get this information in front of the guideline committees for the ESC, ACC [American College of Cardiology], and AHA [American Heart Association], because this is very interesting,” said Dr. Smith, professor of medicine at the University of North Carolina, Chapel Hill.
The MESA analysis included 3,398 adults followed for an average of 10.3 years. During that time 264 incident CHD events and 126 hard stroke events occurred.
“You find that as the calcium volume gets higher, the CHD risk gets much higher – up to fourfold higher for the fourth quartile. But we all knew that before. The new concept is that as your density score gets higher your risk goes way down. In the fourth quartile of density, you have only half the risk of developing a coronary event at any given calcium volume,” according to Dr. Criqui.
This confirms an earlier preliminary report by Dr. Criqui and coinvestigators based upon 7.6 years of MESA follow-up (JAMA. 2014 Jan 15;311[3]:271-8). The number of cardiovascular events in the update is 47% greater than in the initial report, considerably strengthening the findings.
The predictive power of the combined CAC volume and density score was underscored by the finding that the area under the receiver operating curve for CHD events was 0.674. To put that in perspective, when the investigators applied the ACC/AHA risk calculator tool to the MESA data, the area under the receiver operating characteristic curve was less impressive at 0.654. Combining the risk prediction score and the CAC volume/density score further increases the predictive power, he noted.
Plaque calcium density was similarly predictive in men and women, in younger and older adults, and in all four ethnic groups participating in MESA: Hispanics, African Americans, non-Hispanic whites, and Asians.
For CHD, the hazard ratio was 1.83 for each standard deviation of CAC volume and 0.71 for each standard deviation of CAC density. For stroke, the impacts were slightly less: a hazard ratio of 1.46 for each standard deviation of CAC volume and 0.83 for each standard deviation of density.
Asked if any biomarkers are related to CAC density, Dr. Criqui replied, “Preliminary data show that most of the risk factors we know are bad for us, like diabetes and smoking, are associated with lower CAC density. And the things that are good for us, like exercise and statins, are associated with higher density.”
He and his coworkers are now looking at plaque calcium density versus volume in the abdominal and thoracic aorta to learn if the same relationships seen in the coronary arteries hold true.
MESA is funded by the National Heart, Lung, and Blood Institute. Dr. Criqui reported having no financial conflicts of interest.
LONDON – Coronary artery calcium as assessed by CT scan, widely considered the best marker of cardiovascular risk, just got significantly better.
The standard measure of coronary artery calcium (CAC) has been the Agatson score, which evaluates plaque calcium volume. But new evidence from the large, multicenter, prospective, observational Multi-Ethnic Study of Atherosclerosis (MESA) demonstrates that plaque calcium density is independently and inversely associated with both CHD and stroke risk. In other words, greater calcium density is protective against cardiovascular disease and counteracts the increased risk associated with greater calcium volume, Dr. Michael H. Criqui said at the annual congress of the European Society of Cardiology.
“We no longer believe in the Agatson score. We took a look at it and found out that at any given level of plaque calcium volume, a higher density score is protective. So when we look at our scans now, we no longer use the Agatson. We take the volume, then measure density separately, and we calculate a score that’s based on both,” explained Dr. Criqui, professor and chief of the division of preventive medicine at the University of California, San Diego.
Session moderator Dr. Sidney C. Smith Jr., was favorably impressed by the new analysis.
“Somehow we need to get this information in front of the guideline committees for the ESC, ACC [American College of Cardiology], and AHA [American Heart Association], because this is very interesting,” said Dr. Smith, professor of medicine at the University of North Carolina, Chapel Hill.
The MESA analysis included 3,398 adults followed for an average of 10.3 years. During that time 264 incident CHD events and 126 hard stroke events occurred.
“You find that as the calcium volume gets higher, the CHD risk gets much higher – up to fourfold higher for the fourth quartile. But we all knew that before. The new concept is that as your density score gets higher your risk goes way down. In the fourth quartile of density, you have only half the risk of developing a coronary event at any given calcium volume,” according to Dr. Criqui.
This confirms an earlier preliminary report by Dr. Criqui and coinvestigators based upon 7.6 years of MESA follow-up (JAMA. 2014 Jan 15;311[3]:271-8). The number of cardiovascular events in the update is 47% greater than in the initial report, considerably strengthening the findings.
The predictive power of the combined CAC volume and density score was underscored by the finding that the area under the receiver operating curve for CHD events was 0.674. To put that in perspective, when the investigators applied the ACC/AHA risk calculator tool to the MESA data, the area under the receiver operating characteristic curve was less impressive at 0.654. Combining the risk prediction score and the CAC volume/density score further increases the predictive power, he noted.
Plaque calcium density was similarly predictive in men and women, in younger and older adults, and in all four ethnic groups participating in MESA: Hispanics, African Americans, non-Hispanic whites, and Asians.
For CHD, the hazard ratio was 1.83 for each standard deviation of CAC volume and 0.71 for each standard deviation of CAC density. For stroke, the impacts were slightly less: a hazard ratio of 1.46 for each standard deviation of CAC volume and 0.83 for each standard deviation of density.
Asked if any biomarkers are related to CAC density, Dr. Criqui replied, “Preliminary data show that most of the risk factors we know are bad for us, like diabetes and smoking, are associated with lower CAC density. And the things that are good for us, like exercise and statins, are associated with higher density.”
He and his coworkers are now looking at plaque calcium density versus volume in the abdominal and thoracic aorta to learn if the same relationships seen in the coronary arteries hold true.
MESA is funded by the National Heart, Lung, and Blood Institute. Dr. Criqui reported having no financial conflicts of interest.
LONDON – Coronary artery calcium as assessed by CT scan, widely considered the best marker of cardiovascular risk, just got significantly better.
The standard measure of coronary artery calcium (CAC) has been the Agatson score, which evaluates plaque calcium volume. But new evidence from the large, multicenter, prospective, observational Multi-Ethnic Study of Atherosclerosis (MESA) demonstrates that plaque calcium density is independently and inversely associated with both CHD and stroke risk. In other words, greater calcium density is protective against cardiovascular disease and counteracts the increased risk associated with greater calcium volume, Dr. Michael H. Criqui said at the annual congress of the European Society of Cardiology.
“We no longer believe in the Agatson score. We took a look at it and found out that at any given level of plaque calcium volume, a higher density score is protective. So when we look at our scans now, we no longer use the Agatson. We take the volume, then measure density separately, and we calculate a score that’s based on both,” explained Dr. Criqui, professor and chief of the division of preventive medicine at the University of California, San Diego.
Session moderator Dr. Sidney C. Smith Jr., was favorably impressed by the new analysis.
“Somehow we need to get this information in front of the guideline committees for the ESC, ACC [American College of Cardiology], and AHA [American Heart Association], because this is very interesting,” said Dr. Smith, professor of medicine at the University of North Carolina, Chapel Hill.
The MESA analysis included 3,398 adults followed for an average of 10.3 years. During that time 264 incident CHD events and 126 hard stroke events occurred.
“You find that as the calcium volume gets higher, the CHD risk gets much higher – up to fourfold higher for the fourth quartile. But we all knew that before. The new concept is that as your density score gets higher your risk goes way down. In the fourth quartile of density, you have only half the risk of developing a coronary event at any given calcium volume,” according to Dr. Criqui.
This confirms an earlier preliminary report by Dr. Criqui and coinvestigators based upon 7.6 years of MESA follow-up (JAMA. 2014 Jan 15;311[3]:271-8). The number of cardiovascular events in the update is 47% greater than in the initial report, considerably strengthening the findings.
The predictive power of the combined CAC volume and density score was underscored by the finding that the area under the receiver operating curve for CHD events was 0.674. To put that in perspective, when the investigators applied the ACC/AHA risk calculator tool to the MESA data, the area under the receiver operating characteristic curve was less impressive at 0.654. Combining the risk prediction score and the CAC volume/density score further increases the predictive power, he noted.
Plaque calcium density was similarly predictive in men and women, in younger and older adults, and in all four ethnic groups participating in MESA: Hispanics, African Americans, non-Hispanic whites, and Asians.
For CHD, the hazard ratio was 1.83 for each standard deviation of CAC volume and 0.71 for each standard deviation of CAC density. For stroke, the impacts were slightly less: a hazard ratio of 1.46 for each standard deviation of CAC volume and 0.83 for each standard deviation of density.
Asked if any biomarkers are related to CAC density, Dr. Criqui replied, “Preliminary data show that most of the risk factors we know are bad for us, like diabetes and smoking, are associated with lower CAC density. And the things that are good for us, like exercise and statins, are associated with higher density.”
He and his coworkers are now looking at plaque calcium density versus volume in the abdominal and thoracic aorta to learn if the same relationships seen in the coronary arteries hold true.
MESA is funded by the National Heart, Lung, and Blood Institute. Dr. Criqui reported having no financial conflicts of interest.
AT THE ESC CONGRESS 2015
Key clinical point: Greater coronary artery plaque calcium density protects against cardiovascular events.
Major finding: The risk of a coronary heart disease event decreases by 29% for each standard deviation increase in coronary artery calcium plaque density and rises by 83% with each standard deviation increase in plaque volume.
Data source: This analysis from the multicenter, prospective, observational Multi-Ethnic Study of Atherosclerosis included 3,398 adults followed for an average of 10.3 years.
Disclosures: The MESA study is funded by the National Heart, Lung, and Blood Institute. The presenter reported having no financial conflicts.
ESC: Cancer itself may cause cardiotoxicity
LONDON – Cancer itself has cardiotoxic effects independent of those caused by chemotherapy, Dr. Stephan von Haehling said at the annual congress of the European Society of Cardiology.
Evidence from both animal and human studies indicates that the malignancy itself may be exerting adverse cardiac effects even before chemotherapy provides an additional hit to the heart, according to Dr. von Haehling, who is a cardiologist at Charity Medical School, Berlin.
“In patients with advanced cancer, significant alterations exist in several markers of cardiovascular perturbation independent of high-dose chemotherapy. So it looks like the cancer is doing something that’s further worsened when chemotherapy starts,” he explained.
Dr. von Haehling and his coinvestigators first demonstrated this phenomenon in a rat model of liver cancer (Eur Heart J. 2014 Apr;35[14]:932-41). The tumor-bearing rats had the classic symptoms of cancer cachexia, including fatigue, impaired exercise capacity, loss of body weight, and dyspnea, as well as progressive wasting of left ventricular mass, even before exposure to chemotherapy. Strikingly, administration of the cardioselective beta-blocker bisoprolol and the aldosterone inhibitor spironolactone reduced left ventricular wasting, curbed cardiac dysfunction, improved a validated measure of rat quality of life, and significantly prolonged rat survival, compared with placebo.
Further exploration of these findings in clinical trials deserves to be a priority in light of the potential quality-of-life benefits for cancer patients, Dr. von Haehling observed.
He and his coworkers followed up the rat study with a prospective study of 50 patients with colorectal cancer, 51 with heart failure, and 51 healthy controls. Of the colorectal cancer patients, 24 underwent echocardiography and other cardiovascular function studies before they went on chemotherapy, while the other 26 did so after starting chemotherapy.
The colorectal cancer patients had a mildly elevated heart rate: an average of 73 beats per minute, compared with 65 bpm in controls and in heart failure patients on beta-blocker therapy. “This is something I see quite often. These patients usually have a mildly elevated heart rate in the range of 80-90 [bpms] or even slightly above,” he said.
Heart rate variability, exercise capacity as measured by treadmill VO2 max testing, and left ventricular ejection fraction were significantly lower in cancer patients than controls, and lower still in the heart failure patients. More interesting were the differences between chemotherapy-naive and on-treatment colorectal cancer patients. Several major determinants of cardiovascular function were impaired in chemotherapy-naive cancer patients, compared with controls, and even more severely impaired in cancer patients on chemotherapy.
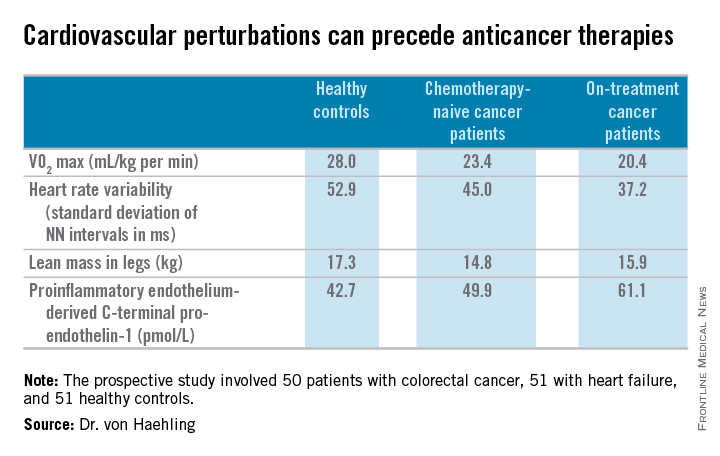
For more about current thinking regarding the prevention, monitoring, and treatment of cardiac side effects of anticancer therapies, Dr. von Haehling recommended the multidisciplinary clinical practice guidelines developed by the European Society for Medical Oncology (Ann Oncol. 2012 Oct;23 Suppl 7:vii155-66).
He reported having no financial conflicts regarding his cardio-oncology studies.
LONDON – Cancer itself has cardiotoxic effects independent of those caused by chemotherapy, Dr. Stephan von Haehling said at the annual congress of the European Society of Cardiology.
Evidence from both animal and human studies indicates that the malignancy itself may be exerting adverse cardiac effects even before chemotherapy provides an additional hit to the heart, according to Dr. von Haehling, who is a cardiologist at Charity Medical School, Berlin.
“In patients with advanced cancer, significant alterations exist in several markers of cardiovascular perturbation independent of high-dose chemotherapy. So it looks like the cancer is doing something that’s further worsened when chemotherapy starts,” he explained.
Dr. von Haehling and his coinvestigators first demonstrated this phenomenon in a rat model of liver cancer (Eur Heart J. 2014 Apr;35[14]:932-41). The tumor-bearing rats had the classic symptoms of cancer cachexia, including fatigue, impaired exercise capacity, loss of body weight, and dyspnea, as well as progressive wasting of left ventricular mass, even before exposure to chemotherapy. Strikingly, administration of the cardioselective beta-blocker bisoprolol and the aldosterone inhibitor spironolactone reduced left ventricular wasting, curbed cardiac dysfunction, improved a validated measure of rat quality of life, and significantly prolonged rat survival, compared with placebo.
Further exploration of these findings in clinical trials deserves to be a priority in light of the potential quality-of-life benefits for cancer patients, Dr. von Haehling observed.
He and his coworkers followed up the rat study with a prospective study of 50 patients with colorectal cancer, 51 with heart failure, and 51 healthy controls. Of the colorectal cancer patients, 24 underwent echocardiography and other cardiovascular function studies before they went on chemotherapy, while the other 26 did so after starting chemotherapy.
The colorectal cancer patients had a mildly elevated heart rate: an average of 73 beats per minute, compared with 65 bpm in controls and in heart failure patients on beta-blocker therapy. “This is something I see quite often. These patients usually have a mildly elevated heart rate in the range of 80-90 [bpms] or even slightly above,” he said.
Heart rate variability, exercise capacity as measured by treadmill VO2 max testing, and left ventricular ejection fraction were significantly lower in cancer patients than controls, and lower still in the heart failure patients. More interesting were the differences between chemotherapy-naive and on-treatment colorectal cancer patients. Several major determinants of cardiovascular function were impaired in chemotherapy-naive cancer patients, compared with controls, and even more severely impaired in cancer patients on chemotherapy.
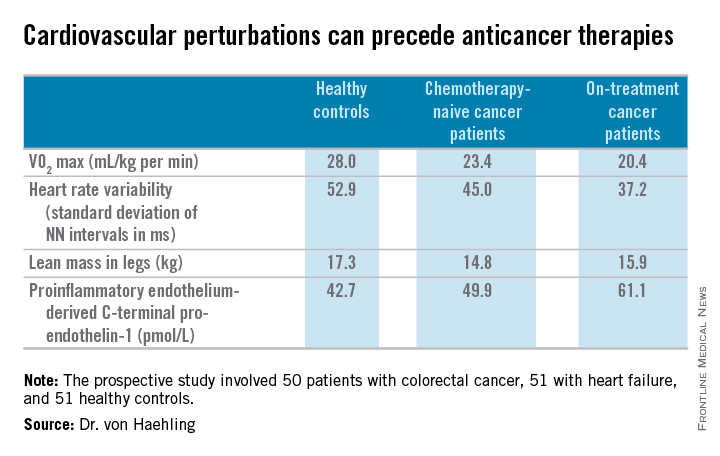
For more about current thinking regarding the prevention, monitoring, and treatment of cardiac side effects of anticancer therapies, Dr. von Haehling recommended the multidisciplinary clinical practice guidelines developed by the European Society for Medical Oncology (Ann Oncol. 2012 Oct;23 Suppl 7:vii155-66).
He reported having no financial conflicts regarding his cardio-oncology studies.
LONDON – Cancer itself has cardiotoxic effects independent of those caused by chemotherapy, Dr. Stephan von Haehling said at the annual congress of the European Society of Cardiology.
Evidence from both animal and human studies indicates that the malignancy itself may be exerting adverse cardiac effects even before chemotherapy provides an additional hit to the heart, according to Dr. von Haehling, who is a cardiologist at Charity Medical School, Berlin.
“In patients with advanced cancer, significant alterations exist in several markers of cardiovascular perturbation independent of high-dose chemotherapy. So it looks like the cancer is doing something that’s further worsened when chemotherapy starts,” he explained.
Dr. von Haehling and his coinvestigators first demonstrated this phenomenon in a rat model of liver cancer (Eur Heart J. 2014 Apr;35[14]:932-41). The tumor-bearing rats had the classic symptoms of cancer cachexia, including fatigue, impaired exercise capacity, loss of body weight, and dyspnea, as well as progressive wasting of left ventricular mass, even before exposure to chemotherapy. Strikingly, administration of the cardioselective beta-blocker bisoprolol and the aldosterone inhibitor spironolactone reduced left ventricular wasting, curbed cardiac dysfunction, improved a validated measure of rat quality of life, and significantly prolonged rat survival, compared with placebo.
Further exploration of these findings in clinical trials deserves to be a priority in light of the potential quality-of-life benefits for cancer patients, Dr. von Haehling observed.
He and his coworkers followed up the rat study with a prospective study of 50 patients with colorectal cancer, 51 with heart failure, and 51 healthy controls. Of the colorectal cancer patients, 24 underwent echocardiography and other cardiovascular function studies before they went on chemotherapy, while the other 26 did so after starting chemotherapy.
The colorectal cancer patients had a mildly elevated heart rate: an average of 73 beats per minute, compared with 65 bpm in controls and in heart failure patients on beta-blocker therapy. “This is something I see quite often. These patients usually have a mildly elevated heart rate in the range of 80-90 [bpms] or even slightly above,” he said.
Heart rate variability, exercise capacity as measured by treadmill VO2 max testing, and left ventricular ejection fraction were significantly lower in cancer patients than controls, and lower still in the heart failure patients. More interesting were the differences between chemotherapy-naive and on-treatment colorectal cancer patients. Several major determinants of cardiovascular function were impaired in chemotherapy-naive cancer patients, compared with controls, and even more severely impaired in cancer patients on chemotherapy.
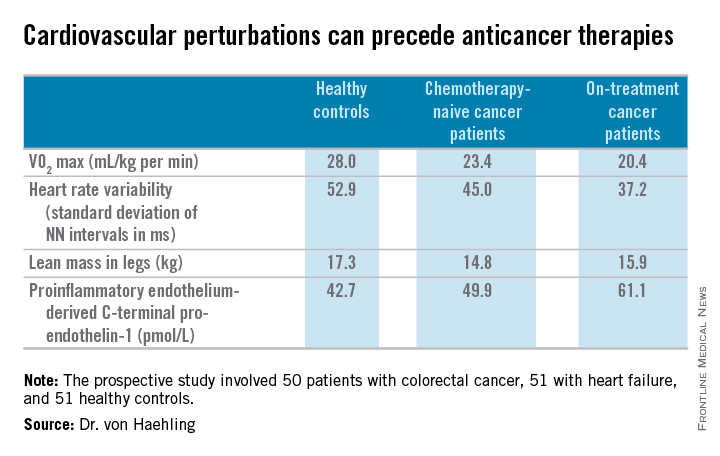
For more about current thinking regarding the prevention, monitoring, and treatment of cardiac side effects of anticancer therapies, Dr. von Haehling recommended the multidisciplinary clinical practice guidelines developed by the European Society for Medical Oncology (Ann Oncol. 2012 Oct;23 Suppl 7:vii155-66).
He reported having no financial conflicts regarding his cardio-oncology studies.
EXPERT ANALYSIS FROM THE ESC CONGRESS 2015
ESC: Heart failure patients have increased cancer incidence
LONDON – Adult patients with chronic heart failure had an average 51% increased incidence of all forms of cancer, compared with the general population in an analysis of more than 9,000 Danish patients treated for heart failure during 2002-2009.
Although the study did not address causality, the elevated risk for new-onset cancers in heart failure patients may stem from shared risk factors for the two diseases, Dr. Ann Banke said at the annual congress of the European Society of Cardiology. Smoking, for example, is a potential etiologic factor for both heart failure and certain cancers. Other potential shared risk factors could include other types of unhealthy lifestyle choices, and a heightened inflammatory state, suggested Dr. Banke, a researcher in the department of cardiology at Odense (Denmark) University Hospital.
“Increased awareness of the risk for development of cancer in heart failure patients is warranted,” especially given the relatively long life expectancy now seen among many patients with chronic heart failure, Dr. Banke said.
She and her associates reviewed 9,307 Danish patients with chronic heart failure and no history of cancer who entered a national heart failure cohort during 2002-2009. Their average age was 68 years, 73% were men, 89% had heart failure with reduced ejection fraction, 80% had New York Heart Association class I or II heart failure, and 15% had diabetes. During follow-up through 2013, a total of 975 of these patients received a diagnosis of cancer. The researchers compared the incidence rate of cancer among these heart failure patients with the rate in the general Danish adult population in the same 2002-2013 period, during which the general population developed 330,843 cancers.
In an analysis that adjusted for age and sex, the heart failure patients had a statistically significant 51% increased rate of incidence cancers of all types (P less than .0001). When broken down by cancer site, the heart failure patients showed significantly increased rates for all types of cancers except prostate cancer (see chart). Dr. Banke speculated that the absence of an increased incidence rate in prostate cancer among heart failure patients may reflect the age of the heart failure patients, or perhaps because prostate cancer does not share as many risk factors with heart failure as do the other cancer types.
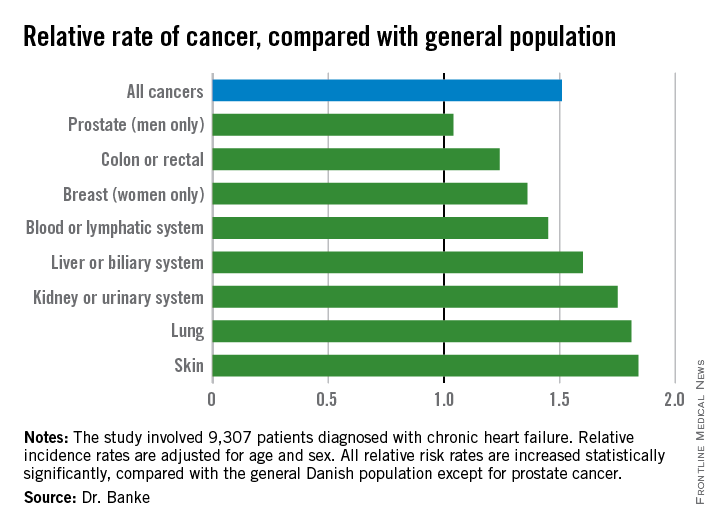
On Twitter @mitchelzoler
LONDON – Adult patients with chronic heart failure had an average 51% increased incidence of all forms of cancer, compared with the general population in an analysis of more than 9,000 Danish patients treated for heart failure during 2002-2009.
Although the study did not address causality, the elevated risk for new-onset cancers in heart failure patients may stem from shared risk factors for the two diseases, Dr. Ann Banke said at the annual congress of the European Society of Cardiology. Smoking, for example, is a potential etiologic factor for both heart failure and certain cancers. Other potential shared risk factors could include other types of unhealthy lifestyle choices, and a heightened inflammatory state, suggested Dr. Banke, a researcher in the department of cardiology at Odense (Denmark) University Hospital.
“Increased awareness of the risk for development of cancer in heart failure patients is warranted,” especially given the relatively long life expectancy now seen among many patients with chronic heart failure, Dr. Banke said.
She and her associates reviewed 9,307 Danish patients with chronic heart failure and no history of cancer who entered a national heart failure cohort during 2002-2009. Their average age was 68 years, 73% were men, 89% had heart failure with reduced ejection fraction, 80% had New York Heart Association class I or II heart failure, and 15% had diabetes. During follow-up through 2013, a total of 975 of these patients received a diagnosis of cancer. The researchers compared the incidence rate of cancer among these heart failure patients with the rate in the general Danish adult population in the same 2002-2013 period, during which the general population developed 330,843 cancers.
In an analysis that adjusted for age and sex, the heart failure patients had a statistically significant 51% increased rate of incidence cancers of all types (P less than .0001). When broken down by cancer site, the heart failure patients showed significantly increased rates for all types of cancers except prostate cancer (see chart). Dr. Banke speculated that the absence of an increased incidence rate in prostate cancer among heart failure patients may reflect the age of the heart failure patients, or perhaps because prostate cancer does not share as many risk factors with heart failure as do the other cancer types.
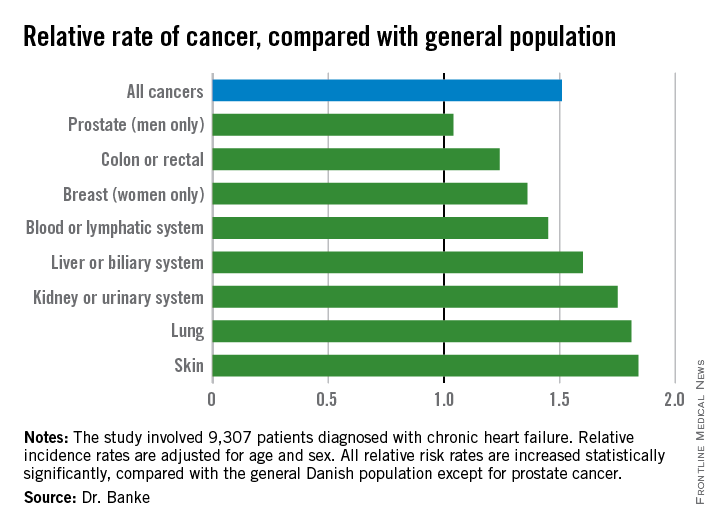
On Twitter @mitchelzoler
LONDON – Adult patients with chronic heart failure had an average 51% increased incidence of all forms of cancer, compared with the general population in an analysis of more than 9,000 Danish patients treated for heart failure during 2002-2009.
Although the study did not address causality, the elevated risk for new-onset cancers in heart failure patients may stem from shared risk factors for the two diseases, Dr. Ann Banke said at the annual congress of the European Society of Cardiology. Smoking, for example, is a potential etiologic factor for both heart failure and certain cancers. Other potential shared risk factors could include other types of unhealthy lifestyle choices, and a heightened inflammatory state, suggested Dr. Banke, a researcher in the department of cardiology at Odense (Denmark) University Hospital.
“Increased awareness of the risk for development of cancer in heart failure patients is warranted,” especially given the relatively long life expectancy now seen among many patients with chronic heart failure, Dr. Banke said.
She and her associates reviewed 9,307 Danish patients with chronic heart failure and no history of cancer who entered a national heart failure cohort during 2002-2009. Their average age was 68 years, 73% were men, 89% had heart failure with reduced ejection fraction, 80% had New York Heart Association class I or II heart failure, and 15% had diabetes. During follow-up through 2013, a total of 975 of these patients received a diagnosis of cancer. The researchers compared the incidence rate of cancer among these heart failure patients with the rate in the general Danish adult population in the same 2002-2013 period, during which the general population developed 330,843 cancers.
In an analysis that adjusted for age and sex, the heart failure patients had a statistically significant 51% increased rate of incidence cancers of all types (P less than .0001). When broken down by cancer site, the heart failure patients showed significantly increased rates for all types of cancers except prostate cancer (see chart). Dr. Banke speculated that the absence of an increased incidence rate in prostate cancer among heart failure patients may reflect the age of the heart failure patients, or perhaps because prostate cancer does not share as many risk factors with heart failure as do the other cancer types.
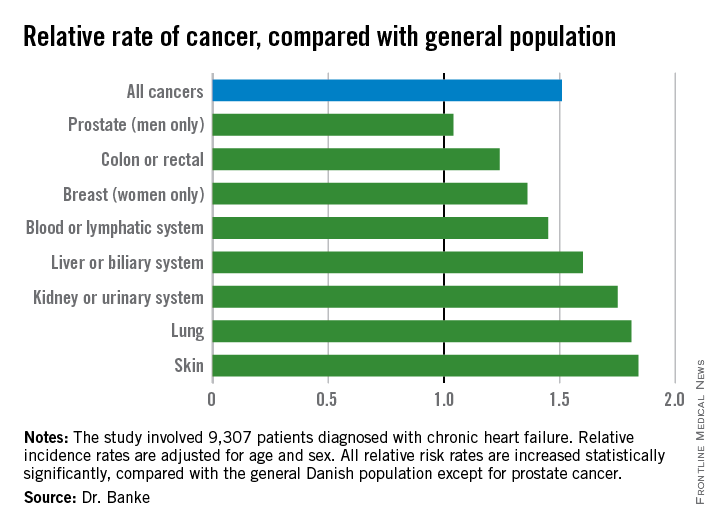
On Twitter @mitchelzoler
AT THE ESC CONGRESS 2015
Key clinical point: Adults with chronic heart failure had a significantly increased incidence of cancer, compared with the general population.
Major finding: Patients with chronic heart failure had an average 51% higher incidence of cancer, compared with the general population.
Data source: A nationwide Danish cohort with 9,307 patients diagnosed with chronic heart failure.
Disclosures: Dr. Banke had no disclosures.