User login
The Official Newspaper of the American Association for Thoracic Surgery
AMA: Patient mix has become less uninsured since 2012
Uninsured patients made up a smaller share of the average physician’s practice in 2016 than in 2012, according to a survey by the American Medical Association.
For the average practice in 2016, 6.1% of patients were uninsured, compared with 6.9% in 2012. That significant drop of 0.8 percentage points was accompanied by significant increases in the number of patients covered by Medicaid and by private insurance, the AMA said in a report released Oct. 30.
“The overall picture from new physician-reported data is of more patients covered and fewer uninsured, but the findings also indicate that the improvement along those lines was concentrated in states that expanded their Medicaid programs under the ACA,” said David O. Barbe, MD, AMA president.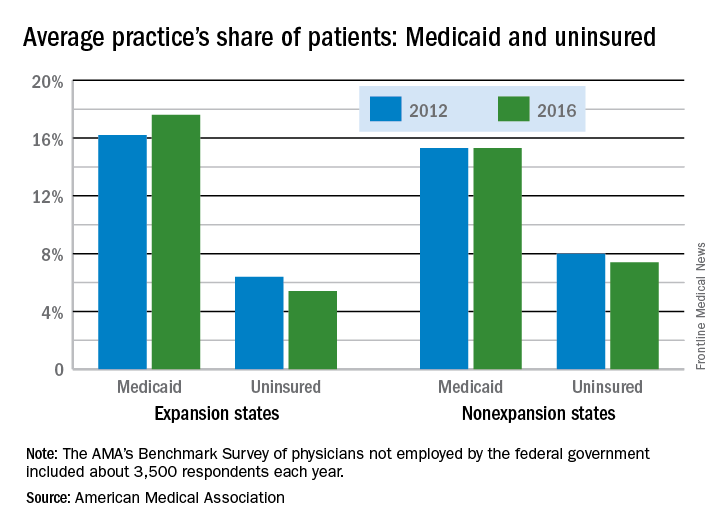
In the 31 states and the District of Columbia that expanded Medicaid, the average patient share dropped from 6.4% uninsured in 2012 to 5.4% in 2016, which was significant. In the states that did not expand Medicaid, the average share of uninsured patients went from 8.0% to 7.4% over that period, a drop that did not reach significance, the AMA said.
The changes involving Medicaid itself were of somewhat greater magnitude, in both directions: nonexpansion states saw a smaller increase and expansion states had a larger increase. In nonexpansion states the average share of a practice’s patients covered by Medicaid basically held steady at 15.3% (there was actually a very slight increase, but the AMA reported the figures for both 2012 and 2016 as 15.3%). In expansion states, the average Medicaid share went from 16.2% to 17.6% – a statistically significant increase of 1.4 percentage points, the AMA analysis shows.
The AMA report covers data from its 2012 and 2016 Benchmark Surveys, which each year involved approximately 3,500 physicians in patient care who were not employed by the federal government.
Uninsured patients made up a smaller share of the average physician’s practice in 2016 than in 2012, according to a survey by the American Medical Association.
For the average practice in 2016, 6.1% of patients were uninsured, compared with 6.9% in 2012. That significant drop of 0.8 percentage points was accompanied by significant increases in the number of patients covered by Medicaid and by private insurance, the AMA said in a report released Oct. 30.
“The overall picture from new physician-reported data is of more patients covered and fewer uninsured, but the findings also indicate that the improvement along those lines was concentrated in states that expanded their Medicaid programs under the ACA,” said David O. Barbe, MD, AMA president.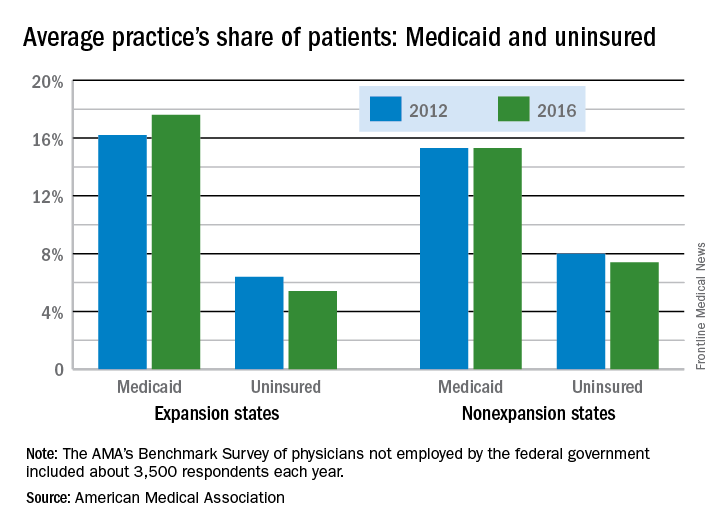
In the 31 states and the District of Columbia that expanded Medicaid, the average patient share dropped from 6.4% uninsured in 2012 to 5.4% in 2016, which was significant. In the states that did not expand Medicaid, the average share of uninsured patients went from 8.0% to 7.4% over that period, a drop that did not reach significance, the AMA said.
The changes involving Medicaid itself were of somewhat greater magnitude, in both directions: nonexpansion states saw a smaller increase and expansion states had a larger increase. In nonexpansion states the average share of a practice’s patients covered by Medicaid basically held steady at 15.3% (there was actually a very slight increase, but the AMA reported the figures for both 2012 and 2016 as 15.3%). In expansion states, the average Medicaid share went from 16.2% to 17.6% – a statistically significant increase of 1.4 percentage points, the AMA analysis shows.
The AMA report covers data from its 2012 and 2016 Benchmark Surveys, which each year involved approximately 3,500 physicians in patient care who were not employed by the federal government.
Uninsured patients made up a smaller share of the average physician’s practice in 2016 than in 2012, according to a survey by the American Medical Association.
For the average practice in 2016, 6.1% of patients were uninsured, compared with 6.9% in 2012. That significant drop of 0.8 percentage points was accompanied by significant increases in the number of patients covered by Medicaid and by private insurance, the AMA said in a report released Oct. 30.
“The overall picture from new physician-reported data is of more patients covered and fewer uninsured, but the findings also indicate that the improvement along those lines was concentrated in states that expanded their Medicaid programs under the ACA,” said David O. Barbe, MD, AMA president.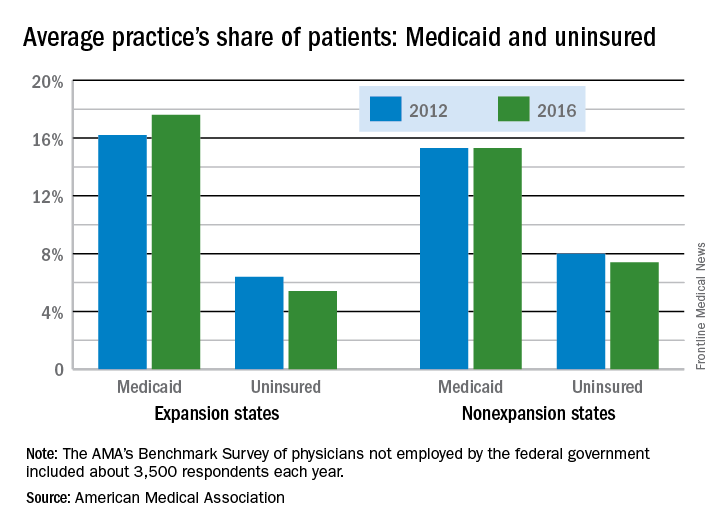
In the 31 states and the District of Columbia that expanded Medicaid, the average patient share dropped from 6.4% uninsured in 2012 to 5.4% in 2016, which was significant. In the states that did not expand Medicaid, the average share of uninsured patients went from 8.0% to 7.4% over that period, a drop that did not reach significance, the AMA said.
The changes involving Medicaid itself were of somewhat greater magnitude, in both directions: nonexpansion states saw a smaller increase and expansion states had a larger increase. In nonexpansion states the average share of a practice’s patients covered by Medicaid basically held steady at 15.3% (there was actually a very slight increase, but the AMA reported the figures for both 2012 and 2016 as 15.3%). In expansion states, the average Medicaid share went from 16.2% to 17.6% – a statistically significant increase of 1.4 percentage points, the AMA analysis shows.
The AMA report covers data from its 2012 and 2016 Benchmark Surveys, which each year involved approximately 3,500 physicians in patient care who were not employed by the federal government.
Cold stored platelets control bleeding after complex cardiac surgery
SAN DIEGO – Cold stored leukoreduced apheresis platelets in platelet additive solution were effective for controlling bleeding in a small study of patients undergoing complex cardiothoracic surgery, according to findings presented at the annual meeting of the American Association of Blood Banks.
The volume of postoperative bleeding was significantly lower among patients who received cold stored platelets compared with those who received standard room temperature storage platelets. Thromboembolic events did not differ between the two groups, nor did measures of coagulation at varying time points. Platelet counts and blood usage were also similar in the two groups. The study was small, however, and further studies are needed to confirm the findings.
“These patients are undergoing major surgery and are at high risk in every aspect,” said Torunn Oveland Apelseth, MD, PhD, of the Laboratory of Clinical Biochemistry, Haukeland (Norway) University Hospital. “They are at high risk for bleeding, at high risk for thromboembolic events and high blood usage, and there is a need for optimized blood components.”
There has been debate over the use of cold stored platelets, she noted. While storage at 4° C shortens platelet circulation time, some research shows that cold stored platelets have better hemostatic function.
In this study, one patient cohort was transfused with leukoreduced apheresis platelets stored at 4° C in platelet additive solution for up to 7 days under constant agitation, while the other group received platelets stored at standard room temperature. The study endpoints were comparisons between the two groups of postoperative bleeding, total blood usage, and laboratory measures of coagulation and blood cell counts within the first postoperative day. Thromboembolic events in the 28 days after surgery were also evaluated.
The study evaluated 17 patients who received cold stored platelets and 22 who received room temperature storage platelets. Patient demographics for the two groups were similar – as were their international normalized ratios, activated partial thromboplastin times, and fibrinogen levels – before surgery, immediately after heparin reversal, and the morning following the procedure.
Platelet counts and hemoglobin levels also did not significantly differ between groups.
As measured by chest drain output after chest closure, patients who received cold stored platelets had a significantly lower median amount of bleeding in the postoperative period compared with patients given room temperature storage platelets: 576 mL vs. 838 mL. Average chest drain output after chest closure was 594 mL in those who did not receive any transfusions.
Thromboembolic events occurred in 3 patients (18%) who received cold stored platelets and 7 (31%) of those given room temperature storage platelets. The difference was not statistically significant. In addition, blood usage – platelets, red blood cells, and solvent/detergent-treated pooled plasma – was similar for the two cohorts.
“There were also no differences in the number of thromboembolic episodes or length of stay in ICU,” said Dr. Apelseth, who recommended larger studies to explore the use of use of cold stored platelet transfusion in the critical care setting.
SAN DIEGO – Cold stored leukoreduced apheresis platelets in platelet additive solution were effective for controlling bleeding in a small study of patients undergoing complex cardiothoracic surgery, according to findings presented at the annual meeting of the American Association of Blood Banks.
The volume of postoperative bleeding was significantly lower among patients who received cold stored platelets compared with those who received standard room temperature storage platelets. Thromboembolic events did not differ between the two groups, nor did measures of coagulation at varying time points. Platelet counts and blood usage were also similar in the two groups. The study was small, however, and further studies are needed to confirm the findings.
“These patients are undergoing major surgery and are at high risk in every aspect,” said Torunn Oveland Apelseth, MD, PhD, of the Laboratory of Clinical Biochemistry, Haukeland (Norway) University Hospital. “They are at high risk for bleeding, at high risk for thromboembolic events and high blood usage, and there is a need for optimized blood components.”
There has been debate over the use of cold stored platelets, she noted. While storage at 4° C shortens platelet circulation time, some research shows that cold stored platelets have better hemostatic function.
In this study, one patient cohort was transfused with leukoreduced apheresis platelets stored at 4° C in platelet additive solution for up to 7 days under constant agitation, while the other group received platelets stored at standard room temperature. The study endpoints were comparisons between the two groups of postoperative bleeding, total blood usage, and laboratory measures of coagulation and blood cell counts within the first postoperative day. Thromboembolic events in the 28 days after surgery were also evaluated.
The study evaluated 17 patients who received cold stored platelets and 22 who received room temperature storage platelets. Patient demographics for the two groups were similar – as were their international normalized ratios, activated partial thromboplastin times, and fibrinogen levels – before surgery, immediately after heparin reversal, and the morning following the procedure.
Platelet counts and hemoglobin levels also did not significantly differ between groups.
As measured by chest drain output after chest closure, patients who received cold stored platelets had a significantly lower median amount of bleeding in the postoperative period compared with patients given room temperature storage platelets: 576 mL vs. 838 mL. Average chest drain output after chest closure was 594 mL in those who did not receive any transfusions.
Thromboembolic events occurred in 3 patients (18%) who received cold stored platelets and 7 (31%) of those given room temperature storage platelets. The difference was not statistically significant. In addition, blood usage – platelets, red blood cells, and solvent/detergent-treated pooled plasma – was similar for the two cohorts.
“There were also no differences in the number of thromboembolic episodes or length of stay in ICU,” said Dr. Apelseth, who recommended larger studies to explore the use of use of cold stored platelet transfusion in the critical care setting.
SAN DIEGO – Cold stored leukoreduced apheresis platelets in platelet additive solution were effective for controlling bleeding in a small study of patients undergoing complex cardiothoracic surgery, according to findings presented at the annual meeting of the American Association of Blood Banks.
The volume of postoperative bleeding was significantly lower among patients who received cold stored platelets compared with those who received standard room temperature storage platelets. Thromboembolic events did not differ between the two groups, nor did measures of coagulation at varying time points. Platelet counts and blood usage were also similar in the two groups. The study was small, however, and further studies are needed to confirm the findings.
“These patients are undergoing major surgery and are at high risk in every aspect,” said Torunn Oveland Apelseth, MD, PhD, of the Laboratory of Clinical Biochemistry, Haukeland (Norway) University Hospital. “They are at high risk for bleeding, at high risk for thromboembolic events and high blood usage, and there is a need for optimized blood components.”
There has been debate over the use of cold stored platelets, she noted. While storage at 4° C shortens platelet circulation time, some research shows that cold stored platelets have better hemostatic function.
In this study, one patient cohort was transfused with leukoreduced apheresis platelets stored at 4° C in platelet additive solution for up to 7 days under constant agitation, while the other group received platelets stored at standard room temperature. The study endpoints were comparisons between the two groups of postoperative bleeding, total blood usage, and laboratory measures of coagulation and blood cell counts within the first postoperative day. Thromboembolic events in the 28 days after surgery were also evaluated.
The study evaluated 17 patients who received cold stored platelets and 22 who received room temperature storage platelets. Patient demographics for the two groups were similar – as were their international normalized ratios, activated partial thromboplastin times, and fibrinogen levels – before surgery, immediately after heparin reversal, and the morning following the procedure.
Platelet counts and hemoglobin levels also did not significantly differ between groups.
As measured by chest drain output after chest closure, patients who received cold stored platelets had a significantly lower median amount of bleeding in the postoperative period compared with patients given room temperature storage platelets: 576 mL vs. 838 mL. Average chest drain output after chest closure was 594 mL in those who did not receive any transfusions.
Thromboembolic events occurred in 3 patients (18%) who received cold stored platelets and 7 (31%) of those given room temperature storage platelets. The difference was not statistically significant. In addition, blood usage – platelets, red blood cells, and solvent/detergent-treated pooled plasma – was similar for the two cohorts.
“There were also no differences in the number of thromboembolic episodes or length of stay in ICU,” said Dr. Apelseth, who recommended larger studies to explore the use of use of cold stored platelet transfusion in the critical care setting.
AT AABB17
Key clinical point: Cold stored leukoreduced apheresis platelets in platelet additive solution are effective for treating bleeding in patients undergoing complex cardiothoracic surgery.
Major finding: Patients who underwent procedures requiring cardiopulmonary bypass circulation had a significantly lower median amount of bleeding in the postoperative period with cold stored platelets compared with standard room temperature platelets: 576 mL vs. 838 mL.
Data source: Randomized two-arm pilot trial of cardiothoracic surgery patients.
Disclosures: The authors have no relevant financial disclosures.
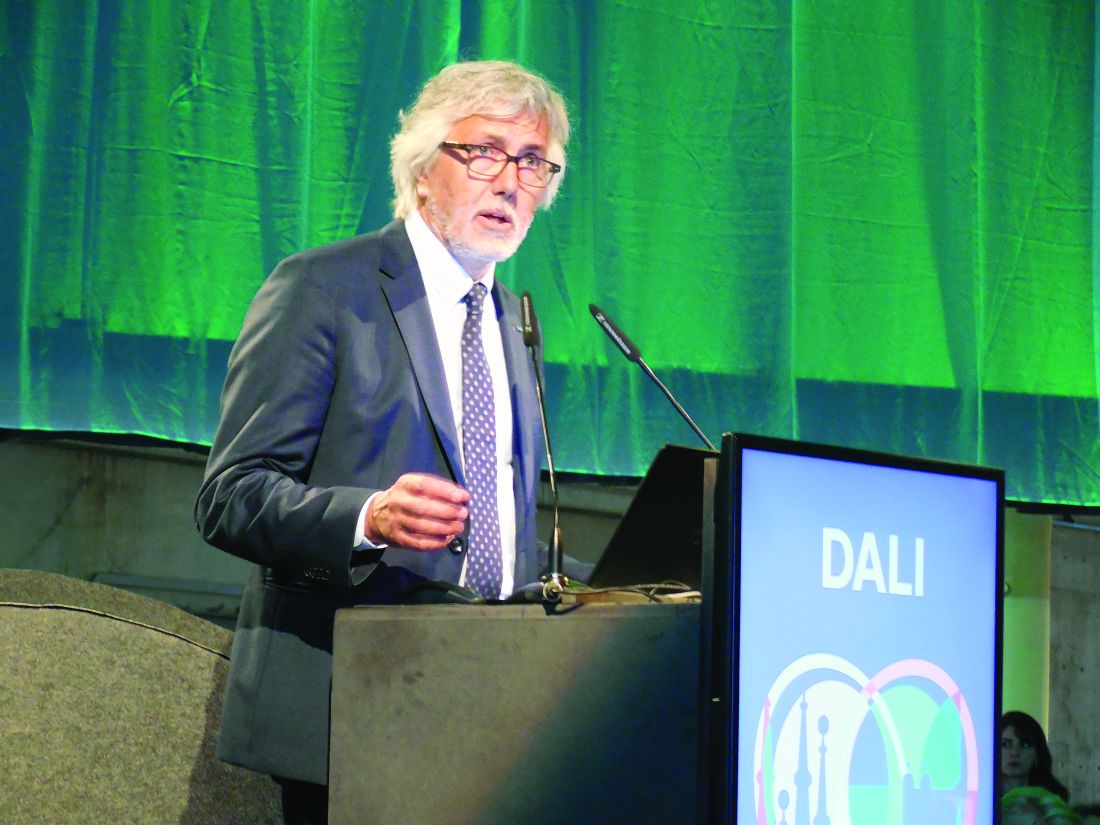
AF patients without oral anticoagulation face higher dementia risk
BARCELONA – The risk of developing dementia was reduced by 48% in patients with atrial fibrillation who were adherent to oral anticoagulation compared with those who were not, according to a Swedish propensity-matched registry study involving nearly 162,000 patients with the arrhythmia.
The study also addressed whether patients with atrial fibrillation (AF) are better off in terms of reducing their dementia risk if they’re on warfarin versus one of the novel oral anticoagulants. The answer is that it makes absolutely no difference, Leif Friberg, MD, reported at the annual congress of the European Society of Cardiology.
“We found no difference whatsoever in any of the subgroups. It appears that it is more important that you have some kind of oral treatment than exactly what kind to have,” said Dr. Friberg, a cardiologist at the Karolinska Institute in Stockholm.
It’s well established that AF is associated with increased risk of dementia, presumably because the arrhythmia kicks out microemboli that get distributed throughout the brain. But it has been unclear whether oral anticoagulation (OAC) prescribed for stroke prevention has the side benefit of reducing the elevated dementia risk.
“A randomized, controlled trial would be ideal to look at this, but it would be impractical and unethical. Second best [would be] a registry study with propensity matching,” according to Dr. Friberg.
And that’s just what he and his coinvestigators carried out. The study included 80,948 AF patients with no baseline diagnosis of dementia who were prescribed an OAC and an equal number of propensity-matched, dementia-free AF patients not on OAC therapy. During up to 8 years of follow-up, the unadjusted risk of a new diagnosis of dementia was 29% lower in the group on an OAC at baseline.
But the Swedish registries also enabled investigators to zero in on the impact of OAC in patients who were actually medication adherent over time. Dr. Friberg and his coworkers identified a subgroup of 50,406 AF patients who regularly filled their OAC prescriptions and took the medication at least 80% of the time, as well as 48,947 propensity-matched controls who never used OACs. In this on-treatment analysis, the OAC users had a robust 48% relative risk reduction in new diagnosis of dementia. The dementia curves diverged almost immediately and the gap between the two curves continued to widen throughout follow-up. All examined subgroups benefited, regardless of age, gender, AF duration, CHA2DS2-VASc score, or the presence or absence of diabetes, renal failure, or frequent falling.
“This is an important issue,” Dr. Friberg declared. “You may say, ‘What do we care about these findings? These patients are all supposed to be on an oral anticoagulant anyway.’ But you know, patients stop taking their oral anticoagulant. We’re pretty good at initiating treatment when we meet patients for the first time, if they have stroke risk factors, but annually, 10%-15% of patients drop out of treatment. And if patients aren’t concerned enough about their risk of stroke, they might be more concerned about the risk of becoming demented. So these data provide an additional argument for the need to persevere with oral anticoagulation therapy.”
Session cochair Gabriel Tatu-Chitoiu, MD, was skeptical.
“I’ve been working in the atrial fibrillation field for 40 years, and I have to say I haven’t seen a strong dementia possibility in my patients,” said Dr. Tatu-Chitoiu, a cardiologist in Bucharest, Romania, and immediate past president of the Romanian Cardiology Society.
Dr. Friberg replied that AF patients are elderly, and many of them may stop going to their cardiologist when they develop dementia.
“I don’t think you can make extensions from personal experience on this. You have to trust in statistical evidence,” he observed.
Dr. Friberg reported receiving research funding from Bayer, Bristol-Myers Squibb, Pfizer, and Sanofi. However, the registry study was carried out without commercial support.
BARCELONA – The risk of developing dementia was reduced by 48% in patients with atrial fibrillation who were adherent to oral anticoagulation compared with those who were not, according to a Swedish propensity-matched registry study involving nearly 162,000 patients with the arrhythmia.
The study also addressed whether patients with atrial fibrillation (AF) are better off in terms of reducing their dementia risk if they’re on warfarin versus one of the novel oral anticoagulants. The answer is that it makes absolutely no difference, Leif Friberg, MD, reported at the annual congress of the European Society of Cardiology.
“We found no difference whatsoever in any of the subgroups. It appears that it is more important that you have some kind of oral treatment than exactly what kind to have,” said Dr. Friberg, a cardiologist at the Karolinska Institute in Stockholm.
It’s well established that AF is associated with increased risk of dementia, presumably because the arrhythmia kicks out microemboli that get distributed throughout the brain. But it has been unclear whether oral anticoagulation (OAC) prescribed for stroke prevention has the side benefit of reducing the elevated dementia risk.
“A randomized, controlled trial would be ideal to look at this, but it would be impractical and unethical. Second best [would be] a registry study with propensity matching,” according to Dr. Friberg.
And that’s just what he and his coinvestigators carried out. The study included 80,948 AF patients with no baseline diagnosis of dementia who were prescribed an OAC and an equal number of propensity-matched, dementia-free AF patients not on OAC therapy. During up to 8 years of follow-up, the unadjusted risk of a new diagnosis of dementia was 29% lower in the group on an OAC at baseline.
But the Swedish registries also enabled investigators to zero in on the impact of OAC in patients who were actually medication adherent over time. Dr. Friberg and his coworkers identified a subgroup of 50,406 AF patients who regularly filled their OAC prescriptions and took the medication at least 80% of the time, as well as 48,947 propensity-matched controls who never used OACs. In this on-treatment analysis, the OAC users had a robust 48% relative risk reduction in new diagnosis of dementia. The dementia curves diverged almost immediately and the gap between the two curves continued to widen throughout follow-up. All examined subgroups benefited, regardless of age, gender, AF duration, CHA2DS2-VASc score, or the presence or absence of diabetes, renal failure, or frequent falling.
“This is an important issue,” Dr. Friberg declared. “You may say, ‘What do we care about these findings? These patients are all supposed to be on an oral anticoagulant anyway.’ But you know, patients stop taking their oral anticoagulant. We’re pretty good at initiating treatment when we meet patients for the first time, if they have stroke risk factors, but annually, 10%-15% of patients drop out of treatment. And if patients aren’t concerned enough about their risk of stroke, they might be more concerned about the risk of becoming demented. So these data provide an additional argument for the need to persevere with oral anticoagulation therapy.”
Session cochair Gabriel Tatu-Chitoiu, MD, was skeptical.
“I’ve been working in the atrial fibrillation field for 40 years, and I have to say I haven’t seen a strong dementia possibility in my patients,” said Dr. Tatu-Chitoiu, a cardiologist in Bucharest, Romania, and immediate past president of the Romanian Cardiology Society.
Dr. Friberg replied that AF patients are elderly, and many of them may stop going to their cardiologist when they develop dementia.
“I don’t think you can make extensions from personal experience on this. You have to trust in statistical evidence,” he observed.
Dr. Friberg reported receiving research funding from Bayer, Bristol-Myers Squibb, Pfizer, and Sanofi. However, the registry study was carried out without commercial support.
BARCELONA – The risk of developing dementia was reduced by 48% in patients with atrial fibrillation who were adherent to oral anticoagulation compared with those who were not, according to a Swedish propensity-matched registry study involving nearly 162,000 patients with the arrhythmia.
The study also addressed whether patients with atrial fibrillation (AF) are better off in terms of reducing their dementia risk if they’re on warfarin versus one of the novel oral anticoagulants. The answer is that it makes absolutely no difference, Leif Friberg, MD, reported at the annual congress of the European Society of Cardiology.
“We found no difference whatsoever in any of the subgroups. It appears that it is more important that you have some kind of oral treatment than exactly what kind to have,” said Dr. Friberg, a cardiologist at the Karolinska Institute in Stockholm.
It’s well established that AF is associated with increased risk of dementia, presumably because the arrhythmia kicks out microemboli that get distributed throughout the brain. But it has been unclear whether oral anticoagulation (OAC) prescribed for stroke prevention has the side benefit of reducing the elevated dementia risk.
“A randomized, controlled trial would be ideal to look at this, but it would be impractical and unethical. Second best [would be] a registry study with propensity matching,” according to Dr. Friberg.
And that’s just what he and his coinvestigators carried out. The study included 80,948 AF patients with no baseline diagnosis of dementia who were prescribed an OAC and an equal number of propensity-matched, dementia-free AF patients not on OAC therapy. During up to 8 years of follow-up, the unadjusted risk of a new diagnosis of dementia was 29% lower in the group on an OAC at baseline.
But the Swedish registries also enabled investigators to zero in on the impact of OAC in patients who were actually medication adherent over time. Dr. Friberg and his coworkers identified a subgroup of 50,406 AF patients who regularly filled their OAC prescriptions and took the medication at least 80% of the time, as well as 48,947 propensity-matched controls who never used OACs. In this on-treatment analysis, the OAC users had a robust 48% relative risk reduction in new diagnosis of dementia. The dementia curves diverged almost immediately and the gap between the two curves continued to widen throughout follow-up. All examined subgroups benefited, regardless of age, gender, AF duration, CHA2DS2-VASc score, or the presence or absence of diabetes, renal failure, or frequent falling.
“This is an important issue,” Dr. Friberg declared. “You may say, ‘What do we care about these findings? These patients are all supposed to be on an oral anticoagulant anyway.’ But you know, patients stop taking their oral anticoagulant. We’re pretty good at initiating treatment when we meet patients for the first time, if they have stroke risk factors, but annually, 10%-15% of patients drop out of treatment. And if patients aren’t concerned enough about their risk of stroke, they might be more concerned about the risk of becoming demented. So these data provide an additional argument for the need to persevere with oral anticoagulation therapy.”
Session cochair Gabriel Tatu-Chitoiu, MD, was skeptical.
“I’ve been working in the atrial fibrillation field for 40 years, and I have to say I haven’t seen a strong dementia possibility in my patients,” said Dr. Tatu-Chitoiu, a cardiologist in Bucharest, Romania, and immediate past president of the Romanian Cardiology Society.
Dr. Friberg replied that AF patients are elderly, and many of them may stop going to their cardiologist when they develop dementia.
“I don’t think you can make extensions from personal experience on this. You have to trust in statistical evidence,” he observed.
Dr. Friberg reported receiving research funding from Bayer, Bristol-Myers Squibb, Pfizer, and Sanofi. However, the registry study was carried out without commercial support.
AT THE ESC CONGRESS 2017
Key clinical point:
Major finding: The risk of new diagnosis of dementia during up to 8 years of follow-up was 48% lower in AF patients on an oral anticoagulant at least 80% of the time, compared with those not on the medication.
Data source: This was a Swedish registry study including nearly 162,000 propensity-matched patients with atrial fibrillation free of baseline dementia.
Disclosures: The study was conducted without commercial support.
Hypothyroidism carries higher surgical risk not captured by calculator
VICTORIA, B.C. – Even with contemporary anesthesia and surgical techniques, patients who are overtly hypothyroid at the time of major surgery have a rockier course, suggests a retrospective cohort study of 58 patients in a poster presentation at the annual meeting of the American Thyroid Association.
Actual length of stay for hypothyroid patients was twice that predicted by a commonly used risk calculator, whereas actual and predicted stays aligned well for euthyroid patients. The hypothyroid group had more cases of postoperative atrial fibrillation, ileus, reintubation, and death, although numbers were too small for statistical comparison.
“This will have an impact on how we look at patients, especially from a hospital standpoint and management. That’s quite a bit longer stay and quite a bit more cost. And the longer you stay, the more complications you have, too, so it could be riskier for the patient as well,” said first author Raquel Villavicencio, MD, a fellow at Indiana University at the time of the study, and now a clinical endocrinologist at Community Hospital in Indianapolis.
“Although we don’t consider hypothyroidism an absolute contraindication to surgery, especially if it’s necessary surgery, certainly anybody who is having elective surgery should have it postponed, in our opinion, until they are rendered euthyroid,” she said. “More studies are needed to look at this a little bit closer.”
Explaining the study’s rationale, Dr. Villavicencio noted, “This was a question that came up maybe three or four times a year, where we would get a hypothyroid patient and had to decide whether or not to clear them for surgery.”
Previous studies conducted at large institutions, the Mayo Clinic and Massachusetts General Hospital, had conflicting findings and were done about 30 years ago, she said. Anesthesia and surgical care have improved substantially since then, leading the investigators to hypothesize that hypothyroidism would not carry higher surgical risk today.
Dr. Villavicencio and her coinvestigator, Cary Mariash, MD, used their institutional database to identify 29 adult patients with a thyroid-stimulating hormone (TSH) level of greater than 10 mcU/mL alone or with a TSH level exceeding the upper limit of normal along with a free thyroxine (T4) level of less than 0.6 ng/dL who underwent surgery during 2010-2015. They matched each patient on age, sex, and surgical procedure with a control euthyroid patient.
The mean TSH level in the hypothyroid group was 29.2 mcU/mL. The majority of patients in each group – 59% of the hypothyroid group and 62% of the euthyroid group – had an American Surgical Association class of 3, denoting that this was a fairly sick population. The groups were generally similar on rates of comorbidity, except that the euthyroid patients had a slightly higher prevalence of obstructive sleep apnea.
In both groups, the majority of procedures were laparotomy and/or bowel resection; pharyngolaryngectomy and esophagectomy/esophagoplasty; and wound or bone debridement.
Main results showed that in the hypothyroid group, hospital length of stay predicted with the American College of Surgeons National Surgical Quality Improvement Program surgical risk calculator was 6.9 days, but actual length of stay was 14.4 days (P = .0004). In contrast, in the euthyroid group, predicted length of stay was a similar at 7.1 days, and actual length of stay was statistically indistinguishable at 9.2 days (P = .1).
“Hypothyroidism is not taken into account with this calculator,” Dr. Villavicencio noted, adding that she was unaware of any surgical calculators that do.
One patient in the hypothyroid group died, compared with none in the euthyroid group. In terms of postoperative cardiac complications, two patients in the hypothyroid group experienced atrial fibrillation, and there was one case of pulseless electrical–activity arrest in each group.
The groups did not differ on incidence of hypothermia, bradycardia, hyponatremia, time to extubation, and hypotension. However, mean arterial pressure tended to be lower in the hypothyroid group (51 mm Hg) than in the euthyroid group (56 mm Hg), and the former more often needed vasopressors. Furthermore, postoperative ileus and reintubation were more common in the hypothyroid group.
“I think that there are kind of a lot of little things that add up to explain [the longer stay],” said Dr. Villavicencio, who disclosed that she had no relevant conflicts of interest.
VICTORIA, B.C. – Even with contemporary anesthesia and surgical techniques, patients who are overtly hypothyroid at the time of major surgery have a rockier course, suggests a retrospective cohort study of 58 patients in a poster presentation at the annual meeting of the American Thyroid Association.
Actual length of stay for hypothyroid patients was twice that predicted by a commonly used risk calculator, whereas actual and predicted stays aligned well for euthyroid patients. The hypothyroid group had more cases of postoperative atrial fibrillation, ileus, reintubation, and death, although numbers were too small for statistical comparison.
“This will have an impact on how we look at patients, especially from a hospital standpoint and management. That’s quite a bit longer stay and quite a bit more cost. And the longer you stay, the more complications you have, too, so it could be riskier for the patient as well,” said first author Raquel Villavicencio, MD, a fellow at Indiana University at the time of the study, and now a clinical endocrinologist at Community Hospital in Indianapolis.
“Although we don’t consider hypothyroidism an absolute contraindication to surgery, especially if it’s necessary surgery, certainly anybody who is having elective surgery should have it postponed, in our opinion, until they are rendered euthyroid,” she said. “More studies are needed to look at this a little bit closer.”
Explaining the study’s rationale, Dr. Villavicencio noted, “This was a question that came up maybe three or four times a year, where we would get a hypothyroid patient and had to decide whether or not to clear them for surgery.”
Previous studies conducted at large institutions, the Mayo Clinic and Massachusetts General Hospital, had conflicting findings and were done about 30 years ago, she said. Anesthesia and surgical care have improved substantially since then, leading the investigators to hypothesize that hypothyroidism would not carry higher surgical risk today.
Dr. Villavicencio and her coinvestigator, Cary Mariash, MD, used their institutional database to identify 29 adult patients with a thyroid-stimulating hormone (TSH) level of greater than 10 mcU/mL alone or with a TSH level exceeding the upper limit of normal along with a free thyroxine (T4) level of less than 0.6 ng/dL who underwent surgery during 2010-2015. They matched each patient on age, sex, and surgical procedure with a control euthyroid patient.
The mean TSH level in the hypothyroid group was 29.2 mcU/mL. The majority of patients in each group – 59% of the hypothyroid group and 62% of the euthyroid group – had an American Surgical Association class of 3, denoting that this was a fairly sick population. The groups were generally similar on rates of comorbidity, except that the euthyroid patients had a slightly higher prevalence of obstructive sleep apnea.
In both groups, the majority of procedures were laparotomy and/or bowel resection; pharyngolaryngectomy and esophagectomy/esophagoplasty; and wound or bone debridement.
Main results showed that in the hypothyroid group, hospital length of stay predicted with the American College of Surgeons National Surgical Quality Improvement Program surgical risk calculator was 6.9 days, but actual length of stay was 14.4 days (P = .0004). In contrast, in the euthyroid group, predicted length of stay was a similar at 7.1 days, and actual length of stay was statistically indistinguishable at 9.2 days (P = .1).
“Hypothyroidism is not taken into account with this calculator,” Dr. Villavicencio noted, adding that she was unaware of any surgical calculators that do.
One patient in the hypothyroid group died, compared with none in the euthyroid group. In terms of postoperative cardiac complications, two patients in the hypothyroid group experienced atrial fibrillation, and there was one case of pulseless electrical–activity arrest in each group.
The groups did not differ on incidence of hypothermia, bradycardia, hyponatremia, time to extubation, and hypotension. However, mean arterial pressure tended to be lower in the hypothyroid group (51 mm Hg) than in the euthyroid group (56 mm Hg), and the former more often needed vasopressors. Furthermore, postoperative ileus and reintubation were more common in the hypothyroid group.
“I think that there are kind of a lot of little things that add up to explain [the longer stay],” said Dr. Villavicencio, who disclosed that she had no relevant conflicts of interest.
VICTORIA, B.C. – Even with contemporary anesthesia and surgical techniques, patients who are overtly hypothyroid at the time of major surgery have a rockier course, suggests a retrospective cohort study of 58 patients in a poster presentation at the annual meeting of the American Thyroid Association.
Actual length of stay for hypothyroid patients was twice that predicted by a commonly used risk calculator, whereas actual and predicted stays aligned well for euthyroid patients. The hypothyroid group had more cases of postoperative atrial fibrillation, ileus, reintubation, and death, although numbers were too small for statistical comparison.
“This will have an impact on how we look at patients, especially from a hospital standpoint and management. That’s quite a bit longer stay and quite a bit more cost. And the longer you stay, the more complications you have, too, so it could be riskier for the patient as well,” said first author Raquel Villavicencio, MD, a fellow at Indiana University at the time of the study, and now a clinical endocrinologist at Community Hospital in Indianapolis.
“Although we don’t consider hypothyroidism an absolute contraindication to surgery, especially if it’s necessary surgery, certainly anybody who is having elective surgery should have it postponed, in our opinion, until they are rendered euthyroid,” she said. “More studies are needed to look at this a little bit closer.”
Explaining the study’s rationale, Dr. Villavicencio noted, “This was a question that came up maybe three or four times a year, where we would get a hypothyroid patient and had to decide whether or not to clear them for surgery.”
Previous studies conducted at large institutions, the Mayo Clinic and Massachusetts General Hospital, had conflicting findings and were done about 30 years ago, she said. Anesthesia and surgical care have improved substantially since then, leading the investigators to hypothesize that hypothyroidism would not carry higher surgical risk today.
Dr. Villavicencio and her coinvestigator, Cary Mariash, MD, used their institutional database to identify 29 adult patients with a thyroid-stimulating hormone (TSH) level of greater than 10 mcU/mL alone or with a TSH level exceeding the upper limit of normal along with a free thyroxine (T4) level of less than 0.6 ng/dL who underwent surgery during 2010-2015. They matched each patient on age, sex, and surgical procedure with a control euthyroid patient.
The mean TSH level in the hypothyroid group was 29.2 mcU/mL. The majority of patients in each group – 59% of the hypothyroid group and 62% of the euthyroid group – had an American Surgical Association class of 3, denoting that this was a fairly sick population. The groups were generally similar on rates of comorbidity, except that the euthyroid patients had a slightly higher prevalence of obstructive sleep apnea.
In both groups, the majority of procedures were laparotomy and/or bowel resection; pharyngolaryngectomy and esophagectomy/esophagoplasty; and wound or bone debridement.
Main results showed that in the hypothyroid group, hospital length of stay predicted with the American College of Surgeons National Surgical Quality Improvement Program surgical risk calculator was 6.9 days, but actual length of stay was 14.4 days (P = .0004). In contrast, in the euthyroid group, predicted length of stay was a similar at 7.1 days, and actual length of stay was statistically indistinguishable at 9.2 days (P = .1).
“Hypothyroidism is not taken into account with this calculator,” Dr. Villavicencio noted, adding that she was unaware of any surgical calculators that do.
One patient in the hypothyroid group died, compared with none in the euthyroid group. In terms of postoperative cardiac complications, two patients in the hypothyroid group experienced atrial fibrillation, and there was one case of pulseless electrical–activity arrest in each group.
The groups did not differ on incidence of hypothermia, bradycardia, hyponatremia, time to extubation, and hypotension. However, mean arterial pressure tended to be lower in the hypothyroid group (51 mm Hg) than in the euthyroid group (56 mm Hg), and the former more often needed vasopressors. Furthermore, postoperative ileus and reintubation were more common in the hypothyroid group.
“I think that there are kind of a lot of little things that add up to explain [the longer stay],” said Dr. Villavicencio, who disclosed that she had no relevant conflicts of interest.
AT ATA 2017
Key clinical point:
Major finding: Actual length of stay was significantly longer than calculator-predicted length of stay among hypothyroid patients (14.4 vs. 6.9 days, P = .0004) but not among euthyroid patients (9.2 vs. 7.1 days; P = .1).
Data source: A retrospective cohort study of 29 hypothyroid patients and 29 matched euthyroid patients undergoing major surgery.
Disclosures: Dr. Villavicencio disclosed that she had no relevant conflicts of interest.
Yoga benefits lung cancer patients and caregivers alike
Yoga provides physical and mental benefits for both lung cancer patients and their caregivers, according to results of a randomized study presented at the Palliative and Supportive Care in Oncology Symposium.
“Overall, we are encouraged by the findings,” said lead study author, Kathrin Milbury, PhD, of University of Texas MD Anderson Cancer Center, Houston.
This study provides preliminary evidence that a yoga program can provide a “buffer” and improve physical function for patients, as well as self-reported improved quality of life for both patients and their caregivers, she added.
All patients in the study had non–small cell lung cancer and were undergoing thoracic radiation therapy, which can cause respiratory toxicities that negatively affect quality of life and physical activity, according to Dr. Milbury and her coinvestigators.
A total of 32 patient-caregiver dyads were randomized to participate in 15 yoga sessions or to be in a “wait-list” control group, and 26 dyads completed all assessments.
Patients who practiced yoga had significantly better scores on a 6-minute walking test (478 vs. 402 for wait-list enrollees; P less than .05), plus better stamina and mental health. Caregivers had improved fatigue and better stamina at work.
Almost all patients (96%) rated the program as “very useful,” investigators reported at the symposium, which was cosponsored by AAHPM, ASCO, ASTRO, and MASCC.
This study provides additional evidence that yoga and other nonpharmacologic supportive therapies “can be integrated into not only the care of cancer patients, but also the family caregivers who support them,” according to Andrew S. Epstein, MD, of Memorial Sloan Kettering Cancer Center, New York.
Next, the researchers plan to conduct a larger, randomized, controlled trial with a more stringent comparison group, according to Dr. Milbury.
Yoga provides physical and mental benefits for both lung cancer patients and their caregivers, according to results of a randomized study presented at the Palliative and Supportive Care in Oncology Symposium.
“Overall, we are encouraged by the findings,” said lead study author, Kathrin Milbury, PhD, of University of Texas MD Anderson Cancer Center, Houston.
This study provides preliminary evidence that a yoga program can provide a “buffer” and improve physical function for patients, as well as self-reported improved quality of life for both patients and their caregivers, she added.
All patients in the study had non–small cell lung cancer and were undergoing thoracic radiation therapy, which can cause respiratory toxicities that negatively affect quality of life and physical activity, according to Dr. Milbury and her coinvestigators.
A total of 32 patient-caregiver dyads were randomized to participate in 15 yoga sessions or to be in a “wait-list” control group, and 26 dyads completed all assessments.
Patients who practiced yoga had significantly better scores on a 6-minute walking test (478 vs. 402 for wait-list enrollees; P less than .05), plus better stamina and mental health. Caregivers had improved fatigue and better stamina at work.
Almost all patients (96%) rated the program as “very useful,” investigators reported at the symposium, which was cosponsored by AAHPM, ASCO, ASTRO, and MASCC.
This study provides additional evidence that yoga and other nonpharmacologic supportive therapies “can be integrated into not only the care of cancer patients, but also the family caregivers who support them,” according to Andrew S. Epstein, MD, of Memorial Sloan Kettering Cancer Center, New York.
Next, the researchers plan to conduct a larger, randomized, controlled trial with a more stringent comparison group, according to Dr. Milbury.
Yoga provides physical and mental benefits for both lung cancer patients and their caregivers, according to results of a randomized study presented at the Palliative and Supportive Care in Oncology Symposium.
“Overall, we are encouraged by the findings,” said lead study author, Kathrin Milbury, PhD, of University of Texas MD Anderson Cancer Center, Houston.
This study provides preliminary evidence that a yoga program can provide a “buffer” and improve physical function for patients, as well as self-reported improved quality of life for both patients and their caregivers, she added.
All patients in the study had non–small cell lung cancer and were undergoing thoracic radiation therapy, which can cause respiratory toxicities that negatively affect quality of life and physical activity, according to Dr. Milbury and her coinvestigators.
A total of 32 patient-caregiver dyads were randomized to participate in 15 yoga sessions or to be in a “wait-list” control group, and 26 dyads completed all assessments.
Patients who practiced yoga had significantly better scores on a 6-minute walking test (478 vs. 402 for wait-list enrollees; P less than .05), plus better stamina and mental health. Caregivers had improved fatigue and better stamina at work.
Almost all patients (96%) rated the program as “very useful,” investigators reported at the symposium, which was cosponsored by AAHPM, ASCO, ASTRO, and MASCC.
This study provides additional evidence that yoga and other nonpharmacologic supportive therapies “can be integrated into not only the care of cancer patients, but also the family caregivers who support them,” according to Andrew S. Epstein, MD, of Memorial Sloan Kettering Cancer Center, New York.
Next, the researchers plan to conduct a larger, randomized, controlled trial with a more stringent comparison group, according to Dr. Milbury.
FROM PALLONC 2017
Key clinical point: Yoga provides both physical and mental benefits for lung cancer patients undergoing radiotherapy and their caregivers.
Major finding: Patients who practiced yoga had significantly better scores on a 6-minute walking test (478 vs. 402 for wait-list enrollees; P less than .05), plus better stamina and mental health. Caregivers had improved fatigue and better stamina at work.
Data source: Randomized study including 47 patient-caregiver dyads, of which 32 consented and 26 completed all assessments.
Disclosures: Funding for this study came from the National Institutes of Health. Lead author Kathrin Milbury, PhD, reported no potential conflicts of interest.
Federal judge skeptical of claims that dropping subsidies hurts consumers
SAN FRANCISCO – A federal judge Monday expressed skepticism that President Donald Trump’s decision to halt certain health law insurance subsidies would cause consumers immediate harm, as California and many other states claim in a lawsuit.
U.S. District Judge Vince Chhabria said he would issue a ruling in the case Tuesday.
Earlier this month, Trump announced that the administration would stop payments that compensate insurers for discounts given to low-income consumers to help cover their out-of-pocket expenses under policies sold on the Affordable Care Act’s insurance marketplaces. These subsidies are different from the tax credits many consumers get, depending on their income, to pay Obamacare premiums.
The lawsuit was filed by 18 states and the District of Columbia, led by California Attorney General Xavier Becerra. It seeks an emergency restraining order compelling the Trump administration to resume the Obamacare payments. Nationwide, cost-sharing payments were expected to total $7 billion this year.
Since assuming office in January, Trump has repeatedly threatened to stop the subsidies, known as cost-sharing reduction payments. But he held off while Republicans in Congress were working to replace the ACA. Republicans have argued that the subsidies are illegal because they have not been approved by Congress and that they amount to a bailout for insurers.
Responding to the uncertainty, a number of states have allowed insurers to raise their premiums. California earlier this month ordered insurers to add a surcharge to some policies next year, to offset the potential loss in federal funding and keep the individual insurance market stable. The 12.4% surcharge was added to silver plans only, the second-least-expensive tier.
“California is doing a really good job in responding to the termination of [cost-sharing reduction] payments in a way that is avoiding harm for people and actually benefiting people,” said Judge Chhabria.
He said that the vast majority of states have “seen the writing on the wall” and chosen to respond by increasing premiums for silver plans. That, in turn, will force the federal government to give higher tax credits to most consumers, so they won’t feel any financial pinch.
Under intense questioning by the judge, California Deputy Attorney General Gregory Brown acknowledged that California has done a lot to mitigate the harm to consumers. But he said the administration’s actions are destabilizing the exchanges and the individual insurance market, and causing chaos for states and consumers just eight days before enrollment begins Nov. 1.
Some experts and states are concerned jumpy insurers will bolt from the market and leave some regions with minimal or no choices for coverage. However, a bipartisan bill in Congress would restore the cost-sharing subsidies and aims to stabilize the insurance markets. But it’s not clear the bill will muster the support it needs to pass both the Senate and House or whether Trump would sign it.
In California, 1.4 million people buy their own coverage through the state marketplace, and 90 percent receive federal subsidies that reduce what they pay.
During the hearing, Chhabria read from a Covered California press release that predicts how the changes will affect consumers in 2018. It notes that even though silver plan premiums will rise as a result of the surcharge, the federal tax credits will also increase to cover the rise in premiums. That would leave 4 out of 5 consumers with monthly premiums that stay the same or decrease.
The judge also said ruling in favor of the restraining order would mean insurance companies could essentially “double collect” – benefiting from both the premium increases from the surcharge on silver plans and the cost-sharing subsidies.
Brown said a restraining order to resume the cost-sharing payments would bring back the status quo. If insurance companies double collect, the state would compensate by reducing rates down the line, he said.
“We’re not looking to give insurance companies a windfall ... but the stability is important to insurance companies,” he said.
This story was produced by Kaiser Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
SAN FRANCISCO – A federal judge Monday expressed skepticism that President Donald Trump’s decision to halt certain health law insurance subsidies would cause consumers immediate harm, as California and many other states claim in a lawsuit.
U.S. District Judge Vince Chhabria said he would issue a ruling in the case Tuesday.
Earlier this month, Trump announced that the administration would stop payments that compensate insurers for discounts given to low-income consumers to help cover their out-of-pocket expenses under policies sold on the Affordable Care Act’s insurance marketplaces. These subsidies are different from the tax credits many consumers get, depending on their income, to pay Obamacare premiums.
The lawsuit was filed by 18 states and the District of Columbia, led by California Attorney General Xavier Becerra. It seeks an emergency restraining order compelling the Trump administration to resume the Obamacare payments. Nationwide, cost-sharing payments were expected to total $7 billion this year.
Since assuming office in January, Trump has repeatedly threatened to stop the subsidies, known as cost-sharing reduction payments. But he held off while Republicans in Congress were working to replace the ACA. Republicans have argued that the subsidies are illegal because they have not been approved by Congress and that they amount to a bailout for insurers.
Responding to the uncertainty, a number of states have allowed insurers to raise their premiums. California earlier this month ordered insurers to add a surcharge to some policies next year, to offset the potential loss in federal funding and keep the individual insurance market stable. The 12.4% surcharge was added to silver plans only, the second-least-expensive tier.
“California is doing a really good job in responding to the termination of [cost-sharing reduction] payments in a way that is avoiding harm for people and actually benefiting people,” said Judge Chhabria.
He said that the vast majority of states have “seen the writing on the wall” and chosen to respond by increasing premiums for silver plans. That, in turn, will force the federal government to give higher tax credits to most consumers, so they won’t feel any financial pinch.
Under intense questioning by the judge, California Deputy Attorney General Gregory Brown acknowledged that California has done a lot to mitigate the harm to consumers. But he said the administration’s actions are destabilizing the exchanges and the individual insurance market, and causing chaos for states and consumers just eight days before enrollment begins Nov. 1.
Some experts and states are concerned jumpy insurers will bolt from the market and leave some regions with minimal or no choices for coverage. However, a bipartisan bill in Congress would restore the cost-sharing subsidies and aims to stabilize the insurance markets. But it’s not clear the bill will muster the support it needs to pass both the Senate and House or whether Trump would sign it.
In California, 1.4 million people buy their own coverage through the state marketplace, and 90 percent receive federal subsidies that reduce what they pay.
During the hearing, Chhabria read from a Covered California press release that predicts how the changes will affect consumers in 2018. It notes that even though silver plan premiums will rise as a result of the surcharge, the federal tax credits will also increase to cover the rise in premiums. That would leave 4 out of 5 consumers with monthly premiums that stay the same or decrease.
The judge also said ruling in favor of the restraining order would mean insurance companies could essentially “double collect” – benefiting from both the premium increases from the surcharge on silver plans and the cost-sharing subsidies.
Brown said a restraining order to resume the cost-sharing payments would bring back the status quo. If insurance companies double collect, the state would compensate by reducing rates down the line, he said.
“We’re not looking to give insurance companies a windfall ... but the stability is important to insurance companies,” he said.
This story was produced by Kaiser Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
SAN FRANCISCO – A federal judge Monday expressed skepticism that President Donald Trump’s decision to halt certain health law insurance subsidies would cause consumers immediate harm, as California and many other states claim in a lawsuit.
U.S. District Judge Vince Chhabria said he would issue a ruling in the case Tuesday.
Earlier this month, Trump announced that the administration would stop payments that compensate insurers for discounts given to low-income consumers to help cover their out-of-pocket expenses under policies sold on the Affordable Care Act’s insurance marketplaces. These subsidies are different from the tax credits many consumers get, depending on their income, to pay Obamacare premiums.
The lawsuit was filed by 18 states and the District of Columbia, led by California Attorney General Xavier Becerra. It seeks an emergency restraining order compelling the Trump administration to resume the Obamacare payments. Nationwide, cost-sharing payments were expected to total $7 billion this year.
Since assuming office in January, Trump has repeatedly threatened to stop the subsidies, known as cost-sharing reduction payments. But he held off while Republicans in Congress were working to replace the ACA. Republicans have argued that the subsidies are illegal because they have not been approved by Congress and that they amount to a bailout for insurers.
Responding to the uncertainty, a number of states have allowed insurers to raise their premiums. California earlier this month ordered insurers to add a surcharge to some policies next year, to offset the potential loss in federal funding and keep the individual insurance market stable. The 12.4% surcharge was added to silver plans only, the second-least-expensive tier.
“California is doing a really good job in responding to the termination of [cost-sharing reduction] payments in a way that is avoiding harm for people and actually benefiting people,” said Judge Chhabria.
He said that the vast majority of states have “seen the writing on the wall” and chosen to respond by increasing premiums for silver plans. That, in turn, will force the federal government to give higher tax credits to most consumers, so they won’t feel any financial pinch.
Under intense questioning by the judge, California Deputy Attorney General Gregory Brown acknowledged that California has done a lot to mitigate the harm to consumers. But he said the administration’s actions are destabilizing the exchanges and the individual insurance market, and causing chaos for states and consumers just eight days before enrollment begins Nov. 1.
Some experts and states are concerned jumpy insurers will bolt from the market and leave some regions with minimal or no choices for coverage. However, a bipartisan bill in Congress would restore the cost-sharing subsidies and aims to stabilize the insurance markets. But it’s not clear the bill will muster the support it needs to pass both the Senate and House or whether Trump would sign it.
In California, 1.4 million people buy their own coverage through the state marketplace, and 90 percent receive federal subsidies that reduce what they pay.
During the hearing, Chhabria read from a Covered California press release that predicts how the changes will affect consumers in 2018. It notes that even though silver plan premiums will rise as a result of the surcharge, the federal tax credits will also increase to cover the rise in premiums. That would leave 4 out of 5 consumers with monthly premiums that stay the same or decrease.
The judge also said ruling in favor of the restraining order would mean insurance companies could essentially “double collect” – benefiting from both the premium increases from the surcharge on silver plans and the cost-sharing subsidies.
Brown said a restraining order to resume the cost-sharing payments would bring back the status quo. If insurance companies double collect, the state would compensate by reducing rates down the line, he said.
“We’re not looking to give insurance companies a windfall ... but the stability is important to insurance companies,” he said.
This story was produced by Kaiser Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
PCI advances produce CABG-like 1-year outcomes
BARCELONA – Improvements in percutaneous coronary intervention over the past decade have made a difference. Coronary stenting to treat triple-vessel disease produced roughly the same 1-year results as coronary artery bypass surgery, based on results from 454 patients in an uncontrolled, prospective trial.
With state-of-the-art percutaneous coronary intervention (PCI), the 1-year incidence of major cardiac and cerebrovascular events was 11% in the Synergy Between PCI with Taxus and Cardiac Surgery (SYNTAX) II trial, a PCI outcome substantially better than the 18% rate with PCI seen in the original SYNTAX trial, run during 2005-2007. That incidence was similar to the 11% 1-year major adverse event rate seen in patients who underwent coronary artery bypass grafting (CABG) in the first SYNTAX trial (N Engl J Med. 2009 Mar 5;360[10]:961-72), said Javier Escaned, MD, who reported the results at the annual congress of the European Society of Cardiology.
- Initial assessment of patients using both clinical and anatomic criteria with the SYNTAX score II (Lancet. 2013 Feb 23;381[9867]:639-50), an improvement over the original SYNTAX score that only used anatomic data.
- Assessment of each coronary stenosis for its physiologic impact using a pressure wire to measure the instantaneous wave-free ratio and fractional flow reserve of each suspicious lesion.
- Performing PCI with a second-generation everolimus-eluting stent with a bioabsorbable polymer stent (Synergy) instead of the paclitaxel-eluting first-generation stent (Taxus) used in the first SYNTAX trial.
- Optimization of stent placement with intravascular ultrasound.
- Application of contemporary methods for treating total chronic occlusions that produce higher success rates than a decade ago.
- Prescription of current guideline-directed medical therapy to each patient following PCI.
“To get the best results you need to do all of this; none of these steps takes full credit by itself,” said Dr. Escaned, an interventional cardiologist at the Hospital Clinic San Carlos in Madrid. “The message from SYNTAX II is that if you put all of these steps together, this is the result,” he said in an interview.
An underlying assumption of the single-arm design of SYNTAX II and its “exploratory” comparison to a 334-patient subset of the 897 patients who underwent CABG in the original SYNTAX trial who retrospectively met the SYNTAX score II enrollment criteria used in the current trial was that “CABG has not changed much” since the first SYNTAX trial, Dr. Escaned said. Although he acknowledged that some progress also occurred with CABG in the subsequent 10 years, “it has not been as big a change” as going to second-generation drug-eluting stents, using a pressure wire assessment to target physiologically important stenoses, and improved techniques for treating chronic total occlusions that have nearly doubled success rates in patients with these lesions.
The SYNTAX II trial enrolled 454 patients with de novo triple-vessel coronary disease without left main stem involvement at 22 centers in four European countries during 2014 and 2015. The improvement in the primary 1-year endpoint in the current patients compared with PCI patients from the first SYNTAX trial was driven primarily by reductions in MI and in repeat revascularizations. The SYNTAX II patients also had a 0.7% rate of definite stent thrombosis events, compared with a 2.4% rate in the original SYNTAX PCI patients, a statistically significant difference. Concurrently with Dr. Escaned’s report at the meeting an article with the results appeared online (Eur Heart J. 2017 Aug 26;doi: 10.1093/eurheartj/ehx512).
Dr. Escaned cautioned that longer-term follow-up is needed to more fully compare the PCI results with CABG.
SYNTAX II received unrestricted grant support from Philips/Volcano and Boston Scientific, the companies that market the pressure wires and stents used in the study. Dr. Escaned reported ties to Abbott, AstraZeneca, Biosensors, Boston Scientific, Medtronic, OrbusNeich, Philips/Volcano, and Boston Scientific.
[email protected]
On Twitter @mitchelzoler
BARCELONA – Improvements in percutaneous coronary intervention over the past decade have made a difference. Coronary stenting to treat triple-vessel disease produced roughly the same 1-year results as coronary artery bypass surgery, based on results from 454 patients in an uncontrolled, prospective trial.
With state-of-the-art percutaneous coronary intervention (PCI), the 1-year incidence of major cardiac and cerebrovascular events was 11% in the Synergy Between PCI with Taxus and Cardiac Surgery (SYNTAX) II trial, a PCI outcome substantially better than the 18% rate with PCI seen in the original SYNTAX trial, run during 2005-2007. That incidence was similar to the 11% 1-year major adverse event rate seen in patients who underwent coronary artery bypass grafting (CABG) in the first SYNTAX trial (N Engl J Med. 2009 Mar 5;360[10]:961-72), said Javier Escaned, MD, who reported the results at the annual congress of the European Society of Cardiology.
- Initial assessment of patients using both clinical and anatomic criteria with the SYNTAX score II (Lancet. 2013 Feb 23;381[9867]:639-50), an improvement over the original SYNTAX score that only used anatomic data.
- Assessment of each coronary stenosis for its physiologic impact using a pressure wire to measure the instantaneous wave-free ratio and fractional flow reserve of each suspicious lesion.
- Performing PCI with a second-generation everolimus-eluting stent with a bioabsorbable polymer stent (Synergy) instead of the paclitaxel-eluting first-generation stent (Taxus) used in the first SYNTAX trial.
- Optimization of stent placement with intravascular ultrasound.
- Application of contemporary methods for treating total chronic occlusions that produce higher success rates than a decade ago.
- Prescription of current guideline-directed medical therapy to each patient following PCI.
“To get the best results you need to do all of this; none of these steps takes full credit by itself,” said Dr. Escaned, an interventional cardiologist at the Hospital Clinic San Carlos in Madrid. “The message from SYNTAX II is that if you put all of these steps together, this is the result,” he said in an interview.
An underlying assumption of the single-arm design of SYNTAX II and its “exploratory” comparison to a 334-patient subset of the 897 patients who underwent CABG in the original SYNTAX trial who retrospectively met the SYNTAX score II enrollment criteria used in the current trial was that “CABG has not changed much” since the first SYNTAX trial, Dr. Escaned said. Although he acknowledged that some progress also occurred with CABG in the subsequent 10 years, “it has not been as big a change” as going to second-generation drug-eluting stents, using a pressure wire assessment to target physiologically important stenoses, and improved techniques for treating chronic total occlusions that have nearly doubled success rates in patients with these lesions.
The SYNTAX II trial enrolled 454 patients with de novo triple-vessel coronary disease without left main stem involvement at 22 centers in four European countries during 2014 and 2015. The improvement in the primary 1-year endpoint in the current patients compared with PCI patients from the first SYNTAX trial was driven primarily by reductions in MI and in repeat revascularizations. The SYNTAX II patients also had a 0.7% rate of definite stent thrombosis events, compared with a 2.4% rate in the original SYNTAX PCI patients, a statistically significant difference. Concurrently with Dr. Escaned’s report at the meeting an article with the results appeared online (Eur Heart J. 2017 Aug 26;doi: 10.1093/eurheartj/ehx512).
Dr. Escaned cautioned that longer-term follow-up is needed to more fully compare the PCI results with CABG.
SYNTAX II received unrestricted grant support from Philips/Volcano and Boston Scientific, the companies that market the pressure wires and stents used in the study. Dr. Escaned reported ties to Abbott, AstraZeneca, Biosensors, Boston Scientific, Medtronic, OrbusNeich, Philips/Volcano, and Boston Scientific.
[email protected]
On Twitter @mitchelzoler
BARCELONA – Improvements in percutaneous coronary intervention over the past decade have made a difference. Coronary stenting to treat triple-vessel disease produced roughly the same 1-year results as coronary artery bypass surgery, based on results from 454 patients in an uncontrolled, prospective trial.
With state-of-the-art percutaneous coronary intervention (PCI), the 1-year incidence of major cardiac and cerebrovascular events was 11% in the Synergy Between PCI with Taxus and Cardiac Surgery (SYNTAX) II trial, a PCI outcome substantially better than the 18% rate with PCI seen in the original SYNTAX trial, run during 2005-2007. That incidence was similar to the 11% 1-year major adverse event rate seen in patients who underwent coronary artery bypass grafting (CABG) in the first SYNTAX trial (N Engl J Med. 2009 Mar 5;360[10]:961-72), said Javier Escaned, MD, who reported the results at the annual congress of the European Society of Cardiology.
- Initial assessment of patients using both clinical and anatomic criteria with the SYNTAX score II (Lancet. 2013 Feb 23;381[9867]:639-50), an improvement over the original SYNTAX score that only used anatomic data.
- Assessment of each coronary stenosis for its physiologic impact using a pressure wire to measure the instantaneous wave-free ratio and fractional flow reserve of each suspicious lesion.
- Performing PCI with a second-generation everolimus-eluting stent with a bioabsorbable polymer stent (Synergy) instead of the paclitaxel-eluting first-generation stent (Taxus) used in the first SYNTAX trial.
- Optimization of stent placement with intravascular ultrasound.
- Application of contemporary methods for treating total chronic occlusions that produce higher success rates than a decade ago.
- Prescription of current guideline-directed medical therapy to each patient following PCI.
“To get the best results you need to do all of this; none of these steps takes full credit by itself,” said Dr. Escaned, an interventional cardiologist at the Hospital Clinic San Carlos in Madrid. “The message from SYNTAX II is that if you put all of these steps together, this is the result,” he said in an interview.
An underlying assumption of the single-arm design of SYNTAX II and its “exploratory” comparison to a 334-patient subset of the 897 patients who underwent CABG in the original SYNTAX trial who retrospectively met the SYNTAX score II enrollment criteria used in the current trial was that “CABG has not changed much” since the first SYNTAX trial, Dr. Escaned said. Although he acknowledged that some progress also occurred with CABG in the subsequent 10 years, “it has not been as big a change” as going to second-generation drug-eluting stents, using a pressure wire assessment to target physiologically important stenoses, and improved techniques for treating chronic total occlusions that have nearly doubled success rates in patients with these lesions.
The SYNTAX II trial enrolled 454 patients with de novo triple-vessel coronary disease without left main stem involvement at 22 centers in four European countries during 2014 and 2015. The improvement in the primary 1-year endpoint in the current patients compared with PCI patients from the first SYNTAX trial was driven primarily by reductions in MI and in repeat revascularizations. The SYNTAX II patients also had a 0.7% rate of definite stent thrombosis events, compared with a 2.4% rate in the original SYNTAX PCI patients, a statistically significant difference. Concurrently with Dr. Escaned’s report at the meeting an article with the results appeared online (Eur Heart J. 2017 Aug 26;doi: 10.1093/eurheartj/ehx512).
Dr. Escaned cautioned that longer-term follow-up is needed to more fully compare the PCI results with CABG.
SYNTAX II received unrestricted grant support from Philips/Volcano and Boston Scientific, the companies that market the pressure wires and stents used in the study. Dr. Escaned reported ties to Abbott, AstraZeneca, Biosensors, Boston Scientific, Medtronic, OrbusNeich, Philips/Volcano, and Boston Scientific.
[email protected]
On Twitter @mitchelzoler
AT THE ESC CONGRESS 2017
Key clinical point:
Major finding: At 1 year, the combined major adverse event rate was 11%, similar to the CABG rate in the original SYNTAX trial.
Data source: SYNTAX II, a prospective, multicenter, single-arm study with 454 patients.
Disclosures: SYNTAX II received unrestricted grant support from Philips/Volcano and Boston Scientific, the companies that market the pressure wires and stents used in the study. Dr. Escaned reported ties to Abbott, AstraZeneca, Biosensors, Boston Scientific, Medtronic, OrbusNeich, Philips/Volcano, and Boston Scientific.
Robotic-assisted pulmonary lobectomy effective for large tumors
Robotic-assisted pulmonary lobectomy is a safe and effective way to remove large tumors in patients with non–small cell lung cancer (NSCLC), according to the abstract of a study scheduled to be presented at the CHEST annual meeting.
The study covers a retrospective analysis of 345 NSCLC patients with tumors who underwent robotic-assisted pulmonary lobectomy performed by one surgeon from September 2010 through August 2016. The participants were grouped into the following three cohorts: patients with tumors less than 5 cm in diameter, patients with tumors from 5 to 7 cm, and patients with tumors larger than 7 cm. The researchers excluded patients with pulmonary metastases or benign lesions from the study.
Patients with smaller tumors were more likely to have simple lobectomy or lobectomy plus wedge, while patients with larger tumors were more likely to require lobectomy with chest wall resection. Increased tumor size was also associated with increased intraoperative estimated blood loss, skin-to-skin operative time, hospital length of stay, and overall conversion to open lobectomy.
There was no association found between tumor size and increased overall intraoperative or postoperative complications, or in-hospital mortality.
Nirav Patel, MD, FCCP, of the Tampa Bay Sleep Center is scheduled to present his abstract on Sunday Oct. 29th, between 2:15 and 2:30 p.m. in Convention Center – 606. Dr. Patel’s research is part of the Cardiothoracic Surgery session, running from 1:30 p.m. to 3:00 p.m. at the CHEST annual meeting.
Robotic-assisted pulmonary lobectomy is a safe and effective way to remove large tumors in patients with non–small cell lung cancer (NSCLC), according to the abstract of a study scheduled to be presented at the CHEST annual meeting.
The study covers a retrospective analysis of 345 NSCLC patients with tumors who underwent robotic-assisted pulmonary lobectomy performed by one surgeon from September 2010 through August 2016. The participants were grouped into the following three cohorts: patients with tumors less than 5 cm in diameter, patients with tumors from 5 to 7 cm, and patients with tumors larger than 7 cm. The researchers excluded patients with pulmonary metastases or benign lesions from the study.
Patients with smaller tumors were more likely to have simple lobectomy or lobectomy plus wedge, while patients with larger tumors were more likely to require lobectomy with chest wall resection. Increased tumor size was also associated with increased intraoperative estimated blood loss, skin-to-skin operative time, hospital length of stay, and overall conversion to open lobectomy.
There was no association found between tumor size and increased overall intraoperative or postoperative complications, or in-hospital mortality.
Nirav Patel, MD, FCCP, of the Tampa Bay Sleep Center is scheduled to present his abstract on Sunday Oct. 29th, between 2:15 and 2:30 p.m. in Convention Center – 606. Dr. Patel’s research is part of the Cardiothoracic Surgery session, running from 1:30 p.m. to 3:00 p.m. at the CHEST annual meeting.
Robotic-assisted pulmonary lobectomy is a safe and effective way to remove large tumors in patients with non–small cell lung cancer (NSCLC), according to the abstract of a study scheduled to be presented at the CHEST annual meeting.
The study covers a retrospective analysis of 345 NSCLC patients with tumors who underwent robotic-assisted pulmonary lobectomy performed by one surgeon from September 2010 through August 2016. The participants were grouped into the following three cohorts: patients with tumors less than 5 cm in diameter, patients with tumors from 5 to 7 cm, and patients with tumors larger than 7 cm. The researchers excluded patients with pulmonary metastases or benign lesions from the study.
Patients with smaller tumors were more likely to have simple lobectomy or lobectomy plus wedge, while patients with larger tumors were more likely to require lobectomy with chest wall resection. Increased tumor size was also associated with increased intraoperative estimated blood loss, skin-to-skin operative time, hospital length of stay, and overall conversion to open lobectomy.
There was no association found between tumor size and increased overall intraoperative or postoperative complications, or in-hospital mortality.
Nirav Patel, MD, FCCP, of the Tampa Bay Sleep Center is scheduled to present his abstract on Sunday Oct. 29th, between 2:15 and 2:30 p.m. in Convention Center – 606. Dr. Patel’s research is part of the Cardiothoracic Surgery session, running from 1:30 p.m. to 3:00 p.m. at the CHEST annual meeting.
FROM CHEST 2017
Abnormal potassium plus suspected ACS spell trouble
BARCELONA – A serum potassium level of at least 5.0 mmol/L or 3.5 mmol/L or less at admission for suspected acute coronary syndrome is a red flag for increased risk of in-hospital mortality and cardiac arrest, according to a Swedish study of nearly 33,000 consecutive patients.
That’s true even if, as so often ultimately proves to be the case, the patient turns out not to have ACS, Jonas Faxén, MD, of the Karolinska Institute, Stockholm, reported at the annual congress of the European Society of Cardiology.
“This study highlights that, if you have a patient in the emergency department with a possible ACS and potassium imbalance, you should really be cautious,” Dr. Faxén said.
He reported on 32,955 consecutive patients admitted to Stockholm County hospitals for suspected ACS during 2006-2011 and thereby enrolled in the SWEDEHEART (Swedish Web System for Enhancement and Development of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies) registry.
Overall in-hospital mortality was 2.7%. In-hospital cardiac arrest occurred in 1.5% of patients. New-onset atrial fibrillation occurred in 2.4% of patients. These key outcomes were compared between the reference group – defined as patients with an admission serum potassium of 3.5 to less than 4.0 mmol/L – and patients with an admission serum potassium above or below those cutoffs.
In a multivariate logistic regression analysis adjusted for 24 potential confounders, including demographics, presentation characteristics, main diagnosis, comorbid conditions, medications on admission, and estimated glomerular filtration rate, patients with a serum potassium of 5.0 to less than 5.5 mmol/L were at 1.8-fold increased risk of in-hospital mortality. Those with a potassium of 5.5 mmol/L or greater were at 2.3-fold increased risk.
In contrast, a low rather than a high serum potassium was an independent risk factor cardiac arrest. An admission potassium of 3.0 to less than 3.5 mmol/L carried a 1.8-fold increased risk of in-hospital cardiac arrest, while a potassium of less than 3.0 was associated with a 2.7-fold increased risk.
A serum potassium below 3.0 mmol/L at admission also was associated with a 1.7-fold increased risk of new-onset atrial fibrillation.
These elevated risks of bad outcomes didn’t differ significantly between patients with ST-elevation MI, non-STEMI ACS, and those whose final diagnosis was not ACS, Dr. Faxén noted.
Session cochair David W. Walker, MD, medical director of the East Sussex (England) Healthcare NHS Trust, observed, “When I was a junior doctor I was always taught that when patients came onto coronary care we had to get their potassium to 4.5-5.0 mmol/L. I think you might want to change that advice now.”
“The implication would be that, if you intervene quickly in a patient with an abnormal potassium level, you might make a difference. Clearly, a potassium that’s too high is much worse than too low, since patients with in-hospital cardiac arrest can often be resuscitated,” Dr. Walker commented.
Dr. Faxén reported having no financial conflicts regarding his study, which was funded by the Swedish Heart and Lung Foundation and the Stockholm County Council.
BARCELONA – A serum potassium level of at least 5.0 mmol/L or 3.5 mmol/L or less at admission for suspected acute coronary syndrome is a red flag for increased risk of in-hospital mortality and cardiac arrest, according to a Swedish study of nearly 33,000 consecutive patients.
That’s true even if, as so often ultimately proves to be the case, the patient turns out not to have ACS, Jonas Faxén, MD, of the Karolinska Institute, Stockholm, reported at the annual congress of the European Society of Cardiology.
“This study highlights that, if you have a patient in the emergency department with a possible ACS and potassium imbalance, you should really be cautious,” Dr. Faxén said.
He reported on 32,955 consecutive patients admitted to Stockholm County hospitals for suspected ACS during 2006-2011 and thereby enrolled in the SWEDEHEART (Swedish Web System for Enhancement and Development of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies) registry.
Overall in-hospital mortality was 2.7%. In-hospital cardiac arrest occurred in 1.5% of patients. New-onset atrial fibrillation occurred in 2.4% of patients. These key outcomes were compared between the reference group – defined as patients with an admission serum potassium of 3.5 to less than 4.0 mmol/L – and patients with an admission serum potassium above or below those cutoffs.
In a multivariate logistic regression analysis adjusted for 24 potential confounders, including demographics, presentation characteristics, main diagnosis, comorbid conditions, medications on admission, and estimated glomerular filtration rate, patients with a serum potassium of 5.0 to less than 5.5 mmol/L were at 1.8-fold increased risk of in-hospital mortality. Those with a potassium of 5.5 mmol/L or greater were at 2.3-fold increased risk.
In contrast, a low rather than a high serum potassium was an independent risk factor cardiac arrest. An admission potassium of 3.0 to less than 3.5 mmol/L carried a 1.8-fold increased risk of in-hospital cardiac arrest, while a potassium of less than 3.0 was associated with a 2.7-fold increased risk.
A serum potassium below 3.0 mmol/L at admission also was associated with a 1.7-fold increased risk of new-onset atrial fibrillation.
These elevated risks of bad outcomes didn’t differ significantly between patients with ST-elevation MI, non-STEMI ACS, and those whose final diagnosis was not ACS, Dr. Faxén noted.
Session cochair David W. Walker, MD, medical director of the East Sussex (England) Healthcare NHS Trust, observed, “When I was a junior doctor I was always taught that when patients came onto coronary care we had to get their potassium to 4.5-5.0 mmol/L. I think you might want to change that advice now.”
“The implication would be that, if you intervene quickly in a patient with an abnormal potassium level, you might make a difference. Clearly, a potassium that’s too high is much worse than too low, since patients with in-hospital cardiac arrest can often be resuscitated,” Dr. Walker commented.
Dr. Faxén reported having no financial conflicts regarding his study, which was funded by the Swedish Heart and Lung Foundation and the Stockholm County Council.
BARCELONA – A serum potassium level of at least 5.0 mmol/L or 3.5 mmol/L or less at admission for suspected acute coronary syndrome is a red flag for increased risk of in-hospital mortality and cardiac arrest, according to a Swedish study of nearly 33,000 consecutive patients.
That’s true even if, as so often ultimately proves to be the case, the patient turns out not to have ACS, Jonas Faxén, MD, of the Karolinska Institute, Stockholm, reported at the annual congress of the European Society of Cardiology.
“This study highlights that, if you have a patient in the emergency department with a possible ACS and potassium imbalance, you should really be cautious,” Dr. Faxén said.
He reported on 32,955 consecutive patients admitted to Stockholm County hospitals for suspected ACS during 2006-2011 and thereby enrolled in the SWEDEHEART (Swedish Web System for Enhancement and Development of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies) registry.
Overall in-hospital mortality was 2.7%. In-hospital cardiac arrest occurred in 1.5% of patients. New-onset atrial fibrillation occurred in 2.4% of patients. These key outcomes were compared between the reference group – defined as patients with an admission serum potassium of 3.5 to less than 4.0 mmol/L – and patients with an admission serum potassium above or below those cutoffs.
In a multivariate logistic regression analysis adjusted for 24 potential confounders, including demographics, presentation characteristics, main diagnosis, comorbid conditions, medications on admission, and estimated glomerular filtration rate, patients with a serum potassium of 5.0 to less than 5.5 mmol/L were at 1.8-fold increased risk of in-hospital mortality. Those with a potassium of 5.5 mmol/L or greater were at 2.3-fold increased risk.
In contrast, a low rather than a high serum potassium was an independent risk factor cardiac arrest. An admission potassium of 3.0 to less than 3.5 mmol/L carried a 1.8-fold increased risk of in-hospital cardiac arrest, while a potassium of less than 3.0 was associated with a 2.7-fold increased risk.
A serum potassium below 3.0 mmol/L at admission also was associated with a 1.7-fold increased risk of new-onset atrial fibrillation.
These elevated risks of bad outcomes didn’t differ significantly between patients with ST-elevation MI, non-STEMI ACS, and those whose final diagnosis was not ACS, Dr. Faxén noted.
Session cochair David W. Walker, MD, medical director of the East Sussex (England) Healthcare NHS Trust, observed, “When I was a junior doctor I was always taught that when patients came onto coronary care we had to get their potassium to 4.5-5.0 mmol/L. I think you might want to change that advice now.”
“The implication would be that, if you intervene quickly in a patient with an abnormal potassium level, you might make a difference. Clearly, a potassium that’s too high is much worse than too low, since patients with in-hospital cardiac arrest can often be resuscitated,” Dr. Walker commented.
Dr. Faxén reported having no financial conflicts regarding his study, which was funded by the Swedish Heart and Lung Foundation and the Stockholm County Council.
AT THE ESC CONGRESS 2017
Key clinical point:
Major finding: Hyperkalemia of 5.0 to less than 5.5 mmol/L at admission for suspected ACS was associated with close to a twofold increased risk of in-hospital mortality.
Data source: The SWEDEHEART study is an ongoing prospective registry of patients with cardiovascular disease admitted to Stockholm County hospitals.
Disclosures: The presenter reported having no financial conflicts regarding his study, which was funded by the Swedish Heart and Lung Foundation and the Stockholm County Council.
Study: EHR malpractice claims rising
Malpractice claims involving the use of electronic health records (EHRs) are on the rise, according to data from The Doctors Company.
Cases in which EHRs were a factor grew from 2 claims during 2007-2010 to 161 claims from 2011 to December 2016, according an analysis published Oct. 16 by The Doctors Company, a national medical malpractice insurer.
The majority of EHR-related claims during 2014-2016 stemmed from incidents in a doctor’s office or a hospital clinic (35%), while the second most common location was a patient’s room. Malpractice claims involving EHRs were most commonly alleged against ob.gyns, followed by family physicians, and orthopedists. Diagnosis errors and improper medication management were the top most frequent allegations associated with EHR claims.
The analysis shows that while digitization of medicine has improved patient safety, it also has a dark side – as evidenced by the emergence of new kinds of errors, said Robert M. Wachter, MD, a professor at the University of California, San Francisco, and a member of the board of governors for The Doctors Company.
“This study makes an important contribution by chronicling actual errors, such as wrong medications selected from an autopick list, and helps point the way to changes ranging from physician education to EHR software design,” Dr. Wachter said in a statement.
[email protected]
On Twitter @legal_med
Malpractice claims involving the use of electronic health records (EHRs) are on the rise, according to data from The Doctors Company.
Cases in which EHRs were a factor grew from 2 claims during 2007-2010 to 161 claims from 2011 to December 2016, according an analysis published Oct. 16 by The Doctors Company, a national medical malpractice insurer.
The majority of EHR-related claims during 2014-2016 stemmed from incidents in a doctor’s office or a hospital clinic (35%), while the second most common location was a patient’s room. Malpractice claims involving EHRs were most commonly alleged against ob.gyns, followed by family physicians, and orthopedists. Diagnosis errors and improper medication management were the top most frequent allegations associated with EHR claims.
The analysis shows that while digitization of medicine has improved patient safety, it also has a dark side – as evidenced by the emergence of new kinds of errors, said Robert M. Wachter, MD, a professor at the University of California, San Francisco, and a member of the board of governors for The Doctors Company.
“This study makes an important contribution by chronicling actual errors, such as wrong medications selected from an autopick list, and helps point the way to changes ranging from physician education to EHR software design,” Dr. Wachter said in a statement.
[email protected]
On Twitter @legal_med
Malpractice claims involving the use of electronic health records (EHRs) are on the rise, according to data from The Doctors Company.
Cases in which EHRs were a factor grew from 2 claims during 2007-2010 to 161 claims from 2011 to December 2016, according an analysis published Oct. 16 by The Doctors Company, a national medical malpractice insurer.
The majority of EHR-related claims during 2014-2016 stemmed from incidents in a doctor’s office or a hospital clinic (35%), while the second most common location was a patient’s room. Malpractice claims involving EHRs were most commonly alleged against ob.gyns, followed by family physicians, and orthopedists. Diagnosis errors and improper medication management were the top most frequent allegations associated with EHR claims.
The analysis shows that while digitization of medicine has improved patient safety, it also has a dark side – as evidenced by the emergence of new kinds of errors, said Robert M. Wachter, MD, a professor at the University of California, San Francisco, and a member of the board of governors for The Doctors Company.
“This study makes an important contribution by chronicling actual errors, such as wrong medications selected from an autopick list, and helps point the way to changes ranging from physician education to EHR software design,” Dr. Wachter said in a statement.
[email protected]
On Twitter @legal_med
Key clinical point:
Major finding: Cases in which EHRs were a factor grew from 2 claims during 2007-2010 to 161 claims from 2011 to December 2016
Data source: Review of 163 claims from 2007 to 2016 in The Doctors Company database.
Disclosures: The study was funded by The Doctors Company.