User login
New Guidance on Genetic Testing for Kidney Disease
A new consensus statement recommended genetic testing for all categories of kidney diseases whenever a genetic cause is suspected and offered guidance on who to test, which tests are the most useful, and how to talk to patients about results.
The statement, published online in the American Journal of Kidney Diseases, is the work of four dozen authors — including patients, nephrologists, experts in clinical and laboratory genetics, kidney pathology, genetic counseling, and ethics. The experts were brought together by the National Kidney Foundation (NKF) with the goal of broadening use and understanding of the tests.
About 10% or more of kidney diseases in adults and 70% of selected chronic kidney diseases (CKDs) in children have genetic causes. But nephrologists have reported a lack of education about genetic testing, and other barriers to wider use, including limited access to testing, cost, insurance coverage, and a small number of genetic counselors who are versed in kidney genetics.
Genetic testing “in the kidney field is a little less developed than in other fields,” said co–lead author Nora Franceschini, MD, MPH, a professor of epidemiology at the University of North Carolina Gillings School of Global Public Health, Chapel Hill, and a nephrologist who studies the genetic epidemiology of hypertension and kidney and cardiovascular diseases.
There are already many known variants that play a role in various kidney diseases and more are on the horizon, Dr. Franceschini told this news organization. More genetic tests will be available in the near future. “The workforce needs to be prepared,” she said.
The statement is an initial step that gets clinicians thinking about testing in a more systematic way, said Dr. Franceschini. “Genetic testing is just another test that physicians can use to complete the story when evaluating patients.
“I think clinicians are ready to implement” testing, said Dr. Franceschini. “We just need to have better guidance.”
Who, When, What to Test
The NKF statement is not the first to try to address gaps in use and knowledge. A European Renal Association Working Group published guidelines in 2022.
The NKF Working Group came up with 56 recommendations and separate algorithms to guide testing for adult and pediatric individuals who are considered at-risk (and currently asymptomatic) and for those who already have clinical disease.
Testing can help determine a cause if there’s an atypical clinical presentation, and it can help avoid biopsies, said the group. Tests can also guide choice of therapy.
For at-risk individuals, there are two broad situations in which testing might be considered: In family members of a patient who already has kidney disease and in potential kidney donors. But testing at-risk children younger than 18 years should only be done if there is an intervention available that could prevent, treat, or slow progression of disease, said the authors.
For patients with an established genetic diagnosis, at-risk family members should be tested with the known single-gene variant diagnostic instead of a broad panel, said the group.
Single-gene variant testing is most appropriate in situations when clinical disease is already evident or when there is known genetic disease in the family, according to the NKF panel. A large diagnostic panel that covers the many common genetic causes of kidney disease is recommended for the majority of patients.
The group recommended that apolipoprotein L1 (APOL1) testing should be included in gene panels for CKD, and it should be offered to any patient “with clinical findings suggestive of APOL1-association nephropathy, regardless of race and ethnicity.”
High-risk APOL1 genotypes confer a 5- to 10-fold increased risk for CKD and are found in one out of seven individuals of African ancestry, which means the focus has largely been on testing those with that ancestry.
However, with many unknowns about APOL1, the NKF panel did not want to “profile” individuals and suggest that testing should not be based on skin color or race/ethnicity, said Dr. Franceschini.
In addition, only about 10% of those with the variant develop disease, so testing is not currently warranted for those who do not already have kidney disease, said the group.
They also recommended against the use of polygenic risk scores, saying that there are not enough data from diverse populations in genome-wide association studies for kidney disease or on their clinical utility.
More Education Needed; Many Barriers
The authors acknowledged that nephrologists generally receive little education in genetics and lack support for interpreting and discussing results.
“Nephrologists should be provided with training and best practice resources to interpret genetic testing and discuss the results with individuals and their families,” they wrote, adding that there’s a need for genomic medicine boards at academic centers that would be available to help nephrologists interpret results and plot clinical management.
The group did not, however, cite some of the other barriers to adoption of testing, including a limited number of sites offering testing, cost, and lack of insurance coverage for the diagnostics.
Medicare may cover genetic testing for kidney disease when an individual has symptoms and there is a Food and Drug Administration–approved test. Joseph Vassalotti, MD, chief medical officer for the NKF, said private insurance may cover the testing if the nephrologist deems it medically necessary, but that he usually confirms coverage before initiating testing. The often-used Renasight panel, which tests for 385 genes related to kidney diseases, costs $300-$400 out of pocket, Dr. Vassalotti told this news organization.
In a survey of 149 nephrologists conducted in 2021, both users (46%) and nonusers of the tests (69%) said that high cost was the most significant perceived barrier to implementing widespread testing. A third of users and almost two thirds of nonusers said that poor availability or lack of ease of testing was the second most significant barrier.
Clinics that test for kidney genes “are largely confined to large academic centers and some specialty clinics,” said Dominic Raj, MD, the Bert B. Brooks chair, and Divya Shankaranarayanan, MD, director of the Kidney Precision Medicine Clinic, both at George Washington University School of Medicine & Health Sciences, Washington, DC, in an email.
Testing is also limited by cultural barriers, lack of genetic literacy, and patients’ concerns that a positive result could lead to a loss of health insurance coverage, said Dr. Raj and Dr. Shankaranarayanan.
Paper Will Help Expand Use
A lack of consensus has also held back expansion. The new statement “may lead to increased and possibly judicious utilization of genetic testing in nephrology practices,” said Dr. Raj and Dr. Shankaranarayanan. “Most importantly, the panel has given specific guidance as to what type of genetic test platform is likely to yield the best and most cost-effective yield.”
The most effective use is “in monogenic kidney diseases and to a lesser extent in oligogenic kidney disease,” said Dr. Raj and Dr. Shankaranarayanan, adding that testing is of less-certain utility in polygenic kidney diseases, “where complex genetic and epigenetic factors determine the phenotype.”
Genetic testing might be especially useful “in atypical clinical presentations” and can help clinicians avoid unnecessary expensive and extensive investigations when multiple organ systems are involved, they said.
“Most importantly, [testing] might prevent unnecessary and potentially harmful treatment and enable targeted specific treatment, when available,” said Dr. Raj and Dr. Shankaranarayanan.
Dr. Franceschini and Dr. Shankaranarayanan reported no relevant financial relationships. Dr. Raj disclosed that he received consulting fees and honoraria from Novo Nordisk and is a national leader for the company’s Zeus trial, studying whether ziltivekimab reduces the risk for cardiovascular events in cardiovascular disease, CKD, and inflammation. He also participated in a study of Natera’s Renasight, a 385-gene panel for kidney disease.
A version of this article first appeared on Medscape.com.
A new consensus statement recommended genetic testing for all categories of kidney diseases whenever a genetic cause is suspected and offered guidance on who to test, which tests are the most useful, and how to talk to patients about results.
The statement, published online in the American Journal of Kidney Diseases, is the work of four dozen authors — including patients, nephrologists, experts in clinical and laboratory genetics, kidney pathology, genetic counseling, and ethics. The experts were brought together by the National Kidney Foundation (NKF) with the goal of broadening use and understanding of the tests.
About 10% or more of kidney diseases in adults and 70% of selected chronic kidney diseases (CKDs) in children have genetic causes. But nephrologists have reported a lack of education about genetic testing, and other barriers to wider use, including limited access to testing, cost, insurance coverage, and a small number of genetic counselors who are versed in kidney genetics.
Genetic testing “in the kidney field is a little less developed than in other fields,” said co–lead author Nora Franceschini, MD, MPH, a professor of epidemiology at the University of North Carolina Gillings School of Global Public Health, Chapel Hill, and a nephrologist who studies the genetic epidemiology of hypertension and kidney and cardiovascular diseases.
There are already many known variants that play a role in various kidney diseases and more are on the horizon, Dr. Franceschini told this news organization. More genetic tests will be available in the near future. “The workforce needs to be prepared,” she said.
The statement is an initial step that gets clinicians thinking about testing in a more systematic way, said Dr. Franceschini. “Genetic testing is just another test that physicians can use to complete the story when evaluating patients.
“I think clinicians are ready to implement” testing, said Dr. Franceschini. “We just need to have better guidance.”
Who, When, What to Test
The NKF statement is not the first to try to address gaps in use and knowledge. A European Renal Association Working Group published guidelines in 2022.
The NKF Working Group came up with 56 recommendations and separate algorithms to guide testing for adult and pediatric individuals who are considered at-risk (and currently asymptomatic) and for those who already have clinical disease.
Testing can help determine a cause if there’s an atypical clinical presentation, and it can help avoid biopsies, said the group. Tests can also guide choice of therapy.
For at-risk individuals, there are two broad situations in which testing might be considered: In family members of a patient who already has kidney disease and in potential kidney donors. But testing at-risk children younger than 18 years should only be done if there is an intervention available that could prevent, treat, or slow progression of disease, said the authors.
For patients with an established genetic diagnosis, at-risk family members should be tested with the known single-gene variant diagnostic instead of a broad panel, said the group.
Single-gene variant testing is most appropriate in situations when clinical disease is already evident or when there is known genetic disease in the family, according to the NKF panel. A large diagnostic panel that covers the many common genetic causes of kidney disease is recommended for the majority of patients.
The group recommended that apolipoprotein L1 (APOL1) testing should be included in gene panels for CKD, and it should be offered to any patient “with clinical findings suggestive of APOL1-association nephropathy, regardless of race and ethnicity.”
High-risk APOL1 genotypes confer a 5- to 10-fold increased risk for CKD and are found in one out of seven individuals of African ancestry, which means the focus has largely been on testing those with that ancestry.
However, with many unknowns about APOL1, the NKF panel did not want to “profile” individuals and suggest that testing should not be based on skin color or race/ethnicity, said Dr. Franceschini.
In addition, only about 10% of those with the variant develop disease, so testing is not currently warranted for those who do not already have kidney disease, said the group.
They also recommended against the use of polygenic risk scores, saying that there are not enough data from diverse populations in genome-wide association studies for kidney disease or on their clinical utility.
More Education Needed; Many Barriers
The authors acknowledged that nephrologists generally receive little education in genetics and lack support for interpreting and discussing results.
“Nephrologists should be provided with training and best practice resources to interpret genetic testing and discuss the results with individuals and their families,” they wrote, adding that there’s a need for genomic medicine boards at academic centers that would be available to help nephrologists interpret results and plot clinical management.
The group did not, however, cite some of the other barriers to adoption of testing, including a limited number of sites offering testing, cost, and lack of insurance coverage for the diagnostics.
Medicare may cover genetic testing for kidney disease when an individual has symptoms and there is a Food and Drug Administration–approved test. Joseph Vassalotti, MD, chief medical officer for the NKF, said private insurance may cover the testing if the nephrologist deems it medically necessary, but that he usually confirms coverage before initiating testing. The often-used Renasight panel, which tests for 385 genes related to kidney diseases, costs $300-$400 out of pocket, Dr. Vassalotti told this news organization.
In a survey of 149 nephrologists conducted in 2021, both users (46%) and nonusers of the tests (69%) said that high cost was the most significant perceived barrier to implementing widespread testing. A third of users and almost two thirds of nonusers said that poor availability or lack of ease of testing was the second most significant barrier.
Clinics that test for kidney genes “are largely confined to large academic centers and some specialty clinics,” said Dominic Raj, MD, the Bert B. Brooks chair, and Divya Shankaranarayanan, MD, director of the Kidney Precision Medicine Clinic, both at George Washington University School of Medicine & Health Sciences, Washington, DC, in an email.
Testing is also limited by cultural barriers, lack of genetic literacy, and patients’ concerns that a positive result could lead to a loss of health insurance coverage, said Dr. Raj and Dr. Shankaranarayanan.
Paper Will Help Expand Use
A lack of consensus has also held back expansion. The new statement “may lead to increased and possibly judicious utilization of genetic testing in nephrology practices,” said Dr. Raj and Dr. Shankaranarayanan. “Most importantly, the panel has given specific guidance as to what type of genetic test platform is likely to yield the best and most cost-effective yield.”
The most effective use is “in monogenic kidney diseases and to a lesser extent in oligogenic kidney disease,” said Dr. Raj and Dr. Shankaranarayanan, adding that testing is of less-certain utility in polygenic kidney diseases, “where complex genetic and epigenetic factors determine the phenotype.”
Genetic testing might be especially useful “in atypical clinical presentations” and can help clinicians avoid unnecessary expensive and extensive investigations when multiple organ systems are involved, they said.
“Most importantly, [testing] might prevent unnecessary and potentially harmful treatment and enable targeted specific treatment, when available,” said Dr. Raj and Dr. Shankaranarayanan.
Dr. Franceschini and Dr. Shankaranarayanan reported no relevant financial relationships. Dr. Raj disclosed that he received consulting fees and honoraria from Novo Nordisk and is a national leader for the company’s Zeus trial, studying whether ziltivekimab reduces the risk for cardiovascular events in cardiovascular disease, CKD, and inflammation. He also participated in a study of Natera’s Renasight, a 385-gene panel for kidney disease.
A version of this article first appeared on Medscape.com.
A new consensus statement recommended genetic testing for all categories of kidney diseases whenever a genetic cause is suspected and offered guidance on who to test, which tests are the most useful, and how to talk to patients about results.
The statement, published online in the American Journal of Kidney Diseases, is the work of four dozen authors — including patients, nephrologists, experts in clinical and laboratory genetics, kidney pathology, genetic counseling, and ethics. The experts were brought together by the National Kidney Foundation (NKF) with the goal of broadening use and understanding of the tests.
About 10% or more of kidney diseases in adults and 70% of selected chronic kidney diseases (CKDs) in children have genetic causes. But nephrologists have reported a lack of education about genetic testing, and other barriers to wider use, including limited access to testing, cost, insurance coverage, and a small number of genetic counselors who are versed in kidney genetics.
Genetic testing “in the kidney field is a little less developed than in other fields,” said co–lead author Nora Franceschini, MD, MPH, a professor of epidemiology at the University of North Carolina Gillings School of Global Public Health, Chapel Hill, and a nephrologist who studies the genetic epidemiology of hypertension and kidney and cardiovascular diseases.
There are already many known variants that play a role in various kidney diseases and more are on the horizon, Dr. Franceschini told this news organization. More genetic tests will be available in the near future. “The workforce needs to be prepared,” she said.
The statement is an initial step that gets clinicians thinking about testing in a more systematic way, said Dr. Franceschini. “Genetic testing is just another test that physicians can use to complete the story when evaluating patients.
“I think clinicians are ready to implement” testing, said Dr. Franceschini. “We just need to have better guidance.”
Who, When, What to Test
The NKF statement is not the first to try to address gaps in use and knowledge. A European Renal Association Working Group published guidelines in 2022.
The NKF Working Group came up with 56 recommendations and separate algorithms to guide testing for adult and pediatric individuals who are considered at-risk (and currently asymptomatic) and for those who already have clinical disease.
Testing can help determine a cause if there’s an atypical clinical presentation, and it can help avoid biopsies, said the group. Tests can also guide choice of therapy.
For at-risk individuals, there are two broad situations in which testing might be considered: In family members of a patient who already has kidney disease and in potential kidney donors. But testing at-risk children younger than 18 years should only be done if there is an intervention available that could prevent, treat, or slow progression of disease, said the authors.
For patients with an established genetic diagnosis, at-risk family members should be tested with the known single-gene variant diagnostic instead of a broad panel, said the group.
Single-gene variant testing is most appropriate in situations when clinical disease is already evident or when there is known genetic disease in the family, according to the NKF panel. A large diagnostic panel that covers the many common genetic causes of kidney disease is recommended for the majority of patients.
The group recommended that apolipoprotein L1 (APOL1) testing should be included in gene panels for CKD, and it should be offered to any patient “with clinical findings suggestive of APOL1-association nephropathy, regardless of race and ethnicity.”
High-risk APOL1 genotypes confer a 5- to 10-fold increased risk for CKD and are found in one out of seven individuals of African ancestry, which means the focus has largely been on testing those with that ancestry.
However, with many unknowns about APOL1, the NKF panel did not want to “profile” individuals and suggest that testing should not be based on skin color or race/ethnicity, said Dr. Franceschini.
In addition, only about 10% of those with the variant develop disease, so testing is not currently warranted for those who do not already have kidney disease, said the group.
They also recommended against the use of polygenic risk scores, saying that there are not enough data from diverse populations in genome-wide association studies for kidney disease or on their clinical utility.
More Education Needed; Many Barriers
The authors acknowledged that nephrologists generally receive little education in genetics and lack support for interpreting and discussing results.
“Nephrologists should be provided with training and best practice resources to interpret genetic testing and discuss the results with individuals and their families,” they wrote, adding that there’s a need for genomic medicine boards at academic centers that would be available to help nephrologists interpret results and plot clinical management.
The group did not, however, cite some of the other barriers to adoption of testing, including a limited number of sites offering testing, cost, and lack of insurance coverage for the diagnostics.
Medicare may cover genetic testing for kidney disease when an individual has symptoms and there is a Food and Drug Administration–approved test. Joseph Vassalotti, MD, chief medical officer for the NKF, said private insurance may cover the testing if the nephrologist deems it medically necessary, but that he usually confirms coverage before initiating testing. The often-used Renasight panel, which tests for 385 genes related to kidney diseases, costs $300-$400 out of pocket, Dr. Vassalotti told this news organization.
In a survey of 149 nephrologists conducted in 2021, both users (46%) and nonusers of the tests (69%) said that high cost was the most significant perceived barrier to implementing widespread testing. A third of users and almost two thirds of nonusers said that poor availability or lack of ease of testing was the second most significant barrier.
Clinics that test for kidney genes “are largely confined to large academic centers and some specialty clinics,” said Dominic Raj, MD, the Bert B. Brooks chair, and Divya Shankaranarayanan, MD, director of the Kidney Precision Medicine Clinic, both at George Washington University School of Medicine & Health Sciences, Washington, DC, in an email.
Testing is also limited by cultural barriers, lack of genetic literacy, and patients’ concerns that a positive result could lead to a loss of health insurance coverage, said Dr. Raj and Dr. Shankaranarayanan.
Paper Will Help Expand Use
A lack of consensus has also held back expansion. The new statement “may lead to increased and possibly judicious utilization of genetic testing in nephrology practices,” said Dr. Raj and Dr. Shankaranarayanan. “Most importantly, the panel has given specific guidance as to what type of genetic test platform is likely to yield the best and most cost-effective yield.”
The most effective use is “in monogenic kidney diseases and to a lesser extent in oligogenic kidney disease,” said Dr. Raj and Dr. Shankaranarayanan, adding that testing is of less-certain utility in polygenic kidney diseases, “where complex genetic and epigenetic factors determine the phenotype.”
Genetic testing might be especially useful “in atypical clinical presentations” and can help clinicians avoid unnecessary expensive and extensive investigations when multiple organ systems are involved, they said.
“Most importantly, [testing] might prevent unnecessary and potentially harmful treatment and enable targeted specific treatment, when available,” said Dr. Raj and Dr. Shankaranarayanan.
Dr. Franceschini and Dr. Shankaranarayanan reported no relevant financial relationships. Dr. Raj disclosed that he received consulting fees and honoraria from Novo Nordisk and is a national leader for the company’s Zeus trial, studying whether ziltivekimab reduces the risk for cardiovascular events in cardiovascular disease, CKD, and inflammation. He also participated in a study of Natera’s Renasight, a 385-gene panel for kidney disease.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF KIDNEY DISEASES
Can Addressing Depression Reduce Chemo Toxicity in Older Adults?
TOPLINE:
METHODOLOGY:
- Researchers conducted a secondary analysis of a randomized controlled trial to evaluate whether greater reductions in grade 3 chemotherapy-related toxicities occurred with geriatric assessment-driven interventions vs standard care.
- A total of 605 patients aged 65 years and older with any stage of solid malignancy were included, with 402 randomized to the intervention arm and 203 to the standard-of-care arm.
- Mental health was assessed using the Mental Health Inventory 13, and chemotherapy toxicity was graded by the National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0.
- Patients in the intervention arm received recommendations from a multidisciplinary team based on their baseline GA, while those in the standard-of-care arm received only the baseline assessment results.
- The study was conducted at City of Hope National Medical Center in Duarte, California, and patients were followed throughout treatment or for up to 6 months from starting chemotherapy.
TAKEAWAY:
- According to the authors, patients with depression had increased chemotherapy toxicity in the standard-of-care arm (70.7% vs 54.3%; P = .02) but not in the GA-driven intervention arm (54.3% vs 48.5%; P = .27).
- The association between depression and chemotherapy toxicity was also seen after adjustment for the Cancer and Aging Research Group toxicity score (odds ratio, [OR], 1.98; 95% CI, 1.07-3.65) and for demographic, disease, and treatment factors (OR, 2.00; 95% CI, 1.03-3.85).
- No significant association was found between anxiety and chemotherapy toxicity in either the standard-of-care arm (univariate OR, 1.07; 95% CI, 0.61-1.88) or the GA-driven intervention arm (univariate OR, 1.15; 95% CI, 0.78-1.71).
- The authors stated that depression was associated with increased odds of hematologic-only toxicities (OR, 2.50; 95% CI, 1.13-5.56) in the standard-of-care arm.
- An analysis of a small subgroup found associations between elevated anxiety symptoms and increased risk for hematologic and nonhematologic chemotherapy toxicities.
IN PRACTICE:
“The current study showed that elevated depression symptoms are associated with increased risk of severe chemotherapy toxicities in older adults with cancer. This risk was mitigated in those in the GA intervention arm, which suggests that addressing elevated depression symptoms may lower the risk of toxicities,” the authors wrote. “Overall, elevated anxiety symptoms were not associated with risk for severe chemotherapy toxicity.”
SOURCE:
Reena V. Jayani, MD, MSCI, of Vanderbilt University Medical Center in Nashville, Tennessee, was the first and corresponding author for this paper. This study was published online August 4, 2024, in Cancer.
LIMITATIONS:
The thresholds for depression and anxiety used in the Mental Health Inventory 13 were based on an English-speaking population, which may not be fully applicable to Chinese- and Spanish-speaking patients included in the study. Depression and anxiety were not evaluated by a mental health professional or with a structured interview to assess formal diagnostic criteria. Psychiatric medication used at the time of baseline GA was not included in the analysis. The study is a secondary analysis of a randomized controlled trial, and it is not known which components of the interventions affected mental health.
DISCLOSURES:
This research project was supported by the UniHealth Foundation, the City of Hope Center for Cancer and Aging, and the National Institutes of Health. One coauthor disclosed receiving institutional research funding from AstraZeneca and Brooklyn ImmunoTherapeutics and consulting for multiple pharmaceutical companies, including AbbVie, Adagene, and Bayer HealthCare Pharmaceuticals. William Dale, MD, PhD, of City of Hope National Medical Center, served as senior author and a principal investigator. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers conducted a secondary analysis of a randomized controlled trial to evaluate whether greater reductions in grade 3 chemotherapy-related toxicities occurred with geriatric assessment-driven interventions vs standard care.
- A total of 605 patients aged 65 years and older with any stage of solid malignancy were included, with 402 randomized to the intervention arm and 203 to the standard-of-care arm.
- Mental health was assessed using the Mental Health Inventory 13, and chemotherapy toxicity was graded by the National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0.
- Patients in the intervention arm received recommendations from a multidisciplinary team based on their baseline GA, while those in the standard-of-care arm received only the baseline assessment results.
- The study was conducted at City of Hope National Medical Center in Duarte, California, and patients were followed throughout treatment or for up to 6 months from starting chemotherapy.
TAKEAWAY:
- According to the authors, patients with depression had increased chemotherapy toxicity in the standard-of-care arm (70.7% vs 54.3%; P = .02) but not in the GA-driven intervention arm (54.3% vs 48.5%; P = .27).
- The association between depression and chemotherapy toxicity was also seen after adjustment for the Cancer and Aging Research Group toxicity score (odds ratio, [OR], 1.98; 95% CI, 1.07-3.65) and for demographic, disease, and treatment factors (OR, 2.00; 95% CI, 1.03-3.85).
- No significant association was found between anxiety and chemotherapy toxicity in either the standard-of-care arm (univariate OR, 1.07; 95% CI, 0.61-1.88) or the GA-driven intervention arm (univariate OR, 1.15; 95% CI, 0.78-1.71).
- The authors stated that depression was associated with increased odds of hematologic-only toxicities (OR, 2.50; 95% CI, 1.13-5.56) in the standard-of-care arm.
- An analysis of a small subgroup found associations between elevated anxiety symptoms and increased risk for hematologic and nonhematologic chemotherapy toxicities.
IN PRACTICE:
“The current study showed that elevated depression symptoms are associated with increased risk of severe chemotherapy toxicities in older adults with cancer. This risk was mitigated in those in the GA intervention arm, which suggests that addressing elevated depression symptoms may lower the risk of toxicities,” the authors wrote. “Overall, elevated anxiety symptoms were not associated with risk for severe chemotherapy toxicity.”
SOURCE:
Reena V. Jayani, MD, MSCI, of Vanderbilt University Medical Center in Nashville, Tennessee, was the first and corresponding author for this paper. This study was published online August 4, 2024, in Cancer.
LIMITATIONS:
The thresholds for depression and anxiety used in the Mental Health Inventory 13 were based on an English-speaking population, which may not be fully applicable to Chinese- and Spanish-speaking patients included in the study. Depression and anxiety were not evaluated by a mental health professional or with a structured interview to assess formal diagnostic criteria. Psychiatric medication used at the time of baseline GA was not included in the analysis. The study is a secondary analysis of a randomized controlled trial, and it is not known which components of the interventions affected mental health.
DISCLOSURES:
This research project was supported by the UniHealth Foundation, the City of Hope Center for Cancer and Aging, and the National Institutes of Health. One coauthor disclosed receiving institutional research funding from AstraZeneca and Brooklyn ImmunoTherapeutics and consulting for multiple pharmaceutical companies, including AbbVie, Adagene, and Bayer HealthCare Pharmaceuticals. William Dale, MD, PhD, of City of Hope National Medical Center, served as senior author and a principal investigator. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers conducted a secondary analysis of a randomized controlled trial to evaluate whether greater reductions in grade 3 chemotherapy-related toxicities occurred with geriatric assessment-driven interventions vs standard care.
- A total of 605 patients aged 65 years and older with any stage of solid malignancy were included, with 402 randomized to the intervention arm and 203 to the standard-of-care arm.
- Mental health was assessed using the Mental Health Inventory 13, and chemotherapy toxicity was graded by the National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0.
- Patients in the intervention arm received recommendations from a multidisciplinary team based on their baseline GA, while those in the standard-of-care arm received only the baseline assessment results.
- The study was conducted at City of Hope National Medical Center in Duarte, California, and patients were followed throughout treatment or for up to 6 months from starting chemotherapy.
TAKEAWAY:
- According to the authors, patients with depression had increased chemotherapy toxicity in the standard-of-care arm (70.7% vs 54.3%; P = .02) but not in the GA-driven intervention arm (54.3% vs 48.5%; P = .27).
- The association between depression and chemotherapy toxicity was also seen after adjustment for the Cancer and Aging Research Group toxicity score (odds ratio, [OR], 1.98; 95% CI, 1.07-3.65) and for demographic, disease, and treatment factors (OR, 2.00; 95% CI, 1.03-3.85).
- No significant association was found between anxiety and chemotherapy toxicity in either the standard-of-care arm (univariate OR, 1.07; 95% CI, 0.61-1.88) or the GA-driven intervention arm (univariate OR, 1.15; 95% CI, 0.78-1.71).
- The authors stated that depression was associated with increased odds of hematologic-only toxicities (OR, 2.50; 95% CI, 1.13-5.56) in the standard-of-care arm.
- An analysis of a small subgroup found associations between elevated anxiety symptoms and increased risk for hematologic and nonhematologic chemotherapy toxicities.
IN PRACTICE:
“The current study showed that elevated depression symptoms are associated with increased risk of severe chemotherapy toxicities in older adults with cancer. This risk was mitigated in those in the GA intervention arm, which suggests that addressing elevated depression symptoms may lower the risk of toxicities,” the authors wrote. “Overall, elevated anxiety symptoms were not associated with risk for severe chemotherapy toxicity.”
SOURCE:
Reena V. Jayani, MD, MSCI, of Vanderbilt University Medical Center in Nashville, Tennessee, was the first and corresponding author for this paper. This study was published online August 4, 2024, in Cancer.
LIMITATIONS:
The thresholds for depression and anxiety used in the Mental Health Inventory 13 were based on an English-speaking population, which may not be fully applicable to Chinese- and Spanish-speaking patients included in the study. Depression and anxiety were not evaluated by a mental health professional or with a structured interview to assess formal diagnostic criteria. Psychiatric medication used at the time of baseline GA was not included in the analysis. The study is a secondary analysis of a randomized controlled trial, and it is not known which components of the interventions affected mental health.
DISCLOSURES:
This research project was supported by the UniHealth Foundation, the City of Hope Center for Cancer and Aging, and the National Institutes of Health. One coauthor disclosed receiving institutional research funding from AstraZeneca and Brooklyn ImmunoTherapeutics and consulting for multiple pharmaceutical companies, including AbbVie, Adagene, and Bayer HealthCare Pharmaceuticals. William Dale, MD, PhD, of City of Hope National Medical Center, served as senior author and a principal investigator. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Support Researchers with a Donation to the AGA Research Foundation
By joining others in donating to the AGA Research Foundation, you will ensure that researchers have opportunities to continue their lifesaving work.
The AGA Research Foundation remains committed to providing young researchers with unprecedented research opportunities. Each year, we receive a caliber of nominations for AGA research awards. You can help gifted investigators as they work to advance the understanding of digestive diseases through their novel research objectives.
As an AGA member, you can help fund discoveries that will continue to improve GI practice and better patient care.
AGA grants have led to discoveries, including new approaches to down-regulate intestinal inflammation, a test for genetic predisposition to colon cancer and autoimmune liver disease treatments. The importance of these awards is evidenced by the fact that virtually every major advance leading to the understanding, prevention, treatment, and cure of digestive diseases has been made in the research laboratory of a talented young investigator.
Donate to the AGA Research Foundation to ensure that researchers have opportunities to continue their lifesaving work.
Three Easy Ways To Give
Online: Donate at www.foundation.gastro.org.
Through the mail:
AGA Research Foundation
4930 Del Ray Avenue
Bethesda, MD 20814
Over the phone: 301-222-4002
All gifts are tax-deductible to the fullest extent of U.S. law.
By joining others in donating to the AGA Research Foundation, you will ensure that researchers have opportunities to continue their lifesaving work.
The AGA Research Foundation remains committed to providing young researchers with unprecedented research opportunities. Each year, we receive a caliber of nominations for AGA research awards. You can help gifted investigators as they work to advance the understanding of digestive diseases through their novel research objectives.
As an AGA member, you can help fund discoveries that will continue to improve GI practice and better patient care.
AGA grants have led to discoveries, including new approaches to down-regulate intestinal inflammation, a test for genetic predisposition to colon cancer and autoimmune liver disease treatments. The importance of these awards is evidenced by the fact that virtually every major advance leading to the understanding, prevention, treatment, and cure of digestive diseases has been made in the research laboratory of a talented young investigator.
Donate to the AGA Research Foundation to ensure that researchers have opportunities to continue their lifesaving work.
Three Easy Ways To Give
Online: Donate at www.foundation.gastro.org.
Through the mail:
AGA Research Foundation
4930 Del Ray Avenue
Bethesda, MD 20814
Over the phone: 301-222-4002
All gifts are tax-deductible to the fullest extent of U.S. law.
By joining others in donating to the AGA Research Foundation, you will ensure that researchers have opportunities to continue their lifesaving work.
The AGA Research Foundation remains committed to providing young researchers with unprecedented research opportunities. Each year, we receive a caliber of nominations for AGA research awards. You can help gifted investigators as they work to advance the understanding of digestive diseases through their novel research objectives.
As an AGA member, you can help fund discoveries that will continue to improve GI practice and better patient care.
AGA grants have led to discoveries, including new approaches to down-regulate intestinal inflammation, a test for genetic predisposition to colon cancer and autoimmune liver disease treatments. The importance of these awards is evidenced by the fact that virtually every major advance leading to the understanding, prevention, treatment, and cure of digestive diseases has been made in the research laboratory of a talented young investigator.
Donate to the AGA Research Foundation to ensure that researchers have opportunities to continue their lifesaving work.
Three Easy Ways To Give
Online: Donate at www.foundation.gastro.org.
Through the mail:
AGA Research Foundation
4930 Del Ray Avenue
Bethesda, MD 20814
Over the phone: 301-222-4002
All gifts are tax-deductible to the fullest extent of U.S. law.
FDA Approves First Blood Test for Colorectal Cancer
In late July, the US Food and Drug Administration (FDA) approved the first use of a liquid biopsy (blood test) for colorectal cancer (CRC) screening. The test, called Shield, launched commercially the first week of August and is the first blood test to be approved by the FDA as a primary screening option for CRC that meets requirements for Medicare reimbursement.
While the convenience of a blood test could potentially encourage more people to get screened, expert consensus is that blood tests can’t prevent CRC and should not be considered a replacement for a colonoscopy. Modeling studies and expert consensus published earlier this year in Gastroenterology and in Clinical Gastroenterology and Hepatology shed light on the perils of liquid biopsy.
“Based on their current characteristics, blood tests should not be recommended to replace established colorectal cancer screening tests, since blood tests are neither as effective nor as cost-effective, and would worsen outcomes,” said David Lieberman, MD, AGAF, chair, AGA CRC Workshop chair and lead author of an expert commentary on liquid biopsy for CRC screening.
Five Key Takeaways
- A blood test for CRC that meets minimal CMS criteria for sensitivity and performed every 3 years would likely result in better outcomes than no screening.
- A blood test for CRC offers a simple process that could encourage more people to participate in screening. Patients who may have declined colonoscopy should understand the need for a colonoscopy if findings are abnormal.
- Because blood tests for CRC are predicted to be less effective and more costly than currently established screening programs, they cannot be recommended to replace established effective screening methods.
- Although blood tests would improve outcomes in currently unscreened people, substituting blood tests for a currently effective test would worsen patient outcomes and increase cost.
- Potential benchmarks that industry might use to assess an effective blood test for CRC going forward would be sensitivity for stage I-III CRC of > 90%, with sensitivity for advanced adenomas of > 40%-50%.
“Unless we have the expectation of high sensitivity and specificity, blood-based colorectal cancer tests could lead to false positive and false negative results, which are both bad for patient outcomes,” said John M. Carethers, MD, AGAF, AGA past president and vice chancellor for health sciences at the University of California San Diego.
In late July, the US Food and Drug Administration (FDA) approved the first use of a liquid biopsy (blood test) for colorectal cancer (CRC) screening. The test, called Shield, launched commercially the first week of August and is the first blood test to be approved by the FDA as a primary screening option for CRC that meets requirements for Medicare reimbursement.
While the convenience of a blood test could potentially encourage more people to get screened, expert consensus is that blood tests can’t prevent CRC and should not be considered a replacement for a colonoscopy. Modeling studies and expert consensus published earlier this year in Gastroenterology and in Clinical Gastroenterology and Hepatology shed light on the perils of liquid biopsy.
“Based on their current characteristics, blood tests should not be recommended to replace established colorectal cancer screening tests, since blood tests are neither as effective nor as cost-effective, and would worsen outcomes,” said David Lieberman, MD, AGAF, chair, AGA CRC Workshop chair and lead author of an expert commentary on liquid biopsy for CRC screening.
Five Key Takeaways
- A blood test for CRC that meets minimal CMS criteria for sensitivity and performed every 3 years would likely result in better outcomes than no screening.
- A blood test for CRC offers a simple process that could encourage more people to participate in screening. Patients who may have declined colonoscopy should understand the need for a colonoscopy if findings are abnormal.
- Because blood tests for CRC are predicted to be less effective and more costly than currently established screening programs, they cannot be recommended to replace established effective screening methods.
- Although blood tests would improve outcomes in currently unscreened people, substituting blood tests for a currently effective test would worsen patient outcomes and increase cost.
- Potential benchmarks that industry might use to assess an effective blood test for CRC going forward would be sensitivity for stage I-III CRC of > 90%, with sensitivity for advanced adenomas of > 40%-50%.
“Unless we have the expectation of high sensitivity and specificity, blood-based colorectal cancer tests could lead to false positive and false negative results, which are both bad for patient outcomes,” said John M. Carethers, MD, AGAF, AGA past president and vice chancellor for health sciences at the University of California San Diego.
In late July, the US Food and Drug Administration (FDA) approved the first use of a liquid biopsy (blood test) for colorectal cancer (CRC) screening. The test, called Shield, launched commercially the first week of August and is the first blood test to be approved by the FDA as a primary screening option for CRC that meets requirements for Medicare reimbursement.
While the convenience of a blood test could potentially encourage more people to get screened, expert consensus is that blood tests can’t prevent CRC and should not be considered a replacement for a colonoscopy. Modeling studies and expert consensus published earlier this year in Gastroenterology and in Clinical Gastroenterology and Hepatology shed light on the perils of liquid biopsy.
“Based on their current characteristics, blood tests should not be recommended to replace established colorectal cancer screening tests, since blood tests are neither as effective nor as cost-effective, and would worsen outcomes,” said David Lieberman, MD, AGAF, chair, AGA CRC Workshop chair and lead author of an expert commentary on liquid biopsy for CRC screening.
Five Key Takeaways
- A blood test for CRC that meets minimal CMS criteria for sensitivity and performed every 3 years would likely result in better outcomes than no screening.
- A blood test for CRC offers a simple process that could encourage more people to participate in screening. Patients who may have declined colonoscopy should understand the need for a colonoscopy if findings are abnormal.
- Because blood tests for CRC are predicted to be less effective and more costly than currently established screening programs, they cannot be recommended to replace established effective screening methods.
- Although blood tests would improve outcomes in currently unscreened people, substituting blood tests for a currently effective test would worsen patient outcomes and increase cost.
- Potential benchmarks that industry might use to assess an effective blood test for CRC going forward would be sensitivity for stage I-III CRC of > 90%, with sensitivity for advanced adenomas of > 40%-50%.
“Unless we have the expectation of high sensitivity and specificity, blood-based colorectal cancer tests could lead to false positive and false negative results, which are both bad for patient outcomes,” said John M. Carethers, MD, AGAF, AGA past president and vice chancellor for health sciences at the University of California San Diego.
Free Med School Alone Won’t Boost Diversity
This transcript has been edited for clarity.
We need more diverse students — more students from disadvantaged and underrepresented backgrounds in medical school. That is not a controversial take. That’s not even a new thought.
What is a hot take, however, is that free medical school alone is not going to accomplish this goal. In fact, based on data and what people think and are saying, that’s just reality.
I recently chatted about whether or not free medical school would motivate more students to pursue primary care. That was New York University’s (NYU’s) goal. If you haven’t seen that video, check it out. Now I want to explore whether free medical school would actually create a more diverse medical student body.
This topic is especially important now because, in 2023, the Supreme Court ended affirmative action for college admissions, and this naturally has a downstream effect when it comes to getting into medical school. Right now, about 6% of US physicians are Black or Hispanic/Latina, and around 0.1%-0.3% identify as Indigenous Americans, Native Hawaiians, or Pacific Islanders.
Is free medical school the answer? Well, that’s based on a huge assumption that the cost of medical school — incoming debt — is the single greatest barrier for students from diverse backgrounds, as if every single student from every background had the same level of resources in the same opportunity and were all equally competitive prior to applying, and just the prospect of debt is what caused the disparity. I don’t know if that’s reality. Let’s take a look at NYU.
After the free tuition announcement, total applications to the medical school went up nearly 50%. And from underrepresented groups, it was 100%. In 2019, the associate dean for admissions said, “A key driver was to remove a financial disincentive that dissuades people from pursuing a path in medicine.” But the acceptance rate stayed under 3%, and the average Medical College Admission Test (MCAT) and grade point average (GPA) to get in went up. Basically, the school just became more competitive.
I will always commend anyone, anywhere, who is making medical school more affordable and more accessible. With NYU, it seems a tuition gift just made it harder for students from disadvantaged backgrounds to actually get in. I mean, congratulations, you got more applications. This probably helped in ratings, and you got mentioned in news headlines, but are you actually achieving your mission?
At NYU, over the last few years, Black students made up about 11% of the medical school class, which is actually down from 2017 before the tuition gift. Students from low-income backgrounds, whom this would really benefit, used to make up around 12% of the class prior to the free tuition announcement, and now it’s around 3%-7%.
According to students from underrepresented backgrounds, the outreach and the equal opportunity need to start way earlier. The K-12 process needs to be addressed, as do mentorship opportunities and guidance throughout college, MCAT prep, resources for interviews, research opportunities, and so much more.
The following quote is from an interview with an interventional cardiology fellow who came here as a refugee: “For me, growing up, basic necessities like a quiet study space, high-speed internet, healthy meals and proper sleep were luxuries of which I could only dream. After resettling in the US as a political refugee, I lived in circumstances where such comforts were out of reach, and my path to medical school seemed insurmountable.”
I also spoke to a friend in pediatric cancer, Michael Galvez, MD, who was outspoken about the need to improve representation in medicine, about what he thought would actually work to diversify medical schools. He mentioned adversity scores or looking at the distance traveled for applicants, as well as efforts to recruit from local, state, and community colleges, which often reflect local underserved populations.
Dr. Galvez also agreed that although such metrics as GPA and MCAT are important, medical schools should also consider the impact applicants may have had for local, underserved communities and life experiences that may represent significant potential contributions applicants can make for public health.
The effort needs to start early. If we take a look at one of the most diverse medical schools in the country, UC Davis, we can see how this makes a difference. At UC Davis, in the class of 2026, about half of the 133 students come from underrepresented backgrounds in medicine. I’m taking a look at their website from the Office of Student and Resident Diversity, and it lists:
- K-12 outreach programs
- Undergraduate and community college programs
- Specific plans for postbaccalaureate students
- Support systems
- Resources for students that extend far beyond just premedical students
My home institution, Stanford School of Medicine, has similar programs as well, with similar ways for students from underrepresented backgrounds to find support and mentorship. This all makes a huge difference.
Regarding the actual admissions process for medical school, I’ll highlight the Johns Hopkins School of Medicine and the adaptions they’ve made to create a more fair and holistic process. It includes:
- A clear mission statement about diversity enhancement
- Anonymous voting
- A larger group to avoid bias
- Not showing academic metrics to interviewers
- Implicit association tests and trainings
- Removing photos from applications
- Appointing women, minorities, and young people with less implicit bias to the committees
Does this seem like a lot? It is, because a comprehensive approach is what it takes to build a more diverse US physician workforce, which will provide more culturally competent care, empower future generations, break down barriers and disparities in health care, and ultimately improve public health. Free tuition is awesome. I’m jealous. But on its own to solve these problems? This all feels like a misguided attempt.
Dr. Patel is clinical instructor, Department of Pediatrics, Columbia University College of Physicians and Surgeons, and pediatric hospitalist at Morgan Stanley Children’s Hospital of NewYork-Presbyterian, New York, and Benioff Children’s Hospital, University of California, San Francisco. He disclosed ties with Medumo Inc.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
We need more diverse students — more students from disadvantaged and underrepresented backgrounds in medical school. That is not a controversial take. That’s not even a new thought.
What is a hot take, however, is that free medical school alone is not going to accomplish this goal. In fact, based on data and what people think and are saying, that’s just reality.
I recently chatted about whether or not free medical school would motivate more students to pursue primary care. That was New York University’s (NYU’s) goal. If you haven’t seen that video, check it out. Now I want to explore whether free medical school would actually create a more diverse medical student body.
This topic is especially important now because, in 2023, the Supreme Court ended affirmative action for college admissions, and this naturally has a downstream effect when it comes to getting into medical school. Right now, about 6% of US physicians are Black or Hispanic/Latina, and around 0.1%-0.3% identify as Indigenous Americans, Native Hawaiians, or Pacific Islanders.
Is free medical school the answer? Well, that’s based on a huge assumption that the cost of medical school — incoming debt — is the single greatest barrier for students from diverse backgrounds, as if every single student from every background had the same level of resources in the same opportunity and were all equally competitive prior to applying, and just the prospect of debt is what caused the disparity. I don’t know if that’s reality. Let’s take a look at NYU.
After the free tuition announcement, total applications to the medical school went up nearly 50%. And from underrepresented groups, it was 100%. In 2019, the associate dean for admissions said, “A key driver was to remove a financial disincentive that dissuades people from pursuing a path in medicine.” But the acceptance rate stayed under 3%, and the average Medical College Admission Test (MCAT) and grade point average (GPA) to get in went up. Basically, the school just became more competitive.
I will always commend anyone, anywhere, who is making medical school more affordable and more accessible. With NYU, it seems a tuition gift just made it harder for students from disadvantaged backgrounds to actually get in. I mean, congratulations, you got more applications. This probably helped in ratings, and you got mentioned in news headlines, but are you actually achieving your mission?
At NYU, over the last few years, Black students made up about 11% of the medical school class, which is actually down from 2017 before the tuition gift. Students from low-income backgrounds, whom this would really benefit, used to make up around 12% of the class prior to the free tuition announcement, and now it’s around 3%-7%.
According to students from underrepresented backgrounds, the outreach and the equal opportunity need to start way earlier. The K-12 process needs to be addressed, as do mentorship opportunities and guidance throughout college, MCAT prep, resources for interviews, research opportunities, and so much more.
The following quote is from an interview with an interventional cardiology fellow who came here as a refugee: “For me, growing up, basic necessities like a quiet study space, high-speed internet, healthy meals and proper sleep were luxuries of which I could only dream. After resettling in the US as a political refugee, I lived in circumstances where such comforts were out of reach, and my path to medical school seemed insurmountable.”
I also spoke to a friend in pediatric cancer, Michael Galvez, MD, who was outspoken about the need to improve representation in medicine, about what he thought would actually work to diversify medical schools. He mentioned adversity scores or looking at the distance traveled for applicants, as well as efforts to recruit from local, state, and community colleges, which often reflect local underserved populations.
Dr. Galvez also agreed that although such metrics as GPA and MCAT are important, medical schools should also consider the impact applicants may have had for local, underserved communities and life experiences that may represent significant potential contributions applicants can make for public health.
The effort needs to start early. If we take a look at one of the most diverse medical schools in the country, UC Davis, we can see how this makes a difference. At UC Davis, in the class of 2026, about half of the 133 students come from underrepresented backgrounds in medicine. I’m taking a look at their website from the Office of Student and Resident Diversity, and it lists:
- K-12 outreach programs
- Undergraduate and community college programs
- Specific plans for postbaccalaureate students
- Support systems
- Resources for students that extend far beyond just premedical students
My home institution, Stanford School of Medicine, has similar programs as well, with similar ways for students from underrepresented backgrounds to find support and mentorship. This all makes a huge difference.
Regarding the actual admissions process for medical school, I’ll highlight the Johns Hopkins School of Medicine and the adaptions they’ve made to create a more fair and holistic process. It includes:
- A clear mission statement about diversity enhancement
- Anonymous voting
- A larger group to avoid bias
- Not showing academic metrics to interviewers
- Implicit association tests and trainings
- Removing photos from applications
- Appointing women, minorities, and young people with less implicit bias to the committees
Does this seem like a lot? It is, because a comprehensive approach is what it takes to build a more diverse US physician workforce, which will provide more culturally competent care, empower future generations, break down barriers and disparities in health care, and ultimately improve public health. Free tuition is awesome. I’m jealous. But on its own to solve these problems? This all feels like a misguided attempt.
Dr. Patel is clinical instructor, Department of Pediatrics, Columbia University College of Physicians and Surgeons, and pediatric hospitalist at Morgan Stanley Children’s Hospital of NewYork-Presbyterian, New York, and Benioff Children’s Hospital, University of California, San Francisco. He disclosed ties with Medumo Inc.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
We need more diverse students — more students from disadvantaged and underrepresented backgrounds in medical school. That is not a controversial take. That’s not even a new thought.
What is a hot take, however, is that free medical school alone is not going to accomplish this goal. In fact, based on data and what people think and are saying, that’s just reality.
I recently chatted about whether or not free medical school would motivate more students to pursue primary care. That was New York University’s (NYU’s) goal. If you haven’t seen that video, check it out. Now I want to explore whether free medical school would actually create a more diverse medical student body.
This topic is especially important now because, in 2023, the Supreme Court ended affirmative action for college admissions, and this naturally has a downstream effect when it comes to getting into medical school. Right now, about 6% of US physicians are Black or Hispanic/Latina, and around 0.1%-0.3% identify as Indigenous Americans, Native Hawaiians, or Pacific Islanders.
Is free medical school the answer? Well, that’s based on a huge assumption that the cost of medical school — incoming debt — is the single greatest barrier for students from diverse backgrounds, as if every single student from every background had the same level of resources in the same opportunity and were all equally competitive prior to applying, and just the prospect of debt is what caused the disparity. I don’t know if that’s reality. Let’s take a look at NYU.
After the free tuition announcement, total applications to the medical school went up nearly 50%. And from underrepresented groups, it was 100%. In 2019, the associate dean for admissions said, “A key driver was to remove a financial disincentive that dissuades people from pursuing a path in medicine.” But the acceptance rate stayed under 3%, and the average Medical College Admission Test (MCAT) and grade point average (GPA) to get in went up. Basically, the school just became more competitive.
I will always commend anyone, anywhere, who is making medical school more affordable and more accessible. With NYU, it seems a tuition gift just made it harder for students from disadvantaged backgrounds to actually get in. I mean, congratulations, you got more applications. This probably helped in ratings, and you got mentioned in news headlines, but are you actually achieving your mission?
At NYU, over the last few years, Black students made up about 11% of the medical school class, which is actually down from 2017 before the tuition gift. Students from low-income backgrounds, whom this would really benefit, used to make up around 12% of the class prior to the free tuition announcement, and now it’s around 3%-7%.
According to students from underrepresented backgrounds, the outreach and the equal opportunity need to start way earlier. The K-12 process needs to be addressed, as do mentorship opportunities and guidance throughout college, MCAT prep, resources for interviews, research opportunities, and so much more.
The following quote is from an interview with an interventional cardiology fellow who came here as a refugee: “For me, growing up, basic necessities like a quiet study space, high-speed internet, healthy meals and proper sleep were luxuries of which I could only dream. After resettling in the US as a political refugee, I lived in circumstances where such comforts were out of reach, and my path to medical school seemed insurmountable.”
I also spoke to a friend in pediatric cancer, Michael Galvez, MD, who was outspoken about the need to improve representation in medicine, about what he thought would actually work to diversify medical schools. He mentioned adversity scores or looking at the distance traveled for applicants, as well as efforts to recruit from local, state, and community colleges, which often reflect local underserved populations.
Dr. Galvez also agreed that although such metrics as GPA and MCAT are important, medical schools should also consider the impact applicants may have had for local, underserved communities and life experiences that may represent significant potential contributions applicants can make for public health.
The effort needs to start early. If we take a look at one of the most diverse medical schools in the country, UC Davis, we can see how this makes a difference. At UC Davis, in the class of 2026, about half of the 133 students come from underrepresented backgrounds in medicine. I’m taking a look at their website from the Office of Student and Resident Diversity, and it lists:
- K-12 outreach programs
- Undergraduate and community college programs
- Specific plans for postbaccalaureate students
- Support systems
- Resources for students that extend far beyond just premedical students
My home institution, Stanford School of Medicine, has similar programs as well, with similar ways for students from underrepresented backgrounds to find support and mentorship. This all makes a huge difference.
Regarding the actual admissions process for medical school, I’ll highlight the Johns Hopkins School of Medicine and the adaptions they’ve made to create a more fair and holistic process. It includes:
- A clear mission statement about diversity enhancement
- Anonymous voting
- A larger group to avoid bias
- Not showing academic metrics to interviewers
- Implicit association tests and trainings
- Removing photos from applications
- Appointing women, minorities, and young people with less implicit bias to the committees
Does this seem like a lot? It is, because a comprehensive approach is what it takes to build a more diverse US physician workforce, which will provide more culturally competent care, empower future generations, break down barriers and disparities in health care, and ultimately improve public health. Free tuition is awesome. I’m jealous. But on its own to solve these problems? This all feels like a misguided attempt.
Dr. Patel is clinical instructor, Department of Pediatrics, Columbia University College of Physicians and Surgeons, and pediatric hospitalist at Morgan Stanley Children’s Hospital of NewYork-Presbyterian, New York, and Benioff Children’s Hospital, University of California, San Francisco. He disclosed ties with Medumo Inc.
A version of this article first appeared on Medscape.com.
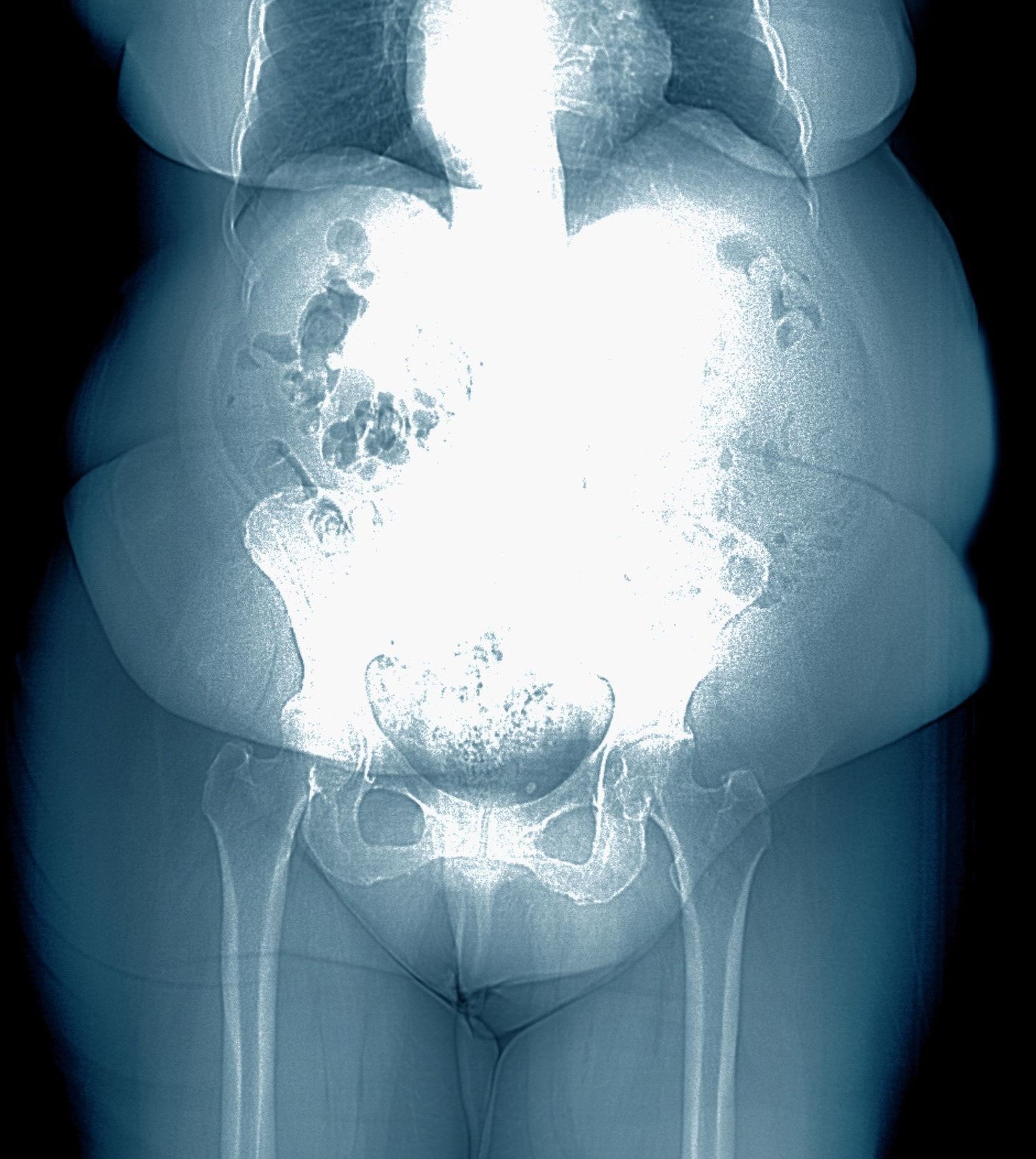
Weight gain despite dieting
Binge-eating disorder is more prevalent in women than men and has one of the strongest associations with obesity; among patients with obesity, lifetime prevalence of binge eating is approximately 5.5%. Large population studies suggest that binge-eating disorder may be present in 2%-4% of adolescents, with a mean age of onset of 12-13 years. This patient probably had milder binge-eating disorder as an adolescent and young adult, which was exacerbated by the pandemic.
Both new diagnoses and reports of clinical worsening in patients with preexisting diagnoses of binge-eating disorder during the pandemic have been documented. Food insecurity has been associated with binge eating, consistent with this patient's anxiety over food and grocery availability during the pandemic. The definition of binge-eating disorder includes recurrent specific episodes of overeating that are not consistent with the patient's usual behavior, eating to the point of being uncomfortably full, eating more quickly or when not hungry, and having feelings of loss of control during episodes and of guilt or disgust afterward.
Obesity and eating disorders share some common risk factors and approaches to management. Binge eating has been associated with type 2 diabetes, hypertension, asthma, sleep disorders, and menstrual disorders, all of which are also affected by obesity. The presence of both conditions increases the adverse outcomes associated with each, including negative impacts on cardiometabolic and psychological health. Workup of patients presenting with binge eating and obesity should always include complete blood/metabolic panels and cardiovascular and renal health, as well as assessments of nutrition status, electrolyte imbalances, gastrointestinal reflux disease, and chronic pain.
In general, where binge-eating disorder and obesity are concurrent, cognitive-behavioral therapy (CBT) for binge-eating disorder should be the first priority, with obesity management (medication or surgery) to follow. CBT has the strongest evidence of benefit for patients with binge-eating disorder and is the recommended treatment approach. Other psychotherapeutic interventions that may be of benefit include dialectical behavioral therapy (to reduce binge-eating frequency), technology-based options, and family-based therapy when symptoms are recognized in children or adolescents. Structured behavioral weight management strategies for management of obesity and overweight do not increase symptoms of eating disorders and may instead relieve some symptoms. An emerging approach to binge eating in patients with obesity is CBT that integrates therapeutic approaches to both issues.
Medications to treat binge-eating disorder are limited and should not be used without concurrent psychotherapy; lisdexamfetamine has demonstrated benefit, is recommended by the American Psychiatric Association, and is approved by the US Food and Drug Administration specifically to treat adults with binge-eating disorder.
The success of psychological interventions and lifestyle modifications for obesity is heavily dependent on the individual's ability and motivation to comply with recommended interventions. The American Gastroenterological Association and other organizations recommend treatment with antiobesity medications along with lifestyle modifications for patients with obesity (BMI ≥ 30) and weight-related complications (BMI > 27). Recommended medications include phentermine-topiramate and bupropion-naltrexone (which may benefit those with binge-eating disorder), as well as injectable glucagon-like peptide receptor agonists (GLP-1 RAs) at the approved dosage for obesity management (semaglutide 2.4 mg weekly or liraglutide 3.0 mg daily). Orlistat is not recommended. Ongoing research on the potential benefit of GLP-1 RAs in management of binge eating offers additional support for a role in patients, like this one, with binge-eating disorder and obesity.
Carolyn Newberry, MD, Assistant Professor of Medicine, Director of GI Nutrition, Innovative Center for Health and Nutrition in Gastroenterology (ICHANGE), Division of Gastroenterology, Weill Cornell Medical Center, New York, NY.
Disclosure: Carolyn Newberry, MD, has disclosed the following relevant financial relationships:
Serve(d) as a speaker or a member of a speakers bureau for: Baster International; InBody.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Binge-eating disorder is more prevalent in women than men and has one of the strongest associations with obesity; among patients with obesity, lifetime prevalence of binge eating is approximately 5.5%. Large population studies suggest that binge-eating disorder may be present in 2%-4% of adolescents, with a mean age of onset of 12-13 years. This patient probably had milder binge-eating disorder as an adolescent and young adult, which was exacerbated by the pandemic.
Both new diagnoses and reports of clinical worsening in patients with preexisting diagnoses of binge-eating disorder during the pandemic have been documented. Food insecurity has been associated with binge eating, consistent with this patient's anxiety over food and grocery availability during the pandemic. The definition of binge-eating disorder includes recurrent specific episodes of overeating that are not consistent with the patient's usual behavior, eating to the point of being uncomfortably full, eating more quickly or when not hungry, and having feelings of loss of control during episodes and of guilt or disgust afterward.
Obesity and eating disorders share some common risk factors and approaches to management. Binge eating has been associated with type 2 diabetes, hypertension, asthma, sleep disorders, and menstrual disorders, all of which are also affected by obesity. The presence of both conditions increases the adverse outcomes associated with each, including negative impacts on cardiometabolic and psychological health. Workup of patients presenting with binge eating and obesity should always include complete blood/metabolic panels and cardiovascular and renal health, as well as assessments of nutrition status, electrolyte imbalances, gastrointestinal reflux disease, and chronic pain.
In general, where binge-eating disorder and obesity are concurrent, cognitive-behavioral therapy (CBT) for binge-eating disorder should be the first priority, with obesity management (medication or surgery) to follow. CBT has the strongest evidence of benefit for patients with binge-eating disorder and is the recommended treatment approach. Other psychotherapeutic interventions that may be of benefit include dialectical behavioral therapy (to reduce binge-eating frequency), technology-based options, and family-based therapy when symptoms are recognized in children or adolescents. Structured behavioral weight management strategies for management of obesity and overweight do not increase symptoms of eating disorders and may instead relieve some symptoms. An emerging approach to binge eating in patients with obesity is CBT that integrates therapeutic approaches to both issues.
Medications to treat binge-eating disorder are limited and should not be used without concurrent psychotherapy; lisdexamfetamine has demonstrated benefit, is recommended by the American Psychiatric Association, and is approved by the US Food and Drug Administration specifically to treat adults with binge-eating disorder.
The success of psychological interventions and lifestyle modifications for obesity is heavily dependent on the individual's ability and motivation to comply with recommended interventions. The American Gastroenterological Association and other organizations recommend treatment with antiobesity medications along with lifestyle modifications for patients with obesity (BMI ≥ 30) and weight-related complications (BMI > 27). Recommended medications include phentermine-topiramate and bupropion-naltrexone (which may benefit those with binge-eating disorder), as well as injectable glucagon-like peptide receptor agonists (GLP-1 RAs) at the approved dosage for obesity management (semaglutide 2.4 mg weekly or liraglutide 3.0 mg daily). Orlistat is not recommended. Ongoing research on the potential benefit of GLP-1 RAs in management of binge eating offers additional support for a role in patients, like this one, with binge-eating disorder and obesity.
Carolyn Newberry, MD, Assistant Professor of Medicine, Director of GI Nutrition, Innovative Center for Health and Nutrition in Gastroenterology (ICHANGE), Division of Gastroenterology, Weill Cornell Medical Center, New York, NY.
Disclosure: Carolyn Newberry, MD, has disclosed the following relevant financial relationships:
Serve(d) as a speaker or a member of a speakers bureau for: Baster International; InBody.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Binge-eating disorder is more prevalent in women than men and has one of the strongest associations with obesity; among patients with obesity, lifetime prevalence of binge eating is approximately 5.5%. Large population studies suggest that binge-eating disorder may be present in 2%-4% of adolescents, with a mean age of onset of 12-13 years. This patient probably had milder binge-eating disorder as an adolescent and young adult, which was exacerbated by the pandemic.
Both new diagnoses and reports of clinical worsening in patients with preexisting diagnoses of binge-eating disorder during the pandemic have been documented. Food insecurity has been associated with binge eating, consistent with this patient's anxiety over food and grocery availability during the pandemic. The definition of binge-eating disorder includes recurrent specific episodes of overeating that are not consistent with the patient's usual behavior, eating to the point of being uncomfortably full, eating more quickly or when not hungry, and having feelings of loss of control during episodes and of guilt or disgust afterward.
Obesity and eating disorders share some common risk factors and approaches to management. Binge eating has been associated with type 2 diabetes, hypertension, asthma, sleep disorders, and menstrual disorders, all of which are also affected by obesity. The presence of both conditions increases the adverse outcomes associated with each, including negative impacts on cardiometabolic and psychological health. Workup of patients presenting with binge eating and obesity should always include complete blood/metabolic panels and cardiovascular and renal health, as well as assessments of nutrition status, electrolyte imbalances, gastrointestinal reflux disease, and chronic pain.
In general, where binge-eating disorder and obesity are concurrent, cognitive-behavioral therapy (CBT) for binge-eating disorder should be the first priority, with obesity management (medication or surgery) to follow. CBT has the strongest evidence of benefit for patients with binge-eating disorder and is the recommended treatment approach. Other psychotherapeutic interventions that may be of benefit include dialectical behavioral therapy (to reduce binge-eating frequency), technology-based options, and family-based therapy when symptoms are recognized in children or adolescents. Structured behavioral weight management strategies for management of obesity and overweight do not increase symptoms of eating disorders and may instead relieve some symptoms. An emerging approach to binge eating in patients with obesity is CBT that integrates therapeutic approaches to both issues.
Medications to treat binge-eating disorder are limited and should not be used without concurrent psychotherapy; lisdexamfetamine has demonstrated benefit, is recommended by the American Psychiatric Association, and is approved by the US Food and Drug Administration specifically to treat adults with binge-eating disorder.
The success of psychological interventions and lifestyle modifications for obesity is heavily dependent on the individual's ability and motivation to comply with recommended interventions. The American Gastroenterological Association and other organizations recommend treatment with antiobesity medications along with lifestyle modifications for patients with obesity (BMI ≥ 30) and weight-related complications (BMI > 27). Recommended medications include phentermine-topiramate and bupropion-naltrexone (which may benefit those with binge-eating disorder), as well as injectable glucagon-like peptide receptor agonists (GLP-1 RAs) at the approved dosage for obesity management (semaglutide 2.4 mg weekly or liraglutide 3.0 mg daily). Orlistat is not recommended. Ongoing research on the potential benefit of GLP-1 RAs in management of binge eating offers additional support for a role in patients, like this one, with binge-eating disorder and obesity.
Carolyn Newberry, MD, Assistant Professor of Medicine, Director of GI Nutrition, Innovative Center for Health and Nutrition in Gastroenterology (ICHANGE), Division of Gastroenterology, Weill Cornell Medical Center, New York, NY.
Disclosure: Carolyn Newberry, MD, has disclosed the following relevant financial relationships:
Serve(d) as a speaker or a member of a speakers bureau for: Baster International; InBody.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 28-year-old woman presents with concerns about weight gain despite dieting. She is 5 ft 4 in and weighs 180 lb (BMI 30.9). The patient lives alone and says she often feels isolated and has ongoing anxiety. She states that she has been overweight since her early teen years and had rare episodes of overeating. As an adult, her weight remained relatively stable (BMI ~26) until she began working remotely because of the COVID-19 pandemic in March 2020. She admits to becoming increasingly anxious and worried about food availability and grocery shopping during the early pandemic closures, feelings that have not completely resolved. While working from home, she has had more days where she compulsively overeats, even while trying to diet or use supplements she saw on TV or the internet. She stopped participating in a regular exercise walking group in mid-2020 and has not returned to it.
At presentation, she appears anxious and nervous. Her blood pressure is elevated (140/90 mm Hg), heart rate is 110 beats/min, and respiratory rate is 18 breaths/min. Her results on the Generalized Anxiety Disorder assessment indicate moderate symptoms of anxiety. Lab results indicate A1c = 6.5%, low-density lipoprotein cholesterol = 105 mg/dL, and estimated glomerular filtration rate = 90 mL/min/1.73 m2; all other results are within normal.
Artera Launches AI Test for Decision-Making on Prostate Cancer Treatment Course
Artera, the Los Altos, California–based developer of tools to diagnose cancer, has launched the first artificial intelligence (AI) test to guide patients in making informed decisions between active surveillance and active treatment based on an analysis of digital pathology images.
Trevor Royce, MD, MPH, senior medical director of Artera, said the new version of the ArteraAI Prostate Test helps patients with low-risk (Grade Group 1/Gleason 6) to favorable intermediate-risk (Grade Group 2/Gleason 3+4) prostate cancer choose between treatment or active surveillance.
The test estimates how a patient’s cancer may progress and predicts the benefit of treatment for localized prostate cancer.
“The prognostic performance of the test has now been validated in a diverse cohort of patients, including those who have undergone active surveillance, radiation therapy, or had a radical prostatectomy,” said Dr. Royce, a faculty member in radiation oncology at Wake Forest University School of Medicine in Winston-Salem, North Carolina. “The prognostic risk result reflects the patient’s prognosis regardless of the treatment path chosen.”
Dr. Royce said the new test predicts the risk for developing distant metastasis in 10 years. For the population considering active surveillance, it also can predict the likelihood their cancer will show more aggressive features. The test does not make a clinical recommendation, he added.
“Ultimately, that’s a very personal decision between the patient and their physician, and we view it as supporting that decision-making process,” he said.
The test is available in all states but New York and California, where the company is now, in discussions with regulators for approval, according to Dr. Royce. He said the company is in discussion with private insurers to set reimbursement and payment rates. In January 2024, Medicare set a payment rate of $700 for the AI test, which carries no out-of-pocket costs for patients.
The first indication for the test was for localized prostate cancer, prognosticating the risk for distant metastases and death from prostate cancer. It can also predict if an individual will benefit from androgen deprivation therapy (ADT). Dr. Royce said up to 60% of patients with intermediate risk prostate cancer now can avoid ADT and its serious side effects, such as brain fog, weight gain, and reduction in muscle mass.
In March, the National Comprehensive Cancer Network, an alliance of 33 cancer centers included Artera as the first AI test in its Clinical Practice Guidelines in Oncology.
Dr. Royce said active surveillance is a new application of the test. The test was initially developed on a foundational study of almost 22,000 pathology slides from nearly 7000 patients published in npj Digital Medicine in 2022.
Todd Morgan, MD, chief of the Division of Urologic Oncology at the University of Michigan in Ann Arbor, and coauthor of the foundational study, said the AI test adds another layer of data to making clinical decisions for lower-risk patients.
“The technology is a big deal. The ability to use digital images to make accurate prognostic estimates is pretty remarkable, and this is the first test in any disease site to do this,” Dr. Morgan said. “Ultimately, this means tests may someday be performed by just sending images rather than sending actual tissue to an outside laboratory. Is the AI test dramatically more accurate than the genomic platforms? That’s TBD [to be determined].”
Dr. Royce said Artera is now working on a version of its test to inform men with higher-risk prostate cancer how long ADT should last and what the prognosis is for patients who have undergone prostatectomy based on their surgical specimen. The current test uses samples from the prostate biopsy, which are processed in a central lab.
Dr. Royce said the company would like to eventually perform the test using digital images of pathology slides only.
Dr. Morgan reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Artera, the Los Altos, California–based developer of tools to diagnose cancer, has launched the first artificial intelligence (AI) test to guide patients in making informed decisions between active surveillance and active treatment based on an analysis of digital pathology images.
Trevor Royce, MD, MPH, senior medical director of Artera, said the new version of the ArteraAI Prostate Test helps patients with low-risk (Grade Group 1/Gleason 6) to favorable intermediate-risk (Grade Group 2/Gleason 3+4) prostate cancer choose between treatment or active surveillance.
The test estimates how a patient’s cancer may progress and predicts the benefit of treatment for localized prostate cancer.
“The prognostic performance of the test has now been validated in a diverse cohort of patients, including those who have undergone active surveillance, radiation therapy, or had a radical prostatectomy,” said Dr. Royce, a faculty member in radiation oncology at Wake Forest University School of Medicine in Winston-Salem, North Carolina. “The prognostic risk result reflects the patient’s prognosis regardless of the treatment path chosen.”
Dr. Royce said the new test predicts the risk for developing distant metastasis in 10 years. For the population considering active surveillance, it also can predict the likelihood their cancer will show more aggressive features. The test does not make a clinical recommendation, he added.
“Ultimately, that’s a very personal decision between the patient and their physician, and we view it as supporting that decision-making process,” he said.
The test is available in all states but New York and California, where the company is now, in discussions with regulators for approval, according to Dr. Royce. He said the company is in discussion with private insurers to set reimbursement and payment rates. In January 2024, Medicare set a payment rate of $700 for the AI test, which carries no out-of-pocket costs for patients.
The first indication for the test was for localized prostate cancer, prognosticating the risk for distant metastases and death from prostate cancer. It can also predict if an individual will benefit from androgen deprivation therapy (ADT). Dr. Royce said up to 60% of patients with intermediate risk prostate cancer now can avoid ADT and its serious side effects, such as brain fog, weight gain, and reduction in muscle mass.
In March, the National Comprehensive Cancer Network, an alliance of 33 cancer centers included Artera as the first AI test in its Clinical Practice Guidelines in Oncology.
Dr. Royce said active surveillance is a new application of the test. The test was initially developed on a foundational study of almost 22,000 pathology slides from nearly 7000 patients published in npj Digital Medicine in 2022.
Todd Morgan, MD, chief of the Division of Urologic Oncology at the University of Michigan in Ann Arbor, and coauthor of the foundational study, said the AI test adds another layer of data to making clinical decisions for lower-risk patients.
“The technology is a big deal. The ability to use digital images to make accurate prognostic estimates is pretty remarkable, and this is the first test in any disease site to do this,” Dr. Morgan said. “Ultimately, this means tests may someday be performed by just sending images rather than sending actual tissue to an outside laboratory. Is the AI test dramatically more accurate than the genomic platforms? That’s TBD [to be determined].”
Dr. Royce said Artera is now working on a version of its test to inform men with higher-risk prostate cancer how long ADT should last and what the prognosis is for patients who have undergone prostatectomy based on their surgical specimen. The current test uses samples from the prostate biopsy, which are processed in a central lab.
Dr. Royce said the company would like to eventually perform the test using digital images of pathology slides only.
Dr. Morgan reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Artera, the Los Altos, California–based developer of tools to diagnose cancer, has launched the first artificial intelligence (AI) test to guide patients in making informed decisions between active surveillance and active treatment based on an analysis of digital pathology images.
Trevor Royce, MD, MPH, senior medical director of Artera, said the new version of the ArteraAI Prostate Test helps patients with low-risk (Grade Group 1/Gleason 6) to favorable intermediate-risk (Grade Group 2/Gleason 3+4) prostate cancer choose between treatment or active surveillance.
The test estimates how a patient’s cancer may progress and predicts the benefit of treatment for localized prostate cancer.
“The prognostic performance of the test has now been validated in a diverse cohort of patients, including those who have undergone active surveillance, radiation therapy, or had a radical prostatectomy,” said Dr. Royce, a faculty member in radiation oncology at Wake Forest University School of Medicine in Winston-Salem, North Carolina. “The prognostic risk result reflects the patient’s prognosis regardless of the treatment path chosen.”
Dr. Royce said the new test predicts the risk for developing distant metastasis in 10 years. For the population considering active surveillance, it also can predict the likelihood their cancer will show more aggressive features. The test does not make a clinical recommendation, he added.
“Ultimately, that’s a very personal decision between the patient and their physician, and we view it as supporting that decision-making process,” he said.
The test is available in all states but New York and California, where the company is now, in discussions with regulators for approval, according to Dr. Royce. He said the company is in discussion with private insurers to set reimbursement and payment rates. In January 2024, Medicare set a payment rate of $700 for the AI test, which carries no out-of-pocket costs for patients.
The first indication for the test was for localized prostate cancer, prognosticating the risk for distant metastases and death from prostate cancer. It can also predict if an individual will benefit from androgen deprivation therapy (ADT). Dr. Royce said up to 60% of patients with intermediate risk prostate cancer now can avoid ADT and its serious side effects, such as brain fog, weight gain, and reduction in muscle mass.
In March, the National Comprehensive Cancer Network, an alliance of 33 cancer centers included Artera as the first AI test in its Clinical Practice Guidelines in Oncology.
Dr. Royce said active surveillance is a new application of the test. The test was initially developed on a foundational study of almost 22,000 pathology slides from nearly 7000 patients published in npj Digital Medicine in 2022.
Todd Morgan, MD, chief of the Division of Urologic Oncology at the University of Michigan in Ann Arbor, and coauthor of the foundational study, said the AI test adds another layer of data to making clinical decisions for lower-risk patients.
“The technology is a big deal. The ability to use digital images to make accurate prognostic estimates is pretty remarkable, and this is the first test in any disease site to do this,” Dr. Morgan said. “Ultimately, this means tests may someday be performed by just sending images rather than sending actual tissue to an outside laboratory. Is the AI test dramatically more accurate than the genomic platforms? That’s TBD [to be determined].”
Dr. Royce said Artera is now working on a version of its test to inform men with higher-risk prostate cancer how long ADT should last and what the prognosis is for patients who have undergone prostatectomy based on their surgical specimen. The current test uses samples from the prostate biopsy, which are processed in a central lab.
Dr. Royce said the company would like to eventually perform the test using digital images of pathology slides only.
Dr. Morgan reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Electroconvulsive Therapy Works, Now Scientists Believe They Know How
For years, electroconvulsive therapy (ECT) has been a lifesaving treatment for patients with treatment-resistant depression (TRD), yet exactly how it works has largely remained a mystery. Now researchers believe they have uncovered the underlying mechanisms behind its therapeutic effects — a discovery that may help clinicians better predict treatment response in individual patients and quell much of the fear and stigma associated with one of psychiatry’s most effective, yet misunderstood, treatments.
Two recent papers published in Translational Psychiatry have highlighted the significance of aperiodic neural activity. The first study showed this activity increased following ECT treatment. The second study expanded on these data by demonstrating a significant increase in aperiodic activity after patients received either ECT or magnetic seizure therapy (MST), which has a better side-effect profile than ECT but lower efficacy.
Aperiodic activity is “like the brain’s background noise, and for years scientists treated it that way and didn’t pay much attention to it,” first author Sydney E. Smith, a PhD candidate at the Voytek Lab in the Neuroscience Graduate Program at the University of California San Diego (UCSD), said in a press release.
However, aperiodic activity boosts inhibitory activity in the brain, effectively slowing it down,” the investigators noted.
In an interview with this news organization, Ms. Smith used a car analogy to explain the mechanism behind ECT. “ECT might be increasing the activity levels in the brain cells that help calm it down. It taps on the brakes that tend to malfunction in depression. By restoring the balance between the gas and the brakes in the brain, some of those depressive symptoms are alleviated,” she said.
Ms. Smith added her team’s research helps demystify one of the most effective yet stigmatized treatments for severe depression.
“Aperiodic activity as a physiologically interpretable EEG metric could be a really valuable new predictive indicator for treatment response,” she added.
Fear and Stigma
ECT is primarily used for TRD and is effective in up to 80% of patients, yet it remains one of the least prescribed treatments.
Although it’s been around for almost 90 years, fear and concern about its potential cognitive side effects have contributed to its poor uptake. It is estimated that less than 1% of patients with TRD receive ECT.
Smith noted that the 1970s movie One Flew Over the Cuckoo’s Nest still contributes to ECT’s stigma. In the film, actor Jack Nicholson’s character is forced to undergo ECT as a punishment.
It’s important for clinicians to acknowledge the stigma while advising patients that “the actual treatment doesn’t look anything like what’s in the movies,” noted Ms. Smith. Patients must give informed consent for the procedure, and it’s delivered with the lowest level of effective stimulation.
“So many steps are taken to consider comfort and efficacy for patients and to minimize how scary it can be,” she said.
ECT uses an electrical current to induce a seizure that spreads to deep subcortical structures. MST, which was developed as an alternative to ECT, uses a magnetic field to induce a more focal seizure primarily confined to the cortex.
Although MST has a better side-effect profile, experts noted it has remission rates of 30%-60% compared with ECT. Even one of MST’s inventors, Harold Sackeim, PhD, professor in the Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, Charleston, is skeptical about its efficacy for TRD.
“I don’t think it works,” Dr. Sackeim, founding editor of Brain Stimulation: Basic, Translational, and Clinical Research in Neuromodulation, told this news organization.
In addition to being more expensive, MST produces a peak electrical intensity at one-tenth of what a typical ECT stimulus produces. “We’re limited by electrical engineering at this point with MST. That’s my view; others are more optimistic,” he said.
A Lifesaving Treatment
One of the reasons ECT isn’t more popular is because for many patients, it’s easier and more convenient to just take a pill, senior investigator Bradley Voytek, PhD, professor of cognitive science at UCSD, said in the release.
“However, in people for whom medications don’t work, [ECT] can be lifesaving. Understanding how it works will help us discover ways to increase the benefits while minimizing side effects,” he added.
In the first study, which included nine patients with major depressive disorder (MDD), EEG results showed an increase in aperiodic activity following ECT.
The investigators then wanted to test whether these findings could be replicated in a larger study. They retrospectively assessed two previous datasets — 1 of 22 patients with MDD who received ECT and 1 of 23 patients who received MST. After treatment, both groups showed increased aperiodic activity.
“Although not directly related to clinical efficacy in this dataset, increased aperiodic activity is linked to greater amounts of neural inhibition, which is suggestive of a potential shared neural mechanism of action across ECT and MST,” the investigators wrote.
The researchers noted that this increase in aperiodic activity is a more parsimonious explanation for observations of clinical slowing than delta band power or delta oscillations for both ECT and MST.”
So why is it important to know exactly how ECT works, and is there any clinical utility to these research findings?
“It’s important for clinicians to give a patient who has questions, a meaningful understanding of what the treatment is going to do, especially with something so scary and stigmatized. The ability to tell a patient why this treatment is working could provide a level of comfort that can assuage some of these fears,” Ms. Smith said.
A New Predictor of Response?
In addition, she noted that psychiatry is becoming more focused on predictive indicators for treatment.
“It’s asking: Are there any biological measures that can be used to predict whether someone is going to respond to a treatment or not?” said Ms. Smith.
“Aperiodic activity might be a valuable asset to add to that arsenal. Maybe we can better predict which patients might respond to ECT by using this as an additional biological indicator,” she added.
Smith noted that while more studies are needed, it’s exciting that some investigators are already starting to include aperiodic activity as a variable in their research analyses on a variety of topics, such as pharmacological intervention and transcranial magnetic stimulation.
“I don’t know exactly how much utility aperiodic activity is going to have in terms of being a great biological indicator, but I hope that the research will start to play out and reveal a little bit more,” she said.
Dr. Sackeim noted that ECT is one of the most misunderstood, controversial, and infrequently used treatments in psychiatry.
“But there’s also no doubt that when you look at ECT, it saves the lives of people with psychiatric illness. Period, full stop,” he said.
He added that although restarting a patient’s heart doesn’t seem to cause unease in the public, the idea of applying electricity to the brain under anesthesia in order to provoke a seizure for therapeutic purpose causes anxiety.
Still, the benefits and harms of a treatment are more important than how it looks, Sackeim said. “If it was only about how it looks, we’d never have surgery,” he added.
‘A Huge Success Story’
ECT was first introduced by Hungarian neuropsychiatrist László Meduna in 1935, and today clinicians “know where the current goes in the brain, at what dosage, and with what path you can get 70%, 80% fully remitted,” said Dr. Sackeim.
He noted that in a randomized study published in JAMA Psychiatry, investigators compared the outcomes of MST vs ECT for major depressive episodes in 73 patients. They reported that although depression symptom scores decreased for both treatments, there was “no significant difference” between the two in response or remission rates.
However, in an opinion letter the journal published in April, Dr. Sackeim and colleagues Mark S. George, MD, Medical University of South Carolina, and William V. McCall, MD, Augusta University, Augusta, Georgia, strongly questioned the findings.
At less than 30%, “the ECT remission rate after acute treatment was exceptionally low, limiting confidence in the validity and/or generalizability of the findings,” they wrote.
“It’s undoubtedly the case that either if you recruited a sample from whom the treatment may not be as efficacious or if there are issues in delivering them, then you may be finding equivalence” between ECT and MST, Dr. Sackeim said.
In addition, he noted that although there have been concerns about cognitive side effects with ECT, they have improved over the years. Sackeim reported that when he entered the field, the average time for a patient to remember their name or the day of the week was 6 hours after receiving unilateral ECT and 8 hours after bilateral ECT. “With modern methods, that’s now down to 10 minutes,” he said.
“The fundamental knowledge is that this treatment can be administered far softer than it ever was in the past. Impressions from the 50s and 60s and portrayed in movies have very little to do with modern practice and with the real effects of the treatment,” Dr. Sackeim said.
As for the new studies about aperiodic activity, the investigators are “essentially saying, ‘We have a better marker’ of the process. That way of thinking had in many ways been left behind in the run to study connectivity,” Dr. Sackeim said.
He noted that years ago, while he was with Columbia University, his team found that patients who had frontal inhibition were more likely to get well after ECT.
“And that’s essentially the same thing you’re hearing from the UCSD group. They’re saying that the aperiodic measure is hopefully of clearer physiological significance than simply delta [waves] in the EEG,” Dr. Sackeim said.
“The idea that inhibition was the key to its efficacy has been around. This is saying it’s a better measure of that, and that may be true. It’s certainly an interesting contribution,” he added.
Dr. Sackeim said the takeaway message for clinicians regarding ECT today is that it can be lifesaving but is still often only used as a last resort and reserved for those who have run out of options.
However, he said, ECT is “a huge success story: Maintaining its efficacy, reducing its side effects, getting an understanding as to what the physics of it are. We have some compelling stories about ECT, but even more so, we know what’s not true. And what’s not true are most of the assumptions people have about the treatment,” he concluded.
Ms. Smith and Dr. Voytek reported no relevant conflicts of interest. Dr. Sackeim reported holding patents in ECT technology and consulting with the MECTA Corporation and SigmaStim LLC and other neuromodulation companies.
A version of this article appeared on Medscape.com.
For years, electroconvulsive therapy (ECT) has been a lifesaving treatment for patients with treatment-resistant depression (TRD), yet exactly how it works has largely remained a mystery. Now researchers believe they have uncovered the underlying mechanisms behind its therapeutic effects — a discovery that may help clinicians better predict treatment response in individual patients and quell much of the fear and stigma associated with one of psychiatry’s most effective, yet misunderstood, treatments.
Two recent papers published in Translational Psychiatry have highlighted the significance of aperiodic neural activity. The first study showed this activity increased following ECT treatment. The second study expanded on these data by demonstrating a significant increase in aperiodic activity after patients received either ECT or magnetic seizure therapy (MST), which has a better side-effect profile than ECT but lower efficacy.
Aperiodic activity is “like the brain’s background noise, and for years scientists treated it that way and didn’t pay much attention to it,” first author Sydney E. Smith, a PhD candidate at the Voytek Lab in the Neuroscience Graduate Program at the University of California San Diego (UCSD), said in a press release.
However, aperiodic activity boosts inhibitory activity in the brain, effectively slowing it down,” the investigators noted.
In an interview with this news organization, Ms. Smith used a car analogy to explain the mechanism behind ECT. “ECT might be increasing the activity levels in the brain cells that help calm it down. It taps on the brakes that tend to malfunction in depression. By restoring the balance between the gas and the brakes in the brain, some of those depressive symptoms are alleviated,” she said.
Ms. Smith added her team’s research helps demystify one of the most effective yet stigmatized treatments for severe depression.
“Aperiodic activity as a physiologically interpretable EEG metric could be a really valuable new predictive indicator for treatment response,” she added.
Fear and Stigma
ECT is primarily used for TRD and is effective in up to 80% of patients, yet it remains one of the least prescribed treatments.
Although it’s been around for almost 90 years, fear and concern about its potential cognitive side effects have contributed to its poor uptake. It is estimated that less than 1% of patients with TRD receive ECT.
Smith noted that the 1970s movie One Flew Over the Cuckoo’s Nest still contributes to ECT’s stigma. In the film, actor Jack Nicholson’s character is forced to undergo ECT as a punishment.
It’s important for clinicians to acknowledge the stigma while advising patients that “the actual treatment doesn’t look anything like what’s in the movies,” noted Ms. Smith. Patients must give informed consent for the procedure, and it’s delivered with the lowest level of effective stimulation.
“So many steps are taken to consider comfort and efficacy for patients and to minimize how scary it can be,” she said.
ECT uses an electrical current to induce a seizure that spreads to deep subcortical structures. MST, which was developed as an alternative to ECT, uses a magnetic field to induce a more focal seizure primarily confined to the cortex.
Although MST has a better side-effect profile, experts noted it has remission rates of 30%-60% compared with ECT. Even one of MST’s inventors, Harold Sackeim, PhD, professor in the Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, Charleston, is skeptical about its efficacy for TRD.
“I don’t think it works,” Dr. Sackeim, founding editor of Brain Stimulation: Basic, Translational, and Clinical Research in Neuromodulation, told this news organization.
In addition to being more expensive, MST produces a peak electrical intensity at one-tenth of what a typical ECT stimulus produces. “We’re limited by electrical engineering at this point with MST. That’s my view; others are more optimistic,” he said.
A Lifesaving Treatment
One of the reasons ECT isn’t more popular is because for many patients, it’s easier and more convenient to just take a pill, senior investigator Bradley Voytek, PhD, professor of cognitive science at UCSD, said in the release.
“However, in people for whom medications don’t work, [ECT] can be lifesaving. Understanding how it works will help us discover ways to increase the benefits while minimizing side effects,” he added.
In the first study, which included nine patients with major depressive disorder (MDD), EEG results showed an increase in aperiodic activity following ECT.
The investigators then wanted to test whether these findings could be replicated in a larger study. They retrospectively assessed two previous datasets — 1 of 22 patients with MDD who received ECT and 1 of 23 patients who received MST. After treatment, both groups showed increased aperiodic activity.
“Although not directly related to clinical efficacy in this dataset, increased aperiodic activity is linked to greater amounts of neural inhibition, which is suggestive of a potential shared neural mechanism of action across ECT and MST,” the investigators wrote.
The researchers noted that this increase in aperiodic activity is a more parsimonious explanation for observations of clinical slowing than delta band power or delta oscillations for both ECT and MST.”
So why is it important to know exactly how ECT works, and is there any clinical utility to these research findings?
“It’s important for clinicians to give a patient who has questions, a meaningful understanding of what the treatment is going to do, especially with something so scary and stigmatized. The ability to tell a patient why this treatment is working could provide a level of comfort that can assuage some of these fears,” Ms. Smith said.
A New Predictor of Response?
In addition, she noted that psychiatry is becoming more focused on predictive indicators for treatment.
“It’s asking: Are there any biological measures that can be used to predict whether someone is going to respond to a treatment or not?” said Ms. Smith.
“Aperiodic activity might be a valuable asset to add to that arsenal. Maybe we can better predict which patients might respond to ECT by using this as an additional biological indicator,” she added.
Smith noted that while more studies are needed, it’s exciting that some investigators are already starting to include aperiodic activity as a variable in their research analyses on a variety of topics, such as pharmacological intervention and transcranial magnetic stimulation.
“I don’t know exactly how much utility aperiodic activity is going to have in terms of being a great biological indicator, but I hope that the research will start to play out and reveal a little bit more,” she said.
Dr. Sackeim noted that ECT is one of the most misunderstood, controversial, and infrequently used treatments in psychiatry.
“But there’s also no doubt that when you look at ECT, it saves the lives of people with psychiatric illness. Period, full stop,” he said.
He added that although restarting a patient’s heart doesn’t seem to cause unease in the public, the idea of applying electricity to the brain under anesthesia in order to provoke a seizure for therapeutic purpose causes anxiety.
Still, the benefits and harms of a treatment are more important than how it looks, Sackeim said. “If it was only about how it looks, we’d never have surgery,” he added.
‘A Huge Success Story’
ECT was first introduced by Hungarian neuropsychiatrist László Meduna in 1935, and today clinicians “know where the current goes in the brain, at what dosage, and with what path you can get 70%, 80% fully remitted,” said Dr. Sackeim.
He noted that in a randomized study published in JAMA Psychiatry, investigators compared the outcomes of MST vs ECT for major depressive episodes in 73 patients. They reported that although depression symptom scores decreased for both treatments, there was “no significant difference” between the two in response or remission rates.
However, in an opinion letter the journal published in April, Dr. Sackeim and colleagues Mark S. George, MD, Medical University of South Carolina, and William V. McCall, MD, Augusta University, Augusta, Georgia, strongly questioned the findings.
At less than 30%, “the ECT remission rate after acute treatment was exceptionally low, limiting confidence in the validity and/or generalizability of the findings,” they wrote.
“It’s undoubtedly the case that either if you recruited a sample from whom the treatment may not be as efficacious or if there are issues in delivering them, then you may be finding equivalence” between ECT and MST, Dr. Sackeim said.
In addition, he noted that although there have been concerns about cognitive side effects with ECT, they have improved over the years. Sackeim reported that when he entered the field, the average time for a patient to remember their name or the day of the week was 6 hours after receiving unilateral ECT and 8 hours after bilateral ECT. “With modern methods, that’s now down to 10 minutes,” he said.
“The fundamental knowledge is that this treatment can be administered far softer than it ever was in the past. Impressions from the 50s and 60s and portrayed in movies have very little to do with modern practice and with the real effects of the treatment,” Dr. Sackeim said.
As for the new studies about aperiodic activity, the investigators are “essentially saying, ‘We have a better marker’ of the process. That way of thinking had in many ways been left behind in the run to study connectivity,” Dr. Sackeim said.
He noted that years ago, while he was with Columbia University, his team found that patients who had frontal inhibition were more likely to get well after ECT.
“And that’s essentially the same thing you’re hearing from the UCSD group. They’re saying that the aperiodic measure is hopefully of clearer physiological significance than simply delta [waves] in the EEG,” Dr. Sackeim said.
“The idea that inhibition was the key to its efficacy has been around. This is saying it’s a better measure of that, and that may be true. It’s certainly an interesting contribution,” he added.
Dr. Sackeim said the takeaway message for clinicians regarding ECT today is that it can be lifesaving but is still often only used as a last resort and reserved for those who have run out of options.
However, he said, ECT is “a huge success story: Maintaining its efficacy, reducing its side effects, getting an understanding as to what the physics of it are. We have some compelling stories about ECT, but even more so, we know what’s not true. And what’s not true are most of the assumptions people have about the treatment,” he concluded.
Ms. Smith and Dr. Voytek reported no relevant conflicts of interest. Dr. Sackeim reported holding patents in ECT technology and consulting with the MECTA Corporation and SigmaStim LLC and other neuromodulation companies.
A version of this article appeared on Medscape.com.
For years, electroconvulsive therapy (ECT) has been a lifesaving treatment for patients with treatment-resistant depression (TRD), yet exactly how it works has largely remained a mystery. Now researchers believe they have uncovered the underlying mechanisms behind its therapeutic effects — a discovery that may help clinicians better predict treatment response in individual patients and quell much of the fear and stigma associated with one of psychiatry’s most effective, yet misunderstood, treatments.
Two recent papers published in Translational Psychiatry have highlighted the significance of aperiodic neural activity. The first study showed this activity increased following ECT treatment. The second study expanded on these data by demonstrating a significant increase in aperiodic activity after patients received either ECT or magnetic seizure therapy (MST), which has a better side-effect profile than ECT but lower efficacy.
Aperiodic activity is “like the brain’s background noise, and for years scientists treated it that way and didn’t pay much attention to it,” first author Sydney E. Smith, a PhD candidate at the Voytek Lab in the Neuroscience Graduate Program at the University of California San Diego (UCSD), said in a press release.
However, aperiodic activity boosts inhibitory activity in the brain, effectively slowing it down,” the investigators noted.
In an interview with this news organization, Ms. Smith used a car analogy to explain the mechanism behind ECT. “ECT might be increasing the activity levels in the brain cells that help calm it down. It taps on the brakes that tend to malfunction in depression. By restoring the balance between the gas and the brakes in the brain, some of those depressive symptoms are alleviated,” she said.
Ms. Smith added her team’s research helps demystify one of the most effective yet stigmatized treatments for severe depression.
“Aperiodic activity as a physiologically interpretable EEG metric could be a really valuable new predictive indicator for treatment response,” she added.
Fear and Stigma
ECT is primarily used for TRD and is effective in up to 80% of patients, yet it remains one of the least prescribed treatments.
Although it’s been around for almost 90 years, fear and concern about its potential cognitive side effects have contributed to its poor uptake. It is estimated that less than 1% of patients with TRD receive ECT.
Smith noted that the 1970s movie One Flew Over the Cuckoo’s Nest still contributes to ECT’s stigma. In the film, actor Jack Nicholson’s character is forced to undergo ECT as a punishment.
It’s important for clinicians to acknowledge the stigma while advising patients that “the actual treatment doesn’t look anything like what’s in the movies,” noted Ms. Smith. Patients must give informed consent for the procedure, and it’s delivered with the lowest level of effective stimulation.
“So many steps are taken to consider comfort and efficacy for patients and to minimize how scary it can be,” she said.
ECT uses an electrical current to induce a seizure that spreads to deep subcortical structures. MST, which was developed as an alternative to ECT, uses a magnetic field to induce a more focal seizure primarily confined to the cortex.
Although MST has a better side-effect profile, experts noted it has remission rates of 30%-60% compared with ECT. Even one of MST’s inventors, Harold Sackeim, PhD, professor in the Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, Charleston, is skeptical about its efficacy for TRD.
“I don’t think it works,” Dr. Sackeim, founding editor of Brain Stimulation: Basic, Translational, and Clinical Research in Neuromodulation, told this news organization.
In addition to being more expensive, MST produces a peak electrical intensity at one-tenth of what a typical ECT stimulus produces. “We’re limited by electrical engineering at this point with MST. That’s my view; others are more optimistic,” he said.
A Lifesaving Treatment
One of the reasons ECT isn’t more popular is because for many patients, it’s easier and more convenient to just take a pill, senior investigator Bradley Voytek, PhD, professor of cognitive science at UCSD, said in the release.
“However, in people for whom medications don’t work, [ECT] can be lifesaving. Understanding how it works will help us discover ways to increase the benefits while minimizing side effects,” he added.
In the first study, which included nine patients with major depressive disorder (MDD), EEG results showed an increase in aperiodic activity following ECT.
The investigators then wanted to test whether these findings could be replicated in a larger study. They retrospectively assessed two previous datasets — 1 of 22 patients with MDD who received ECT and 1 of 23 patients who received MST. After treatment, both groups showed increased aperiodic activity.
“Although not directly related to clinical efficacy in this dataset, increased aperiodic activity is linked to greater amounts of neural inhibition, which is suggestive of a potential shared neural mechanism of action across ECT and MST,” the investigators wrote.
The researchers noted that this increase in aperiodic activity is a more parsimonious explanation for observations of clinical slowing than delta band power or delta oscillations for both ECT and MST.”
So why is it important to know exactly how ECT works, and is there any clinical utility to these research findings?
“It’s important for clinicians to give a patient who has questions, a meaningful understanding of what the treatment is going to do, especially with something so scary and stigmatized. The ability to tell a patient why this treatment is working could provide a level of comfort that can assuage some of these fears,” Ms. Smith said.
A New Predictor of Response?
In addition, she noted that psychiatry is becoming more focused on predictive indicators for treatment.
“It’s asking: Are there any biological measures that can be used to predict whether someone is going to respond to a treatment or not?” said Ms. Smith.
“Aperiodic activity might be a valuable asset to add to that arsenal. Maybe we can better predict which patients might respond to ECT by using this as an additional biological indicator,” she added.
Smith noted that while more studies are needed, it’s exciting that some investigators are already starting to include aperiodic activity as a variable in their research analyses on a variety of topics, such as pharmacological intervention and transcranial magnetic stimulation.
“I don’t know exactly how much utility aperiodic activity is going to have in terms of being a great biological indicator, but I hope that the research will start to play out and reveal a little bit more,” she said.
Dr. Sackeim noted that ECT is one of the most misunderstood, controversial, and infrequently used treatments in psychiatry.
“But there’s also no doubt that when you look at ECT, it saves the lives of people with psychiatric illness. Period, full stop,” he said.
He added that although restarting a patient’s heart doesn’t seem to cause unease in the public, the idea of applying electricity to the brain under anesthesia in order to provoke a seizure for therapeutic purpose causes anxiety.
Still, the benefits and harms of a treatment are more important than how it looks, Sackeim said. “If it was only about how it looks, we’d never have surgery,” he added.
‘A Huge Success Story’
ECT was first introduced by Hungarian neuropsychiatrist László Meduna in 1935, and today clinicians “know where the current goes in the brain, at what dosage, and with what path you can get 70%, 80% fully remitted,” said Dr. Sackeim.
He noted that in a randomized study published in JAMA Psychiatry, investigators compared the outcomes of MST vs ECT for major depressive episodes in 73 patients. They reported that although depression symptom scores decreased for both treatments, there was “no significant difference” between the two in response or remission rates.
However, in an opinion letter the journal published in April, Dr. Sackeim and colleagues Mark S. George, MD, Medical University of South Carolina, and William V. McCall, MD, Augusta University, Augusta, Georgia, strongly questioned the findings.
At less than 30%, “the ECT remission rate after acute treatment was exceptionally low, limiting confidence in the validity and/or generalizability of the findings,” they wrote.
“It’s undoubtedly the case that either if you recruited a sample from whom the treatment may not be as efficacious or if there are issues in delivering them, then you may be finding equivalence” between ECT and MST, Dr. Sackeim said.
In addition, he noted that although there have been concerns about cognitive side effects with ECT, they have improved over the years. Sackeim reported that when he entered the field, the average time for a patient to remember their name or the day of the week was 6 hours after receiving unilateral ECT and 8 hours after bilateral ECT. “With modern methods, that’s now down to 10 minutes,” he said.
“The fundamental knowledge is that this treatment can be administered far softer than it ever was in the past. Impressions from the 50s and 60s and portrayed in movies have very little to do with modern practice and with the real effects of the treatment,” Dr. Sackeim said.
As for the new studies about aperiodic activity, the investigators are “essentially saying, ‘We have a better marker’ of the process. That way of thinking had in many ways been left behind in the run to study connectivity,” Dr. Sackeim said.
He noted that years ago, while he was with Columbia University, his team found that patients who had frontal inhibition were more likely to get well after ECT.
“And that’s essentially the same thing you’re hearing from the UCSD group. They’re saying that the aperiodic measure is hopefully of clearer physiological significance than simply delta [waves] in the EEG,” Dr. Sackeim said.
“The idea that inhibition was the key to its efficacy has been around. This is saying it’s a better measure of that, and that may be true. It’s certainly an interesting contribution,” he added.
Dr. Sackeim said the takeaway message for clinicians regarding ECT today is that it can be lifesaving but is still often only used as a last resort and reserved for those who have run out of options.
However, he said, ECT is “a huge success story: Maintaining its efficacy, reducing its side effects, getting an understanding as to what the physics of it are. We have some compelling stories about ECT, but even more so, we know what’s not true. And what’s not true are most of the assumptions people have about the treatment,” he concluded.
Ms. Smith and Dr. Voytek reported no relevant conflicts of interest. Dr. Sackeim reported holding patents in ECT technology and consulting with the MECTA Corporation and SigmaStim LLC and other neuromodulation companies.
A version of this article appeared on Medscape.com.
How Does ‘Eat Less, Move More’ Promote Obesity Bias?
Experts are debating whether and how to define obesity, but clinicians’ attitudes and behavior toward patients with obesity don’t seem to be undergoing similar scrutiny.
“Despite scientific evidence to the contrary, the prevailing view in society is that obesity is a choice that can be reversed by voluntary decisions to eat less and exercise more,” a multidisciplinary group of 36 international experts wrote in a joint consensus statement for ending the stigma of obesity, published a few years ago in Nature Medicine. “These assumptions mislead public health policies, confuse messages in popular media, undermine access to evidence-based treatments, and compromise advances in research.”
These assumptions also affect how clinicians view and treat their patients.
A systematic review and meta-analysis from Australia using 27 different outcomes to assess weight bias found that “medical doctors, nurses, dietitians, psychologists, physiotherapists, occupational therapists, speech pathologists, podiatrists, and exercise physiologists hold implicit and/or explicit weight-biased attitudes toward people with obesity.”
Another recent systematic review, this one from Brazil, found that obesity bias affected both clinical decision-making and quality of care. Patients with obesity had fewer screening exams for cancer, less-frequent treatment intensification in the management of obesity, and fewer pelvic exams. The authors concluded that their findings “reveal the urgent necessity for reflection and development of strategies to mitigate the adverse impacts” of obesity bias.
“Weight is one of those things that gets judged because it can be seen,” Obesity Society Spokesperson Peminda Cabandugama, MD, of Cleveland Clinic, told this news organization. “People just look at someone with overweight and say, ‘That person needs to eat less and exercise more.’ ”
How Obesity Bias Manifests
The Obesity Action Coalition (OAC), a partner organization to the consensus statement, defines weight bias as “negative attitudes, beliefs, judgments, stereotypes, and discriminatory acts aimed at individuals simply because of their weight. It can be overt or subtle and occur in any setting, including employment, healthcare, education, mass media, and relationships with family and friends.”
The organization notes that weight bias takes many forms, including verbal, written, media, and online.
The consensus statement authors offer these definitions, which encompass the manifestations of obesity bias: Weight stigma refers to “social devaluation and denigration of individuals because of their excess body weight and can lead to negative attitudes, stereotypes, prejudice, and discrimination.”
Weight discrimination refers to “overt forms of weight-based prejudice and unfair treatment (biased behaviors) toward individuals with overweight or obesity.” The authors noted that some public health efforts “openly embrace stigmatization of individuals with obesity based on the assumption that shame will motivate them to change behavior and achieve weight loss through a self-directed diet and increased physical exercise.”
The result: “Individuals with obesity face not only increased risk of serious medical complications but also a pervasive, resilient form of social stigma. Often perceived (without evidence) as lazy, gluttonous, lacking will power and self-discipline, individuals with overweight or obesity are vulnerable to stigma and discrimination in the workplace, education, healthcare settings, and society in general.”
“Obesity bias is so pervasive that the most common thing I hear when I ask a patient why they’re referred to me is ‘my doctor wants me to lose weight,’” Dr. Cabandugama said. “And the first thing I ask them is ‘what do you want to do?’ They come in because they’ve already been judged, and more often than not, in ways that come across as derogatory or punitive — like it’s their fault.”
Why It Persists
Experts say a big part of the problem is the lack of obesity education in medical school. A recent survey study found that medical schools are not prioritizing obesity in their curricula. Among 40 medical schools responding to the survey, only 10% said they believed their students were “very prepared” to manage patients with obesity, and one third had no obesity education program in place with no plans to develop one.
“Most healthcare providers do not get much meaningful education on obesity during medical school or postgraduate training, and many of their opinions may be influenced by the pervasive weight bias that exists in society,” affirmed Jaime Almandoz, MD, medical director of Weight Wellness Program and associate professor of internal medicine at UT Southwestern Medical Center in Dallas. “We need to prioritize updating education and certification curricula to reflect the current science.”
Small wonder that a recent comparison of explicit weight bias among US resident physicians from 49 medical schools across 16 clinical specialties found “problematic levels” of weight bias — eg, anti-fat blame, anti-fat dislike, and other negative attitudes toward patients — in all specialties.
What to Do
To counteract the stigma, when working with patients who have overweight, “We need to be respectful of them, their bodies, and their health wishes,” Dr. Almandoz told this news organization. “Clinicians should always ask for permission to discuss their weight and frame weight or BMI in the context of health, not just an arbitrary number or goal.”
“Many people with obesity have had traumatic and stigmatizing experiences with well-intentioned healthcare providers,” he noted. “This can lead to the avoidance of routine healthcare and screenings and potential exacerbations and maladaptive health behaviors.”
“Be mindful of the environment that you and your office create for people with obesity,” he advised. “Consider getting additional education and information about weight bias.”
The OAC has resources on obesity bias, including steps clinicians can take to reduce the impact. These include, among others: Encouraging patients to share their experiences of stigma to help them feel less isolated in these experiences; helping them identify ways to effectively cope with stigma, such as using positive “self-talk” and obtaining social support from others; and encouraging participation in activities that they may have restricted due to feelings of shame about their weight.
Clinicians can also improve the physical and social environment of their practice by having bathrooms that are easily negotiated by heavier individuals, sturdy armless chairs in waiting rooms, offices with large exam tables, gowns and blood pressure cuffs in appropriate sizes, and “weight-friendly” reading materials rather than fashion magazines with thin supermodels.
Importantly, clinicians need to address the issue of weight bias within themselves, their medical staff, and colleagues, according to the OAC. To be effective and empathic with individuals affected by obesity “requires honest self-examination of one’s own attitudes and weight bias.”
Dr. Almandoz reported being a consultant/advisory board member for Novo Nordisk, Boehringer Ingelheim, and Eli Lilly and Company. Dr. Cabandugama reported no competing interests.
A version of this article first appeared on Medscape.com.
Experts are debating whether and how to define obesity, but clinicians’ attitudes and behavior toward patients with obesity don’t seem to be undergoing similar scrutiny.
“Despite scientific evidence to the contrary, the prevailing view in society is that obesity is a choice that can be reversed by voluntary decisions to eat less and exercise more,” a multidisciplinary group of 36 international experts wrote in a joint consensus statement for ending the stigma of obesity, published a few years ago in Nature Medicine. “These assumptions mislead public health policies, confuse messages in popular media, undermine access to evidence-based treatments, and compromise advances in research.”
These assumptions also affect how clinicians view and treat their patients.
A systematic review and meta-analysis from Australia using 27 different outcomes to assess weight bias found that “medical doctors, nurses, dietitians, psychologists, physiotherapists, occupational therapists, speech pathologists, podiatrists, and exercise physiologists hold implicit and/or explicit weight-biased attitudes toward people with obesity.”
Another recent systematic review, this one from Brazil, found that obesity bias affected both clinical decision-making and quality of care. Patients with obesity had fewer screening exams for cancer, less-frequent treatment intensification in the management of obesity, and fewer pelvic exams. The authors concluded that their findings “reveal the urgent necessity for reflection and development of strategies to mitigate the adverse impacts” of obesity bias.
“Weight is one of those things that gets judged because it can be seen,” Obesity Society Spokesperson Peminda Cabandugama, MD, of Cleveland Clinic, told this news organization. “People just look at someone with overweight and say, ‘That person needs to eat less and exercise more.’ ”
How Obesity Bias Manifests
The Obesity Action Coalition (OAC), a partner organization to the consensus statement, defines weight bias as “negative attitudes, beliefs, judgments, stereotypes, and discriminatory acts aimed at individuals simply because of their weight. It can be overt or subtle and occur in any setting, including employment, healthcare, education, mass media, and relationships with family and friends.”
The organization notes that weight bias takes many forms, including verbal, written, media, and online.
The consensus statement authors offer these definitions, which encompass the manifestations of obesity bias: Weight stigma refers to “social devaluation and denigration of individuals because of their excess body weight and can lead to negative attitudes, stereotypes, prejudice, and discrimination.”
Weight discrimination refers to “overt forms of weight-based prejudice and unfair treatment (biased behaviors) toward individuals with overweight or obesity.” The authors noted that some public health efforts “openly embrace stigmatization of individuals with obesity based on the assumption that shame will motivate them to change behavior and achieve weight loss through a self-directed diet and increased physical exercise.”
The result: “Individuals with obesity face not only increased risk of serious medical complications but also a pervasive, resilient form of social stigma. Often perceived (without evidence) as lazy, gluttonous, lacking will power and self-discipline, individuals with overweight or obesity are vulnerable to stigma and discrimination in the workplace, education, healthcare settings, and society in general.”
“Obesity bias is so pervasive that the most common thing I hear when I ask a patient why they’re referred to me is ‘my doctor wants me to lose weight,’” Dr. Cabandugama said. “And the first thing I ask them is ‘what do you want to do?’ They come in because they’ve already been judged, and more often than not, in ways that come across as derogatory or punitive — like it’s their fault.”
Why It Persists
Experts say a big part of the problem is the lack of obesity education in medical school. A recent survey study found that medical schools are not prioritizing obesity in their curricula. Among 40 medical schools responding to the survey, only 10% said they believed their students were “very prepared” to manage patients with obesity, and one third had no obesity education program in place with no plans to develop one.
“Most healthcare providers do not get much meaningful education on obesity during medical school or postgraduate training, and many of their opinions may be influenced by the pervasive weight bias that exists in society,” affirmed Jaime Almandoz, MD, medical director of Weight Wellness Program and associate professor of internal medicine at UT Southwestern Medical Center in Dallas. “We need to prioritize updating education and certification curricula to reflect the current science.”
Small wonder that a recent comparison of explicit weight bias among US resident physicians from 49 medical schools across 16 clinical specialties found “problematic levels” of weight bias — eg, anti-fat blame, anti-fat dislike, and other negative attitudes toward patients — in all specialties.
What to Do
To counteract the stigma, when working with patients who have overweight, “We need to be respectful of them, their bodies, and their health wishes,” Dr. Almandoz told this news organization. “Clinicians should always ask for permission to discuss their weight and frame weight or BMI in the context of health, not just an arbitrary number or goal.”
“Many people with obesity have had traumatic and stigmatizing experiences with well-intentioned healthcare providers,” he noted. “This can lead to the avoidance of routine healthcare and screenings and potential exacerbations and maladaptive health behaviors.”
“Be mindful of the environment that you and your office create for people with obesity,” he advised. “Consider getting additional education and information about weight bias.”
The OAC has resources on obesity bias, including steps clinicians can take to reduce the impact. These include, among others: Encouraging patients to share their experiences of stigma to help them feel less isolated in these experiences; helping them identify ways to effectively cope with stigma, such as using positive “self-talk” and obtaining social support from others; and encouraging participation in activities that they may have restricted due to feelings of shame about their weight.
Clinicians can also improve the physical and social environment of their practice by having bathrooms that are easily negotiated by heavier individuals, sturdy armless chairs in waiting rooms, offices with large exam tables, gowns and blood pressure cuffs in appropriate sizes, and “weight-friendly” reading materials rather than fashion magazines with thin supermodels.
Importantly, clinicians need to address the issue of weight bias within themselves, their medical staff, and colleagues, according to the OAC. To be effective and empathic with individuals affected by obesity “requires honest self-examination of one’s own attitudes and weight bias.”
Dr. Almandoz reported being a consultant/advisory board member for Novo Nordisk, Boehringer Ingelheim, and Eli Lilly and Company. Dr. Cabandugama reported no competing interests.
A version of this article first appeared on Medscape.com.
Experts are debating whether and how to define obesity, but clinicians’ attitudes and behavior toward patients with obesity don’t seem to be undergoing similar scrutiny.
“Despite scientific evidence to the contrary, the prevailing view in society is that obesity is a choice that can be reversed by voluntary decisions to eat less and exercise more,” a multidisciplinary group of 36 international experts wrote in a joint consensus statement for ending the stigma of obesity, published a few years ago in Nature Medicine. “These assumptions mislead public health policies, confuse messages in popular media, undermine access to evidence-based treatments, and compromise advances in research.”
These assumptions also affect how clinicians view and treat their patients.
A systematic review and meta-analysis from Australia using 27 different outcomes to assess weight bias found that “medical doctors, nurses, dietitians, psychologists, physiotherapists, occupational therapists, speech pathologists, podiatrists, and exercise physiologists hold implicit and/or explicit weight-biased attitudes toward people with obesity.”
Another recent systematic review, this one from Brazil, found that obesity bias affected both clinical decision-making and quality of care. Patients with obesity had fewer screening exams for cancer, less-frequent treatment intensification in the management of obesity, and fewer pelvic exams. The authors concluded that their findings “reveal the urgent necessity for reflection and development of strategies to mitigate the adverse impacts” of obesity bias.
“Weight is one of those things that gets judged because it can be seen,” Obesity Society Spokesperson Peminda Cabandugama, MD, of Cleveland Clinic, told this news organization. “People just look at someone with overweight and say, ‘That person needs to eat less and exercise more.’ ”
How Obesity Bias Manifests
The Obesity Action Coalition (OAC), a partner organization to the consensus statement, defines weight bias as “negative attitudes, beliefs, judgments, stereotypes, and discriminatory acts aimed at individuals simply because of their weight. It can be overt or subtle and occur in any setting, including employment, healthcare, education, mass media, and relationships with family and friends.”
The organization notes that weight bias takes many forms, including verbal, written, media, and online.
The consensus statement authors offer these definitions, which encompass the manifestations of obesity bias: Weight stigma refers to “social devaluation and denigration of individuals because of their excess body weight and can lead to negative attitudes, stereotypes, prejudice, and discrimination.”
Weight discrimination refers to “overt forms of weight-based prejudice and unfair treatment (biased behaviors) toward individuals with overweight or obesity.” The authors noted that some public health efforts “openly embrace stigmatization of individuals with obesity based on the assumption that shame will motivate them to change behavior and achieve weight loss through a self-directed diet and increased physical exercise.”
The result: “Individuals with obesity face not only increased risk of serious medical complications but also a pervasive, resilient form of social stigma. Often perceived (without evidence) as lazy, gluttonous, lacking will power and self-discipline, individuals with overweight or obesity are vulnerable to stigma and discrimination in the workplace, education, healthcare settings, and society in general.”
“Obesity bias is so pervasive that the most common thing I hear when I ask a patient why they’re referred to me is ‘my doctor wants me to lose weight,’” Dr. Cabandugama said. “And the first thing I ask them is ‘what do you want to do?’ They come in because they’ve already been judged, and more often than not, in ways that come across as derogatory or punitive — like it’s their fault.”
Why It Persists
Experts say a big part of the problem is the lack of obesity education in medical school. A recent survey study found that medical schools are not prioritizing obesity in their curricula. Among 40 medical schools responding to the survey, only 10% said they believed their students were “very prepared” to manage patients with obesity, and one third had no obesity education program in place with no plans to develop one.
“Most healthcare providers do not get much meaningful education on obesity during medical school or postgraduate training, and many of their opinions may be influenced by the pervasive weight bias that exists in society,” affirmed Jaime Almandoz, MD, medical director of Weight Wellness Program and associate professor of internal medicine at UT Southwestern Medical Center in Dallas. “We need to prioritize updating education and certification curricula to reflect the current science.”
Small wonder that a recent comparison of explicit weight bias among US resident physicians from 49 medical schools across 16 clinical specialties found “problematic levels” of weight bias — eg, anti-fat blame, anti-fat dislike, and other negative attitudes toward patients — in all specialties.
What to Do
To counteract the stigma, when working with patients who have overweight, “We need to be respectful of them, their bodies, and their health wishes,” Dr. Almandoz told this news organization. “Clinicians should always ask for permission to discuss their weight and frame weight or BMI in the context of health, not just an arbitrary number or goal.”
“Many people with obesity have had traumatic and stigmatizing experiences with well-intentioned healthcare providers,” he noted. “This can lead to the avoidance of routine healthcare and screenings and potential exacerbations and maladaptive health behaviors.”
“Be mindful of the environment that you and your office create for people with obesity,” he advised. “Consider getting additional education and information about weight bias.”
The OAC has resources on obesity bias, including steps clinicians can take to reduce the impact. These include, among others: Encouraging patients to share their experiences of stigma to help them feel less isolated in these experiences; helping them identify ways to effectively cope with stigma, such as using positive “self-talk” and obtaining social support from others; and encouraging participation in activities that they may have restricted due to feelings of shame about their weight.
Clinicians can also improve the physical and social environment of their practice by having bathrooms that are easily negotiated by heavier individuals, sturdy armless chairs in waiting rooms, offices with large exam tables, gowns and blood pressure cuffs in appropriate sizes, and “weight-friendly” reading materials rather than fashion magazines with thin supermodels.
Importantly, clinicians need to address the issue of weight bias within themselves, their medical staff, and colleagues, according to the OAC. To be effective and empathic with individuals affected by obesity “requires honest self-examination of one’s own attitudes and weight bias.”
Dr. Almandoz reported being a consultant/advisory board member for Novo Nordisk, Boehringer Ingelheim, and Eli Lilly and Company. Dr. Cabandugama reported no competing interests.
A version of this article first appeared on Medscape.com.
It’s in the Juice: Cranberries for UTI Prevention
TOPLINE:
A systematic review and network meta-analysis found cranberry juice can help prevent urinary tract infections (UTIs).
METHODOLOGY:
- With an increasing prevalence of antimicrobial resistance and over 50% women reporting at least one episode of UTI each year, identifying evidence supporting possible nondrug interventions is necessary, according to the study researchers from Bond University, the University of Helsinki, and the University of Oxford.
- The primary study outcome was number of UTIs in each treatment or placebo group; the secondary outcomes were UTI symptoms such as increased bladder sensation, urgency, frequency, dysuria, and consumption of antimicrobial drugs.
- Studies analyzed included people of any age and gender at a risk for UTI.
- Researchers included 3091 participants from 18 randomized controlled trials and two nonrandomized controlled trials.
TAKEAWAY:
- Studies used one of the following interventions: Cranberry nonliquid products (tablet, capsule, or fruit), cranberry liquid, liquid other than cranberry, and no treatment.
- A total of 18 studies showed a 27% lower rate of UTIs with the consumption of cranberry juice than with placebo liquid (moderate certainty evidence) and a 54% lower rate of UTIs with the consumption of cranberry juice than with no treatment (very low certainty evidence).
- Based on a meta-analysis of six studies, antibiotic use was 49% lower with the consumption of cranberry juice than with placebo liquid and 59% lower than with no treatment.
- Cranberry compounds also were associated with a decrease in prevalence of UTI symptoms.
IN PRACTICE:
“The evidence supports the use of cranberry juice for the prevention of UTIs. While increased liquids benefit the rate of UTIs and reduce antibiotic use, and cranberry compounds benefit symptoms of infection, the combination of these, in cranberry juice, provides clear and significant clinical outcomes for the reduction in UTIs and antibiotic use and should be considered for the management of UTIs,” the authors wrote.
SOURCE:
The study was led by Christian Moro, PhD, faculty of health sciences and medicine at Bond University in Gold Coast, Australia, and was published online in European Urology Focus on July 18, 2024.
LIMITATIONS:
The authors noted that some planned findings such as the impact on antibiotic use were reduced due to limited studies. Some studies on cranberry tablets also provided education with the intervention, which could have affected UTI recurrence rates. Nearly all the 20 studies that were analyzed included mostly women; thus, comparisons between genders were not possible.
DISCLOSURES:
Dr. Moro reported no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
A systematic review and network meta-analysis found cranberry juice can help prevent urinary tract infections (UTIs).
METHODOLOGY:
- With an increasing prevalence of antimicrobial resistance and over 50% women reporting at least one episode of UTI each year, identifying evidence supporting possible nondrug interventions is necessary, according to the study researchers from Bond University, the University of Helsinki, and the University of Oxford.
- The primary study outcome was number of UTIs in each treatment or placebo group; the secondary outcomes were UTI symptoms such as increased bladder sensation, urgency, frequency, dysuria, and consumption of antimicrobial drugs.
- Studies analyzed included people of any age and gender at a risk for UTI.
- Researchers included 3091 participants from 18 randomized controlled trials and two nonrandomized controlled trials.
TAKEAWAY:
- Studies used one of the following interventions: Cranberry nonliquid products (tablet, capsule, or fruit), cranberry liquid, liquid other than cranberry, and no treatment.
- A total of 18 studies showed a 27% lower rate of UTIs with the consumption of cranberry juice than with placebo liquid (moderate certainty evidence) and a 54% lower rate of UTIs with the consumption of cranberry juice than with no treatment (very low certainty evidence).
- Based on a meta-analysis of six studies, antibiotic use was 49% lower with the consumption of cranberry juice than with placebo liquid and 59% lower than with no treatment.
- Cranberry compounds also were associated with a decrease in prevalence of UTI symptoms.
IN PRACTICE:
“The evidence supports the use of cranberry juice for the prevention of UTIs. While increased liquids benefit the rate of UTIs and reduce antibiotic use, and cranberry compounds benefit symptoms of infection, the combination of these, in cranberry juice, provides clear and significant clinical outcomes for the reduction in UTIs and antibiotic use and should be considered for the management of UTIs,” the authors wrote.
SOURCE:
The study was led by Christian Moro, PhD, faculty of health sciences and medicine at Bond University in Gold Coast, Australia, and was published online in European Urology Focus on July 18, 2024.
LIMITATIONS:
The authors noted that some planned findings such as the impact on antibiotic use were reduced due to limited studies. Some studies on cranberry tablets also provided education with the intervention, which could have affected UTI recurrence rates. Nearly all the 20 studies that were analyzed included mostly women; thus, comparisons between genders were not possible.
DISCLOSURES:
Dr. Moro reported no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
A systematic review and network meta-analysis found cranberry juice can help prevent urinary tract infections (UTIs).
METHODOLOGY:
- With an increasing prevalence of antimicrobial resistance and over 50% women reporting at least one episode of UTI each year, identifying evidence supporting possible nondrug interventions is necessary, according to the study researchers from Bond University, the University of Helsinki, and the University of Oxford.
- The primary study outcome was number of UTIs in each treatment or placebo group; the secondary outcomes were UTI symptoms such as increased bladder sensation, urgency, frequency, dysuria, and consumption of antimicrobial drugs.
- Studies analyzed included people of any age and gender at a risk for UTI.
- Researchers included 3091 participants from 18 randomized controlled trials and two nonrandomized controlled trials.
TAKEAWAY:
- Studies used one of the following interventions: Cranberry nonliquid products (tablet, capsule, or fruit), cranberry liquid, liquid other than cranberry, and no treatment.
- A total of 18 studies showed a 27% lower rate of UTIs with the consumption of cranberry juice than with placebo liquid (moderate certainty evidence) and a 54% lower rate of UTIs with the consumption of cranberry juice than with no treatment (very low certainty evidence).
- Based on a meta-analysis of six studies, antibiotic use was 49% lower with the consumption of cranberry juice than with placebo liquid and 59% lower than with no treatment.
- Cranberry compounds also were associated with a decrease in prevalence of UTI symptoms.
IN PRACTICE:
“The evidence supports the use of cranberry juice for the prevention of UTIs. While increased liquids benefit the rate of UTIs and reduce antibiotic use, and cranberry compounds benefit symptoms of infection, the combination of these, in cranberry juice, provides clear and significant clinical outcomes for the reduction in UTIs and antibiotic use and should be considered for the management of UTIs,” the authors wrote.
SOURCE:
The study was led by Christian Moro, PhD, faculty of health sciences and medicine at Bond University in Gold Coast, Australia, and was published online in European Urology Focus on July 18, 2024.
LIMITATIONS:
The authors noted that some planned findings such as the impact on antibiotic use were reduced due to limited studies. Some studies on cranberry tablets also provided education with the intervention, which could have affected UTI recurrence rates. Nearly all the 20 studies that were analyzed included mostly women; thus, comparisons between genders were not possible.
DISCLOSURES:
Dr. Moro reported no disclosures.
A version of this article appeared on Medscape.com.