User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Psychcast: Nursing home consultations supporting documents
Body Text
Body Text
Body Text
New evidence shows that COVID-19 invades the brain
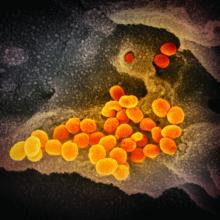
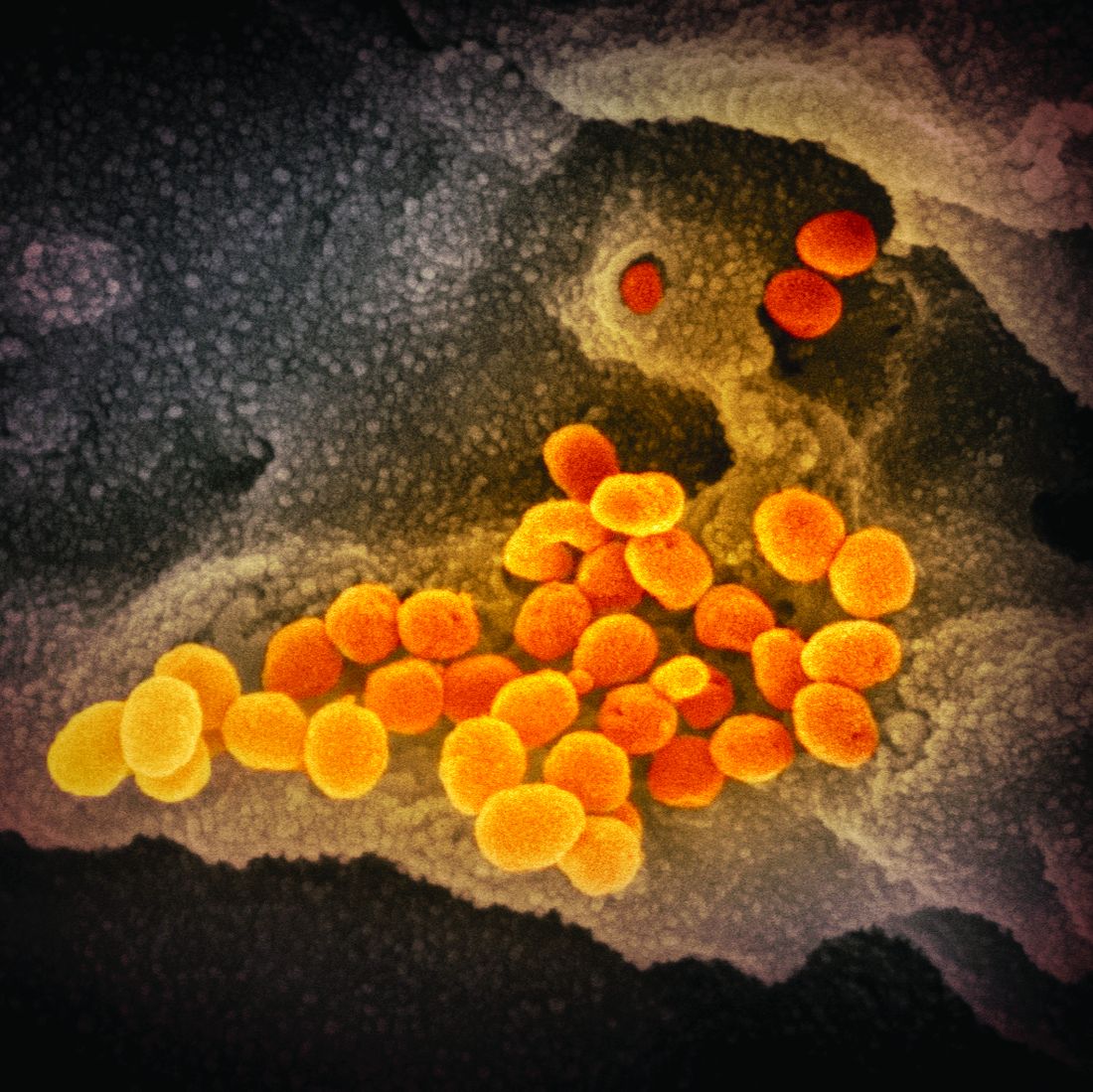
, new animal research suggests. Investigators injected spike 1 (S1), which is found on the tufts of the “red spikes” of the virus, into mice and found that it crossed the blood-brain barrier (BBB) and was taken up not only by brain regions and the brain space but also by other organs – specifically, the lungs, spleen, liver, and kidneys.
“We found that the S1 protein, which is the protein COVID-19 uses to ‘grab onto’ cells, crosses the BBB and is a good model of what the virus does when it enters the brain,” lead author William A. Banks, MD, professor of medicine, University of Washington, Seattle, said in an interview.
“When proteins such as the S1 protein become detached from the virus, they can enter the brain and cause mayhem, causing the brain to release cytokines, which, in turn, cause inflammation and subsequent neurotoxicity,” said Dr. Banks, associate chief of staff and a researcher at the Puget Sound Veterans Affairs Healthcare System.
The study was published online in Nature Neuroscience.
Neurologic symptoms
COVID-19 is associated with a variety of central nervous system symptoms, including the loss of taste and smell, headaches, confusion, stroke, and cerebral hemorrhage, the investigators noted.
Dr. Banks explained that SARS-CoV-2 may enter the brain by crossing the BBB, acting directly on the brain centers responsible for other body functions. The respiratory symptoms of COVID-19 may therefore result partly from the invasion of the areas of the brain responsible for respiratory functions, not only from the virus’ action at the site of the lungs.
The researchers set out to assess whether a particular viral protein – S1, which is a subunit of the viral spike protein – could cross the BBB or enter other organs when injected into mice. They found that, when intravenously injected S1 (I-S1) was cleared from the blood, tissues in multiple organs, including the lung, spleen, kidney, and liver, took it up.
Notably, uptake of I-S1 was higher in the liver, “suggesting that this protein is cleared from the blood predominantly by the liver,” Dr. Banks said. In addition, uptake by the lungs is “important, because that’s where many of the effects of the virus are,” he added.
The researchers found that I-S1 in the brains of the mice was “mostly degraded” 30 minutes following injection. “This indicates that I-S1 enters the BBB intact but is eventually degraded in the brain,” they wrote.
Moreover, by 30 minutes, more than half of the I-S1 proteins had crossed the capillary wall and had fully entered into the brain parenchymal and interstitial fluid spaces, as well as other regions.
More severe outcomes in men
The researchers then induced an inflammatory state in the mice through injection of lipopolysaccharide (LPS) and found that inflammation increased I-S1 uptake in both the brain and the lung (where uptake was increased by 101%). “These results show that inflammation could increase S1 toxicity for lung tissue by increasing its uptake,” the authors suggested. Moreover, inflammation also increased the entry of I-S1 into the brain, “likely due to BBB disruption.”
In human beings, male sex and APOE4 genotype are risk factors for both contracting COVID-19 and having a poor outcome, the authors noted. As a result, they examined I-S1 uptake in male and female mice that expressed human APOE3 or APOE4 (induced by a mouse ApoE promoter).
Multiple-comparison tests showed that among male mice that expressed human APOE3, the “fastest I-S1 uptake” was in the olfactory bulb, liver, and kidney. Female mice displayed increased APOE3 uptake in the spleen.
“This observation might relate to the increased susceptibility of men to more severe COVID-19 outcomes,” coauthor Jacob Raber, PhD, professor, departments of behavioral neuroscience, neurology, and radiation medicine, Oregon Health & Science University, Portland, said in a press release.
In addition to intravenous I-S1 injection, the researchers also investigated the effects of intranasal administration. They found that, although it also entered the brain, it did so at levels roughly 10 times lower than those induced by intravenous administration.
“Frightening tricks”
Dr. Banks said his laboratory has studied the BBB in conditions such as Alzheimer’s disease, obesity, diabetes, and HIV. “Our experience with viruses is that they do an incredible number of things and have a frightening number of tricks,” he said. In this case, “the virus is probably causing inflammation by releasing cytokines elsewhere in the body that get into the brain through the BBB.” Conversely, “the virus itself may enter the brain by crossing the BBB and directly cause brain cells to release their own cytokines,” he added.
An additional finding of the study is that, whatever the S1 protein does in the brain is a model for what the entire virus itself does, because these proteins often bring the viruses along with them, he added.
Dr. Banks said the clinical implications of the findings are that antibodies from those who have already had COVID-19 could potentially be directed against S1. Similarly, he added, so can COVID-19 vaccines, which induce production of S1.
“When an antibody locks onto something, it prevents it from crossing the BBB,” Dr. Banks noted.
Confirmatory findings
Commenting on the study, Howard E. Gendelman, MD, Margaret R. Larson Professor of Internal Medicine and Infectious Diseases and professor and chair of the department of pharmacology and experimental neuroscience, University of Nebraska, Omaha, said the study is confirmatory.
“What this paper highlights, and we have known for a long time, is that COVID-19 is a systemic, not only a respiratory, disease involving many organs and tissues and can yield not only pulmonary problems but also a whole host of cardiac, brain, and kidney problems,” he said.
“So the fact that these proteins are getting in [the brain] and are able to induce a reaction in the brain itself, and this is part of the complex progressive nature of COVID-19, is an important finding,” added Dr. Gendelman, director of the center for neurodegenerative disorders at the university. He was not involved with the study.
The study was supported by the Veterans Affairs Puget Sound Healthcare System and by grants from the National Institutes of Health. The authors and Dr. Gendelman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new animal research suggests. Investigators injected spike 1 (S1), which is found on the tufts of the “red spikes” of the virus, into mice and found that it crossed the blood-brain barrier (BBB) and was taken up not only by brain regions and the brain space but also by other organs – specifically, the lungs, spleen, liver, and kidneys.
“We found that the S1 protein, which is the protein COVID-19 uses to ‘grab onto’ cells, crosses the BBB and is a good model of what the virus does when it enters the brain,” lead author William A. Banks, MD, professor of medicine, University of Washington, Seattle, said in an interview.
“When proteins such as the S1 protein become detached from the virus, they can enter the brain and cause mayhem, causing the brain to release cytokines, which, in turn, cause inflammation and subsequent neurotoxicity,” said Dr. Banks, associate chief of staff and a researcher at the Puget Sound Veterans Affairs Healthcare System.
The study was published online in Nature Neuroscience.
Neurologic symptoms
COVID-19 is associated with a variety of central nervous system symptoms, including the loss of taste and smell, headaches, confusion, stroke, and cerebral hemorrhage, the investigators noted.
Dr. Banks explained that SARS-CoV-2 may enter the brain by crossing the BBB, acting directly on the brain centers responsible for other body functions. The respiratory symptoms of COVID-19 may therefore result partly from the invasion of the areas of the brain responsible for respiratory functions, not only from the virus’ action at the site of the lungs.
The researchers set out to assess whether a particular viral protein – S1, which is a subunit of the viral spike protein – could cross the BBB or enter other organs when injected into mice. They found that, when intravenously injected S1 (I-S1) was cleared from the blood, tissues in multiple organs, including the lung, spleen, kidney, and liver, took it up.
Notably, uptake of I-S1 was higher in the liver, “suggesting that this protein is cleared from the blood predominantly by the liver,” Dr. Banks said. In addition, uptake by the lungs is “important, because that’s where many of the effects of the virus are,” he added.
The researchers found that I-S1 in the brains of the mice was “mostly degraded” 30 minutes following injection. “This indicates that I-S1 enters the BBB intact but is eventually degraded in the brain,” they wrote.
Moreover, by 30 minutes, more than half of the I-S1 proteins had crossed the capillary wall and had fully entered into the brain parenchymal and interstitial fluid spaces, as well as other regions.
More severe outcomes in men
The researchers then induced an inflammatory state in the mice through injection of lipopolysaccharide (LPS) and found that inflammation increased I-S1 uptake in both the brain and the lung (where uptake was increased by 101%). “These results show that inflammation could increase S1 toxicity for lung tissue by increasing its uptake,” the authors suggested. Moreover, inflammation also increased the entry of I-S1 into the brain, “likely due to BBB disruption.”
In human beings, male sex and APOE4 genotype are risk factors for both contracting COVID-19 and having a poor outcome, the authors noted. As a result, they examined I-S1 uptake in male and female mice that expressed human APOE3 or APOE4 (induced by a mouse ApoE promoter).
Multiple-comparison tests showed that among male mice that expressed human APOE3, the “fastest I-S1 uptake” was in the olfactory bulb, liver, and kidney. Female mice displayed increased APOE3 uptake in the spleen.
“This observation might relate to the increased susceptibility of men to more severe COVID-19 outcomes,” coauthor Jacob Raber, PhD, professor, departments of behavioral neuroscience, neurology, and radiation medicine, Oregon Health & Science University, Portland, said in a press release.
In addition to intravenous I-S1 injection, the researchers also investigated the effects of intranasal administration. They found that, although it also entered the brain, it did so at levels roughly 10 times lower than those induced by intravenous administration.
“Frightening tricks”
Dr. Banks said his laboratory has studied the BBB in conditions such as Alzheimer’s disease, obesity, diabetes, and HIV. “Our experience with viruses is that they do an incredible number of things and have a frightening number of tricks,” he said. In this case, “the virus is probably causing inflammation by releasing cytokines elsewhere in the body that get into the brain through the BBB.” Conversely, “the virus itself may enter the brain by crossing the BBB and directly cause brain cells to release their own cytokines,” he added.
An additional finding of the study is that, whatever the S1 protein does in the brain is a model for what the entire virus itself does, because these proteins often bring the viruses along with them, he added.
Dr. Banks said the clinical implications of the findings are that antibodies from those who have already had COVID-19 could potentially be directed against S1. Similarly, he added, so can COVID-19 vaccines, which induce production of S1.
“When an antibody locks onto something, it prevents it from crossing the BBB,” Dr. Banks noted.
Confirmatory findings
Commenting on the study, Howard E. Gendelman, MD, Margaret R. Larson Professor of Internal Medicine and Infectious Diseases and professor and chair of the department of pharmacology and experimental neuroscience, University of Nebraska, Omaha, said the study is confirmatory.
“What this paper highlights, and we have known for a long time, is that COVID-19 is a systemic, not only a respiratory, disease involving many organs and tissues and can yield not only pulmonary problems but also a whole host of cardiac, brain, and kidney problems,” he said.
“So the fact that these proteins are getting in [the brain] and are able to induce a reaction in the brain itself, and this is part of the complex progressive nature of COVID-19, is an important finding,” added Dr. Gendelman, director of the center for neurodegenerative disorders at the university. He was not involved with the study.
The study was supported by the Veterans Affairs Puget Sound Healthcare System and by grants from the National Institutes of Health. The authors and Dr. Gendelman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new animal research suggests. Investigators injected spike 1 (S1), which is found on the tufts of the “red spikes” of the virus, into mice and found that it crossed the blood-brain barrier (BBB) and was taken up not only by brain regions and the brain space but also by other organs – specifically, the lungs, spleen, liver, and kidneys.
“We found that the S1 protein, which is the protein COVID-19 uses to ‘grab onto’ cells, crosses the BBB and is a good model of what the virus does when it enters the brain,” lead author William A. Banks, MD, professor of medicine, University of Washington, Seattle, said in an interview.
“When proteins such as the S1 protein become detached from the virus, they can enter the brain and cause mayhem, causing the brain to release cytokines, which, in turn, cause inflammation and subsequent neurotoxicity,” said Dr. Banks, associate chief of staff and a researcher at the Puget Sound Veterans Affairs Healthcare System.
The study was published online in Nature Neuroscience.
Neurologic symptoms
COVID-19 is associated with a variety of central nervous system symptoms, including the loss of taste and smell, headaches, confusion, stroke, and cerebral hemorrhage, the investigators noted.
Dr. Banks explained that SARS-CoV-2 may enter the brain by crossing the BBB, acting directly on the brain centers responsible for other body functions. The respiratory symptoms of COVID-19 may therefore result partly from the invasion of the areas of the brain responsible for respiratory functions, not only from the virus’ action at the site of the lungs.
The researchers set out to assess whether a particular viral protein – S1, which is a subunit of the viral spike protein – could cross the BBB or enter other organs when injected into mice. They found that, when intravenously injected S1 (I-S1) was cleared from the blood, tissues in multiple organs, including the lung, spleen, kidney, and liver, took it up.
Notably, uptake of I-S1 was higher in the liver, “suggesting that this protein is cleared from the blood predominantly by the liver,” Dr. Banks said. In addition, uptake by the lungs is “important, because that’s where many of the effects of the virus are,” he added.
The researchers found that I-S1 in the brains of the mice was “mostly degraded” 30 minutes following injection. “This indicates that I-S1 enters the BBB intact but is eventually degraded in the brain,” they wrote.
Moreover, by 30 minutes, more than half of the I-S1 proteins had crossed the capillary wall and had fully entered into the brain parenchymal and interstitial fluid spaces, as well as other regions.
More severe outcomes in men
The researchers then induced an inflammatory state in the mice through injection of lipopolysaccharide (LPS) and found that inflammation increased I-S1 uptake in both the brain and the lung (where uptake was increased by 101%). “These results show that inflammation could increase S1 toxicity for lung tissue by increasing its uptake,” the authors suggested. Moreover, inflammation also increased the entry of I-S1 into the brain, “likely due to BBB disruption.”
In human beings, male sex and APOE4 genotype are risk factors for both contracting COVID-19 and having a poor outcome, the authors noted. As a result, they examined I-S1 uptake in male and female mice that expressed human APOE3 or APOE4 (induced by a mouse ApoE promoter).
Multiple-comparison tests showed that among male mice that expressed human APOE3, the “fastest I-S1 uptake” was in the olfactory bulb, liver, and kidney. Female mice displayed increased APOE3 uptake in the spleen.
“This observation might relate to the increased susceptibility of men to more severe COVID-19 outcomes,” coauthor Jacob Raber, PhD, professor, departments of behavioral neuroscience, neurology, and radiation medicine, Oregon Health & Science University, Portland, said in a press release.
In addition to intravenous I-S1 injection, the researchers also investigated the effects of intranasal administration. They found that, although it also entered the brain, it did so at levels roughly 10 times lower than those induced by intravenous administration.
“Frightening tricks”
Dr. Banks said his laboratory has studied the BBB in conditions such as Alzheimer’s disease, obesity, diabetes, and HIV. “Our experience with viruses is that they do an incredible number of things and have a frightening number of tricks,” he said. In this case, “the virus is probably causing inflammation by releasing cytokines elsewhere in the body that get into the brain through the BBB.” Conversely, “the virus itself may enter the brain by crossing the BBB and directly cause brain cells to release their own cytokines,” he added.
An additional finding of the study is that, whatever the S1 protein does in the brain is a model for what the entire virus itself does, because these proteins often bring the viruses along with them, he added.
Dr. Banks said the clinical implications of the findings are that antibodies from those who have already had COVID-19 could potentially be directed against S1. Similarly, he added, so can COVID-19 vaccines, which induce production of S1.
“When an antibody locks onto something, it prevents it from crossing the BBB,” Dr. Banks noted.
Confirmatory findings
Commenting on the study, Howard E. Gendelman, MD, Margaret R. Larson Professor of Internal Medicine and Infectious Diseases and professor and chair of the department of pharmacology and experimental neuroscience, University of Nebraska, Omaha, said the study is confirmatory.
“What this paper highlights, and we have known for a long time, is that COVID-19 is a systemic, not only a respiratory, disease involving many organs and tissues and can yield not only pulmonary problems but also a whole host of cardiac, brain, and kidney problems,” he said.
“So the fact that these proteins are getting in [the brain] and are able to induce a reaction in the brain itself, and this is part of the complex progressive nature of COVID-19, is an important finding,” added Dr. Gendelman, director of the center for neurodegenerative disorders at the university. He was not involved with the study.
The study was supported by the Veterans Affairs Puget Sound Healthcare System and by grants from the National Institutes of Health. The authors and Dr. Gendelman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NATURE NEUROSCIENCE
U.S. hits 20 million cases as COVID variant spreads
The United States started 2021 they way it ended 2020: Setting new records amidst the coronavirus pandemic.
The country passed the 20 million mark for coronavirus cases on Friday, setting the mark sometime around noon, according to Johns Hopkins University’s COVID-19 tracker. The total is nearly twice as many as the next worst country – India, which has 10.28 million cases.
Along with the case count, more than 346,000 Americans have now died of COVID-19, the disease caused by the coronavirus. That is 77% more fatalities than Brazil, which ranks second globally with 194,949 deaths.
More than 125,370 coronavirus patients were hospitalized on Thursday, the fourth record-setting day in a row, according to the COVID Tracking Project.
Going by official tallies, it took 292 days for the United States to reach its first 10 million cases, and just 54 more days to double it, CNN reported.
Meanwhile, 12.41 million doses of COVID-19 vaccines have been distributed in the United States as of Wednesday, according to the Centers for Disease Control and Prevention. Yet only 2.8 million people have received the first of a two-shot regimen.
The slower-than-hoped-for rollout of the Pfizer and Moderna vaccines comes as a new variant of the coronavirus has emerged in a third state. Florida officials announced a confirmed case of the new variant – believed to have originated in the United Kingdom – in Martin County in southeast Florida.
The state health department said on Twitter that the patient is a man in his 20s with no history of travel. The department said it is working with the CDC to investigate.
The variant has also been confirmed in cases in Colorado and California. It is believed to be more contagious. The BBC reported that the new variant increases the reproduction, or “R number,” by 0.4 and 0.7. The UK’s most recent R number has been estimated at 1.1-1.3, meaning anyone who has the coronavirus could be assumed to spread it to up to 1.3 people.
The R number needs to be below 1.0 for the spread of the virus to fall.
“There is a huge difference in how easily the variant virus spreads,” Professor Axel Gandy of London’s Imperial College told BBC News. “This is the most serious change in the virus since the epidemic began.”
A version of this article first appeared on WebMD.com.
The United States started 2021 they way it ended 2020: Setting new records amidst the coronavirus pandemic.
The country passed the 20 million mark for coronavirus cases on Friday, setting the mark sometime around noon, according to Johns Hopkins University’s COVID-19 tracker. The total is nearly twice as many as the next worst country – India, which has 10.28 million cases.
Along with the case count, more than 346,000 Americans have now died of COVID-19, the disease caused by the coronavirus. That is 77% more fatalities than Brazil, which ranks second globally with 194,949 deaths.
More than 125,370 coronavirus patients were hospitalized on Thursday, the fourth record-setting day in a row, according to the COVID Tracking Project.
Going by official tallies, it took 292 days for the United States to reach its first 10 million cases, and just 54 more days to double it, CNN reported.
Meanwhile, 12.41 million doses of COVID-19 vaccines have been distributed in the United States as of Wednesday, according to the Centers for Disease Control and Prevention. Yet only 2.8 million people have received the first of a two-shot regimen.
The slower-than-hoped-for rollout of the Pfizer and Moderna vaccines comes as a new variant of the coronavirus has emerged in a third state. Florida officials announced a confirmed case of the new variant – believed to have originated in the United Kingdom – in Martin County in southeast Florida.
The state health department said on Twitter that the patient is a man in his 20s with no history of travel. The department said it is working with the CDC to investigate.
The variant has also been confirmed in cases in Colorado and California. It is believed to be more contagious. The BBC reported that the new variant increases the reproduction, or “R number,” by 0.4 and 0.7. The UK’s most recent R number has been estimated at 1.1-1.3, meaning anyone who has the coronavirus could be assumed to spread it to up to 1.3 people.
The R number needs to be below 1.0 for the spread of the virus to fall.
“There is a huge difference in how easily the variant virus spreads,” Professor Axel Gandy of London’s Imperial College told BBC News. “This is the most serious change in the virus since the epidemic began.”
A version of this article first appeared on WebMD.com.
The United States started 2021 they way it ended 2020: Setting new records amidst the coronavirus pandemic.
The country passed the 20 million mark for coronavirus cases on Friday, setting the mark sometime around noon, according to Johns Hopkins University’s COVID-19 tracker. The total is nearly twice as many as the next worst country – India, which has 10.28 million cases.
Along with the case count, more than 346,000 Americans have now died of COVID-19, the disease caused by the coronavirus. That is 77% more fatalities than Brazil, which ranks second globally with 194,949 deaths.
More than 125,370 coronavirus patients were hospitalized on Thursday, the fourth record-setting day in a row, according to the COVID Tracking Project.
Going by official tallies, it took 292 days for the United States to reach its first 10 million cases, and just 54 more days to double it, CNN reported.
Meanwhile, 12.41 million doses of COVID-19 vaccines have been distributed in the United States as of Wednesday, according to the Centers for Disease Control and Prevention. Yet only 2.8 million people have received the first of a two-shot regimen.
The slower-than-hoped-for rollout of the Pfizer and Moderna vaccines comes as a new variant of the coronavirus has emerged in a third state. Florida officials announced a confirmed case of the new variant – believed to have originated in the United Kingdom – in Martin County in southeast Florida.
The state health department said on Twitter that the patient is a man in his 20s with no history of travel. The department said it is working with the CDC to investigate.
The variant has also been confirmed in cases in Colorado and California. It is believed to be more contagious. The BBC reported that the new variant increases the reproduction, or “R number,” by 0.4 and 0.7. The UK’s most recent R number has been estimated at 1.1-1.3, meaning anyone who has the coronavirus could be assumed to spread it to up to 1.3 people.
The R number needs to be below 1.0 for the spread of the virus to fall.
“There is a huge difference in how easily the variant virus spreads,” Professor Axel Gandy of London’s Imperial College told BBC News. “This is the most serious change in the virus since the epidemic began.”
A version of this article first appeared on WebMD.com.
Medicaid to cover routine costs for patients in trials
A boost for patients with cancer and other serious illnesses.
Congress has ordered the holdouts among U.S. states to have their Medicaid programs cover expenses related to participation in certain clinical trials, a move that was hailed by the American Society of Clinical Oncology and other groups as a boost to trials as well as to patients with serious illness who have lower incomes.
A massive wrap-up spending/COVID-19 relief bill that was signed into law Dec. 27 carried with it a mandate on Medicaid. States are ordered to put in place Medicaid payment policies for routine items and services, such as the cost of physician visits or laboratory tests, that are provided in connection with participation in clinical trials for serious and life-threatening conditions. The law includes a January 2022 target date for this coverage through Medicaid.
Medicare and other large insurers already pick up the tab for these kinds of expenses, leaving Medicaid as an outlier, ASCO noted in a press statement. ASCO and other cancer groups have for years pressed Medicaid to cover routine expenses for people participating in clinical trials. Already, 15 states, including California, require their Medicaid programs to cover these expenses, according to ASCO.
“We believe that the trials can bring extra benefits to patients,” said Monica M. Bertagnolli, MD, of Dana-Farber Cancer Institute, Boston. Dr. Bertagnolli has worked for years to secure Medicaid coverage for expenses connected to clinical trials.
Although Medicaid covers costs of standard care for cancer patients, people enrolled in the program may have concerns about participating in clinical studies, said Dr. Bertagnolli, chair of the Association for Clinical Oncology, which was established by ASCO to promote wider access to cancer care. Having extra medical expenses may be more than these patients can tolerate.
“Many of them just say, ‘I can’t take that financial risk, so I’ll just stay with standard of care,’ “ Dr. Bertagnolli said in an interview.
Equity issues
Medicaid has expanded greatly, owing to financial aid provided to states through the Affordable Care Act of 2010.
To date, 38 of 50 U.S. states have accepted federal aid to lift income limits for Medicaid eligibility, according to a tally kept by the nonprofit Kaiser Family Foundation. This Medicaid expansion has given more of the nation’s working poor access to health.care, including cancer treatment. Between 2013 and January 2020, enrollment in Medicaid in expansion states increased by about 12.4 million, according to the Medicaid and CHIP Payment and Access Commission.
Medicaid is the nation’s dominant health insurer. Enrollment has been around 70 million in recent months.
That tops the 61 million enrolled in Medicare, the federal program for people aged 65 and older and those with disabilities. (There’s some overlap between Medicare and Medicaid. About 12.8 million persons were dually eligible for these programs in 2018.) UnitedHealth, a giant private insurer, has about 43 million domestic customers.
Medicaid also serves many of the groups of people for which researchers have been seeking to increase participation in clinical trials. ASCO’s Association for Clinical Oncology and dozens of its partners raised this point in a letter to congressional leaders on Feb. 15, 2020.
“Lack of participation in clinical trials from the Medicaid population means these patients are being excluded from potentially life-saving trials and are not reflected in the outcome of the clinical research,” the groups wrote. “Increased access to clinical trial participation for Medicaid enrollees helps ensure medical research results more accurately capture and reflect the populations of this country.”
The ACA’s Medicaid expansion is working to address some of the racial gaps in insurance coverage, according to a January 2020 report from the nonprofit Commonwealth Fund.
Black and Hispanic adults are almost twice as likely as are White adults to have incomes that are less than 200% of the federal poverty level, according to the Commonwealth Fund report. The report also said that people in these groups reported significantly higher rates of cost-related problems in receiving care before the Medicaid expansion began in 2014.
The uninsured rate for Black adults dropped from 24.4% in 2013 to 14.4% in 2018; the rate for Hispanic adults fell from 40.2% to 24.9%, according to the Commonwealth Fund report.
There are concerns, though, about attempts by some governors to impose onerous restrictions on adults enrolled in Medicaid, Dr. Bertagnolli said. She was president of ASCO in 2018 when the group called on the Centers for Medicare & Medicaid Services to reject state requests to create restrictions that could hinder people’s access to cancer screening or care.
The Trump administration encouraged governors to adopt work requirements. As a result, a dozen states approved these policies, according to a November report from the nonprofit Center on Budget and Policy Priorities. The efforts were blocked by courts.
Data from the limited period of implementation in Arkansas, Michigan, and New Hampshire provide evidence that these kinds of requirements don’t work as intended, according to the CBPP report.
“In all three states, evidence suggests that people who were working and people with serious health needs who should have been eligible for exemptions lost coverage or were at risk of losing coverage due to red tape,” CBPP analysts Jennifer Wagner and Jessica Schubel wrote in their report.
In 2019, The New England Journal of Medicine published an article about the early stages of the Arkansas experiment with Medicaid work rules. Almost 17,000 adults lost their health care coverage in the initial months of implementation, but there appeared to be no significant difference in employment, Benjamin Sommers, MD, PhD, of the Harvard School of Public Health, Boston, and colleagues wrote in their article.
For many people in Arkansas, coverage was lost because of difficulties in reporting compliance with the Medicaid work rule, not because of the employment mandate itself, according to the authors. More than 95% of persons who were targeted by Arkansas’ Medicaid work policy already met its requirements or should have been exempt, they wrote.
Democrats have tended to oppose efforts to attach work requirements, which can include volunteer activities or career training, to Medicaid. Dr. Bertagnolli said there is a need to guard against any future bid to add work requirements to the program.
Extra bureaucratic hurdles may pose an especially tough burden on working adults enrolled in Medicaid, she said.
People who qualify for the program may already be worried about their finances while juggling continued demands of child care and employment, she said. They don’t need to be put at risk of losing access to medical care over administrative rules while undergoing cancer treatment, she said.
“We have to take care of people who are sick. That’s just the way it is,” Dr. Bertagnolli said.
A version of this article first appeared on Medscape.com.
A boost for patients with cancer and other serious illnesses.
A boost for patients with cancer and other serious illnesses.
Congress has ordered the holdouts among U.S. states to have their Medicaid programs cover expenses related to participation in certain clinical trials, a move that was hailed by the American Society of Clinical Oncology and other groups as a boost to trials as well as to patients with serious illness who have lower incomes.
A massive wrap-up spending/COVID-19 relief bill that was signed into law Dec. 27 carried with it a mandate on Medicaid. States are ordered to put in place Medicaid payment policies for routine items and services, such as the cost of physician visits or laboratory tests, that are provided in connection with participation in clinical trials for serious and life-threatening conditions. The law includes a January 2022 target date for this coverage through Medicaid.
Medicare and other large insurers already pick up the tab for these kinds of expenses, leaving Medicaid as an outlier, ASCO noted in a press statement. ASCO and other cancer groups have for years pressed Medicaid to cover routine expenses for people participating in clinical trials. Already, 15 states, including California, require their Medicaid programs to cover these expenses, according to ASCO.
“We believe that the trials can bring extra benefits to patients,” said Monica M. Bertagnolli, MD, of Dana-Farber Cancer Institute, Boston. Dr. Bertagnolli has worked for years to secure Medicaid coverage for expenses connected to clinical trials.
Although Medicaid covers costs of standard care for cancer patients, people enrolled in the program may have concerns about participating in clinical studies, said Dr. Bertagnolli, chair of the Association for Clinical Oncology, which was established by ASCO to promote wider access to cancer care. Having extra medical expenses may be more than these patients can tolerate.
“Many of them just say, ‘I can’t take that financial risk, so I’ll just stay with standard of care,’ “ Dr. Bertagnolli said in an interview.
Equity issues
Medicaid has expanded greatly, owing to financial aid provided to states through the Affordable Care Act of 2010.
To date, 38 of 50 U.S. states have accepted federal aid to lift income limits for Medicaid eligibility, according to a tally kept by the nonprofit Kaiser Family Foundation. This Medicaid expansion has given more of the nation’s working poor access to health.care, including cancer treatment. Between 2013 and January 2020, enrollment in Medicaid in expansion states increased by about 12.4 million, according to the Medicaid and CHIP Payment and Access Commission.
Medicaid is the nation’s dominant health insurer. Enrollment has been around 70 million in recent months.
That tops the 61 million enrolled in Medicare, the federal program for people aged 65 and older and those with disabilities. (There’s some overlap between Medicare and Medicaid. About 12.8 million persons were dually eligible for these programs in 2018.) UnitedHealth, a giant private insurer, has about 43 million domestic customers.
Medicaid also serves many of the groups of people for which researchers have been seeking to increase participation in clinical trials. ASCO’s Association for Clinical Oncology and dozens of its partners raised this point in a letter to congressional leaders on Feb. 15, 2020.
“Lack of participation in clinical trials from the Medicaid population means these patients are being excluded from potentially life-saving trials and are not reflected in the outcome of the clinical research,” the groups wrote. “Increased access to clinical trial participation for Medicaid enrollees helps ensure medical research results more accurately capture and reflect the populations of this country.”
The ACA’s Medicaid expansion is working to address some of the racial gaps in insurance coverage, according to a January 2020 report from the nonprofit Commonwealth Fund.
Black and Hispanic adults are almost twice as likely as are White adults to have incomes that are less than 200% of the federal poverty level, according to the Commonwealth Fund report. The report also said that people in these groups reported significantly higher rates of cost-related problems in receiving care before the Medicaid expansion began in 2014.
The uninsured rate for Black adults dropped from 24.4% in 2013 to 14.4% in 2018; the rate for Hispanic adults fell from 40.2% to 24.9%, according to the Commonwealth Fund report.
There are concerns, though, about attempts by some governors to impose onerous restrictions on adults enrolled in Medicaid, Dr. Bertagnolli said. She was president of ASCO in 2018 when the group called on the Centers for Medicare & Medicaid Services to reject state requests to create restrictions that could hinder people’s access to cancer screening or care.
The Trump administration encouraged governors to adopt work requirements. As a result, a dozen states approved these policies, according to a November report from the nonprofit Center on Budget and Policy Priorities. The efforts were blocked by courts.
Data from the limited period of implementation in Arkansas, Michigan, and New Hampshire provide evidence that these kinds of requirements don’t work as intended, according to the CBPP report.
“In all three states, evidence suggests that people who were working and people with serious health needs who should have been eligible for exemptions lost coverage or were at risk of losing coverage due to red tape,” CBPP analysts Jennifer Wagner and Jessica Schubel wrote in their report.
In 2019, The New England Journal of Medicine published an article about the early stages of the Arkansas experiment with Medicaid work rules. Almost 17,000 adults lost their health care coverage in the initial months of implementation, but there appeared to be no significant difference in employment, Benjamin Sommers, MD, PhD, of the Harvard School of Public Health, Boston, and colleagues wrote in their article.
For many people in Arkansas, coverage was lost because of difficulties in reporting compliance with the Medicaid work rule, not because of the employment mandate itself, according to the authors. More than 95% of persons who were targeted by Arkansas’ Medicaid work policy already met its requirements or should have been exempt, they wrote.
Democrats have tended to oppose efforts to attach work requirements, which can include volunteer activities or career training, to Medicaid. Dr. Bertagnolli said there is a need to guard against any future bid to add work requirements to the program.
Extra bureaucratic hurdles may pose an especially tough burden on working adults enrolled in Medicaid, she said.
People who qualify for the program may already be worried about their finances while juggling continued demands of child care and employment, she said. They don’t need to be put at risk of losing access to medical care over administrative rules while undergoing cancer treatment, she said.
“We have to take care of people who are sick. That’s just the way it is,” Dr. Bertagnolli said.
A version of this article first appeared on Medscape.com.
Congress has ordered the holdouts among U.S. states to have their Medicaid programs cover expenses related to participation in certain clinical trials, a move that was hailed by the American Society of Clinical Oncology and other groups as a boost to trials as well as to patients with serious illness who have lower incomes.
A massive wrap-up spending/COVID-19 relief bill that was signed into law Dec. 27 carried with it a mandate on Medicaid. States are ordered to put in place Medicaid payment policies for routine items and services, such as the cost of physician visits or laboratory tests, that are provided in connection with participation in clinical trials for serious and life-threatening conditions. The law includes a January 2022 target date for this coverage through Medicaid.
Medicare and other large insurers already pick up the tab for these kinds of expenses, leaving Medicaid as an outlier, ASCO noted in a press statement. ASCO and other cancer groups have for years pressed Medicaid to cover routine expenses for people participating in clinical trials. Already, 15 states, including California, require their Medicaid programs to cover these expenses, according to ASCO.
“We believe that the trials can bring extra benefits to patients,” said Monica M. Bertagnolli, MD, of Dana-Farber Cancer Institute, Boston. Dr. Bertagnolli has worked for years to secure Medicaid coverage for expenses connected to clinical trials.
Although Medicaid covers costs of standard care for cancer patients, people enrolled in the program may have concerns about participating in clinical studies, said Dr. Bertagnolli, chair of the Association for Clinical Oncology, which was established by ASCO to promote wider access to cancer care. Having extra medical expenses may be more than these patients can tolerate.
“Many of them just say, ‘I can’t take that financial risk, so I’ll just stay with standard of care,’ “ Dr. Bertagnolli said in an interview.
Equity issues
Medicaid has expanded greatly, owing to financial aid provided to states through the Affordable Care Act of 2010.
To date, 38 of 50 U.S. states have accepted federal aid to lift income limits for Medicaid eligibility, according to a tally kept by the nonprofit Kaiser Family Foundation. This Medicaid expansion has given more of the nation’s working poor access to health.care, including cancer treatment. Between 2013 and January 2020, enrollment in Medicaid in expansion states increased by about 12.4 million, according to the Medicaid and CHIP Payment and Access Commission.
Medicaid is the nation’s dominant health insurer. Enrollment has been around 70 million in recent months.
That tops the 61 million enrolled in Medicare, the federal program for people aged 65 and older and those with disabilities. (There’s some overlap between Medicare and Medicaid. About 12.8 million persons were dually eligible for these programs in 2018.) UnitedHealth, a giant private insurer, has about 43 million domestic customers.
Medicaid also serves many of the groups of people for which researchers have been seeking to increase participation in clinical trials. ASCO’s Association for Clinical Oncology and dozens of its partners raised this point in a letter to congressional leaders on Feb. 15, 2020.
“Lack of participation in clinical trials from the Medicaid population means these patients are being excluded from potentially life-saving trials and are not reflected in the outcome of the clinical research,” the groups wrote. “Increased access to clinical trial participation for Medicaid enrollees helps ensure medical research results more accurately capture and reflect the populations of this country.”
The ACA’s Medicaid expansion is working to address some of the racial gaps in insurance coverage, according to a January 2020 report from the nonprofit Commonwealth Fund.
Black and Hispanic adults are almost twice as likely as are White adults to have incomes that are less than 200% of the federal poverty level, according to the Commonwealth Fund report. The report also said that people in these groups reported significantly higher rates of cost-related problems in receiving care before the Medicaid expansion began in 2014.
The uninsured rate for Black adults dropped from 24.4% in 2013 to 14.4% in 2018; the rate for Hispanic adults fell from 40.2% to 24.9%, according to the Commonwealth Fund report.
There are concerns, though, about attempts by some governors to impose onerous restrictions on adults enrolled in Medicaid, Dr. Bertagnolli said. She was president of ASCO in 2018 when the group called on the Centers for Medicare & Medicaid Services to reject state requests to create restrictions that could hinder people’s access to cancer screening or care.
The Trump administration encouraged governors to adopt work requirements. As a result, a dozen states approved these policies, according to a November report from the nonprofit Center on Budget and Policy Priorities. The efforts were blocked by courts.
Data from the limited period of implementation in Arkansas, Michigan, and New Hampshire provide evidence that these kinds of requirements don’t work as intended, according to the CBPP report.
“In all three states, evidence suggests that people who were working and people with serious health needs who should have been eligible for exemptions lost coverage or were at risk of losing coverage due to red tape,” CBPP analysts Jennifer Wagner and Jessica Schubel wrote in their report.
In 2019, The New England Journal of Medicine published an article about the early stages of the Arkansas experiment with Medicaid work rules. Almost 17,000 adults lost their health care coverage in the initial months of implementation, but there appeared to be no significant difference in employment, Benjamin Sommers, MD, PhD, of the Harvard School of Public Health, Boston, and colleagues wrote in their article.
For many people in Arkansas, coverage was lost because of difficulties in reporting compliance with the Medicaid work rule, not because of the employment mandate itself, according to the authors. More than 95% of persons who were targeted by Arkansas’ Medicaid work policy already met its requirements or should have been exempt, they wrote.
Democrats have tended to oppose efforts to attach work requirements, which can include volunteer activities or career training, to Medicaid. Dr. Bertagnolli said there is a need to guard against any future bid to add work requirements to the program.
Extra bureaucratic hurdles may pose an especially tough burden on working adults enrolled in Medicaid, she said.
People who qualify for the program may already be worried about their finances while juggling continued demands of child care and employment, she said. They don’t need to be put at risk of losing access to medical care over administrative rules while undergoing cancer treatment, she said.
“We have to take care of people who are sick. That’s just the way it is,” Dr. Bertagnolli said.
A version of this article first appeared on Medscape.com.
Collective trauma could lead to posttraumatic growth
Reflections for 2021
When we went to medical school, how many of us thought we would practice through a pandemic? For most of us, 2020 was the most challenging professional year of our lives. As a psychiatrist, I found it particularly odd to be struggling with the same issues as all of my patients and to have all my patients in crisis at the same time. I was repeatedly asked by friends, “How are your patients doing?” My reply, “About the same as the rest of us.” After a period of adapting, I felt truly blessed to be able to practice online. I know many of my colleagues did not have that luxury, and the stress you endured is hard to fathom.
Yet, as Friedrich Nietzsche said in so many words, “What doesn’t kill you, makes you stronger,” and here we are in a new year. As we enter 2021, we know so much more about COVID-19 than we did mere months ago, and many of us have been fortunate enough to be vaccinated already.
We should be very proud of our medical and scientific community, which has worked so hard to prevent and treat COVID-19. It is indeed a miracle of modern medicine that two vaccines made their way through development to distribution in under a year. It is a great relief that health care workers are first in line: Of the 4 million vaccine doses given worldwide, 2 million were to U.S. medical personnel. We can now track the number of people vaccinated around the globe.
Yet, “the darkest hour is just before the dawn.” We are currently in the riskiest part of the pandemic, and we must continue to work hard.
As 2021 progresses, we can expect to begin the long recovery process. We know we are innately wired to adapt to adversity and are therefore resilient. The key is to tap into this wiring by developing behaviors, habits, and strategies that support us.
Posttraumatic growth (PTG) is a theory in mental health that explains a kind of transformation following trauma. It was developed by psychologists Richard Tedeschi, PhD, and Lawrence Calhoun, PhD, in the mid-1990s. They studied how people experienced positive growth following adversity. Dr. Tedeschi has said: “People develop new understandings of themselves, the world they live in, how to relate to other people, the kind of future they might have and a better understanding of how to live life.” One-half to two-thirds of individuals experiencing trauma will experience PTG. Given that our entire profession has gone through this collective trauma, far better times may indeed be ahead.
Resilience expert Eva Selhub, MD, suggests cultivating these six pillars:
- Physical vitality: The toll of 2020 has been enormous. If we are to rebound, we must care for ourselves. In our training, we were taught to put our health aside and work grueling hours. But to recover from trauma, we must attend to our own needs. Even after we are vaccinated, we must keep our nutritional status and immunity functioning at optimal levels. Let’s not get COVID-19 complacency. Clearly, health matters most. Ours included!
- Mental toughness: We made it through an incredibly grueling year, and we had to “build it as we sailed.” We figured out how to save as many lives as we could and simultaneously keep ourselves and our families safe. We have seen things previously unimaginable. We have adjusted to telemedicine. We have lived with far fewer pleasures. We have cultivated multiple ways to tame our anxieties. The year 2020 is one we can be proud of for ourselves and our colleagues. We have come a long way in a short time.
- Emotional balance: Anxiety and depression were easy to fall into in 2020. But as the pandemic subsides, the pendulum will swing the other way. The 1918 pandemic gave rise to the Roaring Twenties. What will the next chapter in our civilization bring?
- Loving and strong connections. Our relationships are what give depth and meaning to our lives, and these relationships are crucial now so we can heal. How can we nourish our connections? What toll has the pandemic taken on those closest to you? Did some friends or family step up and help? Can we move out of our caretaker role and allow others to care for us?
- Spiritual connection: Facing so much grief and suffering, we have had an opportunity to look at our own lives from a different perspective. It has been an important year for reflection. How can we cultivate a deeper appreciation recognizing that every day is truly a gift? Did you find more purpose in your work last year? What sustained you in your time of need?
- Inspiring leadership: As health care professionals, we must set an example. We must show our patients and our families how resilient we can be. Let’s grow from trauma and avoid succumbing to depression, self-destructive tendencies, and divisiveness. We must continue to care for ourselves, our patients, and our community and work together to ensure a brighter and safer future for all.
Wishing you a safe, happy and healthy 2021.
“I am not what happened to me, I am what I choose to become.”
– Carl Jung, PhD
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Mimosa Publishing, 2018). She has no conflicts of interest.
Reflections for 2021
Reflections for 2021
When we went to medical school, how many of us thought we would practice through a pandemic? For most of us, 2020 was the most challenging professional year of our lives. As a psychiatrist, I found it particularly odd to be struggling with the same issues as all of my patients and to have all my patients in crisis at the same time. I was repeatedly asked by friends, “How are your patients doing?” My reply, “About the same as the rest of us.” After a period of adapting, I felt truly blessed to be able to practice online. I know many of my colleagues did not have that luxury, and the stress you endured is hard to fathom.
Yet, as Friedrich Nietzsche said in so many words, “What doesn’t kill you, makes you stronger,” and here we are in a new year. As we enter 2021, we know so much more about COVID-19 than we did mere months ago, and many of us have been fortunate enough to be vaccinated already.
We should be very proud of our medical and scientific community, which has worked so hard to prevent and treat COVID-19. It is indeed a miracle of modern medicine that two vaccines made their way through development to distribution in under a year. It is a great relief that health care workers are first in line: Of the 4 million vaccine doses given worldwide, 2 million were to U.S. medical personnel. We can now track the number of people vaccinated around the globe.
Yet, “the darkest hour is just before the dawn.” We are currently in the riskiest part of the pandemic, and we must continue to work hard.
As 2021 progresses, we can expect to begin the long recovery process. We know we are innately wired to adapt to adversity and are therefore resilient. The key is to tap into this wiring by developing behaviors, habits, and strategies that support us.
Posttraumatic growth (PTG) is a theory in mental health that explains a kind of transformation following trauma. It was developed by psychologists Richard Tedeschi, PhD, and Lawrence Calhoun, PhD, in the mid-1990s. They studied how people experienced positive growth following adversity. Dr. Tedeschi has said: “People develop new understandings of themselves, the world they live in, how to relate to other people, the kind of future they might have and a better understanding of how to live life.” One-half to two-thirds of individuals experiencing trauma will experience PTG. Given that our entire profession has gone through this collective trauma, far better times may indeed be ahead.
Resilience expert Eva Selhub, MD, suggests cultivating these six pillars:
- Physical vitality: The toll of 2020 has been enormous. If we are to rebound, we must care for ourselves. In our training, we were taught to put our health aside and work grueling hours. But to recover from trauma, we must attend to our own needs. Even after we are vaccinated, we must keep our nutritional status and immunity functioning at optimal levels. Let’s not get COVID-19 complacency. Clearly, health matters most. Ours included!
- Mental toughness: We made it through an incredibly grueling year, and we had to “build it as we sailed.” We figured out how to save as many lives as we could and simultaneously keep ourselves and our families safe. We have seen things previously unimaginable. We have adjusted to telemedicine. We have lived with far fewer pleasures. We have cultivated multiple ways to tame our anxieties. The year 2020 is one we can be proud of for ourselves and our colleagues. We have come a long way in a short time.
- Emotional balance: Anxiety and depression were easy to fall into in 2020. But as the pandemic subsides, the pendulum will swing the other way. The 1918 pandemic gave rise to the Roaring Twenties. What will the next chapter in our civilization bring?
- Loving and strong connections. Our relationships are what give depth and meaning to our lives, and these relationships are crucial now so we can heal. How can we nourish our connections? What toll has the pandemic taken on those closest to you? Did some friends or family step up and help? Can we move out of our caretaker role and allow others to care for us?
- Spiritual connection: Facing so much grief and suffering, we have had an opportunity to look at our own lives from a different perspective. It has been an important year for reflection. How can we cultivate a deeper appreciation recognizing that every day is truly a gift? Did you find more purpose in your work last year? What sustained you in your time of need?
- Inspiring leadership: As health care professionals, we must set an example. We must show our patients and our families how resilient we can be. Let’s grow from trauma and avoid succumbing to depression, self-destructive tendencies, and divisiveness. We must continue to care for ourselves, our patients, and our community and work together to ensure a brighter and safer future for all.
Wishing you a safe, happy and healthy 2021.
“I am not what happened to me, I am what I choose to become.”
– Carl Jung, PhD
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Mimosa Publishing, 2018). She has no conflicts of interest.
When we went to medical school, how many of us thought we would practice through a pandemic? For most of us, 2020 was the most challenging professional year of our lives. As a psychiatrist, I found it particularly odd to be struggling with the same issues as all of my patients and to have all my patients in crisis at the same time. I was repeatedly asked by friends, “How are your patients doing?” My reply, “About the same as the rest of us.” After a period of adapting, I felt truly blessed to be able to practice online. I know many of my colleagues did not have that luxury, and the stress you endured is hard to fathom.
Yet, as Friedrich Nietzsche said in so many words, “What doesn’t kill you, makes you stronger,” and here we are in a new year. As we enter 2021, we know so much more about COVID-19 than we did mere months ago, and many of us have been fortunate enough to be vaccinated already.
We should be very proud of our medical and scientific community, which has worked so hard to prevent and treat COVID-19. It is indeed a miracle of modern medicine that two vaccines made their way through development to distribution in under a year. It is a great relief that health care workers are first in line: Of the 4 million vaccine doses given worldwide, 2 million were to U.S. medical personnel. We can now track the number of people vaccinated around the globe.
Yet, “the darkest hour is just before the dawn.” We are currently in the riskiest part of the pandemic, and we must continue to work hard.
As 2021 progresses, we can expect to begin the long recovery process. We know we are innately wired to adapt to adversity and are therefore resilient. The key is to tap into this wiring by developing behaviors, habits, and strategies that support us.
Posttraumatic growth (PTG) is a theory in mental health that explains a kind of transformation following trauma. It was developed by psychologists Richard Tedeschi, PhD, and Lawrence Calhoun, PhD, in the mid-1990s. They studied how people experienced positive growth following adversity. Dr. Tedeschi has said: “People develop new understandings of themselves, the world they live in, how to relate to other people, the kind of future they might have and a better understanding of how to live life.” One-half to two-thirds of individuals experiencing trauma will experience PTG. Given that our entire profession has gone through this collective trauma, far better times may indeed be ahead.
Resilience expert Eva Selhub, MD, suggests cultivating these six pillars:
- Physical vitality: The toll of 2020 has been enormous. If we are to rebound, we must care for ourselves. In our training, we were taught to put our health aside and work grueling hours. But to recover from trauma, we must attend to our own needs. Even after we are vaccinated, we must keep our nutritional status and immunity functioning at optimal levels. Let’s not get COVID-19 complacency. Clearly, health matters most. Ours included!
- Mental toughness: We made it through an incredibly grueling year, and we had to “build it as we sailed.” We figured out how to save as many lives as we could and simultaneously keep ourselves and our families safe. We have seen things previously unimaginable. We have adjusted to telemedicine. We have lived with far fewer pleasures. We have cultivated multiple ways to tame our anxieties. The year 2020 is one we can be proud of for ourselves and our colleagues. We have come a long way in a short time.
- Emotional balance: Anxiety and depression were easy to fall into in 2020. But as the pandemic subsides, the pendulum will swing the other way. The 1918 pandemic gave rise to the Roaring Twenties. What will the next chapter in our civilization bring?
- Loving and strong connections. Our relationships are what give depth and meaning to our lives, and these relationships are crucial now so we can heal. How can we nourish our connections? What toll has the pandemic taken on those closest to you? Did some friends or family step up and help? Can we move out of our caretaker role and allow others to care for us?
- Spiritual connection: Facing so much grief and suffering, we have had an opportunity to look at our own lives from a different perspective. It has been an important year for reflection. How can we cultivate a deeper appreciation recognizing that every day is truly a gift? Did you find more purpose in your work last year? What sustained you in your time of need?
- Inspiring leadership: As health care professionals, we must set an example. We must show our patients and our families how resilient we can be. Let’s grow from trauma and avoid succumbing to depression, self-destructive tendencies, and divisiveness. We must continue to care for ourselves, our patients, and our community and work together to ensure a brighter and safer future for all.
Wishing you a safe, happy and healthy 2021.
“I am not what happened to me, I am what I choose to become.”
– Carl Jung, PhD
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Mimosa Publishing, 2018). She has no conflicts of interest.
Zoom Zoom Zoom: An end-of-year update from a virtual psychiatrist
In mid-April, a month into pandemic life with a stay-at-home order, I wrote about my experiences as a virtual outpatient psychiatrist in private practice. It’s been 10 months now and with this tragic year drawing to a close, it seems like a good time for an update.
In that April column, I describe how I created a makeshift home office. This entailed pushing my son’s baseball card collection and dusty sports trophies to the side of the room, bringing in a desk and a rug, a house plant, and a statue of a Buddha. I enjoyed watching out the window behind my computer screen as the neighbors and their dogs walked by, and I loved seeing the tree out the window blossom into gorgeous flowers.
With time, my physical space has changed. The remnants of my son’s childhood have all been moved to a closet, artwork has been added to the wall behind me, and the space is now clearly an office, though my laptop remains propped on a pile of books so that no one is looking up my nose. The room, with four large windows facing north and west, has issues with temperature control. In an old house, the heat works all too well in the adjacent bedroom (while the rest of the occupants in other rooms freeze), but the office itself has no heat: I have added both a fan and a space heater, and there are some very cold days where I’ve propped open one of the windows. And with the shortened days, large windows on two walls have presented a challenge as the sun changes positions throughout the day – there are times when the sun’s rays streak across my face in such a way that I look rather ethereal, and between sessions I have lowered, raised, and adjusted the blinds to avoid this. I finally pulled off the thin metal venetian blinds and took them to Lowe’s, where a partially masked young woman cut me new blinds with larger slats. An ergonomic office chair has replaced the wicker Ikea chair I was using, and between all these machinations, I am now physically comfortable most of the time. I believe I am still a bit too pixelated on the screen, but my patients are not complaining, and when the natural lighting fades at 4:30 p.m., the overhead lighting is all wrong again. These all are things I never considered – or long ago addressed – in my real-life practice of psychiatry in a office I have loved for years.
With time, I’ve grown more comfortable working from home on a screen and there are things about this life I’ve grown to like. My husband no longer travels, my daughter – my gift of the pandemic – returned home from New York City where she was in her final months of graduate school, and these unexpected months with her (and her cat) have been a pleasure. There is something nice about being trapped at home with people I love, even if we are all in our respective places, in front of our separate screens. There has been time for long walks, trips to the beach, and long bike rides. And as my daughter now prepares to move to Denver, I have been heartened by the hope of vaccines, and the knowledge that I will likely be able to see her again in the coming months. The people are not the only ones who have benefited from this time at home together – I have no idea how we would have managed with our elderly dog if we were not home to care for him.
My life has become more efficient. I used to find myself aggravated when patients forgot their appointments, a not-infrequent occurrence. People no longer get caught in traffic, they come on time, and they don’t complain about my crowded parking lot. When there is down time, I use it more efficiently at home – a load of laundry gets done, I get a chance to turn on the news or exercise, or make dinner early. And because I have two other family members working from home, I am not the only one mixing work with chores or exercise.
While my medical colleagues who work in settings where they must see patients in person have struggled or functioned in some state of denial, I have felt safe and protected, a bit cocooned with my family in a house big enough to give us all space, in a neighborhood with sidewalks and places to walk, and to protect my sanity, I am lucky to have a patio that has now been equipped with lights, patio heaters, a fire pit, and socially distanced tables so that I can still see friends outside.
Telemedicine has added a new dimension to treatment. I’ve had family sessions with multiple people joining a zoom link from different locations – so much easier than coordinating a time when everyone can travel to my office. I’ve had patients call in from cars and from closets in search of privacy, and from their gardens and poolsides. I’ve met spouses, children, many a dog and cat, plus the more unusual of pets and farm animals, including a goat, ferret, lizard, African grey parrot, and guinea pigs.
These are the good things, and while I wish I could say it was all good, so much of what remains is laden with anxiety. My son lives nearby, but he has shared a house with a hospital worker for much of the past year and there were COVID scares, months at a time without so much as a hug, and my husband has not seen his parents or brother for a year now. There are the awkward waves or salutes with friends I once gave carefree hugs, the constant thoughts of how far away is that person standing, and each person’s “beliefs” about what is safe when we still don’t fully understand how this virus spreads. I worry for myself, I worry for my family and friends, and I worry for my patients when they tell me about behaviors that clearly are not safe.
At first, I found my work as a telepsychiatrist to be exhausting, and I assumed it was because my patients were now just faces, inches from my own eyes, and no longer diffused by a visual field that included my whole office and the opportunity to break eye contact while I still listened with full attention. This has gotten much better – I’ve adjusted to my on-screen relationships, but what has not gotten better is both the acuity, and sometimes the boredom.
Patients are struggling; they are sad, lonely, and missing the richness of their former lives. They miss friends, meeting new people, cultural experiences, diversity in how they spend their time, and travel. They have all the same human experiences of loss, illness, and grief, but with the added burden of struggling alone or within the confines of pandemic life that has destroyed our ability to mark events with social and religious customs that guide healing. People who had done well for years are now needing more, and those who were not doing well are doing worse. It makes for long days.
I mentioned boredom: With less time spent with other people, so many sessions are about COVID – who has it, who might have it, what people are doing to avoid it, and still, how they get their groceries. The second most popular psychotherapy topic includes what they are watching on Netflix, and as human beings trudging through this together, I have appreciated my patients’ suggestions as much as they have appreciated mine.* Life for all of us has come to be more about survival, and less about self-discovery and striving. Many sessions have started to feel the same from 1 hour to the next, in ways they never did before.
There are other aspects to telepsychiatry that I have found difficult. The site I have used most – Doxy.me – works well with some patients, but with others there are technical problems. Sessions freeze, the sound goes in or out, and we end up switching to another platform, which may or may not work better. Sometimes patients have the camera at odd angles, or they bounce a laptop on their knees to the point that I get seasick. One of my family members has said that I can sometimes be overheard, so I now have a radio playing classical music outside my door, and I often use earbuds so that the patient can’t be overheard and I speak more softly with them – this has all been good in terms of improving privacy, but after a while I find that it’s stressful to have people talking to me inside my own ears! These are little kinks, but when you do it for hours a day, they add up to a sense of being stressed in ways that in-person psychiatry does not lend itself to.
Finally, three seasons into my work-at-home life, I still have not found a new rhythm for some of the logistical aspects of private practice that came so easily in my office. My mail still goes to the office, the plants there still need water, my files and computer are there, but tasks that were once a seamless part of my work day now spill into my time off and I go into the office each week to file, log medications, and attend to the business of my practice. My smartphone, with its ability to e-prescribe, invoice, and fax, has made it possible for me to manage and certainly, outpatient psychiatrists are very lucky that we have the option to continue our work with patients remotely during such difficult times.
I have sent people for virtual intensive substance treatment, and to virtual couples’ counseling, and these remote treatments have been useful. The one treatment that has been very difficult for patients to negotiate has been outpatient electroconvulsive therapy – this requires coordination with another person to drive the patient to treatments (and to wait outside in the parking lot), and also for separate weekly COVID testing. Transcranial magnetic stimulation, which also is still being done in person, has not been any different – patients can drive themselves and the one center I referred to has not required preprocedure COVID testing.
What does the future hold? Will we ever go back to practicing the way we did? While some of my patients miss real-life therapy, most do not; they too like the added efficiency, getting treatment from the comfort of their home without the stress of finding the time to travel. I’ve taken on new patients during this time, and while I anticipated that it would be difficult, it has gone surprisingly well – people I have never met in real life talk to me with ease, and both psychotherapy and medication management have gone well. The one area that I have found most difficult is assessing tremors and dyskinesias, and one patient mentioned she has gained nearly 50 pounds over the past year – something I certainly would have noticed and attended to sooner in real life. I have mixed feelings about returning to a completely live practice. I think I would like a combination where I see all my patients in person once in a while, but would like to be able to offer some times where I see people virtually from home at least one day a week.
Time will tell how that plays out with insurers. My best guess is that, with the lowered no-show rates that everyone is seeing and the higher levels of depression and anxiety that people are having, this may have been a costly time for mental health care. At the same time, inpatient psychiatric units have decreased their capacity, and perhaps more efficient delivery of outpatient care has lowered the overall cost. I suppose we will wait to hear, but for many, the transition to virtual care has allowed many people to get treatment who would have otherwise gone without care.
In my April article, I mentioned that I was having daily Facetime check-in visits with a distressed patient who was on a COVID unit with pneumonia. Since then, I have had several more patients contract COVID, and many of my patients have had family members who have tested positive or become symptomatic with COVID. It has been nice to have sessions with people during this time, and thankfully, I have not had any more patients who have required hospitalization for the virus.
I still catch myself thinking that, of all the things I have worried about over the years, “pandemic” was never on my list. It seems so strange that I left my office on a Friday with no idea that I would not be returning to work the following Monday, or that life would change in such a radical way. As we leave this awful year behind and greet the new one with the hope that vaccines and a new administration might offer solutions, I’d like to wish my readers the best for a healthy, safe, and gentle New Year.
*My top viewing picks for now are “The Queen’s Gambit” (Netflix), and “A Place to Call Home” (Acorn).
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
In mid-April, a month into pandemic life with a stay-at-home order, I wrote about my experiences as a virtual outpatient psychiatrist in private practice. It’s been 10 months now and with this tragic year drawing to a close, it seems like a good time for an update.
In that April column, I describe how I created a makeshift home office. This entailed pushing my son’s baseball card collection and dusty sports trophies to the side of the room, bringing in a desk and a rug, a house plant, and a statue of a Buddha. I enjoyed watching out the window behind my computer screen as the neighbors and their dogs walked by, and I loved seeing the tree out the window blossom into gorgeous flowers.
With time, my physical space has changed. The remnants of my son’s childhood have all been moved to a closet, artwork has been added to the wall behind me, and the space is now clearly an office, though my laptop remains propped on a pile of books so that no one is looking up my nose. The room, with four large windows facing north and west, has issues with temperature control. In an old house, the heat works all too well in the adjacent bedroom (while the rest of the occupants in other rooms freeze), but the office itself has no heat: I have added both a fan and a space heater, and there are some very cold days where I’ve propped open one of the windows. And with the shortened days, large windows on two walls have presented a challenge as the sun changes positions throughout the day – there are times when the sun’s rays streak across my face in such a way that I look rather ethereal, and between sessions I have lowered, raised, and adjusted the blinds to avoid this. I finally pulled off the thin metal venetian blinds and took them to Lowe’s, where a partially masked young woman cut me new blinds with larger slats. An ergonomic office chair has replaced the wicker Ikea chair I was using, and between all these machinations, I am now physically comfortable most of the time. I believe I am still a bit too pixelated on the screen, but my patients are not complaining, and when the natural lighting fades at 4:30 p.m., the overhead lighting is all wrong again. These all are things I never considered – or long ago addressed – in my real-life practice of psychiatry in a office I have loved for years.
With time, I’ve grown more comfortable working from home on a screen and there are things about this life I’ve grown to like. My husband no longer travels, my daughter – my gift of the pandemic – returned home from New York City where she was in her final months of graduate school, and these unexpected months with her (and her cat) have been a pleasure. There is something nice about being trapped at home with people I love, even if we are all in our respective places, in front of our separate screens. There has been time for long walks, trips to the beach, and long bike rides. And as my daughter now prepares to move to Denver, I have been heartened by the hope of vaccines, and the knowledge that I will likely be able to see her again in the coming months. The people are not the only ones who have benefited from this time at home together – I have no idea how we would have managed with our elderly dog if we were not home to care for him.
My life has become more efficient. I used to find myself aggravated when patients forgot their appointments, a not-infrequent occurrence. People no longer get caught in traffic, they come on time, and they don’t complain about my crowded parking lot. When there is down time, I use it more efficiently at home – a load of laundry gets done, I get a chance to turn on the news or exercise, or make dinner early. And because I have two other family members working from home, I am not the only one mixing work with chores or exercise.
While my medical colleagues who work in settings where they must see patients in person have struggled or functioned in some state of denial, I have felt safe and protected, a bit cocooned with my family in a house big enough to give us all space, in a neighborhood with sidewalks and places to walk, and to protect my sanity, I am lucky to have a patio that has now been equipped with lights, patio heaters, a fire pit, and socially distanced tables so that I can still see friends outside.
Telemedicine has added a new dimension to treatment. I’ve had family sessions with multiple people joining a zoom link from different locations – so much easier than coordinating a time when everyone can travel to my office. I’ve had patients call in from cars and from closets in search of privacy, and from their gardens and poolsides. I’ve met spouses, children, many a dog and cat, plus the more unusual of pets and farm animals, including a goat, ferret, lizard, African grey parrot, and guinea pigs.
These are the good things, and while I wish I could say it was all good, so much of what remains is laden with anxiety. My son lives nearby, but he has shared a house with a hospital worker for much of the past year and there were COVID scares, months at a time without so much as a hug, and my husband has not seen his parents or brother for a year now. There are the awkward waves or salutes with friends I once gave carefree hugs, the constant thoughts of how far away is that person standing, and each person’s “beliefs” about what is safe when we still don’t fully understand how this virus spreads. I worry for myself, I worry for my family and friends, and I worry for my patients when they tell me about behaviors that clearly are not safe.
At first, I found my work as a telepsychiatrist to be exhausting, and I assumed it was because my patients were now just faces, inches from my own eyes, and no longer diffused by a visual field that included my whole office and the opportunity to break eye contact while I still listened with full attention. This has gotten much better – I’ve adjusted to my on-screen relationships, but what has not gotten better is both the acuity, and sometimes the boredom.
Patients are struggling; they are sad, lonely, and missing the richness of their former lives. They miss friends, meeting new people, cultural experiences, diversity in how they spend their time, and travel. They have all the same human experiences of loss, illness, and grief, but with the added burden of struggling alone or within the confines of pandemic life that has destroyed our ability to mark events with social and religious customs that guide healing. People who had done well for years are now needing more, and those who were not doing well are doing worse. It makes for long days.
I mentioned boredom: With less time spent with other people, so many sessions are about COVID – who has it, who might have it, what people are doing to avoid it, and still, how they get their groceries. The second most popular psychotherapy topic includes what they are watching on Netflix, and as human beings trudging through this together, I have appreciated my patients’ suggestions as much as they have appreciated mine.* Life for all of us has come to be more about survival, and less about self-discovery and striving. Many sessions have started to feel the same from 1 hour to the next, in ways they never did before.
There are other aspects to telepsychiatry that I have found difficult. The site I have used most – Doxy.me – works well with some patients, but with others there are technical problems. Sessions freeze, the sound goes in or out, and we end up switching to another platform, which may or may not work better. Sometimes patients have the camera at odd angles, or they bounce a laptop on their knees to the point that I get seasick. One of my family members has said that I can sometimes be overheard, so I now have a radio playing classical music outside my door, and I often use earbuds so that the patient can’t be overheard and I speak more softly with them – this has all been good in terms of improving privacy, but after a while I find that it’s stressful to have people talking to me inside my own ears! These are little kinks, but when you do it for hours a day, they add up to a sense of being stressed in ways that in-person psychiatry does not lend itself to.
Finally, three seasons into my work-at-home life, I still have not found a new rhythm for some of the logistical aspects of private practice that came so easily in my office. My mail still goes to the office, the plants there still need water, my files and computer are there, but tasks that were once a seamless part of my work day now spill into my time off and I go into the office each week to file, log medications, and attend to the business of my practice. My smartphone, with its ability to e-prescribe, invoice, and fax, has made it possible for me to manage and certainly, outpatient psychiatrists are very lucky that we have the option to continue our work with patients remotely during such difficult times.
I have sent people for virtual intensive substance treatment, and to virtual couples’ counseling, and these remote treatments have been useful. The one treatment that has been very difficult for patients to negotiate has been outpatient electroconvulsive therapy – this requires coordination with another person to drive the patient to treatments (and to wait outside in the parking lot), and also for separate weekly COVID testing. Transcranial magnetic stimulation, which also is still being done in person, has not been any different – patients can drive themselves and the one center I referred to has not required preprocedure COVID testing.
What does the future hold? Will we ever go back to practicing the way we did? While some of my patients miss real-life therapy, most do not; they too like the added efficiency, getting treatment from the comfort of their home without the stress of finding the time to travel. I’ve taken on new patients during this time, and while I anticipated that it would be difficult, it has gone surprisingly well – people I have never met in real life talk to me with ease, and both psychotherapy and medication management have gone well. The one area that I have found most difficult is assessing tremors and dyskinesias, and one patient mentioned she has gained nearly 50 pounds over the past year – something I certainly would have noticed and attended to sooner in real life. I have mixed feelings about returning to a completely live practice. I think I would like a combination where I see all my patients in person once in a while, but would like to be able to offer some times where I see people virtually from home at least one day a week.
Time will tell how that plays out with insurers. My best guess is that, with the lowered no-show rates that everyone is seeing and the higher levels of depression and anxiety that people are having, this may have been a costly time for mental health care. At the same time, inpatient psychiatric units have decreased their capacity, and perhaps more efficient delivery of outpatient care has lowered the overall cost. I suppose we will wait to hear, but for many, the transition to virtual care has allowed many people to get treatment who would have otherwise gone without care.
In my April article, I mentioned that I was having daily Facetime check-in visits with a distressed patient who was on a COVID unit with pneumonia. Since then, I have had several more patients contract COVID, and many of my patients have had family members who have tested positive or become symptomatic with COVID. It has been nice to have sessions with people during this time, and thankfully, I have not had any more patients who have required hospitalization for the virus.
I still catch myself thinking that, of all the things I have worried about over the years, “pandemic” was never on my list. It seems so strange that I left my office on a Friday with no idea that I would not be returning to work the following Monday, or that life would change in such a radical way. As we leave this awful year behind and greet the new one with the hope that vaccines and a new administration might offer solutions, I’d like to wish my readers the best for a healthy, safe, and gentle New Year.
*My top viewing picks for now are “The Queen’s Gambit” (Netflix), and “A Place to Call Home” (Acorn).
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
In mid-April, a month into pandemic life with a stay-at-home order, I wrote about my experiences as a virtual outpatient psychiatrist in private practice. It’s been 10 months now and with this tragic year drawing to a close, it seems like a good time for an update.
In that April column, I describe how I created a makeshift home office. This entailed pushing my son’s baseball card collection and dusty sports trophies to the side of the room, bringing in a desk and a rug, a house plant, and a statue of a Buddha. I enjoyed watching out the window behind my computer screen as the neighbors and their dogs walked by, and I loved seeing the tree out the window blossom into gorgeous flowers.
With time, my physical space has changed. The remnants of my son’s childhood have all been moved to a closet, artwork has been added to the wall behind me, and the space is now clearly an office, though my laptop remains propped on a pile of books so that no one is looking up my nose. The room, with four large windows facing north and west, has issues with temperature control. In an old house, the heat works all too well in the adjacent bedroom (while the rest of the occupants in other rooms freeze), but the office itself has no heat: I have added both a fan and a space heater, and there are some very cold days where I’ve propped open one of the windows. And with the shortened days, large windows on two walls have presented a challenge as the sun changes positions throughout the day – there are times when the sun’s rays streak across my face in such a way that I look rather ethereal, and between sessions I have lowered, raised, and adjusted the blinds to avoid this. I finally pulled off the thin metal venetian blinds and took them to Lowe’s, where a partially masked young woman cut me new blinds with larger slats. An ergonomic office chair has replaced the wicker Ikea chair I was using, and between all these machinations, I am now physically comfortable most of the time. I believe I am still a bit too pixelated on the screen, but my patients are not complaining, and when the natural lighting fades at 4:30 p.m., the overhead lighting is all wrong again. These all are things I never considered – or long ago addressed – in my real-life practice of psychiatry in a office I have loved for years.
With time, I’ve grown more comfortable working from home on a screen and there are things about this life I’ve grown to like. My husband no longer travels, my daughter – my gift of the pandemic – returned home from New York City where she was in her final months of graduate school, and these unexpected months with her (and her cat) have been a pleasure. There is something nice about being trapped at home with people I love, even if we are all in our respective places, in front of our separate screens. There has been time for long walks, trips to the beach, and long bike rides. And as my daughter now prepares to move to Denver, I have been heartened by the hope of vaccines, and the knowledge that I will likely be able to see her again in the coming months. The people are not the only ones who have benefited from this time at home together – I have no idea how we would have managed with our elderly dog if we were not home to care for him.
My life has become more efficient. I used to find myself aggravated when patients forgot their appointments, a not-infrequent occurrence. People no longer get caught in traffic, they come on time, and they don’t complain about my crowded parking lot. When there is down time, I use it more efficiently at home – a load of laundry gets done, I get a chance to turn on the news or exercise, or make dinner early. And because I have two other family members working from home, I am not the only one mixing work with chores or exercise.
While my medical colleagues who work in settings where they must see patients in person have struggled or functioned in some state of denial, I have felt safe and protected, a bit cocooned with my family in a house big enough to give us all space, in a neighborhood with sidewalks and places to walk, and to protect my sanity, I am lucky to have a patio that has now been equipped with lights, patio heaters, a fire pit, and socially distanced tables so that I can still see friends outside.
Telemedicine has added a new dimension to treatment. I’ve had family sessions with multiple people joining a zoom link from different locations – so much easier than coordinating a time when everyone can travel to my office. I’ve had patients call in from cars and from closets in search of privacy, and from their gardens and poolsides. I’ve met spouses, children, many a dog and cat, plus the more unusual of pets and farm animals, including a goat, ferret, lizard, African grey parrot, and guinea pigs.
These are the good things, and while I wish I could say it was all good, so much of what remains is laden with anxiety. My son lives nearby, but he has shared a house with a hospital worker for much of the past year and there were COVID scares, months at a time without so much as a hug, and my husband has not seen his parents or brother for a year now. There are the awkward waves or salutes with friends I once gave carefree hugs, the constant thoughts of how far away is that person standing, and each person’s “beliefs” about what is safe when we still don’t fully understand how this virus spreads. I worry for myself, I worry for my family and friends, and I worry for my patients when they tell me about behaviors that clearly are not safe.
At first, I found my work as a telepsychiatrist to be exhausting, and I assumed it was because my patients were now just faces, inches from my own eyes, and no longer diffused by a visual field that included my whole office and the opportunity to break eye contact while I still listened with full attention. This has gotten much better – I’ve adjusted to my on-screen relationships, but what has not gotten better is both the acuity, and sometimes the boredom.
Patients are struggling; they are sad, lonely, and missing the richness of their former lives. They miss friends, meeting new people, cultural experiences, diversity in how they spend their time, and travel. They have all the same human experiences of loss, illness, and grief, but with the added burden of struggling alone or within the confines of pandemic life that has destroyed our ability to mark events with social and religious customs that guide healing. People who had done well for years are now needing more, and those who were not doing well are doing worse. It makes for long days.
I mentioned boredom: With less time spent with other people, so many sessions are about COVID – who has it, who might have it, what people are doing to avoid it, and still, how they get their groceries. The second most popular psychotherapy topic includes what they are watching on Netflix, and as human beings trudging through this together, I have appreciated my patients’ suggestions as much as they have appreciated mine.* Life for all of us has come to be more about survival, and less about self-discovery and striving. Many sessions have started to feel the same from 1 hour to the next, in ways they never did before.
There are other aspects to telepsychiatry that I have found difficult. The site I have used most – Doxy.me – works well with some patients, but with others there are technical problems. Sessions freeze, the sound goes in or out, and we end up switching to another platform, which may or may not work better. Sometimes patients have the camera at odd angles, or they bounce a laptop on their knees to the point that I get seasick. One of my family members has said that I can sometimes be overheard, so I now have a radio playing classical music outside my door, and I often use earbuds so that the patient can’t be overheard and I speak more softly with them – this has all been good in terms of improving privacy, but after a while I find that it’s stressful to have people talking to me inside my own ears! These are little kinks, but when you do it for hours a day, they add up to a sense of being stressed in ways that in-person psychiatry does not lend itself to.
Finally, three seasons into my work-at-home life, I still have not found a new rhythm for some of the logistical aspects of private practice that came so easily in my office. My mail still goes to the office, the plants there still need water, my files and computer are there, but tasks that were once a seamless part of my work day now spill into my time off and I go into the office each week to file, log medications, and attend to the business of my practice. My smartphone, with its ability to e-prescribe, invoice, and fax, has made it possible for me to manage and certainly, outpatient psychiatrists are very lucky that we have the option to continue our work with patients remotely during such difficult times.
I have sent people for virtual intensive substance treatment, and to virtual couples’ counseling, and these remote treatments have been useful. The one treatment that has been very difficult for patients to negotiate has been outpatient electroconvulsive therapy – this requires coordination with another person to drive the patient to treatments (and to wait outside in the parking lot), and also for separate weekly COVID testing. Transcranial magnetic stimulation, which also is still being done in person, has not been any different – patients can drive themselves and the one center I referred to has not required preprocedure COVID testing.
What does the future hold? Will we ever go back to practicing the way we did? While some of my patients miss real-life therapy, most do not; they too like the added efficiency, getting treatment from the comfort of their home without the stress of finding the time to travel. I’ve taken on new patients during this time, and while I anticipated that it would be difficult, it has gone surprisingly well – people I have never met in real life talk to me with ease, and both psychotherapy and medication management have gone well. The one area that I have found most difficult is assessing tremors and dyskinesias, and one patient mentioned she has gained nearly 50 pounds over the past year – something I certainly would have noticed and attended to sooner in real life. I have mixed feelings about returning to a completely live practice. I think I would like a combination where I see all my patients in person once in a while, but would like to be able to offer some times where I see people virtually from home at least one day a week.
Time will tell how that plays out with insurers. My best guess is that, with the lowered no-show rates that everyone is seeing and the higher levels of depression and anxiety that people are having, this may have been a costly time for mental health care. At the same time, inpatient psychiatric units have decreased their capacity, and perhaps more efficient delivery of outpatient care has lowered the overall cost. I suppose we will wait to hear, but for many, the transition to virtual care has allowed many people to get treatment who would have otherwise gone without care.
In my April article, I mentioned that I was having daily Facetime check-in visits with a distressed patient who was on a COVID unit with pneumonia. Since then, I have had several more patients contract COVID, and many of my patients have had family members who have tested positive or become symptomatic with COVID. It has been nice to have sessions with people during this time, and thankfully, I have not had any more patients who have required hospitalization for the virus.
I still catch myself thinking that, of all the things I have worried about over the years, “pandemic” was never on my list. It seems so strange that I left my office on a Friday with no idea that I would not be returning to work the following Monday, or that life would change in such a radical way. As we leave this awful year behind and greet the new one with the hope that vaccines and a new administration might offer solutions, I’d like to wish my readers the best for a healthy, safe, and gentle New Year.
*My top viewing picks for now are “The Queen’s Gambit” (Netflix), and “A Place to Call Home” (Acorn).
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
COVID-19 vaccine rollout faces delays
If the current pace of vaccination continues, “it’s going to take years, not months, to vaccinate the American people,” President-elect Joe Biden said during a briefing Dec. 29.
In fact, at the current rate, it would take nearly 10 years to vaccinate enough Americans to bring the pandemic under control, according to NBC News. To reach 80% of the country by late June, 3 million people would need to receive a COVID-19 vaccine each day.
“As I long feared and warned, the effort to distribute and administer the vaccine is not progressing as it should,” Mr. Biden said, reemphasizing his pledge to get 100 million doses to Americans during his first 100 days as president.
So far, 11.4 million doses have been distributed and 2.1 million people have received a vaccine, according to the Centers for Disease Control and Prevention. Most states have administered a fraction of the doses they’ve received, according to data compiled by The New York Times.
Federal officials have said there’s an “expected lag” between delivery of doses, shots going into arms, and the data being reported to the CDC, according to CNN. The Food and Drug Administration must assess each shipment for quality control, which has slowed down distribution, and the CDC data are just now beginning to include the Moderna vaccine, which the FDA authorized for emergency use on Dec. 18.
The 2.1 million number is “an underestimate,” Brett Giroir, MD, the assistant secretary of the U.S. Department of Health & Human Services, told NBC News Dec. 29. At the same time, the U.S. won’t meet the goal of vaccinating 20 million people in the next few days, he said.
Another 30 million doses will go out in January, Dr. Giroir said, followed by 50 million in February.
Some vaccine experts have said they’re not surprised by the speed of vaccine distribution.
“It had to go this way,” Paul Offit, MD, a professor of pediatrics at Children’s Hospital of Philadelphia, told STAT. “We had to trip and fall and stumble and figure this out.”
To speed up distribution in 2021, the federal government will need to help states, Mr. Biden said Dec. 29. He plans to use the Defense Authorization Act to ramp up production of vaccine supplies. Even still, the process will take months, he said.
A version of this article first appeared on WebMD.com .
If the current pace of vaccination continues, “it’s going to take years, not months, to vaccinate the American people,” President-elect Joe Biden said during a briefing Dec. 29.
In fact, at the current rate, it would take nearly 10 years to vaccinate enough Americans to bring the pandemic under control, according to NBC News. To reach 80% of the country by late June, 3 million people would need to receive a COVID-19 vaccine each day.
“As I long feared and warned, the effort to distribute and administer the vaccine is not progressing as it should,” Mr. Biden said, reemphasizing his pledge to get 100 million doses to Americans during his first 100 days as president.
So far, 11.4 million doses have been distributed and 2.1 million people have received a vaccine, according to the Centers for Disease Control and Prevention. Most states have administered a fraction of the doses they’ve received, according to data compiled by The New York Times.
Federal officials have said there’s an “expected lag” between delivery of doses, shots going into arms, and the data being reported to the CDC, according to CNN. The Food and Drug Administration must assess each shipment for quality control, which has slowed down distribution, and the CDC data are just now beginning to include the Moderna vaccine, which the FDA authorized for emergency use on Dec. 18.
The 2.1 million number is “an underestimate,” Brett Giroir, MD, the assistant secretary of the U.S. Department of Health & Human Services, told NBC News Dec. 29. At the same time, the U.S. won’t meet the goal of vaccinating 20 million people in the next few days, he said.
Another 30 million doses will go out in January, Dr. Giroir said, followed by 50 million in February.
Some vaccine experts have said they’re not surprised by the speed of vaccine distribution.
“It had to go this way,” Paul Offit, MD, a professor of pediatrics at Children’s Hospital of Philadelphia, told STAT. “We had to trip and fall and stumble and figure this out.”
To speed up distribution in 2021, the federal government will need to help states, Mr. Biden said Dec. 29. He plans to use the Defense Authorization Act to ramp up production of vaccine supplies. Even still, the process will take months, he said.
A version of this article first appeared on WebMD.com .
If the current pace of vaccination continues, “it’s going to take years, not months, to vaccinate the American people,” President-elect Joe Biden said during a briefing Dec. 29.
In fact, at the current rate, it would take nearly 10 years to vaccinate enough Americans to bring the pandemic under control, according to NBC News. To reach 80% of the country by late June, 3 million people would need to receive a COVID-19 vaccine each day.
“As I long feared and warned, the effort to distribute and administer the vaccine is not progressing as it should,” Mr. Biden said, reemphasizing his pledge to get 100 million doses to Americans during his first 100 days as president.
So far, 11.4 million doses have been distributed and 2.1 million people have received a vaccine, according to the Centers for Disease Control and Prevention. Most states have administered a fraction of the doses they’ve received, according to data compiled by The New York Times.
Federal officials have said there’s an “expected lag” between delivery of doses, shots going into arms, and the data being reported to the CDC, according to CNN. The Food and Drug Administration must assess each shipment for quality control, which has slowed down distribution, and the CDC data are just now beginning to include the Moderna vaccine, which the FDA authorized for emergency use on Dec. 18.
The 2.1 million number is “an underestimate,” Brett Giroir, MD, the assistant secretary of the U.S. Department of Health & Human Services, told NBC News Dec. 29. At the same time, the U.S. won’t meet the goal of vaccinating 20 million people in the next few days, he said.
Another 30 million doses will go out in January, Dr. Giroir said, followed by 50 million in February.
Some vaccine experts have said they’re not surprised by the speed of vaccine distribution.
“It had to go this way,” Paul Offit, MD, a professor of pediatrics at Children’s Hospital of Philadelphia, told STAT. “We had to trip and fall and stumble and figure this out.”
To speed up distribution in 2021, the federal government will need to help states, Mr. Biden said Dec. 29. He plans to use the Defense Authorization Act to ramp up production of vaccine supplies. Even still, the process will take months, he said.
A version of this article first appeared on WebMD.com .
2.1 Million COVID Vaccine Doses Given in U.S.
The U.S. has distributed more than 11.4 million doses of the Pfizer and Moderna COVID-19 vaccines, and more than 2.1 million of those had been given to people as of December 28, according to the CDC.
The CDC’s COVID Data Tracker showed the updated numbers as of 9 a.m. on that day. The distribution total is based on the CDC’s Vaccine Tracking System, and the administered total is based on reports from state and local public health departments, as well as updates from five federal agencies: the Bureau of Prisons, Veterans Administration, Department of Defense, Department of State, and Indian Health Services.
Health care providers report to public health agencies up to 72 hours after the vaccine is given, and public health agencies report to the CDC after that, so there may be a lag in the data. The CDC’s numbers will be updated on Mondays, Wednesdays, and Fridays.
“A large difference between the number of doses distributed and the number of doses administered is expected at this point in the COVID vaccination program due to several factors,” the CDC says.
Delays could occur due to the reporting of doses given, how states and local vaccine sites are managing vaccines, and the pending launch of vaccination through the federal Pharmacy Partnership for Long-Term Care Program.
“Numbers reported on other websites may differ from what is posted on CDC’s website because CDC’s overall numbers are validated through a data submission process with each jurisdiction,” the CDC says.
On Dec. 26, the agency’s tally showed that 9.5 million doses had been distributed and 1.9 million had been given, according to Reuters.
Public health officials and health care workers have begun to voice their concerns about the delay in giving the vaccines.
“We certainly are not at the numbers that we wanted to be at the end of December,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, told CNNDec. 29.
Operation Warp Speed had planned for 20 million people to be vaccinated by the end of the year. Fauci said he hopes that number will be achieved next month.
“I believe that as we get into January, we are going to see an increase in the momentum,” he said.
Shipment delays have affected other priority groups as well. The New York Police Department anticipated a rollout Dec. 29, but it’s now been delayed since the department hasn’t received enough Moderna doses to start giving the shots, according to the New York Daily News.
“We’ve made numerous attempts to get updated information, and when we get further word on its availability, we will immediately keep our members appraised of the new date and the method of distribution,” Paul DiGiacomo, president of the Detectives’ Endowment Association, wrote in a memo to members on Dec. 28.
“Every detective squad has been crushed with [COVID-19],” he told the newspaper. “Within the last couple of weeks, we’ve had at least two detectives hospitalized.”
President-elect Joe Biden will receive a briefing from his COVID-19 advisory team, provide a general update on the pandemic, and describe his own plan for vaccinating people quickly during an address Dec. 29, a transition official told Axios. Biden has pledged to administer 100 million vaccine doses in his first 100 days in office.
A version of this article originally appeared on WebMd.
The U.S. has distributed more than 11.4 million doses of the Pfizer and Moderna COVID-19 vaccines, and more than 2.1 million of those had been given to people as of December 28, according to the CDC.
The CDC’s COVID Data Tracker showed the updated numbers as of 9 a.m. on that day. The distribution total is based on the CDC’s Vaccine Tracking System, and the administered total is based on reports from state and local public health departments, as well as updates from five federal agencies: the Bureau of Prisons, Veterans Administration, Department of Defense, Department of State, and Indian Health Services.
Health care providers report to public health agencies up to 72 hours after the vaccine is given, and public health agencies report to the CDC after that, so there may be a lag in the data. The CDC’s numbers will be updated on Mondays, Wednesdays, and Fridays.
“A large difference between the number of doses distributed and the number of doses administered is expected at this point in the COVID vaccination program due to several factors,” the CDC says.
Delays could occur due to the reporting of doses given, how states and local vaccine sites are managing vaccines, and the pending launch of vaccination through the federal Pharmacy Partnership for Long-Term Care Program.
“Numbers reported on other websites may differ from what is posted on CDC’s website because CDC’s overall numbers are validated through a data submission process with each jurisdiction,” the CDC says.
On Dec. 26, the agency’s tally showed that 9.5 million doses had been distributed and 1.9 million had been given, according to Reuters.
Public health officials and health care workers have begun to voice their concerns about the delay in giving the vaccines.
“We certainly are not at the numbers that we wanted to be at the end of December,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, told CNNDec. 29.
Operation Warp Speed had planned for 20 million people to be vaccinated by the end of the year. Fauci said he hopes that number will be achieved next month.
“I believe that as we get into January, we are going to see an increase in the momentum,” he said.
Shipment delays have affected other priority groups as well. The New York Police Department anticipated a rollout Dec. 29, but it’s now been delayed since the department hasn’t received enough Moderna doses to start giving the shots, according to the New York Daily News.
“We’ve made numerous attempts to get updated information, and when we get further word on its availability, we will immediately keep our members appraised of the new date and the method of distribution,” Paul DiGiacomo, president of the Detectives’ Endowment Association, wrote in a memo to members on Dec. 28.
“Every detective squad has been crushed with [COVID-19],” he told the newspaper. “Within the last couple of weeks, we’ve had at least two detectives hospitalized.”
President-elect Joe Biden will receive a briefing from his COVID-19 advisory team, provide a general update on the pandemic, and describe his own plan for vaccinating people quickly during an address Dec. 29, a transition official told Axios. Biden has pledged to administer 100 million vaccine doses in his first 100 days in office.
A version of this article originally appeared on WebMd.
The U.S. has distributed more than 11.4 million doses of the Pfizer and Moderna COVID-19 vaccines, and more than 2.1 million of those had been given to people as of December 28, according to the CDC.
The CDC’s COVID Data Tracker showed the updated numbers as of 9 a.m. on that day. The distribution total is based on the CDC’s Vaccine Tracking System, and the administered total is based on reports from state and local public health departments, as well as updates from five federal agencies: the Bureau of Prisons, Veterans Administration, Department of Defense, Department of State, and Indian Health Services.
Health care providers report to public health agencies up to 72 hours after the vaccine is given, and public health agencies report to the CDC after that, so there may be a lag in the data. The CDC’s numbers will be updated on Mondays, Wednesdays, and Fridays.
“A large difference between the number of doses distributed and the number of doses administered is expected at this point in the COVID vaccination program due to several factors,” the CDC says.
Delays could occur due to the reporting of doses given, how states and local vaccine sites are managing vaccines, and the pending launch of vaccination through the federal Pharmacy Partnership for Long-Term Care Program.
“Numbers reported on other websites may differ from what is posted on CDC’s website because CDC’s overall numbers are validated through a data submission process with each jurisdiction,” the CDC says.
On Dec. 26, the agency’s tally showed that 9.5 million doses had been distributed and 1.9 million had been given, according to Reuters.
Public health officials and health care workers have begun to voice their concerns about the delay in giving the vaccines.
“We certainly are not at the numbers that we wanted to be at the end of December,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, told CNNDec. 29.
Operation Warp Speed had planned for 20 million people to be vaccinated by the end of the year. Fauci said he hopes that number will be achieved next month.
“I believe that as we get into January, we are going to see an increase in the momentum,” he said.
Shipment delays have affected other priority groups as well. The New York Police Department anticipated a rollout Dec. 29, but it’s now been delayed since the department hasn’t received enough Moderna doses to start giving the shots, according to the New York Daily News.
“We’ve made numerous attempts to get updated information, and when we get further word on its availability, we will immediately keep our members appraised of the new date and the method of distribution,” Paul DiGiacomo, president of the Detectives’ Endowment Association, wrote in a memo to members on Dec. 28.
“Every detective squad has been crushed with [COVID-19],” he told the newspaper. “Within the last couple of weeks, we’ve had at least two detectives hospitalized.”
President-elect Joe Biden will receive a briefing from his COVID-19 advisory team, provide a general update on the pandemic, and describe his own plan for vaccinating people quickly during an address Dec. 29, a transition official told Axios. Biden has pledged to administer 100 million vaccine doses in his first 100 days in office.
A version of this article originally appeared on WebMd.
Reducing COVID-19 opioid deaths
Editor's Note: Due to updated statistics from the CDC, the online version of this article has been modified from the version that appears in the printed edition of the January 2021 issue of Current Psychiatry.
Individuals with mental health and substance use disorders (SUDs) are particularly susceptible to negative effects of the coronavirus disease 2019 (COVID-19) pandemic. The collision of the COVID-19 pandemic and the drug overdose epidemic has highlighted the urgent need for physicians, policymakers, and health care professionals to optimize care for individuals with SUDs because they may be particularly vulnerable to the effects of the virus due to compromised respiratory and immune function, and poor social support.1 In this commentary, we highlight the challenges of the drug overdose epidemic, and recommend strategies to mitigate the impact of the COVID-19 pandemic among patients with SUDs.
A crisis exacerbated by COVID-19
The current drug overdose epidemic has become an American public health nightmare. According to preliminary data released by the CDC on December 17, 2020, there were more than 81,000 drug overdose deaths in the United States in the 12 months ending May 2020.2,3 This is the highest number of overdose deaths ever recorded in a 12-month period. The CDC also noted that while overdose deaths were already increasing in the months preceding the COVID-19 pandemic, the latest numbers suggest an acceleration of overdose deaths during the pandemic.
What is causing this significant loss of life? Prescription opioids and illegal opioids such as heroin and illicitly manufactured fentanyl are the main agents associated with overdose deaths. These opioids were responsible for 61% (28,647) of drug overdose deaths in the United States in 2014.4 In 2015, the opioid overdose death rate increased by 15.6%.5
The increase in the number of opioid overdose deaths in part coincides with a sharp increase in the availability and use of heroin. Heroin overdose deaths have more than tripled since 2010, but heroin is not the only opiate involved. Fentanyl, a synthetic, short-acting opioid that is approved for managing pain in patients with advanced cancers, is 50 times more potent than heroin. The abuse of prescribed fentanyl has been accelerating over the past decade, as is the use of illicitly produced fentanyl. Evidence from US Drug Enforcement Administration (DEA) seizure records shows heroin is being adulterated with illicit fentanyl to enhance the potency of the heroin.6,7 Mixing illicit fentanyl with heroin may be contributing to the recent increase in heroin overdose fatalities. According to the CDC, overdose deaths related to synthetic opioids increased 38.4% from the 12-month period leading up to June 2019 compared with the 12-month period leading up to May 2020.2,3 Postmortem studies of individuals who died from a heroin overdose have frequently found the presence of fentanyl along with heroin.8 Overdose deaths involving heroin may be occurring because individuals may be unknowingly using heroin adulterated with fentanyl.9 In addition, carfentanil, a powerful new synthetic fentanyl, has been recently identified in heroin mixtures. Carfentanil is 10,000 times stronger than morphine. Even in miniscule amounts, carfentanil can suppress breathing to the degree that multiple doses of naloxone are needed to restore respirations.
Initial studies indicate that the COVID-19 pandemic has been exacerbating this situation. Wainwright et al10 conducted an analysis of urine drug test results of patients with SUDs from 4 months before and 4 months after COVID-19 was declared a national emergency on March 13, 2020. Compared with before COVID-19, the proportion of specimens testing positive since COVID-19 increased from 3.80% to 7.32% for fentanyl and from 1.29% to 2.09% for heroin.10
A similar drug testing study found that during the pandemic, the proportion of positive results (positivity) increased by 35% for non-prescribed fentanyl and 44% for heroin.11 Positivity for non-prescribed fentanyl increased significantly among patients who tested positive for other drugs, including by 89% for amphetamines; 48% for benzodiazepines; 34% for cocaine; and 39% for opiates (P < .1 for all).11
In a review of electronic medical records, Ochalek et al12 found that the number of nonfatal opioid overdoses in an emergency department in Virginia increased from 102 in March-June 2019 to 227 in March-June 2020. In an issue brief published on October 31, 2020, the American Medical Association reported increase in opioid and other drug-related overdoses in more than 40 states during the COVID-19 pandemic.13
Continue to: Strategies for intervention...
Strategies for intervention
A multi-dimensional approach is needed to protect the public from this growing opioid overdose epidemic. To address this challenging task, we recommend several strategies:
Enhance access to virtual treatment
Even when in-person treatment cannot take place due to COVID-19-related restrictions, it is vital that services are accessible to patients with SUDs during this pandemic. Examples of virtual treatment include:
- Telehealth for medication-assisted treatment (MAT) using buprenorphine (recently updated guidance from the US DEA and Substance Abuse and Mental Health Services Administration [SAMHSA] allows this method of prescribing)
- Teletherapy to prevent relapse
- Remote drug screens by sending saliva or urine kits to patients' homes, visiting patients to collect fluid samples, or asking patients to come to a "drive-through" facility to provide samples
- Virtual (online) Alcoholics Anonymous, Narcotics Anonymous, SMART Recovery, and similar meetings to provide support in the absence of in-person meetings.
The American Society of Addiction Medicine (ASAM) offers guidance to treatment programs to focus on infection control and mitigation. The Table14 summarizes the ASAM recommendations for office-based opioid treatment during COVID-19.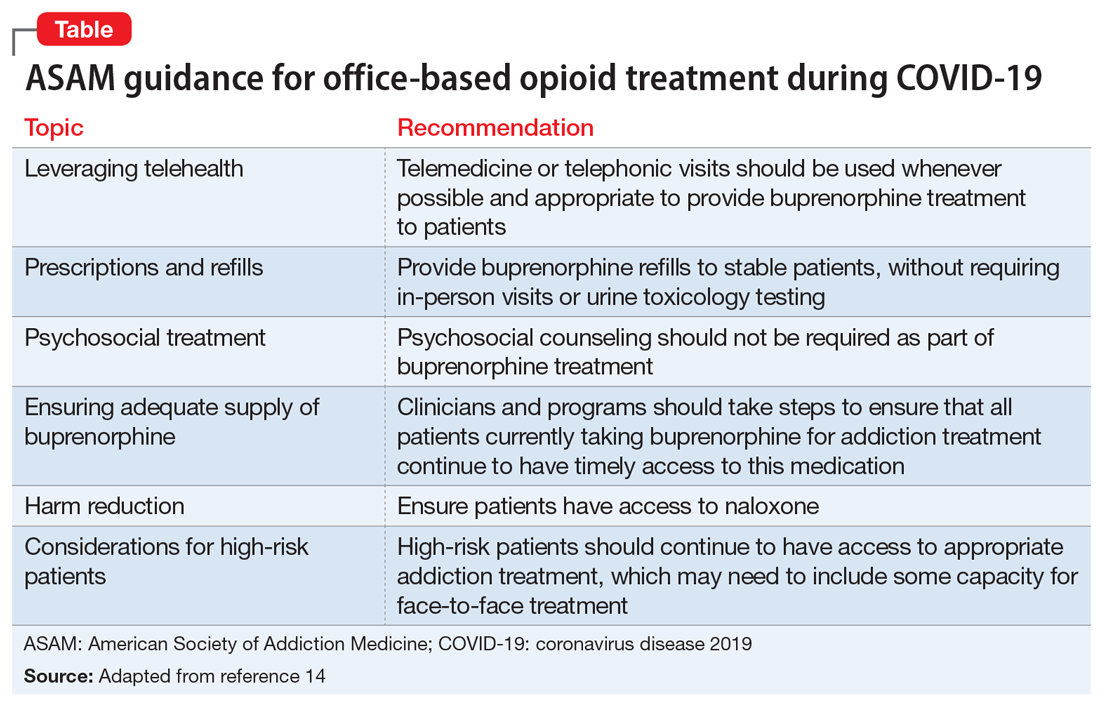
Expand access to treatment
This includes access to MAT (such as buprenorphine/naloxone, methadone, naltrexone, and depot naltrexone) and, equally important, to psychosocial treatment, counseling, and/or recovery services. Recent legislative changes have increased the number of patients that a qualified physician can treat with buprenorphine/naloxone from 100 to 275, and allowed physician extenders to prescribe buprenorphine/naloxone in office-based settings. A recent population-based, retrospective Canadian study showed that opioid agonist treatment decreased the risk of mortality among opioid users, and the protective effects of this treatment increased as fentanyl and other synthetic opioids became common in the illicit drug supply.15 However, because of the shortage of psychiatrists and addiction medicine specialists in several regions of the United States, access to treatment is extremely limited and often inadequate. This constitutes a major public health crisis and contributes to our inability to intervene effectively in the opioid epidemic. Telepsychiatry programs can bring needed services to underserved areas, but they need additional support and development. Further, involving other specialties is paramount for treating this epidemic. Integrating MAT in primary care settings can improve access to treatment. Harm-reduction approaches, such as syringe exchange programs, can play an important role in reducing the adverse consequences associated with heroin use and establish health care relationships with at-risk individuals. Syringe exchange programs can also reduce the rate of infections associated with IV drug use, such as human immunodeficiency virus and hepatitis C virus.
Continue to: Increase education on naloxone...
Increase education on naloxone
Naloxone is a safe and effective opioid antagonist used to treat opioid overdoses. Timely access to naloxone is of the essence when treating opioid-related overdoses. Many states have enacted laws allowing health care professionals, law enforcement officers, and patients and relatives to obtain naloxone without a physician's prescription. It appears this approach may be yielding results. For example, the North Carolina Harm Reduction Coalition distributed >101,000 free overdose rescue kits that included naloxone and recorded 13,392 confirmed cases of overdose rescue with naloxone from 2013 to 2019.16
Divert patients with SUDs from the criminal justice system to treatment
We need to develop programs to divert patients with SUDs from the criminal justice system, which is focused on punishment, to interventions that focus on treatment. Data indicates high recidivism rates for incarcerated individuals with SUDs who do not have access to treatment after they are released. Recognizing this, communities are developing programs that divert low-level offenders from the criminal justice system into treatment. For instance, in Seattle, the Law Enforcement Assisted Diversion is a pilot program developed to divert low-level drug and prostitution offenders into community-based treatment and support services. This helps provide housing, health care, job training, treatment, and mental health support. Innovative programs are needed to provide SUD treatment in the rehabilitation programs of correctional facilities and ensure case managers and discharge planners can transition participants to community treatment programs upon their release.
Develop early identification and prevention programs
These programs should focus on individuals at high risk, such as patients with comorbid SUDs and psychiatric disorders, those with chronic pain, and at-risk children whose parents abuse opiates. Traditional addiction treatment programs typically do not address patients with complex conditions or special populations, such as adolescents or pregnant women with substance use issues. Evidence-based approaches such as Screening, Brief Intervention, and Referral to Treatment (SBIRT), Integrated Dual Diagnosis Treatment (IDDT), and prevention approaches that target students in middle schools and high schools need to be more widely available.
Improve education on opioid prescribing
Responsible opioid prescribing for clinicians should include education about the regular use of prescription drug monitoring programs, urine drug screening, avoiding co-prescription of opioids with sedative-hypnotic medications, and better linkage with addiction treatment.
Treat comorbid psychiatric conditions
It is critical to both identify and effectively treat underlying affective, anxiety, and psychotic disorders in patients with SUDs. Anxiety, depression, and emotional dysregulation often contribute to worsening substance abuse, abuse of prescription drugs, diversion of prescribed drugs, and an increased risk of overdoses and suicides. Effective treatment of comorbid psychiatric conditions also may reduce relapses.
Increase research on causes and treatments
Through research, we must expand our knowledge to better understand the factors that contribute to this epidemic and develop better treatments. These efforts may allow for the development of prevention mechanisms. For example, a recent study found that the continued use of opioid medications after an overdose was associated with a high risk of a repeated overdosecall out material?.17 At the end of a 2-year observation, 17% (confidence interval [CI]: 14% to 20%) of patients receiving a high daily dosage of a prescribed opioid had a repeat overdose compared with 15% (CI: 10% to 21%) of those receiving a moderate dosage, 9% (CI: 6% to 14%) of those receiving a low dosage, and 8% (CI: 6% to 11%) of those receiving no opioids.17 Of the patients who overdosed on prescribed opiates, 30% switched to a new prescriber after their overdose, many of whom may not have been aware of the previous overdose. From a public health perspective, it would make sense for prescribers to know of prior opioid and/or benzodiazepine overdoses. This could be reported by emergency department clinicians, law enforcement, and hospitals into a prescription drug monitoring program, which is readily available to prescribers in most states.
Acknowledgment
The authors thank Scott Proescholdbell, MPH, Injury and Violence Prevention Branch, Chronic Disease and Injury Section, Division of Public Health, North Carolina Department of Health and Human Services, for his assistance.
Bottom Line
The collision of the coronavirus disease 2019 pandemic and the drug overdose epidemic has highlighted the urgent need for health care professionals to optimize care for individuals with substance use disorders. Suggested interventions include enhancing access to medication-assisted treatment and virtual treatment, improving education about naloxone and safe opioid prescribing practices, and diverting at-risk patients from the criminal justice system to interventions that focus on treatment.
1. Volkow ND. Collision of the COVID-19 and addiction epidemics. Ann Intern Med. 2020;173(1):61-62.
2.Centers for Disease Control and Prevention. Overdose deaths accelerating during COVID-19. Accessed December 23, 2020. https://www.cdc.gov/media/releases/2020/p1218-overdose-deaths-covid-19.html
3.Centers for Disease Control and Prevention. National Center for Health Statistics Vital Statistics Rapid Release. Provisional drug overdose death counts. Accessed December 30, 2020. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
4.Rudd RA, Aleshire N, Zibbell JE, et al. Increases in drug and opioid overdose deaths -- United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2016;64(50-51):1378-1382.
5.Rudd RA, Seth P, David F, et al. Increases in drug and opioid-involved overdose deaths -- United States, 2010-2015. MMWR Morb Mortal Wkly Rep. 2016;65(50-51):1445-1452.
6.US Drug Enforcement Administration. DEA issues nationwide alert on fentanyl as threat to health and public safety. Published March 19, 2015. Accessed October 28, 2020. http://www.dea.gov/divisions/hq/2015/hq031815.shtml
7.Gladden RM, Martinez P, Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-involved overdose deaths - 27 states, 2013-2014. MMWR Morb Mortal Wkly Rep. 2016;65(33):837-843.
8.Algren DA, Monteilh CP, Punja M, et al. Fentanyl-associated fatalities among illicit drug users in Wayne County, Michigan (July 2005-May 2006). J Med Toxicol. 2013;9(1):106-115.
9.Centers for Disease Control and Prevention. Increases in fentanyl drug confiscations and fentanyl-related overdose fatalities. HAN Health Advisory. Published October 26, 2015. Accessed October 28, 2020. http://emergency.cdc.gov/han/han00384.asp
10.Wainwright JJ, Mikre M, Whitley P, et al. Analysis of drug test results before and after the us declaration of a national emergency concerning the COVID-19 outbreak. JAMA. 2020;324(16):1674-1677.
11.Niles JK, Gudin J, Radliff J, et al. The opioid epidemic within the COVID-19 pandemic: drug testing in 2020 [published online October 8, 2020]. Population Health Management. doi: 10.1089/pop.2020.0230
12.Ochalek TA, Cumpston KL, Wills BK, et al. Nonfatal opioid overdoses at an urban emergency department during the COVID-19 pandemic. JAMA. 2020;324(16):1673-1674.
13.American Medical Association. Issue brief: reports of increases in opioid- and other drug-related overdose and other concerns during COVID pandemic. Published October 31, 2020. Accessed November 9, 2020. https://www.ama-assn.org/system/files/2020-11/issue-brief-increases-in-opioid-related-overdose.pdf
14.American Society of Addiction Medicine. Caring for patients during the COVID-19 pandemic: ASAM COVID-19 Task Force recommendations. Accessed October 30, 2020. https://www.asam.org/docs/default-source/covid-19/medication-formulation-and-dosage-guidance-(1).pdf
15.Pearce LA, Min JE, Piske M, et al. Opioid agonist treatment and risk of mortality during opioid overdose public health emergency: population based retrospective cohort study. BMJ. 2020;368:m772. doi: 10.1136/bmj.m772
16.North Carolina Harm Reduction Coalition. NCHRC'S community-based overdose prevention project. Accessed March 29, 2020. http://www.nchrc.org/programs-and-services
17.Larochelle MR, Liebschutz JM, Zhang F, et al. Opioid prescribing after nonfatal overdose and association with repeated overdose: a cohort study. Ann Intern Med. 2016;164(1):1-9.
Editor's Note: Due to updated statistics from the CDC, the online version of this article has been modified from the version that appears in the printed edition of the January 2021 issue of Current Psychiatry.
Individuals with mental health and substance use disorders (SUDs) are particularly susceptible to negative effects of the coronavirus disease 2019 (COVID-19) pandemic. The collision of the COVID-19 pandemic and the drug overdose epidemic has highlighted the urgent need for physicians, policymakers, and health care professionals to optimize care for individuals with SUDs because they may be particularly vulnerable to the effects of the virus due to compromised respiratory and immune function, and poor social support.1 In this commentary, we highlight the challenges of the drug overdose epidemic, and recommend strategies to mitigate the impact of the COVID-19 pandemic among patients with SUDs.
A crisis exacerbated by COVID-19
The current drug overdose epidemic has become an American public health nightmare. According to preliminary data released by the CDC on December 17, 2020, there were more than 81,000 drug overdose deaths in the United States in the 12 months ending May 2020.2,3 This is the highest number of overdose deaths ever recorded in a 12-month period. The CDC also noted that while overdose deaths were already increasing in the months preceding the COVID-19 pandemic, the latest numbers suggest an acceleration of overdose deaths during the pandemic.
What is causing this significant loss of life? Prescription opioids and illegal opioids such as heroin and illicitly manufactured fentanyl are the main agents associated with overdose deaths. These opioids were responsible for 61% (28,647) of drug overdose deaths in the United States in 2014.4 In 2015, the opioid overdose death rate increased by 15.6%.5
The increase in the number of opioid overdose deaths in part coincides with a sharp increase in the availability and use of heroin. Heroin overdose deaths have more than tripled since 2010, but heroin is not the only opiate involved. Fentanyl, a synthetic, short-acting opioid that is approved for managing pain in patients with advanced cancers, is 50 times more potent than heroin. The abuse of prescribed fentanyl has been accelerating over the past decade, as is the use of illicitly produced fentanyl. Evidence from US Drug Enforcement Administration (DEA) seizure records shows heroin is being adulterated with illicit fentanyl to enhance the potency of the heroin.6,7 Mixing illicit fentanyl with heroin may be contributing to the recent increase in heroin overdose fatalities. According to the CDC, overdose deaths related to synthetic opioids increased 38.4% from the 12-month period leading up to June 2019 compared with the 12-month period leading up to May 2020.2,3 Postmortem studies of individuals who died from a heroin overdose have frequently found the presence of fentanyl along with heroin.8 Overdose deaths involving heroin may be occurring because individuals may be unknowingly using heroin adulterated with fentanyl.9 In addition, carfentanil, a powerful new synthetic fentanyl, has been recently identified in heroin mixtures. Carfentanil is 10,000 times stronger than morphine. Even in miniscule amounts, carfentanil can suppress breathing to the degree that multiple doses of naloxone are needed to restore respirations.
Initial studies indicate that the COVID-19 pandemic has been exacerbating this situation. Wainwright et al10 conducted an analysis of urine drug test results of patients with SUDs from 4 months before and 4 months after COVID-19 was declared a national emergency on March 13, 2020. Compared with before COVID-19, the proportion of specimens testing positive since COVID-19 increased from 3.80% to 7.32% for fentanyl and from 1.29% to 2.09% for heroin.10
A similar drug testing study found that during the pandemic, the proportion of positive results (positivity) increased by 35% for non-prescribed fentanyl and 44% for heroin.11 Positivity for non-prescribed fentanyl increased significantly among patients who tested positive for other drugs, including by 89% for amphetamines; 48% for benzodiazepines; 34% for cocaine; and 39% for opiates (P < .1 for all).11
In a review of electronic medical records, Ochalek et al12 found that the number of nonfatal opioid overdoses in an emergency department in Virginia increased from 102 in March-June 2019 to 227 in March-June 2020. In an issue brief published on October 31, 2020, the American Medical Association reported increase in opioid and other drug-related overdoses in more than 40 states during the COVID-19 pandemic.13
Continue to: Strategies for intervention...
Strategies for intervention
A multi-dimensional approach is needed to protect the public from this growing opioid overdose epidemic. To address this challenging task, we recommend several strategies:
Enhance access to virtual treatment
Even when in-person treatment cannot take place due to COVID-19-related restrictions, it is vital that services are accessible to patients with SUDs during this pandemic. Examples of virtual treatment include:
- Telehealth for medication-assisted treatment (MAT) using buprenorphine (recently updated guidance from the US DEA and Substance Abuse and Mental Health Services Administration [SAMHSA] allows this method of prescribing)
- Teletherapy to prevent relapse
- Remote drug screens by sending saliva or urine kits to patients' homes, visiting patients to collect fluid samples, or asking patients to come to a "drive-through" facility to provide samples
- Virtual (online) Alcoholics Anonymous, Narcotics Anonymous, SMART Recovery, and similar meetings to provide support in the absence of in-person meetings.
The American Society of Addiction Medicine (ASAM) offers guidance to treatment programs to focus on infection control and mitigation. The Table14 summarizes the ASAM recommendations for office-based opioid treatment during COVID-19.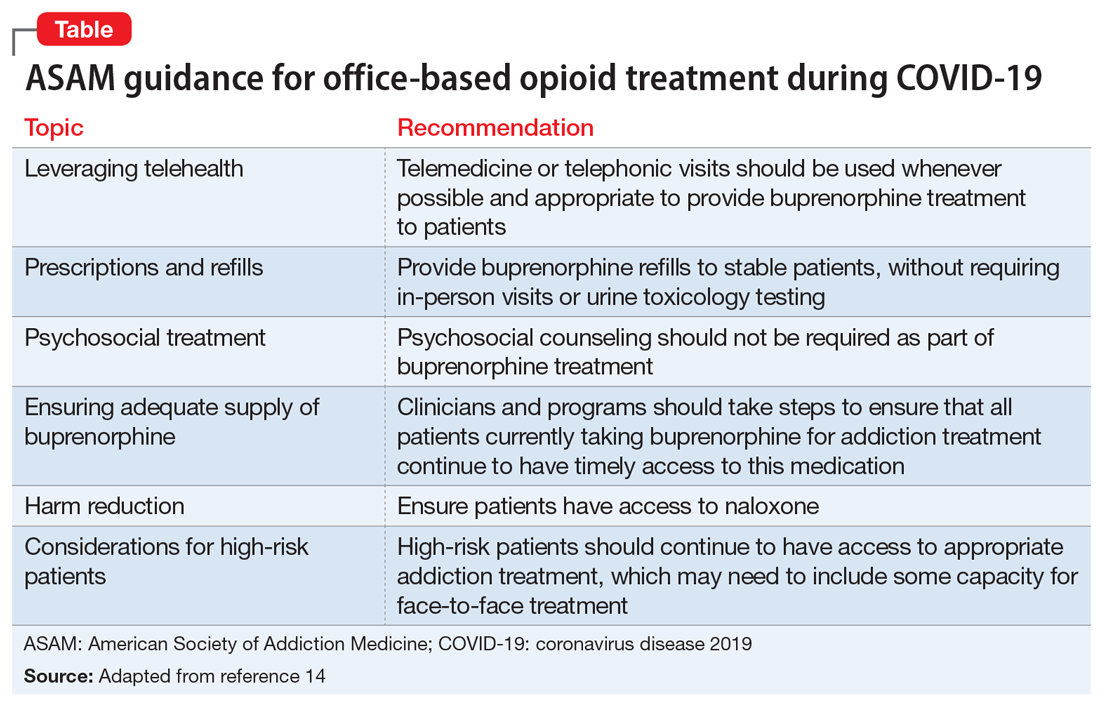
Expand access to treatment
This includes access to MAT (such as buprenorphine/naloxone, methadone, naltrexone, and depot naltrexone) and, equally important, to psychosocial treatment, counseling, and/or recovery services. Recent legislative changes have increased the number of patients that a qualified physician can treat with buprenorphine/naloxone from 100 to 275, and allowed physician extenders to prescribe buprenorphine/naloxone in office-based settings. A recent population-based, retrospective Canadian study showed that opioid agonist treatment decreased the risk of mortality among opioid users, and the protective effects of this treatment increased as fentanyl and other synthetic opioids became common in the illicit drug supply.15 However, because of the shortage of psychiatrists and addiction medicine specialists in several regions of the United States, access to treatment is extremely limited and often inadequate. This constitutes a major public health crisis and contributes to our inability to intervene effectively in the opioid epidemic. Telepsychiatry programs can bring needed services to underserved areas, but they need additional support and development. Further, involving other specialties is paramount for treating this epidemic. Integrating MAT in primary care settings can improve access to treatment. Harm-reduction approaches, such as syringe exchange programs, can play an important role in reducing the adverse consequences associated with heroin use and establish health care relationships with at-risk individuals. Syringe exchange programs can also reduce the rate of infections associated with IV drug use, such as human immunodeficiency virus and hepatitis C virus.
Continue to: Increase education on naloxone...
Increase education on naloxone
Naloxone is a safe and effective opioid antagonist used to treat opioid overdoses. Timely access to naloxone is of the essence when treating opioid-related overdoses. Many states have enacted laws allowing health care professionals, law enforcement officers, and patients and relatives to obtain naloxone without a physician's prescription. It appears this approach may be yielding results. For example, the North Carolina Harm Reduction Coalition distributed >101,000 free overdose rescue kits that included naloxone and recorded 13,392 confirmed cases of overdose rescue with naloxone from 2013 to 2019.16
Divert patients with SUDs from the criminal justice system to treatment
We need to develop programs to divert patients with SUDs from the criminal justice system, which is focused on punishment, to interventions that focus on treatment. Data indicates high recidivism rates for incarcerated individuals with SUDs who do not have access to treatment after they are released. Recognizing this, communities are developing programs that divert low-level offenders from the criminal justice system into treatment. For instance, in Seattle, the Law Enforcement Assisted Diversion is a pilot program developed to divert low-level drug and prostitution offenders into community-based treatment and support services. This helps provide housing, health care, job training, treatment, and mental health support. Innovative programs are needed to provide SUD treatment in the rehabilitation programs of correctional facilities and ensure case managers and discharge planners can transition participants to community treatment programs upon their release.
Develop early identification and prevention programs
These programs should focus on individuals at high risk, such as patients with comorbid SUDs and psychiatric disorders, those with chronic pain, and at-risk children whose parents abuse opiates. Traditional addiction treatment programs typically do not address patients with complex conditions or special populations, such as adolescents or pregnant women with substance use issues. Evidence-based approaches such as Screening, Brief Intervention, and Referral to Treatment (SBIRT), Integrated Dual Diagnosis Treatment (IDDT), and prevention approaches that target students in middle schools and high schools need to be more widely available.
Improve education on opioid prescribing
Responsible opioid prescribing for clinicians should include education about the regular use of prescription drug monitoring programs, urine drug screening, avoiding co-prescription of opioids with sedative-hypnotic medications, and better linkage with addiction treatment.
Treat comorbid psychiatric conditions
It is critical to both identify and effectively treat underlying affective, anxiety, and psychotic disorders in patients with SUDs. Anxiety, depression, and emotional dysregulation often contribute to worsening substance abuse, abuse of prescription drugs, diversion of prescribed drugs, and an increased risk of overdoses and suicides. Effective treatment of comorbid psychiatric conditions also may reduce relapses.
Increase research on causes and treatments
Through research, we must expand our knowledge to better understand the factors that contribute to this epidemic and develop better treatments. These efforts may allow for the development of prevention mechanisms. For example, a recent study found that the continued use of opioid medications after an overdose was associated with a high risk of a repeated overdosecall out material?.17 At the end of a 2-year observation, 17% (confidence interval [CI]: 14% to 20%) of patients receiving a high daily dosage of a prescribed opioid had a repeat overdose compared with 15% (CI: 10% to 21%) of those receiving a moderate dosage, 9% (CI: 6% to 14%) of those receiving a low dosage, and 8% (CI: 6% to 11%) of those receiving no opioids.17 Of the patients who overdosed on prescribed opiates, 30% switched to a new prescriber after their overdose, many of whom may not have been aware of the previous overdose. From a public health perspective, it would make sense for prescribers to know of prior opioid and/or benzodiazepine overdoses. This could be reported by emergency department clinicians, law enforcement, and hospitals into a prescription drug monitoring program, which is readily available to prescribers in most states.
Acknowledgment
The authors thank Scott Proescholdbell, MPH, Injury and Violence Prevention Branch, Chronic Disease and Injury Section, Division of Public Health, North Carolina Department of Health and Human Services, for his assistance.
Bottom Line
The collision of the coronavirus disease 2019 pandemic and the drug overdose epidemic has highlighted the urgent need for health care professionals to optimize care for individuals with substance use disorders. Suggested interventions include enhancing access to medication-assisted treatment and virtual treatment, improving education about naloxone and safe opioid prescribing practices, and diverting at-risk patients from the criminal justice system to interventions that focus on treatment.
Editor's Note: Due to updated statistics from the CDC, the online version of this article has been modified from the version that appears in the printed edition of the January 2021 issue of Current Psychiatry.
Individuals with mental health and substance use disorders (SUDs) are particularly susceptible to negative effects of the coronavirus disease 2019 (COVID-19) pandemic. The collision of the COVID-19 pandemic and the drug overdose epidemic has highlighted the urgent need for physicians, policymakers, and health care professionals to optimize care for individuals with SUDs because they may be particularly vulnerable to the effects of the virus due to compromised respiratory and immune function, and poor social support.1 In this commentary, we highlight the challenges of the drug overdose epidemic, and recommend strategies to mitigate the impact of the COVID-19 pandemic among patients with SUDs.
A crisis exacerbated by COVID-19
The current drug overdose epidemic has become an American public health nightmare. According to preliminary data released by the CDC on December 17, 2020, there were more than 81,000 drug overdose deaths in the United States in the 12 months ending May 2020.2,3 This is the highest number of overdose deaths ever recorded in a 12-month period. The CDC also noted that while overdose deaths were already increasing in the months preceding the COVID-19 pandemic, the latest numbers suggest an acceleration of overdose deaths during the pandemic.
What is causing this significant loss of life? Prescription opioids and illegal opioids such as heroin and illicitly manufactured fentanyl are the main agents associated with overdose deaths. These opioids were responsible for 61% (28,647) of drug overdose deaths in the United States in 2014.4 In 2015, the opioid overdose death rate increased by 15.6%.5
The increase in the number of opioid overdose deaths in part coincides with a sharp increase in the availability and use of heroin. Heroin overdose deaths have more than tripled since 2010, but heroin is not the only opiate involved. Fentanyl, a synthetic, short-acting opioid that is approved for managing pain in patients with advanced cancers, is 50 times more potent than heroin. The abuse of prescribed fentanyl has been accelerating over the past decade, as is the use of illicitly produced fentanyl. Evidence from US Drug Enforcement Administration (DEA) seizure records shows heroin is being adulterated with illicit fentanyl to enhance the potency of the heroin.6,7 Mixing illicit fentanyl with heroin may be contributing to the recent increase in heroin overdose fatalities. According to the CDC, overdose deaths related to synthetic opioids increased 38.4% from the 12-month period leading up to June 2019 compared with the 12-month period leading up to May 2020.2,3 Postmortem studies of individuals who died from a heroin overdose have frequently found the presence of fentanyl along with heroin.8 Overdose deaths involving heroin may be occurring because individuals may be unknowingly using heroin adulterated with fentanyl.9 In addition, carfentanil, a powerful new synthetic fentanyl, has been recently identified in heroin mixtures. Carfentanil is 10,000 times stronger than morphine. Even in miniscule amounts, carfentanil can suppress breathing to the degree that multiple doses of naloxone are needed to restore respirations.
Initial studies indicate that the COVID-19 pandemic has been exacerbating this situation. Wainwright et al10 conducted an analysis of urine drug test results of patients with SUDs from 4 months before and 4 months after COVID-19 was declared a national emergency on March 13, 2020. Compared with before COVID-19, the proportion of specimens testing positive since COVID-19 increased from 3.80% to 7.32% for fentanyl and from 1.29% to 2.09% for heroin.10
A similar drug testing study found that during the pandemic, the proportion of positive results (positivity) increased by 35% for non-prescribed fentanyl and 44% for heroin.11 Positivity for non-prescribed fentanyl increased significantly among patients who tested positive for other drugs, including by 89% for amphetamines; 48% for benzodiazepines; 34% for cocaine; and 39% for opiates (P < .1 for all).11
In a review of electronic medical records, Ochalek et al12 found that the number of nonfatal opioid overdoses in an emergency department in Virginia increased from 102 in March-June 2019 to 227 in March-June 2020. In an issue brief published on October 31, 2020, the American Medical Association reported increase in opioid and other drug-related overdoses in more than 40 states during the COVID-19 pandemic.13
Continue to: Strategies for intervention...
Strategies for intervention
A multi-dimensional approach is needed to protect the public from this growing opioid overdose epidemic. To address this challenging task, we recommend several strategies:
Enhance access to virtual treatment
Even when in-person treatment cannot take place due to COVID-19-related restrictions, it is vital that services are accessible to patients with SUDs during this pandemic. Examples of virtual treatment include:
- Telehealth for medication-assisted treatment (MAT) using buprenorphine (recently updated guidance from the US DEA and Substance Abuse and Mental Health Services Administration [SAMHSA] allows this method of prescribing)
- Teletherapy to prevent relapse
- Remote drug screens by sending saliva or urine kits to patients' homes, visiting patients to collect fluid samples, or asking patients to come to a "drive-through" facility to provide samples
- Virtual (online) Alcoholics Anonymous, Narcotics Anonymous, SMART Recovery, and similar meetings to provide support in the absence of in-person meetings.
The American Society of Addiction Medicine (ASAM) offers guidance to treatment programs to focus on infection control and mitigation. The Table14 summarizes the ASAM recommendations for office-based opioid treatment during COVID-19.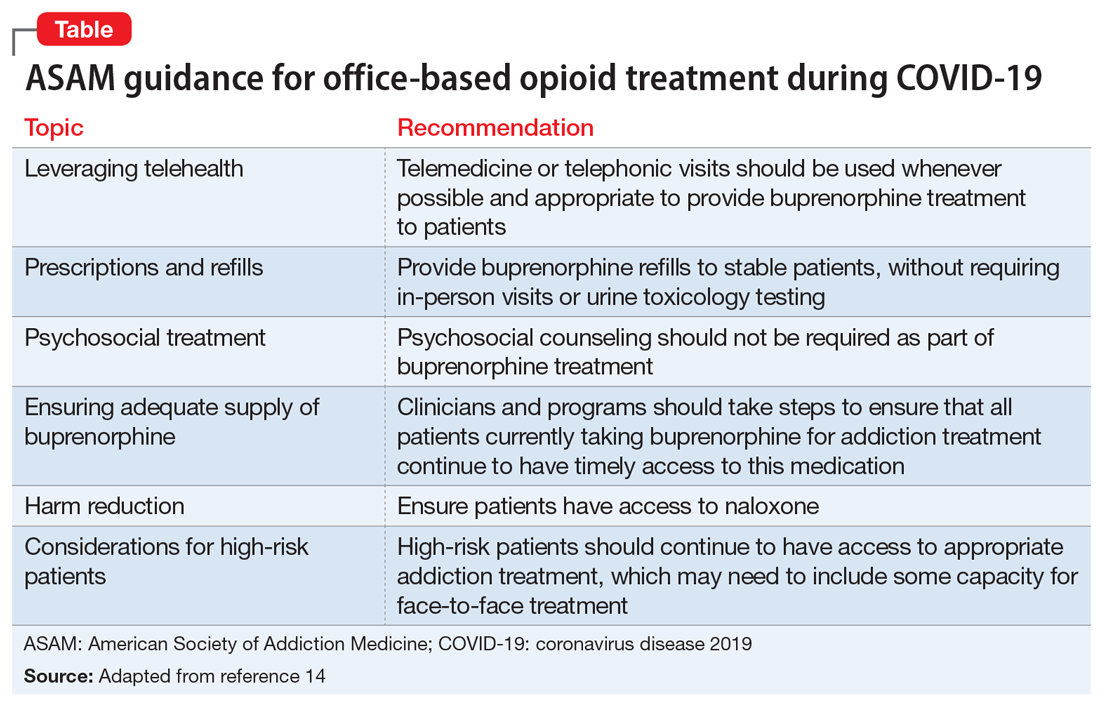
Expand access to treatment
This includes access to MAT (such as buprenorphine/naloxone, methadone, naltrexone, and depot naltrexone) and, equally important, to psychosocial treatment, counseling, and/or recovery services. Recent legislative changes have increased the number of patients that a qualified physician can treat with buprenorphine/naloxone from 100 to 275, and allowed physician extenders to prescribe buprenorphine/naloxone in office-based settings. A recent population-based, retrospective Canadian study showed that opioid agonist treatment decreased the risk of mortality among opioid users, and the protective effects of this treatment increased as fentanyl and other synthetic opioids became common in the illicit drug supply.15 However, because of the shortage of psychiatrists and addiction medicine specialists in several regions of the United States, access to treatment is extremely limited and often inadequate. This constitutes a major public health crisis and contributes to our inability to intervene effectively in the opioid epidemic. Telepsychiatry programs can bring needed services to underserved areas, but they need additional support and development. Further, involving other specialties is paramount for treating this epidemic. Integrating MAT in primary care settings can improve access to treatment. Harm-reduction approaches, such as syringe exchange programs, can play an important role in reducing the adverse consequences associated with heroin use and establish health care relationships with at-risk individuals. Syringe exchange programs can also reduce the rate of infections associated with IV drug use, such as human immunodeficiency virus and hepatitis C virus.
Continue to: Increase education on naloxone...
Increase education on naloxone
Naloxone is a safe and effective opioid antagonist used to treat opioid overdoses. Timely access to naloxone is of the essence when treating opioid-related overdoses. Many states have enacted laws allowing health care professionals, law enforcement officers, and patients and relatives to obtain naloxone without a physician's prescription. It appears this approach may be yielding results. For example, the North Carolina Harm Reduction Coalition distributed >101,000 free overdose rescue kits that included naloxone and recorded 13,392 confirmed cases of overdose rescue with naloxone from 2013 to 2019.16
Divert patients with SUDs from the criminal justice system to treatment
We need to develop programs to divert patients with SUDs from the criminal justice system, which is focused on punishment, to interventions that focus on treatment. Data indicates high recidivism rates for incarcerated individuals with SUDs who do not have access to treatment after they are released. Recognizing this, communities are developing programs that divert low-level offenders from the criminal justice system into treatment. For instance, in Seattle, the Law Enforcement Assisted Diversion is a pilot program developed to divert low-level drug and prostitution offenders into community-based treatment and support services. This helps provide housing, health care, job training, treatment, and mental health support. Innovative programs are needed to provide SUD treatment in the rehabilitation programs of correctional facilities and ensure case managers and discharge planners can transition participants to community treatment programs upon their release.
Develop early identification and prevention programs
These programs should focus on individuals at high risk, such as patients with comorbid SUDs and psychiatric disorders, those with chronic pain, and at-risk children whose parents abuse opiates. Traditional addiction treatment programs typically do not address patients with complex conditions or special populations, such as adolescents or pregnant women with substance use issues. Evidence-based approaches such as Screening, Brief Intervention, and Referral to Treatment (SBIRT), Integrated Dual Diagnosis Treatment (IDDT), and prevention approaches that target students in middle schools and high schools need to be more widely available.
Improve education on opioid prescribing
Responsible opioid prescribing for clinicians should include education about the regular use of prescription drug monitoring programs, urine drug screening, avoiding co-prescription of opioids with sedative-hypnotic medications, and better linkage with addiction treatment.
Treat comorbid psychiatric conditions
It is critical to both identify and effectively treat underlying affective, anxiety, and psychotic disorders in patients with SUDs. Anxiety, depression, and emotional dysregulation often contribute to worsening substance abuse, abuse of prescription drugs, diversion of prescribed drugs, and an increased risk of overdoses and suicides. Effective treatment of comorbid psychiatric conditions also may reduce relapses.
Increase research on causes and treatments
Through research, we must expand our knowledge to better understand the factors that contribute to this epidemic and develop better treatments. These efforts may allow for the development of prevention mechanisms. For example, a recent study found that the continued use of opioid medications after an overdose was associated with a high risk of a repeated overdosecall out material?.17 At the end of a 2-year observation, 17% (confidence interval [CI]: 14% to 20%) of patients receiving a high daily dosage of a prescribed opioid had a repeat overdose compared with 15% (CI: 10% to 21%) of those receiving a moderate dosage, 9% (CI: 6% to 14%) of those receiving a low dosage, and 8% (CI: 6% to 11%) of those receiving no opioids.17 Of the patients who overdosed on prescribed opiates, 30% switched to a new prescriber after their overdose, many of whom may not have been aware of the previous overdose. From a public health perspective, it would make sense for prescribers to know of prior opioid and/or benzodiazepine overdoses. This could be reported by emergency department clinicians, law enforcement, and hospitals into a prescription drug monitoring program, which is readily available to prescribers in most states.
Acknowledgment
The authors thank Scott Proescholdbell, MPH, Injury and Violence Prevention Branch, Chronic Disease and Injury Section, Division of Public Health, North Carolina Department of Health and Human Services, for his assistance.
Bottom Line
The collision of the coronavirus disease 2019 pandemic and the drug overdose epidemic has highlighted the urgent need for health care professionals to optimize care for individuals with substance use disorders. Suggested interventions include enhancing access to medication-assisted treatment and virtual treatment, improving education about naloxone and safe opioid prescribing practices, and diverting at-risk patients from the criminal justice system to interventions that focus on treatment.
1. Volkow ND. Collision of the COVID-19 and addiction epidemics. Ann Intern Med. 2020;173(1):61-62.
2.Centers for Disease Control and Prevention. Overdose deaths accelerating during COVID-19. Accessed December 23, 2020. https://www.cdc.gov/media/releases/2020/p1218-overdose-deaths-covid-19.html
3.Centers for Disease Control and Prevention. National Center for Health Statistics Vital Statistics Rapid Release. Provisional drug overdose death counts. Accessed December 30, 2020. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
4.Rudd RA, Aleshire N, Zibbell JE, et al. Increases in drug and opioid overdose deaths -- United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2016;64(50-51):1378-1382.
5.Rudd RA, Seth P, David F, et al. Increases in drug and opioid-involved overdose deaths -- United States, 2010-2015. MMWR Morb Mortal Wkly Rep. 2016;65(50-51):1445-1452.
6.US Drug Enforcement Administration. DEA issues nationwide alert on fentanyl as threat to health and public safety. Published March 19, 2015. Accessed October 28, 2020. http://www.dea.gov/divisions/hq/2015/hq031815.shtml
7.Gladden RM, Martinez P, Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-involved overdose deaths - 27 states, 2013-2014. MMWR Morb Mortal Wkly Rep. 2016;65(33):837-843.
8.Algren DA, Monteilh CP, Punja M, et al. Fentanyl-associated fatalities among illicit drug users in Wayne County, Michigan (July 2005-May 2006). J Med Toxicol. 2013;9(1):106-115.
9.Centers for Disease Control and Prevention. Increases in fentanyl drug confiscations and fentanyl-related overdose fatalities. HAN Health Advisory. Published October 26, 2015. Accessed October 28, 2020. http://emergency.cdc.gov/han/han00384.asp
10.Wainwright JJ, Mikre M, Whitley P, et al. Analysis of drug test results before and after the us declaration of a national emergency concerning the COVID-19 outbreak. JAMA. 2020;324(16):1674-1677.
11.Niles JK, Gudin J, Radliff J, et al. The opioid epidemic within the COVID-19 pandemic: drug testing in 2020 [published online October 8, 2020]. Population Health Management. doi: 10.1089/pop.2020.0230
12.Ochalek TA, Cumpston KL, Wills BK, et al. Nonfatal opioid overdoses at an urban emergency department during the COVID-19 pandemic. JAMA. 2020;324(16):1673-1674.
13.American Medical Association. Issue brief: reports of increases in opioid- and other drug-related overdose and other concerns during COVID pandemic. Published October 31, 2020. Accessed November 9, 2020. https://www.ama-assn.org/system/files/2020-11/issue-brief-increases-in-opioid-related-overdose.pdf
14.American Society of Addiction Medicine. Caring for patients during the COVID-19 pandemic: ASAM COVID-19 Task Force recommendations. Accessed October 30, 2020. https://www.asam.org/docs/default-source/covid-19/medication-formulation-and-dosage-guidance-(1).pdf
15.Pearce LA, Min JE, Piske M, et al. Opioid agonist treatment and risk of mortality during opioid overdose public health emergency: population based retrospective cohort study. BMJ. 2020;368:m772. doi: 10.1136/bmj.m772
16.North Carolina Harm Reduction Coalition. NCHRC'S community-based overdose prevention project. Accessed March 29, 2020. http://www.nchrc.org/programs-and-services
17.Larochelle MR, Liebschutz JM, Zhang F, et al. Opioid prescribing after nonfatal overdose and association with repeated overdose: a cohort study. Ann Intern Med. 2016;164(1):1-9.
1. Volkow ND. Collision of the COVID-19 and addiction epidemics. Ann Intern Med. 2020;173(1):61-62.
2.Centers for Disease Control and Prevention. Overdose deaths accelerating during COVID-19. Accessed December 23, 2020. https://www.cdc.gov/media/releases/2020/p1218-overdose-deaths-covid-19.html
3.Centers for Disease Control and Prevention. National Center for Health Statistics Vital Statistics Rapid Release. Provisional drug overdose death counts. Accessed December 30, 2020. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
4.Rudd RA, Aleshire N, Zibbell JE, et al. Increases in drug and opioid overdose deaths -- United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2016;64(50-51):1378-1382.
5.Rudd RA, Seth P, David F, et al. Increases in drug and opioid-involved overdose deaths -- United States, 2010-2015. MMWR Morb Mortal Wkly Rep. 2016;65(50-51):1445-1452.
6.US Drug Enforcement Administration. DEA issues nationwide alert on fentanyl as threat to health and public safety. Published March 19, 2015. Accessed October 28, 2020. http://www.dea.gov/divisions/hq/2015/hq031815.shtml
7.Gladden RM, Martinez P, Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-involved overdose deaths - 27 states, 2013-2014. MMWR Morb Mortal Wkly Rep. 2016;65(33):837-843.
8.Algren DA, Monteilh CP, Punja M, et al. Fentanyl-associated fatalities among illicit drug users in Wayne County, Michigan (July 2005-May 2006). J Med Toxicol. 2013;9(1):106-115.
9.Centers for Disease Control and Prevention. Increases in fentanyl drug confiscations and fentanyl-related overdose fatalities. HAN Health Advisory. Published October 26, 2015. Accessed October 28, 2020. http://emergency.cdc.gov/han/han00384.asp
10.Wainwright JJ, Mikre M, Whitley P, et al. Analysis of drug test results before and after the us declaration of a national emergency concerning the COVID-19 outbreak. JAMA. 2020;324(16):1674-1677.
11.Niles JK, Gudin J, Radliff J, et al. The opioid epidemic within the COVID-19 pandemic: drug testing in 2020 [published online October 8, 2020]. Population Health Management. doi: 10.1089/pop.2020.0230
12.Ochalek TA, Cumpston KL, Wills BK, et al. Nonfatal opioid overdoses at an urban emergency department during the COVID-19 pandemic. JAMA. 2020;324(16):1673-1674.
13.American Medical Association. Issue brief: reports of increases in opioid- and other drug-related overdose and other concerns during COVID pandemic. Published October 31, 2020. Accessed November 9, 2020. https://www.ama-assn.org/system/files/2020-11/issue-brief-increases-in-opioid-related-overdose.pdf
14.American Society of Addiction Medicine. Caring for patients during the COVID-19 pandemic: ASAM COVID-19 Task Force recommendations. Accessed October 30, 2020. https://www.asam.org/docs/default-source/covid-19/medication-formulation-and-dosage-guidance-(1).pdf
15.Pearce LA, Min JE, Piske M, et al. Opioid agonist treatment and risk of mortality during opioid overdose public health emergency: population based retrospective cohort study. BMJ. 2020;368:m772. doi: 10.1136/bmj.m772
16.North Carolina Harm Reduction Coalition. NCHRC'S community-based overdose prevention project. Accessed March 29, 2020. http://www.nchrc.org/programs-and-services
17.Larochelle MR, Liebschutz JM, Zhang F, et al. Opioid prescribing after nonfatal overdose and association with repeated overdose: a cohort study. Ann Intern Med. 2016;164(1):1-9.