User login
At 10 years, reintervention rate for EVAR is 20%
NEW YORK – A clever strategy to evaluate long term outcomes in patients undergoing endovascular abdominal aortic aneurysm repair identified a 20% rate of reintervention, according to data presented at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation by Philip P. Goodney, MD.
In this video interview with Dr. Goodney, an associate professor of vascular surgery at Geisel School of Medicine at Dartmouth, Hanover, N.H., he explains how Medicare data were employed to track patients long term, even when they had moved to other hospital systems.
The main message from the long-term follow-up is that there is a persistent risk of recurrence and need for reintervention, according to Dr. Goodney. The hypothesis was that there would be an early risk of failure, followed by a diminishing need for reintervention over time, but this was not what was observed.Rather, the findings suggest that the rate of reinterventions was relatively steady over the course of follow-up, suggesting that patients should be informed of a persistent risk. However, Dr. Goodney reports that age was not a predictor of reintervention, so that older patients were at no greater risk.
NEW YORK – A clever strategy to evaluate long term outcomes in patients undergoing endovascular abdominal aortic aneurysm repair identified a 20% rate of reintervention, according to data presented at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation by Philip P. Goodney, MD.
In this video interview with Dr. Goodney, an associate professor of vascular surgery at Geisel School of Medicine at Dartmouth, Hanover, N.H., he explains how Medicare data were employed to track patients long term, even when they had moved to other hospital systems.
The main message from the long-term follow-up is that there is a persistent risk of recurrence and need for reintervention, according to Dr. Goodney. The hypothesis was that there would be an early risk of failure, followed by a diminishing need for reintervention over time, but this was not what was observed.Rather, the findings suggest that the rate of reinterventions was relatively steady over the course of follow-up, suggesting that patients should be informed of a persistent risk. However, Dr. Goodney reports that age was not a predictor of reintervention, so that older patients were at no greater risk.
NEW YORK – A clever strategy to evaluate long term outcomes in patients undergoing endovascular abdominal aortic aneurysm repair identified a 20% rate of reintervention, according to data presented at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation by Philip P. Goodney, MD.
In this video interview with Dr. Goodney, an associate professor of vascular surgery at Geisel School of Medicine at Dartmouth, Hanover, N.H., he explains how Medicare data were employed to track patients long term, even when they had moved to other hospital systems.
The main message from the long-term follow-up is that there is a persistent risk of recurrence and need for reintervention, according to Dr. Goodney. The hypothesis was that there would be an early risk of failure, followed by a diminishing need for reintervention over time, but this was not what was observed.Rather, the findings suggest that the rate of reinterventions was relatively steady over the course of follow-up, suggesting that patients should be informed of a persistent risk. However, Dr. Goodney reports that age was not a predictor of reintervention, so that older patients were at no greater risk.
FROM 2018 VEITH SYMPOSIUM
Snorkel/chimney repair of aortic aneurysms is still effective after 4 years
NEW YORK – With a median follow-up of almost 4 years in more than 200 patients, the snorkel/chimney technique of endovascular repair of complex abdominal aortic aneurysms continues to generate very good results, according data presented at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
In a video interview with Jason T. Lee, MD, professor of vascular surgery, Stanford (Calif.) University, who presented the long-term results, he explains why these findings are important.
After several single-center studies associated the snorkel/chimney technique with good rates of patency and durability, the PERICLES Registry was created almost 10 years ago to test whether these data could be reproduced in the real world.The data presented by Dr. Lee involved outcomes in 244 patients who were followed for at least 2.5 years. The median follow-up is 47 months.
The results overall confirm that this is a viable technique, according to Dr. Lee who noted very little diminution of patency rates in this long-term cohort relative to the previously published follow-up of 17.1 months.
He acknowledged that the snorkel/chimney repair is not free of potential complications, particularly gutter endovascular leaks, but he recounted that at least some resolve over time. Moreover, he suggests that several strategies are being pursued that appear promising for avoiding this risk.
Most importantly, the registry, which captured the experience at 13 centers in the United States and Europe, shows outcomes that are similar to those reported at centers where the techniques were developed and championed.
NEW YORK – With a median follow-up of almost 4 years in more than 200 patients, the snorkel/chimney technique of endovascular repair of complex abdominal aortic aneurysms continues to generate very good results, according data presented at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
In a video interview with Jason T. Lee, MD, professor of vascular surgery, Stanford (Calif.) University, who presented the long-term results, he explains why these findings are important.
After several single-center studies associated the snorkel/chimney technique with good rates of patency and durability, the PERICLES Registry was created almost 10 years ago to test whether these data could be reproduced in the real world.The data presented by Dr. Lee involved outcomes in 244 patients who were followed for at least 2.5 years. The median follow-up is 47 months.
The results overall confirm that this is a viable technique, according to Dr. Lee who noted very little diminution of patency rates in this long-term cohort relative to the previously published follow-up of 17.1 months.
He acknowledged that the snorkel/chimney repair is not free of potential complications, particularly gutter endovascular leaks, but he recounted that at least some resolve over time. Moreover, he suggests that several strategies are being pursued that appear promising for avoiding this risk.
Most importantly, the registry, which captured the experience at 13 centers in the United States and Europe, shows outcomes that are similar to those reported at centers where the techniques were developed and championed.
NEW YORK – With a median follow-up of almost 4 years in more than 200 patients, the snorkel/chimney technique of endovascular repair of complex abdominal aortic aneurysms continues to generate very good results, according data presented at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
In a video interview with Jason T. Lee, MD, professor of vascular surgery, Stanford (Calif.) University, who presented the long-term results, he explains why these findings are important.
After several single-center studies associated the snorkel/chimney technique with good rates of patency and durability, the PERICLES Registry was created almost 10 years ago to test whether these data could be reproduced in the real world.The data presented by Dr. Lee involved outcomes in 244 patients who were followed for at least 2.5 years. The median follow-up is 47 months.
The results overall confirm that this is a viable technique, according to Dr. Lee who noted very little diminution of patency rates in this long-term cohort relative to the previously published follow-up of 17.1 months.
He acknowledged that the snorkel/chimney repair is not free of potential complications, particularly gutter endovascular leaks, but he recounted that at least some resolve over time. Moreover, he suggests that several strategies are being pursued that appear promising for avoiding this risk.
Most importantly, the registry, which captured the experience at 13 centers in the United States and Europe, shows outcomes that are similar to those reported at centers where the techniques were developed and championed.
FROM 2018 VEITH SYMPOSIUM
Will AI or robotics steal your job?
NEW YORK – Artificial intelligence is currently linked to specific problem solving and is not some form of Terminator model capable of handling multiple tasks with autonomy. In other words, each time you hear the term “AI,” it is a computer solving a specific problem or task using algorithms “and not ‘thinking’ like you and me,” said Ido Weinberg, MD, assistant professor, Harvard Medical School, Boston.
AI is present in daily life – everything from cellphones to the Alexa voice interface on a smart speaker. That AI system, however, is amassing data, learning about you, and using that data intelligently, Dr. Weinberg said at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
AI in health care make sense, he said, because the health sector is a vast consumer market with potential for financial gain. Repetition, which is common in the health sector, is one of the foundations required for using AI and robotics. If a task can be repeated, then it means a machine can do it, said Dr. Weinberg.
The spread of AI and robotics one day may improve health care accessibility in remote areas where physicians with the appropriate training may not be available.
AI is already at work in the health care industry. “Pulmonary nodule detection can be done better with machines than by people, pathological identification and scanning of various slides can be done better by a machine than by a humans,” he said.
Artificial intelligence also can be designed to detect emotion by assessing various cues in phrasing, key words, and tone. These AI functions already are being used by sales reps on the phone to defuse and control interactions with customers and complainants. AI also can be implemented in interactions with people, which is an important part of dealing with patients, Dr. Weinberg said. Drug discovery is a key area where AI is flourishing, as well.
Luckily, in terms of physicians keeping their jobs, there are barriers to the use of AI to replace clinicians, Dr. Weinberg pointed out. Health care is not a monolith, and every specialty is different, meaning AI would have to be tailored to each task and specialty for each unique field. Quick proliferation of AI across the board is unlikely, especially when the varying roles of nurses and physician assistants are included.
Although robots in science fiction stories and films often are capable of multitasking a variety of needs, robots at present are much more limited in real life. In surgical situations, for example, they can perform specifically tailored tasks but cannot extend beyond those defined parameters as a real surgeon can, according to Dr. Weinberg, and this lack of flexibility is a severe limitation on the expansion of AI into health care.
Despite these limitations, Dr. Weinberg urged attendees to consider how AI can be used to facilitate their work.
“Believe in the roadblocks, but be a fast adopter – an early adopter – and understand where AI can currently augment you and make you better and more productive,” he said. “And keep doing procedures; AI and robotics currently have a problem with most of those,” Dr. Weinberg concluded.
Dr. Weinberg reported no conflicts relevant to his talk.
NEW YORK – Artificial intelligence is currently linked to specific problem solving and is not some form of Terminator model capable of handling multiple tasks with autonomy. In other words, each time you hear the term “AI,” it is a computer solving a specific problem or task using algorithms “and not ‘thinking’ like you and me,” said Ido Weinberg, MD, assistant professor, Harvard Medical School, Boston.
AI is present in daily life – everything from cellphones to the Alexa voice interface on a smart speaker. That AI system, however, is amassing data, learning about you, and using that data intelligently, Dr. Weinberg said at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
AI in health care make sense, he said, because the health sector is a vast consumer market with potential for financial gain. Repetition, which is common in the health sector, is one of the foundations required for using AI and robotics. If a task can be repeated, then it means a machine can do it, said Dr. Weinberg.
The spread of AI and robotics one day may improve health care accessibility in remote areas where physicians with the appropriate training may not be available.
AI is already at work in the health care industry. “Pulmonary nodule detection can be done better with machines than by people, pathological identification and scanning of various slides can be done better by a machine than by a humans,” he said.
Artificial intelligence also can be designed to detect emotion by assessing various cues in phrasing, key words, and tone. These AI functions already are being used by sales reps on the phone to defuse and control interactions with customers and complainants. AI also can be implemented in interactions with people, which is an important part of dealing with patients, Dr. Weinberg said. Drug discovery is a key area where AI is flourishing, as well.
Luckily, in terms of physicians keeping their jobs, there are barriers to the use of AI to replace clinicians, Dr. Weinberg pointed out. Health care is not a monolith, and every specialty is different, meaning AI would have to be tailored to each task and specialty for each unique field. Quick proliferation of AI across the board is unlikely, especially when the varying roles of nurses and physician assistants are included.
Although robots in science fiction stories and films often are capable of multitasking a variety of needs, robots at present are much more limited in real life. In surgical situations, for example, they can perform specifically tailored tasks but cannot extend beyond those defined parameters as a real surgeon can, according to Dr. Weinberg, and this lack of flexibility is a severe limitation on the expansion of AI into health care.
Despite these limitations, Dr. Weinberg urged attendees to consider how AI can be used to facilitate their work.
“Believe in the roadblocks, but be a fast adopter – an early adopter – and understand where AI can currently augment you and make you better and more productive,” he said. “And keep doing procedures; AI and robotics currently have a problem with most of those,” Dr. Weinberg concluded.
Dr. Weinberg reported no conflicts relevant to his talk.
NEW YORK – Artificial intelligence is currently linked to specific problem solving and is not some form of Terminator model capable of handling multiple tasks with autonomy. In other words, each time you hear the term “AI,” it is a computer solving a specific problem or task using algorithms “and not ‘thinking’ like you and me,” said Ido Weinberg, MD, assistant professor, Harvard Medical School, Boston.
AI is present in daily life – everything from cellphones to the Alexa voice interface on a smart speaker. That AI system, however, is amassing data, learning about you, and using that data intelligently, Dr. Weinberg said at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
AI in health care make sense, he said, because the health sector is a vast consumer market with potential for financial gain. Repetition, which is common in the health sector, is one of the foundations required for using AI and robotics. If a task can be repeated, then it means a machine can do it, said Dr. Weinberg.
The spread of AI and robotics one day may improve health care accessibility in remote areas where physicians with the appropriate training may not be available.
AI is already at work in the health care industry. “Pulmonary nodule detection can be done better with machines than by people, pathological identification and scanning of various slides can be done better by a machine than by a humans,” he said.
Artificial intelligence also can be designed to detect emotion by assessing various cues in phrasing, key words, and tone. These AI functions already are being used by sales reps on the phone to defuse and control interactions with customers and complainants. AI also can be implemented in interactions with people, which is an important part of dealing with patients, Dr. Weinberg said. Drug discovery is a key area where AI is flourishing, as well.
Luckily, in terms of physicians keeping their jobs, there are barriers to the use of AI to replace clinicians, Dr. Weinberg pointed out. Health care is not a monolith, and every specialty is different, meaning AI would have to be tailored to each task and specialty for each unique field. Quick proliferation of AI across the board is unlikely, especially when the varying roles of nurses and physician assistants are included.
Although robots in science fiction stories and films often are capable of multitasking a variety of needs, robots at present are much more limited in real life. In surgical situations, for example, they can perform specifically tailored tasks but cannot extend beyond those defined parameters as a real surgeon can, according to Dr. Weinberg, and this lack of flexibility is a severe limitation on the expansion of AI into health care.
Despite these limitations, Dr. Weinberg urged attendees to consider how AI can be used to facilitate their work.
“Believe in the roadblocks, but be a fast adopter – an early adopter – and understand where AI can currently augment you and make you better and more productive,” he said. “And keep doing procedures; AI and robotics currently have a problem with most of those,” Dr. Weinberg concluded.
Dr. Weinberg reported no conflicts relevant to his talk.
REPORTING FROM THE VEITHSYMPOSIUM
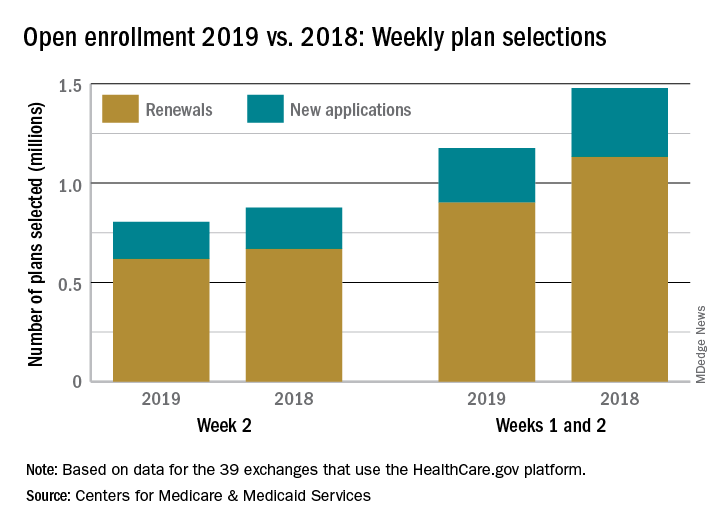
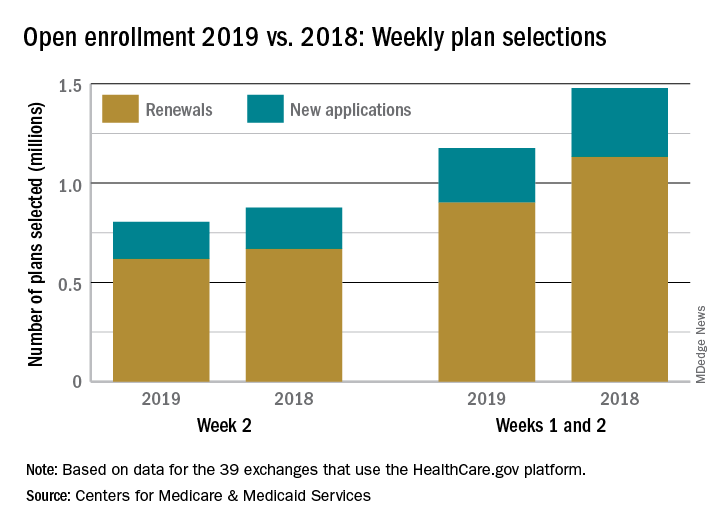
Open enrollment: HealthCare.gov busier in week 2
but the gap has closed since week 1, according to the Centers for Medicare & Medicaid Services.
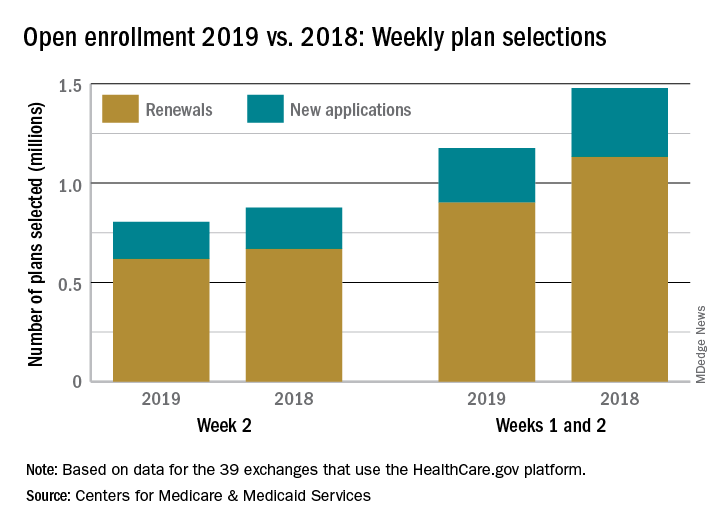
With almost 805,000 plans selected this year during the second week (Nov. 4-10) of open enrollment, the total for the 2019 coverage year stands at nearly 1.18 million for the 39 states that use the HealthCare.gov platform, which is down 20.4% from the 1.48 million plans selected through the first 2 weeks of last year’s enrollment period. After week 1, this year’s total enrollment was down by 38%, compared with last year, CMS data show.
Consumers renewing their insurance plans account for the majority selected for 2019 coverage – 619,000 in week 2 and 901,000 for weeks 1 and 2 (close to 77% in each case) – with the rest coming from new consumers – 186,000 in week 2 and 275,000 overall. The figures reported in the weekly enrollment snapshot could change later since they represent selections only and not “consumers who have paid premiums to effectuate their enrollment,” CMS said.
but the gap has closed since week 1, according to the Centers for Medicare & Medicaid Services.
With almost 805,000 plans selected this year during the second week (Nov. 4-10) of open enrollment, the total for the 2019 coverage year stands at nearly 1.18 million for the 39 states that use the HealthCare.gov platform, which is down 20.4% from the 1.48 million plans selected through the first 2 weeks of last year’s enrollment period. After week 1, this year’s total enrollment was down by 38%, compared with last year, CMS data show.
Consumers renewing their insurance plans account for the majority selected for 2019 coverage – 619,000 in week 2 and 901,000 for weeks 1 and 2 (close to 77% in each case) – with the rest coming from new consumers – 186,000 in week 2 and 275,000 overall. The figures reported in the weekly enrollment snapshot could change later since they represent selections only and not “consumers who have paid premiums to effectuate their enrollment,” CMS said.
but the gap has closed since week 1, according to the Centers for Medicare & Medicaid Services.
With almost 805,000 plans selected this year during the second week (Nov. 4-10) of open enrollment, the total for the 2019 coverage year stands at nearly 1.18 million for the 39 states that use the HealthCare.gov platform, which is down 20.4% from the 1.48 million plans selected through the first 2 weeks of last year’s enrollment period. After week 1, this year’s total enrollment was down by 38%, compared with last year, CMS data show.
Consumers renewing their insurance plans account for the majority selected for 2019 coverage – 619,000 in week 2 and 901,000 for weeks 1 and 2 (close to 77% in each case) – with the rest coming from new consumers – 186,000 in week 2 and 275,000 overall. The figures reported in the weekly enrollment snapshot could change later since they represent selections only and not “consumers who have paid premiums to effectuate their enrollment,” CMS said.
VQI-VVR registry data eyed for guiding development of ethical standards
NEW YORK – Registry data can be used to craft guidance for determining the appropriateness of procedures at vein centers, based on data presented by Thomas W. Wakefield, MD at the 2018 Veith Symposium.
The Vascular Quality Initiative Varicose Vein Registry (VQI-VVR), initiated in 2014 by the Society for Vascular Surgery in conjunction with the American Venous Forum, captures procedures that are performed in vein centers, office-based practices, and ambulatory or inpatient settings. The VVR looks at ablation and phlebectomy techniques and captures data including patient demographics, history, procedure data, plus early and late office-based and patient-reported follow-up in order to benchmark and improve outcomes and develop best practices and to help meet vein center certification requirements. The VVR includes 39 centers and more than 23,000 procedures.
Dr. Wakefield, who heads the VVR, used this registry as a means to illustrate how VQIs could be used to establish whether “the expected health benefit exceeds the expected negative consequences by a sufficiently wide margin that the procedure is worth doing.” This can be considered to be “appropriateness, which is part of ethical treatment.” Dr. Wakefield is the Stanley Professor of Vascular Surgery at the University of Michigan and section head, vascular surgery, University of Michigan Cardiovascular Center, Ann Arbor.
Data from the VQI registry (of which the VVR is a component) are now being used to generate appropriateness reports, said Dr. Wakefield.
The VQI represents a large comprehensive database of long-term data to define appropriate care. In addition, the VQI infrastructure is already geared to producing these reports both at a center and at a surgeon level. One disadvantage of the VVR registry, however, is low participation – only the 39 centers – and that it doesn’t capture cosmetic procedures and lesser (C1) disease. Further, it’s “likely the VQI participants are the ‘good actors,’ ” he added.
Targets for appropriateness include the proportion of patients undergoing ablation C2 or C4 disease or greater, the mean number of ablations per patient, the mean number of ablations per limb, and the proportion of perforated ablations for greater than C4 disease. Plotting out the data for these procedures at the center level can be assessed against current thinking on best practices in the various areas. For example, “the mean number of ablations per patient has been suggested at 1.8 to be about the right number,” and he used the graph of the center performance in this area to show that most of the centers were below this objective.
In an even more appropriate example of how this kind of data could be used to determine appropriateness, Dr. Wakefield described how perforated ablations should be performed for greater than C4 disease, but not for C2 disease. He described how, according to the actual data in the registry, there have been 870 total perforated treatments recorded, 38% for C2 disease, and of these 332 procedures, almost half of these were performed at one center only, with two other centers reporting 30 such procedures. “So clearly there are three centers that are doing perforated ablations for patients that are outside the guidelines,” Dr. Wakefield pointed out.
In future, payer demand is likely to demand that each treating physician provide evidence of the appropriateness of procedures performed, as well as appropriate patient selection and adherence to best practices, and good outcomes, which is part of what a society-based registry such as the VVR can provide.
“I believe the VQI-VVR is well-positioned to meet these needs. And if we ask the question ‘can VQI be used as a benchmark for setting ethical standards,’ I think it can certainly be used to help set appropriate standards, and since appropriateness is one part of ethical standards, I believe it has a role,” he concluded.
Dr. Wakefield reported that he had no disclosures.
NEW YORK – Registry data can be used to craft guidance for determining the appropriateness of procedures at vein centers, based on data presented by Thomas W. Wakefield, MD at the 2018 Veith Symposium.
The Vascular Quality Initiative Varicose Vein Registry (VQI-VVR), initiated in 2014 by the Society for Vascular Surgery in conjunction with the American Venous Forum, captures procedures that are performed in vein centers, office-based practices, and ambulatory or inpatient settings. The VVR looks at ablation and phlebectomy techniques and captures data including patient demographics, history, procedure data, plus early and late office-based and patient-reported follow-up in order to benchmark and improve outcomes and develop best practices and to help meet vein center certification requirements. The VVR includes 39 centers and more than 23,000 procedures.
Dr. Wakefield, who heads the VVR, used this registry as a means to illustrate how VQIs could be used to establish whether “the expected health benefit exceeds the expected negative consequences by a sufficiently wide margin that the procedure is worth doing.” This can be considered to be “appropriateness, which is part of ethical treatment.” Dr. Wakefield is the Stanley Professor of Vascular Surgery at the University of Michigan and section head, vascular surgery, University of Michigan Cardiovascular Center, Ann Arbor.
Data from the VQI registry (of which the VVR is a component) are now being used to generate appropriateness reports, said Dr. Wakefield.
The VQI represents a large comprehensive database of long-term data to define appropriate care. In addition, the VQI infrastructure is already geared to producing these reports both at a center and at a surgeon level. One disadvantage of the VVR registry, however, is low participation – only the 39 centers – and that it doesn’t capture cosmetic procedures and lesser (C1) disease. Further, it’s “likely the VQI participants are the ‘good actors,’ ” he added.
Targets for appropriateness include the proportion of patients undergoing ablation C2 or C4 disease or greater, the mean number of ablations per patient, the mean number of ablations per limb, and the proportion of perforated ablations for greater than C4 disease. Plotting out the data for these procedures at the center level can be assessed against current thinking on best practices in the various areas. For example, “the mean number of ablations per patient has been suggested at 1.8 to be about the right number,” and he used the graph of the center performance in this area to show that most of the centers were below this objective.
In an even more appropriate example of how this kind of data could be used to determine appropriateness, Dr. Wakefield described how perforated ablations should be performed for greater than C4 disease, but not for C2 disease. He described how, according to the actual data in the registry, there have been 870 total perforated treatments recorded, 38% for C2 disease, and of these 332 procedures, almost half of these were performed at one center only, with two other centers reporting 30 such procedures. “So clearly there are three centers that are doing perforated ablations for patients that are outside the guidelines,” Dr. Wakefield pointed out.
In future, payer demand is likely to demand that each treating physician provide evidence of the appropriateness of procedures performed, as well as appropriate patient selection and adherence to best practices, and good outcomes, which is part of what a society-based registry such as the VVR can provide.
“I believe the VQI-VVR is well-positioned to meet these needs. And if we ask the question ‘can VQI be used as a benchmark for setting ethical standards,’ I think it can certainly be used to help set appropriate standards, and since appropriateness is one part of ethical standards, I believe it has a role,” he concluded.
Dr. Wakefield reported that he had no disclosures.
NEW YORK – Registry data can be used to craft guidance for determining the appropriateness of procedures at vein centers, based on data presented by Thomas W. Wakefield, MD at the 2018 Veith Symposium.
The Vascular Quality Initiative Varicose Vein Registry (VQI-VVR), initiated in 2014 by the Society for Vascular Surgery in conjunction with the American Venous Forum, captures procedures that are performed in vein centers, office-based practices, and ambulatory or inpatient settings. The VVR looks at ablation and phlebectomy techniques and captures data including patient demographics, history, procedure data, plus early and late office-based and patient-reported follow-up in order to benchmark and improve outcomes and develop best practices and to help meet vein center certification requirements. The VVR includes 39 centers and more than 23,000 procedures.
Dr. Wakefield, who heads the VVR, used this registry as a means to illustrate how VQIs could be used to establish whether “the expected health benefit exceeds the expected negative consequences by a sufficiently wide margin that the procedure is worth doing.” This can be considered to be “appropriateness, which is part of ethical treatment.” Dr. Wakefield is the Stanley Professor of Vascular Surgery at the University of Michigan and section head, vascular surgery, University of Michigan Cardiovascular Center, Ann Arbor.
Data from the VQI registry (of which the VVR is a component) are now being used to generate appropriateness reports, said Dr. Wakefield.
The VQI represents a large comprehensive database of long-term data to define appropriate care. In addition, the VQI infrastructure is already geared to producing these reports both at a center and at a surgeon level. One disadvantage of the VVR registry, however, is low participation – only the 39 centers – and that it doesn’t capture cosmetic procedures and lesser (C1) disease. Further, it’s “likely the VQI participants are the ‘good actors,’ ” he added.
Targets for appropriateness include the proportion of patients undergoing ablation C2 or C4 disease or greater, the mean number of ablations per patient, the mean number of ablations per limb, and the proportion of perforated ablations for greater than C4 disease. Plotting out the data for these procedures at the center level can be assessed against current thinking on best practices in the various areas. For example, “the mean number of ablations per patient has been suggested at 1.8 to be about the right number,” and he used the graph of the center performance in this area to show that most of the centers were below this objective.
In an even more appropriate example of how this kind of data could be used to determine appropriateness, Dr. Wakefield described how perforated ablations should be performed for greater than C4 disease, but not for C2 disease. He described how, according to the actual data in the registry, there have been 870 total perforated treatments recorded, 38% for C2 disease, and of these 332 procedures, almost half of these were performed at one center only, with two other centers reporting 30 such procedures. “So clearly there are three centers that are doing perforated ablations for patients that are outside the guidelines,” Dr. Wakefield pointed out.
In future, payer demand is likely to demand that each treating physician provide evidence of the appropriateness of procedures performed, as well as appropriate patient selection and adherence to best practices, and good outcomes, which is part of what a society-based registry such as the VVR can provide.
“I believe the VQI-VVR is well-positioned to meet these needs. And if we ask the question ‘can VQI be used as a benchmark for setting ethical standards,’ I think it can certainly be used to help set appropriate standards, and since appropriateness is one part of ethical standards, I believe it has a role,” he concluded.
Dr. Wakefield reported that he had no disclosures.
REPORTING FROM THE 2018 VEITH SYMPOSIUM
Education can improve adherence to VTE prophylaxis
Education can improve adherence to venous thromboembolism (VTE) prophylaxis among hospitalized patients, according to researchers.
They assessed data from more than 19,000 hospital stays and found that “real-time” educational interventions directed toward patients and nurses significantly reduced nonadministration of prescribed VTE prophylaxis.
However, this did not translate to a significant reduction in VTE incidence.
Elliott Haut, MD, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland, and his colleagues reported these results in JAMA Network Open.
For this study, the researchers evaluated patients who were prescribed VTE prophylaxis while admitted to Johns Hopkins Hospital between April 1, 2015, and December 31, 2015.
The researchers evaluated patients in 16 hospital units. Four units were targeted for educational intervention, and the remaining 12 units served as controls.
The educational interventions were given only when patients did not receive prescribed VTE prophylaxis. A bedside nurse would document nonadministration, and an alert built into the hospital’s electronic medical record would email and page a health educator.
If the patient had refused prophylaxis, the patient would receive an educational bundle on VTE, which could consist of any or all of the following (patient’s choice):
- A one-on-one discussion with the health educator
- A two-page paper handout (available in eight languages)
- A 10-minute educational video (on a tablet).
If the nonadministration of prophylaxis was not due to patient refusal or contraindication, the health educator would educate the bedside nurse about the importance of giving all prescribed doses of VTE prophylaxis.
The study included 19,652 patient visits during which VTE prophylaxis was prescribed.
Of these, 726 visits were targeted for educational intervention. In 272 visits, the intervention was administered to a nurse alone (n=45) or the nurse and the patient (n=227).
For the remaining 454 visits, the patient was discharged before the intervention (n=123), there was an order to discontinue prophylaxis (n=111), there was a technical error (n=55), the patient (n=43) or health educator (n=41) was off unit, or “other” reasons (n=81).
Results
The proportion of nonadministered doses of VTE prophylaxis declined significantly in the hospital units targeted with educational intervention—from 9.1% pre-intervention to 5.6% post-intervention (odds ratio [OR]=0.57, P<0.001).
However, there was no significant change in the control units—13.6% and 13.3%, respectively (OR=0.98, P=0.62).
The proportion of nonadministered doses for reasons other than patient refusal decreased significantly in the intervention units—from 2.3% to 1.7% (OR, 0.74, P=0.01)—but not in control units—from 3.4% to 3.3% (OR=0.98, P=0.69).
The proportion of nonadministered doses due to patient refusal decreased significantly in the intervention units—from 5.9% to 3.4% (OR=0.53, P<0.001)—but not in control units—from 8.7% to 8.5% (OR=0.98, P=0.71).
“Our study demonstrates that educating patients quickly, as soon as we learn about a missed dose, is not only possible to implement at a large hospital but is effective in ensuring that patients take the drugs that can save their lives,” Dr. Haut said.
“The educational bundles we created are effective and optimize busy clinicians’ already packed schedules,” added study author Brandyn Lau, of the Johns Hopkins University School of Medicine.
“At the end of the day, we’re here to deliver high quality care and keep patients safe, and this is one method of achieving that mission.”
However, the improved adherence to VTE prophylaxis did not translate to a significant reduction in VTE in this study.
The incidence of VTE decreased from 0.30% to 0.18% (OR=0.60) in intervention units and from 0.24% to 0.20% in control units (OR=0.81).
For all patients, the incidence of VTE was 0.26% pre-intervention and 0.19% post-intervention (P=0.46).
This research was supported by a contract from the Patient-Centered Outcomes Research Institute. The study authors reported support from various government agencies and private organizations.
Education can improve adherence to venous thromboembolism (VTE) prophylaxis among hospitalized patients, according to researchers.
They assessed data from more than 19,000 hospital stays and found that “real-time” educational interventions directed toward patients and nurses significantly reduced nonadministration of prescribed VTE prophylaxis.
However, this did not translate to a significant reduction in VTE incidence.
Elliott Haut, MD, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland, and his colleagues reported these results in JAMA Network Open.
For this study, the researchers evaluated patients who were prescribed VTE prophylaxis while admitted to Johns Hopkins Hospital between April 1, 2015, and December 31, 2015.
The researchers evaluated patients in 16 hospital units. Four units were targeted for educational intervention, and the remaining 12 units served as controls.
The educational interventions were given only when patients did not receive prescribed VTE prophylaxis. A bedside nurse would document nonadministration, and an alert built into the hospital’s electronic medical record would email and page a health educator.
If the patient had refused prophylaxis, the patient would receive an educational bundle on VTE, which could consist of any or all of the following (patient’s choice):
- A one-on-one discussion with the health educator
- A two-page paper handout (available in eight languages)
- A 10-minute educational video (on a tablet).
If the nonadministration of prophylaxis was not due to patient refusal or contraindication, the health educator would educate the bedside nurse about the importance of giving all prescribed doses of VTE prophylaxis.
The study included 19,652 patient visits during which VTE prophylaxis was prescribed.
Of these, 726 visits were targeted for educational intervention. In 272 visits, the intervention was administered to a nurse alone (n=45) or the nurse and the patient (n=227).
For the remaining 454 visits, the patient was discharged before the intervention (n=123), there was an order to discontinue prophylaxis (n=111), there was a technical error (n=55), the patient (n=43) or health educator (n=41) was off unit, or “other” reasons (n=81).
Results
The proportion of nonadministered doses of VTE prophylaxis declined significantly in the hospital units targeted with educational intervention—from 9.1% pre-intervention to 5.6% post-intervention (odds ratio [OR]=0.57, P<0.001).
However, there was no significant change in the control units—13.6% and 13.3%, respectively (OR=0.98, P=0.62).
The proportion of nonadministered doses for reasons other than patient refusal decreased significantly in the intervention units—from 2.3% to 1.7% (OR, 0.74, P=0.01)—but not in control units—from 3.4% to 3.3% (OR=0.98, P=0.69).
The proportion of nonadministered doses due to patient refusal decreased significantly in the intervention units—from 5.9% to 3.4% (OR=0.53, P<0.001)—but not in control units—from 8.7% to 8.5% (OR=0.98, P=0.71).
“Our study demonstrates that educating patients quickly, as soon as we learn about a missed dose, is not only possible to implement at a large hospital but is effective in ensuring that patients take the drugs that can save their lives,” Dr. Haut said.
“The educational bundles we created are effective and optimize busy clinicians’ already packed schedules,” added study author Brandyn Lau, of the Johns Hopkins University School of Medicine.
“At the end of the day, we’re here to deliver high quality care and keep patients safe, and this is one method of achieving that mission.”
However, the improved adherence to VTE prophylaxis did not translate to a significant reduction in VTE in this study.
The incidence of VTE decreased from 0.30% to 0.18% (OR=0.60) in intervention units and from 0.24% to 0.20% in control units (OR=0.81).
For all patients, the incidence of VTE was 0.26% pre-intervention and 0.19% post-intervention (P=0.46).
This research was supported by a contract from the Patient-Centered Outcomes Research Institute. The study authors reported support from various government agencies and private organizations.
Education can improve adherence to venous thromboembolism (VTE) prophylaxis among hospitalized patients, according to researchers.
They assessed data from more than 19,000 hospital stays and found that “real-time” educational interventions directed toward patients and nurses significantly reduced nonadministration of prescribed VTE prophylaxis.
However, this did not translate to a significant reduction in VTE incidence.
Elliott Haut, MD, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland, and his colleagues reported these results in JAMA Network Open.
For this study, the researchers evaluated patients who were prescribed VTE prophylaxis while admitted to Johns Hopkins Hospital between April 1, 2015, and December 31, 2015.
The researchers evaluated patients in 16 hospital units. Four units were targeted for educational intervention, and the remaining 12 units served as controls.
The educational interventions were given only when patients did not receive prescribed VTE prophylaxis. A bedside nurse would document nonadministration, and an alert built into the hospital’s electronic medical record would email and page a health educator.
If the patient had refused prophylaxis, the patient would receive an educational bundle on VTE, which could consist of any or all of the following (patient’s choice):
- A one-on-one discussion with the health educator
- A two-page paper handout (available in eight languages)
- A 10-minute educational video (on a tablet).
If the nonadministration of prophylaxis was not due to patient refusal or contraindication, the health educator would educate the bedside nurse about the importance of giving all prescribed doses of VTE prophylaxis.
The study included 19,652 patient visits during which VTE prophylaxis was prescribed.
Of these, 726 visits were targeted for educational intervention. In 272 visits, the intervention was administered to a nurse alone (n=45) or the nurse and the patient (n=227).
For the remaining 454 visits, the patient was discharged before the intervention (n=123), there was an order to discontinue prophylaxis (n=111), there was a technical error (n=55), the patient (n=43) or health educator (n=41) was off unit, or “other” reasons (n=81).
Results
The proportion of nonadministered doses of VTE prophylaxis declined significantly in the hospital units targeted with educational intervention—from 9.1% pre-intervention to 5.6% post-intervention (odds ratio [OR]=0.57, P<0.001).
However, there was no significant change in the control units—13.6% and 13.3%, respectively (OR=0.98, P=0.62).
The proportion of nonadministered doses for reasons other than patient refusal decreased significantly in the intervention units—from 2.3% to 1.7% (OR, 0.74, P=0.01)—but not in control units—from 3.4% to 3.3% (OR=0.98, P=0.69).
The proportion of nonadministered doses due to patient refusal decreased significantly in the intervention units—from 5.9% to 3.4% (OR=0.53, P<0.001)—but not in control units—from 8.7% to 8.5% (OR=0.98, P=0.71).
“Our study demonstrates that educating patients quickly, as soon as we learn about a missed dose, is not only possible to implement at a large hospital but is effective in ensuring that patients take the drugs that can save their lives,” Dr. Haut said.
“The educational bundles we created are effective and optimize busy clinicians’ already packed schedules,” added study author Brandyn Lau, of the Johns Hopkins University School of Medicine.
“At the end of the day, we’re here to deliver high quality care and keep patients safe, and this is one method of achieving that mission.”
However, the improved adherence to VTE prophylaxis did not translate to a significant reduction in VTE in this study.
The incidence of VTE decreased from 0.30% to 0.18% (OR=0.60) in intervention units and from 0.24% to 0.20% in control units (OR=0.81).
For all patients, the incidence of VTE was 0.26% pre-intervention and 0.19% post-intervention (P=0.46).
This research was supported by a contract from the Patient-Centered Outcomes Research Institute. The study authors reported support from various government agencies and private organizations.
Procalcitonin testing does not decrease antibiotic use for LRTIs
Clinical question: Does testing procalcitonin for lower respiratory tract infections (LRTIs) decrease total antibiotic days without a resultant increase in adverse events?
Background: LRTIs are frequently overtreated with antibiotics. Procalcitonin may indicate bacterial infection and promote antibacterial stewardship. Studies to evaluate how testing procalcitonin affects antibiotic use for suspected lower respiratory tract infections are limited.
Study design: Randomized 1:1 intention-to-treat, multicenter trial.
Setting: 14 U.S. urban academic hospitals.

Synopsis: 1,656 patients across 14 U.S. hospitals were randomized to initial procalcitonin results available prior to clinical decision making versus usual care. All providers were given Food and Drug Administration–approved guidelines to interpret procalcitonin results. In the procalcitonin group, procalcitonin levels were followed serially. Within 30 days of the initial encounter, total antibiotic days did not differ significantly between the two groups. Procalcitonin use did not significantly affect adverse outcomes including organ system failure, death, ICU admission, hospital readmission, or ED visits. A total of 20% of antibiotic prescriptions were written prior to the procalcitonin result. Providers who did not adhere to guidelines either cited a diagnosis of chronic obstructive pulmonary disease or discounted the value of procalcitonin and presumptively diagnosed bacterial infection (40% of cases).
Bottom line: Procalcitonin testing did not change provider practice patterns for antibiotic prescriptions for LRTIs.
Citation: Huang DT et al. Procalcitonin-guided use of antibiotics for lower respiratory tract infection. N Engl J Med. 2018 Jul 19;379(3):236-49.
Dr. Naderi is assistant professor in the division of hospital medicine, University of Colorado, Denver.
Clinical question: Does testing procalcitonin for lower respiratory tract infections (LRTIs) decrease total antibiotic days without a resultant increase in adverse events?
Background: LRTIs are frequently overtreated with antibiotics. Procalcitonin may indicate bacterial infection and promote antibacterial stewardship. Studies to evaluate how testing procalcitonin affects antibiotic use for suspected lower respiratory tract infections are limited.
Study design: Randomized 1:1 intention-to-treat, multicenter trial.
Setting: 14 U.S. urban academic hospitals.

Synopsis: 1,656 patients across 14 U.S. hospitals were randomized to initial procalcitonin results available prior to clinical decision making versus usual care. All providers were given Food and Drug Administration–approved guidelines to interpret procalcitonin results. In the procalcitonin group, procalcitonin levels were followed serially. Within 30 days of the initial encounter, total antibiotic days did not differ significantly between the two groups. Procalcitonin use did not significantly affect adverse outcomes including organ system failure, death, ICU admission, hospital readmission, or ED visits. A total of 20% of antibiotic prescriptions were written prior to the procalcitonin result. Providers who did not adhere to guidelines either cited a diagnosis of chronic obstructive pulmonary disease or discounted the value of procalcitonin and presumptively diagnosed bacterial infection (40% of cases).
Bottom line: Procalcitonin testing did not change provider practice patterns for antibiotic prescriptions for LRTIs.
Citation: Huang DT et al. Procalcitonin-guided use of antibiotics for lower respiratory tract infection. N Engl J Med. 2018 Jul 19;379(3):236-49.
Dr. Naderi is assistant professor in the division of hospital medicine, University of Colorado, Denver.
Clinical question: Does testing procalcitonin for lower respiratory tract infections (LRTIs) decrease total antibiotic days without a resultant increase in adverse events?
Background: LRTIs are frequently overtreated with antibiotics. Procalcitonin may indicate bacterial infection and promote antibacterial stewardship. Studies to evaluate how testing procalcitonin affects antibiotic use for suspected lower respiratory tract infections are limited.
Study design: Randomized 1:1 intention-to-treat, multicenter trial.
Setting: 14 U.S. urban academic hospitals.

Synopsis: 1,656 patients across 14 U.S. hospitals were randomized to initial procalcitonin results available prior to clinical decision making versus usual care. All providers were given Food and Drug Administration–approved guidelines to interpret procalcitonin results. In the procalcitonin group, procalcitonin levels were followed serially. Within 30 days of the initial encounter, total antibiotic days did not differ significantly between the two groups. Procalcitonin use did not significantly affect adverse outcomes including organ system failure, death, ICU admission, hospital readmission, or ED visits. A total of 20% of antibiotic prescriptions were written prior to the procalcitonin result. Providers who did not adhere to guidelines either cited a diagnosis of chronic obstructive pulmonary disease or discounted the value of procalcitonin and presumptively diagnosed bacterial infection (40% of cases).
Bottom line: Procalcitonin testing did not change provider practice patterns for antibiotic prescriptions for LRTIs.
Citation: Huang DT et al. Procalcitonin-guided use of antibiotics for lower respiratory tract infection. N Engl J Med. 2018 Jul 19;379(3):236-49.
Dr. Naderi is assistant professor in the division of hospital medicine, University of Colorado, Denver.
Craig Getting, Luis Aguilar-Montalva: Part I
Thomas Jefferson University in Philadelphia partnered with the Lantern Theater Company to offer a class that teaches staging, acting, and playwriting. The class is designed specifically for med students, current residents, attending physicians, and any other medical professionals. The class eliminates hierarchy, encourages artistic exploration, and can lead to increased empathy when dealing with patients and their families. Nick, Luis, and Craig recognize the similarities between medicine and art but also highlight what we can learn from different passions.
Apple Podcasts
Google Podcasts
Thomas Jefferson University in Philadelphia partnered with the Lantern Theater Company to offer a class that teaches staging, acting, and playwriting. The class is designed specifically for med students, current residents, attending physicians, and any other medical professionals. The class eliminates hierarchy, encourages artistic exploration, and can lead to increased empathy when dealing with patients and their families. Nick, Luis, and Craig recognize the similarities between medicine and art but also highlight what we can learn from different passions.
Apple Podcasts
Google Podcasts
Thomas Jefferson University in Philadelphia partnered with the Lantern Theater Company to offer a class that teaches staging, acting, and playwriting. The class is designed specifically for med students, current residents, attending physicians, and any other medical professionals. The class eliminates hierarchy, encourages artistic exploration, and can lead to increased empathy when dealing with patients and their families. Nick, Luis, and Craig recognize the similarities between medicine and art but also highlight what we can learn from different passions.
Apple Podcasts
Google Podcasts
Panel Provides Recommendations for Managing Cognitive Changes in MS
Baseline screening and periodic reassessments aid in the monitoring of treatment response and disease progression.
The National Multiple Sclerosis (MS) Society has developed recommendations for the identification and management of cognitive impairment in MS. The recommendations, which were endorsed by the Consortium of MS Centers and the International MS Cognition Society, were published online ahead of print October 10 in Multiple Sclerosis Journal.
Cognitive change may affect between 34% and 65% of adults with MS. Decreases in information processing and memory are the most common changes, and cognitive impairment may arise before MRI abnormalities that indicate MS. These changes can affect patients’ ability to work, drive, manage money, and participate in activities.
Patients and Clinicians Need Information
Patients and caregivers should receive information about common cognitive changes in MS and how they affect everyday life, said Rosalind Kalb, PhD, Vice President of the Professional Resource Center at the National MS Society in New York, and coauthors. Patients and caregivers also should be told about the high prevalence of cognitive symptoms in MS and the need for ongoing assessments. Similarly, clinicians need information about how cognitive impairments affect medical decision-making and adherence, said the authors. Clinicians also need referral resources for cognitive assessment and treatment.
All adults and children age 8 or older diagnosed with MS should, as a minimum, undergo early baseline screening with the Symbol Digit Modalities Test (SDMT) or another validated screening tool, according to the recommendations. These patients should be reassessed with the same instrument annually or more often, as needed, to detect disease activity, assess for treatment effects or relapse recovery, monitor progression of cognitive impairment, and screen for new cognitive problems.
In addition to the SDMT, screening tools that have been validated in patients with MS include the Processing Speed Test, Computerized Speed Cognitive Test, MS Neuropsychological Screening Questionnaire, Brief International Cognitive Assessment for MS, Brief Repeatable Neuropsychological Battery, and Minimal Assessment of Cognitive Function in MS.
Interventions May Improve or Maintain Function
An adult who tests positive for cognitive impairment on initial screening should undergo a more comprehensive assessment, especially if the person has comorbidities that raise concerns or is applying for disability due to cognitive impairment. A child with an unexplained change in school performance should receive a neuropsychologic evaluation, said Dr. Kalb and colleagues.
Furthermore, adults and children should be offered remedial interventions or accommodations to improve function at home, work, or school. Appropriately trained professionals should deliver these interventions to address “objectively measured deficits in attention, processing speed, memory and learning, and performance of everyday functional tasks,” said the authors. Clinicians can consider contextualized treatment (eg, self-generated learning tasks) and noncontextualized treatment (eg, memory-retrieval practice and computer-based attention interventions) for remediation of everyday activities, according to the recommendations.
Emerging research supports the potential for exercise to benefit cognitive processing speed in patients with MS. Trials of symptomatic pharmacologic treatments for cognitive impairment related to MS have yielded inconclusive results, however. In addition, few pivotal trials of disease-modifying therapies have incorporated cognitive outcome measures.
—Erik Greb
Suggested Reading
Kalb R, Beier M, Benedict RH, et al. Recommendations for cognitive screening and management in multiple sclerosis care. Mult Scler. 2018 Oct 10 [Epub ahead of print].
Baseline screening and periodic reassessments aid in the monitoring of treatment response and disease progression.
Baseline screening and periodic reassessments aid in the monitoring of treatment response and disease progression.
The National Multiple Sclerosis (MS) Society has developed recommendations for the identification and management of cognitive impairment in MS. The recommendations, which were endorsed by the Consortium of MS Centers and the International MS Cognition Society, were published online ahead of print October 10 in Multiple Sclerosis Journal.
Cognitive change may affect between 34% and 65% of adults with MS. Decreases in information processing and memory are the most common changes, and cognitive impairment may arise before MRI abnormalities that indicate MS. These changes can affect patients’ ability to work, drive, manage money, and participate in activities.
Patients and Clinicians Need Information
Patients and caregivers should receive information about common cognitive changes in MS and how they affect everyday life, said Rosalind Kalb, PhD, Vice President of the Professional Resource Center at the National MS Society in New York, and coauthors. Patients and caregivers also should be told about the high prevalence of cognitive symptoms in MS and the need for ongoing assessments. Similarly, clinicians need information about how cognitive impairments affect medical decision-making and adherence, said the authors. Clinicians also need referral resources for cognitive assessment and treatment.
All adults and children age 8 or older diagnosed with MS should, as a minimum, undergo early baseline screening with the Symbol Digit Modalities Test (SDMT) or another validated screening tool, according to the recommendations. These patients should be reassessed with the same instrument annually or more often, as needed, to detect disease activity, assess for treatment effects or relapse recovery, monitor progression of cognitive impairment, and screen for new cognitive problems.
In addition to the SDMT, screening tools that have been validated in patients with MS include the Processing Speed Test, Computerized Speed Cognitive Test, MS Neuropsychological Screening Questionnaire, Brief International Cognitive Assessment for MS, Brief Repeatable Neuropsychological Battery, and Minimal Assessment of Cognitive Function in MS.
Interventions May Improve or Maintain Function
An adult who tests positive for cognitive impairment on initial screening should undergo a more comprehensive assessment, especially if the person has comorbidities that raise concerns or is applying for disability due to cognitive impairment. A child with an unexplained change in school performance should receive a neuropsychologic evaluation, said Dr. Kalb and colleagues.
Furthermore, adults and children should be offered remedial interventions or accommodations to improve function at home, work, or school. Appropriately trained professionals should deliver these interventions to address “objectively measured deficits in attention, processing speed, memory and learning, and performance of everyday functional tasks,” said the authors. Clinicians can consider contextualized treatment (eg, self-generated learning tasks) and noncontextualized treatment (eg, memory-retrieval practice and computer-based attention interventions) for remediation of everyday activities, according to the recommendations.
Emerging research supports the potential for exercise to benefit cognitive processing speed in patients with MS. Trials of symptomatic pharmacologic treatments for cognitive impairment related to MS have yielded inconclusive results, however. In addition, few pivotal trials of disease-modifying therapies have incorporated cognitive outcome measures.
—Erik Greb
Suggested Reading
Kalb R, Beier M, Benedict RH, et al. Recommendations for cognitive screening and management in multiple sclerosis care. Mult Scler. 2018 Oct 10 [Epub ahead of print].
The National Multiple Sclerosis (MS) Society has developed recommendations for the identification and management of cognitive impairment in MS. The recommendations, which were endorsed by the Consortium of MS Centers and the International MS Cognition Society, were published online ahead of print October 10 in Multiple Sclerosis Journal.
Cognitive change may affect between 34% and 65% of adults with MS. Decreases in information processing and memory are the most common changes, and cognitive impairment may arise before MRI abnormalities that indicate MS. These changes can affect patients’ ability to work, drive, manage money, and participate in activities.
Patients and Clinicians Need Information
Patients and caregivers should receive information about common cognitive changes in MS and how they affect everyday life, said Rosalind Kalb, PhD, Vice President of the Professional Resource Center at the National MS Society in New York, and coauthors. Patients and caregivers also should be told about the high prevalence of cognitive symptoms in MS and the need for ongoing assessments. Similarly, clinicians need information about how cognitive impairments affect medical decision-making and adherence, said the authors. Clinicians also need referral resources for cognitive assessment and treatment.
All adults and children age 8 or older diagnosed with MS should, as a minimum, undergo early baseline screening with the Symbol Digit Modalities Test (SDMT) or another validated screening tool, according to the recommendations. These patients should be reassessed with the same instrument annually or more often, as needed, to detect disease activity, assess for treatment effects or relapse recovery, monitor progression of cognitive impairment, and screen for new cognitive problems.
In addition to the SDMT, screening tools that have been validated in patients with MS include the Processing Speed Test, Computerized Speed Cognitive Test, MS Neuropsychological Screening Questionnaire, Brief International Cognitive Assessment for MS, Brief Repeatable Neuropsychological Battery, and Minimal Assessment of Cognitive Function in MS.
Interventions May Improve or Maintain Function
An adult who tests positive for cognitive impairment on initial screening should undergo a more comprehensive assessment, especially if the person has comorbidities that raise concerns or is applying for disability due to cognitive impairment. A child with an unexplained change in school performance should receive a neuropsychologic evaluation, said Dr. Kalb and colleagues.
Furthermore, adults and children should be offered remedial interventions or accommodations to improve function at home, work, or school. Appropriately trained professionals should deliver these interventions to address “objectively measured deficits in attention, processing speed, memory and learning, and performance of everyday functional tasks,” said the authors. Clinicians can consider contextualized treatment (eg, self-generated learning tasks) and noncontextualized treatment (eg, memory-retrieval practice and computer-based attention interventions) for remediation of everyday activities, according to the recommendations.
Emerging research supports the potential for exercise to benefit cognitive processing speed in patients with MS. Trials of symptomatic pharmacologic treatments for cognitive impairment related to MS have yielded inconclusive results, however. In addition, few pivotal trials of disease-modifying therapies have incorporated cognitive outcome measures.
—Erik Greb
Suggested Reading
Kalb R, Beier M, Benedict RH, et al. Recommendations for cognitive screening and management in multiple sclerosis care. Mult Scler. 2018 Oct 10 [Epub ahead of print].
Change is upon us
It shouldn’t be a surprise. Although we don’t necessarily welcome change, change is a constant in our world. Nothing new here – it has always been so. Most of us dread change, because of our natural apprehension of the unknown. New ideas and ways of functioning that disrupt the status quo require effort, adjustment, and learning with no guarantee of success.
In my lifetime alone, ways of communicating with one another have undergone so many changes that it’s dizzying to contemplate. When I was a child in rural Oregon, our means of communicating with friends and family was the “party line” (by which was meant, not the political party, but the community’s telephone connection). We didn’t have a separate phone number, but rather a ring that was specific to our family. Most people on the line knew each other’s ring and could surreptitiously listen in if curiosity got the best of them. Privacy was not a big consideration.
Fast forward just over a half-century, and our system of communication is barely recognizable: 24/7 connectivity on hand-held electronic devices to any part of the world, SMS, Skype, Facebook, texting. Instantaneous worldwide communication is a given from anywhere, even the golf course.
Yes, there are hazards in this convenience. Recent events have demonstrated the lack of privacy and security of our communications, and what you see is not necessarily what it appears to be. It has become abundantly clear just how fragile the process of exchanging valid information can be. And yet, who would wish to erase all of this convenience to go back to the old days before the Internet? I doubt seriously that many surgeons would exchange the old world of limited access to information and communication for our era of immersive connectivity.
A comparable progression has occurred in our methods of professional learning and moving our corpus of knowledge forward. For the past half-century and more, new techniques, knowledge, and ideas have been presented in meetings of established societies and published in peer-reviewed journals. Unfortunately, not all who might benefit from these new ideas have access to them. If you belong to the society, can afford the time and money to attend the meeting, and work in an institution that subscribes to online access to all of the major journals, you can read them. Surgeons in independent practice in rural, remote communities likely do not have that luxury. ACS Surgery News has had many functions but one of the most important has been to serve surgeons in those remote communities as well as for others who simply wanted the convenience of ready access to new information all in one place.
Unfortunately, print publications are becoming more expensive to produce and mail, and advertising dollars to subsidize them are shrinking. Thus, Tyler Hughes and I, the coeditors of ACS Surgery News, were informed that our publication will cease production after the December 2018 issue. We and the ACS leadership huddled to find a way to continue what we all believe is a benefit to our ACS Fellows, particularly those who practice in small rural hospitals. The answer was right in front of us: The ACS Communities, to which all Fellows have online access. So that is our plan: Tyler and I will continue to write our “homespun” commentaries, and our editorial board will contribute concise articles that summarize the “latest and greatest” presentations at meetings they attend or from recently published articles in major journals across the spectrum of general surgery and surgical specialties. If readers have questions or comments, they will be able to communicate with the authors for clarification. We hope that this structure and content will benefit our surgical colleagues. Look for our new ACS Communities presence in January 2019.
Dr. Deveney is professor of surgery emerita in the department of surgery at Oregon Health & Science University, Portland. She is the coeditor of ACS Surgery News.
It shouldn’t be a surprise. Although we don’t necessarily welcome change, change is a constant in our world. Nothing new here – it has always been so. Most of us dread change, because of our natural apprehension of the unknown. New ideas and ways of functioning that disrupt the status quo require effort, adjustment, and learning with no guarantee of success.
In my lifetime alone, ways of communicating with one another have undergone so many changes that it’s dizzying to contemplate. When I was a child in rural Oregon, our means of communicating with friends and family was the “party line” (by which was meant, not the political party, but the community’s telephone connection). We didn’t have a separate phone number, but rather a ring that was specific to our family. Most people on the line knew each other’s ring and could surreptitiously listen in if curiosity got the best of them. Privacy was not a big consideration.
Fast forward just over a half-century, and our system of communication is barely recognizable: 24/7 connectivity on hand-held electronic devices to any part of the world, SMS, Skype, Facebook, texting. Instantaneous worldwide communication is a given from anywhere, even the golf course.
Yes, there are hazards in this convenience. Recent events have demonstrated the lack of privacy and security of our communications, and what you see is not necessarily what it appears to be. It has become abundantly clear just how fragile the process of exchanging valid information can be. And yet, who would wish to erase all of this convenience to go back to the old days before the Internet? I doubt seriously that many surgeons would exchange the old world of limited access to information and communication for our era of immersive connectivity.
A comparable progression has occurred in our methods of professional learning and moving our corpus of knowledge forward. For the past half-century and more, new techniques, knowledge, and ideas have been presented in meetings of established societies and published in peer-reviewed journals. Unfortunately, not all who might benefit from these new ideas have access to them. If you belong to the society, can afford the time and money to attend the meeting, and work in an institution that subscribes to online access to all of the major journals, you can read them. Surgeons in independent practice in rural, remote communities likely do not have that luxury. ACS Surgery News has had many functions but one of the most important has been to serve surgeons in those remote communities as well as for others who simply wanted the convenience of ready access to new information all in one place.
Unfortunately, print publications are becoming more expensive to produce and mail, and advertising dollars to subsidize them are shrinking. Thus, Tyler Hughes and I, the coeditors of ACS Surgery News, were informed that our publication will cease production after the December 2018 issue. We and the ACS leadership huddled to find a way to continue what we all believe is a benefit to our ACS Fellows, particularly those who practice in small rural hospitals. The answer was right in front of us: The ACS Communities, to which all Fellows have online access. So that is our plan: Tyler and I will continue to write our “homespun” commentaries, and our editorial board will contribute concise articles that summarize the “latest and greatest” presentations at meetings they attend or from recently published articles in major journals across the spectrum of general surgery and surgical specialties. If readers have questions or comments, they will be able to communicate with the authors for clarification. We hope that this structure and content will benefit our surgical colleagues. Look for our new ACS Communities presence in January 2019.
Dr. Deveney is professor of surgery emerita in the department of surgery at Oregon Health & Science University, Portland. She is the coeditor of ACS Surgery News.
It shouldn’t be a surprise. Although we don’t necessarily welcome change, change is a constant in our world. Nothing new here – it has always been so. Most of us dread change, because of our natural apprehension of the unknown. New ideas and ways of functioning that disrupt the status quo require effort, adjustment, and learning with no guarantee of success.
In my lifetime alone, ways of communicating with one another have undergone so many changes that it’s dizzying to contemplate. When I was a child in rural Oregon, our means of communicating with friends and family was the “party line” (by which was meant, not the political party, but the community’s telephone connection). We didn’t have a separate phone number, but rather a ring that was specific to our family. Most people on the line knew each other’s ring and could surreptitiously listen in if curiosity got the best of them. Privacy was not a big consideration.
Fast forward just over a half-century, and our system of communication is barely recognizable: 24/7 connectivity on hand-held electronic devices to any part of the world, SMS, Skype, Facebook, texting. Instantaneous worldwide communication is a given from anywhere, even the golf course.
Yes, there are hazards in this convenience. Recent events have demonstrated the lack of privacy and security of our communications, and what you see is not necessarily what it appears to be. It has become abundantly clear just how fragile the process of exchanging valid information can be. And yet, who would wish to erase all of this convenience to go back to the old days before the Internet? I doubt seriously that many surgeons would exchange the old world of limited access to information and communication for our era of immersive connectivity.
A comparable progression has occurred in our methods of professional learning and moving our corpus of knowledge forward. For the past half-century and more, new techniques, knowledge, and ideas have been presented in meetings of established societies and published in peer-reviewed journals. Unfortunately, not all who might benefit from these new ideas have access to them. If you belong to the society, can afford the time and money to attend the meeting, and work in an institution that subscribes to online access to all of the major journals, you can read them. Surgeons in independent practice in rural, remote communities likely do not have that luxury. ACS Surgery News has had many functions but one of the most important has been to serve surgeons in those remote communities as well as for others who simply wanted the convenience of ready access to new information all in one place.
Unfortunately, print publications are becoming more expensive to produce and mail, and advertising dollars to subsidize them are shrinking. Thus, Tyler Hughes and I, the coeditors of ACS Surgery News, were informed that our publication will cease production after the December 2018 issue. We and the ACS leadership huddled to find a way to continue what we all believe is a benefit to our ACS Fellows, particularly those who practice in small rural hospitals. The answer was right in front of us: The ACS Communities, to which all Fellows have online access. So that is our plan: Tyler and I will continue to write our “homespun” commentaries, and our editorial board will contribute concise articles that summarize the “latest and greatest” presentations at meetings they attend or from recently published articles in major journals across the spectrum of general surgery and surgical specialties. If readers have questions or comments, they will be able to communicate with the authors for clarification. We hope that this structure and content will benefit our surgical colleagues. Look for our new ACS Communities presence in January 2019.
Dr. Deveney is professor of surgery emerita in the department of surgery at Oregon Health & Science University, Portland. She is the coeditor of ACS Surgery News.