User login
Two-thirds of abortions occur by 8 weeks’ gestation
, although there was variation by maternal age and race/ethnicity, according to the Centers for Disease Control and Prevention.
That year, 65.3% of abortions were performed at a gestational age of 8 weeks or earlier, with 25.6% occurring at 9-13 weeks. Gestational distribution of the remaining abortions was fairly even: 3.4% at 14-15 weeks, 2.2% at 16-17 weeks, 2.0% at 18-20 weeks, and 1.4% at 21 weeks or later, the CDC investigators reported (MMWR Surveill Summ. 2017 Nov 25;66[24]:1-48).
The percentage of abortions occurring at 8 weeks or earlier was lowest for the youngest age group and increased along with maternal age: 43% for those under 15 years of age and progressing up to 72.5% for women over age 40. That scenario was basically reversed for all of the other gestational periods, as the under-15 group had the highest percentage for 9-13 weeks (34.4%), 14-15 (6.7%), 16-17 (3.6%), 18-20 (5.0%), and 21 weeks and later (7.3%). Those over age 40 had the lowest or almost the lowest percentage in each period, reported Tara C. Jatlaoui, MD, and her associates.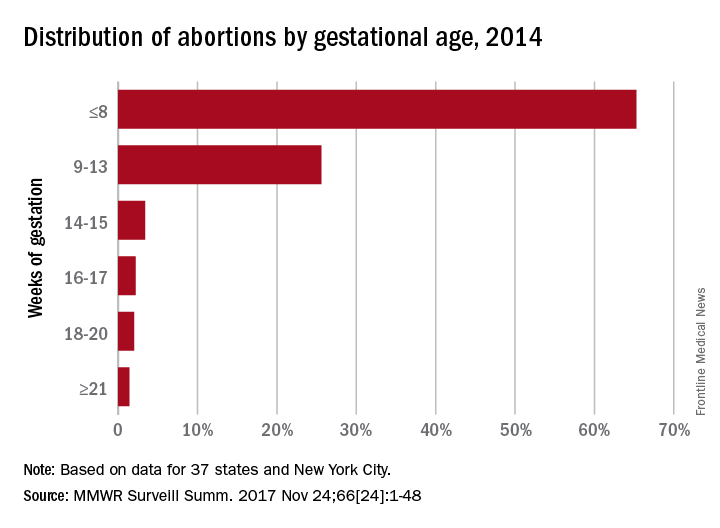
The data for gestational period analysis came from 37 states and New York City. New York State, along with 12 other states, did not report, did not report by gestational age, or did not meet reporting standards.
, although there was variation by maternal age and race/ethnicity, according to the Centers for Disease Control and Prevention.
That year, 65.3% of abortions were performed at a gestational age of 8 weeks or earlier, with 25.6% occurring at 9-13 weeks. Gestational distribution of the remaining abortions was fairly even: 3.4% at 14-15 weeks, 2.2% at 16-17 weeks, 2.0% at 18-20 weeks, and 1.4% at 21 weeks or later, the CDC investigators reported (MMWR Surveill Summ. 2017 Nov 25;66[24]:1-48).
The percentage of abortions occurring at 8 weeks or earlier was lowest for the youngest age group and increased along with maternal age: 43% for those under 15 years of age and progressing up to 72.5% for women over age 40. That scenario was basically reversed for all of the other gestational periods, as the under-15 group had the highest percentage for 9-13 weeks (34.4%), 14-15 (6.7%), 16-17 (3.6%), 18-20 (5.0%), and 21 weeks and later (7.3%). Those over age 40 had the lowest or almost the lowest percentage in each period, reported Tara C. Jatlaoui, MD, and her associates.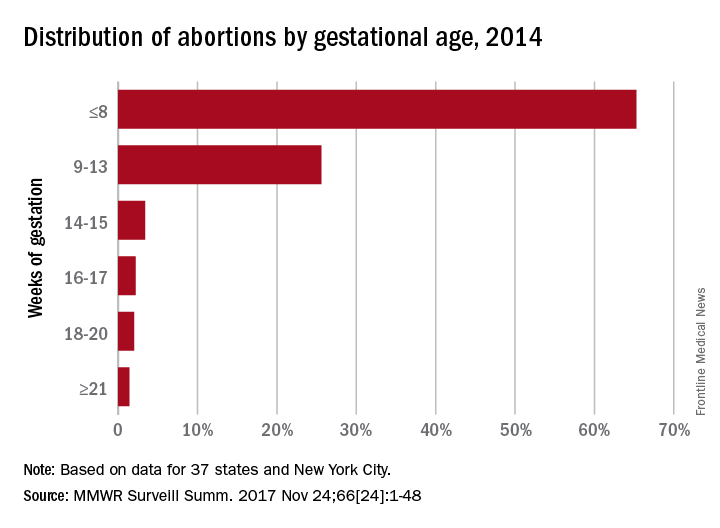
The data for gestational period analysis came from 37 states and New York City. New York State, along with 12 other states, did not report, did not report by gestational age, or did not meet reporting standards.
, although there was variation by maternal age and race/ethnicity, according to the Centers for Disease Control and Prevention.
That year, 65.3% of abortions were performed at a gestational age of 8 weeks or earlier, with 25.6% occurring at 9-13 weeks. Gestational distribution of the remaining abortions was fairly even: 3.4% at 14-15 weeks, 2.2% at 16-17 weeks, 2.0% at 18-20 weeks, and 1.4% at 21 weeks or later, the CDC investigators reported (MMWR Surveill Summ. 2017 Nov 25;66[24]:1-48).
The percentage of abortions occurring at 8 weeks or earlier was lowest for the youngest age group and increased along with maternal age: 43% for those under 15 years of age and progressing up to 72.5% for women over age 40. That scenario was basically reversed for all of the other gestational periods, as the under-15 group had the highest percentage for 9-13 weeks (34.4%), 14-15 (6.7%), 16-17 (3.6%), 18-20 (5.0%), and 21 weeks and later (7.3%). Those over age 40 had the lowest or almost the lowest percentage in each period, reported Tara C. Jatlaoui, MD, and her associates.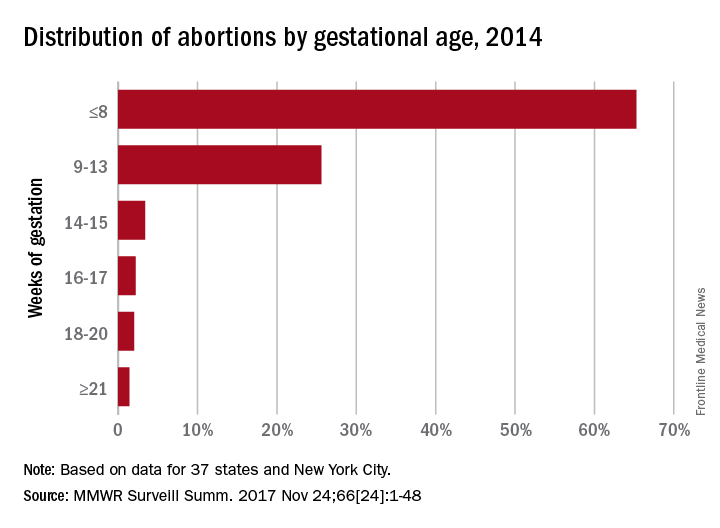
The data for gestational period analysis came from 37 states and New York City. New York State, along with 12 other states, did not report, did not report by gestational age, or did not meet reporting standards.
FROM MMWR SURVEILLANCE SUMMARIES
The clear and present future: Telehealth and telemedicine in obstetrics and gynecology
I recently spoke with 2 outstanding leaders in our field, members of the American College of Obstetricians and Gynecologists (ACOG) task force on telehealth and telemedicine, about the future of providing health care to women in remote locations.
Haywood Brown, MD, is President of ACOG for 2017–2018 and is F. Bayard Carter Professor of Obstetrics and Gynecology at Duke University Medical Center in Durham, North Carolina, and Peter Nielsen, MD, is Professor and Vice Chair of the Department of Obstetrics and Gynecology at Baylor College of Medicine in Houston, Texas, and Obstetrician-in-Chief at Children’s Hospital of San Antonio. Dr. Nielsen is a retired US Army colonel.
Why an ACOG telehealth task force?
Haywood Brown, MD: Our overall goals in telehealth and telemedicine are to coordinate and better facilitate the health care of women in remote locations and to improve maternal morbidity and mortality. Telehealth can be used on both an outpatient and an inpatient basis.
Outpatient telehealth is used for consultations. In maternal-fetal medicine, for instance, we use it for ultrasonography consultations. I also have used telehealth technology to “see” a pregnant patient with type 1diabetes. During our sessions, I managed her blood sugar levels and did all the other things I would have done if we had been together at my clinic. Without telehealth technology, however, this patient would have needed to drive 4 hours round-trip for each appointment.
Our colleagues in rural communities and at lower-level hospitals can use telehealth and telemedicine as aids in treating their high-risk patients, such as those with preeclampsia, prematurity risk, or other conditions. Physicians can consult with specialists through a face-to-face conversation that takes place through telecommunications. The result is that the quality of care for women in our communities is improved.
Genetic counseling, infertility consultation, and fetal anomaly management are some of the other applications. Our task force is discussing different ways to improve patient care and ways to collaborate with our colleagues around the country. Ultimately, we are developing best practices—a model for the best uses of technology to improve women’s health care in the United States.
Task force focus: Telehealth technology, billing, services
Dr. Brown: Our task force, a diverse group of members from all over the country, represents the spectrum of ObGyns. Although task force members have various levels of telehealth experience, all are very interested in these new channels of communication. The task force also includes billers, who understand billing ramifications, and payers, who know firsthand what will and will not be paid.
Technology and its availability is the most important topic for the task force. While some communities have Internet service, not all do. We need to determine which areas need service, how much it would cost, and who pays for it. Can a hospital afford it? A practice? Their partners? Identifying partners in tertiary care settings is a task force goal.
We are engaging a broad range of experts to study all the components and associated costs of technology, licensing, and cross-state credentialing. Gathering this information will help in developing a best practices model that general ObGyns can use.
Telehealth is redefining aspects of care: prenatal care (how many visits are required?), postpartum care, and other types of services that can be done remotely. Genetic counseling—who can provide it, what education is required—is another topic of discussion. Once we surmount the billing obstacles, we can do much with teleconferencing, such as provide genetic consultation with ObGyns in various settings.
The terms "telehealth" and "telemedicine" are often used interchangeably. Telemedicine is the older phrase, while telehealth entered the vernacular more recently and encompasses a broader definition.
The HealthIT.gov website explains the differences in terminology this way1:
- The Health Resources Services Administration defines telehealth as the use of electronic information and telecommunications technologies to support long-distance clinical health care, patient and professional health-related education, public health and health administration. Technologies include videoconferencing, the Internet, store-and-forward imaging, streaming media, and terrestrial and wireless communications.
- Telehealth is different from telemedicine because it refers to a broader scope of remote health care services than telemedicine. While telemedicine refers specifically to remote clinical services, telehealth can refer to remote nonclinical services, such as provider training, administrative meetings, and continuing medical education, in addition to clinical services.
A World Health Organization report, however, uses the 2 terms synonymously and interchangeably, defining telemedicine as2:
- The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.
The American Telemedicine Association (ATA) describes their use of the terms this way3:
- ATA largely views telemedicine and telehealth to be interchangeable terms, encompassing a wide definition of remote healthcare, although telehealth may not always involve clinical care.
References
- HealthIT.gov website. Frequently asked questions. https://www.healthit.gov/providers-professionals/frequently-asked-questions/485. Accessed November 15, 2017.
- World Health Organization. Telemedicine: opportunities and developments in member states. 2010. http://www.who.int/goe/publications/goe_telemedicine_2010.pdf. Accessed November 15, 2017.
- American Telemedicine Association. About telemedicine: the ultimate frontier for superior healthcare delivery. http://www.americantelemed.org/about/about-telemedicine. Accessed November 15, 2017.
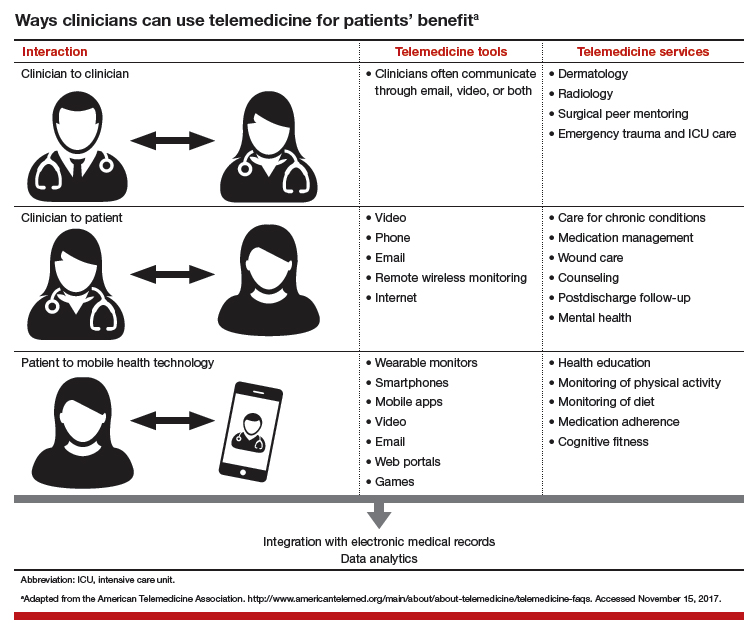
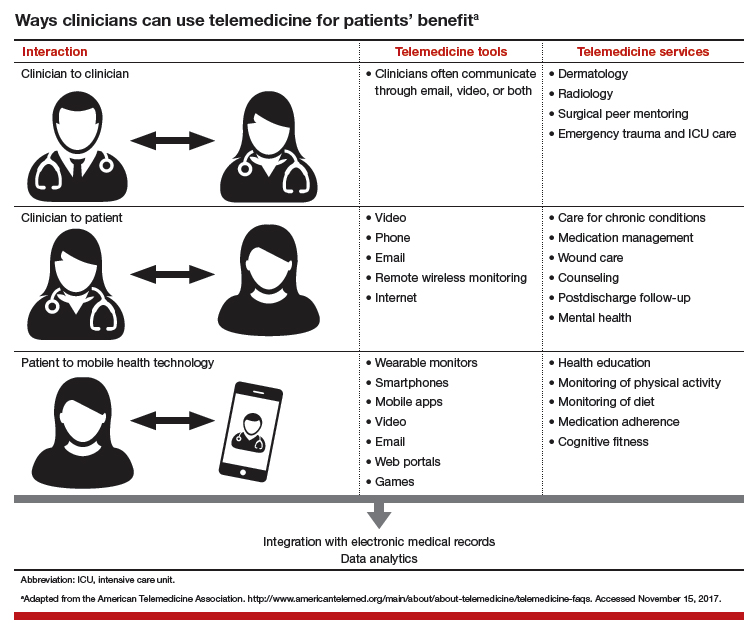
Learn about ways clinicians can use telemedicine.
Making progress in rural and underserved communities
Peter Nielsen, MD: When we saw that some high-risk obstetrics patients were having a difficult time getting to our downtown San Antonio office—the trip from surrounding communities was taking too long, or city driving and parking were stressful or too costly—we looked to improve access to care. Collaborating with a health care network that has a hospital in a town north of San Antonio, we set up a pilot program to provide telemedicine perinatal consultation services.
In this kind of service, which occurs entirely in real time, ultrasound images taken at the hospital are streamed by high-speed fiberoptic cable to our office, where a maternal-fetal medicine physician views them. If a repeat image or a different image is needed, the physician requests another scan. Linked to the physician and listening through an earpiece, the ultrasonographer performs the new scan with little delay and without disturbing the patient. The conversation between physician and ultrasonographer is private.
After ultrasound scanning is complete, the patient goes to a private room at the hospital for a video conference with our physician in San Antonio, who has reviewed the images in the PACS (picture archiving and communication system) or ultrasound recording system. They discuss the images, the findings, and the follow-up.
We tested the technology during a 6-month pilot program to make sure it worked at the highest quality and safety levels. Then the program went live and we started seeing patients remotely. Now we have a robust telemedicine training capability at that hospital outside San Antonio, and we are looking to expand to other south and west Texas areas, some even farther from our office.
I have done some of these remote consultations. In response to my informal queries about the experience, patients said that no one else was offering it, and they were participating for the first time. Naturally they had questions and concerns. Nevertheless, patients, family members, and the ultrasonographer and physicians in the communities seem to think this is a high-quality, safe program that makes it easier for patients to access health care.
Patients uniformly describe these consultations in positive terms. They do not have to drive far, into the city, and deal with traffic; parking is easy and free; and less travel means much less time off from work. Given these very practical advantages, patients are interested in having more appointments done remotely. In addition, they say the appointment itself is easy, being there is effortless, and they feel their physician is sitting in the same room. It is like video chatting with family members—they are comfortable with the technology.
Related article:
Landmark women’s health care remains law of the land
The patients’ perspective
Dr. Brown: Patient satisfaction is an important issue. In psychiatry, dermatology, and other disciplines, patients have indicated that they are very satisfied with telehealth sessions. Telehealth in obstetrics and gynecology, I think, will receive similar positive feedback.
The issue of driving distance led us to reconsider the number of face-to-face prenatal visits a normal, healthy patient needs. These days, a patient can use a prenatal care app to track her weight and blood pressure and send the data to her physician. Besides being convenient, these monitoring apps can give a patient an important sense of control. Our pilot programs found that a patient who self-monitors understands her weight gain better and is more in tune with it. Apps and other technologies can thus improve quality of care and, in reducing the number of trips to an office, increase patient satisfaction.
Many people use or are familiar with the programs Skype and FaceTime (audiovideo chat software), and I envision that our postpartum task force will recommend using such programs for follow-up appointments. For each visit, the question to ask is whether the patient really needs to meet with her physician in person, or can she stay with her new baby and receive postpartum counseling at home. I am excited about the potential of telehealth in obstetrics and gynecology. Our task force is exploring that potential.
Telehealth for both routine and specialized care
Dr. Brown: Specialized care applications are here. In a pilot program in Wisconsin, a colleague has been providing remote psychiatric care. Perhaps such a program can be used to follow up on patients with postpartum depression. In addition, other psychiatry colleagues have long been using telehealth for adolescent behavior follow-ups, and we can do this too.
Another colleague has been performing remote perinatal follow-up for children with congenital anomalies. The physician interacts with the parent or parents as well as the patient. This seems to represent only the tip of the iceberg of what can be done in terms of follow-up.
We can also use telehealth in infertility settings. High-risk patients can benefit, too. Our guidelines say patients with preeclampsia should be seen within 3 days to 1 week. Many are transferred from low-access hospitals to our office. This follow-up, however, also can be done remotely, with patients at health department clinics or even at home. Reporting blood pressure readings and health-related feelings to a physician during a teleconsultation removes driving as a potential inconvenience or obstacle.
Telemedicine can be advantageous in gynecology. Physicians are doing important work with telecolposcopy as a follow-up to abnormal Pap test findings in patients in sub-Saharan Africa.
Routine wound care, which is commonly needed, can be performed in the home by a home health nurse telecommunicating with a physician. I can see broad telehealth use, and indeed our dermatology colleagues have been practicing telemedicine for quite some time.
Read about solving financial barriers and physician shortages.
An affordable solution to financial barriers and physician shortages
Dr. Nielsen: Telehealth can reduce barriers to care. For example, knowing that our teleconsultation services are covered by insurance, referring physicians and patients are more likely to try them and continue to use them. Payers are on board as well. Other barriers can be harder to overcome, particularly for patients at risk for complex diagnoses and medical decisions. Our pilot program, however, has demonstrated success in this area. It has provided safe, high-quality imaging, accurate diagnoses, productive discussions, and helpful management recommendations.
Telehealth also helps address relative and absolute physician shortages. In some areas, a relative shortage may indicate misdistribution. In other areas, specialists simply are too few in number. This absolute shortage of specialists likely will increase, as many communities are too small to sustain and support having them in person.
Outpatients can obtain care 5 days a week with telemedicine, as opposed to only 1 to 3 times a month in person. Physicians travel to remote clinics that are staffed only 1 or 2 days a month. Where the window for care is so small, patients and physicians are likely to turn to telemedicine. In addition, that utility results in better use of resources. For example, studies that were performed earlier would not need to be repeated, since you could access centrally located archives.
Related article:
ICD-10-CM code changes: What's new for 2018
Dr. Brown: For teleconsultations and televisits, all that payers need do is modify the billing codes they use for our usual services. Once that is done, payers can develop a payment model that works for both themselves and the teleconsultants.
The US health care system is fragmented. Health care is provided in various facilities, including federally qualified health centers and health department clinics. As Dr. Nielsen said, physicians travel to remote facilities once or twice a week or even a month, whereas telehealth can be offered 5 days a week. Many residents go to remote clinics, where an attending physician is required. Instead of an attending driving there, he or she could be teleconsulting—interacting with residents and patients from afar. So, telehealth is a win-win situation. It increases access to physicians and facilitates appropriate interactions with them, wherever they are. Telehealth can be an important contribution to developing a more effective health care delivery system than the fragmented one we have now.
Effective health care delivery is so important for obstetrics and gynecology, and the reported workforce challenges are real. A maternal-fetal medicine physician is unlikely to travel to remote communities once a week or even every 2 weeks, but that same physician can teleconsult multiple days each week.
How telehealth can close service gaps
Dr. Brown: Having established relationships with physicians in other clinics and communities paves the way for teleconsultation and remote supervision. Technology can help Planned Parenthood and other clinics continue to provide contraceptive counseling and other health care services. Even medical abortions can be supervised through teleconsultation.
With funds to Medicaid being cut, with the potential for Planned Parenthood to be defunded, physicians must think of ways they can continue to provide care to all patients and communities. By addressing these issues now, we will be ready to take charge of patient care, wherever it is needed.
But, we need partners, no question. We need hospital partners in all communities, and especially in rural communities. Rural hospitals and maternity care are at risk. Health care in rural communities faces many challenges. Telehealth, teleconferencing, and teleconsultation not only can improve access to services, but also can curb travel costs as well as costs to the communities and hospitals.
Who pays the operating costs, and who benefits
Dr. Brown: Payers are already discovering that teleconsultations are as billable as in-person visits. In addition, physicians are realizing that remote consultation can work as well as in-person consultation, with its own merits and advantages. Education is key—education about billing and about what is doable in telehealth. We can learn from colleagues in other specialties.
Dr. Nielsen: Several entities and groups must start covering the technology costs. Federal and state entities need to determine how the country’s information infrastructure can be improved to give rural areas access to high-quality, high-speed, wide-bandwidth communications, which will help expand telehealth and increase other industries’ opportunities to grow and sustain these communities. Improving the infrastructure also can help keep rural areas sustainable.
Health care systems themselves can join federal, state, and local governments in building this infrastructure. They can also start identifying opportunities to support and sustain physicians and hospitals in smaller towns and start combating the perception that the infrastructure is being developed only to migrate patients over to accessing their care through telehealth provided by physicians in the larger cities.
Many payers see telehealth as improving access and outcomes and already support it, but more payers need to become involved. All need to understand how routine and complex consultations, even inpatient consultations, can be performed remotely and can be properly reimbursed, and incentivized with payments for improved outcomes and value.
As barriers fall and telehealth improves, acceptance by patients and physicians will increase. In addition, telehealth will enter medical education in a significant way. The instruction that students, residents, and Fellows receive will be enhanced by new telehealth approaches in various specialties, and residents will come out of these programs with telehealth experience and a sense of both financial benefits and payment structures. This early exposure will pique their interest in using telehealth and advocating its use where it may never before have been considered, owing to real and perceived barriers.
Read about telehealth solutions for ObGyns.
Learning from other specialties and agencies
Dr. Brown: The physician shortage negatively affects access to health care in rural areas. Many city and suburban physicians, including ObGyns, want to stay where they are. Education is needed to show them that a rural practice can be successful. They would have a good patient base and be able to use telehealth to improve care and maintain contact with tertiary care centers.
Several task force members have described their experience within their health systems, and we hope to borrow from that. A health system in South Dakota received a Health Resources and Services Administration grant to use telehealth and teleconsultation in the Indian Health Service (IHS). To women who access their health care through the IHS, being able to remain in the community is culturally important. Telehealth and teleconsultation bring care to these women where they live.
To develop the best telehealth and teleconsultation model, we are borrowing from these health systems and from the experience of our colleagues in dermatology, behavioral health, psychiatry, and other disciplines. These physicians already have overcome many hurdles and discovered the importance of patient satisfaction in providing remote health care.
Patients will benefit in various ways, and here is another example: A clinic refers a patient to an ObGyn to discuss whether it is possible to have a vaginal birth after a cesarean delivery. The drive to the ObGyn’s office takes an hour, but the patient just as easily could have had all her questions answered during a teleconsultation.
Related articles:
Telehealth and you (4-part audiocast)
Telehealth recommendations for ObGyns
Dr. Brown: Our task force will develop recommended best practices for telehealth. We will outline how a practice can engage with telehealth and will address licensing requirements, as a practice must be licensed in each state where it uses telehealth. Our goal is to help our specialty get started in telehealth and telemedicine.
In practices with telehealth, it will be incumbent on ObGyns to identify any barriers to care. For example, we are concerned about early discontinuation of breastfeeding, particularly among African American communities. Fortunately, we have learned that video chat follow-ups can help improve breastfeeding continuation rates.
It also will be incumbent on ObGyns to think differently about how best to follow up. For a patient who calls to say she thinks she has mastitis, much of the consultation can be handled by telephone or video conference with the physician and a nurse practi‑tioner, and then medication can be prescribed without the need for in-person follow-up. We must then determine how to ensure these follow-up methods are compensated.
Direct-to-patient virtual visits
- Virtual home visits
- Low-risk pregnancy
- Postpartum visits
- Lactation support
- Routine gynecologic care
- Postoperative follow-up
Remote patient monitoring
- Chronic disease management
- Antenatal testing
- Fetal heart rate monitoring
- Transfer of care
Final thoughts
Dr. Nielsen: It is time for all US health care players to more seriously and aggressively consider how telehealth can improve health care access, quality, and safety. Even more important, patients and physicians in small communities need to feel that they can access specialists and care that is as good as those available in larger communities without having to pull up stakes and move.
Telehealth can help small communities become sustainable over the long term. As the majority of the people in this country are born in and receive health care in community hospitals, not large tertiary care centers, the state of US health care should be measured by the ability to provide as much care as is technically possible in the small communities where patients live and work and raise their kids.
Dr. Brown: More than 50% of all babies are born in hospitals where fewer than 1,000 deliveries are performed, and almost 40% are born in hospitals where fewer than 500 are performed. To provide high-level care and have patients feel comfortable, to improve morbidity and mortality, we need telehealth and telemedicine.
If I can help a physician in East Africa place a Bakri balloon for postpartum hemorrhaging, surely I can help a physician in rural areas of Wyoming, South Dakota, or North Carolina deal with this obstetric emergency. In obstetrics and gynecology, telehealth and telemedicine have great potential in terms of morbidity and mortality, but we are also doing genetic counseling and a great deal of patient follow-up, and so much more can be done.
That is the key, and the reason for the training, the task force, the deliberations, and the best practices model that we will be sharing with our colleagues.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
I recently spoke with 2 outstanding leaders in our field, members of the American College of Obstetricians and Gynecologists (ACOG) task force on telehealth and telemedicine, about the future of providing health care to women in remote locations.
Haywood Brown, MD, is President of ACOG for 2017–2018 and is F. Bayard Carter Professor of Obstetrics and Gynecology at Duke University Medical Center in Durham, North Carolina, and Peter Nielsen, MD, is Professor and Vice Chair of the Department of Obstetrics and Gynecology at Baylor College of Medicine in Houston, Texas, and Obstetrician-in-Chief at Children’s Hospital of San Antonio. Dr. Nielsen is a retired US Army colonel.
Why an ACOG telehealth task force?
Haywood Brown, MD: Our overall goals in telehealth and telemedicine are to coordinate and better facilitate the health care of women in remote locations and to improve maternal morbidity and mortality. Telehealth can be used on both an outpatient and an inpatient basis.
Outpatient telehealth is used for consultations. In maternal-fetal medicine, for instance, we use it for ultrasonography consultations. I also have used telehealth technology to “see” a pregnant patient with type 1diabetes. During our sessions, I managed her blood sugar levels and did all the other things I would have done if we had been together at my clinic. Without telehealth technology, however, this patient would have needed to drive 4 hours round-trip for each appointment.
Our colleagues in rural communities and at lower-level hospitals can use telehealth and telemedicine as aids in treating their high-risk patients, such as those with preeclampsia, prematurity risk, or other conditions. Physicians can consult with specialists through a face-to-face conversation that takes place through telecommunications. The result is that the quality of care for women in our communities is improved.
Genetic counseling, infertility consultation, and fetal anomaly management are some of the other applications. Our task force is discussing different ways to improve patient care and ways to collaborate with our colleagues around the country. Ultimately, we are developing best practices—a model for the best uses of technology to improve women’s health care in the United States.
Task force focus: Telehealth technology, billing, services
Dr. Brown: Our task force, a diverse group of members from all over the country, represents the spectrum of ObGyns. Although task force members have various levels of telehealth experience, all are very interested in these new channels of communication. The task force also includes billers, who understand billing ramifications, and payers, who know firsthand what will and will not be paid.
Technology and its availability is the most important topic for the task force. While some communities have Internet service, not all do. We need to determine which areas need service, how much it would cost, and who pays for it. Can a hospital afford it? A practice? Their partners? Identifying partners in tertiary care settings is a task force goal.
We are engaging a broad range of experts to study all the components and associated costs of technology, licensing, and cross-state credentialing. Gathering this information will help in developing a best practices model that general ObGyns can use.
Telehealth is redefining aspects of care: prenatal care (how many visits are required?), postpartum care, and other types of services that can be done remotely. Genetic counseling—who can provide it, what education is required—is another topic of discussion. Once we surmount the billing obstacles, we can do much with teleconferencing, such as provide genetic consultation with ObGyns in various settings.
The terms "telehealth" and "telemedicine" are often used interchangeably. Telemedicine is the older phrase, while telehealth entered the vernacular more recently and encompasses a broader definition.
The HealthIT.gov website explains the differences in terminology this way1:
- The Health Resources Services Administration defines telehealth as the use of electronic information and telecommunications technologies to support long-distance clinical health care, patient and professional health-related education, public health and health administration. Technologies include videoconferencing, the Internet, store-and-forward imaging, streaming media, and terrestrial and wireless communications.
- Telehealth is different from telemedicine because it refers to a broader scope of remote health care services than telemedicine. While telemedicine refers specifically to remote clinical services, telehealth can refer to remote nonclinical services, such as provider training, administrative meetings, and continuing medical education, in addition to clinical services.
A World Health Organization report, however, uses the 2 terms synonymously and interchangeably, defining telemedicine as2:
- The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.
The American Telemedicine Association (ATA) describes their use of the terms this way3:
- ATA largely views telemedicine and telehealth to be interchangeable terms, encompassing a wide definition of remote healthcare, although telehealth may not always involve clinical care.
References
- HealthIT.gov website. Frequently asked questions. https://www.healthit.gov/providers-professionals/frequently-asked-questions/485. Accessed November 15, 2017.
- World Health Organization. Telemedicine: opportunities and developments in member states. 2010. http://www.who.int/goe/publications/goe_telemedicine_2010.pdf. Accessed November 15, 2017.
- American Telemedicine Association. About telemedicine: the ultimate frontier for superior healthcare delivery. http://www.americantelemed.org/about/about-telemedicine. Accessed November 15, 2017.
Learn about ways clinicians can use telemedicine.
Making progress in rural and underserved communities
Peter Nielsen, MD: When we saw that some high-risk obstetrics patients were having a difficult time getting to our downtown San Antonio office—the trip from surrounding communities was taking too long, or city driving and parking were stressful or too costly—we looked to improve access to care. Collaborating with a health care network that has a hospital in a town north of San Antonio, we set up a pilot program to provide telemedicine perinatal consultation services.
In this kind of service, which occurs entirely in real time, ultrasound images taken at the hospital are streamed by high-speed fiberoptic cable to our office, where a maternal-fetal medicine physician views them. If a repeat image or a different image is needed, the physician requests another scan. Linked to the physician and listening through an earpiece, the ultrasonographer performs the new scan with little delay and without disturbing the patient. The conversation between physician and ultrasonographer is private.
After ultrasound scanning is complete, the patient goes to a private room at the hospital for a video conference with our physician in San Antonio, who has reviewed the images in the PACS (picture archiving and communication system) or ultrasound recording system. They discuss the images, the findings, and the follow-up.
We tested the technology during a 6-month pilot program to make sure it worked at the highest quality and safety levels. Then the program went live and we started seeing patients remotely. Now we have a robust telemedicine training capability at that hospital outside San Antonio, and we are looking to expand to other south and west Texas areas, some even farther from our office.
I have done some of these remote consultations. In response to my informal queries about the experience, patients said that no one else was offering it, and they were participating for the first time. Naturally they had questions and concerns. Nevertheless, patients, family members, and the ultrasonographer and physicians in the communities seem to think this is a high-quality, safe program that makes it easier for patients to access health care.
Patients uniformly describe these consultations in positive terms. They do not have to drive far, into the city, and deal with traffic; parking is easy and free; and less travel means much less time off from work. Given these very practical advantages, patients are interested in having more appointments done remotely. In addition, they say the appointment itself is easy, being there is effortless, and they feel their physician is sitting in the same room. It is like video chatting with family members—they are comfortable with the technology.
Related article:
Landmark women’s health care remains law of the land
The patients’ perspective
Dr. Brown: Patient satisfaction is an important issue. In psychiatry, dermatology, and other disciplines, patients have indicated that they are very satisfied with telehealth sessions. Telehealth in obstetrics and gynecology, I think, will receive similar positive feedback.
The issue of driving distance led us to reconsider the number of face-to-face prenatal visits a normal, healthy patient needs. These days, a patient can use a prenatal care app to track her weight and blood pressure and send the data to her physician. Besides being convenient, these monitoring apps can give a patient an important sense of control. Our pilot programs found that a patient who self-monitors understands her weight gain better and is more in tune with it. Apps and other technologies can thus improve quality of care and, in reducing the number of trips to an office, increase patient satisfaction.
Many people use or are familiar with the programs Skype and FaceTime (audiovideo chat software), and I envision that our postpartum task force will recommend using such programs for follow-up appointments. For each visit, the question to ask is whether the patient really needs to meet with her physician in person, or can she stay with her new baby and receive postpartum counseling at home. I am excited about the potential of telehealth in obstetrics and gynecology. Our task force is exploring that potential.
Telehealth for both routine and specialized care
Dr. Brown: Specialized care applications are here. In a pilot program in Wisconsin, a colleague has been providing remote psychiatric care. Perhaps such a program can be used to follow up on patients with postpartum depression. In addition, other psychiatry colleagues have long been using telehealth for adolescent behavior follow-ups, and we can do this too.
Another colleague has been performing remote perinatal follow-up for children with congenital anomalies. The physician interacts with the parent or parents as well as the patient. This seems to represent only the tip of the iceberg of what can be done in terms of follow-up.
We can also use telehealth in infertility settings. High-risk patients can benefit, too. Our guidelines say patients with preeclampsia should be seen within 3 days to 1 week. Many are transferred from low-access hospitals to our office. This follow-up, however, also can be done remotely, with patients at health department clinics or even at home. Reporting blood pressure readings and health-related feelings to a physician during a teleconsultation removes driving as a potential inconvenience or obstacle.
Telemedicine can be advantageous in gynecology. Physicians are doing important work with telecolposcopy as a follow-up to abnormal Pap test findings in patients in sub-Saharan Africa.
Routine wound care, which is commonly needed, can be performed in the home by a home health nurse telecommunicating with a physician. I can see broad telehealth use, and indeed our dermatology colleagues have been practicing telemedicine for quite some time.
Read about solving financial barriers and physician shortages.
An affordable solution to financial barriers and physician shortages
Dr. Nielsen: Telehealth can reduce barriers to care. For example, knowing that our teleconsultation services are covered by insurance, referring physicians and patients are more likely to try them and continue to use them. Payers are on board as well. Other barriers can be harder to overcome, particularly for patients at risk for complex diagnoses and medical decisions. Our pilot program, however, has demonstrated success in this area. It has provided safe, high-quality imaging, accurate diagnoses, productive discussions, and helpful management recommendations.
Telehealth also helps address relative and absolute physician shortages. In some areas, a relative shortage may indicate misdistribution. In other areas, specialists simply are too few in number. This absolute shortage of specialists likely will increase, as many communities are too small to sustain and support having them in person.
Outpatients can obtain care 5 days a week with telemedicine, as opposed to only 1 to 3 times a month in person. Physicians travel to remote clinics that are staffed only 1 or 2 days a month. Where the window for care is so small, patients and physicians are likely to turn to telemedicine. In addition, that utility results in better use of resources. For example, studies that were performed earlier would not need to be repeated, since you could access centrally located archives.
Related article:
ICD-10-CM code changes: What's new for 2018
Dr. Brown: For teleconsultations and televisits, all that payers need do is modify the billing codes they use for our usual services. Once that is done, payers can develop a payment model that works for both themselves and the teleconsultants.
The US health care system is fragmented. Health care is provided in various facilities, including federally qualified health centers and health department clinics. As Dr. Nielsen said, physicians travel to remote facilities once or twice a week or even a month, whereas telehealth can be offered 5 days a week. Many residents go to remote clinics, where an attending physician is required. Instead of an attending driving there, he or she could be teleconsulting—interacting with residents and patients from afar. So, telehealth is a win-win situation. It increases access to physicians and facilitates appropriate interactions with them, wherever they are. Telehealth can be an important contribution to developing a more effective health care delivery system than the fragmented one we have now.
Effective health care delivery is so important for obstetrics and gynecology, and the reported workforce challenges are real. A maternal-fetal medicine physician is unlikely to travel to remote communities once a week or even every 2 weeks, but that same physician can teleconsult multiple days each week.
How telehealth can close service gaps
Dr. Brown: Having established relationships with physicians in other clinics and communities paves the way for teleconsultation and remote supervision. Technology can help Planned Parenthood and other clinics continue to provide contraceptive counseling and other health care services. Even medical abortions can be supervised through teleconsultation.
With funds to Medicaid being cut, with the potential for Planned Parenthood to be defunded, physicians must think of ways they can continue to provide care to all patients and communities. By addressing these issues now, we will be ready to take charge of patient care, wherever it is needed.
But, we need partners, no question. We need hospital partners in all communities, and especially in rural communities. Rural hospitals and maternity care are at risk. Health care in rural communities faces many challenges. Telehealth, teleconferencing, and teleconsultation not only can improve access to services, but also can curb travel costs as well as costs to the communities and hospitals.
Who pays the operating costs, and who benefits
Dr. Brown: Payers are already discovering that teleconsultations are as billable as in-person visits. In addition, physicians are realizing that remote consultation can work as well as in-person consultation, with its own merits and advantages. Education is key—education about billing and about what is doable in telehealth. We can learn from colleagues in other specialties.
Dr. Nielsen: Several entities and groups must start covering the technology costs. Federal and state entities need to determine how the country’s information infrastructure can be improved to give rural areas access to high-quality, high-speed, wide-bandwidth communications, which will help expand telehealth and increase other industries’ opportunities to grow and sustain these communities. Improving the infrastructure also can help keep rural areas sustainable.
Health care systems themselves can join federal, state, and local governments in building this infrastructure. They can also start identifying opportunities to support and sustain physicians and hospitals in smaller towns and start combating the perception that the infrastructure is being developed only to migrate patients over to accessing their care through telehealth provided by physicians in the larger cities.
Many payers see telehealth as improving access and outcomes and already support it, but more payers need to become involved. All need to understand how routine and complex consultations, even inpatient consultations, can be performed remotely and can be properly reimbursed, and incentivized with payments for improved outcomes and value.
As barriers fall and telehealth improves, acceptance by patients and physicians will increase. In addition, telehealth will enter medical education in a significant way. The instruction that students, residents, and Fellows receive will be enhanced by new telehealth approaches in various specialties, and residents will come out of these programs with telehealth experience and a sense of both financial benefits and payment structures. This early exposure will pique their interest in using telehealth and advocating its use where it may never before have been considered, owing to real and perceived barriers.
Read about telehealth solutions for ObGyns.
Learning from other specialties and agencies
Dr. Brown: The physician shortage negatively affects access to health care in rural areas. Many city and suburban physicians, including ObGyns, want to stay where they are. Education is needed to show them that a rural practice can be successful. They would have a good patient base and be able to use telehealth to improve care and maintain contact with tertiary care centers.
Several task force members have described their experience within their health systems, and we hope to borrow from that. A health system in South Dakota received a Health Resources and Services Administration grant to use telehealth and teleconsultation in the Indian Health Service (IHS). To women who access their health care through the IHS, being able to remain in the community is culturally important. Telehealth and teleconsultation bring care to these women where they live.
To develop the best telehealth and teleconsultation model, we are borrowing from these health systems and from the experience of our colleagues in dermatology, behavioral health, psychiatry, and other disciplines. These physicians already have overcome many hurdles and discovered the importance of patient satisfaction in providing remote health care.
Patients will benefit in various ways, and here is another example: A clinic refers a patient to an ObGyn to discuss whether it is possible to have a vaginal birth after a cesarean delivery. The drive to the ObGyn’s office takes an hour, but the patient just as easily could have had all her questions answered during a teleconsultation.
Related articles:
Telehealth and you (4-part audiocast)
Telehealth recommendations for ObGyns
Dr. Brown: Our task force will develop recommended best practices for telehealth. We will outline how a practice can engage with telehealth and will address licensing requirements, as a practice must be licensed in each state where it uses telehealth. Our goal is to help our specialty get started in telehealth and telemedicine.
In practices with telehealth, it will be incumbent on ObGyns to identify any barriers to care. For example, we are concerned about early discontinuation of breastfeeding, particularly among African American communities. Fortunately, we have learned that video chat follow-ups can help improve breastfeeding continuation rates.
It also will be incumbent on ObGyns to think differently about how best to follow up. For a patient who calls to say she thinks she has mastitis, much of the consultation can be handled by telephone or video conference with the physician and a nurse practi‑tioner, and then medication can be prescribed without the need for in-person follow-up. We must then determine how to ensure these follow-up methods are compensated.
Direct-to-patient virtual visits
- Virtual home visits
- Low-risk pregnancy
- Postpartum visits
- Lactation support
- Routine gynecologic care
- Postoperative follow-up
Remote patient monitoring
- Chronic disease management
- Antenatal testing
- Fetal heart rate monitoring
- Transfer of care
Final thoughts
Dr. Nielsen: It is time for all US health care players to more seriously and aggressively consider how telehealth can improve health care access, quality, and safety. Even more important, patients and physicians in small communities need to feel that they can access specialists and care that is as good as those available in larger communities without having to pull up stakes and move.
Telehealth can help small communities become sustainable over the long term. As the majority of the people in this country are born in and receive health care in community hospitals, not large tertiary care centers, the state of US health care should be measured by the ability to provide as much care as is technically possible in the small communities where patients live and work and raise their kids.
Dr. Brown: More than 50% of all babies are born in hospitals where fewer than 1,000 deliveries are performed, and almost 40% are born in hospitals where fewer than 500 are performed. To provide high-level care and have patients feel comfortable, to improve morbidity and mortality, we need telehealth and telemedicine.
If I can help a physician in East Africa place a Bakri balloon for postpartum hemorrhaging, surely I can help a physician in rural areas of Wyoming, South Dakota, or North Carolina deal with this obstetric emergency. In obstetrics and gynecology, telehealth and telemedicine have great potential in terms of morbidity and mortality, but we are also doing genetic counseling and a great deal of patient follow-up, and so much more can be done.
That is the key, and the reason for the training, the task force, the deliberations, and the best practices model that we will be sharing with our colleagues.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
I recently spoke with 2 outstanding leaders in our field, members of the American College of Obstetricians and Gynecologists (ACOG) task force on telehealth and telemedicine, about the future of providing health care to women in remote locations.
Haywood Brown, MD, is President of ACOG for 2017–2018 and is F. Bayard Carter Professor of Obstetrics and Gynecology at Duke University Medical Center in Durham, North Carolina, and Peter Nielsen, MD, is Professor and Vice Chair of the Department of Obstetrics and Gynecology at Baylor College of Medicine in Houston, Texas, and Obstetrician-in-Chief at Children’s Hospital of San Antonio. Dr. Nielsen is a retired US Army colonel.
Why an ACOG telehealth task force?
Haywood Brown, MD: Our overall goals in telehealth and telemedicine are to coordinate and better facilitate the health care of women in remote locations and to improve maternal morbidity and mortality. Telehealth can be used on both an outpatient and an inpatient basis.
Outpatient telehealth is used for consultations. In maternal-fetal medicine, for instance, we use it for ultrasonography consultations. I also have used telehealth technology to “see” a pregnant patient with type 1diabetes. During our sessions, I managed her blood sugar levels and did all the other things I would have done if we had been together at my clinic. Without telehealth technology, however, this patient would have needed to drive 4 hours round-trip for each appointment.
Our colleagues in rural communities and at lower-level hospitals can use telehealth and telemedicine as aids in treating their high-risk patients, such as those with preeclampsia, prematurity risk, or other conditions. Physicians can consult with specialists through a face-to-face conversation that takes place through telecommunications. The result is that the quality of care for women in our communities is improved.
Genetic counseling, infertility consultation, and fetal anomaly management are some of the other applications. Our task force is discussing different ways to improve patient care and ways to collaborate with our colleagues around the country. Ultimately, we are developing best practices—a model for the best uses of technology to improve women’s health care in the United States.
Task force focus: Telehealth technology, billing, services
Dr. Brown: Our task force, a diverse group of members from all over the country, represents the spectrum of ObGyns. Although task force members have various levels of telehealth experience, all are very interested in these new channels of communication. The task force also includes billers, who understand billing ramifications, and payers, who know firsthand what will and will not be paid.
Technology and its availability is the most important topic for the task force. While some communities have Internet service, not all do. We need to determine which areas need service, how much it would cost, and who pays for it. Can a hospital afford it? A practice? Their partners? Identifying partners in tertiary care settings is a task force goal.
We are engaging a broad range of experts to study all the components and associated costs of technology, licensing, and cross-state credentialing. Gathering this information will help in developing a best practices model that general ObGyns can use.
Telehealth is redefining aspects of care: prenatal care (how many visits are required?), postpartum care, and other types of services that can be done remotely. Genetic counseling—who can provide it, what education is required—is another topic of discussion. Once we surmount the billing obstacles, we can do much with teleconferencing, such as provide genetic consultation with ObGyns in various settings.
The terms "telehealth" and "telemedicine" are often used interchangeably. Telemedicine is the older phrase, while telehealth entered the vernacular more recently and encompasses a broader definition.
The HealthIT.gov website explains the differences in terminology this way1:
- The Health Resources Services Administration defines telehealth as the use of electronic information and telecommunications technologies to support long-distance clinical health care, patient and professional health-related education, public health and health administration. Technologies include videoconferencing, the Internet, store-and-forward imaging, streaming media, and terrestrial and wireless communications.
- Telehealth is different from telemedicine because it refers to a broader scope of remote health care services than telemedicine. While telemedicine refers specifically to remote clinical services, telehealth can refer to remote nonclinical services, such as provider training, administrative meetings, and continuing medical education, in addition to clinical services.
A World Health Organization report, however, uses the 2 terms synonymously and interchangeably, defining telemedicine as2:
- The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.
The American Telemedicine Association (ATA) describes their use of the terms this way3:
- ATA largely views telemedicine and telehealth to be interchangeable terms, encompassing a wide definition of remote healthcare, although telehealth may not always involve clinical care.
References
- HealthIT.gov website. Frequently asked questions. https://www.healthit.gov/providers-professionals/frequently-asked-questions/485. Accessed November 15, 2017.
- World Health Organization. Telemedicine: opportunities and developments in member states. 2010. http://www.who.int/goe/publications/goe_telemedicine_2010.pdf. Accessed November 15, 2017.
- American Telemedicine Association. About telemedicine: the ultimate frontier for superior healthcare delivery. http://www.americantelemed.org/about/about-telemedicine. Accessed November 15, 2017.
Learn about ways clinicians can use telemedicine.
Making progress in rural and underserved communities
Peter Nielsen, MD: When we saw that some high-risk obstetrics patients were having a difficult time getting to our downtown San Antonio office—the trip from surrounding communities was taking too long, or city driving and parking were stressful or too costly—we looked to improve access to care. Collaborating with a health care network that has a hospital in a town north of San Antonio, we set up a pilot program to provide telemedicine perinatal consultation services.
In this kind of service, which occurs entirely in real time, ultrasound images taken at the hospital are streamed by high-speed fiberoptic cable to our office, where a maternal-fetal medicine physician views them. If a repeat image or a different image is needed, the physician requests another scan. Linked to the physician and listening through an earpiece, the ultrasonographer performs the new scan with little delay and without disturbing the patient. The conversation between physician and ultrasonographer is private.
After ultrasound scanning is complete, the patient goes to a private room at the hospital for a video conference with our physician in San Antonio, who has reviewed the images in the PACS (picture archiving and communication system) or ultrasound recording system. They discuss the images, the findings, and the follow-up.
We tested the technology during a 6-month pilot program to make sure it worked at the highest quality and safety levels. Then the program went live and we started seeing patients remotely. Now we have a robust telemedicine training capability at that hospital outside San Antonio, and we are looking to expand to other south and west Texas areas, some even farther from our office.
I have done some of these remote consultations. In response to my informal queries about the experience, patients said that no one else was offering it, and they were participating for the first time. Naturally they had questions and concerns. Nevertheless, patients, family members, and the ultrasonographer and physicians in the communities seem to think this is a high-quality, safe program that makes it easier for patients to access health care.
Patients uniformly describe these consultations in positive terms. They do not have to drive far, into the city, and deal with traffic; parking is easy and free; and less travel means much less time off from work. Given these very practical advantages, patients are interested in having more appointments done remotely. In addition, they say the appointment itself is easy, being there is effortless, and they feel their physician is sitting in the same room. It is like video chatting with family members—they are comfortable with the technology.
Related article:
Landmark women’s health care remains law of the land
The patients’ perspective
Dr. Brown: Patient satisfaction is an important issue. In psychiatry, dermatology, and other disciplines, patients have indicated that they are very satisfied with telehealth sessions. Telehealth in obstetrics and gynecology, I think, will receive similar positive feedback.
The issue of driving distance led us to reconsider the number of face-to-face prenatal visits a normal, healthy patient needs. These days, a patient can use a prenatal care app to track her weight and blood pressure and send the data to her physician. Besides being convenient, these monitoring apps can give a patient an important sense of control. Our pilot programs found that a patient who self-monitors understands her weight gain better and is more in tune with it. Apps and other technologies can thus improve quality of care and, in reducing the number of trips to an office, increase patient satisfaction.
Many people use or are familiar with the programs Skype and FaceTime (audiovideo chat software), and I envision that our postpartum task force will recommend using such programs for follow-up appointments. For each visit, the question to ask is whether the patient really needs to meet with her physician in person, or can she stay with her new baby and receive postpartum counseling at home. I am excited about the potential of telehealth in obstetrics and gynecology. Our task force is exploring that potential.
Telehealth for both routine and specialized care
Dr. Brown: Specialized care applications are here. In a pilot program in Wisconsin, a colleague has been providing remote psychiatric care. Perhaps such a program can be used to follow up on patients with postpartum depression. In addition, other psychiatry colleagues have long been using telehealth for adolescent behavior follow-ups, and we can do this too.
Another colleague has been performing remote perinatal follow-up for children with congenital anomalies. The physician interacts with the parent or parents as well as the patient. This seems to represent only the tip of the iceberg of what can be done in terms of follow-up.
We can also use telehealth in infertility settings. High-risk patients can benefit, too. Our guidelines say patients with preeclampsia should be seen within 3 days to 1 week. Many are transferred from low-access hospitals to our office. This follow-up, however, also can be done remotely, with patients at health department clinics or even at home. Reporting blood pressure readings and health-related feelings to a physician during a teleconsultation removes driving as a potential inconvenience or obstacle.
Telemedicine can be advantageous in gynecology. Physicians are doing important work with telecolposcopy as a follow-up to abnormal Pap test findings in patients in sub-Saharan Africa.
Routine wound care, which is commonly needed, can be performed in the home by a home health nurse telecommunicating with a physician. I can see broad telehealth use, and indeed our dermatology colleagues have been practicing telemedicine for quite some time.
Read about solving financial barriers and physician shortages.
An affordable solution to financial barriers and physician shortages
Dr. Nielsen: Telehealth can reduce barriers to care. For example, knowing that our teleconsultation services are covered by insurance, referring physicians and patients are more likely to try them and continue to use them. Payers are on board as well. Other barriers can be harder to overcome, particularly for patients at risk for complex diagnoses and medical decisions. Our pilot program, however, has demonstrated success in this area. It has provided safe, high-quality imaging, accurate diagnoses, productive discussions, and helpful management recommendations.
Telehealth also helps address relative and absolute physician shortages. In some areas, a relative shortage may indicate misdistribution. In other areas, specialists simply are too few in number. This absolute shortage of specialists likely will increase, as many communities are too small to sustain and support having them in person.
Outpatients can obtain care 5 days a week with telemedicine, as opposed to only 1 to 3 times a month in person. Physicians travel to remote clinics that are staffed only 1 or 2 days a month. Where the window for care is so small, patients and physicians are likely to turn to telemedicine. In addition, that utility results in better use of resources. For example, studies that were performed earlier would not need to be repeated, since you could access centrally located archives.
Related article:
ICD-10-CM code changes: What's new for 2018
Dr. Brown: For teleconsultations and televisits, all that payers need do is modify the billing codes they use for our usual services. Once that is done, payers can develop a payment model that works for both themselves and the teleconsultants.
The US health care system is fragmented. Health care is provided in various facilities, including federally qualified health centers and health department clinics. As Dr. Nielsen said, physicians travel to remote facilities once or twice a week or even a month, whereas telehealth can be offered 5 days a week. Many residents go to remote clinics, where an attending physician is required. Instead of an attending driving there, he or she could be teleconsulting—interacting with residents and patients from afar. So, telehealth is a win-win situation. It increases access to physicians and facilitates appropriate interactions with them, wherever they are. Telehealth can be an important contribution to developing a more effective health care delivery system than the fragmented one we have now.
Effective health care delivery is so important for obstetrics and gynecology, and the reported workforce challenges are real. A maternal-fetal medicine physician is unlikely to travel to remote communities once a week or even every 2 weeks, but that same physician can teleconsult multiple days each week.
How telehealth can close service gaps
Dr. Brown: Having established relationships with physicians in other clinics and communities paves the way for teleconsultation and remote supervision. Technology can help Planned Parenthood and other clinics continue to provide contraceptive counseling and other health care services. Even medical abortions can be supervised through teleconsultation.
With funds to Medicaid being cut, with the potential for Planned Parenthood to be defunded, physicians must think of ways they can continue to provide care to all patients and communities. By addressing these issues now, we will be ready to take charge of patient care, wherever it is needed.
But, we need partners, no question. We need hospital partners in all communities, and especially in rural communities. Rural hospitals and maternity care are at risk. Health care in rural communities faces many challenges. Telehealth, teleconferencing, and teleconsultation not only can improve access to services, but also can curb travel costs as well as costs to the communities and hospitals.
Who pays the operating costs, and who benefits
Dr. Brown: Payers are already discovering that teleconsultations are as billable as in-person visits. In addition, physicians are realizing that remote consultation can work as well as in-person consultation, with its own merits and advantages. Education is key—education about billing and about what is doable in telehealth. We can learn from colleagues in other specialties.
Dr. Nielsen: Several entities and groups must start covering the technology costs. Federal and state entities need to determine how the country’s information infrastructure can be improved to give rural areas access to high-quality, high-speed, wide-bandwidth communications, which will help expand telehealth and increase other industries’ opportunities to grow and sustain these communities. Improving the infrastructure also can help keep rural areas sustainable.
Health care systems themselves can join federal, state, and local governments in building this infrastructure. They can also start identifying opportunities to support and sustain physicians and hospitals in smaller towns and start combating the perception that the infrastructure is being developed only to migrate patients over to accessing their care through telehealth provided by physicians in the larger cities.
Many payers see telehealth as improving access and outcomes and already support it, but more payers need to become involved. All need to understand how routine and complex consultations, even inpatient consultations, can be performed remotely and can be properly reimbursed, and incentivized with payments for improved outcomes and value.
As barriers fall and telehealth improves, acceptance by patients and physicians will increase. In addition, telehealth will enter medical education in a significant way. The instruction that students, residents, and Fellows receive will be enhanced by new telehealth approaches in various specialties, and residents will come out of these programs with telehealth experience and a sense of both financial benefits and payment structures. This early exposure will pique their interest in using telehealth and advocating its use where it may never before have been considered, owing to real and perceived barriers.
Read about telehealth solutions for ObGyns.
Learning from other specialties and agencies
Dr. Brown: The physician shortage negatively affects access to health care in rural areas. Many city and suburban physicians, including ObGyns, want to stay where they are. Education is needed to show them that a rural practice can be successful. They would have a good patient base and be able to use telehealth to improve care and maintain contact with tertiary care centers.
Several task force members have described their experience within their health systems, and we hope to borrow from that. A health system in South Dakota received a Health Resources and Services Administration grant to use telehealth and teleconsultation in the Indian Health Service (IHS). To women who access their health care through the IHS, being able to remain in the community is culturally important. Telehealth and teleconsultation bring care to these women where they live.
To develop the best telehealth and teleconsultation model, we are borrowing from these health systems and from the experience of our colleagues in dermatology, behavioral health, psychiatry, and other disciplines. These physicians already have overcome many hurdles and discovered the importance of patient satisfaction in providing remote health care.
Patients will benefit in various ways, and here is another example: A clinic refers a patient to an ObGyn to discuss whether it is possible to have a vaginal birth after a cesarean delivery. The drive to the ObGyn’s office takes an hour, but the patient just as easily could have had all her questions answered during a teleconsultation.
Related articles:
Telehealth and you (4-part audiocast)
Telehealth recommendations for ObGyns
Dr. Brown: Our task force will develop recommended best practices for telehealth. We will outline how a practice can engage with telehealth and will address licensing requirements, as a practice must be licensed in each state where it uses telehealth. Our goal is to help our specialty get started in telehealth and telemedicine.
In practices with telehealth, it will be incumbent on ObGyns to identify any barriers to care. For example, we are concerned about early discontinuation of breastfeeding, particularly among African American communities. Fortunately, we have learned that video chat follow-ups can help improve breastfeeding continuation rates.
It also will be incumbent on ObGyns to think differently about how best to follow up. For a patient who calls to say she thinks she has mastitis, much of the consultation can be handled by telephone or video conference with the physician and a nurse practi‑tioner, and then medication can be prescribed without the need for in-person follow-up. We must then determine how to ensure these follow-up methods are compensated.
Direct-to-patient virtual visits
- Virtual home visits
- Low-risk pregnancy
- Postpartum visits
- Lactation support
- Routine gynecologic care
- Postoperative follow-up
Remote patient monitoring
- Chronic disease management
- Antenatal testing
- Fetal heart rate monitoring
- Transfer of care
Final thoughts
Dr. Nielsen: It is time for all US health care players to more seriously and aggressively consider how telehealth can improve health care access, quality, and safety. Even more important, patients and physicians in small communities need to feel that they can access specialists and care that is as good as those available in larger communities without having to pull up stakes and move.
Telehealth can help small communities become sustainable over the long term. As the majority of the people in this country are born in and receive health care in community hospitals, not large tertiary care centers, the state of US health care should be measured by the ability to provide as much care as is technically possible in the small communities where patients live and work and raise their kids.
Dr. Brown: More than 50% of all babies are born in hospitals where fewer than 1,000 deliveries are performed, and almost 40% are born in hospitals where fewer than 500 are performed. To provide high-level care and have patients feel comfortable, to improve morbidity and mortality, we need telehealth and telemedicine.
If I can help a physician in East Africa place a Bakri balloon for postpartum hemorrhaging, surely I can help a physician in rural areas of Wyoming, South Dakota, or North Carolina deal with this obstetric emergency. In obstetrics and gynecology, telehealth and telemedicine have great potential in terms of morbidity and mortality, but we are also doing genetic counseling and a great deal of patient follow-up, and so much more can be done.
That is the key, and the reason for the training, the task force, the deliberations, and the best practices model that we will be sharing with our colleagues.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Supreme Court decisions in 2017 that affected your practice
Despite being short-handed (there were only 8 justices for most of the Term), the United States Supreme Court decided a number of important cases during its most recent Term, which concluded on June 27, 2017. Among the 69 cases, several are of particular interest to ObGyns.
1. Arbitration in health care
In Kindred Nursing Centers v Clark, the Court decided an important case involving arbitration in health care.1
At stake. The families of 2 people who died after being in a long-term care facility filed lawsuits against the facility, claiming personal injury, violations of Kentucky statutes regarding long-term care facilities, and wrongful death. However, during admission to the facility, the patients (technically, their agents under a power of attorney) signed an agreement that any disputes would be taken to arbitration. The facility successfully had the lawsuits dismissed.
Final ruling. The Supreme Court agreed that the case had to go to arbitration rather than to court, even though the arbitration clause violated state law. The Federal Arbitration Act (FAA) preempts state law. The Court has been very aggressive in enforcing arbitration agreements and striking down state laws that are inconsistent with the FAA. This case emphasizes that the FAA applies in the health care context.
The case suggests both a warning and an opportunity for health care providers. The warning is that arbitration clauses will be enforced; thoughtlessly entering into arbitration for future disputes may be dangerous. Among other things, the decision of arbitrators is essentially unreviewable. Appellate courts review the decisions of lower courts, but there is no such review in arbitration. Furthermore, arbitration may be stacked in favor of commercial entities that often use arbitrators.
The opportunity for health care providers lies in that it may be possible to include arbitration clauses in agreements with patients. This should be considered only after obtaining legal advice. The agreements should, for example, be consistent with the obligations to patients (in the case of the Kentucky facility, it made clear that accepting the arbitration agreement was not necessary in order to receive care or be admitted to the facility). Because arbitration agreements are becoming ubiquitous and rigorously enforced by federal courts, arbitration is bound to have an important function in health care.
2. Pharmaceuticals
Biologics and biosimilars
Biologics play an important role in health care. Eight of the top 10 selling drugs in 2016 were biologics.2 The case of Sandoz v Amgen involved biosimilar pharmaceuticals, essentially the generics of biologic drugs.3
At stake. While biologics hold great promise in medicine, they are generally very expensive. Just as with generics, brand-name companies (generally referred to as “reference” biologics) want to keep biosimilars off the market for as long as possible, thereby extending the advantages of monopolistic pricing. This Term the Supreme Court considered the statutory rules for licensing biosimilar drugs.
Final ruling. The Court’s decision will allow biosimilar companies to speed up the licensing process by at least 180 days. This is a modest win for patients and their physicians, but the legal issues around biosimilars will need additional attention.
Class action suits
In another case, the Court made it more difficult to file class action suits against pharmaceutical companies in state courts.4 Although this is a fairly technical decision, it is likely to have a significant impact in pharmaceutical liability by limiting classactions.
3. The travel ban
The American College of Obstetricians and Gynecologists joined other medical organizations in an amicus curiae (friend of the court) brief to challenge President Trump’s “travel ban.”5
At stake. The brief argued that the United States “relies upon a significant number of health professionals and scientists who have entered the country through the immigration system.”5
Final ruling. The Court allowed most of the travel ban to stay in place, but did permit entry into the United States by foreign nationals “with a close familial relationship,” or pre-existing ties to US businesses or institutions (such as students who have been admitted to American colleges, workers who have accepted US employment, or lecturers invited to address American audiences).6 Following the Term, the Administration issued a different travel ban, so the issue was taken off the Court’s calendar for the moment. There undoubtedly will be additional chapters to come.
4. Birth certificates and same-sex marriage
In Pavan v Smith, the legal question concerned whether married same-sex couples may have both parents listed on the birth certificate of children born during the marriage.7 Two same-sex couples conceived children through anonymous sperm donation and gave birth in Arkansas. The Department of Health in Arkansas issued birth certificates listing the mother’s name, but refused to list the spouse on the birth certificate.
At stake. The couples brought suit claiming a constitutional right to have both parents listed. In particular, they noted that under Arkansas law, the woman who gives birth is deemed to be the mother. When the woman is married, the husband’s name is “entered on the certificate as the father of the child.”8 The same-sex parents argued that a 2015 decision of the Supreme Court, which held that the Constitution requires states to recognize same-sex marriages, made it clear that same-sex couples should have the benefits of marriage.9 Eventually the case wound its way to the Supreme Court.
Final ruling. The Court held that if the state ordinarily lists the names of both husband and wife on such certificates, then same-sex couples are entitled to have birth certificates listing both parents. The Court noted that laws are unconstitutional if they treat same-sex couples differently than opposite-sex couples. Based on this principle, the Court held that parental birth certificate registration is part of the “constellations of benefits” linked to marriage that the Constitution affords same-sex couples. This ruling applies as a matter of constitutional right in all states.
Read about more interesting Supreme Court decisions
5. Sexual offenders and social media
States struggle to protect children from convicted sex offenders. North Carolina, for example, made it a felony for sex offenders (who had completed their sentences) to use social media sites that “permit minor children to become members or create and maintain personal web pages.”10
At stake. In Packingham v North Carolina, the Court was asked to decide whether this statute violates the First Amendment (free speech) rights of sex offenders.11
Final ruling. The Court held that the North Carolina limitation on sex offenders’ use of social media was too broad. It noted the wide range of political, employment, news, personal, commercial, and religious websites that are off limits to sex offenders under the statute—hardly narrowly tailored. It suggested, however, that it probably would be constitutional for a state to prohibit sex offenders “from engaging in conduct that often presages a sexual crime, like contacting a minor or using a website to gather information about a minor.”11
It was important in this case that the defendant had already served his entire sentence and was “no longer subject to the supervision of the criminal justice system.”11 If he had still been in prison, the state could limit or prohibit his Internet use. Even if he had been on probation or parole (under the supervision of the criminal justice system) the restrictions may well have been permitted. In addition, the state could impose new, narrowly tailored restrictions.
This case is also a reminder that ObGyns are very important in the efforts to eliminate child sexual abuse. All states have laws that require the reporting of known or suspected sexual abuse. In addition to complying with the law, such reports are often critical to discovering and ending the abuse.
6. Transgender rights
The Court had accepted a “transgender bathroom case” in Gloucester County School Board v G.G.12
At stake. This case essentially challenged the Obama Administration’s requirement that schools allow transgender students to use the restrooms in which they feel most comfortable. It was one of the most anticipated cases of the Term, but it essentially disappeared. Following the presidential election, the Department of Education rescinded the earlier guidance on which the case was based.
Final ruling. The Court returned the case to the Fourth Circuit for reconsideration. This issue, however, may reappear before the Court in the form of a claim that the states must provide this accommodation as a matter of federal statutory right, or even Equal Protection.
- In an important First Amendment decision, the Court held that it is a violation of the Freedom of Religion to deny a church-related school access to generally available state grant funds solely because of its religious status (in this case the program funded playground surfacing grants).1
- In several cases, it was apparent that the Court is uncomfortable with the way death penalty cases are handled in some states.2
- Juries may be questioned about racial bias that was expressed during jury deliberations--a substantial change for many courts.3
- The failure of the Patent and Trademark Office (PTO) to register the trademark for the band "The Slants" was a First Amendment violation. One reason that this case was watched was because of the effort of the PTO to deregister the trademark of the Washington Redskins.4
- The Court considered 9 cases involving revoking citizenship, deportation, and cross-border liability (an extraordinary number). Two cases that could change the nature and process of deportation were held over to the next Term for reargument.
- Individualized educational plans under the federal Individuals with Disabilities Education Act (IDEA) must target more than trivial progress for the students.5
References
- Trinity Lutheran Church of Columbia, Inc. v Comer, 582 US 15 577 (2017).
- McAllister S. Death-penalty symposium: A court increasingly uncomfortable with the death penalty. SCOTUSblog.com. http://www.scotusblog.com/2017/06/death-penalty-symposium-court-increasingly-uncomfortable-death-penalty/. Published June 29, 2017. Accessed November 2, 2017.
- Pena-Rodriguez v Colorado, 580 US 15 606 (2017).
- Matal v Tam, 582 US 15 1293 (2017).
- Endrew F v Douglas County School District, RE-1, 580 US 15 827 (2017).
Summary of the Term
The Term was notable for the level of agreement. With 69 decided cases, 41 (69%) were unanimous. In 59 cases (85%), there was a strong consensus, with no more than 2 justices dissenting. Only 7 decisions (10%) were 5 to 4. Justice Kennedy was, as usual, the deciding vote in most of the close cases. He voted in the majority in 97% of the decisions. Justice Gorsuch took the place of Justice Scalia (who passed away in February 2016), so arguably the Court is ideologically close to where it has been for a number of years. Despite rumors that Justice Kennedy would announce his resignation from the Court, neither he nor any other justice has left. The Supreme Court began its new Term on October 2, 2017, with a full complement of 9 justices.
What’s to come
The Court will add cases through much of its new Term, but it has already accepted cases dealing with arbitration agreements (again); public employees’ union dues; immigration (again); the privacy of information held by mobile phone companies; a constitutional challenge to political gerrymandering; bakeries and gay-marriage ceremonies; whistleblowers and Dodd-Frank regulations; sports gambling and the NCAA; and more.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Kindred Nursing Centers, LP v Clark, 581 US 16 32 (2017).
- Anderson L. Looking Ahead: Pharma Projections for 2016 - & Beyond. Perma.cc Website. . Reviewed March 30, 2017. Accessed November 2, 2017.
- Sandoz Inc v Amgen Inc, 581 US 15 1039 1195 (2017).
- Bristol-Myers Squibb Co v Superior Court of California, San Francisco County, 582 US 16 466 (2017).
- Trinity FR, Sterling AM, Rogaczewski JD, et al. Motion for Leave to File and Brief for the Association of American Medical Colleges and Others as Amici Curiae Supporting Respondents. SCOTUSblog. http://www.scotusblog.com/wp-content/uploads/2017/06/16-1436-ac-AAMC-supporting-respondents.pdf. Accessed November 2, 2017.
- Donald J. Trump, President of the United States v International Refugee Assistance Project, 582 US 16 1436 (2017).
- Pavan v Smith, 582 US 16 992 (2017).
- Arkansas Code, §20 18 401(f)(1) (2014).
- Obergefell v Hodges, 576 US ___ (2015).
- NC Gen. Stat. Ann. §§14-202.5(a),(e).
- Packingham v North Carolina, 582 US 15 1194 (2017).
- Gloucester County School Board v G.G. SCOTUSblog. http://www.scotusblog.com/case-files/cases/gloucester-county-school-board-v-g-g/. Published March 6, 2017. Accessed November 2, 2017.
Despite being short-handed (there were only 8 justices for most of the Term), the United States Supreme Court decided a number of important cases during its most recent Term, which concluded on June 27, 2017. Among the 69 cases, several are of particular interest to ObGyns.
1. Arbitration in health care
In Kindred Nursing Centers v Clark, the Court decided an important case involving arbitration in health care.1
At stake. The families of 2 people who died after being in a long-term care facility filed lawsuits against the facility, claiming personal injury, violations of Kentucky statutes regarding long-term care facilities, and wrongful death. However, during admission to the facility, the patients (technically, their agents under a power of attorney) signed an agreement that any disputes would be taken to arbitration. The facility successfully had the lawsuits dismissed.
Final ruling. The Supreme Court agreed that the case had to go to arbitration rather than to court, even though the arbitration clause violated state law. The Federal Arbitration Act (FAA) preempts state law. The Court has been very aggressive in enforcing arbitration agreements and striking down state laws that are inconsistent with the FAA. This case emphasizes that the FAA applies in the health care context.
The case suggests both a warning and an opportunity for health care providers. The warning is that arbitration clauses will be enforced; thoughtlessly entering into arbitration for future disputes may be dangerous. Among other things, the decision of arbitrators is essentially unreviewable. Appellate courts review the decisions of lower courts, but there is no such review in arbitration. Furthermore, arbitration may be stacked in favor of commercial entities that often use arbitrators.
The opportunity for health care providers lies in that it may be possible to include arbitration clauses in agreements with patients. This should be considered only after obtaining legal advice. The agreements should, for example, be consistent with the obligations to patients (in the case of the Kentucky facility, it made clear that accepting the arbitration agreement was not necessary in order to receive care or be admitted to the facility). Because arbitration agreements are becoming ubiquitous and rigorously enforced by federal courts, arbitration is bound to have an important function in health care.
2. Pharmaceuticals
Biologics and biosimilars
Biologics play an important role in health care. Eight of the top 10 selling drugs in 2016 were biologics.2 The case of Sandoz v Amgen involved biosimilar pharmaceuticals, essentially the generics of biologic drugs.3
At stake. While biologics hold great promise in medicine, they are generally very expensive. Just as with generics, brand-name companies (generally referred to as “reference” biologics) want to keep biosimilars off the market for as long as possible, thereby extending the advantages of monopolistic pricing. This Term the Supreme Court considered the statutory rules for licensing biosimilar drugs.
Final ruling. The Court’s decision will allow biosimilar companies to speed up the licensing process by at least 180 days. This is a modest win for patients and their physicians, but the legal issues around biosimilars will need additional attention.
Class action suits
In another case, the Court made it more difficult to file class action suits against pharmaceutical companies in state courts.4 Although this is a fairly technical decision, it is likely to have a significant impact in pharmaceutical liability by limiting classactions.
3. The travel ban
The American College of Obstetricians and Gynecologists joined other medical organizations in an amicus curiae (friend of the court) brief to challenge President Trump’s “travel ban.”5
At stake. The brief argued that the United States “relies upon a significant number of health professionals and scientists who have entered the country through the immigration system.”5
Final ruling. The Court allowed most of the travel ban to stay in place, but did permit entry into the United States by foreign nationals “with a close familial relationship,” or pre-existing ties to US businesses or institutions (such as students who have been admitted to American colleges, workers who have accepted US employment, or lecturers invited to address American audiences).6 Following the Term, the Administration issued a different travel ban, so the issue was taken off the Court’s calendar for the moment. There undoubtedly will be additional chapters to come.
4. Birth certificates and same-sex marriage
In Pavan v Smith, the legal question concerned whether married same-sex couples may have both parents listed on the birth certificate of children born during the marriage.7 Two same-sex couples conceived children through anonymous sperm donation and gave birth in Arkansas. The Department of Health in Arkansas issued birth certificates listing the mother’s name, but refused to list the spouse on the birth certificate.
At stake. The couples brought suit claiming a constitutional right to have both parents listed. In particular, they noted that under Arkansas law, the woman who gives birth is deemed to be the mother. When the woman is married, the husband’s name is “entered on the certificate as the father of the child.”8 The same-sex parents argued that a 2015 decision of the Supreme Court, which held that the Constitution requires states to recognize same-sex marriages, made it clear that same-sex couples should have the benefits of marriage.9 Eventually the case wound its way to the Supreme Court.
Final ruling. The Court held that if the state ordinarily lists the names of both husband and wife on such certificates, then same-sex couples are entitled to have birth certificates listing both parents. The Court noted that laws are unconstitutional if they treat same-sex couples differently than opposite-sex couples. Based on this principle, the Court held that parental birth certificate registration is part of the “constellations of benefits” linked to marriage that the Constitution affords same-sex couples. This ruling applies as a matter of constitutional right in all states.
Read about more interesting Supreme Court decisions
5. Sexual offenders and social media
States struggle to protect children from convicted sex offenders. North Carolina, for example, made it a felony for sex offenders (who had completed their sentences) to use social media sites that “permit minor children to become members or create and maintain personal web pages.”10
At stake. In Packingham v North Carolina, the Court was asked to decide whether this statute violates the First Amendment (free speech) rights of sex offenders.11
Final ruling. The Court held that the North Carolina limitation on sex offenders’ use of social media was too broad. It noted the wide range of political, employment, news, personal, commercial, and religious websites that are off limits to sex offenders under the statute—hardly narrowly tailored. It suggested, however, that it probably would be constitutional for a state to prohibit sex offenders “from engaging in conduct that often presages a sexual crime, like contacting a minor or using a website to gather information about a minor.”11
It was important in this case that the defendant had already served his entire sentence and was “no longer subject to the supervision of the criminal justice system.”11 If he had still been in prison, the state could limit or prohibit his Internet use. Even if he had been on probation or parole (under the supervision of the criminal justice system) the restrictions may well have been permitted. In addition, the state could impose new, narrowly tailored restrictions.
This case is also a reminder that ObGyns are very important in the efforts to eliminate child sexual abuse. All states have laws that require the reporting of known or suspected sexual abuse. In addition to complying with the law, such reports are often critical to discovering and ending the abuse.
6. Transgender rights
The Court had accepted a “transgender bathroom case” in Gloucester County School Board v G.G.12
At stake. This case essentially challenged the Obama Administration’s requirement that schools allow transgender students to use the restrooms in which they feel most comfortable. It was one of the most anticipated cases of the Term, but it essentially disappeared. Following the presidential election, the Department of Education rescinded the earlier guidance on which the case was based.
Final ruling. The Court returned the case to the Fourth Circuit for reconsideration. This issue, however, may reappear before the Court in the form of a claim that the states must provide this accommodation as a matter of federal statutory right, or even Equal Protection.
- In an important First Amendment decision, the Court held that it is a violation of the Freedom of Religion to deny a church-related school access to generally available state grant funds solely because of its religious status (in this case the program funded playground surfacing grants).1
- In several cases, it was apparent that the Court is uncomfortable with the way death penalty cases are handled in some states.2
- Juries may be questioned about racial bias that was expressed during jury deliberations--a substantial change for many courts.3
- The failure of the Patent and Trademark Office (PTO) to register the trademark for the band "The Slants" was a First Amendment violation. One reason that this case was watched was because of the effort of the PTO to deregister the trademark of the Washington Redskins.4
- The Court considered 9 cases involving revoking citizenship, deportation, and cross-border liability (an extraordinary number). Two cases that could change the nature and process of deportation were held over to the next Term for reargument.
- Individualized educational plans under the federal Individuals with Disabilities Education Act (IDEA) must target more than trivial progress for the students.5
References
- Trinity Lutheran Church of Columbia, Inc. v Comer, 582 US 15 577 (2017).
- McAllister S. Death-penalty symposium: A court increasingly uncomfortable with the death penalty. SCOTUSblog.com. http://www.scotusblog.com/2017/06/death-penalty-symposium-court-increasingly-uncomfortable-death-penalty/. Published June 29, 2017. Accessed November 2, 2017.
- Pena-Rodriguez v Colorado, 580 US 15 606 (2017).
- Matal v Tam, 582 US 15 1293 (2017).
- Endrew F v Douglas County School District, RE-1, 580 US 15 827 (2017).
Summary of the Term
The Term was notable for the level of agreement. With 69 decided cases, 41 (69%) were unanimous. In 59 cases (85%), there was a strong consensus, with no more than 2 justices dissenting. Only 7 decisions (10%) were 5 to 4. Justice Kennedy was, as usual, the deciding vote in most of the close cases. He voted in the majority in 97% of the decisions. Justice Gorsuch took the place of Justice Scalia (who passed away in February 2016), so arguably the Court is ideologically close to where it has been for a number of years. Despite rumors that Justice Kennedy would announce his resignation from the Court, neither he nor any other justice has left. The Supreme Court began its new Term on October 2, 2017, with a full complement of 9 justices.
What’s to come
The Court will add cases through much of its new Term, but it has already accepted cases dealing with arbitration agreements (again); public employees’ union dues; immigration (again); the privacy of information held by mobile phone companies; a constitutional challenge to political gerrymandering; bakeries and gay-marriage ceremonies; whistleblowers and Dodd-Frank regulations; sports gambling and the NCAA; and more.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Despite being short-handed (there were only 8 justices for most of the Term), the United States Supreme Court decided a number of important cases during its most recent Term, which concluded on June 27, 2017. Among the 69 cases, several are of particular interest to ObGyns.
1. Arbitration in health care
In Kindred Nursing Centers v Clark, the Court decided an important case involving arbitration in health care.1
At stake. The families of 2 people who died after being in a long-term care facility filed lawsuits against the facility, claiming personal injury, violations of Kentucky statutes regarding long-term care facilities, and wrongful death. However, during admission to the facility, the patients (technically, their agents under a power of attorney) signed an agreement that any disputes would be taken to arbitration. The facility successfully had the lawsuits dismissed.
Final ruling. The Supreme Court agreed that the case had to go to arbitration rather than to court, even though the arbitration clause violated state law. The Federal Arbitration Act (FAA) preempts state law. The Court has been very aggressive in enforcing arbitration agreements and striking down state laws that are inconsistent with the FAA. This case emphasizes that the FAA applies in the health care context.
The case suggests both a warning and an opportunity for health care providers. The warning is that arbitration clauses will be enforced; thoughtlessly entering into arbitration for future disputes may be dangerous. Among other things, the decision of arbitrators is essentially unreviewable. Appellate courts review the decisions of lower courts, but there is no such review in arbitration. Furthermore, arbitration may be stacked in favor of commercial entities that often use arbitrators.
The opportunity for health care providers lies in that it may be possible to include arbitration clauses in agreements with patients. This should be considered only after obtaining legal advice. The agreements should, for example, be consistent with the obligations to patients (in the case of the Kentucky facility, it made clear that accepting the arbitration agreement was not necessary in order to receive care or be admitted to the facility). Because arbitration agreements are becoming ubiquitous and rigorously enforced by federal courts, arbitration is bound to have an important function in health care.
2. Pharmaceuticals
Biologics and biosimilars
Biologics play an important role in health care. Eight of the top 10 selling drugs in 2016 were biologics.2 The case of Sandoz v Amgen involved biosimilar pharmaceuticals, essentially the generics of biologic drugs.3
At stake. While biologics hold great promise in medicine, they are generally very expensive. Just as with generics, brand-name companies (generally referred to as “reference” biologics) want to keep biosimilars off the market for as long as possible, thereby extending the advantages of monopolistic pricing. This Term the Supreme Court considered the statutory rules for licensing biosimilar drugs.
Final ruling. The Court’s decision will allow biosimilar companies to speed up the licensing process by at least 180 days. This is a modest win for patients and their physicians, but the legal issues around biosimilars will need additional attention.
Class action suits
In another case, the Court made it more difficult to file class action suits against pharmaceutical companies in state courts.4 Although this is a fairly technical decision, it is likely to have a significant impact in pharmaceutical liability by limiting classactions.
3. The travel ban
The American College of Obstetricians and Gynecologists joined other medical organizations in an amicus curiae (friend of the court) brief to challenge President Trump’s “travel ban.”5
At stake. The brief argued that the United States “relies upon a significant number of health professionals and scientists who have entered the country through the immigration system.”5
Final ruling. The Court allowed most of the travel ban to stay in place, but did permit entry into the United States by foreign nationals “with a close familial relationship,” or pre-existing ties to US businesses or institutions (such as students who have been admitted to American colleges, workers who have accepted US employment, or lecturers invited to address American audiences).6 Following the Term, the Administration issued a different travel ban, so the issue was taken off the Court’s calendar for the moment. There undoubtedly will be additional chapters to come.
4. Birth certificates and same-sex marriage
In Pavan v Smith, the legal question concerned whether married same-sex couples may have both parents listed on the birth certificate of children born during the marriage.7 Two same-sex couples conceived children through anonymous sperm donation and gave birth in Arkansas. The Department of Health in Arkansas issued birth certificates listing the mother’s name, but refused to list the spouse on the birth certificate.
At stake. The couples brought suit claiming a constitutional right to have both parents listed. In particular, they noted that under Arkansas law, the woman who gives birth is deemed to be the mother. When the woman is married, the husband’s name is “entered on the certificate as the father of the child.”8 The same-sex parents argued that a 2015 decision of the Supreme Court, which held that the Constitution requires states to recognize same-sex marriages, made it clear that same-sex couples should have the benefits of marriage.9 Eventually the case wound its way to the Supreme Court.
Final ruling. The Court held that if the state ordinarily lists the names of both husband and wife on such certificates, then same-sex couples are entitled to have birth certificates listing both parents. The Court noted that laws are unconstitutional if they treat same-sex couples differently than opposite-sex couples. Based on this principle, the Court held that parental birth certificate registration is part of the “constellations of benefits” linked to marriage that the Constitution affords same-sex couples. This ruling applies as a matter of constitutional right in all states.
Read about more interesting Supreme Court decisions
5. Sexual offenders and social media
States struggle to protect children from convicted sex offenders. North Carolina, for example, made it a felony for sex offenders (who had completed their sentences) to use social media sites that “permit minor children to become members or create and maintain personal web pages.”10
At stake. In Packingham v North Carolina, the Court was asked to decide whether this statute violates the First Amendment (free speech) rights of sex offenders.11
Final ruling. The Court held that the North Carolina limitation on sex offenders’ use of social media was too broad. It noted the wide range of political, employment, news, personal, commercial, and religious websites that are off limits to sex offenders under the statute—hardly narrowly tailored. It suggested, however, that it probably would be constitutional for a state to prohibit sex offenders “from engaging in conduct that often presages a sexual crime, like contacting a minor or using a website to gather information about a minor.”11
It was important in this case that the defendant had already served his entire sentence and was “no longer subject to the supervision of the criminal justice system.”11 If he had still been in prison, the state could limit or prohibit his Internet use. Even if he had been on probation or parole (under the supervision of the criminal justice system) the restrictions may well have been permitted. In addition, the state could impose new, narrowly tailored restrictions.
This case is also a reminder that ObGyns are very important in the efforts to eliminate child sexual abuse. All states have laws that require the reporting of known or suspected sexual abuse. In addition to complying with the law, such reports are often critical to discovering and ending the abuse.
6. Transgender rights
The Court had accepted a “transgender bathroom case” in Gloucester County School Board v G.G.12
At stake. This case essentially challenged the Obama Administration’s requirement that schools allow transgender students to use the restrooms in which they feel most comfortable. It was one of the most anticipated cases of the Term, but it essentially disappeared. Following the presidential election, the Department of Education rescinded the earlier guidance on which the case was based.
Final ruling. The Court returned the case to the Fourth Circuit for reconsideration. This issue, however, may reappear before the Court in the form of a claim that the states must provide this accommodation as a matter of federal statutory right, or even Equal Protection.
- In an important First Amendment decision, the Court held that it is a violation of the Freedom of Religion to deny a church-related school access to generally available state grant funds solely because of its religious status (in this case the program funded playground surfacing grants).1
- In several cases, it was apparent that the Court is uncomfortable with the way death penalty cases are handled in some states.2
- Juries may be questioned about racial bias that was expressed during jury deliberations--a substantial change for many courts.3
- The failure of the Patent and Trademark Office (PTO) to register the trademark for the band "The Slants" was a First Amendment violation. One reason that this case was watched was because of the effort of the PTO to deregister the trademark of the Washington Redskins.4
- The Court considered 9 cases involving revoking citizenship, deportation, and cross-border liability (an extraordinary number). Two cases that could change the nature and process of deportation were held over to the next Term for reargument.
- Individualized educational plans under the federal Individuals with Disabilities Education Act (IDEA) must target more than trivial progress for the students.5
References
- Trinity Lutheran Church of Columbia, Inc. v Comer, 582 US 15 577 (2017).
- McAllister S. Death-penalty symposium: A court increasingly uncomfortable with the death penalty. SCOTUSblog.com. http://www.scotusblog.com/2017/06/death-penalty-symposium-court-increasingly-uncomfortable-death-penalty/. Published June 29, 2017. Accessed November 2, 2017.
- Pena-Rodriguez v Colorado, 580 US 15 606 (2017).
- Matal v Tam, 582 US 15 1293 (2017).
- Endrew F v Douglas County School District, RE-1, 580 US 15 827 (2017).
Summary of the Term
The Term was notable for the level of agreement. With 69 decided cases, 41 (69%) were unanimous. In 59 cases (85%), there was a strong consensus, with no more than 2 justices dissenting. Only 7 decisions (10%) were 5 to 4. Justice Kennedy was, as usual, the deciding vote in most of the close cases. He voted in the majority in 97% of the decisions. Justice Gorsuch took the place of Justice Scalia (who passed away in February 2016), so arguably the Court is ideologically close to where it has been for a number of years. Despite rumors that Justice Kennedy would announce his resignation from the Court, neither he nor any other justice has left. The Supreme Court began its new Term on October 2, 2017, with a full complement of 9 justices.
What’s to come
The Court will add cases through much of its new Term, but it has already accepted cases dealing with arbitration agreements (again); public employees’ union dues; immigration (again); the privacy of information held by mobile phone companies; a constitutional challenge to political gerrymandering; bakeries and gay-marriage ceremonies; whistleblowers and Dodd-Frank regulations; sports gambling and the NCAA; and more.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Kindred Nursing Centers, LP v Clark, 581 US 16 32 (2017).
- Anderson L. Looking Ahead: Pharma Projections for 2016 - & Beyond. Perma.cc Website. . Reviewed March 30, 2017. Accessed November 2, 2017.
- Sandoz Inc v Amgen Inc, 581 US 15 1039 1195 (2017).
- Bristol-Myers Squibb Co v Superior Court of California, San Francisco County, 582 US 16 466 (2017).
- Trinity FR, Sterling AM, Rogaczewski JD, et al. Motion for Leave to File and Brief for the Association of American Medical Colleges and Others as Amici Curiae Supporting Respondents. SCOTUSblog. http://www.scotusblog.com/wp-content/uploads/2017/06/16-1436-ac-AAMC-supporting-respondents.pdf. Accessed November 2, 2017.
- Donald J. Trump, President of the United States v International Refugee Assistance Project, 582 US 16 1436 (2017).
- Pavan v Smith, 582 US 16 992 (2017).
- Arkansas Code, §20 18 401(f)(1) (2014).
- Obergefell v Hodges, 576 US ___ (2015).
- NC Gen. Stat. Ann. §§14-202.5(a),(e).
- Packingham v North Carolina, 582 US 15 1194 (2017).
- Gloucester County School Board v G.G. SCOTUSblog. http://www.scotusblog.com/case-files/cases/gloucester-county-school-board-v-g-g/. Published March 6, 2017. Accessed November 2, 2017.
- Kindred Nursing Centers, LP v Clark, 581 US 16 32 (2017).
- Anderson L. Looking Ahead: Pharma Projections for 2016 - & Beyond. Perma.cc Website. . Reviewed March 30, 2017. Accessed November 2, 2017.
- Sandoz Inc v Amgen Inc, 581 US 15 1039 1195 (2017).
- Bristol-Myers Squibb Co v Superior Court of California, San Francisco County, 582 US 16 466 (2017).
- Trinity FR, Sterling AM, Rogaczewski JD, et al. Motion for Leave to File and Brief for the Association of American Medical Colleges and Others as Amici Curiae Supporting Respondents. SCOTUSblog. http://www.scotusblog.com/wp-content/uploads/2017/06/16-1436-ac-AAMC-supporting-respondents.pdf. Accessed November 2, 2017.
- Donald J. Trump, President of the United States v International Refugee Assistance Project, 582 US 16 1436 (2017).
- Pavan v Smith, 582 US 16 992 (2017).
- Arkansas Code, §20 18 401(f)(1) (2014).
- Obergefell v Hodges, 576 US ___ (2015).
- NC Gen. Stat. Ann. §§14-202.5(a),(e).
- Packingham v North Carolina, 582 US 15 1194 (2017).
- Gloucester County School Board v G.G. SCOTUSblog. http://www.scotusblog.com/case-files/cases/gloucester-county-school-board-v-g-g/. Published March 6, 2017. Accessed November 2, 2017.
Is Change in Personality an Early Sign of Dementia?
Evidence does not support the hypothesis that change in personality is a marker for preclinical mild cognitive impairment or dementia, according to research published online ahead of print September 20 in JAMA Psychiatry. Patients who subsequently develop dementia, however, appear to score higher on neuroticism and lower on conscientiousness and extraversion than people who remain cognitively healthy.
“These findings suggest that tracking change in self-rated personality as an early indicator of dementia is unlikely to be fruitful, while a single assessment provides reliable information on the personality traits that increase resilience (eg, conscientiousness) or vulnerability (eg, neuroticism) to clinical dementia,” said Antonio Terracciano, PhD, Associate Professor of Geriatrics at Florida State University College of Medicine in Tallahassee.
Changes in behavior and personality are one criterion for the diagnosis of dementia. It is uncertain whether such changes begin before the clinical onset of the disease, however. Prospective studies of this question have either not assessed all five major dimensions of personality or administered assessments too close in time to the diagnosis of dementia.
Examining Change in Personality Traits
Dr. Terracciano and colleagues conducted a study to determine whether increases in neuroticism, declines in conscientiousness, and changes in other personality traits occur before the onset of mild cognitive impairment or dementia. They examined data for a cohort of 2,046 community-dwelling older adults who participated in the Baltimore Longitudinal Study of Aging. In the latter study, participants with no cognitive impairment underwent periodic personality and clinical assessments between 1980 and July 13, 2016. Follow-up lasted for as long as 36 years.
Participants completed the self-report version of the Revised NEO Personality Inventory (NEO-PI-R), or an earlier version, in 1980 and 1986. The NEO-PI-R is a 240-item questionnaire that assesses 30 facets of personality, including six for each of the following five major dimensions: neuroticism, extraversion, openness, agreeableness, and conscientiousness. In addition, participants were evaluated at enrollment for history of neurologic or cerebrovascular disease and for impairment of cognitive or behavioral functioning. Follow-up evaluations included a neuropsychologic battery and clinical examination, including an informant-and-participant-structured interview.
Patients With Dementia Had Higher Neuroticism Scores
Participants’ mean age at baseline was 62. In all, 931 participants (46%) were women. The population sample included 374 blacks (18%), 1,582 whites (77%), and 55 Asians or Pacific Islanders (3%). During the study, 104 participants (5%) developed mild cognitive impairment, and 255 (13%) developed all-cause dementia, including 194 (10%) who developed Alzheimer’s disease.
Change in personality before the onset of mild cognitive impairment or dementia was not significantly different between participants who remained unimpaired and those who developed Alzheimer’s disease. Change in personality for participants who developed mild cognitive impairment and all-cause dementia also was similar to that in unimpaired participants. Neuroticism and conscientiousness did not change significantly as disease onset approached.
One limitation of this study was that the population sample was selective and highly educated, said the authors. Another limitation was that the unimpaired participants were relatively young and could develop dementia in the future. “More research is needed on personality and Alzheimer’s disease biomarkers and how personality may increase resilience against neuropathology and forestall the emergence of clinical dementia,” said Dr. Terracciano.
—Erica Tricarico
Suggested Reading
Terracciano A, An Y, Sutin AR, et al. Personality change in the preclinical phase of Alzheimer disease. JAMA Psychiatry. 2017 Sep 20 [Epub ahead of print].
Evidence does not support the hypothesis that change in personality is a marker for preclinical mild cognitive impairment or dementia, according to research published online ahead of print September 20 in JAMA Psychiatry. Patients who subsequently develop dementia, however, appear to score higher on neuroticism and lower on conscientiousness and extraversion than people who remain cognitively healthy.
“These findings suggest that tracking change in self-rated personality as an early indicator of dementia is unlikely to be fruitful, while a single assessment provides reliable information on the personality traits that increase resilience (eg, conscientiousness) or vulnerability (eg, neuroticism) to clinical dementia,” said Antonio Terracciano, PhD, Associate Professor of Geriatrics at Florida State University College of Medicine in Tallahassee.
Changes in behavior and personality are one criterion for the diagnosis of dementia. It is uncertain whether such changes begin before the clinical onset of the disease, however. Prospective studies of this question have either not assessed all five major dimensions of personality or administered assessments too close in time to the diagnosis of dementia.
Examining Change in Personality Traits
Dr. Terracciano and colleagues conducted a study to determine whether increases in neuroticism, declines in conscientiousness, and changes in other personality traits occur before the onset of mild cognitive impairment or dementia. They examined data for a cohort of 2,046 community-dwelling older adults who participated in the Baltimore Longitudinal Study of Aging. In the latter study, participants with no cognitive impairment underwent periodic personality and clinical assessments between 1980 and July 13, 2016. Follow-up lasted for as long as 36 years.
Participants completed the self-report version of the Revised NEO Personality Inventory (NEO-PI-R), or an earlier version, in 1980 and 1986. The NEO-PI-R is a 240-item questionnaire that assesses 30 facets of personality, including six for each of the following five major dimensions: neuroticism, extraversion, openness, agreeableness, and conscientiousness. In addition, participants were evaluated at enrollment for history of neurologic or cerebrovascular disease and for impairment of cognitive or behavioral functioning. Follow-up evaluations included a neuropsychologic battery and clinical examination, including an informant-and-participant-structured interview.
Patients With Dementia Had Higher Neuroticism Scores
Participants’ mean age at baseline was 62. In all, 931 participants (46%) were women. The population sample included 374 blacks (18%), 1,582 whites (77%), and 55 Asians or Pacific Islanders (3%). During the study, 104 participants (5%) developed mild cognitive impairment, and 255 (13%) developed all-cause dementia, including 194 (10%) who developed Alzheimer’s disease.
Change in personality before the onset of mild cognitive impairment or dementia was not significantly different between participants who remained unimpaired and those who developed Alzheimer’s disease. Change in personality for participants who developed mild cognitive impairment and all-cause dementia also was similar to that in unimpaired participants. Neuroticism and conscientiousness did not change significantly as disease onset approached.
One limitation of this study was that the population sample was selective and highly educated, said the authors. Another limitation was that the unimpaired participants were relatively young and could develop dementia in the future. “More research is needed on personality and Alzheimer’s disease biomarkers and how personality may increase resilience against neuropathology and forestall the emergence of clinical dementia,” said Dr. Terracciano.
—Erica Tricarico
Suggested Reading
Terracciano A, An Y, Sutin AR, et al. Personality change in the preclinical phase of Alzheimer disease. JAMA Psychiatry. 2017 Sep 20 [Epub ahead of print].
Evidence does not support the hypothesis that change in personality is a marker for preclinical mild cognitive impairment or dementia, according to research published online ahead of print September 20 in JAMA Psychiatry. Patients who subsequently develop dementia, however, appear to score higher on neuroticism and lower on conscientiousness and extraversion than people who remain cognitively healthy.
“These findings suggest that tracking change in self-rated personality as an early indicator of dementia is unlikely to be fruitful, while a single assessment provides reliable information on the personality traits that increase resilience (eg, conscientiousness) or vulnerability (eg, neuroticism) to clinical dementia,” said Antonio Terracciano, PhD, Associate Professor of Geriatrics at Florida State University College of Medicine in Tallahassee.
Changes in behavior and personality are one criterion for the diagnosis of dementia. It is uncertain whether such changes begin before the clinical onset of the disease, however. Prospective studies of this question have either not assessed all five major dimensions of personality or administered assessments too close in time to the diagnosis of dementia.
Examining Change in Personality Traits
Dr. Terracciano and colleagues conducted a study to determine whether increases in neuroticism, declines in conscientiousness, and changes in other personality traits occur before the onset of mild cognitive impairment or dementia. They examined data for a cohort of 2,046 community-dwelling older adults who participated in the Baltimore Longitudinal Study of Aging. In the latter study, participants with no cognitive impairment underwent periodic personality and clinical assessments between 1980 and July 13, 2016. Follow-up lasted for as long as 36 years.
Participants completed the self-report version of the Revised NEO Personality Inventory (NEO-PI-R), or an earlier version, in 1980 and 1986. The NEO-PI-R is a 240-item questionnaire that assesses 30 facets of personality, including six for each of the following five major dimensions: neuroticism, extraversion, openness, agreeableness, and conscientiousness. In addition, participants were evaluated at enrollment for history of neurologic or cerebrovascular disease and for impairment of cognitive or behavioral functioning. Follow-up evaluations included a neuropsychologic battery and clinical examination, including an informant-and-participant-structured interview.
Patients With Dementia Had Higher Neuroticism Scores
Participants’ mean age at baseline was 62. In all, 931 participants (46%) were women. The population sample included 374 blacks (18%), 1,582 whites (77%), and 55 Asians or Pacific Islanders (3%). During the study, 104 participants (5%) developed mild cognitive impairment, and 255 (13%) developed all-cause dementia, including 194 (10%) who developed Alzheimer’s disease.
Change in personality before the onset of mild cognitive impairment or dementia was not significantly different between participants who remained unimpaired and those who developed Alzheimer’s disease. Change in personality for participants who developed mild cognitive impairment and all-cause dementia also was similar to that in unimpaired participants. Neuroticism and conscientiousness did not change significantly as disease onset approached.
One limitation of this study was that the population sample was selective and highly educated, said the authors. Another limitation was that the unimpaired participants were relatively young and could develop dementia in the future. “More research is needed on personality and Alzheimer’s disease biomarkers and how personality may increase resilience against neuropathology and forestall the emergence of clinical dementia,” said Dr. Terracciano.
—Erica Tricarico
Suggested Reading
Terracciano A, An Y, Sutin AR, et al. Personality change in the preclinical phase of Alzheimer disease. JAMA Psychiatry. 2017 Sep 20 [Epub ahead of print].
2017 Update on bone health
Bone health remains one of the most important health care concerns in the United States today. In 2004, the Surgeon General released a report on bone health and osteoporosis. According to the report’s introduction:
This first-ever Surgeon General’s Report on bone health and osteoporosis illustrates the large burden that bone disease places on our Nation and its citizens. Like other chronic diseases that disproportionately affect the elderly, the prevalence of bone disease and fractures is projected to increase markedly as the population ages. If these predictions come true, bone disease and fractures will have a tremendous negative impact on the future well-being of Americans. But as this report makes clear, they need not come true: by working together we can change the picture of aging in America. Osteoporosis and fractures…no longer should be thought of as an inevitable part of growing old. By focusing on prevention and lifestyle changes, including physical activity and nutrition, as well as early diagnosis and appropriate treatment, Americans can avoid much of the damaging impact of bone disease.1
Related article:
2016 Update on bone health
Although men also experience osteoporosis as they age, in women the rapid loss of bone at menopause makes their disease burden much greater. As women’s health care providers, we stand at the front line for preventing, diagnosing, and treating osteoporosis to reduce the impact of this disease. In this Update I focus on important information that has emerged in the past year.
Read about new ACP guidelines to assess fracture risk
Guidelines for therapy: How to assess fracture risk and when to treat
American College of Obstetricians and Gynecologists Committee on Practice Bulletins--Gynecology. ACOG Practice Bulletin No. 129: Osteoporosis. Obstet Gynecol. 2012;120(3):718-734.
Qaseem A, Forciea MA, McLean RM, Denberg TD; Clinical Guidelines Committee of the American College of Physicians. Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166(11):818-839.
A crucial component for good bone health maintenance and osteoporotic fracture prevention is understanding the current guidelines for therapy. The most recent practice bulletin of the American College of Obstetricians and Gynecologists (ACOG) on osteoporosis was published in 2012. ACOG states that treatment be recommended for women who have a bone mineral density (BMD) T-score of -2.5 or lower.
For women in the low bone mass category (T-score between -1 and -2.5), use of the Fracture Risk Assessment Tool (FRAX) calculator can assist in making an informed treatment decision.2 Based on the FRAX calculator, women who have a 10-year risk of major osteoporotic fracture of 20% or greater, or a risk of hip fracture of 3% or greater, are candidates for pharmacologic therapy.
Women who have experienced a low-trauma fracture (especially of the vertebra or hip) also are candidates for treatment, even in the absence of osteoporosis on a dual-energy x-ray absorptiometry (DXA) report.
Related article:
Women’s Preventive Services Initiative Guidelines provide consensus for practicing ObGyns
Updated recommendations from the ACP
The 2017 guideline published by the American College of Physicians (ACP), whose target audience is "all clinicians," recommends that, for women who have known osteoporosis, clinicians offer pharmacologic treatment with alendronate, risedronate, zoledronic acid, or denosumab to reduce the risk for hip and vertebral fractures.
In addition, the ACP recommends that clinicians make the decision whether or not to treat osteopenic women 65 years of age or older who are at a high risk for fracture based on a discussion of patient preferences, fracture risk profile, and benefits, harms, and costs of medications. This may seem somewhat contradictory to ACOG's guidance vis-a-vis women younger than 65 years of age.
The ACP further states that given the limited evidence supporting the benefit of treatment, the balance of benefits and harms in treating osteopenic women is most favorable when the risk for fracture is high. Women younger than 65 years with osteopenia and women older than 65 years with mild osteopenia (T-score between -1.0 and -1.5) will benefit less than women who are 65 years of age or older with severe osteopenia (T-score <-2.0).
Risk factors and risk assessment tools
Clinicians can use their own judgment based on risk factors for fracture (lower body weight, smoking, weight loss, family history of fractures, decreased physical activity, alcohol or caffeine use, low calcium and vitamin D intake, corticosteroid use), or they can use a risk assessment tool. Several risk assessment tools, such as the FRAX calculator mentioned earlier, are available to predict fracture risk among untreated people with low bone density. Although the FRAX calculator is widely used, there is no evidence from randomized controlled trials demonstrating a benefit of fracture reduction when FRAX scores are used in treatment decision making.
Duration of therapy. The ACP recommends that clinicians treat osteoporotic women with pharmacologic therapy for 5 years. Bone density monitoring is not recommended during the 5-year treatment period for osteoporosis in women; current evidence does not show any benefit for bone density monitoring during treatment.
Moderate-quality evidence demonstrated that women treated with antiresorptive therapies (including bisphosphonates, raloxifene, and teriparatide) benefited from reduced fractures, even if no increase in BMD occurred or if BMD decreased.
As before, all women with osteoporosis or a previous low-trauma fracture should be treated. Use of the FRAX calculator should involve clinician judgment, and other risk factors should be taken into account. For most women, treatment should be continued for 5 years. There is no benefit in continued bone mass assessment (DXA testing) while a patient is on pharmacologic therapy.
Read about fracture risk after stopping HT
Another WHI update: No increase in fractures after stopping HT
Watts NB, Cauley JA, Jackson RD, et al; Women's Health Initiative Investigators. No increase in fractures after stopping hormone therapy: results from the Women's Health Initiative. J Clin Endocrinol Metab. 2017;102(1):302-308.
The analysis and reanalysis of the Women's Health Initiative (WHI) trial data seems never-ending, yet the article by Watts and colleagues is important. Although the WHI hormone therapy (HT) trials showed that treatment protects against hip and total fractures, a later observational report suggested loss of benefit and rebound increased risk after HT was discontinued.3 The purpose of the Watts' study was to examine fractures after stopping HT.
Related article:
Did long-term follow-up of WHI participants reveal any mortality increase among women who received HT?
Details of the study
Two placebo-controlled randomized trials served as the study setting. The study included WHI participants (n = 15,187) who continued to take active HT or placebo through the intervention period and who did not take HT in the postintervention period. The trial interventions included conjugated equine estrogen (CEE) plus medroxyprogesterone acetate (MPA) for women with natural menopause and CEE alone for women with prior hysterectomy. The investigators recorded total fractures and hip fractures through 5 years after HT discontinuation.
Findings on fractures. Hip fractures occurred infrequently, with approximately 2.5 per 1,000 person-years. This finding was similar between trials and in former HT users and placebo groups.
No difference was found in total fractures in the CEE plus MPA trial for former HT users compared with former placebo users (28.9 per 1,000 person-years and 29.9 per 1,000 person-years, respectively; hazard ratio [HR], 0.97; 95% confidence interval [CI], 0.87-1.09; P = .63). In the CEE-alone trial, however, total fractures were higher in former placebo users (36.9 per 1,000 person-years) compared with the former active-treatment group (31.1 per 1,000 person-years). This finding suggests a residual benefit of CEE in reducing total fractures (HR, 0.85; 95% CI, 0.73-0.98; P = .03).
Investigators' takeaway. The authors concluded that, after discontinuing HT, there was no evidence of increased fracture risk (sustained or transient) in former HT users compared with former placebo users. In the CEE-alone trial, there was a residual benefit for total fracture reduction in former HT users compared with placebo users.
Gynecologists have long believed that on stopping HT, the loss of bone mass will follow at the same rate as it would at natural menopause. These WHI trials demonstrate, however, that through 5 years, women who stopped HT had no increase in hip or total fractures, and hysterectomized women who stopped estrogen therapy actually had fewer fractures than the placebo group. Keep in mind that this large cohort was not chosen based on risk of osteoporotic fractures. In fact, baseline bone mass was not even measured in these women, making the results even more "real world."
Read about reassessing FRAX scores
A new look at fracture risk assessment scores
Gourlay ML, Overman RA, Fine JP, et al; Women's Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-e23.
Jiang X, Gruner M, Trémollieres F, et al. Diagnostic accuracy of FRAX in predicting the 10-year risk of osteoporotic fractures using the USA treatment thresholds: a systematic review and meta-analysis. Bone. 2017;99:20-25.
The FRAX score has become a popular form of triage for women who do not yet meet the bone mass criteria of osteoporosis. Current practice guidelines recommend use of fracture risk scores for screening and pharmacologic therapeutic decision making. Some newer data, however, may give rise to questions about its utility, especially in younger women.
Fracture risk analysis in a large postmenopausal population
Gourlay and colleagues conducted a retrospective competing risk analysis of new occurrence of treatment-level and screening-level fracture risk scores. Study participants were postmenopausal women aged 50 years and older who had not previously received pharmacologic treatment and had not had a first hip or clinical vertebral facture.
Details of the study
In 54,280 postmenopausal women aged 50 to 64 years who did not have a bone mineral density test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because the incidence of treatment-level scores was rare.
A total of 6,096 women had FRAX scores calculated with bone mineral density testing. In this group, the estimated unadjusted time to treatment-level FRAX scores was 7.6 years (95% CI, 6.6-8.7) for those aged 65 to 69, and 5.1 years (95% CI, 3.5-7.5) for women aged 75 to 79 at baseline.
Of 17,967 women aged 50 to 64 who had a screening-level FRAX at baseline, 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65 years.
Age is key factor. Gourlay and colleagues concluded that postmenopausal women who had subthreshold fracture risk scores at baseline would be unlikely to develop a treatment-level FRAX score between ages 50 and 64. The increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture after age 65, however, supports more frequent consideration of FRAX assessment and bone mineral density testing.
Related article:
2015 Update on osteoporosis
Meta-analysis of FRAX tool accuracy
In another study, Jiang and colleagues conducted a systematic review and meta-analysis to determine how the FRAX score performed in predicting the 10-year risk of major osteoporotic fractures and hip fractures. The investigators used the US treatment thresholds.
Details of the study
Seven studies (n = 57,027) were analyzed to assess the diagnostic accuracy of FRAX in predicting major osteoporotic fractures; 20% was used as the 10-year fracture risk threshold for intervention. The mean sensitivity and specificity, along with their 95% CIs, were 10.25% (3.76%-25.06%) and 97.02% (91.17%-99.03%), respectively.
For hip fracture prediction, 6 studies (n = 50,944) were analyzed, and 3% was used as the 10-year fracture risk threshold. The mean sensitivity and specificity, along with their 95% CIs, were 45.70% (24.88%-68.13%) and 84.70% (76.41%-90.44%), respectively.
Predictive value of FRAX. The authors concluded that, using the 10-year intervention thresholds of 20% for major osteoporotic fracture and 3% for hip fracture, FRAX performed better in identifying individuals who will not have a major osteoporotic fracture or hip fracture within 10 years than in identifying those who will experience a fracture. A substantial number of those who developed fractures, especially major osteoporotic fracture within 10 years of follow up, were missed by the baseline FRAX assessment.
Increasing age is still arguably among the most important factors for decreasing bone health. Older women are more likely to develop treatment-level FRAX scores more quickly than younger women. In addition, the FRAX tool is better in predicting which women will not develop a fracture in the next 10 years than in predicting those who will experience a fracture.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- United States Office of the Surgeon General. Bone health and osteoporosis: a report of the Surgeon General. Rockville, Maryland: Office of the Surgeon General (US); 2004. https://www.ncbi.nlm.nih.gov/books/NBK45513/. Accessed November 6, 2017.
- Centre for Metabolic Bone Diseases, University of Sheffield, United Kingdom. FRAX Fracture Risk Assessment Tool website. www.sheffield.ac.uk/FRAX. Accessed November 6, 2017.
- Yates J, Barrett-Connor E, Barlas S, Chen YT, Miller PD, Siris ES. Rapid loss of hip fracture protection after estrogen cessation: evidence from the National Osteoporosis Risk Assessment. Obstet Gynecol. 2004;103(3):440–446.
Bone health remains one of the most important health care concerns in the United States today. In 2004, the Surgeon General released a report on bone health and osteoporosis. According to the report’s introduction:
This first-ever Surgeon General’s Report on bone health and osteoporosis illustrates the large burden that bone disease places on our Nation and its citizens. Like other chronic diseases that disproportionately affect the elderly, the prevalence of bone disease and fractures is projected to increase markedly as the population ages. If these predictions come true, bone disease and fractures will have a tremendous negative impact on the future well-being of Americans. But as this report makes clear, they need not come true: by working together we can change the picture of aging in America. Osteoporosis and fractures…no longer should be thought of as an inevitable part of growing old. By focusing on prevention and lifestyle changes, including physical activity and nutrition, as well as early diagnosis and appropriate treatment, Americans can avoid much of the damaging impact of bone disease.1
Related article:
2016 Update on bone health
Although men also experience osteoporosis as they age, in women the rapid loss of bone at menopause makes their disease burden much greater. As women’s health care providers, we stand at the front line for preventing, diagnosing, and treating osteoporosis to reduce the impact of this disease. In this Update I focus on important information that has emerged in the past year.
Read about new ACP guidelines to assess fracture risk
Guidelines for therapy: How to assess fracture risk and when to treat
American College of Obstetricians and Gynecologists Committee on Practice Bulletins--Gynecology. ACOG Practice Bulletin No. 129: Osteoporosis. Obstet Gynecol. 2012;120(3):718-734.
Qaseem A, Forciea MA, McLean RM, Denberg TD; Clinical Guidelines Committee of the American College of Physicians. Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166(11):818-839.
A crucial component for good bone health maintenance and osteoporotic fracture prevention is understanding the current guidelines for therapy. The most recent practice bulletin of the American College of Obstetricians and Gynecologists (ACOG) on osteoporosis was published in 2012. ACOG states that treatment be recommended for women who have a bone mineral density (BMD) T-score of -2.5 or lower.
For women in the low bone mass category (T-score between -1 and -2.5), use of the Fracture Risk Assessment Tool (FRAX) calculator can assist in making an informed treatment decision.2 Based on the FRAX calculator, women who have a 10-year risk of major osteoporotic fracture of 20% or greater, or a risk of hip fracture of 3% or greater, are candidates for pharmacologic therapy.
Women who have experienced a low-trauma fracture (especially of the vertebra or hip) also are candidates for treatment, even in the absence of osteoporosis on a dual-energy x-ray absorptiometry (DXA) report.
Related article:
Women’s Preventive Services Initiative Guidelines provide consensus for practicing ObGyns
Updated recommendations from the ACP
The 2017 guideline published by the American College of Physicians (ACP), whose target audience is "all clinicians," recommends that, for women who have known osteoporosis, clinicians offer pharmacologic treatment with alendronate, risedronate, zoledronic acid, or denosumab to reduce the risk for hip and vertebral fractures.
In addition, the ACP recommends that clinicians make the decision whether or not to treat osteopenic women 65 years of age or older who are at a high risk for fracture based on a discussion of patient preferences, fracture risk profile, and benefits, harms, and costs of medications. This may seem somewhat contradictory to ACOG's guidance vis-a-vis women younger than 65 years of age.
The ACP further states that given the limited evidence supporting the benefit of treatment, the balance of benefits and harms in treating osteopenic women is most favorable when the risk for fracture is high. Women younger than 65 years with osteopenia and women older than 65 years with mild osteopenia (T-score between -1.0 and -1.5) will benefit less than women who are 65 years of age or older with severe osteopenia (T-score <-2.0).
Risk factors and risk assessment tools
Clinicians can use their own judgment based on risk factors for fracture (lower body weight, smoking, weight loss, family history of fractures, decreased physical activity, alcohol or caffeine use, low calcium and vitamin D intake, corticosteroid use), or they can use a risk assessment tool. Several risk assessment tools, such as the FRAX calculator mentioned earlier, are available to predict fracture risk among untreated people with low bone density. Although the FRAX calculator is widely used, there is no evidence from randomized controlled trials demonstrating a benefit of fracture reduction when FRAX scores are used in treatment decision making.
Duration of therapy. The ACP recommends that clinicians treat osteoporotic women with pharmacologic therapy for 5 years. Bone density monitoring is not recommended during the 5-year treatment period for osteoporosis in women; current evidence does not show any benefit for bone density monitoring during treatment.
Moderate-quality evidence demonstrated that women treated with antiresorptive therapies (including bisphosphonates, raloxifene, and teriparatide) benefited from reduced fractures, even if no increase in BMD occurred or if BMD decreased.
As before, all women with osteoporosis or a previous low-trauma fracture should be treated. Use of the FRAX calculator should involve clinician judgment, and other risk factors should be taken into account. For most women, treatment should be continued for 5 years. There is no benefit in continued bone mass assessment (DXA testing) while a patient is on pharmacologic therapy.
Read about fracture risk after stopping HT
Another WHI update: No increase in fractures after stopping HT
Watts NB, Cauley JA, Jackson RD, et al; Women's Health Initiative Investigators. No increase in fractures after stopping hormone therapy: results from the Women's Health Initiative. J Clin Endocrinol Metab. 2017;102(1):302-308.
The analysis and reanalysis of the Women's Health Initiative (WHI) trial data seems never-ending, yet the article by Watts and colleagues is important. Although the WHI hormone therapy (HT) trials showed that treatment protects against hip and total fractures, a later observational report suggested loss of benefit and rebound increased risk after HT was discontinued.3 The purpose of the Watts' study was to examine fractures after stopping HT.
Related article:
Did long-term follow-up of WHI participants reveal any mortality increase among women who received HT?
Details of the study
Two placebo-controlled randomized trials served as the study setting. The study included WHI participants (n = 15,187) who continued to take active HT or placebo through the intervention period and who did not take HT in the postintervention period. The trial interventions included conjugated equine estrogen (CEE) plus medroxyprogesterone acetate (MPA) for women with natural menopause and CEE alone for women with prior hysterectomy. The investigators recorded total fractures and hip fractures through 5 years after HT discontinuation.
Findings on fractures. Hip fractures occurred infrequently, with approximately 2.5 per 1,000 person-years. This finding was similar between trials and in former HT users and placebo groups.
No difference was found in total fractures in the CEE plus MPA trial for former HT users compared with former placebo users (28.9 per 1,000 person-years and 29.9 per 1,000 person-years, respectively; hazard ratio [HR], 0.97; 95% confidence interval [CI], 0.87-1.09; P = .63). In the CEE-alone trial, however, total fractures were higher in former placebo users (36.9 per 1,000 person-years) compared with the former active-treatment group (31.1 per 1,000 person-years). This finding suggests a residual benefit of CEE in reducing total fractures (HR, 0.85; 95% CI, 0.73-0.98; P = .03).
Investigators' takeaway. The authors concluded that, after discontinuing HT, there was no evidence of increased fracture risk (sustained or transient) in former HT users compared with former placebo users. In the CEE-alone trial, there was a residual benefit for total fracture reduction in former HT users compared with placebo users.
Gynecologists have long believed that on stopping HT, the loss of bone mass will follow at the same rate as it would at natural menopause. These WHI trials demonstrate, however, that through 5 years, women who stopped HT had no increase in hip or total fractures, and hysterectomized women who stopped estrogen therapy actually had fewer fractures than the placebo group. Keep in mind that this large cohort was not chosen based on risk of osteoporotic fractures. In fact, baseline bone mass was not even measured in these women, making the results even more "real world."
Read about reassessing FRAX scores
A new look at fracture risk assessment scores
Gourlay ML, Overman RA, Fine JP, et al; Women's Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-e23.
Jiang X, Gruner M, Trémollieres F, et al. Diagnostic accuracy of FRAX in predicting the 10-year risk of osteoporotic fractures using the USA treatment thresholds: a systematic review and meta-analysis. Bone. 2017;99:20-25.
The FRAX score has become a popular form of triage for women who do not yet meet the bone mass criteria of osteoporosis. Current practice guidelines recommend use of fracture risk scores for screening and pharmacologic therapeutic decision making. Some newer data, however, may give rise to questions about its utility, especially in younger women.
Fracture risk analysis in a large postmenopausal population
Gourlay and colleagues conducted a retrospective competing risk analysis of new occurrence of treatment-level and screening-level fracture risk scores. Study participants were postmenopausal women aged 50 years and older who had not previously received pharmacologic treatment and had not had a first hip or clinical vertebral facture.
Details of the study
In 54,280 postmenopausal women aged 50 to 64 years who did not have a bone mineral density test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because the incidence of treatment-level scores was rare.
A total of 6,096 women had FRAX scores calculated with bone mineral density testing. In this group, the estimated unadjusted time to treatment-level FRAX scores was 7.6 years (95% CI, 6.6-8.7) for those aged 65 to 69, and 5.1 years (95% CI, 3.5-7.5) for women aged 75 to 79 at baseline.
Of 17,967 women aged 50 to 64 who had a screening-level FRAX at baseline, 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65 years.
Age is key factor. Gourlay and colleagues concluded that postmenopausal women who had subthreshold fracture risk scores at baseline would be unlikely to develop a treatment-level FRAX score between ages 50 and 64. The increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture after age 65, however, supports more frequent consideration of FRAX assessment and bone mineral density testing.
Related article:
2015 Update on osteoporosis
Meta-analysis of FRAX tool accuracy
In another study, Jiang and colleagues conducted a systematic review and meta-analysis to determine how the FRAX score performed in predicting the 10-year risk of major osteoporotic fractures and hip fractures. The investigators used the US treatment thresholds.
Details of the study
Seven studies (n = 57,027) were analyzed to assess the diagnostic accuracy of FRAX in predicting major osteoporotic fractures; 20% was used as the 10-year fracture risk threshold for intervention. The mean sensitivity and specificity, along with their 95% CIs, were 10.25% (3.76%-25.06%) and 97.02% (91.17%-99.03%), respectively.
For hip fracture prediction, 6 studies (n = 50,944) were analyzed, and 3% was used as the 10-year fracture risk threshold. The mean sensitivity and specificity, along with their 95% CIs, were 45.70% (24.88%-68.13%) and 84.70% (76.41%-90.44%), respectively.
Predictive value of FRAX. The authors concluded that, using the 10-year intervention thresholds of 20% for major osteoporotic fracture and 3% for hip fracture, FRAX performed better in identifying individuals who will not have a major osteoporotic fracture or hip fracture within 10 years than in identifying those who will experience a fracture. A substantial number of those who developed fractures, especially major osteoporotic fracture within 10 years of follow up, were missed by the baseline FRAX assessment.
Increasing age is still arguably among the most important factors for decreasing bone health. Older women are more likely to develop treatment-level FRAX scores more quickly than younger women. In addition, the FRAX tool is better in predicting which women will not develop a fracture in the next 10 years than in predicting those who will experience a fracture.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Bone health remains one of the most important health care concerns in the United States today. In 2004, the Surgeon General released a report on bone health and osteoporosis. According to the report’s introduction:
This first-ever Surgeon General’s Report on bone health and osteoporosis illustrates the large burden that bone disease places on our Nation and its citizens. Like other chronic diseases that disproportionately affect the elderly, the prevalence of bone disease and fractures is projected to increase markedly as the population ages. If these predictions come true, bone disease and fractures will have a tremendous negative impact on the future well-being of Americans. But as this report makes clear, they need not come true: by working together we can change the picture of aging in America. Osteoporosis and fractures…no longer should be thought of as an inevitable part of growing old. By focusing on prevention and lifestyle changes, including physical activity and nutrition, as well as early diagnosis and appropriate treatment, Americans can avoid much of the damaging impact of bone disease.1
Related article:
2016 Update on bone health
Although men also experience osteoporosis as they age, in women the rapid loss of bone at menopause makes their disease burden much greater. As women’s health care providers, we stand at the front line for preventing, diagnosing, and treating osteoporosis to reduce the impact of this disease. In this Update I focus on important information that has emerged in the past year.
Read about new ACP guidelines to assess fracture risk
Guidelines for therapy: How to assess fracture risk and when to treat
American College of Obstetricians and Gynecologists Committee on Practice Bulletins--Gynecology. ACOG Practice Bulletin No. 129: Osteoporosis. Obstet Gynecol. 2012;120(3):718-734.
Qaseem A, Forciea MA, McLean RM, Denberg TD; Clinical Guidelines Committee of the American College of Physicians. Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166(11):818-839.
A crucial component for good bone health maintenance and osteoporotic fracture prevention is understanding the current guidelines for therapy. The most recent practice bulletin of the American College of Obstetricians and Gynecologists (ACOG) on osteoporosis was published in 2012. ACOG states that treatment be recommended for women who have a bone mineral density (BMD) T-score of -2.5 or lower.
For women in the low bone mass category (T-score between -1 and -2.5), use of the Fracture Risk Assessment Tool (FRAX) calculator can assist in making an informed treatment decision.2 Based on the FRAX calculator, women who have a 10-year risk of major osteoporotic fracture of 20% or greater, or a risk of hip fracture of 3% or greater, are candidates for pharmacologic therapy.
Women who have experienced a low-trauma fracture (especially of the vertebra or hip) also are candidates for treatment, even in the absence of osteoporosis on a dual-energy x-ray absorptiometry (DXA) report.
Related article:
Women’s Preventive Services Initiative Guidelines provide consensus for practicing ObGyns
Updated recommendations from the ACP
The 2017 guideline published by the American College of Physicians (ACP), whose target audience is "all clinicians," recommends that, for women who have known osteoporosis, clinicians offer pharmacologic treatment with alendronate, risedronate, zoledronic acid, or denosumab to reduce the risk for hip and vertebral fractures.
In addition, the ACP recommends that clinicians make the decision whether or not to treat osteopenic women 65 years of age or older who are at a high risk for fracture based on a discussion of patient preferences, fracture risk profile, and benefits, harms, and costs of medications. This may seem somewhat contradictory to ACOG's guidance vis-a-vis women younger than 65 years of age.
The ACP further states that given the limited evidence supporting the benefit of treatment, the balance of benefits and harms in treating osteopenic women is most favorable when the risk for fracture is high. Women younger than 65 years with osteopenia and women older than 65 years with mild osteopenia (T-score between -1.0 and -1.5) will benefit less than women who are 65 years of age or older with severe osteopenia (T-score <-2.0).
Risk factors and risk assessment tools
Clinicians can use their own judgment based on risk factors for fracture (lower body weight, smoking, weight loss, family history of fractures, decreased physical activity, alcohol or caffeine use, low calcium and vitamin D intake, corticosteroid use), or they can use a risk assessment tool. Several risk assessment tools, such as the FRAX calculator mentioned earlier, are available to predict fracture risk among untreated people with low bone density. Although the FRAX calculator is widely used, there is no evidence from randomized controlled trials demonstrating a benefit of fracture reduction when FRAX scores are used in treatment decision making.
Duration of therapy. The ACP recommends that clinicians treat osteoporotic women with pharmacologic therapy for 5 years. Bone density monitoring is not recommended during the 5-year treatment period for osteoporosis in women; current evidence does not show any benefit for bone density monitoring during treatment.
Moderate-quality evidence demonstrated that women treated with antiresorptive therapies (including bisphosphonates, raloxifene, and teriparatide) benefited from reduced fractures, even if no increase in BMD occurred or if BMD decreased.
As before, all women with osteoporosis or a previous low-trauma fracture should be treated. Use of the FRAX calculator should involve clinician judgment, and other risk factors should be taken into account. For most women, treatment should be continued for 5 years. There is no benefit in continued bone mass assessment (DXA testing) while a patient is on pharmacologic therapy.
Read about fracture risk after stopping HT
Another WHI update: No increase in fractures after stopping HT
Watts NB, Cauley JA, Jackson RD, et al; Women's Health Initiative Investigators. No increase in fractures after stopping hormone therapy: results from the Women's Health Initiative. J Clin Endocrinol Metab. 2017;102(1):302-308.
The analysis and reanalysis of the Women's Health Initiative (WHI) trial data seems never-ending, yet the article by Watts and colleagues is important. Although the WHI hormone therapy (HT) trials showed that treatment protects against hip and total fractures, a later observational report suggested loss of benefit and rebound increased risk after HT was discontinued.3 The purpose of the Watts' study was to examine fractures after stopping HT.
Related article:
Did long-term follow-up of WHI participants reveal any mortality increase among women who received HT?
Details of the study
Two placebo-controlled randomized trials served as the study setting. The study included WHI participants (n = 15,187) who continued to take active HT or placebo through the intervention period and who did not take HT in the postintervention period. The trial interventions included conjugated equine estrogen (CEE) plus medroxyprogesterone acetate (MPA) for women with natural menopause and CEE alone for women with prior hysterectomy. The investigators recorded total fractures and hip fractures through 5 years after HT discontinuation.
Findings on fractures. Hip fractures occurred infrequently, with approximately 2.5 per 1,000 person-years. This finding was similar between trials and in former HT users and placebo groups.
No difference was found in total fractures in the CEE plus MPA trial for former HT users compared with former placebo users (28.9 per 1,000 person-years and 29.9 per 1,000 person-years, respectively; hazard ratio [HR], 0.97; 95% confidence interval [CI], 0.87-1.09; P = .63). In the CEE-alone trial, however, total fractures were higher in former placebo users (36.9 per 1,000 person-years) compared with the former active-treatment group (31.1 per 1,000 person-years). This finding suggests a residual benefit of CEE in reducing total fractures (HR, 0.85; 95% CI, 0.73-0.98; P = .03).
Investigators' takeaway. The authors concluded that, after discontinuing HT, there was no evidence of increased fracture risk (sustained or transient) in former HT users compared with former placebo users. In the CEE-alone trial, there was a residual benefit for total fracture reduction in former HT users compared with placebo users.
Gynecologists have long believed that on stopping HT, the loss of bone mass will follow at the same rate as it would at natural menopause. These WHI trials demonstrate, however, that through 5 years, women who stopped HT had no increase in hip or total fractures, and hysterectomized women who stopped estrogen therapy actually had fewer fractures than the placebo group. Keep in mind that this large cohort was not chosen based on risk of osteoporotic fractures. In fact, baseline bone mass was not even measured in these women, making the results even more "real world."
Read about reassessing FRAX scores
A new look at fracture risk assessment scores
Gourlay ML, Overman RA, Fine JP, et al; Women's Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-e23.
Jiang X, Gruner M, Trémollieres F, et al. Diagnostic accuracy of FRAX in predicting the 10-year risk of osteoporotic fractures using the USA treatment thresholds: a systematic review and meta-analysis. Bone. 2017;99:20-25.
The FRAX score has become a popular form of triage for women who do not yet meet the bone mass criteria of osteoporosis. Current practice guidelines recommend use of fracture risk scores for screening and pharmacologic therapeutic decision making. Some newer data, however, may give rise to questions about its utility, especially in younger women.
Fracture risk analysis in a large postmenopausal population
Gourlay and colleagues conducted a retrospective competing risk analysis of new occurrence of treatment-level and screening-level fracture risk scores. Study participants were postmenopausal women aged 50 years and older who had not previously received pharmacologic treatment and had not had a first hip or clinical vertebral facture.
Details of the study
In 54,280 postmenopausal women aged 50 to 64 years who did not have a bone mineral density test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because the incidence of treatment-level scores was rare.
A total of 6,096 women had FRAX scores calculated with bone mineral density testing. In this group, the estimated unadjusted time to treatment-level FRAX scores was 7.6 years (95% CI, 6.6-8.7) for those aged 65 to 69, and 5.1 years (95% CI, 3.5-7.5) for women aged 75 to 79 at baseline.
Of 17,967 women aged 50 to 64 who had a screening-level FRAX at baseline, 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65 years.
Age is key factor. Gourlay and colleagues concluded that postmenopausal women who had subthreshold fracture risk scores at baseline would be unlikely to develop a treatment-level FRAX score between ages 50 and 64. The increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture after age 65, however, supports more frequent consideration of FRAX assessment and bone mineral density testing.
Related article:
2015 Update on osteoporosis
Meta-analysis of FRAX tool accuracy
In another study, Jiang and colleagues conducted a systematic review and meta-analysis to determine how the FRAX score performed in predicting the 10-year risk of major osteoporotic fractures and hip fractures. The investigators used the US treatment thresholds.
Details of the study
Seven studies (n = 57,027) were analyzed to assess the diagnostic accuracy of FRAX in predicting major osteoporotic fractures; 20% was used as the 10-year fracture risk threshold for intervention. The mean sensitivity and specificity, along with their 95% CIs, were 10.25% (3.76%-25.06%) and 97.02% (91.17%-99.03%), respectively.
For hip fracture prediction, 6 studies (n = 50,944) were analyzed, and 3% was used as the 10-year fracture risk threshold. The mean sensitivity and specificity, along with their 95% CIs, were 45.70% (24.88%-68.13%) and 84.70% (76.41%-90.44%), respectively.
Predictive value of FRAX. The authors concluded that, using the 10-year intervention thresholds of 20% for major osteoporotic fracture and 3% for hip fracture, FRAX performed better in identifying individuals who will not have a major osteoporotic fracture or hip fracture within 10 years than in identifying those who will experience a fracture. A substantial number of those who developed fractures, especially major osteoporotic fracture within 10 years of follow up, were missed by the baseline FRAX assessment.
Increasing age is still arguably among the most important factors for decreasing bone health. Older women are more likely to develop treatment-level FRAX scores more quickly than younger women. In addition, the FRAX tool is better in predicting which women will not develop a fracture in the next 10 years than in predicting those who will experience a fracture.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- United States Office of the Surgeon General. Bone health and osteoporosis: a report of the Surgeon General. Rockville, Maryland: Office of the Surgeon General (US); 2004. https://www.ncbi.nlm.nih.gov/books/NBK45513/. Accessed November 6, 2017.
- Centre for Metabolic Bone Diseases, University of Sheffield, United Kingdom. FRAX Fracture Risk Assessment Tool website. www.sheffield.ac.uk/FRAX. Accessed November 6, 2017.
- Yates J, Barrett-Connor E, Barlas S, Chen YT, Miller PD, Siris ES. Rapid loss of hip fracture protection after estrogen cessation: evidence from the National Osteoporosis Risk Assessment. Obstet Gynecol. 2004;103(3):440–446.
- United States Office of the Surgeon General. Bone health and osteoporosis: a report of the Surgeon General. Rockville, Maryland: Office of the Surgeon General (US); 2004. https://www.ncbi.nlm.nih.gov/books/NBK45513/. Accessed November 6, 2017.
- Centre for Metabolic Bone Diseases, University of Sheffield, United Kingdom. FRAX Fracture Risk Assessment Tool website. www.sheffield.ac.uk/FRAX. Accessed November 6, 2017.
- Yates J, Barrett-Connor E, Barlas S, Chen YT, Miller PD, Siris ES. Rapid loss of hip fracture protection after estrogen cessation: evidence from the National Osteoporosis Risk Assessment. Obstet Gynecol. 2004;103(3):440–446.
Recognize and treat iron deficiency anemia in pregnant women
All mammalian life is dependent on a continuous supply of molecular oxygen. Molecular oxygen is carried to cells by noncovalent binding to the iron moiety in the hemoglobin of red blood cells. It is utilized within cells by noncovalent binding to the iron moiety in various microsomal and mitochondrial proteins, including myoglobin and cytochromes. Consequently, to efficiently utilize molecular oxygen all mammalian life is dependent on an adequate supply of iron. Surprisingly, in an era of high technology precision medicine, many pregnant women are iron deficient, anemic, and not receiving adequate iron supplementation.
Iron deficiency is prevalent in women and pregnant women
Women often become iron deficient because of pregnancy or heavy menstrual bleeding. During pregnancy, maternal iron is provided to supply the needs of the fetus and placenta. Additional iron is needed to expand maternal red blood cell volume and replace iron lost due to bleeding at delivery. In the National Health and Nutrition Examination Survey (NHANES) of 1988–1994, 11% of women aged 16 to 49 years were iron deficient. By contrast, less than 1% of men aged 16 to 49 years were iron deficient.1
In a NHANES study from 1999–2006, risk factors for iron deficiency included multiparity, current pregnancy, and regular menstrual cycles. Use of hormonal contraception reduced the rate of iron deficiency.2 Using the same data, the prevalences of iron deficiency during the first, second, and third trimesters of pregnancy were reported to be 7%, 14%, and 30%, respectively.3 In addition to pregnancy and menstrual bleeding there are many other medical problems that may contribute to iron deficiency, including Helicobacter pylori (H pylori) infection, gastritis, celiac disease, and bariatric surgery.
Iron deficiency anemia may be associated with adverse pregnancy outcomes
In a retrospective study of 75,660 singleton pregnancies, 7,977 women were diagnosed with iron deficiency anemia when they were admitted for delivery. Compared with pregnant women without iron deficiency, the presence of iron deficiency increased the risk of:
- blood transfusion (odds ratio [OR], 5.48; 95% confidence interval [CI], 4.57–6.58)
- preterm delivery (OR, 1.54; 95% CI, 1.36–1.76)
- cesarean delivery (OR, 1.30; 95% CI, 1.13–1.49)
- 5-minute Apgar score <7 (OR, 2.21; 95% CI, 1.84–2.64)
- intensive care unit (ICU) admission (OR, 1.28; 95% CI, 1.20–1.39).4
In a systematic review and meta-analysis of 26 studies, maternal anemia (mostly iron deficiency anemia) was associated with a higher risk of low birth weight (relative risk [RR], 1.31; 95% CI, 1.13–1.51), preterm birth (RR, 1.63; 95% CI, 1.33–2.01), perinatal mortality (RR, 1.51; 95% CI, 1.30–1.76), and neonatal mortality (RR, 2.72; 95% CI, 1.19–6.25).5
In a clinical trial, pregnant women were randomly assigned to receive folic acid alone; folic acid plus iron supplements; or 15 vitamins and minerals, including folic acid and iron. At delivery, women in the iron-folic acid and the 15 vitamin and minerals groups had higher hemoglobin concentrations than the folic acid monotherapy group. Among 4,697 live births, women in the iron-folic acid group had significantly fewer preterm births (<34 weeks’ gestation) than the folic acid group (RR, 0.50; 95% CI, 0.27–0.94; P = .031).6 Data from additional randomized trials are needed to further clarify the effect of iron supplementation on obstetric outcomes.
Related article:
Treating polycystic ovary syndrome: Start using dual medical therapy
The diagnosis of iron deficiency is optimized by measuring serum ferritin
Serum ferritin measurement is an excellent test of iron deficiency. We recommend that all pregnant women have serum ferritin measured at the first prenatal visit and at the beginning of the third trimester to assess maternal iron stores. In pregnancy, the Centers for Disease Control and Prevention and the World Health Organization define anemia as a hemoglobin level of less than 11 g/dL or hematocrit less than 33% in the first and third trimesters. If a pregnant woman is not anemic, a serum ferritin level less than 15 ng/mL indicates iron deficiency.7 Some experts believe that in pregnant women who are not anemic, a serum ferritin level between 15 and 30 ng/mL may also indicate iron deficiency.8 If the pregnant woman is anemic and does not have another cause of the anemia, a serum ferritin level less than 40 ng/mL is indicative of iron deficiency.7
Ferritin is an acute phase reactant and levels may be falsely elevated due to chronic or acute inflammation, liver disease, renal failure, metabolic syndrome, or malignancy. Some women with iron deficiency due to bariatric surgery or malabsorption also have vitamin B12 and, less commonly, folate deficiency, which can contribute to the development of anemia (see “Diagnosis of anemia, iron deficiency, and iron deficiency anemia in pregnancy.”) Clinicians are often advised that a mean corpuscular volume demonstrating microcytosis is the “best test” to assess a patient for iron deficiency. However, reduced iron availability and low ferritin precede microcytosis. Hence microcytosis is a lagging measure and iron deficiency is diagnosed at an earlier stage by ferritin.
Requirements for a diagnosis of anemia in pregnancy
The American College of Obstetricians and Gynecologists recommends obtaining a hemoglobin and hematocrit test at the first prenatal visit and at the beginning of the third trimester of pregnancy.1
If the hemoglobin concentration is less than 11 g/dL, or hematocrit is less than 33%, anemia is present.2,3
If anemia is diagnosed, additional testing to investigate potential causes of anemia includes hemoglobin electrophoresis and measurement of vitamin B12 and folate levels. Many obstetricians perform hemoglobin electrophoresis on all their pregnant patients as part of the routine prenatal screen.
Requirements for a diagnosis of iron deficiency in pregnancy
We recommend obtaining a ferritin measurement at the first prenatal visit and at the beginning of the third trimester.
In pregnant women with anemia, iron deficiency is present if the ferritin is less than 40 ng/mL.
If a pregnant woman is not anemic, iron deficiency is present if the ferritin is less than 15 ng/mL.4
Requirements for a diagnosis of iron deficiency anemia
Hemoglobin concentration less than 11 g/dL, or hematocrit less than 33% (diagnosis of anemia).
PLUS
Ferritin less than 40 ng/mL (diagnosis of iron deficiency in an anemic woman)
PLUS
Evaluation for other known major causes of anemia, including blood loss, hemolysis, bone marrow disease, medications that suppress bone marrow function, kidney disease, malignancy, hemoglobinopathy, and vitamin B12 or folate deficiency.
References
- Guidelines for Perinatal Care. 8th ed. Washington DC: American Academy of Pediatrics, American College of Obstetricians and Gynecologists;2017.
- Centers for Disease Control and Prevention. CDC criteria for anemia in children and childbearing-aged women. MMWR Morb Mortal Wkly Rep. 1989;38(22):400-404.
- World Health Organization. Iron deficiency anaemia: assessment, prevention and control. A guide for programme managers. World Health Organization: Geneva, Switzerland; 2001. http://www.who.int/nutrition/publications/en/ida_assessment_prevention_control.pdf. Accessed November 8, 2017.
- Guyatt GH, Oxman AD, Ali M, Willan A, McIlroy W, Patterson C. Laboratory diagnosis of iron-deficiency: an overview. J Gen Intern Med. 1992;7(2):145-153.
Dietary iron
Iron in food is present in heme (meat, poultry, fish) and non-heme forms (grains, plant food, supplements). Heme iron is better absorbed than non-heme iron. Foods rich in non-heme iron include spinach, lentils, prune juice, dried prunes, and fortified cereals. Absorption of non-heme iron can be increased by vitamin C or vitamin C–rich foods (broccoli, bell peppers, cantaloupe, grapefruit, oranges, strawberries, and tomatoes). Absorption of non-heme iron is reduced by consumption of dairy products, coffee, tea, and chocolate.
Oral iron treatment
Oral iron is an effective treatment for iron deficiency9,10 and is inexpensive, safe, and widely available. The CDC recommends that all pregnant women take a 30 mg/day iron supplement, unless they have hemochromatosis.11 For women with a low ferritin level and anemia, iron supplementation should be increased to 30 to 120 mg daily.11 Not all prenatal vitamins contain iron; those that do typically contain 17 to 28 mg of elemental iron per dose.
Many pregnant women taking oral iron, especially at doses greater than 30 mg daily, have gastrointestinal side effects, which cause them to discontinue the iron therapy.12 Taking iron supplementation on an intermittent basis may help to reduce gastrointestinal side effects and improve iron stores.13
In the past, a standard approach to the treatment of iron deficiency anemia was oral ferrous sulfate 325 mg (65 mg elemental iron) spaced in 3 doses each day for a total daily dose of 195 mg elemental iron. However, recent absorption studies concluded that maximal absorption of iron occurs with a dose in the range of 40 to 80 mg of elemental iron daily. Greater doses do not result in more iron absorption and are associated with more side effects.14,15 (See “Start using alternate-day oral iron dosing, and stop using daily iron dosing.”)
Recent research reports alternate-day oral iron dosing compared with daily oral iron dosing results in higher absorption of iron.
Details of the study
A total of 40 iron deficient women (mean serum ferritin level, 14 ng/mL) were randomly assigned to receive a daily dose of 60 mg of elemental iron (325 mg of ferrous sulfate) for 14 days or an alternate-day dose of 60 mg for 28 days. A small amount of radioactive iron was added to the oral medication to assess iron absorption. The primary outcome was fractional and total iron absorption, calculated by measuring radioactive iron in circulating red blood cells 14 days after the final oral iron dose.
Alternate-day iron dosing, compared with daily dosing, resulted in a higher fraction of the iron dose being absorbed (22% vs 16%; P = .0013). In addition, alternate-day iron dosing resulted in greater cumulative total iron absorption (175 mg vs 131 mg; P = .001). Nausea was reported less frequently by women in the alternate-day dosing group (11%) than in the daily iron dose group (29%).
The investigators concluded that prescribing iron as a single alternate-day
dose may be a superior dosing regimen compared with daily dosing.
Reference
- Stoffel NU, Cercamondi CI, Brittenham G, et al. Iron absorption from oral iron supplements given on consecutive versus alternate days and as single morning doses versus twice-daily split dosing in iron-depleted women: two open-label, randomised controlled trials. Lancet Haematol. 2017;4(11):e524–e533.
Oral iron should not be taken in close approximation to the consumption of milk, cereals, tea, coffee, eggs, or calcium supplements. The absorption of oral iron is enhanced by the consumption of orange juice or 250 mg of vitamin C. Gastrointestinal side effects include nausea, flatulence, constipation, diarrhea, epigastric distress, and vomiting. If gastrointestinal side effects occur, interventions that might improve tolerability include: reduce the dose of iron or administer intermittently or use a low dose of oral iron, where dosing can be more easily titrated.
We re-check ferritin and hemoglobin levels 2 to 4 weeks after initiation of oral iron therapy and expect to see a hemoglobin rise of 1 g/dL if the therapy is effective.
Intravenous iron treatment
For women with iron deficiency anemia who cannot tolerate oral iron or in whom oral iron treatment has not resolved their anemia, intravenous (IV) iron treatment may be an optimal approach. Women in the third trimester of pregnancy with iron deficiency anemia have very little time to consume sufficient quantities of oral iron in food and supplements to restore their deficiency and reverse their anemia. Consequently, treatment with IV iron may be especially appropriate for women with iron deficiency anemia in the third trimester of pregnancy. Prior gastric surgery, including gastric bypass, results in reduced gastric acid production and causes severe impairment of intestinal absorption of iron. Patients with malabsorption syndromes, including celiac disease, also may have limited absorption of oral iron. These populations of pregnant women may particularly benefit from the use of IV iron. In pregnant women IV iron has fewer gastrointestinal side effects than oral iron.16
Many severely iron deficient patients need 1,000 mg of iron to resolve their deficit. In order to avoid giving multiple standard doses (200 mg per infusion, with 5 infusions over many days), some centers have explored the use of 1 large dose of IV iron (1,000 mg of low molecular weight iron dextran administered over 1 hour) (INFeD, Watson Pharma).17–19 This is not a regimen that is specifically approved by the US Food and Drug Administration. An alternative regimen is to administer 750 mg of ferrous carboxymaltose (Injectafer, Luitpold Pharmaceuticals) over 15 minutes, which is an FDA-approved regimen.18 Many hematologists prefer to administer multiple smaller doses of iron. For example, in our practice, pregnant women are commonly treated with IV iron sucrose (300 mg) every 2 weeks for 3 doses. To increase access of pregnant women to IV iron treatment, obstetricians need to work with hematologists and infusion centers to create collaborative protocols to expeditiously treat women in the third trimester.
There is an epidemic of iron deficiency in pregnant women in the United States. In an era of high technology medicine, it is surprising that iron deficiency remains an unsolved obstetric problem in our country.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Looker AC, Dallman PR, Carroll MD, Gunter EW, Johnson CL. Prevalence of iron deficiency in the United States. JAMA. 1997;277(12):973–976.
- Miller EM. Iron status and reproduction in US women: National Health and Nutrition Examination Survey 1999–2006. PLoS One. 2014;9(11):e112216.
- Mei Z, Cogswell ME, Looker AC, et al. Assessment of iron status in US pregnant women from the National Health and Nutrition Examination Survey (NHANES), 1999–2006. Am J Clin Nutr. 2011;93(6):1312–1320.
- Drukker L, Hants Y, Farkash R, Ruchlemer R, Samueloff A, Grisaru-Granovsky S. Iron deficiency anemia at admission for labor and delivery is associated with an increased risk for Cesarean section and adverse maternal and neonatal outcomes. Transfusion. 2015;55(12):2799–2806.
- Rahmann MM, Abe SK, Rahman MS, et al. Maternal anemia and risk of adverse birth and health outcomes in low- and middle-income countries: systematic review and meta-analysis. Am J Clin Nutr. 2016;103(2):495–504.
- Zeng L, Dibley MJ, Cheng Y, et al. Impact of micronutrient supplementation during pregnancy on birth weight, duration of gestation, and perinatal mortality in rural western China: double blind cluster randomised controlled trial. BMJ. 2008;337:a2001.
- Guyatt GH, Oxman AD, Ali M, Willan A, McIlroy W, Patterson C. Laboratory diagnosis of iron-deficiency: an overview. J Gen Intern Med. 1992;7(2):145–153.
- van den Broek NR, Letsky EA, White SA, Shenkin A. Iron status in pregnant women: which measurements are valid? Br J Haematol. 1998;103(3):817–824.
- Peña-Rosas JP, De-Regil LM, Garcia-Casal MN, Dowswell T. Daily oral iron supplementation during pregnancy. Cochrane Database Syst Rev. 2015(7);CD004736.
- Cantor AG, Bougatsos C, Dana T, Blazina I, McDonagh M. Routine iron supplementation and screening for iron deficiency anemia in pregnancy: a systematic review for the US Preventive Services Task Force. Ann Intern Med. 2015;162(8):566–576.
- Centers for Disease Control and Prevention. Recommendations to prevent and control iron deficiency in the United States. MMWR Recomm Rep. 1998;47(RR-3):1–29.
- Tolkien Z, Stecher L, Mander AP, Pereira DI, Powell JJ. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis. PLoS One. 2015;10(2):e0117383.
- Peña-Rosas JP, De-Regil LM, Gomez Malave H, Flores-Urrutia MC, Dowswell T. Intermittent oral iron supplementation during pregnancy. Cochrane Database Syst Rev. 2015(10);CD009997.
- Moretti D, Goede JS, Zeder C, et al. Oral iron supplements increase hepcidin and decrease iron absorption from daily or twice-daily doses in iron-depleted young women. Blood. 2015;126(17):1981–1989.
- Schrier SL. So you know how to treat iron deficiency anemia. Blood. 2015;126(17):1971.
- Breymann C, Milman N, Mezzacasa A, Bernard R, Dudenhausen J; FER-ASAP investigators. Ferric carboxymaltose vs oral iron in the treatment of pregnant women with iron deficiency anemia: an international, open-label, randomized controlled trial (FER-ASAP). J Perinatal Med. 2017;45(4):443–453.
- Auerbach M, Pappadakis JA, Bahrain H, Auerbach SA, Ballard H, Dahl NV. Safety and efficacy of rapidly administered (one hour) one gram of low molecular weight iron dextran (INFeD) for the treatment of iron deficient anemia. Am J Hematol. 2011;86(10):860–862.
- Auerbach M, Adamson JW. How we diagnose and treat iron deficiency anemia. Am J Hematol. 2016;91(1):31–38.
- Wong L, Smith S, Gilstrop M, et al. Safety and efficacy of rapid (1,000 mg in 1 hr) intravenous iron dextran for treatment of maternal iron deficient anemia of pregnancy. Am J Hematol. 2016;91(6):590–593.
All mammalian life is dependent on a continuous supply of molecular oxygen. Molecular oxygen is carried to cells by noncovalent binding to the iron moiety in the hemoglobin of red blood cells. It is utilized within cells by noncovalent binding to the iron moiety in various microsomal and mitochondrial proteins, including myoglobin and cytochromes. Consequently, to efficiently utilize molecular oxygen all mammalian life is dependent on an adequate supply of iron. Surprisingly, in an era of high technology precision medicine, many pregnant women are iron deficient, anemic, and not receiving adequate iron supplementation.
Iron deficiency is prevalent in women and pregnant women
Women often become iron deficient because of pregnancy or heavy menstrual bleeding. During pregnancy, maternal iron is provided to supply the needs of the fetus and placenta. Additional iron is needed to expand maternal red blood cell volume and replace iron lost due to bleeding at delivery. In the National Health and Nutrition Examination Survey (NHANES) of 1988–1994, 11% of women aged 16 to 49 years were iron deficient. By contrast, less than 1% of men aged 16 to 49 years were iron deficient.1
In a NHANES study from 1999–2006, risk factors for iron deficiency included multiparity, current pregnancy, and regular menstrual cycles. Use of hormonal contraception reduced the rate of iron deficiency.2 Using the same data, the prevalences of iron deficiency during the first, second, and third trimesters of pregnancy were reported to be 7%, 14%, and 30%, respectively.3 In addition to pregnancy and menstrual bleeding there are many other medical problems that may contribute to iron deficiency, including Helicobacter pylori (H pylori) infection, gastritis, celiac disease, and bariatric surgery.
Iron deficiency anemia may be associated with adverse pregnancy outcomes
In a retrospective study of 75,660 singleton pregnancies, 7,977 women were diagnosed with iron deficiency anemia when they were admitted for delivery. Compared with pregnant women without iron deficiency, the presence of iron deficiency increased the risk of:
- blood transfusion (odds ratio [OR], 5.48; 95% confidence interval [CI], 4.57–6.58)
- preterm delivery (OR, 1.54; 95% CI, 1.36–1.76)
- cesarean delivery (OR, 1.30; 95% CI, 1.13–1.49)
- 5-minute Apgar score <7 (OR, 2.21; 95% CI, 1.84–2.64)
- intensive care unit (ICU) admission (OR, 1.28; 95% CI, 1.20–1.39).4
In a systematic review and meta-analysis of 26 studies, maternal anemia (mostly iron deficiency anemia) was associated with a higher risk of low birth weight (relative risk [RR], 1.31; 95% CI, 1.13–1.51), preterm birth (RR, 1.63; 95% CI, 1.33–2.01), perinatal mortality (RR, 1.51; 95% CI, 1.30–1.76), and neonatal mortality (RR, 2.72; 95% CI, 1.19–6.25).5
In a clinical trial, pregnant women were randomly assigned to receive folic acid alone; folic acid plus iron supplements; or 15 vitamins and minerals, including folic acid and iron. At delivery, women in the iron-folic acid and the 15 vitamin and minerals groups had higher hemoglobin concentrations than the folic acid monotherapy group. Among 4,697 live births, women in the iron-folic acid group had significantly fewer preterm births (<34 weeks’ gestation) than the folic acid group (RR, 0.50; 95% CI, 0.27–0.94; P = .031).6 Data from additional randomized trials are needed to further clarify the effect of iron supplementation on obstetric outcomes.
Related article:
Treating polycystic ovary syndrome: Start using dual medical therapy
The diagnosis of iron deficiency is optimized by measuring serum ferritin
Serum ferritin measurement is an excellent test of iron deficiency. We recommend that all pregnant women have serum ferritin measured at the first prenatal visit and at the beginning of the third trimester to assess maternal iron stores. In pregnancy, the Centers for Disease Control and Prevention and the World Health Organization define anemia as a hemoglobin level of less than 11 g/dL or hematocrit less than 33% in the first and third trimesters. If a pregnant woman is not anemic, a serum ferritin level less than 15 ng/mL indicates iron deficiency.7 Some experts believe that in pregnant women who are not anemic, a serum ferritin level between 15 and 30 ng/mL may also indicate iron deficiency.8 If the pregnant woman is anemic and does not have another cause of the anemia, a serum ferritin level less than 40 ng/mL is indicative of iron deficiency.7
Ferritin is an acute phase reactant and levels may be falsely elevated due to chronic or acute inflammation, liver disease, renal failure, metabolic syndrome, or malignancy. Some women with iron deficiency due to bariatric surgery or malabsorption also have vitamin B12 and, less commonly, folate deficiency, which can contribute to the development of anemia (see “Diagnosis of anemia, iron deficiency, and iron deficiency anemia in pregnancy.”) Clinicians are often advised that a mean corpuscular volume demonstrating microcytosis is the “best test” to assess a patient for iron deficiency. However, reduced iron availability and low ferritin precede microcytosis. Hence microcytosis is a lagging measure and iron deficiency is diagnosed at an earlier stage by ferritin.
Requirements for a diagnosis of anemia in pregnancy
The American College of Obstetricians and Gynecologists recommends obtaining a hemoglobin and hematocrit test at the first prenatal visit and at the beginning of the third trimester of pregnancy.1
If the hemoglobin concentration is less than 11 g/dL, or hematocrit is less than 33%, anemia is present.2,3
If anemia is diagnosed, additional testing to investigate potential causes of anemia includes hemoglobin electrophoresis and measurement of vitamin B12 and folate levels. Many obstetricians perform hemoglobin electrophoresis on all their pregnant patients as part of the routine prenatal screen.
Requirements for a diagnosis of iron deficiency in pregnancy
We recommend obtaining a ferritin measurement at the first prenatal visit and at the beginning of the third trimester.
In pregnant women with anemia, iron deficiency is present if the ferritin is less than 40 ng/mL.
If a pregnant woman is not anemic, iron deficiency is present if the ferritin is less than 15 ng/mL.4
Requirements for a diagnosis of iron deficiency anemia
Hemoglobin concentration less than 11 g/dL, or hematocrit less than 33% (diagnosis of anemia).
PLUS
Ferritin less than 40 ng/mL (diagnosis of iron deficiency in an anemic woman)
PLUS
Evaluation for other known major causes of anemia, including blood loss, hemolysis, bone marrow disease, medications that suppress bone marrow function, kidney disease, malignancy, hemoglobinopathy, and vitamin B12 or folate deficiency.
References
- Guidelines for Perinatal Care. 8th ed. Washington DC: American Academy of Pediatrics, American College of Obstetricians and Gynecologists;2017.
- Centers for Disease Control and Prevention. CDC criteria for anemia in children and childbearing-aged women. MMWR Morb Mortal Wkly Rep. 1989;38(22):400-404.
- World Health Organization. Iron deficiency anaemia: assessment, prevention and control. A guide for programme managers. World Health Organization: Geneva, Switzerland; 2001. http://www.who.int/nutrition/publications/en/ida_assessment_prevention_control.pdf. Accessed November 8, 2017.
- Guyatt GH, Oxman AD, Ali M, Willan A, McIlroy W, Patterson C. Laboratory diagnosis of iron-deficiency: an overview. J Gen Intern Med. 1992;7(2):145-153.
Dietary iron
Iron in food is present in heme (meat, poultry, fish) and non-heme forms (grains, plant food, supplements). Heme iron is better absorbed than non-heme iron. Foods rich in non-heme iron include spinach, lentils, prune juice, dried prunes, and fortified cereals. Absorption of non-heme iron can be increased by vitamin C or vitamin C–rich foods (broccoli, bell peppers, cantaloupe, grapefruit, oranges, strawberries, and tomatoes). Absorption of non-heme iron is reduced by consumption of dairy products, coffee, tea, and chocolate.
Oral iron treatment
Oral iron is an effective treatment for iron deficiency9,10 and is inexpensive, safe, and widely available. The CDC recommends that all pregnant women take a 30 mg/day iron supplement, unless they have hemochromatosis.11 For women with a low ferritin level and anemia, iron supplementation should be increased to 30 to 120 mg daily.11 Not all prenatal vitamins contain iron; those that do typically contain 17 to 28 mg of elemental iron per dose.
Many pregnant women taking oral iron, especially at doses greater than 30 mg daily, have gastrointestinal side effects, which cause them to discontinue the iron therapy.12 Taking iron supplementation on an intermittent basis may help to reduce gastrointestinal side effects and improve iron stores.13
In the past, a standard approach to the treatment of iron deficiency anemia was oral ferrous sulfate 325 mg (65 mg elemental iron) spaced in 3 doses each day for a total daily dose of 195 mg elemental iron. However, recent absorption studies concluded that maximal absorption of iron occurs with a dose in the range of 40 to 80 mg of elemental iron daily. Greater doses do not result in more iron absorption and are associated with more side effects.14,15 (See “Start using alternate-day oral iron dosing, and stop using daily iron dosing.”)
Recent research reports alternate-day oral iron dosing compared with daily oral iron dosing results in higher absorption of iron.
Details of the study
A total of 40 iron deficient women (mean serum ferritin level, 14 ng/mL) were randomly assigned to receive a daily dose of 60 mg of elemental iron (325 mg of ferrous sulfate) for 14 days or an alternate-day dose of 60 mg for 28 days. A small amount of radioactive iron was added to the oral medication to assess iron absorption. The primary outcome was fractional and total iron absorption, calculated by measuring radioactive iron in circulating red blood cells 14 days after the final oral iron dose.
Alternate-day iron dosing, compared with daily dosing, resulted in a higher fraction of the iron dose being absorbed (22% vs 16%; P = .0013). In addition, alternate-day iron dosing resulted in greater cumulative total iron absorption (175 mg vs 131 mg; P = .001). Nausea was reported less frequently by women in the alternate-day dosing group (11%) than in the daily iron dose group (29%).
The investigators concluded that prescribing iron as a single alternate-day
dose may be a superior dosing regimen compared with daily dosing.
Reference
- Stoffel NU, Cercamondi CI, Brittenham G, et al. Iron absorption from oral iron supplements given on consecutive versus alternate days and as single morning doses versus twice-daily split dosing in iron-depleted women: two open-label, randomised controlled trials. Lancet Haematol. 2017;4(11):e524–e533.
Oral iron should not be taken in close approximation to the consumption of milk, cereals, tea, coffee, eggs, or calcium supplements. The absorption of oral iron is enhanced by the consumption of orange juice or 250 mg of vitamin C. Gastrointestinal side effects include nausea, flatulence, constipation, diarrhea, epigastric distress, and vomiting. If gastrointestinal side effects occur, interventions that might improve tolerability include: reduce the dose of iron or administer intermittently or use a low dose of oral iron, where dosing can be more easily titrated.
We re-check ferritin and hemoglobin levels 2 to 4 weeks after initiation of oral iron therapy and expect to see a hemoglobin rise of 1 g/dL if the therapy is effective.
Intravenous iron treatment
For women with iron deficiency anemia who cannot tolerate oral iron or in whom oral iron treatment has not resolved their anemia, intravenous (IV) iron treatment may be an optimal approach. Women in the third trimester of pregnancy with iron deficiency anemia have very little time to consume sufficient quantities of oral iron in food and supplements to restore their deficiency and reverse their anemia. Consequently, treatment with IV iron may be especially appropriate for women with iron deficiency anemia in the third trimester of pregnancy. Prior gastric surgery, including gastric bypass, results in reduced gastric acid production and causes severe impairment of intestinal absorption of iron. Patients with malabsorption syndromes, including celiac disease, also may have limited absorption of oral iron. These populations of pregnant women may particularly benefit from the use of IV iron. In pregnant women IV iron has fewer gastrointestinal side effects than oral iron.16
Many severely iron deficient patients need 1,000 mg of iron to resolve their deficit. In order to avoid giving multiple standard doses (200 mg per infusion, with 5 infusions over many days), some centers have explored the use of 1 large dose of IV iron (1,000 mg of low molecular weight iron dextran administered over 1 hour) (INFeD, Watson Pharma).17–19 This is not a regimen that is specifically approved by the US Food and Drug Administration. An alternative regimen is to administer 750 mg of ferrous carboxymaltose (Injectafer, Luitpold Pharmaceuticals) over 15 minutes, which is an FDA-approved regimen.18 Many hematologists prefer to administer multiple smaller doses of iron. For example, in our practice, pregnant women are commonly treated with IV iron sucrose (300 mg) every 2 weeks for 3 doses. To increase access of pregnant women to IV iron treatment, obstetricians need to work with hematologists and infusion centers to create collaborative protocols to expeditiously treat women in the third trimester.
There is an epidemic of iron deficiency in pregnant women in the United States. In an era of high technology medicine, it is surprising that iron deficiency remains an unsolved obstetric problem in our country.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
All mammalian life is dependent on a continuous supply of molecular oxygen. Molecular oxygen is carried to cells by noncovalent binding to the iron moiety in the hemoglobin of red blood cells. It is utilized within cells by noncovalent binding to the iron moiety in various microsomal and mitochondrial proteins, including myoglobin and cytochromes. Consequently, to efficiently utilize molecular oxygen all mammalian life is dependent on an adequate supply of iron. Surprisingly, in an era of high technology precision medicine, many pregnant women are iron deficient, anemic, and not receiving adequate iron supplementation.
Iron deficiency is prevalent in women and pregnant women
Women often become iron deficient because of pregnancy or heavy menstrual bleeding. During pregnancy, maternal iron is provided to supply the needs of the fetus and placenta. Additional iron is needed to expand maternal red blood cell volume and replace iron lost due to bleeding at delivery. In the National Health and Nutrition Examination Survey (NHANES) of 1988–1994, 11% of women aged 16 to 49 years were iron deficient. By contrast, less than 1% of men aged 16 to 49 years were iron deficient.1
In a NHANES study from 1999–2006, risk factors for iron deficiency included multiparity, current pregnancy, and regular menstrual cycles. Use of hormonal contraception reduced the rate of iron deficiency.2 Using the same data, the prevalences of iron deficiency during the first, second, and third trimesters of pregnancy were reported to be 7%, 14%, and 30%, respectively.3 In addition to pregnancy and menstrual bleeding there are many other medical problems that may contribute to iron deficiency, including Helicobacter pylori (H pylori) infection, gastritis, celiac disease, and bariatric surgery.
Iron deficiency anemia may be associated with adverse pregnancy outcomes
In a retrospective study of 75,660 singleton pregnancies, 7,977 women were diagnosed with iron deficiency anemia when they were admitted for delivery. Compared with pregnant women without iron deficiency, the presence of iron deficiency increased the risk of:
- blood transfusion (odds ratio [OR], 5.48; 95% confidence interval [CI], 4.57–6.58)
- preterm delivery (OR, 1.54; 95% CI, 1.36–1.76)
- cesarean delivery (OR, 1.30; 95% CI, 1.13–1.49)
- 5-minute Apgar score <7 (OR, 2.21; 95% CI, 1.84–2.64)
- intensive care unit (ICU) admission (OR, 1.28; 95% CI, 1.20–1.39).4
In a systematic review and meta-analysis of 26 studies, maternal anemia (mostly iron deficiency anemia) was associated with a higher risk of low birth weight (relative risk [RR], 1.31; 95% CI, 1.13–1.51), preterm birth (RR, 1.63; 95% CI, 1.33–2.01), perinatal mortality (RR, 1.51; 95% CI, 1.30–1.76), and neonatal mortality (RR, 2.72; 95% CI, 1.19–6.25).5
In a clinical trial, pregnant women were randomly assigned to receive folic acid alone; folic acid plus iron supplements; or 15 vitamins and minerals, including folic acid and iron. At delivery, women in the iron-folic acid and the 15 vitamin and minerals groups had higher hemoglobin concentrations than the folic acid monotherapy group. Among 4,697 live births, women in the iron-folic acid group had significantly fewer preterm births (<34 weeks’ gestation) than the folic acid group (RR, 0.50; 95% CI, 0.27–0.94; P = .031).6 Data from additional randomized trials are needed to further clarify the effect of iron supplementation on obstetric outcomes.
Related article:
Treating polycystic ovary syndrome: Start using dual medical therapy
The diagnosis of iron deficiency is optimized by measuring serum ferritin
Serum ferritin measurement is an excellent test of iron deficiency. We recommend that all pregnant women have serum ferritin measured at the first prenatal visit and at the beginning of the third trimester to assess maternal iron stores. In pregnancy, the Centers for Disease Control and Prevention and the World Health Organization define anemia as a hemoglobin level of less than 11 g/dL or hematocrit less than 33% in the first and third trimesters. If a pregnant woman is not anemic, a serum ferritin level less than 15 ng/mL indicates iron deficiency.7 Some experts believe that in pregnant women who are not anemic, a serum ferritin level between 15 and 30 ng/mL may also indicate iron deficiency.8 If the pregnant woman is anemic and does not have another cause of the anemia, a serum ferritin level less than 40 ng/mL is indicative of iron deficiency.7
Ferritin is an acute phase reactant and levels may be falsely elevated due to chronic or acute inflammation, liver disease, renal failure, metabolic syndrome, or malignancy. Some women with iron deficiency due to bariatric surgery or malabsorption also have vitamin B12 and, less commonly, folate deficiency, which can contribute to the development of anemia (see “Diagnosis of anemia, iron deficiency, and iron deficiency anemia in pregnancy.”) Clinicians are often advised that a mean corpuscular volume demonstrating microcytosis is the “best test” to assess a patient for iron deficiency. However, reduced iron availability and low ferritin precede microcytosis. Hence microcytosis is a lagging measure and iron deficiency is diagnosed at an earlier stage by ferritin.
Requirements for a diagnosis of anemia in pregnancy
The American College of Obstetricians and Gynecologists recommends obtaining a hemoglobin and hematocrit test at the first prenatal visit and at the beginning of the third trimester of pregnancy.1
If the hemoglobin concentration is less than 11 g/dL, or hematocrit is less than 33%, anemia is present.2,3
If anemia is diagnosed, additional testing to investigate potential causes of anemia includes hemoglobin electrophoresis and measurement of vitamin B12 and folate levels. Many obstetricians perform hemoglobin electrophoresis on all their pregnant patients as part of the routine prenatal screen.
Requirements for a diagnosis of iron deficiency in pregnancy
We recommend obtaining a ferritin measurement at the first prenatal visit and at the beginning of the third trimester.
In pregnant women with anemia, iron deficiency is present if the ferritin is less than 40 ng/mL.
If a pregnant woman is not anemic, iron deficiency is present if the ferritin is less than 15 ng/mL.4
Requirements for a diagnosis of iron deficiency anemia
Hemoglobin concentration less than 11 g/dL, or hematocrit less than 33% (diagnosis of anemia).
PLUS
Ferritin less than 40 ng/mL (diagnosis of iron deficiency in an anemic woman)
PLUS
Evaluation for other known major causes of anemia, including blood loss, hemolysis, bone marrow disease, medications that suppress bone marrow function, kidney disease, malignancy, hemoglobinopathy, and vitamin B12 or folate deficiency.
References
- Guidelines for Perinatal Care. 8th ed. Washington DC: American Academy of Pediatrics, American College of Obstetricians and Gynecologists;2017.
- Centers for Disease Control and Prevention. CDC criteria for anemia in children and childbearing-aged women. MMWR Morb Mortal Wkly Rep. 1989;38(22):400-404.
- World Health Organization. Iron deficiency anaemia: assessment, prevention and control. A guide for programme managers. World Health Organization: Geneva, Switzerland; 2001. http://www.who.int/nutrition/publications/en/ida_assessment_prevention_control.pdf. Accessed November 8, 2017.
- Guyatt GH, Oxman AD, Ali M, Willan A, McIlroy W, Patterson C. Laboratory diagnosis of iron-deficiency: an overview. J Gen Intern Med. 1992;7(2):145-153.
Dietary iron
Iron in food is present in heme (meat, poultry, fish) and non-heme forms (grains, plant food, supplements). Heme iron is better absorbed than non-heme iron. Foods rich in non-heme iron include spinach, lentils, prune juice, dried prunes, and fortified cereals. Absorption of non-heme iron can be increased by vitamin C or vitamin C–rich foods (broccoli, bell peppers, cantaloupe, grapefruit, oranges, strawberries, and tomatoes). Absorption of non-heme iron is reduced by consumption of dairy products, coffee, tea, and chocolate.
Oral iron treatment
Oral iron is an effective treatment for iron deficiency9,10 and is inexpensive, safe, and widely available. The CDC recommends that all pregnant women take a 30 mg/day iron supplement, unless they have hemochromatosis.11 For women with a low ferritin level and anemia, iron supplementation should be increased to 30 to 120 mg daily.11 Not all prenatal vitamins contain iron; those that do typically contain 17 to 28 mg of elemental iron per dose.
Many pregnant women taking oral iron, especially at doses greater than 30 mg daily, have gastrointestinal side effects, which cause them to discontinue the iron therapy.12 Taking iron supplementation on an intermittent basis may help to reduce gastrointestinal side effects and improve iron stores.13
In the past, a standard approach to the treatment of iron deficiency anemia was oral ferrous sulfate 325 mg (65 mg elemental iron) spaced in 3 doses each day for a total daily dose of 195 mg elemental iron. However, recent absorption studies concluded that maximal absorption of iron occurs with a dose in the range of 40 to 80 mg of elemental iron daily. Greater doses do not result in more iron absorption and are associated with more side effects.14,15 (See “Start using alternate-day oral iron dosing, and stop using daily iron dosing.”)
Recent research reports alternate-day oral iron dosing compared with daily oral iron dosing results in higher absorption of iron.
Details of the study
A total of 40 iron deficient women (mean serum ferritin level, 14 ng/mL) were randomly assigned to receive a daily dose of 60 mg of elemental iron (325 mg of ferrous sulfate) for 14 days or an alternate-day dose of 60 mg for 28 days. A small amount of radioactive iron was added to the oral medication to assess iron absorption. The primary outcome was fractional and total iron absorption, calculated by measuring radioactive iron in circulating red blood cells 14 days after the final oral iron dose.
Alternate-day iron dosing, compared with daily dosing, resulted in a higher fraction of the iron dose being absorbed (22% vs 16%; P = .0013). In addition, alternate-day iron dosing resulted in greater cumulative total iron absorption (175 mg vs 131 mg; P = .001). Nausea was reported less frequently by women in the alternate-day dosing group (11%) than in the daily iron dose group (29%).
The investigators concluded that prescribing iron as a single alternate-day
dose may be a superior dosing regimen compared with daily dosing.
Reference
- Stoffel NU, Cercamondi CI, Brittenham G, et al. Iron absorption from oral iron supplements given on consecutive versus alternate days and as single morning doses versus twice-daily split dosing in iron-depleted women: two open-label, randomised controlled trials. Lancet Haematol. 2017;4(11):e524–e533.
Oral iron should not be taken in close approximation to the consumption of milk, cereals, tea, coffee, eggs, or calcium supplements. The absorption of oral iron is enhanced by the consumption of orange juice or 250 mg of vitamin C. Gastrointestinal side effects include nausea, flatulence, constipation, diarrhea, epigastric distress, and vomiting. If gastrointestinal side effects occur, interventions that might improve tolerability include: reduce the dose of iron or administer intermittently or use a low dose of oral iron, where dosing can be more easily titrated.
We re-check ferritin and hemoglobin levels 2 to 4 weeks after initiation of oral iron therapy and expect to see a hemoglobin rise of 1 g/dL if the therapy is effective.
Intravenous iron treatment
For women with iron deficiency anemia who cannot tolerate oral iron or in whom oral iron treatment has not resolved their anemia, intravenous (IV) iron treatment may be an optimal approach. Women in the third trimester of pregnancy with iron deficiency anemia have very little time to consume sufficient quantities of oral iron in food and supplements to restore their deficiency and reverse their anemia. Consequently, treatment with IV iron may be especially appropriate for women with iron deficiency anemia in the third trimester of pregnancy. Prior gastric surgery, including gastric bypass, results in reduced gastric acid production and causes severe impairment of intestinal absorption of iron. Patients with malabsorption syndromes, including celiac disease, also may have limited absorption of oral iron. These populations of pregnant women may particularly benefit from the use of IV iron. In pregnant women IV iron has fewer gastrointestinal side effects than oral iron.16
Many severely iron deficient patients need 1,000 mg of iron to resolve their deficit. In order to avoid giving multiple standard doses (200 mg per infusion, with 5 infusions over many days), some centers have explored the use of 1 large dose of IV iron (1,000 mg of low molecular weight iron dextran administered over 1 hour) (INFeD, Watson Pharma).17–19 This is not a regimen that is specifically approved by the US Food and Drug Administration. An alternative regimen is to administer 750 mg of ferrous carboxymaltose (Injectafer, Luitpold Pharmaceuticals) over 15 minutes, which is an FDA-approved regimen.18 Many hematologists prefer to administer multiple smaller doses of iron. For example, in our practice, pregnant women are commonly treated with IV iron sucrose (300 mg) every 2 weeks for 3 doses. To increase access of pregnant women to IV iron treatment, obstetricians need to work with hematologists and infusion centers to create collaborative protocols to expeditiously treat women in the third trimester.
There is an epidemic of iron deficiency in pregnant women in the United States. In an era of high technology medicine, it is surprising that iron deficiency remains an unsolved obstetric problem in our country.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Looker AC, Dallman PR, Carroll MD, Gunter EW, Johnson CL. Prevalence of iron deficiency in the United States. JAMA. 1997;277(12):973–976.
- Miller EM. Iron status and reproduction in US women: National Health and Nutrition Examination Survey 1999–2006. PLoS One. 2014;9(11):e112216.
- Mei Z, Cogswell ME, Looker AC, et al. Assessment of iron status in US pregnant women from the National Health and Nutrition Examination Survey (NHANES), 1999–2006. Am J Clin Nutr. 2011;93(6):1312–1320.
- Drukker L, Hants Y, Farkash R, Ruchlemer R, Samueloff A, Grisaru-Granovsky S. Iron deficiency anemia at admission for labor and delivery is associated with an increased risk for Cesarean section and adverse maternal and neonatal outcomes. Transfusion. 2015;55(12):2799–2806.
- Rahmann MM, Abe SK, Rahman MS, et al. Maternal anemia and risk of adverse birth and health outcomes in low- and middle-income countries: systematic review and meta-analysis. Am J Clin Nutr. 2016;103(2):495–504.
- Zeng L, Dibley MJ, Cheng Y, et al. Impact of micronutrient supplementation during pregnancy on birth weight, duration of gestation, and perinatal mortality in rural western China: double blind cluster randomised controlled trial. BMJ. 2008;337:a2001.
- Guyatt GH, Oxman AD, Ali M, Willan A, McIlroy W, Patterson C. Laboratory diagnosis of iron-deficiency: an overview. J Gen Intern Med. 1992;7(2):145–153.
- van den Broek NR, Letsky EA, White SA, Shenkin A. Iron status in pregnant women: which measurements are valid? Br J Haematol. 1998;103(3):817–824.
- Peña-Rosas JP, De-Regil LM, Garcia-Casal MN, Dowswell T. Daily oral iron supplementation during pregnancy. Cochrane Database Syst Rev. 2015(7);CD004736.
- Cantor AG, Bougatsos C, Dana T, Blazina I, McDonagh M. Routine iron supplementation and screening for iron deficiency anemia in pregnancy: a systematic review for the US Preventive Services Task Force. Ann Intern Med. 2015;162(8):566–576.
- Centers for Disease Control and Prevention. Recommendations to prevent and control iron deficiency in the United States. MMWR Recomm Rep. 1998;47(RR-3):1–29.
- Tolkien Z, Stecher L, Mander AP, Pereira DI, Powell JJ. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis. PLoS One. 2015;10(2):e0117383.
- Peña-Rosas JP, De-Regil LM, Gomez Malave H, Flores-Urrutia MC, Dowswell T. Intermittent oral iron supplementation during pregnancy. Cochrane Database Syst Rev. 2015(10);CD009997.
- Moretti D, Goede JS, Zeder C, et al. Oral iron supplements increase hepcidin and decrease iron absorption from daily or twice-daily doses in iron-depleted young women. Blood. 2015;126(17):1981–1989.
- Schrier SL. So you know how to treat iron deficiency anemia. Blood. 2015;126(17):1971.
- Breymann C, Milman N, Mezzacasa A, Bernard R, Dudenhausen J; FER-ASAP investigators. Ferric carboxymaltose vs oral iron in the treatment of pregnant women with iron deficiency anemia: an international, open-label, randomized controlled trial (FER-ASAP). J Perinatal Med. 2017;45(4):443–453.
- Auerbach M, Pappadakis JA, Bahrain H, Auerbach SA, Ballard H, Dahl NV. Safety and efficacy of rapidly administered (one hour) one gram of low molecular weight iron dextran (INFeD) for the treatment of iron deficient anemia. Am J Hematol. 2011;86(10):860–862.
- Auerbach M, Adamson JW. How we diagnose and treat iron deficiency anemia. Am J Hematol. 2016;91(1):31–38.
- Wong L, Smith S, Gilstrop M, et al. Safety and efficacy of rapid (1,000 mg in 1 hr) intravenous iron dextran for treatment of maternal iron deficient anemia of pregnancy. Am J Hematol. 2016;91(6):590–593.
- Looker AC, Dallman PR, Carroll MD, Gunter EW, Johnson CL. Prevalence of iron deficiency in the United States. JAMA. 1997;277(12):973–976.
- Miller EM. Iron status and reproduction in US women: National Health and Nutrition Examination Survey 1999–2006. PLoS One. 2014;9(11):e112216.
- Mei Z, Cogswell ME, Looker AC, et al. Assessment of iron status in US pregnant women from the National Health and Nutrition Examination Survey (NHANES), 1999–2006. Am J Clin Nutr. 2011;93(6):1312–1320.
- Drukker L, Hants Y, Farkash R, Ruchlemer R, Samueloff A, Grisaru-Granovsky S. Iron deficiency anemia at admission for labor and delivery is associated with an increased risk for Cesarean section and adverse maternal and neonatal outcomes. Transfusion. 2015;55(12):2799–2806.
- Rahmann MM, Abe SK, Rahman MS, et al. Maternal anemia and risk of adverse birth and health outcomes in low- and middle-income countries: systematic review and meta-analysis. Am J Clin Nutr. 2016;103(2):495–504.
- Zeng L, Dibley MJ, Cheng Y, et al. Impact of micronutrient supplementation during pregnancy on birth weight, duration of gestation, and perinatal mortality in rural western China: double blind cluster randomised controlled trial. BMJ. 2008;337:a2001.
- Guyatt GH, Oxman AD, Ali M, Willan A, McIlroy W, Patterson C. Laboratory diagnosis of iron-deficiency: an overview. J Gen Intern Med. 1992;7(2):145–153.
- van den Broek NR, Letsky EA, White SA, Shenkin A. Iron status in pregnant women: which measurements are valid? Br J Haematol. 1998;103(3):817–824.
- Peña-Rosas JP, De-Regil LM, Garcia-Casal MN, Dowswell T. Daily oral iron supplementation during pregnancy. Cochrane Database Syst Rev. 2015(7);CD004736.
- Cantor AG, Bougatsos C, Dana T, Blazina I, McDonagh M. Routine iron supplementation and screening for iron deficiency anemia in pregnancy: a systematic review for the US Preventive Services Task Force. Ann Intern Med. 2015;162(8):566–576.
- Centers for Disease Control and Prevention. Recommendations to prevent and control iron deficiency in the United States. MMWR Recomm Rep. 1998;47(RR-3):1–29.
- Tolkien Z, Stecher L, Mander AP, Pereira DI, Powell JJ. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis. PLoS One. 2015;10(2):e0117383.
- Peña-Rosas JP, De-Regil LM, Gomez Malave H, Flores-Urrutia MC, Dowswell T. Intermittent oral iron supplementation during pregnancy. Cochrane Database Syst Rev. 2015(10);CD009997.
- Moretti D, Goede JS, Zeder C, et al. Oral iron supplements increase hepcidin and decrease iron absorption from daily or twice-daily doses in iron-depleted young women. Blood. 2015;126(17):1981–1989.
- Schrier SL. So you know how to treat iron deficiency anemia. Blood. 2015;126(17):1971.
- Breymann C, Milman N, Mezzacasa A, Bernard R, Dudenhausen J; FER-ASAP investigators. Ferric carboxymaltose vs oral iron in the treatment of pregnant women with iron deficiency anemia: an international, open-label, randomized controlled trial (FER-ASAP). J Perinatal Med. 2017;45(4):443–453.
- Auerbach M, Pappadakis JA, Bahrain H, Auerbach SA, Ballard H, Dahl NV. Safety and efficacy of rapidly administered (one hour) one gram of low molecular weight iron dextran (INFeD) for the treatment of iron deficient anemia. Am J Hematol. 2011;86(10):860–862.
- Auerbach M, Adamson JW. How we diagnose and treat iron deficiency anemia. Am J Hematol. 2016;91(1):31–38.
- Wong L, Smith S, Gilstrop M, et al. Safety and efficacy of rapid (1,000 mg in 1 hr) intravenous iron dextran for treatment of maternal iron deficient anemia of pregnancy. Am J Hematol. 2016;91(6):590–593.
The importance of weight management and exercise: Practical advice for your patients
Over the past 3 decades, the prevalence of overweight and obesity has increased dramatically in the United States. A study published in 2016 showed the age-adjusted prevalence of obesity in 2013–2014 was 35% among men and 40.4% among women.1 It comes as no surprise that increased reliance on inexpensive fast foods coupled with progressively more sedentary lifestyles have been implicated as causative factors.2
With the rise in obesity also has come an attendant rise in related chronic diseases, such as type 2 diabetes mellitus and cardiovascular disease. Women who are obese are also at risk for certain women’s health conditions, such as polycystic ovary syndrome, breast cancer, and endometrial cancer.
It is clear that curbing this public health crisis will require concerted efforts from individuals, clinicians, and policy makers, as well as changes in societal norms.
Linda D. Bradley, MD: I think it is important for us not to lecture our patients. I could list all of the things that patients should or could do to prevent or even reverse disease states, in terms of eating right and exercising, but I think motivational interviewing is a more productive approach to elicit and evoke change (see “Principles and practice of motivational interviewing”). I used to preach to my patients. I would say, “You know, if you stay at this weight, you’re going to get diabetes, you’re going to increase your breast cancer risk, you’re going to have abnormal bleeding, you’re not going to be able to get pregnant,” and so on. It is easy to slip into that in the 7 minutes that you have with your patient, but to me, that is not the right way.
With motivational interviewing, our interactions with patients are shaped by:
- asking
- advising
- assisting
- arranging.
We begin by asking permission: “Do you mind if we talk about your weight?” or “Can we talk about your level of exercise?” Once the patient has granted permission, we ask open-ended questions and use reflective listening: “What I hear you saying is that you are concerned you will not be able to lose the weight,” or “It sounds like you don’t like to exercise, but you are worried about the health consequences of that.”
Utilizing motivational interviewing to help patients identify thoughts and feelings that contribute to unhealthy behaviors--and replacing those thoughts and feelings with new thought patterns that aid in behavior change--has been shown to be an effective and efficient facilitator for change. By incorporating the following principles of motivational interviewing into practice, clinicians can have an important impact on the prevention or management of serious diseases in women1:
- Express empathy and avoid arguments. "I know it has been difficult for you to take the first step to losing weight. That is something that is difficult for a lot of my patients. How can I help you take that first step?"
- Develop discrepancies to help the patient understand the difference between her behavior and her goals. "You have said that you would like to lose some weight. I think you know that exercise would help with that. Why do you think it has been hard for you to start exercising more?"
- Roll with resistance and provide personalized feedback to help the patient find ways to succeed. "What I hear you saying is your work schedule does not allow you time to work out at the gym. What about walking during lunch breaks or taking the stairs instead of the elevator--is that something you think you can commit to doing?"
- Support self-efficacy and elicit self-motivation. "What would you like to see differently about your health? What makes you think you need to change? What happens if you don't change?"
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 423: Motivational interviewing: a tool for behavioral change. Obstet Gynecol. 2009;113(1):243-246.
I find these skills useful for addressing anything from smoking to drinking to weight management to excessive shopping—any extreme behavior that is affecting a patient negatively. When a patient is not ready to talk about her clinical problems or make changes, I let her know my door is always open to her and that I have many resources available to help her when she is ready (TABLE).4 In those cases, I might say something like, “I have many patients who really don’t want to talk about this when I first ask them, but I just want you to know, Mrs. Jones, that I want you to succeed and I want you to be healthy. We have a team approach to taking care of all of you, and when you are ready, we are here to help.”
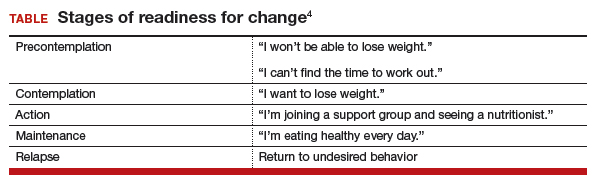
Related article:
2017 Update on fertility: Effects of obesity on reproduction
It is important to provide practical advice to patients—including how much to exercise, the importance of keeping a food journal, and determining a goal for slow, safe weight loss—and provide resources as necessary (such as for Weight Watchers, nutrition, and dieticians). Each day we have more than 30 opportunities to select foods to eat, drink, or purchase. Have a plan and advise your patients do the same. Recommend patients cook their own meals. Suggest weight loss apps. Counsel them to celebrate successes, find a buddy (for social support), practice positive self-talk (positive language), and plan for challenges (travel, parties, working late) and setbacks, which do not need to become a fall. Find an activity or exercise that the patient enjoys and tell them to seek professional help if needed.
Read about how to educate your patients on wellness.
Dr. Bradley: About 86% of the health care dollars spent in the United States are due to chronic diseases, and chronic diseases are the leading cause of death and disability in the country.5 The most common chronic diseases—cardiovascular disease, hypertension, type 2 diabetes, colon cancer, depression, dementia, cognitive problems, higher rates of fractures—all have been associated, at least in part, with unhealthy food choices and lack of exercise. That applies to breast cancer, too.
The good news is, we can prevent and even reverse disease. As Hippocrates said, let food be thy medicine and medicine be thy food. We have all seen success stories where consistent exercise and dietary changes definitely change the paradigm for what the disease state represents. A multiplicity of factors affect poor health—noncompliance, obesity, smoking—but when we begin to make consistent, healthy changes with diet and exercise, this creates a sort of domino effect.
In the book Us! Our Life. Our Health. Our Legacy,1 co-authored by Dr. Bradley and her colleague, Margaret L. McKenzie, MD, the authors highlight the 10 healthiest behaviors to bring about youthfulness and robust health:
- Walk at least 30-45 minutes per day most days of the week.
- Engage in resistance training 2-3 days per week.
- Eat a primarily plant-based diet made up of a variety of whole foods.
- Do not smoke.
- Maintain a waist line that measures less than half your height.
- Drink alcohol only in moderation.
- Get 7-8 hours of sleep most nights.
- Forgive.
- Have gratitude.
- Believe in something greater than yourself.
- Bradley LD, McKenzie ML. Us! Our life. Our health. Our legacy. Las Vegas, Nevada: The Literary Front Publishing Co., LLC; 2016.
Dr. Bradley: I think we need to get to the root cause of these clinical problems and provide the resources and support that patients need to reverse or even prevent these diseases. Clinicians need to become more aware—be an example and a role model. Our patients are watching us as much as we are watching them. Together, we can form good partnerships in order to promote better health.
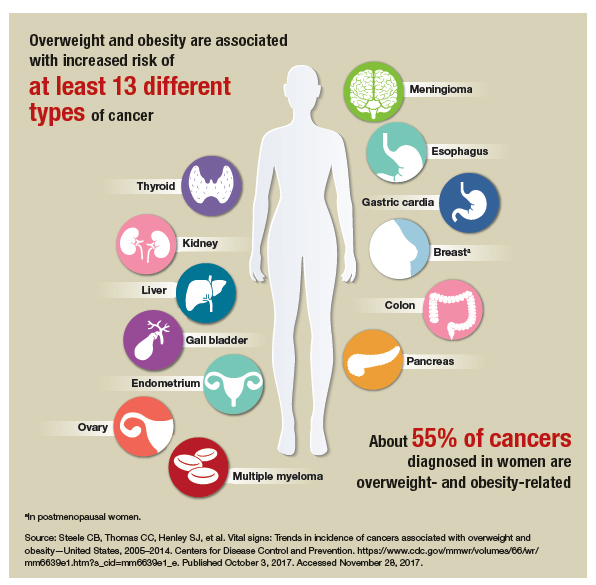
Dr. Bradley: I think when you are about to be a change agent for your body and become what I call the best version of yourself, you can have these great ideas, but you need to turn those ideas into actions and make them consistent. And we know that is difficult to do, so I do try to have patients write down specific goals, their plan for achieving them, and list the reasons why it is important for them to reach their goals. That gives them something tangible to look at when the going gets tough. It is also important to work into the contract ways to reward positive behaviors when goals are met, and to plan for challenges and setbacks and how to get back on track.
I also encourage patients to document their progress and learn how to make quick adjustments when necessary to get back on track. Another important element involves setting milestones—by what date are you going to reach this goal? Like any other contract, I have my patients date and sign their wellness contracts. I also encourage them to visualize what their new self is going to look like, how they will feel when they reach their goal, what they will wear, and what activities they will engage in.
Related article:
Obesity medicine: How to incorporate it into your practice
Dr. Bradley: I do, but the amount of nutrition education that most of us get in medical school is minimal to nonexistent and not practical. As physicians, we know that food is health, exercise is fitness, and that our patients need both of them. We also know that we did not get this information in school and that our education was more about treating disease than preventing disease. Many of us were not trained in robot surgery either, because it did not exist. So what did we do? We took classes, attended lectures, read books, and learned. We can do the same with wellness. There are many courses around the country. We have to begin to relearn and reteach ourselves about health, nutrition, and exercise and then pass that information on to our patients—be a resource and a guide. We should be able to write a prescription for health as quickly as we can write a prescription for insulin or a statin.
I also bring up portion distortion with my patients. The National Institutes of Health has resources on their website (https://www.nhlbi.nih.gov/health/educational /wecan/eat-right/portion-distortion.html) that include great visuals that show portion sizes 20 years ago and what they are now. For instance, 20 years ago a bagel was 3 inches and 140 calories; today’s bagel is 6 inches and 350 calories (plus whatever toppings are added). I tell that to my patients and then explain how much more exercise is needed to burn off just that 1 bagel.
Related article:
How to help your patients control gestational weight gain
Dr. Bradley: They may not know that term directly, but I think people understand that you have the potential to pass on poor lifestyle and/or health issues related to how things are when you are in utero and later in life. It gets back to letting people know to be healthy in pregnancy and even pre-pregnancy, and that includes one’s emotional state, physical state, and spiritual state. We are what we are in our mother’s womb. Getting the best start in life starts with a healthy mom, healthy dad, and a healthy environment.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in obesity among adults in the United States, 2005 to 2014. JAMA.2016;315(21):2284Arial–2291.
- Sturm R, An R. Obesity and economic environments. CA Cancer J Clin. 2014;64(5):337Arial–350.
- Bradley LD, McKenzie ML. Us! Our life. Our health. Our legacy. Las Vegas, Nevada: The Literary Front Publishing Co., LLC; 2016.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 423: Motivational interviewing: a tool for behavioral change. Obstet Gynecol. 2009;113(1):243–246.
- Centers for Disease Control and Prevention. Chronic disease overview. https://www.cdc.gov/chronicdisease/overview/index.htm. Updated June 28, 2017. Accessed November 3, 2017.
Over the past 3 decades, the prevalence of overweight and obesity has increased dramatically in the United States. A study published in 2016 showed the age-adjusted prevalence of obesity in 2013–2014 was 35% among men and 40.4% among women.1 It comes as no surprise that increased reliance on inexpensive fast foods coupled with progressively more sedentary lifestyles have been implicated as causative factors.2
With the rise in obesity also has come an attendant rise in related chronic diseases, such as type 2 diabetes mellitus and cardiovascular disease. Women who are obese are also at risk for certain women’s health conditions, such as polycystic ovary syndrome, breast cancer, and endometrial cancer.
It is clear that curbing this public health crisis will require concerted efforts from individuals, clinicians, and policy makers, as well as changes in societal norms.
Linda D. Bradley, MD: I think it is important for us not to lecture our patients. I could list all of the things that patients should or could do to prevent or even reverse disease states, in terms of eating right and exercising, but I think motivational interviewing is a more productive approach to elicit and evoke change (see “Principles and practice of motivational interviewing”). I used to preach to my patients. I would say, “You know, if you stay at this weight, you’re going to get diabetes, you’re going to increase your breast cancer risk, you’re going to have abnormal bleeding, you’re not going to be able to get pregnant,” and so on. It is easy to slip into that in the 7 minutes that you have with your patient, but to me, that is not the right way.
With motivational interviewing, our interactions with patients are shaped by:
- asking
- advising
- assisting
- arranging.
We begin by asking permission: “Do you mind if we talk about your weight?” or “Can we talk about your level of exercise?” Once the patient has granted permission, we ask open-ended questions and use reflective listening: “What I hear you saying is that you are concerned you will not be able to lose the weight,” or “It sounds like you don’t like to exercise, but you are worried about the health consequences of that.”
Utilizing motivational interviewing to help patients identify thoughts and feelings that contribute to unhealthy behaviors--and replacing those thoughts and feelings with new thought patterns that aid in behavior change--has been shown to be an effective and efficient facilitator for change. By incorporating the following principles of motivational interviewing into practice, clinicians can have an important impact on the prevention or management of serious diseases in women1:
- Express empathy and avoid arguments. "I know it has been difficult for you to take the first step to losing weight. That is something that is difficult for a lot of my patients. How can I help you take that first step?"
- Develop discrepancies to help the patient understand the difference between her behavior and her goals. "You have said that you would like to lose some weight. I think you know that exercise would help with that. Why do you think it has been hard for you to start exercising more?"
- Roll with resistance and provide personalized feedback to help the patient find ways to succeed. "What I hear you saying is your work schedule does not allow you time to work out at the gym. What about walking during lunch breaks or taking the stairs instead of the elevator--is that something you think you can commit to doing?"
- Support self-efficacy and elicit self-motivation. "What would you like to see differently about your health? What makes you think you need to change? What happens if you don't change?"
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 423: Motivational interviewing: a tool for behavioral change. Obstet Gynecol. 2009;113(1):243-246.
I find these skills useful for addressing anything from smoking to drinking to weight management to excessive shopping—any extreme behavior that is affecting a patient negatively. When a patient is not ready to talk about her clinical problems or make changes, I let her know my door is always open to her and that I have many resources available to help her when she is ready (TABLE).4 In those cases, I might say something like, “I have many patients who really don’t want to talk about this when I first ask them, but I just want you to know, Mrs. Jones, that I want you to succeed and I want you to be healthy. We have a team approach to taking care of all of you, and when you are ready, we are here to help.”
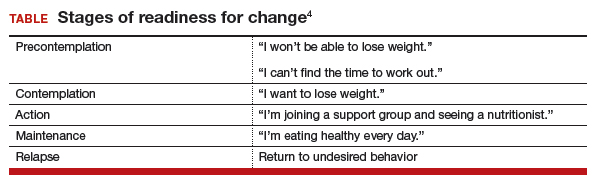
Related article:
2017 Update on fertility: Effects of obesity on reproduction
It is important to provide practical advice to patients—including how much to exercise, the importance of keeping a food journal, and determining a goal for slow, safe weight loss—and provide resources as necessary (such as for Weight Watchers, nutrition, and dieticians). Each day we have more than 30 opportunities to select foods to eat, drink, or purchase. Have a plan and advise your patients do the same. Recommend patients cook their own meals. Suggest weight loss apps. Counsel them to celebrate successes, find a buddy (for social support), practice positive self-talk (positive language), and plan for challenges (travel, parties, working late) and setbacks, which do not need to become a fall. Find an activity or exercise that the patient enjoys and tell them to seek professional help if needed.
Read about how to educate your patients on wellness.
Dr. Bradley: About 86% of the health care dollars spent in the United States are due to chronic diseases, and chronic diseases are the leading cause of death and disability in the country.5 The most common chronic diseases—cardiovascular disease, hypertension, type 2 diabetes, colon cancer, depression, dementia, cognitive problems, higher rates of fractures—all have been associated, at least in part, with unhealthy food choices and lack of exercise. That applies to breast cancer, too.
The good news is, we can prevent and even reverse disease. As Hippocrates said, let food be thy medicine and medicine be thy food. We have all seen success stories where consistent exercise and dietary changes definitely change the paradigm for what the disease state represents. A multiplicity of factors affect poor health—noncompliance, obesity, smoking—but when we begin to make consistent, healthy changes with diet and exercise, this creates a sort of domino effect.
In the book Us! Our Life. Our Health. Our Legacy,1 co-authored by Dr. Bradley and her colleague, Margaret L. McKenzie, MD, the authors highlight the 10 healthiest behaviors to bring about youthfulness and robust health:
- Walk at least 30-45 minutes per day most days of the week.
- Engage in resistance training 2-3 days per week.
- Eat a primarily plant-based diet made up of a variety of whole foods.
- Do not smoke.
- Maintain a waist line that measures less than half your height.
- Drink alcohol only in moderation.
- Get 7-8 hours of sleep most nights.
- Forgive.
- Have gratitude.
- Believe in something greater than yourself.
- Bradley LD, McKenzie ML. Us! Our life. Our health. Our legacy. Las Vegas, Nevada: The Literary Front Publishing Co., LLC; 2016.
Dr. Bradley: I think we need to get to the root cause of these clinical problems and provide the resources and support that patients need to reverse or even prevent these diseases. Clinicians need to become more aware—be an example and a role model. Our patients are watching us as much as we are watching them. Together, we can form good partnerships in order to promote better health.
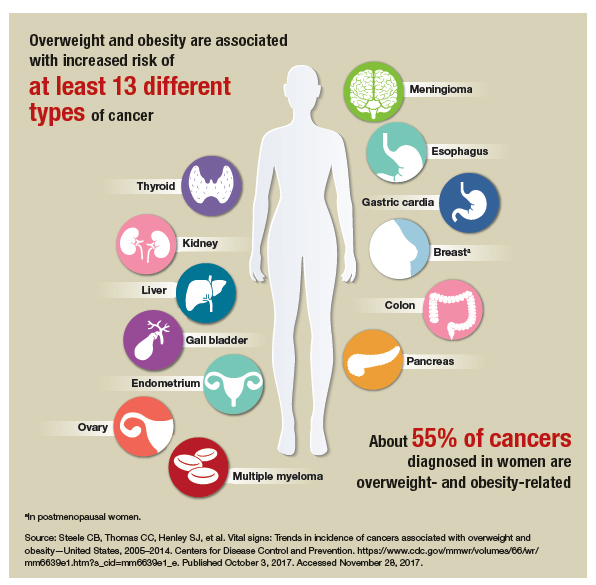
Dr. Bradley: I think when you are about to be a change agent for your body and become what I call the best version of yourself, you can have these great ideas, but you need to turn those ideas into actions and make them consistent. And we know that is difficult to do, so I do try to have patients write down specific goals, their plan for achieving them, and list the reasons why it is important for them to reach their goals. That gives them something tangible to look at when the going gets tough. It is also important to work into the contract ways to reward positive behaviors when goals are met, and to plan for challenges and setbacks and how to get back on track.
I also encourage patients to document their progress and learn how to make quick adjustments when necessary to get back on track. Another important element involves setting milestones—by what date are you going to reach this goal? Like any other contract, I have my patients date and sign their wellness contracts. I also encourage them to visualize what their new self is going to look like, how they will feel when they reach their goal, what they will wear, and what activities they will engage in.
Related article:
Obesity medicine: How to incorporate it into your practice
Dr. Bradley: I do, but the amount of nutrition education that most of us get in medical school is minimal to nonexistent and not practical. As physicians, we know that food is health, exercise is fitness, and that our patients need both of them. We also know that we did not get this information in school and that our education was more about treating disease than preventing disease. Many of us were not trained in robot surgery either, because it did not exist. So what did we do? We took classes, attended lectures, read books, and learned. We can do the same with wellness. There are many courses around the country. We have to begin to relearn and reteach ourselves about health, nutrition, and exercise and then pass that information on to our patients—be a resource and a guide. We should be able to write a prescription for health as quickly as we can write a prescription for insulin or a statin.
I also bring up portion distortion with my patients. The National Institutes of Health has resources on their website (https://www.nhlbi.nih.gov/health/educational /wecan/eat-right/portion-distortion.html) that include great visuals that show portion sizes 20 years ago and what they are now. For instance, 20 years ago a bagel was 3 inches and 140 calories; today’s bagel is 6 inches and 350 calories (plus whatever toppings are added). I tell that to my patients and then explain how much more exercise is needed to burn off just that 1 bagel.
Related article:
How to help your patients control gestational weight gain
Dr. Bradley: They may not know that term directly, but I think people understand that you have the potential to pass on poor lifestyle and/or health issues related to how things are when you are in utero and later in life. It gets back to letting people know to be healthy in pregnancy and even pre-pregnancy, and that includes one’s emotional state, physical state, and spiritual state. We are what we are in our mother’s womb. Getting the best start in life starts with a healthy mom, healthy dad, and a healthy environment.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Over the past 3 decades, the prevalence of overweight and obesity has increased dramatically in the United States. A study published in 2016 showed the age-adjusted prevalence of obesity in 2013–2014 was 35% among men and 40.4% among women.1 It comes as no surprise that increased reliance on inexpensive fast foods coupled with progressively more sedentary lifestyles have been implicated as causative factors.2
With the rise in obesity also has come an attendant rise in related chronic diseases, such as type 2 diabetes mellitus and cardiovascular disease. Women who are obese are also at risk for certain women’s health conditions, such as polycystic ovary syndrome, breast cancer, and endometrial cancer.
It is clear that curbing this public health crisis will require concerted efforts from individuals, clinicians, and policy makers, as well as changes in societal norms.
Linda D. Bradley, MD: I think it is important for us not to lecture our patients. I could list all of the things that patients should or could do to prevent or even reverse disease states, in terms of eating right and exercising, but I think motivational interviewing is a more productive approach to elicit and evoke change (see “Principles and practice of motivational interviewing”). I used to preach to my patients. I would say, “You know, if you stay at this weight, you’re going to get diabetes, you’re going to increase your breast cancer risk, you’re going to have abnormal bleeding, you’re not going to be able to get pregnant,” and so on. It is easy to slip into that in the 7 minutes that you have with your patient, but to me, that is not the right way.
With motivational interviewing, our interactions with patients are shaped by:
- asking
- advising
- assisting
- arranging.
We begin by asking permission: “Do you mind if we talk about your weight?” or “Can we talk about your level of exercise?” Once the patient has granted permission, we ask open-ended questions and use reflective listening: “What I hear you saying is that you are concerned you will not be able to lose the weight,” or “It sounds like you don’t like to exercise, but you are worried about the health consequences of that.”
Utilizing motivational interviewing to help patients identify thoughts and feelings that contribute to unhealthy behaviors--and replacing those thoughts and feelings with new thought patterns that aid in behavior change--has been shown to be an effective and efficient facilitator for change. By incorporating the following principles of motivational interviewing into practice, clinicians can have an important impact on the prevention or management of serious diseases in women1:
- Express empathy and avoid arguments. "I know it has been difficult for you to take the first step to losing weight. That is something that is difficult for a lot of my patients. How can I help you take that first step?"
- Develop discrepancies to help the patient understand the difference between her behavior and her goals. "You have said that you would like to lose some weight. I think you know that exercise would help with that. Why do you think it has been hard for you to start exercising more?"
- Roll with resistance and provide personalized feedback to help the patient find ways to succeed. "What I hear you saying is your work schedule does not allow you time to work out at the gym. What about walking during lunch breaks or taking the stairs instead of the elevator--is that something you think you can commit to doing?"
- Support self-efficacy and elicit self-motivation. "What would you like to see differently about your health? What makes you think you need to change? What happens if you don't change?"
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 423: Motivational interviewing: a tool for behavioral change. Obstet Gynecol. 2009;113(1):243-246.
I find these skills useful for addressing anything from smoking to drinking to weight management to excessive shopping—any extreme behavior that is affecting a patient negatively. When a patient is not ready to talk about her clinical problems or make changes, I let her know my door is always open to her and that I have many resources available to help her when she is ready (TABLE).4 In those cases, I might say something like, “I have many patients who really don’t want to talk about this when I first ask them, but I just want you to know, Mrs. Jones, that I want you to succeed and I want you to be healthy. We have a team approach to taking care of all of you, and when you are ready, we are here to help.”
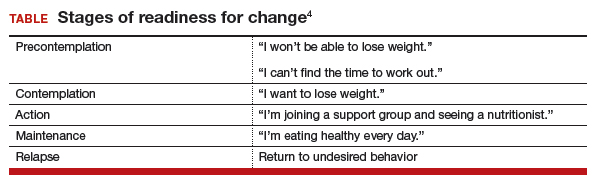
Related article:
2017 Update on fertility: Effects of obesity on reproduction
It is important to provide practical advice to patients—including how much to exercise, the importance of keeping a food journal, and determining a goal for slow, safe weight loss—and provide resources as necessary (such as for Weight Watchers, nutrition, and dieticians). Each day we have more than 30 opportunities to select foods to eat, drink, or purchase. Have a plan and advise your patients do the same. Recommend patients cook their own meals. Suggest weight loss apps. Counsel them to celebrate successes, find a buddy (for social support), practice positive self-talk (positive language), and plan for challenges (travel, parties, working late) and setbacks, which do not need to become a fall. Find an activity or exercise that the patient enjoys and tell them to seek professional help if needed.
Read about how to educate your patients on wellness.
Dr. Bradley: About 86% of the health care dollars spent in the United States are due to chronic diseases, and chronic diseases are the leading cause of death and disability in the country.5 The most common chronic diseases—cardiovascular disease, hypertension, type 2 diabetes, colon cancer, depression, dementia, cognitive problems, higher rates of fractures—all have been associated, at least in part, with unhealthy food choices and lack of exercise. That applies to breast cancer, too.
The good news is, we can prevent and even reverse disease. As Hippocrates said, let food be thy medicine and medicine be thy food. We have all seen success stories where consistent exercise and dietary changes definitely change the paradigm for what the disease state represents. A multiplicity of factors affect poor health—noncompliance, obesity, smoking—but when we begin to make consistent, healthy changes with diet and exercise, this creates a sort of domino effect.
In the book Us! Our Life. Our Health. Our Legacy,1 co-authored by Dr. Bradley and her colleague, Margaret L. McKenzie, MD, the authors highlight the 10 healthiest behaviors to bring about youthfulness and robust health:
- Walk at least 30-45 minutes per day most days of the week.
- Engage in resistance training 2-3 days per week.
- Eat a primarily plant-based diet made up of a variety of whole foods.
- Do not smoke.
- Maintain a waist line that measures less than half your height.
- Drink alcohol only in moderation.
- Get 7-8 hours of sleep most nights.
- Forgive.
- Have gratitude.
- Believe in something greater than yourself.
- Bradley LD, McKenzie ML. Us! Our life. Our health. Our legacy. Las Vegas, Nevada: The Literary Front Publishing Co., LLC; 2016.
Dr. Bradley: I think we need to get to the root cause of these clinical problems and provide the resources and support that patients need to reverse or even prevent these diseases. Clinicians need to become more aware—be an example and a role model. Our patients are watching us as much as we are watching them. Together, we can form good partnerships in order to promote better health.
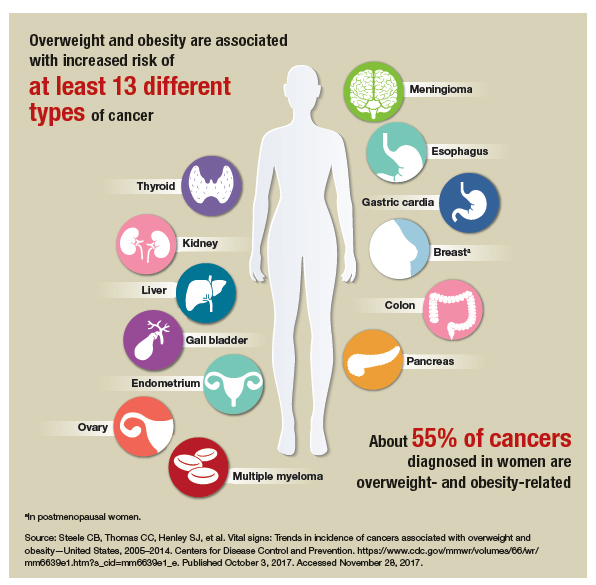
Dr. Bradley: I think when you are about to be a change agent for your body and become what I call the best version of yourself, you can have these great ideas, but you need to turn those ideas into actions and make them consistent. And we know that is difficult to do, so I do try to have patients write down specific goals, their plan for achieving them, and list the reasons why it is important for them to reach their goals. That gives them something tangible to look at when the going gets tough. It is also important to work into the contract ways to reward positive behaviors when goals are met, and to plan for challenges and setbacks and how to get back on track.
I also encourage patients to document their progress and learn how to make quick adjustments when necessary to get back on track. Another important element involves setting milestones—by what date are you going to reach this goal? Like any other contract, I have my patients date and sign their wellness contracts. I also encourage them to visualize what their new self is going to look like, how they will feel when they reach their goal, what they will wear, and what activities they will engage in.
Related article:
Obesity medicine: How to incorporate it into your practice
Dr. Bradley: I do, but the amount of nutrition education that most of us get in medical school is minimal to nonexistent and not practical. As physicians, we know that food is health, exercise is fitness, and that our patients need both of them. We also know that we did not get this information in school and that our education was more about treating disease than preventing disease. Many of us were not trained in robot surgery either, because it did not exist. So what did we do? We took classes, attended lectures, read books, and learned. We can do the same with wellness. There are many courses around the country. We have to begin to relearn and reteach ourselves about health, nutrition, and exercise and then pass that information on to our patients—be a resource and a guide. We should be able to write a prescription for health as quickly as we can write a prescription for insulin or a statin.
I also bring up portion distortion with my patients. The National Institutes of Health has resources on their website (https://www.nhlbi.nih.gov/health/educational /wecan/eat-right/portion-distortion.html) that include great visuals that show portion sizes 20 years ago and what they are now. For instance, 20 years ago a bagel was 3 inches and 140 calories; today’s bagel is 6 inches and 350 calories (plus whatever toppings are added). I tell that to my patients and then explain how much more exercise is needed to burn off just that 1 bagel.
Related article:
How to help your patients control gestational weight gain
Dr. Bradley: They may not know that term directly, but I think people understand that you have the potential to pass on poor lifestyle and/or health issues related to how things are when you are in utero and later in life. It gets back to letting people know to be healthy in pregnancy and even pre-pregnancy, and that includes one’s emotional state, physical state, and spiritual state. We are what we are in our mother’s womb. Getting the best start in life starts with a healthy mom, healthy dad, and a healthy environment.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in obesity among adults in the United States, 2005 to 2014. JAMA.2016;315(21):2284Arial–2291.
- Sturm R, An R. Obesity and economic environments. CA Cancer J Clin. 2014;64(5):337Arial–350.
- Bradley LD, McKenzie ML. Us! Our life. Our health. Our legacy. Las Vegas, Nevada: The Literary Front Publishing Co., LLC; 2016.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 423: Motivational interviewing: a tool for behavioral change. Obstet Gynecol. 2009;113(1):243–246.
- Centers for Disease Control and Prevention. Chronic disease overview. https://www.cdc.gov/chronicdisease/overview/index.htm. Updated June 28, 2017. Accessed November 3, 2017.
- Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in obesity among adults in the United States, 2005 to 2014. JAMA.2016;315(21):2284Arial–2291.
- Sturm R, An R. Obesity and economic environments. CA Cancer J Clin. 2014;64(5):337Arial–350.
- Bradley LD, McKenzie ML. Us! Our life. Our health. Our legacy. Las Vegas, Nevada: The Literary Front Publishing Co., LLC; 2016.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 423: Motivational interviewing: a tool for behavioral change. Obstet Gynecol. 2009;113(1):243–246.
- Centers for Disease Control and Prevention. Chronic disease overview. https://www.cdc.gov/chronicdisease/overview/index.htm. Updated June 28, 2017. Accessed November 3, 2017.
Luxury drug treatment centers: Close scrutiny advised
About 2.5 million people received mental and/or substance use disorder treatment last year, according to the Substance Abuse and Mental Health Services Administration.1 Of those, a small but significant percentage chose support from a luxury type facility. This article intends to provide clinicians with guidance in addressing medically supervised luxury detox and/or rehabilitation programs for drug and alcohol abuse.
We recommend that individuals entering substance abuse services pursue these treatments with “eyes wide open.” A vast amount of literature indicates a rise in programs designed to attract vulnerable clients seeking treatment.2 They offer an array of luxury services such as equine, massage, and yoga therapy, as well as holistic approaches. These services are all packaged in a five-star hotel–like environment in a desirable area (by the sea, mountains, etc.).
The question is whether a $50,000-per-month treatment center is better at keeping its clients in remission than a facility that charges a fraction of the price per month. We believe that success rates may be less a function of financial cost and more a function of evidenced-based treatment strategies that are specific to recovery.
We would like to advise individuals to look for the following elements when reviewing a potential treatment center:
• Accepted by major insurance companies such as Blue Cross/Blue Shield and United Healthcare, to name a few.
• No cookie-cutter approaches: Programs allowing for inter-individual flexibility regarding length of stay (not specifically 21, 30, or 45 days), as well as flexibility of services.
• Group therapy should have no more than 15 clients. Some individuals may not be appropriate for group therapy or may have a strong aversion to this modality.
• Licensed and/or certified staff (not peer coaching and/or paraprofessionals alone).
• Minimum of 20 hours per week, per client, of clinically supervised evidence-based methods, techniques, and/or practices including individual counseling, group therapies, and family involvement.
• If the length of stay is longer, fewer staff members may be more appropriate.
• Availability of higher level of professional staff, psychologists, psychiatrists, and other physicians to address all comorbid concerns.
• Adequate aftercare treatment.
After reviewing social media that rate treatment facilities, one common thread we noticed was the total absence of aftercare services.3 Aftercare services were something that clients may not think of at the initial intake.
References
1 Substance Abuse and Mental Health Services Administration (SAMHSA). “Behavioral Health Treatments and Services.”
2 The Verge, Sept. 6, 2017
3 Rehabs.com
4. The New York Times, Sept. 14, 2017
Dr. Lesser is executive director of RANE, Medical & Mental Health, in New York City. In his recent positions as medical director for New York City and State, he was instrumental in developing and implementing nationally recognized emergency and response programs. Dr. Brenner is chief of Behavioral Health Service Line for Catholic Health Services of Long Island, in New York. He is a clinical professor of psychiatry for the State University of New York, Brooklyn, and medical director and CEO of Neurobehavioral Research Inc. Dr. Ferber is a licensed psychologist in New York and California. He has been the director of Behavioral Health Central Intake at Catholic Health Services of Long Island for the last 2 years. Dr. Ferber specializes in addiction treatment. Ms. Howard is a psychologist in training with specialization in clinical psychology. She currently treats numerous dual-diagnosed patients with comorbidities on an acute psychiatric ward.
About 2.5 million people received mental and/or substance use disorder treatment last year, according to the Substance Abuse and Mental Health Services Administration.1 Of those, a small but significant percentage chose support from a luxury type facility. This article intends to provide clinicians with guidance in addressing medically supervised luxury detox and/or rehabilitation programs for drug and alcohol abuse.
We recommend that individuals entering substance abuse services pursue these treatments with “eyes wide open.” A vast amount of literature indicates a rise in programs designed to attract vulnerable clients seeking treatment.2 They offer an array of luxury services such as equine, massage, and yoga therapy, as well as holistic approaches. These services are all packaged in a five-star hotel–like environment in a desirable area (by the sea, mountains, etc.).
The question is whether a $50,000-per-month treatment center is better at keeping its clients in remission than a facility that charges a fraction of the price per month. We believe that success rates may be less a function of financial cost and more a function of evidenced-based treatment strategies that are specific to recovery.
We would like to advise individuals to look for the following elements when reviewing a potential treatment center:
• Accepted by major insurance companies such as Blue Cross/Blue Shield and United Healthcare, to name a few.
• No cookie-cutter approaches: Programs allowing for inter-individual flexibility regarding length of stay (not specifically 21, 30, or 45 days), as well as flexibility of services.
• Group therapy should have no more than 15 clients. Some individuals may not be appropriate for group therapy or may have a strong aversion to this modality.
• Licensed and/or certified staff (not peer coaching and/or paraprofessionals alone).
• Minimum of 20 hours per week, per client, of clinically supervised evidence-based methods, techniques, and/or practices including individual counseling, group therapies, and family involvement.
• If the length of stay is longer, fewer staff members may be more appropriate.
• Availability of higher level of professional staff, psychologists, psychiatrists, and other physicians to address all comorbid concerns.
• Adequate aftercare treatment.
After reviewing social media that rate treatment facilities, one common thread we noticed was the total absence of aftercare services.3 Aftercare services were something that clients may not think of at the initial intake.
References
1 Substance Abuse and Mental Health Services Administration (SAMHSA). “Behavioral Health Treatments and Services.”
2 The Verge, Sept. 6, 2017
3 Rehabs.com
4. The New York Times, Sept. 14, 2017
Dr. Lesser is executive director of RANE, Medical & Mental Health, in New York City. In his recent positions as medical director for New York City and State, he was instrumental in developing and implementing nationally recognized emergency and response programs. Dr. Brenner is chief of Behavioral Health Service Line for Catholic Health Services of Long Island, in New York. He is a clinical professor of psychiatry for the State University of New York, Brooklyn, and medical director and CEO of Neurobehavioral Research Inc. Dr. Ferber is a licensed psychologist in New York and California. He has been the director of Behavioral Health Central Intake at Catholic Health Services of Long Island for the last 2 years. Dr. Ferber specializes in addiction treatment. Ms. Howard is a psychologist in training with specialization in clinical psychology. She currently treats numerous dual-diagnosed patients with comorbidities on an acute psychiatric ward.
About 2.5 million people received mental and/or substance use disorder treatment last year, according to the Substance Abuse and Mental Health Services Administration.1 Of those, a small but significant percentage chose support from a luxury type facility. This article intends to provide clinicians with guidance in addressing medically supervised luxury detox and/or rehabilitation programs for drug and alcohol abuse.
We recommend that individuals entering substance abuse services pursue these treatments with “eyes wide open.” A vast amount of literature indicates a rise in programs designed to attract vulnerable clients seeking treatment.2 They offer an array of luxury services such as equine, massage, and yoga therapy, as well as holistic approaches. These services are all packaged in a five-star hotel–like environment in a desirable area (by the sea, mountains, etc.).
The question is whether a $50,000-per-month treatment center is better at keeping its clients in remission than a facility that charges a fraction of the price per month. We believe that success rates may be less a function of financial cost and more a function of evidenced-based treatment strategies that are specific to recovery.
We would like to advise individuals to look for the following elements when reviewing a potential treatment center:
• Accepted by major insurance companies such as Blue Cross/Blue Shield and United Healthcare, to name a few.
• No cookie-cutter approaches: Programs allowing for inter-individual flexibility regarding length of stay (not specifically 21, 30, or 45 days), as well as flexibility of services.
• Group therapy should have no more than 15 clients. Some individuals may not be appropriate for group therapy or may have a strong aversion to this modality.
• Licensed and/or certified staff (not peer coaching and/or paraprofessionals alone).
• Minimum of 20 hours per week, per client, of clinically supervised evidence-based methods, techniques, and/or practices including individual counseling, group therapies, and family involvement.
• If the length of stay is longer, fewer staff members may be more appropriate.
• Availability of higher level of professional staff, psychologists, psychiatrists, and other physicians to address all comorbid concerns.
• Adequate aftercare treatment.
After reviewing social media that rate treatment facilities, one common thread we noticed was the total absence of aftercare services.3 Aftercare services were something that clients may not think of at the initial intake.
References
1 Substance Abuse and Mental Health Services Administration (SAMHSA). “Behavioral Health Treatments and Services.”
2 The Verge, Sept. 6, 2017
3 Rehabs.com
4. The New York Times, Sept. 14, 2017
Dr. Lesser is executive director of RANE, Medical & Mental Health, in New York City. In his recent positions as medical director for New York City and State, he was instrumental in developing and implementing nationally recognized emergency and response programs. Dr. Brenner is chief of Behavioral Health Service Line for Catholic Health Services of Long Island, in New York. He is a clinical professor of psychiatry for the State University of New York, Brooklyn, and medical director and CEO of Neurobehavioral Research Inc. Dr. Ferber is a licensed psychologist in New York and California. He has been the director of Behavioral Health Central Intake at Catholic Health Services of Long Island for the last 2 years. Dr. Ferber specializes in addiction treatment. Ms. Howard is a psychologist in training with specialization in clinical psychology. She currently treats numerous dual-diagnosed patients with comorbidities on an acute psychiatric ward.
Are fewer nonpregnant women seeing ObGyns?
EXPERT COMMENTARY
Health care services for women are fragmented due to multiple types of providers who offer a variety of care. Simon and Uddin’s recent research analysis indicates that the percentage of nonpregnant women who visit a general ObGyn, whether alone or in combination with an internist, family physician, or general practitioner, has declined.
Details of the study
The authors used data from the National Health Interview Survey of a representative sample of US women age 18 or older. They sought to identify whether the women saw or talked to a physician who either specialized in women’s health (presumably an ObGyn) or treated a variety of illnesses during the previous 12 months.
While the percentage of women who saw a general physician remained essentially the same (70%–74%), it declined for seeing an ObGyn from 45% to 41% between 2003 and 2007, and from 42% to 38% between 2011 and 2015. Furthermore, the percentage of women who saw both an ObGyn and a general physician declined from a peak of 35% in 2003 to 30% in 2015.
Study strengths and weaknesses
The data used in this study were from a nationally representative, cross-sectional, multistage sample, population health survey conducted by the Centers for Disease Control and Prevention. The study period was sufficient to draw conclusions.
From my perspective, the study had 2 major limitations: 1) only physicians, not mid-level providers, were included in the analysis, and 2) no breakdown of the women’s age groups was provided.
Many ObGyn offices employ nurse practitioners and midwives, and these providers’ roles are increasingly important for improving frontline access to care and different levels of care. Women aged 19 to 39 seek almost all their health care from ObGyns or family physicians, and significant sharing of care exists across these provider groups.1 Women aged 45 to 64 are more likely to obtain care exclusively at the offices of family physicians or general internists than at those of ObGyns.2 Most ObGyns are engaged to some degree with women aged 65 years or older, especially for preventive care, disease screening and early detection, and urogenital conditions.3
The decline in the percentage of women seeking care from ObGyns is likely related to the patient's age, reason for seeking care, and access to care. The US population of adult women, especially those who are beyond the reproductive years, is rising in relation to the number of physicians in general ObGyn practice. Providing a team-based collaborative model of care should allow for improved access and value. Defining the roles of what constitutes evidence-based care also will impact when a person needs to see a women's health care specialist. Geographic distribution of ObGyns in relation to the patient population will invariably impact on the percentage of women who seek care at the office of an ObGyn alone, in combination with another general physician, or not at all. Given the overlap in care provided at more than one physician's office, continued surveillance is needed to minimize redundant costs and optimize resource utilization. I look forward to what unfolds over the next 15 years.
-- William F. Rayburn, MD, MBA
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Petterson SM, Bazemore AW, Phillips RL, Rayburn WF. Trends in office-based care for reproductive-aged women according to physician specialty: a ten-year study. J Womens Health (Larchmt). 2014;23(12):1021–1026.
- Raffoul MC, Petterson SM, Rayburn WF, Wingrove P, Bazemore AW. Office visits for women aged 45–64 years according to physician specialties. J Womens Health (Larchmt). 2016:25(12):1231–1236.
- Rayburn WF, Raglan GB, Herman CJ, Schulkin J. A survey of obstetrician-gynecologists regarding their care of women 65 years or older. J Geriatr Med Gerontol. 2015;1:2-5.
EXPERT COMMENTARY
Health care services for women are fragmented due to multiple types of providers who offer a variety of care. Simon and Uddin’s recent research analysis indicates that the percentage of nonpregnant women who visit a general ObGyn, whether alone or in combination with an internist, family physician, or general practitioner, has declined.
Details of the study
The authors used data from the National Health Interview Survey of a representative sample of US women age 18 or older. They sought to identify whether the women saw or talked to a physician who either specialized in women’s health (presumably an ObGyn) or treated a variety of illnesses during the previous 12 months.
While the percentage of women who saw a general physician remained essentially the same (70%–74%), it declined for seeing an ObGyn from 45% to 41% between 2003 and 2007, and from 42% to 38% between 2011 and 2015. Furthermore, the percentage of women who saw both an ObGyn and a general physician declined from a peak of 35% in 2003 to 30% in 2015.
Study strengths and weaknesses
The data used in this study were from a nationally representative, cross-sectional, multistage sample, population health survey conducted by the Centers for Disease Control and Prevention. The study period was sufficient to draw conclusions.
From my perspective, the study had 2 major limitations: 1) only physicians, not mid-level providers, were included in the analysis, and 2) no breakdown of the women’s age groups was provided.
Many ObGyn offices employ nurse practitioners and midwives, and these providers’ roles are increasingly important for improving frontline access to care and different levels of care. Women aged 19 to 39 seek almost all their health care from ObGyns or family physicians, and significant sharing of care exists across these provider groups.1 Women aged 45 to 64 are more likely to obtain care exclusively at the offices of family physicians or general internists than at those of ObGyns.2 Most ObGyns are engaged to some degree with women aged 65 years or older, especially for preventive care, disease screening and early detection, and urogenital conditions.3
The decline in the percentage of women seeking care from ObGyns is likely related to the patient's age, reason for seeking care, and access to care. The US population of adult women, especially those who are beyond the reproductive years, is rising in relation to the number of physicians in general ObGyn practice. Providing a team-based collaborative model of care should allow for improved access and value. Defining the roles of what constitutes evidence-based care also will impact when a person needs to see a women's health care specialist. Geographic distribution of ObGyns in relation to the patient population will invariably impact on the percentage of women who seek care at the office of an ObGyn alone, in combination with another general physician, or not at all. Given the overlap in care provided at more than one physician's office, continued surveillance is needed to minimize redundant costs and optimize resource utilization. I look forward to what unfolds over the next 15 years.
-- William F. Rayburn, MD, MBA
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
EXPERT COMMENTARY
Health care services for women are fragmented due to multiple types of providers who offer a variety of care. Simon and Uddin’s recent research analysis indicates that the percentage of nonpregnant women who visit a general ObGyn, whether alone or in combination with an internist, family physician, or general practitioner, has declined.
Details of the study
The authors used data from the National Health Interview Survey of a representative sample of US women age 18 or older. They sought to identify whether the women saw or talked to a physician who either specialized in women’s health (presumably an ObGyn) or treated a variety of illnesses during the previous 12 months.
While the percentage of women who saw a general physician remained essentially the same (70%–74%), it declined for seeing an ObGyn from 45% to 41% between 2003 and 2007, and from 42% to 38% between 2011 and 2015. Furthermore, the percentage of women who saw both an ObGyn and a general physician declined from a peak of 35% in 2003 to 30% in 2015.
Study strengths and weaknesses
The data used in this study were from a nationally representative, cross-sectional, multistage sample, population health survey conducted by the Centers for Disease Control and Prevention. The study period was sufficient to draw conclusions.
From my perspective, the study had 2 major limitations: 1) only physicians, not mid-level providers, were included in the analysis, and 2) no breakdown of the women’s age groups was provided.
Many ObGyn offices employ nurse practitioners and midwives, and these providers’ roles are increasingly important for improving frontline access to care and different levels of care. Women aged 19 to 39 seek almost all their health care from ObGyns or family physicians, and significant sharing of care exists across these provider groups.1 Women aged 45 to 64 are more likely to obtain care exclusively at the offices of family physicians or general internists than at those of ObGyns.2 Most ObGyns are engaged to some degree with women aged 65 years or older, especially for preventive care, disease screening and early detection, and urogenital conditions.3
The decline in the percentage of women seeking care from ObGyns is likely related to the patient's age, reason for seeking care, and access to care. The US population of adult women, especially those who are beyond the reproductive years, is rising in relation to the number of physicians in general ObGyn practice. Providing a team-based collaborative model of care should allow for improved access and value. Defining the roles of what constitutes evidence-based care also will impact when a person needs to see a women's health care specialist. Geographic distribution of ObGyns in relation to the patient population will invariably impact on the percentage of women who seek care at the office of an ObGyn alone, in combination with another general physician, or not at all. Given the overlap in care provided at more than one physician's office, continued surveillance is needed to minimize redundant costs and optimize resource utilization. I look forward to what unfolds over the next 15 years.
-- William F. Rayburn, MD, MBA
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Petterson SM, Bazemore AW, Phillips RL, Rayburn WF. Trends in office-based care for reproductive-aged women according to physician specialty: a ten-year study. J Womens Health (Larchmt). 2014;23(12):1021–1026.
- Raffoul MC, Petterson SM, Rayburn WF, Wingrove P, Bazemore AW. Office visits for women aged 45–64 years according to physician specialties. J Womens Health (Larchmt). 2016:25(12):1231–1236.
- Rayburn WF, Raglan GB, Herman CJ, Schulkin J. A survey of obstetrician-gynecologists regarding their care of women 65 years or older. J Geriatr Med Gerontol. 2015;1:2-5.
- Petterson SM, Bazemore AW, Phillips RL, Rayburn WF. Trends in office-based care for reproductive-aged women according to physician specialty: a ten-year study. J Womens Health (Larchmt). 2014;23(12):1021–1026.
- Raffoul MC, Petterson SM, Rayburn WF, Wingrove P, Bazemore AW. Office visits for women aged 45–64 years according to physician specialties. J Womens Health (Larchmt). 2016:25(12):1231–1236.
- Rayburn WF, Raglan GB, Herman CJ, Schulkin J. A survey of obstetrician-gynecologists regarding their care of women 65 years or older. J Geriatr Med Gerontol. 2015;1:2-5.
Shulkin: VA Focused on Transparency and Modernization
After a concerted effort, the VA is now approaching its goal of 100% treatment for patients infected with hepatitis C virus (HCV), VA Secretary David J. Shulkin, MD noted at a speech at the AMSUS Annual Meeting. More than 100,000 veterans have been treated for HCV infection, and 90% have been cured. According to Dr. Shulkin, the VA also has seen significant drops in measures of opioid use and homelessness among veterans. Although the VA is no longer focused on completely ending veteran homelessness, the rate has dropped 50% since 2010, and 3 states (Virginia, Connecticut, and Delaware) have eliminated homelessness completely.
According to Dr. Shulkin, the VA currently is the only health care system that publishes its wait times, quality scores, and disciplinary actions taken against employees. That level of transparency is not only unusual in health care systems, but also unprecedented in the federal government, Dr. Shulkin noted. “I am the only cabinet member that publishes my travel schedule,” Dr. Shulkin told the VA, DoD, and PHS audience.
In addition to promoting current VA progress, Dr. Shulkin also outlined his priorities for the VA moving forward. The priorities included:
- Greater Choice. Dr. Shulkin maintained that the VA should not only provide more options for veterans seeking health care, but also facilitate their ability to make better health care decisions. Choice for veterans will mean being able to access care both inside and outside the VA system.
- Modernize the VA. The signature part of VA’s modernization effort has been its decision to adopt the Cerner/GENESIS electronic health record (EHR) system, but it also includes the VA decision to close 1,100 facilities and focus its resources on the remaining facilities. Dr. Shulkin hopes that the combined power of the VA and DoD on a single EHR system will force EHR providers to improve interoperability. In addition, a new program will allow PHS officers to serve in the VA, bringing in much needed public health experience.
- Improve the Timeliness of Services. Currently, 97% of VA appointments are completed within 30 days, 86% are within a week, and 21% are same day. Improving those metrics will require the VA to “double down on technology,” Dr. Shulkin insisted. The VA now sees 700,000 veterans via telehealth.
- Focus Resources More Efficiently. The VA can and should be “world class” in areas where it matters most, Dr. Shulkin argued, including areas like prosthetics, traumatic brain injury, posttraumatic stress disorder, and spinal cord injury. Better coordination with the DoD also will help both health care systems to improve efficiency. A “Caregivers Moonshot” initiative also will allow more veterans to remain at home at end of life.
- Suicide Prevention. While suicide is a public health crisis across the U.S., it is especially acute amongst veterans. According to Dr. Shulkin, reducing veteran suicide will require action both inside and outside the VA. The VA needs to connect with community mental health providers and provide more services to other than honorable discharges.
After a concerted effort, the VA is now approaching its goal of 100% treatment for patients infected with hepatitis C virus (HCV), VA Secretary David J. Shulkin, MD noted at a speech at the AMSUS Annual Meeting. More than 100,000 veterans have been treated for HCV infection, and 90% have been cured. According to Dr. Shulkin, the VA also has seen significant drops in measures of opioid use and homelessness among veterans. Although the VA is no longer focused on completely ending veteran homelessness, the rate has dropped 50% since 2010, and 3 states (Virginia, Connecticut, and Delaware) have eliminated homelessness completely.
According to Dr. Shulkin, the VA currently is the only health care system that publishes its wait times, quality scores, and disciplinary actions taken against employees. That level of transparency is not only unusual in health care systems, but also unprecedented in the federal government, Dr. Shulkin noted. “I am the only cabinet member that publishes my travel schedule,” Dr. Shulkin told the VA, DoD, and PHS audience.
In addition to promoting current VA progress, Dr. Shulkin also outlined his priorities for the VA moving forward. The priorities included:
- Greater Choice. Dr. Shulkin maintained that the VA should not only provide more options for veterans seeking health care, but also facilitate their ability to make better health care decisions. Choice for veterans will mean being able to access care both inside and outside the VA system.
- Modernize the VA. The signature part of VA’s modernization effort has been its decision to adopt the Cerner/GENESIS electronic health record (EHR) system, but it also includes the VA decision to close 1,100 facilities and focus its resources on the remaining facilities. Dr. Shulkin hopes that the combined power of the VA and DoD on a single EHR system will force EHR providers to improve interoperability. In addition, a new program will allow PHS officers to serve in the VA, bringing in much needed public health experience.
- Improve the Timeliness of Services. Currently, 97% of VA appointments are completed within 30 days, 86% are within a week, and 21% are same day. Improving those metrics will require the VA to “double down on technology,” Dr. Shulkin insisted. The VA now sees 700,000 veterans via telehealth.
- Focus Resources More Efficiently. The VA can and should be “world class” in areas where it matters most, Dr. Shulkin argued, including areas like prosthetics, traumatic brain injury, posttraumatic stress disorder, and spinal cord injury. Better coordination with the DoD also will help both health care systems to improve efficiency. A “Caregivers Moonshot” initiative also will allow more veterans to remain at home at end of life.
- Suicide Prevention. While suicide is a public health crisis across the U.S., it is especially acute amongst veterans. According to Dr. Shulkin, reducing veteran suicide will require action both inside and outside the VA. The VA needs to connect with community mental health providers and provide more services to other than honorable discharges.
After a concerted effort, the VA is now approaching its goal of 100% treatment for patients infected with hepatitis C virus (HCV), VA Secretary David J. Shulkin, MD noted at a speech at the AMSUS Annual Meeting. More than 100,000 veterans have been treated for HCV infection, and 90% have been cured. According to Dr. Shulkin, the VA also has seen significant drops in measures of opioid use and homelessness among veterans. Although the VA is no longer focused on completely ending veteran homelessness, the rate has dropped 50% since 2010, and 3 states (Virginia, Connecticut, and Delaware) have eliminated homelessness completely.
According to Dr. Shulkin, the VA currently is the only health care system that publishes its wait times, quality scores, and disciplinary actions taken against employees. That level of transparency is not only unusual in health care systems, but also unprecedented in the federal government, Dr. Shulkin noted. “I am the only cabinet member that publishes my travel schedule,” Dr. Shulkin told the VA, DoD, and PHS audience.
In addition to promoting current VA progress, Dr. Shulkin also outlined his priorities for the VA moving forward. The priorities included:
- Greater Choice. Dr. Shulkin maintained that the VA should not only provide more options for veterans seeking health care, but also facilitate their ability to make better health care decisions. Choice for veterans will mean being able to access care both inside and outside the VA system.
- Modernize the VA. The signature part of VA’s modernization effort has been its decision to adopt the Cerner/GENESIS electronic health record (EHR) system, but it also includes the VA decision to close 1,100 facilities and focus its resources on the remaining facilities. Dr. Shulkin hopes that the combined power of the VA and DoD on a single EHR system will force EHR providers to improve interoperability. In addition, a new program will allow PHS officers to serve in the VA, bringing in much needed public health experience.
- Improve the Timeliness of Services. Currently, 97% of VA appointments are completed within 30 days, 86% are within a week, and 21% are same day. Improving those metrics will require the VA to “double down on technology,” Dr. Shulkin insisted. The VA now sees 700,000 veterans via telehealth.
- Focus Resources More Efficiently. The VA can and should be “world class” in areas where it matters most, Dr. Shulkin argued, including areas like prosthetics, traumatic brain injury, posttraumatic stress disorder, and spinal cord injury. Better coordination with the DoD also will help both health care systems to improve efficiency. A “Caregivers Moonshot” initiative also will allow more veterans to remain at home at end of life.
- Suicide Prevention. While suicide is a public health crisis across the U.S., it is especially acute amongst veterans. According to Dr. Shulkin, reducing veteran suicide will require action both inside and outside the VA. The VA needs to connect with community mental health providers and provide more services to other than honorable discharges.


























