User login
The Child With Persistent Hives
Persistent hives, or chronic urticaria, can be challenging to diagnose, treat, and manage. This condition is also somewhat common—I see it often at Miami Children's Hospital.
Persistent hives are distinctive from an acute presentation because they typically last 6 weeks or longer. They are not only frustrating for physicians—the etiology is identified in only a minority of affected children, but this disease can significantly impair quality of life for patients and their families.
Infections are a common cause of persistent hives. Other conditions to consider in your differential diagnosis include drug and food allergies, physical urticaria (caused by exposure to heat or cold), autoimmune disease, erythema multiforme minor, and dermatographism. Dermatographism is a condition in which stroking or scratching the skin with a dull instrument causes a raised welt, or wheal, to appear because of increased mast cell activation. The skin generally appears pale in the center with a red flare on either side. A physical allergy causes this type of urticaria.
In conjunction with the physical examination, review all medications taken in the last 6 weeks, including but not limited to new agents. Also ask the patient and parents about the type of foods the child consumed within the last several weeks with regularity.
A long-acting antihistamine, with 24-hour coverage, can be helpful. For some children with persistent hives, you may need to think outside the box and prescribe both a short-acting and long-acting antihistamine. The short-acting agent can be used to control an acute presentation while the long-acting drug provides maintenance.
If the condition improves with antihistamines and the hives are not interfering with quality of life or sleep, then you should feel comfortable treating the child.
If antihistamine therapy is not helpful, the lesions are interfering with lifestyle or sleep, or the patient complains of swelling, it is appropriate to refer the child to a specialist for additional work-up. Swelling is often a presenting sign with chronic urticaria, and typically it is generalized or affects the hands or face. The swelling often makes the patient and family uncomfortable.
If you decide to order laboratory testing prior to a specialist referral, a complete blood count, an erythrocyte sedimentation rate assay, a liver function test, and thyroid studies can be useful. But you also can simply refer the patient to an allergist or immunologist, and we can order the testing.
In contrast, a food-specific immunoglobulin G test is not helpful for the assessment of a child with persistent hives. This laboratory assay should not be ordered because it only adds to the cost of the diagnosis without aiding in the clinical diagnosis.
If you are fortunate and can identify the cause of the chronic urticaria—which only occurs in 5%-20% of cases—it calls for strict avoidance. This is another aspect where persistent hives differ from an acute presentation, because the etiology of an acute condition is more frequently found and subsequently may be avoided by the child.
Also educate the patient that persistent hives can be daily or episodic. Again, if the patient is lucky, the lesions resolve in less than 1 year. However, inform the patient that—in some cases—the hives can persist for several years.
Persistent hives, or chronic urticaria, can be challenging to diagnose, treat, and manage. This condition is also somewhat common—I see it often at Miami Children's Hospital.
Persistent hives are distinctive from an acute presentation because they typically last 6 weeks or longer. They are not only frustrating for physicians—the etiology is identified in only a minority of affected children, but this disease can significantly impair quality of life for patients and their families.
Infections are a common cause of persistent hives. Other conditions to consider in your differential diagnosis include drug and food allergies, physical urticaria (caused by exposure to heat or cold), autoimmune disease, erythema multiforme minor, and dermatographism. Dermatographism is a condition in which stroking or scratching the skin with a dull instrument causes a raised welt, or wheal, to appear because of increased mast cell activation. The skin generally appears pale in the center with a red flare on either side. A physical allergy causes this type of urticaria.
In conjunction with the physical examination, review all medications taken in the last 6 weeks, including but not limited to new agents. Also ask the patient and parents about the type of foods the child consumed within the last several weeks with regularity.
A long-acting antihistamine, with 24-hour coverage, can be helpful. For some children with persistent hives, you may need to think outside the box and prescribe both a short-acting and long-acting antihistamine. The short-acting agent can be used to control an acute presentation while the long-acting drug provides maintenance.
If the condition improves with antihistamines and the hives are not interfering with quality of life or sleep, then you should feel comfortable treating the child.
If antihistamine therapy is not helpful, the lesions are interfering with lifestyle or sleep, or the patient complains of swelling, it is appropriate to refer the child to a specialist for additional work-up. Swelling is often a presenting sign with chronic urticaria, and typically it is generalized or affects the hands or face. The swelling often makes the patient and family uncomfortable.
If you decide to order laboratory testing prior to a specialist referral, a complete blood count, an erythrocyte sedimentation rate assay, a liver function test, and thyroid studies can be useful. But you also can simply refer the patient to an allergist or immunologist, and we can order the testing.
In contrast, a food-specific immunoglobulin G test is not helpful for the assessment of a child with persistent hives. This laboratory assay should not be ordered because it only adds to the cost of the diagnosis without aiding in the clinical diagnosis.
If you are fortunate and can identify the cause of the chronic urticaria—which only occurs in 5%-20% of cases—it calls for strict avoidance. This is another aspect where persistent hives differ from an acute presentation, because the etiology of an acute condition is more frequently found and subsequently may be avoided by the child.
Also educate the patient that persistent hives can be daily or episodic. Again, if the patient is lucky, the lesions resolve in less than 1 year. However, inform the patient that—in some cases—the hives can persist for several years.
Persistent hives, or chronic urticaria, can be challenging to diagnose, treat, and manage. This condition is also somewhat common—I see it often at Miami Children's Hospital.
Persistent hives are distinctive from an acute presentation because they typically last 6 weeks or longer. They are not only frustrating for physicians—the etiology is identified in only a minority of affected children, but this disease can significantly impair quality of life for patients and their families.
Infections are a common cause of persistent hives. Other conditions to consider in your differential diagnosis include drug and food allergies, physical urticaria (caused by exposure to heat or cold), autoimmune disease, erythema multiforme minor, and dermatographism. Dermatographism is a condition in which stroking or scratching the skin with a dull instrument causes a raised welt, or wheal, to appear because of increased mast cell activation. The skin generally appears pale in the center with a red flare on either side. A physical allergy causes this type of urticaria.
In conjunction with the physical examination, review all medications taken in the last 6 weeks, including but not limited to new agents. Also ask the patient and parents about the type of foods the child consumed within the last several weeks with regularity.
A long-acting antihistamine, with 24-hour coverage, can be helpful. For some children with persistent hives, you may need to think outside the box and prescribe both a short-acting and long-acting antihistamine. The short-acting agent can be used to control an acute presentation while the long-acting drug provides maintenance.
If the condition improves with antihistamines and the hives are not interfering with quality of life or sleep, then you should feel comfortable treating the child.
If antihistamine therapy is not helpful, the lesions are interfering with lifestyle or sleep, or the patient complains of swelling, it is appropriate to refer the child to a specialist for additional work-up. Swelling is often a presenting sign with chronic urticaria, and typically it is generalized or affects the hands or face. The swelling often makes the patient and family uncomfortable.
If you decide to order laboratory testing prior to a specialist referral, a complete blood count, an erythrocyte sedimentation rate assay, a liver function test, and thyroid studies can be useful. But you also can simply refer the patient to an allergist or immunologist, and we can order the testing.
In contrast, a food-specific immunoglobulin G test is not helpful for the assessment of a child with persistent hives. This laboratory assay should not be ordered because it only adds to the cost of the diagnosis without aiding in the clinical diagnosis.
If you are fortunate and can identify the cause of the chronic urticaria—which only occurs in 5%-20% of cases—it calls for strict avoidance. This is another aspect where persistent hives differ from an acute presentation, because the etiology of an acute condition is more frequently found and subsequently may be avoided by the child.
Also educate the patient that persistent hives can be daily or episodic. Again, if the patient is lucky, the lesions resolve in less than 1 year. However, inform the patient that—in some cases—the hives can persist for several years.
Pediatric VTE Surge Draws Skeptical Response
In the wake of a study that showed a 70% spike in the rate of VTE in pediatric hospitals, pediatric hospitalists and others are calling for a deeper analysis of the data.
The seven-year, multicenter study measured 11,337 hospitalized patients under the age of 18. Researchers found the annual rate of VTE increased by 70%, to 58 cases from 34 cases per 10,000 (P<0.001) (Pediatrics 2009;124(4):1001-1008). Several pediatricians note that the increase looks outsized because there has been little research on the topic over the past decade. Those interviewed say they expect more research in the future to define the breadth of the problem and potential solutions.
“I don’t think we think there’s been a seven-fold increase,” says Janna Journeycake, MD, MSCS, director of the Hemophilia and Thrombosis Program at Children's Medical Center, University of Texas Southwestern Medical Center at Dallas. “It was there all along. We just didn’t know how to recognize it.”
Mark Shen, MD, medical director of hospital medicine at Dell Children’s Medical Center in Austin, Texas, and The Hospitalist's pediatric editor, attributes a large part of the study’s findings to more awareness of VTE in the pediatric community and increases in serious bone and joint infections that lead to more central lines, a risk factor for VTE. Dr. Shen also points out that as physicians learn more about pediatric VTE, it is expected that the rate of its incidence will increase. “Before, we wouldn’t look for signs of a clot unless there were physical signs of swelling, discomfort, or shortness of breath,” he adds. “Now we are much quicker to go and do an ultrasound or look for some kind of thromboembolism.”
Dr. Journeycake sees pediatric hospitalists as the vanguard in moving forward, as long as they stay vigilant to recognize the warning signs. “The job of the hospitalist is to recognize the certain medical conditions in which VTE are most likely,” she says. “They are going to be the most critically ill kids, the ones with deep-seated infection, such as osteomyelitis, mastoiditis. … Those are going to be children with central venous catheters. Hospitalists need to realize this complication exists.”
In the wake of a study that showed a 70% spike in the rate of VTE in pediatric hospitals, pediatric hospitalists and others are calling for a deeper analysis of the data.
The seven-year, multicenter study measured 11,337 hospitalized patients under the age of 18. Researchers found the annual rate of VTE increased by 70%, to 58 cases from 34 cases per 10,000 (P<0.001) (Pediatrics 2009;124(4):1001-1008). Several pediatricians note that the increase looks outsized because there has been little research on the topic over the past decade. Those interviewed say they expect more research in the future to define the breadth of the problem and potential solutions.
“I don’t think we think there’s been a seven-fold increase,” says Janna Journeycake, MD, MSCS, director of the Hemophilia and Thrombosis Program at Children's Medical Center, University of Texas Southwestern Medical Center at Dallas. “It was there all along. We just didn’t know how to recognize it.”
Mark Shen, MD, medical director of hospital medicine at Dell Children’s Medical Center in Austin, Texas, and The Hospitalist's pediatric editor, attributes a large part of the study’s findings to more awareness of VTE in the pediatric community and increases in serious bone and joint infections that lead to more central lines, a risk factor for VTE. Dr. Shen also points out that as physicians learn more about pediatric VTE, it is expected that the rate of its incidence will increase. “Before, we wouldn’t look for signs of a clot unless there were physical signs of swelling, discomfort, or shortness of breath,” he adds. “Now we are much quicker to go and do an ultrasound or look for some kind of thromboembolism.”
Dr. Journeycake sees pediatric hospitalists as the vanguard in moving forward, as long as they stay vigilant to recognize the warning signs. “The job of the hospitalist is to recognize the certain medical conditions in which VTE are most likely,” she says. “They are going to be the most critically ill kids, the ones with deep-seated infection, such as osteomyelitis, mastoiditis. … Those are going to be children with central venous catheters. Hospitalists need to realize this complication exists.”
In the wake of a study that showed a 70% spike in the rate of VTE in pediatric hospitals, pediatric hospitalists and others are calling for a deeper analysis of the data.
The seven-year, multicenter study measured 11,337 hospitalized patients under the age of 18. Researchers found the annual rate of VTE increased by 70%, to 58 cases from 34 cases per 10,000 (P<0.001) (Pediatrics 2009;124(4):1001-1008). Several pediatricians note that the increase looks outsized because there has been little research on the topic over the past decade. Those interviewed say they expect more research in the future to define the breadth of the problem and potential solutions.
“I don’t think we think there’s been a seven-fold increase,” says Janna Journeycake, MD, MSCS, director of the Hemophilia and Thrombosis Program at Children's Medical Center, University of Texas Southwestern Medical Center at Dallas. “It was there all along. We just didn’t know how to recognize it.”
Mark Shen, MD, medical director of hospital medicine at Dell Children’s Medical Center in Austin, Texas, and The Hospitalist's pediatric editor, attributes a large part of the study’s findings to more awareness of VTE in the pediatric community and increases in serious bone and joint infections that lead to more central lines, a risk factor for VTE. Dr. Shen also points out that as physicians learn more about pediatric VTE, it is expected that the rate of its incidence will increase. “Before, we wouldn’t look for signs of a clot unless there were physical signs of swelling, discomfort, or shortness of breath,” he adds. “Now we are much quicker to go and do an ultrasound or look for some kind of thromboembolism.”
Dr. Journeycake sees pediatric hospitalists as the vanguard in moving forward, as long as they stay vigilant to recognize the warning signs. “The job of the hospitalist is to recognize the certain medical conditions in which VTE are most likely,” she says. “They are going to be the most critically ill kids, the ones with deep-seated infection, such as osteomyelitis, mastoiditis. … Those are going to be children with central venous catheters. Hospitalists need to realize this complication exists.”
Prevention Prowess
Three medical centers have been nationally recognized for innovative approaches to preventing DVT and its potentially fatal complications. Central to each of the prevention strategies is a risk assessment tool that is easy to use, built directly into routine care, and linked directly to guideline-recommended choices for prophylaxis.
The North American Thrombosis Forum (NATF), in coordination with the pharmaceutical company Eisai Inc., recognized the following centers with the first DVTeamCare Hospital Award:
- The University of California at San Diego Medical Center was awarded as a representative of medical centers with more than 200 beds. The hospital embedded its VTE prevention protocol into admission, transfer, and perioperative order sets across all medical and surgical services, says Gregory A. Maynard, MD, chief of the division of hospital medicine. The protocol flags three levels of DVT risk, notes possible contraindications for a particular kind of patient, and presents a set of options for guideline-recommended prophylaxis. The protocol can be paper- or computer-based.
- The Johns Hopkins Hospital in Baltimore, also awarded as a representative for medical centers with more than 200 beds, developed a mandatory computer-based decision support system to facilitate specialty-specific risk factor assessment and the application of risk-appropriate VTE prophylaxis.
- The Washington, D.C., Veterans Affairs Medical Center won in the category representing medical centers with fewer than 200 beds. The hospital designed a seven-step process that walks providers through an evidence-based risk-factor assessment to determine appropriate thromboprophylactic therapy.
The DVTeamCare Hospital Award reflects NATF's goal of enhancing thrombosis education, prevention, diagnosis, and treatment to improve patient outcomes, says NATF Executive Director Ilene Sussman, PhD.
Dr. Maynard and his UCSD colleagues have made their DVT prophylaxis toolkit available to other hospitalists wanting to lead similar efforts in their own hospital. The toolkit is posted both on the AHRQ and SHM Web sites.
"SHM and AHRQ should feel proud about this because we were one of the first places to do this successfully at such a high level," Dr. Maynard says. "We partnered with others and with SHM to build similar toolkits. SHM built VTE prevention collaboratives that enroll hospitalist leaders and mentor them through the process of VTE prevention performance improvement, tracking results longitudinally. Divya Shroff and her group in Washington, D.C., were enrolled in that VTE prevention collaborative. Their team won an award in VTE prevention by following the road map and by coming up with a good order set for DVT prevention that could be used in their VA hospital and in many other VAs across the country. I think that speaks to the strength of the concepts that we're using."
Each of the award-winning protocols will be presented at an NATF-sponsored program April 9 at Harvard Medical School in Boston. After the presentation, the winning protocols and implementation plans will be available at www.DVTeamCareAward.com to help other hospitals enhance their efforts to prevent DVT.
Three medical centers have been nationally recognized for innovative approaches to preventing DVT and its potentially fatal complications. Central to each of the prevention strategies is a risk assessment tool that is easy to use, built directly into routine care, and linked directly to guideline-recommended choices for prophylaxis.
The North American Thrombosis Forum (NATF), in coordination with the pharmaceutical company Eisai Inc., recognized the following centers with the first DVTeamCare Hospital Award:
- The University of California at San Diego Medical Center was awarded as a representative of medical centers with more than 200 beds. The hospital embedded its VTE prevention protocol into admission, transfer, and perioperative order sets across all medical and surgical services, says Gregory A. Maynard, MD, chief of the division of hospital medicine. The protocol flags three levels of DVT risk, notes possible contraindications for a particular kind of patient, and presents a set of options for guideline-recommended prophylaxis. The protocol can be paper- or computer-based.
- The Johns Hopkins Hospital in Baltimore, also awarded as a representative for medical centers with more than 200 beds, developed a mandatory computer-based decision support system to facilitate specialty-specific risk factor assessment and the application of risk-appropriate VTE prophylaxis.
- The Washington, D.C., Veterans Affairs Medical Center won in the category representing medical centers with fewer than 200 beds. The hospital designed a seven-step process that walks providers through an evidence-based risk-factor assessment to determine appropriate thromboprophylactic therapy.
The DVTeamCare Hospital Award reflects NATF's goal of enhancing thrombosis education, prevention, diagnosis, and treatment to improve patient outcomes, says NATF Executive Director Ilene Sussman, PhD.
Dr. Maynard and his UCSD colleagues have made their DVT prophylaxis toolkit available to other hospitalists wanting to lead similar efforts in their own hospital. The toolkit is posted both on the AHRQ and SHM Web sites.
"SHM and AHRQ should feel proud about this because we were one of the first places to do this successfully at such a high level," Dr. Maynard says. "We partnered with others and with SHM to build similar toolkits. SHM built VTE prevention collaboratives that enroll hospitalist leaders and mentor them through the process of VTE prevention performance improvement, tracking results longitudinally. Divya Shroff and her group in Washington, D.C., were enrolled in that VTE prevention collaborative. Their team won an award in VTE prevention by following the road map and by coming up with a good order set for DVT prevention that could be used in their VA hospital and in many other VAs across the country. I think that speaks to the strength of the concepts that we're using."
Each of the award-winning protocols will be presented at an NATF-sponsored program April 9 at Harvard Medical School in Boston. After the presentation, the winning protocols and implementation plans will be available at www.DVTeamCareAward.com to help other hospitals enhance their efforts to prevent DVT.
Three medical centers have been nationally recognized for innovative approaches to preventing DVT and its potentially fatal complications. Central to each of the prevention strategies is a risk assessment tool that is easy to use, built directly into routine care, and linked directly to guideline-recommended choices for prophylaxis.
The North American Thrombosis Forum (NATF), in coordination with the pharmaceutical company Eisai Inc., recognized the following centers with the first DVTeamCare Hospital Award:
- The University of California at San Diego Medical Center was awarded as a representative of medical centers with more than 200 beds. The hospital embedded its VTE prevention protocol into admission, transfer, and perioperative order sets across all medical and surgical services, says Gregory A. Maynard, MD, chief of the division of hospital medicine. The protocol flags three levels of DVT risk, notes possible contraindications for a particular kind of patient, and presents a set of options for guideline-recommended prophylaxis. The protocol can be paper- or computer-based.
- The Johns Hopkins Hospital in Baltimore, also awarded as a representative for medical centers with more than 200 beds, developed a mandatory computer-based decision support system to facilitate specialty-specific risk factor assessment and the application of risk-appropriate VTE prophylaxis.
- The Washington, D.C., Veterans Affairs Medical Center won in the category representing medical centers with fewer than 200 beds. The hospital designed a seven-step process that walks providers through an evidence-based risk-factor assessment to determine appropriate thromboprophylactic therapy.
The DVTeamCare Hospital Award reflects NATF's goal of enhancing thrombosis education, prevention, diagnosis, and treatment to improve patient outcomes, says NATF Executive Director Ilene Sussman, PhD.
Dr. Maynard and his UCSD colleagues have made their DVT prophylaxis toolkit available to other hospitalists wanting to lead similar efforts in their own hospital. The toolkit is posted both on the AHRQ and SHM Web sites.
"SHM and AHRQ should feel proud about this because we were one of the first places to do this successfully at such a high level," Dr. Maynard says. "We partnered with others and with SHM to build similar toolkits. SHM built VTE prevention collaboratives that enroll hospitalist leaders and mentor them through the process of VTE prevention performance improvement, tracking results longitudinally. Divya Shroff and her group in Washington, D.C., were enrolled in that VTE prevention collaborative. Their team won an award in VTE prevention by following the road map and by coming up with a good order set for DVT prevention that could be used in their VA hospital and in many other VAs across the country. I think that speaks to the strength of the concepts that we're using."
Each of the award-winning protocols will be presented at an NATF-sponsored program April 9 at Harvard Medical School in Boston. After the presentation, the winning protocols and implementation plans will be available at www.DVTeamCareAward.com to help other hospitals enhance their efforts to prevent DVT.
Injury Predictors After Inpatient Falls
An estimated 2% to 15% of all hospitalized patients experience at least one fall.1 Approximately 30% of such falls result in injury and up to 6% may be serious in nature.1, 2 These injuries can result in pain, functional impairment, disability, or even death, and can contribute to longer lengths of stay, increased health care costs, and nursing home placement.25 As a result, inpatient falls have become a major priority for hospital quality assurance programs, and hospital risk management departments have begun to target inpatient falls as a source of legal liability.13, 6, 7 Recently, the Centers for Medicare and Medicaid Services announced that it will no longer pay for preventable complications of hospitalizations, including falls and fall‐related injury.8
Much of the literature on falls comes from community and long‐term care settings, and only a few studies have investigated falls during acute care hospitalization.3, 9, 10 From these studies, risk factors for inpatient falls have been identified and various models have been developed to predict an individual patient's risk of falling. However, unlike in the community setting, interventions to prevent falls in the acute care setting have not proven to be beneficial.11, 12 Commonly used approaches including restraints, alarms, bracelets, or having a volunteer sit with high‐risk patients have not been found to be effective.13, 14 Only 1 study found a multicomponent care plan that targeted specific risk factors in older inpatients to be associated with a reduced relative risk of recorded falls.15 Given this dearth of consistent evidence for the prevention of falls in hospitalized inpatients, the American Geriatrics Society has identified this as a gap area for future research.16
There are also limited data regarding predictors of injury after inpatient falls. A few small studies have identified potential risk factors for sustaining an injury after a fall in acute care, such as age >75 years, altered mental status, increased comorbidities, visual impairment, falls in the bathroom, and admission to a geriatric psychiatry floor.2, 5, 17 However, to our knowledge, there are no studies that have identified potential characteristics of inpatients found immediately after a fall that predict an injury. Providers who assess inpatients who have fallen need guidance on how to identify those in need of further evaluation and testing. This study sought to quantify the types and severity of injuries resulting from inpatient falls and to identify predictors of injury after a fall among a cohort of patients who fell at an urban academic medical center.
Patients and Methods
Patient Population
The study population included all inpatients on 13 medical and surgical units who experienced a fall between January 1, 2006 and December 31, 2006, while hospitalized at an 1171‐bed urban academic medical center. Telemetry, intensive care, pediatric, psychiatric, rehabilitation, and obstetrics or gynecology units were excluded from this analysis; the patients on these units are special populations that are qualitatively different than other acute care patients and have a different set of risk factor for falls and predictors of fall‐related injury. The study was approved by the institutional review board of the Mount Sinai School of Medicine.
Data Collection
Inpatient falls were identified retrospectively by review of hospital incident reports, which are most often completed by the unit nurses. In our institution, all falls generate an incident report. Using a standardized abstraction form, patient characteristics, circumstances surrounding falls, and fall‐related injuries were collected from the reports.
Laboratory data for anemia (hemoglobin < 12.0 g/dL), low albumin (<3.5 g/dL), elevated creatinine (>1.5 mg/dL), prolonged partial thromboplastin time (>35 seconds), and elevated international normalized ratio (INR > 1.3), were extracted from the patient's computerized medical record, if available. Number of days from admission to the fall, length of stay to the nearest hundredth of a day, and discharge disposition were also recorded for each patient.
Results of all radiographic studies, including x‐ray, ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI), performed within 2 weeks after the fall were obtained. The indication for the imaging study was assessed from the order given to the radiology department and from the patient's medical record. A positive finding on an imaging study was defined as evidence of intracranial hemorrhage, fracture, joint effusion, soft‐tissue swelling, or any other injury potentially caused by trauma. Fall‐related injury was defined as positive findings on any of these imaging studies that were performed as a result of the fall. Evaluation of fall‐related injuries was conducted by a reviewer blinded to the baseline patient characteristics and laboratory data.
Statistical Analyses
Baseline characteristics and risk factors of patients with and without fall‐related injuries were compared using the chi square test or Student t test as appropriate. Univariate and multivariate logistic regression were used to calculate adjusted odds ratios (ORs) for injury after an inpatient fall. The multivariate model was developed using a manual forward method. Prior research shows that patients with recurrent falls do so in the same manner and for the same reasons.2, 3, 17 Thus, analyses were performed including only the first fall episode as the outcome of interest. Analyses were performed with SPSS statistical software (SPSS Inc., Chicago, IL) using 2‐sided P values.
Results
During the study period, 513 inpatients sustained 636 falls at the Mount Sinai Medical Center. There were 54,257 admissions to the hospital with 322,670 total patient days during this time. Therefore the fall incidence rate was 1.97 falls per 1,000 patient days. Characteristics of inpatients who fell are shown in Table 1. Most patients had 1 fall episode; however, 95 patients (19%) fell multiple times (range, 2‐6 events). There were no significant differences between recurrent fallers and those who fell once with respect to baseline characteristics, injuries sustained, or discharge disposition.
| Characteristic | Number of Patients (n = 513) [number (%)] |
|---|---|
| |
| Age (years) | 70 (21‐104) |
| Age >75 years | 202 (39) |
| Male gender | 255 (50) |
| Assessed at risk of falling | |
| Yes | 378 (74) |
| No | 2 (5) |
| Unknown | 110 (21) |
| Number of falls | |
| 1 | 418 (82) |
| 2 | 78 (15) |
| 3 | 10 (2) |
| 4 | 4 (1) |
| 5 | 2 (0.4) |
| 6 | 1 (0.2) |
| Multiple falls | 95 (19) |
Fall Circumstances
The majority of patients who fell (74%) had been assessed by the nursing staff as being at risk for falling prior to the event. Overall, most falls (73%) occurred on medical rather than surgical units. The units with the most falls were geriatrics, neurology, and general medicine. Details about circumstances surrounding the falls are shown in Table 2. In most instances (71%) patients were found on the floor after the fall while less than 8% of falls were witnessed. Approximately 12% of patients received sedatives within 4 hours of falling (40% opioids, 30% benzodiazepines, 16% zolpidem, and 14% other). Laboratory values at the time of fall revealed that 70% of patients who fell were anemic, 62% had low albumin, and 19% had an elevated creatinine. Almost 20% of the patients had a prolonged partial thromboplastin time (PTT) and 18% had an elevated INR.
| Characteristic | Number of Falls (n = 513) [number (%)]* |
|---|---|
| |
| Location | |
| Medical unit | 374 (73) |
| Surgical unit | 139 (27) |
| Time | |
| Day shift (7:00 AM to 6:59 PM) | 225 (44) |
| Night shift (7:00 PM to 6:59 AM) | 282 (56) |
| Character of fall | |
| Assisted to floor | 15 (3) |
| Fall alleged | 92 (18) |
| Fall witnessed | 39 (8) |
| Found on Floor | 363 (71) |
| Unknown | 4 (<1) |
| Fall‐related activity | |
| Ambulation | 164 (32) |
| Bathroom | 122 (24) |
| Bed | 21 (4) |
| Chair | 19 (4) |
| Other/unknown | 187 (36) |
| Mental status | |
| Oriented | 274 (53) |
| Confused | 151 (29) |
| Unknown | 88 (17) |
| Activity level ordered | |
| Ambulatory | 246 (48) |
| Nonambulatory | 135 (26) |
| Unknown | 132 (26) |
| Siderails | |
| Complete | 15 (3) |
| Partial | 352 (69) |
| None | 15 (3) |
| Unknown | 126 (25) |
| Environmental obstacle | |
| None | 355 (69) |
| Wet | 20 (4) |
| Debris | 2 (<1) |
| Unknown | 136 (27) |
| Restraints | |
| Yes | 3 (<1) |
| No | 374 (73) |
| Unknown | 136 (27) |
| Sedative use | |
| Total | 64 (12) |
| Opioids | 28 (6) |
| Benzos | 21 (4) |
| Antipsychotics | 7 (1) |
| Other | 8 (2) |
| Evidence of trauma | |
| Yes | 25 (5) |
| No | 285 (56) |
| Unknown | 203 (40) |
The median number of days from patient admission until they fell was 4 days (range, 0‐134), with 70% of patients falling within the first week of admission. In general, there was no difference in fall rate by time of day, though slightly more falls (56%) occurred during the night shift (7 PM to 7 AM).
Fall‐related Outcomes
Twenty‐five patients (5%) had evidence of trauma on physical exam after the fall, including lacerations, swelling, and ecchymoses, as documented by the evaluating nurse. A total of 120 imaging procedures were ordered following the first fall; when all inpatient falls were included, 145 imaging procedures were ordered. Most imaging studies (87%) did not show significant findings. Among studies with positive findings, the most common abnormality was fracture, including 3 hip, 1 humeral, 1 vertebral, 1 nasal, and 1 rib fracture. Other injuries found on imaging studies included 1 subdural hematoma, 1 acute cerebral infarct, 2 soft‐tissue hematomas, and 2 knee effusions. The acute cerebral infarct was not considered to be a result of the fall. Additionally, 3 patients had soft‐tissue swelling noted on head CT and 1 had Foley catheter‐related trauma.
The average length of stay for the 513 inpatients who fell was 20 days (range, 7‐444) compared to 6 days for all patients admitted to the hospital during the same period. Among inpatients who fell, there was no statistical difference in length of stay between those who did and those who did not have a fall‐related injury found on imaging. More than one‐half (53%) of the patients who fell were discharged to home, 21% to rehabilitation facilities, 12% to nursing homes, and 9% died during the hospitalization.
Results of Univariate Analysis
Univariate predictors of injury after a fall are shown in Table 3. Patients having evidence of trauma indicated by the evaluating nurse after a fall had an increased risk for having an abnormal imaging study (OR = 14.7, P < 0.001). Having an activity level of ambulatory ordered by the provider (OR = 2.5, P = 0.09), falling during the night shift (OR = 2.5, P = 0.11), having ambulation as the fall‐related activity (OR = 2.2, P = 0.12), and older age (P = 0.19) all showed a trend toward higher rates of injury being found after a fall. There was no significant association between fall‐related injury and being an elderly patient (age > 75 years), sedative use, falling in the bathroom, or having an elevated PTT or INR.
| Variable | Patients without injury (n = 497) [number (%)] | Patients with injury (n = 16) [number (%)] | OR | P Value |
|---|---|---|---|---|
| ||||
| Elderly | 195 (39) | 7 (44) | 1.2 | 0.72 |
| Gender male | 245 (49) | 10 (63) | 1.7 | 0.30 |
| Location surgical unit | 142 (29) | 6 (38) | 1.5 | 0.44 |
| At risk of falling prior to event | 365 (73) | 13 (8) | 1.6 | 0.49 |
| Protocol in place | 338 (68) | 11 (69) | 1.0 | 0.95 |
| Activity level ambulatory | 235 (47) | 11 (69) | 2.5 | 0.09 |
| Occurrence on night shift | 270 (54) | 12 (75) | 2.5 | 0.11 |
| Restraint use | 3 (1) | 0 (0) | ||
| Sedative within 4 hours | 61 (12) | 3 (19) | 1.6 | 0.44 |
| Fall related to ambulation | 156 (31) | 8 (50) | 2.2 | 0.12 |
| Evidence of trauma | 19 (4) | 6 (38) | 14.7 | <0.001 |
| Prolonged PTT | 93 (19) | 5 (31) | 1.9 | 0.29 |
| Elevated INR | 90 (18) | 3 (19) | 1.0 | 0.96 |
| Anemia | 351 (71) | 9 (56) | 0.6 | 0.32 |
| Elevated creatinine | 97 (20) | 2 (13) | 0.7 | 0.60 |
| Low albumin | 309 (62) | 8 (50) | 1.6 | 0.58 |
Multivariate Predictors of Injury
In multivariate analysis, after adjusting for age and sex, evidence of trauma after a fall (OR = 24.6, P < 0.001) and having an activity level of ambulatory ordered by the provider (OR = 7.3, P = 0.01) were independent predictors of injury being found on imaging studies (Table 4). Analyses limited to the 120 patients who had imaging found that the association between evidence of trauma (OR = 6.22, P = 0.02) and having an activity level of ambulatory ordered (OR = 5.53, P = 0.04) remained statistically significant.
| Variable | All Patients (n = 513) | Patients with Imaging (n = 120)* | ||
|---|---|---|---|---|
| OR | P Value | OR | P Value | |
| ||||
| Age | 1.03 | 0.17 | 1.016 | 0.52 |
| Gender | 3.19 | 0.11 | 2.843 | 0.17 |
| Evidence of trauma | 24.63 | <0.001 | 6.22 | 0.02 |
| Activity level ambulatory | 7.33 | 0.01 | 5.53 | 0.04 |
Discussion
Inpatient falls are common and result in significant patient morbidity and increased healthcare costs. Falls in the acute care setting have also proven to be difficult to prevent and as a result have become a priority for patient safety and hospital quality.
Our study confirms that a high percentage of patients with an initial fall will have recurrent falls.1 Additionally, the majority of patients in this cohort fell despite having been assessed as at risk for falling prior to the event. The types of injuries sustained after inpatient falls (eg, subdural hematoma, multiple fractures, joint effusions, other hematomas, and soft‐tissue swelling) are similar to those found by other authors.2, 3, 17, 18
In this study, inpatient falls were associated with an almost 2‐week increase in length of stay. Though we cannot say that this was directly due to falls, and an increased length of stay may just be a marker of severity of illness, this association warrants further study, perhaps with a matched control group of patients who did not fall, and has implications for healthcare cost containment.
We found that having evidence of trauma after a fall and having an activity level of ambulatory ordered by the provider were independent predictors of injury being found after an inpatient fall. It seems intuitive that patients who have physical evidence of trauma, such as lacerations or bruising, would be more likely to have an underlying injury. Clinically, this confirms that providers should have a high index of suspicion for injury being found on imaging studies in such patients. Similar findings have been noted in the emergency medicine literature that further support the validity of our findings.19
Less clear are the reasons for the observed association between having an activity level of ambulatory ordered and higher risk of injury after an inpatient fall. Prior studies have found that ambulatory inpatients are less likely to use assistive devices that they use at home while hospitalized and are less likely to call for help; these factors may contribute to falls.2, 3 However, the interpretation of this finding is limited by the fact that 26% of the patients who fell had an unknown activity level ordered.
Altered mental status, comorbidity, age > 75 years, visual impairment, falling in the bathroom, and being on a geriatric psychiatry floor have previously been found to be risk factors for sustaining an injury after an inpatient fall.2, 5, 17 Conversely, this study did not find altered mental status to be a significant predictor of injury. One reason may be that this was subjectively determined by the evaluating nurse and not by a standardized measure of cognitive impairment. Patients who are oriented may also be more likely to report unwitnessed falls and injuries than patients with altered mental status.3
There was also no association between age and fall‐related injury in our cohort. On univariate analysis, patients who were older in age were more likely to have an injury found after an inpatient fall but this was not statistically significant. Previous authors have suggested that today's inpatients are increasingly ill and may have risk factors for falls and injuries that are independent of age, such as multiple comorbid conditions or deconditioning.3
We hypothesized that patients who are anticoagulated and had an elevated INR or PTT would be more likely to sustain an injury. Anemic inpatients have also been found to be at increased risk of falls.20 We found no significant association between fall‐related injury being found on imaging studies and anemia, low albumin, elevated creatinine, prolonged PTT, or elevated INR. Not every patient who fell had these laboratory values available. However, even when only inpatients who fell and had laboratory tests were included in the analysis, there was still no association with fall‐related injury.
This study has several limitations. First, a low number of serious injuries was found on imaging studies after inpatient falls in this cohort; this limited the power of the study to identify predictors of fall‐related injury.
Second, fall‐related injury was defined as a positive finding on imaging studies within 2 weeks of an inpatient fall. Thus, some fall‐related injuries may have been missed in patients who did not have imaging. However, any patient who had a serious injury after a fall and remained hospitalized would likely have had symptoms such as pain or altered mental status that would have led to an imaging study. Moreover, the analysis was repeated including only inpatients who fell and had imaging, and the association between having evidence of trauma and having an activity level of ambulatory ordered and sustaining a fall‐related injury remained significant.
Third, we relied on hospital incident reports to identify inpatient falls. These reports yield a limited amount of information and may be inaccurate or incomplete. A recent study also raised concern that incident reports significantly underreport actual fall incidence.21 However, previous studies have found no indication that falls are underreported and suggest that incident reports are an established custom in hospital culture.1, 22 Medical staff are aware that administrators want to keep track of hospital fall rates for both quality improvement and documentation for risk management.1, 22 It is unlikely that severe falls or falls leading to serious injury are not reported. A different source of underreporting may actually be failure of patients to tell the medical team about an unwitnessed fall. Older patients may be concerned they will be placed in nursing homes and those with memory loss may forget to report a minor fall. Education of patients and family members could improve reporting of inpatient falls and further our understanding of contributing factors.
Finally, although the evaluation of fall‐related injuries was conducted by a blinded reviewer, the potential for bias does exist among even the best‐intentioned reviewers. Additionally, there may be some degree of variability within the reviewer's data abstraction.
This study adds valuable information about the epidemiology of inpatient falls at large, urban, tertiary‐care academic medical centers, including characteristics of patients who fell, circumstances surrounding falls, injuries sustained, and predictors of fall‐related injury found on imaging. Although additional research is essential to identify methods to effectively prevent inpatient falls, this study contributes to the limited data in this area, can guide providers who are evaluating inpatients who have fallen, and may be used to design future investigations. It is imperative that measures are identified to avoid the frequent adverse outcomes that result from inpatient falls. Insurance companies, hospital administrators, patients, and providers will be demanding that a safe environment be a key component of quality of care measures.
This study draws attention to the scope of the problem at our institution that is common to hospitals across the country. In our study, our academic medical center had a fall rate consistent with published reports, but new efforts have been focused on quality improvement in this area. An interdisciplinary fall prevention committee has been formed that includes physicians, nurses, patient care assistants, physical therapists, pharmacists, and representatives from information technology (IT). Currently, a program of a fall risk‐factor assessment with targeted interventions to reduce those risk factors is being developed for all high‐risk patients and will be piloted on inpatient units.
Acknowledgements
The authors thank Susan Emro, BS, Department of Health Policy, Susan Davis, MS, MPH, RN, CNAA, Department of Nursing, and Albert Siu, MD, MSPH, Brookdale Department of Geriatrics and Adult Development, for their review of this article. Author contributions were as followsconception and design: S.M.B, R.K., and T.M.; collection and assembly of data: S.M.B.; analysis and interpretation of the data: S.M.B, R.K., and J.W.; drafting of the article: S.M.B.; critical revision of the article for important intellectual content: R.K. and J.W.; final approval of the article: S.M.B, R.K., and J.W.; statistical expertise: J.W.; obtaining of funding: S.M.B.
- ,,,.Risk of falls for hospitalized patients: a predictive model based on routinely available data.J Clin Epidemiol.2001;54(12):1258–1266.
- ,,, et al.A case‐control study of patient, medication, and care‐related risk factors for inpatient falls.J Gen Intern Med.2005;20(2):116–122.
- ,,, et al.Characteristics and circumstances of falls in a hospital setting: a prospective analysis.J Gen Intern Med.2004;19(7):732–739.
- ,,,.Falls and consequent injuries in hospitalized patients: effects of an interdisciplinary falls prevention program.BMC Health Serv Res.2006;6:69.
- ,,,.Serious falls in hospitalized patients: correlates and resource utilization.Am J Med.1995;99(2):137–143.
- ,.Using tools to assess and prevent inpatient falls.Jt Comm J Qual Saf.2003;29(7):363–368.
- ,,.Incidence and risk factors for inpatient falls in an academic acute‐care hospital.J Nippon Med Sch.2006;73(5):265–270.
- .Nonpayment for performance? Medicare's new reimbursement rule.N Engl J Med.2007;357(16):1573–1575.
- .Clinical practice. preventing falls in elderly persons.N Engl J Med.2003;348(1):42–49.
- .Building the science of falls‐prevention research.J Am Geriatr Soc.2004;52(3):461–462.
- ,,,,,.Interventions for preventing falls in acute‐ and chronic‐care hospitals: a systematic review and meta‐analysis.J Am Geriatr Soc.2008;56(1):29–36.
- ,,, et al.Interventions for the prevention of falls in older adults: systematic review and meta‐analysis of randomised clinical trials.BMJ.2004;328(7441):680.
- ,,, et al.Acceptability of fall prevention measures for hospital inpatients.Age Ageing.2004;33(4):400–401.
- ,,, et al.Can volunteer companions prevent falls among inpatients? A feasibility study using a pre‐post comparative design.BMC Geriatr.2006;6:11.
- ,,,,.Using targeted risk factor reduction to prevent falls in older in‐patients: a randomised controlled trial.Age Ageing.2004;33(4):390–395.
- .Prevention of falls in hospital inpatients: agendas for research and practice.Age Ageing.2004;33(4):328–330.
- ,,, et al.Patterns and predictors of inpatient falls and fall‐related injuries in a large academic hospital.Infect Control Hosp Epidemiol.2005;26(10):822–827.
- ,,,,.The relationship of falls to injury among hospital in‐patients.Int J Clin Pract.2005;59(1):17–20.
- ,,,,,.Indications for computed tomography in patients with minor head injury.N Engl J Med.2000;343(2):100–105.
- ,,.Anemia increases risk for falls in hospitalized older adults: an evaluation of falls in 362 hospitalized, ambulatory, long‐term care, and community patients.J Am Med Dir Assoc.2006;7(5):287–293.
- ,,,,,.Improving the capture of fall events in hospitals: combining a service for evaluating inpatient falls with an incident report system.J Am Geriatr Soc.2008;56(4):701–704.
- ,,, et al.Attitudes and barriers to incident reporting: a collaborative hospital study.Qual Saf Health Care.2006;15(1):39–43.
An estimated 2% to 15% of all hospitalized patients experience at least one fall.1 Approximately 30% of such falls result in injury and up to 6% may be serious in nature.1, 2 These injuries can result in pain, functional impairment, disability, or even death, and can contribute to longer lengths of stay, increased health care costs, and nursing home placement.25 As a result, inpatient falls have become a major priority for hospital quality assurance programs, and hospital risk management departments have begun to target inpatient falls as a source of legal liability.13, 6, 7 Recently, the Centers for Medicare and Medicaid Services announced that it will no longer pay for preventable complications of hospitalizations, including falls and fall‐related injury.8
Much of the literature on falls comes from community and long‐term care settings, and only a few studies have investigated falls during acute care hospitalization.3, 9, 10 From these studies, risk factors for inpatient falls have been identified and various models have been developed to predict an individual patient's risk of falling. However, unlike in the community setting, interventions to prevent falls in the acute care setting have not proven to be beneficial.11, 12 Commonly used approaches including restraints, alarms, bracelets, or having a volunteer sit with high‐risk patients have not been found to be effective.13, 14 Only 1 study found a multicomponent care plan that targeted specific risk factors in older inpatients to be associated with a reduced relative risk of recorded falls.15 Given this dearth of consistent evidence for the prevention of falls in hospitalized inpatients, the American Geriatrics Society has identified this as a gap area for future research.16
There are also limited data regarding predictors of injury after inpatient falls. A few small studies have identified potential risk factors for sustaining an injury after a fall in acute care, such as age >75 years, altered mental status, increased comorbidities, visual impairment, falls in the bathroom, and admission to a geriatric psychiatry floor.2, 5, 17 However, to our knowledge, there are no studies that have identified potential characteristics of inpatients found immediately after a fall that predict an injury. Providers who assess inpatients who have fallen need guidance on how to identify those in need of further evaluation and testing. This study sought to quantify the types and severity of injuries resulting from inpatient falls and to identify predictors of injury after a fall among a cohort of patients who fell at an urban academic medical center.
Patients and Methods
Patient Population
The study population included all inpatients on 13 medical and surgical units who experienced a fall between January 1, 2006 and December 31, 2006, while hospitalized at an 1171‐bed urban academic medical center. Telemetry, intensive care, pediatric, psychiatric, rehabilitation, and obstetrics or gynecology units were excluded from this analysis; the patients on these units are special populations that are qualitatively different than other acute care patients and have a different set of risk factor for falls and predictors of fall‐related injury. The study was approved by the institutional review board of the Mount Sinai School of Medicine.
Data Collection
Inpatient falls were identified retrospectively by review of hospital incident reports, which are most often completed by the unit nurses. In our institution, all falls generate an incident report. Using a standardized abstraction form, patient characteristics, circumstances surrounding falls, and fall‐related injuries were collected from the reports.
Laboratory data for anemia (hemoglobin < 12.0 g/dL), low albumin (<3.5 g/dL), elevated creatinine (>1.5 mg/dL), prolonged partial thromboplastin time (>35 seconds), and elevated international normalized ratio (INR > 1.3), were extracted from the patient's computerized medical record, if available. Number of days from admission to the fall, length of stay to the nearest hundredth of a day, and discharge disposition were also recorded for each patient.
Results of all radiographic studies, including x‐ray, ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI), performed within 2 weeks after the fall were obtained. The indication for the imaging study was assessed from the order given to the radiology department and from the patient's medical record. A positive finding on an imaging study was defined as evidence of intracranial hemorrhage, fracture, joint effusion, soft‐tissue swelling, or any other injury potentially caused by trauma. Fall‐related injury was defined as positive findings on any of these imaging studies that were performed as a result of the fall. Evaluation of fall‐related injuries was conducted by a reviewer blinded to the baseline patient characteristics and laboratory data.
Statistical Analyses
Baseline characteristics and risk factors of patients with and without fall‐related injuries were compared using the chi square test or Student t test as appropriate. Univariate and multivariate logistic regression were used to calculate adjusted odds ratios (ORs) for injury after an inpatient fall. The multivariate model was developed using a manual forward method. Prior research shows that patients with recurrent falls do so in the same manner and for the same reasons.2, 3, 17 Thus, analyses were performed including only the first fall episode as the outcome of interest. Analyses were performed with SPSS statistical software (SPSS Inc., Chicago, IL) using 2‐sided P values.
Results
During the study period, 513 inpatients sustained 636 falls at the Mount Sinai Medical Center. There were 54,257 admissions to the hospital with 322,670 total patient days during this time. Therefore the fall incidence rate was 1.97 falls per 1,000 patient days. Characteristics of inpatients who fell are shown in Table 1. Most patients had 1 fall episode; however, 95 patients (19%) fell multiple times (range, 2‐6 events). There were no significant differences between recurrent fallers and those who fell once with respect to baseline characteristics, injuries sustained, or discharge disposition.
| Characteristic | Number of Patients (n = 513) [number (%)] |
|---|---|
| |
| Age (years) | 70 (21‐104) |
| Age >75 years | 202 (39) |
| Male gender | 255 (50) |
| Assessed at risk of falling | |
| Yes | 378 (74) |
| No | 2 (5) |
| Unknown | 110 (21) |
| Number of falls | |
| 1 | 418 (82) |
| 2 | 78 (15) |
| 3 | 10 (2) |
| 4 | 4 (1) |
| 5 | 2 (0.4) |
| 6 | 1 (0.2) |
| Multiple falls | 95 (19) |
Fall Circumstances
The majority of patients who fell (74%) had been assessed by the nursing staff as being at risk for falling prior to the event. Overall, most falls (73%) occurred on medical rather than surgical units. The units with the most falls were geriatrics, neurology, and general medicine. Details about circumstances surrounding the falls are shown in Table 2. In most instances (71%) patients were found on the floor after the fall while less than 8% of falls were witnessed. Approximately 12% of patients received sedatives within 4 hours of falling (40% opioids, 30% benzodiazepines, 16% zolpidem, and 14% other). Laboratory values at the time of fall revealed that 70% of patients who fell were anemic, 62% had low albumin, and 19% had an elevated creatinine. Almost 20% of the patients had a prolonged partial thromboplastin time (PTT) and 18% had an elevated INR.
| Characteristic | Number of Falls (n = 513) [number (%)]* |
|---|---|
| |
| Location | |
| Medical unit | 374 (73) |
| Surgical unit | 139 (27) |
| Time | |
| Day shift (7:00 AM to 6:59 PM) | 225 (44) |
| Night shift (7:00 PM to 6:59 AM) | 282 (56) |
| Character of fall | |
| Assisted to floor | 15 (3) |
| Fall alleged | 92 (18) |
| Fall witnessed | 39 (8) |
| Found on Floor | 363 (71) |
| Unknown | 4 (<1) |
| Fall‐related activity | |
| Ambulation | 164 (32) |
| Bathroom | 122 (24) |
| Bed | 21 (4) |
| Chair | 19 (4) |
| Other/unknown | 187 (36) |
| Mental status | |
| Oriented | 274 (53) |
| Confused | 151 (29) |
| Unknown | 88 (17) |
| Activity level ordered | |
| Ambulatory | 246 (48) |
| Nonambulatory | 135 (26) |
| Unknown | 132 (26) |
| Siderails | |
| Complete | 15 (3) |
| Partial | 352 (69) |
| None | 15 (3) |
| Unknown | 126 (25) |
| Environmental obstacle | |
| None | 355 (69) |
| Wet | 20 (4) |
| Debris | 2 (<1) |
| Unknown | 136 (27) |
| Restraints | |
| Yes | 3 (<1) |
| No | 374 (73) |
| Unknown | 136 (27) |
| Sedative use | |
| Total | 64 (12) |
| Opioids | 28 (6) |
| Benzos | 21 (4) |
| Antipsychotics | 7 (1) |
| Other | 8 (2) |
| Evidence of trauma | |
| Yes | 25 (5) |
| No | 285 (56) |
| Unknown | 203 (40) |
The median number of days from patient admission until they fell was 4 days (range, 0‐134), with 70% of patients falling within the first week of admission. In general, there was no difference in fall rate by time of day, though slightly more falls (56%) occurred during the night shift (7 PM to 7 AM).
Fall‐related Outcomes
Twenty‐five patients (5%) had evidence of trauma on physical exam after the fall, including lacerations, swelling, and ecchymoses, as documented by the evaluating nurse. A total of 120 imaging procedures were ordered following the first fall; when all inpatient falls were included, 145 imaging procedures were ordered. Most imaging studies (87%) did not show significant findings. Among studies with positive findings, the most common abnormality was fracture, including 3 hip, 1 humeral, 1 vertebral, 1 nasal, and 1 rib fracture. Other injuries found on imaging studies included 1 subdural hematoma, 1 acute cerebral infarct, 2 soft‐tissue hematomas, and 2 knee effusions. The acute cerebral infarct was not considered to be a result of the fall. Additionally, 3 patients had soft‐tissue swelling noted on head CT and 1 had Foley catheter‐related trauma.
The average length of stay for the 513 inpatients who fell was 20 days (range, 7‐444) compared to 6 days for all patients admitted to the hospital during the same period. Among inpatients who fell, there was no statistical difference in length of stay between those who did and those who did not have a fall‐related injury found on imaging. More than one‐half (53%) of the patients who fell were discharged to home, 21% to rehabilitation facilities, 12% to nursing homes, and 9% died during the hospitalization.
Results of Univariate Analysis
Univariate predictors of injury after a fall are shown in Table 3. Patients having evidence of trauma indicated by the evaluating nurse after a fall had an increased risk for having an abnormal imaging study (OR = 14.7, P < 0.001). Having an activity level of ambulatory ordered by the provider (OR = 2.5, P = 0.09), falling during the night shift (OR = 2.5, P = 0.11), having ambulation as the fall‐related activity (OR = 2.2, P = 0.12), and older age (P = 0.19) all showed a trend toward higher rates of injury being found after a fall. There was no significant association between fall‐related injury and being an elderly patient (age > 75 years), sedative use, falling in the bathroom, or having an elevated PTT or INR.
| Variable | Patients without injury (n = 497) [number (%)] | Patients with injury (n = 16) [number (%)] | OR | P Value |
|---|---|---|---|---|
| ||||
| Elderly | 195 (39) | 7 (44) | 1.2 | 0.72 |
| Gender male | 245 (49) | 10 (63) | 1.7 | 0.30 |
| Location surgical unit | 142 (29) | 6 (38) | 1.5 | 0.44 |
| At risk of falling prior to event | 365 (73) | 13 (8) | 1.6 | 0.49 |
| Protocol in place | 338 (68) | 11 (69) | 1.0 | 0.95 |
| Activity level ambulatory | 235 (47) | 11 (69) | 2.5 | 0.09 |
| Occurrence on night shift | 270 (54) | 12 (75) | 2.5 | 0.11 |
| Restraint use | 3 (1) | 0 (0) | ||
| Sedative within 4 hours | 61 (12) | 3 (19) | 1.6 | 0.44 |
| Fall related to ambulation | 156 (31) | 8 (50) | 2.2 | 0.12 |
| Evidence of trauma | 19 (4) | 6 (38) | 14.7 | <0.001 |
| Prolonged PTT | 93 (19) | 5 (31) | 1.9 | 0.29 |
| Elevated INR | 90 (18) | 3 (19) | 1.0 | 0.96 |
| Anemia | 351 (71) | 9 (56) | 0.6 | 0.32 |
| Elevated creatinine | 97 (20) | 2 (13) | 0.7 | 0.60 |
| Low albumin | 309 (62) | 8 (50) | 1.6 | 0.58 |
Multivariate Predictors of Injury
In multivariate analysis, after adjusting for age and sex, evidence of trauma after a fall (OR = 24.6, P < 0.001) and having an activity level of ambulatory ordered by the provider (OR = 7.3, P = 0.01) were independent predictors of injury being found on imaging studies (Table 4). Analyses limited to the 120 patients who had imaging found that the association between evidence of trauma (OR = 6.22, P = 0.02) and having an activity level of ambulatory ordered (OR = 5.53, P = 0.04) remained statistically significant.
| Variable | All Patients (n = 513) | Patients with Imaging (n = 120)* | ||
|---|---|---|---|---|
| OR | P Value | OR | P Value | |
| ||||
| Age | 1.03 | 0.17 | 1.016 | 0.52 |
| Gender | 3.19 | 0.11 | 2.843 | 0.17 |
| Evidence of trauma | 24.63 | <0.001 | 6.22 | 0.02 |
| Activity level ambulatory | 7.33 | 0.01 | 5.53 | 0.04 |
Discussion
Inpatient falls are common and result in significant patient morbidity and increased healthcare costs. Falls in the acute care setting have also proven to be difficult to prevent and as a result have become a priority for patient safety and hospital quality.
Our study confirms that a high percentage of patients with an initial fall will have recurrent falls.1 Additionally, the majority of patients in this cohort fell despite having been assessed as at risk for falling prior to the event. The types of injuries sustained after inpatient falls (eg, subdural hematoma, multiple fractures, joint effusions, other hematomas, and soft‐tissue swelling) are similar to those found by other authors.2, 3, 17, 18
In this study, inpatient falls were associated with an almost 2‐week increase in length of stay. Though we cannot say that this was directly due to falls, and an increased length of stay may just be a marker of severity of illness, this association warrants further study, perhaps with a matched control group of patients who did not fall, and has implications for healthcare cost containment.
We found that having evidence of trauma after a fall and having an activity level of ambulatory ordered by the provider were independent predictors of injury being found after an inpatient fall. It seems intuitive that patients who have physical evidence of trauma, such as lacerations or bruising, would be more likely to have an underlying injury. Clinically, this confirms that providers should have a high index of suspicion for injury being found on imaging studies in such patients. Similar findings have been noted in the emergency medicine literature that further support the validity of our findings.19
Less clear are the reasons for the observed association between having an activity level of ambulatory ordered and higher risk of injury after an inpatient fall. Prior studies have found that ambulatory inpatients are less likely to use assistive devices that they use at home while hospitalized and are less likely to call for help; these factors may contribute to falls.2, 3 However, the interpretation of this finding is limited by the fact that 26% of the patients who fell had an unknown activity level ordered.
Altered mental status, comorbidity, age > 75 years, visual impairment, falling in the bathroom, and being on a geriatric psychiatry floor have previously been found to be risk factors for sustaining an injury after an inpatient fall.2, 5, 17 Conversely, this study did not find altered mental status to be a significant predictor of injury. One reason may be that this was subjectively determined by the evaluating nurse and not by a standardized measure of cognitive impairment. Patients who are oriented may also be more likely to report unwitnessed falls and injuries than patients with altered mental status.3
There was also no association between age and fall‐related injury in our cohort. On univariate analysis, patients who were older in age were more likely to have an injury found after an inpatient fall but this was not statistically significant. Previous authors have suggested that today's inpatients are increasingly ill and may have risk factors for falls and injuries that are independent of age, such as multiple comorbid conditions or deconditioning.3
We hypothesized that patients who are anticoagulated and had an elevated INR or PTT would be more likely to sustain an injury. Anemic inpatients have also been found to be at increased risk of falls.20 We found no significant association between fall‐related injury being found on imaging studies and anemia, low albumin, elevated creatinine, prolonged PTT, or elevated INR. Not every patient who fell had these laboratory values available. However, even when only inpatients who fell and had laboratory tests were included in the analysis, there was still no association with fall‐related injury.
This study has several limitations. First, a low number of serious injuries was found on imaging studies after inpatient falls in this cohort; this limited the power of the study to identify predictors of fall‐related injury.
Second, fall‐related injury was defined as a positive finding on imaging studies within 2 weeks of an inpatient fall. Thus, some fall‐related injuries may have been missed in patients who did not have imaging. However, any patient who had a serious injury after a fall and remained hospitalized would likely have had symptoms such as pain or altered mental status that would have led to an imaging study. Moreover, the analysis was repeated including only inpatients who fell and had imaging, and the association between having evidence of trauma and having an activity level of ambulatory ordered and sustaining a fall‐related injury remained significant.
Third, we relied on hospital incident reports to identify inpatient falls. These reports yield a limited amount of information and may be inaccurate or incomplete. A recent study also raised concern that incident reports significantly underreport actual fall incidence.21 However, previous studies have found no indication that falls are underreported and suggest that incident reports are an established custom in hospital culture.1, 22 Medical staff are aware that administrators want to keep track of hospital fall rates for both quality improvement and documentation for risk management.1, 22 It is unlikely that severe falls or falls leading to serious injury are not reported. A different source of underreporting may actually be failure of patients to tell the medical team about an unwitnessed fall. Older patients may be concerned they will be placed in nursing homes and those with memory loss may forget to report a minor fall. Education of patients and family members could improve reporting of inpatient falls and further our understanding of contributing factors.
Finally, although the evaluation of fall‐related injuries was conducted by a blinded reviewer, the potential for bias does exist among even the best‐intentioned reviewers. Additionally, there may be some degree of variability within the reviewer's data abstraction.
This study adds valuable information about the epidemiology of inpatient falls at large, urban, tertiary‐care academic medical centers, including characteristics of patients who fell, circumstances surrounding falls, injuries sustained, and predictors of fall‐related injury found on imaging. Although additional research is essential to identify methods to effectively prevent inpatient falls, this study contributes to the limited data in this area, can guide providers who are evaluating inpatients who have fallen, and may be used to design future investigations. It is imperative that measures are identified to avoid the frequent adverse outcomes that result from inpatient falls. Insurance companies, hospital administrators, patients, and providers will be demanding that a safe environment be a key component of quality of care measures.
This study draws attention to the scope of the problem at our institution that is common to hospitals across the country. In our study, our academic medical center had a fall rate consistent with published reports, but new efforts have been focused on quality improvement in this area. An interdisciplinary fall prevention committee has been formed that includes physicians, nurses, patient care assistants, physical therapists, pharmacists, and representatives from information technology (IT). Currently, a program of a fall risk‐factor assessment with targeted interventions to reduce those risk factors is being developed for all high‐risk patients and will be piloted on inpatient units.
Acknowledgements
The authors thank Susan Emro, BS, Department of Health Policy, Susan Davis, MS, MPH, RN, CNAA, Department of Nursing, and Albert Siu, MD, MSPH, Brookdale Department of Geriatrics and Adult Development, for their review of this article. Author contributions were as followsconception and design: S.M.B, R.K., and T.M.; collection and assembly of data: S.M.B.; analysis and interpretation of the data: S.M.B, R.K., and J.W.; drafting of the article: S.M.B.; critical revision of the article for important intellectual content: R.K. and J.W.; final approval of the article: S.M.B, R.K., and J.W.; statistical expertise: J.W.; obtaining of funding: S.M.B.
An estimated 2% to 15% of all hospitalized patients experience at least one fall.1 Approximately 30% of such falls result in injury and up to 6% may be serious in nature.1, 2 These injuries can result in pain, functional impairment, disability, or even death, and can contribute to longer lengths of stay, increased health care costs, and nursing home placement.25 As a result, inpatient falls have become a major priority for hospital quality assurance programs, and hospital risk management departments have begun to target inpatient falls as a source of legal liability.13, 6, 7 Recently, the Centers for Medicare and Medicaid Services announced that it will no longer pay for preventable complications of hospitalizations, including falls and fall‐related injury.8
Much of the literature on falls comes from community and long‐term care settings, and only a few studies have investigated falls during acute care hospitalization.3, 9, 10 From these studies, risk factors for inpatient falls have been identified and various models have been developed to predict an individual patient's risk of falling. However, unlike in the community setting, interventions to prevent falls in the acute care setting have not proven to be beneficial.11, 12 Commonly used approaches including restraints, alarms, bracelets, or having a volunteer sit with high‐risk patients have not been found to be effective.13, 14 Only 1 study found a multicomponent care plan that targeted specific risk factors in older inpatients to be associated with a reduced relative risk of recorded falls.15 Given this dearth of consistent evidence for the prevention of falls in hospitalized inpatients, the American Geriatrics Society has identified this as a gap area for future research.16
There are also limited data regarding predictors of injury after inpatient falls. A few small studies have identified potential risk factors for sustaining an injury after a fall in acute care, such as age >75 years, altered mental status, increased comorbidities, visual impairment, falls in the bathroom, and admission to a geriatric psychiatry floor.2, 5, 17 However, to our knowledge, there are no studies that have identified potential characteristics of inpatients found immediately after a fall that predict an injury. Providers who assess inpatients who have fallen need guidance on how to identify those in need of further evaluation and testing. This study sought to quantify the types and severity of injuries resulting from inpatient falls and to identify predictors of injury after a fall among a cohort of patients who fell at an urban academic medical center.
Patients and Methods
Patient Population
The study population included all inpatients on 13 medical and surgical units who experienced a fall between January 1, 2006 and December 31, 2006, while hospitalized at an 1171‐bed urban academic medical center. Telemetry, intensive care, pediatric, psychiatric, rehabilitation, and obstetrics or gynecology units were excluded from this analysis; the patients on these units are special populations that are qualitatively different than other acute care patients and have a different set of risk factor for falls and predictors of fall‐related injury. The study was approved by the institutional review board of the Mount Sinai School of Medicine.
Data Collection
Inpatient falls were identified retrospectively by review of hospital incident reports, which are most often completed by the unit nurses. In our institution, all falls generate an incident report. Using a standardized abstraction form, patient characteristics, circumstances surrounding falls, and fall‐related injuries were collected from the reports.
Laboratory data for anemia (hemoglobin < 12.0 g/dL), low albumin (<3.5 g/dL), elevated creatinine (>1.5 mg/dL), prolonged partial thromboplastin time (>35 seconds), and elevated international normalized ratio (INR > 1.3), were extracted from the patient's computerized medical record, if available. Number of days from admission to the fall, length of stay to the nearest hundredth of a day, and discharge disposition were also recorded for each patient.
Results of all radiographic studies, including x‐ray, ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI), performed within 2 weeks after the fall were obtained. The indication for the imaging study was assessed from the order given to the radiology department and from the patient's medical record. A positive finding on an imaging study was defined as evidence of intracranial hemorrhage, fracture, joint effusion, soft‐tissue swelling, or any other injury potentially caused by trauma. Fall‐related injury was defined as positive findings on any of these imaging studies that were performed as a result of the fall. Evaluation of fall‐related injuries was conducted by a reviewer blinded to the baseline patient characteristics and laboratory data.
Statistical Analyses
Baseline characteristics and risk factors of patients with and without fall‐related injuries were compared using the chi square test or Student t test as appropriate. Univariate and multivariate logistic regression were used to calculate adjusted odds ratios (ORs) for injury after an inpatient fall. The multivariate model was developed using a manual forward method. Prior research shows that patients with recurrent falls do so in the same manner and for the same reasons.2, 3, 17 Thus, analyses were performed including only the first fall episode as the outcome of interest. Analyses were performed with SPSS statistical software (SPSS Inc., Chicago, IL) using 2‐sided P values.
Results
During the study period, 513 inpatients sustained 636 falls at the Mount Sinai Medical Center. There were 54,257 admissions to the hospital with 322,670 total patient days during this time. Therefore the fall incidence rate was 1.97 falls per 1,000 patient days. Characteristics of inpatients who fell are shown in Table 1. Most patients had 1 fall episode; however, 95 patients (19%) fell multiple times (range, 2‐6 events). There were no significant differences between recurrent fallers and those who fell once with respect to baseline characteristics, injuries sustained, or discharge disposition.
| Characteristic | Number of Patients (n = 513) [number (%)] |
|---|---|
| |
| Age (years) | 70 (21‐104) |
| Age >75 years | 202 (39) |
| Male gender | 255 (50) |
| Assessed at risk of falling | |
| Yes | 378 (74) |
| No | 2 (5) |
| Unknown | 110 (21) |
| Number of falls | |
| 1 | 418 (82) |
| 2 | 78 (15) |
| 3 | 10 (2) |
| 4 | 4 (1) |
| 5 | 2 (0.4) |
| 6 | 1 (0.2) |
| Multiple falls | 95 (19) |
Fall Circumstances
The majority of patients who fell (74%) had been assessed by the nursing staff as being at risk for falling prior to the event. Overall, most falls (73%) occurred on medical rather than surgical units. The units with the most falls were geriatrics, neurology, and general medicine. Details about circumstances surrounding the falls are shown in Table 2. In most instances (71%) patients were found on the floor after the fall while less than 8% of falls were witnessed. Approximately 12% of patients received sedatives within 4 hours of falling (40% opioids, 30% benzodiazepines, 16% zolpidem, and 14% other). Laboratory values at the time of fall revealed that 70% of patients who fell were anemic, 62% had low albumin, and 19% had an elevated creatinine. Almost 20% of the patients had a prolonged partial thromboplastin time (PTT) and 18% had an elevated INR.
| Characteristic | Number of Falls (n = 513) [number (%)]* |
|---|---|
| |
| Location | |
| Medical unit | 374 (73) |
| Surgical unit | 139 (27) |
| Time | |
| Day shift (7:00 AM to 6:59 PM) | 225 (44) |
| Night shift (7:00 PM to 6:59 AM) | 282 (56) |
| Character of fall | |
| Assisted to floor | 15 (3) |
| Fall alleged | 92 (18) |
| Fall witnessed | 39 (8) |
| Found on Floor | 363 (71) |
| Unknown | 4 (<1) |
| Fall‐related activity | |
| Ambulation | 164 (32) |
| Bathroom | 122 (24) |
| Bed | 21 (4) |
| Chair | 19 (4) |
| Other/unknown | 187 (36) |
| Mental status | |
| Oriented | 274 (53) |
| Confused | 151 (29) |
| Unknown | 88 (17) |
| Activity level ordered | |
| Ambulatory | 246 (48) |
| Nonambulatory | 135 (26) |
| Unknown | 132 (26) |
| Siderails | |
| Complete | 15 (3) |
| Partial | 352 (69) |
| None | 15 (3) |
| Unknown | 126 (25) |
| Environmental obstacle | |
| None | 355 (69) |
| Wet | 20 (4) |
| Debris | 2 (<1) |
| Unknown | 136 (27) |
| Restraints | |
| Yes | 3 (<1) |
| No | 374 (73) |
| Unknown | 136 (27) |
| Sedative use | |
| Total | 64 (12) |
| Opioids | 28 (6) |
| Benzos | 21 (4) |
| Antipsychotics | 7 (1) |
| Other | 8 (2) |
| Evidence of trauma | |
| Yes | 25 (5) |
| No | 285 (56) |
| Unknown | 203 (40) |
The median number of days from patient admission until they fell was 4 days (range, 0‐134), with 70% of patients falling within the first week of admission. In general, there was no difference in fall rate by time of day, though slightly more falls (56%) occurred during the night shift (7 PM to 7 AM).
Fall‐related Outcomes
Twenty‐five patients (5%) had evidence of trauma on physical exam after the fall, including lacerations, swelling, and ecchymoses, as documented by the evaluating nurse. A total of 120 imaging procedures were ordered following the first fall; when all inpatient falls were included, 145 imaging procedures were ordered. Most imaging studies (87%) did not show significant findings. Among studies with positive findings, the most common abnormality was fracture, including 3 hip, 1 humeral, 1 vertebral, 1 nasal, and 1 rib fracture. Other injuries found on imaging studies included 1 subdural hematoma, 1 acute cerebral infarct, 2 soft‐tissue hematomas, and 2 knee effusions. The acute cerebral infarct was not considered to be a result of the fall. Additionally, 3 patients had soft‐tissue swelling noted on head CT and 1 had Foley catheter‐related trauma.
The average length of stay for the 513 inpatients who fell was 20 days (range, 7‐444) compared to 6 days for all patients admitted to the hospital during the same period. Among inpatients who fell, there was no statistical difference in length of stay between those who did and those who did not have a fall‐related injury found on imaging. More than one‐half (53%) of the patients who fell were discharged to home, 21% to rehabilitation facilities, 12% to nursing homes, and 9% died during the hospitalization.
Results of Univariate Analysis
Univariate predictors of injury after a fall are shown in Table 3. Patients having evidence of trauma indicated by the evaluating nurse after a fall had an increased risk for having an abnormal imaging study (OR = 14.7, P < 0.001). Having an activity level of ambulatory ordered by the provider (OR = 2.5, P = 0.09), falling during the night shift (OR = 2.5, P = 0.11), having ambulation as the fall‐related activity (OR = 2.2, P = 0.12), and older age (P = 0.19) all showed a trend toward higher rates of injury being found after a fall. There was no significant association between fall‐related injury and being an elderly patient (age > 75 years), sedative use, falling in the bathroom, or having an elevated PTT or INR.
| Variable | Patients without injury (n = 497) [number (%)] | Patients with injury (n = 16) [number (%)] | OR | P Value |
|---|---|---|---|---|
| ||||
| Elderly | 195 (39) | 7 (44) | 1.2 | 0.72 |
| Gender male | 245 (49) | 10 (63) | 1.7 | 0.30 |
| Location surgical unit | 142 (29) | 6 (38) | 1.5 | 0.44 |
| At risk of falling prior to event | 365 (73) | 13 (8) | 1.6 | 0.49 |
| Protocol in place | 338 (68) | 11 (69) | 1.0 | 0.95 |
| Activity level ambulatory | 235 (47) | 11 (69) | 2.5 | 0.09 |
| Occurrence on night shift | 270 (54) | 12 (75) | 2.5 | 0.11 |
| Restraint use | 3 (1) | 0 (0) | ||
| Sedative within 4 hours | 61 (12) | 3 (19) | 1.6 | 0.44 |
| Fall related to ambulation | 156 (31) | 8 (50) | 2.2 | 0.12 |
| Evidence of trauma | 19 (4) | 6 (38) | 14.7 | <0.001 |
| Prolonged PTT | 93 (19) | 5 (31) | 1.9 | 0.29 |
| Elevated INR | 90 (18) | 3 (19) | 1.0 | 0.96 |
| Anemia | 351 (71) | 9 (56) | 0.6 | 0.32 |
| Elevated creatinine | 97 (20) | 2 (13) | 0.7 | 0.60 |
| Low albumin | 309 (62) | 8 (50) | 1.6 | 0.58 |
Multivariate Predictors of Injury
In multivariate analysis, after adjusting for age and sex, evidence of trauma after a fall (OR = 24.6, P < 0.001) and having an activity level of ambulatory ordered by the provider (OR = 7.3, P = 0.01) were independent predictors of injury being found on imaging studies (Table 4). Analyses limited to the 120 patients who had imaging found that the association between evidence of trauma (OR = 6.22, P = 0.02) and having an activity level of ambulatory ordered (OR = 5.53, P = 0.04) remained statistically significant.
| Variable | All Patients (n = 513) | Patients with Imaging (n = 120)* | ||
|---|---|---|---|---|
| OR | P Value | OR | P Value | |
| ||||
| Age | 1.03 | 0.17 | 1.016 | 0.52 |
| Gender | 3.19 | 0.11 | 2.843 | 0.17 |
| Evidence of trauma | 24.63 | <0.001 | 6.22 | 0.02 |
| Activity level ambulatory | 7.33 | 0.01 | 5.53 | 0.04 |
Discussion
Inpatient falls are common and result in significant patient morbidity and increased healthcare costs. Falls in the acute care setting have also proven to be difficult to prevent and as a result have become a priority for patient safety and hospital quality.
Our study confirms that a high percentage of patients with an initial fall will have recurrent falls.1 Additionally, the majority of patients in this cohort fell despite having been assessed as at risk for falling prior to the event. The types of injuries sustained after inpatient falls (eg, subdural hematoma, multiple fractures, joint effusions, other hematomas, and soft‐tissue swelling) are similar to those found by other authors.2, 3, 17, 18
In this study, inpatient falls were associated with an almost 2‐week increase in length of stay. Though we cannot say that this was directly due to falls, and an increased length of stay may just be a marker of severity of illness, this association warrants further study, perhaps with a matched control group of patients who did not fall, and has implications for healthcare cost containment.
We found that having evidence of trauma after a fall and having an activity level of ambulatory ordered by the provider were independent predictors of injury being found after an inpatient fall. It seems intuitive that patients who have physical evidence of trauma, such as lacerations or bruising, would be more likely to have an underlying injury. Clinically, this confirms that providers should have a high index of suspicion for injury being found on imaging studies in such patients. Similar findings have been noted in the emergency medicine literature that further support the validity of our findings.19
Less clear are the reasons for the observed association between having an activity level of ambulatory ordered and higher risk of injury after an inpatient fall. Prior studies have found that ambulatory inpatients are less likely to use assistive devices that they use at home while hospitalized and are less likely to call for help; these factors may contribute to falls.2, 3 However, the interpretation of this finding is limited by the fact that 26% of the patients who fell had an unknown activity level ordered.
Altered mental status, comorbidity, age > 75 years, visual impairment, falling in the bathroom, and being on a geriatric psychiatry floor have previously been found to be risk factors for sustaining an injury after an inpatient fall.2, 5, 17 Conversely, this study did not find altered mental status to be a significant predictor of injury. One reason may be that this was subjectively determined by the evaluating nurse and not by a standardized measure of cognitive impairment. Patients who are oriented may also be more likely to report unwitnessed falls and injuries than patients with altered mental status.3
There was also no association between age and fall‐related injury in our cohort. On univariate analysis, patients who were older in age were more likely to have an injury found after an inpatient fall but this was not statistically significant. Previous authors have suggested that today's inpatients are increasingly ill and may have risk factors for falls and injuries that are independent of age, such as multiple comorbid conditions or deconditioning.3
We hypothesized that patients who are anticoagulated and had an elevated INR or PTT would be more likely to sustain an injury. Anemic inpatients have also been found to be at increased risk of falls.20 We found no significant association between fall‐related injury being found on imaging studies and anemia, low albumin, elevated creatinine, prolonged PTT, or elevated INR. Not every patient who fell had these laboratory values available. However, even when only inpatients who fell and had laboratory tests were included in the analysis, there was still no association with fall‐related injury.
This study has several limitations. First, a low number of serious injuries was found on imaging studies after inpatient falls in this cohort; this limited the power of the study to identify predictors of fall‐related injury.
Second, fall‐related injury was defined as a positive finding on imaging studies within 2 weeks of an inpatient fall. Thus, some fall‐related injuries may have been missed in patients who did not have imaging. However, any patient who had a serious injury after a fall and remained hospitalized would likely have had symptoms such as pain or altered mental status that would have led to an imaging study. Moreover, the analysis was repeated including only inpatients who fell and had imaging, and the association between having evidence of trauma and having an activity level of ambulatory ordered and sustaining a fall‐related injury remained significant.
Third, we relied on hospital incident reports to identify inpatient falls. These reports yield a limited amount of information and may be inaccurate or incomplete. A recent study also raised concern that incident reports significantly underreport actual fall incidence.21 However, previous studies have found no indication that falls are underreported and suggest that incident reports are an established custom in hospital culture.1, 22 Medical staff are aware that administrators want to keep track of hospital fall rates for both quality improvement and documentation for risk management.1, 22 It is unlikely that severe falls or falls leading to serious injury are not reported. A different source of underreporting may actually be failure of patients to tell the medical team about an unwitnessed fall. Older patients may be concerned they will be placed in nursing homes and those with memory loss may forget to report a minor fall. Education of patients and family members could improve reporting of inpatient falls and further our understanding of contributing factors.
Finally, although the evaluation of fall‐related injuries was conducted by a blinded reviewer, the potential for bias does exist among even the best‐intentioned reviewers. Additionally, there may be some degree of variability within the reviewer's data abstraction.
This study adds valuable information about the epidemiology of inpatient falls at large, urban, tertiary‐care academic medical centers, including characteristics of patients who fell, circumstances surrounding falls, injuries sustained, and predictors of fall‐related injury found on imaging. Although additional research is essential to identify methods to effectively prevent inpatient falls, this study contributes to the limited data in this area, can guide providers who are evaluating inpatients who have fallen, and may be used to design future investigations. It is imperative that measures are identified to avoid the frequent adverse outcomes that result from inpatient falls. Insurance companies, hospital administrators, patients, and providers will be demanding that a safe environment be a key component of quality of care measures.
This study draws attention to the scope of the problem at our institution that is common to hospitals across the country. In our study, our academic medical center had a fall rate consistent with published reports, but new efforts have been focused on quality improvement in this area. An interdisciplinary fall prevention committee has been formed that includes physicians, nurses, patient care assistants, physical therapists, pharmacists, and representatives from information technology (IT). Currently, a program of a fall risk‐factor assessment with targeted interventions to reduce those risk factors is being developed for all high‐risk patients and will be piloted on inpatient units.
Acknowledgements
The authors thank Susan Emro, BS, Department of Health Policy, Susan Davis, MS, MPH, RN, CNAA, Department of Nursing, and Albert Siu, MD, MSPH, Brookdale Department of Geriatrics and Adult Development, for their review of this article. Author contributions were as followsconception and design: S.M.B, R.K., and T.M.; collection and assembly of data: S.M.B.; analysis and interpretation of the data: S.M.B, R.K., and J.W.; drafting of the article: S.M.B.; critical revision of the article for important intellectual content: R.K. and J.W.; final approval of the article: S.M.B, R.K., and J.W.; statistical expertise: J.W.; obtaining of funding: S.M.B.
- ,,,.Risk of falls for hospitalized patients: a predictive model based on routinely available data.J Clin Epidemiol.2001;54(12):1258–1266.
- ,,, et al.A case‐control study of patient, medication, and care‐related risk factors for inpatient falls.J Gen Intern Med.2005;20(2):116–122.
- ,,, et al.Characteristics and circumstances of falls in a hospital setting: a prospective analysis.J Gen Intern Med.2004;19(7):732–739.
- ,,,.Falls and consequent injuries in hospitalized patients: effects of an interdisciplinary falls prevention program.BMC Health Serv Res.2006;6:69.
- ,,,.Serious falls in hospitalized patients: correlates and resource utilization.Am J Med.1995;99(2):137–143.
- ,.Using tools to assess and prevent inpatient falls.Jt Comm J Qual Saf.2003;29(7):363–368.
- ,,.Incidence and risk factors for inpatient falls in an academic acute‐care hospital.J Nippon Med Sch.2006;73(5):265–270.
- .Nonpayment for performance? Medicare's new reimbursement rule.N Engl J Med.2007;357(16):1573–1575.
- .Clinical practice. preventing falls in elderly persons.N Engl J Med.2003;348(1):42–49.
- .Building the science of falls‐prevention research.J Am Geriatr Soc.2004;52(3):461–462.
- ,,,,,.Interventions for preventing falls in acute‐ and chronic‐care hospitals: a systematic review and meta‐analysis.J Am Geriatr Soc.2008;56(1):29–36.
- ,,, et al.Interventions for the prevention of falls in older adults: systematic review and meta‐analysis of randomised clinical trials.BMJ.2004;328(7441):680.
- ,,, et al.Acceptability of fall prevention measures for hospital inpatients.Age Ageing.2004;33(4):400–401.
- ,,, et al.Can volunteer companions prevent falls among inpatients? A feasibility study using a pre‐post comparative design.BMC Geriatr.2006;6:11.
- ,,,,.Using targeted risk factor reduction to prevent falls in older in‐patients: a randomised controlled trial.Age Ageing.2004;33(4):390–395.
- .Prevention of falls in hospital inpatients: agendas for research and practice.Age Ageing.2004;33(4):328–330.
- ,,, et al.Patterns and predictors of inpatient falls and fall‐related injuries in a large academic hospital.Infect Control Hosp Epidemiol.2005;26(10):822–827.
- ,,,,.The relationship of falls to injury among hospital in‐patients.Int J Clin Pract.2005;59(1):17–20.
- ,,,,,.Indications for computed tomography in patients with minor head injury.N Engl J Med.2000;343(2):100–105.
- ,,.Anemia increases risk for falls in hospitalized older adults: an evaluation of falls in 362 hospitalized, ambulatory, long‐term care, and community patients.J Am Med Dir Assoc.2006;7(5):287–293.
- ,,,,,.Improving the capture of fall events in hospitals: combining a service for evaluating inpatient falls with an incident report system.J Am Geriatr Soc.2008;56(4):701–704.
- ,,, et al.Attitudes and barriers to incident reporting: a collaborative hospital study.Qual Saf Health Care.2006;15(1):39–43.
- ,,,.Risk of falls for hospitalized patients: a predictive model based on routinely available data.J Clin Epidemiol.2001;54(12):1258–1266.
- ,,, et al.A case‐control study of patient, medication, and care‐related risk factors for inpatient falls.J Gen Intern Med.2005;20(2):116–122.
- ,,, et al.Characteristics and circumstances of falls in a hospital setting: a prospective analysis.J Gen Intern Med.2004;19(7):732–739.
- ,,,.Falls and consequent injuries in hospitalized patients: effects of an interdisciplinary falls prevention program.BMC Health Serv Res.2006;6:69.
- ,,,.Serious falls in hospitalized patients: correlates and resource utilization.Am J Med.1995;99(2):137–143.
- ,.Using tools to assess and prevent inpatient falls.Jt Comm J Qual Saf.2003;29(7):363–368.
- ,,.Incidence and risk factors for inpatient falls in an academic acute‐care hospital.J Nippon Med Sch.2006;73(5):265–270.
- .Nonpayment for performance? Medicare's new reimbursement rule.N Engl J Med.2007;357(16):1573–1575.
- .Clinical practice. preventing falls in elderly persons.N Engl J Med.2003;348(1):42–49.
- .Building the science of falls‐prevention research.J Am Geriatr Soc.2004;52(3):461–462.
- ,,,,,.Interventions for preventing falls in acute‐ and chronic‐care hospitals: a systematic review and meta‐analysis.J Am Geriatr Soc.2008;56(1):29–36.
- ,,, et al.Interventions for the prevention of falls in older adults: systematic review and meta‐analysis of randomised clinical trials.BMJ.2004;328(7441):680.
- ,,, et al.Acceptability of fall prevention measures for hospital inpatients.Age Ageing.2004;33(4):400–401.
- ,,, et al.Can volunteer companions prevent falls among inpatients? A feasibility study using a pre‐post comparative design.BMC Geriatr.2006;6:11.
- ,,,,.Using targeted risk factor reduction to prevent falls in older in‐patients: a randomised controlled trial.Age Ageing.2004;33(4):390–395.
- .Prevention of falls in hospital inpatients: agendas for research and practice.Age Ageing.2004;33(4):328–330.
- ,,, et al.Patterns and predictors of inpatient falls and fall‐related injuries in a large academic hospital.Infect Control Hosp Epidemiol.2005;26(10):822–827.
- ,,,,.The relationship of falls to injury among hospital in‐patients.Int J Clin Pract.2005;59(1):17–20.
- ,,,,,.Indications for computed tomography in patients with minor head injury.N Engl J Med.2000;343(2):100–105.
- ,,.Anemia increases risk for falls in hospitalized older adults: an evaluation of falls in 362 hospitalized, ambulatory, long‐term care, and community patients.J Am Med Dir Assoc.2006;7(5):287–293.
- ,,,,,.Improving the capture of fall events in hospitals: combining a service for evaluating inpatient falls with an incident report system.J Am Geriatr Soc.2008;56(4):701–704.
- ,,, et al.Attitudes and barriers to incident reporting: a collaborative hospital study.Qual Saf Health Care.2006;15(1):39–43.
Copyright © 2010 Society of Hospital Medicine
AMI Treatment for PAC/LTC Residents
The American College of Cardiology (ACC) and the American Heart Association (AHA) recommend early intervention for older persons with acute coronary syndrome (ACS) to improve prognosis. However, numerous studies demonstrate that elderly patients with acute myocardial infarction (AMI) are less likely than their younger counterparts to receive guideline‐recommended therapies.13 No prior studies specifically demonstrate that adherence to AMI guidelines is effective in patients admitted from post‐acute or long‐term care (PAC/LTC) settings such as nursing homes, intermediate care facilities, and LTC hospitals. Recognizing that the barriers to guideline‐adherent care among the elderly may also be present for clinically‐complex PAC/LTC patients, we examined whether hospitalized patients with AMI admitted from PAC/LTC settings were less likely to receive guideline‐recommended therapies and if guideline‐concordant treatment was associated with short‐term (30‐day) survival in this relatively vulnerable subgroup of patients.
Medical decision making, including applicability of guidelines, is not exclusively based on empirical evidence but is also related to morally complex issues such as patient age, social status, and other unknown factors. However, lack of outcome expectancy may limit adherence for AMI care in PAC/LTC populations.4 In particular, treating physicians may not expect that desired outcomes will result when guidelines are followed in the PAC/LTC group compared to community‐based patients. This notion is supported by other research indicating that physicians caring for nursing home residents' chronic health conditions often tailor the care approach according to the patients' functional and cognitive status rather than adhering to recommended guidelines.5 In a study that used hypothetical scenarios, nursing home patients with a better physical condition, a more obvious social role, and a lower age were more likely to be treated with life‐sustaining treatments than were other patients.6 For AMI care, some physicians provide care that is not guideline‐adherent due to concerns that reduced renal function is an absolute rather than relative contraindication to angiography.7, 8 And, because the clinical trials that informed practice guidelines for AMI care did not explicitly include individuals with the chronic complex medical problems prevalent among the PAC/LTC population, treating clinicians may be reluctant to apply acute care guidelines to this subgroup.9 However, we know of no prior research demonstrating that guideline‐adherent care for either chronic or acute conditions results in differential outcomes for PAC/LTC patients cared for in the hospital setting.
For the present study, we examined whether admission source was an independent predictor of AMI treatment and whether guideline‐concordant care was related to mortality for those admitted from PAC/LTC and community settings. We hypothesized that rates of guideline‐concordant care would be higher for patients admitted from community settings vs. PAC/LTC and that differences between the groups would be greater for more intensive interventions such as reperfusion compared to aspirin. The data included detailed clinical eligibility information for treatments based on contemporary ACC/AHA guidelines,10 along with numerous other patient demographic and clinical characteristics, thus allowing us to address the presumptive concern that PAC/LTC patients were sicker or otherwise less‐suited for treatment than other patients.
Methods
This retrospective cohort study relied on existing observational data. The primary data source for this research was the Cooperative Cardiovascular Project (CCP) national baseline data. The CCP was sponsored by the Centers for Medicare & Medicaid Services (CMS) to measure the quality of care provided to a national cohort of Medicare patients hospitalized with AMI. The national data collection and reporting effort was administered through the 53 Medicare Quality Improvement Organization (QIO) contracts established to serve each State, the District of Columbia, Puerto Rico, and the U.S. Virgin Islands. Hospital medical records were requested under QIO authority and then abstracted by centrally‐contracted Clinical Data Abstraction Centers (CDACs). Data quality monitoring involved random reabstraction of records with double entry of the information to ensure consistency across personnel, and data were found to be very reliable. Detailed data collection procedures and main findings from these data have been reported elsewhere.1126
The CCP baseline data included an initial sample of 234,754 records abstracted from inpatient medical charts for fee‐for‐services Medicare beneficiaries hospitalized in 1 of 6684 hospitals located in any of the 50 states, the District of Columbia, Puerto Rico, the U.S. Virgin Islands, American Samoa, Guam, and the Northern Mariana Islands between February 1994 and July 1995. Although the data analyzed for this research relate to hospitalizations for AMI in 1994‐1995, the 2008 ACC/AHA report regarding AMI performance measures retains recommendations for both early aspirin and reperfusion treatments.27 Even though the data are not derived from recent years, the CCP baseline data represent a unique dataset to address questions related to both clinical eligibility and guideline compliance for both community and PAC/LTC patients. The inclusion of PAC/LTC admissions and detailed information regarding clinical eligibility for treatment are particularly important to adequately address the research aim; the CCP baseline data are the single extant U.S. data source we identified that has both features.
AMI cases were identified through inpatient hospital claims using an International Classification of Diseases, 9th Revision, Clinical Modification (ICD‐9‐CM) principal discharge diagnosis of 410 (ACS) for extended chart review to verify AMI and determine clinical eligibility for treatments. CCP records were subsequently linked with the Medicare Denominator File, Area Resource File (ARF), and Medicare PPS cost reports for hospitals (PPS) to obtain additional information regarding patients, local health resources, and admitting hospital.
For the present study, we excluded cases without a confirmed AMI diagnosis; cases with missing geographic information to allow us to control for local practice variation including all cases from outside the Continental U.S.; cases admitted to nonacute facilities or with inadequate information to link with provider data; and cases that originated in states selected for the CCP pilot study due to differences in record abstraction timing and some of the measures. Clinical eligibility for treatments relied on the standardized criteria established by the CCP advisory panel and used in other research.10, 14, 2831
To test whether admission from a LTC setting was negatively associated with guideline adherence and if the relationship varied according to the intensity of the treatment, we examined 2 guidelines related to early interventions care during the hospital stay: (1) administration of aspirin; and (2) reperfusion through either thrombolytic drugs or percutaneous intervention (PTCA). We chose these measures because they range from a simple and readily‐available medical intervention (aspirin), to a clinically complex and costly intervention for a more clinically‐select group of patients (reperfusion). The hypothesis that more intensive acute treatment would be less likely for patients admitted from PAC/LTC settings was empirically tested by examining the differences in overall probabilities and adjusted probabilities of receiving each of these interventions. We then modeled the odds ratios (ORs) for survival based on receiving these treatments.
Guideline adherence and clinical eligibility indicators for the CCP data have been presented elsewhere.10, 20, 23, 29, 32 Using these criteria, we divided patients into clinical eligibility groups, including ideal candidates, eligible candidates, and candidates for whom the care was not indicated. For the present research, all eligible patients were included in the sample; with ideal eligibility included as a covariate in the regression models. All patients in the study sample were at least minimally eligible to receive aspirin during their hospital stay. Ideal candidates for aspirin did not have: a gastrointestinal (GI) ulcer, same day admission/discharge, history of bleeding disorder, risk of bleeding, anemia, allergy to aspirin, warfarin, or terminal illness. Eligible candidates for reperfusion via PTCA or thrombolysis were not transferred from another hospital or emergency department. Ideal eligibility for reperfusion required, in addition, that the patient: was under age 80 years; arrived at the hospital within 6 hours of symptom onset; showed evidence of a transmural (Q‐wave) MI or ST elevation in 2 contiguous leads on arrival electrocardiogram (ECG); was not taking warfarin; did not have cardiac arrest requiring cardiopulmonary resuscitation (CPR), cardioversion, defibrillation, or chemical cardioversion in the 6 hours prior; did not refuse a thrombolytic; did not have cardiac catheterization without PTCA within 12 hours of arrival; had no evidence of hepatic failure or cirrhosis; had no history of active ulcer disease, internal bleeding, trauma, or injury in the month prior to arrival; and had no bleeding risk, cerebral vascular accident, or surgery/biopsy within 2 months of admission.
Prearrival setting was of particular interest for the present study; this information was derived from the patient's medical chart using a standardized chart abstraction process for the CCP. From the original admission source categories, we created a single dichotomous variable that indicated PAC/LTC vs. community setting prior to arrival. We defined PAC/LTC settings to include patients admitted from either a skilled nursing facility (SNF) or intermediate care facility (ICF), chronic hospital, or other residential care facility. Three categories of admission source were used to identify the comparison sample: home, noninstitutional setting, and outpatient setting.
Because differences in care according to admission source could result from observable causes, multiple regression analysis was incorporated to control for observed factors previously shown to be associated with guideline adherence. These included: ideal eligibility for treatment; age; Caucasian (vs. other) ethnicity; gender; limitation of aggressive treatment orders (eg, do not resuscitate, do not intubate, chemical code only, no cardiac monitoring, no invasive procedures, no vasopressor, no antiarrhythmic therapy, no feeding tube, palliative care measures only); Charlson comorbidity index and Acute Physiology, Age, Chronic Health Evaluation assessment (3rd revision) (APACHE III) score, body mass index (BMI), rural hospital location, hospital teaching status, and number of full‐time equivalent cardiologists on staff at the treating hospital. The regression methods also included adjustment for clustering of patients within health services area to account for geographic variation in practice patterns.33
In developing the regression model, we predicted whether the patient received care in accord with guidelines and 30‐day mortality. We also tested whether the regression errors terms (unobserved variables) for these equations were significantly related to error terms in a regression to predict source of admission, which would indicate rejecting the hypothesis that admission source and treatments were determined independently of each other. In particular, admission source may be a proxy for underlying health status (severity of illness), care preferences, or other unobserved factors that differ systematically between patients admitted from the community vs. those admitted from PAC/LTC. In testing the models, we found that the error terms for both treatments (aspirin and reperfusion) and admission source models were significantly negatively correlated (rho or chi‐square P value <0.001), indicating the need to adjust regression estimates to account for unobserved variables related to both admission source and guideline concordant treatment. Because we rejected the hypothesis that admission source was exogenous to treatments, a seemingly‐unrelated regressions (SUR) bivariate probit model was deemed appropriate, as this methodology corrects for correlation between unobserved variables that are related to both admission source and treatment decisions (eg, residual confounding).34 And, since coefficients from SUR bivariate probit models are not directly interpretable as either ORs or relative risks with respect to the outcome variables, we converted the coefficients to reflect marginal probabilities. The correlation in error terms for models predicting 30‐day mortality and admission source was not substantively or statistically significant. As such, we utilized standard logistic regression methods for assessing mortality. Mortality models were predicted separately according to admission source and treatment to allow presentation of ORs associated with each treatment for each group.
Analyses used the Stata statistical package (version 10.1 SE).35 Approval for this use of the CCP data was received from the CMS. Approval for the data analysis protocol was received from the authors' institutional review board.
Results
Of the 128,183 patients in the analytic sample, 7.6% (n = 8151) were admitted from PAC/LTC (Table 1). The members of the PAC/LTC cohort were older on average than the community‐dwelling cohort (83 vs. 76 years, P < 0.001) and more likely to be female (69% vs. 48%, P < 0.001). Limitation of aggressive treatment orders (LAT/DNR) were in place for 55% of the PAC/LTC cohort compared to only 16% of the community‐dwelling cohort (P < 0.001). Severity of illness scores were higher among the PAC/LTC cohort with APACHE III scores of 50.8 in the PAC/LTC cohort vs. 36.8 in the community‐dwelling cohort (P < 0.001). The PAC/LTC cohort also had lower BMI (P < 0.001). Mortality at 30 days and 1 year was 39.5% and 65.4%, respectively, in the PAC/LTC cohort vs. 17.6% and 33.4%, respectively, in the community‐dwelling cohort. These differences across groups were significant at both time points (P < 0.001). PAC/LTC admissions were significantly more likely to be admitted to a hospital located in a rural area (P < 0.001), though the numbers of full‐time equivalent residents and presence of cardiologists in the treating hospitals were similar across groups.
| Sample Characteristics | Overall | PAC/LTC | Community | P Value (2‐sided test) |
|---|---|---|---|---|
| ||||
| Number of cases | 128,183 | 8,151 | 120,032 | |
| Percentage of sample | 100 | 6.4 | 93.6 | |
| Average age, years (mean SD) | 76.7 7.4 | 82.6 7.6 | 76.3 7.2 | <0.001 |
| Female (%) | 49.6 | 69.1 | 48.3 | <0.001 |
| Non‐White (%) | 9.7 | 9.1 | 9.7 | 0.09 |
| Length of stay, days (mean SD) | 7.3 7.2 | 7.4 7.1 | 7.3 7.2 | 0.33 |
| With LAT/DNR order in place (%) | 18.1 | 55.4 | 15.6 | <0.001 |
| APACHE III score (mean SD) | 37.7 17.5 | 50.8 21.0 | 36.8 16.8 | <0.001 |
| Charlson comorbidity index (mean SD) | 2.2 1.2 | 2.7 1.3 | 2.2 1.2 | <0.001 |
| BMI (mean SD) | 26.2 5.2 | 24.2 5.9 | 26.2 5.2 | <0.001 |
| Hospital residents, FTE (mean SD) | 29.3 78.4 | 29.0 78.7 | 29.3 78.3 | 0.75 |
| Hospital cardiologists, FTE (mean SD) | 11.3 13.5 | 11.0 13.9 | 11.3 13.5 | 0.03* |
| Admitted to rural hospital (%) | 20.1 | 22.3 | 20.0 | <0.001 |
| Number of secondary diagnosis codes (0‐8) (mean SD) | 5.1 2.3 | 5.8 2.1 | 5.0 2.26 | <0.001 |
| 30‐day mortality (%) | 18.9 0.39 | 39.5 0.49 | 17.6 0.38 | <0.001 |
| 1‐year mortality (%) | 33.5 0.47 | 65.4 0.48 | 31.4 0.46 | <0.001 |
Table 2 provides overall unadjusted data comparing eligibility and treatment information for PAC/LTC and community admissions. Rates of guideline adherence were uniformly higher for patients admitted from the community. Guideline adherence rates were higher for aspirin compared to reperfusion, and followed the predicted pattern that more resource‐intensive treatments would be less common for both groups and that PAC/LTC admissions would be less likely to receive treatments compared to patients admitted from community settings. Though all 8151 PAC/LTC patients were eligible to receive aspirin, only 4370 were ideally eligible and 3015 (69%) received acetylsalicylic acid (ASA). There were 1418 PAC/LTC patients (17% of the PAC/LTC sample) meeting at least minimal eligibility requirements for reperfusion. Among the 214 PAC/LTC cases that were ideally eligible for reperfusion, 65 (30%) received the treatment; 12 patients received PTCA and 53 received thrombolytic agents. Eligibility and treatment rates for reperfusion were substantially higher for the community sample, with almost 27% meeting minimum eligibility requirements and 60% of the ideally‐eligible group receiving the treatment.
| Aspirin (ASA) [n (% received)] | Reperfusion (PTCA or thrombolysis) [n (% received)] | |
|---|---|---|
| ||
| Eligible sample* | ||
| PAC/LTC | 8151 (60) | 1418 (13) |
| Community | 120,032 (79) | 34,501 (45) |
| Ideal sample* | ||
| PAC/LTC | 4370 (69) | 214 (30) |
| Community | 78,973 (86) | 16,557 (60) |
Table 3 presents the adjusted probability of treatment based upon the SUR bivariate probit regression model. As with the unadjusted results presented in Table 2, PAC/LTC patients had a lower probability of treatment even after controlling for important patient and hospital characteristics. Compared to the unadjusted results, the adjusted probabilities calculated with the SUR bivariate probit model indicated a relatively higher predicted probability of treatment for the PAC/LTC patients and a relatively lower predicted probability of treatment among the community patients. In other words, the probability of treatment becomes more similar across groups once the adjustments for both observed and unobserved differences in patient characteristics are considered. Nonetheless, a difference in probability of treatment remains across the 2 groups.
| Aspirin (ASA) | Reperfusion | |
|---|---|---|
| ||
| PAC/LTC (%) | 64 | 12 |
| Community (%) | 77 | 23 |
| Rho (P value)* | 0.069 (<0.001) | 0.17 (<0.001) |
To determine whether there was survival difference associated with treatment in these data, we conducted a logistic regression analyses to predict 30‐day mortality for both groups (Tables 4 and 5). Table 4 presents results (ORs) of our models emphasizing the relationship between aspirin and 30‐day mortality, while Table 5 presents the models with reperfusion. Model discrimination was tested using a C‐statistic and was at least 0.70 for all models, indicating good predictive validity. However, for the reperfusion models (Table 5) there were relatively few PAC/LTC patients ideally eligible for treatment, which limited statistical power. There was an association between aspirin provision and improved survival for both the PAC/LTC and community admissions (95% confidence intervals [CIs] were less than 1.0) for all eligible patients. For the eligible samples, we did not find the anticipated relationship between reperfusion and 30‐day survival. The ORs and CIs for community admissions were significantly greater than 1.0. However, we noted lower ORs of mortality for the subgroups of ideally eligible patients, with 95% CIs under 1.0 for both PAC/LTC and community admissions, indicating better survival among those who were ideally eligible for reperfusion treatment. The unadjusted data indicated that PAC/LTC patients were much more likely than their community counterparts to die within 30 days of AMI (Table 1). The multiple logistic regression results indicates PAC/LTC patients had similar ORs for mortality compared to community patients when aspirin was given to eligible patients and when reperfusion was given to ideally eligible patients (Tables 4 and 5). Based on the logistic regression results, we calculated that the adjusted probability of 30‐day mortality among eligible PAC/LTC patients who received aspirin was 0.14 compared to 0.32 for those who did not, which is a difference in probability of 0.18. For eligible community admissions, the adjusted probability of mortality with aspirin was 0.09 with aspirin treatment compared to 0.26 without. For reperfusion, the adjusted probability of 30‐day mortality for ideally eligible PAC/LTC admissions falls from 0.27 to 0.15 if treatment is given, representing a difference in probability of 0.12. Similarly, the adjusted probability difference for community admissions who were ideally eligible and received reperfusion was approximately 0.08 (P = 0.16 without treatment and P = 0.08 with treatment).
| Explanatory Variables | PAC/LTC Admissions | Community Admissions | ||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| ||||
| Aspirin (ASA) given during hospital stay | 0.50 | 0.43‐0.58 | 0.57 | 0.54‐0.60 |
| Ideal eligibility for ASA | 0.88 | 0.76‐1.01 | 0.70 | 0.67‐0.73 |
| Female (vs. Male) | 0.85 | 0.73‐0.99 | 0.94 | 0.90‐0.98 |
| Patient age, 5‐year increments | 0.99 | 0.94‐1.04 | 1.04 | 1.02‐1.05 |
| Non‐white Ethnicity (vs. White) | 0.98 | 0.76‐1.28 | 0.95 | 0.89‐1.03 |
| Current Smoker (vs. non‐smoker) | 0.93 | 0.71‐1.22 | 0.97 | 0.91‐1.03 |
| Body mass index | 0.99 | 0.97‐1.00 | 0.99 | 0.99‐1.00 |
| LAT/DNR Order | 4.09 | 3.53‐4.73 | 7.83 | 7.46‐8.21 |
| APACHE 3 Score, 5 point increments | 1.10 | 1.08‐1.12 | 1.13 | 1.12‐1.13 |
| Charlson Index, 3 point increments | 0.87 | 0.74‐1.03 | 1.06 | 1.00‐1.11 |
| Patient received in transfer | 0.99 | 0.65‐1.51 | 1.18 | 0.95‐1.46 |
| Number of hospital residents, 5 FTE increments | 1.00 | 1.00‐1.00 | 1.00 | 1.00‐1.00 |
| Hospital located in rural area | 1.10 | 0.92‐1.31 | 1.09 | 1.03‐1.15 |
| Number of cardiologists on staff, 5 FTE increments | 0.97 | 0.94‐1.00 | 1.00 | 1.00‐1.02 |
| C‐statistic | 0.76 | 0.79 | ||
| Number of observations | 4,559 | 92,004 | ||
| Explanatory Variables | PAC/LTC Admissions | Community Admissions | ||
|---|---|---|---|---|
| OR | 95% CI* | OR | 95% CI* | |
| ||||
| Reperfusion via thrombolytics or PTCA | 1.33 | 0.85‐.10 | 1.24 | 1.13‐1.35 |
| Ideal eligibility for reperfusion | 0.58 | 0.35‐0.95 | 0.74 | 0.68‐0.81 |
| Female (vs. male) | 0.92 | 0.66‐1.29 | 1.05 | 0.97‐1.14 |
| Patient age, 5‐year increments | 0.97 | 0.85‐1.10 | 1.03 | 0.99‐1.06 |
| Non‐White ethnicity (vs. White) | 1.11 | 0.59‐2.10 | 1.10 | 0.95‐1.28 |
| Current smoker (vs. nonsmoker) | 1.13 | 0.66‐1.94 | 0.87 | 0.78‐0.98 |
| BMI | 1.01 | 0.98‐1.04 | 1.00 | 0.99‐1.01 |
| LAT/DNR order | 3.41 | 2.48‐4.70 | 8.26 | 7.52‐9.06 |
| APACHE III score, 5‐point increments | 1.13 | 1.07‐1.19 | 1.15 | 1.14‐1.17 |
| Charlson comorbidity index, 3‐point increments | 0.84 | 0.58‐1.22 | 1.30 | 1.17‐1.44 |
| Patient received in transfer | 1.08 | 0.27‐4.43 | 1.49 | 0.85‐2.60 |
| Number of hospital residents, 5‐FTE increments | 0.99 | 0.98‐1.01 | 1.00 | 1.00‐1.00 |
| Hospital located in rural area | 0.90 | 0.61‐1.34 | 1.12 | 1.01‐1.25 |
| Number of cardiologists on staff, 5‐FTE increments | 0.97 | 0.90‐1.05 | 1.00 | 0.98‐1.01 |
| C‐statistic | 0.71 | 0.78 | ||
| Number of observations | 856 | 26,720 | ||
Discussion
This investigation has important implications. The results suggest systematic differences in care for PAC/LTC compared to community‐based patients hospitalized with AMI. It is possible that short‐term mortality was impacted by guideline adherence differences according to admission source. The analytic methods accounted for clinical eligibility, tested for residual confounding and used econometric methods (SUR bivariate probit) to correct it where found, and excluded patients who refused treatments. Therefore, poor eligibility and treatment refusal are inadequate explanations for the observed differences in treatment according to admission source from a PAC/LTC facility.
Providers may not to follow AMI treatment guidelines because the perceived risks for patients transferred from PAC/LTC were too great or due to a limited clinical evidence base. Even though PAC/LTC patients were not included in clinical trials for AMI care, studies that carefully use observational data may help guide applicability of clinical recommendations for acute care to subgroups of clinically complex patients. This study offers observational evidence and information to guide additional studies regarding of the clinical benefit of treating a particularly vulnerable subgroup of patients.
Other research has noted that adherence to clinical practice guidelines in PAC/LTC facilities is low.36, 37 LTC practitioners have been reluctant to apply clinical practice guidelines to residents with chronic illnesses because these regimens often do not take into consideration individuals with the multiple chronic diseases prevalent among PAC/LTC patients9 and the complexity of the PAC/LTC environment.38, 39 Rather than dismiss the utility of clinical practice guidelines in the PAC/LTC population, this study is one of the first to demonstrate that use of acute care clinical practice guidelines, particularly aspirin, was associated with improved acute care outcomes among PAC/LTC patients transferred to acute care hospitals with AMI. Thus, guidelines for acute inpatient care may be more readily applied to the PAC/LTC population than studies aimed at treating chronic illnesses.9, 38, 40 Our results indicate that reperfusion might not be indicated for the preponderance of PAC/LTC patients, but many would agree that treatments such as aspirin would be a low‐burden intervention for most PAC/LTC patients. This investigation supports considering AMI treatment guidelines even for frail subpopulations such as those transferred from PAC/LTC. Further, the findings suggest there may be important information obtained by including PAC/LTC patients in future clinical trials.
This study has several limitations. First, the data were collected during 1995, and may not adequately reflect the current state of the art for AMI treatment or other changes in the organization, financing, and delivery of care for AMI. Nevertheless, care guidelines for AMI have not changed in ways that we anticipate altering the patterns of care examined in this study. For example, in the 2004 National Healthcare Disparities Report,41 receipt of aspirin among elderly individuals ranged from 79.6% to 86%, which closely resembles our results. Despite overall care improvements from 1990 to 2006, women, minorities, and patients ages 75 years and older remain significantly less likely to receive revascularization or discharge lipid‐lowering therapy relative to their counterparts indicating that differences in care persist today.42 While the data used in these analyses existed before recommendations included specific guidance regarding the care of older adults, other researchers examined data collected from January 1, 2005 to June 30, 2006 and demonstrated that elderly individuals remained less likely to receive indicated therapies.43 Further, this is the only dataset we identified that included an adequate presence of both PAC/LTC and community admission sources and sufficient data to assess guideline adherence and other covariates for our models. Second, The SUR bivariate probit models that account for correlation of error terms in models predicting both admission source and treatment were included to minimize issues related to residual confounding, but may not completely eliminate all systematic variation related to the underlying health status of community vs. PAC/LTC residents. Third, limitation of aggressive treatments was not recorded as to specific type of directives but research has shown that orders to forego treatments other than CPR are written for fewer than 8 % of nursing home residents.44, 45 Furthermore, all of these patients were transferred to a hospital; these transfers almost certainly occurred with an expectation that acute treatment would be offered. Fourth, we were unable to distinguish PAC vs. LTC based on admission source categories provided in the original data source. Finally, PTCA and thrombolysis were considered as a single variable because separating the 2 procedures would result in inadequate sample size to detect statistical differences between the 2 groups.
Conclusions
Patients admitted from PAC/LTC settings were less likely to receive early guideline‐recommended treatment for AMI compared to community‐dwelling patients. Our study finds evidence that following the aspirin guideline may improve survival for most patients, but that reperfusion improved survival only for a clinically‐select subgroup of patients. As such, a possible recommendation for further clinical study is that low‐burden treatments such as aspirin should be offered to most patients with AMI, including those from PAC/LTC. Higher‐burden treatments with have greater associated risks, such as reperfusion, also require more study to inform situations applicable to PAC/LTC patients. Clinical trials data would be indicated to strengthen evidence regarding which AMI treatment guidelines should be followed in frail populations from PAC/LTC settings; we identified no randomized trials that specifically demonstrate efficacy of AMI guidelines for this subgroup of vulnerable patients.
- ,,,.The Characteristics of Long‐Term Care Users. Agency for Healthcare Research and Quality (AHRQ) Publication No. 00–0049.Rockville, MD:Agency for Healthcare Research and Quality;2000.
- U.S. Bureau of the Census.Current Population Reports, P23–190, 65+ in the United States.Washington, DC:U.S. Government Printing Office;1996.
- ,,, et al.Older emergency department patients with acute myocardial infarction receive lower quality of care than younger patients.Ann Emerg Med.2005;46(1):14–21.
- ,,, et al.Why don't physicians follow clinical practice guidelines? A framework for improvement.JAMA.1999;282(15):1458–1465.
- ,,, et al.Differences in diabetes management of nursing home patients based on functional and cognitive status.J Am Med Dir Assoc.2005;6(6):375–382.
- ,,,,.Medical and nonmedical determinants of decision making about potentially life‐prolonging interventions.Med Decis Making.2004;24(5):518–524.
- .Hidden barriers to improvement in the quality of care.N Engl J Med.2001;345(22):1612–1620.
- ,,.“Renalism”: inappropriately low rates of coronary angiography in elderly individuals with renal insufficiency.J Am Soc Nephrol.2004;15(9):2462–2468.
- ,,,,,.Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance.JAMA.2005;294(6):716–724.
- ,,, et al.ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction).J Am Coll Cardiol.1996;28(5):1328–1428.
- ,,,,.Racial differences in the medical treatment of elderly Medicare patients with acute myocardial infarction.J Gen Intern Med.1996;11(12):736–743.
- ,,,,,.Resource use and quality of care for Medicare patients with acute myocardial infarction in Maryland and the District of Columbia: analysis of data from the Cooperative Cardiovascular Project.Am Heart J.1998;135(2 pt 1):349–356.
- ,,, et al.ACC/AHA 2002 guideline update for the management of patients with unstable angina and non‐ST‐segment elevation myocardial infarction—summary article: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the Management of Patients With Unstable Angina).J Am Coll Cardiol.2002;40(7):1366–1374.
- ,,,,.Impact of managed care on the treatment, costs, and outcomes of fee‐for‐service Medicare patients with acute myocardial infarction.Health Serv Res.2005;39(1):131–152.
- ,,, et al.Quality of care for Medicare patients with acute myocardial infarction. A four‐state pilot study from the Cooperative Cardiovascular Project.JAMA.1995;273(19):1509–1514.
- ,,,,.Regionalization of cardiac surgery in the United States and Canada: geographic access, choice, and outcomes.JAMA.1995;274(16):1282–1288.
- .HCFA's Health Care Quality Improvement Program and the Cooperative Cardiovascular Project.Ann Thorac Surg.1994;58(6):1858–1862.
- ,,, et al.Quality of medical care delivered to Medicare beneficiaries: a profile at state and national levels.JAMA.2000;284(13):1670–1676.
- .Cooperative Cardiovascular Project: committee updates.Iowa Med.1993;83(10):379.
- ,,, et al.Aspirin in the treatment of acute myocardial infarction in elderly Medicare beneficiaries. Patterns of use and outcomes.Circulation.1995;92(10):2841–2847.
- ,,,,,.Validation of a clinical prediction rule for left ventricular ejection fraction after myocardial infarction in patients > or = 65 years old.Am J Cardiol.1997;80(1):11–15.
- ,,,,.Clinical correlates of in‐hospital costs for acute myocardial infarction in patients 65 years of age and older.Am Heart J.1998;135(3):523–531.
- ,,, et al.Improving the quality of care for Medicare patients with acute myocardial infarction: results from the Cooperative Cardiovascular Project.JAMA.1998;279(17):1351–1357.
- ,,, et al.Geographic variation in the treatment of acute myocardial infarction.JAMA.1999;281(7):627–633.
- .HCFA's Cooperative Cardiovascular Project: a nationwide quality assessment of acute myocardial infarction.Clin Cardiol.1994;17(7):354–356.
- ,,.Long‐term outcomes of regional variations in intensity of invasive vs medical management of Medicare Patients with acute myocardial infarction.JAMA.2005;293(11):1329–1337.
- ,,, et al.ACC/AHA 2008 performance measures for adults with ST‐elevation and non‐ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to develop performance measures for ST‐elevation and non‐ST‐elevation myocardial infarction): developed in collaboration with the American Academy of Family Physicians and the American College of Emergency Physicians: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation, Society for Cardiovascular Angiography and Interventions, and Society of Hospital Medicine.Circulation.2008;118(24):2596–2648.
- ,,,,.Do “America's best hospitals” perform better for acute myocardial infarction?N Engl J Med.1999;340(4):286–292.
- ,,,.Does the ownership of the admitting hospital make a difference? Outcomes and process of care for Medicare beneficiaries admitted with acute myocardial infarction.Med Care.2003;41(10):1193–1205.
- American Academy of Hospice and Palliative Medicine. Position Statements. Statement on Clinical Practice Guidelines for Quality Palliative Care. Approved by the Board of Directors, June 2006. Available at: http://www.aahpm.org/positions/quality.html. Accessed October 2009.
- .Assessing the relationship between hospital competition and guideline adherence for acute myocardial infarction.University of Minnesota;2000.
- ,,, et al.Quality of care for Medicare patients with acute myocardial infarction. A four‐state pilot study from the Cooperative Cardiovascular Project. [see Comment].JAMA.1995;273(19):1509–1514.
- , et al.Vital and Health Statistics: Health Service Areas for the United States. DHHS (PHS)92–1386.Hyattsville, MD:National Center for Health Statistics, Centers for Disease Control, U.S. Department of Health and Human Services;1991.
- .Econometric Analysis of Cross Section and Panel Data.1st ed.Cambridge, MA:MIT Press;2002.
- StataCorp.Stata Statistical Software: Release 10.1 SE.College Station, TX:Stata Corporation,2008.
- ,,,,,.Hypertension guideline adherence among nursing home patients.J Gen Intern Med.2009;24(4):499–503.
- ,,.Testing the feasibility of implementation of clinical practice guidelines in long‐term care facilities.J Am Med Dir Assoc.2004;5(1):1–8.
- ,,,,.Improving care for nursing home‐acquired pneumonia in a managed care environment.Am J Manag Care.2004;10(10):681–686.
- ,,, et al.Barriers to and facilitators of clinical practice guideline use in nursing homes.J Am Geriatr Soc.2007;55(9):1404–1409.
- ,,.Potential pitfalls of disease‐specific guidelines for patients with multiple conditions.N Engl J Med.2004;351(27):2870–2874.
- ,,.Heart disease and prevention: race and age differences in heart disease prevention, treatment, and mortality.Med Care.2005;43(3 suppl):I33–I41.
- ,,, et al.Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006.Am Heart J.2008;156(6):1045–1055.
- ,,, et al.Evolution in cardiovascular care for elderly patients with non‐ST‐segment elevation acute coronary syndromes: results from the CRUSADE National Quality Improvement Initiative.J Am Coll Cardiol.2005;46(8):1479–1487.
- ,,.Discussions about end‐of‐life care in nursing homes.J Am Geriatr Soc.1998;46:1235–1241.
- ,,, et al.Changes in advance care planning in nursing homes before and after the Patient Self‐Determination Act: report of a 10‐state survey.J Am Geriatr Soc.1997;45(8):939–944.
The American College of Cardiology (ACC) and the American Heart Association (AHA) recommend early intervention for older persons with acute coronary syndrome (ACS) to improve prognosis. However, numerous studies demonstrate that elderly patients with acute myocardial infarction (AMI) are less likely than their younger counterparts to receive guideline‐recommended therapies.13 No prior studies specifically demonstrate that adherence to AMI guidelines is effective in patients admitted from post‐acute or long‐term care (PAC/LTC) settings such as nursing homes, intermediate care facilities, and LTC hospitals. Recognizing that the barriers to guideline‐adherent care among the elderly may also be present for clinically‐complex PAC/LTC patients, we examined whether hospitalized patients with AMI admitted from PAC/LTC settings were less likely to receive guideline‐recommended therapies and if guideline‐concordant treatment was associated with short‐term (30‐day) survival in this relatively vulnerable subgroup of patients.
Medical decision making, including applicability of guidelines, is not exclusively based on empirical evidence but is also related to morally complex issues such as patient age, social status, and other unknown factors. However, lack of outcome expectancy may limit adherence for AMI care in PAC/LTC populations.4 In particular, treating physicians may not expect that desired outcomes will result when guidelines are followed in the PAC/LTC group compared to community‐based patients. This notion is supported by other research indicating that physicians caring for nursing home residents' chronic health conditions often tailor the care approach according to the patients' functional and cognitive status rather than adhering to recommended guidelines.5 In a study that used hypothetical scenarios, nursing home patients with a better physical condition, a more obvious social role, and a lower age were more likely to be treated with life‐sustaining treatments than were other patients.6 For AMI care, some physicians provide care that is not guideline‐adherent due to concerns that reduced renal function is an absolute rather than relative contraindication to angiography.7, 8 And, because the clinical trials that informed practice guidelines for AMI care did not explicitly include individuals with the chronic complex medical problems prevalent among the PAC/LTC population, treating clinicians may be reluctant to apply acute care guidelines to this subgroup.9 However, we know of no prior research demonstrating that guideline‐adherent care for either chronic or acute conditions results in differential outcomes for PAC/LTC patients cared for in the hospital setting.
For the present study, we examined whether admission source was an independent predictor of AMI treatment and whether guideline‐concordant care was related to mortality for those admitted from PAC/LTC and community settings. We hypothesized that rates of guideline‐concordant care would be higher for patients admitted from community settings vs. PAC/LTC and that differences between the groups would be greater for more intensive interventions such as reperfusion compared to aspirin. The data included detailed clinical eligibility information for treatments based on contemporary ACC/AHA guidelines,10 along with numerous other patient demographic and clinical characteristics, thus allowing us to address the presumptive concern that PAC/LTC patients were sicker or otherwise less‐suited for treatment than other patients.
Methods
This retrospective cohort study relied on existing observational data. The primary data source for this research was the Cooperative Cardiovascular Project (CCP) national baseline data. The CCP was sponsored by the Centers for Medicare & Medicaid Services (CMS) to measure the quality of care provided to a national cohort of Medicare patients hospitalized with AMI. The national data collection and reporting effort was administered through the 53 Medicare Quality Improvement Organization (QIO) contracts established to serve each State, the District of Columbia, Puerto Rico, and the U.S. Virgin Islands. Hospital medical records were requested under QIO authority and then abstracted by centrally‐contracted Clinical Data Abstraction Centers (CDACs). Data quality monitoring involved random reabstraction of records with double entry of the information to ensure consistency across personnel, and data were found to be very reliable. Detailed data collection procedures and main findings from these data have been reported elsewhere.1126
The CCP baseline data included an initial sample of 234,754 records abstracted from inpatient medical charts for fee‐for‐services Medicare beneficiaries hospitalized in 1 of 6684 hospitals located in any of the 50 states, the District of Columbia, Puerto Rico, the U.S. Virgin Islands, American Samoa, Guam, and the Northern Mariana Islands between February 1994 and July 1995. Although the data analyzed for this research relate to hospitalizations for AMI in 1994‐1995, the 2008 ACC/AHA report regarding AMI performance measures retains recommendations for both early aspirin and reperfusion treatments.27 Even though the data are not derived from recent years, the CCP baseline data represent a unique dataset to address questions related to both clinical eligibility and guideline compliance for both community and PAC/LTC patients. The inclusion of PAC/LTC admissions and detailed information regarding clinical eligibility for treatment are particularly important to adequately address the research aim; the CCP baseline data are the single extant U.S. data source we identified that has both features.
AMI cases were identified through inpatient hospital claims using an International Classification of Diseases, 9th Revision, Clinical Modification (ICD‐9‐CM) principal discharge diagnosis of 410 (ACS) for extended chart review to verify AMI and determine clinical eligibility for treatments. CCP records were subsequently linked with the Medicare Denominator File, Area Resource File (ARF), and Medicare PPS cost reports for hospitals (PPS) to obtain additional information regarding patients, local health resources, and admitting hospital.
For the present study, we excluded cases without a confirmed AMI diagnosis; cases with missing geographic information to allow us to control for local practice variation including all cases from outside the Continental U.S.; cases admitted to nonacute facilities or with inadequate information to link with provider data; and cases that originated in states selected for the CCP pilot study due to differences in record abstraction timing and some of the measures. Clinical eligibility for treatments relied on the standardized criteria established by the CCP advisory panel and used in other research.10, 14, 2831
To test whether admission from a LTC setting was negatively associated with guideline adherence and if the relationship varied according to the intensity of the treatment, we examined 2 guidelines related to early interventions care during the hospital stay: (1) administration of aspirin; and (2) reperfusion through either thrombolytic drugs or percutaneous intervention (PTCA). We chose these measures because they range from a simple and readily‐available medical intervention (aspirin), to a clinically complex and costly intervention for a more clinically‐select group of patients (reperfusion). The hypothesis that more intensive acute treatment would be less likely for patients admitted from PAC/LTC settings was empirically tested by examining the differences in overall probabilities and adjusted probabilities of receiving each of these interventions. We then modeled the odds ratios (ORs) for survival based on receiving these treatments.
Guideline adherence and clinical eligibility indicators for the CCP data have been presented elsewhere.10, 20, 23, 29, 32 Using these criteria, we divided patients into clinical eligibility groups, including ideal candidates, eligible candidates, and candidates for whom the care was not indicated. For the present research, all eligible patients were included in the sample; with ideal eligibility included as a covariate in the regression models. All patients in the study sample were at least minimally eligible to receive aspirin during their hospital stay. Ideal candidates for aspirin did not have: a gastrointestinal (GI) ulcer, same day admission/discharge, history of bleeding disorder, risk of bleeding, anemia, allergy to aspirin, warfarin, or terminal illness. Eligible candidates for reperfusion via PTCA or thrombolysis were not transferred from another hospital or emergency department. Ideal eligibility for reperfusion required, in addition, that the patient: was under age 80 years; arrived at the hospital within 6 hours of symptom onset; showed evidence of a transmural (Q‐wave) MI or ST elevation in 2 contiguous leads on arrival electrocardiogram (ECG); was not taking warfarin; did not have cardiac arrest requiring cardiopulmonary resuscitation (CPR), cardioversion, defibrillation, or chemical cardioversion in the 6 hours prior; did not refuse a thrombolytic; did not have cardiac catheterization without PTCA within 12 hours of arrival; had no evidence of hepatic failure or cirrhosis; had no history of active ulcer disease, internal bleeding, trauma, or injury in the month prior to arrival; and had no bleeding risk, cerebral vascular accident, or surgery/biopsy within 2 months of admission.
Prearrival setting was of particular interest for the present study; this information was derived from the patient's medical chart using a standardized chart abstraction process for the CCP. From the original admission source categories, we created a single dichotomous variable that indicated PAC/LTC vs. community setting prior to arrival. We defined PAC/LTC settings to include patients admitted from either a skilled nursing facility (SNF) or intermediate care facility (ICF), chronic hospital, or other residential care facility. Three categories of admission source were used to identify the comparison sample: home, noninstitutional setting, and outpatient setting.
Because differences in care according to admission source could result from observable causes, multiple regression analysis was incorporated to control for observed factors previously shown to be associated with guideline adherence. These included: ideal eligibility for treatment; age; Caucasian (vs. other) ethnicity; gender; limitation of aggressive treatment orders (eg, do not resuscitate, do not intubate, chemical code only, no cardiac monitoring, no invasive procedures, no vasopressor, no antiarrhythmic therapy, no feeding tube, palliative care measures only); Charlson comorbidity index and Acute Physiology, Age, Chronic Health Evaluation assessment (3rd revision) (APACHE III) score, body mass index (BMI), rural hospital location, hospital teaching status, and number of full‐time equivalent cardiologists on staff at the treating hospital. The regression methods also included adjustment for clustering of patients within health services area to account for geographic variation in practice patterns.33
In developing the regression model, we predicted whether the patient received care in accord with guidelines and 30‐day mortality. We also tested whether the regression errors terms (unobserved variables) for these equations were significantly related to error terms in a regression to predict source of admission, which would indicate rejecting the hypothesis that admission source and treatments were determined independently of each other. In particular, admission source may be a proxy for underlying health status (severity of illness), care preferences, or other unobserved factors that differ systematically between patients admitted from the community vs. those admitted from PAC/LTC. In testing the models, we found that the error terms for both treatments (aspirin and reperfusion) and admission source models were significantly negatively correlated (rho or chi‐square P value <0.001), indicating the need to adjust regression estimates to account for unobserved variables related to both admission source and guideline concordant treatment. Because we rejected the hypothesis that admission source was exogenous to treatments, a seemingly‐unrelated regressions (SUR) bivariate probit model was deemed appropriate, as this methodology corrects for correlation between unobserved variables that are related to both admission source and treatment decisions (eg, residual confounding).34 And, since coefficients from SUR bivariate probit models are not directly interpretable as either ORs or relative risks with respect to the outcome variables, we converted the coefficients to reflect marginal probabilities. The correlation in error terms for models predicting 30‐day mortality and admission source was not substantively or statistically significant. As such, we utilized standard logistic regression methods for assessing mortality. Mortality models were predicted separately according to admission source and treatment to allow presentation of ORs associated with each treatment for each group.
Analyses used the Stata statistical package (version 10.1 SE).35 Approval for this use of the CCP data was received from the CMS. Approval for the data analysis protocol was received from the authors' institutional review board.
Results
Of the 128,183 patients in the analytic sample, 7.6% (n = 8151) were admitted from PAC/LTC (Table 1). The members of the PAC/LTC cohort were older on average than the community‐dwelling cohort (83 vs. 76 years, P < 0.001) and more likely to be female (69% vs. 48%, P < 0.001). Limitation of aggressive treatment orders (LAT/DNR) were in place for 55% of the PAC/LTC cohort compared to only 16% of the community‐dwelling cohort (P < 0.001). Severity of illness scores were higher among the PAC/LTC cohort with APACHE III scores of 50.8 in the PAC/LTC cohort vs. 36.8 in the community‐dwelling cohort (P < 0.001). The PAC/LTC cohort also had lower BMI (P < 0.001). Mortality at 30 days and 1 year was 39.5% and 65.4%, respectively, in the PAC/LTC cohort vs. 17.6% and 33.4%, respectively, in the community‐dwelling cohort. These differences across groups were significant at both time points (P < 0.001). PAC/LTC admissions were significantly more likely to be admitted to a hospital located in a rural area (P < 0.001), though the numbers of full‐time equivalent residents and presence of cardiologists in the treating hospitals were similar across groups.
| Sample Characteristics | Overall | PAC/LTC | Community | P Value (2‐sided test) |
|---|---|---|---|---|
| ||||
| Number of cases | 128,183 | 8,151 | 120,032 | |
| Percentage of sample | 100 | 6.4 | 93.6 | |
| Average age, years (mean SD) | 76.7 7.4 | 82.6 7.6 | 76.3 7.2 | <0.001 |
| Female (%) | 49.6 | 69.1 | 48.3 | <0.001 |
| Non‐White (%) | 9.7 | 9.1 | 9.7 | 0.09 |
| Length of stay, days (mean SD) | 7.3 7.2 | 7.4 7.1 | 7.3 7.2 | 0.33 |
| With LAT/DNR order in place (%) | 18.1 | 55.4 | 15.6 | <0.001 |
| APACHE III score (mean SD) | 37.7 17.5 | 50.8 21.0 | 36.8 16.8 | <0.001 |
| Charlson comorbidity index (mean SD) | 2.2 1.2 | 2.7 1.3 | 2.2 1.2 | <0.001 |
| BMI (mean SD) | 26.2 5.2 | 24.2 5.9 | 26.2 5.2 | <0.001 |
| Hospital residents, FTE (mean SD) | 29.3 78.4 | 29.0 78.7 | 29.3 78.3 | 0.75 |
| Hospital cardiologists, FTE (mean SD) | 11.3 13.5 | 11.0 13.9 | 11.3 13.5 | 0.03* |
| Admitted to rural hospital (%) | 20.1 | 22.3 | 20.0 | <0.001 |
| Number of secondary diagnosis codes (0‐8) (mean SD) | 5.1 2.3 | 5.8 2.1 | 5.0 2.26 | <0.001 |
| 30‐day mortality (%) | 18.9 0.39 | 39.5 0.49 | 17.6 0.38 | <0.001 |
| 1‐year mortality (%) | 33.5 0.47 | 65.4 0.48 | 31.4 0.46 | <0.001 |
Table 2 provides overall unadjusted data comparing eligibility and treatment information for PAC/LTC and community admissions. Rates of guideline adherence were uniformly higher for patients admitted from the community. Guideline adherence rates were higher for aspirin compared to reperfusion, and followed the predicted pattern that more resource‐intensive treatments would be less common for both groups and that PAC/LTC admissions would be less likely to receive treatments compared to patients admitted from community settings. Though all 8151 PAC/LTC patients were eligible to receive aspirin, only 4370 were ideally eligible and 3015 (69%) received acetylsalicylic acid (ASA). There were 1418 PAC/LTC patients (17% of the PAC/LTC sample) meeting at least minimal eligibility requirements for reperfusion. Among the 214 PAC/LTC cases that were ideally eligible for reperfusion, 65 (30%) received the treatment; 12 patients received PTCA and 53 received thrombolytic agents. Eligibility and treatment rates for reperfusion were substantially higher for the community sample, with almost 27% meeting minimum eligibility requirements and 60% of the ideally‐eligible group receiving the treatment.
| Aspirin (ASA) [n (% received)] | Reperfusion (PTCA or thrombolysis) [n (% received)] | |
|---|---|---|
| ||
| Eligible sample* | ||
| PAC/LTC | 8151 (60) | 1418 (13) |
| Community | 120,032 (79) | 34,501 (45) |
| Ideal sample* | ||
| PAC/LTC | 4370 (69) | 214 (30) |
| Community | 78,973 (86) | 16,557 (60) |
Table 3 presents the adjusted probability of treatment based upon the SUR bivariate probit regression model. As with the unadjusted results presented in Table 2, PAC/LTC patients had a lower probability of treatment even after controlling for important patient and hospital characteristics. Compared to the unadjusted results, the adjusted probabilities calculated with the SUR bivariate probit model indicated a relatively higher predicted probability of treatment for the PAC/LTC patients and a relatively lower predicted probability of treatment among the community patients. In other words, the probability of treatment becomes more similar across groups once the adjustments for both observed and unobserved differences in patient characteristics are considered. Nonetheless, a difference in probability of treatment remains across the 2 groups.
| Aspirin (ASA) | Reperfusion | |
|---|---|---|
| ||
| PAC/LTC (%) | 64 | 12 |
| Community (%) | 77 | 23 |
| Rho (P value)* | 0.069 (<0.001) | 0.17 (<0.001) |
To determine whether there was survival difference associated with treatment in these data, we conducted a logistic regression analyses to predict 30‐day mortality for both groups (Tables 4 and 5). Table 4 presents results (ORs) of our models emphasizing the relationship between aspirin and 30‐day mortality, while Table 5 presents the models with reperfusion. Model discrimination was tested using a C‐statistic and was at least 0.70 for all models, indicating good predictive validity. However, for the reperfusion models (Table 5) there were relatively few PAC/LTC patients ideally eligible for treatment, which limited statistical power. There was an association between aspirin provision and improved survival for both the PAC/LTC and community admissions (95% confidence intervals [CIs] were less than 1.0) for all eligible patients. For the eligible samples, we did not find the anticipated relationship between reperfusion and 30‐day survival. The ORs and CIs for community admissions were significantly greater than 1.0. However, we noted lower ORs of mortality for the subgroups of ideally eligible patients, with 95% CIs under 1.0 for both PAC/LTC and community admissions, indicating better survival among those who were ideally eligible for reperfusion treatment. The unadjusted data indicated that PAC/LTC patients were much more likely than their community counterparts to die within 30 days of AMI (Table 1). The multiple logistic regression results indicates PAC/LTC patients had similar ORs for mortality compared to community patients when aspirin was given to eligible patients and when reperfusion was given to ideally eligible patients (Tables 4 and 5). Based on the logistic regression results, we calculated that the adjusted probability of 30‐day mortality among eligible PAC/LTC patients who received aspirin was 0.14 compared to 0.32 for those who did not, which is a difference in probability of 0.18. For eligible community admissions, the adjusted probability of mortality with aspirin was 0.09 with aspirin treatment compared to 0.26 without. For reperfusion, the adjusted probability of 30‐day mortality for ideally eligible PAC/LTC admissions falls from 0.27 to 0.15 if treatment is given, representing a difference in probability of 0.12. Similarly, the adjusted probability difference for community admissions who were ideally eligible and received reperfusion was approximately 0.08 (P = 0.16 without treatment and P = 0.08 with treatment).
| Explanatory Variables | PAC/LTC Admissions | Community Admissions | ||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| ||||
| Aspirin (ASA) given during hospital stay | 0.50 | 0.43‐0.58 | 0.57 | 0.54‐0.60 |
| Ideal eligibility for ASA | 0.88 | 0.76‐1.01 | 0.70 | 0.67‐0.73 |
| Female (vs. Male) | 0.85 | 0.73‐0.99 | 0.94 | 0.90‐0.98 |
| Patient age, 5‐year increments | 0.99 | 0.94‐1.04 | 1.04 | 1.02‐1.05 |
| Non‐white Ethnicity (vs. White) | 0.98 | 0.76‐1.28 | 0.95 | 0.89‐1.03 |
| Current Smoker (vs. non‐smoker) | 0.93 | 0.71‐1.22 | 0.97 | 0.91‐1.03 |
| Body mass index | 0.99 | 0.97‐1.00 | 0.99 | 0.99‐1.00 |
| LAT/DNR Order | 4.09 | 3.53‐4.73 | 7.83 | 7.46‐8.21 |
| APACHE 3 Score, 5 point increments | 1.10 | 1.08‐1.12 | 1.13 | 1.12‐1.13 |
| Charlson Index, 3 point increments | 0.87 | 0.74‐1.03 | 1.06 | 1.00‐1.11 |
| Patient received in transfer | 0.99 | 0.65‐1.51 | 1.18 | 0.95‐1.46 |
| Number of hospital residents, 5 FTE increments | 1.00 | 1.00‐1.00 | 1.00 | 1.00‐1.00 |
| Hospital located in rural area | 1.10 | 0.92‐1.31 | 1.09 | 1.03‐1.15 |
| Number of cardiologists on staff, 5 FTE increments | 0.97 | 0.94‐1.00 | 1.00 | 1.00‐1.02 |
| C‐statistic | 0.76 | 0.79 | ||
| Number of observations | 4,559 | 92,004 | ||
| Explanatory Variables | PAC/LTC Admissions | Community Admissions | ||
|---|---|---|---|---|
| OR | 95% CI* | OR | 95% CI* | |
| ||||
| Reperfusion via thrombolytics or PTCA | 1.33 | 0.85‐.10 | 1.24 | 1.13‐1.35 |
| Ideal eligibility for reperfusion | 0.58 | 0.35‐0.95 | 0.74 | 0.68‐0.81 |
| Female (vs. male) | 0.92 | 0.66‐1.29 | 1.05 | 0.97‐1.14 |
| Patient age, 5‐year increments | 0.97 | 0.85‐1.10 | 1.03 | 0.99‐1.06 |
| Non‐White ethnicity (vs. White) | 1.11 | 0.59‐2.10 | 1.10 | 0.95‐1.28 |
| Current smoker (vs. nonsmoker) | 1.13 | 0.66‐1.94 | 0.87 | 0.78‐0.98 |
| BMI | 1.01 | 0.98‐1.04 | 1.00 | 0.99‐1.01 |
| LAT/DNR order | 3.41 | 2.48‐4.70 | 8.26 | 7.52‐9.06 |
| APACHE III score, 5‐point increments | 1.13 | 1.07‐1.19 | 1.15 | 1.14‐1.17 |
| Charlson comorbidity index, 3‐point increments | 0.84 | 0.58‐1.22 | 1.30 | 1.17‐1.44 |
| Patient received in transfer | 1.08 | 0.27‐4.43 | 1.49 | 0.85‐2.60 |
| Number of hospital residents, 5‐FTE increments | 0.99 | 0.98‐1.01 | 1.00 | 1.00‐1.00 |
| Hospital located in rural area | 0.90 | 0.61‐1.34 | 1.12 | 1.01‐1.25 |
| Number of cardiologists on staff, 5‐FTE increments | 0.97 | 0.90‐1.05 | 1.00 | 0.98‐1.01 |
| C‐statistic | 0.71 | 0.78 | ||
| Number of observations | 856 | 26,720 | ||
Discussion
This investigation has important implications. The results suggest systematic differences in care for PAC/LTC compared to community‐based patients hospitalized with AMI. It is possible that short‐term mortality was impacted by guideline adherence differences according to admission source. The analytic methods accounted for clinical eligibility, tested for residual confounding and used econometric methods (SUR bivariate probit) to correct it where found, and excluded patients who refused treatments. Therefore, poor eligibility and treatment refusal are inadequate explanations for the observed differences in treatment according to admission source from a PAC/LTC facility.
Providers may not to follow AMI treatment guidelines because the perceived risks for patients transferred from PAC/LTC were too great or due to a limited clinical evidence base. Even though PAC/LTC patients were not included in clinical trials for AMI care, studies that carefully use observational data may help guide applicability of clinical recommendations for acute care to subgroups of clinically complex patients. This study offers observational evidence and information to guide additional studies regarding of the clinical benefit of treating a particularly vulnerable subgroup of patients.
Other research has noted that adherence to clinical practice guidelines in PAC/LTC facilities is low.36, 37 LTC practitioners have been reluctant to apply clinical practice guidelines to residents with chronic illnesses because these regimens often do not take into consideration individuals with the multiple chronic diseases prevalent among PAC/LTC patients9 and the complexity of the PAC/LTC environment.38, 39 Rather than dismiss the utility of clinical practice guidelines in the PAC/LTC population, this study is one of the first to demonstrate that use of acute care clinical practice guidelines, particularly aspirin, was associated with improved acute care outcomes among PAC/LTC patients transferred to acute care hospitals with AMI. Thus, guidelines for acute inpatient care may be more readily applied to the PAC/LTC population than studies aimed at treating chronic illnesses.9, 38, 40 Our results indicate that reperfusion might not be indicated for the preponderance of PAC/LTC patients, but many would agree that treatments such as aspirin would be a low‐burden intervention for most PAC/LTC patients. This investigation supports considering AMI treatment guidelines even for frail subpopulations such as those transferred from PAC/LTC. Further, the findings suggest there may be important information obtained by including PAC/LTC patients in future clinical trials.
This study has several limitations. First, the data were collected during 1995, and may not adequately reflect the current state of the art for AMI treatment or other changes in the organization, financing, and delivery of care for AMI. Nevertheless, care guidelines for AMI have not changed in ways that we anticipate altering the patterns of care examined in this study. For example, in the 2004 National Healthcare Disparities Report,41 receipt of aspirin among elderly individuals ranged from 79.6% to 86%, which closely resembles our results. Despite overall care improvements from 1990 to 2006, women, minorities, and patients ages 75 years and older remain significantly less likely to receive revascularization or discharge lipid‐lowering therapy relative to their counterparts indicating that differences in care persist today.42 While the data used in these analyses existed before recommendations included specific guidance regarding the care of older adults, other researchers examined data collected from January 1, 2005 to June 30, 2006 and demonstrated that elderly individuals remained less likely to receive indicated therapies.43 Further, this is the only dataset we identified that included an adequate presence of both PAC/LTC and community admission sources and sufficient data to assess guideline adherence and other covariates for our models. Second, The SUR bivariate probit models that account for correlation of error terms in models predicting both admission source and treatment were included to minimize issues related to residual confounding, but may not completely eliminate all systematic variation related to the underlying health status of community vs. PAC/LTC residents. Third, limitation of aggressive treatments was not recorded as to specific type of directives but research has shown that orders to forego treatments other than CPR are written for fewer than 8 % of nursing home residents.44, 45 Furthermore, all of these patients were transferred to a hospital; these transfers almost certainly occurred with an expectation that acute treatment would be offered. Fourth, we were unable to distinguish PAC vs. LTC based on admission source categories provided in the original data source. Finally, PTCA and thrombolysis were considered as a single variable because separating the 2 procedures would result in inadequate sample size to detect statistical differences between the 2 groups.
Conclusions
Patients admitted from PAC/LTC settings were less likely to receive early guideline‐recommended treatment for AMI compared to community‐dwelling patients. Our study finds evidence that following the aspirin guideline may improve survival for most patients, but that reperfusion improved survival only for a clinically‐select subgroup of patients. As such, a possible recommendation for further clinical study is that low‐burden treatments such as aspirin should be offered to most patients with AMI, including those from PAC/LTC. Higher‐burden treatments with have greater associated risks, such as reperfusion, also require more study to inform situations applicable to PAC/LTC patients. Clinical trials data would be indicated to strengthen evidence regarding which AMI treatment guidelines should be followed in frail populations from PAC/LTC settings; we identified no randomized trials that specifically demonstrate efficacy of AMI guidelines for this subgroup of vulnerable patients.
The American College of Cardiology (ACC) and the American Heart Association (AHA) recommend early intervention for older persons with acute coronary syndrome (ACS) to improve prognosis. However, numerous studies demonstrate that elderly patients with acute myocardial infarction (AMI) are less likely than their younger counterparts to receive guideline‐recommended therapies.13 No prior studies specifically demonstrate that adherence to AMI guidelines is effective in patients admitted from post‐acute or long‐term care (PAC/LTC) settings such as nursing homes, intermediate care facilities, and LTC hospitals. Recognizing that the barriers to guideline‐adherent care among the elderly may also be present for clinically‐complex PAC/LTC patients, we examined whether hospitalized patients with AMI admitted from PAC/LTC settings were less likely to receive guideline‐recommended therapies and if guideline‐concordant treatment was associated with short‐term (30‐day) survival in this relatively vulnerable subgroup of patients.
Medical decision making, including applicability of guidelines, is not exclusively based on empirical evidence but is also related to morally complex issues such as patient age, social status, and other unknown factors. However, lack of outcome expectancy may limit adherence for AMI care in PAC/LTC populations.4 In particular, treating physicians may not expect that desired outcomes will result when guidelines are followed in the PAC/LTC group compared to community‐based patients. This notion is supported by other research indicating that physicians caring for nursing home residents' chronic health conditions often tailor the care approach according to the patients' functional and cognitive status rather than adhering to recommended guidelines.5 In a study that used hypothetical scenarios, nursing home patients with a better physical condition, a more obvious social role, and a lower age were more likely to be treated with life‐sustaining treatments than were other patients.6 For AMI care, some physicians provide care that is not guideline‐adherent due to concerns that reduced renal function is an absolute rather than relative contraindication to angiography.7, 8 And, because the clinical trials that informed practice guidelines for AMI care did not explicitly include individuals with the chronic complex medical problems prevalent among the PAC/LTC population, treating clinicians may be reluctant to apply acute care guidelines to this subgroup.9 However, we know of no prior research demonstrating that guideline‐adherent care for either chronic or acute conditions results in differential outcomes for PAC/LTC patients cared for in the hospital setting.
For the present study, we examined whether admission source was an independent predictor of AMI treatment and whether guideline‐concordant care was related to mortality for those admitted from PAC/LTC and community settings. We hypothesized that rates of guideline‐concordant care would be higher for patients admitted from community settings vs. PAC/LTC and that differences between the groups would be greater for more intensive interventions such as reperfusion compared to aspirin. The data included detailed clinical eligibility information for treatments based on contemporary ACC/AHA guidelines,10 along with numerous other patient demographic and clinical characteristics, thus allowing us to address the presumptive concern that PAC/LTC patients were sicker or otherwise less‐suited for treatment than other patients.
Methods
This retrospective cohort study relied on existing observational data. The primary data source for this research was the Cooperative Cardiovascular Project (CCP) national baseline data. The CCP was sponsored by the Centers for Medicare & Medicaid Services (CMS) to measure the quality of care provided to a national cohort of Medicare patients hospitalized with AMI. The national data collection and reporting effort was administered through the 53 Medicare Quality Improvement Organization (QIO) contracts established to serve each State, the District of Columbia, Puerto Rico, and the U.S. Virgin Islands. Hospital medical records were requested under QIO authority and then abstracted by centrally‐contracted Clinical Data Abstraction Centers (CDACs). Data quality monitoring involved random reabstraction of records with double entry of the information to ensure consistency across personnel, and data were found to be very reliable. Detailed data collection procedures and main findings from these data have been reported elsewhere.1126
The CCP baseline data included an initial sample of 234,754 records abstracted from inpatient medical charts for fee‐for‐services Medicare beneficiaries hospitalized in 1 of 6684 hospitals located in any of the 50 states, the District of Columbia, Puerto Rico, the U.S. Virgin Islands, American Samoa, Guam, and the Northern Mariana Islands between February 1994 and July 1995. Although the data analyzed for this research relate to hospitalizations for AMI in 1994‐1995, the 2008 ACC/AHA report regarding AMI performance measures retains recommendations for both early aspirin and reperfusion treatments.27 Even though the data are not derived from recent years, the CCP baseline data represent a unique dataset to address questions related to both clinical eligibility and guideline compliance for both community and PAC/LTC patients. The inclusion of PAC/LTC admissions and detailed information regarding clinical eligibility for treatment are particularly important to adequately address the research aim; the CCP baseline data are the single extant U.S. data source we identified that has both features.
AMI cases were identified through inpatient hospital claims using an International Classification of Diseases, 9th Revision, Clinical Modification (ICD‐9‐CM) principal discharge diagnosis of 410 (ACS) for extended chart review to verify AMI and determine clinical eligibility for treatments. CCP records were subsequently linked with the Medicare Denominator File, Area Resource File (ARF), and Medicare PPS cost reports for hospitals (PPS) to obtain additional information regarding patients, local health resources, and admitting hospital.
For the present study, we excluded cases without a confirmed AMI diagnosis; cases with missing geographic information to allow us to control for local practice variation including all cases from outside the Continental U.S.; cases admitted to nonacute facilities or with inadequate information to link with provider data; and cases that originated in states selected for the CCP pilot study due to differences in record abstraction timing and some of the measures. Clinical eligibility for treatments relied on the standardized criteria established by the CCP advisory panel and used in other research.10, 14, 2831
To test whether admission from a LTC setting was negatively associated with guideline adherence and if the relationship varied according to the intensity of the treatment, we examined 2 guidelines related to early interventions care during the hospital stay: (1) administration of aspirin; and (2) reperfusion through either thrombolytic drugs or percutaneous intervention (PTCA). We chose these measures because they range from a simple and readily‐available medical intervention (aspirin), to a clinically complex and costly intervention for a more clinically‐select group of patients (reperfusion). The hypothesis that more intensive acute treatment would be less likely for patients admitted from PAC/LTC settings was empirically tested by examining the differences in overall probabilities and adjusted probabilities of receiving each of these interventions. We then modeled the odds ratios (ORs) for survival based on receiving these treatments.
Guideline adherence and clinical eligibility indicators for the CCP data have been presented elsewhere.10, 20, 23, 29, 32 Using these criteria, we divided patients into clinical eligibility groups, including ideal candidates, eligible candidates, and candidates for whom the care was not indicated. For the present research, all eligible patients were included in the sample; with ideal eligibility included as a covariate in the regression models. All patients in the study sample were at least minimally eligible to receive aspirin during their hospital stay. Ideal candidates for aspirin did not have: a gastrointestinal (GI) ulcer, same day admission/discharge, history of bleeding disorder, risk of bleeding, anemia, allergy to aspirin, warfarin, or terminal illness. Eligible candidates for reperfusion via PTCA or thrombolysis were not transferred from another hospital or emergency department. Ideal eligibility for reperfusion required, in addition, that the patient: was under age 80 years; arrived at the hospital within 6 hours of symptom onset; showed evidence of a transmural (Q‐wave) MI or ST elevation in 2 contiguous leads on arrival electrocardiogram (ECG); was not taking warfarin; did not have cardiac arrest requiring cardiopulmonary resuscitation (CPR), cardioversion, defibrillation, or chemical cardioversion in the 6 hours prior; did not refuse a thrombolytic; did not have cardiac catheterization without PTCA within 12 hours of arrival; had no evidence of hepatic failure or cirrhosis; had no history of active ulcer disease, internal bleeding, trauma, or injury in the month prior to arrival; and had no bleeding risk, cerebral vascular accident, or surgery/biopsy within 2 months of admission.
Prearrival setting was of particular interest for the present study; this information was derived from the patient's medical chart using a standardized chart abstraction process for the CCP. From the original admission source categories, we created a single dichotomous variable that indicated PAC/LTC vs. community setting prior to arrival. We defined PAC/LTC settings to include patients admitted from either a skilled nursing facility (SNF) or intermediate care facility (ICF), chronic hospital, or other residential care facility. Three categories of admission source were used to identify the comparison sample: home, noninstitutional setting, and outpatient setting.
Because differences in care according to admission source could result from observable causes, multiple regression analysis was incorporated to control for observed factors previously shown to be associated with guideline adherence. These included: ideal eligibility for treatment; age; Caucasian (vs. other) ethnicity; gender; limitation of aggressive treatment orders (eg, do not resuscitate, do not intubate, chemical code only, no cardiac monitoring, no invasive procedures, no vasopressor, no antiarrhythmic therapy, no feeding tube, palliative care measures only); Charlson comorbidity index and Acute Physiology, Age, Chronic Health Evaluation assessment (3rd revision) (APACHE III) score, body mass index (BMI), rural hospital location, hospital teaching status, and number of full‐time equivalent cardiologists on staff at the treating hospital. The regression methods also included adjustment for clustering of patients within health services area to account for geographic variation in practice patterns.33
In developing the regression model, we predicted whether the patient received care in accord with guidelines and 30‐day mortality. We also tested whether the regression errors terms (unobserved variables) for these equations were significantly related to error terms in a regression to predict source of admission, which would indicate rejecting the hypothesis that admission source and treatments were determined independently of each other. In particular, admission source may be a proxy for underlying health status (severity of illness), care preferences, or other unobserved factors that differ systematically between patients admitted from the community vs. those admitted from PAC/LTC. In testing the models, we found that the error terms for both treatments (aspirin and reperfusion) and admission source models were significantly negatively correlated (rho or chi‐square P value <0.001), indicating the need to adjust regression estimates to account for unobserved variables related to both admission source and guideline concordant treatment. Because we rejected the hypothesis that admission source was exogenous to treatments, a seemingly‐unrelated regressions (SUR) bivariate probit model was deemed appropriate, as this methodology corrects for correlation between unobserved variables that are related to both admission source and treatment decisions (eg, residual confounding).34 And, since coefficients from SUR bivariate probit models are not directly interpretable as either ORs or relative risks with respect to the outcome variables, we converted the coefficients to reflect marginal probabilities. The correlation in error terms for models predicting 30‐day mortality and admission source was not substantively or statistically significant. As such, we utilized standard logistic regression methods for assessing mortality. Mortality models were predicted separately according to admission source and treatment to allow presentation of ORs associated with each treatment for each group.
Analyses used the Stata statistical package (version 10.1 SE).35 Approval for this use of the CCP data was received from the CMS. Approval for the data analysis protocol was received from the authors' institutional review board.
Results
Of the 128,183 patients in the analytic sample, 7.6% (n = 8151) were admitted from PAC/LTC (Table 1). The members of the PAC/LTC cohort were older on average than the community‐dwelling cohort (83 vs. 76 years, P < 0.001) and more likely to be female (69% vs. 48%, P < 0.001). Limitation of aggressive treatment orders (LAT/DNR) were in place for 55% of the PAC/LTC cohort compared to only 16% of the community‐dwelling cohort (P < 0.001). Severity of illness scores were higher among the PAC/LTC cohort with APACHE III scores of 50.8 in the PAC/LTC cohort vs. 36.8 in the community‐dwelling cohort (P < 0.001). The PAC/LTC cohort also had lower BMI (P < 0.001). Mortality at 30 days and 1 year was 39.5% and 65.4%, respectively, in the PAC/LTC cohort vs. 17.6% and 33.4%, respectively, in the community‐dwelling cohort. These differences across groups were significant at both time points (P < 0.001). PAC/LTC admissions were significantly more likely to be admitted to a hospital located in a rural area (P < 0.001), though the numbers of full‐time equivalent residents and presence of cardiologists in the treating hospitals were similar across groups.
| Sample Characteristics | Overall | PAC/LTC | Community | P Value (2‐sided test) |
|---|---|---|---|---|
| ||||
| Number of cases | 128,183 | 8,151 | 120,032 | |
| Percentage of sample | 100 | 6.4 | 93.6 | |
| Average age, years (mean SD) | 76.7 7.4 | 82.6 7.6 | 76.3 7.2 | <0.001 |
| Female (%) | 49.6 | 69.1 | 48.3 | <0.001 |
| Non‐White (%) | 9.7 | 9.1 | 9.7 | 0.09 |
| Length of stay, days (mean SD) | 7.3 7.2 | 7.4 7.1 | 7.3 7.2 | 0.33 |
| With LAT/DNR order in place (%) | 18.1 | 55.4 | 15.6 | <0.001 |
| APACHE III score (mean SD) | 37.7 17.5 | 50.8 21.0 | 36.8 16.8 | <0.001 |
| Charlson comorbidity index (mean SD) | 2.2 1.2 | 2.7 1.3 | 2.2 1.2 | <0.001 |
| BMI (mean SD) | 26.2 5.2 | 24.2 5.9 | 26.2 5.2 | <0.001 |
| Hospital residents, FTE (mean SD) | 29.3 78.4 | 29.0 78.7 | 29.3 78.3 | 0.75 |
| Hospital cardiologists, FTE (mean SD) | 11.3 13.5 | 11.0 13.9 | 11.3 13.5 | 0.03* |
| Admitted to rural hospital (%) | 20.1 | 22.3 | 20.0 | <0.001 |
| Number of secondary diagnosis codes (0‐8) (mean SD) | 5.1 2.3 | 5.8 2.1 | 5.0 2.26 | <0.001 |
| 30‐day mortality (%) | 18.9 0.39 | 39.5 0.49 | 17.6 0.38 | <0.001 |
| 1‐year mortality (%) | 33.5 0.47 | 65.4 0.48 | 31.4 0.46 | <0.001 |
Table 2 provides overall unadjusted data comparing eligibility and treatment information for PAC/LTC and community admissions. Rates of guideline adherence were uniformly higher for patients admitted from the community. Guideline adherence rates were higher for aspirin compared to reperfusion, and followed the predicted pattern that more resource‐intensive treatments would be less common for both groups and that PAC/LTC admissions would be less likely to receive treatments compared to patients admitted from community settings. Though all 8151 PAC/LTC patients were eligible to receive aspirin, only 4370 were ideally eligible and 3015 (69%) received acetylsalicylic acid (ASA). There were 1418 PAC/LTC patients (17% of the PAC/LTC sample) meeting at least minimal eligibility requirements for reperfusion. Among the 214 PAC/LTC cases that were ideally eligible for reperfusion, 65 (30%) received the treatment; 12 patients received PTCA and 53 received thrombolytic agents. Eligibility and treatment rates for reperfusion were substantially higher for the community sample, with almost 27% meeting minimum eligibility requirements and 60% of the ideally‐eligible group receiving the treatment.
| Aspirin (ASA) [n (% received)] | Reperfusion (PTCA or thrombolysis) [n (% received)] | |
|---|---|---|
| ||
| Eligible sample* | ||
| PAC/LTC | 8151 (60) | 1418 (13) |
| Community | 120,032 (79) | 34,501 (45) |
| Ideal sample* | ||
| PAC/LTC | 4370 (69) | 214 (30) |
| Community | 78,973 (86) | 16,557 (60) |
Table 3 presents the adjusted probability of treatment based upon the SUR bivariate probit regression model. As with the unadjusted results presented in Table 2, PAC/LTC patients had a lower probability of treatment even after controlling for important patient and hospital characteristics. Compared to the unadjusted results, the adjusted probabilities calculated with the SUR bivariate probit model indicated a relatively higher predicted probability of treatment for the PAC/LTC patients and a relatively lower predicted probability of treatment among the community patients. In other words, the probability of treatment becomes more similar across groups once the adjustments for both observed and unobserved differences in patient characteristics are considered. Nonetheless, a difference in probability of treatment remains across the 2 groups.
| Aspirin (ASA) | Reperfusion | |
|---|---|---|
| ||
| PAC/LTC (%) | 64 | 12 |
| Community (%) | 77 | 23 |
| Rho (P value)* | 0.069 (<0.001) | 0.17 (<0.001) |
To determine whether there was survival difference associated with treatment in these data, we conducted a logistic regression analyses to predict 30‐day mortality for both groups (Tables 4 and 5). Table 4 presents results (ORs) of our models emphasizing the relationship between aspirin and 30‐day mortality, while Table 5 presents the models with reperfusion. Model discrimination was tested using a C‐statistic and was at least 0.70 for all models, indicating good predictive validity. However, for the reperfusion models (Table 5) there were relatively few PAC/LTC patients ideally eligible for treatment, which limited statistical power. There was an association between aspirin provision and improved survival for both the PAC/LTC and community admissions (95% confidence intervals [CIs] were less than 1.0) for all eligible patients. For the eligible samples, we did not find the anticipated relationship between reperfusion and 30‐day survival. The ORs and CIs for community admissions were significantly greater than 1.0. However, we noted lower ORs of mortality for the subgroups of ideally eligible patients, with 95% CIs under 1.0 for both PAC/LTC and community admissions, indicating better survival among those who were ideally eligible for reperfusion treatment. The unadjusted data indicated that PAC/LTC patients were much more likely than their community counterparts to die within 30 days of AMI (Table 1). The multiple logistic regression results indicates PAC/LTC patients had similar ORs for mortality compared to community patients when aspirin was given to eligible patients and when reperfusion was given to ideally eligible patients (Tables 4 and 5). Based on the logistic regression results, we calculated that the adjusted probability of 30‐day mortality among eligible PAC/LTC patients who received aspirin was 0.14 compared to 0.32 for those who did not, which is a difference in probability of 0.18. For eligible community admissions, the adjusted probability of mortality with aspirin was 0.09 with aspirin treatment compared to 0.26 without. For reperfusion, the adjusted probability of 30‐day mortality for ideally eligible PAC/LTC admissions falls from 0.27 to 0.15 if treatment is given, representing a difference in probability of 0.12. Similarly, the adjusted probability difference for community admissions who were ideally eligible and received reperfusion was approximately 0.08 (P = 0.16 without treatment and P = 0.08 with treatment).
| Explanatory Variables | PAC/LTC Admissions | Community Admissions | ||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| ||||
| Aspirin (ASA) given during hospital stay | 0.50 | 0.43‐0.58 | 0.57 | 0.54‐0.60 |
| Ideal eligibility for ASA | 0.88 | 0.76‐1.01 | 0.70 | 0.67‐0.73 |
| Female (vs. Male) | 0.85 | 0.73‐0.99 | 0.94 | 0.90‐0.98 |
| Patient age, 5‐year increments | 0.99 | 0.94‐1.04 | 1.04 | 1.02‐1.05 |
| Non‐white Ethnicity (vs. White) | 0.98 | 0.76‐1.28 | 0.95 | 0.89‐1.03 |
| Current Smoker (vs. non‐smoker) | 0.93 | 0.71‐1.22 | 0.97 | 0.91‐1.03 |
| Body mass index | 0.99 | 0.97‐1.00 | 0.99 | 0.99‐1.00 |
| LAT/DNR Order | 4.09 | 3.53‐4.73 | 7.83 | 7.46‐8.21 |
| APACHE 3 Score, 5 point increments | 1.10 | 1.08‐1.12 | 1.13 | 1.12‐1.13 |
| Charlson Index, 3 point increments | 0.87 | 0.74‐1.03 | 1.06 | 1.00‐1.11 |
| Patient received in transfer | 0.99 | 0.65‐1.51 | 1.18 | 0.95‐1.46 |
| Number of hospital residents, 5 FTE increments | 1.00 | 1.00‐1.00 | 1.00 | 1.00‐1.00 |
| Hospital located in rural area | 1.10 | 0.92‐1.31 | 1.09 | 1.03‐1.15 |
| Number of cardiologists on staff, 5 FTE increments | 0.97 | 0.94‐1.00 | 1.00 | 1.00‐1.02 |
| C‐statistic | 0.76 | 0.79 | ||
| Number of observations | 4,559 | 92,004 | ||
| Explanatory Variables | PAC/LTC Admissions | Community Admissions | ||
|---|---|---|---|---|
| OR | 95% CI* | OR | 95% CI* | |
| ||||
| Reperfusion via thrombolytics or PTCA | 1.33 | 0.85‐.10 | 1.24 | 1.13‐1.35 |
| Ideal eligibility for reperfusion | 0.58 | 0.35‐0.95 | 0.74 | 0.68‐0.81 |
| Female (vs. male) | 0.92 | 0.66‐1.29 | 1.05 | 0.97‐1.14 |
| Patient age, 5‐year increments | 0.97 | 0.85‐1.10 | 1.03 | 0.99‐1.06 |
| Non‐White ethnicity (vs. White) | 1.11 | 0.59‐2.10 | 1.10 | 0.95‐1.28 |
| Current smoker (vs. nonsmoker) | 1.13 | 0.66‐1.94 | 0.87 | 0.78‐0.98 |
| BMI | 1.01 | 0.98‐1.04 | 1.00 | 0.99‐1.01 |
| LAT/DNR order | 3.41 | 2.48‐4.70 | 8.26 | 7.52‐9.06 |
| APACHE III score, 5‐point increments | 1.13 | 1.07‐1.19 | 1.15 | 1.14‐1.17 |
| Charlson comorbidity index, 3‐point increments | 0.84 | 0.58‐1.22 | 1.30 | 1.17‐1.44 |
| Patient received in transfer | 1.08 | 0.27‐4.43 | 1.49 | 0.85‐2.60 |
| Number of hospital residents, 5‐FTE increments | 0.99 | 0.98‐1.01 | 1.00 | 1.00‐1.00 |
| Hospital located in rural area | 0.90 | 0.61‐1.34 | 1.12 | 1.01‐1.25 |
| Number of cardiologists on staff, 5‐FTE increments | 0.97 | 0.90‐1.05 | 1.00 | 0.98‐1.01 |
| C‐statistic | 0.71 | 0.78 | ||
| Number of observations | 856 | 26,720 | ||
Discussion
This investigation has important implications. The results suggest systematic differences in care for PAC/LTC compared to community‐based patients hospitalized with AMI. It is possible that short‐term mortality was impacted by guideline adherence differences according to admission source. The analytic methods accounted for clinical eligibility, tested for residual confounding and used econometric methods (SUR bivariate probit) to correct it where found, and excluded patients who refused treatments. Therefore, poor eligibility and treatment refusal are inadequate explanations for the observed differences in treatment according to admission source from a PAC/LTC facility.
Providers may not to follow AMI treatment guidelines because the perceived risks for patients transferred from PAC/LTC were too great or due to a limited clinical evidence base. Even though PAC/LTC patients were not included in clinical trials for AMI care, studies that carefully use observational data may help guide applicability of clinical recommendations for acute care to subgroups of clinically complex patients. This study offers observational evidence and information to guide additional studies regarding of the clinical benefit of treating a particularly vulnerable subgroup of patients.
Other research has noted that adherence to clinical practice guidelines in PAC/LTC facilities is low.36, 37 LTC practitioners have been reluctant to apply clinical practice guidelines to residents with chronic illnesses because these regimens often do not take into consideration individuals with the multiple chronic diseases prevalent among PAC/LTC patients9 and the complexity of the PAC/LTC environment.38, 39 Rather than dismiss the utility of clinical practice guidelines in the PAC/LTC population, this study is one of the first to demonstrate that use of acute care clinical practice guidelines, particularly aspirin, was associated with improved acute care outcomes among PAC/LTC patients transferred to acute care hospitals with AMI. Thus, guidelines for acute inpatient care may be more readily applied to the PAC/LTC population than studies aimed at treating chronic illnesses.9, 38, 40 Our results indicate that reperfusion might not be indicated for the preponderance of PAC/LTC patients, but many would agree that treatments such as aspirin would be a low‐burden intervention for most PAC/LTC patients. This investigation supports considering AMI treatment guidelines even for frail subpopulations such as those transferred from PAC/LTC. Further, the findings suggest there may be important information obtained by including PAC/LTC patients in future clinical trials.
This study has several limitations. First, the data were collected during 1995, and may not adequately reflect the current state of the art for AMI treatment or other changes in the organization, financing, and delivery of care for AMI. Nevertheless, care guidelines for AMI have not changed in ways that we anticipate altering the patterns of care examined in this study. For example, in the 2004 National Healthcare Disparities Report,41 receipt of aspirin among elderly individuals ranged from 79.6% to 86%, which closely resembles our results. Despite overall care improvements from 1990 to 2006, women, minorities, and patients ages 75 years and older remain significantly less likely to receive revascularization or discharge lipid‐lowering therapy relative to their counterparts indicating that differences in care persist today.42 While the data used in these analyses existed before recommendations included specific guidance regarding the care of older adults, other researchers examined data collected from January 1, 2005 to June 30, 2006 and demonstrated that elderly individuals remained less likely to receive indicated therapies.43 Further, this is the only dataset we identified that included an adequate presence of both PAC/LTC and community admission sources and sufficient data to assess guideline adherence and other covariates for our models. Second, The SUR bivariate probit models that account for correlation of error terms in models predicting both admission source and treatment were included to minimize issues related to residual confounding, but may not completely eliminate all systematic variation related to the underlying health status of community vs. PAC/LTC residents. Third, limitation of aggressive treatments was not recorded as to specific type of directives but research has shown that orders to forego treatments other than CPR are written for fewer than 8 % of nursing home residents.44, 45 Furthermore, all of these patients were transferred to a hospital; these transfers almost certainly occurred with an expectation that acute treatment would be offered. Fourth, we were unable to distinguish PAC vs. LTC based on admission source categories provided in the original data source. Finally, PTCA and thrombolysis were considered as a single variable because separating the 2 procedures would result in inadequate sample size to detect statistical differences between the 2 groups.
Conclusions
Patients admitted from PAC/LTC settings were less likely to receive early guideline‐recommended treatment for AMI compared to community‐dwelling patients. Our study finds evidence that following the aspirin guideline may improve survival for most patients, but that reperfusion improved survival only for a clinically‐select subgroup of patients. As such, a possible recommendation for further clinical study is that low‐burden treatments such as aspirin should be offered to most patients with AMI, including those from PAC/LTC. Higher‐burden treatments with have greater associated risks, such as reperfusion, also require more study to inform situations applicable to PAC/LTC patients. Clinical trials data would be indicated to strengthen evidence regarding which AMI treatment guidelines should be followed in frail populations from PAC/LTC settings; we identified no randomized trials that specifically demonstrate efficacy of AMI guidelines for this subgroup of vulnerable patients.
- ,,,.The Characteristics of Long‐Term Care Users. Agency for Healthcare Research and Quality (AHRQ) Publication No. 00–0049.Rockville, MD:Agency for Healthcare Research and Quality;2000.
- U.S. Bureau of the Census.Current Population Reports, P23–190, 65+ in the United States.Washington, DC:U.S. Government Printing Office;1996.
- ,,, et al.Older emergency department patients with acute myocardial infarction receive lower quality of care than younger patients.Ann Emerg Med.2005;46(1):14–21.
- ,,, et al.Why don't physicians follow clinical practice guidelines? A framework for improvement.JAMA.1999;282(15):1458–1465.
- ,,, et al.Differences in diabetes management of nursing home patients based on functional and cognitive status.J Am Med Dir Assoc.2005;6(6):375–382.
- ,,,,.Medical and nonmedical determinants of decision making about potentially life‐prolonging interventions.Med Decis Making.2004;24(5):518–524.
- .Hidden barriers to improvement in the quality of care.N Engl J Med.2001;345(22):1612–1620.
- ,,.“Renalism”: inappropriately low rates of coronary angiography in elderly individuals with renal insufficiency.J Am Soc Nephrol.2004;15(9):2462–2468.
- ,,,,,.Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance.JAMA.2005;294(6):716–724.
- ,,, et al.ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction).J Am Coll Cardiol.1996;28(5):1328–1428.
- ,,,,.Racial differences in the medical treatment of elderly Medicare patients with acute myocardial infarction.J Gen Intern Med.1996;11(12):736–743.
- ,,,,,.Resource use and quality of care for Medicare patients with acute myocardial infarction in Maryland and the District of Columbia: analysis of data from the Cooperative Cardiovascular Project.Am Heart J.1998;135(2 pt 1):349–356.
- ,,, et al.ACC/AHA 2002 guideline update for the management of patients with unstable angina and non‐ST‐segment elevation myocardial infarction—summary article: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the Management of Patients With Unstable Angina).J Am Coll Cardiol.2002;40(7):1366–1374.
- ,,,,.Impact of managed care on the treatment, costs, and outcomes of fee‐for‐service Medicare patients with acute myocardial infarction.Health Serv Res.2005;39(1):131–152.
- ,,, et al.Quality of care for Medicare patients with acute myocardial infarction. A four‐state pilot study from the Cooperative Cardiovascular Project.JAMA.1995;273(19):1509–1514.
- ,,,,.Regionalization of cardiac surgery in the United States and Canada: geographic access, choice, and outcomes.JAMA.1995;274(16):1282–1288.
- .HCFA's Health Care Quality Improvement Program and the Cooperative Cardiovascular Project.Ann Thorac Surg.1994;58(6):1858–1862.
- ,,, et al.Quality of medical care delivered to Medicare beneficiaries: a profile at state and national levels.JAMA.2000;284(13):1670–1676.
- .Cooperative Cardiovascular Project: committee updates.Iowa Med.1993;83(10):379.
- ,,, et al.Aspirin in the treatment of acute myocardial infarction in elderly Medicare beneficiaries. Patterns of use and outcomes.Circulation.1995;92(10):2841–2847.
- ,,,,,.Validation of a clinical prediction rule for left ventricular ejection fraction after myocardial infarction in patients > or = 65 years old.Am J Cardiol.1997;80(1):11–15.
- ,,,,.Clinical correlates of in‐hospital costs for acute myocardial infarction in patients 65 years of age and older.Am Heart J.1998;135(3):523–531.
- ,,, et al.Improving the quality of care for Medicare patients with acute myocardial infarction: results from the Cooperative Cardiovascular Project.JAMA.1998;279(17):1351–1357.
- ,,, et al.Geographic variation in the treatment of acute myocardial infarction.JAMA.1999;281(7):627–633.
- .HCFA's Cooperative Cardiovascular Project: a nationwide quality assessment of acute myocardial infarction.Clin Cardiol.1994;17(7):354–356.
- ,,.Long‐term outcomes of regional variations in intensity of invasive vs medical management of Medicare Patients with acute myocardial infarction.JAMA.2005;293(11):1329–1337.
- ,,, et al.ACC/AHA 2008 performance measures for adults with ST‐elevation and non‐ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to develop performance measures for ST‐elevation and non‐ST‐elevation myocardial infarction): developed in collaboration with the American Academy of Family Physicians and the American College of Emergency Physicians: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation, Society for Cardiovascular Angiography and Interventions, and Society of Hospital Medicine.Circulation.2008;118(24):2596–2648.
- ,,,,.Do “America's best hospitals” perform better for acute myocardial infarction?N Engl J Med.1999;340(4):286–292.
- ,,,.Does the ownership of the admitting hospital make a difference? Outcomes and process of care for Medicare beneficiaries admitted with acute myocardial infarction.Med Care.2003;41(10):1193–1205.
- American Academy of Hospice and Palliative Medicine. Position Statements. Statement on Clinical Practice Guidelines for Quality Palliative Care. Approved by the Board of Directors, June 2006. Available at: http://www.aahpm.org/positions/quality.html. Accessed October 2009.
- .Assessing the relationship between hospital competition and guideline adherence for acute myocardial infarction.University of Minnesota;2000.
- ,,, et al.Quality of care for Medicare patients with acute myocardial infarction. A four‐state pilot study from the Cooperative Cardiovascular Project. [see Comment].JAMA.1995;273(19):1509–1514.
- , et al.Vital and Health Statistics: Health Service Areas for the United States. DHHS (PHS)92–1386.Hyattsville, MD:National Center for Health Statistics, Centers for Disease Control, U.S. Department of Health and Human Services;1991.
- .Econometric Analysis of Cross Section and Panel Data.1st ed.Cambridge, MA:MIT Press;2002.
- StataCorp.Stata Statistical Software: Release 10.1 SE.College Station, TX:Stata Corporation,2008.
- ,,,,,.Hypertension guideline adherence among nursing home patients.J Gen Intern Med.2009;24(4):499–503.
- ,,.Testing the feasibility of implementation of clinical practice guidelines in long‐term care facilities.J Am Med Dir Assoc.2004;5(1):1–8.
- ,,,,.Improving care for nursing home‐acquired pneumonia in a managed care environment.Am J Manag Care.2004;10(10):681–686.
- ,,, et al.Barriers to and facilitators of clinical practice guideline use in nursing homes.J Am Geriatr Soc.2007;55(9):1404–1409.
- ,,.Potential pitfalls of disease‐specific guidelines for patients with multiple conditions.N Engl J Med.2004;351(27):2870–2874.
- ,,.Heart disease and prevention: race and age differences in heart disease prevention, treatment, and mortality.Med Care.2005;43(3 suppl):I33–I41.
- ,,, et al.Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006.Am Heart J.2008;156(6):1045–1055.
- ,,, et al.Evolution in cardiovascular care for elderly patients with non‐ST‐segment elevation acute coronary syndromes: results from the CRUSADE National Quality Improvement Initiative.J Am Coll Cardiol.2005;46(8):1479–1487.
- ,,.Discussions about end‐of‐life care in nursing homes.J Am Geriatr Soc.1998;46:1235–1241.
- ,,, et al.Changes in advance care planning in nursing homes before and after the Patient Self‐Determination Act: report of a 10‐state survey.J Am Geriatr Soc.1997;45(8):939–944.
- ,,,.The Characteristics of Long‐Term Care Users. Agency for Healthcare Research and Quality (AHRQ) Publication No. 00–0049.Rockville, MD:Agency for Healthcare Research and Quality;2000.
- U.S. Bureau of the Census.Current Population Reports, P23–190, 65+ in the United States.Washington, DC:U.S. Government Printing Office;1996.
- ,,, et al.Older emergency department patients with acute myocardial infarction receive lower quality of care than younger patients.Ann Emerg Med.2005;46(1):14–21.
- ,,, et al.Why don't physicians follow clinical practice guidelines? A framework for improvement.JAMA.1999;282(15):1458–1465.
- ,,, et al.Differences in diabetes management of nursing home patients based on functional and cognitive status.J Am Med Dir Assoc.2005;6(6):375–382.
- ,,,,.Medical and nonmedical determinants of decision making about potentially life‐prolonging interventions.Med Decis Making.2004;24(5):518–524.
- .Hidden barriers to improvement in the quality of care.N Engl J Med.2001;345(22):1612–1620.
- ,,.“Renalism”: inappropriately low rates of coronary angiography in elderly individuals with renal insufficiency.J Am Soc Nephrol.2004;15(9):2462–2468.
- ,,,,,.Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance.JAMA.2005;294(6):716–724.
- ,,, et al.ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction).J Am Coll Cardiol.1996;28(5):1328–1428.
- ,,,,.Racial differences in the medical treatment of elderly Medicare patients with acute myocardial infarction.J Gen Intern Med.1996;11(12):736–743.
- ,,,,,.Resource use and quality of care for Medicare patients with acute myocardial infarction in Maryland and the District of Columbia: analysis of data from the Cooperative Cardiovascular Project.Am Heart J.1998;135(2 pt 1):349–356.
- ,,, et al.ACC/AHA 2002 guideline update for the management of patients with unstable angina and non‐ST‐segment elevation myocardial infarction—summary article: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the Management of Patients With Unstable Angina).J Am Coll Cardiol.2002;40(7):1366–1374.
- ,,,,.Impact of managed care on the treatment, costs, and outcomes of fee‐for‐service Medicare patients with acute myocardial infarction.Health Serv Res.2005;39(1):131–152.
- ,,, et al.Quality of care for Medicare patients with acute myocardial infarction. A four‐state pilot study from the Cooperative Cardiovascular Project.JAMA.1995;273(19):1509–1514.
- ,,,,.Regionalization of cardiac surgery in the United States and Canada: geographic access, choice, and outcomes.JAMA.1995;274(16):1282–1288.
- .HCFA's Health Care Quality Improvement Program and the Cooperative Cardiovascular Project.Ann Thorac Surg.1994;58(6):1858–1862.
- ,,, et al.Quality of medical care delivered to Medicare beneficiaries: a profile at state and national levels.JAMA.2000;284(13):1670–1676.
- .Cooperative Cardiovascular Project: committee updates.Iowa Med.1993;83(10):379.
- ,,, et al.Aspirin in the treatment of acute myocardial infarction in elderly Medicare beneficiaries. Patterns of use and outcomes.Circulation.1995;92(10):2841–2847.
- ,,,,,.Validation of a clinical prediction rule for left ventricular ejection fraction after myocardial infarction in patients > or = 65 years old.Am J Cardiol.1997;80(1):11–15.
- ,,,,.Clinical correlates of in‐hospital costs for acute myocardial infarction in patients 65 years of age and older.Am Heart J.1998;135(3):523–531.
- ,,, et al.Improving the quality of care for Medicare patients with acute myocardial infarction: results from the Cooperative Cardiovascular Project.JAMA.1998;279(17):1351–1357.
- ,,, et al.Geographic variation in the treatment of acute myocardial infarction.JAMA.1999;281(7):627–633.
- .HCFA's Cooperative Cardiovascular Project: a nationwide quality assessment of acute myocardial infarction.Clin Cardiol.1994;17(7):354–356.
- ,,.Long‐term outcomes of regional variations in intensity of invasive vs medical management of Medicare Patients with acute myocardial infarction.JAMA.2005;293(11):1329–1337.
- ,,, et al.ACC/AHA 2008 performance measures for adults with ST‐elevation and non‐ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to develop performance measures for ST‐elevation and non‐ST‐elevation myocardial infarction): developed in collaboration with the American Academy of Family Physicians and the American College of Emergency Physicians: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation, Society for Cardiovascular Angiography and Interventions, and Society of Hospital Medicine.Circulation.2008;118(24):2596–2648.
- ,,,,.Do “America's best hospitals” perform better for acute myocardial infarction?N Engl J Med.1999;340(4):286–292.
- ,,,.Does the ownership of the admitting hospital make a difference? Outcomes and process of care for Medicare beneficiaries admitted with acute myocardial infarction.Med Care.2003;41(10):1193–1205.
- American Academy of Hospice and Palliative Medicine. Position Statements. Statement on Clinical Practice Guidelines for Quality Palliative Care. Approved by the Board of Directors, June 2006. Available at: http://www.aahpm.org/positions/quality.html. Accessed October 2009.
- .Assessing the relationship between hospital competition and guideline adherence for acute myocardial infarction.University of Minnesota;2000.
- ,,, et al.Quality of care for Medicare patients with acute myocardial infarction. A four‐state pilot study from the Cooperative Cardiovascular Project. [see Comment].JAMA.1995;273(19):1509–1514.
- , et al.Vital and Health Statistics: Health Service Areas for the United States. DHHS (PHS)92–1386.Hyattsville, MD:National Center for Health Statistics, Centers for Disease Control, U.S. Department of Health and Human Services;1991.
- .Econometric Analysis of Cross Section and Panel Data.1st ed.Cambridge, MA:MIT Press;2002.
- StataCorp.Stata Statistical Software: Release 10.1 SE.College Station, TX:Stata Corporation,2008.
- ,,,,,.Hypertension guideline adherence among nursing home patients.J Gen Intern Med.2009;24(4):499–503.
- ,,.Testing the feasibility of implementation of clinical practice guidelines in long‐term care facilities.J Am Med Dir Assoc.2004;5(1):1–8.
- ,,,,.Improving care for nursing home‐acquired pneumonia in a managed care environment.Am J Manag Care.2004;10(10):681–686.
- ,,, et al.Barriers to and facilitators of clinical practice guideline use in nursing homes.J Am Geriatr Soc.2007;55(9):1404–1409.
- ,,.Potential pitfalls of disease‐specific guidelines for patients with multiple conditions.N Engl J Med.2004;351(27):2870–2874.
- ,,.Heart disease and prevention: race and age differences in heart disease prevention, treatment, and mortality.Med Care.2005;43(3 suppl):I33–I41.
- ,,, et al.Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006.Am Heart J.2008;156(6):1045–1055.
- ,,, et al.Evolution in cardiovascular care for elderly patients with non‐ST‐segment elevation acute coronary syndromes: results from the CRUSADE National Quality Improvement Initiative.J Am Coll Cardiol.2005;46(8):1479–1487.
- ,,.Discussions about end‐of‐life care in nursing homes.J Am Geriatr Soc.1998;46:1235–1241.
- ,,, et al.Changes in advance care planning in nursing homes before and after the Patient Self‐Determination Act: report of a 10‐state survey.J Am Geriatr Soc.1997;45(8):939–944.
Copyright © 2010 Society of Hospital Medicine
Wearing White—Right or Wrong
Physicians wear white coats. In many medical centers, the length of one's coat grows with seniority; medical students, interns, and residents wear short white coats, while attending staff graduate to long white coats with their names embroidered on the front. This traditional uniform serves a similar role to the stripes on a military sleeve. That is, by examining the length of a person's coat, a nurse or other hospital employee can rapidly determine the seniority, and theoretically the increased medical knowledge, of the person inside.
Of course, it isn't quite this simple. In many places, all residents wear long coats (with embroidered names). In other hospitals, attending staff wear short coats. The problem of distinguishing between a medical student, resident, and attending physician can be quite vexing, particularly after the summer months when the anxiety visible on the faces of new house staff and third‐year medical students fades away into the more seasoned look of fatigue and malaise. As hospital‐based practitioners, what are we to do?
To be certain there are clues one can use to identify one's rank in the medical profession. Often medical students wear a medical school pin bestowed upon them at a robing ceremony or other coming‐of‐age festivity to mark the transition to the clinical training years.1 (Little do they know that the primary utility of such adornments is to mark them, as though with a scarlet letter, for easy identification when one wishes to pimp the medical team.)2 Similarly, one can look for an arm patch. Just as a mother hen has the need to identify her own chicks, so too is it helpful for the residency director to have each of his or her own residents easily identifiable by the residency patch emblazoned upon the arm of their (long) white coat. The patch test can fail, though, for too often the residency emblem is merely a simple modification of the hospital or medical center logo, and thus not easily distinguishable.
When all else fails, of course, you can look to the pockets. As one's medical knowledge and training rank increases, the number of papers, pens, and instruments in the pockets of the white coat decreases. This inverse relationship provides some increased ability to identify medical students and junior house staff. For example, a short white coat, busting with oversized index cards held together by a large metal ring, several tattered and folded journal articles, and a worn spiral‐bound text suggests a medical student or intern. If they have an electrocardiogram (ECG), calipers, and tuning fork visible, safe bet is you've found a medical student. Conversely, if the white coat sports several free pens (with medication logos embossed on their stems) and has more than a few stains, chances are you've spotted an intern.
Unfortunately, none of this is of much utility in identifying a physician, as the initial premise that physicians wear white coats may be false. The problem is 2‐fold. First of all, not all physicians wear white coats (or any coat for that matter), and, many nonphysicians wear white coats. Commonly, phlebotomists, pharmacists, and respiratory technicians wear white coats; long white coats, in fact. So do nutritionists, speech pathologists, the clerk at the radiology file room, and even the cashiers in the cafeteria. And why not? Each of these persons has an important role to play in the operation of a modern medical center. The long white coat serves as professional uniform to identify the wearer as contributing to the mission of the medical center. It engenders confidence and suggests cleanliness and purity.
The problem remains, however, what should I, as an attending physician wear? You see, patients encounter so many persons in their visits to the hospital that it is not clear who their doctor is. (It's not statistically likely to be the man in a long white coat.) Being able to identify the attending physician is important. The attending physician is ultimately responsible for the patient's care.
There are many guidelines for how to dress. For example, don't wear white after Labor Day. The pleats on a cummerbund point so that the folds open pointing up (apparently it was originally meant to serve as a ticket holder, perhaps in the days before pockets?). Match your belt to your shoes. The list goes on. However, physicians are not commonly associated with natty attire, so fashion help for the MD is hard to find, though nonetheless necessary.
Even wearing white is questionable. White robes have been associated with purity and sanctity for centuries. Religious leaders have donned white for spiritual cleansing of their communities on the most holy of days. I like the idea of appearing pure and holy. Of course, I don't want to mislead anybody, either.
Brides have traditionally worn white dresses. But, while many believe this is to convey a sense of premarital purity, more likely the tradition stems from an ancient Roman practice of wearing white as a symbol of joyous celebration. Interestingly, in some parts of Asia, people at a funeral wear white while the deceased is dressed in red.
In some environments, the culture of the medical center prescribes appropriate apparel. The Mayo Clinic in Minnesota, for example, has had a tradition of having their physician staff dress in business attire. By this, they mean conservative sport coats or suits with ties for men, and similar appropriate women's business clothing. As noted by Leonard L. Berry and Neeli Bendapudi in their article Why Docs Don't Wear White Coats or Polo Shirts at the Mayo Clinic3 in the Harvard Business School publication Working Knowledge for Business Leaders, while some may consider this semiformal business dress pretentious, it should be considered no more pretentious than, say, the dress code for airline pilots. Airline passengers don't want to see their pilot in a polo shirt, and patients feel the same way about their doctors. The business attire is a uniform; it's a visible clue that communicates respect to patients and their families. But, isn't a white coat a uniform that conveys respect? Perhaps a white coat isn't safe if the physician wants to stand out to oncoming traffic in his snowy Minnesota environs.
Besides, is it true that patients don't want their physician to wear a polo shirt? Perhaps casual dress will break down 1 of the patient‐doctor barriers to communication and allow for improved comfort with greater honesty in patientphysician interactions? Prior to designing a prospective controlled randomized trial to answer this question myself, I reviewed the available literature.
It turns out, that an evaluation of polo‐shirt‐wearing physicians has been carried out. Drs. Barrett and Booth4 from the Birmingham Maternity Hospital in England questioned 203 groups of parents and children (406 individuals) about various levels of physician dress. Seventy percent of participants thought that how the doctor dressed was important. Among children, a male physician in a polo shirt was considered more friendly and gentle than the male physician in a white coat (who did get points for being more competent and more concerned). Women physicians in T‐shirts were also though to be friendlier than if in a white coat, but similarly less competent. Parents were more likely to prefer casually‐dressed physicians and were poor at predicting what their children would want.
So, a polo shirt makes me look friendly, gentle, and less competent? What about a polo shirt under a white coatis that the whole package? What about business attire, as per the Mayo Clinic requirements? These questions remain unanswered. So, back to the literature.
In the Journal of the American Medical Association, in 1987, Dunn et al.5 evaluated 200 medical patients in Boston and San Francisco regarding their preference for physician dress. Sixty‐five percent believed physicians should wear a white coat, 27% said no tennis shoes, one‐half said no blue jeans, and about one‐third thought male physicians should wear ties and female physicians should be in a skirt or dress. I suppose the conclusion here is to wear a white coat with or without jeans and most of the time without a tie, though almost always with proper shoes, or at least without tennis shoes. (I practice in Boston and trained partly in San Francisco so this advice seems particularly valid for me.)
It may be more obvious what to do in Japan. Ikusaka et al.6 evaluated the experience of patients at a university clinic seen by a consulting physician in either a white coat, or private clothes. To me, private clothes imply pajamas and a bathrobe, but we must assume this means some form of professional dress lacking a white coat. It turns out that 71% of the Japanese patients seeing a doctor in a white coat preferred a white coat, though more patients seeing a physician in a white coat (vs. private clothes) felt tense during their consultation. The researchers stress that the presence of a white coat did not increase satisfaction with the consultation. They conclude, that while patients may say they prefer a white coat, maybe it would be better not to wear one since it makes patients feel tense.
In addition to feeling tense, white coats may cause hypertension. The phenomenon of elevated blood pressure when in the presence of the physician (or other hospital staff in a white coat) has been long documented. This white coat hypertension can be found in more than 15% of the population who have a measured blood pressure in the office of over 140/90 mmHg with normal daytime mean ambulatory blood pressure readings (when not around a white‐coat‐wearing stress‐inducing medical worker).7 Older adults, females, and nonsmokers were more likely to have white coat hypertension than other persons.
And yet, older adults prefer white coats. The Japanese study (Ikusaka et al.6) concluded that elderly patients prefer a white coat to other attire. Similarly, a study from the Royal Free Hospital, London, showed that white coats were twice as popular with patients as they were with physicians.8 Specifically, patients found the white coats made doctors easier to identify. In an article by the British Broadcasting Corporation (BBC) on the subject, it was noted that the elderly largely preferred physicians in white coats, while children preferred physicians without white coats. British children must prefer a friendly doctor to a competent one.
The article further suggests that only 1 in 8 physicians wears a white coat, complaining that they are too hot and uncomfortable, and may carry the risk of transmitting infections. The white coat, the symbol of cleanliness and purity, a source of infection? To add hypocrisy to the equation, one‐half of physicians who thought white coats should be worn admitted to never actually wearing a white coat. In fact, only 7 of 86 physicians surveyed wore their white coat on a daily basis. The BBC goes on to note that in Australia, the white coat is gaining momentum as there seems to be a movement towards rediscovering the white coat as a symbol of purpose and pride as a profession.8
Really? Let's consult the literature! According to Dr. D.A. Watson,9 White coats have largely disappeared from Australian teaching hospitals and the majority of junior doctors in Australia oppose the wearing of white coats. In a survey of 337 junior medical officers, only 16% preferred to wear a white coat. Peer pressure seems to have something to do with this, as 70% say they don't wear a white coat because nobody else wears a white coat. This is indeed a compelling argument.
Of course, a better argument against wearing a white coat may be that it causes tension (at least in Japanese patients) and may cause white‐coat‐hypertension, resulting in the inappropriate diagnosis and treatment of elevated blood pressure. In Australia, however, it seems that wearing a white coat may make patients too relaxed. Wing et al.10 noted that in 21% to 45% of elderly patients, blood pressure was atypically low when checked in the physician's office as compared to mean ambulatory blood pressure. This reverse‐white‐coat‐hypertension could result in the omission of necessary blood pressure treatment.
In the United States, residentsour own version of the Australian junior medical officercommonly wear scrubs covered by a white coat. Scrub clothes are typically available without charge from the hospital, limit the amount of laundry a busy resident needs to do, and can be put on with little concern as to pressed pleats or matching colors. The overlying white coat adds a moderate degree of formality to what could otherwise be mistaken as pajamas, while providing convenient pockets for the aforementioned papers and miscellaneous equipment and souvenirs. This outfit is likely one of practicality rather than a desire to be most appealing to patients. But, what do you know? It seems that patients prefer their resident physicians to dress this way. Dr. A. Cha et al.11 at the Northeastern Ohio College of Medicine found that patients in an obstetrics and gynecology clinic overall felt that resident physicians dressed in surgical scrubs with a white coat made them feel more comfortable and confident than if dressed otherwise. On the question of a white coat specifically, the majority had no preference that their physician wear one.
So, it's very much unclear whether a white coat is a tension‐causing, blood‐pressure‐elevating, infection risk or a competence‐implying blood‐pressure‐lowering way to identify a physician. As a result, the jury is still out on whether physicians should wear white.
One thing I do know, however, is that patients shouldn't wear white. But they do. As an OtolaryngologistHead and Neck Surgeon, my clinical practice is split between surgical procedures and office visits. Commonly, patients with sinus or nasal surgery will require some form of cotton gauze or foam material within the nose in order to tamponade bleeding. Similarly, patients presenting to the emergency department or urgent care center with epistaxis may have their noses packed and then be told to see an otolaryngologist (eg, me) in 3 or 4 days to have the packing removed. I also commonly remove facial skin lesions, biopsy tongue masses, reduce nasal fractures, and otherwise engage in activities with an above average propensity to result in a mess. More often than happenstance will allow, patients come to see me for such visits in their white Sunday best. I truly care for my patients. I respect them as individuals and desire to do no harm. This includes not staining their shirts, ties, or pants. However, there is no amount of blue towels or gauze pads than can keep a white shirt clean when you have that first sneeze after removal of your nasal packing.12
So what is it that makes so many patients come to the office in a white shirt? Perhaps patients subconsciously associate healthcare with the color white since their doctors wear white coats and the nurses wear starched white dresses with tight white folded caps on top of their head. I've never seen a nurse in a white dress and hat, but believe television programs have shown this in the past.
Maybe the answer lies in an adaptation of data from another Australian study. In a survey of 180 oncology patients about white coats on physicians, the most common argument against wearing the white coat was that it represented a barrier between the physician and the patient.13 However, it is indeed the sane patient who desires to have a barrier between their physician and the removal of nasal packing, a skin lesion, or a tongue mass. Another possibility is that as fewer and fewer physicians wear white, patients are gravitating toward this color as a way of distinguishing themselves from the medical staff. Perhaps a person dressed in white is less likely to be grabbed in the hallway with a Doctor come quick! and more likely to be allowed to just sit peacefully in the waiting room with a 1997 issue of Ladies Home Journal or Senior Fisherman magazine.
Of course, perhaps patients believe the fashion experts who expound that white goes with everything. If so, they soon learn that white doesn't go so well with blotchy splattered red.
The truth is, I don't want my patients to wear white. Between making certain I project myself as approachable and easy to speak with, remembering to cover all the appropriate irrelevant parts of the history and physical to comply with billing requirements, entering data in our easy‐to‐navigate electronic medical record, and attempting to both diagnose the problem and discern an acceptable and effective treatment, the last thing I need is to worry about staining patient shirts! I believe that this phenomenon is widespread among medical practitioners and should be called white‐shirt‐hypertension.
Conclusion
After reviewing the available literature, I've determined that patients should not wear white. However, I'm still not certain how I should dress. For now, I'll stick with whatever is clean and professional and make sure my belt and shoes match. I may or may not wear a tie, since another study showed that 30% of patients believed their physician wore a tie even if they didn't.14 Of course, I'll put on the white coat for the semiannual meeting with the chairman, or if I'm having something messy for lunch and wore a tie that day.
I'll also wear my name badge. It says I'm an attending physician and not a resident. It opens doors around the hospital. Literally. It's got a magnetic stripe.
- .Deconstructing the white coat.Ann Intern Med.1998;129:740–742.
- .The art of pimping.JAMA.1989;262(1):89–90.
- ,. “Why Docs don't wear white coats or Polo Shirts at the Mayo Clinic” working knowledge for business leaders. Available at:http://hbswk.hbs.edu/pubitem.jhtml?id=3380309(6970):1710–1712.
- ,,,,.Patient and house officer attitudes on physician attire and etiquette.JAMA.1987;257(1):65–68.
- ,,, et al.Patients' attitude toward consultations by a physician without a white coat in Japan.Intern Med.1999;38(7):533–536.
- ,,, et al.Determinants of white‐coat hypertension.Blood Press Monit.2004;9(6):307–309.
- Doctors ‘should wear white coats.’ BBC news, Thursday, 13 May, 2004. Available at:http://news.bbc.co.uk/2/hi/health/3706783.stm. Accessed May2009.
- .What do Australian junior doctors think of white coats?Med Educ.2002;36(12):1209–1213.
- ,,, ,;ANBP2 Management Committee and Investigators.Second Australian National Blood Pressure Study. ‘Reverse white‐coat hypertension’ in older hypertensives.J Hypertens.2002;20(4):639–644.
- ,,,.Resident physician attire: does it make a difference to our patients?Am J Obstet Gynecol.2004;190(5):1484–1488.
- . Personal communication.1994–2008.
- .Should doctors wear white coats?Med J Aust.2001;174:343–344.
- ,,,,.Does wearing a necktie influence patient perceptions of emergency department care?J Emerg Med.1998;16(4):541–543.
Physicians wear white coats. In many medical centers, the length of one's coat grows with seniority; medical students, interns, and residents wear short white coats, while attending staff graduate to long white coats with their names embroidered on the front. This traditional uniform serves a similar role to the stripes on a military sleeve. That is, by examining the length of a person's coat, a nurse or other hospital employee can rapidly determine the seniority, and theoretically the increased medical knowledge, of the person inside.
Of course, it isn't quite this simple. In many places, all residents wear long coats (with embroidered names). In other hospitals, attending staff wear short coats. The problem of distinguishing between a medical student, resident, and attending physician can be quite vexing, particularly after the summer months when the anxiety visible on the faces of new house staff and third‐year medical students fades away into the more seasoned look of fatigue and malaise. As hospital‐based practitioners, what are we to do?
To be certain there are clues one can use to identify one's rank in the medical profession. Often medical students wear a medical school pin bestowed upon them at a robing ceremony or other coming‐of‐age festivity to mark the transition to the clinical training years.1 (Little do they know that the primary utility of such adornments is to mark them, as though with a scarlet letter, for easy identification when one wishes to pimp the medical team.)2 Similarly, one can look for an arm patch. Just as a mother hen has the need to identify her own chicks, so too is it helpful for the residency director to have each of his or her own residents easily identifiable by the residency patch emblazoned upon the arm of their (long) white coat. The patch test can fail, though, for too often the residency emblem is merely a simple modification of the hospital or medical center logo, and thus not easily distinguishable.
When all else fails, of course, you can look to the pockets. As one's medical knowledge and training rank increases, the number of papers, pens, and instruments in the pockets of the white coat decreases. This inverse relationship provides some increased ability to identify medical students and junior house staff. For example, a short white coat, busting with oversized index cards held together by a large metal ring, several tattered and folded journal articles, and a worn spiral‐bound text suggests a medical student or intern. If they have an electrocardiogram (ECG), calipers, and tuning fork visible, safe bet is you've found a medical student. Conversely, if the white coat sports several free pens (with medication logos embossed on their stems) and has more than a few stains, chances are you've spotted an intern.
Unfortunately, none of this is of much utility in identifying a physician, as the initial premise that physicians wear white coats may be false. The problem is 2‐fold. First of all, not all physicians wear white coats (or any coat for that matter), and, many nonphysicians wear white coats. Commonly, phlebotomists, pharmacists, and respiratory technicians wear white coats; long white coats, in fact. So do nutritionists, speech pathologists, the clerk at the radiology file room, and even the cashiers in the cafeteria. And why not? Each of these persons has an important role to play in the operation of a modern medical center. The long white coat serves as professional uniform to identify the wearer as contributing to the mission of the medical center. It engenders confidence and suggests cleanliness and purity.
The problem remains, however, what should I, as an attending physician wear? You see, patients encounter so many persons in their visits to the hospital that it is not clear who their doctor is. (It's not statistically likely to be the man in a long white coat.) Being able to identify the attending physician is important. The attending physician is ultimately responsible for the patient's care.
There are many guidelines for how to dress. For example, don't wear white after Labor Day. The pleats on a cummerbund point so that the folds open pointing up (apparently it was originally meant to serve as a ticket holder, perhaps in the days before pockets?). Match your belt to your shoes. The list goes on. However, physicians are not commonly associated with natty attire, so fashion help for the MD is hard to find, though nonetheless necessary.
Even wearing white is questionable. White robes have been associated with purity and sanctity for centuries. Religious leaders have donned white for spiritual cleansing of their communities on the most holy of days. I like the idea of appearing pure and holy. Of course, I don't want to mislead anybody, either.
Brides have traditionally worn white dresses. But, while many believe this is to convey a sense of premarital purity, more likely the tradition stems from an ancient Roman practice of wearing white as a symbol of joyous celebration. Interestingly, in some parts of Asia, people at a funeral wear white while the deceased is dressed in red.
In some environments, the culture of the medical center prescribes appropriate apparel. The Mayo Clinic in Minnesota, for example, has had a tradition of having their physician staff dress in business attire. By this, they mean conservative sport coats or suits with ties for men, and similar appropriate women's business clothing. As noted by Leonard L. Berry and Neeli Bendapudi in their article Why Docs Don't Wear White Coats or Polo Shirts at the Mayo Clinic3 in the Harvard Business School publication Working Knowledge for Business Leaders, while some may consider this semiformal business dress pretentious, it should be considered no more pretentious than, say, the dress code for airline pilots. Airline passengers don't want to see their pilot in a polo shirt, and patients feel the same way about their doctors. The business attire is a uniform; it's a visible clue that communicates respect to patients and their families. But, isn't a white coat a uniform that conveys respect? Perhaps a white coat isn't safe if the physician wants to stand out to oncoming traffic in his snowy Minnesota environs.
Besides, is it true that patients don't want their physician to wear a polo shirt? Perhaps casual dress will break down 1 of the patient‐doctor barriers to communication and allow for improved comfort with greater honesty in patientphysician interactions? Prior to designing a prospective controlled randomized trial to answer this question myself, I reviewed the available literature.
It turns out, that an evaluation of polo‐shirt‐wearing physicians has been carried out. Drs. Barrett and Booth4 from the Birmingham Maternity Hospital in England questioned 203 groups of parents and children (406 individuals) about various levels of physician dress. Seventy percent of participants thought that how the doctor dressed was important. Among children, a male physician in a polo shirt was considered more friendly and gentle than the male physician in a white coat (who did get points for being more competent and more concerned). Women physicians in T‐shirts were also though to be friendlier than if in a white coat, but similarly less competent. Parents were more likely to prefer casually‐dressed physicians and were poor at predicting what their children would want.
So, a polo shirt makes me look friendly, gentle, and less competent? What about a polo shirt under a white coatis that the whole package? What about business attire, as per the Mayo Clinic requirements? These questions remain unanswered. So, back to the literature.
In the Journal of the American Medical Association, in 1987, Dunn et al.5 evaluated 200 medical patients in Boston and San Francisco regarding their preference for physician dress. Sixty‐five percent believed physicians should wear a white coat, 27% said no tennis shoes, one‐half said no blue jeans, and about one‐third thought male physicians should wear ties and female physicians should be in a skirt or dress. I suppose the conclusion here is to wear a white coat with or without jeans and most of the time without a tie, though almost always with proper shoes, or at least without tennis shoes. (I practice in Boston and trained partly in San Francisco so this advice seems particularly valid for me.)
It may be more obvious what to do in Japan. Ikusaka et al.6 evaluated the experience of patients at a university clinic seen by a consulting physician in either a white coat, or private clothes. To me, private clothes imply pajamas and a bathrobe, but we must assume this means some form of professional dress lacking a white coat. It turns out that 71% of the Japanese patients seeing a doctor in a white coat preferred a white coat, though more patients seeing a physician in a white coat (vs. private clothes) felt tense during their consultation. The researchers stress that the presence of a white coat did not increase satisfaction with the consultation. They conclude, that while patients may say they prefer a white coat, maybe it would be better not to wear one since it makes patients feel tense.
In addition to feeling tense, white coats may cause hypertension. The phenomenon of elevated blood pressure when in the presence of the physician (or other hospital staff in a white coat) has been long documented. This white coat hypertension can be found in more than 15% of the population who have a measured blood pressure in the office of over 140/90 mmHg with normal daytime mean ambulatory blood pressure readings (when not around a white‐coat‐wearing stress‐inducing medical worker).7 Older adults, females, and nonsmokers were more likely to have white coat hypertension than other persons.
And yet, older adults prefer white coats. The Japanese study (Ikusaka et al.6) concluded that elderly patients prefer a white coat to other attire. Similarly, a study from the Royal Free Hospital, London, showed that white coats were twice as popular with patients as they were with physicians.8 Specifically, patients found the white coats made doctors easier to identify. In an article by the British Broadcasting Corporation (BBC) on the subject, it was noted that the elderly largely preferred physicians in white coats, while children preferred physicians without white coats. British children must prefer a friendly doctor to a competent one.
The article further suggests that only 1 in 8 physicians wears a white coat, complaining that they are too hot and uncomfortable, and may carry the risk of transmitting infections. The white coat, the symbol of cleanliness and purity, a source of infection? To add hypocrisy to the equation, one‐half of physicians who thought white coats should be worn admitted to never actually wearing a white coat. In fact, only 7 of 86 physicians surveyed wore their white coat on a daily basis. The BBC goes on to note that in Australia, the white coat is gaining momentum as there seems to be a movement towards rediscovering the white coat as a symbol of purpose and pride as a profession.8
Really? Let's consult the literature! According to Dr. D.A. Watson,9 White coats have largely disappeared from Australian teaching hospitals and the majority of junior doctors in Australia oppose the wearing of white coats. In a survey of 337 junior medical officers, only 16% preferred to wear a white coat. Peer pressure seems to have something to do with this, as 70% say they don't wear a white coat because nobody else wears a white coat. This is indeed a compelling argument.
Of course, a better argument against wearing a white coat may be that it causes tension (at least in Japanese patients) and may cause white‐coat‐hypertension, resulting in the inappropriate diagnosis and treatment of elevated blood pressure. In Australia, however, it seems that wearing a white coat may make patients too relaxed. Wing et al.10 noted that in 21% to 45% of elderly patients, blood pressure was atypically low when checked in the physician's office as compared to mean ambulatory blood pressure. This reverse‐white‐coat‐hypertension could result in the omission of necessary blood pressure treatment.
In the United States, residentsour own version of the Australian junior medical officercommonly wear scrubs covered by a white coat. Scrub clothes are typically available without charge from the hospital, limit the amount of laundry a busy resident needs to do, and can be put on with little concern as to pressed pleats or matching colors. The overlying white coat adds a moderate degree of formality to what could otherwise be mistaken as pajamas, while providing convenient pockets for the aforementioned papers and miscellaneous equipment and souvenirs. This outfit is likely one of practicality rather than a desire to be most appealing to patients. But, what do you know? It seems that patients prefer their resident physicians to dress this way. Dr. A. Cha et al.11 at the Northeastern Ohio College of Medicine found that patients in an obstetrics and gynecology clinic overall felt that resident physicians dressed in surgical scrubs with a white coat made them feel more comfortable and confident than if dressed otherwise. On the question of a white coat specifically, the majority had no preference that their physician wear one.
So, it's very much unclear whether a white coat is a tension‐causing, blood‐pressure‐elevating, infection risk or a competence‐implying blood‐pressure‐lowering way to identify a physician. As a result, the jury is still out on whether physicians should wear white.
One thing I do know, however, is that patients shouldn't wear white. But they do. As an OtolaryngologistHead and Neck Surgeon, my clinical practice is split between surgical procedures and office visits. Commonly, patients with sinus or nasal surgery will require some form of cotton gauze or foam material within the nose in order to tamponade bleeding. Similarly, patients presenting to the emergency department or urgent care center with epistaxis may have their noses packed and then be told to see an otolaryngologist (eg, me) in 3 or 4 days to have the packing removed. I also commonly remove facial skin lesions, biopsy tongue masses, reduce nasal fractures, and otherwise engage in activities with an above average propensity to result in a mess. More often than happenstance will allow, patients come to see me for such visits in their white Sunday best. I truly care for my patients. I respect them as individuals and desire to do no harm. This includes not staining their shirts, ties, or pants. However, there is no amount of blue towels or gauze pads than can keep a white shirt clean when you have that first sneeze after removal of your nasal packing.12
So what is it that makes so many patients come to the office in a white shirt? Perhaps patients subconsciously associate healthcare with the color white since their doctors wear white coats and the nurses wear starched white dresses with tight white folded caps on top of their head. I've never seen a nurse in a white dress and hat, but believe television programs have shown this in the past.
Maybe the answer lies in an adaptation of data from another Australian study. In a survey of 180 oncology patients about white coats on physicians, the most common argument against wearing the white coat was that it represented a barrier between the physician and the patient.13 However, it is indeed the sane patient who desires to have a barrier between their physician and the removal of nasal packing, a skin lesion, or a tongue mass. Another possibility is that as fewer and fewer physicians wear white, patients are gravitating toward this color as a way of distinguishing themselves from the medical staff. Perhaps a person dressed in white is less likely to be grabbed in the hallway with a Doctor come quick! and more likely to be allowed to just sit peacefully in the waiting room with a 1997 issue of Ladies Home Journal or Senior Fisherman magazine.
Of course, perhaps patients believe the fashion experts who expound that white goes with everything. If so, they soon learn that white doesn't go so well with blotchy splattered red.
The truth is, I don't want my patients to wear white. Between making certain I project myself as approachable and easy to speak with, remembering to cover all the appropriate irrelevant parts of the history and physical to comply with billing requirements, entering data in our easy‐to‐navigate electronic medical record, and attempting to both diagnose the problem and discern an acceptable and effective treatment, the last thing I need is to worry about staining patient shirts! I believe that this phenomenon is widespread among medical practitioners and should be called white‐shirt‐hypertension.
Conclusion
After reviewing the available literature, I've determined that patients should not wear white. However, I'm still not certain how I should dress. For now, I'll stick with whatever is clean and professional and make sure my belt and shoes match. I may or may not wear a tie, since another study showed that 30% of patients believed their physician wore a tie even if they didn't.14 Of course, I'll put on the white coat for the semiannual meeting with the chairman, or if I'm having something messy for lunch and wore a tie that day.
I'll also wear my name badge. It says I'm an attending physician and not a resident. It opens doors around the hospital. Literally. It's got a magnetic stripe.
Physicians wear white coats. In many medical centers, the length of one's coat grows with seniority; medical students, interns, and residents wear short white coats, while attending staff graduate to long white coats with their names embroidered on the front. This traditional uniform serves a similar role to the stripes on a military sleeve. That is, by examining the length of a person's coat, a nurse or other hospital employee can rapidly determine the seniority, and theoretically the increased medical knowledge, of the person inside.
Of course, it isn't quite this simple. In many places, all residents wear long coats (with embroidered names). In other hospitals, attending staff wear short coats. The problem of distinguishing between a medical student, resident, and attending physician can be quite vexing, particularly after the summer months when the anxiety visible on the faces of new house staff and third‐year medical students fades away into the more seasoned look of fatigue and malaise. As hospital‐based practitioners, what are we to do?
To be certain there are clues one can use to identify one's rank in the medical profession. Often medical students wear a medical school pin bestowed upon them at a robing ceremony or other coming‐of‐age festivity to mark the transition to the clinical training years.1 (Little do they know that the primary utility of such adornments is to mark them, as though with a scarlet letter, for easy identification when one wishes to pimp the medical team.)2 Similarly, one can look for an arm patch. Just as a mother hen has the need to identify her own chicks, so too is it helpful for the residency director to have each of his or her own residents easily identifiable by the residency patch emblazoned upon the arm of their (long) white coat. The patch test can fail, though, for too often the residency emblem is merely a simple modification of the hospital or medical center logo, and thus not easily distinguishable.
When all else fails, of course, you can look to the pockets. As one's medical knowledge and training rank increases, the number of papers, pens, and instruments in the pockets of the white coat decreases. This inverse relationship provides some increased ability to identify medical students and junior house staff. For example, a short white coat, busting with oversized index cards held together by a large metal ring, several tattered and folded journal articles, and a worn spiral‐bound text suggests a medical student or intern. If they have an electrocardiogram (ECG), calipers, and tuning fork visible, safe bet is you've found a medical student. Conversely, if the white coat sports several free pens (with medication logos embossed on their stems) and has more than a few stains, chances are you've spotted an intern.
Unfortunately, none of this is of much utility in identifying a physician, as the initial premise that physicians wear white coats may be false. The problem is 2‐fold. First of all, not all physicians wear white coats (or any coat for that matter), and, many nonphysicians wear white coats. Commonly, phlebotomists, pharmacists, and respiratory technicians wear white coats; long white coats, in fact. So do nutritionists, speech pathologists, the clerk at the radiology file room, and even the cashiers in the cafeteria. And why not? Each of these persons has an important role to play in the operation of a modern medical center. The long white coat serves as professional uniform to identify the wearer as contributing to the mission of the medical center. It engenders confidence and suggests cleanliness and purity.
The problem remains, however, what should I, as an attending physician wear? You see, patients encounter so many persons in their visits to the hospital that it is not clear who their doctor is. (It's not statistically likely to be the man in a long white coat.) Being able to identify the attending physician is important. The attending physician is ultimately responsible for the patient's care.
There are many guidelines for how to dress. For example, don't wear white after Labor Day. The pleats on a cummerbund point so that the folds open pointing up (apparently it was originally meant to serve as a ticket holder, perhaps in the days before pockets?). Match your belt to your shoes. The list goes on. However, physicians are not commonly associated with natty attire, so fashion help for the MD is hard to find, though nonetheless necessary.
Even wearing white is questionable. White robes have been associated with purity and sanctity for centuries. Religious leaders have donned white for spiritual cleansing of their communities on the most holy of days. I like the idea of appearing pure and holy. Of course, I don't want to mislead anybody, either.
Brides have traditionally worn white dresses. But, while many believe this is to convey a sense of premarital purity, more likely the tradition stems from an ancient Roman practice of wearing white as a symbol of joyous celebration. Interestingly, in some parts of Asia, people at a funeral wear white while the deceased is dressed in red.
In some environments, the culture of the medical center prescribes appropriate apparel. The Mayo Clinic in Minnesota, for example, has had a tradition of having their physician staff dress in business attire. By this, they mean conservative sport coats or suits with ties for men, and similar appropriate women's business clothing. As noted by Leonard L. Berry and Neeli Bendapudi in their article Why Docs Don't Wear White Coats or Polo Shirts at the Mayo Clinic3 in the Harvard Business School publication Working Knowledge for Business Leaders, while some may consider this semiformal business dress pretentious, it should be considered no more pretentious than, say, the dress code for airline pilots. Airline passengers don't want to see their pilot in a polo shirt, and patients feel the same way about their doctors. The business attire is a uniform; it's a visible clue that communicates respect to patients and their families. But, isn't a white coat a uniform that conveys respect? Perhaps a white coat isn't safe if the physician wants to stand out to oncoming traffic in his snowy Minnesota environs.
Besides, is it true that patients don't want their physician to wear a polo shirt? Perhaps casual dress will break down 1 of the patient‐doctor barriers to communication and allow for improved comfort with greater honesty in patientphysician interactions? Prior to designing a prospective controlled randomized trial to answer this question myself, I reviewed the available literature.
It turns out, that an evaluation of polo‐shirt‐wearing physicians has been carried out. Drs. Barrett and Booth4 from the Birmingham Maternity Hospital in England questioned 203 groups of parents and children (406 individuals) about various levels of physician dress. Seventy percent of participants thought that how the doctor dressed was important. Among children, a male physician in a polo shirt was considered more friendly and gentle than the male physician in a white coat (who did get points for being more competent and more concerned). Women physicians in T‐shirts were also though to be friendlier than if in a white coat, but similarly less competent. Parents were more likely to prefer casually‐dressed physicians and were poor at predicting what their children would want.
So, a polo shirt makes me look friendly, gentle, and less competent? What about a polo shirt under a white coatis that the whole package? What about business attire, as per the Mayo Clinic requirements? These questions remain unanswered. So, back to the literature.
In the Journal of the American Medical Association, in 1987, Dunn et al.5 evaluated 200 medical patients in Boston and San Francisco regarding their preference for physician dress. Sixty‐five percent believed physicians should wear a white coat, 27% said no tennis shoes, one‐half said no blue jeans, and about one‐third thought male physicians should wear ties and female physicians should be in a skirt or dress. I suppose the conclusion here is to wear a white coat with or without jeans and most of the time without a tie, though almost always with proper shoes, or at least without tennis shoes. (I practice in Boston and trained partly in San Francisco so this advice seems particularly valid for me.)
It may be more obvious what to do in Japan. Ikusaka et al.6 evaluated the experience of patients at a university clinic seen by a consulting physician in either a white coat, or private clothes. To me, private clothes imply pajamas and a bathrobe, but we must assume this means some form of professional dress lacking a white coat. It turns out that 71% of the Japanese patients seeing a doctor in a white coat preferred a white coat, though more patients seeing a physician in a white coat (vs. private clothes) felt tense during their consultation. The researchers stress that the presence of a white coat did not increase satisfaction with the consultation. They conclude, that while patients may say they prefer a white coat, maybe it would be better not to wear one since it makes patients feel tense.
In addition to feeling tense, white coats may cause hypertension. The phenomenon of elevated blood pressure when in the presence of the physician (or other hospital staff in a white coat) has been long documented. This white coat hypertension can be found in more than 15% of the population who have a measured blood pressure in the office of over 140/90 mmHg with normal daytime mean ambulatory blood pressure readings (when not around a white‐coat‐wearing stress‐inducing medical worker).7 Older adults, females, and nonsmokers were more likely to have white coat hypertension than other persons.
And yet, older adults prefer white coats. The Japanese study (Ikusaka et al.6) concluded that elderly patients prefer a white coat to other attire. Similarly, a study from the Royal Free Hospital, London, showed that white coats were twice as popular with patients as they were with physicians.8 Specifically, patients found the white coats made doctors easier to identify. In an article by the British Broadcasting Corporation (BBC) on the subject, it was noted that the elderly largely preferred physicians in white coats, while children preferred physicians without white coats. British children must prefer a friendly doctor to a competent one.
The article further suggests that only 1 in 8 physicians wears a white coat, complaining that they are too hot and uncomfortable, and may carry the risk of transmitting infections. The white coat, the symbol of cleanliness and purity, a source of infection? To add hypocrisy to the equation, one‐half of physicians who thought white coats should be worn admitted to never actually wearing a white coat. In fact, only 7 of 86 physicians surveyed wore their white coat on a daily basis. The BBC goes on to note that in Australia, the white coat is gaining momentum as there seems to be a movement towards rediscovering the white coat as a symbol of purpose and pride as a profession.8
Really? Let's consult the literature! According to Dr. D.A. Watson,9 White coats have largely disappeared from Australian teaching hospitals and the majority of junior doctors in Australia oppose the wearing of white coats. In a survey of 337 junior medical officers, only 16% preferred to wear a white coat. Peer pressure seems to have something to do with this, as 70% say they don't wear a white coat because nobody else wears a white coat. This is indeed a compelling argument.
Of course, a better argument against wearing a white coat may be that it causes tension (at least in Japanese patients) and may cause white‐coat‐hypertension, resulting in the inappropriate diagnosis and treatment of elevated blood pressure. In Australia, however, it seems that wearing a white coat may make patients too relaxed. Wing et al.10 noted that in 21% to 45% of elderly patients, blood pressure was atypically low when checked in the physician's office as compared to mean ambulatory blood pressure. This reverse‐white‐coat‐hypertension could result in the omission of necessary blood pressure treatment.
In the United States, residentsour own version of the Australian junior medical officercommonly wear scrubs covered by a white coat. Scrub clothes are typically available without charge from the hospital, limit the amount of laundry a busy resident needs to do, and can be put on with little concern as to pressed pleats or matching colors. The overlying white coat adds a moderate degree of formality to what could otherwise be mistaken as pajamas, while providing convenient pockets for the aforementioned papers and miscellaneous equipment and souvenirs. This outfit is likely one of practicality rather than a desire to be most appealing to patients. But, what do you know? It seems that patients prefer their resident physicians to dress this way. Dr. A. Cha et al.11 at the Northeastern Ohio College of Medicine found that patients in an obstetrics and gynecology clinic overall felt that resident physicians dressed in surgical scrubs with a white coat made them feel more comfortable and confident than if dressed otherwise. On the question of a white coat specifically, the majority had no preference that their physician wear one.
So, it's very much unclear whether a white coat is a tension‐causing, blood‐pressure‐elevating, infection risk or a competence‐implying blood‐pressure‐lowering way to identify a physician. As a result, the jury is still out on whether physicians should wear white.
One thing I do know, however, is that patients shouldn't wear white. But they do. As an OtolaryngologistHead and Neck Surgeon, my clinical practice is split between surgical procedures and office visits. Commonly, patients with sinus or nasal surgery will require some form of cotton gauze or foam material within the nose in order to tamponade bleeding. Similarly, patients presenting to the emergency department or urgent care center with epistaxis may have their noses packed and then be told to see an otolaryngologist (eg, me) in 3 or 4 days to have the packing removed. I also commonly remove facial skin lesions, biopsy tongue masses, reduce nasal fractures, and otherwise engage in activities with an above average propensity to result in a mess. More often than happenstance will allow, patients come to see me for such visits in their white Sunday best. I truly care for my patients. I respect them as individuals and desire to do no harm. This includes not staining their shirts, ties, or pants. However, there is no amount of blue towels or gauze pads than can keep a white shirt clean when you have that first sneeze after removal of your nasal packing.12
So what is it that makes so many patients come to the office in a white shirt? Perhaps patients subconsciously associate healthcare with the color white since their doctors wear white coats and the nurses wear starched white dresses with tight white folded caps on top of their head. I've never seen a nurse in a white dress and hat, but believe television programs have shown this in the past.
Maybe the answer lies in an adaptation of data from another Australian study. In a survey of 180 oncology patients about white coats on physicians, the most common argument against wearing the white coat was that it represented a barrier between the physician and the patient.13 However, it is indeed the sane patient who desires to have a barrier between their physician and the removal of nasal packing, a skin lesion, or a tongue mass. Another possibility is that as fewer and fewer physicians wear white, patients are gravitating toward this color as a way of distinguishing themselves from the medical staff. Perhaps a person dressed in white is less likely to be grabbed in the hallway with a Doctor come quick! and more likely to be allowed to just sit peacefully in the waiting room with a 1997 issue of Ladies Home Journal or Senior Fisherman magazine.
Of course, perhaps patients believe the fashion experts who expound that white goes with everything. If so, they soon learn that white doesn't go so well with blotchy splattered red.
The truth is, I don't want my patients to wear white. Between making certain I project myself as approachable and easy to speak with, remembering to cover all the appropriate irrelevant parts of the history and physical to comply with billing requirements, entering data in our easy‐to‐navigate electronic medical record, and attempting to both diagnose the problem and discern an acceptable and effective treatment, the last thing I need is to worry about staining patient shirts! I believe that this phenomenon is widespread among medical practitioners and should be called white‐shirt‐hypertension.
Conclusion
After reviewing the available literature, I've determined that patients should not wear white. However, I'm still not certain how I should dress. For now, I'll stick with whatever is clean and professional and make sure my belt and shoes match. I may or may not wear a tie, since another study showed that 30% of patients believed their physician wore a tie even if they didn't.14 Of course, I'll put on the white coat for the semiannual meeting with the chairman, or if I'm having something messy for lunch and wore a tie that day.
I'll also wear my name badge. It says I'm an attending physician and not a resident. It opens doors around the hospital. Literally. It's got a magnetic stripe.
- .Deconstructing the white coat.Ann Intern Med.1998;129:740–742.
- .The art of pimping.JAMA.1989;262(1):89–90.
- ,. “Why Docs don't wear white coats or Polo Shirts at the Mayo Clinic” working knowledge for business leaders. Available at:http://hbswk.hbs.edu/pubitem.jhtml?id=3380309(6970):1710–1712.
- ,,,,.Patient and house officer attitudes on physician attire and etiquette.JAMA.1987;257(1):65–68.
- ,,, et al.Patients' attitude toward consultations by a physician without a white coat in Japan.Intern Med.1999;38(7):533–536.
- ,,, et al.Determinants of white‐coat hypertension.Blood Press Monit.2004;9(6):307–309.
- Doctors ‘should wear white coats.’ BBC news, Thursday, 13 May, 2004. Available at:http://news.bbc.co.uk/2/hi/health/3706783.stm. Accessed May2009.
- .What do Australian junior doctors think of white coats?Med Educ.2002;36(12):1209–1213.
- ,,, ,;ANBP2 Management Committee and Investigators.Second Australian National Blood Pressure Study. ‘Reverse white‐coat hypertension’ in older hypertensives.J Hypertens.2002;20(4):639–644.
- ,,,.Resident physician attire: does it make a difference to our patients?Am J Obstet Gynecol.2004;190(5):1484–1488.
- . Personal communication.1994–2008.
- .Should doctors wear white coats?Med J Aust.2001;174:343–344.
- ,,,,.Does wearing a necktie influence patient perceptions of emergency department care?J Emerg Med.1998;16(4):541–543.
- .Deconstructing the white coat.Ann Intern Med.1998;129:740–742.
- .The art of pimping.JAMA.1989;262(1):89–90.
- ,. “Why Docs don't wear white coats or Polo Shirts at the Mayo Clinic” working knowledge for business leaders. Available at:http://hbswk.hbs.edu/pubitem.jhtml?id=3380309(6970):1710–1712.
- ,,,,.Patient and house officer attitudes on physician attire and etiquette.JAMA.1987;257(1):65–68.
- ,,, et al.Patients' attitude toward consultations by a physician without a white coat in Japan.Intern Med.1999;38(7):533–536.
- ,,, et al.Determinants of white‐coat hypertension.Blood Press Monit.2004;9(6):307–309.
- Doctors ‘should wear white coats.’ BBC news, Thursday, 13 May, 2004. Available at:http://news.bbc.co.uk/2/hi/health/3706783.stm. Accessed May2009.
- .What do Australian junior doctors think of white coats?Med Educ.2002;36(12):1209–1213.
- ,,, ,;ANBP2 Management Committee and Investigators.Second Australian National Blood Pressure Study. ‘Reverse white‐coat hypertension’ in older hypertensives.J Hypertens.2002;20(4):639–644.
- ,,,.Resident physician attire: does it make a difference to our patients?Am J Obstet Gynecol.2004;190(5):1484–1488.
- . Personal communication.1994–2008.
- .Should doctors wear white coats?Med J Aust.2001;174:343–344.
- ,,,,.Does wearing a necktie influence patient perceptions of emergency department care?J Emerg Med.1998;16(4):541–543.
Port‐A‐Cath Embolization
A 59‐year‐old white female, with a 3‐year history of Port‐A‐Cath (PAC) placement for abdominal mesothelioma, presented with 2 episodes of cardiac palpitations. The onset of palpitations occurred 2 days prior to admission, following 15 minutes of vigorous but failed attempts to access the PAC with normal saline and tissue plasminogen activator at her oncologist's office. Although asymptomatic at the time of manipulation, each episode was triggered by subsequent exertion, lasting for about 1 minute, and not associated with chest pain. Electrocardiogram showed normal sinus rhythm and occasional premature ventricular contractions. A chest x‐ray showed a catheter fragment spanning the right atrium and ventricle (Figure 1). Computed tomography (CT) scan confirmed a 10‐cm dislodged catheter (Figure 2). Following emergent catheter retrieval via right‐sided heart catheterization, the patient's symptoms resolved. At least 42 cases of catheter embolization have been reported in the recent literature.1 Of these cases, only 7% had palpitations. Although rare, catheter fracture should be considered in patients with palpitations and history of indwelling venous catheter.
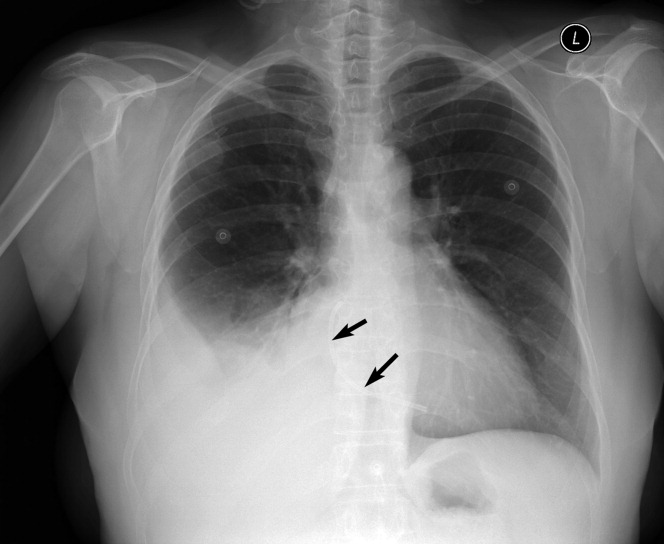

- ,.Ventricular tachycardia secondary to Port‐A‐Cath fracture and embolization.J Emerg Med.2003;24:29–34.
A 59‐year‐old white female, with a 3‐year history of Port‐A‐Cath (PAC) placement for abdominal mesothelioma, presented with 2 episodes of cardiac palpitations. The onset of palpitations occurred 2 days prior to admission, following 15 minutes of vigorous but failed attempts to access the PAC with normal saline and tissue plasminogen activator at her oncologist's office. Although asymptomatic at the time of manipulation, each episode was triggered by subsequent exertion, lasting for about 1 minute, and not associated with chest pain. Electrocardiogram showed normal sinus rhythm and occasional premature ventricular contractions. A chest x‐ray showed a catheter fragment spanning the right atrium and ventricle (Figure 1). Computed tomography (CT) scan confirmed a 10‐cm dislodged catheter (Figure 2). Following emergent catheter retrieval via right‐sided heart catheterization, the patient's symptoms resolved. At least 42 cases of catheter embolization have been reported in the recent literature.1 Of these cases, only 7% had palpitations. Although rare, catheter fracture should be considered in patients with palpitations and history of indwelling venous catheter.
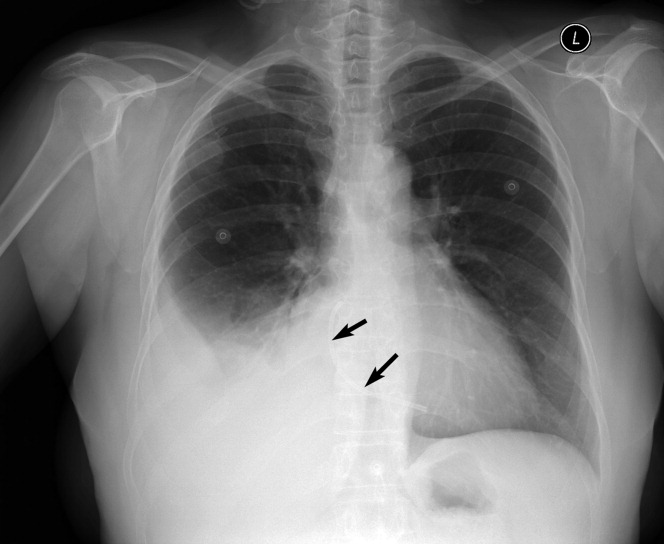

A 59‐year‐old white female, with a 3‐year history of Port‐A‐Cath (PAC) placement for abdominal mesothelioma, presented with 2 episodes of cardiac palpitations. The onset of palpitations occurred 2 days prior to admission, following 15 minutes of vigorous but failed attempts to access the PAC with normal saline and tissue plasminogen activator at her oncologist's office. Although asymptomatic at the time of manipulation, each episode was triggered by subsequent exertion, lasting for about 1 minute, and not associated with chest pain. Electrocardiogram showed normal sinus rhythm and occasional premature ventricular contractions. A chest x‐ray showed a catheter fragment spanning the right atrium and ventricle (Figure 1). Computed tomography (CT) scan confirmed a 10‐cm dislodged catheter (Figure 2). Following emergent catheter retrieval via right‐sided heart catheterization, the patient's symptoms resolved. At least 42 cases of catheter embolization have been reported in the recent literature.1 Of these cases, only 7% had palpitations. Although rare, catheter fracture should be considered in patients with palpitations and history of indwelling venous catheter.
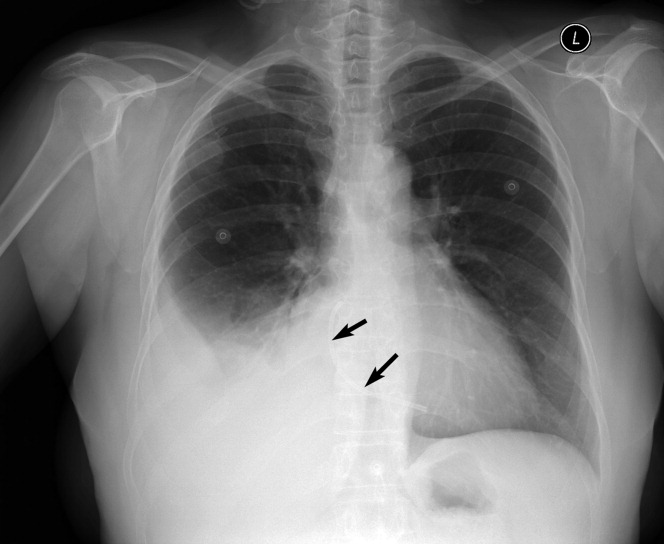

- ,.Ventricular tachycardia secondary to Port‐A‐Cath fracture and embolization.J Emerg Med.2003;24:29–34.
- ,.Ventricular tachycardia secondary to Port‐A‐Cath fracture and embolization.J Emerg Med.2003;24:29–34.
CSI Risk in Infants with Focal Infection
Focal bacterial infections (FBIs), including otitis media (OM), cellulitis, and lymphadenitis, can occur at any age and are usually treated with oral antibiotics. When patients with focal infections present as a young infant, healthcare providers often worry about the risk of coexisting or concomitant systemic infections (CSIs), often termed serious bacterial infections (SBIs) in the published literature.1, 2 Risk of CSI becomes more worrisome when young infants have fever as part of their presentation, especially within the traditional rule‐out sepsis age range of less than 2 months. Often, these patients are well‐appearing and lack prenatal and neonatal risk factors for systemic infections, but are assumed to be at high risk for CSI based on the presence of focal bacterial infection.1, 3, 4
FBIs have been the subject of multiple studies, especially OM and cellulitis. However, few investigations have looked specifically at infants less than 60 days of age, lending uncertainty to medical decision‐making for both community and emergency physicians. Therefore, no standardized evidence‐based practice exists for treating young infants with FBIs. While some clinicians treat these infections using systemic antibiotics without performing laboratory tests, others opt for a full diagnostic evaluation for CSI; including serum blood counts, blood cultures, lumbar punctures (LPs), and bladder catheterizations. Also, some clinicians opt for treatment with oral antibiotics at home, while others choose intravenous (IV) antibiotics and hospitalization.
These decisions are likely due to studies of febrile infants under 60 days of age who present to an emergency department (ED), appear well, and have no focal source of infection on exam, yet are known to have a risk of systemic or occult bacterial infection of roughly 10%.310 There are no such studies documenting the risk of CSI in well‐appearing, afebrile patients, as fever is regarded as the main risk factor for CSI in this age.
Based on our clinical experience and review of the literature, we felt that afebrile, well‐appearing infants less than 60 days of age with an FBI on exam would have a very low risk of CSI. The primary objectives of this study were to determine the risk of CSI when presented with a well‐appearing infant who has an FBI on exam and to examine that risk in relation to the presence of fever. Other objectives were to describe the clinical presentation of FBIs in well‐appearing infants in this age group and to describe the current management and resource utilization of such infections in the ED.
Patients and Methods
Study Population
Cincinnati Children's Hospital Medical Center (CCHMC) is a 423‐bed tertiary‐care hospital located in southwestern Ohio. The medical center serves as the sole pediatric hospital in a 70‐mile radius, serving a metropolitan population of roughly 1 million. In addition, CCHMC cares for patients from a wide demographic and socioeconomic spectrum, including the urban, suburban, and rural areas of Cincinnati, southwestern Ohio, northern Kentucky, and southeastern Indiana. The ED sees an average of 90,000 patients annually, with an average of 15,000 admissions.
Patient Selection
Data were retrospectively collected from a consecutive series of infants age 0 to 59 days who presented to the CCHMC ED between January 1, 2000 and December 31, 2005. Patients met inclusion criteria if they were documented to be well‐appearing on exam; had normal‐for‐age heart rate, respiratory rate, blood pressure, and oxygen saturation (if measured); were discharged from their hospital of birth to home before presentation to the ED; and received a discharge diagnosis consistent with an FBI. Specifically, FBIs included the following diagnoses: soft tissue infection, cellulitis, mastoiditis, abscess, OM, omphalitis, mastitis, mammitis, paronychia, balanitis, posthitis, impetigo, or lymphadenitis. We excluded patients with a history of immunodeficiency, central venous catheter, tracheostomy, gastrostomy tube, chronic lung disease, previous admission for a documented bacterial infection, or if they had been taking systemic antibiotics at the time of evaluation. We also excluded infants noted to be toxic or ill‐appearing on examination.
Definitions
Fever was defined as a temperature greater than or equal to 38C (100.4F), recorded by the ED or by parental report. All infants seen in the CCHMC ED had rectal temperatures measured per protocol. A nontoxic infant was defined by chart review as documentation of: nontoxic, well‐appearing, or alert infant without signs of respiratory distress or hemodynamic instability. Patients were excluded from the nontoxic category with the following parameters: heart rate >180 beats per minute, respiratory rate >60 breaths per minute, oxygen saturation <90% on pulse oximetry, or systolic blood pressure <60 mmHg on 2 or more measurements. CSIs were defined as any of the following: bacteremia, urinary tract infection (UTI) identified by catheterized urine specimen, meningitis, septic arthritis, or osteomyelitis. Additionally, pneumonia was included as a CSI if confirmed by radiographs, based on final reading by an attending radiologist. Pneumonia is included as an SBI in a number of prior publications in this age group; therefore, we felt it was important to include it in our definition of CSI.7, 1115
Procedures
The chart review consisted of both electronic and paper medical records. We searched the electronic database for all the infants in this age group receiving a discharge diagnosis of an FBI as defined above. Information from the medical record was entered onto a standardized data sheet by one of the investigators or a research assistant. Data gathered included baseline demographic information (age at ED evaluation, gestational age at birth, gender, race), presence or absence of fever, vital signs on ED presentation, use of diagnostic evaluation (complete blood count [CBC], blood culture, C‐reactive protein, erythrocyte sedimentation rate, urinalysis, urine culture, LP, wound culture, radiographic studies), laboratory test results, therapeutic interventions (including antibiotics and subspecialty consultation), initial disposition (home, admission to hospital), and clinical outcome of both admitted and discharged patients. The results of all bacterial cultures were obtained from computerized microbiology records. Bacterial isolates from blood cultures that are considered skin flora, such as Staphylococcus epidermidis or Viridans group Streptococcus, were considered contaminants unless they were positive for growth within 24 hours of initial culture.1618 Radiology results were based on final interpretation by an attending radiologist.
Statistical Analysis
The primary objectives of this study were to determine the risk of CSI when presented with a well‐appearing infant who has an FBI on exam and to examine that risk in relation to the presence of fever. Thus, this study was powered to investigate the difference in CSI between febrile and afebrile patients. Again, we hypothesized that in afebrile, well‐appearing infants less than 60 days of age with an FBI on exam there is a very low risk of CSI. For statistical purposes and power calculations we used <1% risk as very low. Using the approximate risk of 10% CSI in well‐appearing, febrile infants this age without CSI, we assumed there would be approximately 10% less CSIs in the afebrile patients compared to the febrile patients. As per consultation with our statistician, for a significance level of = 0.05 and = 0.2 a 2‐sided t test required a total of 188 subjects to be enrolled.
Additional outcome measures (such as use of laboratory testing, IV antibiotics, subspecialty consultation, and admission) were reported as descriptive statistics with frequencies. Fisher's Exact test was used for these nominal variables to test significance of relationship between febrile and afebrile patients. The Exact method was used to calculate 95% confidence intervals (CIs) around the primary outcome point estimates. A P value < 0.05 was considered significant. All data were entered into a Microsoft Excel (Microsoft, Redmond, WA) database.
Results
Study Population
We identified 246 patients less than 60 days of age who were diagnosed in the ED with an FBI during the study period. Thirty‐seven patients met the exclusion criteria, leaving 209 patients for potential enrollment. Twelve (5.7%) charts were not located, resulting in a study population of 197 infants. Of these, 158 patients were afebrile and 39 were febrile. To put these numbers into context, over the study period our ED evaluated 2341 infants less than 60 days of age whose diagnosis included the word fever, febrile, or sepsis. The febrile infants included in our study group were part of these 2341 found in the retrospective search, but the afebrile infants included were not.
The mean age of these 197 infants was 29.6 days, with a standard deviation (SD) of 15.9 days. On average, the febrile patients (mean 40.7 days, SD 15.3 days) were older than the afebrile patients (mean 26.8 days, SD 16.1 days). No statistical differences were found between febrile and afebrile patients in respect to gender, race, and gestational age.
Primary Study OutcomeRisk of SBI
Four patients had a documented CSI, for an overall risk of CSI in our study population of 2.0% (Table 1). Statistically, febrile infants had a significantly higher risk of CSI (odds ratio [OR], 13.08; 95% CI, 1.32‐129.46) than afebrile infants. The febrile infants with a coexisting CSI included the following: a 32‐day‐old male with a buttock abscess and E. coli UTI; a 47‐day‐old male with periorbital cellulitis and Streptococcus pneumoniae bacteremia; and a 21‐day‐old female with trunk cellulitis and E. coli UTI. The afebrile infant with a CSI was an 11‐day‐old male with acute OM (AOM) and E. coli UTI. No cases of bacterial meningitis, septic arthritis, osteomyelitis, radiographic pneumonia, or death occurred.
| CSI | No CSI | Risk (%) | 95% CI (%) | |
|---|---|---|---|---|
| ||||
| Febrile (n = 39) | 3 | 36 | 7.69 | 1.62‐20.87 |
| Afebrile (n = 158) | 1 | 157 | 0.63 | 0.02‐3.48 |
| Total (n = 197) | 4 | 193 | 2.03 | 0.56‐5.12 |
Eight other patients had positive culture results, all of which were considered contaminants. Four patients had peripheral blood cultures that were deemed contaminants: 2 cases of Viridans group streptococcus and 2 cases of coagulase‐negative staphylococcus. Four urine cultures were considered contaminants: 1 staphylococcus species; 1 mixed flora specimen; 1 lactobacillus species, and 1 E. coli.
This positive culture for E. coli occurred in an 11‐day‐old female who presented without fever, was diagnosed clinically and by ultrasound with mastitis, and was admitted to the hospital. She underwent a full diagnostic workup for CSI. Initial screening laboratory test results were normal, including a negative urinalysis and 1 to 2 white blood cells (WBCs)/high‐powered field on the microscopic exam. The catheterized urine specimen grew the following: (1) 10,000 to 100,000 colony forming units (CFU)/mL of E. coli; and (2) normal flora 1000 to 9000 CFU/mL. Her blood and cerebrospinal fluid (CSF) culture were negative. The primary team did not diagnose or treat this patient as a UTI despite the positive culture. According to their documentation, it was a suspected contaminant because of negative chemical and microscopic urinalysis. If this were considered a true positive culture, which seem practical clinically, clinically the overall risk of CSI would be 2.5% (5/197 infants) and the risk of coexisting CSI in afebrile patients would be 1.3% (2/158 infants); however, febrile infants would still had a significantly higher risk of CSI (OR, 6.5; 95% CI, 1.05‐40.34) than afebrile infants.
Secondary Study OutcomeClinical Presentation of FBI in Well‐appearing Infants in This Age Group
Among the 197 study infants, there were multiple types of FBIs found on examination (Table 2). Soft tissue infections were the most common cause in afebrile patients, whereas AOM was the most common cause in the febrile patients. Overall, cellulitis and abscess were the leading causes of focal infections in this age group. A total of 46 patients were diagnosed with abscesses, the buttock being the site in 24 (52%) cases. Abscesses were drained and sent for culture in 13 patients. Methicillin‐resistant Staphylococcus aureus (MRSA) was found in 4 of these 13 cultures. Of the 55 patients diagnosed with cellulitis, 20 (36%) had cultures drawn from the cellulitis site, of which 5 cultures grew MRSA.
| Focal Infection | Afebrile (n = 158) [n (%)] | Febrile (n = 39) [n (%)] | Totals (n = 197) [n (%)] |
|---|---|---|---|
| |||
| AOM | 19 (12) | 22 (56) | 41 (21) |
| Cellulitis | 49 (31) | 6 (15) | 55 (28) |
| Abscess | 40 (25) | 6 (15) | 46 (23) |
| Impetigo | 20 (13) | 1 (3) | 21 (11) |
| Mastitis | 11 (7) | 2 (5) | 13 (7) |
| Lymphadenitis | 4 (3) | 1 (3) | 5 (3) |
| Omphalitis | 2 (1) | 0 (0) | 2 (1) |
| SSSS | 2 (1) | 0 (0) | 2 (1) |
| Paronychia | 1 (1) | 0 (0) | 1 (0) |
| Other | 10 (6) | 1 (3) | 11 (6) |
Of note, a 13‐day‐old male presenting without fever but with a scalp lesion had herpes simplex virus grown from his wound culture. His diagnostic workup was negative for CSI. Omphalitis, uncommon in the United States, was diagnosed in 2 patients in our study and neither of these patients developed necrotizing fasciitis. Mastitis was not a significant focal infection in either group; and no patient was diagnosed with mastoiditis, balanitis, or posthitis.
Secondary Study OutcomeCurrent Management of FBI in the ED: Resource Utilization
Febrile patients underwent significantly more diagnostic testing procedures than afebrile infants. Specifically, CBCs, peripheral blood cultures, urine analyses with cultures, LPs, and radiographic imaging were performed more often in infants with fever (Figure 1). Fifty‐seven infants had urine cultures performed: 32 of 158 afebrile infants and 25 of 39 febrile infants. Among these selected infants, again 3 UTIs occurred: 1 of 32 tested (3.1%) in the afebrile group and 2 of 25 tested (8%) in the febrile group. A total of 115 infants had blood cultures performed: 82 of the 158 afebrile infants and 33 of the 39 febrile infants. Among these selected infants, again 1 positive blood culture occurred: 0 of 82 tested (0%) in the afebrile group and 1 of 33 tested (3%) in the febrile group. Fifty‐five infants had LP performed: 35 of 158 afebrile infants and 30 of 39 febrile infants. No case of meningitis occurred in these selected infants. Twenty infants had diagnostic radiographs performed, 10 in the febrile group and 10 in the afebrile group. None of the radiographs showed signs of pneumonia on final radiology attending reading.
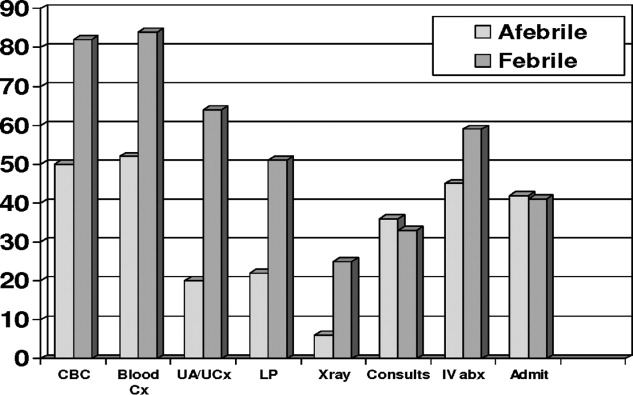
Overall, 33 of 39 febrile infants had cultures drawn and/or radiographs performed, with 3 CSIs discovered, and 87 of 158 afebrile infants had cultures drawn and/or radiographs performed, with 1 CSI discovered (Table 3). This means that 77 infants diagnosed with FBIs did not have any diagnostic testing for CSI performed while in the ED. The overall risk of CSI in patients who were tested was 3.3%. Comparing febrile and afebrile patients who had diagnostic workups performed, febrile infants had a trend toward increased risk of CSI (OR, 8.6; 95% CI, 0.8613‐85.8686).
| CSI | No CSI | Risk (%) | |
|---|---|---|---|
| |||
| Febrile (n = 33) | 3 | 30 | 9.1 |
| Afebrile (n = 87) | 1 | 86 | 1.1 |
| Totals (n = 120) | 4 | 116 | 3.3 |
No significant differences existed in the use of consultants, use of IV antibiotics, or admission rate. Sixty‐six (42%) of the 158 afebrile infants were admitted. The average length of stay for these infants was 2.59 days (range, 1‐22 days). This included a 22‐day‐old female with mastitis who required multiple surgeries and a protracted hospital course. Sixteen (41%) of the febrile infants were admitted and had an average stay of 2.87 days (range, 1‐6 days).
Patient Outcomes
Ninety‐two (58%) of the afebrile infants were discharged home from the ED, of which 5 (5.4%) returned to the ED within 72 hours after discharge. Three of these were planned ED returns as follow‐up with a primary care physician could not be guaranteed. The fourth was a 47‐day‐old with a buttock abscess who returned for reevaluation because of parental concern. The fifth was the 11‐day‐old male initially diagnosed with AOM who was called back to the ED when his urine culture grew E. coli, at which point he was admitted to the hospital. Twenty‐three (59%) of the febrile infants were discharged home from the ED. Two (8.7%) of these 23 returned to the ED within 72 hours; both were initially diagnosed with AOM and had planned follow‐ups as no primary care was available. No admitted patients required transfer to the pediatric intensive care unit and no deaths occurred.
Discussion
This study is the first to investigate the risk of CSI specifically in well‐appearing infants under 60 days of age presenting with FBI. Inclusion criteria were not limited to 1 specific infection, ie, OM, but included all FBI. This study demonstrated that the risk of CSI in afebrile infants is small (0.6%), which is similar to what has been shown in the OM literature.19, 20 However, the risk of CSI among febrile infants is not negligible (7.7%), and is similar to the risk of SBIs among young infants presenting with a fever of unknown source.57
AOM
A total of 41 infants were diagnoses with AOM. Indeed, AOM was the most common discharge diagnosis among the febrile cohort. No febrile infants with AOM were diagnosed with a CSI. However, as noted above, an 11‐day‐old afebrile infant with AOM did have a UTI diagnosed. This male underwent blood, urine, and CSF cultures on initial presentation. He was discharged home from the ED, and called back for further evaluation once the urine culture grew E. coli.
We relied on the diagnostic skills of the ED attending physician for determination of OM, and no rigorous diagnostic criteria were established for an AOM in this young age group. However, on chart review of those patients with AOM who were admitted, otolaryngology was often consulted and confirmed the diagnosis of OM.
AOM has been the most commonly studied focal infection studied most in this age group.1, 2, 11, 2123 More recent studies have investigated the risk of CSI with AOM among febrile and afebrile cohorts. These authors found that in infants under 2 months with AOM, febrile infants had a 6% to 13% risk of CSI, whereas no cases of CSI were found in afebrile patients.19, 20 These results suggest that afebrile, nontoxic infants with AOM could be treated as outpatients without need for further systemic evaluation. Our study strengthens this argument if close follow‐up can be assured.
Cellulitis and Abscess
A total of 106 infants were diagnosed with either abscess and/or cellulitis, with the vast majority of them presenting without fever. Moreover, cellulitis and abscess comprised more than one‐half of all infants in the afebrile cohort. The buttocks were the most common site for abscess (23 cases), followed next by the scalp (8 cases). In our study population, there were 29 positive abscess, wound, lesion, or skin aspirate cultures for Staphylococcus aureus, with 13 (45%) being MRSA. None of these patients had a CSI.
Community‐acquired staphylococcal infections have been studied in the newborn population, with MRSA accounting for up to 69% of soft‐tissue infections in one recent study involving 89 neonates.24 The authors found 4 cases of bacteremia, 3 cases of UTI, and 2 cases of CSF pleocytosis. Application of these results to our patients is difficult, as there was no mention of fever or well‐appearance stratification and there is no specific mention of any of the 77 skin and soft‐tissue infections having a CSI.
The frequency of bacteremia in pediatric patients with periorbital cellulitis has been studied, with some authors suggested more selective use of LP in patients with these localized soft‐tissue infections in the older infant or child.25, 26 Unfortunately, there were not enough patients under 60 days of age in either study from which to draw conclusions. In our study, a total of 5 patients presented with periorbital cellulitis: 2 afebrile and 3 febrile, including the 47‐day‐old febrile infant with coexisting pneumococcal bacteremia.
Group B streptococcus (GBS) cellulitis‐adenitis syndrome has also been identified in neonates, with meningitis occurring in up to 24% of infants in 1 review of 32 cases.27 These studies only included patients with positive blood cultures, providing no denominator for assessing a true CSI risk in young infants with cellulitis. No infants in our study had GBS infections.
Impetigo was diagnosed in 21 patients, with 17 patients being discharged home from the ED. In addition, 2 infants with staphylococcal scalded skin syndrome were identified. None of these infants had a CSI.
Other Infections
Mastitis in the young infant has been studied, with the risk of CSI being 3% in 1 review.2830 In our study, there were 18 patients diagnosed with either mastitis or breast abscess, of which 4 (22%) had fever and none had positive blood or CSF cultures. Multiple studies, either from older literature in the United States or more contemporary from abroad, have investigated omphalitis and necrotizing fasciitis in the newborn.31, 32 These show that infants presenting with omphalitis have a lower mortality and morbidity than those with necrotizing fasciitis. In our study, we had 2 patients with omphalitis, both were afebrile and neither had a coexisting CSI. We had no patients with necrotizing fasciitis. We also found no patients with mastoiditis, balanitis, or posthitis as the listed diagnosis in our study.
UTI
Of the 4 cases of CSI in our study, UTI was the most common, occurring in 3 of the 4 cases. This predominance of UTI as the cause of CSI is well‐recognized in young febrile infants with OM and infants with fever of unknown origin; however, it has not been reported with other FBIs in this age group.1, 5, 9, 11, 19, 33 Specifically, there has not been a reported relationship between UTI and skin or soft tissue infections. However, 2 of our 4 infants with a CSI had a UTI in addition to their skin or soft tissue infection: the 32‐day‐old male with a buttock abscess and E. coli UTI; and the 21‐day‐old female with truncal cellulitis and E. coli UTI.
Resource Utilization
Young infants with FBI and fever underwent significantly more resource utilization than afebrile infants in our ED (Figure 1). Physicians of febrile infants ordered more serum blood counts and blood cultures, urinalysis and urine cultures, and performed more LPs and radiographic studies. This is not surprising given that fever is a risk factor for CSI in this age group; however, resource utilization is not as well‐described in previous reports on infants with FBIs. In 1 retrospective study of 137 infants less than 8 weeks of age with AOM, 88% had diagnostic blood cultures, 66% had LP, and 81% had urine cultures drawn.19 Additionally, in our study the decision to hospitalize infants, use of IV antibiotics, and hospital length of stay was not statistically different between febrile and afebrile groups. This potentially suggests that diagnostic testing for infants with FBIs did not affect management and outcome. Another study showed hospital admission is costly and not without safety risks, with a complication rate as high as 19% in infants.34 Given these results, in addition to the presumption that all FBIs would be treated with antibiotics, one could infer that a number of well‐appearing, afebrile infants underwent unwarranted testing.
Limitations
The main limitation of our study was the retrospective design. A research assistant utilizing a computerized database program of ED patients performed the initial query based upon search criteria. A local expert using an established list of International Statistical Classification of Diseases and Related Health Problems (ICD) codes for any and all of the FBIs performed the chart review. Secondary diagnoses may have been omitted as a result of limited physician charting, which could have resulted in missed patients. CCHMC is currently transitioning from paper records to electronic medical records, which may explain why 12 charts were not found, despite exhaustive searches for them. Ultimately, 94% of all the eligible patients were found. Yet, with so few CSI diagnosed, 1 or 2 could conceivably change our results. As noted above, focal infections in infants under 2 months of age seem to be uncommon, not only in the ED setting, but also in a large cohort of primary care patients.35 With only a small number FBIs present over 6 years and so few having CSIs, we were limited to a univariate analysis, which limited our potential results and conclusions. Performing this study prospectively would have addressed these limitations, but would have required years of recruitment or multicenter collaboration.
Another potential limitation was the search strategy to identify eligible infants. Specifically, we did not search the records for infants diagnosed with UTI, bacteremia, or meningitis. Infants with these more serious conditions may have been coded as the primary or only problem, even if other problems such as OM were also present. Therefore, we may have underestimated the occurrence of systemic bacterial complications in a systematic way. This form of spectrum bias was a potential limitation. We approached this clinical question from the eye of the emergency department practitioner and thus used a search strategy based on the discharge diagnosis from the ED. If we were to look back to see if any patients discharged from the hospital with CSI also had FBI, we doubt our retrospective design would have allowed identification of patients with FBIs.
Other limitations may be our definition of CSI and the potential for missed CSIs. We defined meningitis, bacteremia, and UTI as a positive CSF, blood, or urine culture, respectively. Many studies are now defining culture‐negative meningitis or UTI based on WBC findings on a screening cell count or urine microscopy. However, because no patients were pretreated with antibiotics, we felt that a positive culture from a sterile site was a reasonable definition. Also, not all of the enrolled patients received full diagnostic workups to screen for CSI. In the smaller cohort of infants who received diagnostic testing, febrile infants still seemed to be at higher risk for CSI. To capture all possible CSIs, one would have needed to perform blood culture, suprapubic bladder aspiration, or catheterization for urine culture, LP, and chest radiograph on all patients with an FBI. Given the low risk of CSI in the United States, the previous literature's hinting at low risk for CSI in afebrile patients, and the presence of multiple clinical trials defining low risk characteristics for CSI, such a protocol would not receive support as being standard clinical practice and have difficulty being permitted by an institutional review board.
Another limitation of our study was follow‐up. Ideally, every patient would have been contacted to ensure reliable outcomes measurement. Patients may have been seen after their initial evaluation at their primary care provider's office or at another healthcare facility and had more diagnostic studies performed. However, because our institution is the sole admitting pediatric center in the area, particularly in infants, and most CSIs in this age group require admission; we feel that a reasonable degree of reliability for the outcomes of interest was maintained.
Last, we could not establish the rationale of clinical decision making, as our study was retrospective. For example, staff physicians may have foregone diagnostic testing if they had committed to a therapeutic course of antibiotics and felt diagnostic cultures would not change management. Also, we cannot ensure that interpretation of culture results was consistent with national standards. As described previously, 1 afebrile infant in our study potentially had a CSI that was clinically felt to be a contaminant by the inpatient healthcare team. This 11‐day‐old female was admitted with mastitis and had a negative urinalysis, but grew E. coli on urine culture. This was treated as a contaminant by the ward team, despite her age.
Conclusions
CSI is very uncommon in afebrile, well‐appearing infants under 2 months of age with an FBI. However, febrile infants have a greater risk of CSI. UTI is the most common CSI in well‐appearing infants less than 2 months of age with an FBI found on examination. Prospective, multicentered studies need to be performed to determine whether diagnostic evaluation should change the management of well‐appearing infants with an FBI found on examination.
- ,,, et al.Febrile infants at low risk for serious bacterial infection—an appraisal of the Rochester Criteria and implications for management.Pediatrics.1994;94:390–396.
- ,,, et al.Identification of infants unlikely to have serious bacterial infection although hospitalized for suspected sepsis.J Pediatr.1985;107:855–860.
- ,,.Outpatient management without antibiotics of fever in selected infants.N Engl J Med.1993;329:1437–1441.
- ,,.Outpatient treatment of febrile infants 28 to 89 days of age with intramuscular administration of ceftriaxone.J Pediatr.1992;120:22–27.
- ,.Predictive model for serious bacterial infections among infants younger than 3 months of age.Pediatrics.2001;108:311–316.
- ,,, et al.Applying outpatient protocols to febrile infants 1–28 days of age: can the threshold be lowered?Clin Pediatr.2000;39:81–88.
- ,,.The efficacy of routine outpatient management without antibiotics of fever in selected infants.Pediatrics.1999;103:627–631.
- ,.Evaluation of the infant with fever without source: an evidence based approach.Emerg Med Clin North Am.1999;17:97–126.
- ,,, et al.Risk of serious bacterial infection in young febrile infants with respiratory syncytial virus infections.Pediatrics.2004;113:1728–1734.
- ,,, et al.Relationship of fever magnitude to rate of serious bacterial infections in infants 4–8 weeks.Clin Pediatr (Phila).1991;30:478–480.
- ,,, et al.Enhanced urinalysis improved identification of febrile infants ages 60 days and younger at low risk for serious bacterial illness.Pediatrics.2001;108:866–871.
- ,,.C‐reactive protein in febrile children 1 to 36 months of age with clinically undetectable serious bacterial infection.Pediatrics.2001;108:1275–1279.
- ,.Utility of the serum C‐reactive protein for detection of occult bacterial infection in children.Arch Pediatr Adolesc Med.2002;156:905–909.
- ,,, et al.Procalcitonin and C‐reactive protein as diagnostic markers of severe bacterial infections in febrile infants and children in the emergency department.Pediatr Infect Dis J.2007;26:672–677.
- ,,.Neonatal fever: utility of the Rochester criteria in determining low risk for serious bacterial infections.Am J Emerg Med.1997;15:299–302.
- ,,.Evaluation of false positive blood cultures: guidelines for early detection of contaminated cultures in febrile children.Pediatr Emerg Care.1994;10:20–22.
- ,,.Outpatient pediatric blood cultures: time to positivity.Pediatrics.2000;106:251–255.
- ,,, et al.Occult bacteremia from a pediatric emergency department: current prevalence, time to detection and outcome.Pediatrics.2000;106:505–511.
- ,,, et al.Acute otitis media in infants younger than two months of age: microbiology, clinical presentation and therapeutic approach.Pediatr Infect Dis J.2002;21:669–674.
- ,,, et al.Otitis media in infants aged 0–8 weeks: frequency of associated serious bacterial disease.Pediatr Emerg Care.1999;15:252–254.
- ,,.Otitis media in children less than 12 weeks of age.Pediatrics.1977;59:827–832.
- ,,.Are well‐appearing febrile infants with otitis media at risk for serious bacterial illness? [Abstract].Am J Dis Child.1992;146:468.
- ,,, et al.Streptococcus pneumoniae infections in the neonate.Pediatrics.2003;112:1095–1102.
- ,,, et al.Community‐acquired Staphylococcus aureus infections in term and near‐term previously health neonates.Pediatrics.2007;118:874–881.
- ,.Blood cultures in the evaluation of children with cellulitis.Pediatrics.1997;101:e4.
- ,.Lumbar puncture in children with periorbital and orbital cellulitis.J Pediatr.1993;122:355–359.
- ,.Is lumbar puncture necessary to exclude meningitis in neonates and young infants: lessons from the Group B streptococcus cellulitis‐adenitis syndrome.Pediatrics.1998;102:985–986.
- ,.Neonatal mastitis.Clin Pediatr.1986;25:395–399.
- ,.Pseudomonas aeruginosa mastitis in a neonate.Pediatr Infect Dis J.1993;12:104.
- ,,.Group D streptococcal neonatal mastitis.Pediatr Infect Dis J.1998;7:362.
- ,,, et al.Early recognition of neonatal abdominal wall necrotizing fasciitis.Am J Surg.1994;167:481–484.
- ,,, et al.Necrotizing fasciitis: a serious complication of omphalitis in neonates.J Pediatr Surg.1994;29:1414–1416.
- ,,, et al.Acute otitis media in infants less than three months of age: clinical presentation, etiology and concomitant diseases.Int J Pediatr Otorhinolaryngol.2006;70:613–617.
- ,,, et al.Iatrogenic risks and financial costs of hospitalizing febrile infants.Am J Dis Child.1983;137:1146–1149.
- ,,, et al.Management and outcomes of care of fever in early infancy.JAMA.2004;291:1203–1212.
Focal bacterial infections (FBIs), including otitis media (OM), cellulitis, and lymphadenitis, can occur at any age and are usually treated with oral antibiotics. When patients with focal infections present as a young infant, healthcare providers often worry about the risk of coexisting or concomitant systemic infections (CSIs), often termed serious bacterial infections (SBIs) in the published literature.1, 2 Risk of CSI becomes more worrisome when young infants have fever as part of their presentation, especially within the traditional rule‐out sepsis age range of less than 2 months. Often, these patients are well‐appearing and lack prenatal and neonatal risk factors for systemic infections, but are assumed to be at high risk for CSI based on the presence of focal bacterial infection.1, 3, 4
FBIs have been the subject of multiple studies, especially OM and cellulitis. However, few investigations have looked specifically at infants less than 60 days of age, lending uncertainty to medical decision‐making for both community and emergency physicians. Therefore, no standardized evidence‐based practice exists for treating young infants with FBIs. While some clinicians treat these infections using systemic antibiotics without performing laboratory tests, others opt for a full diagnostic evaluation for CSI; including serum blood counts, blood cultures, lumbar punctures (LPs), and bladder catheterizations. Also, some clinicians opt for treatment with oral antibiotics at home, while others choose intravenous (IV) antibiotics and hospitalization.
These decisions are likely due to studies of febrile infants under 60 days of age who present to an emergency department (ED), appear well, and have no focal source of infection on exam, yet are known to have a risk of systemic or occult bacterial infection of roughly 10%.310 There are no such studies documenting the risk of CSI in well‐appearing, afebrile patients, as fever is regarded as the main risk factor for CSI in this age.
Based on our clinical experience and review of the literature, we felt that afebrile, well‐appearing infants less than 60 days of age with an FBI on exam would have a very low risk of CSI. The primary objectives of this study were to determine the risk of CSI when presented with a well‐appearing infant who has an FBI on exam and to examine that risk in relation to the presence of fever. Other objectives were to describe the clinical presentation of FBIs in well‐appearing infants in this age group and to describe the current management and resource utilization of such infections in the ED.
Patients and Methods
Study Population
Cincinnati Children's Hospital Medical Center (CCHMC) is a 423‐bed tertiary‐care hospital located in southwestern Ohio. The medical center serves as the sole pediatric hospital in a 70‐mile radius, serving a metropolitan population of roughly 1 million. In addition, CCHMC cares for patients from a wide demographic and socioeconomic spectrum, including the urban, suburban, and rural areas of Cincinnati, southwestern Ohio, northern Kentucky, and southeastern Indiana. The ED sees an average of 90,000 patients annually, with an average of 15,000 admissions.
Patient Selection
Data were retrospectively collected from a consecutive series of infants age 0 to 59 days who presented to the CCHMC ED between January 1, 2000 and December 31, 2005. Patients met inclusion criteria if they were documented to be well‐appearing on exam; had normal‐for‐age heart rate, respiratory rate, blood pressure, and oxygen saturation (if measured); were discharged from their hospital of birth to home before presentation to the ED; and received a discharge diagnosis consistent with an FBI. Specifically, FBIs included the following diagnoses: soft tissue infection, cellulitis, mastoiditis, abscess, OM, omphalitis, mastitis, mammitis, paronychia, balanitis, posthitis, impetigo, or lymphadenitis. We excluded patients with a history of immunodeficiency, central venous catheter, tracheostomy, gastrostomy tube, chronic lung disease, previous admission for a documented bacterial infection, or if they had been taking systemic antibiotics at the time of evaluation. We also excluded infants noted to be toxic or ill‐appearing on examination.
Definitions
Fever was defined as a temperature greater than or equal to 38C (100.4F), recorded by the ED or by parental report. All infants seen in the CCHMC ED had rectal temperatures measured per protocol. A nontoxic infant was defined by chart review as documentation of: nontoxic, well‐appearing, or alert infant without signs of respiratory distress or hemodynamic instability. Patients were excluded from the nontoxic category with the following parameters: heart rate >180 beats per minute, respiratory rate >60 breaths per minute, oxygen saturation <90% on pulse oximetry, or systolic blood pressure <60 mmHg on 2 or more measurements. CSIs were defined as any of the following: bacteremia, urinary tract infection (UTI) identified by catheterized urine specimen, meningitis, septic arthritis, or osteomyelitis. Additionally, pneumonia was included as a CSI if confirmed by radiographs, based on final reading by an attending radiologist. Pneumonia is included as an SBI in a number of prior publications in this age group; therefore, we felt it was important to include it in our definition of CSI.7, 1115
Procedures
The chart review consisted of both electronic and paper medical records. We searched the electronic database for all the infants in this age group receiving a discharge diagnosis of an FBI as defined above. Information from the medical record was entered onto a standardized data sheet by one of the investigators or a research assistant. Data gathered included baseline demographic information (age at ED evaluation, gestational age at birth, gender, race), presence or absence of fever, vital signs on ED presentation, use of diagnostic evaluation (complete blood count [CBC], blood culture, C‐reactive protein, erythrocyte sedimentation rate, urinalysis, urine culture, LP, wound culture, radiographic studies), laboratory test results, therapeutic interventions (including antibiotics and subspecialty consultation), initial disposition (home, admission to hospital), and clinical outcome of both admitted and discharged patients. The results of all bacterial cultures were obtained from computerized microbiology records. Bacterial isolates from blood cultures that are considered skin flora, such as Staphylococcus epidermidis or Viridans group Streptococcus, were considered contaminants unless they were positive for growth within 24 hours of initial culture.1618 Radiology results were based on final interpretation by an attending radiologist.
Statistical Analysis
The primary objectives of this study were to determine the risk of CSI when presented with a well‐appearing infant who has an FBI on exam and to examine that risk in relation to the presence of fever. Thus, this study was powered to investigate the difference in CSI between febrile and afebrile patients. Again, we hypothesized that in afebrile, well‐appearing infants less than 60 days of age with an FBI on exam there is a very low risk of CSI. For statistical purposes and power calculations we used <1% risk as very low. Using the approximate risk of 10% CSI in well‐appearing, febrile infants this age without CSI, we assumed there would be approximately 10% less CSIs in the afebrile patients compared to the febrile patients. As per consultation with our statistician, for a significance level of = 0.05 and = 0.2 a 2‐sided t test required a total of 188 subjects to be enrolled.
Additional outcome measures (such as use of laboratory testing, IV antibiotics, subspecialty consultation, and admission) were reported as descriptive statistics with frequencies. Fisher's Exact test was used for these nominal variables to test significance of relationship between febrile and afebrile patients. The Exact method was used to calculate 95% confidence intervals (CIs) around the primary outcome point estimates. A P value < 0.05 was considered significant. All data were entered into a Microsoft Excel (Microsoft, Redmond, WA) database.
Results
Study Population
We identified 246 patients less than 60 days of age who were diagnosed in the ED with an FBI during the study period. Thirty‐seven patients met the exclusion criteria, leaving 209 patients for potential enrollment. Twelve (5.7%) charts were not located, resulting in a study population of 197 infants. Of these, 158 patients were afebrile and 39 were febrile. To put these numbers into context, over the study period our ED evaluated 2341 infants less than 60 days of age whose diagnosis included the word fever, febrile, or sepsis. The febrile infants included in our study group were part of these 2341 found in the retrospective search, but the afebrile infants included were not.
The mean age of these 197 infants was 29.6 days, with a standard deviation (SD) of 15.9 days. On average, the febrile patients (mean 40.7 days, SD 15.3 days) were older than the afebrile patients (mean 26.8 days, SD 16.1 days). No statistical differences were found between febrile and afebrile patients in respect to gender, race, and gestational age.
Primary Study OutcomeRisk of SBI
Four patients had a documented CSI, for an overall risk of CSI in our study population of 2.0% (Table 1). Statistically, febrile infants had a significantly higher risk of CSI (odds ratio [OR], 13.08; 95% CI, 1.32‐129.46) than afebrile infants. The febrile infants with a coexisting CSI included the following: a 32‐day‐old male with a buttock abscess and E. coli UTI; a 47‐day‐old male with periorbital cellulitis and Streptococcus pneumoniae bacteremia; and a 21‐day‐old female with trunk cellulitis and E. coli UTI. The afebrile infant with a CSI was an 11‐day‐old male with acute OM (AOM) and E. coli UTI. No cases of bacterial meningitis, septic arthritis, osteomyelitis, radiographic pneumonia, or death occurred.
| CSI | No CSI | Risk (%) | 95% CI (%) | |
|---|---|---|---|---|
| ||||
| Febrile (n = 39) | 3 | 36 | 7.69 | 1.62‐20.87 |
| Afebrile (n = 158) | 1 | 157 | 0.63 | 0.02‐3.48 |
| Total (n = 197) | 4 | 193 | 2.03 | 0.56‐5.12 |
Eight other patients had positive culture results, all of which were considered contaminants. Four patients had peripheral blood cultures that were deemed contaminants: 2 cases of Viridans group streptococcus and 2 cases of coagulase‐negative staphylococcus. Four urine cultures were considered contaminants: 1 staphylococcus species; 1 mixed flora specimen; 1 lactobacillus species, and 1 E. coli.
This positive culture for E. coli occurred in an 11‐day‐old female who presented without fever, was diagnosed clinically and by ultrasound with mastitis, and was admitted to the hospital. She underwent a full diagnostic workup for CSI. Initial screening laboratory test results were normal, including a negative urinalysis and 1 to 2 white blood cells (WBCs)/high‐powered field on the microscopic exam. The catheterized urine specimen grew the following: (1) 10,000 to 100,000 colony forming units (CFU)/mL of E. coli; and (2) normal flora 1000 to 9000 CFU/mL. Her blood and cerebrospinal fluid (CSF) culture were negative. The primary team did not diagnose or treat this patient as a UTI despite the positive culture. According to their documentation, it was a suspected contaminant because of negative chemical and microscopic urinalysis. If this were considered a true positive culture, which seem practical clinically, clinically the overall risk of CSI would be 2.5% (5/197 infants) and the risk of coexisting CSI in afebrile patients would be 1.3% (2/158 infants); however, febrile infants would still had a significantly higher risk of CSI (OR, 6.5; 95% CI, 1.05‐40.34) than afebrile infants.
Secondary Study OutcomeClinical Presentation of FBI in Well‐appearing Infants in This Age Group
Among the 197 study infants, there were multiple types of FBIs found on examination (Table 2). Soft tissue infections were the most common cause in afebrile patients, whereas AOM was the most common cause in the febrile patients. Overall, cellulitis and abscess were the leading causes of focal infections in this age group. A total of 46 patients were diagnosed with abscesses, the buttock being the site in 24 (52%) cases. Abscesses were drained and sent for culture in 13 patients. Methicillin‐resistant Staphylococcus aureus (MRSA) was found in 4 of these 13 cultures. Of the 55 patients diagnosed with cellulitis, 20 (36%) had cultures drawn from the cellulitis site, of which 5 cultures grew MRSA.
| Focal Infection | Afebrile (n = 158) [n (%)] | Febrile (n = 39) [n (%)] | Totals (n = 197) [n (%)] |
|---|---|---|---|
| |||
| AOM | 19 (12) | 22 (56) | 41 (21) |
| Cellulitis | 49 (31) | 6 (15) | 55 (28) |
| Abscess | 40 (25) | 6 (15) | 46 (23) |
| Impetigo | 20 (13) | 1 (3) | 21 (11) |
| Mastitis | 11 (7) | 2 (5) | 13 (7) |
| Lymphadenitis | 4 (3) | 1 (3) | 5 (3) |
| Omphalitis | 2 (1) | 0 (0) | 2 (1) |
| SSSS | 2 (1) | 0 (0) | 2 (1) |
| Paronychia | 1 (1) | 0 (0) | 1 (0) |
| Other | 10 (6) | 1 (3) | 11 (6) |
Of note, a 13‐day‐old male presenting without fever but with a scalp lesion had herpes simplex virus grown from his wound culture. His diagnostic workup was negative for CSI. Omphalitis, uncommon in the United States, was diagnosed in 2 patients in our study and neither of these patients developed necrotizing fasciitis. Mastitis was not a significant focal infection in either group; and no patient was diagnosed with mastoiditis, balanitis, or posthitis.
Secondary Study OutcomeCurrent Management of FBI in the ED: Resource Utilization
Febrile patients underwent significantly more diagnostic testing procedures than afebrile infants. Specifically, CBCs, peripheral blood cultures, urine analyses with cultures, LPs, and radiographic imaging were performed more often in infants with fever (Figure 1). Fifty‐seven infants had urine cultures performed: 32 of 158 afebrile infants and 25 of 39 febrile infants. Among these selected infants, again 3 UTIs occurred: 1 of 32 tested (3.1%) in the afebrile group and 2 of 25 tested (8%) in the febrile group. A total of 115 infants had blood cultures performed: 82 of the 158 afebrile infants and 33 of the 39 febrile infants. Among these selected infants, again 1 positive blood culture occurred: 0 of 82 tested (0%) in the afebrile group and 1 of 33 tested (3%) in the febrile group. Fifty‐five infants had LP performed: 35 of 158 afebrile infants and 30 of 39 febrile infants. No case of meningitis occurred in these selected infants. Twenty infants had diagnostic radiographs performed, 10 in the febrile group and 10 in the afebrile group. None of the radiographs showed signs of pneumonia on final radiology attending reading.
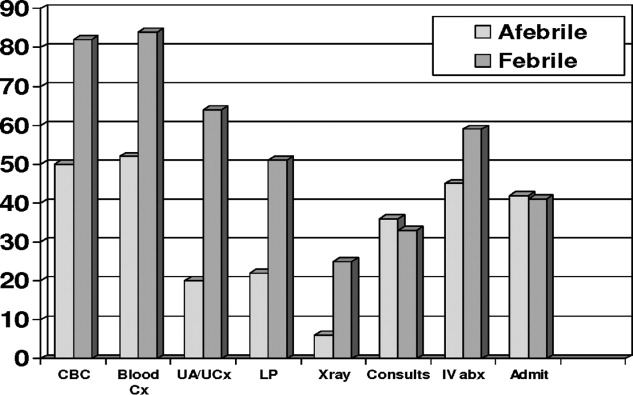
Overall, 33 of 39 febrile infants had cultures drawn and/or radiographs performed, with 3 CSIs discovered, and 87 of 158 afebrile infants had cultures drawn and/or radiographs performed, with 1 CSI discovered (Table 3). This means that 77 infants diagnosed with FBIs did not have any diagnostic testing for CSI performed while in the ED. The overall risk of CSI in patients who were tested was 3.3%. Comparing febrile and afebrile patients who had diagnostic workups performed, febrile infants had a trend toward increased risk of CSI (OR, 8.6; 95% CI, 0.8613‐85.8686).
| CSI | No CSI | Risk (%) | |
|---|---|---|---|
| |||
| Febrile (n = 33) | 3 | 30 | 9.1 |
| Afebrile (n = 87) | 1 | 86 | 1.1 |
| Totals (n = 120) | 4 | 116 | 3.3 |
No significant differences existed in the use of consultants, use of IV antibiotics, or admission rate. Sixty‐six (42%) of the 158 afebrile infants were admitted. The average length of stay for these infants was 2.59 days (range, 1‐22 days). This included a 22‐day‐old female with mastitis who required multiple surgeries and a protracted hospital course. Sixteen (41%) of the febrile infants were admitted and had an average stay of 2.87 days (range, 1‐6 days).
Patient Outcomes
Ninety‐two (58%) of the afebrile infants were discharged home from the ED, of which 5 (5.4%) returned to the ED within 72 hours after discharge. Three of these were planned ED returns as follow‐up with a primary care physician could not be guaranteed. The fourth was a 47‐day‐old with a buttock abscess who returned for reevaluation because of parental concern. The fifth was the 11‐day‐old male initially diagnosed with AOM who was called back to the ED when his urine culture grew E. coli, at which point he was admitted to the hospital. Twenty‐three (59%) of the febrile infants were discharged home from the ED. Two (8.7%) of these 23 returned to the ED within 72 hours; both were initially diagnosed with AOM and had planned follow‐ups as no primary care was available. No admitted patients required transfer to the pediatric intensive care unit and no deaths occurred.
Discussion
This study is the first to investigate the risk of CSI specifically in well‐appearing infants under 60 days of age presenting with FBI. Inclusion criteria were not limited to 1 specific infection, ie, OM, but included all FBI. This study demonstrated that the risk of CSI in afebrile infants is small (0.6%), which is similar to what has been shown in the OM literature.19, 20 However, the risk of CSI among febrile infants is not negligible (7.7%), and is similar to the risk of SBIs among young infants presenting with a fever of unknown source.57
AOM
A total of 41 infants were diagnoses with AOM. Indeed, AOM was the most common discharge diagnosis among the febrile cohort. No febrile infants with AOM were diagnosed with a CSI. However, as noted above, an 11‐day‐old afebrile infant with AOM did have a UTI diagnosed. This male underwent blood, urine, and CSF cultures on initial presentation. He was discharged home from the ED, and called back for further evaluation once the urine culture grew E. coli.
We relied on the diagnostic skills of the ED attending physician for determination of OM, and no rigorous diagnostic criteria were established for an AOM in this young age group. However, on chart review of those patients with AOM who were admitted, otolaryngology was often consulted and confirmed the diagnosis of OM.
AOM has been the most commonly studied focal infection studied most in this age group.1, 2, 11, 2123 More recent studies have investigated the risk of CSI with AOM among febrile and afebrile cohorts. These authors found that in infants under 2 months with AOM, febrile infants had a 6% to 13% risk of CSI, whereas no cases of CSI were found in afebrile patients.19, 20 These results suggest that afebrile, nontoxic infants with AOM could be treated as outpatients without need for further systemic evaluation. Our study strengthens this argument if close follow‐up can be assured.
Cellulitis and Abscess
A total of 106 infants were diagnosed with either abscess and/or cellulitis, with the vast majority of them presenting without fever. Moreover, cellulitis and abscess comprised more than one‐half of all infants in the afebrile cohort. The buttocks were the most common site for abscess (23 cases), followed next by the scalp (8 cases). In our study population, there were 29 positive abscess, wound, lesion, or skin aspirate cultures for Staphylococcus aureus, with 13 (45%) being MRSA. None of these patients had a CSI.
Community‐acquired staphylococcal infections have been studied in the newborn population, with MRSA accounting for up to 69% of soft‐tissue infections in one recent study involving 89 neonates.24 The authors found 4 cases of bacteremia, 3 cases of UTI, and 2 cases of CSF pleocytosis. Application of these results to our patients is difficult, as there was no mention of fever or well‐appearance stratification and there is no specific mention of any of the 77 skin and soft‐tissue infections having a CSI.
The frequency of bacteremia in pediatric patients with periorbital cellulitis has been studied, with some authors suggested more selective use of LP in patients with these localized soft‐tissue infections in the older infant or child.25, 26 Unfortunately, there were not enough patients under 60 days of age in either study from which to draw conclusions. In our study, a total of 5 patients presented with periorbital cellulitis: 2 afebrile and 3 febrile, including the 47‐day‐old febrile infant with coexisting pneumococcal bacteremia.
Group B streptococcus (GBS) cellulitis‐adenitis syndrome has also been identified in neonates, with meningitis occurring in up to 24% of infants in 1 review of 32 cases.27 These studies only included patients with positive blood cultures, providing no denominator for assessing a true CSI risk in young infants with cellulitis. No infants in our study had GBS infections.
Impetigo was diagnosed in 21 patients, with 17 patients being discharged home from the ED. In addition, 2 infants with staphylococcal scalded skin syndrome were identified. None of these infants had a CSI.
Other Infections
Mastitis in the young infant has been studied, with the risk of CSI being 3% in 1 review.2830 In our study, there were 18 patients diagnosed with either mastitis or breast abscess, of which 4 (22%) had fever and none had positive blood or CSF cultures. Multiple studies, either from older literature in the United States or more contemporary from abroad, have investigated omphalitis and necrotizing fasciitis in the newborn.31, 32 These show that infants presenting with omphalitis have a lower mortality and morbidity than those with necrotizing fasciitis. In our study, we had 2 patients with omphalitis, both were afebrile and neither had a coexisting CSI. We had no patients with necrotizing fasciitis. We also found no patients with mastoiditis, balanitis, or posthitis as the listed diagnosis in our study.
UTI
Of the 4 cases of CSI in our study, UTI was the most common, occurring in 3 of the 4 cases. This predominance of UTI as the cause of CSI is well‐recognized in young febrile infants with OM and infants with fever of unknown origin; however, it has not been reported with other FBIs in this age group.1, 5, 9, 11, 19, 33 Specifically, there has not been a reported relationship between UTI and skin or soft tissue infections. However, 2 of our 4 infants with a CSI had a UTI in addition to their skin or soft tissue infection: the 32‐day‐old male with a buttock abscess and E. coli UTI; and the 21‐day‐old female with truncal cellulitis and E. coli UTI.
Resource Utilization
Young infants with FBI and fever underwent significantly more resource utilization than afebrile infants in our ED (Figure 1). Physicians of febrile infants ordered more serum blood counts and blood cultures, urinalysis and urine cultures, and performed more LPs and radiographic studies. This is not surprising given that fever is a risk factor for CSI in this age group; however, resource utilization is not as well‐described in previous reports on infants with FBIs. In 1 retrospective study of 137 infants less than 8 weeks of age with AOM, 88% had diagnostic blood cultures, 66% had LP, and 81% had urine cultures drawn.19 Additionally, in our study the decision to hospitalize infants, use of IV antibiotics, and hospital length of stay was not statistically different between febrile and afebrile groups. This potentially suggests that diagnostic testing for infants with FBIs did not affect management and outcome. Another study showed hospital admission is costly and not without safety risks, with a complication rate as high as 19% in infants.34 Given these results, in addition to the presumption that all FBIs would be treated with antibiotics, one could infer that a number of well‐appearing, afebrile infants underwent unwarranted testing.
Limitations
The main limitation of our study was the retrospective design. A research assistant utilizing a computerized database program of ED patients performed the initial query based upon search criteria. A local expert using an established list of International Statistical Classification of Diseases and Related Health Problems (ICD) codes for any and all of the FBIs performed the chart review. Secondary diagnoses may have been omitted as a result of limited physician charting, which could have resulted in missed patients. CCHMC is currently transitioning from paper records to electronic medical records, which may explain why 12 charts were not found, despite exhaustive searches for them. Ultimately, 94% of all the eligible patients were found. Yet, with so few CSI diagnosed, 1 or 2 could conceivably change our results. As noted above, focal infections in infants under 2 months of age seem to be uncommon, not only in the ED setting, but also in a large cohort of primary care patients.35 With only a small number FBIs present over 6 years and so few having CSIs, we were limited to a univariate analysis, which limited our potential results and conclusions. Performing this study prospectively would have addressed these limitations, but would have required years of recruitment or multicenter collaboration.
Another potential limitation was the search strategy to identify eligible infants. Specifically, we did not search the records for infants diagnosed with UTI, bacteremia, or meningitis. Infants with these more serious conditions may have been coded as the primary or only problem, even if other problems such as OM were also present. Therefore, we may have underestimated the occurrence of systemic bacterial complications in a systematic way. This form of spectrum bias was a potential limitation. We approached this clinical question from the eye of the emergency department practitioner and thus used a search strategy based on the discharge diagnosis from the ED. If we were to look back to see if any patients discharged from the hospital with CSI also had FBI, we doubt our retrospective design would have allowed identification of patients with FBIs.
Other limitations may be our definition of CSI and the potential for missed CSIs. We defined meningitis, bacteremia, and UTI as a positive CSF, blood, or urine culture, respectively. Many studies are now defining culture‐negative meningitis or UTI based on WBC findings on a screening cell count or urine microscopy. However, because no patients were pretreated with antibiotics, we felt that a positive culture from a sterile site was a reasonable definition. Also, not all of the enrolled patients received full diagnostic workups to screen for CSI. In the smaller cohort of infants who received diagnostic testing, febrile infants still seemed to be at higher risk for CSI. To capture all possible CSIs, one would have needed to perform blood culture, suprapubic bladder aspiration, or catheterization for urine culture, LP, and chest radiograph on all patients with an FBI. Given the low risk of CSI in the United States, the previous literature's hinting at low risk for CSI in afebrile patients, and the presence of multiple clinical trials defining low risk characteristics for CSI, such a protocol would not receive support as being standard clinical practice and have difficulty being permitted by an institutional review board.
Another limitation of our study was follow‐up. Ideally, every patient would have been contacted to ensure reliable outcomes measurement. Patients may have been seen after their initial evaluation at their primary care provider's office or at another healthcare facility and had more diagnostic studies performed. However, because our institution is the sole admitting pediatric center in the area, particularly in infants, and most CSIs in this age group require admission; we feel that a reasonable degree of reliability for the outcomes of interest was maintained.
Last, we could not establish the rationale of clinical decision making, as our study was retrospective. For example, staff physicians may have foregone diagnostic testing if they had committed to a therapeutic course of antibiotics and felt diagnostic cultures would not change management. Also, we cannot ensure that interpretation of culture results was consistent with national standards. As described previously, 1 afebrile infant in our study potentially had a CSI that was clinically felt to be a contaminant by the inpatient healthcare team. This 11‐day‐old female was admitted with mastitis and had a negative urinalysis, but grew E. coli on urine culture. This was treated as a contaminant by the ward team, despite her age.
Conclusions
CSI is very uncommon in afebrile, well‐appearing infants under 2 months of age with an FBI. However, febrile infants have a greater risk of CSI. UTI is the most common CSI in well‐appearing infants less than 2 months of age with an FBI found on examination. Prospective, multicentered studies need to be performed to determine whether diagnostic evaluation should change the management of well‐appearing infants with an FBI found on examination.
Focal bacterial infections (FBIs), including otitis media (OM), cellulitis, and lymphadenitis, can occur at any age and are usually treated with oral antibiotics. When patients with focal infections present as a young infant, healthcare providers often worry about the risk of coexisting or concomitant systemic infections (CSIs), often termed serious bacterial infections (SBIs) in the published literature.1, 2 Risk of CSI becomes more worrisome when young infants have fever as part of their presentation, especially within the traditional rule‐out sepsis age range of less than 2 months. Often, these patients are well‐appearing and lack prenatal and neonatal risk factors for systemic infections, but are assumed to be at high risk for CSI based on the presence of focal bacterial infection.1, 3, 4
FBIs have been the subject of multiple studies, especially OM and cellulitis. However, few investigations have looked specifically at infants less than 60 days of age, lending uncertainty to medical decision‐making for both community and emergency physicians. Therefore, no standardized evidence‐based practice exists for treating young infants with FBIs. While some clinicians treat these infections using systemic antibiotics without performing laboratory tests, others opt for a full diagnostic evaluation for CSI; including serum blood counts, blood cultures, lumbar punctures (LPs), and bladder catheterizations. Also, some clinicians opt for treatment with oral antibiotics at home, while others choose intravenous (IV) antibiotics and hospitalization.
These decisions are likely due to studies of febrile infants under 60 days of age who present to an emergency department (ED), appear well, and have no focal source of infection on exam, yet are known to have a risk of systemic or occult bacterial infection of roughly 10%.310 There are no such studies documenting the risk of CSI in well‐appearing, afebrile patients, as fever is regarded as the main risk factor for CSI in this age.
Based on our clinical experience and review of the literature, we felt that afebrile, well‐appearing infants less than 60 days of age with an FBI on exam would have a very low risk of CSI. The primary objectives of this study were to determine the risk of CSI when presented with a well‐appearing infant who has an FBI on exam and to examine that risk in relation to the presence of fever. Other objectives were to describe the clinical presentation of FBIs in well‐appearing infants in this age group and to describe the current management and resource utilization of such infections in the ED.
Patients and Methods
Study Population
Cincinnati Children's Hospital Medical Center (CCHMC) is a 423‐bed tertiary‐care hospital located in southwestern Ohio. The medical center serves as the sole pediatric hospital in a 70‐mile radius, serving a metropolitan population of roughly 1 million. In addition, CCHMC cares for patients from a wide demographic and socioeconomic spectrum, including the urban, suburban, and rural areas of Cincinnati, southwestern Ohio, northern Kentucky, and southeastern Indiana. The ED sees an average of 90,000 patients annually, with an average of 15,000 admissions.
Patient Selection
Data were retrospectively collected from a consecutive series of infants age 0 to 59 days who presented to the CCHMC ED between January 1, 2000 and December 31, 2005. Patients met inclusion criteria if they were documented to be well‐appearing on exam; had normal‐for‐age heart rate, respiratory rate, blood pressure, and oxygen saturation (if measured); were discharged from their hospital of birth to home before presentation to the ED; and received a discharge diagnosis consistent with an FBI. Specifically, FBIs included the following diagnoses: soft tissue infection, cellulitis, mastoiditis, abscess, OM, omphalitis, mastitis, mammitis, paronychia, balanitis, posthitis, impetigo, or lymphadenitis. We excluded patients with a history of immunodeficiency, central venous catheter, tracheostomy, gastrostomy tube, chronic lung disease, previous admission for a documented bacterial infection, or if they had been taking systemic antibiotics at the time of evaluation. We also excluded infants noted to be toxic or ill‐appearing on examination.
Definitions
Fever was defined as a temperature greater than or equal to 38C (100.4F), recorded by the ED or by parental report. All infants seen in the CCHMC ED had rectal temperatures measured per protocol. A nontoxic infant was defined by chart review as documentation of: nontoxic, well‐appearing, or alert infant without signs of respiratory distress or hemodynamic instability. Patients were excluded from the nontoxic category with the following parameters: heart rate >180 beats per minute, respiratory rate >60 breaths per minute, oxygen saturation <90% on pulse oximetry, or systolic blood pressure <60 mmHg on 2 or more measurements. CSIs were defined as any of the following: bacteremia, urinary tract infection (UTI) identified by catheterized urine specimen, meningitis, septic arthritis, or osteomyelitis. Additionally, pneumonia was included as a CSI if confirmed by radiographs, based on final reading by an attending radiologist. Pneumonia is included as an SBI in a number of prior publications in this age group; therefore, we felt it was important to include it in our definition of CSI.7, 1115
Procedures
The chart review consisted of both electronic and paper medical records. We searched the electronic database for all the infants in this age group receiving a discharge diagnosis of an FBI as defined above. Information from the medical record was entered onto a standardized data sheet by one of the investigators or a research assistant. Data gathered included baseline demographic information (age at ED evaluation, gestational age at birth, gender, race), presence or absence of fever, vital signs on ED presentation, use of diagnostic evaluation (complete blood count [CBC], blood culture, C‐reactive protein, erythrocyte sedimentation rate, urinalysis, urine culture, LP, wound culture, radiographic studies), laboratory test results, therapeutic interventions (including antibiotics and subspecialty consultation), initial disposition (home, admission to hospital), and clinical outcome of both admitted and discharged patients. The results of all bacterial cultures were obtained from computerized microbiology records. Bacterial isolates from blood cultures that are considered skin flora, such as Staphylococcus epidermidis or Viridans group Streptococcus, were considered contaminants unless they were positive for growth within 24 hours of initial culture.1618 Radiology results were based on final interpretation by an attending radiologist.
Statistical Analysis
The primary objectives of this study were to determine the risk of CSI when presented with a well‐appearing infant who has an FBI on exam and to examine that risk in relation to the presence of fever. Thus, this study was powered to investigate the difference in CSI between febrile and afebrile patients. Again, we hypothesized that in afebrile, well‐appearing infants less than 60 days of age with an FBI on exam there is a very low risk of CSI. For statistical purposes and power calculations we used <1% risk as very low. Using the approximate risk of 10% CSI in well‐appearing, febrile infants this age without CSI, we assumed there would be approximately 10% less CSIs in the afebrile patients compared to the febrile patients. As per consultation with our statistician, for a significance level of = 0.05 and = 0.2 a 2‐sided t test required a total of 188 subjects to be enrolled.
Additional outcome measures (such as use of laboratory testing, IV antibiotics, subspecialty consultation, and admission) were reported as descriptive statistics with frequencies. Fisher's Exact test was used for these nominal variables to test significance of relationship between febrile and afebrile patients. The Exact method was used to calculate 95% confidence intervals (CIs) around the primary outcome point estimates. A P value < 0.05 was considered significant. All data were entered into a Microsoft Excel (Microsoft, Redmond, WA) database.
Results
Study Population
We identified 246 patients less than 60 days of age who were diagnosed in the ED with an FBI during the study period. Thirty‐seven patients met the exclusion criteria, leaving 209 patients for potential enrollment. Twelve (5.7%) charts were not located, resulting in a study population of 197 infants. Of these, 158 patients were afebrile and 39 were febrile. To put these numbers into context, over the study period our ED evaluated 2341 infants less than 60 days of age whose diagnosis included the word fever, febrile, or sepsis. The febrile infants included in our study group were part of these 2341 found in the retrospective search, but the afebrile infants included were not.
The mean age of these 197 infants was 29.6 days, with a standard deviation (SD) of 15.9 days. On average, the febrile patients (mean 40.7 days, SD 15.3 days) were older than the afebrile patients (mean 26.8 days, SD 16.1 days). No statistical differences were found between febrile and afebrile patients in respect to gender, race, and gestational age.
Primary Study OutcomeRisk of SBI
Four patients had a documented CSI, for an overall risk of CSI in our study population of 2.0% (Table 1). Statistically, febrile infants had a significantly higher risk of CSI (odds ratio [OR], 13.08; 95% CI, 1.32‐129.46) than afebrile infants. The febrile infants with a coexisting CSI included the following: a 32‐day‐old male with a buttock abscess and E. coli UTI; a 47‐day‐old male with periorbital cellulitis and Streptococcus pneumoniae bacteremia; and a 21‐day‐old female with trunk cellulitis and E. coli UTI. The afebrile infant with a CSI was an 11‐day‐old male with acute OM (AOM) and E. coli UTI. No cases of bacterial meningitis, septic arthritis, osteomyelitis, radiographic pneumonia, or death occurred.
| CSI | No CSI | Risk (%) | 95% CI (%) | |
|---|---|---|---|---|
| ||||
| Febrile (n = 39) | 3 | 36 | 7.69 | 1.62‐20.87 |
| Afebrile (n = 158) | 1 | 157 | 0.63 | 0.02‐3.48 |
| Total (n = 197) | 4 | 193 | 2.03 | 0.56‐5.12 |
Eight other patients had positive culture results, all of which were considered contaminants. Four patients had peripheral blood cultures that were deemed contaminants: 2 cases of Viridans group streptococcus and 2 cases of coagulase‐negative staphylococcus. Four urine cultures were considered contaminants: 1 staphylococcus species; 1 mixed flora specimen; 1 lactobacillus species, and 1 E. coli.
This positive culture for E. coli occurred in an 11‐day‐old female who presented without fever, was diagnosed clinically and by ultrasound with mastitis, and was admitted to the hospital. She underwent a full diagnostic workup for CSI. Initial screening laboratory test results were normal, including a negative urinalysis and 1 to 2 white blood cells (WBCs)/high‐powered field on the microscopic exam. The catheterized urine specimen grew the following: (1) 10,000 to 100,000 colony forming units (CFU)/mL of E. coli; and (2) normal flora 1000 to 9000 CFU/mL. Her blood and cerebrospinal fluid (CSF) culture were negative. The primary team did not diagnose or treat this patient as a UTI despite the positive culture. According to their documentation, it was a suspected contaminant because of negative chemical and microscopic urinalysis. If this were considered a true positive culture, which seem practical clinically, clinically the overall risk of CSI would be 2.5% (5/197 infants) and the risk of coexisting CSI in afebrile patients would be 1.3% (2/158 infants); however, febrile infants would still had a significantly higher risk of CSI (OR, 6.5; 95% CI, 1.05‐40.34) than afebrile infants.
Secondary Study OutcomeClinical Presentation of FBI in Well‐appearing Infants in This Age Group
Among the 197 study infants, there were multiple types of FBIs found on examination (Table 2). Soft tissue infections were the most common cause in afebrile patients, whereas AOM was the most common cause in the febrile patients. Overall, cellulitis and abscess were the leading causes of focal infections in this age group. A total of 46 patients were diagnosed with abscesses, the buttock being the site in 24 (52%) cases. Abscesses were drained and sent for culture in 13 patients. Methicillin‐resistant Staphylococcus aureus (MRSA) was found in 4 of these 13 cultures. Of the 55 patients diagnosed with cellulitis, 20 (36%) had cultures drawn from the cellulitis site, of which 5 cultures grew MRSA.
| Focal Infection | Afebrile (n = 158) [n (%)] | Febrile (n = 39) [n (%)] | Totals (n = 197) [n (%)] |
|---|---|---|---|
| |||
| AOM | 19 (12) | 22 (56) | 41 (21) |
| Cellulitis | 49 (31) | 6 (15) | 55 (28) |
| Abscess | 40 (25) | 6 (15) | 46 (23) |
| Impetigo | 20 (13) | 1 (3) | 21 (11) |
| Mastitis | 11 (7) | 2 (5) | 13 (7) |
| Lymphadenitis | 4 (3) | 1 (3) | 5 (3) |
| Omphalitis | 2 (1) | 0 (0) | 2 (1) |
| SSSS | 2 (1) | 0 (0) | 2 (1) |
| Paronychia | 1 (1) | 0 (0) | 1 (0) |
| Other | 10 (6) | 1 (3) | 11 (6) |
Of note, a 13‐day‐old male presenting without fever but with a scalp lesion had herpes simplex virus grown from his wound culture. His diagnostic workup was negative for CSI. Omphalitis, uncommon in the United States, was diagnosed in 2 patients in our study and neither of these patients developed necrotizing fasciitis. Mastitis was not a significant focal infection in either group; and no patient was diagnosed with mastoiditis, balanitis, or posthitis.
Secondary Study OutcomeCurrent Management of FBI in the ED: Resource Utilization
Febrile patients underwent significantly more diagnostic testing procedures than afebrile infants. Specifically, CBCs, peripheral blood cultures, urine analyses with cultures, LPs, and radiographic imaging were performed more often in infants with fever (Figure 1). Fifty‐seven infants had urine cultures performed: 32 of 158 afebrile infants and 25 of 39 febrile infants. Among these selected infants, again 3 UTIs occurred: 1 of 32 tested (3.1%) in the afebrile group and 2 of 25 tested (8%) in the febrile group. A total of 115 infants had blood cultures performed: 82 of the 158 afebrile infants and 33 of the 39 febrile infants. Among these selected infants, again 1 positive blood culture occurred: 0 of 82 tested (0%) in the afebrile group and 1 of 33 tested (3%) in the febrile group. Fifty‐five infants had LP performed: 35 of 158 afebrile infants and 30 of 39 febrile infants. No case of meningitis occurred in these selected infants. Twenty infants had diagnostic radiographs performed, 10 in the febrile group and 10 in the afebrile group. None of the radiographs showed signs of pneumonia on final radiology attending reading.
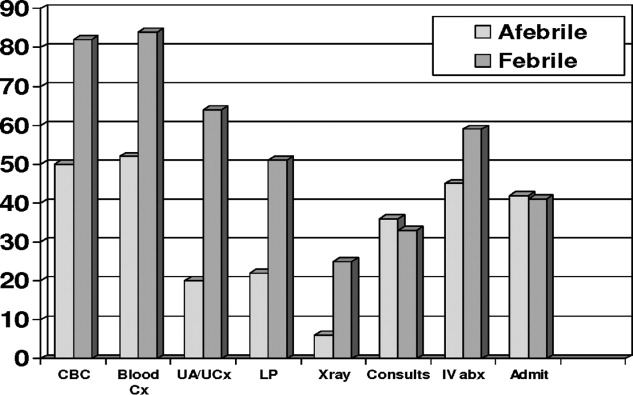
Overall, 33 of 39 febrile infants had cultures drawn and/or radiographs performed, with 3 CSIs discovered, and 87 of 158 afebrile infants had cultures drawn and/or radiographs performed, with 1 CSI discovered (Table 3). This means that 77 infants diagnosed with FBIs did not have any diagnostic testing for CSI performed while in the ED. The overall risk of CSI in patients who were tested was 3.3%. Comparing febrile and afebrile patients who had diagnostic workups performed, febrile infants had a trend toward increased risk of CSI (OR, 8.6; 95% CI, 0.8613‐85.8686).
| CSI | No CSI | Risk (%) | |
|---|---|---|---|
| |||
| Febrile (n = 33) | 3 | 30 | 9.1 |
| Afebrile (n = 87) | 1 | 86 | 1.1 |
| Totals (n = 120) | 4 | 116 | 3.3 |
No significant differences existed in the use of consultants, use of IV antibiotics, or admission rate. Sixty‐six (42%) of the 158 afebrile infants were admitted. The average length of stay for these infants was 2.59 days (range, 1‐22 days). This included a 22‐day‐old female with mastitis who required multiple surgeries and a protracted hospital course. Sixteen (41%) of the febrile infants were admitted and had an average stay of 2.87 days (range, 1‐6 days).
Patient Outcomes
Ninety‐two (58%) of the afebrile infants were discharged home from the ED, of which 5 (5.4%) returned to the ED within 72 hours after discharge. Three of these were planned ED returns as follow‐up with a primary care physician could not be guaranteed. The fourth was a 47‐day‐old with a buttock abscess who returned for reevaluation because of parental concern. The fifth was the 11‐day‐old male initially diagnosed with AOM who was called back to the ED when his urine culture grew E. coli, at which point he was admitted to the hospital. Twenty‐three (59%) of the febrile infants were discharged home from the ED. Two (8.7%) of these 23 returned to the ED within 72 hours; both were initially diagnosed with AOM and had planned follow‐ups as no primary care was available. No admitted patients required transfer to the pediatric intensive care unit and no deaths occurred.
Discussion
This study is the first to investigate the risk of CSI specifically in well‐appearing infants under 60 days of age presenting with FBI. Inclusion criteria were not limited to 1 specific infection, ie, OM, but included all FBI. This study demonstrated that the risk of CSI in afebrile infants is small (0.6%), which is similar to what has been shown in the OM literature.19, 20 However, the risk of CSI among febrile infants is not negligible (7.7%), and is similar to the risk of SBIs among young infants presenting with a fever of unknown source.57
AOM
A total of 41 infants were diagnoses with AOM. Indeed, AOM was the most common discharge diagnosis among the febrile cohort. No febrile infants with AOM were diagnosed with a CSI. However, as noted above, an 11‐day‐old afebrile infant with AOM did have a UTI diagnosed. This male underwent blood, urine, and CSF cultures on initial presentation. He was discharged home from the ED, and called back for further evaluation once the urine culture grew E. coli.
We relied on the diagnostic skills of the ED attending physician for determination of OM, and no rigorous diagnostic criteria were established for an AOM in this young age group. However, on chart review of those patients with AOM who were admitted, otolaryngology was often consulted and confirmed the diagnosis of OM.
AOM has been the most commonly studied focal infection studied most in this age group.1, 2, 11, 2123 More recent studies have investigated the risk of CSI with AOM among febrile and afebrile cohorts. These authors found that in infants under 2 months with AOM, febrile infants had a 6% to 13% risk of CSI, whereas no cases of CSI were found in afebrile patients.19, 20 These results suggest that afebrile, nontoxic infants with AOM could be treated as outpatients without need for further systemic evaluation. Our study strengthens this argument if close follow‐up can be assured.
Cellulitis and Abscess
A total of 106 infants were diagnosed with either abscess and/or cellulitis, with the vast majority of them presenting without fever. Moreover, cellulitis and abscess comprised more than one‐half of all infants in the afebrile cohort. The buttocks were the most common site for abscess (23 cases), followed next by the scalp (8 cases). In our study population, there were 29 positive abscess, wound, lesion, or skin aspirate cultures for Staphylococcus aureus, with 13 (45%) being MRSA. None of these patients had a CSI.
Community‐acquired staphylococcal infections have been studied in the newborn population, with MRSA accounting for up to 69% of soft‐tissue infections in one recent study involving 89 neonates.24 The authors found 4 cases of bacteremia, 3 cases of UTI, and 2 cases of CSF pleocytosis. Application of these results to our patients is difficult, as there was no mention of fever or well‐appearance stratification and there is no specific mention of any of the 77 skin and soft‐tissue infections having a CSI.
The frequency of bacteremia in pediatric patients with periorbital cellulitis has been studied, with some authors suggested more selective use of LP in patients with these localized soft‐tissue infections in the older infant or child.25, 26 Unfortunately, there were not enough patients under 60 days of age in either study from which to draw conclusions. In our study, a total of 5 patients presented with periorbital cellulitis: 2 afebrile and 3 febrile, including the 47‐day‐old febrile infant with coexisting pneumococcal bacteremia.
Group B streptococcus (GBS) cellulitis‐adenitis syndrome has also been identified in neonates, with meningitis occurring in up to 24% of infants in 1 review of 32 cases.27 These studies only included patients with positive blood cultures, providing no denominator for assessing a true CSI risk in young infants with cellulitis. No infants in our study had GBS infections.
Impetigo was diagnosed in 21 patients, with 17 patients being discharged home from the ED. In addition, 2 infants with staphylococcal scalded skin syndrome were identified. None of these infants had a CSI.
Other Infections
Mastitis in the young infant has been studied, with the risk of CSI being 3% in 1 review.2830 In our study, there were 18 patients diagnosed with either mastitis or breast abscess, of which 4 (22%) had fever and none had positive blood or CSF cultures. Multiple studies, either from older literature in the United States or more contemporary from abroad, have investigated omphalitis and necrotizing fasciitis in the newborn.31, 32 These show that infants presenting with omphalitis have a lower mortality and morbidity than those with necrotizing fasciitis. In our study, we had 2 patients with omphalitis, both were afebrile and neither had a coexisting CSI. We had no patients with necrotizing fasciitis. We also found no patients with mastoiditis, balanitis, or posthitis as the listed diagnosis in our study.
UTI
Of the 4 cases of CSI in our study, UTI was the most common, occurring in 3 of the 4 cases. This predominance of UTI as the cause of CSI is well‐recognized in young febrile infants with OM and infants with fever of unknown origin; however, it has not been reported with other FBIs in this age group.1, 5, 9, 11, 19, 33 Specifically, there has not been a reported relationship between UTI and skin or soft tissue infections. However, 2 of our 4 infants with a CSI had a UTI in addition to their skin or soft tissue infection: the 32‐day‐old male with a buttock abscess and E. coli UTI; and the 21‐day‐old female with truncal cellulitis and E. coli UTI.
Resource Utilization
Young infants with FBI and fever underwent significantly more resource utilization than afebrile infants in our ED (Figure 1). Physicians of febrile infants ordered more serum blood counts and blood cultures, urinalysis and urine cultures, and performed more LPs and radiographic studies. This is not surprising given that fever is a risk factor for CSI in this age group; however, resource utilization is not as well‐described in previous reports on infants with FBIs. In 1 retrospective study of 137 infants less than 8 weeks of age with AOM, 88% had diagnostic blood cultures, 66% had LP, and 81% had urine cultures drawn.19 Additionally, in our study the decision to hospitalize infants, use of IV antibiotics, and hospital length of stay was not statistically different between febrile and afebrile groups. This potentially suggests that diagnostic testing for infants with FBIs did not affect management and outcome. Another study showed hospital admission is costly and not without safety risks, with a complication rate as high as 19% in infants.34 Given these results, in addition to the presumption that all FBIs would be treated with antibiotics, one could infer that a number of well‐appearing, afebrile infants underwent unwarranted testing.
Limitations
The main limitation of our study was the retrospective design. A research assistant utilizing a computerized database program of ED patients performed the initial query based upon search criteria. A local expert using an established list of International Statistical Classification of Diseases and Related Health Problems (ICD) codes for any and all of the FBIs performed the chart review. Secondary diagnoses may have been omitted as a result of limited physician charting, which could have resulted in missed patients. CCHMC is currently transitioning from paper records to electronic medical records, which may explain why 12 charts were not found, despite exhaustive searches for them. Ultimately, 94% of all the eligible patients were found. Yet, with so few CSI diagnosed, 1 or 2 could conceivably change our results. As noted above, focal infections in infants under 2 months of age seem to be uncommon, not only in the ED setting, but also in a large cohort of primary care patients.35 With only a small number FBIs present over 6 years and so few having CSIs, we were limited to a univariate analysis, which limited our potential results and conclusions. Performing this study prospectively would have addressed these limitations, but would have required years of recruitment or multicenter collaboration.
Another potential limitation was the search strategy to identify eligible infants. Specifically, we did not search the records for infants diagnosed with UTI, bacteremia, or meningitis. Infants with these more serious conditions may have been coded as the primary or only problem, even if other problems such as OM were also present. Therefore, we may have underestimated the occurrence of systemic bacterial complications in a systematic way. This form of spectrum bias was a potential limitation. We approached this clinical question from the eye of the emergency department practitioner and thus used a search strategy based on the discharge diagnosis from the ED. If we were to look back to see if any patients discharged from the hospital with CSI also had FBI, we doubt our retrospective design would have allowed identification of patients with FBIs.
Other limitations may be our definition of CSI and the potential for missed CSIs. We defined meningitis, bacteremia, and UTI as a positive CSF, blood, or urine culture, respectively. Many studies are now defining culture‐negative meningitis or UTI based on WBC findings on a screening cell count or urine microscopy. However, because no patients were pretreated with antibiotics, we felt that a positive culture from a sterile site was a reasonable definition. Also, not all of the enrolled patients received full diagnostic workups to screen for CSI. In the smaller cohort of infants who received diagnostic testing, febrile infants still seemed to be at higher risk for CSI. To capture all possible CSIs, one would have needed to perform blood culture, suprapubic bladder aspiration, or catheterization for urine culture, LP, and chest radiograph on all patients with an FBI. Given the low risk of CSI in the United States, the previous literature's hinting at low risk for CSI in afebrile patients, and the presence of multiple clinical trials defining low risk characteristics for CSI, such a protocol would not receive support as being standard clinical practice and have difficulty being permitted by an institutional review board.
Another limitation of our study was follow‐up. Ideally, every patient would have been contacted to ensure reliable outcomes measurement. Patients may have been seen after their initial evaluation at their primary care provider's office or at another healthcare facility and had more diagnostic studies performed. However, because our institution is the sole admitting pediatric center in the area, particularly in infants, and most CSIs in this age group require admission; we feel that a reasonable degree of reliability for the outcomes of interest was maintained.
Last, we could not establish the rationale of clinical decision making, as our study was retrospective. For example, staff physicians may have foregone diagnostic testing if they had committed to a therapeutic course of antibiotics and felt diagnostic cultures would not change management. Also, we cannot ensure that interpretation of culture results was consistent with national standards. As described previously, 1 afebrile infant in our study potentially had a CSI that was clinically felt to be a contaminant by the inpatient healthcare team. This 11‐day‐old female was admitted with mastitis and had a negative urinalysis, but grew E. coli on urine culture. This was treated as a contaminant by the ward team, despite her age.
Conclusions
CSI is very uncommon in afebrile, well‐appearing infants under 2 months of age with an FBI. However, febrile infants have a greater risk of CSI. UTI is the most common CSI in well‐appearing infants less than 2 months of age with an FBI found on examination. Prospective, multicentered studies need to be performed to determine whether diagnostic evaluation should change the management of well‐appearing infants with an FBI found on examination.
- ,,, et al.Febrile infants at low risk for serious bacterial infection—an appraisal of the Rochester Criteria and implications for management.Pediatrics.1994;94:390–396.
- ,,, et al.Identification of infants unlikely to have serious bacterial infection although hospitalized for suspected sepsis.J Pediatr.1985;107:855–860.
- ,,.Outpatient management without antibiotics of fever in selected infants.N Engl J Med.1993;329:1437–1441.
- ,,.Outpatient treatment of febrile infants 28 to 89 days of age with intramuscular administration of ceftriaxone.J Pediatr.1992;120:22–27.
- ,.Predictive model for serious bacterial infections among infants younger than 3 months of age.Pediatrics.2001;108:311–316.
- ,,, et al.Applying outpatient protocols to febrile infants 1–28 days of age: can the threshold be lowered?Clin Pediatr.2000;39:81–88.
- ,,.The efficacy of routine outpatient management without antibiotics of fever in selected infants.Pediatrics.1999;103:627–631.
- ,.Evaluation of the infant with fever without source: an evidence based approach.Emerg Med Clin North Am.1999;17:97–126.
- ,,, et al.Risk of serious bacterial infection in young febrile infants with respiratory syncytial virus infections.Pediatrics.2004;113:1728–1734.
- ,,, et al.Relationship of fever magnitude to rate of serious bacterial infections in infants 4–8 weeks.Clin Pediatr (Phila).1991;30:478–480.
- ,,, et al.Enhanced urinalysis improved identification of febrile infants ages 60 days and younger at low risk for serious bacterial illness.Pediatrics.2001;108:866–871.
- ,,.C‐reactive protein in febrile children 1 to 36 months of age with clinically undetectable serious bacterial infection.Pediatrics.2001;108:1275–1279.
- ,.Utility of the serum C‐reactive protein for detection of occult bacterial infection in children.Arch Pediatr Adolesc Med.2002;156:905–909.
- ,,, et al.Procalcitonin and C‐reactive protein as diagnostic markers of severe bacterial infections in febrile infants and children in the emergency department.Pediatr Infect Dis J.2007;26:672–677.
- ,,.Neonatal fever: utility of the Rochester criteria in determining low risk for serious bacterial infections.Am J Emerg Med.1997;15:299–302.
- ,,.Evaluation of false positive blood cultures: guidelines for early detection of contaminated cultures in febrile children.Pediatr Emerg Care.1994;10:20–22.
- ,,.Outpatient pediatric blood cultures: time to positivity.Pediatrics.2000;106:251–255.
- ,,, et al.Occult bacteremia from a pediatric emergency department: current prevalence, time to detection and outcome.Pediatrics.2000;106:505–511.
- ,,, et al.Acute otitis media in infants younger than two months of age: microbiology, clinical presentation and therapeutic approach.Pediatr Infect Dis J.2002;21:669–674.
- ,,, et al.Otitis media in infants aged 0–8 weeks: frequency of associated serious bacterial disease.Pediatr Emerg Care.1999;15:252–254.
- ,,.Otitis media in children less than 12 weeks of age.Pediatrics.1977;59:827–832.
- ,,.Are well‐appearing febrile infants with otitis media at risk for serious bacterial illness? [Abstract].Am J Dis Child.1992;146:468.
- ,,, et al.Streptococcus pneumoniae infections in the neonate.Pediatrics.2003;112:1095–1102.
- ,,, et al.Community‐acquired Staphylococcus aureus infections in term and near‐term previously health neonates.Pediatrics.2007;118:874–881.
- ,.Blood cultures in the evaluation of children with cellulitis.Pediatrics.1997;101:e4.
- ,.Lumbar puncture in children with periorbital and orbital cellulitis.J Pediatr.1993;122:355–359.
- ,.Is lumbar puncture necessary to exclude meningitis in neonates and young infants: lessons from the Group B streptococcus cellulitis‐adenitis syndrome.Pediatrics.1998;102:985–986.
- ,.Neonatal mastitis.Clin Pediatr.1986;25:395–399.
- ,.Pseudomonas aeruginosa mastitis in a neonate.Pediatr Infect Dis J.1993;12:104.
- ,,.Group D streptococcal neonatal mastitis.Pediatr Infect Dis J.1998;7:362.
- ,,, et al.Early recognition of neonatal abdominal wall necrotizing fasciitis.Am J Surg.1994;167:481–484.
- ,,, et al.Necrotizing fasciitis: a serious complication of omphalitis in neonates.J Pediatr Surg.1994;29:1414–1416.
- ,,, et al.Acute otitis media in infants less than three months of age: clinical presentation, etiology and concomitant diseases.Int J Pediatr Otorhinolaryngol.2006;70:613–617.
- ,,, et al.Iatrogenic risks and financial costs of hospitalizing febrile infants.Am J Dis Child.1983;137:1146–1149.
- ,,, et al.Management and outcomes of care of fever in early infancy.JAMA.2004;291:1203–1212.
- ,,, et al.Febrile infants at low risk for serious bacterial infection—an appraisal of the Rochester Criteria and implications for management.Pediatrics.1994;94:390–396.
- ,,, et al.Identification of infants unlikely to have serious bacterial infection although hospitalized for suspected sepsis.J Pediatr.1985;107:855–860.
- ,,.Outpatient management without antibiotics of fever in selected infants.N Engl J Med.1993;329:1437–1441.
- ,,.Outpatient treatment of febrile infants 28 to 89 days of age with intramuscular administration of ceftriaxone.J Pediatr.1992;120:22–27.
- ,.Predictive model for serious bacterial infections among infants younger than 3 months of age.Pediatrics.2001;108:311–316.
- ,,, et al.Applying outpatient protocols to febrile infants 1–28 days of age: can the threshold be lowered?Clin Pediatr.2000;39:81–88.
- ,,.The efficacy of routine outpatient management without antibiotics of fever in selected infants.Pediatrics.1999;103:627–631.
- ,.Evaluation of the infant with fever without source: an evidence based approach.Emerg Med Clin North Am.1999;17:97–126.
- ,,, et al.Risk of serious bacterial infection in young febrile infants with respiratory syncytial virus infections.Pediatrics.2004;113:1728–1734.
- ,,, et al.Relationship of fever magnitude to rate of serious bacterial infections in infants 4–8 weeks.Clin Pediatr (Phila).1991;30:478–480.
- ,,, et al.Enhanced urinalysis improved identification of febrile infants ages 60 days and younger at low risk for serious bacterial illness.Pediatrics.2001;108:866–871.
- ,,.C‐reactive protein in febrile children 1 to 36 months of age with clinically undetectable serious bacterial infection.Pediatrics.2001;108:1275–1279.
- ,.Utility of the serum C‐reactive protein for detection of occult bacterial infection in children.Arch Pediatr Adolesc Med.2002;156:905–909.
- ,,, et al.Procalcitonin and C‐reactive protein as diagnostic markers of severe bacterial infections in febrile infants and children in the emergency department.Pediatr Infect Dis J.2007;26:672–677.
- ,,.Neonatal fever: utility of the Rochester criteria in determining low risk for serious bacterial infections.Am J Emerg Med.1997;15:299–302.
- ,,.Evaluation of false positive blood cultures: guidelines for early detection of contaminated cultures in febrile children.Pediatr Emerg Care.1994;10:20–22.
- ,,.Outpatient pediatric blood cultures: time to positivity.Pediatrics.2000;106:251–255.
- ,,, et al.Occult bacteremia from a pediatric emergency department: current prevalence, time to detection and outcome.Pediatrics.2000;106:505–511.
- ,,, et al.Acute otitis media in infants younger than two months of age: microbiology, clinical presentation and therapeutic approach.Pediatr Infect Dis J.2002;21:669–674.
- ,,, et al.Otitis media in infants aged 0–8 weeks: frequency of associated serious bacterial disease.Pediatr Emerg Care.1999;15:252–254.
- ,,.Otitis media in children less than 12 weeks of age.Pediatrics.1977;59:827–832.
- ,,.Are well‐appearing febrile infants with otitis media at risk for serious bacterial illness? [Abstract].Am J Dis Child.1992;146:468.
- ,,, et al.Streptococcus pneumoniae infections in the neonate.Pediatrics.2003;112:1095–1102.
- ,,, et al.Community‐acquired Staphylococcus aureus infections in term and near‐term previously health neonates.Pediatrics.2007;118:874–881.
- ,.Blood cultures in the evaluation of children with cellulitis.Pediatrics.1997;101:e4.
- ,.Lumbar puncture in children with periorbital and orbital cellulitis.J Pediatr.1993;122:355–359.
- ,.Is lumbar puncture necessary to exclude meningitis in neonates and young infants: lessons from the Group B streptococcus cellulitis‐adenitis syndrome.Pediatrics.1998;102:985–986.
- ,.Neonatal mastitis.Clin Pediatr.1986;25:395–399.
- ,.Pseudomonas aeruginosa mastitis in a neonate.Pediatr Infect Dis J.1993;12:104.
- ,,.Group D streptococcal neonatal mastitis.Pediatr Infect Dis J.1998;7:362.
- ,,, et al.Early recognition of neonatal abdominal wall necrotizing fasciitis.Am J Surg.1994;167:481–484.
- ,,, et al.Necrotizing fasciitis: a serious complication of omphalitis in neonates.J Pediatr Surg.1994;29:1414–1416.
- ,,, et al.Acute otitis media in infants less than three months of age: clinical presentation, etiology and concomitant diseases.Int J Pediatr Otorhinolaryngol.2006;70:613–617.
- ,,, et al.Iatrogenic risks and financial costs of hospitalizing febrile infants.Am J Dis Child.1983;137:1146–1149.
- ,,, et al.Management and outcomes of care of fever in early infancy.JAMA.2004;291:1203–1212.
Copyright © 2010 Society of Hospital Medicine
Gary L. Geis, Division of Emergency Medicine, Assistant Medical Director, Center for Simulation and Research, Cincinnati Childrens Hospital Medical Center, University of Cincinnati, College of Medicine, 333 Burnet Avenue, MLC 12000 Cincinnati, Ohio 45229‐3039
Continuing Medical Education Program in
If you wish to receive credit for this activity, which beginson the next page, please refer to the website:
Accreditation and Designation Statement
Blackwell Futura Media Services designates this educational activity for a 1 AMA PRA Category 1 Credit. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Blackwell Futura Media Services is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Educational Objectives
Continuous participation in the Journal of Hospital Medicine CME program will enable learners to be better able to:
-
Interpret clinical guidelines and their applications for higher quality and more efficient care for all hospitalized patients.
-
Describe the standard of care for common illnesses and conditions treated in the hospital; such as pneumonia, COPD exacerbation, acute coronary syndrome, HF exacerbation, glycemic control, venous thromboembolic disease, stroke, etc.
-
Discuss evidence‐based recommendations involving transitions of care, including the hospital discharge process.
-
Gain insights into the roles of hospitalists as medical educators, researchers, medical ethicists, palliative care providers, and hospital‐based geriatricians.
-
Incorporate best practices for hospitalist administration, including quality improvement, patient safety, practice management, leadership, and demonstrating hospitalist value.
-
Identify evidence‐based best practices and trends for both adult and pediatric hospital medicine.
Instructions on Receiving Credit
For information on applicability and acceptance of continuing medical education credit for this activity, please consult your professional licensing board.
This activity is designed to be completed within the time designated on the title page; physicians should claim only those credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the activity during the valid credit period that is noted on the title page.
Follow these steps to earn credit:
-
Log on to www.blackwellpublishing.com/cme.
-
Read the target audience, learning objectives, and author disclosures.
-
Read the article in print or online format.
-
Reflect on the article.
-
Access the CME Exam, and choose the best answer to each question.
-
Complete the required evaluation component of the activity.
If you wish to receive credit for this activity, which beginson the next page, please refer to the website:
Accreditation and Designation Statement
Blackwell Futura Media Services designates this educational activity for a 1 AMA PRA Category 1 Credit. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Blackwell Futura Media Services is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Educational Objectives
Continuous participation in the Journal of Hospital Medicine CME program will enable learners to be better able to:
-
Interpret clinical guidelines and their applications for higher quality and more efficient care for all hospitalized patients.
-
Describe the standard of care for common illnesses and conditions treated in the hospital; such as pneumonia, COPD exacerbation, acute coronary syndrome, HF exacerbation, glycemic control, venous thromboembolic disease, stroke, etc.
-
Discuss evidence‐based recommendations involving transitions of care, including the hospital discharge process.
-
Gain insights into the roles of hospitalists as medical educators, researchers, medical ethicists, palliative care providers, and hospital‐based geriatricians.
-
Incorporate best practices for hospitalist administration, including quality improvement, patient safety, practice management, leadership, and demonstrating hospitalist value.
-
Identify evidence‐based best practices and trends for both adult and pediatric hospital medicine.
Instructions on Receiving Credit
For information on applicability and acceptance of continuing medical education credit for this activity, please consult your professional licensing board.
This activity is designed to be completed within the time designated on the title page; physicians should claim only those credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the activity during the valid credit period that is noted on the title page.
Follow these steps to earn credit:
-
Log on to www.blackwellpublishing.com/cme.
-
Read the target audience, learning objectives, and author disclosures.
-
Read the article in print or online format.
-
Reflect on the article.
-
Access the CME Exam, and choose the best answer to each question.
-
Complete the required evaluation component of the activity.
If you wish to receive credit for this activity, which beginson the next page, please refer to the website:
Accreditation and Designation Statement
Blackwell Futura Media Services designates this educational activity for a 1 AMA PRA Category 1 Credit. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Blackwell Futura Media Services is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Educational Objectives
Continuous participation in the Journal of Hospital Medicine CME program will enable learners to be better able to:
-
Interpret clinical guidelines and their applications for higher quality and more efficient care for all hospitalized patients.
-
Describe the standard of care for common illnesses and conditions treated in the hospital; such as pneumonia, COPD exacerbation, acute coronary syndrome, HF exacerbation, glycemic control, venous thromboembolic disease, stroke, etc.
-
Discuss evidence‐based recommendations involving transitions of care, including the hospital discharge process.
-
Gain insights into the roles of hospitalists as medical educators, researchers, medical ethicists, palliative care providers, and hospital‐based geriatricians.
-
Incorporate best practices for hospitalist administration, including quality improvement, patient safety, practice management, leadership, and demonstrating hospitalist value.
-
Identify evidence‐based best practices and trends for both adult and pediatric hospital medicine.
Instructions on Receiving Credit
For information on applicability and acceptance of continuing medical education credit for this activity, please consult your professional licensing board.
This activity is designed to be completed within the time designated on the title page; physicians should claim only those credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the activity during the valid credit period that is noted on the title page.
Follow these steps to earn credit:
-
Log on to www.blackwellpublishing.com/cme.
-
Read the target audience, learning objectives, and author disclosures.
-
Read the article in print or online format.
-
Reflect on the article.
-
Access the CME Exam, and choose the best answer to each question.
-
Complete the required evaluation component of the activity.
Hypercalcemia and Milk‐Alkali Syndrome
Historically, the milk‐alkali syndrome developed as an adverse reaction to the Sippy regimen of frequent feedings of milk, cream, and alkaline powders as treatment for peptic ulcer disease.1 The classic description includes hypercalcemia, metabolic alkalosis, and renal failure. This syndrome seemingly disappeared when modern acid suppression therapies such as histamine‐2 blockers and proton pump inhibitors improved dyspepsia treatment. Over the past 20 years, milk‐alkali syndrome has had a resurgence, as consumption of supplements containing calcium has increased.2 Calcium carbonate supplements are a popular over‐the‐counter treatment for osteoporosis, dyspepsia, hypocalcemia, and hyperphosphatemia; these supplements provide both the calcium and alkali required for the development of milk‐alkali syndrome.
A 46‐year‐old man presented to the emergency department after his physician ordered outpatient laboratory tests to evaluate his fatigue. The patient was found to have acute renal failure and hypercalcemia. His serum creatinine was 3.6 mg/dL, increased from his baseline of 1.1 mg/dL several months prior, and his serum calcium was 14.9 mg/dL. Ten days prior to admission he developed increasing fatigue, decreased appetite, and decreased urine output, which he attributed to recent manual labor during summer. He reported taking an occasional calcium carbonate (Tums) for dyspepsia. He did not report pain or other complaints.
His medical history included hypertension and hyperlipidemia. He had a colonoscopy 1 year prior to presentation that was significant for a high‐grade dysplastic polyp and was currently due for repeat colonoscopy. His medications included clonidine, lisinopril, and aspirin. He had no recent medication changes. He had a 30 pack/year history of cigarette smoking and drank occasionally.
On physical exam, his temperature was 99.8F, blood pressure 97/48 mmHg, heart rate 89 beats per minute, respirations 20 breaths per minute, with a room air saturation of 97%. He had dry mucus membranes and the remainder of the physical exam was unremarkable.
In the emergency department laboratory testing revealed a creatinine of 4.6 mg/dL, serum total calcium of 15.9 mg/dL, serum bicarbonate level of 26 mmol/L, phosphate of 3.9 mg/dL, albumin of 4.4 gm/dL, and alkaline phosphatase of 92 IU/L. The urine specific gravity was 1.019 gm/mL (see Table 1 for the patient's complete admission laboratory values).
| Result (Normal Range) | |
|---|---|
| |
| At admission | |
| Sodium (mmol/L) | 135 (135‐145) |
| Potassium (mmol/L) | 4.4 (3.8‐5.0) |
| Chloride (mmol/L) | 97 (98‐107) |
| Bicarbonate (mmol/L) | 25 (22‐31) |
| BUN (mg/dL) | 64 (9‐20) |
| Creatinine (mg/dL) | 4.6 (0.5‐1.5) |
| Calcium (mg/dL) | 15.9 (8.4‐10.2) |
| Albumin (g/dL) | 4.4 (3.5‐5.0) |
| Alkaline phosphatase (U/L) | 92 (38‐126) |
| ALT (U/L) | 24 (11‐66) |
| AST (U/L) | 17 (15‐46) |
| Bilirubin, total (mg/dL) | 0.3 (0.3‐1.2) |
| Ionized calcium (mmol/L) | 1.58 (1.13‐1.32) |
| Creatinine kinase (U/L) | 83 (35‐232) |
| WBC (thousands/cm2) | 12.1 (4‐11) |
| Hemoglobin (g/dL) | 16.5 (14‐18) |
| Hematocrit (%) | 48.6 (40‐54) |
| Platelets (thousands/cm2) | 224 (150‐350) |
| Intact PTH (pg/mL) | 18.78 (15‐65) |
| PTHrP (pmol/L) | 2.5 (5) |
| 25‐OH‐Vitamin D (ng/mL) | 23 (16‐74) |
| H. pylori antibody | Negative |
| SPEP | No M‐spike |
| UPEP | No M‐spike |
| Hospital Day 4 (date of discharge) | |
| BUN (mg/dL) | 21 (9‐20) |
| Creatinine (mg/dL) | 1.6 (0.5‐1.5) |
| Calcium(mg/dL) | 8.4 (8.4‐10.2) |
| WBC (thousands/cm2) | 6.5 (4‐11) |
| Hemoglobin (g/dL) | 14.1 (14‐18) |
| Hematocrit (%) | 40.8 (40‐54) |
| Day 10 (at follow‐up) | |
| BUN (mg/dL) | 16 (9‐20) |
| Creatinine (mg/dL) | 0.9 (0.5‐1.5) |
| Calcium (mg/dL) | 8.1 (8.4‐10.2) |
| Intact PTH (pg/mL) | 240 (15‐65) |
His intact parathyroid (PTH) hormone was 18.8 pg/mL (normal, 15‐65). PTH hormone‐related peptide (PTHrP) was 2.5 pmol/L. After reviewing these laboratory test results, we proceeded with further questioning, during which he admitted to taking approximately 15 to 20 Tums (>7.5 gm of calcium carbonate) daily for dyspepsia rather than the occasional Tums he had originally reported. Over the next 3 days, his calcium decreased to 8.4 mg/dL and his creatinine decreased to 1.6 mg/dL with intravenous hydration. His fatigue improved. His 25‐hydroxy vitamin D (25‐OH‐Vitamin D) level was 23 ng/mL (normal, 16‐74 ng/mL).
At his 1 week follow‐up, his calcium was 8.1 mg/dL, and his creatinine had returned to normal at 0.9 mg/dL. His intact PTH level was elevated at 240 pg/mL.
Discussion
Milk‐alkali syndrome is now believed to be the third most common reason for hypercalcemia hospital admission.2, 3 Malignancy and primary hyperparathyroidism are the only 2 causes of hypercalcemia more common than milk‐alkali syndrome in hospitalized patients; these must be excluded before making a definitive diagnosis of milk‐alkali syndrome. The differential diagnosis for hypercalcemia also includes other less common etiologies such as medications (hydrochlorothiazide and lithium), as well as familial hypocalciuric hypercalcemia, hyperthyroidism, Addison's disease, acromegaly, tertiary hyperparathyroidism, and vitamin D intoxication. Physicians often discover hypercalcemia incidentally on routine laboratory tests, and diagnostic workup should include a thorough history and physical examination, as well as further laboratory evaluation.
The diagnosis of milk‐alkali syndrome requires a history of increased calcium and alkali intake, but is otherwise a diagnosis of exclusion. Given the increasing consumption of nonprescribed calcium supplements, one should have a high index of suspicion for the diagnosis of milk‐alkali syndrome, as patients may not consider calcium carbonate to be hazardous or even a medication and thus may not report calcium carbonate consumption. Patients often view calcium carbonate as a benign treatment for dyspepsia. Its over‐the‐counter availability and economical price make it a common self‐treatment for minor dyspepsia or as prevention of osteoporosis. Calcium supplementation is increasingly added to many products, making it easy for patients to consume large quantities of calcium unknowingly. Of note, without the absorbable alkali supplied by the carbonate in calcium carbonate (Tums), milk‐alkali syndrome does not occur. The amount of calcium carbonate necessary to cause milk‐alkali syndrome is not well known, though it is speculated to be as little as 5 to 10 g of calcium in the form of calcium carbonate, especially in those with other risk factors for hypercalcemia such as chronic renal insufficiency or vomiting.2 Workup of hypercalcemia should entail careful questioning about medications, as well as over‐the‐counter supplements, vitamins, and foods.
Manifestations of the milk‐alkali syndrome include renal failure, metabolic alkalosis, and volume contraction. Normally, the kidneys prevent hypercalcemia by excretion of excess calcium. Hypercalcemia can cause tubular damage and vasoconstriction of the renal afferent arteriole leading to acute renal failure.2, 4 Hypercalcemia can also cause nephrogenic diabetes insipidus, causing impaired renal concentrating ability, leading to increased sodium excretion and volume contraction.2 In addition, alkalosis further impairs calciuresis.2 Laboratory values usually reveal suppressed PTH and vitamin D levels due to hypercalcemia caused by exogenous intake of calcium.5 Hypercalcemia causes suppression of PTH, which can lead to hyperphosphatemia, as well as decreased conversion of vitamin D to the active 1,25‐dihyroxyvitamin‐D form.
The management of hypercalcemia due to milk‐alkali syndrome is supportive and includes saline hydration as well as withholding calcium carbonate. Management of hypercalcemia due to malignancy and hyperparathyroidism includes bisphosphonates with the addition of calcitonin if symptoms are severe.6, 7 There is no evidence that supports the use of bisphosphonates in the treatment of milk‐alkali syndrome. Loop diuretics are sometimes used to promote calciuresis, though evidence is lacking to support this, and it may worsen renal failure.6
In this case, a middle‐aged man took greater than the recommended dose of calcium carbonate for dyspepsia, which led to the development of acute renal failure and hypercalcemia. At first, the patient did not provide an accurate history of the extent of his calcium carbonate ingestion, leading us to focus on hyperparathyroidism or malignancy. With aggressive hydration and cessation of calcium carbonate, his renal function and serum calcium returned to baseline. Because we initially assumed occult malignancy as the most likely diagnosis, we gave the patient pamidronate. The patient did not have a significant alkalemia (serum bicarbonate level was normal). This was thought to be due to the patient's degree of renal failure causing a concomitant metabolic acidosis. The patient's follow‐up elevated PTH level may be explained by bisphosphonate administration or underlying primary hyperparathyroidism. Of note, decreasing calcium levels have also been speculated to be a cause of high PTH levels.8
In conclusion, physicians should have a high index of suspicion for milk‐alkali syndrome in patients with hypercalcemia. Calcium carbonate is responsible for most cases of milk‐alkali syndrome, and clinicians should inquire about the use of this supplement in all patients with hypercalcemia. Milk‐alkali syndrome is no longer a merely a historical curiosity; it is currently the third most common cause of hospital admissions for hypercalcemia.
- .Landmark article May 15, 1915: Gastric and duodenal ulcer. Medical cure by an efficient removal of gastric juice corrosion. By Bertram W. Sippy.JAMA.1983;250(16):2192–2197.
- ,,,.Milk‐alkali syndrome: a historical review and description of the modern version of the syndrome.Am J Med Sci.2006;331(5):233–242.
- ,,.Milk‐alkali syndrome is a major cause of hypercalcaemia among non‐end‐stage renal disease (non‐ESRD) inpatients.Clin Endocrinol (Oxf).2005;63(5):566–576.
- ,.Milk‐alkali syndrome associated with calcium carbonate consumption. Report of 7 patients with parathyroid hormone levels and an estimate of prevalence among patients hospitalized with hypercalcemia.Medicine (Baltimore).1995;74(2):89–96.
- ,,,,,.The milk‐alkali syndrome. A reversible form of acute renal failure.Arch Intern Med.1993;153(8):1005–1010.
- ,,.Narrative review: furosemide for hypercalcemia: an unproven yet common practice.Ann Intern Med.2008;149(4):259–263.
- .Salmon calcitonin in the acute management of hypercalcemia.Calcif Tissue Int.1990;46(suppl):S26–S30.
- ,.Milk alkali syndrome. Does it exist and can it be differentiated from primary hyperparathyroidism?Ann Surg.1983;197(4):427–433.
Historically, the milk‐alkali syndrome developed as an adverse reaction to the Sippy regimen of frequent feedings of milk, cream, and alkaline powders as treatment for peptic ulcer disease.1 The classic description includes hypercalcemia, metabolic alkalosis, and renal failure. This syndrome seemingly disappeared when modern acid suppression therapies such as histamine‐2 blockers and proton pump inhibitors improved dyspepsia treatment. Over the past 20 years, milk‐alkali syndrome has had a resurgence, as consumption of supplements containing calcium has increased.2 Calcium carbonate supplements are a popular over‐the‐counter treatment for osteoporosis, dyspepsia, hypocalcemia, and hyperphosphatemia; these supplements provide both the calcium and alkali required for the development of milk‐alkali syndrome.
A 46‐year‐old man presented to the emergency department after his physician ordered outpatient laboratory tests to evaluate his fatigue. The patient was found to have acute renal failure and hypercalcemia. His serum creatinine was 3.6 mg/dL, increased from his baseline of 1.1 mg/dL several months prior, and his serum calcium was 14.9 mg/dL. Ten days prior to admission he developed increasing fatigue, decreased appetite, and decreased urine output, which he attributed to recent manual labor during summer. He reported taking an occasional calcium carbonate (Tums) for dyspepsia. He did not report pain or other complaints.
His medical history included hypertension and hyperlipidemia. He had a colonoscopy 1 year prior to presentation that was significant for a high‐grade dysplastic polyp and was currently due for repeat colonoscopy. His medications included clonidine, lisinopril, and aspirin. He had no recent medication changes. He had a 30 pack/year history of cigarette smoking and drank occasionally.
On physical exam, his temperature was 99.8F, blood pressure 97/48 mmHg, heart rate 89 beats per minute, respirations 20 breaths per minute, with a room air saturation of 97%. He had dry mucus membranes and the remainder of the physical exam was unremarkable.
In the emergency department laboratory testing revealed a creatinine of 4.6 mg/dL, serum total calcium of 15.9 mg/dL, serum bicarbonate level of 26 mmol/L, phosphate of 3.9 mg/dL, albumin of 4.4 gm/dL, and alkaline phosphatase of 92 IU/L. The urine specific gravity was 1.019 gm/mL (see Table 1 for the patient's complete admission laboratory values).
| Result (Normal Range) | |
|---|---|
| |
| At admission | |
| Sodium (mmol/L) | 135 (135‐145) |
| Potassium (mmol/L) | 4.4 (3.8‐5.0) |
| Chloride (mmol/L) | 97 (98‐107) |
| Bicarbonate (mmol/L) | 25 (22‐31) |
| BUN (mg/dL) | 64 (9‐20) |
| Creatinine (mg/dL) | 4.6 (0.5‐1.5) |
| Calcium (mg/dL) | 15.9 (8.4‐10.2) |
| Albumin (g/dL) | 4.4 (3.5‐5.0) |
| Alkaline phosphatase (U/L) | 92 (38‐126) |
| ALT (U/L) | 24 (11‐66) |
| AST (U/L) | 17 (15‐46) |
| Bilirubin, total (mg/dL) | 0.3 (0.3‐1.2) |
| Ionized calcium (mmol/L) | 1.58 (1.13‐1.32) |
| Creatinine kinase (U/L) | 83 (35‐232) |
| WBC (thousands/cm2) | 12.1 (4‐11) |
| Hemoglobin (g/dL) | 16.5 (14‐18) |
| Hematocrit (%) | 48.6 (40‐54) |
| Platelets (thousands/cm2) | 224 (150‐350) |
| Intact PTH (pg/mL) | 18.78 (15‐65) |
| PTHrP (pmol/L) | 2.5 (5) |
| 25‐OH‐Vitamin D (ng/mL) | 23 (16‐74) |
| H. pylori antibody | Negative |
| SPEP | No M‐spike |
| UPEP | No M‐spike |
| Hospital Day 4 (date of discharge) | |
| BUN (mg/dL) | 21 (9‐20) |
| Creatinine (mg/dL) | 1.6 (0.5‐1.5) |
| Calcium(mg/dL) | 8.4 (8.4‐10.2) |
| WBC (thousands/cm2) | 6.5 (4‐11) |
| Hemoglobin (g/dL) | 14.1 (14‐18) |
| Hematocrit (%) | 40.8 (40‐54) |
| Day 10 (at follow‐up) | |
| BUN (mg/dL) | 16 (9‐20) |
| Creatinine (mg/dL) | 0.9 (0.5‐1.5) |
| Calcium (mg/dL) | 8.1 (8.4‐10.2) |
| Intact PTH (pg/mL) | 240 (15‐65) |
His intact parathyroid (PTH) hormone was 18.8 pg/mL (normal, 15‐65). PTH hormone‐related peptide (PTHrP) was 2.5 pmol/L. After reviewing these laboratory test results, we proceeded with further questioning, during which he admitted to taking approximately 15 to 20 Tums (>7.5 gm of calcium carbonate) daily for dyspepsia rather than the occasional Tums he had originally reported. Over the next 3 days, his calcium decreased to 8.4 mg/dL and his creatinine decreased to 1.6 mg/dL with intravenous hydration. His fatigue improved. His 25‐hydroxy vitamin D (25‐OH‐Vitamin D) level was 23 ng/mL (normal, 16‐74 ng/mL).
At his 1 week follow‐up, his calcium was 8.1 mg/dL, and his creatinine had returned to normal at 0.9 mg/dL. His intact PTH level was elevated at 240 pg/mL.
Discussion
Milk‐alkali syndrome is now believed to be the third most common reason for hypercalcemia hospital admission.2, 3 Malignancy and primary hyperparathyroidism are the only 2 causes of hypercalcemia more common than milk‐alkali syndrome in hospitalized patients; these must be excluded before making a definitive diagnosis of milk‐alkali syndrome. The differential diagnosis for hypercalcemia also includes other less common etiologies such as medications (hydrochlorothiazide and lithium), as well as familial hypocalciuric hypercalcemia, hyperthyroidism, Addison's disease, acromegaly, tertiary hyperparathyroidism, and vitamin D intoxication. Physicians often discover hypercalcemia incidentally on routine laboratory tests, and diagnostic workup should include a thorough history and physical examination, as well as further laboratory evaluation.
The diagnosis of milk‐alkali syndrome requires a history of increased calcium and alkali intake, but is otherwise a diagnosis of exclusion. Given the increasing consumption of nonprescribed calcium supplements, one should have a high index of suspicion for the diagnosis of milk‐alkali syndrome, as patients may not consider calcium carbonate to be hazardous or even a medication and thus may not report calcium carbonate consumption. Patients often view calcium carbonate as a benign treatment for dyspepsia. Its over‐the‐counter availability and economical price make it a common self‐treatment for minor dyspepsia or as prevention of osteoporosis. Calcium supplementation is increasingly added to many products, making it easy for patients to consume large quantities of calcium unknowingly. Of note, without the absorbable alkali supplied by the carbonate in calcium carbonate (Tums), milk‐alkali syndrome does not occur. The amount of calcium carbonate necessary to cause milk‐alkali syndrome is not well known, though it is speculated to be as little as 5 to 10 g of calcium in the form of calcium carbonate, especially in those with other risk factors for hypercalcemia such as chronic renal insufficiency or vomiting.2 Workup of hypercalcemia should entail careful questioning about medications, as well as over‐the‐counter supplements, vitamins, and foods.
Manifestations of the milk‐alkali syndrome include renal failure, metabolic alkalosis, and volume contraction. Normally, the kidneys prevent hypercalcemia by excretion of excess calcium. Hypercalcemia can cause tubular damage and vasoconstriction of the renal afferent arteriole leading to acute renal failure.2, 4 Hypercalcemia can also cause nephrogenic diabetes insipidus, causing impaired renal concentrating ability, leading to increased sodium excretion and volume contraction.2 In addition, alkalosis further impairs calciuresis.2 Laboratory values usually reveal suppressed PTH and vitamin D levels due to hypercalcemia caused by exogenous intake of calcium.5 Hypercalcemia causes suppression of PTH, which can lead to hyperphosphatemia, as well as decreased conversion of vitamin D to the active 1,25‐dihyroxyvitamin‐D form.
The management of hypercalcemia due to milk‐alkali syndrome is supportive and includes saline hydration as well as withholding calcium carbonate. Management of hypercalcemia due to malignancy and hyperparathyroidism includes bisphosphonates with the addition of calcitonin if symptoms are severe.6, 7 There is no evidence that supports the use of bisphosphonates in the treatment of milk‐alkali syndrome. Loop diuretics are sometimes used to promote calciuresis, though evidence is lacking to support this, and it may worsen renal failure.6
In this case, a middle‐aged man took greater than the recommended dose of calcium carbonate for dyspepsia, which led to the development of acute renal failure and hypercalcemia. At first, the patient did not provide an accurate history of the extent of his calcium carbonate ingestion, leading us to focus on hyperparathyroidism or malignancy. With aggressive hydration and cessation of calcium carbonate, his renal function and serum calcium returned to baseline. Because we initially assumed occult malignancy as the most likely diagnosis, we gave the patient pamidronate. The patient did not have a significant alkalemia (serum bicarbonate level was normal). This was thought to be due to the patient's degree of renal failure causing a concomitant metabolic acidosis. The patient's follow‐up elevated PTH level may be explained by bisphosphonate administration or underlying primary hyperparathyroidism. Of note, decreasing calcium levels have also been speculated to be a cause of high PTH levels.8
In conclusion, physicians should have a high index of suspicion for milk‐alkali syndrome in patients with hypercalcemia. Calcium carbonate is responsible for most cases of milk‐alkali syndrome, and clinicians should inquire about the use of this supplement in all patients with hypercalcemia. Milk‐alkali syndrome is no longer a merely a historical curiosity; it is currently the third most common cause of hospital admissions for hypercalcemia.
Historically, the milk‐alkali syndrome developed as an adverse reaction to the Sippy regimen of frequent feedings of milk, cream, and alkaline powders as treatment for peptic ulcer disease.1 The classic description includes hypercalcemia, metabolic alkalosis, and renal failure. This syndrome seemingly disappeared when modern acid suppression therapies such as histamine‐2 blockers and proton pump inhibitors improved dyspepsia treatment. Over the past 20 years, milk‐alkali syndrome has had a resurgence, as consumption of supplements containing calcium has increased.2 Calcium carbonate supplements are a popular over‐the‐counter treatment for osteoporosis, dyspepsia, hypocalcemia, and hyperphosphatemia; these supplements provide both the calcium and alkali required for the development of milk‐alkali syndrome.
A 46‐year‐old man presented to the emergency department after his physician ordered outpatient laboratory tests to evaluate his fatigue. The patient was found to have acute renal failure and hypercalcemia. His serum creatinine was 3.6 mg/dL, increased from his baseline of 1.1 mg/dL several months prior, and his serum calcium was 14.9 mg/dL. Ten days prior to admission he developed increasing fatigue, decreased appetite, and decreased urine output, which he attributed to recent manual labor during summer. He reported taking an occasional calcium carbonate (Tums) for dyspepsia. He did not report pain or other complaints.
His medical history included hypertension and hyperlipidemia. He had a colonoscopy 1 year prior to presentation that was significant for a high‐grade dysplastic polyp and was currently due for repeat colonoscopy. His medications included clonidine, lisinopril, and aspirin. He had no recent medication changes. He had a 30 pack/year history of cigarette smoking and drank occasionally.
On physical exam, his temperature was 99.8F, blood pressure 97/48 mmHg, heart rate 89 beats per minute, respirations 20 breaths per minute, with a room air saturation of 97%. He had dry mucus membranes and the remainder of the physical exam was unremarkable.
In the emergency department laboratory testing revealed a creatinine of 4.6 mg/dL, serum total calcium of 15.9 mg/dL, serum bicarbonate level of 26 mmol/L, phosphate of 3.9 mg/dL, albumin of 4.4 gm/dL, and alkaline phosphatase of 92 IU/L. The urine specific gravity was 1.019 gm/mL (see Table 1 for the patient's complete admission laboratory values).
| Result (Normal Range) | |
|---|---|
| |
| At admission | |
| Sodium (mmol/L) | 135 (135‐145) |
| Potassium (mmol/L) | 4.4 (3.8‐5.0) |
| Chloride (mmol/L) | 97 (98‐107) |
| Bicarbonate (mmol/L) | 25 (22‐31) |
| BUN (mg/dL) | 64 (9‐20) |
| Creatinine (mg/dL) | 4.6 (0.5‐1.5) |
| Calcium (mg/dL) | 15.9 (8.4‐10.2) |
| Albumin (g/dL) | 4.4 (3.5‐5.0) |
| Alkaline phosphatase (U/L) | 92 (38‐126) |
| ALT (U/L) | 24 (11‐66) |
| AST (U/L) | 17 (15‐46) |
| Bilirubin, total (mg/dL) | 0.3 (0.3‐1.2) |
| Ionized calcium (mmol/L) | 1.58 (1.13‐1.32) |
| Creatinine kinase (U/L) | 83 (35‐232) |
| WBC (thousands/cm2) | 12.1 (4‐11) |
| Hemoglobin (g/dL) | 16.5 (14‐18) |
| Hematocrit (%) | 48.6 (40‐54) |
| Platelets (thousands/cm2) | 224 (150‐350) |
| Intact PTH (pg/mL) | 18.78 (15‐65) |
| PTHrP (pmol/L) | 2.5 (5) |
| 25‐OH‐Vitamin D (ng/mL) | 23 (16‐74) |
| H. pylori antibody | Negative |
| SPEP | No M‐spike |
| UPEP | No M‐spike |
| Hospital Day 4 (date of discharge) | |
| BUN (mg/dL) | 21 (9‐20) |
| Creatinine (mg/dL) | 1.6 (0.5‐1.5) |
| Calcium(mg/dL) | 8.4 (8.4‐10.2) |
| WBC (thousands/cm2) | 6.5 (4‐11) |
| Hemoglobin (g/dL) | 14.1 (14‐18) |
| Hematocrit (%) | 40.8 (40‐54) |
| Day 10 (at follow‐up) | |
| BUN (mg/dL) | 16 (9‐20) |
| Creatinine (mg/dL) | 0.9 (0.5‐1.5) |
| Calcium (mg/dL) | 8.1 (8.4‐10.2) |
| Intact PTH (pg/mL) | 240 (15‐65) |
His intact parathyroid (PTH) hormone was 18.8 pg/mL (normal, 15‐65). PTH hormone‐related peptide (PTHrP) was 2.5 pmol/L. After reviewing these laboratory test results, we proceeded with further questioning, during which he admitted to taking approximately 15 to 20 Tums (>7.5 gm of calcium carbonate) daily for dyspepsia rather than the occasional Tums he had originally reported. Over the next 3 days, his calcium decreased to 8.4 mg/dL and his creatinine decreased to 1.6 mg/dL with intravenous hydration. His fatigue improved. His 25‐hydroxy vitamin D (25‐OH‐Vitamin D) level was 23 ng/mL (normal, 16‐74 ng/mL).
At his 1 week follow‐up, his calcium was 8.1 mg/dL, and his creatinine had returned to normal at 0.9 mg/dL. His intact PTH level was elevated at 240 pg/mL.
Discussion
Milk‐alkali syndrome is now believed to be the third most common reason for hypercalcemia hospital admission.2, 3 Malignancy and primary hyperparathyroidism are the only 2 causes of hypercalcemia more common than milk‐alkali syndrome in hospitalized patients; these must be excluded before making a definitive diagnosis of milk‐alkali syndrome. The differential diagnosis for hypercalcemia also includes other less common etiologies such as medications (hydrochlorothiazide and lithium), as well as familial hypocalciuric hypercalcemia, hyperthyroidism, Addison's disease, acromegaly, tertiary hyperparathyroidism, and vitamin D intoxication. Physicians often discover hypercalcemia incidentally on routine laboratory tests, and diagnostic workup should include a thorough history and physical examination, as well as further laboratory evaluation.
The diagnosis of milk‐alkali syndrome requires a history of increased calcium and alkali intake, but is otherwise a diagnosis of exclusion. Given the increasing consumption of nonprescribed calcium supplements, one should have a high index of suspicion for the diagnosis of milk‐alkali syndrome, as patients may not consider calcium carbonate to be hazardous or even a medication and thus may not report calcium carbonate consumption. Patients often view calcium carbonate as a benign treatment for dyspepsia. Its over‐the‐counter availability and economical price make it a common self‐treatment for minor dyspepsia or as prevention of osteoporosis. Calcium supplementation is increasingly added to many products, making it easy for patients to consume large quantities of calcium unknowingly. Of note, without the absorbable alkali supplied by the carbonate in calcium carbonate (Tums), milk‐alkali syndrome does not occur. The amount of calcium carbonate necessary to cause milk‐alkali syndrome is not well known, though it is speculated to be as little as 5 to 10 g of calcium in the form of calcium carbonate, especially in those with other risk factors for hypercalcemia such as chronic renal insufficiency or vomiting.2 Workup of hypercalcemia should entail careful questioning about medications, as well as over‐the‐counter supplements, vitamins, and foods.
Manifestations of the milk‐alkali syndrome include renal failure, metabolic alkalosis, and volume contraction. Normally, the kidneys prevent hypercalcemia by excretion of excess calcium. Hypercalcemia can cause tubular damage and vasoconstriction of the renal afferent arteriole leading to acute renal failure.2, 4 Hypercalcemia can also cause nephrogenic diabetes insipidus, causing impaired renal concentrating ability, leading to increased sodium excretion and volume contraction.2 In addition, alkalosis further impairs calciuresis.2 Laboratory values usually reveal suppressed PTH and vitamin D levels due to hypercalcemia caused by exogenous intake of calcium.5 Hypercalcemia causes suppression of PTH, which can lead to hyperphosphatemia, as well as decreased conversion of vitamin D to the active 1,25‐dihyroxyvitamin‐D form.
The management of hypercalcemia due to milk‐alkali syndrome is supportive and includes saline hydration as well as withholding calcium carbonate. Management of hypercalcemia due to malignancy and hyperparathyroidism includes bisphosphonates with the addition of calcitonin if symptoms are severe.6, 7 There is no evidence that supports the use of bisphosphonates in the treatment of milk‐alkali syndrome. Loop diuretics are sometimes used to promote calciuresis, though evidence is lacking to support this, and it may worsen renal failure.6
In this case, a middle‐aged man took greater than the recommended dose of calcium carbonate for dyspepsia, which led to the development of acute renal failure and hypercalcemia. At first, the patient did not provide an accurate history of the extent of his calcium carbonate ingestion, leading us to focus on hyperparathyroidism or malignancy. With aggressive hydration and cessation of calcium carbonate, his renal function and serum calcium returned to baseline. Because we initially assumed occult malignancy as the most likely diagnosis, we gave the patient pamidronate. The patient did not have a significant alkalemia (serum bicarbonate level was normal). This was thought to be due to the patient's degree of renal failure causing a concomitant metabolic acidosis. The patient's follow‐up elevated PTH level may be explained by bisphosphonate administration or underlying primary hyperparathyroidism. Of note, decreasing calcium levels have also been speculated to be a cause of high PTH levels.8
In conclusion, physicians should have a high index of suspicion for milk‐alkali syndrome in patients with hypercalcemia. Calcium carbonate is responsible for most cases of milk‐alkali syndrome, and clinicians should inquire about the use of this supplement in all patients with hypercalcemia. Milk‐alkali syndrome is no longer a merely a historical curiosity; it is currently the third most common cause of hospital admissions for hypercalcemia.
- .Landmark article May 15, 1915: Gastric and duodenal ulcer. Medical cure by an efficient removal of gastric juice corrosion. By Bertram W. Sippy.JAMA.1983;250(16):2192–2197.
- ,,,.Milk‐alkali syndrome: a historical review and description of the modern version of the syndrome.Am J Med Sci.2006;331(5):233–242.
- ,,.Milk‐alkali syndrome is a major cause of hypercalcaemia among non‐end‐stage renal disease (non‐ESRD) inpatients.Clin Endocrinol (Oxf).2005;63(5):566–576.
- ,.Milk‐alkali syndrome associated with calcium carbonate consumption. Report of 7 patients with parathyroid hormone levels and an estimate of prevalence among patients hospitalized with hypercalcemia.Medicine (Baltimore).1995;74(2):89–96.
- ,,,,,.The milk‐alkali syndrome. A reversible form of acute renal failure.Arch Intern Med.1993;153(8):1005–1010.
- ,,.Narrative review: furosemide for hypercalcemia: an unproven yet common practice.Ann Intern Med.2008;149(4):259–263.
- .Salmon calcitonin in the acute management of hypercalcemia.Calcif Tissue Int.1990;46(suppl):S26–S30.
- ,.Milk alkali syndrome. Does it exist and can it be differentiated from primary hyperparathyroidism?Ann Surg.1983;197(4):427–433.
- .Landmark article May 15, 1915: Gastric and duodenal ulcer. Medical cure by an efficient removal of gastric juice corrosion. By Bertram W. Sippy.JAMA.1983;250(16):2192–2197.
- ,,,.Milk‐alkali syndrome: a historical review and description of the modern version of the syndrome.Am J Med Sci.2006;331(5):233–242.
- ,,.Milk‐alkali syndrome is a major cause of hypercalcaemia among non‐end‐stage renal disease (non‐ESRD) inpatients.Clin Endocrinol (Oxf).2005;63(5):566–576.
- ,.Milk‐alkali syndrome associated with calcium carbonate consumption. Report of 7 patients with parathyroid hormone levels and an estimate of prevalence among patients hospitalized with hypercalcemia.Medicine (Baltimore).1995;74(2):89–96.
- ,,,,,.The milk‐alkali syndrome. A reversible form of acute renal failure.Arch Intern Med.1993;153(8):1005–1010.
- ,,.Narrative review: furosemide for hypercalcemia: an unproven yet common practice.Ann Intern Med.2008;149(4):259–263.
- .Salmon calcitonin in the acute management of hypercalcemia.Calcif Tissue Int.1990;46(suppl):S26–S30.
- ,.Milk alkali syndrome. Does it exist and can it be differentiated from primary hyperparathyroidism?Ann Surg.1983;197(4):427–433.