User login
HM: A Difference-Maker
The author of a new study that shows 20% of Medicare patient discharges are readmitted within 30 days thinks hospitalists can—and should—take a lead role in reducing those rates by improving patient transitions from hospital to home.
The study, released today in the New England Journal of Medicine, also shows that half of nonsurgical patients are readmitted to the hospital without seeing an outpatient doctor, and the unplanned rehospitalizations cost Medicare $17.4 billion in 2004.
“This is not a problem that is limited to the elderly. Going home after being in the hospital is scary,” says Stephen Jencks, MD, MPh, a psychiatrist who worked for the Centers for Medicare & Medicaid Services for more than 20 years. “We need to treat that transition as being as dangerous as going through the operating room.”
Dr. Jencks thinks HM, because of its full-time presence in hospitals, is positioned to make a difference by working with all levels of hospital staff and maintaining relationships with primary-care physicians.
“Hospitalists should say: We are in the middle of this; we are in a position to do this; and if we don’t, a lot of people will continue to get hurt,” Dr. Jencks says. “I think if they can make the re-hospitalization problem better, they will have a real feather in their cap.”
Researchers found most patients were rehospitalized for conditions other than those they were originally hospitalized for but might have been controlled prior to discharge. Rehospitalization rates varied widely by state: Maryland, New Jersey, Louisiana, Illinois, and Mississippi had rates 45% higher than Idaho, Utah, Oregon, Colorado, and New Mexico.
Study co-author Mark Williams, MD, a professor in the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago, also is leader of SHM’s transitional care mentoring program, Project BOOST.
The authors suggest several steps to reduce rehospitalizations: interventions to optimize the discharge process; sharing readmission information between hospitals; and physician collaboration to ensure follow-up care.
The author of a new study that shows 20% of Medicare patient discharges are readmitted within 30 days thinks hospitalists can—and should—take a lead role in reducing those rates by improving patient transitions from hospital to home.
The study, released today in the New England Journal of Medicine, also shows that half of nonsurgical patients are readmitted to the hospital without seeing an outpatient doctor, and the unplanned rehospitalizations cost Medicare $17.4 billion in 2004.
“This is not a problem that is limited to the elderly. Going home after being in the hospital is scary,” says Stephen Jencks, MD, MPh, a psychiatrist who worked for the Centers for Medicare & Medicaid Services for more than 20 years. “We need to treat that transition as being as dangerous as going through the operating room.”
Dr. Jencks thinks HM, because of its full-time presence in hospitals, is positioned to make a difference by working with all levels of hospital staff and maintaining relationships with primary-care physicians.
“Hospitalists should say: We are in the middle of this; we are in a position to do this; and if we don’t, a lot of people will continue to get hurt,” Dr. Jencks says. “I think if they can make the re-hospitalization problem better, they will have a real feather in their cap.”
Researchers found most patients were rehospitalized for conditions other than those they were originally hospitalized for but might have been controlled prior to discharge. Rehospitalization rates varied widely by state: Maryland, New Jersey, Louisiana, Illinois, and Mississippi had rates 45% higher than Idaho, Utah, Oregon, Colorado, and New Mexico.
Study co-author Mark Williams, MD, a professor in the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago, also is leader of SHM’s transitional care mentoring program, Project BOOST.
The authors suggest several steps to reduce rehospitalizations: interventions to optimize the discharge process; sharing readmission information between hospitals; and physician collaboration to ensure follow-up care.
The author of a new study that shows 20% of Medicare patient discharges are readmitted within 30 days thinks hospitalists can—and should—take a lead role in reducing those rates by improving patient transitions from hospital to home.
The study, released today in the New England Journal of Medicine, also shows that half of nonsurgical patients are readmitted to the hospital without seeing an outpatient doctor, and the unplanned rehospitalizations cost Medicare $17.4 billion in 2004.
“This is not a problem that is limited to the elderly. Going home after being in the hospital is scary,” says Stephen Jencks, MD, MPh, a psychiatrist who worked for the Centers for Medicare & Medicaid Services for more than 20 years. “We need to treat that transition as being as dangerous as going through the operating room.”
Dr. Jencks thinks HM, because of its full-time presence in hospitals, is positioned to make a difference by working with all levels of hospital staff and maintaining relationships with primary-care physicians.
“Hospitalists should say: We are in the middle of this; we are in a position to do this; and if we don’t, a lot of people will continue to get hurt,” Dr. Jencks says. “I think if they can make the re-hospitalization problem better, they will have a real feather in their cap.”
Researchers found most patients were rehospitalized for conditions other than those they were originally hospitalized for but might have been controlled prior to discharge. Rehospitalization rates varied widely by state: Maryland, New Jersey, Louisiana, Illinois, and Mississippi had rates 45% higher than Idaho, Utah, Oregon, Colorado, and New Mexico.
Study co-author Mark Williams, MD, a professor in the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago, also is leader of SHM’s transitional care mentoring program, Project BOOST.
The authors suggest several steps to reduce rehospitalizations: interventions to optimize the discharge process; sharing readmission information between hospitals; and physician collaboration to ensure follow-up care.
There Until the End
Patients with advanced cancer who have end-of-life conversations with palliative-care physicians have lower treatment costs, according to a March 9 report in the Archives of Internal Medicine (2009;169(5):480-488). Two other articles in the same issue examine dying patients' feelings of abandonment by physicians.
As more hospitalists move into palliative care, these studies confirm that working with patients in their final days is beneficial for the patient and the hospital.
Take a recent case at Meriter Hospital in Madison, Wis.: A ventilated patient in the hospital's ICU had been receiving aggressive treatment until a palliative-care hospitalist was brought in for a consult. The patient could barely communicate because of the tube in his trachea and an inability to raise his arms; however, the hospitalist took the time to understand the patient's wishes.
"It was very clear he [the patient] had had enough," says hospitalist Amanda duPreez, MD, medical director of Meriter's palliative-care team. "He was ready to die. Had we not been invited into that conversation, it would have been several more days."
Dr. DuPreez thinks hospitalists on palliative-care teams are a natural extension of HM's goal to reduce patient length of stay and contribute to fiscal efficiencies.
"First and foremost, how do we help improve the quality of your life?" Dr. duPreez asks. "Just by nature of [asking that question], there are subsequent cost savings. The intent is never to go out and slash costs across the board. It's a natural byproduct of sitting down with your patients and asking where they're at."
Dr. DuPreez's palliative-care team is looking to recruit another hospitalist because its five-member group has seen its consultations nearly double to more than 30 per week.
Patients with advanced cancer who have end-of-life conversations with palliative-care physicians have lower treatment costs, according to a March 9 report in the Archives of Internal Medicine (2009;169(5):480-488). Two other articles in the same issue examine dying patients' feelings of abandonment by physicians.
As more hospitalists move into palliative care, these studies confirm that working with patients in their final days is beneficial for the patient and the hospital.
Take a recent case at Meriter Hospital in Madison, Wis.: A ventilated patient in the hospital's ICU had been receiving aggressive treatment until a palliative-care hospitalist was brought in for a consult. The patient could barely communicate because of the tube in his trachea and an inability to raise his arms; however, the hospitalist took the time to understand the patient's wishes.
"It was very clear he [the patient] had had enough," says hospitalist Amanda duPreez, MD, medical director of Meriter's palliative-care team. "He was ready to die. Had we not been invited into that conversation, it would have been several more days."
Dr. DuPreez thinks hospitalists on palliative-care teams are a natural extension of HM's goal to reduce patient length of stay and contribute to fiscal efficiencies.
"First and foremost, how do we help improve the quality of your life?" Dr. duPreez asks. "Just by nature of [asking that question], there are subsequent cost savings. The intent is never to go out and slash costs across the board. It's a natural byproduct of sitting down with your patients and asking where they're at."
Dr. DuPreez's palliative-care team is looking to recruit another hospitalist because its five-member group has seen its consultations nearly double to more than 30 per week.
Patients with advanced cancer who have end-of-life conversations with palliative-care physicians have lower treatment costs, according to a March 9 report in the Archives of Internal Medicine (2009;169(5):480-488). Two other articles in the same issue examine dying patients' feelings of abandonment by physicians.
As more hospitalists move into palliative care, these studies confirm that working with patients in their final days is beneficial for the patient and the hospital.
Take a recent case at Meriter Hospital in Madison, Wis.: A ventilated patient in the hospital's ICU had been receiving aggressive treatment until a palliative-care hospitalist was brought in for a consult. The patient could barely communicate because of the tube in his trachea and an inability to raise his arms; however, the hospitalist took the time to understand the patient's wishes.
"It was very clear he [the patient] had had enough," says hospitalist Amanda duPreez, MD, medical director of Meriter's palliative-care team. "He was ready to die. Had we not been invited into that conversation, it would have been several more days."
Dr. DuPreez thinks hospitalists on palliative-care teams are a natural extension of HM's goal to reduce patient length of stay and contribute to fiscal efficiencies.
"First and foremost, how do we help improve the quality of your life?" Dr. duPreez asks. "Just by nature of [asking that question], there are subsequent cost savings. The intent is never to go out and slash costs across the board. It's a natural byproduct of sitting down with your patients and asking where they're at."
Dr. DuPreez's palliative-care team is looking to recruit another hospitalist because its five-member group has seen its consultations nearly double to more than 30 per week.
When Is GI Bleeding Prophylaxis Indicated in Hospitalized Patients?
Case
A 69-year-old man with Type 2 diabetes mellitus and chronic obstructive pulmonary disease is admitted to the ICU with respiratory compromise related to community-acquired pneumonia (CAP), accompanied by delirium, hyperglycemia, and hypovolemia. He responds well to supportive, noninvasive ventilatory therapy, but develops positive stool occult blood testing during the second day in the ICU. Upon clinical improvement, you transfer him to the general medical floor. What is the best strategy for preventing clinically significant gastrointestinal (GI) bleeding during his hospitalization?
Background
Stress-related mucosal disease (SRMD) refers to superficial erosions or focal ulceration of the proximal gastrointestinal mucosa resulting from physiologic demand in acute illness. Multiple factors contribute to its development, including disruption of the protective mucosal barrier, splanchnic vasculature hypoperfusion, and release of inflammatory mediators.1,2 Increasing severity and number of lesions are associated with the propensity for stress-related mucosal bleeding (SRMB). Based on severity, GI hemorrhage can be defined as occult (detected on chemical testing), overt (grossly evident), or clinically important (overt with compromised hemodynamics or requiring transfusion).3
The majority of clinically significant GI bleeding events occur in critically ill patients. Although more than 75% of patients have endoscopic evidence of SRMD within 24 hours of ICU admission, lesions often resolve spontaneously as patients stabilize, and the average frequency of significant bleeding is only 6%. However, when present, SRMB in ICU patients increases the length of hospitalization, cost, and mortality rates.1,3 By contrast, significant GI bleeding occurs in less than 1% of inpatients without critical illness.4
While preventing clinically important bleeding in hospitalized patients is a crucial objective, current practice reflects significant stress ulcer phophylaxis (SUP) overutilization, with substantial economic impact and potential for harm. One in three patients takes antisecretory therapy (AST) upon admission.5 Additionally, SUP is prescribed in 32% to 54% of general medical inpatients, despite the low risk for SRMB. Importantly, these prophylactic agents are continued on discharge in more than half of these patients.6-9 Clinician prescribing practices potentially can set an unfounded standard of care for obligatory prophylaxis among inpatients.
Data for Clinical Decision-Making
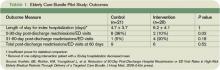
Several studies report the risks for gastrointestinal hemorrhage related to acute illness. In a prospective study of 2,252 ICU patients, two independent predictors of clinically important, new-onset SRMB were identified: mechanical ventilation for more than 48 hours and coagulopathy (see Table 1). Of these risk factors, respiratory failure was present in virtually all patients with GI hemorrhage; only one patient had coagulopathy alone. Mechanical ventilation or coagulopathy was associated with a 4% risk of clinically important GI bleeding, whereas patients with neither symptom had a 0.1% risk.
Though GI bleeding was uncommon, mortality associated with bleeding was 49%, compared with 9% in the nonbleeding group. In the absence of one of these two risk factors, 900 ICU patients would need to be treated to prevent one clinically important GI bleeding event.3 Other studies identify an increased risk of GI bleeding in subsets of patients with trauma, thermal injury, and organ transplantation. Additional possible risk factors might include septic shock, glucocorticoid or NSAID use, renal or hepatic failure, and prior GI bleeding or ulcer.10 The likelihood of GI bleeding increases proportionate to the number of risk factors present.
Limited data for non-ICU patients demonstrate an increased bleeding risk in the presence of ischemic heart disease, chronic renal failure, mechanical ventilation, or prior ICU stay.11 One study of 17,707 general medical patients found a low overall incidence (0.4%) of overt or clinically important GI bleeding, mainly in patients treated with anticoagulants without a mortality difference related to bleeding events.4
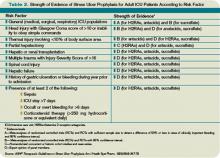
The 1999 American Society of Health System Pharmacists (ASHP) Therapeutic Guidelines on Stress Ulcer Prophylaxis reviewed extensive data by level of evidence to identify clinical indicators of patients at higher risk (see Table 2, p. 31).10 The bottom line is that stress-related bleeding depends on the type and severity of illness. Independent risk factors for critically ill patients include mechanical ventilation or coagulopathy. Stable general medical inpatients are at very low risk of clinically significant GI bleeding.
Clinical predictors help define patients at the greatest risk of SRMB. However, to be meaningful, SUP must improve clinical outcomes. Despite extensive studies on the efficacy of pharmacologic agents in the prevention of significant bleeding, several trials do not show a benefit of SUP over placebo, even in patients with major risk factors.4,12,13 Other independent studies and meta-analyses demonstrate that H2-receptor antagonists (H2RAs) prevent ICU bleeding, reducing events by approximately 50%.10 Of all the available prophylactic agents, H2RAs are FDA-approved for this use, proton pump inhibitors (PPIs) are likely as effective, and both are well-tolerated. However, data suggest that the use of AST is associated with C. difficile-associated disease, hip fracture, and pneumonia.
Outside of the ICU, there is no difference in de novo GI bleeding among general medical patients prescribed SUP. The ASHP guidelines thus conclude there is no indication for SUP in stable, general medical inpatients.10
Prevention Strategies
A subset of seriously ill patients has an increased risk for significant SRMB, but ideal prevention is not well-defined. As noted in the ASHP guidelines, “prophylaxis does not necessarily prevent bleeding in patients with documented risk factors, and the efficacy of prophylaxis varies in different patient populations.”
Given the effect of SRMB, it is reasonable to provide preventive agents to subgroups of critically ill patients with significant risk factors of mechanical ventilation for more than 48 hours and underlying coagulopathy. Studies report that judicious SUP prescription when these risks are present reduces cost without increasing morbidity or mortality in the ICU.14
Back to the Case
Our case addresses a patient in both an ICU and general medical setting. Based on his lack of risk factors for significant GI bleeding, SUP was not indicated. In this case, the patient improved. Had he developed ventilatory failure requiring intubation, the risk of clinically important GI bleeding would have approached 4%, and H2RA prophylaxis would have been recommended. Although the optimal length of prophylaxis is unknown, SUP likely can be discontinued on transfer out of the ICU, as clinical stability is associated with a substantially lower risk of clinically important bleeding.
Bottom Line
Literature supports the limited use of SUP in hospitalized medical inpatients. SUP can be reserved for critically-ill patients with major risk factors, including prolonged mechanical ventilation or coagulopathy. TH
Dr. Wright is associate professor and head of the section of hospital medicine of the Department of Medicine at the University of Wisconsin School of Medicine and Public Health.
References
1. Stollman N, Metz D. Pathophysiology and prophylaxis of stress ulcer in intensive care unit patients. J Crit Care. 2005;20:35-45.
2. Fennerty M. Pathophysiology of the upper gastrointestinal tract in the critically ill patient: rationale for the therapeutic benefits of acid suppression. Crit Care Med. 2002;30(6 Suppl):S351-S355.
3. Cook D, Fuller H, Guyatt G, et al. Risk factors for gastrointestinal bleeding in critically ill patients. New Engl J Med. 1994;330:377-381.
4. Qadeer M, Richter J, Brotman D. Hospital-acquired gastrointestinal bleeding outside the critical care unit: risk factors, role of acid suppression, and endoscopy findings. J Hosp Med. 2006;1:13-20.
5. Heidelbaugh J, Inadomi J. Magnitude and economic impact of inappropriate use of stress ulcer prophylaxis in non-ICU hospitalized patients. Am J Gastroenterol. 2006;101:2200-2205.
6. Nardino R, Vender R, Herbert P. Overuse of acid-suppressive therapy in hospitalized patients. Am J Gastroenterol. 2000;95:3118-3122.
7. Pham C, Regal R, Bostwick T, Knauf K. Acid suppressive therapy use on an inpatient internal medicine service. Ann Pharmacother. 2006;40:1261-1266.
8. Hwang K, Kolarov S, Cheng L, Griffith R. Stress ulcer prophylaxis for non-critically ill patients on a teaching service. J Eval Clin Pract. 2007;13:716-721.
9. Wohlt P, Hansen L, Fish J. Inappropriate continuation of stress ulcer prophylactic therapy after discharge. Ann Pharmachother. 2007;41:1611-1616.
10. ASHP therapeutic guidelines on stress ulcer prophylaxis. Am J Health Syst Pharm. 1999;56:347-379.
11. Janicki T, Stewart S. Stress-ulcer prophylaxis for general medical patients: a review of the evidence. J Hosp Med. 2007;2:86-92.
12. Faisy C, Guerot E, Diehl J, Iftimovici E, Fagon J. Clinically significant gastrointestinal bleeding in critically ill patients with and without stress-ulcer prophylaxis. Intensive Care Med. 2003;29:1306-1313.
13. Kantorova I, Svoboda P, Scheer P, et al. Stress ulcer prophylaxis in critically ill patients: a randomized controlled trial. Hepatogastroenterology. 2004;51:757-761.
14. Coursol C, Sanzari S. Impact of stress ulcer prophylaxis algorithm study. Ann Pharmacother. 2005;39:810-816.
Case
A 69-year-old man with Type 2 diabetes mellitus and chronic obstructive pulmonary disease is admitted to the ICU with respiratory compromise related to community-acquired pneumonia (CAP), accompanied by delirium, hyperglycemia, and hypovolemia. He responds well to supportive, noninvasive ventilatory therapy, but develops positive stool occult blood testing during the second day in the ICU. Upon clinical improvement, you transfer him to the general medical floor. What is the best strategy for preventing clinically significant gastrointestinal (GI) bleeding during his hospitalization?
Background
Stress-related mucosal disease (SRMD) refers to superficial erosions or focal ulceration of the proximal gastrointestinal mucosa resulting from physiologic demand in acute illness. Multiple factors contribute to its development, including disruption of the protective mucosal barrier, splanchnic vasculature hypoperfusion, and release of inflammatory mediators.1,2 Increasing severity and number of lesions are associated with the propensity for stress-related mucosal bleeding (SRMB). Based on severity, GI hemorrhage can be defined as occult (detected on chemical testing), overt (grossly evident), or clinically important (overt with compromised hemodynamics or requiring transfusion).3
The majority of clinically significant GI bleeding events occur in critically ill patients. Although more than 75% of patients have endoscopic evidence of SRMD within 24 hours of ICU admission, lesions often resolve spontaneously as patients stabilize, and the average frequency of significant bleeding is only 6%. However, when present, SRMB in ICU patients increases the length of hospitalization, cost, and mortality rates.1,3 By contrast, significant GI bleeding occurs in less than 1% of inpatients without critical illness.4
While preventing clinically important bleeding in hospitalized patients is a crucial objective, current practice reflects significant stress ulcer phophylaxis (SUP) overutilization, with substantial economic impact and potential for harm. One in three patients takes antisecretory therapy (AST) upon admission.5 Additionally, SUP is prescribed in 32% to 54% of general medical inpatients, despite the low risk for SRMB. Importantly, these prophylactic agents are continued on discharge in more than half of these patients.6-9 Clinician prescribing practices potentially can set an unfounded standard of care for obligatory prophylaxis among inpatients.
Data for Clinical Decision-Making
Several studies report the risks for gastrointestinal hemorrhage related to acute illness. In a prospective study of 2,252 ICU patients, two independent predictors of clinically important, new-onset SRMB were identified: mechanical ventilation for more than 48 hours and coagulopathy (see Table 1). Of these risk factors, respiratory failure was present in virtually all patients with GI hemorrhage; only one patient had coagulopathy alone. Mechanical ventilation or coagulopathy was associated with a 4% risk of clinically important GI bleeding, whereas patients with neither symptom had a 0.1% risk.
Though GI bleeding was uncommon, mortality associated with bleeding was 49%, compared with 9% in the nonbleeding group. In the absence of one of these two risk factors, 900 ICU patients would need to be treated to prevent one clinically important GI bleeding event.3 Other studies identify an increased risk of GI bleeding in subsets of patients with trauma, thermal injury, and organ transplantation. Additional possible risk factors might include septic shock, glucocorticoid or NSAID use, renal or hepatic failure, and prior GI bleeding or ulcer.10 The likelihood of GI bleeding increases proportionate to the number of risk factors present.
Limited data for non-ICU patients demonstrate an increased bleeding risk in the presence of ischemic heart disease, chronic renal failure, mechanical ventilation, or prior ICU stay.11 One study of 17,707 general medical patients found a low overall incidence (0.4%) of overt or clinically important GI bleeding, mainly in patients treated with anticoagulants without a mortality difference related to bleeding events.4
The 1999 American Society of Health System Pharmacists (ASHP) Therapeutic Guidelines on Stress Ulcer Prophylaxis reviewed extensive data by level of evidence to identify clinical indicators of patients at higher risk (see Table 2, p. 31).10 The bottom line is that stress-related bleeding depends on the type and severity of illness. Independent risk factors for critically ill patients include mechanical ventilation or coagulopathy. Stable general medical inpatients are at very low risk of clinically significant GI bleeding.
Clinical predictors help define patients at the greatest risk of SRMB. However, to be meaningful, SUP must improve clinical outcomes. Despite extensive studies on the efficacy of pharmacologic agents in the prevention of significant bleeding, several trials do not show a benefit of SUP over placebo, even in patients with major risk factors.4,12,13 Other independent studies and meta-analyses demonstrate that H2-receptor antagonists (H2RAs) prevent ICU bleeding, reducing events by approximately 50%.10 Of all the available prophylactic agents, H2RAs are FDA-approved for this use, proton pump inhibitors (PPIs) are likely as effective, and both are well-tolerated. However, data suggest that the use of AST is associated with C. difficile-associated disease, hip fracture, and pneumonia.
Outside of the ICU, there is no difference in de novo GI bleeding among general medical patients prescribed SUP. The ASHP guidelines thus conclude there is no indication for SUP in stable, general medical inpatients.10
Prevention Strategies
A subset of seriously ill patients has an increased risk for significant SRMB, but ideal prevention is not well-defined. As noted in the ASHP guidelines, “prophylaxis does not necessarily prevent bleeding in patients with documented risk factors, and the efficacy of prophylaxis varies in different patient populations.”
Given the effect of SRMB, it is reasonable to provide preventive agents to subgroups of critically ill patients with significant risk factors of mechanical ventilation for more than 48 hours and underlying coagulopathy. Studies report that judicious SUP prescription when these risks are present reduces cost without increasing morbidity or mortality in the ICU.14
Back to the Case
Our case addresses a patient in both an ICU and general medical setting. Based on his lack of risk factors for significant GI bleeding, SUP was not indicated. In this case, the patient improved. Had he developed ventilatory failure requiring intubation, the risk of clinically important GI bleeding would have approached 4%, and H2RA prophylaxis would have been recommended. Although the optimal length of prophylaxis is unknown, SUP likely can be discontinued on transfer out of the ICU, as clinical stability is associated with a substantially lower risk of clinically important bleeding.
Bottom Line
Literature supports the limited use of SUP in hospitalized medical inpatients. SUP can be reserved for critically-ill patients with major risk factors, including prolonged mechanical ventilation or coagulopathy. TH
Dr. Wright is associate professor and head of the section of hospital medicine of the Department of Medicine at the University of Wisconsin School of Medicine and Public Health.
References
1. Stollman N, Metz D. Pathophysiology and prophylaxis of stress ulcer in intensive care unit patients. J Crit Care. 2005;20:35-45.
2. Fennerty M. Pathophysiology of the upper gastrointestinal tract in the critically ill patient: rationale for the therapeutic benefits of acid suppression. Crit Care Med. 2002;30(6 Suppl):S351-S355.
3. Cook D, Fuller H, Guyatt G, et al. Risk factors for gastrointestinal bleeding in critically ill patients. New Engl J Med. 1994;330:377-381.
4. Qadeer M, Richter J, Brotman D. Hospital-acquired gastrointestinal bleeding outside the critical care unit: risk factors, role of acid suppression, and endoscopy findings. J Hosp Med. 2006;1:13-20.
5. Heidelbaugh J, Inadomi J. Magnitude and economic impact of inappropriate use of stress ulcer prophylaxis in non-ICU hospitalized patients. Am J Gastroenterol. 2006;101:2200-2205.
6. Nardino R, Vender R, Herbert P. Overuse of acid-suppressive therapy in hospitalized patients. Am J Gastroenterol. 2000;95:3118-3122.
7. Pham C, Regal R, Bostwick T, Knauf K. Acid suppressive therapy use on an inpatient internal medicine service. Ann Pharmacother. 2006;40:1261-1266.
8. Hwang K, Kolarov S, Cheng L, Griffith R. Stress ulcer prophylaxis for non-critically ill patients on a teaching service. J Eval Clin Pract. 2007;13:716-721.
9. Wohlt P, Hansen L, Fish J. Inappropriate continuation of stress ulcer prophylactic therapy after discharge. Ann Pharmachother. 2007;41:1611-1616.
10. ASHP therapeutic guidelines on stress ulcer prophylaxis. Am J Health Syst Pharm. 1999;56:347-379.
11. Janicki T, Stewart S. Stress-ulcer prophylaxis for general medical patients: a review of the evidence. J Hosp Med. 2007;2:86-92.
12. Faisy C, Guerot E, Diehl J, Iftimovici E, Fagon J. Clinically significant gastrointestinal bleeding in critically ill patients with and without stress-ulcer prophylaxis. Intensive Care Med. 2003;29:1306-1313.
13. Kantorova I, Svoboda P, Scheer P, et al. Stress ulcer prophylaxis in critically ill patients: a randomized controlled trial. Hepatogastroenterology. 2004;51:757-761.
14. Coursol C, Sanzari S. Impact of stress ulcer prophylaxis algorithm study. Ann Pharmacother. 2005;39:810-816.
Case
A 69-year-old man with Type 2 diabetes mellitus and chronic obstructive pulmonary disease is admitted to the ICU with respiratory compromise related to community-acquired pneumonia (CAP), accompanied by delirium, hyperglycemia, and hypovolemia. He responds well to supportive, noninvasive ventilatory therapy, but develops positive stool occult blood testing during the second day in the ICU. Upon clinical improvement, you transfer him to the general medical floor. What is the best strategy for preventing clinically significant gastrointestinal (GI) bleeding during his hospitalization?
Background
Stress-related mucosal disease (SRMD) refers to superficial erosions or focal ulceration of the proximal gastrointestinal mucosa resulting from physiologic demand in acute illness. Multiple factors contribute to its development, including disruption of the protective mucosal barrier, splanchnic vasculature hypoperfusion, and release of inflammatory mediators.1,2 Increasing severity and number of lesions are associated with the propensity for stress-related mucosal bleeding (SRMB). Based on severity, GI hemorrhage can be defined as occult (detected on chemical testing), overt (grossly evident), or clinically important (overt with compromised hemodynamics or requiring transfusion).3
The majority of clinically significant GI bleeding events occur in critically ill patients. Although more than 75% of patients have endoscopic evidence of SRMD within 24 hours of ICU admission, lesions often resolve spontaneously as patients stabilize, and the average frequency of significant bleeding is only 6%. However, when present, SRMB in ICU patients increases the length of hospitalization, cost, and mortality rates.1,3 By contrast, significant GI bleeding occurs in less than 1% of inpatients without critical illness.4
While preventing clinically important bleeding in hospitalized patients is a crucial objective, current practice reflects significant stress ulcer phophylaxis (SUP) overutilization, with substantial economic impact and potential for harm. One in three patients takes antisecretory therapy (AST) upon admission.5 Additionally, SUP is prescribed in 32% to 54% of general medical inpatients, despite the low risk for SRMB. Importantly, these prophylactic agents are continued on discharge in more than half of these patients.6-9 Clinician prescribing practices potentially can set an unfounded standard of care for obligatory prophylaxis among inpatients.
Data for Clinical Decision-Making
Several studies report the risks for gastrointestinal hemorrhage related to acute illness. In a prospective study of 2,252 ICU patients, two independent predictors of clinically important, new-onset SRMB were identified: mechanical ventilation for more than 48 hours and coagulopathy (see Table 1). Of these risk factors, respiratory failure was present in virtually all patients with GI hemorrhage; only one patient had coagulopathy alone. Mechanical ventilation or coagulopathy was associated with a 4% risk of clinically important GI bleeding, whereas patients with neither symptom had a 0.1% risk.
Though GI bleeding was uncommon, mortality associated with bleeding was 49%, compared with 9% in the nonbleeding group. In the absence of one of these two risk factors, 900 ICU patients would need to be treated to prevent one clinically important GI bleeding event.3 Other studies identify an increased risk of GI bleeding in subsets of patients with trauma, thermal injury, and organ transplantation. Additional possible risk factors might include septic shock, glucocorticoid or NSAID use, renal or hepatic failure, and prior GI bleeding or ulcer.10 The likelihood of GI bleeding increases proportionate to the number of risk factors present.
Limited data for non-ICU patients demonstrate an increased bleeding risk in the presence of ischemic heart disease, chronic renal failure, mechanical ventilation, or prior ICU stay.11 One study of 17,707 general medical patients found a low overall incidence (0.4%) of overt or clinically important GI bleeding, mainly in patients treated with anticoagulants without a mortality difference related to bleeding events.4
The 1999 American Society of Health System Pharmacists (ASHP) Therapeutic Guidelines on Stress Ulcer Prophylaxis reviewed extensive data by level of evidence to identify clinical indicators of patients at higher risk (see Table 2, p. 31).10 The bottom line is that stress-related bleeding depends on the type and severity of illness. Independent risk factors for critically ill patients include mechanical ventilation or coagulopathy. Stable general medical inpatients are at very low risk of clinically significant GI bleeding.
Clinical predictors help define patients at the greatest risk of SRMB. However, to be meaningful, SUP must improve clinical outcomes. Despite extensive studies on the efficacy of pharmacologic agents in the prevention of significant bleeding, several trials do not show a benefit of SUP over placebo, even in patients with major risk factors.4,12,13 Other independent studies and meta-analyses demonstrate that H2-receptor antagonists (H2RAs) prevent ICU bleeding, reducing events by approximately 50%.10 Of all the available prophylactic agents, H2RAs are FDA-approved for this use, proton pump inhibitors (PPIs) are likely as effective, and both are well-tolerated. However, data suggest that the use of AST is associated with C. difficile-associated disease, hip fracture, and pneumonia.
Outside of the ICU, there is no difference in de novo GI bleeding among general medical patients prescribed SUP. The ASHP guidelines thus conclude there is no indication for SUP in stable, general medical inpatients.10
Prevention Strategies
A subset of seriously ill patients has an increased risk for significant SRMB, but ideal prevention is not well-defined. As noted in the ASHP guidelines, “prophylaxis does not necessarily prevent bleeding in patients with documented risk factors, and the efficacy of prophylaxis varies in different patient populations.”
Given the effect of SRMB, it is reasonable to provide preventive agents to subgroups of critically ill patients with significant risk factors of mechanical ventilation for more than 48 hours and underlying coagulopathy. Studies report that judicious SUP prescription when these risks are present reduces cost without increasing morbidity or mortality in the ICU.14
Back to the Case
Our case addresses a patient in both an ICU and general medical setting. Based on his lack of risk factors for significant GI bleeding, SUP was not indicated. In this case, the patient improved. Had he developed ventilatory failure requiring intubation, the risk of clinically important GI bleeding would have approached 4%, and H2RA prophylaxis would have been recommended. Although the optimal length of prophylaxis is unknown, SUP likely can be discontinued on transfer out of the ICU, as clinical stability is associated with a substantially lower risk of clinically important bleeding.
Bottom Line
Literature supports the limited use of SUP in hospitalized medical inpatients. SUP can be reserved for critically-ill patients with major risk factors, including prolonged mechanical ventilation or coagulopathy. TH
Dr. Wright is associate professor and head of the section of hospital medicine of the Department of Medicine at the University of Wisconsin School of Medicine and Public Health.
References
1. Stollman N, Metz D. Pathophysiology and prophylaxis of stress ulcer in intensive care unit patients. J Crit Care. 2005;20:35-45.
2. Fennerty M. Pathophysiology of the upper gastrointestinal tract in the critically ill patient: rationale for the therapeutic benefits of acid suppression. Crit Care Med. 2002;30(6 Suppl):S351-S355.
3. Cook D, Fuller H, Guyatt G, et al. Risk factors for gastrointestinal bleeding in critically ill patients. New Engl J Med. 1994;330:377-381.
4. Qadeer M, Richter J, Brotman D. Hospital-acquired gastrointestinal bleeding outside the critical care unit: risk factors, role of acid suppression, and endoscopy findings. J Hosp Med. 2006;1:13-20.
5. Heidelbaugh J, Inadomi J. Magnitude and economic impact of inappropriate use of stress ulcer prophylaxis in non-ICU hospitalized patients. Am J Gastroenterol. 2006;101:2200-2205.
6. Nardino R, Vender R, Herbert P. Overuse of acid-suppressive therapy in hospitalized patients. Am J Gastroenterol. 2000;95:3118-3122.
7. Pham C, Regal R, Bostwick T, Knauf K. Acid suppressive therapy use on an inpatient internal medicine service. Ann Pharmacother. 2006;40:1261-1266.
8. Hwang K, Kolarov S, Cheng L, Griffith R. Stress ulcer prophylaxis for non-critically ill patients on a teaching service. J Eval Clin Pract. 2007;13:716-721.
9. Wohlt P, Hansen L, Fish J. Inappropriate continuation of stress ulcer prophylactic therapy after discharge. Ann Pharmachother. 2007;41:1611-1616.
10. ASHP therapeutic guidelines on stress ulcer prophylaxis. Am J Health Syst Pharm. 1999;56:347-379.
11. Janicki T, Stewart S. Stress-ulcer prophylaxis for general medical patients: a review of the evidence. J Hosp Med. 2007;2:86-92.
12. Faisy C, Guerot E, Diehl J, Iftimovici E, Fagon J. Clinically significant gastrointestinal bleeding in critically ill patients with and without stress-ulcer prophylaxis. Intensive Care Med. 2003;29:1306-1313.
13. Kantorova I, Svoboda P, Scheer P, et al. Stress ulcer prophylaxis in critically ill patients: a randomized controlled trial. Hepatogastroenterology. 2004;51:757-761.
14. Coursol C, Sanzari S. Impact of stress ulcer prophylaxis algorithm study. Ann Pharmacother. 2005;39:810-816.
Misunderstood Modifiers
Modifiers are two-digit representations used in conjunction with a service or procedure code (e.g., 99233-25) during claim submission to alert payors that the service or procedure was performed under a special circumstance. Modifiers can:
- Identify body areas;
- Distinguish multiple, separately identifiable services;
- Identify reduced or multiple services of the same or a different nature; or
- Categorize unusual events surrounding a particular service.1
Many questions arise over appropriate modifier use. Hospitalist misconceptions typically involve surgical comanagement or multiple services on the same day. Understanding when to use modifiers is imperative for proper claim submission and reimbursement.
Multiple Visits
Most hospitalists know payors allow reimbursement for only one visit per specialty, per patient, per day; however, some payors further limit coverage to a single service (i.e., a visit or a procedure) unless physician documentation demonstrates a medical necessity for each billed service. When two visits are performed on the same date by the same physician, or by two physicians of the same specialty within the same group, only one cumulative service should be reported.2
Consideration of two notes during visit-level selection does not authorize physicians to report a higher visit level (e.g., 99233 for two notes instead of 99232 for one note). If the cumulative documentation does not include the necessary elements of history, exam, or medical decision-making that are associated with 99233, the physician must report the lower visit level that accurately reflects the content of the progress note (for more information on documentation guidelines, visit www.cms.hhs.gov/MLNEdWebGuide/25_EMDOC.asp).
One exception to this “single cumulative service” rule occurs when a physician provides a typical inpatient service (e.g., admission or subsequent hospital care) for chronic obstructive bronchitis with acute exacerbation (diagnosis code 491.21) early in the day, and later the patient requires a second, more intense encounter for acute respiratory distress (diagnosis code 518.82) that meets the definition of critical care (99291). In this scenario, the physician is allowed to report both services on the same date, appending modifier 25 to the initial service (i.e., 99233-25) because each service was performed for distinct reasons.
If different physicians in the same provider group and specialty provided the initial and follow-up services, each physician reports the corresponding service in their own name with modifier 25 appended to the subsequent hospital care service (as above). Please note that physicians may not report both services if critical care is the initial service of the day. In this latter scenario, the physician reports critical-care codes (99291, 99292) for all of his or other group members’ encounters provided in one calendar day.3
Visits and Procedures
When a physician bills for a procedure and a visit (inpatient or outpatient) on the same day, most payors “bundle” the visit payment into that of the procedure. Some payors do provide separate payment for the visit, if the service is separately identifiable from the procedure (i.e., performed for a separate reason). To electronically demonstrate this on the claim form, the physician appends modifier 25 to the visit. Although not required, it is strongly suggested that, when possible, the primary diagnosis for the visit differs from the one used with the procedure. This will further distinguish the services. However, different diagnoses may not be possible when the physician evaluates the patient and decides, during the course of the evaluation, that a procedure is warranted. In this case, the physician may only have a single diagnosis to list with the procedure and the visit.
Payors may request documentation prior to payment to ensure that the visit is not associated with the required preprocedure history and physical. Modifier 57 is not to be confused with modifier 25. Modifier 57 indicates that the physician made the decision for “surgery” during the visit, but this modifier is used with preprocedural visits involving major surgical procedures (i.e., procedures associated with 90-day global periods). Since hospitalists do not perform major surgical procedures, they would not use this modifier with preprocedural visits.
Keep in mind that this “bundling” concept only applies when same-day visits and procedures are performed by the same physician or members of the same provider group with the same specialty designation. In other words, hospitalist visits are typically considered separate from procedures performed by a surgeon, and there is no need to append a modifier to visits on the same day as the surgeon’s procedure. The surgeon’s packaged payment includes preoperative visits after the decision for surgery is made beginning one day prior to surgery, and postoperative visits by the surgeon related to recovery from surgery, postoperative pain management, and discharge care.4 The surgeon is entitled to the full global payment if he provides the preoperative, intraoperative, and postoperative management.
If the surgeon relinquishes care and formally transfers the preoperative or postoperative management to another physician not associated with the surgical group, the other physician may bill for his portion of the perioperative management by appending modifier 56 (preop) or 55 (postop) to the procedure code. Unfortunately, the hospitalist is subject to the surgeon’s claim reporting. If the surgeon fails to solely report his intraoperative management (modifier 54 appended to the procedure code), the surgeon receives the full packaged payment. The payor will deny the hospitalist’s claim.
The payor is unlikely to retrieve money from one provider to pay another provider, unless a pattern of inappropriate claim submission is detected. Surgical intraoperative responsibilities are not typically reassigned to other provider groups unless special circumstances occur (e.g., geographical restrictions). Therefore, if the surgeon does not relinquish care but merely wants the hospitalist to assist in medical management, the hospitalist reports his medically necessary services with the appropriate inpatient visit code (subsequent hospital care, 99231-99233). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Holmes A. Appropriate Use of Modifiers In: Coding for Chest Medicine 2009. Northbrook, Ill.: American College of Chest Physicians; 2008:273-282.
2. Centers for Medicare and Medicaid Services. Medicare claims processing manual. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Feb. 10, 2009.
3. Centers for Medicare and Medicaid Services. Medicare claims processing manual. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Feb. 10, 2009.
4. Pohlig, C. Sort out surgical cases. The Hospitalist. 2008;12(8):19.
Modifiers are two-digit representations used in conjunction with a service or procedure code (e.g., 99233-25) during claim submission to alert payors that the service or procedure was performed under a special circumstance. Modifiers can:
- Identify body areas;
- Distinguish multiple, separately identifiable services;
- Identify reduced or multiple services of the same or a different nature; or
- Categorize unusual events surrounding a particular service.1
Many questions arise over appropriate modifier use. Hospitalist misconceptions typically involve surgical comanagement or multiple services on the same day. Understanding when to use modifiers is imperative for proper claim submission and reimbursement.
Multiple Visits
Most hospitalists know payors allow reimbursement for only one visit per specialty, per patient, per day; however, some payors further limit coverage to a single service (i.e., a visit or a procedure) unless physician documentation demonstrates a medical necessity for each billed service. When two visits are performed on the same date by the same physician, or by two physicians of the same specialty within the same group, only one cumulative service should be reported.2
Consideration of two notes during visit-level selection does not authorize physicians to report a higher visit level (e.g., 99233 for two notes instead of 99232 for one note). If the cumulative documentation does not include the necessary elements of history, exam, or medical decision-making that are associated with 99233, the physician must report the lower visit level that accurately reflects the content of the progress note (for more information on documentation guidelines, visit www.cms.hhs.gov/MLNEdWebGuide/25_EMDOC.asp).
One exception to this “single cumulative service” rule occurs when a physician provides a typical inpatient service (e.g., admission or subsequent hospital care) for chronic obstructive bronchitis with acute exacerbation (diagnosis code 491.21) early in the day, and later the patient requires a second, more intense encounter for acute respiratory distress (diagnosis code 518.82) that meets the definition of critical care (99291). In this scenario, the physician is allowed to report both services on the same date, appending modifier 25 to the initial service (i.e., 99233-25) because each service was performed for distinct reasons.
If different physicians in the same provider group and specialty provided the initial and follow-up services, each physician reports the corresponding service in their own name with modifier 25 appended to the subsequent hospital care service (as above). Please note that physicians may not report both services if critical care is the initial service of the day. In this latter scenario, the physician reports critical-care codes (99291, 99292) for all of his or other group members’ encounters provided in one calendar day.3
Visits and Procedures
When a physician bills for a procedure and a visit (inpatient or outpatient) on the same day, most payors “bundle” the visit payment into that of the procedure. Some payors do provide separate payment for the visit, if the service is separately identifiable from the procedure (i.e., performed for a separate reason). To electronically demonstrate this on the claim form, the physician appends modifier 25 to the visit. Although not required, it is strongly suggested that, when possible, the primary diagnosis for the visit differs from the one used with the procedure. This will further distinguish the services. However, different diagnoses may not be possible when the physician evaluates the patient and decides, during the course of the evaluation, that a procedure is warranted. In this case, the physician may only have a single diagnosis to list with the procedure and the visit.
Payors may request documentation prior to payment to ensure that the visit is not associated with the required preprocedure history and physical. Modifier 57 is not to be confused with modifier 25. Modifier 57 indicates that the physician made the decision for “surgery” during the visit, but this modifier is used with preprocedural visits involving major surgical procedures (i.e., procedures associated with 90-day global periods). Since hospitalists do not perform major surgical procedures, they would not use this modifier with preprocedural visits.
Keep in mind that this “bundling” concept only applies when same-day visits and procedures are performed by the same physician or members of the same provider group with the same specialty designation. In other words, hospitalist visits are typically considered separate from procedures performed by a surgeon, and there is no need to append a modifier to visits on the same day as the surgeon’s procedure. The surgeon’s packaged payment includes preoperative visits after the decision for surgery is made beginning one day prior to surgery, and postoperative visits by the surgeon related to recovery from surgery, postoperative pain management, and discharge care.4 The surgeon is entitled to the full global payment if he provides the preoperative, intraoperative, and postoperative management.
If the surgeon relinquishes care and formally transfers the preoperative or postoperative management to another physician not associated with the surgical group, the other physician may bill for his portion of the perioperative management by appending modifier 56 (preop) or 55 (postop) to the procedure code. Unfortunately, the hospitalist is subject to the surgeon’s claim reporting. If the surgeon fails to solely report his intraoperative management (modifier 54 appended to the procedure code), the surgeon receives the full packaged payment. The payor will deny the hospitalist’s claim.
The payor is unlikely to retrieve money from one provider to pay another provider, unless a pattern of inappropriate claim submission is detected. Surgical intraoperative responsibilities are not typically reassigned to other provider groups unless special circumstances occur (e.g., geographical restrictions). Therefore, if the surgeon does not relinquish care but merely wants the hospitalist to assist in medical management, the hospitalist reports his medically necessary services with the appropriate inpatient visit code (subsequent hospital care, 99231-99233). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Holmes A. Appropriate Use of Modifiers In: Coding for Chest Medicine 2009. Northbrook, Ill.: American College of Chest Physicians; 2008:273-282.
2. Centers for Medicare and Medicaid Services. Medicare claims processing manual. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Feb. 10, 2009.
3. Centers for Medicare and Medicaid Services. Medicare claims processing manual. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Feb. 10, 2009.
4. Pohlig, C. Sort out surgical cases. The Hospitalist. 2008;12(8):19.
Modifiers are two-digit representations used in conjunction with a service or procedure code (e.g., 99233-25) during claim submission to alert payors that the service or procedure was performed under a special circumstance. Modifiers can:
- Identify body areas;
- Distinguish multiple, separately identifiable services;
- Identify reduced or multiple services of the same or a different nature; or
- Categorize unusual events surrounding a particular service.1
Many questions arise over appropriate modifier use. Hospitalist misconceptions typically involve surgical comanagement or multiple services on the same day. Understanding when to use modifiers is imperative for proper claim submission and reimbursement.
Multiple Visits
Most hospitalists know payors allow reimbursement for only one visit per specialty, per patient, per day; however, some payors further limit coverage to a single service (i.e., a visit or a procedure) unless physician documentation demonstrates a medical necessity for each billed service. When two visits are performed on the same date by the same physician, or by two physicians of the same specialty within the same group, only one cumulative service should be reported.2
Consideration of two notes during visit-level selection does not authorize physicians to report a higher visit level (e.g., 99233 for two notes instead of 99232 for one note). If the cumulative documentation does not include the necessary elements of history, exam, or medical decision-making that are associated with 99233, the physician must report the lower visit level that accurately reflects the content of the progress note (for more information on documentation guidelines, visit www.cms.hhs.gov/MLNEdWebGuide/25_EMDOC.asp).
One exception to this “single cumulative service” rule occurs when a physician provides a typical inpatient service (e.g., admission or subsequent hospital care) for chronic obstructive bronchitis with acute exacerbation (diagnosis code 491.21) early in the day, and later the patient requires a second, more intense encounter for acute respiratory distress (diagnosis code 518.82) that meets the definition of critical care (99291). In this scenario, the physician is allowed to report both services on the same date, appending modifier 25 to the initial service (i.e., 99233-25) because each service was performed for distinct reasons.
If different physicians in the same provider group and specialty provided the initial and follow-up services, each physician reports the corresponding service in their own name with modifier 25 appended to the subsequent hospital care service (as above). Please note that physicians may not report both services if critical care is the initial service of the day. In this latter scenario, the physician reports critical-care codes (99291, 99292) for all of his or other group members’ encounters provided in one calendar day.3
Visits and Procedures
When a physician bills for a procedure and a visit (inpatient or outpatient) on the same day, most payors “bundle” the visit payment into that of the procedure. Some payors do provide separate payment for the visit, if the service is separately identifiable from the procedure (i.e., performed for a separate reason). To electronically demonstrate this on the claim form, the physician appends modifier 25 to the visit. Although not required, it is strongly suggested that, when possible, the primary diagnosis for the visit differs from the one used with the procedure. This will further distinguish the services. However, different diagnoses may not be possible when the physician evaluates the patient and decides, during the course of the evaluation, that a procedure is warranted. In this case, the physician may only have a single diagnosis to list with the procedure and the visit.
Payors may request documentation prior to payment to ensure that the visit is not associated with the required preprocedure history and physical. Modifier 57 is not to be confused with modifier 25. Modifier 57 indicates that the physician made the decision for “surgery” during the visit, but this modifier is used with preprocedural visits involving major surgical procedures (i.e., procedures associated with 90-day global periods). Since hospitalists do not perform major surgical procedures, they would not use this modifier with preprocedural visits.
Keep in mind that this “bundling” concept only applies when same-day visits and procedures are performed by the same physician or members of the same provider group with the same specialty designation. In other words, hospitalist visits are typically considered separate from procedures performed by a surgeon, and there is no need to append a modifier to visits on the same day as the surgeon’s procedure. The surgeon’s packaged payment includes preoperative visits after the decision for surgery is made beginning one day prior to surgery, and postoperative visits by the surgeon related to recovery from surgery, postoperative pain management, and discharge care.4 The surgeon is entitled to the full global payment if he provides the preoperative, intraoperative, and postoperative management.
If the surgeon relinquishes care and formally transfers the preoperative or postoperative management to another physician not associated with the surgical group, the other physician may bill for his portion of the perioperative management by appending modifier 56 (preop) or 55 (postop) to the procedure code. Unfortunately, the hospitalist is subject to the surgeon’s claim reporting. If the surgeon fails to solely report his intraoperative management (modifier 54 appended to the procedure code), the surgeon receives the full packaged payment. The payor will deny the hospitalist’s claim.
The payor is unlikely to retrieve money from one provider to pay another provider, unless a pattern of inappropriate claim submission is detected. Surgical intraoperative responsibilities are not typically reassigned to other provider groups unless special circumstances occur (e.g., geographical restrictions). Therefore, if the surgeon does not relinquish care but merely wants the hospitalist to assist in medical management, the hospitalist reports his medically necessary services with the appropriate inpatient visit code (subsequent hospital care, 99231-99233). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Holmes A. Appropriate Use of Modifiers In: Coding for Chest Medicine 2009. Northbrook, Ill.: American College of Chest Physicians; 2008:273-282.
2. Centers for Medicare and Medicaid Services. Medicare claims processing manual. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Feb. 10, 2009.
3. Centers for Medicare and Medicaid Services. Medicare claims processing manual. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Feb. 10, 2009.
4. Pohlig, C. Sort out surgical cases. The Hospitalist. 2008;12(8):19.
Armed with HM Knowledge
Many physicians use traditional practice as their stepping stone to a hospitalist career. David M. Grace, MD, took a far more unconventional path.
He served as a combat medic in the Army National Guard, joined a disaster medical assistance team at the Federal Emergency Management Agency (FEMA), and volunteered to help the American Red Cross in times of crisis—all before entering medical school.
Dr. Grace became a hospitalist in 2002, and now serves as hospitalist division area medical officer for The Schumacher Group, a staffing and consulting firm in Lafayette, La., that hires physicians as independent contractors to work in hospitals across the country.
But 21 years into his healthcare career, he continues to seek opportunities that offer the same two rewards: “I want to be filled with Adrenalin,” he says, “but I still want to use my brains.”
—David M. Grace, MD, The Schumacher Group, Lafayette, La.
Question: Given your varied background, how did you wind up becoming a hospitalist?
Answer: My predoctoring resume reads like a fast track of becoming an emergency physician. In residency, I had heard the term “hospitalist.” I knew I liked dealing with sick patients. Emergency departments act as a fairly good filter, and anyone who gets through and upstairs truly is a sick patient. I figured if I were a hospitalist, all my patients would be sick, as opposed to just some. That really drove me to hospital medicine.
Q: You founded your own hospitalist company in 2005, but within two years, you joined The Schumacher Group. Why did you make the switch?
A: With the speed with which hospital medicine is growing, I thought if I could tap into their resources and infrastructure … I’d be able to do things I couldn’t do in my own group for years, if not decades. I really thought I would be able to impact a far larger portion of patient lives with them than I could in my own smaller, somewhat homemade group.
Q: When The Schumacher Group formed, it focused on emergency departments. In 2007, it launched a hospitalist service. What’s the benefit?
A: If you put good hospitalist systems under the same umbrella as good emergency department systems, you can do things to boost the synergy between the two disciplines and improve patient care. In the facilities where we’re managing both the ED and the hospitalists, we can effect patient care from the moment the patient swings through the ambulance bay doors until the moment they are discharged.
Q: How successful has the HM effort been?
A: The hospitalist side, by the end of the year, will have about 20 to 25 practices up and running, with growth in the neighborhood of 10 to 15 practices a year expected to come on line.
Q: What are the advantages to a private corporation setup?
A: At the end of the day, doctors need to be patient-care advocates. But if you are employed by a hospital, they sign your check. When push comes to shove on a quality issue, I think there’s a tendency not to shove as hard when the person you’re shoving is the person employing you.
Q: Could this approach be the wave of the future?
A: I think so. It goes back to the idea of focusing all of your resources into one small area, such as hospital medicine or inpatient medicine, so there’s far fewer distractions than for a hospital that runs its own hospitalist program. We saw that in the 1970s, when hospitals were buying primary-care practices left and right. They realized they didn’t have the skills or the resources to make that effective, and they rapidly divested.
Q: Most doctors at the executive level of The Schumacher Group—including yourself—still practice medicine. Why is that so integral to the mission?
A: When I served in the military, the best officers I served under were officers who had been enlisted men earlier in their career. The same follows suit in hospital medicine. When I make an administrative decision, it can affect thousands of patient lives tomorrow. I can mentally track the effects of my decision all the way back to how it will affect the patient laying in the bed. If you’re not having that constantly reinforced by seeing patients, it’s very easy to lose track of it, and that has such a profound effect on patient care.
Q: SHM recently designated you one of the inaugural “Fellows in Hospital Medicine.” What is the biggest reward of a HM career?
A: For me, there are two. One is the ability to see the fruits of your labor much more rapidly than in the outpatient world. I can have a patient in bed in front of me actively dying and watch them a week later walk out of hospital in good condition. That’s a very different timetable than the outpatient world, when you may put a patient on all the right medicines to reduce the risk of a heart attack and, over 60 years, watch them not have a heart attack. The other thing I find very rewarding is the amount of measurements and data collected on what we do. We get feedback ranging from patient satisfaction scores to referring physician scores to readmission rates to data that shows if we are able to get patients better outcomes at lower costs. You just don’t get that type of feedback in many other fields.
Q: What is the greatest challenge facing the profession?
A: One of the biggest is the supply and demand mismatch. Right now, one of the hardest jobs is a hospitalist recruiter. With every physician having five to 10 open job offers …recruiting is difficult, and recruiting the right physician is extremely difficult.
Q: How can that be addressed?
A: One way is to be efficient. Can we see more patients in the same amount of time with no decrease in quality? For us, it involves the use of what we call a practice coordinator. It’s an employee of The Schumacher Group who is located in the individual hospital who does everything from assisting with managing the practice to answering telephone calls. This really allows us to help us organize our time better, so we don’t get bogged down in nonclinical work. Every minute spent on the phone with an insurance company or home health agency is a minute not spent at the bedside. Another way is expanding the use of midlevel providers. The key is not to use them as a replacement for a physician, but as an assistant to the physician—again, to boost capacity.
Q: How did your background with the military, FEMA, and the Red Cross prepare you for what you’re doing now?
A: Business as usual is very difficult to do in a chaotic environment, so I began to appreciate the importance of systems. If you’re relying on an individual and that individual leaves, your entity is in trouble. If you put good systems into place, you’re not so reliant on any one individual. Systems can function long after any individual doctor has come and gone. In the world of hospitalists—where there’s still fairly high turnover, being a young field and there are many opportunities—it’s imperative the systems approach is taken. TH
Mark Leiser is a freelance writer in New Jersey.
Many physicians use traditional practice as their stepping stone to a hospitalist career. David M. Grace, MD, took a far more unconventional path.
He served as a combat medic in the Army National Guard, joined a disaster medical assistance team at the Federal Emergency Management Agency (FEMA), and volunteered to help the American Red Cross in times of crisis—all before entering medical school.
Dr. Grace became a hospitalist in 2002, and now serves as hospitalist division area medical officer for The Schumacher Group, a staffing and consulting firm in Lafayette, La., that hires physicians as independent contractors to work in hospitals across the country.
But 21 years into his healthcare career, he continues to seek opportunities that offer the same two rewards: “I want to be filled with Adrenalin,” he says, “but I still want to use my brains.”
—David M. Grace, MD, The Schumacher Group, Lafayette, La.
Question: Given your varied background, how did you wind up becoming a hospitalist?
Answer: My predoctoring resume reads like a fast track of becoming an emergency physician. In residency, I had heard the term “hospitalist.” I knew I liked dealing with sick patients. Emergency departments act as a fairly good filter, and anyone who gets through and upstairs truly is a sick patient. I figured if I were a hospitalist, all my patients would be sick, as opposed to just some. That really drove me to hospital medicine.
Q: You founded your own hospitalist company in 2005, but within two years, you joined The Schumacher Group. Why did you make the switch?
A: With the speed with which hospital medicine is growing, I thought if I could tap into their resources and infrastructure … I’d be able to do things I couldn’t do in my own group for years, if not decades. I really thought I would be able to impact a far larger portion of patient lives with them than I could in my own smaller, somewhat homemade group.
Q: When The Schumacher Group formed, it focused on emergency departments. In 2007, it launched a hospitalist service. What’s the benefit?
A: If you put good hospitalist systems under the same umbrella as good emergency department systems, you can do things to boost the synergy between the two disciplines and improve patient care. In the facilities where we’re managing both the ED and the hospitalists, we can effect patient care from the moment the patient swings through the ambulance bay doors until the moment they are discharged.
Q: How successful has the HM effort been?
A: The hospitalist side, by the end of the year, will have about 20 to 25 practices up and running, with growth in the neighborhood of 10 to 15 practices a year expected to come on line.
Q: What are the advantages to a private corporation setup?
A: At the end of the day, doctors need to be patient-care advocates. But if you are employed by a hospital, they sign your check. When push comes to shove on a quality issue, I think there’s a tendency not to shove as hard when the person you’re shoving is the person employing you.
Q: Could this approach be the wave of the future?
A: I think so. It goes back to the idea of focusing all of your resources into one small area, such as hospital medicine or inpatient medicine, so there’s far fewer distractions than for a hospital that runs its own hospitalist program. We saw that in the 1970s, when hospitals were buying primary-care practices left and right. They realized they didn’t have the skills or the resources to make that effective, and they rapidly divested.
Q: Most doctors at the executive level of The Schumacher Group—including yourself—still practice medicine. Why is that so integral to the mission?
A: When I served in the military, the best officers I served under were officers who had been enlisted men earlier in their career. The same follows suit in hospital medicine. When I make an administrative decision, it can affect thousands of patient lives tomorrow. I can mentally track the effects of my decision all the way back to how it will affect the patient laying in the bed. If you’re not having that constantly reinforced by seeing patients, it’s very easy to lose track of it, and that has such a profound effect on patient care.
Q: SHM recently designated you one of the inaugural “Fellows in Hospital Medicine.” What is the biggest reward of a HM career?
A: For me, there are two. One is the ability to see the fruits of your labor much more rapidly than in the outpatient world. I can have a patient in bed in front of me actively dying and watch them a week later walk out of hospital in good condition. That’s a very different timetable than the outpatient world, when you may put a patient on all the right medicines to reduce the risk of a heart attack and, over 60 years, watch them not have a heart attack. The other thing I find very rewarding is the amount of measurements and data collected on what we do. We get feedback ranging from patient satisfaction scores to referring physician scores to readmission rates to data that shows if we are able to get patients better outcomes at lower costs. You just don’t get that type of feedback in many other fields.
Q: What is the greatest challenge facing the profession?
A: One of the biggest is the supply and demand mismatch. Right now, one of the hardest jobs is a hospitalist recruiter. With every physician having five to 10 open job offers …recruiting is difficult, and recruiting the right physician is extremely difficult.
Q: How can that be addressed?
A: One way is to be efficient. Can we see more patients in the same amount of time with no decrease in quality? For us, it involves the use of what we call a practice coordinator. It’s an employee of The Schumacher Group who is located in the individual hospital who does everything from assisting with managing the practice to answering telephone calls. This really allows us to help us organize our time better, so we don’t get bogged down in nonclinical work. Every minute spent on the phone with an insurance company or home health agency is a minute not spent at the bedside. Another way is expanding the use of midlevel providers. The key is not to use them as a replacement for a physician, but as an assistant to the physician—again, to boost capacity.
Q: How did your background with the military, FEMA, and the Red Cross prepare you for what you’re doing now?
A: Business as usual is very difficult to do in a chaotic environment, so I began to appreciate the importance of systems. If you’re relying on an individual and that individual leaves, your entity is in trouble. If you put good systems into place, you’re not so reliant on any one individual. Systems can function long after any individual doctor has come and gone. In the world of hospitalists—where there’s still fairly high turnover, being a young field and there are many opportunities—it’s imperative the systems approach is taken. TH
Mark Leiser is a freelance writer in New Jersey.
Many physicians use traditional practice as their stepping stone to a hospitalist career. David M. Grace, MD, took a far more unconventional path.
He served as a combat medic in the Army National Guard, joined a disaster medical assistance team at the Federal Emergency Management Agency (FEMA), and volunteered to help the American Red Cross in times of crisis—all before entering medical school.
Dr. Grace became a hospitalist in 2002, and now serves as hospitalist division area medical officer for The Schumacher Group, a staffing and consulting firm in Lafayette, La., that hires physicians as independent contractors to work in hospitals across the country.
But 21 years into his healthcare career, he continues to seek opportunities that offer the same two rewards: “I want to be filled with Adrenalin,” he says, “but I still want to use my brains.”
—David M. Grace, MD, The Schumacher Group, Lafayette, La.
Question: Given your varied background, how did you wind up becoming a hospitalist?
Answer: My predoctoring resume reads like a fast track of becoming an emergency physician. In residency, I had heard the term “hospitalist.” I knew I liked dealing with sick patients. Emergency departments act as a fairly good filter, and anyone who gets through and upstairs truly is a sick patient. I figured if I were a hospitalist, all my patients would be sick, as opposed to just some. That really drove me to hospital medicine.
Q: You founded your own hospitalist company in 2005, but within two years, you joined The Schumacher Group. Why did you make the switch?
A: With the speed with which hospital medicine is growing, I thought if I could tap into their resources and infrastructure … I’d be able to do things I couldn’t do in my own group for years, if not decades. I really thought I would be able to impact a far larger portion of patient lives with them than I could in my own smaller, somewhat homemade group.
Q: When The Schumacher Group formed, it focused on emergency departments. In 2007, it launched a hospitalist service. What’s the benefit?
A: If you put good hospitalist systems under the same umbrella as good emergency department systems, you can do things to boost the synergy between the two disciplines and improve patient care. In the facilities where we’re managing both the ED and the hospitalists, we can effect patient care from the moment the patient swings through the ambulance bay doors until the moment they are discharged.
Q: How successful has the HM effort been?
A: The hospitalist side, by the end of the year, will have about 20 to 25 practices up and running, with growth in the neighborhood of 10 to 15 practices a year expected to come on line.
Q: What are the advantages to a private corporation setup?
A: At the end of the day, doctors need to be patient-care advocates. But if you are employed by a hospital, they sign your check. When push comes to shove on a quality issue, I think there’s a tendency not to shove as hard when the person you’re shoving is the person employing you.
Q: Could this approach be the wave of the future?
A: I think so. It goes back to the idea of focusing all of your resources into one small area, such as hospital medicine or inpatient medicine, so there’s far fewer distractions than for a hospital that runs its own hospitalist program. We saw that in the 1970s, when hospitals were buying primary-care practices left and right. They realized they didn’t have the skills or the resources to make that effective, and they rapidly divested.
Q: Most doctors at the executive level of The Schumacher Group—including yourself—still practice medicine. Why is that so integral to the mission?
A: When I served in the military, the best officers I served under were officers who had been enlisted men earlier in their career. The same follows suit in hospital medicine. When I make an administrative decision, it can affect thousands of patient lives tomorrow. I can mentally track the effects of my decision all the way back to how it will affect the patient laying in the bed. If you’re not having that constantly reinforced by seeing patients, it’s very easy to lose track of it, and that has such a profound effect on patient care.
Q: SHM recently designated you one of the inaugural “Fellows in Hospital Medicine.” What is the biggest reward of a HM career?
A: For me, there are two. One is the ability to see the fruits of your labor much more rapidly than in the outpatient world. I can have a patient in bed in front of me actively dying and watch them a week later walk out of hospital in good condition. That’s a very different timetable than the outpatient world, when you may put a patient on all the right medicines to reduce the risk of a heart attack and, over 60 years, watch them not have a heart attack. The other thing I find very rewarding is the amount of measurements and data collected on what we do. We get feedback ranging from patient satisfaction scores to referring physician scores to readmission rates to data that shows if we are able to get patients better outcomes at lower costs. You just don’t get that type of feedback in many other fields.
Q: What is the greatest challenge facing the profession?
A: One of the biggest is the supply and demand mismatch. Right now, one of the hardest jobs is a hospitalist recruiter. With every physician having five to 10 open job offers …recruiting is difficult, and recruiting the right physician is extremely difficult.
Q: How can that be addressed?
A: One way is to be efficient. Can we see more patients in the same amount of time with no decrease in quality? For us, it involves the use of what we call a practice coordinator. It’s an employee of The Schumacher Group who is located in the individual hospital who does everything from assisting with managing the practice to answering telephone calls. This really allows us to help us organize our time better, so we don’t get bogged down in nonclinical work. Every minute spent on the phone with an insurance company or home health agency is a minute not spent at the bedside. Another way is expanding the use of midlevel providers. The key is not to use them as a replacement for a physician, but as an assistant to the physician—again, to boost capacity.
Q: How did your background with the military, FEMA, and the Red Cross prepare you for what you’re doing now?
A: Business as usual is very difficult to do in a chaotic environment, so I began to appreciate the importance of systems. If you’re relying on an individual and that individual leaves, your entity is in trouble. If you put good systems into place, you’re not so reliant on any one individual. Systems can function long after any individual doctor has come and gone. In the world of hospitalists—where there’s still fairly high turnover, being a young field and there are many opportunities—it’s imperative the systems approach is taken. TH
Mark Leiser is a freelance writer in New Jersey.
The ABCs of CMS
Now, more than ever, major changes in the way healthcare is provided, measured, and paid for seem to be coming from a single source: the Centers for Medicare and Medicaid Services (CMS). From the Physician Quality Reporting Initiative (PQRI) to last summer’s Medicare Physician Fee Schedule, CMS has an ever-growing influence on U.S. healthcare.
Although it has published numerous articles about CMS and its policies, The Hospitalist has never offered an explanatory overview of one of the largest healthcare agencies in the world. In order to help hospitalists understand the policies, payments, and trends that affect them every day, we have prepared this CMS fact sheet.
Agency Background
CMS falls under the jurisdiction of the U.S. Department of Health and Human Services, and is tasked primarily with administering the Medicare program and working in partnership with state governments to administer Medicaid and the State Children’s Health Insurance Program (SCHIP). CMS’ current mission is “to ensure effective, up-to-date healthcare coverage and to promote quality care for beneficiaries,” which is a more modern focus than when the Medicare and Medicaid programs were first signed into law in 1965. Those programs were created solely to provide healthcare coverage to Americans over the age of 65, as well as low-income children and people with certain disabilities.
CMS has grown in size and scope since its inception. “First and foremost, CMS is the largest single payor for healthcare in the United States,” says Patrick J. Torcson, MD, MMM, FACP, director of hospital medicine at St. Tammany Parish Hospital in Covington, La., and chair of SHM’s Performance and Standards Committee. Insurance companies model their coverage and fee schedules after CMS. “That makes it very important for reimbursement.”
Approximately 45 million Americans are Medicare beneficiaries, and CMS pays reimbursements for more than 90 million people through the Medicare, Medicaid, and SCHIP programs. Hospitalists treat so many of these beneficiaries that Dr. Torcson estimates CMS represents “at least a third” of the payor mix for most adult hospitalists. For hospitals, the percentage is larger: “For acute-care public hospitals, I’d estimate that Medicare is probably 50% of the payor mix,” Dr. Torcson says.
Part A and Part B
When a beneficiary is hospitalized, Medicare pays separately for hospital services (Part A) and physician services (Part B). Because of their unique role in the hospital, most hospitalists receive payment through both Medicare reimbursement plans. “Physicians are never paid under Part A, but most hospital medicine groups receive some subsidy from their hospital, and, of course, that money originally comes from Part A,” Dr. Torcson explains.
Medicare Part A reimbursement applies to inpatient care in hospitals, critical-access hospitals, and skilled nursing facilities. It does not apply to custodial or long-term care, but it does help cover hospice care and some home healthcare.
Medicare Part B covers medically necessary services and supplies. Most beneficiaries pay a premium to receive this coverage, which includes outpatient care, doctor services, physical or occupational therapists, and additional home healthcare. Part B also covers nonphysician services and procedures.
Part B reimbursement is dictated by the CMS Physician Fee Schedule, which is released every year in the agency’s Final Rule (see “Medicare Modifications,” January 2009, p. 17). You may recall the scramble each of the past three years to urge Congress to avert a 10.6% cut in Part B payments to doctors.
“From the physician side, we still have this …hanging over our heads,” Dr. Torcson says. “Every year, we manage to avert a 10% cut in pay. Now we only have until this summer to block that cut again, unless there is a complete reform of how Part B is reimbursed.”
Congress Calls the Shots
Although CMS administers the Medicare programs and writes the checks, Congress sets the agency’s budgets and directives. Congress must pass into law every CMS initiative, including the Physician Compare Web site that publicizes PQRI data and reimbursement for follow-up inpatient telehealth consultations.
Congress is advised on healthcare issues by an independent agency, the Medicare Payment Advisory Commission (MedPAC). The 17-member MedPAC board advises Congress about payments to providers in Medicare’s traditional fee-for-service program as well as private health plans participating in Medicare. MedPAC also is tasked with analyzing access to care, quality of care, and other issues relating to Medicare. “They’re not a governing board,” Dr. Torcson says. “MedPAC clearly functions as an advisory panel. The final authority is through Congress.”
CMS Sets the Direction
In addition to putting money in hospitalists’ pockets, CMS plays an important role in setting nationwide trends for healthcare payment and policies. As the largest and most powerful payor in the U.S., the agency often acts as a model for other payors—namely, private insurance companies.
Dr. Torcson points to two historic changes in payment reform: “By 1983, there was a turning point when hospitals began getting payment through the DRG [diagnosis-related group] system. Private payors started following along.” And when the Medicare physician fee schedule was introduced in the 1990s, “private payors began basing their physician payments on the physician fee schedule.”
Private payors are watching CMS initiatives (e.g., PQRI and value-based purchasing) to see how physician payment develops in the future.
“CMS is powerful and it’s going to become more so,” Dr. Torcson predicts. “It’s going to continue to be a model of healthcare reform, with its focus on aligning quality and cost in concepts like value-based purchasing.”
For the time being, no one knows the exact shape U.S. healthcare reform will take or how fast it might happen. But one thing is certain: CMS will be at the forefront of changes that have a major effect on how hospitalists work, as well as how they are compensated. TH
Jane Jerrard is a medical writer based in Chicago.
Now, more than ever, major changes in the way healthcare is provided, measured, and paid for seem to be coming from a single source: the Centers for Medicare and Medicaid Services (CMS). From the Physician Quality Reporting Initiative (PQRI) to last summer’s Medicare Physician Fee Schedule, CMS has an ever-growing influence on U.S. healthcare.
Although it has published numerous articles about CMS and its policies, The Hospitalist has never offered an explanatory overview of one of the largest healthcare agencies in the world. In order to help hospitalists understand the policies, payments, and trends that affect them every day, we have prepared this CMS fact sheet.
Agency Background
CMS falls under the jurisdiction of the U.S. Department of Health and Human Services, and is tasked primarily with administering the Medicare program and working in partnership with state governments to administer Medicaid and the State Children’s Health Insurance Program (SCHIP). CMS’ current mission is “to ensure effective, up-to-date healthcare coverage and to promote quality care for beneficiaries,” which is a more modern focus than when the Medicare and Medicaid programs were first signed into law in 1965. Those programs were created solely to provide healthcare coverage to Americans over the age of 65, as well as low-income children and people with certain disabilities.
CMS has grown in size and scope since its inception. “First and foremost, CMS is the largest single payor for healthcare in the United States,” says Patrick J. Torcson, MD, MMM, FACP, director of hospital medicine at St. Tammany Parish Hospital in Covington, La., and chair of SHM’s Performance and Standards Committee. Insurance companies model their coverage and fee schedules after CMS. “That makes it very important for reimbursement.”
Approximately 45 million Americans are Medicare beneficiaries, and CMS pays reimbursements for more than 90 million people through the Medicare, Medicaid, and SCHIP programs. Hospitalists treat so many of these beneficiaries that Dr. Torcson estimates CMS represents “at least a third” of the payor mix for most adult hospitalists. For hospitals, the percentage is larger: “For acute-care public hospitals, I’d estimate that Medicare is probably 50% of the payor mix,” Dr. Torcson says.
Part A and Part B
When a beneficiary is hospitalized, Medicare pays separately for hospital services (Part A) and physician services (Part B). Because of their unique role in the hospital, most hospitalists receive payment through both Medicare reimbursement plans. “Physicians are never paid under Part A, but most hospital medicine groups receive some subsidy from their hospital, and, of course, that money originally comes from Part A,” Dr. Torcson explains.
Medicare Part A reimbursement applies to inpatient care in hospitals, critical-access hospitals, and skilled nursing facilities. It does not apply to custodial or long-term care, but it does help cover hospice care and some home healthcare.
Medicare Part B covers medically necessary services and supplies. Most beneficiaries pay a premium to receive this coverage, which includes outpatient care, doctor services, physical or occupational therapists, and additional home healthcare. Part B also covers nonphysician services and procedures.
Part B reimbursement is dictated by the CMS Physician Fee Schedule, which is released every year in the agency’s Final Rule (see “Medicare Modifications,” January 2009, p. 17). You may recall the scramble each of the past three years to urge Congress to avert a 10.6% cut in Part B payments to doctors.
“From the physician side, we still have this …hanging over our heads,” Dr. Torcson says. “Every year, we manage to avert a 10% cut in pay. Now we only have until this summer to block that cut again, unless there is a complete reform of how Part B is reimbursed.”
Congress Calls the Shots
Although CMS administers the Medicare programs and writes the checks, Congress sets the agency’s budgets and directives. Congress must pass into law every CMS initiative, including the Physician Compare Web site that publicizes PQRI data and reimbursement for follow-up inpatient telehealth consultations.
Congress is advised on healthcare issues by an independent agency, the Medicare Payment Advisory Commission (MedPAC). The 17-member MedPAC board advises Congress about payments to providers in Medicare’s traditional fee-for-service program as well as private health plans participating in Medicare. MedPAC also is tasked with analyzing access to care, quality of care, and other issues relating to Medicare. “They’re not a governing board,” Dr. Torcson says. “MedPAC clearly functions as an advisory panel. The final authority is through Congress.”
CMS Sets the Direction
In addition to putting money in hospitalists’ pockets, CMS plays an important role in setting nationwide trends for healthcare payment and policies. As the largest and most powerful payor in the U.S., the agency often acts as a model for other payors—namely, private insurance companies.
Dr. Torcson points to two historic changes in payment reform: “By 1983, there was a turning point when hospitals began getting payment through the DRG [diagnosis-related group] system. Private payors started following along.” And when the Medicare physician fee schedule was introduced in the 1990s, “private payors began basing their physician payments on the physician fee schedule.”
Private payors are watching CMS initiatives (e.g., PQRI and value-based purchasing) to see how physician payment develops in the future.
“CMS is powerful and it’s going to become more so,” Dr. Torcson predicts. “It’s going to continue to be a model of healthcare reform, with its focus on aligning quality and cost in concepts like value-based purchasing.”
For the time being, no one knows the exact shape U.S. healthcare reform will take or how fast it might happen. But one thing is certain: CMS will be at the forefront of changes that have a major effect on how hospitalists work, as well as how they are compensated. TH
Jane Jerrard is a medical writer based in Chicago.
Now, more than ever, major changes in the way healthcare is provided, measured, and paid for seem to be coming from a single source: the Centers for Medicare and Medicaid Services (CMS). From the Physician Quality Reporting Initiative (PQRI) to last summer’s Medicare Physician Fee Schedule, CMS has an ever-growing influence on U.S. healthcare.
Although it has published numerous articles about CMS and its policies, The Hospitalist has never offered an explanatory overview of one of the largest healthcare agencies in the world. In order to help hospitalists understand the policies, payments, and trends that affect them every day, we have prepared this CMS fact sheet.
Agency Background
CMS falls under the jurisdiction of the U.S. Department of Health and Human Services, and is tasked primarily with administering the Medicare program and working in partnership with state governments to administer Medicaid and the State Children’s Health Insurance Program (SCHIP). CMS’ current mission is “to ensure effective, up-to-date healthcare coverage and to promote quality care for beneficiaries,” which is a more modern focus than when the Medicare and Medicaid programs were first signed into law in 1965. Those programs were created solely to provide healthcare coverage to Americans over the age of 65, as well as low-income children and people with certain disabilities.
CMS has grown in size and scope since its inception. “First and foremost, CMS is the largest single payor for healthcare in the United States,” says Patrick J. Torcson, MD, MMM, FACP, director of hospital medicine at St. Tammany Parish Hospital in Covington, La., and chair of SHM’s Performance and Standards Committee. Insurance companies model their coverage and fee schedules after CMS. “That makes it very important for reimbursement.”
Approximately 45 million Americans are Medicare beneficiaries, and CMS pays reimbursements for more than 90 million people through the Medicare, Medicaid, and SCHIP programs. Hospitalists treat so many of these beneficiaries that Dr. Torcson estimates CMS represents “at least a third” of the payor mix for most adult hospitalists. For hospitals, the percentage is larger: “For acute-care public hospitals, I’d estimate that Medicare is probably 50% of the payor mix,” Dr. Torcson says.
Part A and Part B
When a beneficiary is hospitalized, Medicare pays separately for hospital services (Part A) and physician services (Part B). Because of their unique role in the hospital, most hospitalists receive payment through both Medicare reimbursement plans. “Physicians are never paid under Part A, but most hospital medicine groups receive some subsidy from their hospital, and, of course, that money originally comes from Part A,” Dr. Torcson explains.
Medicare Part A reimbursement applies to inpatient care in hospitals, critical-access hospitals, and skilled nursing facilities. It does not apply to custodial or long-term care, but it does help cover hospice care and some home healthcare.
Medicare Part B covers medically necessary services and supplies. Most beneficiaries pay a premium to receive this coverage, which includes outpatient care, doctor services, physical or occupational therapists, and additional home healthcare. Part B also covers nonphysician services and procedures.
Part B reimbursement is dictated by the CMS Physician Fee Schedule, which is released every year in the agency’s Final Rule (see “Medicare Modifications,” January 2009, p. 17). You may recall the scramble each of the past three years to urge Congress to avert a 10.6% cut in Part B payments to doctors.
“From the physician side, we still have this …hanging over our heads,” Dr. Torcson says. “Every year, we manage to avert a 10% cut in pay. Now we only have until this summer to block that cut again, unless there is a complete reform of how Part B is reimbursed.”
Congress Calls the Shots
Although CMS administers the Medicare programs and writes the checks, Congress sets the agency’s budgets and directives. Congress must pass into law every CMS initiative, including the Physician Compare Web site that publicizes PQRI data and reimbursement for follow-up inpatient telehealth consultations.
Congress is advised on healthcare issues by an independent agency, the Medicare Payment Advisory Commission (MedPAC). The 17-member MedPAC board advises Congress about payments to providers in Medicare’s traditional fee-for-service program as well as private health plans participating in Medicare. MedPAC also is tasked with analyzing access to care, quality of care, and other issues relating to Medicare. “They’re not a governing board,” Dr. Torcson says. “MedPAC clearly functions as an advisory panel. The final authority is through Congress.”
CMS Sets the Direction
In addition to putting money in hospitalists’ pockets, CMS plays an important role in setting nationwide trends for healthcare payment and policies. As the largest and most powerful payor in the U.S., the agency often acts as a model for other payors—namely, private insurance companies.
Dr. Torcson points to two historic changes in payment reform: “By 1983, there was a turning point when hospitals began getting payment through the DRG [diagnosis-related group] system. Private payors started following along.” And when the Medicare physician fee schedule was introduced in the 1990s, “private payors began basing their physician payments on the physician fee schedule.”
Private payors are watching CMS initiatives (e.g., PQRI and value-based purchasing) to see how physician payment develops in the future.
“CMS is powerful and it’s going to become more so,” Dr. Torcson predicts. “It’s going to continue to be a model of healthcare reform, with its focus on aligning quality and cost in concepts like value-based purchasing.”
For the time being, no one knows the exact shape U.S. healthcare reform will take or how fast it might happen. But one thing is certain: CMS will be at the forefront of changes that have a major effect on how hospitalists work, as well as how they are compensated. TH
Jane Jerrard is a medical writer based in Chicago.
Multiply Your Contacts
Networking is crucial to career advancement, no matter what your long-term goals are. Connecting with others in hospital medicine, general healthcare, and business can build your knowledge base, your support system, and your reputation. But how—and why—should hospitalists present themselves to the influential people they need to know?
The Need to Network
You may think it’s not necessary to expand your list of contacts within hospital medicine. Put another way, why bother to network? Vineet Arora, MD, MA, assistant professor of medicine at the Pritzker School of Medicine at University of Chicago, points to a paper, “Strength of Weak Ties,” published in the May 1973 American Journal of Sociology by sociologist Mark Granovetter. In the paper, he presents a social science theory that says “the people who are most helpful to you are those who you don’t know well,” Dr. Arora says. Granovetter’s theory suggests that in marketing or politics, the weak ties enable individuals to reach populations and audiences that are not accessible via strong ties.
“It’s not your friends or the people you know the best who are most likely to help you get a job,” Dr. Arora says. “Those people have already helped you as much as they can.” The main lesson here, she says, is to “think carefully about reaching outside your comfort zone. Introduce yourself to a stranger; it’s to your advantage to cultivate these weak ties.”
To increase your number of “weak ties” in hospital medicine, follow these simple steps:
Step 1: Establish Goals
Consider why you’re networking in order to focus your efforts and target your contacts. Are you looking for a new position? Do you want to transform yourself into the go-to hospitalist in a specific clinical area? Are you looking to learn leadership skills?
Once you’ve determined what you want to get out of networking—and it might be more than one goal—outline a brief elevator speech. It’s a one-minute explanation of who you are and what you’re interested in. It will prepare you to open a conversation with a stranger. “You should present yourself in a concise way,” Dr. Arora stresses. “State who you are and what your interests are.”
Step 2: Make a Plan
Once you know your goals and are able to state them clearly and eloquently, map out your networking strategy. You may simply keep this in the back of your mind for the short term, or you may specifically plan on attending events that will allow you to network with the appropriate people, such as hiring managers, experts in your area of interest, or HM movers and shakers.
“Figure out who the people are in your field of interest who are making waves, and go where they are,” Dr. Arora says. But “don’t just attend the meetings. Be proactive.”
Choose your conferences wisely. For example, if you’re interested in leadership skills or a leadership position, consider SHM’s biannual Leadership Academy. “Not only is this a terrific learning opportunity, it’s a very strong networking environment,” says Russell L. Holman, MD, chief operating officer for Cogent Healthcare in Nashville, Tenn., and past president of SHM. “You’re sharing a room with 120 or 130 leaders or leaders-in-training.”
Dozens of annual conferences and courses are available for networking, including clinical CME courses offered by universities. “The American College of Physician Executives [ACPE] has advanced training courses not only in management, but in quality improvement and a variety of other interests,” Dr. Holman explains.
Networking at industry events may not have an immediate payoff, Dr. Arora warns. “You’re probably not going to land a job or land an opportunity at a meeting,” she says, “but you float your name and get to know people.”
Step 3: Let the Networking Begin
With your short speech ready to go, attend a conference or meeting with key industry leaders and simply approach influential individuals you’d like to meet.
“The way it’s done is even more important than where and when you do it,” Dr. Holman says. “You don’t want to come across as pushy, aggressive, or needy.” Simply introduce yourself with a handshake, rely on your elevator speech for a brief explanation, then give that person a chance to talk. Ask questions about how their career advanced, then ask if they know of any opportunities for you, he says.
If your initial conversation is rushed—say, you’re approaching a speaker after a presentation—keep your conversation brief. “At an event like an SHM meeting, it may be difficult to catch certain people,” Dr. Holman says. “If you can, at least shake their hand and exchange business cards, then follow up with an e-mail and ask for 15 minutes of their time. This is very acceptable; it happens to me all the time.”
Another key piece of advice: “Don’t ask them to contact you—you be the one to send an e-mail,” Dr. Holman says.
Step 4: Follow Up
Soon after the in-person meeting, send a follow-up e-mail. Carefully consider your subject line to ensure your message is read. Reference your encounter in the message (e.g., “We met after your presentation at the conference in Miami”) to remind the person who you are. Depending on your goals, you may ask for information to be forwarded, contacts for additional networking, or request a brief telephone conversation.
“A lot of speakers post their e-mail in their presentation,” Dr. Arora points out. “If you don’t get a chance to talk to them in person, send them a message after you get home. People love to get feedback. Comment on their presentation and introduce yourself that way.”
Hospitalists can strengthen their connections with an offer to reciprocate: “You want to be as helpful as you are helped,” Dr. Holman says. “End the conversation with the offer: ‘If there is any way that I can help you, let me know.’ ”
Set goals, practice your elevator speech, venture out and introduce yourself, and follow up.
These simple steps will help you in your networking efforts, and likely will help advance your career. TH
Jane Jerrard is a medical writer based in Chicago. She also writes “Public Policy” for The Hospitalist.
Networking is crucial to career advancement, no matter what your long-term goals are. Connecting with others in hospital medicine, general healthcare, and business can build your knowledge base, your support system, and your reputation. But how—and why—should hospitalists present themselves to the influential people they need to know?
The Need to Network
You may think it’s not necessary to expand your list of contacts within hospital medicine. Put another way, why bother to network? Vineet Arora, MD, MA, assistant professor of medicine at the Pritzker School of Medicine at University of Chicago, points to a paper, “Strength of Weak Ties,” published in the May 1973 American Journal of Sociology by sociologist Mark Granovetter. In the paper, he presents a social science theory that says “the people who are most helpful to you are those who you don’t know well,” Dr. Arora says. Granovetter’s theory suggests that in marketing or politics, the weak ties enable individuals to reach populations and audiences that are not accessible via strong ties.
“It’s not your friends or the people you know the best who are most likely to help you get a job,” Dr. Arora says. “Those people have already helped you as much as they can.” The main lesson here, she says, is to “think carefully about reaching outside your comfort zone. Introduce yourself to a stranger; it’s to your advantage to cultivate these weak ties.”
To increase your number of “weak ties” in hospital medicine, follow these simple steps:
Step 1: Establish Goals
Consider why you’re networking in order to focus your efforts and target your contacts. Are you looking for a new position? Do you want to transform yourself into the go-to hospitalist in a specific clinical area? Are you looking to learn leadership skills?
Once you’ve determined what you want to get out of networking—and it might be more than one goal—outline a brief elevator speech. It’s a one-minute explanation of who you are and what you’re interested in. It will prepare you to open a conversation with a stranger. “You should present yourself in a concise way,” Dr. Arora stresses. “State who you are and what your interests are.”
Step 2: Make a Plan
Once you know your goals and are able to state them clearly and eloquently, map out your networking strategy. You may simply keep this in the back of your mind for the short term, or you may specifically plan on attending events that will allow you to network with the appropriate people, such as hiring managers, experts in your area of interest, or HM movers and shakers.
“Figure out who the people are in your field of interest who are making waves, and go where they are,” Dr. Arora says. But “don’t just attend the meetings. Be proactive.”
Choose your conferences wisely. For example, if you’re interested in leadership skills or a leadership position, consider SHM’s biannual Leadership Academy. “Not only is this a terrific learning opportunity, it’s a very strong networking environment,” says Russell L. Holman, MD, chief operating officer for Cogent Healthcare in Nashville, Tenn., and past president of SHM. “You’re sharing a room with 120 or 130 leaders or leaders-in-training.”
Dozens of annual conferences and courses are available for networking, including clinical CME courses offered by universities. “The American College of Physician Executives [ACPE] has advanced training courses not only in management, but in quality improvement and a variety of other interests,” Dr. Holman explains.
Networking at industry events may not have an immediate payoff, Dr. Arora warns. “You’re probably not going to land a job or land an opportunity at a meeting,” she says, “but you float your name and get to know people.”
Step 3: Let the Networking Begin
With your short speech ready to go, attend a conference or meeting with key industry leaders and simply approach influential individuals you’d like to meet.
“The way it’s done is even more important than where and when you do it,” Dr. Holman says. “You don’t want to come across as pushy, aggressive, or needy.” Simply introduce yourself with a handshake, rely on your elevator speech for a brief explanation, then give that person a chance to talk. Ask questions about how their career advanced, then ask if they know of any opportunities for you, he says.
If your initial conversation is rushed—say, you’re approaching a speaker after a presentation—keep your conversation brief. “At an event like an SHM meeting, it may be difficult to catch certain people,” Dr. Holman says. “If you can, at least shake their hand and exchange business cards, then follow up with an e-mail and ask for 15 minutes of their time. This is very acceptable; it happens to me all the time.”
Another key piece of advice: “Don’t ask them to contact you—you be the one to send an e-mail,” Dr. Holman says.
Step 4: Follow Up
Soon after the in-person meeting, send a follow-up e-mail. Carefully consider your subject line to ensure your message is read. Reference your encounter in the message (e.g., “We met after your presentation at the conference in Miami”) to remind the person who you are. Depending on your goals, you may ask for information to be forwarded, contacts for additional networking, or request a brief telephone conversation.
“A lot of speakers post their e-mail in their presentation,” Dr. Arora points out. “If you don’t get a chance to talk to them in person, send them a message after you get home. People love to get feedback. Comment on their presentation and introduce yourself that way.”
Hospitalists can strengthen their connections with an offer to reciprocate: “You want to be as helpful as you are helped,” Dr. Holman says. “End the conversation with the offer: ‘If there is any way that I can help you, let me know.’ ”
Set goals, practice your elevator speech, venture out and introduce yourself, and follow up.
These simple steps will help you in your networking efforts, and likely will help advance your career. TH
Jane Jerrard is a medical writer based in Chicago. She also writes “Public Policy” for The Hospitalist.
Networking is crucial to career advancement, no matter what your long-term goals are. Connecting with others in hospital medicine, general healthcare, and business can build your knowledge base, your support system, and your reputation. But how—and why—should hospitalists present themselves to the influential people they need to know?
The Need to Network
You may think it’s not necessary to expand your list of contacts within hospital medicine. Put another way, why bother to network? Vineet Arora, MD, MA, assistant professor of medicine at the Pritzker School of Medicine at University of Chicago, points to a paper, “Strength of Weak Ties,” published in the May 1973 American Journal of Sociology by sociologist Mark Granovetter. In the paper, he presents a social science theory that says “the people who are most helpful to you are those who you don’t know well,” Dr. Arora says. Granovetter’s theory suggests that in marketing or politics, the weak ties enable individuals to reach populations and audiences that are not accessible via strong ties.
“It’s not your friends or the people you know the best who are most likely to help you get a job,” Dr. Arora says. “Those people have already helped you as much as they can.” The main lesson here, she says, is to “think carefully about reaching outside your comfort zone. Introduce yourself to a stranger; it’s to your advantage to cultivate these weak ties.”
To increase your number of “weak ties” in hospital medicine, follow these simple steps:
Step 1: Establish Goals
Consider why you’re networking in order to focus your efforts and target your contacts. Are you looking for a new position? Do you want to transform yourself into the go-to hospitalist in a specific clinical area? Are you looking to learn leadership skills?
Once you’ve determined what you want to get out of networking—and it might be more than one goal—outline a brief elevator speech. It’s a one-minute explanation of who you are and what you’re interested in. It will prepare you to open a conversation with a stranger. “You should present yourself in a concise way,” Dr. Arora stresses. “State who you are and what your interests are.”
Step 2: Make a Plan
Once you know your goals and are able to state them clearly and eloquently, map out your networking strategy. You may simply keep this in the back of your mind for the short term, or you may specifically plan on attending events that will allow you to network with the appropriate people, such as hiring managers, experts in your area of interest, or HM movers and shakers.
“Figure out who the people are in your field of interest who are making waves, and go where they are,” Dr. Arora says. But “don’t just attend the meetings. Be proactive.”
Choose your conferences wisely. For example, if you’re interested in leadership skills or a leadership position, consider SHM’s biannual Leadership Academy. “Not only is this a terrific learning opportunity, it’s a very strong networking environment,” says Russell L. Holman, MD, chief operating officer for Cogent Healthcare in Nashville, Tenn., and past president of SHM. “You’re sharing a room with 120 or 130 leaders or leaders-in-training.”
Dozens of annual conferences and courses are available for networking, including clinical CME courses offered by universities. “The American College of Physician Executives [ACPE] has advanced training courses not only in management, but in quality improvement and a variety of other interests,” Dr. Holman explains.
Networking at industry events may not have an immediate payoff, Dr. Arora warns. “You’re probably not going to land a job or land an opportunity at a meeting,” she says, “but you float your name and get to know people.”
Step 3: Let the Networking Begin
With your short speech ready to go, attend a conference or meeting with key industry leaders and simply approach influential individuals you’d like to meet.
“The way it’s done is even more important than where and when you do it,” Dr. Holman says. “You don’t want to come across as pushy, aggressive, or needy.” Simply introduce yourself with a handshake, rely on your elevator speech for a brief explanation, then give that person a chance to talk. Ask questions about how their career advanced, then ask if they know of any opportunities for you, he says.
If your initial conversation is rushed—say, you’re approaching a speaker after a presentation—keep your conversation brief. “At an event like an SHM meeting, it may be difficult to catch certain people,” Dr. Holman says. “If you can, at least shake their hand and exchange business cards, then follow up with an e-mail and ask for 15 minutes of their time. This is very acceptable; it happens to me all the time.”
Another key piece of advice: “Don’t ask them to contact you—you be the one to send an e-mail,” Dr. Holman says.
Step 4: Follow Up
Soon after the in-person meeting, send a follow-up e-mail. Carefully consider your subject line to ensure your message is read. Reference your encounter in the message (e.g., “We met after your presentation at the conference in Miami”) to remind the person who you are. Depending on your goals, you may ask for information to be forwarded, contacts for additional networking, or request a brief telephone conversation.
“A lot of speakers post their e-mail in their presentation,” Dr. Arora points out. “If you don’t get a chance to talk to them in person, send them a message after you get home. People love to get feedback. Comment on their presentation and introduce yourself that way.”
Hospitalists can strengthen their connections with an offer to reciprocate: “You want to be as helpful as you are helped,” Dr. Holman says. “End the conversation with the offer: ‘If there is any way that I can help you, let me know.’ ”
Set goals, practice your elevator speech, venture out and introduce yourself, and follow up.
These simple steps will help you in your networking efforts, and likely will help advance your career. TH
Jane Jerrard is a medical writer based in Chicago. She also writes “Public Policy” for The Hospitalist.
To Crush or Not to Crush
There are multiple reasons for crushing tablets or capsule contents before administering medications, but there are numerous medications that should not be crushed. These medications should not be chewed, either, usually due to their specific formulations and their pharmacokinetic properties.1 Most of the no-crush medications are sustained-release, oral-dosage formulas. The majority of extended-release products should not be crushed or chewed, although there are some newer slow-release tablet formulations available that are scored and can be divided or halved (e.g., Toprol XL).
A common reason for crushing a tablet or capsule is for use by a hospitalized patient with an enteral feeding tube. A recent review in the American Journal of Health-System Pharmacy provides more details about administering medications in patients with enteral feeding tubes.2 Oral solutions can be used when commercially available and medically appropriate. If an oral solution or suspension is not available, the hospital pharmacy should be consulted to determine if a liquid formulation of the product can be extemporaneously prepared. In some cases, after careful consideration of compatibility, stability, and drug absorption changes, an injectable formulation of a product may be used. You should always consult your hospital pharmacist for information on this modality of drug administration.
Some patients have difficulty swallowing tablets or capsules; some dislike the taste. In these cases, crushing of medication for powdered delivery (to be mixed with food or beverages) should be considered. But beware of certain caveats, as not all medications are suitable for crushing. Generally, meds that should not be crushed fall into one of these categories:
- Sustained-release tablets, which can be composed of multiple layers for different drug release times, as can beads within capsules. Some of the more common prefixes or suffixes for sustained-release, controlled-release, or controlled-delivery products include: 12-hour, 24-hour, CC, CD, CR, ER, LA, Retard, SA, Slo-, SR, XL, XR, or XT.
- Enteric-coated tablets, which are formulated because certain drugs can be irritating to the stomach or are degraded by stomach acid. By enteric-coating tablets or capsule beads, the drug’s release can be delayed until it reaches the small intestine. Prefixes include EN- and EC-.
Other medications have objectionable tastes and are sugar-coated to improve tolerability. If this type of medication is crushed, the patient would be subject to its unpleasant taste, which could significantly impair medication adherence. Additionally, both sublingual and effervescent medications should not be crushed because it will decrease the medication’s effectiveness.
Hospital Pharmacy publishes a wall chart that includes many of these types of formulations, along with their do’s and don’ts. If there is ever any doubt about the best way to administer a particular product or whether it can be halved or crushed, ask your pharmacist.3 TH
Michele B. Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City.
References
1. Mitchell J. Oral dosage forms that should not be crushed or chewed: facts and comparisons 4.0. Hospital Pharmacy Web site. Available at: online.factsandcomparisons.com/Viewer.aspx?book=atoz&monoID=fandc-atoz1040. Accessed March 5, 2009.
2. Williams NT. Medication administration through enteral feeding tubes. Am J Health Syst Pharm. 2008;65(24):2347-2357.
3. Mitchell JF. Oral dosage forms that should not be crushed: wall chart. Wolters Kluwer Health Web site. Available at: www.factsandcomparisons.com/Products/product.aspx?id=1111. Accessed Jan. 26, 2009.
4. Mylan's Matrix receives final FDA approval for the generic version of the antiretroviral Zerit capsules. Wolters Kluwer Health Web site. Available at: http://mylan.mediaroom.com/index.php?s=43&item=399. Accessed Jan. 23, 2009.
5. Product approval information. U.S. Food and Drug Administration Web site. Available at: www.fda.gov/Cber/products/Cinryze.htm. Accessed Jan. 14, 2009.
6. FDA licenses for marketing new therapy for rare genetic disease. U.S. Food and Drug Administration Web site. Available at: www.fda.gov/bbs/topics/NEWS/2008/NEW01903.html. Accessed Jan. 14, 2009.
7. Sancuso patch approved for nausea and vomiting. Monthly Prescribing Reference Web site. Available at: www.empr.com/Sancusopatchapprovedfornauseaandvomiting/article/122384/. Accessed Jan. 14, 2009.
8. TussiCaps now available for cough suppression. Monthly Prescribing Reference Web site. Available at: www.empr.com/TussiCapsnowavailableforcoughsuppression/article/122377/. Accessed Jan. 14, 2009.
9. UCB’s Vimpat approved by U.S. FDA as adjunctive therapy for partial onset seizures in adults. Medical News Today Web site. Available at: www.medicalnewstoday.com/articles/127354.php. Accessed Jan. 14, 2009.
10. Apriso granted FDA marketing approval for maintenance of remission of ulcerative colitis. Medical News Today Web site. Available at: http://www.medicalnewstoday.com/articles/127839.php. Accessed Jan. 14, 2009.
11. http://biz.yahoo.com/ap/081106/cv_therapeutics _ranexa.html?.v=1. Accessed February 2, 2009.
12. FDA approves Seroquel for bipolar maintenance. Monthly Prescribing Reference Web site. Available at: www.prescribingreference.com/news/showNews/which/SeroquelXRForBipolar10101. Accessed Jan. 14, 2009.
13. Seroquel XR Web site. Available at: www.pharmacistelink.com/news/2009/01/14_seroquel.pdf. Accessed Jan. 23, 2009.
14. Peck P. Smoking cessation drug linked to 1,001 new serious adverse events. Medpage Today Web site. Available at: www.medpagetoday.com/PrimaryCare/Smoking/11428. Accessed Jan. 14, 2009.
15. Public health advisory: important information on Chantix (varenicline). U.S. Food and Drug Administration Web site. Available at: www.fda.gov/CDER/Drug/advisory/varenicline.htm. Accessed Jan. 14, 2009.
There are multiple reasons for crushing tablets or capsule contents before administering medications, but there are numerous medications that should not be crushed. These medications should not be chewed, either, usually due to their specific formulations and their pharmacokinetic properties.1 Most of the no-crush medications are sustained-release, oral-dosage formulas. The majority of extended-release products should not be crushed or chewed, although there are some newer slow-release tablet formulations available that are scored and can be divided or halved (e.g., Toprol XL).
A common reason for crushing a tablet or capsule is for use by a hospitalized patient with an enteral feeding tube. A recent review in the American Journal of Health-System Pharmacy provides more details about administering medications in patients with enteral feeding tubes.2 Oral solutions can be used when commercially available and medically appropriate. If an oral solution or suspension is not available, the hospital pharmacy should be consulted to determine if a liquid formulation of the product can be extemporaneously prepared. In some cases, after careful consideration of compatibility, stability, and drug absorption changes, an injectable formulation of a product may be used. You should always consult your hospital pharmacist for information on this modality of drug administration.
Some patients have difficulty swallowing tablets or capsules; some dislike the taste. In these cases, crushing of medication for powdered delivery (to be mixed with food or beverages) should be considered. But beware of certain caveats, as not all medications are suitable for crushing. Generally, meds that should not be crushed fall into one of these categories:
- Sustained-release tablets, which can be composed of multiple layers for different drug release times, as can beads within capsules. Some of the more common prefixes or suffixes for sustained-release, controlled-release, or controlled-delivery products include: 12-hour, 24-hour, CC, CD, CR, ER, LA, Retard, SA, Slo-, SR, XL, XR, or XT.
- Enteric-coated tablets, which are formulated because certain drugs can be irritating to the stomach or are degraded by stomach acid. By enteric-coating tablets or capsule beads, the drug’s release can be delayed until it reaches the small intestine. Prefixes include EN- and EC-.
Other medications have objectionable tastes and are sugar-coated to improve tolerability. If this type of medication is crushed, the patient would be subject to its unpleasant taste, which could significantly impair medication adherence. Additionally, both sublingual and effervescent medications should not be crushed because it will decrease the medication’s effectiveness.
Hospital Pharmacy publishes a wall chart that includes many of these types of formulations, along with their do’s and don’ts. If there is ever any doubt about the best way to administer a particular product or whether it can be halved or crushed, ask your pharmacist.3 TH
Michele B. Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City.
References
1. Mitchell J. Oral dosage forms that should not be crushed or chewed: facts and comparisons 4.0. Hospital Pharmacy Web site. Available at: online.factsandcomparisons.com/Viewer.aspx?book=atoz&monoID=fandc-atoz1040. Accessed March 5, 2009.
2. Williams NT. Medication administration through enteral feeding tubes. Am J Health Syst Pharm. 2008;65(24):2347-2357.
3. Mitchell JF. Oral dosage forms that should not be crushed: wall chart. Wolters Kluwer Health Web site. Available at: www.factsandcomparisons.com/Products/product.aspx?id=1111. Accessed Jan. 26, 2009.
4. Mylan's Matrix receives final FDA approval for the generic version of the antiretroviral Zerit capsules. Wolters Kluwer Health Web site. Available at: http://mylan.mediaroom.com/index.php?s=43&item=399. Accessed Jan. 23, 2009.
5. Product approval information. U.S. Food and Drug Administration Web site. Available at: www.fda.gov/Cber/products/Cinryze.htm. Accessed Jan. 14, 2009.
6. FDA licenses for marketing new therapy for rare genetic disease. U.S. Food and Drug Administration Web site. Available at: www.fda.gov/bbs/topics/NEWS/2008/NEW01903.html. Accessed Jan. 14, 2009.
7. Sancuso patch approved for nausea and vomiting. Monthly Prescribing Reference Web site. Available at: www.empr.com/Sancusopatchapprovedfornauseaandvomiting/article/122384/. Accessed Jan. 14, 2009.
8. TussiCaps now available for cough suppression. Monthly Prescribing Reference Web site. Available at: www.empr.com/TussiCapsnowavailableforcoughsuppression/article/122377/. Accessed Jan. 14, 2009.
9. UCB’s Vimpat approved by U.S. FDA as adjunctive therapy for partial onset seizures in adults. Medical News Today Web site. Available at: www.medicalnewstoday.com/articles/127354.php. Accessed Jan. 14, 2009.
10. Apriso granted FDA marketing approval for maintenance of remission of ulcerative colitis. Medical News Today Web site. Available at: http://www.medicalnewstoday.com/articles/127839.php. Accessed Jan. 14, 2009.
11. http://biz.yahoo.com/ap/081106/cv_therapeutics _ranexa.html?.v=1. Accessed February 2, 2009.
12. FDA approves Seroquel for bipolar maintenance. Monthly Prescribing Reference Web site. Available at: www.prescribingreference.com/news/showNews/which/SeroquelXRForBipolar10101. Accessed Jan. 14, 2009.
13. Seroquel XR Web site. Available at: www.pharmacistelink.com/news/2009/01/14_seroquel.pdf. Accessed Jan. 23, 2009.
14. Peck P. Smoking cessation drug linked to 1,001 new serious adverse events. Medpage Today Web site. Available at: www.medpagetoday.com/PrimaryCare/Smoking/11428. Accessed Jan. 14, 2009.
15. Public health advisory: important information on Chantix (varenicline). U.S. Food and Drug Administration Web site. Available at: www.fda.gov/CDER/Drug/advisory/varenicline.htm. Accessed Jan. 14, 2009.
There are multiple reasons for crushing tablets or capsule contents before administering medications, but there are numerous medications that should not be crushed. These medications should not be chewed, either, usually due to their specific formulations and their pharmacokinetic properties.1 Most of the no-crush medications are sustained-release, oral-dosage formulas. The majority of extended-release products should not be crushed or chewed, although there are some newer slow-release tablet formulations available that are scored and can be divided or halved (e.g., Toprol XL).
A common reason for crushing a tablet or capsule is for use by a hospitalized patient with an enteral feeding tube. A recent review in the American Journal of Health-System Pharmacy provides more details about administering medications in patients with enteral feeding tubes.2 Oral solutions can be used when commercially available and medically appropriate. If an oral solution or suspension is not available, the hospital pharmacy should be consulted to determine if a liquid formulation of the product can be extemporaneously prepared. In some cases, after careful consideration of compatibility, stability, and drug absorption changes, an injectable formulation of a product may be used. You should always consult your hospital pharmacist for information on this modality of drug administration.
Some patients have difficulty swallowing tablets or capsules; some dislike the taste. In these cases, crushing of medication for powdered delivery (to be mixed with food or beverages) should be considered. But beware of certain caveats, as not all medications are suitable for crushing. Generally, meds that should not be crushed fall into one of these categories:
- Sustained-release tablets, which can be composed of multiple layers for different drug release times, as can beads within capsules. Some of the more common prefixes or suffixes for sustained-release, controlled-release, or controlled-delivery products include: 12-hour, 24-hour, CC, CD, CR, ER, LA, Retard, SA, Slo-, SR, XL, XR, or XT.
- Enteric-coated tablets, which are formulated because certain drugs can be irritating to the stomach or are degraded by stomach acid. By enteric-coating tablets or capsule beads, the drug’s release can be delayed until it reaches the small intestine. Prefixes include EN- and EC-.
Other medications have objectionable tastes and are sugar-coated to improve tolerability. If this type of medication is crushed, the patient would be subject to its unpleasant taste, which could significantly impair medication adherence. Additionally, both sublingual and effervescent medications should not be crushed because it will decrease the medication’s effectiveness.
Hospital Pharmacy publishes a wall chart that includes many of these types of formulations, along with their do’s and don’ts. If there is ever any doubt about the best way to administer a particular product or whether it can be halved or crushed, ask your pharmacist.3 TH
Michele B. Kaufman, PharmD, BSc, RPh, is a freelance medical writer based in New York City.
References
1. Mitchell J. Oral dosage forms that should not be crushed or chewed: facts and comparisons 4.0. Hospital Pharmacy Web site. Available at: online.factsandcomparisons.com/Viewer.aspx?book=atoz&monoID=fandc-atoz1040. Accessed March 5, 2009.
2. Williams NT. Medication administration through enteral feeding tubes. Am J Health Syst Pharm. 2008;65(24):2347-2357.
3. Mitchell JF. Oral dosage forms that should not be crushed: wall chart. Wolters Kluwer Health Web site. Available at: www.factsandcomparisons.com/Products/product.aspx?id=1111. Accessed Jan. 26, 2009.
4. Mylan's Matrix receives final FDA approval for the generic version of the antiretroviral Zerit capsules. Wolters Kluwer Health Web site. Available at: http://mylan.mediaroom.com/index.php?s=43&item=399. Accessed Jan. 23, 2009.
5. Product approval information. U.S. Food and Drug Administration Web site. Available at: www.fda.gov/Cber/products/Cinryze.htm. Accessed Jan. 14, 2009.
6. FDA licenses for marketing new therapy for rare genetic disease. U.S. Food and Drug Administration Web site. Available at: www.fda.gov/bbs/topics/NEWS/2008/NEW01903.html. Accessed Jan. 14, 2009.
7. Sancuso patch approved for nausea and vomiting. Monthly Prescribing Reference Web site. Available at: www.empr.com/Sancusopatchapprovedfornauseaandvomiting/article/122384/. Accessed Jan. 14, 2009.
8. TussiCaps now available for cough suppression. Monthly Prescribing Reference Web site. Available at: www.empr.com/TussiCapsnowavailableforcoughsuppression/article/122377/. Accessed Jan. 14, 2009.
9. UCB’s Vimpat approved by U.S. FDA as adjunctive therapy for partial onset seizures in adults. Medical News Today Web site. Available at: www.medicalnewstoday.com/articles/127354.php. Accessed Jan. 14, 2009.
10. Apriso granted FDA marketing approval for maintenance of remission of ulcerative colitis. Medical News Today Web site. Available at: http://www.medicalnewstoday.com/articles/127839.php. Accessed Jan. 14, 2009.
11. http://biz.yahoo.com/ap/081106/cv_therapeutics _ranexa.html?.v=1. Accessed February 2, 2009.
12. FDA approves Seroquel for bipolar maintenance. Monthly Prescribing Reference Web site. Available at: www.prescribingreference.com/news/showNews/which/SeroquelXRForBipolar10101. Accessed Jan. 14, 2009.
13. Seroquel XR Web site. Available at: www.pharmacistelink.com/news/2009/01/14_seroquel.pdf. Accessed Jan. 23, 2009.
14. Peck P. Smoking cessation drug linked to 1,001 new serious adverse events. Medpage Today Web site. Available at: www.medpagetoday.com/PrimaryCare/Smoking/11428. Accessed Jan. 14, 2009.
15. Public health advisory: important information on Chantix (varenicline). U.S. Food and Drug Administration Web site. Available at: www.fda.gov/CDER/Drug/advisory/varenicline.htm. Accessed Jan. 14, 2009.
Eliminate Inconsistency
Three years ago, Andrew Masica, MD, MSCI, joined the MedProvider Inpatient Care Unit hospitalist group at Baylor University Medical Center (BUMC) in Dallas just as the national debate on Medicare recidivism rates was focusing on high-risk populations.
Dr. Masica’s master’s degree in clinical investigation, combined with the roughly 35 hospitalists operating at the 900-bed BUMC, suggested it made sense to see what Baylor’s doctors could add to the conversation. And a study was born: “Reduction of 30-Day Post-Discharge Hospital Readmission or ED Visit Rates in High-Risk Elderly Medical Patients Through Delivery of a Targeted Care Bundle.” The single-center study will be published in this month’s Journal of Hospital Medicine.
The study found readmission/ED visit rates were lower after 30 days for those given an individualized care bundle of educational information compared with those who received the center’s standard treatment (10% individualized care bundle compared with 38.1% for standard treatment, P=0.04). Analysis also showed that for those patients who had a readmission or post-discharge ED visit, the time interval to the second event was longer in the intervention group compared with the control group (36.2 days to 15.7 days, P=0.05). At 60 days, however, readmission/ED visit rates were not affected positively for the intervention group versus the control group (42.9% vs. 30%, P=0.52).
The study team emphasizes that its small sample size—20 in the intervention group, 21 in the control—make it nearly impossible to extrapolate the results to large population sets; however, the results fuel the debate. “We don’t want to overstate our conclusions,” says Dr. Masica, the principal study investigator. “Important questions need to be asked. Is it the specific characteristics of the care coordinators? Can you reproduce this at other facilities? Is it the care bundle or the personnel? …We view this as early-phase work that people can build upon.”
Expansion Opportunity
Still, Dr. Masica believes hospitalist-centric conclusions can be reached. Since the study used in-house personnel only, other HM groups could easily reproduce the bundle without added expense. Additionally, because the coordinated-care approach involves a checklist of patient interaction activities, not medical procedures, the barrier to replication is further reduced. However, hospitalists will need the cooperation of more than their own medical directors.
In BUMC’s case, that meant the assistance of patient-care support services and the pharmacy department. Liz Youngblood, RN, MBA, supervised the care coordination in her role as vice president of patient-care support services for the Baylor Health Care System. Brian Cohen, PharmD, MS, was the pharmacy lead. Dr. Masica notes the confluence between departments was one of the keys to the reduction in recidivism over the first 30 days post-discharge.
“If you pick the high-risk patients and deliver the care in a bundle, you would be able to improve outcomes,” Dr. Masica says. “When you deliver just pieces of the care—just the coordinated care or just the pharmacist—you get inconsistencies.”
The first struggle BUMC researchers encountered—once they secured funding from Baylor’s Institute for Health Care Research and Improvement—was enrolling enough patients who met the criteria set for the study. The high-risk patient thresholds were:
- At least 70 years old;
- Regular use of at least five medications;
- At least three chronic, comorbid conditions;
- Assistance with at least one activity of daily living; and
- Preadmission residence at home or at an assisted-living facility with a reasonable expectation of disposition back to that residence.
Researchers also wanted patients with common DRGs admitted, and set exclusion criteria as well: lack of fluency in English; admission primarily for a surgical procedure; terminal diagnosis with life expectancy of less than six months; and residency in a long-term care facility. Patients who could not be enrolled within 72 hours of admission were excluded.
Dr. Masica notes hospitalists interested in replicating the research should pay attention to the consent forms they used. When the Baylor team conducted its research from March to September 2007, they used a long-form consent waiver. Baylor’s consent form for similar studies has since been shortened, and Dr. Masica says a less complicated form would have helped encourage more patients to enroll. In the end, 60 patients declined to enroll in the Baylor study and 56 were unable to give their consent due to impairment.
Once enrolled, the patients were delivered the care bundle in stages (see Table 1). Care coordinators (CCs) saw patients daily, instructing them on specific health conditions with an eye toward teaching home care, should post-discharge problems arise. Clinical pharmacists (CPs) visited patients to focus on medication reconciliation and education. CCs and CPs would follow up with post-discharge phone calls to confirm receipt of medical equipment and medications, use and affects of those medications, home-health arrangements, and to schedule follow-up appointments. If patients indicated any issues, the coordinators recommended action plans.
“It would be surprising to find out how little patients really understand about why they’re in the hospital and what they’re being treated for,” Youngblood says. “To have the reinforcement is really valuable.”
Care Continuum
One topic the study skirts is the ever-contentious realm of post-discharge care and who takes over responsibility for patient care. While the Baylor study examined readmission/ED visit rates through 60 days, Dr. Masica says a transitional-care program is the best way to manage that care continuum.
“We did see a difference at 30 days,” Dr. Masica says. “At 60 days, that effectively washed out. That makes sense. You can only control things so much from the hospital side. After 30 days, you need transitional care, good primary care.”
Baylor’s research team is working on a follow-up study that would apply the coordinated-care bundle to specific disease management. Youngblood notes that directing specific services at a targeted population—for example, congestive heart failure patients—should show an even more concentrated reduction of 30-day recidivism. “The key is to identify the high-risk groups,” he says. “You can’t apply this to every single patient. That would be low-yield. Your yield is going to come in on the very high-risk folks.” TH
Richard Quinn is a freelance writer based in New Jersey.
Three years ago, Andrew Masica, MD, MSCI, joined the MedProvider Inpatient Care Unit hospitalist group at Baylor University Medical Center (BUMC) in Dallas just as the national debate on Medicare recidivism rates was focusing on high-risk populations.
Dr. Masica’s master’s degree in clinical investigation, combined with the roughly 35 hospitalists operating at the 900-bed BUMC, suggested it made sense to see what Baylor’s doctors could add to the conversation. And a study was born: “Reduction of 30-Day Post-Discharge Hospital Readmission or ED Visit Rates in High-Risk Elderly Medical Patients Through Delivery of a Targeted Care Bundle.” The single-center study will be published in this month’s Journal of Hospital Medicine.
The study found readmission/ED visit rates were lower after 30 days for those given an individualized care bundle of educational information compared with those who received the center’s standard treatment (10% individualized care bundle compared with 38.1% for standard treatment, P=0.04). Analysis also showed that for those patients who had a readmission or post-discharge ED visit, the time interval to the second event was longer in the intervention group compared with the control group (36.2 days to 15.7 days, P=0.05). At 60 days, however, readmission/ED visit rates were not affected positively for the intervention group versus the control group (42.9% vs. 30%, P=0.52).
The study team emphasizes that its small sample size—20 in the intervention group, 21 in the control—make it nearly impossible to extrapolate the results to large population sets; however, the results fuel the debate. “We don’t want to overstate our conclusions,” says Dr. Masica, the principal study investigator. “Important questions need to be asked. Is it the specific characteristics of the care coordinators? Can you reproduce this at other facilities? Is it the care bundle or the personnel? …We view this as early-phase work that people can build upon.”
Expansion Opportunity
Still, Dr. Masica believes hospitalist-centric conclusions can be reached. Since the study used in-house personnel only, other HM groups could easily reproduce the bundle without added expense. Additionally, because the coordinated-care approach involves a checklist of patient interaction activities, not medical procedures, the barrier to replication is further reduced. However, hospitalists will need the cooperation of more than their own medical directors.
In BUMC’s case, that meant the assistance of patient-care support services and the pharmacy department. Liz Youngblood, RN, MBA, supervised the care coordination in her role as vice president of patient-care support services for the Baylor Health Care System. Brian Cohen, PharmD, MS, was the pharmacy lead. Dr. Masica notes the confluence between departments was one of the keys to the reduction in recidivism over the first 30 days post-discharge.
“If you pick the high-risk patients and deliver the care in a bundle, you would be able to improve outcomes,” Dr. Masica says. “When you deliver just pieces of the care—just the coordinated care or just the pharmacist—you get inconsistencies.”
The first struggle BUMC researchers encountered—once they secured funding from Baylor’s Institute for Health Care Research and Improvement—was enrolling enough patients who met the criteria set for the study. The high-risk patient thresholds were:
- At least 70 years old;
- Regular use of at least five medications;
- At least three chronic, comorbid conditions;
- Assistance with at least one activity of daily living; and
- Preadmission residence at home or at an assisted-living facility with a reasonable expectation of disposition back to that residence.
Researchers also wanted patients with common DRGs admitted, and set exclusion criteria as well: lack of fluency in English; admission primarily for a surgical procedure; terminal diagnosis with life expectancy of less than six months; and residency in a long-term care facility. Patients who could not be enrolled within 72 hours of admission were excluded.
Dr. Masica notes hospitalists interested in replicating the research should pay attention to the consent forms they used. When the Baylor team conducted its research from March to September 2007, they used a long-form consent waiver. Baylor’s consent form for similar studies has since been shortened, and Dr. Masica says a less complicated form would have helped encourage more patients to enroll. In the end, 60 patients declined to enroll in the Baylor study and 56 were unable to give their consent due to impairment.
Once enrolled, the patients were delivered the care bundle in stages (see Table 1). Care coordinators (CCs) saw patients daily, instructing them on specific health conditions with an eye toward teaching home care, should post-discharge problems arise. Clinical pharmacists (CPs) visited patients to focus on medication reconciliation and education. CCs and CPs would follow up with post-discharge phone calls to confirm receipt of medical equipment and medications, use and affects of those medications, home-health arrangements, and to schedule follow-up appointments. If patients indicated any issues, the coordinators recommended action plans.
“It would be surprising to find out how little patients really understand about why they’re in the hospital and what they’re being treated for,” Youngblood says. “To have the reinforcement is really valuable.”
Care Continuum
One topic the study skirts is the ever-contentious realm of post-discharge care and who takes over responsibility for patient care. While the Baylor study examined readmission/ED visit rates through 60 days, Dr. Masica says a transitional-care program is the best way to manage that care continuum.
“We did see a difference at 30 days,” Dr. Masica says. “At 60 days, that effectively washed out. That makes sense. You can only control things so much from the hospital side. After 30 days, you need transitional care, good primary care.”
Baylor’s research team is working on a follow-up study that would apply the coordinated-care bundle to specific disease management. Youngblood notes that directing specific services at a targeted population—for example, congestive heart failure patients—should show an even more concentrated reduction of 30-day recidivism. “The key is to identify the high-risk groups,” he says. “You can’t apply this to every single patient. That would be low-yield. Your yield is going to come in on the very high-risk folks.” TH
Richard Quinn is a freelance writer based in New Jersey.
Three years ago, Andrew Masica, MD, MSCI, joined the MedProvider Inpatient Care Unit hospitalist group at Baylor University Medical Center (BUMC) in Dallas just as the national debate on Medicare recidivism rates was focusing on high-risk populations.
Dr. Masica’s master’s degree in clinical investigation, combined with the roughly 35 hospitalists operating at the 900-bed BUMC, suggested it made sense to see what Baylor’s doctors could add to the conversation. And a study was born: “Reduction of 30-Day Post-Discharge Hospital Readmission or ED Visit Rates in High-Risk Elderly Medical Patients Through Delivery of a Targeted Care Bundle.” The single-center study will be published in this month’s Journal of Hospital Medicine.
The study found readmission/ED visit rates were lower after 30 days for those given an individualized care bundle of educational information compared with those who received the center’s standard treatment (10% individualized care bundle compared with 38.1% for standard treatment, P=0.04). Analysis also showed that for those patients who had a readmission or post-discharge ED visit, the time interval to the second event was longer in the intervention group compared with the control group (36.2 days to 15.7 days, P=0.05). At 60 days, however, readmission/ED visit rates were not affected positively for the intervention group versus the control group (42.9% vs. 30%, P=0.52).
The study team emphasizes that its small sample size—20 in the intervention group, 21 in the control—make it nearly impossible to extrapolate the results to large population sets; however, the results fuel the debate. “We don’t want to overstate our conclusions,” says Dr. Masica, the principal study investigator. “Important questions need to be asked. Is it the specific characteristics of the care coordinators? Can you reproduce this at other facilities? Is it the care bundle or the personnel? …We view this as early-phase work that people can build upon.”
Expansion Opportunity
Still, Dr. Masica believes hospitalist-centric conclusions can be reached. Since the study used in-house personnel only, other HM groups could easily reproduce the bundle without added expense. Additionally, because the coordinated-care approach involves a checklist of patient interaction activities, not medical procedures, the barrier to replication is further reduced. However, hospitalists will need the cooperation of more than their own medical directors.
In BUMC’s case, that meant the assistance of patient-care support services and the pharmacy department. Liz Youngblood, RN, MBA, supervised the care coordination in her role as vice president of patient-care support services for the Baylor Health Care System. Brian Cohen, PharmD, MS, was the pharmacy lead. Dr. Masica notes the confluence between departments was one of the keys to the reduction in recidivism over the first 30 days post-discharge.
“If you pick the high-risk patients and deliver the care in a bundle, you would be able to improve outcomes,” Dr. Masica says. “When you deliver just pieces of the care—just the coordinated care or just the pharmacist—you get inconsistencies.”
The first struggle BUMC researchers encountered—once they secured funding from Baylor’s Institute for Health Care Research and Improvement—was enrolling enough patients who met the criteria set for the study. The high-risk patient thresholds were:
- At least 70 years old;
- Regular use of at least five medications;
- At least three chronic, comorbid conditions;
- Assistance with at least one activity of daily living; and
- Preadmission residence at home or at an assisted-living facility with a reasonable expectation of disposition back to that residence.
Researchers also wanted patients with common DRGs admitted, and set exclusion criteria as well: lack of fluency in English; admission primarily for a surgical procedure; terminal diagnosis with life expectancy of less than six months; and residency in a long-term care facility. Patients who could not be enrolled within 72 hours of admission were excluded.
Dr. Masica notes hospitalists interested in replicating the research should pay attention to the consent forms they used. When the Baylor team conducted its research from March to September 2007, they used a long-form consent waiver. Baylor’s consent form for similar studies has since been shortened, and Dr. Masica says a less complicated form would have helped encourage more patients to enroll. In the end, 60 patients declined to enroll in the Baylor study and 56 were unable to give their consent due to impairment.
Once enrolled, the patients were delivered the care bundle in stages (see Table 1). Care coordinators (CCs) saw patients daily, instructing them on specific health conditions with an eye toward teaching home care, should post-discharge problems arise. Clinical pharmacists (CPs) visited patients to focus on medication reconciliation and education. CCs and CPs would follow up with post-discharge phone calls to confirm receipt of medical equipment and medications, use and affects of those medications, home-health arrangements, and to schedule follow-up appointments. If patients indicated any issues, the coordinators recommended action plans.
“It would be surprising to find out how little patients really understand about why they’re in the hospital and what they’re being treated for,” Youngblood says. “To have the reinforcement is really valuable.”
Care Continuum
One topic the study skirts is the ever-contentious realm of post-discharge care and who takes over responsibility for patient care. While the Baylor study examined readmission/ED visit rates through 60 days, Dr. Masica says a transitional-care program is the best way to manage that care continuum.
“We did see a difference at 30 days,” Dr. Masica says. “At 60 days, that effectively washed out. That makes sense. You can only control things so much from the hospital side. After 30 days, you need transitional care, good primary care.”
Baylor’s research team is working on a follow-up study that would apply the coordinated-care bundle to specific disease management. Youngblood notes that directing specific services at a targeted population—for example, congestive heart failure patients—should show an even more concentrated reduction of 30-day recidivism. “The key is to identify the high-risk groups,” he says. “You can’t apply this to every single patient. That would be low-yield. Your yield is going to come in on the very high-risk folks.” TH
Richard Quinn is a freelance writer based in New Jersey.
The latest research you need to know
In This Edition
- Generic vs. brand-name drugs.
- Rapid-response teams and mortality.
- A new prediction rule for mortality in acute pancreatitis.
- Viral causes of community-acquired pneumonia.
- Intensive insulin therapy in the ICU.
- New preoperative and intraoperative risk factors.
- Timing of ICU feedings and mortality.
- Aspirin as primary prevention in diabetics.
Generic, Brand-Name Drugs Used for Cardiovascular Disease Are Clinically Equivalent
Clinical question: Is there a clinical risk when substituting generic drugs for brand-name drugs in the treatment of cardiovascular disease?
Background: Spending on healthcare in the U.S. has reached critical levels. Increasing prescription drug costs make up a large portion of healthcare expenditures. The high cost of medicines directly affect adherence to treatment regimens and contribute to poor health outcomes. Cardiovascular drugs make up the largest portion of outpatient prescription drug spending.
Study design: Systematic review of relevant articles with a meta-analysis performed to determine an aggregate effect size.
Setting: Multiple locations and varied patient populations.
Synopsis: A total of 47 articles were included in the review, of which 38 were randomized controlled trials (RCTs). The studies measured both clinical efficacy and safety end points. More than half the articles were published prior to 2000. Clinical equivalence was noted in all seven beta-blocker RCTs; 10 of 11 diuretic RCTs; five of seven calcium-channel-blocker RCTs; all three antiplatelet-agent RCTs (clopidogrel, enteric-coated aspirin); two statin RCTs; one ACE-inhibitor RCT; and one alpha-blocker RCT. For drugs with a narrow therapeutic index, clinical equivalence was noted in all five warfarin RCTs and a single Class 1 anti-arrhythmic-agent RCT.
The aggregate effect size was -0.03 (95% CI, -0.15 to 0.08), which indicates nearly complete overlap of the generic and brand-name distributions. The data show no evidence of superiority of brand-name to generic drugs in clinical outcomes measured in the various studies.
In a separate review of editorials addressing generic substitution for cardiovascular drugs, 53% expressed a negative view of generic-drug substitution.
Bottom line: There is clinical equivalency between generic and brand-name drugs used in the treatment of cardiovascular disease. Despite this conclusion, a substantial number of editorials advise against generic substitution, which affects both patient and physician drug preferences.
Citation: Kesselheim A, Misono A, Lee J, et al. Clinical equivalence of generic and brand-name drugs used in cardiovascular disease: a systematic review and meta-analysis. JAMA. 2008; 300(21):2514-2526.
RRT Implement-ation Doesn’t Affect Hospitalwide Code Rates or Mortality
Clinical question: Does the use of a rapid-response team (RRT) affect hospitalwide code rates and mortality?
Background: In the 100,000 Lives campaign, the Institute for Healthcare Improvement recommended that hospitals implement RRTs to help reduce preventable, in-hospital deaths. Studies have demonstrated that rates of non-ICU codes decrease after RRT implementation. It is unclear if this translates to changes in mortality rates.
Study design: Prospective cohort study of adult inpatients.
Setting: Saint Luke’s Hospital, a 404-bed tertiary-care academic hospital in Kansas City, Mo.
Synopsis: The hospital documented a total of 376 RRT activations. After RRT implementation, mean hospitalwide code rates decreased to 7.5 per 1,000 admissions from 11.2 per 1,000 admissions. This was not associated with a statistically significant reduction in hospitalwide code rates (adjusted odds ratio 0.76; 95% CI; 0.57-1.01; P=0.06). Secondary analyses noted lower rates of non-ICU codes (0.59; 95% CI, 0.40-0.89) compared with ICU codes (0.95; 95% CI; 0.64-1.43; P=0.03 for interaction). Finally, the RRT implementation was not associated with lower hospital-wide mortality (0.95; 95% CI; 0.81-1.11; P=0.52).
Secondary analyses also revealed few instances of RRT undertreatment or underutilization that may have affected the mortality numbers.
A limitation of this study is that it was slightly underpowered (78%) to detect a significant mortality difference. The findings also represent a single institution experience, and may not be generalized to other adult hospital settings or RRT programs.
Bottom line: Implementation of an RRT does not confer lower rates of hospital-wide code arrests or mortality.
Citation: Chan P, Khalid A, Longmore L, et al. Hospital-wide code rates and mortality before and after implementation of a rapid response team. JAMA. 2008;300(21):2506-2513.
Simple Scoring System Provides Timely Prediction of Mortality in Acute Pancreatitis
Clinical question: How can physicians predict mortality in acute pancreatitis?
Background: Historical predictors of mortality in acute pancreatitis require up to 48 hours of data, such as with the Ranson Criteria, or extensive amounts of data, such as with the APACHE II score. An easier tool is needed to predict which patients are at higher risk of mortality.
Study design: Retrospective cohort.
Setting: Patients in the Cardinal Health clinical outcomes research database, which supports public reporting of hospital performance.
Synopsis: The authors identified patients with the principal diagnosis of pancreatitis from 2000-2001 and explored numerous diagnostic findings available within the first 24 hours. Ultimately, BUN >25, impaired mental status, presence of SIRS (systemic inflammatory response syndrome), age >60, and presence of a pleural effusion were found to be predictive of mortality. These diagnostic findings correspond to the mnemonic BISAP. The BISAP score was then validated in a second cohort that included patients from 2004-2005.
Each finding in the BISAP score was given one point. A score of less than 2 was present in approximately 60% of patients admitted with acute pancreatitis, and corresponded to a mortality of less than 1%. A score of 2 corresponded to a mortality of 2%. Higher scores were associated with steeply increasing mortality, with a score of 5 corresponding with greater than 20% mortality.
The BISAP score performed similarly to the APACHE II score, but the former is easier to calculate on the day of admission and has fewer parameters. A more challenging research step will be to demonstrate that using the BISAP score to determine treatment strategies can affect patient outcomes.
Bottom line: The easy-to-calculate BISAP score is a new method for predicting mortality in patients with acute pancreatitis. This tool should help hospitalists determine, on the day of admission, to what extent patients with acute pancreatitis need aggressive management, such as ICU admission and early involvement of specialists.
Citation: Wu B, Johannes R, Sun X, Tabak Y, Conwell D, Banks P. The early prediction of mortality in acute pancreatitis: a large population-based study. Gut. 2008;57(12): 1698-1703.
Nasal Swabs Identify Viral Causes in CAP Patients
Clinical question: How often is viral infection associated with community-acquired pneumonia (CAP) in adults?
Background: CAP is a clinically important disease that is associated with significant hospitalization and mortality. CAP treatment guidelines acknowledge respiratory viruses as an etiology for pneumonia, but few recommendations are made regarding management of these viral infections.
Study design: Prospective study.
Setting: Five hospitals in Edmonton, Alberta, from 2004-2006.
Synopsis: The authors enrolled 193 hospitalized adults, median age 71. Nucleic amplification tests (NATs) from nasopharyngeal swab specimens were tested for human metapneumovirus, respiratory syncytial virus, rhinovirus, parainfluenza virus 1-4, coronaviruses, and adenovirus.
Fifteen percent of these patients had a nasal swab positive for a viral infection. Interestingly, 4% of patients had both a positive viral nasal swab and positive bacterial cultures. Compared with bacterial infection, patients with viral infection tended to be older (76 vs. 64 years, P=0.01), have limited ambulation (66% vs. 32%, P=0.006), and have a history of cardiac disease (66% vs. 32%, P=0.02). Patients with bacterial pneumonia showed a statistically significant trend toward having chest pain, an abnormal white blood count, and a lobar infiltrate on chest X-ray.
Further investigations might look at how nasal swab data could be used to improve infection control within the hospital for patients found to have easily transmissible viruses. Further research could explore the feasibility of avoiding antibiotic use in patients found to have viral pneumonia, assuming bacterial co-infection is reliably excluded.
Bottom line: Nasal swabs using NAT technology could play a significant role in identifying pathogens in CAP patients. How this technology should affect clinical decision-making and how it might improve outcomes remains unknown.
Citation: Johnstone J, Majumdar S, Fox J, Marrie T. Viral infection in adults hospitalized with community-acquired pneumonia: prevalence, pathogens, and presentation. Chest. 2008;134(6):1141-1148.
Intensive Insulin Therapy Doesn’t Reduce ICU Mortality
Clinical question: Does the use of intensive insulin therapy decrease mortality in the intensive-care unit (ICU)?
Background: In 2001, Van den Berghe et al (N Engl J Med. 2001;345(19):1359-67) reported a reduction in morbidity and mortality with intensive insulin therapy (IIT) in surgical ICU patients. This study led to the adoption of IIT protocols in many hospitals. Since 2001, further studies have failed to reproduce the same dramatic benefit of IIT.
Study design: Randomized, controlled trial.
Setting: National Guard King Abdulaziz Medical City, a tertiary-care teaching hospital in Saudi Arabia.
Synopsis: Patients were included in this study if they were 18 years or older with serum glucose levels greater than 110 mg/dL during the first 24 hours of ICU admission. There were multiple exclusion criteria, including patients with Type I diabetes, documented hypoglycemia on ICU admission (glucose <40), or diabetic ketoacidosis.
Enrolled patients were randomized to IIT or conventional insulin therapy (CIT). A multidisciplinary team designed the protocols to maintain glucose levels of 80 to 110 mg/dL and 180 to 200 mg/dL in the IIT and the CIT groups, respectively. The primary endpoint measured was ICU mortality.
The study did not produce a statistically significant difference in ICU mortality (13.5% for IIT vs. 17.1% for CIT; P=0.30). The adjusted hypoglycemia rate was 6.8 per 100 treatment days with IIT and 0.4 per 100 treatment days with CIT (P<0.0001). Patients with hypoglycemia had higher ICU mortality (23.8% vs. 13.7%, P=0.02).
In the measurement of secondary endpoints, there was a trend toward lower episodes of severe sepsis and septic shock in the IIT group (20.7% in IIT vs. 27.2% in CIT, P=0.08). However, this result was not statistically significant.
Bottom line: This well-designed study failed to show a survival benefit with IIT use in the critical-care setting. Given the findings of this and several other recent studies, one should question whether IIT should be prescribed as the standard of care in all critically-ill patients.
Citation: Arabi Y, Dabbagh O, Tamim H, et al. Intensive versus conventional insulin therapy: a randomized controlled trial in medical and surgical critically ill patients. Crit Care Med. 2008;36(12):3190-3197.
Preoperative and Intraoperative Predictors of Cardiac Adverse Events
Clinical question: What are the incidence and risk factors for perioperative cardiac adverse events after noncardiac surgery?
Background: In the past few decades, the incidence of cardiac adverse events (CAEs) for a general surgery population has remained largely unchanged (approximately 1%). This is in spite of multiple studies evaluating predictive models and attempts at preventive treatment, including preoperative coronary revascularization and perioperative beta blockers.
Study design: Prospective observational study.
Setting: Single, large, tertiary-care university hospital.
Synopsis: A total of 7,740 cases were reviewed in this study, which consisted of general surgery (4,937), vascular surgery (1,846), and urological surgery (957). A trained nurse followed up for perioperative CAEs as many as 30 days after the operation via medical chart review, phone calls, and letters. CAEs were defined as: Q-wave myocardial infarction (MI), non-ST elevation MI, cardiac arrest, or new cardiac dysrhythmia. A total of 83 CAEs (1.1% of patients) had cardiac arrest, with cardiac dysrhythmia being most common.
A total of seven preoperative risk factors were identified as independent predictors for CAEs: age 68, BMI 30, emergent surgery, prior coronary intervention or cardiac surgery, active congestive heart failure, cerebrovascular disease, and hypertension. In addition, two intraoperative risk factors were identified: intraoperative transfusion of packed red blood cells and operative duration of 3.8 hours. (The P value was 0.05 for all independent predictors.)
A further evaluation of intraoperative parameters of high-risk patients experiencing a CAE showed that these patients were more likely to have an episode of mean arterial pressure (MAP) <50 mmHg, an episode of 40% decrease in MAP, and an episode of tachycardia (heart rate >100).
Bottom line: A combination of preoperative predictors and intraoperative elements can help improve risk assessment for perioperative CAEs after noncardiac surgery.
Citation: Kheterpal S, O’Reilly M, Englesbe M, et al. Preoperative and intraoperative predictors of cardiac adverse events after general, vascular, and urological surgery. Anesthesiology. 2009;110(1):58-66.
Early Feeding in the ICU Does Not Affect Hospital Mortality
Clinical question: Will implementing evidence-based feeding guidelines improve feeding practices and reduce mortality in ICU patients?
Background: There is evidence suggesting that providing nutritional support to ICU patients within 24 hours of admission may decrease mortality. It is widely understood that patient care varies between ICUs, and there exist no uniform, evidence-based guidelines for nutritional support. Many patients remain unfed after 48 hours.
Study design: Cluster, randomized-controlled trial.
Setting: ICUs in 27 community and tertiary-care hospitals in Australia and New Zealand.
Synopsis: Hospitals were randomized to intervention or control groups. Dietitian and intensivist co-investigators from intervention ICUs developed guidelines using the Clinical Practice Guideline Development Cycle. Control ICUs were requested to make no new ICU nutritional management changes. The study enrolled 1,118 eligible patients and included adults expected to stay longer than two days. Excluded were patients taking oral diets, patients receiving palliative care or with suspected brain death, and patients sent from other facilities.
Guidelines were implemented using several methods—educational outreach visits, one-on-one conversations, active reminders, passive reminders, and educational in-services. The guidelines were successful in evoking significant practice changes in all of the intervention ICUs. Significantly more patients received nutritional support during their ICU stays in guideline ICUs, and patients in these ICUs were fed significantly earlier. There were, however, no significant differences between guideline and control ICUs with regard to hospital discharge mortality (28.9% vs. 27.4%; 95% CI; -6.3% to 12.0%; P=0.75). The groups also showed no statistical difference in hospital or ICU length of stay.
Bottom line: Significantly more patients in the guideline ICUs were fed within 24 hours, but this did not translate into improvements in mortality or other clinical outcomes.
Citation: Doig G, Simpson F, Finfer S, et al. Effect of evidence-based feeding guidelines on mortality of critically ill adults: a cluster randomized controlled trial. JAMA. 2008;300(23):2731-2741.
Low-Dose Aspirin Doesn’t Reduce Cardiovascular Events in Type 2 Diabetes Patients
Clinical question: Is low-dose aspirin effective for the primary prevention of atherosclerotic events in patients with Type 2 diabetes?
Background: Diabetes is a significant risk factor for cardiovascular events. Several prior studies have shown that aspirin therapy is effective as a secondary prevention strategy for cardiovascular events. The American Diabetes Association also recommends use of aspirin as a primary prevention strategy. Clinical trial data is currently insufficient in this area.
Study design: Prospective, randomized, open-label, controlled trial with blinded endpoint assessment.
Setting: 163 institutions in Japan.
Synopsis: The study enrolled 2,539 diabetic patients between 30 and 85 years old—mean age was 65—and included patients without EKG changes or a significant history or ongoing treatment of atherosclerotic disease. Patients were randomly assigned into an aspirin group (81 mg or 100 mg once daily) or a nonaspirin group. Patients had a median follow up of 4.37 years.
The primary endpoint was any atherosclerotic event, ranging from sudden death to ischemic heart disease or stroke. The incidence of atherosclerotic events was not statistically different in the aspirin group (68 events, 5.4%) than in the nonaspirin group (86 events, 6.7%) (HR, 0.80; 95% CI; 0.58-1.10; log-rank test, P=0.16). However, there was a suggested benefit of primary prevention in the subgroup aged 65 years or older. In addition, the combined endpoint of fatal coronary and cerebrovascular events occurred in one patient in the aspirin group and 10 patients in the nonaspirin group (HR, 0.10; 95 % CI, 0.01-0.79; P=.0037). This study is limited by the low incidence of atherosclerotic disease in Japan.
Bottom line: Low-dose aspirin used in patients with Type 2 diabetes does not significantly demonstrate primary prevention of cardiovascular events.
Citation: Ogawa H, Nakayama M, Morimoto T, et al. Low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA. 2008;300(18):2134-2141. TH
In This Edition
- Generic vs. brand-name drugs.
- Rapid-response teams and mortality.
- A new prediction rule for mortality in acute pancreatitis.
- Viral causes of community-acquired pneumonia.
- Intensive insulin therapy in the ICU.
- New preoperative and intraoperative risk factors.
- Timing of ICU feedings and mortality.
- Aspirin as primary prevention in diabetics.
Generic, Brand-Name Drugs Used for Cardiovascular Disease Are Clinically Equivalent
Clinical question: Is there a clinical risk when substituting generic drugs for brand-name drugs in the treatment of cardiovascular disease?
Background: Spending on healthcare in the U.S. has reached critical levels. Increasing prescription drug costs make up a large portion of healthcare expenditures. The high cost of medicines directly affect adherence to treatment regimens and contribute to poor health outcomes. Cardiovascular drugs make up the largest portion of outpatient prescription drug spending.
Study design: Systematic review of relevant articles with a meta-analysis performed to determine an aggregate effect size.
Setting: Multiple locations and varied patient populations.
Synopsis: A total of 47 articles were included in the review, of which 38 were randomized controlled trials (RCTs). The studies measured both clinical efficacy and safety end points. More than half the articles were published prior to 2000. Clinical equivalence was noted in all seven beta-blocker RCTs; 10 of 11 diuretic RCTs; five of seven calcium-channel-blocker RCTs; all three antiplatelet-agent RCTs (clopidogrel, enteric-coated aspirin); two statin RCTs; one ACE-inhibitor RCT; and one alpha-blocker RCT. For drugs with a narrow therapeutic index, clinical equivalence was noted in all five warfarin RCTs and a single Class 1 anti-arrhythmic-agent RCT.
The aggregate effect size was -0.03 (95% CI, -0.15 to 0.08), which indicates nearly complete overlap of the generic and brand-name distributions. The data show no evidence of superiority of brand-name to generic drugs in clinical outcomes measured in the various studies.
In a separate review of editorials addressing generic substitution for cardiovascular drugs, 53% expressed a negative view of generic-drug substitution.
Bottom line: There is clinical equivalency between generic and brand-name drugs used in the treatment of cardiovascular disease. Despite this conclusion, a substantial number of editorials advise against generic substitution, which affects both patient and physician drug preferences.
Citation: Kesselheim A, Misono A, Lee J, et al. Clinical equivalence of generic and brand-name drugs used in cardiovascular disease: a systematic review and meta-analysis. JAMA. 2008; 300(21):2514-2526.
RRT Implement-ation Doesn’t Affect Hospitalwide Code Rates or Mortality
Clinical question: Does the use of a rapid-response team (RRT) affect hospitalwide code rates and mortality?
Background: In the 100,000 Lives campaign, the Institute for Healthcare Improvement recommended that hospitals implement RRTs to help reduce preventable, in-hospital deaths. Studies have demonstrated that rates of non-ICU codes decrease after RRT implementation. It is unclear if this translates to changes in mortality rates.
Study design: Prospective cohort study of adult inpatients.
Setting: Saint Luke’s Hospital, a 404-bed tertiary-care academic hospital in Kansas City, Mo.
Synopsis: The hospital documented a total of 376 RRT activations. After RRT implementation, mean hospitalwide code rates decreased to 7.5 per 1,000 admissions from 11.2 per 1,000 admissions. This was not associated with a statistically significant reduction in hospitalwide code rates (adjusted odds ratio 0.76; 95% CI; 0.57-1.01; P=0.06). Secondary analyses noted lower rates of non-ICU codes (0.59; 95% CI, 0.40-0.89) compared with ICU codes (0.95; 95% CI; 0.64-1.43; P=0.03 for interaction). Finally, the RRT implementation was not associated with lower hospital-wide mortality (0.95; 95% CI; 0.81-1.11; P=0.52).
Secondary analyses also revealed few instances of RRT undertreatment or underutilization that may have affected the mortality numbers.
A limitation of this study is that it was slightly underpowered (78%) to detect a significant mortality difference. The findings also represent a single institution experience, and may not be generalized to other adult hospital settings or RRT programs.
Bottom line: Implementation of an RRT does not confer lower rates of hospital-wide code arrests or mortality.
Citation: Chan P, Khalid A, Longmore L, et al. Hospital-wide code rates and mortality before and after implementation of a rapid response team. JAMA. 2008;300(21):2506-2513.
Simple Scoring System Provides Timely Prediction of Mortality in Acute Pancreatitis
Clinical question: How can physicians predict mortality in acute pancreatitis?
Background: Historical predictors of mortality in acute pancreatitis require up to 48 hours of data, such as with the Ranson Criteria, or extensive amounts of data, such as with the APACHE II score. An easier tool is needed to predict which patients are at higher risk of mortality.
Study design: Retrospective cohort.
Setting: Patients in the Cardinal Health clinical outcomes research database, which supports public reporting of hospital performance.
Synopsis: The authors identified patients with the principal diagnosis of pancreatitis from 2000-2001 and explored numerous diagnostic findings available within the first 24 hours. Ultimately, BUN >25, impaired mental status, presence of SIRS (systemic inflammatory response syndrome), age >60, and presence of a pleural effusion were found to be predictive of mortality. These diagnostic findings correspond to the mnemonic BISAP. The BISAP score was then validated in a second cohort that included patients from 2004-2005.
Each finding in the BISAP score was given one point. A score of less than 2 was present in approximately 60% of patients admitted with acute pancreatitis, and corresponded to a mortality of less than 1%. A score of 2 corresponded to a mortality of 2%. Higher scores were associated with steeply increasing mortality, with a score of 5 corresponding with greater than 20% mortality.
The BISAP score performed similarly to the APACHE II score, but the former is easier to calculate on the day of admission and has fewer parameters. A more challenging research step will be to demonstrate that using the BISAP score to determine treatment strategies can affect patient outcomes.
Bottom line: The easy-to-calculate BISAP score is a new method for predicting mortality in patients with acute pancreatitis. This tool should help hospitalists determine, on the day of admission, to what extent patients with acute pancreatitis need aggressive management, such as ICU admission and early involvement of specialists.
Citation: Wu B, Johannes R, Sun X, Tabak Y, Conwell D, Banks P. The early prediction of mortality in acute pancreatitis: a large population-based study. Gut. 2008;57(12): 1698-1703.
Nasal Swabs Identify Viral Causes in CAP Patients
Clinical question: How often is viral infection associated with community-acquired pneumonia (CAP) in adults?
Background: CAP is a clinically important disease that is associated with significant hospitalization and mortality. CAP treatment guidelines acknowledge respiratory viruses as an etiology for pneumonia, but few recommendations are made regarding management of these viral infections.
Study design: Prospective study.
Setting: Five hospitals in Edmonton, Alberta, from 2004-2006.
Synopsis: The authors enrolled 193 hospitalized adults, median age 71. Nucleic amplification tests (NATs) from nasopharyngeal swab specimens were tested for human metapneumovirus, respiratory syncytial virus, rhinovirus, parainfluenza virus 1-4, coronaviruses, and adenovirus.
Fifteen percent of these patients had a nasal swab positive for a viral infection. Interestingly, 4% of patients had both a positive viral nasal swab and positive bacterial cultures. Compared with bacterial infection, patients with viral infection tended to be older (76 vs. 64 years, P=0.01), have limited ambulation (66% vs. 32%, P=0.006), and have a history of cardiac disease (66% vs. 32%, P=0.02). Patients with bacterial pneumonia showed a statistically significant trend toward having chest pain, an abnormal white blood count, and a lobar infiltrate on chest X-ray.
Further investigations might look at how nasal swab data could be used to improve infection control within the hospital for patients found to have easily transmissible viruses. Further research could explore the feasibility of avoiding antibiotic use in patients found to have viral pneumonia, assuming bacterial co-infection is reliably excluded.
Bottom line: Nasal swabs using NAT technology could play a significant role in identifying pathogens in CAP patients. How this technology should affect clinical decision-making and how it might improve outcomes remains unknown.
Citation: Johnstone J, Majumdar S, Fox J, Marrie T. Viral infection in adults hospitalized with community-acquired pneumonia: prevalence, pathogens, and presentation. Chest. 2008;134(6):1141-1148.
Intensive Insulin Therapy Doesn’t Reduce ICU Mortality
Clinical question: Does the use of intensive insulin therapy decrease mortality in the intensive-care unit (ICU)?
Background: In 2001, Van den Berghe et al (N Engl J Med. 2001;345(19):1359-67) reported a reduction in morbidity and mortality with intensive insulin therapy (IIT) in surgical ICU patients. This study led to the adoption of IIT protocols in many hospitals. Since 2001, further studies have failed to reproduce the same dramatic benefit of IIT.
Study design: Randomized, controlled trial.
Setting: National Guard King Abdulaziz Medical City, a tertiary-care teaching hospital in Saudi Arabia.
Synopsis: Patients were included in this study if they were 18 years or older with serum glucose levels greater than 110 mg/dL during the first 24 hours of ICU admission. There were multiple exclusion criteria, including patients with Type I diabetes, documented hypoglycemia on ICU admission (glucose <40), or diabetic ketoacidosis.
Enrolled patients were randomized to IIT or conventional insulin therapy (CIT). A multidisciplinary team designed the protocols to maintain glucose levels of 80 to 110 mg/dL and 180 to 200 mg/dL in the IIT and the CIT groups, respectively. The primary endpoint measured was ICU mortality.
The study did not produce a statistically significant difference in ICU mortality (13.5% for IIT vs. 17.1% for CIT; P=0.30). The adjusted hypoglycemia rate was 6.8 per 100 treatment days with IIT and 0.4 per 100 treatment days with CIT (P<0.0001). Patients with hypoglycemia had higher ICU mortality (23.8% vs. 13.7%, P=0.02).
In the measurement of secondary endpoints, there was a trend toward lower episodes of severe sepsis and septic shock in the IIT group (20.7% in IIT vs. 27.2% in CIT, P=0.08). However, this result was not statistically significant.
Bottom line: This well-designed study failed to show a survival benefit with IIT use in the critical-care setting. Given the findings of this and several other recent studies, one should question whether IIT should be prescribed as the standard of care in all critically-ill patients.
Citation: Arabi Y, Dabbagh O, Tamim H, et al. Intensive versus conventional insulin therapy: a randomized controlled trial in medical and surgical critically ill patients. Crit Care Med. 2008;36(12):3190-3197.
Preoperative and Intraoperative Predictors of Cardiac Adverse Events
Clinical question: What are the incidence and risk factors for perioperative cardiac adverse events after noncardiac surgery?
Background: In the past few decades, the incidence of cardiac adverse events (CAEs) for a general surgery population has remained largely unchanged (approximately 1%). This is in spite of multiple studies evaluating predictive models and attempts at preventive treatment, including preoperative coronary revascularization and perioperative beta blockers.
Study design: Prospective observational study.
Setting: Single, large, tertiary-care university hospital.
Synopsis: A total of 7,740 cases were reviewed in this study, which consisted of general surgery (4,937), vascular surgery (1,846), and urological surgery (957). A trained nurse followed up for perioperative CAEs as many as 30 days after the operation via medical chart review, phone calls, and letters. CAEs were defined as: Q-wave myocardial infarction (MI), non-ST elevation MI, cardiac arrest, or new cardiac dysrhythmia. A total of 83 CAEs (1.1% of patients) had cardiac arrest, with cardiac dysrhythmia being most common.
A total of seven preoperative risk factors were identified as independent predictors for CAEs: age 68, BMI 30, emergent surgery, prior coronary intervention or cardiac surgery, active congestive heart failure, cerebrovascular disease, and hypertension. In addition, two intraoperative risk factors were identified: intraoperative transfusion of packed red blood cells and operative duration of 3.8 hours. (The P value was 0.05 for all independent predictors.)
A further evaluation of intraoperative parameters of high-risk patients experiencing a CAE showed that these patients were more likely to have an episode of mean arterial pressure (MAP) <50 mmHg, an episode of 40% decrease in MAP, and an episode of tachycardia (heart rate >100).
Bottom line: A combination of preoperative predictors and intraoperative elements can help improve risk assessment for perioperative CAEs after noncardiac surgery.
Citation: Kheterpal S, O’Reilly M, Englesbe M, et al. Preoperative and intraoperative predictors of cardiac adverse events after general, vascular, and urological surgery. Anesthesiology. 2009;110(1):58-66.
Early Feeding in the ICU Does Not Affect Hospital Mortality
Clinical question: Will implementing evidence-based feeding guidelines improve feeding practices and reduce mortality in ICU patients?
Background: There is evidence suggesting that providing nutritional support to ICU patients within 24 hours of admission may decrease mortality. It is widely understood that patient care varies between ICUs, and there exist no uniform, evidence-based guidelines for nutritional support. Many patients remain unfed after 48 hours.
Study design: Cluster, randomized-controlled trial.
Setting: ICUs in 27 community and tertiary-care hospitals in Australia and New Zealand.
Synopsis: Hospitals were randomized to intervention or control groups. Dietitian and intensivist co-investigators from intervention ICUs developed guidelines using the Clinical Practice Guideline Development Cycle. Control ICUs were requested to make no new ICU nutritional management changes. The study enrolled 1,118 eligible patients and included adults expected to stay longer than two days. Excluded were patients taking oral diets, patients receiving palliative care or with suspected brain death, and patients sent from other facilities.
Guidelines were implemented using several methods—educational outreach visits, one-on-one conversations, active reminders, passive reminders, and educational in-services. The guidelines were successful in evoking significant practice changes in all of the intervention ICUs. Significantly more patients received nutritional support during their ICU stays in guideline ICUs, and patients in these ICUs were fed significantly earlier. There were, however, no significant differences between guideline and control ICUs with regard to hospital discharge mortality (28.9% vs. 27.4%; 95% CI; -6.3% to 12.0%; P=0.75). The groups also showed no statistical difference in hospital or ICU length of stay.
Bottom line: Significantly more patients in the guideline ICUs were fed within 24 hours, but this did not translate into improvements in mortality or other clinical outcomes.
Citation: Doig G, Simpson F, Finfer S, et al. Effect of evidence-based feeding guidelines on mortality of critically ill adults: a cluster randomized controlled trial. JAMA. 2008;300(23):2731-2741.
Low-Dose Aspirin Doesn’t Reduce Cardiovascular Events in Type 2 Diabetes Patients
Clinical question: Is low-dose aspirin effective for the primary prevention of atherosclerotic events in patients with Type 2 diabetes?
Background: Diabetes is a significant risk factor for cardiovascular events. Several prior studies have shown that aspirin therapy is effective as a secondary prevention strategy for cardiovascular events. The American Diabetes Association also recommends use of aspirin as a primary prevention strategy. Clinical trial data is currently insufficient in this area.
Study design: Prospective, randomized, open-label, controlled trial with blinded endpoint assessment.
Setting: 163 institutions in Japan.
Synopsis: The study enrolled 2,539 diabetic patients between 30 and 85 years old—mean age was 65—and included patients without EKG changes or a significant history or ongoing treatment of atherosclerotic disease. Patients were randomly assigned into an aspirin group (81 mg or 100 mg once daily) or a nonaspirin group. Patients had a median follow up of 4.37 years.
The primary endpoint was any atherosclerotic event, ranging from sudden death to ischemic heart disease or stroke. The incidence of atherosclerotic events was not statistically different in the aspirin group (68 events, 5.4%) than in the nonaspirin group (86 events, 6.7%) (HR, 0.80; 95% CI; 0.58-1.10; log-rank test, P=0.16). However, there was a suggested benefit of primary prevention in the subgroup aged 65 years or older. In addition, the combined endpoint of fatal coronary and cerebrovascular events occurred in one patient in the aspirin group and 10 patients in the nonaspirin group (HR, 0.10; 95 % CI, 0.01-0.79; P=.0037). This study is limited by the low incidence of atherosclerotic disease in Japan.
Bottom line: Low-dose aspirin used in patients with Type 2 diabetes does not significantly demonstrate primary prevention of cardiovascular events.
Citation: Ogawa H, Nakayama M, Morimoto T, et al. Low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA. 2008;300(18):2134-2141. TH
In This Edition
- Generic vs. brand-name drugs.
- Rapid-response teams and mortality.
- A new prediction rule for mortality in acute pancreatitis.
- Viral causes of community-acquired pneumonia.
- Intensive insulin therapy in the ICU.
- New preoperative and intraoperative risk factors.
- Timing of ICU feedings and mortality.
- Aspirin as primary prevention in diabetics.
Generic, Brand-Name Drugs Used for Cardiovascular Disease Are Clinically Equivalent
Clinical question: Is there a clinical risk when substituting generic drugs for brand-name drugs in the treatment of cardiovascular disease?
Background: Spending on healthcare in the U.S. has reached critical levels. Increasing prescription drug costs make up a large portion of healthcare expenditures. The high cost of medicines directly affect adherence to treatment regimens and contribute to poor health outcomes. Cardiovascular drugs make up the largest portion of outpatient prescription drug spending.
Study design: Systematic review of relevant articles with a meta-analysis performed to determine an aggregate effect size.
Setting: Multiple locations and varied patient populations.
Synopsis: A total of 47 articles were included in the review, of which 38 were randomized controlled trials (RCTs). The studies measured both clinical efficacy and safety end points. More than half the articles were published prior to 2000. Clinical equivalence was noted in all seven beta-blocker RCTs; 10 of 11 diuretic RCTs; five of seven calcium-channel-blocker RCTs; all three antiplatelet-agent RCTs (clopidogrel, enteric-coated aspirin); two statin RCTs; one ACE-inhibitor RCT; and one alpha-blocker RCT. For drugs with a narrow therapeutic index, clinical equivalence was noted in all five warfarin RCTs and a single Class 1 anti-arrhythmic-agent RCT.
The aggregate effect size was -0.03 (95% CI, -0.15 to 0.08), which indicates nearly complete overlap of the generic and brand-name distributions. The data show no evidence of superiority of brand-name to generic drugs in clinical outcomes measured in the various studies.
In a separate review of editorials addressing generic substitution for cardiovascular drugs, 53% expressed a negative view of generic-drug substitution.
Bottom line: There is clinical equivalency between generic and brand-name drugs used in the treatment of cardiovascular disease. Despite this conclusion, a substantial number of editorials advise against generic substitution, which affects both patient and physician drug preferences.
Citation: Kesselheim A, Misono A, Lee J, et al. Clinical equivalence of generic and brand-name drugs used in cardiovascular disease: a systematic review and meta-analysis. JAMA. 2008; 300(21):2514-2526.
RRT Implement-ation Doesn’t Affect Hospitalwide Code Rates or Mortality
Clinical question: Does the use of a rapid-response team (RRT) affect hospitalwide code rates and mortality?
Background: In the 100,000 Lives campaign, the Institute for Healthcare Improvement recommended that hospitals implement RRTs to help reduce preventable, in-hospital deaths. Studies have demonstrated that rates of non-ICU codes decrease after RRT implementation. It is unclear if this translates to changes in mortality rates.
Study design: Prospective cohort study of adult inpatients.
Setting: Saint Luke’s Hospital, a 404-bed tertiary-care academic hospital in Kansas City, Mo.
Synopsis: The hospital documented a total of 376 RRT activations. After RRT implementation, mean hospitalwide code rates decreased to 7.5 per 1,000 admissions from 11.2 per 1,000 admissions. This was not associated with a statistically significant reduction in hospitalwide code rates (adjusted odds ratio 0.76; 95% CI; 0.57-1.01; P=0.06). Secondary analyses noted lower rates of non-ICU codes (0.59; 95% CI, 0.40-0.89) compared with ICU codes (0.95; 95% CI; 0.64-1.43; P=0.03 for interaction). Finally, the RRT implementation was not associated with lower hospital-wide mortality (0.95; 95% CI; 0.81-1.11; P=0.52).
Secondary analyses also revealed few instances of RRT undertreatment or underutilization that may have affected the mortality numbers.
A limitation of this study is that it was slightly underpowered (78%) to detect a significant mortality difference. The findings also represent a single institution experience, and may not be generalized to other adult hospital settings or RRT programs.
Bottom line: Implementation of an RRT does not confer lower rates of hospital-wide code arrests or mortality.
Citation: Chan P, Khalid A, Longmore L, et al. Hospital-wide code rates and mortality before and after implementation of a rapid response team. JAMA. 2008;300(21):2506-2513.
Simple Scoring System Provides Timely Prediction of Mortality in Acute Pancreatitis
Clinical question: How can physicians predict mortality in acute pancreatitis?
Background: Historical predictors of mortality in acute pancreatitis require up to 48 hours of data, such as with the Ranson Criteria, or extensive amounts of data, such as with the APACHE II score. An easier tool is needed to predict which patients are at higher risk of mortality.
Study design: Retrospective cohort.
Setting: Patients in the Cardinal Health clinical outcomes research database, which supports public reporting of hospital performance.
Synopsis: The authors identified patients with the principal diagnosis of pancreatitis from 2000-2001 and explored numerous diagnostic findings available within the first 24 hours. Ultimately, BUN >25, impaired mental status, presence of SIRS (systemic inflammatory response syndrome), age >60, and presence of a pleural effusion were found to be predictive of mortality. These diagnostic findings correspond to the mnemonic BISAP. The BISAP score was then validated in a second cohort that included patients from 2004-2005.
Each finding in the BISAP score was given one point. A score of less than 2 was present in approximately 60% of patients admitted with acute pancreatitis, and corresponded to a mortality of less than 1%. A score of 2 corresponded to a mortality of 2%. Higher scores were associated with steeply increasing mortality, with a score of 5 corresponding with greater than 20% mortality.
The BISAP score performed similarly to the APACHE II score, but the former is easier to calculate on the day of admission and has fewer parameters. A more challenging research step will be to demonstrate that using the BISAP score to determine treatment strategies can affect patient outcomes.
Bottom line: The easy-to-calculate BISAP score is a new method for predicting mortality in patients with acute pancreatitis. This tool should help hospitalists determine, on the day of admission, to what extent patients with acute pancreatitis need aggressive management, such as ICU admission and early involvement of specialists.
Citation: Wu B, Johannes R, Sun X, Tabak Y, Conwell D, Banks P. The early prediction of mortality in acute pancreatitis: a large population-based study. Gut. 2008;57(12): 1698-1703.
Nasal Swabs Identify Viral Causes in CAP Patients
Clinical question: How often is viral infection associated with community-acquired pneumonia (CAP) in adults?
Background: CAP is a clinically important disease that is associated with significant hospitalization and mortality. CAP treatment guidelines acknowledge respiratory viruses as an etiology for pneumonia, but few recommendations are made regarding management of these viral infections.
Study design: Prospective study.
Setting: Five hospitals in Edmonton, Alberta, from 2004-2006.
Synopsis: The authors enrolled 193 hospitalized adults, median age 71. Nucleic amplification tests (NATs) from nasopharyngeal swab specimens were tested for human metapneumovirus, respiratory syncytial virus, rhinovirus, parainfluenza virus 1-4, coronaviruses, and adenovirus.
Fifteen percent of these patients had a nasal swab positive for a viral infection. Interestingly, 4% of patients had both a positive viral nasal swab and positive bacterial cultures. Compared with bacterial infection, patients with viral infection tended to be older (76 vs. 64 years, P=0.01), have limited ambulation (66% vs. 32%, P=0.006), and have a history of cardiac disease (66% vs. 32%, P=0.02). Patients with bacterial pneumonia showed a statistically significant trend toward having chest pain, an abnormal white blood count, and a lobar infiltrate on chest X-ray.
Further investigations might look at how nasal swab data could be used to improve infection control within the hospital for patients found to have easily transmissible viruses. Further research could explore the feasibility of avoiding antibiotic use in patients found to have viral pneumonia, assuming bacterial co-infection is reliably excluded.
Bottom line: Nasal swabs using NAT technology could play a significant role in identifying pathogens in CAP patients. How this technology should affect clinical decision-making and how it might improve outcomes remains unknown.
Citation: Johnstone J, Majumdar S, Fox J, Marrie T. Viral infection in adults hospitalized with community-acquired pneumonia: prevalence, pathogens, and presentation. Chest. 2008;134(6):1141-1148.
Intensive Insulin Therapy Doesn’t Reduce ICU Mortality
Clinical question: Does the use of intensive insulin therapy decrease mortality in the intensive-care unit (ICU)?
Background: In 2001, Van den Berghe et al (N Engl J Med. 2001;345(19):1359-67) reported a reduction in morbidity and mortality with intensive insulin therapy (IIT) in surgical ICU patients. This study led to the adoption of IIT protocols in many hospitals. Since 2001, further studies have failed to reproduce the same dramatic benefit of IIT.
Study design: Randomized, controlled trial.
Setting: National Guard King Abdulaziz Medical City, a tertiary-care teaching hospital in Saudi Arabia.
Synopsis: Patients were included in this study if they were 18 years or older with serum glucose levels greater than 110 mg/dL during the first 24 hours of ICU admission. There were multiple exclusion criteria, including patients with Type I diabetes, documented hypoglycemia on ICU admission (glucose <40), or diabetic ketoacidosis.
Enrolled patients were randomized to IIT or conventional insulin therapy (CIT). A multidisciplinary team designed the protocols to maintain glucose levels of 80 to 110 mg/dL and 180 to 200 mg/dL in the IIT and the CIT groups, respectively. The primary endpoint measured was ICU mortality.
The study did not produce a statistically significant difference in ICU mortality (13.5% for IIT vs. 17.1% for CIT; P=0.30). The adjusted hypoglycemia rate was 6.8 per 100 treatment days with IIT and 0.4 per 100 treatment days with CIT (P<0.0001). Patients with hypoglycemia had higher ICU mortality (23.8% vs. 13.7%, P=0.02).
In the measurement of secondary endpoints, there was a trend toward lower episodes of severe sepsis and septic shock in the IIT group (20.7% in IIT vs. 27.2% in CIT, P=0.08). However, this result was not statistically significant.
Bottom line: This well-designed study failed to show a survival benefit with IIT use in the critical-care setting. Given the findings of this and several other recent studies, one should question whether IIT should be prescribed as the standard of care in all critically-ill patients.
Citation: Arabi Y, Dabbagh O, Tamim H, et al. Intensive versus conventional insulin therapy: a randomized controlled trial in medical and surgical critically ill patients. Crit Care Med. 2008;36(12):3190-3197.
Preoperative and Intraoperative Predictors of Cardiac Adverse Events
Clinical question: What are the incidence and risk factors for perioperative cardiac adverse events after noncardiac surgery?
Background: In the past few decades, the incidence of cardiac adverse events (CAEs) for a general surgery population has remained largely unchanged (approximately 1%). This is in spite of multiple studies evaluating predictive models and attempts at preventive treatment, including preoperative coronary revascularization and perioperative beta blockers.
Study design: Prospective observational study.
Setting: Single, large, tertiary-care university hospital.
Synopsis: A total of 7,740 cases were reviewed in this study, which consisted of general surgery (4,937), vascular surgery (1,846), and urological surgery (957). A trained nurse followed up for perioperative CAEs as many as 30 days after the operation via medical chart review, phone calls, and letters. CAEs were defined as: Q-wave myocardial infarction (MI), non-ST elevation MI, cardiac arrest, or new cardiac dysrhythmia. A total of 83 CAEs (1.1% of patients) had cardiac arrest, with cardiac dysrhythmia being most common.
A total of seven preoperative risk factors were identified as independent predictors for CAEs: age 68, BMI 30, emergent surgery, prior coronary intervention or cardiac surgery, active congestive heart failure, cerebrovascular disease, and hypertension. In addition, two intraoperative risk factors were identified: intraoperative transfusion of packed red blood cells and operative duration of 3.8 hours. (The P value was 0.05 for all independent predictors.)
A further evaluation of intraoperative parameters of high-risk patients experiencing a CAE showed that these patients were more likely to have an episode of mean arterial pressure (MAP) <50 mmHg, an episode of 40% decrease in MAP, and an episode of tachycardia (heart rate >100).
Bottom line: A combination of preoperative predictors and intraoperative elements can help improve risk assessment for perioperative CAEs after noncardiac surgery.
Citation: Kheterpal S, O’Reilly M, Englesbe M, et al. Preoperative and intraoperative predictors of cardiac adverse events after general, vascular, and urological surgery. Anesthesiology. 2009;110(1):58-66.
Early Feeding in the ICU Does Not Affect Hospital Mortality
Clinical question: Will implementing evidence-based feeding guidelines improve feeding practices and reduce mortality in ICU patients?
Background: There is evidence suggesting that providing nutritional support to ICU patients within 24 hours of admission may decrease mortality. It is widely understood that patient care varies between ICUs, and there exist no uniform, evidence-based guidelines for nutritional support. Many patients remain unfed after 48 hours.
Study design: Cluster, randomized-controlled trial.
Setting: ICUs in 27 community and tertiary-care hospitals in Australia and New Zealand.
Synopsis: Hospitals were randomized to intervention or control groups. Dietitian and intensivist co-investigators from intervention ICUs developed guidelines using the Clinical Practice Guideline Development Cycle. Control ICUs were requested to make no new ICU nutritional management changes. The study enrolled 1,118 eligible patients and included adults expected to stay longer than two days. Excluded were patients taking oral diets, patients receiving palliative care or with suspected brain death, and patients sent from other facilities.
Guidelines were implemented using several methods—educational outreach visits, one-on-one conversations, active reminders, passive reminders, and educational in-services. The guidelines were successful in evoking significant practice changes in all of the intervention ICUs. Significantly more patients received nutritional support during their ICU stays in guideline ICUs, and patients in these ICUs were fed significantly earlier. There were, however, no significant differences between guideline and control ICUs with regard to hospital discharge mortality (28.9% vs. 27.4%; 95% CI; -6.3% to 12.0%; P=0.75). The groups also showed no statistical difference in hospital or ICU length of stay.
Bottom line: Significantly more patients in the guideline ICUs were fed within 24 hours, but this did not translate into improvements in mortality or other clinical outcomes.
Citation: Doig G, Simpson F, Finfer S, et al. Effect of evidence-based feeding guidelines on mortality of critically ill adults: a cluster randomized controlled trial. JAMA. 2008;300(23):2731-2741.
Low-Dose Aspirin Doesn’t Reduce Cardiovascular Events in Type 2 Diabetes Patients
Clinical question: Is low-dose aspirin effective for the primary prevention of atherosclerotic events in patients with Type 2 diabetes?
Background: Diabetes is a significant risk factor for cardiovascular events. Several prior studies have shown that aspirin therapy is effective as a secondary prevention strategy for cardiovascular events. The American Diabetes Association also recommends use of aspirin as a primary prevention strategy. Clinical trial data is currently insufficient in this area.
Study design: Prospective, randomized, open-label, controlled trial with blinded endpoint assessment.
Setting: 163 institutions in Japan.
Synopsis: The study enrolled 2,539 diabetic patients between 30 and 85 years old—mean age was 65—and included patients without EKG changes or a significant history or ongoing treatment of atherosclerotic disease. Patients were randomly assigned into an aspirin group (81 mg or 100 mg once daily) or a nonaspirin group. Patients had a median follow up of 4.37 years.
The primary endpoint was any atherosclerotic event, ranging from sudden death to ischemic heart disease or stroke. The incidence of atherosclerotic events was not statistically different in the aspirin group (68 events, 5.4%) than in the nonaspirin group (86 events, 6.7%) (HR, 0.80; 95% CI; 0.58-1.10; log-rank test, P=0.16). However, there was a suggested benefit of primary prevention in the subgroup aged 65 years or older. In addition, the combined endpoint of fatal coronary and cerebrovascular events occurred in one patient in the aspirin group and 10 patients in the nonaspirin group (HR, 0.10; 95 % CI, 0.01-0.79; P=.0037). This study is limited by the low incidence of atherosclerotic disease in Japan.
Bottom line: Low-dose aspirin used in patients with Type 2 diabetes does not significantly demonstrate primary prevention of cardiovascular events.
Citation: Ogawa H, Nakayama M, Morimoto T, et al. Low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA. 2008;300(18):2134-2141. TH