User login
Celiac disease most common among Indians from Punjab study found
Americans from the Punjab region of India had the highest prevalence of celiac disease in a national cross-sectional study of duodenal mucosal biopsies according to a study reported in the August issue of Clinical Gastroenterology and Hepatology.
In contrast, persons of South Asian, East Asian, and Hispanic descent are significantly less likely to receive a biopsy-based diagnosis of celiac disease than were other Americans, Anna Krigel, MD, at Columbia University, New York, reported with her associates. The prevalence of celiac disease among Jewish and Middle Eastern individuals resembled that of other Americans and did not differ by sex, the researchers added. “These findings may have clinical relevance to gastroenterologists across the United States and may aid in their diagnostic practices.”
Dr. Krigel and her associates analyzed a national laboratory pathology registry of 454,885 patients who underwent esophagogastroduodenoscopy with duodenal biopsy between January 2008 and April 2015. Mucosal biopsy specimens were analyzed at three laboratories by histopathologists who had completed fellowships in gastrointestinal pathology. Patients were categorized based on their first and last names as North Indian, South Indian, East Asian, Hispanic, Middle Eastern, Jewish, or as “other Americans,” using a published algorithm. The researchers further validated this algorithm by adjusting it against a list of individuals of known ethnicities until its specificity reached 95%. Two-thirds of patients in the cohort were female, and the median age was 53 years (Clin Gastroenterol Hepatol. 2016 May 31. doi: 10.1016/j.cgh.2016.04.032).
Overall, 7,928 patients (1.7%) had duodenal villous atrophy indicative of disease, including 2% of North Indians, 1.8% of Jewish individuals, 1.8% of other Americans, 1.5% of Middle Easterners, 1.1% of Hispanics, and 0.15% of East Asians, said the investigators. Thus, Jewish persons and Middle Eastern persons had a prevalence of celiac disease similar to that of other Americans. Prevalence also was similar among Ashkenazi and Sephardic Jews. In contrast, none of the 177 South Indians in the study were diagnosed with celiac disease, and both East Asians and Hispanics were significantly less likely to be receive a diagnosis than other Americans, with odds ratios of 0.08 (95% confidence interval, 0.04-0.17) and 0.58 (0.52-0.64), respectively, and P values less than .0001.
Importantly, celiac disease was significantly more common among patients from the Punjab region of India (3.1%) than among other North Indians (1.5%; P = .02). Past studies of celiac disease in India reported similar prevalences of compatible human leukocyte antigen (HLA) haplotypes as in Western countries, without notable regional trends within India, the researchers noted. Substantial regional variations in wheat consumption in India are more likely to explain their findings and patterns of case reports in past studies, they added.
Because the registry lacked serology data, patients diagnosed with celiac disease could have actually had tropical sprue or sprue-like enteropathy due to olmesartan, the researchers acknowledged. “In particular, multiple studies have shown that tropical sprue is still the most common cause of malabsorption syndrome in India, whereas celiac disease is emerging as a more important cause of malabsorption than previously thought,” they said. “However, such cases of tropical sprue and sprue-like enteropathy due to olmesartan are far less common than celiac disease in the United States.” The study also did not account for patients whose celiac disease only was diagnosed by serology and clinical symptoms, and the algorithm probably assigned some individuals who were Hispanic to other ethnicities, because only 7% of the cohort was classified as Hispanic, compared with about 16% of Americans in the 2010 U.S. Census, they noted. But ethnic misclassification was unlikely to have differed by celiac disease status, they said.
The National Institutes of Health partially supported the work. The authors had no disclosures.
Americans from the Punjab region of India had the highest prevalence of celiac disease in a national cross-sectional study of duodenal mucosal biopsies according to a study reported in the August issue of Clinical Gastroenterology and Hepatology.
In contrast, persons of South Asian, East Asian, and Hispanic descent are significantly less likely to receive a biopsy-based diagnosis of celiac disease than were other Americans, Anna Krigel, MD, at Columbia University, New York, reported with her associates. The prevalence of celiac disease among Jewish and Middle Eastern individuals resembled that of other Americans and did not differ by sex, the researchers added. “These findings may have clinical relevance to gastroenterologists across the United States and may aid in their diagnostic practices.”
Dr. Krigel and her associates analyzed a national laboratory pathology registry of 454,885 patients who underwent esophagogastroduodenoscopy with duodenal biopsy between January 2008 and April 2015. Mucosal biopsy specimens were analyzed at three laboratories by histopathologists who had completed fellowships in gastrointestinal pathology. Patients were categorized based on their first and last names as North Indian, South Indian, East Asian, Hispanic, Middle Eastern, Jewish, or as “other Americans,” using a published algorithm. The researchers further validated this algorithm by adjusting it against a list of individuals of known ethnicities until its specificity reached 95%. Two-thirds of patients in the cohort were female, and the median age was 53 years (Clin Gastroenterol Hepatol. 2016 May 31. doi: 10.1016/j.cgh.2016.04.032).
Overall, 7,928 patients (1.7%) had duodenal villous atrophy indicative of disease, including 2% of North Indians, 1.8% of Jewish individuals, 1.8% of other Americans, 1.5% of Middle Easterners, 1.1% of Hispanics, and 0.15% of East Asians, said the investigators. Thus, Jewish persons and Middle Eastern persons had a prevalence of celiac disease similar to that of other Americans. Prevalence also was similar among Ashkenazi and Sephardic Jews. In contrast, none of the 177 South Indians in the study were diagnosed with celiac disease, and both East Asians and Hispanics were significantly less likely to be receive a diagnosis than other Americans, with odds ratios of 0.08 (95% confidence interval, 0.04-0.17) and 0.58 (0.52-0.64), respectively, and P values less than .0001.
Importantly, celiac disease was significantly more common among patients from the Punjab region of India (3.1%) than among other North Indians (1.5%; P = .02). Past studies of celiac disease in India reported similar prevalences of compatible human leukocyte antigen (HLA) haplotypes as in Western countries, without notable regional trends within India, the researchers noted. Substantial regional variations in wheat consumption in India are more likely to explain their findings and patterns of case reports in past studies, they added.
Because the registry lacked serology data, patients diagnosed with celiac disease could have actually had tropical sprue or sprue-like enteropathy due to olmesartan, the researchers acknowledged. “In particular, multiple studies have shown that tropical sprue is still the most common cause of malabsorption syndrome in India, whereas celiac disease is emerging as a more important cause of malabsorption than previously thought,” they said. “However, such cases of tropical sprue and sprue-like enteropathy due to olmesartan are far less common than celiac disease in the United States.” The study also did not account for patients whose celiac disease only was diagnosed by serology and clinical symptoms, and the algorithm probably assigned some individuals who were Hispanic to other ethnicities, because only 7% of the cohort was classified as Hispanic, compared with about 16% of Americans in the 2010 U.S. Census, they noted. But ethnic misclassification was unlikely to have differed by celiac disease status, they said.
The National Institutes of Health partially supported the work. The authors had no disclosures.
Americans from the Punjab region of India had the highest prevalence of celiac disease in a national cross-sectional study of duodenal mucosal biopsies according to a study reported in the August issue of Clinical Gastroenterology and Hepatology.
In contrast, persons of South Asian, East Asian, and Hispanic descent are significantly less likely to receive a biopsy-based diagnosis of celiac disease than were other Americans, Anna Krigel, MD, at Columbia University, New York, reported with her associates. The prevalence of celiac disease among Jewish and Middle Eastern individuals resembled that of other Americans and did not differ by sex, the researchers added. “These findings may have clinical relevance to gastroenterologists across the United States and may aid in their diagnostic practices.”
Dr. Krigel and her associates analyzed a national laboratory pathology registry of 454,885 patients who underwent esophagogastroduodenoscopy with duodenal biopsy between January 2008 and April 2015. Mucosal biopsy specimens were analyzed at three laboratories by histopathologists who had completed fellowships in gastrointestinal pathology. Patients were categorized based on their first and last names as North Indian, South Indian, East Asian, Hispanic, Middle Eastern, Jewish, or as “other Americans,” using a published algorithm. The researchers further validated this algorithm by adjusting it against a list of individuals of known ethnicities until its specificity reached 95%. Two-thirds of patients in the cohort were female, and the median age was 53 years (Clin Gastroenterol Hepatol. 2016 May 31. doi: 10.1016/j.cgh.2016.04.032).
Overall, 7,928 patients (1.7%) had duodenal villous atrophy indicative of disease, including 2% of North Indians, 1.8% of Jewish individuals, 1.8% of other Americans, 1.5% of Middle Easterners, 1.1% of Hispanics, and 0.15% of East Asians, said the investigators. Thus, Jewish persons and Middle Eastern persons had a prevalence of celiac disease similar to that of other Americans. Prevalence also was similar among Ashkenazi and Sephardic Jews. In contrast, none of the 177 South Indians in the study were diagnosed with celiac disease, and both East Asians and Hispanics were significantly less likely to be receive a diagnosis than other Americans, with odds ratios of 0.08 (95% confidence interval, 0.04-0.17) and 0.58 (0.52-0.64), respectively, and P values less than .0001.
Importantly, celiac disease was significantly more common among patients from the Punjab region of India (3.1%) than among other North Indians (1.5%; P = .02). Past studies of celiac disease in India reported similar prevalences of compatible human leukocyte antigen (HLA) haplotypes as in Western countries, without notable regional trends within India, the researchers noted. Substantial regional variations in wheat consumption in India are more likely to explain their findings and patterns of case reports in past studies, they added.
Because the registry lacked serology data, patients diagnosed with celiac disease could have actually had tropical sprue or sprue-like enteropathy due to olmesartan, the researchers acknowledged. “In particular, multiple studies have shown that tropical sprue is still the most common cause of malabsorption syndrome in India, whereas celiac disease is emerging as a more important cause of malabsorption than previously thought,” they said. “However, such cases of tropical sprue and sprue-like enteropathy due to olmesartan are far less common than celiac disease in the United States.” The study also did not account for patients whose celiac disease only was diagnosed by serology and clinical symptoms, and the algorithm probably assigned some individuals who were Hispanic to other ethnicities, because only 7% of the cohort was classified as Hispanic, compared with about 16% of Americans in the 2010 U.S. Census, they noted. But ethnic misclassification was unlikely to have differed by celiac disease status, they said.
The National Institutes of Health partially supported the work. The authors had no disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Duodenal villous atrophy consistent with celiac disease was most common among Americans from, or descended from, the Punjab region of India.
Major finding: The prevalence of celiac disease was highest among Punjabis (3.1%), and lowest among South Indians (0%).
Data source: A cross-sectional study of duodenal biopsies and associated demographic data for 454,885 patients in the United States.
Disclosures: The National Institutes of Health partially supported the work. The authors had no disclosures.
Study highlights cardiovascular benefits, lower GI risks of low-dose aspirin
Resuming low-dose aspirin after an initial lower gastrointestinal bleed significantly increased the chances of recurrence but protected against serious cardiovascular events, based on a single-center retrospective study published in the August issue of Gastroenterology.
In contrast, “we did not find concomitant use of anticoagulants, antiplatelets, and steroids as a predictor of recurrent lower GI bleeding,” said Dr. Francis Chan of the Prince of Wales Hospital in Hong Kong and his associates. “This may be due to the low percentage of concomitant drug use in both groups. Multicenter studies with a large number of patients will be required to identify additional risk factors for recurrent lower GI bleeding with aspirin use.”
Low-dose aspirin has long been known to help prevent coronary artery and cerebrovascular disease, and more recently has been found to potentially reduce the risk of several types of cancer, the researchers noted. Aspirin is well known to increase the risk of upper GI bleeding, but some studies have also linked it to lower GI bleeding. However, “patients with underlying cardiovascular diseases often require lifelong aspirin,” they added. The risks and benefits of stopping or remaining on aspirin after an initial lower GI bleed are unclear (Gastroenterology 2016 Apr 26. doi: 10.1053/j.gastro.2016.04.013).
Accordingly, the researchers retrospectively studied 295 patients who had an initial aspirin-associated lower GI bleed, defined as 325 mg aspirin a day within a week of bleeding onset. All patients had melena or hematochezia documented by an attending physician and had no endoscopic evidence of upper GI bleeding.
For patients who continued using aspirin at least half the time, the 5-year cumulative incidence of recurrent lower GI bleeding was 19% (95% confidence interval [CI], 13%-25%) – more than double the rate among patients who used aspirin 20% or less of the time (5-year cumulative incidence, 7%; 95% CI, 3%-13%; P = .01). However, the 5-year cumulative incidence of serious cardiovascular events among nonusers was 37% (95% CI, 27%-46%), while the rate among aspirin users was 23% (95% CI, 17%-30%; P = .02). Mortality from noncardiovascular causes was also higher among nonusers (27%) than users (8%; P less than .001), probably because nonusers of aspirin tended to be older than users, but perhaps also because aspirin had a “nonvascular protective effect,” the researchers said.
A multivariate analysis confirmed these findings, linking lower GI bleeding to aspirin but not to use of steroids, anticoagulants, or antiplatelet drugs, or to age, sex, alcohol consumption, smoking, comorbidities, or cardiovascular risks. Indeed, continued aspirin use nearly tripled the chances of a recurrent lower GI bleed (hazard ratio, 2.76; 95% CI, 1.3-6.0; P = .01), but cut the risk of serious cardiovascular events by about 40% (HR, 0.59; 95% CI, 0.4-0.9; P = .02).
Deciding whether to resume aspirin after a severe lower GI bleed “presents a management dilemma for physicians, patients, and their families, particularly in the absence of risk-mitigating therapies and a lack of data on the risks and benefits of resuming aspirin,” the investigators emphasized. Their findings highlight the importance of weighing the cardiovascular benefits of aspirin against GI toxicity, they said. “Since there is substantial risk of recurrent bleeding, physicians should critically evaluate individual patients’ cardiovascular risk before resuming aspirin therapy. Our findings also suggest a need for a composite endpoint to evaluate clinically significant events throughout the GI tract in patients receiving antiplatelet drugs.”
The Chinese University of Hong Kong funded the study. Dr. Chan reported financial ties to Pfizer, Eisai, Takeda, Otsuka, and Astrazeneca.
Resuming low-dose aspirin after an initial lower gastrointestinal bleed significantly increased the chances of recurrence but protected against serious cardiovascular events, based on a single-center retrospective study published in the August issue of Gastroenterology.
In contrast, “we did not find concomitant use of anticoagulants, antiplatelets, and steroids as a predictor of recurrent lower GI bleeding,” said Dr. Francis Chan of the Prince of Wales Hospital in Hong Kong and his associates. “This may be due to the low percentage of concomitant drug use in both groups. Multicenter studies with a large number of patients will be required to identify additional risk factors for recurrent lower GI bleeding with aspirin use.”
Low-dose aspirin has long been known to help prevent coronary artery and cerebrovascular disease, and more recently has been found to potentially reduce the risk of several types of cancer, the researchers noted. Aspirin is well known to increase the risk of upper GI bleeding, but some studies have also linked it to lower GI bleeding. However, “patients with underlying cardiovascular diseases often require lifelong aspirin,” they added. The risks and benefits of stopping or remaining on aspirin after an initial lower GI bleed are unclear (Gastroenterology 2016 Apr 26. doi: 10.1053/j.gastro.2016.04.013).
Accordingly, the researchers retrospectively studied 295 patients who had an initial aspirin-associated lower GI bleed, defined as 325 mg aspirin a day within a week of bleeding onset. All patients had melena or hematochezia documented by an attending physician and had no endoscopic evidence of upper GI bleeding.
For patients who continued using aspirin at least half the time, the 5-year cumulative incidence of recurrent lower GI bleeding was 19% (95% confidence interval [CI], 13%-25%) – more than double the rate among patients who used aspirin 20% or less of the time (5-year cumulative incidence, 7%; 95% CI, 3%-13%; P = .01). However, the 5-year cumulative incidence of serious cardiovascular events among nonusers was 37% (95% CI, 27%-46%), while the rate among aspirin users was 23% (95% CI, 17%-30%; P = .02). Mortality from noncardiovascular causes was also higher among nonusers (27%) than users (8%; P less than .001), probably because nonusers of aspirin tended to be older than users, but perhaps also because aspirin had a “nonvascular protective effect,” the researchers said.
A multivariate analysis confirmed these findings, linking lower GI bleeding to aspirin but not to use of steroids, anticoagulants, or antiplatelet drugs, or to age, sex, alcohol consumption, smoking, comorbidities, or cardiovascular risks. Indeed, continued aspirin use nearly tripled the chances of a recurrent lower GI bleed (hazard ratio, 2.76; 95% CI, 1.3-6.0; P = .01), but cut the risk of serious cardiovascular events by about 40% (HR, 0.59; 95% CI, 0.4-0.9; P = .02).
Deciding whether to resume aspirin after a severe lower GI bleed “presents a management dilemma for physicians, patients, and their families, particularly in the absence of risk-mitigating therapies and a lack of data on the risks and benefits of resuming aspirin,” the investigators emphasized. Their findings highlight the importance of weighing the cardiovascular benefits of aspirin against GI toxicity, they said. “Since there is substantial risk of recurrent bleeding, physicians should critically evaluate individual patients’ cardiovascular risk before resuming aspirin therapy. Our findings also suggest a need for a composite endpoint to evaluate clinically significant events throughout the GI tract in patients receiving antiplatelet drugs.”
The Chinese University of Hong Kong funded the study. Dr. Chan reported financial ties to Pfizer, Eisai, Takeda, Otsuka, and Astrazeneca.
Resuming low-dose aspirin after an initial lower gastrointestinal bleed significantly increased the chances of recurrence but protected against serious cardiovascular events, based on a single-center retrospective study published in the August issue of Gastroenterology.
In contrast, “we did not find concomitant use of anticoagulants, antiplatelets, and steroids as a predictor of recurrent lower GI bleeding,” said Dr. Francis Chan of the Prince of Wales Hospital in Hong Kong and his associates. “This may be due to the low percentage of concomitant drug use in both groups. Multicenter studies with a large number of patients will be required to identify additional risk factors for recurrent lower GI bleeding with aspirin use.”
Low-dose aspirin has long been known to help prevent coronary artery and cerebrovascular disease, and more recently has been found to potentially reduce the risk of several types of cancer, the researchers noted. Aspirin is well known to increase the risk of upper GI bleeding, but some studies have also linked it to lower GI bleeding. However, “patients with underlying cardiovascular diseases often require lifelong aspirin,” they added. The risks and benefits of stopping or remaining on aspirin after an initial lower GI bleed are unclear (Gastroenterology 2016 Apr 26. doi: 10.1053/j.gastro.2016.04.013).
Accordingly, the researchers retrospectively studied 295 patients who had an initial aspirin-associated lower GI bleed, defined as 325 mg aspirin a day within a week of bleeding onset. All patients had melena or hematochezia documented by an attending physician and had no endoscopic evidence of upper GI bleeding.
For patients who continued using aspirin at least half the time, the 5-year cumulative incidence of recurrent lower GI bleeding was 19% (95% confidence interval [CI], 13%-25%) – more than double the rate among patients who used aspirin 20% or less of the time (5-year cumulative incidence, 7%; 95% CI, 3%-13%; P = .01). However, the 5-year cumulative incidence of serious cardiovascular events among nonusers was 37% (95% CI, 27%-46%), while the rate among aspirin users was 23% (95% CI, 17%-30%; P = .02). Mortality from noncardiovascular causes was also higher among nonusers (27%) than users (8%; P less than .001), probably because nonusers of aspirin tended to be older than users, but perhaps also because aspirin had a “nonvascular protective effect,” the researchers said.
A multivariate analysis confirmed these findings, linking lower GI bleeding to aspirin but not to use of steroids, anticoagulants, or antiplatelet drugs, or to age, sex, alcohol consumption, smoking, comorbidities, or cardiovascular risks. Indeed, continued aspirin use nearly tripled the chances of a recurrent lower GI bleed (hazard ratio, 2.76; 95% CI, 1.3-6.0; P = .01), but cut the risk of serious cardiovascular events by about 40% (HR, 0.59; 95% CI, 0.4-0.9; P = .02).
Deciding whether to resume aspirin after a severe lower GI bleed “presents a management dilemma for physicians, patients, and their families, particularly in the absence of risk-mitigating therapies and a lack of data on the risks and benefits of resuming aspirin,” the investigators emphasized. Their findings highlight the importance of weighing the cardiovascular benefits of aspirin against GI toxicity, they said. “Since there is substantial risk of recurrent bleeding, physicians should critically evaluate individual patients’ cardiovascular risk before resuming aspirin therapy. Our findings also suggest a need for a composite endpoint to evaluate clinically significant events throughout the GI tract in patients receiving antiplatelet drugs.”
The Chinese University of Hong Kong funded the study. Dr. Chan reported financial ties to Pfizer, Eisai, Takeda, Otsuka, and Astrazeneca.
FROM GASTROENTEROLOGY
Key clinical point: Resuming low-dose aspirin after a lower gastrointestinal bleed increased the risk of recurrence but protected against cardiovascular events.
Major finding: At 5 years, the cumulative incidence of recurrent lower GI bleeding was 19% for patients who stayed on aspirin and 7% for patients who largely stopped it (P = .01). The cumulative incidence of serious cardiovascular events was 25% for users and 37% for nonusers (P = .02).
Data source: A single-center 5-year retrospective cohort study of 295 patients with aspirin-associated melena or hematochezia and no upper gastrointestinal bleeding.
Disclosures: The Chinese University of Hong Kong funded the study. Dr. Chan reported financial ties to Pfizer, Eisai, Takeda, Otsuka, and Astrazeneca.
Rectal indomethacin cut odds of post-ERCP pancreatitis in real-world study
A single, 100-mg rectal dose of indomethacin cut the odds of moderate to severe pancreatitis after endoscopic retrograde cholangiopancreatography (ERCP) by 85% in a single-center retrospective study of more than 4,000 patients reported in the August issue of Gastroenterology.
The effect extended to low-risk patients and those with malignant biliary obstruction, who make up the majority of ERCP patients in community practice, said Nikhil R. Thiruvengadam, MD, and his associates at the University of Pennsylvania. “Usage of rectal indomethacin in current clinical practice is low, as most endoscopists outside of referral centers perform ERCP for indications that are considered low-risk for PEP [post-ERCP pancreatitis], and until now, there were no data to support a benefit of rectal NSAIDs in this population,” they wrote in Gastroenterology. Their “real-world analysis” clearly shows the benefits of rectal indomethacin in low-risk patients and supports its increased use after ERCP, they added.
Pancreatitis, the most common complication of ERCP, affected 2%-9% of patients in prior studies and costs about $200 million in the United States annually, the investigators noted. Pancreatic duct stents help prevent post-ERCP pancreatitis, but require experience to place and have their own complications that limit their use in low-risk patients. Past studies of rectal indomethacin after ERCP reported mixed results and mainly focused on high-risk patients, leaving questions about whether to routinely use this NSAID after ERCP, said the researchers (Gastroenterology. 2016 May 20. doi: 10.1053/j.gastro.2016.04.048). Their study included 4,017 patients who underwent ERCP at the University of Pennsylvania between 2009 and 2015. From 2012 onward, nearly all patients received 100 mg rectal indomethacin immediately after the duodenoscope was withdrawn. This indomethacin group included 2,007 patients, while 2,010 patients in the study did not receive rectal indomethacin. In all, 95 (4.73%) untreated patients developed post-ERCP pancreatitis, compared with only 40 (1.99%) patients who received indomethacin, for a 65% reduction in the odds of post-ERCP pancreatitis (odds ratio, 0.35; 95% confidence interval, 0.24-0.51; P less than .001). Rectal indomethacin also led to an 83% drop in the odds of moderate to severe post-ERCP pancreatitis (OR, 0.17; 95% CI, 0.09-0.32; P less than .001) and showed very similar protective effects for patients with malignant obstruction (OR, 0.35; 95% CI, 0.17-0.75; P less than .001] and 0.20; 95% CI, 0.07-0.63; P less than 0.001, respectively).
Rectal indomethacin was particularly beneficial for patients with malignant obstruction and pancreatic adenocarcinoma, the investigators noted. Such patients had post-ERCP rates of 2.31% when they received rectal indomethacin and 7.53% otherwise (P less than .001). They also had a nearly sevenfold lower rate of moderate to severe post-ERCP pancreatitis when they received rectal indomethacin (P = .001).
Treatment did not affect the chances of perforation and did not cause anaphylaxis, but was tied to a slightly higher rate of postprocedural gastrointestinal bleeding among sphincterotomy patients (0.65% with treatment versus 0.45% without; P = .52). However, sphincterotomy patients were much less likely to develop pancreatitis when they received rectal indomethacin than when they did not (0% and 9.58% of patients, respectively; P = .003).
“The majority of ERCPs were performed by experienced endoscopists at a tertiary care center, which may have limited the effects of variable procedural skills on the risk of PEP,” the researchers said. “Therefore, generalizability of our findings to other populations may be limited. However, it should be noted that the overall PEP rate in both the unexposed and indomethacin groups was fairly low and similar to large community-based estimates, suggesting that our overall patient population was of similar overall risk.” The study was not powered to assess the combined effects of rectal indomethacin and pancreatic duct stents, they noted.
The investigators reported no funding sources and had no disclosures.
A single, 100-mg rectal dose of indomethacin cut the odds of moderate to severe pancreatitis after endoscopic retrograde cholangiopancreatography (ERCP) by 85% in a single-center retrospective study of more than 4,000 patients reported in the August issue of Gastroenterology.
The effect extended to low-risk patients and those with malignant biliary obstruction, who make up the majority of ERCP patients in community practice, said Nikhil R. Thiruvengadam, MD, and his associates at the University of Pennsylvania. “Usage of rectal indomethacin in current clinical practice is low, as most endoscopists outside of referral centers perform ERCP for indications that are considered low-risk for PEP [post-ERCP pancreatitis], and until now, there were no data to support a benefit of rectal NSAIDs in this population,” they wrote in Gastroenterology. Their “real-world analysis” clearly shows the benefits of rectal indomethacin in low-risk patients and supports its increased use after ERCP, they added.
Pancreatitis, the most common complication of ERCP, affected 2%-9% of patients in prior studies and costs about $200 million in the United States annually, the investigators noted. Pancreatic duct stents help prevent post-ERCP pancreatitis, but require experience to place and have their own complications that limit their use in low-risk patients. Past studies of rectal indomethacin after ERCP reported mixed results and mainly focused on high-risk patients, leaving questions about whether to routinely use this NSAID after ERCP, said the researchers (Gastroenterology. 2016 May 20. doi: 10.1053/j.gastro.2016.04.048). Their study included 4,017 patients who underwent ERCP at the University of Pennsylvania between 2009 and 2015. From 2012 onward, nearly all patients received 100 mg rectal indomethacin immediately after the duodenoscope was withdrawn. This indomethacin group included 2,007 patients, while 2,010 patients in the study did not receive rectal indomethacin. In all, 95 (4.73%) untreated patients developed post-ERCP pancreatitis, compared with only 40 (1.99%) patients who received indomethacin, for a 65% reduction in the odds of post-ERCP pancreatitis (odds ratio, 0.35; 95% confidence interval, 0.24-0.51; P less than .001). Rectal indomethacin also led to an 83% drop in the odds of moderate to severe post-ERCP pancreatitis (OR, 0.17; 95% CI, 0.09-0.32; P less than .001) and showed very similar protective effects for patients with malignant obstruction (OR, 0.35; 95% CI, 0.17-0.75; P less than .001] and 0.20; 95% CI, 0.07-0.63; P less than 0.001, respectively).
Rectal indomethacin was particularly beneficial for patients with malignant obstruction and pancreatic adenocarcinoma, the investigators noted. Such patients had post-ERCP rates of 2.31% when they received rectal indomethacin and 7.53% otherwise (P less than .001). They also had a nearly sevenfold lower rate of moderate to severe post-ERCP pancreatitis when they received rectal indomethacin (P = .001).
Treatment did not affect the chances of perforation and did not cause anaphylaxis, but was tied to a slightly higher rate of postprocedural gastrointestinal bleeding among sphincterotomy patients (0.65% with treatment versus 0.45% without; P = .52). However, sphincterotomy patients were much less likely to develop pancreatitis when they received rectal indomethacin than when they did not (0% and 9.58% of patients, respectively; P = .003).
“The majority of ERCPs were performed by experienced endoscopists at a tertiary care center, which may have limited the effects of variable procedural skills on the risk of PEP,” the researchers said. “Therefore, generalizability of our findings to other populations may be limited. However, it should be noted that the overall PEP rate in both the unexposed and indomethacin groups was fairly low and similar to large community-based estimates, suggesting that our overall patient population was of similar overall risk.” The study was not powered to assess the combined effects of rectal indomethacin and pancreatic duct stents, they noted.
The investigators reported no funding sources and had no disclosures.
A single, 100-mg rectal dose of indomethacin cut the odds of moderate to severe pancreatitis after endoscopic retrograde cholangiopancreatography (ERCP) by 85% in a single-center retrospective study of more than 4,000 patients reported in the August issue of Gastroenterology.
The effect extended to low-risk patients and those with malignant biliary obstruction, who make up the majority of ERCP patients in community practice, said Nikhil R. Thiruvengadam, MD, and his associates at the University of Pennsylvania. “Usage of rectal indomethacin in current clinical practice is low, as most endoscopists outside of referral centers perform ERCP for indications that are considered low-risk for PEP [post-ERCP pancreatitis], and until now, there were no data to support a benefit of rectal NSAIDs in this population,” they wrote in Gastroenterology. Their “real-world analysis” clearly shows the benefits of rectal indomethacin in low-risk patients and supports its increased use after ERCP, they added.
Pancreatitis, the most common complication of ERCP, affected 2%-9% of patients in prior studies and costs about $200 million in the United States annually, the investigators noted. Pancreatic duct stents help prevent post-ERCP pancreatitis, but require experience to place and have their own complications that limit their use in low-risk patients. Past studies of rectal indomethacin after ERCP reported mixed results and mainly focused on high-risk patients, leaving questions about whether to routinely use this NSAID after ERCP, said the researchers (Gastroenterology. 2016 May 20. doi: 10.1053/j.gastro.2016.04.048). Their study included 4,017 patients who underwent ERCP at the University of Pennsylvania between 2009 and 2015. From 2012 onward, nearly all patients received 100 mg rectal indomethacin immediately after the duodenoscope was withdrawn. This indomethacin group included 2,007 patients, while 2,010 patients in the study did not receive rectal indomethacin. In all, 95 (4.73%) untreated patients developed post-ERCP pancreatitis, compared with only 40 (1.99%) patients who received indomethacin, for a 65% reduction in the odds of post-ERCP pancreatitis (odds ratio, 0.35; 95% confidence interval, 0.24-0.51; P less than .001). Rectal indomethacin also led to an 83% drop in the odds of moderate to severe post-ERCP pancreatitis (OR, 0.17; 95% CI, 0.09-0.32; P less than .001) and showed very similar protective effects for patients with malignant obstruction (OR, 0.35; 95% CI, 0.17-0.75; P less than .001] and 0.20; 95% CI, 0.07-0.63; P less than 0.001, respectively).
Rectal indomethacin was particularly beneficial for patients with malignant obstruction and pancreatic adenocarcinoma, the investigators noted. Such patients had post-ERCP rates of 2.31% when they received rectal indomethacin and 7.53% otherwise (P less than .001). They also had a nearly sevenfold lower rate of moderate to severe post-ERCP pancreatitis when they received rectal indomethacin (P = .001).
Treatment did not affect the chances of perforation and did not cause anaphylaxis, but was tied to a slightly higher rate of postprocedural gastrointestinal bleeding among sphincterotomy patients (0.65% with treatment versus 0.45% without; P = .52). However, sphincterotomy patients were much less likely to develop pancreatitis when they received rectal indomethacin than when they did not (0% and 9.58% of patients, respectively; P = .003).
“The majority of ERCPs were performed by experienced endoscopists at a tertiary care center, which may have limited the effects of variable procedural skills on the risk of PEP,” the researchers said. “Therefore, generalizability of our findings to other populations may be limited. However, it should be noted that the overall PEP rate in both the unexposed and indomethacin groups was fairly low and similar to large community-based estimates, suggesting that our overall patient population was of similar overall risk.” The study was not powered to assess the combined effects of rectal indomethacin and pancreatic duct stents, they noted.
The investigators reported no funding sources and had no disclosures.
FROM GASTROENTEROLOGY
Key clinical point: A single 100-mg rectal dose of indomethacin given immediately after endoscopic retrograde cholangiopancreatography significantly reduced the odds of postprocedural pancreatitis, including in low-risk patients and those with malignant obstruction.
Major finding: The odds of pancreatitis were 65% lower when patients received rectal indomethacin than otherwise.
Data source: A single-center retrospective cohort study of 4,017 patients undergoing ERCP.
Disclosures: The investigators reported no funding sources and had no disclosures.
Measles: More than the rash
To the Editor: I read the excellent overview article on measles by Drs. Kumar and Sabella.1 However, there are additional important clinical points regarding measles diagnosis that deserve further comment. Prior to definitive diagnosis, measles is a clinical diagnosis. Properly, much attention is given to the rash, but there are important clinical clues besides the rash that are helpful diagnostically.
Some clinical findings are more characteristic of a disease than others, eg, eye findings in measles, and clinicians should specifically look for them. Other findings not characteristic but consistent with the diagnosis are less helpful, eg, measles with diarrhea.2 Measles is a systemic infection with several extradermatologic manifestations. Characteristically, measles involves the respiratory tract, manifested by runny nose, dry cough, or shortness of breath, ie, measles pneumonia.2
Gastrointestinal involvement may be manifested as nausea, vomiting, diarrhea, or abdominal pain. Abdominal pain, when located in the right lower quadrant, may mimic acute appendicitis, ie, pseudoappendicitis. In patients undergoing appendectomy, pathologically the appendix is normal but contains multinucleated giant cells (Warthin-Finkeldey cells). Measles pseudoappendicitis can be perplexing because it presents before the rash. Even without appendiceal involvement (pseudoappendicitis), Warthin-Finkeldey cells are also present in the nasal mucosa. If nasal swab cytology shows Warthin-Finkeldey cells, an early diagnosis of measles may be made days before IgM measles antibodies are reported.3
Other often-overlooked important clues are eye findings, eg, watery eyes, lower lid edema, conjunctival suffusion, and keratitis. No other disease in the differential diagnosis of measles presents with watery eyes with bilateral lower lid edema and conjunctival suffusion. Headache, mental confusion or oral ulcers may suggest alternate diagnoses. Typically, nonspecific laboratory abnormalities include leukopenia and thrombocytopenia, and importantly, the erythrocyte sedimentation rate is not elevated (Table 1).4,5
In measles, much is made of Koplik spots, which are found early on dark red buccal mucosa (vs Fordyce spots).1 However, if these are missed or not present, clinicians can use other characteristic findings to make a presumptive diagnosis of measles.
- Kumar D, Sabella C. Measles: back again. Cleve Clin J Med 2016; 83:340–344.
- Leibovici L, Sharir T, Kalter-Leibovici O, Alpert G, Epstein LM. An outbreak of measles among young adults. Clinical and laboratory features in 461 patients. J Adolesc Health Care 1988; 9:203–207.
- Cunha BA, Hage JE, Turi GK. A 45-year-old male with rash, fever and diarrhea. J Clin Microbiol 2012; 50:1835,2184.
- Cunha BA, Mickail N. Fever and rash in an adult traveler: the many masquerades of measles. Travel Med Inf Dis 2011; 9:255–257.
- Cunha CB, Cunha BA. Rash and fever in the intensive care unit. In: Fink MP, Abraham E, Vincent JL, Kochanek P, editors. Textbook of Critical Care Medicine (7th Ed). Elsevier, Philadelphia, 2016:97–115.
To the Editor: I read the excellent overview article on measles by Drs. Kumar and Sabella.1 However, there are additional important clinical points regarding measles diagnosis that deserve further comment. Prior to definitive diagnosis, measles is a clinical diagnosis. Properly, much attention is given to the rash, but there are important clinical clues besides the rash that are helpful diagnostically.
Some clinical findings are more characteristic of a disease than others, eg, eye findings in measles, and clinicians should specifically look for them. Other findings not characteristic but consistent with the diagnosis are less helpful, eg, measles with diarrhea.2 Measles is a systemic infection with several extradermatologic manifestations. Characteristically, measles involves the respiratory tract, manifested by runny nose, dry cough, or shortness of breath, ie, measles pneumonia.2
Gastrointestinal involvement may be manifested as nausea, vomiting, diarrhea, or abdominal pain. Abdominal pain, when located in the right lower quadrant, may mimic acute appendicitis, ie, pseudoappendicitis. In patients undergoing appendectomy, pathologically the appendix is normal but contains multinucleated giant cells (Warthin-Finkeldey cells). Measles pseudoappendicitis can be perplexing because it presents before the rash. Even without appendiceal involvement (pseudoappendicitis), Warthin-Finkeldey cells are also present in the nasal mucosa. If nasal swab cytology shows Warthin-Finkeldey cells, an early diagnosis of measles may be made days before IgM measles antibodies are reported.3
Other often-overlooked important clues are eye findings, eg, watery eyes, lower lid edema, conjunctival suffusion, and keratitis. No other disease in the differential diagnosis of measles presents with watery eyes with bilateral lower lid edema and conjunctival suffusion. Headache, mental confusion or oral ulcers may suggest alternate diagnoses. Typically, nonspecific laboratory abnormalities include leukopenia and thrombocytopenia, and importantly, the erythrocyte sedimentation rate is not elevated (Table 1).4,5
In measles, much is made of Koplik spots, which are found early on dark red buccal mucosa (vs Fordyce spots).1 However, if these are missed or not present, clinicians can use other characteristic findings to make a presumptive diagnosis of measles.
To the Editor: I read the excellent overview article on measles by Drs. Kumar and Sabella.1 However, there are additional important clinical points regarding measles diagnosis that deserve further comment. Prior to definitive diagnosis, measles is a clinical diagnosis. Properly, much attention is given to the rash, but there are important clinical clues besides the rash that are helpful diagnostically.
Some clinical findings are more characteristic of a disease than others, eg, eye findings in measles, and clinicians should specifically look for them. Other findings not characteristic but consistent with the diagnosis are less helpful, eg, measles with diarrhea.2 Measles is a systemic infection with several extradermatologic manifestations. Characteristically, measles involves the respiratory tract, manifested by runny nose, dry cough, or shortness of breath, ie, measles pneumonia.2
Gastrointestinal involvement may be manifested as nausea, vomiting, diarrhea, or abdominal pain. Abdominal pain, when located in the right lower quadrant, may mimic acute appendicitis, ie, pseudoappendicitis. In patients undergoing appendectomy, pathologically the appendix is normal but contains multinucleated giant cells (Warthin-Finkeldey cells). Measles pseudoappendicitis can be perplexing because it presents before the rash. Even without appendiceal involvement (pseudoappendicitis), Warthin-Finkeldey cells are also present in the nasal mucosa. If nasal swab cytology shows Warthin-Finkeldey cells, an early diagnosis of measles may be made days before IgM measles antibodies are reported.3
Other often-overlooked important clues are eye findings, eg, watery eyes, lower lid edema, conjunctival suffusion, and keratitis. No other disease in the differential diagnosis of measles presents with watery eyes with bilateral lower lid edema and conjunctival suffusion. Headache, mental confusion or oral ulcers may suggest alternate diagnoses. Typically, nonspecific laboratory abnormalities include leukopenia and thrombocytopenia, and importantly, the erythrocyte sedimentation rate is not elevated (Table 1).4,5
In measles, much is made of Koplik spots, which are found early on dark red buccal mucosa (vs Fordyce spots).1 However, if these are missed or not present, clinicians can use other characteristic findings to make a presumptive diagnosis of measles.
- Kumar D, Sabella C. Measles: back again. Cleve Clin J Med 2016; 83:340–344.
- Leibovici L, Sharir T, Kalter-Leibovici O, Alpert G, Epstein LM. An outbreak of measles among young adults. Clinical and laboratory features in 461 patients. J Adolesc Health Care 1988; 9:203–207.
- Cunha BA, Hage JE, Turi GK. A 45-year-old male with rash, fever and diarrhea. J Clin Microbiol 2012; 50:1835,2184.
- Cunha BA, Mickail N. Fever and rash in an adult traveler: the many masquerades of measles. Travel Med Inf Dis 2011; 9:255–257.
- Cunha CB, Cunha BA. Rash and fever in the intensive care unit. In: Fink MP, Abraham E, Vincent JL, Kochanek P, editors. Textbook of Critical Care Medicine (7th Ed). Elsevier, Philadelphia, 2016:97–115.
- Kumar D, Sabella C. Measles: back again. Cleve Clin J Med 2016; 83:340–344.
- Leibovici L, Sharir T, Kalter-Leibovici O, Alpert G, Epstein LM. An outbreak of measles among young adults. Clinical and laboratory features in 461 patients. J Adolesc Health Care 1988; 9:203–207.
- Cunha BA, Hage JE, Turi GK. A 45-year-old male with rash, fever and diarrhea. J Clin Microbiol 2012; 50:1835,2184.
- Cunha BA, Mickail N. Fever and rash in an adult traveler: the many masquerades of measles. Travel Med Inf Dis 2011; 9:255–257.
- Cunha CB, Cunha BA. Rash and fever in the intensive care unit. In: Fink MP, Abraham E, Vincent JL, Kochanek P, editors. Textbook of Critical Care Medicine (7th Ed). Elsevier, Philadelphia, 2016:97–115.
In reply: Measles: More than the rash
In Reply: We thank Dr. Cunha for his comments and appreciate the opportunity to emphasize important points that he highlights.
We agree that measles is a systemic illness with important extradermatologic manifestations that are critical to the diagnosis, and that the nondermatologic manifestations often precede the rash and serve to distinguish measles from other systemic illnesses. As discussed in our review, the respiratory prodrome of cough, coryza, and conjunctivitis is very distinctive and serves as an important clue to the diagnosis. Likewise, we acknowledge the importance of gastrointestinal findings in measles and note appendicitis as an important complication that is well described. Although Koplik spots are pathognomonic, we do stress that these often are not present at the time of presentation.
Finally, we agree that measles is a clinical diagnosis, and that the clinical manifestations beyond the dermatologic manifestations noted in our review and highlighted by Dr. Cunha are extremely helpful to the clinician in considering the diagnosis.
In Reply: We thank Dr. Cunha for his comments and appreciate the opportunity to emphasize important points that he highlights.
We agree that measles is a systemic illness with important extradermatologic manifestations that are critical to the diagnosis, and that the nondermatologic manifestations often precede the rash and serve to distinguish measles from other systemic illnesses. As discussed in our review, the respiratory prodrome of cough, coryza, and conjunctivitis is very distinctive and serves as an important clue to the diagnosis. Likewise, we acknowledge the importance of gastrointestinal findings in measles and note appendicitis as an important complication that is well described. Although Koplik spots are pathognomonic, we do stress that these often are not present at the time of presentation.
Finally, we agree that measles is a clinical diagnosis, and that the clinical manifestations beyond the dermatologic manifestations noted in our review and highlighted by Dr. Cunha are extremely helpful to the clinician in considering the diagnosis.
In Reply: We thank Dr. Cunha for his comments and appreciate the opportunity to emphasize important points that he highlights.
We agree that measles is a systemic illness with important extradermatologic manifestations that are critical to the diagnosis, and that the nondermatologic manifestations often precede the rash and serve to distinguish measles from other systemic illnesses. As discussed in our review, the respiratory prodrome of cough, coryza, and conjunctivitis is very distinctive and serves as an important clue to the diagnosis. Likewise, we acknowledge the importance of gastrointestinal findings in measles and note appendicitis as an important complication that is well described. Although Koplik spots are pathognomonic, we do stress that these often are not present at the time of presentation.
Finally, we agree that measles is a clinical diagnosis, and that the clinical manifestations beyond the dermatologic manifestations noted in our review and highlighted by Dr. Cunha are extremely helpful to the clinician in considering the diagnosis.
Prescribing opioids
To the Editor: As a primary care physician who has practiced for 31 years, I have a few concerns about the article “Prescribing opioids in primary care: Safely starting, monitoring, and stopping” by Drs. Daniel Tobin, Rebecca Andrews, and William Becker in your March 2016 issue.
Prescribing narcotics and other controlled medications has become a hot topic with legal implications. Many physicians have lost their license, and some have lost their freedom as well.
The article notes that primary care physicians provide most of the care for chronic pain but implies that we don’t know what we are doing. Although we might not have completed a residency in the management of chronic pain, we were required to attend a graduate medical school and to complete residency programs. We are also required to read the medical literature and keep up with our CME requirements. We too strive to keep up with and practice the latest cutting-edge medicine. And we have experience. After seeing thousands of patients and writing millions of prescriptions, I think I do know something about whether or not a medicine is safe, effective, and cost-effective. I have encountered quite a few patients with pain, and not one of them has overdosed by taking the medications as prescribed.
Most of what is being said and published about pain medication focuses on the epidemic of young people who are getting pain medications (prescription narcotics) and street narcotics (heroin) illegally. Directly, it has nothing to do with conscientious physicians prescribing narcotics for pain, but indirectly, it has to do with all adults in society. We are allowing our young people to be destroyed by drugs and by a lack of proper discipline in our homes that spills over into society. Where are our children getting these drugs, and who is bringing them into our neighborhoods? The practice of medicine is not the primary problem. I am for scientific, conscientious regulations concerning controlled substances. Medicine needs to inform all doctors about the changing laws surrounding the prescribing of controlled substances.
Cigarettes and alcohol are sold on every corner, and places selling marijuana are popping up everywhere. The former two drugs are harming and killing more young people than all the illegal drugs combined, and marijuana is fast approaching number three. I feel we need to stop picking on the medical profession and stop trying to blame it for all the woes that our young people are encountering every day. The reality is that legal and illegal drugs are not going to go away. We need to love our children more and better prepare them while in our homes to deal with the evils in our society.
To the Editor: As a primary care physician who has practiced for 31 years, I have a few concerns about the article “Prescribing opioids in primary care: Safely starting, monitoring, and stopping” by Drs. Daniel Tobin, Rebecca Andrews, and William Becker in your March 2016 issue.
Prescribing narcotics and other controlled medications has become a hot topic with legal implications. Many physicians have lost their license, and some have lost their freedom as well.
The article notes that primary care physicians provide most of the care for chronic pain but implies that we don’t know what we are doing. Although we might not have completed a residency in the management of chronic pain, we were required to attend a graduate medical school and to complete residency programs. We are also required to read the medical literature and keep up with our CME requirements. We too strive to keep up with and practice the latest cutting-edge medicine. And we have experience. After seeing thousands of patients and writing millions of prescriptions, I think I do know something about whether or not a medicine is safe, effective, and cost-effective. I have encountered quite a few patients with pain, and not one of them has overdosed by taking the medications as prescribed.
Most of what is being said and published about pain medication focuses on the epidemic of young people who are getting pain medications (prescription narcotics) and street narcotics (heroin) illegally. Directly, it has nothing to do with conscientious physicians prescribing narcotics for pain, but indirectly, it has to do with all adults in society. We are allowing our young people to be destroyed by drugs and by a lack of proper discipline in our homes that spills over into society. Where are our children getting these drugs, and who is bringing them into our neighborhoods? The practice of medicine is not the primary problem. I am for scientific, conscientious regulations concerning controlled substances. Medicine needs to inform all doctors about the changing laws surrounding the prescribing of controlled substances.
Cigarettes and alcohol are sold on every corner, and places selling marijuana are popping up everywhere. The former two drugs are harming and killing more young people than all the illegal drugs combined, and marijuana is fast approaching number three. I feel we need to stop picking on the medical profession and stop trying to blame it for all the woes that our young people are encountering every day. The reality is that legal and illegal drugs are not going to go away. We need to love our children more and better prepare them while in our homes to deal with the evils in our society.
To the Editor: As a primary care physician who has practiced for 31 years, I have a few concerns about the article “Prescribing opioids in primary care: Safely starting, monitoring, and stopping” by Drs. Daniel Tobin, Rebecca Andrews, and William Becker in your March 2016 issue.
Prescribing narcotics and other controlled medications has become a hot topic with legal implications. Many physicians have lost their license, and some have lost their freedom as well.
The article notes that primary care physicians provide most of the care for chronic pain but implies that we don’t know what we are doing. Although we might not have completed a residency in the management of chronic pain, we were required to attend a graduate medical school and to complete residency programs. We are also required to read the medical literature and keep up with our CME requirements. We too strive to keep up with and practice the latest cutting-edge medicine. And we have experience. After seeing thousands of patients and writing millions of prescriptions, I think I do know something about whether or not a medicine is safe, effective, and cost-effective. I have encountered quite a few patients with pain, and not one of them has overdosed by taking the medications as prescribed.
Most of what is being said and published about pain medication focuses on the epidemic of young people who are getting pain medications (prescription narcotics) and street narcotics (heroin) illegally. Directly, it has nothing to do with conscientious physicians prescribing narcotics for pain, but indirectly, it has to do with all adults in society. We are allowing our young people to be destroyed by drugs and by a lack of proper discipline in our homes that spills over into society. Where are our children getting these drugs, and who is bringing them into our neighborhoods? The practice of medicine is not the primary problem. I am for scientific, conscientious regulations concerning controlled substances. Medicine needs to inform all doctors about the changing laws surrounding the prescribing of controlled substances.
Cigarettes and alcohol are sold on every corner, and places selling marijuana are popping up everywhere. The former two drugs are harming and killing more young people than all the illegal drugs combined, and marijuana is fast approaching number three. I feel we need to stop picking on the medical profession and stop trying to blame it for all the woes that our young people are encountering every day. The reality is that legal and illegal drugs are not going to go away. We need to love our children more and better prepare them while in our homes to deal with the evils in our society.
In reply: Prescribing opioids
In Reply: We thank Dr. Pettiway for his remarks. The intent of our article was to identify common challenges when prescribing opioids for chronic pain and offer tips to the provider struggling with how to do so safely. We hope these comments will offer additional clarity.
First, as general internists who are essentially “self-trained” in the management of chronic pain, we fully acknowledge the importance of practical experience in learning how to prescribe opioids safely and effectively. Dr. Pettiway is correct that a dedicated physician who keeps up with the medical literature, attends relevant continuing medical education courses, and strives to provide deliberate, rational, and evidence-based care to his or her patients can do so effectively. However, the medical literature suggests that medical school training in the management of chronic pain is sparse; one review found that in 2011 only 5 out of 133 US medical schools required coursework on pain management, and only 13 offered it as an elective.1 Many primary care providers do feel unprepared to handle this challenge.
Additionally, Dr. Pettiway raises a good question about where misused prescription opioids originate and whether prescribers are responsible. The data show that the majority of misused prescription opioids are obtained from a family member or friend and not directly from a physician.2,3 However, this supply does generally originate from a prescription. Providers need to educate their patients about the risk for diversion, the need to keep pills safely hidden and locked away, and the importance of safely discarding unused supplies. Responsible prescribers need to anticipate these concerns and educate patients about them.
In summary, we firmly believe that primary care providers are capable of safe, effective, and responsible opioid prescribing and hope that our paper provides additional guidance on how to do so.
- Roehr B. US needs new strategy to help 116 million patients in chronic pain. BMJ 2011; 343:d4206.
- Becker WC, Tobin DG, Fiellin DA. Nonmedical use of opioid analgesics obtained directly from physicians: prevalence and correlates. Arch Intern Med 2011; 171:1034–1036.
- Substance Abuse and Mental health Services Administration. Results from the 2013 National Survey on Drug Use and Health: summary of national findings. HHS Publication No. (SMA) 14-4863. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.htm. Accessed June 29, 2016.
In Reply: We thank Dr. Pettiway for his remarks. The intent of our article was to identify common challenges when prescribing opioids for chronic pain and offer tips to the provider struggling with how to do so safely. We hope these comments will offer additional clarity.
First, as general internists who are essentially “self-trained” in the management of chronic pain, we fully acknowledge the importance of practical experience in learning how to prescribe opioids safely and effectively. Dr. Pettiway is correct that a dedicated physician who keeps up with the medical literature, attends relevant continuing medical education courses, and strives to provide deliberate, rational, and evidence-based care to his or her patients can do so effectively. However, the medical literature suggests that medical school training in the management of chronic pain is sparse; one review found that in 2011 only 5 out of 133 US medical schools required coursework on pain management, and only 13 offered it as an elective.1 Many primary care providers do feel unprepared to handle this challenge.
Additionally, Dr. Pettiway raises a good question about where misused prescription opioids originate and whether prescribers are responsible. The data show that the majority of misused prescription opioids are obtained from a family member or friend and not directly from a physician.2,3 However, this supply does generally originate from a prescription. Providers need to educate their patients about the risk for diversion, the need to keep pills safely hidden and locked away, and the importance of safely discarding unused supplies. Responsible prescribers need to anticipate these concerns and educate patients about them.
In summary, we firmly believe that primary care providers are capable of safe, effective, and responsible opioid prescribing and hope that our paper provides additional guidance on how to do so.
In Reply: We thank Dr. Pettiway for his remarks. The intent of our article was to identify common challenges when prescribing opioids for chronic pain and offer tips to the provider struggling with how to do so safely. We hope these comments will offer additional clarity.
First, as general internists who are essentially “self-trained” in the management of chronic pain, we fully acknowledge the importance of practical experience in learning how to prescribe opioids safely and effectively. Dr. Pettiway is correct that a dedicated physician who keeps up with the medical literature, attends relevant continuing medical education courses, and strives to provide deliberate, rational, and evidence-based care to his or her patients can do so effectively. However, the medical literature suggests that medical school training in the management of chronic pain is sparse; one review found that in 2011 only 5 out of 133 US medical schools required coursework on pain management, and only 13 offered it as an elective.1 Many primary care providers do feel unprepared to handle this challenge.
Additionally, Dr. Pettiway raises a good question about where misused prescription opioids originate and whether prescribers are responsible. The data show that the majority of misused prescription opioids are obtained from a family member or friend and not directly from a physician.2,3 However, this supply does generally originate from a prescription. Providers need to educate their patients about the risk for diversion, the need to keep pills safely hidden and locked away, and the importance of safely discarding unused supplies. Responsible prescribers need to anticipate these concerns and educate patients about them.
In summary, we firmly believe that primary care providers are capable of safe, effective, and responsible opioid prescribing and hope that our paper provides additional guidance on how to do so.
- Roehr B. US needs new strategy to help 116 million patients in chronic pain. BMJ 2011; 343:d4206.
- Becker WC, Tobin DG, Fiellin DA. Nonmedical use of opioid analgesics obtained directly from physicians: prevalence and correlates. Arch Intern Med 2011; 171:1034–1036.
- Substance Abuse and Mental health Services Administration. Results from the 2013 National Survey on Drug Use and Health: summary of national findings. HHS Publication No. (SMA) 14-4863. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.htm. Accessed June 29, 2016.
- Roehr B. US needs new strategy to help 116 million patients in chronic pain. BMJ 2011; 343:d4206.
- Becker WC, Tobin DG, Fiellin DA. Nonmedical use of opioid analgesics obtained directly from physicians: prevalence and correlates. Arch Intern Med 2011; 171:1034–1036.
- Substance Abuse and Mental health Services Administration. Results from the 2013 National Survey on Drug Use and Health: summary of national findings. HHS Publication No. (SMA) 14-4863. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.htm. Accessed June 29, 2016.
Anemia of chronic kidney disease: Treat it, but not too aggressively
Anemia is a frequent complication of chronic kidney disease, occurring in over 90% of patients receiving renal replacement therapy. It is associated with significant morbidity and mortality. While its pathogenesis is typically multifactorial, the predominant cause is failure of the kidneys to produce enough endogenous erythropoietin. The clinical approval of recombinant human erythropoietin in 1989 dramatically changed the treatment of anemia of chronic kidney disease, but randomized controlled trials yielded disappointing results when erythropoiesis-stimulating agents (ESAs) were used to raise hemoglobin to normal levels.
This article reviews the epidemiology and pathophysiology of anemia of chronic kidney disease and discusses the complicated and conflicting evidence regarding its treatment.
DEFINITION AND PREVALENCE
Anemia is defined as a hemoglobin concentration less than 13.0 g/dL for men and less than 12.0 g/dL for premenopausal women.1 It is more common in patients with impaired kidney function, especially when the glomerular filtration rate (GFR) falls below 60 mL/min. It is rare at GFRs higher than 80 mL/min,2 but as the GFR falls, the severity of the anemia worsens3 and its prevalence increases: almost 90% of patients with a GFR less than 30 mL/min are anemic.4
RENAL ANEMIA IS ASSOCIATED WITH BAD OUTCOMES
Anemia in chronic kidney disease is independently associated with risk of death. It is also an all-cause mortality multiplier, ie, it magnifies the risk of death from other disease states.5
In observational studies, anemia was associated with faster progression of left ventricular hypertrophy, inflammation, and increased myocardial and peripheral oxygen demand, thereby leading to worse cardiac outcomes with increased risk of myocardial infarction, coronary revascularization, and readmission for heart failure.6–8 Anemia is also associated with fatigue, depression, reduced exercise tolerance, stroke, and increased risk of rehospitalization.9–13
RENAL ANEMIA IS MULTIFACTORIAL
Anemia of chronic kidney disease is typically attributed to the decrease of erythropoietin production that accompanies the fall in GFR. However, the process is multifactorial, with several other contributing factors: absolute and functional iron deficiency, folate and vitamin B12 deficiencies, reduced red blood cell life span, and suppression of erythropoiesis by the uremic milieu.14
While it was once thought that chronic kidney disease leads to loss of erythropoietin-producing cells, it is now known that downregulation of hypoxia-inducible factor (HIF; a transcription factor) is at least partially responsible for the decrease in erythropoietin production15,16 and that this downregulation is reversible (see below).
ERYTHROPOIETIN, IRON, AND RED BLOOD CELLS
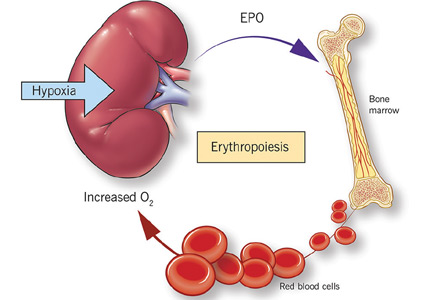
Erythropoietin production is triggered by hypoxia, mediated by HIF
Erythropoietin is produced primarily in the deep cortex and outer medulla of the kidneys by a special population of peritubular interstitial cells.17 The parenchymal cells of the liver also produce erythropoietin, but much less.18
The rate of renal erythropoietin synthesis is determined by tissue oxygenation rather than by renal blood flow; production increases as the hemoglobin concentration drops and the arterial oxygen tension decreases (Figure 1).19
The gene for erythropoietin is located on chromosome 7 and is regulated by HIF. HIF molecules are composed of an alpha subunit, which is unstable at high Po2, and a beta subunit, constitutively present in the nucleus.20
In hypoxic conditions, the HIF dimer is transcriptionally active and binds to specific DNA recognition sequences called hypoxia-response elements. Gene transcription is upregulated, leading to increased production of erythropoietin.21
Under normal oxygen tension, on the other hand, the proline residue of the HIF alpha subunit is hydroxylated. The hydroxylated HIF alpha subunit is then degraded by proteasomal ubiquitylation, which is mediated by the von Hippel-Lindau tumor-suppressor gene pVHL.22 Degradation of HIF alpha prevents formation of the HIF heterodimers. HIF therefore cannot bind to the hypoxia-response elements, and erythropoietin gene transcription does not occur.23
Thus, in states of hypoxia, erythropoietin production is upregulated, whereas with normal oxygen tension, production is downregulated.
Erythropoietin is essential for terminal maturation of erythrocytes
Erythropoietin is essential for terminal maturation of erythrocytes.24 It is thought to stimulate the growth of erythrogenic progenitors: burst-forming units-erythroid (BFU-E) and colony-forming units-erythroid (CFU-E). In the absence of erythropoietin, BFU-E and CFU-E fail to differentiate into mature erythrocytes.25
Binding of erythropoietin to its receptor sets off a series of downstream signals, the most important being the signal transducer and activator of transcription 5 (STAT5). In animal studies, STAT5 was found to inhibit apoptosis through the early induction of an antiapoptotic gene, Bcl-xL.26
Iron metabolism is controlled by several proteins
Iron is characterized by its capacity to accept or donate electrons. This unique property makes it a crucial element in many biochemical reactions such as enzymatic activity, DNA synthesis, oxygen transport, and cell respiration.
Iron metabolism is under the control of several proteins that play different roles in its absorption, recycling, and loss (Figure 2).27
Dietary iron exists primarily in its poorly soluble trivalent ferric form (Fe3+), and it needs to be reduced to its soluble divalent ferrous form (Fe2+) by ferric reductase to be absorbed. Ferrous iron is taken up at the apical side of enterocytes by a divalent metal transporter (DMT1) and is transported across the brush border.28
To enter the circulation, iron has to be transported across the basolateral membrane by a transporter called ferroportin.29 Ferroportin is also found in placental syncitiotrophoblasts, where it transfers iron from mother to fetus, and in macrophages, where it allows recycling of iron scavenged from damaged cells back into the circulation.30 Upon its release, the ferrous iron is oxidized to the ferric form and loaded onto transferrin. This oxidation process involves hephaestin, a homologue of the ferroxidase ceruloplasmin.31
In the plasma, iron is bound to transferrin, and under normal circumstances one-third of transferrin is saturated with iron.32 Transferrin receptors are present on most cells but are most dense on erythroid precursors. Each transferrin receptor can bind two transferrin molecules. After binding to transferrin, the transferrin receptor is endocytosed, and the iron is released into acidified vacuoles. The transferrin-receptor complex is then recycled to the surface.33
Ferritin is the cellular storage protein for iron, and it can store up to 4,500 atoms of iron within its spherical cavity.34 The serum level of ferritin reflects overall storage, with 1 ng/mL of ferritin indicating 10 mg of total iron stores.35 Ferritin is also an acute-phase reactant, and plasma levels can increase in inflammatory states such as infection or malignancy. As such, elevated ferritin does not necessarily indicate elevated iron stores.
Iron is lost in sweat, shed skin cells, and sloughed intestinal mucosal cells. However, there is no specific mechanism of iron excretion from the human body. Thus, iron is mainly regulated at the level of intestinal absorption. The iron exporter ferroportin is upregulated by the amount of available iron and is degraded by hepcidin.36
Hepcidin is a small cysteine-rich cationic peptide that is primarily produced in the liver, with some minor production also occurring in the kidneys.37 Transcription of the gene encoding hepcidin is downregulated by anemia and hypoxia and upregulated by inflammation and elevated iron levels.38 Transcription of hepcidin leads to degradation of ferroportin and a decrease in intestinal iron absorption. On the other hand, anemia and hypoxia inhibit hepcidin transcription, which allows ferroportin to facilitate intestinal iron absorption.
TREATMENT OF RENAL ANEMIA
Early enthusiasm for erythropoietin agents
Androgens started to be used to treat anemia of end-stage renal disease in 1970,39,40 and before the advent of recombinant human erythropoietin, they were a mainstay of nontransfusional therapy for anemic patients on dialysis.
The approval of recombinant human erythropoietin in 1989 drastically shifted the treatment of renal anemia. While the initial goal of treating anemia of chronic kidney disease with erythropoietin was to prevent blood transfusions,41 subsequent studies showed that the benefits might be far greater. Indeed, an initial observational trial showed that erythropoiesis-stimulating agents (ESAs) were associated with improved quality of life,42 improved neurocognitive function,43,44 and even cost savings.45 The benefits also extended to major outcomes such as regression of left ventricular hypertrophy,46 improvement in New York Heart Association class and cardiac function,47 fewer hospitalizations,48 and even reduction of cardiovascular mortality rates.49
As a result, ESA use gained popularity, and by 2006 an estimated 90% of dialysis patients were receiving these agents.50 The target and achieved hemoglobin levels also increased, with mean hemoglobin levels in hemodialysis patients being raised from 9.7 to 12 g/dL.51
Disappointing results in clinical trials of ESAs to normalize hemoglobin
To prospectively study the effects of normalized hemoglobin targets, four randomized controlled trials were conducted (Table 1):
- The Normal Hematocrit Study (NHCT)52
- The Correction of Hemoglobin and Outcomes in Renal Insufficiency (CHOIR) trial53
- The Cardiovascular Risk Reduction by Early Anemia Treatment (CREATE) trial54
- The Trial to Reduce Cardiovascular Events With Aranesp Therapy (TREAT).55
These trials randomized patients to either higher “normal-range” hemoglobin targets or to lower target hemoglobin levels.
Their findings were disappointing and raised several red flags about excessive use of ESAs. The trials found no benefit in higher hemoglobin targets, and in fact, some of them demonstrated harm in patients randomized to higher targets. Notably, higher hemoglobin targets were associated with significant side effects such as access-site thrombosis,52 strokes,55 and possibly cardiovascular events.54,55 Only the CREATE trial was able to demonstrate a quality-of-life benefit for the high-target group.54
It remains unclear whether these adverse events were from the therapy itself or from an increased morbidity burden in the treated patients. Erythropoietin use is associated with hypertension,56 thought to be related to endothelin-mediated vasoconstriction.57 In our experience, this is most evident when hemoglobin levels are normalized with ESA therapy. Cycling of erythropoietin levels between extreme levels can lead to vascular remodeling, which may also be related to its cardiovascular effects.57
A noticeable finding in several of these trials was that patients failed to achieve the higher hemoglobin target despite the use of very high doses of ESA. Reanalysis of data from the CHOIR and CREATE trials showed that the patients who had worse outcomes were more likely to have required very high doses without achieving their target hemoglobin.58,59 Indeed, patients who achieved the higher target hemoglobin levels, usually at lower ESA doses, had better outcomes. This suggested that the need for a higher dose was associated with poorer outcomes, either as a marker of comorbidity or due to yet undocumented side effects of such high doses.
General approach to therapy
Before attributing anemia to chronic kidney disease, a thorough evaluation should be conducted to look for any reversible process that could be contributing to the anemia.
The causes of anemia are numerous and beyond the scope of this review. However, among the common causes of anemia in chronic kidney disease are deficiencies of iron, vitamin B12, and folate. Therefore, guidelines recommend checking iron, vitamin B12, and folate levels in the initial evaluation of anemia.60
Iron deficiency in particular is very common in chronic kidney disease patients and is present in nearly all dialysis patients.61 Hemodialysis patients are estimated to lose 1 to 3 g of iron per year as a result of blood loss in the dialysis circuit and increased iron utilization secondary to ESA therapy.62
However, in contrast to the general population, in which the upper limits of normal for iron indices are well defined, high serum ferritin levels appear to be poorly predictive of hemoglobin responsiveness in dialysis patients.63,64 Thus, the cutoffs that define iron responsiveness are much higher than standard definitions for iron deficiency.65,66 The Dialysis Patients’ Response to IV Iron With Elevated Ferritin (DRIVE) study showed that dialysis patients benefit from intravenous iron therapy even if their ferritin is as high as 1,200 ng/mL, provided their transferrin saturation is below 30%.67
Of note, erythropoietin levels cannot be used to distinguish renal anemia from other causes of anemia. Indeed, patients with renal failure may have “relative erythropoietin deficiency,” ie, “normal” erythropoietin levels that are actually too low in view of the degree of anemia.68,69 In addition to the decreased production capacity by the kidney, there appears to be a component of resistance to the action of erythropoietin in the bone marrow.
For these reasons, there is no erythropoietin level that can be considered “inadequate” or defining of renal anemia. Thus, measuring erythropoietin levels is not routinely recommended in the evaluation of renal anemia.
Two ESA preparations
The two ESAs that have traditionally been used in the treatment of renal anemia are recombinant human erythropoietin and darbepoietin alfa. They appear to be equivalent in terms of safety and efficacy.70 However, darbepoietin alfa has more sialic acid molecules, giving it a higher potency and longer half-life and allowing for less-frequent injections.71,72
In nondialysis patients, recombinant human erythropoietin is typically given every 1 to 2 weeks, whereas darbepoietin alfa can be given every 2 to 4 weeks. In dialysis patients, recombinant human erythropoietin is typically given 3 times per week with every dialysis treatment, while darbepoietin alfa is given once a week.
Target hemoglobin levels: ≤ 11.5 g/dL
In light of the four trials described in Table 1, the international Kidney Disease: Improving Global Outcomes (KDIGO) guidelines60 recommend the following (Table 2):
For patients with chronic kidney disease who are not on dialysis, ESA therapy should not be initiated if the hemoglobin level is higher than 10 g/dL. If the hemoglobin level is lower than 10 g/dL, ESA therapy can be initiated, but the decision needs to be individualized based on the rate of fall of hemoglobin concentration, prior response to iron therapy, the risk of needing a transfusion, the risks related to ESA therapy, and the presence of symptoms attributable to anemia.
For patients on dialysis, ESA therapy should be used when the hemoglobin level is between 9 and 10 g/dL to avoid having the hemoglobin fall below 9 g/dL.
In all adult patients, ESAs should not be used to intentionally increase the hemoglobin level above 13 g/dL but rather to maintain levels no higher than 11.5 g/dL. This target is based on the observation that adverse outcomes were associated with ESA use with hemoglobin targets higher than 13 g/dL (Table 1).
Target iron levels
Regarding iron stores, the guidelines recommend the following:
For adult patients with chronic kidney disease who are not on dialysis, iron should be given to keep transferrin saturation above 20% and ferritin above 100 ng/mL. Transferrin saturation should not exceed 30%, and ferritin levels should not exceed 500 ng/mL.
For adult patients on dialysis, iron should be given to maintain transferrin saturation above 30% and ferritin above 200 ng/mL.
The upper limits of ferritin and transferrin saturation are somewhat controversial, as the safety of intentionally maintaining respective levels greater than 30% and 500 ng/mL has been studied in very few patients. Transferrin saturation should in general not exceed 50%.
High ferritin levels are associated with higher death rates, but whether elevation of ferritin levels is a marker of excessive iron administration rather than a nonspecific acute-phase reactant is not clear. The 2006 guidelines60 cited upper ferritin limits of 500 to 800 ng/mL. However, the more recent DRIVE trial67 showed that patients with ferritin levels of 500 to 1,200 ng/mL will respond to intravenous administration of iron with an increase in their hemoglobin levels. This has led many clinicians to adopt a higher ferritin limit of 1,200 ng/mL.
Hemosiderosis, or excess iron deposition, was a known consequence of frequent transfusions in patients with end-stage renal disease before ESA therapy was available. However, there have been no documented cases of clinical iron overload from iron therapy using current guidelines.73
These algorithms are nuanced, and the benefit of giving intravenous iron should always be weighed against the risks of short-term acute toxicity and infection. Treatment of renal anemia not only requires in-depth knowledge of the topic, but also familiarity with the patient’s specific situation. As such, it is not recommended that clinicians unfamiliar with the treatment of renal anemia manage its treatment.
PARTICULAR CIRCUMSTANCES
Inflammation and ESA resistance
While ESAs are effective in treating anemia in many cases, in many patients the anemia fails to respond. This is of particular importance, since ESA hyporesponsiveness has been found to be a powerful predictor of cardiovascular events and death.74 It is unclear, however, whether high doses of ESA are inherently toxic or whether hyporesponsiveness is a marker of adverse outcomes related to comorbidities.
KDIGO defines initial hyporesponsiveness as having no increase in hemoglobin concentration after the first month of appropriate weight-based dosing, and acquired hyporesponsiveness as requiring two increases in ESA doses up to 50% beyond the dose at which the patient had originally been stable.60 Identifying ESA hyporesponsiveness should lead to an intensive search for potentially correctable factors.
The two major factors accounting for the state of hyporesponsiveness are inflammation and iron deficiency.75,76
Inflammation. High C-reactive protein levels have been shown to predict resistance to erythropoietin in dialysis patients.77 The release of cytokines such as tumor necrosis factor alpha, interleukin 1, and interferon gamma has an inhibitory effect on erythropoiesis.78 Additionally, inflammation can alter the response to ESAs by disrupting the metabolism of iron79 through the release of hepcidin, as previously discussed.38 These reasons likely account for the observed lower response to ESAs in the setting of acute illness and explain why ESAs are not recommended for correcting acute anemia.80
Iron deficiency also can blunt the response to ESAs. Large amounts of iron are needed for effective erythropoietic bursts. As such, iron supplementation is now a recognized treatment of renal anemia.81
Other factors associated with hyporesponsiveness include chronic occult blood loss, aluminum toxicity, cobalamin or folate deficiencies, testosterone deficiency, inadequate dialysis, hyperparathyroidism, and superimposed primary bone marrow disease,82,83 and these should be addressed in patients whose anemia does not respond as expected to ESA therapy. A summary of the main causes of ESA hyporesponsiveness, their reversibility, and recommended treatments is presented in Table 3.
Antibody-mediated pure red-cell aplasia. Rarely, patients receiving ESA therapy develop antibodies that neutralize both the ESA and endogenous erythropoietin. The resulting syndrome, called antibody-mediated pure red-cell aplasia, is characterized by the sudden development of severe transfusion-dependent anemia. This has historically been connected to epoetin beta, a formulation not in use in the United States. However, cases have been documented with epoetin alfa and darbepoetin. The incidence rate is low with subcutaneous ESA use, estimated at 0.5 cases per 10,000 patient-years84 and anecdotal with intravenous ESA.85 The definitive diagnosis requires demonstration of neutralizing antibodies against erythropoietin. Parvovirus infection should be excluded as an alternative cause of pure redcell aplasia.
ANEMIA IN CANCER PATIENTS
ESAs are effective in raising hemoglobin levels and reducing transfusion requirements in patients with chemotherapy-induced anemia.86 However, there are data linking the use of ESAs to shortened survival in patients who have a variety of solid tumors.87
Several mechanisms have been proposed to explain this rapid disease progression, most notably acceleration in tumor growth88–90 by stimulation of erythropoietin receptors on the surface of the tumor cells, leading to increased tumor angiogenesis.91,92
For these reasons, treatment of renal anemia in the setting of active malignancy should be referred to an oncologist.
NOVEL TREATMENTS
Several new agents for treating renal anemia are currently under review.
Continuous erythropoiesis receptor activator
Continuous erythropoiesis receptor activator is a pegylated form of recombinant human erythropoietin that has the ability to repeatedly activate the erythropoietin receptor. It appears to be similar to the other forms of erythropoietin in terms of safety and efficacy in both end-stage renal disease93 and chronic kidney disease.94 It has the advantage of an extended serum half-life, which allows for longer dosing intervals, ie, every 2 weeks. Its use is currently gaining popularity in the dialysis community.
HIF stabilizers
Our growing understanding of the physiology of erythropoietin offers new potential treatment targets. As previously described, production of erythropoietin is stimulated by HIFs. In order to be degraded, these HIFs are hydroxylated at their proline residues by a prolyl hydroxylase. A new category of drugs called prolyl-hydroxylase inhibitors (PDIs) offers the advantage of stabilizing the HIFs, leading to an increase in erythropoietin production.
In phase 1 and 2 clinical trials, these agents have been shown to increase hemoglobin in both end-stage renal disease and chronic kidney disease patients15,16 but not in anephric patients, demonstrating a renal source of the erythropoietin production even in nonfunctioning kidneys. The study of one PDI agent (FG 2216) was halted temporarily after a report of death from fulminant hepatitis, but the other (FG 4592) continues to be studied in a phase 2 clinical trial.95,96
TAKE-HOME POINTS
- Anemia of renal disease is a common condition that is mainly caused by a decrease in erythropoietin production by the kidneys.
- While anemia of renal disease can be corrected with ESAs, it is necessary to investigate and rule out underlying treatable conditions such as iron or vitamin deficiencies before giving an ESA.
- Anemia of renal disease is associated with significant morbidity such as increased risk of left ventricular hypertrophy, myocardial infarction, and heart failure, and has been described as an all-cause mortality multiplier.
- Unfortunately, the only undisputed benefit of treatment to date remains the avoidance of blood transfusions. Furthermore, the large randomized controlled trials that looked at the benefits of ESA have shown that their use can be associated with increased risk of cardiovascular events. Therefore, use of an ESA in end-stage renal disease should never target a normal hemoglobin levels but rather aim for a hemoglobin level of no more than 11.5 g/dL.
- Use of an ESA in chronic kidney disease should be individualized and is not recommended to be started unless the hemoglobin level is less than 10 g/dL.
- Several newer agents for renal anemia are currently under review. A pegylated form of recombinant human erythropoietin has an extended half-life, and a new and promising category of drugs called HIF stabilizers is currently under study.
- World Health Organization (WHO). Nutritional anaemias: report of a WHO scientific group. Geneva, Switzerland: World Health Organization, 1968.
- Hsu CY, McCulloch CE, Curhan GC, et al. Epidemiology of anemia associated with chronic renal insufficiency among adults in the United States: results from the Third National Health and Nutrition Examination Survey. J Am Soc Nephrol 2002; 13:504–510.
- Radtke HW, Claussner A, Erbes PM, Scheuermann EH, Schoeppe W, Koch KM. Serum erythropoetin concentration in chronic renal failure: relationship to degree of anemia and excretory renal function. Blood 1979; 54:877–884.
- Kazmi WH, Kausz AT, Khan S, et al. Anemia: an early complication of chronic renal insufficiency. Am J Kidney Dis 2001; 38:803–812.
- United States Renal Data System. Chapter 3. Morbidity & mortality in patients with CKD. www.usrds.org/2012/view/v1_03.aspx. Accessed June 9, 2016.
- Horwich TB, Fonarow GC, Hamilton MA, MacLellan WR, Borenstein J. Anemia is associated with worse symptoms, greater impairment in functional capacity and a significant increase in mortality in patients with advanced heart failure. J Am Coll Cardiol 2002; 39:1780–1786.
- Mark DB, Felker GM. B-type natriuretic peptide: a biomarker for all seasons? N Engl J Med 2004; 350:718–720.
- Walker AM, Schneider G, Yeaw J, Nordstrom B, Robbins S, Pettitt D. Anemia as a predictor of cardiovascular events in patients with elevated serum creatinine. J Am Soc Nephrol 2006; 17:2293–2298.
- Abramson JL, Jurkovitz CT, Vaccarino V, Weintraub WS, McClellan W. Chronic kidney disease, anemia, and incident stroke in a middle-aged, community-based population: the ARIC Study. Kidney Int 2003; 64:610–615.
- Sarnak MJ, Tighiouart H, Manjunath G, et al. Anemia as a risk factor for cardiovascular disease in the Atherosclerosis Risk in Communities (ARIC) study. J Am Coll Cardiol 2002; 40:27–33.
- McClellan WM, Flanders WD, Langston RD, Jurkovitz C, Presley R. Anemia and renal insufficiency are independent risk factors for death among patients with congestive heart failure admitted to community hospitals: a population-based study. J Am Soc Nephrol 2002; 13:1928–1936.
- Xia H, Ebben J, Ma JZ, Collins AJ. Hematocrit levels and hospitalization risks in hemodialysis patients. J Am Soc Nephrol 1999; 10:1309–1316.
- Collins AJ, Li S, St Peter W, et al. Death, hospitalization, and economic associations among incident hemodialysis patients with hematocrit values of 36 to 39%. J Am Soc Nephrol 2001; 12:2465–2473.
- Agarwal AK. Practical approach to the diagnosis and treatment of anemia associated with CKD in elderly. J Am Med Dir Assoc 2006; 7(suppl 9):S7–S12.
- Bernhardt WM, Wiesener MS, Scigalla P, et al. Inhibition of prolyl hydroxylases increases erythropoietin production in ESRD. J Am Soc Nephrol 2010; 21:2151–2156.
- Provenzano R, Fadda G, Bernardo M, et al. FG-2216, a novel oral HIF-PHI, stimulates erythropoiesis and increases hemoglobin concentration in patients with non-dialysis CKD. Am J Kidney Dis 2008; 51:B80.
- Maxwell PH, Osmond MK, Pugh CW, et al. Identification of the renal erythropoietin-producing cells using transgenic mice. Kidney Int 1993; 44:1149–1162.
- Maxwell PH, Ferguson DJ, Nicholls LG, et al. Sites of erythropoietin production. Kidney Int 1997; 51:393–401.
- Jelkmann W. Erythropoeitin: structure, control of production and function. Physiol Rev 1992; 72:449–489.
- Wang GL, Jiang BH, Rue EA, Semenza GL. Hypoxia-inducible factor 1 is a basic-helix-loop-helix-PAS heterodimer regulated by cellular O2 tension. Proc Natl Acad Sci USA 1995; 92:5510–5514.
- Wang GL, Semenza GL. Purification and characterization of hypoxia-inducible factor 1. J Biol Chem 1995; 270:1230–1237.
- Maxwell PH, Wiesener MS, Chang GW, et al. The tumour suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis. Nature 1999; 399:271–275.
- Salceda S, Caro J. Hypoxia-inducible factor 1alpha protein is rapidly degraded by the ubiquitin-proteasome system under normoxic conditions. Its stabilization by hypoxia depends on redox-induced changes. J Biol Chem 1997; 272:22642–22647.
- Malik J, Kim AR, Tyre KA, Cherukuri AR, Palis J. Erythropoietin critically regulates the terminal maturation of murine and human primitive erythroblasts. Haematologica 2013; 98:1778–1787.
- Wu H, Liu X, Jaenisch R, Lodish HF. Generation of committed erythroid BFU-E and CFU-E progenitors does not require erythropoietin or the erythropoietin receptor. Cell 1995; 83:59–67.
- Socolovsky M, Nam H, Fleming MD, Haase VH, Brugnara C, Lodish HF. Ineffective erythropoiesis in Stat5a(-/-)5b(-/-) mice due to decreased survival of early erythroblasts. Blood 2001; 98:3261–3273.
- Papanikolaou G, Pantopoulos K. Iron metabolism and toxicity. Toxicol Appl Pharmacol 2005; 202:199–211.
- Conrad ME, Umbreit JN. Pathways of iron absorption. Blood Cells Mol Dis 2002; 29:336–355.
- Frazer DM, Anderson GJ. The orchestration of body iron intake: how and where do enterocytes receive their cues? Blood Cells Moll Dis 2003; 30:288–297.
- Donovan A, Lima CA, Pinkus JL, et al. The iron exporter ferroportin/Slc40a1 is essential for iron homeostasis. Cell Metab 2005; 1:191–200.
- Vulpe CD, Kuo YM, Murphy TL, et al. Hephaestin, a ceruloplasmin homologue implicated in intestinal iron transport, is defective in the sla mouse. Nat Genet 1999; 21:195–199.
- Bothwell TH. Overview and mechanisms of iron regulation. Nutr Rev 1995: 53:237–245.
- Kawabata H, Nakamaki T, Ikonomi P, Smith RD, Germain RS, Koeffler HP. Expression of transferrin receptor 2 in normal and neoplastic hematopoietic cells. Blood 2001; 98:2714–2719.
- Arosio P, Levi S. Cytosolic and mitochondrial ferritins in the regulation of cellular iron homeostasis and oxidative damage. Biochim Biophys Acta 2010; 1800:783–792.
- Finch CA, Bellotti V, Stray S, et al. Plasma ferritin determination as a diagnostic tool. West J Med 1986; 145:657–663.
- Delaby C, Pilard N, Goncalves AS, Beaumont C, Canonne-Hergaux F. Presence of the iron exporter ferroportin at the plasma membrane of macrophages is enhanced by iron loading and down-regulated by hepcidin. Blood 2005; 106:3979–3984.
- Ganz T. Hepcidin, a key regulator of iron metabolism and mediator of anemia of inflammation. Blood 2003; 102:783–788.
- Nicolas G, Chauvet C, Viatte L, et al. The gene encoding the iron regulatory peptide hepcidin is regulated by anemia, hypoxia, and inflammation. J Clin Invest 2002; 110:1037–1044.
- DeGowin RL, Lavender AR, Forland M, Charleston D, Gottschalk A. Erythropoiesis and erythropoietin in patients with chronic renal failure treated with hemodialysis and testosterone. Ann Intern Med 1970; 72:913–918.
- Richardson JR Jr, Weinstein MB. Erythropoietic response of dialyzed patients to testosterone administration. Ann Intern Med 1970; 73:403–407
- Eschbach JW, Abdulhadi MH, Browne JK, et al. Recombinant human erythropoietin in anemic patients with end-stage renal disease. Results of a phase III multicenter clinical trial. Ann Intern Med 1989; 111:992–1000.
- Moreno F, Aracil FJ, Pérez R, Valderrábano F. Controlled study on the improvement of quality of life in elderly hemodialysis patients after correcting end-stage renal disease-related anemia with erythropoietin. Am J Kidney Dis 1996; 27:548–556.
- Nissenson AR, Nimer SD, Wolcott DL. Recombinant human erythropoietin and renal anemia: molecular biology, clinical efficacy, and nervous system effects. Ann Intern Med 1991; 114:402–416.
- Stivelman JC. Benefits of anaemia treatment on cognitive function. Nephrol Dial Transplant 2000; 15(suppl 3):29–35.
- Maddux FW, Shetty S, del Aguila MA, Nelson MA, Murray BM. Effect of erythropoiesis-stimulating agents on healthcare utilization, costs, and outcomes in chronic kidney disease. Ann Pharmacother 2007; 41:1761–1769.
- Macdougall IC, Lewis NP, Saunders MJ, et al. Long-term cardiorespiratory effects of amelioration of renal anaemia by erythropoietin. Lancet 1990; 335:489–493.
- Silverberg DS, Wexler D, Blum M, et al. Effects of treatment with epoetin beta on outcomes in patients with anaemia and chronic heart failure. Kidney Blood Press Res 2005; 28:41–47.
- Perkins R, Olson S, Hansen J, Lee J, Stiles K, Lebrun C. Impact of an anemia clinic on emergency room visits and hospitalizations in patients with anemia of CKD pre-dialysis. Nephrol Nurs J 2007; 34:167–173, 182.
- Locatelli F, Conte F, Marcelli D. The impact of haematocrit levels and erythropoietin treatment on overall and cardiovascular mortality and morbidity—the experience of the Lombardy Dialysis Registry. Nephrol Dial Transplant 1998; 13:1642–1644.
- Centers for Medicare and Medicaid Services; Kinney R. 2005 Annual Report: ESRD Clinical Performance Measures Project. Am J Kidney Dis 2006; 48(suppl 2):S1–S106.
- US Renal Data System. Annual Data Report 2006. www.usrds.org/adr.aspx. Accessed July 3, 2016.
- Besarab A, Bolton WK, Browne JK, et al. The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med 1998; 339:584–590.
- Singh AK, Szczech L, Tang KL, et al; CHOIR Investigators. Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med 2006; 355:2085–2098.
- Drüeke TB, Locatelli F, Clyne N, et al; CREATE Investigators. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med 2006; 355:2071–2084.
- Pfeffer MA, Burdmann EA, Chen CY, et al; TREAT Investigators. A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N Engl J Med 2009; 361:2019–2032.
- Kirkpantur A, Kahraman S, Yilmaz R, et al. The effects of maintenance recombinant human erythropoietin therapy on ambulatory blood pressure recordings: conventional, Doppler, and tissue Doppler echocardiographic parameters. Artif Organs 2005; 29:965–972.
- Fishbane S, Berns JS. Hemoglobin cycling in hemodialysis patients treated with recombinant human erythropoietin. Kidney Int 2005; 68:1337–1343.
- Szczech LA, Barnhart HX, Inrig JK, et al. Secondary analysis of the CHOIR trial epoetin-alpha dose and achieved hemoglobin outcomes. Kidney Int 2008; 74:791–798.
- Solomon SD, Uno H, Lewis EF, et al; Trial to Reduce Cardiovascular Events with Aranesp Therapy (TREAT) Investigators. Erythropoietic response and outcomes in kidney disease and type 2 diabetes. N Engl J Med 2010; 363:1146–1155.
- Kidney Disease: Improving Global Outcomes (KDIGO). KDIGO Clinical Practice Guideline for Anemia in Chronic Kidney Disease. Kidney Int Suppl 2012; 2:279–335.
- Fernández-Rodríguez AM, Guindeo-Casasús MC, Molero-Labarta T, et al. Diagnosis of iron deficiency in chronic renal failure. Am J Kidney Dis 1999; 34:508–513.
- Eschbach JW, Cook JD, Scribner BH, Finch CA. Iron balance in hemodialysis patients. Ann Intern Med 1977; 87:710–713.
- Mittman N, Sreedhara R, Mushnick R, et al. Reticulocyte hemoglobin content predicts functional iron deficiency in hemodialysis patients receiving rHuEPO. Am J Kidney Dis 1997; 30:912–922.
- Tessitore N, Solero GP, Lippi G, et al. The role of iron status markers in predicting response to intravenous iron in haemodialysis patients on maintenance erythropoietin. Nephrol Dial Transplant 2001; 16:1416–1423.
- Coyne DW. Iron indices: what do they really mean? Kidney Int Suppl 2006; 101:S4–S8.
- Fishbane S, Kowalski EA, Imbriano LJ, Maesaka JK. The evaluation of iron status in hemodialysis patients. J Am Soc Nephrol 1996; 7:2654–2657.
- Coyne DW, Kapoian T, Suki W, et al; DRIVE Study Group. Ferric gluconate is highly efficacious in anemic hemodialysis patients with high serum ferritin and low transferrin saturation: results of the Dialysis Patients’ Response to IV Iron with Elevated Ferritin (DRIVE) Study. J Am Soc Nephrol 2007; 18:975–984.
- Radtke HW, Claussner A, Erbes PM, Scheuermann EH, Schoeppe W, Koch KM. Serum erythropoietin concentration in chronic renal failure: relationship to degree of anemia and excretory renal function. Blood 1979; 54:877–884.
- Korte W, Cogliatti SB, Jung K, Riesen W. Mild renal dysfunction is sufficient to induce erythropoietin deficiency in patients with unexplained anaemia. Clin Chim Acta 2000; 292:149–154.
- Locatelli F, Olivares J, Walker R, et al; European/Australian NESP 980202 Study Group. Novel erythropoiesis stimulating protein for treatment of anemia in chronic renal insufficiency. Kidney Int 2001; 60:741–747.
- Carrera F, Burnier M. Use of darbepoetin alfa in the treatment of anaemia of chronic kidney disease: clinical and pharmacoeconomic considerations. NDT Plus 2009; 2(suppl 1):i9–i17.
- Egrie JC, Browne JK. Development and characterization of novel erythropoiesis stimulating protein (NESP). Nephrol Dial Transplant 2001; 16(suppl 3):3–13.
- Nissenson AR, Charytan C. Controversies in iron management. Kidney Int Suppl 2003; 87:S64–S71.
- Kilpatrick RD, Critchlow CW, Fishbane S, et al. Greater epoetin alpha responsiveness is associated with improved survival in hemodialysis patients. Clin J Am Soc Nephrol 2008; 3:1077–1083.
- Locatelli F, Aljama P, Barany P, et al; European Best Practice Guidelines Working Group. Revised European best practice guidelines for the management of anaemia in patients with chronic renal failure. Nephrol Dial Transplant 2004; 19(suppl 2):ii1–ii47.
- Stenvinkel P. The role of inflammation in the anaemia of end-stage renal disease. Nephrol Dial Transplant 2001; 16(suppl 7):36–40.
- Barany P, Divino Filho JC, Bergstrom J. High C-reactive protein is a strong predictor of resistance to erythropoietin in hemodialysis patients. Am J Kidney Dis 1997; 29:565–568.
- Drueke T. Hyporesponsiveness to recombinant human erythropoietin. Nephrol Dial Transplant 2001; 16(suppl 7):25–28.
- Casadevall N. Cellular mechanism of resistance to erythropoietin. Nephrol Dial Transplant 1995; 10(suppl 6):27–30.
- Kraus E, Rabb H. EPO therapy during acute kidney disease: to use or not to use, that is the question. Am J Kidney Dis 2005; 46:967–969.
- Gotloib L, Silverberg D, Fudin R, Shostak A. Iron deficiency is a common cause of anemia in chronic kidney disease and can often be corrected with intravenous iron. J Nephrol 2006; 19:161–167.
- Tarng DC, Huang TP, Chen TW, Yang WC. Erythropoietin hyporesponsiveness: from iron deficiency to iron overload. Kidney Int Suppl 1999; 69:S107–S118.
- Drüeke TB. Modulating factors in the hematopoietic response to erythropoietin. Am J Kidney Dis 1991; 18(suppl 1):87–92.
- Boven K, Stryker S, Knight J, et al. The increased incidence of pure red cell aplasia with an Eprex formulation in uncoated rubber stopper syringes. Kidney Int 2005; 67:2346–2353.
- Shimizu H, Saitoh T, Ota F, et al. Pure red cell aplasia induced only by intravenous administration of recombinant human erythropoietin. Acta Haematol 2011; 126:114–118.
- Tonia T, Mettler A, Robert N, et al. Erythropoietin or darbepoetin for patients with cancer. Cochrane Database Syst Rev 2012; 12:CD003407.
- Bohlius J, Langensiepen S, Schwarzer G, et al. Recombinant human erythropoietin and overall survival in cancer patients: results of a comprehensive meta-analysis. J Natl Cancer Inst 2005; 97:489–498.
- Henke M, Laszig R, Rübe C, et al. Erythropoietin to treat head and neck cancer patients with anaemia undergoing radiotherapy: randomised, double-blind, placebo-controlled trial. Lancet 2003; 362:1255–1260.
- Leyland-Jones B, Semiglazov V, Pawlicki M, et al. Maintaining normal hemoglobin levels with epoetin alfa in mainly nonanemic patients with metastatic breast cancer receiving first-line chemotherapy: a survival study. J Clin Oncol 2005; 23:5960–5972.
- Brower V. Erythropoietin may impair, not improve, cancer survival. Nat Med 2003; 9:1439.
- Acs G, Acs P, Beckwith SM, et al. Erythropoietin and erythropoietin receptor expression in human cancer. Cancer Res 2001; 61:3561–3565.
- Yasuda Y, Fujita Y, Matsuo T, et al. Erythropoietin regulates tumour growth of human malignancies. Carcinogenesis 2003; 24:1021–1029.
- Levin NW, Fishbane S, Cañedo FV, et al; MAXIMA Study Investigators. Intravenous methoxy polyethylene glycol-epoetin beta for haemoglobin control in patients with chronic kidney disease who are on dialysis: a randomised non-inferiority trial (MAXIMA). Lancet 2007; 370:1415–1421.
- Macdougall IC, Walker R, Provenzano R, et al; ARCTOS Study Investigators. C.E.R.A. corrects anemia in patients with chronic kidney disease not on dialysis: results of a randomized clinical trial. Clin J Am Soc Nephrol 2008; 3:337–347.
- Frohna PA, Milwee S, Pinkett J, et al. Preliminary results from a randomized, single-blind, placebo-controlled trial of FG-4592, a novel hypoxia inducible factor prolyl hydroxylase inhibitor, in subjects with CKD anemia (abstract). J Am Soc Nephrol 2007; 18:763.
- Holdstock L, Meadowcroft AM, Maier R, et al. Four-week studies of oral hypoxia-inducible factor-prolyl hydroxylase inhibitor GSK1278863 for treatment of anemia. J Am Soc Nephrol 2016; 27:1234–1244.
Anemia is a frequent complication of chronic kidney disease, occurring in over 90% of patients receiving renal replacement therapy. It is associated with significant morbidity and mortality. While its pathogenesis is typically multifactorial, the predominant cause is failure of the kidneys to produce enough endogenous erythropoietin. The clinical approval of recombinant human erythropoietin in 1989 dramatically changed the treatment of anemia of chronic kidney disease, but randomized controlled trials yielded disappointing results when erythropoiesis-stimulating agents (ESAs) were used to raise hemoglobin to normal levels.
This article reviews the epidemiology and pathophysiology of anemia of chronic kidney disease and discusses the complicated and conflicting evidence regarding its treatment.
DEFINITION AND PREVALENCE
Anemia is defined as a hemoglobin concentration less than 13.0 g/dL for men and less than 12.0 g/dL for premenopausal women.1 It is more common in patients with impaired kidney function, especially when the glomerular filtration rate (GFR) falls below 60 mL/min. It is rare at GFRs higher than 80 mL/min,2 but as the GFR falls, the severity of the anemia worsens3 and its prevalence increases: almost 90% of patients with a GFR less than 30 mL/min are anemic.4
RENAL ANEMIA IS ASSOCIATED WITH BAD OUTCOMES
Anemia in chronic kidney disease is independently associated with risk of death. It is also an all-cause mortality multiplier, ie, it magnifies the risk of death from other disease states.5
In observational studies, anemia was associated with faster progression of left ventricular hypertrophy, inflammation, and increased myocardial and peripheral oxygen demand, thereby leading to worse cardiac outcomes with increased risk of myocardial infarction, coronary revascularization, and readmission for heart failure.6–8 Anemia is also associated with fatigue, depression, reduced exercise tolerance, stroke, and increased risk of rehospitalization.9–13
RENAL ANEMIA IS MULTIFACTORIAL
Anemia of chronic kidney disease is typically attributed to the decrease of erythropoietin production that accompanies the fall in GFR. However, the process is multifactorial, with several other contributing factors: absolute and functional iron deficiency, folate and vitamin B12 deficiencies, reduced red blood cell life span, and suppression of erythropoiesis by the uremic milieu.14
While it was once thought that chronic kidney disease leads to loss of erythropoietin-producing cells, it is now known that downregulation of hypoxia-inducible factor (HIF; a transcription factor) is at least partially responsible for the decrease in erythropoietin production15,16 and that this downregulation is reversible (see below).
ERYTHROPOIETIN, IRON, AND RED BLOOD CELLS
Erythropoietin production is triggered by hypoxia, mediated by HIF
Erythropoietin is produced primarily in the deep cortex and outer medulla of the kidneys by a special population of peritubular interstitial cells.17 The parenchymal cells of the liver also produce erythropoietin, but much less.18
The rate of renal erythropoietin synthesis is determined by tissue oxygenation rather than by renal blood flow; production increases as the hemoglobin concentration drops and the arterial oxygen tension decreases (Figure 1).19
The gene for erythropoietin is located on chromosome 7 and is regulated by HIF. HIF molecules are composed of an alpha subunit, which is unstable at high Po2, and a beta subunit, constitutively present in the nucleus.20
In hypoxic conditions, the HIF dimer is transcriptionally active and binds to specific DNA recognition sequences called hypoxia-response elements. Gene transcription is upregulated, leading to increased production of erythropoietin.21
Under normal oxygen tension, on the other hand, the proline residue of the HIF alpha subunit is hydroxylated. The hydroxylated HIF alpha subunit is then degraded by proteasomal ubiquitylation, which is mediated by the von Hippel-Lindau tumor-suppressor gene pVHL.22 Degradation of HIF alpha prevents formation of the HIF heterodimers. HIF therefore cannot bind to the hypoxia-response elements, and erythropoietin gene transcription does not occur.23
Thus, in states of hypoxia, erythropoietin production is upregulated, whereas with normal oxygen tension, production is downregulated.
Erythropoietin is essential for terminal maturation of erythrocytes
Erythropoietin is essential for terminal maturation of erythrocytes.24 It is thought to stimulate the growth of erythrogenic progenitors: burst-forming units-erythroid (BFU-E) and colony-forming units-erythroid (CFU-E). In the absence of erythropoietin, BFU-E and CFU-E fail to differentiate into mature erythrocytes.25
Binding of erythropoietin to its receptor sets off a series of downstream signals, the most important being the signal transducer and activator of transcription 5 (STAT5). In animal studies, STAT5 was found to inhibit apoptosis through the early induction of an antiapoptotic gene, Bcl-xL.26
Iron metabolism is controlled by several proteins
Iron is characterized by its capacity to accept or donate electrons. This unique property makes it a crucial element in many biochemical reactions such as enzymatic activity, DNA synthesis, oxygen transport, and cell respiration.
Iron metabolism is under the control of several proteins that play different roles in its absorption, recycling, and loss (Figure 2).27
Dietary iron exists primarily in its poorly soluble trivalent ferric form (Fe3+), and it needs to be reduced to its soluble divalent ferrous form (Fe2+) by ferric reductase to be absorbed. Ferrous iron is taken up at the apical side of enterocytes by a divalent metal transporter (DMT1) and is transported across the brush border.28
To enter the circulation, iron has to be transported across the basolateral membrane by a transporter called ferroportin.29 Ferroportin is also found in placental syncitiotrophoblasts, where it transfers iron from mother to fetus, and in macrophages, where it allows recycling of iron scavenged from damaged cells back into the circulation.30 Upon its release, the ferrous iron is oxidized to the ferric form and loaded onto transferrin. This oxidation process involves hephaestin, a homologue of the ferroxidase ceruloplasmin.31
In the plasma, iron is bound to transferrin, and under normal circumstances one-third of transferrin is saturated with iron.32 Transferrin receptors are present on most cells but are most dense on erythroid precursors. Each transferrin receptor can bind two transferrin molecules. After binding to transferrin, the transferrin receptor is endocytosed, and the iron is released into acidified vacuoles. The transferrin-receptor complex is then recycled to the surface.33
Ferritin is the cellular storage protein for iron, and it can store up to 4,500 atoms of iron within its spherical cavity.34 The serum level of ferritin reflects overall storage, with 1 ng/mL of ferritin indicating 10 mg of total iron stores.35 Ferritin is also an acute-phase reactant, and plasma levels can increase in inflammatory states such as infection or malignancy. As such, elevated ferritin does not necessarily indicate elevated iron stores.
Iron is lost in sweat, shed skin cells, and sloughed intestinal mucosal cells. However, there is no specific mechanism of iron excretion from the human body. Thus, iron is mainly regulated at the level of intestinal absorption. The iron exporter ferroportin is upregulated by the amount of available iron and is degraded by hepcidin.36
Hepcidin is a small cysteine-rich cationic peptide that is primarily produced in the liver, with some minor production also occurring in the kidneys.37 Transcription of the gene encoding hepcidin is downregulated by anemia and hypoxia and upregulated by inflammation and elevated iron levels.38 Transcription of hepcidin leads to degradation of ferroportin and a decrease in intestinal iron absorption. On the other hand, anemia and hypoxia inhibit hepcidin transcription, which allows ferroportin to facilitate intestinal iron absorption.
TREATMENT OF RENAL ANEMIA
Early enthusiasm for erythropoietin agents
Androgens started to be used to treat anemia of end-stage renal disease in 1970,39,40 and before the advent of recombinant human erythropoietin, they were a mainstay of nontransfusional therapy for anemic patients on dialysis.
The approval of recombinant human erythropoietin in 1989 drastically shifted the treatment of renal anemia. While the initial goal of treating anemia of chronic kidney disease with erythropoietin was to prevent blood transfusions,41 subsequent studies showed that the benefits might be far greater. Indeed, an initial observational trial showed that erythropoiesis-stimulating agents (ESAs) were associated with improved quality of life,42 improved neurocognitive function,43,44 and even cost savings.45 The benefits also extended to major outcomes such as regression of left ventricular hypertrophy,46 improvement in New York Heart Association class and cardiac function,47 fewer hospitalizations,48 and even reduction of cardiovascular mortality rates.49
As a result, ESA use gained popularity, and by 2006 an estimated 90% of dialysis patients were receiving these agents.50 The target and achieved hemoglobin levels also increased, with mean hemoglobin levels in hemodialysis patients being raised from 9.7 to 12 g/dL.51
Disappointing results in clinical trials of ESAs to normalize hemoglobin
To prospectively study the effects of normalized hemoglobin targets, four randomized controlled trials were conducted (Table 1):
- The Normal Hematocrit Study (NHCT)52
- The Correction of Hemoglobin and Outcomes in Renal Insufficiency (CHOIR) trial53
- The Cardiovascular Risk Reduction by Early Anemia Treatment (CREATE) trial54
- The Trial to Reduce Cardiovascular Events With Aranesp Therapy (TREAT).55
These trials randomized patients to either higher “normal-range” hemoglobin targets or to lower target hemoglobin levels.
Their findings were disappointing and raised several red flags about excessive use of ESAs. The trials found no benefit in higher hemoglobin targets, and in fact, some of them demonstrated harm in patients randomized to higher targets. Notably, higher hemoglobin targets were associated with significant side effects such as access-site thrombosis,52 strokes,55 and possibly cardiovascular events.54,55 Only the CREATE trial was able to demonstrate a quality-of-life benefit for the high-target group.54
It remains unclear whether these adverse events were from the therapy itself or from an increased morbidity burden in the treated patients. Erythropoietin use is associated with hypertension,56 thought to be related to endothelin-mediated vasoconstriction.57 In our experience, this is most evident when hemoglobin levels are normalized with ESA therapy. Cycling of erythropoietin levels between extreme levels can lead to vascular remodeling, which may also be related to its cardiovascular effects.57
A noticeable finding in several of these trials was that patients failed to achieve the higher hemoglobin target despite the use of very high doses of ESA. Reanalysis of data from the CHOIR and CREATE trials showed that the patients who had worse outcomes were more likely to have required very high doses without achieving their target hemoglobin.58,59 Indeed, patients who achieved the higher target hemoglobin levels, usually at lower ESA doses, had better outcomes. This suggested that the need for a higher dose was associated with poorer outcomes, either as a marker of comorbidity or due to yet undocumented side effects of such high doses.
General approach to therapy
Before attributing anemia to chronic kidney disease, a thorough evaluation should be conducted to look for any reversible process that could be contributing to the anemia.
The causes of anemia are numerous and beyond the scope of this review. However, among the common causes of anemia in chronic kidney disease are deficiencies of iron, vitamin B12, and folate. Therefore, guidelines recommend checking iron, vitamin B12, and folate levels in the initial evaluation of anemia.60
Iron deficiency in particular is very common in chronic kidney disease patients and is present in nearly all dialysis patients.61 Hemodialysis patients are estimated to lose 1 to 3 g of iron per year as a result of blood loss in the dialysis circuit and increased iron utilization secondary to ESA therapy.62
However, in contrast to the general population, in which the upper limits of normal for iron indices are well defined, high serum ferritin levels appear to be poorly predictive of hemoglobin responsiveness in dialysis patients.63,64 Thus, the cutoffs that define iron responsiveness are much higher than standard definitions for iron deficiency.65,66 The Dialysis Patients’ Response to IV Iron With Elevated Ferritin (DRIVE) study showed that dialysis patients benefit from intravenous iron therapy even if their ferritin is as high as 1,200 ng/mL, provided their transferrin saturation is below 30%.67
Of note, erythropoietin levels cannot be used to distinguish renal anemia from other causes of anemia. Indeed, patients with renal failure may have “relative erythropoietin deficiency,” ie, “normal” erythropoietin levels that are actually too low in view of the degree of anemia.68,69 In addition to the decreased production capacity by the kidney, there appears to be a component of resistance to the action of erythropoietin in the bone marrow.
For these reasons, there is no erythropoietin level that can be considered “inadequate” or defining of renal anemia. Thus, measuring erythropoietin levels is not routinely recommended in the evaluation of renal anemia.
Two ESA preparations
The two ESAs that have traditionally been used in the treatment of renal anemia are recombinant human erythropoietin and darbepoietin alfa. They appear to be equivalent in terms of safety and efficacy.70 However, darbepoietin alfa has more sialic acid molecules, giving it a higher potency and longer half-life and allowing for less-frequent injections.71,72
In nondialysis patients, recombinant human erythropoietin is typically given every 1 to 2 weeks, whereas darbepoietin alfa can be given every 2 to 4 weeks. In dialysis patients, recombinant human erythropoietin is typically given 3 times per week with every dialysis treatment, while darbepoietin alfa is given once a week.
Target hemoglobin levels: ≤ 11.5 g/dL
In light of the four trials described in Table 1, the international Kidney Disease: Improving Global Outcomes (KDIGO) guidelines60 recommend the following (Table 2):
For patients with chronic kidney disease who are not on dialysis, ESA therapy should not be initiated if the hemoglobin level is higher than 10 g/dL. If the hemoglobin level is lower than 10 g/dL, ESA therapy can be initiated, but the decision needs to be individualized based on the rate of fall of hemoglobin concentration, prior response to iron therapy, the risk of needing a transfusion, the risks related to ESA therapy, and the presence of symptoms attributable to anemia.
For patients on dialysis, ESA therapy should be used when the hemoglobin level is between 9 and 10 g/dL to avoid having the hemoglobin fall below 9 g/dL.
In all adult patients, ESAs should not be used to intentionally increase the hemoglobin level above 13 g/dL but rather to maintain levels no higher than 11.5 g/dL. This target is based on the observation that adverse outcomes were associated with ESA use with hemoglobin targets higher than 13 g/dL (Table 1).
Target iron levels
Regarding iron stores, the guidelines recommend the following:
For adult patients with chronic kidney disease who are not on dialysis, iron should be given to keep transferrin saturation above 20% and ferritin above 100 ng/mL. Transferrin saturation should not exceed 30%, and ferritin levels should not exceed 500 ng/mL.
For adult patients on dialysis, iron should be given to maintain transferrin saturation above 30% and ferritin above 200 ng/mL.
The upper limits of ferritin and transferrin saturation are somewhat controversial, as the safety of intentionally maintaining respective levels greater than 30% and 500 ng/mL has been studied in very few patients. Transferrin saturation should in general not exceed 50%.
High ferritin levels are associated with higher death rates, but whether elevation of ferritin levels is a marker of excessive iron administration rather than a nonspecific acute-phase reactant is not clear. The 2006 guidelines60 cited upper ferritin limits of 500 to 800 ng/mL. However, the more recent DRIVE trial67 showed that patients with ferritin levels of 500 to 1,200 ng/mL will respond to intravenous administration of iron with an increase in their hemoglobin levels. This has led many clinicians to adopt a higher ferritin limit of 1,200 ng/mL.
Hemosiderosis, or excess iron deposition, was a known consequence of frequent transfusions in patients with end-stage renal disease before ESA therapy was available. However, there have been no documented cases of clinical iron overload from iron therapy using current guidelines.73
These algorithms are nuanced, and the benefit of giving intravenous iron should always be weighed against the risks of short-term acute toxicity and infection. Treatment of renal anemia not only requires in-depth knowledge of the topic, but also familiarity with the patient’s specific situation. As such, it is not recommended that clinicians unfamiliar with the treatment of renal anemia manage its treatment.
PARTICULAR CIRCUMSTANCES
Inflammation and ESA resistance
While ESAs are effective in treating anemia in many cases, in many patients the anemia fails to respond. This is of particular importance, since ESA hyporesponsiveness has been found to be a powerful predictor of cardiovascular events and death.74 It is unclear, however, whether high doses of ESA are inherently toxic or whether hyporesponsiveness is a marker of adverse outcomes related to comorbidities.
KDIGO defines initial hyporesponsiveness as having no increase in hemoglobin concentration after the first month of appropriate weight-based dosing, and acquired hyporesponsiveness as requiring two increases in ESA doses up to 50% beyond the dose at which the patient had originally been stable.60 Identifying ESA hyporesponsiveness should lead to an intensive search for potentially correctable factors.
The two major factors accounting for the state of hyporesponsiveness are inflammation and iron deficiency.75,76
Inflammation. High C-reactive protein levels have been shown to predict resistance to erythropoietin in dialysis patients.77 The release of cytokines such as tumor necrosis factor alpha, interleukin 1, and interferon gamma has an inhibitory effect on erythropoiesis.78 Additionally, inflammation can alter the response to ESAs by disrupting the metabolism of iron79 through the release of hepcidin, as previously discussed.38 These reasons likely account for the observed lower response to ESAs in the setting of acute illness and explain why ESAs are not recommended for correcting acute anemia.80
Iron deficiency also can blunt the response to ESAs. Large amounts of iron are needed for effective erythropoietic bursts. As such, iron supplementation is now a recognized treatment of renal anemia.81
Other factors associated with hyporesponsiveness include chronic occult blood loss, aluminum toxicity, cobalamin or folate deficiencies, testosterone deficiency, inadequate dialysis, hyperparathyroidism, and superimposed primary bone marrow disease,82,83 and these should be addressed in patients whose anemia does not respond as expected to ESA therapy. A summary of the main causes of ESA hyporesponsiveness, their reversibility, and recommended treatments is presented in Table 3.
Antibody-mediated pure red-cell aplasia. Rarely, patients receiving ESA therapy develop antibodies that neutralize both the ESA and endogenous erythropoietin. The resulting syndrome, called antibody-mediated pure red-cell aplasia, is characterized by the sudden development of severe transfusion-dependent anemia. This has historically been connected to epoetin beta, a formulation not in use in the United States. However, cases have been documented with epoetin alfa and darbepoetin. The incidence rate is low with subcutaneous ESA use, estimated at 0.5 cases per 10,000 patient-years84 and anecdotal with intravenous ESA.85 The definitive diagnosis requires demonstration of neutralizing antibodies against erythropoietin. Parvovirus infection should be excluded as an alternative cause of pure redcell aplasia.
ANEMIA IN CANCER PATIENTS
ESAs are effective in raising hemoglobin levels and reducing transfusion requirements in patients with chemotherapy-induced anemia.86 However, there are data linking the use of ESAs to shortened survival in patients who have a variety of solid tumors.87
Several mechanisms have been proposed to explain this rapid disease progression, most notably acceleration in tumor growth88–90 by stimulation of erythropoietin receptors on the surface of the tumor cells, leading to increased tumor angiogenesis.91,92
For these reasons, treatment of renal anemia in the setting of active malignancy should be referred to an oncologist.
NOVEL TREATMENTS
Several new agents for treating renal anemia are currently under review.
Continuous erythropoiesis receptor activator
Continuous erythropoiesis receptor activator is a pegylated form of recombinant human erythropoietin that has the ability to repeatedly activate the erythropoietin receptor. It appears to be similar to the other forms of erythropoietin in terms of safety and efficacy in both end-stage renal disease93 and chronic kidney disease.94 It has the advantage of an extended serum half-life, which allows for longer dosing intervals, ie, every 2 weeks. Its use is currently gaining popularity in the dialysis community.
HIF stabilizers
Our growing understanding of the physiology of erythropoietin offers new potential treatment targets. As previously described, production of erythropoietin is stimulated by HIFs. In order to be degraded, these HIFs are hydroxylated at their proline residues by a prolyl hydroxylase. A new category of drugs called prolyl-hydroxylase inhibitors (PDIs) offers the advantage of stabilizing the HIFs, leading to an increase in erythropoietin production.
In phase 1 and 2 clinical trials, these agents have been shown to increase hemoglobin in both end-stage renal disease and chronic kidney disease patients15,16 but not in anephric patients, demonstrating a renal source of the erythropoietin production even in nonfunctioning kidneys. The study of one PDI agent (FG 2216) was halted temporarily after a report of death from fulminant hepatitis, but the other (FG 4592) continues to be studied in a phase 2 clinical trial.95,96
TAKE-HOME POINTS
- Anemia of renal disease is a common condition that is mainly caused by a decrease in erythropoietin production by the kidneys.
- While anemia of renal disease can be corrected with ESAs, it is necessary to investigate and rule out underlying treatable conditions such as iron or vitamin deficiencies before giving an ESA.
- Anemia of renal disease is associated with significant morbidity such as increased risk of left ventricular hypertrophy, myocardial infarction, and heart failure, and has been described as an all-cause mortality multiplier.
- Unfortunately, the only undisputed benefit of treatment to date remains the avoidance of blood transfusions. Furthermore, the large randomized controlled trials that looked at the benefits of ESA have shown that their use can be associated with increased risk of cardiovascular events. Therefore, use of an ESA in end-stage renal disease should never target a normal hemoglobin levels but rather aim for a hemoglobin level of no more than 11.5 g/dL.
- Use of an ESA in chronic kidney disease should be individualized and is not recommended to be started unless the hemoglobin level is less than 10 g/dL.
- Several newer agents for renal anemia are currently under review. A pegylated form of recombinant human erythropoietin has an extended half-life, and a new and promising category of drugs called HIF stabilizers is currently under study.
Anemia is a frequent complication of chronic kidney disease, occurring in over 90% of patients receiving renal replacement therapy. It is associated with significant morbidity and mortality. While its pathogenesis is typically multifactorial, the predominant cause is failure of the kidneys to produce enough endogenous erythropoietin. The clinical approval of recombinant human erythropoietin in 1989 dramatically changed the treatment of anemia of chronic kidney disease, but randomized controlled trials yielded disappointing results when erythropoiesis-stimulating agents (ESAs) were used to raise hemoglobin to normal levels.
This article reviews the epidemiology and pathophysiology of anemia of chronic kidney disease and discusses the complicated and conflicting evidence regarding its treatment.
DEFINITION AND PREVALENCE
Anemia is defined as a hemoglobin concentration less than 13.0 g/dL for men and less than 12.0 g/dL for premenopausal women.1 It is more common in patients with impaired kidney function, especially when the glomerular filtration rate (GFR) falls below 60 mL/min. It is rare at GFRs higher than 80 mL/min,2 but as the GFR falls, the severity of the anemia worsens3 and its prevalence increases: almost 90% of patients with a GFR less than 30 mL/min are anemic.4
RENAL ANEMIA IS ASSOCIATED WITH BAD OUTCOMES
Anemia in chronic kidney disease is independently associated with risk of death. It is also an all-cause mortality multiplier, ie, it magnifies the risk of death from other disease states.5
In observational studies, anemia was associated with faster progression of left ventricular hypertrophy, inflammation, and increased myocardial and peripheral oxygen demand, thereby leading to worse cardiac outcomes with increased risk of myocardial infarction, coronary revascularization, and readmission for heart failure.6–8 Anemia is also associated with fatigue, depression, reduced exercise tolerance, stroke, and increased risk of rehospitalization.9–13
RENAL ANEMIA IS MULTIFACTORIAL
Anemia of chronic kidney disease is typically attributed to the decrease of erythropoietin production that accompanies the fall in GFR. However, the process is multifactorial, with several other contributing factors: absolute and functional iron deficiency, folate and vitamin B12 deficiencies, reduced red blood cell life span, and suppression of erythropoiesis by the uremic milieu.14
While it was once thought that chronic kidney disease leads to loss of erythropoietin-producing cells, it is now known that downregulation of hypoxia-inducible factor (HIF; a transcription factor) is at least partially responsible for the decrease in erythropoietin production15,16 and that this downregulation is reversible (see below).
ERYTHROPOIETIN, IRON, AND RED BLOOD CELLS
Erythropoietin production is triggered by hypoxia, mediated by HIF
Erythropoietin is produced primarily in the deep cortex and outer medulla of the kidneys by a special population of peritubular interstitial cells.17 The parenchymal cells of the liver also produce erythropoietin, but much less.18
The rate of renal erythropoietin synthesis is determined by tissue oxygenation rather than by renal blood flow; production increases as the hemoglobin concentration drops and the arterial oxygen tension decreases (Figure 1).19
The gene for erythropoietin is located on chromosome 7 and is regulated by HIF. HIF molecules are composed of an alpha subunit, which is unstable at high Po2, and a beta subunit, constitutively present in the nucleus.20
In hypoxic conditions, the HIF dimer is transcriptionally active and binds to specific DNA recognition sequences called hypoxia-response elements. Gene transcription is upregulated, leading to increased production of erythropoietin.21
Under normal oxygen tension, on the other hand, the proline residue of the HIF alpha subunit is hydroxylated. The hydroxylated HIF alpha subunit is then degraded by proteasomal ubiquitylation, which is mediated by the von Hippel-Lindau tumor-suppressor gene pVHL.22 Degradation of HIF alpha prevents formation of the HIF heterodimers. HIF therefore cannot bind to the hypoxia-response elements, and erythropoietin gene transcription does not occur.23
Thus, in states of hypoxia, erythropoietin production is upregulated, whereas with normal oxygen tension, production is downregulated.
Erythropoietin is essential for terminal maturation of erythrocytes
Erythropoietin is essential for terminal maturation of erythrocytes.24 It is thought to stimulate the growth of erythrogenic progenitors: burst-forming units-erythroid (BFU-E) and colony-forming units-erythroid (CFU-E). In the absence of erythropoietin, BFU-E and CFU-E fail to differentiate into mature erythrocytes.25
Binding of erythropoietin to its receptor sets off a series of downstream signals, the most important being the signal transducer and activator of transcription 5 (STAT5). In animal studies, STAT5 was found to inhibit apoptosis through the early induction of an antiapoptotic gene, Bcl-xL.26
Iron metabolism is controlled by several proteins
Iron is characterized by its capacity to accept or donate electrons. This unique property makes it a crucial element in many biochemical reactions such as enzymatic activity, DNA synthesis, oxygen transport, and cell respiration.
Iron metabolism is under the control of several proteins that play different roles in its absorption, recycling, and loss (Figure 2).27
Dietary iron exists primarily in its poorly soluble trivalent ferric form (Fe3+), and it needs to be reduced to its soluble divalent ferrous form (Fe2+) by ferric reductase to be absorbed. Ferrous iron is taken up at the apical side of enterocytes by a divalent metal transporter (DMT1) and is transported across the brush border.28
To enter the circulation, iron has to be transported across the basolateral membrane by a transporter called ferroportin.29 Ferroportin is also found in placental syncitiotrophoblasts, where it transfers iron from mother to fetus, and in macrophages, where it allows recycling of iron scavenged from damaged cells back into the circulation.30 Upon its release, the ferrous iron is oxidized to the ferric form and loaded onto transferrin. This oxidation process involves hephaestin, a homologue of the ferroxidase ceruloplasmin.31
In the plasma, iron is bound to transferrin, and under normal circumstances one-third of transferrin is saturated with iron.32 Transferrin receptors are present on most cells but are most dense on erythroid precursors. Each transferrin receptor can bind two transferrin molecules. After binding to transferrin, the transferrin receptor is endocytosed, and the iron is released into acidified vacuoles. The transferrin-receptor complex is then recycled to the surface.33
Ferritin is the cellular storage protein for iron, and it can store up to 4,500 atoms of iron within its spherical cavity.34 The serum level of ferritin reflects overall storage, with 1 ng/mL of ferritin indicating 10 mg of total iron stores.35 Ferritin is also an acute-phase reactant, and plasma levels can increase in inflammatory states such as infection or malignancy. As such, elevated ferritin does not necessarily indicate elevated iron stores.
Iron is lost in sweat, shed skin cells, and sloughed intestinal mucosal cells. However, there is no specific mechanism of iron excretion from the human body. Thus, iron is mainly regulated at the level of intestinal absorption. The iron exporter ferroportin is upregulated by the amount of available iron and is degraded by hepcidin.36
Hepcidin is a small cysteine-rich cationic peptide that is primarily produced in the liver, with some minor production also occurring in the kidneys.37 Transcription of the gene encoding hepcidin is downregulated by anemia and hypoxia and upregulated by inflammation and elevated iron levels.38 Transcription of hepcidin leads to degradation of ferroportin and a decrease in intestinal iron absorption. On the other hand, anemia and hypoxia inhibit hepcidin transcription, which allows ferroportin to facilitate intestinal iron absorption.
TREATMENT OF RENAL ANEMIA
Early enthusiasm for erythropoietin agents
Androgens started to be used to treat anemia of end-stage renal disease in 1970,39,40 and before the advent of recombinant human erythropoietin, they were a mainstay of nontransfusional therapy for anemic patients on dialysis.
The approval of recombinant human erythropoietin in 1989 drastically shifted the treatment of renal anemia. While the initial goal of treating anemia of chronic kidney disease with erythropoietin was to prevent blood transfusions,41 subsequent studies showed that the benefits might be far greater. Indeed, an initial observational trial showed that erythropoiesis-stimulating agents (ESAs) were associated with improved quality of life,42 improved neurocognitive function,43,44 and even cost savings.45 The benefits also extended to major outcomes such as regression of left ventricular hypertrophy,46 improvement in New York Heart Association class and cardiac function,47 fewer hospitalizations,48 and even reduction of cardiovascular mortality rates.49
As a result, ESA use gained popularity, and by 2006 an estimated 90% of dialysis patients were receiving these agents.50 The target and achieved hemoglobin levels also increased, with mean hemoglobin levels in hemodialysis patients being raised from 9.7 to 12 g/dL.51
Disappointing results in clinical trials of ESAs to normalize hemoglobin
To prospectively study the effects of normalized hemoglobin targets, four randomized controlled trials were conducted (Table 1):
- The Normal Hematocrit Study (NHCT)52
- The Correction of Hemoglobin and Outcomes in Renal Insufficiency (CHOIR) trial53
- The Cardiovascular Risk Reduction by Early Anemia Treatment (CREATE) trial54
- The Trial to Reduce Cardiovascular Events With Aranesp Therapy (TREAT).55
These trials randomized patients to either higher “normal-range” hemoglobin targets or to lower target hemoglobin levels.
Their findings were disappointing and raised several red flags about excessive use of ESAs. The trials found no benefit in higher hemoglobin targets, and in fact, some of them demonstrated harm in patients randomized to higher targets. Notably, higher hemoglobin targets were associated with significant side effects such as access-site thrombosis,52 strokes,55 and possibly cardiovascular events.54,55 Only the CREATE trial was able to demonstrate a quality-of-life benefit for the high-target group.54
It remains unclear whether these adverse events were from the therapy itself or from an increased morbidity burden in the treated patients. Erythropoietin use is associated with hypertension,56 thought to be related to endothelin-mediated vasoconstriction.57 In our experience, this is most evident when hemoglobin levels are normalized with ESA therapy. Cycling of erythropoietin levels between extreme levels can lead to vascular remodeling, which may also be related to its cardiovascular effects.57
A noticeable finding in several of these trials was that patients failed to achieve the higher hemoglobin target despite the use of very high doses of ESA. Reanalysis of data from the CHOIR and CREATE trials showed that the patients who had worse outcomes were more likely to have required very high doses without achieving their target hemoglobin.58,59 Indeed, patients who achieved the higher target hemoglobin levels, usually at lower ESA doses, had better outcomes. This suggested that the need for a higher dose was associated with poorer outcomes, either as a marker of comorbidity or due to yet undocumented side effects of such high doses.
General approach to therapy
Before attributing anemia to chronic kidney disease, a thorough evaluation should be conducted to look for any reversible process that could be contributing to the anemia.
The causes of anemia are numerous and beyond the scope of this review. However, among the common causes of anemia in chronic kidney disease are deficiencies of iron, vitamin B12, and folate. Therefore, guidelines recommend checking iron, vitamin B12, and folate levels in the initial evaluation of anemia.60
Iron deficiency in particular is very common in chronic kidney disease patients and is present in nearly all dialysis patients.61 Hemodialysis patients are estimated to lose 1 to 3 g of iron per year as a result of blood loss in the dialysis circuit and increased iron utilization secondary to ESA therapy.62
However, in contrast to the general population, in which the upper limits of normal for iron indices are well defined, high serum ferritin levels appear to be poorly predictive of hemoglobin responsiveness in dialysis patients.63,64 Thus, the cutoffs that define iron responsiveness are much higher than standard definitions for iron deficiency.65,66 The Dialysis Patients’ Response to IV Iron With Elevated Ferritin (DRIVE) study showed that dialysis patients benefit from intravenous iron therapy even if their ferritin is as high as 1,200 ng/mL, provided their transferrin saturation is below 30%.67
Of note, erythropoietin levels cannot be used to distinguish renal anemia from other causes of anemia. Indeed, patients with renal failure may have “relative erythropoietin deficiency,” ie, “normal” erythropoietin levels that are actually too low in view of the degree of anemia.68,69 In addition to the decreased production capacity by the kidney, there appears to be a component of resistance to the action of erythropoietin in the bone marrow.
For these reasons, there is no erythropoietin level that can be considered “inadequate” or defining of renal anemia. Thus, measuring erythropoietin levels is not routinely recommended in the evaluation of renal anemia.
Two ESA preparations
The two ESAs that have traditionally been used in the treatment of renal anemia are recombinant human erythropoietin and darbepoietin alfa. They appear to be equivalent in terms of safety and efficacy.70 However, darbepoietin alfa has more sialic acid molecules, giving it a higher potency and longer half-life and allowing for less-frequent injections.71,72
In nondialysis patients, recombinant human erythropoietin is typically given every 1 to 2 weeks, whereas darbepoietin alfa can be given every 2 to 4 weeks. In dialysis patients, recombinant human erythropoietin is typically given 3 times per week with every dialysis treatment, while darbepoietin alfa is given once a week.
Target hemoglobin levels: ≤ 11.5 g/dL
In light of the four trials described in Table 1, the international Kidney Disease: Improving Global Outcomes (KDIGO) guidelines60 recommend the following (Table 2):
For patients with chronic kidney disease who are not on dialysis, ESA therapy should not be initiated if the hemoglobin level is higher than 10 g/dL. If the hemoglobin level is lower than 10 g/dL, ESA therapy can be initiated, but the decision needs to be individualized based on the rate of fall of hemoglobin concentration, prior response to iron therapy, the risk of needing a transfusion, the risks related to ESA therapy, and the presence of symptoms attributable to anemia.
For patients on dialysis, ESA therapy should be used when the hemoglobin level is between 9 and 10 g/dL to avoid having the hemoglobin fall below 9 g/dL.
In all adult patients, ESAs should not be used to intentionally increase the hemoglobin level above 13 g/dL but rather to maintain levels no higher than 11.5 g/dL. This target is based on the observation that adverse outcomes were associated with ESA use with hemoglobin targets higher than 13 g/dL (Table 1).
Target iron levels
Regarding iron stores, the guidelines recommend the following:
For adult patients with chronic kidney disease who are not on dialysis, iron should be given to keep transferrin saturation above 20% and ferritin above 100 ng/mL. Transferrin saturation should not exceed 30%, and ferritin levels should not exceed 500 ng/mL.
For adult patients on dialysis, iron should be given to maintain transferrin saturation above 30% and ferritin above 200 ng/mL.
The upper limits of ferritin and transferrin saturation are somewhat controversial, as the safety of intentionally maintaining respective levels greater than 30% and 500 ng/mL has been studied in very few patients. Transferrin saturation should in general not exceed 50%.
High ferritin levels are associated with higher death rates, but whether elevation of ferritin levels is a marker of excessive iron administration rather than a nonspecific acute-phase reactant is not clear. The 2006 guidelines60 cited upper ferritin limits of 500 to 800 ng/mL. However, the more recent DRIVE trial67 showed that patients with ferritin levels of 500 to 1,200 ng/mL will respond to intravenous administration of iron with an increase in their hemoglobin levels. This has led many clinicians to adopt a higher ferritin limit of 1,200 ng/mL.
Hemosiderosis, or excess iron deposition, was a known consequence of frequent transfusions in patients with end-stage renal disease before ESA therapy was available. However, there have been no documented cases of clinical iron overload from iron therapy using current guidelines.73
These algorithms are nuanced, and the benefit of giving intravenous iron should always be weighed against the risks of short-term acute toxicity and infection. Treatment of renal anemia not only requires in-depth knowledge of the topic, but also familiarity with the patient’s specific situation. As such, it is not recommended that clinicians unfamiliar with the treatment of renal anemia manage its treatment.
PARTICULAR CIRCUMSTANCES
Inflammation and ESA resistance
While ESAs are effective in treating anemia in many cases, in many patients the anemia fails to respond. This is of particular importance, since ESA hyporesponsiveness has been found to be a powerful predictor of cardiovascular events and death.74 It is unclear, however, whether high doses of ESA are inherently toxic or whether hyporesponsiveness is a marker of adverse outcomes related to comorbidities.
KDIGO defines initial hyporesponsiveness as having no increase in hemoglobin concentration after the first month of appropriate weight-based dosing, and acquired hyporesponsiveness as requiring two increases in ESA doses up to 50% beyond the dose at which the patient had originally been stable.60 Identifying ESA hyporesponsiveness should lead to an intensive search for potentially correctable factors.
The two major factors accounting for the state of hyporesponsiveness are inflammation and iron deficiency.75,76
Inflammation. High C-reactive protein levels have been shown to predict resistance to erythropoietin in dialysis patients.77 The release of cytokines such as tumor necrosis factor alpha, interleukin 1, and interferon gamma has an inhibitory effect on erythropoiesis.78 Additionally, inflammation can alter the response to ESAs by disrupting the metabolism of iron79 through the release of hepcidin, as previously discussed.38 These reasons likely account for the observed lower response to ESAs in the setting of acute illness and explain why ESAs are not recommended for correcting acute anemia.80
Iron deficiency also can blunt the response to ESAs. Large amounts of iron are needed for effective erythropoietic bursts. As such, iron supplementation is now a recognized treatment of renal anemia.81
Other factors associated with hyporesponsiveness include chronic occult blood loss, aluminum toxicity, cobalamin or folate deficiencies, testosterone deficiency, inadequate dialysis, hyperparathyroidism, and superimposed primary bone marrow disease,82,83 and these should be addressed in patients whose anemia does not respond as expected to ESA therapy. A summary of the main causes of ESA hyporesponsiveness, their reversibility, and recommended treatments is presented in Table 3.
Antibody-mediated pure red-cell aplasia. Rarely, patients receiving ESA therapy develop antibodies that neutralize both the ESA and endogenous erythropoietin. The resulting syndrome, called antibody-mediated pure red-cell aplasia, is characterized by the sudden development of severe transfusion-dependent anemia. This has historically been connected to epoetin beta, a formulation not in use in the United States. However, cases have been documented with epoetin alfa and darbepoetin. The incidence rate is low with subcutaneous ESA use, estimated at 0.5 cases per 10,000 patient-years84 and anecdotal with intravenous ESA.85 The definitive diagnosis requires demonstration of neutralizing antibodies against erythropoietin. Parvovirus infection should be excluded as an alternative cause of pure redcell aplasia.
ANEMIA IN CANCER PATIENTS
ESAs are effective in raising hemoglobin levels and reducing transfusion requirements in patients with chemotherapy-induced anemia.86 However, there are data linking the use of ESAs to shortened survival in patients who have a variety of solid tumors.87
Several mechanisms have been proposed to explain this rapid disease progression, most notably acceleration in tumor growth88–90 by stimulation of erythropoietin receptors on the surface of the tumor cells, leading to increased tumor angiogenesis.91,92
For these reasons, treatment of renal anemia in the setting of active malignancy should be referred to an oncologist.
NOVEL TREATMENTS
Several new agents for treating renal anemia are currently under review.
Continuous erythropoiesis receptor activator
Continuous erythropoiesis receptor activator is a pegylated form of recombinant human erythropoietin that has the ability to repeatedly activate the erythropoietin receptor. It appears to be similar to the other forms of erythropoietin in terms of safety and efficacy in both end-stage renal disease93 and chronic kidney disease.94 It has the advantage of an extended serum half-life, which allows for longer dosing intervals, ie, every 2 weeks. Its use is currently gaining popularity in the dialysis community.
HIF stabilizers
Our growing understanding of the physiology of erythropoietin offers new potential treatment targets. As previously described, production of erythropoietin is stimulated by HIFs. In order to be degraded, these HIFs are hydroxylated at their proline residues by a prolyl hydroxylase. A new category of drugs called prolyl-hydroxylase inhibitors (PDIs) offers the advantage of stabilizing the HIFs, leading to an increase in erythropoietin production.
In phase 1 and 2 clinical trials, these agents have been shown to increase hemoglobin in both end-stage renal disease and chronic kidney disease patients15,16 but not in anephric patients, demonstrating a renal source of the erythropoietin production even in nonfunctioning kidneys. The study of one PDI agent (FG 2216) was halted temporarily after a report of death from fulminant hepatitis, but the other (FG 4592) continues to be studied in a phase 2 clinical trial.95,96
TAKE-HOME POINTS
- Anemia of renal disease is a common condition that is mainly caused by a decrease in erythropoietin production by the kidneys.
- While anemia of renal disease can be corrected with ESAs, it is necessary to investigate and rule out underlying treatable conditions such as iron or vitamin deficiencies before giving an ESA.
- Anemia of renal disease is associated with significant morbidity such as increased risk of left ventricular hypertrophy, myocardial infarction, and heart failure, and has been described as an all-cause mortality multiplier.
- Unfortunately, the only undisputed benefit of treatment to date remains the avoidance of blood transfusions. Furthermore, the large randomized controlled trials that looked at the benefits of ESA have shown that their use can be associated with increased risk of cardiovascular events. Therefore, use of an ESA in end-stage renal disease should never target a normal hemoglobin levels but rather aim for a hemoglobin level of no more than 11.5 g/dL.
- Use of an ESA in chronic kidney disease should be individualized and is not recommended to be started unless the hemoglobin level is less than 10 g/dL.
- Several newer agents for renal anemia are currently under review. A pegylated form of recombinant human erythropoietin has an extended half-life, and a new and promising category of drugs called HIF stabilizers is currently under study.
- World Health Organization (WHO). Nutritional anaemias: report of a WHO scientific group. Geneva, Switzerland: World Health Organization, 1968.
- Hsu CY, McCulloch CE, Curhan GC, et al. Epidemiology of anemia associated with chronic renal insufficiency among adults in the United States: results from the Third National Health and Nutrition Examination Survey. J Am Soc Nephrol 2002; 13:504–510.
- Radtke HW, Claussner A, Erbes PM, Scheuermann EH, Schoeppe W, Koch KM. Serum erythropoetin concentration in chronic renal failure: relationship to degree of anemia and excretory renal function. Blood 1979; 54:877–884.
- Kazmi WH, Kausz AT, Khan S, et al. Anemia: an early complication of chronic renal insufficiency. Am J Kidney Dis 2001; 38:803–812.
- United States Renal Data System. Chapter 3. Morbidity & mortality in patients with CKD. www.usrds.org/2012/view/v1_03.aspx. Accessed June 9, 2016.
- Horwich TB, Fonarow GC, Hamilton MA, MacLellan WR, Borenstein J. Anemia is associated with worse symptoms, greater impairment in functional capacity and a significant increase in mortality in patients with advanced heart failure. J Am Coll Cardiol 2002; 39:1780–1786.
- Mark DB, Felker GM. B-type natriuretic peptide: a biomarker for all seasons? N Engl J Med 2004; 350:718–720.
- Walker AM, Schneider G, Yeaw J, Nordstrom B, Robbins S, Pettitt D. Anemia as a predictor of cardiovascular events in patients with elevated serum creatinine. J Am Soc Nephrol 2006; 17:2293–2298.
- Abramson JL, Jurkovitz CT, Vaccarino V, Weintraub WS, McClellan W. Chronic kidney disease, anemia, and incident stroke in a middle-aged, community-based population: the ARIC Study. Kidney Int 2003; 64:610–615.
- Sarnak MJ, Tighiouart H, Manjunath G, et al. Anemia as a risk factor for cardiovascular disease in the Atherosclerosis Risk in Communities (ARIC) study. J Am Coll Cardiol 2002; 40:27–33.
- McClellan WM, Flanders WD, Langston RD, Jurkovitz C, Presley R. Anemia and renal insufficiency are independent risk factors for death among patients with congestive heart failure admitted to community hospitals: a population-based study. J Am Soc Nephrol 2002; 13:1928–1936.
- Xia H, Ebben J, Ma JZ, Collins AJ. Hematocrit levels and hospitalization risks in hemodialysis patients. J Am Soc Nephrol 1999; 10:1309–1316.
- Collins AJ, Li S, St Peter W, et al. Death, hospitalization, and economic associations among incident hemodialysis patients with hematocrit values of 36 to 39%. J Am Soc Nephrol 2001; 12:2465–2473.
- Agarwal AK. Practical approach to the diagnosis and treatment of anemia associated with CKD in elderly. J Am Med Dir Assoc 2006; 7(suppl 9):S7–S12.
- Bernhardt WM, Wiesener MS, Scigalla P, et al. Inhibition of prolyl hydroxylases increases erythropoietin production in ESRD. J Am Soc Nephrol 2010; 21:2151–2156.
- Provenzano R, Fadda G, Bernardo M, et al. FG-2216, a novel oral HIF-PHI, stimulates erythropoiesis and increases hemoglobin concentration in patients with non-dialysis CKD. Am J Kidney Dis 2008; 51:B80.
- Maxwell PH, Osmond MK, Pugh CW, et al. Identification of the renal erythropoietin-producing cells using transgenic mice. Kidney Int 1993; 44:1149–1162.
- Maxwell PH, Ferguson DJ, Nicholls LG, et al. Sites of erythropoietin production. Kidney Int 1997; 51:393–401.
- Jelkmann W. Erythropoeitin: structure, control of production and function. Physiol Rev 1992; 72:449–489.
- Wang GL, Jiang BH, Rue EA, Semenza GL. Hypoxia-inducible factor 1 is a basic-helix-loop-helix-PAS heterodimer regulated by cellular O2 tension. Proc Natl Acad Sci USA 1995; 92:5510–5514.
- Wang GL, Semenza GL. Purification and characterization of hypoxia-inducible factor 1. J Biol Chem 1995; 270:1230–1237.
- Maxwell PH, Wiesener MS, Chang GW, et al. The tumour suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis. Nature 1999; 399:271–275.
- Salceda S, Caro J. Hypoxia-inducible factor 1alpha protein is rapidly degraded by the ubiquitin-proteasome system under normoxic conditions. Its stabilization by hypoxia depends on redox-induced changes. J Biol Chem 1997; 272:22642–22647.
- Malik J, Kim AR, Tyre KA, Cherukuri AR, Palis J. Erythropoietin critically regulates the terminal maturation of murine and human primitive erythroblasts. Haematologica 2013; 98:1778–1787.
- Wu H, Liu X, Jaenisch R, Lodish HF. Generation of committed erythroid BFU-E and CFU-E progenitors does not require erythropoietin or the erythropoietin receptor. Cell 1995; 83:59–67.
- Socolovsky M, Nam H, Fleming MD, Haase VH, Brugnara C, Lodish HF. Ineffective erythropoiesis in Stat5a(-/-)5b(-/-) mice due to decreased survival of early erythroblasts. Blood 2001; 98:3261–3273.
- Papanikolaou G, Pantopoulos K. Iron metabolism and toxicity. Toxicol Appl Pharmacol 2005; 202:199–211.
- Conrad ME, Umbreit JN. Pathways of iron absorption. Blood Cells Mol Dis 2002; 29:336–355.
- Frazer DM, Anderson GJ. The orchestration of body iron intake: how and where do enterocytes receive their cues? Blood Cells Moll Dis 2003; 30:288–297.
- Donovan A, Lima CA, Pinkus JL, et al. The iron exporter ferroportin/Slc40a1 is essential for iron homeostasis. Cell Metab 2005; 1:191–200.
- Vulpe CD, Kuo YM, Murphy TL, et al. Hephaestin, a ceruloplasmin homologue implicated in intestinal iron transport, is defective in the sla mouse. Nat Genet 1999; 21:195–199.
- Bothwell TH. Overview and mechanisms of iron regulation. Nutr Rev 1995: 53:237–245.
- Kawabata H, Nakamaki T, Ikonomi P, Smith RD, Germain RS, Koeffler HP. Expression of transferrin receptor 2 in normal and neoplastic hematopoietic cells. Blood 2001; 98:2714–2719.
- Arosio P, Levi S. Cytosolic and mitochondrial ferritins in the regulation of cellular iron homeostasis and oxidative damage. Biochim Biophys Acta 2010; 1800:783–792.
- Finch CA, Bellotti V, Stray S, et al. Plasma ferritin determination as a diagnostic tool. West J Med 1986; 145:657–663.
- Delaby C, Pilard N, Goncalves AS, Beaumont C, Canonne-Hergaux F. Presence of the iron exporter ferroportin at the plasma membrane of macrophages is enhanced by iron loading and down-regulated by hepcidin. Blood 2005; 106:3979–3984.
- Ganz T. Hepcidin, a key regulator of iron metabolism and mediator of anemia of inflammation. Blood 2003; 102:783–788.
- Nicolas G, Chauvet C, Viatte L, et al. The gene encoding the iron regulatory peptide hepcidin is regulated by anemia, hypoxia, and inflammation. J Clin Invest 2002; 110:1037–1044.
- DeGowin RL, Lavender AR, Forland M, Charleston D, Gottschalk A. Erythropoiesis and erythropoietin in patients with chronic renal failure treated with hemodialysis and testosterone. Ann Intern Med 1970; 72:913–918.
- Richardson JR Jr, Weinstein MB. Erythropoietic response of dialyzed patients to testosterone administration. Ann Intern Med 1970; 73:403–407
- Eschbach JW, Abdulhadi MH, Browne JK, et al. Recombinant human erythropoietin in anemic patients with end-stage renal disease. Results of a phase III multicenter clinical trial. Ann Intern Med 1989; 111:992–1000.
- Moreno F, Aracil FJ, Pérez R, Valderrábano F. Controlled study on the improvement of quality of life in elderly hemodialysis patients after correcting end-stage renal disease-related anemia with erythropoietin. Am J Kidney Dis 1996; 27:548–556.
- Nissenson AR, Nimer SD, Wolcott DL. Recombinant human erythropoietin and renal anemia: molecular biology, clinical efficacy, and nervous system effects. Ann Intern Med 1991; 114:402–416.
- Stivelman JC. Benefits of anaemia treatment on cognitive function. Nephrol Dial Transplant 2000; 15(suppl 3):29–35.
- Maddux FW, Shetty S, del Aguila MA, Nelson MA, Murray BM. Effect of erythropoiesis-stimulating agents on healthcare utilization, costs, and outcomes in chronic kidney disease. Ann Pharmacother 2007; 41:1761–1769.
- Macdougall IC, Lewis NP, Saunders MJ, et al. Long-term cardiorespiratory effects of amelioration of renal anaemia by erythropoietin. Lancet 1990; 335:489–493.
- Silverberg DS, Wexler D, Blum M, et al. Effects of treatment with epoetin beta on outcomes in patients with anaemia and chronic heart failure. Kidney Blood Press Res 2005; 28:41–47.
- Perkins R, Olson S, Hansen J, Lee J, Stiles K, Lebrun C. Impact of an anemia clinic on emergency room visits and hospitalizations in patients with anemia of CKD pre-dialysis. Nephrol Nurs J 2007; 34:167–173, 182.
- Locatelli F, Conte F, Marcelli D. The impact of haematocrit levels and erythropoietin treatment on overall and cardiovascular mortality and morbidity—the experience of the Lombardy Dialysis Registry. Nephrol Dial Transplant 1998; 13:1642–1644.
- Centers for Medicare and Medicaid Services; Kinney R. 2005 Annual Report: ESRD Clinical Performance Measures Project. Am J Kidney Dis 2006; 48(suppl 2):S1–S106.
- US Renal Data System. Annual Data Report 2006. www.usrds.org/adr.aspx. Accessed July 3, 2016.
- Besarab A, Bolton WK, Browne JK, et al. The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med 1998; 339:584–590.
- Singh AK, Szczech L, Tang KL, et al; CHOIR Investigators. Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med 2006; 355:2085–2098.
- Drüeke TB, Locatelli F, Clyne N, et al; CREATE Investigators. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med 2006; 355:2071–2084.
- Pfeffer MA, Burdmann EA, Chen CY, et al; TREAT Investigators. A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N Engl J Med 2009; 361:2019–2032.
- Kirkpantur A, Kahraman S, Yilmaz R, et al. The effects of maintenance recombinant human erythropoietin therapy on ambulatory blood pressure recordings: conventional, Doppler, and tissue Doppler echocardiographic parameters. Artif Organs 2005; 29:965–972.
- Fishbane S, Berns JS. Hemoglobin cycling in hemodialysis patients treated with recombinant human erythropoietin. Kidney Int 2005; 68:1337–1343.
- Szczech LA, Barnhart HX, Inrig JK, et al. Secondary analysis of the CHOIR trial epoetin-alpha dose and achieved hemoglobin outcomes. Kidney Int 2008; 74:791–798.
- Solomon SD, Uno H, Lewis EF, et al; Trial to Reduce Cardiovascular Events with Aranesp Therapy (TREAT) Investigators. Erythropoietic response and outcomes in kidney disease and type 2 diabetes. N Engl J Med 2010; 363:1146–1155.
- Kidney Disease: Improving Global Outcomes (KDIGO). KDIGO Clinical Practice Guideline for Anemia in Chronic Kidney Disease. Kidney Int Suppl 2012; 2:279–335.
- Fernández-Rodríguez AM, Guindeo-Casasús MC, Molero-Labarta T, et al. Diagnosis of iron deficiency in chronic renal failure. Am J Kidney Dis 1999; 34:508–513.
- Eschbach JW, Cook JD, Scribner BH, Finch CA. Iron balance in hemodialysis patients. Ann Intern Med 1977; 87:710–713.
- Mittman N, Sreedhara R, Mushnick R, et al. Reticulocyte hemoglobin content predicts functional iron deficiency in hemodialysis patients receiving rHuEPO. Am J Kidney Dis 1997; 30:912–922.
- Tessitore N, Solero GP, Lippi G, et al. The role of iron status markers in predicting response to intravenous iron in haemodialysis patients on maintenance erythropoietin. Nephrol Dial Transplant 2001; 16:1416–1423.
- Coyne DW. Iron indices: what do they really mean? Kidney Int Suppl 2006; 101:S4–S8.
- Fishbane S, Kowalski EA, Imbriano LJ, Maesaka JK. The evaluation of iron status in hemodialysis patients. J Am Soc Nephrol 1996; 7:2654–2657.
- Coyne DW, Kapoian T, Suki W, et al; DRIVE Study Group. Ferric gluconate is highly efficacious in anemic hemodialysis patients with high serum ferritin and low transferrin saturation: results of the Dialysis Patients’ Response to IV Iron with Elevated Ferritin (DRIVE) Study. J Am Soc Nephrol 2007; 18:975–984.
- Radtke HW, Claussner A, Erbes PM, Scheuermann EH, Schoeppe W, Koch KM. Serum erythropoietin concentration in chronic renal failure: relationship to degree of anemia and excretory renal function. Blood 1979; 54:877–884.
- Korte W, Cogliatti SB, Jung K, Riesen W. Mild renal dysfunction is sufficient to induce erythropoietin deficiency in patients with unexplained anaemia. Clin Chim Acta 2000; 292:149–154.
- Locatelli F, Olivares J, Walker R, et al; European/Australian NESP 980202 Study Group. Novel erythropoiesis stimulating protein for treatment of anemia in chronic renal insufficiency. Kidney Int 2001; 60:741–747.
- Carrera F, Burnier M. Use of darbepoetin alfa in the treatment of anaemia of chronic kidney disease: clinical and pharmacoeconomic considerations. NDT Plus 2009; 2(suppl 1):i9–i17.
- Egrie JC, Browne JK. Development and characterization of novel erythropoiesis stimulating protein (NESP). Nephrol Dial Transplant 2001; 16(suppl 3):3–13.
- Nissenson AR, Charytan C. Controversies in iron management. Kidney Int Suppl 2003; 87:S64–S71.
- Kilpatrick RD, Critchlow CW, Fishbane S, et al. Greater epoetin alpha responsiveness is associated with improved survival in hemodialysis patients. Clin J Am Soc Nephrol 2008; 3:1077–1083.
- Locatelli F, Aljama P, Barany P, et al; European Best Practice Guidelines Working Group. Revised European best practice guidelines for the management of anaemia in patients with chronic renal failure. Nephrol Dial Transplant 2004; 19(suppl 2):ii1–ii47.
- Stenvinkel P. The role of inflammation in the anaemia of end-stage renal disease. Nephrol Dial Transplant 2001; 16(suppl 7):36–40.
- Barany P, Divino Filho JC, Bergstrom J. High C-reactive protein is a strong predictor of resistance to erythropoietin in hemodialysis patients. Am J Kidney Dis 1997; 29:565–568.
- Drueke T. Hyporesponsiveness to recombinant human erythropoietin. Nephrol Dial Transplant 2001; 16(suppl 7):25–28.
- Casadevall N. Cellular mechanism of resistance to erythropoietin. Nephrol Dial Transplant 1995; 10(suppl 6):27–30.
- Kraus E, Rabb H. EPO therapy during acute kidney disease: to use or not to use, that is the question. Am J Kidney Dis 2005; 46:967–969.
- Gotloib L, Silverberg D, Fudin R, Shostak A. Iron deficiency is a common cause of anemia in chronic kidney disease and can often be corrected with intravenous iron. J Nephrol 2006; 19:161–167.
- Tarng DC, Huang TP, Chen TW, Yang WC. Erythropoietin hyporesponsiveness: from iron deficiency to iron overload. Kidney Int Suppl 1999; 69:S107–S118.
- Drüeke TB. Modulating factors in the hematopoietic response to erythropoietin. Am J Kidney Dis 1991; 18(suppl 1):87–92.
- Boven K, Stryker S, Knight J, et al. The increased incidence of pure red cell aplasia with an Eprex formulation in uncoated rubber stopper syringes. Kidney Int 2005; 67:2346–2353.
- Shimizu H, Saitoh T, Ota F, et al. Pure red cell aplasia induced only by intravenous administration of recombinant human erythropoietin. Acta Haematol 2011; 126:114–118.
- Tonia T, Mettler A, Robert N, et al. Erythropoietin or darbepoetin for patients with cancer. Cochrane Database Syst Rev 2012; 12:CD003407.
- Bohlius J, Langensiepen S, Schwarzer G, et al. Recombinant human erythropoietin and overall survival in cancer patients: results of a comprehensive meta-analysis. J Natl Cancer Inst 2005; 97:489–498.
- Henke M, Laszig R, Rübe C, et al. Erythropoietin to treat head and neck cancer patients with anaemia undergoing radiotherapy: randomised, double-blind, placebo-controlled trial. Lancet 2003; 362:1255–1260.
- Leyland-Jones B, Semiglazov V, Pawlicki M, et al. Maintaining normal hemoglobin levels with epoetin alfa in mainly nonanemic patients with metastatic breast cancer receiving first-line chemotherapy: a survival study. J Clin Oncol 2005; 23:5960–5972.
- Brower V. Erythropoietin may impair, not improve, cancer survival. Nat Med 2003; 9:1439.
- Acs G, Acs P, Beckwith SM, et al. Erythropoietin and erythropoietin receptor expression in human cancer. Cancer Res 2001; 61:3561–3565.
- Yasuda Y, Fujita Y, Matsuo T, et al. Erythropoietin regulates tumour growth of human malignancies. Carcinogenesis 2003; 24:1021–1029.
- Levin NW, Fishbane S, Cañedo FV, et al; MAXIMA Study Investigators. Intravenous methoxy polyethylene glycol-epoetin beta for haemoglobin control in patients with chronic kidney disease who are on dialysis: a randomised non-inferiority trial (MAXIMA). Lancet 2007; 370:1415–1421.
- Macdougall IC, Walker R, Provenzano R, et al; ARCTOS Study Investigators. C.E.R.A. corrects anemia in patients with chronic kidney disease not on dialysis: results of a randomized clinical trial. Clin J Am Soc Nephrol 2008; 3:337–347.
- Frohna PA, Milwee S, Pinkett J, et al. Preliminary results from a randomized, single-blind, placebo-controlled trial of FG-4592, a novel hypoxia inducible factor prolyl hydroxylase inhibitor, in subjects with CKD anemia (abstract). J Am Soc Nephrol 2007; 18:763.
- Holdstock L, Meadowcroft AM, Maier R, et al. Four-week studies of oral hypoxia-inducible factor-prolyl hydroxylase inhibitor GSK1278863 for treatment of anemia. J Am Soc Nephrol 2016; 27:1234–1244.
- World Health Organization (WHO). Nutritional anaemias: report of a WHO scientific group. Geneva, Switzerland: World Health Organization, 1968.
- Hsu CY, McCulloch CE, Curhan GC, et al. Epidemiology of anemia associated with chronic renal insufficiency among adults in the United States: results from the Third National Health and Nutrition Examination Survey. J Am Soc Nephrol 2002; 13:504–510.
- Radtke HW, Claussner A, Erbes PM, Scheuermann EH, Schoeppe W, Koch KM. Serum erythropoetin concentration in chronic renal failure: relationship to degree of anemia and excretory renal function. Blood 1979; 54:877–884.
- Kazmi WH, Kausz AT, Khan S, et al. Anemia: an early complication of chronic renal insufficiency. Am J Kidney Dis 2001; 38:803–812.
- United States Renal Data System. Chapter 3. Morbidity & mortality in patients with CKD. www.usrds.org/2012/view/v1_03.aspx. Accessed June 9, 2016.
- Horwich TB, Fonarow GC, Hamilton MA, MacLellan WR, Borenstein J. Anemia is associated with worse symptoms, greater impairment in functional capacity and a significant increase in mortality in patients with advanced heart failure. J Am Coll Cardiol 2002; 39:1780–1786.
- Mark DB, Felker GM. B-type natriuretic peptide: a biomarker for all seasons? N Engl J Med 2004; 350:718–720.
- Walker AM, Schneider G, Yeaw J, Nordstrom B, Robbins S, Pettitt D. Anemia as a predictor of cardiovascular events in patients with elevated serum creatinine. J Am Soc Nephrol 2006; 17:2293–2298.
- Abramson JL, Jurkovitz CT, Vaccarino V, Weintraub WS, McClellan W. Chronic kidney disease, anemia, and incident stroke in a middle-aged, community-based population: the ARIC Study. Kidney Int 2003; 64:610–615.
- Sarnak MJ, Tighiouart H, Manjunath G, et al. Anemia as a risk factor for cardiovascular disease in the Atherosclerosis Risk in Communities (ARIC) study. J Am Coll Cardiol 2002; 40:27–33.
- McClellan WM, Flanders WD, Langston RD, Jurkovitz C, Presley R. Anemia and renal insufficiency are independent risk factors for death among patients with congestive heart failure admitted to community hospitals: a population-based study. J Am Soc Nephrol 2002; 13:1928–1936.
- Xia H, Ebben J, Ma JZ, Collins AJ. Hematocrit levels and hospitalization risks in hemodialysis patients. J Am Soc Nephrol 1999; 10:1309–1316.
- Collins AJ, Li S, St Peter W, et al. Death, hospitalization, and economic associations among incident hemodialysis patients with hematocrit values of 36 to 39%. J Am Soc Nephrol 2001; 12:2465–2473.
- Agarwal AK. Practical approach to the diagnosis and treatment of anemia associated with CKD in elderly. J Am Med Dir Assoc 2006; 7(suppl 9):S7–S12.
- Bernhardt WM, Wiesener MS, Scigalla P, et al. Inhibition of prolyl hydroxylases increases erythropoietin production in ESRD. J Am Soc Nephrol 2010; 21:2151–2156.
- Provenzano R, Fadda G, Bernardo M, et al. FG-2216, a novel oral HIF-PHI, stimulates erythropoiesis and increases hemoglobin concentration in patients with non-dialysis CKD. Am J Kidney Dis 2008; 51:B80.
- Maxwell PH, Osmond MK, Pugh CW, et al. Identification of the renal erythropoietin-producing cells using transgenic mice. Kidney Int 1993; 44:1149–1162.
- Maxwell PH, Ferguson DJ, Nicholls LG, et al. Sites of erythropoietin production. Kidney Int 1997; 51:393–401.
- Jelkmann W. Erythropoeitin: structure, control of production and function. Physiol Rev 1992; 72:449–489.
- Wang GL, Jiang BH, Rue EA, Semenza GL. Hypoxia-inducible factor 1 is a basic-helix-loop-helix-PAS heterodimer regulated by cellular O2 tension. Proc Natl Acad Sci USA 1995; 92:5510–5514.
- Wang GL, Semenza GL. Purification and characterization of hypoxia-inducible factor 1. J Biol Chem 1995; 270:1230–1237.
- Maxwell PH, Wiesener MS, Chang GW, et al. The tumour suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis. Nature 1999; 399:271–275.
- Salceda S, Caro J. Hypoxia-inducible factor 1alpha protein is rapidly degraded by the ubiquitin-proteasome system under normoxic conditions. Its stabilization by hypoxia depends on redox-induced changes. J Biol Chem 1997; 272:22642–22647.
- Malik J, Kim AR, Tyre KA, Cherukuri AR, Palis J. Erythropoietin critically regulates the terminal maturation of murine and human primitive erythroblasts. Haematologica 2013; 98:1778–1787.
- Wu H, Liu X, Jaenisch R, Lodish HF. Generation of committed erythroid BFU-E and CFU-E progenitors does not require erythropoietin or the erythropoietin receptor. Cell 1995; 83:59–67.
- Socolovsky M, Nam H, Fleming MD, Haase VH, Brugnara C, Lodish HF. Ineffective erythropoiesis in Stat5a(-/-)5b(-/-) mice due to decreased survival of early erythroblasts. Blood 2001; 98:3261–3273.
- Papanikolaou G, Pantopoulos K. Iron metabolism and toxicity. Toxicol Appl Pharmacol 2005; 202:199–211.
- Conrad ME, Umbreit JN. Pathways of iron absorption. Blood Cells Mol Dis 2002; 29:336–355.
- Frazer DM, Anderson GJ. The orchestration of body iron intake: how and where do enterocytes receive their cues? Blood Cells Moll Dis 2003; 30:288–297.
- Donovan A, Lima CA, Pinkus JL, et al. The iron exporter ferroportin/Slc40a1 is essential for iron homeostasis. Cell Metab 2005; 1:191–200.
- Vulpe CD, Kuo YM, Murphy TL, et al. Hephaestin, a ceruloplasmin homologue implicated in intestinal iron transport, is defective in the sla mouse. Nat Genet 1999; 21:195–199.
- Bothwell TH. Overview and mechanisms of iron regulation. Nutr Rev 1995: 53:237–245.
- Kawabata H, Nakamaki T, Ikonomi P, Smith RD, Germain RS, Koeffler HP. Expression of transferrin receptor 2 in normal and neoplastic hematopoietic cells. Blood 2001; 98:2714–2719.
- Arosio P, Levi S. Cytosolic and mitochondrial ferritins in the regulation of cellular iron homeostasis and oxidative damage. Biochim Biophys Acta 2010; 1800:783–792.
- Finch CA, Bellotti V, Stray S, et al. Plasma ferritin determination as a diagnostic tool. West J Med 1986; 145:657–663.
- Delaby C, Pilard N, Goncalves AS, Beaumont C, Canonne-Hergaux F. Presence of the iron exporter ferroportin at the plasma membrane of macrophages is enhanced by iron loading and down-regulated by hepcidin. Blood 2005; 106:3979–3984.
- Ganz T. Hepcidin, a key regulator of iron metabolism and mediator of anemia of inflammation. Blood 2003; 102:783–788.
- Nicolas G, Chauvet C, Viatte L, et al. The gene encoding the iron regulatory peptide hepcidin is regulated by anemia, hypoxia, and inflammation. J Clin Invest 2002; 110:1037–1044.
- DeGowin RL, Lavender AR, Forland M, Charleston D, Gottschalk A. Erythropoiesis and erythropoietin in patients with chronic renal failure treated with hemodialysis and testosterone. Ann Intern Med 1970; 72:913–918.
- Richardson JR Jr, Weinstein MB. Erythropoietic response of dialyzed patients to testosterone administration. Ann Intern Med 1970; 73:403–407
- Eschbach JW, Abdulhadi MH, Browne JK, et al. Recombinant human erythropoietin in anemic patients with end-stage renal disease. Results of a phase III multicenter clinical trial. Ann Intern Med 1989; 111:992–1000.
- Moreno F, Aracil FJ, Pérez R, Valderrábano F. Controlled study on the improvement of quality of life in elderly hemodialysis patients after correcting end-stage renal disease-related anemia with erythropoietin. Am J Kidney Dis 1996; 27:548–556.
- Nissenson AR, Nimer SD, Wolcott DL. Recombinant human erythropoietin and renal anemia: molecular biology, clinical efficacy, and nervous system effects. Ann Intern Med 1991; 114:402–416.
- Stivelman JC. Benefits of anaemia treatment on cognitive function. Nephrol Dial Transplant 2000; 15(suppl 3):29–35.
- Maddux FW, Shetty S, del Aguila MA, Nelson MA, Murray BM. Effect of erythropoiesis-stimulating agents on healthcare utilization, costs, and outcomes in chronic kidney disease. Ann Pharmacother 2007; 41:1761–1769.
- Macdougall IC, Lewis NP, Saunders MJ, et al. Long-term cardiorespiratory effects of amelioration of renal anaemia by erythropoietin. Lancet 1990; 335:489–493.
- Silverberg DS, Wexler D, Blum M, et al. Effects of treatment with epoetin beta on outcomes in patients with anaemia and chronic heart failure. Kidney Blood Press Res 2005; 28:41–47.
- Perkins R, Olson S, Hansen J, Lee J, Stiles K, Lebrun C. Impact of an anemia clinic on emergency room visits and hospitalizations in patients with anemia of CKD pre-dialysis. Nephrol Nurs J 2007; 34:167–173, 182.
- Locatelli F, Conte F, Marcelli D. The impact of haematocrit levels and erythropoietin treatment on overall and cardiovascular mortality and morbidity—the experience of the Lombardy Dialysis Registry. Nephrol Dial Transplant 1998; 13:1642–1644.
- Centers for Medicare and Medicaid Services; Kinney R. 2005 Annual Report: ESRD Clinical Performance Measures Project. Am J Kidney Dis 2006; 48(suppl 2):S1–S106.
- US Renal Data System. Annual Data Report 2006. www.usrds.org/adr.aspx. Accessed July 3, 2016.
- Besarab A, Bolton WK, Browne JK, et al. The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med 1998; 339:584–590.
- Singh AK, Szczech L, Tang KL, et al; CHOIR Investigators. Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med 2006; 355:2085–2098.
- Drüeke TB, Locatelli F, Clyne N, et al; CREATE Investigators. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med 2006; 355:2071–2084.
- Pfeffer MA, Burdmann EA, Chen CY, et al; TREAT Investigators. A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N Engl J Med 2009; 361:2019–2032.
- Kirkpantur A, Kahraman S, Yilmaz R, et al. The effects of maintenance recombinant human erythropoietin therapy on ambulatory blood pressure recordings: conventional, Doppler, and tissue Doppler echocardiographic parameters. Artif Organs 2005; 29:965–972.
- Fishbane S, Berns JS. Hemoglobin cycling in hemodialysis patients treated with recombinant human erythropoietin. Kidney Int 2005; 68:1337–1343.
- Szczech LA, Barnhart HX, Inrig JK, et al. Secondary analysis of the CHOIR trial epoetin-alpha dose and achieved hemoglobin outcomes. Kidney Int 2008; 74:791–798.
- Solomon SD, Uno H, Lewis EF, et al; Trial to Reduce Cardiovascular Events with Aranesp Therapy (TREAT) Investigators. Erythropoietic response and outcomes in kidney disease and type 2 diabetes. N Engl J Med 2010; 363:1146–1155.
- Kidney Disease: Improving Global Outcomes (KDIGO). KDIGO Clinical Practice Guideline for Anemia in Chronic Kidney Disease. Kidney Int Suppl 2012; 2:279–335.
- Fernández-Rodríguez AM, Guindeo-Casasús MC, Molero-Labarta T, et al. Diagnosis of iron deficiency in chronic renal failure. Am J Kidney Dis 1999; 34:508–513.
- Eschbach JW, Cook JD, Scribner BH, Finch CA. Iron balance in hemodialysis patients. Ann Intern Med 1977; 87:710–713.
- Mittman N, Sreedhara R, Mushnick R, et al. Reticulocyte hemoglobin content predicts functional iron deficiency in hemodialysis patients receiving rHuEPO. Am J Kidney Dis 1997; 30:912–922.
- Tessitore N, Solero GP, Lippi G, et al. The role of iron status markers in predicting response to intravenous iron in haemodialysis patients on maintenance erythropoietin. Nephrol Dial Transplant 2001; 16:1416–1423.
- Coyne DW. Iron indices: what do they really mean? Kidney Int Suppl 2006; 101:S4–S8.
- Fishbane S, Kowalski EA, Imbriano LJ, Maesaka JK. The evaluation of iron status in hemodialysis patients. J Am Soc Nephrol 1996; 7:2654–2657.
- Coyne DW, Kapoian T, Suki W, et al; DRIVE Study Group. Ferric gluconate is highly efficacious in anemic hemodialysis patients with high serum ferritin and low transferrin saturation: results of the Dialysis Patients’ Response to IV Iron with Elevated Ferritin (DRIVE) Study. J Am Soc Nephrol 2007; 18:975–984.
- Radtke HW, Claussner A, Erbes PM, Scheuermann EH, Schoeppe W, Koch KM. Serum erythropoietin concentration in chronic renal failure: relationship to degree of anemia and excretory renal function. Blood 1979; 54:877–884.
- Korte W, Cogliatti SB, Jung K, Riesen W. Mild renal dysfunction is sufficient to induce erythropoietin deficiency in patients with unexplained anaemia. Clin Chim Acta 2000; 292:149–154.
- Locatelli F, Olivares J, Walker R, et al; European/Australian NESP 980202 Study Group. Novel erythropoiesis stimulating protein for treatment of anemia in chronic renal insufficiency. Kidney Int 2001; 60:741–747.
- Carrera F, Burnier M. Use of darbepoetin alfa in the treatment of anaemia of chronic kidney disease: clinical and pharmacoeconomic considerations. NDT Plus 2009; 2(suppl 1):i9–i17.
- Egrie JC, Browne JK. Development and characterization of novel erythropoiesis stimulating protein (NESP). Nephrol Dial Transplant 2001; 16(suppl 3):3–13.
- Nissenson AR, Charytan C. Controversies in iron management. Kidney Int Suppl 2003; 87:S64–S71.
- Kilpatrick RD, Critchlow CW, Fishbane S, et al. Greater epoetin alpha responsiveness is associated with improved survival in hemodialysis patients. Clin J Am Soc Nephrol 2008; 3:1077–1083.
- Locatelli F, Aljama P, Barany P, et al; European Best Practice Guidelines Working Group. Revised European best practice guidelines for the management of anaemia in patients with chronic renal failure. Nephrol Dial Transplant 2004; 19(suppl 2):ii1–ii47.
- Stenvinkel P. The role of inflammation in the anaemia of end-stage renal disease. Nephrol Dial Transplant 2001; 16(suppl 7):36–40.
- Barany P, Divino Filho JC, Bergstrom J. High C-reactive protein is a strong predictor of resistance to erythropoietin in hemodialysis patients. Am J Kidney Dis 1997; 29:565–568.
- Drueke T. Hyporesponsiveness to recombinant human erythropoietin. Nephrol Dial Transplant 2001; 16(suppl 7):25–28.
- Casadevall N. Cellular mechanism of resistance to erythropoietin. Nephrol Dial Transplant 1995; 10(suppl 6):27–30.
- Kraus E, Rabb H. EPO therapy during acute kidney disease: to use or not to use, that is the question. Am J Kidney Dis 2005; 46:967–969.
- Gotloib L, Silverberg D, Fudin R, Shostak A. Iron deficiency is a common cause of anemia in chronic kidney disease and can often be corrected with intravenous iron. J Nephrol 2006; 19:161–167.
- Tarng DC, Huang TP, Chen TW, Yang WC. Erythropoietin hyporesponsiveness: from iron deficiency to iron overload. Kidney Int Suppl 1999; 69:S107–S118.
- Drüeke TB. Modulating factors in the hematopoietic response to erythropoietin. Am J Kidney Dis 1991; 18(suppl 1):87–92.
- Boven K, Stryker S, Knight J, et al. The increased incidence of pure red cell aplasia with an Eprex formulation in uncoated rubber stopper syringes. Kidney Int 2005; 67:2346–2353.
- Shimizu H, Saitoh T, Ota F, et al. Pure red cell aplasia induced only by intravenous administration of recombinant human erythropoietin. Acta Haematol 2011; 126:114–118.
- Tonia T, Mettler A, Robert N, et al. Erythropoietin or darbepoetin for patients with cancer. Cochrane Database Syst Rev 2012; 12:CD003407.
- Bohlius J, Langensiepen S, Schwarzer G, et al. Recombinant human erythropoietin and overall survival in cancer patients: results of a comprehensive meta-analysis. J Natl Cancer Inst 2005; 97:489–498.
- Henke M, Laszig R, Rübe C, et al. Erythropoietin to treat head and neck cancer patients with anaemia undergoing radiotherapy: randomised, double-blind, placebo-controlled trial. Lancet 2003; 362:1255–1260.
- Leyland-Jones B, Semiglazov V, Pawlicki M, et al. Maintaining normal hemoglobin levels with epoetin alfa in mainly nonanemic patients with metastatic breast cancer receiving first-line chemotherapy: a survival study. J Clin Oncol 2005; 23:5960–5972.
- Brower V. Erythropoietin may impair, not improve, cancer survival. Nat Med 2003; 9:1439.
- Acs G, Acs P, Beckwith SM, et al. Erythropoietin and erythropoietin receptor expression in human cancer. Cancer Res 2001; 61:3561–3565.
- Yasuda Y, Fujita Y, Matsuo T, et al. Erythropoietin regulates tumour growth of human malignancies. Carcinogenesis 2003; 24:1021–1029.
- Levin NW, Fishbane S, Cañedo FV, et al; MAXIMA Study Investigators. Intravenous methoxy polyethylene glycol-epoetin beta for haemoglobin control in patients with chronic kidney disease who are on dialysis: a randomised non-inferiority trial (MAXIMA). Lancet 2007; 370:1415–1421.
- Macdougall IC, Walker R, Provenzano R, et al; ARCTOS Study Investigators. C.E.R.A. corrects anemia in patients with chronic kidney disease not on dialysis: results of a randomized clinical trial. Clin J Am Soc Nephrol 2008; 3:337–347.
- Frohna PA, Milwee S, Pinkett J, et al. Preliminary results from a randomized, single-blind, placebo-controlled trial of FG-4592, a novel hypoxia inducible factor prolyl hydroxylase inhibitor, in subjects with CKD anemia (abstract). J Am Soc Nephrol 2007; 18:763.
- Holdstock L, Meadowcroft AM, Maier R, et al. Four-week studies of oral hypoxia-inducible factor-prolyl hydroxylase inhibitor GSK1278863 for treatment of anemia. J Am Soc Nephrol 2016; 27:1234–1244.
KEY POINTS
- Before treating with ESAs, it is necessary to investigate and rule out underlying treatable conditions such as iron or vitamin deficiencies.
- Recognizing anemia in chronic kidney disease is important and often involves participation by the primary care physician, especially in early disease when chronic kidney disease may be mild.
- The only proven benefit of ESA therapy is avoidance of blood transfusions.
- ESAs should not be used to increase the hemoglobin concentration above 13 g/dL. In end-stage renal disease, the goal of therapy is to maintain levels at a target no higher than 11.5 g/dL. In nondialysis-dependent chronic kidney disease, the decision to prescribe ESA therapy should be individualized.
Information management for clinicians
Accessing, absorbing, organizing, storing, and retrieving potentially useful medical information is a challenge. Physicians used to try meet this challenge with personal libraries of journal articles in their file cabinet. Today, that is inadequate to combat the deluge of digital information. In 2013, the Institute of Medicine acknowledged this problem, stating, “The ever-increasing volume of evidence makes it difficult for clinicians to maintain a working knowledge of new clinical information.”1
The sheer volume of data has meant that, rather than try to maintain a regular diet of professional reading (proactive scanning2), many of us now seek information only when we need answers to specific clinical questions (reactive searching). This approach promotes lifelong problem-based learning but assumes that we are consciously aware of this need and are aware of the need to search for new information.
We need to constantly scan for new evidence in our area of practice to avoid becoming falsely assured of our knowledge. We also need to be able to find information we have seen before we need to use it. The following are examples of how using this approach could dramatically empower a busy clinician.
On a recent clinic day, a colleague pokes his head into your office and asks, “Have you heard anything about niacin in the news? I have a patient who is asking me if we should discontinue it.” You respond: “Yes, there was something that just came out. I am not sure where I read it or heard about it. Give me a couple of seconds and I can find it.” True to your word, a few seconds later you find and share the latest article on the HPS2-THRIVE trial and a commentary on the results.
Later, your first patient of the day asks you, “When we switched to dabigatran, you mentioned that, unlike warfarin, there was no specific reversal agent. I heard that there is one now?” Instead of being taken aback, you nod your head. “Yes, I saw that recent article showing that the medication rapidly and completely reverses the effect of dabigatran in the majority of patients. While I hope we don’t need it, this is good news, particularly as there did not seem to be any major adverse events.”
Sounds too good to be true? Can this really be you? In this article, we outline an information management strategy (Figure 1) and tools to help busy clinicians stay up to date with new medical evidence in their areas of interest or expertise. In addition, we provide a strategy for leveraging technology to easily retrieve previously viewed information. A future article will specifically show how to best access information at the point of patient care.
THE NEED TO MANAGE INFORMATION
Physicians are expected to practice evidence-based medicine. When faced with a clinical question, we should search for evidence using focused queries of primary and secondary sources such as PubMed or the Cochrane Library. This is an important skill and is appropriate when we take time to look for an evidence-based answer to a specific question. In many cases, it is appropriate to continue with a current practice until newer information has been reviewed and validated.
Unfortunately, indexing and adding new recommendations to these information sources takes time. We may also be unaware that new information is available and may continue to practice as usual until faced with a situation like those outlined above or until we attend a continuing medical education activity, often quite by chance.
Today we can proactively update ourselves in a manner tailored to our own interests and focus and retrieve important information easily when we need it.
A STRATEGY FOR INFORMATION MANAGEMENT
In general, we come across new information in one of three ways:
- Proactive scanning of personalized sources of information—as discussed above, a habit of regular scanning is critical to information management
- Reactive searching for information to answer clinical problems or when doing research
- Incidentally—an e-mail from a colleague, information shared on a social network or encountered while surfing the Internet.
In each case, we may find information that is potentially useful, something we may need to find again in the future. But unless we use this information often, we will not remember the details or may even forget we had seen it. Thus, we need a strategy to store this information so we can retrieve it easily at any time with any device; neuroscientists call this the “externalization” of memory.3 Ideally, even if we forget that we ever saw this information or where we stored it, a search would retrieve the location and details of this formerly viewed information.
In the following sections, we outline steps and tools of a strategy for managing clinical information relevant to your practice.
STEP 1: SETTING UP INFORMATION FEEDS
The first step in this information management strategy is to become aware of relevant new information in your area of practice or research. To do this, you proactively set up feeds of information from reliable and authentic sources. These feeds can be browsed on any computer or smart mobile device.
There are several possibilities for creating these feeds. One option is to subscribe to the table of contents (TOC) of relevant journals via e-mail.
A more versatile and full-featured option is a research site summary (RSS) feed-reader. RSS is a standard for publishing summaries (feeds) of frequently updated content on the World Wide Web, such as journal TOCs and items from medical journal news sites (Table 1 shows what this looks like on screen), as well as aggregators like the American College of Physicians Journal Club. You can subscribe to these using feed-reader software from Feedly (www.feedly.com) or Inoreader (www.inoreader.com), which can be used with any browser on a desktop or laptop. They are also available as apps for mobile devices such as smartphones and tablets. The feed-reader periodically checks for new content and automatically downloads it to the device. Thus, you do not need to check multiple websites for updates or have e-mail inboxes fill with content; the content is delivered to your device for perusal at your convenience. (See online supplement “Information Management for Clinicians” for step-by-step instructions on creating a free Inoreader account and subscribing to feeds.)

RSS feed-readers have several advantages over e-mailed TOCs:
- RSS feeds create a centralized searchable repository of all subscribed information.
- The software keeps track of what you have read and displays only unread items; after a journal TOC e-mail is opened, the entire TOC is marked as having been read.
- You can organize news items into folders by tagging key words.
- Most journals and medical news sites like Medscape and the health section of the New York Times provide RSS feeds at no cost.
- An unlimited number of feed items, or articles, are stored in the cloud and do not affect e-mail storage capacity.
- The feed is automatically updated multiple times a day instead of once a week or once a month.
- In addition, one can create RSS feeds on PubMed for custom searches. Thus, a physician can get automatic regular updates of new articles indexed in MEDLINE in their area of interest.
Users can thus build their own personalized magazine of constantly updated information for access and can search from any web-enabled device. (Note: It is advisable to turn off notifications generated by these apps on mobile devices to reduce distraction.)
STEP 2: BOOKMARKING EVIDENCE
When you find something useful or interesting, bookmarks help you find the information again quickly when you need it. But while the browsers Firefox, Chrome, Internet Explorer, and Safari allow bookmarking, they have significant limitations. Bookmarks may be available only on the device they were created on, and because people use more than one device to go online, they may not remember which device they used to bookmark or view the web page.
Browser bookmarks generally store the address (URL) of the web page and a label that you create, but they do not do much else. Sharing bookmarks with others is also difficult or impossible.
Social bookmarking
Social bookmarking lets you create bookmarks you can share across other devices and with other people. Diigo (www.diigo.com) and Delicious (www.delicious.com) are two social bookmarking services that let you integrate with all popular browsers through a button or toolbar. They allow you to save displayed web pages with labels, descriptions, and tags.
Diigo offers two additional features. It allows web pages to be annotated with highlights and notes. And during a Google search, relevant results from the Diigo library are simultaneously displayed.
If you forget you bookmarked something and saved it in your Diigo library, when you search for the information again on Google, Diigo will automatically display any results from your Diigo library next to the Google search results. This is very helpful as it is much easier to review information you have already read, marked up, and saved than it is to start over.
Bookmarks and annotations are stored in the cloud and can be accessed by any device. (See “Information Management for Clinicians” to learn how to sign up for a free Diigo account, and how to use it.)
STEP 3: STORING YOUR INFORMATION
You may want the option to store full-text information in your personal library. This information was once stored in file cabinets and, more recently, on hard drives and USB flash drives. But information stored with these methods is not available or searchable on multiple devices from any location.
Cloud storage
Cloud storage services meet the need for access to stored information at any time and with any device. Options include Dropbox (www.dropbox.com), Box (www.box.com), Google Drive (drive.google.com), OneDrive (onedrive.live.com), and Evernote (www.evernote.com). Each provides different amounts of free storage and has apps available for most platforms and devices. They provide search tools and the ability to share articles or “folders” with other users. The information on these online drives is “synced” between all devices so that the most up-to-date version is always available to the user regardless of location and device.
Evernote offers multiple folders called notebooks to store and segregate data. The open notebook shown in Figure 2 is named “reference articles.” It has the HPS2-Thrive article from the New England Journal of Medicine (N Engl J Med) tagged with the terms “niacin” and “lipid” to facilitate retrieval. The article was saved from that journal’s website using an Evernote browser extension that allows entire web pages or selections to be saved to Evernote with a single click. Evernote also has a powerful search feature that can find text in images or in PDF documents. In addition, it allows easy sharing of a note or an entire notebook. Once a note or notebook is shared, all parties can add to it. In The Evernote app also allows tablet and smartphone access to the shareable content.
The other services listed here have similar feature sets. Dropbox is perhaps the easiest to adopt, but it offers the least amount of free storage. If you use Microsoft Office software, OneDrive lets you edit documents online, and an Office 365 subscription includes 1 terabyte of storage. Google Drive is probably the best solution for online collaboration, such as coauthoring a paper. Box is one of the few online storage solutions that complies with the Health Insurance Portability and Accountability privacy rules.
PUTTING IT ALL INTO PRACTICE
Once you have become familiar with Inoreader and Diigo (see Information Management for Clinicians for step-by-step instructions), the following scenario shows how to adapt them into an efficient workflow.
Dr. Smith has a smartphone, a tablet, a laptop at home, and a desktop at work. She signs onto Google Chrome as her preferred browser on all devices. This seamlessly loads her Diigo extension when she is using a laptop or desktop. She has set her RSS feeds for her preferred journal TOCs and medical news sites to be downloaded to Inoreader. (For details on how to add a medical journals feed bundle and a medical news feed bundle, visit Information Management for Clinicians.)
Instead of reading paper journals, Dr. Smith browses her customized up-to-date “magazine” on Inoreader. When she comes across a relevant article, she marks it as “favorite.” If she has more time, she visits the web page, reviews the information, and saves it to her Diigo library with annotations if appropriate.
When searching for information on the web, she uses Google—without having to remember if she bookmarked information related to the search term. The Diigo extension in her browser automatically searches and displays information from her Diigo library next to her Google search results, and she can instantly see her notes from the last time she read the article.
Relating this workflow to the example of the dabigatran story above, Dr. Smith sees an article about dabigatran reversal while viewing her N Engl J Med medical news feed on her feed-reader. She marks it as a favorite and tags it with the key terms “cardiology” and “vascular” (Figure 3).
Dr. Smith later returns to look at her favorite feed items and visits the article on the N Engl J Med website. She annotates the article and saves it to her Diigo library (Figure 4).
Since this information is highly relevant to her practice, she also visits the N Engl J Med website to read the full article and the accompanying editorial (Figure 5). She annotates these and also saves them to her Diigo library.
Later, if she searches Google for dabigatran (using her default Google Chrome browser with Diigo extension), she will see the usual Google search results and twinned Diigo bookmarks (Figure 6).
If she clicks on one of the links, the browser will load the web page with all the annotations that she made when she first visited.
CONCLUSION
The strategies and tools we describe here let you create a personalized and constantly updated medical news “magazine,” accessible from any of your web-enabled devices. They can transform the Internet into a searchable notebook of personally selected, annotated information, helping you to more easily stay up to date with advances in your field of practice, and to more easily manage the modern information overload.
- Institute of Medicine (IOM). Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: National Academies Press; 2013. www.nap.edu/openbook.php?record_id=13444&page=R1. Accessed May 17, 2016.
- Slotnick HB. Physicians’ learning strategies. Chest 2000; 118(suppl 2):18S–23S.
- Levitin DJ. The Organized Mind: Thinking Straight in the Age of Information Overload. New York, NY: Dutton; 2014:528.
Accessing, absorbing, organizing, storing, and retrieving potentially useful medical information is a challenge. Physicians used to try meet this challenge with personal libraries of journal articles in their file cabinet. Today, that is inadequate to combat the deluge of digital information. In 2013, the Institute of Medicine acknowledged this problem, stating, “The ever-increasing volume of evidence makes it difficult for clinicians to maintain a working knowledge of new clinical information.”1
The sheer volume of data has meant that, rather than try to maintain a regular diet of professional reading (proactive scanning2), many of us now seek information only when we need answers to specific clinical questions (reactive searching). This approach promotes lifelong problem-based learning but assumes that we are consciously aware of this need and are aware of the need to search for new information.
We need to constantly scan for new evidence in our area of practice to avoid becoming falsely assured of our knowledge. We also need to be able to find information we have seen before we need to use it. The following are examples of how using this approach could dramatically empower a busy clinician.
On a recent clinic day, a colleague pokes his head into your office and asks, “Have you heard anything about niacin in the news? I have a patient who is asking me if we should discontinue it.” You respond: “Yes, there was something that just came out. I am not sure where I read it or heard about it. Give me a couple of seconds and I can find it.” True to your word, a few seconds later you find and share the latest article on the HPS2-THRIVE trial and a commentary on the results.
Later, your first patient of the day asks you, “When we switched to dabigatran, you mentioned that, unlike warfarin, there was no specific reversal agent. I heard that there is one now?” Instead of being taken aback, you nod your head. “Yes, I saw that recent article showing that the medication rapidly and completely reverses the effect of dabigatran in the majority of patients. While I hope we don’t need it, this is good news, particularly as there did not seem to be any major adverse events.”
Sounds too good to be true? Can this really be you? In this article, we outline an information management strategy (Figure 1) and tools to help busy clinicians stay up to date with new medical evidence in their areas of interest or expertise. In addition, we provide a strategy for leveraging technology to easily retrieve previously viewed information. A future article will specifically show how to best access information at the point of patient care.
THE NEED TO MANAGE INFORMATION
Physicians are expected to practice evidence-based medicine. When faced with a clinical question, we should search for evidence using focused queries of primary and secondary sources such as PubMed or the Cochrane Library. This is an important skill and is appropriate when we take time to look for an evidence-based answer to a specific question. In many cases, it is appropriate to continue with a current practice until newer information has been reviewed and validated.
Unfortunately, indexing and adding new recommendations to these information sources takes time. We may also be unaware that new information is available and may continue to practice as usual until faced with a situation like those outlined above or until we attend a continuing medical education activity, often quite by chance.
Today we can proactively update ourselves in a manner tailored to our own interests and focus and retrieve important information easily when we need it.
A STRATEGY FOR INFORMATION MANAGEMENT
In general, we come across new information in one of three ways:
- Proactive scanning of personalized sources of information—as discussed above, a habit of regular scanning is critical to information management
- Reactive searching for information to answer clinical problems or when doing research
- Incidentally—an e-mail from a colleague, information shared on a social network or encountered while surfing the Internet.
In each case, we may find information that is potentially useful, something we may need to find again in the future. But unless we use this information often, we will not remember the details or may even forget we had seen it. Thus, we need a strategy to store this information so we can retrieve it easily at any time with any device; neuroscientists call this the “externalization” of memory.3 Ideally, even if we forget that we ever saw this information or where we stored it, a search would retrieve the location and details of this formerly viewed information.
In the following sections, we outline steps and tools of a strategy for managing clinical information relevant to your practice.
STEP 1: SETTING UP INFORMATION FEEDS
The first step in this information management strategy is to become aware of relevant new information in your area of practice or research. To do this, you proactively set up feeds of information from reliable and authentic sources. These feeds can be browsed on any computer or smart mobile device.
There are several possibilities for creating these feeds. One option is to subscribe to the table of contents (TOC) of relevant journals via e-mail.
A more versatile and full-featured option is a research site summary (RSS) feed-reader. RSS is a standard for publishing summaries (feeds) of frequently updated content on the World Wide Web, such as journal TOCs and items from medical journal news sites (Table 1 shows what this looks like on screen), as well as aggregators like the American College of Physicians Journal Club. You can subscribe to these using feed-reader software from Feedly (www.feedly.com) or Inoreader (www.inoreader.com), which can be used with any browser on a desktop or laptop. They are also available as apps for mobile devices such as smartphones and tablets. The feed-reader periodically checks for new content and automatically downloads it to the device. Thus, you do not need to check multiple websites for updates or have e-mail inboxes fill with content; the content is delivered to your device for perusal at your convenience. (See online supplement “Information Management for Clinicians” for step-by-step instructions on creating a free Inoreader account and subscribing to feeds.)

RSS feed-readers have several advantages over e-mailed TOCs:
- RSS feeds create a centralized searchable repository of all subscribed information.
- The software keeps track of what you have read and displays only unread items; after a journal TOC e-mail is opened, the entire TOC is marked as having been read.
- You can organize news items into folders by tagging key words.
- Most journals and medical news sites like Medscape and the health section of the New York Times provide RSS feeds at no cost.
- An unlimited number of feed items, or articles, are stored in the cloud and do not affect e-mail storage capacity.
- The feed is automatically updated multiple times a day instead of once a week or once a month.
- In addition, one can create RSS feeds on PubMed for custom searches. Thus, a physician can get automatic regular updates of new articles indexed in MEDLINE in their area of interest.
Users can thus build their own personalized magazine of constantly updated information for access and can search from any web-enabled device. (Note: It is advisable to turn off notifications generated by these apps on mobile devices to reduce distraction.)
STEP 2: BOOKMARKING EVIDENCE
When you find something useful or interesting, bookmarks help you find the information again quickly when you need it. But while the browsers Firefox, Chrome, Internet Explorer, and Safari allow bookmarking, they have significant limitations. Bookmarks may be available only on the device they were created on, and because people use more than one device to go online, they may not remember which device they used to bookmark or view the web page.
Browser bookmarks generally store the address (URL) of the web page and a label that you create, but they do not do much else. Sharing bookmarks with others is also difficult or impossible.
Social bookmarking
Social bookmarking lets you create bookmarks you can share across other devices and with other people. Diigo (www.diigo.com) and Delicious (www.delicious.com) are two social bookmarking services that let you integrate with all popular browsers through a button or toolbar. They allow you to save displayed web pages with labels, descriptions, and tags.
Diigo offers two additional features. It allows web pages to be annotated with highlights and notes. And during a Google search, relevant results from the Diigo library are simultaneously displayed.
If you forget you bookmarked something and saved it in your Diigo library, when you search for the information again on Google, Diigo will automatically display any results from your Diigo library next to the Google search results. This is very helpful as it is much easier to review information you have already read, marked up, and saved than it is to start over.
Bookmarks and annotations are stored in the cloud and can be accessed by any device. (See “Information Management for Clinicians” to learn how to sign up for a free Diigo account, and how to use it.)
STEP 3: STORING YOUR INFORMATION
You may want the option to store full-text information in your personal library. This information was once stored in file cabinets and, more recently, on hard drives and USB flash drives. But information stored with these methods is not available or searchable on multiple devices from any location.
Cloud storage
Cloud storage services meet the need for access to stored information at any time and with any device. Options include Dropbox (www.dropbox.com), Box (www.box.com), Google Drive (drive.google.com), OneDrive (onedrive.live.com), and Evernote (www.evernote.com). Each provides different amounts of free storage and has apps available for most platforms and devices. They provide search tools and the ability to share articles or “folders” with other users. The information on these online drives is “synced” between all devices so that the most up-to-date version is always available to the user regardless of location and device.
Evernote offers multiple folders called notebooks to store and segregate data. The open notebook shown in Figure 2 is named “reference articles.” It has the HPS2-Thrive article from the New England Journal of Medicine (N Engl J Med) tagged with the terms “niacin” and “lipid” to facilitate retrieval. The article was saved from that journal’s website using an Evernote browser extension that allows entire web pages or selections to be saved to Evernote with a single click. Evernote also has a powerful search feature that can find text in images or in PDF documents. In addition, it allows easy sharing of a note or an entire notebook. Once a note or notebook is shared, all parties can add to it. In The Evernote app also allows tablet and smartphone access to the shareable content.
The other services listed here have similar feature sets. Dropbox is perhaps the easiest to adopt, but it offers the least amount of free storage. If you use Microsoft Office software, OneDrive lets you edit documents online, and an Office 365 subscription includes 1 terabyte of storage. Google Drive is probably the best solution for online collaboration, such as coauthoring a paper. Box is one of the few online storage solutions that complies with the Health Insurance Portability and Accountability privacy rules.
PUTTING IT ALL INTO PRACTICE
Once you have become familiar with Inoreader and Diigo (see Information Management for Clinicians for step-by-step instructions), the following scenario shows how to adapt them into an efficient workflow.
Dr. Smith has a smartphone, a tablet, a laptop at home, and a desktop at work. She signs onto Google Chrome as her preferred browser on all devices. This seamlessly loads her Diigo extension when she is using a laptop or desktop. She has set her RSS feeds for her preferred journal TOCs and medical news sites to be downloaded to Inoreader. (For details on how to add a medical journals feed bundle and a medical news feed bundle, visit Information Management for Clinicians.)
Instead of reading paper journals, Dr. Smith browses her customized up-to-date “magazine” on Inoreader. When she comes across a relevant article, she marks it as “favorite.” If she has more time, she visits the web page, reviews the information, and saves it to her Diigo library with annotations if appropriate.
When searching for information on the web, she uses Google—without having to remember if she bookmarked information related to the search term. The Diigo extension in her browser automatically searches and displays information from her Diigo library next to her Google search results, and she can instantly see her notes from the last time she read the article.
Relating this workflow to the example of the dabigatran story above, Dr. Smith sees an article about dabigatran reversal while viewing her N Engl J Med medical news feed on her feed-reader. She marks it as a favorite and tags it with the key terms “cardiology” and “vascular” (Figure 3).
Dr. Smith later returns to look at her favorite feed items and visits the article on the N Engl J Med website. She annotates the article and saves it to her Diigo library (Figure 4).
Since this information is highly relevant to her practice, she also visits the N Engl J Med website to read the full article and the accompanying editorial (Figure 5). She annotates these and also saves them to her Diigo library.
Later, if she searches Google for dabigatran (using her default Google Chrome browser with Diigo extension), she will see the usual Google search results and twinned Diigo bookmarks (Figure 6).
If she clicks on one of the links, the browser will load the web page with all the annotations that she made when she first visited.
CONCLUSION
The strategies and tools we describe here let you create a personalized and constantly updated medical news “magazine,” accessible from any of your web-enabled devices. They can transform the Internet into a searchable notebook of personally selected, annotated information, helping you to more easily stay up to date with advances in your field of practice, and to more easily manage the modern information overload.
Accessing, absorbing, organizing, storing, and retrieving potentially useful medical information is a challenge. Physicians used to try meet this challenge with personal libraries of journal articles in their file cabinet. Today, that is inadequate to combat the deluge of digital information. In 2013, the Institute of Medicine acknowledged this problem, stating, “The ever-increasing volume of evidence makes it difficult for clinicians to maintain a working knowledge of new clinical information.”1
The sheer volume of data has meant that, rather than try to maintain a regular diet of professional reading (proactive scanning2), many of us now seek information only when we need answers to specific clinical questions (reactive searching). This approach promotes lifelong problem-based learning but assumes that we are consciously aware of this need and are aware of the need to search for new information.
We need to constantly scan for new evidence in our area of practice to avoid becoming falsely assured of our knowledge. We also need to be able to find information we have seen before we need to use it. The following are examples of how using this approach could dramatically empower a busy clinician.
On a recent clinic day, a colleague pokes his head into your office and asks, “Have you heard anything about niacin in the news? I have a patient who is asking me if we should discontinue it.” You respond: “Yes, there was something that just came out. I am not sure where I read it or heard about it. Give me a couple of seconds and I can find it.” True to your word, a few seconds later you find and share the latest article on the HPS2-THRIVE trial and a commentary on the results.
Later, your first patient of the day asks you, “When we switched to dabigatran, you mentioned that, unlike warfarin, there was no specific reversal agent. I heard that there is one now?” Instead of being taken aback, you nod your head. “Yes, I saw that recent article showing that the medication rapidly and completely reverses the effect of dabigatran in the majority of patients. While I hope we don’t need it, this is good news, particularly as there did not seem to be any major adverse events.”
Sounds too good to be true? Can this really be you? In this article, we outline an information management strategy (Figure 1) and tools to help busy clinicians stay up to date with new medical evidence in their areas of interest or expertise. In addition, we provide a strategy for leveraging technology to easily retrieve previously viewed information. A future article will specifically show how to best access information at the point of patient care.
THE NEED TO MANAGE INFORMATION
Physicians are expected to practice evidence-based medicine. When faced with a clinical question, we should search for evidence using focused queries of primary and secondary sources such as PubMed or the Cochrane Library. This is an important skill and is appropriate when we take time to look for an evidence-based answer to a specific question. In many cases, it is appropriate to continue with a current practice until newer information has been reviewed and validated.
Unfortunately, indexing and adding new recommendations to these information sources takes time. We may also be unaware that new information is available and may continue to practice as usual until faced with a situation like those outlined above or until we attend a continuing medical education activity, often quite by chance.
Today we can proactively update ourselves in a manner tailored to our own interests and focus and retrieve important information easily when we need it.
A STRATEGY FOR INFORMATION MANAGEMENT
In general, we come across new information in one of three ways:
- Proactive scanning of personalized sources of information—as discussed above, a habit of regular scanning is critical to information management
- Reactive searching for information to answer clinical problems or when doing research
- Incidentally—an e-mail from a colleague, information shared on a social network or encountered while surfing the Internet.
In each case, we may find information that is potentially useful, something we may need to find again in the future. But unless we use this information often, we will not remember the details or may even forget we had seen it. Thus, we need a strategy to store this information so we can retrieve it easily at any time with any device; neuroscientists call this the “externalization” of memory.3 Ideally, even if we forget that we ever saw this information or where we stored it, a search would retrieve the location and details of this formerly viewed information.
In the following sections, we outline steps and tools of a strategy for managing clinical information relevant to your practice.
STEP 1: SETTING UP INFORMATION FEEDS
The first step in this information management strategy is to become aware of relevant new information in your area of practice or research. To do this, you proactively set up feeds of information from reliable and authentic sources. These feeds can be browsed on any computer or smart mobile device.
There are several possibilities for creating these feeds. One option is to subscribe to the table of contents (TOC) of relevant journals via e-mail.
A more versatile and full-featured option is a research site summary (RSS) feed-reader. RSS is a standard for publishing summaries (feeds) of frequently updated content on the World Wide Web, such as journal TOCs and items from medical journal news sites (Table 1 shows what this looks like on screen), as well as aggregators like the American College of Physicians Journal Club. You can subscribe to these using feed-reader software from Feedly (www.feedly.com) or Inoreader (www.inoreader.com), which can be used with any browser on a desktop or laptop. They are also available as apps for mobile devices such as smartphones and tablets. The feed-reader periodically checks for new content and automatically downloads it to the device. Thus, you do not need to check multiple websites for updates or have e-mail inboxes fill with content; the content is delivered to your device for perusal at your convenience. (See online supplement “Information Management for Clinicians” for step-by-step instructions on creating a free Inoreader account and subscribing to feeds.)

RSS feed-readers have several advantages over e-mailed TOCs:
- RSS feeds create a centralized searchable repository of all subscribed information.
- The software keeps track of what you have read and displays only unread items; after a journal TOC e-mail is opened, the entire TOC is marked as having been read.
- You can organize news items into folders by tagging key words.
- Most journals and medical news sites like Medscape and the health section of the New York Times provide RSS feeds at no cost.
- An unlimited number of feed items, or articles, are stored in the cloud and do not affect e-mail storage capacity.
- The feed is automatically updated multiple times a day instead of once a week or once a month.
- In addition, one can create RSS feeds on PubMed for custom searches. Thus, a physician can get automatic regular updates of new articles indexed in MEDLINE in their area of interest.
Users can thus build their own personalized magazine of constantly updated information for access and can search from any web-enabled device. (Note: It is advisable to turn off notifications generated by these apps on mobile devices to reduce distraction.)
STEP 2: BOOKMARKING EVIDENCE
When you find something useful or interesting, bookmarks help you find the information again quickly when you need it. But while the browsers Firefox, Chrome, Internet Explorer, and Safari allow bookmarking, they have significant limitations. Bookmarks may be available only on the device they were created on, and because people use more than one device to go online, they may not remember which device they used to bookmark or view the web page.
Browser bookmarks generally store the address (URL) of the web page and a label that you create, but they do not do much else. Sharing bookmarks with others is also difficult or impossible.
Social bookmarking
Social bookmarking lets you create bookmarks you can share across other devices and with other people. Diigo (www.diigo.com) and Delicious (www.delicious.com) are two social bookmarking services that let you integrate with all popular browsers through a button or toolbar. They allow you to save displayed web pages with labels, descriptions, and tags.
Diigo offers two additional features. It allows web pages to be annotated with highlights and notes. And during a Google search, relevant results from the Diigo library are simultaneously displayed.
If you forget you bookmarked something and saved it in your Diigo library, when you search for the information again on Google, Diigo will automatically display any results from your Diigo library next to the Google search results. This is very helpful as it is much easier to review information you have already read, marked up, and saved than it is to start over.
Bookmarks and annotations are stored in the cloud and can be accessed by any device. (See “Information Management for Clinicians” to learn how to sign up for a free Diigo account, and how to use it.)
STEP 3: STORING YOUR INFORMATION
You may want the option to store full-text information in your personal library. This information was once stored in file cabinets and, more recently, on hard drives and USB flash drives. But information stored with these methods is not available or searchable on multiple devices from any location.
Cloud storage
Cloud storage services meet the need for access to stored information at any time and with any device. Options include Dropbox (www.dropbox.com), Box (www.box.com), Google Drive (drive.google.com), OneDrive (onedrive.live.com), and Evernote (www.evernote.com). Each provides different amounts of free storage and has apps available for most platforms and devices. They provide search tools and the ability to share articles or “folders” with other users. The information on these online drives is “synced” between all devices so that the most up-to-date version is always available to the user regardless of location and device.
Evernote offers multiple folders called notebooks to store and segregate data. The open notebook shown in Figure 2 is named “reference articles.” It has the HPS2-Thrive article from the New England Journal of Medicine (N Engl J Med) tagged with the terms “niacin” and “lipid” to facilitate retrieval. The article was saved from that journal’s website using an Evernote browser extension that allows entire web pages or selections to be saved to Evernote with a single click. Evernote also has a powerful search feature that can find text in images or in PDF documents. In addition, it allows easy sharing of a note or an entire notebook. Once a note or notebook is shared, all parties can add to it. In The Evernote app also allows tablet and smartphone access to the shareable content.
The other services listed here have similar feature sets. Dropbox is perhaps the easiest to adopt, but it offers the least amount of free storage. If you use Microsoft Office software, OneDrive lets you edit documents online, and an Office 365 subscription includes 1 terabyte of storage. Google Drive is probably the best solution for online collaboration, such as coauthoring a paper. Box is one of the few online storage solutions that complies with the Health Insurance Portability and Accountability privacy rules.
PUTTING IT ALL INTO PRACTICE
Once you have become familiar with Inoreader and Diigo (see Information Management for Clinicians for step-by-step instructions), the following scenario shows how to adapt them into an efficient workflow.
Dr. Smith has a smartphone, a tablet, a laptop at home, and a desktop at work. She signs onto Google Chrome as her preferred browser on all devices. This seamlessly loads her Diigo extension when she is using a laptop or desktop. She has set her RSS feeds for her preferred journal TOCs and medical news sites to be downloaded to Inoreader. (For details on how to add a medical journals feed bundle and a medical news feed bundle, visit Information Management for Clinicians.)
Instead of reading paper journals, Dr. Smith browses her customized up-to-date “magazine” on Inoreader. When she comes across a relevant article, she marks it as “favorite.” If she has more time, she visits the web page, reviews the information, and saves it to her Diigo library with annotations if appropriate.
When searching for information on the web, she uses Google—without having to remember if she bookmarked information related to the search term. The Diigo extension in her browser automatically searches and displays information from her Diigo library next to her Google search results, and she can instantly see her notes from the last time she read the article.
Relating this workflow to the example of the dabigatran story above, Dr. Smith sees an article about dabigatran reversal while viewing her N Engl J Med medical news feed on her feed-reader. She marks it as a favorite and tags it with the key terms “cardiology” and “vascular” (Figure 3).
Dr. Smith later returns to look at her favorite feed items and visits the article on the N Engl J Med website. She annotates the article and saves it to her Diigo library (Figure 4).
Since this information is highly relevant to her practice, she also visits the N Engl J Med website to read the full article and the accompanying editorial (Figure 5). She annotates these and also saves them to her Diigo library.
Later, if she searches Google for dabigatran (using her default Google Chrome browser with Diigo extension), she will see the usual Google search results and twinned Diigo bookmarks (Figure 6).
If she clicks on one of the links, the browser will load the web page with all the annotations that she made when she first visited.
CONCLUSION
The strategies and tools we describe here let you create a personalized and constantly updated medical news “magazine,” accessible from any of your web-enabled devices. They can transform the Internet into a searchable notebook of personally selected, annotated information, helping you to more easily stay up to date with advances in your field of practice, and to more easily manage the modern information overload.
- Institute of Medicine (IOM). Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: National Academies Press; 2013. www.nap.edu/openbook.php?record_id=13444&page=R1. Accessed May 17, 2016.
- Slotnick HB. Physicians’ learning strategies. Chest 2000; 118(suppl 2):18S–23S.
- Levitin DJ. The Organized Mind: Thinking Straight in the Age of Information Overload. New York, NY: Dutton; 2014:528.
- Institute of Medicine (IOM). Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: National Academies Press; 2013. www.nap.edu/openbook.php?record_id=13444&page=R1. Accessed May 17, 2016.
- Slotnick HB. Physicians’ learning strategies. Chest 2000; 118(suppl 2):18S–23S.
- Levitin DJ. The Organized Mind: Thinking Straight in the Age of Information Overload. New York, NY: Dutton; 2014:528.
KEY POINTS
- The first step in information management is to become aware of relevant new information in your area of practice and set up feeds of information from reliable and authentic sources. These feeds should be accessible from any computer or mobile device and scanned regularly.
- Useful information you come across in various digital streams needs to be bookmarked for future search and retrieval. Social bookmarking lets you create bookmarks you can share across other devices and with other people and retrieve with an Internet search.
- Cloud storage services have apps for most platforms and devices, providing search tools and the ability to share articles or “folders” with other users. The information is “synced” between all devices so that the most up-to-date version is always available, regardless of location and device.
Should patients with stable ischemic heart disease undergo revascularization?
The answer is less clear for these patients than for patients with acute coronary syndromes. In the latter group, percutaneous or surgical revascularization reduces the rates of morbidity and mortality, whereas in patients with stable ischemic heart disease, benefits may be limited to the improvement of angina. Certain markers and criteria may help us in this decision, and trials are ongoing.
Of importance, all patients with coronary artery disease should receive guideline-directed medical therapy as tolerated, regardless of whether they undergo revascularization.
MEDICAL THERAPY FOR ALL
In all the relevant trials, patients with stable ischemic heart disease in both the revascularization groups and the unrevascularized groups received guideline-directed medical therapy. Current guidelines1 give class I recommendations (ie, treatment should be given) for:
- Lipid management
- Blood pressure management
- Physical activity
- Weight management
- Smoking cessation
- Antiplatelet therapy
- Beta-blockers for patients with normal left ventricular function after an acute coronary syndrome event, and for those with an ejection fraction of 40% or less
- Angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers for patients who have hypertension, diabetes mellitus, a left ventricular ejection fraction of 40% or less, or chronic kidney disease
- Annual influenza vaccination
- Anti-ischemic medications (beta-blockers, calcium channel blockers, nitrates) for relief of symptoms.
REVASCULARIZATION FOR SOME?
Results of the studies outlined below will help in deciding when to use guideline-directed medical therapy alone or medical therapy plus revascularization.
COURAGE trial: No added benefit in patients at low risk
The findings of the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE), published in 2007, suggested that in select patients, percutaneous coronary intervention for stable coronary artery disease was no better than guideline-directed medical therapy alone for reducing the outcomes of death, myocardial infarction, or hospitalization for acute coronary syndrome.2
Of note, however, is that the 2,287 patients included in COURAGE were a low-risk subset of the more than 35,000 patients initially evaluated. The investigators reviewed the patients’ coronary angiograms before enrollment, and thus many patients with complex or high-risk anatomy were likely excluded based on an a priori assessment of angiographic images.
Also, coronary stent technology has substantially improved since COURAGE (which primarily used bare-metal stents and early drug-eluting stents), and this brings into question whether the results are applicable to current patients.
Moreover, in subsequent substudies from COURAGE, revascularization significantly improved symptoms of angina and quality-of-life scores compared with medical therapy alone.3,4
Also important is that more than one-third of the patients in the medical therapy group crossed over to revascularization during the study, most often for worsening symptoms of angina.
Regardless of its limitations, COURAGE played an important role in delineating the use of guideline-directed medical therapy alone in certain low-risk patients and sparked debate about when and if to revascularize other patients.
BARI 2D trial: CABG may benefit those with diabetes
The Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial, published in 2009, aimed to find out if revascularization in patients with stable ischemic heart disease and diabetes was beneficial compared with medical therapy alone.5
While it was not designed to directly compare percutaneous coronary intervention vs coronary artery bypass grafting (CABG), it did find that medical therapy plus CABG might reduce the rate of adverse cardiovascular events in this population compared with medical therapy alone or medical therapy plus percutaneous intervention.
As with COURAGE, however, the patients in the medical therapy group in BARI 2D also had a high rate of crossover to revascularization, primarily driven by worsening anginal symptoms.
FREEDOM and the 2014 updated guideline
Based on the findings of BARI 2D and those of FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus: Optimal Management of Multivessel Disease),6 the American College of Cardiology and American Heart Association updated their recommendations in 2014.7 This focused update states that for patients with diabetes and multivessel coronary artery disease, if revascularization is likely to improve survival (for example, in three-vessel disease or complex two-vessel disease involving the proximal left anterior descending artery), then CABG should be performed if a left internal mammary artery graft can be anastomosed to the left anterior descending artery. Otherwise, percutaneous coronary intervention should be reserved for those patients with diabetes and high-risk or complex multivessel coronary artery disease who are not good surgical candidates.
FAME 2 trial: Fractional flow reserve as a guide
The Fractional Flow Reserve Versus Angiography for Multivessel Evaluation 2 (FAME 2) trial,8 published in 2012, evaluated whether clinical outcomes differ between patients who undergo percutaneous revascularization plus medical therapy and those who are treated with medical therapy alone, using fractional flow reserve as a means to determine which stenoses should be considered for intervention. Fractional flow reserve performed during invasive angiography determines the ratio of intracoronary pressure to aortic pressure using a wire advanced across a coronary obstruction.
FAME 2 found a markedly lower incidence of the primary composite end point of death, myocardial infarction, and urgent revascularization with randomization to percutaneous revascularization plus medical therapy compared with medical therapy only (4.3% vs 12.7%, P = .001) in patients with a fractional flow reserve less than 0.80 (considered a hemodynamically significant obstruction). The trial was stopped early because of the markedly different outcomes.
Of note, however, the reduction in adverse clinical outcomes was driven primarily by a reduction in urgent revascularizations in those treated with percutaneous coronary intervention in the revascularization arm. Regardless, using fractional flow reserve to guide whether obstructive coronary lesions should be treated with percutaneous coronary intervention has appropriately become a mainstay in interventional cardiology.
Stress testing
Noninvasive stress testing has played a role in helping to guide revascularization decisions in stable ischemic heart disease. In particular, revascularization in the setting of greater than 10% ischemia on perfusion imaging has been associated with a lower risk of cardiac death than in those who were revascularized with an ischemic burden less than 10%.9
A substudy of COURAGE found that percutaneous coronary intervention reduced ischemia to a greater degree than medical therapy alone on serial nuclear stress tests in patients with stable ischemic heart disease.10 In this substudy, when both groups were combined, the investigators also found that there were fewer adverse events in those who had an overall reduction of ischemia regardless of treatment strategy.
ISCHEMIA: Revascularize those with ischemia?
While COURAGE, BARI 2D, and FAME 2 suggested that early revascularization for low-risk patients with coronary artery disease does not confer a benefit over medical treatment alone with regard to hard clinical end points, it remains unclear whether an early revascularization strategy is advantageous in patients with stable ischemic heart disease who have at least a moderate amount of ischemia on noninvasive stress testing.
The ongoing ISCHEMIA (International Study of Comparative Effectiveness With Medical and Invasive Approaches) trial will help to answer that question. In this study, 8,000 patients with stable angina and at least moderate ischemia on noninvasive stress testing are being randomized before coronary angiography either to guideline-directed medical therapy plus revascularization (percutaneous or surgical) or to medical therapy alone.11 The ISCHEMIA study population reflects current practice more closely than the previous studies discussed above in its inclusion of fractional flow reserve and later-generation drug-eluting stents.
The results of ISCHEMIA will be an important piece of the puzzle to answer whether patients with stable ischemic heart disease benefit from revascularization in terms of cardiovascular mortality or myocardial infarction (the primary end point of the study).
Studies in additional subsets
It is important to recognize that there are additional subsets of patients with stable ischemic heart disease (those with multivessel disease, left main coronary disease, or low ejection fractions, for example) who have been studied to help determine when and how to perform revascularization. In addition, there are guidelines12 for both interventional cardiologists and cardiac surgeons that help delineate which patients should undergo revascularization. While a complete review is beyond the scope of this discussion, three trials are worth mentioning:
The Coronary Artery Surgery Study (CASS)13 revealed that revascularization in left main coronary artery disease is associated with lower mortality rates than medical therapy alone. This study, along with others, eventually led to recommendations for revascularization to be performed in all patients with significant left main coronary disease, regardless of symptoms or stress test findings.14,15
The Surgical Treatment for Ischemic Heart Failure (STICH) trial16 found that patients with a low ejection fraction (< 35%) and ischemic heart disease had no difference in all-cause mortality rates when treated with CABG plus medical therapy compared with medical therapy alone (although the study’s design has been heavily criticized).
The Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) study17 found that CABG was associated with fewer adverse events in three-vessel coronary artery disease or complex left main coronary artery disease compared with percutaneous coronary intervention. The study used early-generation paclitaxel drug-eluting stents that are no longer used in contemporary practice. This study established the SYNTAX score, which is often used to help make revascularization decisions. A low SYNTAX score of 0 to 22 (meaning less-severe coronary artery disease) was associated with equivalent outcomes for both percutaneous coronary intervention and CABG. Thus, even if there is multivessel disease or left main disease, if the SYNTAX score is low, then percutaneous coronary intervention is an acceptable method for revascularization with similar results as for CABG.
A TEAM APPROACH
Due to the complexity of stable ischemic heart disease and the subtleties of managing these patients, a multidisciplinary “heart team” approach may be the best way to navigate treating stable ischemic heart disease via revascularization or with medical therapy alone. The heart team approach could take advantage of the particular expertise that the primary care physician, cardiologist, interventional cardiologist, and cardiac surgeon provide.
The upcoming results of studies such as the ISCHEMIA trial will help to provide additional guidance for these teams in long-term management of patients with stable ischemic heart disease.
- Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease. Circulation 2012; 126:e354–e471.
- Boden WE, O’Rourke RA, Teo KK, et al; COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007; 356:1503–1516.
- Weintraub WS, Spertus JA, Kolm P, et al. Effect of PCI on quality of life in patients with stable coronary disease. N Engl J Med 2008; 359:677–687.
- Blankenship J, Marshall JJ, Pinto DS, et al; Society for Cardiovascular Angiography and Interventions. Effect of percutaneous coronary intervention on quality of life: a consensus statement from the Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv 2013; 81:243–249.
- BARI 2D Study Group; Frye RL, August P, Brooks MM, et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med 2009; 360:2503–2515.
- Farkouh ME, Domanski M, Sleep LA, et al; FREEDOM Trial Investigators. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med 2012; 367:2375–2384.
- Fihn SD, Blankenship JC, Alexander KP, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 2014; 64:1929–1949.
- De Bruyne B, Pijls NH, Kalesan B, et al; FAME 2 Trial Investigators. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012; 367:991–1001.
- Hachamovitch R, Berman DS, Shaw LJ, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation 1998; 97:535–543.
- Shaw LJ, Berman DS, Maron DJ, et al; COURAGE Investigators. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation 2008; 117:1283–1291.
- Stone GW, Hochman JS, Williams DO, et al. Medical therapy with versus without revascularization in stable patients with moderate and severe ischemia: the case for community equipoise. J Am Coll Cardiol 2016; 67:81–99.
- Patel M, Dehmer G, Hirshfeld J, Smith PK, Spertus JA. ACCF/SCAI/STS/AATS/AHA/ASNC/HFSA/SCCT 2012 appropriate use criteria for coronary revascularization focused update. J Am Coll Cardiol 2012; 59:857–881.
- Alderman EL, Bourassa MG, Cohen LS, et al. Ten-year follow-up of survival and myocardial infarction in the randomized Coronary Artery Surgery Study. Circulation 1990; 82:1629–1646.
- Hillis L, Smith P, Anderson J, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2011; 58:e123–e210.
- Levine G, Bates E, Blankenship J, et al. 2011 ACCF/AHA guideline for percutaneous coronary intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 2011; 58:e44–e122.
- Velazquez EJ, Lee KL, Deja MA, et al, for the STICH Investigators. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med 2011; 364:1607–1616.
- Serruys PW, Morice M-C, Kappetein AP, et al, for the SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009; 360:961–972.
The answer is less clear for these patients than for patients with acute coronary syndromes. In the latter group, percutaneous or surgical revascularization reduces the rates of morbidity and mortality, whereas in patients with stable ischemic heart disease, benefits may be limited to the improvement of angina. Certain markers and criteria may help us in this decision, and trials are ongoing.
Of importance, all patients with coronary artery disease should receive guideline-directed medical therapy as tolerated, regardless of whether they undergo revascularization.
MEDICAL THERAPY FOR ALL
In all the relevant trials, patients with stable ischemic heart disease in both the revascularization groups and the unrevascularized groups received guideline-directed medical therapy. Current guidelines1 give class I recommendations (ie, treatment should be given) for:
- Lipid management
- Blood pressure management
- Physical activity
- Weight management
- Smoking cessation
- Antiplatelet therapy
- Beta-blockers for patients with normal left ventricular function after an acute coronary syndrome event, and for those with an ejection fraction of 40% or less
- Angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers for patients who have hypertension, diabetes mellitus, a left ventricular ejection fraction of 40% or less, or chronic kidney disease
- Annual influenza vaccination
- Anti-ischemic medications (beta-blockers, calcium channel blockers, nitrates) for relief of symptoms.
REVASCULARIZATION FOR SOME?
Results of the studies outlined below will help in deciding when to use guideline-directed medical therapy alone or medical therapy plus revascularization.
COURAGE trial: No added benefit in patients at low risk
The findings of the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE), published in 2007, suggested that in select patients, percutaneous coronary intervention for stable coronary artery disease was no better than guideline-directed medical therapy alone for reducing the outcomes of death, myocardial infarction, or hospitalization for acute coronary syndrome.2
Of note, however, is that the 2,287 patients included in COURAGE were a low-risk subset of the more than 35,000 patients initially evaluated. The investigators reviewed the patients’ coronary angiograms before enrollment, and thus many patients with complex or high-risk anatomy were likely excluded based on an a priori assessment of angiographic images.
Also, coronary stent technology has substantially improved since COURAGE (which primarily used bare-metal stents and early drug-eluting stents), and this brings into question whether the results are applicable to current patients.
Moreover, in subsequent substudies from COURAGE, revascularization significantly improved symptoms of angina and quality-of-life scores compared with medical therapy alone.3,4
Also important is that more than one-third of the patients in the medical therapy group crossed over to revascularization during the study, most often for worsening symptoms of angina.
Regardless of its limitations, COURAGE played an important role in delineating the use of guideline-directed medical therapy alone in certain low-risk patients and sparked debate about when and if to revascularize other patients.
BARI 2D trial: CABG may benefit those with diabetes
The Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial, published in 2009, aimed to find out if revascularization in patients with stable ischemic heart disease and diabetes was beneficial compared with medical therapy alone.5
While it was not designed to directly compare percutaneous coronary intervention vs coronary artery bypass grafting (CABG), it did find that medical therapy plus CABG might reduce the rate of adverse cardiovascular events in this population compared with medical therapy alone or medical therapy plus percutaneous intervention.
As with COURAGE, however, the patients in the medical therapy group in BARI 2D also had a high rate of crossover to revascularization, primarily driven by worsening anginal symptoms.
FREEDOM and the 2014 updated guideline
Based on the findings of BARI 2D and those of FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus: Optimal Management of Multivessel Disease),6 the American College of Cardiology and American Heart Association updated their recommendations in 2014.7 This focused update states that for patients with diabetes and multivessel coronary artery disease, if revascularization is likely to improve survival (for example, in three-vessel disease or complex two-vessel disease involving the proximal left anterior descending artery), then CABG should be performed if a left internal mammary artery graft can be anastomosed to the left anterior descending artery. Otherwise, percutaneous coronary intervention should be reserved for those patients with diabetes and high-risk or complex multivessel coronary artery disease who are not good surgical candidates.
FAME 2 trial: Fractional flow reserve as a guide
The Fractional Flow Reserve Versus Angiography for Multivessel Evaluation 2 (FAME 2) trial,8 published in 2012, evaluated whether clinical outcomes differ between patients who undergo percutaneous revascularization plus medical therapy and those who are treated with medical therapy alone, using fractional flow reserve as a means to determine which stenoses should be considered for intervention. Fractional flow reserve performed during invasive angiography determines the ratio of intracoronary pressure to aortic pressure using a wire advanced across a coronary obstruction.
FAME 2 found a markedly lower incidence of the primary composite end point of death, myocardial infarction, and urgent revascularization with randomization to percutaneous revascularization plus medical therapy compared with medical therapy only (4.3% vs 12.7%, P = .001) in patients with a fractional flow reserve less than 0.80 (considered a hemodynamically significant obstruction). The trial was stopped early because of the markedly different outcomes.
Of note, however, the reduction in adverse clinical outcomes was driven primarily by a reduction in urgent revascularizations in those treated with percutaneous coronary intervention in the revascularization arm. Regardless, using fractional flow reserve to guide whether obstructive coronary lesions should be treated with percutaneous coronary intervention has appropriately become a mainstay in interventional cardiology.
Stress testing
Noninvasive stress testing has played a role in helping to guide revascularization decisions in stable ischemic heart disease. In particular, revascularization in the setting of greater than 10% ischemia on perfusion imaging has been associated with a lower risk of cardiac death than in those who were revascularized with an ischemic burden less than 10%.9
A substudy of COURAGE found that percutaneous coronary intervention reduced ischemia to a greater degree than medical therapy alone on serial nuclear stress tests in patients with stable ischemic heart disease.10 In this substudy, when both groups were combined, the investigators also found that there were fewer adverse events in those who had an overall reduction of ischemia regardless of treatment strategy.
ISCHEMIA: Revascularize those with ischemia?
While COURAGE, BARI 2D, and FAME 2 suggested that early revascularization for low-risk patients with coronary artery disease does not confer a benefit over medical treatment alone with regard to hard clinical end points, it remains unclear whether an early revascularization strategy is advantageous in patients with stable ischemic heart disease who have at least a moderate amount of ischemia on noninvasive stress testing.
The ongoing ISCHEMIA (International Study of Comparative Effectiveness With Medical and Invasive Approaches) trial will help to answer that question. In this study, 8,000 patients with stable angina and at least moderate ischemia on noninvasive stress testing are being randomized before coronary angiography either to guideline-directed medical therapy plus revascularization (percutaneous or surgical) or to medical therapy alone.11 The ISCHEMIA study population reflects current practice more closely than the previous studies discussed above in its inclusion of fractional flow reserve and later-generation drug-eluting stents.
The results of ISCHEMIA will be an important piece of the puzzle to answer whether patients with stable ischemic heart disease benefit from revascularization in terms of cardiovascular mortality or myocardial infarction (the primary end point of the study).
Studies in additional subsets
It is important to recognize that there are additional subsets of patients with stable ischemic heart disease (those with multivessel disease, left main coronary disease, or low ejection fractions, for example) who have been studied to help determine when and how to perform revascularization. In addition, there are guidelines12 for both interventional cardiologists and cardiac surgeons that help delineate which patients should undergo revascularization. While a complete review is beyond the scope of this discussion, three trials are worth mentioning:
The Coronary Artery Surgery Study (CASS)13 revealed that revascularization in left main coronary artery disease is associated with lower mortality rates than medical therapy alone. This study, along with others, eventually led to recommendations for revascularization to be performed in all patients with significant left main coronary disease, regardless of symptoms or stress test findings.14,15
The Surgical Treatment for Ischemic Heart Failure (STICH) trial16 found that patients with a low ejection fraction (< 35%) and ischemic heart disease had no difference in all-cause mortality rates when treated with CABG plus medical therapy compared with medical therapy alone (although the study’s design has been heavily criticized).
The Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) study17 found that CABG was associated with fewer adverse events in three-vessel coronary artery disease or complex left main coronary artery disease compared with percutaneous coronary intervention. The study used early-generation paclitaxel drug-eluting stents that are no longer used in contemporary practice. This study established the SYNTAX score, which is often used to help make revascularization decisions. A low SYNTAX score of 0 to 22 (meaning less-severe coronary artery disease) was associated with equivalent outcomes for both percutaneous coronary intervention and CABG. Thus, even if there is multivessel disease or left main disease, if the SYNTAX score is low, then percutaneous coronary intervention is an acceptable method for revascularization with similar results as for CABG.
A TEAM APPROACH
Due to the complexity of stable ischemic heart disease and the subtleties of managing these patients, a multidisciplinary “heart team” approach may be the best way to navigate treating stable ischemic heart disease via revascularization or with medical therapy alone. The heart team approach could take advantage of the particular expertise that the primary care physician, cardiologist, interventional cardiologist, and cardiac surgeon provide.
The upcoming results of studies such as the ISCHEMIA trial will help to provide additional guidance for these teams in long-term management of patients with stable ischemic heart disease.
The answer is less clear for these patients than for patients with acute coronary syndromes. In the latter group, percutaneous or surgical revascularization reduces the rates of morbidity and mortality, whereas in patients with stable ischemic heart disease, benefits may be limited to the improvement of angina. Certain markers and criteria may help us in this decision, and trials are ongoing.
Of importance, all patients with coronary artery disease should receive guideline-directed medical therapy as tolerated, regardless of whether they undergo revascularization.
MEDICAL THERAPY FOR ALL
In all the relevant trials, patients with stable ischemic heart disease in both the revascularization groups and the unrevascularized groups received guideline-directed medical therapy. Current guidelines1 give class I recommendations (ie, treatment should be given) for:
- Lipid management
- Blood pressure management
- Physical activity
- Weight management
- Smoking cessation
- Antiplatelet therapy
- Beta-blockers for patients with normal left ventricular function after an acute coronary syndrome event, and for those with an ejection fraction of 40% or less
- Angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers for patients who have hypertension, diabetes mellitus, a left ventricular ejection fraction of 40% or less, or chronic kidney disease
- Annual influenza vaccination
- Anti-ischemic medications (beta-blockers, calcium channel blockers, nitrates) for relief of symptoms.
REVASCULARIZATION FOR SOME?
Results of the studies outlined below will help in deciding when to use guideline-directed medical therapy alone or medical therapy plus revascularization.
COURAGE trial: No added benefit in patients at low risk
The findings of the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE), published in 2007, suggested that in select patients, percutaneous coronary intervention for stable coronary artery disease was no better than guideline-directed medical therapy alone for reducing the outcomes of death, myocardial infarction, or hospitalization for acute coronary syndrome.2
Of note, however, is that the 2,287 patients included in COURAGE were a low-risk subset of the more than 35,000 patients initially evaluated. The investigators reviewed the patients’ coronary angiograms before enrollment, and thus many patients with complex or high-risk anatomy were likely excluded based on an a priori assessment of angiographic images.
Also, coronary stent technology has substantially improved since COURAGE (which primarily used bare-metal stents and early drug-eluting stents), and this brings into question whether the results are applicable to current patients.
Moreover, in subsequent substudies from COURAGE, revascularization significantly improved symptoms of angina and quality-of-life scores compared with medical therapy alone.3,4
Also important is that more than one-third of the patients in the medical therapy group crossed over to revascularization during the study, most often for worsening symptoms of angina.
Regardless of its limitations, COURAGE played an important role in delineating the use of guideline-directed medical therapy alone in certain low-risk patients and sparked debate about when and if to revascularize other patients.
BARI 2D trial: CABG may benefit those with diabetes
The Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial, published in 2009, aimed to find out if revascularization in patients with stable ischemic heart disease and diabetes was beneficial compared with medical therapy alone.5
While it was not designed to directly compare percutaneous coronary intervention vs coronary artery bypass grafting (CABG), it did find that medical therapy plus CABG might reduce the rate of adverse cardiovascular events in this population compared with medical therapy alone or medical therapy plus percutaneous intervention.
As with COURAGE, however, the patients in the medical therapy group in BARI 2D also had a high rate of crossover to revascularization, primarily driven by worsening anginal symptoms.
FREEDOM and the 2014 updated guideline
Based on the findings of BARI 2D and those of FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus: Optimal Management of Multivessel Disease),6 the American College of Cardiology and American Heart Association updated their recommendations in 2014.7 This focused update states that for patients with diabetes and multivessel coronary artery disease, if revascularization is likely to improve survival (for example, in three-vessel disease or complex two-vessel disease involving the proximal left anterior descending artery), then CABG should be performed if a left internal mammary artery graft can be anastomosed to the left anterior descending artery. Otherwise, percutaneous coronary intervention should be reserved for those patients with diabetes and high-risk or complex multivessel coronary artery disease who are not good surgical candidates.
FAME 2 trial: Fractional flow reserve as a guide
The Fractional Flow Reserve Versus Angiography for Multivessel Evaluation 2 (FAME 2) trial,8 published in 2012, evaluated whether clinical outcomes differ between patients who undergo percutaneous revascularization plus medical therapy and those who are treated with medical therapy alone, using fractional flow reserve as a means to determine which stenoses should be considered for intervention. Fractional flow reserve performed during invasive angiography determines the ratio of intracoronary pressure to aortic pressure using a wire advanced across a coronary obstruction.
FAME 2 found a markedly lower incidence of the primary composite end point of death, myocardial infarction, and urgent revascularization with randomization to percutaneous revascularization plus medical therapy compared with medical therapy only (4.3% vs 12.7%, P = .001) in patients with a fractional flow reserve less than 0.80 (considered a hemodynamically significant obstruction). The trial was stopped early because of the markedly different outcomes.
Of note, however, the reduction in adverse clinical outcomes was driven primarily by a reduction in urgent revascularizations in those treated with percutaneous coronary intervention in the revascularization arm. Regardless, using fractional flow reserve to guide whether obstructive coronary lesions should be treated with percutaneous coronary intervention has appropriately become a mainstay in interventional cardiology.
Stress testing
Noninvasive stress testing has played a role in helping to guide revascularization decisions in stable ischemic heart disease. In particular, revascularization in the setting of greater than 10% ischemia on perfusion imaging has been associated with a lower risk of cardiac death than in those who were revascularized with an ischemic burden less than 10%.9
A substudy of COURAGE found that percutaneous coronary intervention reduced ischemia to a greater degree than medical therapy alone on serial nuclear stress tests in patients with stable ischemic heart disease.10 In this substudy, when both groups were combined, the investigators also found that there were fewer adverse events in those who had an overall reduction of ischemia regardless of treatment strategy.
ISCHEMIA: Revascularize those with ischemia?
While COURAGE, BARI 2D, and FAME 2 suggested that early revascularization for low-risk patients with coronary artery disease does not confer a benefit over medical treatment alone with regard to hard clinical end points, it remains unclear whether an early revascularization strategy is advantageous in patients with stable ischemic heart disease who have at least a moderate amount of ischemia on noninvasive stress testing.
The ongoing ISCHEMIA (International Study of Comparative Effectiveness With Medical and Invasive Approaches) trial will help to answer that question. In this study, 8,000 patients with stable angina and at least moderate ischemia on noninvasive stress testing are being randomized before coronary angiography either to guideline-directed medical therapy plus revascularization (percutaneous or surgical) or to medical therapy alone.11 The ISCHEMIA study population reflects current practice more closely than the previous studies discussed above in its inclusion of fractional flow reserve and later-generation drug-eluting stents.
The results of ISCHEMIA will be an important piece of the puzzle to answer whether patients with stable ischemic heart disease benefit from revascularization in terms of cardiovascular mortality or myocardial infarction (the primary end point of the study).
Studies in additional subsets
It is important to recognize that there are additional subsets of patients with stable ischemic heart disease (those with multivessel disease, left main coronary disease, or low ejection fractions, for example) who have been studied to help determine when and how to perform revascularization. In addition, there are guidelines12 for both interventional cardiologists and cardiac surgeons that help delineate which patients should undergo revascularization. While a complete review is beyond the scope of this discussion, three trials are worth mentioning:
The Coronary Artery Surgery Study (CASS)13 revealed that revascularization in left main coronary artery disease is associated with lower mortality rates than medical therapy alone. This study, along with others, eventually led to recommendations for revascularization to be performed in all patients with significant left main coronary disease, regardless of symptoms or stress test findings.14,15
The Surgical Treatment for Ischemic Heart Failure (STICH) trial16 found that patients with a low ejection fraction (< 35%) and ischemic heart disease had no difference in all-cause mortality rates when treated with CABG plus medical therapy compared with medical therapy alone (although the study’s design has been heavily criticized).
The Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) study17 found that CABG was associated with fewer adverse events in three-vessel coronary artery disease or complex left main coronary artery disease compared with percutaneous coronary intervention. The study used early-generation paclitaxel drug-eluting stents that are no longer used in contemporary practice. This study established the SYNTAX score, which is often used to help make revascularization decisions. A low SYNTAX score of 0 to 22 (meaning less-severe coronary artery disease) was associated with equivalent outcomes for both percutaneous coronary intervention and CABG. Thus, even if there is multivessel disease or left main disease, if the SYNTAX score is low, then percutaneous coronary intervention is an acceptable method for revascularization with similar results as for CABG.
A TEAM APPROACH
Due to the complexity of stable ischemic heart disease and the subtleties of managing these patients, a multidisciplinary “heart team” approach may be the best way to navigate treating stable ischemic heart disease via revascularization or with medical therapy alone. The heart team approach could take advantage of the particular expertise that the primary care physician, cardiologist, interventional cardiologist, and cardiac surgeon provide.
The upcoming results of studies such as the ISCHEMIA trial will help to provide additional guidance for these teams in long-term management of patients with stable ischemic heart disease.
- Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease. Circulation 2012; 126:e354–e471.
- Boden WE, O’Rourke RA, Teo KK, et al; COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007; 356:1503–1516.
- Weintraub WS, Spertus JA, Kolm P, et al. Effect of PCI on quality of life in patients with stable coronary disease. N Engl J Med 2008; 359:677–687.
- Blankenship J, Marshall JJ, Pinto DS, et al; Society for Cardiovascular Angiography and Interventions. Effect of percutaneous coronary intervention on quality of life: a consensus statement from the Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv 2013; 81:243–249.
- BARI 2D Study Group; Frye RL, August P, Brooks MM, et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med 2009; 360:2503–2515.
- Farkouh ME, Domanski M, Sleep LA, et al; FREEDOM Trial Investigators. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med 2012; 367:2375–2384.
- Fihn SD, Blankenship JC, Alexander KP, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 2014; 64:1929–1949.
- De Bruyne B, Pijls NH, Kalesan B, et al; FAME 2 Trial Investigators. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012; 367:991–1001.
- Hachamovitch R, Berman DS, Shaw LJ, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation 1998; 97:535–543.
- Shaw LJ, Berman DS, Maron DJ, et al; COURAGE Investigators. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation 2008; 117:1283–1291.
- Stone GW, Hochman JS, Williams DO, et al. Medical therapy with versus without revascularization in stable patients with moderate and severe ischemia: the case for community equipoise. J Am Coll Cardiol 2016; 67:81–99.
- Patel M, Dehmer G, Hirshfeld J, Smith PK, Spertus JA. ACCF/SCAI/STS/AATS/AHA/ASNC/HFSA/SCCT 2012 appropriate use criteria for coronary revascularization focused update. J Am Coll Cardiol 2012; 59:857–881.
- Alderman EL, Bourassa MG, Cohen LS, et al. Ten-year follow-up of survival and myocardial infarction in the randomized Coronary Artery Surgery Study. Circulation 1990; 82:1629–1646.
- Hillis L, Smith P, Anderson J, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2011; 58:e123–e210.
- Levine G, Bates E, Blankenship J, et al. 2011 ACCF/AHA guideline for percutaneous coronary intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 2011; 58:e44–e122.
- Velazquez EJ, Lee KL, Deja MA, et al, for the STICH Investigators. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med 2011; 364:1607–1616.
- Serruys PW, Morice M-C, Kappetein AP, et al, for the SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009; 360:961–972.
- Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease. Circulation 2012; 126:e354–e471.
- Boden WE, O’Rourke RA, Teo KK, et al; COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007; 356:1503–1516.
- Weintraub WS, Spertus JA, Kolm P, et al. Effect of PCI on quality of life in patients with stable coronary disease. N Engl J Med 2008; 359:677–687.
- Blankenship J, Marshall JJ, Pinto DS, et al; Society for Cardiovascular Angiography and Interventions. Effect of percutaneous coronary intervention on quality of life: a consensus statement from the Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv 2013; 81:243–249.
- BARI 2D Study Group; Frye RL, August P, Brooks MM, et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med 2009; 360:2503–2515.
- Farkouh ME, Domanski M, Sleep LA, et al; FREEDOM Trial Investigators. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med 2012; 367:2375–2384.
- Fihn SD, Blankenship JC, Alexander KP, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 2014; 64:1929–1949.
- De Bruyne B, Pijls NH, Kalesan B, et al; FAME 2 Trial Investigators. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012; 367:991–1001.
- Hachamovitch R, Berman DS, Shaw LJ, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation 1998; 97:535–543.
- Shaw LJ, Berman DS, Maron DJ, et al; COURAGE Investigators. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation 2008; 117:1283–1291.
- Stone GW, Hochman JS, Williams DO, et al. Medical therapy with versus without revascularization in stable patients with moderate and severe ischemia: the case for community equipoise. J Am Coll Cardiol 2016; 67:81–99.
- Patel M, Dehmer G, Hirshfeld J, Smith PK, Spertus JA. ACCF/SCAI/STS/AATS/AHA/ASNC/HFSA/SCCT 2012 appropriate use criteria for coronary revascularization focused update. J Am Coll Cardiol 2012; 59:857–881.
- Alderman EL, Bourassa MG, Cohen LS, et al. Ten-year follow-up of survival and myocardial infarction in the randomized Coronary Artery Surgery Study. Circulation 1990; 82:1629–1646.
- Hillis L, Smith P, Anderson J, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2011; 58:e123–e210.
- Levine G, Bates E, Blankenship J, et al. 2011 ACCF/AHA guideline for percutaneous coronary intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 2011; 58:e44–e122.
- Velazquez EJ, Lee KL, Deja MA, et al, for the STICH Investigators. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med 2011; 364:1607–1616.
- Serruys PW, Morice M-C, Kappetein AP, et al, for the SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009; 360:961–972.