User login
American Headache Society (AHS): Scottsdale Headache Symposium
Periodic childhood syndromes may precede or shift to migraine
SCOTTSDALE, ARIZ. – At least five episodic syndromes in children can precede pediatric and adult migraine, including infant colic, benign paroxysmal torticollis, benign paroxysmal vertigo, abdominal migraine, and cyclical vomiting syndrome, said Dr. Amy Gelfand.
Some patients progress from one syndrome to the next as they age, and then ultimately develop classical migraine, said Dr. Gelfand, a child neurologist specializing in headache and related syndromes at the University of California, San Francisco (UCSF). “I don’t know if it makes sense to think of these as migraine precursors or as age-sensitive phenotypes of migraine itself,” she said at a symposium sponsored by the American Headache Society.
Children with pediatric migraine, according to the International Classification of Headache Disorders, 3rd edition, have had at least five headache attacks lasting 2-72 hours that were untreated or unsuccessfully treated and caused nausea and vomiting or photophobia and phonophobia. The headaches also need to be characterized by at least two of the following: a pulsating quality, moderate or severe intensity, and worsening during physical activity or causing avoidance of physical activity, she noted.
Each of the following syndromes has been linked with migraine, according to Dr. Gelfand.
Infant colic
Colic affects 5%-19% of infants and is defined as frequent and excessive crying in an otherwise healthy and well-nourished baby, Dr. Gelfand said. Clinicians often assume that colic has a gastrointestinal etiology, even though probiotics typically do not help, she said. Understanding the true cause of colic is crucial because by age 6 months, at least 5.6% of affected babies have been shaken, slapped, or smothered in an attempt to stop their crying, she noted.
In a recently published meta-analysis by Dr. Gelfand and her associates at UCSF, the odds ratio for the link between migraine and infant colic was 3.2 (95% confidence interval, 1.7-7.6), even though the authors removed the study with the largest effect size. “I think that this association between the two [syndromes] is quite robust,” she commented. “I think it’s justified that infant colic is included in the episodic syndromes that might be associated with migraine. What we really need going forward are prospective cohort studies in which we enroll babies with and without colic. We would have to follow them for about a decade, but I think it’s worth doing.”
Benign paroxysmal torticollis
This syndrome typically begins at about 4-6 months of age and resolves by age 3-4 years. Affected patients have recurrent attacks of head tilt to either side, sometimes with a slight rotation, that remit spontaneously after minutes to days and are not caused by another disorder, Dr. Gelfand said.
For a diagnosis, attacks also must have at least one of the following characteristics: pallor, irritability, malaise, vomiting, or ataxia. Treatments for the syndrome “have not been well studied,” she added.
Benign paroxysmal vertigo
The syndrome is diagnosed after at least five attacks of unexpected vertigo that is worst when it begins, spontaneously resolves minutes to hours later, and is not caused by another disorder. Attacks do not cause loss of consciousness and include at least one of the following: nystagmus, ataxia, vomiting, pallor, and fearfulness, Dr. Gelfand said.
In one study, age of onset averaged 3.9 years and ranged from 1.5 to 8 years, while age at resolution averaged 5 years and ranged from 2.5 to 9.5 years. Fully 70% of patients had a family history of migraine, and 33% went on to develop migraine as adults, she said.
Like benign paroxysmal torticollis, children have a normal neurologic examination as well as normal audiometric and vestibular function between attacks.
Abdominal migraine
Children with abdominal migraine have had at least five attacks of abdominal pain with at least two of the following being true: The pain is located at the abdominal midline, is periumbilical, or is poorly localized; the child has dull, “sore” pain; the pain is moderate or severe in intensity, said Dr. Gelfand. Attacks also must include at least two of the following: nausea, vomiting, and pallor. Attacks last 2-72 hours when untreated or unsuccessfully treated, and children are symptom free between attacks, Dr. Gelfand said.
Off-label use of pizotifen, propranolol, cyproheptadine, and flunarizine can be helpful in these children, said Dr. Gelfand. Case reports also support the off-label use of sumatriptan and intravenous dihydroergotamine during attacks, she added. But evidence also suggests that medication overuse can worsen abdominal migraine, she said.
Cyclical vomiting syndrome
A diagnosis of cyclical vomiting syndrome requires at least five attacks of predictable, severe, periodic nausea and vomiting occurring at least four times an hour, lasting at least an hour and up to 10 days, and spaced at least a week apart. Children are completely asymptomatic between attacks, and as with the other syndromes, symptoms are not attributable to another disorder, Dr. Gelfand said.
Mean age of onset of cyclical vomiting syndrome is about 5 years, and attacks typically last about 3.5 days. Children may have comorbid headaches or migraine, she added.
There have been no randomized, controlled trials of treatments, but limited data support the off-label use of amitriptyline, propranolol, coenzyme Q10, L-carnitine, cyproheptadine, flunarizine, and valproate as preventives, and the off-label use of sumatriptan (especially subcutaneously) and ondansetron as acute treatments. Some data also support the off-label use of the neurokinin-1 receptor antagonist aprepitant as an acute and preventive treatment, she said.
Dr. Gelfand reported no relevant financial conflicts.
SCOTTSDALE, ARIZ. – At least five episodic syndromes in children can precede pediatric and adult migraine, including infant colic, benign paroxysmal torticollis, benign paroxysmal vertigo, abdominal migraine, and cyclical vomiting syndrome, said Dr. Amy Gelfand.
Some patients progress from one syndrome to the next as they age, and then ultimately develop classical migraine, said Dr. Gelfand, a child neurologist specializing in headache and related syndromes at the University of California, San Francisco (UCSF). “I don’t know if it makes sense to think of these as migraine precursors or as age-sensitive phenotypes of migraine itself,” she said at a symposium sponsored by the American Headache Society.
Children with pediatric migraine, according to the International Classification of Headache Disorders, 3rd edition, have had at least five headache attacks lasting 2-72 hours that were untreated or unsuccessfully treated and caused nausea and vomiting or photophobia and phonophobia. The headaches also need to be characterized by at least two of the following: a pulsating quality, moderate or severe intensity, and worsening during physical activity or causing avoidance of physical activity, she noted.
Each of the following syndromes has been linked with migraine, according to Dr. Gelfand.
Infant colic
Colic affects 5%-19% of infants and is defined as frequent and excessive crying in an otherwise healthy and well-nourished baby, Dr. Gelfand said. Clinicians often assume that colic has a gastrointestinal etiology, even though probiotics typically do not help, she said. Understanding the true cause of colic is crucial because by age 6 months, at least 5.6% of affected babies have been shaken, slapped, or smothered in an attempt to stop their crying, she noted.
In a recently published meta-analysis by Dr. Gelfand and her associates at UCSF, the odds ratio for the link between migraine and infant colic was 3.2 (95% confidence interval, 1.7-7.6), even though the authors removed the study with the largest effect size. “I think that this association between the two [syndromes] is quite robust,” she commented. “I think it’s justified that infant colic is included in the episodic syndromes that might be associated with migraine. What we really need going forward are prospective cohort studies in which we enroll babies with and without colic. We would have to follow them for about a decade, but I think it’s worth doing.”
Benign paroxysmal torticollis
This syndrome typically begins at about 4-6 months of age and resolves by age 3-4 years. Affected patients have recurrent attacks of head tilt to either side, sometimes with a slight rotation, that remit spontaneously after minutes to days and are not caused by another disorder, Dr. Gelfand said.
For a diagnosis, attacks also must have at least one of the following characteristics: pallor, irritability, malaise, vomiting, or ataxia. Treatments for the syndrome “have not been well studied,” she added.
Benign paroxysmal vertigo
The syndrome is diagnosed after at least five attacks of unexpected vertigo that is worst when it begins, spontaneously resolves minutes to hours later, and is not caused by another disorder. Attacks do not cause loss of consciousness and include at least one of the following: nystagmus, ataxia, vomiting, pallor, and fearfulness, Dr. Gelfand said.
In one study, age of onset averaged 3.9 years and ranged from 1.5 to 8 years, while age at resolution averaged 5 years and ranged from 2.5 to 9.5 years. Fully 70% of patients had a family history of migraine, and 33% went on to develop migraine as adults, she said.
Like benign paroxysmal torticollis, children have a normal neurologic examination as well as normal audiometric and vestibular function between attacks.
Abdominal migraine
Children with abdominal migraine have had at least five attacks of abdominal pain with at least two of the following being true: The pain is located at the abdominal midline, is periumbilical, or is poorly localized; the child has dull, “sore” pain; the pain is moderate or severe in intensity, said Dr. Gelfand. Attacks also must include at least two of the following: nausea, vomiting, and pallor. Attacks last 2-72 hours when untreated or unsuccessfully treated, and children are symptom free between attacks, Dr. Gelfand said.
Off-label use of pizotifen, propranolol, cyproheptadine, and flunarizine can be helpful in these children, said Dr. Gelfand. Case reports also support the off-label use of sumatriptan and intravenous dihydroergotamine during attacks, she added. But evidence also suggests that medication overuse can worsen abdominal migraine, she said.
Cyclical vomiting syndrome
A diagnosis of cyclical vomiting syndrome requires at least five attacks of predictable, severe, periodic nausea and vomiting occurring at least four times an hour, lasting at least an hour and up to 10 days, and spaced at least a week apart. Children are completely asymptomatic between attacks, and as with the other syndromes, symptoms are not attributable to another disorder, Dr. Gelfand said.
Mean age of onset of cyclical vomiting syndrome is about 5 years, and attacks typically last about 3.5 days. Children may have comorbid headaches or migraine, she added.
There have been no randomized, controlled trials of treatments, but limited data support the off-label use of amitriptyline, propranolol, coenzyme Q10, L-carnitine, cyproheptadine, flunarizine, and valproate as preventives, and the off-label use of sumatriptan (especially subcutaneously) and ondansetron as acute treatments. Some data also support the off-label use of the neurokinin-1 receptor antagonist aprepitant as an acute and preventive treatment, she said.
Dr. Gelfand reported no relevant financial conflicts.
SCOTTSDALE, ARIZ. – At least five episodic syndromes in children can precede pediatric and adult migraine, including infant colic, benign paroxysmal torticollis, benign paroxysmal vertigo, abdominal migraine, and cyclical vomiting syndrome, said Dr. Amy Gelfand.
Some patients progress from one syndrome to the next as they age, and then ultimately develop classical migraine, said Dr. Gelfand, a child neurologist specializing in headache and related syndromes at the University of California, San Francisco (UCSF). “I don’t know if it makes sense to think of these as migraine precursors or as age-sensitive phenotypes of migraine itself,” she said at a symposium sponsored by the American Headache Society.
Children with pediatric migraine, according to the International Classification of Headache Disorders, 3rd edition, have had at least five headache attacks lasting 2-72 hours that were untreated or unsuccessfully treated and caused nausea and vomiting or photophobia and phonophobia. The headaches also need to be characterized by at least two of the following: a pulsating quality, moderate or severe intensity, and worsening during physical activity or causing avoidance of physical activity, she noted.
Each of the following syndromes has been linked with migraine, according to Dr. Gelfand.
Infant colic
Colic affects 5%-19% of infants and is defined as frequent and excessive crying in an otherwise healthy and well-nourished baby, Dr. Gelfand said. Clinicians often assume that colic has a gastrointestinal etiology, even though probiotics typically do not help, she said. Understanding the true cause of colic is crucial because by age 6 months, at least 5.6% of affected babies have been shaken, slapped, or smothered in an attempt to stop their crying, she noted.
In a recently published meta-analysis by Dr. Gelfand and her associates at UCSF, the odds ratio for the link between migraine and infant colic was 3.2 (95% confidence interval, 1.7-7.6), even though the authors removed the study with the largest effect size. “I think that this association between the two [syndromes] is quite robust,” she commented. “I think it’s justified that infant colic is included in the episodic syndromes that might be associated with migraine. What we really need going forward are prospective cohort studies in which we enroll babies with and without colic. We would have to follow them for about a decade, but I think it’s worth doing.”
Benign paroxysmal torticollis
This syndrome typically begins at about 4-6 months of age and resolves by age 3-4 years. Affected patients have recurrent attacks of head tilt to either side, sometimes with a slight rotation, that remit spontaneously after minutes to days and are not caused by another disorder, Dr. Gelfand said.
For a diagnosis, attacks also must have at least one of the following characteristics: pallor, irritability, malaise, vomiting, or ataxia. Treatments for the syndrome “have not been well studied,” she added.
Benign paroxysmal vertigo
The syndrome is diagnosed after at least five attacks of unexpected vertigo that is worst when it begins, spontaneously resolves minutes to hours later, and is not caused by another disorder. Attacks do not cause loss of consciousness and include at least one of the following: nystagmus, ataxia, vomiting, pallor, and fearfulness, Dr. Gelfand said.
In one study, age of onset averaged 3.9 years and ranged from 1.5 to 8 years, while age at resolution averaged 5 years and ranged from 2.5 to 9.5 years. Fully 70% of patients had a family history of migraine, and 33% went on to develop migraine as adults, she said.
Like benign paroxysmal torticollis, children have a normal neurologic examination as well as normal audiometric and vestibular function between attacks.
Abdominal migraine
Children with abdominal migraine have had at least five attacks of abdominal pain with at least two of the following being true: The pain is located at the abdominal midline, is periumbilical, or is poorly localized; the child has dull, “sore” pain; the pain is moderate or severe in intensity, said Dr. Gelfand. Attacks also must include at least two of the following: nausea, vomiting, and pallor. Attacks last 2-72 hours when untreated or unsuccessfully treated, and children are symptom free between attacks, Dr. Gelfand said.
Off-label use of pizotifen, propranolol, cyproheptadine, and flunarizine can be helpful in these children, said Dr. Gelfand. Case reports also support the off-label use of sumatriptan and intravenous dihydroergotamine during attacks, she added. But evidence also suggests that medication overuse can worsen abdominal migraine, she said.
Cyclical vomiting syndrome
A diagnosis of cyclical vomiting syndrome requires at least five attacks of predictable, severe, periodic nausea and vomiting occurring at least four times an hour, lasting at least an hour and up to 10 days, and spaced at least a week apart. Children are completely asymptomatic between attacks, and as with the other syndromes, symptoms are not attributable to another disorder, Dr. Gelfand said.
Mean age of onset of cyclical vomiting syndrome is about 5 years, and attacks typically last about 3.5 days. Children may have comorbid headaches or migraine, she added.
There have been no randomized, controlled trials of treatments, but limited data support the off-label use of amitriptyline, propranolol, coenzyme Q10, L-carnitine, cyproheptadine, flunarizine, and valproate as preventives, and the off-label use of sumatriptan (especially subcutaneously) and ondansetron as acute treatments. Some data also support the off-label use of the neurokinin-1 receptor antagonist aprepitant as an acute and preventive treatment, she said.
Dr. Gelfand reported no relevant financial conflicts.
EXPERT ANALYSIS AT THE SCOTTSDALE HEADACHE SYMPOSIUM
Experts debate venous sinus stenting for intracranial hypertension
SCOTTSDALE, ARIZ. – Venous sinus stenting remains a controversial treatment for headache associated with benign intracranial hypertension. Opponents highlight potentially serious adverse effects and a lack of rigorous studies on the procedure, while supporters describe it as safe and effective. Experts recently debated the procedure at a symposium sponsored by the American Headache Society.
Which came first?
Stenting is based on the rationale that lowering venous sinus pressure might lower intracranial pressure, said Dr. Deborah Friedman, a neuro-ophthalmologist at the University of Texas Southwestern Medical Center in Dallas.
“Other surgical techniques create a fistula the body wants to close,” she said. “Stenting may provide a permanent solution.”
The crux of the debate on stenting is whether venous sinus stenosis is a cause or outcome of benign intracranial hypertension (BIH), said Dr. Felipe Albuquerque, an endovascular neurosurgeon at the Barrow Neurological Institute in Phoenix. The fact that 90% of affected patients have venous sinus stenosis on MRI suggests stenosis is a valid etiology the condition, he said.
But Dr. Friedman disagreed. In a retrospective study of 51 patients with BIH and transverse sinus stenosis, 71% had more than 50% stenosis, but the degree and location of stenosis did not predict clinical outcome. The analysis also found no link between cerebrospinal fluid pressure and the location, degree, or residual area of stenosis. Nonetheless, the procedure may be useful in patients who have persistent transverse sinus stenosis after undergoing a shunt procedure, she said.
The cons of stenting
“Stenting carries a high risk of morbidity and mortality, compared with currently used treatments, and should only be used as a last resort in patients who are losing vision,” Dr. Friedman asserted. Most patients do well, but others suffer serious complications, including life-threatening anaphylaxis, subdural hematomas, subarachnoid hemorrhage, and brain herniation, she said.
In contrast, optic nerve sheath fenestration for BIH has no associated fatalities, according to Dr. Friedman. And in a National Inpatient Sample database analysis of 1,224 shunts, mortality was only 0.9% for ventriculoperitoneal shunt and 0.3% for lumbar-peritoneal shunt. No deaths were recorded for shunts performed for BIH or pseudotumor cerebri, she added.
The literature on venous sinus stenting “is a mess,” Dr. Friedman continued. “All data are from retrospective case series, and the diagnosis of idiopathic intracranial hypertension is questionable in some cases,” she said. “The indication for stenting is not well defined.”
Studies on the safety and efficacy of stenting have lacked a common primary outcome variable and may reflect reporting bias, Dr. Friedman said. Studies have been heterogeneous with regard to disease duration and the presence or absence of papilledema, visual status, previous treatments, and definitions of treatment failure, she added. No randomized, controlled trials have been carried out with sham stenting to assess the possibility of placebo effect, she noted.
“I think stenting may have utility in patients who have failed conventional therapy and have had another procedure that did not work. I think it very likely that there is a strong placebo effect in this group,” Dr. Friedman said.
“It’s not like our existing procedures are wonderful,” she added. “I wish we had something better to offer our patients.”
The pros
Venous sinus stenting “is usually effective in ameliorating both subjective headache and objective papilledema symptoms,” Dr. Albuquerque said. “One could argue that both ventriculoperitoneal shunt and lumbar-peritoneal shunt, the most commonly performed surgical interventions for benign intracranial hypertension, are substantially more invasive than stenting is and associated with far more severe complications.”
Dr. Albuquerque described a prospective study he conducted with his associates on 15 patients with BIH who underwent venous sinus stenting. In all, 80% of patients said their headaches improved, and 60% reported at least a 50% decrease in headache pain. Rates of patency and technical success were 100%, and no patients had permanent complications from the procedure, although one patient developed acute retroperitoneal hematoma, he said.
Dr. Albuquerque also reported his long-term follow-up of 27 patients who underwent venous sinus stenting to treat pseudotumors. All patients had more than 50% stenosis confirmed by retrograde venogram and a transstenotic pressure gradient that was greater than 12 mm Hg. Fully 70% of patients improved symptomatically, but five underwent a shunt procedure after they failed to improve. Patients experienced no permanent complications, although one required a stent for femoral artery pseudoaneurysm. Angiographies performed an average of 23 months later showed that all stents remained patent, although four patients had mild (less than 25%) stenosis. Five patients had narrowing of the sinus proximal to the stent.
Patients need dual antiplatelet therapy after venous sinus stenting, and the rate of chronic patency after the procedure is unknown, Dr. Albuquerque noted. Patients can develop scalp pain over the stented segment, he added.
“I think if you limit this procedure to a very select group of patients, I think its efficacy is tremendous,” Dr. Albuquerque concluded.
Dr. Albuquerque declared no conflicts of interest. Dr. Friedman reported serving on the speakers bureau of Allergan, receiving research grants from the National Eye Institute, Merck & Co., and ElectroCore, and having served as an expert witness (for the plaintiff and defense) on idiopathic intracranial hypertension.
SCOTTSDALE, ARIZ. – Venous sinus stenting remains a controversial treatment for headache associated with benign intracranial hypertension. Opponents highlight potentially serious adverse effects and a lack of rigorous studies on the procedure, while supporters describe it as safe and effective. Experts recently debated the procedure at a symposium sponsored by the American Headache Society.
Which came first?
Stenting is based on the rationale that lowering venous sinus pressure might lower intracranial pressure, said Dr. Deborah Friedman, a neuro-ophthalmologist at the University of Texas Southwestern Medical Center in Dallas.
“Other surgical techniques create a fistula the body wants to close,” she said. “Stenting may provide a permanent solution.”
The crux of the debate on stenting is whether venous sinus stenosis is a cause or outcome of benign intracranial hypertension (BIH), said Dr. Felipe Albuquerque, an endovascular neurosurgeon at the Barrow Neurological Institute in Phoenix. The fact that 90% of affected patients have venous sinus stenosis on MRI suggests stenosis is a valid etiology the condition, he said.
But Dr. Friedman disagreed. In a retrospective study of 51 patients with BIH and transverse sinus stenosis, 71% had more than 50% stenosis, but the degree and location of stenosis did not predict clinical outcome. The analysis also found no link between cerebrospinal fluid pressure and the location, degree, or residual area of stenosis. Nonetheless, the procedure may be useful in patients who have persistent transverse sinus stenosis after undergoing a shunt procedure, she said.
The cons of stenting
“Stenting carries a high risk of morbidity and mortality, compared with currently used treatments, and should only be used as a last resort in patients who are losing vision,” Dr. Friedman asserted. Most patients do well, but others suffer serious complications, including life-threatening anaphylaxis, subdural hematomas, subarachnoid hemorrhage, and brain herniation, she said.
In contrast, optic nerve sheath fenestration for BIH has no associated fatalities, according to Dr. Friedman. And in a National Inpatient Sample database analysis of 1,224 shunts, mortality was only 0.9% for ventriculoperitoneal shunt and 0.3% for lumbar-peritoneal shunt. No deaths were recorded for shunts performed for BIH or pseudotumor cerebri, she added.
The literature on venous sinus stenting “is a mess,” Dr. Friedman continued. “All data are from retrospective case series, and the diagnosis of idiopathic intracranial hypertension is questionable in some cases,” she said. “The indication for stenting is not well defined.”
Studies on the safety and efficacy of stenting have lacked a common primary outcome variable and may reflect reporting bias, Dr. Friedman said. Studies have been heterogeneous with regard to disease duration and the presence or absence of papilledema, visual status, previous treatments, and definitions of treatment failure, she added. No randomized, controlled trials have been carried out with sham stenting to assess the possibility of placebo effect, she noted.
“I think stenting may have utility in patients who have failed conventional therapy and have had another procedure that did not work. I think it very likely that there is a strong placebo effect in this group,” Dr. Friedman said.
“It’s not like our existing procedures are wonderful,” she added. “I wish we had something better to offer our patients.”
The pros
Venous sinus stenting “is usually effective in ameliorating both subjective headache and objective papilledema symptoms,” Dr. Albuquerque said. “One could argue that both ventriculoperitoneal shunt and lumbar-peritoneal shunt, the most commonly performed surgical interventions for benign intracranial hypertension, are substantially more invasive than stenting is and associated with far more severe complications.”
Dr. Albuquerque described a prospective study he conducted with his associates on 15 patients with BIH who underwent venous sinus stenting. In all, 80% of patients said their headaches improved, and 60% reported at least a 50% decrease in headache pain. Rates of patency and technical success were 100%, and no patients had permanent complications from the procedure, although one patient developed acute retroperitoneal hematoma, he said.
Dr. Albuquerque also reported his long-term follow-up of 27 patients who underwent venous sinus stenting to treat pseudotumors. All patients had more than 50% stenosis confirmed by retrograde venogram and a transstenotic pressure gradient that was greater than 12 mm Hg. Fully 70% of patients improved symptomatically, but five underwent a shunt procedure after they failed to improve. Patients experienced no permanent complications, although one required a stent for femoral artery pseudoaneurysm. Angiographies performed an average of 23 months later showed that all stents remained patent, although four patients had mild (less than 25%) stenosis. Five patients had narrowing of the sinus proximal to the stent.
Patients need dual antiplatelet therapy after venous sinus stenting, and the rate of chronic patency after the procedure is unknown, Dr. Albuquerque noted. Patients can develop scalp pain over the stented segment, he added.
“I think if you limit this procedure to a very select group of patients, I think its efficacy is tremendous,” Dr. Albuquerque concluded.
Dr. Albuquerque declared no conflicts of interest. Dr. Friedman reported serving on the speakers bureau of Allergan, receiving research grants from the National Eye Institute, Merck & Co., and ElectroCore, and having served as an expert witness (for the plaintiff and defense) on idiopathic intracranial hypertension.
SCOTTSDALE, ARIZ. – Venous sinus stenting remains a controversial treatment for headache associated with benign intracranial hypertension. Opponents highlight potentially serious adverse effects and a lack of rigorous studies on the procedure, while supporters describe it as safe and effective. Experts recently debated the procedure at a symposium sponsored by the American Headache Society.
Which came first?
Stenting is based on the rationale that lowering venous sinus pressure might lower intracranial pressure, said Dr. Deborah Friedman, a neuro-ophthalmologist at the University of Texas Southwestern Medical Center in Dallas.
“Other surgical techniques create a fistula the body wants to close,” she said. “Stenting may provide a permanent solution.”
The crux of the debate on stenting is whether venous sinus stenosis is a cause or outcome of benign intracranial hypertension (BIH), said Dr. Felipe Albuquerque, an endovascular neurosurgeon at the Barrow Neurological Institute in Phoenix. The fact that 90% of affected patients have venous sinus stenosis on MRI suggests stenosis is a valid etiology the condition, he said.
But Dr. Friedman disagreed. In a retrospective study of 51 patients with BIH and transverse sinus stenosis, 71% had more than 50% stenosis, but the degree and location of stenosis did not predict clinical outcome. The analysis also found no link between cerebrospinal fluid pressure and the location, degree, or residual area of stenosis. Nonetheless, the procedure may be useful in patients who have persistent transverse sinus stenosis after undergoing a shunt procedure, she said.
The cons of stenting
“Stenting carries a high risk of morbidity and mortality, compared with currently used treatments, and should only be used as a last resort in patients who are losing vision,” Dr. Friedman asserted. Most patients do well, but others suffer serious complications, including life-threatening anaphylaxis, subdural hematomas, subarachnoid hemorrhage, and brain herniation, she said.
In contrast, optic nerve sheath fenestration for BIH has no associated fatalities, according to Dr. Friedman. And in a National Inpatient Sample database analysis of 1,224 shunts, mortality was only 0.9% for ventriculoperitoneal shunt and 0.3% for lumbar-peritoneal shunt. No deaths were recorded for shunts performed for BIH or pseudotumor cerebri, she added.
The literature on venous sinus stenting “is a mess,” Dr. Friedman continued. “All data are from retrospective case series, and the diagnosis of idiopathic intracranial hypertension is questionable in some cases,” she said. “The indication for stenting is not well defined.”
Studies on the safety and efficacy of stenting have lacked a common primary outcome variable and may reflect reporting bias, Dr. Friedman said. Studies have been heterogeneous with regard to disease duration and the presence or absence of papilledema, visual status, previous treatments, and definitions of treatment failure, she added. No randomized, controlled trials have been carried out with sham stenting to assess the possibility of placebo effect, she noted.
“I think stenting may have utility in patients who have failed conventional therapy and have had another procedure that did not work. I think it very likely that there is a strong placebo effect in this group,” Dr. Friedman said.
“It’s not like our existing procedures are wonderful,” she added. “I wish we had something better to offer our patients.”
The pros
Venous sinus stenting “is usually effective in ameliorating both subjective headache and objective papilledema symptoms,” Dr. Albuquerque said. “One could argue that both ventriculoperitoneal shunt and lumbar-peritoneal shunt, the most commonly performed surgical interventions for benign intracranial hypertension, are substantially more invasive than stenting is and associated with far more severe complications.”
Dr. Albuquerque described a prospective study he conducted with his associates on 15 patients with BIH who underwent venous sinus stenting. In all, 80% of patients said their headaches improved, and 60% reported at least a 50% decrease in headache pain. Rates of patency and technical success were 100%, and no patients had permanent complications from the procedure, although one patient developed acute retroperitoneal hematoma, he said.
Dr. Albuquerque also reported his long-term follow-up of 27 patients who underwent venous sinus stenting to treat pseudotumors. All patients had more than 50% stenosis confirmed by retrograde venogram and a transstenotic pressure gradient that was greater than 12 mm Hg. Fully 70% of patients improved symptomatically, but five underwent a shunt procedure after they failed to improve. Patients experienced no permanent complications, although one required a stent for femoral artery pseudoaneurysm. Angiographies performed an average of 23 months later showed that all stents remained patent, although four patients had mild (less than 25%) stenosis. Five patients had narrowing of the sinus proximal to the stent.
Patients need dual antiplatelet therapy after venous sinus stenting, and the rate of chronic patency after the procedure is unknown, Dr. Albuquerque noted. Patients can develop scalp pain over the stented segment, he added.
“I think if you limit this procedure to a very select group of patients, I think its efficacy is tremendous,” Dr. Albuquerque concluded.
Dr. Albuquerque declared no conflicts of interest. Dr. Friedman reported serving on the speakers bureau of Allergan, receiving research grants from the National Eye Institute, Merck & Co., and ElectroCore, and having served as an expert witness (for the plaintiff and defense) on idiopathic intracranial hypertension.
EXPERT ANALYSIS AT THE SCOTTSDALE HEADACHE SYMPOSIUM
Most papers on headache randomized trials skipped ICMJE guidelines
SCOTTSDALE, ARIZ. – Since 2005, only 26% of randomized trials published in the leading headache medicine journals have followed registration reporting guidelines from the International Committee of Medical Journal Editors, a study found.
“The three major headache journals should pursue consensus regarding ICMJE registration requirements and their enforcement,” lead author Dr. Melissa Rayhill said at a symposium sponsored by the American Headache Society.
Instructions for authors should state that the journals require abstracts about randomized trials to report trial registration numbers, said Dr. Rayhill, a neurologist at Brigham and Women’s Hospital, Boston.
She and her coauthors found that paper titles did not consistently identify randomized trials as such, making them less likely to appear in PubMed searches.
“This has implications for meta-analyses and other efforts to synthesize trial information,” she said.
To address the problem of selective reporting of results, since 2005 the ICMJE has required member journals to only publish reports of clinical trials that were prospectively registered in an approved clinical trial registry. Other journals later followed suite, and the journal Headache adopted the policy in 2009. As a result, the number of registered studies rose from less than 4,000 in 2000 to more than 177,000 in 2014, Dr. Rayhill and her associates reported.
To assess the extent to which trials reported in headache medicine journals have complied with ICMJE requirements, Dr. Rayhill and her colleagues manually reviewed all issues of the three leading journals – Headache, Cephalalgia, and the Journal of Headache and Pain – from July 2005 through June 2014. After identifying papers on randomized clinical trials, they determined which manuscripts reported valid trial registration numbers, and then cross-checked the relevant website to see if the trial was registered.
The three journals published 226 reports of randomized trials between 2005 and 2014, Dr. Rayhill and her associates reported. A total of 46% of these papers appeared in Cephalalgia, 38% in Headache, and 16% in the Journal of Headache and Pain, they said. Only 59 (26%) manuscripts reported a trial registration number that linked to corresponding entry on the clinicaltrials.gov website, they added.
The proportion of published trials that reported a registration number “steadily increased” for the journals Headache and Cephalalgia during the study period, but not for the Journal of Headache and Pain, the investigators reported. In fact, only 8% of trials published in the Journal of Headache and Pain reported a registration number, they added.
Authors should know that trials can be registered retrospectively in cases where prospective registration is not required, Dr. Rayhill and her associates said. They declared no relevant conflicts of interest.
SCOTTSDALE, ARIZ. – Since 2005, only 26% of randomized trials published in the leading headache medicine journals have followed registration reporting guidelines from the International Committee of Medical Journal Editors, a study found.
“The three major headache journals should pursue consensus regarding ICMJE registration requirements and their enforcement,” lead author Dr. Melissa Rayhill said at a symposium sponsored by the American Headache Society.
Instructions for authors should state that the journals require abstracts about randomized trials to report trial registration numbers, said Dr. Rayhill, a neurologist at Brigham and Women’s Hospital, Boston.
She and her coauthors found that paper titles did not consistently identify randomized trials as such, making them less likely to appear in PubMed searches.
“This has implications for meta-analyses and other efforts to synthesize trial information,” she said.
To address the problem of selective reporting of results, since 2005 the ICMJE has required member journals to only publish reports of clinical trials that were prospectively registered in an approved clinical trial registry. Other journals later followed suite, and the journal Headache adopted the policy in 2009. As a result, the number of registered studies rose from less than 4,000 in 2000 to more than 177,000 in 2014, Dr. Rayhill and her associates reported.
To assess the extent to which trials reported in headache medicine journals have complied with ICMJE requirements, Dr. Rayhill and her colleagues manually reviewed all issues of the three leading journals – Headache, Cephalalgia, and the Journal of Headache and Pain – from July 2005 through June 2014. After identifying papers on randomized clinical trials, they determined which manuscripts reported valid trial registration numbers, and then cross-checked the relevant website to see if the trial was registered.
The three journals published 226 reports of randomized trials between 2005 and 2014, Dr. Rayhill and her associates reported. A total of 46% of these papers appeared in Cephalalgia, 38% in Headache, and 16% in the Journal of Headache and Pain, they said. Only 59 (26%) manuscripts reported a trial registration number that linked to corresponding entry on the clinicaltrials.gov website, they added.
The proportion of published trials that reported a registration number “steadily increased” for the journals Headache and Cephalalgia during the study period, but not for the Journal of Headache and Pain, the investigators reported. In fact, only 8% of trials published in the Journal of Headache and Pain reported a registration number, they added.
Authors should know that trials can be registered retrospectively in cases where prospective registration is not required, Dr. Rayhill and her associates said. They declared no relevant conflicts of interest.
SCOTTSDALE, ARIZ. – Since 2005, only 26% of randomized trials published in the leading headache medicine journals have followed registration reporting guidelines from the International Committee of Medical Journal Editors, a study found.
“The three major headache journals should pursue consensus regarding ICMJE registration requirements and their enforcement,” lead author Dr. Melissa Rayhill said at a symposium sponsored by the American Headache Society.
Instructions for authors should state that the journals require abstracts about randomized trials to report trial registration numbers, said Dr. Rayhill, a neurologist at Brigham and Women’s Hospital, Boston.
She and her coauthors found that paper titles did not consistently identify randomized trials as such, making them less likely to appear in PubMed searches.
“This has implications for meta-analyses and other efforts to synthesize trial information,” she said.
To address the problem of selective reporting of results, since 2005 the ICMJE has required member journals to only publish reports of clinical trials that were prospectively registered in an approved clinical trial registry. Other journals later followed suite, and the journal Headache adopted the policy in 2009. As a result, the number of registered studies rose from less than 4,000 in 2000 to more than 177,000 in 2014, Dr. Rayhill and her associates reported.
To assess the extent to which trials reported in headache medicine journals have complied with ICMJE requirements, Dr. Rayhill and her colleagues manually reviewed all issues of the three leading journals – Headache, Cephalalgia, and the Journal of Headache and Pain – from July 2005 through June 2014. After identifying papers on randomized clinical trials, they determined which manuscripts reported valid trial registration numbers, and then cross-checked the relevant website to see if the trial was registered.
The three journals published 226 reports of randomized trials between 2005 and 2014, Dr. Rayhill and her associates reported. A total of 46% of these papers appeared in Cephalalgia, 38% in Headache, and 16% in the Journal of Headache and Pain, they said. Only 59 (26%) manuscripts reported a trial registration number that linked to corresponding entry on the clinicaltrials.gov website, they added.
The proportion of published trials that reported a registration number “steadily increased” for the journals Headache and Cephalalgia during the study period, but not for the Journal of Headache and Pain, the investigators reported. In fact, only 8% of trials published in the Journal of Headache and Pain reported a registration number, they added.
Authors should know that trials can be registered retrospectively in cases where prospective registration is not required, Dr. Rayhill and her associates said. They declared no relevant conflicts of interest.
EXPERT ANALYSIS AT THE SCOTTSDALE HEADACHE SYMPOSIUM
Key clinical point: A minority of randomized trials published in major headache journals follow registration reporting guidelines.
Major finding: Only 59 (26%) of 226 manuscripts reported a trial registration number that linked to corresponding entry on the clinicaltrials.gov website.
Data source: A review of randomized trial manuscripts published in Headache, Cephalalgia, and the Journal of Headache and Pain during July 2005-June 2014.
Disclosures: The authors declared no relevant conflicts of interest.
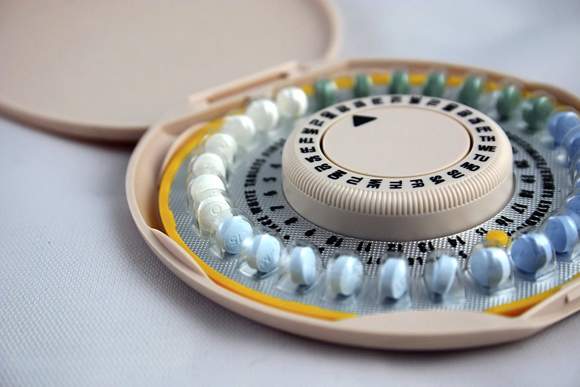
Recommendations mixed on oral contraceptives for female migraineurs
SCOTTSDALE, ARIZ. – Experts have not reached consensus on prescribing oral contraceptives for women with migraine, revealing the need for better studies of stroke risk in these patients, said Dr. Huma Sheikh, a neurologist at Brigham and Women’s Hospital in Boston.
“During the years that women are most likely to need a reliable form of birth control, the prevalence rates of migraine are also considerable,” Dr. Sheikh said at a symposium sponsored by the American Headache Society. The annual prevalence of migraine is about 18%, and most cases occur in women, she noted. “What is not known is how much these two conditions overlap, and who will develop adverse cardiovascular and cerebral outcomes, including stroke.”
Taking combined oral contraceptives can increase stroke risk, although the absolute rate of stroke in oral contraceptive users remains low at 5-11.3 events per 100,000 woman-years. Migraine with aura increases the risk of stroke by 2.3-3.6 times in women younger than 45 years. And in past studies, taking combined oral contraceptives increased the odds of stroke by 5-17 times in women with migraine, she said.
These findings led the World Health Organization and the American Congress of Obstetricians and Gynecologists to regard migraine with aura as an “absolute contraindication” against the use of combined oral contraceptives, Dr. Sheikh said. “But these recommendations are really based on previous studies that included both low-dose and high-dose oral contraceptives that may not be pertinent to this new era,” she said. “The individual studies had low power, and heterogeneity is a problem.”
Unlike WHO and ACOG, the International Headache Society recommends assessing risk individually when deciding whether to prescribe oral contraceptives for women who have migraine with aura, Dr. Sheikh noted. The IHS advises clinicians to identify and treat other risk factors for stroke, such as hypertension and hyperlipidemia; to diagnose the subtype of migraine; to advise smokers to quit; and to consider contraceptives without ethinyl estradiol for women who have multiple risk factors for stroke.
For women with migraine without aura, WHO and ACOG have cited no contraindication against oral contraceptives as long as patients are under 35 years of age. But both organizations state that the risk usually outweighs the benefits in older women. And the IHS again recommends an individualized risk assessment, she said.
“There is a need to develop an updated guideline for the use of hormones in women with migraine,” Dr. Sheikh emphasized. She is planning a systematic literature review to determine if the previously described increased risk of stroke in young women with migraine still holds true for newer, lower-dose estrogen oral contraceptives and oral contraceptives that contain progestin, she said. Her review also will assess the purported link between migraine or migraine with aura and other cardiovascular outcomes, such as myocardial infarction and overall mortality, she added.
Dr. Sheikh declared no conflicts of interest.
SCOTTSDALE, ARIZ. – Experts have not reached consensus on prescribing oral contraceptives for women with migraine, revealing the need for better studies of stroke risk in these patients, said Dr. Huma Sheikh, a neurologist at Brigham and Women’s Hospital in Boston.
“During the years that women are most likely to need a reliable form of birth control, the prevalence rates of migraine are also considerable,” Dr. Sheikh said at a symposium sponsored by the American Headache Society. The annual prevalence of migraine is about 18%, and most cases occur in women, she noted. “What is not known is how much these two conditions overlap, and who will develop adverse cardiovascular and cerebral outcomes, including stroke.”
Taking combined oral contraceptives can increase stroke risk, although the absolute rate of stroke in oral contraceptive users remains low at 5-11.3 events per 100,000 woman-years. Migraine with aura increases the risk of stroke by 2.3-3.6 times in women younger than 45 years. And in past studies, taking combined oral contraceptives increased the odds of stroke by 5-17 times in women with migraine, she said.
These findings led the World Health Organization and the American Congress of Obstetricians and Gynecologists to regard migraine with aura as an “absolute contraindication” against the use of combined oral contraceptives, Dr. Sheikh said. “But these recommendations are really based on previous studies that included both low-dose and high-dose oral contraceptives that may not be pertinent to this new era,” she said. “The individual studies had low power, and heterogeneity is a problem.”
Unlike WHO and ACOG, the International Headache Society recommends assessing risk individually when deciding whether to prescribe oral contraceptives for women who have migraine with aura, Dr. Sheikh noted. The IHS advises clinicians to identify and treat other risk factors for stroke, such as hypertension and hyperlipidemia; to diagnose the subtype of migraine; to advise smokers to quit; and to consider contraceptives without ethinyl estradiol for women who have multiple risk factors for stroke.
For women with migraine without aura, WHO and ACOG have cited no contraindication against oral contraceptives as long as patients are under 35 years of age. But both organizations state that the risk usually outweighs the benefits in older women. And the IHS again recommends an individualized risk assessment, she said.
“There is a need to develop an updated guideline for the use of hormones in women with migraine,” Dr. Sheikh emphasized. She is planning a systematic literature review to determine if the previously described increased risk of stroke in young women with migraine still holds true for newer, lower-dose estrogen oral contraceptives and oral contraceptives that contain progestin, she said. Her review also will assess the purported link between migraine or migraine with aura and other cardiovascular outcomes, such as myocardial infarction and overall mortality, she added.
Dr. Sheikh declared no conflicts of interest.
SCOTTSDALE, ARIZ. – Experts have not reached consensus on prescribing oral contraceptives for women with migraine, revealing the need for better studies of stroke risk in these patients, said Dr. Huma Sheikh, a neurologist at Brigham and Women’s Hospital in Boston.
“During the years that women are most likely to need a reliable form of birth control, the prevalence rates of migraine are also considerable,” Dr. Sheikh said at a symposium sponsored by the American Headache Society. The annual prevalence of migraine is about 18%, and most cases occur in women, she noted. “What is not known is how much these two conditions overlap, and who will develop adverse cardiovascular and cerebral outcomes, including stroke.”
Taking combined oral contraceptives can increase stroke risk, although the absolute rate of stroke in oral contraceptive users remains low at 5-11.3 events per 100,000 woman-years. Migraine with aura increases the risk of stroke by 2.3-3.6 times in women younger than 45 years. And in past studies, taking combined oral contraceptives increased the odds of stroke by 5-17 times in women with migraine, she said.
These findings led the World Health Organization and the American Congress of Obstetricians and Gynecologists to regard migraine with aura as an “absolute contraindication” against the use of combined oral contraceptives, Dr. Sheikh said. “But these recommendations are really based on previous studies that included both low-dose and high-dose oral contraceptives that may not be pertinent to this new era,” she said. “The individual studies had low power, and heterogeneity is a problem.”
Unlike WHO and ACOG, the International Headache Society recommends assessing risk individually when deciding whether to prescribe oral contraceptives for women who have migraine with aura, Dr. Sheikh noted. The IHS advises clinicians to identify and treat other risk factors for stroke, such as hypertension and hyperlipidemia; to diagnose the subtype of migraine; to advise smokers to quit; and to consider contraceptives without ethinyl estradiol for women who have multiple risk factors for stroke.
For women with migraine without aura, WHO and ACOG have cited no contraindication against oral contraceptives as long as patients are under 35 years of age. But both organizations state that the risk usually outweighs the benefits in older women. And the IHS again recommends an individualized risk assessment, she said.
“There is a need to develop an updated guideline for the use of hormones in women with migraine,” Dr. Sheikh emphasized. She is planning a systematic literature review to determine if the previously described increased risk of stroke in young women with migraine still holds true for newer, lower-dose estrogen oral contraceptives and oral contraceptives that contain progestin, she said. Her review also will assess the purported link between migraine or migraine with aura and other cardiovascular outcomes, such as myocardial infarction and overall mortality, she added.
Dr. Sheikh declared no conflicts of interest.
EXPERT ANALYSIS AT THE SCOTTSDALE HEADACHE SYMPOSIUM
Consider graded exercise before medications for postural orthostatic tachycardia syndrome
SCOTTSDALE, ARIZ. – Exercise is a cornerstone of treating postural orthostatic tachycardia syndrome, according to Dr. Deborah Tepper.
“Exercise training is really the hot new way to treat this disorder. It’s been found to be very effective,” she said at a symposium sponsored by the American Headache Society.
Postural orthostatic tachycardia syndrome (POTS) is an autonomic disorder that causes symptoms resembling panic attacks, said Dr. Tepper, who is an internist at the Cleveland Clinic Neurological Center for Pain. Patients may report syncope, dizziness, palpitations, rapid or irregular breathing, fatigue, and chest pain, she said. But to be diagnosed with POTS, they must have an increase of at least 30 beats per minute within 10 minutes of standing or with the 60-degree tilt table test. Patients aged 12-19 years must have an increase in heart rate of at least 40 beats per minute. Blood pressure may drop or stay the same, but will not fall to the extent seen in orthostatic hypotension (that is, a systolic drop of 20 mm Hg or a diastolic fall of at least 10 mm Hg), Dr. Tepper noted.
Deconditioning, chronic fatigue, anxiety, dehydration, and various medications increase the frequency and severity of POTS-related symptoms, Dr. Tepper said. Patients sometimes severely restrict exercise in an effort to control symptoms, but lying on the couch or going to bed “is the worst thing you can do with POTS,” she said. Instead, patients should start a graded exercise program by swimming or exercising in recumbent or seated positions. Exercise training increases the aldosterone-to-renin ratio, can reduce migraine, improves overall health and stamina, supports independent functioning, and can help restore the sleep-wake cycle.
Increasing salt and fluid intake and wearing compression socks also can improve symptoms – often to the extent that patients will not need new medications. But this conservative approach is inadequate in patients with risky occupations and is less effective when patients have frequent episodes of syncope, Dr. Tepper said.
“Beta-blockers remain an option if salts, fluids, and patient education are not enough,” she added.
Beta-blockers inhibit epinephrine release and therefore can improve the migraine and anxiety symptoms that can occur in patients with POTS, although they should not be used in patients with asthma, Dr. Tepper emphasized.
Medications such as fludrocortisone and midodrine should be reserved for patients with recurrent or resistant symptoms, according to Dr. Tepper. “Midodrine can be helpful in some people, although the evidence overall rates it as low to moderate,” she said. Midodrine is a direct vasoconstrictor and alpha-adrenergic agonist that increases vasomotor tone, but also can exacerbate headaches and may cause supine hypertension, urinary retention, and insomnia, she noted. Fludrocortisone increases plasma volume, but worsens migraine, increases fluid retention, and cannot be used in diabetic patients, she said.
Clinicians should refer patients for a cardiology evaluation if they do not improve or have risk factors such as a history of cardiac disease or a family history of sudden cardiac death, chest pain, a QRS interval of more than 120 ms, a corrected QT interval of more than 450 ms or less than 300 ms, or syncope with no warning or while lying down, Dr. Tepper said. She declared no conflicts of interest.
SCOTTSDALE, ARIZ. – Exercise is a cornerstone of treating postural orthostatic tachycardia syndrome, according to Dr. Deborah Tepper.
“Exercise training is really the hot new way to treat this disorder. It’s been found to be very effective,” she said at a symposium sponsored by the American Headache Society.
Postural orthostatic tachycardia syndrome (POTS) is an autonomic disorder that causes symptoms resembling panic attacks, said Dr. Tepper, who is an internist at the Cleveland Clinic Neurological Center for Pain. Patients may report syncope, dizziness, palpitations, rapid or irregular breathing, fatigue, and chest pain, she said. But to be diagnosed with POTS, they must have an increase of at least 30 beats per minute within 10 minutes of standing or with the 60-degree tilt table test. Patients aged 12-19 years must have an increase in heart rate of at least 40 beats per minute. Blood pressure may drop or stay the same, but will not fall to the extent seen in orthostatic hypotension (that is, a systolic drop of 20 mm Hg or a diastolic fall of at least 10 mm Hg), Dr. Tepper noted.
Deconditioning, chronic fatigue, anxiety, dehydration, and various medications increase the frequency and severity of POTS-related symptoms, Dr. Tepper said. Patients sometimes severely restrict exercise in an effort to control symptoms, but lying on the couch or going to bed “is the worst thing you can do with POTS,” she said. Instead, patients should start a graded exercise program by swimming or exercising in recumbent or seated positions. Exercise training increases the aldosterone-to-renin ratio, can reduce migraine, improves overall health and stamina, supports independent functioning, and can help restore the sleep-wake cycle.
Increasing salt and fluid intake and wearing compression socks also can improve symptoms – often to the extent that patients will not need new medications. But this conservative approach is inadequate in patients with risky occupations and is less effective when patients have frequent episodes of syncope, Dr. Tepper said.
“Beta-blockers remain an option if salts, fluids, and patient education are not enough,” she added.
Beta-blockers inhibit epinephrine release and therefore can improve the migraine and anxiety symptoms that can occur in patients with POTS, although they should not be used in patients with asthma, Dr. Tepper emphasized.
Medications such as fludrocortisone and midodrine should be reserved for patients with recurrent or resistant symptoms, according to Dr. Tepper. “Midodrine can be helpful in some people, although the evidence overall rates it as low to moderate,” she said. Midodrine is a direct vasoconstrictor and alpha-adrenergic agonist that increases vasomotor tone, but also can exacerbate headaches and may cause supine hypertension, urinary retention, and insomnia, she noted. Fludrocortisone increases plasma volume, but worsens migraine, increases fluid retention, and cannot be used in diabetic patients, she said.
Clinicians should refer patients for a cardiology evaluation if they do not improve or have risk factors such as a history of cardiac disease or a family history of sudden cardiac death, chest pain, a QRS interval of more than 120 ms, a corrected QT interval of more than 450 ms or less than 300 ms, or syncope with no warning or while lying down, Dr. Tepper said. She declared no conflicts of interest.
SCOTTSDALE, ARIZ. – Exercise is a cornerstone of treating postural orthostatic tachycardia syndrome, according to Dr. Deborah Tepper.
“Exercise training is really the hot new way to treat this disorder. It’s been found to be very effective,” she said at a symposium sponsored by the American Headache Society.
Postural orthostatic tachycardia syndrome (POTS) is an autonomic disorder that causes symptoms resembling panic attacks, said Dr. Tepper, who is an internist at the Cleveland Clinic Neurological Center for Pain. Patients may report syncope, dizziness, palpitations, rapid or irregular breathing, fatigue, and chest pain, she said. But to be diagnosed with POTS, they must have an increase of at least 30 beats per minute within 10 minutes of standing or with the 60-degree tilt table test. Patients aged 12-19 years must have an increase in heart rate of at least 40 beats per minute. Blood pressure may drop or stay the same, but will not fall to the extent seen in orthostatic hypotension (that is, a systolic drop of 20 mm Hg or a diastolic fall of at least 10 mm Hg), Dr. Tepper noted.
Deconditioning, chronic fatigue, anxiety, dehydration, and various medications increase the frequency and severity of POTS-related symptoms, Dr. Tepper said. Patients sometimes severely restrict exercise in an effort to control symptoms, but lying on the couch or going to bed “is the worst thing you can do with POTS,” she said. Instead, patients should start a graded exercise program by swimming or exercising in recumbent or seated positions. Exercise training increases the aldosterone-to-renin ratio, can reduce migraine, improves overall health and stamina, supports independent functioning, and can help restore the sleep-wake cycle.
Increasing salt and fluid intake and wearing compression socks also can improve symptoms – often to the extent that patients will not need new medications. But this conservative approach is inadequate in patients with risky occupations and is less effective when patients have frequent episodes of syncope, Dr. Tepper said.
“Beta-blockers remain an option if salts, fluids, and patient education are not enough,” she added.
Beta-blockers inhibit epinephrine release and therefore can improve the migraine and anxiety symptoms that can occur in patients with POTS, although they should not be used in patients with asthma, Dr. Tepper emphasized.
Medications such as fludrocortisone and midodrine should be reserved for patients with recurrent or resistant symptoms, according to Dr. Tepper. “Midodrine can be helpful in some people, although the evidence overall rates it as low to moderate,” she said. Midodrine is a direct vasoconstrictor and alpha-adrenergic agonist that increases vasomotor tone, but also can exacerbate headaches and may cause supine hypertension, urinary retention, and insomnia, she noted. Fludrocortisone increases plasma volume, but worsens migraine, increases fluid retention, and cannot be used in diabetic patients, she said.
Clinicians should refer patients for a cardiology evaluation if they do not improve or have risk factors such as a history of cardiac disease or a family history of sudden cardiac death, chest pain, a QRS interval of more than 120 ms, a corrected QT interval of more than 450 ms or less than 300 ms, or syncope with no warning or while lying down, Dr. Tepper said. She declared no conflicts of interest.
Anxiety disorders drive, worsen migraine symptoms
SCOTTSDALE, ARIZ. – Patients with migraine often have comorbid psychiatric conditions, but anxiety disorders particularly exacerbate pain, hypervigilance, and the tendency to catastrophize, said Steven Baskin, Ph.D.
“Anxiety is the driver of distress across most emotional disorders,” said Dr. Baskin, a psychologist at the New England Institute for Neurology and Headache in Stamford, Conn. The lifetime prevalence of anxiety disorders among migraineurs is 51%-58%, which is almost twice their lifetime rate of major depression, he added.
Panic disorder is particularly common in migraine patients, with an odds ratio of approximately 10 for migraine with aura and 3 for migraine without aura. However, community studies have also linked migraine to increased odds of generalized anxiety disorder, phobias, and obsessive-compulsive disorder, he said at a symposium sponsored by the American Headache Society.
Anxiety tends to worsen headache symptoms and disability, erodes short-term treatment satisfaction, and decreases therapeutic compliance to a greater extent than depression does, Dr. Baskin said. “Psychological interventions that target anxiety sensitivity may be helpful for headache,” he added.
These therapies include a “top down” approach based on cognitive-behavioral therapy, and a “bottom up” approach based on mindfulness, said Dr. Cynthia Stonnington, chair of the department of psychiatry and psychology at the Mayo Clinic, Phoenix. Cognitive therapy teaches migraineurs to reappraise their situation by focusing on past examples of their resilience and support system instead of catastrophizing their pain, she said. And mindfulness-based therapy trains patients to “make room by breathing, by being aware of what is happening in the body,” she added. “The more you can accept without judgment, and without all that stress and anxiety, the more you will be able to cope with that situation.”
Both therapeutic approaches help to lower the stress response, thereby helping to improve headache symptoms, Dr. Stonnington added. “Patients may be operating outside of their window of tolerance for much of their life without realizing it.”
Taking a longitudinal history also is important to accurately assess psychiatric disorders in migraineurs, Dr. Baskin emphasized. For example, anxiety disorders generally emerge before the onset of episodic migraine, while major depressive disorder typically follows it, he noted.
Genetics, early childhood trauma, and somatic sensitivity all affect the likelihood of anxiety disorders, Dr. Baskin said. Patients can be genetically more likely to develop neurotic personality traits, while severe illness or abuse during childhood can erode perceptions of control in adulthood, he said. Headache in patients who were mistreated as children “is more disabling and more likely to transform from episodic to chronic,” he noted.
In addition, some patients are acutely sensitive to bodily signals of stress or anxiety, such as increased heart rate, Dr. Baskin said. “These patients can feel their bodies, they notice something awry, and they fear it; they think this benign sensation is harmful, is potentially catastrophic,” he said. They are more likely to fear pain, to be affected by headache triggers, to have more frequent and disabling headaches, and to engage in maladaptive thoughts and behaviors, compared with patients with migraine who do not have a comorbid anxiety disorder, he said. Examples of maladaptive thoughts include, “I need to be completely headache free,” “Having migraines is intolerable,” “All these medications have horrible side effects,” and, “If I worry about it, I might prevent it,” he noted.
Patients with comorbid migraine and anxiety disorders also may view themselves as fragile, debilitated, easily unnerved, and helpless in the face of their condition, which tends to further worsen their disability, Dr. Baskin added. Patients also may frequently seek to control situations, see themselves as too special to deserve headaches or, conversely, worry about public humiliation about their migraines, he said.
Dr. Baskin reported serving on advisory boards and speakers bureaus and receiving research support from Allergan, Depomed, and Teva.
SCOTTSDALE, ARIZ. – Patients with migraine often have comorbid psychiatric conditions, but anxiety disorders particularly exacerbate pain, hypervigilance, and the tendency to catastrophize, said Steven Baskin, Ph.D.
“Anxiety is the driver of distress across most emotional disorders,” said Dr. Baskin, a psychologist at the New England Institute for Neurology and Headache in Stamford, Conn. The lifetime prevalence of anxiety disorders among migraineurs is 51%-58%, which is almost twice their lifetime rate of major depression, he added.
Panic disorder is particularly common in migraine patients, with an odds ratio of approximately 10 for migraine with aura and 3 for migraine without aura. However, community studies have also linked migraine to increased odds of generalized anxiety disorder, phobias, and obsessive-compulsive disorder, he said at a symposium sponsored by the American Headache Society.
Anxiety tends to worsen headache symptoms and disability, erodes short-term treatment satisfaction, and decreases therapeutic compliance to a greater extent than depression does, Dr. Baskin said. “Psychological interventions that target anxiety sensitivity may be helpful for headache,” he added.
These therapies include a “top down” approach based on cognitive-behavioral therapy, and a “bottom up” approach based on mindfulness, said Dr. Cynthia Stonnington, chair of the department of psychiatry and psychology at the Mayo Clinic, Phoenix. Cognitive therapy teaches migraineurs to reappraise their situation by focusing on past examples of their resilience and support system instead of catastrophizing their pain, she said. And mindfulness-based therapy trains patients to “make room by breathing, by being aware of what is happening in the body,” she added. “The more you can accept without judgment, and without all that stress and anxiety, the more you will be able to cope with that situation.”
Both therapeutic approaches help to lower the stress response, thereby helping to improve headache symptoms, Dr. Stonnington added. “Patients may be operating outside of their window of tolerance for much of their life without realizing it.”
Taking a longitudinal history also is important to accurately assess psychiatric disorders in migraineurs, Dr. Baskin emphasized. For example, anxiety disorders generally emerge before the onset of episodic migraine, while major depressive disorder typically follows it, he noted.
Genetics, early childhood trauma, and somatic sensitivity all affect the likelihood of anxiety disorders, Dr. Baskin said. Patients can be genetically more likely to develop neurotic personality traits, while severe illness or abuse during childhood can erode perceptions of control in adulthood, he said. Headache in patients who were mistreated as children “is more disabling and more likely to transform from episodic to chronic,” he noted.
In addition, some patients are acutely sensitive to bodily signals of stress or anxiety, such as increased heart rate, Dr. Baskin said. “These patients can feel their bodies, they notice something awry, and they fear it; they think this benign sensation is harmful, is potentially catastrophic,” he said. They are more likely to fear pain, to be affected by headache triggers, to have more frequent and disabling headaches, and to engage in maladaptive thoughts and behaviors, compared with patients with migraine who do not have a comorbid anxiety disorder, he said. Examples of maladaptive thoughts include, “I need to be completely headache free,” “Having migraines is intolerable,” “All these medications have horrible side effects,” and, “If I worry about it, I might prevent it,” he noted.
Patients with comorbid migraine and anxiety disorders also may view themselves as fragile, debilitated, easily unnerved, and helpless in the face of their condition, which tends to further worsen their disability, Dr. Baskin added. Patients also may frequently seek to control situations, see themselves as too special to deserve headaches or, conversely, worry about public humiliation about their migraines, he said.
Dr. Baskin reported serving on advisory boards and speakers bureaus and receiving research support from Allergan, Depomed, and Teva.
SCOTTSDALE, ARIZ. – Patients with migraine often have comorbid psychiatric conditions, but anxiety disorders particularly exacerbate pain, hypervigilance, and the tendency to catastrophize, said Steven Baskin, Ph.D.
“Anxiety is the driver of distress across most emotional disorders,” said Dr. Baskin, a psychologist at the New England Institute for Neurology and Headache in Stamford, Conn. The lifetime prevalence of anxiety disorders among migraineurs is 51%-58%, which is almost twice their lifetime rate of major depression, he added.
Panic disorder is particularly common in migraine patients, with an odds ratio of approximately 10 for migraine with aura and 3 for migraine without aura. However, community studies have also linked migraine to increased odds of generalized anxiety disorder, phobias, and obsessive-compulsive disorder, he said at a symposium sponsored by the American Headache Society.
Anxiety tends to worsen headache symptoms and disability, erodes short-term treatment satisfaction, and decreases therapeutic compliance to a greater extent than depression does, Dr. Baskin said. “Psychological interventions that target anxiety sensitivity may be helpful for headache,” he added.
These therapies include a “top down” approach based on cognitive-behavioral therapy, and a “bottom up” approach based on mindfulness, said Dr. Cynthia Stonnington, chair of the department of psychiatry and psychology at the Mayo Clinic, Phoenix. Cognitive therapy teaches migraineurs to reappraise their situation by focusing on past examples of their resilience and support system instead of catastrophizing their pain, she said. And mindfulness-based therapy trains patients to “make room by breathing, by being aware of what is happening in the body,” she added. “The more you can accept without judgment, and without all that stress and anxiety, the more you will be able to cope with that situation.”
Both therapeutic approaches help to lower the stress response, thereby helping to improve headache symptoms, Dr. Stonnington added. “Patients may be operating outside of their window of tolerance for much of their life without realizing it.”
Taking a longitudinal history also is important to accurately assess psychiatric disorders in migraineurs, Dr. Baskin emphasized. For example, anxiety disorders generally emerge before the onset of episodic migraine, while major depressive disorder typically follows it, he noted.
Genetics, early childhood trauma, and somatic sensitivity all affect the likelihood of anxiety disorders, Dr. Baskin said. Patients can be genetically more likely to develop neurotic personality traits, while severe illness or abuse during childhood can erode perceptions of control in adulthood, he said. Headache in patients who were mistreated as children “is more disabling and more likely to transform from episodic to chronic,” he noted.
In addition, some patients are acutely sensitive to bodily signals of stress or anxiety, such as increased heart rate, Dr. Baskin said. “These patients can feel their bodies, they notice something awry, and they fear it; they think this benign sensation is harmful, is potentially catastrophic,” he said. They are more likely to fear pain, to be affected by headache triggers, to have more frequent and disabling headaches, and to engage in maladaptive thoughts and behaviors, compared with patients with migraine who do not have a comorbid anxiety disorder, he said. Examples of maladaptive thoughts include, “I need to be completely headache free,” “Having migraines is intolerable,” “All these medications have horrible side effects,” and, “If I worry about it, I might prevent it,” he noted.
Patients with comorbid migraine and anxiety disorders also may view themselves as fragile, debilitated, easily unnerved, and helpless in the face of their condition, which tends to further worsen their disability, Dr. Baskin added. Patients also may frequently seek to control situations, see themselves as too special to deserve headaches or, conversely, worry about public humiliation about their migraines, he said.
Dr. Baskin reported serving on advisory boards and speakers bureaus and receiving research support from Allergan, Depomed, and Teva.
EXPERT ANALYSIS AT THE SCOTTSDALE HEADACHE SYMPOSIUM
Randomized trial assesses behavioral weight loss as migraine treatment
SCOTTSDALE, ARIZ. - The first randomized, controlled trial of behavioral weight loss as a treatment for migraine in women is underway, with results expected in mid-2016.
The trial “provides an empirical framework for the recent clinical recommendation that behavioral weight loss strategies be incorporated within treatment plans for patients with migraine and obesity,” said principal investigator Dale Bond, Ph.D., of the department of psychiatry and human behavior at Brown University, Providence, R.I.
Prior research has repeatedly linked obesity to more frequent and severe migraine attacks and worse headache-related disability, but results from the Women’s Health and Migraine (WHAM) trial could help clinicians to motivate patients with migraine to actually lose weight, Dr. Bond said at a symposium sponsored by the American Headache Society.
For the single-site trial, investigators are randomizing overweight and obese female migraineurs aged 18-50 years to either a 16-week behavioral weight loss intervention or to a migraine education control condition, Dr. Bond said. Patients are selected by a “rigorous” 60-minute phone interview and must have had no changes in their headache medications for at least 2 months before the start of the study, he added.
Both groups are using smartphones to record headaches for 4 consecutive weeks during three time periods: at baseline, immediately after the 16-week treatment or control period, and after a 16-week nontreatment follow-up period. “This is one of the more innovative features of this trial – we can look at the data in real time, and if they don’t complete diary, we can prompt them,” Dr. Bond said.
Women in the behavioral weight loss group are asked to lose at least 7% of their initial body weight by weighing themselves daily and recording what they eat, following a 1,200- to 1,500-calorie diet with no more than 25% of calories from fat, attending group meetings, and engaging in moderate to vigorous exercise for at least 250 minutes per week. Participants wear armband pedometers that monitor their physical activity. They also are undergoing behavioral therapy focused on controlling stimuli to eat and learning to set goals and develop problem-solving skills, he added.
In contrast, the control condition “provides the same amount of therapist attention, but no active intervention strategies to produce weight loss,” Dr. Bond said. “We’re using this condition to control for the amount of therapist contact,” he added. These individuals are attending education sessions about migraine, stress, communication with health care providers, relaxation techniques, cognitive restructuring, healthy eating, physical activity, sleep, and developing a personal migraine treatment plan, he added.
The primary outcome number is number of migraine days. Additional outcome measures include height, weight, waist circumference, inflammatory biomarkers, depression, anxiety, pain catastrophizing, cognitive functioning, physical activity, diet, and sleep quality and duration, he said.
The obesity-migraine connection
Several physiologic mechanisms help to explain how weight loss might mitigate the frequency and severity of migraine attacks, Dr. Bond said. Adipocytes secrete inflammatory mediators, which are relatively high in obese individuals and also are high at the start of a migraine attack. Obesity also is linked with increased leptin levels and with low levels of anti-inflammatory oligomers, and these conditions induce release of proinflammatory cytokines. Obese individuals also have relatively low levels of the neuropeptide hormone orexin A, which might contribute to a proinflammatory state within the trigeminal nerve system. Also, high dietary fat intake increases levels of calcitonin gene-related peptide (CGRP), and high CGRP levels can trigger migraine attacks, he noted.
Psychological factors also help explain the migraine-obesity connection, he said. Depression, anxiety, and stress all increase the risk of migraine attacks, progression to chronic migraine, obesity, weight gain, and regain of lost weight. Patients who catastrophize pain typically have decreased functioning, treatment response, and quality of life, as well as higher levels of obesity and decreased ability to control their weight.
“After weight loss treatment, we see improvement in all these psychological mechanisms: depression and anxiety, stress, and pain catastrophizing,” he said. “Weight loss treatment might improve mood and pain perception, leading to better efficacy in terms of trying to manage migraine and decrease attack frequency and severity.”
Additionally, a sedentary lifestyle and sleep disturbances all contribute to obesity and can increase the frequency and potentially the severity of migraine attacks, he added.
Dr. Bond reported receiving grant funding for the WHAM trial from the National Institute of Neurological Disorders and Stroke, the National Institute of Diabetes and Digestive and Kidney Diseases, and Weight Watchers International Inc.
SCOTTSDALE, ARIZ. - The first randomized, controlled trial of behavioral weight loss as a treatment for migraine in women is underway, with results expected in mid-2016.
The trial “provides an empirical framework for the recent clinical recommendation that behavioral weight loss strategies be incorporated within treatment plans for patients with migraine and obesity,” said principal investigator Dale Bond, Ph.D., of the department of psychiatry and human behavior at Brown University, Providence, R.I.
Prior research has repeatedly linked obesity to more frequent and severe migraine attacks and worse headache-related disability, but results from the Women’s Health and Migraine (WHAM) trial could help clinicians to motivate patients with migraine to actually lose weight, Dr. Bond said at a symposium sponsored by the American Headache Society.
For the single-site trial, investigators are randomizing overweight and obese female migraineurs aged 18-50 years to either a 16-week behavioral weight loss intervention or to a migraine education control condition, Dr. Bond said. Patients are selected by a “rigorous” 60-minute phone interview and must have had no changes in their headache medications for at least 2 months before the start of the study, he added.
Both groups are using smartphones to record headaches for 4 consecutive weeks during three time periods: at baseline, immediately after the 16-week treatment or control period, and after a 16-week nontreatment follow-up period. “This is one of the more innovative features of this trial – we can look at the data in real time, and if they don’t complete diary, we can prompt them,” Dr. Bond said.
Women in the behavioral weight loss group are asked to lose at least 7% of their initial body weight by weighing themselves daily and recording what they eat, following a 1,200- to 1,500-calorie diet with no more than 25% of calories from fat, attending group meetings, and engaging in moderate to vigorous exercise for at least 250 minutes per week. Participants wear armband pedometers that monitor their physical activity. They also are undergoing behavioral therapy focused on controlling stimuli to eat and learning to set goals and develop problem-solving skills, he added.
In contrast, the control condition “provides the same amount of therapist attention, but no active intervention strategies to produce weight loss,” Dr. Bond said. “We’re using this condition to control for the amount of therapist contact,” he added. These individuals are attending education sessions about migraine, stress, communication with health care providers, relaxation techniques, cognitive restructuring, healthy eating, physical activity, sleep, and developing a personal migraine treatment plan, he added.
The primary outcome number is number of migraine days. Additional outcome measures include height, weight, waist circumference, inflammatory biomarkers, depression, anxiety, pain catastrophizing, cognitive functioning, physical activity, diet, and sleep quality and duration, he said.
The obesity-migraine connection
Several physiologic mechanisms help to explain how weight loss might mitigate the frequency and severity of migraine attacks, Dr. Bond said. Adipocytes secrete inflammatory mediators, which are relatively high in obese individuals and also are high at the start of a migraine attack. Obesity also is linked with increased leptin levels and with low levels of anti-inflammatory oligomers, and these conditions induce release of proinflammatory cytokines. Obese individuals also have relatively low levels of the neuropeptide hormone orexin A, which might contribute to a proinflammatory state within the trigeminal nerve system. Also, high dietary fat intake increases levels of calcitonin gene-related peptide (CGRP), and high CGRP levels can trigger migraine attacks, he noted.
Psychological factors also help explain the migraine-obesity connection, he said. Depression, anxiety, and stress all increase the risk of migraine attacks, progression to chronic migraine, obesity, weight gain, and regain of lost weight. Patients who catastrophize pain typically have decreased functioning, treatment response, and quality of life, as well as higher levels of obesity and decreased ability to control their weight.
“After weight loss treatment, we see improvement in all these psychological mechanisms: depression and anxiety, stress, and pain catastrophizing,” he said. “Weight loss treatment might improve mood and pain perception, leading to better efficacy in terms of trying to manage migraine and decrease attack frequency and severity.”
Additionally, a sedentary lifestyle and sleep disturbances all contribute to obesity and can increase the frequency and potentially the severity of migraine attacks, he added.
Dr. Bond reported receiving grant funding for the WHAM trial from the National Institute of Neurological Disorders and Stroke, the National Institute of Diabetes and Digestive and Kidney Diseases, and Weight Watchers International Inc.
SCOTTSDALE, ARIZ. - The first randomized, controlled trial of behavioral weight loss as a treatment for migraine in women is underway, with results expected in mid-2016.
The trial “provides an empirical framework for the recent clinical recommendation that behavioral weight loss strategies be incorporated within treatment plans for patients with migraine and obesity,” said principal investigator Dale Bond, Ph.D., of the department of psychiatry and human behavior at Brown University, Providence, R.I.
Prior research has repeatedly linked obesity to more frequent and severe migraine attacks and worse headache-related disability, but results from the Women’s Health and Migraine (WHAM) trial could help clinicians to motivate patients with migraine to actually lose weight, Dr. Bond said at a symposium sponsored by the American Headache Society.
For the single-site trial, investigators are randomizing overweight and obese female migraineurs aged 18-50 years to either a 16-week behavioral weight loss intervention or to a migraine education control condition, Dr. Bond said. Patients are selected by a “rigorous” 60-minute phone interview and must have had no changes in their headache medications for at least 2 months before the start of the study, he added.
Both groups are using smartphones to record headaches for 4 consecutive weeks during three time periods: at baseline, immediately after the 16-week treatment or control period, and after a 16-week nontreatment follow-up period. “This is one of the more innovative features of this trial – we can look at the data in real time, and if they don’t complete diary, we can prompt them,” Dr. Bond said.
Women in the behavioral weight loss group are asked to lose at least 7% of their initial body weight by weighing themselves daily and recording what they eat, following a 1,200- to 1,500-calorie diet with no more than 25% of calories from fat, attending group meetings, and engaging in moderate to vigorous exercise for at least 250 minutes per week. Participants wear armband pedometers that monitor their physical activity. They also are undergoing behavioral therapy focused on controlling stimuli to eat and learning to set goals and develop problem-solving skills, he added.
In contrast, the control condition “provides the same amount of therapist attention, but no active intervention strategies to produce weight loss,” Dr. Bond said. “We’re using this condition to control for the amount of therapist contact,” he added. These individuals are attending education sessions about migraine, stress, communication with health care providers, relaxation techniques, cognitive restructuring, healthy eating, physical activity, sleep, and developing a personal migraine treatment plan, he added.
The primary outcome number is number of migraine days. Additional outcome measures include height, weight, waist circumference, inflammatory biomarkers, depression, anxiety, pain catastrophizing, cognitive functioning, physical activity, diet, and sleep quality and duration, he said.
The obesity-migraine connection
Several physiologic mechanisms help to explain how weight loss might mitigate the frequency and severity of migraine attacks, Dr. Bond said. Adipocytes secrete inflammatory mediators, which are relatively high in obese individuals and also are high at the start of a migraine attack. Obesity also is linked with increased leptin levels and with low levels of anti-inflammatory oligomers, and these conditions induce release of proinflammatory cytokines. Obese individuals also have relatively low levels of the neuropeptide hormone orexin A, which might contribute to a proinflammatory state within the trigeminal nerve system. Also, high dietary fat intake increases levels of calcitonin gene-related peptide (CGRP), and high CGRP levels can trigger migraine attacks, he noted.
Psychological factors also help explain the migraine-obesity connection, he said. Depression, anxiety, and stress all increase the risk of migraine attacks, progression to chronic migraine, obesity, weight gain, and regain of lost weight. Patients who catastrophize pain typically have decreased functioning, treatment response, and quality of life, as well as higher levels of obesity and decreased ability to control their weight.
“After weight loss treatment, we see improvement in all these psychological mechanisms: depression and anxiety, stress, and pain catastrophizing,” he said. “Weight loss treatment might improve mood and pain perception, leading to better efficacy in terms of trying to manage migraine and decrease attack frequency and severity.”
Additionally, a sedentary lifestyle and sleep disturbances all contribute to obesity and can increase the frequency and potentially the severity of migraine attacks, he added.
Dr. Bond reported receiving grant funding for the WHAM trial from the National Institute of Neurological Disorders and Stroke, the National Institute of Diabetes and Digestive and Kidney Diseases, and Weight Watchers International Inc.
EXPERT ANALYSIS AT THE SCOTTSDALE HEADACHE SYMPOSIUM
Dihydroergotamine has a key role in migraine and daily headache, despite its underuse
SCOTTSDALE, ARIZ. – Dihydroergotamine remains underused in the treatment of migraine and daily severe headaches, especially in inpatient settings, according to Dr. Priyanka Chaudhry.
The drug offers several clinical advantages, said Dr. Chaudhry, a neurologist specializing in headache treatment at the University of Texas Southwestern Medical Center in Dallas.
When used in combination with an antiemetic such as metoclopramide, dihydroergotamine (DHE) has been found to be as effective as opiates, valproate, and ketorolac in relieving migraine headache and preventing relapses, Dr. Chaudhry said. Its bioavailability is 100% when given intramuscularly or intravenously, and about 40% when given as a nasal spray, she added.
With its relatively long half-life of 10-13 hours, DHE also poses less risk of physical dependence than does ergotamine, Dr. Chaudhry noted. And in a recent uncontrolled retrospective study, its cumulative positive effects persisted for up to 1 month after patient discharge, she said at a symposium sponsored by the American Headache Society.
Dr. Chaudhry typically starts patients on an infusion of 0.3 mg DHE given over a period of 45 minutes, and if the patient tolerates this dose, increases it to 0.5 mg, then 0.75 mg, and then 1 mg spaced every 6-8 hours, she said. When the patient is free of headaches, she reduces the dose to 0.5 mg. She prefers that patients be headache free for 24 hours before discontinuing DHE, although this goal is not always achievable, she noted.
Treatment with DHE for 5 days seems to be more effective than shorter courses, Dr. Chaudhry added. She, therefore, will admit patients to the infusion clinic for 5 days, and then readmit them later for follow-up treatment with lidocaine, she said.
Dihydroergotamine was associated with several potentially serious adverse effects. “It can be very harsh on veins, so if you’re admitting somebody in an inpatient setting, it is preferable to order a midline catheter or a PICC [peripherally inserted central catheter] line,” said Dr. Chaudhry. Patients also can experience chest pain or a feeling of warmth or pressure in the neck during DHE infusion, especially the first time they are exposed to a given dose of the drug, she noted. “This side effect is not a contraindication for use,” she emphasized. “But consider a slow infusion, and do not bolus.” She orders electrocardiograms for such patients but sees no need to monitor cardiac enzymes, she said.
Nausea is the most common side effect of DHE, and can be treated with 8 mg odansetron, said Dr. Chaudhry. She adds a second antiemetic such as promethazine on an as-needed basis, decreases the rate of DHE infusion, and cuts the dose if nothing else works, she said. Clinicians might also consider adding 50 mg hydroxyzine orally or IM every 6 hours, starting at 25 mg if patients are relatively small or sensitive to medications, she said.
Dihydroergotamine also can cause light-headedness, diarrhea, abdominal cramping, and leg cramps, Dr. Chaudhry noted. Patients who are pregnant or have renal or hepatic failure, uncontrolled hypertension, sepsis, or vascular disease, should not take DHE, she cautioned.
She said she had no relevant financial disclosures.
SCOTTSDALE, ARIZ. – Dihydroergotamine remains underused in the treatment of migraine and daily severe headaches, especially in inpatient settings, according to Dr. Priyanka Chaudhry.
The drug offers several clinical advantages, said Dr. Chaudhry, a neurologist specializing in headache treatment at the University of Texas Southwestern Medical Center in Dallas.
When used in combination with an antiemetic such as metoclopramide, dihydroergotamine (DHE) has been found to be as effective as opiates, valproate, and ketorolac in relieving migraine headache and preventing relapses, Dr. Chaudhry said. Its bioavailability is 100% when given intramuscularly or intravenously, and about 40% when given as a nasal spray, she added.
With its relatively long half-life of 10-13 hours, DHE also poses less risk of physical dependence than does ergotamine, Dr. Chaudhry noted. And in a recent uncontrolled retrospective study, its cumulative positive effects persisted for up to 1 month after patient discharge, she said at a symposium sponsored by the American Headache Society.
Dr. Chaudhry typically starts patients on an infusion of 0.3 mg DHE given over a period of 45 minutes, and if the patient tolerates this dose, increases it to 0.5 mg, then 0.75 mg, and then 1 mg spaced every 6-8 hours, she said. When the patient is free of headaches, she reduces the dose to 0.5 mg. She prefers that patients be headache free for 24 hours before discontinuing DHE, although this goal is not always achievable, she noted.
Treatment with DHE for 5 days seems to be more effective than shorter courses, Dr. Chaudhry added. She, therefore, will admit patients to the infusion clinic for 5 days, and then readmit them later for follow-up treatment with lidocaine, she said.
Dihydroergotamine was associated with several potentially serious adverse effects. “It can be very harsh on veins, so if you’re admitting somebody in an inpatient setting, it is preferable to order a midline catheter or a PICC [peripherally inserted central catheter] line,” said Dr. Chaudhry. Patients also can experience chest pain or a feeling of warmth or pressure in the neck during DHE infusion, especially the first time they are exposed to a given dose of the drug, she noted. “This side effect is not a contraindication for use,” she emphasized. “But consider a slow infusion, and do not bolus.” She orders electrocardiograms for such patients but sees no need to monitor cardiac enzymes, she said.
Nausea is the most common side effect of DHE, and can be treated with 8 mg odansetron, said Dr. Chaudhry. She adds a second antiemetic such as promethazine on an as-needed basis, decreases the rate of DHE infusion, and cuts the dose if nothing else works, she said. Clinicians might also consider adding 50 mg hydroxyzine orally or IM every 6 hours, starting at 25 mg if patients are relatively small or sensitive to medications, she said.
Dihydroergotamine also can cause light-headedness, diarrhea, abdominal cramping, and leg cramps, Dr. Chaudhry noted. Patients who are pregnant or have renal or hepatic failure, uncontrolled hypertension, sepsis, or vascular disease, should not take DHE, she cautioned.
She said she had no relevant financial disclosures.
SCOTTSDALE, ARIZ. – Dihydroergotamine remains underused in the treatment of migraine and daily severe headaches, especially in inpatient settings, according to Dr. Priyanka Chaudhry.
The drug offers several clinical advantages, said Dr. Chaudhry, a neurologist specializing in headache treatment at the University of Texas Southwestern Medical Center in Dallas.
When used in combination with an antiemetic such as metoclopramide, dihydroergotamine (DHE) has been found to be as effective as opiates, valproate, and ketorolac in relieving migraine headache and preventing relapses, Dr. Chaudhry said. Its bioavailability is 100% when given intramuscularly or intravenously, and about 40% when given as a nasal spray, she added.
With its relatively long half-life of 10-13 hours, DHE also poses less risk of physical dependence than does ergotamine, Dr. Chaudhry noted. And in a recent uncontrolled retrospective study, its cumulative positive effects persisted for up to 1 month after patient discharge, she said at a symposium sponsored by the American Headache Society.
Dr. Chaudhry typically starts patients on an infusion of 0.3 mg DHE given over a period of 45 minutes, and if the patient tolerates this dose, increases it to 0.5 mg, then 0.75 mg, and then 1 mg spaced every 6-8 hours, she said. When the patient is free of headaches, she reduces the dose to 0.5 mg. She prefers that patients be headache free for 24 hours before discontinuing DHE, although this goal is not always achievable, she noted.
Treatment with DHE for 5 days seems to be more effective than shorter courses, Dr. Chaudhry added. She, therefore, will admit patients to the infusion clinic for 5 days, and then readmit them later for follow-up treatment with lidocaine, she said.
Dihydroergotamine was associated with several potentially serious adverse effects. “It can be very harsh on veins, so if you’re admitting somebody in an inpatient setting, it is preferable to order a midline catheter or a PICC [peripherally inserted central catheter] line,” said Dr. Chaudhry. Patients also can experience chest pain or a feeling of warmth or pressure in the neck during DHE infusion, especially the first time they are exposed to a given dose of the drug, she noted. “This side effect is not a contraindication for use,” she emphasized. “But consider a slow infusion, and do not bolus.” She orders electrocardiograms for such patients but sees no need to monitor cardiac enzymes, she said.
Nausea is the most common side effect of DHE, and can be treated with 8 mg odansetron, said Dr. Chaudhry. She adds a second antiemetic such as promethazine on an as-needed basis, decreases the rate of DHE infusion, and cuts the dose if nothing else works, she said. Clinicians might also consider adding 50 mg hydroxyzine orally or IM every 6 hours, starting at 25 mg if patients are relatively small or sensitive to medications, she said.
Dihydroergotamine also can cause light-headedness, diarrhea, abdominal cramping, and leg cramps, Dr. Chaudhry noted. Patients who are pregnant or have renal or hepatic failure, uncontrolled hypertension, sepsis, or vascular disease, should not take DHE, she cautioned.
She said she had no relevant financial disclosures.
AT A SYMPOSIUM SPONSORED BY THE AMERICAN HEADACHE SOCIETY
Take these five key steps to limit reimbursement headaches
SCOTTSDALE, ARIZ. – Headache specialists can take five key steps related to coding and billing that can protect their financial investment in their practice, said Stacy Girard, M.B.A., a certified professional coder and revenue analyst at Mayo Clinic Arizona in Phoenix.
Those steps include reviewing annual changes in Current Procedural Terminology (CPT) codes, understanding code descriptions and how to use modifiers, consistently tracking reimbursement denials and intervening if they trend out of control, reviewing medical and reimbursement policies at least once 1 year, and determining their financial liability when services are not covered, Ms. Girard said at a symposium sponsored by the American Headache Society.
The CPT codes for neurologic procedures will not change in the upcoming year, Ms. Girard said. In headache and migraine treatment, some of the most common codes include 64405, for unilateral occipital nerve block; 64450, for unilateral block of another peripheral nerve; 64612, for unilateral facial nerve chemodenervation; and 64615, for bilateral chemodenervation of the facial nerve, trigeminal nerve, cervical spinal nerve, and accessory nerves, she added. Code 64615 was introduced in January 2013 and has “greatly simplified billing for a number of procedures for chronic migraine,” she said.
Payers routinely deny reimbursement claims, Ms. Girard noted. To avoid a reimbursement denial, clinicians and coders must use modifiers correctly when appending claims, she said. For example, they should use modifier 25 only if the same physician performed a completely separate evaluation and management (E/M) service for a patient on the same day of a procedure. And CPT code 64615 already signifies bilateral chemodenervation, so coders should not add modifier 50 to indicate that the service was bilateral, she added.
“You cannot expect what you don’t inspect,” said Ms. Girard. “You cannot expect to be paid for everything if you are not on the back end, inspecting your denials.” She creates a chart to track reimbursement denials by type and month, and reports the results to her practice, highlighting areas “that are really getting out of control,” she said.
Several denial reason codes worth tracking include CO50, CO55, and CO56, for treatments that are deemed “not a medical necessity,” “experimental/investigational,” or “not proven to be effective,” and CO151, in which the payer decides that there is insufficient support for the number or frequency of services provided, Ms. Girard said. “Take action on denials,” she emphasized. “Work with your payers and make a connection with them. We meet with our payers on a regular basis and show them what’s routinely being denied. Maybe you need to understand where they are coming from, and maybe you need to say to them that I really don’t agree with this, and here’s why.”
To minimize denials, practices also need to understand reimbursement policies and who is responsible for paying for services, she said. Information on coverage determinations can be found on payer websites under “medical policies,” or “reimbursement policies,” she noted. Medical policies list the payer’s criteria for covering specific services and diagnosis codes, while reimbursement policies specify how the payer handles issues such as bundling rules, global surgery, and multiple procedures for a single patient.
Practices can further limit their financial liability by obtaining signed advanced beneficiary notices (ABNs) from Medicare patients, Ms. Girard said. Without a signed ABN, patients cannot be billed for services that Medicare does not cover, leaving the practice holding the bill, she said. “Are you going to give away your services for free, or is it something the patient is going to pay for because they’ve signed an ABN?”
Ms. Girard declared no conflicts of interest.
SCOTTSDALE, ARIZ. – Headache specialists can take five key steps related to coding and billing that can protect their financial investment in their practice, said Stacy Girard, M.B.A., a certified professional coder and revenue analyst at Mayo Clinic Arizona in Phoenix.
Those steps include reviewing annual changes in Current Procedural Terminology (CPT) codes, understanding code descriptions and how to use modifiers, consistently tracking reimbursement denials and intervening if they trend out of control, reviewing medical and reimbursement policies at least once 1 year, and determining their financial liability when services are not covered, Ms. Girard said at a symposium sponsored by the American Headache Society.
The CPT codes for neurologic procedures will not change in the upcoming year, Ms. Girard said. In headache and migraine treatment, some of the most common codes include 64405, for unilateral occipital nerve block; 64450, for unilateral block of another peripheral nerve; 64612, for unilateral facial nerve chemodenervation; and 64615, for bilateral chemodenervation of the facial nerve, trigeminal nerve, cervical spinal nerve, and accessory nerves, she added. Code 64615 was introduced in January 2013 and has “greatly simplified billing for a number of procedures for chronic migraine,” she said.
Payers routinely deny reimbursement claims, Ms. Girard noted. To avoid a reimbursement denial, clinicians and coders must use modifiers correctly when appending claims, she said. For example, they should use modifier 25 only if the same physician performed a completely separate evaluation and management (E/M) service for a patient on the same day of a procedure. And CPT code 64615 already signifies bilateral chemodenervation, so coders should not add modifier 50 to indicate that the service was bilateral, she added.
“You cannot expect what you don’t inspect,” said Ms. Girard. “You cannot expect to be paid for everything if you are not on the back end, inspecting your denials.” She creates a chart to track reimbursement denials by type and month, and reports the results to her practice, highlighting areas “that are really getting out of control,” she said.
Several denial reason codes worth tracking include CO50, CO55, and CO56, for treatments that are deemed “not a medical necessity,” “experimental/investigational,” or “not proven to be effective,” and CO151, in which the payer decides that there is insufficient support for the number or frequency of services provided, Ms. Girard said. “Take action on denials,” she emphasized. “Work with your payers and make a connection with them. We meet with our payers on a regular basis and show them what’s routinely being denied. Maybe you need to understand where they are coming from, and maybe you need to say to them that I really don’t agree with this, and here’s why.”
To minimize denials, practices also need to understand reimbursement policies and who is responsible for paying for services, she said. Information on coverage determinations can be found on payer websites under “medical policies,” or “reimbursement policies,” she noted. Medical policies list the payer’s criteria for covering specific services and diagnosis codes, while reimbursement policies specify how the payer handles issues such as bundling rules, global surgery, and multiple procedures for a single patient.
Practices can further limit their financial liability by obtaining signed advanced beneficiary notices (ABNs) from Medicare patients, Ms. Girard said. Without a signed ABN, patients cannot be billed for services that Medicare does not cover, leaving the practice holding the bill, she said. “Are you going to give away your services for free, or is it something the patient is going to pay for because they’ve signed an ABN?”
Ms. Girard declared no conflicts of interest.
SCOTTSDALE, ARIZ. – Headache specialists can take five key steps related to coding and billing that can protect their financial investment in their practice, said Stacy Girard, M.B.A., a certified professional coder and revenue analyst at Mayo Clinic Arizona in Phoenix.
Those steps include reviewing annual changes in Current Procedural Terminology (CPT) codes, understanding code descriptions and how to use modifiers, consistently tracking reimbursement denials and intervening if they trend out of control, reviewing medical and reimbursement policies at least once 1 year, and determining their financial liability when services are not covered, Ms. Girard said at a symposium sponsored by the American Headache Society.
The CPT codes for neurologic procedures will not change in the upcoming year, Ms. Girard said. In headache and migraine treatment, some of the most common codes include 64405, for unilateral occipital nerve block; 64450, for unilateral block of another peripheral nerve; 64612, for unilateral facial nerve chemodenervation; and 64615, for bilateral chemodenervation of the facial nerve, trigeminal nerve, cervical spinal nerve, and accessory nerves, she added. Code 64615 was introduced in January 2013 and has “greatly simplified billing for a number of procedures for chronic migraine,” she said.
Payers routinely deny reimbursement claims, Ms. Girard noted. To avoid a reimbursement denial, clinicians and coders must use modifiers correctly when appending claims, she said. For example, they should use modifier 25 only if the same physician performed a completely separate evaluation and management (E/M) service for a patient on the same day of a procedure. And CPT code 64615 already signifies bilateral chemodenervation, so coders should not add modifier 50 to indicate that the service was bilateral, she added.
“You cannot expect what you don’t inspect,” said Ms. Girard. “You cannot expect to be paid for everything if you are not on the back end, inspecting your denials.” She creates a chart to track reimbursement denials by type and month, and reports the results to her practice, highlighting areas “that are really getting out of control,” she said.
Several denial reason codes worth tracking include CO50, CO55, and CO56, for treatments that are deemed “not a medical necessity,” “experimental/investigational,” or “not proven to be effective,” and CO151, in which the payer decides that there is insufficient support for the number or frequency of services provided, Ms. Girard said. “Take action on denials,” she emphasized. “Work with your payers and make a connection with them. We meet with our payers on a regular basis and show them what’s routinely being denied. Maybe you need to understand where they are coming from, and maybe you need to say to them that I really don’t agree with this, and here’s why.”
To minimize denials, practices also need to understand reimbursement policies and who is responsible for paying for services, she said. Information on coverage determinations can be found on payer websites under “medical policies,” or “reimbursement policies,” she noted. Medical policies list the payer’s criteria for covering specific services and diagnosis codes, while reimbursement policies specify how the payer handles issues such as bundling rules, global surgery, and multiple procedures for a single patient.
Practices can further limit their financial liability by obtaining signed advanced beneficiary notices (ABNs) from Medicare patients, Ms. Girard said. Without a signed ABN, patients cannot be billed for services that Medicare does not cover, leaving the practice holding the bill, she said. “Are you going to give away your services for free, or is it something the patient is going to pay for because they’ve signed an ABN?”
Ms. Girard declared no conflicts of interest.
FROM A SYMPOSIUM SPONSORED BY THE AMERICAN HEADACHE SOCIETY
Use PEARLS to build relationships with patients
SCOTTSDALE – Reasoning with patients can be challenging when they are demanding, have unrealistic expectations about their treatment, are emotionally reactive, or are seeking prescriptions for narcotics, Dr. David Gullen said. “These patients tax our patience and often our clinical skills, because they often don’t respond to the usual logic or presentation of treatment options,” Dr. Gullen said at a symposium sponsored by the American Headache Society.
But by switching the focus from logic to empathy, clinicians can transform relationships, even with very difficult patients who are dealing with migraine and other types of chronic pain, said Dr. Gullen, an internist who teaches communication skills to faculty, fellows, and residents at Mayo Clinic Arizona, Phoenix. Using empathy and other skills to improve relationships enhances physician and patient satisfaction, increases compliance, and improves clinical outcomes, he said.
“The question is, can the patient join you on a cognitive level?” Dr. Gullen concluded. “Often they can’t, but they may be able to join you on another level. It’s a noncognitive way of responding to them.”
Relationship building can also help clinicians heal the patient when they “don’t have a lot of medical options,” Dr. Gullen added. “I think that’s something our forebears knew 200 and 300 years ago,” he said. “Healers in the past had to use this approach because they didn’t have a lot of the tools we have today.”
To build relationships with patients, clinicians can use the mnemonic PEARLS – which stands for partnership, empathy, apology/acknowledgment, respect, legitimation, and support, Dr. Gullen said. For example, when seeing a new patient with migraine who has already tried and “failed” numerous medications, the clinician can use a partnership statement, such as, “I really want us to work on this together.” This approach increases the odds of creating a working relationship with the patient, he said.
“Empathy is probably the most important of all, because it’s your ability to convey to the patient that you understand their position,” Dr. Gullen emphasized. “Showing empathy for a patient’s perspective is not the same as endorsing it,” he added. “They may misunderstand what you’re telling them, or you may disagree with them. By showing that you understand their perspective, you’re not saying it’s correct, but you are saying you understand.”
An apology or acknowledgement could simply mean apologizing for running behind schedule or acknowledging a patient’s frustration with a treatment outcome.
Respecting a patient’s efforts to cope with the pain, and legitimizing the emotional response by letting the patient know it is normal and understandable also helps build trust. “Be aware of when you’re emotionally activated, so that you can use some of the PEARLS or respond with empathy, and take time to calm yourself down,” Dr. Gullen added.
How something is said to a patient matters as much as the words used, he said. “Think of a time in your life when you got a piece of advice that was really important for you to hear, but when you first heard it, it landed on you really badly,” he added. “Now think about getting that advice from someone you thought did not understand you or did not have your best interests at heart, compared with someone who you thought got you and really understood you. That’s why we emphasize the importance of relationship.”
Dr. Gullen declared no financial disclosures.
SCOTTSDALE – Reasoning with patients can be challenging when they are demanding, have unrealistic expectations about their treatment, are emotionally reactive, or are seeking prescriptions for narcotics, Dr. David Gullen said. “These patients tax our patience and often our clinical skills, because they often don’t respond to the usual logic or presentation of treatment options,” Dr. Gullen said at a symposium sponsored by the American Headache Society.
But by switching the focus from logic to empathy, clinicians can transform relationships, even with very difficult patients who are dealing with migraine and other types of chronic pain, said Dr. Gullen, an internist who teaches communication skills to faculty, fellows, and residents at Mayo Clinic Arizona, Phoenix. Using empathy and other skills to improve relationships enhances physician and patient satisfaction, increases compliance, and improves clinical outcomes, he said.
“The question is, can the patient join you on a cognitive level?” Dr. Gullen concluded. “Often they can’t, but they may be able to join you on another level. It’s a noncognitive way of responding to them.”
Relationship building can also help clinicians heal the patient when they “don’t have a lot of medical options,” Dr. Gullen added. “I think that’s something our forebears knew 200 and 300 years ago,” he said. “Healers in the past had to use this approach because they didn’t have a lot of the tools we have today.”
To build relationships with patients, clinicians can use the mnemonic PEARLS – which stands for partnership, empathy, apology/acknowledgment, respect, legitimation, and support, Dr. Gullen said. For example, when seeing a new patient with migraine who has already tried and “failed” numerous medications, the clinician can use a partnership statement, such as, “I really want us to work on this together.” This approach increases the odds of creating a working relationship with the patient, he said.
“Empathy is probably the most important of all, because it’s your ability to convey to the patient that you understand their position,” Dr. Gullen emphasized. “Showing empathy for a patient’s perspective is not the same as endorsing it,” he added. “They may misunderstand what you’re telling them, or you may disagree with them. By showing that you understand their perspective, you’re not saying it’s correct, but you are saying you understand.”
An apology or acknowledgement could simply mean apologizing for running behind schedule or acknowledging a patient’s frustration with a treatment outcome.
Respecting a patient’s efforts to cope with the pain, and legitimizing the emotional response by letting the patient know it is normal and understandable also helps build trust. “Be aware of when you’re emotionally activated, so that you can use some of the PEARLS or respond with empathy, and take time to calm yourself down,” Dr. Gullen added.
How something is said to a patient matters as much as the words used, he said. “Think of a time in your life when you got a piece of advice that was really important for you to hear, but when you first heard it, it landed on you really badly,” he added. “Now think about getting that advice from someone you thought did not understand you or did not have your best interests at heart, compared with someone who you thought got you and really understood you. That’s why we emphasize the importance of relationship.”
Dr. Gullen declared no financial disclosures.
SCOTTSDALE – Reasoning with patients can be challenging when they are demanding, have unrealistic expectations about their treatment, are emotionally reactive, or are seeking prescriptions for narcotics, Dr. David Gullen said. “These patients tax our patience and often our clinical skills, because they often don’t respond to the usual logic or presentation of treatment options,” Dr. Gullen said at a symposium sponsored by the American Headache Society.
But by switching the focus from logic to empathy, clinicians can transform relationships, even with very difficult patients who are dealing with migraine and other types of chronic pain, said Dr. Gullen, an internist who teaches communication skills to faculty, fellows, and residents at Mayo Clinic Arizona, Phoenix. Using empathy and other skills to improve relationships enhances physician and patient satisfaction, increases compliance, and improves clinical outcomes, he said.
“The question is, can the patient join you on a cognitive level?” Dr. Gullen concluded. “Often they can’t, but they may be able to join you on another level. It’s a noncognitive way of responding to them.”
Relationship building can also help clinicians heal the patient when they “don’t have a lot of medical options,” Dr. Gullen added. “I think that’s something our forebears knew 200 and 300 years ago,” he said. “Healers in the past had to use this approach because they didn’t have a lot of the tools we have today.”
To build relationships with patients, clinicians can use the mnemonic PEARLS – which stands for partnership, empathy, apology/acknowledgment, respect, legitimation, and support, Dr. Gullen said. For example, when seeing a new patient with migraine who has already tried and “failed” numerous medications, the clinician can use a partnership statement, such as, “I really want us to work on this together.” This approach increases the odds of creating a working relationship with the patient, he said.
“Empathy is probably the most important of all, because it’s your ability to convey to the patient that you understand their position,” Dr. Gullen emphasized. “Showing empathy for a patient’s perspective is not the same as endorsing it,” he added. “They may misunderstand what you’re telling them, or you may disagree with them. By showing that you understand their perspective, you’re not saying it’s correct, but you are saying you understand.”
An apology or acknowledgement could simply mean apologizing for running behind schedule or acknowledging a patient’s frustration with a treatment outcome.
Respecting a patient’s efforts to cope with the pain, and legitimizing the emotional response by letting the patient know it is normal and understandable also helps build trust. “Be aware of when you’re emotionally activated, so that you can use some of the PEARLS or respond with empathy, and take time to calm yourself down,” Dr. Gullen added.
How something is said to a patient matters as much as the words used, he said. “Think of a time in your life when you got a piece of advice that was really important for you to hear, but when you first heard it, it landed on you really badly,” he added. “Now think about getting that advice from someone you thought did not understand you or did not have your best interests at heart, compared with someone who you thought got you and really understood you. That’s why we emphasize the importance of relationship.”
Dr. Gullen declared no financial disclosures.
EXPERT ANALYSIS FROM A SYMPOSIUM SPONSORED BY THE AMERICAN HEADACHE SOCIETY