User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Diminishing number of clerkship sites poses threat to psychiatry training
Medical school clinical rotations are a rite of passage as students emerge from their basic science courses and first board exam to the clinical world where the patients vaguely resemble the question stem descriptions. Finally, intangible theory can be put into practice. Yet, it is becoming increasingly difficult for 3rd-year medical student clerkship directors to find enough clinical sites to support the growing number of medical students as enrollment numbers steadily increase and outpace the current clinical resources.
In a 2019 Association of American Medical Colleges report, 84% of medical school deans were concerned about the diminishing number of clerkship sites, and there was additional worry about lack of qualified specialty preceptors. This lack of clerkship availability is especially true for psychiatry sites.
Psychiatry clerkship directors are in need of more clinical sites to address the educational needs of medical students, and psychiatrists in the broader clinical community are positioned to help medical schools expand their clinical sites.
Inpatient psychiatric units and consult services continue to be popular sites for medical student rotations, but it has been hard to expand into other settings, where psychiatric treatment is seen as more private and intimate than other specialties. Reasons for falling site availability are varied and include 1) financial disincentive to take students – because they can be seen as a burden on supervisors who must meet revenue-generating patient quotas; 2) competition with other learners, including residents, PA students, NPs, and NP students; and 3) the general financial and operational obstacles to clinical practice inflicted by the pandemic. COVID-19 affected medical education – for better and worse (JAMA. 2020;324[11]:1033-4). Psychiatry clerkships particularly suffered from restricted patient access as inpatient units reduced their census to comply with COVID-19 safety protocols, and during the height of the pandemic inpatient units provided psychiatric care to COVID-19–positive patients, which precluded student involvement. On the other hand, many more students were introduced to telepsychiatry and witnessed creative forms of mental health intervention as clinicians adapted their practices to the pandemic.
When rotations began
Clinical rotations entered the American medical school curriculum in the 1890s when Sir William Osler brought the European standard of medical education with him as Physician in Chief at the newly opened Johns Hopkins University Hospital. He formalized the traditional apprenticeship model by standardizing 3rd- and 4th-year clerkships as rotations in which medical students worked in clinics and on the wards, learning from residents and attendings.
Clinical rotations, their location, the supervisors, and the patients and their ailments all go in to influence a student’s specialty choice. Some students enter medical school knowing they want to be a surgeon, a pediatrician, or a psychiatrist. And some are compelled by a specific rotation, when they realize that it’s not at all what they expected and maybe they could dedicate their professional life to this area of medicine.
High-quality clinical clerkship sites are essential to the future of psychiatry. At clerkship sites, undecided students interested in psychiatry may affirm their commitment to psychiatry. Other students will have their only dedicated exposure to psychiatrically ill patients. This represents students’ only opportunity to learn the skills to treat comorbid psychiatric and medical illness. Regardless of specialty, nearly every physician will have to treat patients with some psychiatric illnesses.
What constitutes a “high-quality clinical site” is difficult to measure and define. Some measures of quality include a safe learning environment, a reasonable ratio of students to supervisors (including residents, fellows, and attendings), and an adequate number and diversity of patients. Many medical schools may prefer an affiliated academic medical center or Veterans’ Affairs hospitals for their rotating students. Private psychiatric hospitals are proliferating, and if these are to be sites for medical students, the following standards are suggested: Private psychiatric hospitals must follow standard safety precautions with sufficient staff presence, ensure willing preceptors who can provide adequate student supervision, and adjust their expectations to students who can carry a few patients of diverse background, but are not to be treated merely as scribes.
Psychiatrists, whether they consider themselves “academic” or not, have a role to play in expanding access to clinical sites. Students are eager to learn in any setting. Inpatient settings have long been seen as the norm for clinical education in psychiatry. Yet inpatient settings perpetuate the idea that those with severe mental illness or individuals with psychosocial stressors or disabling, comorbid substance use disorders are the only people who seek help from a psychiatrist. without an academic affiliation to explore the possibility of creating space for a medical student in their clinical practice.
We cannot deny the demands on psychiatrists’ time – every minute is counted by the patient and doctor, and every encounter is accounted for in some revenue stream. However, the academic world is running out of space for its students, and there’s a serious question as to whether an academic center is the only place for students. If you are a psychiatrist who still loves to learn and prides themselves on high-quality patient care, then you have an essential role in shaping the students who will one day be your peers in psychiatry, or the physicians treating your patients’ comorbid medical illnesses.
There are upfront challenges to teaching 3rd-year medical students, including teaching the psychiatric interview, note writing, persuading patients to allow students into their care, and setting time aside at the end of the workday to provide feedback on performance. Yet, after learning the ropes of psychiatric patient care, medical students can provide help in writing notes, calling collateral, contacting patients with their laboratory results, and even helping with the tedious but necessary administrative tasks like prior authorizations. In exchange for training students, some medical schools may offer perks, such as a volunteer faculty position that comes with access to usually expensive library resources, such as medical databases.
You can help expand clinical sites in psychiatry rotations by contacting your alma mater or the medical school closest to your community and asking about their need for clerkship sites. Many medical schools are branching out by sending students to stay near the clinical sites and immerse themselves in the community where their site director practices. Even one-half day a week in an outpatient setting provides patient and setting diversity to students and helps spread out students to different sites, easing the burden on inpatient supervisors while providing students more individualized supervision.
The practice of medicine is built on apprenticeship and teaching wisdom through patient care. Just because we leave residency doesn’t mean we leave academics. Taking students into your practice is an invaluable service to the medical education community and future physicians.
Dr. Posada is assistant clinical professor in the department of psychiatry and behavioral sciences at George Washington University in Washington, and staff physician at George Washington Medical Faculty Associates, also in Washington. She has no conflicts of interest. Dr. Ortiz is assistant professor and clerkship director in the department of psychiatry at Texas Tech University Health Sciences Center – El Paso. She has no conflicts of interest.
Medical school clinical rotations are a rite of passage as students emerge from their basic science courses and first board exam to the clinical world where the patients vaguely resemble the question stem descriptions. Finally, intangible theory can be put into practice. Yet, it is becoming increasingly difficult for 3rd-year medical student clerkship directors to find enough clinical sites to support the growing number of medical students as enrollment numbers steadily increase and outpace the current clinical resources.
In a 2019 Association of American Medical Colleges report, 84% of medical school deans were concerned about the diminishing number of clerkship sites, and there was additional worry about lack of qualified specialty preceptors. This lack of clerkship availability is especially true for psychiatry sites.
Psychiatry clerkship directors are in need of more clinical sites to address the educational needs of medical students, and psychiatrists in the broader clinical community are positioned to help medical schools expand their clinical sites.
Inpatient psychiatric units and consult services continue to be popular sites for medical student rotations, but it has been hard to expand into other settings, where psychiatric treatment is seen as more private and intimate than other specialties. Reasons for falling site availability are varied and include 1) financial disincentive to take students – because they can be seen as a burden on supervisors who must meet revenue-generating patient quotas; 2) competition with other learners, including residents, PA students, NPs, and NP students; and 3) the general financial and operational obstacles to clinical practice inflicted by the pandemic. COVID-19 affected medical education – for better and worse (JAMA. 2020;324[11]:1033-4). Psychiatry clerkships particularly suffered from restricted patient access as inpatient units reduced their census to comply with COVID-19 safety protocols, and during the height of the pandemic inpatient units provided psychiatric care to COVID-19–positive patients, which precluded student involvement. On the other hand, many more students were introduced to telepsychiatry and witnessed creative forms of mental health intervention as clinicians adapted their practices to the pandemic.
When rotations began
Clinical rotations entered the American medical school curriculum in the 1890s when Sir William Osler brought the European standard of medical education with him as Physician in Chief at the newly opened Johns Hopkins University Hospital. He formalized the traditional apprenticeship model by standardizing 3rd- and 4th-year clerkships as rotations in which medical students worked in clinics and on the wards, learning from residents and attendings.
Clinical rotations, their location, the supervisors, and the patients and their ailments all go in to influence a student’s specialty choice. Some students enter medical school knowing they want to be a surgeon, a pediatrician, or a psychiatrist. And some are compelled by a specific rotation, when they realize that it’s not at all what they expected and maybe they could dedicate their professional life to this area of medicine.
High-quality clinical clerkship sites are essential to the future of psychiatry. At clerkship sites, undecided students interested in psychiatry may affirm their commitment to psychiatry. Other students will have their only dedicated exposure to psychiatrically ill patients. This represents students’ only opportunity to learn the skills to treat comorbid psychiatric and medical illness. Regardless of specialty, nearly every physician will have to treat patients with some psychiatric illnesses.
What constitutes a “high-quality clinical site” is difficult to measure and define. Some measures of quality include a safe learning environment, a reasonable ratio of students to supervisors (including residents, fellows, and attendings), and an adequate number and diversity of patients. Many medical schools may prefer an affiliated academic medical center or Veterans’ Affairs hospitals for their rotating students. Private psychiatric hospitals are proliferating, and if these are to be sites for medical students, the following standards are suggested: Private psychiatric hospitals must follow standard safety precautions with sufficient staff presence, ensure willing preceptors who can provide adequate student supervision, and adjust their expectations to students who can carry a few patients of diverse background, but are not to be treated merely as scribes.
Psychiatrists, whether they consider themselves “academic” or not, have a role to play in expanding access to clinical sites. Students are eager to learn in any setting. Inpatient settings have long been seen as the norm for clinical education in psychiatry. Yet inpatient settings perpetuate the idea that those with severe mental illness or individuals with psychosocial stressors or disabling, comorbid substance use disorders are the only people who seek help from a psychiatrist. without an academic affiliation to explore the possibility of creating space for a medical student in their clinical practice.
We cannot deny the demands on psychiatrists’ time – every minute is counted by the patient and doctor, and every encounter is accounted for in some revenue stream. However, the academic world is running out of space for its students, and there’s a serious question as to whether an academic center is the only place for students. If you are a psychiatrist who still loves to learn and prides themselves on high-quality patient care, then you have an essential role in shaping the students who will one day be your peers in psychiatry, or the physicians treating your patients’ comorbid medical illnesses.
There are upfront challenges to teaching 3rd-year medical students, including teaching the psychiatric interview, note writing, persuading patients to allow students into their care, and setting time aside at the end of the workday to provide feedback on performance. Yet, after learning the ropes of psychiatric patient care, medical students can provide help in writing notes, calling collateral, contacting patients with their laboratory results, and even helping with the tedious but necessary administrative tasks like prior authorizations. In exchange for training students, some medical schools may offer perks, such as a volunteer faculty position that comes with access to usually expensive library resources, such as medical databases.
You can help expand clinical sites in psychiatry rotations by contacting your alma mater or the medical school closest to your community and asking about their need for clerkship sites. Many medical schools are branching out by sending students to stay near the clinical sites and immerse themselves in the community where their site director practices. Even one-half day a week in an outpatient setting provides patient and setting diversity to students and helps spread out students to different sites, easing the burden on inpatient supervisors while providing students more individualized supervision.
The practice of medicine is built on apprenticeship and teaching wisdom through patient care. Just because we leave residency doesn’t mean we leave academics. Taking students into your practice is an invaluable service to the medical education community and future physicians.
Dr. Posada is assistant clinical professor in the department of psychiatry and behavioral sciences at George Washington University in Washington, and staff physician at George Washington Medical Faculty Associates, also in Washington. She has no conflicts of interest. Dr. Ortiz is assistant professor and clerkship director in the department of psychiatry at Texas Tech University Health Sciences Center – El Paso. She has no conflicts of interest.
Medical school clinical rotations are a rite of passage as students emerge from their basic science courses and first board exam to the clinical world where the patients vaguely resemble the question stem descriptions. Finally, intangible theory can be put into practice. Yet, it is becoming increasingly difficult for 3rd-year medical student clerkship directors to find enough clinical sites to support the growing number of medical students as enrollment numbers steadily increase and outpace the current clinical resources.
In a 2019 Association of American Medical Colleges report, 84% of medical school deans were concerned about the diminishing number of clerkship sites, and there was additional worry about lack of qualified specialty preceptors. This lack of clerkship availability is especially true for psychiatry sites.
Psychiatry clerkship directors are in need of more clinical sites to address the educational needs of medical students, and psychiatrists in the broader clinical community are positioned to help medical schools expand their clinical sites.
Inpatient psychiatric units and consult services continue to be popular sites for medical student rotations, but it has been hard to expand into other settings, where psychiatric treatment is seen as more private and intimate than other specialties. Reasons for falling site availability are varied and include 1) financial disincentive to take students – because they can be seen as a burden on supervisors who must meet revenue-generating patient quotas; 2) competition with other learners, including residents, PA students, NPs, and NP students; and 3) the general financial and operational obstacles to clinical practice inflicted by the pandemic. COVID-19 affected medical education – for better and worse (JAMA. 2020;324[11]:1033-4). Psychiatry clerkships particularly suffered from restricted patient access as inpatient units reduced their census to comply with COVID-19 safety protocols, and during the height of the pandemic inpatient units provided psychiatric care to COVID-19–positive patients, which precluded student involvement. On the other hand, many more students were introduced to telepsychiatry and witnessed creative forms of mental health intervention as clinicians adapted their practices to the pandemic.
When rotations began
Clinical rotations entered the American medical school curriculum in the 1890s when Sir William Osler brought the European standard of medical education with him as Physician in Chief at the newly opened Johns Hopkins University Hospital. He formalized the traditional apprenticeship model by standardizing 3rd- and 4th-year clerkships as rotations in which medical students worked in clinics and on the wards, learning from residents and attendings.
Clinical rotations, their location, the supervisors, and the patients and their ailments all go in to influence a student’s specialty choice. Some students enter medical school knowing they want to be a surgeon, a pediatrician, or a psychiatrist. And some are compelled by a specific rotation, when they realize that it’s not at all what they expected and maybe they could dedicate their professional life to this area of medicine.
High-quality clinical clerkship sites are essential to the future of psychiatry. At clerkship sites, undecided students interested in psychiatry may affirm their commitment to psychiatry. Other students will have their only dedicated exposure to psychiatrically ill patients. This represents students’ only opportunity to learn the skills to treat comorbid psychiatric and medical illness. Regardless of specialty, nearly every physician will have to treat patients with some psychiatric illnesses.
What constitutes a “high-quality clinical site” is difficult to measure and define. Some measures of quality include a safe learning environment, a reasonable ratio of students to supervisors (including residents, fellows, and attendings), and an adequate number and diversity of patients. Many medical schools may prefer an affiliated academic medical center or Veterans’ Affairs hospitals for their rotating students. Private psychiatric hospitals are proliferating, and if these are to be sites for medical students, the following standards are suggested: Private psychiatric hospitals must follow standard safety precautions with sufficient staff presence, ensure willing preceptors who can provide adequate student supervision, and adjust their expectations to students who can carry a few patients of diverse background, but are not to be treated merely as scribes.
Psychiatrists, whether they consider themselves “academic” or not, have a role to play in expanding access to clinical sites. Students are eager to learn in any setting. Inpatient settings have long been seen as the norm for clinical education in psychiatry. Yet inpatient settings perpetuate the idea that those with severe mental illness or individuals with psychosocial stressors or disabling, comorbid substance use disorders are the only people who seek help from a psychiatrist. without an academic affiliation to explore the possibility of creating space for a medical student in their clinical practice.
We cannot deny the demands on psychiatrists’ time – every minute is counted by the patient and doctor, and every encounter is accounted for in some revenue stream. However, the academic world is running out of space for its students, and there’s a serious question as to whether an academic center is the only place for students. If you are a psychiatrist who still loves to learn and prides themselves on high-quality patient care, then you have an essential role in shaping the students who will one day be your peers in psychiatry, or the physicians treating your patients’ comorbid medical illnesses.
There are upfront challenges to teaching 3rd-year medical students, including teaching the psychiatric interview, note writing, persuading patients to allow students into their care, and setting time aside at the end of the workday to provide feedback on performance. Yet, after learning the ropes of psychiatric patient care, medical students can provide help in writing notes, calling collateral, contacting patients with their laboratory results, and even helping with the tedious but necessary administrative tasks like prior authorizations. In exchange for training students, some medical schools may offer perks, such as a volunteer faculty position that comes with access to usually expensive library resources, such as medical databases.
You can help expand clinical sites in psychiatry rotations by contacting your alma mater or the medical school closest to your community and asking about their need for clerkship sites. Many medical schools are branching out by sending students to stay near the clinical sites and immerse themselves in the community where their site director practices. Even one-half day a week in an outpatient setting provides patient and setting diversity to students and helps spread out students to different sites, easing the burden on inpatient supervisors while providing students more individualized supervision.
The practice of medicine is built on apprenticeship and teaching wisdom through patient care. Just because we leave residency doesn’t mean we leave academics. Taking students into your practice is an invaluable service to the medical education community and future physicians.
Dr. Posada is assistant clinical professor in the department of psychiatry and behavioral sciences at George Washington University in Washington, and staff physician at George Washington Medical Faculty Associates, also in Washington. She has no conflicts of interest. Dr. Ortiz is assistant professor and clerkship director in the department of psychiatry at Texas Tech University Health Sciences Center – El Paso. She has no conflicts of interest.
Merck’s new COVID-19 pill: ‘Game changer’ or just one more tool?
Soon after Merck announced on Oct. 1 that it would ask federal regulators for emergency use authorization (EUA) for its auspicious new COVID-19 pill, the accolades began.
Former Food and Drug Administration chief Scott Gottlieb, MD, told CNBC the drug was “a profound game changer.” Top infectious disease expert Anthony S. Fauci, MD, called the early data “impressive.” The World Health Organization termed it “certainly good news,” while saying it awaits more data.
Merck, partnering with Ridgeback Biotherapeutics on the investigational oral antiviral medicine molnupiravir, plans to submit applications to regulatory agencies worldwide, hoping to deliver the first oral antiviral medication for COVID-19.
Interim clinical trial results show that the drug may slash the risk for hospitalization or death by 50% in those with mild to moderate COVID-19.
When the results were found to be so favorable, the study was halted at the recommendation of an independent data-monitoring committee and in consultation with the FDA.
“This anticipated drug has gotten a little more hype than it deserves,” said William Schaffner, MD, professor of preventive medicine and infectious disease specialist at Vanderbilt University Medical Center in Nashville, Tenn. He and others suggest a reality check.
“It’s not exactly a home run, like penicillin for strep throat,” agreed Carl Fichtenbaum, MD, professor of infectious diseases at the University of Cincinnati, who is investigating a similar pill for a rival company, Atea, partnering with Roche.
“But it is encouraging,” he said. “It will probably be an incremental improvement on what we have.” The fact that it can be taken at home is a plus: “Anything we can do to keep people from getting sicker is a good thing.”
“The data show in this higher risk group [those who were studied had at least one risk factor for severe COVID-19, such as age or a medical condition], it reduces the risk of advancing to severe disease by 50%,” Dr. Schaffner said. While that’s a clear benefit for half, it of course leaves the other half without benefit, he said.
Others critiqued the predicted cost of the drug. The U.S. government has already agreed to pay about $700 per patient, according to a new report from Harvard T. H. Chan School of Public Health, Boston, and King’s College Hospital, London. That analysis concluded that the actual cost of production for the 5-day course is $17.74.
“We fully expect that having an oral treatment that reduces the risk of hospitalizations will be significantly cost effective for society,” Melissa Moody, a Merck spokesperson, told this news organization. “We are optimistic that molnupiravir can become an important medicine as part of the global effort to fight the pandemic.”
Merck expects to produce 10 million courses of treatment by the end of the year, with additional doses expected to be produced in 2022, according to a company press release. Earlier in 2021, Merck finalized its agreement with the U.S. government to supply about 1.7 million courses of the drug at the $700 price, once an EUA or FDA approval is given.
Merck also has supply and purchase agreements with other governments worldwide, pending regulatory approval.
Study details
Details about the study findings came from a Merck press release. In the planned interim analysis, Merck and Ridgeback evaluated data from 775 patients initially enrolled in the phase 3 MOVe-OUT trial.
All adults had lab-confirmed mild to moderate COVID-19, and reported onset of symptoms within 5 days of being randomly assigned to the drug or placebo. All had at least one risk factor linked with poor disease outcome (such as older age or obesity).
The drug is a ribonucleoside and works by creating mutations in the virus’s genome, halting the ability of the virus to replicate.
Through day 29 of the study, the drug reduced the risk or hospitalization or death by about 50%. While 7.3% of those who received the drug either died or were hospitalized by day 29, 14.1% of those on placebo did, a statistically significant difference (P = .0012).
Side effects were similar in both groups, with 35% of the drug-treated and 40% of the placebo group reporting some side effect, Merck reported. Adverse drug-related events were 12% in the drug group and 11% in the placebo group. While 1.3% of the drug-treated group quit the study because of an adverse event, 3.4% of the placebo group quit.
Pros, cons, and unknowns
The ability to take the drug orally, and at home, is a definite plus, Dr. Schaffner said, compared with the monoclonal antibody treatment currently approved that must be given intravenously or subcutaneously and in certain locations.
More people could be reached and helped with the option of an at-home, oral medicine, he and others agreed.
The regimen for molnupiravir is four pills, two times daily, for 5 days, even if symptoms are mild. As with other prescription drugs, “there will always be folks who don’t comply completely” with the prescribed regimen, Dr. Schaffner said. With this pill, that might be especially true if the symptoms are very mild.
The 50% reduction is not as effective as the benefit often quoted for monoclonal antibody treatment. In clinical trials of Regeneron’s monoclonal antibody treatment, the regimen reduced COVID-19–related hospitalization or death in high-risk patients by 70%.
Even so, the new pill could change the pandemic’s course, others say. “I think molnupiravir has the potential to change how we take care of people who have COVID and risk factors for developing severe disease,” Rajesh Tim Gandhi, MD, an infectious disease physician at Massachusetts General Hospital and Harvard Medical School in Boston, told this news organization.
“What we’ll need to do, however, is make sure that people get tested quickly after they develop symptoms and, if they’re confirmed to have COVID, start on the pills within 5 days of developing symptoms,” he said, while warning that more data are needed about the drug and the trial results.
Another concern is that the promise of a pill will stall vaccination rates, with some people figuring why get vaccinated when they can obtain the pill if they do get sick.
Relying on treatment alone won’t work, Dr. Schaffner said. “Let’s [also] focus on prevention, which is the vaccine. We have to keep working both sides of the street.”
Dr. Gandhi added: “It’s important to remember that even though molnupiravir reduced the likelihood of hospitalization and death, a number of people who received the drug still got sick enough to end up in the hospital.”
Also unknown, he said, is how severe their disease was and whether they will develop long COVID.
The Merck study included only unvaccinated people. Might it work for those vaccinated people who get a breakthrough infection? “From a purely scientific perspective, there is no reason to believe molnupiravir would not work in people who are vaccinated, but the overall efficacy on top of the vaccine is likely dependent on how well they were able to mount a protective immune response to the vaccine,” Ms. Moody said. Still, Merck believes the pill could be of benefit for these infections too, she added.
As for the expected cost, Ms. Moody said that the company takes into account a number of factors in setting pricing, “but fundamentally we look at the impact of the disease, the benefits that the drug delivers to patients and to society, and at supporting ongoing drug development.”
On Merck’s heels: Pfizer, Roche, Atea
Pfizer is studying an antiviral pill, PF-07321332, a protease inhibitor that blocks the protease enzymes and halts replication of the virus.
In addition to studying the drug in infected patients at high risk of severe illness and in those at typical risk, Pfizer launched a phase 2-3 study in late September that will enroll people who live in the same household as a person with a confirmed, symptomatic COVID-19 infection to see if the drug can prevent disease in those who have been exposed.
Atea and Roche’s COVID pill, AT527, is in phase 3 trials as well. AT527 is an inhibitor of polymerase, an enzyme many viruses have, to stop replications. Atea is evaluating the drug to reduce disease “burden” and for both pre- and postexposure prevention.
Big picture: Role of COVID-19 pills
It may be necessary to target the coronavirus with more than one antiviral agent, said Dr. Fichtenbaum, a principal investigator for the AT527 trials.
“Sometimes viruses require two or three active agents to control their replication,” he said, citing information gleaned from other viral research, such as HIV. For control of HIV infection, a cocktail or combination of antivirals is often recommended.
That may well be the case for COVID-19, Dr. Fichtenbaum said. The goal would be to attack the virus at more than one pathway.
A version of this article first appeared on Medscape.com.
Soon after Merck announced on Oct. 1 that it would ask federal regulators for emergency use authorization (EUA) for its auspicious new COVID-19 pill, the accolades began.
Former Food and Drug Administration chief Scott Gottlieb, MD, told CNBC the drug was “a profound game changer.” Top infectious disease expert Anthony S. Fauci, MD, called the early data “impressive.” The World Health Organization termed it “certainly good news,” while saying it awaits more data.
Merck, partnering with Ridgeback Biotherapeutics on the investigational oral antiviral medicine molnupiravir, plans to submit applications to regulatory agencies worldwide, hoping to deliver the first oral antiviral medication for COVID-19.
Interim clinical trial results show that the drug may slash the risk for hospitalization or death by 50% in those with mild to moderate COVID-19.
When the results were found to be so favorable, the study was halted at the recommendation of an independent data-monitoring committee and in consultation with the FDA.
“This anticipated drug has gotten a little more hype than it deserves,” said William Schaffner, MD, professor of preventive medicine and infectious disease specialist at Vanderbilt University Medical Center in Nashville, Tenn. He and others suggest a reality check.
“It’s not exactly a home run, like penicillin for strep throat,” agreed Carl Fichtenbaum, MD, professor of infectious diseases at the University of Cincinnati, who is investigating a similar pill for a rival company, Atea, partnering with Roche.
“But it is encouraging,” he said. “It will probably be an incremental improvement on what we have.” The fact that it can be taken at home is a plus: “Anything we can do to keep people from getting sicker is a good thing.”
“The data show in this higher risk group [those who were studied had at least one risk factor for severe COVID-19, such as age or a medical condition], it reduces the risk of advancing to severe disease by 50%,” Dr. Schaffner said. While that’s a clear benefit for half, it of course leaves the other half without benefit, he said.
Others critiqued the predicted cost of the drug. The U.S. government has already agreed to pay about $700 per patient, according to a new report from Harvard T. H. Chan School of Public Health, Boston, and King’s College Hospital, London. That analysis concluded that the actual cost of production for the 5-day course is $17.74.
“We fully expect that having an oral treatment that reduces the risk of hospitalizations will be significantly cost effective for society,” Melissa Moody, a Merck spokesperson, told this news organization. “We are optimistic that molnupiravir can become an important medicine as part of the global effort to fight the pandemic.”
Merck expects to produce 10 million courses of treatment by the end of the year, with additional doses expected to be produced in 2022, according to a company press release. Earlier in 2021, Merck finalized its agreement with the U.S. government to supply about 1.7 million courses of the drug at the $700 price, once an EUA or FDA approval is given.
Merck also has supply and purchase agreements with other governments worldwide, pending regulatory approval.
Study details
Details about the study findings came from a Merck press release. In the planned interim analysis, Merck and Ridgeback evaluated data from 775 patients initially enrolled in the phase 3 MOVe-OUT trial.
All adults had lab-confirmed mild to moderate COVID-19, and reported onset of symptoms within 5 days of being randomly assigned to the drug or placebo. All had at least one risk factor linked with poor disease outcome (such as older age or obesity).
The drug is a ribonucleoside and works by creating mutations in the virus’s genome, halting the ability of the virus to replicate.
Through day 29 of the study, the drug reduced the risk or hospitalization or death by about 50%. While 7.3% of those who received the drug either died or were hospitalized by day 29, 14.1% of those on placebo did, a statistically significant difference (P = .0012).
Side effects were similar in both groups, with 35% of the drug-treated and 40% of the placebo group reporting some side effect, Merck reported. Adverse drug-related events were 12% in the drug group and 11% in the placebo group. While 1.3% of the drug-treated group quit the study because of an adverse event, 3.4% of the placebo group quit.
Pros, cons, and unknowns
The ability to take the drug orally, and at home, is a definite plus, Dr. Schaffner said, compared with the monoclonal antibody treatment currently approved that must be given intravenously or subcutaneously and in certain locations.
More people could be reached and helped with the option of an at-home, oral medicine, he and others agreed.
The regimen for molnupiravir is four pills, two times daily, for 5 days, even if symptoms are mild. As with other prescription drugs, “there will always be folks who don’t comply completely” with the prescribed regimen, Dr. Schaffner said. With this pill, that might be especially true if the symptoms are very mild.
The 50% reduction is not as effective as the benefit often quoted for monoclonal antibody treatment. In clinical trials of Regeneron’s monoclonal antibody treatment, the regimen reduced COVID-19–related hospitalization or death in high-risk patients by 70%.
Even so, the new pill could change the pandemic’s course, others say. “I think molnupiravir has the potential to change how we take care of people who have COVID and risk factors for developing severe disease,” Rajesh Tim Gandhi, MD, an infectious disease physician at Massachusetts General Hospital and Harvard Medical School in Boston, told this news organization.
“What we’ll need to do, however, is make sure that people get tested quickly after they develop symptoms and, if they’re confirmed to have COVID, start on the pills within 5 days of developing symptoms,” he said, while warning that more data are needed about the drug and the trial results.
Another concern is that the promise of a pill will stall vaccination rates, with some people figuring why get vaccinated when they can obtain the pill if they do get sick.
Relying on treatment alone won’t work, Dr. Schaffner said. “Let’s [also] focus on prevention, which is the vaccine. We have to keep working both sides of the street.”
Dr. Gandhi added: “It’s important to remember that even though molnupiravir reduced the likelihood of hospitalization and death, a number of people who received the drug still got sick enough to end up in the hospital.”
Also unknown, he said, is how severe their disease was and whether they will develop long COVID.
The Merck study included only unvaccinated people. Might it work for those vaccinated people who get a breakthrough infection? “From a purely scientific perspective, there is no reason to believe molnupiravir would not work in people who are vaccinated, but the overall efficacy on top of the vaccine is likely dependent on how well they were able to mount a protective immune response to the vaccine,” Ms. Moody said. Still, Merck believes the pill could be of benefit for these infections too, she added.
As for the expected cost, Ms. Moody said that the company takes into account a number of factors in setting pricing, “but fundamentally we look at the impact of the disease, the benefits that the drug delivers to patients and to society, and at supporting ongoing drug development.”
On Merck’s heels: Pfizer, Roche, Atea
Pfizer is studying an antiviral pill, PF-07321332, a protease inhibitor that blocks the protease enzymes and halts replication of the virus.
In addition to studying the drug in infected patients at high risk of severe illness and in those at typical risk, Pfizer launched a phase 2-3 study in late September that will enroll people who live in the same household as a person with a confirmed, symptomatic COVID-19 infection to see if the drug can prevent disease in those who have been exposed.
Atea and Roche’s COVID pill, AT527, is in phase 3 trials as well. AT527 is an inhibitor of polymerase, an enzyme many viruses have, to stop replications. Atea is evaluating the drug to reduce disease “burden” and for both pre- and postexposure prevention.
Big picture: Role of COVID-19 pills
It may be necessary to target the coronavirus with more than one antiviral agent, said Dr. Fichtenbaum, a principal investigator for the AT527 trials.
“Sometimes viruses require two or three active agents to control their replication,” he said, citing information gleaned from other viral research, such as HIV. For control of HIV infection, a cocktail or combination of antivirals is often recommended.
That may well be the case for COVID-19, Dr. Fichtenbaum said. The goal would be to attack the virus at more than one pathway.
A version of this article first appeared on Medscape.com.
Soon after Merck announced on Oct. 1 that it would ask federal regulators for emergency use authorization (EUA) for its auspicious new COVID-19 pill, the accolades began.
Former Food and Drug Administration chief Scott Gottlieb, MD, told CNBC the drug was “a profound game changer.” Top infectious disease expert Anthony S. Fauci, MD, called the early data “impressive.” The World Health Organization termed it “certainly good news,” while saying it awaits more data.
Merck, partnering with Ridgeback Biotherapeutics on the investigational oral antiviral medicine molnupiravir, plans to submit applications to regulatory agencies worldwide, hoping to deliver the first oral antiviral medication for COVID-19.
Interim clinical trial results show that the drug may slash the risk for hospitalization or death by 50% in those with mild to moderate COVID-19.
When the results were found to be so favorable, the study was halted at the recommendation of an independent data-monitoring committee and in consultation with the FDA.
“This anticipated drug has gotten a little more hype than it deserves,” said William Schaffner, MD, professor of preventive medicine and infectious disease specialist at Vanderbilt University Medical Center in Nashville, Tenn. He and others suggest a reality check.
“It’s not exactly a home run, like penicillin for strep throat,” agreed Carl Fichtenbaum, MD, professor of infectious diseases at the University of Cincinnati, who is investigating a similar pill for a rival company, Atea, partnering with Roche.
“But it is encouraging,” he said. “It will probably be an incremental improvement on what we have.” The fact that it can be taken at home is a plus: “Anything we can do to keep people from getting sicker is a good thing.”
“The data show in this higher risk group [those who were studied had at least one risk factor for severe COVID-19, such as age or a medical condition], it reduces the risk of advancing to severe disease by 50%,” Dr. Schaffner said. While that’s a clear benefit for half, it of course leaves the other half without benefit, he said.
Others critiqued the predicted cost of the drug. The U.S. government has already agreed to pay about $700 per patient, according to a new report from Harvard T. H. Chan School of Public Health, Boston, and King’s College Hospital, London. That analysis concluded that the actual cost of production for the 5-day course is $17.74.
“We fully expect that having an oral treatment that reduces the risk of hospitalizations will be significantly cost effective for society,” Melissa Moody, a Merck spokesperson, told this news organization. “We are optimistic that molnupiravir can become an important medicine as part of the global effort to fight the pandemic.”
Merck expects to produce 10 million courses of treatment by the end of the year, with additional doses expected to be produced in 2022, according to a company press release. Earlier in 2021, Merck finalized its agreement with the U.S. government to supply about 1.7 million courses of the drug at the $700 price, once an EUA or FDA approval is given.
Merck also has supply and purchase agreements with other governments worldwide, pending regulatory approval.
Study details
Details about the study findings came from a Merck press release. In the planned interim analysis, Merck and Ridgeback evaluated data from 775 patients initially enrolled in the phase 3 MOVe-OUT trial.
All adults had lab-confirmed mild to moderate COVID-19, and reported onset of symptoms within 5 days of being randomly assigned to the drug or placebo. All had at least one risk factor linked with poor disease outcome (such as older age or obesity).
The drug is a ribonucleoside and works by creating mutations in the virus’s genome, halting the ability of the virus to replicate.
Through day 29 of the study, the drug reduced the risk or hospitalization or death by about 50%. While 7.3% of those who received the drug either died or were hospitalized by day 29, 14.1% of those on placebo did, a statistically significant difference (P = .0012).
Side effects were similar in both groups, with 35% of the drug-treated and 40% of the placebo group reporting some side effect, Merck reported. Adverse drug-related events were 12% in the drug group and 11% in the placebo group. While 1.3% of the drug-treated group quit the study because of an adverse event, 3.4% of the placebo group quit.
Pros, cons, and unknowns
The ability to take the drug orally, and at home, is a definite plus, Dr. Schaffner said, compared with the monoclonal antibody treatment currently approved that must be given intravenously or subcutaneously and in certain locations.
More people could be reached and helped with the option of an at-home, oral medicine, he and others agreed.
The regimen for molnupiravir is four pills, two times daily, for 5 days, even if symptoms are mild. As with other prescription drugs, “there will always be folks who don’t comply completely” with the prescribed regimen, Dr. Schaffner said. With this pill, that might be especially true if the symptoms are very mild.
The 50% reduction is not as effective as the benefit often quoted for monoclonal antibody treatment. In clinical trials of Regeneron’s monoclonal antibody treatment, the regimen reduced COVID-19–related hospitalization or death in high-risk patients by 70%.
Even so, the new pill could change the pandemic’s course, others say. “I think molnupiravir has the potential to change how we take care of people who have COVID and risk factors for developing severe disease,” Rajesh Tim Gandhi, MD, an infectious disease physician at Massachusetts General Hospital and Harvard Medical School in Boston, told this news organization.
“What we’ll need to do, however, is make sure that people get tested quickly after they develop symptoms and, if they’re confirmed to have COVID, start on the pills within 5 days of developing symptoms,” he said, while warning that more data are needed about the drug and the trial results.
Another concern is that the promise of a pill will stall vaccination rates, with some people figuring why get vaccinated when they can obtain the pill if they do get sick.
Relying on treatment alone won’t work, Dr. Schaffner said. “Let’s [also] focus on prevention, which is the vaccine. We have to keep working both sides of the street.”
Dr. Gandhi added: “It’s important to remember that even though molnupiravir reduced the likelihood of hospitalization and death, a number of people who received the drug still got sick enough to end up in the hospital.”
Also unknown, he said, is how severe their disease was and whether they will develop long COVID.
The Merck study included only unvaccinated people. Might it work for those vaccinated people who get a breakthrough infection? “From a purely scientific perspective, there is no reason to believe molnupiravir would not work in people who are vaccinated, but the overall efficacy on top of the vaccine is likely dependent on how well they were able to mount a protective immune response to the vaccine,” Ms. Moody said. Still, Merck believes the pill could be of benefit for these infections too, she added.
As for the expected cost, Ms. Moody said that the company takes into account a number of factors in setting pricing, “but fundamentally we look at the impact of the disease, the benefits that the drug delivers to patients and to society, and at supporting ongoing drug development.”
On Merck’s heels: Pfizer, Roche, Atea
Pfizer is studying an antiviral pill, PF-07321332, a protease inhibitor that blocks the protease enzymes and halts replication of the virus.
In addition to studying the drug in infected patients at high risk of severe illness and in those at typical risk, Pfizer launched a phase 2-3 study in late September that will enroll people who live in the same household as a person with a confirmed, symptomatic COVID-19 infection to see if the drug can prevent disease in those who have been exposed.
Atea and Roche’s COVID pill, AT527, is in phase 3 trials as well. AT527 is an inhibitor of polymerase, an enzyme many viruses have, to stop replications. Atea is evaluating the drug to reduce disease “burden” and for both pre- and postexposure prevention.
Big picture: Role of COVID-19 pills
It may be necessary to target the coronavirus with more than one antiviral agent, said Dr. Fichtenbaum, a principal investigator for the AT527 trials.
“Sometimes viruses require two or three active agents to control their replication,” he said, citing information gleaned from other viral research, such as HIV. For control of HIV infection, a cocktail or combination of antivirals is often recommended.
That may well be the case for COVID-19, Dr. Fichtenbaum said. The goal would be to attack the virus at more than one pathway.
A version of this article first appeared on Medscape.com.
Web of antimicrobials doesn’t hold water
Music plus mushrooms equals therapy
Magic mushrooms have been used recreationally and medicinally for thousands of years, but researchers have found adding music could be a game changer in antidepressant treatment.
The ingredient that makes these mushrooms so magical is psilocybin. It works well for the clinical treatment of mental health conditions and some forms of depression because the “trip” can be contained to one work day, making it easy to administer under supervision. With the accompaniment of music, scientists have found that psilocybin evokes emotion.
This recent study, presented at the European College of Neuropsychopharmacology Congress in Lisbon, tested participants’ emotional response to music before and after the psilocybin. Ketanserin, an antihypertensive drug, was used to test against the effects of psilocybin. The scientist played Mozart and Elgar and found that participants on psilocybin had an emotional response increase of 60%. That response was even greater, compared with ketanserin, which actually lessened the emotional response to music.
“This shows that combination of psilocybin and music has a strong emotional effect, and we believe that this will be important for the therapeutic application of psychedelics if they are approved for clinical use,” said lead researcher Dea Siggaard Stenbæk of the University of Copenhagen.
Professor David J. Nutt of Imperial College in London, who was not involved in the study, said that it supports the use of music for treatment efficacy with psychedelics and suggested that the next step is to “optimise this approach probably through individualising and personalising music tracks in therapy.”
Cue the 1960s LSD music montage.
Chicken ‘white striping is not a disease’
Have you ever sliced open a new pack of chicken breasts to start dinner and noticed white fatty lines running through the chicken? Maybe you thought it was just some extra fat to trim off, but the Humane League calls it “white striping disease.”
Chicken is the No. 1 meat consumed by Americans, so it’s not surprising that chickens are factory farmed and raised to be ready for slaughter quickly, according to CBSNews.com, which reported that the Humane League claims white striping is found in 70% of the chicken in popular grocery stores. The league expressed concern for the chickens’ welfare as they are bred to grow bigger quickly, which is causing the white striping and increasing the fat content of the meat by as much as 224%.
The National Chicken Council told CBS that the league’s findings were unscientific. A spokesperson said, “White striping is not a disease. It is a quality factor in chicken breast meat caused by deposits of fat in the muscle during the bird’s growth and development.” He went on to say that severe white striping happens in 3%-6% of birds, which are mostly used in further processed products, not in chicken breast packages.
Somehow, that’s not making us feel any better.
The itsy bitsy spider lets us all down
Most people do not like spiders. That’s too bad, because spiders are generally nothing but helpful little creatures that prey upon annoying flies and other pests. Then there’s the silk they produce. The ancient Romans used it to treat conditions such as warts and skin lesions. Spiders wrap their eggs in silk to protect them from harmful bacteria.
Of course, we can hardly trust the medical opinions of people from 2,000 years ago, but modern-day studies have not definitively proved whether or not spider silk has any antimicrobial properties.
To settle the matter once and for all, researchers from Denmark built a silk-harvesting machine using the most famous of Danish inventions: Legos. The contraption, sort of a paddle wheel, pulled the silk from several different species of spider pinned down by the researchers. The silk was then tested against three different bacteria species, including good old Escherichia coli.
Unfortunately for our spider friends, their silk has no antimicrobial activity. The researchers suspected that any such activity seen in previous studies was actually caused by improper control for the solvents used to extract the silk; those solvents can have antimicrobial properties on their own. As for protecting their eggs, rather than killing bacteria, the silk likely provides a physical barrier alone.
It is bad news for spiders on the benefit-to-humanity front, but look at the bright side: If their silk had antimicrobial activity, we’d have to start farming them to acquire more silk. And that’s no good. Spiders deserve to roam free, hunt as they please, and drop down on your head from the ceiling.
Anxiety and allergies: Cause, effect, confusion
We’re big fans of science, but as longtime, totally impartial (Science rules!) observers of science’s medical realm, we can see that the day-to-day process of practicing the scientific method occasionally gets a bit messy. And no, we’re not talking about COVID-19.
We’re talking allergies. We’re talking mental health. We’re talking allergic disease and mental health.
We’re talking about a pair of press releases we came across during our never-ending search for material to educate, entertain, and astound our fabulously wonderful and loyal readers. (We say that, of course, in the most impartial way possible.)
The first release was titled, “Allergies including asthma and hay fever not linked to mental health traits” and covered research from the University of Bristol (England). The investigators were trying to determine if “allergic diseases actually causes mental health traits including anxiety, depression, bipolar disorder, and schizophrenia, or vice versa,” according to the release.
What they found, however, was “little evidence of a causal relationship between the onset of allergic disease and mental health.” Again, this is the press release talking.
The second release seemed to suggest the exact opposite: “Study uncovers link between allergies and mental health conditions.” That got our attention. A little more reading revealed that “people with asthma, atopic dermatitis, and hay fever also had a higher likelihood of having depression, anxiety, bipolar disorder, or neuroticism.”
One of the investigators was quoted as saying, “Establishing whether allergic disease causes mental health problems, or vice versa, is important to ensure that resources and treatment strategies are targeted appropriately.”
Did you notice the “vice versa”? Did you notice that it appeared in quotes from both releases? We did, so we took a closer look at the source. The second release covered a group of investigators from the University of Bristol – the same group, and the same study, in fact, as the first one.
So there you have it. One study, two press releases, and one confused journalist. Thank you, science.
Music plus mushrooms equals therapy
Magic mushrooms have been used recreationally and medicinally for thousands of years, but researchers have found adding music could be a game changer in antidepressant treatment.
The ingredient that makes these mushrooms so magical is psilocybin. It works well for the clinical treatment of mental health conditions and some forms of depression because the “trip” can be contained to one work day, making it easy to administer under supervision. With the accompaniment of music, scientists have found that psilocybin evokes emotion.
This recent study, presented at the European College of Neuropsychopharmacology Congress in Lisbon, tested participants’ emotional response to music before and after the psilocybin. Ketanserin, an antihypertensive drug, was used to test against the effects of psilocybin. The scientist played Mozart and Elgar and found that participants on psilocybin had an emotional response increase of 60%. That response was even greater, compared with ketanserin, which actually lessened the emotional response to music.
“This shows that combination of psilocybin and music has a strong emotional effect, and we believe that this will be important for the therapeutic application of psychedelics if they are approved for clinical use,” said lead researcher Dea Siggaard Stenbæk of the University of Copenhagen.
Professor David J. Nutt of Imperial College in London, who was not involved in the study, said that it supports the use of music for treatment efficacy with psychedelics and suggested that the next step is to “optimise this approach probably through individualising and personalising music tracks in therapy.”
Cue the 1960s LSD music montage.
Chicken ‘white striping is not a disease’
Have you ever sliced open a new pack of chicken breasts to start dinner and noticed white fatty lines running through the chicken? Maybe you thought it was just some extra fat to trim off, but the Humane League calls it “white striping disease.”
Chicken is the No. 1 meat consumed by Americans, so it’s not surprising that chickens are factory farmed and raised to be ready for slaughter quickly, according to CBSNews.com, which reported that the Humane League claims white striping is found in 70% of the chicken in popular grocery stores. The league expressed concern for the chickens’ welfare as they are bred to grow bigger quickly, which is causing the white striping and increasing the fat content of the meat by as much as 224%.
The National Chicken Council told CBS that the league’s findings were unscientific. A spokesperson said, “White striping is not a disease. It is a quality factor in chicken breast meat caused by deposits of fat in the muscle during the bird’s growth and development.” He went on to say that severe white striping happens in 3%-6% of birds, which are mostly used in further processed products, not in chicken breast packages.
Somehow, that’s not making us feel any better.
The itsy bitsy spider lets us all down
Most people do not like spiders. That’s too bad, because spiders are generally nothing but helpful little creatures that prey upon annoying flies and other pests. Then there’s the silk they produce. The ancient Romans used it to treat conditions such as warts and skin lesions. Spiders wrap their eggs in silk to protect them from harmful bacteria.
Of course, we can hardly trust the medical opinions of people from 2,000 years ago, but modern-day studies have not definitively proved whether or not spider silk has any antimicrobial properties.
To settle the matter once and for all, researchers from Denmark built a silk-harvesting machine using the most famous of Danish inventions: Legos. The contraption, sort of a paddle wheel, pulled the silk from several different species of spider pinned down by the researchers. The silk was then tested against three different bacteria species, including good old Escherichia coli.
Unfortunately for our spider friends, their silk has no antimicrobial activity. The researchers suspected that any such activity seen in previous studies was actually caused by improper control for the solvents used to extract the silk; those solvents can have antimicrobial properties on their own. As for protecting their eggs, rather than killing bacteria, the silk likely provides a physical barrier alone.
It is bad news for spiders on the benefit-to-humanity front, but look at the bright side: If their silk had antimicrobial activity, we’d have to start farming them to acquire more silk. And that’s no good. Spiders deserve to roam free, hunt as they please, and drop down on your head from the ceiling.
Anxiety and allergies: Cause, effect, confusion
We’re big fans of science, but as longtime, totally impartial (Science rules!) observers of science’s medical realm, we can see that the day-to-day process of practicing the scientific method occasionally gets a bit messy. And no, we’re not talking about COVID-19.
We’re talking allergies. We’re talking mental health. We’re talking allergic disease and mental health.
We’re talking about a pair of press releases we came across during our never-ending search for material to educate, entertain, and astound our fabulously wonderful and loyal readers. (We say that, of course, in the most impartial way possible.)
The first release was titled, “Allergies including asthma and hay fever not linked to mental health traits” and covered research from the University of Bristol (England). The investigators were trying to determine if “allergic diseases actually causes mental health traits including anxiety, depression, bipolar disorder, and schizophrenia, or vice versa,” according to the release.
What they found, however, was “little evidence of a causal relationship between the onset of allergic disease and mental health.” Again, this is the press release talking.
The second release seemed to suggest the exact opposite: “Study uncovers link between allergies and mental health conditions.” That got our attention. A little more reading revealed that “people with asthma, atopic dermatitis, and hay fever also had a higher likelihood of having depression, anxiety, bipolar disorder, or neuroticism.”
One of the investigators was quoted as saying, “Establishing whether allergic disease causes mental health problems, or vice versa, is important to ensure that resources and treatment strategies are targeted appropriately.”
Did you notice the “vice versa”? Did you notice that it appeared in quotes from both releases? We did, so we took a closer look at the source. The second release covered a group of investigators from the University of Bristol – the same group, and the same study, in fact, as the first one.
So there you have it. One study, two press releases, and one confused journalist. Thank you, science.
Music plus mushrooms equals therapy
Magic mushrooms have been used recreationally and medicinally for thousands of years, but researchers have found adding music could be a game changer in antidepressant treatment.
The ingredient that makes these mushrooms so magical is psilocybin. It works well for the clinical treatment of mental health conditions and some forms of depression because the “trip” can be contained to one work day, making it easy to administer under supervision. With the accompaniment of music, scientists have found that psilocybin evokes emotion.
This recent study, presented at the European College of Neuropsychopharmacology Congress in Lisbon, tested participants’ emotional response to music before and after the psilocybin. Ketanserin, an antihypertensive drug, was used to test against the effects of psilocybin. The scientist played Mozart and Elgar and found that participants on psilocybin had an emotional response increase of 60%. That response was even greater, compared with ketanserin, which actually lessened the emotional response to music.
“This shows that combination of psilocybin and music has a strong emotional effect, and we believe that this will be important for the therapeutic application of psychedelics if they are approved for clinical use,” said lead researcher Dea Siggaard Stenbæk of the University of Copenhagen.
Professor David J. Nutt of Imperial College in London, who was not involved in the study, said that it supports the use of music for treatment efficacy with psychedelics and suggested that the next step is to “optimise this approach probably through individualising and personalising music tracks in therapy.”
Cue the 1960s LSD music montage.
Chicken ‘white striping is not a disease’
Have you ever sliced open a new pack of chicken breasts to start dinner and noticed white fatty lines running through the chicken? Maybe you thought it was just some extra fat to trim off, but the Humane League calls it “white striping disease.”
Chicken is the No. 1 meat consumed by Americans, so it’s not surprising that chickens are factory farmed and raised to be ready for slaughter quickly, according to CBSNews.com, which reported that the Humane League claims white striping is found in 70% of the chicken in popular grocery stores. The league expressed concern for the chickens’ welfare as they are bred to grow bigger quickly, which is causing the white striping and increasing the fat content of the meat by as much as 224%.
The National Chicken Council told CBS that the league’s findings were unscientific. A spokesperson said, “White striping is not a disease. It is a quality factor in chicken breast meat caused by deposits of fat in the muscle during the bird’s growth and development.” He went on to say that severe white striping happens in 3%-6% of birds, which are mostly used in further processed products, not in chicken breast packages.
Somehow, that’s not making us feel any better.
The itsy bitsy spider lets us all down
Most people do not like spiders. That’s too bad, because spiders are generally nothing but helpful little creatures that prey upon annoying flies and other pests. Then there’s the silk they produce. The ancient Romans used it to treat conditions such as warts and skin lesions. Spiders wrap their eggs in silk to protect them from harmful bacteria.
Of course, we can hardly trust the medical opinions of people from 2,000 years ago, but modern-day studies have not definitively proved whether or not spider silk has any antimicrobial properties.
To settle the matter once and for all, researchers from Denmark built a silk-harvesting machine using the most famous of Danish inventions: Legos. The contraption, sort of a paddle wheel, pulled the silk from several different species of spider pinned down by the researchers. The silk was then tested against three different bacteria species, including good old Escherichia coli.
Unfortunately for our spider friends, their silk has no antimicrobial activity. The researchers suspected that any such activity seen in previous studies was actually caused by improper control for the solvents used to extract the silk; those solvents can have antimicrobial properties on their own. As for protecting their eggs, rather than killing bacteria, the silk likely provides a physical barrier alone.
It is bad news for spiders on the benefit-to-humanity front, but look at the bright side: If their silk had antimicrobial activity, we’d have to start farming them to acquire more silk. And that’s no good. Spiders deserve to roam free, hunt as they please, and drop down on your head from the ceiling.
Anxiety and allergies: Cause, effect, confusion
We’re big fans of science, but as longtime, totally impartial (Science rules!) observers of science’s medical realm, we can see that the day-to-day process of practicing the scientific method occasionally gets a bit messy. And no, we’re not talking about COVID-19.
We’re talking allergies. We’re talking mental health. We’re talking allergic disease and mental health.
We’re talking about a pair of press releases we came across during our never-ending search for material to educate, entertain, and astound our fabulously wonderful and loyal readers. (We say that, of course, in the most impartial way possible.)
The first release was titled, “Allergies including asthma and hay fever not linked to mental health traits” and covered research from the University of Bristol (England). The investigators were trying to determine if “allergic diseases actually causes mental health traits including anxiety, depression, bipolar disorder, and schizophrenia, or vice versa,” according to the release.
What they found, however, was “little evidence of a causal relationship between the onset of allergic disease and mental health.” Again, this is the press release talking.
The second release seemed to suggest the exact opposite: “Study uncovers link between allergies and mental health conditions.” That got our attention. A little more reading revealed that “people with asthma, atopic dermatitis, and hay fever also had a higher likelihood of having depression, anxiety, bipolar disorder, or neuroticism.”
One of the investigators was quoted as saying, “Establishing whether allergic disease causes mental health problems, or vice versa, is important to ensure that resources and treatment strategies are targeted appropriately.”
Did you notice the “vice versa”? Did you notice that it appeared in quotes from both releases? We did, so we took a closer look at the source. The second release covered a group of investigators from the University of Bristol – the same group, and the same study, in fact, as the first one.
So there you have it. One study, two press releases, and one confused journalist. Thank you, science.
Customized brain stimulation: New hope for severe depression
Personalized deep brain stimulation (DBS) appears to rapidly and effectively improve symptoms of treatment-resistant depression, new research suggests.
In a proof-of-concept study, investigators identified specific brain activity patterns responsible for a single patient’s severe depression and customized a DBS protocol to modulate the patterns. Results showed rapid and sustained improvement in depression scores.
“This study points the way to a new paradigm that is desperately needed in psychiatry,” Andrew Krystal, PhD, Weill Institute for Neurosciences, University of California, San Francisco, said in a news release.
“ by identifying and modulating the circuit in her brain that’s uniquely associated with her symptoms,” Dr. Krystal added.
The findings were published online Oct. 4 in Nature Medicine.
Closed-loop, on-demand stimulation
The patient was a 36-year-old woman with longstanding, severe, and treatment-resistant major depressive disorder. She was unresponsive to multiple antidepressant combinations and electroconvulsive therapy.
The researchers used intracranial electrophysiology and focal electrical stimulation to identify the specific pattern of electrical brain activity that correlated with her depressed mood.
They identified the right ventral striatum – which is involved in emotion, motivation, and reward – as the stimulation site that led to consistent, sustained, and dose-dependent improvement of symptoms and served as the neural biomarker.
In addition, the investigators identified a neural activity pattern in the amygdala that predicted both the mood symptoms, symptom severity, and stimulation efficacy.
The patient was implanted with the Food and Drug Administration–approved NeuroPace RNS System. The device was placed in the right hemisphere. A single sensing lead was positioned in the amygdala and the second stimulation lead was placed in the ventral striatum.
When the sensing lead detected the activity pattern associated with depression, the other lead delivered a tiny dose (1 milliampere/1 mA) of electricity for 6 seconds, which altered the neural activity and relieved mood symptoms.
Remission achieved
Once this personalized, closed-loop therapy was fully operational, the patient’s depression score on the Montgomery-Åsberg Depression Rating Scale (MADRS) dropped from 33 before turning treatment ON to 14 at the first ON-treatment assessment carried out after 12 days of stimulation. The score dropped below 10, representing remission, several months later.
The treatment also rapidly improved symptom severity, as measured daily with Hamilton Depression Rating Scale (HAMD-6) and visual analog scales.
“Success was predicated on a clinical mapping stage before chronic device placement, a strategy that has been utilized in epilepsy to map seizure foci in a personalized manner but has not previously been performed in other neuropsychiatric conditions,” the investigators wrote.
This patient represents “one of the first examples of precision psychiatry – a treatment tailored to an individual,” the study’s lead author, Katherine Scangos, MD, also with UCSF Weill Institute, said in an interview.
She added that the treatment “was personally tailored both spatially,” meaning at the brain location, and temporally – the time it was delivered.
“This is the first time a neural biomarker has been used to automatically trigger therapeutic stimulation in depression as a successful long-term treatment,” said Dr. Scangos. However, “we have a lot of work left to do,” she added.
“This study provides proof-of-principle that we can utilize a multimodal brain mapping approach to identify a personalized depression circuit and target that circuit with successful treatment. We will need to test the approach in more patients before we can determine its efficacy,” Dr. Scangos said.
First reliable biomarker in psychiatry
In a statement from the UK nonprofit Science Media Centre, Vladimir Litvak, PhD, with the Wellcome Centre for Human Neuroimaging, University College London, said that the study is interesting, noting that it is from “one of the leading groups in the field.”
The fact that depression symptoms can be treated in some patients by electrical stimulation of the ventral striatum is not new, Dr. Litvak said. However, what is “exciting” is that the authors identified a particular neural activity pattern in the amygdala as a reliable predictor of both symptom severity and stimulation effectiveness, he noted.
“Patterns of brain activity correlated with disease symptoms when testing over a large group of patients are commonly discovered. But there are just a handful of examples of patterns that are reliable enough to be predictive on a short time scale in a single patient,” said Dr. Litvak, who was not associated with the research.
“Furthermore, to my knowledge, this is the first example of such a reliable biomarker for psychiatric symptoms. The other examples were all for neurological disorders such as Parkinson’s disease, dystonia, and epilepsy,” he added.
He cautioned that this is a single case, but “if reproduced in additional patients, it will bring at least some psychiatric conditions into the domain of brain diseases that can be characterized and diagnosed objectively rather than based on symptoms alone.”
Dr. Litvak pointed out two other critical aspects of the study: the use of exploratory recordings and stimulation to determine the most effective treatment strategy, and the use of a closed-loop device that stimulates only when detecting the amygdala biomarker.
“It is hard to say based on this single case how important these will be in the future. There is no comparison to constant stimulation that might have worked as well because the implanted device used in the study is not suitable for that,” Dr. Litvak said.
It should also be noted that implanting multiple depth electrodes at different brain sites is a “traumatic invasive procedure only reserved to date for severe cases of drug-resistant epilepsy,” he said. “Furthermore, it only allows [researchers] to test a small number of candidate sites, so it relies heavily on prior knowledge.
“Once clinicians know better what to look for, it might be possible to avoid this procedure altogether by using noninvasive methods,” such as functional MRI or EEG, to match the right treatment option to a patient, Dr. Litvak concluded.
The research was funded by the National Institutes of Health, the Brain & Behavior Research Foundation, and the Ray and Dagmar Dolby Family Fund through the department of psychiatry at UCSF. Dr. Scangos has reported no relevant financial relationships. A complete list of author disclosures is available in the original article. Dr. Litvak is participating in a research funding application to search for electrophysiological biomarkers of depression symptoms using invasive recordings.
A version of this article first appeared on Medscape.com.
Personalized deep brain stimulation (DBS) appears to rapidly and effectively improve symptoms of treatment-resistant depression, new research suggests.
In a proof-of-concept study, investigators identified specific brain activity patterns responsible for a single patient’s severe depression and customized a DBS protocol to modulate the patterns. Results showed rapid and sustained improvement in depression scores.
“This study points the way to a new paradigm that is desperately needed in psychiatry,” Andrew Krystal, PhD, Weill Institute for Neurosciences, University of California, San Francisco, said in a news release.
“ by identifying and modulating the circuit in her brain that’s uniquely associated with her symptoms,” Dr. Krystal added.
The findings were published online Oct. 4 in Nature Medicine.
Closed-loop, on-demand stimulation
The patient was a 36-year-old woman with longstanding, severe, and treatment-resistant major depressive disorder. She was unresponsive to multiple antidepressant combinations and electroconvulsive therapy.
The researchers used intracranial electrophysiology and focal electrical stimulation to identify the specific pattern of electrical brain activity that correlated with her depressed mood.
They identified the right ventral striatum – which is involved in emotion, motivation, and reward – as the stimulation site that led to consistent, sustained, and dose-dependent improvement of symptoms and served as the neural biomarker.
In addition, the investigators identified a neural activity pattern in the amygdala that predicted both the mood symptoms, symptom severity, and stimulation efficacy.
The patient was implanted with the Food and Drug Administration–approved NeuroPace RNS System. The device was placed in the right hemisphere. A single sensing lead was positioned in the amygdala and the second stimulation lead was placed in the ventral striatum.
When the sensing lead detected the activity pattern associated with depression, the other lead delivered a tiny dose (1 milliampere/1 mA) of electricity for 6 seconds, which altered the neural activity and relieved mood symptoms.
Remission achieved
Once this personalized, closed-loop therapy was fully operational, the patient’s depression score on the Montgomery-Åsberg Depression Rating Scale (MADRS) dropped from 33 before turning treatment ON to 14 at the first ON-treatment assessment carried out after 12 days of stimulation. The score dropped below 10, representing remission, several months later.
The treatment also rapidly improved symptom severity, as measured daily with Hamilton Depression Rating Scale (HAMD-6) and visual analog scales.
“Success was predicated on a clinical mapping stage before chronic device placement, a strategy that has been utilized in epilepsy to map seizure foci in a personalized manner but has not previously been performed in other neuropsychiatric conditions,” the investigators wrote.
This patient represents “one of the first examples of precision psychiatry – a treatment tailored to an individual,” the study’s lead author, Katherine Scangos, MD, also with UCSF Weill Institute, said in an interview.
She added that the treatment “was personally tailored both spatially,” meaning at the brain location, and temporally – the time it was delivered.
“This is the first time a neural biomarker has been used to automatically trigger therapeutic stimulation in depression as a successful long-term treatment,” said Dr. Scangos. However, “we have a lot of work left to do,” she added.
“This study provides proof-of-principle that we can utilize a multimodal brain mapping approach to identify a personalized depression circuit and target that circuit with successful treatment. We will need to test the approach in more patients before we can determine its efficacy,” Dr. Scangos said.
First reliable biomarker in psychiatry
In a statement from the UK nonprofit Science Media Centre, Vladimir Litvak, PhD, with the Wellcome Centre for Human Neuroimaging, University College London, said that the study is interesting, noting that it is from “one of the leading groups in the field.”
The fact that depression symptoms can be treated in some patients by electrical stimulation of the ventral striatum is not new, Dr. Litvak said. However, what is “exciting” is that the authors identified a particular neural activity pattern in the amygdala as a reliable predictor of both symptom severity and stimulation effectiveness, he noted.
“Patterns of brain activity correlated with disease symptoms when testing over a large group of patients are commonly discovered. But there are just a handful of examples of patterns that are reliable enough to be predictive on a short time scale in a single patient,” said Dr. Litvak, who was not associated with the research.
“Furthermore, to my knowledge, this is the first example of such a reliable biomarker for psychiatric symptoms. The other examples were all for neurological disorders such as Parkinson’s disease, dystonia, and epilepsy,” he added.
He cautioned that this is a single case, but “if reproduced in additional patients, it will bring at least some psychiatric conditions into the domain of brain diseases that can be characterized and diagnosed objectively rather than based on symptoms alone.”
Dr. Litvak pointed out two other critical aspects of the study: the use of exploratory recordings and stimulation to determine the most effective treatment strategy, and the use of a closed-loop device that stimulates only when detecting the amygdala biomarker.
“It is hard to say based on this single case how important these will be in the future. There is no comparison to constant stimulation that might have worked as well because the implanted device used in the study is not suitable for that,” Dr. Litvak said.
It should also be noted that implanting multiple depth electrodes at different brain sites is a “traumatic invasive procedure only reserved to date for severe cases of drug-resistant epilepsy,” he said. “Furthermore, it only allows [researchers] to test a small number of candidate sites, so it relies heavily on prior knowledge.
“Once clinicians know better what to look for, it might be possible to avoid this procedure altogether by using noninvasive methods,” such as functional MRI or EEG, to match the right treatment option to a patient, Dr. Litvak concluded.
The research was funded by the National Institutes of Health, the Brain & Behavior Research Foundation, and the Ray and Dagmar Dolby Family Fund through the department of psychiatry at UCSF. Dr. Scangos has reported no relevant financial relationships. A complete list of author disclosures is available in the original article. Dr. Litvak is participating in a research funding application to search for electrophysiological biomarkers of depression symptoms using invasive recordings.
A version of this article first appeared on Medscape.com.
Personalized deep brain stimulation (DBS) appears to rapidly and effectively improve symptoms of treatment-resistant depression, new research suggests.
In a proof-of-concept study, investigators identified specific brain activity patterns responsible for a single patient’s severe depression and customized a DBS protocol to modulate the patterns. Results showed rapid and sustained improvement in depression scores.
“This study points the way to a new paradigm that is desperately needed in psychiatry,” Andrew Krystal, PhD, Weill Institute for Neurosciences, University of California, San Francisco, said in a news release.
“ by identifying and modulating the circuit in her brain that’s uniquely associated with her symptoms,” Dr. Krystal added.
The findings were published online Oct. 4 in Nature Medicine.
Closed-loop, on-demand stimulation
The patient was a 36-year-old woman with longstanding, severe, and treatment-resistant major depressive disorder. She was unresponsive to multiple antidepressant combinations and electroconvulsive therapy.
The researchers used intracranial electrophysiology and focal electrical stimulation to identify the specific pattern of electrical brain activity that correlated with her depressed mood.
They identified the right ventral striatum – which is involved in emotion, motivation, and reward – as the stimulation site that led to consistent, sustained, and dose-dependent improvement of symptoms and served as the neural biomarker.
In addition, the investigators identified a neural activity pattern in the amygdala that predicted both the mood symptoms, symptom severity, and stimulation efficacy.
The patient was implanted with the Food and Drug Administration–approved NeuroPace RNS System. The device was placed in the right hemisphere. A single sensing lead was positioned in the amygdala and the second stimulation lead was placed in the ventral striatum.
When the sensing lead detected the activity pattern associated with depression, the other lead delivered a tiny dose (1 milliampere/1 mA) of electricity for 6 seconds, which altered the neural activity and relieved mood symptoms.
Remission achieved
Once this personalized, closed-loop therapy was fully operational, the patient’s depression score on the Montgomery-Åsberg Depression Rating Scale (MADRS) dropped from 33 before turning treatment ON to 14 at the first ON-treatment assessment carried out after 12 days of stimulation. The score dropped below 10, representing remission, several months later.
The treatment also rapidly improved symptom severity, as measured daily with Hamilton Depression Rating Scale (HAMD-6) and visual analog scales.
“Success was predicated on a clinical mapping stage before chronic device placement, a strategy that has been utilized in epilepsy to map seizure foci in a personalized manner but has not previously been performed in other neuropsychiatric conditions,” the investigators wrote.
This patient represents “one of the first examples of precision psychiatry – a treatment tailored to an individual,” the study’s lead author, Katherine Scangos, MD, also with UCSF Weill Institute, said in an interview.
She added that the treatment “was personally tailored both spatially,” meaning at the brain location, and temporally – the time it was delivered.
“This is the first time a neural biomarker has been used to automatically trigger therapeutic stimulation in depression as a successful long-term treatment,” said Dr. Scangos. However, “we have a lot of work left to do,” she added.
“This study provides proof-of-principle that we can utilize a multimodal brain mapping approach to identify a personalized depression circuit and target that circuit with successful treatment. We will need to test the approach in more patients before we can determine its efficacy,” Dr. Scangos said.
First reliable biomarker in psychiatry
In a statement from the UK nonprofit Science Media Centre, Vladimir Litvak, PhD, with the Wellcome Centre for Human Neuroimaging, University College London, said that the study is interesting, noting that it is from “one of the leading groups in the field.”
The fact that depression symptoms can be treated in some patients by electrical stimulation of the ventral striatum is not new, Dr. Litvak said. However, what is “exciting” is that the authors identified a particular neural activity pattern in the amygdala as a reliable predictor of both symptom severity and stimulation effectiveness, he noted.
“Patterns of brain activity correlated with disease symptoms when testing over a large group of patients are commonly discovered. But there are just a handful of examples of patterns that are reliable enough to be predictive on a short time scale in a single patient,” said Dr. Litvak, who was not associated with the research.
“Furthermore, to my knowledge, this is the first example of such a reliable biomarker for psychiatric symptoms. The other examples were all for neurological disorders such as Parkinson’s disease, dystonia, and epilepsy,” he added.
He cautioned that this is a single case, but “if reproduced in additional patients, it will bring at least some psychiatric conditions into the domain of brain diseases that can be characterized and diagnosed objectively rather than based on symptoms alone.”
Dr. Litvak pointed out two other critical aspects of the study: the use of exploratory recordings and stimulation to determine the most effective treatment strategy, and the use of a closed-loop device that stimulates only when detecting the amygdala biomarker.
“It is hard to say based on this single case how important these will be in the future. There is no comparison to constant stimulation that might have worked as well because the implanted device used in the study is not suitable for that,” Dr. Litvak said.
It should also be noted that implanting multiple depth electrodes at different brain sites is a “traumatic invasive procedure only reserved to date for severe cases of drug-resistant epilepsy,” he said. “Furthermore, it only allows [researchers] to test a small number of candidate sites, so it relies heavily on prior knowledge.
“Once clinicians know better what to look for, it might be possible to avoid this procedure altogether by using noninvasive methods,” such as functional MRI or EEG, to match the right treatment option to a patient, Dr. Litvak concluded.
The research was funded by the National Institutes of Health, the Brain & Behavior Research Foundation, and the Ray and Dagmar Dolby Family Fund through the department of psychiatry at UCSF. Dr. Scangos has reported no relevant financial relationships. A complete list of author disclosures is available in the original article. Dr. Litvak is participating in a research funding application to search for electrophysiological biomarkers of depression symptoms using invasive recordings.
A version of this article first appeared on Medscape.com.
New York’s largest health care provider fires 1,400 unvaccinated employees
The employees represented less than 2% of Northwell’s 76,000 employees, who are now all fully vaccinated against COVID-19, Joe Kemp, the assistant vice president of public relations for the company, told The Hill.
“Northwell Health is proud to announce that our workforce -- the largest in New York State -- is 100% vaccinated,” the company said in a statement to several news outlets.
“This allows us to continue to provide exceptional care at all of our facilities, without interruption and remain open and fully operational,” Northwell Health said.
Having a fully vaccinated workforce is part of the health system’s duty to protect others, the company said. Northwell Health includes 23 hospitals and more than 830 outpatient facilities, according to ABC News.
“Northwell regrets losing any employee under such circumstances,” the company said. “We owe it to our staff, our patients, and the communities we serve to be 100% vaccinated against COVID-19.”
Former New York Gov. Andrew Cuomo announced in August that the state would require health care workers to receive at least one COVID-19 vaccine shot by Sept. 27. Employees didn’t have the option for weekly testing or religious exemptions, which is being challenged in several lawsuits, according to The New York Times.
The order went into effect last week, prompting tens of thousands of employees to get vaccinated. As of last week, 87% of hospital staff were fully vaccinated, and 92% of hospital and retirement home workers had received at least one dose, according to state health data.
Northwell announced its own vaccine mandate in August as well, which sparked protests among some workers. The order applied to both clinical and non-clinical staff.
A few thousand Northwell employees got vaccinated as the deadline approached, Mr. Kemp told The New York Times. Some who lost their jobs at first were able to return to work, and those who have been terminated can interview for reinstatement for 30 days. The hospital system is also “openly recruiting” for the vacant positions.
“The goal was to get people vaccinated, not to get people terminated,” Mr. Kemp said.
Hospitalized COVID-19 patients in New York hit a low of 350 in mid-July, according to state hospitalization data. Now, about 2,200 people are hospitalized throughout the state, most of whom are unvaccinated.
As of Oct. 3, nearly 72% of New York residents had received at least one vaccine dose, according to the latest state data. About 64% are fully vaccinated.
A version of this article first appeared on WebMD.com.
The employees represented less than 2% of Northwell’s 76,000 employees, who are now all fully vaccinated against COVID-19, Joe Kemp, the assistant vice president of public relations for the company, told The Hill.
“Northwell Health is proud to announce that our workforce -- the largest in New York State -- is 100% vaccinated,” the company said in a statement to several news outlets.
“This allows us to continue to provide exceptional care at all of our facilities, without interruption and remain open and fully operational,” Northwell Health said.
Having a fully vaccinated workforce is part of the health system’s duty to protect others, the company said. Northwell Health includes 23 hospitals and more than 830 outpatient facilities, according to ABC News.
“Northwell regrets losing any employee under such circumstances,” the company said. “We owe it to our staff, our patients, and the communities we serve to be 100% vaccinated against COVID-19.”
Former New York Gov. Andrew Cuomo announced in August that the state would require health care workers to receive at least one COVID-19 vaccine shot by Sept. 27. Employees didn’t have the option for weekly testing or religious exemptions, which is being challenged in several lawsuits, according to The New York Times.
The order went into effect last week, prompting tens of thousands of employees to get vaccinated. As of last week, 87% of hospital staff were fully vaccinated, and 92% of hospital and retirement home workers had received at least one dose, according to state health data.
Northwell announced its own vaccine mandate in August as well, which sparked protests among some workers. The order applied to both clinical and non-clinical staff.
A few thousand Northwell employees got vaccinated as the deadline approached, Mr. Kemp told The New York Times. Some who lost their jobs at first were able to return to work, and those who have been terminated can interview for reinstatement for 30 days. The hospital system is also “openly recruiting” for the vacant positions.
“The goal was to get people vaccinated, not to get people terminated,” Mr. Kemp said.
Hospitalized COVID-19 patients in New York hit a low of 350 in mid-July, according to state hospitalization data. Now, about 2,200 people are hospitalized throughout the state, most of whom are unvaccinated.
As of Oct. 3, nearly 72% of New York residents had received at least one vaccine dose, according to the latest state data. About 64% are fully vaccinated.
A version of this article first appeared on WebMD.com.
The employees represented less than 2% of Northwell’s 76,000 employees, who are now all fully vaccinated against COVID-19, Joe Kemp, the assistant vice president of public relations for the company, told The Hill.
“Northwell Health is proud to announce that our workforce -- the largest in New York State -- is 100% vaccinated,” the company said in a statement to several news outlets.
“This allows us to continue to provide exceptional care at all of our facilities, without interruption and remain open and fully operational,” Northwell Health said.
Having a fully vaccinated workforce is part of the health system’s duty to protect others, the company said. Northwell Health includes 23 hospitals and more than 830 outpatient facilities, according to ABC News.
“Northwell regrets losing any employee under such circumstances,” the company said. “We owe it to our staff, our patients, and the communities we serve to be 100% vaccinated against COVID-19.”
Former New York Gov. Andrew Cuomo announced in August that the state would require health care workers to receive at least one COVID-19 vaccine shot by Sept. 27. Employees didn’t have the option for weekly testing or religious exemptions, which is being challenged in several lawsuits, according to The New York Times.
The order went into effect last week, prompting tens of thousands of employees to get vaccinated. As of last week, 87% of hospital staff were fully vaccinated, and 92% of hospital and retirement home workers had received at least one dose, according to state health data.
Northwell announced its own vaccine mandate in August as well, which sparked protests among some workers. The order applied to both clinical and non-clinical staff.
A few thousand Northwell employees got vaccinated as the deadline approached, Mr. Kemp told The New York Times. Some who lost their jobs at first were able to return to work, and those who have been terminated can interview for reinstatement for 30 days. The hospital system is also “openly recruiting” for the vacant positions.
“The goal was to get people vaccinated, not to get people terminated,” Mr. Kemp said.
Hospitalized COVID-19 patients in New York hit a low of 350 in mid-July, according to state hospitalization data. Now, about 2,200 people are hospitalized throughout the state, most of whom are unvaccinated.
As of Oct. 3, nearly 72% of New York residents had received at least one vaccine dose, according to the latest state data. About 64% are fully vaccinated.
A version of this article first appeared on WebMD.com.
ADHD med may reduce apathy in Alzheimer’s disease
Methylphenidate is safe and effective for treating apathy in patients with Alzheimer’s disease (AD), new research suggests.
Results from a phase 3 randomized trial showed that, after 6 months of treatment, mean score on the Neuropsychiatric Inventory (NPI) apathy subscale decreased by 4.5 points for patients who received methylphenidate vs. a decrease of 3.1 points for those who received placebo.
In addition, the safety profile showed no significant between-group differences.
“Methylphenidate offers a treatment approach providing a modest but potentially clinically significant benefit for patients and caregivers,” said the investigators, led by Jacobo E. Mintzer, MD, MBA, professor of health studies at the Medical University of South Carolina in Charleston.
The findings were published online Sept. 27 in JAMA Neurology.
Common problem
Apathy, which is common among patients with AD, is associated with increased risk for mortality, financial burden, and caregiver burden. No treatment has proved effective for apathy in this population.
Two trials of methylphenidate, a catecholaminergic agent, have provided preliminary evidence of efficacy. Findings from the Apathy in Dementia Methylphenidate trial (ADMET) suggested the drug was associated with improved cognition and few adverse events. However, both trials had small patient populations and short durations.
The current investigators conducted ADMET 2, a 6-month, phase 3 trial, to investigate methylphenidate further. They recruited 200 patients (mean age, 76 years; 66% men; 90% White) at nine clinical centers that specialized in dementia care in the United States and one in Canada.
Eligible patients had a diagnosis of possible or probable AD and a Mini-Mental State Examination (MMSE) score between 10 and 28. They also had clinically significant apathy for at least 4 weeks and an available caregiver who spent more than 10 hours a week with the patient.
The researchers randomly assigned patients to receive methylphenidate (n = 99) or placebo (n = 101). For 3 days, participants in the active group received 10 mg/day of methylphenidate. After that point, they received 20 mg/day of methylphenidate for the rest of the study.
Patients in both treatment groups were given the same number of identical-appearing capsules each day.
In-person follow-up visits took place monthly for 6 months. Participants also were contacted by telephone at days 15, 45, and 75 after treatment assignment.
Participants underwent cognitive testing at baseline and at 2, 4, and 6 months. The battery of tests included the MMSE, Hopkins Verbal Learning Test, and Wechsler Adult Intelligence Scale – Revised Digit Span.
The trial’s two primary outcomes were mean change in NPI apathy score from baseline to 6 months and the odds of an improved rating on the Alzheimer’s Disease Cooperative Study Clinical Global Impression of Change (ADCS-CGIC) between baseline and 6 months.
Significant change on either outcome was to be considered a signal of effective treatment.
Treatment-specific benefit
Ten patients in the methylphenidate group and seven in the placebo group withdrew during the study.
Mean baseline score on the NPI apathy subscale was 8.0 vs. 7.6, respectively.
In an adjusted, longitudinal model, mean between-group difference in change in NPI apathy score at 6 months was –1.25 (P = .002). The mean NPI apathy score decreased by 4.5 points in the methylphenidate group vs. 3.1 points in the placebo group.
The largest change in apathy score occurred during the first 2 months of treatment. At 6 months, 27% of the methylphenidate group vs. 14% of the placebo group had an NPI apathy score of 0.
In addition, 43.8% of the methylphenidate group had improvement on the ADCS-CGIC compared with 35.2% of the placebo group. The odds ratio (OR) for improvement on ADCS-CGIC for methylphenidate vs. placebo was 1.90 (P = .07).
There was also a strong association between score improvement on the NPI apathy subscale and improvement on the ADCS-CGIC subscale (OR, 2.95; P = .002).
“It is important to note that there were no group differences in any of the cognitive measures, suggesting that the effect of the treatment is specific to the treatment of apathy and not a secondary effect of improvement in cognition,” the researchers wrote.
In all, 17 serious adverse events occurred in the methylphenidate group and 10 occurred in the placebo group. However, all events were found to be hospitalizations for events not related to treatment.
‘Enduring effect’
Commenting on the findings, Jeffrey L. Cummings, MD, ScD, professor of brain sciences at the University of Nevada, Las Vegas, noted that the reduction in NPI apathy subscale score of more than 50% was clinically meaningful.
A more robust outcome on the ADCS-CGIC would have been desirable, he added, although that instrument is not designed specifically for apathy.
Methylphenidate’s effect on apathy observed at 2 months and remaining stable throughout the study makes it appear to be “an enduring effect, and not something that the patient accommodates to,” said Dr. Cummings, who was not involved with the research. Such a change may manifest itself in a patient’s greater willingness to help voluntarily with housework or to suggest going for a walk, he noted.
“These are not dramatic changes in cognition, of course, but they are changes in initiative and that is very important,” Dr. Cummings said. Decreased apathy also may improve quality of life for the patient’s caregiver, he added.
Overall, the findings raise the question of whether the Food and Drug Administration should recognize apathy as an indication for which drugs can be approved, said Dr. Cummings.
“For me, that would be the next major step in this line of investigation,” he concluded.
The study was funded by the National Institute on Aging. Dr. Mintzer has served as an adviser to Praxis Bioresearch and Cerevel Therapeutics on matters unrelated to this study. Dr. Cummings is the author of the Neuropsychiatric Inventory but does not receive payments for it from academic trials such as ADMET 2.
A version of this article first appeared on Medscape.com.
Methylphenidate is safe and effective for treating apathy in patients with Alzheimer’s disease (AD), new research suggests.
Results from a phase 3 randomized trial showed that, after 6 months of treatment, mean score on the Neuropsychiatric Inventory (NPI) apathy subscale decreased by 4.5 points for patients who received methylphenidate vs. a decrease of 3.1 points for those who received placebo.
In addition, the safety profile showed no significant between-group differences.
“Methylphenidate offers a treatment approach providing a modest but potentially clinically significant benefit for patients and caregivers,” said the investigators, led by Jacobo E. Mintzer, MD, MBA, professor of health studies at the Medical University of South Carolina in Charleston.
The findings were published online Sept. 27 in JAMA Neurology.
Common problem
Apathy, which is common among patients with AD, is associated with increased risk for mortality, financial burden, and caregiver burden. No treatment has proved effective for apathy in this population.
Two trials of methylphenidate, a catecholaminergic agent, have provided preliminary evidence of efficacy. Findings from the Apathy in Dementia Methylphenidate trial (ADMET) suggested the drug was associated with improved cognition and few adverse events. However, both trials had small patient populations and short durations.
The current investigators conducted ADMET 2, a 6-month, phase 3 trial, to investigate methylphenidate further. They recruited 200 patients (mean age, 76 years; 66% men; 90% White) at nine clinical centers that specialized in dementia care in the United States and one in Canada.
Eligible patients had a diagnosis of possible or probable AD and a Mini-Mental State Examination (MMSE) score between 10 and 28. They also had clinically significant apathy for at least 4 weeks and an available caregiver who spent more than 10 hours a week with the patient.
The researchers randomly assigned patients to receive methylphenidate (n = 99) or placebo (n = 101). For 3 days, participants in the active group received 10 mg/day of methylphenidate. After that point, they received 20 mg/day of methylphenidate for the rest of the study.
Patients in both treatment groups were given the same number of identical-appearing capsules each day.
In-person follow-up visits took place monthly for 6 months. Participants also were contacted by telephone at days 15, 45, and 75 after treatment assignment.
Participants underwent cognitive testing at baseline and at 2, 4, and 6 months. The battery of tests included the MMSE, Hopkins Verbal Learning Test, and Wechsler Adult Intelligence Scale – Revised Digit Span.
The trial’s two primary outcomes were mean change in NPI apathy score from baseline to 6 months and the odds of an improved rating on the Alzheimer’s Disease Cooperative Study Clinical Global Impression of Change (ADCS-CGIC) between baseline and 6 months.
Significant change on either outcome was to be considered a signal of effective treatment.
Treatment-specific benefit
Ten patients in the methylphenidate group and seven in the placebo group withdrew during the study.
Mean baseline score on the NPI apathy subscale was 8.0 vs. 7.6, respectively.
In an adjusted, longitudinal model, mean between-group difference in change in NPI apathy score at 6 months was –1.25 (P = .002). The mean NPI apathy score decreased by 4.5 points in the methylphenidate group vs. 3.1 points in the placebo group.
The largest change in apathy score occurred during the first 2 months of treatment. At 6 months, 27% of the methylphenidate group vs. 14% of the placebo group had an NPI apathy score of 0.
In addition, 43.8% of the methylphenidate group had improvement on the ADCS-CGIC compared with 35.2% of the placebo group. The odds ratio (OR) for improvement on ADCS-CGIC for methylphenidate vs. placebo was 1.90 (P = .07).
There was also a strong association between score improvement on the NPI apathy subscale and improvement on the ADCS-CGIC subscale (OR, 2.95; P = .002).
“It is important to note that there were no group differences in any of the cognitive measures, suggesting that the effect of the treatment is specific to the treatment of apathy and not a secondary effect of improvement in cognition,” the researchers wrote.
In all, 17 serious adverse events occurred in the methylphenidate group and 10 occurred in the placebo group. However, all events were found to be hospitalizations for events not related to treatment.
‘Enduring effect’
Commenting on the findings, Jeffrey L. Cummings, MD, ScD, professor of brain sciences at the University of Nevada, Las Vegas, noted that the reduction in NPI apathy subscale score of more than 50% was clinically meaningful.
A more robust outcome on the ADCS-CGIC would have been desirable, he added, although that instrument is not designed specifically for apathy.
Methylphenidate’s effect on apathy observed at 2 months and remaining stable throughout the study makes it appear to be “an enduring effect, and not something that the patient accommodates to,” said Dr. Cummings, who was not involved with the research. Such a change may manifest itself in a patient’s greater willingness to help voluntarily with housework or to suggest going for a walk, he noted.
“These are not dramatic changes in cognition, of course, but they are changes in initiative and that is very important,” Dr. Cummings said. Decreased apathy also may improve quality of life for the patient’s caregiver, he added.
Overall, the findings raise the question of whether the Food and Drug Administration should recognize apathy as an indication for which drugs can be approved, said Dr. Cummings.
“For me, that would be the next major step in this line of investigation,” he concluded.
The study was funded by the National Institute on Aging. Dr. Mintzer has served as an adviser to Praxis Bioresearch and Cerevel Therapeutics on matters unrelated to this study. Dr. Cummings is the author of the Neuropsychiatric Inventory but does not receive payments for it from academic trials such as ADMET 2.
A version of this article first appeared on Medscape.com.
Methylphenidate is safe and effective for treating apathy in patients with Alzheimer’s disease (AD), new research suggests.
Results from a phase 3 randomized trial showed that, after 6 months of treatment, mean score on the Neuropsychiatric Inventory (NPI) apathy subscale decreased by 4.5 points for patients who received methylphenidate vs. a decrease of 3.1 points for those who received placebo.
In addition, the safety profile showed no significant between-group differences.
“Methylphenidate offers a treatment approach providing a modest but potentially clinically significant benefit for patients and caregivers,” said the investigators, led by Jacobo E. Mintzer, MD, MBA, professor of health studies at the Medical University of South Carolina in Charleston.
The findings were published online Sept. 27 in JAMA Neurology.
Common problem
Apathy, which is common among patients with AD, is associated with increased risk for mortality, financial burden, and caregiver burden. No treatment has proved effective for apathy in this population.
Two trials of methylphenidate, a catecholaminergic agent, have provided preliminary evidence of efficacy. Findings from the Apathy in Dementia Methylphenidate trial (ADMET) suggested the drug was associated with improved cognition and few adverse events. However, both trials had small patient populations and short durations.
The current investigators conducted ADMET 2, a 6-month, phase 3 trial, to investigate methylphenidate further. They recruited 200 patients (mean age, 76 years; 66% men; 90% White) at nine clinical centers that specialized in dementia care in the United States and one in Canada.
Eligible patients had a diagnosis of possible or probable AD and a Mini-Mental State Examination (MMSE) score between 10 and 28. They also had clinically significant apathy for at least 4 weeks and an available caregiver who spent more than 10 hours a week with the patient.
The researchers randomly assigned patients to receive methylphenidate (n = 99) or placebo (n = 101). For 3 days, participants in the active group received 10 mg/day of methylphenidate. After that point, they received 20 mg/day of methylphenidate for the rest of the study.
Patients in both treatment groups were given the same number of identical-appearing capsules each day.
In-person follow-up visits took place monthly for 6 months. Participants also were contacted by telephone at days 15, 45, and 75 after treatment assignment.
Participants underwent cognitive testing at baseline and at 2, 4, and 6 months. The battery of tests included the MMSE, Hopkins Verbal Learning Test, and Wechsler Adult Intelligence Scale – Revised Digit Span.
The trial’s two primary outcomes were mean change in NPI apathy score from baseline to 6 months and the odds of an improved rating on the Alzheimer’s Disease Cooperative Study Clinical Global Impression of Change (ADCS-CGIC) between baseline and 6 months.
Significant change on either outcome was to be considered a signal of effective treatment.
Treatment-specific benefit
Ten patients in the methylphenidate group and seven in the placebo group withdrew during the study.
Mean baseline score on the NPI apathy subscale was 8.0 vs. 7.6, respectively.
In an adjusted, longitudinal model, mean between-group difference in change in NPI apathy score at 6 months was –1.25 (P = .002). The mean NPI apathy score decreased by 4.5 points in the methylphenidate group vs. 3.1 points in the placebo group.
The largest change in apathy score occurred during the first 2 months of treatment. At 6 months, 27% of the methylphenidate group vs. 14% of the placebo group had an NPI apathy score of 0.
In addition, 43.8% of the methylphenidate group had improvement on the ADCS-CGIC compared with 35.2% of the placebo group. The odds ratio (OR) for improvement on ADCS-CGIC for methylphenidate vs. placebo was 1.90 (P = .07).
There was also a strong association between score improvement on the NPI apathy subscale and improvement on the ADCS-CGIC subscale (OR, 2.95; P = .002).
“It is important to note that there were no group differences in any of the cognitive measures, suggesting that the effect of the treatment is specific to the treatment of apathy and not a secondary effect of improvement in cognition,” the researchers wrote.
In all, 17 serious adverse events occurred in the methylphenidate group and 10 occurred in the placebo group. However, all events were found to be hospitalizations for events not related to treatment.
‘Enduring effect’
Commenting on the findings, Jeffrey L. Cummings, MD, ScD, professor of brain sciences at the University of Nevada, Las Vegas, noted that the reduction in NPI apathy subscale score of more than 50% was clinically meaningful.
A more robust outcome on the ADCS-CGIC would have been desirable, he added, although that instrument is not designed specifically for apathy.
Methylphenidate’s effect on apathy observed at 2 months and remaining stable throughout the study makes it appear to be “an enduring effect, and not something that the patient accommodates to,” said Dr. Cummings, who was not involved with the research. Such a change may manifest itself in a patient’s greater willingness to help voluntarily with housework or to suggest going for a walk, he noted.
“These are not dramatic changes in cognition, of course, but they are changes in initiative and that is very important,” Dr. Cummings said. Decreased apathy also may improve quality of life for the patient’s caregiver, he added.
Overall, the findings raise the question of whether the Food and Drug Administration should recognize apathy as an indication for which drugs can be approved, said Dr. Cummings.
“For me, that would be the next major step in this line of investigation,” he concluded.
The study was funded by the National Institute on Aging. Dr. Mintzer has served as an adviser to Praxis Bioresearch and Cerevel Therapeutics on matters unrelated to this study. Dr. Cummings is the author of the Neuropsychiatric Inventory but does not receive payments for it from academic trials such as ADMET 2.
A version of this article first appeared on Medscape.com.
Johnson & Johnson requests FDA approval for vaccine booster doses
The company said it filed a request for people ages 18 and older who have received the one-shot vaccine. Johnson & Johnson submitted data for several different booster intervals -- ranging from 2 months to 6 months -- but didn’t formally recommend one to the FDA, The Associated Press reported.
“We’re describing the data to them,” Mathai Mammen, MD, head of global research and development for Janssen, the company’s vaccine division, told CNN.
“The process is not that we asked for a very specific interval -- we’re providing them data and we’re going to be presenting to the committee,” he said. “They’ll take all that into consideration when they ultimately decide on an appropriate interval.”
The FDA’s independent vaccine advisory committee meets next week to review data on booster shots from both Johnson & Johnson and Moderna. It’s the first step in the review process, which then requires approval from leaders at the FDA and Centers for Disease Control and Prevention. If both agencies authorize the extra shots, Americans could receive boosters from Johnson & Johnson and Moderna later this month, the AP reported.
Johnson & Johnson previously released data that showed the vaccine remains highly effective against COVID-19 at least 5 months after vaccination, with 81% efficacy against hospitalizations in the United States.
Two weeks ago, the company reported that a booster dose at 2 months or 6 months further lifted immunity, with a booster at 2 months providing 94% protection against moderate and severe COVID-19. The company said the 6-month booster raised antibodies by 12 times but didn’t release additional data at that time.
In September, the FDA authorized booster shots of the Pfizer vaccine for ages 65 and older, those who live in long-term care facilities, and those with higher risks for contracting COVID-19. The Biden administration is supporting a booster campaign to address potential waning vaccine immunity and remaining surges of the more contagious Delta variant, the AP reported.
A version of this article first appeared on WebMD.com.
The company said it filed a request for people ages 18 and older who have received the one-shot vaccine. Johnson & Johnson submitted data for several different booster intervals -- ranging from 2 months to 6 months -- but didn’t formally recommend one to the FDA, The Associated Press reported.
“We’re describing the data to them,” Mathai Mammen, MD, head of global research and development for Janssen, the company’s vaccine division, told CNN.
“The process is not that we asked for a very specific interval -- we’re providing them data and we’re going to be presenting to the committee,” he said. “They’ll take all that into consideration when they ultimately decide on an appropriate interval.”
The FDA’s independent vaccine advisory committee meets next week to review data on booster shots from both Johnson & Johnson and Moderna. It’s the first step in the review process, which then requires approval from leaders at the FDA and Centers for Disease Control and Prevention. If both agencies authorize the extra shots, Americans could receive boosters from Johnson & Johnson and Moderna later this month, the AP reported.
Johnson & Johnson previously released data that showed the vaccine remains highly effective against COVID-19 at least 5 months after vaccination, with 81% efficacy against hospitalizations in the United States.
Two weeks ago, the company reported that a booster dose at 2 months or 6 months further lifted immunity, with a booster at 2 months providing 94% protection against moderate and severe COVID-19. The company said the 6-month booster raised antibodies by 12 times but didn’t release additional data at that time.
In September, the FDA authorized booster shots of the Pfizer vaccine for ages 65 and older, those who live in long-term care facilities, and those with higher risks for contracting COVID-19. The Biden administration is supporting a booster campaign to address potential waning vaccine immunity and remaining surges of the more contagious Delta variant, the AP reported.
A version of this article first appeared on WebMD.com.
The company said it filed a request for people ages 18 and older who have received the one-shot vaccine. Johnson & Johnson submitted data for several different booster intervals -- ranging from 2 months to 6 months -- but didn’t formally recommend one to the FDA, The Associated Press reported.
“We’re describing the data to them,” Mathai Mammen, MD, head of global research and development for Janssen, the company’s vaccine division, told CNN.
“The process is not that we asked for a very specific interval -- we’re providing them data and we’re going to be presenting to the committee,” he said. “They’ll take all that into consideration when they ultimately decide on an appropriate interval.”
The FDA’s independent vaccine advisory committee meets next week to review data on booster shots from both Johnson & Johnson and Moderna. It’s the first step in the review process, which then requires approval from leaders at the FDA and Centers for Disease Control and Prevention. If both agencies authorize the extra shots, Americans could receive boosters from Johnson & Johnson and Moderna later this month, the AP reported.
Johnson & Johnson previously released data that showed the vaccine remains highly effective against COVID-19 at least 5 months after vaccination, with 81% efficacy against hospitalizations in the United States.
Two weeks ago, the company reported that a booster dose at 2 months or 6 months further lifted immunity, with a booster at 2 months providing 94% protection against moderate and severe COVID-19. The company said the 6-month booster raised antibodies by 12 times but didn’t release additional data at that time.
In September, the FDA authorized booster shots of the Pfizer vaccine for ages 65 and older, those who live in long-term care facilities, and those with higher risks for contracting COVID-19. The Biden administration is supporting a booster campaign to address potential waning vaccine immunity and remaining surges of the more contagious Delta variant, the AP reported.
A version of this article first appeared on WebMD.com.
Vaccine holdouts embrace COVID antibody treatment, mystifying doctors
Houston architect Lanson Jones is one of the nearly 80 million Americans who refuse to get a COVID-19 vaccine, arguing the shots are experimental, were rushed to market, may cause side effects, and aren’t all fully approved by federal officials.
But when he contracted COVID in September, he didn’t hesitate to seek treatment with monoclonal antibodies -- a year-old, laboratory-created therapy no less experimental than the vaccines that is not fully approved by the FDA and can also cause rare side effects.
“I haven’t done the shot because I hear a lot -- a lot -- of information about what are some of the effects of these vaccines and how it’s really not being reported, and I just felt I didn’t want to put something in me that has some question,” says Mr. Jones, 65.
“But with this monoclonal antibody treatment, I didn’t hesitate. I had no doubt in my mind -- not even one ounce of doubt about it. Not one person said, ‘Oh, well some people have had a reaction to it.’”
Mr. Jones, who was treated at Houston Methodist Hospital, is one of more than a million Americans who have received antibody IVs after getting the virus.
Those numbers are growing, with the federal government recently taking over distribution of the supplies of the drugs, which are limited in many states.
The treatment has been effective against COVID, in helping patients recover, stay out of the hospital, or die from the illness.
But what doctors and public health experts say is most surprising is that , as well.
“I think it’s irrational, quite frankly, if you have to boil it down to one word,” says Howard Huang, MD, who heads up Houston Methodist’s infusion program, which is providing up to 900 doses a week. “It really doesn’t make any sense on multiple levels.”
For one thing, he says, the FDA has just granted full approval for the COVID vaccine produced by Pfizer and BioNTech, upgrading its status from its emergency use authorization (EUA). Many experts expect the FDA to grant similar full approvals to the Moderna vaccine and possibly the Johnson and Johnson shot, which currently have EUA designations.
Many vaccine holdouts have cited the EUA status of the COVID vaccines -- one step shy of full approval -- as a reason they don’t trust the shot. But the antibody treatments have also been granted only EUA approval, which hasn’t stopped vaccine-resistant Americans from seeking them.
“So, they’re refusing an FDA-approved and tested [vaccine], and then they’re seeking something that’s still under an FDA EUA,” says Dr. Huang. “I just don’t get it. I really don’t.”
Amesh Adalja, MD, an emerging infectious diseases specialist with the Johns Hopkins University Center for Health Security, calls it “paradoxical” thinking for vaccine holdouts to refuse a shot that boosts your natural antibodies to prevent COVID, but take an antibody drug to treat it after infection.
“I don’t understand it, I can’t,” he says. “But the pandemic has been politicized and … I think consistency is not something to expect from people who are thinking about this irrationally [and] for people engaging in these conspiracies about the vaccine.
“I do think the fact that people like Joe Rogan and Gov. Abbot and Donald Trump received the monoclonal antibodies does probably play a role in some of the thinking in some of these individuals.”
Terry Scoggin, CEO of Titus Regional Medical Center in Mount Pleasant, Tex., says even the hospital’s doctors have been shocked by the demand for the new therapy among unvaccinated Texans.
“It’s mind-blowing that there’s been such resistance to the vaccine, but that demand for the monoclonal antibodies is so high,” he says, noting only 47% of adults in the region have received at least one dose of the shot. That’s far below CDC estimates that say 75.2% of American adults have received one shot, while 64.7% are fully vaccinated.
“But our doctors believe in the monoclonal antibodies, so it’s a trust factor -- they trust our community physicians,” Mr. Scoggin says. “I’ve never put the two and two together about the fear of the vaccine vs. [lack of fear] of the treatment. But it’s really interesting.”
Treatments effective, costly
Like the COVID vaccines given to nearly 214 million Americans, the antibody treatments taken by more than 1 million in the United States are highly effective and cause only rare (and usually minor) side effects.
Federal health officials say the infusions have helped keep the U.S. death toll -- now about 2,000 per day-- from soaring even higher, even as vaccine hesitancy persists, particularly in Southern states.
The FDA first authorized monoclonal antibody drugs in November 2020 -- just weeks before the vaccines were approved. But their popularity has soared as the Delta variant of the virus that causes COVID-19 has surged in recent months.
Clinical trials show that the drugs can cut COVID-related hospitalization or death in high-risk patients by as much as 70%-80%. They also can prevent infection in healthy people who have been exposed to an infected person, according to research published this month in The New England Journal of Medicine.
Monoclonal antibodies have been used for decades to treat cancer, autoimmune disorders, and other diseases, with the FDA approving nearly 100 such treatments since 1994.
The FDA has granted EUA approvals to four antibody treatments for COVID-19.
A two-antibody drug combination from Regeneron -- containing casirivimab and imdevimab -- has been shown to reduce the risk of hospitalization and death by 70% in people infected with COVID. Sotrovimab, made by GlaxoSmithKline and Vir, has had similar results.
The FDA approved a third treatment -- Eli Lilly’s combination of bamlanivimab and etesevimab -- in 2020, but the agency recommended against its use earlier this year after it proved ineffective against the Delta variant. The combination came back on the market in late August, but only in states where fewer than 5% of COVID infections are from strains, such as Delta, that are resistant to the treatment.
In June, the FDA authorized a fourth drug combination, Genentech’s tocilizumab, for people already hospitalized with COVID. But it is only moderately effective against the disease.
Lab-made monoclonal antibodies mimic the antibodies the body makes to fight viruses and illnesses. They work by targeting the spike protein on the surface of the virus. COVID vaccines work by priming the body’s immune system to recognize this very same spike protein and block it from entering your body’s cells, preventing infection.
Antibody treatments are given as an IV to treat an infection but can also be given as shots into the belly for people who have been exposed to the virus but have not yet been sickened by it, Dr. Huang says.
Timing is critical, he says, noting antibodies are most effective when given in the first few days after symptoms emerge.
Demands, concerns on the rise
Orders for monoclonal antibodies have skyrocketed in recent weeks -- to 168,000 doses per week in late August, up from 27,000 in July. The Biden administration, which has been covering the cost of the treatment for most patients, took over its distribution as well this week.
But experts foresee potential problems as patient demand increases.
Federal officials have already warned states of potential shortages ahead. Only about 2.4 million monoclonal antibody doses have been shipped nationally so far, less than half of which have been administered.
More supplies are on the way, with the federal government recently buying another 1.8 million doses for delivery in the months ahead. But for now, some hospitals are uncertain of supplies and are already struggling to meet the demand for the treatments.
Seven Southern states account for 70% of orders: Texas, Alabama, Florida, Mississippi, Tennessee, Georgia, and Louisiana. Those states have among the nation’s lowest vaccine rates and highest infection numbers.
Florida officials said the state’s latest weekly allotment left clinics 41,000 doses short of what they need. Tennessee has begun limiting treatments for unvaccinated patients to give priority to those most at risk of dying from COVID. And in Texas, elective surgeries have been postponed to make room for COVID-19 patients at some hospitals, as operating room nurses have been enlisted to give IVs.
Some strong proponents of monoclonal antibody treatments have been frustrated by Republican governors who are scrambling to push and deliver them, while opposing vaccine and mask mandates.
Raising vaccination rates, scientists say, would make the antibody treatments unnecessary in many cases.
Experts also note the drugs are far more costly than the vaccines -- with a price tag of about $2,100 for each IV, compared to $20-$40 for the shot.
“When you’re talking about just the cost to society as a whole -- turning down a [vaccine] that costs a couple dozen dollars for therapies that cost thousands of dollars -- it just doesn’t make any sense,” says Dr. Huang.
“And the tragedy is that a lot of these infections right now are preventable. It’s not like the pre-vaccine days, when we didn’t have anything better. And for these people, it’s just hard to justify that line of thinking. And so, the challenge is changing people’s minds. And that’s really been the difficult thing.”
In addition, the treatments take 90 minutes to administer, taxing health care workers in hard-hit states that have been slammed by the influx of patients.
Beyond these issues, Dr. Huang cites other public health costs of people choosing treatment over vaccination. The vaccine protects others because it limits transmission of the virus. By contrast, a single antibody IV helps only that patient and does not keep people from infecting others or becoming reinfected, requiring another IV.
“Getting the vaccine helps people beyond yourself; it helps the community, too,” he notes. “There’s just a strong argument for getting the vaccine. I obviously have a very biased opinion, but I would hope I have more of a scientific or expert opinion, but that doesn’t seem to matter these days.”
Vaccine resistance still remains for some
Seth Thurman, an IT technician from Mount Pleasant, Tex., acknowledges he was hesitant to get the vaccine at first because he felt it was fast-tracked, “experimental,” might cause unknown side effects, was developed quickly, and was being pushed by government officials.
“I shared the same sentiments as a lot of other people [as] some of the reasons why I might have been hesitant in the beginning to get the vaccine, says Mr. Thurman, 47. “A lot of people don’t trust what’s out there, maybe what the government is pushing, so I was taking a wait-and-see approach.”
In August, he relented and received the first of the two-shot Moderna vaccine. But several weeks later, he developed COVID and took his doctor’s advice to receive antibody therapy at Titus Regional Medical Center.
The results were almost immediate.
“I noticed within just a few hours of getting that infusion I was feeling better,” he says. “And by the next day, I was feeling great. No more temperature and no cough and no loss of taste and smell. And today, I’m 100%.”
Having had COVID convinced him of the importance of getting the vaccine, and he plans to get the second dose of the shot after the prescribed 90-day waiting period.
But Mr. Jones, the Houston architect, remains unconvinced, even after suffering what he describes as a “horrible” experience with COVID.
“It’s something I’m still thinking about,” he says of the vaccine. “But I can’t imagine that there wouldn’t be some sort of side effects from something that was developed so fast and had not gone through 4 or 5 years of vetting or trials. So that kind of just leaves doubt in my mind.
“And it’s just so weird that something so personal has become so public -- like people’s medical decisions now are on the front page of The New York Times. When did we think something like that would ever happen?”
The quick results of his treatment were so “remarkable” that he’d recommend it to anyone without hesitation, he says.
“If my story can help people be willing to seek out this infusion and take it early on in their COVID experience, I think it would not only save lives and keep people out of our hospitals and not overwhelm our hospital systems,” he says.
Dr. Huang agrees that the IV therapy is a great “fallback option” for people who’ve been infected, who have weakened immune systems, or can’t receive the vaccine for other health reasons. But for most people, he argues, the vaccine is the best way to go. That’s why Houston Methodist advises the shot for every patient like Mr. Jones, who’s been treated for COVID.
“Getting the vaccine is the way to go for the vast number of people,” he says.
Frederick Thurmond, MD, who oversees COVID-related care at Titus Regional Medical Center, believes it will take more than just doctors’ recommendations to move some patients to get the vaccine. The only thing that will motivate some will be contracting COVID, or knowing someone who does, he says.
“It’s clear that at least here in Texas, I swear man, you tell people they need to do something, and they just say, ‘Well, then I’m NOT going to do it,’” he says. “But once you’ve got COVID, the game becomes a whole lot more serious. And I think most people in the U.S. know someone who’s died from COVID at this point.”
Dr. Thurmond says that for some patients, stubborn resistance to legitimate medical advice persists -- on the vaccine and even treatment -- even after infection.
“We have seen more than one person avoid any medical care whatsoever after they knew they had COVID,” he says. “They languish in private and eventually come to the emergency room extremely sick and doing things with little to no medical value -- such as taking a friend’s hydroxychloroquine, random antibiotics, a horse de-worming dose of ivermectin, and gargling with Betadine and even bleach.”
But most of his patients who have the IV therapy take his advice to get the vaccine afterward.
“The only way to end the pandemic is to vaccinate everybody,” he says.
Dr. Adalja agrees.
“The monoclonal antibodies work, they are great drugs, so I think it is appropriate to praise them,” says Dr. Adalja, who’s given them to his own patients. “But it’s not appropriate to use them as an alternative to vaccination or to think, you know, don’t worry about the getting the vaccine because if you get infected and get the monoclonal antibodies to get through this -- that’s not the way to approach it.
He also worries about what he calls “dark-age mentalities” that have fueled the anti-vaccine movement, which has sought to heighten fears of modern medicine and doctors.
“The anti-vaccine movement has really capitalized on COVID-19, and it’s really a much more virulent form of the anti-vaccine movement than what we’ve seen with measles and other diseases in the past,” he notes. “And I think it’s going to be very difficult to contend with in the future, because no one thought we’d be battling the anti-vaccine movement this late in the pandemic.”
The biggest takeaway?
“When it comes to an infectious disease, prevention is always much better than treatment,” Dr. Adalja says. “If you don’t even need to get to the treatment stage because you prevent people from getting infected, that’s the goal.”
A version of this article first appeared on WebMD.com.
Houston architect Lanson Jones is one of the nearly 80 million Americans who refuse to get a COVID-19 vaccine, arguing the shots are experimental, were rushed to market, may cause side effects, and aren’t all fully approved by federal officials.
But when he contracted COVID in September, he didn’t hesitate to seek treatment with monoclonal antibodies -- a year-old, laboratory-created therapy no less experimental than the vaccines that is not fully approved by the FDA and can also cause rare side effects.
“I haven’t done the shot because I hear a lot -- a lot -- of information about what are some of the effects of these vaccines and how it’s really not being reported, and I just felt I didn’t want to put something in me that has some question,” says Mr. Jones, 65.
“But with this monoclonal antibody treatment, I didn’t hesitate. I had no doubt in my mind -- not even one ounce of doubt about it. Not one person said, ‘Oh, well some people have had a reaction to it.’”
Mr. Jones, who was treated at Houston Methodist Hospital, is one of more than a million Americans who have received antibody IVs after getting the virus.
Those numbers are growing, with the federal government recently taking over distribution of the supplies of the drugs, which are limited in many states.
The treatment has been effective against COVID, in helping patients recover, stay out of the hospital, or die from the illness.
But what doctors and public health experts say is most surprising is that , as well.
“I think it’s irrational, quite frankly, if you have to boil it down to one word,” says Howard Huang, MD, who heads up Houston Methodist’s infusion program, which is providing up to 900 doses a week. “It really doesn’t make any sense on multiple levels.”
For one thing, he says, the FDA has just granted full approval for the COVID vaccine produced by Pfizer and BioNTech, upgrading its status from its emergency use authorization (EUA). Many experts expect the FDA to grant similar full approvals to the Moderna vaccine and possibly the Johnson and Johnson shot, which currently have EUA designations.
Many vaccine holdouts have cited the EUA status of the COVID vaccines -- one step shy of full approval -- as a reason they don’t trust the shot. But the antibody treatments have also been granted only EUA approval, which hasn’t stopped vaccine-resistant Americans from seeking them.
“So, they’re refusing an FDA-approved and tested [vaccine], and then they’re seeking something that’s still under an FDA EUA,” says Dr. Huang. “I just don’t get it. I really don’t.”
Amesh Adalja, MD, an emerging infectious diseases specialist with the Johns Hopkins University Center for Health Security, calls it “paradoxical” thinking for vaccine holdouts to refuse a shot that boosts your natural antibodies to prevent COVID, but take an antibody drug to treat it after infection.
“I don’t understand it, I can’t,” he says. “But the pandemic has been politicized and … I think consistency is not something to expect from people who are thinking about this irrationally [and] for people engaging in these conspiracies about the vaccine.
“I do think the fact that people like Joe Rogan and Gov. Abbot and Donald Trump received the monoclonal antibodies does probably play a role in some of the thinking in some of these individuals.”
Terry Scoggin, CEO of Titus Regional Medical Center in Mount Pleasant, Tex., says even the hospital’s doctors have been shocked by the demand for the new therapy among unvaccinated Texans.
“It’s mind-blowing that there’s been such resistance to the vaccine, but that demand for the monoclonal antibodies is so high,” he says, noting only 47% of adults in the region have received at least one dose of the shot. That’s far below CDC estimates that say 75.2% of American adults have received one shot, while 64.7% are fully vaccinated.
“But our doctors believe in the monoclonal antibodies, so it’s a trust factor -- they trust our community physicians,” Mr. Scoggin says. “I’ve never put the two and two together about the fear of the vaccine vs. [lack of fear] of the treatment. But it’s really interesting.”
Treatments effective, costly
Like the COVID vaccines given to nearly 214 million Americans, the antibody treatments taken by more than 1 million in the United States are highly effective and cause only rare (and usually minor) side effects.
Federal health officials say the infusions have helped keep the U.S. death toll -- now about 2,000 per day-- from soaring even higher, even as vaccine hesitancy persists, particularly in Southern states.
The FDA first authorized monoclonal antibody drugs in November 2020 -- just weeks before the vaccines were approved. But their popularity has soared as the Delta variant of the virus that causes COVID-19 has surged in recent months.
Clinical trials show that the drugs can cut COVID-related hospitalization or death in high-risk patients by as much as 70%-80%. They also can prevent infection in healthy people who have been exposed to an infected person, according to research published this month in The New England Journal of Medicine.
Monoclonal antibodies have been used for decades to treat cancer, autoimmune disorders, and other diseases, with the FDA approving nearly 100 such treatments since 1994.
The FDA has granted EUA approvals to four antibody treatments for COVID-19.
A two-antibody drug combination from Regeneron -- containing casirivimab and imdevimab -- has been shown to reduce the risk of hospitalization and death by 70% in people infected with COVID. Sotrovimab, made by GlaxoSmithKline and Vir, has had similar results.
The FDA approved a third treatment -- Eli Lilly’s combination of bamlanivimab and etesevimab -- in 2020, but the agency recommended against its use earlier this year after it proved ineffective against the Delta variant. The combination came back on the market in late August, but only in states where fewer than 5% of COVID infections are from strains, such as Delta, that are resistant to the treatment.
In June, the FDA authorized a fourth drug combination, Genentech’s tocilizumab, for people already hospitalized with COVID. But it is only moderately effective against the disease.
Lab-made monoclonal antibodies mimic the antibodies the body makes to fight viruses and illnesses. They work by targeting the spike protein on the surface of the virus. COVID vaccines work by priming the body’s immune system to recognize this very same spike protein and block it from entering your body’s cells, preventing infection.
Antibody treatments are given as an IV to treat an infection but can also be given as shots into the belly for people who have been exposed to the virus but have not yet been sickened by it, Dr. Huang says.
Timing is critical, he says, noting antibodies are most effective when given in the first few days after symptoms emerge.
Demands, concerns on the rise
Orders for monoclonal antibodies have skyrocketed in recent weeks -- to 168,000 doses per week in late August, up from 27,000 in July. The Biden administration, which has been covering the cost of the treatment for most patients, took over its distribution as well this week.
But experts foresee potential problems as patient demand increases.
Federal officials have already warned states of potential shortages ahead. Only about 2.4 million monoclonal antibody doses have been shipped nationally so far, less than half of which have been administered.
More supplies are on the way, with the federal government recently buying another 1.8 million doses for delivery in the months ahead. But for now, some hospitals are uncertain of supplies and are already struggling to meet the demand for the treatments.
Seven Southern states account for 70% of orders: Texas, Alabama, Florida, Mississippi, Tennessee, Georgia, and Louisiana. Those states have among the nation’s lowest vaccine rates and highest infection numbers.
Florida officials said the state’s latest weekly allotment left clinics 41,000 doses short of what they need. Tennessee has begun limiting treatments for unvaccinated patients to give priority to those most at risk of dying from COVID. And in Texas, elective surgeries have been postponed to make room for COVID-19 patients at some hospitals, as operating room nurses have been enlisted to give IVs.
Some strong proponents of monoclonal antibody treatments have been frustrated by Republican governors who are scrambling to push and deliver them, while opposing vaccine and mask mandates.
Raising vaccination rates, scientists say, would make the antibody treatments unnecessary in many cases.
Experts also note the drugs are far more costly than the vaccines -- with a price tag of about $2,100 for each IV, compared to $20-$40 for the shot.
“When you’re talking about just the cost to society as a whole -- turning down a [vaccine] that costs a couple dozen dollars for therapies that cost thousands of dollars -- it just doesn’t make any sense,” says Dr. Huang.
“And the tragedy is that a lot of these infections right now are preventable. It’s not like the pre-vaccine days, when we didn’t have anything better. And for these people, it’s just hard to justify that line of thinking. And so, the challenge is changing people’s minds. And that’s really been the difficult thing.”
In addition, the treatments take 90 minutes to administer, taxing health care workers in hard-hit states that have been slammed by the influx of patients.
Beyond these issues, Dr. Huang cites other public health costs of people choosing treatment over vaccination. The vaccine protects others because it limits transmission of the virus. By contrast, a single antibody IV helps only that patient and does not keep people from infecting others or becoming reinfected, requiring another IV.
“Getting the vaccine helps people beyond yourself; it helps the community, too,” he notes. “There’s just a strong argument for getting the vaccine. I obviously have a very biased opinion, but I would hope I have more of a scientific or expert opinion, but that doesn’t seem to matter these days.”
Vaccine resistance still remains for some
Seth Thurman, an IT technician from Mount Pleasant, Tex., acknowledges he was hesitant to get the vaccine at first because he felt it was fast-tracked, “experimental,” might cause unknown side effects, was developed quickly, and was being pushed by government officials.
“I shared the same sentiments as a lot of other people [as] some of the reasons why I might have been hesitant in the beginning to get the vaccine, says Mr. Thurman, 47. “A lot of people don’t trust what’s out there, maybe what the government is pushing, so I was taking a wait-and-see approach.”
In August, he relented and received the first of the two-shot Moderna vaccine. But several weeks later, he developed COVID and took his doctor’s advice to receive antibody therapy at Titus Regional Medical Center.
The results were almost immediate.
“I noticed within just a few hours of getting that infusion I was feeling better,” he says. “And by the next day, I was feeling great. No more temperature and no cough and no loss of taste and smell. And today, I’m 100%.”
Having had COVID convinced him of the importance of getting the vaccine, and he plans to get the second dose of the shot after the prescribed 90-day waiting period.
But Mr. Jones, the Houston architect, remains unconvinced, even after suffering what he describes as a “horrible” experience with COVID.
“It’s something I’m still thinking about,” he says of the vaccine. “But I can’t imagine that there wouldn’t be some sort of side effects from something that was developed so fast and had not gone through 4 or 5 years of vetting or trials. So that kind of just leaves doubt in my mind.
“And it’s just so weird that something so personal has become so public -- like people’s medical decisions now are on the front page of The New York Times. When did we think something like that would ever happen?”
The quick results of his treatment were so “remarkable” that he’d recommend it to anyone without hesitation, he says.
“If my story can help people be willing to seek out this infusion and take it early on in their COVID experience, I think it would not only save lives and keep people out of our hospitals and not overwhelm our hospital systems,” he says.
Dr. Huang agrees that the IV therapy is a great “fallback option” for people who’ve been infected, who have weakened immune systems, or can’t receive the vaccine for other health reasons. But for most people, he argues, the vaccine is the best way to go. That’s why Houston Methodist advises the shot for every patient like Mr. Jones, who’s been treated for COVID.
“Getting the vaccine is the way to go for the vast number of people,” he says.
Frederick Thurmond, MD, who oversees COVID-related care at Titus Regional Medical Center, believes it will take more than just doctors’ recommendations to move some patients to get the vaccine. The only thing that will motivate some will be contracting COVID, or knowing someone who does, he says.
“It’s clear that at least here in Texas, I swear man, you tell people they need to do something, and they just say, ‘Well, then I’m NOT going to do it,’” he says. “But once you’ve got COVID, the game becomes a whole lot more serious. And I think most people in the U.S. know someone who’s died from COVID at this point.”
Dr. Thurmond says that for some patients, stubborn resistance to legitimate medical advice persists -- on the vaccine and even treatment -- even after infection.
“We have seen more than one person avoid any medical care whatsoever after they knew they had COVID,” he says. “They languish in private and eventually come to the emergency room extremely sick and doing things with little to no medical value -- such as taking a friend’s hydroxychloroquine, random antibiotics, a horse de-worming dose of ivermectin, and gargling with Betadine and even bleach.”
But most of his patients who have the IV therapy take his advice to get the vaccine afterward.
“The only way to end the pandemic is to vaccinate everybody,” he says.
Dr. Adalja agrees.
“The monoclonal antibodies work, they are great drugs, so I think it is appropriate to praise them,” says Dr. Adalja, who’s given them to his own patients. “But it’s not appropriate to use them as an alternative to vaccination or to think, you know, don’t worry about the getting the vaccine because if you get infected and get the monoclonal antibodies to get through this -- that’s not the way to approach it.
He also worries about what he calls “dark-age mentalities” that have fueled the anti-vaccine movement, which has sought to heighten fears of modern medicine and doctors.
“The anti-vaccine movement has really capitalized on COVID-19, and it’s really a much more virulent form of the anti-vaccine movement than what we’ve seen with measles and other diseases in the past,” he notes. “And I think it’s going to be very difficult to contend with in the future, because no one thought we’d be battling the anti-vaccine movement this late in the pandemic.”
The biggest takeaway?
“When it comes to an infectious disease, prevention is always much better than treatment,” Dr. Adalja says. “If you don’t even need to get to the treatment stage because you prevent people from getting infected, that’s the goal.”
A version of this article first appeared on WebMD.com.
Houston architect Lanson Jones is one of the nearly 80 million Americans who refuse to get a COVID-19 vaccine, arguing the shots are experimental, were rushed to market, may cause side effects, and aren’t all fully approved by federal officials.
But when he contracted COVID in September, he didn’t hesitate to seek treatment with monoclonal antibodies -- a year-old, laboratory-created therapy no less experimental than the vaccines that is not fully approved by the FDA and can also cause rare side effects.
“I haven’t done the shot because I hear a lot -- a lot -- of information about what are some of the effects of these vaccines and how it’s really not being reported, and I just felt I didn’t want to put something in me that has some question,” says Mr. Jones, 65.
“But with this monoclonal antibody treatment, I didn’t hesitate. I had no doubt in my mind -- not even one ounce of doubt about it. Not one person said, ‘Oh, well some people have had a reaction to it.’”
Mr. Jones, who was treated at Houston Methodist Hospital, is one of more than a million Americans who have received antibody IVs after getting the virus.
Those numbers are growing, with the federal government recently taking over distribution of the supplies of the drugs, which are limited in many states.
The treatment has been effective against COVID, in helping patients recover, stay out of the hospital, or die from the illness.
But what doctors and public health experts say is most surprising is that , as well.
“I think it’s irrational, quite frankly, if you have to boil it down to one word,” says Howard Huang, MD, who heads up Houston Methodist’s infusion program, which is providing up to 900 doses a week. “It really doesn’t make any sense on multiple levels.”
For one thing, he says, the FDA has just granted full approval for the COVID vaccine produced by Pfizer and BioNTech, upgrading its status from its emergency use authorization (EUA). Many experts expect the FDA to grant similar full approvals to the Moderna vaccine and possibly the Johnson and Johnson shot, which currently have EUA designations.
Many vaccine holdouts have cited the EUA status of the COVID vaccines -- one step shy of full approval -- as a reason they don’t trust the shot. But the antibody treatments have also been granted only EUA approval, which hasn’t stopped vaccine-resistant Americans from seeking them.
“So, they’re refusing an FDA-approved and tested [vaccine], and then they’re seeking something that’s still under an FDA EUA,” says Dr. Huang. “I just don’t get it. I really don’t.”
Amesh Adalja, MD, an emerging infectious diseases specialist with the Johns Hopkins University Center for Health Security, calls it “paradoxical” thinking for vaccine holdouts to refuse a shot that boosts your natural antibodies to prevent COVID, but take an antibody drug to treat it after infection.
“I don’t understand it, I can’t,” he says. “But the pandemic has been politicized and … I think consistency is not something to expect from people who are thinking about this irrationally [and] for people engaging in these conspiracies about the vaccine.
“I do think the fact that people like Joe Rogan and Gov. Abbot and Donald Trump received the monoclonal antibodies does probably play a role in some of the thinking in some of these individuals.”
Terry Scoggin, CEO of Titus Regional Medical Center in Mount Pleasant, Tex., says even the hospital’s doctors have been shocked by the demand for the new therapy among unvaccinated Texans.
“It’s mind-blowing that there’s been such resistance to the vaccine, but that demand for the monoclonal antibodies is so high,” he says, noting only 47% of adults in the region have received at least one dose of the shot. That’s far below CDC estimates that say 75.2% of American adults have received one shot, while 64.7% are fully vaccinated.
“But our doctors believe in the monoclonal antibodies, so it’s a trust factor -- they trust our community physicians,” Mr. Scoggin says. “I’ve never put the two and two together about the fear of the vaccine vs. [lack of fear] of the treatment. But it’s really interesting.”
Treatments effective, costly
Like the COVID vaccines given to nearly 214 million Americans, the antibody treatments taken by more than 1 million in the United States are highly effective and cause only rare (and usually minor) side effects.
Federal health officials say the infusions have helped keep the U.S. death toll -- now about 2,000 per day-- from soaring even higher, even as vaccine hesitancy persists, particularly in Southern states.
The FDA first authorized monoclonal antibody drugs in November 2020 -- just weeks before the vaccines were approved. But their popularity has soared as the Delta variant of the virus that causes COVID-19 has surged in recent months.
Clinical trials show that the drugs can cut COVID-related hospitalization or death in high-risk patients by as much as 70%-80%. They also can prevent infection in healthy people who have been exposed to an infected person, according to research published this month in The New England Journal of Medicine.
Monoclonal antibodies have been used for decades to treat cancer, autoimmune disorders, and other diseases, with the FDA approving nearly 100 such treatments since 1994.
The FDA has granted EUA approvals to four antibody treatments for COVID-19.
A two-antibody drug combination from Regeneron -- containing casirivimab and imdevimab -- has been shown to reduce the risk of hospitalization and death by 70% in people infected with COVID. Sotrovimab, made by GlaxoSmithKline and Vir, has had similar results.
The FDA approved a third treatment -- Eli Lilly’s combination of bamlanivimab and etesevimab -- in 2020, but the agency recommended against its use earlier this year after it proved ineffective against the Delta variant. The combination came back on the market in late August, but only in states where fewer than 5% of COVID infections are from strains, such as Delta, that are resistant to the treatment.
In June, the FDA authorized a fourth drug combination, Genentech’s tocilizumab, for people already hospitalized with COVID. But it is only moderately effective against the disease.
Lab-made monoclonal antibodies mimic the antibodies the body makes to fight viruses and illnesses. They work by targeting the spike protein on the surface of the virus. COVID vaccines work by priming the body’s immune system to recognize this very same spike protein and block it from entering your body’s cells, preventing infection.
Antibody treatments are given as an IV to treat an infection but can also be given as shots into the belly for people who have been exposed to the virus but have not yet been sickened by it, Dr. Huang says.
Timing is critical, he says, noting antibodies are most effective when given in the first few days after symptoms emerge.
Demands, concerns on the rise
Orders for monoclonal antibodies have skyrocketed in recent weeks -- to 168,000 doses per week in late August, up from 27,000 in July. The Biden administration, which has been covering the cost of the treatment for most patients, took over its distribution as well this week.
But experts foresee potential problems as patient demand increases.
Federal officials have already warned states of potential shortages ahead. Only about 2.4 million monoclonal antibody doses have been shipped nationally so far, less than half of which have been administered.
More supplies are on the way, with the federal government recently buying another 1.8 million doses for delivery in the months ahead. But for now, some hospitals are uncertain of supplies and are already struggling to meet the demand for the treatments.
Seven Southern states account for 70% of orders: Texas, Alabama, Florida, Mississippi, Tennessee, Georgia, and Louisiana. Those states have among the nation’s lowest vaccine rates and highest infection numbers.
Florida officials said the state’s latest weekly allotment left clinics 41,000 doses short of what they need. Tennessee has begun limiting treatments for unvaccinated patients to give priority to those most at risk of dying from COVID. And in Texas, elective surgeries have been postponed to make room for COVID-19 patients at some hospitals, as operating room nurses have been enlisted to give IVs.
Some strong proponents of monoclonal antibody treatments have been frustrated by Republican governors who are scrambling to push and deliver them, while opposing vaccine and mask mandates.
Raising vaccination rates, scientists say, would make the antibody treatments unnecessary in many cases.
Experts also note the drugs are far more costly than the vaccines -- with a price tag of about $2,100 for each IV, compared to $20-$40 for the shot.
“When you’re talking about just the cost to society as a whole -- turning down a [vaccine] that costs a couple dozen dollars for therapies that cost thousands of dollars -- it just doesn’t make any sense,” says Dr. Huang.
“And the tragedy is that a lot of these infections right now are preventable. It’s not like the pre-vaccine days, when we didn’t have anything better. And for these people, it’s just hard to justify that line of thinking. And so, the challenge is changing people’s minds. And that’s really been the difficult thing.”
In addition, the treatments take 90 minutes to administer, taxing health care workers in hard-hit states that have been slammed by the influx of patients.
Beyond these issues, Dr. Huang cites other public health costs of people choosing treatment over vaccination. The vaccine protects others because it limits transmission of the virus. By contrast, a single antibody IV helps only that patient and does not keep people from infecting others or becoming reinfected, requiring another IV.
“Getting the vaccine helps people beyond yourself; it helps the community, too,” he notes. “There’s just a strong argument for getting the vaccine. I obviously have a very biased opinion, but I would hope I have more of a scientific or expert opinion, but that doesn’t seem to matter these days.”
Vaccine resistance still remains for some
Seth Thurman, an IT technician from Mount Pleasant, Tex., acknowledges he was hesitant to get the vaccine at first because he felt it was fast-tracked, “experimental,” might cause unknown side effects, was developed quickly, and was being pushed by government officials.
“I shared the same sentiments as a lot of other people [as] some of the reasons why I might have been hesitant in the beginning to get the vaccine, says Mr. Thurman, 47. “A lot of people don’t trust what’s out there, maybe what the government is pushing, so I was taking a wait-and-see approach.”
In August, he relented and received the first of the two-shot Moderna vaccine. But several weeks later, he developed COVID and took his doctor’s advice to receive antibody therapy at Titus Regional Medical Center.
The results were almost immediate.
“I noticed within just a few hours of getting that infusion I was feeling better,” he says. “And by the next day, I was feeling great. No more temperature and no cough and no loss of taste and smell. And today, I’m 100%.”
Having had COVID convinced him of the importance of getting the vaccine, and he plans to get the second dose of the shot after the prescribed 90-day waiting period.
But Mr. Jones, the Houston architect, remains unconvinced, even after suffering what he describes as a “horrible” experience with COVID.
“It’s something I’m still thinking about,” he says of the vaccine. “But I can’t imagine that there wouldn’t be some sort of side effects from something that was developed so fast and had not gone through 4 or 5 years of vetting or trials. So that kind of just leaves doubt in my mind.
“And it’s just so weird that something so personal has become so public -- like people’s medical decisions now are on the front page of The New York Times. When did we think something like that would ever happen?”
The quick results of his treatment were so “remarkable” that he’d recommend it to anyone without hesitation, he says.
“If my story can help people be willing to seek out this infusion and take it early on in their COVID experience, I think it would not only save lives and keep people out of our hospitals and not overwhelm our hospital systems,” he says.
Dr. Huang agrees that the IV therapy is a great “fallback option” for people who’ve been infected, who have weakened immune systems, or can’t receive the vaccine for other health reasons. But for most people, he argues, the vaccine is the best way to go. That’s why Houston Methodist advises the shot for every patient like Mr. Jones, who’s been treated for COVID.
“Getting the vaccine is the way to go for the vast number of people,” he says.
Frederick Thurmond, MD, who oversees COVID-related care at Titus Regional Medical Center, believes it will take more than just doctors’ recommendations to move some patients to get the vaccine. The only thing that will motivate some will be contracting COVID, or knowing someone who does, he says.
“It’s clear that at least here in Texas, I swear man, you tell people they need to do something, and they just say, ‘Well, then I’m NOT going to do it,’” he says. “But once you’ve got COVID, the game becomes a whole lot more serious. And I think most people in the U.S. know someone who’s died from COVID at this point.”
Dr. Thurmond says that for some patients, stubborn resistance to legitimate medical advice persists -- on the vaccine and even treatment -- even after infection.
“We have seen more than one person avoid any medical care whatsoever after they knew they had COVID,” he says. “They languish in private and eventually come to the emergency room extremely sick and doing things with little to no medical value -- such as taking a friend’s hydroxychloroquine, random antibiotics, a horse de-worming dose of ivermectin, and gargling with Betadine and even bleach.”
But most of his patients who have the IV therapy take his advice to get the vaccine afterward.
“The only way to end the pandemic is to vaccinate everybody,” he says.
Dr. Adalja agrees.
“The monoclonal antibodies work, they are great drugs, so I think it is appropriate to praise them,” says Dr. Adalja, who’s given them to his own patients. “But it’s not appropriate to use them as an alternative to vaccination or to think, you know, don’t worry about the getting the vaccine because if you get infected and get the monoclonal antibodies to get through this -- that’s not the way to approach it.
He also worries about what he calls “dark-age mentalities” that have fueled the anti-vaccine movement, which has sought to heighten fears of modern medicine and doctors.
“The anti-vaccine movement has really capitalized on COVID-19, and it’s really a much more virulent form of the anti-vaccine movement than what we’ve seen with measles and other diseases in the past,” he notes. “And I think it’s going to be very difficult to contend with in the future, because no one thought we’d be battling the anti-vaccine movement this late in the pandemic.”
The biggest takeaway?
“When it comes to an infectious disease, prevention is always much better than treatment,” Dr. Adalja says. “If you don’t even need to get to the treatment stage because you prevent people from getting infected, that’s the goal.”
A version of this article first appeared on WebMD.com.
Pfizer COVID vaccine antibodies may disappear in 7 months, study says
, according to a new study published on the bioRxiv preprint server.
In the study, which hasn’t yet been peer-reviewed or formally published in a medical journal, researchers analyzed blood samples from 46 healthy young or middle-aged adults after receiving two doses, and then 6 months after the second dose.
“Our study shows vaccination with the Pfizer-BioNTech vaccine induces high levels of neutralizing antibodies against the original vaccine strain, but these levels drop by nearly 10-fold by 7 months,” the researchers told Reuters.
In about half of the adults, neutralizing antibodies were undetectable at 6 months after the second dose, particularly against coronavirus variants such as Delta, Beta, and Mu.
Neutralizing antibodies only make up part of the body’s immune defense against the virus, Reuters noted, but they are still “critically important” in protecting against coronavirus infections.
“These findings suggest that administering a booster dose at around 6 to 7 months following the initial immunization will likely enhance protection,” the study authors wrote.
BioNTech said a new vaccine formula will likely be needed by mid-2022 to protect against future mutations of the virus, according to the Financial Times.
“This year, [a different vaccine] is completely unneeded, but by mid-next year, it could be a different situation,” Ugur Sahin, MD, cofounder and CEO of BioNTech, told the news outlet.
Current variants, namely the Delta variant, are more contagious than the original coronavirus strain but not different enough to evade current vaccines, he said. But new strains may be able to evade boosters.
“This virus will stay, and the virus will further adapt,” Dr. Sahin said. “This is a continuous evolution, and that evolution has just started.”
A version of this article first appeared on WebMD.com.
, according to a new study published on the bioRxiv preprint server.
In the study, which hasn’t yet been peer-reviewed or formally published in a medical journal, researchers analyzed blood samples from 46 healthy young or middle-aged adults after receiving two doses, and then 6 months after the second dose.
“Our study shows vaccination with the Pfizer-BioNTech vaccine induces high levels of neutralizing antibodies against the original vaccine strain, but these levels drop by nearly 10-fold by 7 months,” the researchers told Reuters.
In about half of the adults, neutralizing antibodies were undetectable at 6 months after the second dose, particularly against coronavirus variants such as Delta, Beta, and Mu.
Neutralizing antibodies only make up part of the body’s immune defense against the virus, Reuters noted, but they are still “critically important” in protecting against coronavirus infections.
“These findings suggest that administering a booster dose at around 6 to 7 months following the initial immunization will likely enhance protection,” the study authors wrote.
BioNTech said a new vaccine formula will likely be needed by mid-2022 to protect against future mutations of the virus, according to the Financial Times.
“This year, [a different vaccine] is completely unneeded, but by mid-next year, it could be a different situation,” Ugur Sahin, MD, cofounder and CEO of BioNTech, told the news outlet.
Current variants, namely the Delta variant, are more contagious than the original coronavirus strain but not different enough to evade current vaccines, he said. But new strains may be able to evade boosters.
“This virus will stay, and the virus will further adapt,” Dr. Sahin said. “This is a continuous evolution, and that evolution has just started.”
A version of this article first appeared on WebMD.com.
, according to a new study published on the bioRxiv preprint server.
In the study, which hasn’t yet been peer-reviewed or formally published in a medical journal, researchers analyzed blood samples from 46 healthy young or middle-aged adults after receiving two doses, and then 6 months after the second dose.
“Our study shows vaccination with the Pfizer-BioNTech vaccine induces high levels of neutralizing antibodies against the original vaccine strain, but these levels drop by nearly 10-fold by 7 months,” the researchers told Reuters.
In about half of the adults, neutralizing antibodies were undetectable at 6 months after the second dose, particularly against coronavirus variants such as Delta, Beta, and Mu.
Neutralizing antibodies only make up part of the body’s immune defense against the virus, Reuters noted, but they are still “critically important” in protecting against coronavirus infections.
“These findings suggest that administering a booster dose at around 6 to 7 months following the initial immunization will likely enhance protection,” the study authors wrote.
BioNTech said a new vaccine formula will likely be needed by mid-2022 to protect against future mutations of the virus, according to the Financial Times.
“This year, [a different vaccine] is completely unneeded, but by mid-next year, it could be a different situation,” Ugur Sahin, MD, cofounder and CEO of BioNTech, told the news outlet.
Current variants, namely the Delta variant, are more contagious than the original coronavirus strain but not different enough to evade current vaccines, he said. But new strains may be able to evade boosters.
“This virus will stay, and the virus will further adapt,” Dr. Sahin said. “This is a continuous evolution, and that evolution has just started.”
A version of this article first appeared on WebMD.com.
Opioid prescribing mapped: Alabama highest, New York lowest
Medicare beneficiaries in Alabama were more likely to get a prescription for an opioid than in any other state in 2019, based on newly released data.
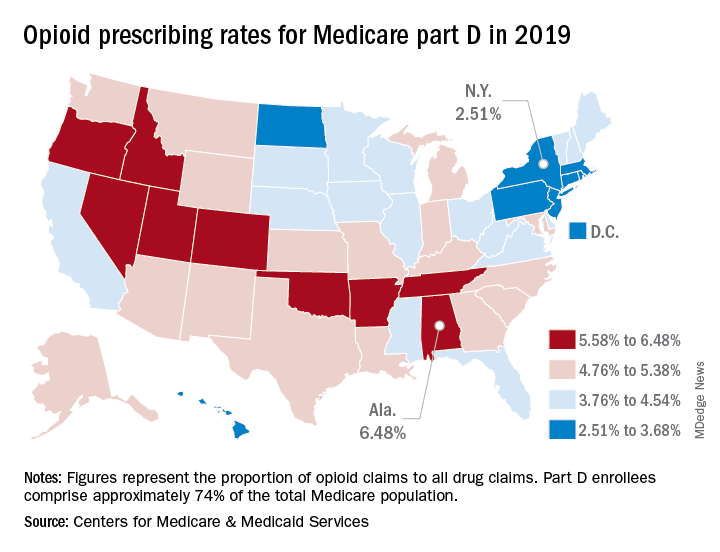
That year, opioids represented 6.48% of all drug claims for part D enrollees in the state, just ahead of Utah at 6.41%. Idaho, at 6.07%, was the only other state with an opioid prescribing rate over 6%, while Oklahoma came in at an even 6.0%, according to the latest update of the Centers for Medicare & Medicaid Services’ dataset.
The lowest rate in 2019 belonged to New York, where 2.51% of drug claims, including original prescriptions and refills, involved an opioid. Rhode Island was next at 2.87%, followed by New Jersey (3.23%), Massachusetts (3.26%), and North Dakota (3.39%),
Altogether, Medicare part D processed 1.5 billion drug claims in 2019, of which 66.1 million, or 4.41%, involved opioids. Both of the opioid numbers were down from 2018, when opioids represented 4.68% (70.2 million) of the 1.5 billion total claims, and from 2014, when opioids were involved in 5.73% (81,026,831) of the 1.41 billion drug claims, the CMS data show. That works out to 5.77% fewer opioids in 2019, compared with 2014, despite the increase in total volume.
from 2014 to 2019, with Hawaii showing the smallest decline as it slipped 0.41 percentage points from 3.9% to 3.49%, according to the CMS.
In 2019, part D beneficiaries in Vermont were the most likely to receive a long-acting opioid, which accounted for 20.14% of all opioid prescriptions in the state, while Kentucky had the lowest share of prescriptions written for long-acting forms at 6.41%. The national average was 11.02%, dropping from 11.79% in 2018 and 12.75% in 2014, the CMS reported.
Medicare beneficiaries in Alabama were more likely to get a prescription for an opioid than in any other state in 2019, based on newly released data.
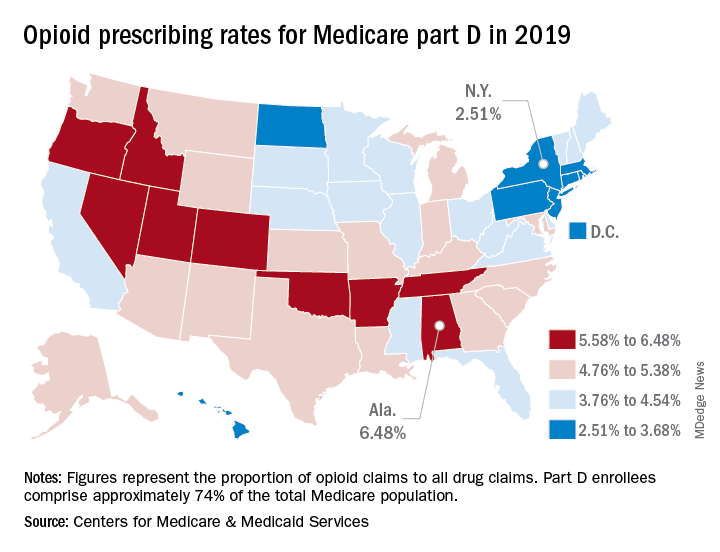
That year, opioids represented 6.48% of all drug claims for part D enrollees in the state, just ahead of Utah at 6.41%. Idaho, at 6.07%, was the only other state with an opioid prescribing rate over 6%, while Oklahoma came in at an even 6.0%, according to the latest update of the Centers for Medicare & Medicaid Services’ dataset.
The lowest rate in 2019 belonged to New York, where 2.51% of drug claims, including original prescriptions and refills, involved an opioid. Rhode Island was next at 2.87%, followed by New Jersey (3.23%), Massachusetts (3.26%), and North Dakota (3.39%),
Altogether, Medicare part D processed 1.5 billion drug claims in 2019, of which 66.1 million, or 4.41%, involved opioids. Both of the opioid numbers were down from 2018, when opioids represented 4.68% (70.2 million) of the 1.5 billion total claims, and from 2014, when opioids were involved in 5.73% (81,026,831) of the 1.41 billion drug claims, the CMS data show. That works out to 5.77% fewer opioids in 2019, compared with 2014, despite the increase in total volume.
from 2014 to 2019, with Hawaii showing the smallest decline as it slipped 0.41 percentage points from 3.9% to 3.49%, according to the CMS.
In 2019, part D beneficiaries in Vermont were the most likely to receive a long-acting opioid, which accounted for 20.14% of all opioid prescriptions in the state, while Kentucky had the lowest share of prescriptions written for long-acting forms at 6.41%. The national average was 11.02%, dropping from 11.79% in 2018 and 12.75% in 2014, the CMS reported.
Medicare beneficiaries in Alabama were more likely to get a prescription for an opioid than in any other state in 2019, based on newly released data.
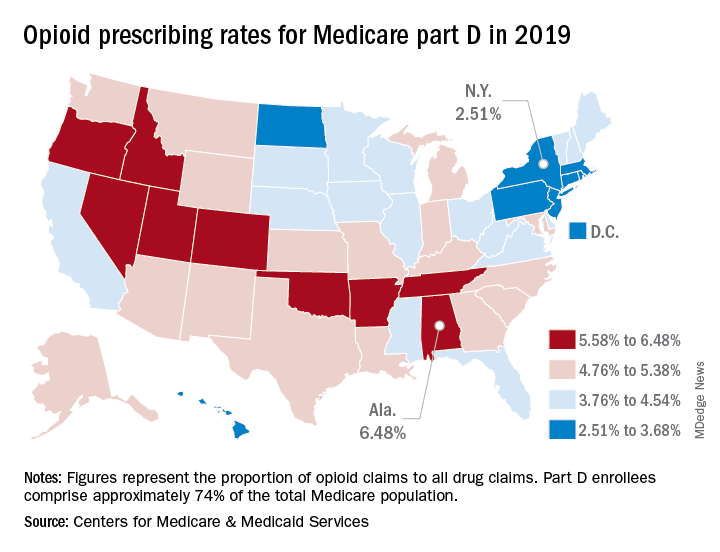
That year, opioids represented 6.48% of all drug claims for part D enrollees in the state, just ahead of Utah at 6.41%. Idaho, at 6.07%, was the only other state with an opioid prescribing rate over 6%, while Oklahoma came in at an even 6.0%, according to the latest update of the Centers for Medicare & Medicaid Services’ dataset.
The lowest rate in 2019 belonged to New York, where 2.51% of drug claims, including original prescriptions and refills, involved an opioid. Rhode Island was next at 2.87%, followed by New Jersey (3.23%), Massachusetts (3.26%), and North Dakota (3.39%),
Altogether, Medicare part D processed 1.5 billion drug claims in 2019, of which 66.1 million, or 4.41%, involved opioids. Both of the opioid numbers were down from 2018, when opioids represented 4.68% (70.2 million) of the 1.5 billion total claims, and from 2014, when opioids were involved in 5.73% (81,026,831) of the 1.41 billion drug claims, the CMS data show. That works out to 5.77% fewer opioids in 2019, compared with 2014, despite the increase in total volume.
from 2014 to 2019, with Hawaii showing the smallest decline as it slipped 0.41 percentage points from 3.9% to 3.49%, according to the CMS.
In 2019, part D beneficiaries in Vermont were the most likely to receive a long-acting opioid, which accounted for 20.14% of all opioid prescriptions in the state, while Kentucky had the lowest share of prescriptions written for long-acting forms at 6.41%. The national average was 11.02%, dropping from 11.79% in 2018 and 12.75% in 2014, the CMS reported.












