User login
The Official Newspaper of the American Association for Thoracic Surgery
Take Part in the Heart Valve Summit: Medical, Surgical and Interventional Decision Making
Join the American College of Cardiology and the American Association for Thoracic Surgery as they once again bring together cardiologists and surgeons in a cooperative, case-based course to address the rapid advances in the treatment of valvular heart disease.
October 5-7, 2017
Radisson Blu Aqua Hotel
Chicago, IL, USA
Program Overview
With the tradition of interactivity and practical decision making, the unique Heart Valve Summit is designed to engage participants in discussions, debates and potential controversies surrounding real-world cases. A renowned faculty on the cutting edge of clinically relevant data for valvular heart disease management will lead this interdisciplinary course that combines the most relevant medical, surgical and interventional options for patient care.
Course Directors
David H. Adams
Steven F. Bolling
Robert O. Bonow
Howard C. Herrmann
Nurse Planner
Michele Mistovich
To register and reserve housing, visit: www.aats.org/valve
Join the American College of Cardiology and the American Association for Thoracic Surgery as they once again bring together cardiologists and surgeons in a cooperative, case-based course to address the rapid advances in the treatment of valvular heart disease.
October 5-7, 2017
Radisson Blu Aqua Hotel
Chicago, IL, USA
Program Overview
With the tradition of interactivity and practical decision making, the unique Heart Valve Summit is designed to engage participants in discussions, debates and potential controversies surrounding real-world cases. A renowned faculty on the cutting edge of clinically relevant data for valvular heart disease management will lead this interdisciplinary course that combines the most relevant medical, surgical and interventional options for patient care.
Course Directors
David H. Adams
Steven F. Bolling
Robert O. Bonow
Howard C. Herrmann
Nurse Planner
Michele Mistovich
To register and reserve housing, visit: www.aats.org/valve
Join the American College of Cardiology and the American Association for Thoracic Surgery as they once again bring together cardiologists and surgeons in a cooperative, case-based course to address the rapid advances in the treatment of valvular heart disease.
October 5-7, 2017
Radisson Blu Aqua Hotel
Chicago, IL, USA
Program Overview
With the tradition of interactivity and practical decision making, the unique Heart Valve Summit is designed to engage participants in discussions, debates and potential controversies surrounding real-world cases. A renowned faculty on the cutting edge of clinically relevant data for valvular heart disease management will lead this interdisciplinary course that combines the most relevant medical, surgical and interventional options for patient care.
Course Directors
David H. Adams
Steven F. Bolling
Robert O. Bonow
Howard C. Herrmann
Nurse Planner
Michele Mistovich
To register and reserve housing, visit: www.aats.org/valve
FDA: Fluoroquinolone use not linked to retina detachment, aortic problems
The Food and Drug Administration has found no evidence of a link between fluoroquinolone usage and retinal detachment or aortic aneurysm and dissection, according to a new Drug Safety Communication update on potential serious, disabling side effects of oral and injectable fluoroquinolone antibiotics.
Fluoroquinolones are used to treat acute bacterial sinusitis, acute bacterial exacerbation of chronic bronchitis, and uncomplicated urinary tract infections.
However, after reviewing patient cases and study findings, the FDA said the evidence didn’t support an association between fluoroquinolone usage and potential retinal or aortic dangers, according to its May 10, 2017, Drug Safety Communication update.
Serious side effects associated with fluoroquinolone use include hallucination, depression, suicidal thoughts, tendinitis and tendon rupture, a “pins and needles” feeling in the arms and legs, joint pain and swelling, skin rash, and severe diarrhea.
“We will continue to assess safety issues with fluoroquinolones, and will update the public if additional actions are needed,” the FDA said in a statement.
The Food and Drug Administration has found no evidence of a link between fluoroquinolone usage and retinal detachment or aortic aneurysm and dissection, according to a new Drug Safety Communication update on potential serious, disabling side effects of oral and injectable fluoroquinolone antibiotics.
Fluoroquinolones are used to treat acute bacterial sinusitis, acute bacterial exacerbation of chronic bronchitis, and uncomplicated urinary tract infections.
However, after reviewing patient cases and study findings, the FDA said the evidence didn’t support an association between fluoroquinolone usage and potential retinal or aortic dangers, according to its May 10, 2017, Drug Safety Communication update.
Serious side effects associated with fluoroquinolone use include hallucination, depression, suicidal thoughts, tendinitis and tendon rupture, a “pins and needles” feeling in the arms and legs, joint pain and swelling, skin rash, and severe diarrhea.
“We will continue to assess safety issues with fluoroquinolones, and will update the public if additional actions are needed,” the FDA said in a statement.
The Food and Drug Administration has found no evidence of a link between fluoroquinolone usage and retinal detachment or aortic aneurysm and dissection, according to a new Drug Safety Communication update on potential serious, disabling side effects of oral and injectable fluoroquinolone antibiotics.
Fluoroquinolones are used to treat acute bacterial sinusitis, acute bacterial exacerbation of chronic bronchitis, and uncomplicated urinary tract infections.
However, after reviewing patient cases and study findings, the FDA said the evidence didn’t support an association between fluoroquinolone usage and potential retinal or aortic dangers, according to its May 10, 2017, Drug Safety Communication update.
Serious side effects associated with fluoroquinolone use include hallucination, depression, suicidal thoughts, tendinitis and tendon rupture, a “pins and needles” feeling in the arms and legs, joint pain and swelling, skin rash, and severe diarrhea.
“We will continue to assess safety issues with fluoroquinolones, and will update the public if additional actions are needed,” the FDA said in a statement.
Lung cancer metastatic sites differ by histology, tumor factors
GENEVA – A review of data on more than 75,000 patients with lung cancer has revealed distinct patterns of metastasis according to subtype, a finding that could help in surveillance, treatment planning, and prophylaxis, an investigator contends.
Patients with small cell lung cancer (SCLC) had significantly higher rates of liver metastases than patients with non–small cell lung cancer (NSCLC), while patients with NSCLC had significantly higher rates of metastases to bone, reported Mohamed Hendawi, MD, a visiting scholar at the Ohio State University Medical Center in Columbus.
“Predictors for liver metastasis were small cell and adenocarcinoma histology, lower and upper lobe locations, and high grade tumors. Predictors for metastasis to brain were advanced age at diagnosis, adenocarcinoma and small-cell histology, lower lobe [and] main bronchus locations, and high grade tumors,” he wrote in a scientific poster presented at the European Lung Cancer Conference.
Dr. Hendawi drew records on all patients with metastatic lung cancer included in the 2010-2013 Surveillance, Epidemiology, and End Results database. He used univariate and multivariate logistic regression models to evaluate predictors of metastasis.
The data set included a total of 76,254 patients with metastatic lung cancer, of which 17% were SCLC and 83% were NSCLC tumors. In 54% of patients, the primary tumor was in the right lung; in 38%, it was in the left lung; and, in 8% of patients, the primary tumor was bilateral.
The rates of metastases to bone were high in both major lung cancer types but, as noted before, were significantly higher in patients with NSCLC: 37% compared with 34% for patients with SCLC (P less than .001).
In contrast, the incidence of liver metastases in SCLC was more than double that of NSCLC: 46% vs. 20%, respectively (P less than .001). There were slightly, but significantly, fewer cases of brain metastases at the time of diagnosis among patients with SCLC: 25% vs. 26% (P = .003).
Histologic subtypes significantly associated with both brain and liver metastases were, in descending order, adenocarcinomas, small cell, and squamous cell cancers.
Although carcinoid lung cancers accounted for only 2.1% of all tumors, they were associated with a high rate of metastasis to brain at diagnosis (44.8%).
As noted, independent risk factors for liver metastasis were small cell and adenocarcinoma histologies (P less than .001), tumors in the upper lobe (P = .028), and high-grade tumor (P less than .001).
Independent predictors for brain metastases were advanced age at diagnosis (P less than .001), adenocarcinoma and small-cell histologies (P less than .001), lower lobe or main bronchus locations (P = .004), and higher-grade tumors (P less than .001).
In a poster discussion session, Paolo Boffetta, MD, MPH, from the Icahn School of Medicine at Mount Sinai in New York City, the invited discussant, commented that, while he thought that the data were interesting, “the main issue I had with this poster is that it’s limited to patients with metastasis, so we cannot really evaluate the risk of metastasis according to the different histological types and the absolute risk of developing metastases in one or the other organ but only the relative risk of developing metastasis in one organ versus the other having one or the other histology.”
“So, we really don’t know whether the risk is increased in one group or decreased in the other one that generates these differences,” he said.
The study did not receive outside support. Dr. Hendawi declared no conflicts of interest.
GENEVA – A review of data on more than 75,000 patients with lung cancer has revealed distinct patterns of metastasis according to subtype, a finding that could help in surveillance, treatment planning, and prophylaxis, an investigator contends.
Patients with small cell lung cancer (SCLC) had significantly higher rates of liver metastases than patients with non–small cell lung cancer (NSCLC), while patients with NSCLC had significantly higher rates of metastases to bone, reported Mohamed Hendawi, MD, a visiting scholar at the Ohio State University Medical Center in Columbus.
“Predictors for liver metastasis were small cell and adenocarcinoma histology, lower and upper lobe locations, and high grade tumors. Predictors for metastasis to brain were advanced age at diagnosis, adenocarcinoma and small-cell histology, lower lobe [and] main bronchus locations, and high grade tumors,” he wrote in a scientific poster presented at the European Lung Cancer Conference.
Dr. Hendawi drew records on all patients with metastatic lung cancer included in the 2010-2013 Surveillance, Epidemiology, and End Results database. He used univariate and multivariate logistic regression models to evaluate predictors of metastasis.
The data set included a total of 76,254 patients with metastatic lung cancer, of which 17% were SCLC and 83% were NSCLC tumors. In 54% of patients, the primary tumor was in the right lung; in 38%, it was in the left lung; and, in 8% of patients, the primary tumor was bilateral.
The rates of metastases to bone were high in both major lung cancer types but, as noted before, were significantly higher in patients with NSCLC: 37% compared with 34% for patients with SCLC (P less than .001).
In contrast, the incidence of liver metastases in SCLC was more than double that of NSCLC: 46% vs. 20%, respectively (P less than .001). There were slightly, but significantly, fewer cases of brain metastases at the time of diagnosis among patients with SCLC: 25% vs. 26% (P = .003).
Histologic subtypes significantly associated with both brain and liver metastases were, in descending order, adenocarcinomas, small cell, and squamous cell cancers.
Although carcinoid lung cancers accounted for only 2.1% of all tumors, they were associated with a high rate of metastasis to brain at diagnosis (44.8%).
As noted, independent risk factors for liver metastasis were small cell and adenocarcinoma histologies (P less than .001), tumors in the upper lobe (P = .028), and high-grade tumor (P less than .001).
Independent predictors for brain metastases were advanced age at diagnosis (P less than .001), adenocarcinoma and small-cell histologies (P less than .001), lower lobe or main bronchus locations (P = .004), and higher-grade tumors (P less than .001).
In a poster discussion session, Paolo Boffetta, MD, MPH, from the Icahn School of Medicine at Mount Sinai in New York City, the invited discussant, commented that, while he thought that the data were interesting, “the main issue I had with this poster is that it’s limited to patients with metastasis, so we cannot really evaluate the risk of metastasis according to the different histological types and the absolute risk of developing metastases in one or the other organ but only the relative risk of developing metastasis in one organ versus the other having one or the other histology.”
“So, we really don’t know whether the risk is increased in one group or decreased in the other one that generates these differences,” he said.
The study did not receive outside support. Dr. Hendawi declared no conflicts of interest.
GENEVA – A review of data on more than 75,000 patients with lung cancer has revealed distinct patterns of metastasis according to subtype, a finding that could help in surveillance, treatment planning, and prophylaxis, an investigator contends.
Patients with small cell lung cancer (SCLC) had significantly higher rates of liver metastases than patients with non–small cell lung cancer (NSCLC), while patients with NSCLC had significantly higher rates of metastases to bone, reported Mohamed Hendawi, MD, a visiting scholar at the Ohio State University Medical Center in Columbus.
“Predictors for liver metastasis were small cell and adenocarcinoma histology, lower and upper lobe locations, and high grade tumors. Predictors for metastasis to brain were advanced age at diagnosis, adenocarcinoma and small-cell histology, lower lobe [and] main bronchus locations, and high grade tumors,” he wrote in a scientific poster presented at the European Lung Cancer Conference.
Dr. Hendawi drew records on all patients with metastatic lung cancer included in the 2010-2013 Surveillance, Epidemiology, and End Results database. He used univariate and multivariate logistic regression models to evaluate predictors of metastasis.
The data set included a total of 76,254 patients with metastatic lung cancer, of which 17% were SCLC and 83% were NSCLC tumors. In 54% of patients, the primary tumor was in the right lung; in 38%, it was in the left lung; and, in 8% of patients, the primary tumor was bilateral.
The rates of metastases to bone were high in both major lung cancer types but, as noted before, were significantly higher in patients with NSCLC: 37% compared with 34% for patients with SCLC (P less than .001).
In contrast, the incidence of liver metastases in SCLC was more than double that of NSCLC: 46% vs. 20%, respectively (P less than .001). There were slightly, but significantly, fewer cases of brain metastases at the time of diagnosis among patients with SCLC: 25% vs. 26% (P = .003).
Histologic subtypes significantly associated with both brain and liver metastases were, in descending order, adenocarcinomas, small cell, and squamous cell cancers.
Although carcinoid lung cancers accounted for only 2.1% of all tumors, they were associated with a high rate of metastasis to brain at diagnosis (44.8%).
As noted, independent risk factors for liver metastasis were small cell and adenocarcinoma histologies (P less than .001), tumors in the upper lobe (P = .028), and high-grade tumor (P less than .001).
Independent predictors for brain metastases were advanced age at diagnosis (P less than .001), adenocarcinoma and small-cell histologies (P less than .001), lower lobe or main bronchus locations (P = .004), and higher-grade tumors (P less than .001).
In a poster discussion session, Paolo Boffetta, MD, MPH, from the Icahn School of Medicine at Mount Sinai in New York City, the invited discussant, commented that, while he thought that the data were interesting, “the main issue I had with this poster is that it’s limited to patients with metastasis, so we cannot really evaluate the risk of metastasis according to the different histological types and the absolute risk of developing metastases in one or the other organ but only the relative risk of developing metastasis in one organ versus the other having one or the other histology.”
“So, we really don’t know whether the risk is increased in one group or decreased in the other one that generates these differences,” he said.
The study did not receive outside support. Dr. Hendawi declared no conflicts of interest.
FROM ELCC
Key clinical point: Lung cancers tend to metastasize to different organs based on histology and other clinical factors.
Major finding: The incidence of metastasis to bone was higher in patients with NSCLC than SCLC, while liver metastases were more than twice as high among patients with SCLC.
Data source: Review of Surveillance, Epidemiology, and End Results data on 76,254 patients with metastatic lung cancer.
Disclosures: The study did not receive outside support. Dr. Hendawi declared no conflicts of interest.
G-CSF safe, but antibiotics are more concerning in SCLC
GENEVA – In patients with limited stage–small cell lung cancer (LS-SCLC) treated with concurrent chemotherapy and radiation, the use of antibiotics to prevent febrile neutropenia was associated with worse outcomes, but granulocyte-colony stimulating factor (G-CSF) prescribed for the same purposes appeared to be safe, reported investigators.
In a subanalysis of data on patients with early SCLC enrolled in the phase III CONVERT trial comparing chemotherapy with concurrent once-daily vs. twice-daily radiation, the use of antibiotic prophylaxis of neutropenia was associated with worse overall survival (OS) and progression-free survival, (PFS) compared with no antibiotics, reported Fabio Gomes, MD, from the Christie NHS Foundation Trust Hospital in Manchester, England.
The use of G-CSF was, however, associated with higher rates of grade 3 or 4 thrombocytopenia and anemia, requiring supportive measures, he acknowledged.
The role of G-CSF with concurrent thoracic radiotherapy is controversial because of safety concerns, but data are scarce, Dr. Gomes said. He noted that the American Society of Clinical Oncology guidelines on the use of white blood cell growth factors recommend against their routine use.
However, some of those concerns arose in the mid-1990s when granulocyt macrophage–stimulating colony factor (GM-CSF) was used, rather than G-CSF, which acts on only a single blood lineage, namely neutrophils. Additionally, modern radiology techniques are more precise than they were 20 years ago, reducing the risk of toxicity, he noted.
In the CONVERT trial, 547 patients with LS-SCLC were randomly assigned to receive four to six cycles of cisplatin and etoposide chemotherapy concurrently with either once daily thoracic radiation for a total dose of 66 Gy divided into 33 fractions delivered over 45 days or to twice-daily radiation at a total dose of 45 Gy divided into 30 fractions delivered over 19 days.
There was no difference between the groups in the primary endpoint of overall survival.
In the subanalysis reported here, Gomes et al. looked at the use of G-CSF, delivered at the investigator’s discretion, in 487 patients. Approximately 40% of patients in the subanalysis received G-CSF during at least one treatment cycle.
Prophylactic antibiotics were recommended by the investigators for use in association with at least one chemotherapy cycle, and 49% of patients in the subanalysis received them during at least one cycle.
Hematological toxicities included grade 3 or 4 thrombocytopenia occurring in 29.9% of patients who received G-CSF, vs. 13.3% of those who did not (P less than .001). The rates were similar between the once-daily and twice-daily radiation groups.
Grade 3 or 4 anemia occurred in 16.9% of patients who received G-CSF, vs. 10.7% of those who didn’t (P = .027). The difference was significant only among patients in the twice-daily radiation arm (20.9% vs. 8.3%, respectively; P = .004).
Patients in the twice-daily radiation arms who received G-CSF also required more platelet transfusion, compared with the once-daily arm (P less than .001), and, in both arms, G-CSF was associated with more red-cell transfusions (P = .007 for once-daily and .001 for twice daily).
G-CSF was not associated with either pneumonitis or esophagitis, and there were no differences in treatment-related deaths with either G-CSF or antibiotics.
Median OS by G-CSF use was 29 months with and 27 months without, a difference that was not significant (P = .08). Median PFS also did not differ by G-CSF use or nonuse.
When it came to antibiotic prophylaxis, however, both median OS and PFS were significant worse with antibiotic use (OS, 24 months with vs. 33 months without; P = .016; PFS, P = .03).
“We are very reassured that there are no significant additional toxicities [with G-CSF] from radiation in the acute setting,” commented Sanjay Popat, FRCP, PhD, from the Royal Marsden Hospital in London, the invited discussant.
“However, we have no data as yet on the impact of G-CSF usage on febrile neutropenia, which is of course the fundamental that we’re aiming to improve in the hope that this will contribute to [lowering] costs,” he added.
The study was sponsored by the Christie Hospital National Health Service Foundation Trust, Cancer Research UK, EORTC, GECP, GFPC, and IFCT. Dr. Gomes reported no relevant disclosures. Dr. Popat reported consultation, honoraria, travel expenses, and institutional research from multiple entities.
GENEVA – In patients with limited stage–small cell lung cancer (LS-SCLC) treated with concurrent chemotherapy and radiation, the use of antibiotics to prevent febrile neutropenia was associated with worse outcomes, but granulocyte-colony stimulating factor (G-CSF) prescribed for the same purposes appeared to be safe, reported investigators.
In a subanalysis of data on patients with early SCLC enrolled in the phase III CONVERT trial comparing chemotherapy with concurrent once-daily vs. twice-daily radiation, the use of antibiotic prophylaxis of neutropenia was associated with worse overall survival (OS) and progression-free survival, (PFS) compared with no antibiotics, reported Fabio Gomes, MD, from the Christie NHS Foundation Trust Hospital in Manchester, England.
The use of G-CSF was, however, associated with higher rates of grade 3 or 4 thrombocytopenia and anemia, requiring supportive measures, he acknowledged.
The role of G-CSF with concurrent thoracic radiotherapy is controversial because of safety concerns, but data are scarce, Dr. Gomes said. He noted that the American Society of Clinical Oncology guidelines on the use of white blood cell growth factors recommend against their routine use.
However, some of those concerns arose in the mid-1990s when granulocyt macrophage–stimulating colony factor (GM-CSF) was used, rather than G-CSF, which acts on only a single blood lineage, namely neutrophils. Additionally, modern radiology techniques are more precise than they were 20 years ago, reducing the risk of toxicity, he noted.
In the CONVERT trial, 547 patients with LS-SCLC were randomly assigned to receive four to six cycles of cisplatin and etoposide chemotherapy concurrently with either once daily thoracic radiation for a total dose of 66 Gy divided into 33 fractions delivered over 45 days or to twice-daily radiation at a total dose of 45 Gy divided into 30 fractions delivered over 19 days.
There was no difference between the groups in the primary endpoint of overall survival.
In the subanalysis reported here, Gomes et al. looked at the use of G-CSF, delivered at the investigator’s discretion, in 487 patients. Approximately 40% of patients in the subanalysis received G-CSF during at least one treatment cycle.
Prophylactic antibiotics were recommended by the investigators for use in association with at least one chemotherapy cycle, and 49% of patients in the subanalysis received them during at least one cycle.
Hematological toxicities included grade 3 or 4 thrombocytopenia occurring in 29.9% of patients who received G-CSF, vs. 13.3% of those who did not (P less than .001). The rates were similar between the once-daily and twice-daily radiation groups.
Grade 3 or 4 anemia occurred in 16.9% of patients who received G-CSF, vs. 10.7% of those who didn’t (P = .027). The difference was significant only among patients in the twice-daily radiation arm (20.9% vs. 8.3%, respectively; P = .004).
Patients in the twice-daily radiation arms who received G-CSF also required more platelet transfusion, compared with the once-daily arm (P less than .001), and, in both arms, G-CSF was associated with more red-cell transfusions (P = .007 for once-daily and .001 for twice daily).
G-CSF was not associated with either pneumonitis or esophagitis, and there were no differences in treatment-related deaths with either G-CSF or antibiotics.
Median OS by G-CSF use was 29 months with and 27 months without, a difference that was not significant (P = .08). Median PFS also did not differ by G-CSF use or nonuse.
When it came to antibiotic prophylaxis, however, both median OS and PFS were significant worse with antibiotic use (OS, 24 months with vs. 33 months without; P = .016; PFS, P = .03).
“We are very reassured that there are no significant additional toxicities [with G-CSF] from radiation in the acute setting,” commented Sanjay Popat, FRCP, PhD, from the Royal Marsden Hospital in London, the invited discussant.
“However, we have no data as yet on the impact of G-CSF usage on febrile neutropenia, which is of course the fundamental that we’re aiming to improve in the hope that this will contribute to [lowering] costs,” he added.
The study was sponsored by the Christie Hospital National Health Service Foundation Trust, Cancer Research UK, EORTC, GECP, GFPC, and IFCT. Dr. Gomes reported no relevant disclosures. Dr. Popat reported consultation, honoraria, travel expenses, and institutional research from multiple entities.
GENEVA – In patients with limited stage–small cell lung cancer (LS-SCLC) treated with concurrent chemotherapy and radiation, the use of antibiotics to prevent febrile neutropenia was associated with worse outcomes, but granulocyte-colony stimulating factor (G-CSF) prescribed for the same purposes appeared to be safe, reported investigators.
In a subanalysis of data on patients with early SCLC enrolled in the phase III CONVERT trial comparing chemotherapy with concurrent once-daily vs. twice-daily radiation, the use of antibiotic prophylaxis of neutropenia was associated with worse overall survival (OS) and progression-free survival, (PFS) compared with no antibiotics, reported Fabio Gomes, MD, from the Christie NHS Foundation Trust Hospital in Manchester, England.
The use of G-CSF was, however, associated with higher rates of grade 3 or 4 thrombocytopenia and anemia, requiring supportive measures, he acknowledged.
The role of G-CSF with concurrent thoracic radiotherapy is controversial because of safety concerns, but data are scarce, Dr. Gomes said. He noted that the American Society of Clinical Oncology guidelines on the use of white blood cell growth factors recommend against their routine use.
However, some of those concerns arose in the mid-1990s when granulocyt macrophage–stimulating colony factor (GM-CSF) was used, rather than G-CSF, which acts on only a single blood lineage, namely neutrophils. Additionally, modern radiology techniques are more precise than they were 20 years ago, reducing the risk of toxicity, he noted.
In the CONVERT trial, 547 patients with LS-SCLC were randomly assigned to receive four to six cycles of cisplatin and etoposide chemotherapy concurrently with either once daily thoracic radiation for a total dose of 66 Gy divided into 33 fractions delivered over 45 days or to twice-daily radiation at a total dose of 45 Gy divided into 30 fractions delivered over 19 days.
There was no difference between the groups in the primary endpoint of overall survival.
In the subanalysis reported here, Gomes et al. looked at the use of G-CSF, delivered at the investigator’s discretion, in 487 patients. Approximately 40% of patients in the subanalysis received G-CSF during at least one treatment cycle.
Prophylactic antibiotics were recommended by the investigators for use in association with at least one chemotherapy cycle, and 49% of patients in the subanalysis received them during at least one cycle.
Hematological toxicities included grade 3 or 4 thrombocytopenia occurring in 29.9% of patients who received G-CSF, vs. 13.3% of those who did not (P less than .001). The rates were similar between the once-daily and twice-daily radiation groups.
Grade 3 or 4 anemia occurred in 16.9% of patients who received G-CSF, vs. 10.7% of those who didn’t (P = .027). The difference was significant only among patients in the twice-daily radiation arm (20.9% vs. 8.3%, respectively; P = .004).
Patients in the twice-daily radiation arms who received G-CSF also required more platelet transfusion, compared with the once-daily arm (P less than .001), and, in both arms, G-CSF was associated with more red-cell transfusions (P = .007 for once-daily and .001 for twice daily).
G-CSF was not associated with either pneumonitis or esophagitis, and there were no differences in treatment-related deaths with either G-CSF or antibiotics.
Median OS by G-CSF use was 29 months with and 27 months without, a difference that was not significant (P = .08). Median PFS also did not differ by G-CSF use or nonuse.
When it came to antibiotic prophylaxis, however, both median OS and PFS were significant worse with antibiotic use (OS, 24 months with vs. 33 months without; P = .016; PFS, P = .03).
“We are very reassured that there are no significant additional toxicities [with G-CSF] from radiation in the acute setting,” commented Sanjay Popat, FRCP, PhD, from the Royal Marsden Hospital in London, the invited discussant.
“However, we have no data as yet on the impact of G-CSF usage on febrile neutropenia, which is of course the fundamental that we’re aiming to improve in the hope that this will contribute to [lowering] costs,” he added.
The study was sponsored by the Christie Hospital National Health Service Foundation Trust, Cancer Research UK, EORTC, GECP, GFPC, and IFCT. Dr. Gomes reported no relevant disclosures. Dr. Popat reported consultation, honoraria, travel expenses, and institutional research from multiple entities.
FROM ELCC
Key clinical point: Febrile neutropenia prophylaxis with G-CSF was safe, but prophylactic antibiotics were associated with worse overall survival in patients with limited stage–small cell lung cancer.
Major finding: Both median overall and progression-free survival were lower among patients who received prophylactic antibiotics. There were no differences in survival by G-CSF use.
Data source: Subanalysis of data on 487 patients in the phase III CONVERT trial comparing once-daily and twice daily radiation concurrent with chemotherapy in LS-SCLC.
Disclosures: The study was sponsored by the Christie Hospital National Health Service Foundation Trust, Cancer Research UK, EORTC, GECP, GFPC, and IFCT. Dr. Gomes reported no relevant disclosures. Dr. Popat reported consultation, honoraria, travel expenses, and institutional research from multiple entities.
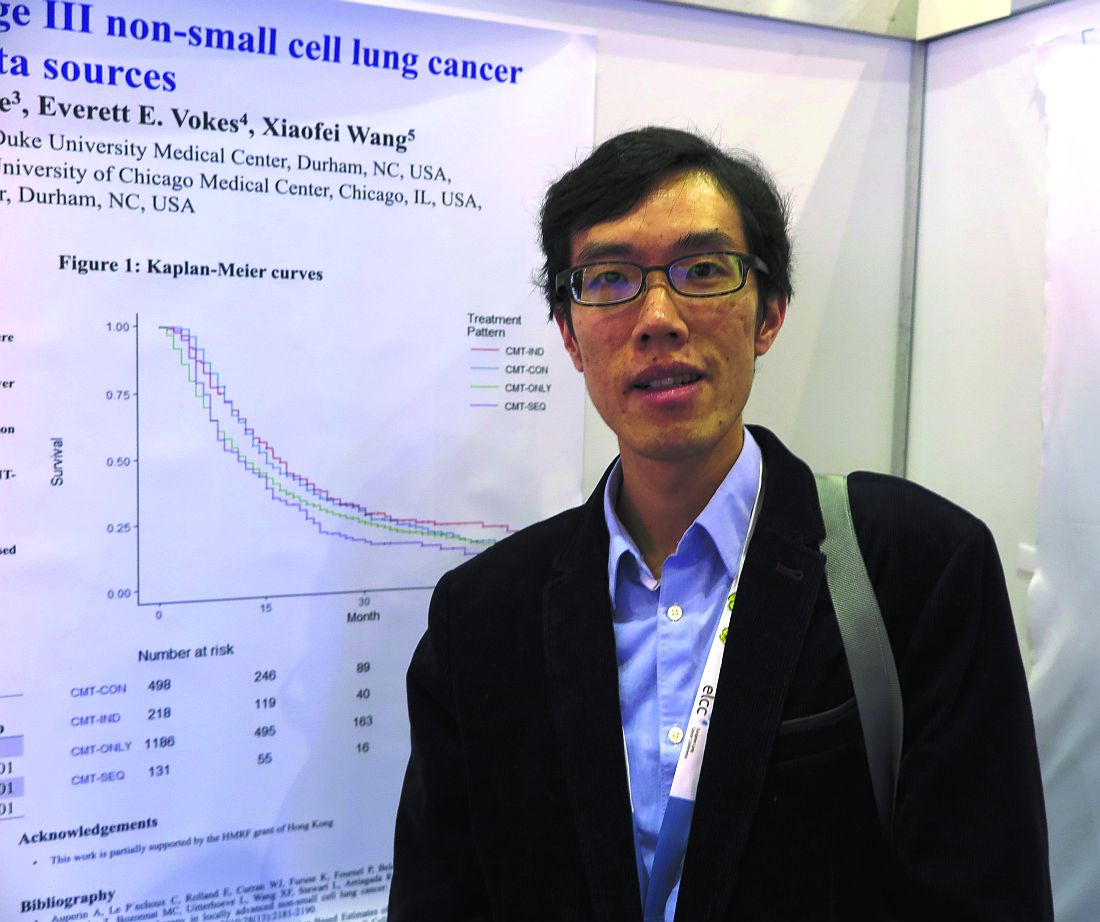
Chemo sequencing in elderly adults with NSCLC linked with survival
GENEVA – Among older adults with stage III non–small cell lung cancer (NSCLC), the sequencing of chemotherapy and radiation has a significant effect on overall survival, a team of investigators from Hong Kong and the United States reported.
Among 2,033 adults who were 65 years or older with locally advanced NSCLC and treated with one of four combined-modality therapy (CMT) schedules, both chemotherapy induction followed by concurrent therapy (CMT-IND) and concurrent therapy followed by consolidation chemoradiation (CMT-CON) were associated with an approximately 30% improvement in survival, compared with either sequential chemotherapy followed by radiation (CMT-SEQ) or concurrent therapy only (CMT-ONLY), reported Hei Man Herbert Pang, MD, of the University of Hong Kong and his colleagues.
The investigators used retrospective data from U.S. and Chinese sources to compare the relative survival benefits with various combined modality therapies. These included a Surveillance, Epidemiology, and End Results–Medicare cohort of patients 65 years and older with stage IIIA or IIIB NSCLC treated with CMT from 2006 through 2010 and a cohort of patients with the same age and NSCLC treated at Queen Mary Hospital in Hong Kong from 2007 through 2016.
They assessed neutropenia using inpatient claims data for episodes occurring within 130 days of the first chemotherapy cycle.
In an unadjusted analysis, they found that median overall survival, in descending order, was 16.1 months for CMT-SEQ,15.0 months for CMT-ONLY, 12.0 months for CMT-IND, and 11.0 months for CMT-CON.
When they controlled for variables, however, a different picture began to emerge.
For example, patients who were treated with CMT-SEQ had lower Charlson Comorbidity Index scores and, thus, were comparatively healthier than patients treated with other combined modalities.
Hospitalizations for neutropenia were most common with CMT-CON, occurring in 13.3% of patients, compared with 9.8% of patients treated with CMT-ONLY, 9.2% with CMT-IND, and 2.3% with CMT-SEQ.
In multivariable models controlling for sex, race, ethnicity, histology, and Charlson score, CMT-CON and CMT-IND were associated with significantly better overall, compared with CMT-SEQ, with respective hazard ratios for death of 0.68 (P less than .001) and 0.67 (P = .001). In this model, CMT-ONLY was not associated with significantly better survival.
In a propensity score model adjusted for the same factors, the respective HRs for CMT-CON, CMT-IND, and CMT-ONLY vs. CMT-SEQ were 0.69, 0.70, and 0.86 (P less than .001 for all three comparisons).
“The findings on efficacy and toxicity are quite consistent with previously reported studies based on clinical trials or observational databases,” the investigators said.
The study was supported by grants from the U.S. National Institutes of Health and the Hong Kong Health and Medical Research Fund. All authors have declared no conflicts of interest.
GENEVA – Among older adults with stage III non–small cell lung cancer (NSCLC), the sequencing of chemotherapy and radiation has a significant effect on overall survival, a team of investigators from Hong Kong and the United States reported.
Among 2,033 adults who were 65 years or older with locally advanced NSCLC and treated with one of four combined-modality therapy (CMT) schedules, both chemotherapy induction followed by concurrent therapy (CMT-IND) and concurrent therapy followed by consolidation chemoradiation (CMT-CON) were associated with an approximately 30% improvement in survival, compared with either sequential chemotherapy followed by radiation (CMT-SEQ) or concurrent therapy only (CMT-ONLY), reported Hei Man Herbert Pang, MD, of the University of Hong Kong and his colleagues.
The investigators used retrospective data from U.S. and Chinese sources to compare the relative survival benefits with various combined modality therapies. These included a Surveillance, Epidemiology, and End Results–Medicare cohort of patients 65 years and older with stage IIIA or IIIB NSCLC treated with CMT from 2006 through 2010 and a cohort of patients with the same age and NSCLC treated at Queen Mary Hospital in Hong Kong from 2007 through 2016.
They assessed neutropenia using inpatient claims data for episodes occurring within 130 days of the first chemotherapy cycle.
In an unadjusted analysis, they found that median overall survival, in descending order, was 16.1 months for CMT-SEQ,15.0 months for CMT-ONLY, 12.0 months for CMT-IND, and 11.0 months for CMT-CON.
When they controlled for variables, however, a different picture began to emerge.
For example, patients who were treated with CMT-SEQ had lower Charlson Comorbidity Index scores and, thus, were comparatively healthier than patients treated with other combined modalities.
Hospitalizations for neutropenia were most common with CMT-CON, occurring in 13.3% of patients, compared with 9.8% of patients treated with CMT-ONLY, 9.2% with CMT-IND, and 2.3% with CMT-SEQ.
In multivariable models controlling for sex, race, ethnicity, histology, and Charlson score, CMT-CON and CMT-IND were associated with significantly better overall, compared with CMT-SEQ, with respective hazard ratios for death of 0.68 (P less than .001) and 0.67 (P = .001). In this model, CMT-ONLY was not associated with significantly better survival.
In a propensity score model adjusted for the same factors, the respective HRs for CMT-CON, CMT-IND, and CMT-ONLY vs. CMT-SEQ were 0.69, 0.70, and 0.86 (P less than .001 for all three comparisons).
“The findings on efficacy and toxicity are quite consistent with previously reported studies based on clinical trials or observational databases,” the investigators said.
The study was supported by grants from the U.S. National Institutes of Health and the Hong Kong Health and Medical Research Fund. All authors have declared no conflicts of interest.
GENEVA – Among older adults with stage III non–small cell lung cancer (NSCLC), the sequencing of chemotherapy and radiation has a significant effect on overall survival, a team of investigators from Hong Kong and the United States reported.
Among 2,033 adults who were 65 years or older with locally advanced NSCLC and treated with one of four combined-modality therapy (CMT) schedules, both chemotherapy induction followed by concurrent therapy (CMT-IND) and concurrent therapy followed by consolidation chemoradiation (CMT-CON) were associated with an approximately 30% improvement in survival, compared with either sequential chemotherapy followed by radiation (CMT-SEQ) or concurrent therapy only (CMT-ONLY), reported Hei Man Herbert Pang, MD, of the University of Hong Kong and his colleagues.
The investigators used retrospective data from U.S. and Chinese sources to compare the relative survival benefits with various combined modality therapies. These included a Surveillance, Epidemiology, and End Results–Medicare cohort of patients 65 years and older with stage IIIA or IIIB NSCLC treated with CMT from 2006 through 2010 and a cohort of patients with the same age and NSCLC treated at Queen Mary Hospital in Hong Kong from 2007 through 2016.
They assessed neutropenia using inpatient claims data for episodes occurring within 130 days of the first chemotherapy cycle.
In an unadjusted analysis, they found that median overall survival, in descending order, was 16.1 months for CMT-SEQ,15.0 months for CMT-ONLY, 12.0 months for CMT-IND, and 11.0 months for CMT-CON.
When they controlled for variables, however, a different picture began to emerge.
For example, patients who were treated with CMT-SEQ had lower Charlson Comorbidity Index scores and, thus, were comparatively healthier than patients treated with other combined modalities.
Hospitalizations for neutropenia were most common with CMT-CON, occurring in 13.3% of patients, compared with 9.8% of patients treated with CMT-ONLY, 9.2% with CMT-IND, and 2.3% with CMT-SEQ.
In multivariable models controlling for sex, race, ethnicity, histology, and Charlson score, CMT-CON and CMT-IND were associated with significantly better overall, compared with CMT-SEQ, with respective hazard ratios for death of 0.68 (P less than .001) and 0.67 (P = .001). In this model, CMT-ONLY was not associated with significantly better survival.
In a propensity score model adjusted for the same factors, the respective HRs for CMT-CON, CMT-IND, and CMT-ONLY vs. CMT-SEQ were 0.69, 0.70, and 0.86 (P less than .001 for all three comparisons).
“The findings on efficacy and toxicity are quite consistent with previously reported studies based on clinical trials or observational databases,” the investigators said.
The study was supported by grants from the U.S. National Institutes of Health and the Hong Kong Health and Medical Research Fund. All authors have declared no conflicts of interest.
FROM ELCC
Key clinical point: Some combined modality therapy options for older adults with NSCLC are associated with better overall survival.
Major finding: CMT-IND and CMT-CON were associated with a 30% improvement in overall survival, compared with CMT-SEQ.
Data source: Retrospective review of data on 2,033 adults 65 years and older with NSCLC in the United States and Hong Kong.
Disclosures: The study was supported by grants from the U.S. National Institutes of Health and the Hong Kong Health and Medical Research Fund. All authors have declared no conflicts of interest.
OR staff perception of safety linked to better surgical outcomes
PHILADELPHIA – No large-scale study has evaluated the culture of operating room safety and 30-day postoperative death, but a statewide evaluation of South Carolina hospitals found that those in which operating-room personnel perceived a high degree of safety reported lower all-cause 30-day postoperative mortality rates.
“Reducing postoperative death rates and improving patient safety require that, in addition to technical competence, surgeons lead surgical teams in ways that foster the creation of a culture in operating rooms where personnel feel respected and invited to speak up on behalf of patient safety,” George Molina, MD, MPH, said at the annual meeting of the American Surgical Association. Dr. Molina is with Brigham and Women’s Hospital, Harvard T.H. Chan School of Public Health, and Massachusetts General Hospital, Boston.
The study drew on a statewide quality and safety program of the South Carolina Hospital Association known as Safe Surgery 2015, one component of which was a survey sent to operating-room (OR) personnel to measure baseline culture of surgical safety. The survey evaluated five teamwork factors: mutual respect, clinical leadership, assertiveness, coordination, and effective communication. The overall response rate of OR staff at 31 surveyed hospitals was 38.1% with 1,793 completed surveys, with a physicians response rate of 29%.
The researchers analyzed statewide claims data of nearly all surgery in the state (except for operations at Veterans Affairs, military and Shriners’ centers) and a state-level death registry to identify patients who died within 30 days after an inpatient operation. The unadjusted median 30-day postoperative death rate at the 31 participating hospitals was 3.2%, Dr. Molina said.
The study evaluated the association between hospital-level mean scores for each survey statement and postoperative death, and used machine learning to adjust for potential confounders. The analysis also took into account hospital-level variables such as patient gender, Charlson Comorbidity Index, primary payer status, and procedure type.
“Among the factors that make up the teamwork dimension, respect, leadership and assertiveness on behalf of patient safety were significantly associated with lower 30-day postoperative death rates,” Dr. Molina said. “For every one-point increase on a seven-point Likert scale and the hospital level mean score for respect, clinical leadership, and assertiveness among all survey respondents, there were associated decreases in postoperative mortality following surgery, ranging from 14% to 29%.”
Of the five teamwork variables, assertiveness had the lowest relative risk, 0.71 (P = .01), whereas communication had the highest, 0.98 (P = .77).
Dr. Molina noted a number of limitations to the study, such as the inability to generalize findings from a single state and the use of cross-sectional data, which precludes a causal link between culture and mortality. “Postoperative mortality is most likely due to multiple factors that take place not only in the operating room, but also during the course of preoperative and postoperative course,” he said.
In his discussion, Justin Dimick, MD, of the University of Michigan, Ann Arbor, asked Dr. Molina what interventions beyond OR checklists are available to improve safety culture.
“It’s not a matter of changing perceptions but actually changing behaviors and then actually improving the culture,” Dr. Molina said. OR team training that includes simulated emergency response is one such intervention. Other strategies he offered: “Working on communication, in particular closed-loop communication among health care providers working in the operating room, and then also quality and safety programs such as Safe Surgery 2015.”
Dr. Molina reported no financial disclosures. Dr. Dimick is cofounder of Arbor Metrix and receives royalties.
The complete manuscript of this study and its presentation at the American Surgical Association’s 137th Annual Meeting, April 2017, in Philadelphia, Pennsylvania, is anticipated to be published in the Annals of Surgery pending editorial review.
PHILADELPHIA – No large-scale study has evaluated the culture of operating room safety and 30-day postoperative death, but a statewide evaluation of South Carolina hospitals found that those in which operating-room personnel perceived a high degree of safety reported lower all-cause 30-day postoperative mortality rates.
“Reducing postoperative death rates and improving patient safety require that, in addition to technical competence, surgeons lead surgical teams in ways that foster the creation of a culture in operating rooms where personnel feel respected and invited to speak up on behalf of patient safety,” George Molina, MD, MPH, said at the annual meeting of the American Surgical Association. Dr. Molina is with Brigham and Women’s Hospital, Harvard T.H. Chan School of Public Health, and Massachusetts General Hospital, Boston.
The study drew on a statewide quality and safety program of the South Carolina Hospital Association known as Safe Surgery 2015, one component of which was a survey sent to operating-room (OR) personnel to measure baseline culture of surgical safety. The survey evaluated five teamwork factors: mutual respect, clinical leadership, assertiveness, coordination, and effective communication. The overall response rate of OR staff at 31 surveyed hospitals was 38.1% with 1,793 completed surveys, with a physicians response rate of 29%.
The researchers analyzed statewide claims data of nearly all surgery in the state (except for operations at Veterans Affairs, military and Shriners’ centers) and a state-level death registry to identify patients who died within 30 days after an inpatient operation. The unadjusted median 30-day postoperative death rate at the 31 participating hospitals was 3.2%, Dr. Molina said.
The study evaluated the association between hospital-level mean scores for each survey statement and postoperative death, and used machine learning to adjust for potential confounders. The analysis also took into account hospital-level variables such as patient gender, Charlson Comorbidity Index, primary payer status, and procedure type.
“Among the factors that make up the teamwork dimension, respect, leadership and assertiveness on behalf of patient safety were significantly associated with lower 30-day postoperative death rates,” Dr. Molina said. “For every one-point increase on a seven-point Likert scale and the hospital level mean score for respect, clinical leadership, and assertiveness among all survey respondents, there were associated decreases in postoperative mortality following surgery, ranging from 14% to 29%.”
Of the five teamwork variables, assertiveness had the lowest relative risk, 0.71 (P = .01), whereas communication had the highest, 0.98 (P = .77).
Dr. Molina noted a number of limitations to the study, such as the inability to generalize findings from a single state and the use of cross-sectional data, which precludes a causal link between culture and mortality. “Postoperative mortality is most likely due to multiple factors that take place not only in the operating room, but also during the course of preoperative and postoperative course,” he said.
In his discussion, Justin Dimick, MD, of the University of Michigan, Ann Arbor, asked Dr. Molina what interventions beyond OR checklists are available to improve safety culture.
“It’s not a matter of changing perceptions but actually changing behaviors and then actually improving the culture,” Dr. Molina said. OR team training that includes simulated emergency response is one such intervention. Other strategies he offered: “Working on communication, in particular closed-loop communication among health care providers working in the operating room, and then also quality and safety programs such as Safe Surgery 2015.”
Dr. Molina reported no financial disclosures. Dr. Dimick is cofounder of Arbor Metrix and receives royalties.
The complete manuscript of this study and its presentation at the American Surgical Association’s 137th Annual Meeting, April 2017, in Philadelphia, Pennsylvania, is anticipated to be published in the Annals of Surgery pending editorial review.
PHILADELPHIA – No large-scale study has evaluated the culture of operating room safety and 30-day postoperative death, but a statewide evaluation of South Carolina hospitals found that those in which operating-room personnel perceived a high degree of safety reported lower all-cause 30-day postoperative mortality rates.
“Reducing postoperative death rates and improving patient safety require that, in addition to technical competence, surgeons lead surgical teams in ways that foster the creation of a culture in operating rooms where personnel feel respected and invited to speak up on behalf of patient safety,” George Molina, MD, MPH, said at the annual meeting of the American Surgical Association. Dr. Molina is with Brigham and Women’s Hospital, Harvard T.H. Chan School of Public Health, and Massachusetts General Hospital, Boston.
The study drew on a statewide quality and safety program of the South Carolina Hospital Association known as Safe Surgery 2015, one component of which was a survey sent to operating-room (OR) personnel to measure baseline culture of surgical safety. The survey evaluated five teamwork factors: mutual respect, clinical leadership, assertiveness, coordination, and effective communication. The overall response rate of OR staff at 31 surveyed hospitals was 38.1% with 1,793 completed surveys, with a physicians response rate of 29%.
The researchers analyzed statewide claims data of nearly all surgery in the state (except for operations at Veterans Affairs, military and Shriners’ centers) and a state-level death registry to identify patients who died within 30 days after an inpatient operation. The unadjusted median 30-day postoperative death rate at the 31 participating hospitals was 3.2%, Dr. Molina said.
The study evaluated the association between hospital-level mean scores for each survey statement and postoperative death, and used machine learning to adjust for potential confounders. The analysis also took into account hospital-level variables such as patient gender, Charlson Comorbidity Index, primary payer status, and procedure type.
“Among the factors that make up the teamwork dimension, respect, leadership and assertiveness on behalf of patient safety were significantly associated with lower 30-day postoperative death rates,” Dr. Molina said. “For every one-point increase on a seven-point Likert scale and the hospital level mean score for respect, clinical leadership, and assertiveness among all survey respondents, there were associated decreases in postoperative mortality following surgery, ranging from 14% to 29%.”
Of the five teamwork variables, assertiveness had the lowest relative risk, 0.71 (P = .01), whereas communication had the highest, 0.98 (P = .77).
Dr. Molina noted a number of limitations to the study, such as the inability to generalize findings from a single state and the use of cross-sectional data, which precludes a causal link between culture and mortality. “Postoperative mortality is most likely due to multiple factors that take place not only in the operating room, but also during the course of preoperative and postoperative course,” he said.
In his discussion, Justin Dimick, MD, of the University of Michigan, Ann Arbor, asked Dr. Molina what interventions beyond OR checklists are available to improve safety culture.
“It’s not a matter of changing perceptions but actually changing behaviors and then actually improving the culture,” Dr. Molina said. OR team training that includes simulated emergency response is one such intervention. Other strategies he offered: “Working on communication, in particular closed-loop communication among health care providers working in the operating room, and then also quality and safety programs such as Safe Surgery 2015.”
Dr. Molina reported no financial disclosures. Dr. Dimick is cofounder of Arbor Metrix and receives royalties.
The complete manuscript of this study and its presentation at the American Surgical Association’s 137th Annual Meeting, April 2017, in Philadelphia, Pennsylvania, is anticipated to be published in the Annals of Surgery pending editorial review.
Key clinical point: Perceptions of safety among operating room personnel may influence postoperative death rates.
Major finding: Higher scores for key teamwork variables were associated with decreases in postoperative hospital death rates ranging from 14% to 29%.
Data source: Survey responses of 1,793 operating room personnel at 31 member hospitals of the South Carolina Hospital Association.
Disclosures: Dr. Molina reported no financial disclosures. Dr. Dimick is cofounder of Arbor Metrix and receives royalties.
Sex-based differences in lung cancer screening intervals suggested
GENEVA – A lung-cancer screening CT interval of once-yearly for men and once every 3 years for women appears to be the optimum schedule for detecting most early-stage lung cancers while minimizing radiation exposure, results of a retrospective study suggest.
Among 96 patients (85 men and 11 women) with lung cancers detected on follow-up screening CT, the mean interval time between initial CT and diagnostic CT was significantly longer among women than among men, at 5.6 vs. 3.6 years (P = .02), reported Mi-Young Kim, MD, a radiologist at Asan Medical Center in Seoul, South Korea.
Men tended to have a higher stage at diagnosis, however. Stage I cancers were diagnosed in 82% of women, but only 49% of men. Tumor size was also larger among men at presentation at a mean of 29.5 mm vs. 15.5 mm, Dr. Kim and her colleagues found.
Current lung cancer screening guidelines vary somewhat, but most recommend annual screening for people aged 55-80 years who have a 30 pack-year or greater smoking history and are current smokers or have quit within the last 15 years.
Prior studies to see whether longer screening intervals were safe have yielded mixed results, possibly because of differences in clinical and radiologic presentation between men and women, Dr. Kim said.
To explore sex differences in lung cancer at the time of diagnosis, she and her colleagues retrospectively reviewed records for 46,766 patients who underwent screening at their center from January 2000 through February 2016, during which time, 282 patients were diagnosed with lung cancer. Of this group, 186 were diagnosed from the initial screening CT scan, and 96 – the cohort included in the study – were diagnosed from subsequent scans.
The authors found that the majority of men (72%) had solid nodules as the primary pathology. In contrast, ground-glass opacities were the most common nodular finding among women, occurring in 45% of the cases. The most common histology among men was adenocarcinoma (42%), followed by squamous-cell carcinoma (35%), small cell lung cancer (18%), and others (5%). All women presented with adenocarcinoma histology.
“Because ground-glass opacity nodule is the most common feature of lung cancer in women, and all cases are adenocarcinoma, the growth rate of cancers might be low,” Dr. Kim said in a statement.
Only 2 of the 11 women in the study were smokers, compared with 74 of the 85 men.
Looking at the operability of lung cancer according to screening intervals, the investigators found that 100% of tumors detected at 1 year in men were operable, compared with 94% of those detected at 2 years, and 55% for those detected at the 3-year interval. In contrast, among women, there were no tumors detected at 1 year, one operable tumor and no inoperable tumors at 2 years, and two operable and no inoperable tumors at 3 years. Beyond 3 years, however, the rate of inoperable tumors at the time of diagnosis was 32% in men and 25% in women.
“We included all patients screened for lung cancer in a 17-year period, but the number of women patients was low and further studies are needed to confirm the sex differences we found,” Dr. Kim acknowledged.
“Only when this is adjusted for – when we compare smokers of the same pack-year history – then we can look at whether women and men do have different rates of appearance of nodules,” he said.
“To me, this is a very interesting suggestion that indeed the biology of the growth of these nodules may be different in men and women, but only if we are sure that the main environmental factor is taken care of.”
The study funding source was not disclosed.
Dr. Kim and Dr. Boffetta reported no relevant disclosures.
GENEVA – A lung-cancer screening CT interval of once-yearly for men and once every 3 years for women appears to be the optimum schedule for detecting most early-stage lung cancers while minimizing radiation exposure, results of a retrospective study suggest.
Among 96 patients (85 men and 11 women) with lung cancers detected on follow-up screening CT, the mean interval time between initial CT and diagnostic CT was significantly longer among women than among men, at 5.6 vs. 3.6 years (P = .02), reported Mi-Young Kim, MD, a radiologist at Asan Medical Center in Seoul, South Korea.
Men tended to have a higher stage at diagnosis, however. Stage I cancers were diagnosed in 82% of women, but only 49% of men. Tumor size was also larger among men at presentation at a mean of 29.5 mm vs. 15.5 mm, Dr. Kim and her colleagues found.
Current lung cancer screening guidelines vary somewhat, but most recommend annual screening for people aged 55-80 years who have a 30 pack-year or greater smoking history and are current smokers or have quit within the last 15 years.
Prior studies to see whether longer screening intervals were safe have yielded mixed results, possibly because of differences in clinical and radiologic presentation between men and women, Dr. Kim said.
To explore sex differences in lung cancer at the time of diagnosis, she and her colleagues retrospectively reviewed records for 46,766 patients who underwent screening at their center from January 2000 through February 2016, during which time, 282 patients were diagnosed with lung cancer. Of this group, 186 were diagnosed from the initial screening CT scan, and 96 – the cohort included in the study – were diagnosed from subsequent scans.
The authors found that the majority of men (72%) had solid nodules as the primary pathology. In contrast, ground-glass opacities were the most common nodular finding among women, occurring in 45% of the cases. The most common histology among men was adenocarcinoma (42%), followed by squamous-cell carcinoma (35%), small cell lung cancer (18%), and others (5%). All women presented with adenocarcinoma histology.
“Because ground-glass opacity nodule is the most common feature of lung cancer in women, and all cases are adenocarcinoma, the growth rate of cancers might be low,” Dr. Kim said in a statement.
Only 2 of the 11 women in the study were smokers, compared with 74 of the 85 men.
Looking at the operability of lung cancer according to screening intervals, the investigators found that 100% of tumors detected at 1 year in men were operable, compared with 94% of those detected at 2 years, and 55% for those detected at the 3-year interval. In contrast, among women, there were no tumors detected at 1 year, one operable tumor and no inoperable tumors at 2 years, and two operable and no inoperable tumors at 3 years. Beyond 3 years, however, the rate of inoperable tumors at the time of diagnosis was 32% in men and 25% in women.
“We included all patients screened for lung cancer in a 17-year period, but the number of women patients was low and further studies are needed to confirm the sex differences we found,” Dr. Kim acknowledged.
“Only when this is adjusted for – when we compare smokers of the same pack-year history – then we can look at whether women and men do have different rates of appearance of nodules,” he said.
“To me, this is a very interesting suggestion that indeed the biology of the growth of these nodules may be different in men and women, but only if we are sure that the main environmental factor is taken care of.”
The study funding source was not disclosed.
Dr. Kim and Dr. Boffetta reported no relevant disclosures.
GENEVA – A lung-cancer screening CT interval of once-yearly for men and once every 3 years for women appears to be the optimum schedule for detecting most early-stage lung cancers while minimizing radiation exposure, results of a retrospective study suggest.
Among 96 patients (85 men and 11 women) with lung cancers detected on follow-up screening CT, the mean interval time between initial CT and diagnostic CT was significantly longer among women than among men, at 5.6 vs. 3.6 years (P = .02), reported Mi-Young Kim, MD, a radiologist at Asan Medical Center in Seoul, South Korea.
Men tended to have a higher stage at diagnosis, however. Stage I cancers were diagnosed in 82% of women, but only 49% of men. Tumor size was also larger among men at presentation at a mean of 29.5 mm vs. 15.5 mm, Dr. Kim and her colleagues found.
Current lung cancer screening guidelines vary somewhat, but most recommend annual screening for people aged 55-80 years who have a 30 pack-year or greater smoking history and are current smokers or have quit within the last 15 years.
Prior studies to see whether longer screening intervals were safe have yielded mixed results, possibly because of differences in clinical and radiologic presentation between men and women, Dr. Kim said.
To explore sex differences in lung cancer at the time of diagnosis, she and her colleagues retrospectively reviewed records for 46,766 patients who underwent screening at their center from January 2000 through February 2016, during which time, 282 patients were diagnosed with lung cancer. Of this group, 186 were diagnosed from the initial screening CT scan, and 96 – the cohort included in the study – were diagnosed from subsequent scans.
The authors found that the majority of men (72%) had solid nodules as the primary pathology. In contrast, ground-glass opacities were the most common nodular finding among women, occurring in 45% of the cases. The most common histology among men was adenocarcinoma (42%), followed by squamous-cell carcinoma (35%), small cell lung cancer (18%), and others (5%). All women presented with adenocarcinoma histology.
“Because ground-glass opacity nodule is the most common feature of lung cancer in women, and all cases are adenocarcinoma, the growth rate of cancers might be low,” Dr. Kim said in a statement.
Only 2 of the 11 women in the study were smokers, compared with 74 of the 85 men.
Looking at the operability of lung cancer according to screening intervals, the investigators found that 100% of tumors detected at 1 year in men were operable, compared with 94% of those detected at 2 years, and 55% for those detected at the 3-year interval. In contrast, among women, there were no tumors detected at 1 year, one operable tumor and no inoperable tumors at 2 years, and two operable and no inoperable tumors at 3 years. Beyond 3 years, however, the rate of inoperable tumors at the time of diagnosis was 32% in men and 25% in women.
“We included all patients screened for lung cancer in a 17-year period, but the number of women patients was low and further studies are needed to confirm the sex differences we found,” Dr. Kim acknowledged.
“Only when this is adjusted for – when we compare smokers of the same pack-year history – then we can look at whether women and men do have different rates of appearance of nodules,” he said.
“To me, this is a very interesting suggestion that indeed the biology of the growth of these nodules may be different in men and women, but only if we are sure that the main environmental factor is taken care of.”
The study funding source was not disclosed.
Dr. Kim and Dr. Boffetta reported no relevant disclosures.
FROM ELCC
Key clinical point:
Major finding: A repeated CT scan for lung cancer every year in men and every 3 years in women picked up most new, operable lesions.
Data source: Retrospective review of data on 96 patients with lung cancer diagnosed at a second or subsequent CT screening.
Disclosures: The study funding source was not disclosed. Dr. Kim and Dr. Boffetta reported no relevant disclosures.
Low-income uninsured trauma patients at risk for ruinous medical costs
Almost three-quarters of uninsured adults admitted for traumatic injury are at risk of catastrophic health expenditures (CHEs), according to a large retrospective study from a national patient database.
Since enactment of the Affordable Care Act in 2010, the number of uninsured individuals has dropped substantially, but there remains a large population of younger adults, many from low-income areas, who still are not covered. The Centers for Disease Control and Prevention reported in 2015 that 12.8% of individuals aged 18-64 years were uninsured. The financial impact of a traumatic injury is likely to be significant for those paying out of pocket, but the question of who is at risk and to what degree is understudied, according to John W. Scott, MD, of Brigham and Women’s Hospital, Boston, and his colleagues.
“Defining populations at risk of financial catastrophe after medical expense is a necessary step towards elucidating the effect of health care reforms intended to increase access to healthcare through insurance expansion,” they wrote in the Annals of Surgery (2017 Apr 7. doi: 10.1097/SLA.0000000000002254).
Dr. Scott and his colleagues analyzed trauma diagnoses in adults aged 18-64 years from Nationwide Inpatient Sample 2007-2011. They used the U.S. Census data to estimate post-subsistence income (income remaining after paying for food) and hospital charges for trauma diagnoses. The sample of 117,502 patient encounters was weighted to represent 579,683 trauma patients in the national database.
CHEs were defined conservatively as expenses that exceed 40% of a patient’s post-subsistence income; they also applied a lower threshold of CHEs – 10% of a patient’s entire income – without accounting for subsistence needs.
The investigators wanted to look at who was at greatest risk for CHEs and used the Census data to sort trauma patients by residential zip code to identify the distribution of income in the sample.
Costs to trauma patients varied by injury severity score (ISS) and by income quartile. Patients in the 25th income quartile paid less for their treatment, even accounting for ISS, but despite this difference, poorer patients were at a much greater risk for CHEs.
The median charge for all of these uninsured trauma patients was $27,420. Those trauma patients in the 25th percentile of income were charged an average of $15,196, while those in 75th quartile were charged $49,696. The difference in costs also was evident when comparing patients in different ISS categories: for ISS 9-15, median trauma costs for the lower-quartile patients was $31,095, but costs for the upper quartile patients was $52,639.
With cost, income, and injury severity data, the investigators found that overall the proportion of adults aged 18-64 years at risk for CHEs was 70.8% (95% confidence interval, 70.7%-71.1%). Subpopulations (ethnicity/race, age, sex) were within a few percentage point of each other.
Risk of CHEs varied widely by income quartile and ISS. Uninsured trauma patients in the highest income quartile had a 52.9% risk of CHEs, compared with 77.5% of those in the lowest-income quartile. Overall, 81.8% of patients with ISS greater than 24 were at risk for CHEs. In addition, the study found that patients treated at large or urban teaching hospitals – those most likely to handle the most-severely injured patients – were at a heightened risk for CHEs.
When the investigators conducted the same analysis with a lower threshold of CHEs (10% of income, not including subsistence expenses), the overall risk for uninsured trauma patients for catastrophic health expenses was more than 90%.
“Trauma patients are at particularly high risk for CHE because trauma disproportionately affects uninsured patients with little disposable income and because trauma injuries commonly affect multiple organ systems and incur expensive, multispecialty care,” Dr. Scott and his colleagues wrote. “Large unpaid medical debts may have longstanding impacts on patients’ financial well-being, affecting credit ratings and overall financial solvency. These financial stresses may be further compounded by an inability to return to work caused by injury.”
Dr. Scott and his coauthors added that having health insurance does not entirely eliminate the risk for CHEs and that individuals in the lower income brackets covered by employer-based plans or Medicaid had difficulty paying medical bills.
Only hospital costs were examined, which may not reflect forgiven debts, the investigators noted. In addition, the costs may be underreported because they do not include physician charges, postacute care, home health care, or rehabilitation. Incomes were estimated by zip code analysis, which may misclassify some individuals.
“Efforts are needed to ensure that the lifesaving care provided by our highly coordinated trauma systems do not have the unintended consequence of curing patients into destitution,” Dr. Scott and his colleagues wrote
The authors declared no conflicts of interest.
Almost three-quarters of uninsured adults admitted for traumatic injury are at risk of catastrophic health expenditures (CHEs), according to a large retrospective study from a national patient database.
Since enactment of the Affordable Care Act in 2010, the number of uninsured individuals has dropped substantially, but there remains a large population of younger adults, many from low-income areas, who still are not covered. The Centers for Disease Control and Prevention reported in 2015 that 12.8% of individuals aged 18-64 years were uninsured. The financial impact of a traumatic injury is likely to be significant for those paying out of pocket, but the question of who is at risk and to what degree is understudied, according to John W. Scott, MD, of Brigham and Women’s Hospital, Boston, and his colleagues.
“Defining populations at risk of financial catastrophe after medical expense is a necessary step towards elucidating the effect of health care reforms intended to increase access to healthcare through insurance expansion,” they wrote in the Annals of Surgery (2017 Apr 7. doi: 10.1097/SLA.0000000000002254).
Dr. Scott and his colleagues analyzed trauma diagnoses in adults aged 18-64 years from Nationwide Inpatient Sample 2007-2011. They used the U.S. Census data to estimate post-subsistence income (income remaining after paying for food) and hospital charges for trauma diagnoses. The sample of 117,502 patient encounters was weighted to represent 579,683 trauma patients in the national database.
CHEs were defined conservatively as expenses that exceed 40% of a patient’s post-subsistence income; they also applied a lower threshold of CHEs – 10% of a patient’s entire income – without accounting for subsistence needs.
The investigators wanted to look at who was at greatest risk for CHEs and used the Census data to sort trauma patients by residential zip code to identify the distribution of income in the sample.
Costs to trauma patients varied by injury severity score (ISS) and by income quartile. Patients in the 25th income quartile paid less for their treatment, even accounting for ISS, but despite this difference, poorer patients were at a much greater risk for CHEs.
The median charge for all of these uninsured trauma patients was $27,420. Those trauma patients in the 25th percentile of income were charged an average of $15,196, while those in 75th quartile were charged $49,696. The difference in costs also was evident when comparing patients in different ISS categories: for ISS 9-15, median trauma costs for the lower-quartile patients was $31,095, but costs for the upper quartile patients was $52,639.
With cost, income, and injury severity data, the investigators found that overall the proportion of adults aged 18-64 years at risk for CHEs was 70.8% (95% confidence interval, 70.7%-71.1%). Subpopulations (ethnicity/race, age, sex) were within a few percentage point of each other.
Risk of CHEs varied widely by income quartile and ISS. Uninsured trauma patients in the highest income quartile had a 52.9% risk of CHEs, compared with 77.5% of those in the lowest-income quartile. Overall, 81.8% of patients with ISS greater than 24 were at risk for CHEs. In addition, the study found that patients treated at large or urban teaching hospitals – those most likely to handle the most-severely injured patients – were at a heightened risk for CHEs.
When the investigators conducted the same analysis with a lower threshold of CHEs (10% of income, not including subsistence expenses), the overall risk for uninsured trauma patients for catastrophic health expenses was more than 90%.
“Trauma patients are at particularly high risk for CHE because trauma disproportionately affects uninsured patients with little disposable income and because trauma injuries commonly affect multiple organ systems and incur expensive, multispecialty care,” Dr. Scott and his colleagues wrote. “Large unpaid medical debts may have longstanding impacts on patients’ financial well-being, affecting credit ratings and overall financial solvency. These financial stresses may be further compounded by an inability to return to work caused by injury.”
Dr. Scott and his coauthors added that having health insurance does not entirely eliminate the risk for CHEs and that individuals in the lower income brackets covered by employer-based plans or Medicaid had difficulty paying medical bills.
Only hospital costs were examined, which may not reflect forgiven debts, the investigators noted. In addition, the costs may be underreported because they do not include physician charges, postacute care, home health care, or rehabilitation. Incomes were estimated by zip code analysis, which may misclassify some individuals.
“Efforts are needed to ensure that the lifesaving care provided by our highly coordinated trauma systems do not have the unintended consequence of curing patients into destitution,” Dr. Scott and his colleagues wrote
The authors declared no conflicts of interest.
Almost three-quarters of uninsured adults admitted for traumatic injury are at risk of catastrophic health expenditures (CHEs), according to a large retrospective study from a national patient database.
Since enactment of the Affordable Care Act in 2010, the number of uninsured individuals has dropped substantially, but there remains a large population of younger adults, many from low-income areas, who still are not covered. The Centers for Disease Control and Prevention reported in 2015 that 12.8% of individuals aged 18-64 years were uninsured. The financial impact of a traumatic injury is likely to be significant for those paying out of pocket, but the question of who is at risk and to what degree is understudied, according to John W. Scott, MD, of Brigham and Women’s Hospital, Boston, and his colleagues.
“Defining populations at risk of financial catastrophe after medical expense is a necessary step towards elucidating the effect of health care reforms intended to increase access to healthcare through insurance expansion,” they wrote in the Annals of Surgery (2017 Apr 7. doi: 10.1097/SLA.0000000000002254).
Dr. Scott and his colleagues analyzed trauma diagnoses in adults aged 18-64 years from Nationwide Inpatient Sample 2007-2011. They used the U.S. Census data to estimate post-subsistence income (income remaining after paying for food) and hospital charges for trauma diagnoses. The sample of 117,502 patient encounters was weighted to represent 579,683 trauma patients in the national database.
CHEs were defined conservatively as expenses that exceed 40% of a patient’s post-subsistence income; they also applied a lower threshold of CHEs – 10% of a patient’s entire income – without accounting for subsistence needs.
The investigators wanted to look at who was at greatest risk for CHEs and used the Census data to sort trauma patients by residential zip code to identify the distribution of income in the sample.
Costs to trauma patients varied by injury severity score (ISS) and by income quartile. Patients in the 25th income quartile paid less for their treatment, even accounting for ISS, but despite this difference, poorer patients were at a much greater risk for CHEs.
The median charge for all of these uninsured trauma patients was $27,420. Those trauma patients in the 25th percentile of income were charged an average of $15,196, while those in 75th quartile were charged $49,696. The difference in costs also was evident when comparing patients in different ISS categories: for ISS 9-15, median trauma costs for the lower-quartile patients was $31,095, but costs for the upper quartile patients was $52,639.
With cost, income, and injury severity data, the investigators found that overall the proportion of adults aged 18-64 years at risk for CHEs was 70.8% (95% confidence interval, 70.7%-71.1%). Subpopulations (ethnicity/race, age, sex) were within a few percentage point of each other.
Risk of CHEs varied widely by income quartile and ISS. Uninsured trauma patients in the highest income quartile had a 52.9% risk of CHEs, compared with 77.5% of those in the lowest-income quartile. Overall, 81.8% of patients with ISS greater than 24 were at risk for CHEs. In addition, the study found that patients treated at large or urban teaching hospitals – those most likely to handle the most-severely injured patients – were at a heightened risk for CHEs.
When the investigators conducted the same analysis with a lower threshold of CHEs (10% of income, not including subsistence expenses), the overall risk for uninsured trauma patients for catastrophic health expenses was more than 90%.
“Trauma patients are at particularly high risk for CHE because trauma disproportionately affects uninsured patients with little disposable income and because trauma injuries commonly affect multiple organ systems and incur expensive, multispecialty care,” Dr. Scott and his colleagues wrote. “Large unpaid medical debts may have longstanding impacts on patients’ financial well-being, affecting credit ratings and overall financial solvency. These financial stresses may be further compounded by an inability to return to work caused by injury.”
Dr. Scott and his coauthors added that having health insurance does not entirely eliminate the risk for CHEs and that individuals in the lower income brackets covered by employer-based plans or Medicaid had difficulty paying medical bills.
Only hospital costs were examined, which may not reflect forgiven debts, the investigators noted. In addition, the costs may be underreported because they do not include physician charges, postacute care, home health care, or rehabilitation. Incomes were estimated by zip code analysis, which may misclassify some individuals.
“Efforts are needed to ensure that the lifesaving care provided by our highly coordinated trauma systems do not have the unintended consequence of curing patients into destitution,” Dr. Scott and his colleagues wrote
The authors declared no conflicts of interest.
FROM ANNALS OF SURGERY
Postop pain may be a predictor for readmission
PHILADELPHIA – How a patient reacts to postoperative pain and how the pain progresses or regresses can be key predictors for 30-day hospital readmissions and emergency department visits after hospital discharge, according to an analysis of more than 200,000 operations in a national database.
The study sample included 211,213 operations in the Veterans Affairs Surgical Quality Improvement Program during 2008-2014, 45% of which were orthopedic in nature, 37% general, and 18% vascular. The overall 30-day unplanned readmission rate was 10.8% and the 30-day ED utilization rate was 14.2%, Dr. Hawn said.
The study identified six distinct postoperative inpatient pain trajectories based on postop pain scores: persistently low (4.5%); mild to low (9%); persistently mild (15.3%); moderate to low (12.1%); persistently moderate (40.2%); and persistently high (18.9%). One of the study objectives, Dr. Hawn said, “was to see if we could identify patterns of postoperative pain trajectories in a surgical cohort, and to describe these subpopulations by their trajectories, and then to determine whether there was an association with postdischarge health care utilization.” The hypothesis was that inpatient postoperative pain trajectory would be associated with 30-day readmission and ED visits as well as postop complications, Dr. Hawn added.
Patients with high pain trajectories had highest rates of postdischarge readmission and ED visits, 14.4% and 16.3%, respectively, Dr. Hawn said.
“Patients in the low-pain categories were more likely to undergo general and vascular procedures compared to orthopedic procedures in the high-pain categories,” Dr. Hawn said. “In the low-pain categories, they were older and less likely to be female. They were less likely to have independent functional status whereas patients in the high-pain category had a 26% prevalence of preoperative diagnosis of depression.”
Those in the high-pain category had a 1.5 times greater risk of an unplanned readmission and a 4 times greater risk in pain-related readmission, according to an odds ratio analysis of the data.
“As for the prevalence of our outcomes, 10.7% had an unplanned readmission. A total of 1.5% from the overall cohort had a pain-related readmission, 8.6% had an emergency visit within 30 days of discharge that did not result in a readmission, and 4.4% had at least one postdischarge complication,” Dr. Hawn said.
In his discussion, Clifford Y. Ko, MD, FACS, of the University of California, Los Angeles, asked what was the take-home for surgeons managing patients postoperatively in the era of the opioid epidemic. “For these types of patients, we need to get our colleagues, the pain specialists, involved much earlier,” Dr. Hawn said. “We need to rethink that strategy of treating the pain-score number. And I think there’s been so much national attention to this that we will stop focusing on that number as a measure of quality of care and patient satisfaction. Those are some trends we’ll see in the future.”
Neither Dr. Hawn nor Dr. Ko reported any financial disclosures
The complete manuscript of this study and its presentation at the American Surgical Association’s 137th Annual Meeting, April 2017, in Philadelphia, is anticipated to be published in the Annals of Surgery pending editorial review.
PHILADELPHIA – How a patient reacts to postoperative pain and how the pain progresses or regresses can be key predictors for 30-day hospital readmissions and emergency department visits after hospital discharge, according to an analysis of more than 200,000 operations in a national database.
The study sample included 211,213 operations in the Veterans Affairs Surgical Quality Improvement Program during 2008-2014, 45% of which were orthopedic in nature, 37% general, and 18% vascular. The overall 30-day unplanned readmission rate was 10.8% and the 30-day ED utilization rate was 14.2%, Dr. Hawn said.
The study identified six distinct postoperative inpatient pain trajectories based on postop pain scores: persistently low (4.5%); mild to low (9%); persistently mild (15.3%); moderate to low (12.1%); persistently moderate (40.2%); and persistently high (18.9%). One of the study objectives, Dr. Hawn said, “was to see if we could identify patterns of postoperative pain trajectories in a surgical cohort, and to describe these subpopulations by their trajectories, and then to determine whether there was an association with postdischarge health care utilization.” The hypothesis was that inpatient postoperative pain trajectory would be associated with 30-day readmission and ED visits as well as postop complications, Dr. Hawn added.
Patients with high pain trajectories had highest rates of postdischarge readmission and ED visits, 14.4% and 16.3%, respectively, Dr. Hawn said.
“Patients in the low-pain categories were more likely to undergo general and vascular procedures compared to orthopedic procedures in the high-pain categories,” Dr. Hawn said. “In the low-pain categories, they were older and less likely to be female. They were less likely to have independent functional status whereas patients in the high-pain category had a 26% prevalence of preoperative diagnosis of depression.”
Those in the high-pain category had a 1.5 times greater risk of an unplanned readmission and a 4 times greater risk in pain-related readmission, according to an odds ratio analysis of the data.
“As for the prevalence of our outcomes, 10.7% had an unplanned readmission. A total of 1.5% from the overall cohort had a pain-related readmission, 8.6% had an emergency visit within 30 days of discharge that did not result in a readmission, and 4.4% had at least one postdischarge complication,” Dr. Hawn said.
In his discussion, Clifford Y. Ko, MD, FACS, of the University of California, Los Angeles, asked what was the take-home for surgeons managing patients postoperatively in the era of the opioid epidemic. “For these types of patients, we need to get our colleagues, the pain specialists, involved much earlier,” Dr. Hawn said. “We need to rethink that strategy of treating the pain-score number. And I think there’s been so much national attention to this that we will stop focusing on that number as a measure of quality of care and patient satisfaction. Those are some trends we’ll see in the future.”
Neither Dr. Hawn nor Dr. Ko reported any financial disclosures
The complete manuscript of this study and its presentation at the American Surgical Association’s 137th Annual Meeting, April 2017, in Philadelphia, is anticipated to be published in the Annals of Surgery pending editorial review.
PHILADELPHIA – How a patient reacts to postoperative pain and how the pain progresses or regresses can be key predictors for 30-day hospital readmissions and emergency department visits after hospital discharge, according to an analysis of more than 200,000 operations in a national database.
The study sample included 211,213 operations in the Veterans Affairs Surgical Quality Improvement Program during 2008-2014, 45% of which were orthopedic in nature, 37% general, and 18% vascular. The overall 30-day unplanned readmission rate was 10.8% and the 30-day ED utilization rate was 14.2%, Dr. Hawn said.
The study identified six distinct postoperative inpatient pain trajectories based on postop pain scores: persistently low (4.5%); mild to low (9%); persistently mild (15.3%); moderate to low (12.1%); persistently moderate (40.2%); and persistently high (18.9%). One of the study objectives, Dr. Hawn said, “was to see if we could identify patterns of postoperative pain trajectories in a surgical cohort, and to describe these subpopulations by their trajectories, and then to determine whether there was an association with postdischarge health care utilization.” The hypothesis was that inpatient postoperative pain trajectory would be associated with 30-day readmission and ED visits as well as postop complications, Dr. Hawn added.
Patients with high pain trajectories had highest rates of postdischarge readmission and ED visits, 14.4% and 16.3%, respectively, Dr. Hawn said.
“Patients in the low-pain categories were more likely to undergo general and vascular procedures compared to orthopedic procedures in the high-pain categories,” Dr. Hawn said. “In the low-pain categories, they were older and less likely to be female. They were less likely to have independent functional status whereas patients in the high-pain category had a 26% prevalence of preoperative diagnosis of depression.”
Those in the high-pain category had a 1.5 times greater risk of an unplanned readmission and a 4 times greater risk in pain-related readmission, according to an odds ratio analysis of the data.
“As for the prevalence of our outcomes, 10.7% had an unplanned readmission. A total of 1.5% from the overall cohort had a pain-related readmission, 8.6% had an emergency visit within 30 days of discharge that did not result in a readmission, and 4.4% had at least one postdischarge complication,” Dr. Hawn said.
In his discussion, Clifford Y. Ko, MD, FACS, of the University of California, Los Angeles, asked what was the take-home for surgeons managing patients postoperatively in the era of the opioid epidemic. “For these types of patients, we need to get our colleagues, the pain specialists, involved much earlier,” Dr. Hawn said. “We need to rethink that strategy of treating the pain-score number. And I think there’s been so much national attention to this that we will stop focusing on that number as a measure of quality of care and patient satisfaction. Those are some trends we’ll see in the future.”
Neither Dr. Hawn nor Dr. Ko reported any financial disclosures
The complete manuscript of this study and its presentation at the American Surgical Association’s 137th Annual Meeting, April 2017, in Philadelphia, is anticipated to be published in the Annals of Surgery pending editorial review.
AT THE ASA ANNUAL
Key clinical point: A higher trajectory of postoperative pain scores may be a predictor of 30-day readmission and emergency department utilization.
Major finding: Patients with high pain trajectories had the highest rates of post-discharge readmission and emergency department visits, 14.4% and 16.3%, respectively.
Data source: Retrospective cohort study of Veterans Affairs’ data on operations on 211,213 operations performed during 2008-2014.
Disclosures: Dr. Hawn and her coauthors reported having no financial disclosures.
House barely passes ACA repeal/replace bill
A few additional tweaks to the American Health Care Act helped garner just enough Republican votes to pass the first phase of the party’s three-part effort to repeal and replace the Affordable Care Act.
The bill passed May 4 by a 217-213 margin, with one Republican member not voting. The vote came after a false start in March when House Speaker Paul Ryan (R-Wisc.) canceled consideration because Republicans could not muster enough votes to pass it. All votes in favor of the bill came from GOP members, while all House Democrats plus 20 Republicans voted against passage.
Two amendments helped to make the bill palatable enough to gain enough votes for passage. New amendments from Rep. Gary Palmer (R-Ala.) and Rep. Fred Upton (R-Mich.) targeted high-risk pools. They were added to an April amendment from Rep. Tom MacArthur (R-N.J.) that would allow states to seek waivers for coverage of the essential health benefits and from community rating provisions to allow for higher premiums for those who are sicker or older.
The American Health Care Act (H.R. 1629) in its amended form has not been yet been scored by the Congressional Budget Office (CBO) to determine its effects on the federal budget. However, an earlier CBO analysis of the original, unamended bill predicted an estimated 58 million people would be uninsured by 2026, compared with 28 million under the Affordable Care Act. It is also predicting large premium increases for some groups of patients.
A CBO score is required of all legislation because, under Senate rules, anything that adds to the budget must be offset by additional revenue-generating provisions or cuts elsewhere in the federal budget. The bill, if passed and sent to the president’s desk for signature, is at minimum budget neutral if not deficit reducing.
The amended AHCA was roundly rejected by most physician organizations, including the American Medical Association and many specialty societies.
“The bill passed by the House today will result in millions of Americans losing access to quality, affordable health insurance and those with preexisting health conditions face the possibility of going back to the time when insurers could charge them premiums that made access to coverage out of the question,” AMA President Andrew Gurman, MD, said in a statement. “The AMA urges the Senate and the Administration to work with physician, patient, hospital, and other provider groups to craft bipartisan solutions so all American families can access affordable and meaningful coverage, while preserving the safety net for vulnerable patients.”
House Minority Leader Nancy Pelosi (D-Calif.), in addition to criticizing the bill for its predicted effects in increasing premiums and decreasing coverage for those with preexisting conditions, called out the bill for being nothing more than a means to help cover the cost of a separate tax bill when she described the AHCA as providing “tax cuts for the rich at the expense of health insurance for tens of millions of working families across America” during the debate prior to passage. “Trumpcare is a billionaire’s tax cut disguised as a health care bill.”
Speaker Ryan continued to highlight the continual coverage issues that have been growing in the individual health insurance marketplace, spotlighting Iowa, where insurer Medica has announced that it will likely discontinue providing coverage in 2018, leaving most counties in the state with no option to purchase coverage following the announced withdrawal of Aetna and Wellmark Blue Cross Blue Shield.
“This is a crisis,” Speaker Ryan said during the debate. “What protection is Obamacare if there is no health care plan to purchase in your state? This is the direction Obamacare is rapidly heading.”
In helping to get the AHCA barely over the final hurdle, the Palmer amendment creates an “invisible risk-sharing program” under which the federal government would subsidize insurers to the tune of $15 billion over 9 years. The program would allow insurers to make a prospective determination of who might be a cost-intensive user and move them to the high-risk pool with the federal funding joining insurer funding to help pay for coverage. The amendment also would change the ACA’s reinsurance provisions, which retroactively reimburse insurers for high-utilizing customers.
Neither invisible risk sharing nor retroactive reinsurance are “inherently superior at reducing premiums,” according to an April 12 blog post by the journal Health Affairs. “Premium reductions depend entirely on how much funding the program receives in relation to the risks being insured. Rep. Palmer’s amendment leaves all the critical details of this new, invisible program unspecified, making it hard to generate precise estimate.”
Authors Mark Hall, senior fellow at Brookings Institute, and Nicholas Bagely, law professor at the University of Michigan, Ann Arbor, note that the funding in the amendment “is no more than 2% of total premiums in the market.”
The Upton amendment would add an additional $8 billion in funding for high-risk pools, bringing the total amount potentially available to help cover people with preexisting conditions to $123 billion.
Analysis from Avalere finds that the funding specifically allocated to assist those with preexisting conditions ($23 billion, including the additional $8 billion from the Upton amendment) “will only cover 110,000 individuals with preexisting, chronic condition. If states were to allocate all the other funds [available in the AHCA] toward providing insurance to people with preexisting conditions ... 600,000 with preexisting chronic conditions could be covered.” The analysis notes approximately “2.2 million enrollees in the individual market today have some sort of preexisting chronic condition.”
“Given the amount of funding in the bill, the program can only afford a few small states to opt into medical underwriting,” Caroline Pearson, senior vice president at Avalere, said in a statement. “If any large states receive a waiver, many chronically ill individuals could be left without access to insurance.”
Because the AHCA focuses solely on reforming revenue-related aspects of the ACA and was passed using budget reconciliation procedures, it will need only a simple majority to pass the Senate. However, keeping the bill budget neutral will make it difficult to pass in its current form, even though Republicans hold 52 of the chamber’s 100 seats.
Phase two of the repeal and replace plan will be a full examination of federal regulations and phase three, which will require at least 60 votes in the Senate, will be changes to other provisions in the health care law that are not directly revenue generating. President Donald Trump in the past has suggested that this will include his goals of opening the sale of insurance across state lines and other key priorities.
A few additional tweaks to the American Health Care Act helped garner just enough Republican votes to pass the first phase of the party’s three-part effort to repeal and replace the Affordable Care Act.
The bill passed May 4 by a 217-213 margin, with one Republican member not voting. The vote came after a false start in March when House Speaker Paul Ryan (R-Wisc.) canceled consideration because Republicans could not muster enough votes to pass it. All votes in favor of the bill came from GOP members, while all House Democrats plus 20 Republicans voted against passage.
Two amendments helped to make the bill palatable enough to gain enough votes for passage. New amendments from Rep. Gary Palmer (R-Ala.) and Rep. Fred Upton (R-Mich.) targeted high-risk pools. They were added to an April amendment from Rep. Tom MacArthur (R-N.J.) that would allow states to seek waivers for coverage of the essential health benefits and from community rating provisions to allow for higher premiums for those who are sicker or older.
The American Health Care Act (H.R. 1629) in its amended form has not been yet been scored by the Congressional Budget Office (CBO) to determine its effects on the federal budget. However, an earlier CBO analysis of the original, unamended bill predicted an estimated 58 million people would be uninsured by 2026, compared with 28 million under the Affordable Care Act. It is also predicting large premium increases for some groups of patients.
A CBO score is required of all legislation because, under Senate rules, anything that adds to the budget must be offset by additional revenue-generating provisions or cuts elsewhere in the federal budget. The bill, if passed and sent to the president’s desk for signature, is at minimum budget neutral if not deficit reducing.
The amended AHCA was roundly rejected by most physician organizations, including the American Medical Association and many specialty societies.
“The bill passed by the House today will result in millions of Americans losing access to quality, affordable health insurance and those with preexisting health conditions face the possibility of going back to the time when insurers could charge them premiums that made access to coverage out of the question,” AMA President Andrew Gurman, MD, said in a statement. “The AMA urges the Senate and the Administration to work with physician, patient, hospital, and other provider groups to craft bipartisan solutions so all American families can access affordable and meaningful coverage, while preserving the safety net for vulnerable patients.”
House Minority Leader Nancy Pelosi (D-Calif.), in addition to criticizing the bill for its predicted effects in increasing premiums and decreasing coverage for those with preexisting conditions, called out the bill for being nothing more than a means to help cover the cost of a separate tax bill when she described the AHCA as providing “tax cuts for the rich at the expense of health insurance for tens of millions of working families across America” during the debate prior to passage. “Trumpcare is a billionaire’s tax cut disguised as a health care bill.”
Speaker Ryan continued to highlight the continual coverage issues that have been growing in the individual health insurance marketplace, spotlighting Iowa, where insurer Medica has announced that it will likely discontinue providing coverage in 2018, leaving most counties in the state with no option to purchase coverage following the announced withdrawal of Aetna and Wellmark Blue Cross Blue Shield.
“This is a crisis,” Speaker Ryan said during the debate. “What protection is Obamacare if there is no health care plan to purchase in your state? This is the direction Obamacare is rapidly heading.”
In helping to get the AHCA barely over the final hurdle, the Palmer amendment creates an “invisible risk-sharing program” under which the federal government would subsidize insurers to the tune of $15 billion over 9 years. The program would allow insurers to make a prospective determination of who might be a cost-intensive user and move them to the high-risk pool with the federal funding joining insurer funding to help pay for coverage. The amendment also would change the ACA’s reinsurance provisions, which retroactively reimburse insurers for high-utilizing customers.
Neither invisible risk sharing nor retroactive reinsurance are “inherently superior at reducing premiums,” according to an April 12 blog post by the journal Health Affairs. “Premium reductions depend entirely on how much funding the program receives in relation to the risks being insured. Rep. Palmer’s amendment leaves all the critical details of this new, invisible program unspecified, making it hard to generate precise estimate.”
Authors Mark Hall, senior fellow at Brookings Institute, and Nicholas Bagely, law professor at the University of Michigan, Ann Arbor, note that the funding in the amendment “is no more than 2% of total premiums in the market.”
The Upton amendment would add an additional $8 billion in funding for high-risk pools, bringing the total amount potentially available to help cover people with preexisting conditions to $123 billion.
Analysis from Avalere finds that the funding specifically allocated to assist those with preexisting conditions ($23 billion, including the additional $8 billion from the Upton amendment) “will only cover 110,000 individuals with preexisting, chronic condition. If states were to allocate all the other funds [available in the AHCA] toward providing insurance to people with preexisting conditions ... 600,000 with preexisting chronic conditions could be covered.” The analysis notes approximately “2.2 million enrollees in the individual market today have some sort of preexisting chronic condition.”
“Given the amount of funding in the bill, the program can only afford a few small states to opt into medical underwriting,” Caroline Pearson, senior vice president at Avalere, said in a statement. “If any large states receive a waiver, many chronically ill individuals could be left without access to insurance.”
Because the AHCA focuses solely on reforming revenue-related aspects of the ACA and was passed using budget reconciliation procedures, it will need only a simple majority to pass the Senate. However, keeping the bill budget neutral will make it difficult to pass in its current form, even though Republicans hold 52 of the chamber’s 100 seats.
Phase two of the repeal and replace plan will be a full examination of federal regulations and phase three, which will require at least 60 votes in the Senate, will be changes to other provisions in the health care law that are not directly revenue generating. President Donald Trump in the past has suggested that this will include his goals of opening the sale of insurance across state lines and other key priorities.
A few additional tweaks to the American Health Care Act helped garner just enough Republican votes to pass the first phase of the party’s three-part effort to repeal and replace the Affordable Care Act.
The bill passed May 4 by a 217-213 margin, with one Republican member not voting. The vote came after a false start in March when House Speaker Paul Ryan (R-Wisc.) canceled consideration because Republicans could not muster enough votes to pass it. All votes in favor of the bill came from GOP members, while all House Democrats plus 20 Republicans voted against passage.
Two amendments helped to make the bill palatable enough to gain enough votes for passage. New amendments from Rep. Gary Palmer (R-Ala.) and Rep. Fred Upton (R-Mich.) targeted high-risk pools. They were added to an April amendment from Rep. Tom MacArthur (R-N.J.) that would allow states to seek waivers for coverage of the essential health benefits and from community rating provisions to allow for higher premiums for those who are sicker or older.
The American Health Care Act (H.R. 1629) in its amended form has not been yet been scored by the Congressional Budget Office (CBO) to determine its effects on the federal budget. However, an earlier CBO analysis of the original, unamended bill predicted an estimated 58 million people would be uninsured by 2026, compared with 28 million under the Affordable Care Act. It is also predicting large premium increases for some groups of patients.
A CBO score is required of all legislation because, under Senate rules, anything that adds to the budget must be offset by additional revenue-generating provisions or cuts elsewhere in the federal budget. The bill, if passed and sent to the president’s desk for signature, is at minimum budget neutral if not deficit reducing.
The amended AHCA was roundly rejected by most physician organizations, including the American Medical Association and many specialty societies.
“The bill passed by the House today will result in millions of Americans losing access to quality, affordable health insurance and those with preexisting health conditions face the possibility of going back to the time when insurers could charge them premiums that made access to coverage out of the question,” AMA President Andrew Gurman, MD, said in a statement. “The AMA urges the Senate and the Administration to work with physician, patient, hospital, and other provider groups to craft bipartisan solutions so all American families can access affordable and meaningful coverage, while preserving the safety net for vulnerable patients.”
House Minority Leader Nancy Pelosi (D-Calif.), in addition to criticizing the bill for its predicted effects in increasing premiums and decreasing coverage for those with preexisting conditions, called out the bill for being nothing more than a means to help cover the cost of a separate tax bill when she described the AHCA as providing “tax cuts for the rich at the expense of health insurance for tens of millions of working families across America” during the debate prior to passage. “Trumpcare is a billionaire’s tax cut disguised as a health care bill.”
Speaker Ryan continued to highlight the continual coverage issues that have been growing in the individual health insurance marketplace, spotlighting Iowa, where insurer Medica has announced that it will likely discontinue providing coverage in 2018, leaving most counties in the state with no option to purchase coverage following the announced withdrawal of Aetna and Wellmark Blue Cross Blue Shield.
“This is a crisis,” Speaker Ryan said during the debate. “What protection is Obamacare if there is no health care plan to purchase in your state? This is the direction Obamacare is rapidly heading.”
In helping to get the AHCA barely over the final hurdle, the Palmer amendment creates an “invisible risk-sharing program” under which the federal government would subsidize insurers to the tune of $15 billion over 9 years. The program would allow insurers to make a prospective determination of who might be a cost-intensive user and move them to the high-risk pool with the federal funding joining insurer funding to help pay for coverage. The amendment also would change the ACA’s reinsurance provisions, which retroactively reimburse insurers for high-utilizing customers.
Neither invisible risk sharing nor retroactive reinsurance are “inherently superior at reducing premiums,” according to an April 12 blog post by the journal Health Affairs. “Premium reductions depend entirely on how much funding the program receives in relation to the risks being insured. Rep. Palmer’s amendment leaves all the critical details of this new, invisible program unspecified, making it hard to generate precise estimate.”
Authors Mark Hall, senior fellow at Brookings Institute, and Nicholas Bagely, law professor at the University of Michigan, Ann Arbor, note that the funding in the amendment “is no more than 2% of total premiums in the market.”
The Upton amendment would add an additional $8 billion in funding for high-risk pools, bringing the total amount potentially available to help cover people with preexisting conditions to $123 billion.
Analysis from Avalere finds that the funding specifically allocated to assist those with preexisting conditions ($23 billion, including the additional $8 billion from the Upton amendment) “will only cover 110,000 individuals with preexisting, chronic condition. If states were to allocate all the other funds [available in the AHCA] toward providing insurance to people with preexisting conditions ... 600,000 with preexisting chronic conditions could be covered.” The analysis notes approximately “2.2 million enrollees in the individual market today have some sort of preexisting chronic condition.”
“Given the amount of funding in the bill, the program can only afford a few small states to opt into medical underwriting,” Caroline Pearson, senior vice president at Avalere, said in a statement. “If any large states receive a waiver, many chronically ill individuals could be left without access to insurance.”
Because the AHCA focuses solely on reforming revenue-related aspects of the ACA and was passed using budget reconciliation procedures, it will need only a simple majority to pass the Senate. However, keeping the bill budget neutral will make it difficult to pass in its current form, even though Republicans hold 52 of the chamber’s 100 seats.
Phase two of the repeal and replace plan will be a full examination of federal regulations and phase three, which will require at least 60 votes in the Senate, will be changes to other provisions in the health care law that are not directly revenue generating. President Donald Trump in the past has suggested that this will include his goals of opening the sale of insurance across state lines and other key priorities.