User login
Children with uncontrolled asthma at higher risk of being bullied
The risk of bullying and teasing is higher in children and young people with poorer asthma control, an international study reported. Published online in the Archives of Disease in Childhood, the Room to Breathe survey of 943 children in six countries found 9.9% had experienced asthma-related bullying or teasing (n = 93).
Children with well-controlled disease, however, were less likely to report being victimized by asthma-related bullying/teasing: odds ratio, 0.51; 95% confidence interval, 0.23-0.84; P = .006).
“It’s important for pediatricians to recognize that children and young people with asthma commonly report bullying or teasing as a result of their condition,” Will Carroll, MD, of the Paediatric Respiratory Service at Staffordshire Children’s Hospital at Royal Stoke, Stoke-on-Trent, England, told this news organization. “Pediatricians should talk to children themselves with asthma about this and not just their parents, and efforts should be made to improve asthma control whenever possible.”
Though common and potentially long-lasting in its effects, bullying is rarely addressed by health care professionals, the U.K. authors said.
But things may differ in the United States. According to Mark Welles, MD, a pediatrician at Cohen Children’s Medical Center at Northwell Health in Queen’s, N.Y., and regional cochair of the American Academy of Pediatrics antibullying committee, young doctors here are trained to ask about bullying when seeing a child, no matter what the reason for the visit. “It’s important to build a rapport with the child, and you need to ask about the disease they may have but also generally ask, ‘How are things at school? Is everyone nice to you?’ It is becoming more common practice to ask this,” said Dr. Welles, who was not involved with the U.K. research.
The U.K. study drew on unpublished data from the Room to Breathe survey conducted by Dr. Carroll’s group during 2008-2009 in Canada, the United Kingdom, Greece, Hungary, South Africa, and the Netherlands. Only 358 of 930 (38.5%) children were found to be well controlled according to current Global Initiative for Asthma symptom-control criteria.
The analysis also found a highly significant association (P < .0001) between Childhood Asthma Control Test (C-ACT) score and reported bullying/teasing, with bullied children having lower scores. C-ACT–defined controlled asthma scores of 20 or higher were significantly associated with a lower risk of bullying (OR, 0.46; 95% CI, 0.28-0.76; P = .001).
In other study findings, harassment was more common in children whose asthma was serious enough to entail activity restriction (OR, 1.74; 95% CI, 1.11-2.75; P = .010) and who described their asthma as “bad” (OR, 3.02; 95% CI, 1.86-4.85; P < .001), as well as those whose parents reported ongoing asthma-related health worries (OR, 1.64; 95% CI, 1.04-2.58; P = .024).
“When a child is clearly different from others, such as having bad asthma or being limited in activities due to asthma, they stand out more and are more frequently bullied,” said Tracy Evian Waasdorp, PhD, MSEd, director of research for school-based bullying and social-emotional learning at Children’s Hospital of Philadelphia, and also not a participant in the U.K. study.
In contrast to the 10% bullying rate in Dr. Carroll’s study, Dr. Waasdorp referred to a CHOP analysis of more than 64,000 youth from a Northeastern state in which those with asthma were 40% more likely to be victims of in-person bullying and 70% were more likely to be cyberbullied than youth without asthma. “Having a medical condition can therefore put you at risk of being bullied regardless of what country you live in,” she said.
CHOP policy encourages practitioners to routinely ask about bullying and to provide handouts and resources for parents, she added.
Interestingly, the U.K. investigators found that open public use of spacers was not associated with asthma-related bullying, nor was parental worry at diagnosis or parental concern about steroid use.
But according to Dr. Welles, “Kids may be using the inhaler in front of other kids, and they may be embarrassed and not want to be seen as different. So they may not use the inhaler when needed for gym class or sports, forcing them to sit out and then potentially be bullied again. It’s a vicious cycle.”
Previous research has identified the bullying and teasing of children with food allergies.
Behaviors have included allergy-specific harassment such as smearing peanut butter on a youngster’s forehead or putting peanut butter cookie crumbs in a child’s lunch box.
“In our survey we asked the question ‘Have you been teased or bullied because of your asthma?’ but we didn’t ask what form this took,” Dr. Carroll said. “But we were surprised at just how many children said yes. It’s time for more research, I think.”
“There are never enough studies around this,” added Dr. Welles. “Bullying, whether because of asthma or otherwise, has the potential for long-term effects well into adulthood.”
In the meantime, asthma consultations should incorporate specific questions about bullying. They should also be child focused in order to gain a representative appreciation of asthma control and its effect on the child’s life.
“As pediatricians, we need to be continuously supporting parents and find the help they need to address any mental health issues,” Dr. Welles said. “Every pediatrician and parent needs to be aware and recognize when something is different in their child’s life. Please don’t ignore it.”
Dr. Waasdorp stressed that school and other communities should be aware that children with asthma may be at increased risk for aggression and harmful interactions related to their asthma. “Programming to reduce bullying should focus broadly on shifting the climate so that bullying is not perceived to be normative and on improving ‘upstander,’ or positive bystander, responses.” she said.
The original survey was funded by Nycomed (Zurich). No additional funding was requested for the current analysis. Dr. Carroll reported personal fees from GlaxoSmithKline, Novartis, and Trudell Medical International outside the submitted work. Dr. Welles and Dr. Waasdorp disclosed no competing interests relevant to their comments.
The risk of bullying and teasing is higher in children and young people with poorer asthma control, an international study reported. Published online in the Archives of Disease in Childhood, the Room to Breathe survey of 943 children in six countries found 9.9% had experienced asthma-related bullying or teasing (n = 93).
Children with well-controlled disease, however, were less likely to report being victimized by asthma-related bullying/teasing: odds ratio, 0.51; 95% confidence interval, 0.23-0.84; P = .006).
“It’s important for pediatricians to recognize that children and young people with asthma commonly report bullying or teasing as a result of their condition,” Will Carroll, MD, of the Paediatric Respiratory Service at Staffordshire Children’s Hospital at Royal Stoke, Stoke-on-Trent, England, told this news organization. “Pediatricians should talk to children themselves with asthma about this and not just their parents, and efforts should be made to improve asthma control whenever possible.”
Though common and potentially long-lasting in its effects, bullying is rarely addressed by health care professionals, the U.K. authors said.
But things may differ in the United States. According to Mark Welles, MD, a pediatrician at Cohen Children’s Medical Center at Northwell Health in Queen’s, N.Y., and regional cochair of the American Academy of Pediatrics antibullying committee, young doctors here are trained to ask about bullying when seeing a child, no matter what the reason for the visit. “It’s important to build a rapport with the child, and you need to ask about the disease they may have but also generally ask, ‘How are things at school? Is everyone nice to you?’ It is becoming more common practice to ask this,” said Dr. Welles, who was not involved with the U.K. research.
The U.K. study drew on unpublished data from the Room to Breathe survey conducted by Dr. Carroll’s group during 2008-2009 in Canada, the United Kingdom, Greece, Hungary, South Africa, and the Netherlands. Only 358 of 930 (38.5%) children were found to be well controlled according to current Global Initiative for Asthma symptom-control criteria.
The analysis also found a highly significant association (P < .0001) between Childhood Asthma Control Test (C-ACT) score and reported bullying/teasing, with bullied children having lower scores. C-ACT–defined controlled asthma scores of 20 or higher were significantly associated with a lower risk of bullying (OR, 0.46; 95% CI, 0.28-0.76; P = .001).
In other study findings, harassment was more common in children whose asthma was serious enough to entail activity restriction (OR, 1.74; 95% CI, 1.11-2.75; P = .010) and who described their asthma as “bad” (OR, 3.02; 95% CI, 1.86-4.85; P < .001), as well as those whose parents reported ongoing asthma-related health worries (OR, 1.64; 95% CI, 1.04-2.58; P = .024).
“When a child is clearly different from others, such as having bad asthma or being limited in activities due to asthma, they stand out more and are more frequently bullied,” said Tracy Evian Waasdorp, PhD, MSEd, director of research for school-based bullying and social-emotional learning at Children’s Hospital of Philadelphia, and also not a participant in the U.K. study.
In contrast to the 10% bullying rate in Dr. Carroll’s study, Dr. Waasdorp referred to a CHOP analysis of more than 64,000 youth from a Northeastern state in which those with asthma were 40% more likely to be victims of in-person bullying and 70% were more likely to be cyberbullied than youth without asthma. “Having a medical condition can therefore put you at risk of being bullied regardless of what country you live in,” she said.
CHOP policy encourages practitioners to routinely ask about bullying and to provide handouts and resources for parents, she added.
Interestingly, the U.K. investigators found that open public use of spacers was not associated with asthma-related bullying, nor was parental worry at diagnosis or parental concern about steroid use.
But according to Dr. Welles, “Kids may be using the inhaler in front of other kids, and they may be embarrassed and not want to be seen as different. So they may not use the inhaler when needed for gym class or sports, forcing them to sit out and then potentially be bullied again. It’s a vicious cycle.”
Previous research has identified the bullying and teasing of children with food allergies.
Behaviors have included allergy-specific harassment such as smearing peanut butter on a youngster’s forehead or putting peanut butter cookie crumbs in a child’s lunch box.
“In our survey we asked the question ‘Have you been teased or bullied because of your asthma?’ but we didn’t ask what form this took,” Dr. Carroll said. “But we were surprised at just how many children said yes. It’s time for more research, I think.”
“There are never enough studies around this,” added Dr. Welles. “Bullying, whether because of asthma or otherwise, has the potential for long-term effects well into adulthood.”
In the meantime, asthma consultations should incorporate specific questions about bullying. They should also be child focused in order to gain a representative appreciation of asthma control and its effect on the child’s life.
“As pediatricians, we need to be continuously supporting parents and find the help they need to address any mental health issues,” Dr. Welles said. “Every pediatrician and parent needs to be aware and recognize when something is different in their child’s life. Please don’t ignore it.”
Dr. Waasdorp stressed that school and other communities should be aware that children with asthma may be at increased risk for aggression and harmful interactions related to their asthma. “Programming to reduce bullying should focus broadly on shifting the climate so that bullying is not perceived to be normative and on improving ‘upstander,’ or positive bystander, responses.” she said.
The original survey was funded by Nycomed (Zurich). No additional funding was requested for the current analysis. Dr. Carroll reported personal fees from GlaxoSmithKline, Novartis, and Trudell Medical International outside the submitted work. Dr. Welles and Dr. Waasdorp disclosed no competing interests relevant to their comments.
The risk of bullying and teasing is higher in children and young people with poorer asthma control, an international study reported. Published online in the Archives of Disease in Childhood, the Room to Breathe survey of 943 children in six countries found 9.9% had experienced asthma-related bullying or teasing (n = 93).
Children with well-controlled disease, however, were less likely to report being victimized by asthma-related bullying/teasing: odds ratio, 0.51; 95% confidence interval, 0.23-0.84; P = .006).
“It’s important for pediatricians to recognize that children and young people with asthma commonly report bullying or teasing as a result of their condition,” Will Carroll, MD, of the Paediatric Respiratory Service at Staffordshire Children’s Hospital at Royal Stoke, Stoke-on-Trent, England, told this news organization. “Pediatricians should talk to children themselves with asthma about this and not just their parents, and efforts should be made to improve asthma control whenever possible.”
Though common and potentially long-lasting in its effects, bullying is rarely addressed by health care professionals, the U.K. authors said.
But things may differ in the United States. According to Mark Welles, MD, a pediatrician at Cohen Children’s Medical Center at Northwell Health in Queen’s, N.Y., and regional cochair of the American Academy of Pediatrics antibullying committee, young doctors here are trained to ask about bullying when seeing a child, no matter what the reason for the visit. “It’s important to build a rapport with the child, and you need to ask about the disease they may have but also generally ask, ‘How are things at school? Is everyone nice to you?’ It is becoming more common practice to ask this,” said Dr. Welles, who was not involved with the U.K. research.
The U.K. study drew on unpublished data from the Room to Breathe survey conducted by Dr. Carroll’s group during 2008-2009 in Canada, the United Kingdom, Greece, Hungary, South Africa, and the Netherlands. Only 358 of 930 (38.5%) children were found to be well controlled according to current Global Initiative for Asthma symptom-control criteria.
The analysis also found a highly significant association (P < .0001) between Childhood Asthma Control Test (C-ACT) score and reported bullying/teasing, with bullied children having lower scores. C-ACT–defined controlled asthma scores of 20 or higher were significantly associated with a lower risk of bullying (OR, 0.46; 95% CI, 0.28-0.76; P = .001).
In other study findings, harassment was more common in children whose asthma was serious enough to entail activity restriction (OR, 1.74; 95% CI, 1.11-2.75; P = .010) and who described their asthma as “bad” (OR, 3.02; 95% CI, 1.86-4.85; P < .001), as well as those whose parents reported ongoing asthma-related health worries (OR, 1.64; 95% CI, 1.04-2.58; P = .024).
“When a child is clearly different from others, such as having bad asthma or being limited in activities due to asthma, they stand out more and are more frequently bullied,” said Tracy Evian Waasdorp, PhD, MSEd, director of research for school-based bullying and social-emotional learning at Children’s Hospital of Philadelphia, and also not a participant in the U.K. study.
In contrast to the 10% bullying rate in Dr. Carroll’s study, Dr. Waasdorp referred to a CHOP analysis of more than 64,000 youth from a Northeastern state in which those with asthma were 40% more likely to be victims of in-person bullying and 70% were more likely to be cyberbullied than youth without asthma. “Having a medical condition can therefore put you at risk of being bullied regardless of what country you live in,” she said.
CHOP policy encourages practitioners to routinely ask about bullying and to provide handouts and resources for parents, she added.
Interestingly, the U.K. investigators found that open public use of spacers was not associated with asthma-related bullying, nor was parental worry at diagnosis or parental concern about steroid use.
But according to Dr. Welles, “Kids may be using the inhaler in front of other kids, and they may be embarrassed and not want to be seen as different. So they may not use the inhaler when needed for gym class or sports, forcing them to sit out and then potentially be bullied again. It’s a vicious cycle.”
Previous research has identified the bullying and teasing of children with food allergies.
Behaviors have included allergy-specific harassment such as smearing peanut butter on a youngster’s forehead or putting peanut butter cookie crumbs in a child’s lunch box.
“In our survey we asked the question ‘Have you been teased or bullied because of your asthma?’ but we didn’t ask what form this took,” Dr. Carroll said. “But we were surprised at just how many children said yes. It’s time for more research, I think.”
“There are never enough studies around this,” added Dr. Welles. “Bullying, whether because of asthma or otherwise, has the potential for long-term effects well into adulthood.”
In the meantime, asthma consultations should incorporate specific questions about bullying. They should also be child focused in order to gain a representative appreciation of asthma control and its effect on the child’s life.
“As pediatricians, we need to be continuously supporting parents and find the help they need to address any mental health issues,” Dr. Welles said. “Every pediatrician and parent needs to be aware and recognize when something is different in their child’s life. Please don’t ignore it.”
Dr. Waasdorp stressed that school and other communities should be aware that children with asthma may be at increased risk for aggression and harmful interactions related to their asthma. “Programming to reduce bullying should focus broadly on shifting the climate so that bullying is not perceived to be normative and on improving ‘upstander,’ or positive bystander, responses.” she said.
The original survey was funded by Nycomed (Zurich). No additional funding was requested for the current analysis. Dr. Carroll reported personal fees from GlaxoSmithKline, Novartis, and Trudell Medical International outside the submitted work. Dr. Welles and Dr. Waasdorp disclosed no competing interests relevant to their comments.
FROM ARCHIVES OF DISEASE IN CHILDHOOD
Single-dose HPV vaccination highly effective
A single dose of human papillomavirus (HPV) vaccine was highly effective at preventing oncogenic infection, rivaling the protection offered by multidose regimens, according to results from the KEN SHE trial, based in Kenya.
The findings, published on the preprint server Research Square and presented Nov. 17 at the 34th International Papillomavirus Conference in Toronto, bring “renewed energy to the push to make cervical cancer the first cancer to be wiped out globally,” according to co–principal investigator Ruanne V. Barnabas, PhD, a professor of global health at the University of Washington, Seattle.
Decision-makers will consider these findings, which have not yet been peer-reviewed, along with other evidence to determine if dosing-schedule changes are warranted, she told this news organization.
In a press release, Samuel Kariuki, PhD, acting director general, Kenya Medical Research Institute, who was not involved in the research, called the findings a “game changer” that could “substantially reduce the incidence of HPV-attributable cervical cancer.”
Between 2018 and 2019, Dr. Barnabas and her colleagues enrolled 2,275 sexually active, HPV-vaccine–naive women in Kenya in their study. The women, 15-20 years of age, were randomly assigned to receive a bivalent vaccine (HPV 16/18), a nonavalent vaccine (HPV 16/18/31/33/45/52/58/6/11), or a vaccine against meningococcal meningitis.
Most participants (57%) were between 15 and 17 years of age, and 61% reported one lifetime sexual partner. The women underwent genital and cervical swabs at enrollment to test for HPV DNA and had blood drawn to test for antibodies. During 18 months of follow-up, they had cervical swabs every 6 months and a vaginal swab at 3 months to test for HPV DNA.
The researchers detected 38 persistent HPV 16/18 infections in women who had tested negative for HPV 16/18 antibodies at enrollment and for HPV 16/18 DNA at enrollment and month 3 – one in each of the HPV-vaccine groups and 36 in the meningococcal group. This infection rate corresponded to a vaccine efficacy of 97.5% (P < .001) against HPV 16/18 for both the bivalent and nonavalent vaccines, which is “comparable to that seen in multidose vaccine trials,” the researchers write.
Among women negative for HPV 16/18/31/33/45/52/58 at the beginning of the trial, 33 had persistent infections: four in the nonavalent vaccine group and 29 in the meningococcal group, demonstrating an efficacy of 89% (P < .001) against all seven oncogenic strains contained in the vaccine.
Even if women tested positive for one strain of HPV, the vaccine protected them from other strains of the virus, the investigators noted.
Serious adverse events occurred in 4.5%-5.2% of participants across the study arms.
The KEN SHE trial comes 15 years after the U.S. Food and Drug Administration approved the first HPV vaccine – Merck’s Gardasil. Two others, Cervarix and Gardasil-9, have since been approved, but cost and supply issues have inhibited coverage, particularly in areas where the cervical cancer burden is high, the researchers noted.
Recent data indicate that just 15% of girls globally are vaccinated against HPV, but a single-dose vaccine would “simplify logistics and decrease costs,” thereby improving the chances of reaching the World Health Organization goal of vaccinating 90% of 15-year-old girls against HPV by 2030, Dr. Barnabas said in a press release about the trial.
Co–principal investigator Nelly Mugo, MBChB, MPH, senior principal clinical research scientist with the Center for Clinical Research at the Kenya Medical Research Institute in Nairobi, further emphasized the importance of the findings, noting in the press release that the “trial brings new energy to the elimination of cervical cancer. It brings great hope to the women living in countries like Kenya, who have a high burden of the disease.”
Dr. Mugo is also an associate research professor of global health at the University of Washington, Seattle.
Dr. Barnabas said women have been given multiple doses of the HPV vaccine because of “gaps in evidence for the effectiveness of a single-dose vaccine and concerns about clinically meaningful differences in efficacy.
“Observational data suggested that the single-dose HPV vaccine could have good efficacy, but because the data were not from randomized trials, that could have been from chance,” she explained, noting, however, that “sufficient evidence supported the decrease in doses from three to two doses for girls 15 years of age and younger.”
Going forward, the researchers will conduct immunobridging studies to other populations and will continue follow-up to assess the durability of single-dose efficacy, Dr. Barnabas said.
“The results from the KEN SHE trial support the use of single-dose HPV vaccination to increase access and coverage,” she concluded.
The KEN SHE trial was funded by the Bill & Melinda Gates Foundation (BMGF). Dr. Barnabas reports grants from BMGF and grants from King K. Holmes Professorship in STDs and AIDS during the conduct of the study, and grants from BMGF, National Institutes of Health, and manuscript and abstract writing support from Regeneron Pharmaceuticals outside the submitted work.
A version of this article first appeared on Medscape.com.
A single dose of human papillomavirus (HPV) vaccine was highly effective at preventing oncogenic infection, rivaling the protection offered by multidose regimens, according to results from the KEN SHE trial, based in Kenya.
The findings, published on the preprint server Research Square and presented Nov. 17 at the 34th International Papillomavirus Conference in Toronto, bring “renewed energy to the push to make cervical cancer the first cancer to be wiped out globally,” according to co–principal investigator Ruanne V. Barnabas, PhD, a professor of global health at the University of Washington, Seattle.
Decision-makers will consider these findings, which have not yet been peer-reviewed, along with other evidence to determine if dosing-schedule changes are warranted, she told this news organization.
In a press release, Samuel Kariuki, PhD, acting director general, Kenya Medical Research Institute, who was not involved in the research, called the findings a “game changer” that could “substantially reduce the incidence of HPV-attributable cervical cancer.”
Between 2018 and 2019, Dr. Barnabas and her colleagues enrolled 2,275 sexually active, HPV-vaccine–naive women in Kenya in their study. The women, 15-20 years of age, were randomly assigned to receive a bivalent vaccine (HPV 16/18), a nonavalent vaccine (HPV 16/18/31/33/45/52/58/6/11), or a vaccine against meningococcal meningitis.
Most participants (57%) were between 15 and 17 years of age, and 61% reported one lifetime sexual partner. The women underwent genital and cervical swabs at enrollment to test for HPV DNA and had blood drawn to test for antibodies. During 18 months of follow-up, they had cervical swabs every 6 months and a vaginal swab at 3 months to test for HPV DNA.
The researchers detected 38 persistent HPV 16/18 infections in women who had tested negative for HPV 16/18 antibodies at enrollment and for HPV 16/18 DNA at enrollment and month 3 – one in each of the HPV-vaccine groups and 36 in the meningococcal group. This infection rate corresponded to a vaccine efficacy of 97.5% (P < .001) against HPV 16/18 for both the bivalent and nonavalent vaccines, which is “comparable to that seen in multidose vaccine trials,” the researchers write.
Among women negative for HPV 16/18/31/33/45/52/58 at the beginning of the trial, 33 had persistent infections: four in the nonavalent vaccine group and 29 in the meningococcal group, demonstrating an efficacy of 89% (P < .001) against all seven oncogenic strains contained in the vaccine.
Even if women tested positive for one strain of HPV, the vaccine protected them from other strains of the virus, the investigators noted.
Serious adverse events occurred in 4.5%-5.2% of participants across the study arms.
The KEN SHE trial comes 15 years after the U.S. Food and Drug Administration approved the first HPV vaccine – Merck’s Gardasil. Two others, Cervarix and Gardasil-9, have since been approved, but cost and supply issues have inhibited coverage, particularly in areas where the cervical cancer burden is high, the researchers noted.
Recent data indicate that just 15% of girls globally are vaccinated against HPV, but a single-dose vaccine would “simplify logistics and decrease costs,” thereby improving the chances of reaching the World Health Organization goal of vaccinating 90% of 15-year-old girls against HPV by 2030, Dr. Barnabas said in a press release about the trial.
Co–principal investigator Nelly Mugo, MBChB, MPH, senior principal clinical research scientist with the Center for Clinical Research at the Kenya Medical Research Institute in Nairobi, further emphasized the importance of the findings, noting in the press release that the “trial brings new energy to the elimination of cervical cancer. It brings great hope to the women living in countries like Kenya, who have a high burden of the disease.”
Dr. Mugo is also an associate research professor of global health at the University of Washington, Seattle.
Dr. Barnabas said women have been given multiple doses of the HPV vaccine because of “gaps in evidence for the effectiveness of a single-dose vaccine and concerns about clinically meaningful differences in efficacy.
“Observational data suggested that the single-dose HPV vaccine could have good efficacy, but because the data were not from randomized trials, that could have been from chance,” she explained, noting, however, that “sufficient evidence supported the decrease in doses from three to two doses for girls 15 years of age and younger.”
Going forward, the researchers will conduct immunobridging studies to other populations and will continue follow-up to assess the durability of single-dose efficacy, Dr. Barnabas said.
“The results from the KEN SHE trial support the use of single-dose HPV vaccination to increase access and coverage,” she concluded.
The KEN SHE trial was funded by the Bill & Melinda Gates Foundation (BMGF). Dr. Barnabas reports grants from BMGF and grants from King K. Holmes Professorship in STDs and AIDS during the conduct of the study, and grants from BMGF, National Institutes of Health, and manuscript and abstract writing support from Regeneron Pharmaceuticals outside the submitted work.
A version of this article first appeared on Medscape.com.
A single dose of human papillomavirus (HPV) vaccine was highly effective at preventing oncogenic infection, rivaling the protection offered by multidose regimens, according to results from the KEN SHE trial, based in Kenya.
The findings, published on the preprint server Research Square and presented Nov. 17 at the 34th International Papillomavirus Conference in Toronto, bring “renewed energy to the push to make cervical cancer the first cancer to be wiped out globally,” according to co–principal investigator Ruanne V. Barnabas, PhD, a professor of global health at the University of Washington, Seattle.
Decision-makers will consider these findings, which have not yet been peer-reviewed, along with other evidence to determine if dosing-schedule changes are warranted, she told this news organization.
In a press release, Samuel Kariuki, PhD, acting director general, Kenya Medical Research Institute, who was not involved in the research, called the findings a “game changer” that could “substantially reduce the incidence of HPV-attributable cervical cancer.”
Between 2018 and 2019, Dr. Barnabas and her colleagues enrolled 2,275 sexually active, HPV-vaccine–naive women in Kenya in their study. The women, 15-20 years of age, were randomly assigned to receive a bivalent vaccine (HPV 16/18), a nonavalent vaccine (HPV 16/18/31/33/45/52/58/6/11), or a vaccine against meningococcal meningitis.
Most participants (57%) were between 15 and 17 years of age, and 61% reported one lifetime sexual partner. The women underwent genital and cervical swabs at enrollment to test for HPV DNA and had blood drawn to test for antibodies. During 18 months of follow-up, they had cervical swabs every 6 months and a vaginal swab at 3 months to test for HPV DNA.
The researchers detected 38 persistent HPV 16/18 infections in women who had tested negative for HPV 16/18 antibodies at enrollment and for HPV 16/18 DNA at enrollment and month 3 – one in each of the HPV-vaccine groups and 36 in the meningococcal group. This infection rate corresponded to a vaccine efficacy of 97.5% (P < .001) against HPV 16/18 for both the bivalent and nonavalent vaccines, which is “comparable to that seen in multidose vaccine trials,” the researchers write.
Among women negative for HPV 16/18/31/33/45/52/58 at the beginning of the trial, 33 had persistent infections: four in the nonavalent vaccine group and 29 in the meningococcal group, demonstrating an efficacy of 89% (P < .001) against all seven oncogenic strains contained in the vaccine.
Even if women tested positive for one strain of HPV, the vaccine protected them from other strains of the virus, the investigators noted.
Serious adverse events occurred in 4.5%-5.2% of participants across the study arms.
The KEN SHE trial comes 15 years after the U.S. Food and Drug Administration approved the first HPV vaccine – Merck’s Gardasil. Two others, Cervarix and Gardasil-9, have since been approved, but cost and supply issues have inhibited coverage, particularly in areas where the cervical cancer burden is high, the researchers noted.
Recent data indicate that just 15% of girls globally are vaccinated against HPV, but a single-dose vaccine would “simplify logistics and decrease costs,” thereby improving the chances of reaching the World Health Organization goal of vaccinating 90% of 15-year-old girls against HPV by 2030, Dr. Barnabas said in a press release about the trial.
Co–principal investigator Nelly Mugo, MBChB, MPH, senior principal clinical research scientist with the Center for Clinical Research at the Kenya Medical Research Institute in Nairobi, further emphasized the importance of the findings, noting in the press release that the “trial brings new energy to the elimination of cervical cancer. It brings great hope to the women living in countries like Kenya, who have a high burden of the disease.”
Dr. Mugo is also an associate research professor of global health at the University of Washington, Seattle.
Dr. Barnabas said women have been given multiple doses of the HPV vaccine because of “gaps in evidence for the effectiveness of a single-dose vaccine and concerns about clinically meaningful differences in efficacy.
“Observational data suggested that the single-dose HPV vaccine could have good efficacy, but because the data were not from randomized trials, that could have been from chance,” she explained, noting, however, that “sufficient evidence supported the decrease in doses from three to two doses for girls 15 years of age and younger.”
Going forward, the researchers will conduct immunobridging studies to other populations and will continue follow-up to assess the durability of single-dose efficacy, Dr. Barnabas said.
“The results from the KEN SHE trial support the use of single-dose HPV vaccination to increase access and coverage,” she concluded.
The KEN SHE trial was funded by the Bill & Melinda Gates Foundation (BMGF). Dr. Barnabas reports grants from BMGF and grants from King K. Holmes Professorship in STDs and AIDS during the conduct of the study, and grants from BMGF, National Institutes of Health, and manuscript and abstract writing support from Regeneron Pharmaceuticals outside the submitted work.
A version of this article first appeared on Medscape.com.
DRESS Syndrome Due to Cefdinir Mimicking Superinfected Eczema in a Pediatric Patient
To the Editor:
Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome, or drug-induced hypersensitivity syndrome, is a serious and potentially fatal multiorgan drug hypersensitivity reaction. Drug reaction with eosinophilia and systemic symptoms syndrome shares many clinical features with viral exanthems and may be difficult to diagnose in the setting of atopic dermatitis (AD) in which children may have baseline eosinophilia from an atopic diathesis. The cutaneous exanthema also may be variable in presentation, further complicating diagnosis.1,2
A 3-year-old boy with AD since infancy and a history of anaphylaxis to peanuts presented to the emergency department with reported fever, rash, sore throat, and decreased oral intake. Ten days prior, the patient was treated for cellulitis of the left foot with a 7-day course of cefdinir with complete resolution of symptoms. Four days prior to admission, the patient started developing “bumps” on the face and fevers. He was seen at an outside facility, where a rapid test for Streptococcus was negative, and the patient was treated with ibuprofen and fluids for a presumed viral exanthem. The rash subsequently spread to involve the trunk and extremities. On the day of admission, the patient had a positive rapid test for Streptococcus and was referred to the emergency department with concern for superinfected eczema and eczema herpeticum. The patient recently traveled to Puerto Rico, where he had contact with an aunt with active herpes zoster but no other sick contacts. The patient’s immunizations were reported to be up-to-date.
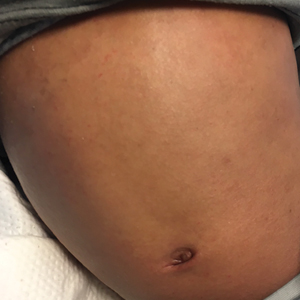
Physical examination revealed the patient was afebrile but irritable and had erythematous crusted papules and patches on the face, arms, and legs, as well as erythematous dry patches on the chest, abdomen, and back (Figure). There were no conjunctival erythematous or oral erosions. The patient was admitted to the hospital for presumed superinfected AD and possible eczema herpeticum. He was started on intravenous clindamycin and acyclovir.

The following day, the patient had new facial edema and fever (temperature, 102.8 °F [39.36 °C]) in addition to palpable mobile cervical, axillary, and inguinal lymphadenopathy. He also was noted to have notably worsening eosinophilia from 1288 (14%) to 2570 (29.2%) cells/µL (reference range, 0%–5%) and new-onset transaminitis. Herpes and varicella-zoster direct fluorescent antibody tests, culture, and serum polymerase chain reaction were all negative, and acyclovir was discontinued. Repeat laboratory tests 12 hours later showed a continued uptrend in transaminitis. Serologies for acute and chronic cytomegalovirus; Epstein-Barr virus; and hepatitis A, B, and C were all nonreactive. The patient was started on intravenous methylprednisolone 1 mg/kg daily for suspected DRESS syndrome likely due to cefdinir.
The patient’s eosinophilia completely resolved (from approximately 2600 to 100 cells/µL) after 1 dose of steroids, and his transaminitis trended down over the next few days. He remained afebrile for the remainder of his admission, and his facial swelling and rash continued to improve. Bacterial culture from the skin grew oxacillin-susceptible Staphylococcus aureus and group A Streptococcus pyogenes. A blood culture was negative. The patient was discharged home to complete a 10-day course of clindamycin and was given topical steroids for the eczema. He continued on oral prednisolone 1 mg/kg daily for 10 days, after which the dose was tapered down for a total 1-month course of systemic corticosteroids. At 1-month follow-up after completing the course of steroids, he was doing well with normal hepatic enzyme levels and no recurrence of fever, facial edema, or rash. He continues to be followed for management of the AD.
Drug reaction with eosinophilia and systemic symptoms syndrome is a serious systemic adverse drug reaction, with high morbidity and even mortality, estimated at 10% in the adult population, though more specific pediatric mortality data are not available.1,2 The exact pathogenesis of DRESS syndrome has not been elucidated. Certain human leukocyte antigen class I alleles are predisposed to the development of DRESS syndrome, but there has not been a human leukocyte antigen subtype identified with beta-lactam–associated DRESS syndrome. Some studies have demonstrated a reactivation of human herpesvirus 6, human herpesvirus 7, and Epstein-Barr virus.3 One study involving 40 patients with DRESS syndrome identified viremia in 76% (29/38) of patients and identified CD8+ T-cell populations directed toward viral epitopes.3 Finally, DRESS syndrome may be related to the slow detoxification and elimination of intermediary products of offending medications that serve as an immunogenic stimulus for the inflammatory cascade.2
In adults, DRESS syndrome was first identified in association with phenytoin, but more recently other drugs have been identified, including other aromatic anticonvulsants (ie, lamotrigine, phenobarbital, carbamazepine), allopurinol, sulfonamides, antiretrovirals (particularly abacavir), and minocycline.2 In a 3-year pediatric prospective study, 11 cases of DRESS syndrome were identified: 4 cases due to lamotrigine, and 3 caused by penicillins.4 The trigger in our patient’s case was the beta-lactam, third-generation cephalosporin cefdinir, and his symptoms developed within 6 days of starting the medication. Many articles report that beta-lactams are a rare cause of DRESS syndrome, with only a handful of cases reported.1,5,6
The diagnosis of DRESS syndrome often can be delayed, as children present acutely febrile and toxic appearing. Unlike many adverse drug reactions, DRESS syndrome does not show rapid resolution with withdrawal of the causative agent, further complicating the diagnosis. The typical onset of DRESS syndrome generally ranges from 2 to 6 weeks after the initiation of the offending drug; however, faster onset of symptoms, similar to our case, has been noted in antibiotic-triggered cases. In the prospective pediatric series by Sasidharanpillai et al,4 the average time to onset among 3 antibiotic-triggered DRESS cases was 5.8 days vs 23.9 days among the 4 cases of lamotrigine-associated DRESS syndrome.
Our patient demonstrated the classic features of DRESS syndrome, including fever, rash, lymphadenopathy, facial edema, peripheral eosinophilia, atypical lymphocytosis, and hepatitis. Based on the proposed RegiSCAR scoring system, our patient was classified as a “definite” case of DRESS syndrome.1,7 Other hematologic findings in DRESS syndrome may include thrombocytopenia and anemia. The liver is the most commonly affected internal organ in DRESS syndrome, with pneumonitis, carditis, and nephritis reported less frequently.1 The pattern of liver injury in our patient was mixed (hepatocellular and cholestatic), the second most common pattern in patients with DRESS syndrome (the cholestatic pattern is most common).8
The exanthem of DRESS syndrome can vary in morphology, with up to 7% of patients reported to have eczemalike lesions in the multinational prospective RegiSCAR study.1 Other entities in the differential diagnosis for our patient included Kawasaki disease, where conjunctivitis and strawberry tongue are classically present, as well as erythrodermic AD, where internal organ involvement is not common.2 Our patient’s exanthem initially was considered to be a flare of AD with superimposed bacterial infection and possible eczema herpeticum. Although bacterial cultures did grow Staphylococcus and Streptococcus, viral studies were all negative, and this alone would not have explained the facial edema, rapidly rising eosinophil count, and transaminitis. The dramatic drop in his eosinophil count and decrease in hepatic enzymes after 1 dose of intravenous methylprednisolone also supported the diagnosis of DRESS syndrome.
Treatment recommendations remain largely anecdotal. Early systemic steroids generally are accepted as the first line of therapy, with a slow taper. Although the average required duration of systemic steroids in 1 series of adults was reported at 50.1 days,9 the duration was shorter (21–35 days) in a series of pediatric patients.4 Our patient’s clinical symptoms and laboratory values normalized after completing a 1-month steroid taper. Other therapies have been tried for recalcitrant cases, including intravenous immunoglobulin, plasmapheresis, rituximab, and valganciclovir.2
Early clinical recognition of the signs and symptoms of DRESS syndrome in the setting of a new medication can decrease morbidity and mortality. Although DRESS syndrome in pediatric patients presents with many similar clinical features as in adults, it may be a greater diagnostic challenge. As in adult cases, timely administration of systemic corticosteroids and tapering based on clinical signs and symptoms can lead to resolution of the hypersensitivity syndrome.
- Kardaun SH, Sekula P, Valeyrie-Allanore L, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. results from the prospective RegiSCAR study. Br J Dermatol. 2013;169:1071-1080.
- Fernando SL. Drug-reaction eosinophilia and systemic symptoms and drug-induced hypersensitivity syndrome. Australas J Dermatol. 2014;55:15-23.
- Picard D, Janela B, Descamps V, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): a multiorgan antiviral T cell response. Sci Transl Med. 2010;2:46ra62.
- Sasidharanpillai S, Sabitha S, Riyaz N, et al. Drug reaction with eosinophilia and systemic symptoms in children: a prospective study. Pediatr Dermatol. 2016;33:E162-E165.
- Aouam K, Chaabane A, Toumi A, et al. Drug rash with eosinophilia and systemic symptoms (DRESS) probably induced by cefotaxime: a report of two cases. Clin Med Res. 2012;10:32-35.
- Guleria VS, Dhillon M, Gill S, et al. Ceftriaxone induced drug rash with eosinophilia and systemic symptoms. J Res Pharm Pract. 2014;3:72-74.
- Kardaun SH, Sidoroff A, Valeyrie-Allanore L, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2007;156:609-611.
- Lin IC, Yang HC, Strong C, et al. Liver injury in patients with DRESS: a clinical study of 72 cases. J Am Acad Dermatol. 2015;72:984-991.
- Ang CC, Wang YS, Yoosuff EL, et al. Retrospective analysis of drug-induced hypersensitivity syndrome: a study of 27 patients. J Am Acad Dermatol. 2010;63:219-227.
To the Editor:
Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome, or drug-induced hypersensitivity syndrome, is a serious and potentially fatal multiorgan drug hypersensitivity reaction. Drug reaction with eosinophilia and systemic symptoms syndrome shares many clinical features with viral exanthems and may be difficult to diagnose in the setting of atopic dermatitis (AD) in which children may have baseline eosinophilia from an atopic diathesis. The cutaneous exanthema also may be variable in presentation, further complicating diagnosis.1,2
A 3-year-old boy with AD since infancy and a history of anaphylaxis to peanuts presented to the emergency department with reported fever, rash, sore throat, and decreased oral intake. Ten days prior, the patient was treated for cellulitis of the left foot with a 7-day course of cefdinir with complete resolution of symptoms. Four days prior to admission, the patient started developing “bumps” on the face and fevers. He was seen at an outside facility, where a rapid test for Streptococcus was negative, and the patient was treated with ibuprofen and fluids for a presumed viral exanthem. The rash subsequently spread to involve the trunk and extremities. On the day of admission, the patient had a positive rapid test for Streptococcus and was referred to the emergency department with concern for superinfected eczema and eczema herpeticum. The patient recently traveled to Puerto Rico, where he had contact with an aunt with active herpes zoster but no other sick contacts. The patient’s immunizations were reported to be up-to-date.
Physical examination revealed the patient was afebrile but irritable and had erythematous crusted papules and patches on the face, arms, and legs, as well as erythematous dry patches on the chest, abdomen, and back (Figure). There were no conjunctival erythematous or oral erosions. The patient was admitted to the hospital for presumed superinfected AD and possible eczema herpeticum. He was started on intravenous clindamycin and acyclovir.

The following day, the patient had new facial edema and fever (temperature, 102.8 °F [39.36 °C]) in addition to palpable mobile cervical, axillary, and inguinal lymphadenopathy. He also was noted to have notably worsening eosinophilia from 1288 (14%) to 2570 (29.2%) cells/µL (reference range, 0%–5%) and new-onset transaminitis. Herpes and varicella-zoster direct fluorescent antibody tests, culture, and serum polymerase chain reaction were all negative, and acyclovir was discontinued. Repeat laboratory tests 12 hours later showed a continued uptrend in transaminitis. Serologies for acute and chronic cytomegalovirus; Epstein-Barr virus; and hepatitis A, B, and C were all nonreactive. The patient was started on intravenous methylprednisolone 1 mg/kg daily for suspected DRESS syndrome likely due to cefdinir.
The patient’s eosinophilia completely resolved (from approximately 2600 to 100 cells/µL) after 1 dose of steroids, and his transaminitis trended down over the next few days. He remained afebrile for the remainder of his admission, and his facial swelling and rash continued to improve. Bacterial culture from the skin grew oxacillin-susceptible Staphylococcus aureus and group A Streptococcus pyogenes. A blood culture was negative. The patient was discharged home to complete a 10-day course of clindamycin and was given topical steroids for the eczema. He continued on oral prednisolone 1 mg/kg daily for 10 days, after which the dose was tapered down for a total 1-month course of systemic corticosteroids. At 1-month follow-up after completing the course of steroids, he was doing well with normal hepatic enzyme levels and no recurrence of fever, facial edema, or rash. He continues to be followed for management of the AD.
Drug reaction with eosinophilia and systemic symptoms syndrome is a serious systemic adverse drug reaction, with high morbidity and even mortality, estimated at 10% in the adult population, though more specific pediatric mortality data are not available.1,2 The exact pathogenesis of DRESS syndrome has not been elucidated. Certain human leukocyte antigen class I alleles are predisposed to the development of DRESS syndrome, but there has not been a human leukocyte antigen subtype identified with beta-lactam–associated DRESS syndrome. Some studies have demonstrated a reactivation of human herpesvirus 6, human herpesvirus 7, and Epstein-Barr virus.3 One study involving 40 patients with DRESS syndrome identified viremia in 76% (29/38) of patients and identified CD8+ T-cell populations directed toward viral epitopes.3 Finally, DRESS syndrome may be related to the slow detoxification and elimination of intermediary products of offending medications that serve as an immunogenic stimulus for the inflammatory cascade.2
In adults, DRESS syndrome was first identified in association with phenytoin, but more recently other drugs have been identified, including other aromatic anticonvulsants (ie, lamotrigine, phenobarbital, carbamazepine), allopurinol, sulfonamides, antiretrovirals (particularly abacavir), and minocycline.2 In a 3-year pediatric prospective study, 11 cases of DRESS syndrome were identified: 4 cases due to lamotrigine, and 3 caused by penicillins.4 The trigger in our patient’s case was the beta-lactam, third-generation cephalosporin cefdinir, and his symptoms developed within 6 days of starting the medication. Many articles report that beta-lactams are a rare cause of DRESS syndrome, with only a handful of cases reported.1,5,6
The diagnosis of DRESS syndrome often can be delayed, as children present acutely febrile and toxic appearing. Unlike many adverse drug reactions, DRESS syndrome does not show rapid resolution with withdrawal of the causative agent, further complicating the diagnosis. The typical onset of DRESS syndrome generally ranges from 2 to 6 weeks after the initiation of the offending drug; however, faster onset of symptoms, similar to our case, has been noted in antibiotic-triggered cases. In the prospective pediatric series by Sasidharanpillai et al,4 the average time to onset among 3 antibiotic-triggered DRESS cases was 5.8 days vs 23.9 days among the 4 cases of lamotrigine-associated DRESS syndrome.
Our patient demonstrated the classic features of DRESS syndrome, including fever, rash, lymphadenopathy, facial edema, peripheral eosinophilia, atypical lymphocytosis, and hepatitis. Based on the proposed RegiSCAR scoring system, our patient was classified as a “definite” case of DRESS syndrome.1,7 Other hematologic findings in DRESS syndrome may include thrombocytopenia and anemia. The liver is the most commonly affected internal organ in DRESS syndrome, with pneumonitis, carditis, and nephritis reported less frequently.1 The pattern of liver injury in our patient was mixed (hepatocellular and cholestatic), the second most common pattern in patients with DRESS syndrome (the cholestatic pattern is most common).8
The exanthem of DRESS syndrome can vary in morphology, with up to 7% of patients reported to have eczemalike lesions in the multinational prospective RegiSCAR study.1 Other entities in the differential diagnosis for our patient included Kawasaki disease, where conjunctivitis and strawberry tongue are classically present, as well as erythrodermic AD, where internal organ involvement is not common.2 Our patient’s exanthem initially was considered to be a flare of AD with superimposed bacterial infection and possible eczema herpeticum. Although bacterial cultures did grow Staphylococcus and Streptococcus, viral studies were all negative, and this alone would not have explained the facial edema, rapidly rising eosinophil count, and transaminitis. The dramatic drop in his eosinophil count and decrease in hepatic enzymes after 1 dose of intravenous methylprednisolone also supported the diagnosis of DRESS syndrome.
Treatment recommendations remain largely anecdotal. Early systemic steroids generally are accepted as the first line of therapy, with a slow taper. Although the average required duration of systemic steroids in 1 series of adults was reported at 50.1 days,9 the duration was shorter (21–35 days) in a series of pediatric patients.4 Our patient’s clinical symptoms and laboratory values normalized after completing a 1-month steroid taper. Other therapies have been tried for recalcitrant cases, including intravenous immunoglobulin, plasmapheresis, rituximab, and valganciclovir.2
Early clinical recognition of the signs and symptoms of DRESS syndrome in the setting of a new medication can decrease morbidity and mortality. Although DRESS syndrome in pediatric patients presents with many similar clinical features as in adults, it may be a greater diagnostic challenge. As in adult cases, timely administration of systemic corticosteroids and tapering based on clinical signs and symptoms can lead to resolution of the hypersensitivity syndrome.
To the Editor:
Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome, or drug-induced hypersensitivity syndrome, is a serious and potentially fatal multiorgan drug hypersensitivity reaction. Drug reaction with eosinophilia and systemic symptoms syndrome shares many clinical features with viral exanthems and may be difficult to diagnose in the setting of atopic dermatitis (AD) in which children may have baseline eosinophilia from an atopic diathesis. The cutaneous exanthema also may be variable in presentation, further complicating diagnosis.1,2
A 3-year-old boy with AD since infancy and a history of anaphylaxis to peanuts presented to the emergency department with reported fever, rash, sore throat, and decreased oral intake. Ten days prior, the patient was treated for cellulitis of the left foot with a 7-day course of cefdinir with complete resolution of symptoms. Four days prior to admission, the patient started developing “bumps” on the face and fevers. He was seen at an outside facility, where a rapid test for Streptococcus was negative, and the patient was treated with ibuprofen and fluids for a presumed viral exanthem. The rash subsequently spread to involve the trunk and extremities. On the day of admission, the patient had a positive rapid test for Streptococcus and was referred to the emergency department with concern for superinfected eczema and eczema herpeticum. The patient recently traveled to Puerto Rico, where he had contact with an aunt with active herpes zoster but no other sick contacts. The patient’s immunizations were reported to be up-to-date.
Physical examination revealed the patient was afebrile but irritable and had erythematous crusted papules and patches on the face, arms, and legs, as well as erythematous dry patches on the chest, abdomen, and back (Figure). There were no conjunctival erythematous or oral erosions. The patient was admitted to the hospital for presumed superinfected AD and possible eczema herpeticum. He was started on intravenous clindamycin and acyclovir.

The following day, the patient had new facial edema and fever (temperature, 102.8 °F [39.36 °C]) in addition to palpable mobile cervical, axillary, and inguinal lymphadenopathy. He also was noted to have notably worsening eosinophilia from 1288 (14%) to 2570 (29.2%) cells/µL (reference range, 0%–5%) and new-onset transaminitis. Herpes and varicella-zoster direct fluorescent antibody tests, culture, and serum polymerase chain reaction were all negative, and acyclovir was discontinued. Repeat laboratory tests 12 hours later showed a continued uptrend in transaminitis. Serologies for acute and chronic cytomegalovirus; Epstein-Barr virus; and hepatitis A, B, and C were all nonreactive. The patient was started on intravenous methylprednisolone 1 mg/kg daily for suspected DRESS syndrome likely due to cefdinir.
The patient’s eosinophilia completely resolved (from approximately 2600 to 100 cells/µL) after 1 dose of steroids, and his transaminitis trended down over the next few days. He remained afebrile for the remainder of his admission, and his facial swelling and rash continued to improve. Bacterial culture from the skin grew oxacillin-susceptible Staphylococcus aureus and group A Streptococcus pyogenes. A blood culture was negative. The patient was discharged home to complete a 10-day course of clindamycin and was given topical steroids for the eczema. He continued on oral prednisolone 1 mg/kg daily for 10 days, after which the dose was tapered down for a total 1-month course of systemic corticosteroids. At 1-month follow-up after completing the course of steroids, he was doing well with normal hepatic enzyme levels and no recurrence of fever, facial edema, or rash. He continues to be followed for management of the AD.
Drug reaction with eosinophilia and systemic symptoms syndrome is a serious systemic adverse drug reaction, with high morbidity and even mortality, estimated at 10% in the adult population, though more specific pediatric mortality data are not available.1,2 The exact pathogenesis of DRESS syndrome has not been elucidated. Certain human leukocyte antigen class I alleles are predisposed to the development of DRESS syndrome, but there has not been a human leukocyte antigen subtype identified with beta-lactam–associated DRESS syndrome. Some studies have demonstrated a reactivation of human herpesvirus 6, human herpesvirus 7, and Epstein-Barr virus.3 One study involving 40 patients with DRESS syndrome identified viremia in 76% (29/38) of patients and identified CD8+ T-cell populations directed toward viral epitopes.3 Finally, DRESS syndrome may be related to the slow detoxification and elimination of intermediary products of offending medications that serve as an immunogenic stimulus for the inflammatory cascade.2
In adults, DRESS syndrome was first identified in association with phenytoin, but more recently other drugs have been identified, including other aromatic anticonvulsants (ie, lamotrigine, phenobarbital, carbamazepine), allopurinol, sulfonamides, antiretrovirals (particularly abacavir), and minocycline.2 In a 3-year pediatric prospective study, 11 cases of DRESS syndrome were identified: 4 cases due to lamotrigine, and 3 caused by penicillins.4 The trigger in our patient’s case was the beta-lactam, third-generation cephalosporin cefdinir, and his symptoms developed within 6 days of starting the medication. Many articles report that beta-lactams are a rare cause of DRESS syndrome, with only a handful of cases reported.1,5,6
The diagnosis of DRESS syndrome often can be delayed, as children present acutely febrile and toxic appearing. Unlike many adverse drug reactions, DRESS syndrome does not show rapid resolution with withdrawal of the causative agent, further complicating the diagnosis. The typical onset of DRESS syndrome generally ranges from 2 to 6 weeks after the initiation of the offending drug; however, faster onset of symptoms, similar to our case, has been noted in antibiotic-triggered cases. In the prospective pediatric series by Sasidharanpillai et al,4 the average time to onset among 3 antibiotic-triggered DRESS cases was 5.8 days vs 23.9 days among the 4 cases of lamotrigine-associated DRESS syndrome.
Our patient demonstrated the classic features of DRESS syndrome, including fever, rash, lymphadenopathy, facial edema, peripheral eosinophilia, atypical lymphocytosis, and hepatitis. Based on the proposed RegiSCAR scoring system, our patient was classified as a “definite” case of DRESS syndrome.1,7 Other hematologic findings in DRESS syndrome may include thrombocytopenia and anemia. The liver is the most commonly affected internal organ in DRESS syndrome, with pneumonitis, carditis, and nephritis reported less frequently.1 The pattern of liver injury in our patient was mixed (hepatocellular and cholestatic), the second most common pattern in patients with DRESS syndrome (the cholestatic pattern is most common).8
The exanthem of DRESS syndrome can vary in morphology, with up to 7% of patients reported to have eczemalike lesions in the multinational prospective RegiSCAR study.1 Other entities in the differential diagnosis for our patient included Kawasaki disease, where conjunctivitis and strawberry tongue are classically present, as well as erythrodermic AD, where internal organ involvement is not common.2 Our patient’s exanthem initially was considered to be a flare of AD with superimposed bacterial infection and possible eczema herpeticum. Although bacterial cultures did grow Staphylococcus and Streptococcus, viral studies were all negative, and this alone would not have explained the facial edema, rapidly rising eosinophil count, and transaminitis. The dramatic drop in his eosinophil count and decrease in hepatic enzymes after 1 dose of intravenous methylprednisolone also supported the diagnosis of DRESS syndrome.
Treatment recommendations remain largely anecdotal. Early systemic steroids generally are accepted as the first line of therapy, with a slow taper. Although the average required duration of systemic steroids in 1 series of adults was reported at 50.1 days,9 the duration was shorter (21–35 days) in a series of pediatric patients.4 Our patient’s clinical symptoms and laboratory values normalized after completing a 1-month steroid taper. Other therapies have been tried for recalcitrant cases, including intravenous immunoglobulin, plasmapheresis, rituximab, and valganciclovir.2
Early clinical recognition of the signs and symptoms of DRESS syndrome in the setting of a new medication can decrease morbidity and mortality. Although DRESS syndrome in pediatric patients presents with many similar clinical features as in adults, it may be a greater diagnostic challenge. As in adult cases, timely administration of systemic corticosteroids and tapering based on clinical signs and symptoms can lead to resolution of the hypersensitivity syndrome.
- Kardaun SH, Sekula P, Valeyrie-Allanore L, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. results from the prospective RegiSCAR study. Br J Dermatol. 2013;169:1071-1080.
- Fernando SL. Drug-reaction eosinophilia and systemic symptoms and drug-induced hypersensitivity syndrome. Australas J Dermatol. 2014;55:15-23.
- Picard D, Janela B, Descamps V, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): a multiorgan antiviral T cell response. Sci Transl Med. 2010;2:46ra62.
- Sasidharanpillai S, Sabitha S, Riyaz N, et al. Drug reaction with eosinophilia and systemic symptoms in children: a prospective study. Pediatr Dermatol. 2016;33:E162-E165.
- Aouam K, Chaabane A, Toumi A, et al. Drug rash with eosinophilia and systemic symptoms (DRESS) probably induced by cefotaxime: a report of two cases. Clin Med Res. 2012;10:32-35.
- Guleria VS, Dhillon M, Gill S, et al. Ceftriaxone induced drug rash with eosinophilia and systemic symptoms. J Res Pharm Pract. 2014;3:72-74.
- Kardaun SH, Sidoroff A, Valeyrie-Allanore L, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2007;156:609-611.
- Lin IC, Yang HC, Strong C, et al. Liver injury in patients with DRESS: a clinical study of 72 cases. J Am Acad Dermatol. 2015;72:984-991.
- Ang CC, Wang YS, Yoosuff EL, et al. Retrospective analysis of drug-induced hypersensitivity syndrome: a study of 27 patients. J Am Acad Dermatol. 2010;63:219-227.
- Kardaun SH, Sekula P, Valeyrie-Allanore L, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. results from the prospective RegiSCAR study. Br J Dermatol. 2013;169:1071-1080.
- Fernando SL. Drug-reaction eosinophilia and systemic symptoms and drug-induced hypersensitivity syndrome. Australas J Dermatol. 2014;55:15-23.
- Picard D, Janela B, Descamps V, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): a multiorgan antiviral T cell response. Sci Transl Med. 2010;2:46ra62.
- Sasidharanpillai S, Sabitha S, Riyaz N, et al. Drug reaction with eosinophilia and systemic symptoms in children: a prospective study. Pediatr Dermatol. 2016;33:E162-E165.
- Aouam K, Chaabane A, Toumi A, et al. Drug rash with eosinophilia and systemic symptoms (DRESS) probably induced by cefotaxime: a report of two cases. Clin Med Res. 2012;10:32-35.
- Guleria VS, Dhillon M, Gill S, et al. Ceftriaxone induced drug rash with eosinophilia and systemic symptoms. J Res Pharm Pract. 2014;3:72-74.
- Kardaun SH, Sidoroff A, Valeyrie-Allanore L, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2007;156:609-611.
- Lin IC, Yang HC, Strong C, et al. Liver injury in patients with DRESS: a clinical study of 72 cases. J Am Acad Dermatol. 2015;72:984-991.
- Ang CC, Wang YS, Yoosuff EL, et al. Retrospective analysis of drug-induced hypersensitivity syndrome: a study of 27 patients. J Am Acad Dermatol. 2010;63:219-227.
Practice Points
- Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome shares many clinical features with viral exanthems and may be difficult to diagnose in the setting of atopic dermatitis in which children may have baseline eosinophilia from an atopic diathesis.
- Early clinical recognition of the signs and symptoms of DRESS syndrome in the setting of a new medication can decrease morbidity and mortality.
Ten changes that could keep clinicians in the workforce in a pandemic
Indeed, a recent poll of 1,000 health care workers conducted Sept. 2-8 by Morning Consult, showed that 18% of medical workers polled quit their jobs during the pandemic. Additionally, 31% said they had at least thought about leaving their work.
“As physicians, educators, peers and friends of COVID-19 responders, we are gravely concerned about our colleagues’ exhaustion, burnout, and disillusionment,” wrote lead author Eileen Barrett, MD, and coauthors of the new action plan, which was published in the Annals of Internal Medicine.
The 10-point, one-page checklist includes providing “practical support in the areas that clinicians identify as causing emotional stress or moral injury,” such as managing anger and grief when patients have chosen not to be vaccinated or confronting misinformation.
“Those are the things that are making people’s mental health worse” psychiatrist Jessi Gold, MD, MS, said in an interview. “I don’t think I’ve seen that mentioned other places.”
Among the other action items are:
- Reduce administrative tasks that are not “mission critical,” such as mandatory training that has no evidence of improving patient outcomes and meetings that could be skipped.
- Offer free and confidential resources to support clinicians’ mental health, such as easy access to crisis hotlines and peer support groups.
- Maintain transparency about personal protective equipment and contingency plans when there are shortages to restore trust.
- Encourage clinicians to use vacation time; leaders should model this.
- Implement suicide prevention strategies, including wellness check-ins for clinicians in hard-hit areas.
The action plan was based on the authors’ own experiences and the stories of colleagues and information in literature. It includes 10 changes health care leaders could make to help retain providers who may be on the brink of leaving their jobs or leaving medicine
Action items intended to be easily achievable, low cost
Dr. Barrett, who is a hospitalist in Albuquerque, said the goal was to present easily achievable and low-cost action items that clinicians and health care leaders could use as a starting point when change seems insurmountable and evidence on what works is slow to come.
She said one of the things that spurred her to coauthor the list was becoming aware of other clinicians’ “secret shame” in thinking about leaving medicine.
“Maybe a person who is not being listened to could take this journal article and say ‘we don’t know where to start. It looks like we can start here,’ ” said Dr. Barrett, who is also an associate professor in the division of hospital medicine, department of internal medicine, at the University of New Mexico, Albuquerque.
She noted that some of the good ideas floated around did not make the list, because they required daunting budget commitments and too much time to put into place.
Numerous other proposed solutions were of the wrong tone, according to Dr. Barrett.
“It’s not just about a hug or a piece of pizza,” she said.
Dr. Gold, who is an assistant professor at Washington University, St. Louis, and specializes in the mental health of health care workers, noted that, even though the list was pared to 10 action items, it is still hard for health care organizations to prioritize mental health.
“Many hospitals are still struggling with the active bleed of the pandemic and financially recovering,” she said. “If you’re dealing with a full ER and people are still dying of COVID and you don’t have the resources to support them, it’s really hard to then find magic money to deal with mental health. I’d love for that to be true.”
Every organization, however, can start with removing questions about mental and physical health diagnoses from credentialing and employment applications, which is one of the items on the list, she said.
“It’s the lowest-bar thing that you can fix for making people in crisis not fear getting help,” she said. That change must come on a state-by-state and individual hospital level.
Favorable reactions to list
Dr. Barrett, who also serves on the editorial advisory board of Internal Medicine News, said the reactions to the checklist have been “overwhelmingly favorable and appreciative.”
Eric J. Topol, MD, founder and director of the Scripps Research Translational Institute in La Jolla, Calif., and editor-in-chief of Medscape Medical News, tweeted about this list: “For COVID-19, more than ever before, it’s vital to keep clinicians in the U.S. health care workforce. These are 10 steps that will help.” The tweet was retweeted more than 100 times.
Lotte Dyrbye, MD, MHPE, a primary care physician and codirector of the program on physician well-being at the Mayo Clinic in Rochester, Minn., said in an interview that managing the anger around patients who choose to be unvaccinated is critical and something that has gotten little notice since the vaccines became available.
“Physicians and nurses are working extremely hard and seeing a lot of suffering and are taking care of patients very sick with COVID-19, knowing they had access to the vaccine. That is causing anger and frustration. We haven’t prepared health care workers to deal with that,” she said.
Outside expert: Not all items may be easy to implement
Dr. Dyrbye said that, though she found adding time to address COVID misinformation questions in appointments is very important, it may be wishful thinking.
The authors suggested training other members of the care team to answer those questions to free up time, but she said, for patients who have been swayed by misinformation, hearing information from someone other than the physician they have a relationship with won’t be convincing.
According to Dr. Dyrbye, the items on the list are not easy to implement, but the action plan is worthwhile to consider adopting as a multipronged approach.
“Most of these things are hard and we need to be in it for the long run,” she said.
The need is clear for efforts to address the mental health of not just experienced clinicians but those in training as well, she noted.
Related research
A study that was also recently published in the Annals of Internal Medicine suggested that making a few simple changes can help improve the mental health of residents. The research, which included nearly 17,000 first-year residents who started training between 2007 and 2019, addressed indicators of mental health in light of interventions such as limiting residents’ work hours and providing more services.
The investigators found that, though depression remains high among residents, depressive symptoms among first-year residents dropped 24.4% from 2007 to 2019 in parallel with four main factors: an increase in mental health services; restrictions on work hours for residents; more sleep hours; and higher-quality feedback from faculty.
Dr. Barrett said she hopes her colleagues and health care workers everywhere will find some solace in seeing that the new checklist she coauthored was published in a prominent journal.
The message Dr. Barrett said she hopes they see is: “Someone is validating it is not in their head. They are validating we can do better. They are validating that we must.”
Dr. Barrett and coauthors had no conflicts of interest. Dr. Gold and Dr. Dyrbye also disclosed having no relevant financial relationships.
Indeed, a recent poll of 1,000 health care workers conducted Sept. 2-8 by Morning Consult, showed that 18% of medical workers polled quit their jobs during the pandemic. Additionally, 31% said they had at least thought about leaving their work.
“As physicians, educators, peers and friends of COVID-19 responders, we are gravely concerned about our colleagues’ exhaustion, burnout, and disillusionment,” wrote lead author Eileen Barrett, MD, and coauthors of the new action plan, which was published in the Annals of Internal Medicine.
The 10-point, one-page checklist includes providing “practical support in the areas that clinicians identify as causing emotional stress or moral injury,” such as managing anger and grief when patients have chosen not to be vaccinated or confronting misinformation.
“Those are the things that are making people’s mental health worse” psychiatrist Jessi Gold, MD, MS, said in an interview. “I don’t think I’ve seen that mentioned other places.”
Among the other action items are:
- Reduce administrative tasks that are not “mission critical,” such as mandatory training that has no evidence of improving patient outcomes and meetings that could be skipped.
- Offer free and confidential resources to support clinicians’ mental health, such as easy access to crisis hotlines and peer support groups.
- Maintain transparency about personal protective equipment and contingency plans when there are shortages to restore trust.
- Encourage clinicians to use vacation time; leaders should model this.
- Implement suicide prevention strategies, including wellness check-ins for clinicians in hard-hit areas.
The action plan was based on the authors’ own experiences and the stories of colleagues and information in literature. It includes 10 changes health care leaders could make to help retain providers who may be on the brink of leaving their jobs or leaving medicine
Action items intended to be easily achievable, low cost
Dr. Barrett, who is a hospitalist in Albuquerque, said the goal was to present easily achievable and low-cost action items that clinicians and health care leaders could use as a starting point when change seems insurmountable and evidence on what works is slow to come.
She said one of the things that spurred her to coauthor the list was becoming aware of other clinicians’ “secret shame” in thinking about leaving medicine.
“Maybe a person who is not being listened to could take this journal article and say ‘we don’t know where to start. It looks like we can start here,’ ” said Dr. Barrett, who is also an associate professor in the division of hospital medicine, department of internal medicine, at the University of New Mexico, Albuquerque.
She noted that some of the good ideas floated around did not make the list, because they required daunting budget commitments and too much time to put into place.
Numerous other proposed solutions were of the wrong tone, according to Dr. Barrett.
“It’s not just about a hug or a piece of pizza,” she said.
Dr. Gold, who is an assistant professor at Washington University, St. Louis, and specializes in the mental health of health care workers, noted that, even though the list was pared to 10 action items, it is still hard for health care organizations to prioritize mental health.
“Many hospitals are still struggling with the active bleed of the pandemic and financially recovering,” she said. “If you’re dealing with a full ER and people are still dying of COVID and you don’t have the resources to support them, it’s really hard to then find magic money to deal with mental health. I’d love for that to be true.”
Every organization, however, can start with removing questions about mental and physical health diagnoses from credentialing and employment applications, which is one of the items on the list, she said.
“It’s the lowest-bar thing that you can fix for making people in crisis not fear getting help,” she said. That change must come on a state-by-state and individual hospital level.
Favorable reactions to list
Dr. Barrett, who also serves on the editorial advisory board of Internal Medicine News, said the reactions to the checklist have been “overwhelmingly favorable and appreciative.”
Eric J. Topol, MD, founder and director of the Scripps Research Translational Institute in La Jolla, Calif., and editor-in-chief of Medscape Medical News, tweeted about this list: “For COVID-19, more than ever before, it’s vital to keep clinicians in the U.S. health care workforce. These are 10 steps that will help.” The tweet was retweeted more than 100 times.
Lotte Dyrbye, MD, MHPE, a primary care physician and codirector of the program on physician well-being at the Mayo Clinic in Rochester, Minn., said in an interview that managing the anger around patients who choose to be unvaccinated is critical and something that has gotten little notice since the vaccines became available.
“Physicians and nurses are working extremely hard and seeing a lot of suffering and are taking care of patients very sick with COVID-19, knowing they had access to the vaccine. That is causing anger and frustration. We haven’t prepared health care workers to deal with that,” she said.
Outside expert: Not all items may be easy to implement
Dr. Dyrbye said that, though she found adding time to address COVID misinformation questions in appointments is very important, it may be wishful thinking.
The authors suggested training other members of the care team to answer those questions to free up time, but she said, for patients who have been swayed by misinformation, hearing information from someone other than the physician they have a relationship with won’t be convincing.
According to Dr. Dyrbye, the items on the list are not easy to implement, but the action plan is worthwhile to consider adopting as a multipronged approach.
“Most of these things are hard and we need to be in it for the long run,” she said.
The need is clear for efforts to address the mental health of not just experienced clinicians but those in training as well, she noted.
Related research
A study that was also recently published in the Annals of Internal Medicine suggested that making a few simple changes can help improve the mental health of residents. The research, which included nearly 17,000 first-year residents who started training between 2007 and 2019, addressed indicators of mental health in light of interventions such as limiting residents’ work hours and providing more services.
The investigators found that, though depression remains high among residents, depressive symptoms among first-year residents dropped 24.4% from 2007 to 2019 in parallel with four main factors: an increase in mental health services; restrictions on work hours for residents; more sleep hours; and higher-quality feedback from faculty.
Dr. Barrett said she hopes her colleagues and health care workers everywhere will find some solace in seeing that the new checklist she coauthored was published in a prominent journal.
The message Dr. Barrett said she hopes they see is: “Someone is validating it is not in their head. They are validating we can do better. They are validating that we must.”
Dr. Barrett and coauthors had no conflicts of interest. Dr. Gold and Dr. Dyrbye also disclosed having no relevant financial relationships.
Indeed, a recent poll of 1,000 health care workers conducted Sept. 2-8 by Morning Consult, showed that 18% of medical workers polled quit their jobs during the pandemic. Additionally, 31% said they had at least thought about leaving their work.
“As physicians, educators, peers and friends of COVID-19 responders, we are gravely concerned about our colleagues’ exhaustion, burnout, and disillusionment,” wrote lead author Eileen Barrett, MD, and coauthors of the new action plan, which was published in the Annals of Internal Medicine.
The 10-point, one-page checklist includes providing “practical support in the areas that clinicians identify as causing emotional stress or moral injury,” such as managing anger and grief when patients have chosen not to be vaccinated or confronting misinformation.
“Those are the things that are making people’s mental health worse” psychiatrist Jessi Gold, MD, MS, said in an interview. “I don’t think I’ve seen that mentioned other places.”
Among the other action items are:
- Reduce administrative tasks that are not “mission critical,” such as mandatory training that has no evidence of improving patient outcomes and meetings that could be skipped.
- Offer free and confidential resources to support clinicians’ mental health, such as easy access to crisis hotlines and peer support groups.
- Maintain transparency about personal protective equipment and contingency plans when there are shortages to restore trust.
- Encourage clinicians to use vacation time; leaders should model this.
- Implement suicide prevention strategies, including wellness check-ins for clinicians in hard-hit areas.
The action plan was based on the authors’ own experiences and the stories of colleagues and information in literature. It includes 10 changes health care leaders could make to help retain providers who may be on the brink of leaving their jobs or leaving medicine
Action items intended to be easily achievable, low cost
Dr. Barrett, who is a hospitalist in Albuquerque, said the goal was to present easily achievable and low-cost action items that clinicians and health care leaders could use as a starting point when change seems insurmountable and evidence on what works is slow to come.
She said one of the things that spurred her to coauthor the list was becoming aware of other clinicians’ “secret shame” in thinking about leaving medicine.
“Maybe a person who is not being listened to could take this journal article and say ‘we don’t know where to start. It looks like we can start here,’ ” said Dr. Barrett, who is also an associate professor in the division of hospital medicine, department of internal medicine, at the University of New Mexico, Albuquerque.
She noted that some of the good ideas floated around did not make the list, because they required daunting budget commitments and too much time to put into place.
Numerous other proposed solutions were of the wrong tone, according to Dr. Barrett.
“It’s not just about a hug or a piece of pizza,” she said.
Dr. Gold, who is an assistant professor at Washington University, St. Louis, and specializes in the mental health of health care workers, noted that, even though the list was pared to 10 action items, it is still hard for health care organizations to prioritize mental health.
“Many hospitals are still struggling with the active bleed of the pandemic and financially recovering,” she said. “If you’re dealing with a full ER and people are still dying of COVID and you don’t have the resources to support them, it’s really hard to then find magic money to deal with mental health. I’d love for that to be true.”
Every organization, however, can start with removing questions about mental and physical health diagnoses from credentialing and employment applications, which is one of the items on the list, she said.
“It’s the lowest-bar thing that you can fix for making people in crisis not fear getting help,” she said. That change must come on a state-by-state and individual hospital level.
Favorable reactions to list
Dr. Barrett, who also serves on the editorial advisory board of Internal Medicine News, said the reactions to the checklist have been “overwhelmingly favorable and appreciative.”
Eric J. Topol, MD, founder and director of the Scripps Research Translational Institute in La Jolla, Calif., and editor-in-chief of Medscape Medical News, tweeted about this list: “For COVID-19, more than ever before, it’s vital to keep clinicians in the U.S. health care workforce. These are 10 steps that will help.” The tweet was retweeted more than 100 times.
Lotte Dyrbye, MD, MHPE, a primary care physician and codirector of the program on physician well-being at the Mayo Clinic in Rochester, Minn., said in an interview that managing the anger around patients who choose to be unvaccinated is critical and something that has gotten little notice since the vaccines became available.
“Physicians and nurses are working extremely hard and seeing a lot of suffering and are taking care of patients very sick with COVID-19, knowing they had access to the vaccine. That is causing anger and frustration. We haven’t prepared health care workers to deal with that,” she said.
Outside expert: Not all items may be easy to implement
Dr. Dyrbye said that, though she found adding time to address COVID misinformation questions in appointments is very important, it may be wishful thinking.
The authors suggested training other members of the care team to answer those questions to free up time, but she said, for patients who have been swayed by misinformation, hearing information from someone other than the physician they have a relationship with won’t be convincing.
According to Dr. Dyrbye, the items on the list are not easy to implement, but the action plan is worthwhile to consider adopting as a multipronged approach.
“Most of these things are hard and we need to be in it for the long run,” she said.
The need is clear for efforts to address the mental health of not just experienced clinicians but those in training as well, she noted.
Related research
A study that was also recently published in the Annals of Internal Medicine suggested that making a few simple changes can help improve the mental health of residents. The research, which included nearly 17,000 first-year residents who started training between 2007 and 2019, addressed indicators of mental health in light of interventions such as limiting residents’ work hours and providing more services.
The investigators found that, though depression remains high among residents, depressive symptoms among first-year residents dropped 24.4% from 2007 to 2019 in parallel with four main factors: an increase in mental health services; restrictions on work hours for residents; more sleep hours; and higher-quality feedback from faculty.
Dr. Barrett said she hopes her colleagues and health care workers everywhere will find some solace in seeing that the new checklist she coauthored was published in a prominent journal.
The message Dr. Barrett said she hopes they see is: “Someone is validating it is not in their head. They are validating we can do better. They are validating that we must.”
Dr. Barrett and coauthors had no conflicts of interest. Dr. Gold and Dr. Dyrbye also disclosed having no relevant financial relationships.
FROM ANNALS OF INTERNAL MEDICINE
Genomic screening of healthy newborns gets more popular
Even before their baby is born, parents face some tough questions: Home birth or hospital? Cloth or disposable diapers? Breast, bottle, or both? But advances in genetic sequencing technology mean that parents will soon face yet another choice: whether to sequence their newborn’s DNA for an overview of the baby’s entire genome.
Genetic testing has been used for decades to diagnose conditions even before birth. But DNA sequencing technologies, once expensive and tough to access, are now rapid and cheap enough that doctors could order genomic screening for any infant, regardless of health status.
The possibility has raised many questions about the ethical, legal, and social repercussions of doing so. One of the biggest sticking points of sequencing newborns is the potential psychosocial fallout for families of such wide-scale use of genetic screening.
“There’s a narrative of catastrophic distress,” says Robert Green, MD, a geneticist at Harvard Medical School and lead investigator on the BabySeq study, which is evaluating the medical, social, and economic consequences of newborn genetic screening. The concern is that parents learning that their child carries a gene variant related to cancer or heart disease will become “incredibly anxious and distressed,” he says. “And it’s not an unreasonable speculation.”
But Dr. Green’s team found no evidence of such anxiety in the results from a randomized trial it conducted, published in JAMA Pediatrics. In the meantime, Genomics England announced it would begin a pilot study involving whole-genome sequencing of up to 200,000 babies. The first goal is to identify severe disease that starts in childhood, but the information would also be stored and used to detect drug sensitivities and conditions that come up later in life.
The large U.K. project is a bold move, according to David Amor, PhD, a pediatric geneticist at Murdoch Children’s Research Institute in Australia, who says its time has come. Geneticists have been accused of thinking their field involves unique pitfalls, compared with the rest of medicine, he points out, and that doctors need to protect patients and families from the potential harm genetic testing poses.
“But it is becoming apparent that that’s not really the case,” he says, and “maybe there’s not a whole lot special about genetics – it’s just medicine.”
When a first-draft copy of the human genome was published in 2001, scientists and doctors hailed the start of a new era of precision medicine. Knowing our genome sequence was expected to lead to a better grasp on our individual disease risks. Yet even as technologies advanced, clinical genetics remained focused on diagnosis rather than screening, according to Lilian Downie, a clinical genetics PhD candidate at the University of Melbourne. She calls the difference subtle but important.
Diagnostic genetic testing confirms whether a person has a specific condition, whereas genetic screening tests evaluate someone’s risk of getting an illness. Both approaches use sequencing, but they answer different questions, explains Ms. Downie.
Diagnosing disease versus predicting future illness
Genetic testing is on the upswing for both purposes, whether clinically for diagnosis or through direct-to-consumer screening-oriented services like 23andMe. Scientists began to note that many people carried disease-related genetic variants without having signs of disease. In some cases, a variant that is mathematically linked to a disease simply doesn’t cause it. In other cases, though, even if the gene variant contributes to a disease, not everyone who carries the genetic change will get the condition.
This potential disconnect between having a variant and developing the condition is a big problem, says Katie Stoll, a genetic counselor and executive director of the Genetic Support Foundation in Olympia, WA.
“It’s more complicated than just looking at one gene variant and one outcome,” she says. Without a sure link between the two, this information could unnecessarily entail “some pretty big emotional and financial costs.”
Ms. Stoll and others in the genetics field who share similar concerns are one reason the BabySeq project was first funded back in 2015. Although the overall aim of the initiative is to answer questions about the value of genomic sequencing in newborn screening, the media and scientific attention has focused on the psychosocial impact of healthy newborn sequencing, says Dr. Green. In the study published in JAMA Pediatrics, his group focused on these issues, too.
For that randomized trial, they enrolled 325 families, 257 with healthy babies and 68 whose babies had spent time in neonatal intensive care. Enrolled infants were randomly given standard care alone or standard care with genomic sequencing added on. The genomic sequencing report contained information about the presence of genetic variants associated with disease that start in childhood. Parents also could choose whether to learn about genetic risks for conditions that start in adulthood, such as cancer.
Boston-based Tina Moniz was one of those parents. When her first daughter was born in Jan. 2016, someone from the BabySeq study asked her and her husband if they would like to take part. The decision was simple for the couple.
“I didn’t hesitate,” she says. “To me, knowledge is power.”
Using screening tools for parental and marital distress and parent-child bonding, the research evaluated BabySeq families at 3 and 10 months after parents received the sequencing results. The investigators found no significant differences in any of these measures between screened and unscreened families. Ms. Moniz learned that her daughter’s only concerning result was being a carrier for cystic fibrosis. Rather than finding this information anxiety-provoking, Ms. Moniz considered it to be reassuring.
“My mom brain worries about so many things, but at least I know I don’t have to add genetic disease to the list,” she says.
But Ms. Stoll, who wasn’t involved in the BabySeq study, isn’t as convinced. She says that less than 10% of the families approached about the trial ultimately agreed to take part, suggesting potential bias in the selection process. Most participants were white, well-educated, and well-off, making it hard to generalize the study’s results.
What’s more, the standard care involved meeting with a genetic counselor and giving a detailed family history, neither of which is routinely offered to new parents, Ms. Stoll says. These study features leave her unconvinced that healthy newborn genetic screening is beneficial.
“We can’t assume these psychosocial consequences will be true for everyone,” she says.
Follow-up and treatment needed
Traditional newborn screening relies on blood biochemical tests to detect and diagnose metabolic diseases. This approach still outperforms DNA sequencing in trials, says Cynthia Powell, MD, a pediatric geneticist at the University of North Carolina at Chapel Hill, who wasn’t involved with the BabySeq study. Despite the enthusiasm for genomics, this kind of screening won’t replace newborn biochemical screening anytime soon, she says.
“There are some states that have only one geneticist available, so should we really be doing this if we can’t provide the necessary follow-up and treatment for these babies?” she asks.
Still, Dr. Powell says, the BabySeq study helps advance understanding of what the infrastructure needs are for widespread use of DNA sequencing in newborns. She says those needs include appropriate consent processes, access to genetic counselors to discuss testing, and referrals for further testing and treatment in those babies with concerning results.
The BabySeq program will also guide new initiatives, like the pilot program that Genomics England launched in Sept. 2021. As part of that project, the U.K. group intends to look into how practical whole-genome sequencing for newborn screening would be and look at the risks, benefits, and limits of its widespread use.
“For the first time, we’re putting real data into these questions that people have basically just speculated and hypothesized and created narratives about,” Dr. Green says.
But for now, the findings on the psychosocial effects of general newborn genomic screening show that “we should consider genetics to be just one more arrow in our medical quiver.”
A version of this article first appeared on WebMD.com.
Even before their baby is born, parents face some tough questions: Home birth or hospital? Cloth or disposable diapers? Breast, bottle, or both? But advances in genetic sequencing technology mean that parents will soon face yet another choice: whether to sequence their newborn’s DNA for an overview of the baby’s entire genome.
Genetic testing has been used for decades to diagnose conditions even before birth. But DNA sequencing technologies, once expensive and tough to access, are now rapid and cheap enough that doctors could order genomic screening for any infant, regardless of health status.
The possibility has raised many questions about the ethical, legal, and social repercussions of doing so. One of the biggest sticking points of sequencing newborns is the potential psychosocial fallout for families of such wide-scale use of genetic screening.
“There’s a narrative of catastrophic distress,” says Robert Green, MD, a geneticist at Harvard Medical School and lead investigator on the BabySeq study, which is evaluating the medical, social, and economic consequences of newborn genetic screening. The concern is that parents learning that their child carries a gene variant related to cancer or heart disease will become “incredibly anxious and distressed,” he says. “And it’s not an unreasonable speculation.”
But Dr. Green’s team found no evidence of such anxiety in the results from a randomized trial it conducted, published in JAMA Pediatrics. In the meantime, Genomics England announced it would begin a pilot study involving whole-genome sequencing of up to 200,000 babies. The first goal is to identify severe disease that starts in childhood, but the information would also be stored and used to detect drug sensitivities and conditions that come up later in life.
The large U.K. project is a bold move, according to David Amor, PhD, a pediatric geneticist at Murdoch Children’s Research Institute in Australia, who says its time has come. Geneticists have been accused of thinking their field involves unique pitfalls, compared with the rest of medicine, he points out, and that doctors need to protect patients and families from the potential harm genetic testing poses.
“But it is becoming apparent that that’s not really the case,” he says, and “maybe there’s not a whole lot special about genetics – it’s just medicine.”
When a first-draft copy of the human genome was published in 2001, scientists and doctors hailed the start of a new era of precision medicine. Knowing our genome sequence was expected to lead to a better grasp on our individual disease risks. Yet even as technologies advanced, clinical genetics remained focused on diagnosis rather than screening, according to Lilian Downie, a clinical genetics PhD candidate at the University of Melbourne. She calls the difference subtle but important.
Diagnostic genetic testing confirms whether a person has a specific condition, whereas genetic screening tests evaluate someone’s risk of getting an illness. Both approaches use sequencing, but they answer different questions, explains Ms. Downie.
Diagnosing disease versus predicting future illness
Genetic testing is on the upswing for both purposes, whether clinically for diagnosis or through direct-to-consumer screening-oriented services like 23andMe. Scientists began to note that many people carried disease-related genetic variants without having signs of disease. In some cases, a variant that is mathematically linked to a disease simply doesn’t cause it. In other cases, though, even if the gene variant contributes to a disease, not everyone who carries the genetic change will get the condition.
This potential disconnect between having a variant and developing the condition is a big problem, says Katie Stoll, a genetic counselor and executive director of the Genetic Support Foundation in Olympia, WA.
“It’s more complicated than just looking at one gene variant and one outcome,” she says. Without a sure link between the two, this information could unnecessarily entail “some pretty big emotional and financial costs.”
Ms. Stoll and others in the genetics field who share similar concerns are one reason the BabySeq project was first funded back in 2015. Although the overall aim of the initiative is to answer questions about the value of genomic sequencing in newborn screening, the media and scientific attention has focused on the psychosocial impact of healthy newborn sequencing, says Dr. Green. In the study published in JAMA Pediatrics, his group focused on these issues, too.
For that randomized trial, they enrolled 325 families, 257 with healthy babies and 68 whose babies had spent time in neonatal intensive care. Enrolled infants were randomly given standard care alone or standard care with genomic sequencing added on. The genomic sequencing report contained information about the presence of genetic variants associated with disease that start in childhood. Parents also could choose whether to learn about genetic risks for conditions that start in adulthood, such as cancer.
Boston-based Tina Moniz was one of those parents. When her first daughter was born in Jan. 2016, someone from the BabySeq study asked her and her husband if they would like to take part. The decision was simple for the couple.
“I didn’t hesitate,” she says. “To me, knowledge is power.”
Using screening tools for parental and marital distress and parent-child bonding, the research evaluated BabySeq families at 3 and 10 months after parents received the sequencing results. The investigators found no significant differences in any of these measures between screened and unscreened families. Ms. Moniz learned that her daughter’s only concerning result was being a carrier for cystic fibrosis. Rather than finding this information anxiety-provoking, Ms. Moniz considered it to be reassuring.
“My mom brain worries about so many things, but at least I know I don’t have to add genetic disease to the list,” she says.
But Ms. Stoll, who wasn’t involved in the BabySeq study, isn’t as convinced. She says that less than 10% of the families approached about the trial ultimately agreed to take part, suggesting potential bias in the selection process. Most participants were white, well-educated, and well-off, making it hard to generalize the study’s results.
What’s more, the standard care involved meeting with a genetic counselor and giving a detailed family history, neither of which is routinely offered to new parents, Ms. Stoll says. These study features leave her unconvinced that healthy newborn genetic screening is beneficial.
“We can’t assume these psychosocial consequences will be true for everyone,” she says.
Follow-up and treatment needed
Traditional newborn screening relies on blood biochemical tests to detect and diagnose metabolic diseases. This approach still outperforms DNA sequencing in trials, says Cynthia Powell, MD, a pediatric geneticist at the University of North Carolina at Chapel Hill, who wasn’t involved with the BabySeq study. Despite the enthusiasm for genomics, this kind of screening won’t replace newborn biochemical screening anytime soon, she says.
“There are some states that have only one geneticist available, so should we really be doing this if we can’t provide the necessary follow-up and treatment for these babies?” she asks.
Still, Dr. Powell says, the BabySeq study helps advance understanding of what the infrastructure needs are for widespread use of DNA sequencing in newborns. She says those needs include appropriate consent processes, access to genetic counselors to discuss testing, and referrals for further testing and treatment in those babies with concerning results.
The BabySeq program will also guide new initiatives, like the pilot program that Genomics England launched in Sept. 2021. As part of that project, the U.K. group intends to look into how practical whole-genome sequencing for newborn screening would be and look at the risks, benefits, and limits of its widespread use.
“For the first time, we’re putting real data into these questions that people have basically just speculated and hypothesized and created narratives about,” Dr. Green says.
But for now, the findings on the psychosocial effects of general newborn genomic screening show that “we should consider genetics to be just one more arrow in our medical quiver.”
A version of this article first appeared on WebMD.com.
Even before their baby is born, parents face some tough questions: Home birth or hospital? Cloth or disposable diapers? Breast, bottle, or both? But advances in genetic sequencing technology mean that parents will soon face yet another choice: whether to sequence their newborn’s DNA for an overview of the baby’s entire genome.
Genetic testing has been used for decades to diagnose conditions even before birth. But DNA sequencing technologies, once expensive and tough to access, are now rapid and cheap enough that doctors could order genomic screening for any infant, regardless of health status.
The possibility has raised many questions about the ethical, legal, and social repercussions of doing so. One of the biggest sticking points of sequencing newborns is the potential psychosocial fallout for families of such wide-scale use of genetic screening.
“There’s a narrative of catastrophic distress,” says Robert Green, MD, a geneticist at Harvard Medical School and lead investigator on the BabySeq study, which is evaluating the medical, social, and economic consequences of newborn genetic screening. The concern is that parents learning that their child carries a gene variant related to cancer or heart disease will become “incredibly anxious and distressed,” he says. “And it’s not an unreasonable speculation.”
But Dr. Green’s team found no evidence of such anxiety in the results from a randomized trial it conducted, published in JAMA Pediatrics. In the meantime, Genomics England announced it would begin a pilot study involving whole-genome sequencing of up to 200,000 babies. The first goal is to identify severe disease that starts in childhood, but the information would also be stored and used to detect drug sensitivities and conditions that come up later in life.
The large U.K. project is a bold move, according to David Amor, PhD, a pediatric geneticist at Murdoch Children’s Research Institute in Australia, who says its time has come. Geneticists have been accused of thinking their field involves unique pitfalls, compared with the rest of medicine, he points out, and that doctors need to protect patients and families from the potential harm genetic testing poses.
“But it is becoming apparent that that’s not really the case,” he says, and “maybe there’s not a whole lot special about genetics – it’s just medicine.”
When a first-draft copy of the human genome was published in 2001, scientists and doctors hailed the start of a new era of precision medicine. Knowing our genome sequence was expected to lead to a better grasp on our individual disease risks. Yet even as technologies advanced, clinical genetics remained focused on diagnosis rather than screening, according to Lilian Downie, a clinical genetics PhD candidate at the University of Melbourne. She calls the difference subtle but important.
Diagnostic genetic testing confirms whether a person has a specific condition, whereas genetic screening tests evaluate someone’s risk of getting an illness. Both approaches use sequencing, but they answer different questions, explains Ms. Downie.
Diagnosing disease versus predicting future illness
Genetic testing is on the upswing for both purposes, whether clinically for diagnosis or through direct-to-consumer screening-oriented services like 23andMe. Scientists began to note that many people carried disease-related genetic variants without having signs of disease. In some cases, a variant that is mathematically linked to a disease simply doesn’t cause it. In other cases, though, even if the gene variant contributes to a disease, not everyone who carries the genetic change will get the condition.
This potential disconnect between having a variant and developing the condition is a big problem, says Katie Stoll, a genetic counselor and executive director of the Genetic Support Foundation in Olympia, WA.
“It’s more complicated than just looking at one gene variant and one outcome,” she says. Without a sure link between the two, this information could unnecessarily entail “some pretty big emotional and financial costs.”
Ms. Stoll and others in the genetics field who share similar concerns are one reason the BabySeq project was first funded back in 2015. Although the overall aim of the initiative is to answer questions about the value of genomic sequencing in newborn screening, the media and scientific attention has focused on the psychosocial impact of healthy newborn sequencing, says Dr. Green. In the study published in JAMA Pediatrics, his group focused on these issues, too.
For that randomized trial, they enrolled 325 families, 257 with healthy babies and 68 whose babies had spent time in neonatal intensive care. Enrolled infants were randomly given standard care alone or standard care with genomic sequencing added on. The genomic sequencing report contained information about the presence of genetic variants associated with disease that start in childhood. Parents also could choose whether to learn about genetic risks for conditions that start in adulthood, such as cancer.
Boston-based Tina Moniz was one of those parents. When her first daughter was born in Jan. 2016, someone from the BabySeq study asked her and her husband if they would like to take part. The decision was simple for the couple.
“I didn’t hesitate,” she says. “To me, knowledge is power.”
Using screening tools for parental and marital distress and parent-child bonding, the research evaluated BabySeq families at 3 and 10 months after parents received the sequencing results. The investigators found no significant differences in any of these measures between screened and unscreened families. Ms. Moniz learned that her daughter’s only concerning result was being a carrier for cystic fibrosis. Rather than finding this information anxiety-provoking, Ms. Moniz considered it to be reassuring.
“My mom brain worries about so many things, but at least I know I don’t have to add genetic disease to the list,” she says.
But Ms. Stoll, who wasn’t involved in the BabySeq study, isn’t as convinced. She says that less than 10% of the families approached about the trial ultimately agreed to take part, suggesting potential bias in the selection process. Most participants were white, well-educated, and well-off, making it hard to generalize the study’s results.
What’s more, the standard care involved meeting with a genetic counselor and giving a detailed family history, neither of which is routinely offered to new parents, Ms. Stoll says. These study features leave her unconvinced that healthy newborn genetic screening is beneficial.
“We can’t assume these psychosocial consequences will be true for everyone,” she says.
Follow-up and treatment needed
Traditional newborn screening relies on blood biochemical tests to detect and diagnose metabolic diseases. This approach still outperforms DNA sequencing in trials, says Cynthia Powell, MD, a pediatric geneticist at the University of North Carolina at Chapel Hill, who wasn’t involved with the BabySeq study. Despite the enthusiasm for genomics, this kind of screening won’t replace newborn biochemical screening anytime soon, she says.
“There are some states that have only one geneticist available, so should we really be doing this if we can’t provide the necessary follow-up and treatment for these babies?” she asks.
Still, Dr. Powell says, the BabySeq study helps advance understanding of what the infrastructure needs are for widespread use of DNA sequencing in newborns. She says those needs include appropriate consent processes, access to genetic counselors to discuss testing, and referrals for further testing and treatment in those babies with concerning results.
The BabySeq program will also guide new initiatives, like the pilot program that Genomics England launched in Sept. 2021. As part of that project, the U.K. group intends to look into how practical whole-genome sequencing for newborn screening would be and look at the risks, benefits, and limits of its widespread use.
“For the first time, we’re putting real data into these questions that people have basically just speculated and hypothesized and created narratives about,” Dr. Green says.
But for now, the findings on the psychosocial effects of general newborn genomic screening show that “we should consider genetics to be just one more arrow in our medical quiver.”
A version of this article first appeared on WebMD.com.
Second U.S. COVID-19 case caused by Omicron found
A second U.S. case of COVID-19 caused by the Omicron variant has been picked up by genetic testing in Minnesota.
The man, from Hennepin County, Minn., fell ill on Nov. 22 after attending the Anime NYC 2021 conference at the Javits Center in New York City a few days before. He sought testing on Nov. 24. His symptoms have resolved, according to a press release on the case from the Minnesota Department of Health. The man was fully vaccinated, the department said.
He was advised to isolate from others, but it’s unclear if he had contact with anyone else before he learning he was infected.
“This news is concerning, but it is not a surprise,” said Governor Tim Walz in a news release. “We know that this virus is highly infectious and moves quickly throughout the world. Minnesotans know what to do to keep each other safe now — get the vaccine, get tested, wear a mask indoors, and get a booster. Together, we can fight this virus and help keep Minnesotans safe,”
The first case of COVID-19 caused by Omicron was detected Dec. 1 in California. That case was in a traveler who had recently returned from South Africa.
This breaking news story will be updated.
A version of this article first appeared on WebMD.com.
A second U.S. case of COVID-19 caused by the Omicron variant has been picked up by genetic testing in Minnesota.
The man, from Hennepin County, Minn., fell ill on Nov. 22 after attending the Anime NYC 2021 conference at the Javits Center in New York City a few days before. He sought testing on Nov. 24. His symptoms have resolved, according to a press release on the case from the Minnesota Department of Health. The man was fully vaccinated, the department said.
He was advised to isolate from others, but it’s unclear if he had contact with anyone else before he learning he was infected.
“This news is concerning, but it is not a surprise,” said Governor Tim Walz in a news release. “We know that this virus is highly infectious and moves quickly throughout the world. Minnesotans know what to do to keep each other safe now — get the vaccine, get tested, wear a mask indoors, and get a booster. Together, we can fight this virus and help keep Minnesotans safe,”
The first case of COVID-19 caused by Omicron was detected Dec. 1 in California. That case was in a traveler who had recently returned from South Africa.
This breaking news story will be updated.
A version of this article first appeared on WebMD.com.
A second U.S. case of COVID-19 caused by the Omicron variant has been picked up by genetic testing in Minnesota.
The man, from Hennepin County, Minn., fell ill on Nov. 22 after attending the Anime NYC 2021 conference at the Javits Center in New York City a few days before. He sought testing on Nov. 24. His symptoms have resolved, according to a press release on the case from the Minnesota Department of Health. The man was fully vaccinated, the department said.
He was advised to isolate from others, but it’s unclear if he had contact with anyone else before he learning he was infected.
“This news is concerning, but it is not a surprise,” said Governor Tim Walz in a news release. “We know that this virus is highly infectious and moves quickly throughout the world. Minnesotans know what to do to keep each other safe now — get the vaccine, get tested, wear a mask indoors, and get a booster. Together, we can fight this virus and help keep Minnesotans safe,”
The first case of COVID-19 caused by Omicron was detected Dec. 1 in California. That case was in a traveler who had recently returned from South Africa.
This breaking news story will be updated.
A version of this article first appeared on WebMD.com.
Expert shares top five atopic dermatitis–related questions he fields
Will my child outgrow the eczema?
That is perhaps the No. 1 atopic dermatitis–related question that Lawrence F. Eichenfield, MD, fields from parents in his role as chief of pediatric and adolescent dermatology at Rady’s Children’s Hospital, San Diego.
The answer “is pretty tricky,” he said during MedscapeLive’s annual Las Vegas Dermatology Seminar. “We used to say, ‘yeah, your kid will probably outgrow the disease,’ but we now have good data that show there are variable courses.”
Using data from the birth study cohort known as the Avon Longitudinal Study of Parents and Children, researchers in the United Kingdom investigated the existence of different longitudinal phenotypes of AD among 9,894 children. They found that 58% of the children in the cohort were unaffected or had transient AD, while 12.9% had early-onset/early-resolving AD. The remaining AD phenotypes consisted of 7%-8% patients each (early-onset persistent, early-onset late-resolving, mid-onset resolving, and late-onset resolving).
“There have been several studies that looked at the natural course of AD,” said Dr. Eichenfield, distinguished professor of dermatology and pediatrics at the University of California, San Diego. “A cohort study from Thailand showed that 50% of patients with childhood AD lost their AD diagnosis about 5 years into it, while there was an increase in allergic rhino-conjunctivitis and asthma, similar to what’s been seen in atopic march studies,” he noted.
A separate group of investigators analyzed records from The Health Improvement Network in the UK to determine the prevalence of AD among more than 8 million patients seen in primary care between 1994 and 2013. They found that the cumulative lifetime prevalence of atopic eczema was 9.9% and the highest rates of active disease were among children and older adults. “The takeaway was markedly inconsistent in terms of whether AD went away over time or increased over time, so it’s really not especially helpful prevalence data,” Dr. Eichenfield said. “Overall, you have a high prevalence in the first years of life, it decreases, and it may increase again when people are 60 years and older. Whether that’s truly AD or xerotic eczema isn’t known in this data set.”
A separate meta-analysis of 17 studies reported that 26% of adults with AD said they had adult-onset disease, which is characterized by more atopy, more foot dermatitis, and less flexural involvement.
Dr. Eichenfield tells parents, “there’s a really good chance (depending on disease severity) that 60% to 70% of children will outgrow their eczema or most of it,” he said. “If you ask me when, I won’t tell you. The important thing is to treat it to minimize its impact. We want minimal rash, minimal itch, and minimal sleep disturbance. Sometimes I say, ‘that might improve the chance of the eczema getting better over time.’ ”
Following are four other common questions parents and patients ask him:
Can we figure out the allergies causing the eczema? “This is probably one of the most unnerving questions I get asked,” he said. “It’s a loaded question. My answer is that allergies are intertwined with AD. Searching for the secret allergy causing the atopic dermatitis is rarely successful.” Sensitization is much more common with AD, he added, meaning specific IgE testing, whether it be blood testing or skin prick testing. “The more severe your eczema is, the more chance you’ll have of real food allergy,” he said. “About 15% of milder eczema patients will have at least one food allergy, but when you get to the more moderate to severe cases, about 40% will have a true food allergy.”
Food reactions may not cause eczema, though. Food reactions can cause urticaria, angioedema, eczematous dermatitis, allergic contact dermatitis, contact urticaria, and respiratory findings. According to National Institutes of Health guidelines for food allergy, skin prick tests and serum IgE tests are recommended to assist in identification of foods that may be provoking IgE-mediated food reactions, but are not diagnostic of food allergy.
“There’s a huge literature showing that there’s a lot of food allergy testing that’s just not helpful,” he said. In one study, 89% of food challenges administered in patients who were listed as being allergic based on skin prick tests or serum IgE tests did not have a true food allergy.
“Empiric elimination diets aren’t especially useful. However, we occasionally see children who do have AD exacerbated by food allergies in the first year of life,” he said. NIH guidelines suggest that children younger than 5 years of age with moderate to severe AD be considered for food allergy evaluation for milk, egg, peanut, wheat, and soy, if at least one of the following conditions is met: the child has persistent AD in spite of optimized management and topical therapy, and/or the child has a reliable history of an immediate reaction after ingestion of a specific food.
“We do know that there are high rates of comorbid allergic processes, besides food allergy, associated with atopic dermatitis, including allergic rhinitis and asthma both in children and adults,” Dr. Eichenfield said. “I do discuss allergy triggers and their importance in the life of the individual, though not necessarily as factors in AD. There are a variety of environmental allergens and/or environmental triggers that can significantly impact AD. Recently, we have seen studies discussing air pollution and wildfires as exacerbators of AD.”
How should I bathe and moisturize? There are no standard guidelines for the frequency, type, or duration of bathing in patients with AD, he said, though in more severe disease, frequent bathing can be helpful along with standard anti-inflammatory topical medicines. “I keep my general recommendations vague,” Dr. Eichenfield said. “I do explain that we don’t want to use harsh soaps; we want to be gentle in our washing. I usually recommend daily to every other day bathing. It’s important to pat the skin dry and then apply a moisturizer. Applying a moisturizer 2-3 minutes after bathing is important and limited significant cleanser use can be helpful.”
Moisturizers and emollients are a standard of care in U.S. guidelines published in 2013 and 2014, and international guidelines, and are steroid-sparing and useful for both prevention and maintenance. “I tell parents and patients that there is no reason to avoid bathing because of AD as long as you moisturize after,” he said.
Do I have to use topical [name of drug]? “I try to explain that there is skin barrier dysfunction that stimulates the inflammatory milieu, and that inflammation in the skin or blood in AD negatively impacts skin barrier function,” Dr. Eichenfield said. “I explain that if inflammation doesn’t get better with good skin care, moisturizers, and avoidance of triggers, we need anti-inflammatory medication. Then we discuss what the options are, the significant variation in strengths of topical corticosteroids, and topical nonsteroid options.”
When he counsels parents and patients on the use of topical corticosteroids, he tells them that cortisone is a naturally-occurring metabolite, and that “we can work together to let you know how much medicine to use, and how a safe amount is a powerful tool to fix the eczema.” He often says that topical steroids “are like hammers. We have tiny hammers, like over-the-counter hydrocortisone, and sledgehammers like clobetasol. We also have ‘screwdrivers’ and ‘pliers’ with nonsteroidal topical calcineurin and PDE-4 inhibitors, which are especially useful for maintenance therapy. Topical ruxolitinib is a new medicine that we may use for patients as well. The label includes discussion of side effects from oral JAK inhibitors as well as from the drug development program, so it takes some time to talk through.”
Is it time for a stronger systemic medicine? Any conversation about this topic should support the concept that the AD is multifactorial. “We have the rash of eczema,” he said. “We have the itch. We have impact on sleep disturbance. We have the comorbidities. We have other physical changes, which can happen with bacterial infections and other immune system or cardiovascular changes. We have the impact on quality of life and impact on school and work. When we recognize that if patients have significant enough disease that it is not getting better with topicals and is having a negative impact on their lives, we can move our discussion to systemic therapy.”
When counseling patients about systemic therapy, Dr. Eichenfield will conduct a body surface area assessment and document how bad the itch is. “But I’m not just recording the information; I’m bringing it out in the room,” he said. “I’ll do a BSA assessment and say, for example, ‘oh, you have 32% of your body involved with eczema.’ I ask about sleep disturbance, to get the answer ‘out in the room.’ ” He also asks questions such as: “When was the last time your skin was last totally clear? Are there activities that you or your family don’t do because of your eczema, or that you’re living your life around it? Is there anxiety or depression?” Documenting both the impact on quality of life and the severity of disease “makes it easier to discuss systemic therapy,” Dr. Eichenfield said. “Meanwhile, as the provider, I am trying to figure out if the patient should ‘go into the topical therapy bucket’ or into the ‘systemic therapy bucket.’ ”
Counseling about systemic therapy includes shared decision-making regarding the choice of biologics versus oral JAK inhibitors versus traditional systemic agent or phototherapy. Factors to consider in the decision making include patient age, sex, severity, comorbidities, prior therapy, risk aversion, duration, medication access, and desired efficacy. “Evolving therapies can change the conversation, the questions, and the outcomes, but the overarching desired outcome is long-term disease control, minimal eczematous rash, minimal pruritus, and minimal sleep disturbance,” he said.
Dr. Eichenfield disclosed that he has served as a consultant to or investigator for AbbVie; Almirall; Arcutis; Arena; Asana; Termagant; Dermira; Forte Biosciences; Galderma Laboratories; Glenmark/Chinos; Incyte; Kyowa Kirin; Leo Pharma; Eli Lilly and Company; Novartis; Ortho Dermatology; Otsuka; Pfizer; Freestone; Regeneron, and Sanofi Genzyme.
MedscapeLive and this news organization are owned by the same parent company.
Will my child outgrow the eczema?
That is perhaps the No. 1 atopic dermatitis–related question that Lawrence F. Eichenfield, MD, fields from parents in his role as chief of pediatric and adolescent dermatology at Rady’s Children’s Hospital, San Diego.
The answer “is pretty tricky,” he said during MedscapeLive’s annual Las Vegas Dermatology Seminar. “We used to say, ‘yeah, your kid will probably outgrow the disease,’ but we now have good data that show there are variable courses.”
Using data from the birth study cohort known as the Avon Longitudinal Study of Parents and Children, researchers in the United Kingdom investigated the existence of different longitudinal phenotypes of AD among 9,894 children. They found that 58% of the children in the cohort were unaffected or had transient AD, while 12.9% had early-onset/early-resolving AD. The remaining AD phenotypes consisted of 7%-8% patients each (early-onset persistent, early-onset late-resolving, mid-onset resolving, and late-onset resolving).
“There have been several studies that looked at the natural course of AD,” said Dr. Eichenfield, distinguished professor of dermatology and pediatrics at the University of California, San Diego. “A cohort study from Thailand showed that 50% of patients with childhood AD lost their AD diagnosis about 5 years into it, while there was an increase in allergic rhino-conjunctivitis and asthma, similar to what’s been seen in atopic march studies,” he noted.
A separate group of investigators analyzed records from The Health Improvement Network in the UK to determine the prevalence of AD among more than 8 million patients seen in primary care between 1994 and 2013. They found that the cumulative lifetime prevalence of atopic eczema was 9.9% and the highest rates of active disease were among children and older adults. “The takeaway was markedly inconsistent in terms of whether AD went away over time or increased over time, so it’s really not especially helpful prevalence data,” Dr. Eichenfield said. “Overall, you have a high prevalence in the first years of life, it decreases, and it may increase again when people are 60 years and older. Whether that’s truly AD or xerotic eczema isn’t known in this data set.”
A separate meta-analysis of 17 studies reported that 26% of adults with AD said they had adult-onset disease, which is characterized by more atopy, more foot dermatitis, and less flexural involvement.
Dr. Eichenfield tells parents, “there’s a really good chance (depending on disease severity) that 60% to 70% of children will outgrow their eczema or most of it,” he said. “If you ask me when, I won’t tell you. The important thing is to treat it to minimize its impact. We want minimal rash, minimal itch, and minimal sleep disturbance. Sometimes I say, ‘that might improve the chance of the eczema getting better over time.’ ”
Following are four other common questions parents and patients ask him:
Can we figure out the allergies causing the eczema? “This is probably one of the most unnerving questions I get asked,” he said. “It’s a loaded question. My answer is that allergies are intertwined with AD. Searching for the secret allergy causing the atopic dermatitis is rarely successful.” Sensitization is much more common with AD, he added, meaning specific IgE testing, whether it be blood testing or skin prick testing. “The more severe your eczema is, the more chance you’ll have of real food allergy,” he said. “About 15% of milder eczema patients will have at least one food allergy, but when you get to the more moderate to severe cases, about 40% will have a true food allergy.”
Food reactions may not cause eczema, though. Food reactions can cause urticaria, angioedema, eczematous dermatitis, allergic contact dermatitis, contact urticaria, and respiratory findings. According to National Institutes of Health guidelines for food allergy, skin prick tests and serum IgE tests are recommended to assist in identification of foods that may be provoking IgE-mediated food reactions, but are not diagnostic of food allergy.
“There’s a huge literature showing that there’s a lot of food allergy testing that’s just not helpful,” he said. In one study, 89% of food challenges administered in patients who were listed as being allergic based on skin prick tests or serum IgE tests did not have a true food allergy.
“Empiric elimination diets aren’t especially useful. However, we occasionally see children who do have AD exacerbated by food allergies in the first year of life,” he said. NIH guidelines suggest that children younger than 5 years of age with moderate to severe AD be considered for food allergy evaluation for milk, egg, peanut, wheat, and soy, if at least one of the following conditions is met: the child has persistent AD in spite of optimized management and topical therapy, and/or the child has a reliable history of an immediate reaction after ingestion of a specific food.
“We do know that there are high rates of comorbid allergic processes, besides food allergy, associated with atopic dermatitis, including allergic rhinitis and asthma both in children and adults,” Dr. Eichenfield said. “I do discuss allergy triggers and their importance in the life of the individual, though not necessarily as factors in AD. There are a variety of environmental allergens and/or environmental triggers that can significantly impact AD. Recently, we have seen studies discussing air pollution and wildfires as exacerbators of AD.”
How should I bathe and moisturize? There are no standard guidelines for the frequency, type, or duration of bathing in patients with AD, he said, though in more severe disease, frequent bathing can be helpful along with standard anti-inflammatory topical medicines. “I keep my general recommendations vague,” Dr. Eichenfield said. “I do explain that we don’t want to use harsh soaps; we want to be gentle in our washing. I usually recommend daily to every other day bathing. It’s important to pat the skin dry and then apply a moisturizer. Applying a moisturizer 2-3 minutes after bathing is important and limited significant cleanser use can be helpful.”
Moisturizers and emollients are a standard of care in U.S. guidelines published in 2013 and 2014, and international guidelines, and are steroid-sparing and useful for both prevention and maintenance. “I tell parents and patients that there is no reason to avoid bathing because of AD as long as you moisturize after,” he said.
Do I have to use topical [name of drug]? “I try to explain that there is skin barrier dysfunction that stimulates the inflammatory milieu, and that inflammation in the skin or blood in AD negatively impacts skin barrier function,” Dr. Eichenfield said. “I explain that if inflammation doesn’t get better with good skin care, moisturizers, and avoidance of triggers, we need anti-inflammatory medication. Then we discuss what the options are, the significant variation in strengths of topical corticosteroids, and topical nonsteroid options.”
When he counsels parents and patients on the use of topical corticosteroids, he tells them that cortisone is a naturally-occurring metabolite, and that “we can work together to let you know how much medicine to use, and how a safe amount is a powerful tool to fix the eczema.” He often says that topical steroids “are like hammers. We have tiny hammers, like over-the-counter hydrocortisone, and sledgehammers like clobetasol. We also have ‘screwdrivers’ and ‘pliers’ with nonsteroidal topical calcineurin and PDE-4 inhibitors, which are especially useful for maintenance therapy. Topical ruxolitinib is a new medicine that we may use for patients as well. The label includes discussion of side effects from oral JAK inhibitors as well as from the drug development program, so it takes some time to talk through.”
Is it time for a stronger systemic medicine? Any conversation about this topic should support the concept that the AD is multifactorial. “We have the rash of eczema,” he said. “We have the itch. We have impact on sleep disturbance. We have the comorbidities. We have other physical changes, which can happen with bacterial infections and other immune system or cardiovascular changes. We have the impact on quality of life and impact on school and work. When we recognize that if patients have significant enough disease that it is not getting better with topicals and is having a negative impact on their lives, we can move our discussion to systemic therapy.”
When counseling patients about systemic therapy, Dr. Eichenfield will conduct a body surface area assessment and document how bad the itch is. “But I’m not just recording the information; I’m bringing it out in the room,” he said. “I’ll do a BSA assessment and say, for example, ‘oh, you have 32% of your body involved with eczema.’ I ask about sleep disturbance, to get the answer ‘out in the room.’ ” He also asks questions such as: “When was the last time your skin was last totally clear? Are there activities that you or your family don’t do because of your eczema, or that you’re living your life around it? Is there anxiety or depression?” Documenting both the impact on quality of life and the severity of disease “makes it easier to discuss systemic therapy,” Dr. Eichenfield said. “Meanwhile, as the provider, I am trying to figure out if the patient should ‘go into the topical therapy bucket’ or into the ‘systemic therapy bucket.’ ”
Counseling about systemic therapy includes shared decision-making regarding the choice of biologics versus oral JAK inhibitors versus traditional systemic agent or phototherapy. Factors to consider in the decision making include patient age, sex, severity, comorbidities, prior therapy, risk aversion, duration, medication access, and desired efficacy. “Evolving therapies can change the conversation, the questions, and the outcomes, but the overarching desired outcome is long-term disease control, minimal eczematous rash, minimal pruritus, and minimal sleep disturbance,” he said.
Dr. Eichenfield disclosed that he has served as a consultant to or investigator for AbbVie; Almirall; Arcutis; Arena; Asana; Termagant; Dermira; Forte Biosciences; Galderma Laboratories; Glenmark/Chinos; Incyte; Kyowa Kirin; Leo Pharma; Eli Lilly and Company; Novartis; Ortho Dermatology; Otsuka; Pfizer; Freestone; Regeneron, and Sanofi Genzyme.
MedscapeLive and this news organization are owned by the same parent company.
Will my child outgrow the eczema?
That is perhaps the No. 1 atopic dermatitis–related question that Lawrence F. Eichenfield, MD, fields from parents in his role as chief of pediatric and adolescent dermatology at Rady’s Children’s Hospital, San Diego.
The answer “is pretty tricky,” he said during MedscapeLive’s annual Las Vegas Dermatology Seminar. “We used to say, ‘yeah, your kid will probably outgrow the disease,’ but we now have good data that show there are variable courses.”
Using data from the birth study cohort known as the Avon Longitudinal Study of Parents and Children, researchers in the United Kingdom investigated the existence of different longitudinal phenotypes of AD among 9,894 children. They found that 58% of the children in the cohort were unaffected or had transient AD, while 12.9% had early-onset/early-resolving AD. The remaining AD phenotypes consisted of 7%-8% patients each (early-onset persistent, early-onset late-resolving, mid-onset resolving, and late-onset resolving).
“There have been several studies that looked at the natural course of AD,” said Dr. Eichenfield, distinguished professor of dermatology and pediatrics at the University of California, San Diego. “A cohort study from Thailand showed that 50% of patients with childhood AD lost their AD diagnosis about 5 years into it, while there was an increase in allergic rhino-conjunctivitis and asthma, similar to what’s been seen in atopic march studies,” he noted.
A separate group of investigators analyzed records from The Health Improvement Network in the UK to determine the prevalence of AD among more than 8 million patients seen in primary care between 1994 and 2013. They found that the cumulative lifetime prevalence of atopic eczema was 9.9% and the highest rates of active disease were among children and older adults. “The takeaway was markedly inconsistent in terms of whether AD went away over time or increased over time, so it’s really not especially helpful prevalence data,” Dr. Eichenfield said. “Overall, you have a high prevalence in the first years of life, it decreases, and it may increase again when people are 60 years and older. Whether that’s truly AD or xerotic eczema isn’t known in this data set.”
A separate meta-analysis of 17 studies reported that 26% of adults with AD said they had adult-onset disease, which is characterized by more atopy, more foot dermatitis, and less flexural involvement.
Dr. Eichenfield tells parents, “there’s a really good chance (depending on disease severity) that 60% to 70% of children will outgrow their eczema or most of it,” he said. “If you ask me when, I won’t tell you. The important thing is to treat it to minimize its impact. We want minimal rash, minimal itch, and minimal sleep disturbance. Sometimes I say, ‘that might improve the chance of the eczema getting better over time.’ ”
Following are four other common questions parents and patients ask him:
Can we figure out the allergies causing the eczema? “This is probably one of the most unnerving questions I get asked,” he said. “It’s a loaded question. My answer is that allergies are intertwined with AD. Searching for the secret allergy causing the atopic dermatitis is rarely successful.” Sensitization is much more common with AD, he added, meaning specific IgE testing, whether it be blood testing or skin prick testing. “The more severe your eczema is, the more chance you’ll have of real food allergy,” he said. “About 15% of milder eczema patients will have at least one food allergy, but when you get to the more moderate to severe cases, about 40% will have a true food allergy.”
Food reactions may not cause eczema, though. Food reactions can cause urticaria, angioedema, eczematous dermatitis, allergic contact dermatitis, contact urticaria, and respiratory findings. According to National Institutes of Health guidelines for food allergy, skin prick tests and serum IgE tests are recommended to assist in identification of foods that may be provoking IgE-mediated food reactions, but are not diagnostic of food allergy.
“There’s a huge literature showing that there’s a lot of food allergy testing that’s just not helpful,” he said. In one study, 89% of food challenges administered in patients who were listed as being allergic based on skin prick tests or serum IgE tests did not have a true food allergy.
“Empiric elimination diets aren’t especially useful. However, we occasionally see children who do have AD exacerbated by food allergies in the first year of life,” he said. NIH guidelines suggest that children younger than 5 years of age with moderate to severe AD be considered for food allergy evaluation for milk, egg, peanut, wheat, and soy, if at least one of the following conditions is met: the child has persistent AD in spite of optimized management and topical therapy, and/or the child has a reliable history of an immediate reaction after ingestion of a specific food.
“We do know that there are high rates of comorbid allergic processes, besides food allergy, associated with atopic dermatitis, including allergic rhinitis and asthma both in children and adults,” Dr. Eichenfield said. “I do discuss allergy triggers and their importance in the life of the individual, though not necessarily as factors in AD. There are a variety of environmental allergens and/or environmental triggers that can significantly impact AD. Recently, we have seen studies discussing air pollution and wildfires as exacerbators of AD.”
How should I bathe and moisturize? There are no standard guidelines for the frequency, type, or duration of bathing in patients with AD, he said, though in more severe disease, frequent bathing can be helpful along with standard anti-inflammatory topical medicines. “I keep my general recommendations vague,” Dr. Eichenfield said. “I do explain that we don’t want to use harsh soaps; we want to be gentle in our washing. I usually recommend daily to every other day bathing. It’s important to pat the skin dry and then apply a moisturizer. Applying a moisturizer 2-3 minutes after bathing is important and limited significant cleanser use can be helpful.”
Moisturizers and emollients are a standard of care in U.S. guidelines published in 2013 and 2014, and international guidelines, and are steroid-sparing and useful for both prevention and maintenance. “I tell parents and patients that there is no reason to avoid bathing because of AD as long as you moisturize after,” he said.
Do I have to use topical [name of drug]? “I try to explain that there is skin barrier dysfunction that stimulates the inflammatory milieu, and that inflammation in the skin or blood in AD negatively impacts skin barrier function,” Dr. Eichenfield said. “I explain that if inflammation doesn’t get better with good skin care, moisturizers, and avoidance of triggers, we need anti-inflammatory medication. Then we discuss what the options are, the significant variation in strengths of topical corticosteroids, and topical nonsteroid options.”
When he counsels parents and patients on the use of topical corticosteroids, he tells them that cortisone is a naturally-occurring metabolite, and that “we can work together to let you know how much medicine to use, and how a safe amount is a powerful tool to fix the eczema.” He often says that topical steroids “are like hammers. We have tiny hammers, like over-the-counter hydrocortisone, and sledgehammers like clobetasol. We also have ‘screwdrivers’ and ‘pliers’ with nonsteroidal topical calcineurin and PDE-4 inhibitors, which are especially useful for maintenance therapy. Topical ruxolitinib is a new medicine that we may use for patients as well. The label includes discussion of side effects from oral JAK inhibitors as well as from the drug development program, so it takes some time to talk through.”
Is it time for a stronger systemic medicine? Any conversation about this topic should support the concept that the AD is multifactorial. “We have the rash of eczema,” he said. “We have the itch. We have impact on sleep disturbance. We have the comorbidities. We have other physical changes, which can happen with bacterial infections and other immune system or cardiovascular changes. We have the impact on quality of life and impact on school and work. When we recognize that if patients have significant enough disease that it is not getting better with topicals and is having a negative impact on their lives, we can move our discussion to systemic therapy.”
When counseling patients about systemic therapy, Dr. Eichenfield will conduct a body surface area assessment and document how bad the itch is. “But I’m not just recording the information; I’m bringing it out in the room,” he said. “I’ll do a BSA assessment and say, for example, ‘oh, you have 32% of your body involved with eczema.’ I ask about sleep disturbance, to get the answer ‘out in the room.’ ” He also asks questions such as: “When was the last time your skin was last totally clear? Are there activities that you or your family don’t do because of your eczema, or that you’re living your life around it? Is there anxiety or depression?” Documenting both the impact on quality of life and the severity of disease “makes it easier to discuss systemic therapy,” Dr. Eichenfield said. “Meanwhile, as the provider, I am trying to figure out if the patient should ‘go into the topical therapy bucket’ or into the ‘systemic therapy bucket.’ ”
Counseling about systemic therapy includes shared decision-making regarding the choice of biologics versus oral JAK inhibitors versus traditional systemic agent or phototherapy. Factors to consider in the decision making include patient age, sex, severity, comorbidities, prior therapy, risk aversion, duration, medication access, and desired efficacy. “Evolving therapies can change the conversation, the questions, and the outcomes, but the overarching desired outcome is long-term disease control, minimal eczematous rash, minimal pruritus, and minimal sleep disturbance,” he said.
Dr. Eichenfield disclosed that he has served as a consultant to or investigator for AbbVie; Almirall; Arcutis; Arena; Asana; Termagant; Dermira; Forte Biosciences; Galderma Laboratories; Glenmark/Chinos; Incyte; Kyowa Kirin; Leo Pharma; Eli Lilly and Company; Novartis; Ortho Dermatology; Otsuka; Pfizer; Freestone; Regeneron, and Sanofi Genzyme.
MedscapeLive and this news organization are owned by the same parent company.
FROM THE MEDSCAPELIVE LAS VEGAS DERMATOLOGY SEMINAR
Rapid COVID-19 tests will soon be covered by insurance
and mask mandates will be extended for air, rail and bus travelers through at least mid-March.
The measures are part of a suite of new actions President Joe Biden is expected to announce later today, Dec. 2, in the wake of the arrival of the Omicron variant in the United States. The White House’s initiatives are designed to fight an expected winter surge of COVID-19 infections, according to sources familiar with the president’s plans.
At about $24 per package, rapid COVID-19 testing remains prohibitively expensive for many, even after a promise to bring the tests to Americans at a wholesale cost.
Other countries have rapid tests available for free or about $1 per test, and many experts say more frequent use of rapid tests could help stop transmission of COVID-19 virus.
About 150 million Americans would be eligible for reimbursement for rapid tests through their insurance plans.
In addition to those steps, international travelers flying into the United States will soon be required to show proof of a negative COVID-19 test within 24 hours of their departure, whether they are vaccinated or not.
In keeping with the six-part plan to fight COVID-19 the administration outlined in August, the president’s new plan is centered around vaccinations for all eligible Americans, including booster doses for the estimated 100 million adults who are now at least 6 months past their second doses of a Pfizer or Moderna vaccine or 2 months past a Johnson & Johnson shot.
Those plans, which relied on vaccine mandates for most workers, have been stymied by recent court rulings blocking implementation of those requirements.
As the issue makes its way through the courts, Biden is expected to call on companies to voluntarily implement vaccination requirements for their workers, which he says are helping to close vaccination gaps.
Biden is also expected to outline a new push to get booster shots to all adults, with an emphasis on reaching seniors, who are at greatest risk for hospitalization and death from COVID-19.
The president is scheduled to speak at 1:40 PM on Dec. 2 at the National Institutes of Health.
A version of this article first appeared on WebMD.com .
and mask mandates will be extended for air, rail and bus travelers through at least mid-March.
The measures are part of a suite of new actions President Joe Biden is expected to announce later today, Dec. 2, in the wake of the arrival of the Omicron variant in the United States. The White House’s initiatives are designed to fight an expected winter surge of COVID-19 infections, according to sources familiar with the president’s plans.
At about $24 per package, rapid COVID-19 testing remains prohibitively expensive for many, even after a promise to bring the tests to Americans at a wholesale cost.
Other countries have rapid tests available for free or about $1 per test, and many experts say more frequent use of rapid tests could help stop transmission of COVID-19 virus.
About 150 million Americans would be eligible for reimbursement for rapid tests through their insurance plans.
In addition to those steps, international travelers flying into the United States will soon be required to show proof of a negative COVID-19 test within 24 hours of their departure, whether they are vaccinated or not.
In keeping with the six-part plan to fight COVID-19 the administration outlined in August, the president’s new plan is centered around vaccinations for all eligible Americans, including booster doses for the estimated 100 million adults who are now at least 6 months past their second doses of a Pfizer or Moderna vaccine or 2 months past a Johnson & Johnson shot.
Those plans, which relied on vaccine mandates for most workers, have been stymied by recent court rulings blocking implementation of those requirements.
As the issue makes its way through the courts, Biden is expected to call on companies to voluntarily implement vaccination requirements for their workers, which he says are helping to close vaccination gaps.
Biden is also expected to outline a new push to get booster shots to all adults, with an emphasis on reaching seniors, who are at greatest risk for hospitalization and death from COVID-19.
The president is scheduled to speak at 1:40 PM on Dec. 2 at the National Institutes of Health.
A version of this article first appeared on WebMD.com .
and mask mandates will be extended for air, rail and bus travelers through at least mid-March.
The measures are part of a suite of new actions President Joe Biden is expected to announce later today, Dec. 2, in the wake of the arrival of the Omicron variant in the United States. The White House’s initiatives are designed to fight an expected winter surge of COVID-19 infections, according to sources familiar with the president’s plans.
At about $24 per package, rapid COVID-19 testing remains prohibitively expensive for many, even after a promise to bring the tests to Americans at a wholesale cost.
Other countries have rapid tests available for free or about $1 per test, and many experts say more frequent use of rapid tests could help stop transmission of COVID-19 virus.
About 150 million Americans would be eligible for reimbursement for rapid tests through their insurance plans.
In addition to those steps, international travelers flying into the United States will soon be required to show proof of a negative COVID-19 test within 24 hours of their departure, whether they are vaccinated or not.
In keeping with the six-part plan to fight COVID-19 the administration outlined in August, the president’s new plan is centered around vaccinations for all eligible Americans, including booster doses for the estimated 100 million adults who are now at least 6 months past their second doses of a Pfizer or Moderna vaccine or 2 months past a Johnson & Johnson shot.
Those plans, which relied on vaccine mandates for most workers, have been stymied by recent court rulings blocking implementation of those requirements.
As the issue makes its way through the courts, Biden is expected to call on companies to voluntarily implement vaccination requirements for their workers, which he says are helping to close vaccination gaps.
Biden is also expected to outline a new push to get booster shots to all adults, with an emphasis on reaching seniors, who are at greatest risk for hospitalization and death from COVID-19.
The president is scheduled to speak at 1:40 PM on Dec. 2 at the National Institutes of Health.
A version of this article first appeared on WebMD.com .
Retinopathy risk in children higher in T2D than T1D
Children diagnosed with type 2 diabetes (T2D) appear significantly more likely to develop retinopathy and other ocular complications over time than children who are diagnosed with type 1 diabetes (T1D), researchers report.
Among a population-based cohort of children (defined as younger than 22 years), the risk of diabetic retinopathy was 88% greater in those with T2D than T1D within the first 15 years of disease diagnosis.
“The purpose of this study was to assess the risk of developing diabetes-associated ocular complications among a population-based cohort of children diagnosed with either T1D or T2D during a 50-year period,” lead author Patricia Bai, BA, of Mayo Clinic, Phoenix, and colleagues reported in JAMA Ophthalmology.
The researchers retrospectively reviewed medical records from all residents of Olmsted County, Minn., from 1970 to 2019. The study cohort included 606 children with a confirmed a diagnosis of T1D or T2D, 525 (87%) of whom had at least one ocular examination.
The mean age at diabetes diagnosis was 12 years (standard deviation, 5.4 years); most participants were White (95.7% in 1990), and half (50%) were male. Diabetes-associated ocular complications occurred in 31.9% and 26.6% of children with T1D and T2D, respectively.
The hazard ratios illustrating the risk between T2D and T1D rates were 1.88 (95% confidence interval, 1.13-3.12; P = .02) for any diabetic retinopathy, 2.33 (95% CI, 0.99-5.50; P = .048) for proliferative diabetic retinopathy, 1.49 (95% CI, 0.46-4.89; P = .50) for diabetic macular edema, 2.43 (95% CI, 0.54-11.07; P = .24) for a visually significant cataract, and 4.06 (95% CI, 1.34-12.33; P = .007) for requiring pars plana vitrectomy within the first 15 years of diagnosis.
These results suggest that earlier surveillance and intervention may help prevent vision-threatening complications, the researchers explained.
“After adjusting for race using self-identified categories of White or not White, the adjusted HR of developing any retinopathy was 1.63 (95% CI, 0.96-2.79; P = .07), and the adjusted HR of developing proliferative diabetic retinopathy was 2.02 (95% CI, 0.79-5.16; P = .14)” in T2D versus T1D patients, the researchers wrote.
“We would expect the reported rate of type 2 diabetes to be potentially underestimated in our study cohort,” Ms. Bai commented in an interview. “Race has been suggested to be a surrogate for other social determinants of health, such as lower rates of optimal follow-up care received by racial and ethnic minorities, which could influence subsequent retinopathy rates.”
Understanding retinopathy outcomes in youth
In an accompanying editorial, Jennifer K. Sun, MD, MPH, from Harvard Medical School, Boston, wrote that the present study indicates the natural history of retinopathy may differ between patients with T1D and T2D.
While the pathophysiology of diabetic retinopathy in T1D and T2D appears similar, other patient-related factors such as lipid profiles, the presence of hypertension, and body mass index may differ between the two disease states.
She wrote that “there is a particular need to document retinopathy outcomes and risk factors for advanced disease in youth with T2D, for whom there is a paucity of information.”
Ms. Bai and colleagues acknowledged that a key limitation of the study was the retrospective design. As a result, irregular follow-up and incomplete data may limit the applicability of the findings.
“Some children with milder forms of diabetes may have eluded detection, a limitation that is more likely to affect T2D, which may exist undetected for years before a diagnosis,” Bai explained.
Dr. Sun recommended that further epidemiologic studies are needed to help optimize guidelines for screening and follow-up for young people diagnosed with diabetes. “Such efforts may potentially lead to increased understanding of the mechanistic differences between pathology in T1D versus T2D,” she concluded.
This study used the resources of the Rochester Epidemiology Project (REP) medical records linkage system, which is supported by grant funding from the National Institute on Aging, the Mayo Clinic Research Committee, and by fees paid annually by REP users. The study authors disclosed no conflicts of interest.
Children diagnosed with type 2 diabetes (T2D) appear significantly more likely to develop retinopathy and other ocular complications over time than children who are diagnosed with type 1 diabetes (T1D), researchers report.
Among a population-based cohort of children (defined as younger than 22 years), the risk of diabetic retinopathy was 88% greater in those with T2D than T1D within the first 15 years of disease diagnosis.
“The purpose of this study was to assess the risk of developing diabetes-associated ocular complications among a population-based cohort of children diagnosed with either T1D or T2D during a 50-year period,” lead author Patricia Bai, BA, of Mayo Clinic, Phoenix, and colleagues reported in JAMA Ophthalmology.
The researchers retrospectively reviewed medical records from all residents of Olmsted County, Minn., from 1970 to 2019. The study cohort included 606 children with a confirmed a diagnosis of T1D or T2D, 525 (87%) of whom had at least one ocular examination.
The mean age at diabetes diagnosis was 12 years (standard deviation, 5.4 years); most participants were White (95.7% in 1990), and half (50%) were male. Diabetes-associated ocular complications occurred in 31.9% and 26.6% of children with T1D and T2D, respectively.
The hazard ratios illustrating the risk between T2D and T1D rates were 1.88 (95% confidence interval, 1.13-3.12; P = .02) for any diabetic retinopathy, 2.33 (95% CI, 0.99-5.50; P = .048) for proliferative diabetic retinopathy, 1.49 (95% CI, 0.46-4.89; P = .50) for diabetic macular edema, 2.43 (95% CI, 0.54-11.07; P = .24) for a visually significant cataract, and 4.06 (95% CI, 1.34-12.33; P = .007) for requiring pars plana vitrectomy within the first 15 years of diagnosis.
These results suggest that earlier surveillance and intervention may help prevent vision-threatening complications, the researchers explained.
“After adjusting for race using self-identified categories of White or not White, the adjusted HR of developing any retinopathy was 1.63 (95% CI, 0.96-2.79; P = .07), and the adjusted HR of developing proliferative diabetic retinopathy was 2.02 (95% CI, 0.79-5.16; P = .14)” in T2D versus T1D patients, the researchers wrote.
“We would expect the reported rate of type 2 diabetes to be potentially underestimated in our study cohort,” Ms. Bai commented in an interview. “Race has been suggested to be a surrogate for other social determinants of health, such as lower rates of optimal follow-up care received by racial and ethnic minorities, which could influence subsequent retinopathy rates.”
Understanding retinopathy outcomes in youth
In an accompanying editorial, Jennifer K. Sun, MD, MPH, from Harvard Medical School, Boston, wrote that the present study indicates the natural history of retinopathy may differ between patients with T1D and T2D.
While the pathophysiology of diabetic retinopathy in T1D and T2D appears similar, other patient-related factors such as lipid profiles, the presence of hypertension, and body mass index may differ between the two disease states.
She wrote that “there is a particular need to document retinopathy outcomes and risk factors for advanced disease in youth with T2D, for whom there is a paucity of information.”
Ms. Bai and colleagues acknowledged that a key limitation of the study was the retrospective design. As a result, irregular follow-up and incomplete data may limit the applicability of the findings.
“Some children with milder forms of diabetes may have eluded detection, a limitation that is more likely to affect T2D, which may exist undetected for years before a diagnosis,” Bai explained.
Dr. Sun recommended that further epidemiologic studies are needed to help optimize guidelines for screening and follow-up for young people diagnosed with diabetes. “Such efforts may potentially lead to increased understanding of the mechanistic differences between pathology in T1D versus T2D,” she concluded.
This study used the resources of the Rochester Epidemiology Project (REP) medical records linkage system, which is supported by grant funding from the National Institute on Aging, the Mayo Clinic Research Committee, and by fees paid annually by REP users. The study authors disclosed no conflicts of interest.
Children diagnosed with type 2 diabetes (T2D) appear significantly more likely to develop retinopathy and other ocular complications over time than children who are diagnosed with type 1 diabetes (T1D), researchers report.
Among a population-based cohort of children (defined as younger than 22 years), the risk of diabetic retinopathy was 88% greater in those with T2D than T1D within the first 15 years of disease diagnosis.
“The purpose of this study was to assess the risk of developing diabetes-associated ocular complications among a population-based cohort of children diagnosed with either T1D or T2D during a 50-year period,” lead author Patricia Bai, BA, of Mayo Clinic, Phoenix, and colleagues reported in JAMA Ophthalmology.
The researchers retrospectively reviewed medical records from all residents of Olmsted County, Minn., from 1970 to 2019. The study cohort included 606 children with a confirmed a diagnosis of T1D or T2D, 525 (87%) of whom had at least one ocular examination.
The mean age at diabetes diagnosis was 12 years (standard deviation, 5.4 years); most participants were White (95.7% in 1990), and half (50%) were male. Diabetes-associated ocular complications occurred in 31.9% and 26.6% of children with T1D and T2D, respectively.
The hazard ratios illustrating the risk between T2D and T1D rates were 1.88 (95% confidence interval, 1.13-3.12; P = .02) for any diabetic retinopathy, 2.33 (95% CI, 0.99-5.50; P = .048) for proliferative diabetic retinopathy, 1.49 (95% CI, 0.46-4.89; P = .50) for diabetic macular edema, 2.43 (95% CI, 0.54-11.07; P = .24) for a visually significant cataract, and 4.06 (95% CI, 1.34-12.33; P = .007) for requiring pars plana vitrectomy within the first 15 years of diagnosis.
These results suggest that earlier surveillance and intervention may help prevent vision-threatening complications, the researchers explained.
“After adjusting for race using self-identified categories of White or not White, the adjusted HR of developing any retinopathy was 1.63 (95% CI, 0.96-2.79; P = .07), and the adjusted HR of developing proliferative diabetic retinopathy was 2.02 (95% CI, 0.79-5.16; P = .14)” in T2D versus T1D patients, the researchers wrote.
“We would expect the reported rate of type 2 diabetes to be potentially underestimated in our study cohort,” Ms. Bai commented in an interview. “Race has been suggested to be a surrogate for other social determinants of health, such as lower rates of optimal follow-up care received by racial and ethnic minorities, which could influence subsequent retinopathy rates.”
Understanding retinopathy outcomes in youth
In an accompanying editorial, Jennifer K. Sun, MD, MPH, from Harvard Medical School, Boston, wrote that the present study indicates the natural history of retinopathy may differ between patients with T1D and T2D.
While the pathophysiology of diabetic retinopathy in T1D and T2D appears similar, other patient-related factors such as lipid profiles, the presence of hypertension, and body mass index may differ between the two disease states.
She wrote that “there is a particular need to document retinopathy outcomes and risk factors for advanced disease in youth with T2D, for whom there is a paucity of information.”
Ms. Bai and colleagues acknowledged that a key limitation of the study was the retrospective design. As a result, irregular follow-up and incomplete data may limit the applicability of the findings.
“Some children with milder forms of diabetes may have eluded detection, a limitation that is more likely to affect T2D, which may exist undetected for years before a diagnosis,” Bai explained.
Dr. Sun recommended that further epidemiologic studies are needed to help optimize guidelines for screening and follow-up for young people diagnosed with diabetes. “Such efforts may potentially lead to increased understanding of the mechanistic differences between pathology in T1D versus T2D,” she concluded.
This study used the resources of the Rochester Epidemiology Project (REP) medical records linkage system, which is supported by grant funding from the National Institute on Aging, the Mayo Clinic Research Committee, and by fees paid annually by REP users. The study authors disclosed no conflicts of interest.
FROM JAMA OPHTHALMOLOGY
AHA statement on impact of major life events on physical activity
Physical activity levels may decline during major life events, and it’s important for health care professionals to encourage patients to maintain regular physical activity during times of significant changes in their lives, the American Heart Association says in a new scientific statement.
With this statement, “We hope health care providers, public health workers, and individuals understand that a major life change can lead to decreases in physical activity or increases in sedentary behavior,” writing group chair Abbi D. Lane-Cordova, PhD, said in an interview.
The statement includes “tips for screening for physical activity and talking to people about their activity during these big life events and resources that can be used by health care providers to help people achieve healthy levels of physical activity,” said Dr. Lane-Cordova, assistant professor in exercise science, Arnold School of Public Health, University of South Carolina, Columbia.
The statement was published online Dec. 1 in the journal Circulation.
The AHA Committee on Physical Activity, part of the organization’s Council on Lifestyle and Cardiometabolic Health, began discussing this topic back in 2019, Dr. Lane-Cordova explained.
“We spoke as a group about how much activity levels can change when something big happens in life, like becoming a parent or retiring. The change in activity behavior (physical activity or sedentary behavior) is important because these activity behaviors can influence heart health,” she said.
The group started work on the scientific statement in early 2020 – “and then the pandemic hit, and it seemed more important than ever to create awareness and a resource for people to help improve, or at least maintain, favorable activity behaviors when there’s a profound change or event in life,” Dr. Lane-Cordova said.
Some more vulnerable than others
The writing group examined data on 17 different life events or transitions and found evidence that physical activity levels may decline during nine events: beginning a new school (elementary, middle, high school, or college); a first job or career change; a marriage or civil union; pregnancy; parenting; retirement; or moving into a long-term care facility.
The authors also identified individuals who may be particularly susceptible to lower levels of physical activity in general and during important life events. They include those with lower levels of education; those who live alone; those who lack access to a safe outdoor space; Black Americans; some members of the LGBTQ+ community; and women who are pregnant and new parents.
They offer practical strategies for health care professionals to support routine physical activity levels during major life events and transitions. These include asking simple questions about how life transitions may be changing physical activity patterns and encouraging the use of wearable step trackers to monitor levels and changes.
“It’s important to maintain or improve physical activity when major life events happen, which is often a time when exercise is most needed,” Dr. Lane-Cordova said in a news release.
“Clinicians should express compassion as they ask about life transitions and initiate conversations about physical activity during life events and transitions,” the writing group advises.
The group also says its important “to look beyond the health care setting and engage organizations, communities, workplaces, faith-based communities, and assisted living facilities to promote physical activity.”
The statement provides a list of resources for individuals and health care professionals, many of which are free and online.
This research had no commercial funding. Members of the writing group have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Physical activity levels may decline during major life events, and it’s important for health care professionals to encourage patients to maintain regular physical activity during times of significant changes in their lives, the American Heart Association says in a new scientific statement.
With this statement, “We hope health care providers, public health workers, and individuals understand that a major life change can lead to decreases in physical activity or increases in sedentary behavior,” writing group chair Abbi D. Lane-Cordova, PhD, said in an interview.
The statement includes “tips for screening for physical activity and talking to people about their activity during these big life events and resources that can be used by health care providers to help people achieve healthy levels of physical activity,” said Dr. Lane-Cordova, assistant professor in exercise science, Arnold School of Public Health, University of South Carolina, Columbia.
The statement was published online Dec. 1 in the journal Circulation.
The AHA Committee on Physical Activity, part of the organization’s Council on Lifestyle and Cardiometabolic Health, began discussing this topic back in 2019, Dr. Lane-Cordova explained.
“We spoke as a group about how much activity levels can change when something big happens in life, like becoming a parent or retiring. The change in activity behavior (physical activity or sedentary behavior) is important because these activity behaviors can influence heart health,” she said.
The group started work on the scientific statement in early 2020 – “and then the pandemic hit, and it seemed more important than ever to create awareness and a resource for people to help improve, or at least maintain, favorable activity behaviors when there’s a profound change or event in life,” Dr. Lane-Cordova said.
Some more vulnerable than others
The writing group examined data on 17 different life events or transitions and found evidence that physical activity levels may decline during nine events: beginning a new school (elementary, middle, high school, or college); a first job or career change; a marriage or civil union; pregnancy; parenting; retirement; or moving into a long-term care facility.
The authors also identified individuals who may be particularly susceptible to lower levels of physical activity in general and during important life events. They include those with lower levels of education; those who live alone; those who lack access to a safe outdoor space; Black Americans; some members of the LGBTQ+ community; and women who are pregnant and new parents.
They offer practical strategies for health care professionals to support routine physical activity levels during major life events and transitions. These include asking simple questions about how life transitions may be changing physical activity patterns and encouraging the use of wearable step trackers to monitor levels and changes.
“It’s important to maintain or improve physical activity when major life events happen, which is often a time when exercise is most needed,” Dr. Lane-Cordova said in a news release.
“Clinicians should express compassion as they ask about life transitions and initiate conversations about physical activity during life events and transitions,” the writing group advises.
The group also says its important “to look beyond the health care setting and engage organizations, communities, workplaces, faith-based communities, and assisted living facilities to promote physical activity.”
The statement provides a list of resources for individuals and health care professionals, many of which are free and online.
This research had no commercial funding. Members of the writing group have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Physical activity levels may decline during major life events, and it’s important for health care professionals to encourage patients to maintain regular physical activity during times of significant changes in their lives, the American Heart Association says in a new scientific statement.
With this statement, “We hope health care providers, public health workers, and individuals understand that a major life change can lead to decreases in physical activity or increases in sedentary behavior,” writing group chair Abbi D. Lane-Cordova, PhD, said in an interview.
The statement includes “tips for screening for physical activity and talking to people about their activity during these big life events and resources that can be used by health care providers to help people achieve healthy levels of physical activity,” said Dr. Lane-Cordova, assistant professor in exercise science, Arnold School of Public Health, University of South Carolina, Columbia.
The statement was published online Dec. 1 in the journal Circulation.
The AHA Committee on Physical Activity, part of the organization’s Council on Lifestyle and Cardiometabolic Health, began discussing this topic back in 2019, Dr. Lane-Cordova explained.
“We spoke as a group about how much activity levels can change when something big happens in life, like becoming a parent or retiring. The change in activity behavior (physical activity or sedentary behavior) is important because these activity behaviors can influence heart health,” she said.
The group started work on the scientific statement in early 2020 – “and then the pandemic hit, and it seemed more important than ever to create awareness and a resource for people to help improve, or at least maintain, favorable activity behaviors when there’s a profound change or event in life,” Dr. Lane-Cordova said.
Some more vulnerable than others
The writing group examined data on 17 different life events or transitions and found evidence that physical activity levels may decline during nine events: beginning a new school (elementary, middle, high school, or college); a first job or career change; a marriage or civil union; pregnancy; parenting; retirement; or moving into a long-term care facility.
The authors also identified individuals who may be particularly susceptible to lower levels of physical activity in general and during important life events. They include those with lower levels of education; those who live alone; those who lack access to a safe outdoor space; Black Americans; some members of the LGBTQ+ community; and women who are pregnant and new parents.
They offer practical strategies for health care professionals to support routine physical activity levels during major life events and transitions. These include asking simple questions about how life transitions may be changing physical activity patterns and encouraging the use of wearable step trackers to monitor levels and changes.
“It’s important to maintain or improve physical activity when major life events happen, which is often a time when exercise is most needed,” Dr. Lane-Cordova said in a news release.
“Clinicians should express compassion as they ask about life transitions and initiate conversations about physical activity during life events and transitions,” the writing group advises.
The group also says its important “to look beyond the health care setting and engage organizations, communities, workplaces, faith-based communities, and assisted living facilities to promote physical activity.”
The statement provides a list of resources for individuals and health care professionals, many of which are free and online.
This research had no commercial funding. Members of the writing group have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.