User login
Combo treatment may improve quality of life in CTCL
LA JOLLA, CALIF. — Treatment with brentuximab vedotin (BV) and lenalidomide (len) may improve quality of life (QOL) for patients with cutaneous T-cell lymphoma (CTCL), according to the principal investigator of a phase 2 trial.

In this small trial, most CTCL patients experienced relief from pruritus after one cycle of treatment with BV-len.
Investigators also observed durable responses to the combination, although two patients experienced tumor flare prior to response.
“Because of the tumor flare, we decreased the dose of lenalidomide ... and, since then, it has not been a major problem,” said Basem M. William, MD, principal investigator of the trial and a professor at Ohio State University in Columbus.
“We’re trying to be more reassuring to patients that, if they experience a little bit of tumor flare, as long as it’s not dangerous or life-threatening, if they can hold on with the treatment, this might translate to a later durable response.”
Dr. William and his colleagues presented results from this ongoing, phase 2 trial (NCT03409432) at the annual T-cell Lymphoma Forum.
Thus far, the investigators have treated 12 patients with relapsed or refractory CTCL or peripheral T-cell lymphoma (PTCL). The CTCL patients had received at least two lines of skin-directed therapy or one line of systemic therapy, and the PTCL patients had received at least one line of systemic therapy.
Dr. William and his colleagues reported results for 10 patients. Six patients had mycosis fungoides (MF), two had Sézary syndrome (SS), one had CD30+ lymphoproliferative disorder, and one had systemic anaplastic large-cell lymphoma (ALCL).
The patients’ median age was 59 (range, 49-74), there were nine males, and patients had received a median of 2 (range, 1-10) prior therapies.
The first seven patients received BV at 1.2 mg/kg and len at 20 mg daily every 3 weeks. However, after the investigators observed tumor flare in two patients, the dose of len was lowered to 10 mg.
Safety
The investigators said all adverse events (AEs) were reversible by stopping therapy, there were no grade 4 AEs, and none of the patients had grade 3 or higher neuropathy.
“We have not seen an excess of neuropathy, which is very important because both brentuximab and lenalidomide are known to cause neuropathy,” Dr. William said. “So we were fairly concerned that there would be a synergistic neurotoxic effect, which we don’t want, but we haven’t seen that.”
The most common treatment-related AE was neutropenia. Grade 3 neutropenia occurred in four patients.
Other grade 3 AEs, which occurred in patients on the 20 mg dose of len, were thrombocytopenia (n = 1), dyspnea (n = 1), vertigo (n = 1), drug rash with eosinophilia and systemic symptoms (DRESS) syndrome (n = 1), and tumor flare (n = 1).
Three patients discontinued treatment because of AEs — thrombocytopenia, tumor flare, and DRESS syndrome.
Tumor flare and response
“We did see tumor flare in two initial patients treated with the higher dose of lenalidomide, and we had to remove them from the study for their safety,” Dr. William said. “One of them had a full-blown DRESS syndrome. For their safety, we did have to remove them, but both did experience durable remissions after.”
One of the patients with tumor flare, who had MF, didn’t require treatment for 6 months after going off study. The other patient, who had SS, cleared the clone from his blood but developed DRESS syndrome.
In all, three patients achieved a response to treatment. The ALCL patient had a complete response, and two MF patients achieved a partial response.
Two MF patients and one SS patient had stable disease. The remaining four patients — two with MF, one with SS, and one with lymphoproliferative disorder — progressed.
QOL
The investigators used the Skindex-16 to assess the effect of treatment on QOL.
Five of six evaluable patients with CTCL had a 50% or greater reduction in their Skindex-16 scores after two cycles of treatment. In fact, most patients had relief from pruritus after one cycle, Dr. William said.
“Patients with cutaneous T-cell lymphoma, their biggest problem is with the symptom burden, with pruritus,” he said. “They’re really miserable from all the itching they have. They cannot sleep at night. So we’re fairly excited that most of the patients we’ve treated so far had relief from pruritus just after one cycle.”
Dr. William said he and his colleagues are excited about the overall results they have observed with BV-len, although it’s “still pretty early” in the trial. The investigators are planning to enroll a total of 42 patients and may open the trial at a second center.
The study is sponsored by Ohio State University and the lenalidomide is provided by Celgene. Dr. William reported relationships with miRagen Therapeutics, GuidePoint, Kyowa Kirin, and Celgene.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. — Treatment with brentuximab vedotin (BV) and lenalidomide (len) may improve quality of life (QOL) for patients with cutaneous T-cell lymphoma (CTCL), according to the principal investigator of a phase 2 trial.

In this small trial, most CTCL patients experienced relief from pruritus after one cycle of treatment with BV-len.
Investigators also observed durable responses to the combination, although two patients experienced tumor flare prior to response.
“Because of the tumor flare, we decreased the dose of lenalidomide ... and, since then, it has not been a major problem,” said Basem M. William, MD, principal investigator of the trial and a professor at Ohio State University in Columbus.
“We’re trying to be more reassuring to patients that, if they experience a little bit of tumor flare, as long as it’s not dangerous or life-threatening, if they can hold on with the treatment, this might translate to a later durable response.”
Dr. William and his colleagues presented results from this ongoing, phase 2 trial (NCT03409432) at the annual T-cell Lymphoma Forum.
Thus far, the investigators have treated 12 patients with relapsed or refractory CTCL or peripheral T-cell lymphoma (PTCL). The CTCL patients had received at least two lines of skin-directed therapy or one line of systemic therapy, and the PTCL patients had received at least one line of systemic therapy.
Dr. William and his colleagues reported results for 10 patients. Six patients had mycosis fungoides (MF), two had Sézary syndrome (SS), one had CD30+ lymphoproliferative disorder, and one had systemic anaplastic large-cell lymphoma (ALCL).
The patients’ median age was 59 (range, 49-74), there were nine males, and patients had received a median of 2 (range, 1-10) prior therapies.
The first seven patients received BV at 1.2 mg/kg and len at 20 mg daily every 3 weeks. However, after the investigators observed tumor flare in two patients, the dose of len was lowered to 10 mg.
Safety
The investigators said all adverse events (AEs) were reversible by stopping therapy, there were no grade 4 AEs, and none of the patients had grade 3 or higher neuropathy.
“We have not seen an excess of neuropathy, which is very important because both brentuximab and lenalidomide are known to cause neuropathy,” Dr. William said. “So we were fairly concerned that there would be a synergistic neurotoxic effect, which we don’t want, but we haven’t seen that.”
The most common treatment-related AE was neutropenia. Grade 3 neutropenia occurred in four patients.
Other grade 3 AEs, which occurred in patients on the 20 mg dose of len, were thrombocytopenia (n = 1), dyspnea (n = 1), vertigo (n = 1), drug rash with eosinophilia and systemic symptoms (DRESS) syndrome (n = 1), and tumor flare (n = 1).
Three patients discontinued treatment because of AEs — thrombocytopenia, tumor flare, and DRESS syndrome.
Tumor flare and response
“We did see tumor flare in two initial patients treated with the higher dose of lenalidomide, and we had to remove them from the study for their safety,” Dr. William said. “One of them had a full-blown DRESS syndrome. For their safety, we did have to remove them, but both did experience durable remissions after.”
One of the patients with tumor flare, who had MF, didn’t require treatment for 6 months after going off study. The other patient, who had SS, cleared the clone from his blood but developed DRESS syndrome.
In all, three patients achieved a response to treatment. The ALCL patient had a complete response, and two MF patients achieved a partial response.
Two MF patients and one SS patient had stable disease. The remaining four patients — two with MF, one with SS, and one with lymphoproliferative disorder — progressed.
QOL
The investigators used the Skindex-16 to assess the effect of treatment on QOL.
Five of six evaluable patients with CTCL had a 50% or greater reduction in their Skindex-16 scores after two cycles of treatment. In fact, most patients had relief from pruritus after one cycle, Dr. William said.
“Patients with cutaneous T-cell lymphoma, their biggest problem is with the symptom burden, with pruritus,” he said. “They’re really miserable from all the itching they have. They cannot sleep at night. So we’re fairly excited that most of the patients we’ve treated so far had relief from pruritus just after one cycle.”
Dr. William said he and his colleagues are excited about the overall results they have observed with BV-len, although it’s “still pretty early” in the trial. The investigators are planning to enroll a total of 42 patients and may open the trial at a second center.
The study is sponsored by Ohio State University and the lenalidomide is provided by Celgene. Dr. William reported relationships with miRagen Therapeutics, GuidePoint, Kyowa Kirin, and Celgene.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. — Treatment with brentuximab vedotin (BV) and lenalidomide (len) may improve quality of life (QOL) for patients with cutaneous T-cell lymphoma (CTCL), according to the principal investigator of a phase 2 trial.

In this small trial, most CTCL patients experienced relief from pruritus after one cycle of treatment with BV-len.
Investigators also observed durable responses to the combination, although two patients experienced tumor flare prior to response.
“Because of the tumor flare, we decreased the dose of lenalidomide ... and, since then, it has not been a major problem,” said Basem M. William, MD, principal investigator of the trial and a professor at Ohio State University in Columbus.
“We’re trying to be more reassuring to patients that, if they experience a little bit of tumor flare, as long as it’s not dangerous or life-threatening, if they can hold on with the treatment, this might translate to a later durable response.”
Dr. William and his colleagues presented results from this ongoing, phase 2 trial (NCT03409432) at the annual T-cell Lymphoma Forum.
Thus far, the investigators have treated 12 patients with relapsed or refractory CTCL or peripheral T-cell lymphoma (PTCL). The CTCL patients had received at least two lines of skin-directed therapy or one line of systemic therapy, and the PTCL patients had received at least one line of systemic therapy.
Dr. William and his colleagues reported results for 10 patients. Six patients had mycosis fungoides (MF), two had Sézary syndrome (SS), one had CD30+ lymphoproliferative disorder, and one had systemic anaplastic large-cell lymphoma (ALCL).
The patients’ median age was 59 (range, 49-74), there were nine males, and patients had received a median of 2 (range, 1-10) prior therapies.
The first seven patients received BV at 1.2 mg/kg and len at 20 mg daily every 3 weeks. However, after the investigators observed tumor flare in two patients, the dose of len was lowered to 10 mg.
Safety
The investigators said all adverse events (AEs) were reversible by stopping therapy, there were no grade 4 AEs, and none of the patients had grade 3 or higher neuropathy.
“We have not seen an excess of neuropathy, which is very important because both brentuximab and lenalidomide are known to cause neuropathy,” Dr. William said. “So we were fairly concerned that there would be a synergistic neurotoxic effect, which we don’t want, but we haven’t seen that.”
The most common treatment-related AE was neutropenia. Grade 3 neutropenia occurred in four patients.
Other grade 3 AEs, which occurred in patients on the 20 mg dose of len, were thrombocytopenia (n = 1), dyspnea (n = 1), vertigo (n = 1), drug rash with eosinophilia and systemic symptoms (DRESS) syndrome (n = 1), and tumor flare (n = 1).
Three patients discontinued treatment because of AEs — thrombocytopenia, tumor flare, and DRESS syndrome.
Tumor flare and response
“We did see tumor flare in two initial patients treated with the higher dose of lenalidomide, and we had to remove them from the study for their safety,” Dr. William said. “One of them had a full-blown DRESS syndrome. For their safety, we did have to remove them, but both did experience durable remissions after.”
One of the patients with tumor flare, who had MF, didn’t require treatment for 6 months after going off study. The other patient, who had SS, cleared the clone from his blood but developed DRESS syndrome.
In all, three patients achieved a response to treatment. The ALCL patient had a complete response, and two MF patients achieved a partial response.
Two MF patients and one SS patient had stable disease. The remaining four patients — two with MF, one with SS, and one with lymphoproliferative disorder — progressed.
QOL
The investigators used the Skindex-16 to assess the effect of treatment on QOL.
Five of six evaluable patients with CTCL had a 50% or greater reduction in their Skindex-16 scores after two cycles of treatment. In fact, most patients had relief from pruritus after one cycle, Dr. William said.
“Patients with cutaneous T-cell lymphoma, their biggest problem is with the symptom burden, with pruritus,” he said. “They’re really miserable from all the itching they have. They cannot sleep at night. So we’re fairly excited that most of the patients we’ve treated so far had relief from pruritus just after one cycle.”
Dr. William said he and his colleagues are excited about the overall results they have observed with BV-len, although it’s “still pretty early” in the trial. The investigators are planning to enroll a total of 42 patients and may open the trial at a second center.
The study is sponsored by Ohio State University and the lenalidomide is provided by Celgene. Dr. William reported relationships with miRagen Therapeutics, GuidePoint, Kyowa Kirin, and Celgene.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
REPORTING FROM TCLF 2019
Key clinical point:
Major finding: Five of six evaluable CTCL patients had a 50% or greater reduction in their Skindex-16 scores after two cycles of treatment.
Study details: A phase 2 study with results reported for 10 patients.
Disclosures: The study is sponsored by Ohio State University and the lenalidomide is provided by Celgene. The principal investigator reported relationships with miRagen Therapeutics, GuidePoint, Kyowa Kirin, and Celgene.
Are single agents better than chemo for relapsed/refractory PTCL?
LA JOLLA, CALIF. — Results from the COMPLETE registry suggest newer single agents may be more effective than combination chemotherapy for patients with relapsed/refractory peripheral T-cell lymphoma (PTCL).
Complete response (CR) rates and median survival times were significantly better among patients who received single agents than among those who received combination therapy.
Although researchers don’t know what is driving these differences in outcomes, they did find that outcomes were best among patients who received single-agent brentuximab vedotin (BV), and a disproportionate number of patients received BV.
The researchers also found that patients who received single-agent therapy were more likely to proceed to stem cell transplant.
Therefore, it’s still unclear if single-agent treatment is superior to combination therapy for relapsed/refractory PTCL, according to Robert Stuver, MD, of Beth Israel Deaconess Medical Center in Boston.
Dr. Stuver presented data from the COMPLETE (Comprehensive Oncology Measures for Peripheral T-cell Lymphoma Treatment) registry at the annual T-cell Lymphoma Forum.
The registry (NCT01110733) enrolled patients newly diagnosed with PTCL. Dr. Stuver presented results among patients who had relapsed after, or were refractory to, upfront therapy and went on to receive single-agent therapy or any combination regimen excluding those single agents. Outcome data were collected for 5 years or until death.
Patients and treatment
There were 26 patients in the combination treatment group — 10 with PTCL not otherwise specified (NOS), 6 with angioimmunoblastic T-cell lymphoma (AITL), 5 with natural killer T-cell lymphoma (NKTL), 3 with anaplastic large-cell lymphoma (ALCL), 1 with enteropathy-associated T-cell lymphoma (EATL), and 1 with hepatosplenic T-cell lymphoma (HSTCL).
Patients in the combination group received gemcitabine-based therapy (n = 10), ifosfamide-based therapy (n = 7), platinum-based therapy (n = 4), CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone)-like therapy (n = 1), DHAP (dexamethasone, high-dose cytarabine, and cisplatin; n = 1), and other combinations (n = 3).
There were 31 patients in the single-agent group – 13 with PTCL-NOS, 7 with ALCL, 5 with AITL, 2 with EATL, 2 with NKTL, and 2 with HSTCL.
These patients were treated with BV (n = 12), romidepsin (n = 8), pralatrexate (n = 5), alisertib (n = 3), bendamustine (n = 1), denileukin diftitox (n = 1), and lenalidomide (n = 1).
Response
The CR rates were significantly higher among patients who received single-agent treatment than among those who received combination therapy — 41.4% (12/31) and 19.2% (5/26), respectively (P = .02). The partial response rates were 17.2% (5/31) and 26.9% (7/26), respectively. Rates of stable disease were 3.4% (1/31) and 30.8% (8/26), respectively.
Complete responders in the single-agent arm were treated with BV (n = 7), romidepsin (n = 2), pralatrexate (n = 1), alisertib (n = 1), and bendamustine (n = 1). Four of the patients treated with BV had ALCL.
“We had an enrichment of patients treated with brentuximab,” Dr. Stuver said. “So the obvious question this begs is, ‘Are the favorable results that were seen for single agents over combination therapy solely due to patients treated with brentuximab?’ ”
To investigate, Dr. Stuver and his colleagues compared responses among patients who received BV with patients who received other single agents or combination therapies.
The CR rate was 58.3% (7/12) among BV recipients, 29.4% (5/17) among patients who received other single agents, and 19.2% (5/26) among patients who received combination therapy.
“The takeaway here is that, when you do divide the single-agent group into BV and other single agents, you’re seeing that BV is doing much better than every other group,” Dr. Stuver said. “And all the other single agents are doing somewhat similarly to the combination group, although there’s still a 10% difference, 29% versus 19%.”
Survival
The median progression-free survival (PFS) and overall survival (OS) were significantly better among patients who received single-agent therapy. The median PFS was 11.7 months in the single-agent group and 6.7 months in the combination group (P = .0197). The median OS was 38.9 months and 17.1 months, respectively (P = .0170).
A factor that may have affected survival is that patients were more likely to undergo stem cell transplant after single-agent therapy (25.8%, 8/31), compared with those who had received combination therapy (7.7%, 2/26).
Another factor that may have affected the survival differences is the enrichment of patients treated with BV.
The researchers found the median PFS was 11.9 months among BV recipients, 10.4 months among patients who received other single agents, and 6.7 months in the combination-therapy group. The median OS was 44.5 months, 19.1 months, and 17.1 months, respectively.
Dr. Stuver said these results suggest there is a role for single agents as first retreatment in the salvage setting. However, this analysis was limited by the small sample size and the enrichment of patients treated with BV.
Larger, randomized studies are needed to identify the “truly superior” treatment strategy for relapsed/refractory PTCL, Dr. Stuver said.
The COMPLETE registry is sponsored by Spectrum Pharmaceuticals. Dr. Stuver did not declare any conflicts of interest.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. — Results from the COMPLETE registry suggest newer single agents may be more effective than combination chemotherapy for patients with relapsed/refractory peripheral T-cell lymphoma (PTCL).
Complete response (CR) rates and median survival times were significantly better among patients who received single agents than among those who received combination therapy.
Although researchers don’t know what is driving these differences in outcomes, they did find that outcomes were best among patients who received single-agent brentuximab vedotin (BV), and a disproportionate number of patients received BV.
The researchers also found that patients who received single-agent therapy were more likely to proceed to stem cell transplant.
Therefore, it’s still unclear if single-agent treatment is superior to combination therapy for relapsed/refractory PTCL, according to Robert Stuver, MD, of Beth Israel Deaconess Medical Center in Boston.
Dr. Stuver presented data from the COMPLETE (Comprehensive Oncology Measures for Peripheral T-cell Lymphoma Treatment) registry at the annual T-cell Lymphoma Forum.
The registry (NCT01110733) enrolled patients newly diagnosed with PTCL. Dr. Stuver presented results among patients who had relapsed after, or were refractory to, upfront therapy and went on to receive single-agent therapy or any combination regimen excluding those single agents. Outcome data were collected for 5 years or until death.
Patients and treatment
There were 26 patients in the combination treatment group — 10 with PTCL not otherwise specified (NOS), 6 with angioimmunoblastic T-cell lymphoma (AITL), 5 with natural killer T-cell lymphoma (NKTL), 3 with anaplastic large-cell lymphoma (ALCL), 1 with enteropathy-associated T-cell lymphoma (EATL), and 1 with hepatosplenic T-cell lymphoma (HSTCL).
Patients in the combination group received gemcitabine-based therapy (n = 10), ifosfamide-based therapy (n = 7), platinum-based therapy (n = 4), CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone)-like therapy (n = 1), DHAP (dexamethasone, high-dose cytarabine, and cisplatin; n = 1), and other combinations (n = 3).
There were 31 patients in the single-agent group – 13 with PTCL-NOS, 7 with ALCL, 5 with AITL, 2 with EATL, 2 with NKTL, and 2 with HSTCL.
These patients were treated with BV (n = 12), romidepsin (n = 8), pralatrexate (n = 5), alisertib (n = 3), bendamustine (n = 1), denileukin diftitox (n = 1), and lenalidomide (n = 1).
Response
The CR rates were significantly higher among patients who received single-agent treatment than among those who received combination therapy — 41.4% (12/31) and 19.2% (5/26), respectively (P = .02). The partial response rates were 17.2% (5/31) and 26.9% (7/26), respectively. Rates of stable disease were 3.4% (1/31) and 30.8% (8/26), respectively.
Complete responders in the single-agent arm were treated with BV (n = 7), romidepsin (n = 2), pralatrexate (n = 1), alisertib (n = 1), and bendamustine (n = 1). Four of the patients treated with BV had ALCL.
“We had an enrichment of patients treated with brentuximab,” Dr. Stuver said. “So the obvious question this begs is, ‘Are the favorable results that were seen for single agents over combination therapy solely due to patients treated with brentuximab?’ ”
To investigate, Dr. Stuver and his colleagues compared responses among patients who received BV with patients who received other single agents or combination therapies.
The CR rate was 58.3% (7/12) among BV recipients, 29.4% (5/17) among patients who received other single agents, and 19.2% (5/26) among patients who received combination therapy.
“The takeaway here is that, when you do divide the single-agent group into BV and other single agents, you’re seeing that BV is doing much better than every other group,” Dr. Stuver said. “And all the other single agents are doing somewhat similarly to the combination group, although there’s still a 10% difference, 29% versus 19%.”
Survival
The median progression-free survival (PFS) and overall survival (OS) were significantly better among patients who received single-agent therapy. The median PFS was 11.7 months in the single-agent group and 6.7 months in the combination group (P = .0197). The median OS was 38.9 months and 17.1 months, respectively (P = .0170).
A factor that may have affected survival is that patients were more likely to undergo stem cell transplant after single-agent therapy (25.8%, 8/31), compared with those who had received combination therapy (7.7%, 2/26).
Another factor that may have affected the survival differences is the enrichment of patients treated with BV.
The researchers found the median PFS was 11.9 months among BV recipients, 10.4 months among patients who received other single agents, and 6.7 months in the combination-therapy group. The median OS was 44.5 months, 19.1 months, and 17.1 months, respectively.
Dr. Stuver said these results suggest there is a role for single agents as first retreatment in the salvage setting. However, this analysis was limited by the small sample size and the enrichment of patients treated with BV.
Larger, randomized studies are needed to identify the “truly superior” treatment strategy for relapsed/refractory PTCL, Dr. Stuver said.
The COMPLETE registry is sponsored by Spectrum Pharmaceuticals. Dr. Stuver did not declare any conflicts of interest.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. — Results from the COMPLETE registry suggest newer single agents may be more effective than combination chemotherapy for patients with relapsed/refractory peripheral T-cell lymphoma (PTCL).
Complete response (CR) rates and median survival times were significantly better among patients who received single agents than among those who received combination therapy.
Although researchers don’t know what is driving these differences in outcomes, they did find that outcomes were best among patients who received single-agent brentuximab vedotin (BV), and a disproportionate number of patients received BV.
The researchers also found that patients who received single-agent therapy were more likely to proceed to stem cell transplant.
Therefore, it’s still unclear if single-agent treatment is superior to combination therapy for relapsed/refractory PTCL, according to Robert Stuver, MD, of Beth Israel Deaconess Medical Center in Boston.
Dr. Stuver presented data from the COMPLETE (Comprehensive Oncology Measures for Peripheral T-cell Lymphoma Treatment) registry at the annual T-cell Lymphoma Forum.
The registry (NCT01110733) enrolled patients newly diagnosed with PTCL. Dr. Stuver presented results among patients who had relapsed after, or were refractory to, upfront therapy and went on to receive single-agent therapy or any combination regimen excluding those single agents. Outcome data were collected for 5 years or until death.
Patients and treatment
There were 26 patients in the combination treatment group — 10 with PTCL not otherwise specified (NOS), 6 with angioimmunoblastic T-cell lymphoma (AITL), 5 with natural killer T-cell lymphoma (NKTL), 3 with anaplastic large-cell lymphoma (ALCL), 1 with enteropathy-associated T-cell lymphoma (EATL), and 1 with hepatosplenic T-cell lymphoma (HSTCL).
Patients in the combination group received gemcitabine-based therapy (n = 10), ifosfamide-based therapy (n = 7), platinum-based therapy (n = 4), CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone)-like therapy (n = 1), DHAP (dexamethasone, high-dose cytarabine, and cisplatin; n = 1), and other combinations (n = 3).
There were 31 patients in the single-agent group – 13 with PTCL-NOS, 7 with ALCL, 5 with AITL, 2 with EATL, 2 with NKTL, and 2 with HSTCL.
These patients were treated with BV (n = 12), romidepsin (n = 8), pralatrexate (n = 5), alisertib (n = 3), bendamustine (n = 1), denileukin diftitox (n = 1), and lenalidomide (n = 1).
Response
The CR rates were significantly higher among patients who received single-agent treatment than among those who received combination therapy — 41.4% (12/31) and 19.2% (5/26), respectively (P = .02). The partial response rates were 17.2% (5/31) and 26.9% (7/26), respectively. Rates of stable disease were 3.4% (1/31) and 30.8% (8/26), respectively.
Complete responders in the single-agent arm were treated with BV (n = 7), romidepsin (n = 2), pralatrexate (n = 1), alisertib (n = 1), and bendamustine (n = 1). Four of the patients treated with BV had ALCL.
“We had an enrichment of patients treated with brentuximab,” Dr. Stuver said. “So the obvious question this begs is, ‘Are the favorable results that were seen for single agents over combination therapy solely due to patients treated with brentuximab?’ ”
To investigate, Dr. Stuver and his colleagues compared responses among patients who received BV with patients who received other single agents or combination therapies.
The CR rate was 58.3% (7/12) among BV recipients, 29.4% (5/17) among patients who received other single agents, and 19.2% (5/26) among patients who received combination therapy.
“The takeaway here is that, when you do divide the single-agent group into BV and other single agents, you’re seeing that BV is doing much better than every other group,” Dr. Stuver said. “And all the other single agents are doing somewhat similarly to the combination group, although there’s still a 10% difference, 29% versus 19%.”
Survival
The median progression-free survival (PFS) and overall survival (OS) were significantly better among patients who received single-agent therapy. The median PFS was 11.7 months in the single-agent group and 6.7 months in the combination group (P = .0197). The median OS was 38.9 months and 17.1 months, respectively (P = .0170).
A factor that may have affected survival is that patients were more likely to undergo stem cell transplant after single-agent therapy (25.8%, 8/31), compared with those who had received combination therapy (7.7%, 2/26).
Another factor that may have affected the survival differences is the enrichment of patients treated with BV.
The researchers found the median PFS was 11.9 months among BV recipients, 10.4 months among patients who received other single agents, and 6.7 months in the combination-therapy group. The median OS was 44.5 months, 19.1 months, and 17.1 months, respectively.
Dr. Stuver said these results suggest there is a role for single agents as first retreatment in the salvage setting. However, this analysis was limited by the small sample size and the enrichment of patients treated with BV.
Larger, randomized studies are needed to identify the “truly superior” treatment strategy for relapsed/refractory PTCL, Dr. Stuver said.
The COMPLETE registry is sponsored by Spectrum Pharmaceuticals. Dr. Stuver did not declare any conflicts of interest.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
REPORTING FROM TCLF 2019
Key clinical point:
Major finding: The complete response rate was significantly higher among patients who received single-agent treatment than it was among those who received combination therapy – 41.4% and 19.2%, respectively (P = .02).
Study details: Analysis of 57 patients with relapsed/refractory PTCL in the COMPLETE registry.
Disclosures: The COMPLETE registry is sponsored by Spectrum Pharmaceuticals. Dr. Stuver did not declare any conflicts of interest.
Management of hypertensive disorders in pregnancy
In the last installment of the Master Class, I addressed the importance of clarity in the classification of hypertensive disorders in pregnancy, and proposed several key diagnostic definitions. Here, I address the management of “mild” gestational hypertension (GHTN) and preeclampsia without severe features, which I believe should be managed similarly. I also address the management of preeclampsia with severe features, and I share an algorithm that I have developed and fine-tuned over the years to control acute severe hypertension with the use of intravenous labetalol, intravenous hydralazine, or oral nifedipine.
Management of “mild” gestational hypertension/Preeclampsia without severe features
Mild gestational hypertension in and of itself has little effect on maternal or perinatal morbidity and mortality when it develops at or beyond 37 weeks’ gestation. However, approximately 40% of patients diagnosed with preterm GHTN will subsequently develop preeclampsia or progress to severe GHTN. In addition, these pregnancies may result in fetal growth restriction and placental abruption.
Antihypertensive drugs should not be used during ambulatory management of women with GHTN. Patients who receive antihypertensive therapy, including those diagnosed with severe GHTN, should be hospitalized and initially treated as having preeclampsia with or without severe features. Subsequent management will depend on initial response to therapy, blood pressure values after treatment, gestational age, and laboratory findings.
Preeclampsia without severe features is usually managed as in those with GHTN. (See related figure.) 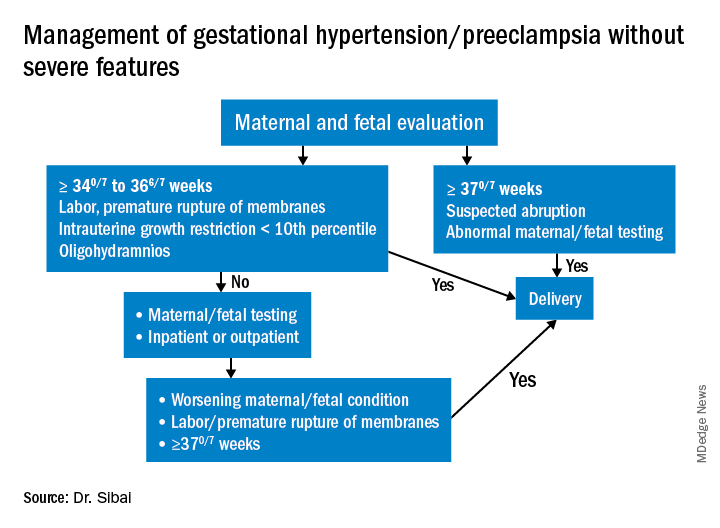
Close surveillance is warranted, as either type may progress to fulminant disease. Maternal surveillance should include blood pressure measurements twice per week, and CBC, liver enzymes, and serum creatinine measurements once every week. Patients also should be instructed to immediately report any of these symptoms: Persistent severe headaches; right upper quadrant or epigastric pain, nausea, and vomiting; scotomata, blurred vision, photophobia, or double vision; shortness of breath or orthopnea; altered mental changes; decreased fetal movement; rupture of membranes; vaginal bleeding; or regular uterine contractions.
Fetal evaluation for patients with GHTN/preeclampsia includes ultrasound at the time of diagnosis for evaluation of fetal growth and amniotic fluid value (deepest vertical pocket, or DVP) as well as fetal movement count and non-stress testing (NST). Subsequently, NST and DVP need to be checked twice per week. A decision for delivery will depend on gestational age, fetal status, and development of severe disease.
Management of preeclampsia with severe features
Any patient who has preeclampsia with severe features should be admitted and initially observed in a labor and delivery unit. (See related figure.) 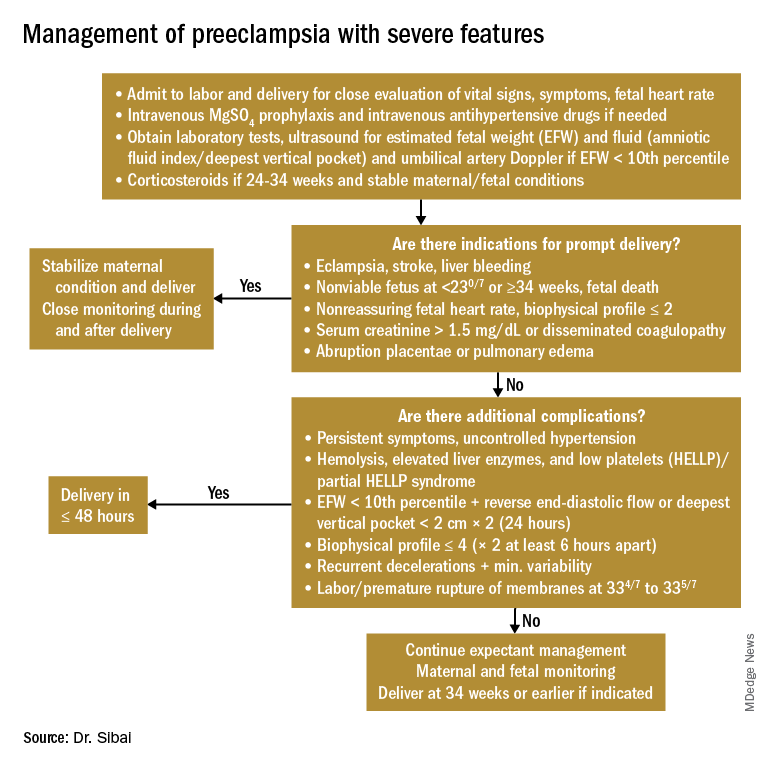
Initial workup should include assessment for fetal well-being, monitoring of maternal blood pressure and symptomatology, and laboratory evaluation. Laboratory assessment should include hematocrit, platelet count, serum creatinine, and aspartate aminotransferase (AST). An ultrasound for fetal growth and amniotic fluid index/DVP also should be obtained. Candidates for expectant management should be carefully selected, counseled regarding its risks and benefits, and managed only at tertiary care hospitals.
Fetal well-being should be assessed on a daily basis by NST and on a weekly basis with amniotic fluid/DVP determination. An ultrasound for fetal growth should be performed every 2-3 weeks. Maternal laboratory evaluation should be done daily or every other day. If the patient maintains a stable maternal and fetal course, she may be expectantly managed until 34 weeks. Worsening maternal or fetal status warrants delivery, regardless of gestational age.
Maternal blood pressure (BP) control is essential with expectant management or during delivery. Medications can be given orally or intravenously, as necessary, to maintain a systolic BP of 140-150 mm Hg and a diastolic BP of 90-100 mm Hg. The most commonly used intravenous medications for this purpose are labetalol and hydralazine. Other medications can include oral rapid-acting nifedipine. Subsequent management can include oral medications such as labetalol and long-acting nifedipine. Care should be taken not to drop the blood pressure too rapidly to avoid reduced renal and placental perfusion.
A trial of labor is indicated in patients with severe preeclampsia if gestational age is greater than 30 weeks and/or if cervical Bishop Score is greater than or equal to 6. However, an appropriate time frame should be established regarding achievement of active labor.
Patients should be closely monitored for at least 24 hours post partum. Post partum eclampsia occurs in 30% of patients; thus, women who are receiving magnesium sulfate should continue it for 24 hours after delivery. In addition, women with preeclampsia who are receiving magnesium sulfate are at risk for postpartum hemorrhage due to uterine atony and should be managed accordingly.
Some patients with severe preeclampsia also are at risk for pulmonary edema and exacerbation of severe hypertension 3-5 days post partum. Therefore, all patients should receive frequent monitoring of intake and output.
Control of acute severe hypertension antepartum, in labor, or post partum
Uncontrolled severe hypertension for several hours may be associated with stroke and pulmonary edema. Therefore, several guidelines recommend initiation of antihypertensive medications for acute lowering of maternal blood pressure within 30-60 minutes. Several antihypertensive agents are available for the control of sustained severe hypertension before, during, and after delivery. It is important to be familiar with the maternal and fetal side effects, as well as mode of action of each agent, to select the best one. Antihypertensive agents can exert an effect by decreasing cardiac output, peripheral vascular resistance, and central blood pressure, or by inhibiting angiotensin production. Indications for therapy and commonly used drugs in pregnancy are listed in the accompanying table.
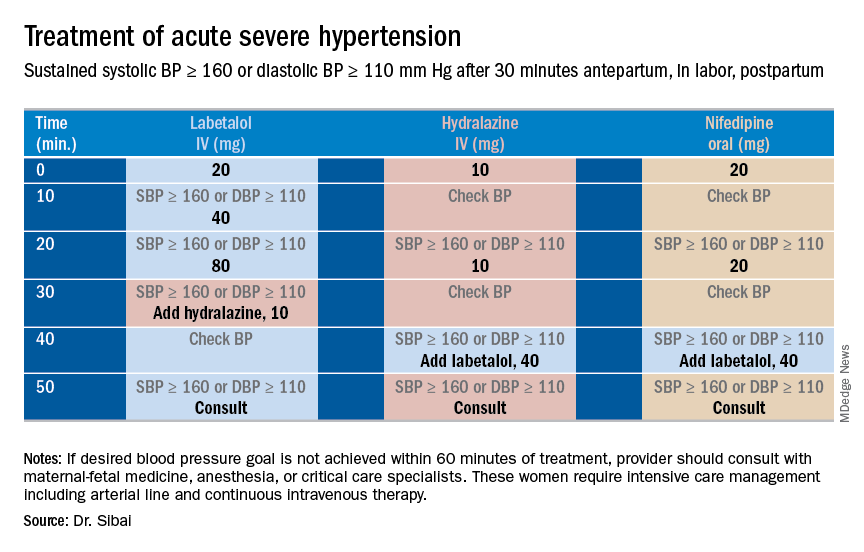
Several trials have compared the efficacy and side effects of intravenous bolus injections of hydralazine to either IV labetalol or oral rapid-acting nifedipine as well as oral nifedipine to IV labetalol. The results of these studies suggest that any of these three medications can be used to treat severe hypertension in pregnancy as long as the physician is familiar with the doses to be used, the expected onset of action, and potential side effects.
Because both hydralazine and nifedipine are associated with tachycardia, it is recommended that these agents not be used in patients with a heart rate above 105-110 beats per minute (bpm). It also is important to be attentive to patients with generalized swelling and/or hemoconcentration (hematocrit great than or equal to 40%), as these patients usually have marked reduction in plasma volume and can develop an excessive hypotensive response, with secondary reduction in tissue perfusion and uteroplacental blood flow, when treated with a combination of rapid-acting vasodilators (hydralazine or nifedipine). Such patients may require a bolus infusion of 250-500 mL of isotonic saline prior to the administration of vasodilators. In these patients, labetalol may be the appropriate drug to use.
Labetalol should be avoided in patients with bradycardia (heart rate less than 60 bpm), in those with moderate to severe asthma, and in those with heart failure. In these patients, either hydralazine or nifedipine is the drug of choice. If an intravenous access is not available or difficult to obtain, oral nifedipine should be the drug of choice. In addition, because nifedipine is associated with improved renal blood flow with resultant increase in urine output, it is the drug of choice for treatment in those with decreased urine output, and for treatment of severe hypertension in the postpartum period.
In a third and final installment, I will elaborate on the postpartum management of women who have experienced hypertension with or without associated symptoms. Recently, postpartum hypertension has become a major cause of hospital readmission, as well as severe maternal morbidity and mortality.
Dr. Sibai is professor of obstetrics, gynecology, and reproductive sciences at the University of Texas McGovern Medical School, Houston.
In the last installment of the Master Class, I addressed the importance of clarity in the classification of hypertensive disorders in pregnancy, and proposed several key diagnostic definitions. Here, I address the management of “mild” gestational hypertension (GHTN) and preeclampsia without severe features, which I believe should be managed similarly. I also address the management of preeclampsia with severe features, and I share an algorithm that I have developed and fine-tuned over the years to control acute severe hypertension with the use of intravenous labetalol, intravenous hydralazine, or oral nifedipine.
Management of “mild” gestational hypertension/Preeclampsia without severe features
Mild gestational hypertension in and of itself has little effect on maternal or perinatal morbidity and mortality when it develops at or beyond 37 weeks’ gestation. However, approximately 40% of patients diagnosed with preterm GHTN will subsequently develop preeclampsia or progress to severe GHTN. In addition, these pregnancies may result in fetal growth restriction and placental abruption.
Antihypertensive drugs should not be used during ambulatory management of women with GHTN. Patients who receive antihypertensive therapy, including those diagnosed with severe GHTN, should be hospitalized and initially treated as having preeclampsia with or without severe features. Subsequent management will depend on initial response to therapy, blood pressure values after treatment, gestational age, and laboratory findings.
Preeclampsia without severe features is usually managed as in those with GHTN. (See related figure.) 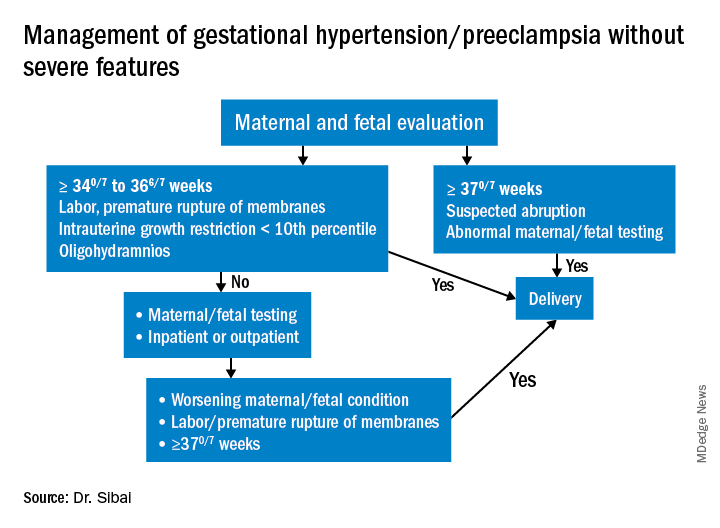
Close surveillance is warranted, as either type may progress to fulminant disease. Maternal surveillance should include blood pressure measurements twice per week, and CBC, liver enzymes, and serum creatinine measurements once every week. Patients also should be instructed to immediately report any of these symptoms: Persistent severe headaches; right upper quadrant or epigastric pain, nausea, and vomiting; scotomata, blurred vision, photophobia, or double vision; shortness of breath or orthopnea; altered mental changes; decreased fetal movement; rupture of membranes; vaginal bleeding; or regular uterine contractions.
Fetal evaluation for patients with GHTN/preeclampsia includes ultrasound at the time of diagnosis for evaluation of fetal growth and amniotic fluid value (deepest vertical pocket, or DVP) as well as fetal movement count and non-stress testing (NST). Subsequently, NST and DVP need to be checked twice per week. A decision for delivery will depend on gestational age, fetal status, and development of severe disease.
Management of preeclampsia with severe features
Any patient who has preeclampsia with severe features should be admitted and initially observed in a labor and delivery unit. (See related figure.) 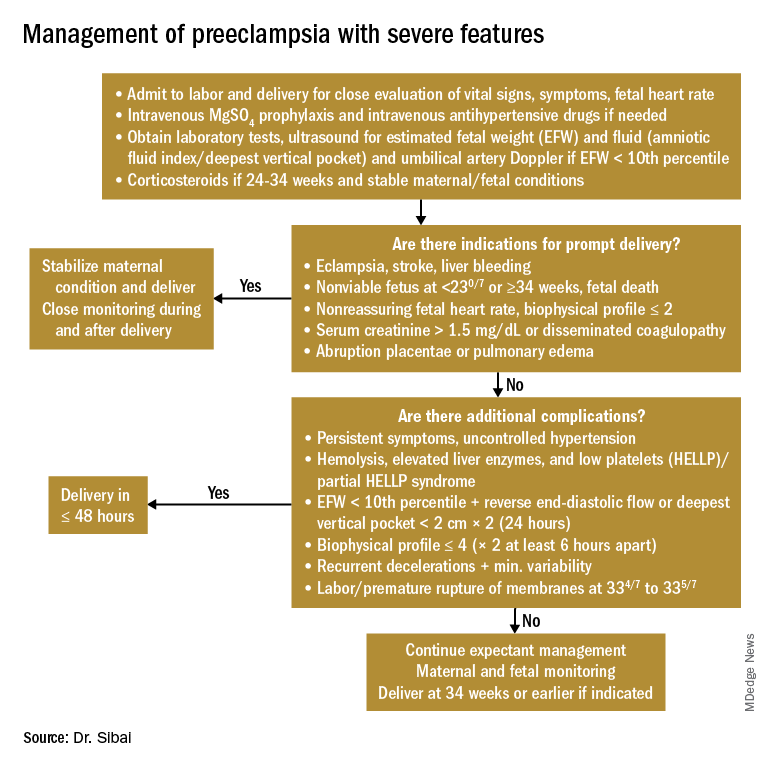
Initial workup should include assessment for fetal well-being, monitoring of maternal blood pressure and symptomatology, and laboratory evaluation. Laboratory assessment should include hematocrit, platelet count, serum creatinine, and aspartate aminotransferase (AST). An ultrasound for fetal growth and amniotic fluid index/DVP also should be obtained. Candidates for expectant management should be carefully selected, counseled regarding its risks and benefits, and managed only at tertiary care hospitals.
Fetal well-being should be assessed on a daily basis by NST and on a weekly basis with amniotic fluid/DVP determination. An ultrasound for fetal growth should be performed every 2-3 weeks. Maternal laboratory evaluation should be done daily or every other day. If the patient maintains a stable maternal and fetal course, she may be expectantly managed until 34 weeks. Worsening maternal or fetal status warrants delivery, regardless of gestational age.
Maternal blood pressure (BP) control is essential with expectant management or during delivery. Medications can be given orally or intravenously, as necessary, to maintain a systolic BP of 140-150 mm Hg and a diastolic BP of 90-100 mm Hg. The most commonly used intravenous medications for this purpose are labetalol and hydralazine. Other medications can include oral rapid-acting nifedipine. Subsequent management can include oral medications such as labetalol and long-acting nifedipine. Care should be taken not to drop the blood pressure too rapidly to avoid reduced renal and placental perfusion.
A trial of labor is indicated in patients with severe preeclampsia if gestational age is greater than 30 weeks and/or if cervical Bishop Score is greater than or equal to 6. However, an appropriate time frame should be established regarding achievement of active labor.
Patients should be closely monitored for at least 24 hours post partum. Post partum eclampsia occurs in 30% of patients; thus, women who are receiving magnesium sulfate should continue it for 24 hours after delivery. In addition, women with preeclampsia who are receiving magnesium sulfate are at risk for postpartum hemorrhage due to uterine atony and should be managed accordingly.
Some patients with severe preeclampsia also are at risk for pulmonary edema and exacerbation of severe hypertension 3-5 days post partum. Therefore, all patients should receive frequent monitoring of intake and output.
Control of acute severe hypertension antepartum, in labor, or post partum
Uncontrolled severe hypertension for several hours may be associated with stroke and pulmonary edema. Therefore, several guidelines recommend initiation of antihypertensive medications for acute lowering of maternal blood pressure within 30-60 minutes. Several antihypertensive agents are available for the control of sustained severe hypertension before, during, and after delivery. It is important to be familiar with the maternal and fetal side effects, as well as mode of action of each agent, to select the best one. Antihypertensive agents can exert an effect by decreasing cardiac output, peripheral vascular resistance, and central blood pressure, or by inhibiting angiotensin production. Indications for therapy and commonly used drugs in pregnancy are listed in the accompanying table.
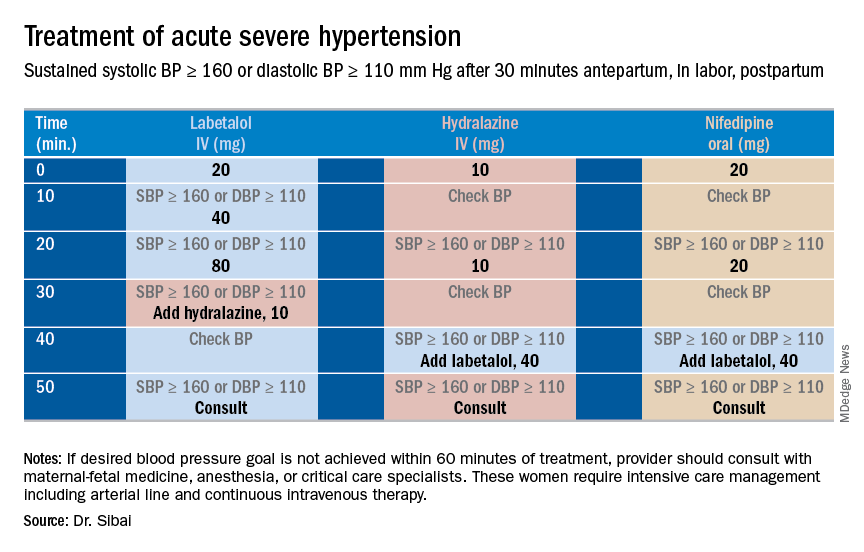
Several trials have compared the efficacy and side effects of intravenous bolus injections of hydralazine to either IV labetalol or oral rapid-acting nifedipine as well as oral nifedipine to IV labetalol. The results of these studies suggest that any of these three medications can be used to treat severe hypertension in pregnancy as long as the physician is familiar with the doses to be used, the expected onset of action, and potential side effects.
Because both hydralazine and nifedipine are associated with tachycardia, it is recommended that these agents not be used in patients with a heart rate above 105-110 beats per minute (bpm). It also is important to be attentive to patients with generalized swelling and/or hemoconcentration (hematocrit great than or equal to 40%), as these patients usually have marked reduction in plasma volume and can develop an excessive hypotensive response, with secondary reduction in tissue perfusion and uteroplacental blood flow, when treated with a combination of rapid-acting vasodilators (hydralazine or nifedipine). Such patients may require a bolus infusion of 250-500 mL of isotonic saline prior to the administration of vasodilators. In these patients, labetalol may be the appropriate drug to use.
Labetalol should be avoided in patients with bradycardia (heart rate less than 60 bpm), in those with moderate to severe asthma, and in those with heart failure. In these patients, either hydralazine or nifedipine is the drug of choice. If an intravenous access is not available or difficult to obtain, oral nifedipine should be the drug of choice. In addition, because nifedipine is associated with improved renal blood flow with resultant increase in urine output, it is the drug of choice for treatment in those with decreased urine output, and for treatment of severe hypertension in the postpartum period.
In a third and final installment, I will elaborate on the postpartum management of women who have experienced hypertension with or without associated symptoms. Recently, postpartum hypertension has become a major cause of hospital readmission, as well as severe maternal morbidity and mortality.
Dr. Sibai is professor of obstetrics, gynecology, and reproductive sciences at the University of Texas McGovern Medical School, Houston.
In the last installment of the Master Class, I addressed the importance of clarity in the classification of hypertensive disorders in pregnancy, and proposed several key diagnostic definitions. Here, I address the management of “mild” gestational hypertension (GHTN) and preeclampsia without severe features, which I believe should be managed similarly. I also address the management of preeclampsia with severe features, and I share an algorithm that I have developed and fine-tuned over the years to control acute severe hypertension with the use of intravenous labetalol, intravenous hydralazine, or oral nifedipine.
Management of “mild” gestational hypertension/Preeclampsia without severe features
Mild gestational hypertension in and of itself has little effect on maternal or perinatal morbidity and mortality when it develops at or beyond 37 weeks’ gestation. However, approximately 40% of patients diagnosed with preterm GHTN will subsequently develop preeclampsia or progress to severe GHTN. In addition, these pregnancies may result in fetal growth restriction and placental abruption.
Antihypertensive drugs should not be used during ambulatory management of women with GHTN. Patients who receive antihypertensive therapy, including those diagnosed with severe GHTN, should be hospitalized and initially treated as having preeclampsia with or without severe features. Subsequent management will depend on initial response to therapy, blood pressure values after treatment, gestational age, and laboratory findings.
Preeclampsia without severe features is usually managed as in those with GHTN. (See related figure.) 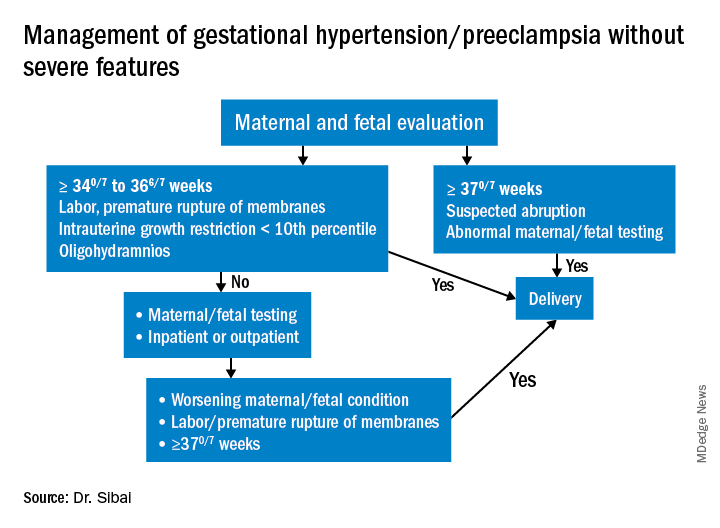
Close surveillance is warranted, as either type may progress to fulminant disease. Maternal surveillance should include blood pressure measurements twice per week, and CBC, liver enzymes, and serum creatinine measurements once every week. Patients also should be instructed to immediately report any of these symptoms: Persistent severe headaches; right upper quadrant or epigastric pain, nausea, and vomiting; scotomata, blurred vision, photophobia, or double vision; shortness of breath or orthopnea; altered mental changes; decreased fetal movement; rupture of membranes; vaginal bleeding; or regular uterine contractions.
Fetal evaluation for patients with GHTN/preeclampsia includes ultrasound at the time of diagnosis for evaluation of fetal growth and amniotic fluid value (deepest vertical pocket, or DVP) as well as fetal movement count and non-stress testing (NST). Subsequently, NST and DVP need to be checked twice per week. A decision for delivery will depend on gestational age, fetal status, and development of severe disease.
Management of preeclampsia with severe features
Any patient who has preeclampsia with severe features should be admitted and initially observed in a labor and delivery unit. (See related figure.) 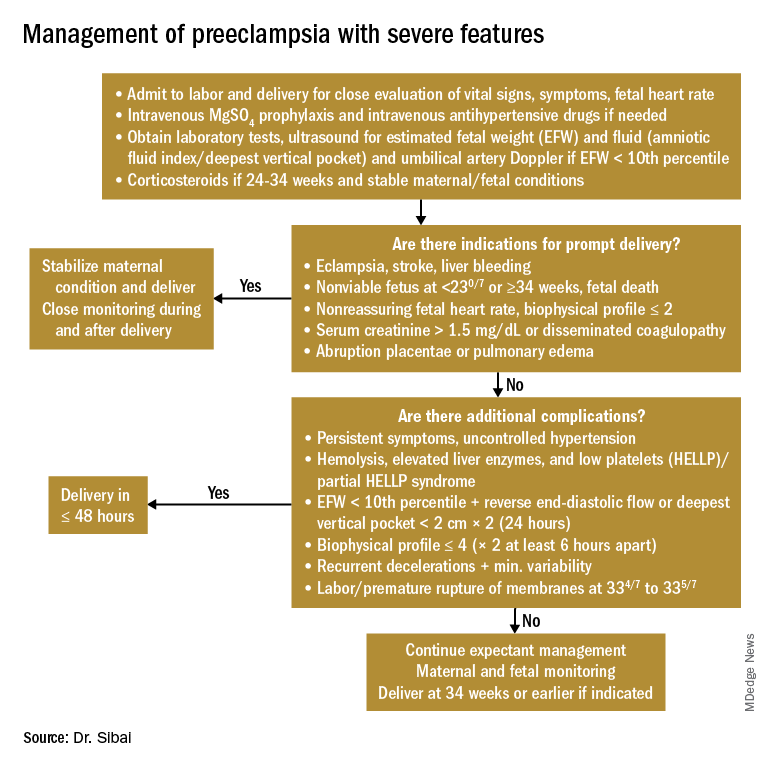
Initial workup should include assessment for fetal well-being, monitoring of maternal blood pressure and symptomatology, and laboratory evaluation. Laboratory assessment should include hematocrit, platelet count, serum creatinine, and aspartate aminotransferase (AST). An ultrasound for fetal growth and amniotic fluid index/DVP also should be obtained. Candidates for expectant management should be carefully selected, counseled regarding its risks and benefits, and managed only at tertiary care hospitals.
Fetal well-being should be assessed on a daily basis by NST and on a weekly basis with amniotic fluid/DVP determination. An ultrasound for fetal growth should be performed every 2-3 weeks. Maternal laboratory evaluation should be done daily or every other day. If the patient maintains a stable maternal and fetal course, she may be expectantly managed until 34 weeks. Worsening maternal or fetal status warrants delivery, regardless of gestational age.
Maternal blood pressure (BP) control is essential with expectant management or during delivery. Medications can be given orally or intravenously, as necessary, to maintain a systolic BP of 140-150 mm Hg and a diastolic BP of 90-100 mm Hg. The most commonly used intravenous medications for this purpose are labetalol and hydralazine. Other medications can include oral rapid-acting nifedipine. Subsequent management can include oral medications such as labetalol and long-acting nifedipine. Care should be taken not to drop the blood pressure too rapidly to avoid reduced renal and placental perfusion.
A trial of labor is indicated in patients with severe preeclampsia if gestational age is greater than 30 weeks and/or if cervical Bishop Score is greater than or equal to 6. However, an appropriate time frame should be established regarding achievement of active labor.
Patients should be closely monitored for at least 24 hours post partum. Post partum eclampsia occurs in 30% of patients; thus, women who are receiving magnesium sulfate should continue it for 24 hours after delivery. In addition, women with preeclampsia who are receiving magnesium sulfate are at risk for postpartum hemorrhage due to uterine atony and should be managed accordingly.
Some patients with severe preeclampsia also are at risk for pulmonary edema and exacerbation of severe hypertension 3-5 days post partum. Therefore, all patients should receive frequent monitoring of intake and output.
Control of acute severe hypertension antepartum, in labor, or post partum
Uncontrolled severe hypertension for several hours may be associated with stroke and pulmonary edema. Therefore, several guidelines recommend initiation of antihypertensive medications for acute lowering of maternal blood pressure within 30-60 minutes. Several antihypertensive agents are available for the control of sustained severe hypertension before, during, and after delivery. It is important to be familiar with the maternal and fetal side effects, as well as mode of action of each agent, to select the best one. Antihypertensive agents can exert an effect by decreasing cardiac output, peripheral vascular resistance, and central blood pressure, or by inhibiting angiotensin production. Indications for therapy and commonly used drugs in pregnancy are listed in the accompanying table.
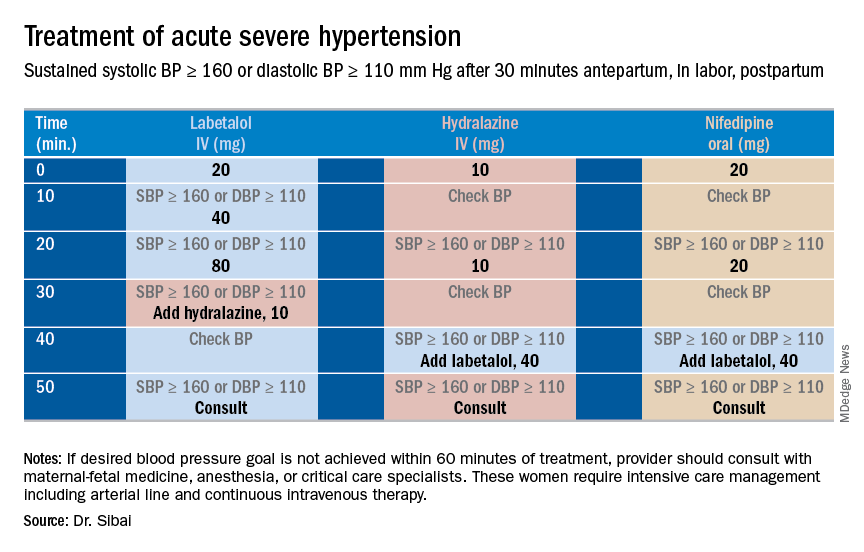
Several trials have compared the efficacy and side effects of intravenous bolus injections of hydralazine to either IV labetalol or oral rapid-acting nifedipine as well as oral nifedipine to IV labetalol. The results of these studies suggest that any of these three medications can be used to treat severe hypertension in pregnancy as long as the physician is familiar with the doses to be used, the expected onset of action, and potential side effects.
Because both hydralazine and nifedipine are associated with tachycardia, it is recommended that these agents not be used in patients with a heart rate above 105-110 beats per minute (bpm). It also is important to be attentive to patients with generalized swelling and/or hemoconcentration (hematocrit great than or equal to 40%), as these patients usually have marked reduction in plasma volume and can develop an excessive hypotensive response, with secondary reduction in tissue perfusion and uteroplacental blood flow, when treated with a combination of rapid-acting vasodilators (hydralazine or nifedipine). Such patients may require a bolus infusion of 250-500 mL of isotonic saline prior to the administration of vasodilators. In these patients, labetalol may be the appropriate drug to use.
Labetalol should be avoided in patients with bradycardia (heart rate less than 60 bpm), in those with moderate to severe asthma, and in those with heart failure. In these patients, either hydralazine or nifedipine is the drug of choice. If an intravenous access is not available or difficult to obtain, oral nifedipine should be the drug of choice. In addition, because nifedipine is associated with improved renal blood flow with resultant increase in urine output, it is the drug of choice for treatment in those with decreased urine output, and for treatment of severe hypertension in the postpartum period.
In a third and final installment, I will elaborate on the postpartum management of women who have experienced hypertension with or without associated symptoms. Recently, postpartum hypertension has become a major cause of hospital readmission, as well as severe maternal morbidity and mortality.
Dr. Sibai is professor of obstetrics, gynecology, and reproductive sciences at the University of Texas McGovern Medical School, Houston.
SNOT-22 may help identify patients with undiagnosed OSA
CORONADO, CALIF. – results from a retrospective analysis demonstrated.
“We know based on experience and prior studies that there is significant overlap in symptoms for obstructive sleep apnea and chronic rhinosinusitis [CRS], which are two common conditions in the general population,” one of the study authors, David W. Jang, MD, said in an interview in advance of the Triological Society’s Combined Sections Meeting. “Therefore, it is important to identify patients with undiagnosed OSA who may present to the physician with nose- and sinus-related symptoms.”
Dr. Jang, assistant professor of rhinology and endoscopic skull surgery in the department of surgery at Duke University, Durham, N.C., and his colleagues conducted a 3-year retrospective analysis of 165 adults who presented with a rhinologic chief complaint and completed the SNOT-22 survey. The researchers compared SNOT-22 survey results between patients with untreated OSA confirmed on polysomnography without chronic rhinosinusitis and a control group of CRS patients. A chi-square test with Bonferroni correction was used for analysis.
Of the 165 patients, 41 met criteria for untreated OSA, based on a mean apnea-hypopnea index of 29.3, while 124 were included in the CRS control group. Sleep and psychological domain scores were not significantly different between the two groups, although patients in the OSA group were more likely to choose a sleep-related symptom as their most important complaint (MIC) (P less than .001). As for the cardinal symptoms of CRS, nasal discharge and loss of smell were significantly higher in the CRS group (P less than .001), while facial pain and nasal obstruction were not significantly different (P = .117 and P = .198, respectively). Facial pain and nasal obstruction were the most common MICs in the rhinologic domain for OSA patients; thick nasal discharge and postnasal discharge were the most common MICs reported by patients in the CRS group.
“It was surprising that, for the cardinal symptoms of CRS, only two of the four were significantly worse for the CRS group and predictive of CRS [nasal discharge and loss of smell],” Dr. Jang said. “Nasal obstruction and facial pain scores were similar between the two groups. Also, there was no significant difference in each of the sleep-related questions when comparing the CRS and OSA groups.”
He concluded that the findings further underscore the “significant overlap in symptoms between CRS and OSA. The SNOT-22 questionnaire may help identify patients with undiagnosed OSA.”
Dr. Jang acknowledged certain limitations of the study, including its retrospective design and relatively small sample size. He reported receiving research funding from Olympus.
The meeting was jointly sponsored by the Triological Society and the American College of Surgeons.
CORONADO, CALIF. – results from a retrospective analysis demonstrated.
“We know based on experience and prior studies that there is significant overlap in symptoms for obstructive sleep apnea and chronic rhinosinusitis [CRS], which are two common conditions in the general population,” one of the study authors, David W. Jang, MD, said in an interview in advance of the Triological Society’s Combined Sections Meeting. “Therefore, it is important to identify patients with undiagnosed OSA who may present to the physician with nose- and sinus-related symptoms.”
Dr. Jang, assistant professor of rhinology and endoscopic skull surgery in the department of surgery at Duke University, Durham, N.C., and his colleagues conducted a 3-year retrospective analysis of 165 adults who presented with a rhinologic chief complaint and completed the SNOT-22 survey. The researchers compared SNOT-22 survey results between patients with untreated OSA confirmed on polysomnography without chronic rhinosinusitis and a control group of CRS patients. A chi-square test with Bonferroni correction was used for analysis.
Of the 165 patients, 41 met criteria for untreated OSA, based on a mean apnea-hypopnea index of 29.3, while 124 were included in the CRS control group. Sleep and psychological domain scores were not significantly different between the two groups, although patients in the OSA group were more likely to choose a sleep-related symptom as their most important complaint (MIC) (P less than .001). As for the cardinal symptoms of CRS, nasal discharge and loss of smell were significantly higher in the CRS group (P less than .001), while facial pain and nasal obstruction were not significantly different (P = .117 and P = .198, respectively). Facial pain and nasal obstruction were the most common MICs in the rhinologic domain for OSA patients; thick nasal discharge and postnasal discharge were the most common MICs reported by patients in the CRS group.
“It was surprising that, for the cardinal symptoms of CRS, only two of the four were significantly worse for the CRS group and predictive of CRS [nasal discharge and loss of smell],” Dr. Jang said. “Nasal obstruction and facial pain scores were similar between the two groups. Also, there was no significant difference in each of the sleep-related questions when comparing the CRS and OSA groups.”
He concluded that the findings further underscore the “significant overlap in symptoms between CRS and OSA. The SNOT-22 questionnaire may help identify patients with undiagnosed OSA.”
Dr. Jang acknowledged certain limitations of the study, including its retrospective design and relatively small sample size. He reported receiving research funding from Olympus.
The meeting was jointly sponsored by the Triological Society and the American College of Surgeons.
CORONADO, CALIF. – results from a retrospective analysis demonstrated.
“We know based on experience and prior studies that there is significant overlap in symptoms for obstructive sleep apnea and chronic rhinosinusitis [CRS], which are two common conditions in the general population,” one of the study authors, David W. Jang, MD, said in an interview in advance of the Triological Society’s Combined Sections Meeting. “Therefore, it is important to identify patients with undiagnosed OSA who may present to the physician with nose- and sinus-related symptoms.”
Dr. Jang, assistant professor of rhinology and endoscopic skull surgery in the department of surgery at Duke University, Durham, N.C., and his colleagues conducted a 3-year retrospective analysis of 165 adults who presented with a rhinologic chief complaint and completed the SNOT-22 survey. The researchers compared SNOT-22 survey results between patients with untreated OSA confirmed on polysomnography without chronic rhinosinusitis and a control group of CRS patients. A chi-square test with Bonferroni correction was used for analysis.
Of the 165 patients, 41 met criteria for untreated OSA, based on a mean apnea-hypopnea index of 29.3, while 124 were included in the CRS control group. Sleep and psychological domain scores were not significantly different between the two groups, although patients in the OSA group were more likely to choose a sleep-related symptom as their most important complaint (MIC) (P less than .001). As for the cardinal symptoms of CRS, nasal discharge and loss of smell were significantly higher in the CRS group (P less than .001), while facial pain and nasal obstruction were not significantly different (P = .117 and P = .198, respectively). Facial pain and nasal obstruction were the most common MICs in the rhinologic domain for OSA patients; thick nasal discharge and postnasal discharge were the most common MICs reported by patients in the CRS group.
“It was surprising that, for the cardinal symptoms of CRS, only two of the four were significantly worse for the CRS group and predictive of CRS [nasal discharge and loss of smell],” Dr. Jang said. “Nasal obstruction and facial pain scores were similar between the two groups. Also, there was no significant difference in each of the sleep-related questions when comparing the CRS and OSA groups.”
He concluded that the findings further underscore the “significant overlap in symptoms between CRS and OSA. The SNOT-22 questionnaire may help identify patients with undiagnosed OSA.”
Dr. Jang acknowledged certain limitations of the study, including its retrospective design and relatively small sample size. He reported receiving research funding from Olympus.
The meeting was jointly sponsored by the Triological Society and the American College of Surgeons.
REPORTING FROM THE TRIOLOGICAL CSM
Key clinical point: Obstructive sleep apnea (OSA) should be suspected in patients with sleep dysfunction as their primary complaint without the significant nasal drainage and anosmia that characterizes chronic rhinosinusitis.
Major finding: Sleep and psychological domain scores on the SNOT-22 were not significantly different between patients with chronic rhinosinusitis and those with OSA, although OSA patients were more likely to choose a sleep-related symptom as their most important complaint (P less than .001).
Study details: A retrospective analysis of 165 adults who presented with a rhinologic chief complaint and completed the SNOT-22 survey.
Disclosures: Dr. Jang reported receiving research funding from Olympus.
Treating preeclampsia
Preeclampsia is such a complicated and insidious disease – and one with such serious implications for the fetus, the infant at birth, and the mother – that we decided to run a three-part series on its diagnosis and management. The complication can have an acute onset in many patients, and this acute onset may rapidly progress to eclampsia and to severe consequences, including maternal death. In addition, the disorder can occur as early as the late second trimester and can thus impact the timing of delivery and fetal age at birth. A full knowledge of the disease state – its pathophysiology, clinical manifestations, and various therapeutic options, both medical and surgical – is critical for obstetricians to be able to affect the health and well-being of both the mother and fetus.
I have invited Dr. Baha M. Sibai, professor of obstetrics, gynecology, and reproductive sciences at the University of Texas McGovern Medical School, Houston, to deliver this series. Our first installment addressed diagnostic criteria and attempted to clarify confusion that may have been introduced with the 2013 publication of the American College of Obstetricians and Gynecologists’ Task Force Report on Hypertension in Pregnancy. It is important that the diagnostic criteria are well established and understood because the management of patients is very much based on accurate placement within these diagnostic criteria.
This second installment of our series focuses on the application of appropriate therapeutic measures for various diagnostic groups. Dr. Sibai has spent decades studying hypertensive disorders in pregnancy and developing practical clinical strategies for management. It is our hope that the guidance and algorithms presented here will be useful for improving patient care and outcomes of this serious obstetrical syndrome. A third installment on postpartum management will come later.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
Preeclampsia is such a complicated and insidious disease – and one with such serious implications for the fetus, the infant at birth, and the mother – that we decided to run a three-part series on its diagnosis and management. The complication can have an acute onset in many patients, and this acute onset may rapidly progress to eclampsia and to severe consequences, including maternal death. In addition, the disorder can occur as early as the late second trimester and can thus impact the timing of delivery and fetal age at birth. A full knowledge of the disease state – its pathophysiology, clinical manifestations, and various therapeutic options, both medical and surgical – is critical for obstetricians to be able to affect the health and well-being of both the mother and fetus.
I have invited Dr. Baha M. Sibai, professor of obstetrics, gynecology, and reproductive sciences at the University of Texas McGovern Medical School, Houston, to deliver this series. Our first installment addressed diagnostic criteria and attempted to clarify confusion that may have been introduced with the 2013 publication of the American College of Obstetricians and Gynecologists’ Task Force Report on Hypertension in Pregnancy. It is important that the diagnostic criteria are well established and understood because the management of patients is very much based on accurate placement within these diagnostic criteria.
This second installment of our series focuses on the application of appropriate therapeutic measures for various diagnostic groups. Dr. Sibai has spent decades studying hypertensive disorders in pregnancy and developing practical clinical strategies for management. It is our hope that the guidance and algorithms presented here will be useful for improving patient care and outcomes of this serious obstetrical syndrome. A third installment on postpartum management will come later.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
Preeclampsia is such a complicated and insidious disease – and one with such serious implications for the fetus, the infant at birth, and the mother – that we decided to run a three-part series on its diagnosis and management. The complication can have an acute onset in many patients, and this acute onset may rapidly progress to eclampsia and to severe consequences, including maternal death. In addition, the disorder can occur as early as the late second trimester and can thus impact the timing of delivery and fetal age at birth. A full knowledge of the disease state – its pathophysiology, clinical manifestations, and various therapeutic options, both medical and surgical – is critical for obstetricians to be able to affect the health and well-being of both the mother and fetus.
I have invited Dr. Baha M. Sibai, professor of obstetrics, gynecology, and reproductive sciences at the University of Texas McGovern Medical School, Houston, to deliver this series. Our first installment addressed diagnostic criteria and attempted to clarify confusion that may have been introduced with the 2013 publication of the American College of Obstetricians and Gynecologists’ Task Force Report on Hypertension in Pregnancy. It is important that the diagnostic criteria are well established and understood because the management of patients is very much based on accurate placement within these diagnostic criteria.
This second installment of our series focuses on the application of appropriate therapeutic measures for various diagnostic groups. Dr. Sibai has spent decades studying hypertensive disorders in pregnancy and developing practical clinical strategies for management. It is our hope that the guidance and algorithms presented here will be useful for improving patient care and outcomes of this serious obstetrical syndrome. A third installment on postpartum management will come later.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
Single-dose tafenoquine appears to prevent malaria relapse
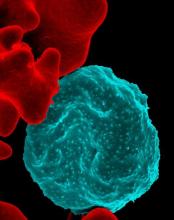
Single-dose tafenoquine therapy safely reduces the risk of Plasmodium vivax relapse in patients with normal glucose-6-phosphate dehydrogenase (G6PD) activity, according to the results of two phase 3, double-blind, randomized controlled trials.
Findings from both studies were published in two separate reports in the New England Journal of Medicine.
In the first study, the Dose and Efficacy Trial Evaluating Chloroquine and Tafenoquine in Vivax Elimination (DETECTIVE), the risk of P. vivax recurrence was approximately 70% lower with tafenoquine versus placebo, wrote Marcus V.G. Lacerda, MD, of Fundação de Medicina Tropical Doutor Heitor Vieira Dourado in Manaus, Brazil, and his colleagues.
The study included 522 patients with confirmed P. vivax infection from Peru, Brazil, Ethiopia, Cambodia, Thailand, and the Philippines. Patients received 3 days of chloroquine therapy (600 mg on days 1 and 2, and 300 mg on day 3) and were randomly assigned on a 2:1:1 basis to receive a single 300-mg dose of tafenoquine on day 1 or 2, primaquine once daily for 14 days, or placebo.
Since primaquine and tafenoquine can cause clinically significant hemolysis in individuals with G6PD deficiency, the study included only patients with normal G6PD activity.
In the intention-to-treat analysis, 62% of tafenoquine recipients were free from P. vivax recurrence (95% confidence interval [CI], 55%-69%) at 6 months, as were 70% of primaquine recipients (95% CI, 60%-77%) and 28% of placebo recipients (95% CI, 20%-37%). Compared with placebo, the reduction in risk of recurrence was 70% with tafenoquine (hazard ratio [HR], 0.30; 95% CI, 0.22-0.40; P less than .001) and 74% with primaquine.
Declines in hemoglobin levels were greatest in the tafenoquine group but were not associated with symptomatic anemia and resolved without intervention, the investigators wrote.
In addition to the quantitative G6PD test, the investigators also evaluated a qualitative test, which “failed to identify 16 patients most at risk for hemolysis,” they reported. “If tafenoquine use is expanded, adoption of reliable quantitative point-of-care G6PD tests will be needed; such tests are not currently available but are in development.”
In the second study, Global Assessment of Tafenoquine Hemolytic Risk (GATHER), Alejandro Llanos-Cuentas, MD, of Universidad Peruana Cayetano Heredia, Lima, Peru, and his colleagues enrolled 251 patients with confirmed P. vivax infection from Peru, Brazil, Columbia, Vietnam, and Thailand. They attempted to recruit women with moderate G6PD levels, but only one participant met this criterion – all others had normal G6PD activity.
Patients received 3-day course of chloroquine and were randomly assigned on a 2:1 basis to either tafenoquine or primaquine at the same doses as in the DETECTIVE trial.
At 6 months, 2% (95% CI, 1%-6%) of tafenoquine recipients and 1% (95% CI, 0.2%-6%) of primaquine recipients had decreased hemoglobin levels, but none consequently needed treatment. The medications also caused a similar degree and time course of hemoglobin decrease, the investigators noted.
A meta-analysis of GATHER and DETECTIVE confirmed that tafenoquine more often led to a decreased hemoglobin level (4% versus 1.5% with primaquine). Tafenoquine also did not meet prespecified criteria for noninferiority compared with primaquine, with respective 6-month recurrence rates of 67% versus 73%.
However, GATHER deployed “extensive” support to help patients adhere to the 15-day primaquine course, Dr. Llanos-Cuentas and his colleagues wrote. “Without such interventions, adherence to primaquine has been reported to be as low as 24% in Southeast Asia, with a corresponding attenuation of efficacy.”
GlaxoSmithKline and Medicines for Malaria Venture funded both studies, and GSK funded and conducted the meta-analysis. Dr. Llanos-Cuentas and several coinvestigators reported ties to GSK, Medicines for Malaria Venture, the Gambia, and LSTMH. Dr. Lacerda reported having no conflicts of interest.
SOURCES: Lacerda MVG et al. N Engl J Med 2019;380:215-28, and Llanos-Cuentas A et al. N Engl J Med 2019;380:229-41.
The studies show that tafenoquine reduces the risk of Plasmodium vivax recurrence in patients with quantitatively confirmed normal glucose-6-phosphate dehydrogenase (G6PD) activity, Nicholas J. White, FRS, wrote in an accompanying editorial.
But the need for this test and current prescribing restrictions will “limit the potential deployment of tafenoquine, at least in the immediate future,” he said. He praised the developers of tafenoquine “for persevering with this potentially valuable antimalarial drug, despite the difficulties,” but cautioned that it’s too soon to conclude that tafenoquine can be used safely and routinely on a large scale “and thus fulfill its promise as a radical improvement in the treatment of malaria.”
Currently, tafenoquine may not be used during pregnancy, lactation, or in patients younger than 16 years, Dr. White noted. Tafenoquine, like primaquine, causes dose-dependent hemolysis in patients with G6PD deficiency, but unlike primaquine, it is given as a single large dose. Hence, pretreatment quantitative G6PD testing is necessary. Point-of-care quantitative G6PD tests have been developed but await extensive field testing, Dr. White said.
Dr. White is with Mahidol University, Bangkok, Thailand, and University of Oxford, England. He reported having no financial disclosures. These comments are from his accompanying editorial ( N Engl J Med. 2019;380:285-6 ).
The studies show that tafenoquine reduces the risk of Plasmodium vivax recurrence in patients with quantitatively confirmed normal glucose-6-phosphate dehydrogenase (G6PD) activity, Nicholas J. White, FRS, wrote in an accompanying editorial.
But the need for this test and current prescribing restrictions will “limit the potential deployment of tafenoquine, at least in the immediate future,” he said. He praised the developers of tafenoquine “for persevering with this potentially valuable antimalarial drug, despite the difficulties,” but cautioned that it’s too soon to conclude that tafenoquine can be used safely and routinely on a large scale “and thus fulfill its promise as a radical improvement in the treatment of malaria.”
Currently, tafenoquine may not be used during pregnancy, lactation, or in patients younger than 16 years, Dr. White noted. Tafenoquine, like primaquine, causes dose-dependent hemolysis in patients with G6PD deficiency, but unlike primaquine, it is given as a single large dose. Hence, pretreatment quantitative G6PD testing is necessary. Point-of-care quantitative G6PD tests have been developed but await extensive field testing, Dr. White said.
Dr. White is with Mahidol University, Bangkok, Thailand, and University of Oxford, England. He reported having no financial disclosures. These comments are from his accompanying editorial ( N Engl J Med. 2019;380:285-6 ).
The studies show that tafenoquine reduces the risk of Plasmodium vivax recurrence in patients with quantitatively confirmed normal glucose-6-phosphate dehydrogenase (G6PD) activity, Nicholas J. White, FRS, wrote in an accompanying editorial.
But the need for this test and current prescribing restrictions will “limit the potential deployment of tafenoquine, at least in the immediate future,” he said. He praised the developers of tafenoquine “for persevering with this potentially valuable antimalarial drug, despite the difficulties,” but cautioned that it’s too soon to conclude that tafenoquine can be used safely and routinely on a large scale “and thus fulfill its promise as a radical improvement in the treatment of malaria.”
Currently, tafenoquine may not be used during pregnancy, lactation, or in patients younger than 16 years, Dr. White noted. Tafenoquine, like primaquine, causes dose-dependent hemolysis in patients with G6PD deficiency, but unlike primaquine, it is given as a single large dose. Hence, pretreatment quantitative G6PD testing is necessary. Point-of-care quantitative G6PD tests have been developed but await extensive field testing, Dr. White said.
Dr. White is with Mahidol University, Bangkok, Thailand, and University of Oxford, England. He reported having no financial disclosures. These comments are from his accompanying editorial ( N Engl J Med. 2019;380:285-6 ).
Single-dose tafenoquine therapy safely reduces the risk of Plasmodium vivax relapse in patients with normal glucose-6-phosphate dehydrogenase (G6PD) activity, according to the results of two phase 3, double-blind, randomized controlled trials.
Findings from both studies were published in two separate reports in the New England Journal of Medicine.
In the first study, the Dose and Efficacy Trial Evaluating Chloroquine and Tafenoquine in Vivax Elimination (DETECTIVE), the risk of P. vivax recurrence was approximately 70% lower with tafenoquine versus placebo, wrote Marcus V.G. Lacerda, MD, of Fundação de Medicina Tropical Doutor Heitor Vieira Dourado in Manaus, Brazil, and his colleagues.
The study included 522 patients with confirmed P. vivax infection from Peru, Brazil, Ethiopia, Cambodia, Thailand, and the Philippines. Patients received 3 days of chloroquine therapy (600 mg on days 1 and 2, and 300 mg on day 3) and were randomly assigned on a 2:1:1 basis to receive a single 300-mg dose of tafenoquine on day 1 or 2, primaquine once daily for 14 days, or placebo.
Since primaquine and tafenoquine can cause clinically significant hemolysis in individuals with G6PD deficiency, the study included only patients with normal G6PD activity.
In the intention-to-treat analysis, 62% of tafenoquine recipients were free from P. vivax recurrence (95% confidence interval [CI], 55%-69%) at 6 months, as were 70% of primaquine recipients (95% CI, 60%-77%) and 28% of placebo recipients (95% CI, 20%-37%). Compared with placebo, the reduction in risk of recurrence was 70% with tafenoquine (hazard ratio [HR], 0.30; 95% CI, 0.22-0.40; P less than .001) and 74% with primaquine.
Declines in hemoglobin levels were greatest in the tafenoquine group but were not associated with symptomatic anemia and resolved without intervention, the investigators wrote.
In addition to the quantitative G6PD test, the investigators also evaluated a qualitative test, which “failed to identify 16 patients most at risk for hemolysis,” they reported. “If tafenoquine use is expanded, adoption of reliable quantitative point-of-care G6PD tests will be needed; such tests are not currently available but are in development.”
In the second study, Global Assessment of Tafenoquine Hemolytic Risk (GATHER), Alejandro Llanos-Cuentas, MD, of Universidad Peruana Cayetano Heredia, Lima, Peru, and his colleagues enrolled 251 patients with confirmed P. vivax infection from Peru, Brazil, Columbia, Vietnam, and Thailand. They attempted to recruit women with moderate G6PD levels, but only one participant met this criterion – all others had normal G6PD activity.
Patients received 3-day course of chloroquine and were randomly assigned on a 2:1 basis to either tafenoquine or primaquine at the same doses as in the DETECTIVE trial.
At 6 months, 2% (95% CI, 1%-6%) of tafenoquine recipients and 1% (95% CI, 0.2%-6%) of primaquine recipients had decreased hemoglobin levels, but none consequently needed treatment. The medications also caused a similar degree and time course of hemoglobin decrease, the investigators noted.
A meta-analysis of GATHER and DETECTIVE confirmed that tafenoquine more often led to a decreased hemoglobin level (4% versus 1.5% with primaquine). Tafenoquine also did not meet prespecified criteria for noninferiority compared with primaquine, with respective 6-month recurrence rates of 67% versus 73%.
However, GATHER deployed “extensive” support to help patients adhere to the 15-day primaquine course, Dr. Llanos-Cuentas and his colleagues wrote. “Without such interventions, adherence to primaquine has been reported to be as low as 24% in Southeast Asia, with a corresponding attenuation of efficacy.”
GlaxoSmithKline and Medicines for Malaria Venture funded both studies, and GSK funded and conducted the meta-analysis. Dr. Llanos-Cuentas and several coinvestigators reported ties to GSK, Medicines for Malaria Venture, the Gambia, and LSTMH. Dr. Lacerda reported having no conflicts of interest.
SOURCES: Lacerda MVG et al. N Engl J Med 2019;380:215-28, and Llanos-Cuentas A et al. N Engl J Med 2019;380:229-41.
Single-dose tafenoquine therapy safely reduces the risk of Plasmodium vivax relapse in patients with normal glucose-6-phosphate dehydrogenase (G6PD) activity, according to the results of two phase 3, double-blind, randomized controlled trials.
Findings from both studies were published in two separate reports in the New England Journal of Medicine.
In the first study, the Dose and Efficacy Trial Evaluating Chloroquine and Tafenoquine in Vivax Elimination (DETECTIVE), the risk of P. vivax recurrence was approximately 70% lower with tafenoquine versus placebo, wrote Marcus V.G. Lacerda, MD, of Fundação de Medicina Tropical Doutor Heitor Vieira Dourado in Manaus, Brazil, and his colleagues.
The study included 522 patients with confirmed P. vivax infection from Peru, Brazil, Ethiopia, Cambodia, Thailand, and the Philippines. Patients received 3 days of chloroquine therapy (600 mg on days 1 and 2, and 300 mg on day 3) and were randomly assigned on a 2:1:1 basis to receive a single 300-mg dose of tafenoquine on day 1 or 2, primaquine once daily for 14 days, or placebo.
Since primaquine and tafenoquine can cause clinically significant hemolysis in individuals with G6PD deficiency, the study included only patients with normal G6PD activity.
In the intention-to-treat analysis, 62% of tafenoquine recipients were free from P. vivax recurrence (95% confidence interval [CI], 55%-69%) at 6 months, as were 70% of primaquine recipients (95% CI, 60%-77%) and 28% of placebo recipients (95% CI, 20%-37%). Compared with placebo, the reduction in risk of recurrence was 70% with tafenoquine (hazard ratio [HR], 0.30; 95% CI, 0.22-0.40; P less than .001) and 74% with primaquine.
Declines in hemoglobin levels were greatest in the tafenoquine group but were not associated with symptomatic anemia and resolved without intervention, the investigators wrote.
In addition to the quantitative G6PD test, the investigators also evaluated a qualitative test, which “failed to identify 16 patients most at risk for hemolysis,” they reported. “If tafenoquine use is expanded, adoption of reliable quantitative point-of-care G6PD tests will be needed; such tests are not currently available but are in development.”
In the second study, Global Assessment of Tafenoquine Hemolytic Risk (GATHER), Alejandro Llanos-Cuentas, MD, of Universidad Peruana Cayetano Heredia, Lima, Peru, and his colleagues enrolled 251 patients with confirmed P. vivax infection from Peru, Brazil, Columbia, Vietnam, and Thailand. They attempted to recruit women with moderate G6PD levels, but only one participant met this criterion – all others had normal G6PD activity.
Patients received 3-day course of chloroquine and were randomly assigned on a 2:1 basis to either tafenoquine or primaquine at the same doses as in the DETECTIVE trial.
At 6 months, 2% (95% CI, 1%-6%) of tafenoquine recipients and 1% (95% CI, 0.2%-6%) of primaquine recipients had decreased hemoglobin levels, but none consequently needed treatment. The medications also caused a similar degree and time course of hemoglobin decrease, the investigators noted.
A meta-analysis of GATHER and DETECTIVE confirmed that tafenoquine more often led to a decreased hemoglobin level (4% versus 1.5% with primaquine). Tafenoquine also did not meet prespecified criteria for noninferiority compared with primaquine, with respective 6-month recurrence rates of 67% versus 73%.
However, GATHER deployed “extensive” support to help patients adhere to the 15-day primaquine course, Dr. Llanos-Cuentas and his colleagues wrote. “Without such interventions, adherence to primaquine has been reported to be as low as 24% in Southeast Asia, with a corresponding attenuation of efficacy.”
GlaxoSmithKline and Medicines for Malaria Venture funded both studies, and GSK funded and conducted the meta-analysis. Dr. Llanos-Cuentas and several coinvestigators reported ties to GSK, Medicines for Malaria Venture, the Gambia, and LSTMH. Dr. Lacerda reported having no conflicts of interest.
SOURCES: Lacerda MVG et al. N Engl J Med 2019;380:215-28, and Llanos-Cuentas A et al. N Engl J Med 2019;380:229-41.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: In DETECTIVE, 6-month rates of freedom from recurrence from Plasmodium vivax infection were 62% with tafenoquine, 70% with primaquine, and 28% with placebo.
Study details: Two randomized, phase 3, double-blind controlled trials of patients with confirmed P. vivax infection (DETECTIVE and GATHER) and without deficient G6PD activity.
Disclosures: GlaxoSmithKline and Medicines for Malaria Venture funded both studies, and GSK funded and conducted the meta-analysis. Dr. Llanos-Cuentas and several coinvestigators reported ties to GSK, Medicines for Malaria Venture, the Gambia, and LSTMH. Dr. Lacerda reported having financial disclosures.
Source: Lacerda MVG et al. N Engl J Med 2019;380:215-28, and Llanos-Cuentas A et al. N Engl J Med 2019;380:229-41.
Oral GLP-1 receptor agonist pioneered in T2DM trial
BERLIN – An investigational oral formulation of the glucagonlike peptide–1 receptor agonist (GLP-1 RA) semaglutide reduced glycated hemoglobin (HbA1c) to a greater extent than did placebo at all doses tested in patients with type 2 diabetes mellitus (T2DM) in the phase 3a PIONEER 1 trial.
The estimated mean change in HbA1c from baseline to week 26 – the primary endpoint – using an on-treatment analysis was –0.8% with a once-daily dose of 3 mg, –1.3% with a once-daily dose of 7 mg, and –1.5% with a once-daily dose of 14 mg. The corresponding value for placebo was –0.1%, with all comparisons statistically significant (P less than .001).
The on-treatment analysis evaluated treatment effects for all randomized patients (n = 703) and assumed that all subjects remained on-treatment and excluded the effect of any rescue medication. Results for an intention-to-treat (ITT) analysis provided similar results, however, with estimated mean changes in HbA1c of –0.9%, –1.2%, and –1.4% for the three respective semaglutide doses and –0.3% for placebo.
“There was a very nice dose-dependent decrease in HbA1c, which was superior to placebo for all doses of semaglutide” said study investigator Martin Haluzík, MD, at the annual meeting of the European Association for the Study of Diabetes.
“I think it’s quite important to stress the magnitude of the decrease of HbA1c, because with the highest dose it was –1.5% from a baseline of 8%, which I believe is something that hasn’t ever really been seen with any other oral antidiabetic medication,” added Dr. Haluzík, professor of internal medicine at the 1st Faculty of Medicine at Charles University and deputy head of the Institute for Clinical and Experimental Medicine, both in Prague.
Currently, GLP-1 RAs are available only in a subcutaneous formulation, Dr. Haluzík reminded his audience, adding that oral semaglutide was the first GLP-1 RA to be developed in a tablet formulation and was in the late stages of clinical development.
PIONEER 1 is the first of 10 phase 3a trials with oral semaglutide to be reported. “Additional studies, across the full spectrum of diabetes care, in special populations, comparing it with active comparators with varied trial duration, have been completed or will be completed in 2018,” said coinvestigator for the study Vanita Aroda, MD, during a separate presentation at a dedicated symposium on the PIONEER program.
Dr. Aroda, the director of the diabetes research program at Brigham and Women’s Hospital in Boston, observed that oral semaglutide was being evaluated from early care as monotherapy in the PIONEER 1 study. The other trials, such as PIONEER 2, PIONEER 3, PIONEER 4, and PIONEER 7 were looking at oral semaglutide in combination with oral antidiabetic agents versus various active comparators; PIONEER 5 and PIONEER 6 were in special populations; and PIONEER 8 was looking at its use on top of basal insulin. Two further trials are also part of the study program.
“I think this is the first time that we actually have completed data of an entire program, including cardiovascular data, all within the same year,” Dr. Aroda said. “All of the studies are in the process of data analysis or data reporting.”
PIONEER 1 was a multicenter, randomized, double-blind, placebo-controlled trial examining efficacy and safety of semaglutide versus placebo in 703 adults with drug-naive T2DM who were being treated with diet and exercise only.
Three doses of oral semaglutide – 3 mg, 7 mg, and 14 mg – were assessed and compared with placebo. There was a fixed 4-week dose escalation period, with all patients starting treatment with 3 mg of semaglutide and then increasing to 7 mg by week 4 and 14 mg by week 8. This was to try to reduce the risk of gastrointestinal side effects, which are known to occur with GLP-1 RAs.
Secondary outcome measures were change in body weight, fasting plasma glucose, HbA1c below a target of 7% (53 mmol/mol), which were all measured from baseline to week 26; adverse events, including severe and blood glucose–confirmed symptomatic hypoglycemic episodes, were assessed out to week 31.
The average age of patients in the trial was around 55 years, around half were female, and the starting HbA1c was approximately 8%.The mean body weight ranged from 86.9 kg to 89 kg in the different treatment groups, with a similar body mass index of about 32 kg/m2.
Clinically meaningful weight loss, compared with placebo, was only achieved with the highest dose of oral semaglutide, with a –4.1 kg reduction versus –1.5 kg for placebo from baseline to week 26 (P less than .001, on-treatment analysis). Reductions in body weight for the 3-mg and 7-mg oral semaglutide doses were a respective –1.7 kg and –2.5 kg. ITT results were again similar, with weight losses of –1.5, –2.3, and –3.7 kg for the 3-, 7-, and 14-mg doses of oral semaglutide, respectively, and –1.4 kg for placebo.
More patients treated with oral semaglutide 3, 7, or 14 mg versus placebo achieved an HbA1c of below 7% (59.1%, 71.9%, and 80.3%, respectively, vs. 33.8%) or a body weight loss of 5% or more (21.3%, 28.7%, and 44.3% vs. 15.7%).
Furthermore, more patients treated with oral semaglutide achieved an HbA1c of or below 7% without hypoglycemic episodes or body weight gain than did those given placebo. There were also more patients who achieved an HbA1c reduction of at least 1% and a weight loss of 3% or higher.
“Oral semaglutide demonstrated a safety and tolerability profile consistent with that of [injectable] GLP-1 RAs,” Dr. Haluzík reported. Adverse events were seen in 57.7%, 53.1%, and 56.6%of patients treated with 3, 7, and 14 mg of oral semaglutide and 55.6% of those treated with placebo.
The most common adverse events seen with oral semaglutide affected the gastrointestinal tract, with nausea affecting 8%, 5.1%, and 16% of 3, 7, and 14 mg–treated patients versus 5.6% of placebo-treated patients. Vomiting affected a respective 2.9%, 4.6%, 6.9%, and 2.1%, and diarrhea a respective 8.6%, 5.1%, 5.1%, and 2.2%.
Severe or blood glucose–confirmed, symptomatic hypoglycemia was reported in 2.9%, 1.1%, and 0.6%of those treated with 3, 7, 14 mg of oral semaglutide and 0.6% of placebo-treated patients.
PIONEER 1 represents a “step change in GLP-1 receptor agonist therapy”, said Cliff Bailey, MD, who discussed the trial aa the EASD’s independent commentator during a symposium on the PIONEER program. These data are “leading to a new delivery route for GLP-1 receptor agonists, from injection to oral,” and “this can be done with good metabolic efficacy, with substantial reductions in A1c and body weight, and with a safety profile that’s comparable to the subcutaneous injection.”
Dr. Bailey, who is professor of clinical science at Aston University in Birmingham, England, noted, however, the oral dosing of semaglutide “requires patient commitment because it needs to be taken before breakfast time, and it may also, to some extent, affect the timing of some of the other medications.”
The study was sponsored by Novo Nordisk. Dr. Haluzík disclosed acting as a consultant to AstraZeneca, Eli Lilly, Johnson & Johnson, Mundipharma, Novatin, Novo Nordisk, and Sanofi Aventis. Dr. Aroda was an investigator in the PIONEER 1 study and disclosed acting as a consultant to Novo Nordisk; she also disclosed relationships with multiple other pharmaceutical companies, including AstraZeneca, BMS, Calbra, Eisai, Elcelyx Therapeutics, Janssen, and Sanofi Aventis. Dr. Bailey acknowledged attending advisory boards, undertaking ad hoc consultancy work, and receiving research and travel support from several pharmaceutical companies that included Novo Nordisk.
SOURCES: Haluzík M et al. EASD 2018, Abstract 38; Aroda V. EASD 2018, Session S18 - PIONEER Trial; Bailey C. EASD 2018, Session S18 - PIONEER Trial.
BERLIN – An investigational oral formulation of the glucagonlike peptide–1 receptor agonist (GLP-1 RA) semaglutide reduced glycated hemoglobin (HbA1c) to a greater extent than did placebo at all doses tested in patients with type 2 diabetes mellitus (T2DM) in the phase 3a PIONEER 1 trial.
The estimated mean change in HbA1c from baseline to week 26 – the primary endpoint – using an on-treatment analysis was –0.8% with a once-daily dose of 3 mg, –1.3% with a once-daily dose of 7 mg, and –1.5% with a once-daily dose of 14 mg. The corresponding value for placebo was –0.1%, with all comparisons statistically significant (P less than .001).
The on-treatment analysis evaluated treatment effects for all randomized patients (n = 703) and assumed that all subjects remained on-treatment and excluded the effect of any rescue medication. Results for an intention-to-treat (ITT) analysis provided similar results, however, with estimated mean changes in HbA1c of –0.9%, –1.2%, and –1.4% for the three respective semaglutide doses and –0.3% for placebo.
“There was a very nice dose-dependent decrease in HbA1c, which was superior to placebo for all doses of semaglutide” said study investigator Martin Haluzík, MD, at the annual meeting of the European Association for the Study of Diabetes.
“I think it’s quite important to stress the magnitude of the decrease of HbA1c, because with the highest dose it was –1.5% from a baseline of 8%, which I believe is something that hasn’t ever really been seen with any other oral antidiabetic medication,” added Dr. Haluzík, professor of internal medicine at the 1st Faculty of Medicine at Charles University and deputy head of the Institute for Clinical and Experimental Medicine, both in Prague.
Currently, GLP-1 RAs are available only in a subcutaneous formulation, Dr. Haluzík reminded his audience, adding that oral semaglutide was the first GLP-1 RA to be developed in a tablet formulation and was in the late stages of clinical development.
PIONEER 1 is the first of 10 phase 3a trials with oral semaglutide to be reported. “Additional studies, across the full spectrum of diabetes care, in special populations, comparing it with active comparators with varied trial duration, have been completed or will be completed in 2018,” said coinvestigator for the study Vanita Aroda, MD, during a separate presentation at a dedicated symposium on the PIONEER program.
Dr. Aroda, the director of the diabetes research program at Brigham and Women’s Hospital in Boston, observed that oral semaglutide was being evaluated from early care as monotherapy in the PIONEER 1 study. The other trials, such as PIONEER 2, PIONEER 3, PIONEER 4, and PIONEER 7 were looking at oral semaglutide in combination with oral antidiabetic agents versus various active comparators; PIONEER 5 and PIONEER 6 were in special populations; and PIONEER 8 was looking at its use on top of basal insulin. Two further trials are also part of the study program.
“I think this is the first time that we actually have completed data of an entire program, including cardiovascular data, all within the same year,” Dr. Aroda said. “All of the studies are in the process of data analysis or data reporting.”
PIONEER 1 was a multicenter, randomized, double-blind, placebo-controlled trial examining efficacy and safety of semaglutide versus placebo in 703 adults with drug-naive T2DM who were being treated with diet and exercise only.
Three doses of oral semaglutide – 3 mg, 7 mg, and 14 mg – were assessed and compared with placebo. There was a fixed 4-week dose escalation period, with all patients starting treatment with 3 mg of semaglutide and then increasing to 7 mg by week 4 and 14 mg by week 8. This was to try to reduce the risk of gastrointestinal side effects, which are known to occur with GLP-1 RAs.
Secondary outcome measures were change in body weight, fasting plasma glucose, HbA1c below a target of 7% (53 mmol/mol), which were all measured from baseline to week 26; adverse events, including severe and blood glucose–confirmed symptomatic hypoglycemic episodes, were assessed out to week 31.
The average age of patients in the trial was around 55 years, around half were female, and the starting HbA1c was approximately 8%.The mean body weight ranged from 86.9 kg to 89 kg in the different treatment groups, with a similar body mass index of about 32 kg/m2.
Clinically meaningful weight loss, compared with placebo, was only achieved with the highest dose of oral semaglutide, with a –4.1 kg reduction versus –1.5 kg for placebo from baseline to week 26 (P less than .001, on-treatment analysis). Reductions in body weight for the 3-mg and 7-mg oral semaglutide doses were a respective –1.7 kg and –2.5 kg. ITT results were again similar, with weight losses of –1.5, –2.3, and –3.7 kg for the 3-, 7-, and 14-mg doses of oral semaglutide, respectively, and –1.4 kg for placebo.
More patients treated with oral semaglutide 3, 7, or 14 mg versus placebo achieved an HbA1c of below 7% (59.1%, 71.9%, and 80.3%, respectively, vs. 33.8%) or a body weight loss of 5% or more (21.3%, 28.7%, and 44.3% vs. 15.7%).
Furthermore, more patients treated with oral semaglutide achieved an HbA1c of or below 7% without hypoglycemic episodes or body weight gain than did those given placebo. There were also more patients who achieved an HbA1c reduction of at least 1% and a weight loss of 3% or higher.
“Oral semaglutide demonstrated a safety and tolerability profile consistent with that of [injectable] GLP-1 RAs,” Dr. Haluzík reported. Adverse events were seen in 57.7%, 53.1%, and 56.6%of patients treated with 3, 7, and 14 mg of oral semaglutide and 55.6% of those treated with placebo.
The most common adverse events seen with oral semaglutide affected the gastrointestinal tract, with nausea affecting 8%, 5.1%, and 16% of 3, 7, and 14 mg–treated patients versus 5.6% of placebo-treated patients. Vomiting affected a respective 2.9%, 4.6%, 6.9%, and 2.1%, and diarrhea a respective 8.6%, 5.1%, 5.1%, and 2.2%.
Severe or blood glucose–confirmed, symptomatic hypoglycemia was reported in 2.9%, 1.1%, and 0.6%of those treated with 3, 7, 14 mg of oral semaglutide and 0.6% of placebo-treated patients.
PIONEER 1 represents a “step change in GLP-1 receptor agonist therapy”, said Cliff Bailey, MD, who discussed the trial aa the EASD’s independent commentator during a symposium on the PIONEER program. These data are “leading to a new delivery route for GLP-1 receptor agonists, from injection to oral,” and “this can be done with good metabolic efficacy, with substantial reductions in A1c and body weight, and with a safety profile that’s comparable to the subcutaneous injection.”
Dr. Bailey, who is professor of clinical science at Aston University in Birmingham, England, noted, however, the oral dosing of semaglutide “requires patient commitment because it needs to be taken before breakfast time, and it may also, to some extent, affect the timing of some of the other medications.”
The study was sponsored by Novo Nordisk. Dr. Haluzík disclosed acting as a consultant to AstraZeneca, Eli Lilly, Johnson & Johnson, Mundipharma, Novatin, Novo Nordisk, and Sanofi Aventis. Dr. Aroda was an investigator in the PIONEER 1 study and disclosed acting as a consultant to Novo Nordisk; she also disclosed relationships with multiple other pharmaceutical companies, including AstraZeneca, BMS, Calbra, Eisai, Elcelyx Therapeutics, Janssen, and Sanofi Aventis. Dr. Bailey acknowledged attending advisory boards, undertaking ad hoc consultancy work, and receiving research and travel support from several pharmaceutical companies that included Novo Nordisk.
SOURCES: Haluzík M et al. EASD 2018, Abstract 38; Aroda V. EASD 2018, Session S18 - PIONEER Trial; Bailey C. EASD 2018, Session S18 - PIONEER Trial.
BERLIN – An investigational oral formulation of the glucagonlike peptide–1 receptor agonist (GLP-1 RA) semaglutide reduced glycated hemoglobin (HbA1c) to a greater extent than did placebo at all doses tested in patients with type 2 diabetes mellitus (T2DM) in the phase 3a PIONEER 1 trial.
The estimated mean change in HbA1c from baseline to week 26 – the primary endpoint – using an on-treatment analysis was –0.8% with a once-daily dose of 3 mg, –1.3% with a once-daily dose of 7 mg, and –1.5% with a once-daily dose of 14 mg. The corresponding value for placebo was –0.1%, with all comparisons statistically significant (P less than .001).
The on-treatment analysis evaluated treatment effects for all randomized patients (n = 703) and assumed that all subjects remained on-treatment and excluded the effect of any rescue medication. Results for an intention-to-treat (ITT) analysis provided similar results, however, with estimated mean changes in HbA1c of –0.9%, –1.2%, and –1.4% for the three respective semaglutide doses and –0.3% for placebo.
“There was a very nice dose-dependent decrease in HbA1c, which was superior to placebo for all doses of semaglutide” said study investigator Martin Haluzík, MD, at the annual meeting of the European Association for the Study of Diabetes.
“I think it’s quite important to stress the magnitude of the decrease of HbA1c, because with the highest dose it was –1.5% from a baseline of 8%, which I believe is something that hasn’t ever really been seen with any other oral antidiabetic medication,” added Dr. Haluzík, professor of internal medicine at the 1st Faculty of Medicine at Charles University and deputy head of the Institute for Clinical and Experimental Medicine, both in Prague.
Currently, GLP-1 RAs are available only in a subcutaneous formulation, Dr. Haluzík reminded his audience, adding that oral semaglutide was the first GLP-1 RA to be developed in a tablet formulation and was in the late stages of clinical development.
PIONEER 1 is the first of 10 phase 3a trials with oral semaglutide to be reported. “Additional studies, across the full spectrum of diabetes care, in special populations, comparing it with active comparators with varied trial duration, have been completed or will be completed in 2018,” said coinvestigator for the study Vanita Aroda, MD, during a separate presentation at a dedicated symposium on the PIONEER program.
Dr. Aroda, the director of the diabetes research program at Brigham and Women’s Hospital in Boston, observed that oral semaglutide was being evaluated from early care as monotherapy in the PIONEER 1 study. The other trials, such as PIONEER 2, PIONEER 3, PIONEER 4, and PIONEER 7 were looking at oral semaglutide in combination with oral antidiabetic agents versus various active comparators; PIONEER 5 and PIONEER 6 were in special populations; and PIONEER 8 was looking at its use on top of basal insulin. Two further trials are also part of the study program.
“I think this is the first time that we actually have completed data of an entire program, including cardiovascular data, all within the same year,” Dr. Aroda said. “All of the studies are in the process of data analysis or data reporting.”
PIONEER 1 was a multicenter, randomized, double-blind, placebo-controlled trial examining efficacy and safety of semaglutide versus placebo in 703 adults with drug-naive T2DM who were being treated with diet and exercise only.
Three doses of oral semaglutide – 3 mg, 7 mg, and 14 mg – were assessed and compared with placebo. There was a fixed 4-week dose escalation period, with all patients starting treatment with 3 mg of semaglutide and then increasing to 7 mg by week 4 and 14 mg by week 8. This was to try to reduce the risk of gastrointestinal side effects, which are known to occur with GLP-1 RAs.
Secondary outcome measures were change in body weight, fasting plasma glucose, HbA1c below a target of 7% (53 mmol/mol), which were all measured from baseline to week 26; adverse events, including severe and blood glucose–confirmed symptomatic hypoglycemic episodes, were assessed out to week 31.
The average age of patients in the trial was around 55 years, around half were female, and the starting HbA1c was approximately 8%.The mean body weight ranged from 86.9 kg to 89 kg in the different treatment groups, with a similar body mass index of about 32 kg/m2.
Clinically meaningful weight loss, compared with placebo, was only achieved with the highest dose of oral semaglutide, with a –4.1 kg reduction versus –1.5 kg for placebo from baseline to week 26 (P less than .001, on-treatment analysis). Reductions in body weight for the 3-mg and 7-mg oral semaglutide doses were a respective –1.7 kg and –2.5 kg. ITT results were again similar, with weight losses of –1.5, –2.3, and –3.7 kg for the 3-, 7-, and 14-mg doses of oral semaglutide, respectively, and –1.4 kg for placebo.
More patients treated with oral semaglutide 3, 7, or 14 mg versus placebo achieved an HbA1c of below 7% (59.1%, 71.9%, and 80.3%, respectively, vs. 33.8%) or a body weight loss of 5% or more (21.3%, 28.7%, and 44.3% vs. 15.7%).
Furthermore, more patients treated with oral semaglutide achieved an HbA1c of or below 7% without hypoglycemic episodes or body weight gain than did those given placebo. There were also more patients who achieved an HbA1c reduction of at least 1% and a weight loss of 3% or higher.
“Oral semaglutide demonstrated a safety and tolerability profile consistent with that of [injectable] GLP-1 RAs,” Dr. Haluzík reported. Adverse events were seen in 57.7%, 53.1%, and 56.6%of patients treated with 3, 7, and 14 mg of oral semaglutide and 55.6% of those treated with placebo.
The most common adverse events seen with oral semaglutide affected the gastrointestinal tract, with nausea affecting 8%, 5.1%, and 16% of 3, 7, and 14 mg–treated patients versus 5.6% of placebo-treated patients. Vomiting affected a respective 2.9%, 4.6%, 6.9%, and 2.1%, and diarrhea a respective 8.6%, 5.1%, 5.1%, and 2.2%.
Severe or blood glucose–confirmed, symptomatic hypoglycemia was reported in 2.9%, 1.1%, and 0.6%of those treated with 3, 7, 14 mg of oral semaglutide and 0.6% of placebo-treated patients.
PIONEER 1 represents a “step change in GLP-1 receptor agonist therapy”, said Cliff Bailey, MD, who discussed the trial aa the EASD’s independent commentator during a symposium on the PIONEER program. These data are “leading to a new delivery route for GLP-1 receptor agonists, from injection to oral,” and “this can be done with good metabolic efficacy, with substantial reductions in A1c and body weight, and with a safety profile that’s comparable to the subcutaneous injection.”
Dr. Bailey, who is professor of clinical science at Aston University in Birmingham, England, noted, however, the oral dosing of semaglutide “requires patient commitment because it needs to be taken before breakfast time, and it may also, to some extent, affect the timing of some of the other medications.”
The study was sponsored by Novo Nordisk. Dr. Haluzík disclosed acting as a consultant to AstraZeneca, Eli Lilly, Johnson & Johnson, Mundipharma, Novatin, Novo Nordisk, and Sanofi Aventis. Dr. Aroda was an investigator in the PIONEER 1 study and disclosed acting as a consultant to Novo Nordisk; she also disclosed relationships with multiple other pharmaceutical companies, including AstraZeneca, BMS, Calbra, Eisai, Elcelyx Therapeutics, Janssen, and Sanofi Aventis. Dr. Bailey acknowledged attending advisory boards, undertaking ad hoc consultancy work, and receiving research and travel support from several pharmaceutical companies that included Novo Nordisk.
SOURCES: Haluzík M et al. EASD 2018, Abstract 38; Aroda V. EASD 2018, Session S18 - PIONEER Trial; Bailey C. EASD 2018, Session S18 - PIONEER Trial.
REPORTING FROM EASD 2018
Key clinical point: A novel oral formulation of semaglutide proved better than placebo for diabetes control and weight loss in patients with T2DM.
Major finding: Mean change in hemoglobin A1c (baseline to week 26) – the primary endpoint – using an on-treatment analysis was –0.8% with a once-daily dose of 3 mg, –1.3% with a once-daily dose of 7 mg, and –1.5% with a once-daily dose of 14 mg. The corresponding value for placebo was –0.1%.
Study details: Phase 3a, multicenter, randomized, double-blind, placebo-controlled trial examining efficacy and safety of semaglutide versus placebo in 703 individuals with T2DM being treated with diet and exercise only.
Disclosures: The study was sponsored by Novo Nordisk. Dr. Haluzík disclosed acting as a consultant to AstraZeneca, Eli Lilly, Johnson & Johnson, Mundipharma, Novatin, Novo Nordisk, and Sanofi Aventis. Dr. Aroda was an investigator in the PIONEER 1 study and disclosed acting as a consultant to Novo Nordisk. She also disclosed relationships with multiple other pharmaceutical companies, including AstraZeneca, BMS, Calbra, Eisai, Elcelyx Therapeutics, Janssen, and Sanofi Aventis. Dr. Bailey acknowledged attending advisory boards of, undertaking ad hoc consultancy work for, and receiving research and travel support from several pharmaceutical companies that included Novo Nordisk.
Source: Haluzík M et al. EASD 2018, Abstract 38; Aroda V. EASD 2018, Session S18 – PIONEER Trial; Bailey C. EASD 2018, Session S18 – PIONEER Trial.
mRECIST response to kinase inhibitors predicts survival in HCC
SAN FRANCISCO – Patients with hepatocellular carcinoma (HCC) who have a response to first-line kinase inhibitors based on modified RECIST (mRECIST) criteria live almost a year longer than counterparts who have stable or progressive disease, finds a retrospective post hoc analysis of the REFLECT trial.
“The inability to accurately evaluate response to targeted or locoregional therapies resulted in the adaptation of RECIST to mRECIST, guidelines specifically designed to evaluate response to treatment in HCC,” noted lead investigator Masatoshi Kudo, MD, PhD, of the department of gastroenterology and hepatology, Kindai University Faculty of Medicine, Osaka, Japan. “Based on recommendations from the EASL [European Association for the Study of the Liver] consensus conference in 2000, mRECIST was developed to assess response based on the reduction of viable tumor burden … rather than overall tumor shrinkage. However, EASL clinical practice guidelines also suggested additional studies are needed to validate this approach.”
The investigators analyzed data from REFLECT, a global phase 3 noninferiority, randomized, controlled trial that showed overall survival with the novel kinase inhibitor lenvatinib (Lenvima) was not inferior to that with the older kinase inhibitor sorafenib (Nexavar) in 954 patients with untreated, unresectable HCC (Lancet. 2018;391:1163-73).
The new analysis, reported at the 2019 GI Cancers Symposium, showed that, among all randomized patients, those having an objective response according to mRECIST criteria were 39% less likely to die after other factors were taken into account. The finding was consistent in a landmark analysis, which addresses the issue of lead-time bias.
“Objective response by mRECIST was an independent predictor of overall survival in patients with HCC regardless of treatment,” Dr. Kudo concluded, adding that the findings are consistent with those of several previous studies. “Thus, patients who achieve an objective response can potentially expect a longer overall survival. However, additional studies are needed to further validate the correlation between objective response and overall survival.”
Findings in context
Although the mRECIST criteria overcome some issues with the size-based RECIST criteria in assessing HCC, the former are not without their limitations, noted invited discussant Andrew X. Zhu, MD, PhD, of Harvard Medical School and Massachusetts General Hospital Cancer Center.
These limitations include, for example, the need for more stringent selection of target lesions and the potential for antiangiogenic agents to cause vasoconstriction, complicating measurement. “There is tremendous intraobserver and interobserver variability, and a tremendous learning curve,” he added, noting that in REFLECT the mRECIST overall response rate assessed by independent reviewers was considerably higher than that assessed by investigators.
To date, three other trials of targeted therapies have similarly found an association between mRECIST response and overall survival. But a fourth did not.
“In the era of immunotherapy being actively applied to HCC, it’s important to recognize that this association actually may be agent dependent,” Dr. Zhu said. “Even though the TKIs with antiangiogenic [activity] have shown an improved overall response [going] from RECIST to mRECIST, this has not been recapitulated, at least based on the current experience that we have, with checkpoint inhibitors.”
The REFLECT investigators’ conclusion “is certainly backed by the large dataset from a positive phase 3 trial. It has very sound statistical methodology, and it may actually provide the initial evidence that this biomarker may serve as a potentially relevant surrogate to predict overall survival,” he said.
At the same time, there is reason to be cautious given the post hoc, retrospective nature of the study; the lack of a comparison with conventional RECIST response; absence of analysis of the potential correlation of stable disease with overall survival; and the lumping together of two agents, among other issues.
“For these reasons, I do think additional studies are warranted for prospective validation of the findings,” Dr. Zhu concluded.
Study details
REFLECT patients had an investigator-assessed mRECIST objective response rate of 16.7% overall (24.1% with lenvatinib and 9.2% with sorafenib) and a median overall survival of 13.0 months (13.6 months with lenvatinib and 12.3 months with sorafenib).
Median overall survival was 22.4 months for mRECIST responders and 11.4 months for nonresponders (P less than .001), Dr. Kudo reported at the symposium, sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
In a multivariate analysis, this difference translated to a 39% reduction in risk of death for responders (hazard ratio, 0.61; P less than .0001).
Moreover, the survival advantage of response was evident in landmark analyses, whether response was assessed at 2 months (HR, 0.75; P = .033), at 4 months (HR, 0.72; P = .009), or at 6 months (HR, 0.73; P = .010).
Dr. Kudo disclosed that he receives honoraria or has a consulting or advisory role with several pharmaceutical companies. The presentation was sponsored by Eisai and Merck.
SOURCE: Kudo M et al. GI Cancers Symposium, Abstract 186.
SAN FRANCISCO – Patients with hepatocellular carcinoma (HCC) who have a response to first-line kinase inhibitors based on modified RECIST (mRECIST) criteria live almost a year longer than counterparts who have stable or progressive disease, finds a retrospective post hoc analysis of the REFLECT trial.
“The inability to accurately evaluate response to targeted or locoregional therapies resulted in the adaptation of RECIST to mRECIST, guidelines specifically designed to evaluate response to treatment in HCC,” noted lead investigator Masatoshi Kudo, MD, PhD, of the department of gastroenterology and hepatology, Kindai University Faculty of Medicine, Osaka, Japan. “Based on recommendations from the EASL [European Association for the Study of the Liver] consensus conference in 2000, mRECIST was developed to assess response based on the reduction of viable tumor burden … rather than overall tumor shrinkage. However, EASL clinical practice guidelines also suggested additional studies are needed to validate this approach.”
The investigators analyzed data from REFLECT, a global phase 3 noninferiority, randomized, controlled trial that showed overall survival with the novel kinase inhibitor lenvatinib (Lenvima) was not inferior to that with the older kinase inhibitor sorafenib (Nexavar) in 954 patients with untreated, unresectable HCC (Lancet. 2018;391:1163-73).
The new analysis, reported at the 2019 GI Cancers Symposium, showed that, among all randomized patients, those having an objective response according to mRECIST criteria were 39% less likely to die after other factors were taken into account. The finding was consistent in a landmark analysis, which addresses the issue of lead-time bias.
“Objective response by mRECIST was an independent predictor of overall survival in patients with HCC regardless of treatment,” Dr. Kudo concluded, adding that the findings are consistent with those of several previous studies. “Thus, patients who achieve an objective response can potentially expect a longer overall survival. However, additional studies are needed to further validate the correlation between objective response and overall survival.”
Findings in context
Although the mRECIST criteria overcome some issues with the size-based RECIST criteria in assessing HCC, the former are not without their limitations, noted invited discussant Andrew X. Zhu, MD, PhD, of Harvard Medical School and Massachusetts General Hospital Cancer Center.
These limitations include, for example, the need for more stringent selection of target lesions and the potential for antiangiogenic agents to cause vasoconstriction, complicating measurement. “There is tremendous intraobserver and interobserver variability, and a tremendous learning curve,” he added, noting that in REFLECT the mRECIST overall response rate assessed by independent reviewers was considerably higher than that assessed by investigators.
To date, three other trials of targeted therapies have similarly found an association between mRECIST response and overall survival. But a fourth did not.
“In the era of immunotherapy being actively applied to HCC, it’s important to recognize that this association actually may be agent dependent,” Dr. Zhu said. “Even though the TKIs with antiangiogenic [activity] have shown an improved overall response [going] from RECIST to mRECIST, this has not been recapitulated, at least based on the current experience that we have, with checkpoint inhibitors.”
The REFLECT investigators’ conclusion “is certainly backed by the large dataset from a positive phase 3 trial. It has very sound statistical methodology, and it may actually provide the initial evidence that this biomarker may serve as a potentially relevant surrogate to predict overall survival,” he said.
At the same time, there is reason to be cautious given the post hoc, retrospective nature of the study; the lack of a comparison with conventional RECIST response; absence of analysis of the potential correlation of stable disease with overall survival; and the lumping together of two agents, among other issues.
“For these reasons, I do think additional studies are warranted for prospective validation of the findings,” Dr. Zhu concluded.
Study details
REFLECT patients had an investigator-assessed mRECIST objective response rate of 16.7% overall (24.1% with lenvatinib and 9.2% with sorafenib) and a median overall survival of 13.0 months (13.6 months with lenvatinib and 12.3 months with sorafenib).
Median overall survival was 22.4 months for mRECIST responders and 11.4 months for nonresponders (P less than .001), Dr. Kudo reported at the symposium, sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
In a multivariate analysis, this difference translated to a 39% reduction in risk of death for responders (hazard ratio, 0.61; P less than .0001).
Moreover, the survival advantage of response was evident in landmark analyses, whether response was assessed at 2 months (HR, 0.75; P = .033), at 4 months (HR, 0.72; P = .009), or at 6 months (HR, 0.73; P = .010).
Dr. Kudo disclosed that he receives honoraria or has a consulting or advisory role with several pharmaceutical companies. The presentation was sponsored by Eisai and Merck.
SOURCE: Kudo M et al. GI Cancers Symposium, Abstract 186.
SAN FRANCISCO – Patients with hepatocellular carcinoma (HCC) who have a response to first-line kinase inhibitors based on modified RECIST (mRECIST) criteria live almost a year longer than counterparts who have stable or progressive disease, finds a retrospective post hoc analysis of the REFLECT trial.
“The inability to accurately evaluate response to targeted or locoregional therapies resulted in the adaptation of RECIST to mRECIST, guidelines specifically designed to evaluate response to treatment in HCC,” noted lead investigator Masatoshi Kudo, MD, PhD, of the department of gastroenterology and hepatology, Kindai University Faculty of Medicine, Osaka, Japan. “Based on recommendations from the EASL [European Association for the Study of the Liver] consensus conference in 2000, mRECIST was developed to assess response based on the reduction of viable tumor burden … rather than overall tumor shrinkage. However, EASL clinical practice guidelines also suggested additional studies are needed to validate this approach.”
The investigators analyzed data from REFLECT, a global phase 3 noninferiority, randomized, controlled trial that showed overall survival with the novel kinase inhibitor lenvatinib (Lenvima) was not inferior to that with the older kinase inhibitor sorafenib (Nexavar) in 954 patients with untreated, unresectable HCC (Lancet. 2018;391:1163-73).
The new analysis, reported at the 2019 GI Cancers Symposium, showed that, among all randomized patients, those having an objective response according to mRECIST criteria were 39% less likely to die after other factors were taken into account. The finding was consistent in a landmark analysis, which addresses the issue of lead-time bias.
“Objective response by mRECIST was an independent predictor of overall survival in patients with HCC regardless of treatment,” Dr. Kudo concluded, adding that the findings are consistent with those of several previous studies. “Thus, patients who achieve an objective response can potentially expect a longer overall survival. However, additional studies are needed to further validate the correlation between objective response and overall survival.”
Findings in context
Although the mRECIST criteria overcome some issues with the size-based RECIST criteria in assessing HCC, the former are not without their limitations, noted invited discussant Andrew X. Zhu, MD, PhD, of Harvard Medical School and Massachusetts General Hospital Cancer Center.
These limitations include, for example, the need for more stringent selection of target lesions and the potential for antiangiogenic agents to cause vasoconstriction, complicating measurement. “There is tremendous intraobserver and interobserver variability, and a tremendous learning curve,” he added, noting that in REFLECT the mRECIST overall response rate assessed by independent reviewers was considerably higher than that assessed by investigators.
To date, three other trials of targeted therapies have similarly found an association between mRECIST response and overall survival. But a fourth did not.
“In the era of immunotherapy being actively applied to HCC, it’s important to recognize that this association actually may be agent dependent,” Dr. Zhu said. “Even though the TKIs with antiangiogenic [activity] have shown an improved overall response [going] from RECIST to mRECIST, this has not been recapitulated, at least based on the current experience that we have, with checkpoint inhibitors.”
The REFLECT investigators’ conclusion “is certainly backed by the large dataset from a positive phase 3 trial. It has very sound statistical methodology, and it may actually provide the initial evidence that this biomarker may serve as a potentially relevant surrogate to predict overall survival,” he said.
At the same time, there is reason to be cautious given the post hoc, retrospective nature of the study; the lack of a comparison with conventional RECIST response; absence of analysis of the potential correlation of stable disease with overall survival; and the lumping together of two agents, among other issues.
“For these reasons, I do think additional studies are warranted for prospective validation of the findings,” Dr. Zhu concluded.
Study details
REFLECT patients had an investigator-assessed mRECIST objective response rate of 16.7% overall (24.1% with lenvatinib and 9.2% with sorafenib) and a median overall survival of 13.0 months (13.6 months with lenvatinib and 12.3 months with sorafenib).
Median overall survival was 22.4 months for mRECIST responders and 11.4 months for nonresponders (P less than .001), Dr. Kudo reported at the symposium, sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
In a multivariate analysis, this difference translated to a 39% reduction in risk of death for responders (hazard ratio, 0.61; P less than .0001).
Moreover, the survival advantage of response was evident in landmark analyses, whether response was assessed at 2 months (HR, 0.75; P = .033), at 4 months (HR, 0.72; P = .009), or at 6 months (HR, 0.73; P = .010).
Dr. Kudo disclosed that he receives honoraria or has a consulting or advisory role with several pharmaceutical companies. The presentation was sponsored by Eisai and Merck.
SOURCE: Kudo M et al. GI Cancers Symposium, Abstract 186.
REPORTING FROM THE 2019 GI CANCERS SYMPOSIUM
Key clinical point: .
Major finding: Median overall survival was a respective 22.4 months and 11.4 months in patients who did and did not have a response according to mRECIST criteria (HR, 0.61; P less than .0001).
Study details: A retrospective post hoc analysis of a phase 3 randomized controlled trial of lenvatinib versus sorafenib among 954 patients with untreated, unresectable HCC (REFLECT trial).
Disclosures: Dr. Kudo disclosed that he receives honoraria or has a consulting or advisory role with several pharmaceutical companies. The presentation was sponsored by Eisai and Merck.
Source: Kudo M et al. 2019 GI Cancers Symposium, Abstract 186.
Coffee shop founder provides mental health intervention
A sign on the wall of the Sip of Hope Coffee Bar in the Logan Square area of Chicago reads: “It’s OK not to be OK.” The slogan is more than a way to distinguish the coffee shop from competitors. According to a report published recently in the Chicago Sun-Times, all money spent on beverages and pastries is donated to suicide prevention and mental health programs in the Windy City.
“Sip of Hope is the brick-and-mortar version of what we do every day,” Jonny Boucher, who started a nonprofit called Hope for the Day in 2011 in an effort to make mental health issues part of the everyday conversation, said in the article. “I’ve lost 16 people to suicide, and I thought if I can just take this pain and I can do something with it, then I can allow others to do something with their pain.”
Mr. Boucher organizes a monthly get-together at the coffee shop where people can talk about their mental health struggles and find help and friendship.
said Mr. Boucher. “There is no magic wand with mental health but I try to tell people – we’re all in this together – it’s not about me, it’s about we.”
Housing First program launched
A housing program being offered in some parts of Kansas, including Wichita, is making housing available to people with mental illness without the traditional requirements of a nightly curfew or adherence to sobriety.
“What we’re doing with a program like this is essentially leveling the playing field so that people who have for some reason become homeless have the same opportunity to have and keep housing as the rest of us,” Sam J. Tsemberis, PhD, a psychologist who founded Pathways to Housing in New York City and is spearheading the program in Kansas, said in an interview with the Topeka Capital-Journal. “Most people in Kansas don’t have sobriety and treatment requirements in order to stay housed. And if they did, we’d be in a lot more trouble on the homelessness front.”
Dr. Tsemberis said his philosophy about providing housing for people with mental illness stems from his work years ago at Bellevue Hospital in New York. During his commute, Dr. Tsemberis said, he “passed people on the sidewalk he had just treated as patients, still wearing the hospital pajamas they were dispatched in.”
“A community’s social structure is impaired when people can walk by somebody who is homeless on the street,” Dr. Tsemberis, a psychiatry professor at Columbia University in New York, said in the interview. “It’s not just the person who is homeless, who is isolated and disconnected. It’s everybody else who walks past them that also has to cut off a part of their humanity in order to tolerate being able to walk past another human being who is sitting there.”
More than 2,000 homeless people live in Kansas, and Wichita is the hub. So far, more than 320 Kansas residents have entered the Housing First program, and more than 240 have found permanent housing.
Some residents shortchanged on services
Policymakers in Chicago are discussing the possibility of reopening some of the city’s mental health clinics.
A city council committee recently unanimously voted to approve a Public Mental Health Clinic Service Expansion Task Force to look into the possibility.
“We are all aware of the anecdotal issues related to the gaps in mental health care that face our wards,” Alderman Sophia King, who sponsored the measure, said in an article published in the Chicago Sun-Times.
According to the article, six of the city’s mental health clinics were shut down in 2012. Mental health clinics said funding for mental health care in the city has continued to decline. A report issued last year by the Collaborative for Community Wellness focusing on mental health services on the city’s southwest side said there were 0.17 licensed mental health clinicians for every 1,000 residents. Meanwhile, on the city’s near north side, also known as the Gold Coast, there were 4.45 clinicians for every 1,000 residents, the report said.
Increase in suicides raising concerns
A recent report from the Tennessee Suicide Prevention Network reveals a dark picture. As reported by the Tennessean, the suicide rate continued to climb last year, continuing an increase that began in 2014. The suicide rate of 17.3 of every 100,000 people is markedly higher than the national rate of 14.5, according to an article in the Tennessean.
For children and adolescents aged 10-17 years, the situation is worse. In that cohort, rate of suicide climbed by more than 24% from 2016 to 2017, and a huge 55% between 2015 and 2017. In 2017, 142 people between 10 and 24 years of age ended their own lives. Overall, there were 1,163 suicides in 2017, an average of 3 every day.
Among the states’ demographics, suicide is three times higher among white non-Hispanics. Whites comprise 79% of the population of Tennessee and account for 91% of the suicides.
A national study in 2015 estimated the total national cost of suicides and suicide attempts at $93.5 billion. A single suicide can cost $1,329,553 in medical treatment and the lost productivity.
But those losses cannot be quantified. “For every number and rate that is provided in the 2019 ‘Status of Suicide in Tennessee’ report, a family member, loved one, neighbor, coworker, and friend suffers an unimaginable loss,” said Scott Ridgway, executive director of the Tennessee Suicide Prevention Network.
Anticonversion therapy bill introduced
A state senator in Arizona has reintroduced legislation aimed at preventing mental health professionals from practicing conversion therapy on minors.
Under the bill reintroduced by state Sen. Sean Bowie, a Democrat, psychotherapists who engage in practices aimed at changing the sexual orientation of a person under age 18 years would be “subject to disciplinary action.”
“This (practice) is completely discredited and actually hurtful for young people,” said state Sen. Bowie, according to azcentral.com, which is part of the USA Today network. “There’s really no medical proof that it’s helpful or effective at all.”
Late last year, the American Psychiatric Association reiterated its strong opposition to the practice. “Conversion therapy is banned in 14 states as well as the District of Columbia,” the group said. “The APA calls upon other lawmakers to ban the harmful and discriminatory practice.”
A sign on the wall of the Sip of Hope Coffee Bar in the Logan Square area of Chicago reads: “It’s OK not to be OK.” The slogan is more than a way to distinguish the coffee shop from competitors. According to a report published recently in the Chicago Sun-Times, all money spent on beverages and pastries is donated to suicide prevention and mental health programs in the Windy City.
“Sip of Hope is the brick-and-mortar version of what we do every day,” Jonny Boucher, who started a nonprofit called Hope for the Day in 2011 in an effort to make mental health issues part of the everyday conversation, said in the article. “I’ve lost 16 people to suicide, and I thought if I can just take this pain and I can do something with it, then I can allow others to do something with their pain.”
Mr. Boucher organizes a monthly get-together at the coffee shop where people can talk about their mental health struggles and find help and friendship.
said Mr. Boucher. “There is no magic wand with mental health but I try to tell people – we’re all in this together – it’s not about me, it’s about we.”
Housing First program launched
A housing program being offered in some parts of Kansas, including Wichita, is making housing available to people with mental illness without the traditional requirements of a nightly curfew or adherence to sobriety.
“What we’re doing with a program like this is essentially leveling the playing field so that people who have for some reason become homeless have the same opportunity to have and keep housing as the rest of us,” Sam J. Tsemberis, PhD, a psychologist who founded Pathways to Housing in New York City and is spearheading the program in Kansas, said in an interview with the Topeka Capital-Journal. “Most people in Kansas don’t have sobriety and treatment requirements in order to stay housed. And if they did, we’d be in a lot more trouble on the homelessness front.”
Dr. Tsemberis said his philosophy about providing housing for people with mental illness stems from his work years ago at Bellevue Hospital in New York. During his commute, Dr. Tsemberis said, he “passed people on the sidewalk he had just treated as patients, still wearing the hospital pajamas they were dispatched in.”
“A community’s social structure is impaired when people can walk by somebody who is homeless on the street,” Dr. Tsemberis, a psychiatry professor at Columbia University in New York, said in the interview. “It’s not just the person who is homeless, who is isolated and disconnected. It’s everybody else who walks past them that also has to cut off a part of their humanity in order to tolerate being able to walk past another human being who is sitting there.”
More than 2,000 homeless people live in Kansas, and Wichita is the hub. So far, more than 320 Kansas residents have entered the Housing First program, and more than 240 have found permanent housing.
Some residents shortchanged on services
Policymakers in Chicago are discussing the possibility of reopening some of the city’s mental health clinics.
A city council committee recently unanimously voted to approve a Public Mental Health Clinic Service Expansion Task Force to look into the possibility.
“We are all aware of the anecdotal issues related to the gaps in mental health care that face our wards,” Alderman Sophia King, who sponsored the measure, said in an article published in the Chicago Sun-Times.
According to the article, six of the city’s mental health clinics were shut down in 2012. Mental health clinics said funding for mental health care in the city has continued to decline. A report issued last year by the Collaborative for Community Wellness focusing on mental health services on the city’s southwest side said there were 0.17 licensed mental health clinicians for every 1,000 residents. Meanwhile, on the city’s near north side, also known as the Gold Coast, there were 4.45 clinicians for every 1,000 residents, the report said.
Increase in suicides raising concerns
A recent report from the Tennessee Suicide Prevention Network reveals a dark picture. As reported by the Tennessean, the suicide rate continued to climb last year, continuing an increase that began in 2014. The suicide rate of 17.3 of every 100,000 people is markedly higher than the national rate of 14.5, according to an article in the Tennessean.
For children and adolescents aged 10-17 years, the situation is worse. In that cohort, rate of suicide climbed by more than 24% from 2016 to 2017, and a huge 55% between 2015 and 2017. In 2017, 142 people between 10 and 24 years of age ended their own lives. Overall, there were 1,163 suicides in 2017, an average of 3 every day.
Among the states’ demographics, suicide is three times higher among white non-Hispanics. Whites comprise 79% of the population of Tennessee and account for 91% of the suicides.
A national study in 2015 estimated the total national cost of suicides and suicide attempts at $93.5 billion. A single suicide can cost $1,329,553 in medical treatment and the lost productivity.
But those losses cannot be quantified. “For every number and rate that is provided in the 2019 ‘Status of Suicide in Tennessee’ report, a family member, loved one, neighbor, coworker, and friend suffers an unimaginable loss,” said Scott Ridgway, executive director of the Tennessee Suicide Prevention Network.
Anticonversion therapy bill introduced
A state senator in Arizona has reintroduced legislation aimed at preventing mental health professionals from practicing conversion therapy on minors.
Under the bill reintroduced by state Sen. Sean Bowie, a Democrat, psychotherapists who engage in practices aimed at changing the sexual orientation of a person under age 18 years would be “subject to disciplinary action.”
“This (practice) is completely discredited and actually hurtful for young people,” said state Sen. Bowie, according to azcentral.com, which is part of the USA Today network. “There’s really no medical proof that it’s helpful or effective at all.”
Late last year, the American Psychiatric Association reiterated its strong opposition to the practice. “Conversion therapy is banned in 14 states as well as the District of Columbia,” the group said. “The APA calls upon other lawmakers to ban the harmful and discriminatory practice.”
A sign on the wall of the Sip of Hope Coffee Bar in the Logan Square area of Chicago reads: “It’s OK not to be OK.” The slogan is more than a way to distinguish the coffee shop from competitors. According to a report published recently in the Chicago Sun-Times, all money spent on beverages and pastries is donated to suicide prevention and mental health programs in the Windy City.
“Sip of Hope is the brick-and-mortar version of what we do every day,” Jonny Boucher, who started a nonprofit called Hope for the Day in 2011 in an effort to make mental health issues part of the everyday conversation, said in the article. “I’ve lost 16 people to suicide, and I thought if I can just take this pain and I can do something with it, then I can allow others to do something with their pain.”
Mr. Boucher organizes a monthly get-together at the coffee shop where people can talk about their mental health struggles and find help and friendship.
said Mr. Boucher. “There is no magic wand with mental health but I try to tell people – we’re all in this together – it’s not about me, it’s about we.”
Housing First program launched
A housing program being offered in some parts of Kansas, including Wichita, is making housing available to people with mental illness without the traditional requirements of a nightly curfew or adherence to sobriety.
“What we’re doing with a program like this is essentially leveling the playing field so that people who have for some reason become homeless have the same opportunity to have and keep housing as the rest of us,” Sam J. Tsemberis, PhD, a psychologist who founded Pathways to Housing in New York City and is spearheading the program in Kansas, said in an interview with the Topeka Capital-Journal. “Most people in Kansas don’t have sobriety and treatment requirements in order to stay housed. And if they did, we’d be in a lot more trouble on the homelessness front.”
Dr. Tsemberis said his philosophy about providing housing for people with mental illness stems from his work years ago at Bellevue Hospital in New York. During his commute, Dr. Tsemberis said, he “passed people on the sidewalk he had just treated as patients, still wearing the hospital pajamas they were dispatched in.”
“A community’s social structure is impaired when people can walk by somebody who is homeless on the street,” Dr. Tsemberis, a psychiatry professor at Columbia University in New York, said in the interview. “It’s not just the person who is homeless, who is isolated and disconnected. It’s everybody else who walks past them that also has to cut off a part of their humanity in order to tolerate being able to walk past another human being who is sitting there.”
More than 2,000 homeless people live in Kansas, and Wichita is the hub. So far, more than 320 Kansas residents have entered the Housing First program, and more than 240 have found permanent housing.
Some residents shortchanged on services
Policymakers in Chicago are discussing the possibility of reopening some of the city’s mental health clinics.
A city council committee recently unanimously voted to approve a Public Mental Health Clinic Service Expansion Task Force to look into the possibility.
“We are all aware of the anecdotal issues related to the gaps in mental health care that face our wards,” Alderman Sophia King, who sponsored the measure, said in an article published in the Chicago Sun-Times.
According to the article, six of the city’s mental health clinics were shut down in 2012. Mental health clinics said funding for mental health care in the city has continued to decline. A report issued last year by the Collaborative for Community Wellness focusing on mental health services on the city’s southwest side said there were 0.17 licensed mental health clinicians for every 1,000 residents. Meanwhile, on the city’s near north side, also known as the Gold Coast, there were 4.45 clinicians for every 1,000 residents, the report said.
Increase in suicides raising concerns
A recent report from the Tennessee Suicide Prevention Network reveals a dark picture. As reported by the Tennessean, the suicide rate continued to climb last year, continuing an increase that began in 2014. The suicide rate of 17.3 of every 100,000 people is markedly higher than the national rate of 14.5, according to an article in the Tennessean.
For children and adolescents aged 10-17 years, the situation is worse. In that cohort, rate of suicide climbed by more than 24% from 2016 to 2017, and a huge 55% between 2015 and 2017. In 2017, 142 people between 10 and 24 years of age ended their own lives. Overall, there were 1,163 suicides in 2017, an average of 3 every day.
Among the states’ demographics, suicide is three times higher among white non-Hispanics. Whites comprise 79% of the population of Tennessee and account for 91% of the suicides.
A national study in 2015 estimated the total national cost of suicides and suicide attempts at $93.5 billion. A single suicide can cost $1,329,553 in medical treatment and the lost productivity.
But those losses cannot be quantified. “For every number and rate that is provided in the 2019 ‘Status of Suicide in Tennessee’ report, a family member, loved one, neighbor, coworker, and friend suffers an unimaginable loss,” said Scott Ridgway, executive director of the Tennessee Suicide Prevention Network.
Anticonversion therapy bill introduced
A state senator in Arizona has reintroduced legislation aimed at preventing mental health professionals from practicing conversion therapy on minors.
Under the bill reintroduced by state Sen. Sean Bowie, a Democrat, psychotherapists who engage in practices aimed at changing the sexual orientation of a person under age 18 years would be “subject to disciplinary action.”
“This (practice) is completely discredited and actually hurtful for young people,” said state Sen. Bowie, according to azcentral.com, which is part of the USA Today network. “There’s really no medical proof that it’s helpful or effective at all.”
Late last year, the American Psychiatric Association reiterated its strong opposition to the practice. “Conversion therapy is banned in 14 states as well as the District of Columbia,” the group said. “The APA calls upon other lawmakers to ban the harmful and discriminatory practice.”
Guideline public comment period framework
AGA is dedicated to integrity and transparency in the development of clinical guidance.
W In addition, to keep academic integrity of the AGA guideline, clinical practice update, and clinical pathway process, AGA follows the framework outlined by the Council of Medical Specialty Societies (CMSS) in The Code for Interaction with Companies.
The Code for Interaction with Companies states:
“7.15. Societies will not permit Guideline development panel members or staff to discuss a Guideline’s development with Company employees or representatives, will not accept unpublished data from Companies, and will not permit Companies to review Guidelines in draft form, except if a Society permits public or member comment on draft Guidelines as a part of the Society’s published Guideline development process.”
The Clinical Guidelines Committee and Clinical Practice Updates Committee strive to keep AGA’s clinical practice tools independent of industry influence and remain solely based on scientific evidence. As a result of this effort, AGA’s writing panels and chairs will have no direct communication with industry. Companies will have the opportunity to submit feedback during the public comment period. The panel will review any comments submitted through the online platform along with feedback from the public. The writing panel will take these suggestions into consideration when making revisions following the public comment period.
AGA is dedicated to integrity and transparency in the development of clinical guidance.
W In addition, to keep academic integrity of the AGA guideline, clinical practice update, and clinical pathway process, AGA follows the framework outlined by the Council of Medical Specialty Societies (CMSS) in The Code for Interaction with Companies.
The Code for Interaction with Companies states:
“7.15. Societies will not permit Guideline development panel members or staff to discuss a Guideline’s development with Company employees or representatives, will not accept unpublished data from Companies, and will not permit Companies to review Guidelines in draft form, except if a Society permits public or member comment on draft Guidelines as a part of the Society’s published Guideline development process.”
The Clinical Guidelines Committee and Clinical Practice Updates Committee strive to keep AGA’s clinical practice tools independent of industry influence and remain solely based on scientific evidence. As a result of this effort, AGA’s writing panels and chairs will have no direct communication with industry. Companies will have the opportunity to submit feedback during the public comment period. The panel will review any comments submitted through the online platform along with feedback from the public. The writing panel will take these suggestions into consideration when making revisions following the public comment period.
AGA is dedicated to integrity and transparency in the development of clinical guidance.
W In addition, to keep academic integrity of the AGA guideline, clinical practice update, and clinical pathway process, AGA follows the framework outlined by the Council of Medical Specialty Societies (CMSS) in The Code for Interaction with Companies.
The Code for Interaction with Companies states:
“7.15. Societies will not permit Guideline development panel members or staff to discuss a Guideline’s development with Company employees or representatives, will not accept unpublished data from Companies, and will not permit Companies to review Guidelines in draft form, except if a Society permits public or member comment on draft Guidelines as a part of the Society’s published Guideline development process.”
The Clinical Guidelines Committee and Clinical Practice Updates Committee strive to keep AGA’s clinical practice tools independent of industry influence and remain solely based on scientific evidence. As a result of this effort, AGA’s writing panels and chairs will have no direct communication with industry. Companies will have the opportunity to submit feedback during the public comment period. The panel will review any comments submitted through the online platform along with feedback from the public. The writing panel will take these suggestions into consideration when making revisions following the public comment period.