User login
Diet modifications highly effective in EoE
An elemental diet was more than 90% effective in inducing histologic remission in eosinophilic esophagitis patients, reported Dr. Ángel Arias and colleagues in the June issue of Gastroenterology.
The Six Food Elimination Diet was also highly efficacious, reinforcing the idea that dietary modification "should be considered as a first-line therapy in both children and adults affected by this disease," wrote the investigators (doi:10.1053/j.gastro.2014.02.006).
Dr. Arias of the Complejo Hospitalario La Mancha Centro, in Alcázar de San Juan, Spain, searched the MEDLINE, EMBASE, and SCOPUS databases for studies performed prior to June 2013 investigating the efficacy of dietary interventions in eosinophilic esophagitis (EoE).
Abstracts and other relevant material from conferences including Digestive Disease Week, the American College of Gastroenterology meeting, and European Gastroenterology Week were also included.
Overall, 33 studies were included, 23 of which were full articles with the remainder being abstracts; there were a total of 1,128 children and 189 adults included in the analysis.
Of the 13 studies that assessed the efficacy of exclusive feeding with an amino acid–based elemental diet (involving 411 children and 18 adults), 90.8% of patients achieved histologic remission of EoE, defined as fewer than 15 eosinophils per high-power field on esophageal biopsy (95% confidence interval, 84.7%-95.5%).
The next best diet, the Six Food Elimination Diet (SFED), offered a 72.1% efficacy rate (95% CI, 65.8%-78.1%) across 75 children and 122 adults and was "the only one assessed in more adults than children."
On the other hand, the strategy of eliminating foods that gave a positive result in skin allergy tests was assessed in 14 studies (594 children and 32 adults), and demonstrated an overall efficacy of just 45.5% (95% CI, 35.4%-55.7%).
Other less-studied diets included gluten-free and cow’s milk elimination diets, both of which seemed to result in histologic remission (58.7% and 68.2%, respectively).
However, "because studies assessing these dietary treatments are still scarce, making conclusions from them can be risky," wrote the authors.
"For example, although the overall efficacy of a gluten-free diet in achieving histologic remission of EoE was 58.7%, the remission rate ranged from 23.1% to 85.6%," they reported.
"Despite its obvious success, the multiple drawbacks of elemental diets, which include the need to avoid all table food, its unpleasant taste, and high cost, and the psychological effects produced by the social limitations that this diet entails, have probably contributed to the fact that this dietary intervention has been restricted almost exclusively to pediatric patients," commented Dr. Arias.
"In fact, no research on adults was available until 2013, with the reported remission rates being comparable with those documented in children."
On the other hand, the relatively high efficacy of the SFED diet, which avoids many of the disadvantages of the elemental diet, seems to make this the best choice for "children and motivated adult patients," added the researchers.
Future studies and meta-analyses should address whether diet adherence results in changes in esophageal fibrosis as well as quality of life issues brought on by diet adherence.
The authors disclosed no relevant financial conflicts.
An elemental diet was more than 90% effective in inducing histologic remission in eosinophilic esophagitis patients, reported Dr. Ángel Arias and colleagues in the June issue of Gastroenterology.
The Six Food Elimination Diet was also highly efficacious, reinforcing the idea that dietary modification "should be considered as a first-line therapy in both children and adults affected by this disease," wrote the investigators (doi:10.1053/j.gastro.2014.02.006).
Dr. Arias of the Complejo Hospitalario La Mancha Centro, in Alcázar de San Juan, Spain, searched the MEDLINE, EMBASE, and SCOPUS databases for studies performed prior to June 2013 investigating the efficacy of dietary interventions in eosinophilic esophagitis (EoE).
Abstracts and other relevant material from conferences including Digestive Disease Week, the American College of Gastroenterology meeting, and European Gastroenterology Week were also included.
Overall, 33 studies were included, 23 of which were full articles with the remainder being abstracts; there were a total of 1,128 children and 189 adults included in the analysis.
Of the 13 studies that assessed the efficacy of exclusive feeding with an amino acid–based elemental diet (involving 411 children and 18 adults), 90.8% of patients achieved histologic remission of EoE, defined as fewer than 15 eosinophils per high-power field on esophageal biopsy (95% confidence interval, 84.7%-95.5%).
The next best diet, the Six Food Elimination Diet (SFED), offered a 72.1% efficacy rate (95% CI, 65.8%-78.1%) across 75 children and 122 adults and was "the only one assessed in more adults than children."
On the other hand, the strategy of eliminating foods that gave a positive result in skin allergy tests was assessed in 14 studies (594 children and 32 adults), and demonstrated an overall efficacy of just 45.5% (95% CI, 35.4%-55.7%).
Other less-studied diets included gluten-free and cow’s milk elimination diets, both of which seemed to result in histologic remission (58.7% and 68.2%, respectively).
However, "because studies assessing these dietary treatments are still scarce, making conclusions from them can be risky," wrote the authors.
"For example, although the overall efficacy of a gluten-free diet in achieving histologic remission of EoE was 58.7%, the remission rate ranged from 23.1% to 85.6%," they reported.
"Despite its obvious success, the multiple drawbacks of elemental diets, which include the need to avoid all table food, its unpleasant taste, and high cost, and the psychological effects produced by the social limitations that this diet entails, have probably contributed to the fact that this dietary intervention has been restricted almost exclusively to pediatric patients," commented Dr. Arias.
"In fact, no research on adults was available until 2013, with the reported remission rates being comparable with those documented in children."
On the other hand, the relatively high efficacy of the SFED diet, which avoids many of the disadvantages of the elemental diet, seems to make this the best choice for "children and motivated adult patients," added the researchers.
Future studies and meta-analyses should address whether diet adherence results in changes in esophageal fibrosis as well as quality of life issues brought on by diet adherence.
The authors disclosed no relevant financial conflicts.
An elemental diet was more than 90% effective in inducing histologic remission in eosinophilic esophagitis patients, reported Dr. Ángel Arias and colleagues in the June issue of Gastroenterology.
The Six Food Elimination Diet was also highly efficacious, reinforcing the idea that dietary modification "should be considered as a first-line therapy in both children and adults affected by this disease," wrote the investigators (doi:10.1053/j.gastro.2014.02.006).
Dr. Arias of the Complejo Hospitalario La Mancha Centro, in Alcázar de San Juan, Spain, searched the MEDLINE, EMBASE, and SCOPUS databases for studies performed prior to June 2013 investigating the efficacy of dietary interventions in eosinophilic esophagitis (EoE).
Abstracts and other relevant material from conferences including Digestive Disease Week, the American College of Gastroenterology meeting, and European Gastroenterology Week were also included.
Overall, 33 studies were included, 23 of which were full articles with the remainder being abstracts; there were a total of 1,128 children and 189 adults included in the analysis.
Of the 13 studies that assessed the efficacy of exclusive feeding with an amino acid–based elemental diet (involving 411 children and 18 adults), 90.8% of patients achieved histologic remission of EoE, defined as fewer than 15 eosinophils per high-power field on esophageal biopsy (95% confidence interval, 84.7%-95.5%).
The next best diet, the Six Food Elimination Diet (SFED), offered a 72.1% efficacy rate (95% CI, 65.8%-78.1%) across 75 children and 122 adults and was "the only one assessed in more adults than children."
On the other hand, the strategy of eliminating foods that gave a positive result in skin allergy tests was assessed in 14 studies (594 children and 32 adults), and demonstrated an overall efficacy of just 45.5% (95% CI, 35.4%-55.7%).
Other less-studied diets included gluten-free and cow’s milk elimination diets, both of which seemed to result in histologic remission (58.7% and 68.2%, respectively).
However, "because studies assessing these dietary treatments are still scarce, making conclusions from them can be risky," wrote the authors.
"For example, although the overall efficacy of a gluten-free diet in achieving histologic remission of EoE was 58.7%, the remission rate ranged from 23.1% to 85.6%," they reported.
"Despite its obvious success, the multiple drawbacks of elemental diets, which include the need to avoid all table food, its unpleasant taste, and high cost, and the psychological effects produced by the social limitations that this diet entails, have probably contributed to the fact that this dietary intervention has been restricted almost exclusively to pediatric patients," commented Dr. Arias.
"In fact, no research on adults was available until 2013, with the reported remission rates being comparable with those documented in children."
On the other hand, the relatively high efficacy of the SFED diet, which avoids many of the disadvantages of the elemental diet, seems to make this the best choice for "children and motivated adult patients," added the researchers.
Future studies and meta-analyses should address whether diet adherence results in changes in esophageal fibrosis as well as quality of life issues brought on by diet adherence.
The authors disclosed no relevant financial conflicts.
FROM GASTROENTEROLOGY
Major finding: Elemental diets effectively induced histologic remission in 90.8% of eosinophilic esophagitis patients.
Data source: A meta-analysis comprising 33 studies and 1,317 patients with EoE.
Disclosures: The authors disclosed no conflicts of interest related to this study.
Prescribing for the pregnant patient
Primum non nocere: First, do no harm—a principle taught across the world to all medical students. It reminds the health care provider to consider the possible harm that any intervention might produce. Never is it more relevant in the mind of a clinician than when prescribing a medication for a pregnant woman. We are, after all, brought up in a society averse to medical risk.
When managing a pregnant patient, should the baby be the highest priority, whatever the mother may face? Or to take the extreme opposite position, should the mother be treated with the best possible options and the baby ignored?
And what about the views of the patient? There is a widespread cultural belief about the vulnerability of the mother and fetus during pregnancy. Therefore, when faced with the decision of whether to use a medication or not, what is the best recourse for the pregnant patient? Should she be the “good mother” and avoid all risk to the baby, or should she be the “responsible mother” who follows medical advice and takes treatment as recommended?
In truth, the path to safe management of a pregnant patient is rarely so dichotomous. In most cases, what is best for the mother is also best for the baby. However, caring for a pregnant or lactating woman can be challenging for clinicians facing insufficient information regarding medication safety, overestimation of the risk of medication by both the patient and the care provider, and increasing litigation costs.
This article provides key principles to guide clinicians caring for pregnant patients, as we find ourselves increasingly dependent on pharmacotherapy. It also includes sources of information clinicians can turn to when they need additional pregnancy safety data about a certain drug and when they want advice about conditions commonly seen in pregnancy and medications that can be justifiably used in those circumstances.
KEY CONCEPTS FOR PRESCRIBING IN PREGNANCY
The following concepts are key to prescribing for a pregnant patient:
No protective barrier exists between the maternal and fetal environments
The placenta contains a semipermeable membrane that selectively allows some substances to pass from the maternal to the fetal blood and excludes others. However, it is not really a “protective mechanism” when it comes to medications. Assume that the fetus will have exposure, at least to some degree.
In general, drugs that are lipophilic, of a low molecular weight, or not ionized at physiologic pH cross the placenta more efficiently than others. Heparin and insulin are notable exceptions to the rule that most drugs cross the placenta. They do not.
The gestational stage may determine the effect of a medication on the fetus
In animals and in humans, exposure of the embryo or fetus to a teratogen may produce a permanent abnormality of structure or function.
First-trimester exposures are most worrisome for structural malformations. However, fetal neurologic and behavioral development, fetal survival, and function of specific organs can be affected even after the first trimester. For example, while first-trimester exposure to angiotensin-converting enzyme inhibitors has been linked to a slight increase in congenital heart defects, exposure in the second or third trimester can result in fetal oligohydramnios, neonatal anuria, pulmonary hypoplasia, intrauterine growth restriction, and fetal death.
Physiologic changes of pregnancy affect the pharmacokinetics of medications
Pregnancy is associated with increased plasma volume, increased glomerular filtration rate, and dilutional hypoalbuminemia, which can all affect the bioavailability of medications. Absorption of oral agents also may be affected by slowed gastric motility in pregnancy.
Although these physiologic alterations do not routinely warrant a change in drug dosage, they may be important considerations when choosing an appropriate agent. For example, medications taken in multiple doses per day are more likely to have a sustained effect than once-daily medications, which would be rapidly cleared in a pregnant patient.
Sole reliance on the FDA pregnancy safety category may be inadequate
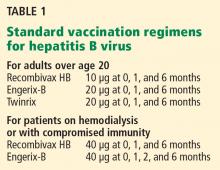
To help clinicians prescribe medications for pregnant women, the US Food and Drug Administration (FDA) assigns medications to one of five categories of risk (A, B, C, D, or X) (Table 1). Unfortunately, this classification system has several shortcomings:
- The categories are often seen as a grading system in which the risk increases from the lowest in category A to highest in category X, and the safety information in the accompanying narrative is not always appreciated by prescribers.
- Clinicians incorrectly assume that drugs in a particular category carry a similar risk. However, 65% to 70% of all medications are in category C. This category includes medications with adverse animal data or no animal data at all. In addition, adverse animal data may vary in severity from decreased fetal weight to major structural malformation and fetal loss, indicating a difference in expected risk.
- Most of the data on medication safety in pregnancy comes from animal studies, case reports, case series, case-control studies, or pregnancy registries, and each of these sources has significant limitations.
- The categories do not distinguish between supporting data from animal studies and human studies. For instance, a category-B drug may have animal studies that show no risk but no adequate human studies, or may have animal studies showing risk but human studies that do not.
Looking at the pregnancy risk classifications used in the United States (ie, the FDA system), Australia, and Sweden, researchers compared the classification of 236 drugs between the three systems and found that only one in four drugs was similarly classified into the same risk category. This discrepancy further brings into question the usefulness and reliability of these classifications.1
Finally, none of the classification systems tells us the potential harm from withholding a medication in pregnancy.
RESOURCES TO ASSESS MEDICATION SAFETY IN PREGNANCY
The FDA has proposed changes in the labeling of medications related to pregnancy and lactation.2 The proposed changes would eliminate the current categories and instead require a summary of the risks, the effects of the drug on the fetus, and clinical considerations for use during pregnancy. In addition, labeling would include a description of the medication’s effects on milk production, the amount of drug present in milk, and possible effects on the infant.
Until such changes are in place, what other resources can a busy clinician turn to for support?
The official drug labeling (or the package insert), also published in the Physicians’ Desk Reference, is one source of information, but it rarely provides up-to-date information about teratogenic risks in human pregnancies.
Several online databases review, summarize, and periodically update information from the peer-reviewed medical literature.3–7 The REPRORISK system4–7 maintained by Micromedex (Greenwood Village, CO) provides access to several databases that contain information about a wide range of individual medications: REPROTEXT, REPROTOX,5 Shepard’s Catalog of Teratogenic Agents,7 and the Teratogen Information System (TERIS).4 Online access and a smartphone “app” for these databases are available for a subscription fee. Summaries for individual medications can be ordered directly from TERIS, also for a fee. Several other resources are available in textbook format.8–10
In addition, health care providers can obtain information from or can refer pregnant and breastfeeding patients to a teratology information service for information and counseling about medication exposures. MotherToBaby,11 a service of the nonprofit Organization of Teratology Information Specialists, provides fact sheets, free phone consultation, risk assessment, and counseling by trained teratogen information specialists about environmental exposures, including prescription and over-the-counter medications and dietary and herbal supplements. Counselors from these services gather and synthesize information about exposures from the databases mentioned above, from the peer-reviewed medical literature, from drug manufacturers, and from other sources.
With the advent of electronic medical records and computerized provider order entry, clinical decision support systems hold promise as an additional resource for safe prescribing in pregnancy.
Fortunately, the list of teratogenic medications that are absolutely contraindicated in pregnancy remains small (Table 2).12,13
THE FOUR-QUESTION APPROACH TO CARING FOR THE PREGNANT PATIENT
Is the symptom self-limited or amenable to nonpharmacologic management?
It has been said that we live in a culture where every symptom warrants a pill. If this is true, there can be no better time for reevaluating this practice than during pregnancy.
Many of the medications most commonly used in pregnancy are for upper-respiratory-tract infections, headache, or psychological distress. Pregnancy is the ideal time to educate patients about the limited effectiveness of most cough-and-cold remedies and the inappropriateness of antibiotics for colds and viral bronchitis. It is also an ideal time for a trial of lifestyle modifications, relaxation, and biofeedback for a chronic headache problem. For cases of mild to moderate depression, it may be worth considering treatment with psychotherapy rather than medications.
Offering patients the option of no treatment or nonpharmacologic treatment for self-limited symptoms is an option worth considering.
How do the patient’s (and your) values and understanding affect the decision?
Is the patient willing to take medication? What are her beliefs with regard to her problem and how it should be managed in pregnancy?
Women and clinicians bring many worries and prejudices to the use of medications in pregnancy. The experiences of the patient and her family and friends may present huge obstacles to needed medication use in pregnancy. Misinformation in the media and from family members, friends, and other health care providers are other obstacles. The only way to deal with this issue is to ask your patient directly about her fears and concerns regarding each prescription written.
Clinicians also need to address fears or prejudices they themselves may have about medication safety in pregnancy. These may arise from a single bad experience in caring for a pregnant woman, discomfort with uncertainty, or a belief that pregnant women should avoid any and all risks of exposures, even when the mother’s condition warrants pharmacologic treatment.
Being informed, both scientifically and about one’s own biases or tendencies, is an essential foundation for rational prescribing in pregnancy.
Is the problem affected by pregnancy, and how?
Pregnancy can affect many medical conditions, and in different ways. Conditions such as asthma, migraine headache, and cardiac arrhythmia are exacerbated in pregnancy, placing the mother and fetus at increased risk of morbidity. Conditions such as Graves disease and hypertension may improve as pregnancy progresses, and medications often can be withdrawn as the patient progresses further along in gestation.
Understanding the effect of pregnancy on a particular problem may help the clinician to make an informed decision about medication use in pregnancy.
How does the problem affect pregnancy?
Considering the risk of untreated disease to the pregnancy may help in decision-making.
Many medical conditions can negatively affect the development of the fetus. A glaring example is diabetes mellitus, with poor glycemic control being linked to congenital malformations, spontaneous abortion, and fetal demise. Chronic conditions with periodic exacerbations such as asthma or epilepsy place the fetus at increased risk during a flare-up.
Therefore, for chronic conditions, continuing maintenance therapy is best. Preconception counseling in such cases is crucial, so that a drug with adequate safety data can be substituted before pregnancy. In this way, any risk to the mother or the embryo from exacerbation of disease as such adjustments are made is avoided.
For conditions arising de novo in pregnancy, the underlying principle remains the same. Is the risk of pharmacotherapy more than the risk of untreated disease? Invariably, the answer to this question supports medication use, and an educated provider will be able to choose a treatment that is justifiable in most circumstances.
CHOOSING A MEDICATION
Fetal well-being depends on maternal well-being. It therefore helps to think of medication use in pregnancy as “justified or not” rather than “safe or not.” Table 3 lists some conditions commonly seen in pregnancy, selected drugs of choice that can be safely used for treating those conditions, and alternates that may be justified in some circumstances.5,6,14–18
GOOD PRACTICES WHEN PRESCRIBING IN PREGNANCY
Prescribing in pregnancy will be most successful when both the patient and the prescribing physician consider the fetal benefit gained from optimizing maternal health. Good prescribing practices to ensure optimum therapeutic benefit when caring for a pregnant patient are to:
- Involve the patient in decision-making. Recognize her concerns, worries, and preferences regarding her illness and its treatment.
- Inform the patient of the risk of an untreated medical condition, weighed against the risk of medication.
- Choose medications with the most available safety data. Let the patient know what resources you have referred to in choosing the medication.
- It is advisable to perform a search each time a prescription is written for a pregnant or lactating woman.
- When possible, have the discussion in the preconception period.
- Consider the dynamic physiology of gestation. Choose the right drug for the right trimester.
- Discuss the plan with the patient and other providers.
- Define clear criteria for when to discontinue the treatment.
- Addis A, Sharabi S, Bonati M. Risk classification systems for drug use during pregnancy: are they a reliable source of information? Drug Saf 2000; 23:245–253.
- US Food and Drug Administration (FDA). Pregnancy and lactation labeling. http://www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/Labeling/ucm093307.htm. Accessed April 4, 2014.
- Lagoy CT, Joshi N, Cragan JD, Rasmussen SA. Medication use during pregnancy and lactation: an urgent call for public health action. J Womens Health (Larchmt) 2005; 14:104–109.
- Clinical Teratology Website. University of Washington. http://depts.washington.edu/terisweb/teris/. Accessed April 4, 2014.
- REPROTOX, An Online Reproductive Toxicology Resource. Reproductive Toxicology Center. www.reprotox.org. Accessed April 4, 2014.
- REPRORISK. Micromedex, Inc. www.micromedex.com/products/reprorisk. Accessed April 4, 2014.
- Shepard TH. Catalog of teratogenic agents. 13th ed. Baltimore, MD: Johns Hopkins University Press; 2010.
- Briggs GG, Freeman RK, Yaffe SJ. Drugs in pregnancy and lactation: A reference guide to fetal and neonatal risk. Philadelphia, PA: Lippincott Williams & Wilkins; 2011.
- Koren G. Medication safety in pregnancy and breastfeeding. McGraw-Hill Professional Publishing; 2007.
- Friedman JM, Polifka JE. Teratogenic effects of drugs: A resource for clinicians (TERIS). Baltimore, MD: Johns Hopkins University Press; 2000.
- MotherToBaby. www.mothertobaby.org. Accessed April 4, 2014.
- Dunlop AL, Gardiner PM, Shellhaas CS, Menard MK, McDiarmid MA. The clinical content of preconception care: the use of medications and supplements among women of reproductive age. Am J Obstet Gynecol 2008; 199(suppl 2):S367–S372.
- Ciarkowski SL, Stalburg CM. Medication safety in obstetrics and gynecology. Clin Obstet Gynecol 2010; 53:482–499.
- Koren G, Pastuszak A, Ito S. Drugs in pregnancy. N Engl J Med 1998; 338:1128–1137.
- Lambert K, Holt RI. The use of insulin analogues in pregnancy. Diabetes Obes Metab 2013; 15:888–900.
- Chan WS, Anand S, Ginsberg JS. Anticoagulation of pregnant women with mechanical heart valves: a systematic review of the literature. Arch Intern Med 2000; 160:191–196.
- Nagler M, Haslauer M, Wuillemin WA. Fondaparinux—data on efficacy and safety in special situations. Thromb Res 2012; 129:407–417.
- Kweder SL, Powrie RO. Prescribing in pregnancy: a practical approach. In:Powrie RO, Greene M, Camann W, editors. De Swiet’s Medical disorders in Obstetric Practice. 5th ed. Hoboken, NJ: Wiley-Blackwell; 2010:633–640.
Primum non nocere: First, do no harm—a principle taught across the world to all medical students. It reminds the health care provider to consider the possible harm that any intervention might produce. Never is it more relevant in the mind of a clinician than when prescribing a medication for a pregnant woman. We are, after all, brought up in a society averse to medical risk.
When managing a pregnant patient, should the baby be the highest priority, whatever the mother may face? Or to take the extreme opposite position, should the mother be treated with the best possible options and the baby ignored?
And what about the views of the patient? There is a widespread cultural belief about the vulnerability of the mother and fetus during pregnancy. Therefore, when faced with the decision of whether to use a medication or not, what is the best recourse for the pregnant patient? Should she be the “good mother” and avoid all risk to the baby, or should she be the “responsible mother” who follows medical advice and takes treatment as recommended?
In truth, the path to safe management of a pregnant patient is rarely so dichotomous. In most cases, what is best for the mother is also best for the baby. However, caring for a pregnant or lactating woman can be challenging for clinicians facing insufficient information regarding medication safety, overestimation of the risk of medication by both the patient and the care provider, and increasing litigation costs.
This article provides key principles to guide clinicians caring for pregnant patients, as we find ourselves increasingly dependent on pharmacotherapy. It also includes sources of information clinicians can turn to when they need additional pregnancy safety data about a certain drug and when they want advice about conditions commonly seen in pregnancy and medications that can be justifiably used in those circumstances.
KEY CONCEPTS FOR PRESCRIBING IN PREGNANCY
The following concepts are key to prescribing for a pregnant patient:
No protective barrier exists between the maternal and fetal environments
The placenta contains a semipermeable membrane that selectively allows some substances to pass from the maternal to the fetal blood and excludes others. However, it is not really a “protective mechanism” when it comes to medications. Assume that the fetus will have exposure, at least to some degree.
In general, drugs that are lipophilic, of a low molecular weight, or not ionized at physiologic pH cross the placenta more efficiently than others. Heparin and insulin are notable exceptions to the rule that most drugs cross the placenta. They do not.
The gestational stage may determine the effect of a medication on the fetus
In animals and in humans, exposure of the embryo or fetus to a teratogen may produce a permanent abnormality of structure or function.
First-trimester exposures are most worrisome for structural malformations. However, fetal neurologic and behavioral development, fetal survival, and function of specific organs can be affected even after the first trimester. For example, while first-trimester exposure to angiotensin-converting enzyme inhibitors has been linked to a slight increase in congenital heart defects, exposure in the second or third trimester can result in fetal oligohydramnios, neonatal anuria, pulmonary hypoplasia, intrauterine growth restriction, and fetal death.
Physiologic changes of pregnancy affect the pharmacokinetics of medications
Pregnancy is associated with increased plasma volume, increased glomerular filtration rate, and dilutional hypoalbuminemia, which can all affect the bioavailability of medications. Absorption of oral agents also may be affected by slowed gastric motility in pregnancy.
Although these physiologic alterations do not routinely warrant a change in drug dosage, they may be important considerations when choosing an appropriate agent. For example, medications taken in multiple doses per day are more likely to have a sustained effect than once-daily medications, which would be rapidly cleared in a pregnant patient.
Sole reliance on the FDA pregnancy safety category may be inadequate
To help clinicians prescribe medications for pregnant women, the US Food and Drug Administration (FDA) assigns medications to one of five categories of risk (A, B, C, D, or X) (Table 1). Unfortunately, this classification system has several shortcomings:
- The categories are often seen as a grading system in which the risk increases from the lowest in category A to highest in category X, and the safety information in the accompanying narrative is not always appreciated by prescribers.
- Clinicians incorrectly assume that drugs in a particular category carry a similar risk. However, 65% to 70% of all medications are in category C. This category includes medications with adverse animal data or no animal data at all. In addition, adverse animal data may vary in severity from decreased fetal weight to major structural malformation and fetal loss, indicating a difference in expected risk.
- Most of the data on medication safety in pregnancy comes from animal studies, case reports, case series, case-control studies, or pregnancy registries, and each of these sources has significant limitations.
- The categories do not distinguish between supporting data from animal studies and human studies. For instance, a category-B drug may have animal studies that show no risk but no adequate human studies, or may have animal studies showing risk but human studies that do not.
Looking at the pregnancy risk classifications used in the United States (ie, the FDA system), Australia, and Sweden, researchers compared the classification of 236 drugs between the three systems and found that only one in four drugs was similarly classified into the same risk category. This discrepancy further brings into question the usefulness and reliability of these classifications.1
Finally, none of the classification systems tells us the potential harm from withholding a medication in pregnancy.
RESOURCES TO ASSESS MEDICATION SAFETY IN PREGNANCY
The FDA has proposed changes in the labeling of medications related to pregnancy and lactation.2 The proposed changes would eliminate the current categories and instead require a summary of the risks, the effects of the drug on the fetus, and clinical considerations for use during pregnancy. In addition, labeling would include a description of the medication’s effects on milk production, the amount of drug present in milk, and possible effects on the infant.
Until such changes are in place, what other resources can a busy clinician turn to for support?
The official drug labeling (or the package insert), also published in the Physicians’ Desk Reference, is one source of information, but it rarely provides up-to-date information about teratogenic risks in human pregnancies.
Several online databases review, summarize, and periodically update information from the peer-reviewed medical literature.3–7 The REPRORISK system4–7 maintained by Micromedex (Greenwood Village, CO) provides access to several databases that contain information about a wide range of individual medications: REPROTEXT, REPROTOX,5 Shepard’s Catalog of Teratogenic Agents,7 and the Teratogen Information System (TERIS).4 Online access and a smartphone “app” for these databases are available for a subscription fee. Summaries for individual medications can be ordered directly from TERIS, also for a fee. Several other resources are available in textbook format.8–10
In addition, health care providers can obtain information from or can refer pregnant and breastfeeding patients to a teratology information service for information and counseling about medication exposures. MotherToBaby,11 a service of the nonprofit Organization of Teratology Information Specialists, provides fact sheets, free phone consultation, risk assessment, and counseling by trained teratogen information specialists about environmental exposures, including prescription and over-the-counter medications and dietary and herbal supplements. Counselors from these services gather and synthesize information about exposures from the databases mentioned above, from the peer-reviewed medical literature, from drug manufacturers, and from other sources.
With the advent of electronic medical records and computerized provider order entry, clinical decision support systems hold promise as an additional resource for safe prescribing in pregnancy.
Fortunately, the list of teratogenic medications that are absolutely contraindicated in pregnancy remains small (Table 2).12,13
THE FOUR-QUESTION APPROACH TO CARING FOR THE PREGNANT PATIENT
Is the symptom self-limited or amenable to nonpharmacologic management?
It has been said that we live in a culture where every symptom warrants a pill. If this is true, there can be no better time for reevaluating this practice than during pregnancy.
Many of the medications most commonly used in pregnancy are for upper-respiratory-tract infections, headache, or psychological distress. Pregnancy is the ideal time to educate patients about the limited effectiveness of most cough-and-cold remedies and the inappropriateness of antibiotics for colds and viral bronchitis. It is also an ideal time for a trial of lifestyle modifications, relaxation, and biofeedback for a chronic headache problem. For cases of mild to moderate depression, it may be worth considering treatment with psychotherapy rather than medications.
Offering patients the option of no treatment or nonpharmacologic treatment for self-limited symptoms is an option worth considering.
How do the patient’s (and your) values and understanding affect the decision?
Is the patient willing to take medication? What are her beliefs with regard to her problem and how it should be managed in pregnancy?
Women and clinicians bring many worries and prejudices to the use of medications in pregnancy. The experiences of the patient and her family and friends may present huge obstacles to needed medication use in pregnancy. Misinformation in the media and from family members, friends, and other health care providers are other obstacles. The only way to deal with this issue is to ask your patient directly about her fears and concerns regarding each prescription written.
Clinicians also need to address fears or prejudices they themselves may have about medication safety in pregnancy. These may arise from a single bad experience in caring for a pregnant woman, discomfort with uncertainty, or a belief that pregnant women should avoid any and all risks of exposures, even when the mother’s condition warrants pharmacologic treatment.
Being informed, both scientifically and about one’s own biases or tendencies, is an essential foundation for rational prescribing in pregnancy.
Is the problem affected by pregnancy, and how?
Pregnancy can affect many medical conditions, and in different ways. Conditions such as asthma, migraine headache, and cardiac arrhythmia are exacerbated in pregnancy, placing the mother and fetus at increased risk of morbidity. Conditions such as Graves disease and hypertension may improve as pregnancy progresses, and medications often can be withdrawn as the patient progresses further along in gestation.
Understanding the effect of pregnancy on a particular problem may help the clinician to make an informed decision about medication use in pregnancy.
How does the problem affect pregnancy?
Considering the risk of untreated disease to the pregnancy may help in decision-making.
Many medical conditions can negatively affect the development of the fetus. A glaring example is diabetes mellitus, with poor glycemic control being linked to congenital malformations, spontaneous abortion, and fetal demise. Chronic conditions with periodic exacerbations such as asthma or epilepsy place the fetus at increased risk during a flare-up.
Therefore, for chronic conditions, continuing maintenance therapy is best. Preconception counseling in such cases is crucial, so that a drug with adequate safety data can be substituted before pregnancy. In this way, any risk to the mother or the embryo from exacerbation of disease as such adjustments are made is avoided.
For conditions arising de novo in pregnancy, the underlying principle remains the same. Is the risk of pharmacotherapy more than the risk of untreated disease? Invariably, the answer to this question supports medication use, and an educated provider will be able to choose a treatment that is justifiable in most circumstances.
CHOOSING A MEDICATION
Fetal well-being depends on maternal well-being. It therefore helps to think of medication use in pregnancy as “justified or not” rather than “safe or not.” Table 3 lists some conditions commonly seen in pregnancy, selected drugs of choice that can be safely used for treating those conditions, and alternates that may be justified in some circumstances.5,6,14–18
GOOD PRACTICES WHEN PRESCRIBING IN PREGNANCY
Prescribing in pregnancy will be most successful when both the patient and the prescribing physician consider the fetal benefit gained from optimizing maternal health. Good prescribing practices to ensure optimum therapeutic benefit when caring for a pregnant patient are to:
- Involve the patient in decision-making. Recognize her concerns, worries, and preferences regarding her illness and its treatment.
- Inform the patient of the risk of an untreated medical condition, weighed against the risk of medication.
- Choose medications with the most available safety data. Let the patient know what resources you have referred to in choosing the medication.
- It is advisable to perform a search each time a prescription is written for a pregnant or lactating woman.
- When possible, have the discussion in the preconception period.
- Consider the dynamic physiology of gestation. Choose the right drug for the right trimester.
- Discuss the plan with the patient and other providers.
- Define clear criteria for when to discontinue the treatment.
Primum non nocere: First, do no harm—a principle taught across the world to all medical students. It reminds the health care provider to consider the possible harm that any intervention might produce. Never is it more relevant in the mind of a clinician than when prescribing a medication for a pregnant woman. We are, after all, brought up in a society averse to medical risk.
When managing a pregnant patient, should the baby be the highest priority, whatever the mother may face? Or to take the extreme opposite position, should the mother be treated with the best possible options and the baby ignored?
And what about the views of the patient? There is a widespread cultural belief about the vulnerability of the mother and fetus during pregnancy. Therefore, when faced with the decision of whether to use a medication or not, what is the best recourse for the pregnant patient? Should she be the “good mother” and avoid all risk to the baby, or should she be the “responsible mother” who follows medical advice and takes treatment as recommended?
In truth, the path to safe management of a pregnant patient is rarely so dichotomous. In most cases, what is best for the mother is also best for the baby. However, caring for a pregnant or lactating woman can be challenging for clinicians facing insufficient information regarding medication safety, overestimation of the risk of medication by both the patient and the care provider, and increasing litigation costs.
This article provides key principles to guide clinicians caring for pregnant patients, as we find ourselves increasingly dependent on pharmacotherapy. It also includes sources of information clinicians can turn to when they need additional pregnancy safety data about a certain drug and when they want advice about conditions commonly seen in pregnancy and medications that can be justifiably used in those circumstances.
KEY CONCEPTS FOR PRESCRIBING IN PREGNANCY
The following concepts are key to prescribing for a pregnant patient:
No protective barrier exists between the maternal and fetal environments
The placenta contains a semipermeable membrane that selectively allows some substances to pass from the maternal to the fetal blood and excludes others. However, it is not really a “protective mechanism” when it comes to medications. Assume that the fetus will have exposure, at least to some degree.
In general, drugs that are lipophilic, of a low molecular weight, or not ionized at physiologic pH cross the placenta more efficiently than others. Heparin and insulin are notable exceptions to the rule that most drugs cross the placenta. They do not.
The gestational stage may determine the effect of a medication on the fetus
In animals and in humans, exposure of the embryo or fetus to a teratogen may produce a permanent abnormality of structure or function.
First-trimester exposures are most worrisome for structural malformations. However, fetal neurologic and behavioral development, fetal survival, and function of specific organs can be affected even after the first trimester. For example, while first-trimester exposure to angiotensin-converting enzyme inhibitors has been linked to a slight increase in congenital heart defects, exposure in the second or third trimester can result in fetal oligohydramnios, neonatal anuria, pulmonary hypoplasia, intrauterine growth restriction, and fetal death.
Physiologic changes of pregnancy affect the pharmacokinetics of medications
Pregnancy is associated with increased plasma volume, increased glomerular filtration rate, and dilutional hypoalbuminemia, which can all affect the bioavailability of medications. Absorption of oral agents also may be affected by slowed gastric motility in pregnancy.
Although these physiologic alterations do not routinely warrant a change in drug dosage, they may be important considerations when choosing an appropriate agent. For example, medications taken in multiple doses per day are more likely to have a sustained effect than once-daily medications, which would be rapidly cleared in a pregnant patient.
Sole reliance on the FDA pregnancy safety category may be inadequate
To help clinicians prescribe medications for pregnant women, the US Food and Drug Administration (FDA) assigns medications to one of five categories of risk (A, B, C, D, or X) (Table 1). Unfortunately, this classification system has several shortcomings:
- The categories are often seen as a grading system in which the risk increases from the lowest in category A to highest in category X, and the safety information in the accompanying narrative is not always appreciated by prescribers.
- Clinicians incorrectly assume that drugs in a particular category carry a similar risk. However, 65% to 70% of all medications are in category C. This category includes medications with adverse animal data or no animal data at all. In addition, adverse animal data may vary in severity from decreased fetal weight to major structural malformation and fetal loss, indicating a difference in expected risk.
- Most of the data on medication safety in pregnancy comes from animal studies, case reports, case series, case-control studies, or pregnancy registries, and each of these sources has significant limitations.
- The categories do not distinguish between supporting data from animal studies and human studies. For instance, a category-B drug may have animal studies that show no risk but no adequate human studies, or may have animal studies showing risk but human studies that do not.
Looking at the pregnancy risk classifications used in the United States (ie, the FDA system), Australia, and Sweden, researchers compared the classification of 236 drugs between the three systems and found that only one in four drugs was similarly classified into the same risk category. This discrepancy further brings into question the usefulness and reliability of these classifications.1
Finally, none of the classification systems tells us the potential harm from withholding a medication in pregnancy.
RESOURCES TO ASSESS MEDICATION SAFETY IN PREGNANCY
The FDA has proposed changes in the labeling of medications related to pregnancy and lactation.2 The proposed changes would eliminate the current categories and instead require a summary of the risks, the effects of the drug on the fetus, and clinical considerations for use during pregnancy. In addition, labeling would include a description of the medication’s effects on milk production, the amount of drug present in milk, and possible effects on the infant.
Until such changes are in place, what other resources can a busy clinician turn to for support?
The official drug labeling (or the package insert), also published in the Physicians’ Desk Reference, is one source of information, but it rarely provides up-to-date information about teratogenic risks in human pregnancies.
Several online databases review, summarize, and periodically update information from the peer-reviewed medical literature.3–7 The REPRORISK system4–7 maintained by Micromedex (Greenwood Village, CO) provides access to several databases that contain information about a wide range of individual medications: REPROTEXT, REPROTOX,5 Shepard’s Catalog of Teratogenic Agents,7 and the Teratogen Information System (TERIS).4 Online access and a smartphone “app” for these databases are available for a subscription fee. Summaries for individual medications can be ordered directly from TERIS, also for a fee. Several other resources are available in textbook format.8–10
In addition, health care providers can obtain information from or can refer pregnant and breastfeeding patients to a teratology information service for information and counseling about medication exposures. MotherToBaby,11 a service of the nonprofit Organization of Teratology Information Specialists, provides fact sheets, free phone consultation, risk assessment, and counseling by trained teratogen information specialists about environmental exposures, including prescription and over-the-counter medications and dietary and herbal supplements. Counselors from these services gather and synthesize information about exposures from the databases mentioned above, from the peer-reviewed medical literature, from drug manufacturers, and from other sources.
With the advent of electronic medical records and computerized provider order entry, clinical decision support systems hold promise as an additional resource for safe prescribing in pregnancy.
Fortunately, the list of teratogenic medications that are absolutely contraindicated in pregnancy remains small (Table 2).12,13
THE FOUR-QUESTION APPROACH TO CARING FOR THE PREGNANT PATIENT
Is the symptom self-limited or amenable to nonpharmacologic management?
It has been said that we live in a culture where every symptom warrants a pill. If this is true, there can be no better time for reevaluating this practice than during pregnancy.
Many of the medications most commonly used in pregnancy are for upper-respiratory-tract infections, headache, or psychological distress. Pregnancy is the ideal time to educate patients about the limited effectiveness of most cough-and-cold remedies and the inappropriateness of antibiotics for colds and viral bronchitis. It is also an ideal time for a trial of lifestyle modifications, relaxation, and biofeedback for a chronic headache problem. For cases of mild to moderate depression, it may be worth considering treatment with psychotherapy rather than medications.
Offering patients the option of no treatment or nonpharmacologic treatment for self-limited symptoms is an option worth considering.
How do the patient’s (and your) values and understanding affect the decision?
Is the patient willing to take medication? What are her beliefs with regard to her problem and how it should be managed in pregnancy?
Women and clinicians bring many worries and prejudices to the use of medications in pregnancy. The experiences of the patient and her family and friends may present huge obstacles to needed medication use in pregnancy. Misinformation in the media and from family members, friends, and other health care providers are other obstacles. The only way to deal with this issue is to ask your patient directly about her fears and concerns regarding each prescription written.
Clinicians also need to address fears or prejudices they themselves may have about medication safety in pregnancy. These may arise from a single bad experience in caring for a pregnant woman, discomfort with uncertainty, or a belief that pregnant women should avoid any and all risks of exposures, even when the mother’s condition warrants pharmacologic treatment.
Being informed, both scientifically and about one’s own biases or tendencies, is an essential foundation for rational prescribing in pregnancy.
Is the problem affected by pregnancy, and how?
Pregnancy can affect many medical conditions, and in different ways. Conditions such as asthma, migraine headache, and cardiac arrhythmia are exacerbated in pregnancy, placing the mother and fetus at increased risk of morbidity. Conditions such as Graves disease and hypertension may improve as pregnancy progresses, and medications often can be withdrawn as the patient progresses further along in gestation.
Understanding the effect of pregnancy on a particular problem may help the clinician to make an informed decision about medication use in pregnancy.
How does the problem affect pregnancy?
Considering the risk of untreated disease to the pregnancy may help in decision-making.
Many medical conditions can negatively affect the development of the fetus. A glaring example is diabetes mellitus, with poor glycemic control being linked to congenital malformations, spontaneous abortion, and fetal demise. Chronic conditions with periodic exacerbations such as asthma or epilepsy place the fetus at increased risk during a flare-up.
Therefore, for chronic conditions, continuing maintenance therapy is best. Preconception counseling in such cases is crucial, so that a drug with adequate safety data can be substituted before pregnancy. In this way, any risk to the mother or the embryo from exacerbation of disease as such adjustments are made is avoided.
For conditions arising de novo in pregnancy, the underlying principle remains the same. Is the risk of pharmacotherapy more than the risk of untreated disease? Invariably, the answer to this question supports medication use, and an educated provider will be able to choose a treatment that is justifiable in most circumstances.
CHOOSING A MEDICATION
Fetal well-being depends on maternal well-being. It therefore helps to think of medication use in pregnancy as “justified or not” rather than “safe or not.” Table 3 lists some conditions commonly seen in pregnancy, selected drugs of choice that can be safely used for treating those conditions, and alternates that may be justified in some circumstances.5,6,14–18
GOOD PRACTICES WHEN PRESCRIBING IN PREGNANCY
Prescribing in pregnancy will be most successful when both the patient and the prescribing physician consider the fetal benefit gained from optimizing maternal health. Good prescribing practices to ensure optimum therapeutic benefit when caring for a pregnant patient are to:
- Involve the patient in decision-making. Recognize her concerns, worries, and preferences regarding her illness and its treatment.
- Inform the patient of the risk of an untreated medical condition, weighed against the risk of medication.
- Choose medications with the most available safety data. Let the patient know what resources you have referred to in choosing the medication.
- It is advisable to perform a search each time a prescription is written for a pregnant or lactating woman.
- When possible, have the discussion in the preconception period.
- Consider the dynamic physiology of gestation. Choose the right drug for the right trimester.
- Discuss the plan with the patient and other providers.
- Define clear criteria for when to discontinue the treatment.
- Addis A, Sharabi S, Bonati M. Risk classification systems for drug use during pregnancy: are they a reliable source of information? Drug Saf 2000; 23:245–253.
- US Food and Drug Administration (FDA). Pregnancy and lactation labeling. http://www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/Labeling/ucm093307.htm. Accessed April 4, 2014.
- Lagoy CT, Joshi N, Cragan JD, Rasmussen SA. Medication use during pregnancy and lactation: an urgent call for public health action. J Womens Health (Larchmt) 2005; 14:104–109.
- Clinical Teratology Website. University of Washington. http://depts.washington.edu/terisweb/teris/. Accessed April 4, 2014.
- REPROTOX, An Online Reproductive Toxicology Resource. Reproductive Toxicology Center. www.reprotox.org. Accessed April 4, 2014.
- REPRORISK. Micromedex, Inc. www.micromedex.com/products/reprorisk. Accessed April 4, 2014.
- Shepard TH. Catalog of teratogenic agents. 13th ed. Baltimore, MD: Johns Hopkins University Press; 2010.
- Briggs GG, Freeman RK, Yaffe SJ. Drugs in pregnancy and lactation: A reference guide to fetal and neonatal risk. Philadelphia, PA: Lippincott Williams & Wilkins; 2011.
- Koren G. Medication safety in pregnancy and breastfeeding. McGraw-Hill Professional Publishing; 2007.
- Friedman JM, Polifka JE. Teratogenic effects of drugs: A resource for clinicians (TERIS). Baltimore, MD: Johns Hopkins University Press; 2000.
- MotherToBaby. www.mothertobaby.org. Accessed April 4, 2014.
- Dunlop AL, Gardiner PM, Shellhaas CS, Menard MK, McDiarmid MA. The clinical content of preconception care: the use of medications and supplements among women of reproductive age. Am J Obstet Gynecol 2008; 199(suppl 2):S367–S372.
- Ciarkowski SL, Stalburg CM. Medication safety in obstetrics and gynecology. Clin Obstet Gynecol 2010; 53:482–499.
- Koren G, Pastuszak A, Ito S. Drugs in pregnancy. N Engl J Med 1998; 338:1128–1137.
- Lambert K, Holt RI. The use of insulin analogues in pregnancy. Diabetes Obes Metab 2013; 15:888–900.
- Chan WS, Anand S, Ginsberg JS. Anticoagulation of pregnant women with mechanical heart valves: a systematic review of the literature. Arch Intern Med 2000; 160:191–196.
- Nagler M, Haslauer M, Wuillemin WA. Fondaparinux—data on efficacy and safety in special situations. Thromb Res 2012; 129:407–417.
- Kweder SL, Powrie RO. Prescribing in pregnancy: a practical approach. In:Powrie RO, Greene M, Camann W, editors. De Swiet’s Medical disorders in Obstetric Practice. 5th ed. Hoboken, NJ: Wiley-Blackwell; 2010:633–640.
- Addis A, Sharabi S, Bonati M. Risk classification systems for drug use during pregnancy: are they a reliable source of information? Drug Saf 2000; 23:245–253.
- US Food and Drug Administration (FDA). Pregnancy and lactation labeling. http://www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/Labeling/ucm093307.htm. Accessed April 4, 2014.
- Lagoy CT, Joshi N, Cragan JD, Rasmussen SA. Medication use during pregnancy and lactation: an urgent call for public health action. J Womens Health (Larchmt) 2005; 14:104–109.
- Clinical Teratology Website. University of Washington. http://depts.washington.edu/terisweb/teris/. Accessed April 4, 2014.
- REPROTOX, An Online Reproductive Toxicology Resource. Reproductive Toxicology Center. www.reprotox.org. Accessed April 4, 2014.
- REPRORISK. Micromedex, Inc. www.micromedex.com/products/reprorisk. Accessed April 4, 2014.
- Shepard TH. Catalog of teratogenic agents. 13th ed. Baltimore, MD: Johns Hopkins University Press; 2010.
- Briggs GG, Freeman RK, Yaffe SJ. Drugs in pregnancy and lactation: A reference guide to fetal and neonatal risk. Philadelphia, PA: Lippincott Williams & Wilkins; 2011.
- Koren G. Medication safety in pregnancy and breastfeeding. McGraw-Hill Professional Publishing; 2007.
- Friedman JM, Polifka JE. Teratogenic effects of drugs: A resource for clinicians (TERIS). Baltimore, MD: Johns Hopkins University Press; 2000.
- MotherToBaby. www.mothertobaby.org. Accessed April 4, 2014.
- Dunlop AL, Gardiner PM, Shellhaas CS, Menard MK, McDiarmid MA. The clinical content of preconception care: the use of medications and supplements among women of reproductive age. Am J Obstet Gynecol 2008; 199(suppl 2):S367–S372.
- Ciarkowski SL, Stalburg CM. Medication safety in obstetrics and gynecology. Clin Obstet Gynecol 2010; 53:482–499.
- Koren G, Pastuszak A, Ito S. Drugs in pregnancy. N Engl J Med 1998; 338:1128–1137.
- Lambert K, Holt RI. The use of insulin analogues in pregnancy. Diabetes Obes Metab 2013; 15:888–900.
- Chan WS, Anand S, Ginsberg JS. Anticoagulation of pregnant women with mechanical heart valves: a systematic review of the literature. Arch Intern Med 2000; 160:191–196.
- Nagler M, Haslauer M, Wuillemin WA. Fondaparinux—data on efficacy and safety in special situations. Thromb Res 2012; 129:407–417.
- Kweder SL, Powrie RO. Prescribing in pregnancy: a practical approach. In:Powrie RO, Greene M, Camann W, editors. De Swiet’s Medical disorders in Obstetric Practice. 5th ed. Hoboken, NJ: Wiley-Blackwell; 2010:633–640.
KEY POINTS
- There is no protective physiologic barrier between the maternal and fetal environments.
- The gestational stage may determine the effect of a medication on the fetus.
- The physiologic changes of pregnancy affect the pharmacokinetics of medications.
- Sole reliance on the US Food and Drug Administration’s pregnancy safety category may be inadequate.
- Key questions: Is the problem self-limited or amenable to nonpharmacologic management? How do the patient’s (and provider’s) presumptions affect decisions about this medication in pregnancy? How does pregnancy affect the problem, and how does the problem affect pregnancy?
Role of imaging in endometriosis
A 32-year-old woman presents with a history of pelvic pain, dysmenorrhea, dyspareunia, dyschezia, and dysuria, with exacerbation of the symptoms during her menstrual cycles. Her menarche occurred at the age of 13 and her menses are regular. She has never undergone surgery and has no relevant pathologic processes. She also reports that for the past 18 months she has been unsuccessfully trying to conceive.
Two months ago, she went to the emergency department because of an acute episode of severe pelvic pain associated with abdominal cramps, vomiting, and dyschezia, occurring at the beginning of her menstrual cycle. At that time, her vital signs were within normal limits, but deep palpation of the right iliac fossa was painful. On that occasion, acute abdomen and bowel obstruction were excluded.
Now, vaginal examination reveals a bluish, painful, bulky induration in the posterior fornix. Digital rectal examination reveals a circular infiltrated area in the anterior rectal wall. Her cancer antigen 125 (CA 125) level is 230 U/mL (normal range 0–35 U/mL).
MENSES-RELATED SYMPTOMS AND THE DIAGNOSIS OF ENDOMETRIOSIS
The diagnosis of endometriosis should be considered in the patient described above. Many of her signs and symptoms can be associated with several diseases. However, the diagnostic hypothesis points strongly toward endometriosis, since her symptoms recur at the beginning of every menstrual cycle.1
Endometriosis is the presence of endometrial tissue outside the uterine cavity. The affected organs usually include the ovaries, fallopian tubes,2 peritoneal surface, vagina, cervix, abdominal wall,3 scar tissue, pouch of Douglas, urinary tract, and bowel. However, any organ can be involved.
So-called deeply infiltrating endometriosis is an endometriotic lesion penetrating into the retroperitoneal space (most often affecting the uterosacral ligaments and the rectovaginal septum) or the pelvic-organ wall to a depth of at least 5 mm and involving structures such as the rectum, vagina, ureters, and bladder.4 Its clinical presentation is highly variable, ranging from no symptoms to severe pain and dysfunction of pelvic organs.
Endometriosis can be diagnosed with certainty only when the endometriotic lesions are observed by laparoscopy or laparotomy and after the histologic examination of surgically resected lesions (Figure 1).1 However, a presumptive diagnosis can be made on the basis of imaging findings, which can be useful in the differential diagnostic process (Table 1).
EXAMINATION AND BLOOD MARKERS PROVIDE LIMITED INFORMATION
Knowing the history of the patient, along with a physical examination that includes speculum and bimanual vaginal and rectal examination, can be helpful in the diagnostic process even if nothing abnormal is found.
Pelvic examination has a poor predictive value, as demonstrated in a study conducted by Nezhat et al5 in 91 patients with surgically confirmed endometriosis, 47% of whom had a normal bimanual examination.
CA 125 is the serologic marker most often used for diagnosing endometriosis. Levels are usually high in the sera of patients with endometriosis, especially in the advanced stages.6 However, levels increase both in the physiologic menstrual cycle and in epithelial ovarian cancers.7 Thus, the diagnostic value of CA 125 is limited in terms of both sensitivity and specificity.
INCLUDE IMAGING IN THE DIAGNOSTIC WORKUP
Surgical treatment is frequently offered to patients who have severe pelvic pain that does not respond to medical treatment, or in cases of infertility. Imaging investigations are mandatory both to ascertain the diagnosis and to assess involvement of internal organs before surgery. Moreover, imaging helps minimize the surgical risks.
The primary aim of the radiologic examination is to describe the precise location, the depth, and the number of pelvic endometriotic lesions. Furthermore, imaging is useful to check for endometriotic foci in pelvic organs such as the bowel, ureters, and bladder, which are often involved in the pathologic process.
Transvaginal ultrasonography and magnetic resonance imaging (MRI) can accurately delineate deeply infiltrating lesions of endometriosis that are not easily accessible laparoscopically.
Transvaginal ultrasonography
Transvaginal ultrasonography is the first-line imaging study when endometriosis is suspected: it is powerful, simple, widely available, and cost-effective. In particular, it is recommended for diagnosing endometriotic ovarian cysts (endometriomas)8,9 and endometriosis of the bladder.10 However, its value for the assessment of superficial peritoneal lesions, ovarian foci, and deeply infiltrating endometriosis is questionable.
Although uncomfortable for the patient, transvaginal ultrasonography should be performed during menses, or when the pain reaches its highest level. In fact, during menstrual bleeding the endometrial implants grow and become easier to detect.
Mais et al8 reported that transvaginal ultrasonography has a sensitivity of 88% in differentiating endometriomas from other ovarian masses, and a specificity of 90% (Figure 2). Furthermore, its specificity is as high as that of MRI.8,9
Endometriotic nodules detected in the uterosacral ligaments, rectovaginal septum, vagina, vesicouterine pouch, bladder (Figure 3), and ureters can be signs of deeply infiltrating endometriosis. Pelvic adhesions can be suspected when pelvic organs appear fixed to each other, when hyperechogenic plaques are found between the serosal surfaces of the different organs, and when the pouch of Douglas is partially or completely obliterated.
The accuracy of transvaginal ultrasonography strongly depends on the operator’s skill. Furthermore, lesions of the sigmoid colon are impossible to visualize by transvaginal ultrasonography; hence, further diagnostic procedures are required. Transvaginal ultrasonography is the most accurate technique in detecting endometriotic nodules of the bladder wall in patients with urinary symptoms.
Transvaginal ultrasonography combined with color Doppler can also demonstrate the flow of urine through the ureters to the bladder, thereby ascertaining the patency of the ureters and clarifying the anatomic relationship between the ureters and any endometriotic lesions in the detrusors.10 Hydronephrosis can arise from ureteral restriction caused by endometriotic nodules. Thus, transabdominal ultrasonography of the kidneys is always recommended when deeply infiltrating endometriosis is suspected.
Some centers use a bowel-preparation protocol consisting of a laxative taken 24 hours before the procedure, combined with a low-residue diet and an enema 1 hour before the examination to cleanse the rectosigmoid colon of fecal content and gas, which can interfere with the visual examination of the pelvic structures.11
Transabdominal ultrasonography
Transabdominal ultrasonography can be used instead of transvaginal ultrasonography, eg, in young girls and women who have never been sexually active. When transabdominal ultrasonography is selected, the patient should have a full bladder to maximize the visualization of the pelvic structures. However, transvaginal ultrasonography is generally more sensitive than transabdominal in detecting adnexal masses and pelvic nodules.12
Magnetic resonance imaging
MRI has been recently introduced in the diagnosis of endometriosis. MRI is less operator-dependent than transvaginal ultrasonography and is more sensitive for detecting foci of deeply infiltrating endometriosis, because of its ability to completely survey the anterior and posterior compartments of the pelvis. However, its diagnostic value in cases of bladder endometriosis, superficial peritoneal lesions, and ovarian foci is still controversial.13–16
On MRI, lesions of deeply infiltrating endometriosis mainly appear as areas or nodules with regular, irregular, indistinct, or stellate margins. A distortion of the normal pelvic anatomy or the detection of a loculated fluid collection can indirectly signal the presence of adhesions.
MRI has high specificity for the diagnosis of endometriomas as a result of its ability to detect aged hemorrhagic content (Figure 4).17 Despite the many studies that point to the limits of MRI in detecting small endometriotic lesions, recent studies demonstrated that MRI also has good sensitivity for small peritoneal implants and adhesions.18,19 The injection of gadolinium contrast is still a debatable measure, because contrast-enhanced imaging cannot differentiate infiltrating lesions from other normal fibromuscular pelvic anatomic structures.15,20
Bowel preparation can be done with an oral laxative the day before imaging, complemented by a low-residue diet. A single dose of a ready-to-use enema is given 30 minutes before the examination to cleanse the terminal section of the intestinal tract. To avoid motion artifacts caused by bowel peristalsis, images are obtained after intramuscular injections of a myorelaxant are given, if there is no contraindication. Bowel preparation is useful to eliminate fecal residue and gas, thereby allowing proper visualization of lesions of deeply infiltrating endometriosis, but it is not routinely prescribed in all centers.11
In most cases, endometriotic lesions have an MRI signal intensity that comes very close to that of the surrounding fibromuscular structures. In this regard, vaginal and rectal distention and opacification using ultrasonographic gel clearly help to delineate the cervix, vaginal fornices, and vaginal wall, as well as the rectum and wall of the rectosigmoid junction (Figure 5).20
PRESURGICAL IMAGING
Rectal endoscopic ultrasonography
Even though it should not be included in the routine diagnostic workup, rectal endoscopic ultrasonography, using a flexible echoendoscope, is suitable in certain presurgical cases. The aim of this imaging technique is to assess the depth of bowel wall infiltration thanks to the visualization of the different layers.21
Double-contrast barium enema and multislice computed tomography
Double-contrast barium enema is extensively used for the diagnosis of bowel endometriosis, once the decision to perform surgery has been made. It allows evaluation of the degree and length of the bowel occlusion at the level of the sigmoid or high rectosigmoid tract, but it does not permit differentiation of bowel endometriosis from other pathologies.
Multislice computed tomography offers the opportunity to evaluate the depth of the lesions with excellent precision. 22
The most relevant disadvantage of both procedures is the exposure of women of reproductive age to ionizing radiation. In addition, multislice computed tomography requires the administration of an intravenous iodinated contrast medium and a retrograde colonic distention with about 2 L of water.
- Attaran M, Falcone T, Goldberg J. Endometriosis: still tough to diagnose and treat. Cleve Clin J Med 2002; 69:647–653.
- Wenger JM, Soave I, Lo Monte G, Petignat P, Marci R. Tubal endometrioma within a twisted fallopian tube: a clinically complex diagnosis. J Pediatr Adolesc Gynecol 2013; 26:e1–e4.
- Marci R, Lo Monte G, Soave I, Bianchi A, Patella A, Wenger JM. Rectus abdominis muscle endometriotic mass in a woman affected by multiple sclerosis. J Obstet Gynaecol Res 2013; 39:462–465.
- Vercellini P, Frontino G, Pietropaolo G, Gattei U, Daguati R, Crosignani PG. Deep endometriosis: definition, pathogenesis, and clinical management. J Am Assoc Gynecol Laparosc 2004; 11:153–161.
- Nezhat C, Santolaya J, Nezhat FR. Comparison of transvaginal sonography and bimanual pelvic examination in patients with laparoscopically confirmed endometriosis. J Am Assoc Gynecol Laparosc 1994; 1:127–130.
- Barbieri RL, Niloff JM, Bast RC, Scaetzl E, Kistner RW, Knapp RC. Elevated serum concentrations of CA-125 in patients with advanced endometriosis. Fertil Steril 1986; 45:630–634.
- Bon GG, Kenemans P, Dekker JJ, et al. Fluctuations in CA 125 and CA 15-3 serum concentrations during spontaneous ovulatory cycles. Hum Reprod 1999; 14:566–570.
- Mais V, Guerriero S, Ajossa S, Angiolucci M, Paoletti AM, Melis GB. The efficiency of transvaginal ultrasonography in the diagnosis of endometrioma. Fertil Steril 1993; 60:776–780.
- Guerriero S, Mais V, Ajossa S, et al. The role of endovaginal ultrasound in differentiating endometriomas from other ovarian cysts. Clin Exp Obstet Gynecol 1995; 22:20–22.
- Fedele L, Bianchi S, Raffaelli R, Portuese A. Pre-operative assessment of bladder endometriosis. Hum Reprod 1997; 12:2519–2522.
- Chamié LP, Blasbalg R, Pereira RM, Warmbrand G, Serafini PC. Findings of pelvic endometriosis at transvaginal US, MR imaging, and laparoscopy. Radiographics 2011; 31:E77–E100.
- Fleischer AC. Transabdominal and transvaginal sonography of ovarian masses. Clin Obstet Gynecol 1991; 34:433–442.
- Zawin M, McCarthy S, Scoutt L, Comite F. Endometriosis: appearance and detection at MR imaging. Radiology 1989; 171:693–696.
- Togashi K, Nishimura K, Kimura I, et al. Endometrial cysts: diagnosis with MR imaging. Radiology 1991; 180:73–78.
- Balleyguier C, Chapron C, Dubuisson JB, et al. Comparison of magnetic resonance imaging and transvaginal ultrasonography in diagnosing bladder endometriosis. J Am Assoc Gynecol Laparosc 2002; 9:15–23.
- Siegelman ES, Oliver ER. MR imaging of endometriosis: ten imaging pearls. Radiographics 2012; 32:1675–1691.
- Takeuchi M, Matsuzaki K, Kubo H, Nishitani H. Magnetic resonance manifestations of endometrial cysts at 3 T compared with 1.5 T. J Comput Assist Tomogr 2008; 32:369–271.
- Zanardi R, Del Frate C, Zuiani C, Del Frate G, Bazzocchi M. Staging of pelvic endometriosis using magnetic resonance imaging compared with the laparoscopic classification of the American Fertility Society: a prospective study. Radiol Med 2003; 105:326–338.
- Takahashi K, Okada M, Okada S, Kitao M, Imaoka I, Sugimura K. Studies on the detection of small endometrial implants by magnetic resonance imaging using a fat saturation technique. Gynecol Obstet Invest 1996; 41:203–206.
- Loubeyre P, Copercini M, Frossard JL, Wenger JM, Petignat P. Pictorial review: rectosigmoid endometriosis on MRI with gel opacification after rectosigmoid colon cleansing. Clin Imaging 2012; 36:295–300.
- Bahr A, de Parades V, Gadonneix P, et al. Endorectal ultrasonography in predicting rectal wall infiltration in patients with deep pelvic endometriosis: a modern tool for an ancient disease. Dis Colon Rectum 2006; 49:869–875.
- Biscaldi E, Ferrero S, Remorgida V, Rollandi GA. Bowel endometriosis: CT-enteroclysis. Abdom Imaging 2007; 32:441–450.
A 32-year-old woman presents with a history of pelvic pain, dysmenorrhea, dyspareunia, dyschezia, and dysuria, with exacerbation of the symptoms during her menstrual cycles. Her menarche occurred at the age of 13 and her menses are regular. She has never undergone surgery and has no relevant pathologic processes. She also reports that for the past 18 months she has been unsuccessfully trying to conceive.
Two months ago, she went to the emergency department because of an acute episode of severe pelvic pain associated with abdominal cramps, vomiting, and dyschezia, occurring at the beginning of her menstrual cycle. At that time, her vital signs were within normal limits, but deep palpation of the right iliac fossa was painful. On that occasion, acute abdomen and bowel obstruction were excluded.
Now, vaginal examination reveals a bluish, painful, bulky induration in the posterior fornix. Digital rectal examination reveals a circular infiltrated area in the anterior rectal wall. Her cancer antigen 125 (CA 125) level is 230 U/mL (normal range 0–35 U/mL).
MENSES-RELATED SYMPTOMS AND THE DIAGNOSIS OF ENDOMETRIOSIS
The diagnosis of endometriosis should be considered in the patient described above. Many of her signs and symptoms can be associated with several diseases. However, the diagnostic hypothesis points strongly toward endometriosis, since her symptoms recur at the beginning of every menstrual cycle.1
Endometriosis is the presence of endometrial tissue outside the uterine cavity. The affected organs usually include the ovaries, fallopian tubes,2 peritoneal surface, vagina, cervix, abdominal wall,3 scar tissue, pouch of Douglas, urinary tract, and bowel. However, any organ can be involved.
So-called deeply infiltrating endometriosis is an endometriotic lesion penetrating into the retroperitoneal space (most often affecting the uterosacral ligaments and the rectovaginal septum) or the pelvic-organ wall to a depth of at least 5 mm and involving structures such as the rectum, vagina, ureters, and bladder.4 Its clinical presentation is highly variable, ranging from no symptoms to severe pain and dysfunction of pelvic organs.
Endometriosis can be diagnosed with certainty only when the endometriotic lesions are observed by laparoscopy or laparotomy and after the histologic examination of surgically resected lesions (Figure 1).1 However, a presumptive diagnosis can be made on the basis of imaging findings, which can be useful in the differential diagnostic process (Table 1).
EXAMINATION AND BLOOD MARKERS PROVIDE LIMITED INFORMATION
Knowing the history of the patient, along with a physical examination that includes speculum and bimanual vaginal and rectal examination, can be helpful in the diagnostic process even if nothing abnormal is found.
Pelvic examination has a poor predictive value, as demonstrated in a study conducted by Nezhat et al5 in 91 patients with surgically confirmed endometriosis, 47% of whom had a normal bimanual examination.
CA 125 is the serologic marker most often used for diagnosing endometriosis. Levels are usually high in the sera of patients with endometriosis, especially in the advanced stages.6 However, levels increase both in the physiologic menstrual cycle and in epithelial ovarian cancers.7 Thus, the diagnostic value of CA 125 is limited in terms of both sensitivity and specificity.
INCLUDE IMAGING IN THE DIAGNOSTIC WORKUP
Surgical treatment is frequently offered to patients who have severe pelvic pain that does not respond to medical treatment, or in cases of infertility. Imaging investigations are mandatory both to ascertain the diagnosis and to assess involvement of internal organs before surgery. Moreover, imaging helps minimize the surgical risks.
The primary aim of the radiologic examination is to describe the precise location, the depth, and the number of pelvic endometriotic lesions. Furthermore, imaging is useful to check for endometriotic foci in pelvic organs such as the bowel, ureters, and bladder, which are often involved in the pathologic process.
Transvaginal ultrasonography and magnetic resonance imaging (MRI) can accurately delineate deeply infiltrating lesions of endometriosis that are not easily accessible laparoscopically.
Transvaginal ultrasonography
Transvaginal ultrasonography is the first-line imaging study when endometriosis is suspected: it is powerful, simple, widely available, and cost-effective. In particular, it is recommended for diagnosing endometriotic ovarian cysts (endometriomas)8,9 and endometriosis of the bladder.10 However, its value for the assessment of superficial peritoneal lesions, ovarian foci, and deeply infiltrating endometriosis is questionable.
Although uncomfortable for the patient, transvaginal ultrasonography should be performed during menses, or when the pain reaches its highest level. In fact, during menstrual bleeding the endometrial implants grow and become easier to detect.
Mais et al8 reported that transvaginal ultrasonography has a sensitivity of 88% in differentiating endometriomas from other ovarian masses, and a specificity of 90% (Figure 2). Furthermore, its specificity is as high as that of MRI.8,9
Endometriotic nodules detected in the uterosacral ligaments, rectovaginal septum, vagina, vesicouterine pouch, bladder (Figure 3), and ureters can be signs of deeply infiltrating endometriosis. Pelvic adhesions can be suspected when pelvic organs appear fixed to each other, when hyperechogenic plaques are found between the serosal surfaces of the different organs, and when the pouch of Douglas is partially or completely obliterated.
The accuracy of transvaginal ultrasonography strongly depends on the operator’s skill. Furthermore, lesions of the sigmoid colon are impossible to visualize by transvaginal ultrasonography; hence, further diagnostic procedures are required. Transvaginal ultrasonography is the most accurate technique in detecting endometriotic nodules of the bladder wall in patients with urinary symptoms.
Transvaginal ultrasonography combined with color Doppler can also demonstrate the flow of urine through the ureters to the bladder, thereby ascertaining the patency of the ureters and clarifying the anatomic relationship between the ureters and any endometriotic lesions in the detrusors.10 Hydronephrosis can arise from ureteral restriction caused by endometriotic nodules. Thus, transabdominal ultrasonography of the kidneys is always recommended when deeply infiltrating endometriosis is suspected.
Some centers use a bowel-preparation protocol consisting of a laxative taken 24 hours before the procedure, combined with a low-residue diet and an enema 1 hour before the examination to cleanse the rectosigmoid colon of fecal content and gas, which can interfere with the visual examination of the pelvic structures.11
Transabdominal ultrasonography
Transabdominal ultrasonography can be used instead of transvaginal ultrasonography, eg, in young girls and women who have never been sexually active. When transabdominal ultrasonography is selected, the patient should have a full bladder to maximize the visualization of the pelvic structures. However, transvaginal ultrasonography is generally more sensitive than transabdominal in detecting adnexal masses and pelvic nodules.12
Magnetic resonance imaging
MRI has been recently introduced in the diagnosis of endometriosis. MRI is less operator-dependent than transvaginal ultrasonography and is more sensitive for detecting foci of deeply infiltrating endometriosis, because of its ability to completely survey the anterior and posterior compartments of the pelvis. However, its diagnostic value in cases of bladder endometriosis, superficial peritoneal lesions, and ovarian foci is still controversial.13–16
On MRI, lesions of deeply infiltrating endometriosis mainly appear as areas or nodules with regular, irregular, indistinct, or stellate margins. A distortion of the normal pelvic anatomy or the detection of a loculated fluid collection can indirectly signal the presence of adhesions.
MRI has high specificity for the diagnosis of endometriomas as a result of its ability to detect aged hemorrhagic content (Figure 4).17 Despite the many studies that point to the limits of MRI in detecting small endometriotic lesions, recent studies demonstrated that MRI also has good sensitivity for small peritoneal implants and adhesions.18,19 The injection of gadolinium contrast is still a debatable measure, because contrast-enhanced imaging cannot differentiate infiltrating lesions from other normal fibromuscular pelvic anatomic structures.15,20
Bowel preparation can be done with an oral laxative the day before imaging, complemented by a low-residue diet. A single dose of a ready-to-use enema is given 30 minutes before the examination to cleanse the terminal section of the intestinal tract. To avoid motion artifacts caused by bowel peristalsis, images are obtained after intramuscular injections of a myorelaxant are given, if there is no contraindication. Bowel preparation is useful to eliminate fecal residue and gas, thereby allowing proper visualization of lesions of deeply infiltrating endometriosis, but it is not routinely prescribed in all centers.11
In most cases, endometriotic lesions have an MRI signal intensity that comes very close to that of the surrounding fibromuscular structures. In this regard, vaginal and rectal distention and opacification using ultrasonographic gel clearly help to delineate the cervix, vaginal fornices, and vaginal wall, as well as the rectum and wall of the rectosigmoid junction (Figure 5).20
PRESURGICAL IMAGING
Rectal endoscopic ultrasonography
Even though it should not be included in the routine diagnostic workup, rectal endoscopic ultrasonography, using a flexible echoendoscope, is suitable in certain presurgical cases. The aim of this imaging technique is to assess the depth of bowel wall infiltration thanks to the visualization of the different layers.21
Double-contrast barium enema and multislice computed tomography
Double-contrast barium enema is extensively used for the diagnosis of bowel endometriosis, once the decision to perform surgery has been made. It allows evaluation of the degree and length of the bowel occlusion at the level of the sigmoid or high rectosigmoid tract, but it does not permit differentiation of bowel endometriosis from other pathologies.
Multislice computed tomography offers the opportunity to evaluate the depth of the lesions with excellent precision. 22
The most relevant disadvantage of both procedures is the exposure of women of reproductive age to ionizing radiation. In addition, multislice computed tomography requires the administration of an intravenous iodinated contrast medium and a retrograde colonic distention with about 2 L of water.
A 32-year-old woman presents with a history of pelvic pain, dysmenorrhea, dyspareunia, dyschezia, and dysuria, with exacerbation of the symptoms during her menstrual cycles. Her menarche occurred at the age of 13 and her menses are regular. She has never undergone surgery and has no relevant pathologic processes. She also reports that for the past 18 months she has been unsuccessfully trying to conceive.
Two months ago, she went to the emergency department because of an acute episode of severe pelvic pain associated with abdominal cramps, vomiting, and dyschezia, occurring at the beginning of her menstrual cycle. At that time, her vital signs were within normal limits, but deep palpation of the right iliac fossa was painful. On that occasion, acute abdomen and bowel obstruction were excluded.
Now, vaginal examination reveals a bluish, painful, bulky induration in the posterior fornix. Digital rectal examination reveals a circular infiltrated area in the anterior rectal wall. Her cancer antigen 125 (CA 125) level is 230 U/mL (normal range 0–35 U/mL).
MENSES-RELATED SYMPTOMS AND THE DIAGNOSIS OF ENDOMETRIOSIS
The diagnosis of endometriosis should be considered in the patient described above. Many of her signs and symptoms can be associated with several diseases. However, the diagnostic hypothesis points strongly toward endometriosis, since her symptoms recur at the beginning of every menstrual cycle.1
Endometriosis is the presence of endometrial tissue outside the uterine cavity. The affected organs usually include the ovaries, fallopian tubes,2 peritoneal surface, vagina, cervix, abdominal wall,3 scar tissue, pouch of Douglas, urinary tract, and bowel. However, any organ can be involved.
So-called deeply infiltrating endometriosis is an endometriotic lesion penetrating into the retroperitoneal space (most often affecting the uterosacral ligaments and the rectovaginal septum) or the pelvic-organ wall to a depth of at least 5 mm and involving structures such as the rectum, vagina, ureters, and bladder.4 Its clinical presentation is highly variable, ranging from no symptoms to severe pain and dysfunction of pelvic organs.
Endometriosis can be diagnosed with certainty only when the endometriotic lesions are observed by laparoscopy or laparotomy and after the histologic examination of surgically resected lesions (Figure 1).1 However, a presumptive diagnosis can be made on the basis of imaging findings, which can be useful in the differential diagnostic process (Table 1).
EXAMINATION AND BLOOD MARKERS PROVIDE LIMITED INFORMATION
Knowing the history of the patient, along with a physical examination that includes speculum and bimanual vaginal and rectal examination, can be helpful in the diagnostic process even if nothing abnormal is found.
Pelvic examination has a poor predictive value, as demonstrated in a study conducted by Nezhat et al5 in 91 patients with surgically confirmed endometriosis, 47% of whom had a normal bimanual examination.
CA 125 is the serologic marker most often used for diagnosing endometriosis. Levels are usually high in the sera of patients with endometriosis, especially in the advanced stages.6 However, levels increase both in the physiologic menstrual cycle and in epithelial ovarian cancers.7 Thus, the diagnostic value of CA 125 is limited in terms of both sensitivity and specificity.
INCLUDE IMAGING IN THE DIAGNOSTIC WORKUP
Surgical treatment is frequently offered to patients who have severe pelvic pain that does not respond to medical treatment, or in cases of infertility. Imaging investigations are mandatory both to ascertain the diagnosis and to assess involvement of internal organs before surgery. Moreover, imaging helps minimize the surgical risks.
The primary aim of the radiologic examination is to describe the precise location, the depth, and the number of pelvic endometriotic lesions. Furthermore, imaging is useful to check for endometriotic foci in pelvic organs such as the bowel, ureters, and bladder, which are often involved in the pathologic process.
Transvaginal ultrasonography and magnetic resonance imaging (MRI) can accurately delineate deeply infiltrating lesions of endometriosis that are not easily accessible laparoscopically.
Transvaginal ultrasonography
Transvaginal ultrasonography is the first-line imaging study when endometriosis is suspected: it is powerful, simple, widely available, and cost-effective. In particular, it is recommended for diagnosing endometriotic ovarian cysts (endometriomas)8,9 and endometriosis of the bladder.10 However, its value for the assessment of superficial peritoneal lesions, ovarian foci, and deeply infiltrating endometriosis is questionable.
Although uncomfortable for the patient, transvaginal ultrasonography should be performed during menses, or when the pain reaches its highest level. In fact, during menstrual bleeding the endometrial implants grow and become easier to detect.
Mais et al8 reported that transvaginal ultrasonography has a sensitivity of 88% in differentiating endometriomas from other ovarian masses, and a specificity of 90% (Figure 2). Furthermore, its specificity is as high as that of MRI.8,9
Endometriotic nodules detected in the uterosacral ligaments, rectovaginal septum, vagina, vesicouterine pouch, bladder (Figure 3), and ureters can be signs of deeply infiltrating endometriosis. Pelvic adhesions can be suspected when pelvic organs appear fixed to each other, when hyperechogenic plaques are found between the serosal surfaces of the different organs, and when the pouch of Douglas is partially or completely obliterated.
The accuracy of transvaginal ultrasonography strongly depends on the operator’s skill. Furthermore, lesions of the sigmoid colon are impossible to visualize by transvaginal ultrasonography; hence, further diagnostic procedures are required. Transvaginal ultrasonography is the most accurate technique in detecting endometriotic nodules of the bladder wall in patients with urinary symptoms.
Transvaginal ultrasonography combined with color Doppler can also demonstrate the flow of urine through the ureters to the bladder, thereby ascertaining the patency of the ureters and clarifying the anatomic relationship between the ureters and any endometriotic lesions in the detrusors.10 Hydronephrosis can arise from ureteral restriction caused by endometriotic nodules. Thus, transabdominal ultrasonography of the kidneys is always recommended when deeply infiltrating endometriosis is suspected.
Some centers use a bowel-preparation protocol consisting of a laxative taken 24 hours before the procedure, combined with a low-residue diet and an enema 1 hour before the examination to cleanse the rectosigmoid colon of fecal content and gas, which can interfere with the visual examination of the pelvic structures.11
Transabdominal ultrasonography
Transabdominal ultrasonography can be used instead of transvaginal ultrasonography, eg, in young girls and women who have never been sexually active. When transabdominal ultrasonography is selected, the patient should have a full bladder to maximize the visualization of the pelvic structures. However, transvaginal ultrasonography is generally more sensitive than transabdominal in detecting adnexal masses and pelvic nodules.12
Magnetic resonance imaging
MRI has been recently introduced in the diagnosis of endometriosis. MRI is less operator-dependent than transvaginal ultrasonography and is more sensitive for detecting foci of deeply infiltrating endometriosis, because of its ability to completely survey the anterior and posterior compartments of the pelvis. However, its diagnostic value in cases of bladder endometriosis, superficial peritoneal lesions, and ovarian foci is still controversial.13–16
On MRI, lesions of deeply infiltrating endometriosis mainly appear as areas or nodules with regular, irregular, indistinct, or stellate margins. A distortion of the normal pelvic anatomy or the detection of a loculated fluid collection can indirectly signal the presence of adhesions.
MRI has high specificity for the diagnosis of endometriomas as a result of its ability to detect aged hemorrhagic content (Figure 4).17 Despite the many studies that point to the limits of MRI in detecting small endometriotic lesions, recent studies demonstrated that MRI also has good sensitivity for small peritoneal implants and adhesions.18,19 The injection of gadolinium contrast is still a debatable measure, because contrast-enhanced imaging cannot differentiate infiltrating lesions from other normal fibromuscular pelvic anatomic structures.15,20
Bowel preparation can be done with an oral laxative the day before imaging, complemented by a low-residue diet. A single dose of a ready-to-use enema is given 30 minutes before the examination to cleanse the terminal section of the intestinal tract. To avoid motion artifacts caused by bowel peristalsis, images are obtained after intramuscular injections of a myorelaxant are given, if there is no contraindication. Bowel preparation is useful to eliminate fecal residue and gas, thereby allowing proper visualization of lesions of deeply infiltrating endometriosis, but it is not routinely prescribed in all centers.11
In most cases, endometriotic lesions have an MRI signal intensity that comes very close to that of the surrounding fibromuscular structures. In this regard, vaginal and rectal distention and opacification using ultrasonographic gel clearly help to delineate the cervix, vaginal fornices, and vaginal wall, as well as the rectum and wall of the rectosigmoid junction (Figure 5).20
PRESURGICAL IMAGING
Rectal endoscopic ultrasonography
Even though it should not be included in the routine diagnostic workup, rectal endoscopic ultrasonography, using a flexible echoendoscope, is suitable in certain presurgical cases. The aim of this imaging technique is to assess the depth of bowel wall infiltration thanks to the visualization of the different layers.21
Double-contrast barium enema and multislice computed tomography
Double-contrast barium enema is extensively used for the diagnosis of bowel endometriosis, once the decision to perform surgery has been made. It allows evaluation of the degree and length of the bowel occlusion at the level of the sigmoid or high rectosigmoid tract, but it does not permit differentiation of bowel endometriosis from other pathologies.
Multislice computed tomography offers the opportunity to evaluate the depth of the lesions with excellent precision. 22
The most relevant disadvantage of both procedures is the exposure of women of reproductive age to ionizing radiation. In addition, multislice computed tomography requires the administration of an intravenous iodinated contrast medium and a retrograde colonic distention with about 2 L of water.
- Attaran M, Falcone T, Goldberg J. Endometriosis: still tough to diagnose and treat. Cleve Clin J Med 2002; 69:647–653.
- Wenger JM, Soave I, Lo Monte G, Petignat P, Marci R. Tubal endometrioma within a twisted fallopian tube: a clinically complex diagnosis. J Pediatr Adolesc Gynecol 2013; 26:e1–e4.
- Marci R, Lo Monte G, Soave I, Bianchi A, Patella A, Wenger JM. Rectus abdominis muscle endometriotic mass in a woman affected by multiple sclerosis. J Obstet Gynaecol Res 2013; 39:462–465.
- Vercellini P, Frontino G, Pietropaolo G, Gattei U, Daguati R, Crosignani PG. Deep endometriosis: definition, pathogenesis, and clinical management. J Am Assoc Gynecol Laparosc 2004; 11:153–161.
- Nezhat C, Santolaya J, Nezhat FR. Comparison of transvaginal sonography and bimanual pelvic examination in patients with laparoscopically confirmed endometriosis. J Am Assoc Gynecol Laparosc 1994; 1:127–130.
- Barbieri RL, Niloff JM, Bast RC, Scaetzl E, Kistner RW, Knapp RC. Elevated serum concentrations of CA-125 in patients with advanced endometriosis. Fertil Steril 1986; 45:630–634.
- Bon GG, Kenemans P, Dekker JJ, et al. Fluctuations in CA 125 and CA 15-3 serum concentrations during spontaneous ovulatory cycles. Hum Reprod 1999; 14:566–570.
- Mais V, Guerriero S, Ajossa S, Angiolucci M, Paoletti AM, Melis GB. The efficiency of transvaginal ultrasonography in the diagnosis of endometrioma. Fertil Steril 1993; 60:776–780.
- Guerriero S, Mais V, Ajossa S, et al. The role of endovaginal ultrasound in differentiating endometriomas from other ovarian cysts. Clin Exp Obstet Gynecol 1995; 22:20–22.
- Fedele L, Bianchi S, Raffaelli R, Portuese A. Pre-operative assessment of bladder endometriosis. Hum Reprod 1997; 12:2519–2522.
- Chamié LP, Blasbalg R, Pereira RM, Warmbrand G, Serafini PC. Findings of pelvic endometriosis at transvaginal US, MR imaging, and laparoscopy. Radiographics 2011; 31:E77–E100.
- Fleischer AC. Transabdominal and transvaginal sonography of ovarian masses. Clin Obstet Gynecol 1991; 34:433–442.
- Zawin M, McCarthy S, Scoutt L, Comite F. Endometriosis: appearance and detection at MR imaging. Radiology 1989; 171:693–696.
- Togashi K, Nishimura K, Kimura I, et al. Endometrial cysts: diagnosis with MR imaging. Radiology 1991; 180:73–78.
- Balleyguier C, Chapron C, Dubuisson JB, et al. Comparison of magnetic resonance imaging and transvaginal ultrasonography in diagnosing bladder endometriosis. J Am Assoc Gynecol Laparosc 2002; 9:15–23.
- Siegelman ES, Oliver ER. MR imaging of endometriosis: ten imaging pearls. Radiographics 2012; 32:1675–1691.
- Takeuchi M, Matsuzaki K, Kubo H, Nishitani H. Magnetic resonance manifestations of endometrial cysts at 3 T compared with 1.5 T. J Comput Assist Tomogr 2008; 32:369–271.
- Zanardi R, Del Frate C, Zuiani C, Del Frate G, Bazzocchi M. Staging of pelvic endometriosis using magnetic resonance imaging compared with the laparoscopic classification of the American Fertility Society: a prospective study. Radiol Med 2003; 105:326–338.
- Takahashi K, Okada M, Okada S, Kitao M, Imaoka I, Sugimura K. Studies on the detection of small endometrial implants by magnetic resonance imaging using a fat saturation technique. Gynecol Obstet Invest 1996; 41:203–206.
- Loubeyre P, Copercini M, Frossard JL, Wenger JM, Petignat P. Pictorial review: rectosigmoid endometriosis on MRI with gel opacification after rectosigmoid colon cleansing. Clin Imaging 2012; 36:295–300.
- Bahr A, de Parades V, Gadonneix P, et al. Endorectal ultrasonography in predicting rectal wall infiltration in patients with deep pelvic endometriosis: a modern tool for an ancient disease. Dis Colon Rectum 2006; 49:869–875.
- Biscaldi E, Ferrero S, Remorgida V, Rollandi GA. Bowel endometriosis: CT-enteroclysis. Abdom Imaging 2007; 32:441–450.
- Attaran M, Falcone T, Goldberg J. Endometriosis: still tough to diagnose and treat. Cleve Clin J Med 2002; 69:647–653.
- Wenger JM, Soave I, Lo Monte G, Petignat P, Marci R. Tubal endometrioma within a twisted fallopian tube: a clinically complex diagnosis. J Pediatr Adolesc Gynecol 2013; 26:e1–e4.
- Marci R, Lo Monte G, Soave I, Bianchi A, Patella A, Wenger JM. Rectus abdominis muscle endometriotic mass in a woman affected by multiple sclerosis. J Obstet Gynaecol Res 2013; 39:462–465.
- Vercellini P, Frontino G, Pietropaolo G, Gattei U, Daguati R, Crosignani PG. Deep endometriosis: definition, pathogenesis, and clinical management. J Am Assoc Gynecol Laparosc 2004; 11:153–161.
- Nezhat C, Santolaya J, Nezhat FR. Comparison of transvaginal sonography and bimanual pelvic examination in patients with laparoscopically confirmed endometriosis. J Am Assoc Gynecol Laparosc 1994; 1:127–130.
- Barbieri RL, Niloff JM, Bast RC, Scaetzl E, Kistner RW, Knapp RC. Elevated serum concentrations of CA-125 in patients with advanced endometriosis. Fertil Steril 1986; 45:630–634.
- Bon GG, Kenemans P, Dekker JJ, et al. Fluctuations in CA 125 and CA 15-3 serum concentrations during spontaneous ovulatory cycles. Hum Reprod 1999; 14:566–570.
- Mais V, Guerriero S, Ajossa S, Angiolucci M, Paoletti AM, Melis GB. The efficiency of transvaginal ultrasonography in the diagnosis of endometrioma. Fertil Steril 1993; 60:776–780.
- Guerriero S, Mais V, Ajossa S, et al. The role of endovaginal ultrasound in differentiating endometriomas from other ovarian cysts. Clin Exp Obstet Gynecol 1995; 22:20–22.
- Fedele L, Bianchi S, Raffaelli R, Portuese A. Pre-operative assessment of bladder endometriosis. Hum Reprod 1997; 12:2519–2522.
- Chamié LP, Blasbalg R, Pereira RM, Warmbrand G, Serafini PC. Findings of pelvic endometriosis at transvaginal US, MR imaging, and laparoscopy. Radiographics 2011; 31:E77–E100.
- Fleischer AC. Transabdominal and transvaginal sonography of ovarian masses. Clin Obstet Gynecol 1991; 34:433–442.
- Zawin M, McCarthy S, Scoutt L, Comite F. Endometriosis: appearance and detection at MR imaging. Radiology 1989; 171:693–696.
- Togashi K, Nishimura K, Kimura I, et al. Endometrial cysts: diagnosis with MR imaging. Radiology 1991; 180:73–78.
- Balleyguier C, Chapron C, Dubuisson JB, et al. Comparison of magnetic resonance imaging and transvaginal ultrasonography in diagnosing bladder endometriosis. J Am Assoc Gynecol Laparosc 2002; 9:15–23.
- Siegelman ES, Oliver ER. MR imaging of endometriosis: ten imaging pearls. Radiographics 2012; 32:1675–1691.
- Takeuchi M, Matsuzaki K, Kubo H, Nishitani H. Magnetic resonance manifestations of endometrial cysts at 3 T compared with 1.5 T. J Comput Assist Tomogr 2008; 32:369–271.
- Zanardi R, Del Frate C, Zuiani C, Del Frate G, Bazzocchi M. Staging of pelvic endometriosis using magnetic resonance imaging compared with the laparoscopic classification of the American Fertility Society: a prospective study. Radiol Med 2003; 105:326–338.
- Takahashi K, Okada M, Okada S, Kitao M, Imaoka I, Sugimura K. Studies on the detection of small endometrial implants by magnetic resonance imaging using a fat saturation technique. Gynecol Obstet Invest 1996; 41:203–206.
- Loubeyre P, Copercini M, Frossard JL, Wenger JM, Petignat P. Pictorial review: rectosigmoid endometriosis on MRI with gel opacification after rectosigmoid colon cleansing. Clin Imaging 2012; 36:295–300.
- Bahr A, de Parades V, Gadonneix P, et al. Endorectal ultrasonography in predicting rectal wall infiltration in patients with deep pelvic endometriosis: a modern tool for an ancient disease. Dis Colon Rectum 2006; 49:869–875.
- Biscaldi E, Ferrero S, Remorgida V, Rollandi GA. Bowel endometriosis: CT-enteroclysis. Abdom Imaging 2007; 32:441–450.
KEY POINTS
- The diagnostic evaluation should always start with transvaginal ultrasonography of the pelvic structures followed by magnetic resonance imaging, especially if deeply infiltrating endometriosis is suspected.
- An inaccurate imaging evaluation may lead to an incomplete excision of lesions if the patient undergoes surgery.
- Transvaginal ultrasonography and magnetic resonance imaging allow the assessment of the size, location, and extent of the lesions.
- Given the multifocal nature of the disease, a thorough evaluation of all pelvic structures, including the bowel, the bladder, and the ureters, is always recommended.
Encephalopathy despite thiamine repletion during alcohol withdrawal
Managing a patient with chronic alcohol abuse who is beginning to withdraw is a situation in which to expect the unexpected.
A 61-year-old man with a 40-year history of alcohol abuse was admitted to the hospital after presenting with a 6-month history of weakness and increasing frequency of falls, as well as a 2-day history of myalgias and fatigue. He had anorexia and chronic diarrhea, and he reported an unintentional 100-lb weight loss over the past year. He consumed at least three to five alcoholic drinks daily, including a daily “eye-opener,” and his diet was essentially devoid of meat, bread, fruits, and vegetables. His last drink had been on the morning of admission.
On physical examination, his vital signs were notable for marked orthostatic hypotension. He had angular cheilitis, an erythematous, scaly facial rash, and poorly healing severe sunburn on the dorsal surface of the left forearm, acquired 1 month earlier after minimal sun exposure while driving his car (Figure 1).
The neurologic examination noted decreased sensation in a stocking distribution, reduced proprioception in both great toes, and an intention tremor. His upper extremities were slightly hyperreflexic, he had down-going toes, he did not have clonus, and his gait was wide-based.
Laboratory results were notable for mild anemia, with an elevated mean corpuscular volume of 109.2 fL and a normal thyrotropin level. Urinalysis and urine culture were normal. Stool testing for Clostridium difficile toxin was negative. Computed tomography of the head was unremarkable.
He was placed on the Clinical Institute Withdrawal Assessment for Alcohol revised protocol,1 and he was started on careful fluid, electrolyte, and nutritional management, including intravenous supplementation with thiamine 100 mg daily, folic acid 1 mg twice daily, and an oral multivitamin. Despite these interventions, he became delirious and developed horizontal nystagmus, visual hallucinations, dizziness, and increasing weakness. Benzodiazepine toxicity, which may cause similar findings, was thought unlikely, as he had received only a maximum of 4 mg of lorazepam in any single 24-hour period. His ongoing confusion, orthostatic hypotension, ataxia, and nystagmus raised concern for Wernicke encephalopathy. Thiamine was increased to 500 mg intravenously three times daily for 2 days, followed by 500 mg daily for 2 days, as recommended for acute Wernicke encephalopathy by the Royal College of Physicians.2
Although his ocular findings resolved and his blood pressure improved with high-dose thiamine, he remained confused. Other causes of delirium were considered, including other micronutrient deficiencies. He was evaluated for magnesium deficiency, as magnesium is a necessary cofactor in thiamine metabolism,3 but his level was within normal limits. The constellation of symptoms, including persistent delirium, diarrhea, and skin findings, appeared to be consistent with pellagra, and niacin deficiency became a concern.
PELLAGRA AND ALCOHOL ABUSE
Niacin is a water-soluble vitamin converted to two important coenzymes involved in carbohydrate metabolism and fatty-acid synthesis.4 Body stores are minimal, although the liver can convert tryptophan to niacin.4
In the United States, pellagra has become rare since niacin enrichment of bread and flour began in the 1940s. However, the risk is increased in those with chronic alcohol dependency, metabolic disease such as carcinoid syndrome, and malabsorptive states such as Crohn disease.5 Alcohol abuse is commonly associated with micronutrient deficiencies. Even in alcoholics with sufficient food intake, their ability to absorb niacin may be impaired both directly and indirectly because of the toxic effects of alcohol on the gastrointestinal tract.5
The three D’s of niacin deficiency
The clinical picture of pellagra includes the three “D’s” of niacin deficiency—diarrhea, dementia, and dermatitis—representing the organ systems most commonly affected (ie, the gastrointestinal tract, nervous system, and skin). Gastrointestinal signs and symptoms may include anorexia, diarrhea, stomatitis, and abdominal discomfort.4 Neurologic signs and symptoms are the most frequent clinical manifestations of pellagra but are often overlooked in alcoholics with altered mental status.5,6 Early neurologic findings may include apathy, depression, paresthesias, dizziness, and falling.4,5 Later findings may include hallucinations, seizures, and psychosis.4,5 If severe enough, this may progress to coma and to a fourth “D”—death—if left untreated.
Skin findings, if present, are typically the most characteristic of pellagra.5,6 They include a photosensitive eruption that most commonly appears on the face, arms, and the “V” of the neck (“Casal’s necklace”).3,6 Erythema develops on areas of sun-exposed skin and may be painful or pruritic.6 It may take up to four times as long to resolve as a normal sunburn.6 On repeated exposure, the skin becomes thickened, hyperkeratotic, and hyperpigmented.6
DIAGNOSIS AND TREATMENT OF PELLAGRA
Suspicion of pellagra should be high in any patient with chronic alcohol abuse with changes in mental status.5 Pellagra is typically diagnosed clinically. Although testing of serum levels of niacin or urine levels of niacin metabolites can be performed,4,5 these tests are not commonly used, as they are neither widely available nor reliable.3,4 Because there is little downside to giving niacin, treatment should be started if there is clinical suspicion of pellagra.3,4 The diagnosis is confirmed by clinical improvement after niacin replacement begins.4
Pellagra is easy and inexpensive to treat once the diagnosis has been established. Supplementation can be given orally at 50 mg to 100 mg three times daily, with a maximum of 500 mg daily for 3 to 4 weeks.3,5 The multivitamin our patient initially received provided only 30 mg of niacin, which was insufficient to treat his deficiency.
Other micronutrient deficiencies are also common in pellagra, such as the suspected thiamine deficiency in this patient. Although rare in adults, pyridoxine deficiency should be considered because pyridoxine plays an important role in niacin metabolism, and in patients such as this, the signs and symptoms of pellagra will not resolve with niacin administration alone.3,4
Neurologic symptoms can begin to resolve as soon as 24 to 48 hours after replacement therapy is started, although skin symptoms take longer to respond.6
OUR PATIENT’S MANAGEMENT AND LESSONS LEARNED
Our patient was treated with extended-release niacin 500 mg daily. He was significantly less confused within 24 hours, and 2 days later he was no longer delirious. His diarrhea resolved, but his peripheral neuropathy improved only modestly, and we believe that this was the result of his long history of alcohol abuse.
Although there are guidelines to help with the management of patients undergoing alcohol withdrawal, our experience with this patient illustrates that important clinical conditions, including micronutrient deficiencies, can easily be overlooked or misattributed, with potentially dangerous consequences. It is crucial to be mindful of these considerations.
- Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). Br J Addict 1989; 84:1353–1357.
- Thomson AD, Cook CC, Touquet R, Henry JA; Royal College of Physicians, London. The Royal College of Physicians report on alcohol: guidelines for managing Wernicke’s encephalopathy in the accident and Emergency Department. Alcohol Alcohol 2002; 37:513–521.
- Weathers AL, Lewis SL. Rare and unusual … or are they? Less commonly diagnosed encephalopathies associated with systemic disease. Semin Neurol 2009; 29:136–153.
- World Health Organization, United Nations High Commissions for Refugees. Pellagra and its prevention and control in major emergencies. 2000. http://www.who.int/nutrition/publications/emergencies/WHO_NHD_00.10/en/index.html. Accessed April 26, 2014.
- Oldham MA, Ivkovic A. Pellagrous encephalopathy presenting as alcohol withdrawal delirium: a case series and literature review. Addict Sci Clin Pract 2012; 7:12.
- Karthikeyan K, Thappa DM. Pellagra and skin. Int J Dermatol 2002; 41:476–481.
Managing a patient with chronic alcohol abuse who is beginning to withdraw is a situation in which to expect the unexpected.
A 61-year-old man with a 40-year history of alcohol abuse was admitted to the hospital after presenting with a 6-month history of weakness and increasing frequency of falls, as well as a 2-day history of myalgias and fatigue. He had anorexia and chronic diarrhea, and he reported an unintentional 100-lb weight loss over the past year. He consumed at least three to five alcoholic drinks daily, including a daily “eye-opener,” and his diet was essentially devoid of meat, bread, fruits, and vegetables. His last drink had been on the morning of admission.
On physical examination, his vital signs were notable for marked orthostatic hypotension. He had angular cheilitis, an erythematous, scaly facial rash, and poorly healing severe sunburn on the dorsal surface of the left forearm, acquired 1 month earlier after minimal sun exposure while driving his car (Figure 1).
The neurologic examination noted decreased sensation in a stocking distribution, reduced proprioception in both great toes, and an intention tremor. His upper extremities were slightly hyperreflexic, he had down-going toes, he did not have clonus, and his gait was wide-based.
Laboratory results were notable for mild anemia, with an elevated mean corpuscular volume of 109.2 fL and a normal thyrotropin level. Urinalysis and urine culture were normal. Stool testing for Clostridium difficile toxin was negative. Computed tomography of the head was unremarkable.
He was placed on the Clinical Institute Withdrawal Assessment for Alcohol revised protocol,1 and he was started on careful fluid, electrolyte, and nutritional management, including intravenous supplementation with thiamine 100 mg daily, folic acid 1 mg twice daily, and an oral multivitamin. Despite these interventions, he became delirious and developed horizontal nystagmus, visual hallucinations, dizziness, and increasing weakness. Benzodiazepine toxicity, which may cause similar findings, was thought unlikely, as he had received only a maximum of 4 mg of lorazepam in any single 24-hour period. His ongoing confusion, orthostatic hypotension, ataxia, and nystagmus raised concern for Wernicke encephalopathy. Thiamine was increased to 500 mg intravenously three times daily for 2 days, followed by 500 mg daily for 2 days, as recommended for acute Wernicke encephalopathy by the Royal College of Physicians.2
Although his ocular findings resolved and his blood pressure improved with high-dose thiamine, he remained confused. Other causes of delirium were considered, including other micronutrient deficiencies. He was evaluated for magnesium deficiency, as magnesium is a necessary cofactor in thiamine metabolism,3 but his level was within normal limits. The constellation of symptoms, including persistent delirium, diarrhea, and skin findings, appeared to be consistent with pellagra, and niacin deficiency became a concern.
PELLAGRA AND ALCOHOL ABUSE
Niacin is a water-soluble vitamin converted to two important coenzymes involved in carbohydrate metabolism and fatty-acid synthesis.4 Body stores are minimal, although the liver can convert tryptophan to niacin.4
In the United States, pellagra has become rare since niacin enrichment of bread and flour began in the 1940s. However, the risk is increased in those with chronic alcohol dependency, metabolic disease such as carcinoid syndrome, and malabsorptive states such as Crohn disease.5 Alcohol abuse is commonly associated with micronutrient deficiencies. Even in alcoholics with sufficient food intake, their ability to absorb niacin may be impaired both directly and indirectly because of the toxic effects of alcohol on the gastrointestinal tract.5
The three D’s of niacin deficiency
The clinical picture of pellagra includes the three “D’s” of niacin deficiency—diarrhea, dementia, and dermatitis—representing the organ systems most commonly affected (ie, the gastrointestinal tract, nervous system, and skin). Gastrointestinal signs and symptoms may include anorexia, diarrhea, stomatitis, and abdominal discomfort.4 Neurologic signs and symptoms are the most frequent clinical manifestations of pellagra but are often overlooked in alcoholics with altered mental status.5,6 Early neurologic findings may include apathy, depression, paresthesias, dizziness, and falling.4,5 Later findings may include hallucinations, seizures, and psychosis.4,5 If severe enough, this may progress to coma and to a fourth “D”—death—if left untreated.
Skin findings, if present, are typically the most characteristic of pellagra.5,6 They include a photosensitive eruption that most commonly appears on the face, arms, and the “V” of the neck (“Casal’s necklace”).3,6 Erythema develops on areas of sun-exposed skin and may be painful or pruritic.6 It may take up to four times as long to resolve as a normal sunburn.6 On repeated exposure, the skin becomes thickened, hyperkeratotic, and hyperpigmented.6
DIAGNOSIS AND TREATMENT OF PELLAGRA
Suspicion of pellagra should be high in any patient with chronic alcohol abuse with changes in mental status.5 Pellagra is typically diagnosed clinically. Although testing of serum levels of niacin or urine levels of niacin metabolites can be performed,4,5 these tests are not commonly used, as they are neither widely available nor reliable.3,4 Because there is little downside to giving niacin, treatment should be started if there is clinical suspicion of pellagra.3,4 The diagnosis is confirmed by clinical improvement after niacin replacement begins.4
Pellagra is easy and inexpensive to treat once the diagnosis has been established. Supplementation can be given orally at 50 mg to 100 mg three times daily, with a maximum of 500 mg daily for 3 to 4 weeks.3,5 The multivitamin our patient initially received provided only 30 mg of niacin, which was insufficient to treat his deficiency.
Other micronutrient deficiencies are also common in pellagra, such as the suspected thiamine deficiency in this patient. Although rare in adults, pyridoxine deficiency should be considered because pyridoxine plays an important role in niacin metabolism, and in patients such as this, the signs and symptoms of pellagra will not resolve with niacin administration alone.3,4
Neurologic symptoms can begin to resolve as soon as 24 to 48 hours after replacement therapy is started, although skin symptoms take longer to respond.6
OUR PATIENT’S MANAGEMENT AND LESSONS LEARNED
Our patient was treated with extended-release niacin 500 mg daily. He was significantly less confused within 24 hours, and 2 days later he was no longer delirious. His diarrhea resolved, but his peripheral neuropathy improved only modestly, and we believe that this was the result of his long history of alcohol abuse.
Although there are guidelines to help with the management of patients undergoing alcohol withdrawal, our experience with this patient illustrates that important clinical conditions, including micronutrient deficiencies, can easily be overlooked or misattributed, with potentially dangerous consequences. It is crucial to be mindful of these considerations.
Managing a patient with chronic alcohol abuse who is beginning to withdraw is a situation in which to expect the unexpected.
A 61-year-old man with a 40-year history of alcohol abuse was admitted to the hospital after presenting with a 6-month history of weakness and increasing frequency of falls, as well as a 2-day history of myalgias and fatigue. He had anorexia and chronic diarrhea, and he reported an unintentional 100-lb weight loss over the past year. He consumed at least three to five alcoholic drinks daily, including a daily “eye-opener,” and his diet was essentially devoid of meat, bread, fruits, and vegetables. His last drink had been on the morning of admission.
On physical examination, his vital signs were notable for marked orthostatic hypotension. He had angular cheilitis, an erythematous, scaly facial rash, and poorly healing severe sunburn on the dorsal surface of the left forearm, acquired 1 month earlier after minimal sun exposure while driving his car (Figure 1).
The neurologic examination noted decreased sensation in a stocking distribution, reduced proprioception in both great toes, and an intention tremor. His upper extremities were slightly hyperreflexic, he had down-going toes, he did not have clonus, and his gait was wide-based.
Laboratory results were notable for mild anemia, with an elevated mean corpuscular volume of 109.2 fL and a normal thyrotropin level. Urinalysis and urine culture were normal. Stool testing for Clostridium difficile toxin was negative. Computed tomography of the head was unremarkable.
He was placed on the Clinical Institute Withdrawal Assessment for Alcohol revised protocol,1 and he was started on careful fluid, electrolyte, and nutritional management, including intravenous supplementation with thiamine 100 mg daily, folic acid 1 mg twice daily, and an oral multivitamin. Despite these interventions, he became delirious and developed horizontal nystagmus, visual hallucinations, dizziness, and increasing weakness. Benzodiazepine toxicity, which may cause similar findings, was thought unlikely, as he had received only a maximum of 4 mg of lorazepam in any single 24-hour period. His ongoing confusion, orthostatic hypotension, ataxia, and nystagmus raised concern for Wernicke encephalopathy. Thiamine was increased to 500 mg intravenously three times daily for 2 days, followed by 500 mg daily for 2 days, as recommended for acute Wernicke encephalopathy by the Royal College of Physicians.2
Although his ocular findings resolved and his blood pressure improved with high-dose thiamine, he remained confused. Other causes of delirium were considered, including other micronutrient deficiencies. He was evaluated for magnesium deficiency, as magnesium is a necessary cofactor in thiamine metabolism,3 but his level was within normal limits. The constellation of symptoms, including persistent delirium, diarrhea, and skin findings, appeared to be consistent with pellagra, and niacin deficiency became a concern.
PELLAGRA AND ALCOHOL ABUSE
Niacin is a water-soluble vitamin converted to two important coenzymes involved in carbohydrate metabolism and fatty-acid synthesis.4 Body stores are minimal, although the liver can convert tryptophan to niacin.4
In the United States, pellagra has become rare since niacin enrichment of bread and flour began in the 1940s. However, the risk is increased in those with chronic alcohol dependency, metabolic disease such as carcinoid syndrome, and malabsorptive states such as Crohn disease.5 Alcohol abuse is commonly associated with micronutrient deficiencies. Even in alcoholics with sufficient food intake, their ability to absorb niacin may be impaired both directly and indirectly because of the toxic effects of alcohol on the gastrointestinal tract.5
The three D’s of niacin deficiency
The clinical picture of pellagra includes the three “D’s” of niacin deficiency—diarrhea, dementia, and dermatitis—representing the organ systems most commonly affected (ie, the gastrointestinal tract, nervous system, and skin). Gastrointestinal signs and symptoms may include anorexia, diarrhea, stomatitis, and abdominal discomfort.4 Neurologic signs and symptoms are the most frequent clinical manifestations of pellagra but are often overlooked in alcoholics with altered mental status.5,6 Early neurologic findings may include apathy, depression, paresthesias, dizziness, and falling.4,5 Later findings may include hallucinations, seizures, and psychosis.4,5 If severe enough, this may progress to coma and to a fourth “D”—death—if left untreated.
Skin findings, if present, are typically the most characteristic of pellagra.5,6 They include a photosensitive eruption that most commonly appears on the face, arms, and the “V” of the neck (“Casal’s necklace”).3,6 Erythema develops on areas of sun-exposed skin and may be painful or pruritic.6 It may take up to four times as long to resolve as a normal sunburn.6 On repeated exposure, the skin becomes thickened, hyperkeratotic, and hyperpigmented.6
DIAGNOSIS AND TREATMENT OF PELLAGRA
Suspicion of pellagra should be high in any patient with chronic alcohol abuse with changes in mental status.5 Pellagra is typically diagnosed clinically. Although testing of serum levels of niacin or urine levels of niacin metabolites can be performed,4,5 these tests are not commonly used, as they are neither widely available nor reliable.3,4 Because there is little downside to giving niacin, treatment should be started if there is clinical suspicion of pellagra.3,4 The diagnosis is confirmed by clinical improvement after niacin replacement begins.4
Pellagra is easy and inexpensive to treat once the diagnosis has been established. Supplementation can be given orally at 50 mg to 100 mg three times daily, with a maximum of 500 mg daily for 3 to 4 weeks.3,5 The multivitamin our patient initially received provided only 30 mg of niacin, which was insufficient to treat his deficiency.
Other micronutrient deficiencies are also common in pellagra, such as the suspected thiamine deficiency in this patient. Although rare in adults, pyridoxine deficiency should be considered because pyridoxine plays an important role in niacin metabolism, and in patients such as this, the signs and symptoms of pellagra will not resolve with niacin administration alone.3,4
Neurologic symptoms can begin to resolve as soon as 24 to 48 hours after replacement therapy is started, although skin symptoms take longer to respond.6
OUR PATIENT’S MANAGEMENT AND LESSONS LEARNED
Our patient was treated with extended-release niacin 500 mg daily. He was significantly less confused within 24 hours, and 2 days later he was no longer delirious. His diarrhea resolved, but his peripheral neuropathy improved only modestly, and we believe that this was the result of his long history of alcohol abuse.
Although there are guidelines to help with the management of patients undergoing alcohol withdrawal, our experience with this patient illustrates that important clinical conditions, including micronutrient deficiencies, can easily be overlooked or misattributed, with potentially dangerous consequences. It is crucial to be mindful of these considerations.
- Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). Br J Addict 1989; 84:1353–1357.
- Thomson AD, Cook CC, Touquet R, Henry JA; Royal College of Physicians, London. The Royal College of Physicians report on alcohol: guidelines for managing Wernicke’s encephalopathy in the accident and Emergency Department. Alcohol Alcohol 2002; 37:513–521.
- Weathers AL, Lewis SL. Rare and unusual … or are they? Less commonly diagnosed encephalopathies associated with systemic disease. Semin Neurol 2009; 29:136–153.
- World Health Organization, United Nations High Commissions for Refugees. Pellagra and its prevention and control in major emergencies. 2000. http://www.who.int/nutrition/publications/emergencies/WHO_NHD_00.10/en/index.html. Accessed April 26, 2014.
- Oldham MA, Ivkovic A. Pellagrous encephalopathy presenting as alcohol withdrawal delirium: a case series and literature review. Addict Sci Clin Pract 2012; 7:12.
- Karthikeyan K, Thappa DM. Pellagra and skin. Int J Dermatol 2002; 41:476–481.
- Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). Br J Addict 1989; 84:1353–1357.
- Thomson AD, Cook CC, Touquet R, Henry JA; Royal College of Physicians, London. The Royal College of Physicians report on alcohol: guidelines for managing Wernicke’s encephalopathy in the accident and Emergency Department. Alcohol Alcohol 2002; 37:513–521.
- Weathers AL, Lewis SL. Rare and unusual … or are they? Less commonly diagnosed encephalopathies associated with systemic disease. Semin Neurol 2009; 29:136–153.
- World Health Organization, United Nations High Commissions for Refugees. Pellagra and its prevention and control in major emergencies. 2000. http://www.who.int/nutrition/publications/emergencies/WHO_NHD_00.10/en/index.html. Accessed April 26, 2014.
- Oldham MA, Ivkovic A. Pellagrous encephalopathy presenting as alcohol withdrawal delirium: a case series and literature review. Addict Sci Clin Pract 2012; 7:12.
- Karthikeyan K, Thappa DM. Pellagra and skin. Int J Dermatol 2002; 41:476–481.
Do patients who received only two doses of hepatitis B vaccine need a booster?
The Advisory Committee on Immunization Practices (ACIP) currently recommends that people who have not completed the three-dose vaccination series against hepatitis B virus (HBV) should receive the missed doses: ie, the three-dose regimen does not need to be restarted.1 However, evidence suggests that a two-dose regimen may provide adequate seroprotection for healthy young adults.
As the three-dose regimen has been shown to protect 90% to 100% of adults,2 it has gained widespread acceptance and is now standard clinical practice.2 However, deviating from the three-dose regimen may not leave healthy young adults vulnerable to HBV infection.
RECOMMENDED DOSES AND SCHEDULES
Widespread use of the three-dose regimen for HBV stemmed from the first clinical evaluation of the recombinant vaccine, in which three 10-μg doses were given at 0, 1, and 6 months to healthy, low-risk adult volunteers.3 This regimen was shown to provide seroprotection in over 95% of adolescents and 90% of healthy adults.2
Currently, three HBV vaccines for adults are approved in the United States: Recombivax HB, Engerix-B, and Twinrix (Table 1). While Recombivax has a seroprotection rate of 89% in healthy adults over age 40, it has higher seroprotection rates in younger people: eg, two doses of Recombivax given 4 to 6 months apart provide seroprotection to 99% of children aged 11 to 15.4 On the other hand, patients on hemodialysis require three 40-μg doses of Recombivax or four 40-μg doses of Engerix-B.
Evidence for a two-dose regimen
Since the development of the recombinant HBV vaccine used today, studies have shown that a two-dose regimen offers seroprotection comparable with, if not better than, the three-dose regimen in adolescents and healthy young adults. Marsano et al5 found that with a two-dose regimen, 96% to 99% of young adults attained seroprotection, with immune memory persisting for up to 2 years.5 Moreover, Cassidy et al6 randomized adolescents to a two-dose or a three-dose regimen and found the two regimens to be equally effective in conferring immunogenicity and immunologic memory.6
Other studies in adolescents have confirmed these findings and offered new evidence in support of the two-dose regimen.7,8 For example, studies found that the two-dose regimen conferred seroprotection at even lower doses than previously studied, and that it conferred immune memory lasting at least 5 years.6,7
However, because these studies were conducted in adolescents and healthy young adults, the findings may not hold true for other populations. Studies suggest that the three-dose regimen is best for those over age 40. Moreover, it is advisable to adhere to a three-dose regimen when treating people at high risk of contracting HBV, such as health care workers; people with chronic liver disease, diabetes mellitus, or end-stage renal disease on hemodialysis; people who have multiple sex partners; and men who have sex with men.
The impact of long intervals between doses
Although the aforementioned studies focused on a two-dose regimen with a 6-month interval, longer intervals between doses do not impair seroprotection and in some cases may even prove beneficial. Heron et al9 demonstrated that a two-dose regimen with a 12-month interval induces seroprotection as effectively as a standard three-dose or two-dose regimen with a 6-month interval.9 Moreover, studies of the impact of deviating from a three-dose regimen found that intervals of longer than 1 year did not impede seroprotection. Not only may seroprotection be attained with intervals of 5 to 10 years before the final dose, but final antibody levels tend to increase with increasing time between doses.10
Nevertheless, even though an extended interval between doses may prove beneficial after the final dose is received, delaying doses may leave patients unprotected. Indeed, alternative three-dose and even four-dose schedules with shorter intervals between doses exist for certain high-risk populations, such as those recently exposed to HBV and travelers to areas of high prevalence. Therefore, intentionally extending intervals between doses may be inappropriate.
SEROPROTECTION AND PROTECTION AGAINST INFECTION
Legitimate concerns exist about the final antibody level attained with a two-dose regimen, which is typically lower than that attained with a three-dose regimen. As HBV antibody levels decline with time, lower final antibody levels theoretically increase the risk of losing seroprotection. Study of vaccine efficacy has defined seroprotection as antibody levels greater than or equal to 10 mIU/mL.11 Yet evidence suggests that even when antibody levels drop below this level, the risk of symptomatic HBV infection does not increase. Evidence also suggests that immune memory outlasts the presence of seroprotective antibody levels, indicating that true protection against significant infection does not necessarily correlate with, and may even exceed, seroprotection.2 This may relate to HBV’s long incubation period, which allows memory cells time to generate an effective immune response.10 For example, Floreani et al12 showed that even though 15% of adults lost seroprotective antibody levels 10 years after vaccination, none demonstrated hepatitis B antigen reactivity or seroconversion.
POSTVACCINATION TESTING AND ADDITIONAL DOSES
At times, it may be wise to measure antibody levels after the final dose to confirm seroprotection. Seroprotection should be documented when knowledge of the patient’s immune status will affect subsequent management. As recommended by the US Centers for Disease Control and Prevention, health care workers, hemodialysis patients, immunocompromised patients, and sexual partners of patients with chronic HBV infection should undergo antibody testing 1 to 2 months after the completion of a three-dose vaccination regimen. Hemodialysis patients require annual confirmation of seroprotection and should receive booster doses of HBV vaccine if necessary.
Postvaccination testing (quantitative HBV surface antibody testing) costs about the same as a single dose of HBV vaccine. Therefore, if postvaccination testing is considered because of missed vaccine doses, it may be more cost-efficient to simply administer the missed dose.
- Department of Health and Human Services. Appendix A Immunization Management Issues. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5516a2.htm. Accessed April 6, 2014.
- Leuridan E, Van Damme P. Hepatitis B and the need for a booster dose. Clin Infect Dis 2011; 53:68–75.
- Scolnick EM, McLean AA, West DJ, McAleer WJ, Miller WJ, Buynak EB. Clinical evaluation in healthy adults of a hepatitis B vaccine made by recombinant DNA. JAMA 1984; 251:2812–2815.
- Merck and Co, Inc. 1998. Recombivax HB. http://www.merck.com/product/usa/pi_circulars/r/recombivax_hb/re-combivax_pi.pdf. Accessed April 7, 2014.
- Marsano LS, West DJ, Chan I, et al. A two-dose hepatitis B vaccine regimen: proof of priming and memory responses in young adults. Vaccine 1998; 16:624–629.
- Cassidy WM, Watson B, Ioli VA, Williams K, Bird S, West DJ. A randomized trial of alternative two- and three-dose hepatitis B vaccination regimens in adolescents: antibody responses, safety, and immunologic memory. Pediatrics 2001; 107:626–631.
- Van Damme P, Moiseeva A, Marichev I, et al. Five years follow-up following two or three doses of a hepatitis B vaccine in adolescents aged 11–15 years: a randomised controlled study. BMC Infect Dis 2010; 10:357.
- Heron L, Selnikova O, Moiseieva A, et al. Immunogenicity, reactogenicity and safety of two-dose versus three-dose (standard care) hepatitis B immunisation of healthy adolescents aged 11–15 years: a randomised controlled trial. Vaccine 2007; 25:2817–2822.
- Heron LG, Chant KG, Jalaludin BB. A novel hepatitis B vaccination regimen for adolescents: two doses 12 months apart. Vaccine 2002; 20:3472–3476.
- Jackson Y, Chappuis F, Mezger N, Kanappa K, Loutan L. High immunogenicity of delayed third dose of hepatitis B vaccine in travellers. Vaccine 2007; 25:3482–3484.
- Jack AD, Hall AJ, Maine N, Mendy M, Whittle HC. What level of hepatitis B antibody is protective? J Infect Dis 1999; 179:489–492.
- Floreani A, Baldo V, Cristofoletti M, et al. Long-term persistence of anti-HBs after vaccination against HBV: an 18 year experience in health care workers. Vaccine 2004; 22:607–610.
The Advisory Committee on Immunization Practices (ACIP) currently recommends that people who have not completed the three-dose vaccination series against hepatitis B virus (HBV) should receive the missed doses: ie, the three-dose regimen does not need to be restarted.1 However, evidence suggests that a two-dose regimen may provide adequate seroprotection for healthy young adults.
As the three-dose regimen has been shown to protect 90% to 100% of adults,2 it has gained widespread acceptance and is now standard clinical practice.2 However, deviating from the three-dose regimen may not leave healthy young adults vulnerable to HBV infection.
RECOMMENDED DOSES AND SCHEDULES
Widespread use of the three-dose regimen for HBV stemmed from the first clinical evaluation of the recombinant vaccine, in which three 10-μg doses were given at 0, 1, and 6 months to healthy, low-risk adult volunteers.3 This regimen was shown to provide seroprotection in over 95% of adolescents and 90% of healthy adults.2
Currently, three HBV vaccines for adults are approved in the United States: Recombivax HB, Engerix-B, and Twinrix (Table 1). While Recombivax has a seroprotection rate of 89% in healthy adults over age 40, it has higher seroprotection rates in younger people: eg, two doses of Recombivax given 4 to 6 months apart provide seroprotection to 99% of children aged 11 to 15.4 On the other hand, patients on hemodialysis require three 40-μg doses of Recombivax or four 40-μg doses of Engerix-B.
Evidence for a two-dose regimen
Since the development of the recombinant HBV vaccine used today, studies have shown that a two-dose regimen offers seroprotection comparable with, if not better than, the three-dose regimen in adolescents and healthy young adults. Marsano et al5 found that with a two-dose regimen, 96% to 99% of young adults attained seroprotection, with immune memory persisting for up to 2 years.5 Moreover, Cassidy et al6 randomized adolescents to a two-dose or a three-dose regimen and found the two regimens to be equally effective in conferring immunogenicity and immunologic memory.6
Other studies in adolescents have confirmed these findings and offered new evidence in support of the two-dose regimen.7,8 For example, studies found that the two-dose regimen conferred seroprotection at even lower doses than previously studied, and that it conferred immune memory lasting at least 5 years.6,7
However, because these studies were conducted in adolescents and healthy young adults, the findings may not hold true for other populations. Studies suggest that the three-dose regimen is best for those over age 40. Moreover, it is advisable to adhere to a three-dose regimen when treating people at high risk of contracting HBV, such as health care workers; people with chronic liver disease, diabetes mellitus, or end-stage renal disease on hemodialysis; people who have multiple sex partners; and men who have sex with men.
The impact of long intervals between doses
Although the aforementioned studies focused on a two-dose regimen with a 6-month interval, longer intervals between doses do not impair seroprotection and in some cases may even prove beneficial. Heron et al9 demonstrated that a two-dose regimen with a 12-month interval induces seroprotection as effectively as a standard three-dose or two-dose regimen with a 6-month interval.9 Moreover, studies of the impact of deviating from a three-dose regimen found that intervals of longer than 1 year did not impede seroprotection. Not only may seroprotection be attained with intervals of 5 to 10 years before the final dose, but final antibody levels tend to increase with increasing time between doses.10
Nevertheless, even though an extended interval between doses may prove beneficial after the final dose is received, delaying doses may leave patients unprotected. Indeed, alternative three-dose and even four-dose schedules with shorter intervals between doses exist for certain high-risk populations, such as those recently exposed to HBV and travelers to areas of high prevalence. Therefore, intentionally extending intervals between doses may be inappropriate.
SEROPROTECTION AND PROTECTION AGAINST INFECTION
Legitimate concerns exist about the final antibody level attained with a two-dose regimen, which is typically lower than that attained with a three-dose regimen. As HBV antibody levels decline with time, lower final antibody levels theoretically increase the risk of losing seroprotection. Study of vaccine efficacy has defined seroprotection as antibody levels greater than or equal to 10 mIU/mL.11 Yet evidence suggests that even when antibody levels drop below this level, the risk of symptomatic HBV infection does not increase. Evidence also suggests that immune memory outlasts the presence of seroprotective antibody levels, indicating that true protection against significant infection does not necessarily correlate with, and may even exceed, seroprotection.2 This may relate to HBV’s long incubation period, which allows memory cells time to generate an effective immune response.10 For example, Floreani et al12 showed that even though 15% of adults lost seroprotective antibody levels 10 years after vaccination, none demonstrated hepatitis B antigen reactivity or seroconversion.
POSTVACCINATION TESTING AND ADDITIONAL DOSES
At times, it may be wise to measure antibody levels after the final dose to confirm seroprotection. Seroprotection should be documented when knowledge of the patient’s immune status will affect subsequent management. As recommended by the US Centers for Disease Control and Prevention, health care workers, hemodialysis patients, immunocompromised patients, and sexual partners of patients with chronic HBV infection should undergo antibody testing 1 to 2 months after the completion of a three-dose vaccination regimen. Hemodialysis patients require annual confirmation of seroprotection and should receive booster doses of HBV vaccine if necessary.
Postvaccination testing (quantitative HBV surface antibody testing) costs about the same as a single dose of HBV vaccine. Therefore, if postvaccination testing is considered because of missed vaccine doses, it may be more cost-efficient to simply administer the missed dose.
The Advisory Committee on Immunization Practices (ACIP) currently recommends that people who have not completed the three-dose vaccination series against hepatitis B virus (HBV) should receive the missed doses: ie, the three-dose regimen does not need to be restarted.1 However, evidence suggests that a two-dose regimen may provide adequate seroprotection for healthy young adults.
As the three-dose regimen has been shown to protect 90% to 100% of adults,2 it has gained widespread acceptance and is now standard clinical practice.2 However, deviating from the three-dose regimen may not leave healthy young adults vulnerable to HBV infection.
RECOMMENDED DOSES AND SCHEDULES
Widespread use of the three-dose regimen for HBV stemmed from the first clinical evaluation of the recombinant vaccine, in which three 10-μg doses were given at 0, 1, and 6 months to healthy, low-risk adult volunteers.3 This regimen was shown to provide seroprotection in over 95% of adolescents and 90% of healthy adults.2
Currently, three HBV vaccines for adults are approved in the United States: Recombivax HB, Engerix-B, and Twinrix (Table 1). While Recombivax has a seroprotection rate of 89% in healthy adults over age 40, it has higher seroprotection rates in younger people: eg, two doses of Recombivax given 4 to 6 months apart provide seroprotection to 99% of children aged 11 to 15.4 On the other hand, patients on hemodialysis require three 40-μg doses of Recombivax or four 40-μg doses of Engerix-B.
Evidence for a two-dose regimen
Since the development of the recombinant HBV vaccine used today, studies have shown that a two-dose regimen offers seroprotection comparable with, if not better than, the three-dose regimen in adolescents and healthy young adults. Marsano et al5 found that with a two-dose regimen, 96% to 99% of young adults attained seroprotection, with immune memory persisting for up to 2 years.5 Moreover, Cassidy et al6 randomized adolescents to a two-dose or a three-dose regimen and found the two regimens to be equally effective in conferring immunogenicity and immunologic memory.6
Other studies in adolescents have confirmed these findings and offered new evidence in support of the two-dose regimen.7,8 For example, studies found that the two-dose regimen conferred seroprotection at even lower doses than previously studied, and that it conferred immune memory lasting at least 5 years.6,7
However, because these studies were conducted in adolescents and healthy young adults, the findings may not hold true for other populations. Studies suggest that the three-dose regimen is best for those over age 40. Moreover, it is advisable to adhere to a three-dose regimen when treating people at high risk of contracting HBV, such as health care workers; people with chronic liver disease, diabetes mellitus, or end-stage renal disease on hemodialysis; people who have multiple sex partners; and men who have sex with men.
The impact of long intervals between doses
Although the aforementioned studies focused on a two-dose regimen with a 6-month interval, longer intervals between doses do not impair seroprotection and in some cases may even prove beneficial. Heron et al9 demonstrated that a two-dose regimen with a 12-month interval induces seroprotection as effectively as a standard three-dose or two-dose regimen with a 6-month interval.9 Moreover, studies of the impact of deviating from a three-dose regimen found that intervals of longer than 1 year did not impede seroprotection. Not only may seroprotection be attained with intervals of 5 to 10 years before the final dose, but final antibody levels tend to increase with increasing time between doses.10
Nevertheless, even though an extended interval between doses may prove beneficial after the final dose is received, delaying doses may leave patients unprotected. Indeed, alternative three-dose and even four-dose schedules with shorter intervals between doses exist for certain high-risk populations, such as those recently exposed to HBV and travelers to areas of high prevalence. Therefore, intentionally extending intervals between doses may be inappropriate.
SEROPROTECTION AND PROTECTION AGAINST INFECTION
Legitimate concerns exist about the final antibody level attained with a two-dose regimen, which is typically lower than that attained with a three-dose regimen. As HBV antibody levels decline with time, lower final antibody levels theoretically increase the risk of losing seroprotection. Study of vaccine efficacy has defined seroprotection as antibody levels greater than or equal to 10 mIU/mL.11 Yet evidence suggests that even when antibody levels drop below this level, the risk of symptomatic HBV infection does not increase. Evidence also suggests that immune memory outlasts the presence of seroprotective antibody levels, indicating that true protection against significant infection does not necessarily correlate with, and may even exceed, seroprotection.2 This may relate to HBV’s long incubation period, which allows memory cells time to generate an effective immune response.10 For example, Floreani et al12 showed that even though 15% of adults lost seroprotective antibody levels 10 years after vaccination, none demonstrated hepatitis B antigen reactivity or seroconversion.
POSTVACCINATION TESTING AND ADDITIONAL DOSES
At times, it may be wise to measure antibody levels after the final dose to confirm seroprotection. Seroprotection should be documented when knowledge of the patient’s immune status will affect subsequent management. As recommended by the US Centers for Disease Control and Prevention, health care workers, hemodialysis patients, immunocompromised patients, and sexual partners of patients with chronic HBV infection should undergo antibody testing 1 to 2 months after the completion of a three-dose vaccination regimen. Hemodialysis patients require annual confirmation of seroprotection and should receive booster doses of HBV vaccine if necessary.
Postvaccination testing (quantitative HBV surface antibody testing) costs about the same as a single dose of HBV vaccine. Therefore, if postvaccination testing is considered because of missed vaccine doses, it may be more cost-efficient to simply administer the missed dose.
- Department of Health and Human Services. Appendix A Immunization Management Issues. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5516a2.htm. Accessed April 6, 2014.
- Leuridan E, Van Damme P. Hepatitis B and the need for a booster dose. Clin Infect Dis 2011; 53:68–75.
- Scolnick EM, McLean AA, West DJ, McAleer WJ, Miller WJ, Buynak EB. Clinical evaluation in healthy adults of a hepatitis B vaccine made by recombinant DNA. JAMA 1984; 251:2812–2815.
- Merck and Co, Inc. 1998. Recombivax HB. http://www.merck.com/product/usa/pi_circulars/r/recombivax_hb/re-combivax_pi.pdf. Accessed April 7, 2014.
- Marsano LS, West DJ, Chan I, et al. A two-dose hepatitis B vaccine regimen: proof of priming and memory responses in young adults. Vaccine 1998; 16:624–629.
- Cassidy WM, Watson B, Ioli VA, Williams K, Bird S, West DJ. A randomized trial of alternative two- and three-dose hepatitis B vaccination regimens in adolescents: antibody responses, safety, and immunologic memory. Pediatrics 2001; 107:626–631.
- Van Damme P, Moiseeva A, Marichev I, et al. Five years follow-up following two or three doses of a hepatitis B vaccine in adolescents aged 11–15 years: a randomised controlled study. BMC Infect Dis 2010; 10:357.
- Heron L, Selnikova O, Moiseieva A, et al. Immunogenicity, reactogenicity and safety of two-dose versus three-dose (standard care) hepatitis B immunisation of healthy adolescents aged 11–15 years: a randomised controlled trial. Vaccine 2007; 25:2817–2822.
- Heron LG, Chant KG, Jalaludin BB. A novel hepatitis B vaccination regimen for adolescents: two doses 12 months apart. Vaccine 2002; 20:3472–3476.
- Jackson Y, Chappuis F, Mezger N, Kanappa K, Loutan L. High immunogenicity of delayed third dose of hepatitis B vaccine in travellers. Vaccine 2007; 25:3482–3484.
- Jack AD, Hall AJ, Maine N, Mendy M, Whittle HC. What level of hepatitis B antibody is protective? J Infect Dis 1999; 179:489–492.
- Floreani A, Baldo V, Cristofoletti M, et al. Long-term persistence of anti-HBs after vaccination against HBV: an 18 year experience in health care workers. Vaccine 2004; 22:607–610.
- Department of Health and Human Services. Appendix A Immunization Management Issues. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5516a2.htm. Accessed April 6, 2014.
- Leuridan E, Van Damme P. Hepatitis B and the need for a booster dose. Clin Infect Dis 2011; 53:68–75.
- Scolnick EM, McLean AA, West DJ, McAleer WJ, Miller WJ, Buynak EB. Clinical evaluation in healthy adults of a hepatitis B vaccine made by recombinant DNA. JAMA 1984; 251:2812–2815.
- Merck and Co, Inc. 1998. Recombivax HB. http://www.merck.com/product/usa/pi_circulars/r/recombivax_hb/re-combivax_pi.pdf. Accessed April 7, 2014.
- Marsano LS, West DJ, Chan I, et al. A two-dose hepatitis B vaccine regimen: proof of priming and memory responses in young adults. Vaccine 1998; 16:624–629.
- Cassidy WM, Watson B, Ioli VA, Williams K, Bird S, West DJ. A randomized trial of alternative two- and three-dose hepatitis B vaccination regimens in adolescents: antibody responses, safety, and immunologic memory. Pediatrics 2001; 107:626–631.
- Van Damme P, Moiseeva A, Marichev I, et al. Five years follow-up following two or three doses of a hepatitis B vaccine in adolescents aged 11–15 years: a randomised controlled study. BMC Infect Dis 2010; 10:357.
- Heron L, Selnikova O, Moiseieva A, et al. Immunogenicity, reactogenicity and safety of two-dose versus three-dose (standard care) hepatitis B immunisation of healthy adolescents aged 11–15 years: a randomised controlled trial. Vaccine 2007; 25:2817–2822.
- Heron LG, Chant KG, Jalaludin BB. A novel hepatitis B vaccination regimen for adolescents: two doses 12 months apart. Vaccine 2002; 20:3472–3476.
- Jackson Y, Chappuis F, Mezger N, Kanappa K, Loutan L. High immunogenicity of delayed third dose of hepatitis B vaccine in travellers. Vaccine 2007; 25:3482–3484.
- Jack AD, Hall AJ, Maine N, Mendy M, Whittle HC. What level of hepatitis B antibody is protective? J Infect Dis 1999; 179:489–492.
- Floreani A, Baldo V, Cristofoletti M, et al. Long-term persistence of anti-HBs after vaccination against HBV: an 18 year experience in health care workers. Vaccine 2004; 22:607–610.
COPD: More options mean potentially better control
Some common diseases outside of my specialty areas of interest have, over time, blended into the background of daily practice. When patients have clearly inadequately controlled disease I refer them back to their internist or relevant subspecialist. Otherwise I find myself accepting the clinical status quo, providing stopgap care when necessary, utilizing my present knowledge of the disease process. But if I am not aware of any paradigm shifts in management, I tend to just peruse the published studies of new drug therapies as they appear in major journals, and not necessarily incorporate new therapies into my practice.
Chronic obstructive pulmonary disease (COPD) is one of those diseases, and the update by Hatipoğlu and Aboussouan in this issue of the Journal provided the opportunity to review some important things I have missed and to take note of the therapeutic principles that haven’t changed that much.
The incidence of COPD seems to be increasing. Cigarette smoking remains the major reversible cause, but one-fourth of current COPD patients have never smoked.
Patients who have early COPD may not be asked about or may not volunteer complaints specific to COPD. Lung examinations are insensitive, and chest radiography, if done, rarely identifies patients with early disease, so it is no surprise that COPD is underdiagnosed. While for many patients it is unclear whether the natural progression of lung damage can be dramatically altered by early diagnosis, other than by stopping smoking, that may not be the case for subsets of patients such as those with alpha-1 antitrypsin deficiency. But COPD generally has to be suspected in order to prompt appropriate screening for it.
COPD is still diagnosed by spirometry, with findings demonstrating incompletely reversible airway obstruction. The forced expiratory volume in 1 second (FEV1), a spirometric measure required to make the diagnosis, has been a useful surrogate marker of drug efficacy, but it is far from the ideal measure of disease progression and risk of death. Patients who have frequent exacerbations requiring hospitalization tend to have a tumultuous clinical course. The best predictor of future exacerbations is the patient’s history of exacerbations. Reducing the exacerbation rate improves the quality of life but may not translate to a benefit in terms of the mortality risk.
A lower risk of death is most consistently attained by helping patients stop smoking and, if they have sustained hypoxemia, giving them supplemental oxygen. The former intervention is the population game-changer—yet the US Centers for Disease Control and Prevention reports that 18% of American adults still smoke cigarettes, a number that dropped only slightly between 2005 and 2012. Americans with less education and less income more frequently smoke cigarettes, and it is estimated that one in 13 Americans currently 17 years or younger will die prematurely from the effects of cigarette smoking.
As for newer therapies, many that are applicable to most patients with COPD represent a fine-tuning of drug therapies we have been using for decades. Thus, it is not surprising that no dramatic increase in survival rates has been achieved. The advantage of several of the newer therapies in terms of FEV1 or exacerbation rate is statistically significant but relatively modest in terms of clinical impact. Their clinical promise (including specific antibiotics in low doses), revealed in recent studies, may be dependent upon using them in the most appropriate patients. Reducing the exacerbation rate is a significant advantage, but I would also like to know which drugs or drug combinations are most likely to permit major reductions in patients’ corticosteroid requirements. Hopefully, these data will come from real-world comparative efficacy studies.
Reading the article by Hatipoğlu and Aboussouan, I was reminded that utilizing our pulmonary colleagues’ expertise is of particular value in individualizing therapy for our patients with COPD—using newer drugs and combinations when most appropriate, not just because they are readily available. As physicians who are not pulmonary specialists, we need to be vigilant in recognizing the treatable comorbidities that contribute to dyspnea and poor outcome in patients with COPD, such as obstructive sleep apnea, congestive heart failure, obesity, and thromboembolism.
But to make the largest impact on the mortality rate, we need to continue to engage in and expand the ongoing war against cigarette use.
Some common diseases outside of my specialty areas of interest have, over time, blended into the background of daily practice. When patients have clearly inadequately controlled disease I refer them back to their internist or relevant subspecialist. Otherwise I find myself accepting the clinical status quo, providing stopgap care when necessary, utilizing my present knowledge of the disease process. But if I am not aware of any paradigm shifts in management, I tend to just peruse the published studies of new drug therapies as they appear in major journals, and not necessarily incorporate new therapies into my practice.
Chronic obstructive pulmonary disease (COPD) is one of those diseases, and the update by Hatipoğlu and Aboussouan in this issue of the Journal provided the opportunity to review some important things I have missed and to take note of the therapeutic principles that haven’t changed that much.
The incidence of COPD seems to be increasing. Cigarette smoking remains the major reversible cause, but one-fourth of current COPD patients have never smoked.
Patients who have early COPD may not be asked about or may not volunteer complaints specific to COPD. Lung examinations are insensitive, and chest radiography, if done, rarely identifies patients with early disease, so it is no surprise that COPD is underdiagnosed. While for many patients it is unclear whether the natural progression of lung damage can be dramatically altered by early diagnosis, other than by stopping smoking, that may not be the case for subsets of patients such as those with alpha-1 antitrypsin deficiency. But COPD generally has to be suspected in order to prompt appropriate screening for it.
COPD is still diagnosed by spirometry, with findings demonstrating incompletely reversible airway obstruction. The forced expiratory volume in 1 second (FEV1), a spirometric measure required to make the diagnosis, has been a useful surrogate marker of drug efficacy, but it is far from the ideal measure of disease progression and risk of death. Patients who have frequent exacerbations requiring hospitalization tend to have a tumultuous clinical course. The best predictor of future exacerbations is the patient’s history of exacerbations. Reducing the exacerbation rate improves the quality of life but may not translate to a benefit in terms of the mortality risk.
A lower risk of death is most consistently attained by helping patients stop smoking and, if they have sustained hypoxemia, giving them supplemental oxygen. The former intervention is the population game-changer—yet the US Centers for Disease Control and Prevention reports that 18% of American adults still smoke cigarettes, a number that dropped only slightly between 2005 and 2012. Americans with less education and less income more frequently smoke cigarettes, and it is estimated that one in 13 Americans currently 17 years or younger will die prematurely from the effects of cigarette smoking.
As for newer therapies, many that are applicable to most patients with COPD represent a fine-tuning of drug therapies we have been using for decades. Thus, it is not surprising that no dramatic increase in survival rates has been achieved. The advantage of several of the newer therapies in terms of FEV1 or exacerbation rate is statistically significant but relatively modest in terms of clinical impact. Their clinical promise (including specific antibiotics in low doses), revealed in recent studies, may be dependent upon using them in the most appropriate patients. Reducing the exacerbation rate is a significant advantage, but I would also like to know which drugs or drug combinations are most likely to permit major reductions in patients’ corticosteroid requirements. Hopefully, these data will come from real-world comparative efficacy studies.
Reading the article by Hatipoğlu and Aboussouan, I was reminded that utilizing our pulmonary colleagues’ expertise is of particular value in individualizing therapy for our patients with COPD—using newer drugs and combinations when most appropriate, not just because they are readily available. As physicians who are not pulmonary specialists, we need to be vigilant in recognizing the treatable comorbidities that contribute to dyspnea and poor outcome in patients with COPD, such as obstructive sleep apnea, congestive heart failure, obesity, and thromboembolism.
But to make the largest impact on the mortality rate, we need to continue to engage in and expand the ongoing war against cigarette use.
Some common diseases outside of my specialty areas of interest have, over time, blended into the background of daily practice. When patients have clearly inadequately controlled disease I refer them back to their internist or relevant subspecialist. Otherwise I find myself accepting the clinical status quo, providing stopgap care when necessary, utilizing my present knowledge of the disease process. But if I am not aware of any paradigm shifts in management, I tend to just peruse the published studies of new drug therapies as they appear in major journals, and not necessarily incorporate new therapies into my practice.
Chronic obstructive pulmonary disease (COPD) is one of those diseases, and the update by Hatipoğlu and Aboussouan in this issue of the Journal provided the opportunity to review some important things I have missed and to take note of the therapeutic principles that haven’t changed that much.
The incidence of COPD seems to be increasing. Cigarette smoking remains the major reversible cause, but one-fourth of current COPD patients have never smoked.
Patients who have early COPD may not be asked about or may not volunteer complaints specific to COPD. Lung examinations are insensitive, and chest radiography, if done, rarely identifies patients with early disease, so it is no surprise that COPD is underdiagnosed. While for many patients it is unclear whether the natural progression of lung damage can be dramatically altered by early diagnosis, other than by stopping smoking, that may not be the case for subsets of patients such as those with alpha-1 antitrypsin deficiency. But COPD generally has to be suspected in order to prompt appropriate screening for it.
COPD is still diagnosed by spirometry, with findings demonstrating incompletely reversible airway obstruction. The forced expiratory volume in 1 second (FEV1), a spirometric measure required to make the diagnosis, has been a useful surrogate marker of drug efficacy, but it is far from the ideal measure of disease progression and risk of death. Patients who have frequent exacerbations requiring hospitalization tend to have a tumultuous clinical course. The best predictor of future exacerbations is the patient’s history of exacerbations. Reducing the exacerbation rate improves the quality of life but may not translate to a benefit in terms of the mortality risk.
A lower risk of death is most consistently attained by helping patients stop smoking and, if they have sustained hypoxemia, giving them supplemental oxygen. The former intervention is the population game-changer—yet the US Centers for Disease Control and Prevention reports that 18% of American adults still smoke cigarettes, a number that dropped only slightly between 2005 and 2012. Americans with less education and less income more frequently smoke cigarettes, and it is estimated that one in 13 Americans currently 17 years or younger will die prematurely from the effects of cigarette smoking.
As for newer therapies, many that are applicable to most patients with COPD represent a fine-tuning of drug therapies we have been using for decades. Thus, it is not surprising that no dramatic increase in survival rates has been achieved. The advantage of several of the newer therapies in terms of FEV1 or exacerbation rate is statistically significant but relatively modest in terms of clinical impact. Their clinical promise (including specific antibiotics in low doses), revealed in recent studies, may be dependent upon using them in the most appropriate patients. Reducing the exacerbation rate is a significant advantage, but I would also like to know which drugs or drug combinations are most likely to permit major reductions in patients’ corticosteroid requirements. Hopefully, these data will come from real-world comparative efficacy studies.
Reading the article by Hatipoğlu and Aboussouan, I was reminded that utilizing our pulmonary colleagues’ expertise is of particular value in individualizing therapy for our patients with COPD—using newer drugs and combinations when most appropriate, not just because they are readily available. As physicians who are not pulmonary specialists, we need to be vigilant in recognizing the treatable comorbidities that contribute to dyspnea and poor outcome in patients with COPD, such as obstructive sleep apnea, congestive heart failure, obesity, and thromboembolism.
But to make the largest impact on the mortality rate, we need to continue to engage in and expand the ongoing war against cigarette use.
Chronic obstructive pulmonary disease: An update for the primary physician
Chronic obstructive pulmonary disease (COPD) has seen several changes in its assessment and treatment in recent years, reflecting advances in our understanding of this common and serious disease.
This review updates busy practitioners on the major advances, including new assessment tools and new therapies.
COMMON AND INCREASING
COPD is the third leading cause of death in the United States, behind heart disease and cancer,1 and of the top five (the others being stroke and accidents), it is the only one that increased in incidence between 2007 and 2010.2 The 11th leading cause of disability-adjusted life years worldwide in 2002, COPD is projected to become the seventh by the year 2030.3
CHARACTERIZED BY OBSTRUCTION
COPD is characterized by persistent and progressive airflow obstruction associated with chronic airway inflammation in response to noxious particles and gases. Disease of the small airways (inflammation, mucus plugging, and fibrosis) and parenchymal destruction (emphysema) limit the flow of air.
COPD is diagnosed by spirometry—specifically, a ratio of forced expiratory volume in 1 second to forced vital capacity (FEV1/FVC) of less than 0.7 after a bronchodilator is given. The severity of airflow limitation is revealed by the FEV1 as a percent of the predicted value.
Cigarette smoking is the major cause of COPD, but the prevalence of COPD is 6.6% in people who have never smoked, and one-fourth of COPD patients in the United States have never smoked.4
GOLDEN GOALS: FEWER SYMPTOMS, LOWER RISK
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) periodically issues evidence-based statements on how to prevent and treat COPD.
In its 2013 update,5 GOLD suggested two goals: improving symptoms and reducing the risk of death, exacerbations, progression of disease, and treatment-related adverse effects. The latter goal—reducing risk—is relatively new.
Exacerbations are acute inflammatory events superimposed on chronic inflammation. The inflammation is often brought on by infection6 and increases the risk of death7 and the risk of a faster decline in lung function.8
Exacerbations may characterize a phenotype of COPD. The Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) analyzed the frequency of COPD exacerbations and associated factors in 2,138 patients with COPD over a period of 3 years.9 Although patients with more severe obstruction tended to have more exacerbations, some patients appeared susceptible to exacerbations irrespective of the severity of obstruction. The best predictor of exacerbations was a history of exacerbations.
HOW DO I ASSESS A PATIENT WITH COPD ON PRESENTATION?
Markers of airflow obstruction such as the FEV1 do not correlate strongly with exertional capacity and health status in patients with COPD.10,11
The BODE index (body mass index, obstruction, dyspnea score, and exercise oximetry) takes into account the multidimensional nature of COPD. It performs better than the FEV1 in predicting the risk of death.12 The propensity for exacerbations and comorbidities further modulates outcome.
Assessing symptoms
The modified British Medical Research Council (mMRC) dyspnea scale, based on work by Fletcher in 1952,13 has five grades, numbered 0 through 4:
- Grade 0—Breathless with strenuous exercise only
- Grade 1—Breathless when hurrying on level ground or walking up a slight hill
- Grade 2—Walks slower than people of the same age on level ground because of shortness of breath or has to stop when walking at own pace on level ground
- Grade 3—Stops for breath after walking about 100 yards or after a few minutes on level ground
- Grade 4—Too breathless to leave the house or breathless when dressing or undressing.
Grade 2 or higher separates symptomatic from asymptomatic COPD.
The COPD Assessment Test (CAT) (www.catestonline.org) is a proprietary questionnaire. Patients use a 6-point scale (numbered 0 though 5) to rate eight symptoms (cough, mucus production, chest tightness, shortness of breath on exertion, limitations in home activities, lack of confidence leaving the home, poor sleep, and lack of energy). A total score of 10 or higher is abnormal.
Four GOLD groups
The new GOLD guidelines (Table 1)5 define four groups of patients according to their severity of airflow obstruction, symptoms, and exacerbation history:
- Group A—fewer symptoms, low risk: Fewer symptoms (“less symptoms,” as worded in the guidelines) means a CAT score less than 10 or an mMRC grade less than 2; “low risk” means no more than one exacerbation per year and an FEV1 of at least 50%
- Group B—more symptoms, low risk: “More symptoms” means a CAT score of 10 or more or an mMRC grade of 2 or more
- Group C—fewer symptoms, high risk: “High risk” means two or more exacerbations per year or an FEV1 less than 50%
- Group D—more symptoms, high risk.
Thus, a patient with an FEV1 of 60% (moderate airflow limitation) who has had one exacerbation during the past year and a CAT score of 8 would be in group A. In contrast, a patient who has an FEV1 of 40% (severe airflow limitation), no history of exacerbations, and a CAT score of 20 would be in group D.
Updated GOLD guidelines suggest utilizing a stepwise approach to treatment, akin to asthma management guidelines, based on patient grouping.5
How accurate is the new GOLD system?
Although practical and suited for use in primary care, the new GOLD system is arbitrary and has not been thoroughly studied, and may therefore need refinement.
Lange et al14 compared the new GOLD system with the previous one in 6,628 patients with COPD. As anticipated, the new system was better at predicting exacerbations, as it incorporates a history of exacerbations in stratification. The presence of symptoms (as determined by an mMRC grade ≥ 2) was a marker of mortality risk that distinguished group A from group B, and group C from group D. Surprisingly, the rate of death was higher in group B (more symptoms, low risk) than in group C (fewer symptoms, high risk).
Notably, most patients in group C qualified for this group because of the severity of airflow obstruction, not because of a history of exacerbations. Therefore, patients whose symptoms are out of proportion to the severity of obstruction may be at higher risk of death, possibly because of comorbidities such as cardiovascular disease.15 Patients who qualified for groups C and D by having both a history of frequent exacerbations (≥ 2 per year) and symptoms rather than either one alone had a higher risk of death in 3 years.
Similarly, the symptom-assessment tool that is used—ie, the mMRC grade or the CAT score—also makes a difference.
The Health-Related Quality of Life in COPD in Europe Study16 retrospectively analyzed data from 1,817 patients to determine whether the cutoff points for symptoms as assessed by mMRC grade and CAT score were equivalent. Although the mMRC grade correlated well with overall health status, the cutoff mMRC grade of 2 or higher did not correspond to a CAT score of 10 or higher, classifying patients with health status impairment as asymptomatic (mean weighted kappa 0.626). The two tools agreed much better when the cutoff was set at an mMRC grade of 1 or higher (mean weighted kappa 0.792).16
Although assessment schemes continue to evolve as data accumulate, we believe the new system is a welcome initiative that reflects the changing notions of COPD.
Comorbidities matter
Another shift is the recognition that certain comorbidities increase the risk of death. In 1,664 patients with COPD who were followed for 51 months, 12 distinct comorbidities were associated with a higher risk of death after multivariate analysis.17
The COTE index (COPD-Specific Comorbidity Test) is based on these findings. It awards points as follows:
- 6 points for cancer of the lung, esophagus, pancreas, or breast, or for anxiety
- 2 points for all other cancers, liver cirrhosis, atrial fibrillation or flutter, diabetes with neuropathy, or pulmonary fibrosis
- 1 point for congestive heart failure, gastric or duodenal ulcer, or coronary artery disease.
A COTE index score of 4 or higher was associated with a risk of death 2.2 times higher in each quartile of the BODE index.
We strongly recommend being aware of comorbidities in COPD patients, particularly when symptoms are out of proportion to the severity of obstruction.
SHOULD I USE ANTIBIOTICS TO TREAT ALL COPD EXACERBATIONS?
Infections are thought to cause more than 80% of acute exacerbations of COPD.
Anthonisen et al,18 in a landmark trial, found broad-spectrum antibiotics to be most helpful if the patient had at least two of the three cardinal symptoms of COPD exacerbation (ie, shortness of breath, increase in sputum volume, and sputum purulence). Antibiotics decreased the rate of treatment failure and led to a more rapid clinical resolution of exacerbation. However, they did not help patients who had milder exacerbations.
Antibiotics may nevertheless have a role in ambulatory patients with mild to moderate COPD who present with exacerbations characterized by one or more cardinal symptoms.
Llor et al,19 in a multicenter randomized double-blind placebo-controlled trial in Spain, concluded that amoxicillin clavulanate (Augmentin) led to higher clinical cure rates and longer time to the next exacerbation in these patients. Most of the benefit was in patients with more symptoms, consistent with the results of the study by Anthonisen et al.18
There is also strong evidence to support the use of antibiotics in addition to systemic corticosteroids in hospitalized patients with acute exacerbations of COPD. A 7-day course of doxycycline (Vibramycin) added to a standard regimen of corticosteroids was associated with higher rates of clinical and microbiological cure on day 10 of the exacerbation.20 In a large retrospective cohort study in 84,621 hospitalized patients with COPD exacerbations, fewer of those who received antibiotics needed mechanical ventilation, died, or were readmitted.21 Although sicker patients received antibiotics more frequently, their mortality rate was lower than in those who did not receive antibiotics, who were presumably less sick.
A meta-analysis confirmed the salutary effect of antibiotics in inpatients and particularly those admitted to the intensive care unit.22 Mortality rates and hospital length of stay were not affected in patients who were not in intensive care.
Biomarkers such as procalcitonin might help reduce the unnecessary use of antibiotics. Stolz et al23 conducted a randomized controlled trial in which they based the decision to give antibiotics on a threshold procalcitonin level of at least 1 μg/L in hospitalized patients with COPD exacerbation. The rate of antibiotic use was reduced by more than 40% in the procalcitonin group without any difference in clinical outcomes, 6-month exacerbation rate, or rehospitalization compared with controls. Nonstandardized procalcitonin assays are a possible barrier to the widespread adoption of this threshold.
Comment. In general, we recommend antibiotics for hospitalized patients with COPD exacerbation and look forward to confirmatory data that support the use of biomarkers. For outpatients, we find the Anthonisen criteria useful for decision-making at the point of care.
ARE THERE ANY NEW INTERVENTIONS TO PREVENT COPD EXACERBATIONS?
Macrolides
Macrolides have a proven role in managing chronic suppurative respiratory diseases such as cystic fibrosis24 and diffuse panbronchiolitis.25 Since they are beneficial at lower doses than those used to treat infection, the mechanism may be anti-inflammatory rather than antimicrobial.
Albert et al26 assigned 1,142 patients who had had a COPD exacerbation within a year before enrollment or who were on home oxygen therapy to receive azithromycin (Zithromax) 250 mg daily or placebo.25 The azithromycin group had fewer acute exacerbations (hazard ratio 0.73, 95% CI 0.63–0.84, P < .001), and more patients in the azithromycin group achieved clinically significant improvements in quality of life, ie, a reduction in the St. George’s Respiratory Questionnaire (SGRQ) score of at least 4 points (43% vs 36%, P = .03). Adverse events that were more common in the azithromycin group were hearing loss (25% vs 20%) and macrolide-resistant strains in nasopharyngeal secretions (81% vs 41%). In subgroup analysis, the benefit in terms of reducing exacerbations was greater in patients over age 65, patients on home oxygen, and patients with moderate or severe obstruction compared with those with very severe obstruction.
Comment. Macrolides are a valuable addition to the agents available for preventing COPD exacerbation (Table 2), but their role is still uncertain. Potential topics of research are whether these drugs have a role in patients already on preventive regimens, whether they would have a greater effect in distinct patient populations (eg, patients who have two or more exacerbations per year), and whether their broader use would lead to a change in the resident flora in the community.
Clinicians should exercise caution in the use of azithromycin in light of recent concern about associated cardiac morbidity and death. All patients should undergo electrocardiography to assess the QTc interval before starting treatment, as in the trial by Albert et al.26
Phosphodiesterase inhibitors
Roflumilast (Daliresp) is an oral phosphodiesterase 4 inhibitor approved for treating exacerbations and symptoms of chronic bronchitis in patients with severe COPD (Table 3). Phosphodiesterase 4, one of the 11 isoforms of the enzyme, is found in immune and inflammatory cells and promotes inflammatory responses. Roflumilast has anti-inflammatory properties but no acute bronchodilatory effect.27 Several phase 3 trials found the compound to have beneficial effects.
Calverley et al28 performed two placebo-controlled double-blind trials in outpatients with the clinical diagnosis of COPD who had chronic cough; increased sputum production; at least one recorded exacerbation requiring corticosteroids or hospitalization, or both; and an FEV1 of 50% or less. Patients were randomized to receive roflumilast 500 μg once a day (n = 1,537) or placebo (n = 1,554) for 1 year. The rate of moderate to severe exacerbations was 1.17 per year with roflumilast vs 1.37 with placebo (P < .0003). Adverse events were significantly more common with roflumilast and were related to the known side effects of the drug, namely, diarrhea, weight loss, decreased appetite, and nausea.
Fabbri et al29 performed two other placebo-controlled double-blind multicenter trials, studying the combinations of roflumilast with salmeterol (Serevent) and roflumilast with tiotropium (Spiriva) compared with placebo in 1,676 patients with COPD who had post-bronchodilator FEV1 values of 40% to 70% of predicted. The mean prebronchodilator FEV1 improved by 49 mL (P < .0001) in the salmeterol-plus-roflumilast trial and by 80 mL (P < .0001) in the tiotropium-plus-roflumilast trial compared with placebo. Fewer patients on roflumilast had exacerbations of any severity in both trials (risk ratio 0.82, P = .0419 and risk ratio 0.75, P = .0169, respectively).
No trial has yet addressed whether roflumilast is better than the combination of a long-acting muscarinic antagonist and a beta agonist, or whether roflumilast can be substituted for inhaled corticosteroids in a new triple-therapy combination. Clinicians should also be aware of psychiatric side effects of roflumilast, which include depression and, possibly, suicide.
ARE THERE ANY NEW BRONCHODILATORS FOR PATIENTS WITH COPD?
Long-acting muscarinic antagonists
Reversible airflow obstruction and mucus secretion are determined by the vagal cholinergic tone in patients with COPD.30 Antagonism of cholinergic (muscarinic) receptors results in bronchodilation and reduction in mucus production. Consequently, inhaled anticholinergic agents are the first-line therapy for COPD (Table 4).
Tiotropium bromide is a long-acting antimuscarinic approved in 2002 by the US Food and Drug Administration (FDA). The UPLIFT trial (Understanding Potential Long-Term Impacts on Function With Tiotropium)31 enrolled 5,993 patients with a mean FEV1 of 48% of predicted. Over a 4-year follow-up, significant improvements in mean FEV1 values (ranging from 87 mL to 103 mL before bronchodilation and 47 mL to 65 mL after bronchodilation, P < .001) in the tiotropium group were observed compared with placebo. The rate of the primary end point—the rate of decline in mean FEV1—was not different between tiotropium and placebo. However, there were important salutary effects in multiple clinical end points in the tiotropium group. Health-related quality of life as measured by the SGRQ improved in a clinically significant manner (> 4 points) in favor of tiotropium in a higher proportion of patients (45% vs 36%, P < .001). Tiotropium reduced the number of exacerbations per patient year (0.73 ± 0.02 vs 0.85 ± 0.02, RR = 0.86 (95% CI 0.81–0.91), P < .001) and the risk of respiratory failure (RR = 0.67, 95% CI 0.51–0.89). There were no significant differences in the risk of myocardial infarction, stroke, or pneumonia.
Aclidinium bromide (Tudorza Pressair) is a long-acting antimuscarinic recently approved by the FDA. Compared with tiotropium, it has a slightly faster onset of action and a considerably shorter half-life (29 hours vs 64 hours).32,33 Its dosage is 400 μg twice daily by inhalation. It provides sustained bronchodilation over 24 hours and may have a favorable side-effect profile, because it undergoes rapid hydrolysis in human plasma.34
ACCORD COPD I35 and ATTAIN,36 two phase 3 trials in patients with moderate-to severe COPD, found that twice-daily aclidinium was associated with statistically and clinically significant (> 100 mL) improvements in trough and peak FEV1 compared with placebo. Health status (assessed by SGRQ) and dyspnea (assessed by transitional dyspnea index) also improved significantly. However, improvements beyond minimum clinically significant thresholds were achieved only with 400 μg twice-daily dosing.
To date, no study has evaluated the impact of aclidinium on COPD exacerbation as a primary end point. Fewer moderate to severe exacerbations were reported in an earlier 52-week study of once-daily aclidinium (ACCLAIM COPD II) but not in ACCLAIM COPD I.37
Aclidinium may offer an advantage over tiotropium in patients who have nocturnal symptoms. Twice-daily aclidinium 400 μg was associated with superior FEV1 area-under-the-curve values compared with placebo and tiotropium, the difference mostly owing to improved nocturnal profile.38
Long-acting beta-2 agonists
Stimulation of airway beta-2 receptors relaxes smooth muscles and consequently dilates bronchioles via a cyclic adenosine monophosphate-dependent pathway.39
Short-acting beta-2 agonists such as albuterol and terbutaline have long been used as rescue medications for obstructive lung disease. Long-acting beta-2 agonists provide sustained bronchodilation and are therefore more efficacious as maintenance medications. Salmeterol, formoterol (Foradil), and arformoterol (Brovana) are long-acting beta-2 agonists in clinical use that are taken twice daily.
Clinical studies indicate that use of long-acting beta-2 agonists leads to significant improvements in FEV1,40–42 dynamic hyperinflation, exercise tolerance,43,44 and dyspnea.45,46 These drugs have also been associated with significant improvements in health-related quality of life and in the frequency of exacerbations.47–49
In patients with asthma, long-acting beta agonists may increase the risk of death.50 In contrast, in patients with COPD, they appear to offer a survival advantage when used in combination with inhaled corticosteroids,51 and some argue that this benefit is entirely from the long-acting beta agonist (a 17% reduction in mortality) rather than the inhaled corticosteroid (0% reduction in mortality).52
Indacaterol (Arcapta), approved in July 2011, is the first once-daily beta agonist or “ultra-long-acting” beta agonist (Table 5). Possibly because it has a high affinity for the lipid raft domain of the cell membrane where beta-2 receptors are coupled to second messengers,53 the drug has a 24-hour duration of action.
In patients with COPD, inhaled indacaterol 150 μg once daily improved airflow obstruction and health status as measured by SGRQ compared with salmeterol 50 μg twice daily and placebo.54 At the higher dose of 300 μg daily, the 52-week INVOLVE trial55 demonstrated early and more sustained improvement in FEV1 compared with placebo and formoterol. In this study, a lower exacerbation rate than with placebo was also noted. The drug has also shown equivalent bronchodilator efficacy at 150 μg and 300 μg daily dosing compared with tiotropium.56
The benefits of a longer-acting bronchodilator such as indacaterol are likely mediated by smoothing out airway bronchomotor tone over 24 hours without the dips seen with shorter-acting agents and by improvement of the FEV1 trough before the subsequent dose is due, aptly named “pharmacologic stenting.”57 Once-daily dosing should also foster better adherence. The safety profile appears excellent with no increase in cardiovascular or cerebrovascular events compared with placebo.58
The FDA approved the 75-μg daily dose instead of the higher doses used in the studies mentioned above. This decision was based on the observation that there appeared to be a flattened dose-response in patients with more severe COPD, with no further improvement in trough FEV1 at higher doses.59
DOES VITAMIN D SUPPLEMENTATION HAVE A ROLE IN COPD MANAGEMENT?
Vitamin D is vital for calcium and phosphate metabolism and bone health. Low vitamin D levels are associated with diminished leg strength and falls in the elderly.60 Osteoporosis, preventable with vitamin D and calcium supplementation, is linked to thoracic vertebral fracture and consequent reduced lung function.61,62
Patients with COPD are at higher risk of vitamin D deficiency, and more so if they also are obese, have advanced airflow obstruction, are depressed, or smoke.62 Therefore, there are sound reasons to look for vitamin D deficiency in patients with COPD and to treat it if the 25-hydroxyvitamin D level is less than 10 ng/ mL (Table 6).
Vitamin D may also have antimicrobial and immunomodulatory effects.63 Since COPD exacerbations are frequently caused by infection, it was hypothesized that vitamin D supplementation might reduce the rate of exacerbations.
In a study in 182 patients with moderate to very severe COPD and a history of recent exacerbations, high-dose vitamin D supplementation (100,000 IU) was given every 4 weeks for 1 year.64 There were no differences in the time to first exacerbation, in the rate of exacerbation, hospitalization, or death, or in quality of life between the placebo and intervention groups. However, subgroup analysis indicated that, in those with severe vitamin D deficiency at baseline, the exacerbation rate was reduced by more than 40%.
Comment. We recommend screening for vitamin D deficiency in patients with COPD. Supplementation is appropriate in those with low levels, but data indicate no role in those with normal levels.
WHAT ARE THE NONPHARMACOLOGIC APPROACHES TO COPD TREATMENT?
Noninvasive positive-pressure ventilation
Nocturnal noninvasive positive-pressure ventilation may be beneficial in patients with severe COPD, daytime hypercapnia, and nocturnal hypoventilation, particularly if higher inspiratory pressures are selected (Table 7).65,66
For instance, a randomized controlled trial of noninvasive positive-pressure ventilation plus long-term oxygen therapy compared with long-term oxygen therapy alone in hypercapnic COPD demonstrated a survival benefit in favor of ventilation (hazard ratio 0.6).67
In another randomized trial,68 settings that aimed to maximally reduce Paco2 (mean inspiratory positive airway pressure 29 cm H2O with a backup rate of 17.5/min) were compared with low-intensity positive airway pressure (mean inspiratory positive airway pressure 14 cm H2O, backup rate 8/min). The high inspiratory pressures increased the daily use of ventilation by 3.6 hours per day and improved exercise-related dyspnea, daytime Paco2, FEV1, vital capacity, and health-related quality of life66 without disrupting sleep quality.68
Caveats are that acclimation to the high pressures was achieved in the hospital, and the high pressures were associated with a significant increase in air leaks.66
Comments. Whether high-pressure noninvasive positive-pressure ventilation can be routinely implemented and adopted in the outpatient setting, and whether it is associated with a survival advantage remains to be determined. The advantages of noninvasive positive-pressure ventilation in the setting of hypercapnic COPD appear to augment those of pulmonary rehabilitation, with improved quality of life, gas exchange, and exercise tolerance, and a slower decline of lung function.69
Pulmonary rehabilitation
Pulmonary rehabilitation is a multidisciplinary approach to managing COPD (Table 8).
Patients participate in three to five supervised sessions per week, each lasting 3 to 4 hours, for 6 to 12 weeks. Less-frequent sessions may not be effective. For instance, in a randomized trial, exercising twice a week was not enough.70 Additionally, a program lasting longer than 12 weeks produced more sustained benefits than shorter programs.71
A key component is an exercise protocol centered on the lower extremities (walking, cycling, treadmill), with progressive exercise intensity to a target of about 60% to 80% of the maximal exercise tolerance,72 though more modest targets of about 50% can also be beneficial.73
Exercise should be tailored to the desired outcome. For instance, training of the upper arms may help with activities of daily living. In one study, unsupported (against gravity) arm training improved upper-extremity function more than supported arm training (by ergometer).74 Ventilatory muscle training is less common, as most randomized trials have not shown conclusive evidence of benefit. Current guidelines do not recommend routine inspiratory muscle training.71
Even though indices of pulmonary function do not improve after an exercise program, randomized trials have shown that pulmonary rehabilitation improves exercise capacity, dyspnea, and health-related quality of life; improves cost-effectiveness of health care utilization; and provides psychosocial benefits that often exceed those of other therapies. Although there is no significant evidence of whether pulmonary rehabilitation improves survival in patients with COPD,71 an observational study documented improvements in BODE scores as well as a reduction in respiratory mortality rates in patients undergoing pulmonary rehabilitation.75
A limitation of pulmonary rehabilitation is that endurance and psychological and cognitive function decline significantly if exercise is not maintained. However, the role of a maintenance program is uncertain, with long-term benefits considered modest.71
Lung-volume reduction surgery
Lung-volume reduction consists of surgical wedge resections of emphysematous areas of the lung (Table 9).
The National Emphysema Treatment Trial76 randomized 1,218 patients to undergo either lung-volume reduction surgery or maximal medical therapy. Surgery improved survival, quality of life, and dyspnea in patients with upper-lobe emphysema and a low exercise capacity (corresponding to < 40 watts for men or < 25 watts for women in the maximal power achieved on cycle ergometry). While conferring no survival benefit in patients with upper-lobe-predominant emphysema and high exercise capacity, this surgery is likely to improve exercise capacity and quality of life in this subset of patients.
Importantly, the procedure is associated with a lower survival rate in patients with an FEV1 lower than 20%, homogeneous emphysema, a diffusing capacity of the lung for carbon monoxide lower than 20%, non-upper-lobe emphysema, or high baseline exercise capacity.
The proposed mechanisms of improvement of lung function include placing the diaphragm in a position with better mechanical advantage, reducing overall lung volume, better size-matching between the lungs and chest cavity, and restoring elastic recoil.76,77
Ongoing trials aim to replicate the success of lung-volume reduction using nonsurgical bronchoscopic techniques with one-way valves, coils, biologic sealants, thermal ablation, and airway stents.
- Miniño AM, Xu J, Kochanek KD. Deaths: preliminary data for 2008. National Vital Statistics Reports 2010; 59:1–52. http://www.cdc.gov/nchs/data/nvsr/nvsr59/nvsr59_02.pdf. Accessed April 10, 2014.
- Murphy SL, Xu J, Kochanek KD. Deaths: preliminary data from 2010. National Vital Statistics Reports 2012; 60:1–51. http://www.cdc.gov/nchs/data/nvsr/nvsr60/nvsr60_04.pdf. Accessed April 10, 2014.
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006; 3:e442.
- Behrendt CE. Mild and moderate-to-severe COPD in nonsmokers: distinct demographic profiles. Chest 2005; 128:1239–1244.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). http://www.goldcopd.org/Guidelines/guidelines-resources.html. Accessed April 10, 2014.
- Papi A, Bellettato CM, Braccioni F, et al. Infections and airway inflammation in chronic obstructive pulmonary disease severe exacerbations. Am J Respir Crit Care Med 2006; 173:1114–1121.
- Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax 2005; 60:925–931.
- Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax 2002; 57:847–852.
- Hurst JR, Vestbo J, Anzueto A, et al; Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Investigators. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med 2010; 363:1128–1138.
- Cooper CB. The connection between chronic obstructive pulmonary disease symptoms and hyperinflation and its impact on exercise and function. Am J Med 2006; 119(suppl 1):21–31.
- Jones PW. Issues concerning health-related quality of life in COPD. Chest 1995; 107(suppl):187S–193S.
- Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004; 350:1005–1012.
- Fletcher CM. The clinical diagnosis of pulmonary emphysema—an experimental study. J Royal Soc Med 1952; 45:577–584.
- Lange P, Marott JL, Vestbo J, et al. Prediction of the clinical course of chronic obstructive pulmonary disease, using the new GOLD classification: a study of the general population. Am J Respir Crit Care Med 2012; 186:975–981.
- Hurst J. Phenotype-based care in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2012; 186:935–936.
- Jones PW, Adamek L, Nadeau G, Banik N. Comparisons of health status scores with MRC grades in COPD: implications for the GOLD 2011 classification. Eur Respir J 2013; 42:647–654.
- Divo M, Cote C, de Torres JP, et al; BODE Collaborative Group. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2012; 186:155–161.
- Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GK, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med 1987; 106:196–204.
- Llor C, Moragas A, Hernández S, Bayona C, Miravitlles M. Efficacy of antibiotic therapy for acute exacerbations of mild to moderate chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2012; 186:716–723.
- Daniels JM, Snijders D, de Graaff CS, Vlaspolder F, Jansen HM, Boersma WG. Antibiotics in addition to systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2010; 181:150–157.
- Rothberg MB, Pekow PS, Lahti M, Brody O, Skiest DJ, Lindenauer PK. Antibiotic therapy and treatment failure in patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease. JAMA 2010; 303:2035–2042.
- Vollenweider DJ, Jarrett H, Steurer-Stey CA, Garcia-Aymerich J, Puhan MA. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012; 12:CD010257.
- Stolz D, Christ-Crain M, Bingisser R, et al. Antibiotic treatment of exacerbations of COPD: a randomized, controlled trial comparing procalcitonin-guidance with standard therapy. Chest 2007; 131:9–19.
- Wolter J, Seeney S, Bell S, Bowler S, Masel P, McCormack J. Effect of long term treatment with azithromycin on disease parameters in cystic fibrosis: a randomised trial. Thorax 2002; 57:212–216.
- Kudoh S, Azuma A, Yamamoto M, Izumi T, Ando M. Improvement of survival in patients with diffuse panbronchiolitis treated with low-dose erythromycin. Am J Respir Crit Care Med 1998; 157:1829–1832.
- Albert RK, Connett J, Bailey WC, et al; COPD Clinical Research Network. Azithromycin for prevention of exacerbations of COPD. N Engl J Med 2011; 365:689–698.
- Gross NJ, Giembycz MA, Rennard SI. Treatment of chronic obstructive pulmonary disease with roflumilast, a new phosphodiesterase 4 inhibitor. COPD 2010; 7:141–153.
- Calverley PM, Rabe KF, Goehring UM, Kristiansen S, Fabbri LM, Martinez FJ; M2-124 and M2-125 study groups. Roflumilast in symptomatic chronic obstructive pulmonary disease: two randomised clinical trials. Lancet 2009; 374:685–694.
- Fabbri LM, Calverley PM, Izquierdo-Alonso JL, et al; M2-127 and M2-128 study groups. Roflumilast in moderate-to-severe chronic obstructive pulmonary disease treated with long acting bronchodilators: two randomised clinical trials. Lancet 2009; 374:695–703.
- Gross NJ, Skorodin MS. Anticholinergic, antimuscarinic bronchodilators. Am Rev Respir Dis 1984; 129:856–870.
- Tashkin DP, Celli B, Senn S, et al; UPLIFT Study Investigators. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med 2008; 359:1543–1554.
- Cazzola M. Aclidinium bromide, a novel long-acting muscarinic M3 antagonist for the treatment of COPD. Curr Opin Investig Drugs 2009; 10:482–490.
- Gavaldà A, Miralpeix M, Ramos I, et al. Characterization of aclidinium bromide, a novel inhaled muscarinic antagonist, with long duration of action and a favorable pharmacological profile. J Pharmacol Exp Ther 2009; 331:740–751.
- Alagha K, Bourdin A, Tummino C, Chanez P. An update on the efficacy and safety of aclidinium bromide in patients with COPD. Ther Adv Respir Dis 2011; 5:19–28.
- Kerwin EM, D’Urzo AD, Gelb AF, Lakkis H, Garcia Gil E, Caracta CF; ACCORD I study investigators. Efficacy and safety of a 12-week treatment with twice-daily aclidinium bromide in COPD patients (ACCORD COPD I). COPD 2012; 9:90–101.
- Jones PW, Singh D, Bateman ED, et al. Efficacy and safety of twice-daily aclidinium bromide in COPD patients: the ATTAIN study. Eur Respir J 2012; 40:830–836.
- Jones PW, Rennard SI, Agusti A, et al. Efficacy and safety of once-daily aclidinium in chronic obstructive pulmonary disease. Respir Res 2011; 12:55.
- Fuhr R, Magnussen H, Sarem K, et al. Efficacy of aclidinium bromide 400 μg twice daily compared with placebo and tiotropium in patients with moderate to severe COPD. Chest 2012; 141:745–752.
- Tashkin DP, Fabbri LM. Long-acting beta-agonists in the management of chronic obstructive pulmonary disease: current and future agents. Respir Res 2010; 11:149.
- Mahler DA, Donohue JF, Barbee RA, et al. Efficacy of salmeterol xinafoate in the treatment of COPD. Chest 1999; 115:957–965.
- Campbell M, Eliraz A, Johansson G, et al. Formoterol for maintenance and as-needed treatment of chronic obstructive pulmonary disease. Respir Med 2005; 99:1511–1520.
- Hanrahan JP, Hanania NA, Calhoun WJ, Sahn SA, Sciarappa K, Baumgartner RA. Effect of nebulized arformoterol on airway function in COPD: results from two randomized trials. COPD 2008; 5:25–34.
- Neder JA, Fuld JP, Overend T, et al. Effects of formoterol on exercise tolerance in severely disabled patients with COPD. Respir Med 2007; 101:2056–2064.
- O’Donnell DE, Voduc N, Fitzpatrick M, Webb KA. Effect of salmeterol on the ventilatory response to exercise in chronic obstructive pulmonary disease. Eur Respir J 2004; 24:86–94.
- Rennard SI, Anderson W, ZuWallack R, et al. Use of a long-acting inhaled beta 2-adrenergic agonist, salmeterol xinafoate, in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2001; 163:1087–1092.
- Schultze-Werninghaus G. Multicenter 1-year trial on formoterol, a new long-acting beta 2-agonist, in chronic obstructive airway disease. Lung 1990; 168(suppl):83–89.
- Rodrigo GJ, Nannini LJ, Rodríguez-Roisin R. Safety of long-acting beta-agonists in stable COPD: a systematic review. Chest 2008; 133:1079–1087.
- Baker WL, Baker EL, Coleman CI. Pharmacologic treatments for chronic obstructive pulmonary disease: a mixed-treatment comparison meta-analysis. Pharmacotherapy 2009; 29:891–905.
- Rodrigo GJ, Castro-Rodriguez JA, Plaza V. Safety and efficacy of combined long-acting beta-agonists and inhaled corticosteroids vs long-acting beta-agonists monotherapy for stable COPD: a systematic review. Chest 2009; 136:1029–1038.
- Nelson HS, Weiss ST, Bleecker ER, Yancey SW, Dorinsky PM; SMART Study Group. The Salmeterol Multicenter Asthma Research Trial: a comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. Chest 2006; 129:15–26.
- Calverley PM, Anderson JA, Celli B, et al; TORCH investigators. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med 2007; 356:775–789.
- Suissa S, Ernst P, Vandemheen KL, Aaron SD. Methodological issues in therapeutic trials of COPD. Eur Respir J 2008; 31:927–933.
- Lombardi D, Cuenoud B, Krämer SD. Lipid membrane interactions of indacaterol and salmeterol: do they influence their pharmacological properties? Eur J Pharm Sci 2009; 38:533–547.
- Kornmann O, Dahl R, Centanni S, et al; INLIGHT-2 (Indacaterol Efficacy Evaluation Using 150-μg Doses with COPD Patients) study investigators. Once-daily indacaterol versus twice-daily salmeterol for COPD: a placebo-controlled comparison. Eur Respir J 2011; 37:273–279.
- Dahl R, Chung KF, Buhl R, et al; INVOLVE (INdacaterol: Value in COPD: Longer Term Validation of Efficacy and Safety) Study Investigators. Efficacy of a new once-daily long-acting inhaled beta2-agonist indacaterol versus twice-daily formoterol in COPD. Thorax 2010; 65:473–479.
- Donohue JF, Fogarty C, Lötvall J, et al; INHANCE Study Investigators. Once-daily bronchodilators for chronic obstructive pulmonary disease: indacaterol versus tiotropium. Am J Respir Crit Care Med 2010; 182:155–162.
- Beeh KM, Beier J. The short, the long and the “ultra-long”: why duration of bronchodilator action matters in chronic obstructive pulmonary disease. Adv Ther 2010; 27:150–159.
- Worth H, Chung KF, Felser JM, Hu H, Rueegg P. Cardio- and cerebrovascular safety of indacaterol vs formoterol, salmeterol, tiotropium and placebo in COPD. Respir Med 2011; 105:571–579.
- Chowdhury BA, Seymour SM, Michele TM, Durmowicz AG, Liu D, Rosebraugh CJ. The risks and benefits of indacaterol--the FDA’s review. N Engl J Med 2011; 365:2247–2249.
- Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, et al. Effect of vitamin D on falls: a meta-analysis. JAMA 2004; 291:1999–2006.
- Leech JA, Dulberg C, Kellie S, Pattee L, Gay J. Relationship of lung function to severity of osteoporosis in women. Am Rev Respir Dis 1990; 141:68–71.
- Persson LJ, Aanerud M, Hiemstra PS, Hardie JA, Bakke PS, Eagan TM. Chronic obstructive pulmonary disease is associated with low levels of vitamin D. PLoS One 2012; 7:e38934.
- Janssens W, Lehouck A, Carremans C, Bouillon R, Mathieu C, Decramer M. Vitamin D beyond bones in chronic obstructive pulmonary disease: time to act. Am J Respir Crit Care Med 2009; 179:630–636.
- Lehouck A, Mathieu C, Carremans C, et al. High doses of vitamin D to reduce exacerbations in chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med 2012; 156:105–114.
- Casanova C, Celli BR, Tost L, et al. Long-term controlled trial of nocturnal nasal positive pressure ventilation in patients with severe COPD. Chest 2000; 118:1582–1590.
- Dreher M, Storre JH, Schmoor C, Windisch W. High-intensity versus low-intensity non-invasive ventilation in patients with stable hypercapnic COPD: a randomised crossover trial. Thorax 2010; 65:303–308.
- McEvoy RD, Pierce RJ, Hillman D, et al; Australian trial of non-invasive Ventilation in Chronic Airflow Limitation (AVCAL) Study Group. Nocturnal non-invasive nasal ventilation in stable hypercapnic COPD: a randomised controlled trial. Thorax 2009; 64:561–566.
- Dreher M, Ekkernkamp E, Walterspacher S, et al. Noninvasive ventilation in COPD: impact of inspiratory pressure levels on sleep quality. Chest 2011; 140:939–945.
- Duiverman ML, Wempe JB, Bladder G, et al. Two-year home-based nocturnal noninvasive ventilation added to rehabilitation in chronic obstructive pulmonary disease patients: a randomized controlled trial. Respir Res 2011; 12:112.
- Ringbaek TJ, Broendum E, Hemmingsen L, et al. Rehabilitation of patients with chronic obstructive pulmonary disease. Exercise twice a week is not sufficient! Respir Med 2000; 94:150–154.
- Ries AL, Bauldoff GS, Carlin BW, et al. Pulmonary Rehabilitation: Joint ACCP/AACVPR Evidence-Based Clinical Practice Guidelines. Chest 2007; 131(suppl):4S–42S.
- Vallet G, Ahmaïdi S, Serres I, et al. Comparison of two training programmes in chronic airway limitation patients: standardized versus individualized protocols. Eur Respir J 1997; 10:114–122.
- Vogiatzis I, Williamson AF, Miles J, Taylor IK. Physiological response to moderate exercise workloads in a pulmonary rehabilitation program in patients with varying degrees of airflow obstruction. Chest 1999; 116:1200–1207.
- Martinez FJ, Vogel PD, Dupont DN, Stanopoulos I, Gray A, Beamis JF. Supported arm exercise vs unsupported arm exercise in the rehabilitation of patients with severe chronic airflow obstruction. Chest 1993; 103:1397–1402.
- Cote CG, Celli BR. Pulmonary rehabilitation and the BODE index in COPD. Eur Respir J 2005; 26:630–636.
- Fishman A, Martinez F, Naunheim K, et al; National Emphysema Treatment Trial Research Group. A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl J Med 2003; 348:2059–2073.
- Naunheim KS, Wood DE, Mohsenifar Z, et al; National Emphysema Treatment Trial Research Group. Long-term follow-up of patients receiving lung-volume-reduction surgery versus medical therapy for severe emphysema by the National Emphysema Treatment Trial Research Group. Ann Thorac Surg 2006; 82:431–443.
Chronic obstructive pulmonary disease (COPD) has seen several changes in its assessment and treatment in recent years, reflecting advances in our understanding of this common and serious disease.
This review updates busy practitioners on the major advances, including new assessment tools and new therapies.
COMMON AND INCREASING
COPD is the third leading cause of death in the United States, behind heart disease and cancer,1 and of the top five (the others being stroke and accidents), it is the only one that increased in incidence between 2007 and 2010.2 The 11th leading cause of disability-adjusted life years worldwide in 2002, COPD is projected to become the seventh by the year 2030.3
CHARACTERIZED BY OBSTRUCTION
COPD is characterized by persistent and progressive airflow obstruction associated with chronic airway inflammation in response to noxious particles and gases. Disease of the small airways (inflammation, mucus plugging, and fibrosis) and parenchymal destruction (emphysema) limit the flow of air.
COPD is diagnosed by spirometry—specifically, a ratio of forced expiratory volume in 1 second to forced vital capacity (FEV1/FVC) of less than 0.7 after a bronchodilator is given. The severity of airflow limitation is revealed by the FEV1 as a percent of the predicted value.
Cigarette smoking is the major cause of COPD, but the prevalence of COPD is 6.6% in people who have never smoked, and one-fourth of COPD patients in the United States have never smoked.4
GOLDEN GOALS: FEWER SYMPTOMS, LOWER RISK
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) periodically issues evidence-based statements on how to prevent and treat COPD.
In its 2013 update,5 GOLD suggested two goals: improving symptoms and reducing the risk of death, exacerbations, progression of disease, and treatment-related adverse effects. The latter goal—reducing risk—is relatively new.
Exacerbations are acute inflammatory events superimposed on chronic inflammation. The inflammation is often brought on by infection6 and increases the risk of death7 and the risk of a faster decline in lung function.8
Exacerbations may characterize a phenotype of COPD. The Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) analyzed the frequency of COPD exacerbations and associated factors in 2,138 patients with COPD over a period of 3 years.9 Although patients with more severe obstruction tended to have more exacerbations, some patients appeared susceptible to exacerbations irrespective of the severity of obstruction. The best predictor of exacerbations was a history of exacerbations.
HOW DO I ASSESS A PATIENT WITH COPD ON PRESENTATION?
Markers of airflow obstruction such as the FEV1 do not correlate strongly with exertional capacity and health status in patients with COPD.10,11
The BODE index (body mass index, obstruction, dyspnea score, and exercise oximetry) takes into account the multidimensional nature of COPD. It performs better than the FEV1 in predicting the risk of death.12 The propensity for exacerbations and comorbidities further modulates outcome.
Assessing symptoms
The modified British Medical Research Council (mMRC) dyspnea scale, based on work by Fletcher in 1952,13 has five grades, numbered 0 through 4:
- Grade 0—Breathless with strenuous exercise only
- Grade 1—Breathless when hurrying on level ground or walking up a slight hill
- Grade 2—Walks slower than people of the same age on level ground because of shortness of breath or has to stop when walking at own pace on level ground
- Grade 3—Stops for breath after walking about 100 yards or after a few minutes on level ground
- Grade 4—Too breathless to leave the house or breathless when dressing or undressing.
Grade 2 or higher separates symptomatic from asymptomatic COPD.
The COPD Assessment Test (CAT) (www.catestonline.org) is a proprietary questionnaire. Patients use a 6-point scale (numbered 0 though 5) to rate eight symptoms (cough, mucus production, chest tightness, shortness of breath on exertion, limitations in home activities, lack of confidence leaving the home, poor sleep, and lack of energy). A total score of 10 or higher is abnormal.
Four GOLD groups
The new GOLD guidelines (Table 1)5 define four groups of patients according to their severity of airflow obstruction, symptoms, and exacerbation history:
- Group A—fewer symptoms, low risk: Fewer symptoms (“less symptoms,” as worded in the guidelines) means a CAT score less than 10 or an mMRC grade less than 2; “low risk” means no more than one exacerbation per year and an FEV1 of at least 50%
- Group B—more symptoms, low risk: “More symptoms” means a CAT score of 10 or more or an mMRC grade of 2 or more
- Group C—fewer symptoms, high risk: “High risk” means two or more exacerbations per year or an FEV1 less than 50%
- Group D—more symptoms, high risk.
Thus, a patient with an FEV1 of 60% (moderate airflow limitation) who has had one exacerbation during the past year and a CAT score of 8 would be in group A. In contrast, a patient who has an FEV1 of 40% (severe airflow limitation), no history of exacerbations, and a CAT score of 20 would be in group D.
Updated GOLD guidelines suggest utilizing a stepwise approach to treatment, akin to asthma management guidelines, based on patient grouping.5
How accurate is the new GOLD system?
Although practical and suited for use in primary care, the new GOLD system is arbitrary and has not been thoroughly studied, and may therefore need refinement.
Lange et al14 compared the new GOLD system with the previous one in 6,628 patients with COPD. As anticipated, the new system was better at predicting exacerbations, as it incorporates a history of exacerbations in stratification. The presence of symptoms (as determined by an mMRC grade ≥ 2) was a marker of mortality risk that distinguished group A from group B, and group C from group D. Surprisingly, the rate of death was higher in group B (more symptoms, low risk) than in group C (fewer symptoms, high risk).
Notably, most patients in group C qualified for this group because of the severity of airflow obstruction, not because of a history of exacerbations. Therefore, patients whose symptoms are out of proportion to the severity of obstruction may be at higher risk of death, possibly because of comorbidities such as cardiovascular disease.15 Patients who qualified for groups C and D by having both a history of frequent exacerbations (≥ 2 per year) and symptoms rather than either one alone had a higher risk of death in 3 years.
Similarly, the symptom-assessment tool that is used—ie, the mMRC grade or the CAT score—also makes a difference.
The Health-Related Quality of Life in COPD in Europe Study16 retrospectively analyzed data from 1,817 patients to determine whether the cutoff points for symptoms as assessed by mMRC grade and CAT score were equivalent. Although the mMRC grade correlated well with overall health status, the cutoff mMRC grade of 2 or higher did not correspond to a CAT score of 10 or higher, classifying patients with health status impairment as asymptomatic (mean weighted kappa 0.626). The two tools agreed much better when the cutoff was set at an mMRC grade of 1 or higher (mean weighted kappa 0.792).16
Although assessment schemes continue to evolve as data accumulate, we believe the new system is a welcome initiative that reflects the changing notions of COPD.
Comorbidities matter
Another shift is the recognition that certain comorbidities increase the risk of death. In 1,664 patients with COPD who were followed for 51 months, 12 distinct comorbidities were associated with a higher risk of death after multivariate analysis.17
The COTE index (COPD-Specific Comorbidity Test) is based on these findings. It awards points as follows:
- 6 points for cancer of the lung, esophagus, pancreas, or breast, or for anxiety
- 2 points for all other cancers, liver cirrhosis, atrial fibrillation or flutter, diabetes with neuropathy, or pulmonary fibrosis
- 1 point for congestive heart failure, gastric or duodenal ulcer, or coronary artery disease.
A COTE index score of 4 or higher was associated with a risk of death 2.2 times higher in each quartile of the BODE index.
We strongly recommend being aware of comorbidities in COPD patients, particularly when symptoms are out of proportion to the severity of obstruction.
SHOULD I USE ANTIBIOTICS TO TREAT ALL COPD EXACERBATIONS?
Infections are thought to cause more than 80% of acute exacerbations of COPD.
Anthonisen et al,18 in a landmark trial, found broad-spectrum antibiotics to be most helpful if the patient had at least two of the three cardinal symptoms of COPD exacerbation (ie, shortness of breath, increase in sputum volume, and sputum purulence). Antibiotics decreased the rate of treatment failure and led to a more rapid clinical resolution of exacerbation. However, they did not help patients who had milder exacerbations.
Antibiotics may nevertheless have a role in ambulatory patients with mild to moderate COPD who present with exacerbations characterized by one or more cardinal symptoms.
Llor et al,19 in a multicenter randomized double-blind placebo-controlled trial in Spain, concluded that amoxicillin clavulanate (Augmentin) led to higher clinical cure rates and longer time to the next exacerbation in these patients. Most of the benefit was in patients with more symptoms, consistent with the results of the study by Anthonisen et al.18
There is also strong evidence to support the use of antibiotics in addition to systemic corticosteroids in hospitalized patients with acute exacerbations of COPD. A 7-day course of doxycycline (Vibramycin) added to a standard regimen of corticosteroids was associated with higher rates of clinical and microbiological cure on day 10 of the exacerbation.20 In a large retrospective cohort study in 84,621 hospitalized patients with COPD exacerbations, fewer of those who received antibiotics needed mechanical ventilation, died, or were readmitted.21 Although sicker patients received antibiotics more frequently, their mortality rate was lower than in those who did not receive antibiotics, who were presumably less sick.
A meta-analysis confirmed the salutary effect of antibiotics in inpatients and particularly those admitted to the intensive care unit.22 Mortality rates and hospital length of stay were not affected in patients who were not in intensive care.
Biomarkers such as procalcitonin might help reduce the unnecessary use of antibiotics. Stolz et al23 conducted a randomized controlled trial in which they based the decision to give antibiotics on a threshold procalcitonin level of at least 1 μg/L in hospitalized patients with COPD exacerbation. The rate of antibiotic use was reduced by more than 40% in the procalcitonin group without any difference in clinical outcomes, 6-month exacerbation rate, or rehospitalization compared with controls. Nonstandardized procalcitonin assays are a possible barrier to the widespread adoption of this threshold.
Comment. In general, we recommend antibiotics for hospitalized patients with COPD exacerbation and look forward to confirmatory data that support the use of biomarkers. For outpatients, we find the Anthonisen criteria useful for decision-making at the point of care.
ARE THERE ANY NEW INTERVENTIONS TO PREVENT COPD EXACERBATIONS?
Macrolides
Macrolides have a proven role in managing chronic suppurative respiratory diseases such as cystic fibrosis24 and diffuse panbronchiolitis.25 Since they are beneficial at lower doses than those used to treat infection, the mechanism may be anti-inflammatory rather than antimicrobial.
Albert et al26 assigned 1,142 patients who had had a COPD exacerbation within a year before enrollment or who were on home oxygen therapy to receive azithromycin (Zithromax) 250 mg daily or placebo.25 The azithromycin group had fewer acute exacerbations (hazard ratio 0.73, 95% CI 0.63–0.84, P < .001), and more patients in the azithromycin group achieved clinically significant improvements in quality of life, ie, a reduction in the St. George’s Respiratory Questionnaire (SGRQ) score of at least 4 points (43% vs 36%, P = .03). Adverse events that were more common in the azithromycin group were hearing loss (25% vs 20%) and macrolide-resistant strains in nasopharyngeal secretions (81% vs 41%). In subgroup analysis, the benefit in terms of reducing exacerbations was greater in patients over age 65, patients on home oxygen, and patients with moderate or severe obstruction compared with those with very severe obstruction.
Comment. Macrolides are a valuable addition to the agents available for preventing COPD exacerbation (Table 2), but their role is still uncertain. Potential topics of research are whether these drugs have a role in patients already on preventive regimens, whether they would have a greater effect in distinct patient populations (eg, patients who have two or more exacerbations per year), and whether their broader use would lead to a change in the resident flora in the community.
Clinicians should exercise caution in the use of azithromycin in light of recent concern about associated cardiac morbidity and death. All patients should undergo electrocardiography to assess the QTc interval before starting treatment, as in the trial by Albert et al.26
Phosphodiesterase inhibitors
Roflumilast (Daliresp) is an oral phosphodiesterase 4 inhibitor approved for treating exacerbations and symptoms of chronic bronchitis in patients with severe COPD (Table 3). Phosphodiesterase 4, one of the 11 isoforms of the enzyme, is found in immune and inflammatory cells and promotes inflammatory responses. Roflumilast has anti-inflammatory properties but no acute bronchodilatory effect.27 Several phase 3 trials found the compound to have beneficial effects.
Calverley et al28 performed two placebo-controlled double-blind trials in outpatients with the clinical diagnosis of COPD who had chronic cough; increased sputum production; at least one recorded exacerbation requiring corticosteroids or hospitalization, or both; and an FEV1 of 50% or less. Patients were randomized to receive roflumilast 500 μg once a day (n = 1,537) or placebo (n = 1,554) for 1 year. The rate of moderate to severe exacerbations was 1.17 per year with roflumilast vs 1.37 with placebo (P < .0003). Adverse events were significantly more common with roflumilast and were related to the known side effects of the drug, namely, diarrhea, weight loss, decreased appetite, and nausea.
Fabbri et al29 performed two other placebo-controlled double-blind multicenter trials, studying the combinations of roflumilast with salmeterol (Serevent) and roflumilast with tiotropium (Spiriva) compared with placebo in 1,676 patients with COPD who had post-bronchodilator FEV1 values of 40% to 70% of predicted. The mean prebronchodilator FEV1 improved by 49 mL (P < .0001) in the salmeterol-plus-roflumilast trial and by 80 mL (P < .0001) in the tiotropium-plus-roflumilast trial compared with placebo. Fewer patients on roflumilast had exacerbations of any severity in both trials (risk ratio 0.82, P = .0419 and risk ratio 0.75, P = .0169, respectively).
No trial has yet addressed whether roflumilast is better than the combination of a long-acting muscarinic antagonist and a beta agonist, or whether roflumilast can be substituted for inhaled corticosteroids in a new triple-therapy combination. Clinicians should also be aware of psychiatric side effects of roflumilast, which include depression and, possibly, suicide.
ARE THERE ANY NEW BRONCHODILATORS FOR PATIENTS WITH COPD?
Long-acting muscarinic antagonists
Reversible airflow obstruction and mucus secretion are determined by the vagal cholinergic tone in patients with COPD.30 Antagonism of cholinergic (muscarinic) receptors results in bronchodilation and reduction in mucus production. Consequently, inhaled anticholinergic agents are the first-line therapy for COPD (Table 4).
Tiotropium bromide is a long-acting antimuscarinic approved in 2002 by the US Food and Drug Administration (FDA). The UPLIFT trial (Understanding Potential Long-Term Impacts on Function With Tiotropium)31 enrolled 5,993 patients with a mean FEV1 of 48% of predicted. Over a 4-year follow-up, significant improvements in mean FEV1 values (ranging from 87 mL to 103 mL before bronchodilation and 47 mL to 65 mL after bronchodilation, P < .001) in the tiotropium group were observed compared with placebo. The rate of the primary end point—the rate of decline in mean FEV1—was not different between tiotropium and placebo. However, there were important salutary effects in multiple clinical end points in the tiotropium group. Health-related quality of life as measured by the SGRQ improved in a clinically significant manner (> 4 points) in favor of tiotropium in a higher proportion of patients (45% vs 36%, P < .001). Tiotropium reduced the number of exacerbations per patient year (0.73 ± 0.02 vs 0.85 ± 0.02, RR = 0.86 (95% CI 0.81–0.91), P < .001) and the risk of respiratory failure (RR = 0.67, 95% CI 0.51–0.89). There were no significant differences in the risk of myocardial infarction, stroke, or pneumonia.
Aclidinium bromide (Tudorza Pressair) is a long-acting antimuscarinic recently approved by the FDA. Compared with tiotropium, it has a slightly faster onset of action and a considerably shorter half-life (29 hours vs 64 hours).32,33 Its dosage is 400 μg twice daily by inhalation. It provides sustained bronchodilation over 24 hours and may have a favorable side-effect profile, because it undergoes rapid hydrolysis in human plasma.34
ACCORD COPD I35 and ATTAIN,36 two phase 3 trials in patients with moderate-to severe COPD, found that twice-daily aclidinium was associated with statistically and clinically significant (> 100 mL) improvements in trough and peak FEV1 compared with placebo. Health status (assessed by SGRQ) and dyspnea (assessed by transitional dyspnea index) also improved significantly. However, improvements beyond minimum clinically significant thresholds were achieved only with 400 μg twice-daily dosing.
To date, no study has evaluated the impact of aclidinium on COPD exacerbation as a primary end point. Fewer moderate to severe exacerbations were reported in an earlier 52-week study of once-daily aclidinium (ACCLAIM COPD II) but not in ACCLAIM COPD I.37
Aclidinium may offer an advantage over tiotropium in patients who have nocturnal symptoms. Twice-daily aclidinium 400 μg was associated with superior FEV1 area-under-the-curve values compared with placebo and tiotropium, the difference mostly owing to improved nocturnal profile.38
Long-acting beta-2 agonists
Stimulation of airway beta-2 receptors relaxes smooth muscles and consequently dilates bronchioles via a cyclic adenosine monophosphate-dependent pathway.39
Short-acting beta-2 agonists such as albuterol and terbutaline have long been used as rescue medications for obstructive lung disease. Long-acting beta-2 agonists provide sustained bronchodilation and are therefore more efficacious as maintenance medications. Salmeterol, formoterol (Foradil), and arformoterol (Brovana) are long-acting beta-2 agonists in clinical use that are taken twice daily.
Clinical studies indicate that use of long-acting beta-2 agonists leads to significant improvements in FEV1,40–42 dynamic hyperinflation, exercise tolerance,43,44 and dyspnea.45,46 These drugs have also been associated with significant improvements in health-related quality of life and in the frequency of exacerbations.47–49
In patients with asthma, long-acting beta agonists may increase the risk of death.50 In contrast, in patients with COPD, they appear to offer a survival advantage when used in combination with inhaled corticosteroids,51 and some argue that this benefit is entirely from the long-acting beta agonist (a 17% reduction in mortality) rather than the inhaled corticosteroid (0% reduction in mortality).52
Indacaterol (Arcapta), approved in July 2011, is the first once-daily beta agonist or “ultra-long-acting” beta agonist (Table 5). Possibly because it has a high affinity for the lipid raft domain of the cell membrane where beta-2 receptors are coupled to second messengers,53 the drug has a 24-hour duration of action.
In patients with COPD, inhaled indacaterol 150 μg once daily improved airflow obstruction and health status as measured by SGRQ compared with salmeterol 50 μg twice daily and placebo.54 At the higher dose of 300 μg daily, the 52-week INVOLVE trial55 demonstrated early and more sustained improvement in FEV1 compared with placebo and formoterol. In this study, a lower exacerbation rate than with placebo was also noted. The drug has also shown equivalent bronchodilator efficacy at 150 μg and 300 μg daily dosing compared with tiotropium.56
The benefits of a longer-acting bronchodilator such as indacaterol are likely mediated by smoothing out airway bronchomotor tone over 24 hours without the dips seen with shorter-acting agents and by improvement of the FEV1 trough before the subsequent dose is due, aptly named “pharmacologic stenting.”57 Once-daily dosing should also foster better adherence. The safety profile appears excellent with no increase in cardiovascular or cerebrovascular events compared with placebo.58
The FDA approved the 75-μg daily dose instead of the higher doses used in the studies mentioned above. This decision was based on the observation that there appeared to be a flattened dose-response in patients with more severe COPD, with no further improvement in trough FEV1 at higher doses.59
DOES VITAMIN D SUPPLEMENTATION HAVE A ROLE IN COPD MANAGEMENT?
Vitamin D is vital for calcium and phosphate metabolism and bone health. Low vitamin D levels are associated with diminished leg strength and falls in the elderly.60 Osteoporosis, preventable with vitamin D and calcium supplementation, is linked to thoracic vertebral fracture and consequent reduced lung function.61,62
Patients with COPD are at higher risk of vitamin D deficiency, and more so if they also are obese, have advanced airflow obstruction, are depressed, or smoke.62 Therefore, there are sound reasons to look for vitamin D deficiency in patients with COPD and to treat it if the 25-hydroxyvitamin D level is less than 10 ng/ mL (Table 6).
Vitamin D may also have antimicrobial and immunomodulatory effects.63 Since COPD exacerbations are frequently caused by infection, it was hypothesized that vitamin D supplementation might reduce the rate of exacerbations.
In a study in 182 patients with moderate to very severe COPD and a history of recent exacerbations, high-dose vitamin D supplementation (100,000 IU) was given every 4 weeks for 1 year.64 There were no differences in the time to first exacerbation, in the rate of exacerbation, hospitalization, or death, or in quality of life between the placebo and intervention groups. However, subgroup analysis indicated that, in those with severe vitamin D deficiency at baseline, the exacerbation rate was reduced by more than 40%.
Comment. We recommend screening for vitamin D deficiency in patients with COPD. Supplementation is appropriate in those with low levels, but data indicate no role in those with normal levels.
WHAT ARE THE NONPHARMACOLOGIC APPROACHES TO COPD TREATMENT?
Noninvasive positive-pressure ventilation
Nocturnal noninvasive positive-pressure ventilation may be beneficial in patients with severe COPD, daytime hypercapnia, and nocturnal hypoventilation, particularly if higher inspiratory pressures are selected (Table 7).65,66
For instance, a randomized controlled trial of noninvasive positive-pressure ventilation plus long-term oxygen therapy compared with long-term oxygen therapy alone in hypercapnic COPD demonstrated a survival benefit in favor of ventilation (hazard ratio 0.6).67
In another randomized trial,68 settings that aimed to maximally reduce Paco2 (mean inspiratory positive airway pressure 29 cm H2O with a backup rate of 17.5/min) were compared with low-intensity positive airway pressure (mean inspiratory positive airway pressure 14 cm H2O, backup rate 8/min). The high inspiratory pressures increased the daily use of ventilation by 3.6 hours per day and improved exercise-related dyspnea, daytime Paco2, FEV1, vital capacity, and health-related quality of life66 without disrupting sleep quality.68
Caveats are that acclimation to the high pressures was achieved in the hospital, and the high pressures were associated with a significant increase in air leaks.66
Comments. Whether high-pressure noninvasive positive-pressure ventilation can be routinely implemented and adopted in the outpatient setting, and whether it is associated with a survival advantage remains to be determined. The advantages of noninvasive positive-pressure ventilation in the setting of hypercapnic COPD appear to augment those of pulmonary rehabilitation, with improved quality of life, gas exchange, and exercise tolerance, and a slower decline of lung function.69
Pulmonary rehabilitation
Pulmonary rehabilitation is a multidisciplinary approach to managing COPD (Table 8).
Patients participate in three to five supervised sessions per week, each lasting 3 to 4 hours, for 6 to 12 weeks. Less-frequent sessions may not be effective. For instance, in a randomized trial, exercising twice a week was not enough.70 Additionally, a program lasting longer than 12 weeks produced more sustained benefits than shorter programs.71
A key component is an exercise protocol centered on the lower extremities (walking, cycling, treadmill), with progressive exercise intensity to a target of about 60% to 80% of the maximal exercise tolerance,72 though more modest targets of about 50% can also be beneficial.73
Exercise should be tailored to the desired outcome. For instance, training of the upper arms may help with activities of daily living. In one study, unsupported (against gravity) arm training improved upper-extremity function more than supported arm training (by ergometer).74 Ventilatory muscle training is less common, as most randomized trials have not shown conclusive evidence of benefit. Current guidelines do not recommend routine inspiratory muscle training.71
Even though indices of pulmonary function do not improve after an exercise program, randomized trials have shown that pulmonary rehabilitation improves exercise capacity, dyspnea, and health-related quality of life; improves cost-effectiveness of health care utilization; and provides psychosocial benefits that often exceed those of other therapies. Although there is no significant evidence of whether pulmonary rehabilitation improves survival in patients with COPD,71 an observational study documented improvements in BODE scores as well as a reduction in respiratory mortality rates in patients undergoing pulmonary rehabilitation.75
A limitation of pulmonary rehabilitation is that endurance and psychological and cognitive function decline significantly if exercise is not maintained. However, the role of a maintenance program is uncertain, with long-term benefits considered modest.71
Lung-volume reduction surgery
Lung-volume reduction consists of surgical wedge resections of emphysematous areas of the lung (Table 9).
The National Emphysema Treatment Trial76 randomized 1,218 patients to undergo either lung-volume reduction surgery or maximal medical therapy. Surgery improved survival, quality of life, and dyspnea in patients with upper-lobe emphysema and a low exercise capacity (corresponding to < 40 watts for men or < 25 watts for women in the maximal power achieved on cycle ergometry). While conferring no survival benefit in patients with upper-lobe-predominant emphysema and high exercise capacity, this surgery is likely to improve exercise capacity and quality of life in this subset of patients.
Importantly, the procedure is associated with a lower survival rate in patients with an FEV1 lower than 20%, homogeneous emphysema, a diffusing capacity of the lung for carbon monoxide lower than 20%, non-upper-lobe emphysema, or high baseline exercise capacity.
The proposed mechanisms of improvement of lung function include placing the diaphragm in a position with better mechanical advantage, reducing overall lung volume, better size-matching between the lungs and chest cavity, and restoring elastic recoil.76,77
Ongoing trials aim to replicate the success of lung-volume reduction using nonsurgical bronchoscopic techniques with one-way valves, coils, biologic sealants, thermal ablation, and airway stents.
Chronic obstructive pulmonary disease (COPD) has seen several changes in its assessment and treatment in recent years, reflecting advances in our understanding of this common and serious disease.
This review updates busy practitioners on the major advances, including new assessment tools and new therapies.
COMMON AND INCREASING
COPD is the third leading cause of death in the United States, behind heart disease and cancer,1 and of the top five (the others being stroke and accidents), it is the only one that increased in incidence between 2007 and 2010.2 The 11th leading cause of disability-adjusted life years worldwide in 2002, COPD is projected to become the seventh by the year 2030.3
CHARACTERIZED BY OBSTRUCTION
COPD is characterized by persistent and progressive airflow obstruction associated with chronic airway inflammation in response to noxious particles and gases. Disease of the small airways (inflammation, mucus plugging, and fibrosis) and parenchymal destruction (emphysema) limit the flow of air.
COPD is diagnosed by spirometry—specifically, a ratio of forced expiratory volume in 1 second to forced vital capacity (FEV1/FVC) of less than 0.7 after a bronchodilator is given. The severity of airflow limitation is revealed by the FEV1 as a percent of the predicted value.
Cigarette smoking is the major cause of COPD, but the prevalence of COPD is 6.6% in people who have never smoked, and one-fourth of COPD patients in the United States have never smoked.4
GOLDEN GOALS: FEWER SYMPTOMS, LOWER RISK
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) periodically issues evidence-based statements on how to prevent and treat COPD.
In its 2013 update,5 GOLD suggested two goals: improving symptoms and reducing the risk of death, exacerbations, progression of disease, and treatment-related adverse effects. The latter goal—reducing risk—is relatively new.
Exacerbations are acute inflammatory events superimposed on chronic inflammation. The inflammation is often brought on by infection6 and increases the risk of death7 and the risk of a faster decline in lung function.8
Exacerbations may characterize a phenotype of COPD. The Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) analyzed the frequency of COPD exacerbations and associated factors in 2,138 patients with COPD over a period of 3 years.9 Although patients with more severe obstruction tended to have more exacerbations, some patients appeared susceptible to exacerbations irrespective of the severity of obstruction. The best predictor of exacerbations was a history of exacerbations.
HOW DO I ASSESS A PATIENT WITH COPD ON PRESENTATION?
Markers of airflow obstruction such as the FEV1 do not correlate strongly with exertional capacity and health status in patients with COPD.10,11
The BODE index (body mass index, obstruction, dyspnea score, and exercise oximetry) takes into account the multidimensional nature of COPD. It performs better than the FEV1 in predicting the risk of death.12 The propensity for exacerbations and comorbidities further modulates outcome.
Assessing symptoms
The modified British Medical Research Council (mMRC) dyspnea scale, based on work by Fletcher in 1952,13 has five grades, numbered 0 through 4:
- Grade 0—Breathless with strenuous exercise only
- Grade 1—Breathless when hurrying on level ground or walking up a slight hill
- Grade 2—Walks slower than people of the same age on level ground because of shortness of breath or has to stop when walking at own pace on level ground
- Grade 3—Stops for breath after walking about 100 yards or after a few minutes on level ground
- Grade 4—Too breathless to leave the house or breathless when dressing or undressing.
Grade 2 or higher separates symptomatic from asymptomatic COPD.
The COPD Assessment Test (CAT) (www.catestonline.org) is a proprietary questionnaire. Patients use a 6-point scale (numbered 0 though 5) to rate eight symptoms (cough, mucus production, chest tightness, shortness of breath on exertion, limitations in home activities, lack of confidence leaving the home, poor sleep, and lack of energy). A total score of 10 or higher is abnormal.
Four GOLD groups
The new GOLD guidelines (Table 1)5 define four groups of patients according to their severity of airflow obstruction, symptoms, and exacerbation history:
- Group A—fewer symptoms, low risk: Fewer symptoms (“less symptoms,” as worded in the guidelines) means a CAT score less than 10 or an mMRC grade less than 2; “low risk” means no more than one exacerbation per year and an FEV1 of at least 50%
- Group B—more symptoms, low risk: “More symptoms” means a CAT score of 10 or more or an mMRC grade of 2 or more
- Group C—fewer symptoms, high risk: “High risk” means two or more exacerbations per year or an FEV1 less than 50%
- Group D—more symptoms, high risk.
Thus, a patient with an FEV1 of 60% (moderate airflow limitation) who has had one exacerbation during the past year and a CAT score of 8 would be in group A. In contrast, a patient who has an FEV1 of 40% (severe airflow limitation), no history of exacerbations, and a CAT score of 20 would be in group D.
Updated GOLD guidelines suggest utilizing a stepwise approach to treatment, akin to asthma management guidelines, based on patient grouping.5
How accurate is the new GOLD system?
Although practical and suited for use in primary care, the new GOLD system is arbitrary and has not been thoroughly studied, and may therefore need refinement.
Lange et al14 compared the new GOLD system with the previous one in 6,628 patients with COPD. As anticipated, the new system was better at predicting exacerbations, as it incorporates a history of exacerbations in stratification. The presence of symptoms (as determined by an mMRC grade ≥ 2) was a marker of mortality risk that distinguished group A from group B, and group C from group D. Surprisingly, the rate of death was higher in group B (more symptoms, low risk) than in group C (fewer symptoms, high risk).
Notably, most patients in group C qualified for this group because of the severity of airflow obstruction, not because of a history of exacerbations. Therefore, patients whose symptoms are out of proportion to the severity of obstruction may be at higher risk of death, possibly because of comorbidities such as cardiovascular disease.15 Patients who qualified for groups C and D by having both a history of frequent exacerbations (≥ 2 per year) and symptoms rather than either one alone had a higher risk of death in 3 years.
Similarly, the symptom-assessment tool that is used—ie, the mMRC grade or the CAT score—also makes a difference.
The Health-Related Quality of Life in COPD in Europe Study16 retrospectively analyzed data from 1,817 patients to determine whether the cutoff points for symptoms as assessed by mMRC grade and CAT score were equivalent. Although the mMRC grade correlated well with overall health status, the cutoff mMRC grade of 2 or higher did not correspond to a CAT score of 10 or higher, classifying patients with health status impairment as asymptomatic (mean weighted kappa 0.626). The two tools agreed much better when the cutoff was set at an mMRC grade of 1 or higher (mean weighted kappa 0.792).16
Although assessment schemes continue to evolve as data accumulate, we believe the new system is a welcome initiative that reflects the changing notions of COPD.
Comorbidities matter
Another shift is the recognition that certain comorbidities increase the risk of death. In 1,664 patients with COPD who were followed for 51 months, 12 distinct comorbidities were associated with a higher risk of death after multivariate analysis.17
The COTE index (COPD-Specific Comorbidity Test) is based on these findings. It awards points as follows:
- 6 points for cancer of the lung, esophagus, pancreas, or breast, or for anxiety
- 2 points for all other cancers, liver cirrhosis, atrial fibrillation or flutter, diabetes with neuropathy, or pulmonary fibrosis
- 1 point for congestive heart failure, gastric or duodenal ulcer, or coronary artery disease.
A COTE index score of 4 or higher was associated with a risk of death 2.2 times higher in each quartile of the BODE index.
We strongly recommend being aware of comorbidities in COPD patients, particularly when symptoms are out of proportion to the severity of obstruction.
SHOULD I USE ANTIBIOTICS TO TREAT ALL COPD EXACERBATIONS?
Infections are thought to cause more than 80% of acute exacerbations of COPD.
Anthonisen et al,18 in a landmark trial, found broad-spectrum antibiotics to be most helpful if the patient had at least two of the three cardinal symptoms of COPD exacerbation (ie, shortness of breath, increase in sputum volume, and sputum purulence). Antibiotics decreased the rate of treatment failure and led to a more rapid clinical resolution of exacerbation. However, they did not help patients who had milder exacerbations.
Antibiotics may nevertheless have a role in ambulatory patients with mild to moderate COPD who present with exacerbations characterized by one or more cardinal symptoms.
Llor et al,19 in a multicenter randomized double-blind placebo-controlled trial in Spain, concluded that amoxicillin clavulanate (Augmentin) led to higher clinical cure rates and longer time to the next exacerbation in these patients. Most of the benefit was in patients with more symptoms, consistent with the results of the study by Anthonisen et al.18
There is also strong evidence to support the use of antibiotics in addition to systemic corticosteroids in hospitalized patients with acute exacerbations of COPD. A 7-day course of doxycycline (Vibramycin) added to a standard regimen of corticosteroids was associated with higher rates of clinical and microbiological cure on day 10 of the exacerbation.20 In a large retrospective cohort study in 84,621 hospitalized patients with COPD exacerbations, fewer of those who received antibiotics needed mechanical ventilation, died, or were readmitted.21 Although sicker patients received antibiotics more frequently, their mortality rate was lower than in those who did not receive antibiotics, who were presumably less sick.
A meta-analysis confirmed the salutary effect of antibiotics in inpatients and particularly those admitted to the intensive care unit.22 Mortality rates and hospital length of stay were not affected in patients who were not in intensive care.
Biomarkers such as procalcitonin might help reduce the unnecessary use of antibiotics. Stolz et al23 conducted a randomized controlled trial in which they based the decision to give antibiotics on a threshold procalcitonin level of at least 1 μg/L in hospitalized patients with COPD exacerbation. The rate of antibiotic use was reduced by more than 40% in the procalcitonin group without any difference in clinical outcomes, 6-month exacerbation rate, or rehospitalization compared with controls. Nonstandardized procalcitonin assays are a possible barrier to the widespread adoption of this threshold.
Comment. In general, we recommend antibiotics for hospitalized patients with COPD exacerbation and look forward to confirmatory data that support the use of biomarkers. For outpatients, we find the Anthonisen criteria useful for decision-making at the point of care.
ARE THERE ANY NEW INTERVENTIONS TO PREVENT COPD EXACERBATIONS?
Macrolides
Macrolides have a proven role in managing chronic suppurative respiratory diseases such as cystic fibrosis24 and diffuse panbronchiolitis.25 Since they are beneficial at lower doses than those used to treat infection, the mechanism may be anti-inflammatory rather than antimicrobial.
Albert et al26 assigned 1,142 patients who had had a COPD exacerbation within a year before enrollment or who were on home oxygen therapy to receive azithromycin (Zithromax) 250 mg daily or placebo.25 The azithromycin group had fewer acute exacerbations (hazard ratio 0.73, 95% CI 0.63–0.84, P < .001), and more patients in the azithromycin group achieved clinically significant improvements in quality of life, ie, a reduction in the St. George’s Respiratory Questionnaire (SGRQ) score of at least 4 points (43% vs 36%, P = .03). Adverse events that were more common in the azithromycin group were hearing loss (25% vs 20%) and macrolide-resistant strains in nasopharyngeal secretions (81% vs 41%). In subgroup analysis, the benefit in terms of reducing exacerbations was greater in patients over age 65, patients on home oxygen, and patients with moderate or severe obstruction compared with those with very severe obstruction.
Comment. Macrolides are a valuable addition to the agents available for preventing COPD exacerbation (Table 2), but their role is still uncertain. Potential topics of research are whether these drugs have a role in patients already on preventive regimens, whether they would have a greater effect in distinct patient populations (eg, patients who have two or more exacerbations per year), and whether their broader use would lead to a change in the resident flora in the community.
Clinicians should exercise caution in the use of azithromycin in light of recent concern about associated cardiac morbidity and death. All patients should undergo electrocardiography to assess the QTc interval before starting treatment, as in the trial by Albert et al.26
Phosphodiesterase inhibitors
Roflumilast (Daliresp) is an oral phosphodiesterase 4 inhibitor approved for treating exacerbations and symptoms of chronic bronchitis in patients with severe COPD (Table 3). Phosphodiesterase 4, one of the 11 isoforms of the enzyme, is found in immune and inflammatory cells and promotes inflammatory responses. Roflumilast has anti-inflammatory properties but no acute bronchodilatory effect.27 Several phase 3 trials found the compound to have beneficial effects.
Calverley et al28 performed two placebo-controlled double-blind trials in outpatients with the clinical diagnosis of COPD who had chronic cough; increased sputum production; at least one recorded exacerbation requiring corticosteroids or hospitalization, or both; and an FEV1 of 50% or less. Patients were randomized to receive roflumilast 500 μg once a day (n = 1,537) or placebo (n = 1,554) for 1 year. The rate of moderate to severe exacerbations was 1.17 per year with roflumilast vs 1.37 with placebo (P < .0003). Adverse events were significantly more common with roflumilast and were related to the known side effects of the drug, namely, diarrhea, weight loss, decreased appetite, and nausea.
Fabbri et al29 performed two other placebo-controlled double-blind multicenter trials, studying the combinations of roflumilast with salmeterol (Serevent) and roflumilast with tiotropium (Spiriva) compared with placebo in 1,676 patients with COPD who had post-bronchodilator FEV1 values of 40% to 70% of predicted. The mean prebronchodilator FEV1 improved by 49 mL (P < .0001) in the salmeterol-plus-roflumilast trial and by 80 mL (P < .0001) in the tiotropium-plus-roflumilast trial compared with placebo. Fewer patients on roflumilast had exacerbations of any severity in both trials (risk ratio 0.82, P = .0419 and risk ratio 0.75, P = .0169, respectively).
No trial has yet addressed whether roflumilast is better than the combination of a long-acting muscarinic antagonist and a beta agonist, or whether roflumilast can be substituted for inhaled corticosteroids in a new triple-therapy combination. Clinicians should also be aware of psychiatric side effects of roflumilast, which include depression and, possibly, suicide.
ARE THERE ANY NEW BRONCHODILATORS FOR PATIENTS WITH COPD?
Long-acting muscarinic antagonists
Reversible airflow obstruction and mucus secretion are determined by the vagal cholinergic tone in patients with COPD.30 Antagonism of cholinergic (muscarinic) receptors results in bronchodilation and reduction in mucus production. Consequently, inhaled anticholinergic agents are the first-line therapy for COPD (Table 4).
Tiotropium bromide is a long-acting antimuscarinic approved in 2002 by the US Food and Drug Administration (FDA). The UPLIFT trial (Understanding Potential Long-Term Impacts on Function With Tiotropium)31 enrolled 5,993 patients with a mean FEV1 of 48% of predicted. Over a 4-year follow-up, significant improvements in mean FEV1 values (ranging from 87 mL to 103 mL before bronchodilation and 47 mL to 65 mL after bronchodilation, P < .001) in the tiotropium group were observed compared with placebo. The rate of the primary end point—the rate of decline in mean FEV1—was not different between tiotropium and placebo. However, there were important salutary effects in multiple clinical end points in the tiotropium group. Health-related quality of life as measured by the SGRQ improved in a clinically significant manner (> 4 points) in favor of tiotropium in a higher proportion of patients (45% vs 36%, P < .001). Tiotropium reduced the number of exacerbations per patient year (0.73 ± 0.02 vs 0.85 ± 0.02, RR = 0.86 (95% CI 0.81–0.91), P < .001) and the risk of respiratory failure (RR = 0.67, 95% CI 0.51–0.89). There were no significant differences in the risk of myocardial infarction, stroke, or pneumonia.
Aclidinium bromide (Tudorza Pressair) is a long-acting antimuscarinic recently approved by the FDA. Compared with tiotropium, it has a slightly faster onset of action and a considerably shorter half-life (29 hours vs 64 hours).32,33 Its dosage is 400 μg twice daily by inhalation. It provides sustained bronchodilation over 24 hours and may have a favorable side-effect profile, because it undergoes rapid hydrolysis in human plasma.34
ACCORD COPD I35 and ATTAIN,36 two phase 3 trials in patients with moderate-to severe COPD, found that twice-daily aclidinium was associated with statistically and clinically significant (> 100 mL) improvements in trough and peak FEV1 compared with placebo. Health status (assessed by SGRQ) and dyspnea (assessed by transitional dyspnea index) also improved significantly. However, improvements beyond minimum clinically significant thresholds were achieved only with 400 μg twice-daily dosing.
To date, no study has evaluated the impact of aclidinium on COPD exacerbation as a primary end point. Fewer moderate to severe exacerbations were reported in an earlier 52-week study of once-daily aclidinium (ACCLAIM COPD II) but not in ACCLAIM COPD I.37
Aclidinium may offer an advantage over tiotropium in patients who have nocturnal symptoms. Twice-daily aclidinium 400 μg was associated with superior FEV1 area-under-the-curve values compared with placebo and tiotropium, the difference mostly owing to improved nocturnal profile.38
Long-acting beta-2 agonists
Stimulation of airway beta-2 receptors relaxes smooth muscles and consequently dilates bronchioles via a cyclic adenosine monophosphate-dependent pathway.39
Short-acting beta-2 agonists such as albuterol and terbutaline have long been used as rescue medications for obstructive lung disease. Long-acting beta-2 agonists provide sustained bronchodilation and are therefore more efficacious as maintenance medications. Salmeterol, formoterol (Foradil), and arformoterol (Brovana) are long-acting beta-2 agonists in clinical use that are taken twice daily.
Clinical studies indicate that use of long-acting beta-2 agonists leads to significant improvements in FEV1,40–42 dynamic hyperinflation, exercise tolerance,43,44 and dyspnea.45,46 These drugs have also been associated with significant improvements in health-related quality of life and in the frequency of exacerbations.47–49
In patients with asthma, long-acting beta agonists may increase the risk of death.50 In contrast, in patients with COPD, they appear to offer a survival advantage when used in combination with inhaled corticosteroids,51 and some argue that this benefit is entirely from the long-acting beta agonist (a 17% reduction in mortality) rather than the inhaled corticosteroid (0% reduction in mortality).52
Indacaterol (Arcapta), approved in July 2011, is the first once-daily beta agonist or “ultra-long-acting” beta agonist (Table 5). Possibly because it has a high affinity for the lipid raft domain of the cell membrane where beta-2 receptors are coupled to second messengers,53 the drug has a 24-hour duration of action.
In patients with COPD, inhaled indacaterol 150 μg once daily improved airflow obstruction and health status as measured by SGRQ compared with salmeterol 50 μg twice daily and placebo.54 At the higher dose of 300 μg daily, the 52-week INVOLVE trial55 demonstrated early and more sustained improvement in FEV1 compared with placebo and formoterol. In this study, a lower exacerbation rate than with placebo was also noted. The drug has also shown equivalent bronchodilator efficacy at 150 μg and 300 μg daily dosing compared with tiotropium.56
The benefits of a longer-acting bronchodilator such as indacaterol are likely mediated by smoothing out airway bronchomotor tone over 24 hours without the dips seen with shorter-acting agents and by improvement of the FEV1 trough before the subsequent dose is due, aptly named “pharmacologic stenting.”57 Once-daily dosing should also foster better adherence. The safety profile appears excellent with no increase in cardiovascular or cerebrovascular events compared with placebo.58
The FDA approved the 75-μg daily dose instead of the higher doses used in the studies mentioned above. This decision was based on the observation that there appeared to be a flattened dose-response in patients with more severe COPD, with no further improvement in trough FEV1 at higher doses.59
DOES VITAMIN D SUPPLEMENTATION HAVE A ROLE IN COPD MANAGEMENT?
Vitamin D is vital for calcium and phosphate metabolism and bone health. Low vitamin D levels are associated with diminished leg strength and falls in the elderly.60 Osteoporosis, preventable with vitamin D and calcium supplementation, is linked to thoracic vertebral fracture and consequent reduced lung function.61,62
Patients with COPD are at higher risk of vitamin D deficiency, and more so if they also are obese, have advanced airflow obstruction, are depressed, or smoke.62 Therefore, there are sound reasons to look for vitamin D deficiency in patients with COPD and to treat it if the 25-hydroxyvitamin D level is less than 10 ng/ mL (Table 6).
Vitamin D may also have antimicrobial and immunomodulatory effects.63 Since COPD exacerbations are frequently caused by infection, it was hypothesized that vitamin D supplementation might reduce the rate of exacerbations.
In a study in 182 patients with moderate to very severe COPD and a history of recent exacerbations, high-dose vitamin D supplementation (100,000 IU) was given every 4 weeks for 1 year.64 There were no differences in the time to first exacerbation, in the rate of exacerbation, hospitalization, or death, or in quality of life between the placebo and intervention groups. However, subgroup analysis indicated that, in those with severe vitamin D deficiency at baseline, the exacerbation rate was reduced by more than 40%.
Comment. We recommend screening for vitamin D deficiency in patients with COPD. Supplementation is appropriate in those with low levels, but data indicate no role in those with normal levels.
WHAT ARE THE NONPHARMACOLOGIC APPROACHES TO COPD TREATMENT?
Noninvasive positive-pressure ventilation
Nocturnal noninvasive positive-pressure ventilation may be beneficial in patients with severe COPD, daytime hypercapnia, and nocturnal hypoventilation, particularly if higher inspiratory pressures are selected (Table 7).65,66
For instance, a randomized controlled trial of noninvasive positive-pressure ventilation plus long-term oxygen therapy compared with long-term oxygen therapy alone in hypercapnic COPD demonstrated a survival benefit in favor of ventilation (hazard ratio 0.6).67
In another randomized trial,68 settings that aimed to maximally reduce Paco2 (mean inspiratory positive airway pressure 29 cm H2O with a backup rate of 17.5/min) were compared with low-intensity positive airway pressure (mean inspiratory positive airway pressure 14 cm H2O, backup rate 8/min). The high inspiratory pressures increased the daily use of ventilation by 3.6 hours per day and improved exercise-related dyspnea, daytime Paco2, FEV1, vital capacity, and health-related quality of life66 without disrupting sleep quality.68
Caveats are that acclimation to the high pressures was achieved in the hospital, and the high pressures were associated with a significant increase in air leaks.66
Comments. Whether high-pressure noninvasive positive-pressure ventilation can be routinely implemented and adopted in the outpatient setting, and whether it is associated with a survival advantage remains to be determined. The advantages of noninvasive positive-pressure ventilation in the setting of hypercapnic COPD appear to augment those of pulmonary rehabilitation, with improved quality of life, gas exchange, and exercise tolerance, and a slower decline of lung function.69
Pulmonary rehabilitation
Pulmonary rehabilitation is a multidisciplinary approach to managing COPD (Table 8).
Patients participate in three to five supervised sessions per week, each lasting 3 to 4 hours, for 6 to 12 weeks. Less-frequent sessions may not be effective. For instance, in a randomized trial, exercising twice a week was not enough.70 Additionally, a program lasting longer than 12 weeks produced more sustained benefits than shorter programs.71
A key component is an exercise protocol centered on the lower extremities (walking, cycling, treadmill), with progressive exercise intensity to a target of about 60% to 80% of the maximal exercise tolerance,72 though more modest targets of about 50% can also be beneficial.73
Exercise should be tailored to the desired outcome. For instance, training of the upper arms may help with activities of daily living. In one study, unsupported (against gravity) arm training improved upper-extremity function more than supported arm training (by ergometer).74 Ventilatory muscle training is less common, as most randomized trials have not shown conclusive evidence of benefit. Current guidelines do not recommend routine inspiratory muscle training.71
Even though indices of pulmonary function do not improve after an exercise program, randomized trials have shown that pulmonary rehabilitation improves exercise capacity, dyspnea, and health-related quality of life; improves cost-effectiveness of health care utilization; and provides psychosocial benefits that often exceed those of other therapies. Although there is no significant evidence of whether pulmonary rehabilitation improves survival in patients with COPD,71 an observational study documented improvements in BODE scores as well as a reduction in respiratory mortality rates in patients undergoing pulmonary rehabilitation.75
A limitation of pulmonary rehabilitation is that endurance and psychological and cognitive function decline significantly if exercise is not maintained. However, the role of a maintenance program is uncertain, with long-term benefits considered modest.71
Lung-volume reduction surgery
Lung-volume reduction consists of surgical wedge resections of emphysematous areas of the lung (Table 9).
The National Emphysema Treatment Trial76 randomized 1,218 patients to undergo either lung-volume reduction surgery or maximal medical therapy. Surgery improved survival, quality of life, and dyspnea in patients with upper-lobe emphysema and a low exercise capacity (corresponding to < 40 watts for men or < 25 watts for women in the maximal power achieved on cycle ergometry). While conferring no survival benefit in patients with upper-lobe-predominant emphysema and high exercise capacity, this surgery is likely to improve exercise capacity and quality of life in this subset of patients.
Importantly, the procedure is associated with a lower survival rate in patients with an FEV1 lower than 20%, homogeneous emphysema, a diffusing capacity of the lung for carbon monoxide lower than 20%, non-upper-lobe emphysema, or high baseline exercise capacity.
The proposed mechanisms of improvement of lung function include placing the diaphragm in a position with better mechanical advantage, reducing overall lung volume, better size-matching between the lungs and chest cavity, and restoring elastic recoil.76,77
Ongoing trials aim to replicate the success of lung-volume reduction using nonsurgical bronchoscopic techniques with one-way valves, coils, biologic sealants, thermal ablation, and airway stents.
- Miniño AM, Xu J, Kochanek KD. Deaths: preliminary data for 2008. National Vital Statistics Reports 2010; 59:1–52. http://www.cdc.gov/nchs/data/nvsr/nvsr59/nvsr59_02.pdf. Accessed April 10, 2014.
- Murphy SL, Xu J, Kochanek KD. Deaths: preliminary data from 2010. National Vital Statistics Reports 2012; 60:1–51. http://www.cdc.gov/nchs/data/nvsr/nvsr60/nvsr60_04.pdf. Accessed April 10, 2014.
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006; 3:e442.
- Behrendt CE. Mild and moderate-to-severe COPD in nonsmokers: distinct demographic profiles. Chest 2005; 128:1239–1244.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). http://www.goldcopd.org/Guidelines/guidelines-resources.html. Accessed April 10, 2014.
- Papi A, Bellettato CM, Braccioni F, et al. Infections and airway inflammation in chronic obstructive pulmonary disease severe exacerbations. Am J Respir Crit Care Med 2006; 173:1114–1121.
- Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax 2005; 60:925–931.
- Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax 2002; 57:847–852.
- Hurst JR, Vestbo J, Anzueto A, et al; Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Investigators. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med 2010; 363:1128–1138.
- Cooper CB. The connection between chronic obstructive pulmonary disease symptoms and hyperinflation and its impact on exercise and function. Am J Med 2006; 119(suppl 1):21–31.
- Jones PW. Issues concerning health-related quality of life in COPD. Chest 1995; 107(suppl):187S–193S.
- Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004; 350:1005–1012.
- Fletcher CM. The clinical diagnosis of pulmonary emphysema—an experimental study. J Royal Soc Med 1952; 45:577–584.
- Lange P, Marott JL, Vestbo J, et al. Prediction of the clinical course of chronic obstructive pulmonary disease, using the new GOLD classification: a study of the general population. Am J Respir Crit Care Med 2012; 186:975–981.
- Hurst J. Phenotype-based care in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2012; 186:935–936.
- Jones PW, Adamek L, Nadeau G, Banik N. Comparisons of health status scores with MRC grades in COPD: implications for the GOLD 2011 classification. Eur Respir J 2013; 42:647–654.
- Divo M, Cote C, de Torres JP, et al; BODE Collaborative Group. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2012; 186:155–161.
- Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GK, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med 1987; 106:196–204.
- Llor C, Moragas A, Hernández S, Bayona C, Miravitlles M. Efficacy of antibiotic therapy for acute exacerbations of mild to moderate chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2012; 186:716–723.
- Daniels JM, Snijders D, de Graaff CS, Vlaspolder F, Jansen HM, Boersma WG. Antibiotics in addition to systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2010; 181:150–157.
- Rothberg MB, Pekow PS, Lahti M, Brody O, Skiest DJ, Lindenauer PK. Antibiotic therapy and treatment failure in patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease. JAMA 2010; 303:2035–2042.
- Vollenweider DJ, Jarrett H, Steurer-Stey CA, Garcia-Aymerich J, Puhan MA. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012; 12:CD010257.
- Stolz D, Christ-Crain M, Bingisser R, et al. Antibiotic treatment of exacerbations of COPD: a randomized, controlled trial comparing procalcitonin-guidance with standard therapy. Chest 2007; 131:9–19.
- Wolter J, Seeney S, Bell S, Bowler S, Masel P, McCormack J. Effect of long term treatment with azithromycin on disease parameters in cystic fibrosis: a randomised trial. Thorax 2002; 57:212–216.
- Kudoh S, Azuma A, Yamamoto M, Izumi T, Ando M. Improvement of survival in patients with diffuse panbronchiolitis treated with low-dose erythromycin. Am J Respir Crit Care Med 1998; 157:1829–1832.
- Albert RK, Connett J, Bailey WC, et al; COPD Clinical Research Network. Azithromycin for prevention of exacerbations of COPD. N Engl J Med 2011; 365:689–698.
- Gross NJ, Giembycz MA, Rennard SI. Treatment of chronic obstructive pulmonary disease with roflumilast, a new phosphodiesterase 4 inhibitor. COPD 2010; 7:141–153.
- Calverley PM, Rabe KF, Goehring UM, Kristiansen S, Fabbri LM, Martinez FJ; M2-124 and M2-125 study groups. Roflumilast in symptomatic chronic obstructive pulmonary disease: two randomised clinical trials. Lancet 2009; 374:685–694.
- Fabbri LM, Calverley PM, Izquierdo-Alonso JL, et al; M2-127 and M2-128 study groups. Roflumilast in moderate-to-severe chronic obstructive pulmonary disease treated with long acting bronchodilators: two randomised clinical trials. Lancet 2009; 374:695–703.
- Gross NJ, Skorodin MS. Anticholinergic, antimuscarinic bronchodilators. Am Rev Respir Dis 1984; 129:856–870.
- Tashkin DP, Celli B, Senn S, et al; UPLIFT Study Investigators. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med 2008; 359:1543–1554.
- Cazzola M. Aclidinium bromide, a novel long-acting muscarinic M3 antagonist for the treatment of COPD. Curr Opin Investig Drugs 2009; 10:482–490.
- Gavaldà A, Miralpeix M, Ramos I, et al. Characterization of aclidinium bromide, a novel inhaled muscarinic antagonist, with long duration of action and a favorable pharmacological profile. J Pharmacol Exp Ther 2009; 331:740–751.
- Alagha K, Bourdin A, Tummino C, Chanez P. An update on the efficacy and safety of aclidinium bromide in patients with COPD. Ther Adv Respir Dis 2011; 5:19–28.
- Kerwin EM, D’Urzo AD, Gelb AF, Lakkis H, Garcia Gil E, Caracta CF; ACCORD I study investigators. Efficacy and safety of a 12-week treatment with twice-daily aclidinium bromide in COPD patients (ACCORD COPD I). COPD 2012; 9:90–101.
- Jones PW, Singh D, Bateman ED, et al. Efficacy and safety of twice-daily aclidinium bromide in COPD patients: the ATTAIN study. Eur Respir J 2012; 40:830–836.
- Jones PW, Rennard SI, Agusti A, et al. Efficacy and safety of once-daily aclidinium in chronic obstructive pulmonary disease. Respir Res 2011; 12:55.
- Fuhr R, Magnussen H, Sarem K, et al. Efficacy of aclidinium bromide 400 μg twice daily compared with placebo and tiotropium in patients with moderate to severe COPD. Chest 2012; 141:745–752.
- Tashkin DP, Fabbri LM. Long-acting beta-agonists in the management of chronic obstructive pulmonary disease: current and future agents. Respir Res 2010; 11:149.
- Mahler DA, Donohue JF, Barbee RA, et al. Efficacy of salmeterol xinafoate in the treatment of COPD. Chest 1999; 115:957–965.
- Campbell M, Eliraz A, Johansson G, et al. Formoterol for maintenance and as-needed treatment of chronic obstructive pulmonary disease. Respir Med 2005; 99:1511–1520.
- Hanrahan JP, Hanania NA, Calhoun WJ, Sahn SA, Sciarappa K, Baumgartner RA. Effect of nebulized arformoterol on airway function in COPD: results from two randomized trials. COPD 2008; 5:25–34.
- Neder JA, Fuld JP, Overend T, et al. Effects of formoterol on exercise tolerance in severely disabled patients with COPD. Respir Med 2007; 101:2056–2064.
- O’Donnell DE, Voduc N, Fitzpatrick M, Webb KA. Effect of salmeterol on the ventilatory response to exercise in chronic obstructive pulmonary disease. Eur Respir J 2004; 24:86–94.
- Rennard SI, Anderson W, ZuWallack R, et al. Use of a long-acting inhaled beta 2-adrenergic agonist, salmeterol xinafoate, in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2001; 163:1087–1092.
- Schultze-Werninghaus G. Multicenter 1-year trial on formoterol, a new long-acting beta 2-agonist, in chronic obstructive airway disease. Lung 1990; 168(suppl):83–89.
- Rodrigo GJ, Nannini LJ, Rodríguez-Roisin R. Safety of long-acting beta-agonists in stable COPD: a systematic review. Chest 2008; 133:1079–1087.
- Baker WL, Baker EL, Coleman CI. Pharmacologic treatments for chronic obstructive pulmonary disease: a mixed-treatment comparison meta-analysis. Pharmacotherapy 2009; 29:891–905.
- Rodrigo GJ, Castro-Rodriguez JA, Plaza V. Safety and efficacy of combined long-acting beta-agonists and inhaled corticosteroids vs long-acting beta-agonists monotherapy for stable COPD: a systematic review. Chest 2009; 136:1029–1038.
- Nelson HS, Weiss ST, Bleecker ER, Yancey SW, Dorinsky PM; SMART Study Group. The Salmeterol Multicenter Asthma Research Trial: a comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. Chest 2006; 129:15–26.
- Calverley PM, Anderson JA, Celli B, et al; TORCH investigators. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med 2007; 356:775–789.
- Suissa S, Ernst P, Vandemheen KL, Aaron SD. Methodological issues in therapeutic trials of COPD. Eur Respir J 2008; 31:927–933.
- Lombardi D, Cuenoud B, Krämer SD. Lipid membrane interactions of indacaterol and salmeterol: do they influence their pharmacological properties? Eur J Pharm Sci 2009; 38:533–547.
- Kornmann O, Dahl R, Centanni S, et al; INLIGHT-2 (Indacaterol Efficacy Evaluation Using 150-μg Doses with COPD Patients) study investigators. Once-daily indacaterol versus twice-daily salmeterol for COPD: a placebo-controlled comparison. Eur Respir J 2011; 37:273–279.
- Dahl R, Chung KF, Buhl R, et al; INVOLVE (INdacaterol: Value in COPD: Longer Term Validation of Efficacy and Safety) Study Investigators. Efficacy of a new once-daily long-acting inhaled beta2-agonist indacaterol versus twice-daily formoterol in COPD. Thorax 2010; 65:473–479.
- Donohue JF, Fogarty C, Lötvall J, et al; INHANCE Study Investigators. Once-daily bronchodilators for chronic obstructive pulmonary disease: indacaterol versus tiotropium. Am J Respir Crit Care Med 2010; 182:155–162.
- Beeh KM, Beier J. The short, the long and the “ultra-long”: why duration of bronchodilator action matters in chronic obstructive pulmonary disease. Adv Ther 2010; 27:150–159.
- Worth H, Chung KF, Felser JM, Hu H, Rueegg P. Cardio- and cerebrovascular safety of indacaterol vs formoterol, salmeterol, tiotropium and placebo in COPD. Respir Med 2011; 105:571–579.
- Chowdhury BA, Seymour SM, Michele TM, Durmowicz AG, Liu D, Rosebraugh CJ. The risks and benefits of indacaterol--the FDA’s review. N Engl J Med 2011; 365:2247–2249.
- Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, et al. Effect of vitamin D on falls: a meta-analysis. JAMA 2004; 291:1999–2006.
- Leech JA, Dulberg C, Kellie S, Pattee L, Gay J. Relationship of lung function to severity of osteoporosis in women. Am Rev Respir Dis 1990; 141:68–71.
- Persson LJ, Aanerud M, Hiemstra PS, Hardie JA, Bakke PS, Eagan TM. Chronic obstructive pulmonary disease is associated with low levels of vitamin D. PLoS One 2012; 7:e38934.
- Janssens W, Lehouck A, Carremans C, Bouillon R, Mathieu C, Decramer M. Vitamin D beyond bones in chronic obstructive pulmonary disease: time to act. Am J Respir Crit Care Med 2009; 179:630–636.
- Lehouck A, Mathieu C, Carremans C, et al. High doses of vitamin D to reduce exacerbations in chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med 2012; 156:105–114.
- Casanova C, Celli BR, Tost L, et al. Long-term controlled trial of nocturnal nasal positive pressure ventilation in patients with severe COPD. Chest 2000; 118:1582–1590.
- Dreher M, Storre JH, Schmoor C, Windisch W. High-intensity versus low-intensity non-invasive ventilation in patients with stable hypercapnic COPD: a randomised crossover trial. Thorax 2010; 65:303–308.
- McEvoy RD, Pierce RJ, Hillman D, et al; Australian trial of non-invasive Ventilation in Chronic Airflow Limitation (AVCAL) Study Group. Nocturnal non-invasive nasal ventilation in stable hypercapnic COPD: a randomised controlled trial. Thorax 2009; 64:561–566.
- Dreher M, Ekkernkamp E, Walterspacher S, et al. Noninvasive ventilation in COPD: impact of inspiratory pressure levels on sleep quality. Chest 2011; 140:939–945.
- Duiverman ML, Wempe JB, Bladder G, et al. Two-year home-based nocturnal noninvasive ventilation added to rehabilitation in chronic obstructive pulmonary disease patients: a randomized controlled trial. Respir Res 2011; 12:112.
- Ringbaek TJ, Broendum E, Hemmingsen L, et al. Rehabilitation of patients with chronic obstructive pulmonary disease. Exercise twice a week is not sufficient! Respir Med 2000; 94:150–154.
- Ries AL, Bauldoff GS, Carlin BW, et al. Pulmonary Rehabilitation: Joint ACCP/AACVPR Evidence-Based Clinical Practice Guidelines. Chest 2007; 131(suppl):4S–42S.
- Vallet G, Ahmaïdi S, Serres I, et al. Comparison of two training programmes in chronic airway limitation patients: standardized versus individualized protocols. Eur Respir J 1997; 10:114–122.
- Vogiatzis I, Williamson AF, Miles J, Taylor IK. Physiological response to moderate exercise workloads in a pulmonary rehabilitation program in patients with varying degrees of airflow obstruction. Chest 1999; 116:1200–1207.
- Martinez FJ, Vogel PD, Dupont DN, Stanopoulos I, Gray A, Beamis JF. Supported arm exercise vs unsupported arm exercise in the rehabilitation of patients with severe chronic airflow obstruction. Chest 1993; 103:1397–1402.
- Cote CG, Celli BR. Pulmonary rehabilitation and the BODE index in COPD. Eur Respir J 2005; 26:630–636.
- Fishman A, Martinez F, Naunheim K, et al; National Emphysema Treatment Trial Research Group. A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl J Med 2003; 348:2059–2073.
- Naunheim KS, Wood DE, Mohsenifar Z, et al; National Emphysema Treatment Trial Research Group. Long-term follow-up of patients receiving lung-volume-reduction surgery versus medical therapy for severe emphysema by the National Emphysema Treatment Trial Research Group. Ann Thorac Surg 2006; 82:431–443.
- Miniño AM, Xu J, Kochanek KD. Deaths: preliminary data for 2008. National Vital Statistics Reports 2010; 59:1–52. http://www.cdc.gov/nchs/data/nvsr/nvsr59/nvsr59_02.pdf. Accessed April 10, 2014.
- Murphy SL, Xu J, Kochanek KD. Deaths: preliminary data from 2010. National Vital Statistics Reports 2012; 60:1–51. http://www.cdc.gov/nchs/data/nvsr/nvsr60/nvsr60_04.pdf. Accessed April 10, 2014.
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006; 3:e442.
- Behrendt CE. Mild and moderate-to-severe COPD in nonsmokers: distinct demographic profiles. Chest 2005; 128:1239–1244.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). http://www.goldcopd.org/Guidelines/guidelines-resources.html. Accessed April 10, 2014.
- Papi A, Bellettato CM, Braccioni F, et al. Infections and airway inflammation in chronic obstructive pulmonary disease severe exacerbations. Am J Respir Crit Care Med 2006; 173:1114–1121.
- Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax 2005; 60:925–931.
- Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax 2002; 57:847–852.
- Hurst JR, Vestbo J, Anzueto A, et al; Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Investigators. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med 2010; 363:1128–1138.
- Cooper CB. The connection between chronic obstructive pulmonary disease symptoms and hyperinflation and its impact on exercise and function. Am J Med 2006; 119(suppl 1):21–31.
- Jones PW. Issues concerning health-related quality of life in COPD. Chest 1995; 107(suppl):187S–193S.
- Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004; 350:1005–1012.
- Fletcher CM. The clinical diagnosis of pulmonary emphysema—an experimental study. J Royal Soc Med 1952; 45:577–584.
- Lange P, Marott JL, Vestbo J, et al. Prediction of the clinical course of chronic obstructive pulmonary disease, using the new GOLD classification: a study of the general population. Am J Respir Crit Care Med 2012; 186:975–981.
- Hurst J. Phenotype-based care in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2012; 186:935–936.
- Jones PW, Adamek L, Nadeau G, Banik N. Comparisons of health status scores with MRC grades in COPD: implications for the GOLD 2011 classification. Eur Respir J 2013; 42:647–654.
- Divo M, Cote C, de Torres JP, et al; BODE Collaborative Group. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2012; 186:155–161.
- Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GK, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med 1987; 106:196–204.
- Llor C, Moragas A, Hernández S, Bayona C, Miravitlles M. Efficacy of antibiotic therapy for acute exacerbations of mild to moderate chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2012; 186:716–723.
- Daniels JM, Snijders D, de Graaff CS, Vlaspolder F, Jansen HM, Boersma WG. Antibiotics in addition to systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2010; 181:150–157.
- Rothberg MB, Pekow PS, Lahti M, Brody O, Skiest DJ, Lindenauer PK. Antibiotic therapy and treatment failure in patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease. JAMA 2010; 303:2035–2042.
- Vollenweider DJ, Jarrett H, Steurer-Stey CA, Garcia-Aymerich J, Puhan MA. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012; 12:CD010257.
- Stolz D, Christ-Crain M, Bingisser R, et al. Antibiotic treatment of exacerbations of COPD: a randomized, controlled trial comparing procalcitonin-guidance with standard therapy. Chest 2007; 131:9–19.
- Wolter J, Seeney S, Bell S, Bowler S, Masel P, McCormack J. Effect of long term treatment with azithromycin on disease parameters in cystic fibrosis: a randomised trial. Thorax 2002; 57:212–216.
- Kudoh S, Azuma A, Yamamoto M, Izumi T, Ando M. Improvement of survival in patients with diffuse panbronchiolitis treated with low-dose erythromycin. Am J Respir Crit Care Med 1998; 157:1829–1832.
- Albert RK, Connett J, Bailey WC, et al; COPD Clinical Research Network. Azithromycin for prevention of exacerbations of COPD. N Engl J Med 2011; 365:689–698.
- Gross NJ, Giembycz MA, Rennard SI. Treatment of chronic obstructive pulmonary disease with roflumilast, a new phosphodiesterase 4 inhibitor. COPD 2010; 7:141–153.
- Calverley PM, Rabe KF, Goehring UM, Kristiansen S, Fabbri LM, Martinez FJ; M2-124 and M2-125 study groups. Roflumilast in symptomatic chronic obstructive pulmonary disease: two randomised clinical trials. Lancet 2009; 374:685–694.
- Fabbri LM, Calverley PM, Izquierdo-Alonso JL, et al; M2-127 and M2-128 study groups. Roflumilast in moderate-to-severe chronic obstructive pulmonary disease treated with long acting bronchodilators: two randomised clinical trials. Lancet 2009; 374:695–703.
- Gross NJ, Skorodin MS. Anticholinergic, antimuscarinic bronchodilators. Am Rev Respir Dis 1984; 129:856–870.
- Tashkin DP, Celli B, Senn S, et al; UPLIFT Study Investigators. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med 2008; 359:1543–1554.
- Cazzola M. Aclidinium bromide, a novel long-acting muscarinic M3 antagonist for the treatment of COPD. Curr Opin Investig Drugs 2009; 10:482–490.
- Gavaldà A, Miralpeix M, Ramos I, et al. Characterization of aclidinium bromide, a novel inhaled muscarinic antagonist, with long duration of action and a favorable pharmacological profile. J Pharmacol Exp Ther 2009; 331:740–751.
- Alagha K, Bourdin A, Tummino C, Chanez P. An update on the efficacy and safety of aclidinium bromide in patients with COPD. Ther Adv Respir Dis 2011; 5:19–28.
- Kerwin EM, D’Urzo AD, Gelb AF, Lakkis H, Garcia Gil E, Caracta CF; ACCORD I study investigators. Efficacy and safety of a 12-week treatment with twice-daily aclidinium bromide in COPD patients (ACCORD COPD I). COPD 2012; 9:90–101.
- Jones PW, Singh D, Bateman ED, et al. Efficacy and safety of twice-daily aclidinium bromide in COPD patients: the ATTAIN study. Eur Respir J 2012; 40:830–836.
- Jones PW, Rennard SI, Agusti A, et al. Efficacy and safety of once-daily aclidinium in chronic obstructive pulmonary disease. Respir Res 2011; 12:55.
- Fuhr R, Magnussen H, Sarem K, et al. Efficacy of aclidinium bromide 400 μg twice daily compared with placebo and tiotropium in patients with moderate to severe COPD. Chest 2012; 141:745–752.
- Tashkin DP, Fabbri LM. Long-acting beta-agonists in the management of chronic obstructive pulmonary disease: current and future agents. Respir Res 2010; 11:149.
- Mahler DA, Donohue JF, Barbee RA, et al. Efficacy of salmeterol xinafoate in the treatment of COPD. Chest 1999; 115:957–965.
- Campbell M, Eliraz A, Johansson G, et al. Formoterol for maintenance and as-needed treatment of chronic obstructive pulmonary disease. Respir Med 2005; 99:1511–1520.
- Hanrahan JP, Hanania NA, Calhoun WJ, Sahn SA, Sciarappa K, Baumgartner RA. Effect of nebulized arformoterol on airway function in COPD: results from two randomized trials. COPD 2008; 5:25–34.
- Neder JA, Fuld JP, Overend T, et al. Effects of formoterol on exercise tolerance in severely disabled patients with COPD. Respir Med 2007; 101:2056–2064.
- O’Donnell DE, Voduc N, Fitzpatrick M, Webb KA. Effect of salmeterol on the ventilatory response to exercise in chronic obstructive pulmonary disease. Eur Respir J 2004; 24:86–94.
- Rennard SI, Anderson W, ZuWallack R, et al. Use of a long-acting inhaled beta 2-adrenergic agonist, salmeterol xinafoate, in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2001; 163:1087–1092.
- Schultze-Werninghaus G. Multicenter 1-year trial on formoterol, a new long-acting beta 2-agonist, in chronic obstructive airway disease. Lung 1990; 168(suppl):83–89.
- Rodrigo GJ, Nannini LJ, Rodríguez-Roisin R. Safety of long-acting beta-agonists in stable COPD: a systematic review. Chest 2008; 133:1079–1087.
- Baker WL, Baker EL, Coleman CI. Pharmacologic treatments for chronic obstructive pulmonary disease: a mixed-treatment comparison meta-analysis. Pharmacotherapy 2009; 29:891–905.
- Rodrigo GJ, Castro-Rodriguez JA, Plaza V. Safety and efficacy of combined long-acting beta-agonists and inhaled corticosteroids vs long-acting beta-agonists monotherapy for stable COPD: a systematic review. Chest 2009; 136:1029–1038.
- Nelson HS, Weiss ST, Bleecker ER, Yancey SW, Dorinsky PM; SMART Study Group. The Salmeterol Multicenter Asthma Research Trial: a comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. Chest 2006; 129:15–26.
- Calverley PM, Anderson JA, Celli B, et al; TORCH investigators. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med 2007; 356:775–789.
- Suissa S, Ernst P, Vandemheen KL, Aaron SD. Methodological issues in therapeutic trials of COPD. Eur Respir J 2008; 31:927–933.
- Lombardi D, Cuenoud B, Krämer SD. Lipid membrane interactions of indacaterol and salmeterol: do they influence their pharmacological properties? Eur J Pharm Sci 2009; 38:533–547.
- Kornmann O, Dahl R, Centanni S, et al; INLIGHT-2 (Indacaterol Efficacy Evaluation Using 150-μg Doses with COPD Patients) study investigators. Once-daily indacaterol versus twice-daily salmeterol for COPD: a placebo-controlled comparison. Eur Respir J 2011; 37:273–279.
- Dahl R, Chung KF, Buhl R, et al; INVOLVE (INdacaterol: Value in COPD: Longer Term Validation of Efficacy and Safety) Study Investigators. Efficacy of a new once-daily long-acting inhaled beta2-agonist indacaterol versus twice-daily formoterol in COPD. Thorax 2010; 65:473–479.
- Donohue JF, Fogarty C, Lötvall J, et al; INHANCE Study Investigators. Once-daily bronchodilators for chronic obstructive pulmonary disease: indacaterol versus tiotropium. Am J Respir Crit Care Med 2010; 182:155–162.
- Beeh KM, Beier J. The short, the long and the “ultra-long”: why duration of bronchodilator action matters in chronic obstructive pulmonary disease. Adv Ther 2010; 27:150–159.
- Worth H, Chung KF, Felser JM, Hu H, Rueegg P. Cardio- and cerebrovascular safety of indacaterol vs formoterol, salmeterol, tiotropium and placebo in COPD. Respir Med 2011; 105:571–579.
- Chowdhury BA, Seymour SM, Michele TM, Durmowicz AG, Liu D, Rosebraugh CJ. The risks and benefits of indacaterol--the FDA’s review. N Engl J Med 2011; 365:2247–2249.
- Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, et al. Effect of vitamin D on falls: a meta-analysis. JAMA 2004; 291:1999–2006.
- Leech JA, Dulberg C, Kellie S, Pattee L, Gay J. Relationship of lung function to severity of osteoporosis in women. Am Rev Respir Dis 1990; 141:68–71.
- Persson LJ, Aanerud M, Hiemstra PS, Hardie JA, Bakke PS, Eagan TM. Chronic obstructive pulmonary disease is associated with low levels of vitamin D. PLoS One 2012; 7:e38934.
- Janssens W, Lehouck A, Carremans C, Bouillon R, Mathieu C, Decramer M. Vitamin D beyond bones in chronic obstructive pulmonary disease: time to act. Am J Respir Crit Care Med 2009; 179:630–636.
- Lehouck A, Mathieu C, Carremans C, et al. High doses of vitamin D to reduce exacerbations in chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med 2012; 156:105–114.
- Casanova C, Celli BR, Tost L, et al. Long-term controlled trial of nocturnal nasal positive pressure ventilation in patients with severe COPD. Chest 2000; 118:1582–1590.
- Dreher M, Storre JH, Schmoor C, Windisch W. High-intensity versus low-intensity non-invasive ventilation in patients with stable hypercapnic COPD: a randomised crossover trial. Thorax 2010; 65:303–308.
- McEvoy RD, Pierce RJ, Hillman D, et al; Australian trial of non-invasive Ventilation in Chronic Airflow Limitation (AVCAL) Study Group. Nocturnal non-invasive nasal ventilation in stable hypercapnic COPD: a randomised controlled trial. Thorax 2009; 64:561–566.
- Dreher M, Ekkernkamp E, Walterspacher S, et al. Noninvasive ventilation in COPD: impact of inspiratory pressure levels on sleep quality. Chest 2011; 140:939–945.
- Duiverman ML, Wempe JB, Bladder G, et al. Two-year home-based nocturnal noninvasive ventilation added to rehabilitation in chronic obstructive pulmonary disease patients: a randomized controlled trial. Respir Res 2011; 12:112.
- Ringbaek TJ, Broendum E, Hemmingsen L, et al. Rehabilitation of patients with chronic obstructive pulmonary disease. Exercise twice a week is not sufficient! Respir Med 2000; 94:150–154.
- Ries AL, Bauldoff GS, Carlin BW, et al. Pulmonary Rehabilitation: Joint ACCP/AACVPR Evidence-Based Clinical Practice Guidelines. Chest 2007; 131(suppl):4S–42S.
- Vallet G, Ahmaïdi S, Serres I, et al. Comparison of two training programmes in chronic airway limitation patients: standardized versus individualized protocols. Eur Respir J 1997; 10:114–122.
- Vogiatzis I, Williamson AF, Miles J, Taylor IK. Physiological response to moderate exercise workloads in a pulmonary rehabilitation program in patients with varying degrees of airflow obstruction. Chest 1999; 116:1200–1207.
- Martinez FJ, Vogel PD, Dupont DN, Stanopoulos I, Gray A, Beamis JF. Supported arm exercise vs unsupported arm exercise in the rehabilitation of patients with severe chronic airflow obstruction. Chest 1993; 103:1397–1402.
- Cote CG, Celli BR. Pulmonary rehabilitation and the BODE index in COPD. Eur Respir J 2005; 26:630–636.
- Fishman A, Martinez F, Naunheim K, et al; National Emphysema Treatment Trial Research Group. A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl J Med 2003; 348:2059–2073.
- Naunheim KS, Wood DE, Mohsenifar Z, et al; National Emphysema Treatment Trial Research Group. Long-term follow-up of patients receiving lung-volume-reduction surgery versus medical therapy for severe emphysema by the National Emphysema Treatment Trial Research Group. Ann Thorac Surg 2006; 82:431–443.
KEY POINTS
- A new COPD classification scheme is based on severity, symptoms, and exacerbations.
- Azithromycin 250 mg daily prevents exacerbations of COPD in those at high risk.
- Long-acting muscarinic antagonists such as aclidinium and tiotropium are first-line therapy.
- Relatively new options include roflumilast, an oral phosphodiesterase inhibitor, and indacaterol, an ultra-long-acting beta agonist that is taken once daily.
- Nondrug interventions include pulmonary rehabilitation, vitamin D supplementation, noninvasive positive-pressure ventilation, and lung-volume reduction surgery.
EMA’s transparency plans criticized

to be used in a clinical trial
Credit: Esther Dyson
Many in the research community have lauded the European Medicines Agency’s (EMA’s) plans to make clinical trial data available to the public.
But the agency has also drawn criticism for the way it plans to go about increasing transparency.
The EMA has said it plans to make trial data available online in a “read-only” mode. So readers will not be able to save or transfer the data, making scientific analysis difficult, if not impossible.
The EMA also plans to allow drug manufacturers to omit some trial data from its public posts.
In response to this news, the European Ombudsman, Emily O’Reilly, wrote a letter to the EMA expressing concern about their seemingly significant change in policy.
“We were pleased when EMA announced, in 2012, a new pro-active transparency policy, giving the broadest possible public access to clinical trial data,” O’Reilly said.
“I am now concerned about what appears to be a significant change in EMA’s policy, which could undermine the fundamental right of public access to documents established by EU law. European citizens, doctors, and researchers need maximum information about the medicines they take, prescribe, and analyze.”
Beate Wieseler, PhD, and her colleagues from the German Institute for Quality and Efficiency in Health Care, echoed this sentiment in a “rapid response” published in the British Medical Journal.
The authors said the proposed read-only mode of accessing data makes scientific analyses, such as risk-benefit assessments of drugs, impossible.
For these assessments, an enormous amount of data must be viewed, annotated and saved, pooled from different studies, analyzed statistically, and shared among researchers. But the read-only mode would not allow for that.
Dr Wieseler and other critics also take issue with EMA’s decision to allow drug manufacturers to omit some trial data from its public posts.
The EMA has said that, within the context of market approval, drug manufacturers will be able to submit 2 versions of a clinical study report to the EMA: a complete one, by means of which the agency will decide on approval, and an incomplete one for the public.
The EMA previously decided that individual patient data, which could allow patients to be identified, would be deleted from the study reports. Now, this step has been extended to cover study results.
For example, the EMA believes deleting information is acceptable in cases of results on exploratory outcomes that are not supportive for the approval decision. However, Dr Weiseler and her colleagues noted that such study results often contain analyses of patient-relevant outcomes such as health-related quality of life.
“We are talking about studies in people who participated in a clinical study because they hoped that, with the information gained, better treatments would be developed,” Dr Wieseler said. “This information can only be used to improve patient care if it is publicly available to all.”
About the policy change
In June 2013, the EMA released for public consultation a draft policy on “publication and access to clinical trial data.” In that draft, the agency proposed publishing data submitted in support of marketing-authorization applications (only for centrally approved medicines from 2014 onward).
The idea was that interested parties would no longer need to invoke the European Freedom of Information Regulation (Regulation [EC] N°1049/2001), when exercising their right to access documents held by the EMA.
However, according to documents the EMA shared during a stakeholder consultation earlier this month, the EMA now plans to allow systematic censorship by pharmaceutical companies and impose both strict confidentiality requirements and restrictions on the use of data.
For more information on the policy, see the EMA website. ![]()

to be used in a clinical trial
Credit: Esther Dyson
Many in the research community have lauded the European Medicines Agency’s (EMA’s) plans to make clinical trial data available to the public.
But the agency has also drawn criticism for the way it plans to go about increasing transparency.
The EMA has said it plans to make trial data available online in a “read-only” mode. So readers will not be able to save or transfer the data, making scientific analysis difficult, if not impossible.
The EMA also plans to allow drug manufacturers to omit some trial data from its public posts.
In response to this news, the European Ombudsman, Emily O’Reilly, wrote a letter to the EMA expressing concern about their seemingly significant change in policy.
“We were pleased when EMA announced, in 2012, a new pro-active transparency policy, giving the broadest possible public access to clinical trial data,” O’Reilly said.
“I am now concerned about what appears to be a significant change in EMA’s policy, which could undermine the fundamental right of public access to documents established by EU law. European citizens, doctors, and researchers need maximum information about the medicines they take, prescribe, and analyze.”
Beate Wieseler, PhD, and her colleagues from the German Institute for Quality and Efficiency in Health Care, echoed this sentiment in a “rapid response” published in the British Medical Journal.
The authors said the proposed read-only mode of accessing data makes scientific analyses, such as risk-benefit assessments of drugs, impossible.
For these assessments, an enormous amount of data must be viewed, annotated and saved, pooled from different studies, analyzed statistically, and shared among researchers. But the read-only mode would not allow for that.
Dr Wieseler and other critics also take issue with EMA’s decision to allow drug manufacturers to omit some trial data from its public posts.
The EMA has said that, within the context of market approval, drug manufacturers will be able to submit 2 versions of a clinical study report to the EMA: a complete one, by means of which the agency will decide on approval, and an incomplete one for the public.
The EMA previously decided that individual patient data, which could allow patients to be identified, would be deleted from the study reports. Now, this step has been extended to cover study results.
For example, the EMA believes deleting information is acceptable in cases of results on exploratory outcomes that are not supportive for the approval decision. However, Dr Weiseler and her colleagues noted that such study results often contain analyses of patient-relevant outcomes such as health-related quality of life.
“We are talking about studies in people who participated in a clinical study because they hoped that, with the information gained, better treatments would be developed,” Dr Wieseler said. “This information can only be used to improve patient care if it is publicly available to all.”
About the policy change
In June 2013, the EMA released for public consultation a draft policy on “publication and access to clinical trial data.” In that draft, the agency proposed publishing data submitted in support of marketing-authorization applications (only for centrally approved medicines from 2014 onward).
The idea was that interested parties would no longer need to invoke the European Freedom of Information Regulation (Regulation [EC] N°1049/2001), when exercising their right to access documents held by the EMA.
However, according to documents the EMA shared during a stakeholder consultation earlier this month, the EMA now plans to allow systematic censorship by pharmaceutical companies and impose both strict confidentiality requirements and restrictions on the use of data.
For more information on the policy, see the EMA website. ![]()

to be used in a clinical trial
Credit: Esther Dyson
Many in the research community have lauded the European Medicines Agency’s (EMA’s) plans to make clinical trial data available to the public.
But the agency has also drawn criticism for the way it plans to go about increasing transparency.
The EMA has said it plans to make trial data available online in a “read-only” mode. So readers will not be able to save or transfer the data, making scientific analysis difficult, if not impossible.
The EMA also plans to allow drug manufacturers to omit some trial data from its public posts.
In response to this news, the European Ombudsman, Emily O’Reilly, wrote a letter to the EMA expressing concern about their seemingly significant change in policy.
“We were pleased when EMA announced, in 2012, a new pro-active transparency policy, giving the broadest possible public access to clinical trial data,” O’Reilly said.
“I am now concerned about what appears to be a significant change in EMA’s policy, which could undermine the fundamental right of public access to documents established by EU law. European citizens, doctors, and researchers need maximum information about the medicines they take, prescribe, and analyze.”
Beate Wieseler, PhD, and her colleagues from the German Institute for Quality and Efficiency in Health Care, echoed this sentiment in a “rapid response” published in the British Medical Journal.
The authors said the proposed read-only mode of accessing data makes scientific analyses, such as risk-benefit assessments of drugs, impossible.
For these assessments, an enormous amount of data must be viewed, annotated and saved, pooled from different studies, analyzed statistically, and shared among researchers. But the read-only mode would not allow for that.
Dr Wieseler and other critics also take issue with EMA’s decision to allow drug manufacturers to omit some trial data from its public posts.
The EMA has said that, within the context of market approval, drug manufacturers will be able to submit 2 versions of a clinical study report to the EMA: a complete one, by means of which the agency will decide on approval, and an incomplete one for the public.
The EMA previously decided that individual patient data, which could allow patients to be identified, would be deleted from the study reports. Now, this step has been extended to cover study results.
For example, the EMA believes deleting information is acceptable in cases of results on exploratory outcomes that are not supportive for the approval decision. However, Dr Weiseler and her colleagues noted that such study results often contain analyses of patient-relevant outcomes such as health-related quality of life.
“We are talking about studies in people who participated in a clinical study because they hoped that, with the information gained, better treatments would be developed,” Dr Wieseler said. “This information can only be used to improve patient care if it is publicly available to all.”
About the policy change
In June 2013, the EMA released for public consultation a draft policy on “publication and access to clinical trial data.” In that draft, the agency proposed publishing data submitted in support of marketing-authorization applications (only for centrally approved medicines from 2014 onward).
The idea was that interested parties would no longer need to invoke the European Freedom of Information Regulation (Regulation [EC] N°1049/2001), when exercising their right to access documents held by the EMA.
However, according to documents the EMA shared during a stakeholder consultation earlier this month, the EMA now plans to allow systematic censorship by pharmaceutical companies and impose both strict confidentiality requirements and restrictions on the use of data.
For more information on the policy, see the EMA website. ![]()
Clipped by an Oncoming Car
A 23-year-old man is brought in after being hit by a car. He was in the process of getting into his car when another vehicle coming from the opposite direction swerved into his lane. He tried to jump onto his hood to avoid the other car but was struck by the side mirror and landed on the ground. He is primarily complaining of left knee and lower leg pain. He denies any medical history. Primary survey appears to be stable except for scalp and facial lacerations. The patient is awake, alert, and oriented, and his vital signs are stable. His left lower extremity is in a splint immobilizer, placed by emergency medical personnel. There is a moderate amount of soft tissue swelling around the knee, which is exquisitely tender to palpation. The patient has limited flexion and extension of the knee due to pain. He is able to wiggle his toes, and distally in the leg and foot there appears to be no neurovascular compromise. Radiographs of the tibia are obtained. What is your impression?
Man, 26, With Sudden-Onset Right Lower Quadrant Pain
A 26-year-old man presented to the emergency department (ED) with a chief complaint of abdominal pain. After triage was complete, he was transported to an examination room, where the clinician obtained the history of presenting illness. The onset of pain was approximately 90 minutes prior to arrival at the ED and woke the patient from a “sound sleep.” He stated that the pain initially started as a “3 out of 10” but had progressed to a “12 out of 10,” and he described it as being in the right lower quadrant of his abdomen, with radiation to his right testicle. However, he was unsure where the pain started or if it was worse in either location. Nausea was the primary associated symptom, but he denied vomiting, diarrhea, fever, dysuria, or hematuria. Last, the patient denied history of trauma.
Medical history was noncontributory: He denied previous gastrointestinal diseases, and there was no history of renal stones, urinary tract infection, or any other genitourinary disease. He had no surgical history. The patient smoked less than a pack of cigarettes per day but denied alcohol or drug use.
Physical examination revealed a young man in moderate discomfort. Despite describing his pain as a “12 out of 10,” he had a blood pressure of 121/72 mm Hg; pulse, 59 beats/min; respiratory rate, 20 breaths/min; and temperature, 96.8°F. HEENT and cardiovascular, respiratory, musculoskeletal, and neurologic exam results were all within normal limits. Abdominal examination revealed a mildly tender right lower quadrant with deep palpation, but no rebound or guarding. Murphy sign was negative.
Because of the complaint of pain radiating to the testicles, a genitourinary examination was performed. The penis appeared unremarkable, with no lesions or discharge. There was no inguinal lymphadenopathy. The scrotum appeared appropriate in size and was also grossly unremarkable. The left testicle was nontender. However, palpation of the right testicle elicited moderate to severe pain. There was no visible swelling, and there were no palpable hernias or other masses. Cremasteric reflex was assessed bilaterally and deemed to be absent on the right side.
A workup was initiated that included a complete blood count, comprehensive metabolic panel, and urinalysis; the results of these tests were unremarkable. A differential diagnosis was formed, with emphasis on appendicitis and testicular torsion. Because of the specific nature and location of the pain, both ultrasound and CT of the abdomen/pelvis were considered. It was decided to order the ultrasound, with a plan to perform CT only if ultrasound was unremarkable. The patient was medicated for his pain and the ultrasound commenced. Halfway through the imaging, the clinician and attending physician were summoned to the examination room to review the image seen in Figure 1.
On the next page: Discussion and diagnosis >>
DISCUSSION
Testicular torsion may occur if the testicle twists or rotates on the spermatic cord. The twisting causes arterial ischemia and venous outflow obstruction, cutting off the testicle’s blood supply.1,2 Torsion may be extravaginal or intravaginal, depending on the extent of involvement of the surrounding structures.2
Extravaginal torsion is most commonly seen in neonates and occurs because the entire testicle may freely rotate prior to fixation to the scrotal wall via the tunica vaginalis.2Intravaginal torsion is more common in adolescents and often occurs as a result of a condition known as bell clapper deformity. This congenital abnormality enables the testicle to rotate within the tunica vaginalis and rest transversely in the scrotum instead of in a more vertical orientation.2,3 Torsion occurs if the testicle rotates 90° to 180°, with complete torsion occurring at 360° (torsion may extend to as much as 720°).2 Torsion may also occur as a result of trauma.1
Peak incidence of testicular torsion occurs at ages 13 to 14, but it can occur at any age; torsion affects approximately 1 in 4,000 males younger than 25.2-5 Ninety-five percent of all torsions are intravaginal.2 Torsion is the most common pathology for males who undergo surgical exploration for scrotal pain.3
The main goal in the diagnosis and treatment of torsion is testicular salvage. Torsion is considered a urologic emergency, making early diagnosis and treatment critical to prevent testicular loss. In fact, a review of the relevant literature reveals that the rate of testicular salvage is much higher if the diagnosis is made within 6 to 12 hours.1,2,5 Potential sequelae from delayed treatment include testicular infarction, loss of testicle, infertility problems, infections, cosmetic deformity, and increased risk for testicular malignancy.2
Because many men hesitate to seek medical attention for symptoms of testicular pain and swelling, the primary care clinician should openly discuss testicular disorders, especially with preadolescent males, during testicular examinations.6
Diagnosis
A testicular examination should be performed on any male presenting with a chief complaint of lower abdominal pain, back/flank pain, or any pain that radiates to the groin. The cremasteric reflex should be assessed because it can help differentiate among the causes of testicular pain.7 It is performed by gently stroking the upper inner thigh and observing for contraction of the ipsilateral testicle. One study found that, in cases of torsion, the absence of a cremasteric reflex had a sensitivity of 96% and a specificity of 88%.7 See the Table for the differential diagnosis for acute testicular pain.
While it is often possible to make the diagnosis of testicular torsion clinically, ultrasound with color Doppler is the diagnostic test of choice in cases for which the cause of acute scrotal pain is unclear.8 Ultrasound provides anatomic detail of the scrotum and its contents, and perfusion is assessed by adding the color Doppler images.8 It is important to note that, while the absence of blood flow is considered diagnostic for testicular torsion, the presence of flow does not necessarily exclude it.4
On the next page: Treatment >>
Treatment
Surgical exploration with intraoperative detorsion and orchiopexy (fixation of the testicle to the scrotal wall) is the mainstay of treatment for testicular torsion.1 Orchiopexy is often performed bilaterally in order to prevent future torsion of the unaffected testicle. In about 40% of males with the bell clapper deformity, the condition is present on both sides.2 Orchiectomy, the complete removal of the testicle, is necessary when the degree of torsion and subsequent ischemia have caused irreversible damage to the testicle.6 In one study in which 2,248 cases of torsion were reviewed, approximately 34% of males required orchiectomy.6
If surgery may be delayed, the clinician may attempt manual detorsion at the bedside. Despite the “open book” method described in many texts—which instructs the practitioner to rotate the testicle laterally—a review of the literature reveals that torsion takes place medially only 70% of the time.1,5 The clinician should always consider this when any attempts at manual detorsion are made and correlate his or her technique with physical examination and the patient’s response.5
Relief of pain and return of the testicle to its natural longitudinal lie are considered indicators of successful detorsion.1 Color Doppler ultrasound should be used to confirm the return of circulation. However, in one case review of pediatric patients who underwent surgical exploration after manual detorsion, some degree of residual torsion remained in 32%.5 Because of this risk, surgery is still indicated even in cases of successful bedside detorsion.5
On the next page: Case continuation >>
CASE CONTINUATION
The decision to perform bedside ultrasound was made because the diagnosis of testicular torsion is a surgical emergency, and the window of time to prevent complications can be extremely narrow. If the ultrasound had been normal, then a CT scan may have provided additional data on which to base the diagnosis.
The patient was given adequate parenteral pain medication. After color Doppler ultrasound confirmed the torsion, the testicle was laterally rotated approximately 360°. The patient reported alleviation of his symptoms. Color Doppler was again performed to confirm the return of hyperemic blood flow to the affected testicle (Figure 2). The urologist arrived shortly thereafter and the patient was taken to the operating room, where he underwent scrotal exploration and bilateral orchiopexy.
On the next page: Conclusion >>
CONCLUSION
A testicular examination should be performed on any male presenting with a chief complaint of lower abdominal pain, back/flank pain, or any pain that radiates to the groin. Testicular torsion is most commonly seen in infants and adolescents but can occur at any age. The condition is a surgical emergency and the goal is testicular salvage, which is most likely to occur before 12 hours have elapsed since the onset of symptoms. An important component of the physical examination is attempting to elicit the cremasteric reflex, which is likely to be absent in the presence of torsion.
The primary care provider’s goal is to rapidly diagnose testicular torsion, then refer the patient immediately to a urologist or ED. The skilled clinician may attempt manual detorsion, based on his/her expertise and comfort level; however, this procedure should never delay prompt surgical intervention.
REFERENCES
1. Eyre RC. Evaluation of the acute scrotum in adults. www.uptodate.com/contents/evaluation-of-the-acute-scrotum-in-adults. Accessed May 16, 2014.
2. Ogunyemi OI, Weiker M, Abel EJ. Testicular torsion. http://emedicine.medscape.com/article/2036003-overview. Accessed May 16, 2014.
3. Khan F, Muoka O, Watson GM. Bell clapper testis, torsion, and detorsion: a case report. Case Rep Urol. 2011;2011:631970.
4. Molokwu CN, Somani BK, Goodman CM. Outcomes of scrotal exploration for acute scrotal pain suspicious of testicular torsion: a consecutive case series of 173 patients. BJU Int. 2011;107(6):990-993.
5. Sessions AE, Rabinowitz R, Hulbert WC, et al. Testicular torsion: direction, degree, duration and disinformation. J Urol. 2003;169(2):663-665.
6. Mansbach JM, Forbes P, Peters C. Testicular torsion and risk factors for orchiectomy. Arch Pediatr Adolesc Med. 2005;159:1167-1171.
7. Schmitz D, Safranek S. How useful is a physical exam in diagnosing testicular torsion? J Fam Pract. 2009;58(8):433-434.
8. D’Andrea A, Coppolino F, Cesarano E, et al. US in the assessment of acute scrotum. Crit Ultrasound J. 2013;5(suppl 1):S8. www.criticalultrasound journal.com/content/5/S1/S8/. Accessed May 16, 2014.
A 26-year-old man presented to the emergency department (ED) with a chief complaint of abdominal pain. After triage was complete, he was transported to an examination room, where the clinician obtained the history of presenting illness. The onset of pain was approximately 90 minutes prior to arrival at the ED and woke the patient from a “sound sleep.” He stated that the pain initially started as a “3 out of 10” but had progressed to a “12 out of 10,” and he described it as being in the right lower quadrant of his abdomen, with radiation to his right testicle. However, he was unsure where the pain started or if it was worse in either location. Nausea was the primary associated symptom, but he denied vomiting, diarrhea, fever, dysuria, or hematuria. Last, the patient denied history of trauma.
Medical history was noncontributory: He denied previous gastrointestinal diseases, and there was no history of renal stones, urinary tract infection, or any other genitourinary disease. He had no surgical history. The patient smoked less than a pack of cigarettes per day but denied alcohol or drug use.
Physical examination revealed a young man in moderate discomfort. Despite describing his pain as a “12 out of 10,” he had a blood pressure of 121/72 mm Hg; pulse, 59 beats/min; respiratory rate, 20 breaths/min; and temperature, 96.8°F. HEENT and cardiovascular, respiratory, musculoskeletal, and neurologic exam results were all within normal limits. Abdominal examination revealed a mildly tender right lower quadrant with deep palpation, but no rebound or guarding. Murphy sign was negative.
Because of the complaint of pain radiating to the testicles, a genitourinary examination was performed. The penis appeared unremarkable, with no lesions or discharge. There was no inguinal lymphadenopathy. The scrotum appeared appropriate in size and was also grossly unremarkable. The left testicle was nontender. However, palpation of the right testicle elicited moderate to severe pain. There was no visible swelling, and there were no palpable hernias or other masses. Cremasteric reflex was assessed bilaterally and deemed to be absent on the right side.
A workup was initiated that included a complete blood count, comprehensive metabolic panel, and urinalysis; the results of these tests were unremarkable. A differential diagnosis was formed, with emphasis on appendicitis and testicular torsion. Because of the specific nature and location of the pain, both ultrasound and CT of the abdomen/pelvis were considered. It was decided to order the ultrasound, with a plan to perform CT only if ultrasound was unremarkable. The patient was medicated for his pain and the ultrasound commenced. Halfway through the imaging, the clinician and attending physician were summoned to the examination room to review the image seen in Figure 1.
On the next page: Discussion and diagnosis >>
DISCUSSION
Testicular torsion may occur if the testicle twists or rotates on the spermatic cord. The twisting causes arterial ischemia and venous outflow obstruction, cutting off the testicle’s blood supply.1,2 Torsion may be extravaginal or intravaginal, depending on the extent of involvement of the surrounding structures.2
Extravaginal torsion is most commonly seen in neonates and occurs because the entire testicle may freely rotate prior to fixation to the scrotal wall via the tunica vaginalis.2Intravaginal torsion is more common in adolescents and often occurs as a result of a condition known as bell clapper deformity. This congenital abnormality enables the testicle to rotate within the tunica vaginalis and rest transversely in the scrotum instead of in a more vertical orientation.2,3 Torsion occurs if the testicle rotates 90° to 180°, with complete torsion occurring at 360° (torsion may extend to as much as 720°).2 Torsion may also occur as a result of trauma.1
Peak incidence of testicular torsion occurs at ages 13 to 14, but it can occur at any age; torsion affects approximately 1 in 4,000 males younger than 25.2-5 Ninety-five percent of all torsions are intravaginal.2 Torsion is the most common pathology for males who undergo surgical exploration for scrotal pain.3
The main goal in the diagnosis and treatment of torsion is testicular salvage. Torsion is considered a urologic emergency, making early diagnosis and treatment critical to prevent testicular loss. In fact, a review of the relevant literature reveals that the rate of testicular salvage is much higher if the diagnosis is made within 6 to 12 hours.1,2,5 Potential sequelae from delayed treatment include testicular infarction, loss of testicle, infertility problems, infections, cosmetic deformity, and increased risk for testicular malignancy.2
Because many men hesitate to seek medical attention for symptoms of testicular pain and swelling, the primary care clinician should openly discuss testicular disorders, especially with preadolescent males, during testicular examinations.6
Diagnosis
A testicular examination should be performed on any male presenting with a chief complaint of lower abdominal pain, back/flank pain, or any pain that radiates to the groin. The cremasteric reflex should be assessed because it can help differentiate among the causes of testicular pain.7 It is performed by gently stroking the upper inner thigh and observing for contraction of the ipsilateral testicle. One study found that, in cases of torsion, the absence of a cremasteric reflex had a sensitivity of 96% and a specificity of 88%.7 See the Table for the differential diagnosis for acute testicular pain.
While it is often possible to make the diagnosis of testicular torsion clinically, ultrasound with color Doppler is the diagnostic test of choice in cases for which the cause of acute scrotal pain is unclear.8 Ultrasound provides anatomic detail of the scrotum and its contents, and perfusion is assessed by adding the color Doppler images.8 It is important to note that, while the absence of blood flow is considered diagnostic for testicular torsion, the presence of flow does not necessarily exclude it.4
On the next page: Treatment >>
Treatment
Surgical exploration with intraoperative detorsion and orchiopexy (fixation of the testicle to the scrotal wall) is the mainstay of treatment for testicular torsion.1 Orchiopexy is often performed bilaterally in order to prevent future torsion of the unaffected testicle. In about 40% of males with the bell clapper deformity, the condition is present on both sides.2 Orchiectomy, the complete removal of the testicle, is necessary when the degree of torsion and subsequent ischemia have caused irreversible damage to the testicle.6 In one study in which 2,248 cases of torsion were reviewed, approximately 34% of males required orchiectomy.6
If surgery may be delayed, the clinician may attempt manual detorsion at the bedside. Despite the “open book” method described in many texts—which instructs the practitioner to rotate the testicle laterally—a review of the literature reveals that torsion takes place medially only 70% of the time.1,5 The clinician should always consider this when any attempts at manual detorsion are made and correlate his or her technique with physical examination and the patient’s response.5
Relief of pain and return of the testicle to its natural longitudinal lie are considered indicators of successful detorsion.1 Color Doppler ultrasound should be used to confirm the return of circulation. However, in one case review of pediatric patients who underwent surgical exploration after manual detorsion, some degree of residual torsion remained in 32%.5 Because of this risk, surgery is still indicated even in cases of successful bedside detorsion.5
On the next page: Case continuation >>
CASE CONTINUATION
The decision to perform bedside ultrasound was made because the diagnosis of testicular torsion is a surgical emergency, and the window of time to prevent complications can be extremely narrow. If the ultrasound had been normal, then a CT scan may have provided additional data on which to base the diagnosis.
The patient was given adequate parenteral pain medication. After color Doppler ultrasound confirmed the torsion, the testicle was laterally rotated approximately 360°. The patient reported alleviation of his symptoms. Color Doppler was again performed to confirm the return of hyperemic blood flow to the affected testicle (Figure 2). The urologist arrived shortly thereafter and the patient was taken to the operating room, where he underwent scrotal exploration and bilateral orchiopexy.
On the next page: Conclusion >>
CONCLUSION
A testicular examination should be performed on any male presenting with a chief complaint of lower abdominal pain, back/flank pain, or any pain that radiates to the groin. Testicular torsion is most commonly seen in infants and adolescents but can occur at any age. The condition is a surgical emergency and the goal is testicular salvage, which is most likely to occur before 12 hours have elapsed since the onset of symptoms. An important component of the physical examination is attempting to elicit the cremasteric reflex, which is likely to be absent in the presence of torsion.
The primary care provider’s goal is to rapidly diagnose testicular torsion, then refer the patient immediately to a urologist or ED. The skilled clinician may attempt manual detorsion, based on his/her expertise and comfort level; however, this procedure should never delay prompt surgical intervention.
REFERENCES
1. Eyre RC. Evaluation of the acute scrotum in adults. www.uptodate.com/contents/evaluation-of-the-acute-scrotum-in-adults. Accessed May 16, 2014.
2. Ogunyemi OI, Weiker M, Abel EJ. Testicular torsion. http://emedicine.medscape.com/article/2036003-overview. Accessed May 16, 2014.
3. Khan F, Muoka O, Watson GM. Bell clapper testis, torsion, and detorsion: a case report. Case Rep Urol. 2011;2011:631970.
4. Molokwu CN, Somani BK, Goodman CM. Outcomes of scrotal exploration for acute scrotal pain suspicious of testicular torsion: a consecutive case series of 173 patients. BJU Int. 2011;107(6):990-993.
5. Sessions AE, Rabinowitz R, Hulbert WC, et al. Testicular torsion: direction, degree, duration and disinformation. J Urol. 2003;169(2):663-665.
6. Mansbach JM, Forbes P, Peters C. Testicular torsion and risk factors for orchiectomy. Arch Pediatr Adolesc Med. 2005;159:1167-1171.
7. Schmitz D, Safranek S. How useful is a physical exam in diagnosing testicular torsion? J Fam Pract. 2009;58(8):433-434.
8. D’Andrea A, Coppolino F, Cesarano E, et al. US in the assessment of acute scrotum. Crit Ultrasound J. 2013;5(suppl 1):S8. www.criticalultrasound journal.com/content/5/S1/S8/. Accessed May 16, 2014.
A 26-year-old man presented to the emergency department (ED) with a chief complaint of abdominal pain. After triage was complete, he was transported to an examination room, where the clinician obtained the history of presenting illness. The onset of pain was approximately 90 minutes prior to arrival at the ED and woke the patient from a “sound sleep.” He stated that the pain initially started as a “3 out of 10” but had progressed to a “12 out of 10,” and he described it as being in the right lower quadrant of his abdomen, with radiation to his right testicle. However, he was unsure where the pain started or if it was worse in either location. Nausea was the primary associated symptom, but he denied vomiting, diarrhea, fever, dysuria, or hematuria. Last, the patient denied history of trauma.
Medical history was noncontributory: He denied previous gastrointestinal diseases, and there was no history of renal stones, urinary tract infection, or any other genitourinary disease. He had no surgical history. The patient smoked less than a pack of cigarettes per day but denied alcohol or drug use.
Physical examination revealed a young man in moderate discomfort. Despite describing his pain as a “12 out of 10,” he had a blood pressure of 121/72 mm Hg; pulse, 59 beats/min; respiratory rate, 20 breaths/min; and temperature, 96.8°F. HEENT and cardiovascular, respiratory, musculoskeletal, and neurologic exam results were all within normal limits. Abdominal examination revealed a mildly tender right lower quadrant with deep palpation, but no rebound or guarding. Murphy sign was negative.
Because of the complaint of pain radiating to the testicles, a genitourinary examination was performed. The penis appeared unremarkable, with no lesions or discharge. There was no inguinal lymphadenopathy. The scrotum appeared appropriate in size and was also grossly unremarkable. The left testicle was nontender. However, palpation of the right testicle elicited moderate to severe pain. There was no visible swelling, and there were no palpable hernias or other masses. Cremasteric reflex was assessed bilaterally and deemed to be absent on the right side.
A workup was initiated that included a complete blood count, comprehensive metabolic panel, and urinalysis; the results of these tests were unremarkable. A differential diagnosis was formed, with emphasis on appendicitis and testicular torsion. Because of the specific nature and location of the pain, both ultrasound and CT of the abdomen/pelvis were considered. It was decided to order the ultrasound, with a plan to perform CT only if ultrasound was unremarkable. The patient was medicated for his pain and the ultrasound commenced. Halfway through the imaging, the clinician and attending physician were summoned to the examination room to review the image seen in Figure 1.
On the next page: Discussion and diagnosis >>
DISCUSSION
Testicular torsion may occur if the testicle twists or rotates on the spermatic cord. The twisting causes arterial ischemia and venous outflow obstruction, cutting off the testicle’s blood supply.1,2 Torsion may be extravaginal or intravaginal, depending on the extent of involvement of the surrounding structures.2
Extravaginal torsion is most commonly seen in neonates and occurs because the entire testicle may freely rotate prior to fixation to the scrotal wall via the tunica vaginalis.2Intravaginal torsion is more common in adolescents and often occurs as a result of a condition known as bell clapper deformity. This congenital abnormality enables the testicle to rotate within the tunica vaginalis and rest transversely in the scrotum instead of in a more vertical orientation.2,3 Torsion occurs if the testicle rotates 90° to 180°, with complete torsion occurring at 360° (torsion may extend to as much as 720°).2 Torsion may also occur as a result of trauma.1
Peak incidence of testicular torsion occurs at ages 13 to 14, but it can occur at any age; torsion affects approximately 1 in 4,000 males younger than 25.2-5 Ninety-five percent of all torsions are intravaginal.2 Torsion is the most common pathology for males who undergo surgical exploration for scrotal pain.3
The main goal in the diagnosis and treatment of torsion is testicular salvage. Torsion is considered a urologic emergency, making early diagnosis and treatment critical to prevent testicular loss. In fact, a review of the relevant literature reveals that the rate of testicular salvage is much higher if the diagnosis is made within 6 to 12 hours.1,2,5 Potential sequelae from delayed treatment include testicular infarction, loss of testicle, infertility problems, infections, cosmetic deformity, and increased risk for testicular malignancy.2
Because many men hesitate to seek medical attention for symptoms of testicular pain and swelling, the primary care clinician should openly discuss testicular disorders, especially with preadolescent males, during testicular examinations.6
Diagnosis
A testicular examination should be performed on any male presenting with a chief complaint of lower abdominal pain, back/flank pain, or any pain that radiates to the groin. The cremasteric reflex should be assessed because it can help differentiate among the causes of testicular pain.7 It is performed by gently stroking the upper inner thigh and observing for contraction of the ipsilateral testicle. One study found that, in cases of torsion, the absence of a cremasteric reflex had a sensitivity of 96% and a specificity of 88%.7 See the Table for the differential diagnosis for acute testicular pain.
While it is often possible to make the diagnosis of testicular torsion clinically, ultrasound with color Doppler is the diagnostic test of choice in cases for which the cause of acute scrotal pain is unclear.8 Ultrasound provides anatomic detail of the scrotum and its contents, and perfusion is assessed by adding the color Doppler images.8 It is important to note that, while the absence of blood flow is considered diagnostic for testicular torsion, the presence of flow does not necessarily exclude it.4
On the next page: Treatment >>
Treatment
Surgical exploration with intraoperative detorsion and orchiopexy (fixation of the testicle to the scrotal wall) is the mainstay of treatment for testicular torsion.1 Orchiopexy is often performed bilaterally in order to prevent future torsion of the unaffected testicle. In about 40% of males with the bell clapper deformity, the condition is present on both sides.2 Orchiectomy, the complete removal of the testicle, is necessary when the degree of torsion and subsequent ischemia have caused irreversible damage to the testicle.6 In one study in which 2,248 cases of torsion were reviewed, approximately 34% of males required orchiectomy.6
If surgery may be delayed, the clinician may attempt manual detorsion at the bedside. Despite the “open book” method described in many texts—which instructs the practitioner to rotate the testicle laterally—a review of the literature reveals that torsion takes place medially only 70% of the time.1,5 The clinician should always consider this when any attempts at manual detorsion are made and correlate his or her technique with physical examination and the patient’s response.5
Relief of pain and return of the testicle to its natural longitudinal lie are considered indicators of successful detorsion.1 Color Doppler ultrasound should be used to confirm the return of circulation. However, in one case review of pediatric patients who underwent surgical exploration after manual detorsion, some degree of residual torsion remained in 32%.5 Because of this risk, surgery is still indicated even in cases of successful bedside detorsion.5
On the next page: Case continuation >>
CASE CONTINUATION
The decision to perform bedside ultrasound was made because the diagnosis of testicular torsion is a surgical emergency, and the window of time to prevent complications can be extremely narrow. If the ultrasound had been normal, then a CT scan may have provided additional data on which to base the diagnosis.
The patient was given adequate parenteral pain medication. After color Doppler ultrasound confirmed the torsion, the testicle was laterally rotated approximately 360°. The patient reported alleviation of his symptoms. Color Doppler was again performed to confirm the return of hyperemic blood flow to the affected testicle (Figure 2). The urologist arrived shortly thereafter and the patient was taken to the operating room, where he underwent scrotal exploration and bilateral orchiopexy.
On the next page: Conclusion >>
CONCLUSION
A testicular examination should be performed on any male presenting with a chief complaint of lower abdominal pain, back/flank pain, or any pain that radiates to the groin. Testicular torsion is most commonly seen in infants and adolescents but can occur at any age. The condition is a surgical emergency and the goal is testicular salvage, which is most likely to occur before 12 hours have elapsed since the onset of symptoms. An important component of the physical examination is attempting to elicit the cremasteric reflex, which is likely to be absent in the presence of torsion.
The primary care provider’s goal is to rapidly diagnose testicular torsion, then refer the patient immediately to a urologist or ED. The skilled clinician may attempt manual detorsion, based on his/her expertise and comfort level; however, this procedure should never delay prompt surgical intervention.
REFERENCES
1. Eyre RC. Evaluation of the acute scrotum in adults. www.uptodate.com/contents/evaluation-of-the-acute-scrotum-in-adults. Accessed May 16, 2014.
2. Ogunyemi OI, Weiker M, Abel EJ. Testicular torsion. http://emedicine.medscape.com/article/2036003-overview. Accessed May 16, 2014.
3. Khan F, Muoka O, Watson GM. Bell clapper testis, torsion, and detorsion: a case report. Case Rep Urol. 2011;2011:631970.
4. Molokwu CN, Somani BK, Goodman CM. Outcomes of scrotal exploration for acute scrotal pain suspicious of testicular torsion: a consecutive case series of 173 patients. BJU Int. 2011;107(6):990-993.
5. Sessions AE, Rabinowitz R, Hulbert WC, et al. Testicular torsion: direction, degree, duration and disinformation. J Urol. 2003;169(2):663-665.
6. Mansbach JM, Forbes P, Peters C. Testicular torsion and risk factors for orchiectomy. Arch Pediatr Adolesc Med. 2005;159:1167-1171.
7. Schmitz D, Safranek S. How useful is a physical exam in diagnosing testicular torsion? J Fam Pract. 2009;58(8):433-434.
8. D’Andrea A, Coppolino F, Cesarano E, et al. US in the assessment of acute scrotum. Crit Ultrasound J. 2013;5(suppl 1):S8. www.criticalultrasound journal.com/content/5/S1/S8/. Accessed May 16, 2014.