User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Welcoming LGBTQ Patients
Imagine going to see your physician and being mistreated for who you are. For LGBTQ patients, this is an everyday reality. According to a new Kaiser Family Foundation report, 33% of LGBT adults experienced unfair or disrespectful treatment from their physician or other healthcare provider compared with only 15% of their non-LGBT counterparts.1
Statistics such as this underscore the importance of ensuring our offices and staff are as welcoming as possible to our LGBTQ patients. When patients feel unwelcome, it can have serious consequences for their health. In a 2022 report, the Center for American Progress found that 23% of LGBTQ patients, and 37% of transgender patients, postponed medically necessary care out of fear that they would experience discrimination in the healthcare setting.2 This compares with 7% of their non-LGBTQ counterparts. In addition, 7% of LGBTQ patients said that their provider refused to see them due to their actual or perceived sexual orientation. While this may not be a problem in major urban areas where there are many physicians or other healthcare providers to see, in rural areas this could lead to loss of access to medically necessary care or require long travel times.
This is not just an adult care problem. In their 2023 LGBTQ+ Youth Report, the Human Rights Campaign found that only 35.9% of LGBTQ+ youth were out to some or all of their doctors and 35.8% of transgender youth were out to some or all of their doctors.3 This could be due to fear of discrimination from their physician, in addition to possible concerns about loss of confidentiality if the physician were to tell their parent about their sexual orientation and/or gender identity. As of the time of the writing of this article, no state requires a physician to “out” their minor patients to their parent(s) or guardian(s). Therefore, it is important to respect the trust that your patient places in your confidentiality. As their physician, you may be the only adult to know about a patient’s sexual orientation and/or gender identity. Research shows that acceptance of one’s gender identity by at least one healthcare professional reduces the odds of a past-year suicide attempt by 32%.4
As of the time of the writing of this article, 10 states have laws that allow medical professionals to decline services to patients who are, or are perceived to be, LGBTQ based on their sincerely held religious beliefs. These laws directly conflict with our ethical obligations as physicians to care for all patients, regardless of their race, gender, culture, sexuality, gender identity, or religion. In fact, the American Medical Association Code of Medical Ethics states that physicians must “respect basic civil liberties and not discriminate against individuals in deciding whether to enter into a professional relationship with a new patient” and “take care that their actions do not discriminate against or unduly burden individual patients or populations of patients and do not adversely affect patient or public trust.” This requires all of us to examine our implicit biases and treat all patients with the dignity and respect that they deserve.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Montero A et al. LGBT Adults’ Experiences With Discrimination and Health Care Disparities: Findings From the KFF Survey of Racism, Discrimination, and Health. KFF 2024 Apr 2.
2. Medina C and Mahowald L. Discrimination and Barriers to Well-Being: The State of the LGBTQI+ Community in 2022. Center for American Progress. 2023, Jan 12.
3. Goldberg SK et al. 2023 LGBTQ+ Youth Report. Human Rights Campaign Foundation. 2023 Aug.
4. Price MN and Green AE. Association of Gender Identity Acceptance With Fewer Suicide Attempts Among Transgender and Nonbinary Youth. Transgend Health. 2023 Feb 8;8(1):56-63. doi: 10.1089/trgh.2021.0079.
Imagine going to see your physician and being mistreated for who you are. For LGBTQ patients, this is an everyday reality. According to a new Kaiser Family Foundation report, 33% of LGBT adults experienced unfair or disrespectful treatment from their physician or other healthcare provider compared with only 15% of their non-LGBT counterparts.1
Statistics such as this underscore the importance of ensuring our offices and staff are as welcoming as possible to our LGBTQ patients. When patients feel unwelcome, it can have serious consequences for their health. In a 2022 report, the Center for American Progress found that 23% of LGBTQ patients, and 37% of transgender patients, postponed medically necessary care out of fear that they would experience discrimination in the healthcare setting.2 This compares with 7% of their non-LGBTQ counterparts. In addition, 7% of LGBTQ patients said that their provider refused to see them due to their actual or perceived sexual orientation. While this may not be a problem in major urban areas where there are many physicians or other healthcare providers to see, in rural areas this could lead to loss of access to medically necessary care or require long travel times.
This is not just an adult care problem. In their 2023 LGBTQ+ Youth Report, the Human Rights Campaign found that only 35.9% of LGBTQ+ youth were out to some or all of their doctors and 35.8% of transgender youth were out to some or all of their doctors.3 This could be due to fear of discrimination from their physician, in addition to possible concerns about loss of confidentiality if the physician were to tell their parent about their sexual orientation and/or gender identity. As of the time of the writing of this article, no state requires a physician to “out” their minor patients to their parent(s) or guardian(s). Therefore, it is important to respect the trust that your patient places in your confidentiality. As their physician, you may be the only adult to know about a patient’s sexual orientation and/or gender identity. Research shows that acceptance of one’s gender identity by at least one healthcare professional reduces the odds of a past-year suicide attempt by 32%.4
As of the time of the writing of this article, 10 states have laws that allow medical professionals to decline services to patients who are, or are perceived to be, LGBTQ based on their sincerely held religious beliefs. These laws directly conflict with our ethical obligations as physicians to care for all patients, regardless of their race, gender, culture, sexuality, gender identity, or religion. In fact, the American Medical Association Code of Medical Ethics states that physicians must “respect basic civil liberties and not discriminate against individuals in deciding whether to enter into a professional relationship with a new patient” and “take care that their actions do not discriminate against or unduly burden individual patients or populations of patients and do not adversely affect patient or public trust.” This requires all of us to examine our implicit biases and treat all patients with the dignity and respect that they deserve.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Montero A et al. LGBT Adults’ Experiences With Discrimination and Health Care Disparities: Findings From the KFF Survey of Racism, Discrimination, and Health. KFF 2024 Apr 2.
2. Medina C and Mahowald L. Discrimination and Barriers to Well-Being: The State of the LGBTQI+ Community in 2022. Center for American Progress. 2023, Jan 12.
3. Goldberg SK et al. 2023 LGBTQ+ Youth Report. Human Rights Campaign Foundation. 2023 Aug.
4. Price MN and Green AE. Association of Gender Identity Acceptance With Fewer Suicide Attempts Among Transgender and Nonbinary Youth. Transgend Health. 2023 Feb 8;8(1):56-63. doi: 10.1089/trgh.2021.0079.
Imagine going to see your physician and being mistreated for who you are. For LGBTQ patients, this is an everyday reality. According to a new Kaiser Family Foundation report, 33% of LGBT adults experienced unfair or disrespectful treatment from their physician or other healthcare provider compared with only 15% of their non-LGBT counterparts.1
Statistics such as this underscore the importance of ensuring our offices and staff are as welcoming as possible to our LGBTQ patients. When patients feel unwelcome, it can have serious consequences for their health. In a 2022 report, the Center for American Progress found that 23% of LGBTQ patients, and 37% of transgender patients, postponed medically necessary care out of fear that they would experience discrimination in the healthcare setting.2 This compares with 7% of their non-LGBTQ counterparts. In addition, 7% of LGBTQ patients said that their provider refused to see them due to their actual or perceived sexual orientation. While this may not be a problem in major urban areas where there are many physicians or other healthcare providers to see, in rural areas this could lead to loss of access to medically necessary care or require long travel times.
This is not just an adult care problem. In their 2023 LGBTQ+ Youth Report, the Human Rights Campaign found that only 35.9% of LGBTQ+ youth were out to some or all of their doctors and 35.8% of transgender youth were out to some or all of their doctors.3 This could be due to fear of discrimination from their physician, in addition to possible concerns about loss of confidentiality if the physician were to tell their parent about their sexual orientation and/or gender identity. As of the time of the writing of this article, no state requires a physician to “out” their minor patients to their parent(s) or guardian(s). Therefore, it is important to respect the trust that your patient places in your confidentiality. As their physician, you may be the only adult to know about a patient’s sexual orientation and/or gender identity. Research shows that acceptance of one’s gender identity by at least one healthcare professional reduces the odds of a past-year suicide attempt by 32%.4
As of the time of the writing of this article, 10 states have laws that allow medical professionals to decline services to patients who are, or are perceived to be, LGBTQ based on their sincerely held religious beliefs. These laws directly conflict with our ethical obligations as physicians to care for all patients, regardless of their race, gender, culture, sexuality, gender identity, or religion. In fact, the American Medical Association Code of Medical Ethics states that physicians must “respect basic civil liberties and not discriminate against individuals in deciding whether to enter into a professional relationship with a new patient” and “take care that their actions do not discriminate against or unduly burden individual patients or populations of patients and do not adversely affect patient or public trust.” This requires all of us to examine our implicit biases and treat all patients with the dignity and respect that they deserve.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Montero A et al. LGBT Adults’ Experiences With Discrimination and Health Care Disparities: Findings From the KFF Survey of Racism, Discrimination, and Health. KFF 2024 Apr 2.
2. Medina C and Mahowald L. Discrimination and Barriers to Well-Being: The State of the LGBTQI+ Community in 2022. Center for American Progress. 2023, Jan 12.
3. Goldberg SK et al. 2023 LGBTQ+ Youth Report. Human Rights Campaign Foundation. 2023 Aug.
4. Price MN and Green AE. Association of Gender Identity Acceptance With Fewer Suicide Attempts Among Transgender and Nonbinary Youth. Transgend Health. 2023 Feb 8;8(1):56-63. doi: 10.1089/trgh.2021.0079.
Physicians Own Less Than Half of US Practices; Federal Agencies Want Outside Input
Physician practice ownership by corporations, including health insurers, private equity firms, and large pharmacy chains, reached 30.1% as of January for the first time surpassing ownership by hospitals and health systems (28.4%), according to a new report.
As a result, about three in five physician practices are now owned by nonphysicians.
In early 2020, corporations owned just about 17% of US medical practices, while hospitals and health systems owned about 25%, according to the report released Thursday by nonprofit Physician Advocacy Institute (PAI). But corporate ownership of medical groups surged during the pandemic.
These trends raise questions about how best to protect patients and physicians in a changing employment landscape, said Kelly Kenney, PAI’s chief executive officer, in a statement.
“Corporate entities are assuming control of physician practices and changing the face of medicine in the United States with little to no scrutiny from regulators,” Ms. Kenney said.
The research, conducted by consulting group Avalere for PAI, used the IQVIA OneKey database that contains physician and practice location information on hospital and health system ownership.
By 2022-2023, there was a 7.3% increase in the percentage of practices owned by hospitals and 5.9% increase in the percentage of physicians employed by these organizations, PAI said. In the same time frame, there was an 11% increase in the percentage of practices owned by corporations and a 3.0% increase in the percentage of physicians employed by these entities.
“Physicians have an ethical responsibility to their patients’ health,” Ms. Kenney said. “Corporate entities have a fiduciary responsibility to their shareholders and are motivated to put profits first…these interests can conflict with providing the best medical care to patients.”
Federal Scrutiny Increases
However, both federal and state regulators are paying more attention to what happens to patients and physicians when corporations acquire practices.
“Given recent trends, we are concerned that some transactions may generate profits for those firms at the expense of patients’ health, workers’ safety, quality of care, and affordable healthcare for patients and taxpayers,” said the Federal Trade Commission (FTC) and the Justice (DOJ) and Health and Human Services (HHS) departments.
This statement appears in those agencies’ joint request for information (RFI) announced in March. An RFI is a tool that federal agencies can use to gauge the level of both support and opposition they would face if they were to try to change policies. Public comments are due May 6.
Corporations and advocacy groups often submit detailed comments outlining reasons why the federal government should or should not act on an issue. But individuals also can make their case in this forum.
The FTC, DOJ, and HHS are looking broadly at consolidation in healthcare, but they also spell out potential concerns related to acquisition of physician practices.
For example, they asked clinicians and support staff to provide feedback about whether acquisitions lead to changes in:
- Take-home pay
- Staffing levels
- Workplace safety
- Compensation model (eg, from fixed salary to volume based)
- Policies regarding patient referrals
- Mix of patients
- The volume of patients
- The way providers practice medicine (eg, incentives, prescribing decisions, forced protocols, restrictions on time spent with patients, or mandatory coding practices)
- Administrative or managerial organization (eg, transition to a management services organization).
A version of this article appeared on Medscape.com.
Physician practice ownership by corporations, including health insurers, private equity firms, and large pharmacy chains, reached 30.1% as of January for the first time surpassing ownership by hospitals and health systems (28.4%), according to a new report.
As a result, about three in five physician practices are now owned by nonphysicians.
In early 2020, corporations owned just about 17% of US medical practices, while hospitals and health systems owned about 25%, according to the report released Thursday by nonprofit Physician Advocacy Institute (PAI). But corporate ownership of medical groups surged during the pandemic.
These trends raise questions about how best to protect patients and physicians in a changing employment landscape, said Kelly Kenney, PAI’s chief executive officer, in a statement.
“Corporate entities are assuming control of physician practices and changing the face of medicine in the United States with little to no scrutiny from regulators,” Ms. Kenney said.
The research, conducted by consulting group Avalere for PAI, used the IQVIA OneKey database that contains physician and practice location information on hospital and health system ownership.
By 2022-2023, there was a 7.3% increase in the percentage of practices owned by hospitals and 5.9% increase in the percentage of physicians employed by these organizations, PAI said. In the same time frame, there was an 11% increase in the percentage of practices owned by corporations and a 3.0% increase in the percentage of physicians employed by these entities.
“Physicians have an ethical responsibility to their patients’ health,” Ms. Kenney said. “Corporate entities have a fiduciary responsibility to their shareholders and are motivated to put profits first…these interests can conflict with providing the best medical care to patients.”
Federal Scrutiny Increases
However, both federal and state regulators are paying more attention to what happens to patients and physicians when corporations acquire practices.
“Given recent trends, we are concerned that some transactions may generate profits for those firms at the expense of patients’ health, workers’ safety, quality of care, and affordable healthcare for patients and taxpayers,” said the Federal Trade Commission (FTC) and the Justice (DOJ) and Health and Human Services (HHS) departments.
This statement appears in those agencies’ joint request for information (RFI) announced in March. An RFI is a tool that federal agencies can use to gauge the level of both support and opposition they would face if they were to try to change policies. Public comments are due May 6.
Corporations and advocacy groups often submit detailed comments outlining reasons why the federal government should or should not act on an issue. But individuals also can make their case in this forum.
The FTC, DOJ, and HHS are looking broadly at consolidation in healthcare, but they also spell out potential concerns related to acquisition of physician practices.
For example, they asked clinicians and support staff to provide feedback about whether acquisitions lead to changes in:
- Take-home pay
- Staffing levels
- Workplace safety
- Compensation model (eg, from fixed salary to volume based)
- Policies regarding patient referrals
- Mix of patients
- The volume of patients
- The way providers practice medicine (eg, incentives, prescribing decisions, forced protocols, restrictions on time spent with patients, or mandatory coding practices)
- Administrative or managerial organization (eg, transition to a management services organization).
A version of this article appeared on Medscape.com.
Physician practice ownership by corporations, including health insurers, private equity firms, and large pharmacy chains, reached 30.1% as of January for the first time surpassing ownership by hospitals and health systems (28.4%), according to a new report.
As a result, about three in five physician practices are now owned by nonphysicians.
In early 2020, corporations owned just about 17% of US medical practices, while hospitals and health systems owned about 25%, according to the report released Thursday by nonprofit Physician Advocacy Institute (PAI). But corporate ownership of medical groups surged during the pandemic.
These trends raise questions about how best to protect patients and physicians in a changing employment landscape, said Kelly Kenney, PAI’s chief executive officer, in a statement.
“Corporate entities are assuming control of physician practices and changing the face of medicine in the United States with little to no scrutiny from regulators,” Ms. Kenney said.
The research, conducted by consulting group Avalere for PAI, used the IQVIA OneKey database that contains physician and practice location information on hospital and health system ownership.
By 2022-2023, there was a 7.3% increase in the percentage of practices owned by hospitals and 5.9% increase in the percentage of physicians employed by these organizations, PAI said. In the same time frame, there was an 11% increase in the percentage of practices owned by corporations and a 3.0% increase in the percentage of physicians employed by these entities.
“Physicians have an ethical responsibility to their patients’ health,” Ms. Kenney said. “Corporate entities have a fiduciary responsibility to their shareholders and are motivated to put profits first…these interests can conflict with providing the best medical care to patients.”
Federal Scrutiny Increases
However, both federal and state regulators are paying more attention to what happens to patients and physicians when corporations acquire practices.
“Given recent trends, we are concerned that some transactions may generate profits for those firms at the expense of patients’ health, workers’ safety, quality of care, and affordable healthcare for patients and taxpayers,” said the Federal Trade Commission (FTC) and the Justice (DOJ) and Health and Human Services (HHS) departments.
This statement appears in those agencies’ joint request for information (RFI) announced in March. An RFI is a tool that federal agencies can use to gauge the level of both support and opposition they would face if they were to try to change policies. Public comments are due May 6.
Corporations and advocacy groups often submit detailed comments outlining reasons why the federal government should or should not act on an issue. But individuals also can make their case in this forum.
The FTC, DOJ, and HHS are looking broadly at consolidation in healthcare, but they also spell out potential concerns related to acquisition of physician practices.
For example, they asked clinicians and support staff to provide feedback about whether acquisitions lead to changes in:
- Take-home pay
- Staffing levels
- Workplace safety
- Compensation model (eg, from fixed salary to volume based)
- Policies regarding patient referrals
- Mix of patients
- The volume of patients
- The way providers practice medicine (eg, incentives, prescribing decisions, forced protocols, restrictions on time spent with patients, or mandatory coding practices)
- Administrative or managerial organization (eg, transition to a management services organization).
A version of this article appeared on Medscape.com.
Cannabis Constituent May Be Key to Easing THC-Induced Anxiety
, new data from a small study suggested.
Participants who inhaled vaporized D-limonene and THC reported significantly greater decreases in anxiogenic effects than did people who received either component alone or a placebo. Reductions were greater as the dose of the D-limonene was increased.
Investigators noted that the findings could have implications for the use of medicinal or recreational cannabis, which has increased in recent years due to state legalization efforts.
“People use cannabis to help reduce anxiety, depression, and posttraumatic stress disorder, but since THC levels vary widely, if a person overshoots their tolerance of THC, cannabis can induce anxiety rather than relieve it,” senior investigator Ryan Vandrey, PhD, professor of psychiatry and behavioral sciences, Johns Hopkins School of Medicine, Baltimore, said in a news release.
“Our study demonstrates that D-limonene can modulate the effects of THC in a meaningful way and make THC more tolerable to people using it for both therapeutic and non-therapeutic purposes,” he added.
The study was published online in Drug and Alcohol Dependence.
Entourage Theory
Cannabis legalization has opened the door to an increased range of medicinal and nonmedicinal uses, but its benefits can be limited by the anxiety and panic some people experience with its use, investigators noted.
Many cannabis plants have been bred to contain higher concentrations of THC, with some dispensaries selling cannabis with more than 20%-30% THC. The plants often include cannabidiol, “minor” cannabinoids, and terpenes, such as D-limonene.
Prior studies pointed to THC as the cause of acute behavioral and psychoactive effects some cannabis users experience. However, a new, untested theory, the “cannabis entourage effect theory,” suggested other components in cannabis, including D-limonene, may contribute to the anxiogenic symptoms.
“We were motivated by scientific publications that hypothesized D-limonene can attenuate the acute anxiogenic effects of cannabis, but for which empirical data did not exist,” Dr. Vandrey said.
Investigators designed a small double-blind, within-subjects crossover study of 20 healthy adults (median age, 26 years; 50% men). About half of participants were Caucasian/non-Hispanic, 30% African American/non-Hispanic, 10% Caucasian/Hispanic, and 10% Asian/non-Hispanic.
All participants completed nine outpatient drug administration sessions, during which they inhaled vaporized D-limonene alone (1 or 5 mg), THC alone (15 or 30 mg), the same doses of THC and D-limonene together, or placebo.
Primary outcomes included subjective drug effects, measured with the Drug Effect Questionnaire (DEQ) and the 20-item state subscale of the State-Trait Anxiety Inventory (STAI-S). Investigators also measured cognitive/psychomotor performance with the Digit Symbol Substitution Task (DSST) and the Paced Serial Addition Task.
Vital signs such as heart rate, systolic blood pressure (SBP), diastolic blood pressure (DBP), and plasma D-limonene and THC concentrations were also tracked.
Participants’ responses were measured at baseline and then an additional nine times after initial exposure over the course of each 6-hour test session. Blood and urine samples were collected from participants before, during, and after each session.
First Evidence
There were no significant differences in outcomes between the D-limonene alone and placebo groups.
Receipt of 15- and 30-mg doses of THC alone was associated with subjective reports of acute cannabis exposure, including cognitive and physiological effects.
A treatment effect was observed for “anxious/nervous” (P < .01), “paranoid” (P < .01), and “heart racing” (P < .0001).
In planned comparisons, ratings of anxiety-like subjective effects qualitatively decreased as D-limonene dose increased, and concurrent administration of 30-mg THC plus 15-mg D-limonene significantly reduced ratings of “anxious/nervous” and “paranoid” on the DEQ compared to 30 mg of THC alone (P < .05).
Findings were similar on the composite score of the STAI-S, and although planned comparisons did not reach the threshold for statistical significance, reductions in anxiety approached significance in the THC plus D-limonene group compared with the THC alone condition (P = .08). The combination group also reported significantly lower subjective ratings of unpleasant drug effects than the THC alone group (P = .03).
In particular, a main effect of treatment was found for the anxious/nervous category on the DEQ (P < .01), as well as the “paranoid” (P < .01) and heart racing (P < .0001) categories.
On the other hand, ratings of anxious/nervous and paranoid categories were significantly lower in the 30-mg THC plus 15-mg D-limonene vs the 30-mg THC alone condition (P < .05, for all).
As for cognition, following drug administration, a significant main effect of treatment was observed for the DSST (P < .05), but no significant differences between THC and THC plus D-limonene combination conditions or between D-limonene alone and placebo were detected.
There were no differences within each THC dose and between D-limonene alone versus placebo conditions. Moreover, there were no main effects of treatment found for SBP or DBP.
The combination condition produced significantly greater concentrations of THC than the THC alone condition (P < .05).
“This study provides the first evidence that there are chemical constituents found naturally in the cannabis plant that can reduce some of the adverse effects of using delta-9-THC,” Dr. Vandrey said.
Although the exact mechanism by which vaporized D-limonene counters the anxiogenic effects of THC is unclear, “our best guess is that D-limonene is producing an anxiolytic effect on its own that is not mediated by cannabinoid receptors,” Dr. Vandrey said.
Significant Impact
Commenting on the research, Joshua Lile, PhD, professor, Department of Behavioral Science, University of Kentucky College of Medicine, Lexington, noted that the study seems to be the first of its kind to study the influence of terpene on THC response.
The research “makes a significant impact on our field,” and is “among the few controlled clinical studies that have demonstrated interactions between THC and other cannabis constituents, supporting the validity of the ‘entourage’ effect,” said Dr. Lile, who was not involved with the current research.
“This work is particularly important, given the unfounded claims sometimes made by the cannabis industry regarding the effects of different cannabis products,” he added.
Also commenting on the study, Ziva Cooper, PhD, professor and director of the UCLA Center for Cannabis and Cannabinoids, University of California Los Angeles, said the findings “have direct implications for improving the safety of cannabis, whether it’s being used for medical or nonmedical purposes, especially in people and patients who do not have experience with cannabis, a group that is at high risk for experiencing anxiety after using cannabis.”
In addition, “an important aspect to this study is that the effects of limonene in reducing anxiety attributed to delta-9-THC were observed at higher concentrations (or doses) than those usually present in the plant,” Dr. Copper said. “This calls for further investigation into new cannabis formulations specifically designed to leverage the potential protective effects of the terpene.”
This research was supported by the National Institute on Drug Abuse. Dr. Vandrey served as a consultant or received honoraria from Mira1a Therapeutics, Inc.; Jazz Pharmaceuticals; Charlotte’s Web; Syqe Medical Ltd.; and WebMD. The other authors’ disclosures are listed on the original paper. Dr. Lile declared no relevant financial relationships. Dr. Cooper reported receiving study drug from Canopy Growth Corp and True Terpenes, study-related materials from Storz & Bickel, and research support from the National Institute on Drug Abuse, National Center for Complementary and Integrative Health, California Department of Cannabis Control, Center for Medicinal Cannabis Research, and California Highway Patrol.
A version of this article appeared on Medscape.com.
, new data from a small study suggested.
Participants who inhaled vaporized D-limonene and THC reported significantly greater decreases in anxiogenic effects than did people who received either component alone or a placebo. Reductions were greater as the dose of the D-limonene was increased.
Investigators noted that the findings could have implications for the use of medicinal or recreational cannabis, which has increased in recent years due to state legalization efforts.
“People use cannabis to help reduce anxiety, depression, and posttraumatic stress disorder, but since THC levels vary widely, if a person overshoots their tolerance of THC, cannabis can induce anxiety rather than relieve it,” senior investigator Ryan Vandrey, PhD, professor of psychiatry and behavioral sciences, Johns Hopkins School of Medicine, Baltimore, said in a news release.
“Our study demonstrates that D-limonene can modulate the effects of THC in a meaningful way and make THC more tolerable to people using it for both therapeutic and non-therapeutic purposes,” he added.
The study was published online in Drug and Alcohol Dependence.
Entourage Theory
Cannabis legalization has opened the door to an increased range of medicinal and nonmedicinal uses, but its benefits can be limited by the anxiety and panic some people experience with its use, investigators noted.
Many cannabis plants have been bred to contain higher concentrations of THC, with some dispensaries selling cannabis with more than 20%-30% THC. The plants often include cannabidiol, “minor” cannabinoids, and terpenes, such as D-limonene.
Prior studies pointed to THC as the cause of acute behavioral and psychoactive effects some cannabis users experience. However, a new, untested theory, the “cannabis entourage effect theory,” suggested other components in cannabis, including D-limonene, may contribute to the anxiogenic symptoms.
“We were motivated by scientific publications that hypothesized D-limonene can attenuate the acute anxiogenic effects of cannabis, but for which empirical data did not exist,” Dr. Vandrey said.
Investigators designed a small double-blind, within-subjects crossover study of 20 healthy adults (median age, 26 years; 50% men). About half of participants were Caucasian/non-Hispanic, 30% African American/non-Hispanic, 10% Caucasian/Hispanic, and 10% Asian/non-Hispanic.
All participants completed nine outpatient drug administration sessions, during which they inhaled vaporized D-limonene alone (1 or 5 mg), THC alone (15 or 30 mg), the same doses of THC and D-limonene together, or placebo.
Primary outcomes included subjective drug effects, measured with the Drug Effect Questionnaire (DEQ) and the 20-item state subscale of the State-Trait Anxiety Inventory (STAI-S). Investigators also measured cognitive/psychomotor performance with the Digit Symbol Substitution Task (DSST) and the Paced Serial Addition Task.
Vital signs such as heart rate, systolic blood pressure (SBP), diastolic blood pressure (DBP), and plasma D-limonene and THC concentrations were also tracked.
Participants’ responses were measured at baseline and then an additional nine times after initial exposure over the course of each 6-hour test session. Blood and urine samples were collected from participants before, during, and after each session.
First Evidence
There were no significant differences in outcomes between the D-limonene alone and placebo groups.
Receipt of 15- and 30-mg doses of THC alone was associated with subjective reports of acute cannabis exposure, including cognitive and physiological effects.
A treatment effect was observed for “anxious/nervous” (P < .01), “paranoid” (P < .01), and “heart racing” (P < .0001).
In planned comparisons, ratings of anxiety-like subjective effects qualitatively decreased as D-limonene dose increased, and concurrent administration of 30-mg THC plus 15-mg D-limonene significantly reduced ratings of “anxious/nervous” and “paranoid” on the DEQ compared to 30 mg of THC alone (P < .05).
Findings were similar on the composite score of the STAI-S, and although planned comparisons did not reach the threshold for statistical significance, reductions in anxiety approached significance in the THC plus D-limonene group compared with the THC alone condition (P = .08). The combination group also reported significantly lower subjective ratings of unpleasant drug effects than the THC alone group (P = .03).
In particular, a main effect of treatment was found for the anxious/nervous category on the DEQ (P < .01), as well as the “paranoid” (P < .01) and heart racing (P < .0001) categories.
On the other hand, ratings of anxious/nervous and paranoid categories were significantly lower in the 30-mg THC plus 15-mg D-limonene vs the 30-mg THC alone condition (P < .05, for all).
As for cognition, following drug administration, a significant main effect of treatment was observed for the DSST (P < .05), but no significant differences between THC and THC plus D-limonene combination conditions or between D-limonene alone and placebo were detected.
There were no differences within each THC dose and between D-limonene alone versus placebo conditions. Moreover, there were no main effects of treatment found for SBP or DBP.
The combination condition produced significantly greater concentrations of THC than the THC alone condition (P < .05).
“This study provides the first evidence that there are chemical constituents found naturally in the cannabis plant that can reduce some of the adverse effects of using delta-9-THC,” Dr. Vandrey said.
Although the exact mechanism by which vaporized D-limonene counters the anxiogenic effects of THC is unclear, “our best guess is that D-limonene is producing an anxiolytic effect on its own that is not mediated by cannabinoid receptors,” Dr. Vandrey said.
Significant Impact
Commenting on the research, Joshua Lile, PhD, professor, Department of Behavioral Science, University of Kentucky College of Medicine, Lexington, noted that the study seems to be the first of its kind to study the influence of terpene on THC response.
The research “makes a significant impact on our field,” and is “among the few controlled clinical studies that have demonstrated interactions between THC and other cannabis constituents, supporting the validity of the ‘entourage’ effect,” said Dr. Lile, who was not involved with the current research.
“This work is particularly important, given the unfounded claims sometimes made by the cannabis industry regarding the effects of different cannabis products,” he added.
Also commenting on the study, Ziva Cooper, PhD, professor and director of the UCLA Center for Cannabis and Cannabinoids, University of California Los Angeles, said the findings “have direct implications for improving the safety of cannabis, whether it’s being used for medical or nonmedical purposes, especially in people and patients who do not have experience with cannabis, a group that is at high risk for experiencing anxiety after using cannabis.”
In addition, “an important aspect to this study is that the effects of limonene in reducing anxiety attributed to delta-9-THC were observed at higher concentrations (or doses) than those usually present in the plant,” Dr. Copper said. “This calls for further investigation into new cannabis formulations specifically designed to leverage the potential protective effects of the terpene.”
This research was supported by the National Institute on Drug Abuse. Dr. Vandrey served as a consultant or received honoraria from Mira1a Therapeutics, Inc.; Jazz Pharmaceuticals; Charlotte’s Web; Syqe Medical Ltd.; and WebMD. The other authors’ disclosures are listed on the original paper. Dr. Lile declared no relevant financial relationships. Dr. Cooper reported receiving study drug from Canopy Growth Corp and True Terpenes, study-related materials from Storz & Bickel, and research support from the National Institute on Drug Abuse, National Center for Complementary and Integrative Health, California Department of Cannabis Control, Center for Medicinal Cannabis Research, and California Highway Patrol.
A version of this article appeared on Medscape.com.
, new data from a small study suggested.
Participants who inhaled vaporized D-limonene and THC reported significantly greater decreases in anxiogenic effects than did people who received either component alone or a placebo. Reductions were greater as the dose of the D-limonene was increased.
Investigators noted that the findings could have implications for the use of medicinal or recreational cannabis, which has increased in recent years due to state legalization efforts.
“People use cannabis to help reduce anxiety, depression, and posttraumatic stress disorder, but since THC levels vary widely, if a person overshoots their tolerance of THC, cannabis can induce anxiety rather than relieve it,” senior investigator Ryan Vandrey, PhD, professor of psychiatry and behavioral sciences, Johns Hopkins School of Medicine, Baltimore, said in a news release.
“Our study demonstrates that D-limonene can modulate the effects of THC in a meaningful way and make THC more tolerable to people using it for both therapeutic and non-therapeutic purposes,” he added.
The study was published online in Drug and Alcohol Dependence.
Entourage Theory
Cannabis legalization has opened the door to an increased range of medicinal and nonmedicinal uses, but its benefits can be limited by the anxiety and panic some people experience with its use, investigators noted.
Many cannabis plants have been bred to contain higher concentrations of THC, with some dispensaries selling cannabis with more than 20%-30% THC. The plants often include cannabidiol, “minor” cannabinoids, and terpenes, such as D-limonene.
Prior studies pointed to THC as the cause of acute behavioral and psychoactive effects some cannabis users experience. However, a new, untested theory, the “cannabis entourage effect theory,” suggested other components in cannabis, including D-limonene, may contribute to the anxiogenic symptoms.
“We were motivated by scientific publications that hypothesized D-limonene can attenuate the acute anxiogenic effects of cannabis, but for which empirical data did not exist,” Dr. Vandrey said.
Investigators designed a small double-blind, within-subjects crossover study of 20 healthy adults (median age, 26 years; 50% men). About half of participants were Caucasian/non-Hispanic, 30% African American/non-Hispanic, 10% Caucasian/Hispanic, and 10% Asian/non-Hispanic.
All participants completed nine outpatient drug administration sessions, during which they inhaled vaporized D-limonene alone (1 or 5 mg), THC alone (15 or 30 mg), the same doses of THC and D-limonene together, or placebo.
Primary outcomes included subjective drug effects, measured with the Drug Effect Questionnaire (DEQ) and the 20-item state subscale of the State-Trait Anxiety Inventory (STAI-S). Investigators also measured cognitive/psychomotor performance with the Digit Symbol Substitution Task (DSST) and the Paced Serial Addition Task.
Vital signs such as heart rate, systolic blood pressure (SBP), diastolic blood pressure (DBP), and plasma D-limonene and THC concentrations were also tracked.
Participants’ responses were measured at baseline and then an additional nine times after initial exposure over the course of each 6-hour test session. Blood and urine samples were collected from participants before, during, and after each session.
First Evidence
There were no significant differences in outcomes between the D-limonene alone and placebo groups.
Receipt of 15- and 30-mg doses of THC alone was associated with subjective reports of acute cannabis exposure, including cognitive and physiological effects.
A treatment effect was observed for “anxious/nervous” (P < .01), “paranoid” (P < .01), and “heart racing” (P < .0001).
In planned comparisons, ratings of anxiety-like subjective effects qualitatively decreased as D-limonene dose increased, and concurrent administration of 30-mg THC plus 15-mg D-limonene significantly reduced ratings of “anxious/nervous” and “paranoid” on the DEQ compared to 30 mg of THC alone (P < .05).
Findings were similar on the composite score of the STAI-S, and although planned comparisons did not reach the threshold for statistical significance, reductions in anxiety approached significance in the THC plus D-limonene group compared with the THC alone condition (P = .08). The combination group also reported significantly lower subjective ratings of unpleasant drug effects than the THC alone group (P = .03).
In particular, a main effect of treatment was found for the anxious/nervous category on the DEQ (P < .01), as well as the “paranoid” (P < .01) and heart racing (P < .0001) categories.
On the other hand, ratings of anxious/nervous and paranoid categories were significantly lower in the 30-mg THC plus 15-mg D-limonene vs the 30-mg THC alone condition (P < .05, for all).
As for cognition, following drug administration, a significant main effect of treatment was observed for the DSST (P < .05), but no significant differences between THC and THC plus D-limonene combination conditions or between D-limonene alone and placebo were detected.
There were no differences within each THC dose and between D-limonene alone versus placebo conditions. Moreover, there were no main effects of treatment found for SBP or DBP.
The combination condition produced significantly greater concentrations of THC than the THC alone condition (P < .05).
“This study provides the first evidence that there are chemical constituents found naturally in the cannabis plant that can reduce some of the adverse effects of using delta-9-THC,” Dr. Vandrey said.
Although the exact mechanism by which vaporized D-limonene counters the anxiogenic effects of THC is unclear, “our best guess is that D-limonene is producing an anxiolytic effect on its own that is not mediated by cannabinoid receptors,” Dr. Vandrey said.
Significant Impact
Commenting on the research, Joshua Lile, PhD, professor, Department of Behavioral Science, University of Kentucky College of Medicine, Lexington, noted that the study seems to be the first of its kind to study the influence of terpene on THC response.
The research “makes a significant impact on our field,” and is “among the few controlled clinical studies that have demonstrated interactions between THC and other cannabis constituents, supporting the validity of the ‘entourage’ effect,” said Dr. Lile, who was not involved with the current research.
“This work is particularly important, given the unfounded claims sometimes made by the cannabis industry regarding the effects of different cannabis products,” he added.
Also commenting on the study, Ziva Cooper, PhD, professor and director of the UCLA Center for Cannabis and Cannabinoids, University of California Los Angeles, said the findings “have direct implications for improving the safety of cannabis, whether it’s being used for medical or nonmedical purposes, especially in people and patients who do not have experience with cannabis, a group that is at high risk for experiencing anxiety after using cannabis.”
In addition, “an important aspect to this study is that the effects of limonene in reducing anxiety attributed to delta-9-THC were observed at higher concentrations (or doses) than those usually present in the plant,” Dr. Copper said. “This calls for further investigation into new cannabis formulations specifically designed to leverage the potential protective effects of the terpene.”
This research was supported by the National Institute on Drug Abuse. Dr. Vandrey served as a consultant or received honoraria from Mira1a Therapeutics, Inc.; Jazz Pharmaceuticals; Charlotte’s Web; Syqe Medical Ltd.; and WebMD. The other authors’ disclosures are listed on the original paper. Dr. Lile declared no relevant financial relationships. Dr. Cooper reported receiving study drug from Canopy Growth Corp and True Terpenes, study-related materials from Storz & Bickel, and research support from the National Institute on Drug Abuse, National Center for Complementary and Integrative Health, California Department of Cannabis Control, Center for Medicinal Cannabis Research, and California Highway Patrol.
A version of this article appeared on Medscape.com.
From Drug and Alcohol Dependence
‘Difficult Patient’: Stigmatizing Words and Medical Error
This transcript has been edited for clarity.
When I was doing my nephrology training, I had an attending who would write notes that were, well, kind of funny. I remember one time we were seeing a patient whose first name was “Lucky.” He dryly opened his section of the consult note as follows: “This is a 56-year-old woman with an ironic name who presents with acute renal failure.”
As an exhausted renal fellow, I appreciated the bit of color amid the ongoing series of tragedies that was the consult service. But let’s be clear — writing like this in the medical record is not a good idea. It wasn’t a good idea then, when any record might end up disclosed during a malpractice suit, and it’s really not a good idea now, when patients have ready and automated access to all the notes we write about them.
And yet, worse language than that of my attending appears in hospital notes all the time; there is research about this. Specifically, I’m talking about language that does not have high clinical utility but telegraphs the biases of the person writing the note. This is known as “stigmatizing language” and it can be overt or subtle.
For example, a physician wrote “I listed several fictitious medication names and she reported she was taking them.”
This casts suspicions about the patient’s credibility, as does the more subtle statement, “he claims nicotine patches don’t work for him.” Stigmatizing language may cast the patient in a difficult light, like this note: “she persevered on the fact that ... ‘you wouldn’t understand.’ ”
Stay with me.
We are going to start by defining a very sick patient population: those admitted to the hospital and who, within 48 hours, have either been transferred to the intensive care unit or died. Because of the severity of illness in this population we’ve just defined, figuring out whether a diagnostic or other error was made would be extremely high yield; these can mean the difference between life and death.
In a letter appearing in JAMA Internal Medicine, researchers examined a group of more than 2300 patients just like this from 29 hospitals, scouring the medical records for evidence of these types of errors.
Nearly one in four (23.2%) had at least one diagnostic error, which could include a missed physical exam finding, failure to ask a key question on history taking, inadequate testing, and so on.
Understanding why we make these errors is clearly critical to improving care for these patients. The researchers hypothesized that stigmatizing language might lead to errors like this. For example, by demonstrating that you don’t find a patient credible, you may ignore statements that would help make a better diagnosis.
Just over 5% of these patients had evidence of stigmatizing language in their medical notes. Like earlier studies, this language was more common if the patient was Black or had unstable housing.
Critically, stigmatizing language was more likely to be found among those who had diagnostic errors — a rate of 8.2% vs 4.1%. After adjustment for factors like race, the presence of stigmatizing language was associated with roughly a doubling of the risk for diagnostic errors.
Now, I’m all for eliminating stigmatizing language from our medical notes. And, given the increased transparency of all medical notes these days, I expect that we’ll see less of this over time. But of course, the fact that a physician doesn’t write something that disparages the patient does not necessarily mean that they don’t retain that bias. That said, those comments have an effect on all the other team members who care for that patient as well; it sets a tone and can entrench an individual’s bias more broadly. We should strive to eliminate our biases when it comes to caring for patients. But perhaps the second best thing is to work to keep those biases to ourselves.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
When I was doing my nephrology training, I had an attending who would write notes that were, well, kind of funny. I remember one time we were seeing a patient whose first name was “Lucky.” He dryly opened his section of the consult note as follows: “This is a 56-year-old woman with an ironic name who presents with acute renal failure.”
As an exhausted renal fellow, I appreciated the bit of color amid the ongoing series of tragedies that was the consult service. But let’s be clear — writing like this in the medical record is not a good idea. It wasn’t a good idea then, when any record might end up disclosed during a malpractice suit, and it’s really not a good idea now, when patients have ready and automated access to all the notes we write about them.
And yet, worse language than that of my attending appears in hospital notes all the time; there is research about this. Specifically, I’m talking about language that does not have high clinical utility but telegraphs the biases of the person writing the note. This is known as “stigmatizing language” and it can be overt or subtle.
For example, a physician wrote “I listed several fictitious medication names and she reported she was taking them.”
This casts suspicions about the patient’s credibility, as does the more subtle statement, “he claims nicotine patches don’t work for him.” Stigmatizing language may cast the patient in a difficult light, like this note: “she persevered on the fact that ... ‘you wouldn’t understand.’ ”
Stay with me.
We are going to start by defining a very sick patient population: those admitted to the hospital and who, within 48 hours, have either been transferred to the intensive care unit or died. Because of the severity of illness in this population we’ve just defined, figuring out whether a diagnostic or other error was made would be extremely high yield; these can mean the difference between life and death.
In a letter appearing in JAMA Internal Medicine, researchers examined a group of more than 2300 patients just like this from 29 hospitals, scouring the medical records for evidence of these types of errors.
Nearly one in four (23.2%) had at least one diagnostic error, which could include a missed physical exam finding, failure to ask a key question on history taking, inadequate testing, and so on.
Understanding why we make these errors is clearly critical to improving care for these patients. The researchers hypothesized that stigmatizing language might lead to errors like this. For example, by demonstrating that you don’t find a patient credible, you may ignore statements that would help make a better diagnosis.
Just over 5% of these patients had evidence of stigmatizing language in their medical notes. Like earlier studies, this language was more common if the patient was Black or had unstable housing.
Critically, stigmatizing language was more likely to be found among those who had diagnostic errors — a rate of 8.2% vs 4.1%. After adjustment for factors like race, the presence of stigmatizing language was associated with roughly a doubling of the risk for diagnostic errors.
Now, I’m all for eliminating stigmatizing language from our medical notes. And, given the increased transparency of all medical notes these days, I expect that we’ll see less of this over time. But of course, the fact that a physician doesn’t write something that disparages the patient does not necessarily mean that they don’t retain that bias. That said, those comments have an effect on all the other team members who care for that patient as well; it sets a tone and can entrench an individual’s bias more broadly. We should strive to eliminate our biases when it comes to caring for patients. But perhaps the second best thing is to work to keep those biases to ourselves.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
When I was doing my nephrology training, I had an attending who would write notes that were, well, kind of funny. I remember one time we were seeing a patient whose first name was “Lucky.” He dryly opened his section of the consult note as follows: “This is a 56-year-old woman with an ironic name who presents with acute renal failure.”
As an exhausted renal fellow, I appreciated the bit of color amid the ongoing series of tragedies that was the consult service. But let’s be clear — writing like this in the medical record is not a good idea. It wasn’t a good idea then, when any record might end up disclosed during a malpractice suit, and it’s really not a good idea now, when patients have ready and automated access to all the notes we write about them.
And yet, worse language than that of my attending appears in hospital notes all the time; there is research about this. Specifically, I’m talking about language that does not have high clinical utility but telegraphs the biases of the person writing the note. This is known as “stigmatizing language” and it can be overt or subtle.
For example, a physician wrote “I listed several fictitious medication names and she reported she was taking them.”
This casts suspicions about the patient’s credibility, as does the more subtle statement, “he claims nicotine patches don’t work for him.” Stigmatizing language may cast the patient in a difficult light, like this note: “she persevered on the fact that ... ‘you wouldn’t understand.’ ”
Stay with me.
We are going to start by defining a very sick patient population: those admitted to the hospital and who, within 48 hours, have either been transferred to the intensive care unit or died. Because of the severity of illness in this population we’ve just defined, figuring out whether a diagnostic or other error was made would be extremely high yield; these can mean the difference between life and death.
In a letter appearing in JAMA Internal Medicine, researchers examined a group of more than 2300 patients just like this from 29 hospitals, scouring the medical records for evidence of these types of errors.
Nearly one in four (23.2%) had at least one diagnostic error, which could include a missed physical exam finding, failure to ask a key question on history taking, inadequate testing, and so on.
Understanding why we make these errors is clearly critical to improving care for these patients. The researchers hypothesized that stigmatizing language might lead to errors like this. For example, by demonstrating that you don’t find a patient credible, you may ignore statements that would help make a better diagnosis.
Just over 5% of these patients had evidence of stigmatizing language in their medical notes. Like earlier studies, this language was more common if the patient was Black or had unstable housing.
Critically, stigmatizing language was more likely to be found among those who had diagnostic errors — a rate of 8.2% vs 4.1%. After adjustment for factors like race, the presence of stigmatizing language was associated with roughly a doubling of the risk for diagnostic errors.
Now, I’m all for eliminating stigmatizing language from our medical notes. And, given the increased transparency of all medical notes these days, I expect that we’ll see less of this over time. But of course, the fact that a physician doesn’t write something that disparages the patient does not necessarily mean that they don’t retain that bias. That said, those comments have an effect on all the other team members who care for that patient as well; it sets a tone and can entrench an individual’s bias more broadly. We should strive to eliminate our biases when it comes to caring for patients. But perhaps the second best thing is to work to keep those biases to ourselves.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Recently Immunized Febrile Infants Have Low Infection Risk
TOPLINE:
METHODOLOGY:
- Researchers evaluated 508 infants aged 6-12 weeks who presented with a fever of 38 °C or greater at two US military academic emergency departments (EDs) over a span of 4 years.
- The infants were categorized as “recently immunized” if they had received immunizations within 72 hours before ED presentation and “not recently immunized” if they had not. Among the 508 infants, 114 were immunized recently.
- The primary outcome was the prevalence of a serious bacterial infection (SBI), categorized into IBI and non-IBI on the basis of culture and radiography findings.
TAKEAWAY:
- The prevalence of SBI was 3.5% in the recently immunized febrile infants and 13.7% in not recently immunized febrile infants.
- Among the recently immunized infants, the prevalence of SBI was lower in those immunized within the first 24 hours than those immunized more than 24 hours before ED presentation (2% vs 14.3%, respectively).
- Almost all identified SBI cases were of urinary tract infection (UTI), with the only non-UTI case being pneumonia in an infant who exhibited respiratory symptoms within 24 hours of receiving immunization.
IN PRACTICE:
Physicians should discuss the possibilities of a less invasive approach for evaluating recently immunized febrile infants. The study findings support the general recommendation to obtain a urinalysis for all recently immunized infants over 60 days presenting with fever, including those presenting less than 24 hours post immunization.
SOURCE:
This study, led by Kyla Casey, MD, Department of Emergency Medicine, Naval Medical Center San Diego, was published online in The American Journal of Emergency Medicine.
LIMITATIONS:
The small sample size and retrospective design might have resulted in an overestimation of outcomes like IBIs within 24 hours after immunization. As the study was conducted in a specific clinical setting with febrile infants from military medical centers, the findings may have limited generalizability. Moreover, the inclusion of premature infants without age correction for prematurity could have impacted the prevalence of IBIs. Factors like missing vaccination history, healthcare referral patterns, and immunization practices in the military system may have introduced bias.
DISCLOSURE:
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors. The authors had no conflicts of interest to disclose.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers evaluated 508 infants aged 6-12 weeks who presented with a fever of 38 °C or greater at two US military academic emergency departments (EDs) over a span of 4 years.
- The infants were categorized as “recently immunized” if they had received immunizations within 72 hours before ED presentation and “not recently immunized” if they had not. Among the 508 infants, 114 were immunized recently.
- The primary outcome was the prevalence of a serious bacterial infection (SBI), categorized into IBI and non-IBI on the basis of culture and radiography findings.
TAKEAWAY:
- The prevalence of SBI was 3.5% in the recently immunized febrile infants and 13.7% in not recently immunized febrile infants.
- Among the recently immunized infants, the prevalence of SBI was lower in those immunized within the first 24 hours than those immunized more than 24 hours before ED presentation (2% vs 14.3%, respectively).
- Almost all identified SBI cases were of urinary tract infection (UTI), with the only non-UTI case being pneumonia in an infant who exhibited respiratory symptoms within 24 hours of receiving immunization.
IN PRACTICE:
Physicians should discuss the possibilities of a less invasive approach for evaluating recently immunized febrile infants. The study findings support the general recommendation to obtain a urinalysis for all recently immunized infants over 60 days presenting with fever, including those presenting less than 24 hours post immunization.
SOURCE:
This study, led by Kyla Casey, MD, Department of Emergency Medicine, Naval Medical Center San Diego, was published online in The American Journal of Emergency Medicine.
LIMITATIONS:
The small sample size and retrospective design might have resulted in an overestimation of outcomes like IBIs within 24 hours after immunization. As the study was conducted in a specific clinical setting with febrile infants from military medical centers, the findings may have limited generalizability. Moreover, the inclusion of premature infants without age correction for prematurity could have impacted the prevalence of IBIs. Factors like missing vaccination history, healthcare referral patterns, and immunization practices in the military system may have introduced bias.
DISCLOSURE:
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors. The authors had no conflicts of interest to disclose.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers evaluated 508 infants aged 6-12 weeks who presented with a fever of 38 °C or greater at two US military academic emergency departments (EDs) over a span of 4 years.
- The infants were categorized as “recently immunized” if they had received immunizations within 72 hours before ED presentation and “not recently immunized” if they had not. Among the 508 infants, 114 were immunized recently.
- The primary outcome was the prevalence of a serious bacterial infection (SBI), categorized into IBI and non-IBI on the basis of culture and radiography findings.
TAKEAWAY:
- The prevalence of SBI was 3.5% in the recently immunized febrile infants and 13.7% in not recently immunized febrile infants.
- Among the recently immunized infants, the prevalence of SBI was lower in those immunized within the first 24 hours than those immunized more than 24 hours before ED presentation (2% vs 14.3%, respectively).
- Almost all identified SBI cases were of urinary tract infection (UTI), with the only non-UTI case being pneumonia in an infant who exhibited respiratory symptoms within 24 hours of receiving immunization.
IN PRACTICE:
Physicians should discuss the possibilities of a less invasive approach for evaluating recently immunized febrile infants. The study findings support the general recommendation to obtain a urinalysis for all recently immunized infants over 60 days presenting with fever, including those presenting less than 24 hours post immunization.
SOURCE:
This study, led by Kyla Casey, MD, Department of Emergency Medicine, Naval Medical Center San Diego, was published online in The American Journal of Emergency Medicine.
LIMITATIONS:
The small sample size and retrospective design might have resulted in an overestimation of outcomes like IBIs within 24 hours after immunization. As the study was conducted in a specific clinical setting with febrile infants from military medical centers, the findings may have limited generalizability. Moreover, the inclusion of premature infants without age correction for prematurity could have impacted the prevalence of IBIs. Factors like missing vaccination history, healthcare referral patterns, and immunization practices in the military system may have introduced bias.
DISCLOSURE:
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors. The authors had no conflicts of interest to disclose.
A version of this article appeared on Medscape.com.
Sugar Substitutes Satisfy Appetite, Blunt Insulin Response
TOPLINE:
but decrease post-meal insulin and glucose levels in adults with overweight or obesity.
METHODOLOGY:
- In 2023, the World Health Organization issued a conditional recommendation that S&SE should not be used for weight control, apparently due to a lack of evidence for a clear benefit and weak evidence linking S&SE intake with excess weight and poorer health outcomes.
- This randomized crossover trial, conducted in England and France between 2021 and 2022, evaluated the acute (1 day) and repeated (daily for 2 weeks) effects of S&SEs vs sucrose in solid food on appetite and endocrine responses in adults with overweight or obesity.
- Overall, 53 adults (33 women, 20 men; aged 18-60 years) with overweight or obesity consumed biscuits with fruit filling containing either sucrose or reformulated with the S&SEs StRebM or neotame, daily for three 2-week intervention periods separated by a washout period of 14-21 days.
- Participants were required to fast for 12 hours before attending a laboratory session at the beginning (day 1) and end (day 14) of each consumption period.
- The primary endpoint was the composite appetite score, while secondary endpoints included food preferences, postprandial glucose and insulin response, and other satiety-related peptides, such as ghrelin, glucagon-like peptide 1, and pancreatic polypeptide.
TAKEAWAY:
- The composite appetite scores were comparable between the sucrose, StRebM, and neotame groups, with lower appetite suppression observed on day 14 than on day 1 for all three formulations.
- Neotame (P < .001) and StRebM (P < .001) lowered postprandial insulin levels compared with sucrose, while glucose levels saw a decline only with StRebM (and not with neotame) compared with sucrose (P < .05).
- The S&SEs had no effect on satiety levels, as any acute or repeated exposures to StRebM or neotame vs sucrose did not affect the ghrelin and glucagon-like peptide-1 responses.
- Gastrointestinal issues were more frequently reported in the neotame and StRebM groups than in the sucrose group.
IN PRACTICE:
“There is no detrimental impact of replacing sugar with S&SE in these endpoints,” the authors wrote. “Additionally, glucose and insulin responses were blunted after acute and repeated consumption of S&SE-reformulated biscuits, which may confer a benefit for blood glucose control, for example, in individuals at risk of developing type 2 diabetes.”
SOURCE:
This study was led by Catherine Gibbons, School of Psychology, Faculty of Medicine and Health, University of Leeds, England. It was published online in eBioMedicine.
LIMITATIONS:
The reformulated products required the addition of polyol bulking agents (8% maltitol and 8% sorbitol) to match the biscuits in sensory qualities as closely as possible. Gastrointestinal symptoms (initial bloating and flatulence) in the neotame and StRebM formulations may be due to the polyols, classed as low-digestible carbohydrates.
DISCLOSURES:
This study received funding from a European Union Horizon 2020 program, SWEET (Sweeteners and sweetness enhancers: Impact on health, obesity, safety, and sustainability). The authors reported receiving funding and honoraria from the food and beverage industry and trade groups from various entities.
A version of this article appeared on Medscape.com.
TOPLINE:
but decrease post-meal insulin and glucose levels in adults with overweight or obesity.
METHODOLOGY:
- In 2023, the World Health Organization issued a conditional recommendation that S&SE should not be used for weight control, apparently due to a lack of evidence for a clear benefit and weak evidence linking S&SE intake with excess weight and poorer health outcomes.
- This randomized crossover trial, conducted in England and France between 2021 and 2022, evaluated the acute (1 day) and repeated (daily for 2 weeks) effects of S&SEs vs sucrose in solid food on appetite and endocrine responses in adults with overweight or obesity.
- Overall, 53 adults (33 women, 20 men; aged 18-60 years) with overweight or obesity consumed biscuits with fruit filling containing either sucrose or reformulated with the S&SEs StRebM or neotame, daily for three 2-week intervention periods separated by a washout period of 14-21 days.
- Participants were required to fast for 12 hours before attending a laboratory session at the beginning (day 1) and end (day 14) of each consumption period.
- The primary endpoint was the composite appetite score, while secondary endpoints included food preferences, postprandial glucose and insulin response, and other satiety-related peptides, such as ghrelin, glucagon-like peptide 1, and pancreatic polypeptide.
TAKEAWAY:
- The composite appetite scores were comparable between the sucrose, StRebM, and neotame groups, with lower appetite suppression observed on day 14 than on day 1 for all three formulations.
- Neotame (P < .001) and StRebM (P < .001) lowered postprandial insulin levels compared with sucrose, while glucose levels saw a decline only with StRebM (and not with neotame) compared with sucrose (P < .05).
- The S&SEs had no effect on satiety levels, as any acute or repeated exposures to StRebM or neotame vs sucrose did not affect the ghrelin and glucagon-like peptide-1 responses.
- Gastrointestinal issues were more frequently reported in the neotame and StRebM groups than in the sucrose group.
IN PRACTICE:
“There is no detrimental impact of replacing sugar with S&SE in these endpoints,” the authors wrote. “Additionally, glucose and insulin responses were blunted after acute and repeated consumption of S&SE-reformulated biscuits, which may confer a benefit for blood glucose control, for example, in individuals at risk of developing type 2 diabetes.”
SOURCE:
This study was led by Catherine Gibbons, School of Psychology, Faculty of Medicine and Health, University of Leeds, England. It was published online in eBioMedicine.
LIMITATIONS:
The reformulated products required the addition of polyol bulking agents (8% maltitol and 8% sorbitol) to match the biscuits in sensory qualities as closely as possible. Gastrointestinal symptoms (initial bloating and flatulence) in the neotame and StRebM formulations may be due to the polyols, classed as low-digestible carbohydrates.
DISCLOSURES:
This study received funding from a European Union Horizon 2020 program, SWEET (Sweeteners and sweetness enhancers: Impact on health, obesity, safety, and sustainability). The authors reported receiving funding and honoraria from the food and beverage industry and trade groups from various entities.
A version of this article appeared on Medscape.com.
TOPLINE:
but decrease post-meal insulin and glucose levels in adults with overweight or obesity.
METHODOLOGY:
- In 2023, the World Health Organization issued a conditional recommendation that S&SE should not be used for weight control, apparently due to a lack of evidence for a clear benefit and weak evidence linking S&SE intake with excess weight and poorer health outcomes.
- This randomized crossover trial, conducted in England and France between 2021 and 2022, evaluated the acute (1 day) and repeated (daily for 2 weeks) effects of S&SEs vs sucrose in solid food on appetite and endocrine responses in adults with overweight or obesity.
- Overall, 53 adults (33 women, 20 men; aged 18-60 years) with overweight or obesity consumed biscuits with fruit filling containing either sucrose or reformulated with the S&SEs StRebM or neotame, daily for three 2-week intervention periods separated by a washout period of 14-21 days.
- Participants were required to fast for 12 hours before attending a laboratory session at the beginning (day 1) and end (day 14) of each consumption period.
- The primary endpoint was the composite appetite score, while secondary endpoints included food preferences, postprandial glucose and insulin response, and other satiety-related peptides, such as ghrelin, glucagon-like peptide 1, and pancreatic polypeptide.
TAKEAWAY:
- The composite appetite scores were comparable between the sucrose, StRebM, and neotame groups, with lower appetite suppression observed on day 14 than on day 1 for all three formulations.
- Neotame (P < .001) and StRebM (P < .001) lowered postprandial insulin levels compared with sucrose, while glucose levels saw a decline only with StRebM (and not with neotame) compared with sucrose (P < .05).
- The S&SEs had no effect on satiety levels, as any acute or repeated exposures to StRebM or neotame vs sucrose did not affect the ghrelin and glucagon-like peptide-1 responses.
- Gastrointestinal issues were more frequently reported in the neotame and StRebM groups than in the sucrose group.
IN PRACTICE:
“There is no detrimental impact of replacing sugar with S&SE in these endpoints,” the authors wrote. “Additionally, glucose and insulin responses were blunted after acute and repeated consumption of S&SE-reformulated biscuits, which may confer a benefit for blood glucose control, for example, in individuals at risk of developing type 2 diabetes.”
SOURCE:
This study was led by Catherine Gibbons, School of Psychology, Faculty of Medicine and Health, University of Leeds, England. It was published online in eBioMedicine.
LIMITATIONS:
The reformulated products required the addition of polyol bulking agents (8% maltitol and 8% sorbitol) to match the biscuits in sensory qualities as closely as possible. Gastrointestinal symptoms (initial bloating and flatulence) in the neotame and StRebM formulations may be due to the polyols, classed as low-digestible carbohydrates.
DISCLOSURES:
This study received funding from a European Union Horizon 2020 program, SWEET (Sweeteners and sweetness enhancers: Impact on health, obesity, safety, and sustainability). The authors reported receiving funding and honoraria from the food and beverage industry and trade groups from various entities.
A version of this article appeared on Medscape.com.
Children With ASD May Have Earlier Onset of Suicidal Thoughts, Behaviors
, according to a research letter in JAMA Pediatrics.
Suicide rates among all US children ages 10-14 years tripled between 2007 and 2021, becoming the second leading cause of death for this age bracket. Between 2018 and 2021, 315 suicides were reported among US children ages 5 to 11 years.
People with ASD show increased rates of STB, although prevalence estimates vary by study, which led the authors to study the issue.
Lead author Benjamin Joffe Schindel, MD, MPH, a fellow in neurodevelopmental medicine at the Kennedy Krieger Institute in Columbia, Maryland, and colleagues, analyzed responses from 968 caregivers of children ages 8-25 with ASD.
They found the following reported lifetime STB incidence:
- 392 (40.5%) reported wanting to die
- 187 (19.3%) reported wanting to end their own lives
- 72 (7.4%) reported having a suicide plan
Among those answering affirmatively to each of the above questions regarding STB, onset at 8 years or younger was reported in 142 (36.2%); 66 (35.3%); and 13 (18.1%) of the children, respectively. Included in the findings was one suicide attempt by cutting in an 8-year-old child.
Dr. Schindel said though there is no direct comparison with age of these thoughts among the general population, a previous study in 2013 showed that through age 10 prevalence of suicide ideation is very low (< 1%), then increases slowly through age 12 and then more rapidly until age 17.
Disturbing Findings
“The unexpectedly high frequency of STBs among children with ASD who were 8 years or younger is particularly disturbing given the lack of validated suicide risk screening tools and interventions for this age group,” the authors wrote. They added that early start of STB in children with ASD is important as this population has been underrepresented in suicide research and prevention efforts.
The average child age in this study was 13.4; 84.8% were White; and 81% were male. More than half of the children (54.8%) were taking medications for emotional, behavioral, or mood-related issues.
Data were collected from May to October 2017 from responses to the Mental Health and Suicidal Behaviors Questionnaire, an online caregiver-answered survey. The survey was created and distributed by the Interactive Autism Network (IAN), an international autism registry, from 2006 to 2019 with approximately 55, 000 participating families.
Thoughts Come at a ‘Shockingly Young Age’
Suzanne Rybczynski, MD, chief medical officer at East Tennessee Children’s Hospital in Knoxville, who was not part of the research, said the study was small but will help get the message out that “kids start thinking about suicide, especially kids with autism,” at a “shockingly young age.”
The results demonstrate the great demand for studying thoughts and behaviors especially in younger children and in children with neurodiversity — autism or other neurodevelopmental disabilities.
Studying children with ASD in relation to suicidal thoughts is difficult, Dr. Rybczynski said, because the way they think about death and how much is understood about the finality of suicide has not been well studied. It’s also uncertain how well the children understood the questions in this study, she added.
This retrospective study also asked for responses from caregivers who may remember or interpret a child’s thoughts and words differently from the child’s true intent, Dr. Rybczynski said.
“We need more studies like this asking questions to kids directly,” she said, so researchers can figure what children think it means to die.
Current Screening Recommendations
Current recommendations from the American Academy of Pediatrics (AAP) are to screen children universally for suicide risk at age 12 using a validated tool and if there are behavioral health concerns, screen as needed from ages 8 to 12.
This study suggests that screening needs to start earlier, Dr. Rybczynski said. “But we also need to know that we’re asking the right questions” and whether questions might be different for children with different abilities.
Children who are less verbal are often not included in screening. Screening studies often specifically exclude children with neurodisabilities, she explained. Getting these youngsters involved and making appropriate screening available “would be lifesaving,” she said.
“There are no validated (screening) tools down to age 8, which is not to say that some organizations don’t use them, but they’re not validated,” she said.
Dr. Rybczynski pointed out that most of the children were White and male and future work investigating these thoughts in girls and other racial/ethnic groups with ASD will be important as well. In addition, it will be important to revisit the issue post-pandemic with the rise in mental health issues with COVID-19.
Identifying children struggling with thoughts of suicide is the key to preventing tragedy, Dr. Rybczynski said, adding, “All those deaths are avoidable.”
Various study coauthors disclosed ties to the Simons Foundation, the Patient-Centered Outcomes Research Institute, the US Social Security Administration, American Foundation for Suicide Prevention, and Sarepta. No other disclosures were reported. Dr. Rybczynski, who provided commentary on the study, has no relevant financial relationships.
, according to a research letter in JAMA Pediatrics.
Suicide rates among all US children ages 10-14 years tripled between 2007 and 2021, becoming the second leading cause of death for this age bracket. Between 2018 and 2021, 315 suicides were reported among US children ages 5 to 11 years.
People with ASD show increased rates of STB, although prevalence estimates vary by study, which led the authors to study the issue.
Lead author Benjamin Joffe Schindel, MD, MPH, a fellow in neurodevelopmental medicine at the Kennedy Krieger Institute in Columbia, Maryland, and colleagues, analyzed responses from 968 caregivers of children ages 8-25 with ASD.
They found the following reported lifetime STB incidence:
- 392 (40.5%) reported wanting to die
- 187 (19.3%) reported wanting to end their own lives
- 72 (7.4%) reported having a suicide plan
Among those answering affirmatively to each of the above questions regarding STB, onset at 8 years or younger was reported in 142 (36.2%); 66 (35.3%); and 13 (18.1%) of the children, respectively. Included in the findings was one suicide attempt by cutting in an 8-year-old child.
Dr. Schindel said though there is no direct comparison with age of these thoughts among the general population, a previous study in 2013 showed that through age 10 prevalence of suicide ideation is very low (< 1%), then increases slowly through age 12 and then more rapidly until age 17.
Disturbing Findings
“The unexpectedly high frequency of STBs among children with ASD who were 8 years or younger is particularly disturbing given the lack of validated suicide risk screening tools and interventions for this age group,” the authors wrote. They added that early start of STB in children with ASD is important as this population has been underrepresented in suicide research and prevention efforts.
The average child age in this study was 13.4; 84.8% were White; and 81% were male. More than half of the children (54.8%) were taking medications for emotional, behavioral, or mood-related issues.
Data were collected from May to October 2017 from responses to the Mental Health and Suicidal Behaviors Questionnaire, an online caregiver-answered survey. The survey was created and distributed by the Interactive Autism Network (IAN), an international autism registry, from 2006 to 2019 with approximately 55, 000 participating families.
Thoughts Come at a ‘Shockingly Young Age’
Suzanne Rybczynski, MD, chief medical officer at East Tennessee Children’s Hospital in Knoxville, who was not part of the research, said the study was small but will help get the message out that “kids start thinking about suicide, especially kids with autism,” at a “shockingly young age.”
The results demonstrate the great demand for studying thoughts and behaviors especially in younger children and in children with neurodiversity — autism or other neurodevelopmental disabilities.
Studying children with ASD in relation to suicidal thoughts is difficult, Dr. Rybczynski said, because the way they think about death and how much is understood about the finality of suicide has not been well studied. It’s also uncertain how well the children understood the questions in this study, she added.
This retrospective study also asked for responses from caregivers who may remember or interpret a child’s thoughts and words differently from the child’s true intent, Dr. Rybczynski said.
“We need more studies like this asking questions to kids directly,” she said, so researchers can figure what children think it means to die.
Current Screening Recommendations
Current recommendations from the American Academy of Pediatrics (AAP) are to screen children universally for suicide risk at age 12 using a validated tool and if there are behavioral health concerns, screen as needed from ages 8 to 12.
This study suggests that screening needs to start earlier, Dr. Rybczynski said. “But we also need to know that we’re asking the right questions” and whether questions might be different for children with different abilities.
Children who are less verbal are often not included in screening. Screening studies often specifically exclude children with neurodisabilities, she explained. Getting these youngsters involved and making appropriate screening available “would be lifesaving,” she said.
“There are no validated (screening) tools down to age 8, which is not to say that some organizations don’t use them, but they’re not validated,” she said.
Dr. Rybczynski pointed out that most of the children were White and male and future work investigating these thoughts in girls and other racial/ethnic groups with ASD will be important as well. In addition, it will be important to revisit the issue post-pandemic with the rise in mental health issues with COVID-19.
Identifying children struggling with thoughts of suicide is the key to preventing tragedy, Dr. Rybczynski said, adding, “All those deaths are avoidable.”
Various study coauthors disclosed ties to the Simons Foundation, the Patient-Centered Outcomes Research Institute, the US Social Security Administration, American Foundation for Suicide Prevention, and Sarepta. No other disclosures were reported. Dr. Rybczynski, who provided commentary on the study, has no relevant financial relationships.
, according to a research letter in JAMA Pediatrics.
Suicide rates among all US children ages 10-14 years tripled between 2007 and 2021, becoming the second leading cause of death for this age bracket. Between 2018 and 2021, 315 suicides were reported among US children ages 5 to 11 years.
People with ASD show increased rates of STB, although prevalence estimates vary by study, which led the authors to study the issue.
Lead author Benjamin Joffe Schindel, MD, MPH, a fellow in neurodevelopmental medicine at the Kennedy Krieger Institute in Columbia, Maryland, and colleagues, analyzed responses from 968 caregivers of children ages 8-25 with ASD.
They found the following reported lifetime STB incidence:
- 392 (40.5%) reported wanting to die
- 187 (19.3%) reported wanting to end their own lives
- 72 (7.4%) reported having a suicide plan
Among those answering affirmatively to each of the above questions regarding STB, onset at 8 years or younger was reported in 142 (36.2%); 66 (35.3%); and 13 (18.1%) of the children, respectively. Included in the findings was one suicide attempt by cutting in an 8-year-old child.
Dr. Schindel said though there is no direct comparison with age of these thoughts among the general population, a previous study in 2013 showed that through age 10 prevalence of suicide ideation is very low (< 1%), then increases slowly through age 12 and then more rapidly until age 17.
Disturbing Findings
“The unexpectedly high frequency of STBs among children with ASD who were 8 years or younger is particularly disturbing given the lack of validated suicide risk screening tools and interventions for this age group,” the authors wrote. They added that early start of STB in children with ASD is important as this population has been underrepresented in suicide research and prevention efforts.
The average child age in this study was 13.4; 84.8% were White; and 81% were male. More than half of the children (54.8%) were taking medications for emotional, behavioral, or mood-related issues.
Data were collected from May to October 2017 from responses to the Mental Health and Suicidal Behaviors Questionnaire, an online caregiver-answered survey. The survey was created and distributed by the Interactive Autism Network (IAN), an international autism registry, from 2006 to 2019 with approximately 55, 000 participating families.
Thoughts Come at a ‘Shockingly Young Age’
Suzanne Rybczynski, MD, chief medical officer at East Tennessee Children’s Hospital in Knoxville, who was not part of the research, said the study was small but will help get the message out that “kids start thinking about suicide, especially kids with autism,” at a “shockingly young age.”
The results demonstrate the great demand for studying thoughts and behaviors especially in younger children and in children with neurodiversity — autism or other neurodevelopmental disabilities.
Studying children with ASD in relation to suicidal thoughts is difficult, Dr. Rybczynski said, because the way they think about death and how much is understood about the finality of suicide has not been well studied. It’s also uncertain how well the children understood the questions in this study, she added.
This retrospective study also asked for responses from caregivers who may remember or interpret a child’s thoughts and words differently from the child’s true intent, Dr. Rybczynski said.
“We need more studies like this asking questions to kids directly,” she said, so researchers can figure what children think it means to die.
Current Screening Recommendations
Current recommendations from the American Academy of Pediatrics (AAP) are to screen children universally for suicide risk at age 12 using a validated tool and if there are behavioral health concerns, screen as needed from ages 8 to 12.
This study suggests that screening needs to start earlier, Dr. Rybczynski said. “But we also need to know that we’re asking the right questions” and whether questions might be different for children with different abilities.
Children who are less verbal are often not included in screening. Screening studies often specifically exclude children with neurodisabilities, she explained. Getting these youngsters involved and making appropriate screening available “would be lifesaving,” she said.
“There are no validated (screening) tools down to age 8, which is not to say that some organizations don’t use them, but they’re not validated,” she said.
Dr. Rybczynski pointed out that most of the children were White and male and future work investigating these thoughts in girls and other racial/ethnic groups with ASD will be important as well. In addition, it will be important to revisit the issue post-pandemic with the rise in mental health issues with COVID-19.
Identifying children struggling with thoughts of suicide is the key to preventing tragedy, Dr. Rybczynski said, adding, “All those deaths are avoidable.”
Various study coauthors disclosed ties to the Simons Foundation, the Patient-Centered Outcomes Research Institute, the US Social Security Administration, American Foundation for Suicide Prevention, and Sarepta. No other disclosures were reported. Dr. Rybczynski, who provided commentary on the study, has no relevant financial relationships.
FROM JAMA PEDIATRICS
The Rise of Positive Psychiatry (and How Pediatrics Can Join the Effort)
Psychiatry, like all medical disciplines, changes over time. For many decades, psychiatrists were primarily psychotherapists. As medications slowly became available, these became a second tool for treatment — so much so that by the 21st century many, if not most, psychiatrists saw themselves primarily as psychopharmacologists and diagnosticians who were skilled at identifying various forms of mental illness and using medications in the hopes of inducing a clinically meaningful “response” in symptoms. While still belonging to the umbrella category of a mental health professional, more and more psychiatrists trained and practiced as mental illness professionals.
Slowly, however, there have been stirrings within the field by many who have found the identity of the psychiatrist as a “prescriber” to be too narrow, and the current “med check” model of treatment too confining. This change was partly inspired by our colleagues in clinical psychology who were challenged in the 1990s by then American Psychological Association President Martin Seligman, PhD, to develop knowledge and expertise not only in alleviating mental suffering but also in promoting true mental well-being, a construct that still was often vaguely defined. One framework of well-being that was advanced at the time was the PERMA model, representing the five well-being dimensions of Positive emotions, Engagement, Relationships, Meaning, and Accomplishment.1
While there have always been those in psychiatry who have advocated for a broad emphasis that incorporates the full spectrum of mental health, there has been a surge of interest in the past 10-15 years, urging a focus on well-being and the tools that can help a person achieve it. This trend has variably been referred to as positive psychiatry, lifestyle psychiatry, and other terms.2 As one might expect, child and adolescent psychiatry has been particularly fertile ground for such principles, and models such as the Vermont Family Based Approach have expanded the concept beyond the individual to the family and even community.3
It is important to note here that embracing the concept of well-being in treatment does not in any way require one to abandon the idea that genetic or environmental factors can lead to negative outcomes in brain development, nor does it mandate that one leaves behind important treatment modalities such as traditional psychotherapy and medication treatment. Further, this approach should not be confused with some “wellness” activities that offer quick fixes and lack scientific rigor. Positive psychiatry does, however, offer a third pathway to advance positive emotional behavioral growth, namely through health promotion activities ranging from exercise to good nutrition to positive parenting in ways that have been shown to benefit both those who are already doing fairly well as well as those who are actively struggling with significant psychiatric disorders.4
Primary care clinicians already have extensive familiarity talking about these kinds of health promoting activities with families. That said, it’s been my observation from many years of doing consultations and reviewing notes that these conversations happen almost exclusively during well-check visits and can get forgotten when a child presents with emotional behavioral challenges.
So how can the primary care clinician who is interested in more fully incorporating the burgeoning science on well-being work these principles into routine practice? Here are three suggestions.
Ask Some New Questions
It’s difficult to treat things that aren’t assessed. To best incorporate true mental health within one’s work with families, it can be very helpful to expand the regular questions one asks to include those that address some of the PERMA and health promotion areas described above. Some examples could include the following:
- Hopes. What would a perfect life look like for you when you’re older?
- Connection. Is there anything that you just love doing, so much so that time sometimes just seems to go away?
- Strengths. What are you good at? What good things would your friends say about you?
- Parenting. What are you most proud of as a parent, and where are your biggest challenges?
- Nutrition. What does a typical school day breakfast look like for you?
- Screens. Do you have any restrictions related to what you do on screens?
- Sleep. Tell me about your typical bedtime routine.
Add Some New Interventions
Counseling and medications can be powerful ways to bring improvement in a child’s life, but thinking about health promotion opens up a whole new avenue for intervention. This domain includes areas like physical activity, nutrition, sleep practices, parenting, participation in music and the arts, practicing kindness towards others, and mindfulness, among others.
For someone newly diagnosed with ADHD, for example, consider expanding your treatment plan to include not only medications but also specific guidance to exercise more, limit screen usage, practice good bedtime routines, eat a real breakfast, and reduce the helicopter parenting. Monitor these areas over time.
Another example relates to common sleep problems. Before making that melatonin recommendation, ask yourself if you understand what is happening in that child’s environment at night. Are they allowed to play video games until 2 a.m.? Are they taking naps during the day because they have nothing to do? Are they downing caffeinated drinks with dinner? Does the child get zero physical activity outside of the PE class? Maybe you still will need the melatonin, but perhaps other areas need to be addressed first.
Find Some New Colleagues
While it can be challenging sometimes to find anyone in mental health who sees new patients, there is value is finding out the approach and methodology that psychiatric clinicians and therapists apply in their practice. Working collaboratively with those who value a well-being orientation and who can work productively with the whole family to increase health promotion can yield benefits for a patient’s long-term physical and mental health.
The renewed interest and attention on well-being and health promotion activities that can optimize brain growth are a welcome and overdue development in mental health treatment. Pediatricians and other primary care clinicians can be a critical part of this growing initiative by gaining knowledge about youth well-being, applying this knowledge in day-to-day practice, and working collaboratively with those who share a similar perspective.
Dr. Rettew is a child & adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Oregon. He is on the psychiatry faculty at Oregon Health & Science University. You can follow him on Facebook and X @PediPsych. His latest book is Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.
References
1. Seligman, MEP. Flourish: a visionary new understanding of happiness and well-being. New York: Simon & Schuster; 2011.
2. Jeste DV, Palmer BW. (Eds.). Positive psychiatry: a clinical handbook. Washington DC: American Psychiatric Publishing; 2015. doi: 10.1176/appi.books.9781615370818.
3. Hudziak J, Ivanova MY. The Vermont family based approach: Family based health promotion, illness prevention, and intervention. Child Adolesc Psychiatr Clin N Am. 2016 Apr;25(2):167-78. doi: 10.1016/j.chc.2015.11.002.
4. Rettew DC. Incorporating positive psychiatry with children and adolescents. Current Psychiatry. 2022 November;21(11):12-16,45. doi: 10.12788/cp.0303.
Psychiatry, like all medical disciplines, changes over time. For many decades, psychiatrists were primarily psychotherapists. As medications slowly became available, these became a second tool for treatment — so much so that by the 21st century many, if not most, psychiatrists saw themselves primarily as psychopharmacologists and diagnosticians who were skilled at identifying various forms of mental illness and using medications in the hopes of inducing a clinically meaningful “response” in symptoms. While still belonging to the umbrella category of a mental health professional, more and more psychiatrists trained and practiced as mental illness professionals.
Slowly, however, there have been stirrings within the field by many who have found the identity of the psychiatrist as a “prescriber” to be too narrow, and the current “med check” model of treatment too confining. This change was partly inspired by our colleagues in clinical psychology who were challenged in the 1990s by then American Psychological Association President Martin Seligman, PhD, to develop knowledge and expertise not only in alleviating mental suffering but also in promoting true mental well-being, a construct that still was often vaguely defined. One framework of well-being that was advanced at the time was the PERMA model, representing the five well-being dimensions of Positive emotions, Engagement, Relationships, Meaning, and Accomplishment.1
While there have always been those in psychiatry who have advocated for a broad emphasis that incorporates the full spectrum of mental health, there has been a surge of interest in the past 10-15 years, urging a focus on well-being and the tools that can help a person achieve it. This trend has variably been referred to as positive psychiatry, lifestyle psychiatry, and other terms.2 As one might expect, child and adolescent psychiatry has been particularly fertile ground for such principles, and models such as the Vermont Family Based Approach have expanded the concept beyond the individual to the family and even community.3
It is important to note here that embracing the concept of well-being in treatment does not in any way require one to abandon the idea that genetic or environmental factors can lead to negative outcomes in brain development, nor does it mandate that one leaves behind important treatment modalities such as traditional psychotherapy and medication treatment. Further, this approach should not be confused with some “wellness” activities that offer quick fixes and lack scientific rigor. Positive psychiatry does, however, offer a third pathway to advance positive emotional behavioral growth, namely through health promotion activities ranging from exercise to good nutrition to positive parenting in ways that have been shown to benefit both those who are already doing fairly well as well as those who are actively struggling with significant psychiatric disorders.4
Primary care clinicians already have extensive familiarity talking about these kinds of health promoting activities with families. That said, it’s been my observation from many years of doing consultations and reviewing notes that these conversations happen almost exclusively during well-check visits and can get forgotten when a child presents with emotional behavioral challenges.
So how can the primary care clinician who is interested in more fully incorporating the burgeoning science on well-being work these principles into routine practice? Here are three suggestions.
Ask Some New Questions
It’s difficult to treat things that aren’t assessed. To best incorporate true mental health within one’s work with families, it can be very helpful to expand the regular questions one asks to include those that address some of the PERMA and health promotion areas described above. Some examples could include the following:
- Hopes. What would a perfect life look like for you when you’re older?
- Connection. Is there anything that you just love doing, so much so that time sometimes just seems to go away?
- Strengths. What are you good at? What good things would your friends say about you?
- Parenting. What are you most proud of as a parent, and where are your biggest challenges?
- Nutrition. What does a typical school day breakfast look like for you?
- Screens. Do you have any restrictions related to what you do on screens?
- Sleep. Tell me about your typical bedtime routine.
Add Some New Interventions
Counseling and medications can be powerful ways to bring improvement in a child’s life, but thinking about health promotion opens up a whole new avenue for intervention. This domain includes areas like physical activity, nutrition, sleep practices, parenting, participation in music and the arts, practicing kindness towards others, and mindfulness, among others.
For someone newly diagnosed with ADHD, for example, consider expanding your treatment plan to include not only medications but also specific guidance to exercise more, limit screen usage, practice good bedtime routines, eat a real breakfast, and reduce the helicopter parenting. Monitor these areas over time.
Another example relates to common sleep problems. Before making that melatonin recommendation, ask yourself if you understand what is happening in that child’s environment at night. Are they allowed to play video games until 2 a.m.? Are they taking naps during the day because they have nothing to do? Are they downing caffeinated drinks with dinner? Does the child get zero physical activity outside of the PE class? Maybe you still will need the melatonin, but perhaps other areas need to be addressed first.
Find Some New Colleagues
While it can be challenging sometimes to find anyone in mental health who sees new patients, there is value is finding out the approach and methodology that psychiatric clinicians and therapists apply in their practice. Working collaboratively with those who value a well-being orientation and who can work productively with the whole family to increase health promotion can yield benefits for a patient’s long-term physical and mental health.
The renewed interest and attention on well-being and health promotion activities that can optimize brain growth are a welcome and overdue development in mental health treatment. Pediatricians and other primary care clinicians can be a critical part of this growing initiative by gaining knowledge about youth well-being, applying this knowledge in day-to-day practice, and working collaboratively with those who share a similar perspective.
Dr. Rettew is a child & adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Oregon. He is on the psychiatry faculty at Oregon Health & Science University. You can follow him on Facebook and X @PediPsych. His latest book is Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.
References
1. Seligman, MEP. Flourish: a visionary new understanding of happiness and well-being. New York: Simon & Schuster; 2011.
2. Jeste DV, Palmer BW. (Eds.). Positive psychiatry: a clinical handbook. Washington DC: American Psychiatric Publishing; 2015. doi: 10.1176/appi.books.9781615370818.
3. Hudziak J, Ivanova MY. The Vermont family based approach: Family based health promotion, illness prevention, and intervention. Child Adolesc Psychiatr Clin N Am. 2016 Apr;25(2):167-78. doi: 10.1016/j.chc.2015.11.002.
4. Rettew DC. Incorporating positive psychiatry with children and adolescents. Current Psychiatry. 2022 November;21(11):12-16,45. doi: 10.12788/cp.0303.
Psychiatry, like all medical disciplines, changes over time. For many decades, psychiatrists were primarily psychotherapists. As medications slowly became available, these became a second tool for treatment — so much so that by the 21st century many, if not most, psychiatrists saw themselves primarily as psychopharmacologists and diagnosticians who were skilled at identifying various forms of mental illness and using medications in the hopes of inducing a clinically meaningful “response” in symptoms. While still belonging to the umbrella category of a mental health professional, more and more psychiatrists trained and practiced as mental illness professionals.
Slowly, however, there have been stirrings within the field by many who have found the identity of the psychiatrist as a “prescriber” to be too narrow, and the current “med check” model of treatment too confining. This change was partly inspired by our colleagues in clinical psychology who were challenged in the 1990s by then American Psychological Association President Martin Seligman, PhD, to develop knowledge and expertise not only in alleviating mental suffering but also in promoting true mental well-being, a construct that still was often vaguely defined. One framework of well-being that was advanced at the time was the PERMA model, representing the five well-being dimensions of Positive emotions, Engagement, Relationships, Meaning, and Accomplishment.1
While there have always been those in psychiatry who have advocated for a broad emphasis that incorporates the full spectrum of mental health, there has been a surge of interest in the past 10-15 years, urging a focus on well-being and the tools that can help a person achieve it. This trend has variably been referred to as positive psychiatry, lifestyle psychiatry, and other terms.2 As one might expect, child and adolescent psychiatry has been particularly fertile ground for such principles, and models such as the Vermont Family Based Approach have expanded the concept beyond the individual to the family and even community.3
It is important to note here that embracing the concept of well-being in treatment does not in any way require one to abandon the idea that genetic or environmental factors can lead to negative outcomes in brain development, nor does it mandate that one leaves behind important treatment modalities such as traditional psychotherapy and medication treatment. Further, this approach should not be confused with some “wellness” activities that offer quick fixes and lack scientific rigor. Positive psychiatry does, however, offer a third pathway to advance positive emotional behavioral growth, namely through health promotion activities ranging from exercise to good nutrition to positive parenting in ways that have been shown to benefit both those who are already doing fairly well as well as those who are actively struggling with significant psychiatric disorders.4
Primary care clinicians already have extensive familiarity talking about these kinds of health promoting activities with families. That said, it’s been my observation from many years of doing consultations and reviewing notes that these conversations happen almost exclusively during well-check visits and can get forgotten when a child presents with emotional behavioral challenges.
So how can the primary care clinician who is interested in more fully incorporating the burgeoning science on well-being work these principles into routine practice? Here are three suggestions.
Ask Some New Questions
It’s difficult to treat things that aren’t assessed. To best incorporate true mental health within one’s work with families, it can be very helpful to expand the regular questions one asks to include those that address some of the PERMA and health promotion areas described above. Some examples could include the following:
- Hopes. What would a perfect life look like for you when you’re older?
- Connection. Is there anything that you just love doing, so much so that time sometimes just seems to go away?
- Strengths. What are you good at? What good things would your friends say about you?
- Parenting. What are you most proud of as a parent, and where are your biggest challenges?
- Nutrition. What does a typical school day breakfast look like for you?
- Screens. Do you have any restrictions related to what you do on screens?
- Sleep. Tell me about your typical bedtime routine.
Add Some New Interventions
Counseling and medications can be powerful ways to bring improvement in a child’s life, but thinking about health promotion opens up a whole new avenue for intervention. This domain includes areas like physical activity, nutrition, sleep practices, parenting, participation in music and the arts, practicing kindness towards others, and mindfulness, among others.
For someone newly diagnosed with ADHD, for example, consider expanding your treatment plan to include not only medications but also specific guidance to exercise more, limit screen usage, practice good bedtime routines, eat a real breakfast, and reduce the helicopter parenting. Monitor these areas over time.
Another example relates to common sleep problems. Before making that melatonin recommendation, ask yourself if you understand what is happening in that child’s environment at night. Are they allowed to play video games until 2 a.m.? Are they taking naps during the day because they have nothing to do? Are they downing caffeinated drinks with dinner? Does the child get zero physical activity outside of the PE class? Maybe you still will need the melatonin, but perhaps other areas need to be addressed first.
Find Some New Colleagues
While it can be challenging sometimes to find anyone in mental health who sees new patients, there is value is finding out the approach and methodology that psychiatric clinicians and therapists apply in their practice. Working collaboratively with those who value a well-being orientation and who can work productively with the whole family to increase health promotion can yield benefits for a patient’s long-term physical and mental health.
The renewed interest and attention on well-being and health promotion activities that can optimize brain growth are a welcome and overdue development in mental health treatment. Pediatricians and other primary care clinicians can be a critical part of this growing initiative by gaining knowledge about youth well-being, applying this knowledge in day-to-day practice, and working collaboratively with those who share a similar perspective.
Dr. Rettew is a child & adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Oregon. He is on the psychiatry faculty at Oregon Health & Science University. You can follow him on Facebook and X @PediPsych. His latest book is Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.
References
1. Seligman, MEP. Flourish: a visionary new understanding of happiness and well-being. New York: Simon & Schuster; 2011.
2. Jeste DV, Palmer BW. (Eds.). Positive psychiatry: a clinical handbook. Washington DC: American Psychiatric Publishing; 2015. doi: 10.1176/appi.books.9781615370818.
3. Hudziak J, Ivanova MY. The Vermont family based approach: Family based health promotion, illness prevention, and intervention. Child Adolesc Psychiatr Clin N Am. 2016 Apr;25(2):167-78. doi: 10.1016/j.chc.2015.11.002.
4. Rettew DC. Incorporating positive psychiatry with children and adolescents. Current Psychiatry. 2022 November;21(11):12-16,45. doi: 10.12788/cp.0303.
Worldwide Uptick in Invasive Group A Streptococcus Disease Post Pandemic — What Should We Know?
Invasive group A streptococcus (iGAS) infections are rare (4-9 cases/100,000 US population annually) but potentially devastating (approximately 2,300 deaths annually in US), and affect all ages. Cases increase in winter-spring, paralleling the “season” of increased noninvasive GAS, e.g., pharyngitis and scarlet fever. iGAS case rates are lower in children than adults. That said, one well-known pediatric iGAS scenario has been deep cellulitis and necrotizing fasciitis during the healing phase of varicella. Other forms of iGAS include bacteremia, pneumonia (particularly when empyema is present), lymphangitis, erysipelas, and toxic shock syndrome. iGAS can occur with/after influenza but has also occurred concurrently with other viral respiratory infections.
Persons with underlying conditions (cancer or immune compromised status; chronic diseases of the heart, kidney or lung; diabetes mellitus) are at higher risk. Other subpopulations at risk for iGAS are illicit drug users, the elderly, homeless persons, nursing home residents, American Indian persons, and Alaska Native persons. Most experts feel that highly toxigenic strains of GAS are responsible for most iGAS. Indeed, most iGAS isolates produce (sometimes hyper-produce) superantigens that cause exaggerated innate immune responses, higher levels of inflammation, and often times tissue destruction, e.g., “flesh eating bacteria.” And who can forget that Jim Henson, creator of the Muppets, died of iGAS?
But why discuss iGAS in 2024? The pattern for iGAS has fluctuated more than usual in the last decade. So much so that the recent upsurge has caught the collective eye of the lay press. So, patients and friends may have questions about why and how iGAS is increasing lately. The bottom line is that no one knows for sure. However, the most recent 2 years of uptick may reflect GAS circulating at relatively high levels even when taking into account that GAS season occurs in winter-spring most years. Yet it seems likely that additional factors may have played a role in the fluctuations noted this past decade, e.g., temporary changes in societal behavior, a new GAS strain with over two dozen mutations, and possibly rapid waning of protection against GAS exotoxins.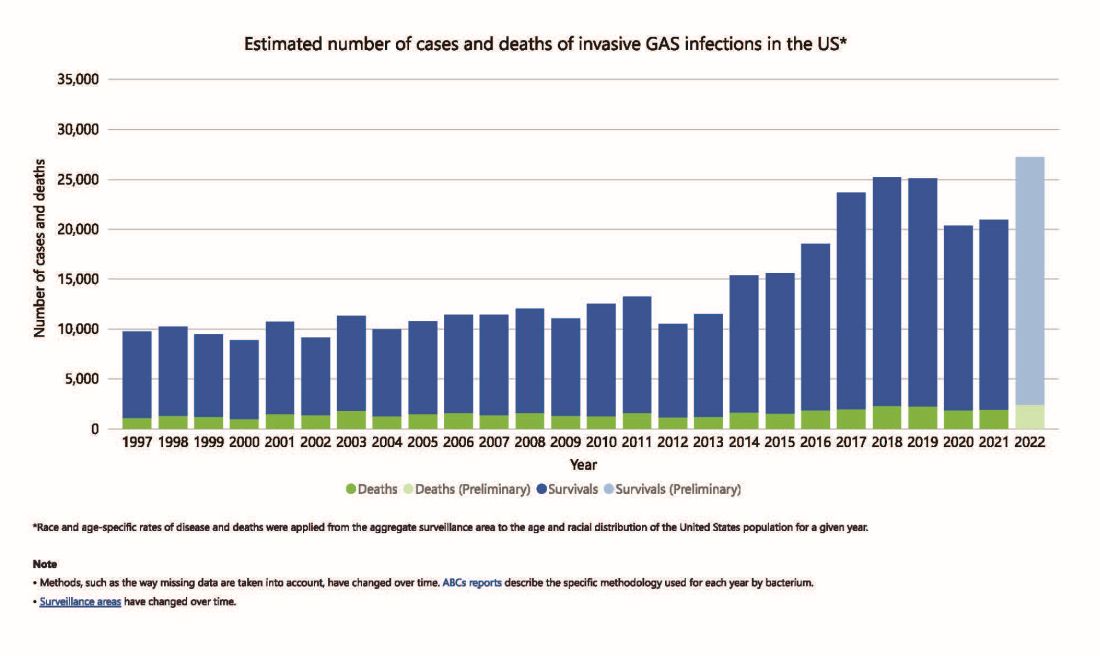
Social Behavior Factor
The SARS-CoV-2 pandemic brought extremes of disease and death to the world and dramatic changes in social behavior. A byproduct was dramatic decreases in nearly all infectious diseases, with numerous reports of near absence of many respiratory and gastrointestinal viruses in the 2020-2021 seasons. Interestingly, we did not see a drop in human rhinovirus infections, justifying its nickname as the cockroach of viruses. Reports also emerged about drops in bacterial diseases during 2020-2021 (although not so much for STIs), including noninvasive and invasive GAS disease, and also GAS-associated deaths (lowest since 2016).1 The drop in iGAS during social restrictions makes sense because GAS is spread by direct contact with infected persons or their secretions, and social contact had dramatically decreased particularly in the first 6 months of the pandemic.
However, since 2022 and the return to “normal” social behaviors, both viral diseases (e.g., RSV, influenza, and Norovirus), and some bacterial diseases have rebounded. That said, something else must be contributing, because iGAS rates had increased 4-5 years pre pandemic. In fact, the fluctuating pattern included “normal” annual rates in the early 2000s rising in ~2015 followed by the explainable pandemic drop (by nearly 25%), and not-too-unexpected 2-year postpandemic rise. But interestingly enough, the rebound is higher than might be expected for iGAS and children were overrepresented in first year’s rise (2022 rate for pediatric iGAS was the highest since 1997) while those older than 65 were overrepresented in second year (2023).1
Emergence of M1UK
One potential factor for the prepandemic rise in iGAS infections worldwide is the emergence and worldwide spread of a new GAS emm type variant designated M1UK.2 GAS isolates can be typed into categories designated as emm types based on DNA sequence. There are more than 240 emm types, with 6 being most common — M1, M3, and M28 (each up to 20% of GAS isolates) and M12, M82, and M89 (each up to 10%). M1, M3 and M28 have also been particularly associated with invasive disease. While emm types vary year to year and region by region, the overall emm type distribution among iGAS isolates in the United States had not been unusual since the turn of the century and the US M1 strain was the same as that which had been predominant worldwide (designated M1GLOBAL). This new M1UK sublineage had emerged around 2010 and had been increasing pre pandemic. The M1UK sequence contained a specific set of 27 SNPs (single nucleoside polymorphisms, i.e., single base mutations) and was associated with an uptick in scarlet fever in the United Kingdom starting around 2010. Its prevalence increased up to around 2015 while spreading internationally. It also had enhanced expression of SpeA, a phage-encoded superantigen. Some of the M1UK mutations also appear to alter GAS metabolic processes to allow better survival (better “fitness”) compared with other GAS. So, a more virulent hardier GAS had arisen and seems a reasonable candidate for contributing to the increased iGAS rates.
Waning Antibody to GAS As Potential Factor in Rebound
No consensus exists on correlates of protection from iGAS. However, adults seem to have less noninvasive GAS than children. One potential reason is that frequent GAS re-exposure, regardless of whether disease results, likely boosts anti-GAS antibodies. Pandemic social restrictions temporarily prevented such boosts. In children with developing antibody repertoires, anti-GAS antibodies may have waned below protective levels faster during a year without frequent boosting. Thus, children were iGAS susceptible soon after pandemic restrictions were dropped (2022). Increased iGAS rates in the elderly in 2023 may have occurred because of diminished GAS exposures accelerating immune senescence with anti-GAS antibodies dropping, but less quickly than in children. These speculations are simply hypotheses until future studies can test them.
All that said, how do we use information on increased iGAS in our daily practices? In addition to standard preventive strategies for viral coinfections (e.g., varicella and influenza vaccine), reminding families about rigorous attention to wound care is the one high-risk scenario we have not yet discussed. During 2024, a time of expected increased prevalence of iGAS, early wound care needs to be fastidious. Further, share warning signs with families (e.g., rapidly expanding painful erythema), “streaks” ascending from extremity wounds, fever and a highly painful wound, darkening almost purple color within cellulitis or soft tissue infection, or loss of sensation in the middle of an otherwise painful soft tissue infection. These presentations require immediate medical attention.
If such a patient presents, the Centers for Disease Control and Prevention (CDC) recommends admission along with blood and, where possible, wound cultures. If in the context of pneumonia with pleural effusion, culturing pleural fluid is also important. Remember, leading edge cultures are not often positive for GAS, seemingly because GAS exotoxins are found at erythema’s leading edge, not the bacteria. The bacteria are somewhere more central in the inflammatory process. Despite not being prominent among recent iGAS cases, another scenario that could sneak up on you is the infected surgical wound as nascent iGAS.
Finally, remember that nationally increasing numbers of iGAS isolates are resistant to erythromycin and clindamycin, the latter usually recommended to reduce tissue damage in iGAS.3 So, it is important to be aware of susceptibility patterns in your locale and consider an ID consultation. My hope is that you do not see an iGAS case this year, but we all need to remain alert. With a high index of suspicion and rapid diagnosis, you can minimize long-term sequelae and potential fatalities.
While it is too early to tell how the rest of 2024 will turn out, preliminary indications are that GAS is circulating at higher than usual levels (30%-35% GAS positive throat swabs in early April 2024 in Kansas City area) and iGAS rates will likely also be relatively high, particularly if Ontario, Canada, data are any indication.4 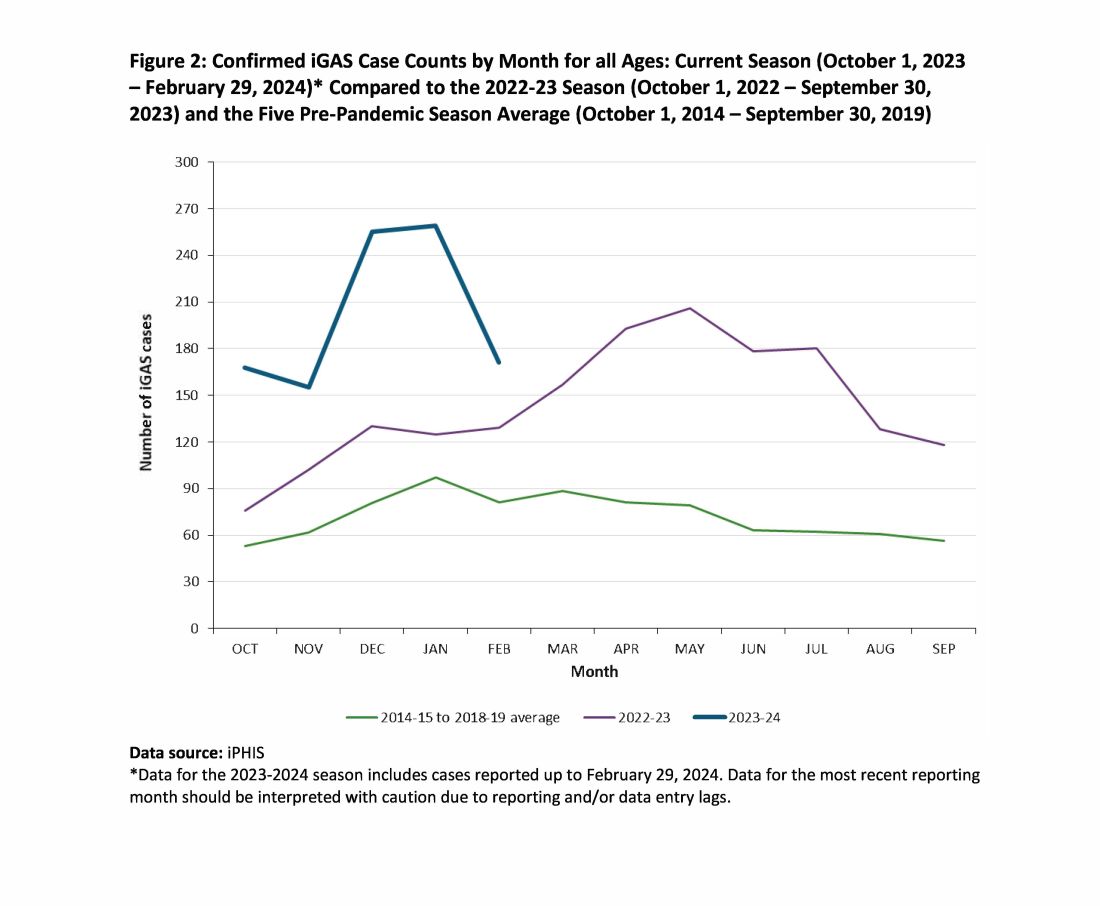
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. Current Group A Strep Activity, Centers for Disease Control and Prevention. April 2024. CDC webpage on current invasive GAS disease. April 2024.
2. Li Y et al. Expansion of Invasive Group A Streptococcus M1UK Lineage in Active Bacterial Core Surveillance, United States, 2019-2021 Emerg Infect Dis. 2023;29(10):2116-2120. doi: 10.3201/eid2910.230675.
3. Andreoni F et al. Clindamycin Affects Group A Streptococcus Virulence Factors and Improves Clinical Outcome. J Infect Dis. 2017 Jan 15;215(2):269-277. doi: 10.1093/infdis/jiw229.
4. Group A Streptococcal Disease, Invasive (iGAS), Public Health Ontario.
Invasive group A streptococcus (iGAS) infections are rare (4-9 cases/100,000 US population annually) but potentially devastating (approximately 2,300 deaths annually in US), and affect all ages. Cases increase in winter-spring, paralleling the “season” of increased noninvasive GAS, e.g., pharyngitis and scarlet fever. iGAS case rates are lower in children than adults. That said, one well-known pediatric iGAS scenario has been deep cellulitis and necrotizing fasciitis during the healing phase of varicella. Other forms of iGAS include bacteremia, pneumonia (particularly when empyema is present), lymphangitis, erysipelas, and toxic shock syndrome. iGAS can occur with/after influenza but has also occurred concurrently with other viral respiratory infections.
Persons with underlying conditions (cancer or immune compromised status; chronic diseases of the heart, kidney or lung; diabetes mellitus) are at higher risk. Other subpopulations at risk for iGAS are illicit drug users, the elderly, homeless persons, nursing home residents, American Indian persons, and Alaska Native persons. Most experts feel that highly toxigenic strains of GAS are responsible for most iGAS. Indeed, most iGAS isolates produce (sometimes hyper-produce) superantigens that cause exaggerated innate immune responses, higher levels of inflammation, and often times tissue destruction, e.g., “flesh eating bacteria.” And who can forget that Jim Henson, creator of the Muppets, died of iGAS?
But why discuss iGAS in 2024? The pattern for iGAS has fluctuated more than usual in the last decade. So much so that the recent upsurge has caught the collective eye of the lay press. So, patients and friends may have questions about why and how iGAS is increasing lately. The bottom line is that no one knows for sure. However, the most recent 2 years of uptick may reflect GAS circulating at relatively high levels even when taking into account that GAS season occurs in winter-spring most years. Yet it seems likely that additional factors may have played a role in the fluctuations noted this past decade, e.g., temporary changes in societal behavior, a new GAS strain with over two dozen mutations, and possibly rapid waning of protection against GAS exotoxins.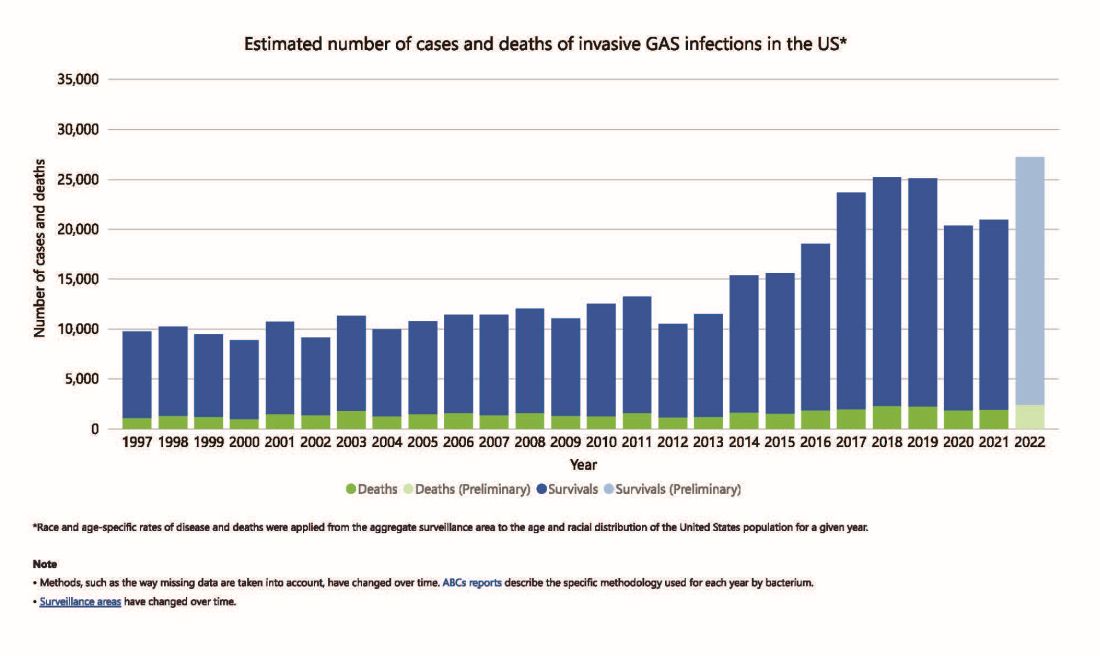
Social Behavior Factor
The SARS-CoV-2 pandemic brought extremes of disease and death to the world and dramatic changes in social behavior. A byproduct was dramatic decreases in nearly all infectious diseases, with numerous reports of near absence of many respiratory and gastrointestinal viruses in the 2020-2021 seasons. Interestingly, we did not see a drop in human rhinovirus infections, justifying its nickname as the cockroach of viruses. Reports also emerged about drops in bacterial diseases during 2020-2021 (although not so much for STIs), including noninvasive and invasive GAS disease, and also GAS-associated deaths (lowest since 2016).1 The drop in iGAS during social restrictions makes sense because GAS is spread by direct contact with infected persons or their secretions, and social contact had dramatically decreased particularly in the first 6 months of the pandemic.
However, since 2022 and the return to “normal” social behaviors, both viral diseases (e.g., RSV, influenza, and Norovirus), and some bacterial diseases have rebounded. That said, something else must be contributing, because iGAS rates had increased 4-5 years pre pandemic. In fact, the fluctuating pattern included “normal” annual rates in the early 2000s rising in ~2015 followed by the explainable pandemic drop (by nearly 25%), and not-too-unexpected 2-year postpandemic rise. But interestingly enough, the rebound is higher than might be expected for iGAS and children were overrepresented in first year’s rise (2022 rate for pediatric iGAS was the highest since 1997) while those older than 65 were overrepresented in second year (2023).1
Emergence of M1UK
One potential factor for the prepandemic rise in iGAS infections worldwide is the emergence and worldwide spread of a new GAS emm type variant designated M1UK.2 GAS isolates can be typed into categories designated as emm types based on DNA sequence. There are more than 240 emm types, with 6 being most common — M1, M3, and M28 (each up to 20% of GAS isolates) and M12, M82, and M89 (each up to 10%). M1, M3 and M28 have also been particularly associated with invasive disease. While emm types vary year to year and region by region, the overall emm type distribution among iGAS isolates in the United States had not been unusual since the turn of the century and the US M1 strain was the same as that which had been predominant worldwide (designated M1GLOBAL). This new M1UK sublineage had emerged around 2010 and had been increasing pre pandemic. The M1UK sequence contained a specific set of 27 SNPs (single nucleoside polymorphisms, i.e., single base mutations) and was associated with an uptick in scarlet fever in the United Kingdom starting around 2010. Its prevalence increased up to around 2015 while spreading internationally. It also had enhanced expression of SpeA, a phage-encoded superantigen. Some of the M1UK mutations also appear to alter GAS metabolic processes to allow better survival (better “fitness”) compared with other GAS. So, a more virulent hardier GAS had arisen and seems a reasonable candidate for contributing to the increased iGAS rates.
Waning Antibody to GAS As Potential Factor in Rebound
No consensus exists on correlates of protection from iGAS. However, adults seem to have less noninvasive GAS than children. One potential reason is that frequent GAS re-exposure, regardless of whether disease results, likely boosts anti-GAS antibodies. Pandemic social restrictions temporarily prevented such boosts. In children with developing antibody repertoires, anti-GAS antibodies may have waned below protective levels faster during a year without frequent boosting. Thus, children were iGAS susceptible soon after pandemic restrictions were dropped (2022). Increased iGAS rates in the elderly in 2023 may have occurred because of diminished GAS exposures accelerating immune senescence with anti-GAS antibodies dropping, but less quickly than in children. These speculations are simply hypotheses until future studies can test them.
All that said, how do we use information on increased iGAS in our daily practices? In addition to standard preventive strategies for viral coinfections (e.g., varicella and influenza vaccine), reminding families about rigorous attention to wound care is the one high-risk scenario we have not yet discussed. During 2024, a time of expected increased prevalence of iGAS, early wound care needs to be fastidious. Further, share warning signs with families (e.g., rapidly expanding painful erythema), “streaks” ascending from extremity wounds, fever and a highly painful wound, darkening almost purple color within cellulitis or soft tissue infection, or loss of sensation in the middle of an otherwise painful soft tissue infection. These presentations require immediate medical attention.
If such a patient presents, the Centers for Disease Control and Prevention (CDC) recommends admission along with blood and, where possible, wound cultures. If in the context of pneumonia with pleural effusion, culturing pleural fluid is also important. Remember, leading edge cultures are not often positive for GAS, seemingly because GAS exotoxins are found at erythema’s leading edge, not the bacteria. The bacteria are somewhere more central in the inflammatory process. Despite not being prominent among recent iGAS cases, another scenario that could sneak up on you is the infected surgical wound as nascent iGAS.
Finally, remember that nationally increasing numbers of iGAS isolates are resistant to erythromycin and clindamycin, the latter usually recommended to reduce tissue damage in iGAS.3 So, it is important to be aware of susceptibility patterns in your locale and consider an ID consultation. My hope is that you do not see an iGAS case this year, but we all need to remain alert. With a high index of suspicion and rapid diagnosis, you can minimize long-term sequelae and potential fatalities.
While it is too early to tell how the rest of 2024 will turn out, preliminary indications are that GAS is circulating at higher than usual levels (30%-35% GAS positive throat swabs in early April 2024 in Kansas City area) and iGAS rates will likely also be relatively high, particularly if Ontario, Canada, data are any indication.4 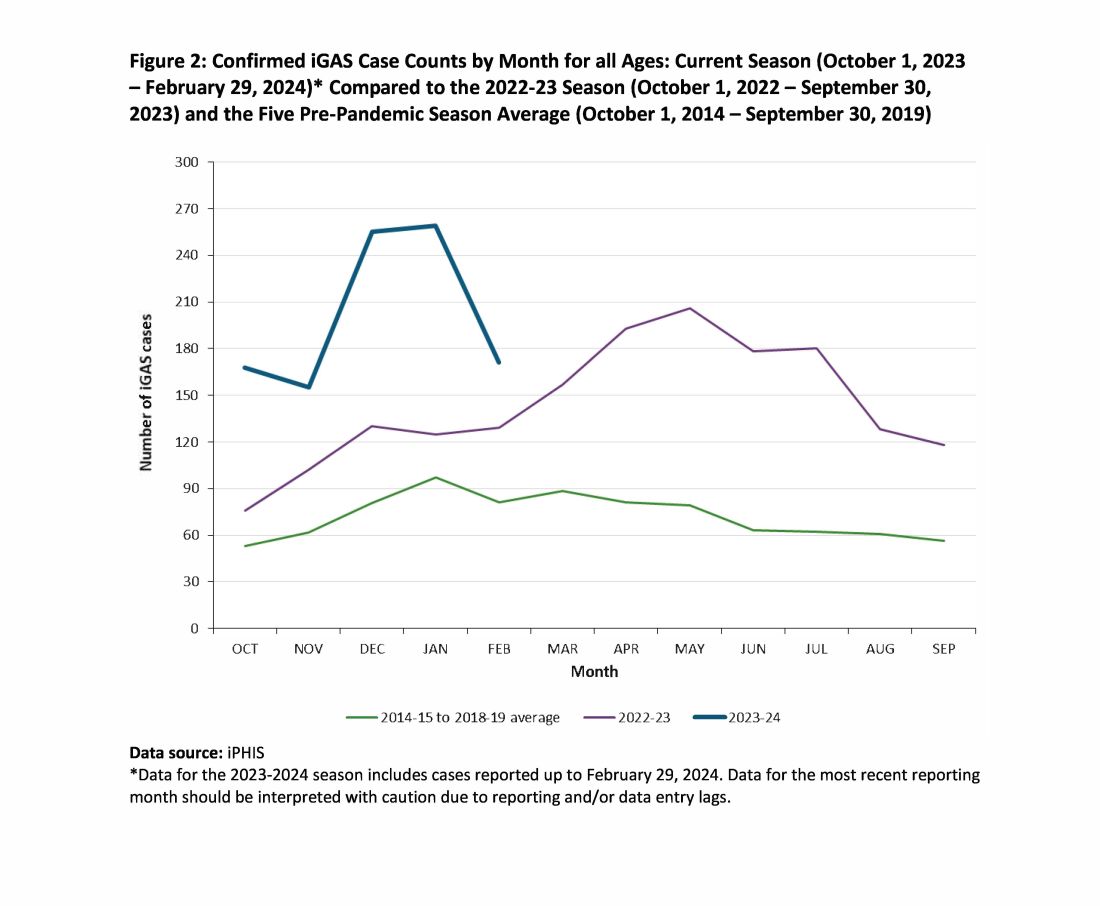
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. Current Group A Strep Activity, Centers for Disease Control and Prevention. April 2024. CDC webpage on current invasive GAS disease. April 2024.
2. Li Y et al. Expansion of Invasive Group A Streptococcus M1UK Lineage in Active Bacterial Core Surveillance, United States, 2019-2021 Emerg Infect Dis. 2023;29(10):2116-2120. doi: 10.3201/eid2910.230675.
3. Andreoni F et al. Clindamycin Affects Group A Streptococcus Virulence Factors and Improves Clinical Outcome. J Infect Dis. 2017 Jan 15;215(2):269-277. doi: 10.1093/infdis/jiw229.
4. Group A Streptococcal Disease, Invasive (iGAS), Public Health Ontario.
Invasive group A streptococcus (iGAS) infections are rare (4-9 cases/100,000 US population annually) but potentially devastating (approximately 2,300 deaths annually in US), and affect all ages. Cases increase in winter-spring, paralleling the “season” of increased noninvasive GAS, e.g., pharyngitis and scarlet fever. iGAS case rates are lower in children than adults. That said, one well-known pediatric iGAS scenario has been deep cellulitis and necrotizing fasciitis during the healing phase of varicella. Other forms of iGAS include bacteremia, pneumonia (particularly when empyema is present), lymphangitis, erysipelas, and toxic shock syndrome. iGAS can occur with/after influenza but has also occurred concurrently with other viral respiratory infections.
Persons with underlying conditions (cancer or immune compromised status; chronic diseases of the heart, kidney or lung; diabetes mellitus) are at higher risk. Other subpopulations at risk for iGAS are illicit drug users, the elderly, homeless persons, nursing home residents, American Indian persons, and Alaska Native persons. Most experts feel that highly toxigenic strains of GAS are responsible for most iGAS. Indeed, most iGAS isolates produce (sometimes hyper-produce) superantigens that cause exaggerated innate immune responses, higher levels of inflammation, and often times tissue destruction, e.g., “flesh eating bacteria.” And who can forget that Jim Henson, creator of the Muppets, died of iGAS?
But why discuss iGAS in 2024? The pattern for iGAS has fluctuated more than usual in the last decade. So much so that the recent upsurge has caught the collective eye of the lay press. So, patients and friends may have questions about why and how iGAS is increasing lately. The bottom line is that no one knows for sure. However, the most recent 2 years of uptick may reflect GAS circulating at relatively high levels even when taking into account that GAS season occurs in winter-spring most years. Yet it seems likely that additional factors may have played a role in the fluctuations noted this past decade, e.g., temporary changes in societal behavior, a new GAS strain with over two dozen mutations, and possibly rapid waning of protection against GAS exotoxins.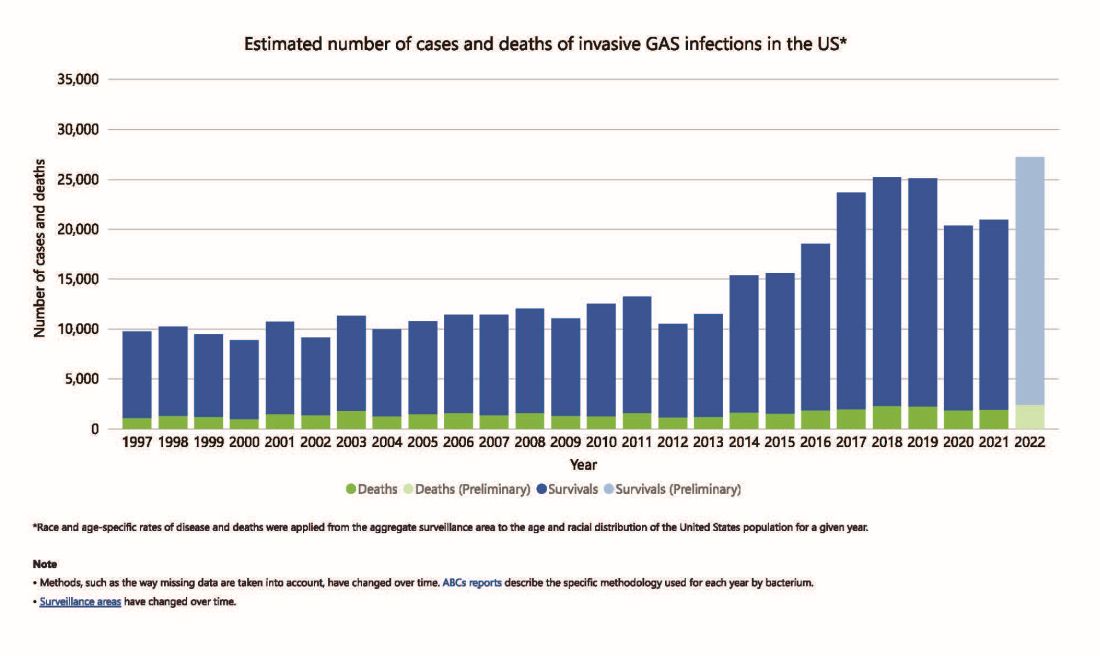
Social Behavior Factor
The SARS-CoV-2 pandemic brought extremes of disease and death to the world and dramatic changes in social behavior. A byproduct was dramatic decreases in nearly all infectious diseases, with numerous reports of near absence of many respiratory and gastrointestinal viruses in the 2020-2021 seasons. Interestingly, we did not see a drop in human rhinovirus infections, justifying its nickname as the cockroach of viruses. Reports also emerged about drops in bacterial diseases during 2020-2021 (although not so much for STIs), including noninvasive and invasive GAS disease, and also GAS-associated deaths (lowest since 2016).1 The drop in iGAS during social restrictions makes sense because GAS is spread by direct contact with infected persons or their secretions, and social contact had dramatically decreased particularly in the first 6 months of the pandemic.
However, since 2022 and the return to “normal” social behaviors, both viral diseases (e.g., RSV, influenza, and Norovirus), and some bacterial diseases have rebounded. That said, something else must be contributing, because iGAS rates had increased 4-5 years pre pandemic. In fact, the fluctuating pattern included “normal” annual rates in the early 2000s rising in ~2015 followed by the explainable pandemic drop (by nearly 25%), and not-too-unexpected 2-year postpandemic rise. But interestingly enough, the rebound is higher than might be expected for iGAS and children were overrepresented in first year’s rise (2022 rate for pediatric iGAS was the highest since 1997) while those older than 65 were overrepresented in second year (2023).1
Emergence of M1UK
One potential factor for the prepandemic rise in iGAS infections worldwide is the emergence and worldwide spread of a new GAS emm type variant designated M1UK.2 GAS isolates can be typed into categories designated as emm types based on DNA sequence. There are more than 240 emm types, with 6 being most common — M1, M3, and M28 (each up to 20% of GAS isolates) and M12, M82, and M89 (each up to 10%). M1, M3 and M28 have also been particularly associated with invasive disease. While emm types vary year to year and region by region, the overall emm type distribution among iGAS isolates in the United States had not been unusual since the turn of the century and the US M1 strain was the same as that which had been predominant worldwide (designated M1GLOBAL). This new M1UK sublineage had emerged around 2010 and had been increasing pre pandemic. The M1UK sequence contained a specific set of 27 SNPs (single nucleoside polymorphisms, i.e., single base mutations) and was associated with an uptick in scarlet fever in the United Kingdom starting around 2010. Its prevalence increased up to around 2015 while spreading internationally. It also had enhanced expression of SpeA, a phage-encoded superantigen. Some of the M1UK mutations also appear to alter GAS metabolic processes to allow better survival (better “fitness”) compared with other GAS. So, a more virulent hardier GAS had arisen and seems a reasonable candidate for contributing to the increased iGAS rates.
Waning Antibody to GAS As Potential Factor in Rebound
No consensus exists on correlates of protection from iGAS. However, adults seem to have less noninvasive GAS than children. One potential reason is that frequent GAS re-exposure, regardless of whether disease results, likely boosts anti-GAS antibodies. Pandemic social restrictions temporarily prevented such boosts. In children with developing antibody repertoires, anti-GAS antibodies may have waned below protective levels faster during a year without frequent boosting. Thus, children were iGAS susceptible soon after pandemic restrictions were dropped (2022). Increased iGAS rates in the elderly in 2023 may have occurred because of diminished GAS exposures accelerating immune senescence with anti-GAS antibodies dropping, but less quickly than in children. These speculations are simply hypotheses until future studies can test them.
All that said, how do we use information on increased iGAS in our daily practices? In addition to standard preventive strategies for viral coinfections (e.g., varicella and influenza vaccine), reminding families about rigorous attention to wound care is the one high-risk scenario we have not yet discussed. During 2024, a time of expected increased prevalence of iGAS, early wound care needs to be fastidious. Further, share warning signs with families (e.g., rapidly expanding painful erythema), “streaks” ascending from extremity wounds, fever and a highly painful wound, darkening almost purple color within cellulitis or soft tissue infection, or loss of sensation in the middle of an otherwise painful soft tissue infection. These presentations require immediate medical attention.
If such a patient presents, the Centers for Disease Control and Prevention (CDC) recommends admission along with blood and, where possible, wound cultures. If in the context of pneumonia with pleural effusion, culturing pleural fluid is also important. Remember, leading edge cultures are not often positive for GAS, seemingly because GAS exotoxins are found at erythema’s leading edge, not the bacteria. The bacteria are somewhere more central in the inflammatory process. Despite not being prominent among recent iGAS cases, another scenario that could sneak up on you is the infected surgical wound as nascent iGAS.
Finally, remember that nationally increasing numbers of iGAS isolates are resistant to erythromycin and clindamycin, the latter usually recommended to reduce tissue damage in iGAS.3 So, it is important to be aware of susceptibility patterns in your locale and consider an ID consultation. My hope is that you do not see an iGAS case this year, but we all need to remain alert. With a high index of suspicion and rapid diagnosis, you can minimize long-term sequelae and potential fatalities.
While it is too early to tell how the rest of 2024 will turn out, preliminary indications are that GAS is circulating at higher than usual levels (30%-35% GAS positive throat swabs in early April 2024 in Kansas City area) and iGAS rates will likely also be relatively high, particularly if Ontario, Canada, data are any indication.4 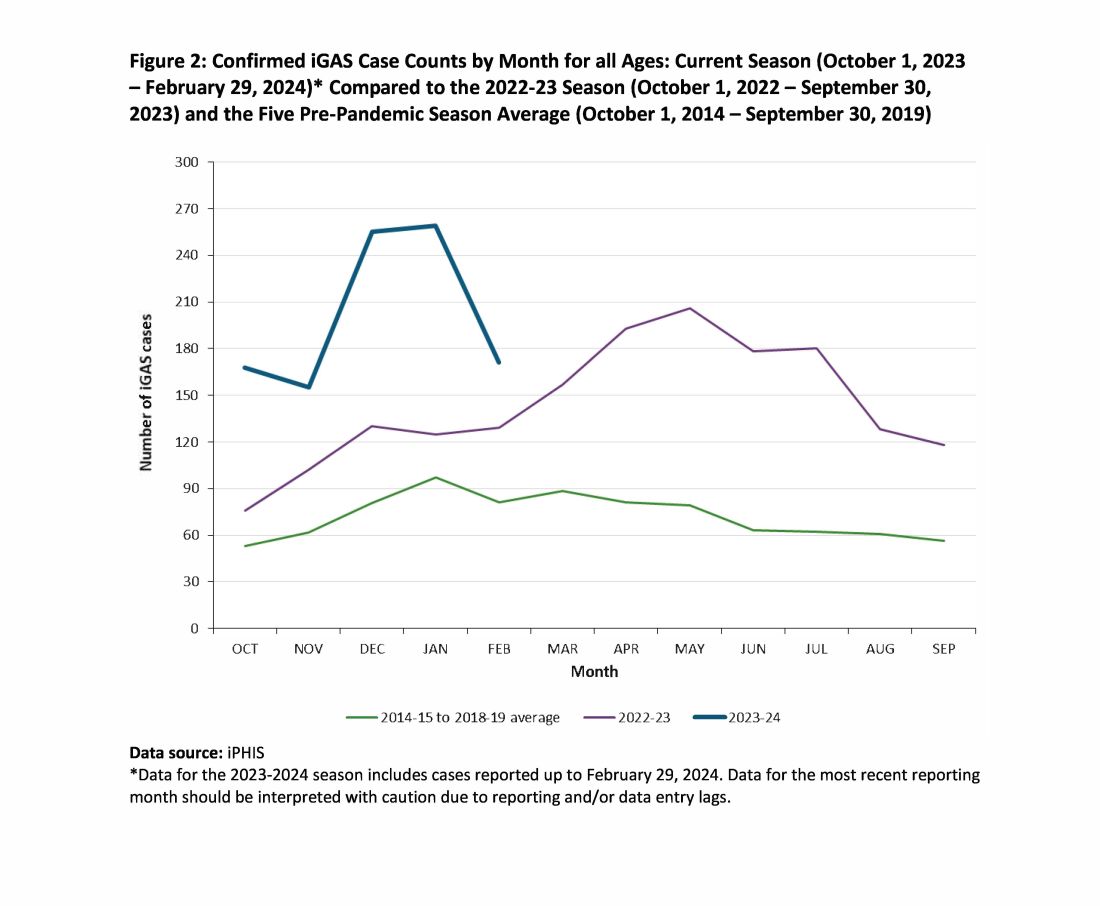
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. Current Group A Strep Activity, Centers for Disease Control and Prevention. April 2024. CDC webpage on current invasive GAS disease. April 2024.
2. Li Y et al. Expansion of Invasive Group A Streptococcus M1UK Lineage in Active Bacterial Core Surveillance, United States, 2019-2021 Emerg Infect Dis. 2023;29(10):2116-2120. doi: 10.3201/eid2910.230675.
3. Andreoni F et al. Clindamycin Affects Group A Streptococcus Virulence Factors and Improves Clinical Outcome. J Infect Dis. 2017 Jan 15;215(2):269-277. doi: 10.1093/infdis/jiw229.
4. Group A Streptococcal Disease, Invasive (iGAS), Public Health Ontario.
Working From Home: Doctors’ Options Are Not Limited to Classic Telemedicine
The appeal of working from home is undeniable. It comes with no daily commute, casual dress, and the ability to manage work-life balance more effectively.
Telemedicine is often the first thing that comes to mind when physicians think about remote medical practice. In its traditional sense, telemedicine entails live video consults, replicating the in-person experience as closely as possible, minus the hands-on component. However, this format is just one of many types of virtual care presenting opportunities to practice medicine from home.
The scope and volume of such opportunities are expanding due to technology, regulatory shifts at the state and federal levels favoring remote healthcare, and a wider move toward remote work. Virtual practice options for physicians range from full-time employment to flexible part-time positions that can be used to earn supplementary income.
Just a few of those virtual options are:
Remote Patient Monitoring
Remote patient monitoring uses technology for tracking patient health data, applicable in real-time or asynchronously, through devices ranging from specialized monitors to consumer wearables. Data are securely transmitted to healthcare providers, enabling them to guide or make treatment choices remotely. This method has proven particularly valuable in managing chronic diseases where continuous monitoring can significantly affect outcomes.
Like standard telemedicine, remote patient monitoring offers flexibility, autonomy, and the ability to work from home. It is picking up steam across the healthcare industry, especially in critical care, surgery, post-acute care, and primary care, so there are opportunities for physicians across a variety of specialties.
Online Medication Management and Text-Based Consults
Gathering necessary information for patient care decisions often doesn’t require a direct, face-to-face visit in person or by telemedicine. Clinical data can be efficiently collected through online forms, HIPAA-compliant messaging, medical record reviews, and information gathered by staff.
An approach that uses all these sources enables effective medication management for stable chronic conditions (such as hypertension), as well as straightforward but simple acute issues (such as urinary tract infections). It also is useful for quick follow-ups with patients after starting new treatments, to address questions between visits, and to give them educational material.
Some medical practices and virtual healthcare corporations have made online medication management and text-based consults the center of their business model. Part-time positions with platforms that offer this type of care let physicians fit consultations into their schedule as time permits, without committing to scheduled appointments.
eConsults
Electronic consultations, or eConsults, facilitate collaboration among healthcare professionals about complex cases without direct patient interaction.
These services operate via online platforms that support asynchronous communication and often bypass the need for a traditional referral. Typically, a primary care provider submits a query that is then assigned to a specialist. Next, the specialist reviews the information and offers recommendations for the patient’s care plan.
Major eConsult platforms such as AristaMD and RubiconMD contract with healthcare systems and medical practices. Physicians can easily join the specialist panels of these companies and complete assigned consultations from their homes or offices, paid on a per-consult basis. They should check their employment contracts to make sure such independent contract work is allowed.
Phone-Only On-Call Positions
On-call rotations for after-hour care bring with them challenges in staffing and scheduling vacations. These challenges have helped trigger as-needed or per diem on-call roles, in which a physician provides recommendations and orders over the phone without needing to visit an office or a hospital.
Examples of workplaces that employ phone-only on-call physicians include smaller jails, mental health facilities, dialysis centers, long-term care facilities, and sporting groups or events needing back-up for on-site nurses or emergency medical technicians.
While these positions can sometimes be challenging for a physician to find, they are out there. They can be a fantastic option to earn additional income through low-stress clinical work performed from home.
Supervision of Nurse Practitioners (NPs) and Physician Assistants (PAs)
In states that mandate such physician oversight, it often be conducted remotely — depending on that state’s rules, the practice type, and the scope of services being provided. This remote option introduces part-time opportunities for physicians to oversee NPs and PAs without being in the medical office. Essentially, the doctor needs to be available for phone or email consultations, complete chart reviews, and meet regularly with the provider.
Remote supervision roles are available across various types of healthcare organizations and medical practices. There also are opportunities with insurers, many of which have established NP-run, in-home member assessment programs that require remote supervision by a doctor.
Remote Medical Directorships
Medical directors are a key part of the clinician team in a wide variety of healthcare settings requiring clinical protocol oversight, regulatory compliance, and guidance for other clinicians making treatment decisions. Many directorships do not require direct patient contact and therefore are conducive to remote work, given technologies such as electronic health record and secure messaging systems.
Organizations such as emergency medical service agencies, hospice services, med spas, blood and plasma donation centers, home health agencies, and substance use disorder treatment programs increasingly rely on remote medical directorships to meet legal requirements and accreditation standards.
Although these positions are often viewed as “nonclinical,” they carry significant clinical responsibilities. Examples are developing and reviewing treatment protocols, ensuring adherence to healthcare regulations, and sometimes intervening in complex patient cases or when adverse outcomes occur.
Keeping a Role in Patient Welfare
Clearly, working from home as a physician doesn’t have to mean taking on a nonclinical job. Beyond the options already mentioned, there are numerous others — for example, working as a medical monitor for clinical trials, in utilization management for insurance companies, or in conducting independent medical exams for insurance claims. While these roles don’t involve direct patient treatment, they require similar skills and affect the quality of care.
If such remote opportunities aren’t currently available in your workplace, consider approaching your management about trying them.
Physicians who are experiencing burnout, seeking a career change, or interested in earning extra income should consider exploring more of the unconventional ways that they can practice medicine.
A version of this article appeared on Medscape.com.
The appeal of working from home is undeniable. It comes with no daily commute, casual dress, and the ability to manage work-life balance more effectively.
Telemedicine is often the first thing that comes to mind when physicians think about remote medical practice. In its traditional sense, telemedicine entails live video consults, replicating the in-person experience as closely as possible, minus the hands-on component. However, this format is just one of many types of virtual care presenting opportunities to practice medicine from home.
The scope and volume of such opportunities are expanding due to technology, regulatory shifts at the state and federal levels favoring remote healthcare, and a wider move toward remote work. Virtual practice options for physicians range from full-time employment to flexible part-time positions that can be used to earn supplementary income.
Just a few of those virtual options are:
Remote Patient Monitoring
Remote patient monitoring uses technology for tracking patient health data, applicable in real-time or asynchronously, through devices ranging from specialized monitors to consumer wearables. Data are securely transmitted to healthcare providers, enabling them to guide or make treatment choices remotely. This method has proven particularly valuable in managing chronic diseases where continuous monitoring can significantly affect outcomes.
Like standard telemedicine, remote patient monitoring offers flexibility, autonomy, and the ability to work from home. It is picking up steam across the healthcare industry, especially in critical care, surgery, post-acute care, and primary care, so there are opportunities for physicians across a variety of specialties.
Online Medication Management and Text-Based Consults
Gathering necessary information for patient care decisions often doesn’t require a direct, face-to-face visit in person or by telemedicine. Clinical data can be efficiently collected through online forms, HIPAA-compliant messaging, medical record reviews, and information gathered by staff.
An approach that uses all these sources enables effective medication management for stable chronic conditions (such as hypertension), as well as straightforward but simple acute issues (such as urinary tract infections). It also is useful for quick follow-ups with patients after starting new treatments, to address questions between visits, and to give them educational material.
Some medical practices and virtual healthcare corporations have made online medication management and text-based consults the center of their business model. Part-time positions with platforms that offer this type of care let physicians fit consultations into their schedule as time permits, without committing to scheduled appointments.
eConsults
Electronic consultations, or eConsults, facilitate collaboration among healthcare professionals about complex cases without direct patient interaction.
These services operate via online platforms that support asynchronous communication and often bypass the need for a traditional referral. Typically, a primary care provider submits a query that is then assigned to a specialist. Next, the specialist reviews the information and offers recommendations for the patient’s care plan.
Major eConsult platforms such as AristaMD and RubiconMD contract with healthcare systems and medical practices. Physicians can easily join the specialist panels of these companies and complete assigned consultations from their homes or offices, paid on a per-consult basis. They should check their employment contracts to make sure such independent contract work is allowed.
Phone-Only On-Call Positions
On-call rotations for after-hour care bring with them challenges in staffing and scheduling vacations. These challenges have helped trigger as-needed or per diem on-call roles, in which a physician provides recommendations and orders over the phone without needing to visit an office or a hospital.
Examples of workplaces that employ phone-only on-call physicians include smaller jails, mental health facilities, dialysis centers, long-term care facilities, and sporting groups or events needing back-up for on-site nurses or emergency medical technicians.
While these positions can sometimes be challenging for a physician to find, they are out there. They can be a fantastic option to earn additional income through low-stress clinical work performed from home.
Supervision of Nurse Practitioners (NPs) and Physician Assistants (PAs)
In states that mandate such physician oversight, it often be conducted remotely — depending on that state’s rules, the practice type, and the scope of services being provided. This remote option introduces part-time opportunities for physicians to oversee NPs and PAs without being in the medical office. Essentially, the doctor needs to be available for phone or email consultations, complete chart reviews, and meet regularly with the provider.
Remote supervision roles are available across various types of healthcare organizations and medical practices. There also are opportunities with insurers, many of which have established NP-run, in-home member assessment programs that require remote supervision by a doctor.
Remote Medical Directorships
Medical directors are a key part of the clinician team in a wide variety of healthcare settings requiring clinical protocol oversight, regulatory compliance, and guidance for other clinicians making treatment decisions. Many directorships do not require direct patient contact and therefore are conducive to remote work, given technologies such as electronic health record and secure messaging systems.
Organizations such as emergency medical service agencies, hospice services, med spas, blood and plasma donation centers, home health agencies, and substance use disorder treatment programs increasingly rely on remote medical directorships to meet legal requirements and accreditation standards.
Although these positions are often viewed as “nonclinical,” they carry significant clinical responsibilities. Examples are developing and reviewing treatment protocols, ensuring adherence to healthcare regulations, and sometimes intervening in complex patient cases or when adverse outcomes occur.
Keeping a Role in Patient Welfare
Clearly, working from home as a physician doesn’t have to mean taking on a nonclinical job. Beyond the options already mentioned, there are numerous others — for example, working as a medical monitor for clinical trials, in utilization management for insurance companies, or in conducting independent medical exams for insurance claims. While these roles don’t involve direct patient treatment, they require similar skills and affect the quality of care.
If such remote opportunities aren’t currently available in your workplace, consider approaching your management about trying them.
Physicians who are experiencing burnout, seeking a career change, or interested in earning extra income should consider exploring more of the unconventional ways that they can practice medicine.
A version of this article appeared on Medscape.com.
The appeal of working from home is undeniable. It comes with no daily commute, casual dress, and the ability to manage work-life balance more effectively.
Telemedicine is often the first thing that comes to mind when physicians think about remote medical practice. In its traditional sense, telemedicine entails live video consults, replicating the in-person experience as closely as possible, minus the hands-on component. However, this format is just one of many types of virtual care presenting opportunities to practice medicine from home.
The scope and volume of such opportunities are expanding due to technology, regulatory shifts at the state and federal levels favoring remote healthcare, and a wider move toward remote work. Virtual practice options for physicians range from full-time employment to flexible part-time positions that can be used to earn supplementary income.
Just a few of those virtual options are:
Remote Patient Monitoring
Remote patient monitoring uses technology for tracking patient health data, applicable in real-time or asynchronously, through devices ranging from specialized monitors to consumer wearables. Data are securely transmitted to healthcare providers, enabling them to guide or make treatment choices remotely. This method has proven particularly valuable in managing chronic diseases where continuous monitoring can significantly affect outcomes.
Like standard telemedicine, remote patient monitoring offers flexibility, autonomy, and the ability to work from home. It is picking up steam across the healthcare industry, especially in critical care, surgery, post-acute care, and primary care, so there are opportunities for physicians across a variety of specialties.
Online Medication Management and Text-Based Consults
Gathering necessary information for patient care decisions often doesn’t require a direct, face-to-face visit in person or by telemedicine. Clinical data can be efficiently collected through online forms, HIPAA-compliant messaging, medical record reviews, and information gathered by staff.
An approach that uses all these sources enables effective medication management for stable chronic conditions (such as hypertension), as well as straightforward but simple acute issues (such as urinary tract infections). It also is useful for quick follow-ups with patients after starting new treatments, to address questions between visits, and to give them educational material.
Some medical practices and virtual healthcare corporations have made online medication management and text-based consults the center of their business model. Part-time positions with platforms that offer this type of care let physicians fit consultations into their schedule as time permits, without committing to scheduled appointments.
eConsults
Electronic consultations, or eConsults, facilitate collaboration among healthcare professionals about complex cases without direct patient interaction.
These services operate via online platforms that support asynchronous communication and often bypass the need for a traditional referral. Typically, a primary care provider submits a query that is then assigned to a specialist. Next, the specialist reviews the information and offers recommendations for the patient’s care plan.
Major eConsult platforms such as AristaMD and RubiconMD contract with healthcare systems and medical practices. Physicians can easily join the specialist panels of these companies and complete assigned consultations from their homes or offices, paid on a per-consult basis. They should check their employment contracts to make sure such independent contract work is allowed.
Phone-Only On-Call Positions
On-call rotations for after-hour care bring with them challenges in staffing and scheduling vacations. These challenges have helped trigger as-needed or per diem on-call roles, in which a physician provides recommendations and orders over the phone without needing to visit an office or a hospital.
Examples of workplaces that employ phone-only on-call physicians include smaller jails, mental health facilities, dialysis centers, long-term care facilities, and sporting groups or events needing back-up for on-site nurses or emergency medical technicians.
While these positions can sometimes be challenging for a physician to find, they are out there. They can be a fantastic option to earn additional income through low-stress clinical work performed from home.
Supervision of Nurse Practitioners (NPs) and Physician Assistants (PAs)
In states that mandate such physician oversight, it often be conducted remotely — depending on that state’s rules, the practice type, and the scope of services being provided. This remote option introduces part-time opportunities for physicians to oversee NPs and PAs without being in the medical office. Essentially, the doctor needs to be available for phone or email consultations, complete chart reviews, and meet regularly with the provider.
Remote supervision roles are available across various types of healthcare organizations and medical practices. There also are opportunities with insurers, many of which have established NP-run, in-home member assessment programs that require remote supervision by a doctor.
Remote Medical Directorships
Medical directors are a key part of the clinician team in a wide variety of healthcare settings requiring clinical protocol oversight, regulatory compliance, and guidance for other clinicians making treatment decisions. Many directorships do not require direct patient contact and therefore are conducive to remote work, given technologies such as electronic health record and secure messaging systems.
Organizations such as emergency medical service agencies, hospice services, med spas, blood and plasma donation centers, home health agencies, and substance use disorder treatment programs increasingly rely on remote medical directorships to meet legal requirements and accreditation standards.
Although these positions are often viewed as “nonclinical,” they carry significant clinical responsibilities. Examples are developing and reviewing treatment protocols, ensuring adherence to healthcare regulations, and sometimes intervening in complex patient cases or when adverse outcomes occur.
Keeping a Role in Patient Welfare
Clearly, working from home as a physician doesn’t have to mean taking on a nonclinical job. Beyond the options already mentioned, there are numerous others — for example, working as a medical monitor for clinical trials, in utilization management for insurance companies, or in conducting independent medical exams for insurance claims. While these roles don’t involve direct patient treatment, they require similar skills and affect the quality of care.
If such remote opportunities aren’t currently available in your workplace, consider approaching your management about trying them.
Physicians who are experiencing burnout, seeking a career change, or interested in earning extra income should consider exploring more of the unconventional ways that they can practice medicine.
A version of this article appeared on Medscape.com.




