User login
Opioid use curbed with patient education and lower prescription quantities
Patients given lower prescription quantities of opioid tablets with and without opioid education used significantly less of the medication compared with those given more tablets and no education, according to data from 264 adults and adolescents who underwent anterior cruciate ligament (ACL) surgery.
Although lower default prescription programs have been shown to reduce the number of tablets prescribed, “the effect of reduced prescription quantities on actual patient opioid consumption remains undetermined,” wrote Kevin X. Farley, BS, of Emory University, Atlanta, and colleagues.
In a study published in JAMA, the researchers examined whether patients took fewer tablets if given fewer, and whether patient education about opioids further reduced the number of tablets taken.
The study population included adults and adolescents who underwent ACL surgery at a single center. The patients were divided into three groups: 109 patients received 50 opioid tablets after surgery, 78 received 30 tablets plus education prior to surgery about appropriate opioid use and alternative pain management, and 77 received 30 tablets but no education on opioid use.
Patients given 50 tablets consumed an average of 25 tablets for an average of 5.8 days. By contrast, patients given 30 tablets but no opioid education consumed an average of 16 tablets for an average of 4.5 days, and those given 30 tablets and preoperative education consumed an average of 12 tablets for an average of 3.5 days.
In addition, patients given 30 tablets reported lower levels of constipation and fatigue compared with patients given 50 tablets. No differences were seen in medication refills among the groups.
The findings were limited by several factors including the use of data from a single center, the lack of randomization, and the potential for recall bias, the researchers noted. However, the results suggest that prescribing fewer tablets may further reduce use, as each group consumed approximately half of the tablets given, the researchers added.
“Further investigation should evaluate whether similar opioid stewardship and education protocols would be successful in other patient populations,” they said.
Corresponding author John Xerogeanes, MD, disclosed personal fees from Arthrex and stock options from Trice. The other researchers had no financial conflicts to disclose.
Patients given lower prescription quantities of opioid tablets with and without opioid education used significantly less of the medication compared with those given more tablets and no education, according to data from 264 adults and adolescents who underwent anterior cruciate ligament (ACL) surgery.
Although lower default prescription programs have been shown to reduce the number of tablets prescribed, “the effect of reduced prescription quantities on actual patient opioid consumption remains undetermined,” wrote Kevin X. Farley, BS, of Emory University, Atlanta, and colleagues.
In a study published in JAMA, the researchers examined whether patients took fewer tablets if given fewer, and whether patient education about opioids further reduced the number of tablets taken.
The study population included adults and adolescents who underwent ACL surgery at a single center. The patients were divided into three groups: 109 patients received 50 opioid tablets after surgery, 78 received 30 tablets plus education prior to surgery about appropriate opioid use and alternative pain management, and 77 received 30 tablets but no education on opioid use.
Patients given 50 tablets consumed an average of 25 tablets for an average of 5.8 days. By contrast, patients given 30 tablets but no opioid education consumed an average of 16 tablets for an average of 4.5 days, and those given 30 tablets and preoperative education consumed an average of 12 tablets for an average of 3.5 days.
In addition, patients given 30 tablets reported lower levels of constipation and fatigue compared with patients given 50 tablets. No differences were seen in medication refills among the groups.
The findings were limited by several factors including the use of data from a single center, the lack of randomization, and the potential for recall bias, the researchers noted. However, the results suggest that prescribing fewer tablets may further reduce use, as each group consumed approximately half of the tablets given, the researchers added.
“Further investigation should evaluate whether similar opioid stewardship and education protocols would be successful in other patient populations,” they said.
Corresponding author John Xerogeanes, MD, disclosed personal fees from Arthrex and stock options from Trice. The other researchers had no financial conflicts to disclose.
Patients given lower prescription quantities of opioid tablets with and without opioid education used significantly less of the medication compared with those given more tablets and no education, according to data from 264 adults and adolescents who underwent anterior cruciate ligament (ACL) surgery.
Although lower default prescription programs have been shown to reduce the number of tablets prescribed, “the effect of reduced prescription quantities on actual patient opioid consumption remains undetermined,” wrote Kevin X. Farley, BS, of Emory University, Atlanta, and colleagues.
In a study published in JAMA, the researchers examined whether patients took fewer tablets if given fewer, and whether patient education about opioids further reduced the number of tablets taken.
The study population included adults and adolescents who underwent ACL surgery at a single center. The patients were divided into three groups: 109 patients received 50 opioid tablets after surgery, 78 received 30 tablets plus education prior to surgery about appropriate opioid use and alternative pain management, and 77 received 30 tablets but no education on opioid use.
Patients given 50 tablets consumed an average of 25 tablets for an average of 5.8 days. By contrast, patients given 30 tablets but no opioid education consumed an average of 16 tablets for an average of 4.5 days, and those given 30 tablets and preoperative education consumed an average of 12 tablets for an average of 3.5 days.
In addition, patients given 30 tablets reported lower levels of constipation and fatigue compared with patients given 50 tablets. No differences were seen in medication refills among the groups.
The findings were limited by several factors including the use of data from a single center, the lack of randomization, and the potential for recall bias, the researchers noted. However, the results suggest that prescribing fewer tablets may further reduce use, as each group consumed approximately half of the tablets given, the researchers added.
“Further investigation should evaluate whether similar opioid stewardship and education protocols would be successful in other patient populations,” they said.
Corresponding author John Xerogeanes, MD, disclosed personal fees from Arthrex and stock options from Trice. The other researchers had no financial conflicts to disclose.
FROM JAMA
Key clinical point: Patient education and fewer tablets prescribed significantly reduced the amount of opioid tablets taken compared with no education and more tablets prescribed.
Major finding: Patients given 50 tablets and no patient education, 30 tablets and no patient education, and 30 tablets plus education consumed an average of 25, 16, and 12 tablets, respectively.
Study details: The data come from 264 adolescents and adults who underwent ACL surgery at a single center.
Disclosures: Corresponding author John Xerogeanes, MD, disclosed personal fees from Arthrex and stock options from Trice. The other researchers had no financial conflicts to disclose.
Source: Farley KX et al. JAMA. 2019 June 25.321(24):2465-7.
Penicillin-susceptible Streptococcus pneumoniae most common cause of bacteremic CAP
A study found that only 2% of children hospitalized with community-acquired pneumonia (CAP) actually had any causative pathogen in their blood culture results, despite national guidelines that recommend blood cultures for all children hospitalized with moderate to severe CAP.

The guidelines are the 2011 guidelines for managing CAP published by the Pediatric Infectious Diseases Society (PIDS) and the Infectious Diseases Society of America (IDSA) (Clin Infect Dis. 2011 Oct;53[7]:617-30).
Cristin O. Fritz, MD, of the Children’s Hospital of Colorado, Aurora, and associates conducted a data analysis of the EPIC (Etiology of Pneumonia in the Community) study to estimate prevalence, risk factors, and clinical outcomes in children hospitalized with bacteremic CAP and to evaluate the relationship between positive blood culture results, empirical antibiotics, and changes in antibiotic treatment regimens.
Data were collected at two Tennessee hospitals and one Utah hospital during Jan. 1, 2010–June 30, 2012. Of the 2,358 children with CAP enrolled in the study, 2,143 (91%) with blood cultures were included in Dr. Fritz’s analysis. Of the 53 patients presenting with positive blood culture results, 46 (2%; 95% confidence interval: 1.6%-2.9%) were identified as having bacteremia. Half of all cases observed were caused by Streptococcus pneumoniae, with Staphylococcus aureus and Streptococcus pyogenes noted less frequently, according to the study published in Pediatrics.
A previous meta-analysis of smaller studies also found that children with CAP rarely had positive blood culture results, a pooled prevalence of 5% (Pediatr Infect Dis J. 2013;32[7]:736-40). Although it is believed that positive blood culture results are key to narrowing the choice of antibiotic and predicting treatment outcomes, the literature – to date – reveals a paucity of data supporting this assumption.
Overall, children in the study presenting with bacteremia experienced more severe clinical outcomes, including longer length of stay, greater likelihood of ICU admission, and invasive mechanical ventilation and/or shock. The authors also observed that bacteremia was less likely to be detected in children given antibiotics after admission but before cultures were obtained (0.8% vs 3%; P = .021). Pleural effusion detected with chest radiograph also consistently indicated bacteremic pneumonia, an observation made within this and other similar studies.
Also of note in detection is the biomarker procalcitonin, which is typically present with bacterial disease. Dr. Fritz and colleagues stressed that because the procalcitonin rate was higher in patients presenting with bacteremia, “this information could influence decisions around culturing if results are rapidly available.” Risk-stratification tools also might serve a valuable purpose in ferreting out those patients presenting with moderate to severe pneumonia most at increased risk for bacterial CAP.
Compared with other studies reporting prevalence ranges of 1%-7%, the prevalence of bacteremia in this study is lower at 2%. The authors attributed the difference to a possible potential limitation with the other studies, for which culture data was only available for a median 47% of enrollees. Dr. Fritz and her colleagues caution that “because cultures were obtained at the discretion of the treating clinician in a majority of studies, blood cultures were likely obtained more often in those with more severe illness or who had not already received antibiotics.” In this scenario, the likelihood that prevalence of bacteremia was overestimated is noteworthy.
The authors observed that penicillin-susceptible S. pneumonia was the most common cause of bacteremic CAP. They further acknowledged that their study and findings by Neuman et al. in 2017 give credence to the joint 2011 PIDS/IDSA guideline recommending narrow-spectrum aminopenicillins specifically to treat children hospitalized due to suspected bacterial CAP.
Despite its small sample size, the results of this study clearly demonstrate that children with bacteremia because of S. pyogenes or S. aureus experience increased morbidity, compared with children with S. pneumoniae, they said
While this is acknowledged to be one of the largest studies of its kind to date, a key limitation was the small number of observable patients with bacteremia, which prevented the researchers from conducting a more in-depth analysis of risk factors and pathogen-specific differences. That one-fourth of patients received in-patient antibiotics before cultures could be collected also likely led to an underestimation of risk factors and misclassification bias. Lastly, the use of blood culture instead of whole-blood polymerase chain reaction, which is known to be more sensitive, also may have led to underestimation of overall bacteremia prevalence.
“In an era with widespread pneumococcal vaccination and low prevalence of bacteremia in the United States, noted Dr. Fritz and associates.
Dr. Fritz had no conflicts of interest to report. Some coauthors cited multiple sources of potential conflict of interest related to consulting fees, grant support, and research support from various pharmaceutical companies and agencies. The study was funded by the National Institutes of Health and in part by a grant from the National Institute of Allergy and Infectious Diseases.
SOURCE: Fritz C et al. Pediatrics. 2019;144(1):e20183090.
A study found that only 2% of children hospitalized with community-acquired pneumonia (CAP) actually had any causative pathogen in their blood culture results, despite national guidelines that recommend blood cultures for all children hospitalized with moderate to severe CAP.

The guidelines are the 2011 guidelines for managing CAP published by the Pediatric Infectious Diseases Society (PIDS) and the Infectious Diseases Society of America (IDSA) (Clin Infect Dis. 2011 Oct;53[7]:617-30).
Cristin O. Fritz, MD, of the Children’s Hospital of Colorado, Aurora, and associates conducted a data analysis of the EPIC (Etiology of Pneumonia in the Community) study to estimate prevalence, risk factors, and clinical outcomes in children hospitalized with bacteremic CAP and to evaluate the relationship between positive blood culture results, empirical antibiotics, and changes in antibiotic treatment regimens.
Data were collected at two Tennessee hospitals and one Utah hospital during Jan. 1, 2010–June 30, 2012. Of the 2,358 children with CAP enrolled in the study, 2,143 (91%) with blood cultures were included in Dr. Fritz’s analysis. Of the 53 patients presenting with positive blood culture results, 46 (2%; 95% confidence interval: 1.6%-2.9%) were identified as having bacteremia. Half of all cases observed were caused by Streptococcus pneumoniae, with Staphylococcus aureus and Streptococcus pyogenes noted less frequently, according to the study published in Pediatrics.
A previous meta-analysis of smaller studies also found that children with CAP rarely had positive blood culture results, a pooled prevalence of 5% (Pediatr Infect Dis J. 2013;32[7]:736-40). Although it is believed that positive blood culture results are key to narrowing the choice of antibiotic and predicting treatment outcomes, the literature – to date – reveals a paucity of data supporting this assumption.
Overall, children in the study presenting with bacteremia experienced more severe clinical outcomes, including longer length of stay, greater likelihood of ICU admission, and invasive mechanical ventilation and/or shock. The authors also observed that bacteremia was less likely to be detected in children given antibiotics after admission but before cultures were obtained (0.8% vs 3%; P = .021). Pleural effusion detected with chest radiograph also consistently indicated bacteremic pneumonia, an observation made within this and other similar studies.
Also of note in detection is the biomarker procalcitonin, which is typically present with bacterial disease. Dr. Fritz and colleagues stressed that because the procalcitonin rate was higher in patients presenting with bacteremia, “this information could influence decisions around culturing if results are rapidly available.” Risk-stratification tools also might serve a valuable purpose in ferreting out those patients presenting with moderate to severe pneumonia most at increased risk for bacterial CAP.
Compared with other studies reporting prevalence ranges of 1%-7%, the prevalence of bacteremia in this study is lower at 2%. The authors attributed the difference to a possible potential limitation with the other studies, for which culture data was only available for a median 47% of enrollees. Dr. Fritz and her colleagues caution that “because cultures were obtained at the discretion of the treating clinician in a majority of studies, blood cultures were likely obtained more often in those with more severe illness or who had not already received antibiotics.” In this scenario, the likelihood that prevalence of bacteremia was overestimated is noteworthy.
The authors observed that penicillin-susceptible S. pneumonia was the most common cause of bacteremic CAP. They further acknowledged that their study and findings by Neuman et al. in 2017 give credence to the joint 2011 PIDS/IDSA guideline recommending narrow-spectrum aminopenicillins specifically to treat children hospitalized due to suspected bacterial CAP.
Despite its small sample size, the results of this study clearly demonstrate that children with bacteremia because of S. pyogenes or S. aureus experience increased morbidity, compared with children with S. pneumoniae, they said
While this is acknowledged to be one of the largest studies of its kind to date, a key limitation was the small number of observable patients with bacteremia, which prevented the researchers from conducting a more in-depth analysis of risk factors and pathogen-specific differences. That one-fourth of patients received in-patient antibiotics before cultures could be collected also likely led to an underestimation of risk factors and misclassification bias. Lastly, the use of blood culture instead of whole-blood polymerase chain reaction, which is known to be more sensitive, also may have led to underestimation of overall bacteremia prevalence.
“In an era with widespread pneumococcal vaccination and low prevalence of bacteremia in the United States, noted Dr. Fritz and associates.
Dr. Fritz had no conflicts of interest to report. Some coauthors cited multiple sources of potential conflict of interest related to consulting fees, grant support, and research support from various pharmaceutical companies and agencies. The study was funded by the National Institutes of Health and in part by a grant from the National Institute of Allergy and Infectious Diseases.
SOURCE: Fritz C et al. Pediatrics. 2019;144(1):e20183090.
A study found that only 2% of children hospitalized with community-acquired pneumonia (CAP) actually had any causative pathogen in their blood culture results, despite national guidelines that recommend blood cultures for all children hospitalized with moderate to severe CAP.

The guidelines are the 2011 guidelines for managing CAP published by the Pediatric Infectious Diseases Society (PIDS) and the Infectious Diseases Society of America (IDSA) (Clin Infect Dis. 2011 Oct;53[7]:617-30).
Cristin O. Fritz, MD, of the Children’s Hospital of Colorado, Aurora, and associates conducted a data analysis of the EPIC (Etiology of Pneumonia in the Community) study to estimate prevalence, risk factors, and clinical outcomes in children hospitalized with bacteremic CAP and to evaluate the relationship between positive blood culture results, empirical antibiotics, and changes in antibiotic treatment regimens.
Data were collected at two Tennessee hospitals and one Utah hospital during Jan. 1, 2010–June 30, 2012. Of the 2,358 children with CAP enrolled in the study, 2,143 (91%) with blood cultures were included in Dr. Fritz’s analysis. Of the 53 patients presenting with positive blood culture results, 46 (2%; 95% confidence interval: 1.6%-2.9%) were identified as having bacteremia. Half of all cases observed were caused by Streptococcus pneumoniae, with Staphylococcus aureus and Streptococcus pyogenes noted less frequently, according to the study published in Pediatrics.
A previous meta-analysis of smaller studies also found that children with CAP rarely had positive blood culture results, a pooled prevalence of 5% (Pediatr Infect Dis J. 2013;32[7]:736-40). Although it is believed that positive blood culture results are key to narrowing the choice of antibiotic and predicting treatment outcomes, the literature – to date – reveals a paucity of data supporting this assumption.
Overall, children in the study presenting with bacteremia experienced more severe clinical outcomes, including longer length of stay, greater likelihood of ICU admission, and invasive mechanical ventilation and/or shock. The authors also observed that bacteremia was less likely to be detected in children given antibiotics after admission but before cultures were obtained (0.8% vs 3%; P = .021). Pleural effusion detected with chest radiograph also consistently indicated bacteremic pneumonia, an observation made within this and other similar studies.
Also of note in detection is the biomarker procalcitonin, which is typically present with bacterial disease. Dr. Fritz and colleagues stressed that because the procalcitonin rate was higher in patients presenting with bacteremia, “this information could influence decisions around culturing if results are rapidly available.” Risk-stratification tools also might serve a valuable purpose in ferreting out those patients presenting with moderate to severe pneumonia most at increased risk for bacterial CAP.
Compared with other studies reporting prevalence ranges of 1%-7%, the prevalence of bacteremia in this study is lower at 2%. The authors attributed the difference to a possible potential limitation with the other studies, for which culture data was only available for a median 47% of enrollees. Dr. Fritz and her colleagues caution that “because cultures were obtained at the discretion of the treating clinician in a majority of studies, blood cultures were likely obtained more often in those with more severe illness or who had not already received antibiotics.” In this scenario, the likelihood that prevalence of bacteremia was overestimated is noteworthy.
The authors observed that penicillin-susceptible S. pneumonia was the most common cause of bacteremic CAP. They further acknowledged that their study and findings by Neuman et al. in 2017 give credence to the joint 2011 PIDS/IDSA guideline recommending narrow-spectrum aminopenicillins specifically to treat children hospitalized due to suspected bacterial CAP.
Despite its small sample size, the results of this study clearly demonstrate that children with bacteremia because of S. pyogenes or S. aureus experience increased morbidity, compared with children with S. pneumoniae, they said
While this is acknowledged to be one of the largest studies of its kind to date, a key limitation was the small number of observable patients with bacteremia, which prevented the researchers from conducting a more in-depth analysis of risk factors and pathogen-specific differences. That one-fourth of patients received in-patient antibiotics before cultures could be collected also likely led to an underestimation of risk factors and misclassification bias. Lastly, the use of blood culture instead of whole-blood polymerase chain reaction, which is known to be more sensitive, also may have led to underestimation of overall bacteremia prevalence.
“In an era with widespread pneumococcal vaccination and low prevalence of bacteremia in the United States, noted Dr. Fritz and associates.
Dr. Fritz had no conflicts of interest to report. Some coauthors cited multiple sources of potential conflict of interest related to consulting fees, grant support, and research support from various pharmaceutical companies and agencies. The study was funded by the National Institutes of Health and in part by a grant from the National Institute of Allergy and Infectious Diseases.
SOURCE: Fritz C et al. Pediatrics. 2019;144(1):e20183090.
FROM PEDIATRICS
Patients concerned about clinician burnout
Almost three-quarters of Americans are concerned about burnout among health care professionals, according to the American Society of Health-System Pharmacists.
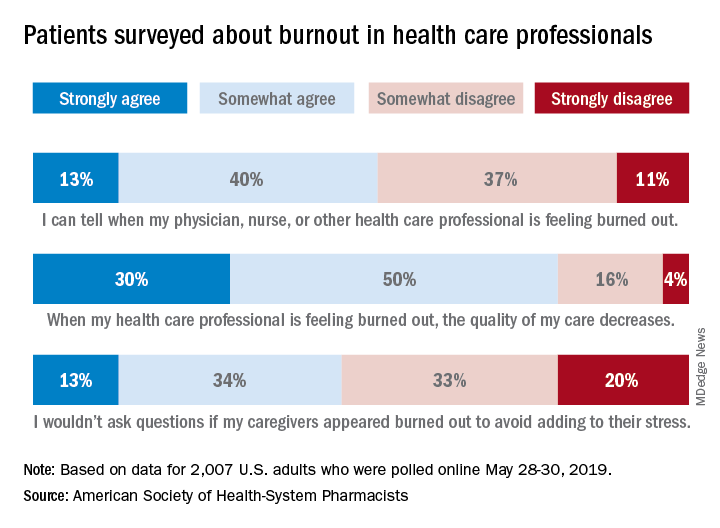
The public is aware “that burnout among pharmacists, physicians, nurses, and other professionals can lead to impaired attention and decreased functioning that threatens to cause medical errors and reduce safety,” the ASHP said when it released data from a survey conducted May 28-30, 2019, by the Harris Poll.
Those data show that 23% of respondents were very concerned and 51% were somewhat concerned about burnout among health care providers. Just over half (53%) of the 2,007 adults involved said that they could tell when a provider was burned out, suggesting that health care professionals “may be conveying signs of burnout to their patients without knowing it,” the society noted.
A majority of respondents (80%) felt that the quality of their care was affected when their physician, nurse, pharmacist, or other health care professional was burned out, and almost half (47%) said that they would avoid asking questions if their provider appeared burned out because they wouldn’t want to add to that person’s stress, the ASHP said.
“A healthy and thriving clinician workforce is essential to ensure optimal patient health outcomes and safety,” said Paul W. Abramowitz, PharmD, chief executive officer of the ASHP. “Within the healthcare industry, we are working to help build a culture of resilience and well-being to ensure that no patient or clinician is harmed due to burnout; but it takes a concerted effort from all entities involved – providers and healthcare organizations.”
Almost three-quarters of Americans are concerned about burnout among health care professionals, according to the American Society of Health-System Pharmacists.
The public is aware “that burnout among pharmacists, physicians, nurses, and other professionals can lead to impaired attention and decreased functioning that threatens to cause medical errors and reduce safety,” the ASHP said when it released data from a survey conducted May 28-30, 2019, by the Harris Poll.
Those data show that 23% of respondents were very concerned and 51% were somewhat concerned about burnout among health care providers. Just over half (53%) of the 2,007 adults involved said that they could tell when a provider was burned out, suggesting that health care professionals “may be conveying signs of burnout to their patients without knowing it,” the society noted.
A majority of respondents (80%) felt that the quality of their care was affected when their physician, nurse, pharmacist, or other health care professional was burned out, and almost half (47%) said that they would avoid asking questions if their provider appeared burned out because they wouldn’t want to add to that person’s stress, the ASHP said.
“A healthy and thriving clinician workforce is essential to ensure optimal patient health outcomes and safety,” said Paul W. Abramowitz, PharmD, chief executive officer of the ASHP. “Within the healthcare industry, we are working to help build a culture of resilience and well-being to ensure that no patient or clinician is harmed due to burnout; but it takes a concerted effort from all entities involved – providers and healthcare organizations.”
Almost three-quarters of Americans are concerned about burnout among health care professionals, according to the American Society of Health-System Pharmacists.
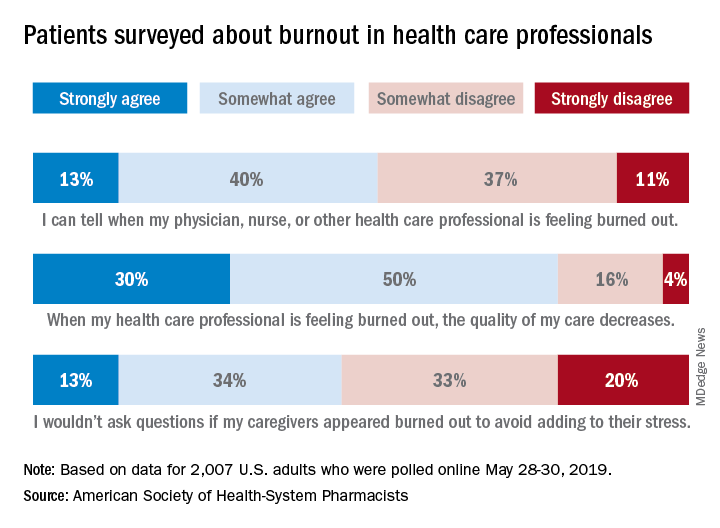
The public is aware “that burnout among pharmacists, physicians, nurses, and other professionals can lead to impaired attention and decreased functioning that threatens to cause medical errors and reduce safety,” the ASHP said when it released data from a survey conducted May 28-30, 2019, by the Harris Poll.
Those data show that 23% of respondents were very concerned and 51% were somewhat concerned about burnout among health care providers. Just over half (53%) of the 2,007 adults involved said that they could tell when a provider was burned out, suggesting that health care professionals “may be conveying signs of burnout to their patients without knowing it,” the society noted.
A majority of respondents (80%) felt that the quality of their care was affected when their physician, nurse, pharmacist, or other health care professional was burned out, and almost half (47%) said that they would avoid asking questions if their provider appeared burned out because they wouldn’t want to add to that person’s stress, the ASHP said.
“A healthy and thriving clinician workforce is essential to ensure optimal patient health outcomes and safety,” said Paul W. Abramowitz, PharmD, chief executive officer of the ASHP. “Within the healthcare industry, we are working to help build a culture of resilience and well-being to ensure that no patient or clinician is harmed due to burnout; but it takes a concerted effort from all entities involved – providers and healthcare organizations.”
New single-dose influenza therapy effective among outpatients
Clinical question: Is baloxavir marboxil, a selective inhibitor of influenza cap-dependent endonuclease, a safe and effective treatment for acute uncomplicated influenza?
Background: The emergence of oseltamivir-resistant influenza A(H1NI) infection in 2007 highlights the risk of future neuraminidase-resistant global pandemics. Baloxavir represents a new class of antiviral agent that may help treat such outbreaks.
Study design: Phase 3 randomized, double-blind, placebo-controlled trial.
Setting: Outpatients in the United States and Japan.
Synopsis: The trial recruited 1,436 otherwise healthy patients aged 12-64 years of age (median age, 33 years) with a clinical diagnosis of acute uncomplicated influenza pneumonia. The patients were randomly assigned to receive either a single dose of oral baloxavir, oseltamivir 75 mg twice daily for 5 days, or matching placebo within 48 hours of symptom onset. The primary outcome was patient self-assessment of symptomatology.
Among the 1,064 adult patients (age 20-64) with influenza diagnosis confirmed by reverse transcription polymerase chain reaction (RT-PCR), the median time to alleviation of symptoms was lower in the baloxavir group than it was in the placebo group (53.7 hours vs. 80.2 hours; P less than .001). There was no significant difference in time to alleviation of symptoms in the baloxavir group when compared with the oseltamivir group. Adverse events were reported in 21% of baloxavir patients, 25% of placebo patients, and 25% of oseltamivir patients.
The enrolled patients were predominantly young, healthy, and treated as an outpatient. Patients hospitalized with influenza pneumonia are often older, have significant comorbidities, and are at higher risk of poor outcomes. This trial does not directly support the safety or efficacy of baloxavir in this population.
Bottom line: A single dose of baloxavir provides similar clinical benefit as 5 days of oseltamivir therapy in the early treatment of healthy patients with acute influenza.
Citation: Hayden FG et al. Baloxavir marboxil for uncomplicated influenza in adults and adolescents. N Eng J Med. 2018:379(10):914-23.
Dr. Holzer is an assistant professor of medicine in the division of hospital medicine at Mount Sinai Hospital, New York.
Clinical question: Is baloxavir marboxil, a selective inhibitor of influenza cap-dependent endonuclease, a safe and effective treatment for acute uncomplicated influenza?
Background: The emergence of oseltamivir-resistant influenza A(H1NI) infection in 2007 highlights the risk of future neuraminidase-resistant global pandemics. Baloxavir represents a new class of antiviral agent that may help treat such outbreaks.
Study design: Phase 3 randomized, double-blind, placebo-controlled trial.
Setting: Outpatients in the United States and Japan.
Synopsis: The trial recruited 1,436 otherwise healthy patients aged 12-64 years of age (median age, 33 years) with a clinical diagnosis of acute uncomplicated influenza pneumonia. The patients were randomly assigned to receive either a single dose of oral baloxavir, oseltamivir 75 mg twice daily for 5 days, or matching placebo within 48 hours of symptom onset. The primary outcome was patient self-assessment of symptomatology.
Among the 1,064 adult patients (age 20-64) with influenza diagnosis confirmed by reverse transcription polymerase chain reaction (RT-PCR), the median time to alleviation of symptoms was lower in the baloxavir group than it was in the placebo group (53.7 hours vs. 80.2 hours; P less than .001). There was no significant difference in time to alleviation of symptoms in the baloxavir group when compared with the oseltamivir group. Adverse events were reported in 21% of baloxavir patients, 25% of placebo patients, and 25% of oseltamivir patients.
The enrolled patients were predominantly young, healthy, and treated as an outpatient. Patients hospitalized with influenza pneumonia are often older, have significant comorbidities, and are at higher risk of poor outcomes. This trial does not directly support the safety or efficacy of baloxavir in this population.
Bottom line: A single dose of baloxavir provides similar clinical benefit as 5 days of oseltamivir therapy in the early treatment of healthy patients with acute influenza.
Citation: Hayden FG et al. Baloxavir marboxil for uncomplicated influenza in adults and adolescents. N Eng J Med. 2018:379(10):914-23.
Dr. Holzer is an assistant professor of medicine in the division of hospital medicine at Mount Sinai Hospital, New York.
Clinical question: Is baloxavir marboxil, a selective inhibitor of influenza cap-dependent endonuclease, a safe and effective treatment for acute uncomplicated influenza?
Background: The emergence of oseltamivir-resistant influenza A(H1NI) infection in 2007 highlights the risk of future neuraminidase-resistant global pandemics. Baloxavir represents a new class of antiviral agent that may help treat such outbreaks.
Study design: Phase 3 randomized, double-blind, placebo-controlled trial.
Setting: Outpatients in the United States and Japan.
Synopsis: The trial recruited 1,436 otherwise healthy patients aged 12-64 years of age (median age, 33 years) with a clinical diagnosis of acute uncomplicated influenza pneumonia. The patients were randomly assigned to receive either a single dose of oral baloxavir, oseltamivir 75 mg twice daily for 5 days, or matching placebo within 48 hours of symptom onset. The primary outcome was patient self-assessment of symptomatology.
Among the 1,064 adult patients (age 20-64) with influenza diagnosis confirmed by reverse transcription polymerase chain reaction (RT-PCR), the median time to alleviation of symptoms was lower in the baloxavir group than it was in the placebo group (53.7 hours vs. 80.2 hours; P less than .001). There was no significant difference in time to alleviation of symptoms in the baloxavir group when compared with the oseltamivir group. Adverse events were reported in 21% of baloxavir patients, 25% of placebo patients, and 25% of oseltamivir patients.
The enrolled patients were predominantly young, healthy, and treated as an outpatient. Patients hospitalized with influenza pneumonia are often older, have significant comorbidities, and are at higher risk of poor outcomes. This trial does not directly support the safety or efficacy of baloxavir in this population.
Bottom line: A single dose of baloxavir provides similar clinical benefit as 5 days of oseltamivir therapy in the early treatment of healthy patients with acute influenza.
Citation: Hayden FG et al. Baloxavir marboxil for uncomplicated influenza in adults and adolescents. N Eng J Med. 2018:379(10):914-23.
Dr. Holzer is an assistant professor of medicine in the division of hospital medicine at Mount Sinai Hospital, New York.
No Pip/Tazo for patients with ESBL blood stream infections
Background: ESBL-producing gram-negative bacilli are becoming increasingly common. Carbapenems are considered the treatment of choice for these infections, but they may in turn select for carbapenem-resistant gram-negative bacilli.
Study design: Open-label, noninferiority, randomized clinical trial.
Setting: Adult inpatients from nine countries (not including the United States).
Synopsis: Patients with at least one positive blood culture for ESBL E. coli or K. pneumoniae were screened. Of the initial 1,646 patients assessed, only 391 were enrolled (866 met exclusion criteria, 218 patients declined, and 123 treating physicians declined). Patients were randomized within 72 hours of the positive blood culture collection to either piperacillin/tazobactam 4.5 g every 6 hours or meropenem 1 g every 8 hours. Patients were treated from 4 to 14 days, with the total duration of antibiotics left up to the treating physician.
The primary outcome was all-cause mortality at 30 days after randomization. The study was stopped early because of a significant mortality difference between the two groups (12.3% in the piperacillin/tazobactam group versus 3.7% in the meropenem group).
The overall mortality rate was lower than expected. The sickest patients may have been excluded because the treating physician needed to approve enrollment. Because of the necessity for empiric antibiotic therapy, there was substantial crossover in antibiotics between the groups, although this would have biased the study toward noninferiority.
Bottom line: For patients with ESBL E. coli or K. pneumoniae blood stream infections, treatment with piperacillin/tazobactam was inferior to meropenem for 30-day mortality.
Citation: Harris PNA et al. Effect of piperacillin-tazobactam vs meropenem on 30-day mortality for patients with E coli or Klebsiella pneumoniae bloodstream infection and ceftriaxone resistance: A randomized clinical trial. JAMA. 2018;320(10):984-94.
Dr. Gabriel is assistant professor of medicine and director of Preoperative Medicine and Medicine Consult Service in the division of hospital medicine at Mount Sinai Hospital, New York.
Background: ESBL-producing gram-negative bacilli are becoming increasingly common. Carbapenems are considered the treatment of choice for these infections, but they may in turn select for carbapenem-resistant gram-negative bacilli.
Study design: Open-label, noninferiority, randomized clinical trial.
Setting: Adult inpatients from nine countries (not including the United States).
Synopsis: Patients with at least one positive blood culture for ESBL E. coli or K. pneumoniae were screened. Of the initial 1,646 patients assessed, only 391 were enrolled (866 met exclusion criteria, 218 patients declined, and 123 treating physicians declined). Patients were randomized within 72 hours of the positive blood culture collection to either piperacillin/tazobactam 4.5 g every 6 hours or meropenem 1 g every 8 hours. Patients were treated from 4 to 14 days, with the total duration of antibiotics left up to the treating physician.
The primary outcome was all-cause mortality at 30 days after randomization. The study was stopped early because of a significant mortality difference between the two groups (12.3% in the piperacillin/tazobactam group versus 3.7% in the meropenem group).
The overall mortality rate was lower than expected. The sickest patients may have been excluded because the treating physician needed to approve enrollment. Because of the necessity for empiric antibiotic therapy, there was substantial crossover in antibiotics between the groups, although this would have biased the study toward noninferiority.
Bottom line: For patients with ESBL E. coli or K. pneumoniae blood stream infections, treatment with piperacillin/tazobactam was inferior to meropenem for 30-day mortality.
Citation: Harris PNA et al. Effect of piperacillin-tazobactam vs meropenem on 30-day mortality for patients with E coli or Klebsiella pneumoniae bloodstream infection and ceftriaxone resistance: A randomized clinical trial. JAMA. 2018;320(10):984-94.
Dr. Gabriel is assistant professor of medicine and director of Preoperative Medicine and Medicine Consult Service in the division of hospital medicine at Mount Sinai Hospital, New York.
Background: ESBL-producing gram-negative bacilli are becoming increasingly common. Carbapenems are considered the treatment of choice for these infections, but they may in turn select for carbapenem-resistant gram-negative bacilli.
Study design: Open-label, noninferiority, randomized clinical trial.
Setting: Adult inpatients from nine countries (not including the United States).
Synopsis: Patients with at least one positive blood culture for ESBL E. coli or K. pneumoniae were screened. Of the initial 1,646 patients assessed, only 391 were enrolled (866 met exclusion criteria, 218 patients declined, and 123 treating physicians declined). Patients were randomized within 72 hours of the positive blood culture collection to either piperacillin/tazobactam 4.5 g every 6 hours or meropenem 1 g every 8 hours. Patients were treated from 4 to 14 days, with the total duration of antibiotics left up to the treating physician.
The primary outcome was all-cause mortality at 30 days after randomization. The study was stopped early because of a significant mortality difference between the two groups (12.3% in the piperacillin/tazobactam group versus 3.7% in the meropenem group).
The overall mortality rate was lower than expected. The sickest patients may have been excluded because the treating physician needed to approve enrollment. Because of the necessity for empiric antibiotic therapy, there was substantial crossover in antibiotics between the groups, although this would have biased the study toward noninferiority.
Bottom line: For patients with ESBL E. coli or K. pneumoniae blood stream infections, treatment with piperacillin/tazobactam was inferior to meropenem for 30-day mortality.
Citation: Harris PNA et al. Effect of piperacillin-tazobactam vs meropenem on 30-day mortality for patients with E coli or Klebsiella pneumoniae bloodstream infection and ceftriaxone resistance: A randomized clinical trial. JAMA. 2018;320(10):984-94.
Dr. Gabriel is assistant professor of medicine and director of Preoperative Medicine and Medicine Consult Service in the division of hospital medicine at Mount Sinai Hospital, New York.
Physician burnout may be jeopardizing patient care
Clinical question: Is physician burnout associated with more patient safety issues, low professionalism, or poor patient satisfaction?
Background: Burnout is common among physicians and has a negative effect on their personal lives. It is unclear whether physician burnout is associated with poor outcomes for patients.
Study design: Meta-analysis.
Setting: Forty-seven published studies from 19 countries assessing inpatient and outpatient physicians and the relationship between physician burnout and patient care.
Synopsis: After a systematic review of the published literature, 47 studies were included to pool data from 42,473 physicians. Study subjects included residents, early-career and late-career physicians, and both hospital and outpatient physicians. All studies used validated measures of physician burnout.
Burnout was associated with a two-fold increased risk of physician-reported safety incidents (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), low professionalism (OR, 2.31; 95% CI, 1.87-2.85), and likelihood of low patient-reported satisfaction (OR, 2.28; 95% CI, 1.42-3.68). There were no significant differences in these results based on country of origin of the study. Early-career physicians were more likely to have burnout associated with low professionalism than were late-career physicians.
Of the components of burnout, depersonalization was most strongly associated with these negative outcomes. Interestingly, the increased risk of patient safety incidents was associated with physician-reported, but not health care system–reported, patient safety outcomes. This raises concerns that the health care systems may not be capturing “near misses” in their metrics.
Bottom line: Physician burnout doubles the risk of being involved in a patient safety incident, low professionalism, and poor patient satisfaction.
Citation: Panagioti M et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction. JAMA Intern Med. 2018;178(10):1317-30.
Dr. Gabriel is assistant professor of medicine and director of Pre-operative Medicine and Medicine Consult Service in the division of hospital medicine at Mount Sinai Hospital, New York.
Clinical question: Is physician burnout associated with more patient safety issues, low professionalism, or poor patient satisfaction?
Background: Burnout is common among physicians and has a negative effect on their personal lives. It is unclear whether physician burnout is associated with poor outcomes for patients.
Study design: Meta-analysis.
Setting: Forty-seven published studies from 19 countries assessing inpatient and outpatient physicians and the relationship between physician burnout and patient care.
Synopsis: After a systematic review of the published literature, 47 studies were included to pool data from 42,473 physicians. Study subjects included residents, early-career and late-career physicians, and both hospital and outpatient physicians. All studies used validated measures of physician burnout.
Burnout was associated with a two-fold increased risk of physician-reported safety incidents (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), low professionalism (OR, 2.31; 95% CI, 1.87-2.85), and likelihood of low patient-reported satisfaction (OR, 2.28; 95% CI, 1.42-3.68). There were no significant differences in these results based on country of origin of the study. Early-career physicians were more likely to have burnout associated with low professionalism than were late-career physicians.
Of the components of burnout, depersonalization was most strongly associated with these negative outcomes. Interestingly, the increased risk of patient safety incidents was associated with physician-reported, but not health care system–reported, patient safety outcomes. This raises concerns that the health care systems may not be capturing “near misses” in their metrics.
Bottom line: Physician burnout doubles the risk of being involved in a patient safety incident, low professionalism, and poor patient satisfaction.
Citation: Panagioti M et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction. JAMA Intern Med. 2018;178(10):1317-30.
Dr. Gabriel is assistant professor of medicine and director of Pre-operative Medicine and Medicine Consult Service in the division of hospital medicine at Mount Sinai Hospital, New York.
Clinical question: Is physician burnout associated with more patient safety issues, low professionalism, or poor patient satisfaction?
Background: Burnout is common among physicians and has a negative effect on their personal lives. It is unclear whether physician burnout is associated with poor outcomes for patients.
Study design: Meta-analysis.
Setting: Forty-seven published studies from 19 countries assessing inpatient and outpatient physicians and the relationship between physician burnout and patient care.
Synopsis: After a systematic review of the published literature, 47 studies were included to pool data from 42,473 physicians. Study subjects included residents, early-career and late-career physicians, and both hospital and outpatient physicians. All studies used validated measures of physician burnout.
Burnout was associated with a two-fold increased risk of physician-reported safety incidents (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), low professionalism (OR, 2.31; 95% CI, 1.87-2.85), and likelihood of low patient-reported satisfaction (OR, 2.28; 95% CI, 1.42-3.68). There were no significant differences in these results based on country of origin of the study. Early-career physicians were more likely to have burnout associated with low professionalism than were late-career physicians.
Of the components of burnout, depersonalization was most strongly associated with these negative outcomes. Interestingly, the increased risk of patient safety incidents was associated with physician-reported, but not health care system–reported, patient safety outcomes. This raises concerns that the health care systems may not be capturing “near misses” in their metrics.
Bottom line: Physician burnout doubles the risk of being involved in a patient safety incident, low professionalism, and poor patient satisfaction.
Citation: Panagioti M et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction. JAMA Intern Med. 2018;178(10):1317-30.
Dr. Gabriel is assistant professor of medicine and director of Pre-operative Medicine and Medicine Consult Service in the division of hospital medicine at Mount Sinai Hospital, New York.
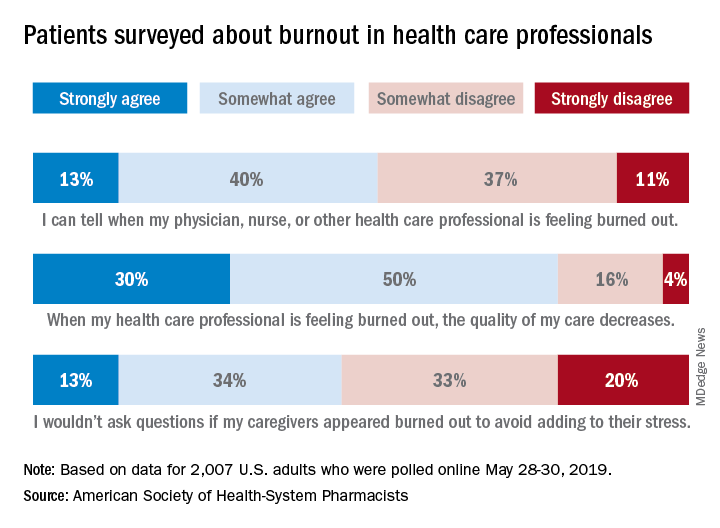
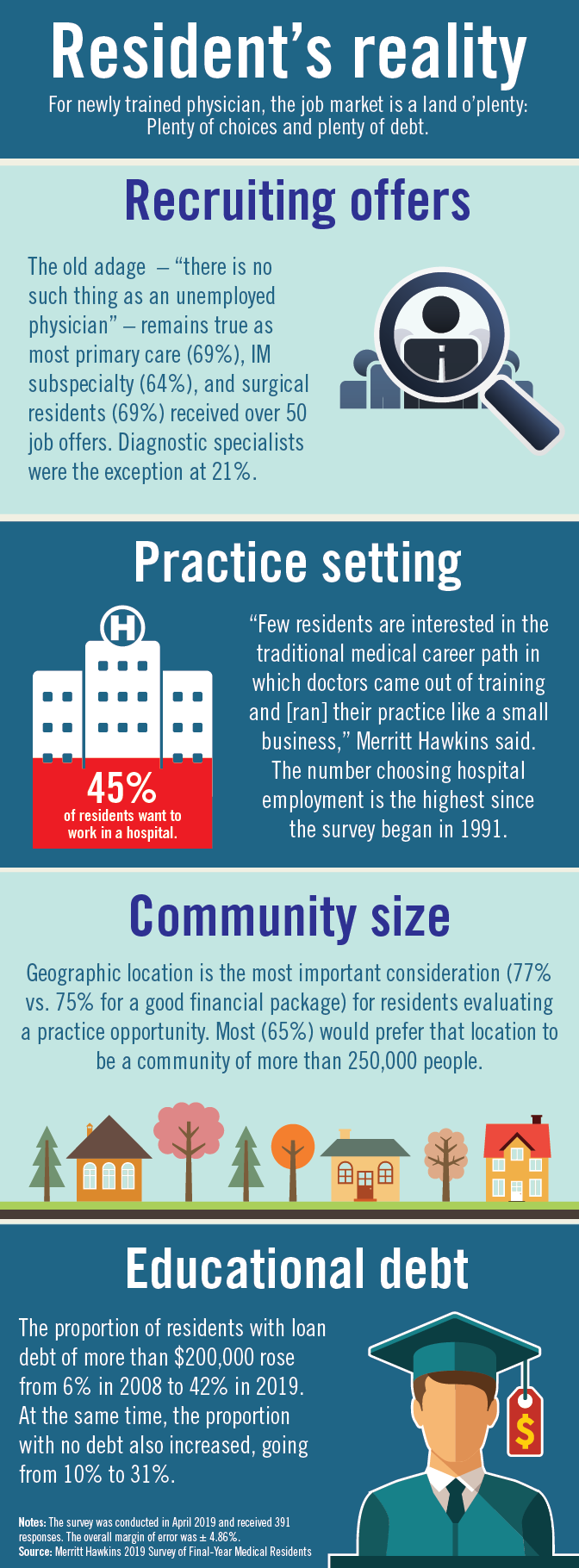
Residents are drowning in job offers – and debt
Physician search firm Merritt Hawkins did – actually, they heard from 391 residents – and 64% said that they had been contacted too many times by recruiters.
“Physicians coming out of training are being recruited like blue-chip athletes,” Travis Singleton, executive vice president of Merritt Hawkins, said in a statement. “There are simply not enough new doctors to go around.”
Merritt Hawkins asked physicians in their final year of residency about career choices, practice plans, and finances. Most said that they would prefer to be employed by a hospital or group practice, and a majority want to practice in a community with a population of 250,000 or more. More than half of the residents owed over $150,000 in student loans, but there were considerable debt differences between U.S. and international medical graduates.
The specialty distribution of respondents was 50% primary care, 30% internal medicine subspecialty/other, 15% surgical, and 5% diagnostic. About three-quarters were U.S. graduates and one-quarter of the residents were international medical graduates in this latest survey in a series that has been conducted periodically since 1991.
The survey was conducted in April 2018.
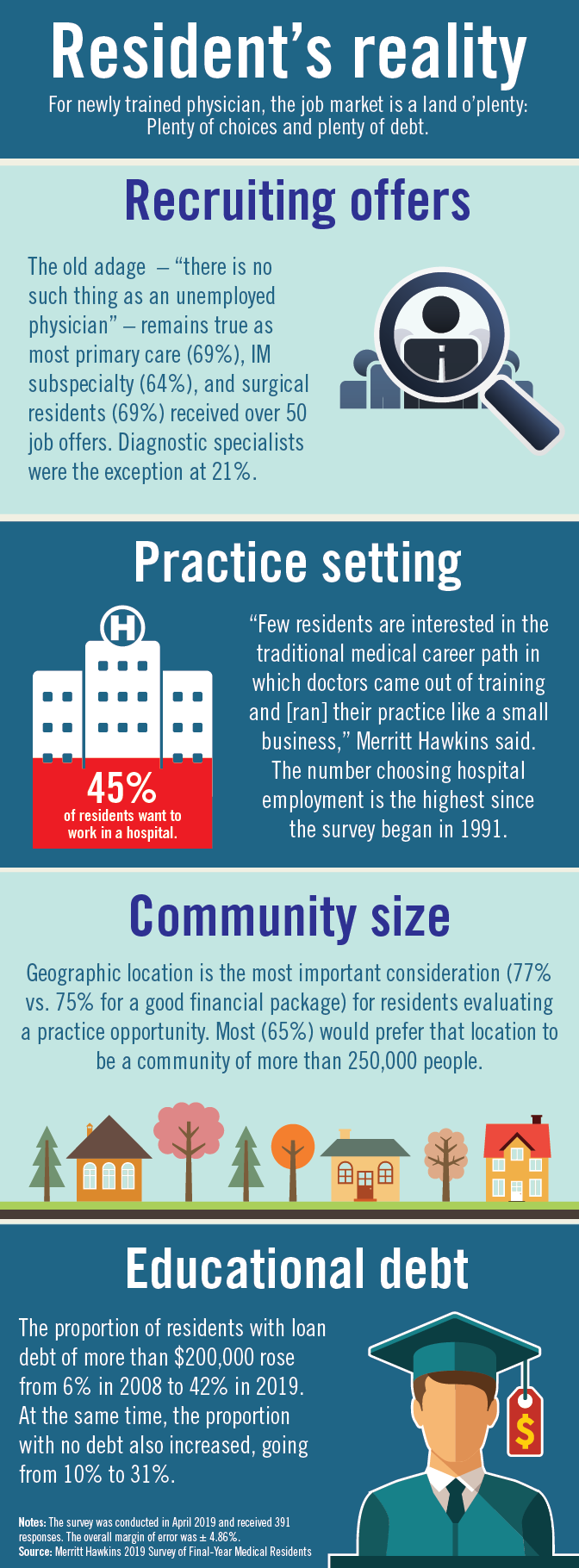
Physician search firm Merritt Hawkins did – actually, they heard from 391 residents – and 64% said that they had been contacted too many times by recruiters.
“Physicians coming out of training are being recruited like blue-chip athletes,” Travis Singleton, executive vice president of Merritt Hawkins, said in a statement. “There are simply not enough new doctors to go around.”
Merritt Hawkins asked physicians in their final year of residency about career choices, practice plans, and finances. Most said that they would prefer to be employed by a hospital or group practice, and a majority want to practice in a community with a population of 250,000 or more. More than half of the residents owed over $150,000 in student loans, but there were considerable debt differences between U.S. and international medical graduates.
The specialty distribution of respondents was 50% primary care, 30% internal medicine subspecialty/other, 15% surgical, and 5% diagnostic. About three-quarters were U.S. graduates and one-quarter of the residents were international medical graduates in this latest survey in a series that has been conducted periodically since 1991.
The survey was conducted in April 2018.
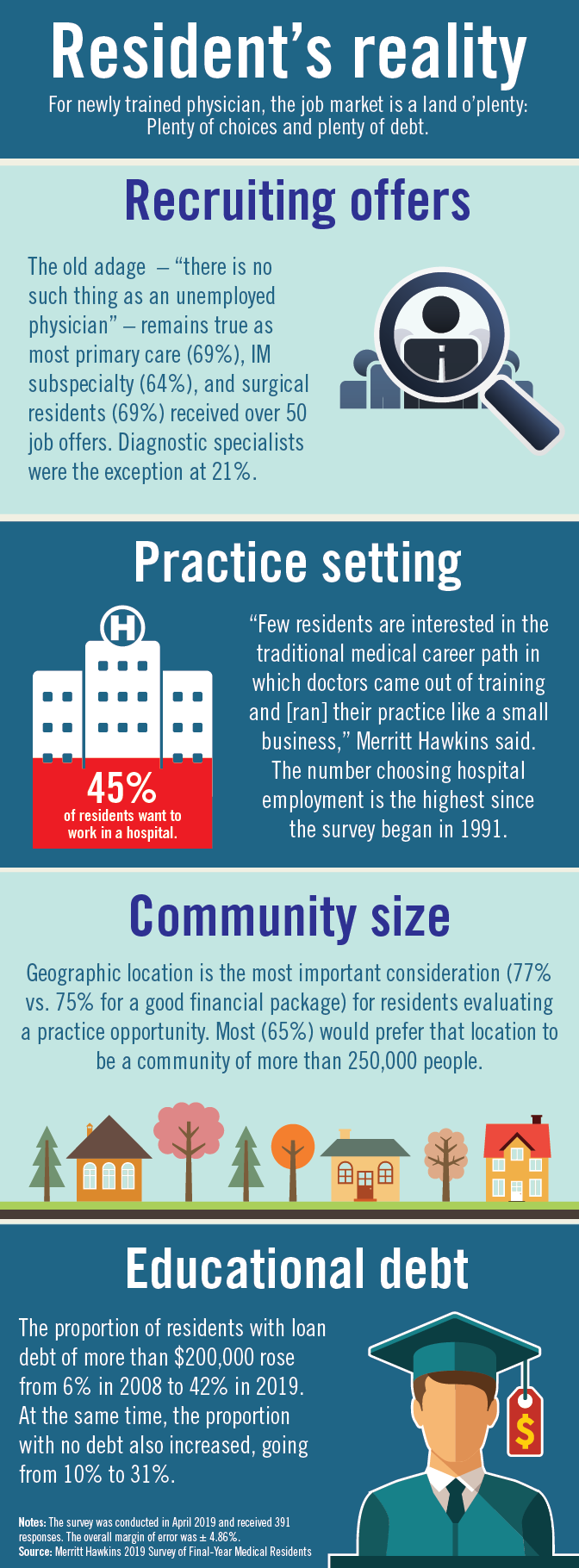
Physician search firm Merritt Hawkins did – actually, they heard from 391 residents – and 64% said that they had been contacted too many times by recruiters.
“Physicians coming out of training are being recruited like blue-chip athletes,” Travis Singleton, executive vice president of Merritt Hawkins, said in a statement. “There are simply not enough new doctors to go around.”
Merritt Hawkins asked physicians in their final year of residency about career choices, practice plans, and finances. Most said that they would prefer to be employed by a hospital or group practice, and a majority want to practice in a community with a population of 250,000 or more. More than half of the residents owed over $150,000 in student loans, but there were considerable debt differences between U.S. and international medical graduates.
The specialty distribution of respondents was 50% primary care, 30% internal medicine subspecialty/other, 15% surgical, and 5% diagnostic. About three-quarters were U.S. graduates and one-quarter of the residents were international medical graduates in this latest survey in a series that has been conducted periodically since 1991.
The survey was conducted in April 2018.
Benefits of Medicare Shared Savings Program ACOs lacking
or improving quality, according to new research.
“Our conclusion that the MSSP was not associated with improvements in spending, quality, or most measures of hospital use differ from that of previous evaluations of Medicare ACOs,” Adam Markovitz, of the University of Michigan, Ann Arbor, and colleagues wrote in a new research report published in Annals of Internal Medicine.
“Our instrumental variable model addresses selection effects not directly captured in previous evaluations,” the researchers continued.
To illustrate the point, the researchers found an association between MSSP and spending when using an adjusted longitudinal model (change, –$118; 95% confidence interval, –$151 to –$85 per beneficiary per quarter), with savings coming from reductions in inpatient services, outpatient services, and skilled nursing facility charges.
However, when employing an instrumental variable model, there was not an association with changes in total spending (change, $5; 95%CI, –$51 to $62 per beneficiary per quarter.
“The instrumental variable estimate for spending differed significantly from the adjusted estimate,” Mr. Markovitz and colleagues noted. “Estimated savings were smaller in instrumental variable models than in adjusted models across each ACO cohort.”
Similar patterns were observed in quality observations.
“The MSSP was associated with improvements in all four clinical quality indicators in the adjusted longitudinal model but not in the instrumental variable model,” the authors wrote. “The MSSP was associated with modest decreases in all-cause hospitalizations and preventable hospitalizations in the longitudinal model but not in the instrumental variable model.”
Overall, the authors noted that the results “challenge the view that MSSP ACOs have lowered spending and improved quality; they indicate that savings by MSSP ACOs may be driven by nonrandom exit of high-cost clinicians and their patient panels from this voluntary program.”
Indeed, the report states that removing “high-cost clinicians from ACO contracts could have large effects on spending estimates and may contribute to reported findings that MSSP savings grow over time.”
Primary sources of funding for the research included the Horowitz Foundation for Social Policy, Agency for Healthcare Research and Quality, and the National Institute on Aging. No relevant disclosures were made by the authors.
SOURCE: Markovitz A et al. Ann Intern Med. 2019 Jun 18. doi: 10.7326/M18-2539.
or improving quality, according to new research.
“Our conclusion that the MSSP was not associated with improvements in spending, quality, or most measures of hospital use differ from that of previous evaluations of Medicare ACOs,” Adam Markovitz, of the University of Michigan, Ann Arbor, and colleagues wrote in a new research report published in Annals of Internal Medicine.
“Our instrumental variable model addresses selection effects not directly captured in previous evaluations,” the researchers continued.
To illustrate the point, the researchers found an association between MSSP and spending when using an adjusted longitudinal model (change, –$118; 95% confidence interval, –$151 to –$85 per beneficiary per quarter), with savings coming from reductions in inpatient services, outpatient services, and skilled nursing facility charges.
However, when employing an instrumental variable model, there was not an association with changes in total spending (change, $5; 95%CI, –$51 to $62 per beneficiary per quarter.
“The instrumental variable estimate for spending differed significantly from the adjusted estimate,” Mr. Markovitz and colleagues noted. “Estimated savings were smaller in instrumental variable models than in adjusted models across each ACO cohort.”
Similar patterns were observed in quality observations.
“The MSSP was associated with improvements in all four clinical quality indicators in the adjusted longitudinal model but not in the instrumental variable model,” the authors wrote. “The MSSP was associated with modest decreases in all-cause hospitalizations and preventable hospitalizations in the longitudinal model but not in the instrumental variable model.”
Overall, the authors noted that the results “challenge the view that MSSP ACOs have lowered spending and improved quality; they indicate that savings by MSSP ACOs may be driven by nonrandom exit of high-cost clinicians and their patient panels from this voluntary program.”
Indeed, the report states that removing “high-cost clinicians from ACO contracts could have large effects on spending estimates and may contribute to reported findings that MSSP savings grow over time.”
Primary sources of funding for the research included the Horowitz Foundation for Social Policy, Agency for Healthcare Research and Quality, and the National Institute on Aging. No relevant disclosures were made by the authors.
SOURCE: Markovitz A et al. Ann Intern Med. 2019 Jun 18. doi: 10.7326/M18-2539.
or improving quality, according to new research.
“Our conclusion that the MSSP was not associated with improvements in spending, quality, or most measures of hospital use differ from that of previous evaluations of Medicare ACOs,” Adam Markovitz, of the University of Michigan, Ann Arbor, and colleagues wrote in a new research report published in Annals of Internal Medicine.
“Our instrumental variable model addresses selection effects not directly captured in previous evaluations,” the researchers continued.
To illustrate the point, the researchers found an association between MSSP and spending when using an adjusted longitudinal model (change, –$118; 95% confidence interval, –$151 to –$85 per beneficiary per quarter), with savings coming from reductions in inpatient services, outpatient services, and skilled nursing facility charges.
However, when employing an instrumental variable model, there was not an association with changes in total spending (change, $5; 95%CI, –$51 to $62 per beneficiary per quarter.
“The instrumental variable estimate for spending differed significantly from the adjusted estimate,” Mr. Markovitz and colleagues noted. “Estimated savings were smaller in instrumental variable models than in adjusted models across each ACO cohort.”
Similar patterns were observed in quality observations.
“The MSSP was associated with improvements in all four clinical quality indicators in the adjusted longitudinal model but not in the instrumental variable model,” the authors wrote. “The MSSP was associated with modest decreases in all-cause hospitalizations and preventable hospitalizations in the longitudinal model but not in the instrumental variable model.”
Overall, the authors noted that the results “challenge the view that MSSP ACOs have lowered spending and improved quality; they indicate that savings by MSSP ACOs may be driven by nonrandom exit of high-cost clinicians and their patient panels from this voluntary program.”
Indeed, the report states that removing “high-cost clinicians from ACO contracts could have large effects on spending estimates and may contribute to reported findings that MSSP savings grow over time.”
Primary sources of funding for the research included the Horowitz Foundation for Social Policy, Agency for Healthcare Research and Quality, and the National Institute on Aging. No relevant disclosures were made by the authors.
SOURCE: Markovitz A et al. Ann Intern Med. 2019 Jun 18. doi: 10.7326/M18-2539.
FROM ANNALS OF INTERNAL MEDICINE
HM19: Sepsis care update
Presenter
Patricia Kritek MD, EdM
Session Title
Sepsis update: From screening to refractory shock
Background
Each year 1.7 million adults in America develop sepsis, and 270,000 Americans die from sepsis annually. Sepsis costs U.S. health care over $27 billion dollars each year. Because of the wide range of etiologies and variation in presentation and intensity, it is a challenge to establish homogeneous evidence based guidelines.1
The definition of sepsis based on the “SIRS” criterion was developed initially in 1992, later revised as Sepsis-2 in 2001. The latest Sepsis-3 definition – “life-threatening organ dysfunction due to a dysregulated host response to infection” – was developed in 2016 by the Third International Consensus Definitions for Sepsis and Septic Shock. This newest definition has renounced the SIRS criterion and adopted the Sequential Organ Failure Assessment (SOFA) score. Treatment guidelines in sepsis were developed by the Surviving Sepsis Campaign starting with the Barcelona Declaration in 2002 and revised multiple times, with the development of 3-hour and 6-hour care bundles in 2012. The latest revision, in 2018, consolidated to a 1-hour bundle.2
Sepsis is a continuum of every severe infection, and with the combined efforts of the Society of Critical Care Medicine and the European Society of Intensive Care Medicine, evidence-based guidelines have been developed over the past 2 decades, with the latest iteration in 2018. The Centers for Medicare & Medicaid Services still uses Sepsis-2 for diagnosis, and the 3-hr/6-hr bundle compliance (2016) for expected care.3
Session summary
Dr. Kritek, of the division of pulmonary, critical care, and sleep medicine at the University of Washington, Seattle, presented to a room of over 1,000 enthusiastic hospitalists. She was able to capture everyone’s attention with a great presentation. As sepsis is one of the most common and serious conditions we encounter, most hospitalists are fairly well versed in evidence-based practices, and Dr. Kritek was able to keep us engaged, describing in detail the evolving definition, pathophysiology, and screening procedures for sepsis. She also spoke about important studies and the latest evidence that will positively impact each hospitalist’s practice in treating sepsis.
Dr. Kritek explained clearly how the Surviving Sepsis Campaign developed a vital and nontraditional guideline that “recommends health systems have a performance improvement program for sepsis including screening for high-risk patients.” In a 1-hour session, Dr. Kritek did a commendable job untangling this bewildering health care challenge, and aligned each component to explain how to best use available resources and address sepsis in individual hospitals.
She talked about the statistics and historical aspects involved in the definition of sepsis, and the Surviving Sepsis Campaign. With three good case scenarios, Dr. Kritek explained how it was difficult to accurately diagnose sepsis using the Sepsis-2/SIRS criterion, and how the SIRS criterion led to several false positives. This created a need for the new Sepsis-3 definition, which used delta SOFA score of 2 indicating “organ failure.”
Key takeaways: Screening
- Sepsis-3 with delta SOFA score of at least 2 and Quick SOFA (qSOFA) of at least 2 was best at predicting in-hospital death, ICU admission, and long ICU stay in ED.
- qSOFA was not helpful in the admitted ICU population. An increase of at least 2 points in SOFA score within 24 hours of admission to the ICU was the best predictor of in-hospital mortality and long ICU stays.
- SIRS has high sensitivity and low specificity. The Early Warning Score has accuracy similar to qSOFA.
- Understanding that there is no perfect answer regarding screening, but having a process is vital for each organization. This approach led to the Surviving Sepsis Campaign guideline: “Recommend health systems have a performance improvement program for sepsis including screening for high-risk patients.”
Key takeaways: Treatment
- Meta-analysis showed that specifically targeted, early goal–directed treatment (specifically, central venous pressure 8-12 mm Hg, central venous oxygen saturation greater than 70%, packed red blood cell inotropes used) did not show any improvement in 90-day mortality, and actually generated worse outcomes, including cirrhosis, as well as higher costs of care.
- Antibiotics: Though part of the 3-hour bundle, antibiotics are recommended to be administered within 1 hour.
- Intravenous fluids: Patients with sepsis-induced hypoperfusion need 30 mL/kg crystalloids. Normal saline and lactated ringer are preferred. Lactated ringer has the advantage over normal saline, with a reduced incidence of major adverse kidney events.
- Importance of bundle compliance: N.Y. study showed use of protocols cut mortality from 30.2% to 25.4%.
Refractory septic shock
- Adding hydrocortisone and fludrocortisone improved mortality at 28 days, helped patients get off vasopressors sooner, and ultimately resulted in less organ failure. But no difference in 90-day mortality.
- A study of vitamin C use in septic patients needs further studies to validate, as it only included 47 patients.
- Early renal replacement therapy showed no difference in mortality or length of stay.
Dr. Kritek’s presentation made a positive impact by helping to explain the reasoning behind the established and evolving best practices and guidelines for care of patients with sepsis and septic shock. Her approach will help hospitalists provide cost-effective care, by understanding which expensive interventions and practices do not make a difference in patient care.
Dr. Odeti is hospitalist medical director at Johnston Memorial Hospital in Abingdon, Va. JMH is part of Ballad Health, a health system operating 21 hospitals in northeast Tennessee and southwest Virginia.
References
1. https://www.sepsis.org/wp-content/uploads/2017/05/Sepsis-Fact-Sheet-2018.pdf.
2. http://www.survivingsepsis.org/News/Pages/SCCM-and-ACEP-Release-Joint-Statement-About-the-Surviving-Sepsis-Campaign-Hour-1-Bundle.aspx
3. Specifications Manual for National Hospital Inpatient Quality Measures Discharges 01-01-17 (1Q17) through 12-31-17 (4Q17).
Presenter
Patricia Kritek MD, EdM
Session Title
Sepsis update: From screening to refractory shock
Background
Each year 1.7 million adults in America develop sepsis, and 270,000 Americans die from sepsis annually. Sepsis costs U.S. health care over $27 billion dollars each year. Because of the wide range of etiologies and variation in presentation and intensity, it is a challenge to establish homogeneous evidence based guidelines.1
The definition of sepsis based on the “SIRS” criterion was developed initially in 1992, later revised as Sepsis-2 in 2001. The latest Sepsis-3 definition – “life-threatening organ dysfunction due to a dysregulated host response to infection” – was developed in 2016 by the Third International Consensus Definitions for Sepsis and Septic Shock. This newest definition has renounced the SIRS criterion and adopted the Sequential Organ Failure Assessment (SOFA) score. Treatment guidelines in sepsis were developed by the Surviving Sepsis Campaign starting with the Barcelona Declaration in 2002 and revised multiple times, with the development of 3-hour and 6-hour care bundles in 2012. The latest revision, in 2018, consolidated to a 1-hour bundle.2
Sepsis is a continuum of every severe infection, and with the combined efforts of the Society of Critical Care Medicine and the European Society of Intensive Care Medicine, evidence-based guidelines have been developed over the past 2 decades, with the latest iteration in 2018. The Centers for Medicare & Medicaid Services still uses Sepsis-2 for diagnosis, and the 3-hr/6-hr bundle compliance (2016) for expected care.3
Session summary
Dr. Kritek, of the division of pulmonary, critical care, and sleep medicine at the University of Washington, Seattle, presented to a room of over 1,000 enthusiastic hospitalists. She was able to capture everyone’s attention with a great presentation. As sepsis is one of the most common and serious conditions we encounter, most hospitalists are fairly well versed in evidence-based practices, and Dr. Kritek was able to keep us engaged, describing in detail the evolving definition, pathophysiology, and screening procedures for sepsis. She also spoke about important studies and the latest evidence that will positively impact each hospitalist’s practice in treating sepsis.
Dr. Kritek explained clearly how the Surviving Sepsis Campaign developed a vital and nontraditional guideline that “recommends health systems have a performance improvement program for sepsis including screening for high-risk patients.” In a 1-hour session, Dr. Kritek did a commendable job untangling this bewildering health care challenge, and aligned each component to explain how to best use available resources and address sepsis in individual hospitals.
She talked about the statistics and historical aspects involved in the definition of sepsis, and the Surviving Sepsis Campaign. With three good case scenarios, Dr. Kritek explained how it was difficult to accurately diagnose sepsis using the Sepsis-2/SIRS criterion, and how the SIRS criterion led to several false positives. This created a need for the new Sepsis-3 definition, which used delta SOFA score of 2 indicating “organ failure.”
Key takeaways: Screening
- Sepsis-3 with delta SOFA score of at least 2 and Quick SOFA (qSOFA) of at least 2 was best at predicting in-hospital death, ICU admission, and long ICU stay in ED.
- qSOFA was not helpful in the admitted ICU population. An increase of at least 2 points in SOFA score within 24 hours of admission to the ICU was the best predictor of in-hospital mortality and long ICU stays.
- SIRS has high sensitivity and low specificity. The Early Warning Score has accuracy similar to qSOFA.
- Understanding that there is no perfect answer regarding screening, but having a process is vital for each organization. This approach led to the Surviving Sepsis Campaign guideline: “Recommend health systems have a performance improvement program for sepsis including screening for high-risk patients.”
Key takeaways: Treatment
- Meta-analysis showed that specifically targeted, early goal–directed treatment (specifically, central venous pressure 8-12 mm Hg, central venous oxygen saturation greater than 70%, packed red blood cell inotropes used) did not show any improvement in 90-day mortality, and actually generated worse outcomes, including cirrhosis, as well as higher costs of care.
- Antibiotics: Though part of the 3-hour bundle, antibiotics are recommended to be administered within 1 hour.
- Intravenous fluids: Patients with sepsis-induced hypoperfusion need 30 mL/kg crystalloids. Normal saline and lactated ringer are preferred. Lactated ringer has the advantage over normal saline, with a reduced incidence of major adverse kidney events.
- Importance of bundle compliance: N.Y. study showed use of protocols cut mortality from 30.2% to 25.4%.
Refractory septic shock
- Adding hydrocortisone and fludrocortisone improved mortality at 28 days, helped patients get off vasopressors sooner, and ultimately resulted in less organ failure. But no difference in 90-day mortality.
- A study of vitamin C use in septic patients needs further studies to validate, as it only included 47 patients.
- Early renal replacement therapy showed no difference in mortality or length of stay.
Dr. Kritek’s presentation made a positive impact by helping to explain the reasoning behind the established and evolving best practices and guidelines for care of patients with sepsis and septic shock. Her approach will help hospitalists provide cost-effective care, by understanding which expensive interventions and practices do not make a difference in patient care.
Dr. Odeti is hospitalist medical director at Johnston Memorial Hospital in Abingdon, Va. JMH is part of Ballad Health, a health system operating 21 hospitals in northeast Tennessee and southwest Virginia.
References
1. https://www.sepsis.org/wp-content/uploads/2017/05/Sepsis-Fact-Sheet-2018.pdf.
2. http://www.survivingsepsis.org/News/Pages/SCCM-and-ACEP-Release-Joint-Statement-About-the-Surviving-Sepsis-Campaign-Hour-1-Bundle.aspx
3. Specifications Manual for National Hospital Inpatient Quality Measures Discharges 01-01-17 (1Q17) through 12-31-17 (4Q17).
Presenter
Patricia Kritek MD, EdM
Session Title
Sepsis update: From screening to refractory shock
Background
Each year 1.7 million adults in America develop sepsis, and 270,000 Americans die from sepsis annually. Sepsis costs U.S. health care over $27 billion dollars each year. Because of the wide range of etiologies and variation in presentation and intensity, it is a challenge to establish homogeneous evidence based guidelines.1
The definition of sepsis based on the “SIRS” criterion was developed initially in 1992, later revised as Sepsis-2 in 2001. The latest Sepsis-3 definition – “life-threatening organ dysfunction due to a dysregulated host response to infection” – was developed in 2016 by the Third International Consensus Definitions for Sepsis and Septic Shock. This newest definition has renounced the SIRS criterion and adopted the Sequential Organ Failure Assessment (SOFA) score. Treatment guidelines in sepsis were developed by the Surviving Sepsis Campaign starting with the Barcelona Declaration in 2002 and revised multiple times, with the development of 3-hour and 6-hour care bundles in 2012. The latest revision, in 2018, consolidated to a 1-hour bundle.2
Sepsis is a continuum of every severe infection, and with the combined efforts of the Society of Critical Care Medicine and the European Society of Intensive Care Medicine, evidence-based guidelines have been developed over the past 2 decades, with the latest iteration in 2018. The Centers for Medicare & Medicaid Services still uses Sepsis-2 for diagnosis, and the 3-hr/6-hr bundle compliance (2016) for expected care.3
Session summary
Dr. Kritek, of the division of pulmonary, critical care, and sleep medicine at the University of Washington, Seattle, presented to a room of over 1,000 enthusiastic hospitalists. She was able to capture everyone’s attention with a great presentation. As sepsis is one of the most common and serious conditions we encounter, most hospitalists are fairly well versed in evidence-based practices, and Dr. Kritek was able to keep us engaged, describing in detail the evolving definition, pathophysiology, and screening procedures for sepsis. She also spoke about important studies and the latest evidence that will positively impact each hospitalist’s practice in treating sepsis.
Dr. Kritek explained clearly how the Surviving Sepsis Campaign developed a vital and nontraditional guideline that “recommends health systems have a performance improvement program for sepsis including screening for high-risk patients.” In a 1-hour session, Dr. Kritek did a commendable job untangling this bewildering health care challenge, and aligned each component to explain how to best use available resources and address sepsis in individual hospitals.
She talked about the statistics and historical aspects involved in the definition of sepsis, and the Surviving Sepsis Campaign. With three good case scenarios, Dr. Kritek explained how it was difficult to accurately diagnose sepsis using the Sepsis-2/SIRS criterion, and how the SIRS criterion led to several false positives. This created a need for the new Sepsis-3 definition, which used delta SOFA score of 2 indicating “organ failure.”
Key takeaways: Screening
- Sepsis-3 with delta SOFA score of at least 2 and Quick SOFA (qSOFA) of at least 2 was best at predicting in-hospital death, ICU admission, and long ICU stay in ED.
- qSOFA was not helpful in the admitted ICU population. An increase of at least 2 points in SOFA score within 24 hours of admission to the ICU was the best predictor of in-hospital mortality and long ICU stays.
- SIRS has high sensitivity and low specificity. The Early Warning Score has accuracy similar to qSOFA.
- Understanding that there is no perfect answer regarding screening, but having a process is vital for each organization. This approach led to the Surviving Sepsis Campaign guideline: “Recommend health systems have a performance improvement program for sepsis including screening for high-risk patients.”
Key takeaways: Treatment
- Meta-analysis showed that specifically targeted, early goal–directed treatment (specifically, central venous pressure 8-12 mm Hg, central venous oxygen saturation greater than 70%, packed red blood cell inotropes used) did not show any improvement in 90-day mortality, and actually generated worse outcomes, including cirrhosis, as well as higher costs of care.
- Antibiotics: Though part of the 3-hour bundle, antibiotics are recommended to be administered within 1 hour.
- Intravenous fluids: Patients with sepsis-induced hypoperfusion need 30 mL/kg crystalloids. Normal saline and lactated ringer are preferred. Lactated ringer has the advantage over normal saline, with a reduced incidence of major adverse kidney events.
- Importance of bundle compliance: N.Y. study showed use of protocols cut mortality from 30.2% to 25.4%.
Refractory septic shock
- Adding hydrocortisone and fludrocortisone improved mortality at 28 days, helped patients get off vasopressors sooner, and ultimately resulted in less organ failure. But no difference in 90-day mortality.
- A study of vitamin C use in septic patients needs further studies to validate, as it only included 47 patients.
- Early renal replacement therapy showed no difference in mortality or length of stay.
Dr. Kritek’s presentation made a positive impact by helping to explain the reasoning behind the established and evolving best practices and guidelines for care of patients with sepsis and septic shock. Her approach will help hospitalists provide cost-effective care, by understanding which expensive interventions and practices do not make a difference in patient care.
Dr. Odeti is hospitalist medical director at Johnston Memorial Hospital in Abingdon, Va. JMH is part of Ballad Health, a health system operating 21 hospitals in northeast Tennessee and southwest Virginia.
References
1. https://www.sepsis.org/wp-content/uploads/2017/05/Sepsis-Fact-Sheet-2018.pdf.
2. http://www.survivingsepsis.org/News/Pages/SCCM-and-ACEP-Release-Joint-Statement-About-the-Surviving-Sepsis-Campaign-Hour-1-Bundle.aspx
3. Specifications Manual for National Hospital Inpatient Quality Measures Discharges 01-01-17 (1Q17) through 12-31-17 (4Q17).
Quick Byte: Conversations about cost
Patients want to talk
Seventy percent of Americans would like to have conversations about the costs of care with their health care providers, but only 28% do so, according to polling conducted for the Robert Wood Johnson Foundation (RWJF) by Avalere Health.
With those polling results in hand, 2 years ago RWJF and Avalere Health launched the Cost Conversation projects to help. Practice briefs for these kinds of conversations are now available on America’s Essential Hospitals’ website (https://essentialhospitals.org/cost-care/practice-briefs/).
Reference
1. Ganos E, Steinberg K, Seidman J, Masi D, Gomez-Rexode A, Fraser A. Talking About Costs: Innovation In Clinician-Patient Conversations. Health Affairs. Published online Nov. 27, 2018. doi: 10.1377/hblog20181126.366161. Accessed Dec. 11, 2018.
Patients want to talk
Patients want to talk
Seventy percent of Americans would like to have conversations about the costs of care with their health care providers, but only 28% do so, according to polling conducted for the Robert Wood Johnson Foundation (RWJF) by Avalere Health.
With those polling results in hand, 2 years ago RWJF and Avalere Health launched the Cost Conversation projects to help. Practice briefs for these kinds of conversations are now available on America’s Essential Hospitals’ website (https://essentialhospitals.org/cost-care/practice-briefs/).
Reference
1. Ganos E, Steinberg K, Seidman J, Masi D, Gomez-Rexode A, Fraser A. Talking About Costs: Innovation In Clinician-Patient Conversations. Health Affairs. Published online Nov. 27, 2018. doi: 10.1377/hblog20181126.366161. Accessed Dec. 11, 2018.
Seventy percent of Americans would like to have conversations about the costs of care with their health care providers, but only 28% do so, according to polling conducted for the Robert Wood Johnson Foundation (RWJF) by Avalere Health.
With those polling results in hand, 2 years ago RWJF and Avalere Health launched the Cost Conversation projects to help. Practice briefs for these kinds of conversations are now available on America’s Essential Hospitals’ website (https://essentialhospitals.org/cost-care/practice-briefs/).
Reference
1. Ganos E, Steinberg K, Seidman J, Masi D, Gomez-Rexode A, Fraser A. Talking About Costs: Innovation In Clinician-Patient Conversations. Health Affairs. Published online Nov. 27, 2018. doi: 10.1377/hblog20181126.366161. Accessed Dec. 11, 2018.













