User login
Tips for taming atopic dermatitis and managing expectations
MIAMI – Tactics for managing patients with atopic dermatitis can go a long way to educate patients, set realistic expectations, and devise strategies for existing therapies, even as clinicians await some promising agents expected on the market soon.
“The good news is this is the Age of Eczema. In the last couple of years we’ve seen an explosion in the literature,” Adam Friedman, MD, of the department of dermatology, George Washington University, Washington, D.C., said at the Orlando Dermatology Aesthetic and Clinical Conference. Some of this research is spurring new therapeutics. a phosphodiesterase 4 inhibitor.
Crisaborole ointment, 2% (Eucrisa), a phosphodiesterase 4 inhibitor, was approved by the Food and Drug Administration in December 2016 for treating patients aged 2 years and older with mild to moderate AD, for example. It is a novel, nonsteroidal anti-inflammatory and the first prescription agent approved in the United States for atopic dermatitis in more than 10 years.
Dr. Friedman has no personal experience with crisaborole, which just became available. “But the data look encouraging. From what I’ve seen this may be a nonburning alternative to calcineurin inhibitors. It will be interesting to see how this will fit in our practices.”
Systemic management of pruritus
There’s also promise for patients troubled by one of the top manifestations of AD – the itch. “We have new targeted therapies coming down the pike, some hopefully [gaining approval] in the next few months. We have biologics going after the cytokines of itch. It’s a very, very exciting time right now,” Dr. Friedman said.
Current clinical trials are not only focusing on AD but also specifically on pruritus, he added.
In the meantime, itch can be managed with prescription and over-the-counter topical agents, as well as systemic therapies such as gabapentin, some antidepressants, and the antiemetic aprepitant. Aprepitant is a substance P antagonist (through blocking neurokinin 1 receptor) and can be effective for some patients when taken three times a week, but it is not indicated for itch, Dr. Friedman said. Because of its off label indication “it’s a little tricky getting [insurance] coverage.”
Back to basics
“Even with all the excitement, even with the new therapeutics, you have to stick with the basics,” he said. “Put the lotion on, put the cream on. You have to put moisturizer on wet skin and be cautious with soaps.” He added, “don’t be afraid to ask for help. The National Eczema Association has a wonderful website with research, education, tools – you name it.”
Keeping it real
For regional eczemas like hand dermatitis, what are the options? “Tell patients they can glove up, there are various latex alternatives … but it probably won’t fly in the real world,” Dr. Friedman said. Zinc oxide “works like armor, and patients will probably do well,” but the aesthetics are unacceptable for most, he added. “Newer alternatives, such as those with aluminum magnesium hydroxide stearate, have similar protecting power, but are not opaque and rub on easier.”
A goal of topical therapy is to get rid of the inflammation, and steroids have a long history of evidence supporting their use, but “topical steroid phobia in parents” is a problem, he said. To counter the reluctance or refusal to use topical steroids, he suggested exploring reasons for noncompliance, dispelling any myths, and working with parent to make it easier to apply the steroids to their child.
Interestingly, there is some evidence that a simpler regimen may work well for some patients. “We always say ‘apply twice a day.’ Why? Because all the clinical trials had participants apply steroids twice a day. But there is no evidence to show twice a day is better than once a day, and in fact, a meta-analysis suggests once a day works just as well” (Br J Dermatol. 2005 Jan;152[1]:130-41).
Topical calcineurin inhibitors are another option. In general, Dr. Friedman prescribes these agents for delicate areas, for patients with thin skin, or for patients who use a topical steroid “on and on and on and can’t seem to get off it.” Calcineurin inhibitors can also be used on in-between days during steroid maintenance therapy, he added. When prescribing, warn patients about the initial burn (due to substance P release) that commonly occurs so that they have realistic expectations.
Education remains essential
“I encourage you to educate your patients and empathize with them,” he said. “Show them how to apply a moisturizer. Also, use your nurses and assistants to help with education – really empower them to be part of the process.”
“Explain, explain, explain, so they have realistic expectations,” and know that there is no cure, so that when they experience a flare, they understand that “it’s not that the steroid didn’t work – this is a chronic disease,” added Dr. Friedman, who recommends providing patients with handouts that answer many of their questions.
Maximize moisturizing
When it comes to moisturizing, more is usually better. Effective products contain all the key ingredients: emollients to soften the skin, an occlusive to keep the water there, and a humectant to bond the water. “Just one or two is not going to cut it,” he said.
“Something we now know is that starting early is key,” he pointed out, referring to recent studies that have shown that in babies at high risk for AD, starting moisturizers early can decrease their risk for developing AD later (J Allergy Clin Immunol. 2014 Oct; 134[4]: 818-23).
“Another study that received a ton of press was in JAMA Pediatrics recently,” Dr. Friedman said. The study concluded that the use of different moisturizers to prevent AD in high risk babies was likely to be cost-effective (JAMA Pediatr. 2017 Feb 6;171[2]:e163909. doi: 10.1001/jamapediatrics.2016.3909). Although some news reports claimed starting babies with Vaseline as a moisturizer will prevent AD, “that’s actually not what the study showed. All the over-the-counter moisturizers they used worked, but Vaseline was the least expensive,” Dr. Friedman noted
Help patients select the right soap
Educate patients to avoid “true soaps” such as Dial, Ivory, Irish Spring, or Lever 2000. “Soaps can be a real enemy here. You want lower pH types of soaps. Depending on skin type, our skin is somewhere between 5.5 and 6.5 pH,” Dr. Friedman explained. “The paradigm shift for your patients is to hydrate, not to clean. Showers are okay if they’re not blaring hot. Baths are okay ... but you should not be sitting in a sudsy bath.”
Also, instruct patients to avoid irritating fabrics, dryer sheets, or harsh laundry detergents that could exacerbate AD.
‘You’re not alone’
Sometimes it’s helpful to assure patients with AD that they’re not alone, and that many researchers and clinicians are working on effective treatment strategies. “We’re all familiar with atopic dermatitis because there’s so much of it. The numbers are surprisingly high,” Dr. Friedman said. Compared with the estimated 2.2 million Americans with psoriasis, AD eclipses their numbers substantially, affecting about 17 million people.
Dr. Friedman disclosed that he is a speaker for Amgen, Janssen, and Promius; receives research grants from Valeant; and is a consultant and/or advisory board member for Amgen, Aveeno, Biogen, Encore, Exeltis, Ferndale, Galderma, G&W Laboratories, Intraderm, La Roche-Posay, Loreal, Microcures, Nano Bio-Med, Novartis, Oakstone Institute, Occulus, Onset, Pfizer, Promius, Sanova Works, and Valeant. Dr. Friedman is also an editorial advisory board member for Dermatology News.
MIAMI – Tactics for managing patients with atopic dermatitis can go a long way to educate patients, set realistic expectations, and devise strategies for existing therapies, even as clinicians await some promising agents expected on the market soon.
“The good news is this is the Age of Eczema. In the last couple of years we’ve seen an explosion in the literature,” Adam Friedman, MD, of the department of dermatology, George Washington University, Washington, D.C., said at the Orlando Dermatology Aesthetic and Clinical Conference. Some of this research is spurring new therapeutics. a phosphodiesterase 4 inhibitor.
Crisaborole ointment, 2% (Eucrisa), a phosphodiesterase 4 inhibitor, was approved by the Food and Drug Administration in December 2016 for treating patients aged 2 years and older with mild to moderate AD, for example. It is a novel, nonsteroidal anti-inflammatory and the first prescription agent approved in the United States for atopic dermatitis in more than 10 years.
Dr. Friedman has no personal experience with crisaborole, which just became available. “But the data look encouraging. From what I’ve seen this may be a nonburning alternative to calcineurin inhibitors. It will be interesting to see how this will fit in our practices.”
Systemic management of pruritus
There’s also promise for patients troubled by one of the top manifestations of AD – the itch. “We have new targeted therapies coming down the pike, some hopefully [gaining approval] in the next few months. We have biologics going after the cytokines of itch. It’s a very, very exciting time right now,” Dr. Friedman said.
Current clinical trials are not only focusing on AD but also specifically on pruritus, he added.
In the meantime, itch can be managed with prescription and over-the-counter topical agents, as well as systemic therapies such as gabapentin, some antidepressants, and the antiemetic aprepitant. Aprepitant is a substance P antagonist (through blocking neurokinin 1 receptor) and can be effective for some patients when taken three times a week, but it is not indicated for itch, Dr. Friedman said. Because of its off label indication “it’s a little tricky getting [insurance] coverage.”
Back to basics
“Even with all the excitement, even with the new therapeutics, you have to stick with the basics,” he said. “Put the lotion on, put the cream on. You have to put moisturizer on wet skin and be cautious with soaps.” He added, “don’t be afraid to ask for help. The National Eczema Association has a wonderful website with research, education, tools – you name it.”
Keeping it real
For regional eczemas like hand dermatitis, what are the options? “Tell patients they can glove up, there are various latex alternatives … but it probably won’t fly in the real world,” Dr. Friedman said. Zinc oxide “works like armor, and patients will probably do well,” but the aesthetics are unacceptable for most, he added. “Newer alternatives, such as those with aluminum magnesium hydroxide stearate, have similar protecting power, but are not opaque and rub on easier.”
A goal of topical therapy is to get rid of the inflammation, and steroids have a long history of evidence supporting their use, but “topical steroid phobia in parents” is a problem, he said. To counter the reluctance or refusal to use topical steroids, he suggested exploring reasons for noncompliance, dispelling any myths, and working with parent to make it easier to apply the steroids to their child.
Interestingly, there is some evidence that a simpler regimen may work well for some patients. “We always say ‘apply twice a day.’ Why? Because all the clinical trials had participants apply steroids twice a day. But there is no evidence to show twice a day is better than once a day, and in fact, a meta-analysis suggests once a day works just as well” (Br J Dermatol. 2005 Jan;152[1]:130-41).
Topical calcineurin inhibitors are another option. In general, Dr. Friedman prescribes these agents for delicate areas, for patients with thin skin, or for patients who use a topical steroid “on and on and on and can’t seem to get off it.” Calcineurin inhibitors can also be used on in-between days during steroid maintenance therapy, he added. When prescribing, warn patients about the initial burn (due to substance P release) that commonly occurs so that they have realistic expectations.
Education remains essential
“I encourage you to educate your patients and empathize with them,” he said. “Show them how to apply a moisturizer. Also, use your nurses and assistants to help with education – really empower them to be part of the process.”
“Explain, explain, explain, so they have realistic expectations,” and know that there is no cure, so that when they experience a flare, they understand that “it’s not that the steroid didn’t work – this is a chronic disease,” added Dr. Friedman, who recommends providing patients with handouts that answer many of their questions.
Maximize moisturizing
When it comes to moisturizing, more is usually better. Effective products contain all the key ingredients: emollients to soften the skin, an occlusive to keep the water there, and a humectant to bond the water. “Just one or two is not going to cut it,” he said.
“Something we now know is that starting early is key,” he pointed out, referring to recent studies that have shown that in babies at high risk for AD, starting moisturizers early can decrease their risk for developing AD later (J Allergy Clin Immunol. 2014 Oct; 134[4]: 818-23).
“Another study that received a ton of press was in JAMA Pediatrics recently,” Dr. Friedman said. The study concluded that the use of different moisturizers to prevent AD in high risk babies was likely to be cost-effective (JAMA Pediatr. 2017 Feb 6;171[2]:e163909. doi: 10.1001/jamapediatrics.2016.3909). Although some news reports claimed starting babies with Vaseline as a moisturizer will prevent AD, “that’s actually not what the study showed. All the over-the-counter moisturizers they used worked, but Vaseline was the least expensive,” Dr. Friedman noted
Help patients select the right soap
Educate patients to avoid “true soaps” such as Dial, Ivory, Irish Spring, or Lever 2000. “Soaps can be a real enemy here. You want lower pH types of soaps. Depending on skin type, our skin is somewhere between 5.5 and 6.5 pH,” Dr. Friedman explained. “The paradigm shift for your patients is to hydrate, not to clean. Showers are okay if they’re not blaring hot. Baths are okay ... but you should not be sitting in a sudsy bath.”
Also, instruct patients to avoid irritating fabrics, dryer sheets, or harsh laundry detergents that could exacerbate AD.
‘You’re not alone’
Sometimes it’s helpful to assure patients with AD that they’re not alone, and that many researchers and clinicians are working on effective treatment strategies. “We’re all familiar with atopic dermatitis because there’s so much of it. The numbers are surprisingly high,” Dr. Friedman said. Compared with the estimated 2.2 million Americans with psoriasis, AD eclipses their numbers substantially, affecting about 17 million people.
Dr. Friedman disclosed that he is a speaker for Amgen, Janssen, and Promius; receives research grants from Valeant; and is a consultant and/or advisory board member for Amgen, Aveeno, Biogen, Encore, Exeltis, Ferndale, Galderma, G&W Laboratories, Intraderm, La Roche-Posay, Loreal, Microcures, Nano Bio-Med, Novartis, Oakstone Institute, Occulus, Onset, Pfizer, Promius, Sanova Works, and Valeant. Dr. Friedman is also an editorial advisory board member for Dermatology News.
MIAMI – Tactics for managing patients with atopic dermatitis can go a long way to educate patients, set realistic expectations, and devise strategies for existing therapies, even as clinicians await some promising agents expected on the market soon.
“The good news is this is the Age of Eczema. In the last couple of years we’ve seen an explosion in the literature,” Adam Friedman, MD, of the department of dermatology, George Washington University, Washington, D.C., said at the Orlando Dermatology Aesthetic and Clinical Conference. Some of this research is spurring new therapeutics. a phosphodiesterase 4 inhibitor.
Crisaborole ointment, 2% (Eucrisa), a phosphodiesterase 4 inhibitor, was approved by the Food and Drug Administration in December 2016 for treating patients aged 2 years and older with mild to moderate AD, for example. It is a novel, nonsteroidal anti-inflammatory and the first prescription agent approved in the United States for atopic dermatitis in more than 10 years.
Dr. Friedman has no personal experience with crisaborole, which just became available. “But the data look encouraging. From what I’ve seen this may be a nonburning alternative to calcineurin inhibitors. It will be interesting to see how this will fit in our practices.”
Systemic management of pruritus
There’s also promise for patients troubled by one of the top manifestations of AD – the itch. “We have new targeted therapies coming down the pike, some hopefully [gaining approval] in the next few months. We have biologics going after the cytokines of itch. It’s a very, very exciting time right now,” Dr. Friedman said.
Current clinical trials are not only focusing on AD but also specifically on pruritus, he added.
In the meantime, itch can be managed with prescription and over-the-counter topical agents, as well as systemic therapies such as gabapentin, some antidepressants, and the antiemetic aprepitant. Aprepitant is a substance P antagonist (through blocking neurokinin 1 receptor) and can be effective for some patients when taken three times a week, but it is not indicated for itch, Dr. Friedman said. Because of its off label indication “it’s a little tricky getting [insurance] coverage.”
Back to basics
“Even with all the excitement, even with the new therapeutics, you have to stick with the basics,” he said. “Put the lotion on, put the cream on. You have to put moisturizer on wet skin and be cautious with soaps.” He added, “don’t be afraid to ask for help. The National Eczema Association has a wonderful website with research, education, tools – you name it.”
Keeping it real
For regional eczemas like hand dermatitis, what are the options? “Tell patients they can glove up, there are various latex alternatives … but it probably won’t fly in the real world,” Dr. Friedman said. Zinc oxide “works like armor, and patients will probably do well,” but the aesthetics are unacceptable for most, he added. “Newer alternatives, such as those with aluminum magnesium hydroxide stearate, have similar protecting power, but are not opaque and rub on easier.”
A goal of topical therapy is to get rid of the inflammation, and steroids have a long history of evidence supporting their use, but “topical steroid phobia in parents” is a problem, he said. To counter the reluctance or refusal to use topical steroids, he suggested exploring reasons for noncompliance, dispelling any myths, and working with parent to make it easier to apply the steroids to their child.
Interestingly, there is some evidence that a simpler regimen may work well for some patients. “We always say ‘apply twice a day.’ Why? Because all the clinical trials had participants apply steroids twice a day. But there is no evidence to show twice a day is better than once a day, and in fact, a meta-analysis suggests once a day works just as well” (Br J Dermatol. 2005 Jan;152[1]:130-41).
Topical calcineurin inhibitors are another option. In general, Dr. Friedman prescribes these agents for delicate areas, for patients with thin skin, or for patients who use a topical steroid “on and on and on and can’t seem to get off it.” Calcineurin inhibitors can also be used on in-between days during steroid maintenance therapy, he added. When prescribing, warn patients about the initial burn (due to substance P release) that commonly occurs so that they have realistic expectations.
Education remains essential
“I encourage you to educate your patients and empathize with them,” he said. “Show them how to apply a moisturizer. Also, use your nurses and assistants to help with education – really empower them to be part of the process.”
“Explain, explain, explain, so they have realistic expectations,” and know that there is no cure, so that when they experience a flare, they understand that “it’s not that the steroid didn’t work – this is a chronic disease,” added Dr. Friedman, who recommends providing patients with handouts that answer many of their questions.
Maximize moisturizing
When it comes to moisturizing, more is usually better. Effective products contain all the key ingredients: emollients to soften the skin, an occlusive to keep the water there, and a humectant to bond the water. “Just one or two is not going to cut it,” he said.
“Something we now know is that starting early is key,” he pointed out, referring to recent studies that have shown that in babies at high risk for AD, starting moisturizers early can decrease their risk for developing AD later (J Allergy Clin Immunol. 2014 Oct; 134[4]: 818-23).
“Another study that received a ton of press was in JAMA Pediatrics recently,” Dr. Friedman said. The study concluded that the use of different moisturizers to prevent AD in high risk babies was likely to be cost-effective (JAMA Pediatr. 2017 Feb 6;171[2]:e163909. doi: 10.1001/jamapediatrics.2016.3909). Although some news reports claimed starting babies with Vaseline as a moisturizer will prevent AD, “that’s actually not what the study showed. All the over-the-counter moisturizers they used worked, but Vaseline was the least expensive,” Dr. Friedman noted
Help patients select the right soap
Educate patients to avoid “true soaps” such as Dial, Ivory, Irish Spring, or Lever 2000. “Soaps can be a real enemy here. You want lower pH types of soaps. Depending on skin type, our skin is somewhere between 5.5 and 6.5 pH,” Dr. Friedman explained. “The paradigm shift for your patients is to hydrate, not to clean. Showers are okay if they’re not blaring hot. Baths are okay ... but you should not be sitting in a sudsy bath.”
Also, instruct patients to avoid irritating fabrics, dryer sheets, or harsh laundry detergents that could exacerbate AD.
‘You’re not alone’
Sometimes it’s helpful to assure patients with AD that they’re not alone, and that many researchers and clinicians are working on effective treatment strategies. “We’re all familiar with atopic dermatitis because there’s so much of it. The numbers are surprisingly high,” Dr. Friedman said. Compared with the estimated 2.2 million Americans with psoriasis, AD eclipses their numbers substantially, affecting about 17 million people.
Dr. Friedman disclosed that he is a speaker for Amgen, Janssen, and Promius; receives research grants from Valeant; and is a consultant and/or advisory board member for Amgen, Aveeno, Biogen, Encore, Exeltis, Ferndale, Galderma, G&W Laboratories, Intraderm, La Roche-Posay, Loreal, Microcures, Nano Bio-Med, Novartis, Oakstone Institute, Occulus, Onset, Pfizer, Promius, Sanova Works, and Valeant. Dr. Friedman is also an editorial advisory board member for Dermatology News.
AT ODAC 2017
Laser resurfacing can effectively minimize post surgery scars
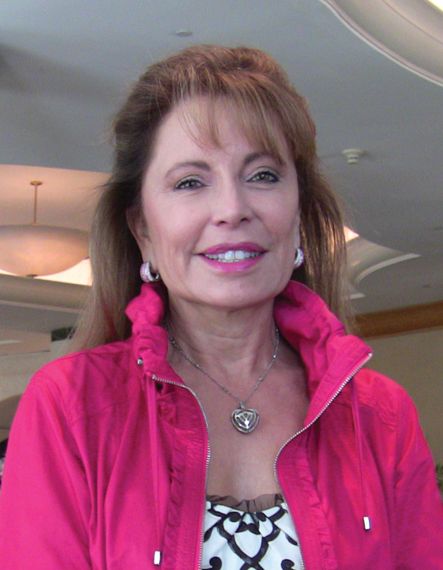
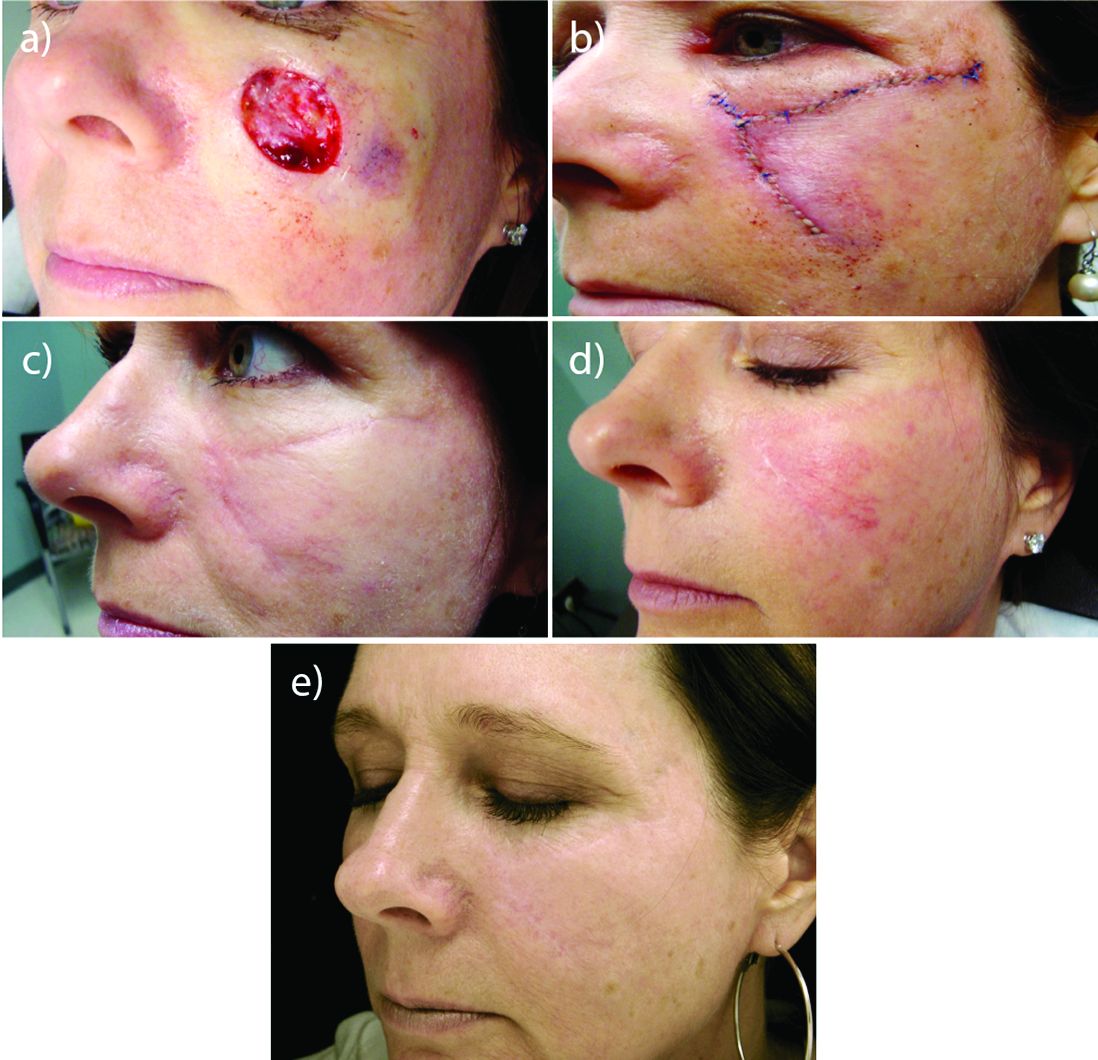
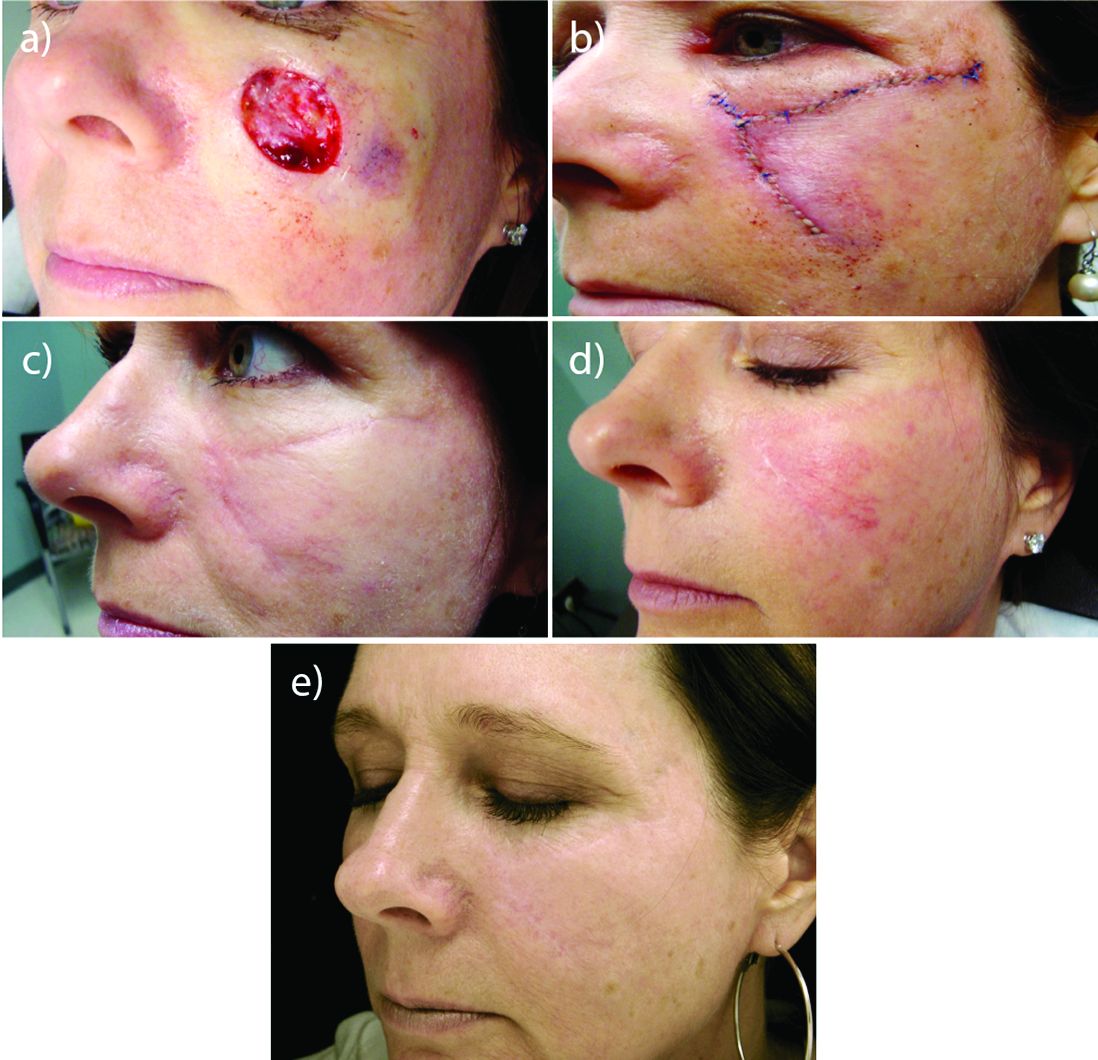
MIAMI – In his practice, Joel L. Cohen, MD, spends a good part of his day doing Mohs surgery, “with the goal of cancer removal, and after surgery, having the patient look good,” he said at the Orlando Dermatology Aesthetic and Clinical Conference.
“Having resurfacing in my practice has allowed me to treat not only wrinkles and etched lines, but also help skin cancer patients by blending and minimizing their skin cancer scars,” said Dr. Cohen, an aesthetic dermatologist and Mohs surgeon in private practice in Denver.
Resurfacing in his practice using a variety of lasers is very helpful, Dr. Cohen said. He published a study in November that compared pulse dye laser, CO2 ablative fractional lasers, or a combination of both for modification of scars following Mohs surgery (J Drugs Dermatol. 2016 Nov 1;15[11]:1315-9).
The prospective, multicenter study revealed that although both monotherapy approaches were safe and effective, the combination of pulse dye laser and fractional ablative laser offered some synergy that was preferred by patients.
Perioral resurfacing possible
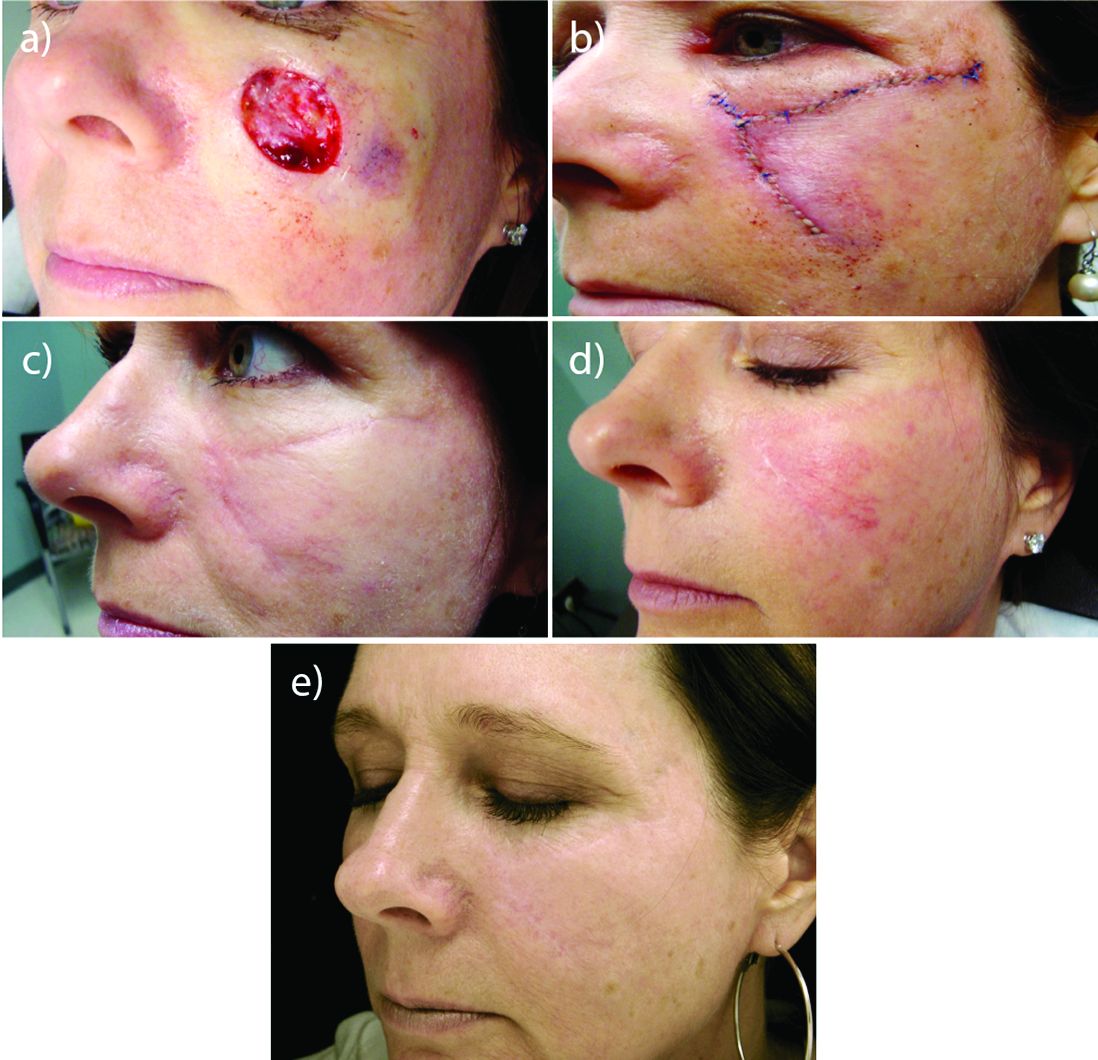
Beyond the world of treating scars, a typical cosmetic patient in Dr. Cohen’s practice presents with numerous lines around the perioral area. “When people think about rejuvenation of the lips, they only think of fillers. But fillers are not the only way to rejuvenate this area, and it is really about choosing the right tool for the right job – where resurfacing lasers are needed.”
Set realistic expectations
Setting the right expectations for people is extremely important, Dr. Cohen said. “You can educate the patient that if you’re putting the needle into the lines, you’re only treating the larger lines that you can get a 30-g needle into, but there are often a host of other lines in that area – many of which are too small to get a needle into.”
As a starting point, neuromodulators can have a role in trying to prevent or delay etched-in lines from forming around the mouth in the first place. “These are the lines between the musculature, the ones you see when you ask the patient to purse their lips,” Dr. Cohen said. He typically injects a medium dose of one of three neuromodulators – such as 6-10 U of onabotulinumtoxinA (Botox), 6-10 U of incobotulinumtoxinA (Xeomin) or 14-18 U of abobotulinumtoxinA (Dysport). “Then somewhere between week 8 and 10, there is an attenuation of the effect, and I often will see patients back then for additional treatment with a neuromodulator,” he added.
“For our every day patient complaining of lots of etched perioral lines, we have laser resurfacing,” Dr. Cohen noted. He is a bigger proponent of full-field erbium treatment versus fractional ablative laser resurfacing for these prominent upper cutaneous lip lines because the results are much more impressive with a single treatment. He added that dermatologists could do fractional treatment around the rest of the face, and reserve the erbium resurfacing to improve the appearance of lines around the mouth and prominent creping skin around the eyes.
Realistic postprocedure expectations are especially essential in the days after erbium laser resurfacing – as it is a tough downtime procedure for patients, often taking 7-9 days to re-epithelialize. “Having photos to show patients what they will look like is really helpful,” Dr. Cohen said. He suggested showing patients a chronologic set of photos of the downtime period as well as the results – so they realize improvement occurs slowly over time. “Getting people to understand they are gong to look terrible for 1.5-2 weeks is superimportant.”
“I like to have them back in the office for a postprocedure check a few days after the bigger laser resurfacing procedures are done, just to check on them,” Dr. Cohen said. “A lot of hand holding is often needed, as there is significantly more healing time with the full-field ablative resurfacing than there is with fractional. Full-field resurfacing patients will experience postprocedure erythema for a few weeks or even months,” Dr. Cohen said. A prescription of topical steroids, and sometimes some brimonidine topical gel (Mirvaso) as well can help reduce the redness.
Toxin injection then laser resurfacing
For some patients, injection of a neuromodulator a week or 2 before laser resurfacing treatment can decrease some of the movement and contraction of the muscle, “and hopefully give them better results,” Dr. Cohen said.
Timing is important. “You don’t want to use neuromodulators on the same day of treatment,” he advised. “The thinking is swelling could potentially cause the neuromodulators to spread to unwanted adjacent muscles.”
Safety first
Another tip for the postprocedure period is to supply patients with very specific written instructions. “I wish they would follow them. Patients don’t always listen to what we advise, demonstrate, and also have written down for them,” he commented. For example, one patient had resurfacing several weeks before leaving on an undisclosed kayaking trip. Despite instructions to use sunscreen, she said she wore a hat for sun protection and developed postinflammatory hyperpigmentation around the mouth that lasted for several months, Dr. Cohen said.*
With heavy resurfacing and ablative resurfacing in general, it is advised to always give patients an antiviral prophylaxis course such as valacyclovir, but it is unfortunate that not all patients will adhere to the recommended regimen, he added.
Another patient had an adverse reaction after resurfacing because she did not follow instructions to apply white petrolatum to her chest following laser resurfacing, Dr. Cohen said. She used Neosporin, “even though in all our paperwork we say never use Neosporin and just use the petrolatum. She had a big contact dermatitis reaction to the Neosporin.”
“So you really need to caution people about the importance of following instructions very carefully,” he emphasized.
Dr. Cohen is a consultant for Sciton and for companies that manufacture injectables, including Allergan, Galderma, and Merz.
Correction 2/24/17: An earlier version of this article mischaracterized the type of pigmentation disorder that the patient developed.
MIAMI – In his practice, Joel L. Cohen, MD, spends a good part of his day doing Mohs surgery, “with the goal of cancer removal, and after surgery, having the patient look good,” he said at the Orlando Dermatology Aesthetic and Clinical Conference.
“Having resurfacing in my practice has allowed me to treat not only wrinkles and etched lines, but also help skin cancer patients by blending and minimizing their skin cancer scars,” said Dr. Cohen, an aesthetic dermatologist and Mohs surgeon in private practice in Denver.
Resurfacing in his practice using a variety of lasers is very helpful, Dr. Cohen said. He published a study in November that compared pulse dye laser, CO2 ablative fractional lasers, or a combination of both for modification of scars following Mohs surgery (J Drugs Dermatol. 2016 Nov 1;15[11]:1315-9).
The prospective, multicenter study revealed that although both monotherapy approaches were safe and effective, the combination of pulse dye laser and fractional ablative laser offered some synergy that was preferred by patients.
Perioral resurfacing possible
Beyond the world of treating scars, a typical cosmetic patient in Dr. Cohen’s practice presents with numerous lines around the perioral area. “When people think about rejuvenation of the lips, they only think of fillers. But fillers are not the only way to rejuvenate this area, and it is really about choosing the right tool for the right job – where resurfacing lasers are needed.”
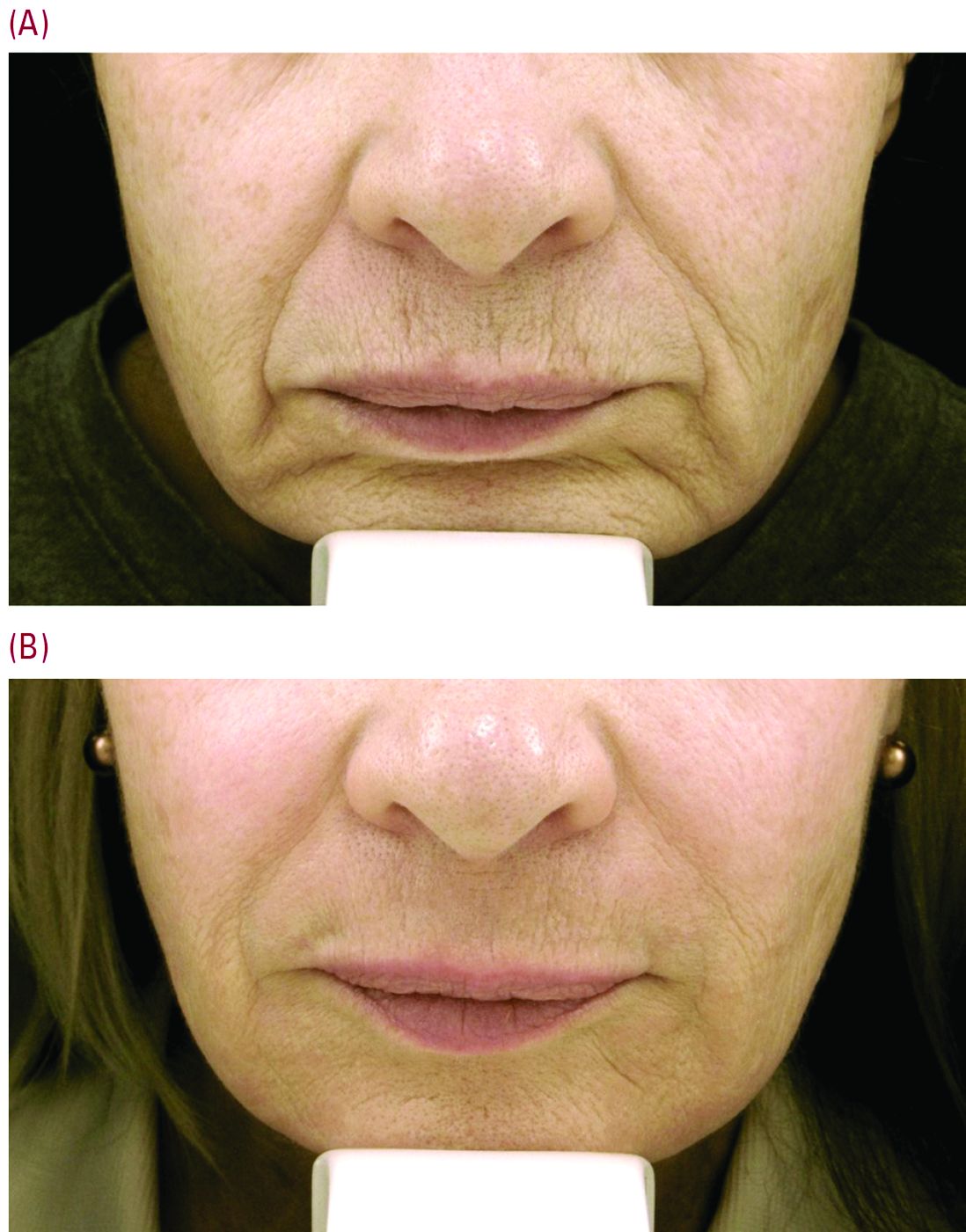
Set realistic expectations
Setting the right expectations for people is extremely important, Dr. Cohen said. “You can educate the patient that if you’re putting the needle into the lines, you’re only treating the larger lines that you can get a 30-g needle into, but there are often a host of other lines in that area – many of which are too small to get a needle into.”
As a starting point, neuromodulators can have a role in trying to prevent or delay etched-in lines from forming around the mouth in the first place. “These are the lines between the musculature, the ones you see when you ask the patient to purse their lips,” Dr. Cohen said. He typically injects a medium dose of one of three neuromodulators – such as 6-10 U of onabotulinumtoxinA (Botox), 6-10 U of incobotulinumtoxinA (Xeomin) or 14-18 U of abobotulinumtoxinA (Dysport). “Then somewhere between week 8 and 10, there is an attenuation of the effect, and I often will see patients back then for additional treatment with a neuromodulator,” he added.
“For our every day patient complaining of lots of etched perioral lines, we have laser resurfacing,” Dr. Cohen noted. He is a bigger proponent of full-field erbium treatment versus fractional ablative laser resurfacing for these prominent upper cutaneous lip lines because the results are much more impressive with a single treatment. He added that dermatologists could do fractional treatment around the rest of the face, and reserve the erbium resurfacing to improve the appearance of lines around the mouth and prominent creping skin around the eyes.
Realistic postprocedure expectations are especially essential in the days after erbium laser resurfacing – as it is a tough downtime procedure for patients, often taking 7-9 days to re-epithelialize. “Having photos to show patients what they will look like is really helpful,” Dr. Cohen said. He suggested showing patients a chronologic set of photos of the downtime period as well as the results – so they realize improvement occurs slowly over time. “Getting people to understand they are gong to look terrible for 1.5-2 weeks is superimportant.”
“I like to have them back in the office for a postprocedure check a few days after the bigger laser resurfacing procedures are done, just to check on them,” Dr. Cohen said. “A lot of hand holding is often needed, as there is significantly more healing time with the full-field ablative resurfacing than there is with fractional. Full-field resurfacing patients will experience postprocedure erythema for a few weeks or even months,” Dr. Cohen said. A prescription of topical steroids, and sometimes some brimonidine topical gel (Mirvaso) as well can help reduce the redness.
Toxin injection then laser resurfacing
For some patients, injection of a neuromodulator a week or 2 before laser resurfacing treatment can decrease some of the movement and contraction of the muscle, “and hopefully give them better results,” Dr. Cohen said.
Timing is important. “You don’t want to use neuromodulators on the same day of treatment,” he advised. “The thinking is swelling could potentially cause the neuromodulators to spread to unwanted adjacent muscles.”
Safety first
Another tip for the postprocedure period is to supply patients with very specific written instructions. “I wish they would follow them. Patients don’t always listen to what we advise, demonstrate, and also have written down for them,” he commented. For example, one patient had resurfacing several weeks before leaving on an undisclosed kayaking trip. Despite instructions to use sunscreen, she said she wore a hat for sun protection and developed postinflammatory hyperpigmentation around the mouth that lasted for several months, Dr. Cohen said.*
With heavy resurfacing and ablative resurfacing in general, it is advised to always give patients an antiviral prophylaxis course such as valacyclovir, but it is unfortunate that not all patients will adhere to the recommended regimen, he added.
Another patient had an adverse reaction after resurfacing because she did not follow instructions to apply white petrolatum to her chest following laser resurfacing, Dr. Cohen said. She used Neosporin, “even though in all our paperwork we say never use Neosporin and just use the petrolatum. She had a big contact dermatitis reaction to the Neosporin.”
“So you really need to caution people about the importance of following instructions very carefully,” he emphasized.
Dr. Cohen is a consultant for Sciton and for companies that manufacture injectables, including Allergan, Galderma, and Merz.
Correction 2/24/17: An earlier version of this article mischaracterized the type of pigmentation disorder that the patient developed.
MIAMI – In his practice, Joel L. Cohen, MD, spends a good part of his day doing Mohs surgery, “with the goal of cancer removal, and after surgery, having the patient look good,” he said at the Orlando Dermatology Aesthetic and Clinical Conference.
“Having resurfacing in my practice has allowed me to treat not only wrinkles and etched lines, but also help skin cancer patients by blending and minimizing their skin cancer scars,” said Dr. Cohen, an aesthetic dermatologist and Mohs surgeon in private practice in Denver.
Resurfacing in his practice using a variety of lasers is very helpful, Dr. Cohen said. He published a study in November that compared pulse dye laser, CO2 ablative fractional lasers, or a combination of both for modification of scars following Mohs surgery (J Drugs Dermatol. 2016 Nov 1;15[11]:1315-9).
The prospective, multicenter study revealed that although both monotherapy approaches were safe and effective, the combination of pulse dye laser and fractional ablative laser offered some synergy that was preferred by patients.
Perioral resurfacing possible
Beyond the world of treating scars, a typical cosmetic patient in Dr. Cohen’s practice presents with numerous lines around the perioral area. “When people think about rejuvenation of the lips, they only think of fillers. But fillers are not the only way to rejuvenate this area, and it is really about choosing the right tool for the right job – where resurfacing lasers are needed.”
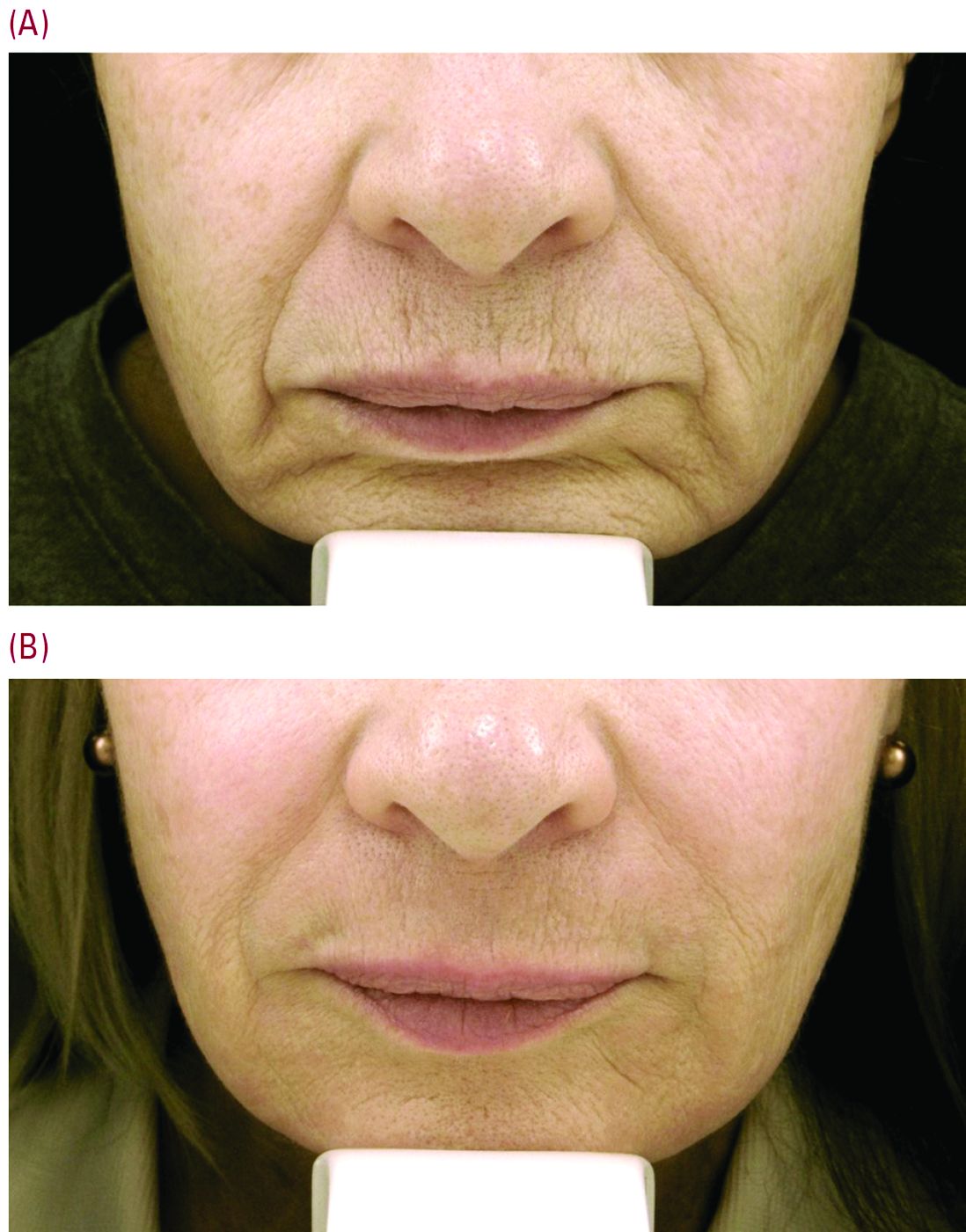
Set realistic expectations
Setting the right expectations for people is extremely important, Dr. Cohen said. “You can educate the patient that if you’re putting the needle into the lines, you’re only treating the larger lines that you can get a 30-g needle into, but there are often a host of other lines in that area – many of which are too small to get a needle into.”
As a starting point, neuromodulators can have a role in trying to prevent or delay etched-in lines from forming around the mouth in the first place. “These are the lines between the musculature, the ones you see when you ask the patient to purse their lips,” Dr. Cohen said. He typically injects a medium dose of one of three neuromodulators – such as 6-10 U of onabotulinumtoxinA (Botox), 6-10 U of incobotulinumtoxinA (Xeomin) or 14-18 U of abobotulinumtoxinA (Dysport). “Then somewhere between week 8 and 10, there is an attenuation of the effect, and I often will see patients back then for additional treatment with a neuromodulator,” he added.
“For our every day patient complaining of lots of etched perioral lines, we have laser resurfacing,” Dr. Cohen noted. He is a bigger proponent of full-field erbium treatment versus fractional ablative laser resurfacing for these prominent upper cutaneous lip lines because the results are much more impressive with a single treatment. He added that dermatologists could do fractional treatment around the rest of the face, and reserve the erbium resurfacing to improve the appearance of lines around the mouth and prominent creping skin around the eyes.
Realistic postprocedure expectations are especially essential in the days after erbium laser resurfacing – as it is a tough downtime procedure for patients, often taking 7-9 days to re-epithelialize. “Having photos to show patients what they will look like is really helpful,” Dr. Cohen said. He suggested showing patients a chronologic set of photos of the downtime period as well as the results – so they realize improvement occurs slowly over time. “Getting people to understand they are gong to look terrible for 1.5-2 weeks is superimportant.”
“I like to have them back in the office for a postprocedure check a few days after the bigger laser resurfacing procedures are done, just to check on them,” Dr. Cohen said. “A lot of hand holding is often needed, as there is significantly more healing time with the full-field ablative resurfacing than there is with fractional. Full-field resurfacing patients will experience postprocedure erythema for a few weeks or even months,” Dr. Cohen said. A prescription of topical steroids, and sometimes some brimonidine topical gel (Mirvaso) as well can help reduce the redness.
Toxin injection then laser resurfacing
For some patients, injection of a neuromodulator a week or 2 before laser resurfacing treatment can decrease some of the movement and contraction of the muscle, “and hopefully give them better results,” Dr. Cohen said.
Timing is important. “You don’t want to use neuromodulators on the same day of treatment,” he advised. “The thinking is swelling could potentially cause the neuromodulators to spread to unwanted adjacent muscles.”
Safety first
Another tip for the postprocedure period is to supply patients with very specific written instructions. “I wish they would follow them. Patients don’t always listen to what we advise, demonstrate, and also have written down for them,” he commented. For example, one patient had resurfacing several weeks before leaving on an undisclosed kayaking trip. Despite instructions to use sunscreen, she said she wore a hat for sun protection and developed postinflammatory hyperpigmentation around the mouth that lasted for several months, Dr. Cohen said.*
With heavy resurfacing and ablative resurfacing in general, it is advised to always give patients an antiviral prophylaxis course such as valacyclovir, but it is unfortunate that not all patients will adhere to the recommended regimen, he added.
Another patient had an adverse reaction after resurfacing because she did not follow instructions to apply white petrolatum to her chest following laser resurfacing, Dr. Cohen said. She used Neosporin, “even though in all our paperwork we say never use Neosporin and just use the petrolatum. She had a big contact dermatitis reaction to the Neosporin.”
“So you really need to caution people about the importance of following instructions very carefully,” he emphasized.
Dr. Cohen is a consultant for Sciton and for companies that manufacture injectables, including Allergan, Galderma, and Merz.
Correction 2/24/17: An earlier version of this article mischaracterized the type of pigmentation disorder that the patient developed.
EXPERT ANALYSIS FROM THE ODAC CONFERENCE
Essential tips to diagnose and intervene early in hair loss
MIAMI – and watch for a new trend – man bun traction alopecia.
These and other clinical pearls on hair loss come courtesy of Wendy E. Roberts, MD.
“Hair loss can be scary,” but if physicians diagnose the underlying cause and treat early, a number of existing and upcoming treatments can be effective, said Dr. Roberts, a dermatologist in private practice in Rancho Mirage, Calif. “Timing is very critical.”
A dermatology full body examination is a perfect opportunity to ask patients about their hair because “you’re checking them from head to toe,” Dr. Roberts said. She recommends asking: “How is your hair doing?” This advice prompted a bit of uproar from the ODAC audience, suggesting this may be too sensitive a subject for some to broach with patients. Dr. Roberts responded, “No, not at all. Your patients will be glad you asked.
“That simple question will open up doors of opportunity” for dermatologists, she said. The condition remains very common: About 80 million people in the United States are affected by its No. 1 cause, hereditary hair loss. An Internet search for “hair loss,” in fact, reveals an overwhelming amount of consumer interest in hair loss treatment and management, yielding approximately 35 million results.
Paying attention to hair loss is not just question of appearance or aesthetics; hair loss can also indicate declining health, Dr. Roberts said at the Orlando Dermatology Aesthetic and Clinical Conference.
Suggest supplements backed by science
Given the millions of online searches, it’s apparent that people continue to look for the latest solutions to treat or prevent further hair loss. But as with many “treatments” and “cures” touted online, caution is warranted – not every claim is backed by solid research, she said. “Go with supplements that do have peer review literature.”
For this reason, Dr. Roberts suggests considering the following three supplements for patients with hair loss:
• Nutrafol – “What I like about this supplement is it has ashwagandha, an Indian herb that reduces stress,” she said.
• Viviscal – This supplement has the marine extract AminoMar, which includes shark cartilage and oyster extract powder.
• Vitalize Hair – Its active ingredient, Redensyl, contains two molecules, Dr. Roberts said, one to boost metabolism of the hair follicle and the other to increase hair volume over time.
Application of platelet rich plasma is another option showing promise for hair loss. It works by activating hair bulb cells. “It kind of whispers to the hair: ‘Be young again.’ Many times it comes in at the original hair color – tell your patients to be prepared to see their hair color from childhood.” Dr. Roberts said.
Man bun alert
There is a new consideration in male hair loss based on changing hairstyles. “One thing that is trending: man bun traction alopecia. We see a lot of this in Southern California where I practice,” Dr. Roberts said. She showed meeting attendees the photo of a man with a tight hair bun whose hairline was starting to recede.
Basics to remember: differential diagnosis
When a patient presents with hair loss, things to consider in a differential diagnosis include chemical hair treatments, hairstyles that can cause traction alopecia, and behaviors such as compulsive hair pulling. Trichotillomania is on the increase. It affects approximately 2% of the population, but 90% of those are women, Dr. Roberts said. To diagnose, “look at the scalp and lower area near the nape of neck, especially in younger patients.”
She suggested that dermatologists show male patients the Norwood Scale illustrations of hair loss. The illustrations can help them understand when their hair loss is progressing over time, she added. For female patients with hair loss, the Ludwig Scale for hair loss in women can be very illustrative.
In the work-up of the patient, conduct a physical exam and consider overall health and nutritional status. Ask about family history as well, because relatives are the best window for insight into hair loss caused by genetics and aging, Dr. Roberts said.
Review patient medications. Older patients, in particular, often take multiple medications, which increases the likelihood for interactions or side effects leading to hair loss.
In addition, she had a few specific recommendations. “When you have male patient with hair loss taking Propecia [finasteride], talk to them about the dangers of exposure to a female partner and pregnancy in particular.” Also ask patients to bring in any supplements they are taking. Watch out for keratin supplements in patients with renal disease, she added, because elevated levels can be associated with kidney problems.
In terms of laboratory testing, consider checking for thyroid function, hormonal imbalance, and anemia. “The most overlooked is hemoglobin levels,” Dr. Roberts said, although anemia can cause hair loss in some patients.
Dr. Roberts is a speaker, consultant, investigator for and/or receives honoraria from Allergan, Colorescience, Galderma, Lytera, MDRejuvena, Restorsea, SkinMedica, Theraplex, Top MD Skincare, Valeant Pharmaceutical International, and Viviscal.
MIAMI – and watch for a new trend – man bun traction alopecia.
These and other clinical pearls on hair loss come courtesy of Wendy E. Roberts, MD.
“Hair loss can be scary,” but if physicians diagnose the underlying cause and treat early, a number of existing and upcoming treatments can be effective, said Dr. Roberts, a dermatologist in private practice in Rancho Mirage, Calif. “Timing is very critical.”
A dermatology full body examination is a perfect opportunity to ask patients about their hair because “you’re checking them from head to toe,” Dr. Roberts said. She recommends asking: “How is your hair doing?” This advice prompted a bit of uproar from the ODAC audience, suggesting this may be too sensitive a subject for some to broach with patients. Dr. Roberts responded, “No, not at all. Your patients will be glad you asked.
“That simple question will open up doors of opportunity” for dermatologists, she said. The condition remains very common: About 80 million people in the United States are affected by its No. 1 cause, hereditary hair loss. An Internet search for “hair loss,” in fact, reveals an overwhelming amount of consumer interest in hair loss treatment and management, yielding approximately 35 million results.
Paying attention to hair loss is not just question of appearance or aesthetics; hair loss can also indicate declining health, Dr. Roberts said at the Orlando Dermatology Aesthetic and Clinical Conference.
Suggest supplements backed by science
Given the millions of online searches, it’s apparent that people continue to look for the latest solutions to treat or prevent further hair loss. But as with many “treatments” and “cures” touted online, caution is warranted – not every claim is backed by solid research, she said. “Go with supplements that do have peer review literature.”
For this reason, Dr. Roberts suggests considering the following three supplements for patients with hair loss:
• Nutrafol – “What I like about this supplement is it has ashwagandha, an Indian herb that reduces stress,” she said.
• Viviscal – This supplement has the marine extract AminoMar, which includes shark cartilage and oyster extract powder.
• Vitalize Hair – Its active ingredient, Redensyl, contains two molecules, Dr. Roberts said, one to boost metabolism of the hair follicle and the other to increase hair volume over time.
Application of platelet rich plasma is another option showing promise for hair loss. It works by activating hair bulb cells. “It kind of whispers to the hair: ‘Be young again.’ Many times it comes in at the original hair color – tell your patients to be prepared to see their hair color from childhood.” Dr. Roberts said.
Man bun alert
There is a new consideration in male hair loss based on changing hairstyles. “One thing that is trending: man bun traction alopecia. We see a lot of this in Southern California where I practice,” Dr. Roberts said. She showed meeting attendees the photo of a man with a tight hair bun whose hairline was starting to recede.
Basics to remember: differential diagnosis
When a patient presents with hair loss, things to consider in a differential diagnosis include chemical hair treatments, hairstyles that can cause traction alopecia, and behaviors such as compulsive hair pulling. Trichotillomania is on the increase. It affects approximately 2% of the population, but 90% of those are women, Dr. Roberts said. To diagnose, “look at the scalp and lower area near the nape of neck, especially in younger patients.”
She suggested that dermatologists show male patients the Norwood Scale illustrations of hair loss. The illustrations can help them understand when their hair loss is progressing over time, she added. For female patients with hair loss, the Ludwig Scale for hair loss in women can be very illustrative.
In the work-up of the patient, conduct a physical exam and consider overall health and nutritional status. Ask about family history as well, because relatives are the best window for insight into hair loss caused by genetics and aging, Dr. Roberts said.
Review patient medications. Older patients, in particular, often take multiple medications, which increases the likelihood for interactions or side effects leading to hair loss.
In addition, she had a few specific recommendations. “When you have male patient with hair loss taking Propecia [finasteride], talk to them about the dangers of exposure to a female partner and pregnancy in particular.” Also ask patients to bring in any supplements they are taking. Watch out for keratin supplements in patients with renal disease, she added, because elevated levels can be associated with kidney problems.
In terms of laboratory testing, consider checking for thyroid function, hormonal imbalance, and anemia. “The most overlooked is hemoglobin levels,” Dr. Roberts said, although anemia can cause hair loss in some patients.
Dr. Roberts is a speaker, consultant, investigator for and/or receives honoraria from Allergan, Colorescience, Galderma, Lytera, MDRejuvena, Restorsea, SkinMedica, Theraplex, Top MD Skincare, Valeant Pharmaceutical International, and Viviscal.
MIAMI – and watch for a new trend – man bun traction alopecia.
These and other clinical pearls on hair loss come courtesy of Wendy E. Roberts, MD.
“Hair loss can be scary,” but if physicians diagnose the underlying cause and treat early, a number of existing and upcoming treatments can be effective, said Dr. Roberts, a dermatologist in private practice in Rancho Mirage, Calif. “Timing is very critical.”
A dermatology full body examination is a perfect opportunity to ask patients about their hair because “you’re checking them from head to toe,” Dr. Roberts said. She recommends asking: “How is your hair doing?” This advice prompted a bit of uproar from the ODAC audience, suggesting this may be too sensitive a subject for some to broach with patients. Dr. Roberts responded, “No, not at all. Your patients will be glad you asked.
“That simple question will open up doors of opportunity” for dermatologists, she said. The condition remains very common: About 80 million people in the United States are affected by its No. 1 cause, hereditary hair loss. An Internet search for “hair loss,” in fact, reveals an overwhelming amount of consumer interest in hair loss treatment and management, yielding approximately 35 million results.
Paying attention to hair loss is not just question of appearance or aesthetics; hair loss can also indicate declining health, Dr. Roberts said at the Orlando Dermatology Aesthetic and Clinical Conference.
Suggest supplements backed by science
Given the millions of online searches, it’s apparent that people continue to look for the latest solutions to treat or prevent further hair loss. But as with many “treatments” and “cures” touted online, caution is warranted – not every claim is backed by solid research, she said. “Go with supplements that do have peer review literature.”
For this reason, Dr. Roberts suggests considering the following three supplements for patients with hair loss:
• Nutrafol – “What I like about this supplement is it has ashwagandha, an Indian herb that reduces stress,” she said.
• Viviscal – This supplement has the marine extract AminoMar, which includes shark cartilage and oyster extract powder.
• Vitalize Hair – Its active ingredient, Redensyl, contains two molecules, Dr. Roberts said, one to boost metabolism of the hair follicle and the other to increase hair volume over time.
Application of platelet rich plasma is another option showing promise for hair loss. It works by activating hair bulb cells. “It kind of whispers to the hair: ‘Be young again.’ Many times it comes in at the original hair color – tell your patients to be prepared to see their hair color from childhood.” Dr. Roberts said.
Man bun alert
There is a new consideration in male hair loss based on changing hairstyles. “One thing that is trending: man bun traction alopecia. We see a lot of this in Southern California where I practice,” Dr. Roberts said. She showed meeting attendees the photo of a man with a tight hair bun whose hairline was starting to recede.
Basics to remember: differential diagnosis
When a patient presents with hair loss, things to consider in a differential diagnosis include chemical hair treatments, hairstyles that can cause traction alopecia, and behaviors such as compulsive hair pulling. Trichotillomania is on the increase. It affects approximately 2% of the population, but 90% of those are women, Dr. Roberts said. To diagnose, “look at the scalp and lower area near the nape of neck, especially in younger patients.”
She suggested that dermatologists show male patients the Norwood Scale illustrations of hair loss. The illustrations can help them understand when their hair loss is progressing over time, she added. For female patients with hair loss, the Ludwig Scale for hair loss in women can be very illustrative.
In the work-up of the patient, conduct a physical exam and consider overall health and nutritional status. Ask about family history as well, because relatives are the best window for insight into hair loss caused by genetics and aging, Dr. Roberts said.
Review patient medications. Older patients, in particular, often take multiple medications, which increases the likelihood for interactions or side effects leading to hair loss.
In addition, she had a few specific recommendations. “When you have male patient with hair loss taking Propecia [finasteride], talk to them about the dangers of exposure to a female partner and pregnancy in particular.” Also ask patients to bring in any supplements they are taking. Watch out for keratin supplements in patients with renal disease, she added, because elevated levels can be associated with kidney problems.
In terms of laboratory testing, consider checking for thyroid function, hormonal imbalance, and anemia. “The most overlooked is hemoglobin levels,” Dr. Roberts said, although anemia can cause hair loss in some patients.
Dr. Roberts is a speaker, consultant, investigator for and/or receives honoraria from Allergan, Colorescience, Galderma, Lytera, MDRejuvena, Restorsea, SkinMedica, Theraplex, Top MD Skincare, Valeant Pharmaceutical International, and Viviscal.
EXPERT ANALYSIS FROM ODAC 2017
Dual fractional laser offers advantages for facial rejuvenation
MIAMI – A device that combines nonablative and ablative laser energies can promote mild to moderate facial photo rejuvenation and improve the appearance of fine lines and wrinkles, according to Jason Pozner, MD.
Clinicians can tailor the depth for the 1470 nm nonablative diode and the 2940 nm Er:YAG lasers for each individual patient, Dr. Pozner said at the Orlando Dermatology Aesthetic and Clinical Conference. Advantages of resurfacing with the device, the HALO laser, include a cost-effective disposable tip and the ability to combine treatment with other therapies, he noted.
Before treatment begins, clinicians use the device to take facial measurements. Many patients find this precision reassuring, Dr. Pozner said during a live patient demonstration. Also, the device uses the information to help clinicians deliver the appropriate duration of therapy.
At this stage, it is a simple procedure, said Dr. Pozner, a plastic surgeon in a group practice in Boca Raton, Fla. Suction is turned on and the probe is then slowly advanced back and forth until the zone is finished, and “the laser beeps at you and you know you’re done,” he explained.
The HALO laser is useful for rejuvenation with little downtime. Most women treated with the device can wear makeup the same day, although more aggressively treated patients generally wait 1 additional day, Dr. Pozner said.
“I’ve never seen anything in our practice that gives this good a clinical result with this little downtime,” he added. He initially expected results to fall in between those associated with typical nonablative and ablative fractional laser treatments. But “in our experience, we get better results than ablative fractional [laser therapy], a story of one plus one equals three,” he said. “No matter what laser setting you use, patients are better by 5 days.”
When combined with intense pulsed light (IPL) treatment you can get a “double whammy effect,” Dr. Pozner said.
A meeting attendee asked about the appropriate order of IPL and HALO treatments. “When you combine the BBL (IPL) and HALO, yes, you do the IPL first,” Joel L. Cohen, MD, a private practice aesthetic dermatologist and Mohs surgeon in Denver who moderated the session at the meeting and also gave his own lecture on resurfacing options for the face.
Aside from the laser itself, the HALO system contains two tubes integrated into the handpiece, one of which is a Zimmer to deliver cooling during the procedure and the other is an air evacuator, he explained. “By having all of this integrated into the handpiece itself, it makes it much easier for the nurse who is circulating in the room to assist.”
Patients may feel warm for about 90 minutes post procedure, Dr. Cohen said. Make sure patients’ hands are clean and that the circulating nurse has given them an ice pack to minimize discomfort. “Even though I practice in Denver, where it is freezing cold right now, I’ve had patients drive home with the air conditioning on – just to try to cool down in the hour or so immediately following the laser treatment.”
Dr. Pozner said that a decrease in pore counts was an unexpected effect of HALO treatment, and he estimated that patients end up with about 20% fewer pores in treated areas, which can be advantage because “nothing else works on pores.” In his experience, most of the pore reduction persists over time.
A HALO disposal tip costs approximately $50, which he said was inexpensive, compared with other devices.
Dr. Cohen said that in his practice, using HALO, “We can give patients a significant improvement in overall photodamage and mild improvement in wrinkles with only about 5 days of redness and swelling, and on the last few days, some coffee-ground appearance.” The nonablative component can promote coagulation, so there is less bleeding when you turn up the erbium component, “offering synergistic results for the patient,” he added.
Dr. Pozner has received equipment, consulting fees, and honoraria from Halo manufacturer Sciton and is a member of the company’s advisory board and speakers bureau. Dr. Cohen is a consultant for Sciton.
MIAMI – A device that combines nonablative and ablative laser energies can promote mild to moderate facial photo rejuvenation and improve the appearance of fine lines and wrinkles, according to Jason Pozner, MD.
Clinicians can tailor the depth for the 1470 nm nonablative diode and the 2940 nm Er:YAG lasers for each individual patient, Dr. Pozner said at the Orlando Dermatology Aesthetic and Clinical Conference. Advantages of resurfacing with the device, the HALO laser, include a cost-effective disposable tip and the ability to combine treatment with other therapies, he noted.
Before treatment begins, clinicians use the device to take facial measurements. Many patients find this precision reassuring, Dr. Pozner said during a live patient demonstration. Also, the device uses the information to help clinicians deliver the appropriate duration of therapy.
At this stage, it is a simple procedure, said Dr. Pozner, a plastic surgeon in a group practice in Boca Raton, Fla. Suction is turned on and the probe is then slowly advanced back and forth until the zone is finished, and “the laser beeps at you and you know you’re done,” he explained.
The HALO laser is useful for rejuvenation with little downtime. Most women treated with the device can wear makeup the same day, although more aggressively treated patients generally wait 1 additional day, Dr. Pozner said.
“I’ve never seen anything in our practice that gives this good a clinical result with this little downtime,” he added. He initially expected results to fall in between those associated with typical nonablative and ablative fractional laser treatments. But “in our experience, we get better results than ablative fractional [laser therapy], a story of one plus one equals three,” he said. “No matter what laser setting you use, patients are better by 5 days.”
When combined with intense pulsed light (IPL) treatment you can get a “double whammy effect,” Dr. Pozner said.
A meeting attendee asked about the appropriate order of IPL and HALO treatments. “When you combine the BBL (IPL) and HALO, yes, you do the IPL first,” Joel L. Cohen, MD, a private practice aesthetic dermatologist and Mohs surgeon in Denver who moderated the session at the meeting and also gave his own lecture on resurfacing options for the face.
Aside from the laser itself, the HALO system contains two tubes integrated into the handpiece, one of which is a Zimmer to deliver cooling during the procedure and the other is an air evacuator, he explained. “By having all of this integrated into the handpiece itself, it makes it much easier for the nurse who is circulating in the room to assist.”
Patients may feel warm for about 90 minutes post procedure, Dr. Cohen said. Make sure patients’ hands are clean and that the circulating nurse has given them an ice pack to minimize discomfort. “Even though I practice in Denver, where it is freezing cold right now, I’ve had patients drive home with the air conditioning on – just to try to cool down in the hour or so immediately following the laser treatment.”
Dr. Pozner said that a decrease in pore counts was an unexpected effect of HALO treatment, and he estimated that patients end up with about 20% fewer pores in treated areas, which can be advantage because “nothing else works on pores.” In his experience, most of the pore reduction persists over time.
A HALO disposal tip costs approximately $50, which he said was inexpensive, compared with other devices.
Dr. Cohen said that in his practice, using HALO, “We can give patients a significant improvement in overall photodamage and mild improvement in wrinkles with only about 5 days of redness and swelling, and on the last few days, some coffee-ground appearance.” The nonablative component can promote coagulation, so there is less bleeding when you turn up the erbium component, “offering synergistic results for the patient,” he added.
Dr. Pozner has received equipment, consulting fees, and honoraria from Halo manufacturer Sciton and is a member of the company’s advisory board and speakers bureau. Dr. Cohen is a consultant for Sciton.
MIAMI – A device that combines nonablative and ablative laser energies can promote mild to moderate facial photo rejuvenation and improve the appearance of fine lines and wrinkles, according to Jason Pozner, MD.
Clinicians can tailor the depth for the 1470 nm nonablative diode and the 2940 nm Er:YAG lasers for each individual patient, Dr. Pozner said at the Orlando Dermatology Aesthetic and Clinical Conference. Advantages of resurfacing with the device, the HALO laser, include a cost-effective disposable tip and the ability to combine treatment with other therapies, he noted.
Before treatment begins, clinicians use the device to take facial measurements. Many patients find this precision reassuring, Dr. Pozner said during a live patient demonstration. Also, the device uses the information to help clinicians deliver the appropriate duration of therapy.
At this stage, it is a simple procedure, said Dr. Pozner, a plastic surgeon in a group practice in Boca Raton, Fla. Suction is turned on and the probe is then slowly advanced back and forth until the zone is finished, and “the laser beeps at you and you know you’re done,” he explained.
The HALO laser is useful for rejuvenation with little downtime. Most women treated with the device can wear makeup the same day, although more aggressively treated patients generally wait 1 additional day, Dr. Pozner said.
“I’ve never seen anything in our practice that gives this good a clinical result with this little downtime,” he added. He initially expected results to fall in between those associated with typical nonablative and ablative fractional laser treatments. But “in our experience, we get better results than ablative fractional [laser therapy], a story of one plus one equals three,” he said. “No matter what laser setting you use, patients are better by 5 days.”
When combined with intense pulsed light (IPL) treatment you can get a “double whammy effect,” Dr. Pozner said.
A meeting attendee asked about the appropriate order of IPL and HALO treatments. “When you combine the BBL (IPL) and HALO, yes, you do the IPL first,” Joel L. Cohen, MD, a private practice aesthetic dermatologist and Mohs surgeon in Denver who moderated the session at the meeting and also gave his own lecture on resurfacing options for the face.
Aside from the laser itself, the HALO system contains two tubes integrated into the handpiece, one of which is a Zimmer to deliver cooling during the procedure and the other is an air evacuator, he explained. “By having all of this integrated into the handpiece itself, it makes it much easier for the nurse who is circulating in the room to assist.”
Patients may feel warm for about 90 minutes post procedure, Dr. Cohen said. Make sure patients’ hands are clean and that the circulating nurse has given them an ice pack to minimize discomfort. “Even though I practice in Denver, where it is freezing cold right now, I’ve had patients drive home with the air conditioning on – just to try to cool down in the hour or so immediately following the laser treatment.”
Dr. Pozner said that a decrease in pore counts was an unexpected effect of HALO treatment, and he estimated that patients end up with about 20% fewer pores in treated areas, which can be advantage because “nothing else works on pores.” In his experience, most of the pore reduction persists over time.
A HALO disposal tip costs approximately $50, which he said was inexpensive, compared with other devices.
Dr. Cohen said that in his practice, using HALO, “We can give patients a significant improvement in overall photodamage and mild improvement in wrinkles with only about 5 days of redness and swelling, and on the last few days, some coffee-ground appearance.” The nonablative component can promote coagulation, so there is less bleeding when you turn up the erbium component, “offering synergistic results for the patient,” he added.
Dr. Pozner has received equipment, consulting fees, and honoraria from Halo manufacturer Sciton and is a member of the company’s advisory board and speakers bureau. Dr. Cohen is a consultant for Sciton.
AT THE ODAC CONFERENCE
Rosacea research reveals advances, promising therapies
MIAMI – Management of rosacea continues to challenge dermatologists and patients alike, although new advances and recent studies shine a light on promising new therapies to target this inflammatory skin condition.
Linda Stein Gold, MD, who directs dermatology clinical trials at the Henry Ford Hospital in Detroit, shared new information about the pathophysiology of rosacea and the controversial associations with cardiovascular disease and addressed the rosacea “genes versus environment” etiology question at the Orlando Dermatology Aesthetic and Clinical Conference.
The topical vasoconstrictor of cutaneous vasculature, oxymetazoline hydrochloride cream 1%, showed a statistically significant improvement in erythema, compared with vehicle only in people with rosacea in a phase III study, Dr. Stein Gold said. The outcome was strict, requiring both physician and patient assessment of at least a two-point improvement on the Erythema Assessment Scale. Investigators observed responses over 12 hours on the same day. “It’s actually kind of fun to do these studies,” she added. “You get to see what happens with patients across a whole day.”
A long-term analysis showed the efficacy of oxymetazoline “actually increased over the course of 52 weeks,” Dr. Stein Gold said. A total of 43% of participants experienced a two-grade improvement in erythema during this time. The agent was generally well tolerated, with dermatitis, pruritus, and headaches the most common treatment-related adverse events reported. (In January, the Food and Drug Administration approved oxymetazoline cream for the treatment of “persistent facial erythema associated with rosacea in adults.”)
Sometimes, a new formulation can make a difference in terms of treatment tolerability, a major consideration for patients with rosacea, Dr. Stein Gold said. Recent evidence suggests azelaic acid foam, 15% (Finacea), approved by the FDA in 2015, provides a well-tolerated option with only 6.2% of patients experiencing any application site pain, compared with 1.5% on vehicle alone, she added.
Cardiovascular comorbidities
“We’ve heard a lot about psoriasis and cardiovascular comorbidities, and we worry that other skin diseases may have similar associations,” Dr. Stein Gold said. New revelations in the pathogenesis of rosacea suggest a comparable association, she added, including findings related to matrix metalloproteinases (MMPs). MMPs have a key role in rosacea, for example, and are also important in the pathogenesis of cardiovascular disease, she noted. Several studies have confirmed this association as well as other links, including to Parkinson’s disease.
Although these studies support associations, more evidence is needed to prove any causal relationship between rosacea and other conditions where inflammation plays a prominent role, she added.
Translating findings into action
Given this emerging evidence, “what are we going to do about it?” Dr. Stein Gold asked attendees at the meeting. Research suggests tetracycline might be protective, she said, because this antibiotic can inhibit MMP activity. In a retrospective cohort study, investigators discovered rosacea patients on tetracycline therapy were at lower risk for developing vascular disease (J Invest Dermatol. 2014 Aug;134[8]:2267-9).
Nature or nurture?
Researchers and clinicians frequently debate the precise etiology of rosacea and whether the underlying causes are primarily genetic versus environmental. Investigators conducted a twin cohort study to find a more concrete answer, specifically looking at identical and fraternal twin pairs to determine how much genetics or environment likely contributes to factors on the National Rosacea Society grading system (JAMA Dermatol. 2015 Nov;151[11]:1213-9).
“The bottom line is it’s really about half and half – about half were associated with genetics, the other half with environment,” Dr. Stein Gold said.
No matter what the etiology, it’s important to diagnose and treat rosacea, Dr. Stein Gold said. Although patients tend to be middle-aged white women, the condition is not limited to this patient population, and “you have to think about it to diagnose it in skin of color,” she added.
Rosacea, which has a high emotional impact, presents an opportunity for dermatologists to improve quality of life, Dr. Stein Gold said. “When people walk around with papules and pustules, [other] people think there is something wrong with them.”
Dr. Stein Gold disclosed that she is a consultant, member of the advisory boards and speaker’s bureaus for, and receives research grants from Galderma, Leo, Novan, Valeant, Novartis, Celgene and Allergan. She is also a consultant, advisory board member, and receives research grants from Dermira and Foamix. She is a consultant to Sol-Gel, Promis, Anacor, and Medimetriks. She is on the advisory board for Promis.
MIAMI – Management of rosacea continues to challenge dermatologists and patients alike, although new advances and recent studies shine a light on promising new therapies to target this inflammatory skin condition.
Linda Stein Gold, MD, who directs dermatology clinical trials at the Henry Ford Hospital in Detroit, shared new information about the pathophysiology of rosacea and the controversial associations with cardiovascular disease and addressed the rosacea “genes versus environment” etiology question at the Orlando Dermatology Aesthetic and Clinical Conference.
The topical vasoconstrictor of cutaneous vasculature, oxymetazoline hydrochloride cream 1%, showed a statistically significant improvement in erythema, compared with vehicle only in people with rosacea in a phase III study, Dr. Stein Gold said. The outcome was strict, requiring both physician and patient assessment of at least a two-point improvement on the Erythema Assessment Scale. Investigators observed responses over 12 hours on the same day. “It’s actually kind of fun to do these studies,” she added. “You get to see what happens with patients across a whole day.”
A long-term analysis showed the efficacy of oxymetazoline “actually increased over the course of 52 weeks,” Dr. Stein Gold said. A total of 43% of participants experienced a two-grade improvement in erythema during this time. The agent was generally well tolerated, with dermatitis, pruritus, and headaches the most common treatment-related adverse events reported. (In January, the Food and Drug Administration approved oxymetazoline cream for the treatment of “persistent facial erythema associated with rosacea in adults.”)
Sometimes, a new formulation can make a difference in terms of treatment tolerability, a major consideration for patients with rosacea, Dr. Stein Gold said. Recent evidence suggests azelaic acid foam, 15% (Finacea), approved by the FDA in 2015, provides a well-tolerated option with only 6.2% of patients experiencing any application site pain, compared with 1.5% on vehicle alone, she added.
Cardiovascular comorbidities
“We’ve heard a lot about psoriasis and cardiovascular comorbidities, and we worry that other skin diseases may have similar associations,” Dr. Stein Gold said. New revelations in the pathogenesis of rosacea suggest a comparable association, she added, including findings related to matrix metalloproteinases (MMPs). MMPs have a key role in rosacea, for example, and are also important in the pathogenesis of cardiovascular disease, she noted. Several studies have confirmed this association as well as other links, including to Parkinson’s disease.
Although these studies support associations, more evidence is needed to prove any causal relationship between rosacea and other conditions where inflammation plays a prominent role, she added.
Translating findings into action
Given this emerging evidence, “what are we going to do about it?” Dr. Stein Gold asked attendees at the meeting. Research suggests tetracycline might be protective, she said, because this antibiotic can inhibit MMP activity. In a retrospective cohort study, investigators discovered rosacea patients on tetracycline therapy were at lower risk for developing vascular disease (J Invest Dermatol. 2014 Aug;134[8]:2267-9).
Nature or nurture?
Researchers and clinicians frequently debate the precise etiology of rosacea and whether the underlying causes are primarily genetic versus environmental. Investigators conducted a twin cohort study to find a more concrete answer, specifically looking at identical and fraternal twin pairs to determine how much genetics or environment likely contributes to factors on the National Rosacea Society grading system (JAMA Dermatol. 2015 Nov;151[11]:1213-9).
“The bottom line is it’s really about half and half – about half were associated with genetics, the other half with environment,” Dr. Stein Gold said.
No matter what the etiology, it’s important to diagnose and treat rosacea, Dr. Stein Gold said. Although patients tend to be middle-aged white women, the condition is not limited to this patient population, and “you have to think about it to diagnose it in skin of color,” she added.
Rosacea, which has a high emotional impact, presents an opportunity for dermatologists to improve quality of life, Dr. Stein Gold said. “When people walk around with papules and pustules, [other] people think there is something wrong with them.”
Dr. Stein Gold disclosed that she is a consultant, member of the advisory boards and speaker’s bureaus for, and receives research grants from Galderma, Leo, Novan, Valeant, Novartis, Celgene and Allergan. She is also a consultant, advisory board member, and receives research grants from Dermira and Foamix. She is a consultant to Sol-Gel, Promis, Anacor, and Medimetriks. She is on the advisory board for Promis.
MIAMI – Management of rosacea continues to challenge dermatologists and patients alike, although new advances and recent studies shine a light on promising new therapies to target this inflammatory skin condition.
Linda Stein Gold, MD, who directs dermatology clinical trials at the Henry Ford Hospital in Detroit, shared new information about the pathophysiology of rosacea and the controversial associations with cardiovascular disease and addressed the rosacea “genes versus environment” etiology question at the Orlando Dermatology Aesthetic and Clinical Conference.
The topical vasoconstrictor of cutaneous vasculature, oxymetazoline hydrochloride cream 1%, showed a statistically significant improvement in erythema, compared with vehicle only in people with rosacea in a phase III study, Dr. Stein Gold said. The outcome was strict, requiring both physician and patient assessment of at least a two-point improvement on the Erythema Assessment Scale. Investigators observed responses over 12 hours on the same day. “It’s actually kind of fun to do these studies,” she added. “You get to see what happens with patients across a whole day.”
A long-term analysis showed the efficacy of oxymetazoline “actually increased over the course of 52 weeks,” Dr. Stein Gold said. A total of 43% of participants experienced a two-grade improvement in erythema during this time. The agent was generally well tolerated, with dermatitis, pruritus, and headaches the most common treatment-related adverse events reported. (In January, the Food and Drug Administration approved oxymetazoline cream for the treatment of “persistent facial erythema associated with rosacea in adults.”)
Sometimes, a new formulation can make a difference in terms of treatment tolerability, a major consideration for patients with rosacea, Dr. Stein Gold said. Recent evidence suggests azelaic acid foam, 15% (Finacea), approved by the FDA in 2015, provides a well-tolerated option with only 6.2% of patients experiencing any application site pain, compared with 1.5% on vehicle alone, she added.
Cardiovascular comorbidities
“We’ve heard a lot about psoriasis and cardiovascular comorbidities, and we worry that other skin diseases may have similar associations,” Dr. Stein Gold said. New revelations in the pathogenesis of rosacea suggest a comparable association, she added, including findings related to matrix metalloproteinases (MMPs). MMPs have a key role in rosacea, for example, and are also important in the pathogenesis of cardiovascular disease, she noted. Several studies have confirmed this association as well as other links, including to Parkinson’s disease.
Although these studies support associations, more evidence is needed to prove any causal relationship between rosacea and other conditions where inflammation plays a prominent role, she added.
Translating findings into action
Given this emerging evidence, “what are we going to do about it?” Dr. Stein Gold asked attendees at the meeting. Research suggests tetracycline might be protective, she said, because this antibiotic can inhibit MMP activity. In a retrospective cohort study, investigators discovered rosacea patients on tetracycline therapy were at lower risk for developing vascular disease (J Invest Dermatol. 2014 Aug;134[8]:2267-9).
Nature or nurture?
Researchers and clinicians frequently debate the precise etiology of rosacea and whether the underlying causes are primarily genetic versus environmental. Investigators conducted a twin cohort study to find a more concrete answer, specifically looking at identical and fraternal twin pairs to determine how much genetics or environment likely contributes to factors on the National Rosacea Society grading system (JAMA Dermatol. 2015 Nov;151[11]:1213-9).
“The bottom line is it’s really about half and half – about half were associated with genetics, the other half with environment,” Dr. Stein Gold said.
No matter what the etiology, it’s important to diagnose and treat rosacea, Dr. Stein Gold said. Although patients tend to be middle-aged white women, the condition is not limited to this patient population, and “you have to think about it to diagnose it in skin of color,” she added.
Rosacea, which has a high emotional impact, presents an opportunity for dermatologists to improve quality of life, Dr. Stein Gold said. “When people walk around with papules and pustules, [other] people think there is something wrong with them.”
Dr. Stein Gold disclosed that she is a consultant, member of the advisory boards and speaker’s bureaus for, and receives research grants from Galderma, Leo, Novan, Valeant, Novartis, Celgene and Allergan. She is also a consultant, advisory board member, and receives research grants from Dermira and Foamix. She is a consultant to Sol-Gel, Promis, Anacor, and Medimetriks. She is on the advisory board for Promis.
EXPERT ANALYSIS FROM ODAC 2017
Tips to maximize minimally invasive lower facial lift procedure
MIAMI – Lifting the lower face using minimally invasive barbed sutures can yield rejuvenation results that last 12-18 months, providing an option for patients who do not wish to undergo full facelift surgery, according to a presentation at ODAC 2017.
“We have something new in our toolbox. The Silhouette InstaLift is a “good new thing to consider adding to your practice. It works really nice for me in combination with other facial rejuvenation strategies,” said Susan Weinkle, MD, a private practice Mohs surgeon and aesthetic dermatologist in Bradenton, Fla.
“Now we can reposition the skin. It works quite nicely in skin of color also,” Dr. Weinkle said during a lecture and live demonstration at the Orlando Dermatology Aesthetic and Clinical Conference.
Procedure tips
Begin by marking where on the patient’s face you intend to place the sutures. The proper vector is a straight lift back toward the upper ear in many cases. Also, take a photo before you start, so you know the location of the sutures in case the patient comes back for more, Dr. Weinkle recommended.
“What I like to do next is to sit the patient up and look at them head-on,” Dr. Weinkle said. “It helps to tweak the placement of the suture markings.” If a patient’s face appears asymmetrical, the dermatologist can place more sutures on one side than the other. Also, when there are neck issues, you can put an exit point for the sutures 1.5 cm below the mandible, she added.
Be patient after you anesthetize the entry and exit points because the epinephrine does not work immediately, Dr. Weinkle advised.
She does not anesthetize along the entire suture tract because the aim is to thread the sutures through the subcutaneous tissue. “You do not want to anesthetize the tract area between entry and exit points. If the patient feels it, you’re probably too superficial and you’re in the dermis.”
The next step is using an 18G needle to form an entry point for the 23G needle. “Pinch the skin, insert and stretch the skin just a bit. If you don’t pinch at the entry point, the cones can be difficult to pop in.” Dr. Weinkle said. Also, if you establish all entry points before inserting the sutures, it can save time.
Dr. Weinkle generally uses a number 8 InstaLift suture, but it also comes in sizes 12 and 16. After you open the package, gently pull the suture to tighten the knots between the cones. “Don’t pull hard from both ends – you can break the suture.”
When inserting the long needle to place the suture, it’s “almost like playing the violin with a bow.” As the clinician advances along tract line, he or she should run the needle between thumb and forefinger to check the positioning. Once the suture is placed and the needle removed, pull medially on the suture until the cones audibly “pop” – they are self anchoring. “I’ve seen some people break the sutures. You can pull them out and start again,” she noted.
“InstaLift is a bit of a misnomer,” Dr. Weinkle said. “Fibroblast stimulation and collagen improves final result over the next 2-3 months.” Improvements can last 12-18 months – it’s not permanent. “I think I would make a great candidate,” she joked. “Unfortunately, this is one thing I cannot do myself.”
There is minimal bruising after the procedure in Dr. Weinkle’s experience. Potential complications include swelling, dimpling at entry points, misplacement, and ecchymosis.
Dr. Weinkle is a consultant and principal investigator for Sinclair Pharma, manufacturer of InstaLift.
MIAMI – Lifting the lower face using minimally invasive barbed sutures can yield rejuvenation results that last 12-18 months, providing an option for patients who do not wish to undergo full facelift surgery, according to a presentation at ODAC 2017.
“We have something new in our toolbox. The Silhouette InstaLift is a “good new thing to consider adding to your practice. It works really nice for me in combination with other facial rejuvenation strategies,” said Susan Weinkle, MD, a private practice Mohs surgeon and aesthetic dermatologist in Bradenton, Fla.
“Now we can reposition the skin. It works quite nicely in skin of color also,” Dr. Weinkle said during a lecture and live demonstration at the Orlando Dermatology Aesthetic and Clinical Conference.
Procedure tips
Begin by marking where on the patient’s face you intend to place the sutures. The proper vector is a straight lift back toward the upper ear in many cases. Also, take a photo before you start, so you know the location of the sutures in case the patient comes back for more, Dr. Weinkle recommended.
“What I like to do next is to sit the patient up and look at them head-on,” Dr. Weinkle said. “It helps to tweak the placement of the suture markings.” If a patient’s face appears asymmetrical, the dermatologist can place more sutures on one side than the other. Also, when there are neck issues, you can put an exit point for the sutures 1.5 cm below the mandible, she added.
Be patient after you anesthetize the entry and exit points because the epinephrine does not work immediately, Dr. Weinkle advised.
She does not anesthetize along the entire suture tract because the aim is to thread the sutures through the subcutaneous tissue. “You do not want to anesthetize the tract area between entry and exit points. If the patient feels it, you’re probably too superficial and you’re in the dermis.”
The next step is using an 18G needle to form an entry point for the 23G needle. “Pinch the skin, insert and stretch the skin just a bit. If you don’t pinch at the entry point, the cones can be difficult to pop in.” Dr. Weinkle said. Also, if you establish all entry points before inserting the sutures, it can save time.
Dr. Weinkle generally uses a number 8 InstaLift suture, but it also comes in sizes 12 and 16. After you open the package, gently pull the suture to tighten the knots between the cones. “Don’t pull hard from both ends – you can break the suture.”
When inserting the long needle to place the suture, it’s “almost like playing the violin with a bow.” As the clinician advances along tract line, he or she should run the needle between thumb and forefinger to check the positioning. Once the suture is placed and the needle removed, pull medially on the suture until the cones audibly “pop” – they are self anchoring. “I’ve seen some people break the sutures. You can pull them out and start again,” she noted.
“InstaLift is a bit of a misnomer,” Dr. Weinkle said. “Fibroblast stimulation and collagen improves final result over the next 2-3 months.” Improvements can last 12-18 months – it’s not permanent. “I think I would make a great candidate,” she joked. “Unfortunately, this is one thing I cannot do myself.”
There is minimal bruising after the procedure in Dr. Weinkle’s experience. Potential complications include swelling, dimpling at entry points, misplacement, and ecchymosis.
Dr. Weinkle is a consultant and principal investigator for Sinclair Pharma, manufacturer of InstaLift.
MIAMI – Lifting the lower face using minimally invasive barbed sutures can yield rejuvenation results that last 12-18 months, providing an option for patients who do not wish to undergo full facelift surgery, according to a presentation at ODAC 2017.
“We have something new in our toolbox. The Silhouette InstaLift is a “good new thing to consider adding to your practice. It works really nice for me in combination with other facial rejuvenation strategies,” said Susan Weinkle, MD, a private practice Mohs surgeon and aesthetic dermatologist in Bradenton, Fla.
“Now we can reposition the skin. It works quite nicely in skin of color also,” Dr. Weinkle said during a lecture and live demonstration at the Orlando Dermatology Aesthetic and Clinical Conference.
Procedure tips
Begin by marking where on the patient’s face you intend to place the sutures. The proper vector is a straight lift back toward the upper ear in many cases. Also, take a photo before you start, so you know the location of the sutures in case the patient comes back for more, Dr. Weinkle recommended.
“What I like to do next is to sit the patient up and look at them head-on,” Dr. Weinkle said. “It helps to tweak the placement of the suture markings.” If a patient’s face appears asymmetrical, the dermatologist can place more sutures on one side than the other. Also, when there are neck issues, you can put an exit point for the sutures 1.5 cm below the mandible, she added.
Be patient after you anesthetize the entry and exit points because the epinephrine does not work immediately, Dr. Weinkle advised.
She does not anesthetize along the entire suture tract because the aim is to thread the sutures through the subcutaneous tissue. “You do not want to anesthetize the tract area between entry and exit points. If the patient feels it, you’re probably too superficial and you’re in the dermis.”
The next step is using an 18G needle to form an entry point for the 23G needle. “Pinch the skin, insert and stretch the skin just a bit. If you don’t pinch at the entry point, the cones can be difficult to pop in.” Dr. Weinkle said. Also, if you establish all entry points before inserting the sutures, it can save time.
Dr. Weinkle generally uses a number 8 InstaLift suture, but it also comes in sizes 12 and 16. After you open the package, gently pull the suture to tighten the knots between the cones. “Don’t pull hard from both ends – you can break the suture.”
When inserting the long needle to place the suture, it’s “almost like playing the violin with a bow.” As the clinician advances along tract line, he or she should run the needle between thumb and forefinger to check the positioning. Once the suture is placed and the needle removed, pull medially on the suture until the cones audibly “pop” – they are self anchoring. “I’ve seen some people break the sutures. You can pull them out and start again,” she noted.
“InstaLift is a bit of a misnomer,” Dr. Weinkle said. “Fibroblast stimulation and collagen improves final result over the next 2-3 months.” Improvements can last 12-18 months – it’s not permanent. “I think I would make a great candidate,” she joked. “Unfortunately, this is one thing I cannot do myself.”
There is minimal bruising after the procedure in Dr. Weinkle’s experience. Potential complications include swelling, dimpling at entry points, misplacement, and ecchymosis.
Dr. Weinkle is a consultant and principal investigator for Sinclair Pharma, manufacturer of InstaLift.
EXPERT ANALYSIS AT ODAC 2017
New auto-grafting techniques could advance wound healing
MIAMI – Pinch grafting can accelerate the healing of chronic, treatment-resistant wounds such as leg ulcers, while at the same time reducing morbidity to the donor skin site. A new epidermal harvesting device also is showing promise, as is a new tool that minces autologous skin grafts prior to application to promote wound healing.
These and other advances in wound healing were presented at the Orlando Dermatology Aesthetic and Clinical Conference. The pinch grafts and minced grafts each rely on the newly added skin to stimulate cytokines. Interestingly, there is evidence that grafts taken from hair-bearing donor sites could be superior for stimulating cytokines and accelerating wound healing, said Robert Kirsner, MD, PhD, of the University of Miami Health System.
Islands of regrowth
Physicians perform pinch grafting by taking small punches of skin from a donor site on the thigh, abdomen, or elsewhere, and then transferring the grafts to serve as islands of regrowth in a wound. Pinch grafting can be faster and less expensive than techniques typically performed in an operating room, such as meshed auto-grafting. In contrast, pinch grafting can be accomplished in an office setting “and patients can do quite well.” Dr. Kirsner said. In terms of outcomes, “our data is typical,” he added. “About 50% of refractory ulcers heal, 25% improve, and a percentage recur.”
Spreadable skin grafts
Another autologous grafting technique that can be performed at the bedside uses the Xpansion Micro-Autografting Kit, which minces autologous, split thickness skin grafts. “Then you apply them like peanut butter to bread,” Dr. Kirsner said.
The micro-autografts can help heal both acute and chronic wounds, including full thickness wounds from trauma, some burn wounds, diabetic foot ulcers, and venous ulcers, according to the manufacturer’s website.
Epidermal harvesting (without anesthesia)
Epidermal grafting can make sense because the epidermis regenerates. “You can lift off just the epidermis with heat or suction, “ Dr. Kirsner said. For the first time, he added, a new tool allows epidermal grafting without the need for anesthesia (Cellutome Epidermal Harvesting System). The device raises little microdomes of epidermis down to the basal layer, including basal keratinocytes and melanocytes, and a dermatologist can use a sterile dressing to transfer them to the wound. Confocal microscopy shows the dermoepidermal junction healing as early as within 2 days.
The epidermal harvesting was initially developed for pigment problems, such as piebaldism. (Dermatol Surg. 2017 Jan;43[1]:159-60). “We quickly realized it might have applicability for nonhealing wounds,” Dr. Kirsner said.
Deeper wound healing
A novel strategy for triggering deeper wound healing evolved from fractional laser technology, which remove columns of skin to generate healing. Instead, Rox Anderson, MD, of Massachusetts General Hospital, Boston, “envisioned pulling up microcolumns of full thickness epidermis, all the way to the fat, placing them into a wound, and the wound would heal with very little donor site morbidity,” Dr. Kirsner said.
This tool is coming out in spring of this year, he noted. It will resemble a fractional laser, “but now you have the skin available to place in another wound.” Prior animal studies revealed a healing benefit with very little scarring, he added.
Is hairier better?
Does the donor site matter? Dr. Kirsner asked. Although dermatologists typically graft skin from an abdomen or thigh, a hair-bearing site may be a better option because of the presence of pluripotent stem cells, according to a case report (Wounds. 2016 Apr;28[4]:109-11). J.D. Fox of the University of Miami, Dr. Kirsner, and their colleagues treated a large, chronic venous leg ulcer, almost 60 cm2, with punch grafts from a variety of donor sites.
“The side that got scalp punch grafts healed better, suggesting with skin taken from richly hairy area, you’ll get better results,” Dr. Kirsner said.
Another study supports this strategy (J Am Acad Dermatol. 2016 Nov;75[5]:1007-14). These researchers reported greater wound size reduction using grafts containing hair follicles versus nonhairy areas, again suggesting follicular stem cells play a role in better wound healing, Dr. Kirsner said. “This may be a better source of donor skin in the future.”
Dr. Kirsner is a consultant for Cardinal Health, Mölnlycke, Amniox, Organogenesis, Kerecis, Keretec, and KCI, an Acelity company.
MIAMI – Pinch grafting can accelerate the healing of chronic, treatment-resistant wounds such as leg ulcers, while at the same time reducing morbidity to the donor skin site. A new epidermal harvesting device also is showing promise, as is a new tool that minces autologous skin grafts prior to application to promote wound healing.
These and other advances in wound healing were presented at the Orlando Dermatology Aesthetic and Clinical Conference. The pinch grafts and minced grafts each rely on the newly added skin to stimulate cytokines. Interestingly, there is evidence that grafts taken from hair-bearing donor sites could be superior for stimulating cytokines and accelerating wound healing, said Robert Kirsner, MD, PhD, of the University of Miami Health System.
Islands of regrowth
Physicians perform pinch grafting by taking small punches of skin from a donor site on the thigh, abdomen, or elsewhere, and then transferring the grafts to serve as islands of regrowth in a wound. Pinch grafting can be faster and less expensive than techniques typically performed in an operating room, such as meshed auto-grafting. In contrast, pinch grafting can be accomplished in an office setting “and patients can do quite well.” Dr. Kirsner said. In terms of outcomes, “our data is typical,” he added. “About 50% of refractory ulcers heal, 25% improve, and a percentage recur.”
Spreadable skin grafts
Another autologous grafting technique that can be performed at the bedside uses the Xpansion Micro-Autografting Kit, which minces autologous, split thickness skin grafts. “Then you apply them like peanut butter to bread,” Dr. Kirsner said.
The micro-autografts can help heal both acute and chronic wounds, including full thickness wounds from trauma, some burn wounds, diabetic foot ulcers, and venous ulcers, according to the manufacturer’s website.
Epidermal harvesting (without anesthesia)
Epidermal grafting can make sense because the epidermis regenerates. “You can lift off just the epidermis with heat or suction, “ Dr. Kirsner said. For the first time, he added, a new tool allows epidermal grafting without the need for anesthesia (Cellutome Epidermal Harvesting System). The device raises little microdomes of epidermis down to the basal layer, including basal keratinocytes and melanocytes, and a dermatologist can use a sterile dressing to transfer them to the wound. Confocal microscopy shows the dermoepidermal junction healing as early as within 2 days.
The epidermal harvesting was initially developed for pigment problems, such as piebaldism. (Dermatol Surg. 2017 Jan;43[1]:159-60). “We quickly realized it might have applicability for nonhealing wounds,” Dr. Kirsner said.
Deeper wound healing
A novel strategy for triggering deeper wound healing evolved from fractional laser technology, which remove columns of skin to generate healing. Instead, Rox Anderson, MD, of Massachusetts General Hospital, Boston, “envisioned pulling up microcolumns of full thickness epidermis, all the way to the fat, placing them into a wound, and the wound would heal with very little donor site morbidity,” Dr. Kirsner said.
This tool is coming out in spring of this year, he noted. It will resemble a fractional laser, “but now you have the skin available to place in another wound.” Prior animal studies revealed a healing benefit with very little scarring, he added.
Is hairier better?
Does the donor site matter? Dr. Kirsner asked. Although dermatologists typically graft skin from an abdomen or thigh, a hair-bearing site may be a better option because of the presence of pluripotent stem cells, according to a case report (Wounds. 2016 Apr;28[4]:109-11). J.D. Fox of the University of Miami, Dr. Kirsner, and their colleagues treated a large, chronic venous leg ulcer, almost 60 cm2, with punch grafts from a variety of donor sites.
“The side that got scalp punch grafts healed better, suggesting with skin taken from richly hairy area, you’ll get better results,” Dr. Kirsner said.
Another study supports this strategy (J Am Acad Dermatol. 2016 Nov;75[5]:1007-14). These researchers reported greater wound size reduction using grafts containing hair follicles versus nonhairy areas, again suggesting follicular stem cells play a role in better wound healing, Dr. Kirsner said. “This may be a better source of donor skin in the future.”
Dr. Kirsner is a consultant for Cardinal Health, Mölnlycke, Amniox, Organogenesis, Kerecis, Keretec, and KCI, an Acelity company.
MIAMI – Pinch grafting can accelerate the healing of chronic, treatment-resistant wounds such as leg ulcers, while at the same time reducing morbidity to the donor skin site. A new epidermal harvesting device also is showing promise, as is a new tool that minces autologous skin grafts prior to application to promote wound healing.
These and other advances in wound healing were presented at the Orlando Dermatology Aesthetic and Clinical Conference. The pinch grafts and minced grafts each rely on the newly added skin to stimulate cytokines. Interestingly, there is evidence that grafts taken from hair-bearing donor sites could be superior for stimulating cytokines and accelerating wound healing, said Robert Kirsner, MD, PhD, of the University of Miami Health System.
Islands of regrowth
Physicians perform pinch grafting by taking small punches of skin from a donor site on the thigh, abdomen, or elsewhere, and then transferring the grafts to serve as islands of regrowth in a wound. Pinch grafting can be faster and less expensive than techniques typically performed in an operating room, such as meshed auto-grafting. In contrast, pinch grafting can be accomplished in an office setting “and patients can do quite well.” Dr. Kirsner said. In terms of outcomes, “our data is typical,” he added. “About 50% of refractory ulcers heal, 25% improve, and a percentage recur.”
Spreadable skin grafts
Another autologous grafting technique that can be performed at the bedside uses the Xpansion Micro-Autografting Kit, which minces autologous, split thickness skin grafts. “Then you apply them like peanut butter to bread,” Dr. Kirsner said.
The micro-autografts can help heal both acute and chronic wounds, including full thickness wounds from trauma, some burn wounds, diabetic foot ulcers, and venous ulcers, according to the manufacturer’s website.
Epidermal harvesting (without anesthesia)
Epidermal grafting can make sense because the epidermis regenerates. “You can lift off just the epidermis with heat or suction, “ Dr. Kirsner said. For the first time, he added, a new tool allows epidermal grafting without the need for anesthesia (Cellutome Epidermal Harvesting System). The device raises little microdomes of epidermis down to the basal layer, including basal keratinocytes and melanocytes, and a dermatologist can use a sterile dressing to transfer them to the wound. Confocal microscopy shows the dermoepidermal junction healing as early as within 2 days.
The epidermal harvesting was initially developed for pigment problems, such as piebaldism. (Dermatol Surg. 2017 Jan;43[1]:159-60). “We quickly realized it might have applicability for nonhealing wounds,” Dr. Kirsner said.
Deeper wound healing
A novel strategy for triggering deeper wound healing evolved from fractional laser technology, which remove columns of skin to generate healing. Instead, Rox Anderson, MD, of Massachusetts General Hospital, Boston, “envisioned pulling up microcolumns of full thickness epidermis, all the way to the fat, placing them into a wound, and the wound would heal with very little donor site morbidity,” Dr. Kirsner said.
This tool is coming out in spring of this year, he noted. It will resemble a fractional laser, “but now you have the skin available to place in another wound.” Prior animal studies revealed a healing benefit with very little scarring, he added.
Is hairier better?
Does the donor site matter? Dr. Kirsner asked. Although dermatologists typically graft skin from an abdomen or thigh, a hair-bearing site may be a better option because of the presence of pluripotent stem cells, according to a case report (Wounds. 2016 Apr;28[4]:109-11). J.D. Fox of the University of Miami, Dr. Kirsner, and their colleagues treated a large, chronic venous leg ulcer, almost 60 cm2, with punch grafts from a variety of donor sites.
“The side that got scalp punch grafts healed better, suggesting with skin taken from richly hairy area, you’ll get better results,” Dr. Kirsner said.
Another study supports this strategy (J Am Acad Dermatol. 2016 Nov;75[5]:1007-14). These researchers reported greater wound size reduction using grafts containing hair follicles versus nonhairy areas, again suggesting follicular stem cells play a role in better wound healing, Dr. Kirsner said. “This may be a better source of donor skin in the future.”
Dr. Kirsner is a consultant for Cardinal Health, Mölnlycke, Amniox, Organogenesis, Kerecis, Keretec, and KCI, an Acelity company.
Evidence supports efficacy of topical skin products for photoaging reversal
MIAMI – Topical skin care products are evolving along with evidence in the literature supporting their efficacy; these products include serums, lotions, and cleansers with DNA repair enzymes or epidermal growth factor as active ingredients, according to Ron Moy, MD.
Importantly, some of these formulations not only show efficacy to reverse the signs of photodamage to skin and to promote rejuvenation, but may have a role in skin cancer prevention as well, said Dr. Moy, a dermatologist and facial plastic surgeon in private practice in Beverly Hills, Calif.
More investigators are assessing the mechanisms and potential advantages of DNA repair, Dr. Moy said at the Orlando Dermatology Aesthetic and Clinical Conference. In 2015, the Nobel Prize in Chemistry was awarded to scientists who discovered key mechanisms underlying DNA repair. “Since then, DNA repair has gotten a lot more attention,” he said.
Evidence suggests a person’s DNA repair capability can modulate colon cancer risk. Also, smokers with a low level of DNA repair enzymes carry a higher risk for lung cancer, and DNA repair genes can predict ovarian cancer and lung cancer survival, Dr. Moy said.
“It is still not entirely understood how everything ties together,” he said. “But the work on DNA repair is convincing, more convincing than work on antioxidants or retinoids.” Although antioxidants look favorable in experimental and animal studies, for example, “generally the published work on antioxidants does not give you good clinical results,” he said.
DNA repair enzymes have a beneficial effect on the proto-oncogene hyperexpression in human skin and ultraviolet light telomere shortening, according to an experimental pilot study in the Journal of Drugs in Dermatology (2013 Sep;12[9]:1017-21).
Also, a DNA repair enzyme derived from bacteria, T4 endonuclease V, showed promise in an older study of 30 patients with xeroderma pigmentosum (Lancet. 2001 Mar 24;357[9260]:926-9). Those affected carry a higher risk overall for any skin cancer, compared with the general population. The DNA repair enzyme group had fewer new actinic keratoses and fewer new basal cell carcinoma, squamous cell carcinomas, and melanoma lesions at 1 year, compared with a vehicle-only group at 1 year.
Another class of DNA repair molecules, photolyases, is newer than T4 endonuclease V and “might work even better,” Dr. Moy said.
“There is evidence that DNA enzymes are very effective and helpful in preventing skin cancer,” he pointed out. One mechanism is the ability of exogenous DNA repair enzymes to bolster intrinsic DNA in the fight against carcinogenesis, according to a review article Dr. Moy and his colleagues published in the Journal of Drugs in Dermatology (2015 Mar;14[3]:297-303).
The role of human epidermal growth factor for improving skin appearance and tightening is another area of active research and promise.
“It basically thickens and tightens skin,” Dr. Moy explained. “It works better on thinner skin, including the eyelids and neck.” Ultrasound objectively demonstrates gains in skin thickness. Studies also show improvement in acne scars following application of epidermal growth factor.
In addition, epidermal growth factor can enhance the appearance of solar purpura. In fact, this is the dermatologic condition with the most convincing evidence supporting its use so far, Dr. Moy said. Clinical studies have shown that epidermal growth factor along with other active ingredients also can improve acne scars and eye bags.
During the question and answer session at the ODAC conference, moderator Susan Weinkle, MD, a dermatologist and Mohs surgeon in private practice in Bradenton, Fla., asked Dr. Moy which epidermal growth factor product he recommends.
“There are a lot of different growth factors. Epidermal growth factors are not all the same,” said Dr. Moy, who is the founder of DNA EGF Renewal, a company that manufactures skin care products containing epidermal growth factor and DNA repair enzymes.
When pressed for the name of his growth factor product by Dr. Weinkle and an uproar from the audience, Dr. Moy chose to stay noncommercial, pointing attendees to his website instead: www.dnaegfrenewal.com.
Dr. Moy is founder of DNA EGF Renewal in Beverly Hills, Calif.
MIAMI – Topical skin care products are evolving along with evidence in the literature supporting their efficacy; these products include serums, lotions, and cleansers with DNA repair enzymes or epidermal growth factor as active ingredients, according to Ron Moy, MD.
Importantly, some of these formulations not only show efficacy to reverse the signs of photodamage to skin and to promote rejuvenation, but may have a role in skin cancer prevention as well, said Dr. Moy, a dermatologist and facial plastic surgeon in private practice in Beverly Hills, Calif.
More investigators are assessing the mechanisms and potential advantages of DNA repair, Dr. Moy said at the Orlando Dermatology Aesthetic and Clinical Conference. In 2015, the Nobel Prize in Chemistry was awarded to scientists who discovered key mechanisms underlying DNA repair. “Since then, DNA repair has gotten a lot more attention,” he said.
Evidence suggests a person’s DNA repair capability can modulate colon cancer risk. Also, smokers with a low level of DNA repair enzymes carry a higher risk for lung cancer, and DNA repair genes can predict ovarian cancer and lung cancer survival, Dr. Moy said.
“It is still not entirely understood how everything ties together,” he said. “But the work on DNA repair is convincing, more convincing than work on antioxidants or retinoids.” Although antioxidants look favorable in experimental and animal studies, for example, “generally the published work on antioxidants does not give you good clinical results,” he said.
DNA repair enzymes have a beneficial effect on the proto-oncogene hyperexpression in human skin and ultraviolet light telomere shortening, according to an experimental pilot study in the Journal of Drugs in Dermatology (2013 Sep;12[9]:1017-21).
Also, a DNA repair enzyme derived from bacteria, T4 endonuclease V, showed promise in an older study of 30 patients with xeroderma pigmentosum (Lancet. 2001 Mar 24;357[9260]:926-9). Those affected carry a higher risk overall for any skin cancer, compared with the general population. The DNA repair enzyme group had fewer new actinic keratoses and fewer new basal cell carcinoma, squamous cell carcinomas, and melanoma lesions at 1 year, compared with a vehicle-only group at 1 year.
Another class of DNA repair molecules, photolyases, is newer than T4 endonuclease V and “might work even better,” Dr. Moy said.
“There is evidence that DNA enzymes are very effective and helpful in preventing skin cancer,” he pointed out. One mechanism is the ability of exogenous DNA repair enzymes to bolster intrinsic DNA in the fight against carcinogenesis, according to a review article Dr. Moy and his colleagues published in the Journal of Drugs in Dermatology (2015 Mar;14[3]:297-303).
The role of human epidermal growth factor for improving skin appearance and tightening is another area of active research and promise.
“It basically thickens and tightens skin,” Dr. Moy explained. “It works better on thinner skin, including the eyelids and neck.” Ultrasound objectively demonstrates gains in skin thickness. Studies also show improvement in acne scars following application of epidermal growth factor.
In addition, epidermal growth factor can enhance the appearance of solar purpura. In fact, this is the dermatologic condition with the most convincing evidence supporting its use so far, Dr. Moy said. Clinical studies have shown that epidermal growth factor along with other active ingredients also can improve acne scars and eye bags.
During the question and answer session at the ODAC conference, moderator Susan Weinkle, MD, a dermatologist and Mohs surgeon in private practice in Bradenton, Fla., asked Dr. Moy which epidermal growth factor product he recommends.
“There are a lot of different growth factors. Epidermal growth factors are not all the same,” said Dr. Moy, who is the founder of DNA EGF Renewal, a company that manufactures skin care products containing epidermal growth factor and DNA repair enzymes.
When pressed for the name of his growth factor product by Dr. Weinkle and an uproar from the audience, Dr. Moy chose to stay noncommercial, pointing attendees to his website instead: www.dnaegfrenewal.com.
Dr. Moy is founder of DNA EGF Renewal in Beverly Hills, Calif.
MIAMI – Topical skin care products are evolving along with evidence in the literature supporting their efficacy; these products include serums, lotions, and cleansers with DNA repair enzymes or epidermal growth factor as active ingredients, according to Ron Moy, MD.
Importantly, some of these formulations not only show efficacy to reverse the signs of photodamage to skin and to promote rejuvenation, but may have a role in skin cancer prevention as well, said Dr. Moy, a dermatologist and facial plastic surgeon in private practice in Beverly Hills, Calif.
More investigators are assessing the mechanisms and potential advantages of DNA repair, Dr. Moy said at the Orlando Dermatology Aesthetic and Clinical Conference. In 2015, the Nobel Prize in Chemistry was awarded to scientists who discovered key mechanisms underlying DNA repair. “Since then, DNA repair has gotten a lot more attention,” he said.
Evidence suggests a person’s DNA repair capability can modulate colon cancer risk. Also, smokers with a low level of DNA repair enzymes carry a higher risk for lung cancer, and DNA repair genes can predict ovarian cancer and lung cancer survival, Dr. Moy said.
“It is still not entirely understood how everything ties together,” he said. “But the work on DNA repair is convincing, more convincing than work on antioxidants or retinoids.” Although antioxidants look favorable in experimental and animal studies, for example, “generally the published work on antioxidants does not give you good clinical results,” he said.
DNA repair enzymes have a beneficial effect on the proto-oncogene hyperexpression in human skin and ultraviolet light telomere shortening, according to an experimental pilot study in the Journal of Drugs in Dermatology (2013 Sep;12[9]:1017-21).
Also, a DNA repair enzyme derived from bacteria, T4 endonuclease V, showed promise in an older study of 30 patients with xeroderma pigmentosum (Lancet. 2001 Mar 24;357[9260]:926-9). Those affected carry a higher risk overall for any skin cancer, compared with the general population. The DNA repair enzyme group had fewer new actinic keratoses and fewer new basal cell carcinoma, squamous cell carcinomas, and melanoma lesions at 1 year, compared with a vehicle-only group at 1 year.
Another class of DNA repair molecules, photolyases, is newer than T4 endonuclease V and “might work even better,” Dr. Moy said.
“There is evidence that DNA enzymes are very effective and helpful in preventing skin cancer,” he pointed out. One mechanism is the ability of exogenous DNA repair enzymes to bolster intrinsic DNA in the fight against carcinogenesis, according to a review article Dr. Moy and his colleagues published in the Journal of Drugs in Dermatology (2015 Mar;14[3]:297-303).
The role of human epidermal growth factor for improving skin appearance and tightening is another area of active research and promise.
“It basically thickens and tightens skin,” Dr. Moy explained. “It works better on thinner skin, including the eyelids and neck.” Ultrasound objectively demonstrates gains in skin thickness. Studies also show improvement in acne scars following application of epidermal growth factor.
In addition, epidermal growth factor can enhance the appearance of solar purpura. In fact, this is the dermatologic condition with the most convincing evidence supporting its use so far, Dr. Moy said. Clinical studies have shown that epidermal growth factor along with other active ingredients also can improve acne scars and eye bags.
During the question and answer session at the ODAC conference, moderator Susan Weinkle, MD, a dermatologist and Mohs surgeon in private practice in Bradenton, Fla., asked Dr. Moy which epidermal growth factor product he recommends.
“There are a lot of different growth factors. Epidermal growth factors are not all the same,” said Dr. Moy, who is the founder of DNA EGF Renewal, a company that manufactures skin care products containing epidermal growth factor and DNA repair enzymes.
When pressed for the name of his growth factor product by Dr. Weinkle and an uproar from the audience, Dr. Moy chose to stay noncommercial, pointing attendees to his website instead: www.dnaegfrenewal.com.
Dr. Moy is founder of DNA EGF Renewal in Beverly Hills, Calif.
EXPERT ANALYSIS FROM ODAC 2017
Recognize, treat, and teach others to spot hidradenitis suppurativa
MIAMI – Clinicians have many options to treat and help people manage hidradenitis suppurativa, but for most patients, an early and accurate diagnosis remains elusive.
“The problem here is because it has so many mimickers, the diagnosis is often delayed, patients can be [treated for an incorrect diagnosis] and in many ways that treatment can be harmful,” said Adam Friedman, MD, of the George Washington University in Washington. Missed or ignored diagnoses can lead to more pain, impaired function, and wasted time and money.
“There are – no question – gaps in clinical care. Patients seek care outside of dermatology and go to urgent care centers, emergency rooms, [and other settings]. That’s why it’s not only important for us to recognize this, but to teach everyone else as well,” Dr. Friedman said at the Orlando Dermatology Aesthetic and Clinical Conference.
Tips for early detection
Look for chronicity in the disease’s presentation, Dr. Friedman said. “Chronicity is key, but the morphology will change, and lesions will look different over time.” Therefore, “the clinical presentation can be challenging, depending on when you catch the patient.”
Hidradenitis suppurativa is characterized by very purulent, indurated, abscesslike structures often on the underarms and groin. Ask patients where and how often they see lesions. Lesions in certain locations can be very disabling for patients not only because of pain, but also from a psychosocial impact. The groin and chest are prime examples. Also, there is a genetic predisposition so it is important to ask patients about family history as well.
Use combination therapy to hit disease ‘from all angles’
It is imperative to treat patients even when they present at a time of mild disease, Dr. Friedman said. “This is a chronic, snowballing disease that will get worse over time, because inflammation begets inflammation. Even if it’s mild disease, you still want to treat. Combinations are king, and we dermatologists are the synergy masters.”
Effective treatment strategies include medications that curtail inflammation and block hormonal influences; dietary changes (a minimal-dairy, low-carbohydrate diet helps some patients, for example); environmental changes and/or eliminating the invasive proliferative gelatinous mass (IPGM). “This is not step therapy,” Dr. Friedman emphasized. “You want to hit all these angles at once.”
In terms of nutritional support, “I usually put my patients on a combination of zinc and vitamin C, both anti-inflammatories, but also good for wound healing,” Dr. Friedman said. “I also get them on board with V-8, which can be a tough sell sometimes.” He recommends patients drink three small cans per week, adding that he has no financial disclosure related to the vegetable juice.
Patient education, smoking cessation, and keeping affected areas dry and cool are other important management strategies. Instruct patients that stress, friction, and obesity can each worsen the condition “I think obesity is an independent risk factor here, like it is in psoriasis, where obesity alone has been shown to increase the risk of psoriasis later on,” he said.
Ease the inflammation
Hidradenitis suppurativa is a disease of “inappropriate inflammation,” Dr. Friedman said, which explains why anti-inflammatory agents remain the mainstay of treatment. These include antibiotics, classic corticosteroids, and biologics, which all can have a role in therapy. He highlighted the potential role of the cutaneous microbiota and possible dysbiosis associated with disease activity. “I also use a lot chlorhexidine washes to wipe the microbial slate clean in high-risk areas; just be careful to avoid the face.”
Intralesional Kenalog (triamcinolone acetonide), in particular, is useful for its rapid results. “This is such a great and easy trick, and it really works quickly,” Dr. Friedman said. He added that a recent case series provides evidence for its efficacy as well (J Amer Acad Dermatol. 2016 Dec;75:1151-5).
Three take-home treatment pointers
Dr. Friedman shared these three take-aways for treatment of hidradenitis suppurativa with antibiotics:
- The combination of oral clindamycin 300 mg twice daily and oral rifampin 300 mg twice daily carries the most evidence for efficacy and safety, with no evidence of resistance.
- Rifampin also acts against Clostridium difficile infections, which decreases the risk of associated colitis.
- Do not give a tetracycline antibiotic as monotherapy.
In terms of retinoids, “I’ve been pretty disappointed. I find them effective [in other conditions], but for hidradenitis suppurativa, I’m just not impressed, unfortunately,” Dr. Friedman said. “Antihormonal therapies such as oral contraceptives and spironolactone for women and finasteride for men have been a useful adjuncts in my practice, with evidence supporting their use in the literature, he added. Biologics are among the new treatment options, but there are cost and insurance coverage issues, Dr. Friedman said. There are small case series evaluating biologics such as infliximab, which are very supportive – and he himself has had good responses – although the Food and Drug Administration indication has been the hurdle.
One exception is the recent FDA approval of adalimumab (Humira) for hidradenitis suppurativa. “Make sure you realize that the dosing is different, more like a ‘whopping’ Crohn’s disease dose. This is a very important medication in our armamentarium – the issue is when you start it,” Dr. Friedman said. He also cautioned, “if a patient has sinus tracts and scarring, it’s not going to be enough. You still need to address that. Adalimumab is only going to get rid of the inflammation. This is why early diagnosis is so important!”
When it comes to surgery, “my philosophy is it’s all or none. If you’re going to do surgery, do surgery. You better cut these things out. Do a wide global excision,” Dr. Friedman emphasized.
Dr. Friedman is a member of the Dermatology News editorial advisory board.
Dr. Friedman had no relevant financial disclosures.
MIAMI – Clinicians have many options to treat and help people manage hidradenitis suppurativa, but for most patients, an early and accurate diagnosis remains elusive.
“The problem here is because it has so many mimickers, the diagnosis is often delayed, patients can be [treated for an incorrect diagnosis] and in many ways that treatment can be harmful,” said Adam Friedman, MD, of the George Washington University in Washington. Missed or ignored diagnoses can lead to more pain, impaired function, and wasted time and money.
“There are – no question – gaps in clinical care. Patients seek care outside of dermatology and go to urgent care centers, emergency rooms, [and other settings]. That’s why it’s not only important for us to recognize this, but to teach everyone else as well,” Dr. Friedman said at the Orlando Dermatology Aesthetic and Clinical Conference.
Tips for early detection
Look for chronicity in the disease’s presentation, Dr. Friedman said. “Chronicity is key, but the morphology will change, and lesions will look different over time.” Therefore, “the clinical presentation can be challenging, depending on when you catch the patient.”
Hidradenitis suppurativa is characterized by very purulent, indurated, abscesslike structures often on the underarms and groin. Ask patients where and how often they see lesions. Lesions in certain locations can be very disabling for patients not only because of pain, but also from a psychosocial impact. The groin and chest are prime examples. Also, there is a genetic predisposition so it is important to ask patients about family history as well.
Use combination therapy to hit disease ‘from all angles’
It is imperative to treat patients even when they present at a time of mild disease, Dr. Friedman said. “This is a chronic, snowballing disease that will get worse over time, because inflammation begets inflammation. Even if it’s mild disease, you still want to treat. Combinations are king, and we dermatologists are the synergy masters.”
Effective treatment strategies include medications that curtail inflammation and block hormonal influences; dietary changes (a minimal-dairy, low-carbohydrate diet helps some patients, for example); environmental changes and/or eliminating the invasive proliferative gelatinous mass (IPGM). “This is not step therapy,” Dr. Friedman emphasized. “You want to hit all these angles at once.”
In terms of nutritional support, “I usually put my patients on a combination of zinc and vitamin C, both anti-inflammatories, but also good for wound healing,” Dr. Friedman said. “I also get them on board with V-8, which can be a tough sell sometimes.” He recommends patients drink three small cans per week, adding that he has no financial disclosure related to the vegetable juice.
Patient education, smoking cessation, and keeping affected areas dry and cool are other important management strategies. Instruct patients that stress, friction, and obesity can each worsen the condition “I think obesity is an independent risk factor here, like it is in psoriasis, where obesity alone has been shown to increase the risk of psoriasis later on,” he said.
Ease the inflammation
Hidradenitis suppurativa is a disease of “inappropriate inflammation,” Dr. Friedman said, which explains why anti-inflammatory agents remain the mainstay of treatment. These include antibiotics, classic corticosteroids, and biologics, which all can have a role in therapy. He highlighted the potential role of the cutaneous microbiota and possible dysbiosis associated with disease activity. “I also use a lot chlorhexidine washes to wipe the microbial slate clean in high-risk areas; just be careful to avoid the face.”
Intralesional Kenalog (triamcinolone acetonide), in particular, is useful for its rapid results. “This is such a great and easy trick, and it really works quickly,” Dr. Friedman said. He added that a recent case series provides evidence for its efficacy as well (J Amer Acad Dermatol. 2016 Dec;75:1151-5).
Three take-home treatment pointers
Dr. Friedman shared these three take-aways for treatment of hidradenitis suppurativa with antibiotics:
- The combination of oral clindamycin 300 mg twice daily and oral rifampin 300 mg twice daily carries the most evidence for efficacy and safety, with no evidence of resistance.
- Rifampin also acts against Clostridium difficile infections, which decreases the risk of associated colitis.
- Do not give a tetracycline antibiotic as monotherapy.
In terms of retinoids, “I’ve been pretty disappointed. I find them effective [in other conditions], but for hidradenitis suppurativa, I’m just not impressed, unfortunately,” Dr. Friedman said. “Antihormonal therapies such as oral contraceptives and spironolactone for women and finasteride for men have been a useful adjuncts in my practice, with evidence supporting their use in the literature, he added. Biologics are among the new treatment options, but there are cost and insurance coverage issues, Dr. Friedman said. There are small case series evaluating biologics such as infliximab, which are very supportive – and he himself has had good responses – although the Food and Drug Administration indication has been the hurdle.
One exception is the recent FDA approval of adalimumab (Humira) for hidradenitis suppurativa. “Make sure you realize that the dosing is different, more like a ‘whopping’ Crohn’s disease dose. This is a very important medication in our armamentarium – the issue is when you start it,” Dr. Friedman said. He also cautioned, “if a patient has sinus tracts and scarring, it’s not going to be enough. You still need to address that. Adalimumab is only going to get rid of the inflammation. This is why early diagnosis is so important!”
When it comes to surgery, “my philosophy is it’s all or none. If you’re going to do surgery, do surgery. You better cut these things out. Do a wide global excision,” Dr. Friedman emphasized.
Dr. Friedman is a member of the Dermatology News editorial advisory board.
Dr. Friedman had no relevant financial disclosures.
MIAMI – Clinicians have many options to treat and help people manage hidradenitis suppurativa, but for most patients, an early and accurate diagnosis remains elusive.
“The problem here is because it has so many mimickers, the diagnosis is often delayed, patients can be [treated for an incorrect diagnosis] and in many ways that treatment can be harmful,” said Adam Friedman, MD, of the George Washington University in Washington. Missed or ignored diagnoses can lead to more pain, impaired function, and wasted time and money.
“There are – no question – gaps in clinical care. Patients seek care outside of dermatology and go to urgent care centers, emergency rooms, [and other settings]. That’s why it’s not only important for us to recognize this, but to teach everyone else as well,” Dr. Friedman said at the Orlando Dermatology Aesthetic and Clinical Conference.
Tips for early detection
Look for chronicity in the disease’s presentation, Dr. Friedman said. “Chronicity is key, but the morphology will change, and lesions will look different over time.” Therefore, “the clinical presentation can be challenging, depending on when you catch the patient.”
Hidradenitis suppurativa is characterized by very purulent, indurated, abscesslike structures often on the underarms and groin. Ask patients where and how often they see lesions. Lesions in certain locations can be very disabling for patients not only because of pain, but also from a psychosocial impact. The groin and chest are prime examples. Also, there is a genetic predisposition so it is important to ask patients about family history as well.
Use combination therapy to hit disease ‘from all angles’
It is imperative to treat patients even when they present at a time of mild disease, Dr. Friedman said. “This is a chronic, snowballing disease that will get worse over time, because inflammation begets inflammation. Even if it’s mild disease, you still want to treat. Combinations are king, and we dermatologists are the synergy masters.”
Effective treatment strategies include medications that curtail inflammation and block hormonal influences; dietary changes (a minimal-dairy, low-carbohydrate diet helps some patients, for example); environmental changes and/or eliminating the invasive proliferative gelatinous mass (IPGM). “This is not step therapy,” Dr. Friedman emphasized. “You want to hit all these angles at once.”
In terms of nutritional support, “I usually put my patients on a combination of zinc and vitamin C, both anti-inflammatories, but also good for wound healing,” Dr. Friedman said. “I also get them on board with V-8, which can be a tough sell sometimes.” He recommends patients drink three small cans per week, adding that he has no financial disclosure related to the vegetable juice.
Patient education, smoking cessation, and keeping affected areas dry and cool are other important management strategies. Instruct patients that stress, friction, and obesity can each worsen the condition “I think obesity is an independent risk factor here, like it is in psoriasis, where obesity alone has been shown to increase the risk of psoriasis later on,” he said.
Ease the inflammation
Hidradenitis suppurativa is a disease of “inappropriate inflammation,” Dr. Friedman said, which explains why anti-inflammatory agents remain the mainstay of treatment. These include antibiotics, classic corticosteroids, and biologics, which all can have a role in therapy. He highlighted the potential role of the cutaneous microbiota and possible dysbiosis associated with disease activity. “I also use a lot chlorhexidine washes to wipe the microbial slate clean in high-risk areas; just be careful to avoid the face.”
Intralesional Kenalog (triamcinolone acetonide), in particular, is useful for its rapid results. “This is such a great and easy trick, and it really works quickly,” Dr. Friedman said. He added that a recent case series provides evidence for its efficacy as well (J Amer Acad Dermatol. 2016 Dec;75:1151-5).
Three take-home treatment pointers
Dr. Friedman shared these three take-aways for treatment of hidradenitis suppurativa with antibiotics:
- The combination of oral clindamycin 300 mg twice daily and oral rifampin 300 mg twice daily carries the most evidence for efficacy and safety, with no evidence of resistance.
- Rifampin also acts against Clostridium difficile infections, which decreases the risk of associated colitis.
- Do not give a tetracycline antibiotic as monotherapy.
In terms of retinoids, “I’ve been pretty disappointed. I find them effective [in other conditions], but for hidradenitis suppurativa, I’m just not impressed, unfortunately,” Dr. Friedman said. “Antihormonal therapies such as oral contraceptives and spironolactone for women and finasteride for men have been a useful adjuncts in my practice, with evidence supporting their use in the literature, he added. Biologics are among the new treatment options, but there are cost and insurance coverage issues, Dr. Friedman said. There are small case series evaluating biologics such as infliximab, which are very supportive – and he himself has had good responses – although the Food and Drug Administration indication has been the hurdle.
One exception is the recent FDA approval of adalimumab (Humira) for hidradenitis suppurativa. “Make sure you realize that the dosing is different, more like a ‘whopping’ Crohn’s disease dose. This is a very important medication in our armamentarium – the issue is when you start it,” Dr. Friedman said. He also cautioned, “if a patient has sinus tracts and scarring, it’s not going to be enough. You still need to address that. Adalimumab is only going to get rid of the inflammation. This is why early diagnosis is so important!”
When it comes to surgery, “my philosophy is it’s all or none. If you’re going to do surgery, do surgery. You better cut these things out. Do a wide global excision,” Dr. Friedman emphasized.
Dr. Friedman is a member of the Dermatology News editorial advisory board.
Dr. Friedman had no relevant financial disclosures.
EXPERT ANALYSIS FROM ODAC 2017
Fixed combination topical shows promise for psoriasis
MIAMI – In an ongoing drive to identify an alternative to the mainstay treatment of psoriasis with topical corticosteroids, researchers evaluated a fixed-dose combination of halobetasol propionate 0.01% and tazarotene 0.045% lotion compared to its monads and vehicle in 212 people with moderate to severe psoriasis.
After 8 weeks of once-daily applications, combination therapy yielded significantly greater reductions in erythema, plaque elevation, and scaling at the target lesion, compared with the other groups in the phase II trial. The investigators also reported at safety profile consistent with halobetasol propionate or tazarotene monotherapy, meaning no new safety concerns emerged with the combination.
Participants were randomized to the combination, halobetasol propionate alone, tazarotene monotherapy, or vehicle in the multicenter, double blind study.
Efficacy evaluation
At 8 weeks, 53% of the combination group achieved treatment success, defined as at least a 2-point gain in Investigator’s Global Assessment of Disease Severity and a score of “clear” or “almost clear.” In contrast, 33% of the halobetasol propionate group, 19% in the tazarotene, and 10% of the vehicle only group achieved those endpoints in the intent-to-treat-analysis. The difference in efficacy between the combination group and vehicle was statistically significant (P less than .001).
On individual clinical efficacy measures, more than half of the patients in the combination treatment group achieved at least a 2-point improvement from baseline: 54% for erythema, 68% for plaque elevation, 65% for scaling. Each of these outcomes was significantly superior compared to the tazarotene or vehicle group (P less than or equal to .001).
“I was not surprised by the findings as the drugs work by complimentary mechanisms of action – so combination therapy should be effective,” Dr. Stein Gold said.
At baseline, IGA severity score of 3 was most common in each group and for each psoriasis sign at the target lesions. In each group, the mean age of participants ranged from 48 to 56 years; the proportion of men ranged from 59% to 68%; and 87% to 95% were white. The median target lesion sizes ranged from 25 to 32 cm2.
Safety outcomes
One patient in the vehicle-only group died. Three other participants experienced serious adverse events – one in each of the noncombination groups. None of these events were related to the study medications, the investigators noted. Application site reactions were the most common treatment-associated adverse events. Some skin atrophy was reported.
“These results show that the fixed combination of halobetasol propionate and tazarotene was effective and well tolerated,” said Dr. Stein Gold, who serves as division head of dermatology at Henry Ford Health System, West Bloomfield, Mich. “This would be a nice addition to our treatment armamentarium for patients with plaque psoriasis.”
Dr. Stein Gold is a speaker, consultant, and study investigator for Valeant Pharmaceuticals, which supported the study.
MIAMI – In an ongoing drive to identify an alternative to the mainstay treatment of psoriasis with topical corticosteroids, researchers evaluated a fixed-dose combination of halobetasol propionate 0.01% and tazarotene 0.045% lotion compared to its monads and vehicle in 212 people with moderate to severe psoriasis.
After 8 weeks of once-daily applications, combination therapy yielded significantly greater reductions in erythema, plaque elevation, and scaling at the target lesion, compared with the other groups in the phase II trial. The investigators also reported at safety profile consistent with halobetasol propionate or tazarotene monotherapy, meaning no new safety concerns emerged with the combination.
Participants were randomized to the combination, halobetasol propionate alone, tazarotene monotherapy, or vehicle in the multicenter, double blind study.
Efficacy evaluation
At 8 weeks, 53% of the combination group achieved treatment success, defined as at least a 2-point gain in Investigator’s Global Assessment of Disease Severity and a score of “clear” or “almost clear.” In contrast, 33% of the halobetasol propionate group, 19% in the tazarotene, and 10% of the vehicle only group achieved those endpoints in the intent-to-treat-analysis. The difference in efficacy between the combination group and vehicle was statistically significant (P less than .001).
On individual clinical efficacy measures, more than half of the patients in the combination treatment group achieved at least a 2-point improvement from baseline: 54% for erythema, 68% for plaque elevation, 65% for scaling. Each of these outcomes was significantly superior compared to the tazarotene or vehicle group (P less than or equal to .001).
“I was not surprised by the findings as the drugs work by complimentary mechanisms of action – so combination therapy should be effective,” Dr. Stein Gold said.
At baseline, IGA severity score of 3 was most common in each group and for each psoriasis sign at the target lesions. In each group, the mean age of participants ranged from 48 to 56 years; the proportion of men ranged from 59% to 68%; and 87% to 95% were white. The median target lesion sizes ranged from 25 to 32 cm2.
Safety outcomes
One patient in the vehicle-only group died. Three other participants experienced serious adverse events – one in each of the noncombination groups. None of these events were related to the study medications, the investigators noted. Application site reactions were the most common treatment-associated adverse events. Some skin atrophy was reported.
“These results show that the fixed combination of halobetasol propionate and tazarotene was effective and well tolerated,” said Dr. Stein Gold, who serves as division head of dermatology at Henry Ford Health System, West Bloomfield, Mich. “This would be a nice addition to our treatment armamentarium for patients with plaque psoriasis.”
Dr. Stein Gold is a speaker, consultant, and study investigator for Valeant Pharmaceuticals, which supported the study.
MIAMI – In an ongoing drive to identify an alternative to the mainstay treatment of psoriasis with topical corticosteroids, researchers evaluated a fixed-dose combination of halobetasol propionate 0.01% and tazarotene 0.045% lotion compared to its monads and vehicle in 212 people with moderate to severe psoriasis.
After 8 weeks of once-daily applications, combination therapy yielded significantly greater reductions in erythema, plaque elevation, and scaling at the target lesion, compared with the other groups in the phase II trial. The investigators also reported at safety profile consistent with halobetasol propionate or tazarotene monotherapy, meaning no new safety concerns emerged with the combination.
Participants were randomized to the combination, halobetasol propionate alone, tazarotene monotherapy, or vehicle in the multicenter, double blind study.
Efficacy evaluation
At 8 weeks, 53% of the combination group achieved treatment success, defined as at least a 2-point gain in Investigator’s Global Assessment of Disease Severity and a score of “clear” or “almost clear.” In contrast, 33% of the halobetasol propionate group, 19% in the tazarotene, and 10% of the vehicle only group achieved those endpoints in the intent-to-treat-analysis. The difference in efficacy between the combination group and vehicle was statistically significant (P less than .001).
On individual clinical efficacy measures, more than half of the patients in the combination treatment group achieved at least a 2-point improvement from baseline: 54% for erythema, 68% for plaque elevation, 65% for scaling. Each of these outcomes was significantly superior compared to the tazarotene or vehicle group (P less than or equal to .001).
“I was not surprised by the findings as the drugs work by complimentary mechanisms of action – so combination therapy should be effective,” Dr. Stein Gold said.
At baseline, IGA severity score of 3 was most common in each group and for each psoriasis sign at the target lesions. In each group, the mean age of participants ranged from 48 to 56 years; the proportion of men ranged from 59% to 68%; and 87% to 95% were white. The median target lesion sizes ranged from 25 to 32 cm2.
Safety outcomes
One patient in the vehicle-only group died. Three other participants experienced serious adverse events – one in each of the noncombination groups. None of these events were related to the study medications, the investigators noted. Application site reactions were the most common treatment-associated adverse events. Some skin atrophy was reported.
“These results show that the fixed combination of halobetasol propionate and tazarotene was effective and well tolerated,” said Dr. Stein Gold, who serves as division head of dermatology at Henry Ford Health System, West Bloomfield, Mich. “This would be a nice addition to our treatment armamentarium for patients with plaque psoriasis.”
Dr. Stein Gold is a speaker, consultant, and study investigator for Valeant Pharmaceuticals, which supported the study.
AT ODAC 2017
Key clinical point: A fixed dose combination of topical halobetasol propionate 0.01% and tazarotene 0.045% proved superior to either monotherapy or vehicle.
Major finding: Treatment success was achieved by 53% of a combination group compared with 33% of a halobetasol propionate group, 19% of a tazarotene group, and 10% of the vehicle-only group in an intent-to-treat-analysis.
Data source: A multicenter, randomized, double blind phase II study of 212 people with moderate to severe psoriasis.
Disclosures: Dr. Stein Gold is a speaker, consultant, and study investigator for Valeant Pharmaceuticals, which supported the study.