User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Metformin fails as early COVID-19 treatment but shows potential
Neither metformin, ivermectin, or fluvoxamine had any impact on reducing disease severity, hospitalization, or death from COVID-19, according to results from more than 1,000 overweight or obese adult patients in the COVID-OUT randomized trial.
However, metformin showed some potential in a secondary analysis.
Early treatment to prevent severe disease remains a goal in managing the ongoing COVID-19 pandemic, and biophysical modeling suggested that metformin, ivermectin, and fluvoxamine may serve as antivirals to help reduce severe disease in COVID-19 patients, Carolyn T. Bramante, MD, of the University of Minnesota, Minneapolis, and colleagues wrote.
“We started enrolling patients at the end of December 2020,” Dr. Bramante said in an interview. “At that time, even though vaccine data were coming out, we thought it was important to test early outpatient treatment with widely available safe medications with no interactions, because the virus would evolve and vaccine availability may be limited.”
In a study published in the New England Journal of Medicine, the researchers used a two-by-three factorial design to test the ability of metformin, ivermectin, and fluvoxamine to prevent severe COVID-19 infection in nonhospitalized adults aged 30-85 years. A total of 1,431 patients at six U.S. sites were enrolled within 3 days of a confirmed infection and less than 7 days after the start of symptoms, then randomized to one of six groups: metformin plus fluvoxamine; metformin plus ivermectin; metformin plus placebo; placebo plus fluvoxamine; placebo plus ivermectin; and placebo plus placebo.
A total of 1,323 patients were included in the primary analysis. The median age of the patients was 46 years, 56% were female (of whom 6% were pregnant), and all individuals met criteria for overweight or obesity. About half (52%) of the patients had been vaccinated against COVID-19.
The primary endpoint was a composite of hypoxemia, ED visit, hospitalization, or death. The analyses were adjusted for COVID-19 vaccination and other trial medications. Overall, the adjusted odds ratios of any primary event, compared with placebo, was 0.84 for metformin (P = .19), 1.05 for ivermectin (P = .78), and 0.94 for fluvoxamine (P = .75).
The researchers also conducted a prespecified secondary analysis of components of the primary endpoint. In this analysis, the aORs for an ED visit, hospitalization, or death was 0.58 for metformin, 1.39 for ivermectin, and 1.17 for fluvoxamine. The aORs for hospitalization or death were 0.47, 0.73, and 1.11 for metformin, ivermectin, and fluvoxamine, respectively. No medication-related serious adverse events were reported with any of the drugs during the study period.
The possible benefit for prevention of severe COVID-19 with metformin was a prespecified secondary endpoint, and therefore not definitive until more research has been completed, the researchers said. Metformin has demonstrated anti-inflammatory actions in previous studies, and has shown protective effects against COVID-19 lung injury in animal studies.
Previous observational studies also have shown an association between metformin use and less severe COVID-19 in patients already taking metformin. “The proposed mechanisms of action against COVID-19 for metformin include anti-inflammatory and antiviral activity and the prevention of hyperglycemia during acute illness,” they added.
The study findings were limited by several factors including the population age range and focus on overweight and obese patients, which may limit generalizability, the researchers noted. Other limitations include the disproportionately small percentage of Black and Latino patients and the potential lack of accuracy in identifying hypoxemia via home oxygen monitors.
However, the results demonstrate that none of the three repurposed drugs – metformin, ivermectin, and fluvoxamine – prevented primary events or reduced symptom severity in COVID-19, compared with placebos, the researchers concluded.
“Metformin had several streams of evidence supporting its use: in vitro, in silico [computer modeled], observational, and in tissue. We were not surprised to see that it reduced emergency department visits, hospitalization, and death,” Dr. Bramante said in an interview.
The take-home message for clinicians is to continue to look to guideline committees for direction on COVID-19 treatments, but to continue to consider metformin along with other treatments, she said.
“All research should be replicated, whether the primary outcome is positive or negative,” Dr. Bramante emphasized. “In this case, when our positive outcome was negative and secondary outcome was positive, a confirmatory trial for metformin is particularly important.”
Ineffective drugs are inefficient use of resources
“The results of the COVID-OUT trial provide persuasive additional data that increase the confidence and degree of certainty that fluvoxamine and ivermectin are not effective in preventing progression to severe disease,” wrote Salim S. Abdool Karim, MB, and Nikita Devnarain, PhD, of the Centre for the AIDS Programme of Research in South Africa, Durban, in an accompanying editorial.
At the start of the study, in 2020, data on the use of the three drugs to prevent severe COVID-19 were “either unavailable or equivocal,” they said. Since then, accumulating data support the current study findings of the nonefficacy of ivermectin and fluvoxamine, and the World Health Organization has advised against their use for COVID-19, although the WHO has not provided guidance for the use of metformin.
The authors called on clinicians to stop using ivermectin and fluvoxamine to treat COVID-19 patients.
“With respect to clinical decisions about COVID-19 treatment, some drug choices, especially those that have negative [World Health Organization] recommendations, are clearly wrong,” they wrote. “In keeping with evidence-based medical practice, patients with COVID-19 must be treated with efficacious medications; they deserve nothing less.”
The study was supported by the Parsemus Foundation, Rainwater Charitable Foundation, Fast Grants, and UnitedHealth Group Foundation. The fluvoxamine placebo tablets were donated by Apotex Pharmaceuticals. The ivermectin placebo and active tablets were donated by Edenbridge Pharmaceuticals. Lead author Dr. Bramante was supported the National Center for Advancing Translational Sciences and the National Institute of Diabetes and Digestive and Kidney Diseases. The researchers had no financial conflicts to disclose. Dr. Abdool Karim serves as a member of the World Health Organization Science Council. Dr. Devnarain had no financial conflicts to disclose.
Neither metformin, ivermectin, or fluvoxamine had any impact on reducing disease severity, hospitalization, or death from COVID-19, according to results from more than 1,000 overweight or obese adult patients in the COVID-OUT randomized trial.
However, metformin showed some potential in a secondary analysis.
Early treatment to prevent severe disease remains a goal in managing the ongoing COVID-19 pandemic, and biophysical modeling suggested that metformin, ivermectin, and fluvoxamine may serve as antivirals to help reduce severe disease in COVID-19 patients, Carolyn T. Bramante, MD, of the University of Minnesota, Minneapolis, and colleagues wrote.
“We started enrolling patients at the end of December 2020,” Dr. Bramante said in an interview. “At that time, even though vaccine data were coming out, we thought it was important to test early outpatient treatment with widely available safe medications with no interactions, because the virus would evolve and vaccine availability may be limited.”
In a study published in the New England Journal of Medicine, the researchers used a two-by-three factorial design to test the ability of metformin, ivermectin, and fluvoxamine to prevent severe COVID-19 infection in nonhospitalized adults aged 30-85 years. A total of 1,431 patients at six U.S. sites were enrolled within 3 days of a confirmed infection and less than 7 days after the start of symptoms, then randomized to one of six groups: metformin plus fluvoxamine; metformin plus ivermectin; metformin plus placebo; placebo plus fluvoxamine; placebo plus ivermectin; and placebo plus placebo.
A total of 1,323 patients were included in the primary analysis. The median age of the patients was 46 years, 56% were female (of whom 6% were pregnant), and all individuals met criteria for overweight or obesity. About half (52%) of the patients had been vaccinated against COVID-19.
The primary endpoint was a composite of hypoxemia, ED visit, hospitalization, or death. The analyses were adjusted for COVID-19 vaccination and other trial medications. Overall, the adjusted odds ratios of any primary event, compared with placebo, was 0.84 for metformin (P = .19), 1.05 for ivermectin (P = .78), and 0.94 for fluvoxamine (P = .75).
The researchers also conducted a prespecified secondary analysis of components of the primary endpoint. In this analysis, the aORs for an ED visit, hospitalization, or death was 0.58 for metformin, 1.39 for ivermectin, and 1.17 for fluvoxamine. The aORs for hospitalization or death were 0.47, 0.73, and 1.11 for metformin, ivermectin, and fluvoxamine, respectively. No medication-related serious adverse events were reported with any of the drugs during the study period.
The possible benefit for prevention of severe COVID-19 with metformin was a prespecified secondary endpoint, and therefore not definitive until more research has been completed, the researchers said. Metformin has demonstrated anti-inflammatory actions in previous studies, and has shown protective effects against COVID-19 lung injury in animal studies.
Previous observational studies also have shown an association between metformin use and less severe COVID-19 in patients already taking metformin. “The proposed mechanisms of action against COVID-19 for metformin include anti-inflammatory and antiviral activity and the prevention of hyperglycemia during acute illness,” they added.
The study findings were limited by several factors including the population age range and focus on overweight and obese patients, which may limit generalizability, the researchers noted. Other limitations include the disproportionately small percentage of Black and Latino patients and the potential lack of accuracy in identifying hypoxemia via home oxygen monitors.
However, the results demonstrate that none of the three repurposed drugs – metformin, ivermectin, and fluvoxamine – prevented primary events or reduced symptom severity in COVID-19, compared with placebos, the researchers concluded.
“Metformin had several streams of evidence supporting its use: in vitro, in silico [computer modeled], observational, and in tissue. We were not surprised to see that it reduced emergency department visits, hospitalization, and death,” Dr. Bramante said in an interview.
The take-home message for clinicians is to continue to look to guideline committees for direction on COVID-19 treatments, but to continue to consider metformin along with other treatments, she said.
“All research should be replicated, whether the primary outcome is positive or negative,” Dr. Bramante emphasized. “In this case, when our positive outcome was negative and secondary outcome was positive, a confirmatory trial for metformin is particularly important.”
Ineffective drugs are inefficient use of resources
“The results of the COVID-OUT trial provide persuasive additional data that increase the confidence and degree of certainty that fluvoxamine and ivermectin are not effective in preventing progression to severe disease,” wrote Salim S. Abdool Karim, MB, and Nikita Devnarain, PhD, of the Centre for the AIDS Programme of Research in South Africa, Durban, in an accompanying editorial.
At the start of the study, in 2020, data on the use of the three drugs to prevent severe COVID-19 were “either unavailable or equivocal,” they said. Since then, accumulating data support the current study findings of the nonefficacy of ivermectin and fluvoxamine, and the World Health Organization has advised against their use for COVID-19, although the WHO has not provided guidance for the use of metformin.
The authors called on clinicians to stop using ivermectin and fluvoxamine to treat COVID-19 patients.
“With respect to clinical decisions about COVID-19 treatment, some drug choices, especially those that have negative [World Health Organization] recommendations, are clearly wrong,” they wrote. “In keeping with evidence-based medical practice, patients with COVID-19 must be treated with efficacious medications; they deserve nothing less.”
The study was supported by the Parsemus Foundation, Rainwater Charitable Foundation, Fast Grants, and UnitedHealth Group Foundation. The fluvoxamine placebo tablets were donated by Apotex Pharmaceuticals. The ivermectin placebo and active tablets were donated by Edenbridge Pharmaceuticals. Lead author Dr. Bramante was supported the National Center for Advancing Translational Sciences and the National Institute of Diabetes and Digestive and Kidney Diseases. The researchers had no financial conflicts to disclose. Dr. Abdool Karim serves as a member of the World Health Organization Science Council. Dr. Devnarain had no financial conflicts to disclose.
Neither metformin, ivermectin, or fluvoxamine had any impact on reducing disease severity, hospitalization, or death from COVID-19, according to results from more than 1,000 overweight or obese adult patients in the COVID-OUT randomized trial.
However, metformin showed some potential in a secondary analysis.
Early treatment to prevent severe disease remains a goal in managing the ongoing COVID-19 pandemic, and biophysical modeling suggested that metformin, ivermectin, and fluvoxamine may serve as antivirals to help reduce severe disease in COVID-19 patients, Carolyn T. Bramante, MD, of the University of Minnesota, Minneapolis, and colleagues wrote.
“We started enrolling patients at the end of December 2020,” Dr. Bramante said in an interview. “At that time, even though vaccine data were coming out, we thought it was important to test early outpatient treatment with widely available safe medications with no interactions, because the virus would evolve and vaccine availability may be limited.”
In a study published in the New England Journal of Medicine, the researchers used a two-by-three factorial design to test the ability of metformin, ivermectin, and fluvoxamine to prevent severe COVID-19 infection in nonhospitalized adults aged 30-85 years. A total of 1,431 patients at six U.S. sites were enrolled within 3 days of a confirmed infection and less than 7 days after the start of symptoms, then randomized to one of six groups: metformin plus fluvoxamine; metformin plus ivermectin; metformin plus placebo; placebo plus fluvoxamine; placebo plus ivermectin; and placebo plus placebo.
A total of 1,323 patients were included in the primary analysis. The median age of the patients was 46 years, 56% were female (of whom 6% were pregnant), and all individuals met criteria for overweight or obesity. About half (52%) of the patients had been vaccinated against COVID-19.
The primary endpoint was a composite of hypoxemia, ED visit, hospitalization, or death. The analyses were adjusted for COVID-19 vaccination and other trial medications. Overall, the adjusted odds ratios of any primary event, compared with placebo, was 0.84 for metformin (P = .19), 1.05 for ivermectin (P = .78), and 0.94 for fluvoxamine (P = .75).
The researchers also conducted a prespecified secondary analysis of components of the primary endpoint. In this analysis, the aORs for an ED visit, hospitalization, or death was 0.58 for metformin, 1.39 for ivermectin, and 1.17 for fluvoxamine. The aORs for hospitalization or death were 0.47, 0.73, and 1.11 for metformin, ivermectin, and fluvoxamine, respectively. No medication-related serious adverse events were reported with any of the drugs during the study period.
The possible benefit for prevention of severe COVID-19 with metformin was a prespecified secondary endpoint, and therefore not definitive until more research has been completed, the researchers said. Metformin has demonstrated anti-inflammatory actions in previous studies, and has shown protective effects against COVID-19 lung injury in animal studies.
Previous observational studies also have shown an association between metformin use and less severe COVID-19 in patients already taking metformin. “The proposed mechanisms of action against COVID-19 for metformin include anti-inflammatory and antiviral activity and the prevention of hyperglycemia during acute illness,” they added.
The study findings were limited by several factors including the population age range and focus on overweight and obese patients, which may limit generalizability, the researchers noted. Other limitations include the disproportionately small percentage of Black and Latino patients and the potential lack of accuracy in identifying hypoxemia via home oxygen monitors.
However, the results demonstrate that none of the three repurposed drugs – metformin, ivermectin, and fluvoxamine – prevented primary events or reduced symptom severity in COVID-19, compared with placebos, the researchers concluded.
“Metformin had several streams of evidence supporting its use: in vitro, in silico [computer modeled], observational, and in tissue. We were not surprised to see that it reduced emergency department visits, hospitalization, and death,” Dr. Bramante said in an interview.
The take-home message for clinicians is to continue to look to guideline committees for direction on COVID-19 treatments, but to continue to consider metformin along with other treatments, she said.
“All research should be replicated, whether the primary outcome is positive or negative,” Dr. Bramante emphasized. “In this case, when our positive outcome was negative and secondary outcome was positive, a confirmatory trial for metformin is particularly important.”
Ineffective drugs are inefficient use of resources
“The results of the COVID-OUT trial provide persuasive additional data that increase the confidence and degree of certainty that fluvoxamine and ivermectin are not effective in preventing progression to severe disease,” wrote Salim S. Abdool Karim, MB, and Nikita Devnarain, PhD, of the Centre for the AIDS Programme of Research in South Africa, Durban, in an accompanying editorial.
At the start of the study, in 2020, data on the use of the three drugs to prevent severe COVID-19 were “either unavailable or equivocal,” they said. Since then, accumulating data support the current study findings of the nonefficacy of ivermectin and fluvoxamine, and the World Health Organization has advised against their use for COVID-19, although the WHO has not provided guidance for the use of metformin.
The authors called on clinicians to stop using ivermectin and fluvoxamine to treat COVID-19 patients.
“With respect to clinical decisions about COVID-19 treatment, some drug choices, especially those that have negative [World Health Organization] recommendations, are clearly wrong,” they wrote. “In keeping with evidence-based medical practice, patients with COVID-19 must be treated with efficacious medications; they deserve nothing less.”
The study was supported by the Parsemus Foundation, Rainwater Charitable Foundation, Fast Grants, and UnitedHealth Group Foundation. The fluvoxamine placebo tablets were donated by Apotex Pharmaceuticals. The ivermectin placebo and active tablets were donated by Edenbridge Pharmaceuticals. Lead author Dr. Bramante was supported the National Center for Advancing Translational Sciences and the National Institute of Diabetes and Digestive and Kidney Diseases. The researchers had no financial conflicts to disclose. Dr. Abdool Karim serves as a member of the World Health Organization Science Council. Dr. Devnarain had no financial conflicts to disclose.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Use of antidotes in pregnancy and lactation
The human pregnancy data reported for these 16 agents are very limited as only 8 of the drugs have this data. However, the 8 reports indicated that the use of these drugs was highly important for the mother and did not cause embryo/fetal harm.
- Acetylcysteine
The need for this antidote in a pregnant or lactating woman is most likely a rare requirement. However, the need for this agent does occur in women who have taken a potentially hepatic toxic dose of acetaminophen (e.g., Tylenol).
- Black widow spider antivenin
Only three reports of the use of this agent in a pregnant woman have been located. In each case, the symptoms from the spider bite did not respond to other therapies but did within 1 hour to the antivenin. There was no fetal harm in these cases.
- Deferasirox
This agent is an oral iron-chelating agent used for the treatment of chronic iron overload. Five case reports have described its use without causing any fetal harm.
- Deferoxamine
This agent has been used in more than 65 pregnancies for acute iron overdose or for transfusion-dependent thalassemia. No reports have observed adverse human developmental effects.
- Digoxin immune FAB (ovine)
Several reports have described the use of this agent in pregnancy. No fetal harm has been observed, but none of the reports involved exposure during organogenesis. However, in cases of digoxin overdose, the maternal benefits of therapy should take priority over the embryo/fetus.
- Dimercaprol
Although the limited animal data suggest low risk, there are no reports of the use of this drug in human organogenesis. The absence of data prevents an assessment of the embryo-fetal risk, but the maternal benefit and indirect embryo-fetal benefit appears to outweigh that risk.
- Edetate calcium disodium
This agent is used to treat acute or chronic lead poisoning. It is compatible in pregnancy because the maternal and possibly the embryo-fetal benefit appears to outweigh any unknown direct or indirect risks.
- Flumazenil
The use of this drug in the third trimester has been reported in two cases. Because the drug is indicated to reverse the effects of benzodiazepines on the central nervous system, the maternal benefit should far outweigh the unknown embryo-fetal risk.
- Glucagon
The embryo-fetal risks appear to be very low. Apparently, the drug does not cross the placenta.
- Glucarpidase
This drug is indicated for the treatment of methotrexate toxicity. There are no reports describing the use of this drug in pregnancy or during breastfeeding.
- Idarucizumab
This agent is a humanized monoclonal antibody fragment that is indicated for the reversal of the anticoagulant effects of dabigatran. No reports describing its use in human or animal pregnancy have been located. However, the maternal benefit appears to be high and probably outweighs the unknown risk to the embryo/fetus.
- Lanthanum carbonate
There are no human pregnancy or lactation data. It is used to reduce blood levels of phosphate in people with kidney disease.
- Pralidoxime
This agent relieves the paralysis of the muscles of respiration caused by an organophosphate pesticide or related compound. The human pregnancy experience is limited to two cases, one at 36 weeks and the other at 16 weeks, both of which delivered normal infants.
- Sapropterin
Four reports have described the use of sapropterin to lower blood phenylalanine levels in 31 pregnancies. There were no embryo-fetal adverse effects attributable to the drug.
- Sevelamer
Sevelamer is used to control high blood levels of phosphorus in people with chronic kidney disease who are on dialysis. There are no human pregnancy or breastfeeding data.
- Succimer
This drug is a heavy metal–chelating agent that is indicated for the treatment of lead poisoning in pediatric patients. The drug was teratogenic in rats and mice. Two reports described the use of the drug in two pregnant women for lead poisoning. It has also been used as an antidote for the treatment of arsenic, mercury, and cadmium poisoning in adults, but there have been no reports of this use in pregnant patients.
Mr. Briggs, now retired, was a clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
The human pregnancy data reported for these 16 agents are very limited as only 8 of the drugs have this data. However, the 8 reports indicated that the use of these drugs was highly important for the mother and did not cause embryo/fetal harm.
- Acetylcysteine
The need for this antidote in a pregnant or lactating woman is most likely a rare requirement. However, the need for this agent does occur in women who have taken a potentially hepatic toxic dose of acetaminophen (e.g., Tylenol).
- Black widow spider antivenin
Only three reports of the use of this agent in a pregnant woman have been located. In each case, the symptoms from the spider bite did not respond to other therapies but did within 1 hour to the antivenin. There was no fetal harm in these cases.
- Deferasirox
This agent is an oral iron-chelating agent used for the treatment of chronic iron overload. Five case reports have described its use without causing any fetal harm.
- Deferoxamine
This agent has been used in more than 65 pregnancies for acute iron overdose or for transfusion-dependent thalassemia. No reports have observed adverse human developmental effects.
- Digoxin immune FAB (ovine)
Several reports have described the use of this agent in pregnancy. No fetal harm has been observed, but none of the reports involved exposure during organogenesis. However, in cases of digoxin overdose, the maternal benefits of therapy should take priority over the embryo/fetus.
- Dimercaprol
Although the limited animal data suggest low risk, there are no reports of the use of this drug in human organogenesis. The absence of data prevents an assessment of the embryo-fetal risk, but the maternal benefit and indirect embryo-fetal benefit appears to outweigh that risk.
- Edetate calcium disodium
This agent is used to treat acute or chronic lead poisoning. It is compatible in pregnancy because the maternal and possibly the embryo-fetal benefit appears to outweigh any unknown direct or indirect risks.
- Flumazenil
The use of this drug in the third trimester has been reported in two cases. Because the drug is indicated to reverse the effects of benzodiazepines on the central nervous system, the maternal benefit should far outweigh the unknown embryo-fetal risk.
- Glucagon
The embryo-fetal risks appear to be very low. Apparently, the drug does not cross the placenta.
- Glucarpidase
This drug is indicated for the treatment of methotrexate toxicity. There are no reports describing the use of this drug in pregnancy or during breastfeeding.
- Idarucizumab
This agent is a humanized monoclonal antibody fragment that is indicated for the reversal of the anticoagulant effects of dabigatran. No reports describing its use in human or animal pregnancy have been located. However, the maternal benefit appears to be high and probably outweighs the unknown risk to the embryo/fetus.
- Lanthanum carbonate
There are no human pregnancy or lactation data. It is used to reduce blood levels of phosphate in people with kidney disease.
- Pralidoxime
This agent relieves the paralysis of the muscles of respiration caused by an organophosphate pesticide or related compound. The human pregnancy experience is limited to two cases, one at 36 weeks and the other at 16 weeks, both of which delivered normal infants.
- Sapropterin
Four reports have described the use of sapropterin to lower blood phenylalanine levels in 31 pregnancies. There were no embryo-fetal adverse effects attributable to the drug.
- Sevelamer
Sevelamer is used to control high blood levels of phosphorus in people with chronic kidney disease who are on dialysis. There are no human pregnancy or breastfeeding data.
- Succimer
This drug is a heavy metal–chelating agent that is indicated for the treatment of lead poisoning in pediatric patients. The drug was teratogenic in rats and mice. Two reports described the use of the drug in two pregnant women for lead poisoning. It has also been used as an antidote for the treatment of arsenic, mercury, and cadmium poisoning in adults, but there have been no reports of this use in pregnant patients.
Mr. Briggs, now retired, was a clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
The human pregnancy data reported for these 16 agents are very limited as only 8 of the drugs have this data. However, the 8 reports indicated that the use of these drugs was highly important for the mother and did not cause embryo/fetal harm.
- Acetylcysteine
The need for this antidote in a pregnant or lactating woman is most likely a rare requirement. However, the need for this agent does occur in women who have taken a potentially hepatic toxic dose of acetaminophen (e.g., Tylenol).
- Black widow spider antivenin
Only three reports of the use of this agent in a pregnant woman have been located. In each case, the symptoms from the spider bite did not respond to other therapies but did within 1 hour to the antivenin. There was no fetal harm in these cases.
- Deferasirox
This agent is an oral iron-chelating agent used for the treatment of chronic iron overload. Five case reports have described its use without causing any fetal harm.
- Deferoxamine
This agent has been used in more than 65 pregnancies for acute iron overdose or for transfusion-dependent thalassemia. No reports have observed adverse human developmental effects.
- Digoxin immune FAB (ovine)
Several reports have described the use of this agent in pregnancy. No fetal harm has been observed, but none of the reports involved exposure during organogenesis. However, in cases of digoxin overdose, the maternal benefits of therapy should take priority over the embryo/fetus.
- Dimercaprol
Although the limited animal data suggest low risk, there are no reports of the use of this drug in human organogenesis. The absence of data prevents an assessment of the embryo-fetal risk, but the maternal benefit and indirect embryo-fetal benefit appears to outweigh that risk.
- Edetate calcium disodium
This agent is used to treat acute or chronic lead poisoning. It is compatible in pregnancy because the maternal and possibly the embryo-fetal benefit appears to outweigh any unknown direct or indirect risks.
- Flumazenil
The use of this drug in the third trimester has been reported in two cases. Because the drug is indicated to reverse the effects of benzodiazepines on the central nervous system, the maternal benefit should far outweigh the unknown embryo-fetal risk.
- Glucagon
The embryo-fetal risks appear to be very low. Apparently, the drug does not cross the placenta.
- Glucarpidase
This drug is indicated for the treatment of methotrexate toxicity. There are no reports describing the use of this drug in pregnancy or during breastfeeding.
- Idarucizumab
This agent is a humanized monoclonal antibody fragment that is indicated for the reversal of the anticoagulant effects of dabigatran. No reports describing its use in human or animal pregnancy have been located. However, the maternal benefit appears to be high and probably outweighs the unknown risk to the embryo/fetus.
- Lanthanum carbonate
There are no human pregnancy or lactation data. It is used to reduce blood levels of phosphate in people with kidney disease.
- Pralidoxime
This agent relieves the paralysis of the muscles of respiration caused by an organophosphate pesticide or related compound. The human pregnancy experience is limited to two cases, one at 36 weeks and the other at 16 weeks, both of which delivered normal infants.
- Sapropterin
Four reports have described the use of sapropterin to lower blood phenylalanine levels in 31 pregnancies. There were no embryo-fetal adverse effects attributable to the drug.
- Sevelamer
Sevelamer is used to control high blood levels of phosphorus in people with chronic kidney disease who are on dialysis. There are no human pregnancy or breastfeeding data.
- Succimer
This drug is a heavy metal–chelating agent that is indicated for the treatment of lead poisoning in pediatric patients. The drug was teratogenic in rats and mice. Two reports described the use of the drug in two pregnant women for lead poisoning. It has also been used as an antidote for the treatment of arsenic, mercury, and cadmium poisoning in adults, but there have been no reports of this use in pregnant patients.
Mr. Briggs, now retired, was a clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
No fish can escape this net ... of COVID testing
Something about this COVID testing smells fishy
The Chinese have been challenging America’s political and economic hegemony (yes, we did have to look that one up – you’re rude to ask) for some time, but now they’ve gone too far. Are we going to just sit here and let China do something more ridiculous than us in response to COVID? No way!
Here’s the deal: The government of the Chinese coastal city of Xiamen has decided that it’s not just the workers on returning fishing boats who have the potential to introduce COVID to the rest of the population. The fish also present a problem. So when the authorities say that everyone needs to be tested before they can enter the city, they mean everyone.
An employee of the municipal ocean development bureau told local media that “all people in Xiamen City need nucleic acid testing, and the fish catches must be tested as well,” according to the Guardian, which also said that “TV news reports showed officials swabbing the mouths of fish and the underside of crabs.”
In the words of George Takei: “Oh my.”
Hold on there a second, George Takei, because we here in the good old US of A have still got Los Angeles, where COVID testing also has taken a nonhuman turn. The LA County public health department recently announced that pets are now eligible for a free SARS-CoV-2 test through veterinarians and other animal care facilities.
“Our goal is to test many different species of animals including wildlife (deer, bats, raccoons), pets (dogs, cats, hamsters, pocket pets), marine mammals (seals), and more,” Veterinary Public Health announced.
Hegemony restored.
Not even God could save them from worms
The Dark Ages may not have been as dark and violent as many people think, but there’s no denying that life in medieval Europe kind of sucked. The only real alternative to serfdom was a job with the Catholic Church. Medieval friars, for example, lived in stone buildings, had access to fresh fruits and vegetables, and even had latrines and running water. Luxuries compared with the life of the average peasant.
So why then, despite having access to more modern sanitation and amenities, did the friars have so many gut parasites? That’s the question raised by a group of researchers from the University of Cambridge, who conducted a study of 19 medieval friars buried at a local friary (Oh, doesn’t your town have one of those?) and 25 local people buried at a nonreligious cemetery during a similar time period. Of those 19 friars, 11 were infected with worms and parasites, compared with just 8 of 25 townspeople.
This doesn’t make a lot of sense. The friars had a good life by old-time standards: They had basic sanitation down and a solid diet. These things should lead to a healthier population. The problem, the researchers found, is two pronged and a vicious cycle. First off, the friars had plenty of fresh food, but they used human feces to fertilize their produce. There’s a reason modern practice for human waste fertilization is to let the waste compost for 6 months: The waiting period allows the parasites a chance to kindly die off, which prevents reinfection.
Secondly, the friars’ diet of fresh fruits and vegetables mixed together into a salad, while appealing to our modern-day sensibilities, was not a great choice. By comparison, laypeople tended to eat a boiled mishmash of whatever they could find, and while that’s kind of gross, the key here is that their food was cooked. And heat kills parasites. The uncooked salads did no such thing, so the monks ate infected food, expelled infected poop, and grew more infected food with their infected poop.
Once the worms arrived, they never left, making them the worst kind of house guest. Read the room, worms, take your dinner and move on. You don’t have to go home, but you can’t stay here.
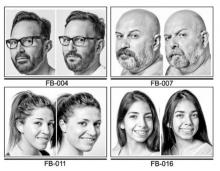
What’s a shared genotype between friends?
Do you find it hard to tell the difference between Katy Perry and Zooey Deschanel? They look alike, but they’re not related. Or are they? According to new research, people who look and act very similar but are not related may share DNA.
“Our study provides a rare insight into human likeness by showing that people with extreme look-alike faces share common genotypes, whereas they are discordant at the epigenome and microbiome levels,” senior author Manel Esteller of the Josep Carreras Leukemia Research Institute in Barcelona said in a written statement. “Genomics clusters them together, and the rest sets them apart.”
The Internet has been a great source in being able to find look-alikes. The research team found photos of doppelgangers photographed by François Brunelle, a Canadian artist. Using facial recognition algorithms, the investigators were able to measure likeness between the each pair of look-alikes. The participants also completed a questionnaire about lifestyle and provided a saliva sample.
The results showed that the look-alikes had similar genotypes but different DNA methylation and microbiome landscapes. The look-alikes also seemed to have similarities in weight, height, and behaviors such as smoking, proving that doppelgangers not only look alike but also share common interests.
Next time someone tells you that you look like their best friend Steve, you won’t have to wonder much what Steve is like.
The secret to a good relationship? It’s a secret
Strong relationships are built on honesty and trust, right? Being open with your partner and/or friends is usually a good practice for keeping the relationship healthy, but the latest evidence suggests that maybe you shouldn’t share everything.
According to the first known study on the emotional, behavioral, and relational aspect of consumer behavior, not disclosing certain purchases to your partner can actually be a good thing for the relationship. How? Well, it all has to do with guilt.
In a series of studies, the researchers asked couples about their secret consumptions. The most commonly hidden thing by far was a product (65%).
“We found that 90% of people have recently kept everyday consumer behaviors a secret from a close other – like a friend or spouse – even though they also report that they don’t think their partner would care if they knew about it,” Kelley Gullo Wight, one of the study’s two lead authors, said in a written statement.
Keeping a hidden stash of chocolate produces guilt, which the researchers found to be the key factor, making the perpetrator want to do more in the relationship to ease that sense of betrayal or dishonesty. They called it a “greater relationship investment,” meaning the person is more likely to do a little extra for their partner, like shell out more money for the next anniversary gift or yield to watching their partner’s favorite program.
So don’t feel too bad about that secret Amazon purchase. As long as the other person doesn’t see the box, nobody has to know. Your relationship can only improve.
Something about this COVID testing smells fishy
The Chinese have been challenging America’s political and economic hegemony (yes, we did have to look that one up – you’re rude to ask) for some time, but now they’ve gone too far. Are we going to just sit here and let China do something more ridiculous than us in response to COVID? No way!
Here’s the deal: The government of the Chinese coastal city of Xiamen has decided that it’s not just the workers on returning fishing boats who have the potential to introduce COVID to the rest of the population. The fish also present a problem. So when the authorities say that everyone needs to be tested before they can enter the city, they mean everyone.
An employee of the municipal ocean development bureau told local media that “all people in Xiamen City need nucleic acid testing, and the fish catches must be tested as well,” according to the Guardian, which also said that “TV news reports showed officials swabbing the mouths of fish and the underside of crabs.”
In the words of George Takei: “Oh my.”
Hold on there a second, George Takei, because we here in the good old US of A have still got Los Angeles, where COVID testing also has taken a nonhuman turn. The LA County public health department recently announced that pets are now eligible for a free SARS-CoV-2 test through veterinarians and other animal care facilities.
“Our goal is to test many different species of animals including wildlife (deer, bats, raccoons), pets (dogs, cats, hamsters, pocket pets), marine mammals (seals), and more,” Veterinary Public Health announced.
Hegemony restored.
Not even God could save them from worms
The Dark Ages may not have been as dark and violent as many people think, but there’s no denying that life in medieval Europe kind of sucked. The only real alternative to serfdom was a job with the Catholic Church. Medieval friars, for example, lived in stone buildings, had access to fresh fruits and vegetables, and even had latrines and running water. Luxuries compared with the life of the average peasant.
So why then, despite having access to more modern sanitation and amenities, did the friars have so many gut parasites? That’s the question raised by a group of researchers from the University of Cambridge, who conducted a study of 19 medieval friars buried at a local friary (Oh, doesn’t your town have one of those?) and 25 local people buried at a nonreligious cemetery during a similar time period. Of those 19 friars, 11 were infected with worms and parasites, compared with just 8 of 25 townspeople.
This doesn’t make a lot of sense. The friars had a good life by old-time standards: They had basic sanitation down and a solid diet. These things should lead to a healthier population. The problem, the researchers found, is two pronged and a vicious cycle. First off, the friars had plenty of fresh food, but they used human feces to fertilize their produce. There’s a reason modern practice for human waste fertilization is to let the waste compost for 6 months: The waiting period allows the parasites a chance to kindly die off, which prevents reinfection.
Secondly, the friars’ diet of fresh fruits and vegetables mixed together into a salad, while appealing to our modern-day sensibilities, was not a great choice. By comparison, laypeople tended to eat a boiled mishmash of whatever they could find, and while that’s kind of gross, the key here is that their food was cooked. And heat kills parasites. The uncooked salads did no such thing, so the monks ate infected food, expelled infected poop, and grew more infected food with their infected poop.
Once the worms arrived, they never left, making them the worst kind of house guest. Read the room, worms, take your dinner and move on. You don’t have to go home, but you can’t stay here.
What’s a shared genotype between friends?
Do you find it hard to tell the difference between Katy Perry and Zooey Deschanel? They look alike, but they’re not related. Or are they? According to new research, people who look and act very similar but are not related may share DNA.
“Our study provides a rare insight into human likeness by showing that people with extreme look-alike faces share common genotypes, whereas they are discordant at the epigenome and microbiome levels,” senior author Manel Esteller of the Josep Carreras Leukemia Research Institute in Barcelona said in a written statement. “Genomics clusters them together, and the rest sets them apart.”
The Internet has been a great source in being able to find look-alikes. The research team found photos of doppelgangers photographed by François Brunelle, a Canadian artist. Using facial recognition algorithms, the investigators were able to measure likeness between the each pair of look-alikes. The participants also completed a questionnaire about lifestyle and provided a saliva sample.
The results showed that the look-alikes had similar genotypes but different DNA methylation and microbiome landscapes. The look-alikes also seemed to have similarities in weight, height, and behaviors such as smoking, proving that doppelgangers not only look alike but also share common interests.
Next time someone tells you that you look like their best friend Steve, you won’t have to wonder much what Steve is like.
The secret to a good relationship? It’s a secret
Strong relationships are built on honesty and trust, right? Being open with your partner and/or friends is usually a good practice for keeping the relationship healthy, but the latest evidence suggests that maybe you shouldn’t share everything.
According to the first known study on the emotional, behavioral, and relational aspect of consumer behavior, not disclosing certain purchases to your partner can actually be a good thing for the relationship. How? Well, it all has to do with guilt.
In a series of studies, the researchers asked couples about their secret consumptions. The most commonly hidden thing by far was a product (65%).
“We found that 90% of people have recently kept everyday consumer behaviors a secret from a close other – like a friend or spouse – even though they also report that they don’t think their partner would care if they knew about it,” Kelley Gullo Wight, one of the study’s two lead authors, said in a written statement.
Keeping a hidden stash of chocolate produces guilt, which the researchers found to be the key factor, making the perpetrator want to do more in the relationship to ease that sense of betrayal or dishonesty. They called it a “greater relationship investment,” meaning the person is more likely to do a little extra for their partner, like shell out more money for the next anniversary gift or yield to watching their partner’s favorite program.
So don’t feel too bad about that secret Amazon purchase. As long as the other person doesn’t see the box, nobody has to know. Your relationship can only improve.
Something about this COVID testing smells fishy
The Chinese have been challenging America’s political and economic hegemony (yes, we did have to look that one up – you’re rude to ask) for some time, but now they’ve gone too far. Are we going to just sit here and let China do something more ridiculous than us in response to COVID? No way!
Here’s the deal: The government of the Chinese coastal city of Xiamen has decided that it’s not just the workers on returning fishing boats who have the potential to introduce COVID to the rest of the population. The fish also present a problem. So when the authorities say that everyone needs to be tested before they can enter the city, they mean everyone.
An employee of the municipal ocean development bureau told local media that “all people in Xiamen City need nucleic acid testing, and the fish catches must be tested as well,” according to the Guardian, which also said that “TV news reports showed officials swabbing the mouths of fish and the underside of crabs.”
In the words of George Takei: “Oh my.”
Hold on there a second, George Takei, because we here in the good old US of A have still got Los Angeles, where COVID testing also has taken a nonhuman turn. The LA County public health department recently announced that pets are now eligible for a free SARS-CoV-2 test through veterinarians and other animal care facilities.
“Our goal is to test many different species of animals including wildlife (deer, bats, raccoons), pets (dogs, cats, hamsters, pocket pets), marine mammals (seals), and more,” Veterinary Public Health announced.
Hegemony restored.
Not even God could save them from worms
The Dark Ages may not have been as dark and violent as many people think, but there’s no denying that life in medieval Europe kind of sucked. The only real alternative to serfdom was a job with the Catholic Church. Medieval friars, for example, lived in stone buildings, had access to fresh fruits and vegetables, and even had latrines and running water. Luxuries compared with the life of the average peasant.
So why then, despite having access to more modern sanitation and amenities, did the friars have so many gut parasites? That’s the question raised by a group of researchers from the University of Cambridge, who conducted a study of 19 medieval friars buried at a local friary (Oh, doesn’t your town have one of those?) and 25 local people buried at a nonreligious cemetery during a similar time period. Of those 19 friars, 11 were infected with worms and parasites, compared with just 8 of 25 townspeople.
This doesn’t make a lot of sense. The friars had a good life by old-time standards: They had basic sanitation down and a solid diet. These things should lead to a healthier population. The problem, the researchers found, is two pronged and a vicious cycle. First off, the friars had plenty of fresh food, but they used human feces to fertilize their produce. There’s a reason modern practice for human waste fertilization is to let the waste compost for 6 months: The waiting period allows the parasites a chance to kindly die off, which prevents reinfection.
Secondly, the friars’ diet of fresh fruits and vegetables mixed together into a salad, while appealing to our modern-day sensibilities, was not a great choice. By comparison, laypeople tended to eat a boiled mishmash of whatever they could find, and while that’s kind of gross, the key here is that their food was cooked. And heat kills parasites. The uncooked salads did no such thing, so the monks ate infected food, expelled infected poop, and grew more infected food with their infected poop.
Once the worms arrived, they never left, making them the worst kind of house guest. Read the room, worms, take your dinner and move on. You don’t have to go home, but you can’t stay here.
What’s a shared genotype between friends?
Do you find it hard to tell the difference between Katy Perry and Zooey Deschanel? They look alike, but they’re not related. Or are they? According to new research, people who look and act very similar but are not related may share DNA.
“Our study provides a rare insight into human likeness by showing that people with extreme look-alike faces share common genotypes, whereas they are discordant at the epigenome and microbiome levels,” senior author Manel Esteller of the Josep Carreras Leukemia Research Institute in Barcelona said in a written statement. “Genomics clusters them together, and the rest sets them apart.”
The Internet has been a great source in being able to find look-alikes. The research team found photos of doppelgangers photographed by François Brunelle, a Canadian artist. Using facial recognition algorithms, the investigators were able to measure likeness between the each pair of look-alikes. The participants also completed a questionnaire about lifestyle and provided a saliva sample.
The results showed that the look-alikes had similar genotypes but different DNA methylation and microbiome landscapes. The look-alikes also seemed to have similarities in weight, height, and behaviors such as smoking, proving that doppelgangers not only look alike but also share common interests.
Next time someone tells you that you look like their best friend Steve, you won’t have to wonder much what Steve is like.
The secret to a good relationship? It’s a secret
Strong relationships are built on honesty and trust, right? Being open with your partner and/or friends is usually a good practice for keeping the relationship healthy, but the latest evidence suggests that maybe you shouldn’t share everything.
According to the first known study on the emotional, behavioral, and relational aspect of consumer behavior, not disclosing certain purchases to your partner can actually be a good thing for the relationship. How? Well, it all has to do with guilt.
In a series of studies, the researchers asked couples about their secret consumptions. The most commonly hidden thing by far was a product (65%).
“We found that 90% of people have recently kept everyday consumer behaviors a secret from a close other – like a friend or spouse – even though they also report that they don’t think their partner would care if they knew about it,” Kelley Gullo Wight, one of the study’s two lead authors, said in a written statement.
Keeping a hidden stash of chocolate produces guilt, which the researchers found to be the key factor, making the perpetrator want to do more in the relationship to ease that sense of betrayal or dishonesty. They called it a “greater relationship investment,” meaning the person is more likely to do a little extra for their partner, like shell out more money for the next anniversary gift or yield to watching their partner’s favorite program.
So don’t feel too bad about that secret Amazon purchase. As long as the other person doesn’t see the box, nobody has to know. Your relationship can only improve.
How much weight does my patient need to lose?
What is the real goal of weight loss? In health care, reducing excess body fat is known to improve many complications faced by patients with obesity. Even modest to moderate weight loss contributes to improvements in health. Normalizing body weight is not required.
While our culture promotes an ideal body size, in the health care setting, our attention must focus on achieving health improvement. We need to be more tolerant of variations in body size if patients are healthy. Of note, varying amounts of weight loss produce improvement in the different complications of obesity, so the amount of weight loss required for improving one condition differs from that required to improve another condition.
When we prescribe weight loss for health improvement, we are trying to reduce both the mechanical burden of fat and the excess ectopic and visceral body fat that is driving disease. The good news about the physiology of weight loss is that we do not need to attain a body mass index (BMI) of 25 or even 30 to have health improvement. The excess abnormal body fat is the first to go!
Losing weight causes a disproportional reduction in ectopic and visceral fat depots. With a 5% weight loss, visceral fat is reduced by 9%. With 16% weight loss, visceral fat is reduced by 30%. Clearing of liver fat is even more dramatic. With 16% weight loss, 65% of liver fat is cleared.
Because ectopic abnormal fat is cleared preferentially with weight loss, it affects different tissues with varying amounts of weight loss.
Weight loss and diabetes
A close relationship exists between weight loss and insulin sensitivity. With just 5% weight loss, insulin sensitivity in the liver and adipose tissue is greatly improved, but while muscle insulin sensitivity is improved at just 5% weight loss, it continues to improve with further weight loss. Indeed, weight loss has enormous benefits in improving glycemia in prediabetes and diabetes.
In patients with impaired glucose tolerance, weight loss of 10% can eliminate progression to type 2 diabetes. In patients with type 2 diabetes who still have beta-cell reserve, 15% weight loss can produce diabetes remission – normoglycemia without diabetes medications.
Weight loss and cardiovascular risk factors
Even very small amounts of weight loss – 3% – can improve triglycerides and glycemia. It takes 5% weight loss to show benefits in systolic and diastolic blood pressure, as well as in HDL and LDL cholesterol levels. For all of these, additional weight loss brings more improvement. Inflammatory markers are more difficult. It takes 10%-15% weight loss to improve most of these – for example, C-reactive protein.
Weight loss and other complications
It takes 10% or more weight loss to demonstrate improvements in symptoms in obstructive sleep apnea and gastroesophageal reflux disease. For knee pain, the relationship to improvement is not based on achieving a percentage loss. Each pound of weight lost can result in a fourfold reduction in the load exerted on the knee per step during daily activities, but it is important to reduce weight before there is structural damage, because weight loss can’t repair damaged knee joints. Moderate weight loss (5%-10%) produces improvements in quality-of-life measures, in urinary stress incontinence symptoms, and in measures of sexual function. It probably takes 15% or more weight loss to demonstrate improvement in cardiovascular events.
Must heavier patients lose more weight?
To answer this question, it is important to think in terms of percent weight loss rather than pounds or kilograms. In large studies of lifestyle intervention, of course individuals with higher BMI lost more weight. But the percentage weight loss was the same across BMI categories: class 1 (BMI 30-35), class 2 (BMI 35-40), class 3 (BMI > 40). Furthermore, the improvement in risk factors was the same across BMI categories. Those with class 3 obesity had the same improvements as those with class 1. This provides further rationale for thinking about weight loss as a percentage from baseline weight rather than as simply a weight-loss goal in pounds.
Goal setting is an important part of any behavioral intervention
At the start of a weight-loss intervention, the health care provider should raise the issue of the goal and the time course for achieving it. Patients often have unrealistic expectations, wanting to achieve large amounts of weight loss rapidly. Unfortunately, popular culture has reinforced this idea with advertisements using “lose 10 pounds the first week” and promoting before-and-after pictures of weight-loss results. The job of the health care provider is to coach and guide the patient in terms of achievable weight loss that can bring health improvement safely. Managing patient expectations is critical to long-term success.
Think in terms of percentage weight loss, not pounds, and set goals at achievable time points
Help patients translate a percent weight-loss goal to a pounds goal at 3, 6, and 12 months. With the emergence of medications approved for chronic weight management with robust weight-loss efficacy, it now is possible to achieve a weight-loss goal of 10% or 15% with regularity, and some patients will be able to achieve 20% or 25% weight loss with newer medications.
We should help our patients set a goal by calculating a goal for certain time points. A good goal for 3 months would be 5% weight loss. For our 200-lb patient, we would translate that to 10 lb in 3 months. For 6 months, the goal should be 10% (20 lb for our 200-lb patient). The usual trajectory of weight loss with lifestyle intervention alone is for a “plateau” at 6 months, although with newer medications, weight loss will continue for more than a year. That 1-year goal might be 15% (30 lb for our 200-lb patient) or even more, based on the patient’s baseline weight and body composition.
Weight-loss calculators can be useful tools for patients and health care providers. They can be found online and include the National Institutes of Health Body Weight Planner and the Pennington Biomedical Weight Loss Predictor Calculator. These tools give patients a realistic expectation of how fast weight loss can occur and provide guidelines to measure success.
Can patients lose too much weight?
In this patient population, losing too much weight is not typically a concern. However, newer medications are achieving average weight losses of 17% and 22% at 62 weeks, as reported by this news organization. There is a wide variation in response to these newer agents which target appetite, and many patients are losing more than the average percentages.
Remembering that the goal of weight loss is the reduction of excess abnormal body fat, we want patients to preserve as much lean mass as possible. Weight-bearing exercise can help during the weight-loss phase, but large or rapid weight loss can be concerning, especially in older individuals. When the BMI drops below 25, we want to watch patients carefully. Measurement of body composition, including bone mineral density, with dual-energy x-ray absorptiometry (DEXA) can help. This is a scenario where dose reduction of antiobesity medication can be indicated, and good clinical judgment is required to keep weight loss at healthy levels.
The future of weight loss
In the past, our strategy has been to promote as much weight loss as possible. With more effective medications, our strategy will have to change to a treat-to-target approach, such as we already use in hypertension and diabetes.
With the ability to produce powerful effects on appetite will come the need to not only target weight loss but to target preservation of lean mass and even to target different approaches for weight-loss maintenance. At present, we have no evidence that stopping medications results in anything other than weight regain. The study of different approaches to weight-loss maintenance will require our full attention.
Dr. Ryan has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, consultant, or trustee for: Altimmune; Amgen; Calibrate; Epitomee; Gila; Lilly; Novo Nordisk; Scientific Intake; Wondr Health; Xeno Biosciences; YSOPIA; Zealand. Received income in an amount equal to or greater than $250 from: Altimmune; Amgen; Calibrate; Epitomee; Gila; Lilly; Novo Nordisk; Scientific Intake; Wondr Health; Xeno Biosciences; YSOPIA; Zealand.
Donna Ryan, MD, is Professor Emerita, Pennington Biomedical Research Center, Louisiana State University, New Orleans.
A version of this article first appeared on Medscape.com.
What is the real goal of weight loss? In health care, reducing excess body fat is known to improve many complications faced by patients with obesity. Even modest to moderate weight loss contributes to improvements in health. Normalizing body weight is not required.
While our culture promotes an ideal body size, in the health care setting, our attention must focus on achieving health improvement. We need to be more tolerant of variations in body size if patients are healthy. Of note, varying amounts of weight loss produce improvement in the different complications of obesity, so the amount of weight loss required for improving one condition differs from that required to improve another condition.
When we prescribe weight loss for health improvement, we are trying to reduce both the mechanical burden of fat and the excess ectopic and visceral body fat that is driving disease. The good news about the physiology of weight loss is that we do not need to attain a body mass index (BMI) of 25 or even 30 to have health improvement. The excess abnormal body fat is the first to go!
Losing weight causes a disproportional reduction in ectopic and visceral fat depots. With a 5% weight loss, visceral fat is reduced by 9%. With 16% weight loss, visceral fat is reduced by 30%. Clearing of liver fat is even more dramatic. With 16% weight loss, 65% of liver fat is cleared.
Because ectopic abnormal fat is cleared preferentially with weight loss, it affects different tissues with varying amounts of weight loss.
Weight loss and diabetes
A close relationship exists between weight loss and insulin sensitivity. With just 5% weight loss, insulin sensitivity in the liver and adipose tissue is greatly improved, but while muscle insulin sensitivity is improved at just 5% weight loss, it continues to improve with further weight loss. Indeed, weight loss has enormous benefits in improving glycemia in prediabetes and diabetes.
In patients with impaired glucose tolerance, weight loss of 10% can eliminate progression to type 2 diabetes. In patients with type 2 diabetes who still have beta-cell reserve, 15% weight loss can produce diabetes remission – normoglycemia without diabetes medications.
Weight loss and cardiovascular risk factors
Even very small amounts of weight loss – 3% – can improve triglycerides and glycemia. It takes 5% weight loss to show benefits in systolic and diastolic blood pressure, as well as in HDL and LDL cholesterol levels. For all of these, additional weight loss brings more improvement. Inflammatory markers are more difficult. It takes 10%-15% weight loss to improve most of these – for example, C-reactive protein.
Weight loss and other complications
It takes 10% or more weight loss to demonstrate improvements in symptoms in obstructive sleep apnea and gastroesophageal reflux disease. For knee pain, the relationship to improvement is not based on achieving a percentage loss. Each pound of weight lost can result in a fourfold reduction in the load exerted on the knee per step during daily activities, but it is important to reduce weight before there is structural damage, because weight loss can’t repair damaged knee joints. Moderate weight loss (5%-10%) produces improvements in quality-of-life measures, in urinary stress incontinence symptoms, and in measures of sexual function. It probably takes 15% or more weight loss to demonstrate improvement in cardiovascular events.
Must heavier patients lose more weight?
To answer this question, it is important to think in terms of percent weight loss rather than pounds or kilograms. In large studies of lifestyle intervention, of course individuals with higher BMI lost more weight. But the percentage weight loss was the same across BMI categories: class 1 (BMI 30-35), class 2 (BMI 35-40), class 3 (BMI > 40). Furthermore, the improvement in risk factors was the same across BMI categories. Those with class 3 obesity had the same improvements as those with class 1. This provides further rationale for thinking about weight loss as a percentage from baseline weight rather than as simply a weight-loss goal in pounds.
Goal setting is an important part of any behavioral intervention
At the start of a weight-loss intervention, the health care provider should raise the issue of the goal and the time course for achieving it. Patients often have unrealistic expectations, wanting to achieve large amounts of weight loss rapidly. Unfortunately, popular culture has reinforced this idea with advertisements using “lose 10 pounds the first week” and promoting before-and-after pictures of weight-loss results. The job of the health care provider is to coach and guide the patient in terms of achievable weight loss that can bring health improvement safely. Managing patient expectations is critical to long-term success.
Think in terms of percentage weight loss, not pounds, and set goals at achievable time points
Help patients translate a percent weight-loss goal to a pounds goal at 3, 6, and 12 months. With the emergence of medications approved for chronic weight management with robust weight-loss efficacy, it now is possible to achieve a weight-loss goal of 10% or 15% with regularity, and some patients will be able to achieve 20% or 25% weight loss with newer medications.
We should help our patients set a goal by calculating a goal for certain time points. A good goal for 3 months would be 5% weight loss. For our 200-lb patient, we would translate that to 10 lb in 3 months. For 6 months, the goal should be 10% (20 lb for our 200-lb patient). The usual trajectory of weight loss with lifestyle intervention alone is for a “plateau” at 6 months, although with newer medications, weight loss will continue for more than a year. That 1-year goal might be 15% (30 lb for our 200-lb patient) or even more, based on the patient’s baseline weight and body composition.
Weight-loss calculators can be useful tools for patients and health care providers. They can be found online and include the National Institutes of Health Body Weight Planner and the Pennington Biomedical Weight Loss Predictor Calculator. These tools give patients a realistic expectation of how fast weight loss can occur and provide guidelines to measure success.
Can patients lose too much weight?
In this patient population, losing too much weight is not typically a concern. However, newer medications are achieving average weight losses of 17% and 22% at 62 weeks, as reported by this news organization. There is a wide variation in response to these newer agents which target appetite, and many patients are losing more than the average percentages.
Remembering that the goal of weight loss is the reduction of excess abnormal body fat, we want patients to preserve as much lean mass as possible. Weight-bearing exercise can help during the weight-loss phase, but large or rapid weight loss can be concerning, especially in older individuals. When the BMI drops below 25, we want to watch patients carefully. Measurement of body composition, including bone mineral density, with dual-energy x-ray absorptiometry (DEXA) can help. This is a scenario where dose reduction of antiobesity medication can be indicated, and good clinical judgment is required to keep weight loss at healthy levels.
The future of weight loss
In the past, our strategy has been to promote as much weight loss as possible. With more effective medications, our strategy will have to change to a treat-to-target approach, such as we already use in hypertension and diabetes.
With the ability to produce powerful effects on appetite will come the need to not only target weight loss but to target preservation of lean mass and even to target different approaches for weight-loss maintenance. At present, we have no evidence that stopping medications results in anything other than weight regain. The study of different approaches to weight-loss maintenance will require our full attention.
Dr. Ryan has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, consultant, or trustee for: Altimmune; Amgen; Calibrate; Epitomee; Gila; Lilly; Novo Nordisk; Scientific Intake; Wondr Health; Xeno Biosciences; YSOPIA; Zealand. Received income in an amount equal to or greater than $250 from: Altimmune; Amgen; Calibrate; Epitomee; Gila; Lilly; Novo Nordisk; Scientific Intake; Wondr Health; Xeno Biosciences; YSOPIA; Zealand.
Donna Ryan, MD, is Professor Emerita, Pennington Biomedical Research Center, Louisiana State University, New Orleans.
A version of this article first appeared on Medscape.com.
What is the real goal of weight loss? In health care, reducing excess body fat is known to improve many complications faced by patients with obesity. Even modest to moderate weight loss contributes to improvements in health. Normalizing body weight is not required.
While our culture promotes an ideal body size, in the health care setting, our attention must focus on achieving health improvement. We need to be more tolerant of variations in body size if patients are healthy. Of note, varying amounts of weight loss produce improvement in the different complications of obesity, so the amount of weight loss required for improving one condition differs from that required to improve another condition.
When we prescribe weight loss for health improvement, we are trying to reduce both the mechanical burden of fat and the excess ectopic and visceral body fat that is driving disease. The good news about the physiology of weight loss is that we do not need to attain a body mass index (BMI) of 25 or even 30 to have health improvement. The excess abnormal body fat is the first to go!
Losing weight causes a disproportional reduction in ectopic and visceral fat depots. With a 5% weight loss, visceral fat is reduced by 9%. With 16% weight loss, visceral fat is reduced by 30%. Clearing of liver fat is even more dramatic. With 16% weight loss, 65% of liver fat is cleared.
Because ectopic abnormal fat is cleared preferentially with weight loss, it affects different tissues with varying amounts of weight loss.
Weight loss and diabetes
A close relationship exists between weight loss and insulin sensitivity. With just 5% weight loss, insulin sensitivity in the liver and adipose tissue is greatly improved, but while muscle insulin sensitivity is improved at just 5% weight loss, it continues to improve with further weight loss. Indeed, weight loss has enormous benefits in improving glycemia in prediabetes and diabetes.
In patients with impaired glucose tolerance, weight loss of 10% can eliminate progression to type 2 diabetes. In patients with type 2 diabetes who still have beta-cell reserve, 15% weight loss can produce diabetes remission – normoglycemia without diabetes medications.
Weight loss and cardiovascular risk factors
Even very small amounts of weight loss – 3% – can improve triglycerides and glycemia. It takes 5% weight loss to show benefits in systolic and diastolic blood pressure, as well as in HDL and LDL cholesterol levels. For all of these, additional weight loss brings more improvement. Inflammatory markers are more difficult. It takes 10%-15% weight loss to improve most of these – for example, C-reactive protein.
Weight loss and other complications
It takes 10% or more weight loss to demonstrate improvements in symptoms in obstructive sleep apnea and gastroesophageal reflux disease. For knee pain, the relationship to improvement is not based on achieving a percentage loss. Each pound of weight lost can result in a fourfold reduction in the load exerted on the knee per step during daily activities, but it is important to reduce weight before there is structural damage, because weight loss can’t repair damaged knee joints. Moderate weight loss (5%-10%) produces improvements in quality-of-life measures, in urinary stress incontinence symptoms, and in measures of sexual function. It probably takes 15% or more weight loss to demonstrate improvement in cardiovascular events.
Must heavier patients lose more weight?
To answer this question, it is important to think in terms of percent weight loss rather than pounds or kilograms. In large studies of lifestyle intervention, of course individuals with higher BMI lost more weight. But the percentage weight loss was the same across BMI categories: class 1 (BMI 30-35), class 2 (BMI 35-40), class 3 (BMI > 40). Furthermore, the improvement in risk factors was the same across BMI categories. Those with class 3 obesity had the same improvements as those with class 1. This provides further rationale for thinking about weight loss as a percentage from baseline weight rather than as simply a weight-loss goal in pounds.
Goal setting is an important part of any behavioral intervention
At the start of a weight-loss intervention, the health care provider should raise the issue of the goal and the time course for achieving it. Patients often have unrealistic expectations, wanting to achieve large amounts of weight loss rapidly. Unfortunately, popular culture has reinforced this idea with advertisements using “lose 10 pounds the first week” and promoting before-and-after pictures of weight-loss results. The job of the health care provider is to coach and guide the patient in terms of achievable weight loss that can bring health improvement safely. Managing patient expectations is critical to long-term success.
Think in terms of percentage weight loss, not pounds, and set goals at achievable time points
Help patients translate a percent weight-loss goal to a pounds goal at 3, 6, and 12 months. With the emergence of medications approved for chronic weight management with robust weight-loss efficacy, it now is possible to achieve a weight-loss goal of 10% or 15% with regularity, and some patients will be able to achieve 20% or 25% weight loss with newer medications.
We should help our patients set a goal by calculating a goal for certain time points. A good goal for 3 months would be 5% weight loss. For our 200-lb patient, we would translate that to 10 lb in 3 months. For 6 months, the goal should be 10% (20 lb for our 200-lb patient). The usual trajectory of weight loss with lifestyle intervention alone is for a “plateau” at 6 months, although with newer medications, weight loss will continue for more than a year. That 1-year goal might be 15% (30 lb for our 200-lb patient) or even more, based on the patient’s baseline weight and body composition.
Weight-loss calculators can be useful tools for patients and health care providers. They can be found online and include the National Institutes of Health Body Weight Planner and the Pennington Biomedical Weight Loss Predictor Calculator. These tools give patients a realistic expectation of how fast weight loss can occur and provide guidelines to measure success.
Can patients lose too much weight?
In this patient population, losing too much weight is not typically a concern. However, newer medications are achieving average weight losses of 17% and 22% at 62 weeks, as reported by this news organization. There is a wide variation in response to these newer agents which target appetite, and many patients are losing more than the average percentages.
Remembering that the goal of weight loss is the reduction of excess abnormal body fat, we want patients to preserve as much lean mass as possible. Weight-bearing exercise can help during the weight-loss phase, but large or rapid weight loss can be concerning, especially in older individuals. When the BMI drops below 25, we want to watch patients carefully. Measurement of body composition, including bone mineral density, with dual-energy x-ray absorptiometry (DEXA) can help. This is a scenario where dose reduction of antiobesity medication can be indicated, and good clinical judgment is required to keep weight loss at healthy levels.
The future of weight loss
In the past, our strategy has been to promote as much weight loss as possible. With more effective medications, our strategy will have to change to a treat-to-target approach, such as we already use in hypertension and diabetes.
With the ability to produce powerful effects on appetite will come the need to not only target weight loss but to target preservation of lean mass and even to target different approaches for weight-loss maintenance. At present, we have no evidence that stopping medications results in anything other than weight regain. The study of different approaches to weight-loss maintenance will require our full attention.
Dr. Ryan has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, consultant, or trustee for: Altimmune; Amgen; Calibrate; Epitomee; Gila; Lilly; Novo Nordisk; Scientific Intake; Wondr Health; Xeno Biosciences; YSOPIA; Zealand. Received income in an amount equal to or greater than $250 from: Altimmune; Amgen; Calibrate; Epitomee; Gila; Lilly; Novo Nordisk; Scientific Intake; Wondr Health; Xeno Biosciences; YSOPIA; Zealand.
Donna Ryan, MD, is Professor Emerita, Pennington Biomedical Research Center, Louisiana State University, New Orleans.
A version of this article first appeared on Medscape.com.
After cancer, abortion experience highlights post-Roe reality
The drive from Texas to the clinic in Albuquerque, N.M., took 10 hours. It was mid-April of this year. There wasn’t much to see along the mostly barren stretch, and there wasn’t much for Kailee DeSpain to do aside from think about where she was going and why.
Her husband was driving. She sensed his nervous glances toward the passenger seat where she sat struggling to quiet her thoughts.
No, she wasn’t having any pain, she told him. No, she wasn’t feeling like she did the last time or the two times before that.
This pregnancy was different. It was the first in which she feared for her own life. Her fetus – Finley – had triploidy, a rare chromosomal abnormality. Because of the condition, which affects 1%-3% of pregnancies, his heart, brain, and kidneys were not developing properly.
At 19 weeks, Finley was already struggling to draw breath from lungs squeezed inside an overcrowded chest cavity. Ms. DeSpain wanted nothing more than to carry Finley to term, hold him, meet him even for a moment before saying goodbye.
But his condition meant he would likely suffocate in utero well before that. And Ms. DeSpain knew that carrying him longer would likely raise her risk of bleeding and of her blood pressure increasing to dangerous highs.
“This could kill you,” her husband told her. “Do you realize you could die bringing a baby into this world who is not going to live? I don’t want to lose you.’”
Unlike her other pregnancies, the timing of this one and the decision she faced to end it put her health in even greater danger.
Imminent danger
On Sept. 1, 2021, a bill went into effect in Texas that banned abortions from as early as 6 weeks’ gestation. Texas Senate Bill 8 (SB8) became one of the most restrictive abortion laws in the country. It prohibited abortions whenever a fetal heartbeat, defined by lawmakers, could be detected on an ultrasound, often before many women knew they were pregnant.
The Texas abortion law was hardly the last word on the topic. Ms. DeSpain didn’t know it on her drive to New Mexico in April, but the U.S. Supreme Court was weeks away from overturning the landmark Roe v. Wade decision.
On June 24, the Supreme Court delivered its 6-3 ruling overturning Roe v. Wade, the 1973 case that granted women the right to abortion.
This decision set in motion “trigger laws” in some states – laws that essentially fully banned abortions. Those states included Ms. DeSpain’s home state of Texas, where abortion is now a felony except when the life of the mother is in peril.
However, legal definitions of what qualifies as “life-threatening” remain murky.
The law is unclear, says Lisa Harris, MD, PhD, professor in the department of obstetrics and gynecology at the University of Michigan, Ann Arbor. “What does the risk of death have to be, and how imminent must it be?” she asked in a recent editorial in the New England Journal of Medicine. Is 25% enough? 50%? Or does a woman have to be moments from dying?
“This whole thing makes me so angry,” says Shikha Jain, MD, a medical oncologist at University of Illinois Health, Chicago. “A patient may not be experiencing an emergency right now, but if we don’t take care of the situation, it may become an emergency in 2 hours or 2 days.”
Even before the Roe v. Wade decision, pregnancy had been a high-stakes endeavor for many women. In 2019, more than 750 women died from pregnancy-related events in the United States. In 2020, that number rose to 850. Each year dozens more suffer pregnancy-related events that require lifesaving interventions.
Now, in a post-Roe world, the number of maternal deaths will likely climb as more abortion bans take effect and fewer women have access to lifesaving care, experts say. A 2021 study that compared 2017 maternal mortality rates in states with different levels of abortion restrictions found that the rate of maternal mortality was almost two times higher in states that restricted abortion access compared with those that protected it – 28.5 per 100,000 women vs. 15.7.
Some women living in states with abortion bans won’t have the resources to cross state lines for care.
“This is just going to widen the health care disparities that are already so prevalent in this country,” Dr. Jain says.
Navigating a crossroads
Ms. DeSpain’s medical history reads like a checklist of pregnancy-related perils: chronic high blood pressure, persistent clotting problems, and a high risk of hemorrhage. She was also diagnosed with cervical cancer in 2020, which left her body more fragile.
Cardiovascular conditions, including hypertension and hemorrhage, are the leading causes of maternal mortality, responsible for more than one-third of pregnancy-related deaths. Preeclampsia, characterized by high blood pressure, accounts for more than 7% of maternal deaths in the United States. Although less common, genetic disorders, such as spinal muscular atrophy and triploidy, or cancer during pregnancy can put a mother and fetus at risk.
Cancer – which affects about 1 in 1,000 pregnant women and results in termination in as many as 28% of cases – brings sharp focus to the new dangers and complex decision-making patients and their doctors face as abortion bans take hold.
Before the Supreme Court decision, a pregnant woman with cancer was already facing great uncertainty. The decision to treat cancer during pregnancy involves “weighing the risk of exposing the fetus to medication vs. the risk to the mother’s untreated illness if you don’t expose the fetus to medication,” Elyce Cardonick, MD, an obstetrician at Cooper University Health Care, Camden, N.J., who specializes in high-risk pregnancies, told the National Cancer Institute.
Oncologists generally agree that it’s safe for pregnant women to receive chemotherapy during the second and third trimesters. But for women with aggressive cancers that are diagnosed in the first trimester, chemotherapy is dangerous. For women who need immunotherapy, the risks of treatment remain unclear.
In these cases, Alice S. Mims, MD, must broach the possibility of terminating the pregnancy.
“Cancer is a very urgent condition,” says Dr. Mims, a hematology specialist at the Ohio State University Comprehensive Cancer Center, Columbus, who sees patients who are pregnant. “These women may have other children at home, and they want to do their best to fight the disease so they can be around for their family long term.”
Now the changing legal landscape on abortion will put hundreds more pregnant women with cancer in danger. In a recent viewpoint article published in JAMA Oncology, Jordyn Silverstein and Katherine Van Loon, MD, MPH, estimate that during the next year, up to 420 pregnant women living in states with restricted abortion access will face threats to their cancer care and potentially their life.
“The repercussions of overturning Roe v. Wade – and the failure of the Supreme Court to provide any guidance on exceptions related to the life and health of the mother – are potentially catastrophic for a subset of women who face a life-threating diagnosis of [pregnancy-associated cancer],” they write.
The choice Ms. DeSpain faced after her cervical cancer diagnosis was different. She was not pregnant at the time, but she was at a crossroads.
Although it was caught early, the cancer was aggressive. Her oncologist recommended that she undergo a hysterectomy – the surgery that would give her the best chance for a cancer-free future. It would also mean she could no longer become pregnant.
With a less invasive procedure, on the other hand, she could still carry a child, but she would face a much greater chance that the cancer would come back.
At 27, Ms. DeSpain was not ready to close the pregnancy door. She opted for a surgery in which part of her cervix was removed, allowing her to try for another baby.
But she faced a ticking clock in the event her cancer returned.
If you want to have a baby, “try soon,” her doctor warned.
A dead end
After her cancer surgery and a third miscarriage, Ms. DeSpain and her husband were surprised and excited when in late 2021 she again became pregnant.
The first trimester seemed blissfully uneventful. As the weeks passed, Finley’s heart started to beat.
But the 16-week ultrasound signaled a turning point. The sonographer was too quiet.
“This is really bad, isn’t it?” Ms. DeSpain asked her sonographer.
The doctors told her he wouldn’t survive. Finley had no heart chambers. His heart couldn’t pump blood properly. He was missing one kidney, and his brain was split in the back. With almost no amniotic fluid, her doctor said he would likely die in utero, crushed to death without support from the protective liquid.
She fought for him anyway. She sought specialty care, followed bed rest orders, and traveled 3 hours to Houston to enroll in a clinical trial.
But every road was a dead end.
Ultimately, testing revealed Finley had triploidy, and all lines led to one point.
“There were too many things wrong, too much wrong for them to fix,” says Ms. DeSpain, recalling the news from her doctor in Houston. “I was in shock. My husband was just sitting with his hands flat on the table, staring at nothing, shaking a little bit.”
However, Finley still had a heartbeat, making an abortion after 6 weeks a felony in Texas. Even a compassionate induction was now out of the question unless her death was imminent.
Ms. DeSpain called the abortion clinic in Albuquerque and made an appointment. She would have to wait 2 weeks because of an influx of pregnant patients coming from Texas.
She welcomed the wait … just in case she changed her mind.
“At that point I wanted to carry him as far as I could,” she says.
For those 2 weeks, Ms. DeSpain remained on bed rest. She cried all day every day. She worried that Finley was experiencing pain.
Through this process, her doctor’s support helped keep her grounded.
“She cried with us in her office and said, ‘I wish that you didn’t have to go, but I think you’re doing the right thing, doing what keeps you safest,’ “ Ms. DeSpain recalls.
Ms. DeSpain declined to share the name of her doctor out of fear that even expressing compassion for a patient’s safety could put the physician in legal jeopardy and provoke harassment.
That fear is warranted. Some doctors will be forced to choose between doing what is legal – even though the law is vague – and doing what is right for patients, says law professor Jamie Abrams, who was recently diagnosed with breast cancer.
To live in a world where there’s talk of criminalizing doctors for taking care of their patients, where there’s “this national movement to position some women to be shunned and exiled for seeking care that’s right for them, their health, and might save their life is staggering and beyond comprehension,” says Ms. Abrams, professor of law at the American University Washington College of Law.
Ms. Abrams, who was diagnosed with hormone receptor–positive invasive breast cancer the same day she read the leaked Supreme Court draft on the decision to end of Roe v. Wade, said that “overnight, I became a person who would need an abortion if I became pregnant, because my treatment would compromise a healthy birth or delay necessary cancer care.” Ms. Abrams was also told she could no longer use hormonal contraception.
Dr. Harris’s advice to clinicians is to try to do what they feel is best for patients, including referring them to centers that have legal resources and protections regarding abortions.
Dr. Mims agrees and recommends that doctors reach out to those with more resources and legal backing for support. “I would advise doctors in [states with restrictive laws] to familiarize themselves with available resources and organizations taking action to deal with questionable cases,” Dr. Mims says.
‘Baby killers work here’
Following her 10-hour drive to Albuquerque, Ms. DeSpain encountered lines of protesters at the clinic. They were holding signs that said, “Abortion is murder,” and “Baby killers work here.”
“Please don’t kill your baby – we have resources for you,” a woman screeched through a megaphone as Ms. DeSpain, nearly 20 weeks’ pregnant, stepped out of the car to enter the clinic.
“I remember turning around, looking at her and making eye contact, and yelling back, ‘My baby has triploidy – he is dying! He is going to suffocate if I carry him full term. You don’t know what you’re talking about!’ “
A nurse held her hand during the procedure.
“He said, ‘You’re doing great, you’re okay,’ “ she recalls. She knew there was a chance that Finley’s face would be crushed by contractions during labor because of the lack of amniotic fluid, but she hoped not. Ms. DeSpain longed for a photo.
There was no photo to take home the next day, but Ms. DeSpain did receive Finley’s footprints, and his heartbeat – as captured by the specialty team in Houston – lives on in a stuffed giraffe.
His ashes arrived a few weeks later.
By then, the Supreme Court draft had been leaked. Ms. DeSpain knew her predicament in Texas would soon affect women across the United States and make any future pregnancy attempt for her even more risky.
The weeks and months that followed were a blur of grief, anger, and medical testing.
But she received some good news. A second triploidy pregnancy was extremely unlikely.
Several weeks later, Ms. DeSpain got more good news.
“I had a follow-up cancer appointment, and everything was completely clear,” she says.
She remains hopeful that she will be able to give birth, but her doctor cautioned that it’s no longer safe to become pregnant in Texas.
“I need you to understand that if you get pregnant and you have complications, we can’t intervene unless the baby doesn’t have a heartbeat, even if it would save your life,” Ms. DeSpain recalls her doctor saying.
If Texas remains a dangerous place to be pregnant, Ms. DeSpain and her husband will have to move.
For now, Ms. DeSpain wants people to know her story and to continue to fight for her right to govern her body.
In a public post to Facebook, she laid bare her pregnancy journey.
“No one should have to share a story like mine to justify abortion,” she wrote. “My choice is not yours to judge, and my rights are not yours to gleefully take away.”
Ms. Abrams, Ms. DeSpain, Dr. Harris, Dr. Jain, and Dr. Mims have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The drive from Texas to the clinic in Albuquerque, N.M., took 10 hours. It was mid-April of this year. There wasn’t much to see along the mostly barren stretch, and there wasn’t much for Kailee DeSpain to do aside from think about where she was going and why.
Her husband was driving. She sensed his nervous glances toward the passenger seat where she sat struggling to quiet her thoughts.
No, she wasn’t having any pain, she told him. No, she wasn’t feeling like she did the last time or the two times before that.
This pregnancy was different. It was the first in which she feared for her own life. Her fetus – Finley – had triploidy, a rare chromosomal abnormality. Because of the condition, which affects 1%-3% of pregnancies, his heart, brain, and kidneys were not developing properly.
At 19 weeks, Finley was already struggling to draw breath from lungs squeezed inside an overcrowded chest cavity. Ms. DeSpain wanted nothing more than to carry Finley to term, hold him, meet him even for a moment before saying goodbye.
But his condition meant he would likely suffocate in utero well before that. And Ms. DeSpain knew that carrying him longer would likely raise her risk of bleeding and of her blood pressure increasing to dangerous highs.
“This could kill you,” her husband told her. “Do you realize you could die bringing a baby into this world who is not going to live? I don’t want to lose you.’”
Unlike her other pregnancies, the timing of this one and the decision she faced to end it put her health in even greater danger.
Imminent danger
On Sept. 1, 2021, a bill went into effect in Texas that banned abortions from as early as 6 weeks’ gestation. Texas Senate Bill 8 (SB8) became one of the most restrictive abortion laws in the country. It prohibited abortions whenever a fetal heartbeat, defined by lawmakers, could be detected on an ultrasound, often before many women knew they were pregnant.
The Texas abortion law was hardly the last word on the topic. Ms. DeSpain didn’t know it on her drive to New Mexico in April, but the U.S. Supreme Court was weeks away from overturning the landmark Roe v. Wade decision.
On June 24, the Supreme Court delivered its 6-3 ruling overturning Roe v. Wade, the 1973 case that granted women the right to abortion.
This decision set in motion “trigger laws” in some states – laws that essentially fully banned abortions. Those states included Ms. DeSpain’s home state of Texas, where abortion is now a felony except when the life of the mother is in peril.
However, legal definitions of what qualifies as “life-threatening” remain murky.
The law is unclear, says Lisa Harris, MD, PhD, professor in the department of obstetrics and gynecology at the University of Michigan, Ann Arbor. “What does the risk of death have to be, and how imminent must it be?” she asked in a recent editorial in the New England Journal of Medicine. Is 25% enough? 50%? Or does a woman have to be moments from dying?
“This whole thing makes me so angry,” says Shikha Jain, MD, a medical oncologist at University of Illinois Health, Chicago. “A patient may not be experiencing an emergency right now, but if we don’t take care of the situation, it may become an emergency in 2 hours or 2 days.”
Even before the Roe v. Wade decision, pregnancy had been a high-stakes endeavor for many women. In 2019, more than 750 women died from pregnancy-related events in the United States. In 2020, that number rose to 850. Each year dozens more suffer pregnancy-related events that require lifesaving interventions.
Now, in a post-Roe world, the number of maternal deaths will likely climb as more abortion bans take effect and fewer women have access to lifesaving care, experts say. A 2021 study that compared 2017 maternal mortality rates in states with different levels of abortion restrictions found that the rate of maternal mortality was almost two times higher in states that restricted abortion access compared with those that protected it – 28.5 per 100,000 women vs. 15.7.
Some women living in states with abortion bans won’t have the resources to cross state lines for care.
“This is just going to widen the health care disparities that are already so prevalent in this country,” Dr. Jain says.
Navigating a crossroads
Ms. DeSpain’s medical history reads like a checklist of pregnancy-related perils: chronic high blood pressure, persistent clotting problems, and a high risk of hemorrhage. She was also diagnosed with cervical cancer in 2020, which left her body more fragile.
Cardiovascular conditions, including hypertension and hemorrhage, are the leading causes of maternal mortality, responsible for more than one-third of pregnancy-related deaths. Preeclampsia, characterized by high blood pressure, accounts for more than 7% of maternal deaths in the United States. Although less common, genetic disorders, such as spinal muscular atrophy and triploidy, or cancer during pregnancy can put a mother and fetus at risk.
Cancer – which affects about 1 in 1,000 pregnant women and results in termination in as many as 28% of cases – brings sharp focus to the new dangers and complex decision-making patients and their doctors face as abortion bans take hold.
Before the Supreme Court decision, a pregnant woman with cancer was already facing great uncertainty. The decision to treat cancer during pregnancy involves “weighing the risk of exposing the fetus to medication vs. the risk to the mother’s untreated illness if you don’t expose the fetus to medication,” Elyce Cardonick, MD, an obstetrician at Cooper University Health Care, Camden, N.J., who specializes in high-risk pregnancies, told the National Cancer Institute.
Oncologists generally agree that it’s safe for pregnant women to receive chemotherapy during the second and third trimesters. But for women with aggressive cancers that are diagnosed in the first trimester, chemotherapy is dangerous. For women who need immunotherapy, the risks of treatment remain unclear.
In these cases, Alice S. Mims, MD, must broach the possibility of terminating the pregnancy.
“Cancer is a very urgent condition,” says Dr. Mims, a hematology specialist at the Ohio State University Comprehensive Cancer Center, Columbus, who sees patients who are pregnant. “These women may have other children at home, and they want to do their best to fight the disease so they can be around for their family long term.”
Now the changing legal landscape on abortion will put hundreds more pregnant women with cancer in danger. In a recent viewpoint article published in JAMA Oncology, Jordyn Silverstein and Katherine Van Loon, MD, MPH, estimate that during the next year, up to 420 pregnant women living in states with restricted abortion access will face threats to their cancer care and potentially their life.
“The repercussions of overturning Roe v. Wade – and the failure of the Supreme Court to provide any guidance on exceptions related to the life and health of the mother – are potentially catastrophic for a subset of women who face a life-threating diagnosis of [pregnancy-associated cancer],” they write.
The choice Ms. DeSpain faced after her cervical cancer diagnosis was different. She was not pregnant at the time, but she was at a crossroads.
Although it was caught early, the cancer was aggressive. Her oncologist recommended that she undergo a hysterectomy – the surgery that would give her the best chance for a cancer-free future. It would also mean she could no longer become pregnant.
With a less invasive procedure, on the other hand, she could still carry a child, but she would face a much greater chance that the cancer would come back.
At 27, Ms. DeSpain was not ready to close the pregnancy door. She opted for a surgery in which part of her cervix was removed, allowing her to try for another baby.
But she faced a ticking clock in the event her cancer returned.
If you want to have a baby, “try soon,” her doctor warned.
A dead end
After her cancer surgery and a third miscarriage, Ms. DeSpain and her husband were surprised and excited when in late 2021 she again became pregnant.
The first trimester seemed blissfully uneventful. As the weeks passed, Finley’s heart started to beat.
But the 16-week ultrasound signaled a turning point. The sonographer was too quiet.
“This is really bad, isn’t it?” Ms. DeSpain asked her sonographer.
The doctors told her he wouldn’t survive. Finley had no heart chambers. His heart couldn’t pump blood properly. He was missing one kidney, and his brain was split in the back. With almost no amniotic fluid, her doctor said he would likely die in utero, crushed to death without support from the protective liquid.
She fought for him anyway. She sought specialty care, followed bed rest orders, and traveled 3 hours to Houston to enroll in a clinical trial.
But every road was a dead end.
Ultimately, testing revealed Finley had triploidy, and all lines led to one point.
“There were too many things wrong, too much wrong for them to fix,” says Ms. DeSpain, recalling the news from her doctor in Houston. “I was in shock. My husband was just sitting with his hands flat on the table, staring at nothing, shaking a little bit.”
However, Finley still had a heartbeat, making an abortion after 6 weeks a felony in Texas. Even a compassionate induction was now out of the question unless her death was imminent.
Ms. DeSpain called the abortion clinic in Albuquerque and made an appointment. She would have to wait 2 weeks because of an influx of pregnant patients coming from Texas.
She welcomed the wait … just in case she changed her mind.
“At that point I wanted to carry him as far as I could,” she says.
For those 2 weeks, Ms. DeSpain remained on bed rest. She cried all day every day. She worried that Finley was experiencing pain.
Through this process, her doctor’s support helped keep her grounded.
“She cried with us in her office and said, ‘I wish that you didn’t have to go, but I think you’re doing the right thing, doing what keeps you safest,’ “ Ms. DeSpain recalls.
Ms. DeSpain declined to share the name of her doctor out of fear that even expressing compassion for a patient’s safety could put the physician in legal jeopardy and provoke harassment.
That fear is warranted. Some doctors will be forced to choose between doing what is legal – even though the law is vague – and doing what is right for patients, says law professor Jamie Abrams, who was recently diagnosed with breast cancer.
To live in a world where there’s talk of criminalizing doctors for taking care of their patients, where there’s “this national movement to position some women to be shunned and exiled for seeking care that’s right for them, their health, and might save their life is staggering and beyond comprehension,” says Ms. Abrams, professor of law at the American University Washington College of Law.
Ms. Abrams, who was diagnosed with hormone receptor–positive invasive breast cancer the same day she read the leaked Supreme Court draft on the decision to end of Roe v. Wade, said that “overnight, I became a person who would need an abortion if I became pregnant, because my treatment would compromise a healthy birth or delay necessary cancer care.” Ms. Abrams was also told she could no longer use hormonal contraception.
Dr. Harris’s advice to clinicians is to try to do what they feel is best for patients, including referring them to centers that have legal resources and protections regarding abortions.
Dr. Mims agrees and recommends that doctors reach out to those with more resources and legal backing for support. “I would advise doctors in [states with restrictive laws] to familiarize themselves with available resources and organizations taking action to deal with questionable cases,” Dr. Mims says.
‘Baby killers work here’
Following her 10-hour drive to Albuquerque, Ms. DeSpain encountered lines of protesters at the clinic. They were holding signs that said, “Abortion is murder,” and “Baby killers work here.”
“Please don’t kill your baby – we have resources for you,” a woman screeched through a megaphone as Ms. DeSpain, nearly 20 weeks’ pregnant, stepped out of the car to enter the clinic.
“I remember turning around, looking at her and making eye contact, and yelling back, ‘My baby has triploidy – he is dying! He is going to suffocate if I carry him full term. You don’t know what you’re talking about!’ “
A nurse held her hand during the procedure.
“He said, ‘You’re doing great, you’re okay,’ “ she recalls. She knew there was a chance that Finley’s face would be crushed by contractions during labor because of the lack of amniotic fluid, but she hoped not. Ms. DeSpain longed for a photo.
There was no photo to take home the next day, but Ms. DeSpain did receive Finley’s footprints, and his heartbeat – as captured by the specialty team in Houston – lives on in a stuffed giraffe.
His ashes arrived a few weeks later.
By then, the Supreme Court draft had been leaked. Ms. DeSpain knew her predicament in Texas would soon affect women across the United States and make any future pregnancy attempt for her even more risky.
The weeks and months that followed were a blur of grief, anger, and medical testing.
But she received some good news. A second triploidy pregnancy was extremely unlikely.
Several weeks later, Ms. DeSpain got more good news.
“I had a follow-up cancer appointment, and everything was completely clear,” she says.
She remains hopeful that she will be able to give birth, but her doctor cautioned that it’s no longer safe to become pregnant in Texas.
“I need you to understand that if you get pregnant and you have complications, we can’t intervene unless the baby doesn’t have a heartbeat, even if it would save your life,” Ms. DeSpain recalls her doctor saying.
If Texas remains a dangerous place to be pregnant, Ms. DeSpain and her husband will have to move.
For now, Ms. DeSpain wants people to know her story and to continue to fight for her right to govern her body.
In a public post to Facebook, she laid bare her pregnancy journey.
“No one should have to share a story like mine to justify abortion,” she wrote. “My choice is not yours to judge, and my rights are not yours to gleefully take away.”
Ms. Abrams, Ms. DeSpain, Dr. Harris, Dr. Jain, and Dr. Mims have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The drive from Texas to the clinic in Albuquerque, N.M., took 10 hours. It was mid-April of this year. There wasn’t much to see along the mostly barren stretch, and there wasn’t much for Kailee DeSpain to do aside from think about where she was going and why.
Her husband was driving. She sensed his nervous glances toward the passenger seat where she sat struggling to quiet her thoughts.
No, she wasn’t having any pain, she told him. No, she wasn’t feeling like she did the last time or the two times before that.
This pregnancy was different. It was the first in which she feared for her own life. Her fetus – Finley – had triploidy, a rare chromosomal abnormality. Because of the condition, which affects 1%-3% of pregnancies, his heart, brain, and kidneys were not developing properly.
At 19 weeks, Finley was already struggling to draw breath from lungs squeezed inside an overcrowded chest cavity. Ms. DeSpain wanted nothing more than to carry Finley to term, hold him, meet him even for a moment before saying goodbye.
But his condition meant he would likely suffocate in utero well before that. And Ms. DeSpain knew that carrying him longer would likely raise her risk of bleeding and of her blood pressure increasing to dangerous highs.
“This could kill you,” her husband told her. “Do you realize you could die bringing a baby into this world who is not going to live? I don’t want to lose you.’”
Unlike her other pregnancies, the timing of this one and the decision she faced to end it put her health in even greater danger.
Imminent danger
On Sept. 1, 2021, a bill went into effect in Texas that banned abortions from as early as 6 weeks’ gestation. Texas Senate Bill 8 (SB8) became one of the most restrictive abortion laws in the country. It prohibited abortions whenever a fetal heartbeat, defined by lawmakers, could be detected on an ultrasound, often before many women knew they were pregnant.
The Texas abortion law was hardly the last word on the topic. Ms. DeSpain didn’t know it on her drive to New Mexico in April, but the U.S. Supreme Court was weeks away from overturning the landmark Roe v. Wade decision.
On June 24, the Supreme Court delivered its 6-3 ruling overturning Roe v. Wade, the 1973 case that granted women the right to abortion.
This decision set in motion “trigger laws” in some states – laws that essentially fully banned abortions. Those states included Ms. DeSpain’s home state of Texas, where abortion is now a felony except when the life of the mother is in peril.
However, legal definitions of what qualifies as “life-threatening” remain murky.
The law is unclear, says Lisa Harris, MD, PhD, professor in the department of obstetrics and gynecology at the University of Michigan, Ann Arbor. “What does the risk of death have to be, and how imminent must it be?” she asked in a recent editorial in the New England Journal of Medicine. Is 25% enough? 50%? Or does a woman have to be moments from dying?
“This whole thing makes me so angry,” says Shikha Jain, MD, a medical oncologist at University of Illinois Health, Chicago. “A patient may not be experiencing an emergency right now, but if we don’t take care of the situation, it may become an emergency in 2 hours or 2 days.”
Even before the Roe v. Wade decision, pregnancy had been a high-stakes endeavor for many women. In 2019, more than 750 women died from pregnancy-related events in the United States. In 2020, that number rose to 850. Each year dozens more suffer pregnancy-related events that require lifesaving interventions.
Now, in a post-Roe world, the number of maternal deaths will likely climb as more abortion bans take effect and fewer women have access to lifesaving care, experts say. A 2021 study that compared 2017 maternal mortality rates in states with different levels of abortion restrictions found that the rate of maternal mortality was almost two times higher in states that restricted abortion access compared with those that protected it – 28.5 per 100,000 women vs. 15.7.
Some women living in states with abortion bans won’t have the resources to cross state lines for care.
“This is just going to widen the health care disparities that are already so prevalent in this country,” Dr. Jain says.
Navigating a crossroads
Ms. DeSpain’s medical history reads like a checklist of pregnancy-related perils: chronic high blood pressure, persistent clotting problems, and a high risk of hemorrhage. She was also diagnosed with cervical cancer in 2020, which left her body more fragile.
Cardiovascular conditions, including hypertension and hemorrhage, are the leading causes of maternal mortality, responsible for more than one-third of pregnancy-related deaths. Preeclampsia, characterized by high blood pressure, accounts for more than 7% of maternal deaths in the United States. Although less common, genetic disorders, such as spinal muscular atrophy and triploidy, or cancer during pregnancy can put a mother and fetus at risk.
Cancer – which affects about 1 in 1,000 pregnant women and results in termination in as many as 28% of cases – brings sharp focus to the new dangers and complex decision-making patients and their doctors face as abortion bans take hold.
Before the Supreme Court decision, a pregnant woman with cancer was already facing great uncertainty. The decision to treat cancer during pregnancy involves “weighing the risk of exposing the fetus to medication vs. the risk to the mother’s untreated illness if you don’t expose the fetus to medication,” Elyce Cardonick, MD, an obstetrician at Cooper University Health Care, Camden, N.J., who specializes in high-risk pregnancies, told the National Cancer Institute.
Oncologists generally agree that it’s safe for pregnant women to receive chemotherapy during the second and third trimesters. But for women with aggressive cancers that are diagnosed in the first trimester, chemotherapy is dangerous. For women who need immunotherapy, the risks of treatment remain unclear.
In these cases, Alice S. Mims, MD, must broach the possibility of terminating the pregnancy.
“Cancer is a very urgent condition,” says Dr. Mims, a hematology specialist at the Ohio State University Comprehensive Cancer Center, Columbus, who sees patients who are pregnant. “These women may have other children at home, and they want to do their best to fight the disease so they can be around for their family long term.”
Now the changing legal landscape on abortion will put hundreds more pregnant women with cancer in danger. In a recent viewpoint article published in JAMA Oncology, Jordyn Silverstein and Katherine Van Loon, MD, MPH, estimate that during the next year, up to 420 pregnant women living in states with restricted abortion access will face threats to their cancer care and potentially their life.
“The repercussions of overturning Roe v. Wade – and the failure of the Supreme Court to provide any guidance on exceptions related to the life and health of the mother – are potentially catastrophic for a subset of women who face a life-threating diagnosis of [pregnancy-associated cancer],” they write.
The choice Ms. DeSpain faced after her cervical cancer diagnosis was different. She was not pregnant at the time, but she was at a crossroads.
Although it was caught early, the cancer was aggressive. Her oncologist recommended that she undergo a hysterectomy – the surgery that would give her the best chance for a cancer-free future. It would also mean she could no longer become pregnant.
With a less invasive procedure, on the other hand, she could still carry a child, but she would face a much greater chance that the cancer would come back.
At 27, Ms. DeSpain was not ready to close the pregnancy door. She opted for a surgery in which part of her cervix was removed, allowing her to try for another baby.
But she faced a ticking clock in the event her cancer returned.
If you want to have a baby, “try soon,” her doctor warned.
A dead end
After her cancer surgery and a third miscarriage, Ms. DeSpain and her husband were surprised and excited when in late 2021 she again became pregnant.
The first trimester seemed blissfully uneventful. As the weeks passed, Finley’s heart started to beat.
But the 16-week ultrasound signaled a turning point. The sonographer was too quiet.
“This is really bad, isn’t it?” Ms. DeSpain asked her sonographer.
The doctors told her he wouldn’t survive. Finley had no heart chambers. His heart couldn’t pump blood properly. He was missing one kidney, and his brain was split in the back. With almost no amniotic fluid, her doctor said he would likely die in utero, crushed to death without support from the protective liquid.
She fought for him anyway. She sought specialty care, followed bed rest orders, and traveled 3 hours to Houston to enroll in a clinical trial.
But every road was a dead end.
Ultimately, testing revealed Finley had triploidy, and all lines led to one point.
“There were too many things wrong, too much wrong for them to fix,” says Ms. DeSpain, recalling the news from her doctor in Houston. “I was in shock. My husband was just sitting with his hands flat on the table, staring at nothing, shaking a little bit.”
However, Finley still had a heartbeat, making an abortion after 6 weeks a felony in Texas. Even a compassionate induction was now out of the question unless her death was imminent.
Ms. DeSpain called the abortion clinic in Albuquerque and made an appointment. She would have to wait 2 weeks because of an influx of pregnant patients coming from Texas.
She welcomed the wait … just in case she changed her mind.
“At that point I wanted to carry him as far as I could,” she says.
For those 2 weeks, Ms. DeSpain remained on bed rest. She cried all day every day. She worried that Finley was experiencing pain.
Through this process, her doctor’s support helped keep her grounded.
“She cried with us in her office and said, ‘I wish that you didn’t have to go, but I think you’re doing the right thing, doing what keeps you safest,’ “ Ms. DeSpain recalls.
Ms. DeSpain declined to share the name of her doctor out of fear that even expressing compassion for a patient’s safety could put the physician in legal jeopardy and provoke harassment.
That fear is warranted. Some doctors will be forced to choose between doing what is legal – even though the law is vague – and doing what is right for patients, says law professor Jamie Abrams, who was recently diagnosed with breast cancer.
To live in a world where there’s talk of criminalizing doctors for taking care of their patients, where there’s “this national movement to position some women to be shunned and exiled for seeking care that’s right for them, their health, and might save their life is staggering and beyond comprehension,” says Ms. Abrams, professor of law at the American University Washington College of Law.
Ms. Abrams, who was diagnosed with hormone receptor–positive invasive breast cancer the same day she read the leaked Supreme Court draft on the decision to end of Roe v. Wade, said that “overnight, I became a person who would need an abortion if I became pregnant, because my treatment would compromise a healthy birth or delay necessary cancer care.” Ms. Abrams was also told she could no longer use hormonal contraception.
Dr. Harris’s advice to clinicians is to try to do what they feel is best for patients, including referring them to centers that have legal resources and protections regarding abortions.
Dr. Mims agrees and recommends that doctors reach out to those with more resources and legal backing for support. “I would advise doctors in [states with restrictive laws] to familiarize themselves with available resources and organizations taking action to deal with questionable cases,” Dr. Mims says.
‘Baby killers work here’
Following her 10-hour drive to Albuquerque, Ms. DeSpain encountered lines of protesters at the clinic. They were holding signs that said, “Abortion is murder,” and “Baby killers work here.”
“Please don’t kill your baby – we have resources for you,” a woman screeched through a megaphone as Ms. DeSpain, nearly 20 weeks’ pregnant, stepped out of the car to enter the clinic.
“I remember turning around, looking at her and making eye contact, and yelling back, ‘My baby has triploidy – he is dying! He is going to suffocate if I carry him full term. You don’t know what you’re talking about!’ “
A nurse held her hand during the procedure.
“He said, ‘You’re doing great, you’re okay,’ “ she recalls. She knew there was a chance that Finley’s face would be crushed by contractions during labor because of the lack of amniotic fluid, but she hoped not. Ms. DeSpain longed for a photo.
There was no photo to take home the next day, but Ms. DeSpain did receive Finley’s footprints, and his heartbeat – as captured by the specialty team in Houston – lives on in a stuffed giraffe.
His ashes arrived a few weeks later.
By then, the Supreme Court draft had been leaked. Ms. DeSpain knew her predicament in Texas would soon affect women across the United States and make any future pregnancy attempt for her even more risky.
The weeks and months that followed were a blur of grief, anger, and medical testing.
But she received some good news. A second triploidy pregnancy was extremely unlikely.
Several weeks later, Ms. DeSpain got more good news.
“I had a follow-up cancer appointment, and everything was completely clear,” she says.
She remains hopeful that she will be able to give birth, but her doctor cautioned that it’s no longer safe to become pregnant in Texas.
“I need you to understand that if you get pregnant and you have complications, we can’t intervene unless the baby doesn’t have a heartbeat, even if it would save your life,” Ms. DeSpain recalls her doctor saying.
If Texas remains a dangerous place to be pregnant, Ms. DeSpain and her husband will have to move.
For now, Ms. DeSpain wants people to know her story and to continue to fight for her right to govern her body.
In a public post to Facebook, she laid bare her pregnancy journey.
“No one should have to share a story like mine to justify abortion,” she wrote. “My choice is not yours to judge, and my rights are not yours to gleefully take away.”
Ms. Abrams, Ms. DeSpain, Dr. Harris, Dr. Jain, and Dr. Mims have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
California wants to snip costs for vasectomies and condoms
SACRAMENTO – California is trying to ease the pain of vasectomies by making them free for millions of residents.
Federal law and state law require most health insurers to cover prescription contraceptives at no cost to the patient. But those provisions apply to only 18 Food and Drug Administration–approved birth control options for women, so anyone with testicles is out of luck.
California lawmakers are now considering a bill that would expand that requirement to male sterilization and non-prescription birth control, including condoms and contraceptive sponges. If the Contraceptive Equity Act of 2022 passes, commercial insurance plans regulated by the state won’t be allowed to impose out-of-pocket costs, like copays, coinsurance, and deductibles, on those modes of birth control.
“It’s pretty groundbreaking in that way – it’s a whole new framework to think about contraception as something that is relevant for people of all genders,” said Liz McCaman Taylor, a senior attorney with the National Health Law Program, a group that advocates for the health rights of low-income people.
A vasectomy is an outpatient surgical procedure in which the patient’s supply of sperm is cut off from his semen by sealing or snipping the tubes that transport sperm from the testes to the penis. Most men need to recover on the couch with an ice pack for a day or 2, and a test a few months later determines whether the procedure worked.
Because vasectomies are elective procedures and usually not urgent, price can be a deciding factor.
For Nathan Songne, cost was the most stressful part of the procedure. For several years, the 31-year-old had known he didn’t want to have kids biologically. Better to adopt a 4-year-old and skip the diaper stage, he thought. He was adopted by his stepfather as a child and knew he didn’t need to be genetically related to his children to love them.
“My only concern was that I had no idea how much it was going to cost me because nobody told me,” said Mr. Songne, who lives in Mission Viejo, in Orange County. If the procedure cost $1,000, as he expected, he wouldn’t be able to afford it.
Mr. Songne’s insurance, which he gets through his work assembling guitars, covered 70% of the Aug. 8 procedure, leaving him with a bill of just under $200. “Cost did affect my decision, but because it was only $200, it made me feel a lot more relieved about continuing on with the vasectomy.”
There are two hot times of year in the vasectomy business, according to Mary Samplaski, MD, an associate professor of urology at the University of Southern California, Los Angeles. First, she sees an uptick during the March Madness college basketball tournament, when men choose to recover on the couch watching hoops.
The end of the year is also busy, she said, because many patients have finally met their annual insurance deductible and can afford the procedure.
Patients discuss out-of-pocket costs in about 20% of her vasectomy consultations. “It’s obviously a nerve-wracking procedure,” Dr. Samplaski said. “And on top of that, if your copay is high, there’s even less reason to want to do it.”
In April, Jacob Elert comparison-shopped for a vasectomy near his home in Sacramento because his health plan doesn’t cover the procedure. He had hoped to schedule one with his regular urologist, but that would have come with a $1,500 price tag.
Instead, he found a chain of vasectomy clinics where he could get the procedure for $850. Three months later, a test confirmed the vasectomy was a success.
Mr. Elert has no regrets, but had price not been a factor, he would have preferred to go to his regular urologist. “That’s the doctor I trust,” Mr. Elert said. “But it was just way too expensive.”
In November, California voters will decide whether to lock rights to abortion and contraception into the state constitution. But Proposition 1 doesn’t address issues such as cost and coverage, said Amy Moy, a spokesperson for Essential Access Health, a group that runs California’s Title X family planning program.
“The constitutional amendment is kind of the long-term protection, and we are still working to reduce barriers for Californians on the short-term and day-to-day level regardless of their gender,” she said.
SB 523 has sailed through preliminary votes in the state legislature, which faces an end-of-August deadline to act on bills. If the measure passes, it would take effect in 2024, and California would join a handful of states that require plans they regulate to completely cover vasectomies or nonprescription birth control.
The California Association of Health Plans is still evaluating the measure, which may be amended in the final days of the legislative session. But the association generally opposes bills that require additional insurance benefits because they could lead to higher premiums, spokesperson Mary Ellen Grant said.
SB 523 applies to more than 14 million Californians who work for the state, have a student health plan through a university, or have state-regulated commercial health plans. They would become eligible to receive free over-the-counter birth control – such as emergency contraception, condoms, spermicide, and contraceptive sponges – in addition to vasectomies. The bill would not apply to the millions of Californians whose health insurance plans are regulated by the federal government.
The specifics of how the benefit would work, including the frequency and amount of birth control that insurers must cover and whether patients would have to pay upfront and be reimbursed later, would be hammered out after the measure is adopted. Ms. McCaman Taylor said allowing people to simply present their insurance card at a pharmacy counter and walk away with the birth control they need would be preferable.
“We kind of learned from the national experiment with COVID over-the-counter tests that reimbursement wasn’t the best model,” she said. “If people can’t afford to pay out of pocket for it, they’re just not going to get it.”
The California Health Benefits Review Program, which analyzes legislation, projected that roughly 14,200 people with state-regulated commercial insurance would get vasectomies in California in 2022. Eliminating cost sharing would increase the number of vasectomies by 252 in the law’s first year, the program estimated.
It’s a small increase. But that, plus a jump in the use of other contraceptives covered by the bill, particularly condoms, could add up to a big reduction in unintended pregnancies. Roughly 12,300 unplanned pregnancies might be averted each year if the mandate takes effect, a reduction of more than 11%, according to the analysis.
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
SACRAMENTO – California is trying to ease the pain of vasectomies by making them free for millions of residents.
Federal law and state law require most health insurers to cover prescription contraceptives at no cost to the patient. But those provisions apply to only 18 Food and Drug Administration–approved birth control options for women, so anyone with testicles is out of luck.
California lawmakers are now considering a bill that would expand that requirement to male sterilization and non-prescription birth control, including condoms and contraceptive sponges. If the Contraceptive Equity Act of 2022 passes, commercial insurance plans regulated by the state won’t be allowed to impose out-of-pocket costs, like copays, coinsurance, and deductibles, on those modes of birth control.
“It’s pretty groundbreaking in that way – it’s a whole new framework to think about contraception as something that is relevant for people of all genders,” said Liz McCaman Taylor, a senior attorney with the National Health Law Program, a group that advocates for the health rights of low-income people.
A vasectomy is an outpatient surgical procedure in which the patient’s supply of sperm is cut off from his semen by sealing or snipping the tubes that transport sperm from the testes to the penis. Most men need to recover on the couch with an ice pack for a day or 2, and a test a few months later determines whether the procedure worked.
Because vasectomies are elective procedures and usually not urgent, price can be a deciding factor.
For Nathan Songne, cost was the most stressful part of the procedure. For several years, the 31-year-old had known he didn’t want to have kids biologically. Better to adopt a 4-year-old and skip the diaper stage, he thought. He was adopted by his stepfather as a child and knew he didn’t need to be genetically related to his children to love them.
“My only concern was that I had no idea how much it was going to cost me because nobody told me,” said Mr. Songne, who lives in Mission Viejo, in Orange County. If the procedure cost $1,000, as he expected, he wouldn’t be able to afford it.
Mr. Songne’s insurance, which he gets through his work assembling guitars, covered 70% of the Aug. 8 procedure, leaving him with a bill of just under $200. “Cost did affect my decision, but because it was only $200, it made me feel a lot more relieved about continuing on with the vasectomy.”
There are two hot times of year in the vasectomy business, according to Mary Samplaski, MD, an associate professor of urology at the University of Southern California, Los Angeles. First, she sees an uptick during the March Madness college basketball tournament, when men choose to recover on the couch watching hoops.
The end of the year is also busy, she said, because many patients have finally met their annual insurance deductible and can afford the procedure.
Patients discuss out-of-pocket costs in about 20% of her vasectomy consultations. “It’s obviously a nerve-wracking procedure,” Dr. Samplaski said. “And on top of that, if your copay is high, there’s even less reason to want to do it.”
In April, Jacob Elert comparison-shopped for a vasectomy near his home in Sacramento because his health plan doesn’t cover the procedure. He had hoped to schedule one with his regular urologist, but that would have come with a $1,500 price tag.
Instead, he found a chain of vasectomy clinics where he could get the procedure for $850. Three months later, a test confirmed the vasectomy was a success.
Mr. Elert has no regrets, but had price not been a factor, he would have preferred to go to his regular urologist. “That’s the doctor I trust,” Mr. Elert said. “But it was just way too expensive.”
In November, California voters will decide whether to lock rights to abortion and contraception into the state constitution. But Proposition 1 doesn’t address issues such as cost and coverage, said Amy Moy, a spokesperson for Essential Access Health, a group that runs California’s Title X family planning program.
“The constitutional amendment is kind of the long-term protection, and we are still working to reduce barriers for Californians on the short-term and day-to-day level regardless of their gender,” she said.
SB 523 has sailed through preliminary votes in the state legislature, which faces an end-of-August deadline to act on bills. If the measure passes, it would take effect in 2024, and California would join a handful of states that require plans they regulate to completely cover vasectomies or nonprescription birth control.
The California Association of Health Plans is still evaluating the measure, which may be amended in the final days of the legislative session. But the association generally opposes bills that require additional insurance benefits because they could lead to higher premiums, spokesperson Mary Ellen Grant said.
SB 523 applies to more than 14 million Californians who work for the state, have a student health plan through a university, or have state-regulated commercial health plans. They would become eligible to receive free over-the-counter birth control – such as emergency contraception, condoms, spermicide, and contraceptive sponges – in addition to vasectomies. The bill would not apply to the millions of Californians whose health insurance plans are regulated by the federal government.
The specifics of how the benefit would work, including the frequency and amount of birth control that insurers must cover and whether patients would have to pay upfront and be reimbursed later, would be hammered out after the measure is adopted. Ms. McCaman Taylor said allowing people to simply present their insurance card at a pharmacy counter and walk away with the birth control they need would be preferable.
“We kind of learned from the national experiment with COVID over-the-counter tests that reimbursement wasn’t the best model,” she said. “If people can’t afford to pay out of pocket for it, they’re just not going to get it.”
The California Health Benefits Review Program, which analyzes legislation, projected that roughly 14,200 people with state-regulated commercial insurance would get vasectomies in California in 2022. Eliminating cost sharing would increase the number of vasectomies by 252 in the law’s first year, the program estimated.
It’s a small increase. But that, plus a jump in the use of other contraceptives covered by the bill, particularly condoms, could add up to a big reduction in unintended pregnancies. Roughly 12,300 unplanned pregnancies might be averted each year if the mandate takes effect, a reduction of more than 11%, according to the analysis.
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
SACRAMENTO – California is trying to ease the pain of vasectomies by making them free for millions of residents.
Federal law and state law require most health insurers to cover prescription contraceptives at no cost to the patient. But those provisions apply to only 18 Food and Drug Administration–approved birth control options for women, so anyone with testicles is out of luck.
California lawmakers are now considering a bill that would expand that requirement to male sterilization and non-prescription birth control, including condoms and contraceptive sponges. If the Contraceptive Equity Act of 2022 passes, commercial insurance plans regulated by the state won’t be allowed to impose out-of-pocket costs, like copays, coinsurance, and deductibles, on those modes of birth control.
“It’s pretty groundbreaking in that way – it’s a whole new framework to think about contraception as something that is relevant for people of all genders,” said Liz McCaman Taylor, a senior attorney with the National Health Law Program, a group that advocates for the health rights of low-income people.
A vasectomy is an outpatient surgical procedure in which the patient’s supply of sperm is cut off from his semen by sealing or snipping the tubes that transport sperm from the testes to the penis. Most men need to recover on the couch with an ice pack for a day or 2, and a test a few months later determines whether the procedure worked.
Because vasectomies are elective procedures and usually not urgent, price can be a deciding factor.
For Nathan Songne, cost was the most stressful part of the procedure. For several years, the 31-year-old had known he didn’t want to have kids biologically. Better to adopt a 4-year-old and skip the diaper stage, he thought. He was adopted by his stepfather as a child and knew he didn’t need to be genetically related to his children to love them.
“My only concern was that I had no idea how much it was going to cost me because nobody told me,” said Mr. Songne, who lives in Mission Viejo, in Orange County. If the procedure cost $1,000, as he expected, he wouldn’t be able to afford it.
Mr. Songne’s insurance, which he gets through his work assembling guitars, covered 70% of the Aug. 8 procedure, leaving him with a bill of just under $200. “Cost did affect my decision, but because it was only $200, it made me feel a lot more relieved about continuing on with the vasectomy.”
There are two hot times of year in the vasectomy business, according to Mary Samplaski, MD, an associate professor of urology at the University of Southern California, Los Angeles. First, she sees an uptick during the March Madness college basketball tournament, when men choose to recover on the couch watching hoops.
The end of the year is also busy, she said, because many patients have finally met their annual insurance deductible and can afford the procedure.
Patients discuss out-of-pocket costs in about 20% of her vasectomy consultations. “It’s obviously a nerve-wracking procedure,” Dr. Samplaski said. “And on top of that, if your copay is high, there’s even less reason to want to do it.”
In April, Jacob Elert comparison-shopped for a vasectomy near his home in Sacramento because his health plan doesn’t cover the procedure. He had hoped to schedule one with his regular urologist, but that would have come with a $1,500 price tag.
Instead, he found a chain of vasectomy clinics where he could get the procedure for $850. Three months later, a test confirmed the vasectomy was a success.
Mr. Elert has no regrets, but had price not been a factor, he would have preferred to go to his regular urologist. “That’s the doctor I trust,” Mr. Elert said. “But it was just way too expensive.”
In November, California voters will decide whether to lock rights to abortion and contraception into the state constitution. But Proposition 1 doesn’t address issues such as cost and coverage, said Amy Moy, a spokesperson for Essential Access Health, a group that runs California’s Title X family planning program.
“The constitutional amendment is kind of the long-term protection, and we are still working to reduce barriers for Californians on the short-term and day-to-day level regardless of their gender,” she said.
SB 523 has sailed through preliminary votes in the state legislature, which faces an end-of-August deadline to act on bills. If the measure passes, it would take effect in 2024, and California would join a handful of states that require plans they regulate to completely cover vasectomies or nonprescription birth control.
The California Association of Health Plans is still evaluating the measure, which may be amended in the final days of the legislative session. But the association generally opposes bills that require additional insurance benefits because they could lead to higher premiums, spokesperson Mary Ellen Grant said.
SB 523 applies to more than 14 million Californians who work for the state, have a student health plan through a university, or have state-regulated commercial health plans. They would become eligible to receive free over-the-counter birth control – such as emergency contraception, condoms, spermicide, and contraceptive sponges – in addition to vasectomies. The bill would not apply to the millions of Californians whose health insurance plans are regulated by the federal government.
The specifics of how the benefit would work, including the frequency and amount of birth control that insurers must cover and whether patients would have to pay upfront and be reimbursed later, would be hammered out after the measure is adopted. Ms. McCaman Taylor said allowing people to simply present their insurance card at a pharmacy counter and walk away with the birth control they need would be preferable.
“We kind of learned from the national experiment with COVID over-the-counter tests that reimbursement wasn’t the best model,” she said. “If people can’t afford to pay out of pocket for it, they’re just not going to get it.”
The California Health Benefits Review Program, which analyzes legislation, projected that roughly 14,200 people with state-regulated commercial insurance would get vasectomies in California in 2022. Eliminating cost sharing would increase the number of vasectomies by 252 in the law’s first year, the program estimated.
It’s a small increase. But that, plus a jump in the use of other contraceptives covered by the bill, particularly condoms, could add up to a big reduction in unintended pregnancies. Roughly 12,300 unplanned pregnancies might be averted each year if the mandate takes effect, a reduction of more than 11%, according to the analysis.
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Higher rates of group B strep disease found in Black and Asian newborns
Health charities called for action to address racial health disparities after population-wide analysis by the UK Health Security Agency found that Black and Asian neonates had a significantly higher risk of early-onset group B streptococcal disease (GBS), compared with White infants.
One support group said more research was now needed to identify the cause of the disparity, and called for pregnant women to be better informed about the disease and what it could mean for them and their baby.
The study, published in Pediatrics, used UKHSA data on laboratory-confirmed infant group B streptococcal (iGBS) disease cases between Jan. 1, 2016, and Dec. 31, 2020, and were linked to hospital ethnicity records.
Cases of iGBS were defined as isolation of Streptococcus agalactiae from a normally sterile site at 0-6 days of life for early-onset iGBS and 7-90 days for late-onset disease.
Hospital data and parent-reported ethnicity
Researchers found 2,512 iGBS cases in England during the study period, 65.3% were early onset and 34.8% late onset, equivalent to 0.52 and 0.28 cases per 1000 live births respectively.
Researchers were able to link 85.6% of those to ethnicity. Among those 2,149 cases, Black infants had a 48% higher risk, and Asian infants a 40% higher risk of early onset iGBS, compared with White infants. Among those from an Asian background, the risk was 87% higher for Bangladeshi and 38% higher for Pakistani neonates.
Rates of early onset iGBS per 1,000 live births were 0.43 for White infants, 0.63 for Black infants, and 0.60 for those of Asian ethnicity.
In contrast, Indian infants had an early-onset rate of 0.47 per 1,000 live births, which was similar to White infants.
Black infants had 57% higher rates of late-onset iGBS (0.37) than White infants (0.24), the researchers reported.
The study authors highlighted previous research which found higher prevalence of group B streptococcal colonization in mothers from Black and some Asian ethnic groups, but lower prevalence in mothers from the Indian subcontinent. More research was needed to establish causes, the researchers said, including whether higher preterm birth rates in minority ethnic groups led to increased iGBS risk in neonates, or whether maternal group B streptococcal disease led to higher preterm birth rates and subsequent neonatal iGBS.
The researchers concluded: “Understanding the factors underpinning differences in rates of early-onset iGBS within south Asian groups in England may lead to new opportunities for prevention such as prioritized antenatal screening. Strategies to prevent neonatal iGBS must be tailored from high-quality quantitative and qualitative data to reach all women and protect all infants, irrespective of racial or ethnic background.”
‘Shocking but not surprising’
Commenting on the study, Edward Morris, president of the Royal College of Obstetricians and Gynaecologists, said: “This research is striking reading, and is yet another example of how far we have to go to tackle health inequalities within women’s health care.”
Philip Steer, professor emeritus at Imperial College London, said that the results were “consistent with previous reports of higher GBS carriage and higher maternal and neonatal mortality rates in minority groups” and “emphasize the importance of studying not just whether, but why, these differences exist.” He added: “We need to understand the reasons for the differences before we can design much-needed intervention to eliminate them.”
Jane Plumb, chief executive of Group B Strep Support, called the findings “shocking, but unfortunately not surprising” and said that they offered “another example of racial disparities in maternal and neonatal health.” She said: “We’re calling for all pregnant women and birthing people to be informed about GBS and its risks, so they can make empowered choices for themselves and their baby. It is also critical that trusts sign up to take part in the internationally significant [National Institute for Health and Care Research]–funded GBS3 clinical trial, designed to improve the prevention of GBS infection.”
Baroness Shaista Gohir, chief executive of the Muslim Women’s Network, said: “With significantly higher rates of group B Strep infection in Black and Asian babies, greater efforts must be made to improve awareness among pregnant women within these communities.”
A version of this article first appeared on Medscape UK.
Health charities called for action to address racial health disparities after population-wide analysis by the UK Health Security Agency found that Black and Asian neonates had a significantly higher risk of early-onset group B streptococcal disease (GBS), compared with White infants.
One support group said more research was now needed to identify the cause of the disparity, and called for pregnant women to be better informed about the disease and what it could mean for them and their baby.
The study, published in Pediatrics, used UKHSA data on laboratory-confirmed infant group B streptococcal (iGBS) disease cases between Jan. 1, 2016, and Dec. 31, 2020, and were linked to hospital ethnicity records.
Cases of iGBS were defined as isolation of Streptococcus agalactiae from a normally sterile site at 0-6 days of life for early-onset iGBS and 7-90 days for late-onset disease.
Hospital data and parent-reported ethnicity
Researchers found 2,512 iGBS cases in England during the study period, 65.3% were early onset and 34.8% late onset, equivalent to 0.52 and 0.28 cases per 1000 live births respectively.
Researchers were able to link 85.6% of those to ethnicity. Among those 2,149 cases, Black infants had a 48% higher risk, and Asian infants a 40% higher risk of early onset iGBS, compared with White infants. Among those from an Asian background, the risk was 87% higher for Bangladeshi and 38% higher for Pakistani neonates.
Rates of early onset iGBS per 1,000 live births were 0.43 for White infants, 0.63 for Black infants, and 0.60 for those of Asian ethnicity.
In contrast, Indian infants had an early-onset rate of 0.47 per 1,000 live births, which was similar to White infants.
Black infants had 57% higher rates of late-onset iGBS (0.37) than White infants (0.24), the researchers reported.
The study authors highlighted previous research which found higher prevalence of group B streptococcal colonization in mothers from Black and some Asian ethnic groups, but lower prevalence in mothers from the Indian subcontinent. More research was needed to establish causes, the researchers said, including whether higher preterm birth rates in minority ethnic groups led to increased iGBS risk in neonates, or whether maternal group B streptococcal disease led to higher preterm birth rates and subsequent neonatal iGBS.
The researchers concluded: “Understanding the factors underpinning differences in rates of early-onset iGBS within south Asian groups in England may lead to new opportunities for prevention such as prioritized antenatal screening. Strategies to prevent neonatal iGBS must be tailored from high-quality quantitative and qualitative data to reach all women and protect all infants, irrespective of racial or ethnic background.”
‘Shocking but not surprising’
Commenting on the study, Edward Morris, president of the Royal College of Obstetricians and Gynaecologists, said: “This research is striking reading, and is yet another example of how far we have to go to tackle health inequalities within women’s health care.”
Philip Steer, professor emeritus at Imperial College London, said that the results were “consistent with previous reports of higher GBS carriage and higher maternal and neonatal mortality rates in minority groups” and “emphasize the importance of studying not just whether, but why, these differences exist.” He added: “We need to understand the reasons for the differences before we can design much-needed intervention to eliminate them.”
Jane Plumb, chief executive of Group B Strep Support, called the findings “shocking, but unfortunately not surprising” and said that they offered “another example of racial disparities in maternal and neonatal health.” She said: “We’re calling for all pregnant women and birthing people to be informed about GBS and its risks, so they can make empowered choices for themselves and their baby. It is also critical that trusts sign up to take part in the internationally significant [National Institute for Health and Care Research]–funded GBS3 clinical trial, designed to improve the prevention of GBS infection.”
Baroness Shaista Gohir, chief executive of the Muslim Women’s Network, said: “With significantly higher rates of group B Strep infection in Black and Asian babies, greater efforts must be made to improve awareness among pregnant women within these communities.”
A version of this article first appeared on Medscape UK.
Health charities called for action to address racial health disparities after population-wide analysis by the UK Health Security Agency found that Black and Asian neonates had a significantly higher risk of early-onset group B streptococcal disease (GBS), compared with White infants.
One support group said more research was now needed to identify the cause of the disparity, and called for pregnant women to be better informed about the disease and what it could mean for them and their baby.
The study, published in Pediatrics, used UKHSA data on laboratory-confirmed infant group B streptococcal (iGBS) disease cases between Jan. 1, 2016, and Dec. 31, 2020, and were linked to hospital ethnicity records.
Cases of iGBS were defined as isolation of Streptococcus agalactiae from a normally sterile site at 0-6 days of life for early-onset iGBS and 7-90 days for late-onset disease.
Hospital data and parent-reported ethnicity
Researchers found 2,512 iGBS cases in England during the study period, 65.3% were early onset and 34.8% late onset, equivalent to 0.52 and 0.28 cases per 1000 live births respectively.
Researchers were able to link 85.6% of those to ethnicity. Among those 2,149 cases, Black infants had a 48% higher risk, and Asian infants a 40% higher risk of early onset iGBS, compared with White infants. Among those from an Asian background, the risk was 87% higher for Bangladeshi and 38% higher for Pakistani neonates.
Rates of early onset iGBS per 1,000 live births were 0.43 for White infants, 0.63 for Black infants, and 0.60 for those of Asian ethnicity.
In contrast, Indian infants had an early-onset rate of 0.47 per 1,000 live births, which was similar to White infants.
Black infants had 57% higher rates of late-onset iGBS (0.37) than White infants (0.24), the researchers reported.
The study authors highlighted previous research which found higher prevalence of group B streptococcal colonization in mothers from Black and some Asian ethnic groups, but lower prevalence in mothers from the Indian subcontinent. More research was needed to establish causes, the researchers said, including whether higher preterm birth rates in minority ethnic groups led to increased iGBS risk in neonates, or whether maternal group B streptococcal disease led to higher preterm birth rates and subsequent neonatal iGBS.
The researchers concluded: “Understanding the factors underpinning differences in rates of early-onset iGBS within south Asian groups in England may lead to new opportunities for prevention such as prioritized antenatal screening. Strategies to prevent neonatal iGBS must be tailored from high-quality quantitative and qualitative data to reach all women and protect all infants, irrespective of racial or ethnic background.”
‘Shocking but not surprising’
Commenting on the study, Edward Morris, president of the Royal College of Obstetricians and Gynaecologists, said: “This research is striking reading, and is yet another example of how far we have to go to tackle health inequalities within women’s health care.”
Philip Steer, professor emeritus at Imperial College London, said that the results were “consistent with previous reports of higher GBS carriage and higher maternal and neonatal mortality rates in minority groups” and “emphasize the importance of studying not just whether, but why, these differences exist.” He added: “We need to understand the reasons for the differences before we can design much-needed intervention to eliminate them.”
Jane Plumb, chief executive of Group B Strep Support, called the findings “shocking, but unfortunately not surprising” and said that they offered “another example of racial disparities in maternal and neonatal health.” She said: “We’re calling for all pregnant women and birthing people to be informed about GBS and its risks, so they can make empowered choices for themselves and their baby. It is also critical that trusts sign up to take part in the internationally significant [National Institute for Health and Care Research]–funded GBS3 clinical trial, designed to improve the prevention of GBS infection.”
Baroness Shaista Gohir, chief executive of the Muslim Women’s Network, said: “With significantly higher rates of group B Strep infection in Black and Asian babies, greater efforts must be made to improve awareness among pregnant women within these communities.”
A version of this article first appeared on Medscape UK.
FROM PEDIATRICS
Indiana’s new abortion ban may drive some young ob.gyns. to leave a state where they’re needed
On a Monday morning, a group of obstetrics and gynecology residents, dressed in blue scrubs and white coats, gathered in an auditorium at Indiana University, Indianapolis. After the usual updates and announcements, Nicole Scott, MD, the residency program director, addressed the elephant in the room. “Any more abortion care questions?” she asked the trainees.
After a few moments of silence, one resident asked: “How’s Dr. Bernard doing?”
“Bernard is actually in really good spirits – I mean, relatively,” Dr. Scott answered. “She has 24/7 security, has her own lawyer.”
They were talking about Caitlin Bernard, MD, an Indiana ob.gyn. who provides abortions and trains residents at the university hospital. Dr. Bernard was recently caught in a political whirlwind after she spoke about an abortion she provided to a 10-year-old rape victim from Ohio. Dr. Bernard was the target of false accusations made on national television by pundits and political leaders, including Indiana’s attorney general.
The doctors interviewed for this article said that they are not speaking on behalf of their school of medicine but rather about their personal experiences during a tumultuous moment that they worry will affect the way they care for their patients.
The vitriol directed at Dr. Bernard hit home for this group of residents. She has mentored most of them for years. Many of the young doctors were certain they wanted to practice in Indiana after their training. But lately, some have been ambivalent about that prospect.
Beatrice Soderholm, DO, a fourth-year ob.gyn. resident, said watching what Dr. Bernard went through was “scary.” “I think that was part of the point for those who were putting her through that,” Dr. Soderholm said. They were trying “to scare other people out of doing the work that she does.”
In early August, Gov. Eric Holcomb, a Republican, signed a near-total abortion ban into law, making Indiana the first state to adopt new restrictions on abortion access since the Supreme Court struck down Roe v. Wade in June. When the ban takes effect Sept. 15, medical providers who violate the law risk losing their licenses or serving up to six years in prison.
These days, Dr. Scott, the residency program director, uses some meeting time with residents to fill them in on political updates and available mental health services. She also reminds them that legal counsel is on call round the clock to help if they’re ever unsure about the care they should provide a patient.
“Our residents are devastated,” Dr. Scott said, holding back tears. “They signed up to provide comprehensive health care to women, and they are being told that they can’t do that.”
She expects this will “deeply impact” how Indiana hospitals recruit and retain medical professionals.
A 2018 report from the March of Dimes found that 27% of Indiana counties are considered maternity care deserts, with no or limited access to maternal care. The state has one of the nation’s highest maternal mortality rates.
Dr. Scott said new laws restricting abortion will only worsen those statistics.
Dr. Scott shared results from a recent survey of nearly 1,400 residents and fellows across all specialties at IU, nearly 80% of the trainees said they were less likely to stay and practice in Indiana after the abortion ban.
Wendy Tian, MD, a third-year resident, said she is worried about her safety. Dr. Tian grew up and went to medical school in Chicago and chose to do her residency in Indiana because the program has a strong family-planning focus. She was open to practicing in Indiana when she completed her training.
But that’s changed.
“I, for sure, don’t know if I would be able to stay in Indiana post graduation with what’s going on,” Dr. Tian said.
Still, she feels guilty for “giving up” on Indiana’s most vulnerable patients.
Even before Roe fell, Dr. Tian said, the climate in Indiana could be hostile and frustrating for ob.gyns. Indiana, like other states with abortion restrictions, allows nearly all health care providers to opt out of providing care to patients having an abortion.
“We encounter other people who we work with on a daily basis who are opposed to what we do,” Dr. Tian said, adding that she and her colleagues have had to cancel scheduled procedures because the nurses on call were not comfortable assisting during an abortion.
Dr. Scott said the ob.gyn. program at the IU has provided residents with comprehensive training, including on abortion care and family planning. Since miscarriages are managed the same way as first-trimester abortions, she said, the training gives residents lots of hands-on experience. “What termination procedures allow you to do is that kind of repetition and that understanding of the female anatomy and how to manage complications that may happen with miscarriages.”
The ban on abortions dramatically reduces the hands-on opportunities for ob.gyn. residents, and that’s a huge concern, she said.
The program is exploring ways to offer training. One option is to send residents to learn in states without abortion restrictions, but Dr. Scott said that would be a logistical nightmare. “This is not as simple as just showing up to an office and saying: ‘Can I observe?’ This includes getting a medical license for out-of-state trainees. This includes funding for travel and lodging,” Dr. Scott said. “It adds a lot to what we already do to educate future ob.gyns.”
Four in 10 of all ob.gyn. residents in the United States are in states where abortion is banned or likely to be banned, so there could be a surge of residents looking to go out of state to make up for lost training opportunities. The Accreditation Council for Graduate Medical Education, the body that accredits residency programs, proposed modifications to the graduation requirements for ob.gyn. residents to account for the changing landscape.
For some of the Indiana ob.gyn. residents – including Veronica Santana, MD, a first-year resident – these political hurdles are a challenge they’re more than willing to take on. Dr. Santana is Latina, grew up in Seattle, and has been involved in community organizing since she was a teenager. One reason she chose obstetrics and gynecology was because of how the field intersects with social justice. “It’s political. It always has been, and it continues to be,” she said, “And, obviously, especially now.”
After Roe was overturned, Dr. Santana, alongside other residents and mentors, took to the streets of Indianapolis to participate in rallies in support of abortion rights.
Indiana could be the perfect battleground for Dr. Santana’s advocacy and social activism. But lately, she said, she is “very unsure” whether staying in Indiana to practice after residency makes sense, since she wants to provide the entire range of ob.gyn. services.
Dr. Soderholm, who grew up in Minnesota, has felt a strong connection to patients at the county hospital in Indianapolis. She had been certain she wanted to practice in Indiana. But her family in Minnesota – where abortion remains largely protected – has recently questioned why she would stay in a state with such a hostile climate for ob.gyns. “There’s been a lot of hesitation,” she said. But the patients make leaving difficult. “Sorry,” she said, starting to cry.
It’s for those patients that Dr. Soderholm decided she’ll likely stay. Other young doctors may make a different decision.
This story is part of a partnership that includes Side Effects Public Media, NPR, and KHN. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
On a Monday morning, a group of obstetrics and gynecology residents, dressed in blue scrubs and white coats, gathered in an auditorium at Indiana University, Indianapolis. After the usual updates and announcements, Nicole Scott, MD, the residency program director, addressed the elephant in the room. “Any more abortion care questions?” she asked the trainees.
After a few moments of silence, one resident asked: “How’s Dr. Bernard doing?”
“Bernard is actually in really good spirits – I mean, relatively,” Dr. Scott answered. “She has 24/7 security, has her own lawyer.”
They were talking about Caitlin Bernard, MD, an Indiana ob.gyn. who provides abortions and trains residents at the university hospital. Dr. Bernard was recently caught in a political whirlwind after she spoke about an abortion she provided to a 10-year-old rape victim from Ohio. Dr. Bernard was the target of false accusations made on national television by pundits and political leaders, including Indiana’s attorney general.
The doctors interviewed for this article said that they are not speaking on behalf of their school of medicine but rather about their personal experiences during a tumultuous moment that they worry will affect the way they care for their patients.
The vitriol directed at Dr. Bernard hit home for this group of residents. She has mentored most of them for years. Many of the young doctors were certain they wanted to practice in Indiana after their training. But lately, some have been ambivalent about that prospect.
Beatrice Soderholm, DO, a fourth-year ob.gyn. resident, said watching what Dr. Bernard went through was “scary.” “I think that was part of the point for those who were putting her through that,” Dr. Soderholm said. They were trying “to scare other people out of doing the work that she does.”
In early August, Gov. Eric Holcomb, a Republican, signed a near-total abortion ban into law, making Indiana the first state to adopt new restrictions on abortion access since the Supreme Court struck down Roe v. Wade in June. When the ban takes effect Sept. 15, medical providers who violate the law risk losing their licenses or serving up to six years in prison.
These days, Dr. Scott, the residency program director, uses some meeting time with residents to fill them in on political updates and available mental health services. She also reminds them that legal counsel is on call round the clock to help if they’re ever unsure about the care they should provide a patient.
“Our residents are devastated,” Dr. Scott said, holding back tears. “They signed up to provide comprehensive health care to women, and they are being told that they can’t do that.”
She expects this will “deeply impact” how Indiana hospitals recruit and retain medical professionals.
A 2018 report from the March of Dimes found that 27% of Indiana counties are considered maternity care deserts, with no or limited access to maternal care. The state has one of the nation’s highest maternal mortality rates.
Dr. Scott said new laws restricting abortion will only worsen those statistics.
Dr. Scott shared results from a recent survey of nearly 1,400 residents and fellows across all specialties at IU, nearly 80% of the trainees said they were less likely to stay and practice in Indiana after the abortion ban.
Wendy Tian, MD, a third-year resident, said she is worried about her safety. Dr. Tian grew up and went to medical school in Chicago and chose to do her residency in Indiana because the program has a strong family-planning focus. She was open to practicing in Indiana when she completed her training.
But that’s changed.
“I, for sure, don’t know if I would be able to stay in Indiana post graduation with what’s going on,” Dr. Tian said.
Still, she feels guilty for “giving up” on Indiana’s most vulnerable patients.
Even before Roe fell, Dr. Tian said, the climate in Indiana could be hostile and frustrating for ob.gyns. Indiana, like other states with abortion restrictions, allows nearly all health care providers to opt out of providing care to patients having an abortion.
“We encounter other people who we work with on a daily basis who are opposed to what we do,” Dr. Tian said, adding that she and her colleagues have had to cancel scheduled procedures because the nurses on call were not comfortable assisting during an abortion.
Dr. Scott said the ob.gyn. program at the IU has provided residents with comprehensive training, including on abortion care and family planning. Since miscarriages are managed the same way as first-trimester abortions, she said, the training gives residents lots of hands-on experience. “What termination procedures allow you to do is that kind of repetition and that understanding of the female anatomy and how to manage complications that may happen with miscarriages.”
The ban on abortions dramatically reduces the hands-on opportunities for ob.gyn. residents, and that’s a huge concern, she said.
The program is exploring ways to offer training. One option is to send residents to learn in states without abortion restrictions, but Dr. Scott said that would be a logistical nightmare. “This is not as simple as just showing up to an office and saying: ‘Can I observe?’ This includes getting a medical license for out-of-state trainees. This includes funding for travel and lodging,” Dr. Scott said. “It adds a lot to what we already do to educate future ob.gyns.”
Four in 10 of all ob.gyn. residents in the United States are in states where abortion is banned or likely to be banned, so there could be a surge of residents looking to go out of state to make up for lost training opportunities. The Accreditation Council for Graduate Medical Education, the body that accredits residency programs, proposed modifications to the graduation requirements for ob.gyn. residents to account for the changing landscape.
For some of the Indiana ob.gyn. residents – including Veronica Santana, MD, a first-year resident – these political hurdles are a challenge they’re more than willing to take on. Dr. Santana is Latina, grew up in Seattle, and has been involved in community organizing since she was a teenager. One reason she chose obstetrics and gynecology was because of how the field intersects with social justice. “It’s political. It always has been, and it continues to be,” she said, “And, obviously, especially now.”
After Roe was overturned, Dr. Santana, alongside other residents and mentors, took to the streets of Indianapolis to participate in rallies in support of abortion rights.
Indiana could be the perfect battleground for Dr. Santana’s advocacy and social activism. But lately, she said, she is “very unsure” whether staying in Indiana to practice after residency makes sense, since she wants to provide the entire range of ob.gyn. services.
Dr. Soderholm, who grew up in Minnesota, has felt a strong connection to patients at the county hospital in Indianapolis. She had been certain she wanted to practice in Indiana. But her family in Minnesota – where abortion remains largely protected – has recently questioned why she would stay in a state with such a hostile climate for ob.gyns. “There’s been a lot of hesitation,” she said. But the patients make leaving difficult. “Sorry,” she said, starting to cry.
It’s for those patients that Dr. Soderholm decided she’ll likely stay. Other young doctors may make a different decision.
This story is part of a partnership that includes Side Effects Public Media, NPR, and KHN. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
On a Monday morning, a group of obstetrics and gynecology residents, dressed in blue scrubs and white coats, gathered in an auditorium at Indiana University, Indianapolis. After the usual updates and announcements, Nicole Scott, MD, the residency program director, addressed the elephant in the room. “Any more abortion care questions?” she asked the trainees.
After a few moments of silence, one resident asked: “How’s Dr. Bernard doing?”
“Bernard is actually in really good spirits – I mean, relatively,” Dr. Scott answered. “She has 24/7 security, has her own lawyer.”
They were talking about Caitlin Bernard, MD, an Indiana ob.gyn. who provides abortions and trains residents at the university hospital. Dr. Bernard was recently caught in a political whirlwind after she spoke about an abortion she provided to a 10-year-old rape victim from Ohio. Dr. Bernard was the target of false accusations made on national television by pundits and political leaders, including Indiana’s attorney general.
The doctors interviewed for this article said that they are not speaking on behalf of their school of medicine but rather about their personal experiences during a tumultuous moment that they worry will affect the way they care for their patients.
The vitriol directed at Dr. Bernard hit home for this group of residents. She has mentored most of them for years. Many of the young doctors were certain they wanted to practice in Indiana after their training. But lately, some have been ambivalent about that prospect.
Beatrice Soderholm, DO, a fourth-year ob.gyn. resident, said watching what Dr. Bernard went through was “scary.” “I think that was part of the point for those who were putting her through that,” Dr. Soderholm said. They were trying “to scare other people out of doing the work that she does.”
In early August, Gov. Eric Holcomb, a Republican, signed a near-total abortion ban into law, making Indiana the first state to adopt new restrictions on abortion access since the Supreme Court struck down Roe v. Wade in June. When the ban takes effect Sept. 15, medical providers who violate the law risk losing their licenses or serving up to six years in prison.
These days, Dr. Scott, the residency program director, uses some meeting time with residents to fill them in on political updates and available mental health services. She also reminds them that legal counsel is on call round the clock to help if they’re ever unsure about the care they should provide a patient.
“Our residents are devastated,” Dr. Scott said, holding back tears. “They signed up to provide comprehensive health care to women, and they are being told that they can’t do that.”
She expects this will “deeply impact” how Indiana hospitals recruit and retain medical professionals.
A 2018 report from the March of Dimes found that 27% of Indiana counties are considered maternity care deserts, with no or limited access to maternal care. The state has one of the nation’s highest maternal mortality rates.
Dr. Scott said new laws restricting abortion will only worsen those statistics.
Dr. Scott shared results from a recent survey of nearly 1,400 residents and fellows across all specialties at IU, nearly 80% of the trainees said they were less likely to stay and practice in Indiana after the abortion ban.
Wendy Tian, MD, a third-year resident, said she is worried about her safety. Dr. Tian grew up and went to medical school in Chicago and chose to do her residency in Indiana because the program has a strong family-planning focus. She was open to practicing in Indiana when she completed her training.
But that’s changed.
“I, for sure, don’t know if I would be able to stay in Indiana post graduation with what’s going on,” Dr. Tian said.
Still, she feels guilty for “giving up” on Indiana’s most vulnerable patients.
Even before Roe fell, Dr. Tian said, the climate in Indiana could be hostile and frustrating for ob.gyns. Indiana, like other states with abortion restrictions, allows nearly all health care providers to opt out of providing care to patients having an abortion.
“We encounter other people who we work with on a daily basis who are opposed to what we do,” Dr. Tian said, adding that she and her colleagues have had to cancel scheduled procedures because the nurses on call were not comfortable assisting during an abortion.
Dr. Scott said the ob.gyn. program at the IU has provided residents with comprehensive training, including on abortion care and family planning. Since miscarriages are managed the same way as first-trimester abortions, she said, the training gives residents lots of hands-on experience. “What termination procedures allow you to do is that kind of repetition and that understanding of the female anatomy and how to manage complications that may happen with miscarriages.”
The ban on abortions dramatically reduces the hands-on opportunities for ob.gyn. residents, and that’s a huge concern, she said.
The program is exploring ways to offer training. One option is to send residents to learn in states without abortion restrictions, but Dr. Scott said that would be a logistical nightmare. “This is not as simple as just showing up to an office and saying: ‘Can I observe?’ This includes getting a medical license for out-of-state trainees. This includes funding for travel and lodging,” Dr. Scott said. “It adds a lot to what we already do to educate future ob.gyns.”
Four in 10 of all ob.gyn. residents in the United States are in states where abortion is banned or likely to be banned, so there could be a surge of residents looking to go out of state to make up for lost training opportunities. The Accreditation Council for Graduate Medical Education, the body that accredits residency programs, proposed modifications to the graduation requirements for ob.gyn. residents to account for the changing landscape.
For some of the Indiana ob.gyn. residents – including Veronica Santana, MD, a first-year resident – these political hurdles are a challenge they’re more than willing to take on. Dr. Santana is Latina, grew up in Seattle, and has been involved in community organizing since she was a teenager. One reason she chose obstetrics and gynecology was because of how the field intersects with social justice. “It’s political. It always has been, and it continues to be,” she said, “And, obviously, especially now.”
After Roe was overturned, Dr. Santana, alongside other residents and mentors, took to the streets of Indianapolis to participate in rallies in support of abortion rights.
Indiana could be the perfect battleground for Dr. Santana’s advocacy and social activism. But lately, she said, she is “very unsure” whether staying in Indiana to practice after residency makes sense, since she wants to provide the entire range of ob.gyn. services.
Dr. Soderholm, who grew up in Minnesota, has felt a strong connection to patients at the county hospital in Indianapolis. She had been certain she wanted to practice in Indiana. But her family in Minnesota – where abortion remains largely protected – has recently questioned why she would stay in a state with such a hostile climate for ob.gyns. “There’s been a lot of hesitation,” she said. But the patients make leaving difficult. “Sorry,” she said, starting to cry.
It’s for those patients that Dr. Soderholm decided she’ll likely stay. Other young doctors may make a different decision.
This story is part of a partnership that includes Side Effects Public Media, NPR, and KHN. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Is it COVID or long COVID? Your organs may know
There’s little doubt long COVID is real. The federal government recognizes long COVID as a condition and said in two reports issued in August that one in five adult COVID-19 survivors have a health condition related to their illness.
COVID-19 can damage multiple organs in the body. Sometimes this damage leads to long COVID; sometimes other reasons are at play. Doctors are beginning to sort it out.
“COVID itself can actually cause prolonged illness, and we don’t really call that long COVID,” said Nisha Viswanathan, MD, a doctor at UCLA Health in Los Angeles. But if symptoms extend beyond 12 weeks, that puts patients in the realm of long COVID.
Symptoms can range from mild to severe and can keep people from resuming their normal lives and jobs. Sometimes they last for months, according to the U.S. Department of Health & Human Services.
Multiorgan damage
Lung scarring and other lung problems are common after COVID, said Leora Horwitz, MD, an internal medicine specialist at New York University. Even after a mild case, people can have breathing issues for months, a team at Johns Hopkins Medicine, Baltimore, said in an online briefing. One study published in the journal Radiology found damage in people a full year after a COVID-19 diagnosis.
Some people have persistent heart, kidney, liver, and nervous system problems after COVID-19. A study published in 2020 in JAMA Cardiology found 60% of people who had COVID-19 had ongoing signs of heart inflammation. Nearly a third of people hospitalized for COVID-19 get kidney damage that can become chronic, and some end up needing dialysis or a transplant, said C. John Sperati, MD, a kidney specialist at Johns Hopkins Medicine.
This might be, in part, because SARS-CoV-2, the virus that causes COVID-19, directly infects the cells in many organs.
Nicole Bhave, MD, a cardiologist at University of Michigan Health, Ann Arbor is concerned that COVID-19 appears to increase the risk of heart problems in some people.
“Some of the uptick may just be recognition bias, in that people with symptoms are seeking care,” she said. “But there’s definitely a biological basis by which COVID could tip people over into a new diagnosis of heart failure.”
Inflammation
Inflammation is probably a key part of the long-term effects of COVID-19.
Some people have a serious immune reaction to COVID-19 called a cytokine storm, said Nitra Aggarwal Gilotra, MD, a cardiologist at Johns Hopkins Medicine. This release of inflammation-causing molecules called cytokines is meant to attack the invading virus. But it can be so severe that it wreaks havoc on healthy tissues and organs and causes lasting damage – if patients even survive it.
In some people, inflammation can affect the heart, causing myocarditis. Myocarditis symptoms include chest pain, breathlessness, and heart palpitations. Though rare, it can be serious and can raise the risk of other heart problems, including heart failure, down the line.
Long COVID may also trigger an autoimmune condition, said Eline Luning Prak, MD, PhD, a pathologist at the Hospital of the University of Pennsylvania, Philadelphia. Long COVID can share many hallmark symptoms with autoimmune diseases, including fatigue, widespread pain, memory problems, and mood disorders.
Blood clots
Studies have shown the overcharged inflammatory response to COVID-19 can cause blood clots. This sometimes overwhelming clotting was an early hallmark of COVID-19 infection, and when clots restrict blood flow in the brain, lungs, kidneys, or limbs, they can cause long-term damage. Some can be deadly. Researchers in Sweden found patients were at risk of deep vein thrombosis – a blood clot usually in the leg – up to 3 months after infection and at higher risk of a blood clot in the lung, called pulmonary embolism, for as long as 3 months.
Viral reservoirs
The virus itself may also linger in a patient’s body, causing continued symptoms and, potentially, new flare-ups. Zoe Swank, PhD, of Harvard Medical School, Boston, and colleagues reported in a preprint study that they found pieces of the SARS-CoV-2 virus in the blood of most patients with long COVID symptoms they tested – some as long as a year after infection. The study has not yet been peer reviewed.
Another team found evidence of the virus in stool up to 7 months later, which suggests the virus hides out in the gut. Other early studies have found bits of viral RNA in the appendix, breast tissue, heart, eyes, and brain.
Diabetes
Diabetes is a risk factor for getting severe COVID-19, and multiple studies have shown people can get diabetes both while battling infection and afterward. One study of veterans, published in The Lancet Diabetes and Endocrinology, found COVID-19 survivors were about 40% more likely to get diabetes over the next year.
There are a few ways this might happen. Insulin-producing cells in the pancreas have SARS-CoV-2 receptors – a type of molecular doorway the coronavirus can attach to. Damage to these cells could make the body less able to produce insulin, which in turn can lead to diabetes. The virus could also disrupt the balance in the body or cause inflammation that leads to insulin resistance, which can develop into diabetes, Ziad Al-Aly, MD, of the Veterans Affairs St. Louis Health Care System, and colleagues wrote.
Nervous system issues
People who get COVID-19 are also more vulnerable to postural orthostatic tachycardia syndrome (POTS). This affects what’s known as the autonomic nervous system, which regulates blood circulation, and includes those things that happen in your body without your having to think about them, like breathing, heartbeat, and digestion. POTS can cause common long COVID neurologic symptoms, including headaches, fatigue, brain fog, insomnia, and problems thinking and concentrating. “This was a known condition prior to COVID, but it was incredibly rare,” said Dr. Viswanathan. “After COVID, I’ve seen it with increasing frequency.”
Long-term outlook
Lasting issues after COVID-19 are much more likely after a moderate or severe infection. Still, plenty of people are battling them even after a mild illness. “As for why, that’s the billion-dollar question,” said Dr. Horwitz. “It’s well known that viral infections can cause long-term dysregulation. Why that is, we really just don’t know.”
Whether it’s virus hiding out in the body, long-term organ damage, or an autoimmune reaction likely differs from person to person. “I’m believing, increasingly, that it’s a combination of all of these, just based on how different patients are responding to different medications,” said Dr. Viswanathan. “One patient will respond to something beautifully, and another patient won’t at all.”
But it’s clear a significant number of people are facing long-term health struggles because of COVID-19, which has infected at least 580 million people globally and 92 million – likely many more – in the United States, according to Johns Hopkins University.
Even a small increased risk of conditions like heart disease or diabetes translates to a huge number of people, Dr. Horwitz said. “If even 1% of people getting COVID have long-term symptoms, that’s a major public health crisis, because that’s 1% of pretty much everybody in the country.”
A version of this article first appeared on WebMD.com.
There’s little doubt long COVID is real. The federal government recognizes long COVID as a condition and said in two reports issued in August that one in five adult COVID-19 survivors have a health condition related to their illness.
COVID-19 can damage multiple organs in the body. Sometimes this damage leads to long COVID; sometimes other reasons are at play. Doctors are beginning to sort it out.
“COVID itself can actually cause prolonged illness, and we don’t really call that long COVID,” said Nisha Viswanathan, MD, a doctor at UCLA Health in Los Angeles. But if symptoms extend beyond 12 weeks, that puts patients in the realm of long COVID.
Symptoms can range from mild to severe and can keep people from resuming their normal lives and jobs. Sometimes they last for months, according to the U.S. Department of Health & Human Services.
Multiorgan damage
Lung scarring and other lung problems are common after COVID, said Leora Horwitz, MD, an internal medicine specialist at New York University. Even after a mild case, people can have breathing issues for months, a team at Johns Hopkins Medicine, Baltimore, said in an online briefing. One study published in the journal Radiology found damage in people a full year after a COVID-19 diagnosis.
Some people have persistent heart, kidney, liver, and nervous system problems after COVID-19. A study published in 2020 in JAMA Cardiology found 60% of people who had COVID-19 had ongoing signs of heart inflammation. Nearly a third of people hospitalized for COVID-19 get kidney damage that can become chronic, and some end up needing dialysis or a transplant, said C. John Sperati, MD, a kidney specialist at Johns Hopkins Medicine.
This might be, in part, because SARS-CoV-2, the virus that causes COVID-19, directly infects the cells in many organs.
Nicole Bhave, MD, a cardiologist at University of Michigan Health, Ann Arbor is concerned that COVID-19 appears to increase the risk of heart problems in some people.
“Some of the uptick may just be recognition bias, in that people with symptoms are seeking care,” she said. “But there’s definitely a biological basis by which COVID could tip people over into a new diagnosis of heart failure.”
Inflammation
Inflammation is probably a key part of the long-term effects of COVID-19.
Some people have a serious immune reaction to COVID-19 called a cytokine storm, said Nitra Aggarwal Gilotra, MD, a cardiologist at Johns Hopkins Medicine. This release of inflammation-causing molecules called cytokines is meant to attack the invading virus. But it can be so severe that it wreaks havoc on healthy tissues and organs and causes lasting damage – if patients even survive it.
In some people, inflammation can affect the heart, causing myocarditis. Myocarditis symptoms include chest pain, breathlessness, and heart palpitations. Though rare, it can be serious and can raise the risk of other heart problems, including heart failure, down the line.
Long COVID may also trigger an autoimmune condition, said Eline Luning Prak, MD, PhD, a pathologist at the Hospital of the University of Pennsylvania, Philadelphia. Long COVID can share many hallmark symptoms with autoimmune diseases, including fatigue, widespread pain, memory problems, and mood disorders.
Blood clots
Studies have shown the overcharged inflammatory response to COVID-19 can cause blood clots. This sometimes overwhelming clotting was an early hallmark of COVID-19 infection, and when clots restrict blood flow in the brain, lungs, kidneys, or limbs, they can cause long-term damage. Some can be deadly. Researchers in Sweden found patients were at risk of deep vein thrombosis – a blood clot usually in the leg – up to 3 months after infection and at higher risk of a blood clot in the lung, called pulmonary embolism, for as long as 3 months.
Viral reservoirs
The virus itself may also linger in a patient’s body, causing continued symptoms and, potentially, new flare-ups. Zoe Swank, PhD, of Harvard Medical School, Boston, and colleagues reported in a preprint study that they found pieces of the SARS-CoV-2 virus in the blood of most patients with long COVID symptoms they tested – some as long as a year after infection. The study has not yet been peer reviewed.
Another team found evidence of the virus in stool up to 7 months later, which suggests the virus hides out in the gut. Other early studies have found bits of viral RNA in the appendix, breast tissue, heart, eyes, and brain.
Diabetes
Diabetes is a risk factor for getting severe COVID-19, and multiple studies have shown people can get diabetes both while battling infection and afterward. One study of veterans, published in The Lancet Diabetes and Endocrinology, found COVID-19 survivors were about 40% more likely to get diabetes over the next year.
There are a few ways this might happen. Insulin-producing cells in the pancreas have SARS-CoV-2 receptors – a type of molecular doorway the coronavirus can attach to. Damage to these cells could make the body less able to produce insulin, which in turn can lead to diabetes. The virus could also disrupt the balance in the body or cause inflammation that leads to insulin resistance, which can develop into diabetes, Ziad Al-Aly, MD, of the Veterans Affairs St. Louis Health Care System, and colleagues wrote.
Nervous system issues
People who get COVID-19 are also more vulnerable to postural orthostatic tachycardia syndrome (POTS). This affects what’s known as the autonomic nervous system, which regulates blood circulation, and includes those things that happen in your body without your having to think about them, like breathing, heartbeat, and digestion. POTS can cause common long COVID neurologic symptoms, including headaches, fatigue, brain fog, insomnia, and problems thinking and concentrating. “This was a known condition prior to COVID, but it was incredibly rare,” said Dr. Viswanathan. “After COVID, I’ve seen it with increasing frequency.”
Long-term outlook
Lasting issues after COVID-19 are much more likely after a moderate or severe infection. Still, plenty of people are battling them even after a mild illness. “As for why, that’s the billion-dollar question,” said Dr. Horwitz. “It’s well known that viral infections can cause long-term dysregulation. Why that is, we really just don’t know.”
Whether it’s virus hiding out in the body, long-term organ damage, or an autoimmune reaction likely differs from person to person. “I’m believing, increasingly, that it’s a combination of all of these, just based on how different patients are responding to different medications,” said Dr. Viswanathan. “One patient will respond to something beautifully, and another patient won’t at all.”
But it’s clear a significant number of people are facing long-term health struggles because of COVID-19, which has infected at least 580 million people globally and 92 million – likely many more – in the United States, according to Johns Hopkins University.
Even a small increased risk of conditions like heart disease or diabetes translates to a huge number of people, Dr. Horwitz said. “If even 1% of people getting COVID have long-term symptoms, that’s a major public health crisis, because that’s 1% of pretty much everybody in the country.”
A version of this article first appeared on WebMD.com.
There’s little doubt long COVID is real. The federal government recognizes long COVID as a condition and said in two reports issued in August that one in five adult COVID-19 survivors have a health condition related to their illness.
COVID-19 can damage multiple organs in the body. Sometimes this damage leads to long COVID; sometimes other reasons are at play. Doctors are beginning to sort it out.
“COVID itself can actually cause prolonged illness, and we don’t really call that long COVID,” said Nisha Viswanathan, MD, a doctor at UCLA Health in Los Angeles. But if symptoms extend beyond 12 weeks, that puts patients in the realm of long COVID.
Symptoms can range from mild to severe and can keep people from resuming their normal lives and jobs. Sometimes they last for months, according to the U.S. Department of Health & Human Services.
Multiorgan damage
Lung scarring and other lung problems are common after COVID, said Leora Horwitz, MD, an internal medicine specialist at New York University. Even after a mild case, people can have breathing issues for months, a team at Johns Hopkins Medicine, Baltimore, said in an online briefing. One study published in the journal Radiology found damage in people a full year after a COVID-19 diagnosis.
Some people have persistent heart, kidney, liver, and nervous system problems after COVID-19. A study published in 2020 in JAMA Cardiology found 60% of people who had COVID-19 had ongoing signs of heart inflammation. Nearly a third of people hospitalized for COVID-19 get kidney damage that can become chronic, and some end up needing dialysis or a transplant, said C. John Sperati, MD, a kidney specialist at Johns Hopkins Medicine.
This might be, in part, because SARS-CoV-2, the virus that causes COVID-19, directly infects the cells in many organs.
Nicole Bhave, MD, a cardiologist at University of Michigan Health, Ann Arbor is concerned that COVID-19 appears to increase the risk of heart problems in some people.
“Some of the uptick may just be recognition bias, in that people with symptoms are seeking care,” she said. “But there’s definitely a biological basis by which COVID could tip people over into a new diagnosis of heart failure.”
Inflammation
Inflammation is probably a key part of the long-term effects of COVID-19.
Some people have a serious immune reaction to COVID-19 called a cytokine storm, said Nitra Aggarwal Gilotra, MD, a cardiologist at Johns Hopkins Medicine. This release of inflammation-causing molecules called cytokines is meant to attack the invading virus. But it can be so severe that it wreaks havoc on healthy tissues and organs and causes lasting damage – if patients even survive it.
In some people, inflammation can affect the heart, causing myocarditis. Myocarditis symptoms include chest pain, breathlessness, and heart palpitations. Though rare, it can be serious and can raise the risk of other heart problems, including heart failure, down the line.
Long COVID may also trigger an autoimmune condition, said Eline Luning Prak, MD, PhD, a pathologist at the Hospital of the University of Pennsylvania, Philadelphia. Long COVID can share many hallmark symptoms with autoimmune diseases, including fatigue, widespread pain, memory problems, and mood disorders.
Blood clots
Studies have shown the overcharged inflammatory response to COVID-19 can cause blood clots. This sometimes overwhelming clotting was an early hallmark of COVID-19 infection, and when clots restrict blood flow in the brain, lungs, kidneys, or limbs, they can cause long-term damage. Some can be deadly. Researchers in Sweden found patients were at risk of deep vein thrombosis – a blood clot usually in the leg – up to 3 months after infection and at higher risk of a blood clot in the lung, called pulmonary embolism, for as long as 3 months.
Viral reservoirs
The virus itself may also linger in a patient’s body, causing continued symptoms and, potentially, new flare-ups. Zoe Swank, PhD, of Harvard Medical School, Boston, and colleagues reported in a preprint study that they found pieces of the SARS-CoV-2 virus in the blood of most patients with long COVID symptoms they tested – some as long as a year after infection. The study has not yet been peer reviewed.
Another team found evidence of the virus in stool up to 7 months later, which suggests the virus hides out in the gut. Other early studies have found bits of viral RNA in the appendix, breast tissue, heart, eyes, and brain.
Diabetes
Diabetes is a risk factor for getting severe COVID-19, and multiple studies have shown people can get diabetes both while battling infection and afterward. One study of veterans, published in The Lancet Diabetes and Endocrinology, found COVID-19 survivors were about 40% more likely to get diabetes over the next year.
There are a few ways this might happen. Insulin-producing cells in the pancreas have SARS-CoV-2 receptors – a type of molecular doorway the coronavirus can attach to. Damage to these cells could make the body less able to produce insulin, which in turn can lead to diabetes. The virus could also disrupt the balance in the body or cause inflammation that leads to insulin resistance, which can develop into diabetes, Ziad Al-Aly, MD, of the Veterans Affairs St. Louis Health Care System, and colleagues wrote.
Nervous system issues
People who get COVID-19 are also more vulnerable to postural orthostatic tachycardia syndrome (POTS). This affects what’s known as the autonomic nervous system, which regulates blood circulation, and includes those things that happen in your body without your having to think about them, like breathing, heartbeat, and digestion. POTS can cause common long COVID neurologic symptoms, including headaches, fatigue, brain fog, insomnia, and problems thinking and concentrating. “This was a known condition prior to COVID, but it was incredibly rare,” said Dr. Viswanathan. “After COVID, I’ve seen it with increasing frequency.”
Long-term outlook
Lasting issues after COVID-19 are much more likely after a moderate or severe infection. Still, plenty of people are battling them even after a mild illness. “As for why, that’s the billion-dollar question,” said Dr. Horwitz. “It’s well known that viral infections can cause long-term dysregulation. Why that is, we really just don’t know.”
Whether it’s virus hiding out in the body, long-term organ damage, or an autoimmune reaction likely differs from person to person. “I’m believing, increasingly, that it’s a combination of all of these, just based on how different patients are responding to different medications,” said Dr. Viswanathan. “One patient will respond to something beautifully, and another patient won’t at all.”
But it’s clear a significant number of people are facing long-term health struggles because of COVID-19, which has infected at least 580 million people globally and 92 million – likely many more – in the United States, according to Johns Hopkins University.
Even a small increased risk of conditions like heart disease or diabetes translates to a huge number of people, Dr. Horwitz said. “If even 1% of people getting COVID have long-term symptoms, that’s a major public health crisis, because that’s 1% of pretty much everybody in the country.”
A version of this article first appeared on WebMD.com.
Most people with Omicron don’t know they’re infected
Most people with Omicron likely don’t know it.
That’s according to a study in JAMA Network Open, which says 56% of people who have the Omicron variant of the coronavirus are unaware of their infection.
And it has an upside and a downside, depending on how you look at it, according to Time magazine.
“It’s good news, in some ways, since ) in vaccinated people,” Time says. “The downside is that many people are likely spreading the virus unintentionally.”
The study looked at 210 hospital patients and employees in the Los Angeles area. More than half who tested positive didn’t know it – because they had no symptoms, or they assumed they merely had a cold or allergies.
“The findings support early data from around the world suggesting that throughout the pandemic, anywhere from 25% to 40% of SARS-CoV-2 infections have been asymptomatic, which presents challenges for public health officials trying to control the spread of the virus,” Time reports.
The study found that awareness of infection rose after at-home tests became available this year. About three-quarters of people in January and February didn’t know their status, for example.
“Findings of this study suggest that low rates of Omicron variant infection awareness may be a key contributor to rapid transmission of the virus within communities,” the authors wrote. “Given that unawareness of active infection precludes self-initiated interventions, such as testing and self-isolation, even modest levels of undiagnosed infection can contribute to substantial population-level transmission.”
A version of this article first appeared on WebMD.com.
Most people with Omicron likely don’t know it.
That’s according to a study in JAMA Network Open, which says 56% of people who have the Omicron variant of the coronavirus are unaware of their infection.
And it has an upside and a downside, depending on how you look at it, according to Time magazine.
“It’s good news, in some ways, since ) in vaccinated people,” Time says. “The downside is that many people are likely spreading the virus unintentionally.”
The study looked at 210 hospital patients and employees in the Los Angeles area. More than half who tested positive didn’t know it – because they had no symptoms, or they assumed they merely had a cold or allergies.
“The findings support early data from around the world suggesting that throughout the pandemic, anywhere from 25% to 40% of SARS-CoV-2 infections have been asymptomatic, which presents challenges for public health officials trying to control the spread of the virus,” Time reports.
The study found that awareness of infection rose after at-home tests became available this year. About three-quarters of people in January and February didn’t know their status, for example.
“Findings of this study suggest that low rates of Omicron variant infection awareness may be a key contributor to rapid transmission of the virus within communities,” the authors wrote. “Given that unawareness of active infection precludes self-initiated interventions, such as testing and self-isolation, even modest levels of undiagnosed infection can contribute to substantial population-level transmission.”
A version of this article first appeared on WebMD.com.
Most people with Omicron likely don’t know it.
That’s according to a study in JAMA Network Open, which says 56% of people who have the Omicron variant of the coronavirus are unaware of their infection.
And it has an upside and a downside, depending on how you look at it, according to Time magazine.
“It’s good news, in some ways, since ) in vaccinated people,” Time says. “The downside is that many people are likely spreading the virus unintentionally.”
The study looked at 210 hospital patients and employees in the Los Angeles area. More than half who tested positive didn’t know it – because they had no symptoms, or they assumed they merely had a cold or allergies.
“The findings support early data from around the world suggesting that throughout the pandemic, anywhere from 25% to 40% of SARS-CoV-2 infections have been asymptomatic, which presents challenges for public health officials trying to control the spread of the virus,” Time reports.
The study found that awareness of infection rose after at-home tests became available this year. About three-quarters of people in January and February didn’t know their status, for example.
“Findings of this study suggest that low rates of Omicron variant infection awareness may be a key contributor to rapid transmission of the virus within communities,” the authors wrote. “Given that unawareness of active infection precludes self-initiated interventions, such as testing and self-isolation, even modest levels of undiagnosed infection can contribute to substantial population-level transmission.”
A version of this article first appeared on WebMD.com.
FROM JAMA NETWORK OPEN