User login
Pfizer seeks approval for updated COVID booster
Pfizer has sent an application to the Food and Drug Administration for emergency use authorization of its updated COVID-19 booster vaccine for the fall of 2022, the company announced on Aug. 22.
The vaccine, which is adapted for the BA.4 and BA.5 Omicron variants, would be meant for ages 12 and older. If authorized by the FDA, the doses could ship as soon as September.
“Having rapidly scaled up production, we are positioned to immediately begin distribution of the bivalent Omicron BA.4/BA.5 boosters, if authorized, to help protect individuals and families as we prepare for potential fall and winter surges,” Albert Bourla, PhD, Pfizer’s chairman and CEO, said in the statement.
Earlier this year, the FDA ordered vaccine makers such as Pfizer and Moderna to update their shots to target BA.4 and BA.5, which are better at escaping immunity from earlier vaccines and previous infections.
The United States has a contract to buy 105 million of the Pfizer doses and 66 million of the Moderna doses, according to The Associated Press. Moderna is expected to file its FDA application soon as well.
The new shots target both the original spike protein on the coronavirus and the spike mutations carried by BA.4 and BA.5. For now, BA.5 is causing 89% of new infections in the United States, followed by BA.4.6 with 6.3% and BA.4 with 4.3%, according to the latest Centers for Disease Control and Prevention data.
There’s no way to tell if BA.5 will still be the dominant strain this winter or if new variant will replace it, the AP reported. But public health officials have supported the updated boosters as a way to target the most recent strains and increase immunity again.
On Aug. 15, Great Britain became the first country to authorize another one of Moderna’s updated vaccines, which adds protection against BA.1, or the original Omicron strain that became dominant in the winter of 2021-2022. European regulators are considering this shot, the AP reported, but the United States opted not to use this version since new Omicron variants have become dominant.
To approve the latest Pfizer shot, the FDA will rely on scientific testing of prior updates to the vaccine, rather than the newest boosters, to decide whether to fast-track the updated shots for fall, the AP reported. This method is like how flu vaccines are updated each year without large studies that take months.
Previously, Pfizer announced results from a study that found the earlier Omicron update significantly boosted antibodies capable of fighting the BA.1 variant and provided some protection against BA.4 and BA.5. The company’s latest FDA application contains that data and animal testing on the newest booster, the AP reported.
Pfizer will start a trial using the BA.4/BA.5 booster in coming weeks to get more data on how well the latest shot works. Moderna has begun a similar study.
The full results from these studies won’t be available before a fall booster campaign, which is why the FDA and public health officials have called for an updated shot to be ready for distribution in September.
“It’s clear that none of these vaccines are going to completely prevent infection,” Rachel Presti, MD, a researcher with the Moderna trial and an infectious diseases specialist at Washington University in St. Louis, told the AP.
But previous studies of variant booster candidates have shown that “you still get a broader immune response giving a variant booster than giving the same booster,” she said.
A version of this article first appeared on WebMD.com.
Pfizer has sent an application to the Food and Drug Administration for emergency use authorization of its updated COVID-19 booster vaccine for the fall of 2022, the company announced on Aug. 22.
The vaccine, which is adapted for the BA.4 and BA.5 Omicron variants, would be meant for ages 12 and older. If authorized by the FDA, the doses could ship as soon as September.
“Having rapidly scaled up production, we are positioned to immediately begin distribution of the bivalent Omicron BA.4/BA.5 boosters, if authorized, to help protect individuals and families as we prepare for potential fall and winter surges,” Albert Bourla, PhD, Pfizer’s chairman and CEO, said in the statement.
Earlier this year, the FDA ordered vaccine makers such as Pfizer and Moderna to update their shots to target BA.4 and BA.5, which are better at escaping immunity from earlier vaccines and previous infections.
The United States has a contract to buy 105 million of the Pfizer doses and 66 million of the Moderna doses, according to The Associated Press. Moderna is expected to file its FDA application soon as well.
The new shots target both the original spike protein on the coronavirus and the spike mutations carried by BA.4 and BA.5. For now, BA.5 is causing 89% of new infections in the United States, followed by BA.4.6 with 6.3% and BA.4 with 4.3%, according to the latest Centers for Disease Control and Prevention data.
There’s no way to tell if BA.5 will still be the dominant strain this winter or if new variant will replace it, the AP reported. But public health officials have supported the updated boosters as a way to target the most recent strains and increase immunity again.
On Aug. 15, Great Britain became the first country to authorize another one of Moderna’s updated vaccines, which adds protection against BA.1, or the original Omicron strain that became dominant in the winter of 2021-2022. European regulators are considering this shot, the AP reported, but the United States opted not to use this version since new Omicron variants have become dominant.
To approve the latest Pfizer shot, the FDA will rely on scientific testing of prior updates to the vaccine, rather than the newest boosters, to decide whether to fast-track the updated shots for fall, the AP reported. This method is like how flu vaccines are updated each year without large studies that take months.
Previously, Pfizer announced results from a study that found the earlier Omicron update significantly boosted antibodies capable of fighting the BA.1 variant and provided some protection against BA.4 and BA.5. The company’s latest FDA application contains that data and animal testing on the newest booster, the AP reported.
Pfizer will start a trial using the BA.4/BA.5 booster in coming weeks to get more data on how well the latest shot works. Moderna has begun a similar study.
The full results from these studies won’t be available before a fall booster campaign, which is why the FDA and public health officials have called for an updated shot to be ready for distribution in September.
“It’s clear that none of these vaccines are going to completely prevent infection,” Rachel Presti, MD, a researcher with the Moderna trial and an infectious diseases specialist at Washington University in St. Louis, told the AP.
But previous studies of variant booster candidates have shown that “you still get a broader immune response giving a variant booster than giving the same booster,” she said.
A version of this article first appeared on WebMD.com.
Pfizer has sent an application to the Food and Drug Administration for emergency use authorization of its updated COVID-19 booster vaccine for the fall of 2022, the company announced on Aug. 22.
The vaccine, which is adapted for the BA.4 and BA.5 Omicron variants, would be meant for ages 12 and older. If authorized by the FDA, the doses could ship as soon as September.
“Having rapidly scaled up production, we are positioned to immediately begin distribution of the bivalent Omicron BA.4/BA.5 boosters, if authorized, to help protect individuals and families as we prepare for potential fall and winter surges,” Albert Bourla, PhD, Pfizer’s chairman and CEO, said in the statement.
Earlier this year, the FDA ordered vaccine makers such as Pfizer and Moderna to update their shots to target BA.4 and BA.5, which are better at escaping immunity from earlier vaccines and previous infections.
The United States has a contract to buy 105 million of the Pfizer doses and 66 million of the Moderna doses, according to The Associated Press. Moderna is expected to file its FDA application soon as well.
The new shots target both the original spike protein on the coronavirus and the spike mutations carried by BA.4 and BA.5. For now, BA.5 is causing 89% of new infections in the United States, followed by BA.4.6 with 6.3% and BA.4 with 4.3%, according to the latest Centers for Disease Control and Prevention data.
There’s no way to tell if BA.5 will still be the dominant strain this winter or if new variant will replace it, the AP reported. But public health officials have supported the updated boosters as a way to target the most recent strains and increase immunity again.
On Aug. 15, Great Britain became the first country to authorize another one of Moderna’s updated vaccines, which adds protection against BA.1, or the original Omicron strain that became dominant in the winter of 2021-2022. European regulators are considering this shot, the AP reported, but the United States opted not to use this version since new Omicron variants have become dominant.
To approve the latest Pfizer shot, the FDA will rely on scientific testing of prior updates to the vaccine, rather than the newest boosters, to decide whether to fast-track the updated shots for fall, the AP reported. This method is like how flu vaccines are updated each year without large studies that take months.
Previously, Pfizer announced results from a study that found the earlier Omicron update significantly boosted antibodies capable of fighting the BA.1 variant and provided some protection against BA.4 and BA.5. The company’s latest FDA application contains that data and animal testing on the newest booster, the AP reported.
Pfizer will start a trial using the BA.4/BA.5 booster in coming weeks to get more data on how well the latest shot works. Moderna has begun a similar study.
The full results from these studies won’t be available before a fall booster campaign, which is why the FDA and public health officials have called for an updated shot to be ready for distribution in September.
“It’s clear that none of these vaccines are going to completely prevent infection,” Rachel Presti, MD, a researcher with the Moderna trial and an infectious diseases specialist at Washington University in St. Louis, told the AP.
But previous studies of variant booster candidates have shown that “you still get a broader immune response giving a variant booster than giving the same booster,” she said.
A version of this article first appeared on WebMD.com.
Young children with leukemia are outliving teens
“Outcomes are improving. However, additional efforts, support, and resources are needed to further improve short- and long-term survival for acute leukemia survivors. Targeted efforts focused on populations that face greater disparities in their survival are needed to move the needle faster,” Michael Roth, MD, codirector of the Adolescent and Young Adult Oncology Program at the University of Texas M.D. Anderson Cancer Center, said in an interview.
In one study, released in The Lancet Child & Adolescent Health, an international team of researchers tracked survival outcomes from various types of leukemia in 61 nations. The study focused on the years 2000-2014 and followed patients aged 0-24.
“Age-standardized 5-year net survival in children, adolescents, and young adults for all leukemias combined during 2010-14 varied widely, ranging from 46% in Mexico to more than 85% in Canada, Cyprus, Belgium, Denmark, Finland, and Australia,” the researchers wrote. “Throughout 2000-14, survival from all leukemias combined remained consistently higher for children than adolescents and young adults, and minimal improvement was seen for adolescents and young adults in most countries.”
The U.S. data came from 41 states that cover 86% of the nation’s population, lead author Naomi Ssenyonga, a research fellow at London School of Hygiene & Tropical Medicine, said in an interview.
The 5-year survival rate for acute lymphoid leukemia (ALL) rose from 80% during 2000-2004 to 86% during 2010-2014. Survival in patients with acute myeloid leukemia (AML) was lower than for other subtypes: 66% in 2010-2014 vs. 57% in 2000-2004.
In regard to all leukemias, “we noted a steady increase in the U.S. of 6 percentage points in 5-year survival, up from 77% for patients diagnosed during 2000-2004 to 83% for those diagnosed during 2010-2014,” Ms. Ssenyonga said. “The gains were largely driven by the improvements seen among children.”
Why haven’t adolescents and young adults gained as much ground in survival?
“They often have unique clinical needs,” Ms. Ssenyonga said. “Over the past few years, adolescents and young adults with leukemia in some parts of the world, including the U.S., have increasingly been treated under pediatric protocols. This has led to higher survival. However, this approach has not been adopted consistently, and survival for adolescents and young adults with leukemia is still generally lower than survival for children.”
Gwen Nichols, MD, chief medical officer of the Leukemia & Lymphoma Society, agreed that pediatric treatment protocols hold promise as treatments for young adults. However, “because we arbitrarily set an age cutoff for being an adult, many of these patients are treated by an adult [nonpediatric] hematologist/oncologist, and some patients in the 20-39 age group do not receive the more intensive treatment regimens given to children,” she said in an interview.
In another study, published in Cancer Epidemiology, Biomarkers, & Prevention, M.D. Anderson Cancer Center’s Dr. Roth and colleagues tracked 1,938 patients with ALL and 2,350 with AML who were diagnosed at ages 15-39 from 1980 to 2009. All lived at least 5 years after diagnosis. In both groups, about 58% were White, and most of the rest were Hispanic. The median age of diagnosis for ALL was 23 (range: 15-39) and 28 years for AML (range: 15-39).
“For ALL, 10-year survival for those diagnosed in the 1980s, 1990s, and 2000s was 83%, 88%, and 88%, respectively,” the researchers reported. “Ten-year survival for AML was 82%, 90%, and 90% for those diagnosed in the 1980s, 1990s, and 2000s, respectively.”
“Early mortality within 10 years of diagnosis was mostly secondary to leukemia progressing or recurring. We believe that later mortality is secondary to the development of late side effects from their cancer treatment,” Dr. Roth said.
He noted that many adolescents and young adults with ALL or AML receive stem-cell transplants. “This treatment approach is effective. However, it is associated with short- and long-term toxicity that impacts patients’ health for many years after treatment.”
Indeed, up to 80% of acute leukemia survivors have significant health complications after therapy, said the Leukemia & Lymphoma Society’s Dr. Nichols, who wasn’t surprised by the findings. According to the society, “even when treatments are effective, more than 70% of childhood cancer survivors have a chronic health condition and 42% have a severe, disabling or life-threatening condition 30 years after diagnosis.”
“It would be interesting to understand the male predominance better,” she added, noting that the study found that male patients had worse long-term survival than females (survival time ratio: 0.61, 95% confidence interval, 0.45-0.82). “While it is tempting to suggest it is due to difference in cardiac disease, I am not aware of data to support why there is this survival difference.”
What’s next? “In ALL, we now have a number of new modalities to treat high-risk and relapsed disease such as antibodies and CAR-T,” Dr. Nichols said. “We anticipate that 5-year survival can improve utilizing these modalities due to getting more patients into remission, hopefully while reducing chemotherapeutic toxicity.”
Dr. Nichol’s also highlighted the society’s new genomic-led Pediatric Acute Leukemia (PedAL) Master Clinical Trial, which began enrolling children with acute leukemia in the United States and Canada this year, in an effort to transform medicine’s traditional high-level chemotherapy strategy to their care. The project was launched in collaboration with the National Cancer Institute, Children’s Oncology Group, and the European Pediatric Acute Leukemia Foundation.
As part of the screening process, the biology of each child’s cancer will be identified, and families will be encouraged to enroll them in appropriate targeted therapy trials.
“Until we are able to decrease the toxicity of leukemia regimens, we won’t see a dramatic shift in late effects and thus in morbidity and mortality,” Dr. Nichols said. “The trial is an effort to test newer, less toxic regimens to begin to change that cycle.”
The 5-year survival study was funded by Children with Cancer UK, Institut National du Cancer, La Ligue Contre le Cancer, Centers for Disease Control and Prevention, Swiss Re, Swiss Cancer Research foundation, Swiss Cancer League, Rossy Family Foundation, National Cancer Institute, and the American Cancer Society. One author reports a grant from Macmillan Cancer Support, consultancy fees from Pfizer, and unsolicited small gifts from Moondance Cancer Initiative for philanthropic work. The other authors report no disclosures.
The long-term survival study was funded by the National Cancer Institute, the Archer Foundation and LyondellBasell Industries. Dr. Roth reports no disclosures; other authors report various disclosures. Dr. Nichols reports no disclosures.
“Outcomes are improving. However, additional efforts, support, and resources are needed to further improve short- and long-term survival for acute leukemia survivors. Targeted efforts focused on populations that face greater disparities in their survival are needed to move the needle faster,” Michael Roth, MD, codirector of the Adolescent and Young Adult Oncology Program at the University of Texas M.D. Anderson Cancer Center, said in an interview.
In one study, released in The Lancet Child & Adolescent Health, an international team of researchers tracked survival outcomes from various types of leukemia in 61 nations. The study focused on the years 2000-2014 and followed patients aged 0-24.
“Age-standardized 5-year net survival in children, adolescents, and young adults for all leukemias combined during 2010-14 varied widely, ranging from 46% in Mexico to more than 85% in Canada, Cyprus, Belgium, Denmark, Finland, and Australia,” the researchers wrote. “Throughout 2000-14, survival from all leukemias combined remained consistently higher for children than adolescents and young adults, and minimal improvement was seen for adolescents and young adults in most countries.”
The U.S. data came from 41 states that cover 86% of the nation’s population, lead author Naomi Ssenyonga, a research fellow at London School of Hygiene & Tropical Medicine, said in an interview.
The 5-year survival rate for acute lymphoid leukemia (ALL) rose from 80% during 2000-2004 to 86% during 2010-2014. Survival in patients with acute myeloid leukemia (AML) was lower than for other subtypes: 66% in 2010-2014 vs. 57% in 2000-2004.
In regard to all leukemias, “we noted a steady increase in the U.S. of 6 percentage points in 5-year survival, up from 77% for patients diagnosed during 2000-2004 to 83% for those diagnosed during 2010-2014,” Ms. Ssenyonga said. “The gains were largely driven by the improvements seen among children.”
Why haven’t adolescents and young adults gained as much ground in survival?
“They often have unique clinical needs,” Ms. Ssenyonga said. “Over the past few years, adolescents and young adults with leukemia in some parts of the world, including the U.S., have increasingly been treated under pediatric protocols. This has led to higher survival. However, this approach has not been adopted consistently, and survival for adolescents and young adults with leukemia is still generally lower than survival for children.”
Gwen Nichols, MD, chief medical officer of the Leukemia & Lymphoma Society, agreed that pediatric treatment protocols hold promise as treatments for young adults. However, “because we arbitrarily set an age cutoff for being an adult, many of these patients are treated by an adult [nonpediatric] hematologist/oncologist, and some patients in the 20-39 age group do not receive the more intensive treatment regimens given to children,” she said in an interview.
In another study, published in Cancer Epidemiology, Biomarkers, & Prevention, M.D. Anderson Cancer Center’s Dr. Roth and colleagues tracked 1,938 patients with ALL and 2,350 with AML who were diagnosed at ages 15-39 from 1980 to 2009. All lived at least 5 years after diagnosis. In both groups, about 58% were White, and most of the rest were Hispanic. The median age of diagnosis for ALL was 23 (range: 15-39) and 28 years for AML (range: 15-39).
“For ALL, 10-year survival for those diagnosed in the 1980s, 1990s, and 2000s was 83%, 88%, and 88%, respectively,” the researchers reported. “Ten-year survival for AML was 82%, 90%, and 90% for those diagnosed in the 1980s, 1990s, and 2000s, respectively.”
“Early mortality within 10 years of diagnosis was mostly secondary to leukemia progressing or recurring. We believe that later mortality is secondary to the development of late side effects from their cancer treatment,” Dr. Roth said.
He noted that many adolescents and young adults with ALL or AML receive stem-cell transplants. “This treatment approach is effective. However, it is associated with short- and long-term toxicity that impacts patients’ health for many years after treatment.”
Indeed, up to 80% of acute leukemia survivors have significant health complications after therapy, said the Leukemia & Lymphoma Society’s Dr. Nichols, who wasn’t surprised by the findings. According to the society, “even when treatments are effective, more than 70% of childhood cancer survivors have a chronic health condition and 42% have a severe, disabling or life-threatening condition 30 years after diagnosis.”
“It would be interesting to understand the male predominance better,” she added, noting that the study found that male patients had worse long-term survival than females (survival time ratio: 0.61, 95% confidence interval, 0.45-0.82). “While it is tempting to suggest it is due to difference in cardiac disease, I am not aware of data to support why there is this survival difference.”
What’s next? “In ALL, we now have a number of new modalities to treat high-risk and relapsed disease such as antibodies and CAR-T,” Dr. Nichols said. “We anticipate that 5-year survival can improve utilizing these modalities due to getting more patients into remission, hopefully while reducing chemotherapeutic toxicity.”
Dr. Nichol’s also highlighted the society’s new genomic-led Pediatric Acute Leukemia (PedAL) Master Clinical Trial, which began enrolling children with acute leukemia in the United States and Canada this year, in an effort to transform medicine’s traditional high-level chemotherapy strategy to their care. The project was launched in collaboration with the National Cancer Institute, Children’s Oncology Group, and the European Pediatric Acute Leukemia Foundation.
As part of the screening process, the biology of each child’s cancer will be identified, and families will be encouraged to enroll them in appropriate targeted therapy trials.
“Until we are able to decrease the toxicity of leukemia regimens, we won’t see a dramatic shift in late effects and thus in morbidity and mortality,” Dr. Nichols said. “The trial is an effort to test newer, less toxic regimens to begin to change that cycle.”
The 5-year survival study was funded by Children with Cancer UK, Institut National du Cancer, La Ligue Contre le Cancer, Centers for Disease Control and Prevention, Swiss Re, Swiss Cancer Research foundation, Swiss Cancer League, Rossy Family Foundation, National Cancer Institute, and the American Cancer Society. One author reports a grant from Macmillan Cancer Support, consultancy fees from Pfizer, and unsolicited small gifts from Moondance Cancer Initiative for philanthropic work. The other authors report no disclosures.
The long-term survival study was funded by the National Cancer Institute, the Archer Foundation and LyondellBasell Industries. Dr. Roth reports no disclosures; other authors report various disclosures. Dr. Nichols reports no disclosures.
“Outcomes are improving. However, additional efforts, support, and resources are needed to further improve short- and long-term survival for acute leukemia survivors. Targeted efforts focused on populations that face greater disparities in their survival are needed to move the needle faster,” Michael Roth, MD, codirector of the Adolescent and Young Adult Oncology Program at the University of Texas M.D. Anderson Cancer Center, said in an interview.
In one study, released in The Lancet Child & Adolescent Health, an international team of researchers tracked survival outcomes from various types of leukemia in 61 nations. The study focused on the years 2000-2014 and followed patients aged 0-24.
“Age-standardized 5-year net survival in children, adolescents, and young adults for all leukemias combined during 2010-14 varied widely, ranging from 46% in Mexico to more than 85% in Canada, Cyprus, Belgium, Denmark, Finland, and Australia,” the researchers wrote. “Throughout 2000-14, survival from all leukemias combined remained consistently higher for children than adolescents and young adults, and minimal improvement was seen for adolescents and young adults in most countries.”
The U.S. data came from 41 states that cover 86% of the nation’s population, lead author Naomi Ssenyonga, a research fellow at London School of Hygiene & Tropical Medicine, said in an interview.
The 5-year survival rate for acute lymphoid leukemia (ALL) rose from 80% during 2000-2004 to 86% during 2010-2014. Survival in patients with acute myeloid leukemia (AML) was lower than for other subtypes: 66% in 2010-2014 vs. 57% in 2000-2004.
In regard to all leukemias, “we noted a steady increase in the U.S. of 6 percentage points in 5-year survival, up from 77% for patients diagnosed during 2000-2004 to 83% for those diagnosed during 2010-2014,” Ms. Ssenyonga said. “The gains were largely driven by the improvements seen among children.”
Why haven’t adolescents and young adults gained as much ground in survival?
“They often have unique clinical needs,” Ms. Ssenyonga said. “Over the past few years, adolescents and young adults with leukemia in some parts of the world, including the U.S., have increasingly been treated under pediatric protocols. This has led to higher survival. However, this approach has not been adopted consistently, and survival for adolescents and young adults with leukemia is still generally lower than survival for children.”
Gwen Nichols, MD, chief medical officer of the Leukemia & Lymphoma Society, agreed that pediatric treatment protocols hold promise as treatments for young adults. However, “because we arbitrarily set an age cutoff for being an adult, many of these patients are treated by an adult [nonpediatric] hematologist/oncologist, and some patients in the 20-39 age group do not receive the more intensive treatment regimens given to children,” she said in an interview.
In another study, published in Cancer Epidemiology, Biomarkers, & Prevention, M.D. Anderson Cancer Center’s Dr. Roth and colleagues tracked 1,938 patients with ALL and 2,350 with AML who were diagnosed at ages 15-39 from 1980 to 2009. All lived at least 5 years after diagnosis. In both groups, about 58% were White, and most of the rest were Hispanic. The median age of diagnosis for ALL was 23 (range: 15-39) and 28 years for AML (range: 15-39).
“For ALL, 10-year survival for those diagnosed in the 1980s, 1990s, and 2000s was 83%, 88%, and 88%, respectively,” the researchers reported. “Ten-year survival for AML was 82%, 90%, and 90% for those diagnosed in the 1980s, 1990s, and 2000s, respectively.”
“Early mortality within 10 years of diagnosis was mostly secondary to leukemia progressing or recurring. We believe that later mortality is secondary to the development of late side effects from their cancer treatment,” Dr. Roth said.
He noted that many adolescents and young adults with ALL or AML receive stem-cell transplants. “This treatment approach is effective. However, it is associated with short- and long-term toxicity that impacts patients’ health for many years after treatment.”
Indeed, up to 80% of acute leukemia survivors have significant health complications after therapy, said the Leukemia & Lymphoma Society’s Dr. Nichols, who wasn’t surprised by the findings. According to the society, “even when treatments are effective, more than 70% of childhood cancer survivors have a chronic health condition and 42% have a severe, disabling or life-threatening condition 30 years after diagnosis.”
“It would be interesting to understand the male predominance better,” she added, noting that the study found that male patients had worse long-term survival than females (survival time ratio: 0.61, 95% confidence interval, 0.45-0.82). “While it is tempting to suggest it is due to difference in cardiac disease, I am not aware of data to support why there is this survival difference.”
What’s next? “In ALL, we now have a number of new modalities to treat high-risk and relapsed disease such as antibodies and CAR-T,” Dr. Nichols said. “We anticipate that 5-year survival can improve utilizing these modalities due to getting more patients into remission, hopefully while reducing chemotherapeutic toxicity.”
Dr. Nichol’s also highlighted the society’s new genomic-led Pediatric Acute Leukemia (PedAL) Master Clinical Trial, which began enrolling children with acute leukemia in the United States and Canada this year, in an effort to transform medicine’s traditional high-level chemotherapy strategy to their care. The project was launched in collaboration with the National Cancer Institute, Children’s Oncology Group, and the European Pediatric Acute Leukemia Foundation.
As part of the screening process, the biology of each child’s cancer will be identified, and families will be encouraged to enroll them in appropriate targeted therapy trials.
“Until we are able to decrease the toxicity of leukemia regimens, we won’t see a dramatic shift in late effects and thus in morbidity and mortality,” Dr. Nichols said. “The trial is an effort to test newer, less toxic regimens to begin to change that cycle.”
The 5-year survival study was funded by Children with Cancer UK, Institut National du Cancer, La Ligue Contre le Cancer, Centers for Disease Control and Prevention, Swiss Re, Swiss Cancer Research foundation, Swiss Cancer League, Rossy Family Foundation, National Cancer Institute, and the American Cancer Society. One author reports a grant from Macmillan Cancer Support, consultancy fees from Pfizer, and unsolicited small gifts from Moondance Cancer Initiative for philanthropic work. The other authors report no disclosures.
The long-term survival study was funded by the National Cancer Institute, the Archer Foundation and LyondellBasell Industries. Dr. Roth reports no disclosures; other authors report various disclosures. Dr. Nichols reports no disclosures.
Are we up the creek without a paddle? What COVID, monkeypox, and nature are trying to tell us
Monkeypox. Polio. Covid. A quick glance at the news on any given day seems to indicate that outbreaks, epidemics, and perhaps even pandemics are increasing in frequency.
Granted, these types of events are hardly new; from the plagues of the 5th and 13th centuries to the Spanish flu in the 20th century and SARS-CoV-2 today, they’ve been with us from time immemorial.
What appears to be different, however, is not their frequency, but their intensity, with research reinforcing that we may be facing unique challenges and smaller windows to intervene as we move forward.
Findings from a modeling study, published in 2021 in Proceedings of the National Academy of Sciences, underscore that without effective intervention, the probability of extreme events like COVID-19 will likely increase threefold in the coming decades.
Amesh Adalja, MD, senior scholar, Johns Hopkins Center for Health Security, Baltimore, told this news organization.
“It’s all been based on some unusual cluster of cases that were causing severe disease and overwhelming local authorities. So often, like Indiana Jones, somebody got dispatched to deal with an outbreak,” Dr. Adalja said.
In a perfect post-COVID world, government bodies, scientists, clinicians, and others would cross silos to coordinate pandemic prevention, not just preparedness. The public would trust those who carry the title “public health” in their daily responsibilities, and in turn, public health experts would get back to their core responsibility – infectious disease preparedness – the role they were initially assigned following Europe’s Black Death during the 14th century. Instead, the world finds itself at a crossroads, with emerging and reemerging infectious disease outbreaks that on the surface appear to arise haphazardly but in reality are the result of decades of reaction and containment policies aimed at putting out fires, not addressing their cause.
Dr. Adalja noted that only when the threat of biological weapons became a reality in the mid-2000s was there a realization that economies of scale could be exploited by merging interests and efforts to develop health security medical countermeasures. For example, it encouraged governments to more closely integrate agencies like the Biomedical Advanced Research and Development Authority and infectious disease research organizations and individuals.
Still, while significant strides have been made in certain areas, the ongoing COVID-19 pandemic has revealed substantial weaknesses remaining in public and private health systems, as well as major gaps in infectious disease preparedness.
The role of spillover events
No matter whom you ask, scientists, public health and conservation experts, and infectious disease clinicians all point to one of the most important threats to human health. As Walt Kelly’s Pogo famously put it, “We have met the enemy, and he is us.”
“The reason why these outbreaks of novel infectious diseases are increasingly occurring is because of human-driven environmental change, particularly land use, unsafe practices when raising farmed animals, and commercial wildlife markets,” Neil M. Vora, MD, a physician specializing in pandemic prevention at Conservation International and a former Centers for Disease Control and Prevention epidemic intelligence officer, said in an interview.
In fact, more than 60% of emerging infections and diseases are due to these “spillover events” (zoonotic spillover) that occur when pathogens that commonly circulate in wildlife jump over to new, human hosts.
Several examples come to mind.
COVID-19 may have begun as an enzootic virus from two undetermined animals, using the Huanan Seafood Market as a possible intermediate reservoir, according to a July 26 preprint in the journal Science.
Likewise, while the Ebola virus was originally attributed to deforestation efforts to create palm oil (which allowed fruit bat carriers to transfer the virus to humans), recent research suggests that bats dwelling in the walls of human dwellings and hospitals are responsible for the 2018 outbreak in the Democratic Republic of Congo.
(Incidentally, just this week, a new Ebola case was confirmed in Eastern Congo, and it has been genetically linked to the previous outbreak, despite that outbreak having been declared over in early July.)
“When we clear forests, we create opportunities for humans to live alongside the forest edge and displace wildlife. There’s evidence that shows when [these] biodiverse areas are cleared, specialist species that evolved to live in the forests first start to disappear, whereas generalist species – rodents and bats – continue to survive and are able to carry pathogens that can be passed on to humans,” Dr. Vora explained.
So far, China’s outbreak of the novel Langya henipavirus is believed to have spread (either directly or indirectly) by rodents and shrews, according to reports from public health authorities like the European Centre for Disease Prevention and Control, which is currently monitoring the situation.
Yet, an overreliance on surveillance and containment only perpetuates what Dr. Vora says are cycles of panic and neglect.
“We saw it with Ebola in 2015, in 2016 to 2017 with Zika, you see it with tuberculosis, with sexually transmitted infections, and with COVID. You have policymakers working on solutions, and once they think that they’ve fixed the problem, they’re going to move on to the next crisis.”
It’s also a question of equity.
Reports detailing the reemergence of monkeypox in Nigeria in 2017 were largely ignored, despite the fact that the United States assisted in diagnosing an early case in an 11-year-old boy. At the time, it was clear that the virus was spreading by human-to-human transmission versus animal-to-human transmission, something that had not been seen previously.
“The current model [is] waiting for pathogens to spill over and then [continuing] to spread signals that rich countries are tolerant of these outbreaks so long as they don’t grow into epidemics or pandemics,” Dr. Vora said.
This model is clearly broken; roughly 5 years after Nigeria reported the resurgence of monkeypox, the United States has more than 14,000 confirmed cases, which represents more than a quarter of the total number of cases reported worldwide.
Public health on the brink
I’s difficult to imagine a future without outbreaks and more pandemics, and if experts are to be believed, we are ill-prepared.
“I think that we are in a situation where this is a major threat, and people have become complacent about it,” said Dr. Adalja, who noted that we should be asking ourselves if the “government is actually in a position to be able to respond in a way that we need them to or is [that response] tied up in bureaucracy and inefficiency?”
COVID-19 should have been seen as a wake-up call, and many of those deaths were preventable. “With monkeypox, they’re faltering; it should have been a layup, not a disaster,” he emphasized.
Ellen Eaton, MD, associate professor of infectious diseases at the University of Alabama at Birmingham, also pointed to the reality that by the time COVID-19 reached North America, the United States had already moved away from the model of the public health department as the epicenter of knowledge, education, awareness, and, ironically, public health.
“Thinking about my community, very few people knew the face and name of our local and state health officers,” she told this news organization.
“There was just this inherent mistrust of these people. If you add in a lot of talking heads, a lot of politicians and messaging from non-experts that countered what was coming out of our public health agencies early, you had this huge disconnect; in the South, it was the perfect storm for vaccine hesitancy.”
At last count, this perfect storm has led to 1.46 million COVID cases and just over 20,000 deaths – many of which were preventable – in Alabama alone.
“In certain parts of America, we were starting with a broken system with limited resources and few providers,” Dr. Eaton explained.
Dr. Eaton said that a lot of fields, not just medicine and public health, have finite resources that have been stretched to capacity by COVID, and now monkeypox, and wondered what was next as we’re headed into autumn and influenza season. But she also mentioned the tremendous implications of climate change on infectious diseases and community health and wellness.
“There’s a tremendous need to have the ability to survey not just humans but also how the disease burden in our environment that is fluctuating with climate change is going to impact communities in really important ways,” Dr. Eaton said.
Upstream prevention
Dr. Vora said he could not agree more and believes that upstream prevention holds the key.
“We have to make sure while there’s tension on this issue that the right solutions are implemented,” he said.
In coming years, postspillover containment strategies – vaccine research and development and strengthening health care surveillance, for example – are likely to become inadequate.
“We saw it with COVID and we are seeing it again with monkeypox,” Dr. Vora said. “We also have to invest further upstream to prevent spillovers in the first place, for example, by addressing deforestation, commercial wildlife markets and trade, [and] infection control when raising farm animals.”
“The thing is, when you invest in those upstream solutions, you are also mitigating climate change and loss of biodiversity. I’m not saying that we should not invest in postspillover containment efforts; we’re never going to contain every spillover. But we also have to invest in prevention,” he added.
In a piece published in Nature, Dr. Vora and his coauthors acknowledge that several international bodies such as the World Health Organization and G7 have invested in initiatives to facilitate coordinated, global responses to climate change, pandemic preparedness, and response. But they point out that these efforts fail to “explicitly address the negative feedback cycle between environmental degradation, wildlife exploitation, and the emergence of pathogens.”
“Environmental conservation is no longer a left-wing fringe issue, it’s moving into public consciousness, and ... it is public health,” Dr. Vora said. “When we destroy nature, we’re destroying our own ability to survive.”
Dr. Adalja, Dr. Vora, and Dr. Eaton report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Monkeypox. Polio. Covid. A quick glance at the news on any given day seems to indicate that outbreaks, epidemics, and perhaps even pandemics are increasing in frequency.
Granted, these types of events are hardly new; from the plagues of the 5th and 13th centuries to the Spanish flu in the 20th century and SARS-CoV-2 today, they’ve been with us from time immemorial.
What appears to be different, however, is not their frequency, but their intensity, with research reinforcing that we may be facing unique challenges and smaller windows to intervene as we move forward.
Findings from a modeling study, published in 2021 in Proceedings of the National Academy of Sciences, underscore that without effective intervention, the probability of extreme events like COVID-19 will likely increase threefold in the coming decades.
Amesh Adalja, MD, senior scholar, Johns Hopkins Center for Health Security, Baltimore, told this news organization.
“It’s all been based on some unusual cluster of cases that were causing severe disease and overwhelming local authorities. So often, like Indiana Jones, somebody got dispatched to deal with an outbreak,” Dr. Adalja said.
In a perfect post-COVID world, government bodies, scientists, clinicians, and others would cross silos to coordinate pandemic prevention, not just preparedness. The public would trust those who carry the title “public health” in their daily responsibilities, and in turn, public health experts would get back to their core responsibility – infectious disease preparedness – the role they were initially assigned following Europe’s Black Death during the 14th century. Instead, the world finds itself at a crossroads, with emerging and reemerging infectious disease outbreaks that on the surface appear to arise haphazardly but in reality are the result of decades of reaction and containment policies aimed at putting out fires, not addressing their cause.
Dr. Adalja noted that only when the threat of biological weapons became a reality in the mid-2000s was there a realization that economies of scale could be exploited by merging interests and efforts to develop health security medical countermeasures. For example, it encouraged governments to more closely integrate agencies like the Biomedical Advanced Research and Development Authority and infectious disease research organizations and individuals.
Still, while significant strides have been made in certain areas, the ongoing COVID-19 pandemic has revealed substantial weaknesses remaining in public and private health systems, as well as major gaps in infectious disease preparedness.
The role of spillover events
No matter whom you ask, scientists, public health and conservation experts, and infectious disease clinicians all point to one of the most important threats to human health. As Walt Kelly’s Pogo famously put it, “We have met the enemy, and he is us.”
“The reason why these outbreaks of novel infectious diseases are increasingly occurring is because of human-driven environmental change, particularly land use, unsafe practices when raising farmed animals, and commercial wildlife markets,” Neil M. Vora, MD, a physician specializing in pandemic prevention at Conservation International and a former Centers for Disease Control and Prevention epidemic intelligence officer, said in an interview.
In fact, more than 60% of emerging infections and diseases are due to these “spillover events” (zoonotic spillover) that occur when pathogens that commonly circulate in wildlife jump over to new, human hosts.
Several examples come to mind.
COVID-19 may have begun as an enzootic virus from two undetermined animals, using the Huanan Seafood Market as a possible intermediate reservoir, according to a July 26 preprint in the journal Science.
Likewise, while the Ebola virus was originally attributed to deforestation efforts to create palm oil (which allowed fruit bat carriers to transfer the virus to humans), recent research suggests that bats dwelling in the walls of human dwellings and hospitals are responsible for the 2018 outbreak in the Democratic Republic of Congo.
(Incidentally, just this week, a new Ebola case was confirmed in Eastern Congo, and it has been genetically linked to the previous outbreak, despite that outbreak having been declared over in early July.)
“When we clear forests, we create opportunities for humans to live alongside the forest edge and displace wildlife. There’s evidence that shows when [these] biodiverse areas are cleared, specialist species that evolved to live in the forests first start to disappear, whereas generalist species – rodents and bats – continue to survive and are able to carry pathogens that can be passed on to humans,” Dr. Vora explained.
So far, China’s outbreak of the novel Langya henipavirus is believed to have spread (either directly or indirectly) by rodents and shrews, according to reports from public health authorities like the European Centre for Disease Prevention and Control, which is currently monitoring the situation.
Yet, an overreliance on surveillance and containment only perpetuates what Dr. Vora says are cycles of panic and neglect.
“We saw it with Ebola in 2015, in 2016 to 2017 with Zika, you see it with tuberculosis, with sexually transmitted infections, and with COVID. You have policymakers working on solutions, and once they think that they’ve fixed the problem, they’re going to move on to the next crisis.”
It’s also a question of equity.
Reports detailing the reemergence of monkeypox in Nigeria in 2017 were largely ignored, despite the fact that the United States assisted in diagnosing an early case in an 11-year-old boy. At the time, it was clear that the virus was spreading by human-to-human transmission versus animal-to-human transmission, something that had not been seen previously.
“The current model [is] waiting for pathogens to spill over and then [continuing] to spread signals that rich countries are tolerant of these outbreaks so long as they don’t grow into epidemics or pandemics,” Dr. Vora said.
This model is clearly broken; roughly 5 years after Nigeria reported the resurgence of monkeypox, the United States has more than 14,000 confirmed cases, which represents more than a quarter of the total number of cases reported worldwide.
Public health on the brink
I’s difficult to imagine a future without outbreaks and more pandemics, and if experts are to be believed, we are ill-prepared.
“I think that we are in a situation where this is a major threat, and people have become complacent about it,” said Dr. Adalja, who noted that we should be asking ourselves if the “government is actually in a position to be able to respond in a way that we need them to or is [that response] tied up in bureaucracy and inefficiency?”
COVID-19 should have been seen as a wake-up call, and many of those deaths were preventable. “With monkeypox, they’re faltering; it should have been a layup, not a disaster,” he emphasized.
Ellen Eaton, MD, associate professor of infectious diseases at the University of Alabama at Birmingham, also pointed to the reality that by the time COVID-19 reached North America, the United States had already moved away from the model of the public health department as the epicenter of knowledge, education, awareness, and, ironically, public health.
“Thinking about my community, very few people knew the face and name of our local and state health officers,” she told this news organization.
“There was just this inherent mistrust of these people. If you add in a lot of talking heads, a lot of politicians and messaging from non-experts that countered what was coming out of our public health agencies early, you had this huge disconnect; in the South, it was the perfect storm for vaccine hesitancy.”
At last count, this perfect storm has led to 1.46 million COVID cases and just over 20,000 deaths – many of which were preventable – in Alabama alone.
“In certain parts of America, we were starting with a broken system with limited resources and few providers,” Dr. Eaton explained.
Dr. Eaton said that a lot of fields, not just medicine and public health, have finite resources that have been stretched to capacity by COVID, and now monkeypox, and wondered what was next as we’re headed into autumn and influenza season. But she also mentioned the tremendous implications of climate change on infectious diseases and community health and wellness.
“There’s a tremendous need to have the ability to survey not just humans but also how the disease burden in our environment that is fluctuating with climate change is going to impact communities in really important ways,” Dr. Eaton said.
Upstream prevention
Dr. Vora said he could not agree more and believes that upstream prevention holds the key.
“We have to make sure while there’s tension on this issue that the right solutions are implemented,” he said.
In coming years, postspillover containment strategies – vaccine research and development and strengthening health care surveillance, for example – are likely to become inadequate.
“We saw it with COVID and we are seeing it again with monkeypox,” Dr. Vora said. “We also have to invest further upstream to prevent spillovers in the first place, for example, by addressing deforestation, commercial wildlife markets and trade, [and] infection control when raising farm animals.”
“The thing is, when you invest in those upstream solutions, you are also mitigating climate change and loss of biodiversity. I’m not saying that we should not invest in postspillover containment efforts; we’re never going to contain every spillover. But we also have to invest in prevention,” he added.
In a piece published in Nature, Dr. Vora and his coauthors acknowledge that several international bodies such as the World Health Organization and G7 have invested in initiatives to facilitate coordinated, global responses to climate change, pandemic preparedness, and response. But they point out that these efforts fail to “explicitly address the negative feedback cycle between environmental degradation, wildlife exploitation, and the emergence of pathogens.”
“Environmental conservation is no longer a left-wing fringe issue, it’s moving into public consciousness, and ... it is public health,” Dr. Vora said. “When we destroy nature, we’re destroying our own ability to survive.”
Dr. Adalja, Dr. Vora, and Dr. Eaton report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Monkeypox. Polio. Covid. A quick glance at the news on any given day seems to indicate that outbreaks, epidemics, and perhaps even pandemics are increasing in frequency.
Granted, these types of events are hardly new; from the plagues of the 5th and 13th centuries to the Spanish flu in the 20th century and SARS-CoV-2 today, they’ve been with us from time immemorial.
What appears to be different, however, is not their frequency, but their intensity, with research reinforcing that we may be facing unique challenges and smaller windows to intervene as we move forward.
Findings from a modeling study, published in 2021 in Proceedings of the National Academy of Sciences, underscore that without effective intervention, the probability of extreme events like COVID-19 will likely increase threefold in the coming decades.
Amesh Adalja, MD, senior scholar, Johns Hopkins Center for Health Security, Baltimore, told this news organization.
“It’s all been based on some unusual cluster of cases that were causing severe disease and overwhelming local authorities. So often, like Indiana Jones, somebody got dispatched to deal with an outbreak,” Dr. Adalja said.
In a perfect post-COVID world, government bodies, scientists, clinicians, and others would cross silos to coordinate pandemic prevention, not just preparedness. The public would trust those who carry the title “public health” in their daily responsibilities, and in turn, public health experts would get back to their core responsibility – infectious disease preparedness – the role they were initially assigned following Europe’s Black Death during the 14th century. Instead, the world finds itself at a crossroads, with emerging and reemerging infectious disease outbreaks that on the surface appear to arise haphazardly but in reality are the result of decades of reaction and containment policies aimed at putting out fires, not addressing their cause.
Dr. Adalja noted that only when the threat of biological weapons became a reality in the mid-2000s was there a realization that economies of scale could be exploited by merging interests and efforts to develop health security medical countermeasures. For example, it encouraged governments to more closely integrate agencies like the Biomedical Advanced Research and Development Authority and infectious disease research organizations and individuals.
Still, while significant strides have been made in certain areas, the ongoing COVID-19 pandemic has revealed substantial weaknesses remaining in public and private health systems, as well as major gaps in infectious disease preparedness.
The role of spillover events
No matter whom you ask, scientists, public health and conservation experts, and infectious disease clinicians all point to one of the most important threats to human health. As Walt Kelly’s Pogo famously put it, “We have met the enemy, and he is us.”
“The reason why these outbreaks of novel infectious diseases are increasingly occurring is because of human-driven environmental change, particularly land use, unsafe practices when raising farmed animals, and commercial wildlife markets,” Neil M. Vora, MD, a physician specializing in pandemic prevention at Conservation International and a former Centers for Disease Control and Prevention epidemic intelligence officer, said in an interview.
In fact, more than 60% of emerging infections and diseases are due to these “spillover events” (zoonotic spillover) that occur when pathogens that commonly circulate in wildlife jump over to new, human hosts.
Several examples come to mind.
COVID-19 may have begun as an enzootic virus from two undetermined animals, using the Huanan Seafood Market as a possible intermediate reservoir, according to a July 26 preprint in the journal Science.
Likewise, while the Ebola virus was originally attributed to deforestation efforts to create palm oil (which allowed fruit bat carriers to transfer the virus to humans), recent research suggests that bats dwelling in the walls of human dwellings and hospitals are responsible for the 2018 outbreak in the Democratic Republic of Congo.
(Incidentally, just this week, a new Ebola case was confirmed in Eastern Congo, and it has been genetically linked to the previous outbreak, despite that outbreak having been declared over in early July.)
“When we clear forests, we create opportunities for humans to live alongside the forest edge and displace wildlife. There’s evidence that shows when [these] biodiverse areas are cleared, specialist species that evolved to live in the forests first start to disappear, whereas generalist species – rodents and bats – continue to survive and are able to carry pathogens that can be passed on to humans,” Dr. Vora explained.
So far, China’s outbreak of the novel Langya henipavirus is believed to have spread (either directly or indirectly) by rodents and shrews, according to reports from public health authorities like the European Centre for Disease Prevention and Control, which is currently monitoring the situation.
Yet, an overreliance on surveillance and containment only perpetuates what Dr. Vora says are cycles of panic and neglect.
“We saw it with Ebola in 2015, in 2016 to 2017 with Zika, you see it with tuberculosis, with sexually transmitted infections, and with COVID. You have policymakers working on solutions, and once they think that they’ve fixed the problem, they’re going to move on to the next crisis.”
It’s also a question of equity.
Reports detailing the reemergence of monkeypox in Nigeria in 2017 were largely ignored, despite the fact that the United States assisted in diagnosing an early case in an 11-year-old boy. At the time, it was clear that the virus was spreading by human-to-human transmission versus animal-to-human transmission, something that had not been seen previously.
“The current model [is] waiting for pathogens to spill over and then [continuing] to spread signals that rich countries are tolerant of these outbreaks so long as they don’t grow into epidemics or pandemics,” Dr. Vora said.
This model is clearly broken; roughly 5 years after Nigeria reported the resurgence of monkeypox, the United States has more than 14,000 confirmed cases, which represents more than a quarter of the total number of cases reported worldwide.
Public health on the brink
I’s difficult to imagine a future without outbreaks and more pandemics, and if experts are to be believed, we are ill-prepared.
“I think that we are in a situation where this is a major threat, and people have become complacent about it,” said Dr. Adalja, who noted that we should be asking ourselves if the “government is actually in a position to be able to respond in a way that we need them to or is [that response] tied up in bureaucracy and inefficiency?”
COVID-19 should have been seen as a wake-up call, and many of those deaths were preventable. “With monkeypox, they’re faltering; it should have been a layup, not a disaster,” he emphasized.
Ellen Eaton, MD, associate professor of infectious diseases at the University of Alabama at Birmingham, also pointed to the reality that by the time COVID-19 reached North America, the United States had already moved away from the model of the public health department as the epicenter of knowledge, education, awareness, and, ironically, public health.
“Thinking about my community, very few people knew the face and name of our local and state health officers,” she told this news organization.
“There was just this inherent mistrust of these people. If you add in a lot of talking heads, a lot of politicians and messaging from non-experts that countered what was coming out of our public health agencies early, you had this huge disconnect; in the South, it was the perfect storm for vaccine hesitancy.”
At last count, this perfect storm has led to 1.46 million COVID cases and just over 20,000 deaths – many of which were preventable – in Alabama alone.
“In certain parts of America, we were starting with a broken system with limited resources and few providers,” Dr. Eaton explained.
Dr. Eaton said that a lot of fields, not just medicine and public health, have finite resources that have been stretched to capacity by COVID, and now monkeypox, and wondered what was next as we’re headed into autumn and influenza season. But she also mentioned the tremendous implications of climate change on infectious diseases and community health and wellness.
“There’s a tremendous need to have the ability to survey not just humans but also how the disease burden in our environment that is fluctuating with climate change is going to impact communities in really important ways,” Dr. Eaton said.
Upstream prevention
Dr. Vora said he could not agree more and believes that upstream prevention holds the key.
“We have to make sure while there’s tension on this issue that the right solutions are implemented,” he said.
In coming years, postspillover containment strategies – vaccine research and development and strengthening health care surveillance, for example – are likely to become inadequate.
“We saw it with COVID and we are seeing it again with monkeypox,” Dr. Vora said. “We also have to invest further upstream to prevent spillovers in the first place, for example, by addressing deforestation, commercial wildlife markets and trade, [and] infection control when raising farm animals.”
“The thing is, when you invest in those upstream solutions, you are also mitigating climate change and loss of biodiversity. I’m not saying that we should not invest in postspillover containment efforts; we’re never going to contain every spillover. But we also have to invest in prevention,” he added.
In a piece published in Nature, Dr. Vora and his coauthors acknowledge that several international bodies such as the World Health Organization and G7 have invested in initiatives to facilitate coordinated, global responses to climate change, pandemic preparedness, and response. But they point out that these efforts fail to “explicitly address the negative feedback cycle between environmental degradation, wildlife exploitation, and the emergence of pathogens.”
“Environmental conservation is no longer a left-wing fringe issue, it’s moving into public consciousness, and ... it is public health,” Dr. Vora said. “When we destroy nature, we’re destroying our own ability to survive.”
Dr. Adalja, Dr. Vora, and Dr. Eaton report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pink Nodule Behind the Ear
The Diagnosis: Acanthoma Fissuratum
Acanthoma fissuratum is a skin lesion that results from consistent pressure, typically from ill-fitting eyeglass frames.1 The chronic irritation leads to collagen deposition and inflammation that gradually creates the lesion. Many patients never seek care, making incidence figures undeterminable.2 It usually presents as a firm, tender, flesh-colored or pink nodule or plaque with a central indentation from where the frame rests. This indentation splits the lesion in half and classically gives the appearance of a coffee bean.1 The repeated minor trauma at this point of contact also may lead to centralized ulceration, which further blurs the diagnosis to include basal cell carcinoma (BCC).3,4 Although the postauricular groove is the most cited location, lesions also may occur at other contact points of the glasses, such as the lateral aspect of the bridge of the nose and the superior auricular sulcus.5 Acanthoma fissuratum is not limited to the external head. Other etiologies of local trauma and pressure have led to its diagnosis in the upper labioalveolar fold, posterior fourchette of the vulva, penis, and external auditory canal.6-9
The diagnosis of acanthoma fissuratum mainly is clinical; however, due to its similar appearance to BCC and other lesions, a biopsy can be taken to support the diagnosis; a biopsy was not performed in our patient. The main features seen on histopathology include acanthosis, hyperkeratosis, variable parakeratosis, and perivascular nonspecific inflammatory infiltration. The epidermis may reflect the macroscopic frame indentation with central attenuation of the epidermis, which potentially is filled with inflammatory cells or keratin.5
Treatment normally encompasses removing the illfitting frames or fixing the fit, which gradually leads to reduction of the lesion.4,5 This occurred in our patient, who changed eyeglasses and saw an 80% resolution of the lesion in 8 months. Such improvement after removal of a trauma-inducing stimulus would not be seen in malignancies (eg, BCC, squamous cell carcinoma [SCC]), keloids, or cylindromas. If the granulation tissue does not regress or recurs, other potential treatments include excision, intralesional corticosteroids, and electrosurgery.5
Basal cell carcinoma is a common nonmelanoma skin cancer that most often presents on the sun-exposed areas of the head and neck, especially the cheeks, nasolabial folds, and forehead. Although the nodular subtype may clinically appear similar to acanthoma fissuratum, it more typically presents as a pearly papule or nodule with a sharp border, small telangiectases, and potential ulceration.10 Squamous cell carcinoma is another common nonmelanoma skin cancer that often arises in sun-exposed areas, which can include the postauricular area. Although the lesion can be associated with chronic wounds and also can grow vertically, SCC typically has a scalier and more hyperkeratotic surface that can ulcerate.1 A cylindroma is a benign sweat gland tumor that most commonly presents on the head and neck (also known as the turban tumor), though it can develop on the ear. It appears as solitary or multiple nodules that often are flesh colored, red, or blue with a shiny surface.1 Cylindromas are not known to be associated with chronic local trauma or irritation,11 such as wearing ill-fitting eyeglasses. Unlike acanthoma fissuratum, the treatment of cylindromas, BCC, and SCC most often involves excision.1 A keloid presents as a flesh-colored, red, or purple exophytic plaque that is composed of dense dermal tissue and progressively forms after local trauma. Although keloids can spontaneously develop, they commonly form on the ears in susceptible individuals after skin excisions including prior keloid removal, piercings, repairment of auricular traumas, or infections.1 The patient’s coffee bean–like lesion that coincided with wearing new eyeglasses better fits the diagnosis of acanthoma fissuratum than a keloid. Additionally, keloids typically do not regress without treatment. Keloid treatment consists of intralesional steroid injections, occlusive silicone dressings, compression, cryotherapy, radiation, and excisional surgery.1
- Sand M, Sand D, Brors D, et al. Cutaneous lesions of the external ear. Head Face Med. 2008;4. doi:10.1186/1746-160X-4-2
- Orengo I, Robbins K, Marsch A. Pathology of the ear. Semin Plast Surg. 2011;25:279-287. doi:10.1055/s-0031-1288920
- Ramroop S. Successful treatment of acanthoma fissuratum with intralesional triamcinolone acetonide. Clin Case Rep. 2020;8:702-703. doi:10.1002/ccr3.2708
- Delaney TJ, Stewart TW. Granuloma fissuratum. Br J Dermatol. 1971;84:373-375. doi:10.1111/j.1365-2133.1971.tb14235.x
- Deshpande NS, Sen A, Vasudevan B, et al. Acanthoma fissuratum: lest we forget. Indian Dermatol Online J. 2017;8:141-143. doi:10.4103/2229- 5178.202267
- Surron RL Jr. A fissured granulomatous lesion of the upper labioalveolar fold. Arch Dermatol Syph. 1932;26:425. doi:10.1001 /archderm.1932.01450030423004
- Kennedy CM, Dewdney S, Galask RP. Vulvar granuloma fissuratum: a description of fissuring of the posterior fourchette and the repair. Obstet Gynecol. 2005;105:1018-1023. doi:10.1097/01. AOG.0000158863.70819.53
- Lee JL, Lee YB, Cho BK, et al. Acanthoma fissuratum on the penis. Int J Dermatol. 2013;52:382-384. doi:10.1111/j.1365-4632.2011.04903.x
- Gonzalez SA, Moore AGN. Acanthoma fissuratum of the outer auditory canal from a hearing aid. J Cutan Pathol. 1989;16:304.
- Fania L, Didona D, Morese R, et al. Basal cell carcinoma: from pathophysiology to novel therapeutic approaches. Biomedicines. 2020;8:449. doi:10.3390/biomedicines8110449
- Chauhan DS, Guruprasad Y. Dermal cylindroma of the scalp. Natl J Maxillofac Surg. 2012;3:59-61. doi:10.4103/0975-5950.102163
The Diagnosis: Acanthoma Fissuratum
Acanthoma fissuratum is a skin lesion that results from consistent pressure, typically from ill-fitting eyeglass frames.1 The chronic irritation leads to collagen deposition and inflammation that gradually creates the lesion. Many patients never seek care, making incidence figures undeterminable.2 It usually presents as a firm, tender, flesh-colored or pink nodule or plaque with a central indentation from where the frame rests. This indentation splits the lesion in half and classically gives the appearance of a coffee bean.1 The repeated minor trauma at this point of contact also may lead to centralized ulceration, which further blurs the diagnosis to include basal cell carcinoma (BCC).3,4 Although the postauricular groove is the most cited location, lesions also may occur at other contact points of the glasses, such as the lateral aspect of the bridge of the nose and the superior auricular sulcus.5 Acanthoma fissuratum is not limited to the external head. Other etiologies of local trauma and pressure have led to its diagnosis in the upper labioalveolar fold, posterior fourchette of the vulva, penis, and external auditory canal.6-9
The diagnosis of acanthoma fissuratum mainly is clinical; however, due to its similar appearance to BCC and other lesions, a biopsy can be taken to support the diagnosis; a biopsy was not performed in our patient. The main features seen on histopathology include acanthosis, hyperkeratosis, variable parakeratosis, and perivascular nonspecific inflammatory infiltration. The epidermis may reflect the macroscopic frame indentation with central attenuation of the epidermis, which potentially is filled with inflammatory cells or keratin.5
Treatment normally encompasses removing the illfitting frames or fixing the fit, which gradually leads to reduction of the lesion.4,5 This occurred in our patient, who changed eyeglasses and saw an 80% resolution of the lesion in 8 months. Such improvement after removal of a trauma-inducing stimulus would not be seen in malignancies (eg, BCC, squamous cell carcinoma [SCC]), keloids, or cylindromas. If the granulation tissue does not regress or recurs, other potential treatments include excision, intralesional corticosteroids, and electrosurgery.5
Basal cell carcinoma is a common nonmelanoma skin cancer that most often presents on the sun-exposed areas of the head and neck, especially the cheeks, nasolabial folds, and forehead. Although the nodular subtype may clinically appear similar to acanthoma fissuratum, it more typically presents as a pearly papule or nodule with a sharp border, small telangiectases, and potential ulceration.10 Squamous cell carcinoma is another common nonmelanoma skin cancer that often arises in sun-exposed areas, which can include the postauricular area. Although the lesion can be associated with chronic wounds and also can grow vertically, SCC typically has a scalier and more hyperkeratotic surface that can ulcerate.1 A cylindroma is a benign sweat gland tumor that most commonly presents on the head and neck (also known as the turban tumor), though it can develop on the ear. It appears as solitary or multiple nodules that often are flesh colored, red, or blue with a shiny surface.1 Cylindromas are not known to be associated with chronic local trauma or irritation,11 such as wearing ill-fitting eyeglasses. Unlike acanthoma fissuratum, the treatment of cylindromas, BCC, and SCC most often involves excision.1 A keloid presents as a flesh-colored, red, or purple exophytic plaque that is composed of dense dermal tissue and progressively forms after local trauma. Although keloids can spontaneously develop, they commonly form on the ears in susceptible individuals after skin excisions including prior keloid removal, piercings, repairment of auricular traumas, or infections.1 The patient’s coffee bean–like lesion that coincided with wearing new eyeglasses better fits the diagnosis of acanthoma fissuratum than a keloid. Additionally, keloids typically do not regress without treatment. Keloid treatment consists of intralesional steroid injections, occlusive silicone dressings, compression, cryotherapy, radiation, and excisional surgery.1
The Diagnosis: Acanthoma Fissuratum
Acanthoma fissuratum is a skin lesion that results from consistent pressure, typically from ill-fitting eyeglass frames.1 The chronic irritation leads to collagen deposition and inflammation that gradually creates the lesion. Many patients never seek care, making incidence figures undeterminable.2 It usually presents as a firm, tender, flesh-colored or pink nodule or plaque with a central indentation from where the frame rests. This indentation splits the lesion in half and classically gives the appearance of a coffee bean.1 The repeated minor trauma at this point of contact also may lead to centralized ulceration, which further blurs the diagnosis to include basal cell carcinoma (BCC).3,4 Although the postauricular groove is the most cited location, lesions also may occur at other contact points of the glasses, such as the lateral aspect of the bridge of the nose and the superior auricular sulcus.5 Acanthoma fissuratum is not limited to the external head. Other etiologies of local trauma and pressure have led to its diagnosis in the upper labioalveolar fold, posterior fourchette of the vulva, penis, and external auditory canal.6-9
The diagnosis of acanthoma fissuratum mainly is clinical; however, due to its similar appearance to BCC and other lesions, a biopsy can be taken to support the diagnosis; a biopsy was not performed in our patient. The main features seen on histopathology include acanthosis, hyperkeratosis, variable parakeratosis, and perivascular nonspecific inflammatory infiltration. The epidermis may reflect the macroscopic frame indentation with central attenuation of the epidermis, which potentially is filled with inflammatory cells or keratin.5
Treatment normally encompasses removing the illfitting frames or fixing the fit, which gradually leads to reduction of the lesion.4,5 This occurred in our patient, who changed eyeglasses and saw an 80% resolution of the lesion in 8 months. Such improvement after removal of a trauma-inducing stimulus would not be seen in malignancies (eg, BCC, squamous cell carcinoma [SCC]), keloids, or cylindromas. If the granulation tissue does not regress or recurs, other potential treatments include excision, intralesional corticosteroids, and electrosurgery.5
Basal cell carcinoma is a common nonmelanoma skin cancer that most often presents on the sun-exposed areas of the head and neck, especially the cheeks, nasolabial folds, and forehead. Although the nodular subtype may clinically appear similar to acanthoma fissuratum, it more typically presents as a pearly papule or nodule with a sharp border, small telangiectases, and potential ulceration.10 Squamous cell carcinoma is another common nonmelanoma skin cancer that often arises in sun-exposed areas, which can include the postauricular area. Although the lesion can be associated with chronic wounds and also can grow vertically, SCC typically has a scalier and more hyperkeratotic surface that can ulcerate.1 A cylindroma is a benign sweat gland tumor that most commonly presents on the head and neck (also known as the turban tumor), though it can develop on the ear. It appears as solitary or multiple nodules that often are flesh colored, red, or blue with a shiny surface.1 Cylindromas are not known to be associated with chronic local trauma or irritation,11 such as wearing ill-fitting eyeglasses. Unlike acanthoma fissuratum, the treatment of cylindromas, BCC, and SCC most often involves excision.1 A keloid presents as a flesh-colored, red, or purple exophytic plaque that is composed of dense dermal tissue and progressively forms after local trauma. Although keloids can spontaneously develop, they commonly form on the ears in susceptible individuals after skin excisions including prior keloid removal, piercings, repairment of auricular traumas, or infections.1 The patient’s coffee bean–like lesion that coincided with wearing new eyeglasses better fits the diagnosis of acanthoma fissuratum than a keloid. Additionally, keloids typically do not regress without treatment. Keloid treatment consists of intralesional steroid injections, occlusive silicone dressings, compression, cryotherapy, radiation, and excisional surgery.1
- Sand M, Sand D, Brors D, et al. Cutaneous lesions of the external ear. Head Face Med. 2008;4. doi:10.1186/1746-160X-4-2
- Orengo I, Robbins K, Marsch A. Pathology of the ear. Semin Plast Surg. 2011;25:279-287. doi:10.1055/s-0031-1288920
- Ramroop S. Successful treatment of acanthoma fissuratum with intralesional triamcinolone acetonide. Clin Case Rep. 2020;8:702-703. doi:10.1002/ccr3.2708
- Delaney TJ, Stewart TW. Granuloma fissuratum. Br J Dermatol. 1971;84:373-375. doi:10.1111/j.1365-2133.1971.tb14235.x
- Deshpande NS, Sen A, Vasudevan B, et al. Acanthoma fissuratum: lest we forget. Indian Dermatol Online J. 2017;8:141-143. doi:10.4103/2229- 5178.202267
- Surron RL Jr. A fissured granulomatous lesion of the upper labioalveolar fold. Arch Dermatol Syph. 1932;26:425. doi:10.1001 /archderm.1932.01450030423004
- Kennedy CM, Dewdney S, Galask RP. Vulvar granuloma fissuratum: a description of fissuring of the posterior fourchette and the repair. Obstet Gynecol. 2005;105:1018-1023. doi:10.1097/01. AOG.0000158863.70819.53
- Lee JL, Lee YB, Cho BK, et al. Acanthoma fissuratum on the penis. Int J Dermatol. 2013;52:382-384. doi:10.1111/j.1365-4632.2011.04903.x
- Gonzalez SA, Moore AGN. Acanthoma fissuratum of the outer auditory canal from a hearing aid. J Cutan Pathol. 1989;16:304.
- Fania L, Didona D, Morese R, et al. Basal cell carcinoma: from pathophysiology to novel therapeutic approaches. Biomedicines. 2020;8:449. doi:10.3390/biomedicines8110449
- Chauhan DS, Guruprasad Y. Dermal cylindroma of the scalp. Natl J Maxillofac Surg. 2012;3:59-61. doi:10.4103/0975-5950.102163
- Sand M, Sand D, Brors D, et al. Cutaneous lesions of the external ear. Head Face Med. 2008;4. doi:10.1186/1746-160X-4-2
- Orengo I, Robbins K, Marsch A. Pathology of the ear. Semin Plast Surg. 2011;25:279-287. doi:10.1055/s-0031-1288920
- Ramroop S. Successful treatment of acanthoma fissuratum with intralesional triamcinolone acetonide. Clin Case Rep. 2020;8:702-703. doi:10.1002/ccr3.2708
- Delaney TJ, Stewart TW. Granuloma fissuratum. Br J Dermatol. 1971;84:373-375. doi:10.1111/j.1365-2133.1971.tb14235.x
- Deshpande NS, Sen A, Vasudevan B, et al. Acanthoma fissuratum: lest we forget. Indian Dermatol Online J. 2017;8:141-143. doi:10.4103/2229- 5178.202267
- Surron RL Jr. A fissured granulomatous lesion of the upper labioalveolar fold. Arch Dermatol Syph. 1932;26:425. doi:10.1001 /archderm.1932.01450030423004
- Kennedy CM, Dewdney S, Galask RP. Vulvar granuloma fissuratum: a description of fissuring of the posterior fourchette and the repair. Obstet Gynecol. 2005;105:1018-1023. doi:10.1097/01. AOG.0000158863.70819.53
- Lee JL, Lee YB, Cho BK, et al. Acanthoma fissuratum on the penis. Int J Dermatol. 2013;52:382-384. doi:10.1111/j.1365-4632.2011.04903.x
- Gonzalez SA, Moore AGN. Acanthoma fissuratum of the outer auditory canal from a hearing aid. J Cutan Pathol. 1989;16:304.
- Fania L, Didona D, Morese R, et al. Basal cell carcinoma: from pathophysiology to novel therapeutic approaches. Biomedicines. 2020;8:449. doi:10.3390/biomedicines8110449
- Chauhan DS, Guruprasad Y. Dermal cylindroma of the scalp. Natl J Maxillofac Surg. 2012;3:59-61. doi:10.4103/0975-5950.102163
A 62-year-old man presented to the dermatology office with a 1.5-cm, pink, rubbery nodule behind the left ear that sometimes was tender. He stated that the lesion gradually grew in size over the last 2 years, and it developed after he was fitted for new glasses.

Parameters of Scratch Pleasurability in the Management of Pruritic Conditions
To the Editor:
The itch-scratch cycle refers to the sequence created when a pruritic skin condition leads to scratching and skin barrier disruption, ultimately facilitating secondary skin changes and neural activation that prolongs pruritus. In patients with pruritic conditions, the itch-scratch cycle often can run unrestrained, with patients unaware of their scratching habits. Understanding what drives a patient to scratch, such as the pleasure gained from scratching, may be beneficial for dermatologists combating a patient’s scratching habits. The earliest documented attempts to understand the mechanism of an itch were made in Greece around the fifth century, but the pathophysiology of this sensation still is not fully understood. The Latin term pruritus refers to itching, irritation, or sexual excitement, while the Greek term knêsmos and related words also denote itch in an irritating or pleasurable sense.1 This paradoxical duality of irritation and pleasure is a phenomenon all too well understood by those affected with pruritic symptoms.
Although there are many measured characteristics of an itch, the pleasure granted from scratching an itch rarely is addressed. Understanding the factors influencing the pleasurability of scratching could help improve management and outcomes of patients’ pruritic conditions.
Pruritus is associated with a wide array of etiologies including dermatologic, infectious, metabolic, and autoimmune, but unanimously it evokes a strong desire to scratch. Scratching an itch often yields temporary relief from the irritation by dispensing a complex sensory concoction between pleasure and pain.2 The neurobiology behind this pleasure phenomenon is inconclusive. Some hypotheses point to how scratching-induced pleasure may be derived from the deactivation or inhibition of the unpleasant sensation of an itch in the central nervous system, the stimulation of the reward signals in the C-fiber system in the peripheral nervous system, the release of pruritis-inhibiting prostaglandin D2, or a combination of these pathways. Levels of sensation and pleasure induced from itch attenuation by scratching even vary based on anatomic location. One study demonstrated that, when compared to the forearms, the ankles and back perceived baseline induced itch most intensely, but no significant difference in perceived itch intensity was found between the ankles and back. Additionally, scratching an itchy back or ankle notably induced more pleasure when compared to the forearms, but there was no significant difference in scratching pleasurability between the ankle and back.3
Although there are adequate questionnaires and scales (eg, ItchyQoL,4 Skindex-16, Skindex-29) to quantify the severity of pruritus and its effects on a patient’s quality of life, these measurements do not assess the pleasure yielded from scratching, the impact of scratch pleasure on the patient experience, or the effect of scratch pleasure on the disease state.4 It appears that there are inadequate assessment tools to define factors associated with the pleasurability of scratching. A PubMed search of articles indexed for MEDLINE using the terms scratching pleasure scale and pruritus pleasure questionnaire yielded scarce results measuring patient perspectives on scratching-associated pleasure. A pertinent study performed by O’Neill et al5 compared the differences in itch characteristics between patients with psoriasis and those with atopic dermatitis using a web-based questionnaire featuring a numerical pleasure scale (ranging from −5 [highly unpleasurable] to +5 [highly pleasurable]) on an 11-point Likert scale. The questionnaire sought to measure the effects of scratching during a typical episode of itch within the past 2 weeks. Scratching was found pleasurable in both groups of patients.5 Another web-based questionnaire that characterized pleasurability in scratching a typical episode of itch in individuals with atopic dermatitis using a −5 to +5 Likert scale (−5 [highly unpleasurable] to +5 [highly pleasurable]) found that most participants perceived scratching as pleasurable and that there was a positive correlation between itch intensity and scratch pleasurability.6 Both of these studies quantified that scratching an itch is pleasurable, a correlation that may not come as a surprise. This direct correlation suggests that a more detailed analysis of this scratch pleasure could be beneficial in the management of pruritic conditions.
Treating the underlying cause of an itch is key to inhibiting the sensation; in some cases, anti-itch medications must be used. Current medications have limited effects on itch relief, but an expanding understanding of itch pathophysiology through clinical and laboratory research in the fields of dermatology, immunology, and neurology is paving the way for promising new therapeutic medications.7-11 In a review of the literature, Sanders and Akiyama12 elucidated the influence of stress and anxiety in scratching an itch and the way in which both pharmacologic and nonpharmacologic (ie, psychological and educational interventions) may be used to help break the itch-scratch cycle. Possible techniques include habit-reversal training, relaxation therapy, and cognitive behavioral therapy.13 Understanding patient perspectives on the pleasure yielded from scratching an itch and the disease factors that influence this pleasure seeking are paramount to reducing patient scratching. In understanding the pleasurability of scratching in pruritic conditions, the itch-scratch cycle and its accompanying deleterious effects (eg, stress, anxiety, pain, infection, secondary skin changes) can be broken.
The pleasure yielded from scratching an itch is a component of patient scratching habits that should be analyzed and quantified to reduce itch in pruritic conditions, mitigate damaging consequences of scratching, and improve the quality of life of patients with pruritic conditions. Furthermore, this understanding may help guide clinicians in management, such as counseling patients on the itch-scratch cycle and deciding which forthcoming medications could ameliorate a patient’s pruritic symptoms.
- Weisshaar E, Grüll V, König A, et al. The symptom of itch in medical history: highlights through the centuries. Int J Dermatol. 2009;48:1385-1394.
- Lavery MJ, Kinney MO, Mochizuki H, et al. Pruritus: an overview. what drives people to scratch an itch? Ulster Med J. 2016;85:164-173.
- Bin Saif GA, Papoiu ADP, Banari L, et al. The pleasurability of scratching an itch: a psychophysical and topographical assessment. Br J Dermatol. 2012;166:981-985.
- Desai NS, Poindexter GB, Monthrope YM, et al. A pilot quality-of-life instrument for pruritus. J Am Acad Dermatol. 2008;59:234-244.
- O’Neill JL, Chan YH, Rapp SR, et al. Differences in itch characteristics between psoriasis and atopic dermatitis patients: results of a web-based questionnaire. Acta Derm Venereol. 2011;91:537-540.
- Dawn A, Papoiu ADP, Chan YH, et al. Itch characteristics in atopic dermatitis: results of a web-based questionnaire. Br J Dermatol. 2009;160:642-644.
- Yosipovitch G, Rosen JD, Hashimoto T. Itch: from mechanism to (novel) therapeutic approaches. J Allergy Clin Immunol. 2018;142:1375-1390.
- Yosipovitch G, Misery L, Proksch E, et al. Skin barrier damage and itch: review of mechanisms, topical management and future directions. Acta Derm Venereol. 2019;99:1201-1209.
- Dong X, Dong X. Peripheral and central mechanisms of itch. Neuron. 2018;98:482-494.
- Lerner EA. Pathophysiology of itch. Dermatol Clin. 2018;36:175-177.
- Cevikbas F, Lerner EA. Physiology and pathophysiology of itch. Physiol Rev. 2020;100:945-982.
- Sanders KM, Akiyama T. The vicious cycle of itch and anxiety. Neurosci Biobehav Rev. 2018;87:17-26.
- Sanders KM, Nattkemper LA, Yosipovitch G. Advances in understanding itching and scratching: a new era of targeted treatments [published online August 22, 2016]. F1000Res. doi:10.12688/f1000research.8659.
To the Editor:
The itch-scratch cycle refers to the sequence created when a pruritic skin condition leads to scratching and skin barrier disruption, ultimately facilitating secondary skin changes and neural activation that prolongs pruritus. In patients with pruritic conditions, the itch-scratch cycle often can run unrestrained, with patients unaware of their scratching habits. Understanding what drives a patient to scratch, such as the pleasure gained from scratching, may be beneficial for dermatologists combating a patient’s scratching habits. The earliest documented attempts to understand the mechanism of an itch were made in Greece around the fifth century, but the pathophysiology of this sensation still is not fully understood. The Latin term pruritus refers to itching, irritation, or sexual excitement, while the Greek term knêsmos and related words also denote itch in an irritating or pleasurable sense.1 This paradoxical duality of irritation and pleasure is a phenomenon all too well understood by those affected with pruritic symptoms.
Although there are many measured characteristics of an itch, the pleasure granted from scratching an itch rarely is addressed. Understanding the factors influencing the pleasurability of scratching could help improve management and outcomes of patients’ pruritic conditions.
Pruritus is associated with a wide array of etiologies including dermatologic, infectious, metabolic, and autoimmune, but unanimously it evokes a strong desire to scratch. Scratching an itch often yields temporary relief from the irritation by dispensing a complex sensory concoction between pleasure and pain.2 The neurobiology behind this pleasure phenomenon is inconclusive. Some hypotheses point to how scratching-induced pleasure may be derived from the deactivation or inhibition of the unpleasant sensation of an itch in the central nervous system, the stimulation of the reward signals in the C-fiber system in the peripheral nervous system, the release of pruritis-inhibiting prostaglandin D2, or a combination of these pathways. Levels of sensation and pleasure induced from itch attenuation by scratching even vary based on anatomic location. One study demonstrated that, when compared to the forearms, the ankles and back perceived baseline induced itch most intensely, but no significant difference in perceived itch intensity was found between the ankles and back. Additionally, scratching an itchy back or ankle notably induced more pleasure when compared to the forearms, but there was no significant difference in scratching pleasurability between the ankle and back.3
Although there are adequate questionnaires and scales (eg, ItchyQoL,4 Skindex-16, Skindex-29) to quantify the severity of pruritus and its effects on a patient’s quality of life, these measurements do not assess the pleasure yielded from scratching, the impact of scratch pleasure on the patient experience, or the effect of scratch pleasure on the disease state.4 It appears that there are inadequate assessment tools to define factors associated with the pleasurability of scratching. A PubMed search of articles indexed for MEDLINE using the terms scratching pleasure scale and pruritus pleasure questionnaire yielded scarce results measuring patient perspectives on scratching-associated pleasure. A pertinent study performed by O’Neill et al5 compared the differences in itch characteristics between patients with psoriasis and those with atopic dermatitis using a web-based questionnaire featuring a numerical pleasure scale (ranging from −5 [highly unpleasurable] to +5 [highly pleasurable]) on an 11-point Likert scale. The questionnaire sought to measure the effects of scratching during a typical episode of itch within the past 2 weeks. Scratching was found pleasurable in both groups of patients.5 Another web-based questionnaire that characterized pleasurability in scratching a typical episode of itch in individuals with atopic dermatitis using a −5 to +5 Likert scale (−5 [highly unpleasurable] to +5 [highly pleasurable]) found that most participants perceived scratching as pleasurable and that there was a positive correlation between itch intensity and scratch pleasurability.6 Both of these studies quantified that scratching an itch is pleasurable, a correlation that may not come as a surprise. This direct correlation suggests that a more detailed analysis of this scratch pleasure could be beneficial in the management of pruritic conditions.
Treating the underlying cause of an itch is key to inhibiting the sensation; in some cases, anti-itch medications must be used. Current medications have limited effects on itch relief, but an expanding understanding of itch pathophysiology through clinical and laboratory research in the fields of dermatology, immunology, and neurology is paving the way for promising new therapeutic medications.7-11 In a review of the literature, Sanders and Akiyama12 elucidated the influence of stress and anxiety in scratching an itch and the way in which both pharmacologic and nonpharmacologic (ie, psychological and educational interventions) may be used to help break the itch-scratch cycle. Possible techniques include habit-reversal training, relaxation therapy, and cognitive behavioral therapy.13 Understanding patient perspectives on the pleasure yielded from scratching an itch and the disease factors that influence this pleasure seeking are paramount to reducing patient scratching. In understanding the pleasurability of scratching in pruritic conditions, the itch-scratch cycle and its accompanying deleterious effects (eg, stress, anxiety, pain, infection, secondary skin changes) can be broken.
The pleasure yielded from scratching an itch is a component of patient scratching habits that should be analyzed and quantified to reduce itch in pruritic conditions, mitigate damaging consequences of scratching, and improve the quality of life of patients with pruritic conditions. Furthermore, this understanding may help guide clinicians in management, such as counseling patients on the itch-scratch cycle and deciding which forthcoming medications could ameliorate a patient’s pruritic symptoms.
To the Editor:
The itch-scratch cycle refers to the sequence created when a pruritic skin condition leads to scratching and skin barrier disruption, ultimately facilitating secondary skin changes and neural activation that prolongs pruritus. In patients with pruritic conditions, the itch-scratch cycle often can run unrestrained, with patients unaware of their scratching habits. Understanding what drives a patient to scratch, such as the pleasure gained from scratching, may be beneficial for dermatologists combating a patient’s scratching habits. The earliest documented attempts to understand the mechanism of an itch were made in Greece around the fifth century, but the pathophysiology of this sensation still is not fully understood. The Latin term pruritus refers to itching, irritation, or sexual excitement, while the Greek term knêsmos and related words also denote itch in an irritating or pleasurable sense.1 This paradoxical duality of irritation and pleasure is a phenomenon all too well understood by those affected with pruritic symptoms.
Although there are many measured characteristics of an itch, the pleasure granted from scratching an itch rarely is addressed. Understanding the factors influencing the pleasurability of scratching could help improve management and outcomes of patients’ pruritic conditions.
Pruritus is associated with a wide array of etiologies including dermatologic, infectious, metabolic, and autoimmune, but unanimously it evokes a strong desire to scratch. Scratching an itch often yields temporary relief from the irritation by dispensing a complex sensory concoction between pleasure and pain.2 The neurobiology behind this pleasure phenomenon is inconclusive. Some hypotheses point to how scratching-induced pleasure may be derived from the deactivation or inhibition of the unpleasant sensation of an itch in the central nervous system, the stimulation of the reward signals in the C-fiber system in the peripheral nervous system, the release of pruritis-inhibiting prostaglandin D2, or a combination of these pathways. Levels of sensation and pleasure induced from itch attenuation by scratching even vary based on anatomic location. One study demonstrated that, when compared to the forearms, the ankles and back perceived baseline induced itch most intensely, but no significant difference in perceived itch intensity was found between the ankles and back. Additionally, scratching an itchy back or ankle notably induced more pleasure when compared to the forearms, but there was no significant difference in scratching pleasurability between the ankle and back.3
Although there are adequate questionnaires and scales (eg, ItchyQoL,4 Skindex-16, Skindex-29) to quantify the severity of pruritus and its effects on a patient’s quality of life, these measurements do not assess the pleasure yielded from scratching, the impact of scratch pleasure on the patient experience, or the effect of scratch pleasure on the disease state.4 It appears that there are inadequate assessment tools to define factors associated with the pleasurability of scratching. A PubMed search of articles indexed for MEDLINE using the terms scratching pleasure scale and pruritus pleasure questionnaire yielded scarce results measuring patient perspectives on scratching-associated pleasure. A pertinent study performed by O’Neill et al5 compared the differences in itch characteristics between patients with psoriasis and those with atopic dermatitis using a web-based questionnaire featuring a numerical pleasure scale (ranging from −5 [highly unpleasurable] to +5 [highly pleasurable]) on an 11-point Likert scale. The questionnaire sought to measure the effects of scratching during a typical episode of itch within the past 2 weeks. Scratching was found pleasurable in both groups of patients.5 Another web-based questionnaire that characterized pleasurability in scratching a typical episode of itch in individuals with atopic dermatitis using a −5 to +5 Likert scale (−5 [highly unpleasurable] to +5 [highly pleasurable]) found that most participants perceived scratching as pleasurable and that there was a positive correlation between itch intensity and scratch pleasurability.6 Both of these studies quantified that scratching an itch is pleasurable, a correlation that may not come as a surprise. This direct correlation suggests that a more detailed analysis of this scratch pleasure could be beneficial in the management of pruritic conditions.
Treating the underlying cause of an itch is key to inhibiting the sensation; in some cases, anti-itch medications must be used. Current medications have limited effects on itch relief, but an expanding understanding of itch pathophysiology through clinical and laboratory research in the fields of dermatology, immunology, and neurology is paving the way for promising new therapeutic medications.7-11 In a review of the literature, Sanders and Akiyama12 elucidated the influence of stress and anxiety in scratching an itch and the way in which both pharmacologic and nonpharmacologic (ie, psychological and educational interventions) may be used to help break the itch-scratch cycle. Possible techniques include habit-reversal training, relaxation therapy, and cognitive behavioral therapy.13 Understanding patient perspectives on the pleasure yielded from scratching an itch and the disease factors that influence this pleasure seeking are paramount to reducing patient scratching. In understanding the pleasurability of scratching in pruritic conditions, the itch-scratch cycle and its accompanying deleterious effects (eg, stress, anxiety, pain, infection, secondary skin changes) can be broken.
The pleasure yielded from scratching an itch is a component of patient scratching habits that should be analyzed and quantified to reduce itch in pruritic conditions, mitigate damaging consequences of scratching, and improve the quality of life of patients with pruritic conditions. Furthermore, this understanding may help guide clinicians in management, such as counseling patients on the itch-scratch cycle and deciding which forthcoming medications could ameliorate a patient’s pruritic symptoms.
- Weisshaar E, Grüll V, König A, et al. The symptom of itch in medical history: highlights through the centuries. Int J Dermatol. 2009;48:1385-1394.
- Lavery MJ, Kinney MO, Mochizuki H, et al. Pruritus: an overview. what drives people to scratch an itch? Ulster Med J. 2016;85:164-173.
- Bin Saif GA, Papoiu ADP, Banari L, et al. The pleasurability of scratching an itch: a psychophysical and topographical assessment. Br J Dermatol. 2012;166:981-985.
- Desai NS, Poindexter GB, Monthrope YM, et al. A pilot quality-of-life instrument for pruritus. J Am Acad Dermatol. 2008;59:234-244.
- O’Neill JL, Chan YH, Rapp SR, et al. Differences in itch characteristics between psoriasis and atopic dermatitis patients: results of a web-based questionnaire. Acta Derm Venereol. 2011;91:537-540.
- Dawn A, Papoiu ADP, Chan YH, et al. Itch characteristics in atopic dermatitis: results of a web-based questionnaire. Br J Dermatol. 2009;160:642-644.
- Yosipovitch G, Rosen JD, Hashimoto T. Itch: from mechanism to (novel) therapeutic approaches. J Allergy Clin Immunol. 2018;142:1375-1390.
- Yosipovitch G, Misery L, Proksch E, et al. Skin barrier damage and itch: review of mechanisms, topical management and future directions. Acta Derm Venereol. 2019;99:1201-1209.
- Dong X, Dong X. Peripheral and central mechanisms of itch. Neuron. 2018;98:482-494.
- Lerner EA. Pathophysiology of itch. Dermatol Clin. 2018;36:175-177.
- Cevikbas F, Lerner EA. Physiology and pathophysiology of itch. Physiol Rev. 2020;100:945-982.
- Sanders KM, Akiyama T. The vicious cycle of itch and anxiety. Neurosci Biobehav Rev. 2018;87:17-26.
- Sanders KM, Nattkemper LA, Yosipovitch G. Advances in understanding itching and scratching: a new era of targeted treatments [published online August 22, 2016]. F1000Res. doi:10.12688/f1000research.8659.
- Weisshaar E, Grüll V, König A, et al. The symptom of itch in medical history: highlights through the centuries. Int J Dermatol. 2009;48:1385-1394.
- Lavery MJ, Kinney MO, Mochizuki H, et al. Pruritus: an overview. what drives people to scratch an itch? Ulster Med J. 2016;85:164-173.
- Bin Saif GA, Papoiu ADP, Banari L, et al. The pleasurability of scratching an itch: a psychophysical and topographical assessment. Br J Dermatol. 2012;166:981-985.
- Desai NS, Poindexter GB, Monthrope YM, et al. A pilot quality-of-life instrument for pruritus. J Am Acad Dermatol. 2008;59:234-244.
- O’Neill JL, Chan YH, Rapp SR, et al. Differences in itch characteristics between psoriasis and atopic dermatitis patients: results of a web-based questionnaire. Acta Derm Venereol. 2011;91:537-540.
- Dawn A, Papoiu ADP, Chan YH, et al. Itch characteristics in atopic dermatitis: results of a web-based questionnaire. Br J Dermatol. 2009;160:642-644.
- Yosipovitch G, Rosen JD, Hashimoto T. Itch: from mechanism to (novel) therapeutic approaches. J Allergy Clin Immunol. 2018;142:1375-1390.
- Yosipovitch G, Misery L, Proksch E, et al. Skin barrier damage and itch: review of mechanisms, topical management and future directions. Acta Derm Venereol. 2019;99:1201-1209.
- Dong X, Dong X. Peripheral and central mechanisms of itch. Neuron. 2018;98:482-494.
- Lerner EA. Pathophysiology of itch. Dermatol Clin. 2018;36:175-177.
- Cevikbas F, Lerner EA. Physiology and pathophysiology of itch. Physiol Rev. 2020;100:945-982.
- Sanders KM, Akiyama T. The vicious cycle of itch and anxiety. Neurosci Biobehav Rev. 2018;87:17-26.
- Sanders KM, Nattkemper LA, Yosipovitch G. Advances in understanding itching and scratching: a new era of targeted treatments [published online August 22, 2016]. F1000Res. doi:10.12688/f1000research.8659.
Practice Points
- In individuals with pruritic skin conditions, the itch-scratch cycle can have damaging consequences such as anxiety, infection, and secondary skin changes.
- Understanding the pleasurability of scratching in pruritic skin conditions allows providers to help patients break the itch-scratch cycle and improve quality of life.
Digital therapy may ‘rewire’ the brain to improve tinnitus
, new research suggests. In a randomized controlled trial, results at 12 weeks showed patients with tinnitus reported clinically meaningful reductions in ratings of annoyance, inability to ignore, unpleasantness, and loudness after using a digital polytherapeutic app prototype that focuses on relief, relaxation, and attention-focused retraining. In addition, their improvements were significantly greater than for the control group, which received a common white noise app.
Researchers called the results “promising” for a condition that has no cure and few successful treatments. “What this therapy does is essentially rewire the brain in a way that de-emphasizes the sound of the tinnitus to a background noise that has no meaning or relevance to the listener,” lead author Grant Searchfield, PhD, associate professor of audiology at the University of Auckland, New Zealand, said in a press release.
The findings were published online in Frontiers in Neurology.
Worldwide problem
A recent study showed more than 740 million adults worldwide (nearly 15% of the population) have experienced at least one symptom of tinnitus – and about 120 million are severely affected. Tinnitus is the perception of a ringing, buzzing, whistling, or hissing noise in one or both ears when no external source of the sound is present. Often caused by damage to the auditory system, tinnitus can also be a symptom of a wide range of medical conditions and has been identified as a side effect of COVID-19 vaccination. In its most severe form, which is associated with hearing loss, tinnitus can also affect a patient’s mental, emotional, and social health.
For the current study, participants with tinnitus were randomly assigned to a popular app that uses white noise (control group, n = 30) or to the UpSilent app (n = 31). The UpSilent group received a smartphone app, Bluetooth bone conduction headphones, a Bluetooth neck pillow speaker for sleep, and written counseling materials. Participants in the control group received a widely available app called “White Noise” and in-ear wired headphones.
‘Quicker and more effective’
Both groups reported reductions in ratings of annoyance, inability to ignore, unpleasantness, and loudness at 12 weeks. But significantly more of the UpSilent group reported clinically meaningful improvement compared with the control group (65% vs. 43%, respectively; P = .049).
“Earlier trials have found white noise, goal-based counseling, goal-oriented games, and other technology-based therapies are effective for some people some of the time,” Dr. Searchfield said. “This is quicker and more effective, taking 12 weeks rather than 12 months for more individuals to gain some control,” he added.
The investigators noted that the study was not designed to determine which of the app’s functions of passive listening, active listening, or counseling contributed to symptom improvement.
The next step will be to refine the prototype and proceed to larger local and international trials with a view toward approval by the U.S. Food and Drug Administration, they reported.
The researchers hope the app will be clinically available in about 6 months.
The study was funded by Return on Science, Auckland UniServices. Dr. Searchfield is a founder and scientific officer for TrueSilence, a spinout company of the University of Auckland, and has a financial interest in TrueSilence. His coauthor has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests. In a randomized controlled trial, results at 12 weeks showed patients with tinnitus reported clinically meaningful reductions in ratings of annoyance, inability to ignore, unpleasantness, and loudness after using a digital polytherapeutic app prototype that focuses on relief, relaxation, and attention-focused retraining. In addition, their improvements were significantly greater than for the control group, which received a common white noise app.
Researchers called the results “promising” for a condition that has no cure and few successful treatments. “What this therapy does is essentially rewire the brain in a way that de-emphasizes the sound of the tinnitus to a background noise that has no meaning or relevance to the listener,” lead author Grant Searchfield, PhD, associate professor of audiology at the University of Auckland, New Zealand, said in a press release.
The findings were published online in Frontiers in Neurology.
Worldwide problem
A recent study showed more than 740 million adults worldwide (nearly 15% of the population) have experienced at least one symptom of tinnitus – and about 120 million are severely affected. Tinnitus is the perception of a ringing, buzzing, whistling, or hissing noise in one or both ears when no external source of the sound is present. Often caused by damage to the auditory system, tinnitus can also be a symptom of a wide range of medical conditions and has been identified as a side effect of COVID-19 vaccination. In its most severe form, which is associated with hearing loss, tinnitus can also affect a patient’s mental, emotional, and social health.
For the current study, participants with tinnitus were randomly assigned to a popular app that uses white noise (control group, n = 30) or to the UpSilent app (n = 31). The UpSilent group received a smartphone app, Bluetooth bone conduction headphones, a Bluetooth neck pillow speaker for sleep, and written counseling materials. Participants in the control group received a widely available app called “White Noise” and in-ear wired headphones.
‘Quicker and more effective’
Both groups reported reductions in ratings of annoyance, inability to ignore, unpleasantness, and loudness at 12 weeks. But significantly more of the UpSilent group reported clinically meaningful improvement compared with the control group (65% vs. 43%, respectively; P = .049).
“Earlier trials have found white noise, goal-based counseling, goal-oriented games, and other technology-based therapies are effective for some people some of the time,” Dr. Searchfield said. “This is quicker and more effective, taking 12 weeks rather than 12 months for more individuals to gain some control,” he added.
The investigators noted that the study was not designed to determine which of the app’s functions of passive listening, active listening, or counseling contributed to symptom improvement.
The next step will be to refine the prototype and proceed to larger local and international trials with a view toward approval by the U.S. Food and Drug Administration, they reported.
The researchers hope the app will be clinically available in about 6 months.
The study was funded by Return on Science, Auckland UniServices. Dr. Searchfield is a founder and scientific officer for TrueSilence, a spinout company of the University of Auckland, and has a financial interest in TrueSilence. His coauthor has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests. In a randomized controlled trial, results at 12 weeks showed patients with tinnitus reported clinically meaningful reductions in ratings of annoyance, inability to ignore, unpleasantness, and loudness after using a digital polytherapeutic app prototype that focuses on relief, relaxation, and attention-focused retraining. In addition, their improvements were significantly greater than for the control group, which received a common white noise app.
Researchers called the results “promising” for a condition that has no cure and few successful treatments. “What this therapy does is essentially rewire the brain in a way that de-emphasizes the sound of the tinnitus to a background noise that has no meaning or relevance to the listener,” lead author Grant Searchfield, PhD, associate professor of audiology at the University of Auckland, New Zealand, said in a press release.
The findings were published online in Frontiers in Neurology.
Worldwide problem
A recent study showed more than 740 million adults worldwide (nearly 15% of the population) have experienced at least one symptom of tinnitus – and about 120 million are severely affected. Tinnitus is the perception of a ringing, buzzing, whistling, or hissing noise in one or both ears when no external source of the sound is present. Often caused by damage to the auditory system, tinnitus can also be a symptom of a wide range of medical conditions and has been identified as a side effect of COVID-19 vaccination. In its most severe form, which is associated with hearing loss, tinnitus can also affect a patient’s mental, emotional, and social health.
For the current study, participants with tinnitus were randomly assigned to a popular app that uses white noise (control group, n = 30) or to the UpSilent app (n = 31). The UpSilent group received a smartphone app, Bluetooth bone conduction headphones, a Bluetooth neck pillow speaker for sleep, and written counseling materials. Participants in the control group received a widely available app called “White Noise” and in-ear wired headphones.
‘Quicker and more effective’
Both groups reported reductions in ratings of annoyance, inability to ignore, unpleasantness, and loudness at 12 weeks. But significantly more of the UpSilent group reported clinically meaningful improvement compared with the control group (65% vs. 43%, respectively; P = .049).
“Earlier trials have found white noise, goal-based counseling, goal-oriented games, and other technology-based therapies are effective for some people some of the time,” Dr. Searchfield said. “This is quicker and more effective, taking 12 weeks rather than 12 months for more individuals to gain some control,” he added.
The investigators noted that the study was not designed to determine which of the app’s functions of passive listening, active listening, or counseling contributed to symptom improvement.
The next step will be to refine the prototype and proceed to larger local and international trials with a view toward approval by the U.S. Food and Drug Administration, they reported.
The researchers hope the app will be clinically available in about 6 months.
The study was funded by Return on Science, Auckland UniServices. Dr. Searchfield is a founder and scientific officer for TrueSilence, a spinout company of the University of Auckland, and has a financial interest in TrueSilence. His coauthor has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM FRONTIERS IN NEUROLOGY
Multiple Eruptive Dermatofibromas Associated With Down Syndrome
To the Editor:
Dermatofibromas (also known as fibrous histiocytomas) are benign fibrous nodules that most often arise as solitary lesions on the lower extremities. Multiple eruptive dermatofibromas (MEDFs) are uncommon and have been defined as more than 15 in number1 or 5 to 8 dermatofibromas appearing within 4 months.2 They have been reported in association with a number of conditions of immune dysregulation such as systemic lupus erythematosus, Sjögren syndrome, HIV infection, and leukemia.3 Multiple eruptive dermatofibromas also have been described in patients with Down syndrome (DS).4-7 We report a case of MEDFs in a patient with DS and review the literature on the association between MEDFs and DS.
A 38-year-old woman with DS, hidradenitis suppurativa, and hypothyroidism presented with multiple cutaneous lesions developing over the last year. The lesions continued to increase in number but were otherwise asymptomatic. Physical examination revealed approximately 20 rubbery, pink-tan papules measuring less than 1 cm in diameter that were scattered along the trunk (Figure, A), arms, and legs (Figure, B).
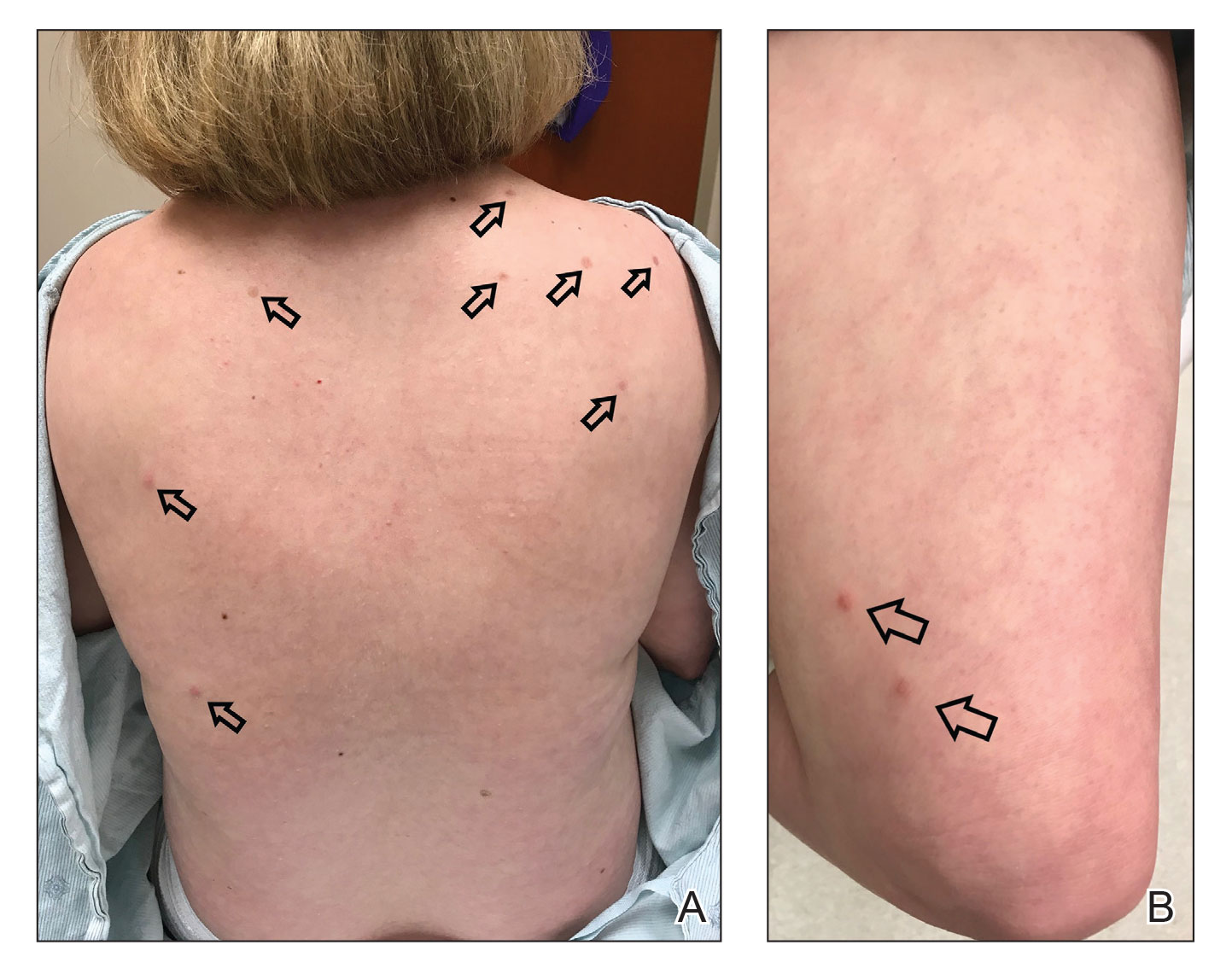
The patient had no known history of immunosuppression or rheumatologic disease and was otherwise healthy. Basic laboratory tests including a complete blood cell count and antinuclear antibody titer were within reference range. The lesions were clinically consistent with dermatofibromas, but due to their increasing number within a short period of time, a biopsy of a representative lesion was performed to confirm the diagnosis.
The exact incidence of MEDFs is unknown, but they are rare, with one review finding only 50 cases reported from 1960 to 2002.8 They are increasingly recognized as a sign of potential immune dysregulation. Approximately 56% to 70% of cases are seen in patients with an underlying disease state; 80% are immune mediated.8,9 Interestingly, DS has long been associated with notable immune dysfunction,10,11 with evidence suggesting that trisomy 21 may result in widespread changes in gene expression that can lead to interferon activation.12
A PubMed search of articles indexed for MEDLINE using the terms dermatofibroma and Down, dermatofibroma and Down syndrome, eruptive dermatofibroma and Down syndrome, and multiple dermatofibroma and Down syndrome revealed 6 cases of MEDFs in patients with DS that have been reported since 2005.4-7 An additional report by Honda et al13 described a patient with DS who developed 7 dermatofibromas, but no time frame of development was specified. We reviewed the characteristics of 8 patients with DS with MEDFs, which included our patient (Table). The average age at time of presentation was 39 years (median age, 40 years). Six patients (75%) were female and 2 (25%) were male. Dermatofibromas were reported to appear over the course of months to years. Comorbidities included psoriatic arthritis (treated with methotrexate),6 thyroid disorders (ie, Graves disease),6 hypercholesterolemia,6 hidradenitis suppurativa, long-standing mild lymphopenia (1.4×109/L [reference range, 1.5−4.0×109/L]),4 and acute megakaryoblastic leukemia13 treated 15 years before the appearance of dermatofibromas.
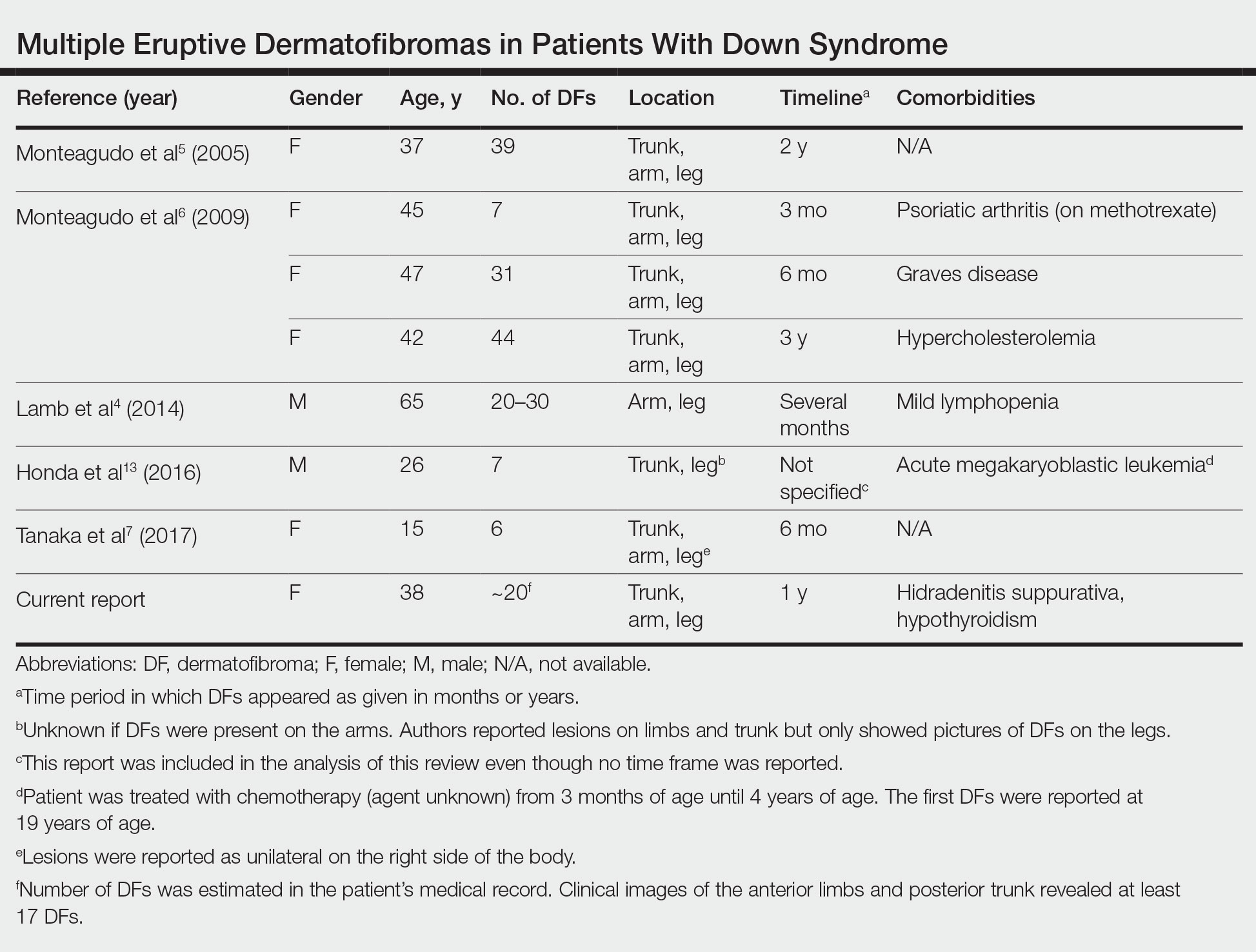
Many dermatologic conditions have been reported at increased rates in individuals with DS, including seborrheic dermatitis, alopecia areata, syringomas, elastosis perforans serpiginosa, cutis marmorata, xerosis, and palmoplantar hyperkeratosis.14,15 Although drawing conclusions about associations between MEDFs and DS is limited by our small sample size, we have reported this case and reviewed existing cases of MEDFs in DS to highlight a potential association that may be underrecognized or underreported. More evidence is needed to determine the strength of the association between MEDFs and DS, but dermatologists should be aware that MEDFs may be an additional skin finding associated with DS that is related to the syndrome’s immune dysregulation.
- Baraf CS, Shapiro L. Multiple histiocytomas: report of a case. Arch Dermatol. 1970;101:588-590.
- Ammirati CT, Mann C, Hornstra IK. Multiple eruptive dermatofibromas in three men with HIV infection. Dermatology. 1997;4:344-348.
- Zaccaria E, Rebora A, Rongioletti F. Multiple eruptive dermatofibromas and immunosuppression: report of two cases and review of the literature. Int J Dermatol. 2008;47:723-727.
- Lamb RC, Gangopadhyay M, MacDonald A. Multiple dermatofibromas in Down syndrome. Int J Dermatol. 2014;53:E274-E275.
- Monteagudo B, Álvarez-Fernández JC, Iglesias B, et al. Multiple eruptive dermatofibromas in a patient with Down’s syndrome [article in Spanish]. Actas Dermosifiliogr. 2005;96:199.
- Monteagudo B, Suárez-Amor O, Cabanillas M, et al. Down syndrome: another cause of immunosuppression associated with multiple eruptive dermatofibroma? [article in Spanish]. Dermatol Online J. 2009;15:15.
- Tanaka M, Hoashi T, Serizawa N, et al. Multiple unilaterally localized dermatofibromas in a patient with Down syndrome. J Dermatol. 2017;44:1074-1076.
- Niiyama S, Katsuoka K, Happle R, et al. Multiple eruptive dermatofibromas: a review of the literature. Acta Derm Venereol. 2002;82:241-244.
- Her Y, Ku SH, Kim KH. A case of multiple eruptive dermatofibromas in a healthy adult. Ann Dermatol. 2014;26:539-540.
- Bertotto A, Arcangeli C, Crupi S, et al. T cell response to anti-CD3 antibody in Down’s syndrome. Arch Dis Child. 1987;62:1148-1151.
- Kusters MA, Verstegen RH, Gemen EF, et al. Intrinsic defect of the immune system in children with Down syndrome: a review. Clin Exp Immunol. 2009;156:189-193.
- Sullivan KD, Evans D, Pandey A, et al. Trisomy 21 causes changes in the circulating proteome indicative of chronic inflammation. Sci Rep. 2017;7:14818.
- Honda M, Tomimura S, de Vega S, et al. Multiple dermatofibromas in a patient with Down syndrome. J Dermatol. 2016;43:346-348.
- Daneshpazhooh M, Nazemi TM, Bigdeloo L, et al. Mucocutaneous findings in 100 children with Down syndrome. Pediatr Dermatol. 2007;24:317-320.
- Madan V, Williams J, Lear JT. Dermatological manifestations of Down’s syndrome. Clin Exp Dermatol. 2006;31:623-629.
To the Editor:
Dermatofibromas (also known as fibrous histiocytomas) are benign fibrous nodules that most often arise as solitary lesions on the lower extremities. Multiple eruptive dermatofibromas (MEDFs) are uncommon and have been defined as more than 15 in number1 or 5 to 8 dermatofibromas appearing within 4 months.2 They have been reported in association with a number of conditions of immune dysregulation such as systemic lupus erythematosus, Sjögren syndrome, HIV infection, and leukemia.3 Multiple eruptive dermatofibromas also have been described in patients with Down syndrome (DS).4-7 We report a case of MEDFs in a patient with DS and review the literature on the association between MEDFs and DS.
A 38-year-old woman with DS, hidradenitis suppurativa, and hypothyroidism presented with multiple cutaneous lesions developing over the last year. The lesions continued to increase in number but were otherwise asymptomatic. Physical examination revealed approximately 20 rubbery, pink-tan papules measuring less than 1 cm in diameter that were scattered along the trunk (Figure, A), arms, and legs (Figure, B).
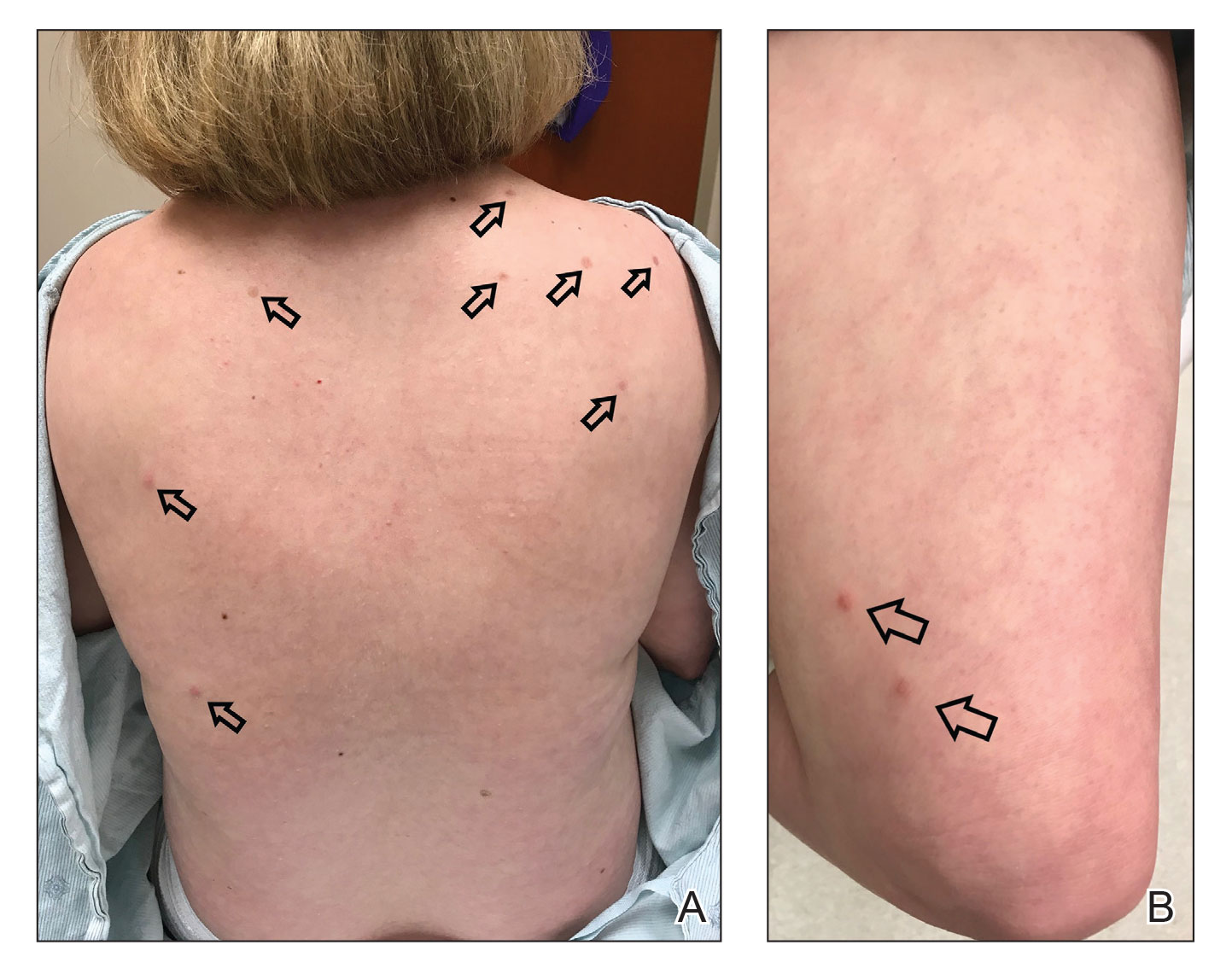
The patient had no known history of immunosuppression or rheumatologic disease and was otherwise healthy. Basic laboratory tests including a complete blood cell count and antinuclear antibody titer were within reference range. The lesions were clinically consistent with dermatofibromas, but due to their increasing number within a short period of time, a biopsy of a representative lesion was performed to confirm the diagnosis.
The exact incidence of MEDFs is unknown, but they are rare, with one review finding only 50 cases reported from 1960 to 2002.8 They are increasingly recognized as a sign of potential immune dysregulation. Approximately 56% to 70% of cases are seen in patients with an underlying disease state; 80% are immune mediated.8,9 Interestingly, DS has long been associated with notable immune dysfunction,10,11 with evidence suggesting that trisomy 21 may result in widespread changes in gene expression that can lead to interferon activation.12
A PubMed search of articles indexed for MEDLINE using the terms dermatofibroma and Down, dermatofibroma and Down syndrome, eruptive dermatofibroma and Down syndrome, and multiple dermatofibroma and Down syndrome revealed 6 cases of MEDFs in patients with DS that have been reported since 2005.4-7 An additional report by Honda et al13 described a patient with DS who developed 7 dermatofibromas, but no time frame of development was specified. We reviewed the characteristics of 8 patients with DS with MEDFs, which included our patient (Table). The average age at time of presentation was 39 years (median age, 40 years). Six patients (75%) were female and 2 (25%) were male. Dermatofibromas were reported to appear over the course of months to years. Comorbidities included psoriatic arthritis (treated with methotrexate),6 thyroid disorders (ie, Graves disease),6 hypercholesterolemia,6 hidradenitis suppurativa, long-standing mild lymphopenia (1.4×109/L [reference range, 1.5−4.0×109/L]),4 and acute megakaryoblastic leukemia13 treated 15 years before the appearance of dermatofibromas.
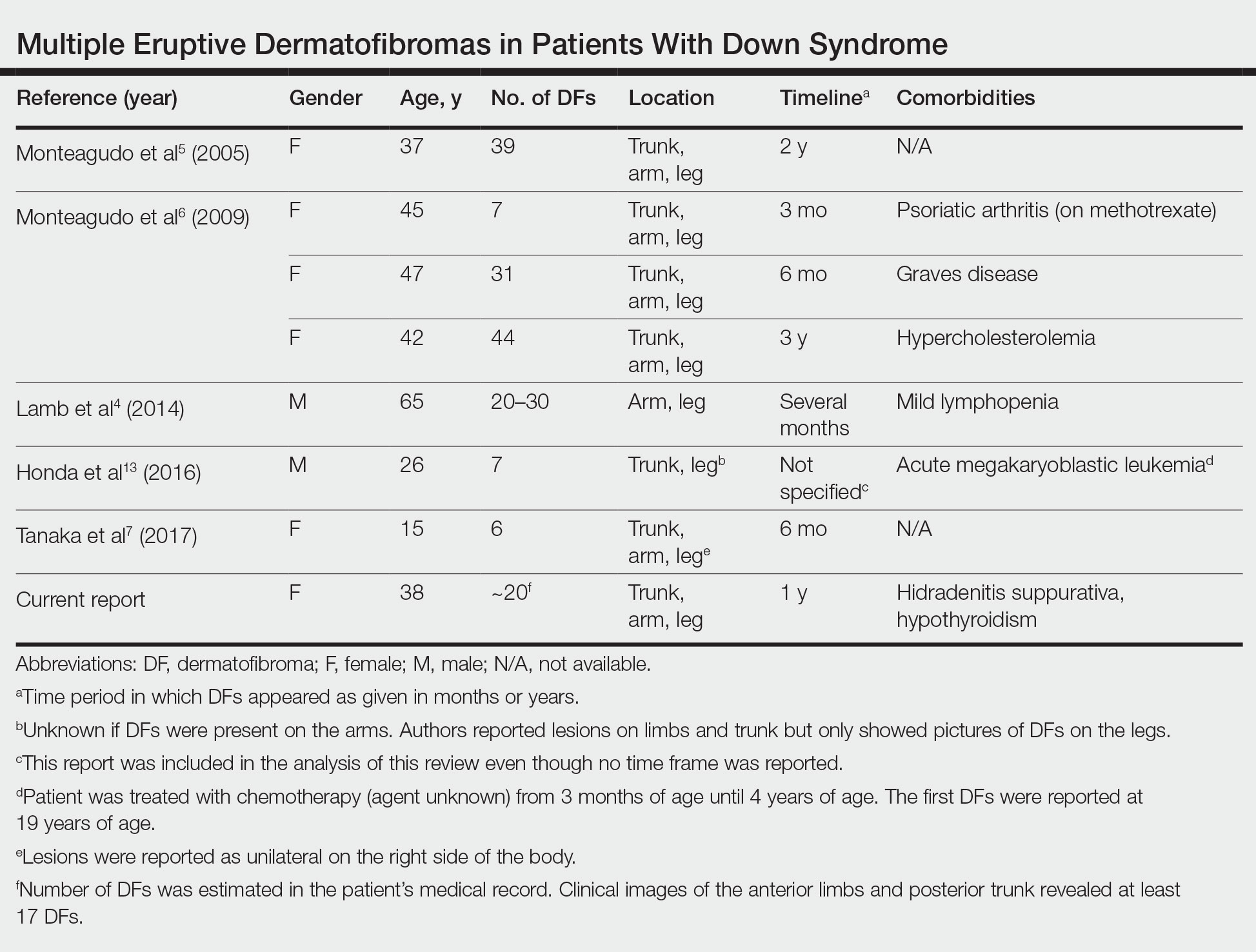
Many dermatologic conditions have been reported at increased rates in individuals with DS, including seborrheic dermatitis, alopecia areata, syringomas, elastosis perforans serpiginosa, cutis marmorata, xerosis, and palmoplantar hyperkeratosis.14,15 Although drawing conclusions about associations between MEDFs and DS is limited by our small sample size, we have reported this case and reviewed existing cases of MEDFs in DS to highlight a potential association that may be underrecognized or underreported. More evidence is needed to determine the strength of the association between MEDFs and DS, but dermatologists should be aware that MEDFs may be an additional skin finding associated with DS that is related to the syndrome’s immune dysregulation.
To the Editor:
Dermatofibromas (also known as fibrous histiocytomas) are benign fibrous nodules that most often arise as solitary lesions on the lower extremities. Multiple eruptive dermatofibromas (MEDFs) are uncommon and have been defined as more than 15 in number1 or 5 to 8 dermatofibromas appearing within 4 months.2 They have been reported in association with a number of conditions of immune dysregulation such as systemic lupus erythematosus, Sjögren syndrome, HIV infection, and leukemia.3 Multiple eruptive dermatofibromas also have been described in patients with Down syndrome (DS).4-7 We report a case of MEDFs in a patient with DS and review the literature on the association between MEDFs and DS.
A 38-year-old woman with DS, hidradenitis suppurativa, and hypothyroidism presented with multiple cutaneous lesions developing over the last year. The lesions continued to increase in number but were otherwise asymptomatic. Physical examination revealed approximately 20 rubbery, pink-tan papules measuring less than 1 cm in diameter that were scattered along the trunk (Figure, A), arms, and legs (Figure, B).
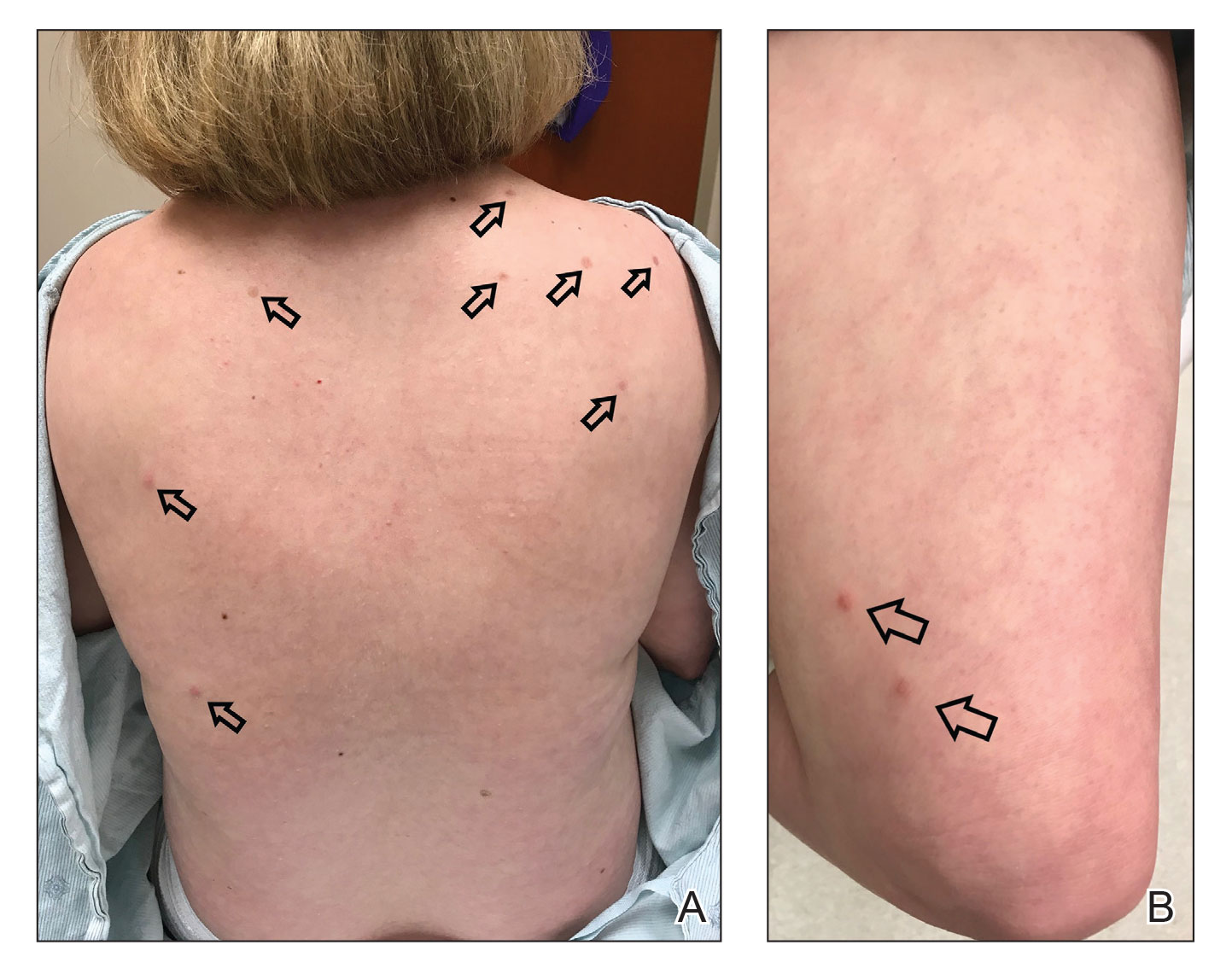
The patient had no known history of immunosuppression or rheumatologic disease and was otherwise healthy. Basic laboratory tests including a complete blood cell count and antinuclear antibody titer were within reference range. The lesions were clinically consistent with dermatofibromas, but due to their increasing number within a short period of time, a biopsy of a representative lesion was performed to confirm the diagnosis.
The exact incidence of MEDFs is unknown, but they are rare, with one review finding only 50 cases reported from 1960 to 2002.8 They are increasingly recognized as a sign of potential immune dysregulation. Approximately 56% to 70% of cases are seen in patients with an underlying disease state; 80% are immune mediated.8,9 Interestingly, DS has long been associated with notable immune dysfunction,10,11 with evidence suggesting that trisomy 21 may result in widespread changes in gene expression that can lead to interferon activation.12
A PubMed search of articles indexed for MEDLINE using the terms dermatofibroma and Down, dermatofibroma and Down syndrome, eruptive dermatofibroma and Down syndrome, and multiple dermatofibroma and Down syndrome revealed 6 cases of MEDFs in patients with DS that have been reported since 2005.4-7 An additional report by Honda et al13 described a patient with DS who developed 7 dermatofibromas, but no time frame of development was specified. We reviewed the characteristics of 8 patients with DS with MEDFs, which included our patient (Table). The average age at time of presentation was 39 years (median age, 40 years). Six patients (75%) were female and 2 (25%) were male. Dermatofibromas were reported to appear over the course of months to years. Comorbidities included psoriatic arthritis (treated with methotrexate),6 thyroid disorders (ie, Graves disease),6 hypercholesterolemia,6 hidradenitis suppurativa, long-standing mild lymphopenia (1.4×109/L [reference range, 1.5−4.0×109/L]),4 and acute megakaryoblastic leukemia13 treated 15 years before the appearance of dermatofibromas.
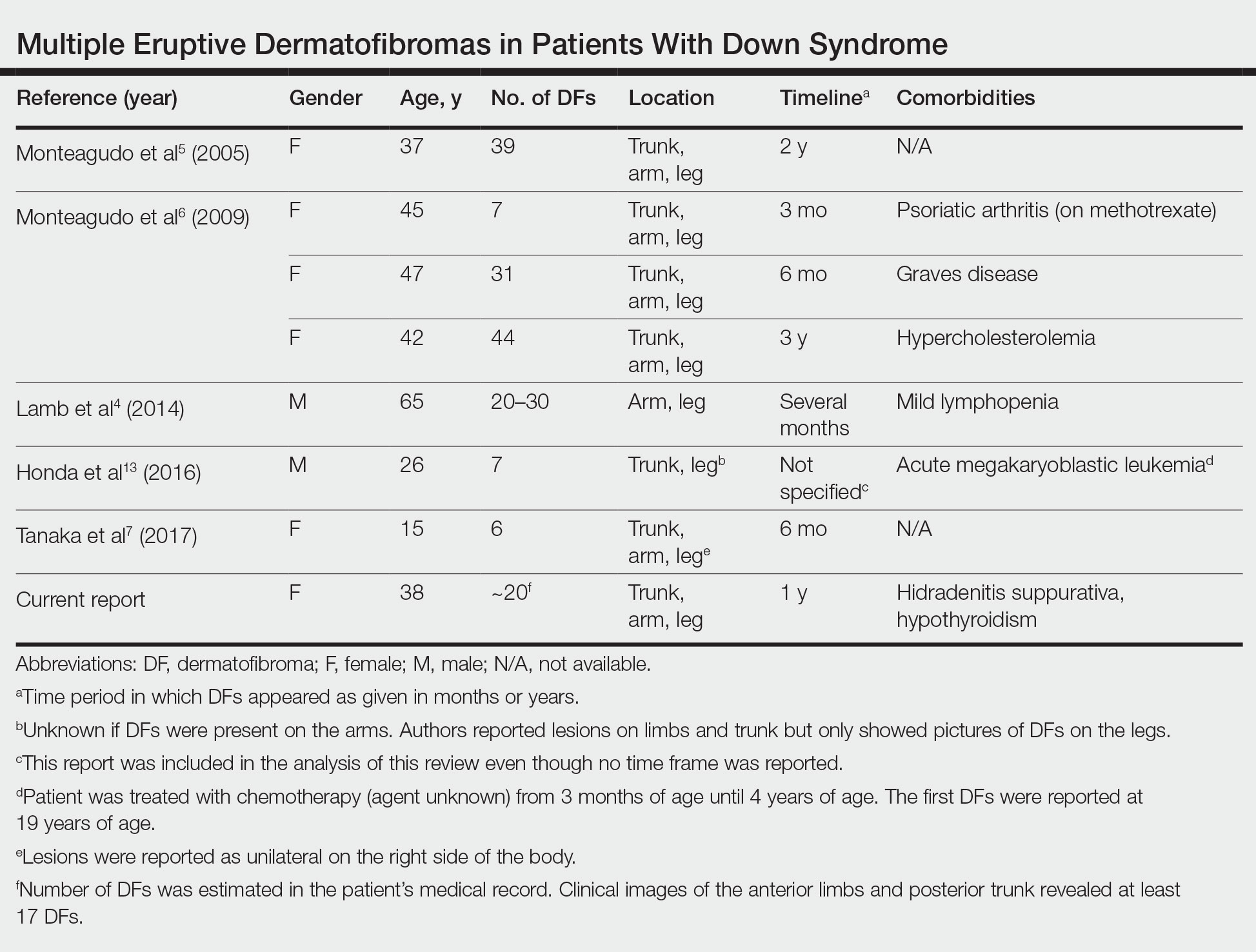
Many dermatologic conditions have been reported at increased rates in individuals with DS, including seborrheic dermatitis, alopecia areata, syringomas, elastosis perforans serpiginosa, cutis marmorata, xerosis, and palmoplantar hyperkeratosis.14,15 Although drawing conclusions about associations between MEDFs and DS is limited by our small sample size, we have reported this case and reviewed existing cases of MEDFs in DS to highlight a potential association that may be underrecognized or underreported. More evidence is needed to determine the strength of the association between MEDFs and DS, but dermatologists should be aware that MEDFs may be an additional skin finding associated with DS that is related to the syndrome’s immune dysregulation.
- Baraf CS, Shapiro L. Multiple histiocytomas: report of a case. Arch Dermatol. 1970;101:588-590.
- Ammirati CT, Mann C, Hornstra IK. Multiple eruptive dermatofibromas in three men with HIV infection. Dermatology. 1997;4:344-348.
- Zaccaria E, Rebora A, Rongioletti F. Multiple eruptive dermatofibromas and immunosuppression: report of two cases and review of the literature. Int J Dermatol. 2008;47:723-727.
- Lamb RC, Gangopadhyay M, MacDonald A. Multiple dermatofibromas in Down syndrome. Int J Dermatol. 2014;53:E274-E275.
- Monteagudo B, Álvarez-Fernández JC, Iglesias B, et al. Multiple eruptive dermatofibromas in a patient with Down’s syndrome [article in Spanish]. Actas Dermosifiliogr. 2005;96:199.
- Monteagudo B, Suárez-Amor O, Cabanillas M, et al. Down syndrome: another cause of immunosuppression associated with multiple eruptive dermatofibroma? [article in Spanish]. Dermatol Online J. 2009;15:15.
- Tanaka M, Hoashi T, Serizawa N, et al. Multiple unilaterally localized dermatofibromas in a patient with Down syndrome. J Dermatol. 2017;44:1074-1076.
- Niiyama S, Katsuoka K, Happle R, et al. Multiple eruptive dermatofibromas: a review of the literature. Acta Derm Venereol. 2002;82:241-244.
- Her Y, Ku SH, Kim KH. A case of multiple eruptive dermatofibromas in a healthy adult. Ann Dermatol. 2014;26:539-540.
- Bertotto A, Arcangeli C, Crupi S, et al. T cell response to anti-CD3 antibody in Down’s syndrome. Arch Dis Child. 1987;62:1148-1151.
- Kusters MA, Verstegen RH, Gemen EF, et al. Intrinsic defect of the immune system in children with Down syndrome: a review. Clin Exp Immunol. 2009;156:189-193.
- Sullivan KD, Evans D, Pandey A, et al. Trisomy 21 causes changes in the circulating proteome indicative of chronic inflammation. Sci Rep. 2017;7:14818.
- Honda M, Tomimura S, de Vega S, et al. Multiple dermatofibromas in a patient with Down syndrome. J Dermatol. 2016;43:346-348.
- Daneshpazhooh M, Nazemi TM, Bigdeloo L, et al. Mucocutaneous findings in 100 children with Down syndrome. Pediatr Dermatol. 2007;24:317-320.
- Madan V, Williams J, Lear JT. Dermatological manifestations of Down’s syndrome. Clin Exp Dermatol. 2006;31:623-629.
- Baraf CS, Shapiro L. Multiple histiocytomas: report of a case. Arch Dermatol. 1970;101:588-590.
- Ammirati CT, Mann C, Hornstra IK. Multiple eruptive dermatofibromas in three men with HIV infection. Dermatology. 1997;4:344-348.
- Zaccaria E, Rebora A, Rongioletti F. Multiple eruptive dermatofibromas and immunosuppression: report of two cases and review of the literature. Int J Dermatol. 2008;47:723-727.
- Lamb RC, Gangopadhyay M, MacDonald A. Multiple dermatofibromas in Down syndrome. Int J Dermatol. 2014;53:E274-E275.
- Monteagudo B, Álvarez-Fernández JC, Iglesias B, et al. Multiple eruptive dermatofibromas in a patient with Down’s syndrome [article in Spanish]. Actas Dermosifiliogr. 2005;96:199.
- Monteagudo B, Suárez-Amor O, Cabanillas M, et al. Down syndrome: another cause of immunosuppression associated with multiple eruptive dermatofibroma? [article in Spanish]. Dermatol Online J. 2009;15:15.
- Tanaka M, Hoashi T, Serizawa N, et al. Multiple unilaterally localized dermatofibromas in a patient with Down syndrome. J Dermatol. 2017;44:1074-1076.
- Niiyama S, Katsuoka K, Happle R, et al. Multiple eruptive dermatofibromas: a review of the literature. Acta Derm Venereol. 2002;82:241-244.
- Her Y, Ku SH, Kim KH. A case of multiple eruptive dermatofibromas in a healthy adult. Ann Dermatol. 2014;26:539-540.
- Bertotto A, Arcangeli C, Crupi S, et al. T cell response to anti-CD3 antibody in Down’s syndrome. Arch Dis Child. 1987;62:1148-1151.
- Kusters MA, Verstegen RH, Gemen EF, et al. Intrinsic defect of the immune system in children with Down syndrome: a review. Clin Exp Immunol. 2009;156:189-193.
- Sullivan KD, Evans D, Pandey A, et al. Trisomy 21 causes changes in the circulating proteome indicative of chronic inflammation. Sci Rep. 2017;7:14818.
- Honda M, Tomimura S, de Vega S, et al. Multiple dermatofibromas in a patient with Down syndrome. J Dermatol. 2016;43:346-348.
- Daneshpazhooh M, Nazemi TM, Bigdeloo L, et al. Mucocutaneous findings in 100 children with Down syndrome. Pediatr Dermatol. 2007;24:317-320.
- Madan V, Williams J, Lear JT. Dermatological manifestations of Down’s syndrome. Clin Exp Dermatol. 2006;31:623-629.
Practice Points
- Although dermatofibromas are common and benign skin lesions, multiple eruptive dermatofibromas have been associated with a number of underlying conditions, particularly those associated with immune dysregulation.
- The immune dysregulation reported in Down syndrome may explain the appearance of multiple dermatofibromas.
Children and COVID: New cases fall again, ED rates rebound for some
The 7-day average percentage of ED visits with diagnosed COVID, which had reached a post-Omicron high of 3.5% in late July for those aged 12-15, began to fall and was down to 3.0% on Aug. 12. That trend reversed, however, and the rate was up to 3.6% on Aug. 19, the last date for which data are available from the Centers for Disease Control and Prevention.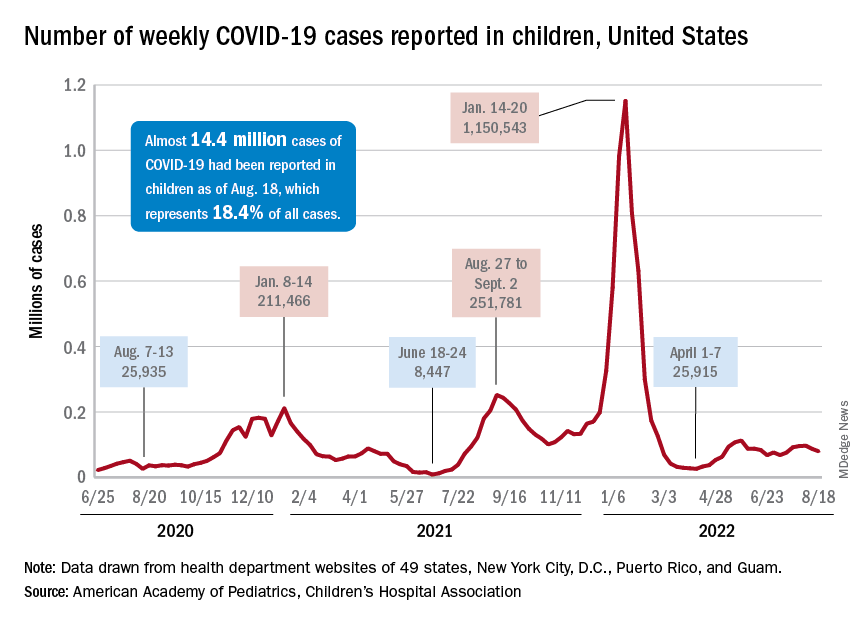
That change of COVID fortunes cannot yet be seen for all children. The 7-day average ED visit rate for those aged 0-11 years peaked at 6.8% during the last week of July and has continued to fall, dropping from 5.7% on Aug. 12 to 5.1% on Aug. 19. Children aged 16-17 years seem to be taking a middle path: Their ED-visit rate declined from late July into mid-August but held steady over the last week, according to the CDC’s COVID Data Tracker.
There is a hint of the same trend regarding new admissions among children aged 0-17 years. The national rate, which had declined in recent weeks, ticked up from 0.42 to 0.43 new admissions per 100,000 population over the last week of available data, the CDC said.
Weekly cases fall below 80,000
New cases in general were down by 8.5% from the previous week, dropping from 87,902 for the week of Aug. 5-11 to 79,525 for Aug. 12-18. That marked the second straight week with fewer cases after a 4-week period that saw weekly totals increase from almost 68,000 to nearly 97,000, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP and CHA put the cumulative number of child COVID-19 cases at just under 14.4 million since the pandemic began, which represents 18.4% of cases among all ages. The CDC estimates that there have been almost 14.7 million cases in children aged 0-17 years, as well as 1,750 deaths, of which 14 were reported in the last week (Aug. 16-22).
The CDC age subgroups indicate that children aged 0-4 years have experienced fewer cases (2.9 million) than children aged 5-11 years (5.6 million cases) and 12-15 (3.0 million cases) but more deaths: 548 so far, versus 432 for 5- to 11-year-olds and 437 for 12- to 15-year-olds, the COVID Data Tracker shows. Those aged 0-4 make up 6% of the total U.S. population, compared with 8.7% and 5.1%, respectively, for the older children.
Most younger children still not vaccinated
Although it may not qualify as a big push to vaccinate children before the start of the new school year, first-time vaccinations did rise somewhat in late July and August for children aged 5-17 years. Among children younger than 5 years, though, initial doses of the vaccine fell during the second full week of August, especially in 2- to 4-year-olds, based on the CDC data.
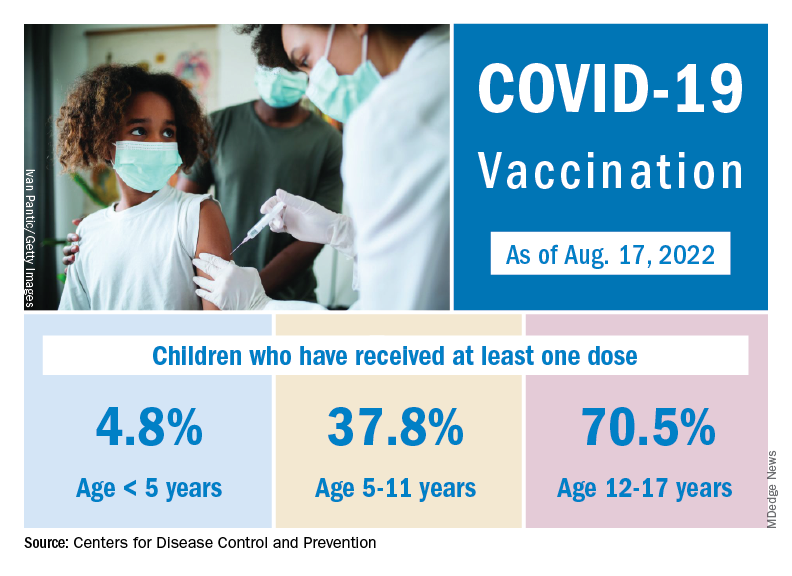
Through almost 2 months of vaccine eligibility, 4.8% of children under age 5 have received at least one dose and 0.9% are fully vaccinated as of Aug. 17. The current rates are 37.8% (one dose) and 30.4% (completed) for those aged 5-11 and 70.5% and 60.3% for 12- to 17-year-olds.
The 7-day average percentage of ED visits with diagnosed COVID, which had reached a post-Omicron high of 3.5% in late July for those aged 12-15, began to fall and was down to 3.0% on Aug. 12. That trend reversed, however, and the rate was up to 3.6% on Aug. 19, the last date for which data are available from the Centers for Disease Control and Prevention.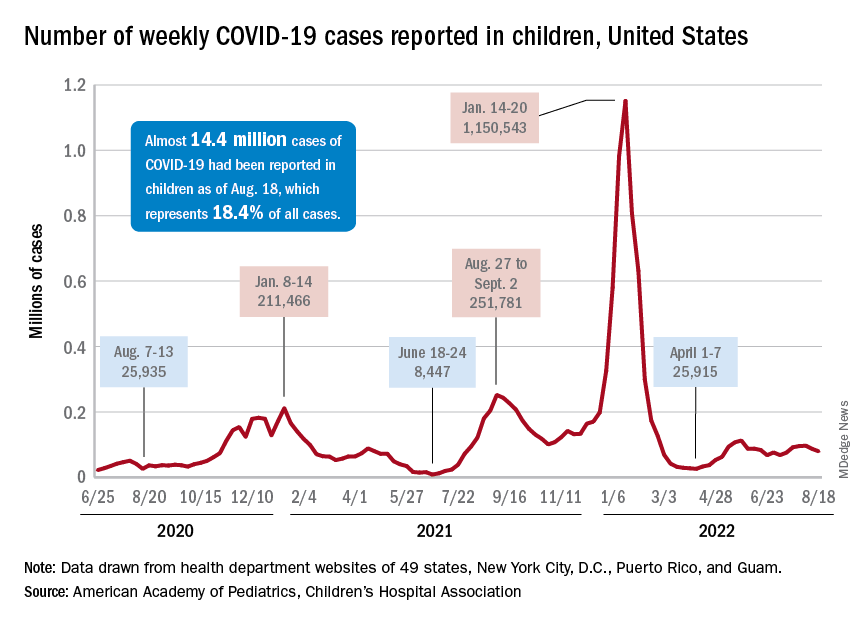
That change of COVID fortunes cannot yet be seen for all children. The 7-day average ED visit rate for those aged 0-11 years peaked at 6.8% during the last week of July and has continued to fall, dropping from 5.7% on Aug. 12 to 5.1% on Aug. 19. Children aged 16-17 years seem to be taking a middle path: Their ED-visit rate declined from late July into mid-August but held steady over the last week, according to the CDC’s COVID Data Tracker.
There is a hint of the same trend regarding new admissions among children aged 0-17 years. The national rate, which had declined in recent weeks, ticked up from 0.42 to 0.43 new admissions per 100,000 population over the last week of available data, the CDC said.
Weekly cases fall below 80,000
New cases in general were down by 8.5% from the previous week, dropping from 87,902 for the week of Aug. 5-11 to 79,525 for Aug. 12-18. That marked the second straight week with fewer cases after a 4-week period that saw weekly totals increase from almost 68,000 to nearly 97,000, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP and CHA put the cumulative number of child COVID-19 cases at just under 14.4 million since the pandemic began, which represents 18.4% of cases among all ages. The CDC estimates that there have been almost 14.7 million cases in children aged 0-17 years, as well as 1,750 deaths, of which 14 were reported in the last week (Aug. 16-22).
The CDC age subgroups indicate that children aged 0-4 years have experienced fewer cases (2.9 million) than children aged 5-11 years (5.6 million cases) and 12-15 (3.0 million cases) but more deaths: 548 so far, versus 432 for 5- to 11-year-olds and 437 for 12- to 15-year-olds, the COVID Data Tracker shows. Those aged 0-4 make up 6% of the total U.S. population, compared with 8.7% and 5.1%, respectively, for the older children.
Most younger children still not vaccinated
Although it may not qualify as a big push to vaccinate children before the start of the new school year, first-time vaccinations did rise somewhat in late July and August for children aged 5-17 years. Among children younger than 5 years, though, initial doses of the vaccine fell during the second full week of August, especially in 2- to 4-year-olds, based on the CDC data.
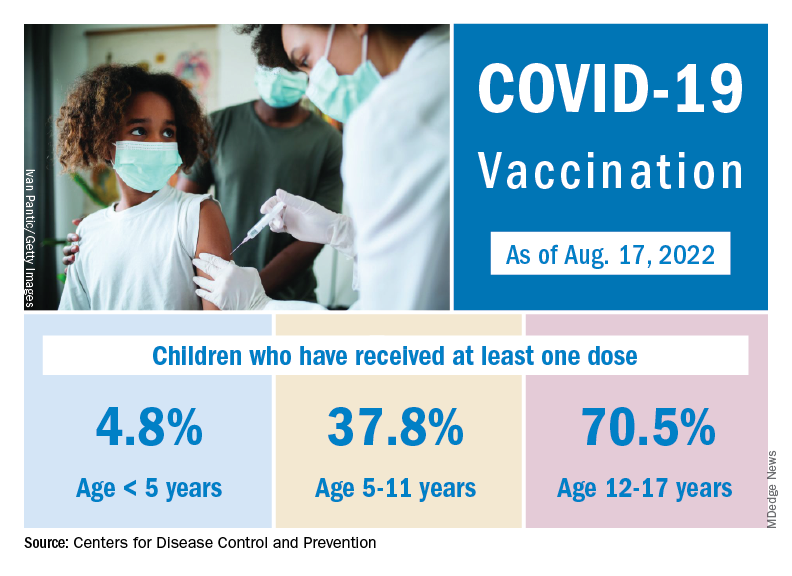
Through almost 2 months of vaccine eligibility, 4.8% of children under age 5 have received at least one dose and 0.9% are fully vaccinated as of Aug. 17. The current rates are 37.8% (one dose) and 30.4% (completed) for those aged 5-11 and 70.5% and 60.3% for 12- to 17-year-olds.
The 7-day average percentage of ED visits with diagnosed COVID, which had reached a post-Omicron high of 3.5% in late July for those aged 12-15, began to fall and was down to 3.0% on Aug. 12. That trend reversed, however, and the rate was up to 3.6% on Aug. 19, the last date for which data are available from the Centers for Disease Control and Prevention.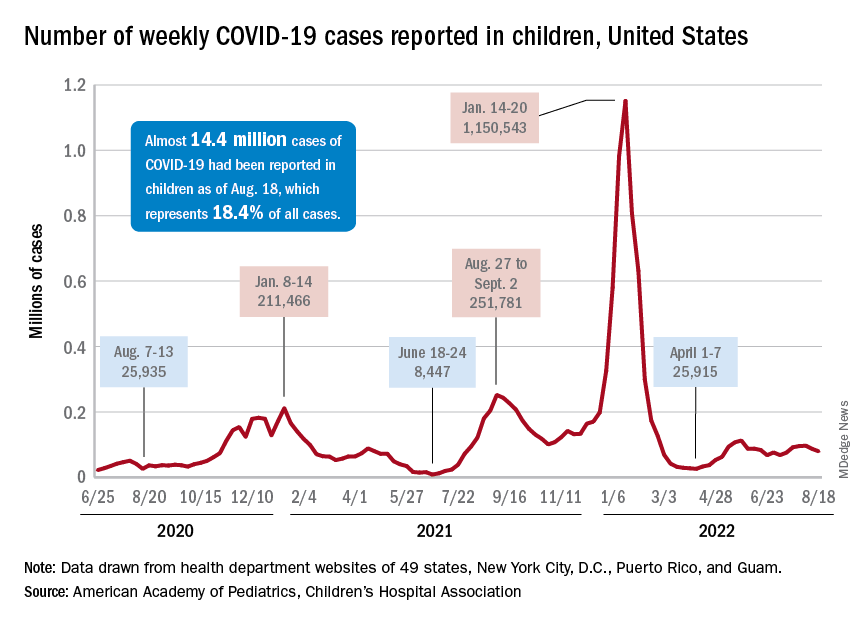
That change of COVID fortunes cannot yet be seen for all children. The 7-day average ED visit rate for those aged 0-11 years peaked at 6.8% during the last week of July and has continued to fall, dropping from 5.7% on Aug. 12 to 5.1% on Aug. 19. Children aged 16-17 years seem to be taking a middle path: Their ED-visit rate declined from late July into mid-August but held steady over the last week, according to the CDC’s COVID Data Tracker.
There is a hint of the same trend regarding new admissions among children aged 0-17 years. The national rate, which had declined in recent weeks, ticked up from 0.42 to 0.43 new admissions per 100,000 population over the last week of available data, the CDC said.
Weekly cases fall below 80,000
New cases in general were down by 8.5% from the previous week, dropping from 87,902 for the week of Aug. 5-11 to 79,525 for Aug. 12-18. That marked the second straight week with fewer cases after a 4-week period that saw weekly totals increase from almost 68,000 to nearly 97,000, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP and CHA put the cumulative number of child COVID-19 cases at just under 14.4 million since the pandemic began, which represents 18.4% of cases among all ages. The CDC estimates that there have been almost 14.7 million cases in children aged 0-17 years, as well as 1,750 deaths, of which 14 were reported in the last week (Aug. 16-22).
The CDC age subgroups indicate that children aged 0-4 years have experienced fewer cases (2.9 million) than children aged 5-11 years (5.6 million cases) and 12-15 (3.0 million cases) but more deaths: 548 so far, versus 432 for 5- to 11-year-olds and 437 for 12- to 15-year-olds, the COVID Data Tracker shows. Those aged 0-4 make up 6% of the total U.S. population, compared with 8.7% and 5.1%, respectively, for the older children.
Most younger children still not vaccinated
Although it may not qualify as a big push to vaccinate children before the start of the new school year, first-time vaccinations did rise somewhat in late July and August for children aged 5-17 years. Among children younger than 5 years, though, initial doses of the vaccine fell during the second full week of August, especially in 2- to 4-year-olds, based on the CDC data.
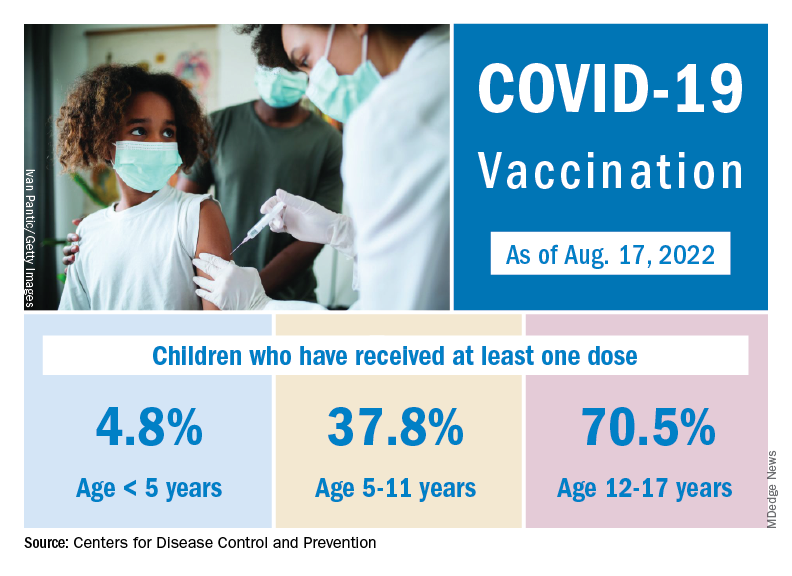
Through almost 2 months of vaccine eligibility, 4.8% of children under age 5 have received at least one dose and 0.9% are fully vaccinated as of Aug. 17. The current rates are 37.8% (one dose) and 30.4% (completed) for those aged 5-11 and 70.5% and 60.3% for 12- to 17-year-olds.
Erlotinib promising for cancer prevention in familial adenomatous polyposis
“If existing data are confirmed and extended through future research, this strategy has the potential for substantial impact on clinical practice by decreasing, delaying, or augmenting endoscopic and surgical interventions as the mainstay for duodenal cancer prevention in this high-risk patient population,” the study team says.
FAP is a rare genetic condition that markedly raises the risk for colorectal polyps and cancer.
“The biological pathway that leads to the development of polyps and colon cancer in patients with FAP is the same biological pathway as patients in the general population,” study investigator Niloy Jewel Samadder, MD, with the Mayo Clinic, Rochester, Minn., said in a news release.
“Our trial looked at opportunities to use chemoprevention agents in patients with FAP to inhibit the development of precancerous polyps in the small bowel and colorectum,” Dr. Samadder explains.
In an earlier study, the researchers found that the combination of the COX-2 inhibitor sulindac (150 mg twice daily) and erlotinib (75 mg daily) reduced duodenal polyp burden.
However, the dual-drug strategy was associated with a relatively high adverse event (AE) rate, which may limit use of the combination for chemoprevention, as reported previously.
This phase 2 study tested whether erlotinib’s AE profile would be improved with a once-weekly dosing schedule while still reducing polyp burden.
The study was first published online in the journal Gut.
In the single-arm, multicenter study, 46 adults with FAP (mean age, 44 years; 48% women) self-administered 350 mg of erlotinib by mouth one time per week for 6 months. All but four participants completed the 6-month study.
After 6 months of weekly erlotinib, duodenal polyp burden was significantly reduced, with a mean percent reduction of 29.6% (95% confidence interval: –39.6% to –19.7%; P < .0001).
The benefit was observed in patients with either Spigelman 2 or Spigelman 3 duodenal polyp burden.
“Though only 12% of patients noted a decrease in Spigelman stage from 3 to 2 associated with therapy, the majority of patients (86%) had stable disease while on treatment,” the study team reports.
GI polyp number (a secondary outcome) was also decreased after 6 months of treatment with erlotinib (median decrease of 30.8%; P = .0256).
While once-weekly erlotinib was “generally” well tolerated, grade 2 or 3 AEs were reported in 72% of patients; two suffered grade 3 toxicity. Nonetheless, the AE rate was significantly more than the expected null hypothesis rate of 50%, the study team states.
Four patients withdrew from the study because of drug-induced AEs, which included grade 3 rash acneiform, grade 2 infections (hand, foot, and mouth disease), grade 1 fatigue, and grade 1 rash acneiform. No grade 4 AEs were reported.
The most common AE was an erlotinib-induced acneiform-like rash, which occurred in 56.5% of study patients. The rash was managed with topical cortisone and/or clindamycin. Additional erlotinib-induced AEs included oral mucositis (6.5%), diarrhea (50%), and nausea (26.1%).
Summing up, Dr. Samadder and colleagues note that FAP “portends a heritable, systemic predisposition to cancer, and the ultimate goal of cancer preventive intervention is to interrupt the development of neoplasia, need for surgery, and ultimately death from cancer, with an acceptable AE profile.”
The findings from this phase 2 trial support further study of erlotinib as “an effective, acceptable cancer preventive agent for FAP-associated gastrointestinal polyposis,” they conclude.
The study was sponsored by the National Cancer Institute. Dr. Samadder is a consultant for Janssen Research and Development, Recursion Pharmaceuticals, and Cancer Prevention Pharmaceuticals.
A version of this article first appeared on Medscape.com.
“If existing data are confirmed and extended through future research, this strategy has the potential for substantial impact on clinical practice by decreasing, delaying, or augmenting endoscopic and surgical interventions as the mainstay for duodenal cancer prevention in this high-risk patient population,” the study team says.
FAP is a rare genetic condition that markedly raises the risk for colorectal polyps and cancer.
“The biological pathway that leads to the development of polyps and colon cancer in patients with FAP is the same biological pathway as patients in the general population,” study investigator Niloy Jewel Samadder, MD, with the Mayo Clinic, Rochester, Minn., said in a news release.
“Our trial looked at opportunities to use chemoprevention agents in patients with FAP to inhibit the development of precancerous polyps in the small bowel and colorectum,” Dr. Samadder explains.
In an earlier study, the researchers found that the combination of the COX-2 inhibitor sulindac (150 mg twice daily) and erlotinib (75 mg daily) reduced duodenal polyp burden.
However, the dual-drug strategy was associated with a relatively high adverse event (AE) rate, which may limit use of the combination for chemoprevention, as reported previously.
This phase 2 study tested whether erlotinib’s AE profile would be improved with a once-weekly dosing schedule while still reducing polyp burden.
The study was first published online in the journal Gut.
In the single-arm, multicenter study, 46 adults with FAP (mean age, 44 years; 48% women) self-administered 350 mg of erlotinib by mouth one time per week for 6 months. All but four participants completed the 6-month study.
After 6 months of weekly erlotinib, duodenal polyp burden was significantly reduced, with a mean percent reduction of 29.6% (95% confidence interval: –39.6% to –19.7%; P < .0001).
The benefit was observed in patients with either Spigelman 2 or Spigelman 3 duodenal polyp burden.
“Though only 12% of patients noted a decrease in Spigelman stage from 3 to 2 associated with therapy, the majority of patients (86%) had stable disease while on treatment,” the study team reports.
GI polyp number (a secondary outcome) was also decreased after 6 months of treatment with erlotinib (median decrease of 30.8%; P = .0256).
While once-weekly erlotinib was “generally” well tolerated, grade 2 or 3 AEs were reported in 72% of patients; two suffered grade 3 toxicity. Nonetheless, the AE rate was significantly more than the expected null hypothesis rate of 50%, the study team states.
Four patients withdrew from the study because of drug-induced AEs, which included grade 3 rash acneiform, grade 2 infections (hand, foot, and mouth disease), grade 1 fatigue, and grade 1 rash acneiform. No grade 4 AEs were reported.
The most common AE was an erlotinib-induced acneiform-like rash, which occurred in 56.5% of study patients. The rash was managed with topical cortisone and/or clindamycin. Additional erlotinib-induced AEs included oral mucositis (6.5%), diarrhea (50%), and nausea (26.1%).
Summing up, Dr. Samadder and colleagues note that FAP “portends a heritable, systemic predisposition to cancer, and the ultimate goal of cancer preventive intervention is to interrupt the development of neoplasia, need for surgery, and ultimately death from cancer, with an acceptable AE profile.”
The findings from this phase 2 trial support further study of erlotinib as “an effective, acceptable cancer preventive agent for FAP-associated gastrointestinal polyposis,” they conclude.
The study was sponsored by the National Cancer Institute. Dr. Samadder is a consultant for Janssen Research and Development, Recursion Pharmaceuticals, and Cancer Prevention Pharmaceuticals.
A version of this article first appeared on Medscape.com.
“If existing data are confirmed and extended through future research, this strategy has the potential for substantial impact on clinical practice by decreasing, delaying, or augmenting endoscopic and surgical interventions as the mainstay for duodenal cancer prevention in this high-risk patient population,” the study team says.
FAP is a rare genetic condition that markedly raises the risk for colorectal polyps and cancer.
“The biological pathway that leads to the development of polyps and colon cancer in patients with FAP is the same biological pathway as patients in the general population,” study investigator Niloy Jewel Samadder, MD, with the Mayo Clinic, Rochester, Minn., said in a news release.
“Our trial looked at opportunities to use chemoprevention agents in patients with FAP to inhibit the development of precancerous polyps in the small bowel and colorectum,” Dr. Samadder explains.
In an earlier study, the researchers found that the combination of the COX-2 inhibitor sulindac (150 mg twice daily) and erlotinib (75 mg daily) reduced duodenal polyp burden.
However, the dual-drug strategy was associated with a relatively high adverse event (AE) rate, which may limit use of the combination for chemoprevention, as reported previously.
This phase 2 study tested whether erlotinib’s AE profile would be improved with a once-weekly dosing schedule while still reducing polyp burden.
The study was first published online in the journal Gut.
In the single-arm, multicenter study, 46 adults with FAP (mean age, 44 years; 48% women) self-administered 350 mg of erlotinib by mouth one time per week for 6 months. All but four participants completed the 6-month study.
After 6 months of weekly erlotinib, duodenal polyp burden was significantly reduced, with a mean percent reduction of 29.6% (95% confidence interval: –39.6% to –19.7%; P < .0001).
The benefit was observed in patients with either Spigelman 2 or Spigelman 3 duodenal polyp burden.
“Though only 12% of patients noted a decrease in Spigelman stage from 3 to 2 associated with therapy, the majority of patients (86%) had stable disease while on treatment,” the study team reports.
GI polyp number (a secondary outcome) was also decreased after 6 months of treatment with erlotinib (median decrease of 30.8%; P = .0256).
While once-weekly erlotinib was “generally” well tolerated, grade 2 or 3 AEs were reported in 72% of patients; two suffered grade 3 toxicity. Nonetheless, the AE rate was significantly more than the expected null hypothesis rate of 50%, the study team states.
Four patients withdrew from the study because of drug-induced AEs, which included grade 3 rash acneiform, grade 2 infections (hand, foot, and mouth disease), grade 1 fatigue, and grade 1 rash acneiform. No grade 4 AEs were reported.
The most common AE was an erlotinib-induced acneiform-like rash, which occurred in 56.5% of study patients. The rash was managed with topical cortisone and/or clindamycin. Additional erlotinib-induced AEs included oral mucositis (6.5%), diarrhea (50%), and nausea (26.1%).
Summing up, Dr. Samadder and colleagues note that FAP “portends a heritable, systemic predisposition to cancer, and the ultimate goal of cancer preventive intervention is to interrupt the development of neoplasia, need for surgery, and ultimately death from cancer, with an acceptable AE profile.”
The findings from this phase 2 trial support further study of erlotinib as “an effective, acceptable cancer preventive agent for FAP-associated gastrointestinal polyposis,” they conclude.
The study was sponsored by the National Cancer Institute. Dr. Samadder is a consultant for Janssen Research and Development, Recursion Pharmaceuticals, and Cancer Prevention Pharmaceuticals.
A version of this article first appeared on Medscape.com.
FROM GUT
Commentary: Appropriate Downstaging and TACE in HCC, September 2022
Liver transplantation has the opportunity to cure both localized HCC as well as underlying liver cirrhosis. Donor organ shortage has led to the implementation of the Milan criteria as a way to identify patients whose tumor burden is low enough to predict a good outcome. Downstaging liver cancer to fit within Milan criteria has been controversial.
Tabrizian and colleagues undertook a retrospective cohort analysis of 2645 adult patients with HCC who underwent liver transplant. Out of those, 2122 patients always had disease that was within the Milan criteria, 341 patients had HCC that was downstaged to fit within the Milan criteria, and 182 patients had HCC that was outside the Milan criteria at the time of liver transplantation. The authors report that the 10-year post-transplant survival and recurrence rates were 61.5% and 13.3%, respectively, in those always within the Milan criteria, 52.1% and 20.6% among those whose disease was downstaged, and 43.3% and 41.1% in those whose disease was never downstaged. Characteristics that predicted recurrence after downstaging were tumor size > 7 cm at diagnosis (odds ratio [OR] 2.62; 95% CI 1.20-5.75; P = .02), more than three tumors at diagnosis (OR 2.34; 95% CI 1.22-4.50; P = .01), and alpha-fetoprotein (AFP) response ≥ 20 ng/mL with < 50% improvement from maximum AFP before transplantation (OR 1.99; 95% CI 1.14-3.46; P = .02). Additionally, patients with recurrent tumors that were surgically resected had improved 5-year post-recurrence survival (31.6% vs 7.3%; P < .001). The conclusion was that the national downstaging policies were valid and should continue.
For patients who have unresectable HCC, systemic therapy is the mainstay of treatment. Peng and colleagues reported the results of the LAUNCH phase 3 clinical trial that randomized patients to receive lenvatinib alone or lenvatinib plus transarterial chemoembolization (TACE). Out of 338 patients, 170 received lenvatinib plus TACE. Unsurprisingly, the response rate was higher with the combination (54.1% vs 25.0%; P < .001); however, so was the median overall survival (17.8 vs 11.5 months; hazard ratio 0.45; P < .001), and median progression-free survival (10.6 vs 6.4 months; hazard ratio 0.43; P < .001). The investigators concluded that the addition of TACE to lenvatinib had manageable toxicities, improved clinical outcomes, and could be used as a potential first-line treatment for some patients with unresectable HCC.
Finally, in patients whose HCC progressed after a single TACE treatment, the question remains whether repeated TACE is worthwhile. Zhao and colleagues retrospectively reviewed the outcomes of 94 patients who underwent at least one TACE. Of these, 28 (29.8%) had a response to the first TACE, and these patients tended to have a longer OS compared with nonresponders (36.7 vs 21.5 months; P = .071). Of the 43 initial nonresponders who underwent a second TACE, 15 of 43 (34.9%) achieved a response and had an improved median overall survival (47.8 v. 13.6 months; P = .01), suggesting that repeat TACE may offer a benefit to some patients, even after no response to the initial treatment.
Liver transplantation has the opportunity to cure both localized HCC as well as underlying liver cirrhosis. Donor organ shortage has led to the implementation of the Milan criteria as a way to identify patients whose tumor burden is low enough to predict a good outcome. Downstaging liver cancer to fit within Milan criteria has been controversial.
Tabrizian and colleagues undertook a retrospective cohort analysis of 2645 adult patients with HCC who underwent liver transplant. Out of those, 2122 patients always had disease that was within the Milan criteria, 341 patients had HCC that was downstaged to fit within the Milan criteria, and 182 patients had HCC that was outside the Milan criteria at the time of liver transplantation. The authors report that the 10-year post-transplant survival and recurrence rates were 61.5% and 13.3%, respectively, in those always within the Milan criteria, 52.1% and 20.6% among those whose disease was downstaged, and 43.3% and 41.1% in those whose disease was never downstaged. Characteristics that predicted recurrence after downstaging were tumor size > 7 cm at diagnosis (odds ratio [OR] 2.62; 95% CI 1.20-5.75; P = .02), more than three tumors at diagnosis (OR 2.34; 95% CI 1.22-4.50; P = .01), and alpha-fetoprotein (AFP) response ≥ 20 ng/mL with < 50% improvement from maximum AFP before transplantation (OR 1.99; 95% CI 1.14-3.46; P = .02). Additionally, patients with recurrent tumors that were surgically resected had improved 5-year post-recurrence survival (31.6% vs 7.3%; P < .001). The conclusion was that the national downstaging policies were valid and should continue.
For patients who have unresectable HCC, systemic therapy is the mainstay of treatment. Peng and colleagues reported the results of the LAUNCH phase 3 clinical trial that randomized patients to receive lenvatinib alone or lenvatinib plus transarterial chemoembolization (TACE). Out of 338 patients, 170 received lenvatinib plus TACE. Unsurprisingly, the response rate was higher with the combination (54.1% vs 25.0%; P < .001); however, so was the median overall survival (17.8 vs 11.5 months; hazard ratio 0.45; P < .001), and median progression-free survival (10.6 vs 6.4 months; hazard ratio 0.43; P < .001). The investigators concluded that the addition of TACE to lenvatinib had manageable toxicities, improved clinical outcomes, and could be used as a potential first-line treatment for some patients with unresectable HCC.
Finally, in patients whose HCC progressed after a single TACE treatment, the question remains whether repeated TACE is worthwhile. Zhao and colleagues retrospectively reviewed the outcomes of 94 patients who underwent at least one TACE. Of these, 28 (29.8%) had a response to the first TACE, and these patients tended to have a longer OS compared with nonresponders (36.7 vs 21.5 months; P = .071). Of the 43 initial nonresponders who underwent a second TACE, 15 of 43 (34.9%) achieved a response and had an improved median overall survival (47.8 v. 13.6 months; P = .01), suggesting that repeat TACE may offer a benefit to some patients, even after no response to the initial treatment.
Liver transplantation has the opportunity to cure both localized HCC as well as underlying liver cirrhosis. Donor organ shortage has led to the implementation of the Milan criteria as a way to identify patients whose tumor burden is low enough to predict a good outcome. Downstaging liver cancer to fit within Milan criteria has been controversial.
Tabrizian and colleagues undertook a retrospective cohort analysis of 2645 adult patients with HCC who underwent liver transplant. Out of those, 2122 patients always had disease that was within the Milan criteria, 341 patients had HCC that was downstaged to fit within the Milan criteria, and 182 patients had HCC that was outside the Milan criteria at the time of liver transplantation. The authors report that the 10-year post-transplant survival and recurrence rates were 61.5% and 13.3%, respectively, in those always within the Milan criteria, 52.1% and 20.6% among those whose disease was downstaged, and 43.3% and 41.1% in those whose disease was never downstaged. Characteristics that predicted recurrence after downstaging were tumor size > 7 cm at diagnosis (odds ratio [OR] 2.62; 95% CI 1.20-5.75; P = .02), more than three tumors at diagnosis (OR 2.34; 95% CI 1.22-4.50; P = .01), and alpha-fetoprotein (AFP) response ≥ 20 ng/mL with < 50% improvement from maximum AFP before transplantation (OR 1.99; 95% CI 1.14-3.46; P = .02). Additionally, patients with recurrent tumors that were surgically resected had improved 5-year post-recurrence survival (31.6% vs 7.3%; P < .001). The conclusion was that the national downstaging policies were valid and should continue.
For patients who have unresectable HCC, systemic therapy is the mainstay of treatment. Peng and colleagues reported the results of the LAUNCH phase 3 clinical trial that randomized patients to receive lenvatinib alone or lenvatinib plus transarterial chemoembolization (TACE). Out of 338 patients, 170 received lenvatinib plus TACE. Unsurprisingly, the response rate was higher with the combination (54.1% vs 25.0%; P < .001); however, so was the median overall survival (17.8 vs 11.5 months; hazard ratio 0.45; P < .001), and median progression-free survival (10.6 vs 6.4 months; hazard ratio 0.43; P < .001). The investigators concluded that the addition of TACE to lenvatinib had manageable toxicities, improved clinical outcomes, and could be used as a potential first-line treatment for some patients with unresectable HCC.
Finally, in patients whose HCC progressed after a single TACE treatment, the question remains whether repeated TACE is worthwhile. Zhao and colleagues retrospectively reviewed the outcomes of 94 patients who underwent at least one TACE. Of these, 28 (29.8%) had a response to the first TACE, and these patients tended to have a longer OS compared with nonresponders (36.7 vs 21.5 months; P = .071). Of the 43 initial nonresponders who underwent a second TACE, 15 of 43 (34.9%) achieved a response and had an improved median overall survival (47.8 v. 13.6 months; P = .01), suggesting that repeat TACE may offer a benefit to some patients, even after no response to the initial treatment.


