User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
‘Substantial’ CVD risks, burden up to a year after COVID-19
People who have had COVID-19 have an increased risk for, and 12-month burden of, cardiovascular disease (CVD) that is substantial and spans an array of cardiovascular disorders, a deep dive into federal data suggests.
“I went into this thinking that this is most likely happening in people to start with who have a higher risk of cardiovascular disorders, smokers, people with high BMI, diabetes, but what we found is something different,” Ziyad Al-Aly, MD, said in an interview. “It’s evident in people at high risk, but it was also as clear as the sun even in people who have no cardiovascular risk whatsoever.”
Rates were increased in younger adults, never smokers, White and Black people, and males and females, he said. “So the risk confirmed by the SARS-CoV-2 virus seems to spare almost no one.”
Although cardiovascular outcomes increased with the severity of the acute infection, the excess risks and burdens were also evident in those who never required hospitalization, a group that represents the majority of people with COVID-19, observed Dr. Al-Aly, who directs the Clinical Epidemiology Center at the Veterans Affairs St. Louis Health Care System.
“This study is very important because it underscores not just the acute cardiovascular risk associated with COVID but the increased risk of chronic cardiovascular outcomes as well,” cardiologist C. Michael Gibson, MD, professor of medicine, Harvard Medical School, Boston, said in an interview. “Given the number of patients in the U.S. who have been infected with COVID, this could represent a significant chronic burden on the health care system, particularly as health care professionals leave the profession.”
For the study, the investigators used national VA databases to build a cohort of 153,760 veterans who were alive 30 days after testing positive for COVID-19 between March 1, 2020, and January 2021. They were compared with a contemporary cohort of 5.6 million veterans with no evidence of SARS-CoV-2 infection and a historical cohort of 5.8 million veterans using the system in 2017 prior to the pandemic. Median follow-up was 347, 348, and 347 days, respectively.
As reported in Nature Medicine, the risk for a major adverse cardiovascular event, a composite of myocardial infarction, stroke, and all-cause mortality, was 4% higher in people who had been infected with COVID-19 than in those who had not.
“People say 4% is small, but actually it’s really, really big if you think about it in the context of the huge number of people who have had COVID-19 in the United States, and also globally,” Dr. Al-Aly said.
Compared with the contemporary control group, people who had COVID-19 had an increased risk (hazard ratio [HR]) and burden per 1,000 people at 1 year for the following cardiovascular outcomes:
- Stroke: HR, 1.52; burden, 4.03
- Transient ischemic attack: HR, 1.49; burden, 1.84
- Dysrhythmias: HR, 1.69; burden, 19.86
- Ischemic heart disease: HR, 1.66; burden, 7.28
- Heart failure: HR, 1.72; burden, 11.61
- Nonischemic cardiomyopathy: HR, 1.62; burden 3.56
- Pulmonary embolism: HR, 2.93; burden, 5.47
- Deep vein thrombosis: HR, 2.09; burden, 4.18
- Pericarditis: HR, 1.85, burden, 0.98
- Myocarditis: HR, 5.38; burden, 0.31
Recent reports have raised concerns about an association between COVID-19 vaccines and myocarditis and pericarditis, particularly in young males. Although very few of the participants were vaccinated prior to becoming infected, as vaccines were not yet widely available, the researchers performed two analyses censoring participants at the time of the first dose of any COVID-19 vaccine and adjusting for vaccination as a time-varying covariate.
The absolute numbers of myocarditis and pericarditis were still higher than the contemporary and historical cohorts. These numbers are much larger than those reported for myocarditis after vaccines, which are generally around 40 cases per 1 million people, observed Dr. Al-Aly.
The overall results were also consistent when compared with the historical control subjects.
“What we’re seeing in our report and others is that SARS-CoV-2 can leave a sort of scar or imprint on people, and some of these conditions are likely chronic conditions,” Dr. Al-Aly said. “So you’re going to have a generation of people who will bear the scar of COVID for their lifetime and I think that requires recognition and attention, so we’re aware of the magnitude of the problem and prepared to deal with it.”
With more than 76 million COVID-19 cases in the United States, that effort will likely have to be at the federal level, similar to President Joe Biden’s recent relaunch of the “Cancer Moonshot,” he added. “We need a greater and broader recognition at the federal level to try and recognize that when you have an earthquake, you don’t just deal with the earthquake when the earth is shaking, but you also need to deal with the aftermath.”
Dr. Gibson pointed out that this was a study of predominantly males and, thus, it’s unclear if the results can be extended to females. Nevertheless, he added, “long COVID may include outcomes beyond the central nervous system and we should educate patients about the risk of late cardiovascular outcomes.”
The authors noted the largely White, male cohort may limit generalizability of the findings. Other limitations include the possibility that some people may have had COVID-19 but were not tested, the datasets lacked information on cause of death, and possible residual confounding not accounted for in the adjusted analyses.
The research was funded by the U.S. Department of Veterans Affairs and two American Society of Nephrology and Kidney Cure fellowship awards. The authors declared no competing interests. Dr. Gibson reports having no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
People who have had COVID-19 have an increased risk for, and 12-month burden of, cardiovascular disease (CVD) that is substantial and spans an array of cardiovascular disorders, a deep dive into federal data suggests.
“I went into this thinking that this is most likely happening in people to start with who have a higher risk of cardiovascular disorders, smokers, people with high BMI, diabetes, but what we found is something different,” Ziyad Al-Aly, MD, said in an interview. “It’s evident in people at high risk, but it was also as clear as the sun even in people who have no cardiovascular risk whatsoever.”
Rates were increased in younger adults, never smokers, White and Black people, and males and females, he said. “So the risk confirmed by the SARS-CoV-2 virus seems to spare almost no one.”
Although cardiovascular outcomes increased with the severity of the acute infection, the excess risks and burdens were also evident in those who never required hospitalization, a group that represents the majority of people with COVID-19, observed Dr. Al-Aly, who directs the Clinical Epidemiology Center at the Veterans Affairs St. Louis Health Care System.
“This study is very important because it underscores not just the acute cardiovascular risk associated with COVID but the increased risk of chronic cardiovascular outcomes as well,” cardiologist C. Michael Gibson, MD, professor of medicine, Harvard Medical School, Boston, said in an interview. “Given the number of patients in the U.S. who have been infected with COVID, this could represent a significant chronic burden on the health care system, particularly as health care professionals leave the profession.”
For the study, the investigators used national VA databases to build a cohort of 153,760 veterans who were alive 30 days after testing positive for COVID-19 between March 1, 2020, and January 2021. They were compared with a contemporary cohort of 5.6 million veterans with no evidence of SARS-CoV-2 infection and a historical cohort of 5.8 million veterans using the system in 2017 prior to the pandemic. Median follow-up was 347, 348, and 347 days, respectively.
As reported in Nature Medicine, the risk for a major adverse cardiovascular event, a composite of myocardial infarction, stroke, and all-cause mortality, was 4% higher in people who had been infected with COVID-19 than in those who had not.
“People say 4% is small, but actually it’s really, really big if you think about it in the context of the huge number of people who have had COVID-19 in the United States, and also globally,” Dr. Al-Aly said.
Compared with the contemporary control group, people who had COVID-19 had an increased risk (hazard ratio [HR]) and burden per 1,000 people at 1 year for the following cardiovascular outcomes:
- Stroke: HR, 1.52; burden, 4.03
- Transient ischemic attack: HR, 1.49; burden, 1.84
- Dysrhythmias: HR, 1.69; burden, 19.86
- Ischemic heart disease: HR, 1.66; burden, 7.28
- Heart failure: HR, 1.72; burden, 11.61
- Nonischemic cardiomyopathy: HR, 1.62; burden 3.56
- Pulmonary embolism: HR, 2.93; burden, 5.47
- Deep vein thrombosis: HR, 2.09; burden, 4.18
- Pericarditis: HR, 1.85, burden, 0.98
- Myocarditis: HR, 5.38; burden, 0.31
Recent reports have raised concerns about an association between COVID-19 vaccines and myocarditis and pericarditis, particularly in young males. Although very few of the participants were vaccinated prior to becoming infected, as vaccines were not yet widely available, the researchers performed two analyses censoring participants at the time of the first dose of any COVID-19 vaccine and adjusting for vaccination as a time-varying covariate.
The absolute numbers of myocarditis and pericarditis were still higher than the contemporary and historical cohorts. These numbers are much larger than those reported for myocarditis after vaccines, which are generally around 40 cases per 1 million people, observed Dr. Al-Aly.
The overall results were also consistent when compared with the historical control subjects.
“What we’re seeing in our report and others is that SARS-CoV-2 can leave a sort of scar or imprint on people, and some of these conditions are likely chronic conditions,” Dr. Al-Aly said. “So you’re going to have a generation of people who will bear the scar of COVID for their lifetime and I think that requires recognition and attention, so we’re aware of the magnitude of the problem and prepared to deal with it.”
With more than 76 million COVID-19 cases in the United States, that effort will likely have to be at the federal level, similar to President Joe Biden’s recent relaunch of the “Cancer Moonshot,” he added. “We need a greater and broader recognition at the federal level to try and recognize that when you have an earthquake, you don’t just deal with the earthquake when the earth is shaking, but you also need to deal with the aftermath.”
Dr. Gibson pointed out that this was a study of predominantly males and, thus, it’s unclear if the results can be extended to females. Nevertheless, he added, “long COVID may include outcomes beyond the central nervous system and we should educate patients about the risk of late cardiovascular outcomes.”
The authors noted the largely White, male cohort may limit generalizability of the findings. Other limitations include the possibility that some people may have had COVID-19 but were not tested, the datasets lacked information on cause of death, and possible residual confounding not accounted for in the adjusted analyses.
The research was funded by the U.S. Department of Veterans Affairs and two American Society of Nephrology and Kidney Cure fellowship awards. The authors declared no competing interests. Dr. Gibson reports having no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
People who have had COVID-19 have an increased risk for, and 12-month burden of, cardiovascular disease (CVD) that is substantial and spans an array of cardiovascular disorders, a deep dive into federal data suggests.
“I went into this thinking that this is most likely happening in people to start with who have a higher risk of cardiovascular disorders, smokers, people with high BMI, diabetes, but what we found is something different,” Ziyad Al-Aly, MD, said in an interview. “It’s evident in people at high risk, but it was also as clear as the sun even in people who have no cardiovascular risk whatsoever.”
Rates were increased in younger adults, never smokers, White and Black people, and males and females, he said. “So the risk confirmed by the SARS-CoV-2 virus seems to spare almost no one.”
Although cardiovascular outcomes increased with the severity of the acute infection, the excess risks and burdens were also evident in those who never required hospitalization, a group that represents the majority of people with COVID-19, observed Dr. Al-Aly, who directs the Clinical Epidemiology Center at the Veterans Affairs St. Louis Health Care System.
“This study is very important because it underscores not just the acute cardiovascular risk associated with COVID but the increased risk of chronic cardiovascular outcomes as well,” cardiologist C. Michael Gibson, MD, professor of medicine, Harvard Medical School, Boston, said in an interview. “Given the number of patients in the U.S. who have been infected with COVID, this could represent a significant chronic burden on the health care system, particularly as health care professionals leave the profession.”
For the study, the investigators used national VA databases to build a cohort of 153,760 veterans who were alive 30 days after testing positive for COVID-19 between March 1, 2020, and January 2021. They were compared with a contemporary cohort of 5.6 million veterans with no evidence of SARS-CoV-2 infection and a historical cohort of 5.8 million veterans using the system in 2017 prior to the pandemic. Median follow-up was 347, 348, and 347 days, respectively.
As reported in Nature Medicine, the risk for a major adverse cardiovascular event, a composite of myocardial infarction, stroke, and all-cause mortality, was 4% higher in people who had been infected with COVID-19 than in those who had not.
“People say 4% is small, but actually it’s really, really big if you think about it in the context of the huge number of people who have had COVID-19 in the United States, and also globally,” Dr. Al-Aly said.
Compared with the contemporary control group, people who had COVID-19 had an increased risk (hazard ratio [HR]) and burden per 1,000 people at 1 year for the following cardiovascular outcomes:
- Stroke: HR, 1.52; burden, 4.03
- Transient ischemic attack: HR, 1.49; burden, 1.84
- Dysrhythmias: HR, 1.69; burden, 19.86
- Ischemic heart disease: HR, 1.66; burden, 7.28
- Heart failure: HR, 1.72; burden, 11.61
- Nonischemic cardiomyopathy: HR, 1.62; burden 3.56
- Pulmonary embolism: HR, 2.93; burden, 5.47
- Deep vein thrombosis: HR, 2.09; burden, 4.18
- Pericarditis: HR, 1.85, burden, 0.98
- Myocarditis: HR, 5.38; burden, 0.31
Recent reports have raised concerns about an association between COVID-19 vaccines and myocarditis and pericarditis, particularly in young males. Although very few of the participants were vaccinated prior to becoming infected, as vaccines were not yet widely available, the researchers performed two analyses censoring participants at the time of the first dose of any COVID-19 vaccine and adjusting for vaccination as a time-varying covariate.
The absolute numbers of myocarditis and pericarditis were still higher than the contemporary and historical cohorts. These numbers are much larger than those reported for myocarditis after vaccines, which are generally around 40 cases per 1 million people, observed Dr. Al-Aly.
The overall results were also consistent when compared with the historical control subjects.
“What we’re seeing in our report and others is that SARS-CoV-2 can leave a sort of scar or imprint on people, and some of these conditions are likely chronic conditions,” Dr. Al-Aly said. “So you’re going to have a generation of people who will bear the scar of COVID for their lifetime and I think that requires recognition and attention, so we’re aware of the magnitude of the problem and prepared to deal with it.”
With more than 76 million COVID-19 cases in the United States, that effort will likely have to be at the federal level, similar to President Joe Biden’s recent relaunch of the “Cancer Moonshot,” he added. “We need a greater and broader recognition at the federal level to try and recognize that when you have an earthquake, you don’t just deal with the earthquake when the earth is shaking, but you also need to deal with the aftermath.”
Dr. Gibson pointed out that this was a study of predominantly males and, thus, it’s unclear if the results can be extended to females. Nevertheless, he added, “long COVID may include outcomes beyond the central nervous system and we should educate patients about the risk of late cardiovascular outcomes.”
The authors noted the largely White, male cohort may limit generalizability of the findings. Other limitations include the possibility that some people may have had COVID-19 but were not tested, the datasets lacked information on cause of death, and possible residual confounding not accounted for in the adjusted analyses.
The research was funded by the U.S. Department of Veterans Affairs and two American Society of Nephrology and Kidney Cure fellowship awards. The authors declared no competing interests. Dr. Gibson reports having no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Scientists see hope in new therapy for COVID-19 brain fog patients
People with long-COVID “brain fog” may be able to recover mental abilities that were dulled or stolen from them by the virus through an approach that has improved the effects of stroke, traumatic brain injury, and other post-viral disorders, doctors and scientists say.
For a lucky portion of the population, COVID-19 lasts a handful of days with minor symptoms. But for an estimated 37% who contract the virus, symptoms can linger for weeks, months, or even years. One of the most common symptoms of long COVID is brain fog: a life-altering condition characterized by slow thinking, confusion, difficulty remembering things, and poor concentration.
The approaches are based on the concept of neuroplasticity: The ability of neural networks in the brain to change, adapt, and strengthen, much like a muscle in the body that has been trained and exercised.
“The brain’s ability to bounce back from injury is what neuroplasticity is, and I’ve worked with people in our rehab clinic who have had brain tumors or suffer the effects of surgery or radiation on the brain, and people who have had West Nile virus, HIV, and meningitis,” said Tom Bergquist, PhD, clinical neuropsychologist at Mayo Clinic in Rochester, Minn. “There’s not a week that goes by that I don’t see someone recovering from COVID-19.”
One of the approaches used in the clinic is errorless learning, or having a patient with memory problems repeat information a certain number of times without error. The repetition helps rebuild those memory skills that were weakened during infection, Dr. Bergquist says.
People who have experienced brain fog after other viral infections have seen improvements with these approaches. Ben Ahrens, co-founder and CEO of re-origin – a company that offers neuroplasticity therapy – says he had long-term cognitive issues after a Lyme disease infection. Posttreatment Lyme disease syndrome, or chronic Lyme disease, occurs in about 1 in 10 people who are infected.
Mr. Ahrens says he was struck with Lyme 10 years ago and had brain fog, joint pain, and brain lesions detectable on scans for several years after infection.
According to Mr. Ahrens, neuroplasticity-based therapies help combat what researchers have found may be a lingering memory of past infections that lead to a heightened immune response, causing lingering symptoms.
“Essentially, what we believe is happening here, is the brain has learned that these symptoms are life-threatening – because, in fact, they can be,” Mr. Ahrens said. “The brain’s one job is to protect the body, and once it’s learned to associate these symptoms with that potentially very dangerous pathogen, even after it’s gone, things like a normal headache can trigger an immune cascade.”
Studies are underway at the University of Alabama at Birmingham to examine whether constraint-induced therapy – an approach rooted in neuroplasticity and historically used for loss of limb and speech function – is also effective for cognitive impairments like brain fog.
One technique they use is called shaping, which requires a person to repeatedly carry out their personal best function of impaired use – for example, remembering household tasks they have previously forgotten. That is done multiple times over several weeks in the clinic, and patients are given ways to transfer those skills to real-life use.
So far, the results are promising, said Edward Taub, PhD, researcher and professor of psychology at the University of Alabama at Birmingham.
When used in the past for physical impairments, researchers have noted not just clinical improvements, but structural changes. It led to an increase in the brain’s gray matter – which allows individuals to control movement, memory, and emotions – and improved white matter, which helps communication between gray matter areas.
Though results of the cognitive studies have not been published, Dr. Taub said patients with brain fog have shown improvement after just 35 hours of therapy and are nearly 100% improved after 6 months.
“The idea behind this is that the brain is responsive to use,” Dr. Taub said. “The amount of brain territory that’s dedicated to supporting or mediating a given behavioral function depends on the demands placed on the brain.”
A version of this article first appeared on WebMD.com.
People with long-COVID “brain fog” may be able to recover mental abilities that were dulled or stolen from them by the virus through an approach that has improved the effects of stroke, traumatic brain injury, and other post-viral disorders, doctors and scientists say.
For a lucky portion of the population, COVID-19 lasts a handful of days with minor symptoms. But for an estimated 37% who contract the virus, symptoms can linger for weeks, months, or even years. One of the most common symptoms of long COVID is brain fog: a life-altering condition characterized by slow thinking, confusion, difficulty remembering things, and poor concentration.
The approaches are based on the concept of neuroplasticity: The ability of neural networks in the brain to change, adapt, and strengthen, much like a muscle in the body that has been trained and exercised.
“The brain’s ability to bounce back from injury is what neuroplasticity is, and I’ve worked with people in our rehab clinic who have had brain tumors or suffer the effects of surgery or radiation on the brain, and people who have had West Nile virus, HIV, and meningitis,” said Tom Bergquist, PhD, clinical neuropsychologist at Mayo Clinic in Rochester, Minn. “There’s not a week that goes by that I don’t see someone recovering from COVID-19.”
One of the approaches used in the clinic is errorless learning, or having a patient with memory problems repeat information a certain number of times without error. The repetition helps rebuild those memory skills that were weakened during infection, Dr. Bergquist says.
People who have experienced brain fog after other viral infections have seen improvements with these approaches. Ben Ahrens, co-founder and CEO of re-origin – a company that offers neuroplasticity therapy – says he had long-term cognitive issues after a Lyme disease infection. Posttreatment Lyme disease syndrome, or chronic Lyme disease, occurs in about 1 in 10 people who are infected.
Mr. Ahrens says he was struck with Lyme 10 years ago and had brain fog, joint pain, and brain lesions detectable on scans for several years after infection.
According to Mr. Ahrens, neuroplasticity-based therapies help combat what researchers have found may be a lingering memory of past infections that lead to a heightened immune response, causing lingering symptoms.
“Essentially, what we believe is happening here, is the brain has learned that these symptoms are life-threatening – because, in fact, they can be,” Mr. Ahrens said. “The brain’s one job is to protect the body, and once it’s learned to associate these symptoms with that potentially very dangerous pathogen, even after it’s gone, things like a normal headache can trigger an immune cascade.”
Studies are underway at the University of Alabama at Birmingham to examine whether constraint-induced therapy – an approach rooted in neuroplasticity and historically used for loss of limb and speech function – is also effective for cognitive impairments like brain fog.
One technique they use is called shaping, which requires a person to repeatedly carry out their personal best function of impaired use – for example, remembering household tasks they have previously forgotten. That is done multiple times over several weeks in the clinic, and patients are given ways to transfer those skills to real-life use.
So far, the results are promising, said Edward Taub, PhD, researcher and professor of psychology at the University of Alabama at Birmingham.
When used in the past for physical impairments, researchers have noted not just clinical improvements, but structural changes. It led to an increase in the brain’s gray matter – which allows individuals to control movement, memory, and emotions – and improved white matter, which helps communication between gray matter areas.
Though results of the cognitive studies have not been published, Dr. Taub said patients with brain fog have shown improvement after just 35 hours of therapy and are nearly 100% improved after 6 months.
“The idea behind this is that the brain is responsive to use,” Dr. Taub said. “The amount of brain territory that’s dedicated to supporting or mediating a given behavioral function depends on the demands placed on the brain.”
A version of this article first appeared on WebMD.com.
People with long-COVID “brain fog” may be able to recover mental abilities that were dulled or stolen from them by the virus through an approach that has improved the effects of stroke, traumatic brain injury, and other post-viral disorders, doctors and scientists say.
For a lucky portion of the population, COVID-19 lasts a handful of days with minor symptoms. But for an estimated 37% who contract the virus, symptoms can linger for weeks, months, or even years. One of the most common symptoms of long COVID is brain fog: a life-altering condition characterized by slow thinking, confusion, difficulty remembering things, and poor concentration.
The approaches are based on the concept of neuroplasticity: The ability of neural networks in the brain to change, adapt, and strengthen, much like a muscle in the body that has been trained and exercised.
“The brain’s ability to bounce back from injury is what neuroplasticity is, and I’ve worked with people in our rehab clinic who have had brain tumors or suffer the effects of surgery or radiation on the brain, and people who have had West Nile virus, HIV, and meningitis,” said Tom Bergquist, PhD, clinical neuropsychologist at Mayo Clinic in Rochester, Minn. “There’s not a week that goes by that I don’t see someone recovering from COVID-19.”
One of the approaches used in the clinic is errorless learning, or having a patient with memory problems repeat information a certain number of times without error. The repetition helps rebuild those memory skills that were weakened during infection, Dr. Bergquist says.
People who have experienced brain fog after other viral infections have seen improvements with these approaches. Ben Ahrens, co-founder and CEO of re-origin – a company that offers neuroplasticity therapy – says he had long-term cognitive issues after a Lyme disease infection. Posttreatment Lyme disease syndrome, or chronic Lyme disease, occurs in about 1 in 10 people who are infected.
Mr. Ahrens says he was struck with Lyme 10 years ago and had brain fog, joint pain, and brain lesions detectable on scans for several years after infection.
According to Mr. Ahrens, neuroplasticity-based therapies help combat what researchers have found may be a lingering memory of past infections that lead to a heightened immune response, causing lingering symptoms.
“Essentially, what we believe is happening here, is the brain has learned that these symptoms are life-threatening – because, in fact, they can be,” Mr. Ahrens said. “The brain’s one job is to protect the body, and once it’s learned to associate these symptoms with that potentially very dangerous pathogen, even after it’s gone, things like a normal headache can trigger an immune cascade.”
Studies are underway at the University of Alabama at Birmingham to examine whether constraint-induced therapy – an approach rooted in neuroplasticity and historically used for loss of limb and speech function – is also effective for cognitive impairments like brain fog.
One technique they use is called shaping, which requires a person to repeatedly carry out their personal best function of impaired use – for example, remembering household tasks they have previously forgotten. That is done multiple times over several weeks in the clinic, and patients are given ways to transfer those skills to real-life use.
So far, the results are promising, said Edward Taub, PhD, researcher and professor of psychology at the University of Alabama at Birmingham.
When used in the past for physical impairments, researchers have noted not just clinical improvements, but structural changes. It led to an increase in the brain’s gray matter – which allows individuals to control movement, memory, and emotions – and improved white matter, which helps communication between gray matter areas.
Though results of the cognitive studies have not been published, Dr. Taub said patients with brain fog have shown improvement after just 35 hours of therapy and are nearly 100% improved after 6 months.
“The idea behind this is that the brain is responsive to use,” Dr. Taub said. “The amount of brain territory that’s dedicated to supporting or mediating a given behavioral function depends on the demands placed on the brain.”
A version of this article first appeared on WebMD.com.
Does endovascular therapy benefit strokes with larger ischemic cores?
The RESCUE-JAPAN LIMIT trial was presented at the International Stroke Conference by Shinichi Yoshimura, MD, Hyogo College of Medicine, Nishinomiya, Japan. The study was also published online in the New England Journal of Medicine to coincide with its presentation at the ISC meeting.
The trial showed that among patients with acute stroke and a large ischemic brain region, functional outcomes at 90 days were better with endovascular therapy and medical care than with medical care alone.
Patients who received endovascular therapy were more than twice as likely to have a good functional outcome, defined as a modified Rankin scale (mRS) score of 0-3 at 90 days, than those who received medical care alone.
While the rate of intracranial hemorrhage increased with endovascular therapy, authors of the study and outside commentators suggested that the benefit appeared to outweigh the risk. “Our results provide strong evidence that endovascular therapy improves patient outcomes when the infarct area is large,” Dr. Yoshimura concluded at the meeting, presented by the American Stroke Association, a division of the American Heart Association.
Commenting on the study at an ISC press conference, Tudor Jovin, MD, chair of neurology at Cooper University Hospital, Cherry Hill, New Jersey, said: “The question of strokes with a large core stroke being an exclusion criteria for endovascular therapy is arguably one of the hottest topics the field is facing at this time. There are several randomized trials ongoing aiming to answer this question.”
“The RESCUE-JAPAN trial is the first of these trials to report and shed some light on this issue,” Dr. Jovin added. “The results appear to show that these patients with large core infarcts have just as much benefit from endovascular therapy as patients with smaller infarcts.”
Dr. Jovin described these findings as encouraging but also surprising. “When these large core randomized trials were planned, there was a belief that there would be benefit at some level. But what is surprising to me is that in this trial the benefit was similar to that seen in trials in patients with moderate or small core infarcts. This begs the question of whether we should care about the size of the infarct when we are considering taking these patients for thrombectomy,” he said.
Confirmation needed
On whether this will change practice, Dr. Jovin cautioned that this was just one study with a relatively small number of patients. “I think it is important that all the other randomized trials ongoing should continue so that we have a definitive answer to this question,” he said.
In his presentation, Dr. Yoshimura explained that current guidelines recommended endovascular therapy for patients with large cerebral vessel occlusion and a small or moderate infarct size – an ASPECTS score (Alberta Stroke Program Early Computed Tomographic Score) of 6 or higher. The ASPECTS score has a scale of 1-10, with lower values indicating larger infarction.
The RESCUE-JAPAN LIMIT study included 203 patients with occlusion of large cerebral vessels and sizable strokes on imaging, as indicated by an ASPECTS score of 3 to 5.
Patients were randomly assigned to receive endovascular therapy with medical care (endovascular-therapy group) or medical therapy alone (medical-care group) within 6 hours after they were last known to be well or within 24 hours if there was no early change on fluid-attenuated inversion recovery images indicating that the infarction was recent.
The percentage of patients with a good outcome as defined by an mRS score of 0 to 3 at 90 days, the primary outcome, was 31.0% in the endovascular-therapy group and 12.7% in the medical-care group (relative risk, 2.43; 95% confidence interval, 1.35 to 4.37; P = .002).
Secondary outcomes were mRS scores of 0 to 2 and 0 to 1, an ordinal shift across the range of mRS scores toward a better outcome at 90 days, and an improvement of at least 8 points in the National Institutes of Health Stroke Scale (NIHSS) score (range, 0 to 42, with higher scores indicating greater deficit) at 48 hours.
An mRS score of 0 to 2 was seen in 14% of patients in the endovascular-therapy group and 6.9% in the medical-care group (RR, 2.04; 95% CI, 0.86 to 4.84), and an mRS score of 0 to 1 was reported in 5% of the endovascular group versus 2.9% of the medical group (RR, 1.70; 95% CI, 0.42 to 6.93).
The ordinal shift across the range of mRS scores also favored endovascular therapy (common odds ratio, 2.42; 95% CI, 1.46 to 4.01).
An improvement of at least 8 points on the NIHSS score at 48 hours was observed in 31.0% of the patients in the endovascular-therapy group and 8.8% of those in the medical-care group (RR, 3.51; 95% CI, 1.76 to 7.00).
In terms of safety, any intracranial hemorrhage occurred in 58.0% of patients in the endovascular group and 31.4% of those in the medical therapy group (RR, 1.85; 95% CI, 1.33 to 2.58; P < .001).
There was also a trend toward an increase in symptomatic intracranial hemorrhage in the endovascular group (9% vs. 4.9%), but this did not reach significance (RR, 1.84; 95% CI, 0.64 to 5.29; P = .25).
In the NEJM paper, the authors pointed out that the ASPECTS value in most of the patients in this study was determined with the use of diffusion-weighted MRI, as MRI is widely used in Japan for the diagnosis of acute ischemic stroke. They noted that differences between ASPECTS values based on CT results and those based on diffusion-weighted MRI results should be considered in the interpretation of the results and that previous studies have suggested that an ASPECTS value determined with the use of diffusion-weighted MRI may be one level lower than that determined with the use of CT.
They also noted that there was a relatively low use of thrombolysis in the trial (27% to 29%), which may have altered the outcomes in both groups and disadvantaged the medical-care group. However, they add that most guidelines recommend against the use of thrombolysis when there is extensive ischemic change on imaging.
Risk/benefit trade-off
Commenting on the trade-off between benefits and risks in the study, Dr. Jovin said the increase in intracranial hemorrhage seen in the endovascular group was similar to that seen in other situations.
“This is not really any different from what is seen when giving tPA [tissue plasminogen activator] to stroke patients or when performing thrombectomy in small or moderate core strokes – we know that intracranial hemorrhage is the price to pay,” he stated.
“While the increase in symptomatic intracranial hemorrhage was nonsignificant, the trend is very clear, and I believe it is real,” Dr. Jovin said. “But I think what matters – and what matters to patients – is that there is a much higher chance of having a good outcome with endovascular therapy. I think most patients will accept the extra risk of intracranial hemorrhage if there is an even higher chance of having a better neurological outcome. This is no different to the approach that we take when we treat patients with IV tPA.”
Dr. Jovin pointed out that the RESCUE-JAPAN study did not include the largest core infarcts (ASPECTS score 0-1), but he added that these very large core infarcts are quite rare – especially in patients in the early time window.
He concluded that the study provided important information but cautioned that, with just 200 patients, the findings needed confirmation from other randomized trials that are ongoing.
Also speaking at the ISC press conference, Mitchell Elkind, MD, immediate past president of the American Heart Association/American Stroke Association, and professor of neurology at Columbia University, New York, said previous trials had established endovascular therapy for patients with large cerebral artery occlusions who have primarily preserved brain tissue and small infarct cores.
“We have picked off the low-lying fruit – the patients with small areas of infarcted brain. But perhaps most patients do not fit into this category and now we are seeing trials addressing these groups,” he said. “This initial study suggests that these patients with larger core infarcts can indeed still benefit from this therapy tremendously.”
The RESCUE-JAPAN LIMIT study was supported in part by the Mihara Cerebrovascular Disorder Research Promotion Fund and the Japanese Society for Neuroendovascular Therapy. There was no industry involvement. Dr. Yoshimura reported research grants from Stryker, Siemens Healthineers, Bristol-Myers Squibb, Sanofi, Eisai, Daiichi Sankyo, Teijin Pharma, Chugai Pharmaceutical, HEALIOS, Asahi Kasei Medical, Kowa, and CSL Behring; and lecturer fees from Stryker, Medtronic, Johnson & Johnson, Kaneka, Terumo, Biomedical Solutions, Boehringer-Ingelheim, Daiichi Sankyo, Bayer, and Bristol-Meyers Squibb.
A version of this article first appeared on Medscape.com.
The RESCUE-JAPAN LIMIT trial was presented at the International Stroke Conference by Shinichi Yoshimura, MD, Hyogo College of Medicine, Nishinomiya, Japan. The study was also published online in the New England Journal of Medicine to coincide with its presentation at the ISC meeting.
The trial showed that among patients with acute stroke and a large ischemic brain region, functional outcomes at 90 days were better with endovascular therapy and medical care than with medical care alone.
Patients who received endovascular therapy were more than twice as likely to have a good functional outcome, defined as a modified Rankin scale (mRS) score of 0-3 at 90 days, than those who received medical care alone.
While the rate of intracranial hemorrhage increased with endovascular therapy, authors of the study and outside commentators suggested that the benefit appeared to outweigh the risk. “Our results provide strong evidence that endovascular therapy improves patient outcomes when the infarct area is large,” Dr. Yoshimura concluded at the meeting, presented by the American Stroke Association, a division of the American Heart Association.
Commenting on the study at an ISC press conference, Tudor Jovin, MD, chair of neurology at Cooper University Hospital, Cherry Hill, New Jersey, said: “The question of strokes with a large core stroke being an exclusion criteria for endovascular therapy is arguably one of the hottest topics the field is facing at this time. There are several randomized trials ongoing aiming to answer this question.”
“The RESCUE-JAPAN trial is the first of these trials to report and shed some light on this issue,” Dr. Jovin added. “The results appear to show that these patients with large core infarcts have just as much benefit from endovascular therapy as patients with smaller infarcts.”
Dr. Jovin described these findings as encouraging but also surprising. “When these large core randomized trials were planned, there was a belief that there would be benefit at some level. But what is surprising to me is that in this trial the benefit was similar to that seen in trials in patients with moderate or small core infarcts. This begs the question of whether we should care about the size of the infarct when we are considering taking these patients for thrombectomy,” he said.
Confirmation needed
On whether this will change practice, Dr. Jovin cautioned that this was just one study with a relatively small number of patients. “I think it is important that all the other randomized trials ongoing should continue so that we have a definitive answer to this question,” he said.
In his presentation, Dr. Yoshimura explained that current guidelines recommended endovascular therapy for patients with large cerebral vessel occlusion and a small or moderate infarct size – an ASPECTS score (Alberta Stroke Program Early Computed Tomographic Score) of 6 or higher. The ASPECTS score has a scale of 1-10, with lower values indicating larger infarction.
The RESCUE-JAPAN LIMIT study included 203 patients with occlusion of large cerebral vessels and sizable strokes on imaging, as indicated by an ASPECTS score of 3 to 5.
Patients were randomly assigned to receive endovascular therapy with medical care (endovascular-therapy group) or medical therapy alone (medical-care group) within 6 hours after they were last known to be well or within 24 hours if there was no early change on fluid-attenuated inversion recovery images indicating that the infarction was recent.
The percentage of patients with a good outcome as defined by an mRS score of 0 to 3 at 90 days, the primary outcome, was 31.0% in the endovascular-therapy group and 12.7% in the medical-care group (relative risk, 2.43; 95% confidence interval, 1.35 to 4.37; P = .002).
Secondary outcomes were mRS scores of 0 to 2 and 0 to 1, an ordinal shift across the range of mRS scores toward a better outcome at 90 days, and an improvement of at least 8 points in the National Institutes of Health Stroke Scale (NIHSS) score (range, 0 to 42, with higher scores indicating greater deficit) at 48 hours.
An mRS score of 0 to 2 was seen in 14% of patients in the endovascular-therapy group and 6.9% in the medical-care group (RR, 2.04; 95% CI, 0.86 to 4.84), and an mRS score of 0 to 1 was reported in 5% of the endovascular group versus 2.9% of the medical group (RR, 1.70; 95% CI, 0.42 to 6.93).
The ordinal shift across the range of mRS scores also favored endovascular therapy (common odds ratio, 2.42; 95% CI, 1.46 to 4.01).
An improvement of at least 8 points on the NIHSS score at 48 hours was observed in 31.0% of the patients in the endovascular-therapy group and 8.8% of those in the medical-care group (RR, 3.51; 95% CI, 1.76 to 7.00).
In terms of safety, any intracranial hemorrhage occurred in 58.0% of patients in the endovascular group and 31.4% of those in the medical therapy group (RR, 1.85; 95% CI, 1.33 to 2.58; P < .001).
There was also a trend toward an increase in symptomatic intracranial hemorrhage in the endovascular group (9% vs. 4.9%), but this did not reach significance (RR, 1.84; 95% CI, 0.64 to 5.29; P = .25).
In the NEJM paper, the authors pointed out that the ASPECTS value in most of the patients in this study was determined with the use of diffusion-weighted MRI, as MRI is widely used in Japan for the diagnosis of acute ischemic stroke. They noted that differences between ASPECTS values based on CT results and those based on diffusion-weighted MRI results should be considered in the interpretation of the results and that previous studies have suggested that an ASPECTS value determined with the use of diffusion-weighted MRI may be one level lower than that determined with the use of CT.
They also noted that there was a relatively low use of thrombolysis in the trial (27% to 29%), which may have altered the outcomes in both groups and disadvantaged the medical-care group. However, they add that most guidelines recommend against the use of thrombolysis when there is extensive ischemic change on imaging.
Risk/benefit trade-off
Commenting on the trade-off between benefits and risks in the study, Dr. Jovin said the increase in intracranial hemorrhage seen in the endovascular group was similar to that seen in other situations.
“This is not really any different from what is seen when giving tPA [tissue plasminogen activator] to stroke patients or when performing thrombectomy in small or moderate core strokes – we know that intracranial hemorrhage is the price to pay,” he stated.
“While the increase in symptomatic intracranial hemorrhage was nonsignificant, the trend is very clear, and I believe it is real,” Dr. Jovin said. “But I think what matters – and what matters to patients – is that there is a much higher chance of having a good outcome with endovascular therapy. I think most patients will accept the extra risk of intracranial hemorrhage if there is an even higher chance of having a better neurological outcome. This is no different to the approach that we take when we treat patients with IV tPA.”
Dr. Jovin pointed out that the RESCUE-JAPAN study did not include the largest core infarcts (ASPECTS score 0-1), but he added that these very large core infarcts are quite rare – especially in patients in the early time window.
He concluded that the study provided important information but cautioned that, with just 200 patients, the findings needed confirmation from other randomized trials that are ongoing.
Also speaking at the ISC press conference, Mitchell Elkind, MD, immediate past president of the American Heart Association/American Stroke Association, and professor of neurology at Columbia University, New York, said previous trials had established endovascular therapy for patients with large cerebral artery occlusions who have primarily preserved brain tissue and small infarct cores.
“We have picked off the low-lying fruit – the patients with small areas of infarcted brain. But perhaps most patients do not fit into this category and now we are seeing trials addressing these groups,” he said. “This initial study suggests that these patients with larger core infarcts can indeed still benefit from this therapy tremendously.”
The RESCUE-JAPAN LIMIT study was supported in part by the Mihara Cerebrovascular Disorder Research Promotion Fund and the Japanese Society for Neuroendovascular Therapy. There was no industry involvement. Dr. Yoshimura reported research grants from Stryker, Siemens Healthineers, Bristol-Myers Squibb, Sanofi, Eisai, Daiichi Sankyo, Teijin Pharma, Chugai Pharmaceutical, HEALIOS, Asahi Kasei Medical, Kowa, and CSL Behring; and lecturer fees from Stryker, Medtronic, Johnson & Johnson, Kaneka, Terumo, Biomedical Solutions, Boehringer-Ingelheim, Daiichi Sankyo, Bayer, and Bristol-Meyers Squibb.
A version of this article first appeared on Medscape.com.
The RESCUE-JAPAN LIMIT trial was presented at the International Stroke Conference by Shinichi Yoshimura, MD, Hyogo College of Medicine, Nishinomiya, Japan. The study was also published online in the New England Journal of Medicine to coincide with its presentation at the ISC meeting.
The trial showed that among patients with acute stroke and a large ischemic brain region, functional outcomes at 90 days were better with endovascular therapy and medical care than with medical care alone.
Patients who received endovascular therapy were more than twice as likely to have a good functional outcome, defined as a modified Rankin scale (mRS) score of 0-3 at 90 days, than those who received medical care alone.
While the rate of intracranial hemorrhage increased with endovascular therapy, authors of the study and outside commentators suggested that the benefit appeared to outweigh the risk. “Our results provide strong evidence that endovascular therapy improves patient outcomes when the infarct area is large,” Dr. Yoshimura concluded at the meeting, presented by the American Stroke Association, a division of the American Heart Association.
Commenting on the study at an ISC press conference, Tudor Jovin, MD, chair of neurology at Cooper University Hospital, Cherry Hill, New Jersey, said: “The question of strokes with a large core stroke being an exclusion criteria for endovascular therapy is arguably one of the hottest topics the field is facing at this time. There are several randomized trials ongoing aiming to answer this question.”
“The RESCUE-JAPAN trial is the first of these trials to report and shed some light on this issue,” Dr. Jovin added. “The results appear to show that these patients with large core infarcts have just as much benefit from endovascular therapy as patients with smaller infarcts.”
Dr. Jovin described these findings as encouraging but also surprising. “When these large core randomized trials were planned, there was a belief that there would be benefit at some level. But what is surprising to me is that in this trial the benefit was similar to that seen in trials in patients with moderate or small core infarcts. This begs the question of whether we should care about the size of the infarct when we are considering taking these patients for thrombectomy,” he said.
Confirmation needed
On whether this will change practice, Dr. Jovin cautioned that this was just one study with a relatively small number of patients. “I think it is important that all the other randomized trials ongoing should continue so that we have a definitive answer to this question,” he said.
In his presentation, Dr. Yoshimura explained that current guidelines recommended endovascular therapy for patients with large cerebral vessel occlusion and a small or moderate infarct size – an ASPECTS score (Alberta Stroke Program Early Computed Tomographic Score) of 6 or higher. The ASPECTS score has a scale of 1-10, with lower values indicating larger infarction.
The RESCUE-JAPAN LIMIT study included 203 patients with occlusion of large cerebral vessels and sizable strokes on imaging, as indicated by an ASPECTS score of 3 to 5.
Patients were randomly assigned to receive endovascular therapy with medical care (endovascular-therapy group) or medical therapy alone (medical-care group) within 6 hours after they were last known to be well or within 24 hours if there was no early change on fluid-attenuated inversion recovery images indicating that the infarction was recent.
The percentage of patients with a good outcome as defined by an mRS score of 0 to 3 at 90 days, the primary outcome, was 31.0% in the endovascular-therapy group and 12.7% in the medical-care group (relative risk, 2.43; 95% confidence interval, 1.35 to 4.37; P = .002).
Secondary outcomes were mRS scores of 0 to 2 and 0 to 1, an ordinal shift across the range of mRS scores toward a better outcome at 90 days, and an improvement of at least 8 points in the National Institutes of Health Stroke Scale (NIHSS) score (range, 0 to 42, with higher scores indicating greater deficit) at 48 hours.
An mRS score of 0 to 2 was seen in 14% of patients in the endovascular-therapy group and 6.9% in the medical-care group (RR, 2.04; 95% CI, 0.86 to 4.84), and an mRS score of 0 to 1 was reported in 5% of the endovascular group versus 2.9% of the medical group (RR, 1.70; 95% CI, 0.42 to 6.93).
The ordinal shift across the range of mRS scores also favored endovascular therapy (common odds ratio, 2.42; 95% CI, 1.46 to 4.01).
An improvement of at least 8 points on the NIHSS score at 48 hours was observed in 31.0% of the patients in the endovascular-therapy group and 8.8% of those in the medical-care group (RR, 3.51; 95% CI, 1.76 to 7.00).
In terms of safety, any intracranial hemorrhage occurred in 58.0% of patients in the endovascular group and 31.4% of those in the medical therapy group (RR, 1.85; 95% CI, 1.33 to 2.58; P < .001).
There was also a trend toward an increase in symptomatic intracranial hemorrhage in the endovascular group (9% vs. 4.9%), but this did not reach significance (RR, 1.84; 95% CI, 0.64 to 5.29; P = .25).
In the NEJM paper, the authors pointed out that the ASPECTS value in most of the patients in this study was determined with the use of diffusion-weighted MRI, as MRI is widely used in Japan for the diagnosis of acute ischemic stroke. They noted that differences between ASPECTS values based on CT results and those based on diffusion-weighted MRI results should be considered in the interpretation of the results and that previous studies have suggested that an ASPECTS value determined with the use of diffusion-weighted MRI may be one level lower than that determined with the use of CT.
They also noted that there was a relatively low use of thrombolysis in the trial (27% to 29%), which may have altered the outcomes in both groups and disadvantaged the medical-care group. However, they add that most guidelines recommend against the use of thrombolysis when there is extensive ischemic change on imaging.
Risk/benefit trade-off
Commenting on the trade-off between benefits and risks in the study, Dr. Jovin said the increase in intracranial hemorrhage seen in the endovascular group was similar to that seen in other situations.
“This is not really any different from what is seen when giving tPA [tissue plasminogen activator] to stroke patients or when performing thrombectomy in small or moderate core strokes – we know that intracranial hemorrhage is the price to pay,” he stated.
“While the increase in symptomatic intracranial hemorrhage was nonsignificant, the trend is very clear, and I believe it is real,” Dr. Jovin said. “But I think what matters – and what matters to patients – is that there is a much higher chance of having a good outcome with endovascular therapy. I think most patients will accept the extra risk of intracranial hemorrhage if there is an even higher chance of having a better neurological outcome. This is no different to the approach that we take when we treat patients with IV tPA.”
Dr. Jovin pointed out that the RESCUE-JAPAN study did not include the largest core infarcts (ASPECTS score 0-1), but he added that these very large core infarcts are quite rare – especially in patients in the early time window.
He concluded that the study provided important information but cautioned that, with just 200 patients, the findings needed confirmation from other randomized trials that are ongoing.
Also speaking at the ISC press conference, Mitchell Elkind, MD, immediate past president of the American Heart Association/American Stroke Association, and professor of neurology at Columbia University, New York, said previous trials had established endovascular therapy for patients with large cerebral artery occlusions who have primarily preserved brain tissue and small infarct cores.
“We have picked off the low-lying fruit – the patients with small areas of infarcted brain. But perhaps most patients do not fit into this category and now we are seeing trials addressing these groups,” he said. “This initial study suggests that these patients with larger core infarcts can indeed still benefit from this therapy tremendously.”
The RESCUE-JAPAN LIMIT study was supported in part by the Mihara Cerebrovascular Disorder Research Promotion Fund and the Japanese Society for Neuroendovascular Therapy. There was no industry involvement. Dr. Yoshimura reported research grants from Stryker, Siemens Healthineers, Bristol-Myers Squibb, Sanofi, Eisai, Daiichi Sankyo, Teijin Pharma, Chugai Pharmaceutical, HEALIOS, Asahi Kasei Medical, Kowa, and CSL Behring; and lecturer fees from Stryker, Medtronic, Johnson & Johnson, Kaneka, Terumo, Biomedical Solutions, Boehringer-Ingelheim, Daiichi Sankyo, Bayer, and Bristol-Meyers Squibb.
A version of this article first appeared on Medscape.com.
FROM ISC 2022
Seniors face higher risk of other medical conditions after COVID-19
The findings of the observational study, which were published in the BMJ, show the risk of a new condition being triggered by COVID is more than twice as high in seniors, compared with younger patients. Plus, the researchers observed an even higher risk among those who were hospitalized, with nearly half (46%) of patients having developed new conditions after the acute COVID-19 infection period.
Respiratory failure with shortness of breath was the most common postacute sequela, but a wide range of heart, kidney, lung, liver, cognitive, mental health, and other conditions were diagnosed at least 3 weeks after initial infection and persisted beyond 30 days.
This is one of the first studies to specifically describe the incidence and severity of new conditions triggered by COVID-19 infection in a general sample of older adults, said study author Ken Cohen MD, FACP, executive director of translational research at Optum Labs and national senior medical director at Optum Care.
“Much of what has been published on the postacute sequelae of COVID-19 has been predominantly from a younger population, and many of the patients had been hospitalized,” Dr. Cohen noted. “This was the first study to focus on a large population of seniors, most of whom did not require hospitalization.”
Dr. Cohen and colleagues reviewed the health insurance records of more than 133,000 Medicare beneficiaries aged 65 or older who were diagnosed with COVID-19 before April 2020. They also matched individuals by age, race, sex, hospitalization status, and other factors to comparison groups without COVID-19 (one from 2020 and one from 2019), and to a group diagnosed with other lower respiratory tract viral infections before the pandemic.
Risk of developing new conditions was higher in hospitalized
After acute COVID-19 infection, 32% of seniors sought medical care for at least one new medical condition in 2020, compared with 21% of uninfected people in the same year.
The most commonly observed conditions included:
- Respiratory failure (7.55% higher risk).
- Fatigue (5.66% higher risk).
- High blood pressure (4.43% higher risk).
- Memory problems (2.63% higher risk).
- Kidney injury (2.59% higher risk).
- Mental health diagnoses (2.5% higher risk).
- Blood-clotting disorders (1.47 % higher risk).
- Heart rhythm disorders (2.9% higher risk).
The risk of developing new conditions was even higher among those 23,486 who were hospitalized in 2020. Those individuals showed a 23.6% higher risk for developing at least one new condition, compared with uninfected seniors in the same year. Also, patients older than 75 had a higher risk for neurological disorders, including dementia, encephalopathy, and memory problems. The researchers also found that respiratory failure and kidney injury were significantly more likely to affect men and Black patients.
When those who had COVID were compared with the group with other lower respiratory viral infections before the pandemic, only the risks of respiratory failure (2.39% higher), dementia (0.71% higher), and fatigue (0.18% higher) were higher.
Primary care providers can learn from these data to better evaluate and manage their geriatric patients with COVID-19 infection, said Amit Shah, MD, a geriatrician with the Mayo Clinic in Phoenix, in an interview.
“We must assess older patients who have had COVID-19 for more than just improvement from the respiratory symptoms of COVID-19 in post-COVID follow-up visits,” he said. “Older individuals with frailty have vulnerability to subsequent complications from severe illnesses and it is common to see post-illness diagnoses, such as new diagnosis of delirium; dementia; or renal, respiratory, or cardiac issues that is precipitated by the original illness. This study confirms that this is likely the case with COVID-19 as well.
“Primary care physicians should be vigilant for these complications, including attention to the rehabilitation needs of older patients with longer-term postviral fatigue from COVID-19,” Dr. Shah added.
Data predates ‘Omicron wave’
It remains uncertain whether sequelae will differ with the Omicron variant, but the findings remain applicable, Dr. Cohen said.
“We know that illness from the Omicron variant is on average less severe in those that have been vaccinated. However, throughout the Omicron wave, individuals who have not been vaccinated continue to have significant rates of serious illness and hospitalization,” he said.
“Our findings showed that serious illness with hospitalization was associated with a higher rate of sequelae. It can therefore be inferred that the rates of sequelae seen in our study would continue to occur in unvaccinated individuals who contract Omicron, but might occur less frequently in vaccinated individuals who contract Omicron and have less severe illness.”
Dr. Cohen serves as a consultant for Pfizer. Dr. Shah has disclosed no relevant financial relationships.
The findings of the observational study, which were published in the BMJ, show the risk of a new condition being triggered by COVID is more than twice as high in seniors, compared with younger patients. Plus, the researchers observed an even higher risk among those who were hospitalized, with nearly half (46%) of patients having developed new conditions after the acute COVID-19 infection period.
Respiratory failure with shortness of breath was the most common postacute sequela, but a wide range of heart, kidney, lung, liver, cognitive, mental health, and other conditions were diagnosed at least 3 weeks after initial infection and persisted beyond 30 days.
This is one of the first studies to specifically describe the incidence and severity of new conditions triggered by COVID-19 infection in a general sample of older adults, said study author Ken Cohen MD, FACP, executive director of translational research at Optum Labs and national senior medical director at Optum Care.
“Much of what has been published on the postacute sequelae of COVID-19 has been predominantly from a younger population, and many of the patients had been hospitalized,” Dr. Cohen noted. “This was the first study to focus on a large population of seniors, most of whom did not require hospitalization.”
Dr. Cohen and colleagues reviewed the health insurance records of more than 133,000 Medicare beneficiaries aged 65 or older who were diagnosed with COVID-19 before April 2020. They also matched individuals by age, race, sex, hospitalization status, and other factors to comparison groups without COVID-19 (one from 2020 and one from 2019), and to a group diagnosed with other lower respiratory tract viral infections before the pandemic.
Risk of developing new conditions was higher in hospitalized
After acute COVID-19 infection, 32% of seniors sought medical care for at least one new medical condition in 2020, compared with 21% of uninfected people in the same year.
The most commonly observed conditions included:
- Respiratory failure (7.55% higher risk).
- Fatigue (5.66% higher risk).
- High blood pressure (4.43% higher risk).
- Memory problems (2.63% higher risk).
- Kidney injury (2.59% higher risk).
- Mental health diagnoses (2.5% higher risk).
- Blood-clotting disorders (1.47 % higher risk).
- Heart rhythm disorders (2.9% higher risk).
The risk of developing new conditions was even higher among those 23,486 who were hospitalized in 2020. Those individuals showed a 23.6% higher risk for developing at least one new condition, compared with uninfected seniors in the same year. Also, patients older than 75 had a higher risk for neurological disorders, including dementia, encephalopathy, and memory problems. The researchers also found that respiratory failure and kidney injury were significantly more likely to affect men and Black patients.
When those who had COVID were compared with the group with other lower respiratory viral infections before the pandemic, only the risks of respiratory failure (2.39% higher), dementia (0.71% higher), and fatigue (0.18% higher) were higher.
Primary care providers can learn from these data to better evaluate and manage their geriatric patients with COVID-19 infection, said Amit Shah, MD, a geriatrician with the Mayo Clinic in Phoenix, in an interview.
“We must assess older patients who have had COVID-19 for more than just improvement from the respiratory symptoms of COVID-19 in post-COVID follow-up visits,” he said. “Older individuals with frailty have vulnerability to subsequent complications from severe illnesses and it is common to see post-illness diagnoses, such as new diagnosis of delirium; dementia; or renal, respiratory, or cardiac issues that is precipitated by the original illness. This study confirms that this is likely the case with COVID-19 as well.
“Primary care physicians should be vigilant for these complications, including attention to the rehabilitation needs of older patients with longer-term postviral fatigue from COVID-19,” Dr. Shah added.
Data predates ‘Omicron wave’
It remains uncertain whether sequelae will differ with the Omicron variant, but the findings remain applicable, Dr. Cohen said.
“We know that illness from the Omicron variant is on average less severe in those that have been vaccinated. However, throughout the Omicron wave, individuals who have not been vaccinated continue to have significant rates of serious illness and hospitalization,” he said.
“Our findings showed that serious illness with hospitalization was associated with a higher rate of sequelae. It can therefore be inferred that the rates of sequelae seen in our study would continue to occur in unvaccinated individuals who contract Omicron, but might occur less frequently in vaccinated individuals who contract Omicron and have less severe illness.”
Dr. Cohen serves as a consultant for Pfizer. Dr. Shah has disclosed no relevant financial relationships.
The findings of the observational study, which were published in the BMJ, show the risk of a new condition being triggered by COVID is more than twice as high in seniors, compared with younger patients. Plus, the researchers observed an even higher risk among those who were hospitalized, with nearly half (46%) of patients having developed new conditions after the acute COVID-19 infection period.
Respiratory failure with shortness of breath was the most common postacute sequela, but a wide range of heart, kidney, lung, liver, cognitive, mental health, and other conditions were diagnosed at least 3 weeks after initial infection and persisted beyond 30 days.
This is one of the first studies to specifically describe the incidence and severity of new conditions triggered by COVID-19 infection in a general sample of older adults, said study author Ken Cohen MD, FACP, executive director of translational research at Optum Labs and national senior medical director at Optum Care.
“Much of what has been published on the postacute sequelae of COVID-19 has been predominantly from a younger population, and many of the patients had been hospitalized,” Dr. Cohen noted. “This was the first study to focus on a large population of seniors, most of whom did not require hospitalization.”
Dr. Cohen and colleagues reviewed the health insurance records of more than 133,000 Medicare beneficiaries aged 65 or older who were diagnosed with COVID-19 before April 2020. They also matched individuals by age, race, sex, hospitalization status, and other factors to comparison groups without COVID-19 (one from 2020 and one from 2019), and to a group diagnosed with other lower respiratory tract viral infections before the pandemic.
Risk of developing new conditions was higher in hospitalized
After acute COVID-19 infection, 32% of seniors sought medical care for at least one new medical condition in 2020, compared with 21% of uninfected people in the same year.
The most commonly observed conditions included:
- Respiratory failure (7.55% higher risk).
- Fatigue (5.66% higher risk).
- High blood pressure (4.43% higher risk).
- Memory problems (2.63% higher risk).
- Kidney injury (2.59% higher risk).
- Mental health diagnoses (2.5% higher risk).
- Blood-clotting disorders (1.47 % higher risk).
- Heart rhythm disorders (2.9% higher risk).
The risk of developing new conditions was even higher among those 23,486 who were hospitalized in 2020. Those individuals showed a 23.6% higher risk for developing at least one new condition, compared with uninfected seniors in the same year. Also, patients older than 75 had a higher risk for neurological disorders, including dementia, encephalopathy, and memory problems. The researchers also found that respiratory failure and kidney injury were significantly more likely to affect men and Black patients.
When those who had COVID were compared with the group with other lower respiratory viral infections before the pandemic, only the risks of respiratory failure (2.39% higher), dementia (0.71% higher), and fatigue (0.18% higher) were higher.
Primary care providers can learn from these data to better evaluate and manage their geriatric patients with COVID-19 infection, said Amit Shah, MD, a geriatrician with the Mayo Clinic in Phoenix, in an interview.
“We must assess older patients who have had COVID-19 for more than just improvement from the respiratory symptoms of COVID-19 in post-COVID follow-up visits,” he said. “Older individuals with frailty have vulnerability to subsequent complications from severe illnesses and it is common to see post-illness diagnoses, such as new diagnosis of delirium; dementia; or renal, respiratory, or cardiac issues that is precipitated by the original illness. This study confirms that this is likely the case with COVID-19 as well.
“Primary care physicians should be vigilant for these complications, including attention to the rehabilitation needs of older patients with longer-term postviral fatigue from COVID-19,” Dr. Shah added.
Data predates ‘Omicron wave’
It remains uncertain whether sequelae will differ with the Omicron variant, but the findings remain applicable, Dr. Cohen said.
“We know that illness from the Omicron variant is on average less severe in those that have been vaccinated. However, throughout the Omicron wave, individuals who have not been vaccinated continue to have significant rates of serious illness and hospitalization,” he said.
“Our findings showed that serious illness with hospitalization was associated with a higher rate of sequelae. It can therefore be inferred that the rates of sequelae seen in our study would continue to occur in unvaccinated individuals who contract Omicron, but might occur less frequently in vaccinated individuals who contract Omicron and have less severe illness.”
Dr. Cohen serves as a consultant for Pfizer. Dr. Shah has disclosed no relevant financial relationships.
FROM BMJ
If you’ve got 3 seconds, then you’ve got time to work out
Goffin’s cockatoo? More like golfin’ cockatoo
Can birds play golf? Of course not; it’s ridiculous. Humans can barely play golf, and we invented the sport. Anyway, moving on to “Brian retraction injury after elective aneurysm clipping.”
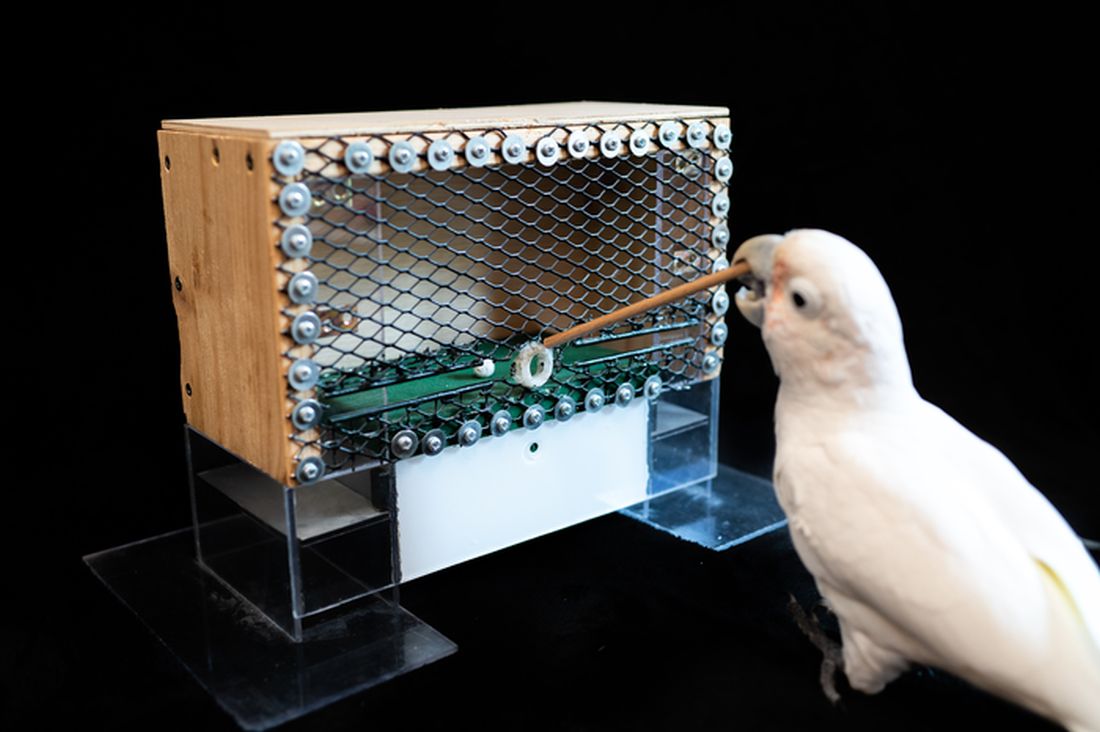
Hang on, we’re now hearing that a group of researchers, as part of a large international project comparing children’s innovation and problem-solving skills with those of cockatoos, have in fact taught a group of Goffin’s cockatoos how to play golf. Huh. What an oddly specific project. All right, fine, I guess we’ll go with the golf-playing birds.
Golf may seem very simple at its core. It is, essentially, whacking a ball with a stick. But the Scots who invented the game were undertaking a complex project involving combined usage of multiple tools, and until now, only primates were thought to be capable of utilizing compound tools to play games such as golf.
For this latest research, published in Scientific Reports, our intrepid birds were given a rudimentary form of golf to play (featuring a stick, a ball, and a closed box to get the ball through). Putting the ball through the hole gave the bird a reward. Not every cockatoo was able to hole out, but three did, with each inventing a unique way to manipulate the stick to hit the ball.
As entertaining as it would be to simply teach some birds how to play golf, we do loop back around to medical relevance. While children are perfectly capable of using tools, young children in particular are actually quite bad at using tools to solve novel solutions. Present a 5-year-old with a stick, a ball, and a hole, and that child might not figure out what the cockatoos did. The research really does give insight into the psychology behind the development of complex tools and technology by our ancient ancestors, according to the researchers.
We’re not entirely convinced this isn’t an elaborate ploy to get a bird out onto the PGA Tour. The LOTME staff can see the future headline already: “Painted bunting wins Valspar Championship in epic playoff.”
Work out now, sweat never
Okay, show of hands: Who’s familiar with “Name that tune?” The TV game show got a reboot last year, but some of us are old enough to remember the 1970s version hosted by national treasure Tom Kennedy.
The contestants try to identify a song as quickly as possible, claiming that they “can name that tune in five notes.” Or four notes, or three. Well, welcome to “Name that exercise study.”
Senior author Masatoshi Nakamura, PhD, and associates gathered together 39 students from Niigata (Japan) University of Health and Welfare and had them perform one isometric, concentric, or eccentric bicep curl with a dumbbell for 3 seconds a day at maximum effort for 5 days a week, over 4 weeks. And yes, we did say 3 seconds.
“Lifting the weight sees the bicep in concentric contraction, lowering the weight sees it in eccentric contraction, while holding the weight parallel to the ground is isometric,” they explained in a statement on Eurekalert.
The three exercise groups were compared with a group that did no exercise, and after 4 weeks of rigorous but brief science, the group doing eccentric contractions had the best results, as their overall muscle strength increased by 11.5%. After a total of just 60 seconds of exercise in 4 weeks. That’s 60 seconds. In 4 weeks.
Big news, but maybe we can do better. “Tom, we can do that exercise in 2 seconds.”
And one! And two! Whoa, feel the burn.
Tingling over anxiety
Apparently there are two kinds of people in this world. Those who love ASMR and those who just don’t get it.
ASMR, for those who don’t know, is the autonomous sensory meridian response. An online community has surfaced, with video creators making tapping sounds, whispering, or brushing mannequin hair to elicit “a pleasant tingling sensation originating from the scalp and neck which can spread to the rest of the body” from viewers, Charlotte M. Eid and associates said in PLOS One.
The people who are into these types of videos are more likely to have higher levels of neuroticism than those who aren’t, which gives ASMR the potential to be a nontraditional form of treatment for anxiety and/or neuroticism, they suggested.
The research involved a group of 64 volunteers who watched an ASMR video meant to trigger the tingles and then completed questionnaires to evaluate their levels of neuroticism, trait anxiety, and state anxiety, said Ms. Eid and associates of Northumbria University in Newcastle-upon-Tyne, England.
The people who had a history of producing tingles from ASMR videos in the past had higher levels of anxiety, compared with those who didn’t. Those who responded to triggers also received some benefit from the video in the study, reporting lower levels of neuroticism and anxiety after watching, the investigators found.
Although people who didn’t have a history of tingles didn’t feel any reduction in anxiety after the video, that didn’t stop the people who weren’t familiar with the genre from catching tingles.
So if you find yourself a little high strung or anxious, or if you can’t sleep, consider watching a person pretending to give you a makeover or using fingernails to tap on books for some relaxation. Don’t knock it until you try it!
Living in the past? Not so far-fetched
It’s usually an insult when people tell us to stop living in the past, but the joke’s on them because we really do live in the past. By 15 seconds, to be exact, according to researchers from the University of California, Berkeley.
But wait, did you just read that last sentence 15 seconds ago, even though it feels like real time? Did we just type these words now, or 15 seconds ago?
Think of your brain as a web page you’re constantly refreshing. We are constantly seeing new pictures, images, and colors, and your brain is responsible for keeping everything in chronological order. This new research suggests that our brains show us images from 15 seconds prior. Is your mind blown yet?
“One could say our brain is procrastinating. It’s too much work to constantly update images, so it sticks to the past because the past is a good predictor of the present. We recycle information from the past because it’s faster, more efficient and less work,” senior author David Whitney explained in a statement from the university.
It seems like the 15-second rule helps us not lose our minds by keeping a steady flow of information, but it could be a bit dangerous if someone, such as a surgeon, needs to see things with extreme precision.
And now we are definitely feeling a bit anxious about our upcoming heart/spleen/gallbladder replacement. … Where’s that link to the ASMR video?
Goffin’s cockatoo? More like golfin’ cockatoo
Can birds play golf? Of course not; it’s ridiculous. Humans can barely play golf, and we invented the sport. Anyway, moving on to “Brian retraction injury after elective aneurysm clipping.”
Hang on, we’re now hearing that a group of researchers, as part of a large international project comparing children’s innovation and problem-solving skills with those of cockatoos, have in fact taught a group of Goffin’s cockatoos how to play golf. Huh. What an oddly specific project. All right, fine, I guess we’ll go with the golf-playing birds.
Golf may seem very simple at its core. It is, essentially, whacking a ball with a stick. But the Scots who invented the game were undertaking a complex project involving combined usage of multiple tools, and until now, only primates were thought to be capable of utilizing compound tools to play games such as golf.
For this latest research, published in Scientific Reports, our intrepid birds were given a rudimentary form of golf to play (featuring a stick, a ball, and a closed box to get the ball through). Putting the ball through the hole gave the bird a reward. Not every cockatoo was able to hole out, but three did, with each inventing a unique way to manipulate the stick to hit the ball.
As entertaining as it would be to simply teach some birds how to play golf, we do loop back around to medical relevance. While children are perfectly capable of using tools, young children in particular are actually quite bad at using tools to solve novel solutions. Present a 5-year-old with a stick, a ball, and a hole, and that child might not figure out what the cockatoos did. The research really does give insight into the psychology behind the development of complex tools and technology by our ancient ancestors, according to the researchers.
We’re not entirely convinced this isn’t an elaborate ploy to get a bird out onto the PGA Tour. The LOTME staff can see the future headline already: “Painted bunting wins Valspar Championship in epic playoff.”
Work out now, sweat never
Okay, show of hands: Who’s familiar with “Name that tune?” The TV game show got a reboot last year, but some of us are old enough to remember the 1970s version hosted by national treasure Tom Kennedy.
The contestants try to identify a song as quickly as possible, claiming that they “can name that tune in five notes.” Or four notes, or three. Well, welcome to “Name that exercise study.”
Senior author Masatoshi Nakamura, PhD, and associates gathered together 39 students from Niigata (Japan) University of Health and Welfare and had them perform one isometric, concentric, or eccentric bicep curl with a dumbbell for 3 seconds a day at maximum effort for 5 days a week, over 4 weeks. And yes, we did say 3 seconds.
“Lifting the weight sees the bicep in concentric contraction, lowering the weight sees it in eccentric contraction, while holding the weight parallel to the ground is isometric,” they explained in a statement on Eurekalert.
The three exercise groups were compared with a group that did no exercise, and after 4 weeks of rigorous but brief science, the group doing eccentric contractions had the best results, as their overall muscle strength increased by 11.5%. After a total of just 60 seconds of exercise in 4 weeks. That’s 60 seconds. In 4 weeks.
Big news, but maybe we can do better. “Tom, we can do that exercise in 2 seconds.”
And one! And two! Whoa, feel the burn.
Tingling over anxiety
Apparently there are two kinds of people in this world. Those who love ASMR and those who just don’t get it.
ASMR, for those who don’t know, is the autonomous sensory meridian response. An online community has surfaced, with video creators making tapping sounds, whispering, or brushing mannequin hair to elicit “a pleasant tingling sensation originating from the scalp and neck which can spread to the rest of the body” from viewers, Charlotte M. Eid and associates said in PLOS One.
The people who are into these types of videos are more likely to have higher levels of neuroticism than those who aren’t, which gives ASMR the potential to be a nontraditional form of treatment for anxiety and/or neuroticism, they suggested.
The research involved a group of 64 volunteers who watched an ASMR video meant to trigger the tingles and then completed questionnaires to evaluate their levels of neuroticism, trait anxiety, and state anxiety, said Ms. Eid and associates of Northumbria University in Newcastle-upon-Tyne, England.
The people who had a history of producing tingles from ASMR videos in the past had higher levels of anxiety, compared with those who didn’t. Those who responded to triggers also received some benefit from the video in the study, reporting lower levels of neuroticism and anxiety after watching, the investigators found.
Although people who didn’t have a history of tingles didn’t feel any reduction in anxiety after the video, that didn’t stop the people who weren’t familiar with the genre from catching tingles.
So if you find yourself a little high strung or anxious, or if you can’t sleep, consider watching a person pretending to give you a makeover or using fingernails to tap on books for some relaxation. Don’t knock it until you try it!
Living in the past? Not so far-fetched
It’s usually an insult when people tell us to stop living in the past, but the joke’s on them because we really do live in the past. By 15 seconds, to be exact, according to researchers from the University of California, Berkeley.
But wait, did you just read that last sentence 15 seconds ago, even though it feels like real time? Did we just type these words now, or 15 seconds ago?
Think of your brain as a web page you’re constantly refreshing. We are constantly seeing new pictures, images, and colors, and your brain is responsible for keeping everything in chronological order. This new research suggests that our brains show us images from 15 seconds prior. Is your mind blown yet?
“One could say our brain is procrastinating. It’s too much work to constantly update images, so it sticks to the past because the past is a good predictor of the present. We recycle information from the past because it’s faster, more efficient and less work,” senior author David Whitney explained in a statement from the university.
It seems like the 15-second rule helps us not lose our minds by keeping a steady flow of information, but it could be a bit dangerous if someone, such as a surgeon, needs to see things with extreme precision.
And now we are definitely feeling a bit anxious about our upcoming heart/spleen/gallbladder replacement. … Where’s that link to the ASMR video?
Goffin’s cockatoo? More like golfin’ cockatoo
Can birds play golf? Of course not; it’s ridiculous. Humans can barely play golf, and we invented the sport. Anyway, moving on to “Brian retraction injury after elective aneurysm clipping.”
Hang on, we’re now hearing that a group of researchers, as part of a large international project comparing children’s innovation and problem-solving skills with those of cockatoos, have in fact taught a group of Goffin’s cockatoos how to play golf. Huh. What an oddly specific project. All right, fine, I guess we’ll go with the golf-playing birds.
Golf may seem very simple at its core. It is, essentially, whacking a ball with a stick. But the Scots who invented the game were undertaking a complex project involving combined usage of multiple tools, and until now, only primates were thought to be capable of utilizing compound tools to play games such as golf.
For this latest research, published in Scientific Reports, our intrepid birds were given a rudimentary form of golf to play (featuring a stick, a ball, and a closed box to get the ball through). Putting the ball through the hole gave the bird a reward. Not every cockatoo was able to hole out, but three did, with each inventing a unique way to manipulate the stick to hit the ball.
As entertaining as it would be to simply teach some birds how to play golf, we do loop back around to medical relevance. While children are perfectly capable of using tools, young children in particular are actually quite bad at using tools to solve novel solutions. Present a 5-year-old with a stick, a ball, and a hole, and that child might not figure out what the cockatoos did. The research really does give insight into the psychology behind the development of complex tools and technology by our ancient ancestors, according to the researchers.
We’re not entirely convinced this isn’t an elaborate ploy to get a bird out onto the PGA Tour. The LOTME staff can see the future headline already: “Painted bunting wins Valspar Championship in epic playoff.”
Work out now, sweat never
Okay, show of hands: Who’s familiar with “Name that tune?” The TV game show got a reboot last year, but some of us are old enough to remember the 1970s version hosted by national treasure Tom Kennedy.
The contestants try to identify a song as quickly as possible, claiming that they “can name that tune in five notes.” Or four notes, or three. Well, welcome to “Name that exercise study.”
Senior author Masatoshi Nakamura, PhD, and associates gathered together 39 students from Niigata (Japan) University of Health and Welfare and had them perform one isometric, concentric, or eccentric bicep curl with a dumbbell for 3 seconds a day at maximum effort for 5 days a week, over 4 weeks. And yes, we did say 3 seconds.
“Lifting the weight sees the bicep in concentric contraction, lowering the weight sees it in eccentric contraction, while holding the weight parallel to the ground is isometric,” they explained in a statement on Eurekalert.
The three exercise groups were compared with a group that did no exercise, and after 4 weeks of rigorous but brief science, the group doing eccentric contractions had the best results, as their overall muscle strength increased by 11.5%. After a total of just 60 seconds of exercise in 4 weeks. That’s 60 seconds. In 4 weeks.
Big news, but maybe we can do better. “Tom, we can do that exercise in 2 seconds.”
And one! And two! Whoa, feel the burn.
Tingling over anxiety
Apparently there are two kinds of people in this world. Those who love ASMR and those who just don’t get it.
ASMR, for those who don’t know, is the autonomous sensory meridian response. An online community has surfaced, with video creators making tapping sounds, whispering, or brushing mannequin hair to elicit “a pleasant tingling sensation originating from the scalp and neck which can spread to the rest of the body” from viewers, Charlotte M. Eid and associates said in PLOS One.
The people who are into these types of videos are more likely to have higher levels of neuroticism than those who aren’t, which gives ASMR the potential to be a nontraditional form of treatment for anxiety and/or neuroticism, they suggested.
The research involved a group of 64 volunteers who watched an ASMR video meant to trigger the tingles and then completed questionnaires to evaluate their levels of neuroticism, trait anxiety, and state anxiety, said Ms. Eid and associates of Northumbria University in Newcastle-upon-Tyne, England.
The people who had a history of producing tingles from ASMR videos in the past had higher levels of anxiety, compared with those who didn’t. Those who responded to triggers also received some benefit from the video in the study, reporting lower levels of neuroticism and anxiety after watching, the investigators found.
Although people who didn’t have a history of tingles didn’t feel any reduction in anxiety after the video, that didn’t stop the people who weren’t familiar with the genre from catching tingles.
So if you find yourself a little high strung or anxious, or if you can’t sleep, consider watching a person pretending to give you a makeover or using fingernails to tap on books for some relaxation. Don’t knock it until you try it!
Living in the past? Not so far-fetched
It’s usually an insult when people tell us to stop living in the past, but the joke’s on them because we really do live in the past. By 15 seconds, to be exact, according to researchers from the University of California, Berkeley.
But wait, did you just read that last sentence 15 seconds ago, even though it feels like real time? Did we just type these words now, or 15 seconds ago?
Think of your brain as a web page you’re constantly refreshing. We are constantly seeing new pictures, images, and colors, and your brain is responsible for keeping everything in chronological order. This new research suggests that our brains show us images from 15 seconds prior. Is your mind blown yet?
“One could say our brain is procrastinating. It’s too much work to constantly update images, so it sticks to the past because the past is a good predictor of the present. We recycle information from the past because it’s faster, more efficient and less work,” senior author David Whitney explained in a statement from the university.
It seems like the 15-second rule helps us not lose our minds by keeping a steady flow of information, but it could be a bit dangerous if someone, such as a surgeon, needs to see things with extreme precision.
And now we are definitely feeling a bit anxious about our upcoming heart/spleen/gallbladder replacement. … Where’s that link to the ASMR video?
Chronic marijuana use linked to recurrent stroke
, new observational research suggests. “Our analysis shows young marijuana users with a history of stroke or transient ischemic attack remain at significantly high risk for future strokes,” said lead study author Akhil Jain, MD, a resident physician at Mercy Fitzgerald Hospital in Darby, Pennsylvania.
“It’s essential to raise awareness among young adults about the impact of chronic habitual use of marijuana, especially if they have established cardiovascular risk factors or previous stroke.”
The study will be presented during the International Stroke Conference, presented by the American Stroke Association, a division of the American Heart Association.
An increasing number of jurisdictions are allowing marijuana use. To date, 18 states and the District of Columbia have legalized recreational cannabis use, the investigators noted.
Research suggests cannabis use disorder – defined as the chronic habitual use of cannabis – is more prevalent in the young adult population. But Dr. Jain said the population of marijuana users is “a changing dynamic.”
Cannabis use has been linked to an increased risk for first-time stroke or transient ischemic attack (TIA). Traditional stroke risk factors include hypertension, diabetes, and diseases related to blood vessels or blood circulation, including atherosclerosis.
Young adults might have additional stroke risk factors, such as behavioral habits like substance abuse, low physical activity, and smoking, oral contraceptives use among females, and brain infections, especially in the immunocompromised, said Dr. Jain.
Research from the American Heart Association shows stroke rates are increasing among adults 18 to 45 years of age. Each year, young adults account for up to 15% of strokes in the United States.
Prevalence and risk for recurrent stroke in patients with previous stroke or TIA in cannabis users have not been clearly established, the researchers pointed out.
A higher rate of recurrent stroke
For this new study, Dr. Jain and colleagues used data from the National Inpatient Sample from October 2015 to December 2017. They identified hospitalizations among young adults 18 to 45 years of age with a previous history of stroke or TIA.
They then grouped these patients into those with cannabis use disorder (4,690) and those without cannabis use disorder (156,700). The median age in both cohorts was 37 years.
The analysis did not include those who were considered in remission from cannabis use disorder.
Results showed that 6.9% of those with cannabis use disorder were hospitalized for a recurrent stroke, compared with 5.4% of those without cannabis use disorder (P < .001).
After adjustment for demographic factors (age, sex, race, household income), and pre-existing conditions, patients with cannabis use disorder were 48% more likely to be hospitalized for recurrent stroke than those without cannabis use disorder (odds ratio, 1.48; 95% confidence interval, 1.28-1.71; P < .001).
Compared with the group without cannabis use disorder, the cannabis use disorder group had more men (55.2% vs. 40.2%), more African American people (44.6% vs. 37.2%), and more use of tobacco (73.9% vs. 39.6%) and alcohol (16.5% vs. 3.6%). They also had a greater percentage of chronic obstructive pulmonary disease, depression, and psychoses.
But a smaller percentage of those with cannabis use disorder had hypertension (51.3% vs. 55.6%; P = .001) and diabetes (16.3% vs. 22.7%; P < .001), which is an “interesting” finding, said Dr. Jain.
“We observed that even with a lower rate of cardiovascular risk factors, after controlling for all the risk factors, we still found the cannabis users had a higher rate of recurrent stroke.”
He noted this was a retrospective study without a control group. “If both groups had comparable hypertension, then this risk might actually be more evident,” said Dr. Jain. “We need a prospective study with comparable groups.”
Living in low-income neighborhoods and in northeast and southern regions of the United States was also more common in the cannabis use disorder group.
Hypothesis-generating research
The study did not investigate the possible mechanisms by which marijuana use might increase stroke risk, but Dr. Jain speculated that these could include factors such as impaired blood vessel function, changes in blood supply, an increased tendency of blood clotting, impaired energy production in brain cells, and an imbalance between molecules that harm healthy tissue and the antioxidant defenses that neutralize them.
As cannabis use may pose a different risk for a new stroke, as opposed a previous stroke, Dr. Jain said it would be interesting to study the amount of “residual function deficit” experienced with the first stroke.
The new study represents “foundational research” upon which other research teams can build, said Dr. Jain. “Our study is hypothesis-generating research for a future prospective randomized controlled trial.”
A limitation of the study is that it did not consider the effect of various doses, duration, and forms of cannabis abuse, or use of medicinal cannabis or other drugs.
Robert L. Page II, PharmD, professor, departments of clinical pharmacy and physical medicine/rehabilitation, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, Aurora, provided a comment on this new research.
A cannabis use disorder diagnosis provides “specific criteria” with regard to chronicity of use and reflects “more of a physical and psychological dependence upon cannabis,” said Dr. Page, who chaired the writing group for the AHA 2020 cannabis and cardiovascular disease scientific statement.
He explained what sets people with cannabis use disorder apart from “run-of-the-mill” recreational cannabis users is that “these are individuals who use a cannabis product, whether it’s smoking it, vaping it, or consuming it via an edible, and are using it on a regular basis, in a chronic fashion.”
The study received no outside funding. The authors report no relevant disclosures.
A version of this article first appeared on Medscape.com.
, new observational research suggests. “Our analysis shows young marijuana users with a history of stroke or transient ischemic attack remain at significantly high risk for future strokes,” said lead study author Akhil Jain, MD, a resident physician at Mercy Fitzgerald Hospital in Darby, Pennsylvania.
“It’s essential to raise awareness among young adults about the impact of chronic habitual use of marijuana, especially if they have established cardiovascular risk factors or previous stroke.”
The study will be presented during the International Stroke Conference, presented by the American Stroke Association, a division of the American Heart Association.
An increasing number of jurisdictions are allowing marijuana use. To date, 18 states and the District of Columbia have legalized recreational cannabis use, the investigators noted.
Research suggests cannabis use disorder – defined as the chronic habitual use of cannabis – is more prevalent in the young adult population. But Dr. Jain said the population of marijuana users is “a changing dynamic.”
Cannabis use has been linked to an increased risk for first-time stroke or transient ischemic attack (TIA). Traditional stroke risk factors include hypertension, diabetes, and diseases related to blood vessels or blood circulation, including atherosclerosis.
Young adults might have additional stroke risk factors, such as behavioral habits like substance abuse, low physical activity, and smoking, oral contraceptives use among females, and brain infections, especially in the immunocompromised, said Dr. Jain.
Research from the American Heart Association shows stroke rates are increasing among adults 18 to 45 years of age. Each year, young adults account for up to 15% of strokes in the United States.
Prevalence and risk for recurrent stroke in patients with previous stroke or TIA in cannabis users have not been clearly established, the researchers pointed out.
A higher rate of recurrent stroke
For this new study, Dr. Jain and colleagues used data from the National Inpatient Sample from October 2015 to December 2017. They identified hospitalizations among young adults 18 to 45 years of age with a previous history of stroke or TIA.
They then grouped these patients into those with cannabis use disorder (4,690) and those without cannabis use disorder (156,700). The median age in both cohorts was 37 years.
The analysis did not include those who were considered in remission from cannabis use disorder.
Results showed that 6.9% of those with cannabis use disorder were hospitalized for a recurrent stroke, compared with 5.4% of those without cannabis use disorder (P < .001).
After adjustment for demographic factors (age, sex, race, household income), and pre-existing conditions, patients with cannabis use disorder were 48% more likely to be hospitalized for recurrent stroke than those without cannabis use disorder (odds ratio, 1.48; 95% confidence interval, 1.28-1.71; P < .001).
Compared with the group without cannabis use disorder, the cannabis use disorder group had more men (55.2% vs. 40.2%), more African American people (44.6% vs. 37.2%), and more use of tobacco (73.9% vs. 39.6%) and alcohol (16.5% vs. 3.6%). They also had a greater percentage of chronic obstructive pulmonary disease, depression, and psychoses.
But a smaller percentage of those with cannabis use disorder had hypertension (51.3% vs. 55.6%; P = .001) and diabetes (16.3% vs. 22.7%; P < .001), which is an “interesting” finding, said Dr. Jain.
“We observed that even with a lower rate of cardiovascular risk factors, after controlling for all the risk factors, we still found the cannabis users had a higher rate of recurrent stroke.”
He noted this was a retrospective study without a control group. “If both groups had comparable hypertension, then this risk might actually be more evident,” said Dr. Jain. “We need a prospective study with comparable groups.”
Living in low-income neighborhoods and in northeast and southern regions of the United States was also more common in the cannabis use disorder group.
Hypothesis-generating research
The study did not investigate the possible mechanisms by which marijuana use might increase stroke risk, but Dr. Jain speculated that these could include factors such as impaired blood vessel function, changes in blood supply, an increased tendency of blood clotting, impaired energy production in brain cells, and an imbalance between molecules that harm healthy tissue and the antioxidant defenses that neutralize them.
As cannabis use may pose a different risk for a new stroke, as opposed a previous stroke, Dr. Jain said it would be interesting to study the amount of “residual function deficit” experienced with the first stroke.
The new study represents “foundational research” upon which other research teams can build, said Dr. Jain. “Our study is hypothesis-generating research for a future prospective randomized controlled trial.”
A limitation of the study is that it did not consider the effect of various doses, duration, and forms of cannabis abuse, or use of medicinal cannabis or other drugs.
Robert L. Page II, PharmD, professor, departments of clinical pharmacy and physical medicine/rehabilitation, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, Aurora, provided a comment on this new research.
A cannabis use disorder diagnosis provides “specific criteria” with regard to chronicity of use and reflects “more of a physical and psychological dependence upon cannabis,” said Dr. Page, who chaired the writing group for the AHA 2020 cannabis and cardiovascular disease scientific statement.
He explained what sets people with cannabis use disorder apart from “run-of-the-mill” recreational cannabis users is that “these are individuals who use a cannabis product, whether it’s smoking it, vaping it, or consuming it via an edible, and are using it on a regular basis, in a chronic fashion.”
The study received no outside funding. The authors report no relevant disclosures.
A version of this article first appeared on Medscape.com.
, new observational research suggests. “Our analysis shows young marijuana users with a history of stroke or transient ischemic attack remain at significantly high risk for future strokes,” said lead study author Akhil Jain, MD, a resident physician at Mercy Fitzgerald Hospital in Darby, Pennsylvania.
“It’s essential to raise awareness among young adults about the impact of chronic habitual use of marijuana, especially if they have established cardiovascular risk factors or previous stroke.”
The study will be presented during the International Stroke Conference, presented by the American Stroke Association, a division of the American Heart Association.
An increasing number of jurisdictions are allowing marijuana use. To date, 18 states and the District of Columbia have legalized recreational cannabis use, the investigators noted.
Research suggests cannabis use disorder – defined as the chronic habitual use of cannabis – is more prevalent in the young adult population. But Dr. Jain said the population of marijuana users is “a changing dynamic.”
Cannabis use has been linked to an increased risk for first-time stroke or transient ischemic attack (TIA). Traditional stroke risk factors include hypertension, diabetes, and diseases related to blood vessels or blood circulation, including atherosclerosis.
Young adults might have additional stroke risk factors, such as behavioral habits like substance abuse, low physical activity, and smoking, oral contraceptives use among females, and brain infections, especially in the immunocompromised, said Dr. Jain.
Research from the American Heart Association shows stroke rates are increasing among adults 18 to 45 years of age. Each year, young adults account for up to 15% of strokes in the United States.
Prevalence and risk for recurrent stroke in patients with previous stroke or TIA in cannabis users have not been clearly established, the researchers pointed out.
A higher rate of recurrent stroke
For this new study, Dr. Jain and colleagues used data from the National Inpatient Sample from October 2015 to December 2017. They identified hospitalizations among young adults 18 to 45 years of age with a previous history of stroke or TIA.
They then grouped these patients into those with cannabis use disorder (4,690) and those without cannabis use disorder (156,700). The median age in both cohorts was 37 years.
The analysis did not include those who were considered in remission from cannabis use disorder.
Results showed that 6.9% of those with cannabis use disorder were hospitalized for a recurrent stroke, compared with 5.4% of those without cannabis use disorder (P < .001).
After adjustment for demographic factors (age, sex, race, household income), and pre-existing conditions, patients with cannabis use disorder were 48% more likely to be hospitalized for recurrent stroke than those without cannabis use disorder (odds ratio, 1.48; 95% confidence interval, 1.28-1.71; P < .001).
Compared with the group without cannabis use disorder, the cannabis use disorder group had more men (55.2% vs. 40.2%), more African American people (44.6% vs. 37.2%), and more use of tobacco (73.9% vs. 39.6%) and alcohol (16.5% vs. 3.6%). They also had a greater percentage of chronic obstructive pulmonary disease, depression, and psychoses.
But a smaller percentage of those with cannabis use disorder had hypertension (51.3% vs. 55.6%; P = .001) and diabetes (16.3% vs. 22.7%; P < .001), which is an “interesting” finding, said Dr. Jain.
“We observed that even with a lower rate of cardiovascular risk factors, after controlling for all the risk factors, we still found the cannabis users had a higher rate of recurrent stroke.”
He noted this was a retrospective study without a control group. “If both groups had comparable hypertension, then this risk might actually be more evident,” said Dr. Jain. “We need a prospective study with comparable groups.”
Living in low-income neighborhoods and in northeast and southern regions of the United States was also more common in the cannabis use disorder group.
Hypothesis-generating research
The study did not investigate the possible mechanisms by which marijuana use might increase stroke risk, but Dr. Jain speculated that these could include factors such as impaired blood vessel function, changes in blood supply, an increased tendency of blood clotting, impaired energy production in brain cells, and an imbalance between molecules that harm healthy tissue and the antioxidant defenses that neutralize them.
As cannabis use may pose a different risk for a new stroke, as opposed a previous stroke, Dr. Jain said it would be interesting to study the amount of “residual function deficit” experienced with the first stroke.
The new study represents “foundational research” upon which other research teams can build, said Dr. Jain. “Our study is hypothesis-generating research for a future prospective randomized controlled trial.”
A limitation of the study is that it did not consider the effect of various doses, duration, and forms of cannabis abuse, or use of medicinal cannabis or other drugs.
Robert L. Page II, PharmD, professor, departments of clinical pharmacy and physical medicine/rehabilitation, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, Aurora, provided a comment on this new research.
A cannabis use disorder diagnosis provides “specific criteria” with regard to chronicity of use and reflects “more of a physical and psychological dependence upon cannabis,” said Dr. Page, who chaired the writing group for the AHA 2020 cannabis and cardiovascular disease scientific statement.
He explained what sets people with cannabis use disorder apart from “run-of-the-mill” recreational cannabis users is that “these are individuals who use a cannabis product, whether it’s smoking it, vaping it, or consuming it via an edible, and are using it on a regular basis, in a chronic fashion.”
The study received no outside funding. The authors report no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM ISC 2022
Brain imaging gives new insight into hoarding disorder
In a neuroimaging study, investigators led by Taro Mizobe, department of neuropsychiatry, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan, compared brain scans of individuals with and without HD.
Results showed that compared with healthy family members, participants with HD had anatomically widespread abnormalities in WM tracts.
In particular, a broad range of alterations were found in frontal WM related to HD symptom severity, as well as cortical regions involved in cognitive dysfunction.
“The finding of a characteristic association between alterations in the prefrontal WM tract, which connects cortical regions involved in cognitive function and the severity of hoarding symptoms, could provide new insights into the neurobiological basis of HD,” the researchers write.
The findings were published online Jan. 18 in the Journal of Psychiatric Research.
Limited information to date
“Although there are no clear neurobiological models of HD, several neuroimaging studies have found specific differences in specific brain regions” between patients with and without HD, the investigators write.
Structural MRI studies and voxel-based morphometry have shown larger volumes of gray matter in several regions of the brain in patients with HD. However, there have been no reports on alterations in the WM tracts – and studies of patients with obsessive-compulsive disorder and hoarding symptoms have yielded only “limited information” regarding WM tracts, the researchers note.
Diffusion tensor imaging (DTI) studies have yielded “inconsistent” findings, “therefore little is known about the microstructure of WM in the brains of patients with HD,” they add.
The current study was designed “to investigate microstructural alterations in the WM tracts of individuals with HD” by using tract-based spatial statistics – a model typically used for whole-brain, voxel-wise analysis of DTI measures.
DTI neuroimaging can assess the microstructure of WM. In the current study, the investigators focused on the three measures yielded by DTI: fractional anisotropy (FA), which is an index of overall WM integrity; axial diffusivity (AD); and radial diffusivity (RD).
Participants underwent MRI and DTI scans. Brain images of 25 individuals with hoarding disorder (mean age, 43 years; 64% women; 96% right-handed) were compared with those of 36 healthy controls matched for age, sex, and handedness.
Participants with HD had higher scores on the Hamilton Rating Scales for depression and anxiety than those without HD (P < .001 for both).
Of the patients with HD, 10 were taking psychiatric medications such as antidepressants, tranquilizers, or nonstimulant agents for attention-deficit/hyperactivity disorder.
Most (n = 18) were concurrently diagnosed with other psychiatric conditions, including ADHD, anxiety disorder, major depressive disorder, posttraumatic stress disorder, or obsessive-compulsive disorder.
The researchers also conducted a post hoc analysis of regions of interest “to detect correlations with clinical features.”
Microstructural alterations
Compared with healthy controls, patients with hoarding disorder showed decreased FA and increased RD in anatomically widespread WM tracts.
Decreased FA areas included the left superior longitudinal fasciculus (SLF), left uncinate fasciculus, left inferior fronto-occipital fasciculus (IFOF), left anterior thalamic radiation (ATR), left corticospinal tract, and left anterior limb of the internal capsule (ALIC).
Increased RD areas included the bilateral SLF, right IFOF, bilateral anterior and superior corona radiata, left posterior corona radiata, right ATR, left posterior thalamic radiation, right external capsule, and right ALIC.
Post hoc analyses of “regions of interest,” revealed “significant negative correlation” between the severity of hoarding symptoms and FA, particularly in the left anterior limb of the internal capsule, and a positive correlation between HD symptom severity and radial diffusivity in the right anterior thalamic radiation.
Those with HD also showed “a broad range of alterations” in the frontal WM tracts, including the frontothalamic circuit, frontoparietal network, and frontolimbic pathway.
“We found anatomically widespread decreases in FA and increases in WD in many major WM tracts and correlations between the severity of hoarding symptoms and DTI parameters (FA and RD) in the left ALIC and right ATR, which is part of the frontothalamic circuit,” the investigators write.
These findings “suggest that patients with HD have microstructural alterations in the prefrontal WM tracts,” they add.
First study
The researchers say that, to their knowledge, this is the first study to find major abnormalities in WM tracts within the brain and correlations between DTI indexes and clinical features in patients with HD.
The frontothalamic circuit is “thought to play an important role in executive functions, including working memory, attention, reward processing, and decision-making,” the investigators write.
Previous research implied that frontothalamic circuit–related cognitive functions are “impaired in patients with HD” and suggested that these impairments “underlie hoarding symptoms such as acquiring, saving, and cluttering relevant to HD.”
The decreased FA in the left SLF “reflects alterations in WM in the frontoparietal network in these patients and may be associated with cognitive impairments, such as task switching and inhibition, as shown in previous studies,” the researchers write.
Additionally, changes in FA and RD often “indicate myelin pathology,” which suggest that HD pathophysiology “may include abnormalities of myelination.”
However, the investigators cite several study limitations, including the “relatively small” sample size, which kept the DTI analysis from being “robust.” Moreover, many patients with HD had comorbid psychiatric disorders, which have also been associated with microstructural abnormalities in WM, the researchers note.
Novel approach
Commenting for this news organization, Michael Stevens, PhD, director, CNDLAB, Olin Neuropsychiatry Research Center, and adjunct professor of psychiatry at Yale University School of Medicine, New Haven, Conn., said the study “provides useful new clues for understanding HD neurobiology” because of its novel approach in assessing microstructural properties of major WM tracts.
The study’s “main contribution is to identify specific WM pathways between brain regions as worth looking at closely in the future. Some of these regions already have been implicated by brain function neuroimaging as abnormal in patients who compulsively hoard,” said Dr. Stevens, who was not involved in the research.
He noted that, when WM pathway integrity is affected, “it is thought to have an impact on how well information is communicated” between the brain regions.
“So once these specific findings are replicated in a separate study, they hopefully can guide researchers to ask new questions to learn exactly how these WM tracts might contribute to hoarding behavior,” Dr. Stevens said.
The study had no specific funding. The investigators and Dr. Stevens have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a neuroimaging study, investigators led by Taro Mizobe, department of neuropsychiatry, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan, compared brain scans of individuals with and without HD.
Results showed that compared with healthy family members, participants with HD had anatomically widespread abnormalities in WM tracts.
In particular, a broad range of alterations were found in frontal WM related to HD symptom severity, as well as cortical regions involved in cognitive dysfunction.
“The finding of a characteristic association between alterations in the prefrontal WM tract, which connects cortical regions involved in cognitive function and the severity of hoarding symptoms, could provide new insights into the neurobiological basis of HD,” the researchers write.
The findings were published online Jan. 18 in the Journal of Psychiatric Research.
Limited information to date
“Although there are no clear neurobiological models of HD, several neuroimaging studies have found specific differences in specific brain regions” between patients with and without HD, the investigators write.
Structural MRI studies and voxel-based morphometry have shown larger volumes of gray matter in several regions of the brain in patients with HD. However, there have been no reports on alterations in the WM tracts – and studies of patients with obsessive-compulsive disorder and hoarding symptoms have yielded only “limited information” regarding WM tracts, the researchers note.
Diffusion tensor imaging (DTI) studies have yielded “inconsistent” findings, “therefore little is known about the microstructure of WM in the brains of patients with HD,” they add.
The current study was designed “to investigate microstructural alterations in the WM tracts of individuals with HD” by using tract-based spatial statistics – a model typically used for whole-brain, voxel-wise analysis of DTI measures.
DTI neuroimaging can assess the microstructure of WM. In the current study, the investigators focused on the three measures yielded by DTI: fractional anisotropy (FA), which is an index of overall WM integrity; axial diffusivity (AD); and radial diffusivity (RD).
Participants underwent MRI and DTI scans. Brain images of 25 individuals with hoarding disorder (mean age, 43 years; 64% women; 96% right-handed) were compared with those of 36 healthy controls matched for age, sex, and handedness.
Participants with HD had higher scores on the Hamilton Rating Scales for depression and anxiety than those without HD (P < .001 for both).
Of the patients with HD, 10 were taking psychiatric medications such as antidepressants, tranquilizers, or nonstimulant agents for attention-deficit/hyperactivity disorder.
Most (n = 18) were concurrently diagnosed with other psychiatric conditions, including ADHD, anxiety disorder, major depressive disorder, posttraumatic stress disorder, or obsessive-compulsive disorder.
The researchers also conducted a post hoc analysis of regions of interest “to detect correlations with clinical features.”
Microstructural alterations
Compared with healthy controls, patients with hoarding disorder showed decreased FA and increased RD in anatomically widespread WM tracts.
Decreased FA areas included the left superior longitudinal fasciculus (SLF), left uncinate fasciculus, left inferior fronto-occipital fasciculus (IFOF), left anterior thalamic radiation (ATR), left corticospinal tract, and left anterior limb of the internal capsule (ALIC).
Increased RD areas included the bilateral SLF, right IFOF, bilateral anterior and superior corona radiata, left posterior corona radiata, right ATR, left posterior thalamic radiation, right external capsule, and right ALIC.
Post hoc analyses of “regions of interest,” revealed “significant negative correlation” between the severity of hoarding symptoms and FA, particularly in the left anterior limb of the internal capsule, and a positive correlation between HD symptom severity and radial diffusivity in the right anterior thalamic radiation.
Those with HD also showed “a broad range of alterations” in the frontal WM tracts, including the frontothalamic circuit, frontoparietal network, and frontolimbic pathway.
“We found anatomically widespread decreases in FA and increases in WD in many major WM tracts and correlations between the severity of hoarding symptoms and DTI parameters (FA and RD) in the left ALIC and right ATR, which is part of the frontothalamic circuit,” the investigators write.
These findings “suggest that patients with HD have microstructural alterations in the prefrontal WM tracts,” they add.
First study
The researchers say that, to their knowledge, this is the first study to find major abnormalities in WM tracts within the brain and correlations between DTI indexes and clinical features in patients with HD.
The frontothalamic circuit is “thought to play an important role in executive functions, including working memory, attention, reward processing, and decision-making,” the investigators write.
Previous research implied that frontothalamic circuit–related cognitive functions are “impaired in patients with HD” and suggested that these impairments “underlie hoarding symptoms such as acquiring, saving, and cluttering relevant to HD.”
The decreased FA in the left SLF “reflects alterations in WM in the frontoparietal network in these patients and may be associated with cognitive impairments, such as task switching and inhibition, as shown in previous studies,” the researchers write.
Additionally, changes in FA and RD often “indicate myelin pathology,” which suggest that HD pathophysiology “may include abnormalities of myelination.”
However, the investigators cite several study limitations, including the “relatively small” sample size, which kept the DTI analysis from being “robust.” Moreover, many patients with HD had comorbid psychiatric disorders, which have also been associated with microstructural abnormalities in WM, the researchers note.
Novel approach
Commenting for this news organization, Michael Stevens, PhD, director, CNDLAB, Olin Neuropsychiatry Research Center, and adjunct professor of psychiatry at Yale University School of Medicine, New Haven, Conn., said the study “provides useful new clues for understanding HD neurobiology” because of its novel approach in assessing microstructural properties of major WM tracts.
The study’s “main contribution is to identify specific WM pathways between brain regions as worth looking at closely in the future. Some of these regions already have been implicated by brain function neuroimaging as abnormal in patients who compulsively hoard,” said Dr. Stevens, who was not involved in the research.
He noted that, when WM pathway integrity is affected, “it is thought to have an impact on how well information is communicated” between the brain regions.
“So once these specific findings are replicated in a separate study, they hopefully can guide researchers to ask new questions to learn exactly how these WM tracts might contribute to hoarding behavior,” Dr. Stevens said.
The study had no specific funding. The investigators and Dr. Stevens have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a neuroimaging study, investigators led by Taro Mizobe, department of neuropsychiatry, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan, compared brain scans of individuals with and without HD.
Results showed that compared with healthy family members, participants with HD had anatomically widespread abnormalities in WM tracts.
In particular, a broad range of alterations were found in frontal WM related to HD symptom severity, as well as cortical regions involved in cognitive dysfunction.
“The finding of a characteristic association between alterations in the prefrontal WM tract, which connects cortical regions involved in cognitive function and the severity of hoarding symptoms, could provide new insights into the neurobiological basis of HD,” the researchers write.
The findings were published online Jan. 18 in the Journal of Psychiatric Research.
Limited information to date
“Although there are no clear neurobiological models of HD, several neuroimaging studies have found specific differences in specific brain regions” between patients with and without HD, the investigators write.
Structural MRI studies and voxel-based morphometry have shown larger volumes of gray matter in several regions of the brain in patients with HD. However, there have been no reports on alterations in the WM tracts – and studies of patients with obsessive-compulsive disorder and hoarding symptoms have yielded only “limited information” regarding WM tracts, the researchers note.
Diffusion tensor imaging (DTI) studies have yielded “inconsistent” findings, “therefore little is known about the microstructure of WM in the brains of patients with HD,” they add.
The current study was designed “to investigate microstructural alterations in the WM tracts of individuals with HD” by using tract-based spatial statistics – a model typically used for whole-brain, voxel-wise analysis of DTI measures.
DTI neuroimaging can assess the microstructure of WM. In the current study, the investigators focused on the three measures yielded by DTI: fractional anisotropy (FA), which is an index of overall WM integrity; axial diffusivity (AD); and radial diffusivity (RD).
Participants underwent MRI and DTI scans. Brain images of 25 individuals with hoarding disorder (mean age, 43 years; 64% women; 96% right-handed) were compared with those of 36 healthy controls matched for age, sex, and handedness.
Participants with HD had higher scores on the Hamilton Rating Scales for depression and anxiety than those without HD (P < .001 for both).
Of the patients with HD, 10 were taking psychiatric medications such as antidepressants, tranquilizers, or nonstimulant agents for attention-deficit/hyperactivity disorder.
Most (n = 18) were concurrently diagnosed with other psychiatric conditions, including ADHD, anxiety disorder, major depressive disorder, posttraumatic stress disorder, or obsessive-compulsive disorder.
The researchers also conducted a post hoc analysis of regions of interest “to detect correlations with clinical features.”
Microstructural alterations
Compared with healthy controls, patients with hoarding disorder showed decreased FA and increased RD in anatomically widespread WM tracts.
Decreased FA areas included the left superior longitudinal fasciculus (SLF), left uncinate fasciculus, left inferior fronto-occipital fasciculus (IFOF), left anterior thalamic radiation (ATR), left corticospinal tract, and left anterior limb of the internal capsule (ALIC).
Increased RD areas included the bilateral SLF, right IFOF, bilateral anterior and superior corona radiata, left posterior corona radiata, right ATR, left posterior thalamic radiation, right external capsule, and right ALIC.
Post hoc analyses of “regions of interest,” revealed “significant negative correlation” between the severity of hoarding symptoms and FA, particularly in the left anterior limb of the internal capsule, and a positive correlation between HD symptom severity and radial diffusivity in the right anterior thalamic radiation.
Those with HD also showed “a broad range of alterations” in the frontal WM tracts, including the frontothalamic circuit, frontoparietal network, and frontolimbic pathway.
“We found anatomically widespread decreases in FA and increases in WD in many major WM tracts and correlations between the severity of hoarding symptoms and DTI parameters (FA and RD) in the left ALIC and right ATR, which is part of the frontothalamic circuit,” the investigators write.
These findings “suggest that patients with HD have microstructural alterations in the prefrontal WM tracts,” they add.
First study
The researchers say that, to their knowledge, this is the first study to find major abnormalities in WM tracts within the brain and correlations between DTI indexes and clinical features in patients with HD.
The frontothalamic circuit is “thought to play an important role in executive functions, including working memory, attention, reward processing, and decision-making,” the investigators write.
Previous research implied that frontothalamic circuit–related cognitive functions are “impaired in patients with HD” and suggested that these impairments “underlie hoarding symptoms such as acquiring, saving, and cluttering relevant to HD.”
The decreased FA in the left SLF “reflects alterations in WM in the frontoparietal network in these patients and may be associated with cognitive impairments, such as task switching and inhibition, as shown in previous studies,” the researchers write.
Additionally, changes in FA and RD often “indicate myelin pathology,” which suggest that HD pathophysiology “may include abnormalities of myelination.”
However, the investigators cite several study limitations, including the “relatively small” sample size, which kept the DTI analysis from being “robust.” Moreover, many patients with HD had comorbid psychiatric disorders, which have also been associated with microstructural abnormalities in WM, the researchers note.
Novel approach
Commenting for this news organization, Michael Stevens, PhD, director, CNDLAB, Olin Neuropsychiatry Research Center, and adjunct professor of psychiatry at Yale University School of Medicine, New Haven, Conn., said the study “provides useful new clues for understanding HD neurobiology” because of its novel approach in assessing microstructural properties of major WM tracts.
The study’s “main contribution is to identify specific WM pathways between brain regions as worth looking at closely in the future. Some of these regions already have been implicated by brain function neuroimaging as abnormal in patients who compulsively hoard,” said Dr. Stevens, who was not involved in the research.
He noted that, when WM pathway integrity is affected, “it is thought to have an impact on how well information is communicated” between the brain regions.
“So once these specific findings are replicated in a separate study, they hopefully can guide researchers to ask new questions to learn exactly how these WM tracts might contribute to hoarding behavior,” Dr. Stevens said.
The study had no specific funding. The investigators and Dr. Stevens have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Potential new neuromodulation treatment for migraines
Most people avoid smartphones when they have a migraine headache, but a noninvasive treatment for episodic migraines may change that.
that can help ease migraine pain.
Tina Montgomery, 58, has suffered from migraines since childhood and spent years looking for something to help manage them. Doctors consider her a “chronic” sufferer in that she has more than 14 migraines a month (fewer than 14 is considered “episodic”). Prescription antidepressants, anticonvulsants, and botulinum toxin shots as preventive treatments helped a little but not enough.
A few years ago, she found some relief using a new preventive injectable medication that targets a peptide known as CGRP, combined with an oral CGRP rescue medication, ubrogepant (Ubrelvy). However, by early 2021, Ms. Montgomery’s chronic migraines were back as she faced stress from the pandemic and her role as a caregiver for her aging parents.
“I was going through so much medication. I just didn’t feel good taking so much,” she said.
Looking for relief, she read about Nerivio, a wearable migraine treatment device that uses remote electrical neuromodulation (REN). She mentioned the device to her neurologist, and he agreed she might benefit from trying it out. Today, she uses the device whenever she feels a migraine may be imminent, she said.
“It really helps me stave off migraines I feel coming on and the milder ones where I would normally hesitate to use prescription medication because [insurance] limits the number of pills they give you in a month,” she said. “I follow through with the Nerivio treatment and usually find that my migraine doesn’t fully develop or is completely gone, and I don’t get a migraine at all.”
Taking it on the arm
The device works by stimulating nerves at the back of the arm right around the triceps. “Those nerve fibers relay information to the brain stem [so it can] work its magic and use the brain’s own natural mechanisms for reducing pain,” said Brian M. Grosberg, MD, director of the Hartford Healthcare Ayer Neuroscience Institute Headache Center, West Hartford, Conn.
These mechanisms are like a bait-and-switch for the brain, said Britany Klenofsky, MD, assistant professor of neurology, Icahn School of Medicine at Mount Sinai, New York. “You’re trying to stimulate pain somewhere else [on the body] to tell the brain to protect itself and release [the neurotransmitter] serotonin,” she said. “You do this by putting the device on your arm, an area that’s away from the head where the pain is actively occurring, turning the device on, and increasing the stimulation to a nearly painful stimulus.”
This pseudo pain prompts the brain to release serotonin, the feel-good hormone along with norepinephrine and noradrenaline. The device works best when it’s used as soon as a migraine starts, so patients should hook up Nerivio within the first 20-30 minutes of onset of pain, said Dr. Grosberg, who was an investigator on the double-blind treatment study that led to FDA clearance. If patients wait too long, the device may not work.
This is why as soon as Ms. Montgomery feels a migraine aura (there are six types of migraine auras, including visual changes and muscle weakness) that occurs right before a migraine strikes, she puts the device armband on her upper arm and launches its smartphone app. Then she turns on the device for a 45-minute treatment, which begins with what she characterizes as tingling and vibration sensations on her arm. She turns up the intensity of the sensations, which are mild electric currents, until they are well-felt but not painful.
Ms. Montgomery said she can use the device and multitask since there’s no need for her to lie down or sit in a darkened room. And since it is worn on the arm, she can wear it under a shirtsleeve while working or out in public without anyone noticing. She also uses the app’s migraine diary and guided meditation to help reduce the anxiety that often accompanies her migraines.
The device is approved for adolescents and adults and can be used for both episodic and chronic migraines. From an efficacy standpoint, the device provides relief about as well as a commonly used pharmaceutical class of drugs, triptans. About 37% of people with episodic migraine achieved complete freedom from pain 2 hours after their treatment. In addition, about two-thirds of people reported pain relief after 2 hours, which is better success than people find with many prescription and nonprescription drugs.
A separate study looked at acute treatment for chronic migraine sufferers and found nearly 60% of people using the device found relief and 21% said they were pain-free after 2 hours. Almost two-thirds of those who experienced pain relief were pain-free 24 hours after the treatment.
Finding the perfect patient
There are other FDA-cleared noninvasive devices to treat migraines. One device, CEFALY, is an external trigeminal nerve stimulation device that sits on the forehead. Another device, SpringTMS, uses transcranial magnetic stimulation on the back of the head. A third option, the gammaCore Sapphire, is placed on the neck to stimulate the vagus nerve. All three have been cleared by the FDA to work as preventive and acute treatments for migraine.
Theranica, the company that developed Nerivio, is trying to boost use of the device by allowing patients to get a prescription via telehealth visits with a physician.
The company, as well as the companies behind the other neuromodulation devices, are marketing their treatments to children ages 12 and up since nonpharmacologic options are often preferable for parents, said Thomas Berk, MD, a clinical associate professor in the division of headache at NYU Langone Health in New York.
Dr. Berk said the devices could be appealing for those people who don’t want or can’t take medication, such as pregnant women or those who don’t respond well to drugs. “[They] could also be used by somebody who needs something in addition to a medication,” he said.
For now, people like Ms. Montgomery say they are happy to have another tool in their migraine arsenal. “Overall, I’m taking less medication because I haven’t had to have my Ubrelvy refilled as often as I used to,” she said. “It’s really helped me manage changes and stresses in my life.”
A version of this article first appeared on Medscape.com.
Most people avoid smartphones when they have a migraine headache, but a noninvasive treatment for episodic migraines may change that.
that can help ease migraine pain.
Tina Montgomery, 58, has suffered from migraines since childhood and spent years looking for something to help manage them. Doctors consider her a “chronic” sufferer in that she has more than 14 migraines a month (fewer than 14 is considered “episodic”). Prescription antidepressants, anticonvulsants, and botulinum toxin shots as preventive treatments helped a little but not enough.
A few years ago, she found some relief using a new preventive injectable medication that targets a peptide known as CGRP, combined with an oral CGRP rescue medication, ubrogepant (Ubrelvy). However, by early 2021, Ms. Montgomery’s chronic migraines were back as she faced stress from the pandemic and her role as a caregiver for her aging parents.
“I was going through so much medication. I just didn’t feel good taking so much,” she said.
Looking for relief, she read about Nerivio, a wearable migraine treatment device that uses remote electrical neuromodulation (REN). She mentioned the device to her neurologist, and he agreed she might benefit from trying it out. Today, she uses the device whenever she feels a migraine may be imminent, she said.
“It really helps me stave off migraines I feel coming on and the milder ones where I would normally hesitate to use prescription medication because [insurance] limits the number of pills they give you in a month,” she said. “I follow through with the Nerivio treatment and usually find that my migraine doesn’t fully develop or is completely gone, and I don’t get a migraine at all.”
Taking it on the arm
The device works by stimulating nerves at the back of the arm right around the triceps. “Those nerve fibers relay information to the brain stem [so it can] work its magic and use the brain’s own natural mechanisms for reducing pain,” said Brian M. Grosberg, MD, director of the Hartford Healthcare Ayer Neuroscience Institute Headache Center, West Hartford, Conn.
These mechanisms are like a bait-and-switch for the brain, said Britany Klenofsky, MD, assistant professor of neurology, Icahn School of Medicine at Mount Sinai, New York. “You’re trying to stimulate pain somewhere else [on the body] to tell the brain to protect itself and release [the neurotransmitter] serotonin,” she said. “You do this by putting the device on your arm, an area that’s away from the head where the pain is actively occurring, turning the device on, and increasing the stimulation to a nearly painful stimulus.”
This pseudo pain prompts the brain to release serotonin, the feel-good hormone along with norepinephrine and noradrenaline. The device works best when it’s used as soon as a migraine starts, so patients should hook up Nerivio within the first 20-30 minutes of onset of pain, said Dr. Grosberg, who was an investigator on the double-blind treatment study that led to FDA clearance. If patients wait too long, the device may not work.
This is why as soon as Ms. Montgomery feels a migraine aura (there are six types of migraine auras, including visual changes and muscle weakness) that occurs right before a migraine strikes, she puts the device armband on her upper arm and launches its smartphone app. Then she turns on the device for a 45-minute treatment, which begins with what she characterizes as tingling and vibration sensations on her arm. She turns up the intensity of the sensations, which are mild electric currents, until they are well-felt but not painful.
Ms. Montgomery said she can use the device and multitask since there’s no need for her to lie down or sit in a darkened room. And since it is worn on the arm, she can wear it under a shirtsleeve while working or out in public without anyone noticing. She also uses the app’s migraine diary and guided meditation to help reduce the anxiety that often accompanies her migraines.
The device is approved for adolescents and adults and can be used for both episodic and chronic migraines. From an efficacy standpoint, the device provides relief about as well as a commonly used pharmaceutical class of drugs, triptans. About 37% of people with episodic migraine achieved complete freedom from pain 2 hours after their treatment. In addition, about two-thirds of people reported pain relief after 2 hours, which is better success than people find with many prescription and nonprescription drugs.
A separate study looked at acute treatment for chronic migraine sufferers and found nearly 60% of people using the device found relief and 21% said they were pain-free after 2 hours. Almost two-thirds of those who experienced pain relief were pain-free 24 hours after the treatment.
Finding the perfect patient
There are other FDA-cleared noninvasive devices to treat migraines. One device, CEFALY, is an external trigeminal nerve stimulation device that sits on the forehead. Another device, SpringTMS, uses transcranial magnetic stimulation on the back of the head. A third option, the gammaCore Sapphire, is placed on the neck to stimulate the vagus nerve. All three have been cleared by the FDA to work as preventive and acute treatments for migraine.
Theranica, the company that developed Nerivio, is trying to boost use of the device by allowing patients to get a prescription via telehealth visits with a physician.
The company, as well as the companies behind the other neuromodulation devices, are marketing their treatments to children ages 12 and up since nonpharmacologic options are often preferable for parents, said Thomas Berk, MD, a clinical associate professor in the division of headache at NYU Langone Health in New York.
Dr. Berk said the devices could be appealing for those people who don’t want or can’t take medication, such as pregnant women or those who don’t respond well to drugs. “[They] could also be used by somebody who needs something in addition to a medication,” he said.
For now, people like Ms. Montgomery say they are happy to have another tool in their migraine arsenal. “Overall, I’m taking less medication because I haven’t had to have my Ubrelvy refilled as often as I used to,” she said. “It’s really helped me manage changes and stresses in my life.”
A version of this article first appeared on Medscape.com.
Most people avoid smartphones when they have a migraine headache, but a noninvasive treatment for episodic migraines may change that.
that can help ease migraine pain.
Tina Montgomery, 58, has suffered from migraines since childhood and spent years looking for something to help manage them. Doctors consider her a “chronic” sufferer in that she has more than 14 migraines a month (fewer than 14 is considered “episodic”). Prescription antidepressants, anticonvulsants, and botulinum toxin shots as preventive treatments helped a little but not enough.
A few years ago, she found some relief using a new preventive injectable medication that targets a peptide known as CGRP, combined with an oral CGRP rescue medication, ubrogepant (Ubrelvy). However, by early 2021, Ms. Montgomery’s chronic migraines were back as she faced stress from the pandemic and her role as a caregiver for her aging parents.
“I was going through so much medication. I just didn’t feel good taking so much,” she said.
Looking for relief, she read about Nerivio, a wearable migraine treatment device that uses remote electrical neuromodulation (REN). She mentioned the device to her neurologist, and he agreed she might benefit from trying it out. Today, she uses the device whenever she feels a migraine may be imminent, she said.
“It really helps me stave off migraines I feel coming on and the milder ones where I would normally hesitate to use prescription medication because [insurance] limits the number of pills they give you in a month,” she said. “I follow through with the Nerivio treatment and usually find that my migraine doesn’t fully develop or is completely gone, and I don’t get a migraine at all.”
Taking it on the arm
The device works by stimulating nerves at the back of the arm right around the triceps. “Those nerve fibers relay information to the brain stem [so it can] work its magic and use the brain’s own natural mechanisms for reducing pain,” said Brian M. Grosberg, MD, director of the Hartford Healthcare Ayer Neuroscience Institute Headache Center, West Hartford, Conn.
These mechanisms are like a bait-and-switch for the brain, said Britany Klenofsky, MD, assistant professor of neurology, Icahn School of Medicine at Mount Sinai, New York. “You’re trying to stimulate pain somewhere else [on the body] to tell the brain to protect itself and release [the neurotransmitter] serotonin,” she said. “You do this by putting the device on your arm, an area that’s away from the head where the pain is actively occurring, turning the device on, and increasing the stimulation to a nearly painful stimulus.”
This pseudo pain prompts the brain to release serotonin, the feel-good hormone along with norepinephrine and noradrenaline. The device works best when it’s used as soon as a migraine starts, so patients should hook up Nerivio within the first 20-30 minutes of onset of pain, said Dr. Grosberg, who was an investigator on the double-blind treatment study that led to FDA clearance. If patients wait too long, the device may not work.
This is why as soon as Ms. Montgomery feels a migraine aura (there are six types of migraine auras, including visual changes and muscle weakness) that occurs right before a migraine strikes, she puts the device armband on her upper arm and launches its smartphone app. Then she turns on the device for a 45-minute treatment, which begins with what she characterizes as tingling and vibration sensations on her arm. She turns up the intensity of the sensations, which are mild electric currents, until they are well-felt but not painful.
Ms. Montgomery said she can use the device and multitask since there’s no need for her to lie down or sit in a darkened room. And since it is worn on the arm, she can wear it under a shirtsleeve while working or out in public without anyone noticing. She also uses the app’s migraine diary and guided meditation to help reduce the anxiety that often accompanies her migraines.
The device is approved for adolescents and adults and can be used for both episodic and chronic migraines. From an efficacy standpoint, the device provides relief about as well as a commonly used pharmaceutical class of drugs, triptans. About 37% of people with episodic migraine achieved complete freedom from pain 2 hours after their treatment. In addition, about two-thirds of people reported pain relief after 2 hours, which is better success than people find with many prescription and nonprescription drugs.
A separate study looked at acute treatment for chronic migraine sufferers and found nearly 60% of people using the device found relief and 21% said they were pain-free after 2 hours. Almost two-thirds of those who experienced pain relief were pain-free 24 hours after the treatment.
Finding the perfect patient
There are other FDA-cleared noninvasive devices to treat migraines. One device, CEFALY, is an external trigeminal nerve stimulation device that sits on the forehead. Another device, SpringTMS, uses transcranial magnetic stimulation on the back of the head. A third option, the gammaCore Sapphire, is placed on the neck to stimulate the vagus nerve. All three have been cleared by the FDA to work as preventive and acute treatments for migraine.
Theranica, the company that developed Nerivio, is trying to boost use of the device by allowing patients to get a prescription via telehealth visits with a physician.
The company, as well as the companies behind the other neuromodulation devices, are marketing their treatments to children ages 12 and up since nonpharmacologic options are often preferable for parents, said Thomas Berk, MD, a clinical associate professor in the division of headache at NYU Langone Health in New York.
Dr. Berk said the devices could be appealing for those people who don’t want or can’t take medication, such as pregnant women or those who don’t respond well to drugs. “[They] could also be used by somebody who needs something in addition to a medication,” he said.
For now, people like Ms. Montgomery say they are happy to have another tool in their migraine arsenal. “Overall, I’m taking less medication because I haven’t had to have my Ubrelvy refilled as often as I used to,” she said. “It’s really helped me manage changes and stresses in my life.”
A version of this article first appeared on Medscape.com.
Enjoy the ride
She was a 20-year-old barista when we first met, working her way through college.
I was a newly minted attending physician. I’d stopped at the place she worked for coffee on the way to my office. When I got up to the front she was wearing sunglasses and apologized for them. She said she was having bad headaches, and couldn’t get into a doctor she’d been referred to. Feeling bad for her, and needing patients, I handed her my card.
She showed up a few days later, a little nervous as she’d never met a “regular” outside the coffee place before, and had brought her sister along for support.
She was back last week. Now she’s head of human resources for the same chain of local coffee shops. She’s married, with kids, a mortgage, and a minivan.
We were talking about our chance meeting and reminiscing. Her migraines had taken a few medication trials to control, but after a year or 2 we’d found the right one for her and she’s been on it since.
Like many of my longtime patients, she moved past calling me “doctor” long ago. Our one to two visits a year are now more social than medical, chatting about our kids, dogs, and lives.
The same passage of time that brings us from grade school, to medical school, to medical practice takes others along with it. We may not see the changes of days, but when they drop by only once a year it’s obvious. Just like the way we don’t see daily changes in family and friends, but when we look at old pictures we’re shocked by how different they (not to mention ourselves) look.
We all follow the same course around the sun, usually facing the same milestones and similar memories on the trip. Our long-term patients, like distant relatives, may only come by infrequently, so the changes are greater. I’m sure they say the same things about me. “I saw Dr. Block today; boy, he’s really gone gray.”
I don’t mind that (too much) anymore. My thinning, graying, hair (I hope) makes me look a little more distinguished, although my complete lack of fashion sense more than goes the other way.
The river only goes in one direction, carrying us, our patients, and our families, all along with it. We often lose track of time’s effects on us until we see the changes it has brought to another.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
She was a 20-year-old barista when we first met, working her way through college.
I was a newly minted attending physician. I’d stopped at the place she worked for coffee on the way to my office. When I got up to the front she was wearing sunglasses and apologized for them. She said she was having bad headaches, and couldn’t get into a doctor she’d been referred to. Feeling bad for her, and needing patients, I handed her my card.
She showed up a few days later, a little nervous as she’d never met a “regular” outside the coffee place before, and had brought her sister along for support.
She was back last week. Now she’s head of human resources for the same chain of local coffee shops. She’s married, with kids, a mortgage, and a minivan.
We were talking about our chance meeting and reminiscing. Her migraines had taken a few medication trials to control, but after a year or 2 we’d found the right one for her and she’s been on it since.
Like many of my longtime patients, she moved past calling me “doctor” long ago. Our one to two visits a year are now more social than medical, chatting about our kids, dogs, and lives.
The same passage of time that brings us from grade school, to medical school, to medical practice takes others along with it. We may not see the changes of days, but when they drop by only once a year it’s obvious. Just like the way we don’t see daily changes in family and friends, but when we look at old pictures we’re shocked by how different they (not to mention ourselves) look.
We all follow the same course around the sun, usually facing the same milestones and similar memories on the trip. Our long-term patients, like distant relatives, may only come by infrequently, so the changes are greater. I’m sure they say the same things about me. “I saw Dr. Block today; boy, he’s really gone gray.”
I don’t mind that (too much) anymore. My thinning, graying, hair (I hope) makes me look a little more distinguished, although my complete lack of fashion sense more than goes the other way.
The river only goes in one direction, carrying us, our patients, and our families, all along with it. We often lose track of time’s effects on us until we see the changes it has brought to another.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
She was a 20-year-old barista when we first met, working her way through college.
I was a newly minted attending physician. I’d stopped at the place she worked for coffee on the way to my office. When I got up to the front she was wearing sunglasses and apologized for them. She said she was having bad headaches, and couldn’t get into a doctor she’d been referred to. Feeling bad for her, and needing patients, I handed her my card.
She showed up a few days later, a little nervous as she’d never met a “regular” outside the coffee place before, and had brought her sister along for support.
She was back last week. Now she’s head of human resources for the same chain of local coffee shops. She’s married, with kids, a mortgage, and a minivan.
We were talking about our chance meeting and reminiscing. Her migraines had taken a few medication trials to control, but after a year or 2 we’d found the right one for her and she’s been on it since.
Like many of my longtime patients, she moved past calling me “doctor” long ago. Our one to two visits a year are now more social than medical, chatting about our kids, dogs, and lives.
The same passage of time that brings us from grade school, to medical school, to medical practice takes others along with it. We may not see the changes of days, but when they drop by only once a year it’s obvious. Just like the way we don’t see daily changes in family and friends, but when we look at old pictures we’re shocked by how different they (not to mention ourselves) look.
We all follow the same course around the sun, usually facing the same milestones and similar memories on the trip. Our long-term patients, like distant relatives, may only come by infrequently, so the changes are greater. I’m sure they say the same things about me. “I saw Dr. Block today; boy, he’s really gone gray.”
I don’t mind that (too much) anymore. My thinning, graying, hair (I hope) makes me look a little more distinguished, although my complete lack of fashion sense more than goes the other way.
The river only goes in one direction, carrying us, our patients, and our families, all along with it. We often lose track of time’s effects on us until we see the changes it has brought to another.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Motor function restored in three men after complete paralysis from spinal cord injury
(SCI), new research shows.
The study demonstrated that an epidural electrical stimulation (EES) system developed specifically for spinal cord injuries enabled three men with complete paralysis to stand, walk, cycle, swim, and move their torso within 1 day.
“Thanks to this technology, we have been able to target individuals with the most serious spinal cord injury, meaning those with clinically complete spinal cord injury, with no sensation and no movement in the legs,” Grégoire Courtine, PhD, professor of neuroscience and neurotechnology at the Swiss Federal Institute of Technology, University Hospital Lausanne (Switzerland), and the University of Lausanne, told reporters attending a press briefing.
The study was published online Feb. 7, 2022, in Nature Medicine.
More rapid, precise, effective
SCIs involve severed connections between the brain and extremities. To compensate for these lost connections, researchers have investigated stem cell therapy, brain-machine interfaces, and powered exoskeletons.
However, these approaches aren’t yet ready for prime time.
In the meantime, researchers discovered even patients with a “complete” injury may have low-functioning connections and started investigating epidural stimulators designed to treat chronic pain. Recent studies – including three published in 2018 – showed promise for these pain-related stimulators in patients with incomplete SCI.
But using such “repurposed” technology meant the electrode array was relatively narrow and short, “so we could not target all the regions of the spinal cord involving control of leg and trunk movements,” said Dr. Courtine. With the newer technology “we are much more precise, effective, and more rapid in delivering therapy.”
To develop this new approach, the researchers designed a paddle lead with an arrangement of electrodes that targets sacral, lumbar, and low-thoracic dorsal roots involved in leg and trunk movements. They also established a personalized computational framework that allows for optimal surgical placement of this paddle lead.
In addition, they developed software that renders the configuration of individualized activity–dependent stimulation programs rapid, simple, and predictable.
They tested these neurotechnologies in three men with complete sensorimotor paralysis as part of an ongoing clinical trial. The participants, aged 29, 32, and 41 years, suffered an SCI from a motor bike accident 3, 9, and 1 year before enrollment.
All three patients exhibited complete sensorimotor paralysis. They were unable to take any step, and muscles remained quiescent during these attempts.
A neurosurgeon implanted electrodes along the spinal cord of study subjects. Wires from these electrodes were connected to a neurostimulator implanted under the skin in the abdomen.
The men can select different activity-based programs from a tablet that sends signals to the implanted device.
Personalized approach
Within a single day of the surgery, the participants were able to stand, walk, cycle, swim, and control trunk movements.
“It was not perfect at the very beginning, but they could train very early on to have a more fluid gait,” said study investigator neurosurgeon Joceylyne Bloch, MD, associate professor, University of Lausanne and University Hospital Lausanne.
At this stage, not all paralyzed patients are eligible for the procedure. Dr. Bloch explained that at least 6 cm of healthy spinal cord under the lesion is needed to implant the electrodes.
“There’s a huge variability of spinal cord anatomy between individuals. That’s why it’s important to study each person individually and to have individual models in order to be precise.”
Researchers envision having “a library of electrode arrays,” added Dr. Courtine. With preoperative imaging of the individual’s spinal cord, “the neurosurgeon can select the more appropriate electrode array for that specific patient.”
Dr. Courtine noted recovery of sensation with the system differs from one individual to another. One study participant, Michel Roccati, now 30, told the briefing he feels a contraction in his muscle during the stimulation.
Currently, only individuals whose injury is more than a year old are included in the study to ensure patients have “a stable lesion” and reached “a plateau of recovery,” said Dr. Bloch. However, animal models show intervening earlier might boost the benefits.
A patient’s age can influence the outcome, as younger patients are likely in better condition and more motivated than older patients, said Dr. Bloch. However, she noted patients closing in on 50 years have responded well to the therapy.
Such stimulation systems may prove useful in treating conditions typically associated with SCI, such as hypertension and bladder control, and perhaps also in patients with Parkinson’s disease, said Dr. Courtine.
The researchers plan to conduct another study that will include a next-generation pulse generator with features that make the stimulation even more effective and user friendly. A voice recognition system could eventually be connected to the system.
“The next step is a minicomputer that you implant in the body that communicates in real time with an external iPhone,” said Dr. Courtine.
ONWARD Medical, which developed the technology, has received a breakthrough device designation from the Food and Drug Administration. The company is in discussions with the FDA to carry out a clinical trial of the device in the United States.
A ‘huge step forward’
Peter J. Grahn, PhD, assistant professor, department of physical medicine and rehabilitation and department of neurologic surgery, Mayo Clinic, Rochester, Minn., an author of one of the 2018 studies, said this technology “is a huge step forward” and “really pushes the field.”
Compared with the device used in his study that’s designed to treat neuropathic pain, this new system “is much more capable of dynamic stimulation,” said Dr. Grahn. “You can tailor the stimulation based on which area of the spinal cord you want to target during a specific function.”
There has been “a lot of hope and hype” recently around stem cells and biological molecules that were supposed to be “magic pills” to cure spinal cord dysfunction, said Dr. Grahn. “I don’t think this is one of those.”
However, he questioned the researchers’ use of the word “walking.”
“They say independent stepping or walking is restored on day 1, but the graphs show day 1 function is having over 60% of their body weight supported when they’re taking these steps,” he said.
In addition, the “big question” is how this technology can “be distilled down” into an approach “applicable across rehabilitation centers,” said Dr. Grahn.
The study was supported by numerous organizations, including ONWARD Medical. Dr. Courtine and Dr. Bloch hold various patents in relation with the present work. Dr. Courtine is a consultant with ONWARD Medical, and he and Dr. Bloch are shareholders of ONWARD Medical, a company with direct relationships with the presented work. Dr. Grahn reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(SCI), new research shows.
The study demonstrated that an epidural electrical stimulation (EES) system developed specifically for spinal cord injuries enabled three men with complete paralysis to stand, walk, cycle, swim, and move their torso within 1 day.
“Thanks to this technology, we have been able to target individuals with the most serious spinal cord injury, meaning those with clinically complete spinal cord injury, with no sensation and no movement in the legs,” Grégoire Courtine, PhD, professor of neuroscience and neurotechnology at the Swiss Federal Institute of Technology, University Hospital Lausanne (Switzerland), and the University of Lausanne, told reporters attending a press briefing.
The study was published online Feb. 7, 2022, in Nature Medicine.
More rapid, precise, effective
SCIs involve severed connections between the brain and extremities. To compensate for these lost connections, researchers have investigated stem cell therapy, brain-machine interfaces, and powered exoskeletons.
However, these approaches aren’t yet ready for prime time.
In the meantime, researchers discovered even patients with a “complete” injury may have low-functioning connections and started investigating epidural stimulators designed to treat chronic pain. Recent studies – including three published in 2018 – showed promise for these pain-related stimulators in patients with incomplete SCI.
But using such “repurposed” technology meant the electrode array was relatively narrow and short, “so we could not target all the regions of the spinal cord involving control of leg and trunk movements,” said Dr. Courtine. With the newer technology “we are much more precise, effective, and more rapid in delivering therapy.”
To develop this new approach, the researchers designed a paddle lead with an arrangement of electrodes that targets sacral, lumbar, and low-thoracic dorsal roots involved in leg and trunk movements. They also established a personalized computational framework that allows for optimal surgical placement of this paddle lead.
In addition, they developed software that renders the configuration of individualized activity–dependent stimulation programs rapid, simple, and predictable.
They tested these neurotechnologies in three men with complete sensorimotor paralysis as part of an ongoing clinical trial. The participants, aged 29, 32, and 41 years, suffered an SCI from a motor bike accident 3, 9, and 1 year before enrollment.
All three patients exhibited complete sensorimotor paralysis. They were unable to take any step, and muscles remained quiescent during these attempts.
A neurosurgeon implanted electrodes along the spinal cord of study subjects. Wires from these electrodes were connected to a neurostimulator implanted under the skin in the abdomen.
The men can select different activity-based programs from a tablet that sends signals to the implanted device.
Personalized approach
Within a single day of the surgery, the participants were able to stand, walk, cycle, swim, and control trunk movements.
“It was not perfect at the very beginning, but they could train very early on to have a more fluid gait,” said study investigator neurosurgeon Joceylyne Bloch, MD, associate professor, University of Lausanne and University Hospital Lausanne.
At this stage, not all paralyzed patients are eligible for the procedure. Dr. Bloch explained that at least 6 cm of healthy spinal cord under the lesion is needed to implant the electrodes.
“There’s a huge variability of spinal cord anatomy between individuals. That’s why it’s important to study each person individually and to have individual models in order to be precise.”
Researchers envision having “a library of electrode arrays,” added Dr. Courtine. With preoperative imaging of the individual’s spinal cord, “the neurosurgeon can select the more appropriate electrode array for that specific patient.”
Dr. Courtine noted recovery of sensation with the system differs from one individual to another. One study participant, Michel Roccati, now 30, told the briefing he feels a contraction in his muscle during the stimulation.
Currently, only individuals whose injury is more than a year old are included in the study to ensure patients have “a stable lesion” and reached “a plateau of recovery,” said Dr. Bloch. However, animal models show intervening earlier might boost the benefits.
A patient’s age can influence the outcome, as younger patients are likely in better condition and more motivated than older patients, said Dr. Bloch. However, she noted patients closing in on 50 years have responded well to the therapy.
Such stimulation systems may prove useful in treating conditions typically associated with SCI, such as hypertension and bladder control, and perhaps also in patients with Parkinson’s disease, said Dr. Courtine.
The researchers plan to conduct another study that will include a next-generation pulse generator with features that make the stimulation even more effective and user friendly. A voice recognition system could eventually be connected to the system.
“The next step is a minicomputer that you implant in the body that communicates in real time with an external iPhone,” said Dr. Courtine.
ONWARD Medical, which developed the technology, has received a breakthrough device designation from the Food and Drug Administration. The company is in discussions with the FDA to carry out a clinical trial of the device in the United States.
A ‘huge step forward’
Peter J. Grahn, PhD, assistant professor, department of physical medicine and rehabilitation and department of neurologic surgery, Mayo Clinic, Rochester, Minn., an author of one of the 2018 studies, said this technology “is a huge step forward” and “really pushes the field.”
Compared with the device used in his study that’s designed to treat neuropathic pain, this new system “is much more capable of dynamic stimulation,” said Dr. Grahn. “You can tailor the stimulation based on which area of the spinal cord you want to target during a specific function.”
There has been “a lot of hope and hype” recently around stem cells and biological molecules that were supposed to be “magic pills” to cure spinal cord dysfunction, said Dr. Grahn. “I don’t think this is one of those.”
However, he questioned the researchers’ use of the word “walking.”
“They say independent stepping or walking is restored on day 1, but the graphs show day 1 function is having over 60% of their body weight supported when they’re taking these steps,” he said.
In addition, the “big question” is how this technology can “be distilled down” into an approach “applicable across rehabilitation centers,” said Dr. Grahn.
The study was supported by numerous organizations, including ONWARD Medical. Dr. Courtine and Dr. Bloch hold various patents in relation with the present work. Dr. Courtine is a consultant with ONWARD Medical, and he and Dr. Bloch are shareholders of ONWARD Medical, a company with direct relationships with the presented work. Dr. Grahn reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(SCI), new research shows.
The study demonstrated that an epidural electrical stimulation (EES) system developed specifically for spinal cord injuries enabled three men with complete paralysis to stand, walk, cycle, swim, and move their torso within 1 day.
“Thanks to this technology, we have been able to target individuals with the most serious spinal cord injury, meaning those with clinically complete spinal cord injury, with no sensation and no movement in the legs,” Grégoire Courtine, PhD, professor of neuroscience and neurotechnology at the Swiss Federal Institute of Technology, University Hospital Lausanne (Switzerland), and the University of Lausanne, told reporters attending a press briefing.
The study was published online Feb. 7, 2022, in Nature Medicine.
More rapid, precise, effective
SCIs involve severed connections between the brain and extremities. To compensate for these lost connections, researchers have investigated stem cell therapy, brain-machine interfaces, and powered exoskeletons.
However, these approaches aren’t yet ready for prime time.
In the meantime, researchers discovered even patients with a “complete” injury may have low-functioning connections and started investigating epidural stimulators designed to treat chronic pain. Recent studies – including three published in 2018 – showed promise for these pain-related stimulators in patients with incomplete SCI.
But using such “repurposed” technology meant the electrode array was relatively narrow and short, “so we could not target all the regions of the spinal cord involving control of leg and trunk movements,” said Dr. Courtine. With the newer technology “we are much more precise, effective, and more rapid in delivering therapy.”
To develop this new approach, the researchers designed a paddle lead with an arrangement of electrodes that targets sacral, lumbar, and low-thoracic dorsal roots involved in leg and trunk movements. They also established a personalized computational framework that allows for optimal surgical placement of this paddle lead.
In addition, they developed software that renders the configuration of individualized activity–dependent stimulation programs rapid, simple, and predictable.
They tested these neurotechnologies in three men with complete sensorimotor paralysis as part of an ongoing clinical trial. The participants, aged 29, 32, and 41 years, suffered an SCI from a motor bike accident 3, 9, and 1 year before enrollment.
All three patients exhibited complete sensorimotor paralysis. They were unable to take any step, and muscles remained quiescent during these attempts.
A neurosurgeon implanted electrodes along the spinal cord of study subjects. Wires from these electrodes were connected to a neurostimulator implanted under the skin in the abdomen.
The men can select different activity-based programs from a tablet that sends signals to the implanted device.
Personalized approach
Within a single day of the surgery, the participants were able to stand, walk, cycle, swim, and control trunk movements.
“It was not perfect at the very beginning, but they could train very early on to have a more fluid gait,” said study investigator neurosurgeon Joceylyne Bloch, MD, associate professor, University of Lausanne and University Hospital Lausanne.
At this stage, not all paralyzed patients are eligible for the procedure. Dr. Bloch explained that at least 6 cm of healthy spinal cord under the lesion is needed to implant the electrodes.
“There’s a huge variability of spinal cord anatomy between individuals. That’s why it’s important to study each person individually and to have individual models in order to be precise.”
Researchers envision having “a library of electrode arrays,” added Dr. Courtine. With preoperative imaging of the individual’s spinal cord, “the neurosurgeon can select the more appropriate electrode array for that specific patient.”
Dr. Courtine noted recovery of sensation with the system differs from one individual to another. One study participant, Michel Roccati, now 30, told the briefing he feels a contraction in his muscle during the stimulation.
Currently, only individuals whose injury is more than a year old are included in the study to ensure patients have “a stable lesion” and reached “a plateau of recovery,” said Dr. Bloch. However, animal models show intervening earlier might boost the benefits.
A patient’s age can influence the outcome, as younger patients are likely in better condition and more motivated than older patients, said Dr. Bloch. However, she noted patients closing in on 50 years have responded well to the therapy.
Such stimulation systems may prove useful in treating conditions typically associated with SCI, such as hypertension and bladder control, and perhaps also in patients with Parkinson’s disease, said Dr. Courtine.
The researchers plan to conduct another study that will include a next-generation pulse generator with features that make the stimulation even more effective and user friendly. A voice recognition system could eventually be connected to the system.
“The next step is a minicomputer that you implant in the body that communicates in real time with an external iPhone,” said Dr. Courtine.
ONWARD Medical, which developed the technology, has received a breakthrough device designation from the Food and Drug Administration. The company is in discussions with the FDA to carry out a clinical trial of the device in the United States.
A ‘huge step forward’
Peter J. Grahn, PhD, assistant professor, department of physical medicine and rehabilitation and department of neurologic surgery, Mayo Clinic, Rochester, Minn., an author of one of the 2018 studies, said this technology “is a huge step forward” and “really pushes the field.”
Compared with the device used in his study that’s designed to treat neuropathic pain, this new system “is much more capable of dynamic stimulation,” said Dr. Grahn. “You can tailor the stimulation based on which area of the spinal cord you want to target during a specific function.”
There has been “a lot of hope and hype” recently around stem cells and biological molecules that were supposed to be “magic pills” to cure spinal cord dysfunction, said Dr. Grahn. “I don’t think this is one of those.”
However, he questioned the researchers’ use of the word “walking.”
“They say independent stepping or walking is restored on day 1, but the graphs show day 1 function is having over 60% of their body weight supported when they’re taking these steps,” he said.
In addition, the “big question” is how this technology can “be distilled down” into an approach “applicable across rehabilitation centers,” said Dr. Grahn.
The study was supported by numerous organizations, including ONWARD Medical. Dr. Courtine and Dr. Bloch hold various patents in relation with the present work. Dr. Courtine is a consultant with ONWARD Medical, and he and Dr. Bloch are shareholders of ONWARD Medical, a company with direct relationships with the presented work. Dr. Grahn reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NATURE MEDICINE