User login
In the Literature - Short Takes
Sepsis Campaign bundles shortened to 1 hour
In response to the 2016 Surviving Sepsis Campaign guidelines, the 3-hour and 6-hour bundles have been combined and shortened into a 1-hour bundle to emphasize the emergent nature of sepsis. Elements of the bundle remain to same: measuring lactate, obtaining blood cultures, administration of broad-spectrume antibiotics, administration of 30mL/kg crystalloid, and vasopressors when necessary.
Citation: Levy MM et al. The Surviving Sepsis Campaign bundle: 2018 update. Crit Care Med. 2018;46(6):997-1000
Early ED discharge for PE
This randomized trial showed that low-risk emergency department patients diagnosed with pulmonary embolism who were discharged from the ED with rivaroxaban within 24 hours of presentation had decreased length of stay and nearly $2,500 in cost savings, compared with patients treated according to standard of care (often including hospitalization) without increased risk of bleeding, recurrent venous thromboembolism, or death.
Citation: Peacock WF et al. Emergency department discharge of pulmonary embolus patients. Acad Emerg Med. 2018. doi: 10.1111/acem.13451.
Outbreak of coagulopathy associated with synthetic cannabinoids
The Centers for Disease Control and Prevention reports a recent outbreak of life-threatening coagulopathy associated with synthetic cannabinoid use, because of contamination with vitmin K antagonist agents. All patients who report synthetic cannabinoid use should be screened with INR testing, especially prior to procedures.
Citation: Outbreak of life-threatening coagulopathy associated with synthetic cannabinoid use. CDC Health Alert Network. June 27, 2018.
Lumbar puncture safe when performed on patients on dual-antiplatelet therapy
In a retrospective review of 100 adult patients who underwent lumbar puncture procedures while taking dual-antiplatelet therapy with aspirin and clopidogrel, Mayo clinic investigators found no epidural hematomas or other serious complications with at least 3 months of follow-up. This study was nto powered to detect the risk of spinal hematoma so caution and open discussion with patients still is recommended.
Citation: Carabenciov ID et al. Safety of lumbar puncture performed on dual anti-platelet therapy. Mayo Clinic Proc. 2018;93(5):627-9.
Sepsis Campaign bundles shortened to 1 hour
In response to the 2016 Surviving Sepsis Campaign guidelines, the 3-hour and 6-hour bundles have been combined and shortened into a 1-hour bundle to emphasize the emergent nature of sepsis. Elements of the bundle remain to same: measuring lactate, obtaining blood cultures, administration of broad-spectrume antibiotics, administration of 30mL/kg crystalloid, and vasopressors when necessary.
Citation: Levy MM et al. The Surviving Sepsis Campaign bundle: 2018 update. Crit Care Med. 2018;46(6):997-1000
Early ED discharge for PE
This randomized trial showed that low-risk emergency department patients diagnosed with pulmonary embolism who were discharged from the ED with rivaroxaban within 24 hours of presentation had decreased length of stay and nearly $2,500 in cost savings, compared with patients treated according to standard of care (often including hospitalization) without increased risk of bleeding, recurrent venous thromboembolism, or death.
Citation: Peacock WF et al. Emergency department discharge of pulmonary embolus patients. Acad Emerg Med. 2018. doi: 10.1111/acem.13451.
Outbreak of coagulopathy associated with synthetic cannabinoids
The Centers for Disease Control and Prevention reports a recent outbreak of life-threatening coagulopathy associated with synthetic cannabinoid use, because of contamination with vitmin K antagonist agents. All patients who report synthetic cannabinoid use should be screened with INR testing, especially prior to procedures.
Citation: Outbreak of life-threatening coagulopathy associated with synthetic cannabinoid use. CDC Health Alert Network. June 27, 2018.
Lumbar puncture safe when performed on patients on dual-antiplatelet therapy
In a retrospective review of 100 adult patients who underwent lumbar puncture procedures while taking dual-antiplatelet therapy with aspirin and clopidogrel, Mayo clinic investigators found no epidural hematomas or other serious complications with at least 3 months of follow-up. This study was nto powered to detect the risk of spinal hematoma so caution and open discussion with patients still is recommended.
Citation: Carabenciov ID et al. Safety of lumbar puncture performed on dual anti-platelet therapy. Mayo Clinic Proc. 2018;93(5):627-9.
Sepsis Campaign bundles shortened to 1 hour
In response to the 2016 Surviving Sepsis Campaign guidelines, the 3-hour and 6-hour bundles have been combined and shortened into a 1-hour bundle to emphasize the emergent nature of sepsis. Elements of the bundle remain to same: measuring lactate, obtaining blood cultures, administration of broad-spectrume antibiotics, administration of 30mL/kg crystalloid, and vasopressors when necessary.
Citation: Levy MM et al. The Surviving Sepsis Campaign bundle: 2018 update. Crit Care Med. 2018;46(6):997-1000
Early ED discharge for PE
This randomized trial showed that low-risk emergency department patients diagnosed with pulmonary embolism who were discharged from the ED with rivaroxaban within 24 hours of presentation had decreased length of stay and nearly $2,500 in cost savings, compared with patients treated according to standard of care (often including hospitalization) without increased risk of bleeding, recurrent venous thromboembolism, or death.
Citation: Peacock WF et al. Emergency department discharge of pulmonary embolus patients. Acad Emerg Med. 2018. doi: 10.1111/acem.13451.
Outbreak of coagulopathy associated with synthetic cannabinoids
The Centers for Disease Control and Prevention reports a recent outbreak of life-threatening coagulopathy associated with synthetic cannabinoid use, because of contamination with vitmin K antagonist agents. All patients who report synthetic cannabinoid use should be screened with INR testing, especially prior to procedures.
Citation: Outbreak of life-threatening coagulopathy associated with synthetic cannabinoid use. CDC Health Alert Network. June 27, 2018.
Lumbar puncture safe when performed on patients on dual-antiplatelet therapy
In a retrospective review of 100 adult patients who underwent lumbar puncture procedures while taking dual-antiplatelet therapy with aspirin and clopidogrel, Mayo clinic investigators found no epidural hematomas or other serious complications with at least 3 months of follow-up. This study was nto powered to detect the risk of spinal hematoma so caution and open discussion with patients still is recommended.
Citation: Carabenciov ID et al. Safety of lumbar puncture performed on dual anti-platelet therapy. Mayo Clinic Proc. 2018;93(5):627-9.
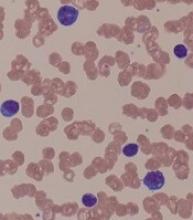
Rituximab biosimilar looks equivalent in follicular lymphoma
The rituximab biosimilar CT-P10 has equivalent efficacy, compared with rituximab, and is well tolerated in the treatment of low–tumor-burden follicular lymphoma, according to results from a multinational, randomized, phase 3 study.
Overall response after 7 months of treatment exceeded 80% for patients assigned to CT-P10 and for those assigned to rituximab, investigators reported in the Lancet Haematology.
Adverse event profiles were comparable for rituximab and the biosimilar over that time period, while pharmacokinetics, pharmacodynamics, and immunogenicity were likewise comparable between arms, according to investigators.
“Thus, CT-P10 monotherapy is suggested as a new therapeutic option for patients with low–tumor-burden follicular lymphoma,” wrote senior author Larry W Kwak, MD, PhD, of the Comprehensive Cancer Center, City of Hope, Duarte, Calif., and his colleagues.
CT-P10, the first rituximab biosimilar to be authorized by the European Medicines Agency, has been recommended for approval in the United States by the Food and Drug Administration’s Oncologic Drugs Advisory Committee.
If approved by the FDA, CT-P10 would be the first rituximab biosimilar available in the United States, according to the company, which noted three proposed indications in non-Hodgkin lymphoma.
In the current randomized, double-blind, parallel-group, phase 3 trial, 258 patients with stage II-IV low–tumor-burden follicular lymphoma were randomly assigned to CT-P10 (130 patients) or rituximab sourced in the United States (128 patients).
Treatment consisted of an induction period of intravenous CT-P10 or rituximab weekly for 4 weeks, while patients experiencing disease control went on to a maintenance phase with their assigned treatment given every 8 weeks for six cycles, followed by another year of maintenance therapy with CT-P10 for those still on study.
The primary endpoint of the study was overall response at 7 months, defined as a complete response, unconfirmed complete response, or partial response.
Overall response was seen in 83% of patients randomized to CT-P10 and 81% of patients randomized to rituximab at 7 months, Dr. Kwak and his colleagues reported.
The two treatments were deemed therapeutically equivalent, as illustrated by 90% confidence intervals within a prespecified equivalence margin of 17%, investigators said.
The most common treatment-emergent adverse events in either group were infusion-related reactions, which were of grade 1-2, except for one grade 3 reaction reported in the CT-P10 group, according to the report. Other common adverse events were upper respiratory tract infections and fatigue.
Serious adverse events were reported in six patients in the CT-P10 arm and three patients in the rituximab arm.
The availability of a rituximab biosimilar is anticipated to reduce the cost of treatment and improve patient access, according to investigators.
Introduction of CT-P10 in the European Union was projected to save between 90 and 150 million euros over a year, enabling more than 12,500 new patients to be treated with the biosimilar, according to results of a budget impact analysis investigators cited in their report.
“Widespread adoption of a rituximab biosimilar could have a substantial effect on health care budgets and might also have effects at a societal level,” Dr. Kwak and his coauthors said in the report.
The trial was sponsored by Celltrion and three coauthors of the study were employees of the company. Dr. Kwak and several other coinvestigators not employed by Celltrion reported disclosures related to the company. Other disclosures provided related to Novartis, Roche, AbbVie, Celgene, and Takeda, among other entities.
SOURCE: Ogura M et al. Lancet Haematol. 2018 Nov;5(11):e543-53.
The rituximab biosimilar CT-P10 has equivalent efficacy, compared with rituximab, and is well tolerated in the treatment of low–tumor-burden follicular lymphoma, according to results from a multinational, randomized, phase 3 study.
Overall response after 7 months of treatment exceeded 80% for patients assigned to CT-P10 and for those assigned to rituximab, investigators reported in the Lancet Haematology.
Adverse event profiles were comparable for rituximab and the biosimilar over that time period, while pharmacokinetics, pharmacodynamics, and immunogenicity were likewise comparable between arms, according to investigators.
“Thus, CT-P10 monotherapy is suggested as a new therapeutic option for patients with low–tumor-burden follicular lymphoma,” wrote senior author Larry W Kwak, MD, PhD, of the Comprehensive Cancer Center, City of Hope, Duarte, Calif., and his colleagues.
CT-P10, the first rituximab biosimilar to be authorized by the European Medicines Agency, has been recommended for approval in the United States by the Food and Drug Administration’s Oncologic Drugs Advisory Committee.
If approved by the FDA, CT-P10 would be the first rituximab biosimilar available in the United States, according to the company, which noted three proposed indications in non-Hodgkin lymphoma.
In the current randomized, double-blind, parallel-group, phase 3 trial, 258 patients with stage II-IV low–tumor-burden follicular lymphoma were randomly assigned to CT-P10 (130 patients) or rituximab sourced in the United States (128 patients).
Treatment consisted of an induction period of intravenous CT-P10 or rituximab weekly for 4 weeks, while patients experiencing disease control went on to a maintenance phase with their assigned treatment given every 8 weeks for six cycles, followed by another year of maintenance therapy with CT-P10 for those still on study.
The primary endpoint of the study was overall response at 7 months, defined as a complete response, unconfirmed complete response, or partial response.
Overall response was seen in 83% of patients randomized to CT-P10 and 81% of patients randomized to rituximab at 7 months, Dr. Kwak and his colleagues reported.
The two treatments were deemed therapeutically equivalent, as illustrated by 90% confidence intervals within a prespecified equivalence margin of 17%, investigators said.
The most common treatment-emergent adverse events in either group were infusion-related reactions, which were of grade 1-2, except for one grade 3 reaction reported in the CT-P10 group, according to the report. Other common adverse events were upper respiratory tract infections and fatigue.
Serious adverse events were reported in six patients in the CT-P10 arm and three patients in the rituximab arm.
The availability of a rituximab biosimilar is anticipated to reduce the cost of treatment and improve patient access, according to investigators.
Introduction of CT-P10 in the European Union was projected to save between 90 and 150 million euros over a year, enabling more than 12,500 new patients to be treated with the biosimilar, according to results of a budget impact analysis investigators cited in their report.
“Widespread adoption of a rituximab biosimilar could have a substantial effect on health care budgets and might also have effects at a societal level,” Dr. Kwak and his coauthors said in the report.
The trial was sponsored by Celltrion and three coauthors of the study were employees of the company. Dr. Kwak and several other coinvestigators not employed by Celltrion reported disclosures related to the company. Other disclosures provided related to Novartis, Roche, AbbVie, Celgene, and Takeda, among other entities.
SOURCE: Ogura M et al. Lancet Haematol. 2018 Nov;5(11):e543-53.
The rituximab biosimilar CT-P10 has equivalent efficacy, compared with rituximab, and is well tolerated in the treatment of low–tumor-burden follicular lymphoma, according to results from a multinational, randomized, phase 3 study.
Overall response after 7 months of treatment exceeded 80% for patients assigned to CT-P10 and for those assigned to rituximab, investigators reported in the Lancet Haematology.
Adverse event profiles were comparable for rituximab and the biosimilar over that time period, while pharmacokinetics, pharmacodynamics, and immunogenicity were likewise comparable between arms, according to investigators.
“Thus, CT-P10 monotherapy is suggested as a new therapeutic option for patients with low–tumor-burden follicular lymphoma,” wrote senior author Larry W Kwak, MD, PhD, of the Comprehensive Cancer Center, City of Hope, Duarte, Calif., and his colleagues.
CT-P10, the first rituximab biosimilar to be authorized by the European Medicines Agency, has been recommended for approval in the United States by the Food and Drug Administration’s Oncologic Drugs Advisory Committee.
If approved by the FDA, CT-P10 would be the first rituximab biosimilar available in the United States, according to the company, which noted three proposed indications in non-Hodgkin lymphoma.
In the current randomized, double-blind, parallel-group, phase 3 trial, 258 patients with stage II-IV low–tumor-burden follicular lymphoma were randomly assigned to CT-P10 (130 patients) or rituximab sourced in the United States (128 patients).
Treatment consisted of an induction period of intravenous CT-P10 or rituximab weekly for 4 weeks, while patients experiencing disease control went on to a maintenance phase with their assigned treatment given every 8 weeks for six cycles, followed by another year of maintenance therapy with CT-P10 for those still on study.
The primary endpoint of the study was overall response at 7 months, defined as a complete response, unconfirmed complete response, or partial response.
Overall response was seen in 83% of patients randomized to CT-P10 and 81% of patients randomized to rituximab at 7 months, Dr. Kwak and his colleagues reported.
The two treatments were deemed therapeutically equivalent, as illustrated by 90% confidence intervals within a prespecified equivalence margin of 17%, investigators said.
The most common treatment-emergent adverse events in either group were infusion-related reactions, which were of grade 1-2, except for one grade 3 reaction reported in the CT-P10 group, according to the report. Other common adverse events were upper respiratory tract infections and fatigue.
Serious adverse events were reported in six patients in the CT-P10 arm and three patients in the rituximab arm.
The availability of a rituximab biosimilar is anticipated to reduce the cost of treatment and improve patient access, according to investigators.
Introduction of CT-P10 in the European Union was projected to save between 90 and 150 million euros over a year, enabling more than 12,500 new patients to be treated with the biosimilar, according to results of a budget impact analysis investigators cited in their report.
“Widespread adoption of a rituximab biosimilar could have a substantial effect on health care budgets and might also have effects at a societal level,” Dr. Kwak and his coauthors said in the report.
The trial was sponsored by Celltrion and three coauthors of the study were employees of the company. Dr. Kwak and several other coinvestigators not employed by Celltrion reported disclosures related to the company. Other disclosures provided related to Novartis, Roche, AbbVie, Celgene, and Takeda, among other entities.
SOURCE: Ogura M et al. Lancet Haematol. 2018 Nov;5(11):e543-53.
FROM LANCET HAEMATOLOGY
Key clinical point:
Major finding: Overall response after 7 months of treatment was seen in 83% of patients randomized to CT-P10 and 81% of patients randomized to rituximab.
Study details: Analysis of 258 patients randomized to CT-P10 or rituximab in a phase 3, double-blind, parallel-group trial.
Disclosures: The trial was sponsored by Celltrion and three coauthors of the study were employees of the company. Other study coauthors reported disclosures related to Celltrion, Novartis, Roche, AbbVie, Celgene, and Takeda, among other companies.
Source: Ogura M et al. Lancet Haematol. 2018 Nov;5(11):e543-53.
PD-L1 correlates with worse sporadic, hereditary ccRCC outcomes
In patients with either sporadic or hereditary clear cell renal cell carcinoma, tumor expression of programmed death–ligand 1 (PD-L1) is associated with aggressive disease, investigators have found.
Analysis of tumor samples from patients with sporadic clear cell renal cell carcinoma (ccRCC) and others with Von Hippel-Lindau (VHL)–associated hereditary ccRCC showed that positive PD-L1 correlated with aggressive clinicopathologic features, reported Baoan Hong, MD, from Peking University First Hospital in Beijing, and colleagues.
“PD-L1 is a promising predictive biomarker for the utilization of PD-1/PD-L1 checkpoint inhibitors in ccRCC patients,” they wrote in Genitourinary Cancer.
The investigators conducted a retrospective analysis of PD-L1 expression and its potential correlation with disease features using samples from 129 patients with sporadic ccRCC and 26 patients with VHL disease who underwent partial or radical nephrectomy at their center from 2010 to 2017.
Sporadic ccRCC
The median age of patients with sporadic ccRCC was 61 years and the median tumor size was 4.3 cm. Of the 129 patients, 56 had pathological stage T1a at diagnosis, 44 had stage T1b, 8 had stage T2, and 21 had stage T3. In all, 25 patients had Fuhrman nuclear grade 3 tumors and 104 had grade 1 or 2 tumors. A total of 7 patients had metastases to lymph nodes, 41 had microvascular invasion, and 16 had tumor necrosis.
In all, 61 of these patients had PD-L1-positive tumors and 68 were PD-L1 negative. Positive PD-L1 was significantly associated with male gender (P = .025) and worse disease features, including higher T stage (P = .0011) and higher Fuhrman nuclear grade (P = .022).
After a median follow-up of 68 months, 9 patients in this group died and 17 others developed distant metastases or recurrent disease. Patients whose tumors were PD-L1 negative had significantly longer disease-free survival than patients with PD-L1-positive tumors, at a median 36 versus 28 months (P = .037).
VHL-associated ccRCC
Of the 26 patients with VHL-associated hereditary ccRCC (13 men and 13 women; median age, 42 years), 13 had pathological stage T1a disease, 7 had T1b, and 2 each has stage T2a, T3a, and T3b tumors. A total of 18 patients had Fuhrman nuclear grade 1 tumors and 8 had grade 2 tumors.
In this cohort, 17 patients had PD-L1-negative tumors, and 9 had PD-L1-positive tumors. PD-L1 expression was more common in patients with Fuhrman nuclear grade 2 tumors (six of eight cases). Patients with Fuhrman nuclear grade 1 tumors were more likely to be PD-L1 negative (15 of 18, P = .008). PD-L1 expression was not significantly correlated with either gender or tumor stage in this cohort.
There were no associations in this population between PD-L1 status and either age, tumor size, microvascular invasion, tumor necrosis, or lymph node metastases.
The investigators also compared the age of onset of all VHL-associated tumors in this cohort in PD-L1-positive versus PD-L1-negative patients, but found no statistically significant differences.
The authors acknowledged that the cohort sizes were small and that follow-up was relatively short, which could have a bearing on the analysis of associations between PD-L1 expression and disease features.
“Whether PD-L1 expression level in ccRCC is related to the effectiveness of PD-1/PD-L1 checkpoint inhibitor immunotherapy needs to be further investigated,” they wrote.
The study was supported by the National Natural Science Foundation of China and Special Health Development Research Project of Capital. The authors reported having no relevant disclosures.
SOURCE: Hong B et al. Clin Genitourin Cancer. 2018 Nov 13. doi: 10.1016/j.clgc.2018.11.001.
In patients with either sporadic or hereditary clear cell renal cell carcinoma, tumor expression of programmed death–ligand 1 (PD-L1) is associated with aggressive disease, investigators have found.
Analysis of tumor samples from patients with sporadic clear cell renal cell carcinoma (ccRCC) and others with Von Hippel-Lindau (VHL)–associated hereditary ccRCC showed that positive PD-L1 correlated with aggressive clinicopathologic features, reported Baoan Hong, MD, from Peking University First Hospital in Beijing, and colleagues.
“PD-L1 is a promising predictive biomarker for the utilization of PD-1/PD-L1 checkpoint inhibitors in ccRCC patients,” they wrote in Genitourinary Cancer.
The investigators conducted a retrospective analysis of PD-L1 expression and its potential correlation with disease features using samples from 129 patients with sporadic ccRCC and 26 patients with VHL disease who underwent partial or radical nephrectomy at their center from 2010 to 2017.
Sporadic ccRCC
The median age of patients with sporadic ccRCC was 61 years and the median tumor size was 4.3 cm. Of the 129 patients, 56 had pathological stage T1a at diagnosis, 44 had stage T1b, 8 had stage T2, and 21 had stage T3. In all, 25 patients had Fuhrman nuclear grade 3 tumors and 104 had grade 1 or 2 tumors. A total of 7 patients had metastases to lymph nodes, 41 had microvascular invasion, and 16 had tumor necrosis.
In all, 61 of these patients had PD-L1-positive tumors and 68 were PD-L1 negative. Positive PD-L1 was significantly associated with male gender (P = .025) and worse disease features, including higher T stage (P = .0011) and higher Fuhrman nuclear grade (P = .022).
After a median follow-up of 68 months, 9 patients in this group died and 17 others developed distant metastases or recurrent disease. Patients whose tumors were PD-L1 negative had significantly longer disease-free survival than patients with PD-L1-positive tumors, at a median 36 versus 28 months (P = .037).
VHL-associated ccRCC
Of the 26 patients with VHL-associated hereditary ccRCC (13 men and 13 women; median age, 42 years), 13 had pathological stage T1a disease, 7 had T1b, and 2 each has stage T2a, T3a, and T3b tumors. A total of 18 patients had Fuhrman nuclear grade 1 tumors and 8 had grade 2 tumors.
In this cohort, 17 patients had PD-L1-negative tumors, and 9 had PD-L1-positive tumors. PD-L1 expression was more common in patients with Fuhrman nuclear grade 2 tumors (six of eight cases). Patients with Fuhrman nuclear grade 1 tumors were more likely to be PD-L1 negative (15 of 18, P = .008). PD-L1 expression was not significantly correlated with either gender or tumor stage in this cohort.
There were no associations in this population between PD-L1 status and either age, tumor size, microvascular invasion, tumor necrosis, or lymph node metastases.
The investigators also compared the age of onset of all VHL-associated tumors in this cohort in PD-L1-positive versus PD-L1-negative patients, but found no statistically significant differences.
The authors acknowledged that the cohort sizes were small and that follow-up was relatively short, which could have a bearing on the analysis of associations between PD-L1 expression and disease features.
“Whether PD-L1 expression level in ccRCC is related to the effectiveness of PD-1/PD-L1 checkpoint inhibitor immunotherapy needs to be further investigated,” they wrote.
The study was supported by the National Natural Science Foundation of China and Special Health Development Research Project of Capital. The authors reported having no relevant disclosures.
SOURCE: Hong B et al. Clin Genitourin Cancer. 2018 Nov 13. doi: 10.1016/j.clgc.2018.11.001.
In patients with either sporadic or hereditary clear cell renal cell carcinoma, tumor expression of programmed death–ligand 1 (PD-L1) is associated with aggressive disease, investigators have found.
Analysis of tumor samples from patients with sporadic clear cell renal cell carcinoma (ccRCC) and others with Von Hippel-Lindau (VHL)–associated hereditary ccRCC showed that positive PD-L1 correlated with aggressive clinicopathologic features, reported Baoan Hong, MD, from Peking University First Hospital in Beijing, and colleagues.
“PD-L1 is a promising predictive biomarker for the utilization of PD-1/PD-L1 checkpoint inhibitors in ccRCC patients,” they wrote in Genitourinary Cancer.
The investigators conducted a retrospective analysis of PD-L1 expression and its potential correlation with disease features using samples from 129 patients with sporadic ccRCC and 26 patients with VHL disease who underwent partial or radical nephrectomy at their center from 2010 to 2017.
Sporadic ccRCC
The median age of patients with sporadic ccRCC was 61 years and the median tumor size was 4.3 cm. Of the 129 patients, 56 had pathological stage T1a at diagnosis, 44 had stage T1b, 8 had stage T2, and 21 had stage T3. In all, 25 patients had Fuhrman nuclear grade 3 tumors and 104 had grade 1 or 2 tumors. A total of 7 patients had metastases to lymph nodes, 41 had microvascular invasion, and 16 had tumor necrosis.
In all, 61 of these patients had PD-L1-positive tumors and 68 were PD-L1 negative. Positive PD-L1 was significantly associated with male gender (P = .025) and worse disease features, including higher T stage (P = .0011) and higher Fuhrman nuclear grade (P = .022).
After a median follow-up of 68 months, 9 patients in this group died and 17 others developed distant metastases or recurrent disease. Patients whose tumors were PD-L1 negative had significantly longer disease-free survival than patients with PD-L1-positive tumors, at a median 36 versus 28 months (P = .037).
VHL-associated ccRCC
Of the 26 patients with VHL-associated hereditary ccRCC (13 men and 13 women; median age, 42 years), 13 had pathological stage T1a disease, 7 had T1b, and 2 each has stage T2a, T3a, and T3b tumors. A total of 18 patients had Fuhrman nuclear grade 1 tumors and 8 had grade 2 tumors.
In this cohort, 17 patients had PD-L1-negative tumors, and 9 had PD-L1-positive tumors. PD-L1 expression was more common in patients with Fuhrman nuclear grade 2 tumors (six of eight cases). Patients with Fuhrman nuclear grade 1 tumors were more likely to be PD-L1 negative (15 of 18, P = .008). PD-L1 expression was not significantly correlated with either gender or tumor stage in this cohort.
There were no associations in this population between PD-L1 status and either age, tumor size, microvascular invasion, tumor necrosis, or lymph node metastases.
The investigators also compared the age of onset of all VHL-associated tumors in this cohort in PD-L1-positive versus PD-L1-negative patients, but found no statistically significant differences.
The authors acknowledged that the cohort sizes were small and that follow-up was relatively short, which could have a bearing on the analysis of associations between PD-L1 expression and disease features.
“Whether PD-L1 expression level in ccRCC is related to the effectiveness of PD-1/PD-L1 checkpoint inhibitor immunotherapy needs to be further investigated,” they wrote.
The study was supported by the National Natural Science Foundation of China and Special Health Development Research Project of Capital. The authors reported having no relevant disclosures.
SOURCE: Hong B et al. Clin Genitourin Cancer. 2018 Nov 13. doi: 10.1016/j.clgc.2018.11.001.
FROM CLINICAL GENITOURINARY CANCER
Key clinical point: Expression of programmed death–ligand 1 (PD-L1) in both sporadic and hereditary clear cell renal cell carcinoma (ccRCC) was associated with worse prognosis.
Major finding: Median disease-free survival of patients with sporadic ccRCC tumors negative for PD-L1 was 36 months, compared with 28 months for patients with PD-L1-positive tumors.
Study details: A retrospective analysis of tissues from 129 patients with sporadic ccRCC and 26 with Von Hippel-Lindau–associated hereditary ccRCC.
Disclosures: The study was supported by the National Natural Science Foundation of China and Special Health Development Research Project of Capital. The authors reported having no relevant disclosures.
Source: Hong B et al. Clin Genitourin Cancer. 2018 Nov 13. doi: 10.1016/j.clgc.2018.11.001.
Development of reversible B-cell inhibitor XmAb5871 for SLE moves forward
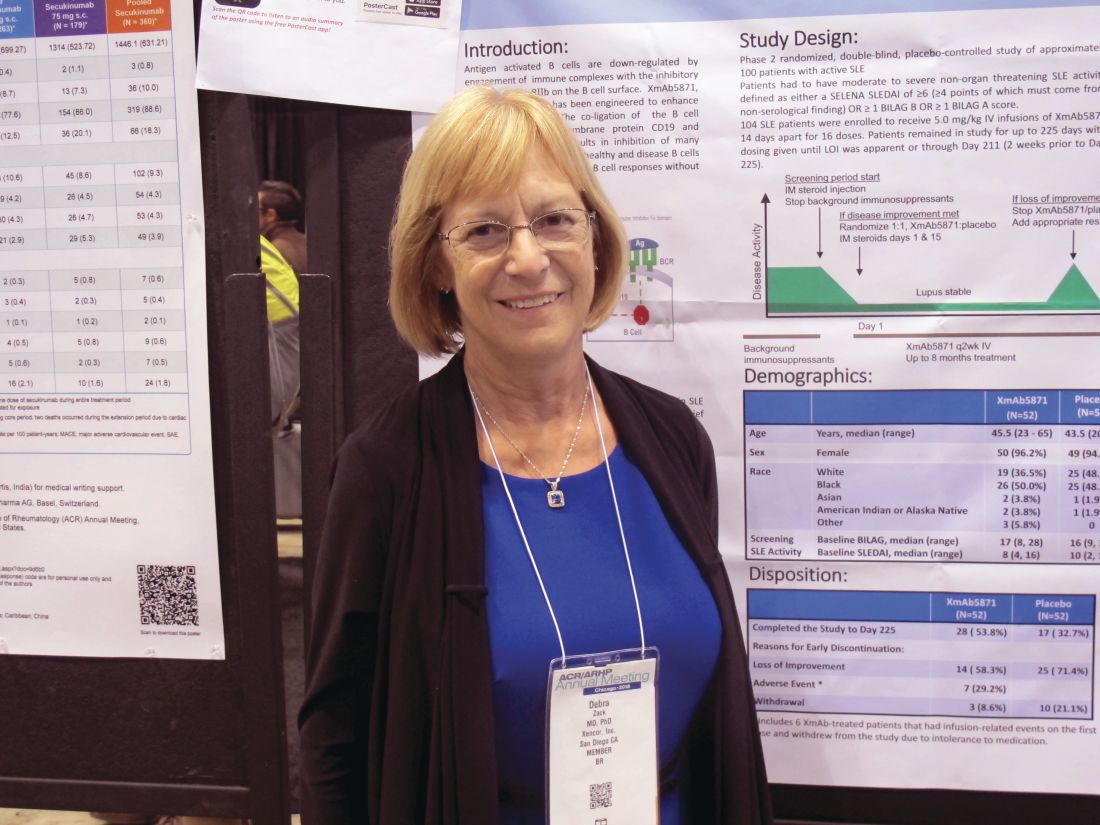
CHICAGO – The novel reversible B-cell inhibitor XmAb5871 showed promise for delaying loss of improvement after steroid therapy in patients with systemic lupus erythematosus in a randomized, placebo-controlled, phase 2 study.
Patients with moderate to severe nonorgan-threatening systemic lupus erythematosus (SLE) who underwent biweekly treatment with XmAb5871 after intramuscular glucocorticoid therapy more often achieved the trial’s primary endpoint of no loss of improvement through day 225 than did patients who took placebo. Overall, 21 (42%) of 50 patients who were randomized to receive active treatment reached this outcome, compared with 12 (29%) of 42 who received placebo based on the “efficacy-evaluable” patient population, defined as those who completed day 225, had a loss of improvement, or discontinued because of a drug-related adverse even. The difference between the treatment and placebo groups with respect to loss of improvement through day 225 reflected a positive trend, but did not reach statistical significance (P = .18), Debra J. Zack, MD, of Xencor in Monrovia, Calif., and her colleagues reported in a poster at the annual meeting of the American College of Rheumatology.
Of the patients who didn’t achieve the primary endpoint, 23 (46%) in the XmAb5871 arm versus 30 (71%) in the placebo arm experienced loss of improvement at any visit, the investigators noted. Six patients in the treatment arm discontinued for toxicity and were also considered nonresponders.
Treatment with XmAb5871 also led to a longer median time to loss of improvement of 230 days in comparison with the 130 days observed in placebo-treated patients. The difference was statistically significant in the efficacy-evaluable population (hazard ratio, 0.53; P = .025) and nearly statistically significant in the intent-to-treat (ITT) population of 52 patients in each group (HR, 0.59; P = .06), they noted.
Maintenance of improvement, which was another secondary endpoint, did not differ significantly between the groups in the efficacy-evaluable population (58.0% vs. 40.5%, respectively; P = .11), but did differ significantly with treatment versus placebo at both day 225 (response rates of 44.0% vs. 23.1%, respectively; P = .06) and at day 169 (57.7% vs. 34.6%; P = .02) in the ITT population, they said.
Of note, patients in the treatment group stayed in the study longer (median of 6.9 vs. 3.6 months) and received more infusions (median of 15.0 vs. 8.5).
“Antigen-activated B cells are down-regulated by engagement of immune complexes with the inhibitory Fcy receptor FcyRIIB on the B cell surface. XmAb5871 is an anti-CD19 monoclonal antibody engineered to enhance binding to FcyRIIB,” they explained, adding that the study was designed using unique methodology to minimize background medication and placebo responses to allow for better interpretation of the results in patients with complex, heterogeneous disease.
Participants were adults with a median age of 44.5 years; most (99 of 104) were women. All received an intramuscular glucocorticoid injection at the start of the screening period as background immunosuppressants were stopped, and those who experienced at least a 4-point decrease on the SLE disease activity index or at least a 1-grade decrease in at least one British Isles Lupus Activity Group A or B score were eligible for enrollment. Background immunosuppressants had to be stopped by the time of enrollment, but patients were allowed to remain on hydroxychloroquine and prednisone 10 mg or less daily or the equivalent.
Those enrolled were randomized to receive intravenous XmAb5871 at a dose of 5 mg/kg or placebo every 14 days for up to 16 doses until day 225 or loss of improvement (at which time patients could receive standard of care and withdraw from the study); all received intramuscular glucocorticoids (Depo-Medrol 80 mg [methylprednisolone acetate]) on days 1 and 15.
XmAb5871 was well tolerated in this study and had a safety profile consistent with that seen in previous SLE studies, with the exception of six withdrawals caused by infusion reactions, the investigators said. They noted that a subcutaneous formulation showed no infusion reactions or gastrointestinal-related infusion reactions in a bioavailability study of 40 healthy subjects, and so a formulation for subcutaneous injection will be used in future studies.
The vast majority of the 149 treatment-related adverse events that occurred in 41 patients in the current study (including 26% in placebo group patients) were mild or moderate in severity. A total of 13 serious adverse events (SAEs) occurred in 11 patients, and included fever, SLE flare (lung), atrial fibrillation, worsening hypertension, iron deficiency anemia, pneumonia (occurring 36 days, or 10 half-lives, after the last dose), infusion-related reaction, and vertigo in the XmAb5871 patients, and anemia SLE flare, SLE flare (enteritis), angioedema, and migraine headache in the placebo group.
“All SAEs were considered not or unlikely related except the infusion-related reaction. There were no deaths and no opportunistic infections,” they wrote.
Although the primary endpoint of loss of improvement by day 225 was not significantly better in the treatment group in this study, a positive trend was noted, the median time to loss of improvement was extended by 76%, and the risk of increased SLE disease activity was reduced by 47% in those who received XmAb5871, they said, concluding that the findings support further evaluation of the agent in patients with SLE.
The study was supported by Xencor.
SOURCE: Zack DJ et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract L14.
CHICAGO – The novel reversible B-cell inhibitor XmAb5871 showed promise for delaying loss of improvement after steroid therapy in patients with systemic lupus erythematosus in a randomized, placebo-controlled, phase 2 study.
Patients with moderate to severe nonorgan-threatening systemic lupus erythematosus (SLE) who underwent biweekly treatment with XmAb5871 after intramuscular glucocorticoid therapy more often achieved the trial’s primary endpoint of no loss of improvement through day 225 than did patients who took placebo. Overall, 21 (42%) of 50 patients who were randomized to receive active treatment reached this outcome, compared with 12 (29%) of 42 who received placebo based on the “efficacy-evaluable” patient population, defined as those who completed day 225, had a loss of improvement, or discontinued because of a drug-related adverse even. The difference between the treatment and placebo groups with respect to loss of improvement through day 225 reflected a positive trend, but did not reach statistical significance (P = .18), Debra J. Zack, MD, of Xencor in Monrovia, Calif., and her colleagues reported in a poster at the annual meeting of the American College of Rheumatology.
Of the patients who didn’t achieve the primary endpoint, 23 (46%) in the XmAb5871 arm versus 30 (71%) in the placebo arm experienced loss of improvement at any visit, the investigators noted. Six patients in the treatment arm discontinued for toxicity and were also considered nonresponders.
Treatment with XmAb5871 also led to a longer median time to loss of improvement of 230 days in comparison with the 130 days observed in placebo-treated patients. The difference was statistically significant in the efficacy-evaluable population (hazard ratio, 0.53; P = .025) and nearly statistically significant in the intent-to-treat (ITT) population of 52 patients in each group (HR, 0.59; P = .06), they noted.
Maintenance of improvement, which was another secondary endpoint, did not differ significantly between the groups in the efficacy-evaluable population (58.0% vs. 40.5%, respectively; P = .11), but did differ significantly with treatment versus placebo at both day 225 (response rates of 44.0% vs. 23.1%, respectively; P = .06) and at day 169 (57.7% vs. 34.6%; P = .02) in the ITT population, they said.
Of note, patients in the treatment group stayed in the study longer (median of 6.9 vs. 3.6 months) and received more infusions (median of 15.0 vs. 8.5).
“Antigen-activated B cells are down-regulated by engagement of immune complexes with the inhibitory Fcy receptor FcyRIIB on the B cell surface. XmAb5871 is an anti-CD19 monoclonal antibody engineered to enhance binding to FcyRIIB,” they explained, adding that the study was designed using unique methodology to minimize background medication and placebo responses to allow for better interpretation of the results in patients with complex, heterogeneous disease.
Participants were adults with a median age of 44.5 years; most (99 of 104) were women. All received an intramuscular glucocorticoid injection at the start of the screening period as background immunosuppressants were stopped, and those who experienced at least a 4-point decrease on the SLE disease activity index or at least a 1-grade decrease in at least one British Isles Lupus Activity Group A or B score were eligible for enrollment. Background immunosuppressants had to be stopped by the time of enrollment, but patients were allowed to remain on hydroxychloroquine and prednisone 10 mg or less daily or the equivalent.
Those enrolled were randomized to receive intravenous XmAb5871 at a dose of 5 mg/kg or placebo every 14 days for up to 16 doses until day 225 or loss of improvement (at which time patients could receive standard of care and withdraw from the study); all received intramuscular glucocorticoids (Depo-Medrol 80 mg [methylprednisolone acetate]) on days 1 and 15.
XmAb5871 was well tolerated in this study and had a safety profile consistent with that seen in previous SLE studies, with the exception of six withdrawals caused by infusion reactions, the investigators said. They noted that a subcutaneous formulation showed no infusion reactions or gastrointestinal-related infusion reactions in a bioavailability study of 40 healthy subjects, and so a formulation for subcutaneous injection will be used in future studies.
The vast majority of the 149 treatment-related adverse events that occurred in 41 patients in the current study (including 26% in placebo group patients) were mild or moderate in severity. A total of 13 serious adverse events (SAEs) occurred in 11 patients, and included fever, SLE flare (lung), atrial fibrillation, worsening hypertension, iron deficiency anemia, pneumonia (occurring 36 days, or 10 half-lives, after the last dose), infusion-related reaction, and vertigo in the XmAb5871 patients, and anemia SLE flare, SLE flare (enteritis), angioedema, and migraine headache in the placebo group.
“All SAEs were considered not or unlikely related except the infusion-related reaction. There were no deaths and no opportunistic infections,” they wrote.
Although the primary endpoint of loss of improvement by day 225 was not significantly better in the treatment group in this study, a positive trend was noted, the median time to loss of improvement was extended by 76%, and the risk of increased SLE disease activity was reduced by 47% in those who received XmAb5871, they said, concluding that the findings support further evaluation of the agent in patients with SLE.
The study was supported by Xencor.
SOURCE: Zack DJ et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract L14.
CHICAGO – The novel reversible B-cell inhibitor XmAb5871 showed promise for delaying loss of improvement after steroid therapy in patients with systemic lupus erythematosus in a randomized, placebo-controlled, phase 2 study.
Patients with moderate to severe nonorgan-threatening systemic lupus erythematosus (SLE) who underwent biweekly treatment with XmAb5871 after intramuscular glucocorticoid therapy more often achieved the trial’s primary endpoint of no loss of improvement through day 225 than did patients who took placebo. Overall, 21 (42%) of 50 patients who were randomized to receive active treatment reached this outcome, compared with 12 (29%) of 42 who received placebo based on the “efficacy-evaluable” patient population, defined as those who completed day 225, had a loss of improvement, or discontinued because of a drug-related adverse even. The difference between the treatment and placebo groups with respect to loss of improvement through day 225 reflected a positive trend, but did not reach statistical significance (P = .18), Debra J. Zack, MD, of Xencor in Monrovia, Calif., and her colleagues reported in a poster at the annual meeting of the American College of Rheumatology.
Of the patients who didn’t achieve the primary endpoint, 23 (46%) in the XmAb5871 arm versus 30 (71%) in the placebo arm experienced loss of improvement at any visit, the investigators noted. Six patients in the treatment arm discontinued for toxicity and were also considered nonresponders.
Treatment with XmAb5871 also led to a longer median time to loss of improvement of 230 days in comparison with the 130 days observed in placebo-treated patients. The difference was statistically significant in the efficacy-evaluable population (hazard ratio, 0.53; P = .025) and nearly statistically significant in the intent-to-treat (ITT) population of 52 patients in each group (HR, 0.59; P = .06), they noted.
Maintenance of improvement, which was another secondary endpoint, did not differ significantly between the groups in the efficacy-evaluable population (58.0% vs. 40.5%, respectively; P = .11), but did differ significantly with treatment versus placebo at both day 225 (response rates of 44.0% vs. 23.1%, respectively; P = .06) and at day 169 (57.7% vs. 34.6%; P = .02) in the ITT population, they said.
Of note, patients in the treatment group stayed in the study longer (median of 6.9 vs. 3.6 months) and received more infusions (median of 15.0 vs. 8.5).
“Antigen-activated B cells are down-regulated by engagement of immune complexes with the inhibitory Fcy receptor FcyRIIB on the B cell surface. XmAb5871 is an anti-CD19 monoclonal antibody engineered to enhance binding to FcyRIIB,” they explained, adding that the study was designed using unique methodology to minimize background medication and placebo responses to allow for better interpretation of the results in patients with complex, heterogeneous disease.
Participants were adults with a median age of 44.5 years; most (99 of 104) were women. All received an intramuscular glucocorticoid injection at the start of the screening period as background immunosuppressants were stopped, and those who experienced at least a 4-point decrease on the SLE disease activity index or at least a 1-grade decrease in at least one British Isles Lupus Activity Group A or B score were eligible for enrollment. Background immunosuppressants had to be stopped by the time of enrollment, but patients were allowed to remain on hydroxychloroquine and prednisone 10 mg or less daily or the equivalent.
Those enrolled were randomized to receive intravenous XmAb5871 at a dose of 5 mg/kg or placebo every 14 days for up to 16 doses until day 225 or loss of improvement (at which time patients could receive standard of care and withdraw from the study); all received intramuscular glucocorticoids (Depo-Medrol 80 mg [methylprednisolone acetate]) on days 1 and 15.
XmAb5871 was well tolerated in this study and had a safety profile consistent with that seen in previous SLE studies, with the exception of six withdrawals caused by infusion reactions, the investigators said. They noted that a subcutaneous formulation showed no infusion reactions or gastrointestinal-related infusion reactions in a bioavailability study of 40 healthy subjects, and so a formulation for subcutaneous injection will be used in future studies.
The vast majority of the 149 treatment-related adverse events that occurred in 41 patients in the current study (including 26% in placebo group patients) were mild or moderate in severity. A total of 13 serious adverse events (SAEs) occurred in 11 patients, and included fever, SLE flare (lung), atrial fibrillation, worsening hypertension, iron deficiency anemia, pneumonia (occurring 36 days, or 10 half-lives, after the last dose), infusion-related reaction, and vertigo in the XmAb5871 patients, and anemia SLE flare, SLE flare (enteritis), angioedema, and migraine headache in the placebo group.
“All SAEs were considered not or unlikely related except the infusion-related reaction. There were no deaths and no opportunistic infections,” they wrote.
Although the primary endpoint of loss of improvement by day 225 was not significantly better in the treatment group in this study, a positive trend was noted, the median time to loss of improvement was extended by 76%, and the risk of increased SLE disease activity was reduced by 47% in those who received XmAb5871, they said, concluding that the findings support further evaluation of the agent in patients with SLE.
The study was supported by Xencor.
SOURCE: Zack DJ et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract L14.
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point: XmAb5871 shows promise in systemic lupus erythematosus.
Major finding: There was no loss of improvement through day 225 in 42% of patients treated with XmAb5871 versus 29% with placebo.
Study details: A randomized, placebo-controlled, phase 2 study.
Disclosures: The study was supported by Xencor. Dr. Zack is an employee of Xencor.
Source: Zack DJ et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract L14.
A paradigm shift in medical research is necessary
ORLANDO – What doctors think they know to be true in medicine has changed dramatically in the past several decades and will be different again in the decades to come, leaving them with a dilemma, according to Kevin T. Powell, MD, PhD, a pediatric hospitalist in St. Louis. If half of what doctors teach or know in medicine today will ultimately end up not being true, how do they know what to believe or accept?
While there is not a single satisfactory answer to that question, researchers can select research that gets doctors closer to reliable findings and steer them away from the barrage of poor-quality research that emerges from the current publish-or-perish system, Dr. Powell told his colleagues at the annual meeting of the American Academy of Pediatrics.
During his talk, Dr. Powell discussed the challenges and flaws with medical research as it is currently conducted, citing Doug Altman’s writings on these problems as early as 1994.
“The poor quality of much medical research is widely acknowledged, yet disturbingly the leaders of the medical profession seem only minimally concerned about the problem and make no apparent effort to find a solution,” wrote Mr. Altman, an English medical statistician (BMJ. 1994;308:283).
“We need less research, better research, and research done for the right reasons,” Mr. Altman concluded. “Abandoning using the number of publications as a measure of ability would be a start.”
In an interview, Dr. Powell described an unfortunate consequence of the publish-or-perish pressure in academic medicine: A glut of short-term, small studies with little clinical utility that researchers can complete in 1 or 2 years rather than the large, multicenter studies that take several years – and produce higher-quality findings – but cannot be turned into as many publications.
“We’re generating a lot of medical research findings that end up being false,” he said. “It’s a random walk in terms of getting to the truth rather than having an accurate process of getting to truth through evidence-based medicine.”
But he was hopeful, not cynical, about the way forward. By persuading people that medical research has changed for the worse over time and can change into something better, Dr. Powell saw potential for future research resulting in the same sort of public health achievements that research produced in the past, such as big reductions in smoking or sudden infant death syndrome.
Dr. Powell concluded his talk with a riff on Martin Luther’s 95 Theses, the 9.5 Theses, for a reformation of evidence-based medicine that together address the various shortcomings he discussed.
1. Recognize academic promotion as a bias, just like drug money.
2. Don’t confound statistically significant and clinically significant.
3. Use only significant figures.
4. Use the phrase “we did not DETECT a difference” and include power calculations.
5. Use confidence intervals instead of P values.
6. Use number needed to harm and number needed to treat instead of relative risk.
7. Absence of proof is not proof of absence. When there is insufficient randomized, controlled trial evidence, have an independent party estimate an effect based on non-RCT articles.
8. Any article implying clinical practice should change must include a counterpoint and a benefit cost analysis. Consider both effectiveness and safety.
9. Use postmarketing peer review.
9.5. Beware of research based on surveys.
Dr. Powell reported no relevant financial disclosures.
ORLANDO – What doctors think they know to be true in medicine has changed dramatically in the past several decades and will be different again in the decades to come, leaving them with a dilemma, according to Kevin T. Powell, MD, PhD, a pediatric hospitalist in St. Louis. If half of what doctors teach or know in medicine today will ultimately end up not being true, how do they know what to believe or accept?
While there is not a single satisfactory answer to that question, researchers can select research that gets doctors closer to reliable findings and steer them away from the barrage of poor-quality research that emerges from the current publish-or-perish system, Dr. Powell told his colleagues at the annual meeting of the American Academy of Pediatrics.
During his talk, Dr. Powell discussed the challenges and flaws with medical research as it is currently conducted, citing Doug Altman’s writings on these problems as early as 1994.
“The poor quality of much medical research is widely acknowledged, yet disturbingly the leaders of the medical profession seem only minimally concerned about the problem and make no apparent effort to find a solution,” wrote Mr. Altman, an English medical statistician (BMJ. 1994;308:283).
“We need less research, better research, and research done for the right reasons,” Mr. Altman concluded. “Abandoning using the number of publications as a measure of ability would be a start.”
In an interview, Dr. Powell described an unfortunate consequence of the publish-or-perish pressure in academic medicine: A glut of short-term, small studies with little clinical utility that researchers can complete in 1 or 2 years rather than the large, multicenter studies that take several years – and produce higher-quality findings – but cannot be turned into as many publications.
“We’re generating a lot of medical research findings that end up being false,” he said. “It’s a random walk in terms of getting to the truth rather than having an accurate process of getting to truth through evidence-based medicine.”
But he was hopeful, not cynical, about the way forward. By persuading people that medical research has changed for the worse over time and can change into something better, Dr. Powell saw potential for future research resulting in the same sort of public health achievements that research produced in the past, such as big reductions in smoking or sudden infant death syndrome.
Dr. Powell concluded his talk with a riff on Martin Luther’s 95 Theses, the 9.5 Theses, for a reformation of evidence-based medicine that together address the various shortcomings he discussed.
1. Recognize academic promotion as a bias, just like drug money.
2. Don’t confound statistically significant and clinically significant.
3. Use only significant figures.
4. Use the phrase “we did not DETECT a difference” and include power calculations.
5. Use confidence intervals instead of P values.
6. Use number needed to harm and number needed to treat instead of relative risk.
7. Absence of proof is not proof of absence. When there is insufficient randomized, controlled trial evidence, have an independent party estimate an effect based on non-RCT articles.
8. Any article implying clinical practice should change must include a counterpoint and a benefit cost analysis. Consider both effectiveness and safety.
9. Use postmarketing peer review.
9.5. Beware of research based on surveys.
Dr. Powell reported no relevant financial disclosures.
ORLANDO – What doctors think they know to be true in medicine has changed dramatically in the past several decades and will be different again in the decades to come, leaving them with a dilemma, according to Kevin T. Powell, MD, PhD, a pediatric hospitalist in St. Louis. If half of what doctors teach or know in medicine today will ultimately end up not being true, how do they know what to believe or accept?
While there is not a single satisfactory answer to that question, researchers can select research that gets doctors closer to reliable findings and steer them away from the barrage of poor-quality research that emerges from the current publish-or-perish system, Dr. Powell told his colleagues at the annual meeting of the American Academy of Pediatrics.
During his talk, Dr. Powell discussed the challenges and flaws with medical research as it is currently conducted, citing Doug Altman’s writings on these problems as early as 1994.
“The poor quality of much medical research is widely acknowledged, yet disturbingly the leaders of the medical profession seem only minimally concerned about the problem and make no apparent effort to find a solution,” wrote Mr. Altman, an English medical statistician (BMJ. 1994;308:283).
“We need less research, better research, and research done for the right reasons,” Mr. Altman concluded. “Abandoning using the number of publications as a measure of ability would be a start.”
In an interview, Dr. Powell described an unfortunate consequence of the publish-or-perish pressure in academic medicine: A glut of short-term, small studies with little clinical utility that researchers can complete in 1 or 2 years rather than the large, multicenter studies that take several years – and produce higher-quality findings – but cannot be turned into as many publications.
“We’re generating a lot of medical research findings that end up being false,” he said. “It’s a random walk in terms of getting to the truth rather than having an accurate process of getting to truth through evidence-based medicine.”
But he was hopeful, not cynical, about the way forward. By persuading people that medical research has changed for the worse over time and can change into something better, Dr. Powell saw potential for future research resulting in the same sort of public health achievements that research produced in the past, such as big reductions in smoking or sudden infant death syndrome.
Dr. Powell concluded his talk with a riff on Martin Luther’s 95 Theses, the 9.5 Theses, for a reformation of evidence-based medicine that together address the various shortcomings he discussed.
1. Recognize academic promotion as a bias, just like drug money.
2. Don’t confound statistically significant and clinically significant.
3. Use only significant figures.
4. Use the phrase “we did not DETECT a difference” and include power calculations.
5. Use confidence intervals instead of P values.
6. Use number needed to harm and number needed to treat instead of relative risk.
7. Absence of proof is not proof of absence. When there is insufficient randomized, controlled trial evidence, have an independent party estimate an effect based on non-RCT articles.
8. Any article implying clinical practice should change must include a counterpoint and a benefit cost analysis. Consider both effectiveness and safety.
9. Use postmarketing peer review.
9.5. Beware of research based on surveys.
Dr. Powell reported no relevant financial disclosures.
EXPERT ANALYSIS FROM AAP 18
Lemons into lemonade: The 2019 Medicare physician fee schedule
Of course, there is a new final rule every year, so it really isn’t very final. I know this is confusing to many of you, I was dazed for several days by this year’s proposed final rule.

Each year, the Centers for Medicare & Medicaid Services receives input from innumerable sources and formulates its payment for physicians. These responses are often in response to requests by CMS itself, which wants to make sure reimbursements are accurate. Generally, input comes from the American Medical Association’s RVS Update Committee (RUC), which values new and existing CPT codes, as well as Congress, the Health & Human Services Office of Inspector General, lobbyists, specialty society organizations, public advocacy groups, and anyone who can wrangle an appointment at or write a letter to CMS headquarters in Baltimore. This conflicted brew is hashed over, and published in late July as a proposed rule. Public comments are then solicited (all letters and emails are considered, dermatologists sent 1,500 responses to this one!) and a final rule is published in the fall. I have constructed a flowchart of this process.
This year’s proposed rule was particularly disturbing because of major changes in reimbursement proposed by CMS. As you may recall, officials proposed to collapse all the evaluation and management (E/M) codes into two levels and pay bonuses to certain specialists (but not dermatologists). This might have been agreeable, except Medicare reimbursements are a zero-sum game. If someone is paid more, someone else will be paid less. Of course, you could always let the increase come out of the general pool, but that would decrease the conversion factor, and some health care professionals (usually primary care) might not see an overall increase. So, the proposed rule was going to “pay” for this increase by way of eliminating the 25 modifier, the CPT modifier that allows you to be paid for the evaluation and management (E/M) service on the same day as a procedure. This has been averted, at least for two years.
The final rule also makes a real effort to eliminate some meaningless documentation. Effective Jan. 1, 2019, for established patients, practitioners can focus their notes on patient changes. With new and established patients, they need not personally reenter the chief complaint and history already recorded by staff or the patient, other than simply indicate that they reviewed and verified the information in the medical record. In addition, teaching physicians do not have to duplicate notations by residents. CMS also included practice expense for additional skin biopsies.
CMS is also going to pay for services using communication technology. These include:
- Brief communication technology-based service, e.g. virtual check-in (HCPCS code G2012). This is provided by a physician or other qualified health care professional who can report E/M services for an established patient, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion. It is important to note that CMS is allowing for this code to include audio-only, real-time telephone interactions, in addition to synchronous, two-way audio interactions that are enhanced with video or other kinds of data transmission.
- Remote evaluation of recorded video and/or images submitted by an established patient (HCPCS code G2010). This is remote evaluation of recorded video and/or images submitted by an established patient (e.g., store and forward), including interpretation with follow-up with the patient within 24 business hours, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment). The code can be reported effective Jan. 1, 2019, for established patients only.
You can use G2012 to decide if an office visit is needed. Similarly, the service of remote evaluation of recorded video and/or images submitted by an established patient would allow health care professionals to be paid separately for reviewing patient-transmitted photo or video information whether or not a visit is needed. The encounter must be synchronous (real-time), two-way audio interactions enhanced with video or other kinds of data transmission.
It appears that these would only be practical for established patients, and don’t forget, your Internet and text responses to patients’ messages are not secure, unless they are on a secure portal, although their messages to you are HIPAA compliant. However, the telephone, some Internet portals, and your electronic medical record portals are secure. It is intriguing to me that I might get paid for all those bad pictures patients send me, at least if it is not in a global period.
It also appears that Rural Health Clinics and Federally Qualified Health Centers will be able to bill for new and established patient visits via communication technology.
This is all great news to physicians. Kudos to dermatologists Jack Resneck Jr., MD, American Medical Association trustee; and George Hruza, MD, the American Academy of Dermatology president-elect; and Sabra Sullivan, MD, PhD, chair of the AAD’s Council on Government Affairs and Health Policy Government, who organized this lemonade-making effort. And once again, the AAD’s Washington office has shown its great value. This also aptly demonstrates why you write letters to CMS.
In 2021, levels 2-4 will be collapsed into one code (levels 5 will remain, but remember, very few dermatologists use level 5) and you will have to document only at level 2 code levels. Special add-on codes will be added for exceptionally difficult cases for primary care and all specialist physicians, including dermatology. What is not clear is how this new reimbursement schemata will be funded. CMS is still suspicious that there is overlapping work when procedures are performed on the same day as an E/M (evaluation and management code). We may end up fighting this battle all over again.
Currently CMS is conducting a survey, sent to 1,500 dermatologists, on follow-up visits. CMS has stated that they will evaluate the public comments received and consider whether to propose action at a future date. CMS plans to send a letter describing the requirements, once again, to health care professionals in nine affected states, who are required to report the global period encounter. If you are one of these practitioners, please do fill this out and contact Faith McNicholas at AAD ([email protected]) if you have questions. The decision to eliminate global periods (disastrous) will be based on this survey.
This is why you need to stay engaged, write letters, join the AMA, donate to SkinPAC, and attend the legislative fly in, the AAD’s legislative conference held every year in Washington. We are a small specialty. If we do not speak up and stay engaged, we will become the lemons for the next pitcher of lemonade.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Of course, there is a new final rule every year, so it really isn’t very final. I know this is confusing to many of you, I was dazed for several days by this year’s proposed final rule.

Each year, the Centers for Medicare & Medicaid Services receives input from innumerable sources and formulates its payment for physicians. These responses are often in response to requests by CMS itself, which wants to make sure reimbursements are accurate. Generally, input comes from the American Medical Association’s RVS Update Committee (RUC), which values new and existing CPT codes, as well as Congress, the Health & Human Services Office of Inspector General, lobbyists, specialty society organizations, public advocacy groups, and anyone who can wrangle an appointment at or write a letter to CMS headquarters in Baltimore. This conflicted brew is hashed over, and published in late July as a proposed rule. Public comments are then solicited (all letters and emails are considered, dermatologists sent 1,500 responses to this one!) and a final rule is published in the fall. I have constructed a flowchart of this process.
This year’s proposed rule was particularly disturbing because of major changes in reimbursement proposed by CMS. As you may recall, officials proposed to collapse all the evaluation and management (E/M) codes into two levels and pay bonuses to certain specialists (but not dermatologists). This might have been agreeable, except Medicare reimbursements are a zero-sum game. If someone is paid more, someone else will be paid less. Of course, you could always let the increase come out of the general pool, but that would decrease the conversion factor, and some health care professionals (usually primary care) might not see an overall increase. So, the proposed rule was going to “pay” for this increase by way of eliminating the 25 modifier, the CPT modifier that allows you to be paid for the evaluation and management (E/M) service on the same day as a procedure. This has been averted, at least for two years.
The final rule also makes a real effort to eliminate some meaningless documentation. Effective Jan. 1, 2019, for established patients, practitioners can focus their notes on patient changes. With new and established patients, they need not personally reenter the chief complaint and history already recorded by staff or the patient, other than simply indicate that they reviewed and verified the information in the medical record. In addition, teaching physicians do not have to duplicate notations by residents. CMS also included practice expense for additional skin biopsies.
CMS is also going to pay for services using communication technology. These include:
- Brief communication technology-based service, e.g. virtual check-in (HCPCS code G2012). This is provided by a physician or other qualified health care professional who can report E/M services for an established patient, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion. It is important to note that CMS is allowing for this code to include audio-only, real-time telephone interactions, in addition to synchronous, two-way audio interactions that are enhanced with video or other kinds of data transmission.
- Remote evaluation of recorded video and/or images submitted by an established patient (HCPCS code G2010). This is remote evaluation of recorded video and/or images submitted by an established patient (e.g., store and forward), including interpretation with follow-up with the patient within 24 business hours, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment). The code can be reported effective Jan. 1, 2019, for established patients only.
You can use G2012 to decide if an office visit is needed. Similarly, the service of remote evaluation of recorded video and/or images submitted by an established patient would allow health care professionals to be paid separately for reviewing patient-transmitted photo or video information whether or not a visit is needed. The encounter must be synchronous (real-time), two-way audio interactions enhanced with video or other kinds of data transmission.
It appears that these would only be practical for established patients, and don’t forget, your Internet and text responses to patients’ messages are not secure, unless they are on a secure portal, although their messages to you are HIPAA compliant. However, the telephone, some Internet portals, and your electronic medical record portals are secure. It is intriguing to me that I might get paid for all those bad pictures patients send me, at least if it is not in a global period.
It also appears that Rural Health Clinics and Federally Qualified Health Centers will be able to bill for new and established patient visits via communication technology.
This is all great news to physicians. Kudos to dermatologists Jack Resneck Jr., MD, American Medical Association trustee; and George Hruza, MD, the American Academy of Dermatology president-elect; and Sabra Sullivan, MD, PhD, chair of the AAD’s Council on Government Affairs and Health Policy Government, who organized this lemonade-making effort. And once again, the AAD’s Washington office has shown its great value. This also aptly demonstrates why you write letters to CMS.
In 2021, levels 2-4 will be collapsed into one code (levels 5 will remain, but remember, very few dermatologists use level 5) and you will have to document only at level 2 code levels. Special add-on codes will be added for exceptionally difficult cases for primary care and all specialist physicians, including dermatology. What is not clear is how this new reimbursement schemata will be funded. CMS is still suspicious that there is overlapping work when procedures are performed on the same day as an E/M (evaluation and management code). We may end up fighting this battle all over again.
Currently CMS is conducting a survey, sent to 1,500 dermatologists, on follow-up visits. CMS has stated that they will evaluate the public comments received and consider whether to propose action at a future date. CMS plans to send a letter describing the requirements, once again, to health care professionals in nine affected states, who are required to report the global period encounter. If you are one of these practitioners, please do fill this out and contact Faith McNicholas at AAD ([email protected]) if you have questions. The decision to eliminate global periods (disastrous) will be based on this survey.
This is why you need to stay engaged, write letters, join the AMA, donate to SkinPAC, and attend the legislative fly in, the AAD’s legislative conference held every year in Washington. We are a small specialty. If we do not speak up and stay engaged, we will become the lemons for the next pitcher of lemonade.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Of course, there is a new final rule every year, so it really isn’t very final. I know this is confusing to many of you, I was dazed for several days by this year’s proposed final rule.

Each year, the Centers for Medicare & Medicaid Services receives input from innumerable sources and formulates its payment for physicians. These responses are often in response to requests by CMS itself, which wants to make sure reimbursements are accurate. Generally, input comes from the American Medical Association’s RVS Update Committee (RUC), which values new and existing CPT codes, as well as Congress, the Health & Human Services Office of Inspector General, lobbyists, specialty society organizations, public advocacy groups, and anyone who can wrangle an appointment at or write a letter to CMS headquarters in Baltimore. This conflicted brew is hashed over, and published in late July as a proposed rule. Public comments are then solicited (all letters and emails are considered, dermatologists sent 1,500 responses to this one!) and a final rule is published in the fall. I have constructed a flowchart of this process.
This year’s proposed rule was particularly disturbing because of major changes in reimbursement proposed by CMS. As you may recall, officials proposed to collapse all the evaluation and management (E/M) codes into two levels and pay bonuses to certain specialists (but not dermatologists). This might have been agreeable, except Medicare reimbursements are a zero-sum game. If someone is paid more, someone else will be paid less. Of course, you could always let the increase come out of the general pool, but that would decrease the conversion factor, and some health care professionals (usually primary care) might not see an overall increase. So, the proposed rule was going to “pay” for this increase by way of eliminating the 25 modifier, the CPT modifier that allows you to be paid for the evaluation and management (E/M) service on the same day as a procedure. This has been averted, at least for two years.
The final rule also makes a real effort to eliminate some meaningless documentation. Effective Jan. 1, 2019, for established patients, practitioners can focus their notes on patient changes. With new and established patients, they need not personally reenter the chief complaint and history already recorded by staff or the patient, other than simply indicate that they reviewed and verified the information in the medical record. In addition, teaching physicians do not have to duplicate notations by residents. CMS also included practice expense for additional skin biopsies.
CMS is also going to pay for services using communication technology. These include:
- Brief communication technology-based service, e.g. virtual check-in (HCPCS code G2012). This is provided by a physician or other qualified health care professional who can report E/M services for an established patient, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion. It is important to note that CMS is allowing for this code to include audio-only, real-time telephone interactions, in addition to synchronous, two-way audio interactions that are enhanced with video or other kinds of data transmission.
- Remote evaluation of recorded video and/or images submitted by an established patient (HCPCS code G2010). This is remote evaluation of recorded video and/or images submitted by an established patient (e.g., store and forward), including interpretation with follow-up with the patient within 24 business hours, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment). The code can be reported effective Jan. 1, 2019, for established patients only.
You can use G2012 to decide if an office visit is needed. Similarly, the service of remote evaluation of recorded video and/or images submitted by an established patient would allow health care professionals to be paid separately for reviewing patient-transmitted photo or video information whether or not a visit is needed. The encounter must be synchronous (real-time), two-way audio interactions enhanced with video or other kinds of data transmission.
It appears that these would only be practical for established patients, and don’t forget, your Internet and text responses to patients’ messages are not secure, unless they are on a secure portal, although their messages to you are HIPAA compliant. However, the telephone, some Internet portals, and your electronic medical record portals are secure. It is intriguing to me that I might get paid for all those bad pictures patients send me, at least if it is not in a global period.
It also appears that Rural Health Clinics and Federally Qualified Health Centers will be able to bill for new and established patient visits via communication technology.
This is all great news to physicians. Kudos to dermatologists Jack Resneck Jr., MD, American Medical Association trustee; and George Hruza, MD, the American Academy of Dermatology president-elect; and Sabra Sullivan, MD, PhD, chair of the AAD’s Council on Government Affairs and Health Policy Government, who organized this lemonade-making effort. And once again, the AAD’s Washington office has shown its great value. This also aptly demonstrates why you write letters to CMS.
In 2021, levels 2-4 will be collapsed into one code (levels 5 will remain, but remember, very few dermatologists use level 5) and you will have to document only at level 2 code levels. Special add-on codes will be added for exceptionally difficult cases for primary care and all specialist physicians, including dermatology. What is not clear is how this new reimbursement schemata will be funded. CMS is still suspicious that there is overlapping work when procedures are performed on the same day as an E/M (evaluation and management code). We may end up fighting this battle all over again.
Currently CMS is conducting a survey, sent to 1,500 dermatologists, on follow-up visits. CMS has stated that they will evaluate the public comments received and consider whether to propose action at a future date. CMS plans to send a letter describing the requirements, once again, to health care professionals in nine affected states, who are required to report the global period encounter. If you are one of these practitioners, please do fill this out and contact Faith McNicholas at AAD ([email protected]) if you have questions. The decision to eliminate global periods (disastrous) will be based on this survey.
This is why you need to stay engaged, write letters, join the AMA, donate to SkinPAC, and attend the legislative fly in, the AAD’s legislative conference held every year in Washington. We are a small specialty. If we do not speak up and stay engaged, we will become the lemons for the next pitcher of lemonade.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Physical fitness guidelines from HHS
Also today, hydroxychloroquine treatment of SLE is hobbled by fears of blindness, antiepileptic drugs are strongly linked to rare serious skin reactions, and the FDA aims to squash vaping and smoking among youth.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, hydroxychloroquine treatment of SLE is hobbled by fears of blindness, antiepileptic drugs are strongly linked to rare serious skin reactions, and the FDA aims to squash vaping and smoking among youth.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, hydroxychloroquine treatment of SLE is hobbled by fears of blindness, antiepileptic drugs are strongly linked to rare serious skin reactions, and the FDA aims to squash vaping and smoking among youth.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Naloxone in the Workplace
According to 2017 data from the CDC’s National Center for Health Statistics, on average 115 Americans die every day from an opioid overdose—and it is happening more often at work. Between 2013 and 2016, the Bureau of Labor Statistics finds overdose deaths at work from nonmedical use of drugs and alcohol increased by at least 38% annually.
Naloxone can be one of the first-aid tools of today’s workplace. To help employers decide whether to supply naloxone at work, NIOSH has released a new fact sheet that outlines questions to consider. Using Naloxone to Reverse Opioid Overdose in the Workplace: Information for Employers and Workers gives an overview of opioids and naloxone, a checklist to determine whether a naloxone program is appropriate, and information about how to implement and maintain a program.
The fact sheet is available at www.cdc.gov/niosh/docs/2019-101/.
According to 2017 data from the CDC’s National Center for Health Statistics, on average 115 Americans die every day from an opioid overdose—and it is happening more often at work. Between 2013 and 2016, the Bureau of Labor Statistics finds overdose deaths at work from nonmedical use of drugs and alcohol increased by at least 38% annually.
Naloxone can be one of the first-aid tools of today’s workplace. To help employers decide whether to supply naloxone at work, NIOSH has released a new fact sheet that outlines questions to consider. Using Naloxone to Reverse Opioid Overdose in the Workplace: Information for Employers and Workers gives an overview of opioids and naloxone, a checklist to determine whether a naloxone program is appropriate, and information about how to implement and maintain a program.
The fact sheet is available at www.cdc.gov/niosh/docs/2019-101/.
According to 2017 data from the CDC’s National Center for Health Statistics, on average 115 Americans die every day from an opioid overdose—and it is happening more often at work. Between 2013 and 2016, the Bureau of Labor Statistics finds overdose deaths at work from nonmedical use of drugs and alcohol increased by at least 38% annually.
Naloxone can be one of the first-aid tools of today’s workplace. To help employers decide whether to supply naloxone at work, NIOSH has released a new fact sheet that outlines questions to consider. Using Naloxone to Reverse Opioid Overdose in the Workplace: Information for Employers and Workers gives an overview of opioids and naloxone, a checklist to determine whether a naloxone program is appropriate, and information about how to implement and maintain a program.
The fact sheet is available at www.cdc.gov/niosh/docs/2019-101/.
Bortezomib may overcome resistance in WM
Bortezomib may help overcome treatment resistance in patients with Waldenström’s macroglobulinemia (WM) and CXCR4 mutations, according to a new study.
Researchers assessed the impact of treatment with bortezomib and rituximab in patients with WM, based on their CXCR4 mutation status.
The team found no significant difference in progression-free survival or overall survival between patients with CXCR4 mutations and those with wild-type CXCR4.
Romanos Sklavenitis-Pistofidis, MD, of Dana-Farber Cancer Institute in Boston, Massachusetts, and his colleagues reported this discovery in Blood.
The researchers’ main analysis included 43 patients with WM, 17 (39.5%) of whom had a CXCR4 mutation.
All patients who carried a CXCR4 mutation also had MYD88 L265P. Ten patients had frameshift mutations, one patient had a nonsense mutation, and six patients had missense mutations.
The patients were treated with bortezomib and rituximab, either upfront (n=14) or in the relapsed/refractory (n=29) setting, as part of a phase 2 trial.
Bortezomib was given at 1.6 mg/m2 on days 1, 8, and 15 every 28 days for six cycles, and rituximab was given at 375 mg/m2 on days 1, 8, 15, and 22 during cycles one and four. Patients were taken off therapy after two cycles if they had progressive disease.
The median follow-up was 90.7 months.
The researchers found no significant difference between CXCR4-mutated and wild-type patients when it came to progression-free survival (P=0.994) or overall survival (P=0.407).
The researchers repeated their analysis after excluding six patients with missense mutations and accounting for different treatment settings and found that survival remained unchanged.
“We report, for the first time, that a bortezomib-based combination is impervious to the impact of CXCR4 mutations in a cohort of patients with WM,” the researchers wrote.
“Previously, we had shown this to be true in WM cell lines, whereby genetically engineering BCWM.1 and MWCL-1 to overexpress CXCR4 had no impact on bortezomib resistance.”
The researchers noted, however, that the mechanism at work here may be different than what is seen with bortezomib in other cancers.
“Different experiments have linked CXCR4 expression and bortezomib in a variety of ways in other hematological malignancies, including multiple myeloma,” the researchers wrote.
“However, despite the complicated association in those cancer types, in WM, there seems to be a consistently neutral effect of CXCR4 mutations on bortezomib resistance in both cell line and patient data.”
The researchers recommended that this theory be tested in a prospective trial of bortezomib-based therapy in WM patients with CXCR4 mutations.
Another thing to be determined, they said, is the role of rituximab in the survival results seen in the current analysis.
This study was supported by the National Institutes of Health, the Leukemia and Lymphoma Society, and the International Waldenström Macroglobulinemia Foundation. One of the authors reported consulting and research funding from Takeda, which markets bortezomib, and other companies.
Bortezomib may help overcome treatment resistance in patients with Waldenström’s macroglobulinemia (WM) and CXCR4 mutations, according to a new study.
Researchers assessed the impact of treatment with bortezomib and rituximab in patients with WM, based on their CXCR4 mutation status.
The team found no significant difference in progression-free survival or overall survival between patients with CXCR4 mutations and those with wild-type CXCR4.
Romanos Sklavenitis-Pistofidis, MD, of Dana-Farber Cancer Institute in Boston, Massachusetts, and his colleagues reported this discovery in Blood.
The researchers’ main analysis included 43 patients with WM, 17 (39.5%) of whom had a CXCR4 mutation.
All patients who carried a CXCR4 mutation also had MYD88 L265P. Ten patients had frameshift mutations, one patient had a nonsense mutation, and six patients had missense mutations.
The patients were treated with bortezomib and rituximab, either upfront (n=14) or in the relapsed/refractory (n=29) setting, as part of a phase 2 trial.
Bortezomib was given at 1.6 mg/m2 on days 1, 8, and 15 every 28 days for six cycles, and rituximab was given at 375 mg/m2 on days 1, 8, 15, and 22 during cycles one and four. Patients were taken off therapy after two cycles if they had progressive disease.
The median follow-up was 90.7 months.
The researchers found no significant difference between CXCR4-mutated and wild-type patients when it came to progression-free survival (P=0.994) or overall survival (P=0.407).
The researchers repeated their analysis after excluding six patients with missense mutations and accounting for different treatment settings and found that survival remained unchanged.
“We report, for the first time, that a bortezomib-based combination is impervious to the impact of CXCR4 mutations in a cohort of patients with WM,” the researchers wrote.
“Previously, we had shown this to be true in WM cell lines, whereby genetically engineering BCWM.1 and MWCL-1 to overexpress CXCR4 had no impact on bortezomib resistance.”
The researchers noted, however, that the mechanism at work here may be different than what is seen with bortezomib in other cancers.
“Different experiments have linked CXCR4 expression and bortezomib in a variety of ways in other hematological malignancies, including multiple myeloma,” the researchers wrote.
“However, despite the complicated association in those cancer types, in WM, there seems to be a consistently neutral effect of CXCR4 mutations on bortezomib resistance in both cell line and patient data.”
The researchers recommended that this theory be tested in a prospective trial of bortezomib-based therapy in WM patients with CXCR4 mutations.
Another thing to be determined, they said, is the role of rituximab in the survival results seen in the current analysis.
This study was supported by the National Institutes of Health, the Leukemia and Lymphoma Society, and the International Waldenström Macroglobulinemia Foundation. One of the authors reported consulting and research funding from Takeda, which markets bortezomib, and other companies.
Bortezomib may help overcome treatment resistance in patients with Waldenström’s macroglobulinemia (WM) and CXCR4 mutations, according to a new study.
Researchers assessed the impact of treatment with bortezomib and rituximab in patients with WM, based on their CXCR4 mutation status.
The team found no significant difference in progression-free survival or overall survival between patients with CXCR4 mutations and those with wild-type CXCR4.
Romanos Sklavenitis-Pistofidis, MD, of Dana-Farber Cancer Institute in Boston, Massachusetts, and his colleagues reported this discovery in Blood.
The researchers’ main analysis included 43 patients with WM, 17 (39.5%) of whom had a CXCR4 mutation.
All patients who carried a CXCR4 mutation also had MYD88 L265P. Ten patients had frameshift mutations, one patient had a nonsense mutation, and six patients had missense mutations.
The patients were treated with bortezomib and rituximab, either upfront (n=14) or in the relapsed/refractory (n=29) setting, as part of a phase 2 trial.
Bortezomib was given at 1.6 mg/m2 on days 1, 8, and 15 every 28 days for six cycles, and rituximab was given at 375 mg/m2 on days 1, 8, 15, and 22 during cycles one and four. Patients were taken off therapy after two cycles if they had progressive disease.
The median follow-up was 90.7 months.
The researchers found no significant difference between CXCR4-mutated and wild-type patients when it came to progression-free survival (P=0.994) or overall survival (P=0.407).
The researchers repeated their analysis after excluding six patients with missense mutations and accounting for different treatment settings and found that survival remained unchanged.
“We report, for the first time, that a bortezomib-based combination is impervious to the impact of CXCR4 mutations in a cohort of patients with WM,” the researchers wrote.
“Previously, we had shown this to be true in WM cell lines, whereby genetically engineering BCWM.1 and MWCL-1 to overexpress CXCR4 had no impact on bortezomib resistance.”
The researchers noted, however, that the mechanism at work here may be different than what is seen with bortezomib in other cancers.
“Different experiments have linked CXCR4 expression and bortezomib in a variety of ways in other hematological malignancies, including multiple myeloma,” the researchers wrote.
“However, despite the complicated association in those cancer types, in WM, there seems to be a consistently neutral effect of CXCR4 mutations on bortezomib resistance in both cell line and patient data.”
The researchers recommended that this theory be tested in a prospective trial of bortezomib-based therapy in WM patients with CXCR4 mutations.
Another thing to be determined, they said, is the role of rituximab in the survival results seen in the current analysis.
This study was supported by the National Institutes of Health, the Leukemia and Lymphoma Society, and the International Waldenström Macroglobulinemia Foundation. One of the authors reported consulting and research funding from Takeda, which markets bortezomib, and other companies.
Residents: Apply for Research Award
The SVS Research and Education Committee encourages eligible members to apply for the prestigious Resident Research Award. The recipient will showcase his or her work at the 2019 Vascular Annual Meeting in June as well as receive a $5,000 award. This award is designed to provide special recognition of original scientific work that has yet to be published in manuscript form. It’s an excellent opportunity for surgical trainees in vascular research laboratories to be recognized and rewarded for their research efforts. The application deadline is Jan. 16, 2019, and the annual meeting will take place June 12 to 15 in National Harbor, Md., outside of Washington, D.C.
The SVS Research and Education Committee encourages eligible members to apply for the prestigious Resident Research Award. The recipient will showcase his or her work at the 2019 Vascular Annual Meeting in June as well as receive a $5,000 award. This award is designed to provide special recognition of original scientific work that has yet to be published in manuscript form. It’s an excellent opportunity for surgical trainees in vascular research laboratories to be recognized and rewarded for their research efforts. The application deadline is Jan. 16, 2019, and the annual meeting will take place June 12 to 15 in National Harbor, Md., outside of Washington, D.C.
The SVS Research and Education Committee encourages eligible members to apply for the prestigious Resident Research Award. The recipient will showcase his or her work at the 2019 Vascular Annual Meeting in June as well as receive a $5,000 award. This award is designed to provide special recognition of original scientific work that has yet to be published in manuscript form. It’s an excellent opportunity for surgical trainees in vascular research laboratories to be recognized and rewarded for their research efforts. The application deadline is Jan. 16, 2019, and the annual meeting will take place June 12 to 15 in National Harbor, Md., outside of Washington, D.C.