User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Post–COVID-19 lung injury: What we know so far
With vaccination rates increasing and new infections declining, we all hope the worst of the COVID-19 pandemic is over (fingers crossed really tight). Regardless, the post–COVID-19 syndrome pandemic has already begun. What is post–COVID-19 syndrome (or long-haulers or long-COVID)? Is it standard postviral fatigue? Prolonged deconditioning following debilitating illness? Permanent lung or vascular injury? Common sense and past experience say it’s all of these.
In theory, the burden of actual lung injury post COVID-19 should be the easiest to quantify, so let’s discuss what we think we know. I’ve heard experts break post–COVID-19 lung injury into three broad categories:
- Preexisting lung disease that is exacerbated by acute COVID-19 infection.
- Acute COVID-19 infection that causes acute respiratory distress syndrome (ARDS) or other acute lung injury (ALI).
- Non–critically ill acute COVID-19 with residual lung damage and abnormal repair.
These categories are necessarily imprecise, making it challenging to fit some patients neatly into a single definition.
For patients in the first category, management will be dictated largely by the nature of the preexisting lung disease. For those in category two, we already know a lot about what their recovery from ARDS will look like. There’s no longer reason to believe that COVID-19–related ARDS is particularly unique, and all things being equal, lung recovery should mimic that seen with non–COVID-19 ARDS.
It’s going to take patience and time, and beyond targeted rehabilitation it’s not clear that we have anything available to expedite the process.
The third category of patients is the most intriguing. Is there a group of patients who have residual lung injury but didn’t have evident ARDS/ALI during their acute COVID-19 infection? Anecdotally we think so, but we know little about prevalence and less about management. A recent study published in Annals of the American Thoracic Society addresses both issues. In an observational report on patients recovering after being hospitalized with COVID-19 infection, the authors found that 3.6% of patients had residual lung injury that improved with 3 weeks of corticosteroid treatment.
The report is timely and helpful but hardly definitive. It’s observational, and patients required extensive screening and identification by a multidisciplinary committee of experts in interstitial lung disease. Patients were diagnosed as having organizing pneumonia (OP) as their “lung injury” if certain radiographic criteria were met. There were no biopsies. Last, there was no control group. Still, this report is critically important. It tells us that at 6 weeks post discharge, about 3.6% of patients who were hospitalized for COVID-19 will have persistent symptoms, radiographic abnormalities, and a plateau in their recovery.
Beyond that, it tells us little. Did these patients really have OP? It’s impossible to know. The CT findings used to establish the diagnosis are nonspecific. Response to steroids is consistent with OP, but the treatment course was quite short. If truly OP, one would expect a high relapse rate after steroid withdrawal. Patients weren’t followed long enough to monitor recurrence rates. Also, as appropriately discussed in the accompanying editorial, there’s no control group so we can’t know whether the patients treated with steroids would have recovered without treatment. There was objective improvement in lung function for the two to three patients they followed who did not receive steroids. However, it was of lesser magnitude than in the steroid group.
Post–COVID-19 symptoms will remain a challenge for the foreseeable future. More than 30 million patients have been diagnosed with COVID-19 in the United States and close to half will experience persistent dyspnea. Putting the numbers together, I conclude that the vast majority will not have identifiable lung injury that will benefit from steroids. I wish I could prescribe patience to both physicians and patients.
Dr. Holley is associate professor of medicine at Uniformed Services University and program director of pulmonary and critical care medicine at Walter Reed National Military Medical Center. He covers a wide range of topics in pulmonary, critical care, and sleep medicine.
A version of this article first appeared on Medscape.com.
With vaccination rates increasing and new infections declining, we all hope the worst of the COVID-19 pandemic is over (fingers crossed really tight). Regardless, the post–COVID-19 syndrome pandemic has already begun. What is post–COVID-19 syndrome (or long-haulers or long-COVID)? Is it standard postviral fatigue? Prolonged deconditioning following debilitating illness? Permanent lung or vascular injury? Common sense and past experience say it’s all of these.
In theory, the burden of actual lung injury post COVID-19 should be the easiest to quantify, so let’s discuss what we think we know. I’ve heard experts break post–COVID-19 lung injury into three broad categories:
- Preexisting lung disease that is exacerbated by acute COVID-19 infection.
- Acute COVID-19 infection that causes acute respiratory distress syndrome (ARDS) or other acute lung injury (ALI).
- Non–critically ill acute COVID-19 with residual lung damage and abnormal repair.
These categories are necessarily imprecise, making it challenging to fit some patients neatly into a single definition.
For patients in the first category, management will be dictated largely by the nature of the preexisting lung disease. For those in category two, we already know a lot about what their recovery from ARDS will look like. There’s no longer reason to believe that COVID-19–related ARDS is particularly unique, and all things being equal, lung recovery should mimic that seen with non–COVID-19 ARDS.
It’s going to take patience and time, and beyond targeted rehabilitation it’s not clear that we have anything available to expedite the process.
The third category of patients is the most intriguing. Is there a group of patients who have residual lung injury but didn’t have evident ARDS/ALI during their acute COVID-19 infection? Anecdotally we think so, but we know little about prevalence and less about management. A recent study published in Annals of the American Thoracic Society addresses both issues. In an observational report on patients recovering after being hospitalized with COVID-19 infection, the authors found that 3.6% of patients had residual lung injury that improved with 3 weeks of corticosteroid treatment.
The report is timely and helpful but hardly definitive. It’s observational, and patients required extensive screening and identification by a multidisciplinary committee of experts in interstitial lung disease. Patients were diagnosed as having organizing pneumonia (OP) as their “lung injury” if certain radiographic criteria were met. There were no biopsies. Last, there was no control group. Still, this report is critically important. It tells us that at 6 weeks post discharge, about 3.6% of patients who were hospitalized for COVID-19 will have persistent symptoms, radiographic abnormalities, and a plateau in their recovery.
Beyond that, it tells us little. Did these patients really have OP? It’s impossible to know. The CT findings used to establish the diagnosis are nonspecific. Response to steroids is consistent with OP, but the treatment course was quite short. If truly OP, one would expect a high relapse rate after steroid withdrawal. Patients weren’t followed long enough to monitor recurrence rates. Also, as appropriately discussed in the accompanying editorial, there’s no control group so we can’t know whether the patients treated with steroids would have recovered without treatment. There was objective improvement in lung function for the two to three patients they followed who did not receive steroids. However, it was of lesser magnitude than in the steroid group.
Post–COVID-19 symptoms will remain a challenge for the foreseeable future. More than 30 million patients have been diagnosed with COVID-19 in the United States and close to half will experience persistent dyspnea. Putting the numbers together, I conclude that the vast majority will not have identifiable lung injury that will benefit from steroids. I wish I could prescribe patience to both physicians and patients.
Dr. Holley is associate professor of medicine at Uniformed Services University and program director of pulmonary and critical care medicine at Walter Reed National Military Medical Center. He covers a wide range of topics in pulmonary, critical care, and sleep medicine.
A version of this article first appeared on Medscape.com.
With vaccination rates increasing and new infections declining, we all hope the worst of the COVID-19 pandemic is over (fingers crossed really tight). Regardless, the post–COVID-19 syndrome pandemic has already begun. What is post–COVID-19 syndrome (or long-haulers or long-COVID)? Is it standard postviral fatigue? Prolonged deconditioning following debilitating illness? Permanent lung or vascular injury? Common sense and past experience say it’s all of these.
In theory, the burden of actual lung injury post COVID-19 should be the easiest to quantify, so let’s discuss what we think we know. I’ve heard experts break post–COVID-19 lung injury into three broad categories:
- Preexisting lung disease that is exacerbated by acute COVID-19 infection.
- Acute COVID-19 infection that causes acute respiratory distress syndrome (ARDS) or other acute lung injury (ALI).
- Non–critically ill acute COVID-19 with residual lung damage and abnormal repair.
These categories are necessarily imprecise, making it challenging to fit some patients neatly into a single definition.
For patients in the first category, management will be dictated largely by the nature of the preexisting lung disease. For those in category two, we already know a lot about what their recovery from ARDS will look like. There’s no longer reason to believe that COVID-19–related ARDS is particularly unique, and all things being equal, lung recovery should mimic that seen with non–COVID-19 ARDS.
It’s going to take patience and time, and beyond targeted rehabilitation it’s not clear that we have anything available to expedite the process.
The third category of patients is the most intriguing. Is there a group of patients who have residual lung injury but didn’t have evident ARDS/ALI during their acute COVID-19 infection? Anecdotally we think so, but we know little about prevalence and less about management. A recent study published in Annals of the American Thoracic Society addresses both issues. In an observational report on patients recovering after being hospitalized with COVID-19 infection, the authors found that 3.6% of patients had residual lung injury that improved with 3 weeks of corticosteroid treatment.
The report is timely and helpful but hardly definitive. It’s observational, and patients required extensive screening and identification by a multidisciplinary committee of experts in interstitial lung disease. Patients were diagnosed as having organizing pneumonia (OP) as their “lung injury” if certain radiographic criteria were met. There were no biopsies. Last, there was no control group. Still, this report is critically important. It tells us that at 6 weeks post discharge, about 3.6% of patients who were hospitalized for COVID-19 will have persistent symptoms, radiographic abnormalities, and a plateau in their recovery.
Beyond that, it tells us little. Did these patients really have OP? It’s impossible to know. The CT findings used to establish the diagnosis are nonspecific. Response to steroids is consistent with OP, but the treatment course was quite short. If truly OP, one would expect a high relapse rate after steroid withdrawal. Patients weren’t followed long enough to monitor recurrence rates. Also, as appropriately discussed in the accompanying editorial, there’s no control group so we can’t know whether the patients treated with steroids would have recovered without treatment. There was objective improvement in lung function for the two to three patients they followed who did not receive steroids. However, it was of lesser magnitude than in the steroid group.
Post–COVID-19 symptoms will remain a challenge for the foreseeable future. More than 30 million patients have been diagnosed with COVID-19 in the United States and close to half will experience persistent dyspnea. Putting the numbers together, I conclude that the vast majority will not have identifiable lung injury that will benefit from steroids. I wish I could prescribe patience to both physicians and patients.
Dr. Holley is associate professor of medicine at Uniformed Services University and program director of pulmonary and critical care medicine at Walter Reed National Military Medical Center. He covers a wide range of topics in pulmonary, critical care, and sleep medicine.
A version of this article first appeared on Medscape.com.
A pacemaker that 'just disappears' and a magnetic diet device
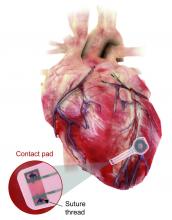
Ignore this pacemaker and it will go away
At some point – and now seems to be that point – we have to say enough is enough. The throwaway culture that produces phones, TVs, and computers that get tossed in the trash because they can’t be repaired has gone too far. That’s right, we’re looking at you, medical science!
This time, it’s a pacemaker that just disappears when it’s no longer needed. Some lazy heart surgeon decided that it was way too much trouble to do another surgery to remove the leads when a temporary pacemaker was no longer needed. You know the type: “It sure would be nice if the pacemaker components were biocompatible and were naturally absorbed by the body over the course of a few weeks and wouldn’t need to be surgically extracted.” Slacker.
Well, get a load of this. Researchers at Northwestern and George Washington universities say that they have come up with a transient pacemaker that “harvests energy from an external, remote antenna using near-field communication protocols – the same technology used in smartphones for electronic payments and in RFID tags.”
That means no batteries and no wires that have to be removed and can cause infections. Because the infectious disease docs also are too lazy to do their jobs, apparently.
The lack of onboard infrastructure means that the device can be very small – it weighs less than half a gram and is only 250 microns thick. And yes, it is bioresorbable and completely harmless. It fully degrades and disappears in 5-7 weeks through the body’s natural biologic processes, “thereby avoiding the need for physical removal of the pacemaker electrodes. This is potentially a major victory for postoperative patients,” said Dr. Rishi Arora, one of the investigators.
A victory for patients, he says. Not a word about the time and effort saved by the surgeons. Typical.
It’s a mask! No, it’s a COVID-19 test!
Mask wearing has gotten more lax as people get vaccinated for COVID-19, but as wearing masks for virus prevention is becoming more normalized in western society, some saw an opportunity to make them work for diagnosis.
Researchers from the Massachusetts Institute of Technology and the Wyss Institute for Biologically Inspired Engineering at Harvard University have found a way to do just that with their wearable freeze-dried cell-free (wFDCF) technology. A single push of a button releases water from a reservoir in the mask that sequentially activates three different freeze-dried biological reactions, which detect the SARS-CoV-2 virus in the wearer’s breath.
Initially meant as a tool for the Zika outbreak in 2015, the team made a quick pivot in May 2020. But this isn’t just some run-of-the-mill, at-home test. The data prove that the wFDCF mask is comparable to polymerase chain reactions tests, the standard in COVID-19 detection. Plus there aren’t any extra factors to deal with, like room or instrument temperature to ensure accuracy. In just 90 minutes, the mask gives results on a readout in a way similar to that of a pregnancy test. Voilà! To have COVID-19 or not to have COVID-19 is an easily answered question.
At LOTME, we think this is a big improvement from having dogs, or even three-foot rats, sniffing out coronavirus.
But wait, there’s more. “In addition to face masks, our programmable biosensors can be integrated into other garments to provide on-the-go detection of dangerous substances including viruses, bacteria, toxins, and chemical agents,” said Peter Nguyen, PhD, study coauthor and research scientist at the Wyss Institute. The technology can be used on lab coats, scrubs, military uniforms, and uniforms of first responders who may come in contact with hazardous pathogens and toxins. Think of all the lives saved and possible avoidances.
If only it could diagnose bad breath.
Finally, an excuse for the all-beer diet
Weight loss is hard work. Extremely hard work, and, as evidenced by the constant inundation and advertisement of quick fixes, crash diets, and expensive gym memberships, there’s not really a solid, 100% solution to the issue. Until now, thanks to a team of doctors from New Zealand, who’ve decided that the best way to combat obesity is to leave you in constant agony.
The DentalSlim Diet Control device is certainly a radical yet comically logical attempt to combat obesity. The creators say that the biggest problem with dieting is compliance, and, well, it’s difficult to eat too much if you can’t actually open your mouth. The metal contraption is mounted onto your teeth and uses magnetic locks to prevent the user from opening their mouths more than 2 mm. That’s less than a tenth of an inch. Which is not a lot. So not a lot that essentially all you can consume is liquid.
Oh, and they’ve got results to back up their madness. In a small study, seven otherwise healthy obese women lost an average of 5.1% of their body weight after using the DentalSlim for 2 weeks, though they did complain that the device was difficult to use, caused discomfort and difficulty speaking, made them more tense, and in general made life “less satisfying.” And one participant was able to cheat the system and consume nonhealthy food like chocolate by melting it.
So, there you are, if you want a weight-loss solution that tortures you and has far bigger holes than the one it leaves for your mouth, try the DentalSlim. Or, you know, don’t eat that eighth slice of pizza and maybe go for a walk later. Your choice.
Ignore this pacemaker and it will go away
At some point – and now seems to be that point – we have to say enough is enough. The throwaway culture that produces phones, TVs, and computers that get tossed in the trash because they can’t be repaired has gone too far. That’s right, we’re looking at you, medical science!
This time, it’s a pacemaker that just disappears when it’s no longer needed. Some lazy heart surgeon decided that it was way too much trouble to do another surgery to remove the leads when a temporary pacemaker was no longer needed. You know the type: “It sure would be nice if the pacemaker components were biocompatible and were naturally absorbed by the body over the course of a few weeks and wouldn’t need to be surgically extracted.” Slacker.
Well, get a load of this. Researchers at Northwestern and George Washington universities say that they have come up with a transient pacemaker that “harvests energy from an external, remote antenna using near-field communication protocols – the same technology used in smartphones for electronic payments and in RFID tags.”
That means no batteries and no wires that have to be removed and can cause infections. Because the infectious disease docs also are too lazy to do their jobs, apparently.
The lack of onboard infrastructure means that the device can be very small – it weighs less than half a gram and is only 250 microns thick. And yes, it is bioresorbable and completely harmless. It fully degrades and disappears in 5-7 weeks through the body’s natural biologic processes, “thereby avoiding the need for physical removal of the pacemaker electrodes. This is potentially a major victory for postoperative patients,” said Dr. Rishi Arora, one of the investigators.
A victory for patients, he says. Not a word about the time and effort saved by the surgeons. Typical.
It’s a mask! No, it’s a COVID-19 test!
Mask wearing has gotten more lax as people get vaccinated for COVID-19, but as wearing masks for virus prevention is becoming more normalized in western society, some saw an opportunity to make them work for diagnosis.
Researchers from the Massachusetts Institute of Technology and the Wyss Institute for Biologically Inspired Engineering at Harvard University have found a way to do just that with their wearable freeze-dried cell-free (wFDCF) technology. A single push of a button releases water from a reservoir in the mask that sequentially activates three different freeze-dried biological reactions, which detect the SARS-CoV-2 virus in the wearer’s breath.
Initially meant as a tool for the Zika outbreak in 2015, the team made a quick pivot in May 2020. But this isn’t just some run-of-the-mill, at-home test. The data prove that the wFDCF mask is comparable to polymerase chain reactions tests, the standard in COVID-19 detection. Plus there aren’t any extra factors to deal with, like room or instrument temperature to ensure accuracy. In just 90 minutes, the mask gives results on a readout in a way similar to that of a pregnancy test. Voilà! To have COVID-19 or not to have COVID-19 is an easily answered question.
At LOTME, we think this is a big improvement from having dogs, or even three-foot rats, sniffing out coronavirus.
But wait, there’s more. “In addition to face masks, our programmable biosensors can be integrated into other garments to provide on-the-go detection of dangerous substances including viruses, bacteria, toxins, and chemical agents,” said Peter Nguyen, PhD, study coauthor and research scientist at the Wyss Institute. The technology can be used on lab coats, scrubs, military uniforms, and uniforms of first responders who may come in contact with hazardous pathogens and toxins. Think of all the lives saved and possible avoidances.
If only it could diagnose bad breath.
Finally, an excuse for the all-beer diet
Weight loss is hard work. Extremely hard work, and, as evidenced by the constant inundation and advertisement of quick fixes, crash diets, and expensive gym memberships, there’s not really a solid, 100% solution to the issue. Until now, thanks to a team of doctors from New Zealand, who’ve decided that the best way to combat obesity is to leave you in constant agony.
The DentalSlim Diet Control device is certainly a radical yet comically logical attempt to combat obesity. The creators say that the biggest problem with dieting is compliance, and, well, it’s difficult to eat too much if you can’t actually open your mouth. The metal contraption is mounted onto your teeth and uses magnetic locks to prevent the user from opening their mouths more than 2 mm. That’s less than a tenth of an inch. Which is not a lot. So not a lot that essentially all you can consume is liquid.
Oh, and they’ve got results to back up their madness. In a small study, seven otherwise healthy obese women lost an average of 5.1% of their body weight after using the DentalSlim for 2 weeks, though they did complain that the device was difficult to use, caused discomfort and difficulty speaking, made them more tense, and in general made life “less satisfying.” And one participant was able to cheat the system and consume nonhealthy food like chocolate by melting it.
So, there you are, if you want a weight-loss solution that tortures you and has far bigger holes than the one it leaves for your mouth, try the DentalSlim. Or, you know, don’t eat that eighth slice of pizza and maybe go for a walk later. Your choice.
Ignore this pacemaker and it will go away
At some point – and now seems to be that point – we have to say enough is enough. The throwaway culture that produces phones, TVs, and computers that get tossed in the trash because they can’t be repaired has gone too far. That’s right, we’re looking at you, medical science!
This time, it’s a pacemaker that just disappears when it’s no longer needed. Some lazy heart surgeon decided that it was way too much trouble to do another surgery to remove the leads when a temporary pacemaker was no longer needed. You know the type: “It sure would be nice if the pacemaker components were biocompatible and were naturally absorbed by the body over the course of a few weeks and wouldn’t need to be surgically extracted.” Slacker.
Well, get a load of this. Researchers at Northwestern and George Washington universities say that they have come up with a transient pacemaker that “harvests energy from an external, remote antenna using near-field communication protocols – the same technology used in smartphones for electronic payments and in RFID tags.”
That means no batteries and no wires that have to be removed and can cause infections. Because the infectious disease docs also are too lazy to do their jobs, apparently.
The lack of onboard infrastructure means that the device can be very small – it weighs less than half a gram and is only 250 microns thick. And yes, it is bioresorbable and completely harmless. It fully degrades and disappears in 5-7 weeks through the body’s natural biologic processes, “thereby avoiding the need for physical removal of the pacemaker electrodes. This is potentially a major victory for postoperative patients,” said Dr. Rishi Arora, one of the investigators.
A victory for patients, he says. Not a word about the time and effort saved by the surgeons. Typical.
It’s a mask! No, it’s a COVID-19 test!
Mask wearing has gotten more lax as people get vaccinated for COVID-19, but as wearing masks for virus prevention is becoming more normalized in western society, some saw an opportunity to make them work for diagnosis.
Researchers from the Massachusetts Institute of Technology and the Wyss Institute for Biologically Inspired Engineering at Harvard University have found a way to do just that with their wearable freeze-dried cell-free (wFDCF) technology. A single push of a button releases water from a reservoir in the mask that sequentially activates three different freeze-dried biological reactions, which detect the SARS-CoV-2 virus in the wearer’s breath.
Initially meant as a tool for the Zika outbreak in 2015, the team made a quick pivot in May 2020. But this isn’t just some run-of-the-mill, at-home test. The data prove that the wFDCF mask is comparable to polymerase chain reactions tests, the standard in COVID-19 detection. Plus there aren’t any extra factors to deal with, like room or instrument temperature to ensure accuracy. In just 90 minutes, the mask gives results on a readout in a way similar to that of a pregnancy test. Voilà! To have COVID-19 or not to have COVID-19 is an easily answered question.
At LOTME, we think this is a big improvement from having dogs, or even three-foot rats, sniffing out coronavirus.
But wait, there’s more. “In addition to face masks, our programmable biosensors can be integrated into other garments to provide on-the-go detection of dangerous substances including viruses, bacteria, toxins, and chemical agents,” said Peter Nguyen, PhD, study coauthor and research scientist at the Wyss Institute. The technology can be used on lab coats, scrubs, military uniforms, and uniforms of first responders who may come in contact with hazardous pathogens and toxins. Think of all the lives saved and possible avoidances.
If only it could diagnose bad breath.
Finally, an excuse for the all-beer diet
Weight loss is hard work. Extremely hard work, and, as evidenced by the constant inundation and advertisement of quick fixes, crash diets, and expensive gym memberships, there’s not really a solid, 100% solution to the issue. Until now, thanks to a team of doctors from New Zealand, who’ve decided that the best way to combat obesity is to leave you in constant agony.
The DentalSlim Diet Control device is certainly a radical yet comically logical attempt to combat obesity. The creators say that the biggest problem with dieting is compliance, and, well, it’s difficult to eat too much if you can’t actually open your mouth. The metal contraption is mounted onto your teeth and uses magnetic locks to prevent the user from opening their mouths more than 2 mm. That’s less than a tenth of an inch. Which is not a lot. So not a lot that essentially all you can consume is liquid.
Oh, and they’ve got results to back up their madness. In a small study, seven otherwise healthy obese women lost an average of 5.1% of their body weight after using the DentalSlim for 2 weeks, though they did complain that the device was difficult to use, caused discomfort and difficulty speaking, made them more tense, and in general made life “less satisfying.” And one participant was able to cheat the system and consume nonhealthy food like chocolate by melting it.
So, there you are, if you want a weight-loss solution that tortures you and has far bigger holes than the one it leaves for your mouth, try the DentalSlim. Or, you know, don’t eat that eighth slice of pizza and maybe go for a walk later. Your choice.
Almost all U.S. COVID-19 deaths now in the unvaccinated
If you, a friend, or a loved one remain unvaccinated against COVID-19 at this point – for whatever reason – you are at higher risk of dying if you become infected.
That’s the conclusion of a new report released by the Associated Press looking at COVID-19 deaths during May 2021.
Of more than 18,000 people who died from COVID-19, for example, only about 150 were fully vaccinated. That’s less than 1%.
“Recently, I was working in the emergency room [and] I saw a 21-year-old African American who came in with shortness of breath,” said Vino K. Palli, MD, MPH, a physician specializing in emergency medicine, internal medicine, and urgent care.
The patient rapidly deteriorated and required intubation and ventilation. She was transferred to a specialized hospital for possible extracorporeal membrane oxygenation (ECMO) treatment.
“This patient was unvaccinated, along with her entire family. This would have been easily preventable,” added Dr. Palli, who is also founder and CEO of MiDoctor Urgent Care in New York City.
“Vaccine misinformation, compounded with vaccine inertia and vaccine access, have contributed to this,” he added. “Even though we have a surplus amount of vaccines at this time, we are only seeing 50% to 55% of completely vaccinated patients.”
Authors of the Associated Press report also acknowledge that some people who are fully vaccinated can get a breakthrough infection. These occurred in fewer than 1,200 of more than 853,000 people hospitalized for COVID-19 in May, or about 0.1%.
The Associated Press came up with these numbers using data from the Centers for Disease Control and Prevention. The CDC tracks the numbers of cases, hospitalizations, and deaths but does not breakdown rates by vaccination status.
Stronger argument for vaccination?
“The fact that only 0.8% of COVID-19 deaths are in the fully vaccinated should persuade those people still hesitant about vaccination,” said Hugh Cassiere, MD, medical director of Respiratory Therapy Services at North Shore University Hospital in Manhasset, New York.
Stuart C. Ray, MD, professor of medicine and oncology in the Division of Infectious Diseases at Johns Hopkins University, Baltimore, agreed. “It seems compelling, even for skeptics, that unvaccinated people represent 99% of those now dying from COVID-19 when they represent less than 50% of the adult population in the United States.”
The findings from the study could be more persuasive than previous arguments made in favor of immunization, Dr. Ray said. “These recent findings of striking reductions in risk of death in the vaccinated are more directly attributable and harder to ignore or dismiss.”
Brian Labus, PhD, MPH, of the University of Nevada Las Vegas (UNLV) is less convinced. “While this might change some peoples’ minds, it probably won’t make a major difference. People have many different reasons for not getting vaccinated, and this is only one of the things they consider.”
The study adds information that was not available before, said Dr. Labus, assistant professor in the Department of Epidemiology and Biostatistics at the UNLV School of Public Health. “We study the vaccine under tightly controlled, ideal conditions. This is the evidence that it works as well in the real world as it did in the trials, and that is what is most important in implementing a vaccination program,” added Dr. Labus.
“The scientific data has honed in on one thing: Vaccines are effective in preventing hospitalizations, ICU admissions, ventilations, and deaths,” agreed Dr. Palli.
“We now know that almost all deaths occurred in patients who were not vaccinated. We also know that all vaccines are effective against various strains that are in circulation right now, including the Delta variant, which is rapidly spreading,” Dr. Palli said.
Dr. Cassiere pointed out that the unvaccinated are not only at higher risk of developing COVID-19 but also of spreading, being hospitalized for, and dying from the infection. Avoiding “long hauler” symptoms is another argument in favor of immunization, he added.
As of June 28, the CDC reports that 63% of Americans 12 years and older have received at least one dose of a COVID-19 vaccine, and 54% are fully vaccinated.
Worldwide worry?
Although overall rates of U.S. COVID-19 hospitalizations and deaths are down, the outlook may not remain as encouraging. “I hope I’m wrong about this, but I anticipate that the coming fall and winter will bring increasingly localized versions of similar findings – severe disease and death due to SARS-CoV-2 infection in regions or groups with lower vaccination rates,” Dr. Ray said.
There could be a silver lining, he added: “If this unfortunate surge occurs, the health and economic consequences seem likely to erode much of the remaining hesitancy regarding vaccination.”
The rise of more infectious SARS-CoV-2 variants, such as the Delta variant, could also throw a wrench in controlling COVID-19. “This isn’t just a domestic issue,” Dr. Ray said. “We have learned that the world is a small place in pandemic times.”
The Associated Press investigators state that their findings support the high efficacy of the vaccine. Also, given the current widespread availability of COVID-19 vaccines in the United States, they believe many of the COVID-19 deaths now occurring are preventable.
Public health measures should have continued longer to protect unvaccinated individuals, especially Black Americans, Hispanic Americans, and other minorities, Dr. Palli said. “Only time will tell if re-opening and abandoning all public health measures by the CDC was premature.”
A version of this article first appeared on Medscape.com.
If you, a friend, or a loved one remain unvaccinated against COVID-19 at this point – for whatever reason – you are at higher risk of dying if you become infected.
That’s the conclusion of a new report released by the Associated Press looking at COVID-19 deaths during May 2021.
Of more than 18,000 people who died from COVID-19, for example, only about 150 were fully vaccinated. That’s less than 1%.
“Recently, I was working in the emergency room [and] I saw a 21-year-old African American who came in with shortness of breath,” said Vino K. Palli, MD, MPH, a physician specializing in emergency medicine, internal medicine, and urgent care.
The patient rapidly deteriorated and required intubation and ventilation. She was transferred to a specialized hospital for possible extracorporeal membrane oxygenation (ECMO) treatment.
“This patient was unvaccinated, along with her entire family. This would have been easily preventable,” added Dr. Palli, who is also founder and CEO of MiDoctor Urgent Care in New York City.
“Vaccine misinformation, compounded with vaccine inertia and vaccine access, have contributed to this,” he added. “Even though we have a surplus amount of vaccines at this time, we are only seeing 50% to 55% of completely vaccinated patients.”
Authors of the Associated Press report also acknowledge that some people who are fully vaccinated can get a breakthrough infection. These occurred in fewer than 1,200 of more than 853,000 people hospitalized for COVID-19 in May, or about 0.1%.
The Associated Press came up with these numbers using data from the Centers for Disease Control and Prevention. The CDC tracks the numbers of cases, hospitalizations, and deaths but does not breakdown rates by vaccination status.
Stronger argument for vaccination?
“The fact that only 0.8% of COVID-19 deaths are in the fully vaccinated should persuade those people still hesitant about vaccination,” said Hugh Cassiere, MD, medical director of Respiratory Therapy Services at North Shore University Hospital in Manhasset, New York.
Stuart C. Ray, MD, professor of medicine and oncology in the Division of Infectious Diseases at Johns Hopkins University, Baltimore, agreed. “It seems compelling, even for skeptics, that unvaccinated people represent 99% of those now dying from COVID-19 when they represent less than 50% of the adult population in the United States.”
The findings from the study could be more persuasive than previous arguments made in favor of immunization, Dr. Ray said. “These recent findings of striking reductions in risk of death in the vaccinated are more directly attributable and harder to ignore or dismiss.”
Brian Labus, PhD, MPH, of the University of Nevada Las Vegas (UNLV) is less convinced. “While this might change some peoples’ minds, it probably won’t make a major difference. People have many different reasons for not getting vaccinated, and this is only one of the things they consider.”
The study adds information that was not available before, said Dr. Labus, assistant professor in the Department of Epidemiology and Biostatistics at the UNLV School of Public Health. “We study the vaccine under tightly controlled, ideal conditions. This is the evidence that it works as well in the real world as it did in the trials, and that is what is most important in implementing a vaccination program,” added Dr. Labus.
“The scientific data has honed in on one thing: Vaccines are effective in preventing hospitalizations, ICU admissions, ventilations, and deaths,” agreed Dr. Palli.
“We now know that almost all deaths occurred in patients who were not vaccinated. We also know that all vaccines are effective against various strains that are in circulation right now, including the Delta variant, which is rapidly spreading,” Dr. Palli said.
Dr. Cassiere pointed out that the unvaccinated are not only at higher risk of developing COVID-19 but also of spreading, being hospitalized for, and dying from the infection. Avoiding “long hauler” symptoms is another argument in favor of immunization, he added.
As of June 28, the CDC reports that 63% of Americans 12 years and older have received at least one dose of a COVID-19 vaccine, and 54% are fully vaccinated.
Worldwide worry?
Although overall rates of U.S. COVID-19 hospitalizations and deaths are down, the outlook may not remain as encouraging. “I hope I’m wrong about this, but I anticipate that the coming fall and winter will bring increasingly localized versions of similar findings – severe disease and death due to SARS-CoV-2 infection in regions or groups with lower vaccination rates,” Dr. Ray said.
There could be a silver lining, he added: “If this unfortunate surge occurs, the health and economic consequences seem likely to erode much of the remaining hesitancy regarding vaccination.”
The rise of more infectious SARS-CoV-2 variants, such as the Delta variant, could also throw a wrench in controlling COVID-19. “This isn’t just a domestic issue,” Dr. Ray said. “We have learned that the world is a small place in pandemic times.”
The Associated Press investigators state that their findings support the high efficacy of the vaccine. Also, given the current widespread availability of COVID-19 vaccines in the United States, they believe many of the COVID-19 deaths now occurring are preventable.
Public health measures should have continued longer to protect unvaccinated individuals, especially Black Americans, Hispanic Americans, and other minorities, Dr. Palli said. “Only time will tell if re-opening and abandoning all public health measures by the CDC was premature.”
A version of this article first appeared on Medscape.com.
If you, a friend, or a loved one remain unvaccinated against COVID-19 at this point – for whatever reason – you are at higher risk of dying if you become infected.
That’s the conclusion of a new report released by the Associated Press looking at COVID-19 deaths during May 2021.
Of more than 18,000 people who died from COVID-19, for example, only about 150 were fully vaccinated. That’s less than 1%.
“Recently, I was working in the emergency room [and] I saw a 21-year-old African American who came in with shortness of breath,” said Vino K. Palli, MD, MPH, a physician specializing in emergency medicine, internal medicine, and urgent care.
The patient rapidly deteriorated and required intubation and ventilation. She was transferred to a specialized hospital for possible extracorporeal membrane oxygenation (ECMO) treatment.
“This patient was unvaccinated, along with her entire family. This would have been easily preventable,” added Dr. Palli, who is also founder and CEO of MiDoctor Urgent Care in New York City.
“Vaccine misinformation, compounded with vaccine inertia and vaccine access, have contributed to this,” he added. “Even though we have a surplus amount of vaccines at this time, we are only seeing 50% to 55% of completely vaccinated patients.”
Authors of the Associated Press report also acknowledge that some people who are fully vaccinated can get a breakthrough infection. These occurred in fewer than 1,200 of more than 853,000 people hospitalized for COVID-19 in May, or about 0.1%.
The Associated Press came up with these numbers using data from the Centers for Disease Control and Prevention. The CDC tracks the numbers of cases, hospitalizations, and deaths but does not breakdown rates by vaccination status.
Stronger argument for vaccination?
“The fact that only 0.8% of COVID-19 deaths are in the fully vaccinated should persuade those people still hesitant about vaccination,” said Hugh Cassiere, MD, medical director of Respiratory Therapy Services at North Shore University Hospital in Manhasset, New York.
Stuart C. Ray, MD, professor of medicine and oncology in the Division of Infectious Diseases at Johns Hopkins University, Baltimore, agreed. “It seems compelling, even for skeptics, that unvaccinated people represent 99% of those now dying from COVID-19 when they represent less than 50% of the adult population in the United States.”
The findings from the study could be more persuasive than previous arguments made in favor of immunization, Dr. Ray said. “These recent findings of striking reductions in risk of death in the vaccinated are more directly attributable and harder to ignore or dismiss.”
Brian Labus, PhD, MPH, of the University of Nevada Las Vegas (UNLV) is less convinced. “While this might change some peoples’ minds, it probably won’t make a major difference. People have many different reasons for not getting vaccinated, and this is only one of the things they consider.”
The study adds information that was not available before, said Dr. Labus, assistant professor in the Department of Epidemiology and Biostatistics at the UNLV School of Public Health. “We study the vaccine under tightly controlled, ideal conditions. This is the evidence that it works as well in the real world as it did in the trials, and that is what is most important in implementing a vaccination program,” added Dr. Labus.
“The scientific data has honed in on one thing: Vaccines are effective in preventing hospitalizations, ICU admissions, ventilations, and deaths,” agreed Dr. Palli.
“We now know that almost all deaths occurred in patients who were not vaccinated. We also know that all vaccines are effective against various strains that are in circulation right now, including the Delta variant, which is rapidly spreading,” Dr. Palli said.
Dr. Cassiere pointed out that the unvaccinated are not only at higher risk of developing COVID-19 but also of spreading, being hospitalized for, and dying from the infection. Avoiding “long hauler” symptoms is another argument in favor of immunization, he added.
As of June 28, the CDC reports that 63% of Americans 12 years and older have received at least one dose of a COVID-19 vaccine, and 54% are fully vaccinated.
Worldwide worry?
Although overall rates of U.S. COVID-19 hospitalizations and deaths are down, the outlook may not remain as encouraging. “I hope I’m wrong about this, but I anticipate that the coming fall and winter will bring increasingly localized versions of similar findings – severe disease and death due to SARS-CoV-2 infection in regions or groups with lower vaccination rates,” Dr. Ray said.
There could be a silver lining, he added: “If this unfortunate surge occurs, the health and economic consequences seem likely to erode much of the remaining hesitancy regarding vaccination.”
The rise of more infectious SARS-CoV-2 variants, such as the Delta variant, could also throw a wrench in controlling COVID-19. “This isn’t just a domestic issue,” Dr. Ray said. “We have learned that the world is a small place in pandemic times.”
The Associated Press investigators state that their findings support the high efficacy of the vaccine. Also, given the current widespread availability of COVID-19 vaccines in the United States, they believe many of the COVID-19 deaths now occurring are preventable.
Public health measures should have continued longer to protect unvaccinated individuals, especially Black Americans, Hispanic Americans, and other minorities, Dr. Palli said. “Only time will tell if re-opening and abandoning all public health measures by the CDC was premature.”
A version of this article first appeared on Medscape.com.
Physician fired after slurs, including ‘cannibalism,’ against Israel
Fidaa Wishah, MD, a pediatric radiologist at Phoenix Children’s Hospital in Arizona, has been fired after the hospital reviewed evidence that included her anti-Israel comments on social media, according to the hospital’s statement.
On May 26, Dr. Wishah posted, “We will uncover your thirst to kill our Palestinian children. … We sense your fear. The fear of your collapse. A state based on atrocity, inhumanity, racism and cannibalism never last long! Hey #israel … your end is coming sooner than you think.”
Phoenix Children’s Hospital did not respond to this news organization’s request for comment but said in a statement to the Jewish News Syndicate : “After a thorough review of the facts related to this matter, this individual is no longer providing care at Phoenix Children’s. All children in the care of Phoenix Children’s receive hope, healing and the best possible health care, regardless of race, color, disability, religion, gender, gender identity, sexual orientation or national origin.”
Dr. Wishah’s profile has been removed from the hospital website. Her LinkedIn profile indicates she had been a pediatric radiology fellow at Stanford (Calif.) University, specializing in advanced magnetic resonance imaging and fetal imaging and had been a senior staff pediatric radiologist at Henry Ford Health System in Detroit.
It wasn’t the first time antisemitic comments have led to the firing of a physician. Last year, this news organization wrote about Lara Kollab, DO, a first-year resident fired for her antisemitic tweets. She was subsequently barred from medicine.
In the same post from May 26, Dr. Wishah also wrote: “We will not be #censored anymore! Bomb our media buildings and we have the phones[.] Bribe the mainstream media and we have our small #socialmedia platforms[.] From our windows ... from our streets ... next the rubble we will expose you to the world[.] We will expose the #massacre and #genocide you #zionists are proud of[.]”
Today, CAIR-AZ, a group whose mission is to “enhance understanding of Islam, protect civil rights, promote justice, and empower American Muslims,” according to its website, announced that it, along with three private law firms, will represent Dr. Wishah in what they referred to as “her wrongful termination case against Phoenix Children’s Hospital.”
The announcement, which mentions that Dr. Wishah was born and raised in Gaza, said, “Dr. Wishah has been a medical doctor since 2010 and has spent the vast majority of her career as a pediatric physician. Despite caring for thousands of children, many of whom are Jewish, she has never been accused of discriminating against any of her patients or colleagues.”
The statement added, “PCH’s decision to terminate Dr. Wishah is shameful and an attack on freedom of speech.”
A version of this article first appeared on Medscape.com.
Fidaa Wishah, MD, a pediatric radiologist at Phoenix Children’s Hospital in Arizona, has been fired after the hospital reviewed evidence that included her anti-Israel comments on social media, according to the hospital’s statement.
On May 26, Dr. Wishah posted, “We will uncover your thirst to kill our Palestinian children. … We sense your fear. The fear of your collapse. A state based on atrocity, inhumanity, racism and cannibalism never last long! Hey #israel … your end is coming sooner than you think.”
Phoenix Children’s Hospital did not respond to this news organization’s request for comment but said in a statement to the Jewish News Syndicate : “After a thorough review of the facts related to this matter, this individual is no longer providing care at Phoenix Children’s. All children in the care of Phoenix Children’s receive hope, healing and the best possible health care, regardless of race, color, disability, religion, gender, gender identity, sexual orientation or national origin.”
Dr. Wishah’s profile has been removed from the hospital website. Her LinkedIn profile indicates she had been a pediatric radiology fellow at Stanford (Calif.) University, specializing in advanced magnetic resonance imaging and fetal imaging and had been a senior staff pediatric radiologist at Henry Ford Health System in Detroit.
It wasn’t the first time antisemitic comments have led to the firing of a physician. Last year, this news organization wrote about Lara Kollab, DO, a first-year resident fired for her antisemitic tweets. She was subsequently barred from medicine.
In the same post from May 26, Dr. Wishah also wrote: “We will not be #censored anymore! Bomb our media buildings and we have the phones[.] Bribe the mainstream media and we have our small #socialmedia platforms[.] From our windows ... from our streets ... next the rubble we will expose you to the world[.] We will expose the #massacre and #genocide you #zionists are proud of[.]”
Today, CAIR-AZ, a group whose mission is to “enhance understanding of Islam, protect civil rights, promote justice, and empower American Muslims,” according to its website, announced that it, along with three private law firms, will represent Dr. Wishah in what they referred to as “her wrongful termination case against Phoenix Children’s Hospital.”
The announcement, which mentions that Dr. Wishah was born and raised in Gaza, said, “Dr. Wishah has been a medical doctor since 2010 and has spent the vast majority of her career as a pediatric physician. Despite caring for thousands of children, many of whom are Jewish, she has never been accused of discriminating against any of her patients or colleagues.”
The statement added, “PCH’s decision to terminate Dr. Wishah is shameful and an attack on freedom of speech.”
A version of this article first appeared on Medscape.com.
Fidaa Wishah, MD, a pediatric radiologist at Phoenix Children’s Hospital in Arizona, has been fired after the hospital reviewed evidence that included her anti-Israel comments on social media, according to the hospital’s statement.
On May 26, Dr. Wishah posted, “We will uncover your thirst to kill our Palestinian children. … We sense your fear. The fear of your collapse. A state based on atrocity, inhumanity, racism and cannibalism never last long! Hey #israel … your end is coming sooner than you think.”
Phoenix Children’s Hospital did not respond to this news organization’s request for comment but said in a statement to the Jewish News Syndicate : “After a thorough review of the facts related to this matter, this individual is no longer providing care at Phoenix Children’s. All children in the care of Phoenix Children’s receive hope, healing and the best possible health care, regardless of race, color, disability, religion, gender, gender identity, sexual orientation or national origin.”
Dr. Wishah’s profile has been removed from the hospital website. Her LinkedIn profile indicates she had been a pediatric radiology fellow at Stanford (Calif.) University, specializing in advanced magnetic resonance imaging and fetal imaging and had been a senior staff pediatric radiologist at Henry Ford Health System in Detroit.
It wasn’t the first time antisemitic comments have led to the firing of a physician. Last year, this news organization wrote about Lara Kollab, DO, a first-year resident fired for her antisemitic tweets. She was subsequently barred from medicine.
In the same post from May 26, Dr. Wishah also wrote: “We will not be #censored anymore! Bomb our media buildings and we have the phones[.] Bribe the mainstream media and we have our small #socialmedia platforms[.] From our windows ... from our streets ... next the rubble we will expose you to the world[.] We will expose the #massacre and #genocide you #zionists are proud of[.]”
Today, CAIR-AZ, a group whose mission is to “enhance understanding of Islam, protect civil rights, promote justice, and empower American Muslims,” according to its website, announced that it, along with three private law firms, will represent Dr. Wishah in what they referred to as “her wrongful termination case against Phoenix Children’s Hospital.”
The announcement, which mentions that Dr. Wishah was born and raised in Gaza, said, “Dr. Wishah has been a medical doctor since 2010 and has spent the vast majority of her career as a pediatric physician. Despite caring for thousands of children, many of whom are Jewish, she has never been accused of discriminating against any of her patients or colleagues.”
The statement added, “PCH’s decision to terminate Dr. Wishah is shameful and an attack on freedom of speech.”
A version of this article first appeared on Medscape.com.
Wrong-site surgery doc says he can’t be sued
A neurosurgeon who operated on the wrong side of his patient’s spine claims he can’t be sued because of a federal law that protects health care professionals during a public health emergency, according to a report by KSDK, an NBC-affiliated television station in St. Louis.
Natalie Avilez, who lives in Missouri with her husband and five children, had been suffering from intense back pain. At some point in the recent past (the story doesn’t identify precisely when), she was referred to Fangxiang Chen, MD, a neurosurgeon affiliated with Mercy Hospital and Mercy Hospital South, in St. Louis. Ms. Avilez reportedly claims that Dr. Chen told her that an “easy” surgery – a hemilaminectomy – could relieve her back pain.
Something went wrong during the procedure, however. Dr. Chen ended up operating on the left side of Avilez’s spine instead of the right side, where he had initially diagnosed disk-related pressure. Dr. Chen realized his mistake while his patient was under anesthesia but couldn’t remedy it.
As the patient awakened, Dr. Chen asked her to authorize an immediate right-side surgery, but, as Ms. Avilez told the TV station, her “charge nurse would not let him get authorization because I wasn’t fully awake.” In the recovery room afterward, Dr. Chen explained what had happened to his patient, who permitted him to redo the surgery the following day.
But the redo didn’t remedy Ms. Avilez’s pain; in fact, the second surgery made things worse. “I’m always in constant pain,” she said. “I kind of feel like I would have been better off not even doing it at all.”
In January of this year, Ms. Avilez filed a medical malpractice suit against Dr. Chen and Mercy. But the neurosurgeon made a surprising claim:
Initially passed in 2005, PREP was intended to shield doctors and other licensed health care professionals from liability during a public health emergency except in cases of willful misconduct. On March 17, 2020, then–Health and Human Services Secretary Alex Azar invoked the PREP Act “for activities related to medical countermeasures against COVID-19.”
But could this declaration – which has since been amended multiple times – shield a physician from a claim of wrong-site surgery?
Ms. Avilez’s attorney, Morgan Murphy, doesn’t think so. “Obviously, we are not claiming that COVID had anything to do with the fact that Dr. Chen operated on the incorrect side of Natalie’s spine. It is a fairly straightforward situation. A doctor should never perform the incorrect surgery, period.”
Other observers are less certain that the Chen defense won’t hold. It’s true the PREP Act doesn’t protect doctors against claims of willful or intentional misconduct, says Deidre Gilbert, who leads a national medical malpractice patient-advocacy group. But such claims are, she quickly adds, very difficult to prove, never more so than during a pandemic.
Several states, including Missouri, have passed or are considering additional measures to protect health care professionals against the expected wave of COVID-related claims. (One estimate places the number of those claims at almost 6,000 as of February 2021.) “We want to make sure that there is a heightened standard for holding somebody liable in ... COVID transmission cases,” said the sponsor of the proposed Show-Me State legislation.
As for Ms. Avilez, she feels lucky that she’s not even worse off than she is now. She worries, though, about other patients who are less fortunate and who are told that the pandemic protects their health care professionals from liability. “That’s just not fair,” she says.
Hidden beliefs about people of color raise liability risks
Clinicians’ “implicit bias” can exacerbate medical disparities and also malpractice claims, a story in the Dayton Daily News reports.
The story’s authors cite La Fleur Small, PhD, a medical sociologist at Wayne State University, in Detroit, who sees “implicit bias” as a set of “unconscious associations and judgments” that affect social behavior, causing people to act in ways that are often contrary to their perceived value system. In the medical profession, such thinking can have unintended consequences, especially for people of color.
Implicit bias can erode the physician-patient relationship, which in turn can make a malpractice suit more likely should an adverse event occur. Studies reported in recent years in the AMA Journal of Ethics, for instance, found that poor communication was a factor in almost three-quarters of closed claims. Other studies have revealed that, of patients seeking legal advice following a medical mishap, more than half cited a poor doctor-patient relationship as a contributing factor in their decision.
To remedy things, it would be helpful to boost the number of doctors of color, at least to the point that it more closely reflects the percentage in the general population, say experts. Currently, although Black and Hispanic persons constitute 13.4% and 18.5%, respectively, of the overall U.S. population, they make up only 5.0% and 5.8% of active physicians. (As of 2018, 56.2% of all physicians were White and 17.2% were Asian, according to data from the Association of American Medical Colleges.)
Father of impaired baby seeks mega damages
An Oregon man whose son sustained permanent neurologic injuries during childbirth has sued the hospital where the 2017 delivery took place, as reported in The Astorian.
In the suit on behalf of his son, Wesley Humphries claims that Columbia Memorial Hospital in Astoria, Oregon, failed to monitor the baby’s heart rate and other aspects of the labor and delivery. As a consequence, the baby needed to be transferred to Oregon Health and Science University Hospital in Portland, approximately 100 miles away, for emergency treatment. Doctors there diagnosed the child as having hypoxic ischemic encephalopathy, which his lawyers say resulted in cerebral palsy, among other neurologic conditions.
Because of his son’s permanent impairment, Mr. Humphries is seeking significant damages: more than $45 million in medical, custodial, and life-care expenses and $65 million in noneconomic damages. Should his claim prove successful, the payout would mark one of the largest awards – if not the largest award – in Oregon State history. The hospital has declined to comment.
At press time, a trial date hadn’t been set.
A version of this article first appeared on Medscape.com.
A neurosurgeon who operated on the wrong side of his patient’s spine claims he can’t be sued because of a federal law that protects health care professionals during a public health emergency, according to a report by KSDK, an NBC-affiliated television station in St. Louis.
Natalie Avilez, who lives in Missouri with her husband and five children, had been suffering from intense back pain. At some point in the recent past (the story doesn’t identify precisely when), she was referred to Fangxiang Chen, MD, a neurosurgeon affiliated with Mercy Hospital and Mercy Hospital South, in St. Louis. Ms. Avilez reportedly claims that Dr. Chen told her that an “easy” surgery – a hemilaminectomy – could relieve her back pain.
Something went wrong during the procedure, however. Dr. Chen ended up operating on the left side of Avilez’s spine instead of the right side, where he had initially diagnosed disk-related pressure. Dr. Chen realized his mistake while his patient was under anesthesia but couldn’t remedy it.
As the patient awakened, Dr. Chen asked her to authorize an immediate right-side surgery, but, as Ms. Avilez told the TV station, her “charge nurse would not let him get authorization because I wasn’t fully awake.” In the recovery room afterward, Dr. Chen explained what had happened to his patient, who permitted him to redo the surgery the following day.
But the redo didn’t remedy Ms. Avilez’s pain; in fact, the second surgery made things worse. “I’m always in constant pain,” she said. “I kind of feel like I would have been better off not even doing it at all.”
In January of this year, Ms. Avilez filed a medical malpractice suit against Dr. Chen and Mercy. But the neurosurgeon made a surprising claim:
Initially passed in 2005, PREP was intended to shield doctors and other licensed health care professionals from liability during a public health emergency except in cases of willful misconduct. On March 17, 2020, then–Health and Human Services Secretary Alex Azar invoked the PREP Act “for activities related to medical countermeasures against COVID-19.”
But could this declaration – which has since been amended multiple times – shield a physician from a claim of wrong-site surgery?
Ms. Avilez’s attorney, Morgan Murphy, doesn’t think so. “Obviously, we are not claiming that COVID had anything to do with the fact that Dr. Chen operated on the incorrect side of Natalie’s spine. It is a fairly straightforward situation. A doctor should never perform the incorrect surgery, period.”
Other observers are less certain that the Chen defense won’t hold. It’s true the PREP Act doesn’t protect doctors against claims of willful or intentional misconduct, says Deidre Gilbert, who leads a national medical malpractice patient-advocacy group. But such claims are, she quickly adds, very difficult to prove, never more so than during a pandemic.
Several states, including Missouri, have passed or are considering additional measures to protect health care professionals against the expected wave of COVID-related claims. (One estimate places the number of those claims at almost 6,000 as of February 2021.) “We want to make sure that there is a heightened standard for holding somebody liable in ... COVID transmission cases,” said the sponsor of the proposed Show-Me State legislation.
As for Ms. Avilez, she feels lucky that she’s not even worse off than she is now. She worries, though, about other patients who are less fortunate and who are told that the pandemic protects their health care professionals from liability. “That’s just not fair,” she says.
Hidden beliefs about people of color raise liability risks
Clinicians’ “implicit bias” can exacerbate medical disparities and also malpractice claims, a story in the Dayton Daily News reports.
The story’s authors cite La Fleur Small, PhD, a medical sociologist at Wayne State University, in Detroit, who sees “implicit bias” as a set of “unconscious associations and judgments” that affect social behavior, causing people to act in ways that are often contrary to their perceived value system. In the medical profession, such thinking can have unintended consequences, especially for people of color.
Implicit bias can erode the physician-patient relationship, which in turn can make a malpractice suit more likely should an adverse event occur. Studies reported in recent years in the AMA Journal of Ethics, for instance, found that poor communication was a factor in almost three-quarters of closed claims. Other studies have revealed that, of patients seeking legal advice following a medical mishap, more than half cited a poor doctor-patient relationship as a contributing factor in their decision.
To remedy things, it would be helpful to boost the number of doctors of color, at least to the point that it more closely reflects the percentage in the general population, say experts. Currently, although Black and Hispanic persons constitute 13.4% and 18.5%, respectively, of the overall U.S. population, they make up only 5.0% and 5.8% of active physicians. (As of 2018, 56.2% of all physicians were White and 17.2% were Asian, according to data from the Association of American Medical Colleges.)
Father of impaired baby seeks mega damages
An Oregon man whose son sustained permanent neurologic injuries during childbirth has sued the hospital where the 2017 delivery took place, as reported in The Astorian.
In the suit on behalf of his son, Wesley Humphries claims that Columbia Memorial Hospital in Astoria, Oregon, failed to monitor the baby’s heart rate and other aspects of the labor and delivery. As a consequence, the baby needed to be transferred to Oregon Health and Science University Hospital in Portland, approximately 100 miles away, for emergency treatment. Doctors there diagnosed the child as having hypoxic ischemic encephalopathy, which his lawyers say resulted in cerebral palsy, among other neurologic conditions.
Because of his son’s permanent impairment, Mr. Humphries is seeking significant damages: more than $45 million in medical, custodial, and life-care expenses and $65 million in noneconomic damages. Should his claim prove successful, the payout would mark one of the largest awards – if not the largest award – in Oregon State history. The hospital has declined to comment.
At press time, a trial date hadn’t been set.
A version of this article first appeared on Medscape.com.
A neurosurgeon who operated on the wrong side of his patient’s spine claims he can’t be sued because of a federal law that protects health care professionals during a public health emergency, according to a report by KSDK, an NBC-affiliated television station in St. Louis.
Natalie Avilez, who lives in Missouri with her husband and five children, had been suffering from intense back pain. At some point in the recent past (the story doesn’t identify precisely when), she was referred to Fangxiang Chen, MD, a neurosurgeon affiliated with Mercy Hospital and Mercy Hospital South, in St. Louis. Ms. Avilez reportedly claims that Dr. Chen told her that an “easy” surgery – a hemilaminectomy – could relieve her back pain.
Something went wrong during the procedure, however. Dr. Chen ended up operating on the left side of Avilez’s spine instead of the right side, where he had initially diagnosed disk-related pressure. Dr. Chen realized his mistake while his patient was under anesthesia but couldn’t remedy it.
As the patient awakened, Dr. Chen asked her to authorize an immediate right-side surgery, but, as Ms. Avilez told the TV station, her “charge nurse would not let him get authorization because I wasn’t fully awake.” In the recovery room afterward, Dr. Chen explained what had happened to his patient, who permitted him to redo the surgery the following day.
But the redo didn’t remedy Ms. Avilez’s pain; in fact, the second surgery made things worse. “I’m always in constant pain,” she said. “I kind of feel like I would have been better off not even doing it at all.”
In January of this year, Ms. Avilez filed a medical malpractice suit against Dr. Chen and Mercy. But the neurosurgeon made a surprising claim:
Initially passed in 2005, PREP was intended to shield doctors and other licensed health care professionals from liability during a public health emergency except in cases of willful misconduct. On March 17, 2020, then–Health and Human Services Secretary Alex Azar invoked the PREP Act “for activities related to medical countermeasures against COVID-19.”
But could this declaration – which has since been amended multiple times – shield a physician from a claim of wrong-site surgery?
Ms. Avilez’s attorney, Morgan Murphy, doesn’t think so. “Obviously, we are not claiming that COVID had anything to do with the fact that Dr. Chen operated on the incorrect side of Natalie’s spine. It is a fairly straightforward situation. A doctor should never perform the incorrect surgery, period.”
Other observers are less certain that the Chen defense won’t hold. It’s true the PREP Act doesn’t protect doctors against claims of willful or intentional misconduct, says Deidre Gilbert, who leads a national medical malpractice patient-advocacy group. But such claims are, she quickly adds, very difficult to prove, never more so than during a pandemic.
Several states, including Missouri, have passed or are considering additional measures to protect health care professionals against the expected wave of COVID-related claims. (One estimate places the number of those claims at almost 6,000 as of February 2021.) “We want to make sure that there is a heightened standard for holding somebody liable in ... COVID transmission cases,” said the sponsor of the proposed Show-Me State legislation.
As for Ms. Avilez, she feels lucky that she’s not even worse off than she is now. She worries, though, about other patients who are less fortunate and who are told that the pandemic protects their health care professionals from liability. “That’s just not fair,” she says.
Hidden beliefs about people of color raise liability risks
Clinicians’ “implicit bias” can exacerbate medical disparities and also malpractice claims, a story in the Dayton Daily News reports.
The story’s authors cite La Fleur Small, PhD, a medical sociologist at Wayne State University, in Detroit, who sees “implicit bias” as a set of “unconscious associations and judgments” that affect social behavior, causing people to act in ways that are often contrary to their perceived value system. In the medical profession, such thinking can have unintended consequences, especially for people of color.
Implicit bias can erode the physician-patient relationship, which in turn can make a malpractice suit more likely should an adverse event occur. Studies reported in recent years in the AMA Journal of Ethics, for instance, found that poor communication was a factor in almost three-quarters of closed claims. Other studies have revealed that, of patients seeking legal advice following a medical mishap, more than half cited a poor doctor-patient relationship as a contributing factor in their decision.
To remedy things, it would be helpful to boost the number of doctors of color, at least to the point that it more closely reflects the percentage in the general population, say experts. Currently, although Black and Hispanic persons constitute 13.4% and 18.5%, respectively, of the overall U.S. population, they make up only 5.0% and 5.8% of active physicians. (As of 2018, 56.2% of all physicians were White and 17.2% were Asian, according to data from the Association of American Medical Colleges.)
Father of impaired baby seeks mega damages
An Oregon man whose son sustained permanent neurologic injuries during childbirth has sued the hospital where the 2017 delivery took place, as reported in The Astorian.
In the suit on behalf of his son, Wesley Humphries claims that Columbia Memorial Hospital in Astoria, Oregon, failed to monitor the baby’s heart rate and other aspects of the labor and delivery. As a consequence, the baby needed to be transferred to Oregon Health and Science University Hospital in Portland, approximately 100 miles away, for emergency treatment. Doctors there diagnosed the child as having hypoxic ischemic encephalopathy, which his lawyers say resulted in cerebral palsy, among other neurologic conditions.
Because of his son’s permanent impairment, Mr. Humphries is seeking significant damages: more than $45 million in medical, custodial, and life-care expenses and $65 million in noneconomic damages. Should his claim prove successful, the payout would mark one of the largest awards – if not the largest award – in Oregon State history. The hospital has declined to comment.
At press time, a trial date hadn’t been set.
A version of this article first appeared on Medscape.com.
Fundamentals of laparoscopic surgery (FLS) manual skills exam: Tips and tricks
Patients’ sexual problems: Be proactive, make discussions routine
If the goal of a clinical encounter is to identify issues that adversely affect health, well-being, and life satisfaction, open-ended questions on sexual problems are essential, according to an expert who provided tips during a session presented by Current Psychiatry and the American Academy of Clinical Psychiatrists about how to begin a productive dialogue.
For identifying and treating the obstacles to sexual health, “the onus is on the provider,” said Anita H. Clayton, MD, chair of psychiatry and neurobehavioral sciences at the University of Virginia, Charlottesville.
In a poll published more than 20 years ago, 91% of men and 84% of women reported that a satisfying sex life is important, while 90% agreed that sexual difficulties cause emotional problems, said Dr. Clayton, who sees no reason to think that those percentages have changed. Yet, patients are traditionally reluctant to raise their concerns about sexual issues to a physician.
In the same poll, about 50% of the respondents characterized themselves as “very concerned” that a clinician would simply dismiss a sexual complaint or that there would be no treatment. Of the other respondents, 40% were somewhat concerned. Dr. Clayton assumes that those numbers are still valid and that they provide the rationale for asking routinely about sexual health, she said at the virtual meeting, presented by MedscapeLive.
Raising sexual health issues
“The clinician has to initiate the discussion and make it part of the routine examination,” said Dr. Clayton, also a professor of obstetrics and gynecology at the university. She indicated that unresolved sexual issues are a common and important but treatable problem, whether the underlying issue has a medical or psychological origin.
Yet, language is critical. Many physicians might have no difficulty discussing sexual problems, but patients often do. Dr. Clayton recommended developing strategies that might it easy if not seamless to elicit information about sexual health in the context of inquiring about other clinical issues.
“Use bridging statements,” Dr. Clayton suggested.
Bridging statements allow an easy transition into a discussion of sexual function from another clinical issue, Dr. Clayton said. As examples, she suggested moving to questions about sex from inquiries about conditions, such as diabetes, or medications, such as antidepressants, that are known to have an impact on sexual dysfunction.
Avoid yes-no questions.
To prompt a dialogue, Dr. Clayton advised against using yes-no questions that allow the patient to quickly dismiss the topic with a negative response. She tries to frame a question that requires a complete thought. In an inquiry addressed to a patient with diabetes, for example, she might first inform the patient that sexual issues are common with this disorder and then ask what types of sexual issues the patient is experiencing.
Once the topic is raised, a checklist approach is appropriate. Patients might be more or less willing to talk any one of the range of issues that influence sexual health, ranging from issues of desire and arousal to discomfort or pain. The door should be opened to a discussion of specific sexual organ function, such as ability to achieve an erection or adequate lubrication.
“Do not assume the patient is heterosexual,” Dr. Clayton cautioned.
It is reasonable and appropriate to bring up sexual health during the intake history. A discussion of sexual health can be initiated by simply posing the question: “Are you sexually active?” Importantly, Dr. Clayton strongly recommended a follow-up question when adults reply that they are not sexually active.
In the ELIXIR study, which evaluated sexual function in patients with depression, more than twice as many patients reported impairments when asked by the physician than who volunteered this information spontaneously, according to Dr. Clayton, citing a study that found sexual issues in more than 70% of the 4,557 participants.
Prioritize choice of language.
Once sexual impairments are uncovered, clinicians will need to determine how to intervene, but Dr. Clayton recommended using clear and frank language to define the problem even if the language is tailored to the patient’s comfort level. Patients should be encouraged to recognize that there are solutions for most problems, but clinicians should recognize and respect cultural issues in directing patients toward solutions.
Dr. Clayton is not alone in recommending that patients be asked routinely about sexual health. Margot Savoy, MD, MPH, chair of family and community medicine, Temple University, Philadelphia, has also advocated for a proactive approach.
“Patients deserve whole-patient care that includes sexual health,” said Dr. Savoy, who was coauthor of a recent article that also outlined techniques for eliciting a sexual history.
She suggested that the need to inquire should not be considered age specific.
“Asking patients about their sexual history and concerns is a critical part of routine primary care across the lifespan,” she said.
“We also need to intentionally create a safe environment where it is as normal to talk about sexual questions or concerns as it is about how to care for a cold or manage a backache,” she added.
MedscapeLive and this news organization are owned by the same company. Dr. Clayton disclosed financial relationships with Acadia, Alkermes, Allergan, AMAG, Astellas, Fabre-Kramer, Janssen, Ovoca Bio, PureTech Health, Relmada, S1 Biopharma, Safe Therapeutics, Takeda, and WCG MedAd-vante-Prophase. Dr. Savoy reported no conflicts of interest.
If the goal of a clinical encounter is to identify issues that adversely affect health, well-being, and life satisfaction, open-ended questions on sexual problems are essential, according to an expert who provided tips during a session presented by Current Psychiatry and the American Academy of Clinical Psychiatrists about how to begin a productive dialogue.
For identifying and treating the obstacles to sexual health, “the onus is on the provider,” said Anita H. Clayton, MD, chair of psychiatry and neurobehavioral sciences at the University of Virginia, Charlottesville.
In a poll published more than 20 years ago, 91% of men and 84% of women reported that a satisfying sex life is important, while 90% agreed that sexual difficulties cause emotional problems, said Dr. Clayton, who sees no reason to think that those percentages have changed. Yet, patients are traditionally reluctant to raise their concerns about sexual issues to a physician.
In the same poll, about 50% of the respondents characterized themselves as “very concerned” that a clinician would simply dismiss a sexual complaint or that there would be no treatment. Of the other respondents, 40% were somewhat concerned. Dr. Clayton assumes that those numbers are still valid and that they provide the rationale for asking routinely about sexual health, she said at the virtual meeting, presented by MedscapeLive.
Raising sexual health issues
“The clinician has to initiate the discussion and make it part of the routine examination,” said Dr. Clayton, also a professor of obstetrics and gynecology at the university. She indicated that unresolved sexual issues are a common and important but treatable problem, whether the underlying issue has a medical or psychological origin.
Yet, language is critical. Many physicians might have no difficulty discussing sexual problems, but patients often do. Dr. Clayton recommended developing strategies that might it easy if not seamless to elicit information about sexual health in the context of inquiring about other clinical issues.
“Use bridging statements,” Dr. Clayton suggested.
Bridging statements allow an easy transition into a discussion of sexual function from another clinical issue, Dr. Clayton said. As examples, she suggested moving to questions about sex from inquiries about conditions, such as diabetes, or medications, such as antidepressants, that are known to have an impact on sexual dysfunction.
Avoid yes-no questions.
To prompt a dialogue, Dr. Clayton advised against using yes-no questions that allow the patient to quickly dismiss the topic with a negative response. She tries to frame a question that requires a complete thought. In an inquiry addressed to a patient with diabetes, for example, she might first inform the patient that sexual issues are common with this disorder and then ask what types of sexual issues the patient is experiencing.
Once the topic is raised, a checklist approach is appropriate. Patients might be more or less willing to talk any one of the range of issues that influence sexual health, ranging from issues of desire and arousal to discomfort or pain. The door should be opened to a discussion of specific sexual organ function, such as ability to achieve an erection or adequate lubrication.
“Do not assume the patient is heterosexual,” Dr. Clayton cautioned.
It is reasonable and appropriate to bring up sexual health during the intake history. A discussion of sexual health can be initiated by simply posing the question: “Are you sexually active?” Importantly, Dr. Clayton strongly recommended a follow-up question when adults reply that they are not sexually active.
In the ELIXIR study, which evaluated sexual function in patients with depression, more than twice as many patients reported impairments when asked by the physician than who volunteered this information spontaneously, according to Dr. Clayton, citing a study that found sexual issues in more than 70% of the 4,557 participants.
Prioritize choice of language.
Once sexual impairments are uncovered, clinicians will need to determine how to intervene, but Dr. Clayton recommended using clear and frank language to define the problem even if the language is tailored to the patient’s comfort level. Patients should be encouraged to recognize that there are solutions for most problems, but clinicians should recognize and respect cultural issues in directing patients toward solutions.
Dr. Clayton is not alone in recommending that patients be asked routinely about sexual health. Margot Savoy, MD, MPH, chair of family and community medicine, Temple University, Philadelphia, has also advocated for a proactive approach.
“Patients deserve whole-patient care that includes sexual health,” said Dr. Savoy, who was coauthor of a recent article that also outlined techniques for eliciting a sexual history.
She suggested that the need to inquire should not be considered age specific.
“Asking patients about their sexual history and concerns is a critical part of routine primary care across the lifespan,” she said.
“We also need to intentionally create a safe environment where it is as normal to talk about sexual questions or concerns as it is about how to care for a cold or manage a backache,” she added.
MedscapeLive and this news organization are owned by the same company. Dr. Clayton disclosed financial relationships with Acadia, Alkermes, Allergan, AMAG, Astellas, Fabre-Kramer, Janssen, Ovoca Bio, PureTech Health, Relmada, S1 Biopharma, Safe Therapeutics, Takeda, and WCG MedAd-vante-Prophase. Dr. Savoy reported no conflicts of interest.
If the goal of a clinical encounter is to identify issues that adversely affect health, well-being, and life satisfaction, open-ended questions on sexual problems are essential, according to an expert who provided tips during a session presented by Current Psychiatry and the American Academy of Clinical Psychiatrists about how to begin a productive dialogue.
For identifying and treating the obstacles to sexual health, “the onus is on the provider,” said Anita H. Clayton, MD, chair of psychiatry and neurobehavioral sciences at the University of Virginia, Charlottesville.
In a poll published more than 20 years ago, 91% of men and 84% of women reported that a satisfying sex life is important, while 90% agreed that sexual difficulties cause emotional problems, said Dr. Clayton, who sees no reason to think that those percentages have changed. Yet, patients are traditionally reluctant to raise their concerns about sexual issues to a physician.
In the same poll, about 50% of the respondents characterized themselves as “very concerned” that a clinician would simply dismiss a sexual complaint or that there would be no treatment. Of the other respondents, 40% were somewhat concerned. Dr. Clayton assumes that those numbers are still valid and that they provide the rationale for asking routinely about sexual health, she said at the virtual meeting, presented by MedscapeLive.
Raising sexual health issues
“The clinician has to initiate the discussion and make it part of the routine examination,” said Dr. Clayton, also a professor of obstetrics and gynecology at the university. She indicated that unresolved sexual issues are a common and important but treatable problem, whether the underlying issue has a medical or psychological origin.
Yet, language is critical. Many physicians might have no difficulty discussing sexual problems, but patients often do. Dr. Clayton recommended developing strategies that might it easy if not seamless to elicit information about sexual health in the context of inquiring about other clinical issues.
“Use bridging statements,” Dr. Clayton suggested.
Bridging statements allow an easy transition into a discussion of sexual function from another clinical issue, Dr. Clayton said. As examples, she suggested moving to questions about sex from inquiries about conditions, such as diabetes, or medications, such as antidepressants, that are known to have an impact on sexual dysfunction.
Avoid yes-no questions.
To prompt a dialogue, Dr. Clayton advised against using yes-no questions that allow the patient to quickly dismiss the topic with a negative response. She tries to frame a question that requires a complete thought. In an inquiry addressed to a patient with diabetes, for example, she might first inform the patient that sexual issues are common with this disorder and then ask what types of sexual issues the patient is experiencing.
Once the topic is raised, a checklist approach is appropriate. Patients might be more or less willing to talk any one of the range of issues that influence sexual health, ranging from issues of desire and arousal to discomfort or pain. The door should be opened to a discussion of specific sexual organ function, such as ability to achieve an erection or adequate lubrication.
“Do not assume the patient is heterosexual,” Dr. Clayton cautioned.
It is reasonable and appropriate to bring up sexual health during the intake history. A discussion of sexual health can be initiated by simply posing the question: “Are you sexually active?” Importantly, Dr. Clayton strongly recommended a follow-up question when adults reply that they are not sexually active.
In the ELIXIR study, which evaluated sexual function in patients with depression, more than twice as many patients reported impairments when asked by the physician than who volunteered this information spontaneously, according to Dr. Clayton, citing a study that found sexual issues in more than 70% of the 4,557 participants.
Prioritize choice of language.
Once sexual impairments are uncovered, clinicians will need to determine how to intervene, but Dr. Clayton recommended using clear and frank language to define the problem even if the language is tailored to the patient’s comfort level. Patients should be encouraged to recognize that there are solutions for most problems, but clinicians should recognize and respect cultural issues in directing patients toward solutions.
Dr. Clayton is not alone in recommending that patients be asked routinely about sexual health. Margot Savoy, MD, MPH, chair of family and community medicine, Temple University, Philadelphia, has also advocated for a proactive approach.
“Patients deserve whole-patient care that includes sexual health,” said Dr. Savoy, who was coauthor of a recent article that also outlined techniques for eliciting a sexual history.
She suggested that the need to inquire should not be considered age specific.
“Asking patients about their sexual history and concerns is a critical part of routine primary care across the lifespan,” she said.
“We also need to intentionally create a safe environment where it is as normal to talk about sexual questions or concerns as it is about how to care for a cold or manage a backache,” she added.
MedscapeLive and this news organization are owned by the same company. Dr. Clayton disclosed financial relationships with Acadia, Alkermes, Allergan, AMAG, Astellas, Fabre-Kramer, Janssen, Ovoca Bio, PureTech Health, Relmada, S1 Biopharma, Safe Therapeutics, Takeda, and WCG MedAd-vante-Prophase. Dr. Savoy reported no conflicts of interest.
FROM CP/AACP PSYCHIATRY UPDATE
No increase in breast cancer risk with fertility treatments
No link between fertility treatment and an increase in the risk for breast cancer was found in the largest study of the issue to date.
This study “provides the evidence needed to reassure women and couples seeking fertility treatments,” commented senior author Sesh Sunkara, MD, a reproductive medicine specialist at King’s College London in a press release.
With an increasing number of women seeking help to become mothers, the question “is a matter of great importance” and a source of considerable concern among patients, the study authors comment.
This is the largest meta-analysis to date, involving 1.8 million women who were followed for an average of 27 years. The investigators found no link with the use of gonadotropins or clomiphene citrate to increase egg production in fertility cycles.
There has been concern over the years that fertility treatment could stimulate estrogen-sensitive precursor breast cancer cells.
More than 4,000 studies of this issue have been conducted since 1990, and results have been conflicting. The investigators analyzed results from the 20 strongest ones.
The new meta-analysis included nine retrospective studies, five case-control studies, five prospective studies, and one comparative study
The team cautioned that the quality of evidence in even these top 20 studies was “very low” but that such an approach is perhaps the best possible on this issue because a randomized trial among women seeking help to have children would be “ethically challenging.”
In the study, the team compared breast cancer incidence among women who underwent ovarian stimulation with the incidence in both age-matched unexposed women in the general population and unexposed infertile women.
There was no significant increase in the risk for breast cancer among women treated with any ovarian stimulation drug (pooled odds ratio, 1.03; 95% confidence interval, 0.86-1.23, but with substantial heterogeneity between study outcomes).
There was also no increased risk when the analysis was limited to the eight studies in which women were treated with both gonadotropins and clomiphene citrate (pooled OR, 0.92; 95% CI, 0.52-1.60, with substantial heterogeneity).
The authors noted that, among the many study limitations, no distinction was made between physiological dosing for anovulation and supraphysiological dosing for in vitro fertilization cycles. In addition, because the treated women were generally young, the follow-up period fell short of the age at which they’d be most at risk for breast cancer.
Individual patient data were also not available, but 14 studies did adjust for confounders, including weight, race, parity, age at first birth, age at menarche, and family history of breast cancer.
Although the findings are reassuring, “further long-term and detailed studies are now needed to confirm” them, Kotryna Temcinaite, PhD, senior research communications manager at the U.K. charity Breast Cancer Now, said in the press release.
A version of this article first appeared on Medscape.com.
No link between fertility treatment and an increase in the risk for breast cancer was found in the largest study of the issue to date.
This study “provides the evidence needed to reassure women and couples seeking fertility treatments,” commented senior author Sesh Sunkara, MD, a reproductive medicine specialist at King’s College London in a press release.
With an increasing number of women seeking help to become mothers, the question “is a matter of great importance” and a source of considerable concern among patients, the study authors comment.
This is the largest meta-analysis to date, involving 1.8 million women who were followed for an average of 27 years. The investigators found no link with the use of gonadotropins or clomiphene citrate to increase egg production in fertility cycles.
There has been concern over the years that fertility treatment could stimulate estrogen-sensitive precursor breast cancer cells.
More than 4,000 studies of this issue have been conducted since 1990, and results have been conflicting. The investigators analyzed results from the 20 strongest ones.
The new meta-analysis included nine retrospective studies, five case-control studies, five prospective studies, and one comparative study
The team cautioned that the quality of evidence in even these top 20 studies was “very low” but that such an approach is perhaps the best possible on this issue because a randomized trial among women seeking help to have children would be “ethically challenging.”
In the study, the team compared breast cancer incidence among women who underwent ovarian stimulation with the incidence in both age-matched unexposed women in the general population and unexposed infertile women.
There was no significant increase in the risk for breast cancer among women treated with any ovarian stimulation drug (pooled odds ratio, 1.03; 95% confidence interval, 0.86-1.23, but with substantial heterogeneity between study outcomes).
There was also no increased risk when the analysis was limited to the eight studies in which women were treated with both gonadotropins and clomiphene citrate (pooled OR, 0.92; 95% CI, 0.52-1.60, with substantial heterogeneity).
The authors noted that, among the many study limitations, no distinction was made between physiological dosing for anovulation and supraphysiological dosing for in vitro fertilization cycles. In addition, because the treated women were generally young, the follow-up period fell short of the age at which they’d be most at risk for breast cancer.
Individual patient data were also not available, but 14 studies did adjust for confounders, including weight, race, parity, age at first birth, age at menarche, and family history of breast cancer.
Although the findings are reassuring, “further long-term and detailed studies are now needed to confirm” them, Kotryna Temcinaite, PhD, senior research communications manager at the U.K. charity Breast Cancer Now, said in the press release.
A version of this article first appeared on Medscape.com.
No link between fertility treatment and an increase in the risk for breast cancer was found in the largest study of the issue to date.
This study “provides the evidence needed to reassure women and couples seeking fertility treatments,” commented senior author Sesh Sunkara, MD, a reproductive medicine specialist at King’s College London in a press release.
With an increasing number of women seeking help to become mothers, the question “is a matter of great importance” and a source of considerable concern among patients, the study authors comment.
This is the largest meta-analysis to date, involving 1.8 million women who were followed for an average of 27 years. The investigators found no link with the use of gonadotropins or clomiphene citrate to increase egg production in fertility cycles.
There has been concern over the years that fertility treatment could stimulate estrogen-sensitive precursor breast cancer cells.
More than 4,000 studies of this issue have been conducted since 1990, and results have been conflicting. The investigators analyzed results from the 20 strongest ones.
The new meta-analysis included nine retrospective studies, five case-control studies, five prospective studies, and one comparative study
The team cautioned that the quality of evidence in even these top 20 studies was “very low” but that such an approach is perhaps the best possible on this issue because a randomized trial among women seeking help to have children would be “ethically challenging.”
In the study, the team compared breast cancer incidence among women who underwent ovarian stimulation with the incidence in both age-matched unexposed women in the general population and unexposed infertile women.
There was no significant increase in the risk for breast cancer among women treated with any ovarian stimulation drug (pooled odds ratio, 1.03; 95% confidence interval, 0.86-1.23, but with substantial heterogeneity between study outcomes).
There was also no increased risk when the analysis was limited to the eight studies in which women were treated with both gonadotropins and clomiphene citrate (pooled OR, 0.92; 95% CI, 0.52-1.60, with substantial heterogeneity).
The authors noted that, among the many study limitations, no distinction was made between physiological dosing for anovulation and supraphysiological dosing for in vitro fertilization cycles. In addition, because the treated women were generally young, the follow-up period fell short of the age at which they’d be most at risk for breast cancer.
Individual patient data were also not available, but 14 studies did adjust for confounders, including weight, race, parity, age at first birth, age at menarche, and family history of breast cancer.
Although the findings are reassuring, “further long-term and detailed studies are now needed to confirm” them, Kotryna Temcinaite, PhD, senior research communications manager at the U.K. charity Breast Cancer Now, said in the press release.
A version of this article first appeared on Medscape.com.
Racial and economic disparities persist in endometrial cancer care
Women who were Black, Latina, American Indian, or Alaska Native were significantly less likely than White women to receive guidelines-adherent treatment for endometrial cancer, based on data from more than 80,000 women.
The incidence of uterine cancer has increased across all ethnicities in recent decades, and adherence to the National Comprehensive Cancer Network treatment guidelines has been associated with improved survival, wrote Victoria A. Rodriguez, MSW, MPH, of the University of California, Irvine, and colleagues. “To date, however, there are few studies that have looked at endometrial cancer disparities with adherence to National Comprehensive Cancer Network treatment guidelines.”
In a retrospective study published in Obstetrics & Gynecology, the researchers used data from the SEER (Surveillance, Epidemiology, and End Results) database between Jan. 1, 2006, and Dec. 31, 2015. The study population included 83,883 women aged 18 years and older who were diagnosed with their first or only endometrial carcinoma. The primary dependent variable was adherence to the NCCN guidelines for the initial course of treatment, which included a combination of therapies based on cancer subtype and the extent of the disease, the researchers said.
The researchers combined the guidelines and the corresponding data from the SEER database to create “a binary variable representing adherence to [NCCN] guidelines (1 = adherent treatment, 0 = nonadherent treatment).”
Approximately 60% of the total patient population received guidelines-adherent treatment. In a multivariate analysis, Black women, Latina women, and American Indian or Alaska Native women were significantly less likely than White women to receive such treatment (odds ratios, 0.88, 0.92, and 0.82, respectively), controlling for factors including neighborhood socioeconomic status, age, and stage at diagnosis, year of diagnosis, histology, and disease grade. Asian women and Native Hawaiian/Pacific Islander women were significantly more likely to received guidelines-adherent treatment, compared with White women (OR, 1.14 and 1.19, respectively).
The researchers also found a significant gradient in guidelines-adherent treatment based on neighborhood socioeconomic status. Relative to the highest neighborhood socioeconomic status group, women in the lower groups had significantly lower odds of receiving guidelines-adherent treatment, with ORs of 0.89, 0.84, 0.80, and 0.73, respectively, for the high-middle neighborhood socioeconomic group, the middle group, the low-middle group, and the lowest group (P < .001 for all).
“Our study is novel in that it examines neighborhood socioeconomic disparities in the understudied context of treatment adherence for endometrial cancer,” the researchers noted.
The study findings were limited by several factors in including the retrospective design and potential for unmeasured confounding variables not included in SEER, such as hospital and physician characteristics, the researchers said. Also, the SEER data set was limited to only the first course of treatment, and did not include information on patient comorbidities that might affect treatment.
“Future research should qualitatively explore reasons for nonadherent treatment within endometrial cancer and other cancer sites among various racial-ethnic groups and socioeconomic status groups, with special attention to low-income women of color,” the researchers emphasized. More research on the impact of comorbidities on a patient’s ability to receive guidelines-based care should be used to inform whether comorbidities should be part of the NCCN guidelines.
However, the results were strengthened by the large sample size and diverse population, so the findings are generalizable to the overall U.S. population, the researchers said.
“Interventions are needed to ensure that equitable cancer treatment practices are available for all individuals regardless of their racial-ethnic or socioeconomic backgrounds,” they concluded.
Pursue optimal treatment to curb mortality
Even more concerning than the increase in the incidence of endometrial cancer in the United States is the increase in mortality from this disease, said Emma C. Rossi, MD, of the University of North Carolina at Chapel Hill, in an interview.
“Therefore, it is critical that we identify factors which might be contributing to the increasing lethality of this cancer,” she emphasized. “One such potential factor is race, as it has been observed that Black race is associated with an increased risk of death from endometrial cancer. Historically, this was attributed to the more aggressive subtypes of endometrial cancer (such as serous) which have a higher incidence among Black women. However, more recently, population-based studies have identified that this worse prognosis is independent of histologic cell type,” which suggests that something in our health care delivery is contributing to these worse outcomes.
“The present study helps to confirm these concerning associations, shedding some light on contributory factors, in this case, modifiable (adherence to recommended guidelines) and less modifiable (neighborhood socioeconomic environments) [ones],” Dr. Rossi noted. “The guidelines that are established by the NCCN are chosen after they have been shown to be associated with improved outcomes (including either survival or quality of life), and therefore lack of adherence to these outcomes may suggest inferior quality care is being delivered.”
Studies such as this are helpful in exposing the problem of treatment disparity to help identify sources of problems to develop solutions, she added.
The results should inspire clinicians “to feel agency in changing these outcomes, albeit by tackling very difficult social, political, and health system shortfalls,” she said.
Identify barriers to care
Barriers to greater adherence to guidelines-based care include varying definitions of such care, Dr. Rossi said.
“This is particularly true for surgical management of endometrial cancer, which remains controversial with respect to lymph node assessment. Lack of surgical staging with lymph node assessment was considered noncompliant care for this study; however, lymphadenectomy has not specifically, in and of itself, been associated with improved outcomes, and therefore some surgeons argue against performing it routinely,” she explained.
“Lack of access to sophisticated surgical tools and advanced surgical techniques may account for nonguidelines-based care in the patients with early-stage endometrial cancer; however, there are likely other differences in the ability to deliver guideline-concordant care (such as chemotherapy and radiation therapy) for advanced-stage cancers,” Dr. Rossi said. “Patient and provider positive attitudes toward adjuvant therapy, access to transportation, supportive home environments, paid sick leave, well-controlled or minimal comorbidities are all factors which promote the administration of complex adjuvant therapies such as chemotherapy and radiation. In low-resource neighborhoods and minority communities, barriers to these factors may be contributing to nonguidelines-concordant care.”
Dr. Rossi emphasized the need to “dive deeper into these data at individual health-system and provider levels.” For example, research is needed to compare the practice patterns and models of high-performing clinical practices with lower-performing practices in terms of factors such as tumor boards, journal review, peer review, dashboards, and metrics. By doing so, “we can ensure that we are understanding where and why variations in care are occurring,” Dr. Rossi said.
The study was supported in part by the Faculty Mentor Program Fellowship from the University of California, Irvine, graduate division. Ms. Rodriguez was supported in part by a grant from the National Cancer Institute. The researchers had no financial conflicts to disclose. Dr. Rossi had no financial conflicts to disclose.
Women who were Black, Latina, American Indian, or Alaska Native were significantly less likely than White women to receive guidelines-adherent treatment for endometrial cancer, based on data from more than 80,000 women.
The incidence of uterine cancer has increased across all ethnicities in recent decades, and adherence to the National Comprehensive Cancer Network treatment guidelines has been associated with improved survival, wrote Victoria A. Rodriguez, MSW, MPH, of the University of California, Irvine, and colleagues. “To date, however, there are few studies that have looked at endometrial cancer disparities with adherence to National Comprehensive Cancer Network treatment guidelines.”
In a retrospective study published in Obstetrics & Gynecology, the researchers used data from the SEER (Surveillance, Epidemiology, and End Results) database between Jan. 1, 2006, and Dec. 31, 2015. The study population included 83,883 women aged 18 years and older who were diagnosed with their first or only endometrial carcinoma. The primary dependent variable was adherence to the NCCN guidelines for the initial course of treatment, which included a combination of therapies based on cancer subtype and the extent of the disease, the researchers said.
The researchers combined the guidelines and the corresponding data from the SEER database to create “a binary variable representing adherence to [NCCN] guidelines (1 = adherent treatment, 0 = nonadherent treatment).”
Approximately 60% of the total patient population received guidelines-adherent treatment. In a multivariate analysis, Black women, Latina women, and American Indian or Alaska Native women were significantly less likely than White women to receive such treatment (odds ratios, 0.88, 0.92, and 0.82, respectively), controlling for factors including neighborhood socioeconomic status, age, and stage at diagnosis, year of diagnosis, histology, and disease grade. Asian women and Native Hawaiian/Pacific Islander women were significantly more likely to received guidelines-adherent treatment, compared with White women (OR, 1.14 and 1.19, respectively).
The researchers also found a significant gradient in guidelines-adherent treatment based on neighborhood socioeconomic status. Relative to the highest neighborhood socioeconomic status group, women in the lower groups had significantly lower odds of receiving guidelines-adherent treatment, with ORs of 0.89, 0.84, 0.80, and 0.73, respectively, for the high-middle neighborhood socioeconomic group, the middle group, the low-middle group, and the lowest group (P < .001 for all).
“Our study is novel in that it examines neighborhood socioeconomic disparities in the understudied context of treatment adherence for endometrial cancer,” the researchers noted.
The study findings were limited by several factors in including the retrospective design and potential for unmeasured confounding variables not included in SEER, such as hospital and physician characteristics, the researchers said. Also, the SEER data set was limited to only the first course of treatment, and did not include information on patient comorbidities that might affect treatment.
“Future research should qualitatively explore reasons for nonadherent treatment within endometrial cancer and other cancer sites among various racial-ethnic groups and socioeconomic status groups, with special attention to low-income women of color,” the researchers emphasized. More research on the impact of comorbidities on a patient’s ability to receive guidelines-based care should be used to inform whether comorbidities should be part of the NCCN guidelines.
However, the results were strengthened by the large sample size and diverse population, so the findings are generalizable to the overall U.S. population, the researchers said.
“Interventions are needed to ensure that equitable cancer treatment practices are available for all individuals regardless of their racial-ethnic or socioeconomic backgrounds,” they concluded.
Pursue optimal treatment to curb mortality
Even more concerning than the increase in the incidence of endometrial cancer in the United States is the increase in mortality from this disease, said Emma C. Rossi, MD, of the University of North Carolina at Chapel Hill, in an interview.
“Therefore, it is critical that we identify factors which might be contributing to the increasing lethality of this cancer,” she emphasized. “One such potential factor is race, as it has been observed that Black race is associated with an increased risk of death from endometrial cancer. Historically, this was attributed to the more aggressive subtypes of endometrial cancer (such as serous) which have a higher incidence among Black women. However, more recently, population-based studies have identified that this worse prognosis is independent of histologic cell type,” which suggests that something in our health care delivery is contributing to these worse outcomes.
“The present study helps to confirm these concerning associations, shedding some light on contributory factors, in this case, modifiable (adherence to recommended guidelines) and less modifiable (neighborhood socioeconomic environments) [ones],” Dr. Rossi noted. “The guidelines that are established by the NCCN are chosen after they have been shown to be associated with improved outcomes (including either survival or quality of life), and therefore lack of adherence to these outcomes may suggest inferior quality care is being delivered.”
Studies such as this are helpful in exposing the problem of treatment disparity to help identify sources of problems to develop solutions, she added.
The results should inspire clinicians “to feel agency in changing these outcomes, albeit by tackling very difficult social, political, and health system shortfalls,” she said.
Identify barriers to care
Barriers to greater adherence to guidelines-based care include varying definitions of such care, Dr. Rossi said.
“This is particularly true for surgical management of endometrial cancer, which remains controversial with respect to lymph node assessment. Lack of surgical staging with lymph node assessment was considered noncompliant care for this study; however, lymphadenectomy has not specifically, in and of itself, been associated with improved outcomes, and therefore some surgeons argue against performing it routinely,” she explained.
“Lack of access to sophisticated surgical tools and advanced surgical techniques may account for nonguidelines-based care in the patients with early-stage endometrial cancer; however, there are likely other differences in the ability to deliver guideline-concordant care (such as chemotherapy and radiation therapy) for advanced-stage cancers,” Dr. Rossi said. “Patient and provider positive attitudes toward adjuvant therapy, access to transportation, supportive home environments, paid sick leave, well-controlled or minimal comorbidities are all factors which promote the administration of complex adjuvant therapies such as chemotherapy and radiation. In low-resource neighborhoods and minority communities, barriers to these factors may be contributing to nonguidelines-concordant care.”
Dr. Rossi emphasized the need to “dive deeper into these data at individual health-system and provider levels.” For example, research is needed to compare the practice patterns and models of high-performing clinical practices with lower-performing practices in terms of factors such as tumor boards, journal review, peer review, dashboards, and metrics. By doing so, “we can ensure that we are understanding where and why variations in care are occurring,” Dr. Rossi said.
The study was supported in part by the Faculty Mentor Program Fellowship from the University of California, Irvine, graduate division. Ms. Rodriguez was supported in part by a grant from the National Cancer Institute. The researchers had no financial conflicts to disclose. Dr. Rossi had no financial conflicts to disclose.
Women who were Black, Latina, American Indian, or Alaska Native were significantly less likely than White women to receive guidelines-adherent treatment for endometrial cancer, based on data from more than 80,000 women.
The incidence of uterine cancer has increased across all ethnicities in recent decades, and adherence to the National Comprehensive Cancer Network treatment guidelines has been associated with improved survival, wrote Victoria A. Rodriguez, MSW, MPH, of the University of California, Irvine, and colleagues. “To date, however, there are few studies that have looked at endometrial cancer disparities with adherence to National Comprehensive Cancer Network treatment guidelines.”
In a retrospective study published in Obstetrics & Gynecology, the researchers used data from the SEER (Surveillance, Epidemiology, and End Results) database between Jan. 1, 2006, and Dec. 31, 2015. The study population included 83,883 women aged 18 years and older who were diagnosed with their first or only endometrial carcinoma. The primary dependent variable was adherence to the NCCN guidelines for the initial course of treatment, which included a combination of therapies based on cancer subtype and the extent of the disease, the researchers said.
The researchers combined the guidelines and the corresponding data from the SEER database to create “a binary variable representing adherence to [NCCN] guidelines (1 = adherent treatment, 0 = nonadherent treatment).”
Approximately 60% of the total patient population received guidelines-adherent treatment. In a multivariate analysis, Black women, Latina women, and American Indian or Alaska Native women were significantly less likely than White women to receive such treatment (odds ratios, 0.88, 0.92, and 0.82, respectively), controlling for factors including neighborhood socioeconomic status, age, and stage at diagnosis, year of diagnosis, histology, and disease grade. Asian women and Native Hawaiian/Pacific Islander women were significantly more likely to received guidelines-adherent treatment, compared with White women (OR, 1.14 and 1.19, respectively).
The researchers also found a significant gradient in guidelines-adherent treatment based on neighborhood socioeconomic status. Relative to the highest neighborhood socioeconomic status group, women in the lower groups had significantly lower odds of receiving guidelines-adherent treatment, with ORs of 0.89, 0.84, 0.80, and 0.73, respectively, for the high-middle neighborhood socioeconomic group, the middle group, the low-middle group, and the lowest group (P < .001 for all).
“Our study is novel in that it examines neighborhood socioeconomic disparities in the understudied context of treatment adherence for endometrial cancer,” the researchers noted.
The study findings were limited by several factors in including the retrospective design and potential for unmeasured confounding variables not included in SEER, such as hospital and physician characteristics, the researchers said. Also, the SEER data set was limited to only the first course of treatment, and did not include information on patient comorbidities that might affect treatment.
“Future research should qualitatively explore reasons for nonadherent treatment within endometrial cancer and other cancer sites among various racial-ethnic groups and socioeconomic status groups, with special attention to low-income women of color,” the researchers emphasized. More research on the impact of comorbidities on a patient’s ability to receive guidelines-based care should be used to inform whether comorbidities should be part of the NCCN guidelines.
However, the results were strengthened by the large sample size and diverse population, so the findings are generalizable to the overall U.S. population, the researchers said.
“Interventions are needed to ensure that equitable cancer treatment practices are available for all individuals regardless of their racial-ethnic or socioeconomic backgrounds,” they concluded.
Pursue optimal treatment to curb mortality
Even more concerning than the increase in the incidence of endometrial cancer in the United States is the increase in mortality from this disease, said Emma C. Rossi, MD, of the University of North Carolina at Chapel Hill, in an interview.
“Therefore, it is critical that we identify factors which might be contributing to the increasing lethality of this cancer,” she emphasized. “One such potential factor is race, as it has been observed that Black race is associated with an increased risk of death from endometrial cancer. Historically, this was attributed to the more aggressive subtypes of endometrial cancer (such as serous) which have a higher incidence among Black women. However, more recently, population-based studies have identified that this worse prognosis is independent of histologic cell type,” which suggests that something in our health care delivery is contributing to these worse outcomes.
“The present study helps to confirm these concerning associations, shedding some light on contributory factors, in this case, modifiable (adherence to recommended guidelines) and less modifiable (neighborhood socioeconomic environments) [ones],” Dr. Rossi noted. “The guidelines that are established by the NCCN are chosen after they have been shown to be associated with improved outcomes (including either survival or quality of life), and therefore lack of adherence to these outcomes may suggest inferior quality care is being delivered.”
Studies such as this are helpful in exposing the problem of treatment disparity to help identify sources of problems to develop solutions, she added.
The results should inspire clinicians “to feel agency in changing these outcomes, albeit by tackling very difficult social, political, and health system shortfalls,” she said.
Identify barriers to care
Barriers to greater adherence to guidelines-based care include varying definitions of such care, Dr. Rossi said.
“This is particularly true for surgical management of endometrial cancer, which remains controversial with respect to lymph node assessment. Lack of surgical staging with lymph node assessment was considered noncompliant care for this study; however, lymphadenectomy has not specifically, in and of itself, been associated with improved outcomes, and therefore some surgeons argue against performing it routinely,” she explained.
“Lack of access to sophisticated surgical tools and advanced surgical techniques may account for nonguidelines-based care in the patients with early-stage endometrial cancer; however, there are likely other differences in the ability to deliver guideline-concordant care (such as chemotherapy and radiation therapy) for advanced-stage cancers,” Dr. Rossi said. “Patient and provider positive attitudes toward adjuvant therapy, access to transportation, supportive home environments, paid sick leave, well-controlled or minimal comorbidities are all factors which promote the administration of complex adjuvant therapies such as chemotherapy and radiation. In low-resource neighborhoods and minority communities, barriers to these factors may be contributing to nonguidelines-concordant care.”
Dr. Rossi emphasized the need to “dive deeper into these data at individual health-system and provider levels.” For example, research is needed to compare the practice patterns and models of high-performing clinical practices with lower-performing practices in terms of factors such as tumor boards, journal review, peer review, dashboards, and metrics. By doing so, “we can ensure that we are understanding where and why variations in care are occurring,” Dr. Rossi said.
The study was supported in part by the Faculty Mentor Program Fellowship from the University of California, Irvine, graduate division. Ms. Rodriguez was supported in part by a grant from the National Cancer Institute. The researchers had no financial conflicts to disclose. Dr. Rossi had no financial conflicts to disclose.
FROM OBSTETRICS & GYNECOLOGY
Daily reporting from the 2021 Society of Gynecologic Surgeons Annual Meeting
TUESDAY, 6/29/21. DAY 3 AT SGS
The third day of the annual SGS meeting started with several academic roundtables hosted by experts in the field. These authorities shared their knowledge on a range of topics including endometriosis, building an academic career, diversity and equity in the workplace, and scientific publishing. The general session got underway with additional oral and video presentations highlighting advancements in our field. This year’s SGS President Dr. Miles Murphy gave the annual presidential address. He spoke genuinely and humbly about our field. Whitney Ross, MD, (@WRossMD), referred to his speech on Twitter as “Best. Presidential. Address. Ever.” –a sentiment felt by many in the crowd!
This year’s Telinde Lecture was given by Janet Dombrowski, the first ever non-physician to present this lecture. She spoke on resiliency in a lecture titled, “Cultivating Resilience: The Power in Connection & Collaboration.” It was an insightful and wise presentation on the power of connection and how connection bolsters our resiliency. She challenged us to all break down “thinking habits” that isolate us into silos and get in the way of powerful connection and collaboration. She reminded us of the African greeting “Sawubona” (I see you) and “Sikhona” (Because you see me, I am here). A gentle reminder that we feel our existence most tangibly when we are seen by others—an idea consistent with other important themes of this conference, focused on diversity, equity, and inclusion of all. The morning session was rounded out with a panel discussion on “Novel GYN Office Procedure,” featuring Drs. Cecile Ferrando (@CFerrandoMD), Abbas Shobeiri (@ShobeiriAbbas), Andrea Pezzela, and Eric Sokol.
The afternoon was filled with leisure activities in beautiful Palm Springs, including the SGS Golf Tournament, mountain biking, aerial tramway tour, and hike. The weather even cooperated with slightly cooler temperatures (think 100℉ instead of 120℉)! The evening was filled with food, drinks, and the excitement around the annual “SGS’ Got Talent” show! Everyone was able to let down, show off their dance moves, and enjoy some of that much needed connection time!
Tomorrow is the last day of #SGS2021! Excited to round out the conference with continued learning.
MONDAY, 6/28/21. DAY 2 AT SGS
The sun is up and working hard here in Palm Springs, and so are we!
Welcome and introduction of new members
The general session started with a warm welcome to the 12 new SGS members. A special shout out to Dr. Kelly Wright who is a new SGS Member and won the #SGS2021 tweetup! She ranked as a top influencer, prolific tweeter, and made more than 250K impressions leading up to SGS! Way to represent @MigsRunner.
General scientific sessions
There were several excellent oral and video presentations throughout the morning session. A range of topics were discussed, including postoperative pain management, strategies for cost-effective surgery, and how racial and ethnic disparities play into our medical education and patient outcomes. Dr. Eva Welch gave a stellar video presentation on straight-stick sacrocolpopexy techniques for the savvy surgeon. I personally will be incorporating some of her needle management tricks!
After a brief break with some refreshments and a stroll around the exhibit hall, the second scientific session initiated with a transformative lecture. Dr. Mark Walters presented "Insights on Surgical Education: How Can I Help You Get Better" in the inaugural Mark D. Walters Lectureship. Dr. Walters shared his experience and insights on how to transform oneself from a good surgeon to an expert and from a teacher to a coach in the operating room. His dedication to our field, years of experience, and wisdom earned him a standing ovation! Additional oral and video presentations followed. Dr. J. Wong shared correlations between surgeon gender and ergonomic strain with laparoscopic devices. Female surgeons more often reported inappropriate fit and expressed physical discomfort compared with male surgeons. Injuries and ergonomic strain lead to less operating and even disability for some surgeons. It is past time for us to have better--we need instruments that fit our hands!
The afternoon session started with a panel on "Perspectives on Race in GYN Surgery." It was another insightful discussion with thought- and action-provoking knowledge. The afternoon session included the SGS Prize Video by Dr. Angela DiCarlo-Meacham on excision of a vulvar cyst.
Fellows' Pelvic Research Network
After adjourning of the scientific sessions, the fellow-ran, multicenter research network (FPRN) met to give updates. This diverse group of both AUGS-SGS and FMIGS-SGS offers mentorship and relationships that are important for future careers and research. The collaboration allows the study of rare outcomes that may not be feasible at single sites. Dr. Amanda Yunker, fellowship director at Vanderbilt University, gave an amazing history lesson on the fields of OB and GYN, and the evolution of gynecologic surgery. We then had fun assigning a "report card grade" on how MIGS is doing comparatively with other subspecialties in the realms of academics and research.
VideoFest
The late afternoon was concluded with a surgical video session. What an amazing and talented group we are here at SGS!
President's awards ceremony and reception
The scientific focused day was rounded out with an evening of honors, awards, and social time as we celebrated all the achievements of our peers and colleagues. The president's reception was filled with food, laughter, networking, and reconnecting with friends and colleagues. We are looking forward to another day of education tomorrow!
Follow @JennaRehmerMD, @GynSurgery, and #SGS2021 on Twitter for updates.
SUNDAY, 6/27/21. DAY 1 AT SGS
Hello live from sunny Palm Spring, CA, and the Annual Scientific Meeting of the Society of Gynecologic Surgeons (SGS)! This year’s conference balances the long-awaited return to in-person events while simultaneously embracing virtual learning with their hybrid meeting format. You can follow me, @JennaRehmerMD, and #SGS2021 in real-time on Twitter.
Dismantling racism
We were incredibly fortunate to take a deep dive into dismantling racism in our personal and professional spheres. The postgraduate course was well researched and presented by Drs. Oluwateniola “Teni” Brown, Cassandra Carberry, Olivia Cardenas-Trowers (@otrowers_md), Annetta Madsen, Moiuri Siddique, and Blair Washington (@Dr_B_Washington). Each presentation provided a succinct and cohesive flow, taking us through what racism is, the historical and active structural racism in medicine, and the actions and steps of becoming anti-racist.
Dr. Brown discussed critical race theory. We learned that the engineered system of oppression is so advanced that it is often hidden in plain sight, and that one’s conscious awareness is not necessary in order to uphold the system of oppression. It is reinforced and supported with minimal effort. This is why not being racist is not enough; active anti-racism is needed to bring about change.
Fibroid management
Across the hall, Drs. Linda Bradley (@BradlelMD), Kimberly Kho (@KimberlyKho1), Cara King (@drcaraking), and Kelly Wright (@MigsRunner) broadened our armamentarium for uterine conservation in fibroid management. Dr. Bradley reviewed medical therapies, including novel treatments, as first-line or adjunct treatment options. Next, the course focused on surgical techniques for hysteroscopic myomectomies, optimization of minilaparotomy for myomectomy, and tissue extraction. Dr. King displayed true grit when giving her lecture from the airport after flight delays prevented her from being in person with us.
Multidisciplinary care within gyn surgery
In this virtual only postgraduate course, Drs. Risal Djohan (@DjohanMD), Cecile Ferrando (@CFerrandoMD), Marie Fidela Paraiso, Sandip Vasavada (@SandipVasavada), and Sarah Vogler showed us the importance of multidisciplinary care within gynecologic surgery practices. They explored how to streamline the approach so it complements your practice, how to co-bill for shared patient care, and tips and tricks for optimizing the surgical experience for the patient.
Industry presentations
Over lunch, Dr. Opoku-Akane presented on using ERAS (enhanced recovery after surgery) protocols for endometriosis and chronic pelvic pain and how to optimize the use of alternative surgical modalities for endometriosis. Following this, Drs. Albert Huany and Craig McCoy taught about a new technology using electrical stimulation to optimize visualization of the ureter.
Harnessing the power of social media
This workshop, organized by SGS Social Media Committee Chair Dr. Amy Park (@dramypark) showed us the importance of having an online identity for the sharing of ideas, networking, professional development, and education. We learned how to optimize our online bios, proper use of GYN ontology for hashtags, and how to maintain professionalism on social media. We reviewed the data on how sharing publications on social media improves altmetric scores and discussed how our social media influence may be tied to performance in the future.
Lessons in leadership
We rounded out the day with after-dinner dessert and drinks at the evening SGS Women’s Council presentation. We had the great honor of hearing from Lori Ryerker, CEO of Celanese Corporation, a Fortune 500 global company. She provided much wisdom on being a leader. She shared several keys to creating a successful work environment:
- being a leader that “provides an environment where people feel like they can bring their best selves every day” (and that being your best self is being your whole self, without reservations)
- allowing all genders, sexual orientations, races, ethnicities, and ages to show up together without reservations (because only then can people feel safe to be their best, because their best self is their true self).
It was a wonderful and successful kick-off to the meeting. I look forward to a full day tomorrow! Follow along as this year’s Fellow Scholars, Drs. Tara Brah (@TaraBrah), Amr El Haraki (@drharaki), Sheena Galhotra (@SheenaGalhotra), Meenal Misal (@meenalmisalMD), and yours truly, post live updates daily.
TUESDAY, 6/29/21. DAY 3 AT SGS
The third day of the annual SGS meeting started with several academic roundtables hosted by experts in the field. These authorities shared their knowledge on a range of topics including endometriosis, building an academic career, diversity and equity in the workplace, and scientific publishing. The general session got underway with additional oral and video presentations highlighting advancements in our field. This year’s SGS President Dr. Miles Murphy gave the annual presidential address. He spoke genuinely and humbly about our field. Whitney Ross, MD, (@WRossMD), referred to his speech on Twitter as “Best. Presidential. Address. Ever.” –a sentiment felt by many in the crowd!
This year’s Telinde Lecture was given by Janet Dombrowski, the first ever non-physician to present this lecture. She spoke on resiliency in a lecture titled, “Cultivating Resilience: The Power in Connection & Collaboration.” It was an insightful and wise presentation on the power of connection and how connection bolsters our resiliency. She challenged us to all break down “thinking habits” that isolate us into silos and get in the way of powerful connection and collaboration. She reminded us of the African greeting “Sawubona” (I see you) and “Sikhona” (Because you see me, I am here). A gentle reminder that we feel our existence most tangibly when we are seen by others—an idea consistent with other important themes of this conference, focused on diversity, equity, and inclusion of all. The morning session was rounded out with a panel discussion on “Novel GYN Office Procedure,” featuring Drs. Cecile Ferrando (@CFerrandoMD), Abbas Shobeiri (@ShobeiriAbbas), Andrea Pezzela, and Eric Sokol.
The afternoon was filled with leisure activities in beautiful Palm Springs, including the SGS Golf Tournament, mountain biking, aerial tramway tour, and hike. The weather even cooperated with slightly cooler temperatures (think 100℉ instead of 120℉)! The evening was filled with food, drinks, and the excitement around the annual “SGS’ Got Talent” show! Everyone was able to let down, show off their dance moves, and enjoy some of that much needed connection time!
Tomorrow is the last day of #SGS2021! Excited to round out the conference with continued learning.
MONDAY, 6/28/21. DAY 2 AT SGS
The sun is up and working hard here in Palm Springs, and so are we!
Welcome and introduction of new members
The general session started with a warm welcome to the 12 new SGS members. A special shout out to Dr. Kelly Wright who is a new SGS Member and won the #SGS2021 tweetup! She ranked as a top influencer, prolific tweeter, and made more than 250K impressions leading up to SGS! Way to represent @MigsRunner.
General scientific sessions
There were several excellent oral and video presentations throughout the morning session. A range of topics were discussed, including postoperative pain management, strategies for cost-effective surgery, and how racial and ethnic disparities play into our medical education and patient outcomes. Dr. Eva Welch gave a stellar video presentation on straight-stick sacrocolpopexy techniques for the savvy surgeon. I personally will be incorporating some of her needle management tricks!
After a brief break with some refreshments and a stroll around the exhibit hall, the second scientific session initiated with a transformative lecture. Dr. Mark Walters presented "Insights on Surgical Education: How Can I Help You Get Better" in the inaugural Mark D. Walters Lectureship. Dr. Walters shared his experience and insights on how to transform oneself from a good surgeon to an expert and from a teacher to a coach in the operating room. His dedication to our field, years of experience, and wisdom earned him a standing ovation! Additional oral and video presentations followed. Dr. J. Wong shared correlations between surgeon gender and ergonomic strain with laparoscopic devices. Female surgeons more often reported inappropriate fit and expressed physical discomfort compared with male surgeons. Injuries and ergonomic strain lead to less operating and even disability for some surgeons. It is past time for us to have better--we need instruments that fit our hands!
The afternoon session started with a panel on "Perspectives on Race in GYN Surgery." It was another insightful discussion with thought- and action-provoking knowledge. The afternoon session included the SGS Prize Video by Dr. Angela DiCarlo-Meacham on excision of a vulvar cyst.
Fellows' Pelvic Research Network
After adjourning of the scientific sessions, the fellow-ran, multicenter research network (FPRN) met to give updates. This diverse group of both AUGS-SGS and FMIGS-SGS offers mentorship and relationships that are important for future careers and research. The collaboration allows the study of rare outcomes that may not be feasible at single sites. Dr. Amanda Yunker, fellowship director at Vanderbilt University, gave an amazing history lesson on the fields of OB and GYN, and the evolution of gynecologic surgery. We then had fun assigning a "report card grade" on how MIGS is doing comparatively with other subspecialties in the realms of academics and research.
VideoFest
The late afternoon was concluded with a surgical video session. What an amazing and talented group we are here at SGS!
President's awards ceremony and reception
The scientific focused day was rounded out with an evening of honors, awards, and social time as we celebrated all the achievements of our peers and colleagues. The president's reception was filled with food, laughter, networking, and reconnecting with friends and colleagues. We are looking forward to another day of education tomorrow!
Follow @JennaRehmerMD, @GynSurgery, and #SGS2021 on Twitter for updates.
SUNDAY, 6/27/21. DAY 1 AT SGS
Hello live from sunny Palm Spring, CA, and the Annual Scientific Meeting of the Society of Gynecologic Surgeons (SGS)! This year’s conference balances the long-awaited return to in-person events while simultaneously embracing virtual learning with their hybrid meeting format. You can follow me, @JennaRehmerMD, and #SGS2021 in real-time on Twitter.
Dismantling racism
We were incredibly fortunate to take a deep dive into dismantling racism in our personal and professional spheres. The postgraduate course was well researched and presented by Drs. Oluwateniola “Teni” Brown, Cassandra Carberry, Olivia Cardenas-Trowers (@otrowers_md), Annetta Madsen, Moiuri Siddique, and Blair Washington (@Dr_B_Washington). Each presentation provided a succinct and cohesive flow, taking us through what racism is, the historical and active structural racism in medicine, and the actions and steps of becoming anti-racist.
Dr. Brown discussed critical race theory. We learned that the engineered system of oppression is so advanced that it is often hidden in plain sight, and that one’s conscious awareness is not necessary in order to uphold the system of oppression. It is reinforced and supported with minimal effort. This is why not being racist is not enough; active anti-racism is needed to bring about change.
Fibroid management
Across the hall, Drs. Linda Bradley (@BradlelMD), Kimberly Kho (@KimberlyKho1), Cara King (@drcaraking), and Kelly Wright (@MigsRunner) broadened our armamentarium for uterine conservation in fibroid management. Dr. Bradley reviewed medical therapies, including novel treatments, as first-line or adjunct treatment options. Next, the course focused on surgical techniques for hysteroscopic myomectomies, optimization of minilaparotomy for myomectomy, and tissue extraction. Dr. King displayed true grit when giving her lecture from the airport after flight delays prevented her from being in person with us.
Multidisciplinary care within gyn surgery
In this virtual only postgraduate course, Drs. Risal Djohan (@DjohanMD), Cecile Ferrando (@CFerrandoMD), Marie Fidela Paraiso, Sandip Vasavada (@SandipVasavada), and Sarah Vogler showed us the importance of multidisciplinary care within gynecologic surgery practices. They explored how to streamline the approach so it complements your practice, how to co-bill for shared patient care, and tips and tricks for optimizing the surgical experience for the patient.
Industry presentations
Over lunch, Dr. Opoku-Akane presented on using ERAS (enhanced recovery after surgery) protocols for endometriosis and chronic pelvic pain and how to optimize the use of alternative surgical modalities for endometriosis. Following this, Drs. Albert Huany and Craig McCoy taught about a new technology using electrical stimulation to optimize visualization of the ureter.
Harnessing the power of social media
This workshop, organized by SGS Social Media Committee Chair Dr. Amy Park (@dramypark) showed us the importance of having an online identity for the sharing of ideas, networking, professional development, and education. We learned how to optimize our online bios, proper use of GYN ontology for hashtags, and how to maintain professionalism on social media. We reviewed the data on how sharing publications on social media improves altmetric scores and discussed how our social media influence may be tied to performance in the future.
Lessons in leadership
We rounded out the day with after-dinner dessert and drinks at the evening SGS Women’s Council presentation. We had the great honor of hearing from Lori Ryerker, CEO of Celanese Corporation, a Fortune 500 global company. She provided much wisdom on being a leader. She shared several keys to creating a successful work environment:
- being a leader that “provides an environment where people feel like they can bring their best selves every day” (and that being your best self is being your whole self, without reservations)
- allowing all genders, sexual orientations, races, ethnicities, and ages to show up together without reservations (because only then can people feel safe to be their best, because their best self is their true self).
It was a wonderful and successful kick-off to the meeting. I look forward to a full day tomorrow! Follow along as this year’s Fellow Scholars, Drs. Tara Brah (@TaraBrah), Amr El Haraki (@drharaki), Sheena Galhotra (@SheenaGalhotra), Meenal Misal (@meenalmisalMD), and yours truly, post live updates daily.
TUESDAY, 6/29/21. DAY 3 AT SGS
The third day of the annual SGS meeting started with several academic roundtables hosted by experts in the field. These authorities shared their knowledge on a range of topics including endometriosis, building an academic career, diversity and equity in the workplace, and scientific publishing. The general session got underway with additional oral and video presentations highlighting advancements in our field. This year’s SGS President Dr. Miles Murphy gave the annual presidential address. He spoke genuinely and humbly about our field. Whitney Ross, MD, (@WRossMD), referred to his speech on Twitter as “Best. Presidential. Address. Ever.” –a sentiment felt by many in the crowd!
This year’s Telinde Lecture was given by Janet Dombrowski, the first ever non-physician to present this lecture. She spoke on resiliency in a lecture titled, “Cultivating Resilience: The Power in Connection & Collaboration.” It was an insightful and wise presentation on the power of connection and how connection bolsters our resiliency. She challenged us to all break down “thinking habits” that isolate us into silos and get in the way of powerful connection and collaboration. She reminded us of the African greeting “Sawubona” (I see you) and “Sikhona” (Because you see me, I am here). A gentle reminder that we feel our existence most tangibly when we are seen by others—an idea consistent with other important themes of this conference, focused on diversity, equity, and inclusion of all. The morning session was rounded out with a panel discussion on “Novel GYN Office Procedure,” featuring Drs. Cecile Ferrando (@CFerrandoMD), Abbas Shobeiri (@ShobeiriAbbas), Andrea Pezzela, and Eric Sokol.
The afternoon was filled with leisure activities in beautiful Palm Springs, including the SGS Golf Tournament, mountain biking, aerial tramway tour, and hike. The weather even cooperated with slightly cooler temperatures (think 100℉ instead of 120℉)! The evening was filled with food, drinks, and the excitement around the annual “SGS’ Got Talent” show! Everyone was able to let down, show off their dance moves, and enjoy some of that much needed connection time!
Tomorrow is the last day of #SGS2021! Excited to round out the conference with continued learning.
MONDAY, 6/28/21. DAY 2 AT SGS
The sun is up and working hard here in Palm Springs, and so are we!
Welcome and introduction of new members
The general session started with a warm welcome to the 12 new SGS members. A special shout out to Dr. Kelly Wright who is a new SGS Member and won the #SGS2021 tweetup! She ranked as a top influencer, prolific tweeter, and made more than 250K impressions leading up to SGS! Way to represent @MigsRunner.
General scientific sessions
There were several excellent oral and video presentations throughout the morning session. A range of topics were discussed, including postoperative pain management, strategies for cost-effective surgery, and how racial and ethnic disparities play into our medical education and patient outcomes. Dr. Eva Welch gave a stellar video presentation on straight-stick sacrocolpopexy techniques for the savvy surgeon. I personally will be incorporating some of her needle management tricks!
After a brief break with some refreshments and a stroll around the exhibit hall, the second scientific session initiated with a transformative lecture. Dr. Mark Walters presented "Insights on Surgical Education: How Can I Help You Get Better" in the inaugural Mark D. Walters Lectureship. Dr. Walters shared his experience and insights on how to transform oneself from a good surgeon to an expert and from a teacher to a coach in the operating room. His dedication to our field, years of experience, and wisdom earned him a standing ovation! Additional oral and video presentations followed. Dr. J. Wong shared correlations between surgeon gender and ergonomic strain with laparoscopic devices. Female surgeons more often reported inappropriate fit and expressed physical discomfort compared with male surgeons. Injuries and ergonomic strain lead to less operating and even disability for some surgeons. It is past time for us to have better--we need instruments that fit our hands!
The afternoon session started with a panel on "Perspectives on Race in GYN Surgery." It was another insightful discussion with thought- and action-provoking knowledge. The afternoon session included the SGS Prize Video by Dr. Angela DiCarlo-Meacham on excision of a vulvar cyst.
Fellows' Pelvic Research Network
After adjourning of the scientific sessions, the fellow-ran, multicenter research network (FPRN) met to give updates. This diverse group of both AUGS-SGS and FMIGS-SGS offers mentorship and relationships that are important for future careers and research. The collaboration allows the study of rare outcomes that may not be feasible at single sites. Dr. Amanda Yunker, fellowship director at Vanderbilt University, gave an amazing history lesson on the fields of OB and GYN, and the evolution of gynecologic surgery. We then had fun assigning a "report card grade" on how MIGS is doing comparatively with other subspecialties in the realms of academics and research.
VideoFest
The late afternoon was concluded with a surgical video session. What an amazing and talented group we are here at SGS!
President's awards ceremony and reception
The scientific focused day was rounded out with an evening of honors, awards, and social time as we celebrated all the achievements of our peers and colleagues. The president's reception was filled with food, laughter, networking, and reconnecting with friends and colleagues. We are looking forward to another day of education tomorrow!
Follow @JennaRehmerMD, @GynSurgery, and #SGS2021 on Twitter for updates.
SUNDAY, 6/27/21. DAY 1 AT SGS
Hello live from sunny Palm Spring, CA, and the Annual Scientific Meeting of the Society of Gynecologic Surgeons (SGS)! This year’s conference balances the long-awaited return to in-person events while simultaneously embracing virtual learning with their hybrid meeting format. You can follow me, @JennaRehmerMD, and #SGS2021 in real-time on Twitter.
Dismantling racism
We were incredibly fortunate to take a deep dive into dismantling racism in our personal and professional spheres. The postgraduate course was well researched and presented by Drs. Oluwateniola “Teni” Brown, Cassandra Carberry, Olivia Cardenas-Trowers (@otrowers_md), Annetta Madsen, Moiuri Siddique, and Blair Washington (@Dr_B_Washington). Each presentation provided a succinct and cohesive flow, taking us through what racism is, the historical and active structural racism in medicine, and the actions and steps of becoming anti-racist.
Dr. Brown discussed critical race theory. We learned that the engineered system of oppression is so advanced that it is often hidden in plain sight, and that one’s conscious awareness is not necessary in order to uphold the system of oppression. It is reinforced and supported with minimal effort. This is why not being racist is not enough; active anti-racism is needed to bring about change.
Fibroid management
Across the hall, Drs. Linda Bradley (@BradlelMD), Kimberly Kho (@KimberlyKho1), Cara King (@drcaraking), and Kelly Wright (@MigsRunner) broadened our armamentarium for uterine conservation in fibroid management. Dr. Bradley reviewed medical therapies, including novel treatments, as first-line or adjunct treatment options. Next, the course focused on surgical techniques for hysteroscopic myomectomies, optimization of minilaparotomy for myomectomy, and tissue extraction. Dr. King displayed true grit when giving her lecture from the airport after flight delays prevented her from being in person with us.
Multidisciplinary care within gyn surgery
In this virtual only postgraduate course, Drs. Risal Djohan (@DjohanMD), Cecile Ferrando (@CFerrandoMD), Marie Fidela Paraiso, Sandip Vasavada (@SandipVasavada), and Sarah Vogler showed us the importance of multidisciplinary care within gynecologic surgery practices. They explored how to streamline the approach so it complements your practice, how to co-bill for shared patient care, and tips and tricks for optimizing the surgical experience for the patient.
Industry presentations
Over lunch, Dr. Opoku-Akane presented on using ERAS (enhanced recovery after surgery) protocols for endometriosis and chronic pelvic pain and how to optimize the use of alternative surgical modalities for endometriosis. Following this, Drs. Albert Huany and Craig McCoy taught about a new technology using electrical stimulation to optimize visualization of the ureter.
Harnessing the power of social media
This workshop, organized by SGS Social Media Committee Chair Dr. Amy Park (@dramypark) showed us the importance of having an online identity for the sharing of ideas, networking, professional development, and education. We learned how to optimize our online bios, proper use of GYN ontology for hashtags, and how to maintain professionalism on social media. We reviewed the data on how sharing publications on social media improves altmetric scores and discussed how our social media influence may be tied to performance in the future.
Lessons in leadership
We rounded out the day with after-dinner dessert and drinks at the evening SGS Women’s Council presentation. We had the great honor of hearing from Lori Ryerker, CEO of Celanese Corporation, a Fortune 500 global company. She provided much wisdom on being a leader. She shared several keys to creating a successful work environment:
- being a leader that “provides an environment where people feel like they can bring their best selves every day” (and that being your best self is being your whole self, without reservations)
- allowing all genders, sexual orientations, races, ethnicities, and ages to show up together without reservations (because only then can people feel safe to be their best, because their best self is their true self).
It was a wonderful and successful kick-off to the meeting. I look forward to a full day tomorrow! Follow along as this year’s Fellow Scholars, Drs. Tara Brah (@TaraBrah), Amr El Haraki (@drharaki), Sheena Galhotra (@SheenaGalhotra), Meenal Misal (@meenalmisalMD), and yours truly, post live updates daily.