User login
The Cutting Edge
Since the beginning of formal medical education, one of the biggest challenges in treating patients has been learning from mistakes. How do providers balance the potentially grave consequences of medical mistakes with the possibilities of improving patient care?
While the conundrum is far from solved, hospitalists at HM11’s “Advanced Interactive Critical Care” pre-course will get hands-on experience in the newest techniques in patient care without affecting real patients. The pre-course will use simulators to replicate real-life situations with critical-care patients.
For the annual meeting’s course director, the simulators are the next step in training hospitalists. “This is really exciting,” says Daniel D. Dressler, MD, MSc, FHM, associate professor and director of internal-medicine teaching services at Emory University Hospital in Atlanta. “As an educator, it’s really something unique. We learn the best by actually doing and sometimes making mistakes; it’s better to do that in simulations with expert advisors offering immediate feedback.
“Not only will pre-course attendees get high-quality didactic information, but they will also participate in the simulation of critical-care events with very experienced faculty,” he says.

Pre-course participants will have the option of having more hands-on time with the simulators in lieu of lectures. Dr. Dressler, an SHM board member, calls the opportunity to work on cutting-edge technology “exceedingly unique.”
The primary simulator will look, feel, and sound like a real person with actual physiological parameters. It breathes and has a pulse—or, in some cases, doesn’t have a pulse. Dressler says participants will be in front of a simulated patient who is going through septic shock or having airway or ventilator problems. While interacting with colleagues and instructors, participants will diagnose and treat the simulated patient. The simulator can replicate real-life complications that can result from treatments.
The pre-course materials state that after completing the course, participants will be able to:
- Explain basic and advanced mechanical ventilator physiology and strategies for complex situations, including acute respiratory distress syndrome (ARDS) and troubleshooting ventilator problems;
- Integrate physiology with treatment of common and less common forms of shock; and
- Apply appropriate sedation and analgesia strategies to minimize delirium in the ICU, and optimize ventilator weaning.
Additionally, the pre-course will present, model, and practice the latest in evidence-based, critical-care practice. Though the pre-course is called “advanced,” it is open to any hospitalist looking to improve their critical-care skills.
“We were getting feedback that people were ready for the next level,” Dr. Dressler says. Along with the basics of critical care (e.g. sepsis, sedation), the pre-course will cover more advanced issues. “We understand that many people have been practicing critical care for a number of years. This course will benefit any hospitalist, regardless of prior critical care experience.”
Led by instructors Kevin Felner, MD, and Brian Kaufman, MD, of New York University Medical Center, “Advanced Interactive Critical Care” begins at 8:50 a.m. May 10. However, the first simulation session begins at 7:20 a.m., and pre-registration is required.
Another new HM11 pre-course will focus solely on using handheld ultrasound devices. The appeal of ultrasounds for use in hospitalists’ rounds is increasing; this course will train hospitalists to use them to look at patients’ vessels, heart, and abdomen.
Hospitalists who take the portable ultrasound pre-course in conjunction with the “Medical Procedures for the Hospitalist” pre-course will receive a full day of the best training in the practice and tools used in medical procedures. The procedures course runs from 8 a.m. to noon May 10. The portable ultrasound course runs from 1:30 to 5:30 p.m. Both pre-courses are taught by Bradley T. Rosen, MD, MBA, FHM, of Cedars-Sinai Medical Center in Los Angeles and Sally Wang, MD, FHM, of Brigham and Women’s Hospital in Boston. TH
Brendon Shank is SHM’s vice president of communications.
Since the beginning of formal medical education, one of the biggest challenges in treating patients has been learning from mistakes. How do providers balance the potentially grave consequences of medical mistakes with the possibilities of improving patient care?
While the conundrum is far from solved, hospitalists at HM11’s “Advanced Interactive Critical Care” pre-course will get hands-on experience in the newest techniques in patient care without affecting real patients. The pre-course will use simulators to replicate real-life situations with critical-care patients.
For the annual meeting’s course director, the simulators are the next step in training hospitalists. “This is really exciting,” says Daniel D. Dressler, MD, MSc, FHM, associate professor and director of internal-medicine teaching services at Emory University Hospital in Atlanta. “As an educator, it’s really something unique. We learn the best by actually doing and sometimes making mistakes; it’s better to do that in simulations with expert advisors offering immediate feedback.
“Not only will pre-course attendees get high-quality didactic information, but they will also participate in the simulation of critical-care events with very experienced faculty,” he says.

Pre-course participants will have the option of having more hands-on time with the simulators in lieu of lectures. Dr. Dressler, an SHM board member, calls the opportunity to work on cutting-edge technology “exceedingly unique.”
The primary simulator will look, feel, and sound like a real person with actual physiological parameters. It breathes and has a pulse—or, in some cases, doesn’t have a pulse. Dressler says participants will be in front of a simulated patient who is going through septic shock or having airway or ventilator problems. While interacting with colleagues and instructors, participants will diagnose and treat the simulated patient. The simulator can replicate real-life complications that can result from treatments.
The pre-course materials state that after completing the course, participants will be able to:
- Explain basic and advanced mechanical ventilator physiology and strategies for complex situations, including acute respiratory distress syndrome (ARDS) and troubleshooting ventilator problems;
- Integrate physiology with treatment of common and less common forms of shock; and
- Apply appropriate sedation and analgesia strategies to minimize delirium in the ICU, and optimize ventilator weaning.
Additionally, the pre-course will present, model, and practice the latest in evidence-based, critical-care practice. Though the pre-course is called “advanced,” it is open to any hospitalist looking to improve their critical-care skills.
“We were getting feedback that people were ready for the next level,” Dr. Dressler says. Along with the basics of critical care (e.g. sepsis, sedation), the pre-course will cover more advanced issues. “We understand that many people have been practicing critical care for a number of years. This course will benefit any hospitalist, regardless of prior critical care experience.”
Led by instructors Kevin Felner, MD, and Brian Kaufman, MD, of New York University Medical Center, “Advanced Interactive Critical Care” begins at 8:50 a.m. May 10. However, the first simulation session begins at 7:20 a.m., and pre-registration is required.
Another new HM11 pre-course will focus solely on using handheld ultrasound devices. The appeal of ultrasounds for use in hospitalists’ rounds is increasing; this course will train hospitalists to use them to look at patients’ vessels, heart, and abdomen.
Hospitalists who take the portable ultrasound pre-course in conjunction with the “Medical Procedures for the Hospitalist” pre-course will receive a full day of the best training in the practice and tools used in medical procedures. The procedures course runs from 8 a.m. to noon May 10. The portable ultrasound course runs from 1:30 to 5:30 p.m. Both pre-courses are taught by Bradley T. Rosen, MD, MBA, FHM, of Cedars-Sinai Medical Center in Los Angeles and Sally Wang, MD, FHM, of Brigham and Women’s Hospital in Boston. TH
Brendon Shank is SHM’s vice president of communications.
Since the beginning of formal medical education, one of the biggest challenges in treating patients has been learning from mistakes. How do providers balance the potentially grave consequences of medical mistakes with the possibilities of improving patient care?
While the conundrum is far from solved, hospitalists at HM11’s “Advanced Interactive Critical Care” pre-course will get hands-on experience in the newest techniques in patient care without affecting real patients. The pre-course will use simulators to replicate real-life situations with critical-care patients.
For the annual meeting’s course director, the simulators are the next step in training hospitalists. “This is really exciting,” says Daniel D. Dressler, MD, MSc, FHM, associate professor and director of internal-medicine teaching services at Emory University Hospital in Atlanta. “As an educator, it’s really something unique. We learn the best by actually doing and sometimes making mistakes; it’s better to do that in simulations with expert advisors offering immediate feedback.
“Not only will pre-course attendees get high-quality didactic information, but they will also participate in the simulation of critical-care events with very experienced faculty,” he says.

Pre-course participants will have the option of having more hands-on time with the simulators in lieu of lectures. Dr. Dressler, an SHM board member, calls the opportunity to work on cutting-edge technology “exceedingly unique.”
The primary simulator will look, feel, and sound like a real person with actual physiological parameters. It breathes and has a pulse—or, in some cases, doesn’t have a pulse. Dressler says participants will be in front of a simulated patient who is going through septic shock or having airway or ventilator problems. While interacting with colleagues and instructors, participants will diagnose and treat the simulated patient. The simulator can replicate real-life complications that can result from treatments.
The pre-course materials state that after completing the course, participants will be able to:
- Explain basic and advanced mechanical ventilator physiology and strategies for complex situations, including acute respiratory distress syndrome (ARDS) and troubleshooting ventilator problems;
- Integrate physiology with treatment of common and less common forms of shock; and
- Apply appropriate sedation and analgesia strategies to minimize delirium in the ICU, and optimize ventilator weaning.
Additionally, the pre-course will present, model, and practice the latest in evidence-based, critical-care practice. Though the pre-course is called “advanced,” it is open to any hospitalist looking to improve their critical-care skills.
“We were getting feedback that people were ready for the next level,” Dr. Dressler says. Along with the basics of critical care (e.g. sepsis, sedation), the pre-course will cover more advanced issues. “We understand that many people have been practicing critical care for a number of years. This course will benefit any hospitalist, regardless of prior critical care experience.”
Led by instructors Kevin Felner, MD, and Brian Kaufman, MD, of New York University Medical Center, “Advanced Interactive Critical Care” begins at 8:50 a.m. May 10. However, the first simulation session begins at 7:20 a.m., and pre-registration is required.
Another new HM11 pre-course will focus solely on using handheld ultrasound devices. The appeal of ultrasounds for use in hospitalists’ rounds is increasing; this course will train hospitalists to use them to look at patients’ vessels, heart, and abdomen.
Hospitalists who take the portable ultrasound pre-course in conjunction with the “Medical Procedures for the Hospitalist” pre-course will receive a full day of the best training in the practice and tools used in medical procedures. The procedures course runs from 8 a.m. to noon May 10. The portable ultrasound course runs from 1:30 to 5:30 p.m. Both pre-courses are taught by Bradley T. Rosen, MD, MBA, FHM, of Cedars-Sinai Medical Center in Los Angeles and Sally Wang, MD, FHM, of Brigham and Women’s Hospital in Boston. TH
Brendon Shank is SHM’s vice president of communications.
In the Literature: HM-Related Research You Need to Know
In This Edition
Literature at a Glance
A guide to this month’s studies
- Effects of extended VTE prophylaxis in medical patients
- Outcomes with and without preprocedural statins
- Association of subclinical hypothyroidism and CHD
- BP treatment after intracerebral hemorrhage
- Outcomes of ICD therapy in the elderly
- Systems delays and outcomes of STEMI
- D-dimer to predict recurrent VTE
- Stocking height and risk of post-stroke DVT
Extending Anticoagulant Prophylaxis after Medical Hospitalization Decreases VTE, Increases Major Bleeding
Clinical question: For patients with acute medical illness, does extending low-molecular-weight heparin (LMWH) administration for up to 28 days after discharge reduce the incidence of venous thromboembolism (VTE)?
Background: DVT and pulmonary embolism (PE) are common hospital-acquired complications. LMWH has been shown to reduce VTE for medical and surgical patients, and extended-duration LMWH reduces VTE in high-risk surgical patients. Whether extending anticoagulant prophylaxis after discharge for acutely ill medical patients with reduced mobility improves outcomes is unknown.
Study design: Randomized, placebo-controlled trial.
Setting: Three hundred seventy hospitals in 20 countries.
Synopsis: Eligible patients were >40 years old, hospitalized with acute medical illness, and had reduced mobility for ≥3 days. Patients received enoxaparin 40 mg SC daily prophylaxis while hospitalized and were then randomized to an additional 28±4 days of enoxaparin or placebo. Patients received a screening ultrasound to assess for asymptomatic DVT. The primary outcome was a composite of asymptomatic proximal DVT, symptomatic DVT or PE, or fatal PE during the period of extended prophylaxis.
An interim analysis indicated that extended prophylaxis was ineffective; at that time, the protocol was amended to target patients with severe immobility or with moderate immobility plus an additional risk factor (e.g. cancer, prior VTE, or age >75).
The study found that extended prophylaxis decreased the composite VTE outcome (2.5% vs 4.0%, P<0.05) and symptomatic VTE (0.2% vs 1.0%, P<0.05). The incidence of major bleeding was increased in the extended prophylaxis group (0.8% vs 0.3%, P<0.05). There was no difference in mortality.
The unplanned, midstudy protocol amendment to target higher-risk patients is a concern, though the final analyses included patients pre- and post-amendment.
Bottom line: Extending LMWH beyond hospitalization for patients admitted with acute medical illness and decreased mobility decreases VTE, but increases major bleeding.
Citation: Hull RD, Schellong SM, Tapson VF, et al. Extended-duration venous thromboembolism prophylaxis in acutely ill medical patients with recently reduced mobility: a randomized trial. Ann Intern Med. 2010;153(1);8-18.
Preprocedural Statin Therapy Reduces Postprocedural Myocardial Infarction
Clinical question: Does statin therapy reduce periprocedural cardiovascular events?
Background: Myocardial infarction (MI) and death are inherent risks of invasive procedures. Reduction of these risks in certain patient populations has been shown with the use of a beta blockade. Statins have shown promise during acute coronary syndrome. Questions remain about the role of statin therapy before invasive procedures in reducing adverse cardiovascular events.
Study design: Meta-analysis of randomized controlled trials.
Setting: Twenty-one studies involving 4,805 patients, published from inception of MEDLINE, Cochrane, and Clinicaltrials to February 2010.
Synopsis: The use of statins one to seven days preprocedure significantly reduced post-procedural MI in percutaneous coronary interventions (PCI) (P<0.0001). Statins given approximately four weeks in advance of noncardiac surgical procedures also significantly reduced postprocedural MI (P=0.004). An absolute risk reduction of 5.8% for postprocedural MI was found after PCI and 4.1% in noncardiac surgical procedures.
Statins did not show a significant reduction in postprocedural MI (P=0.40) or all-cause mortality (P=0.15) in coronary artery bypass graft surgery (CABG). However, statins did reduce post-CABG atrial fibrillation (P<0.0001).
The 21 studies used a variety of drugs and doses. However, the PCI studies favored atorvastatin 40 mg; more than half the CABG studies used atorvastatin 20 mg; and 91% of the noncardiac surgical studies used fluvastatin 80 mg. Dedicated trials are needed to demonstrate optimal statin agent, dose, and timing of therapy.
Bottom line: Preprocedural statin therapy reduces postprocedural MI after both PCI and noncardiac procedures but not after CABG.
Citation: Winchester DE, Wen X, Xie L, Bavry AA. Evidence of pre-procedural statin therapy: a meta-analysis of randomized trials. J Am Coll Cardiol. 2010;56(19); 1099-1109.
Subclinical Hypothyroidism Increases the Risk of Coronary Heart Disease and Mortality
Clinical question: What are the risks of coronary heart disease (CHD) and mortality among adults with subclinical hypothyroidism?
Background: Subclinical hypo-thyroidism is defined as an elevated serum thyroid stimulating hormone (TSH) level with a normal T4 concentration. Controversy exists regarding the treatment of subclinical hypothyroidism. Because of the association with hyperlipidemia and atherosclerosis, treatment of subclinical hypothyroidism is thought to be beneficial. Previous data from large prospective cohort studies regarding this association are conflicting.
Study design: Study-level meta-analysis of prospective cohort studies.
Setting: Eleven prospective cohorts in the U.S., Europe, Australia, Brazil, and Japan from 1972 to 2007.
Synopsis: Among 55,287 adults, 3,450 (6.2%) had subclinical hypothyroidism and 51,837 were euthyroid. Using Cox proportional hazard models, the association of subclinical hypothyroidism with CHD and mortality were determined for each cohort.
The risk of CHD events and CHD mortality increased with higher TSH concentrations.
In age- and sex-adjusted analyses, the hazard ratio (HR) for CHD events were as follows: HR=1.0 (TSH=4.5-6.9 mIU/L); HR=1.17 (TSH=7-9.9 mIU/L), and HR=1.89 (TSH=10-19.9 mIU/L). Similarly, HRs for CHD mortality showed an increasing trend: 1.09, 1.42, and 1.58, respectively.
Although the association is clearly established here, randomized controlled trials are needed to address whether thyroxine replacement can prevent CHD and the TSH threshold that will provide the most clinical benefit.
Bottom line: Subclinical hypo-thyroidism is associated with an increased risk for CHD events and mortality, primarily in patients with TSH concentrations of 10 mIU/L or higher.
Citation: Rodondi N, den Elzen WP, Bauer DC, et al. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA. 2010;304(12): 1365-1374.
Reduction in Hematoma Growth after Acute Intracerebral Hemorrhage Associated with Lower Blood Pressure
Clinical question: Does intensive systolic blood pressure (SBP) <140 mmHg within one hour reduce hematoma growth after acute intracerebral bleeding?
Background: Early elevation of blood pressure after an acute intracerebral bleed is strongly associated with hematoma growth and worse outcomes. The pilot phase of the Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage Trial (INTERACT) showed that early intensive blood pressure lowering reduced hematoma growth within six hours after onset of intracerebral hemorrhage.
Study design: Randomized controlled trial in which patients received an early intensive blood-pressure-lowering treatment (goal SBP<140 mmHg within one hour) or the AHA recommended best practice guidelines (goal SBP <180 mmHg), which were published in 1999.
Setting: Network of hospitals in China, South Korea, and Australia.
Synopsis: From 2005 to 2007, the study examined 404 patients with computed-tomography (CT) evidence of intracerebral hemorrhage, elevated SBP (150 mmHg-220 mmHg), and ability to commence BP lowering treatment within six hours of onset. Hematoma volumes were measured in the intensive treatment and guideline groups based on CT scans done at baseline and after 24 hours.
No significant association was found between the baseline SBP and the absolute or proportional growth of the hematoma. However, in the intensively treated patients who achieved target SBP within the first 24 hours, a significant association was found with the absolute and proportional hematoma growth.
Maximum reduction of hematoma growth occurred in the group with a median SBP of 135 mmHg.
This single-observational study did not include patients with severe intracranial bleeding who died or required surgical evacuation within the first 24 hours.
Hematoma size reduction did not improve survival or outcomes.
Bottom line: Intensive SBP lowering from 140 mmHg to 130 mmHg within one hour reduces hematoma growth after an intracranial hemorrhage.
Citation: Arima H, Anderson CS, Wang JG, et al. Lower treatment blood pressure is associated with the greatest reduction in hematoma growth after acute intracerebral hemorrhage. Hypertension. 2010;56(5):852-858.
Implantable Cardioverter-Defibrillator (ICD) Therapy for Primary Prevention of Sudden Cardiac Death Might Not Provide Survival Benefit to Elderly
Clinical question: Does ICD therapy for primary prevention of sudden cardiac death in individuals with severe left ventricular dysfunction improve survival in elderly patients?
Background: Several clinical trials of select individuals with severe left ventricular dysfunction (EF <40%) have demonstrated that ICD therapy is associated with a reduction in overall mortality. Given the costs and risks associated with ICD placement, it is important to assess how this therapy affects survival in younger versus older individuals.
Study design: Meta-analysis of five randomized controlled trials.
Setting: Five trials (MADIT-II, DEFINITE, DINAMIT, SCDHeFT, and IRIS).
Synopsis: All included studies compared ICD therapy to standard medical care in the primary prevention of sudden cardiac death in individuals with severe left ventricular dysfunction. Elderly patients comprised 44% of the 5,783 patients included in the study; elderly patients were defined as >65 in three studies, and >60 in two studies. Pooled analysis of the three trials examining ICD use for primary prevention found a nonsignificant reduction in all-cause mortality compared with medical therapy in elderly patients (HR 0.81 [95% CI 0.62 to 1.05], P=0.11). The two remaining studies involving post-MI patients showed no statistically significant reduction in mortality in elderly patients.
In contrast, pooled data from younger patients in the five trials showed that prophylactic ICD therapy reduced all-cause mortality.
None of the selected trials demonstrated evidence of selection, performance, detection, or attrition bias. Only a small number of studies were included, and four potentially relevant trials were not included because mortality data by age group were not available.
Trials including cardiac resynchronization therapy (CRT) were excluded from this meta-analysis, and elderly patients meeting criteria for CRT comprise an important group that must be considered separately.
Bottom line: There is no definitive reduction in mortality with prophylactic ICD therapy in elderly patients with severe left ventricular dysfunction.
Citation: Santangeli P, Di Biase L, Dello Russo A, et al. Meta-analysis: age and effectiveness of prophylactic implantable cardioverter-defibrillators. Ann Intern Med. 2010;153(9):592-599.
System Delay Is Mortality Marker in STEMI Patients Treated with Primary PCI
Clinical question: What is the relationship between system delays to reperfusion therapy and mortality in patients with ST-segment-elevation myocardial infarction (STEMI)?
Background: In patients with STEMI, an early reperfusion strategy is often sought, and several studies have focused on the association between door-to-balloon delay and outcomes. Focusing more broadly on the time from first contact with the healthcare system to the initiation of reperfusion therapy (system delay) might be a more relevant approach.
Study design: Historical follow-up study.
Setting: Three high-volume PCI centers in Denmark.
Synopsis: Using population-based medical registries of 6,209 Danish patients treated for STEMI with percutaneous coronary intervention (PCI), the authors examined the association between delays in reperfusion therapy and mortality. System delay encompassed the entire time from first contact with the healthcare system to the initiation of reperfusion therapy.
Overall, shorter system delay was associated with significantly decreased mortality, as were the individual components of system delay (prehospital delay and door-to-balloon delay). The shortest delays (0-60 minutes) corresponded to a mortality rate of 15%, and the longest delays (181-360 minutes) corresponded to a mortality rate of 31%. Patients were followed for a median of 3.4 years.
This study is unique, as it is the first to look at the association between system delay and outcomes in patients with STEMI transported by EMS and treated with primary PCI. The study highlights the harmful impact of longer system delays on mortality. Limitations of this study include possible underestimation of system delay and challenges surrounding the right marker for reperfusion.
Bottom line: System delay might serve as a broad, comprehensive marker for predicting mortality in patients with STEMI treated with primary PCI.
Citation: Terkelsen CJ, Sorensen JT, Maeng M, et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304(7): 763-771.
D-Dimer Is Effective in Determining the Risk of VTE Recurrence after First Unprovoked Event
Clinical question: Does the timing, patient age, or cut point level affect the predictive value of a D-dimer in predicting VTE recurrence after a first unprovoked event?
Background: Anticoagulation duration after a first unprovoked VTE is at least three months, but it can be indefinite in patients with stable anticoagulation and low bleeding risk. Measuring a D-dimer level after discontinuation of anticoagulation is helpful in determining which patients might benefit from prolonged anticoagulation. However, several unanswered questions remain regarding D-dimer testing.
Study design: Patient-level meta-analysis.
Setting: Pooled patient-level data from seven prospective studies.
Synopsis: Patient-level data were obtained for all patients enrolled using post-treatment D-dimer measurement to predict recurrent VTE in patients with a first unprovoked VTE who had completed at least three months of anticoagulation therapy. The mean length of follow-up was 30 months. Patients with a positive D-dimer had recurrent VTE at a rate of 8.8 per 100 patient-years while those with a negative D-dimer had a rate of 3.7 per 100 patient-years.
Univariate analysis revealed an HR of 2.59 for patients with a positive versus a negative test result. The analysis also showed that the timing of the test, the age of the patient, and the actual cut points used for the various D-dimer tests did not affect the analysis significantly.
These studies’ strength is their large sample sizes and the use of prospective studies. The weaknesses include a mostly white patient population and incomplete data on all patients.
Bottom line: D-dimer testing is useful in predicting VTE recurrence after treatment for a first unprovoked event regardless of patient age, post-treatment timing, or the assay cut point used.
Citation: Douketis J, Tosetto A, Marcucci M, et al. Patient-level meta-analysis: effect of measurement timing, threshold, and patient age on ability of D-dimer testing to assess recurrence risk after unprovoked venous thromboembolism. Ann Intern Med. 2010;153(8): 523-531.
Thigh-High Stockings Are Better than Knee-High Stockings for Post-Stroke DVT Prophylaxis
Clinical question: Are thigh-high compression stockings better then knee-high stockings in immobilized acute-stroke patients?
Background: DVT is common in hospitalized stroke patients with immobility. Graduated compression stockings are often used for DVT prophylaxis, but the CLOTS-1 trial recently found that thigh-high stockings were ineffective after acute stroke. It is unclear if the more commonly used knee-high stockings are more effective than thigh-high stockings.
Study design: Parallel-group trial (the CLOTS-2 trial).
Setting: One hundred twelve hospitals in nine countries.
Synopsis: More than 3,100 patients with acute stroke and immobilization were recruited from January 2002 to May 2009. Patients were randomized to receive thigh-high or knee-high stockings. Patients also received usual care, including anticoagulants and a screening ultrasound for asymptomatic proximal DVT at seven to 10 days. Approximately 640 patients in each group also underwent ultrasound at 25-30 days.
Overall, 6.3% of patients in the thigh-high group had DVT, compared with 8.8% in the knee-high group (P=0.007). There were no significant differences in the secondary outcomes of pulmonary embolism or death. The thigh-high stockings had a higher number of adverse skin events. Enrollment was stopped early when the CLOTS-1 trial showed no difference in DVT rates between thigh-high stockings and no stockings.
Bottom line: Knee-high graduated compression stockings lead to worse outcomes than thigh-high stockings for DVT prophylaxis in immobilized acute-stroke patients.
Citation: CLOTS (Clots in Legs Or sTockings after Stroke) Trial Collaboration. Thigh-length versus below-knee stockings for deep venous thrombosis prophylaxis after stroke: a randomized trial. Ann Intern Med. 2010;153(9):553-562. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Effects of extended VTE prophylaxis in medical patients
- Outcomes with and without preprocedural statins
- Association of subclinical hypothyroidism and CHD
- BP treatment after intracerebral hemorrhage
- Outcomes of ICD therapy in the elderly
- Systems delays and outcomes of STEMI
- D-dimer to predict recurrent VTE
- Stocking height and risk of post-stroke DVT
Extending Anticoagulant Prophylaxis after Medical Hospitalization Decreases VTE, Increases Major Bleeding
Clinical question: For patients with acute medical illness, does extending low-molecular-weight heparin (LMWH) administration for up to 28 days after discharge reduce the incidence of venous thromboembolism (VTE)?
Background: DVT and pulmonary embolism (PE) are common hospital-acquired complications. LMWH has been shown to reduce VTE for medical and surgical patients, and extended-duration LMWH reduces VTE in high-risk surgical patients. Whether extending anticoagulant prophylaxis after discharge for acutely ill medical patients with reduced mobility improves outcomes is unknown.
Study design: Randomized, placebo-controlled trial.
Setting: Three hundred seventy hospitals in 20 countries.
Synopsis: Eligible patients were >40 years old, hospitalized with acute medical illness, and had reduced mobility for ≥3 days. Patients received enoxaparin 40 mg SC daily prophylaxis while hospitalized and were then randomized to an additional 28±4 days of enoxaparin or placebo. Patients received a screening ultrasound to assess for asymptomatic DVT. The primary outcome was a composite of asymptomatic proximal DVT, symptomatic DVT or PE, or fatal PE during the period of extended prophylaxis.
An interim analysis indicated that extended prophylaxis was ineffective; at that time, the protocol was amended to target patients with severe immobility or with moderate immobility plus an additional risk factor (e.g. cancer, prior VTE, or age >75).
The study found that extended prophylaxis decreased the composite VTE outcome (2.5% vs 4.0%, P<0.05) and symptomatic VTE (0.2% vs 1.0%, P<0.05). The incidence of major bleeding was increased in the extended prophylaxis group (0.8% vs 0.3%, P<0.05). There was no difference in mortality.
The unplanned, midstudy protocol amendment to target higher-risk patients is a concern, though the final analyses included patients pre- and post-amendment.
Bottom line: Extending LMWH beyond hospitalization for patients admitted with acute medical illness and decreased mobility decreases VTE, but increases major bleeding.
Citation: Hull RD, Schellong SM, Tapson VF, et al. Extended-duration venous thromboembolism prophylaxis in acutely ill medical patients with recently reduced mobility: a randomized trial. Ann Intern Med. 2010;153(1);8-18.
Preprocedural Statin Therapy Reduces Postprocedural Myocardial Infarction
Clinical question: Does statin therapy reduce periprocedural cardiovascular events?
Background: Myocardial infarction (MI) and death are inherent risks of invasive procedures. Reduction of these risks in certain patient populations has been shown with the use of a beta blockade. Statins have shown promise during acute coronary syndrome. Questions remain about the role of statin therapy before invasive procedures in reducing adverse cardiovascular events.
Study design: Meta-analysis of randomized controlled trials.
Setting: Twenty-one studies involving 4,805 patients, published from inception of MEDLINE, Cochrane, and Clinicaltrials to February 2010.
Synopsis: The use of statins one to seven days preprocedure significantly reduced post-procedural MI in percutaneous coronary interventions (PCI) (P<0.0001). Statins given approximately four weeks in advance of noncardiac surgical procedures also significantly reduced postprocedural MI (P=0.004). An absolute risk reduction of 5.8% for postprocedural MI was found after PCI and 4.1% in noncardiac surgical procedures.
Statins did not show a significant reduction in postprocedural MI (P=0.40) or all-cause mortality (P=0.15) in coronary artery bypass graft surgery (CABG). However, statins did reduce post-CABG atrial fibrillation (P<0.0001).
The 21 studies used a variety of drugs and doses. However, the PCI studies favored atorvastatin 40 mg; more than half the CABG studies used atorvastatin 20 mg; and 91% of the noncardiac surgical studies used fluvastatin 80 mg. Dedicated trials are needed to demonstrate optimal statin agent, dose, and timing of therapy.
Bottom line: Preprocedural statin therapy reduces postprocedural MI after both PCI and noncardiac procedures but not after CABG.
Citation: Winchester DE, Wen X, Xie L, Bavry AA. Evidence of pre-procedural statin therapy: a meta-analysis of randomized trials. J Am Coll Cardiol. 2010;56(19); 1099-1109.
Subclinical Hypothyroidism Increases the Risk of Coronary Heart Disease and Mortality
Clinical question: What are the risks of coronary heart disease (CHD) and mortality among adults with subclinical hypothyroidism?
Background: Subclinical hypo-thyroidism is defined as an elevated serum thyroid stimulating hormone (TSH) level with a normal T4 concentration. Controversy exists regarding the treatment of subclinical hypothyroidism. Because of the association with hyperlipidemia and atherosclerosis, treatment of subclinical hypothyroidism is thought to be beneficial. Previous data from large prospective cohort studies regarding this association are conflicting.
Study design: Study-level meta-analysis of prospective cohort studies.
Setting: Eleven prospective cohorts in the U.S., Europe, Australia, Brazil, and Japan from 1972 to 2007.
Synopsis: Among 55,287 adults, 3,450 (6.2%) had subclinical hypothyroidism and 51,837 were euthyroid. Using Cox proportional hazard models, the association of subclinical hypothyroidism with CHD and mortality were determined for each cohort.
The risk of CHD events and CHD mortality increased with higher TSH concentrations.
In age- and sex-adjusted analyses, the hazard ratio (HR) for CHD events were as follows: HR=1.0 (TSH=4.5-6.9 mIU/L); HR=1.17 (TSH=7-9.9 mIU/L), and HR=1.89 (TSH=10-19.9 mIU/L). Similarly, HRs for CHD mortality showed an increasing trend: 1.09, 1.42, and 1.58, respectively.
Although the association is clearly established here, randomized controlled trials are needed to address whether thyroxine replacement can prevent CHD and the TSH threshold that will provide the most clinical benefit.
Bottom line: Subclinical hypo-thyroidism is associated with an increased risk for CHD events and mortality, primarily in patients with TSH concentrations of 10 mIU/L or higher.
Citation: Rodondi N, den Elzen WP, Bauer DC, et al. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA. 2010;304(12): 1365-1374.
Reduction in Hematoma Growth after Acute Intracerebral Hemorrhage Associated with Lower Blood Pressure
Clinical question: Does intensive systolic blood pressure (SBP) <140 mmHg within one hour reduce hematoma growth after acute intracerebral bleeding?
Background: Early elevation of blood pressure after an acute intracerebral bleed is strongly associated with hematoma growth and worse outcomes. The pilot phase of the Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage Trial (INTERACT) showed that early intensive blood pressure lowering reduced hematoma growth within six hours after onset of intracerebral hemorrhage.
Study design: Randomized controlled trial in which patients received an early intensive blood-pressure-lowering treatment (goal SBP<140 mmHg within one hour) or the AHA recommended best practice guidelines (goal SBP <180 mmHg), which were published in 1999.
Setting: Network of hospitals in China, South Korea, and Australia.
Synopsis: From 2005 to 2007, the study examined 404 patients with computed-tomography (CT) evidence of intracerebral hemorrhage, elevated SBP (150 mmHg-220 mmHg), and ability to commence BP lowering treatment within six hours of onset. Hematoma volumes were measured in the intensive treatment and guideline groups based on CT scans done at baseline and after 24 hours.
No significant association was found between the baseline SBP and the absolute or proportional growth of the hematoma. However, in the intensively treated patients who achieved target SBP within the first 24 hours, a significant association was found with the absolute and proportional hematoma growth.
Maximum reduction of hematoma growth occurred in the group with a median SBP of 135 mmHg.
This single-observational study did not include patients with severe intracranial bleeding who died or required surgical evacuation within the first 24 hours.
Hematoma size reduction did not improve survival or outcomes.
Bottom line: Intensive SBP lowering from 140 mmHg to 130 mmHg within one hour reduces hematoma growth after an intracranial hemorrhage.
Citation: Arima H, Anderson CS, Wang JG, et al. Lower treatment blood pressure is associated with the greatest reduction in hematoma growth after acute intracerebral hemorrhage. Hypertension. 2010;56(5):852-858.
Implantable Cardioverter-Defibrillator (ICD) Therapy for Primary Prevention of Sudden Cardiac Death Might Not Provide Survival Benefit to Elderly
Clinical question: Does ICD therapy for primary prevention of sudden cardiac death in individuals with severe left ventricular dysfunction improve survival in elderly patients?
Background: Several clinical trials of select individuals with severe left ventricular dysfunction (EF <40%) have demonstrated that ICD therapy is associated with a reduction in overall mortality. Given the costs and risks associated with ICD placement, it is important to assess how this therapy affects survival in younger versus older individuals.
Study design: Meta-analysis of five randomized controlled trials.
Setting: Five trials (MADIT-II, DEFINITE, DINAMIT, SCDHeFT, and IRIS).
Synopsis: All included studies compared ICD therapy to standard medical care in the primary prevention of sudden cardiac death in individuals with severe left ventricular dysfunction. Elderly patients comprised 44% of the 5,783 patients included in the study; elderly patients were defined as >65 in three studies, and >60 in two studies. Pooled analysis of the three trials examining ICD use for primary prevention found a nonsignificant reduction in all-cause mortality compared with medical therapy in elderly patients (HR 0.81 [95% CI 0.62 to 1.05], P=0.11). The two remaining studies involving post-MI patients showed no statistically significant reduction in mortality in elderly patients.
In contrast, pooled data from younger patients in the five trials showed that prophylactic ICD therapy reduced all-cause mortality.
None of the selected trials demonstrated evidence of selection, performance, detection, or attrition bias. Only a small number of studies were included, and four potentially relevant trials were not included because mortality data by age group were not available.
Trials including cardiac resynchronization therapy (CRT) were excluded from this meta-analysis, and elderly patients meeting criteria for CRT comprise an important group that must be considered separately.
Bottom line: There is no definitive reduction in mortality with prophylactic ICD therapy in elderly patients with severe left ventricular dysfunction.
Citation: Santangeli P, Di Biase L, Dello Russo A, et al. Meta-analysis: age and effectiveness of prophylactic implantable cardioverter-defibrillators. Ann Intern Med. 2010;153(9):592-599.
System Delay Is Mortality Marker in STEMI Patients Treated with Primary PCI
Clinical question: What is the relationship between system delays to reperfusion therapy and mortality in patients with ST-segment-elevation myocardial infarction (STEMI)?
Background: In patients with STEMI, an early reperfusion strategy is often sought, and several studies have focused on the association between door-to-balloon delay and outcomes. Focusing more broadly on the time from first contact with the healthcare system to the initiation of reperfusion therapy (system delay) might be a more relevant approach.
Study design: Historical follow-up study.
Setting: Three high-volume PCI centers in Denmark.
Synopsis: Using population-based medical registries of 6,209 Danish patients treated for STEMI with percutaneous coronary intervention (PCI), the authors examined the association between delays in reperfusion therapy and mortality. System delay encompassed the entire time from first contact with the healthcare system to the initiation of reperfusion therapy.
Overall, shorter system delay was associated with significantly decreased mortality, as were the individual components of system delay (prehospital delay and door-to-balloon delay). The shortest delays (0-60 minutes) corresponded to a mortality rate of 15%, and the longest delays (181-360 minutes) corresponded to a mortality rate of 31%. Patients were followed for a median of 3.4 years.
This study is unique, as it is the first to look at the association between system delay and outcomes in patients with STEMI transported by EMS and treated with primary PCI. The study highlights the harmful impact of longer system delays on mortality. Limitations of this study include possible underestimation of system delay and challenges surrounding the right marker for reperfusion.
Bottom line: System delay might serve as a broad, comprehensive marker for predicting mortality in patients with STEMI treated with primary PCI.
Citation: Terkelsen CJ, Sorensen JT, Maeng M, et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304(7): 763-771.
D-Dimer Is Effective in Determining the Risk of VTE Recurrence after First Unprovoked Event
Clinical question: Does the timing, patient age, or cut point level affect the predictive value of a D-dimer in predicting VTE recurrence after a first unprovoked event?
Background: Anticoagulation duration after a first unprovoked VTE is at least three months, but it can be indefinite in patients with stable anticoagulation and low bleeding risk. Measuring a D-dimer level after discontinuation of anticoagulation is helpful in determining which patients might benefit from prolonged anticoagulation. However, several unanswered questions remain regarding D-dimer testing.
Study design: Patient-level meta-analysis.
Setting: Pooled patient-level data from seven prospective studies.
Synopsis: Patient-level data were obtained for all patients enrolled using post-treatment D-dimer measurement to predict recurrent VTE in patients with a first unprovoked VTE who had completed at least three months of anticoagulation therapy. The mean length of follow-up was 30 months. Patients with a positive D-dimer had recurrent VTE at a rate of 8.8 per 100 patient-years while those with a negative D-dimer had a rate of 3.7 per 100 patient-years.
Univariate analysis revealed an HR of 2.59 for patients with a positive versus a negative test result. The analysis also showed that the timing of the test, the age of the patient, and the actual cut points used for the various D-dimer tests did not affect the analysis significantly.
These studies’ strength is their large sample sizes and the use of prospective studies. The weaknesses include a mostly white patient population and incomplete data on all patients.
Bottom line: D-dimer testing is useful in predicting VTE recurrence after treatment for a first unprovoked event regardless of patient age, post-treatment timing, or the assay cut point used.
Citation: Douketis J, Tosetto A, Marcucci M, et al. Patient-level meta-analysis: effect of measurement timing, threshold, and patient age on ability of D-dimer testing to assess recurrence risk after unprovoked venous thromboembolism. Ann Intern Med. 2010;153(8): 523-531.
Thigh-High Stockings Are Better than Knee-High Stockings for Post-Stroke DVT Prophylaxis
Clinical question: Are thigh-high compression stockings better then knee-high stockings in immobilized acute-stroke patients?
Background: DVT is common in hospitalized stroke patients with immobility. Graduated compression stockings are often used for DVT prophylaxis, but the CLOTS-1 trial recently found that thigh-high stockings were ineffective after acute stroke. It is unclear if the more commonly used knee-high stockings are more effective than thigh-high stockings.
Study design: Parallel-group trial (the CLOTS-2 trial).
Setting: One hundred twelve hospitals in nine countries.
Synopsis: More than 3,100 patients with acute stroke and immobilization were recruited from January 2002 to May 2009. Patients were randomized to receive thigh-high or knee-high stockings. Patients also received usual care, including anticoagulants and a screening ultrasound for asymptomatic proximal DVT at seven to 10 days. Approximately 640 patients in each group also underwent ultrasound at 25-30 days.
Overall, 6.3% of patients in the thigh-high group had DVT, compared with 8.8% in the knee-high group (P=0.007). There were no significant differences in the secondary outcomes of pulmonary embolism or death. The thigh-high stockings had a higher number of adverse skin events. Enrollment was stopped early when the CLOTS-1 trial showed no difference in DVT rates between thigh-high stockings and no stockings.
Bottom line: Knee-high graduated compression stockings lead to worse outcomes than thigh-high stockings for DVT prophylaxis in immobilized acute-stroke patients.
Citation: CLOTS (Clots in Legs Or sTockings after Stroke) Trial Collaboration. Thigh-length versus below-knee stockings for deep venous thrombosis prophylaxis after stroke: a randomized trial. Ann Intern Med. 2010;153(9):553-562. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Effects of extended VTE prophylaxis in medical patients
- Outcomes with and without preprocedural statins
- Association of subclinical hypothyroidism and CHD
- BP treatment after intracerebral hemorrhage
- Outcomes of ICD therapy in the elderly
- Systems delays and outcomes of STEMI
- D-dimer to predict recurrent VTE
- Stocking height and risk of post-stroke DVT
Extending Anticoagulant Prophylaxis after Medical Hospitalization Decreases VTE, Increases Major Bleeding
Clinical question: For patients with acute medical illness, does extending low-molecular-weight heparin (LMWH) administration for up to 28 days after discharge reduce the incidence of venous thromboembolism (VTE)?
Background: DVT and pulmonary embolism (PE) are common hospital-acquired complications. LMWH has been shown to reduce VTE for medical and surgical patients, and extended-duration LMWH reduces VTE in high-risk surgical patients. Whether extending anticoagulant prophylaxis after discharge for acutely ill medical patients with reduced mobility improves outcomes is unknown.
Study design: Randomized, placebo-controlled trial.
Setting: Three hundred seventy hospitals in 20 countries.
Synopsis: Eligible patients were >40 years old, hospitalized with acute medical illness, and had reduced mobility for ≥3 days. Patients received enoxaparin 40 mg SC daily prophylaxis while hospitalized and were then randomized to an additional 28±4 days of enoxaparin or placebo. Patients received a screening ultrasound to assess for asymptomatic DVT. The primary outcome was a composite of asymptomatic proximal DVT, symptomatic DVT or PE, or fatal PE during the period of extended prophylaxis.
An interim analysis indicated that extended prophylaxis was ineffective; at that time, the protocol was amended to target patients with severe immobility or with moderate immobility plus an additional risk factor (e.g. cancer, prior VTE, or age >75).
The study found that extended prophylaxis decreased the composite VTE outcome (2.5% vs 4.0%, P<0.05) and symptomatic VTE (0.2% vs 1.0%, P<0.05). The incidence of major bleeding was increased in the extended prophylaxis group (0.8% vs 0.3%, P<0.05). There was no difference in mortality.
The unplanned, midstudy protocol amendment to target higher-risk patients is a concern, though the final analyses included patients pre- and post-amendment.
Bottom line: Extending LMWH beyond hospitalization for patients admitted with acute medical illness and decreased mobility decreases VTE, but increases major bleeding.
Citation: Hull RD, Schellong SM, Tapson VF, et al. Extended-duration venous thromboembolism prophylaxis in acutely ill medical patients with recently reduced mobility: a randomized trial. Ann Intern Med. 2010;153(1);8-18.
Preprocedural Statin Therapy Reduces Postprocedural Myocardial Infarction
Clinical question: Does statin therapy reduce periprocedural cardiovascular events?
Background: Myocardial infarction (MI) and death are inherent risks of invasive procedures. Reduction of these risks in certain patient populations has been shown with the use of a beta blockade. Statins have shown promise during acute coronary syndrome. Questions remain about the role of statin therapy before invasive procedures in reducing adverse cardiovascular events.
Study design: Meta-analysis of randomized controlled trials.
Setting: Twenty-one studies involving 4,805 patients, published from inception of MEDLINE, Cochrane, and Clinicaltrials to February 2010.
Synopsis: The use of statins one to seven days preprocedure significantly reduced post-procedural MI in percutaneous coronary interventions (PCI) (P<0.0001). Statins given approximately four weeks in advance of noncardiac surgical procedures also significantly reduced postprocedural MI (P=0.004). An absolute risk reduction of 5.8% for postprocedural MI was found after PCI and 4.1% in noncardiac surgical procedures.
Statins did not show a significant reduction in postprocedural MI (P=0.40) or all-cause mortality (P=0.15) in coronary artery bypass graft surgery (CABG). However, statins did reduce post-CABG atrial fibrillation (P<0.0001).
The 21 studies used a variety of drugs and doses. However, the PCI studies favored atorvastatin 40 mg; more than half the CABG studies used atorvastatin 20 mg; and 91% of the noncardiac surgical studies used fluvastatin 80 mg. Dedicated trials are needed to demonstrate optimal statin agent, dose, and timing of therapy.
Bottom line: Preprocedural statin therapy reduces postprocedural MI after both PCI and noncardiac procedures but not after CABG.
Citation: Winchester DE, Wen X, Xie L, Bavry AA. Evidence of pre-procedural statin therapy: a meta-analysis of randomized trials. J Am Coll Cardiol. 2010;56(19); 1099-1109.
Subclinical Hypothyroidism Increases the Risk of Coronary Heart Disease and Mortality
Clinical question: What are the risks of coronary heart disease (CHD) and mortality among adults with subclinical hypothyroidism?
Background: Subclinical hypo-thyroidism is defined as an elevated serum thyroid stimulating hormone (TSH) level with a normal T4 concentration. Controversy exists regarding the treatment of subclinical hypothyroidism. Because of the association with hyperlipidemia and atherosclerosis, treatment of subclinical hypothyroidism is thought to be beneficial. Previous data from large prospective cohort studies regarding this association are conflicting.
Study design: Study-level meta-analysis of prospective cohort studies.
Setting: Eleven prospective cohorts in the U.S., Europe, Australia, Brazil, and Japan from 1972 to 2007.
Synopsis: Among 55,287 adults, 3,450 (6.2%) had subclinical hypothyroidism and 51,837 were euthyroid. Using Cox proportional hazard models, the association of subclinical hypothyroidism with CHD and mortality were determined for each cohort.
The risk of CHD events and CHD mortality increased with higher TSH concentrations.
In age- and sex-adjusted analyses, the hazard ratio (HR) for CHD events were as follows: HR=1.0 (TSH=4.5-6.9 mIU/L); HR=1.17 (TSH=7-9.9 mIU/L), and HR=1.89 (TSH=10-19.9 mIU/L). Similarly, HRs for CHD mortality showed an increasing trend: 1.09, 1.42, and 1.58, respectively.
Although the association is clearly established here, randomized controlled trials are needed to address whether thyroxine replacement can prevent CHD and the TSH threshold that will provide the most clinical benefit.
Bottom line: Subclinical hypo-thyroidism is associated with an increased risk for CHD events and mortality, primarily in patients with TSH concentrations of 10 mIU/L or higher.
Citation: Rodondi N, den Elzen WP, Bauer DC, et al. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA. 2010;304(12): 1365-1374.
Reduction in Hematoma Growth after Acute Intracerebral Hemorrhage Associated with Lower Blood Pressure
Clinical question: Does intensive systolic blood pressure (SBP) <140 mmHg within one hour reduce hematoma growth after acute intracerebral bleeding?
Background: Early elevation of blood pressure after an acute intracerebral bleed is strongly associated with hematoma growth and worse outcomes. The pilot phase of the Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage Trial (INTERACT) showed that early intensive blood pressure lowering reduced hematoma growth within six hours after onset of intracerebral hemorrhage.
Study design: Randomized controlled trial in which patients received an early intensive blood-pressure-lowering treatment (goal SBP<140 mmHg within one hour) or the AHA recommended best practice guidelines (goal SBP <180 mmHg), which were published in 1999.
Setting: Network of hospitals in China, South Korea, and Australia.
Synopsis: From 2005 to 2007, the study examined 404 patients with computed-tomography (CT) evidence of intracerebral hemorrhage, elevated SBP (150 mmHg-220 mmHg), and ability to commence BP lowering treatment within six hours of onset. Hematoma volumes were measured in the intensive treatment and guideline groups based on CT scans done at baseline and after 24 hours.
No significant association was found between the baseline SBP and the absolute or proportional growth of the hematoma. However, in the intensively treated patients who achieved target SBP within the first 24 hours, a significant association was found with the absolute and proportional hematoma growth.
Maximum reduction of hematoma growth occurred in the group with a median SBP of 135 mmHg.
This single-observational study did not include patients with severe intracranial bleeding who died or required surgical evacuation within the first 24 hours.
Hematoma size reduction did not improve survival or outcomes.
Bottom line: Intensive SBP lowering from 140 mmHg to 130 mmHg within one hour reduces hematoma growth after an intracranial hemorrhage.
Citation: Arima H, Anderson CS, Wang JG, et al. Lower treatment blood pressure is associated with the greatest reduction in hematoma growth after acute intracerebral hemorrhage. Hypertension. 2010;56(5):852-858.
Implantable Cardioverter-Defibrillator (ICD) Therapy for Primary Prevention of Sudden Cardiac Death Might Not Provide Survival Benefit to Elderly
Clinical question: Does ICD therapy for primary prevention of sudden cardiac death in individuals with severe left ventricular dysfunction improve survival in elderly patients?
Background: Several clinical trials of select individuals with severe left ventricular dysfunction (EF <40%) have demonstrated that ICD therapy is associated with a reduction in overall mortality. Given the costs and risks associated with ICD placement, it is important to assess how this therapy affects survival in younger versus older individuals.
Study design: Meta-analysis of five randomized controlled trials.
Setting: Five trials (MADIT-II, DEFINITE, DINAMIT, SCDHeFT, and IRIS).
Synopsis: All included studies compared ICD therapy to standard medical care in the primary prevention of sudden cardiac death in individuals with severe left ventricular dysfunction. Elderly patients comprised 44% of the 5,783 patients included in the study; elderly patients were defined as >65 in three studies, and >60 in two studies. Pooled analysis of the three trials examining ICD use for primary prevention found a nonsignificant reduction in all-cause mortality compared with medical therapy in elderly patients (HR 0.81 [95% CI 0.62 to 1.05], P=0.11). The two remaining studies involving post-MI patients showed no statistically significant reduction in mortality in elderly patients.
In contrast, pooled data from younger patients in the five trials showed that prophylactic ICD therapy reduced all-cause mortality.
None of the selected trials demonstrated evidence of selection, performance, detection, or attrition bias. Only a small number of studies were included, and four potentially relevant trials were not included because mortality data by age group were not available.
Trials including cardiac resynchronization therapy (CRT) were excluded from this meta-analysis, and elderly patients meeting criteria for CRT comprise an important group that must be considered separately.
Bottom line: There is no definitive reduction in mortality with prophylactic ICD therapy in elderly patients with severe left ventricular dysfunction.
Citation: Santangeli P, Di Biase L, Dello Russo A, et al. Meta-analysis: age and effectiveness of prophylactic implantable cardioverter-defibrillators. Ann Intern Med. 2010;153(9):592-599.
System Delay Is Mortality Marker in STEMI Patients Treated with Primary PCI
Clinical question: What is the relationship between system delays to reperfusion therapy and mortality in patients with ST-segment-elevation myocardial infarction (STEMI)?
Background: In patients with STEMI, an early reperfusion strategy is often sought, and several studies have focused on the association between door-to-balloon delay and outcomes. Focusing more broadly on the time from first contact with the healthcare system to the initiation of reperfusion therapy (system delay) might be a more relevant approach.
Study design: Historical follow-up study.
Setting: Three high-volume PCI centers in Denmark.
Synopsis: Using population-based medical registries of 6,209 Danish patients treated for STEMI with percutaneous coronary intervention (PCI), the authors examined the association between delays in reperfusion therapy and mortality. System delay encompassed the entire time from first contact with the healthcare system to the initiation of reperfusion therapy.
Overall, shorter system delay was associated with significantly decreased mortality, as were the individual components of system delay (prehospital delay and door-to-balloon delay). The shortest delays (0-60 minutes) corresponded to a mortality rate of 15%, and the longest delays (181-360 minutes) corresponded to a mortality rate of 31%. Patients were followed for a median of 3.4 years.
This study is unique, as it is the first to look at the association between system delay and outcomes in patients with STEMI transported by EMS and treated with primary PCI. The study highlights the harmful impact of longer system delays on mortality. Limitations of this study include possible underestimation of system delay and challenges surrounding the right marker for reperfusion.
Bottom line: System delay might serve as a broad, comprehensive marker for predicting mortality in patients with STEMI treated with primary PCI.
Citation: Terkelsen CJ, Sorensen JT, Maeng M, et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304(7): 763-771.
D-Dimer Is Effective in Determining the Risk of VTE Recurrence after First Unprovoked Event
Clinical question: Does the timing, patient age, or cut point level affect the predictive value of a D-dimer in predicting VTE recurrence after a first unprovoked event?
Background: Anticoagulation duration after a first unprovoked VTE is at least three months, but it can be indefinite in patients with stable anticoagulation and low bleeding risk. Measuring a D-dimer level after discontinuation of anticoagulation is helpful in determining which patients might benefit from prolonged anticoagulation. However, several unanswered questions remain regarding D-dimer testing.
Study design: Patient-level meta-analysis.
Setting: Pooled patient-level data from seven prospective studies.
Synopsis: Patient-level data were obtained for all patients enrolled using post-treatment D-dimer measurement to predict recurrent VTE in patients with a first unprovoked VTE who had completed at least three months of anticoagulation therapy. The mean length of follow-up was 30 months. Patients with a positive D-dimer had recurrent VTE at a rate of 8.8 per 100 patient-years while those with a negative D-dimer had a rate of 3.7 per 100 patient-years.
Univariate analysis revealed an HR of 2.59 for patients with a positive versus a negative test result. The analysis also showed that the timing of the test, the age of the patient, and the actual cut points used for the various D-dimer tests did not affect the analysis significantly.
These studies’ strength is their large sample sizes and the use of prospective studies. The weaknesses include a mostly white patient population and incomplete data on all patients.
Bottom line: D-dimer testing is useful in predicting VTE recurrence after treatment for a first unprovoked event regardless of patient age, post-treatment timing, or the assay cut point used.
Citation: Douketis J, Tosetto A, Marcucci M, et al. Patient-level meta-analysis: effect of measurement timing, threshold, and patient age on ability of D-dimer testing to assess recurrence risk after unprovoked venous thromboembolism. Ann Intern Med. 2010;153(8): 523-531.
Thigh-High Stockings Are Better than Knee-High Stockings for Post-Stroke DVT Prophylaxis
Clinical question: Are thigh-high compression stockings better then knee-high stockings in immobilized acute-stroke patients?
Background: DVT is common in hospitalized stroke patients with immobility. Graduated compression stockings are often used for DVT prophylaxis, but the CLOTS-1 trial recently found that thigh-high stockings were ineffective after acute stroke. It is unclear if the more commonly used knee-high stockings are more effective than thigh-high stockings.
Study design: Parallel-group trial (the CLOTS-2 trial).
Setting: One hundred twelve hospitals in nine countries.
Synopsis: More than 3,100 patients with acute stroke and immobilization were recruited from January 2002 to May 2009. Patients were randomized to receive thigh-high or knee-high stockings. Patients also received usual care, including anticoagulants and a screening ultrasound for asymptomatic proximal DVT at seven to 10 days. Approximately 640 patients in each group also underwent ultrasound at 25-30 days.
Overall, 6.3% of patients in the thigh-high group had DVT, compared with 8.8% in the knee-high group (P=0.007). There were no significant differences in the secondary outcomes of pulmonary embolism or death. The thigh-high stockings had a higher number of adverse skin events. Enrollment was stopped early when the CLOTS-1 trial showed no difference in DVT rates between thigh-high stockings and no stockings.
Bottom line: Knee-high graduated compression stockings lead to worse outcomes than thigh-high stockings for DVT prophylaxis in immobilized acute-stroke patients.
Citation: CLOTS (Clots in Legs Or sTockings after Stroke) Trial Collaboration. Thigh-length versus below-knee stockings for deep venous thrombosis prophylaxis after stroke: a randomized trial. Ann Intern Med. 2010;153(9):553-562. TH
What Is the Role of BNP in Diagnosis and Management of Acutely Decompensated Heart Failure?
Case
A 76-year-old woman with a history of chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), and atrial fibrillation presents with shortness of breath. She is tachypneic, her pulse is 105 beats per minute, and her blood pressure is 105/60 mm/Hg. She is obese and has an immeasurable venous pressure with decreased breath sounds in both lung bases, and irregular and distant heart sounds. What is the role of brain (or B-type) natriuretic peptide (BNP) in the diagnosis and management of this patient?
Overview
Each year, more than 1 million patients are admitted to hospitals with acutely decompensated heart failure (ADHF). Although many of these patients carry a pre-admission diagnosis of CHF, their common presenting symptoms are not specific for ADHF, which leads to delays in diagnosis and therapy initiation, and increased diagnostic costs and potentially worse outcomes. Clinical risk scores from NHANES and the Framingham heart study have limited sensitivity, missing nearly 20% of patients.1,2 Moreover, these scores are underused by clinicians who depend heavily on clinical gestalt.3
Once ADHF is diagnosed, ongoing bedside assessment of volume status is a difficult and inexact science. The physiologic goal is achievement of normal left ventricular end diastolic volume; however, surrogate measures of this status, including weight change, venous pressure, and pulmonary and cardiac auscultatory findings, have significant limitations. After discharge, patients have high and heterogeneous risks of readmission, death, and other adverse events. Identifying patients with the highest risk might allow for intensive strategies to improve outcomes.
BNP is a neurohormone released from the ventricular cells in response to increased cardiac filling pressures. Plasma measurements of BNP have been shown to reflect volume status, to predict risk at admission and discharge, and to serve as a treatment guide in a variety of clinical settings.4 This simple laboratory test increasingly has been used to diagnose and manage ADHF; its utility and limitations deserve critical review.
Review of the Data
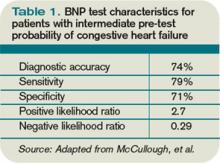
CHF diagnosis. Since introduction of the rapid BNP assay, several trials have evaluated its clinical utility in determining whether ADHF is the cause of a patient’s dyspnea. The largest of these trials, the Breathing Not Properly Multinational Study, conducted by McCullough et al, enrolled nearly 1,600 patients who presented with the primary complaint of dyspnea.5 After reviewing conventional clinical information, ED physicians were asked to determine the likelihood that ADHF was the etiology of a patient’s dyspnea. These likelihoods were classified as low (<20%), intermediate (20%-80%), or high (>80%). The admission BNP was recorded but was not available for the ED physician decisions.
The “gold standard” was the opinion of two adjudicating cardiologists who reviewed the cases retrospectively and determined whether the dyspnea resulted from ADHF. They were blinded to both the ED physician’s opinion and the BNP results. The accuracy of the ED physician’s initial assessment and the impact of the BNP results were compared with this gold standard.
For the entire cohort, the use of BNP (with a cutoff point of 100 pg/mL) would have improved the ED physician’s assessment from 74% diagnostic accuracy to 81%, which is statistically significant. Most important, in those patients initially given an intermediate likelihood of CHF, BNP results correctly classified 75% of these patients and rarely missed ADHF cases (<10%).
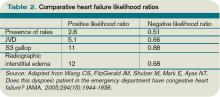
Atrial fibrillation. Since the original trials that established a BNP cutoff of 100 pg/mL for determining the presence of ADHF, several adjustments have been suggested. The presence of atrial fibrillation has been shown to increase BNP values independent of cardiac filling pressures. Breidthardt et al examined patients with atrial fibrillation presenting with dyspnea.4 In their analysis, using a cutoff of 100 pg/mL remained robust in identifying patients without ADHF. However, in the 100 pg/mL-500 pg/mL range, the test was not able to discriminate between atrial fibrillation and ADHF. Values greater than 500 pg/mL proved accurate in supporting the diagnosis of ADHF.
Renal failure. Renal dysfunction also elevates BNP levels independent of filling pressures. McCullough et al re-examined data from their Breathing Not Properly Multinational Study and found that the glomerular filtration rate (GFR) was inversely related to BNP levels.5 They recommend using a cutoff point of 200 pg/mL when the GFR is below 60 mg/dL. Other authors recommend not using BNP levels to diagnose ADHF when the GFR is less than 60 mg/dL due to the lack of data supporting this approach. Until clarified, clinicians should be cautious of interpreting BNP elevations in the setting of kidney disease.
Obesity. Obesity has a negative effect on BNP levels, decreasing the sensitivity of the test in these patients.6 Although no study defines how to adjust for body mass index (BMI), clinicians should be cautious about using a low BNP to rule out ADHF in a dyspneic obese patient.
Historical BNP values. If historical BNP values are available, studies of biological variation have shown that an increase to 123% from 66% from baseline is representative of a clinically meaningful increase in cardiac filling pressures. Less significant changes could merely represent biological variation and should be cautiously interpreted.7
Cost effectiveness. The cost effectiveness of using BNP measurements in dyspneic ED patients has been examined as well. Mueller et al found in a Swiss hospital that BNP testing was associated with a 25% decrease in treatment cost, length of stay (LOS), and ICU usage.8 However, LOS is significantly longer in Switzerland compared with the U.S., and given that much of the cost savings was attributed to reducing LOS, it is not possible to extrapolate these data to the U.S. health system. More evidence is needed to truly evaluate the cost effectiveness of BNP testing.
Serial BNP testing. Once a patient has been diagnosed with ADHF and admitted to the hospital, diuretics are indicated with the goal of achieving euvolemia. The bedside assessment of volume status remains a difficult and inexact science, and failure to appropriately remove fluid is associated with readmissions. Conversely, overdiuresis with a concomitant rise in creatinine has been associated with increased morbidity and mortality.
Several studies have shown that the reduction of volume associated with diuretic administration is coupled with a rapid decrease in BNP levels. Therefore, serial BNP measurement has been evaluated as a tool to guide the daily assessment of volume status in patients admitted with ADHF. Unfortunately, frequent measurements of BNP reveal that a great deal of variance, or “noise,” is present in these repeat measurements. Data do not clearly show how to incorporate serial BNP measurements into daily diuretic management.9
Mortality prediction. Nearly 3.5% of admitted heart failure patients will die during their hospitalization. For perspective, the rate of hospital mortality with acute myocardial infarction is 7%. BNP serves as a powerful and independent predictor of inpatient mortality. The ADHERE (Acute Decompensated Heart Failure National Registry) study showed that when divided into BNP quartiles of <430 pg/mL, 430 pg/mL to 839 pg/mL, 840 pg/mL to 1,729 pg/mL, and >1,730 pg/mL, patients’ risk of inpatient death was accurately predicted as 1.9%, 2.8%, 3.8%, and 6.0%, respectively.10 Even when adjusted for other risk factors, BNP remained a powerful predictor; the mortality rate more than doubled from the lowest to highest quartile.
Different strategies have been proposed to improve the outcomes in these highest-risk patients; however, to date, no evidence-based strategy offers a meaningful way to reduce inpatient mortality beyond the current standard of care.
Readmission and 30-day mortality. The 30-day readmission rate after discharge for ADHF is more than than 25%. A study of Medicare patients showed that more than $17 billion (more than 15% of all Medicare payments to hospitals) was associated with unplanned rehospitalizations.11 As bundling payment trends develop, hospitals have an enormous incentive to identify CHF patients with the highest risk of readmission and attempt to mitigate that risk.
From a patient-centered view, upon hospital discharge a patient with ADHF also realizes a 1 in 10 chance of dying within the first 30 days.
At discharge, BNP serves as a powerful and independent marker of increased risk of readmission, morbidity, and mortality. O’Connor et al developed a discharge risk model in patients with severe left ventricular dysfunction; the ESCAPE risk model and discharge score showed elevated BNP was the single most powerful predictor of six-month mortality.12 For every doubling of the BNP, the odds of death at six months increased by 1.4 times.
After combining discharge BNP with other factors, the ESCAPE discharge score was fairly successful at discriminating between patients who would and would not survive to six months. By identifying these outpatients, intensive management strategies could be focused on individuals with the highest risk. The data support the idea that readmission reductions are significant when outpatients obtain early follow-up. Many healthcare centers struggle to schedule early follow-up for all heart failure patients.
As such, the ability to target individuals with the highest discharge scores for intensive follow-up might improve outcomes. These patients could undergo early evaluation for such advanced therapies as resynchronization, left ventricular assist device implantation, or listing for transplantation. Currently, this strategy is not proven. It also is possible that these high-risk patients might have such advanced diseases that their risk cannot be modified by our current medications and advanced therapies.
Back to the Case
This patient has symptoms and signs that could be caused by ADHF or COPD. Her presentation is consistent with an intermediate probability of ADHF. A rapid BNP reveals a level of 950 pg/mL.
Even considering the higher cutoff required because of her coexistent atrial fibrillation, her BNP is consistent with ADHF. Additionally, her obesity likely has decreased the true value of her BNP. A previous BNP drawn when the patient was not in ADHF was 250 ng/mL, meaning that at least a 70% increase is present.
She was admitted and treated with intravenous diuretics with improvement in her congestion and relief of her symptoms. Daily BNPs were not drawn and her diuretics were titrated based on bedside clinical assessments. Her admission BNP elevation would predict a moderately high risk of short- and intermediate term of morbidity and mortality.
At discharge, a repeat BNP also could add to her risk stratification, though it would not be clear what do with this prognostic information beyond the standard of care.
Bottom Line
BNP measurement in specific situations can complement conventional clinical information in determining the presence of ADHF and also can enhance clinicians’ ability to risk-stratify patients during and after hospitalization. TH
Dr. Wolfe is a hospitalist and assistant professor of medicine at the University of Colorado Denver.
References
- Schocken DD, Arrieta MI, Leaverton PE, Ross EA. Prevalence and mortality of congestive heart failure in the United States. J Am Coll Cardiol. 1992;20(2):301-306.
- McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Eng J Med. 1971;285(26):1441-1446.
- Wang CS, FitzGerald JM, Schulzer M, Mak E, Ayas NT. Does this dyspneic patient in the emergency department have congestive heart failure? JAMA. 2005;294(15):1944-1956.
- Breidthardt T, Noveanu M, Cayir S, et al. The use of B-type natriuretic peptide in the management of patients with atrial fibrillation and dyspnea. Int J Cardiol. 2009;136(2):193-199.
- McCullough PA, Duc P, Omland T, et al. B-type natriuretic peptide and renal function in the diagnosis of heart failure: an analysis from the Breathing Not Properly Multinational Study. Am J Kidney Dis. 2003;41(3):571-579.
- Iwanaga Y, Hihara Y, Nizuma S, et al. BNP in overweight and obese patients with heart failure: an analysis based on the BNP-LV diastolic wall stress relationship. J Card Fail. 2007;13(8):663-667.
- O’Hanlon R, O’Shea P, Ledwidge M. The biologic variability of B-type natriuretic peptide and N-terminal pro-B-type natriuretic peptide in stable heart failure patients. J Card Fail. 2007;13(1):50-55.
- Mueller C, Laule-Kilian K, Schindler C, et al. Cost-effectiveness of B-type natriuretic peptide testing in patients with acute dyspnea. Arch Intern Med. 2006;166(1):1081-1087.
- Wu AH. Serial testing of B-type natriuretic peptide and NTpro-BNP for monitoring therapy of heart failure: the role of biologic variation in the interpretation of results. Am Heart J. 2006;152(5):828-834.
- Fonarow GC, Peacock WF, Phillips CO, et al. ADHERE Scientific Advisory Committee and Investigators. Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol. 2007;48 (19):1943-1950.
- Jencks SF, Williams MC, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428.
- O’Connor CM, Hasselblad V, Mehta RH, et al. Triage after hospitalization with advanced heart failure: the ESCAPE (Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness) risk model and discharge score. J Am Coll Cardiol. 2010;55(9):872-878.
Case
A 76-year-old woman with a history of chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), and atrial fibrillation presents with shortness of breath. She is tachypneic, her pulse is 105 beats per minute, and her blood pressure is 105/60 mm/Hg. She is obese and has an immeasurable venous pressure with decreased breath sounds in both lung bases, and irregular and distant heart sounds. What is the role of brain (or B-type) natriuretic peptide (BNP) in the diagnosis and management of this patient?
Overview
Each year, more than 1 million patients are admitted to hospitals with acutely decompensated heart failure (ADHF). Although many of these patients carry a pre-admission diagnosis of CHF, their common presenting symptoms are not specific for ADHF, which leads to delays in diagnosis and therapy initiation, and increased diagnostic costs and potentially worse outcomes. Clinical risk scores from NHANES and the Framingham heart study have limited sensitivity, missing nearly 20% of patients.1,2 Moreover, these scores are underused by clinicians who depend heavily on clinical gestalt.3
Once ADHF is diagnosed, ongoing bedside assessment of volume status is a difficult and inexact science. The physiologic goal is achievement of normal left ventricular end diastolic volume; however, surrogate measures of this status, including weight change, venous pressure, and pulmonary and cardiac auscultatory findings, have significant limitations. After discharge, patients have high and heterogeneous risks of readmission, death, and other adverse events. Identifying patients with the highest risk might allow for intensive strategies to improve outcomes.
BNP is a neurohormone released from the ventricular cells in response to increased cardiac filling pressures. Plasma measurements of BNP have been shown to reflect volume status, to predict risk at admission and discharge, and to serve as a treatment guide in a variety of clinical settings.4 This simple laboratory test increasingly has been used to diagnose and manage ADHF; its utility and limitations deserve critical review.
Review of the Data
CHF diagnosis. Since introduction of the rapid BNP assay, several trials have evaluated its clinical utility in determining whether ADHF is the cause of a patient’s dyspnea. The largest of these trials, the Breathing Not Properly Multinational Study, conducted by McCullough et al, enrolled nearly 1,600 patients who presented with the primary complaint of dyspnea.5 After reviewing conventional clinical information, ED physicians were asked to determine the likelihood that ADHF was the etiology of a patient’s dyspnea. These likelihoods were classified as low (<20%), intermediate (20%-80%), or high (>80%). The admission BNP was recorded but was not available for the ED physician decisions.
The “gold standard” was the opinion of two adjudicating cardiologists who reviewed the cases retrospectively and determined whether the dyspnea resulted from ADHF. They were blinded to both the ED physician’s opinion and the BNP results. The accuracy of the ED physician’s initial assessment and the impact of the BNP results were compared with this gold standard.
For the entire cohort, the use of BNP (with a cutoff point of 100 pg/mL) would have improved the ED physician’s assessment from 74% diagnostic accuracy to 81%, which is statistically significant. Most important, in those patients initially given an intermediate likelihood of CHF, BNP results correctly classified 75% of these patients and rarely missed ADHF cases (<10%).
Atrial fibrillation. Since the original trials that established a BNP cutoff of 100 pg/mL for determining the presence of ADHF, several adjustments have been suggested. The presence of atrial fibrillation has been shown to increase BNP values independent of cardiac filling pressures. Breidthardt et al examined patients with atrial fibrillation presenting with dyspnea.4 In their analysis, using a cutoff of 100 pg/mL remained robust in identifying patients without ADHF. However, in the 100 pg/mL-500 pg/mL range, the test was not able to discriminate between atrial fibrillation and ADHF. Values greater than 500 pg/mL proved accurate in supporting the diagnosis of ADHF.
Renal failure. Renal dysfunction also elevates BNP levels independent of filling pressures. McCullough et al re-examined data from their Breathing Not Properly Multinational Study and found that the glomerular filtration rate (GFR) was inversely related to BNP levels.5 They recommend using a cutoff point of 200 pg/mL when the GFR is below 60 mg/dL. Other authors recommend not using BNP levels to diagnose ADHF when the GFR is less than 60 mg/dL due to the lack of data supporting this approach. Until clarified, clinicians should be cautious of interpreting BNP elevations in the setting of kidney disease.
Obesity. Obesity has a negative effect on BNP levels, decreasing the sensitivity of the test in these patients.6 Although no study defines how to adjust for body mass index (BMI), clinicians should be cautious about using a low BNP to rule out ADHF in a dyspneic obese patient.
Historical BNP values. If historical BNP values are available, studies of biological variation have shown that an increase to 123% from 66% from baseline is representative of a clinically meaningful increase in cardiac filling pressures. Less significant changes could merely represent biological variation and should be cautiously interpreted.7
Cost effectiveness. The cost effectiveness of using BNP measurements in dyspneic ED patients has been examined as well. Mueller et al found in a Swiss hospital that BNP testing was associated with a 25% decrease in treatment cost, length of stay (LOS), and ICU usage.8 However, LOS is significantly longer in Switzerland compared with the U.S., and given that much of the cost savings was attributed to reducing LOS, it is not possible to extrapolate these data to the U.S. health system. More evidence is needed to truly evaluate the cost effectiveness of BNP testing.
Serial BNP testing. Once a patient has been diagnosed with ADHF and admitted to the hospital, diuretics are indicated with the goal of achieving euvolemia. The bedside assessment of volume status remains a difficult and inexact science, and failure to appropriately remove fluid is associated with readmissions. Conversely, overdiuresis with a concomitant rise in creatinine has been associated with increased morbidity and mortality.
Several studies have shown that the reduction of volume associated with diuretic administration is coupled with a rapid decrease in BNP levels. Therefore, serial BNP measurement has been evaluated as a tool to guide the daily assessment of volume status in patients admitted with ADHF. Unfortunately, frequent measurements of BNP reveal that a great deal of variance, or “noise,” is present in these repeat measurements. Data do not clearly show how to incorporate serial BNP measurements into daily diuretic management.9
Mortality prediction. Nearly 3.5% of admitted heart failure patients will die during their hospitalization. For perspective, the rate of hospital mortality with acute myocardial infarction is 7%. BNP serves as a powerful and independent predictor of inpatient mortality. The ADHERE (Acute Decompensated Heart Failure National Registry) study showed that when divided into BNP quartiles of <430 pg/mL, 430 pg/mL to 839 pg/mL, 840 pg/mL to 1,729 pg/mL, and >1,730 pg/mL, patients’ risk of inpatient death was accurately predicted as 1.9%, 2.8%, 3.8%, and 6.0%, respectively.10 Even when adjusted for other risk factors, BNP remained a powerful predictor; the mortality rate more than doubled from the lowest to highest quartile.
Different strategies have been proposed to improve the outcomes in these highest-risk patients; however, to date, no evidence-based strategy offers a meaningful way to reduce inpatient mortality beyond the current standard of care.
Readmission and 30-day mortality. The 30-day readmission rate after discharge for ADHF is more than than 25%. A study of Medicare patients showed that more than $17 billion (more than 15% of all Medicare payments to hospitals) was associated with unplanned rehospitalizations.11 As bundling payment trends develop, hospitals have an enormous incentive to identify CHF patients with the highest risk of readmission and attempt to mitigate that risk.
From a patient-centered view, upon hospital discharge a patient with ADHF also realizes a 1 in 10 chance of dying within the first 30 days.
At discharge, BNP serves as a powerful and independent marker of increased risk of readmission, morbidity, and mortality. O’Connor et al developed a discharge risk model in patients with severe left ventricular dysfunction; the ESCAPE risk model and discharge score showed elevated BNP was the single most powerful predictor of six-month mortality.12 For every doubling of the BNP, the odds of death at six months increased by 1.4 times.
After combining discharge BNP with other factors, the ESCAPE discharge score was fairly successful at discriminating between patients who would and would not survive to six months. By identifying these outpatients, intensive management strategies could be focused on individuals with the highest risk. The data support the idea that readmission reductions are significant when outpatients obtain early follow-up. Many healthcare centers struggle to schedule early follow-up for all heart failure patients.
As such, the ability to target individuals with the highest discharge scores for intensive follow-up might improve outcomes. These patients could undergo early evaluation for such advanced therapies as resynchronization, left ventricular assist device implantation, or listing for transplantation. Currently, this strategy is not proven. It also is possible that these high-risk patients might have such advanced diseases that their risk cannot be modified by our current medications and advanced therapies.
Back to the Case
This patient has symptoms and signs that could be caused by ADHF or COPD. Her presentation is consistent with an intermediate probability of ADHF. A rapid BNP reveals a level of 950 pg/mL.
Even considering the higher cutoff required because of her coexistent atrial fibrillation, her BNP is consistent with ADHF. Additionally, her obesity likely has decreased the true value of her BNP. A previous BNP drawn when the patient was not in ADHF was 250 ng/mL, meaning that at least a 70% increase is present.
She was admitted and treated with intravenous diuretics with improvement in her congestion and relief of her symptoms. Daily BNPs were not drawn and her diuretics were titrated based on bedside clinical assessments. Her admission BNP elevation would predict a moderately high risk of short- and intermediate term of morbidity and mortality.
At discharge, a repeat BNP also could add to her risk stratification, though it would not be clear what do with this prognostic information beyond the standard of care.
Bottom Line
BNP measurement in specific situations can complement conventional clinical information in determining the presence of ADHF and also can enhance clinicians’ ability to risk-stratify patients during and after hospitalization. TH
Dr. Wolfe is a hospitalist and assistant professor of medicine at the University of Colorado Denver.
References
- Schocken DD, Arrieta MI, Leaverton PE, Ross EA. Prevalence and mortality of congestive heart failure in the United States. J Am Coll Cardiol. 1992;20(2):301-306.
- McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Eng J Med. 1971;285(26):1441-1446.
- Wang CS, FitzGerald JM, Schulzer M, Mak E, Ayas NT. Does this dyspneic patient in the emergency department have congestive heart failure? JAMA. 2005;294(15):1944-1956.
- Breidthardt T, Noveanu M, Cayir S, et al. The use of B-type natriuretic peptide in the management of patients with atrial fibrillation and dyspnea. Int J Cardiol. 2009;136(2):193-199.
- McCullough PA, Duc P, Omland T, et al. B-type natriuretic peptide and renal function in the diagnosis of heart failure: an analysis from the Breathing Not Properly Multinational Study. Am J Kidney Dis. 2003;41(3):571-579.
- Iwanaga Y, Hihara Y, Nizuma S, et al. BNP in overweight and obese patients with heart failure: an analysis based on the BNP-LV diastolic wall stress relationship. J Card Fail. 2007;13(8):663-667.
- O’Hanlon R, O’Shea P, Ledwidge M. The biologic variability of B-type natriuretic peptide and N-terminal pro-B-type natriuretic peptide in stable heart failure patients. J Card Fail. 2007;13(1):50-55.
- Mueller C, Laule-Kilian K, Schindler C, et al. Cost-effectiveness of B-type natriuretic peptide testing in patients with acute dyspnea. Arch Intern Med. 2006;166(1):1081-1087.
- Wu AH. Serial testing of B-type natriuretic peptide and NTpro-BNP for monitoring therapy of heart failure: the role of biologic variation in the interpretation of results. Am Heart J. 2006;152(5):828-834.
- Fonarow GC, Peacock WF, Phillips CO, et al. ADHERE Scientific Advisory Committee and Investigators. Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol. 2007;48 (19):1943-1950.
- Jencks SF, Williams MC, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428.
- O’Connor CM, Hasselblad V, Mehta RH, et al. Triage after hospitalization with advanced heart failure: the ESCAPE (Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness) risk model and discharge score. J Am Coll Cardiol. 2010;55(9):872-878.
Case
A 76-year-old woman with a history of chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), and atrial fibrillation presents with shortness of breath. She is tachypneic, her pulse is 105 beats per minute, and her blood pressure is 105/60 mm/Hg. She is obese and has an immeasurable venous pressure with decreased breath sounds in both lung bases, and irregular and distant heart sounds. What is the role of brain (or B-type) natriuretic peptide (BNP) in the diagnosis and management of this patient?
Overview
Each year, more than 1 million patients are admitted to hospitals with acutely decompensated heart failure (ADHF). Although many of these patients carry a pre-admission diagnosis of CHF, their common presenting symptoms are not specific for ADHF, which leads to delays in diagnosis and therapy initiation, and increased diagnostic costs and potentially worse outcomes. Clinical risk scores from NHANES and the Framingham heart study have limited sensitivity, missing nearly 20% of patients.1,2 Moreover, these scores are underused by clinicians who depend heavily on clinical gestalt.3
Once ADHF is diagnosed, ongoing bedside assessment of volume status is a difficult and inexact science. The physiologic goal is achievement of normal left ventricular end diastolic volume; however, surrogate measures of this status, including weight change, venous pressure, and pulmonary and cardiac auscultatory findings, have significant limitations. After discharge, patients have high and heterogeneous risks of readmission, death, and other adverse events. Identifying patients with the highest risk might allow for intensive strategies to improve outcomes.
BNP is a neurohormone released from the ventricular cells in response to increased cardiac filling pressures. Plasma measurements of BNP have been shown to reflect volume status, to predict risk at admission and discharge, and to serve as a treatment guide in a variety of clinical settings.4 This simple laboratory test increasingly has been used to diagnose and manage ADHF; its utility and limitations deserve critical review.
Review of the Data
CHF diagnosis. Since introduction of the rapid BNP assay, several trials have evaluated its clinical utility in determining whether ADHF is the cause of a patient’s dyspnea. The largest of these trials, the Breathing Not Properly Multinational Study, conducted by McCullough et al, enrolled nearly 1,600 patients who presented with the primary complaint of dyspnea.5 After reviewing conventional clinical information, ED physicians were asked to determine the likelihood that ADHF was the etiology of a patient’s dyspnea. These likelihoods were classified as low (<20%), intermediate (20%-80%), or high (>80%). The admission BNP was recorded but was not available for the ED physician decisions.
The “gold standard” was the opinion of two adjudicating cardiologists who reviewed the cases retrospectively and determined whether the dyspnea resulted from ADHF. They were blinded to both the ED physician’s opinion and the BNP results. The accuracy of the ED physician’s initial assessment and the impact of the BNP results were compared with this gold standard.
For the entire cohort, the use of BNP (with a cutoff point of 100 pg/mL) would have improved the ED physician’s assessment from 74% diagnostic accuracy to 81%, which is statistically significant. Most important, in those patients initially given an intermediate likelihood of CHF, BNP results correctly classified 75% of these patients and rarely missed ADHF cases (<10%).
Atrial fibrillation. Since the original trials that established a BNP cutoff of 100 pg/mL for determining the presence of ADHF, several adjustments have been suggested. The presence of atrial fibrillation has been shown to increase BNP values independent of cardiac filling pressures. Breidthardt et al examined patients with atrial fibrillation presenting with dyspnea.4 In their analysis, using a cutoff of 100 pg/mL remained robust in identifying patients without ADHF. However, in the 100 pg/mL-500 pg/mL range, the test was not able to discriminate between atrial fibrillation and ADHF. Values greater than 500 pg/mL proved accurate in supporting the diagnosis of ADHF.
Renal failure. Renal dysfunction also elevates BNP levels independent of filling pressures. McCullough et al re-examined data from their Breathing Not Properly Multinational Study and found that the glomerular filtration rate (GFR) was inversely related to BNP levels.5 They recommend using a cutoff point of 200 pg/mL when the GFR is below 60 mg/dL. Other authors recommend not using BNP levels to diagnose ADHF when the GFR is less than 60 mg/dL due to the lack of data supporting this approach. Until clarified, clinicians should be cautious of interpreting BNP elevations in the setting of kidney disease.
Obesity. Obesity has a negative effect on BNP levels, decreasing the sensitivity of the test in these patients.6 Although no study defines how to adjust for body mass index (BMI), clinicians should be cautious about using a low BNP to rule out ADHF in a dyspneic obese patient.
Historical BNP values. If historical BNP values are available, studies of biological variation have shown that an increase to 123% from 66% from baseline is representative of a clinically meaningful increase in cardiac filling pressures. Less significant changes could merely represent biological variation and should be cautiously interpreted.7
Cost effectiveness. The cost effectiveness of using BNP measurements in dyspneic ED patients has been examined as well. Mueller et al found in a Swiss hospital that BNP testing was associated with a 25% decrease in treatment cost, length of stay (LOS), and ICU usage.8 However, LOS is significantly longer in Switzerland compared with the U.S., and given that much of the cost savings was attributed to reducing LOS, it is not possible to extrapolate these data to the U.S. health system. More evidence is needed to truly evaluate the cost effectiveness of BNP testing.
Serial BNP testing. Once a patient has been diagnosed with ADHF and admitted to the hospital, diuretics are indicated with the goal of achieving euvolemia. The bedside assessment of volume status remains a difficult and inexact science, and failure to appropriately remove fluid is associated with readmissions. Conversely, overdiuresis with a concomitant rise in creatinine has been associated with increased morbidity and mortality.
Several studies have shown that the reduction of volume associated with diuretic administration is coupled with a rapid decrease in BNP levels. Therefore, serial BNP measurement has been evaluated as a tool to guide the daily assessment of volume status in patients admitted with ADHF. Unfortunately, frequent measurements of BNP reveal that a great deal of variance, or “noise,” is present in these repeat measurements. Data do not clearly show how to incorporate serial BNP measurements into daily diuretic management.9
Mortality prediction. Nearly 3.5% of admitted heart failure patients will die during their hospitalization. For perspective, the rate of hospital mortality with acute myocardial infarction is 7%. BNP serves as a powerful and independent predictor of inpatient mortality. The ADHERE (Acute Decompensated Heart Failure National Registry) study showed that when divided into BNP quartiles of <430 pg/mL, 430 pg/mL to 839 pg/mL, 840 pg/mL to 1,729 pg/mL, and >1,730 pg/mL, patients’ risk of inpatient death was accurately predicted as 1.9%, 2.8%, 3.8%, and 6.0%, respectively.10 Even when adjusted for other risk factors, BNP remained a powerful predictor; the mortality rate more than doubled from the lowest to highest quartile.
Different strategies have been proposed to improve the outcomes in these highest-risk patients; however, to date, no evidence-based strategy offers a meaningful way to reduce inpatient mortality beyond the current standard of care.
Readmission and 30-day mortality. The 30-day readmission rate after discharge for ADHF is more than than 25%. A study of Medicare patients showed that more than $17 billion (more than 15% of all Medicare payments to hospitals) was associated with unplanned rehospitalizations.11 As bundling payment trends develop, hospitals have an enormous incentive to identify CHF patients with the highest risk of readmission and attempt to mitigate that risk.
From a patient-centered view, upon hospital discharge a patient with ADHF also realizes a 1 in 10 chance of dying within the first 30 days.
At discharge, BNP serves as a powerful and independent marker of increased risk of readmission, morbidity, and mortality. O’Connor et al developed a discharge risk model in patients with severe left ventricular dysfunction; the ESCAPE risk model and discharge score showed elevated BNP was the single most powerful predictor of six-month mortality.12 For every doubling of the BNP, the odds of death at six months increased by 1.4 times.
After combining discharge BNP with other factors, the ESCAPE discharge score was fairly successful at discriminating between patients who would and would not survive to six months. By identifying these outpatients, intensive management strategies could be focused on individuals with the highest risk. The data support the idea that readmission reductions are significant when outpatients obtain early follow-up. Many healthcare centers struggle to schedule early follow-up for all heart failure patients.
As such, the ability to target individuals with the highest discharge scores for intensive follow-up might improve outcomes. These patients could undergo early evaluation for such advanced therapies as resynchronization, left ventricular assist device implantation, or listing for transplantation. Currently, this strategy is not proven. It also is possible that these high-risk patients might have such advanced diseases that their risk cannot be modified by our current medications and advanced therapies.
Back to the Case
This patient has symptoms and signs that could be caused by ADHF or COPD. Her presentation is consistent with an intermediate probability of ADHF. A rapid BNP reveals a level of 950 pg/mL.
Even considering the higher cutoff required because of her coexistent atrial fibrillation, her BNP is consistent with ADHF. Additionally, her obesity likely has decreased the true value of her BNP. A previous BNP drawn when the patient was not in ADHF was 250 ng/mL, meaning that at least a 70% increase is present.
She was admitted and treated with intravenous diuretics with improvement in her congestion and relief of her symptoms. Daily BNPs were not drawn and her diuretics were titrated based on bedside clinical assessments. Her admission BNP elevation would predict a moderately high risk of short- and intermediate term of morbidity and mortality.
At discharge, a repeat BNP also could add to her risk stratification, though it would not be clear what do with this prognostic information beyond the standard of care.
Bottom Line
BNP measurement in specific situations can complement conventional clinical information in determining the presence of ADHF and also can enhance clinicians’ ability to risk-stratify patients during and after hospitalization. TH
Dr. Wolfe is a hospitalist and assistant professor of medicine at the University of Colorado Denver.
References
- Schocken DD, Arrieta MI, Leaverton PE, Ross EA. Prevalence and mortality of congestive heart failure in the United States. J Am Coll Cardiol. 1992;20(2):301-306.
- McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Eng J Med. 1971;285(26):1441-1446.
- Wang CS, FitzGerald JM, Schulzer M, Mak E, Ayas NT. Does this dyspneic patient in the emergency department have congestive heart failure? JAMA. 2005;294(15):1944-1956.
- Breidthardt T, Noveanu M, Cayir S, et al. The use of B-type natriuretic peptide in the management of patients with atrial fibrillation and dyspnea. Int J Cardiol. 2009;136(2):193-199.
- McCullough PA, Duc P, Omland T, et al. B-type natriuretic peptide and renal function in the diagnosis of heart failure: an analysis from the Breathing Not Properly Multinational Study. Am J Kidney Dis. 2003;41(3):571-579.
- Iwanaga Y, Hihara Y, Nizuma S, et al. BNP in overweight and obese patients with heart failure: an analysis based on the BNP-LV diastolic wall stress relationship. J Card Fail. 2007;13(8):663-667.
- O’Hanlon R, O’Shea P, Ledwidge M. The biologic variability of B-type natriuretic peptide and N-terminal pro-B-type natriuretic peptide in stable heart failure patients. J Card Fail. 2007;13(1):50-55.
- Mueller C, Laule-Kilian K, Schindler C, et al. Cost-effectiveness of B-type natriuretic peptide testing in patients with acute dyspnea. Arch Intern Med. 2006;166(1):1081-1087.
- Wu AH. Serial testing of B-type natriuretic peptide and NTpro-BNP for monitoring therapy of heart failure: the role of biologic variation in the interpretation of results. Am Heart J. 2006;152(5):828-834.
- Fonarow GC, Peacock WF, Phillips CO, et al. ADHERE Scientific Advisory Committee and Investigators. Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol. 2007;48 (19):1943-1950.
- Jencks SF, Williams MC, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428.
- O’Connor CM, Hasselblad V, Mehta RH, et al. Triage after hospitalization with advanced heart failure: the ESCAPE (Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness) risk model and discharge score. J Am Coll Cardiol. 2010;55(9):872-878.
Communication Counts
Put yourself for a moment in your patient’s situation. You are sick enough to have been thrust out of your normal life and admitted to the hospital. You find yourself attached to unfamiliar objects and machines, listening to unfamiliar words, and watching a revolving door of unfamiliar faces stroll in and out of the room to take blood, ask personal questions, touch your body, and monitor equipment. It would be enough to bear if you were well, but you’re not. You are ill and that makes you feel particularly worried and desperate.
Whether the physician succeeds in this scenario largely depends on their communication skills.
“A hospitalist needs to develop an almost immediate relationship with their patients because they are at their most vulnerable,” says Mark Williams, MD, FACP, FHM, professor and chief of the Division of Hospital Medicine at Northwestern University’s Feinberg School of Medicine in Chicago. “It is proven that if a hospitalist can successfully communicate with their patients, the result is much more satisfied patients.”

CAT: The Doctor-Patient Relationship Exam
This is easier said than done, as new research by Dr. Williams and colleagues at Feinberg, Northwestern Memorial Hospital (NMH) in Chicago, and Saint Francis Hospital and Medical Center in Hartford, Conn., has found. As part of the study, which published in the December issue of the Journal of Hospital Medicine, patients who were admitted to NMH between September 2008 and August 2009 and cared for by a hospitalist or hospitalist-led teaching team were interviewed using the Communication Assessment Tool (CAT). The CAT is a 14-item survey designed to measure a patient’s perception of communication with their hospitalist.
The average excellent rating among the 35 hospitalists involved in the study was 59.1% on a scale of 0 to 100 percent. Collectively, the hospitalists scored highest on such items as paying attention to patients (64.1%), talking in terms patients could understand (64.2%), and showing care and concern for patients (63.8%). The hospitalists scored lowest in greeting patients in a way that made them feel comfortable (54.9%), encouraging patients to ask questions (53.2%), and involving patients in decisions as much as they wanted (52.9%).
“There are a lot of factors working against hospitalists. Hospitalists are first meeting their patients when they are at their weakest, they sometimes don’t know the patient’s history, and, of course, there are all the demands on hospitalists’ time,” says Darlene Ferranti, research coordinator at the Feinberg School of Medicine.
What is particularly fascinating about the research is 13% of the patients eligible for the study could not participate because they weren’t able to identify their hospitalist by name or photo, Ferranti says. “If your patient doesn’t know who you are, how can they recall the information you are sharing with them?” she asks.
The study wasn’t designed to test patient communication techniques and their effectiveness, Dr. Williams explains. “We think future research needs to focus on interventions to improve doctor-patient communication,” he says.
However, the study did demonstrate that the CAT survey can be a valuable tool for HM groups interested in learning how their physicians are doing from the patient’s perspective, Dr. Williams notes. Perhaps more importantly, it can also help hospitalists target those communication areas in need of improvement, Ferranti says. For example, each hospitalist in the study was given a report of their individual scores and where they fell in the chart compared to the group as a whole.
“If you want to improve your career, you need to improve your communication with patients,” says Dr. Williams, who notes that hospitalists often don’t know the areas in which they are weak and strong. “It’s a career killer if you have multiple patient complaints against you.”
Risk Reduction
Being an effective communicator can also reduce one’s risk of being sued for malpractice, says Mitchell Wilson, MD, FHM, chief medical officer of Atlanta-based Eagle Hospital Physicians, which manages hospitalist practices for clients in the Southeast and Mid-Atlantic regions of the U.S. Dr. Wilson’s company believes communication is so important that starting with the very first interview of a hospitalist candidate, it considers the candidate’s ability to communicate by taking note of such things as accents, how they present information, and body language, Dr. Wilson says.
“Communication is one of the top three competencies that are essential to hospitalists,” he says.
Certain aspects of hospitalist work make communication exceedingly important, Dr. Wilson says. Hospitalists are coordinators of a patient’s care; they are caring for patients who are out of their comfort zone; many times the patient is in an extreme health situation; and hospitalized patients are of all different ages and backgrounds.
“If a hospitalist is a poor communicator, I would encourage them to seek additional training,” Dr. Wilson says. TH
Lisa Ryan is a freelance writer based in New Jersey.
Put yourself for a moment in your patient’s situation. You are sick enough to have been thrust out of your normal life and admitted to the hospital. You find yourself attached to unfamiliar objects and machines, listening to unfamiliar words, and watching a revolving door of unfamiliar faces stroll in and out of the room to take blood, ask personal questions, touch your body, and monitor equipment. It would be enough to bear if you were well, but you’re not. You are ill and that makes you feel particularly worried and desperate.
Whether the physician succeeds in this scenario largely depends on their communication skills.
“A hospitalist needs to develop an almost immediate relationship with their patients because they are at their most vulnerable,” says Mark Williams, MD, FACP, FHM, professor and chief of the Division of Hospital Medicine at Northwestern University’s Feinberg School of Medicine in Chicago. “It is proven that if a hospitalist can successfully communicate with their patients, the result is much more satisfied patients.”

CAT: The Doctor-Patient Relationship Exam
This is easier said than done, as new research by Dr. Williams and colleagues at Feinberg, Northwestern Memorial Hospital (NMH) in Chicago, and Saint Francis Hospital and Medical Center in Hartford, Conn., has found. As part of the study, which published in the December issue of the Journal of Hospital Medicine, patients who were admitted to NMH between September 2008 and August 2009 and cared for by a hospitalist or hospitalist-led teaching team were interviewed using the Communication Assessment Tool (CAT). The CAT is a 14-item survey designed to measure a patient’s perception of communication with their hospitalist.
The average excellent rating among the 35 hospitalists involved in the study was 59.1% on a scale of 0 to 100 percent. Collectively, the hospitalists scored highest on such items as paying attention to patients (64.1%), talking in terms patients could understand (64.2%), and showing care and concern for patients (63.8%). The hospitalists scored lowest in greeting patients in a way that made them feel comfortable (54.9%), encouraging patients to ask questions (53.2%), and involving patients in decisions as much as they wanted (52.9%).
“There are a lot of factors working against hospitalists. Hospitalists are first meeting their patients when they are at their weakest, they sometimes don’t know the patient’s history, and, of course, there are all the demands on hospitalists’ time,” says Darlene Ferranti, research coordinator at the Feinberg School of Medicine.
What is particularly fascinating about the research is 13% of the patients eligible for the study could not participate because they weren’t able to identify their hospitalist by name or photo, Ferranti says. “If your patient doesn’t know who you are, how can they recall the information you are sharing with them?” she asks.
The study wasn’t designed to test patient communication techniques and their effectiveness, Dr. Williams explains. “We think future research needs to focus on interventions to improve doctor-patient communication,” he says.
However, the study did demonstrate that the CAT survey can be a valuable tool for HM groups interested in learning how their physicians are doing from the patient’s perspective, Dr. Williams notes. Perhaps more importantly, it can also help hospitalists target those communication areas in need of improvement, Ferranti says. For example, each hospitalist in the study was given a report of their individual scores and where they fell in the chart compared to the group as a whole.
“If you want to improve your career, you need to improve your communication with patients,” says Dr. Williams, who notes that hospitalists often don’t know the areas in which they are weak and strong. “It’s a career killer if you have multiple patient complaints against you.”
Risk Reduction
Being an effective communicator can also reduce one’s risk of being sued for malpractice, says Mitchell Wilson, MD, FHM, chief medical officer of Atlanta-based Eagle Hospital Physicians, which manages hospitalist practices for clients in the Southeast and Mid-Atlantic regions of the U.S. Dr. Wilson’s company believes communication is so important that starting with the very first interview of a hospitalist candidate, it considers the candidate’s ability to communicate by taking note of such things as accents, how they present information, and body language, Dr. Wilson says.
“Communication is one of the top three competencies that are essential to hospitalists,” he says.
Certain aspects of hospitalist work make communication exceedingly important, Dr. Wilson says. Hospitalists are coordinators of a patient’s care; they are caring for patients who are out of their comfort zone; many times the patient is in an extreme health situation; and hospitalized patients are of all different ages and backgrounds.
“If a hospitalist is a poor communicator, I would encourage them to seek additional training,” Dr. Wilson says. TH
Lisa Ryan is a freelance writer based in New Jersey.
Put yourself for a moment in your patient’s situation. You are sick enough to have been thrust out of your normal life and admitted to the hospital. You find yourself attached to unfamiliar objects and machines, listening to unfamiliar words, and watching a revolving door of unfamiliar faces stroll in and out of the room to take blood, ask personal questions, touch your body, and monitor equipment. It would be enough to bear if you were well, but you’re not. You are ill and that makes you feel particularly worried and desperate.
Whether the physician succeeds in this scenario largely depends on their communication skills.
“A hospitalist needs to develop an almost immediate relationship with their patients because they are at their most vulnerable,” says Mark Williams, MD, FACP, FHM, professor and chief of the Division of Hospital Medicine at Northwestern University’s Feinberg School of Medicine in Chicago. “It is proven that if a hospitalist can successfully communicate with their patients, the result is much more satisfied patients.”

CAT: The Doctor-Patient Relationship Exam
This is easier said than done, as new research by Dr. Williams and colleagues at Feinberg, Northwestern Memorial Hospital (NMH) in Chicago, and Saint Francis Hospital and Medical Center in Hartford, Conn., has found. As part of the study, which published in the December issue of the Journal of Hospital Medicine, patients who were admitted to NMH between September 2008 and August 2009 and cared for by a hospitalist or hospitalist-led teaching team were interviewed using the Communication Assessment Tool (CAT). The CAT is a 14-item survey designed to measure a patient’s perception of communication with their hospitalist.
The average excellent rating among the 35 hospitalists involved in the study was 59.1% on a scale of 0 to 100 percent. Collectively, the hospitalists scored highest on such items as paying attention to patients (64.1%), talking in terms patients could understand (64.2%), and showing care and concern for patients (63.8%). The hospitalists scored lowest in greeting patients in a way that made them feel comfortable (54.9%), encouraging patients to ask questions (53.2%), and involving patients in decisions as much as they wanted (52.9%).
“There are a lot of factors working against hospitalists. Hospitalists are first meeting their patients when they are at their weakest, they sometimes don’t know the patient’s history, and, of course, there are all the demands on hospitalists’ time,” says Darlene Ferranti, research coordinator at the Feinberg School of Medicine.
What is particularly fascinating about the research is 13% of the patients eligible for the study could not participate because they weren’t able to identify their hospitalist by name or photo, Ferranti says. “If your patient doesn’t know who you are, how can they recall the information you are sharing with them?” she asks.
The study wasn’t designed to test patient communication techniques and their effectiveness, Dr. Williams explains. “We think future research needs to focus on interventions to improve doctor-patient communication,” he says.
However, the study did demonstrate that the CAT survey can be a valuable tool for HM groups interested in learning how their physicians are doing from the patient’s perspective, Dr. Williams notes. Perhaps more importantly, it can also help hospitalists target those communication areas in need of improvement, Ferranti says. For example, each hospitalist in the study was given a report of their individual scores and where they fell in the chart compared to the group as a whole.
“If you want to improve your career, you need to improve your communication with patients,” says Dr. Williams, who notes that hospitalists often don’t know the areas in which they are weak and strong. “It’s a career killer if you have multiple patient complaints against you.”
Risk Reduction
Being an effective communicator can also reduce one’s risk of being sued for malpractice, says Mitchell Wilson, MD, FHM, chief medical officer of Atlanta-based Eagle Hospital Physicians, which manages hospitalist practices for clients in the Southeast and Mid-Atlantic regions of the U.S. Dr. Wilson’s company believes communication is so important that starting with the very first interview of a hospitalist candidate, it considers the candidate’s ability to communicate by taking note of such things as accents, how they present information, and body language, Dr. Wilson says.
“Communication is one of the top three competencies that are essential to hospitalists,” he says.
Certain aspects of hospitalist work make communication exceedingly important, Dr. Wilson says. Hospitalists are coordinators of a patient’s care; they are caring for patients who are out of their comfort zone; many times the patient is in an extreme health situation; and hospitalized patients are of all different ages and backgrounds.
“If a hospitalist is a poor communicator, I would encourage them to seek additional training,” Dr. Wilson says. TH
Lisa Ryan is a freelance writer based in New Jersey.
On the Road Again?
Necessity, as they say, is the mother of invention, and the growing focus on the need for high-quality and cost-effective care is bringing a host of new innovations to light. One that hospitalists are likely to hear about far more about is the evolving role of an “extensivist,” an inpatient provider who ventures to outpatient settings to assist with care transitions.
In many ways, the expanding discussion of what extensivists are and do reflects the success of hospitalists in coordinating inpatient care and improving such metrics as length of stay (LOS). Why should that coordination end upon discharge? healthcare experts have wondered. Instead of a pure hospitalist system, could the experience and training of hospitalists be extended to include transitional or interim settings that provide a safety net between the hospital and a primary-care physician (PCP)? Might that improved inpatient-outpatient coordination help with other metrics, such as reduced rehospitalizations (see “All Aboard,” p. 1)?

One tangible result of those questions has been the growth of high-risk clinics. Hospitalist programs can provide clinic referrals for discharged patients who still require hands-on care, while PCPs can likewise refer some of their more complex patients. The clinic, then, becomes an alternative to hospitalization, or a preventive measure to avoid rehospitalization.
Philip Sanger, MD, founder and former CEO of Houston-based Inpatient Medical Services (now Intercede Health), is credited with one of the first uses of the term “extensivist.” Initially, it only described a hospitalist or other care provider who sees high-risk patients in an outpatient clinic.
Writing in Managed Healthcare Executive in 2002, Dr. Sanger explained: “To move from generally sick to generally well, high-risk patients need something extra—more attention than a busy PCP can offer [and] more individualized care than most protocol-driven disease management programs can provide. A high-risk clinic system is one way to fill this care gap. Also referred to as transitional-care clinics, these outpatient clinics focus on preventing hospital admissions and stabilizing high-risk patients.”1
Measured Improvements
Adam Singer, MD, CEO of North Hollywood, Calif.-based IPC: The Hospitalist Co., says this extensivist model provides a respite for hospitalists, who typically spend a month at a time in these transitional clinics before heading back into the fray of the hospital. As hospitals, independent physician associations, and managed-care organizations try out new models of care, though, the definition of an extensivist has broadened to include providers in a range of outpatient settings, such as skilled nursing facilities, assistant living communities, and even home health services. California’s CareMore Medicare Advantage plan, in particular, has been cited by the Agency for Healthcare Research and Quality (AHRQ) for using hospitalists as extensivists in both outpatient clinics and skilled nursing facilities to reduce hospital readmission rates, LOS, and inpatient resource use.
The CareMore model reduces the caseload of its hospitalists to about six or eight patients per half-day, giving doctors more time to talk to patients and their family members. Based on those conversations, the extensivist works with a case manager to provide needed resources to each patient after discharge. The doctors also spend roughly half of each day in clinics seeing their own recently discharged patients, and one or two days each week in a skilled nursing facility to visit patients transferred from the hospital (for more details, visit www.innovations.ahrq.gov/content.aspx?id=2903).
Average inpatient LOS among the plan’s 44,000 members dipped to 3.2 days, compared with 5.8 days for Medicare fee-for-service providers and 4.5 days for traditional HM programs in the state. Last April, CareMore’s 30-day readmission rate averaged 13.4%, compared with a 19.6% rate for Medicare.
Baltimore-based Bravo Health has begun opening its own transitional advanced-care centers for members of its Medicare Advantage program, offering case management for complex conditions and immediate care when a PCP is unavailable. Another model has been advanced through team approaches practiced by the likes of Kaiser Permanente, though hospitalists aren’t necessarily the ones providing outpatient follow-up care. No matter what the model is called, Dr. Singer says, the main point is the same: “trying to connect the dots so that we get patients continuing to get better along the continuum without having to be readmitted.”
In December, IPC did some more dot-connecting of its own with its announced acquisition of Senior Care of Colorado, which operates more than 200 geriatric-care facilities in the Denver area. Don Murphy, MD, IPC’s practice group leader for Senior Care of Colorado, says the model emphasizes a continuum of care and information flow from hospitalists in the hospital to affiliated providers in skilled nursing facilities and other outpatient settings. “We think that model, where we tie everything together, will be one of the best that we can do,” Dr. Murphy says.
From Dr. Singer’s perspective, the growing opportunities have sprung from efforts to address a persistent challenge. “We write an order of discharge to a skilled nursing facility, and patients go off into the community and we have no idea where they’re going, who they’re going to, what’s the quality of care out there, what’s the capacity of care,” he says. One of the central ideas of healthcare reform—creating true accountability around an episode of care—will require doctors to be linked “not just during what used to be the episode of care in the hospital,” he adds, “but throughout the continuum until that patient is really returned healthy back to wherever they’re going to be living.”
With a new emphasis on avoidable hospitalizations, hospitals will increasingly need to team up with other providers to avoid fragmentation of care. Using extensivists to help avoid gaps might be a good fit for accountable-care organizations, and Dr. Murphy says the process may be easier for big systems, such as Ochsner in New Orleans or the Cleveland Clinic, which are working in a confined geographic area with a defined patient population.
“The real challenge will be those of us out there in larger metropolitan areas where we’re not under the roof of one big conglomerate but still having to work together creatively and effectively to smooth the continuum,” Dr. Singer says.
Emerging Trends
Other trends are making inpatient-outpatient partnerships, whether formal or informal, an increasingly necessary part of providing high-quality healthcare. “We are seeing folks come out of the hospitals who 30 years ago clearly would have been in the hospital for a prolonged stay,” Dr. Murphy says. “A lot of these [patients], instead of going to SNFs, are going back to their homes and to assisted living with additional services; they require a lot of follow-up.”
Dr. Singer says he’s seeing another trend in which PCPs are likewise transitioning to newly created extensivist roles in sub-acute settings such as nursing homes. The position, he says, offers the attraction of a high-impact, longer-term relationship with patients without the high overhead of standalone clinics. The blurring of lines between outpatient and inpatient providers has created questions for hospitalists, too. For example, at what point does a hospitalist working much of the time in an outpatient clinic or skilled nursing facility no longer fit the traditional definition of a hospitalist? Does that detract from the doctor’s hospital duties? TH
Bryn Nelson is a freelance medical writer based in Seattle.
Reference
- Sanger, P. Health plans juggle precarious patients. Managed Healthcare Executive. 2002:40-41.
Necessity, as they say, is the mother of invention, and the growing focus on the need for high-quality and cost-effective care is bringing a host of new innovations to light. One that hospitalists are likely to hear about far more about is the evolving role of an “extensivist,” an inpatient provider who ventures to outpatient settings to assist with care transitions.
In many ways, the expanding discussion of what extensivists are and do reflects the success of hospitalists in coordinating inpatient care and improving such metrics as length of stay (LOS). Why should that coordination end upon discharge? healthcare experts have wondered. Instead of a pure hospitalist system, could the experience and training of hospitalists be extended to include transitional or interim settings that provide a safety net between the hospital and a primary-care physician (PCP)? Might that improved inpatient-outpatient coordination help with other metrics, such as reduced rehospitalizations (see “All Aboard,” p. 1)?

One tangible result of those questions has been the growth of high-risk clinics. Hospitalist programs can provide clinic referrals for discharged patients who still require hands-on care, while PCPs can likewise refer some of their more complex patients. The clinic, then, becomes an alternative to hospitalization, or a preventive measure to avoid rehospitalization.
Philip Sanger, MD, founder and former CEO of Houston-based Inpatient Medical Services (now Intercede Health), is credited with one of the first uses of the term “extensivist.” Initially, it only described a hospitalist or other care provider who sees high-risk patients in an outpatient clinic.
Writing in Managed Healthcare Executive in 2002, Dr. Sanger explained: “To move from generally sick to generally well, high-risk patients need something extra—more attention than a busy PCP can offer [and] more individualized care than most protocol-driven disease management programs can provide. A high-risk clinic system is one way to fill this care gap. Also referred to as transitional-care clinics, these outpatient clinics focus on preventing hospital admissions and stabilizing high-risk patients.”1
Measured Improvements
Adam Singer, MD, CEO of North Hollywood, Calif.-based IPC: The Hospitalist Co., says this extensivist model provides a respite for hospitalists, who typically spend a month at a time in these transitional clinics before heading back into the fray of the hospital. As hospitals, independent physician associations, and managed-care organizations try out new models of care, though, the definition of an extensivist has broadened to include providers in a range of outpatient settings, such as skilled nursing facilities, assistant living communities, and even home health services. California’s CareMore Medicare Advantage plan, in particular, has been cited by the Agency for Healthcare Research and Quality (AHRQ) for using hospitalists as extensivists in both outpatient clinics and skilled nursing facilities to reduce hospital readmission rates, LOS, and inpatient resource use.
The CareMore model reduces the caseload of its hospitalists to about six or eight patients per half-day, giving doctors more time to talk to patients and their family members. Based on those conversations, the extensivist works with a case manager to provide needed resources to each patient after discharge. The doctors also spend roughly half of each day in clinics seeing their own recently discharged patients, and one or two days each week in a skilled nursing facility to visit patients transferred from the hospital (for more details, visit www.innovations.ahrq.gov/content.aspx?id=2903).
Average inpatient LOS among the plan’s 44,000 members dipped to 3.2 days, compared with 5.8 days for Medicare fee-for-service providers and 4.5 days for traditional HM programs in the state. Last April, CareMore’s 30-day readmission rate averaged 13.4%, compared with a 19.6% rate for Medicare.
Baltimore-based Bravo Health has begun opening its own transitional advanced-care centers for members of its Medicare Advantage program, offering case management for complex conditions and immediate care when a PCP is unavailable. Another model has been advanced through team approaches practiced by the likes of Kaiser Permanente, though hospitalists aren’t necessarily the ones providing outpatient follow-up care. No matter what the model is called, Dr. Singer says, the main point is the same: “trying to connect the dots so that we get patients continuing to get better along the continuum without having to be readmitted.”
In December, IPC did some more dot-connecting of its own with its announced acquisition of Senior Care of Colorado, which operates more than 200 geriatric-care facilities in the Denver area. Don Murphy, MD, IPC’s practice group leader for Senior Care of Colorado, says the model emphasizes a continuum of care and information flow from hospitalists in the hospital to affiliated providers in skilled nursing facilities and other outpatient settings. “We think that model, where we tie everything together, will be one of the best that we can do,” Dr. Murphy says.
From Dr. Singer’s perspective, the growing opportunities have sprung from efforts to address a persistent challenge. “We write an order of discharge to a skilled nursing facility, and patients go off into the community and we have no idea where they’re going, who they’re going to, what’s the quality of care out there, what’s the capacity of care,” he says. One of the central ideas of healthcare reform—creating true accountability around an episode of care—will require doctors to be linked “not just during what used to be the episode of care in the hospital,” he adds, “but throughout the continuum until that patient is really returned healthy back to wherever they’re going to be living.”
With a new emphasis on avoidable hospitalizations, hospitals will increasingly need to team up with other providers to avoid fragmentation of care. Using extensivists to help avoid gaps might be a good fit for accountable-care organizations, and Dr. Murphy says the process may be easier for big systems, such as Ochsner in New Orleans or the Cleveland Clinic, which are working in a confined geographic area with a defined patient population.
“The real challenge will be those of us out there in larger metropolitan areas where we’re not under the roof of one big conglomerate but still having to work together creatively and effectively to smooth the continuum,” Dr. Singer says.
Emerging Trends
Other trends are making inpatient-outpatient partnerships, whether formal or informal, an increasingly necessary part of providing high-quality healthcare. “We are seeing folks come out of the hospitals who 30 years ago clearly would have been in the hospital for a prolonged stay,” Dr. Murphy says. “A lot of these [patients], instead of going to SNFs, are going back to their homes and to assisted living with additional services; they require a lot of follow-up.”
Dr. Singer says he’s seeing another trend in which PCPs are likewise transitioning to newly created extensivist roles in sub-acute settings such as nursing homes. The position, he says, offers the attraction of a high-impact, longer-term relationship with patients without the high overhead of standalone clinics. The blurring of lines between outpatient and inpatient providers has created questions for hospitalists, too. For example, at what point does a hospitalist working much of the time in an outpatient clinic or skilled nursing facility no longer fit the traditional definition of a hospitalist? Does that detract from the doctor’s hospital duties? TH
Bryn Nelson is a freelance medical writer based in Seattle.
Reference
- Sanger, P. Health plans juggle precarious patients. Managed Healthcare Executive. 2002:40-41.
Necessity, as they say, is the mother of invention, and the growing focus on the need for high-quality and cost-effective care is bringing a host of new innovations to light. One that hospitalists are likely to hear about far more about is the evolving role of an “extensivist,” an inpatient provider who ventures to outpatient settings to assist with care transitions.
In many ways, the expanding discussion of what extensivists are and do reflects the success of hospitalists in coordinating inpatient care and improving such metrics as length of stay (LOS). Why should that coordination end upon discharge? healthcare experts have wondered. Instead of a pure hospitalist system, could the experience and training of hospitalists be extended to include transitional or interim settings that provide a safety net between the hospital and a primary-care physician (PCP)? Might that improved inpatient-outpatient coordination help with other metrics, such as reduced rehospitalizations (see “All Aboard,” p. 1)?

One tangible result of those questions has been the growth of high-risk clinics. Hospitalist programs can provide clinic referrals for discharged patients who still require hands-on care, while PCPs can likewise refer some of their more complex patients. The clinic, then, becomes an alternative to hospitalization, or a preventive measure to avoid rehospitalization.
Philip Sanger, MD, founder and former CEO of Houston-based Inpatient Medical Services (now Intercede Health), is credited with one of the first uses of the term “extensivist.” Initially, it only described a hospitalist or other care provider who sees high-risk patients in an outpatient clinic.
Writing in Managed Healthcare Executive in 2002, Dr. Sanger explained: “To move from generally sick to generally well, high-risk patients need something extra—more attention than a busy PCP can offer [and] more individualized care than most protocol-driven disease management programs can provide. A high-risk clinic system is one way to fill this care gap. Also referred to as transitional-care clinics, these outpatient clinics focus on preventing hospital admissions and stabilizing high-risk patients.”1
Measured Improvements
Adam Singer, MD, CEO of North Hollywood, Calif.-based IPC: The Hospitalist Co., says this extensivist model provides a respite for hospitalists, who typically spend a month at a time in these transitional clinics before heading back into the fray of the hospital. As hospitals, independent physician associations, and managed-care organizations try out new models of care, though, the definition of an extensivist has broadened to include providers in a range of outpatient settings, such as skilled nursing facilities, assistant living communities, and even home health services. California’s CareMore Medicare Advantage plan, in particular, has been cited by the Agency for Healthcare Research and Quality (AHRQ) for using hospitalists as extensivists in both outpatient clinics and skilled nursing facilities to reduce hospital readmission rates, LOS, and inpatient resource use.
The CareMore model reduces the caseload of its hospitalists to about six or eight patients per half-day, giving doctors more time to talk to patients and their family members. Based on those conversations, the extensivist works with a case manager to provide needed resources to each patient after discharge. The doctors also spend roughly half of each day in clinics seeing their own recently discharged patients, and one or two days each week in a skilled nursing facility to visit patients transferred from the hospital (for more details, visit www.innovations.ahrq.gov/content.aspx?id=2903).
Average inpatient LOS among the plan’s 44,000 members dipped to 3.2 days, compared with 5.8 days for Medicare fee-for-service providers and 4.5 days for traditional HM programs in the state. Last April, CareMore’s 30-day readmission rate averaged 13.4%, compared with a 19.6% rate for Medicare.
Baltimore-based Bravo Health has begun opening its own transitional advanced-care centers for members of its Medicare Advantage program, offering case management for complex conditions and immediate care when a PCP is unavailable. Another model has been advanced through team approaches practiced by the likes of Kaiser Permanente, though hospitalists aren’t necessarily the ones providing outpatient follow-up care. No matter what the model is called, Dr. Singer says, the main point is the same: “trying to connect the dots so that we get patients continuing to get better along the continuum without having to be readmitted.”
In December, IPC did some more dot-connecting of its own with its announced acquisition of Senior Care of Colorado, which operates more than 200 geriatric-care facilities in the Denver area. Don Murphy, MD, IPC’s practice group leader for Senior Care of Colorado, says the model emphasizes a continuum of care and information flow from hospitalists in the hospital to affiliated providers in skilled nursing facilities and other outpatient settings. “We think that model, where we tie everything together, will be one of the best that we can do,” Dr. Murphy says.
From Dr. Singer’s perspective, the growing opportunities have sprung from efforts to address a persistent challenge. “We write an order of discharge to a skilled nursing facility, and patients go off into the community and we have no idea where they’re going, who they’re going to, what’s the quality of care out there, what’s the capacity of care,” he says. One of the central ideas of healthcare reform—creating true accountability around an episode of care—will require doctors to be linked “not just during what used to be the episode of care in the hospital,” he adds, “but throughout the continuum until that patient is really returned healthy back to wherever they’re going to be living.”
With a new emphasis on avoidable hospitalizations, hospitals will increasingly need to team up with other providers to avoid fragmentation of care. Using extensivists to help avoid gaps might be a good fit for accountable-care organizations, and Dr. Murphy says the process may be easier for big systems, such as Ochsner in New Orleans or the Cleveland Clinic, which are working in a confined geographic area with a defined patient population.
“The real challenge will be those of us out there in larger metropolitan areas where we’re not under the roof of one big conglomerate but still having to work together creatively and effectively to smooth the continuum,” Dr. Singer says.
Emerging Trends
Other trends are making inpatient-outpatient partnerships, whether formal or informal, an increasingly necessary part of providing high-quality healthcare. “We are seeing folks come out of the hospitals who 30 years ago clearly would have been in the hospital for a prolonged stay,” Dr. Murphy says. “A lot of these [patients], instead of going to SNFs, are going back to their homes and to assisted living with additional services; they require a lot of follow-up.”
Dr. Singer says he’s seeing another trend in which PCPs are likewise transitioning to newly created extensivist roles in sub-acute settings such as nursing homes. The position, he says, offers the attraction of a high-impact, longer-term relationship with patients without the high overhead of standalone clinics. The blurring of lines between outpatient and inpatient providers has created questions for hospitalists, too. For example, at what point does a hospitalist working much of the time in an outpatient clinic or skilled nursing facility no longer fit the traditional definition of a hospitalist? Does that detract from the doctor’s hospital duties? TH
Bryn Nelson is a freelance medical writer based in Seattle.
Reference
- Sanger, P. Health plans juggle precarious patients. Managed Healthcare Executive. 2002:40-41.
The Mentalist
Kelly Cunningham, MD, acknowledges she followed a “pretty traditional” path into medicine. She can’t point to one role model or a single experience that sparked her interest in the field. Rather, she felt medical school would be the ideal way to combine her love for biological sciences, her passion for helping others, and her desire to make a difference.
But Dr. Cunningham didn’t have to wait long for career inspiration. “When I was doing my initial clinical rotations, I had very good hospitalist mentors,” she says. “I started thinking, ‘I really like your job, and I can see myself wanting to be like you.’ ”
Those mentors developed Dr. Cunningham’s interest in quality improvement (QI) and patient safety, which tied in well with hospitalists’ evolving role and complemented her interest in caring for medically complex patients. “I’m a thinker, so I realized early on internal medicine was a good fit for me,” says Dr. Cunningham, an assistant professor of medicine at Vanderbilt University in Nashville, Tenn., and an attending physician at Vanderbilt University Hospital and the Veterans Affairs Medical Center in Nashville. “It became clear I wasn’t going to be a surgeon. I don’t like to fix things using my hands. I like to fix things using my mind.”

Question: How do you balance your academic appointment with your clinical responsibilities?
Answer: That’s the biggest challenge for me. I went into hospital medicine first and foremost because I enjoy taking care of patients. But I really like teaching. I’m very interested in working with residents and students. I’m at the point now where I’m starting to have to say no to things and prioritize a bit just to maintain my sanity.
Q: Does one aspect of your career complement the other?
A: Absolutely. You can’t do clinical activities or academic activities in a vacuum. In order to be a good clinician, you need to have the perspective of being able to ask research questions or understand how to teach and be able to tie QI activities into your daily work. On the other hand, I don’t think you can be involved with a residency program without having the knowledge of what it’s like to be on the front line of patient care.
Q: What do you find rewarding about working at the VA?
A: The physicians who are working in the VAs very much appreciate veterans’ service. They enjoy sitting down with them and hearing their stories and seeing them as people. In turn, the veterans are very grateful for the care they receive. Most veterans only receive care within the VA system, so it’s kind of like its own community, and I really like that.
Q: You are passionate about improving the quality of care transitions. What sparked that interest?
A: When I was a resident at Emory University, much of my clinical work was at Grady Hospital in Atlanta. The patient population tends to be underinsured and doesn’t have great access to healthcare. On the day of discharge, we’d give them the right instructions and the right prescriptions, and we’d schedule a follow-up appointment. Two weeks later, they were readmitted. We’d find out they didn’t understand the instructions, couldn’t afford the prescriptions, or didn’t go to the follow-up appointment. It made me realize how important the transition is between hospital and home, and what a vulnerable time it is for patients.
Q: How can hospitalists help improve those transitions?
A: It’s about doing the right thing and providing good customer service. Studies show it’s not uncommon for patients to not know the name of their treating physician in a hospital or to not know their diagnosis or to not know why they’re taking a certain medication. It comes down to taking the time to talk to patients and empower them to take an active part in their medical care.
Q: How do you respond to someone who says there’s not enough time?
A: It’s critical to being a good physician. Sometimes when I’m taking care of 15 or 20 patients, it’s easy to think about cutting corners. But this is one area where it’s not worth it to cut corners.
Q: What is your biggest professional reward?
A: Working with so many trainees and being able to help shape their career path or interest. At the end of a rotation, if they tell me they learned something from me—not necessarily facts but something that they feel will make them a better doctor—that truly is the most rewarding thing.
Q: What advice are you giving to the next generation of hospitalists?
A: It’s important for them to realize that residency is not always completely representative of the real world.
Q: How so?
A: Since the Accreditation Council for Graduate Medical Education is becoming more strict with work hours and workload, the doctors who are graduating from residency now may not have as much clinical experience when they’re coming out of residency and transitioning into their role as an attending physician or practicing hospitalist. … When I was a resident, I was taking care of 12 or 15 patients. As a hospitalist, I’m sometimes taking care of 20 or 25 patients. Being aware of the workload and how to balance work with the rest of your life is something I didn’t have a great perspective into when I started.
Q: How will the ACGME duty-hour changes affect HM?
A: Interns can only work 16-hour shifts. Who is going to take care of patients when interns have to take a nap or go off shift? Who will pick up all of the resident duties? A lot of it is going to fall on the hospitalists. We can increase our workload, but at what cost? We still need to maintain job satisfaction and have a career that is sustainable and desirable.
Q: Do you see any other solution?
A: Doctors spend a lot of time doing activities that don’t require a medical degree. I think a lot of case managers, midlevel providers, and ancillary support will help us improve our efficiency and workload to help our resident teams while still helping us maintain our sanity.
Q: What’s next for you professionally?
A: I’m finally at the point where I’m starting to define my niche academically. On the clinical side, I really enjoy the variety of the work I do. I’d like to get involved more with handovers within the hospital and also medication reconciliation. Those are two things I’m involved in on a small scale, but they are priorities for the medical center.
Beyond that, I want to try to balance everything and be more selective when choosing opportunities that come my way and be thoughtful about how they fit with my work before just saying yes. TH
Mark Leiser is a freelance writer based in New Jersey.
Kelly Cunningham, MD, acknowledges she followed a “pretty traditional” path into medicine. She can’t point to one role model or a single experience that sparked her interest in the field. Rather, she felt medical school would be the ideal way to combine her love for biological sciences, her passion for helping others, and her desire to make a difference.
But Dr. Cunningham didn’t have to wait long for career inspiration. “When I was doing my initial clinical rotations, I had very good hospitalist mentors,” she says. “I started thinking, ‘I really like your job, and I can see myself wanting to be like you.’ ”
Those mentors developed Dr. Cunningham’s interest in quality improvement (QI) and patient safety, which tied in well with hospitalists’ evolving role and complemented her interest in caring for medically complex patients. “I’m a thinker, so I realized early on internal medicine was a good fit for me,” says Dr. Cunningham, an assistant professor of medicine at Vanderbilt University in Nashville, Tenn., and an attending physician at Vanderbilt University Hospital and the Veterans Affairs Medical Center in Nashville. “It became clear I wasn’t going to be a surgeon. I don’t like to fix things using my hands. I like to fix things using my mind.”

Question: How do you balance your academic appointment with your clinical responsibilities?
Answer: That’s the biggest challenge for me. I went into hospital medicine first and foremost because I enjoy taking care of patients. But I really like teaching. I’m very interested in working with residents and students. I’m at the point now where I’m starting to have to say no to things and prioritize a bit just to maintain my sanity.
Q: Does one aspect of your career complement the other?
A: Absolutely. You can’t do clinical activities or academic activities in a vacuum. In order to be a good clinician, you need to have the perspective of being able to ask research questions or understand how to teach and be able to tie QI activities into your daily work. On the other hand, I don’t think you can be involved with a residency program without having the knowledge of what it’s like to be on the front line of patient care.
Q: What do you find rewarding about working at the VA?
A: The physicians who are working in the VAs very much appreciate veterans’ service. They enjoy sitting down with them and hearing their stories and seeing them as people. In turn, the veterans are very grateful for the care they receive. Most veterans only receive care within the VA system, so it’s kind of like its own community, and I really like that.
Q: You are passionate about improving the quality of care transitions. What sparked that interest?
A: When I was a resident at Emory University, much of my clinical work was at Grady Hospital in Atlanta. The patient population tends to be underinsured and doesn’t have great access to healthcare. On the day of discharge, we’d give them the right instructions and the right prescriptions, and we’d schedule a follow-up appointment. Two weeks later, they were readmitted. We’d find out they didn’t understand the instructions, couldn’t afford the prescriptions, or didn’t go to the follow-up appointment. It made me realize how important the transition is between hospital and home, and what a vulnerable time it is for patients.
Q: How can hospitalists help improve those transitions?
A: It’s about doing the right thing and providing good customer service. Studies show it’s not uncommon for patients to not know the name of their treating physician in a hospital or to not know their diagnosis or to not know why they’re taking a certain medication. It comes down to taking the time to talk to patients and empower them to take an active part in their medical care.
Q: How do you respond to someone who says there’s not enough time?
A: It’s critical to being a good physician. Sometimes when I’m taking care of 15 or 20 patients, it’s easy to think about cutting corners. But this is one area where it’s not worth it to cut corners.
Q: What is your biggest professional reward?
A: Working with so many trainees and being able to help shape their career path or interest. At the end of a rotation, if they tell me they learned something from me—not necessarily facts but something that they feel will make them a better doctor—that truly is the most rewarding thing.
Q: What advice are you giving to the next generation of hospitalists?
A: It’s important for them to realize that residency is not always completely representative of the real world.
Q: How so?
A: Since the Accreditation Council for Graduate Medical Education is becoming more strict with work hours and workload, the doctors who are graduating from residency now may not have as much clinical experience when they’re coming out of residency and transitioning into their role as an attending physician or practicing hospitalist. … When I was a resident, I was taking care of 12 or 15 patients. As a hospitalist, I’m sometimes taking care of 20 or 25 patients. Being aware of the workload and how to balance work with the rest of your life is something I didn’t have a great perspective into when I started.
Q: How will the ACGME duty-hour changes affect HM?
A: Interns can only work 16-hour shifts. Who is going to take care of patients when interns have to take a nap or go off shift? Who will pick up all of the resident duties? A lot of it is going to fall on the hospitalists. We can increase our workload, but at what cost? We still need to maintain job satisfaction and have a career that is sustainable and desirable.
Q: Do you see any other solution?
A: Doctors spend a lot of time doing activities that don’t require a medical degree. I think a lot of case managers, midlevel providers, and ancillary support will help us improve our efficiency and workload to help our resident teams while still helping us maintain our sanity.
Q: What’s next for you professionally?
A: I’m finally at the point where I’m starting to define my niche academically. On the clinical side, I really enjoy the variety of the work I do. I’d like to get involved more with handovers within the hospital and also medication reconciliation. Those are two things I’m involved in on a small scale, but they are priorities for the medical center.
Beyond that, I want to try to balance everything and be more selective when choosing opportunities that come my way and be thoughtful about how they fit with my work before just saying yes. TH
Mark Leiser is a freelance writer based in New Jersey.
Kelly Cunningham, MD, acknowledges she followed a “pretty traditional” path into medicine. She can’t point to one role model or a single experience that sparked her interest in the field. Rather, she felt medical school would be the ideal way to combine her love for biological sciences, her passion for helping others, and her desire to make a difference.
But Dr. Cunningham didn’t have to wait long for career inspiration. “When I was doing my initial clinical rotations, I had very good hospitalist mentors,” she says. “I started thinking, ‘I really like your job, and I can see myself wanting to be like you.’ ”
Those mentors developed Dr. Cunningham’s interest in quality improvement (QI) and patient safety, which tied in well with hospitalists’ evolving role and complemented her interest in caring for medically complex patients. “I’m a thinker, so I realized early on internal medicine was a good fit for me,” says Dr. Cunningham, an assistant professor of medicine at Vanderbilt University in Nashville, Tenn., and an attending physician at Vanderbilt University Hospital and the Veterans Affairs Medical Center in Nashville. “It became clear I wasn’t going to be a surgeon. I don’t like to fix things using my hands. I like to fix things using my mind.”

Question: How do you balance your academic appointment with your clinical responsibilities?
Answer: That’s the biggest challenge for me. I went into hospital medicine first and foremost because I enjoy taking care of patients. But I really like teaching. I’m very interested in working with residents and students. I’m at the point now where I’m starting to have to say no to things and prioritize a bit just to maintain my sanity.
Q: Does one aspect of your career complement the other?
A: Absolutely. You can’t do clinical activities or academic activities in a vacuum. In order to be a good clinician, you need to have the perspective of being able to ask research questions or understand how to teach and be able to tie QI activities into your daily work. On the other hand, I don’t think you can be involved with a residency program without having the knowledge of what it’s like to be on the front line of patient care.
Q: What do you find rewarding about working at the VA?
A: The physicians who are working in the VAs very much appreciate veterans’ service. They enjoy sitting down with them and hearing their stories and seeing them as people. In turn, the veterans are very grateful for the care they receive. Most veterans only receive care within the VA system, so it’s kind of like its own community, and I really like that.
Q: You are passionate about improving the quality of care transitions. What sparked that interest?
A: When I was a resident at Emory University, much of my clinical work was at Grady Hospital in Atlanta. The patient population tends to be underinsured and doesn’t have great access to healthcare. On the day of discharge, we’d give them the right instructions and the right prescriptions, and we’d schedule a follow-up appointment. Two weeks later, they were readmitted. We’d find out they didn’t understand the instructions, couldn’t afford the prescriptions, or didn’t go to the follow-up appointment. It made me realize how important the transition is between hospital and home, and what a vulnerable time it is for patients.
Q: How can hospitalists help improve those transitions?
A: It’s about doing the right thing and providing good customer service. Studies show it’s not uncommon for patients to not know the name of their treating physician in a hospital or to not know their diagnosis or to not know why they’re taking a certain medication. It comes down to taking the time to talk to patients and empower them to take an active part in their medical care.
Q: How do you respond to someone who says there’s not enough time?
A: It’s critical to being a good physician. Sometimes when I’m taking care of 15 or 20 patients, it’s easy to think about cutting corners. But this is one area where it’s not worth it to cut corners.
Q: What is your biggest professional reward?
A: Working with so many trainees and being able to help shape their career path or interest. At the end of a rotation, if they tell me they learned something from me—not necessarily facts but something that they feel will make them a better doctor—that truly is the most rewarding thing.
Q: What advice are you giving to the next generation of hospitalists?
A: It’s important for them to realize that residency is not always completely representative of the real world.
Q: How so?
A: Since the Accreditation Council for Graduate Medical Education is becoming more strict with work hours and workload, the doctors who are graduating from residency now may not have as much clinical experience when they’re coming out of residency and transitioning into their role as an attending physician or practicing hospitalist. … When I was a resident, I was taking care of 12 or 15 patients. As a hospitalist, I’m sometimes taking care of 20 or 25 patients. Being aware of the workload and how to balance work with the rest of your life is something I didn’t have a great perspective into when I started.
Q: How will the ACGME duty-hour changes affect HM?
A: Interns can only work 16-hour shifts. Who is going to take care of patients when interns have to take a nap or go off shift? Who will pick up all of the resident duties? A lot of it is going to fall on the hospitalists. We can increase our workload, but at what cost? We still need to maintain job satisfaction and have a career that is sustainable and desirable.
Q: Do you see any other solution?
A: Doctors spend a lot of time doing activities that don’t require a medical degree. I think a lot of case managers, midlevel providers, and ancillary support will help us improve our efficiency and workload to help our resident teams while still helping us maintain our sanity.
Q: What’s next for you professionally?
A: I’m finally at the point where I’m starting to define my niche academically. On the clinical side, I really enjoy the variety of the work I do. I’d like to get involved more with handovers within the hospital and also medication reconciliation. Those are two things I’m involved in on a small scale, but they are priorities for the medical center.
Beyond that, I want to try to balance everything and be more selective when choosing opportunities that come my way and be thoughtful about how they fit with my work before just saying yes. TH
Mark Leiser is a freelance writer based in New Jersey.
The Story of Us, Ch. 2
In the December 2010 issue of The Hospitalist (p. 43), I started the discussion of “The Story of Us” by outlining three threats that could limit our effectiveness in realizing our vision of quality and patient safety. The story continues here, with four additional threats to the culture of quality that is our mutual dream.
Threat 4: Strategy Trumps Tactics and Execution
There is no shortage of “strategery” in the context of healthcare reform, and it is tempting to succumb to the idea that the correct strategy automatically translates into intended results. But anyone who has suffered through a high-school rendition of Hamlet knows that while Shakespeare’s words might be the same, it is hardly a Broadway performance. Put another way, what is written in the coach’s playbook is the first step; execution of the playbook is what wins or loses the game.
Chan et al’s article “Delayed Time to Defibrillation after In-Hospital Cardiac Arrest” makes this point.1 I doubt there is any physician who does not know that defibrillation is indicated in a cardiac arrest, but as the article illustrates, it took more than two minutes for 30% of patients with in-hospital cardiac arrest to be defibrillated. The upshot: If you have a cardiac arrest, you might be safer in a casino than you are in a hospital.
Healthcare reform and the expanding literature in patient safety and quality bring us closer to having the strategy we need, but what lags is execution of that strategy. Tactics, not strategy, is our greatest deficiency now. And while strategy can be designed for virtually all hospitals, tactics rest with each individual hospital, as each individual hospital system is unique.
Enter again the importance of the hospitalist: the physician intimately aware of the intricacies of their hospital system. There are reasons that defibrillation might be delayed in an individual hospital; perhaps it’s the location of the code cart, perhaps it is how patients are determined to need telemetry monitoring, perhaps it is the line of communication between telemetry and the responsible physician. But whatever the reason, it is not likely to be the same for all hospitals.
And here is the new challenge for the hospitalist: Discover the unique systems deficits in your hospital that prevent the perfect strategy from translating into perfect results.
Threat 5: Focus on One Component at a Time
The essence of systems-level change is simple: In a system, changing one component has effects (good or bad) on other components of the system. Unfortunately, our healthcare systems continue to exist in silos, with few people in leadership positions who are empowered with a perspective of the system as a whole.
Case in point: the yin-yang of length of stay (LOS) and hospital readmissions. I doubt there is a hospitalist who has not heard the words “discharge by 11 a.m.,” in large part because of the hospital truism “every medicine bed is a wasted ortho bed.” Patients who leave by 11 a.m. open up more beds for patients coming out of the operating rooms, and that translates into more surgical procedures. But discharge by 11 a.m. is not as simple as it appears. A sound discharge decision that does not result in readmissions is predicated upon multiple components of the system: results from diagnostic testing have to be obtainable early, the physician must not be dual-tasked during the early hours (e.g. receiving patients from the ED or ICU, performing procedures, etc.), and communication with the family and PCP has to be established early.
The hospitalist thus finds herself stuck between the proverbial rock and a hard place: Discharge early (i.e. before you are ready to do so safely) but ensure that patients don’t come back. There is no easy answer to this potential dilemma, except to say that the solution rests with people who do have a systemwide perspective. To this end, it will be the hospitalist “on the ground,” familiar with the need to prevent readmissions but sensitive to the need to discharge early, who will have the unique insight to design solutions, for all elements of the hospital system, that ensure meeting both ends.
Threat 6: Ignoring the Adaptive Unconscious
Think about whether this has ever happened to you: You finish a busy day at work, with many thoughts still on your mind as you begin your car drive home. Thirty minutes later, you find yourself sitting in your car in your driveway, wondering, “Wow, how did I get home? I don’t remember that drive at all.” Such is the benefit of what Timothy Wilson in his book Strangers to Ourselves calls the “adaptive unconscious.” See it as the mind’s ability to go on “autopilot” to accomplish repetitive tasks without requiring conscious thought, freeing up the mind to devote mental energy to something else. It’s adaptive, of course, because without it, it would be impossible to do any physical activity (i.e. collecting your wallet and keys as you leave the house) while simultaneously doing another activity (i.e. talking on the cell phone as you leave the house). The danger, however, is that tasks that are performed by the adaptive unconscious autopilot are quite inaccessible to the conscious mind for inspection and improvement.
Now consider this example. Have you ever seen a patient in the ED, sat down at the nurses’ station with the chart (contemplating all that needs to happen for the patient’s care), only to look down a few minutes later to see a fully completed set of admission orders? And you say, “Wow, how did these orders get done? I don’t remember writing these at all. Well, thanks for that.”
The focus of the quality- and patient-safety movements has been on changing the physician’s “conscious mind” decisions. But the reality is that the vast majority of what we do in our daily lives is performed without conscious thought. You can’t begrudge it, because again, without it, you would be paralyzed. But it has profound implications for the goal of advancing quality and patient safety in our practice of medicine.
There are two points to make in the context of this discussion. First, the adaptive unconscious is not a magical gift; it develops as a product of our repetitive tasks. You can make that drive home, or write those admission orders, without conscious thought only because you have done it hundreds of times before. And here’s the implication: Much of the behavior that is not conducive to optimal patient safety is a product of what we have done for the past five years. And what we do now in changing physician behavior has implications not only for today, but also for what we will do five years from now.
With this in mind, the bad decisions that result in adverse events do not concern me as much as the bad decisions that do not result in adverse events. The adverse outcome has enough drama to immediately bring the decision into the realm of the conscious, making it accessible for the physician to change behavior. But a bad decision (call it a “near miss”) that does not result in an adverse outcome remains inaccessible to the conscious mind. And should the bad decision be repeated again and again, it would insidiously become integrated into the adaptive unconscious, forever coloring the physician’s delivery of care.
The scary part of the adaptive unconscious is that it is inaccessible to the conscious mind because it is unconscious. But there is a way to modify the adaptive unconscious: reflection. I am not advocating candles, incense, and Kenny G. But reflection on physician behavior has to occur, and it must be much more than just focusing upon the adverse events (which, by virtue of being adverse, are fully in the conscious mind). Reflection that meaningfully changes unconscious behavior has to be focused upon what seemingly didn’t happen. It is a step-by-step analysis of a physician’s performance in ordinary time.
Put another way, every quarterback in the NFL leaves the football game thinking about the interceptions thrown (the dramatic mistakes), but only by virtue of reviewing the game film does he become aware of the interceptions he almost threw. Unlike the NFL quarterback, the hospitalist does not have the luxury of reviewing game film, but the need for reflection on the “near miss” events is no less important.
This takes time, and it likely takes an element of external discipline that the ordinary physician cannot provide for himself. Time is addressed in the next threat, but see the summary of this discussion as simply this: In the face of the prevailing culture of peer review and RCAs, there has to be equal attention paid to finding time and structure to reviewing a physician’s performance in the absence of adverse events. Perhaps this is structured alone time; perhaps its structured time with other hospitalists as a group discussion—I don’t know. But some element of reflection in the absence of “what went wrong” has to occur, lest we find ourselves in 2020 repetitively responding to adverse events, wondering why in 10 years’ time, the number of adverse events has not appreciably diminished.
Threat 7: Failure to Optimize Efficiency
Our story began in 1999 with a focus on hospitalists improving efficiency. The second chapter of our story, of course, has been on improving quality and patient safety. Interesting, isn’t it, that we find ourselves where we began? For Chapter 3 begins again with a focus on improving efficiency, not for financial ends, but for the meaningful enactment of quality and patient safety. Two points make the case.
If I were reading the discussion above, and not writing it, I am sure I would have your same response: “Great, more things (reflection time) to do with a fixed amount of time, and no additional money. Thanks for another unfunded mandate.” The reality is that until we get to an ultimately inspired healthcare system, there is unlikely to be financial support, or a discounting of RVU expectations, to support reflection. So with a fixed amount of time, and increasing activities to fit into that time, there is only one answer: We must become more efficient.
Taiichi Ohno, Toyota’s chief engineer, described what are essentially the bones of “LEAN” in optimizing efficiency. The challenge before us, despite what we have already done, is to further eliminate the “Muda”: activity that does not add value. Not only will this save money, but it will also create the additional time necessary for reflection, which is in turn requisite for a meaningful culture of patient safety and quality.
But there is another reason, one that makes improved efficiency essential in advancing patient safety. In the early part of the century, Yerkes and Dodson published the performance vs. stress curve.2 Like preload to the heart, the authors postulated that performance (on the Y axis) was related to stress (on the X axis) in a rainbow curve. With very little stress, there was very little performance. As stress increased, so did performance, at least to the inflection point on the rainbow curve, after which too much stress led to decreased performance. If you have ever stared blankly at a computer screen trying to formulate a response to the simplest of e-mails, you have experienced both tails of the Yerkes-Dodson curve.
I suspect that there are few hospitalists faced with the problem of “not enough to do,” but I equally suspect that more and more hospitalists are finding themselves farther and farther to the right side of the Yerkes-Dodson curve. After the inflection point, with more and more stress comes less and less performance, a phenomenon felt in every performance-based career.
The bottom line is this: We have created more and more things for the hospitalist to consciously think about in ensuring patient safety and quality. If you had an index card for every guideline/core indicator/standard the hospitalist was supposed to remember, the stack would be 6 inches thick. And this list will only grow with time.
However, these admonishments “to the conscious mind” only improve performance if the physician has enough time to consciously think about each of them. If there is not enough time, then the physician’s mind reverts to the adaptive unconscious, which, because these QI measures have not been a part of his practice for the past several years, is unable to enact them. It’s captured by the simple sentiment when your patient has a DVT: “Wow, I knew to do that, but it just slipped my mind.” Moving too far to the right on the Yerkes-Dodson curve is more than just a risk for burnout; it has serious implications to ensuring that we design a strategy in quality and patient safety that actually comes to fruition.
And that’s Chapter 2 in the story of us: the need to ensure that our tactics and execution remain as important as our strategy, that one element of the system is never treated in isolation, that reflection on ordinary practice becomes a habit, and that efficiency remains a priority. TH
Dr. Wiese is president of SHM.
References
- Chan PS, Krumholz HM, Nichol G, Nallamothu BK; American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358(1):9-17.
- Yerkes RM, Dodson JD. The relation of strength of stimulus to rapidity of habit-formation. J Comparative Neuro Psych. 1908;18:459-482.
In the December 2010 issue of The Hospitalist (p. 43), I started the discussion of “The Story of Us” by outlining three threats that could limit our effectiveness in realizing our vision of quality and patient safety. The story continues here, with four additional threats to the culture of quality that is our mutual dream.
Threat 4: Strategy Trumps Tactics and Execution
There is no shortage of “strategery” in the context of healthcare reform, and it is tempting to succumb to the idea that the correct strategy automatically translates into intended results. But anyone who has suffered through a high-school rendition of Hamlet knows that while Shakespeare’s words might be the same, it is hardly a Broadway performance. Put another way, what is written in the coach’s playbook is the first step; execution of the playbook is what wins or loses the game.
Chan et al’s article “Delayed Time to Defibrillation after In-Hospital Cardiac Arrest” makes this point.1 I doubt there is any physician who does not know that defibrillation is indicated in a cardiac arrest, but as the article illustrates, it took more than two minutes for 30% of patients with in-hospital cardiac arrest to be defibrillated. The upshot: If you have a cardiac arrest, you might be safer in a casino than you are in a hospital.
Healthcare reform and the expanding literature in patient safety and quality bring us closer to having the strategy we need, but what lags is execution of that strategy. Tactics, not strategy, is our greatest deficiency now. And while strategy can be designed for virtually all hospitals, tactics rest with each individual hospital, as each individual hospital system is unique.
Enter again the importance of the hospitalist: the physician intimately aware of the intricacies of their hospital system. There are reasons that defibrillation might be delayed in an individual hospital; perhaps it’s the location of the code cart, perhaps it is how patients are determined to need telemetry monitoring, perhaps it is the line of communication between telemetry and the responsible physician. But whatever the reason, it is not likely to be the same for all hospitals.
And here is the new challenge for the hospitalist: Discover the unique systems deficits in your hospital that prevent the perfect strategy from translating into perfect results.
Threat 5: Focus on One Component at a Time
The essence of systems-level change is simple: In a system, changing one component has effects (good or bad) on other components of the system. Unfortunately, our healthcare systems continue to exist in silos, with few people in leadership positions who are empowered with a perspective of the system as a whole.
Case in point: the yin-yang of length of stay (LOS) and hospital readmissions. I doubt there is a hospitalist who has not heard the words “discharge by 11 a.m.,” in large part because of the hospital truism “every medicine bed is a wasted ortho bed.” Patients who leave by 11 a.m. open up more beds for patients coming out of the operating rooms, and that translates into more surgical procedures. But discharge by 11 a.m. is not as simple as it appears. A sound discharge decision that does not result in readmissions is predicated upon multiple components of the system: results from diagnostic testing have to be obtainable early, the physician must not be dual-tasked during the early hours (e.g. receiving patients from the ED or ICU, performing procedures, etc.), and communication with the family and PCP has to be established early.
The hospitalist thus finds herself stuck between the proverbial rock and a hard place: Discharge early (i.e. before you are ready to do so safely) but ensure that patients don’t come back. There is no easy answer to this potential dilemma, except to say that the solution rests with people who do have a systemwide perspective. To this end, it will be the hospitalist “on the ground,” familiar with the need to prevent readmissions but sensitive to the need to discharge early, who will have the unique insight to design solutions, for all elements of the hospital system, that ensure meeting both ends.
Threat 6: Ignoring the Adaptive Unconscious
Think about whether this has ever happened to you: You finish a busy day at work, with many thoughts still on your mind as you begin your car drive home. Thirty minutes later, you find yourself sitting in your car in your driveway, wondering, “Wow, how did I get home? I don’t remember that drive at all.” Such is the benefit of what Timothy Wilson in his book Strangers to Ourselves calls the “adaptive unconscious.” See it as the mind’s ability to go on “autopilot” to accomplish repetitive tasks without requiring conscious thought, freeing up the mind to devote mental energy to something else. It’s adaptive, of course, because without it, it would be impossible to do any physical activity (i.e. collecting your wallet and keys as you leave the house) while simultaneously doing another activity (i.e. talking on the cell phone as you leave the house). The danger, however, is that tasks that are performed by the adaptive unconscious autopilot are quite inaccessible to the conscious mind for inspection and improvement.
Now consider this example. Have you ever seen a patient in the ED, sat down at the nurses’ station with the chart (contemplating all that needs to happen for the patient’s care), only to look down a few minutes later to see a fully completed set of admission orders? And you say, “Wow, how did these orders get done? I don’t remember writing these at all. Well, thanks for that.”
The focus of the quality- and patient-safety movements has been on changing the physician’s “conscious mind” decisions. But the reality is that the vast majority of what we do in our daily lives is performed without conscious thought. You can’t begrudge it, because again, without it, you would be paralyzed. But it has profound implications for the goal of advancing quality and patient safety in our practice of medicine.
There are two points to make in the context of this discussion. First, the adaptive unconscious is not a magical gift; it develops as a product of our repetitive tasks. You can make that drive home, or write those admission orders, without conscious thought only because you have done it hundreds of times before. And here’s the implication: Much of the behavior that is not conducive to optimal patient safety is a product of what we have done for the past five years. And what we do now in changing physician behavior has implications not only for today, but also for what we will do five years from now.
With this in mind, the bad decisions that result in adverse events do not concern me as much as the bad decisions that do not result in adverse events. The adverse outcome has enough drama to immediately bring the decision into the realm of the conscious, making it accessible for the physician to change behavior. But a bad decision (call it a “near miss”) that does not result in an adverse outcome remains inaccessible to the conscious mind. And should the bad decision be repeated again and again, it would insidiously become integrated into the adaptive unconscious, forever coloring the physician’s delivery of care.
The scary part of the adaptive unconscious is that it is inaccessible to the conscious mind because it is unconscious. But there is a way to modify the adaptive unconscious: reflection. I am not advocating candles, incense, and Kenny G. But reflection on physician behavior has to occur, and it must be much more than just focusing upon the adverse events (which, by virtue of being adverse, are fully in the conscious mind). Reflection that meaningfully changes unconscious behavior has to be focused upon what seemingly didn’t happen. It is a step-by-step analysis of a physician’s performance in ordinary time.
Put another way, every quarterback in the NFL leaves the football game thinking about the interceptions thrown (the dramatic mistakes), but only by virtue of reviewing the game film does he become aware of the interceptions he almost threw. Unlike the NFL quarterback, the hospitalist does not have the luxury of reviewing game film, but the need for reflection on the “near miss” events is no less important.
This takes time, and it likely takes an element of external discipline that the ordinary physician cannot provide for himself. Time is addressed in the next threat, but see the summary of this discussion as simply this: In the face of the prevailing culture of peer review and RCAs, there has to be equal attention paid to finding time and structure to reviewing a physician’s performance in the absence of adverse events. Perhaps this is structured alone time; perhaps its structured time with other hospitalists as a group discussion—I don’t know. But some element of reflection in the absence of “what went wrong” has to occur, lest we find ourselves in 2020 repetitively responding to adverse events, wondering why in 10 years’ time, the number of adverse events has not appreciably diminished.
Threat 7: Failure to Optimize Efficiency
Our story began in 1999 with a focus on hospitalists improving efficiency. The second chapter of our story, of course, has been on improving quality and patient safety. Interesting, isn’t it, that we find ourselves where we began? For Chapter 3 begins again with a focus on improving efficiency, not for financial ends, but for the meaningful enactment of quality and patient safety. Two points make the case.
If I were reading the discussion above, and not writing it, I am sure I would have your same response: “Great, more things (reflection time) to do with a fixed amount of time, and no additional money. Thanks for another unfunded mandate.” The reality is that until we get to an ultimately inspired healthcare system, there is unlikely to be financial support, or a discounting of RVU expectations, to support reflection. So with a fixed amount of time, and increasing activities to fit into that time, there is only one answer: We must become more efficient.
Taiichi Ohno, Toyota’s chief engineer, described what are essentially the bones of “LEAN” in optimizing efficiency. The challenge before us, despite what we have already done, is to further eliminate the “Muda”: activity that does not add value. Not only will this save money, but it will also create the additional time necessary for reflection, which is in turn requisite for a meaningful culture of patient safety and quality.
But there is another reason, one that makes improved efficiency essential in advancing patient safety. In the early part of the century, Yerkes and Dodson published the performance vs. stress curve.2 Like preload to the heart, the authors postulated that performance (on the Y axis) was related to stress (on the X axis) in a rainbow curve. With very little stress, there was very little performance. As stress increased, so did performance, at least to the inflection point on the rainbow curve, after which too much stress led to decreased performance. If you have ever stared blankly at a computer screen trying to formulate a response to the simplest of e-mails, you have experienced both tails of the Yerkes-Dodson curve.
I suspect that there are few hospitalists faced with the problem of “not enough to do,” but I equally suspect that more and more hospitalists are finding themselves farther and farther to the right side of the Yerkes-Dodson curve. After the inflection point, with more and more stress comes less and less performance, a phenomenon felt in every performance-based career.
The bottom line is this: We have created more and more things for the hospitalist to consciously think about in ensuring patient safety and quality. If you had an index card for every guideline/core indicator/standard the hospitalist was supposed to remember, the stack would be 6 inches thick. And this list will only grow with time.
However, these admonishments “to the conscious mind” only improve performance if the physician has enough time to consciously think about each of them. If there is not enough time, then the physician’s mind reverts to the adaptive unconscious, which, because these QI measures have not been a part of his practice for the past several years, is unable to enact them. It’s captured by the simple sentiment when your patient has a DVT: “Wow, I knew to do that, but it just slipped my mind.” Moving too far to the right on the Yerkes-Dodson curve is more than just a risk for burnout; it has serious implications to ensuring that we design a strategy in quality and patient safety that actually comes to fruition.
And that’s Chapter 2 in the story of us: the need to ensure that our tactics and execution remain as important as our strategy, that one element of the system is never treated in isolation, that reflection on ordinary practice becomes a habit, and that efficiency remains a priority. TH
Dr. Wiese is president of SHM.
References
- Chan PS, Krumholz HM, Nichol G, Nallamothu BK; American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358(1):9-17.
- Yerkes RM, Dodson JD. The relation of strength of stimulus to rapidity of habit-formation. J Comparative Neuro Psych. 1908;18:459-482.
In the December 2010 issue of The Hospitalist (p. 43), I started the discussion of “The Story of Us” by outlining three threats that could limit our effectiveness in realizing our vision of quality and patient safety. The story continues here, with four additional threats to the culture of quality that is our mutual dream.
Threat 4: Strategy Trumps Tactics and Execution
There is no shortage of “strategery” in the context of healthcare reform, and it is tempting to succumb to the idea that the correct strategy automatically translates into intended results. But anyone who has suffered through a high-school rendition of Hamlet knows that while Shakespeare’s words might be the same, it is hardly a Broadway performance. Put another way, what is written in the coach’s playbook is the first step; execution of the playbook is what wins or loses the game.
Chan et al’s article “Delayed Time to Defibrillation after In-Hospital Cardiac Arrest” makes this point.1 I doubt there is any physician who does not know that defibrillation is indicated in a cardiac arrest, but as the article illustrates, it took more than two minutes for 30% of patients with in-hospital cardiac arrest to be defibrillated. The upshot: If you have a cardiac arrest, you might be safer in a casino than you are in a hospital.
Healthcare reform and the expanding literature in patient safety and quality bring us closer to having the strategy we need, but what lags is execution of that strategy. Tactics, not strategy, is our greatest deficiency now. And while strategy can be designed for virtually all hospitals, tactics rest with each individual hospital, as each individual hospital system is unique.
Enter again the importance of the hospitalist: the physician intimately aware of the intricacies of their hospital system. There are reasons that defibrillation might be delayed in an individual hospital; perhaps it’s the location of the code cart, perhaps it is how patients are determined to need telemetry monitoring, perhaps it is the line of communication between telemetry and the responsible physician. But whatever the reason, it is not likely to be the same for all hospitals.
And here is the new challenge for the hospitalist: Discover the unique systems deficits in your hospital that prevent the perfect strategy from translating into perfect results.
Threat 5: Focus on One Component at a Time
The essence of systems-level change is simple: In a system, changing one component has effects (good or bad) on other components of the system. Unfortunately, our healthcare systems continue to exist in silos, with few people in leadership positions who are empowered with a perspective of the system as a whole.
Case in point: the yin-yang of length of stay (LOS) and hospital readmissions. I doubt there is a hospitalist who has not heard the words “discharge by 11 a.m.,” in large part because of the hospital truism “every medicine bed is a wasted ortho bed.” Patients who leave by 11 a.m. open up more beds for patients coming out of the operating rooms, and that translates into more surgical procedures. But discharge by 11 a.m. is not as simple as it appears. A sound discharge decision that does not result in readmissions is predicated upon multiple components of the system: results from diagnostic testing have to be obtainable early, the physician must not be dual-tasked during the early hours (e.g. receiving patients from the ED or ICU, performing procedures, etc.), and communication with the family and PCP has to be established early.
The hospitalist thus finds herself stuck between the proverbial rock and a hard place: Discharge early (i.e. before you are ready to do so safely) but ensure that patients don’t come back. There is no easy answer to this potential dilemma, except to say that the solution rests with people who do have a systemwide perspective. To this end, it will be the hospitalist “on the ground,” familiar with the need to prevent readmissions but sensitive to the need to discharge early, who will have the unique insight to design solutions, for all elements of the hospital system, that ensure meeting both ends.
Threat 6: Ignoring the Adaptive Unconscious
Think about whether this has ever happened to you: You finish a busy day at work, with many thoughts still on your mind as you begin your car drive home. Thirty minutes later, you find yourself sitting in your car in your driveway, wondering, “Wow, how did I get home? I don’t remember that drive at all.” Such is the benefit of what Timothy Wilson in his book Strangers to Ourselves calls the “adaptive unconscious.” See it as the mind’s ability to go on “autopilot” to accomplish repetitive tasks without requiring conscious thought, freeing up the mind to devote mental energy to something else. It’s adaptive, of course, because without it, it would be impossible to do any physical activity (i.e. collecting your wallet and keys as you leave the house) while simultaneously doing another activity (i.e. talking on the cell phone as you leave the house). The danger, however, is that tasks that are performed by the adaptive unconscious autopilot are quite inaccessible to the conscious mind for inspection and improvement.
Now consider this example. Have you ever seen a patient in the ED, sat down at the nurses’ station with the chart (contemplating all that needs to happen for the patient’s care), only to look down a few minutes later to see a fully completed set of admission orders? And you say, “Wow, how did these orders get done? I don’t remember writing these at all. Well, thanks for that.”
The focus of the quality- and patient-safety movements has been on changing the physician’s “conscious mind” decisions. But the reality is that the vast majority of what we do in our daily lives is performed without conscious thought. You can’t begrudge it, because again, without it, you would be paralyzed. But it has profound implications for the goal of advancing quality and patient safety in our practice of medicine.
There are two points to make in the context of this discussion. First, the adaptive unconscious is not a magical gift; it develops as a product of our repetitive tasks. You can make that drive home, or write those admission orders, without conscious thought only because you have done it hundreds of times before. And here’s the implication: Much of the behavior that is not conducive to optimal patient safety is a product of what we have done for the past five years. And what we do now in changing physician behavior has implications not only for today, but also for what we will do five years from now.
With this in mind, the bad decisions that result in adverse events do not concern me as much as the bad decisions that do not result in adverse events. The adverse outcome has enough drama to immediately bring the decision into the realm of the conscious, making it accessible for the physician to change behavior. But a bad decision (call it a “near miss”) that does not result in an adverse outcome remains inaccessible to the conscious mind. And should the bad decision be repeated again and again, it would insidiously become integrated into the adaptive unconscious, forever coloring the physician’s delivery of care.
The scary part of the adaptive unconscious is that it is inaccessible to the conscious mind because it is unconscious. But there is a way to modify the adaptive unconscious: reflection. I am not advocating candles, incense, and Kenny G. But reflection on physician behavior has to occur, and it must be much more than just focusing upon the adverse events (which, by virtue of being adverse, are fully in the conscious mind). Reflection that meaningfully changes unconscious behavior has to be focused upon what seemingly didn’t happen. It is a step-by-step analysis of a physician’s performance in ordinary time.
Put another way, every quarterback in the NFL leaves the football game thinking about the interceptions thrown (the dramatic mistakes), but only by virtue of reviewing the game film does he become aware of the interceptions he almost threw. Unlike the NFL quarterback, the hospitalist does not have the luxury of reviewing game film, but the need for reflection on the “near miss” events is no less important.
This takes time, and it likely takes an element of external discipline that the ordinary physician cannot provide for himself. Time is addressed in the next threat, but see the summary of this discussion as simply this: In the face of the prevailing culture of peer review and RCAs, there has to be equal attention paid to finding time and structure to reviewing a physician’s performance in the absence of adverse events. Perhaps this is structured alone time; perhaps its structured time with other hospitalists as a group discussion—I don’t know. But some element of reflection in the absence of “what went wrong” has to occur, lest we find ourselves in 2020 repetitively responding to adverse events, wondering why in 10 years’ time, the number of adverse events has not appreciably diminished.
Threat 7: Failure to Optimize Efficiency
Our story began in 1999 with a focus on hospitalists improving efficiency. The second chapter of our story, of course, has been on improving quality and patient safety. Interesting, isn’t it, that we find ourselves where we began? For Chapter 3 begins again with a focus on improving efficiency, not for financial ends, but for the meaningful enactment of quality and patient safety. Two points make the case.
If I were reading the discussion above, and not writing it, I am sure I would have your same response: “Great, more things (reflection time) to do with a fixed amount of time, and no additional money. Thanks for another unfunded mandate.” The reality is that until we get to an ultimately inspired healthcare system, there is unlikely to be financial support, or a discounting of RVU expectations, to support reflection. So with a fixed amount of time, and increasing activities to fit into that time, there is only one answer: We must become more efficient.
Taiichi Ohno, Toyota’s chief engineer, described what are essentially the bones of “LEAN” in optimizing efficiency. The challenge before us, despite what we have already done, is to further eliminate the “Muda”: activity that does not add value. Not only will this save money, but it will also create the additional time necessary for reflection, which is in turn requisite for a meaningful culture of patient safety and quality.
But there is another reason, one that makes improved efficiency essential in advancing patient safety. In the early part of the century, Yerkes and Dodson published the performance vs. stress curve.2 Like preload to the heart, the authors postulated that performance (on the Y axis) was related to stress (on the X axis) in a rainbow curve. With very little stress, there was very little performance. As stress increased, so did performance, at least to the inflection point on the rainbow curve, after which too much stress led to decreased performance. If you have ever stared blankly at a computer screen trying to formulate a response to the simplest of e-mails, you have experienced both tails of the Yerkes-Dodson curve.
I suspect that there are few hospitalists faced with the problem of “not enough to do,” but I equally suspect that more and more hospitalists are finding themselves farther and farther to the right side of the Yerkes-Dodson curve. After the inflection point, with more and more stress comes less and less performance, a phenomenon felt in every performance-based career.
The bottom line is this: We have created more and more things for the hospitalist to consciously think about in ensuring patient safety and quality. If you had an index card for every guideline/core indicator/standard the hospitalist was supposed to remember, the stack would be 6 inches thick. And this list will only grow with time.
However, these admonishments “to the conscious mind” only improve performance if the physician has enough time to consciously think about each of them. If there is not enough time, then the physician’s mind reverts to the adaptive unconscious, which, because these QI measures have not been a part of his practice for the past several years, is unable to enact them. It’s captured by the simple sentiment when your patient has a DVT: “Wow, I knew to do that, but it just slipped my mind.” Moving too far to the right on the Yerkes-Dodson curve is more than just a risk for burnout; it has serious implications to ensuring that we design a strategy in quality and patient safety that actually comes to fruition.
And that’s Chapter 2 in the story of us: the need to ensure that our tactics and execution remain as important as our strategy, that one element of the system is never treated in isolation, that reflection on ordinary practice becomes a habit, and that efficiency remains a priority. TH
Dr. Wiese is president of SHM.
References
- Chan PS, Krumholz HM, Nichol G, Nallamothu BK; American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358(1):9-17.
- Yerkes RM, Dodson JD. The relation of strength of stimulus to rapidity of habit-formation. J Comparative Neuro Psych. 1908;18:459-482.
Surgery’s Waterboys
The query came from the audience: “But isn’t comanagement really about us becoming the surgeon’s waterboy?” Encouraged by the chortling crowd, he furthered, “I mean, think about it: How much more demeaning can it get than to be the admit-ologist and discharge-ologist for the surgeon? They make all the coin and we just follow after them picking up their jock straps.”
Slack-jawed, I mustered what was, under the circumstances, a rather confident “Umm … ?”
This comment, from a talk I gave a couple of years ago at an SHM annual meeting about comanagement, took me a bit by surprise. Not because of the sentiment; that I get. It’s easy to feel that the comanagement we do suffices only to sate the surgeon at the hospitalist’s expense. Rather, I was taken aback because of its indication of the distance with which we’ve missed the comanagement bull’s-eye.
New Comanagement Data
A recent article regarding the comanagement of neurosurgical patients drudged this oratorical memory from its peaceful cerebral resting place between the 1982 Milwaukee Brewers’ starting outfield (Ogilvie, Thomas, Moore), my wife’s least favorite Beatle (Ringo), and the number of macaroni noodles my grade-school friend Mike could stuff into his nostril and cough up through his mouth (nine with aspiration, five without). In the paper, Auerbach et al report a retrospective, before-and-after study of 7,596 patients admitted to the neurosurgery service at the University of California at San Francisco Medical Center.1 The authors compared administrative, financial, and survey data for 4,203 patients before a hospitalist-neurosurgery comanagement arrangement to 3,393 patients after the program implementation—by far the largest trial of hospitalist comanagement to date.
They found:
- Shockingly, surgeons (“hospitalists make it easier for me to do my job”) and nurses (“I can easily and promptly reach a physician”) liked having us around.
- Curiously, patients were rather indifferent (measured via patient satisfaction indicators) to our presence.
- The cost of care decreased by about $1,500 per patient after the intercalation of hospitalists—this despite the fact that the length of stay was unchanged before and after model implementation.
- Unfortunately, such traditional markers of quality as mortality and readmission rate remained stubbornly unchanged.
- Encouragingly, nontraditional-but-likely-important indicators of quality (e.g. nursing and physician perception of improvements in care provision) were achieved.
Perspective
This study adds significantly to our understanding of the comanagement model. The finding of costs savings is as expected (nearly all studies of hospitalist programs have shown cost savings) as it is unexpected (prior studies of comanagement models reported no cost savings).2 Likewise, the lack of improvement of hard quality endpoints (mortality and readmission rates) is consistent with most studies of hospitalist programs, including a previous report of comanagement of orthopedic patients that showed improvements only in minor complications, such as rates of electrolyte abnormalities, while improvement in the softer quality endpoints—nursing and surgeon satisfaction and perceptions of quality—is consistent with most reports and conventional wisdom.2
Within hours of publication, the blogs were throbbing with discussion of what this meant for the field of hospital medicine. Did this prove comanagement to be the godsend many believe (perceptions of improved quality), the complete farce that many believe (no evidence of mortality benefit), or was this just further confirmation that hospitalists are really nothing more than cost reduction-ists?
My opinion? This is just the comanagement MacGuffin.
MacGuffin Explained
Fans of film will know that the MacGuffin is a Hitchcockian plot device that uses a meaningless but often mysterious and intriguing element to drive the plot. So while everyone, it seems, is concerned with the MacGuffin, the MacGuffin exists only to help the story unfold. Think of the “government secrets” driving the plot in Hitchcock’s North by Northwest, or “unobtainium” in the movie Avatar. In both cases, the MacGuffin preoccupied the cast (they had to have it, or defend it), but in the end, the MacGuffin was insignificant except to move the plot forward.
In much the same way, the debate about whether the shared-care model of surgical patients is a good thing is comanagment’s MacGuffin; it definitely drives the plot but ultimately it misses the point. The real comanagement story—indeed, the story of the whole of hospital medicine—is our need to fundamentally improve outcomes through systems improvements. The true benefit of comanagement is not in one doctor (hospitalist) taking over the medical care of another doctor (surgeon). That will only slightly improve outcomes of the medical issues at which the hospitalist is more expert (e.g. minor electrolyte disorders). Meanwhile, this model continues to allow the same harms that the underlying unsafe hospital system imparts. The comanagement model itself won’t fix this. Rather, the model simply acts as a mechanism for us to accomplish our desired goals of system redesign.
Put another way, I am better at internal-medicine care than a neurosurgeon is. As such, I have no doubt that if I manage the medical issues of neurosurgical patients, I will do it better. However, this system of hospitalist provision of internal-medicine care can ultimately only lead to the type of marginal, not meaningful, improvements these comanagement studies have shown.
The real potential for the comanagement model comes when I take off my internal-medicine hat (diabetes care, electrolyte management, etc.) and put on my HM hat (ability to execute systematic quality and process improvements that result in safer systems that effect ALL patients, ALL the time, and is not dependent on the individual provider to do the right thing).
In doing this, the MacGuffin—the comanagement model that cohorts a lot of patients in the hands of a relatively few hospitalists—affords us the opportunity to truly advance the patient-safety plot by building better systems, the type of systems that ensure that every patient systematically gets appropriate VTE prophylaxis, avoids medication errors, has unnecessary urinary and central venous catheters removed, avoids pressure ulcers, doesn’t fall or get delirious, and has expert transitions of care. I have no doubt that if we achieved these kinds of interventions, rather than just managing patients’ medical issues, we’d see the kind of profound changes the comanagement model can offer.
MacGuffin or not, comanagement is likely here to stay. The challenge, then, is to find a way in which these care arrangements can go beyond scut to systematically and comprehensively improve the flawed systems of care that envelop our surgical patients.
Doing this will vastly improve patient outcomes, add significant value to the care we provide, and clearly signal to the surgeon that it’s time to bring us the water bottle. TH
Dr. Glasheen is physician editor of The Hospitalist. He is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Auerbach AD, Wachter RM, Cheng HQ, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170(22):2004-2010.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28-38.
The query came from the audience: “But isn’t comanagement really about us becoming the surgeon’s waterboy?” Encouraged by the chortling crowd, he furthered, “I mean, think about it: How much more demeaning can it get than to be the admit-ologist and discharge-ologist for the surgeon? They make all the coin and we just follow after them picking up their jock straps.”
Slack-jawed, I mustered what was, under the circumstances, a rather confident “Umm … ?”
This comment, from a talk I gave a couple of years ago at an SHM annual meeting about comanagement, took me a bit by surprise. Not because of the sentiment; that I get. It’s easy to feel that the comanagement we do suffices only to sate the surgeon at the hospitalist’s expense. Rather, I was taken aback because of its indication of the distance with which we’ve missed the comanagement bull’s-eye.
New Comanagement Data
A recent article regarding the comanagement of neurosurgical patients drudged this oratorical memory from its peaceful cerebral resting place between the 1982 Milwaukee Brewers’ starting outfield (Ogilvie, Thomas, Moore), my wife’s least favorite Beatle (Ringo), and the number of macaroni noodles my grade-school friend Mike could stuff into his nostril and cough up through his mouth (nine with aspiration, five without). In the paper, Auerbach et al report a retrospective, before-and-after study of 7,596 patients admitted to the neurosurgery service at the University of California at San Francisco Medical Center.1 The authors compared administrative, financial, and survey data for 4,203 patients before a hospitalist-neurosurgery comanagement arrangement to 3,393 patients after the program implementation—by far the largest trial of hospitalist comanagement to date.
They found:
- Shockingly, surgeons (“hospitalists make it easier for me to do my job”) and nurses (“I can easily and promptly reach a physician”) liked having us around.
- Curiously, patients were rather indifferent (measured via patient satisfaction indicators) to our presence.
- The cost of care decreased by about $1,500 per patient after the intercalation of hospitalists—this despite the fact that the length of stay was unchanged before and after model implementation.
- Unfortunately, such traditional markers of quality as mortality and readmission rate remained stubbornly unchanged.
- Encouragingly, nontraditional-but-likely-important indicators of quality (e.g. nursing and physician perception of improvements in care provision) were achieved.
Perspective
This study adds significantly to our understanding of the comanagement model. The finding of costs savings is as expected (nearly all studies of hospitalist programs have shown cost savings) as it is unexpected (prior studies of comanagement models reported no cost savings).2 Likewise, the lack of improvement of hard quality endpoints (mortality and readmission rates) is consistent with most studies of hospitalist programs, including a previous report of comanagement of orthopedic patients that showed improvements only in minor complications, such as rates of electrolyte abnormalities, while improvement in the softer quality endpoints—nursing and surgeon satisfaction and perceptions of quality—is consistent with most reports and conventional wisdom.2
Within hours of publication, the blogs were throbbing with discussion of what this meant for the field of hospital medicine. Did this prove comanagement to be the godsend many believe (perceptions of improved quality), the complete farce that many believe (no evidence of mortality benefit), or was this just further confirmation that hospitalists are really nothing more than cost reduction-ists?
My opinion? This is just the comanagement MacGuffin.
MacGuffin Explained
Fans of film will know that the MacGuffin is a Hitchcockian plot device that uses a meaningless but often mysterious and intriguing element to drive the plot. So while everyone, it seems, is concerned with the MacGuffin, the MacGuffin exists only to help the story unfold. Think of the “government secrets” driving the plot in Hitchcock’s North by Northwest, or “unobtainium” in the movie Avatar. In both cases, the MacGuffin preoccupied the cast (they had to have it, or defend it), but in the end, the MacGuffin was insignificant except to move the plot forward.
In much the same way, the debate about whether the shared-care model of surgical patients is a good thing is comanagment’s MacGuffin; it definitely drives the plot but ultimately it misses the point. The real comanagement story—indeed, the story of the whole of hospital medicine—is our need to fundamentally improve outcomes through systems improvements. The true benefit of comanagement is not in one doctor (hospitalist) taking over the medical care of another doctor (surgeon). That will only slightly improve outcomes of the medical issues at which the hospitalist is more expert (e.g. minor electrolyte disorders). Meanwhile, this model continues to allow the same harms that the underlying unsafe hospital system imparts. The comanagement model itself won’t fix this. Rather, the model simply acts as a mechanism for us to accomplish our desired goals of system redesign.
Put another way, I am better at internal-medicine care than a neurosurgeon is. As such, I have no doubt that if I manage the medical issues of neurosurgical patients, I will do it better. However, this system of hospitalist provision of internal-medicine care can ultimately only lead to the type of marginal, not meaningful, improvements these comanagement studies have shown.
The real potential for the comanagement model comes when I take off my internal-medicine hat (diabetes care, electrolyte management, etc.) and put on my HM hat (ability to execute systematic quality and process improvements that result in safer systems that effect ALL patients, ALL the time, and is not dependent on the individual provider to do the right thing).
In doing this, the MacGuffin—the comanagement model that cohorts a lot of patients in the hands of a relatively few hospitalists—affords us the opportunity to truly advance the patient-safety plot by building better systems, the type of systems that ensure that every patient systematically gets appropriate VTE prophylaxis, avoids medication errors, has unnecessary urinary and central venous catheters removed, avoids pressure ulcers, doesn’t fall or get delirious, and has expert transitions of care. I have no doubt that if we achieved these kinds of interventions, rather than just managing patients’ medical issues, we’d see the kind of profound changes the comanagement model can offer.
MacGuffin or not, comanagement is likely here to stay. The challenge, then, is to find a way in which these care arrangements can go beyond scut to systematically and comprehensively improve the flawed systems of care that envelop our surgical patients.
Doing this will vastly improve patient outcomes, add significant value to the care we provide, and clearly signal to the surgeon that it’s time to bring us the water bottle. TH
Dr. Glasheen is physician editor of The Hospitalist. He is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Auerbach AD, Wachter RM, Cheng HQ, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170(22):2004-2010.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28-38.
The query came from the audience: “But isn’t comanagement really about us becoming the surgeon’s waterboy?” Encouraged by the chortling crowd, he furthered, “I mean, think about it: How much more demeaning can it get than to be the admit-ologist and discharge-ologist for the surgeon? They make all the coin and we just follow after them picking up their jock straps.”
Slack-jawed, I mustered what was, under the circumstances, a rather confident “Umm … ?”
This comment, from a talk I gave a couple of years ago at an SHM annual meeting about comanagement, took me a bit by surprise. Not because of the sentiment; that I get. It’s easy to feel that the comanagement we do suffices only to sate the surgeon at the hospitalist’s expense. Rather, I was taken aback because of its indication of the distance with which we’ve missed the comanagement bull’s-eye.
New Comanagement Data
A recent article regarding the comanagement of neurosurgical patients drudged this oratorical memory from its peaceful cerebral resting place between the 1982 Milwaukee Brewers’ starting outfield (Ogilvie, Thomas, Moore), my wife’s least favorite Beatle (Ringo), and the number of macaroni noodles my grade-school friend Mike could stuff into his nostril and cough up through his mouth (nine with aspiration, five without). In the paper, Auerbach et al report a retrospective, before-and-after study of 7,596 patients admitted to the neurosurgery service at the University of California at San Francisco Medical Center.1 The authors compared administrative, financial, and survey data for 4,203 patients before a hospitalist-neurosurgery comanagement arrangement to 3,393 patients after the program implementation—by far the largest trial of hospitalist comanagement to date.
They found:
- Shockingly, surgeons (“hospitalists make it easier for me to do my job”) and nurses (“I can easily and promptly reach a physician”) liked having us around.
- Curiously, patients were rather indifferent (measured via patient satisfaction indicators) to our presence.
- The cost of care decreased by about $1,500 per patient after the intercalation of hospitalists—this despite the fact that the length of stay was unchanged before and after model implementation.
- Unfortunately, such traditional markers of quality as mortality and readmission rate remained stubbornly unchanged.
- Encouragingly, nontraditional-but-likely-important indicators of quality (e.g. nursing and physician perception of improvements in care provision) were achieved.
Perspective
This study adds significantly to our understanding of the comanagement model. The finding of costs savings is as expected (nearly all studies of hospitalist programs have shown cost savings) as it is unexpected (prior studies of comanagement models reported no cost savings).2 Likewise, the lack of improvement of hard quality endpoints (mortality and readmission rates) is consistent with most studies of hospitalist programs, including a previous report of comanagement of orthopedic patients that showed improvements only in minor complications, such as rates of electrolyte abnormalities, while improvement in the softer quality endpoints—nursing and surgeon satisfaction and perceptions of quality—is consistent with most reports and conventional wisdom.2
Within hours of publication, the blogs were throbbing with discussion of what this meant for the field of hospital medicine. Did this prove comanagement to be the godsend many believe (perceptions of improved quality), the complete farce that many believe (no evidence of mortality benefit), or was this just further confirmation that hospitalists are really nothing more than cost reduction-ists?
My opinion? This is just the comanagement MacGuffin.
MacGuffin Explained
Fans of film will know that the MacGuffin is a Hitchcockian plot device that uses a meaningless but often mysterious and intriguing element to drive the plot. So while everyone, it seems, is concerned with the MacGuffin, the MacGuffin exists only to help the story unfold. Think of the “government secrets” driving the plot in Hitchcock’s North by Northwest, or “unobtainium” in the movie Avatar. In both cases, the MacGuffin preoccupied the cast (they had to have it, or defend it), but in the end, the MacGuffin was insignificant except to move the plot forward.
In much the same way, the debate about whether the shared-care model of surgical patients is a good thing is comanagment’s MacGuffin; it definitely drives the plot but ultimately it misses the point. The real comanagement story—indeed, the story of the whole of hospital medicine—is our need to fundamentally improve outcomes through systems improvements. The true benefit of comanagement is not in one doctor (hospitalist) taking over the medical care of another doctor (surgeon). That will only slightly improve outcomes of the medical issues at which the hospitalist is more expert (e.g. minor electrolyte disorders). Meanwhile, this model continues to allow the same harms that the underlying unsafe hospital system imparts. The comanagement model itself won’t fix this. Rather, the model simply acts as a mechanism for us to accomplish our desired goals of system redesign.
Put another way, I am better at internal-medicine care than a neurosurgeon is. As such, I have no doubt that if I manage the medical issues of neurosurgical patients, I will do it better. However, this system of hospitalist provision of internal-medicine care can ultimately only lead to the type of marginal, not meaningful, improvements these comanagement studies have shown.
The real potential for the comanagement model comes when I take off my internal-medicine hat (diabetes care, electrolyte management, etc.) and put on my HM hat (ability to execute systematic quality and process improvements that result in safer systems that effect ALL patients, ALL the time, and is not dependent on the individual provider to do the right thing).
In doing this, the MacGuffin—the comanagement model that cohorts a lot of patients in the hands of a relatively few hospitalists—affords us the opportunity to truly advance the patient-safety plot by building better systems, the type of systems that ensure that every patient systematically gets appropriate VTE prophylaxis, avoids medication errors, has unnecessary urinary and central venous catheters removed, avoids pressure ulcers, doesn’t fall or get delirious, and has expert transitions of care. I have no doubt that if we achieved these kinds of interventions, rather than just managing patients’ medical issues, we’d see the kind of profound changes the comanagement model can offer.
MacGuffin or not, comanagement is likely here to stay. The challenge, then, is to find a way in which these care arrangements can go beyond scut to systematically and comprehensively improve the flawed systems of care that envelop our surgical patients.
Doing this will vastly improve patient outcomes, add significant value to the care we provide, and clearly signal to the surgeon that it’s time to bring us the water bottle. TH
Dr. Glasheen is physician editor of The Hospitalist. He is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Auerbach AD, Wachter RM, Cheng HQ, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170(22):2004-2010.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28-38.
Referral Lists
I like to ask laypeople what they think “hospitalist” means. For years, I was confident that they had never heard the term, but now my question is more often met with an accurate response.
A hotel desk clerk in 1998 actually made one of the cleverest guesses I’ve ever heard. For the whole day, she and her colleagues had in front of them a sign that read “Hospitalist Meeting in the Ballroom,” which got them talking about what in the world a hospitalist is. Seeing from my badge that I was attending that meeting, she asked me what the term meant, but she first gamely provided her best guess: “Someone who makes lists of hospitals.”
There seems to be no end to the number of healthcare-related nouns and verbs to which someone attaches the suffix “ist.” Some days I request so many consults that I’m just a “referralist” (one who refers patients; surely this is a term we can do without). But don’t let the headline of this column confuse you: I really am addressing the lists used to determine which doctor to refer patients to.
Hospitalist Referrals
The first of two common referral lists for hospitalists is a directory of primary-care physicians (PCPs) and clinics, as well as some other providers that refer patients to the hospitalist. Nearly all hospitalist groups maintain such a list, and they might apply a variety of terms such as “subscriber” (which refers to hospitalists) and “nonsubscriber” physicians.
Because most HM groups care for patients who come from all or nearly all of the PCPs in an area, it is often simpler to just create a short list of those providers who don’t refer to the hospitalists. In many hospitals, there are just four or five providers on that list. ED providers are the ones who most often access this list. When visiting other hospitals, I often see a paper copy of the list taped up at the provider workstations in the ED.
Consult Who?
The other, and much less common, type of referral list governs which doctors the hospitalists are to consult. There are two strategies that come up when thinking about this kind of list.
Do what the ED doctors do. ED physicians typically are constrained by the list of on-call physicians for each specialty, and are to always consult that doctor rather than another. For example, the ED doctor is required to consult Dr. Taylor for any patient in need of a general surgeon and doesn’t have a prior relationship with one. Tomorrow, the ED doctor is required to consult Dr. Simon. Dr. Taylor and Dr. Simon are to be contacted because they are the ones on call for the ED those days. Even if the ED doctor would rather consult Dr. Simon today (maybe she is more able, affable, and available than Dr. Taylor), that isn’t an option, because it is Dr. Taylor’s name on the ED on-call roster today.
Each PCP creates a referral list for hospitalists to follow. New hospitalist practices often agree to follow the consulting patterns of each referring PCP. This can increase PCP acceptance of the HM model, and after all, the GI doctor consulted by the hospitalist during the few days in the hospital is the same one who will be working with the PCP when the patient has outpatient issues requiring GI specialty care. This usually means that the hospitalist carries a list of each PCP, and which GI doctor, orthopedist, etc., that particular PCP likes to consult. When the hospitalist needs an ortho consult, she first verifies the PCP this patient sees, then pulls out the list to see the orthopedist(s) that PCP prefers.
In most settings, either form of a mandated referral list is a poor system for hospitalists and is best avoided. Instead, the hospitalists should be free to deviate from the ED call list as they see fit. And while they should be attentive to the consulting preferences of each PCP, it is best not to promise the PCPs that their preference will always be followed. Providing the hospitalists this latitude means they can tailor the choice of consultant to the patient’s needs and the level of service (i.e. able, affable, available) each provides. And, at least in theory, when there are competing providers in a given specialty, they will have an incentive to provide better service to the hospitalist as a way of ensuring future referrals.
Practical Considerations
Even though I think it is optimal for hospitalists to have a lot of latitude in which doctors they consult, there are some practical considerations to keep in mind. For example, if the patient’s PCP is in a group that also has surgeons, it will be best to call one of them, and not a competing surgeon, when the patient has surgical needs. And the hospitalists as a group should usually make some effort to avoid never consulting a particular provider or group, as that could lead the “blackballed” doctor or group to complain enough that the medical staff or hospital leadership might force the hospitalists to follow the ED call roster when choosing referrals.
The number of physicians seeking hospital employment, which is steadily increasing these days, will in many settings increase sensitivities around referral patterns. For example, if your hospital has had three competing general surgery groups and one chooses to become hospital-employed, then the other two groups are likely to worry a lot that the hospitalists might be directed by the hospital to preferentially refer to the newly employed surgeons. Even if your hospitalist group has never had any sort of encouragement to do this, it could be very hard to convince the non-hospital-employed surgeons of this. This could become such a sensitive issue that it might be necessary to carefully track the number of referrals to each surgical group.
And to prevent arguments like “You just consult us on the bad or uninsured patients,” you might also need to track the nature of the patient’s problem and insurance status, and whether the referral led to a procedure. The best approach will be to try to prevent these sorts of things from coming up by maintaining good communication and relations with other physician groups and thinking deliberately about your referral patterns. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
I like to ask laypeople what they think “hospitalist” means. For years, I was confident that they had never heard the term, but now my question is more often met with an accurate response.
A hotel desk clerk in 1998 actually made one of the cleverest guesses I’ve ever heard. For the whole day, she and her colleagues had in front of them a sign that read “Hospitalist Meeting in the Ballroom,” which got them talking about what in the world a hospitalist is. Seeing from my badge that I was attending that meeting, she asked me what the term meant, but she first gamely provided her best guess: “Someone who makes lists of hospitals.”
There seems to be no end to the number of healthcare-related nouns and verbs to which someone attaches the suffix “ist.” Some days I request so many consults that I’m just a “referralist” (one who refers patients; surely this is a term we can do without). But don’t let the headline of this column confuse you: I really am addressing the lists used to determine which doctor to refer patients to.
Hospitalist Referrals
The first of two common referral lists for hospitalists is a directory of primary-care physicians (PCPs) and clinics, as well as some other providers that refer patients to the hospitalist. Nearly all hospitalist groups maintain such a list, and they might apply a variety of terms such as “subscriber” (which refers to hospitalists) and “nonsubscriber” physicians.
Because most HM groups care for patients who come from all or nearly all of the PCPs in an area, it is often simpler to just create a short list of those providers who don’t refer to the hospitalists. In many hospitals, there are just four or five providers on that list. ED providers are the ones who most often access this list. When visiting other hospitals, I often see a paper copy of the list taped up at the provider workstations in the ED.
Consult Who?
The other, and much less common, type of referral list governs which doctors the hospitalists are to consult. There are two strategies that come up when thinking about this kind of list.
Do what the ED doctors do. ED physicians typically are constrained by the list of on-call physicians for each specialty, and are to always consult that doctor rather than another. For example, the ED doctor is required to consult Dr. Taylor for any patient in need of a general surgeon and doesn’t have a prior relationship with one. Tomorrow, the ED doctor is required to consult Dr. Simon. Dr. Taylor and Dr. Simon are to be contacted because they are the ones on call for the ED those days. Even if the ED doctor would rather consult Dr. Simon today (maybe she is more able, affable, and available than Dr. Taylor), that isn’t an option, because it is Dr. Taylor’s name on the ED on-call roster today.
Each PCP creates a referral list for hospitalists to follow. New hospitalist practices often agree to follow the consulting patterns of each referring PCP. This can increase PCP acceptance of the HM model, and after all, the GI doctor consulted by the hospitalist during the few days in the hospital is the same one who will be working with the PCP when the patient has outpatient issues requiring GI specialty care. This usually means that the hospitalist carries a list of each PCP, and which GI doctor, orthopedist, etc., that particular PCP likes to consult. When the hospitalist needs an ortho consult, she first verifies the PCP this patient sees, then pulls out the list to see the orthopedist(s) that PCP prefers.
In most settings, either form of a mandated referral list is a poor system for hospitalists and is best avoided. Instead, the hospitalists should be free to deviate from the ED call list as they see fit. And while they should be attentive to the consulting preferences of each PCP, it is best not to promise the PCPs that their preference will always be followed. Providing the hospitalists this latitude means they can tailor the choice of consultant to the patient’s needs and the level of service (i.e. able, affable, available) each provides. And, at least in theory, when there are competing providers in a given specialty, they will have an incentive to provide better service to the hospitalist as a way of ensuring future referrals.
Practical Considerations
Even though I think it is optimal for hospitalists to have a lot of latitude in which doctors they consult, there are some practical considerations to keep in mind. For example, if the patient’s PCP is in a group that also has surgeons, it will be best to call one of them, and not a competing surgeon, when the patient has surgical needs. And the hospitalists as a group should usually make some effort to avoid never consulting a particular provider or group, as that could lead the “blackballed” doctor or group to complain enough that the medical staff or hospital leadership might force the hospitalists to follow the ED call roster when choosing referrals.
The number of physicians seeking hospital employment, which is steadily increasing these days, will in many settings increase sensitivities around referral patterns. For example, if your hospital has had three competing general surgery groups and one chooses to become hospital-employed, then the other two groups are likely to worry a lot that the hospitalists might be directed by the hospital to preferentially refer to the newly employed surgeons. Even if your hospitalist group has never had any sort of encouragement to do this, it could be very hard to convince the non-hospital-employed surgeons of this. This could become such a sensitive issue that it might be necessary to carefully track the number of referrals to each surgical group.
And to prevent arguments like “You just consult us on the bad or uninsured patients,” you might also need to track the nature of the patient’s problem and insurance status, and whether the referral led to a procedure. The best approach will be to try to prevent these sorts of things from coming up by maintaining good communication and relations with other physician groups and thinking deliberately about your referral patterns. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
I like to ask laypeople what they think “hospitalist” means. For years, I was confident that they had never heard the term, but now my question is more often met with an accurate response.
A hotel desk clerk in 1998 actually made one of the cleverest guesses I’ve ever heard. For the whole day, she and her colleagues had in front of them a sign that read “Hospitalist Meeting in the Ballroom,” which got them talking about what in the world a hospitalist is. Seeing from my badge that I was attending that meeting, she asked me what the term meant, but she first gamely provided her best guess: “Someone who makes lists of hospitals.”
There seems to be no end to the number of healthcare-related nouns and verbs to which someone attaches the suffix “ist.” Some days I request so many consults that I’m just a “referralist” (one who refers patients; surely this is a term we can do without). But don’t let the headline of this column confuse you: I really am addressing the lists used to determine which doctor to refer patients to.
Hospitalist Referrals
The first of two common referral lists for hospitalists is a directory of primary-care physicians (PCPs) and clinics, as well as some other providers that refer patients to the hospitalist. Nearly all hospitalist groups maintain such a list, and they might apply a variety of terms such as “subscriber” (which refers to hospitalists) and “nonsubscriber” physicians.
Because most HM groups care for patients who come from all or nearly all of the PCPs in an area, it is often simpler to just create a short list of those providers who don’t refer to the hospitalists. In many hospitals, there are just four or five providers on that list. ED providers are the ones who most often access this list. When visiting other hospitals, I often see a paper copy of the list taped up at the provider workstations in the ED.
Consult Who?
The other, and much less common, type of referral list governs which doctors the hospitalists are to consult. There are two strategies that come up when thinking about this kind of list.
Do what the ED doctors do. ED physicians typically are constrained by the list of on-call physicians for each specialty, and are to always consult that doctor rather than another. For example, the ED doctor is required to consult Dr. Taylor for any patient in need of a general surgeon and doesn’t have a prior relationship with one. Tomorrow, the ED doctor is required to consult Dr. Simon. Dr. Taylor and Dr. Simon are to be contacted because they are the ones on call for the ED those days. Even if the ED doctor would rather consult Dr. Simon today (maybe she is more able, affable, and available than Dr. Taylor), that isn’t an option, because it is Dr. Taylor’s name on the ED on-call roster today.
Each PCP creates a referral list for hospitalists to follow. New hospitalist practices often agree to follow the consulting patterns of each referring PCP. This can increase PCP acceptance of the HM model, and after all, the GI doctor consulted by the hospitalist during the few days in the hospital is the same one who will be working with the PCP when the patient has outpatient issues requiring GI specialty care. This usually means that the hospitalist carries a list of each PCP, and which GI doctor, orthopedist, etc., that particular PCP likes to consult. When the hospitalist needs an ortho consult, she first verifies the PCP this patient sees, then pulls out the list to see the orthopedist(s) that PCP prefers.
In most settings, either form of a mandated referral list is a poor system for hospitalists and is best avoided. Instead, the hospitalists should be free to deviate from the ED call list as they see fit. And while they should be attentive to the consulting preferences of each PCP, it is best not to promise the PCPs that their preference will always be followed. Providing the hospitalists this latitude means they can tailor the choice of consultant to the patient’s needs and the level of service (i.e. able, affable, available) each provides. And, at least in theory, when there are competing providers in a given specialty, they will have an incentive to provide better service to the hospitalist as a way of ensuring future referrals.
Practical Considerations
Even though I think it is optimal for hospitalists to have a lot of latitude in which doctors they consult, there are some practical considerations to keep in mind. For example, if the patient’s PCP is in a group that also has surgeons, it will be best to call one of them, and not a competing surgeon, when the patient has surgical needs. And the hospitalists as a group should usually make some effort to avoid never consulting a particular provider or group, as that could lead the “blackballed” doctor or group to complain enough that the medical staff or hospital leadership might force the hospitalists to follow the ED call roster when choosing referrals.
The number of physicians seeking hospital employment, which is steadily increasing these days, will in many settings increase sensitivities around referral patterns. For example, if your hospital has had three competing general surgery groups and one chooses to become hospital-employed, then the other two groups are likely to worry a lot that the hospitalists might be directed by the hospital to preferentially refer to the newly employed surgeons. Even if your hospitalist group has never had any sort of encouragement to do this, it could be very hard to convince the non-hospital-employed surgeons of this. This could become such a sensitive issue that it might be necessary to carefully track the number of referrals to each surgical group.
And to prevent arguments like “You just consult us on the bad or uninsured patients,” you might also need to track the nature of the patient’s problem and insurance status, and whether the referral led to a procedure. The best approach will be to try to prevent these sorts of things from coming up by maintaining good communication and relations with other physician groups and thinking deliberately about your referral patterns. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
Resident Restrictions Fuel HM Program Growth
I heard that there are new resident work-hour rules that preclude interns from spending the night in the hospital. Tell me this isn’t true! I am an old-timer.
Thad Horton, MD
St. Louis
Dr. Hospitalist responds: On Sept. 26, 2010, the Accreditation Council for Graduate Medical Education (ACGME) approved new resident duty-hours and supervision standards; the new rules go into effect July 1. ACGME accredits more than 8,800 medical residency programs in the U.S. in more than 130 specialties and subspecialties. More than 111,000 residents and fellows train in these programs annually. ACGME first instituted duty-hour regulations in 2003; those led to a dramatic decrease in resident work-hours.
Basically, the highlights of the new rules are:
- Residents are limited to 80 hours weekly, averaged over a four-week period, and inclusive of all in-house call activities and moonlighting;
- Residents must be allowed one day free of duty every week (at-home call cannot be assigned on these free days);
- PGY-1 residents cannot work more than 16 hours daily, and residents beyond their PGY-1 year cannot work more than 24 hours daily;
- Residents must have at least eight hours off between shifts, and residents who work a 24-hour shift must have a minimum of 14 hours off before starting another shift;
- Residents cannot work more than six consecutive nights as night float; and
- Residents cannot be scheduled for in-house call more frequently than every third night.
I have not seen any specific prohibition on interns working overnight in the hospital. However, the new rules restrict interns to working no more than 16 hours daily, so that will mean interns who stay overnight in the hospital, until 7 or 8 a.m., cannot begin that overnight shift until 3 or 4 p.m. the day before. That means programs planning to keep their interns in-house overnight will have to be creative in their scheduling.
The demand for innovative scheduling won’t be the only implication of these new regulations. A number of forces have driven the rapid expansion of HM over the past decade. We have seen the development of sizable hospitalist programs at a number of teaching hospitals across the country. Hospitalists at teaching hospitals are not only supervising the care provided by residents, but they are also caring for patients without resident involvement. Since the original ACGME duty-hours cutback in 2002, we have seen the development and expansion of hospitalist-staffed, non-resident-covered medical services at most teaching hospitals across the country. Any further restriction in resident work-hours likely will result in the need to hire additional hospitalists to care for patients.
Virtually all HM programs require financial support to make ends meet. The most recent SHM/MGMA compensation and productivity survey found that the average hospitalist full-time equivalent (FTE) requires a little more than $100,000 of support annually. Regardless of the employer, much of that support comes from the hospital. So it appears that hospitals with teaching programs will end up footing the bill for the new resident regulations. I expect HM programs at teaching hospitals will face pushback from hospital administrators, but hiring additional hospitalists is a cost-effective proposition—and not complying with the ACGME rules is not an option, unless your program wants to risk losing its accreditation.
If you are a hospitalist program leader at a teaching hospital, I encourage you to plan accordingly and discuss the impact of these revisions in duty-hours with your teaching program director and your hospital administration.
Communication, Comfort Zone Key to Managing Hypertensive Emergencies
I just saw a patient in our urgent-care clinic sent from an ophthalmologist’s office with newly diagnosed retinal hemorrhages in both eyes and repeated BPs of 170/115. She had no history of hypertension (HTN) and no other symptoms. Does this qualify as an emergency? I couldn’t find any literature in this regard. My sense was it was an emergency, as her vision seemed to be at risk, so I sent her to the ED for IV meds in a controlled environment. Did I overreact?
Dennis Swanson, MD
Grand Rapids, Mich.
Dr. Hospitalist responds: Thank you for your question. There are numerous potential causes of retinal hemorrhages. Aside from trauma, we most commonly see retinal hemorrhages in patients with diabetic retinopathy and/or HTN. As you know, the retina is the only part of the vasculature that we can visualize noninvasively. This is a good example of why it is always important for providers to perform a fundoscopy on every patient with newly discovered HTN.
Retinal hemorrhage is one of several ocular diseases directly related to HTN. Based on your description, it sounds as if the ophthalmologist discovered the retinal hemorrhages and sent the patient to you, given the concern that uncontrolled HTN was the cause of the hemorrhages. You stated that you sent the patient to the ED because you were concerned the patient’s vision “seemed to be at risk.” Most retinal hemorrhages are asymptomatic unless the macular is affected, in which case the patient experiences a change in their visual acuity. Progressive microvascular changes in the retina can cause a loss of visual acuity. Aside from addressing the underlying problem causing the hemorrhages, laser surgery is the typical treatment of retinal hemorrhages. The laser seals off the abnormally bleeding vessels in the retina.
It would be useful to know about any communication that occurred between you and the ophthalmologist. I imagine the ophthalmologist was going to perform laser surgery but sent the patient to the hospital to address the HTN. If you did not feel comfortable managing the patient’s HTN in the urgent-care clinic, you did the right thing by sending the patient to the ED. It also is important to note that patients with hypertensive retinopathy often have other microvascular diseases, including in the kidneys. This patient should be evaluated for any evidence of proteinuria, which can suggest progressive microvascular renal disease, also as a result of uncontrolled HTN. TH
I heard that there are new resident work-hour rules that preclude interns from spending the night in the hospital. Tell me this isn’t true! I am an old-timer.
Thad Horton, MD
St. Louis
Dr. Hospitalist responds: On Sept. 26, 2010, the Accreditation Council for Graduate Medical Education (ACGME) approved new resident duty-hours and supervision standards; the new rules go into effect July 1. ACGME accredits more than 8,800 medical residency programs in the U.S. in more than 130 specialties and subspecialties. More than 111,000 residents and fellows train in these programs annually. ACGME first instituted duty-hour regulations in 2003; those led to a dramatic decrease in resident work-hours.
Basically, the highlights of the new rules are:
- Residents are limited to 80 hours weekly, averaged over a four-week period, and inclusive of all in-house call activities and moonlighting;
- Residents must be allowed one day free of duty every week (at-home call cannot be assigned on these free days);
- PGY-1 residents cannot work more than 16 hours daily, and residents beyond their PGY-1 year cannot work more than 24 hours daily;
- Residents must have at least eight hours off between shifts, and residents who work a 24-hour shift must have a minimum of 14 hours off before starting another shift;
- Residents cannot work more than six consecutive nights as night float; and
- Residents cannot be scheduled for in-house call more frequently than every third night.
I have not seen any specific prohibition on interns working overnight in the hospital. However, the new rules restrict interns to working no more than 16 hours daily, so that will mean interns who stay overnight in the hospital, until 7 or 8 a.m., cannot begin that overnight shift until 3 or 4 p.m. the day before. That means programs planning to keep their interns in-house overnight will have to be creative in their scheduling.
The demand for innovative scheduling won’t be the only implication of these new regulations. A number of forces have driven the rapid expansion of HM over the past decade. We have seen the development of sizable hospitalist programs at a number of teaching hospitals across the country. Hospitalists at teaching hospitals are not only supervising the care provided by residents, but they are also caring for patients without resident involvement. Since the original ACGME duty-hours cutback in 2002, we have seen the development and expansion of hospitalist-staffed, non-resident-covered medical services at most teaching hospitals across the country. Any further restriction in resident work-hours likely will result in the need to hire additional hospitalists to care for patients.
Virtually all HM programs require financial support to make ends meet. The most recent SHM/MGMA compensation and productivity survey found that the average hospitalist full-time equivalent (FTE) requires a little more than $100,000 of support annually. Regardless of the employer, much of that support comes from the hospital. So it appears that hospitals with teaching programs will end up footing the bill for the new resident regulations. I expect HM programs at teaching hospitals will face pushback from hospital administrators, but hiring additional hospitalists is a cost-effective proposition—and not complying with the ACGME rules is not an option, unless your program wants to risk losing its accreditation.
If you are a hospitalist program leader at a teaching hospital, I encourage you to plan accordingly and discuss the impact of these revisions in duty-hours with your teaching program director and your hospital administration.
Communication, Comfort Zone Key to Managing Hypertensive Emergencies
I just saw a patient in our urgent-care clinic sent from an ophthalmologist’s office with newly diagnosed retinal hemorrhages in both eyes and repeated BPs of 170/115. She had no history of hypertension (HTN) and no other symptoms. Does this qualify as an emergency? I couldn’t find any literature in this regard. My sense was it was an emergency, as her vision seemed to be at risk, so I sent her to the ED for IV meds in a controlled environment. Did I overreact?
Dennis Swanson, MD
Grand Rapids, Mich.
Dr. Hospitalist responds: Thank you for your question. There are numerous potential causes of retinal hemorrhages. Aside from trauma, we most commonly see retinal hemorrhages in patients with diabetic retinopathy and/or HTN. As you know, the retina is the only part of the vasculature that we can visualize noninvasively. This is a good example of why it is always important for providers to perform a fundoscopy on every patient with newly discovered HTN.
Retinal hemorrhage is one of several ocular diseases directly related to HTN. Based on your description, it sounds as if the ophthalmologist discovered the retinal hemorrhages and sent the patient to you, given the concern that uncontrolled HTN was the cause of the hemorrhages. You stated that you sent the patient to the ED because you were concerned the patient’s vision “seemed to be at risk.” Most retinal hemorrhages are asymptomatic unless the macular is affected, in which case the patient experiences a change in their visual acuity. Progressive microvascular changes in the retina can cause a loss of visual acuity. Aside from addressing the underlying problem causing the hemorrhages, laser surgery is the typical treatment of retinal hemorrhages. The laser seals off the abnormally bleeding vessels in the retina.
It would be useful to know about any communication that occurred between you and the ophthalmologist. I imagine the ophthalmologist was going to perform laser surgery but sent the patient to the hospital to address the HTN. If you did not feel comfortable managing the patient’s HTN in the urgent-care clinic, you did the right thing by sending the patient to the ED. It also is important to note that patients with hypertensive retinopathy often have other microvascular diseases, including in the kidneys. This patient should be evaluated for any evidence of proteinuria, which can suggest progressive microvascular renal disease, also as a result of uncontrolled HTN. TH
I heard that there are new resident work-hour rules that preclude interns from spending the night in the hospital. Tell me this isn’t true! I am an old-timer.
Thad Horton, MD
St. Louis
Dr. Hospitalist responds: On Sept. 26, 2010, the Accreditation Council for Graduate Medical Education (ACGME) approved new resident duty-hours and supervision standards; the new rules go into effect July 1. ACGME accredits more than 8,800 medical residency programs in the U.S. in more than 130 specialties and subspecialties. More than 111,000 residents and fellows train in these programs annually. ACGME first instituted duty-hour regulations in 2003; those led to a dramatic decrease in resident work-hours.
Basically, the highlights of the new rules are:
- Residents are limited to 80 hours weekly, averaged over a four-week period, and inclusive of all in-house call activities and moonlighting;
- Residents must be allowed one day free of duty every week (at-home call cannot be assigned on these free days);
- PGY-1 residents cannot work more than 16 hours daily, and residents beyond their PGY-1 year cannot work more than 24 hours daily;
- Residents must have at least eight hours off between shifts, and residents who work a 24-hour shift must have a minimum of 14 hours off before starting another shift;
- Residents cannot work more than six consecutive nights as night float; and
- Residents cannot be scheduled for in-house call more frequently than every third night.
I have not seen any specific prohibition on interns working overnight in the hospital. However, the new rules restrict interns to working no more than 16 hours daily, so that will mean interns who stay overnight in the hospital, until 7 or 8 a.m., cannot begin that overnight shift until 3 or 4 p.m. the day before. That means programs planning to keep their interns in-house overnight will have to be creative in their scheduling.
The demand for innovative scheduling won’t be the only implication of these new regulations. A number of forces have driven the rapid expansion of HM over the past decade. We have seen the development of sizable hospitalist programs at a number of teaching hospitals across the country. Hospitalists at teaching hospitals are not only supervising the care provided by residents, but they are also caring for patients without resident involvement. Since the original ACGME duty-hours cutback in 2002, we have seen the development and expansion of hospitalist-staffed, non-resident-covered medical services at most teaching hospitals across the country. Any further restriction in resident work-hours likely will result in the need to hire additional hospitalists to care for patients.
Virtually all HM programs require financial support to make ends meet. The most recent SHM/MGMA compensation and productivity survey found that the average hospitalist full-time equivalent (FTE) requires a little more than $100,000 of support annually. Regardless of the employer, much of that support comes from the hospital. So it appears that hospitals with teaching programs will end up footing the bill for the new resident regulations. I expect HM programs at teaching hospitals will face pushback from hospital administrators, but hiring additional hospitalists is a cost-effective proposition—and not complying with the ACGME rules is not an option, unless your program wants to risk losing its accreditation.
If you are a hospitalist program leader at a teaching hospital, I encourage you to plan accordingly and discuss the impact of these revisions in duty-hours with your teaching program director and your hospital administration.
Communication, Comfort Zone Key to Managing Hypertensive Emergencies
I just saw a patient in our urgent-care clinic sent from an ophthalmologist’s office with newly diagnosed retinal hemorrhages in both eyes and repeated BPs of 170/115. She had no history of hypertension (HTN) and no other symptoms. Does this qualify as an emergency? I couldn’t find any literature in this regard. My sense was it was an emergency, as her vision seemed to be at risk, so I sent her to the ED for IV meds in a controlled environment. Did I overreact?
Dennis Swanson, MD
Grand Rapids, Mich.
Dr. Hospitalist responds: Thank you for your question. There are numerous potential causes of retinal hemorrhages. Aside from trauma, we most commonly see retinal hemorrhages in patients with diabetic retinopathy and/or HTN. As you know, the retina is the only part of the vasculature that we can visualize noninvasively. This is a good example of why it is always important for providers to perform a fundoscopy on every patient with newly discovered HTN.
Retinal hemorrhage is one of several ocular diseases directly related to HTN. Based on your description, it sounds as if the ophthalmologist discovered the retinal hemorrhages and sent the patient to you, given the concern that uncontrolled HTN was the cause of the hemorrhages. You stated that you sent the patient to the ED because you were concerned the patient’s vision “seemed to be at risk.” Most retinal hemorrhages are asymptomatic unless the macular is affected, in which case the patient experiences a change in their visual acuity. Progressive microvascular changes in the retina can cause a loss of visual acuity. Aside from addressing the underlying problem causing the hemorrhages, laser surgery is the typical treatment of retinal hemorrhages. The laser seals off the abnormally bleeding vessels in the retina.
It would be useful to know about any communication that occurred between you and the ophthalmologist. I imagine the ophthalmologist was going to perform laser surgery but sent the patient to the hospital to address the HTN. If you did not feel comfortable managing the patient’s HTN in the urgent-care clinic, you did the right thing by sending the patient to the ED. It also is important to note that patients with hypertensive retinopathy often have other microvascular diseases, including in the kidneys. This patient should be evaluated for any evidence of proteinuria, which can suggest progressive microvascular renal disease, also as a result of uncontrolled HTN. TH