User login
Pediatric OCD: A case for vigilance
Max is an 8-year-old boy in the third grade, and you have been his pediatrician since birth. Described as “emotional” and “particular” since his early years, Max is prone to prolonged tantrums that have not improved with age. Parents have described a tic that involves repeatedly touching his ear, but this has not been observed in the office setting. Max has struggled with some attention issues at school, and often needs help finishing assignments. The family is feeling increasingly desperate for ways to manage his near-daily meltdowns at home, and parenting strategies you’ve discussed thus far don’t seem to be helping much. Should obsessive-compulsive disorder be in your differential? And at what point do you seek outside evaluation?
OCD is a condition characterized by recurrent, intrusive, and unwanted thoughts, images, and urges (obsessions), and repetitive behaviors or mental acts performed in a particular way to reduce anxiety (compulsions). It affects 1%-3% of children, and onset can be as early as age 3-4 years. While the average age of onset in children is approximately 10 years old, average age of diagnosis is at least several years later.1 A primary care physician’s ability to recognize OCD symptoms in children, perform an initial assessment, and connect the child to appropriate clinical care is key to reducing the years of difficulty that children and families often endure prior to beginning treatment.
Common obsessions in children include contamination, fear of harm to self or others, symmetry, and the belief that bad things will occur if rituals are performed incorrectly. Common compulsions include checking, washing, ordering, and mental acts such as praying or counting to one’s self.1,2 In addition to the fact that OCD presentations are highly heterogeneous, early diagnosis is challenging due to significant overlap of OCD symptoms with developmentally normal behaviors. For example, magical or superstitious thinking is common among school-age children who avoid stepping on cracks or utilize lucky numbers. What differentiates OCD is the presence of obsessions and/or compulsions that are time consuming and cause subjective distress or functional impairment. Children often are adept at keeping OCD symptoms secret. At time of diagnosis, the child may have a complex array of discreet behaviors to manage distress and minimize shame. Children may not have insight into the irrationality of their thoughts or behaviors, but they are certainly aware of how terrible and confused they feel inside, and how it affects their relationship with their parents. Rituals, such as those that delay bedtime or cause school tardiness, may look like oppositional behaviors and cause immense frustration for parents.
Comorbidities are common and include ADHD, oppositional defiant disorder, depression, and Tourette syndrome.3 Nearly 60% of children with OCD meet criteria for a tic disorder at some point in their lifetime.4 Compulsions designed to ease a feeling of internal discomfort, such as touching or tapping, are particularly typical of patients with OCD and comorbid tics. Often these children will express a need for things to be “just right,” with lasting relief from such a feeling rarely found. While sensory intolerances are not part of OCD’s diagnostic criteria, clinical experiences and growing research point to a high prevalence in affected children.5,6 Sensory intolerances may even be the primary presenting problem. Examples include clothing feeling uncomfortable, or inability to tolerate certain smells or innocuous sounds.
The preferred method for assessment of OCD in children is the Children’s Yale–Brown Obsessive Compulsive Scale (CY-BOCS), a semi-structured, clinician-rated interview designed to elicit symptoms, severity, and distress. While time constraints may prevent use of the CY-BOCS in the primary care setting, a handful of screening questions instead can go a long way. These might include:
- Do you have to do things in a certain way, such as washing or making things “just right?”
- What happens if you can’t do things in a certain way?
- Do you have unwanted thoughts that keep coming back and are hard to get rid of?
Equally as important as understanding a child’s OCD symptoms is understanding how the family has, often unwittingly, become intertwined in a web of OCD-driven behaviors. In an effort to soothe the child, prevent emotional outbursts, or simply get through the day, parents may find themselves accommodating behaviors that seem irrational. Despite parents’ best intentions, this is likely reinforcing OCD patterns. Parents may be asked by the child to repeat a reassuring phrase in a certain way, arrange furniture “just so,” or drive a certain route to school. In the case of contamination fears, a child may be taking several showers per day, using two bottles of shampoo per week, and demanding that his or her clothes be washed separately before a parent begins to realize the cumulative impact of these unusual behaviors on the household. In addition to exploring concerns, primary care physicians can provide a sounding board for exhausted parents wondering if other families face the same thing. While connecting the family to treatment, they also can provide reassurances that treatment can dramatically shift the trajectory of the illness.
Treatment of pediatric OCD begins with a specific form of cognitive behavioral therapy (CBT) called Exposure and Response Prevention therapy (ERP). ERP requires a skilled therapist, and a strong alliance with a child and family because the child will be asked to gradually challenge compulsions head-on and tolerate the accompanied distress. CBT/ERP is associated with a 40%-65% reduction in symptoms, but combination with SSRI therapy improves outcomes in more severe cases.3 Despite limited mental health resources and long wait lists in many parts of the country, connection to OCD-specific treatment is increasingly feasible in virtual format via online support groups and telemedicine.
“Max” may experience any number of OCD-related symptoms that a primary care physician could deftly uncover. He may become “stuck” at school because his handwriting accidentally strayed below the line. He may have hours-long meltdowns because his hair never feels right. He may touch his ear to prevent tragic harm coming to his mother. Whatever further exploration reveals, Max and his family stand to benefit immensely from early detection and intervention.
Dr. McGowan is assistant professor of psychiatry and pediatrics at the Vermont Center for Children, Youth, and Families, University of Vermont Medical Center, Burlington. She had no relevant financial disclosures. Email Dr. McGowan at [email protected].
Resources for providers and families*
UNSTUCK: An OCD Kids Movie. Featuring a 23-minute documentary film about children living with OCD, this website also is rich in OCD-related resources.
International OCD Foundation. Has information for families about OCD. Also has a resource directory for therapists, clinics, support groups, and other organizations specializing in OCD and related disorders in different geographic areas.
*Of note, both resources above include COVID-19-specific resources for those struggling with worsening OCD symptoms as a result of the pandemic.
References
1. Lewis’s Child and Adolescent Psychiatry: A Comprehensive Textbook, 4th ed. (Baltimore: Lippincott Williams & Wilkins, 2020, pp. 518-27).
2. J Amer Acad Child Adol Psychiatry. 2012;51(1):98-113.
3. J Clin. Invest. 2009;119(4):737-46.
4. Arch Dis Child. 2015;100(5):495-9.
5. J Develop Behav Pediatr. 2019 Jun;40(5):377-82.
6. Ann Clin Psychiatry. 2008 Oct-Dec;20(4):199-203.
Max is an 8-year-old boy in the third grade, and you have been his pediatrician since birth. Described as “emotional” and “particular” since his early years, Max is prone to prolonged tantrums that have not improved with age. Parents have described a tic that involves repeatedly touching his ear, but this has not been observed in the office setting. Max has struggled with some attention issues at school, and often needs help finishing assignments. The family is feeling increasingly desperate for ways to manage his near-daily meltdowns at home, and parenting strategies you’ve discussed thus far don’t seem to be helping much. Should obsessive-compulsive disorder be in your differential? And at what point do you seek outside evaluation?
OCD is a condition characterized by recurrent, intrusive, and unwanted thoughts, images, and urges (obsessions), and repetitive behaviors or mental acts performed in a particular way to reduce anxiety (compulsions). It affects 1%-3% of children, and onset can be as early as age 3-4 years. While the average age of onset in children is approximately 10 years old, average age of diagnosis is at least several years later.1 A primary care physician’s ability to recognize OCD symptoms in children, perform an initial assessment, and connect the child to appropriate clinical care is key to reducing the years of difficulty that children and families often endure prior to beginning treatment.
Common obsessions in children include contamination, fear of harm to self or others, symmetry, and the belief that bad things will occur if rituals are performed incorrectly. Common compulsions include checking, washing, ordering, and mental acts such as praying or counting to one’s self.1,2 In addition to the fact that OCD presentations are highly heterogeneous, early diagnosis is challenging due to significant overlap of OCD symptoms with developmentally normal behaviors. For example, magical or superstitious thinking is common among school-age children who avoid stepping on cracks or utilize lucky numbers. What differentiates OCD is the presence of obsessions and/or compulsions that are time consuming and cause subjective distress or functional impairment. Children often are adept at keeping OCD symptoms secret. At time of diagnosis, the child may have a complex array of discreet behaviors to manage distress and minimize shame. Children may not have insight into the irrationality of their thoughts or behaviors, but they are certainly aware of how terrible and confused they feel inside, and how it affects their relationship with their parents. Rituals, such as those that delay bedtime or cause school tardiness, may look like oppositional behaviors and cause immense frustration for parents.
Comorbidities are common and include ADHD, oppositional defiant disorder, depression, and Tourette syndrome.3 Nearly 60% of children with OCD meet criteria for a tic disorder at some point in their lifetime.4 Compulsions designed to ease a feeling of internal discomfort, such as touching or tapping, are particularly typical of patients with OCD and comorbid tics. Often these children will express a need for things to be “just right,” with lasting relief from such a feeling rarely found. While sensory intolerances are not part of OCD’s diagnostic criteria, clinical experiences and growing research point to a high prevalence in affected children.5,6 Sensory intolerances may even be the primary presenting problem. Examples include clothing feeling uncomfortable, or inability to tolerate certain smells or innocuous sounds.
The preferred method for assessment of OCD in children is the Children’s Yale–Brown Obsessive Compulsive Scale (CY-BOCS), a semi-structured, clinician-rated interview designed to elicit symptoms, severity, and distress. While time constraints may prevent use of the CY-BOCS in the primary care setting, a handful of screening questions instead can go a long way. These might include:
- Do you have to do things in a certain way, such as washing or making things “just right?”
- What happens if you can’t do things in a certain way?
- Do you have unwanted thoughts that keep coming back and are hard to get rid of?
Equally as important as understanding a child’s OCD symptoms is understanding how the family has, often unwittingly, become intertwined in a web of OCD-driven behaviors. In an effort to soothe the child, prevent emotional outbursts, or simply get through the day, parents may find themselves accommodating behaviors that seem irrational. Despite parents’ best intentions, this is likely reinforcing OCD patterns. Parents may be asked by the child to repeat a reassuring phrase in a certain way, arrange furniture “just so,” or drive a certain route to school. In the case of contamination fears, a child may be taking several showers per day, using two bottles of shampoo per week, and demanding that his or her clothes be washed separately before a parent begins to realize the cumulative impact of these unusual behaviors on the household. In addition to exploring concerns, primary care physicians can provide a sounding board for exhausted parents wondering if other families face the same thing. While connecting the family to treatment, they also can provide reassurances that treatment can dramatically shift the trajectory of the illness.
Treatment of pediatric OCD begins with a specific form of cognitive behavioral therapy (CBT) called Exposure and Response Prevention therapy (ERP). ERP requires a skilled therapist, and a strong alliance with a child and family because the child will be asked to gradually challenge compulsions head-on and tolerate the accompanied distress. CBT/ERP is associated with a 40%-65% reduction in symptoms, but combination with SSRI therapy improves outcomes in more severe cases.3 Despite limited mental health resources and long wait lists in many parts of the country, connection to OCD-specific treatment is increasingly feasible in virtual format via online support groups and telemedicine.
“Max” may experience any number of OCD-related symptoms that a primary care physician could deftly uncover. He may become “stuck” at school because his handwriting accidentally strayed below the line. He may have hours-long meltdowns because his hair never feels right. He may touch his ear to prevent tragic harm coming to his mother. Whatever further exploration reveals, Max and his family stand to benefit immensely from early detection and intervention.
Dr. McGowan is assistant professor of psychiatry and pediatrics at the Vermont Center for Children, Youth, and Families, University of Vermont Medical Center, Burlington. She had no relevant financial disclosures. Email Dr. McGowan at [email protected].
Resources for providers and families*
UNSTUCK: An OCD Kids Movie. Featuring a 23-minute documentary film about children living with OCD, this website also is rich in OCD-related resources.
International OCD Foundation. Has information for families about OCD. Also has a resource directory for therapists, clinics, support groups, and other organizations specializing in OCD and related disorders in different geographic areas.
*Of note, both resources above include COVID-19-specific resources for those struggling with worsening OCD symptoms as a result of the pandemic.
References
1. Lewis’s Child and Adolescent Psychiatry: A Comprehensive Textbook, 4th ed. (Baltimore: Lippincott Williams & Wilkins, 2020, pp. 518-27).
2. J Amer Acad Child Adol Psychiatry. 2012;51(1):98-113.
3. J Clin. Invest. 2009;119(4):737-46.
4. Arch Dis Child. 2015;100(5):495-9.
5. J Develop Behav Pediatr. 2019 Jun;40(5):377-82.
6. Ann Clin Psychiatry. 2008 Oct-Dec;20(4):199-203.
Max is an 8-year-old boy in the third grade, and you have been his pediatrician since birth. Described as “emotional” and “particular” since his early years, Max is prone to prolonged tantrums that have not improved with age. Parents have described a tic that involves repeatedly touching his ear, but this has not been observed in the office setting. Max has struggled with some attention issues at school, and often needs help finishing assignments. The family is feeling increasingly desperate for ways to manage his near-daily meltdowns at home, and parenting strategies you’ve discussed thus far don’t seem to be helping much. Should obsessive-compulsive disorder be in your differential? And at what point do you seek outside evaluation?
OCD is a condition characterized by recurrent, intrusive, and unwanted thoughts, images, and urges (obsessions), and repetitive behaviors or mental acts performed in a particular way to reduce anxiety (compulsions). It affects 1%-3% of children, and onset can be as early as age 3-4 years. While the average age of onset in children is approximately 10 years old, average age of diagnosis is at least several years later.1 A primary care physician’s ability to recognize OCD symptoms in children, perform an initial assessment, and connect the child to appropriate clinical care is key to reducing the years of difficulty that children and families often endure prior to beginning treatment.
Common obsessions in children include contamination, fear of harm to self or others, symmetry, and the belief that bad things will occur if rituals are performed incorrectly. Common compulsions include checking, washing, ordering, and mental acts such as praying or counting to one’s self.1,2 In addition to the fact that OCD presentations are highly heterogeneous, early diagnosis is challenging due to significant overlap of OCD symptoms with developmentally normal behaviors. For example, magical or superstitious thinking is common among school-age children who avoid stepping on cracks or utilize lucky numbers. What differentiates OCD is the presence of obsessions and/or compulsions that are time consuming and cause subjective distress or functional impairment. Children often are adept at keeping OCD symptoms secret. At time of diagnosis, the child may have a complex array of discreet behaviors to manage distress and minimize shame. Children may not have insight into the irrationality of their thoughts or behaviors, but they are certainly aware of how terrible and confused they feel inside, and how it affects their relationship with their parents. Rituals, such as those that delay bedtime or cause school tardiness, may look like oppositional behaviors and cause immense frustration for parents.
Comorbidities are common and include ADHD, oppositional defiant disorder, depression, and Tourette syndrome.3 Nearly 60% of children with OCD meet criteria for a tic disorder at some point in their lifetime.4 Compulsions designed to ease a feeling of internal discomfort, such as touching or tapping, are particularly typical of patients with OCD and comorbid tics. Often these children will express a need for things to be “just right,” with lasting relief from such a feeling rarely found. While sensory intolerances are not part of OCD’s diagnostic criteria, clinical experiences and growing research point to a high prevalence in affected children.5,6 Sensory intolerances may even be the primary presenting problem. Examples include clothing feeling uncomfortable, or inability to tolerate certain smells or innocuous sounds.
The preferred method for assessment of OCD in children is the Children’s Yale–Brown Obsessive Compulsive Scale (CY-BOCS), a semi-structured, clinician-rated interview designed to elicit symptoms, severity, and distress. While time constraints may prevent use of the CY-BOCS in the primary care setting, a handful of screening questions instead can go a long way. These might include:
- Do you have to do things in a certain way, such as washing or making things “just right?”
- What happens if you can’t do things in a certain way?
- Do you have unwanted thoughts that keep coming back and are hard to get rid of?
Equally as important as understanding a child’s OCD symptoms is understanding how the family has, often unwittingly, become intertwined in a web of OCD-driven behaviors. In an effort to soothe the child, prevent emotional outbursts, or simply get through the day, parents may find themselves accommodating behaviors that seem irrational. Despite parents’ best intentions, this is likely reinforcing OCD patterns. Parents may be asked by the child to repeat a reassuring phrase in a certain way, arrange furniture “just so,” or drive a certain route to school. In the case of contamination fears, a child may be taking several showers per day, using two bottles of shampoo per week, and demanding that his or her clothes be washed separately before a parent begins to realize the cumulative impact of these unusual behaviors on the household. In addition to exploring concerns, primary care physicians can provide a sounding board for exhausted parents wondering if other families face the same thing. While connecting the family to treatment, they also can provide reassurances that treatment can dramatically shift the trajectory of the illness.
Treatment of pediatric OCD begins with a specific form of cognitive behavioral therapy (CBT) called Exposure and Response Prevention therapy (ERP). ERP requires a skilled therapist, and a strong alliance with a child and family because the child will be asked to gradually challenge compulsions head-on and tolerate the accompanied distress. CBT/ERP is associated with a 40%-65% reduction in symptoms, but combination with SSRI therapy improves outcomes in more severe cases.3 Despite limited mental health resources and long wait lists in many parts of the country, connection to OCD-specific treatment is increasingly feasible in virtual format via online support groups and telemedicine.
“Max” may experience any number of OCD-related symptoms that a primary care physician could deftly uncover. He may become “stuck” at school because his handwriting accidentally strayed below the line. He may have hours-long meltdowns because his hair never feels right. He may touch his ear to prevent tragic harm coming to his mother. Whatever further exploration reveals, Max and his family stand to benefit immensely from early detection and intervention.
Dr. McGowan is assistant professor of psychiatry and pediatrics at the Vermont Center for Children, Youth, and Families, University of Vermont Medical Center, Burlington. She had no relevant financial disclosures. Email Dr. McGowan at [email protected].
Resources for providers and families*
UNSTUCK: An OCD Kids Movie. Featuring a 23-minute documentary film about children living with OCD, this website also is rich in OCD-related resources.
International OCD Foundation. Has information for families about OCD. Also has a resource directory for therapists, clinics, support groups, and other organizations specializing in OCD and related disorders in different geographic areas.
*Of note, both resources above include COVID-19-specific resources for those struggling with worsening OCD symptoms as a result of the pandemic.
References
1. Lewis’s Child and Adolescent Psychiatry: A Comprehensive Textbook, 4th ed. (Baltimore: Lippincott Williams & Wilkins, 2020, pp. 518-27).
2. J Amer Acad Child Adol Psychiatry. 2012;51(1):98-113.
3. J Clin. Invest. 2009;119(4):737-46.
4. Arch Dis Child. 2015;100(5):495-9.
5. J Develop Behav Pediatr. 2019 Jun;40(5):377-82.
6. Ann Clin Psychiatry. 2008 Oct-Dec;20(4):199-203.
In praise of parents and children
The COVID-19 pandemic has changed the lives of children, teenagers, and parents worldwide. While some families are experiencing the unburdening of overly packed schedules and may be having a romantic or nostalgic “Little House on the Prairie” experience, for most it is at a minimum uncomfortable and inconvenient. For others it’s unbearable as they experience loss and feel relationship strain intensified by social distancing, seclusion, or quarantine. Some children have found respite from bullying at school, while other children have lost their only respite from being mistreated at home. Now may be as critical a time as ever for health care providers to listen carefully, empathize, validate, and proactively reach out to provide encouraging guidance and counsel, as well as express concern for families and children.
Many parents across the country are taking on an enormous, unanticipated task. Many parents have lost employment and income, while many mandatory professionals now struggle to keep up with increased work hours and work stress. Parents are trying to become multitaskers who assume the role of the music teacher, the soccer coach, the drama instructor, the friend, and of course their original role as a parent.
This seems an appropriate time to consider the work of Donald W. Winnicott, FRCP, the English pediatrician known for the concept of the “good enough parent.”1 This notion of parental competence was in part born out of a desire to defend parents against possible erosion of their confidence in following loving instincts by encroachment from professional expertise. The concept of the “good enough” parent is also related to the idea that young children who believe their parent is perfect will eventually know better. Now is a fitting time for pediatricians to buoy up imperfect but striving parents who are plenty “good enough” as they follow loving instincts to support their children during unforeseen changes associated with the pandemic.
Social distancing has led to family condensing. Many parents and children remain within the same four walls all day, every day. For many parents, the outlet of water cooler banter or yoga classes is gone. Even the commute home, with all its frustration, may have allowed decompression in the form of an audiobook, favorite music, or verbal transference of frustration onto the stranger who just cut you off. That commute might be gone too. Now, for many the good, bad, and the ugly is all happening at home. The 3-year-old may still adorably see a parent who can do no wrong, but in the end, the truth will prevail. A timely word of encouragement to parents: It’s okay to not be omnipotent. In fact, it will help children have a richer view of the world and more realistic expectations of themselves.
For children, they’ll need praise too, and the upheaval caused by the pandemic may be a fitting opportunity to make that praise more meaningful. But sports are off, the school musical is canceled, and the spelling bee is gone. The dojo is closed, the art fair is postponed, and the dance recital isn’t happening. Report cards in many schools may now transition from letter grades to pass/fail. Parents may be asking, “How on earth are we going to celebrate and praise the children?”
Research has shown us that praising the process is more valuable than praising the person.2 If Lucy participates in a soccer game and Javier gets his math results back, there are many possible approaches to praise. “You scored a goal!” or “You got an A on your math test!” is outcome- or product-focused praise. “You’re a good soccer player” or “You’re smart at math!” is person-focused praise. Instead, the most effective praise is process-focused praise: “You worked hard and ran hard even when it looked tiring” or “I noticed that you kept trying different strategies on those math problems until you figured them out.”
This may be a time when children face less comparison, less ranking, and receive less direct reward. With help, they can focus more on the process of learning and less on the outcomes of learning. They may more readily enjoy the efforts in their hobbies, not just the outcomes of their hobbies. When children receive praise for their work, effort, and actions rather than outcomes, externally validating things may be pleasantly replaced by internally validating traits. With process praise, children are more likely to feel self-confident, to set higher learning goals, and to accurately believe that intelligence is related to effort rather than a fixed trait that has been divided up among haves and have nots.3
Families currently face immense change, uncertainty, and discouragement largely unprecedented in their lifetimes. As care providers, we can look to lasting principles as we encourage parents in their provision of love. We can effectively provide praise and celebrate effort using evidence-based strategies uniquely fitted to our current circumstances. As we do this, we can provide healing of some of the less visible ailments associated with the COVID-19 pandemic.
Dr. Jackson is in the department of psychiatry at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email Dr. Jackson at [email protected].
References
1. “The Child, the Family, and the Outside World.” London: Penguin; 1973. p. 173.
2. Dev Psychol. 1999;35(3):835-47.
3. J Exp Child Psychol. 2018;173:116-35.
The COVID-19 pandemic has changed the lives of children, teenagers, and parents worldwide. While some families are experiencing the unburdening of overly packed schedules and may be having a romantic or nostalgic “Little House on the Prairie” experience, for most it is at a minimum uncomfortable and inconvenient. For others it’s unbearable as they experience loss and feel relationship strain intensified by social distancing, seclusion, or quarantine. Some children have found respite from bullying at school, while other children have lost their only respite from being mistreated at home. Now may be as critical a time as ever for health care providers to listen carefully, empathize, validate, and proactively reach out to provide encouraging guidance and counsel, as well as express concern for families and children.
Many parents across the country are taking on an enormous, unanticipated task. Many parents have lost employment and income, while many mandatory professionals now struggle to keep up with increased work hours and work stress. Parents are trying to become multitaskers who assume the role of the music teacher, the soccer coach, the drama instructor, the friend, and of course their original role as a parent.
This seems an appropriate time to consider the work of Donald W. Winnicott, FRCP, the English pediatrician known for the concept of the “good enough parent.”1 This notion of parental competence was in part born out of a desire to defend parents against possible erosion of their confidence in following loving instincts by encroachment from professional expertise. The concept of the “good enough” parent is also related to the idea that young children who believe their parent is perfect will eventually know better. Now is a fitting time for pediatricians to buoy up imperfect but striving parents who are plenty “good enough” as they follow loving instincts to support their children during unforeseen changes associated with the pandemic.
Social distancing has led to family condensing. Many parents and children remain within the same four walls all day, every day. For many parents, the outlet of water cooler banter or yoga classes is gone. Even the commute home, with all its frustration, may have allowed decompression in the form of an audiobook, favorite music, or verbal transference of frustration onto the stranger who just cut you off. That commute might be gone too. Now, for many the good, bad, and the ugly is all happening at home. The 3-year-old may still adorably see a parent who can do no wrong, but in the end, the truth will prevail. A timely word of encouragement to parents: It’s okay to not be omnipotent. In fact, it will help children have a richer view of the world and more realistic expectations of themselves.
For children, they’ll need praise too, and the upheaval caused by the pandemic may be a fitting opportunity to make that praise more meaningful. But sports are off, the school musical is canceled, and the spelling bee is gone. The dojo is closed, the art fair is postponed, and the dance recital isn’t happening. Report cards in many schools may now transition from letter grades to pass/fail. Parents may be asking, “How on earth are we going to celebrate and praise the children?”
Research has shown us that praising the process is more valuable than praising the person.2 If Lucy participates in a soccer game and Javier gets his math results back, there are many possible approaches to praise. “You scored a goal!” or “You got an A on your math test!” is outcome- or product-focused praise. “You’re a good soccer player” or “You’re smart at math!” is person-focused praise. Instead, the most effective praise is process-focused praise: “You worked hard and ran hard even when it looked tiring” or “I noticed that you kept trying different strategies on those math problems until you figured them out.”
This may be a time when children face less comparison, less ranking, and receive less direct reward. With help, they can focus more on the process of learning and less on the outcomes of learning. They may more readily enjoy the efforts in their hobbies, not just the outcomes of their hobbies. When children receive praise for their work, effort, and actions rather than outcomes, externally validating things may be pleasantly replaced by internally validating traits. With process praise, children are more likely to feel self-confident, to set higher learning goals, and to accurately believe that intelligence is related to effort rather than a fixed trait that has been divided up among haves and have nots.3
Families currently face immense change, uncertainty, and discouragement largely unprecedented in their lifetimes. As care providers, we can look to lasting principles as we encourage parents in their provision of love. We can effectively provide praise and celebrate effort using evidence-based strategies uniquely fitted to our current circumstances. As we do this, we can provide healing of some of the less visible ailments associated with the COVID-19 pandemic.
Dr. Jackson is in the department of psychiatry at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email Dr. Jackson at [email protected].
References
1. “The Child, the Family, and the Outside World.” London: Penguin; 1973. p. 173.
2. Dev Psychol. 1999;35(3):835-47.
3. J Exp Child Psychol. 2018;173:116-35.
The COVID-19 pandemic has changed the lives of children, teenagers, and parents worldwide. While some families are experiencing the unburdening of overly packed schedules and may be having a romantic or nostalgic “Little House on the Prairie” experience, for most it is at a minimum uncomfortable and inconvenient. For others it’s unbearable as they experience loss and feel relationship strain intensified by social distancing, seclusion, or quarantine. Some children have found respite from bullying at school, while other children have lost their only respite from being mistreated at home. Now may be as critical a time as ever for health care providers to listen carefully, empathize, validate, and proactively reach out to provide encouraging guidance and counsel, as well as express concern for families and children.
Many parents across the country are taking on an enormous, unanticipated task. Many parents have lost employment and income, while many mandatory professionals now struggle to keep up with increased work hours and work stress. Parents are trying to become multitaskers who assume the role of the music teacher, the soccer coach, the drama instructor, the friend, and of course their original role as a parent.
This seems an appropriate time to consider the work of Donald W. Winnicott, FRCP, the English pediatrician known for the concept of the “good enough parent.”1 This notion of parental competence was in part born out of a desire to defend parents against possible erosion of their confidence in following loving instincts by encroachment from professional expertise. The concept of the “good enough” parent is also related to the idea that young children who believe their parent is perfect will eventually know better. Now is a fitting time for pediatricians to buoy up imperfect but striving parents who are plenty “good enough” as they follow loving instincts to support their children during unforeseen changes associated with the pandemic.
Social distancing has led to family condensing. Many parents and children remain within the same four walls all day, every day. For many parents, the outlet of water cooler banter or yoga classes is gone. Even the commute home, with all its frustration, may have allowed decompression in the form of an audiobook, favorite music, or verbal transference of frustration onto the stranger who just cut you off. That commute might be gone too. Now, for many the good, bad, and the ugly is all happening at home. The 3-year-old may still adorably see a parent who can do no wrong, but in the end, the truth will prevail. A timely word of encouragement to parents: It’s okay to not be omnipotent. In fact, it will help children have a richer view of the world and more realistic expectations of themselves.
For children, they’ll need praise too, and the upheaval caused by the pandemic may be a fitting opportunity to make that praise more meaningful. But sports are off, the school musical is canceled, and the spelling bee is gone. The dojo is closed, the art fair is postponed, and the dance recital isn’t happening. Report cards in many schools may now transition from letter grades to pass/fail. Parents may be asking, “How on earth are we going to celebrate and praise the children?”
Research has shown us that praising the process is more valuable than praising the person.2 If Lucy participates in a soccer game and Javier gets his math results back, there are many possible approaches to praise. “You scored a goal!” or “You got an A on your math test!” is outcome- or product-focused praise. “You’re a good soccer player” or “You’re smart at math!” is person-focused praise. Instead, the most effective praise is process-focused praise: “You worked hard and ran hard even when it looked tiring” or “I noticed that you kept trying different strategies on those math problems until you figured them out.”
This may be a time when children face less comparison, less ranking, and receive less direct reward. With help, they can focus more on the process of learning and less on the outcomes of learning. They may more readily enjoy the efforts in their hobbies, not just the outcomes of their hobbies. When children receive praise for their work, effort, and actions rather than outcomes, externally validating things may be pleasantly replaced by internally validating traits. With process praise, children are more likely to feel self-confident, to set higher learning goals, and to accurately believe that intelligence is related to effort rather than a fixed trait that has been divided up among haves and have nots.3
Families currently face immense change, uncertainty, and discouragement largely unprecedented in their lifetimes. As care providers, we can look to lasting principles as we encourage parents in their provision of love. We can effectively provide praise and celebrate effort using evidence-based strategies uniquely fitted to our current circumstances. As we do this, we can provide healing of some of the less visible ailments associated with the COVID-19 pandemic.
Dr. Jackson is in the department of psychiatry at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email Dr. Jackson at [email protected].
References
1. “The Child, the Family, and the Outside World.” London: Penguin; 1973. p. 173.
2. Dev Psychol. 1999;35(3):835-47.
3. J Exp Child Psychol. 2018;173:116-35.
The role of medication in autism spectrum disorder
Efforts toward early identification and treatment are an important facet of the public health work in autism spectrum disorder (ASD).
The prevalence of ASD is rising. With the most recent estimate from the Centers from Disease Control and Prevention of 1 in 59* children aged 8 years,1 it is important for pediatric health care providers to have an understanding of current recommendations for treatment so they can counsel and guide affected families. ASD is a heterogeneous condition, so this article seeks to touch on broad principles, recognizing that clinicians must take into account the full clinical picture of each individual and family.
It is important to acknowledge that while there is no cure for ASD, there are treatment modalities that have an evidence base for addressing specific areas that may be impaired in children with autism. While it is beyond the scope of this article to review all of the potential areas of intervention in children with ASD, it is important to be keep in mind a few important principles.
1. The best evidenced treatment for addressing challenging and problematic behavior as well as improving a host of outcomes in children with ASD is itself behavioral in nature. These treatments are based on the principles of applied behavioral analysis,2 an educational and therapeutic approach which involves looking at antecedents and consequences of behaviors. This approach also looks to shape, motivate, and reinforce functional behaviors while discouraging harmful and disruptive ones.
2. Because communication often is impaired in children with ASD, providers always should investigate for possible medical causes of pain or discomfort that might explain sudden behavior change, as well as environmental changes that could be involved.
3. – because children with ASD often are particularly sensitive to medication side effects.
Irritability/aggression/extreme mood lability
There are only two medications with Food and Drug Administration labeling for an autism specific condition, and those are aripiprazole and risperidone, two second-generation antipsychotic agents approved for irritability associated with ASD on the basis of randomized controlled trials (RCTs) demonstrating their efficacy.3,4 Included under the umbrella of irritability are aggression, deliberate self-injurious behavior, extreme temper tantrums, and quick and extreme mood changes. For aripiprazole the approved ages are 6-17 years; a dosing range of 2-15 mg/day is recommended. For risperidone, the approved age range is 5-17 years; the recommended dosing range is 0.25-4 mg/day. Prior to starting either of these medications, a cardiac history should be obtained, and baseline laboratory values, particularly lipid levels and hemoglobin A1c (HbA1c) are recommended. All second-generation antipsychotics carry the risk of tardive dyskinesia (a movement disorder), as well as risk of weight gain and metabolic effects. Baseline weight prior to medication initiation with routine follow-up measurement is encouraged. In light of the burden of potential side effects, these medications tend to be reserved by clinicians for circumstances where there is a significant impact on functioning. Both medications are available in liquid form for children with difficulty swallowing pills.
ADHD
There are positive RCTs of methylphenidate in co-occurring ASD and ADHD,5 making it the preferred first line agent for treatment. Amphetamine salt based stimulant preparations do not have any RCTs in co-occurring ASD, but theoretically should be similarly effective. Again, the principle of starting low and going slow is applicable. Second line are the alpha 2 adrenergic agonists guanfacine and clonidine, both of whose long-acting formulations are approved for treatment of ADHD in children and adolescents without ASD, as well as atomoxetine, a selective norepinephrine reuptake inhibitor approved for ADHD. Guanfacine and atomoxetine have the stronger evidence base in the co-occurring condition. None of the second-line medications come in liquid preparation, although the immediate-release forms of guanfacine and clonidine both can be crushed and are used in clinical practice when the extended-release forms are not practicable.
Anxiety disorders and depression
Repetitive behaviors and insistence on sameness are broad headings that can be thought of as similar to obsessive compulsive disorder in children without ASD. However, controlled studies of SSRIs and clomipramine (a tricyclic antidepressant) have not shown a clear benefit in these behaviors in children with autism. There are no RCTs looking specifically at treatment of anxiety disorders in children with ASD, but expert consensus is that pharmacologic treatment is similar to that of children without ASD, with the SSRIs fluoxetine and sertraline the first-line agents due to the robust evidence for these two medications in treatment of anxiety disorders in children.6 Especially for kids with higher functioning ASD, cognitive behavioral therapy (CBT) should be considered and has some evidence for the co-occurring condition. Similarly, there are no RCTs for co-occurring depression in ASD, and clinical practice is to treat it as you would depression in the non-ASD population. Be aware that the studies of SSRIs in children with ASD reported higher than typical rates of behavioral activation on these medications, and again the principle of starting low and going slow is emphasized. Fluoxetine and sertraline both come in liquid form.
Insomnia
Insomnia is a common occurrence in children with ASD, and studies suggest melatonin can be effective, with immediate release clonidine a consideration with some limited evidence, if melatonin is not successful.
Finally I would be remiss in not mentioning that there is preliminary evidence from review7 and meta-analysis8 articles to suggest that regular exercise for individuals with ASD has a positive effect on multiple symptom domains, suggesting that this is an important additional treatment recommendation for children and families.
In conclusion, identification and treatment of ASD and co-occurring syndromes is often challenging, and while specialty referral often will be necessary, it is hoped that this overview provides a helpful frame of reference for primary care providers who encounter these conditions in clinical practice.
For further reading on this important subject, I recommend the American Academy of Child and Adolescent Psychiatry Practice Parameter for the Assessment and Treatment of Children and Adolescents with ASD and the Parents Medication Guide for Autism Spectrum Disorders.
Dr. Hoffnung is a pediatric psychiatrist at the University of Vermont Children’s Hospital and an assistant professor of psychiatry at the Robert Larner, M.D. College of Medicine at the University of Vermont, both in Burlington. He has no relevant financial disclosures. Email him at [email protected].
References
1. MMWR Surveill Summ 2018;67(No. SS-6):1–23*
2. National Standards Project, Phase 2. National Autism Center 2015.
3. N Engl J Med. 2002 Aug 1;347(5):314-21.
4. J Am Acad Child Adolesc Psychiatry. 2009 Nov;48(11):1110-9.
5. Arch Gen Psychiatry. 2005 Nov;62(11):1266-74.
6. Pediatrics. 2016 Feb;137(Supplement 2):S115-S123.
7. Research in Autism Spectrum Disorders. 2010 Dec;4(4):565-76.
8. Research in Autism Spectrum Disorders. 2012;6(1):46-57.
*This article was updated 4/2/2020.
Efforts toward early identification and treatment are an important facet of the public health work in autism spectrum disorder (ASD).
The prevalence of ASD is rising. With the most recent estimate from the Centers from Disease Control and Prevention of 1 in 59* children aged 8 years,1 it is important for pediatric health care providers to have an understanding of current recommendations for treatment so they can counsel and guide affected families. ASD is a heterogeneous condition, so this article seeks to touch on broad principles, recognizing that clinicians must take into account the full clinical picture of each individual and family.
It is important to acknowledge that while there is no cure for ASD, there are treatment modalities that have an evidence base for addressing specific areas that may be impaired in children with autism. While it is beyond the scope of this article to review all of the potential areas of intervention in children with ASD, it is important to be keep in mind a few important principles.
1. The best evidenced treatment for addressing challenging and problematic behavior as well as improving a host of outcomes in children with ASD is itself behavioral in nature. These treatments are based on the principles of applied behavioral analysis,2 an educational and therapeutic approach which involves looking at antecedents and consequences of behaviors. This approach also looks to shape, motivate, and reinforce functional behaviors while discouraging harmful and disruptive ones.
2. Because communication often is impaired in children with ASD, providers always should investigate for possible medical causes of pain or discomfort that might explain sudden behavior change, as well as environmental changes that could be involved.
3. – because children with ASD often are particularly sensitive to medication side effects.
Irritability/aggression/extreme mood lability
There are only two medications with Food and Drug Administration labeling for an autism specific condition, and those are aripiprazole and risperidone, two second-generation antipsychotic agents approved for irritability associated with ASD on the basis of randomized controlled trials (RCTs) demonstrating their efficacy.3,4 Included under the umbrella of irritability are aggression, deliberate self-injurious behavior, extreme temper tantrums, and quick and extreme mood changes. For aripiprazole the approved ages are 6-17 years; a dosing range of 2-15 mg/day is recommended. For risperidone, the approved age range is 5-17 years; the recommended dosing range is 0.25-4 mg/day. Prior to starting either of these medications, a cardiac history should be obtained, and baseline laboratory values, particularly lipid levels and hemoglobin A1c (HbA1c) are recommended. All second-generation antipsychotics carry the risk of tardive dyskinesia (a movement disorder), as well as risk of weight gain and metabolic effects. Baseline weight prior to medication initiation with routine follow-up measurement is encouraged. In light of the burden of potential side effects, these medications tend to be reserved by clinicians for circumstances where there is a significant impact on functioning. Both medications are available in liquid form for children with difficulty swallowing pills.
ADHD
There are positive RCTs of methylphenidate in co-occurring ASD and ADHD,5 making it the preferred first line agent for treatment. Amphetamine salt based stimulant preparations do not have any RCTs in co-occurring ASD, but theoretically should be similarly effective. Again, the principle of starting low and going slow is applicable. Second line are the alpha 2 adrenergic agonists guanfacine and clonidine, both of whose long-acting formulations are approved for treatment of ADHD in children and adolescents without ASD, as well as atomoxetine, a selective norepinephrine reuptake inhibitor approved for ADHD. Guanfacine and atomoxetine have the stronger evidence base in the co-occurring condition. None of the second-line medications come in liquid preparation, although the immediate-release forms of guanfacine and clonidine both can be crushed and are used in clinical practice when the extended-release forms are not practicable.
Anxiety disorders and depression
Repetitive behaviors and insistence on sameness are broad headings that can be thought of as similar to obsessive compulsive disorder in children without ASD. However, controlled studies of SSRIs and clomipramine (a tricyclic antidepressant) have not shown a clear benefit in these behaviors in children with autism. There are no RCTs looking specifically at treatment of anxiety disorders in children with ASD, but expert consensus is that pharmacologic treatment is similar to that of children without ASD, with the SSRIs fluoxetine and sertraline the first-line agents due to the robust evidence for these two medications in treatment of anxiety disorders in children.6 Especially for kids with higher functioning ASD, cognitive behavioral therapy (CBT) should be considered and has some evidence for the co-occurring condition. Similarly, there are no RCTs for co-occurring depression in ASD, and clinical practice is to treat it as you would depression in the non-ASD population. Be aware that the studies of SSRIs in children with ASD reported higher than typical rates of behavioral activation on these medications, and again the principle of starting low and going slow is emphasized. Fluoxetine and sertraline both come in liquid form.
Insomnia
Insomnia is a common occurrence in children with ASD, and studies suggest melatonin can be effective, with immediate release clonidine a consideration with some limited evidence, if melatonin is not successful.
Finally I would be remiss in not mentioning that there is preliminary evidence from review7 and meta-analysis8 articles to suggest that regular exercise for individuals with ASD has a positive effect on multiple symptom domains, suggesting that this is an important additional treatment recommendation for children and families.
In conclusion, identification and treatment of ASD and co-occurring syndromes is often challenging, and while specialty referral often will be necessary, it is hoped that this overview provides a helpful frame of reference for primary care providers who encounter these conditions in clinical practice.
For further reading on this important subject, I recommend the American Academy of Child and Adolescent Psychiatry Practice Parameter for the Assessment and Treatment of Children and Adolescents with ASD and the Parents Medication Guide for Autism Spectrum Disorders.
Dr. Hoffnung is a pediatric psychiatrist at the University of Vermont Children’s Hospital and an assistant professor of psychiatry at the Robert Larner, M.D. College of Medicine at the University of Vermont, both in Burlington. He has no relevant financial disclosures. Email him at [email protected].
References
1. MMWR Surveill Summ 2018;67(No. SS-6):1–23*
2. National Standards Project, Phase 2. National Autism Center 2015.
3. N Engl J Med. 2002 Aug 1;347(5):314-21.
4. J Am Acad Child Adolesc Psychiatry. 2009 Nov;48(11):1110-9.
5. Arch Gen Psychiatry. 2005 Nov;62(11):1266-74.
6. Pediatrics. 2016 Feb;137(Supplement 2):S115-S123.
7. Research in Autism Spectrum Disorders. 2010 Dec;4(4):565-76.
8. Research in Autism Spectrum Disorders. 2012;6(1):46-57.
*This article was updated 4/2/2020.
Efforts toward early identification and treatment are an important facet of the public health work in autism spectrum disorder (ASD).
The prevalence of ASD is rising. With the most recent estimate from the Centers from Disease Control and Prevention of 1 in 59* children aged 8 years,1 it is important for pediatric health care providers to have an understanding of current recommendations for treatment so they can counsel and guide affected families. ASD is a heterogeneous condition, so this article seeks to touch on broad principles, recognizing that clinicians must take into account the full clinical picture of each individual and family.
It is important to acknowledge that while there is no cure for ASD, there are treatment modalities that have an evidence base for addressing specific areas that may be impaired in children with autism. While it is beyond the scope of this article to review all of the potential areas of intervention in children with ASD, it is important to be keep in mind a few important principles.
1. The best evidenced treatment for addressing challenging and problematic behavior as well as improving a host of outcomes in children with ASD is itself behavioral in nature. These treatments are based on the principles of applied behavioral analysis,2 an educational and therapeutic approach which involves looking at antecedents and consequences of behaviors. This approach also looks to shape, motivate, and reinforce functional behaviors while discouraging harmful and disruptive ones.
2. Because communication often is impaired in children with ASD, providers always should investigate for possible medical causes of pain or discomfort that might explain sudden behavior change, as well as environmental changes that could be involved.
3. – because children with ASD often are particularly sensitive to medication side effects.
Irritability/aggression/extreme mood lability
There are only two medications with Food and Drug Administration labeling for an autism specific condition, and those are aripiprazole and risperidone, two second-generation antipsychotic agents approved for irritability associated with ASD on the basis of randomized controlled trials (RCTs) demonstrating their efficacy.3,4 Included under the umbrella of irritability are aggression, deliberate self-injurious behavior, extreme temper tantrums, and quick and extreme mood changes. For aripiprazole the approved ages are 6-17 years; a dosing range of 2-15 mg/day is recommended. For risperidone, the approved age range is 5-17 years; the recommended dosing range is 0.25-4 mg/day. Prior to starting either of these medications, a cardiac history should be obtained, and baseline laboratory values, particularly lipid levels and hemoglobin A1c (HbA1c) are recommended. All second-generation antipsychotics carry the risk of tardive dyskinesia (a movement disorder), as well as risk of weight gain and metabolic effects. Baseline weight prior to medication initiation with routine follow-up measurement is encouraged. In light of the burden of potential side effects, these medications tend to be reserved by clinicians for circumstances where there is a significant impact on functioning. Both medications are available in liquid form for children with difficulty swallowing pills.
ADHD
There are positive RCTs of methylphenidate in co-occurring ASD and ADHD,5 making it the preferred first line agent for treatment. Amphetamine salt based stimulant preparations do not have any RCTs in co-occurring ASD, but theoretically should be similarly effective. Again, the principle of starting low and going slow is applicable. Second line are the alpha 2 adrenergic agonists guanfacine and clonidine, both of whose long-acting formulations are approved for treatment of ADHD in children and adolescents without ASD, as well as atomoxetine, a selective norepinephrine reuptake inhibitor approved for ADHD. Guanfacine and atomoxetine have the stronger evidence base in the co-occurring condition. None of the second-line medications come in liquid preparation, although the immediate-release forms of guanfacine and clonidine both can be crushed and are used in clinical practice when the extended-release forms are not practicable.
Anxiety disorders and depression
Repetitive behaviors and insistence on sameness are broad headings that can be thought of as similar to obsessive compulsive disorder in children without ASD. However, controlled studies of SSRIs and clomipramine (a tricyclic antidepressant) have not shown a clear benefit in these behaviors in children with autism. There are no RCTs looking specifically at treatment of anxiety disorders in children with ASD, but expert consensus is that pharmacologic treatment is similar to that of children without ASD, with the SSRIs fluoxetine and sertraline the first-line agents due to the robust evidence for these two medications in treatment of anxiety disorders in children.6 Especially for kids with higher functioning ASD, cognitive behavioral therapy (CBT) should be considered and has some evidence for the co-occurring condition. Similarly, there are no RCTs for co-occurring depression in ASD, and clinical practice is to treat it as you would depression in the non-ASD population. Be aware that the studies of SSRIs in children with ASD reported higher than typical rates of behavioral activation on these medications, and again the principle of starting low and going slow is emphasized. Fluoxetine and sertraline both come in liquid form.
Insomnia
Insomnia is a common occurrence in children with ASD, and studies suggest melatonin can be effective, with immediate release clonidine a consideration with some limited evidence, if melatonin is not successful.
Finally I would be remiss in not mentioning that there is preliminary evidence from review7 and meta-analysis8 articles to suggest that regular exercise for individuals with ASD has a positive effect on multiple symptom domains, suggesting that this is an important additional treatment recommendation for children and families.
In conclusion, identification and treatment of ASD and co-occurring syndromes is often challenging, and while specialty referral often will be necessary, it is hoped that this overview provides a helpful frame of reference for primary care providers who encounter these conditions in clinical practice.
For further reading on this important subject, I recommend the American Academy of Child and Adolescent Psychiatry Practice Parameter for the Assessment and Treatment of Children and Adolescents with ASD and the Parents Medication Guide for Autism Spectrum Disorders.
Dr. Hoffnung is a pediatric psychiatrist at the University of Vermont Children’s Hospital and an assistant professor of psychiatry at the Robert Larner, M.D. College of Medicine at the University of Vermont, both in Burlington. He has no relevant financial disclosures. Email him at [email protected].
References
1. MMWR Surveill Summ 2018;67(No. SS-6):1–23*
2. National Standards Project, Phase 2. National Autism Center 2015.
3. N Engl J Med. 2002 Aug 1;347(5):314-21.
4. J Am Acad Child Adolesc Psychiatry. 2009 Nov;48(11):1110-9.
5. Arch Gen Psychiatry. 2005 Nov;62(11):1266-74.
6. Pediatrics. 2016 Feb;137(Supplement 2):S115-S123.
7. Research in Autism Spectrum Disorders. 2010 Dec;4(4):565-76.
8. Research in Autism Spectrum Disorders. 2012;6(1):46-57.
*This article was updated 4/2/2020.
Psychopharmacology for aggression? Our field’s ‘nonconsensus’ and the risks
A 13-year-old boy with ADHD, combined type, presents to his family physician with his parents. His parents called for an appointment outside of his routine follow-up care to discuss what they should do to address their son’s new “aggressive behaviors.” He will throw objects when angry, yell, and slam doors at home when he is told to turn off video games. He used to play soccer but doesn’t anymore. He has maintained very good grades and friends. There is not a concern for substance abuse at this time.He speaks in curt sentences during the appointment, and he has his arms crossed or is looking out of the window the entire time.
His parents share in front on him that he has always been a “difficult child” (their words), but they now are struggling to adjust to his aggressive tendencies as he ages. He is growing bigger and angrier. He will not attend therapy and will not see a consultation psychiatrist in the office. A variety of stimulant trials including Ritalin and amphetamine preparations to manage impulsivity in ADHD were ineffective to curb his aggression, and he doesn’t want to take any medication.
They ask, what do we do? They are not worried for their safety but living like this is eroding their quality of life as a family, and the dynamic seems destined to get worse before it gets better.
They wonder, is there a next medication step to manage his aggression?
A family physician presented the above situation to me in my role as a child and adolescent psychiatrist in the medical home. It led us to a fruitful discussion of aggression and what can be done to help families who are all too often in situations like the above, then in your office looking for immediate solutions. The questions are, what can be done with an aggressive child, even and especially without the child’s buy-in to work on that as a problem?
Psychoeducation can go a long way in helping families rethink aggression as a symptom of something deeper, either in the environment or a diagnosis, although we all can empathize with the desire to reconcile the above behavior immediately.
Characterize the aggression
First, it can be helpful to identify a child’s aggression type. There are two types of aggression, reactive and proactive. We most often see reactive aggression in our clinics, which is aggression as a defensive and impulsive response to something in the environment (often limit-setting, as above). Proactive aggression is premeditated and may appear as aggression for aggression’s sake without the emotional drive behind it.
Secondly, it also can be helpful to know that externalizing and internalizing symptoms can represent different sides of the same coin, with the proverbial “coin” as “emotion” and the associated behaviors (throwing objects, in the above example) as the “signs” that there is a complex difficulty in managing painful emotions. Some children (and adults too!) tend to “externalize” strong emotions as aggression or irritability with others, while others “internalize” them by retreating with internal suffering such as “anxiety and depression.” These styles also can be similar among children and their parents.
With those two points in mind, it’s important to consider the diagnosis, which would guide treatment. It’s generally agreed upon that “reactive aggression” is more likely to be related to underlying untreated ADHD, or a depressive or anxiety disorder. This is much more amenable to treatment than aggression related to oppositional defiant disorder or conduct disorder, which are more defined by proactive forms of aggression.
You can pick up on family dynamics that may inadvertently reinforce the same behaviors they so wish to change. In the above example, the parents have clearly identified their son as “the problem.” You can imagine the difficulty of going to school and being a “problem,” and then coming home and feeling the same way. This negative perception can erode a child’s self-esteem over time, which may appear as disengagement or simply not caring in an appointment. It may become harder and harder to engage the child in psychotherapy or even in taking a medication as their only means of resistance to that painful notion about oneself as the “problem.”
It can be useful to begin appointments with “what is going well?” (in the example above, he “has friends and is maintaining grades”) and “what do you like most about your child?” As we all know, positive reinforcement is more powerful than its counterpart. Also problems in a family often are complex, and may involve many family members needing to change to meet their goals, not just the child.
Why you should try behavioral interventions first
Behavioral interventions are the first step always. Parents can do behavioral interventions and change their parenting and family environment through their own behavioral changes – commonly called parent management training. They can assess antecedents of aggression and their own responses, which may contribute or perpetuate a cycle of the aggression – such as giving attention or giving in to fewer limitations to avoid a fight. This small but important point can help protect against a feeling of helplessness that a child will not engage in therapy or skills-building.
In answering the clinician’s question about what to do next, I often feel like the question embedded in this is “what medication is next?” There is a felt pressure to do something “right now” conveyed to a clinician. This drives the impulse to prescribe something immediately – and likely more risky and with less of an evidence base – even before trying the known psychotherapy interventions that have the most evidence to change aggressive tendencies.
In looking deeper into this consultation case, I also found more “food for thought” for one’s thinking about aggression and psychopharmacology in cases like the above: Aggression isn’t an uncomplicated symptom that one can address immediately, and therefore we cannot rely on symptom-specific management to eradicate it. This is similar to prescribing Tylenol to manage a general ache or pain; if the pain persists, we want to know the “whys” of the pain persisting.
Thankfully, there are ways that a parent can better understand behaviors with this philosophy in mind. Applied Behavioral Analysis1 offers some helpful ideas, not only for children with autism spectrum disorder, but that can be applied to one’s understanding of other’s behavior in general. ABA pays attention to antecedents, perpetuating factors, and consequences as well as their interplay in understanding behaviors. You can encourage a family – rather than wanting to “get rid of a problem behavior” – to try to understand it and come up, with help from a psychotherapist or other professional, with a deeper evaluation of the behavior and a specific, collaborative plan.
Most experts see that ADHD, anxiety disorders, depressive disorders, and unrecognized learning disabilities, in sum, are more common underpinnings than not with aggressive children. This also can be confounded by an environment with parents who have those diagnoses untreated as well. Aggression should raise a red flag in our clinics to consider the above even if a family or child simply says aggression is the one issue, and it’s only the child with the issue.
While there have been attempts to find a “spot treatment” for aggression in a medication, medications not only fail to address the underlying issues many times, but have little evidence that support them and may do more harm long term than good.2
Kids need outlets for “normal aggressive drives.” And puberty, as in the case above, is a time of intense emotions of all varieties. In the example above, you may notice that the child is no longer playing soccer, which was likely serving some protective function in many ways for him and as a positive outlet for aggression. In the same way, you may see that kids who are more sedentary or idle (playing unrestricted video games now instead of sports, ) would benefit from revisiting outlets or finding new ones as a family.
Consider medications if the underlying diagnosis merits it
We generally seek to find and treat the underlying diagnosis, if it exists, in the following ways.
If a child has ADHD, as in the case above, you can trial a stimulant or an alpha-adrenergic agent to target impulsivity if that is suspected as the driver of aggression. This may include guanfacine (long-acting Intuniv at night, but I would choose lower dosing such as 0.5 mg to 1 mg at bedtime) to manage ADHD. However, the evidence base that management of ADHD improves aggressive behaviors at all or on their own, is scant. In addition, these medications can represent more harm than good as well, although they are perceived as more innocuous than their antipsychotic counterparts. For example, some patients can begin to have bed-wetting accidents in the evening or become sleepy in classes, which can further erode their sense of self-confidence even if this is clearly attributable to a medication side effect and resolves once the agent is reduced or removed.
In the same way to reorient to diagnosis with children with aggression, you can consider an SSRI for an anxiety disorder or irritable depression. But know that it’s a rare thing for children to say specifically that they are struggling with their emotions, whether they are angry, sad, or nervous and that a deeper dive into this may be warranted. Data by Connor DF et al.3 may indicate anxiety disorders should be highest on one’s differential diagnosis in aggression, followed by consideration for ADHD, which may be a different assumption than one would expect.
Mood stabilizers –lamotrigine (Lamictal), divalproex sodium (Depakote), and lithium – and antipsychotics – aripiprazole (Abilify) and risperidone (Risperdal) – are risky medications and the use of them contradicts the first point, agreed upon by most experts, that diagnosis should drive treatment. One is hardly ever treating a young child for psychosis or bipolar disorder in these circumstances of episodic, reactive aggression. Antipsychotics also carry the notorious risks of metabolic syndrome, among other risks to overall health, which becomes an additive risk over time and potentially into adulthood. I once heard in my child adolescent psychiatry training the haunting phase, “yes, they can ‘work’ quickly but they can work ‘almost too well,’ ” meaning they can sedate or tranquilize an aggressive child when the real goal should be to understand, diagnose, and intervene in ways that see the “big picture” of aggression.
Benzodiazepines generally are avoided in children due to disinhibition and often not even considered, in these circumstances, as they are in adults to manage agitation or aggression, due to this fact.
In many instances in working with families, our role in primary care can be one of illuminating children’s behaviors not just as symptoms to treat, but to understand deeply. This is as true for aggression as it is for anxiety.
Finally, I am reminded of the common question I receive from adult patients in primary care who ask me if anyone has yet made a medication to lose weight that’s safe and effective. Then the counseling commences on our fantasies, from our patients and ourselves, about what medications can do for us and our risks therein.
Dr. Pawlowski is an adult, adolescent, and child psychiatrist at the University of Vermont Medical Center and assistant professor of psychiatry at the Larner College of Medicine at UVM in Burlington. Email her at [email protected].
References
1. ABA in the Treatment of Aggressive Behavior Disorder and Lack of Impulse Control.
2. Managing Aggression in Children: A Practical Approach, The Carlat Child Psychiatry Report, May 2010, The Explosive Child.
3. Child Psychiatry Hum Dev. 2006 May;37[1]:1-14.
A 13-year-old boy with ADHD, combined type, presents to his family physician with his parents. His parents called for an appointment outside of his routine follow-up care to discuss what they should do to address their son’s new “aggressive behaviors.” He will throw objects when angry, yell, and slam doors at home when he is told to turn off video games. He used to play soccer but doesn’t anymore. He has maintained very good grades and friends. There is not a concern for substance abuse at this time.He speaks in curt sentences during the appointment, and he has his arms crossed or is looking out of the window the entire time.
His parents share in front on him that he has always been a “difficult child” (their words), but they now are struggling to adjust to his aggressive tendencies as he ages. He is growing bigger and angrier. He will not attend therapy and will not see a consultation psychiatrist in the office. A variety of stimulant trials including Ritalin and amphetamine preparations to manage impulsivity in ADHD were ineffective to curb his aggression, and he doesn’t want to take any medication.
They ask, what do we do? They are not worried for their safety but living like this is eroding their quality of life as a family, and the dynamic seems destined to get worse before it gets better.
They wonder, is there a next medication step to manage his aggression?
A family physician presented the above situation to me in my role as a child and adolescent psychiatrist in the medical home. It led us to a fruitful discussion of aggression and what can be done to help families who are all too often in situations like the above, then in your office looking for immediate solutions. The questions are, what can be done with an aggressive child, even and especially without the child’s buy-in to work on that as a problem?
Psychoeducation can go a long way in helping families rethink aggression as a symptom of something deeper, either in the environment or a diagnosis, although we all can empathize with the desire to reconcile the above behavior immediately.
Characterize the aggression
First, it can be helpful to identify a child’s aggression type. There are two types of aggression, reactive and proactive. We most often see reactive aggression in our clinics, which is aggression as a defensive and impulsive response to something in the environment (often limit-setting, as above). Proactive aggression is premeditated and may appear as aggression for aggression’s sake without the emotional drive behind it.
Secondly, it also can be helpful to know that externalizing and internalizing symptoms can represent different sides of the same coin, with the proverbial “coin” as “emotion” and the associated behaviors (throwing objects, in the above example) as the “signs” that there is a complex difficulty in managing painful emotions. Some children (and adults too!) tend to “externalize” strong emotions as aggression or irritability with others, while others “internalize” them by retreating with internal suffering such as “anxiety and depression.” These styles also can be similar among children and their parents.
With those two points in mind, it’s important to consider the diagnosis, which would guide treatment. It’s generally agreed upon that “reactive aggression” is more likely to be related to underlying untreated ADHD, or a depressive or anxiety disorder. This is much more amenable to treatment than aggression related to oppositional defiant disorder or conduct disorder, which are more defined by proactive forms of aggression.
You can pick up on family dynamics that may inadvertently reinforce the same behaviors they so wish to change. In the above example, the parents have clearly identified their son as “the problem.” You can imagine the difficulty of going to school and being a “problem,” and then coming home and feeling the same way. This negative perception can erode a child’s self-esteem over time, which may appear as disengagement or simply not caring in an appointment. It may become harder and harder to engage the child in psychotherapy or even in taking a medication as their only means of resistance to that painful notion about oneself as the “problem.”
It can be useful to begin appointments with “what is going well?” (in the example above, he “has friends and is maintaining grades”) and “what do you like most about your child?” As we all know, positive reinforcement is more powerful than its counterpart. Also problems in a family often are complex, and may involve many family members needing to change to meet their goals, not just the child.
Why you should try behavioral interventions first
Behavioral interventions are the first step always. Parents can do behavioral interventions and change their parenting and family environment through their own behavioral changes – commonly called parent management training. They can assess antecedents of aggression and their own responses, which may contribute or perpetuate a cycle of the aggression – such as giving attention or giving in to fewer limitations to avoid a fight. This small but important point can help protect against a feeling of helplessness that a child will not engage in therapy or skills-building.
In answering the clinician’s question about what to do next, I often feel like the question embedded in this is “what medication is next?” There is a felt pressure to do something “right now” conveyed to a clinician. This drives the impulse to prescribe something immediately – and likely more risky and with less of an evidence base – even before trying the known psychotherapy interventions that have the most evidence to change aggressive tendencies.
In looking deeper into this consultation case, I also found more “food for thought” for one’s thinking about aggression and psychopharmacology in cases like the above: Aggression isn’t an uncomplicated symptom that one can address immediately, and therefore we cannot rely on symptom-specific management to eradicate it. This is similar to prescribing Tylenol to manage a general ache or pain; if the pain persists, we want to know the “whys” of the pain persisting.
Thankfully, there are ways that a parent can better understand behaviors with this philosophy in mind. Applied Behavioral Analysis1 offers some helpful ideas, not only for children with autism spectrum disorder, but that can be applied to one’s understanding of other’s behavior in general. ABA pays attention to antecedents, perpetuating factors, and consequences as well as their interplay in understanding behaviors. You can encourage a family – rather than wanting to “get rid of a problem behavior” – to try to understand it and come up, with help from a psychotherapist or other professional, with a deeper evaluation of the behavior and a specific, collaborative plan.
Most experts see that ADHD, anxiety disorders, depressive disorders, and unrecognized learning disabilities, in sum, are more common underpinnings than not with aggressive children. This also can be confounded by an environment with parents who have those diagnoses untreated as well. Aggression should raise a red flag in our clinics to consider the above even if a family or child simply says aggression is the one issue, and it’s only the child with the issue.
While there have been attempts to find a “spot treatment” for aggression in a medication, medications not only fail to address the underlying issues many times, but have little evidence that support them and may do more harm long term than good.2
Kids need outlets for “normal aggressive drives.” And puberty, as in the case above, is a time of intense emotions of all varieties. In the example above, you may notice that the child is no longer playing soccer, which was likely serving some protective function in many ways for him and as a positive outlet for aggression. In the same way, you may see that kids who are more sedentary or idle (playing unrestricted video games now instead of sports, ) would benefit from revisiting outlets or finding new ones as a family.
Consider medications if the underlying diagnosis merits it
We generally seek to find and treat the underlying diagnosis, if it exists, in the following ways.
If a child has ADHD, as in the case above, you can trial a stimulant or an alpha-adrenergic agent to target impulsivity if that is suspected as the driver of aggression. This may include guanfacine (long-acting Intuniv at night, but I would choose lower dosing such as 0.5 mg to 1 mg at bedtime) to manage ADHD. However, the evidence base that management of ADHD improves aggressive behaviors at all or on their own, is scant. In addition, these medications can represent more harm than good as well, although they are perceived as more innocuous than their antipsychotic counterparts. For example, some patients can begin to have bed-wetting accidents in the evening or become sleepy in classes, which can further erode their sense of self-confidence even if this is clearly attributable to a medication side effect and resolves once the agent is reduced or removed.
In the same way to reorient to diagnosis with children with aggression, you can consider an SSRI for an anxiety disorder or irritable depression. But know that it’s a rare thing for children to say specifically that they are struggling with their emotions, whether they are angry, sad, or nervous and that a deeper dive into this may be warranted. Data by Connor DF et al.3 may indicate anxiety disorders should be highest on one’s differential diagnosis in aggression, followed by consideration for ADHD, which may be a different assumption than one would expect.
Mood stabilizers –lamotrigine (Lamictal), divalproex sodium (Depakote), and lithium – and antipsychotics – aripiprazole (Abilify) and risperidone (Risperdal) – are risky medications and the use of them contradicts the first point, agreed upon by most experts, that diagnosis should drive treatment. One is hardly ever treating a young child for psychosis or bipolar disorder in these circumstances of episodic, reactive aggression. Antipsychotics also carry the notorious risks of metabolic syndrome, among other risks to overall health, which becomes an additive risk over time and potentially into adulthood. I once heard in my child adolescent psychiatry training the haunting phase, “yes, they can ‘work’ quickly but they can work ‘almost too well,’ ” meaning they can sedate or tranquilize an aggressive child when the real goal should be to understand, diagnose, and intervene in ways that see the “big picture” of aggression.
Benzodiazepines generally are avoided in children due to disinhibition and often not even considered, in these circumstances, as they are in adults to manage agitation or aggression, due to this fact.
In many instances in working with families, our role in primary care can be one of illuminating children’s behaviors not just as symptoms to treat, but to understand deeply. This is as true for aggression as it is for anxiety.
Finally, I am reminded of the common question I receive from adult patients in primary care who ask me if anyone has yet made a medication to lose weight that’s safe and effective. Then the counseling commences on our fantasies, from our patients and ourselves, about what medications can do for us and our risks therein.
Dr. Pawlowski is an adult, adolescent, and child psychiatrist at the University of Vermont Medical Center and assistant professor of psychiatry at the Larner College of Medicine at UVM in Burlington. Email her at [email protected].
References
1. ABA in the Treatment of Aggressive Behavior Disorder and Lack of Impulse Control.
2. Managing Aggression in Children: A Practical Approach, The Carlat Child Psychiatry Report, May 2010, The Explosive Child.
3. Child Psychiatry Hum Dev. 2006 May;37[1]:1-14.
A 13-year-old boy with ADHD, combined type, presents to his family physician with his parents. His parents called for an appointment outside of his routine follow-up care to discuss what they should do to address their son’s new “aggressive behaviors.” He will throw objects when angry, yell, and slam doors at home when he is told to turn off video games. He used to play soccer but doesn’t anymore. He has maintained very good grades and friends. There is not a concern for substance abuse at this time.He speaks in curt sentences during the appointment, and he has his arms crossed or is looking out of the window the entire time.
His parents share in front on him that he has always been a “difficult child” (their words), but they now are struggling to adjust to his aggressive tendencies as he ages. He is growing bigger and angrier. He will not attend therapy and will not see a consultation psychiatrist in the office. A variety of stimulant trials including Ritalin and amphetamine preparations to manage impulsivity in ADHD were ineffective to curb his aggression, and he doesn’t want to take any medication.
They ask, what do we do? They are not worried for their safety but living like this is eroding their quality of life as a family, and the dynamic seems destined to get worse before it gets better.
They wonder, is there a next medication step to manage his aggression?
A family physician presented the above situation to me in my role as a child and adolescent psychiatrist in the medical home. It led us to a fruitful discussion of aggression and what can be done to help families who are all too often in situations like the above, then in your office looking for immediate solutions. The questions are, what can be done with an aggressive child, even and especially without the child’s buy-in to work on that as a problem?
Psychoeducation can go a long way in helping families rethink aggression as a symptom of something deeper, either in the environment or a diagnosis, although we all can empathize with the desire to reconcile the above behavior immediately.
Characterize the aggression
First, it can be helpful to identify a child’s aggression type. There are two types of aggression, reactive and proactive. We most often see reactive aggression in our clinics, which is aggression as a defensive and impulsive response to something in the environment (often limit-setting, as above). Proactive aggression is premeditated and may appear as aggression for aggression’s sake without the emotional drive behind it.
Secondly, it also can be helpful to know that externalizing and internalizing symptoms can represent different sides of the same coin, with the proverbial “coin” as “emotion” and the associated behaviors (throwing objects, in the above example) as the “signs” that there is a complex difficulty in managing painful emotions. Some children (and adults too!) tend to “externalize” strong emotions as aggression or irritability with others, while others “internalize” them by retreating with internal suffering such as “anxiety and depression.” These styles also can be similar among children and their parents.
With those two points in mind, it’s important to consider the diagnosis, which would guide treatment. It’s generally agreed upon that “reactive aggression” is more likely to be related to underlying untreated ADHD, or a depressive or anxiety disorder. This is much more amenable to treatment than aggression related to oppositional defiant disorder or conduct disorder, which are more defined by proactive forms of aggression.
You can pick up on family dynamics that may inadvertently reinforce the same behaviors they so wish to change. In the above example, the parents have clearly identified their son as “the problem.” You can imagine the difficulty of going to school and being a “problem,” and then coming home and feeling the same way. This negative perception can erode a child’s self-esteem over time, which may appear as disengagement or simply not caring in an appointment. It may become harder and harder to engage the child in psychotherapy or even in taking a medication as their only means of resistance to that painful notion about oneself as the “problem.”
It can be useful to begin appointments with “what is going well?” (in the example above, he “has friends and is maintaining grades”) and “what do you like most about your child?” As we all know, positive reinforcement is more powerful than its counterpart. Also problems in a family often are complex, and may involve many family members needing to change to meet their goals, not just the child.
Why you should try behavioral interventions first
Behavioral interventions are the first step always. Parents can do behavioral interventions and change their parenting and family environment through their own behavioral changes – commonly called parent management training. They can assess antecedents of aggression and their own responses, which may contribute or perpetuate a cycle of the aggression – such as giving attention or giving in to fewer limitations to avoid a fight. This small but important point can help protect against a feeling of helplessness that a child will not engage in therapy or skills-building.
In answering the clinician’s question about what to do next, I often feel like the question embedded in this is “what medication is next?” There is a felt pressure to do something “right now” conveyed to a clinician. This drives the impulse to prescribe something immediately – and likely more risky and with less of an evidence base – even before trying the known psychotherapy interventions that have the most evidence to change aggressive tendencies.
In looking deeper into this consultation case, I also found more “food for thought” for one’s thinking about aggression and psychopharmacology in cases like the above: Aggression isn’t an uncomplicated symptom that one can address immediately, and therefore we cannot rely on symptom-specific management to eradicate it. This is similar to prescribing Tylenol to manage a general ache or pain; if the pain persists, we want to know the “whys” of the pain persisting.
Thankfully, there are ways that a parent can better understand behaviors with this philosophy in mind. Applied Behavioral Analysis1 offers some helpful ideas, not only for children with autism spectrum disorder, but that can be applied to one’s understanding of other’s behavior in general. ABA pays attention to antecedents, perpetuating factors, and consequences as well as their interplay in understanding behaviors. You can encourage a family – rather than wanting to “get rid of a problem behavior” – to try to understand it and come up, with help from a psychotherapist or other professional, with a deeper evaluation of the behavior and a specific, collaborative plan.
Most experts see that ADHD, anxiety disorders, depressive disorders, and unrecognized learning disabilities, in sum, are more common underpinnings than not with aggressive children. This also can be confounded by an environment with parents who have those diagnoses untreated as well. Aggression should raise a red flag in our clinics to consider the above even if a family or child simply says aggression is the one issue, and it’s only the child with the issue.
While there have been attempts to find a “spot treatment” for aggression in a medication, medications not only fail to address the underlying issues many times, but have little evidence that support them and may do more harm long term than good.2
Kids need outlets for “normal aggressive drives.” And puberty, as in the case above, is a time of intense emotions of all varieties. In the example above, you may notice that the child is no longer playing soccer, which was likely serving some protective function in many ways for him and as a positive outlet for aggression. In the same way, you may see that kids who are more sedentary or idle (playing unrestricted video games now instead of sports, ) would benefit from revisiting outlets or finding new ones as a family.
Consider medications if the underlying diagnosis merits it
We generally seek to find and treat the underlying diagnosis, if it exists, in the following ways.
If a child has ADHD, as in the case above, you can trial a stimulant or an alpha-adrenergic agent to target impulsivity if that is suspected as the driver of aggression. This may include guanfacine (long-acting Intuniv at night, but I would choose lower dosing such as 0.5 mg to 1 mg at bedtime) to manage ADHD. However, the evidence base that management of ADHD improves aggressive behaviors at all or on their own, is scant. In addition, these medications can represent more harm than good as well, although they are perceived as more innocuous than their antipsychotic counterparts. For example, some patients can begin to have bed-wetting accidents in the evening or become sleepy in classes, which can further erode their sense of self-confidence even if this is clearly attributable to a medication side effect and resolves once the agent is reduced or removed.
In the same way to reorient to diagnosis with children with aggression, you can consider an SSRI for an anxiety disorder or irritable depression. But know that it’s a rare thing for children to say specifically that they are struggling with their emotions, whether they are angry, sad, or nervous and that a deeper dive into this may be warranted. Data by Connor DF et al.3 may indicate anxiety disorders should be highest on one’s differential diagnosis in aggression, followed by consideration for ADHD, which may be a different assumption than one would expect.
Mood stabilizers –lamotrigine (Lamictal), divalproex sodium (Depakote), and lithium – and antipsychotics – aripiprazole (Abilify) and risperidone (Risperdal) – are risky medications and the use of them contradicts the first point, agreed upon by most experts, that diagnosis should drive treatment. One is hardly ever treating a young child for psychosis or bipolar disorder in these circumstances of episodic, reactive aggression. Antipsychotics also carry the notorious risks of metabolic syndrome, among other risks to overall health, which becomes an additive risk over time and potentially into adulthood. I once heard in my child adolescent psychiatry training the haunting phase, “yes, they can ‘work’ quickly but they can work ‘almost too well,’ ” meaning they can sedate or tranquilize an aggressive child when the real goal should be to understand, diagnose, and intervene in ways that see the “big picture” of aggression.
Benzodiazepines generally are avoided in children due to disinhibition and often not even considered, in these circumstances, as they are in adults to manage agitation or aggression, due to this fact.
In many instances in working with families, our role in primary care can be one of illuminating children’s behaviors not just as symptoms to treat, but to understand deeply. This is as true for aggression as it is for anxiety.
Finally, I am reminded of the common question I receive from adult patients in primary care who ask me if anyone has yet made a medication to lose weight that’s safe and effective. Then the counseling commences on our fantasies, from our patients and ourselves, about what medications can do for us and our risks therein.
Dr. Pawlowski is an adult, adolescent, and child psychiatrist at the University of Vermont Medical Center and assistant professor of psychiatry at the Larner College of Medicine at UVM in Burlington. Email her at [email protected].
References
1. ABA in the Treatment of Aggressive Behavior Disorder and Lack of Impulse Control.
2. Managing Aggression in Children: A Practical Approach, The Carlat Child Psychiatry Report, May 2010, The Explosive Child.
3. Child Psychiatry Hum Dev. 2006 May;37[1]:1-14.
Pediatricians take on more mental health care
Assessment and treatment of many of the more common behavioral disorders in childhood, such as ADHD and anxiety, should be considered within a pediatrician’s scope of practice, a stance made very clear by a recent policy statement published by the American Academy of Pediatrics entitled “Mental health competencies for pediatric practice.”1 These competencies include medication treatment. As stated in the article, “certain disorders (ADHD, common anxiety disorders, depression), if associated with no more than moderate impairment, are amenable to primary care medication management because there are indicated medications with a well-established safety profile.”
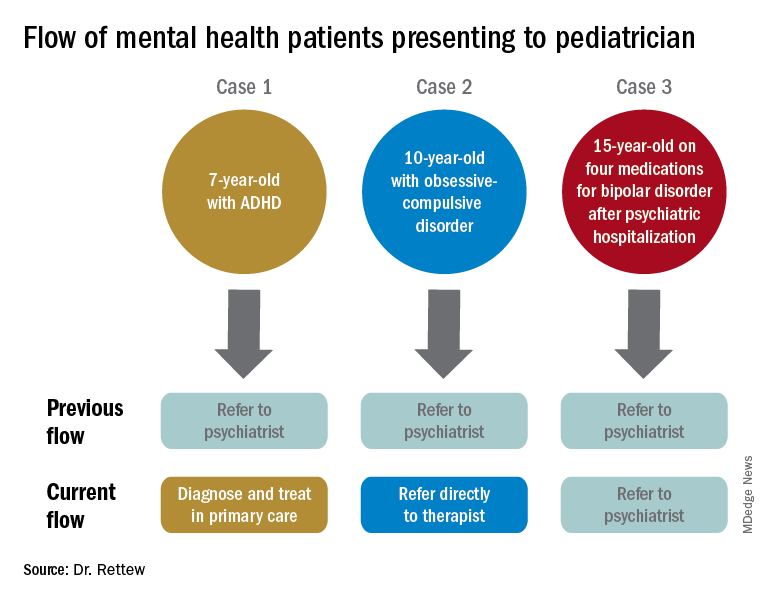
This shift to shared ownership when it comes to mental health care is likely coming from multiple sources, not the least of them being necessity and an acknowledgment that there simply aren’t enough psychiatrists to take over the mental health care of every youth with a diagnosable psychiatric disorder. While the number of child and adolescent psychiatrists remains relatively flat, the youth suicide rate is rising, as are the numbers presenting to emergency departments in crisis – all for reasons still to be fully understood. And these trends all are occurring as the medical community overall is appreciating more and more that good mental health is a cornerstone of all health.
The response from the pediatric community, whether it be because of personal conviction or simply a lack of options, largely has been to step up to the plate and take on these new responsibilities and challenges while trying to get up to speed with the latest information about mental health best practices. From my own experience doing evaluations and consultations from area primary care clinicians for over 15 years, the shift is noticeable. The typical patient now coming in has already seen a mental health counselor and tried at least one medication, while evaluations for diagnosis and treatment recommendations for things like uncomplicated and treatment-naive ADHD symptoms, for example, are becoming much more infrequent – although still far from extinct.
Nevertheless, there remain concerns about the extent of these new charges. Joe Nasca, MD, an experienced pediatrician who has been practicing in rural Vermont for decades, is worried that there is simply too much already for pediatricians to know and do to be able to add extensive mental health care. “There is so much to know in general peds [pediatrics] that I would guess a year or more of additional residency and experience would adequately prepare me to take this on,” he said in an interview. In comparing psychiatric care to other specialties, Dr. Nasca went on to say that, “I would not presume to treat chronic renal failure without the help of a nephrologist or a dilated aortic arch without a cardiologist.”
In a similar vein, however, it also is true that a significant percentage of children presenting to pediatricians for orthopedic problems, infections, asthma, and rashes are managed without referrals to specialists. The right balance, of course, will vary from clinician to clinician based on that pediatrician’s level of interest, experience, and available resources in the community. The AAP position papers don’t mandate or even encourage the notion that all pediatricians need to be at the same place when it comes to competency in assessment and treatment of mental health problems, although it is probably fair to say that there is a push for the pediatric community as a whole to raise the collective bar at least a notch or two.
In response, the mental health community has moved to support the primary care community in their expanded role. These efforts have taken many forms, most notably the model of integrated care, in which mental health clinicians of various types see patients in primary care offices rather than making patients come to them. There also are new consultation programs that provide easy access to a child psychiatrist or other mental health professional for case-related questions delivered by phone, email, or for single in-person consultations. Additional training and educational offerings also are now available for pediatricians either in training and for those already in practice. These initiatives are bolstered by research showing that, not only can good mental health care be delivered in pediatric settings, but there are cost savings that can be realized, particularly for nonpsychiatric medical care.2 Despite these promising leads, however, there will remain some for whom anything less than the increased availability of a psychiatrist to “take over” a patient’s mental health care will be seen as a falling short of the clinical need.
To illustrate how things have and continue to change, consider the following three common clinical scenarios that generally present to a pediatrician:
- New presentation of ADHD symptoms.
- Anxiety or obsessive-compulsive problems.
- Return of a patient who has been psychiatrically hospitalized and now is taking multiple medications.
In the past, all three cases often would have resulted in a referral to a psychiatrist. Today, however, it is quite likely that only one of these cases would be referred because ADHD could be well diagnosed and managed within the primary care setting, and problems like anxiety and obsessive-compulsive disorder are sent first not to a psychiatrist but to a non-MD psychotherapist.
Moving forward, today’s pediatricians are expected to do more for the mental health care of patients themselves instead of referring to a psychiatrist. Most already do, despite having had little in the way of formal training. As the evidence grows that the promotion of mental well-being can be a key to future overall health, as well as to the cost of future health care, there are many reasons to be optimistic that support for pediatricians and collaborative care models for clinicians trying to fulfill these new responsibilities will get only stronger.
References
1. Pediatrics. 2019 Nov;144(5). pii: e20192757.
2. Pediatrics. 2019 Jul;144(1). pii: e20183243.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @PediPsych. Email him at [email protected]. Looking for more mental health training? Attend the 14th annual Child Psychiatry in Primary Care conference in Burlington on May 8, 2020 (http://www.med.uvm.edu/cme/conferences).
Assessment and treatment of many of the more common behavioral disorders in childhood, such as ADHD and anxiety, should be considered within a pediatrician’s scope of practice, a stance made very clear by a recent policy statement published by the American Academy of Pediatrics entitled “Mental health competencies for pediatric practice.”1 These competencies include medication treatment. As stated in the article, “certain disorders (ADHD, common anxiety disorders, depression), if associated with no more than moderate impairment, are amenable to primary care medication management because there are indicated medications with a well-established safety profile.”
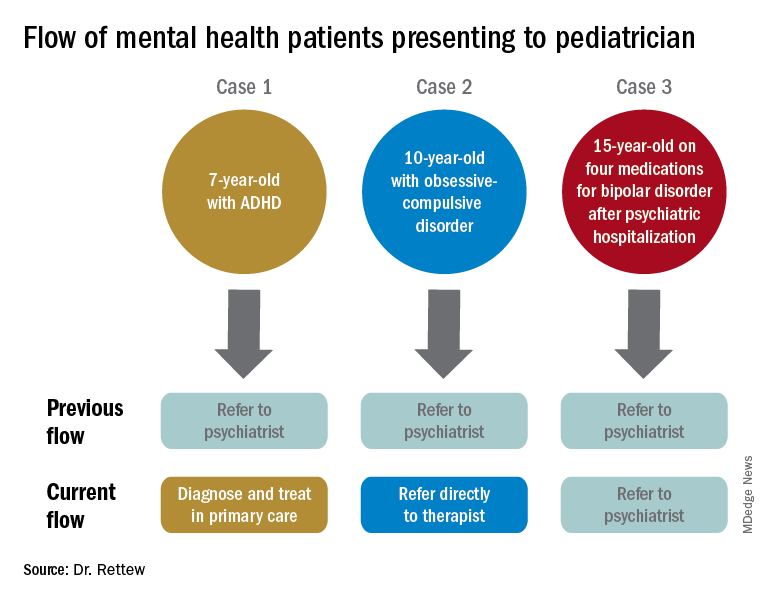
This shift to shared ownership when it comes to mental health care is likely coming from multiple sources, not the least of them being necessity and an acknowledgment that there simply aren’t enough psychiatrists to take over the mental health care of every youth with a diagnosable psychiatric disorder. While the number of child and adolescent psychiatrists remains relatively flat, the youth suicide rate is rising, as are the numbers presenting to emergency departments in crisis – all for reasons still to be fully understood. And these trends all are occurring as the medical community overall is appreciating more and more that good mental health is a cornerstone of all health.
The response from the pediatric community, whether it be because of personal conviction or simply a lack of options, largely has been to step up to the plate and take on these new responsibilities and challenges while trying to get up to speed with the latest information about mental health best practices. From my own experience doing evaluations and consultations from area primary care clinicians for over 15 years, the shift is noticeable. The typical patient now coming in has already seen a mental health counselor and tried at least one medication, while evaluations for diagnosis and treatment recommendations for things like uncomplicated and treatment-naive ADHD symptoms, for example, are becoming much more infrequent – although still far from extinct.
Nevertheless, there remain concerns about the extent of these new charges. Joe Nasca, MD, an experienced pediatrician who has been practicing in rural Vermont for decades, is worried that there is simply too much already for pediatricians to know and do to be able to add extensive mental health care. “There is so much to know in general peds [pediatrics] that I would guess a year or more of additional residency and experience would adequately prepare me to take this on,” he said in an interview. In comparing psychiatric care to other specialties, Dr. Nasca went on to say that, “I would not presume to treat chronic renal failure without the help of a nephrologist or a dilated aortic arch without a cardiologist.”
In a similar vein, however, it also is true that a significant percentage of children presenting to pediatricians for orthopedic problems, infections, asthma, and rashes are managed without referrals to specialists. The right balance, of course, will vary from clinician to clinician based on that pediatrician’s level of interest, experience, and available resources in the community. The AAP position papers don’t mandate or even encourage the notion that all pediatricians need to be at the same place when it comes to competency in assessment and treatment of mental health problems, although it is probably fair to say that there is a push for the pediatric community as a whole to raise the collective bar at least a notch or two.
In response, the mental health community has moved to support the primary care community in their expanded role. These efforts have taken many forms, most notably the model of integrated care, in which mental health clinicians of various types see patients in primary care offices rather than making patients come to them. There also are new consultation programs that provide easy access to a child psychiatrist or other mental health professional for case-related questions delivered by phone, email, or for single in-person consultations. Additional training and educational offerings also are now available for pediatricians either in training and for those already in practice. These initiatives are bolstered by research showing that, not only can good mental health care be delivered in pediatric settings, but there are cost savings that can be realized, particularly for nonpsychiatric medical care.2 Despite these promising leads, however, there will remain some for whom anything less than the increased availability of a psychiatrist to “take over” a patient’s mental health care will be seen as a falling short of the clinical need.
To illustrate how things have and continue to change, consider the following three common clinical scenarios that generally present to a pediatrician:
- New presentation of ADHD symptoms.
- Anxiety or obsessive-compulsive problems.
- Return of a patient who has been psychiatrically hospitalized and now is taking multiple medications.
In the past, all three cases often would have resulted in a referral to a psychiatrist. Today, however, it is quite likely that only one of these cases would be referred because ADHD could be well diagnosed and managed within the primary care setting, and problems like anxiety and obsessive-compulsive disorder are sent first not to a psychiatrist but to a non-MD psychotherapist.
Moving forward, today’s pediatricians are expected to do more for the mental health care of patients themselves instead of referring to a psychiatrist. Most already do, despite having had little in the way of formal training. As the evidence grows that the promotion of mental well-being can be a key to future overall health, as well as to the cost of future health care, there are many reasons to be optimistic that support for pediatricians and collaborative care models for clinicians trying to fulfill these new responsibilities will get only stronger.
References
1. Pediatrics. 2019 Nov;144(5). pii: e20192757.
2. Pediatrics. 2019 Jul;144(1). pii: e20183243.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @PediPsych. Email him at [email protected]. Looking for more mental health training? Attend the 14th annual Child Psychiatry in Primary Care conference in Burlington on May 8, 2020 (http://www.med.uvm.edu/cme/conferences).
Assessment and treatment of many of the more common behavioral disorders in childhood, such as ADHD and anxiety, should be considered within a pediatrician’s scope of practice, a stance made very clear by a recent policy statement published by the American Academy of Pediatrics entitled “Mental health competencies for pediatric practice.”1 These competencies include medication treatment. As stated in the article, “certain disorders (ADHD, common anxiety disorders, depression), if associated with no more than moderate impairment, are amenable to primary care medication management because there are indicated medications with a well-established safety profile.”
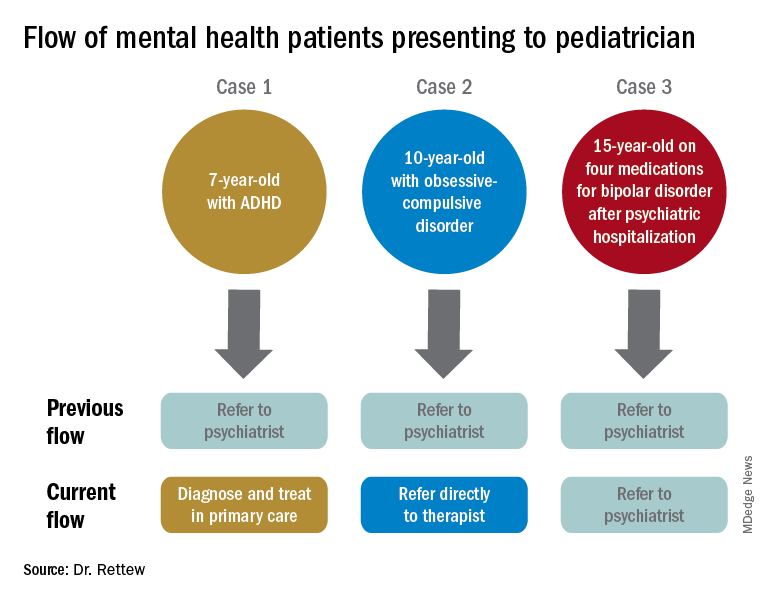
This shift to shared ownership when it comes to mental health care is likely coming from multiple sources, not the least of them being necessity and an acknowledgment that there simply aren’t enough psychiatrists to take over the mental health care of every youth with a diagnosable psychiatric disorder. While the number of child and adolescent psychiatrists remains relatively flat, the youth suicide rate is rising, as are the numbers presenting to emergency departments in crisis – all for reasons still to be fully understood. And these trends all are occurring as the medical community overall is appreciating more and more that good mental health is a cornerstone of all health.
The response from the pediatric community, whether it be because of personal conviction or simply a lack of options, largely has been to step up to the plate and take on these new responsibilities and challenges while trying to get up to speed with the latest information about mental health best practices. From my own experience doing evaluations and consultations from area primary care clinicians for over 15 years, the shift is noticeable. The typical patient now coming in has already seen a mental health counselor and tried at least one medication, while evaluations for diagnosis and treatment recommendations for things like uncomplicated and treatment-naive ADHD symptoms, for example, are becoming much more infrequent – although still far from extinct.
Nevertheless, there remain concerns about the extent of these new charges. Joe Nasca, MD, an experienced pediatrician who has been practicing in rural Vermont for decades, is worried that there is simply too much already for pediatricians to know and do to be able to add extensive mental health care. “There is so much to know in general peds [pediatrics] that I would guess a year or more of additional residency and experience would adequately prepare me to take this on,” he said in an interview. In comparing psychiatric care to other specialties, Dr. Nasca went on to say that, “I would not presume to treat chronic renal failure without the help of a nephrologist or a dilated aortic arch without a cardiologist.”
In a similar vein, however, it also is true that a significant percentage of children presenting to pediatricians for orthopedic problems, infections, asthma, and rashes are managed without referrals to specialists. The right balance, of course, will vary from clinician to clinician based on that pediatrician’s level of interest, experience, and available resources in the community. The AAP position papers don’t mandate or even encourage the notion that all pediatricians need to be at the same place when it comes to competency in assessment and treatment of mental health problems, although it is probably fair to say that there is a push for the pediatric community as a whole to raise the collective bar at least a notch or two.
In response, the mental health community has moved to support the primary care community in their expanded role. These efforts have taken many forms, most notably the model of integrated care, in which mental health clinicians of various types see patients in primary care offices rather than making patients come to them. There also are new consultation programs that provide easy access to a child psychiatrist or other mental health professional for case-related questions delivered by phone, email, or for single in-person consultations. Additional training and educational offerings also are now available for pediatricians either in training and for those already in practice. These initiatives are bolstered by research showing that, not only can good mental health care be delivered in pediatric settings, but there are cost savings that can be realized, particularly for nonpsychiatric medical care.2 Despite these promising leads, however, there will remain some for whom anything less than the increased availability of a psychiatrist to “take over” a patient’s mental health care will be seen as a falling short of the clinical need.
To illustrate how things have and continue to change, consider the following three common clinical scenarios that generally present to a pediatrician:
- New presentation of ADHD symptoms.
- Anxiety or obsessive-compulsive problems.
- Return of a patient who has been psychiatrically hospitalized and now is taking multiple medications.
In the past, all three cases often would have resulted in a referral to a psychiatrist. Today, however, it is quite likely that only one of these cases would be referred because ADHD could be well diagnosed and managed within the primary care setting, and problems like anxiety and obsessive-compulsive disorder are sent first not to a psychiatrist but to a non-MD psychotherapist.
Moving forward, today’s pediatricians are expected to do more for the mental health care of patients themselves instead of referring to a psychiatrist. Most already do, despite having had little in the way of formal training. As the evidence grows that the promotion of mental well-being can be a key to future overall health, as well as to the cost of future health care, there are many reasons to be optimistic that support for pediatricians and collaborative care models for clinicians trying to fulfill these new responsibilities will get only stronger.
References
1. Pediatrics. 2019 Nov;144(5). pii: e20192757.
2. Pediatrics. 2019 Jul;144(1). pii: e20183243.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @PediPsych. Email him at [email protected]. Looking for more mental health training? Attend the 14th annual Child Psychiatry in Primary Care conference in Burlington on May 8, 2020 (http://www.med.uvm.edu/cme/conferences).
An alarming number of bipolar disorder diagnoses or something else?
During a particularly busy day in my inpatient and outpatient practice, I realized that nearly every one of the patients had been given the diagnosis of bipolar disorder at one point or another. The interesting thing is this wasn’t an unusual day.
Nearly all of my patients and their family members have been given the diagnosis of bipolar disorder. Because prevalence of bipolar affective disorders is a little over 2%, this seemed a little odd. Could there be an epidemic of bipolar disorder in the area? Should someone sound the alarm on this unique cluster and get Julia Roberts ready? Unfortunately, the story behind this mystery is a little less sexy but nevertheless interesting.
When I probe more into what symptoms might have led to the diagnosis of bipolar disorder, I most often get some sort of answer about being easily angered (“I’m fine 1 minute and the next minute I’m yelling at my mom”) or mood changing from 1 minute to the next. Rarely do they tell me about sleeping less, increased energy, change in mood (elation, anger, irritability), increase in activity level, and increased pleasurable though dangerous activities all happening around the same time(s). So what is going on?
Beginning in the 1990s, a debate about the phenotypic presentation of pediatric bipolar disorder polarized the field. It was theorized that mania could present with severe nonepisodic irritability with extended periods of very rapid mood cycling within the day as opposed to discrete episodic mood cycles in children and adolescents. With this broader conceptualization in the United States, the rate of bipolar diagnosis increased by over 40 times in less than a decade.1 Similarly, the use of mood stabilizers and atypical antipsychotics in children also rose substantially.2
To help assess if severe nonepisodic irritability belongs in the spectrum of bipolar disorders, the National Institutes of Mental Health proposed a syndrome called “Severe Mood Dysregulation” or SMD, to promote the study of children with this phenotype. In longitudinal studies, Stringaris et al. compared rates of manic episodes in youth with SMD versus bipolar disorder over 2 years and found only one youth (1%) with SMD who presented with manic, hypomanic, or mixed episodes, compared with 58 (62%) with bipolar disorder.3 Leibenluft et al.showed that chronic irritability during early adolescence predicted ADHD at late adolescence and major depressive disorder in early adulthood whereas episodic irritability predicted mania.4 Twenty-year follow-up of the same sample showed chronic irritability in adolescence predicted dysthymia, generalized anxiety disorders, and major depressive disorder.5 Other longitudinal studies essentially have shown the same results.6
At this point, the question of whether chronic irritability is a part of the bipolar spectrum disorder is largely resolved – 7 The diagnosis emphasizes the episodic nature of the illness, and that irritability would wax and wane with other manic symptoms such as changes in energy and sleep. And the ultrarapid mood changes (mood changes within the day) appear to describe mood fluctuations within a manic episode as opposed to each change being a separate episode.
So, most likely, my patients were caught in a time of uncertainty before data were able to clarify their phenotype.
Dr. Chung is a child and adolescent psychiatrist at the University of Vermont Medical Center, Burlington, and practices at Champlain Valley Physician’s Hospital in Plattsburgh, N.Y. Email him at [email protected].
References
1. Biol Psychiatry. 2007 Jul 15;62(2):107–14.
2. JAMA Psychiatry. 2015 Sep;72(9):859-60.
3. J Am Acad Child Adolesc Psychiatry. 2010 Apr;49(4):397-405.
4. J Child Adolesc Psychopharmacol 2006;16(4):456-66.
5. Am J Psychiatry. 2009 Sep;166(9):1048-54.
6. Biol Psychiatry. 2006 Nov 1;60(9):991-7.
7. Bipolar Disord. 2017 Nov;19(7):524-43.
During a particularly busy day in my inpatient and outpatient practice, I realized that nearly every one of the patients had been given the diagnosis of bipolar disorder at one point or another. The interesting thing is this wasn’t an unusual day.
Nearly all of my patients and their family members have been given the diagnosis of bipolar disorder. Because prevalence of bipolar affective disorders is a little over 2%, this seemed a little odd. Could there be an epidemic of bipolar disorder in the area? Should someone sound the alarm on this unique cluster and get Julia Roberts ready? Unfortunately, the story behind this mystery is a little less sexy but nevertheless interesting.
When I probe more into what symptoms might have led to the diagnosis of bipolar disorder, I most often get some sort of answer about being easily angered (“I’m fine 1 minute and the next minute I’m yelling at my mom”) or mood changing from 1 minute to the next. Rarely do they tell me about sleeping less, increased energy, change in mood (elation, anger, irritability), increase in activity level, and increased pleasurable though dangerous activities all happening around the same time(s). So what is going on?
Beginning in the 1990s, a debate about the phenotypic presentation of pediatric bipolar disorder polarized the field. It was theorized that mania could present with severe nonepisodic irritability with extended periods of very rapid mood cycling within the day as opposed to discrete episodic mood cycles in children and adolescents. With this broader conceptualization in the United States, the rate of bipolar diagnosis increased by over 40 times in less than a decade.1 Similarly, the use of mood stabilizers and atypical antipsychotics in children also rose substantially.2
To help assess if severe nonepisodic irritability belongs in the spectrum of bipolar disorders, the National Institutes of Mental Health proposed a syndrome called “Severe Mood Dysregulation” or SMD, to promote the study of children with this phenotype. In longitudinal studies, Stringaris et al. compared rates of manic episodes in youth with SMD versus bipolar disorder over 2 years and found only one youth (1%) with SMD who presented with manic, hypomanic, or mixed episodes, compared with 58 (62%) with bipolar disorder.3 Leibenluft et al.showed that chronic irritability during early adolescence predicted ADHD at late adolescence and major depressive disorder in early adulthood whereas episodic irritability predicted mania.4 Twenty-year follow-up of the same sample showed chronic irritability in adolescence predicted dysthymia, generalized anxiety disorders, and major depressive disorder.5 Other longitudinal studies essentially have shown the same results.6
At this point, the question of whether chronic irritability is a part of the bipolar spectrum disorder is largely resolved – 7 The diagnosis emphasizes the episodic nature of the illness, and that irritability would wax and wane with other manic symptoms such as changes in energy and sleep. And the ultrarapid mood changes (mood changes within the day) appear to describe mood fluctuations within a manic episode as opposed to each change being a separate episode.
So, most likely, my patients were caught in a time of uncertainty before data were able to clarify their phenotype.
Dr. Chung is a child and adolescent psychiatrist at the University of Vermont Medical Center, Burlington, and practices at Champlain Valley Physician’s Hospital in Plattsburgh, N.Y. Email him at [email protected].
References
1. Biol Psychiatry. 2007 Jul 15;62(2):107–14.
2. JAMA Psychiatry. 2015 Sep;72(9):859-60.
3. J Am Acad Child Adolesc Psychiatry. 2010 Apr;49(4):397-405.
4. J Child Adolesc Psychopharmacol 2006;16(4):456-66.
5. Am J Psychiatry. 2009 Sep;166(9):1048-54.
6. Biol Psychiatry. 2006 Nov 1;60(9):991-7.
7. Bipolar Disord. 2017 Nov;19(7):524-43.
During a particularly busy day in my inpatient and outpatient practice, I realized that nearly every one of the patients had been given the diagnosis of bipolar disorder at one point or another. The interesting thing is this wasn’t an unusual day.
Nearly all of my patients and their family members have been given the diagnosis of bipolar disorder. Because prevalence of bipolar affective disorders is a little over 2%, this seemed a little odd. Could there be an epidemic of bipolar disorder in the area? Should someone sound the alarm on this unique cluster and get Julia Roberts ready? Unfortunately, the story behind this mystery is a little less sexy but nevertheless interesting.
When I probe more into what symptoms might have led to the diagnosis of bipolar disorder, I most often get some sort of answer about being easily angered (“I’m fine 1 minute and the next minute I’m yelling at my mom”) or mood changing from 1 minute to the next. Rarely do they tell me about sleeping less, increased energy, change in mood (elation, anger, irritability), increase in activity level, and increased pleasurable though dangerous activities all happening around the same time(s). So what is going on?
Beginning in the 1990s, a debate about the phenotypic presentation of pediatric bipolar disorder polarized the field. It was theorized that mania could present with severe nonepisodic irritability with extended periods of very rapid mood cycling within the day as opposed to discrete episodic mood cycles in children and adolescents. With this broader conceptualization in the United States, the rate of bipolar diagnosis increased by over 40 times in less than a decade.1 Similarly, the use of mood stabilizers and atypical antipsychotics in children also rose substantially.2
To help assess if severe nonepisodic irritability belongs in the spectrum of bipolar disorders, the National Institutes of Mental Health proposed a syndrome called “Severe Mood Dysregulation” or SMD, to promote the study of children with this phenotype. In longitudinal studies, Stringaris et al. compared rates of manic episodes in youth with SMD versus bipolar disorder over 2 years and found only one youth (1%) with SMD who presented with manic, hypomanic, or mixed episodes, compared with 58 (62%) with bipolar disorder.3 Leibenluft et al.showed that chronic irritability during early adolescence predicted ADHD at late adolescence and major depressive disorder in early adulthood whereas episodic irritability predicted mania.4 Twenty-year follow-up of the same sample showed chronic irritability in adolescence predicted dysthymia, generalized anxiety disorders, and major depressive disorder.5 Other longitudinal studies essentially have shown the same results.6
At this point, the question of whether chronic irritability is a part of the bipolar spectrum disorder is largely resolved – 7 The diagnosis emphasizes the episodic nature of the illness, and that irritability would wax and wane with other manic symptoms such as changes in energy and sleep. And the ultrarapid mood changes (mood changes within the day) appear to describe mood fluctuations within a manic episode as opposed to each change being a separate episode.
So, most likely, my patients were caught in a time of uncertainty before data were able to clarify their phenotype.
Dr. Chung is a child and adolescent psychiatrist at the University of Vermont Medical Center, Burlington, and practices at Champlain Valley Physician’s Hospital in Plattsburgh, N.Y. Email him at [email protected].
References
1. Biol Psychiatry. 2007 Jul 15;62(2):107–14.
2. JAMA Psychiatry. 2015 Sep;72(9):859-60.
3. J Am Acad Child Adolesc Psychiatry. 2010 Apr;49(4):397-405.
4. J Child Adolesc Psychopharmacol 2006;16(4):456-66.
5. Am J Psychiatry. 2009 Sep;166(9):1048-54.
6. Biol Psychiatry. 2006 Nov 1;60(9):991-7.
7. Bipolar Disord. 2017 Nov;19(7):524-43.
CBD for sleep and anxiety – A brief review of the evidence
Grace is a 15-year-old girl in the 10th grade whom you have been treating for anxiety. Family history also is notable for her father having an anxiety disorder. She has been taking an SSRI and is engaged in therapy, which has resulted in some improvement in symptoms. She can become overwhelmed when taking tests, and she has breakthrough anxiety in social situations and occasional difficulties with sleep. She denies using any substances. Her parents, who have come to her appointment with her, noted that while they see some progress, they would like to try more natural interventions. They had done some research on cannabidiol (CBD), and Grace’s father said that using it has tremendously helped his sleep. They inquired about Grace using it as well.
Discussion
CBD use has dramatically increased over the past few years, and in many places can be found in gummies, chocolate, tinctures, and other forms at grocery and convenience stores, in addition to being widely available online. It is a nonpsychoactive compound (versus tetrahydrocannabinol or THC) found in the Cannabis sativa plant. The Farm Bill, which was passed in 2018, legalized production of hemp or the cannabis plant with a THC concentration less than 0.3%. This bill additionally maintained the Food and Drug Administration’s oversight with CBD. States may have laws that are more restrictive about use. CBD was approved in 2018 by the FDA for treatment of Lennox-Gastaut syndrome and Dravet syndrome in individuals 2 years of age and older, and is categorized as a schedule I substance due to its being derived from the cannabis plant.
In randomized, double-blind, placebo-controlled trials leading to CBD’s approval, the most common side effects were drowsiness, insomnia, disrupted sleep, sedation, malaise, weakness, decreased appetite, diarrhea, elevated liver enzymes, rash, and infections. CBD also carries a warning about the potential for suicidal ideation, agitation, new or worsening depression, aggression, and panic attacks.1 In in vitro and animal studies, CBD has been found to affect growth of tumor cell lines, to have no effects on embryonic development, and to potentially cause some drug-drug interactions through inhibition of CYP2C9, CYP2C19, and CYP3A4. However, the clinical relevance currently is unknown. Animal studies also indicate potential efficacy in decreasing anxiety.2
CBD has been promoted as being effective in treating a number of ailments including migraines, chronic pain, insomnia, ADHD, and anxiety. Multiple anecdotal reports tout the benefits. In a study exploring abuse potential, there were no significant findings, and CBD was generally well tolerated in open trials exploring potential clinical benefits. A retrospective feasibility study – conducted in Israel – exploring use of CBD to decrease problematic behaviors in youth with autism spectrum disorder demonstrated improvement in communication, anxiety, disruptive behaviors, and parental stress.3
- There is potential lack of clarity regarding legality of use in some states. Based on federal law, it is legal to possess CBD derived from hemp, but state laws may differ.
- There is lack of oversight regarding monitoring what is in each supplement. Lab testing for CBD to determine contents is not mandatory in every state. The amount of active compound as well as other ingredients may not be consistent or accurate. According to the FDA, CBD-containing products cannot claim to have health benefits, treat disease, or be sold as dietary supplements without its approval.
- Clear information about appropriate dosing for children is limited.
- Varying delivery systems could affect absorption and bioavailability of CBD.
- Information is lacking regarding potential drug-drug interactions.
- There is a lack of information regarding effects of long-term use.
Use of CBD is an area with significant interest and potential for growth. Although risks are thought to be low overall, there likely is insufficient evidence at this time to actively recommend its use. Additional research in human subjects exploring effective and safe dosing, tolerability, as well as use in special populations (including children, pregnant women, elderly) is needed.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. She has no relevant financial disclosures. Email her at [email protected].
References
1. “FDA approves first drug comprised of an active ingredient derived from marijuana to treat rare, severe forms of epilepsy,” FDA news release, June 25, 2018.
2. Cannabidiol (CBD) Critical Review Report. Expert Committee on Drug Dependence Fortieth Meeting. World Health Organization. Geneva June 4-7, 2018.
3. J Autism Dev Disord. 2019 Mar;49(3):1284-8.
Grace is a 15-year-old girl in the 10th grade whom you have been treating for anxiety. Family history also is notable for her father having an anxiety disorder. She has been taking an SSRI and is engaged in therapy, which has resulted in some improvement in symptoms. She can become overwhelmed when taking tests, and she has breakthrough anxiety in social situations and occasional difficulties with sleep. She denies using any substances. Her parents, who have come to her appointment with her, noted that while they see some progress, they would like to try more natural interventions. They had done some research on cannabidiol (CBD), and Grace’s father said that using it has tremendously helped his sleep. They inquired about Grace using it as well.
Discussion
CBD use has dramatically increased over the past few years, and in many places can be found in gummies, chocolate, tinctures, and other forms at grocery and convenience stores, in addition to being widely available online. It is a nonpsychoactive compound (versus tetrahydrocannabinol or THC) found in the Cannabis sativa plant. The Farm Bill, which was passed in 2018, legalized production of hemp or the cannabis plant with a THC concentration less than 0.3%. This bill additionally maintained the Food and Drug Administration’s oversight with CBD. States may have laws that are more restrictive about use. CBD was approved in 2018 by the FDA for treatment of Lennox-Gastaut syndrome and Dravet syndrome in individuals 2 years of age and older, and is categorized as a schedule I substance due to its being derived from the cannabis plant.
In randomized, double-blind, placebo-controlled trials leading to CBD’s approval, the most common side effects were drowsiness, insomnia, disrupted sleep, sedation, malaise, weakness, decreased appetite, diarrhea, elevated liver enzymes, rash, and infections. CBD also carries a warning about the potential for suicidal ideation, agitation, new or worsening depression, aggression, and panic attacks.1 In in vitro and animal studies, CBD has been found to affect growth of tumor cell lines, to have no effects on embryonic development, and to potentially cause some drug-drug interactions through inhibition of CYP2C9, CYP2C19, and CYP3A4. However, the clinical relevance currently is unknown. Animal studies also indicate potential efficacy in decreasing anxiety.2
CBD has been promoted as being effective in treating a number of ailments including migraines, chronic pain, insomnia, ADHD, and anxiety. Multiple anecdotal reports tout the benefits. In a study exploring abuse potential, there were no significant findings, and CBD was generally well tolerated in open trials exploring potential clinical benefits. A retrospective feasibility study – conducted in Israel – exploring use of CBD to decrease problematic behaviors in youth with autism spectrum disorder demonstrated improvement in communication, anxiety, disruptive behaviors, and parental stress.3
- There is potential lack of clarity regarding legality of use in some states. Based on federal law, it is legal to possess CBD derived from hemp, but state laws may differ.
- There is lack of oversight regarding monitoring what is in each supplement. Lab testing for CBD to determine contents is not mandatory in every state. The amount of active compound as well as other ingredients may not be consistent or accurate. According to the FDA, CBD-containing products cannot claim to have health benefits, treat disease, or be sold as dietary supplements without its approval.
- Clear information about appropriate dosing for children is limited.
- Varying delivery systems could affect absorption and bioavailability of CBD.
- Information is lacking regarding potential drug-drug interactions.
- There is a lack of information regarding effects of long-term use.
Use of CBD is an area with significant interest and potential for growth. Although risks are thought to be low overall, there likely is insufficient evidence at this time to actively recommend its use. Additional research in human subjects exploring effective and safe dosing, tolerability, as well as use in special populations (including children, pregnant women, elderly) is needed.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. She has no relevant financial disclosures. Email her at [email protected].
References
1. “FDA approves first drug comprised of an active ingredient derived from marijuana to treat rare, severe forms of epilepsy,” FDA news release, June 25, 2018.
2. Cannabidiol (CBD) Critical Review Report. Expert Committee on Drug Dependence Fortieth Meeting. World Health Organization. Geneva June 4-7, 2018.
3. J Autism Dev Disord. 2019 Mar;49(3):1284-8.
Grace is a 15-year-old girl in the 10th grade whom you have been treating for anxiety. Family history also is notable for her father having an anxiety disorder. She has been taking an SSRI and is engaged in therapy, which has resulted in some improvement in symptoms. She can become overwhelmed when taking tests, and she has breakthrough anxiety in social situations and occasional difficulties with sleep. She denies using any substances. Her parents, who have come to her appointment with her, noted that while they see some progress, they would like to try more natural interventions. They had done some research on cannabidiol (CBD), and Grace’s father said that using it has tremendously helped his sleep. They inquired about Grace using it as well.
Discussion
CBD use has dramatically increased over the past few years, and in many places can be found in gummies, chocolate, tinctures, and other forms at grocery and convenience stores, in addition to being widely available online. It is a nonpsychoactive compound (versus tetrahydrocannabinol or THC) found in the Cannabis sativa plant. The Farm Bill, which was passed in 2018, legalized production of hemp or the cannabis plant with a THC concentration less than 0.3%. This bill additionally maintained the Food and Drug Administration’s oversight with CBD. States may have laws that are more restrictive about use. CBD was approved in 2018 by the FDA for treatment of Lennox-Gastaut syndrome and Dravet syndrome in individuals 2 years of age and older, and is categorized as a schedule I substance due to its being derived from the cannabis plant.
In randomized, double-blind, placebo-controlled trials leading to CBD’s approval, the most common side effects were drowsiness, insomnia, disrupted sleep, sedation, malaise, weakness, decreased appetite, diarrhea, elevated liver enzymes, rash, and infections. CBD also carries a warning about the potential for suicidal ideation, agitation, new or worsening depression, aggression, and panic attacks.1 In in vitro and animal studies, CBD has been found to affect growth of tumor cell lines, to have no effects on embryonic development, and to potentially cause some drug-drug interactions through inhibition of CYP2C9, CYP2C19, and CYP3A4. However, the clinical relevance currently is unknown. Animal studies also indicate potential efficacy in decreasing anxiety.2
CBD has been promoted as being effective in treating a number of ailments including migraines, chronic pain, insomnia, ADHD, and anxiety. Multiple anecdotal reports tout the benefits. In a study exploring abuse potential, there were no significant findings, and CBD was generally well tolerated in open trials exploring potential clinical benefits. A retrospective feasibility study – conducted in Israel – exploring use of CBD to decrease problematic behaviors in youth with autism spectrum disorder demonstrated improvement in communication, anxiety, disruptive behaviors, and parental stress.3
- There is potential lack of clarity regarding legality of use in some states. Based on federal law, it is legal to possess CBD derived from hemp, but state laws may differ.
- There is lack of oversight regarding monitoring what is in each supplement. Lab testing for CBD to determine contents is not mandatory in every state. The amount of active compound as well as other ingredients may not be consistent or accurate. According to the FDA, CBD-containing products cannot claim to have health benefits, treat disease, or be sold as dietary supplements without its approval.
- Clear information about appropriate dosing for children is limited.
- Varying delivery systems could affect absorption and bioavailability of CBD.
- Information is lacking regarding potential drug-drug interactions.
- There is a lack of information regarding effects of long-term use.
Use of CBD is an area with significant interest and potential for growth. Although risks are thought to be low overall, there likely is insufficient evidence at this time to actively recommend its use. Additional research in human subjects exploring effective and safe dosing, tolerability, as well as use in special populations (including children, pregnant women, elderly) is needed.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. She has no relevant financial disclosures. Email her at [email protected].
References
1. “FDA approves first drug comprised of an active ingredient derived from marijuana to treat rare, severe forms of epilepsy,” FDA news release, June 25, 2018.
2. Cannabidiol (CBD) Critical Review Report. Expert Committee on Drug Dependence Fortieth Meeting. World Health Organization. Geneva June 4-7, 2018.
3. J Autism Dev Disord. 2019 Mar;49(3):1284-8.
Consider hormones and mood in adolescent girls
Prior to puberty, the rate of mood disorders in males and females is roughly the same; however in adolescence, depression doubles in (biological) girls. While the association isn’t clear, it is reasonable to consider that hormones may be involved, at least for some. For instance, we know that menstrual cycle–related mood changes have been noted since the time of Hippocrates. In this article, I will discuss premenstrual dysphoric disorder (PMDD), as well as potential mood-related side effects of hormonal contraceptives. Because I am talking about physiology, I will be referring to individuals born as biological females in the absence of any hormonal gender treatments, regardless of identified gender.
Many young women will acknowledge somatic and/or psychological symptoms that occur in the luteal phase of their cycle, most commonly in the week before menses begins. The most common somatic symptom is bloating, and mood symptoms are irritability and mood lability.1 To meet criteria for premenstrual syndrome (PMS), a woman must endorse one symptom that causes impairment in their functioning and reoccurs over consecutive cycles. PMDD is more specific and involves five or more affective symptoms, at least one of which is consistent with depressed mood, irritability, anxiety, or mood lability. The other potential symptoms include impaired concentration, fatigue, insomnia or hypersomnia, anhedonia, and appetite issues, all of which are included as criteria for major depression. The population prevalence has been quoted between 2% and 5% and is relatively stable across cultures.1 It tends to be highly genetic, as well as highly comorbid with other psychiatric disorders.2 Girls and women with higher rates of trauma appear to be more likely to experience symptoms,3 which indicates there are environmental influences that can interact with genetic vulnerability.
Interestingly, studies have not found differences in serum hormone levels between those with PMDD and others, which leads to the hypothesis that the main difference is in a woman’s sensitivity to circulating hormones,4 and there has been some evidence of different concentrations of neurotransmitters between affected and unaffected women. Many hormone-neurotransmitter interactions have been described, but two that have received the most attention include the relationship between progesterone, its main metabolite allopregnanolone, and gamma-aminobutyric acid (GABA) receptors. Allopregnanolone, which interacts with GABA receptors similarly to benzodiazepines, tends to be higher in the luteal phase, rising with progesterone, and the concentration quickly recedes at the onset of menses as progesterone levels drop off. The other highly notable relationship is the positive association between estradiol and the expression of the serotonin transporter (SERT) genes, which can potentially lead to higher levels of circulating serotonin in the follicular phase.
When PMDD is suspected in an adolescent who presents with intermittent mood and anxiety symptoms that lessen or disappear at baseline and appear unrelated to circumstances, it is important to check in regarding monthly patterns. It can be challenging for adolescents to make this connection, and even more so prior to achieving cycle regularity. Observational studies suggest that by age 14 years, about 82% of girls have a regular cycle.5 The best way to help a patient make the connection is to suggest a period tracking app on their smartphone or tablet. There are many available period trackers that track mood as well and are free to download. Sometimes, simply the act of tracking and bringing awareness to the pattern is therapeutic in itself; sometimes, more formal treatment is needed.
Once the diagnosis of PMDD has been established, there are several options for treatment that range from supplements and herbal remedies to SSRIs, as well as psychotherapy. Treatment may begin with calcium supplements (1,200 mg have been effective in reducing symptoms)6 and referral for cognitive-behavioral therapy (CBT). CBT appears to be associated with a shift in the ability to attribute symptoms to hormones,7 which can help decrease hopelessness and reactivity. SSRIs are another effective strategy to treat PMDD, both taken daily and continuously and also taken in a pulsed fashion, starting with the onset of symptoms or 7-10 days before the period starts and stopping on the first day of menses. Low doses of sertraline, fluoxetine, paroxetine, escitalopram and citalopram have been studied.8 There is some low-quality evidence for herbal supplements as well, probably the most consistent finding is for Vitex taken the week prior to menses.9 Finally, certain oral contraceptives have been associated with PMDD symptom reduction, specifically formulations with 3 mg of drospirenone (a fourth generation progesterone) and 20 mcg of ethinyl estradiol.10 Other formulations, including progesterone-only pills, have not been helpful and have been demonstrated to have a negative effect on mood.11
The literature on hormonal contraceptives and mood can be confusing. While oral agents containing drospirenone have been helpful for premenstrual dysphoria, other studies outside of the PMDD literature have found positive associations between oral contraceptives and depression in adolescents.11 Girls taking combined oral contraceptives seem to be at a 1.8-fold risk of depression, while girls taking progesterone-only formulations were at 2.2 times the risk of developing depression, compared with girls who weren’t taking anything. These days, more pediatricians are recommending long acting reversible contraceptives (LARCs), and there is some thought that even these may carry some risk, but this remains to be studied.
In conclusion, As a provider, you are in a special position to help your patients by bringing nonjudgmental awareness to the potential contribution of their own cyclical hormones or that of exogenous hormones associated with contraceptive choices. Whether it means switching contraceptives, adding calcium or starting a low dose SSRI for 1 week a month, there are many ways to approach symptoms. Often, simply helping make the connection between physiology and mood can be empowering.
Dr. Guth is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and the University of Vermont, both in Burlington. Email her at [email protected].
References
1. Am J Psychiatry. 2012 May;169(5):465-75.
2. Arch Womens Ment Health. 2004 Feb;7(1):37-47.
3. Arch Womens Ment Health. 2011 Oct;14(5):383-93.
4. Curr Psychiatry Rep. 2015 Nov;17(11):87.
5. Ital J Pediatr. 2012 Aug 14;38:38.
6. Am J Obstet Gynecol. 1998 Aug;179(2):444-52.
7. J Clin Psychol Med Settings. 2012 Sep;19(3):308-19.
8. Cochrane Database Syst Rev. 2013 Jun 7;(6):CD001396.
9. J Psychosom Obstet Gynaecol. 2011 Mar;32(1):42-51.
10. Cochrane Database Syst Rev. 2008 Jan 23;(1):CD006586.
11. PLoS One. 2018 Mar 22;13(3):e0194773.
Prior to puberty, the rate of mood disorders in males and females is roughly the same; however in adolescence, depression doubles in (biological) girls. While the association isn’t clear, it is reasonable to consider that hormones may be involved, at least for some. For instance, we know that menstrual cycle–related mood changes have been noted since the time of Hippocrates. In this article, I will discuss premenstrual dysphoric disorder (PMDD), as well as potential mood-related side effects of hormonal contraceptives. Because I am talking about physiology, I will be referring to individuals born as biological females in the absence of any hormonal gender treatments, regardless of identified gender.
Many young women will acknowledge somatic and/or psychological symptoms that occur in the luteal phase of their cycle, most commonly in the week before menses begins. The most common somatic symptom is bloating, and mood symptoms are irritability and mood lability.1 To meet criteria for premenstrual syndrome (PMS), a woman must endorse one symptom that causes impairment in their functioning and reoccurs over consecutive cycles. PMDD is more specific and involves five or more affective symptoms, at least one of which is consistent with depressed mood, irritability, anxiety, or mood lability. The other potential symptoms include impaired concentration, fatigue, insomnia or hypersomnia, anhedonia, and appetite issues, all of which are included as criteria for major depression. The population prevalence has been quoted between 2% and 5% and is relatively stable across cultures.1 It tends to be highly genetic, as well as highly comorbid with other psychiatric disorders.2 Girls and women with higher rates of trauma appear to be more likely to experience symptoms,3 which indicates there are environmental influences that can interact with genetic vulnerability.
Interestingly, studies have not found differences in serum hormone levels between those with PMDD and others, which leads to the hypothesis that the main difference is in a woman’s sensitivity to circulating hormones,4 and there has been some evidence of different concentrations of neurotransmitters between affected and unaffected women. Many hormone-neurotransmitter interactions have been described, but two that have received the most attention include the relationship between progesterone, its main metabolite allopregnanolone, and gamma-aminobutyric acid (GABA) receptors. Allopregnanolone, which interacts with GABA receptors similarly to benzodiazepines, tends to be higher in the luteal phase, rising with progesterone, and the concentration quickly recedes at the onset of menses as progesterone levels drop off. The other highly notable relationship is the positive association between estradiol and the expression of the serotonin transporter (SERT) genes, which can potentially lead to higher levels of circulating serotonin in the follicular phase.
When PMDD is suspected in an adolescent who presents with intermittent mood and anxiety symptoms that lessen or disappear at baseline and appear unrelated to circumstances, it is important to check in regarding monthly patterns. It can be challenging for adolescents to make this connection, and even more so prior to achieving cycle regularity. Observational studies suggest that by age 14 years, about 82% of girls have a regular cycle.5 The best way to help a patient make the connection is to suggest a period tracking app on their smartphone or tablet. There are many available period trackers that track mood as well and are free to download. Sometimes, simply the act of tracking and bringing awareness to the pattern is therapeutic in itself; sometimes, more formal treatment is needed.
Once the diagnosis of PMDD has been established, there are several options for treatment that range from supplements and herbal remedies to SSRIs, as well as psychotherapy. Treatment may begin with calcium supplements (1,200 mg have been effective in reducing symptoms)6 and referral for cognitive-behavioral therapy (CBT). CBT appears to be associated with a shift in the ability to attribute symptoms to hormones,7 which can help decrease hopelessness and reactivity. SSRIs are another effective strategy to treat PMDD, both taken daily and continuously and also taken in a pulsed fashion, starting with the onset of symptoms or 7-10 days before the period starts and stopping on the first day of menses. Low doses of sertraline, fluoxetine, paroxetine, escitalopram and citalopram have been studied.8 There is some low-quality evidence for herbal supplements as well, probably the most consistent finding is for Vitex taken the week prior to menses.9 Finally, certain oral contraceptives have been associated with PMDD symptom reduction, specifically formulations with 3 mg of drospirenone (a fourth generation progesterone) and 20 mcg of ethinyl estradiol.10 Other formulations, including progesterone-only pills, have not been helpful and have been demonstrated to have a negative effect on mood.11
The literature on hormonal contraceptives and mood can be confusing. While oral agents containing drospirenone have been helpful for premenstrual dysphoria, other studies outside of the PMDD literature have found positive associations between oral contraceptives and depression in adolescents.11 Girls taking combined oral contraceptives seem to be at a 1.8-fold risk of depression, while girls taking progesterone-only formulations were at 2.2 times the risk of developing depression, compared with girls who weren’t taking anything. These days, more pediatricians are recommending long acting reversible contraceptives (LARCs), and there is some thought that even these may carry some risk, but this remains to be studied.
In conclusion, As a provider, you are in a special position to help your patients by bringing nonjudgmental awareness to the potential contribution of their own cyclical hormones or that of exogenous hormones associated with contraceptive choices. Whether it means switching contraceptives, adding calcium or starting a low dose SSRI for 1 week a month, there are many ways to approach symptoms. Often, simply helping make the connection between physiology and mood can be empowering.
Dr. Guth is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and the University of Vermont, both in Burlington. Email her at [email protected].
References
1. Am J Psychiatry. 2012 May;169(5):465-75.
2. Arch Womens Ment Health. 2004 Feb;7(1):37-47.
3. Arch Womens Ment Health. 2011 Oct;14(5):383-93.
4. Curr Psychiatry Rep. 2015 Nov;17(11):87.
5. Ital J Pediatr. 2012 Aug 14;38:38.
6. Am J Obstet Gynecol. 1998 Aug;179(2):444-52.
7. J Clin Psychol Med Settings. 2012 Sep;19(3):308-19.
8. Cochrane Database Syst Rev. 2013 Jun 7;(6):CD001396.
9. J Psychosom Obstet Gynaecol. 2011 Mar;32(1):42-51.
10. Cochrane Database Syst Rev. 2008 Jan 23;(1):CD006586.
11. PLoS One. 2018 Mar 22;13(3):e0194773.
Prior to puberty, the rate of mood disorders in males and females is roughly the same; however in adolescence, depression doubles in (biological) girls. While the association isn’t clear, it is reasonable to consider that hormones may be involved, at least for some. For instance, we know that menstrual cycle–related mood changes have been noted since the time of Hippocrates. In this article, I will discuss premenstrual dysphoric disorder (PMDD), as well as potential mood-related side effects of hormonal contraceptives. Because I am talking about physiology, I will be referring to individuals born as biological females in the absence of any hormonal gender treatments, regardless of identified gender.
Many young women will acknowledge somatic and/or psychological symptoms that occur in the luteal phase of their cycle, most commonly in the week before menses begins. The most common somatic symptom is bloating, and mood symptoms are irritability and mood lability.1 To meet criteria for premenstrual syndrome (PMS), a woman must endorse one symptom that causes impairment in their functioning and reoccurs over consecutive cycles. PMDD is more specific and involves five or more affective symptoms, at least one of which is consistent with depressed mood, irritability, anxiety, or mood lability. The other potential symptoms include impaired concentration, fatigue, insomnia or hypersomnia, anhedonia, and appetite issues, all of which are included as criteria for major depression. The population prevalence has been quoted between 2% and 5% and is relatively stable across cultures.1 It tends to be highly genetic, as well as highly comorbid with other psychiatric disorders.2 Girls and women with higher rates of trauma appear to be more likely to experience symptoms,3 which indicates there are environmental influences that can interact with genetic vulnerability.
Interestingly, studies have not found differences in serum hormone levels between those with PMDD and others, which leads to the hypothesis that the main difference is in a woman’s sensitivity to circulating hormones,4 and there has been some evidence of different concentrations of neurotransmitters between affected and unaffected women. Many hormone-neurotransmitter interactions have been described, but two that have received the most attention include the relationship between progesterone, its main metabolite allopregnanolone, and gamma-aminobutyric acid (GABA) receptors. Allopregnanolone, which interacts with GABA receptors similarly to benzodiazepines, tends to be higher in the luteal phase, rising with progesterone, and the concentration quickly recedes at the onset of menses as progesterone levels drop off. The other highly notable relationship is the positive association between estradiol and the expression of the serotonin transporter (SERT) genes, which can potentially lead to higher levels of circulating serotonin in the follicular phase.
When PMDD is suspected in an adolescent who presents with intermittent mood and anxiety symptoms that lessen or disappear at baseline and appear unrelated to circumstances, it is important to check in regarding monthly patterns. It can be challenging for adolescents to make this connection, and even more so prior to achieving cycle regularity. Observational studies suggest that by age 14 years, about 82% of girls have a regular cycle.5 The best way to help a patient make the connection is to suggest a period tracking app on their smartphone or tablet. There are many available period trackers that track mood as well and are free to download. Sometimes, simply the act of tracking and bringing awareness to the pattern is therapeutic in itself; sometimes, more formal treatment is needed.
Once the diagnosis of PMDD has been established, there are several options for treatment that range from supplements and herbal remedies to SSRIs, as well as psychotherapy. Treatment may begin with calcium supplements (1,200 mg have been effective in reducing symptoms)6 and referral for cognitive-behavioral therapy (CBT). CBT appears to be associated with a shift in the ability to attribute symptoms to hormones,7 which can help decrease hopelessness and reactivity. SSRIs are another effective strategy to treat PMDD, both taken daily and continuously and also taken in a pulsed fashion, starting with the onset of symptoms or 7-10 days before the period starts and stopping on the first day of menses. Low doses of sertraline, fluoxetine, paroxetine, escitalopram and citalopram have been studied.8 There is some low-quality evidence for herbal supplements as well, probably the most consistent finding is for Vitex taken the week prior to menses.9 Finally, certain oral contraceptives have been associated with PMDD symptom reduction, specifically formulations with 3 mg of drospirenone (a fourth generation progesterone) and 20 mcg of ethinyl estradiol.10 Other formulations, including progesterone-only pills, have not been helpful and have been demonstrated to have a negative effect on mood.11
The literature on hormonal contraceptives and mood can be confusing. While oral agents containing drospirenone have been helpful for premenstrual dysphoria, other studies outside of the PMDD literature have found positive associations between oral contraceptives and depression in adolescents.11 Girls taking combined oral contraceptives seem to be at a 1.8-fold risk of depression, while girls taking progesterone-only formulations were at 2.2 times the risk of developing depression, compared with girls who weren’t taking anything. These days, more pediatricians are recommending long acting reversible contraceptives (LARCs), and there is some thought that even these may carry some risk, but this remains to be studied.
In conclusion, As a provider, you are in a special position to help your patients by bringing nonjudgmental awareness to the potential contribution of their own cyclical hormones or that of exogenous hormones associated with contraceptive choices. Whether it means switching contraceptives, adding calcium or starting a low dose SSRI for 1 week a month, there are many ways to approach symptoms. Often, simply helping make the connection between physiology and mood can be empowering.
Dr. Guth is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and the University of Vermont, both in Burlington. Email her at [email protected].
References
1. Am J Psychiatry. 2012 May;169(5):465-75.
2. Arch Womens Ment Health. 2004 Feb;7(1):37-47.
3. Arch Womens Ment Health. 2011 Oct;14(5):383-93.
4. Curr Psychiatry Rep. 2015 Nov;17(11):87.
5. Ital J Pediatr. 2012 Aug 14;38:38.
6. Am J Obstet Gynecol. 1998 Aug;179(2):444-52.
7. J Clin Psychol Med Settings. 2012 Sep;19(3):308-19.
8. Cochrane Database Syst Rev. 2013 Jun 7;(6):CD001396.
9. J Psychosom Obstet Gynaecol. 2011 Mar;32(1):42-51.
10. Cochrane Database Syst Rev. 2008 Jan 23;(1):CD006586.
11. PLoS One. 2018 Mar 22;13(3):e0194773.
Sensitive gray matters in treating teen depression
Carla is an otherwise-healthy 14-year-old female followed by her pediatrician for symptoms of depression and anxiety that have worsened over the past 8 months. Anhedonia, irritability, poor concentration, fatigue, hypersomnolence, and significant weight gain have increasingly led to further dysphoria, social isolation, and obsessive rumination, all of which now contribute to more dysfunction in both her home and school life. Based on Carla’s apprehension over “taking pills,” she was referred for outpatient therapy 5 months ago but because of difficulty maintaining weekly appointments, she stopped attending after 6 weeks, citing difficulty aligning with her therapist.
Carla was seen in an urgent, unscheduled follow-up appointment 2 months prior to address increased thoughts of wishing to be dead. She had neither a plan nor a desire to act on these ideations. During an interview, she was distant with poor eye contact, and her affect was notably blunted. Her mother, who had accompanied her in the waiting room, expressed frustration to the nurse about discovering that Carla was using cannabis, that she often appeared aloof and unmotivated to do much of anything but “sit in her room and play on her phone for hours on end.” She compared Carla with her ex-husband, who had similar mood swings that often led to erratic and violent outbursts towards Carla and her mother, behaviors that ultimately led them to leave him when Carla was 6 years old.
After a discussion over the risks and benefits of various treatment options, Carla was started on low-dose fluoxetine with a plan to titrate the medication after 2 weeks. A referral for outpatient substance use treatment also was initiated. Carla’s mother telephoned 10 days later in an update that things have drastically improved in Carla’s mood and activity. The following week her mother called back again with concerns that Carla is no longer sleeping, appears restless, impulsive, and disinhibited.
Discussion
Carla’s initial presentation is common to primary care settings. Based on her earliest reported symptoms, she would qualify for a diagnosis of major depression. Decisions regarding initial treatment for children and adolescents must take into account the severity of symptoms, risks, autonomy of the patient and family, as well as available evidence. Her response to outpatient therapy is not an anomaly. With an ever-increasing demand on mental health services, the availability of consistent, quality outpatient therapy for this population is not always easy to secure.1,2 Combining targeted therapy with pharmacologic interventions for major depression appear to have the most effective outcomes.3
Carla’s progression also illustrates the challenges and potential pitfalls of attempting to understand and address her symptoms according to a single nosology. Depression is a like a fever. It can be caused by a myriad of factors and, left to linger, may lead to further residual complications. Focusing attention to her symptoms also may lead to a differential including adjustment problems, social anxiety, effects of trauma, surreptitious substance use, or even bipolar depression.
To begin with, a clear delineation of Carla’s historic symptoms and any possible medical contributions to her presentation are necessary to investigate. Specific inquiries into past episodes of activation including hyperarousal, impulsivity, restlessness, and insomnia should be elucidated prior to consideration of medication selection.4 Considering Carla’s age and the known association between antidepressant-induced manic conversion among children aged 10-14 years,5 any pharmacologic intervention will benefit from the maxim “start low and go slow.” Her symptoms of activation arise within the setting of titration of an antidepressant. This may raise considerations to her specific metabolism and physiological concentrations of the medication as well as cumulative day exposure.
Complementary to Carla’s own history is that of family members. Often obtaining a reliable family psychiatric history is an exercise fraught with bias, vagueness, and generalizations.6 However, given the known heritability of bipolar disorders and the implications for treating depression in such individuals, compared with unipolar depressive symptoms, clarifying the nature of family illness may elucidate potential susceptibilities previously unconsidered.7 In this case, descriptions of Carla’s father’s behavior raise concerns for underlying bipolar disorder, as do the accounts of traumatic stress exposure and their compounded preponderance for increased suicide risk.8
Unfortunately, Carla’s current environmental cues and maladaptive behaviors may be perpetuating her symptoms and possibly placing her on a trajectory for further illness. Exploration of her relationship with her caregivers regarding the interpretation of her symptoms, and need for treatment should be undertaken so as to expand supportive roles. Education regarding cannabis use among adolescents and age-specific risks for later depression, anxiety, and suicide is warranted in a climate when accessibility is on the rise.9 Whether or not cannabis use itself leads to amotivation is the subject of current debate.10 A growing body of evidence is clearly illustrating that Carla’s sedentary behaviors and perceived loneliness likely exacerbate her mental well-being. Such patterns indicate the need for environmental intervention to change such cycles.
Finally, Carla’s progression through treatment speak to the need for open and honest discussions regarding realistic benefits as well potential risks. Progressive symptoms of depression left untreated can be life-threatening themselves, just as effects of activation as described in the vignette above can easily and quickly progress into situations that pose safety concerns. Amidst such periods of intervention, close communication and follow up with patients and their supports ameliorate potential adverse events and lead to better outcomes.
Outcome
Carla’s mother was advised to discontinue the medication, closely monitor Carla’s behavior and sleep, and schedule an emergent follow-up appointment for the next day. A safety plan indicating circumstances in which Carla would require closer medical supervision for safety was reviewed with her mother. Carla was later initiated on lamotrigine and restarted interpersonal therapy.
References
1. N Engl J Med. 2015 May 21;372(21):2029-38.
2. J Pediatr. 2010 Nov;157(5):848-51.
3. Arch Gen Psychiatry. 2007 Oct;64(10):1132-43.
4. Curr Probl Pediatr Adolesc Health Care. 2018 Feb;48(2):50-62.
5. Arch Pediatr Adolesc Med. 2004 Aug;158(8):773-80.
6. Can J Psychiatry. 1993 Nov;38(9):590-4.
7. Appl Clin Genet. 2014 Feb 12;7:33-42.
8. J Am Acad Child Adolesc Psychiatry. 2017 Dec;56(12):1073-1080.
9. JAMA Psychiatry. 2019;76(4):426-34.
10. Subst Use Misuse. 2018 Jun 7;53(7):1158-69.
Carla is an otherwise-healthy 14-year-old female followed by her pediatrician for symptoms of depression and anxiety that have worsened over the past 8 months. Anhedonia, irritability, poor concentration, fatigue, hypersomnolence, and significant weight gain have increasingly led to further dysphoria, social isolation, and obsessive rumination, all of which now contribute to more dysfunction in both her home and school life. Based on Carla’s apprehension over “taking pills,” she was referred for outpatient therapy 5 months ago but because of difficulty maintaining weekly appointments, she stopped attending after 6 weeks, citing difficulty aligning with her therapist.
Carla was seen in an urgent, unscheduled follow-up appointment 2 months prior to address increased thoughts of wishing to be dead. She had neither a plan nor a desire to act on these ideations. During an interview, she was distant with poor eye contact, and her affect was notably blunted. Her mother, who had accompanied her in the waiting room, expressed frustration to the nurse about discovering that Carla was using cannabis, that she often appeared aloof and unmotivated to do much of anything but “sit in her room and play on her phone for hours on end.” She compared Carla with her ex-husband, who had similar mood swings that often led to erratic and violent outbursts towards Carla and her mother, behaviors that ultimately led them to leave him when Carla was 6 years old.
After a discussion over the risks and benefits of various treatment options, Carla was started on low-dose fluoxetine with a plan to titrate the medication after 2 weeks. A referral for outpatient substance use treatment also was initiated. Carla’s mother telephoned 10 days later in an update that things have drastically improved in Carla’s mood and activity. The following week her mother called back again with concerns that Carla is no longer sleeping, appears restless, impulsive, and disinhibited.
Discussion
Carla’s initial presentation is common to primary care settings. Based on her earliest reported symptoms, she would qualify for a diagnosis of major depression. Decisions regarding initial treatment for children and adolescents must take into account the severity of symptoms, risks, autonomy of the patient and family, as well as available evidence. Her response to outpatient therapy is not an anomaly. With an ever-increasing demand on mental health services, the availability of consistent, quality outpatient therapy for this population is not always easy to secure.1,2 Combining targeted therapy with pharmacologic interventions for major depression appear to have the most effective outcomes.3
Carla’s progression also illustrates the challenges and potential pitfalls of attempting to understand and address her symptoms according to a single nosology. Depression is a like a fever. It can be caused by a myriad of factors and, left to linger, may lead to further residual complications. Focusing attention to her symptoms also may lead to a differential including adjustment problems, social anxiety, effects of trauma, surreptitious substance use, or even bipolar depression.
To begin with, a clear delineation of Carla’s historic symptoms and any possible medical contributions to her presentation are necessary to investigate. Specific inquiries into past episodes of activation including hyperarousal, impulsivity, restlessness, and insomnia should be elucidated prior to consideration of medication selection.4 Considering Carla’s age and the known association between antidepressant-induced manic conversion among children aged 10-14 years,5 any pharmacologic intervention will benefit from the maxim “start low and go slow.” Her symptoms of activation arise within the setting of titration of an antidepressant. This may raise considerations to her specific metabolism and physiological concentrations of the medication as well as cumulative day exposure.
Complementary to Carla’s own history is that of family members. Often obtaining a reliable family psychiatric history is an exercise fraught with bias, vagueness, and generalizations.6 However, given the known heritability of bipolar disorders and the implications for treating depression in such individuals, compared with unipolar depressive symptoms, clarifying the nature of family illness may elucidate potential susceptibilities previously unconsidered.7 In this case, descriptions of Carla’s father’s behavior raise concerns for underlying bipolar disorder, as do the accounts of traumatic stress exposure and their compounded preponderance for increased suicide risk.8
Unfortunately, Carla’s current environmental cues and maladaptive behaviors may be perpetuating her symptoms and possibly placing her on a trajectory for further illness. Exploration of her relationship with her caregivers regarding the interpretation of her symptoms, and need for treatment should be undertaken so as to expand supportive roles. Education regarding cannabis use among adolescents and age-specific risks for later depression, anxiety, and suicide is warranted in a climate when accessibility is on the rise.9 Whether or not cannabis use itself leads to amotivation is the subject of current debate.10 A growing body of evidence is clearly illustrating that Carla’s sedentary behaviors and perceived loneliness likely exacerbate her mental well-being. Such patterns indicate the need for environmental intervention to change such cycles.
Finally, Carla’s progression through treatment speak to the need for open and honest discussions regarding realistic benefits as well potential risks. Progressive symptoms of depression left untreated can be life-threatening themselves, just as effects of activation as described in the vignette above can easily and quickly progress into situations that pose safety concerns. Amidst such periods of intervention, close communication and follow up with patients and their supports ameliorate potential adverse events and lead to better outcomes.
Outcome
Carla’s mother was advised to discontinue the medication, closely monitor Carla’s behavior and sleep, and schedule an emergent follow-up appointment for the next day. A safety plan indicating circumstances in which Carla would require closer medical supervision for safety was reviewed with her mother. Carla was later initiated on lamotrigine and restarted interpersonal therapy.
References
1. N Engl J Med. 2015 May 21;372(21):2029-38.
2. J Pediatr. 2010 Nov;157(5):848-51.
3. Arch Gen Psychiatry. 2007 Oct;64(10):1132-43.
4. Curr Probl Pediatr Adolesc Health Care. 2018 Feb;48(2):50-62.
5. Arch Pediatr Adolesc Med. 2004 Aug;158(8):773-80.
6. Can J Psychiatry. 1993 Nov;38(9):590-4.
7. Appl Clin Genet. 2014 Feb 12;7:33-42.
8. J Am Acad Child Adolesc Psychiatry. 2017 Dec;56(12):1073-1080.
9. JAMA Psychiatry. 2019;76(4):426-34.
10. Subst Use Misuse. 2018 Jun 7;53(7):1158-69.
Carla is an otherwise-healthy 14-year-old female followed by her pediatrician for symptoms of depression and anxiety that have worsened over the past 8 months. Anhedonia, irritability, poor concentration, fatigue, hypersomnolence, and significant weight gain have increasingly led to further dysphoria, social isolation, and obsessive rumination, all of which now contribute to more dysfunction in both her home and school life. Based on Carla’s apprehension over “taking pills,” she was referred for outpatient therapy 5 months ago but because of difficulty maintaining weekly appointments, she stopped attending after 6 weeks, citing difficulty aligning with her therapist.
Carla was seen in an urgent, unscheduled follow-up appointment 2 months prior to address increased thoughts of wishing to be dead. She had neither a plan nor a desire to act on these ideations. During an interview, she was distant with poor eye contact, and her affect was notably blunted. Her mother, who had accompanied her in the waiting room, expressed frustration to the nurse about discovering that Carla was using cannabis, that she often appeared aloof and unmotivated to do much of anything but “sit in her room and play on her phone for hours on end.” She compared Carla with her ex-husband, who had similar mood swings that often led to erratic and violent outbursts towards Carla and her mother, behaviors that ultimately led them to leave him when Carla was 6 years old.
After a discussion over the risks and benefits of various treatment options, Carla was started on low-dose fluoxetine with a plan to titrate the medication after 2 weeks. A referral for outpatient substance use treatment also was initiated. Carla’s mother telephoned 10 days later in an update that things have drastically improved in Carla’s mood and activity. The following week her mother called back again with concerns that Carla is no longer sleeping, appears restless, impulsive, and disinhibited.
Discussion
Carla’s initial presentation is common to primary care settings. Based on her earliest reported symptoms, she would qualify for a diagnosis of major depression. Decisions regarding initial treatment for children and adolescents must take into account the severity of symptoms, risks, autonomy of the patient and family, as well as available evidence. Her response to outpatient therapy is not an anomaly. With an ever-increasing demand on mental health services, the availability of consistent, quality outpatient therapy for this population is not always easy to secure.1,2 Combining targeted therapy with pharmacologic interventions for major depression appear to have the most effective outcomes.3
Carla’s progression also illustrates the challenges and potential pitfalls of attempting to understand and address her symptoms according to a single nosology. Depression is a like a fever. It can be caused by a myriad of factors and, left to linger, may lead to further residual complications. Focusing attention to her symptoms also may lead to a differential including adjustment problems, social anxiety, effects of trauma, surreptitious substance use, or even bipolar depression.
To begin with, a clear delineation of Carla’s historic symptoms and any possible medical contributions to her presentation are necessary to investigate. Specific inquiries into past episodes of activation including hyperarousal, impulsivity, restlessness, and insomnia should be elucidated prior to consideration of medication selection.4 Considering Carla’s age and the known association between antidepressant-induced manic conversion among children aged 10-14 years,5 any pharmacologic intervention will benefit from the maxim “start low and go slow.” Her symptoms of activation arise within the setting of titration of an antidepressant. This may raise considerations to her specific metabolism and physiological concentrations of the medication as well as cumulative day exposure.
Complementary to Carla’s own history is that of family members. Often obtaining a reliable family psychiatric history is an exercise fraught with bias, vagueness, and generalizations.6 However, given the known heritability of bipolar disorders and the implications for treating depression in such individuals, compared with unipolar depressive symptoms, clarifying the nature of family illness may elucidate potential susceptibilities previously unconsidered.7 In this case, descriptions of Carla’s father’s behavior raise concerns for underlying bipolar disorder, as do the accounts of traumatic stress exposure and their compounded preponderance for increased suicide risk.8
Unfortunately, Carla’s current environmental cues and maladaptive behaviors may be perpetuating her symptoms and possibly placing her on a trajectory for further illness. Exploration of her relationship with her caregivers regarding the interpretation of her symptoms, and need for treatment should be undertaken so as to expand supportive roles. Education regarding cannabis use among adolescents and age-specific risks for later depression, anxiety, and suicide is warranted in a climate when accessibility is on the rise.9 Whether or not cannabis use itself leads to amotivation is the subject of current debate.10 A growing body of evidence is clearly illustrating that Carla’s sedentary behaviors and perceived loneliness likely exacerbate her mental well-being. Such patterns indicate the need for environmental intervention to change such cycles.
Finally, Carla’s progression through treatment speak to the need for open and honest discussions regarding realistic benefits as well potential risks. Progressive symptoms of depression left untreated can be life-threatening themselves, just as effects of activation as described in the vignette above can easily and quickly progress into situations that pose safety concerns. Amidst such periods of intervention, close communication and follow up with patients and their supports ameliorate potential adverse events and lead to better outcomes.
Outcome
Carla’s mother was advised to discontinue the medication, closely monitor Carla’s behavior and sleep, and schedule an emergent follow-up appointment for the next day. A safety plan indicating circumstances in which Carla would require closer medical supervision for safety was reviewed with her mother. Carla was later initiated on lamotrigine and restarted interpersonal therapy.
References
1. N Engl J Med. 2015 May 21;372(21):2029-38.
2. J Pediatr. 2010 Nov;157(5):848-51.
3. Arch Gen Psychiatry. 2007 Oct;64(10):1132-43.
4. Curr Probl Pediatr Adolesc Health Care. 2018 Feb;48(2):50-62.
5. Arch Pediatr Adolesc Med. 2004 Aug;158(8):773-80.
6. Can J Psychiatry. 1993 Nov;38(9):590-4.
7. Appl Clin Genet. 2014 Feb 12;7:33-42.
8. J Am Acad Child Adolesc Psychiatry. 2017 Dec;56(12):1073-1080.
9. JAMA Psychiatry. 2019;76(4):426-34.
10. Subst Use Misuse. 2018 Jun 7;53(7):1158-69.
Beyond symptom improvement: Practicing happiness
Kailah is a 13-year-old cisgender female with two working parents, two younger siblings, and a history of mild asthma and overweight who recently presented for a problem-focused visit related to increasing anxiety. An interview of Kailah and her parents led to a diagnosis of generalized anxiety disorder, and she was referred for cognitive-behavioral therapy (CBT) and started on a low-dose SSRI. She now presents 3 months later with decreased anxiety and is compliant with the SSRI and CBT. What next?
Positive psychology and psychiatry have emerged as scientific disciplines since Seligman et al.1 charged the field of psychology with reclaiming its stake in helping everyday people to thrive, as well as cultivating strengths and talents at each level of society – individual, family, institutional, and beyond. This call to action revealed the shift over time from mental health care toward a focus only on mental illness. And study after study confirmed that being “not depressed,” “not anxious” and so on was not the same as flourishing.2
Returning to Kailah, from a mental-health-as-usual approach, your job may be done. Her symptoms have responded to first-line treatments. Perhaps you even tracked her symptoms with a freely available standardized assessment tool like the Screen for Child Anxiety Related Disorders (SCARED)3 and noted a significant drop in her generalized anxiety score.
After a couple decades of research, the science of well-being has led to some consistent findings that can be translated into office practice with children and families. As with any new science, the first steps to building well-being are defining and measuring what we are talking about. I recommend the Flourishing Scale4 for its brevity, availability, and ease of use. It covers the domains included in Seligman’s formula for thriving: PERMA. This acronym represents a consolidation of the first decades of research on well-being, and stands for Positive Emotions, Engagement, (Positive) Relationships, Meaning, and Accomplishments. For a readable but deeper look at the science behind this, check out Seligman’s “Flourish.”5
With the Flourishing Scale total score as a starting point, the acronym PERMA itself can be a good rubric to guide assessment and treatment planning in the office. You can query each of the elements to understand a youth’s current status and areas for building strengths. What brings positive emotions? What activities bring a sense of harmonious engagement without self-consciousness or awareness of time (such as a flow state)? What supportive relationships exist? Where does the youth find meaning or purpose – connection to something larger than themselves (family, work, community, teams, religion, and so on)? And where does the youth derive a sense of competence or self-esteem – something they are good at (accomplishment)?
Your clinical recommendations can flow from this assessment discussion, melding the patient’s and family’s strengths and priorities with evidence-based interventions. “The Resilience Drive,” by Alexia Michiels,6 is a good source for the latter – each chapter has segments relating research to straightforward happiness practices. The Growing Happy card deck (available online) also has brief and usable recommendations suitable for many young people. You can use these during office visits, loan out cards, gift them to families, or recommend families purchase a deck.
To build relationships, I recommend the StoryCorps and 36 Questions To Fall In Love apps. They are free and can be used with parents, peers, or others to build relationship supports and positive intimacy. Try them out yourself first; they essentially provide a platform to generate vulnerable conversations.
Mindfulness is a great antidote to lack of engagement, and it can be practiced in a variety of forms. Card decks make good office props or giveaways, including Growing Mindful (mindfulness practices for all ages) and the YogaKids Toolbox. Plus, there’s an app for that – in fact, many. Two that are free and include materials accessible for younger age groups are Smiling Mind (a nonprofit) and Insight Timer (searchable). This can build engagement and counter negative emotions.
For increasing engagement and flow, I recommend patients and family members assess their character strengths at Strengths-Based Resilience by the University of Toronto SSQ72. Research shows that using your strengths in novel ways lowers depression risk, increases happiness,7 and may be a key to increasing engagement in everyday activities.
When Kailah came in for her next visit, a discussion of PERMA led to identifying time with her family and time with her dog as significant relationship supports that bring positive emotions. However, she struggled to identify a realm where she felt some sense of mastery or competence. Taking the strengths survey (SSQ72) brought out her strengths of love of learning and curiosity. This led to her volunteering at her local library – assisting with programs and eventually creating and leading a teens’ book group. Her CBT therapist supported her through these challenges, and she was able to taper the frequency of therapy sessions so that Kailah only returns for a booster session now every 6 months or so. While she still identifies as an anxious person, Kailah has broadened her self-image to include her resilience and love of learning as core strengths.
Dr. Andrew J. Rosenfeld is an assistant professor in the departments of psychiatry and pediatrics at the University of Vermont Medical Center, Burlington. He said he has no relevant disclosures. Email him at [email protected].
References
1. Am Psychol. 2000;55(1):5-14.
2. Am Psychol. 2007 Feb-Mar;62(2):95-108.
3. J Am Acad Child Adolesc Psychiatry. 1999 Oct;38(10):1230-6.
4. Soc Indic Res. 2009; 39:247-66.
5. “Flourish: A visionary new understanding of happiness and well-being” (New York: Free Press, 2011).
6. “The Resilience Drive” (Switzerland: Favre, 2017).
7. Am Psychol. 2005 Jul-Aug;60(5):410-21.
Kailah is a 13-year-old cisgender female with two working parents, two younger siblings, and a history of mild asthma and overweight who recently presented for a problem-focused visit related to increasing anxiety. An interview of Kailah and her parents led to a diagnosis of generalized anxiety disorder, and she was referred for cognitive-behavioral therapy (CBT) and started on a low-dose SSRI. She now presents 3 months later with decreased anxiety and is compliant with the SSRI and CBT. What next?
Positive psychology and psychiatry have emerged as scientific disciplines since Seligman et al.1 charged the field of psychology with reclaiming its stake in helping everyday people to thrive, as well as cultivating strengths and talents at each level of society – individual, family, institutional, and beyond. This call to action revealed the shift over time from mental health care toward a focus only on mental illness. And study after study confirmed that being “not depressed,” “not anxious” and so on was not the same as flourishing.2
Returning to Kailah, from a mental-health-as-usual approach, your job may be done. Her symptoms have responded to first-line treatments. Perhaps you even tracked her symptoms with a freely available standardized assessment tool like the Screen for Child Anxiety Related Disorders (SCARED)3 and noted a significant drop in her generalized anxiety score.
After a couple decades of research, the science of well-being has led to some consistent findings that can be translated into office practice with children and families. As with any new science, the first steps to building well-being are defining and measuring what we are talking about. I recommend the Flourishing Scale4 for its brevity, availability, and ease of use. It covers the domains included in Seligman’s formula for thriving: PERMA. This acronym represents a consolidation of the first decades of research on well-being, and stands for Positive Emotions, Engagement, (Positive) Relationships, Meaning, and Accomplishments. For a readable but deeper look at the science behind this, check out Seligman’s “Flourish.”5
With the Flourishing Scale total score as a starting point, the acronym PERMA itself can be a good rubric to guide assessment and treatment planning in the office. You can query each of the elements to understand a youth’s current status and areas for building strengths. What brings positive emotions? What activities bring a sense of harmonious engagement without self-consciousness or awareness of time (such as a flow state)? What supportive relationships exist? Where does the youth find meaning or purpose – connection to something larger than themselves (family, work, community, teams, religion, and so on)? And where does the youth derive a sense of competence or self-esteem – something they are good at (accomplishment)?
Your clinical recommendations can flow from this assessment discussion, melding the patient’s and family’s strengths and priorities with evidence-based interventions. “The Resilience Drive,” by Alexia Michiels,6 is a good source for the latter – each chapter has segments relating research to straightforward happiness practices. The Growing Happy card deck (available online) also has brief and usable recommendations suitable for many young people. You can use these during office visits, loan out cards, gift them to families, or recommend families purchase a deck.
To build relationships, I recommend the StoryCorps and 36 Questions To Fall In Love apps. They are free and can be used with parents, peers, or others to build relationship supports and positive intimacy. Try them out yourself first; they essentially provide a platform to generate vulnerable conversations.
Mindfulness is a great antidote to lack of engagement, and it can be practiced in a variety of forms. Card decks make good office props or giveaways, including Growing Mindful (mindfulness practices for all ages) and the YogaKids Toolbox. Plus, there’s an app for that – in fact, many. Two that are free and include materials accessible for younger age groups are Smiling Mind (a nonprofit) and Insight Timer (searchable). This can build engagement and counter negative emotions.
For increasing engagement and flow, I recommend patients and family members assess their character strengths at Strengths-Based Resilience by the University of Toronto SSQ72. Research shows that using your strengths in novel ways lowers depression risk, increases happiness,7 and may be a key to increasing engagement in everyday activities.
When Kailah came in for her next visit, a discussion of PERMA led to identifying time with her family and time with her dog as significant relationship supports that bring positive emotions. However, she struggled to identify a realm where she felt some sense of mastery or competence. Taking the strengths survey (SSQ72) brought out her strengths of love of learning and curiosity. This led to her volunteering at her local library – assisting with programs and eventually creating and leading a teens’ book group. Her CBT therapist supported her through these challenges, and she was able to taper the frequency of therapy sessions so that Kailah only returns for a booster session now every 6 months or so. While she still identifies as an anxious person, Kailah has broadened her self-image to include her resilience and love of learning as core strengths.
Dr. Andrew J. Rosenfeld is an assistant professor in the departments of psychiatry and pediatrics at the University of Vermont Medical Center, Burlington. He said he has no relevant disclosures. Email him at [email protected].
References
1. Am Psychol. 2000;55(1):5-14.
2. Am Psychol. 2007 Feb-Mar;62(2):95-108.
3. J Am Acad Child Adolesc Psychiatry. 1999 Oct;38(10):1230-6.
4. Soc Indic Res. 2009; 39:247-66.
5. “Flourish: A visionary new understanding of happiness and well-being” (New York: Free Press, 2011).
6. “The Resilience Drive” (Switzerland: Favre, 2017).
7. Am Psychol. 2005 Jul-Aug;60(5):410-21.
Kailah is a 13-year-old cisgender female with two working parents, two younger siblings, and a history of mild asthma and overweight who recently presented for a problem-focused visit related to increasing anxiety. An interview of Kailah and her parents led to a diagnosis of generalized anxiety disorder, and she was referred for cognitive-behavioral therapy (CBT) and started on a low-dose SSRI. She now presents 3 months later with decreased anxiety and is compliant with the SSRI and CBT. What next?
Positive psychology and psychiatry have emerged as scientific disciplines since Seligman et al.1 charged the field of psychology with reclaiming its stake in helping everyday people to thrive, as well as cultivating strengths and talents at each level of society – individual, family, institutional, and beyond. This call to action revealed the shift over time from mental health care toward a focus only on mental illness. And study after study confirmed that being “not depressed,” “not anxious” and so on was not the same as flourishing.2
Returning to Kailah, from a mental-health-as-usual approach, your job may be done. Her symptoms have responded to first-line treatments. Perhaps you even tracked her symptoms with a freely available standardized assessment tool like the Screen for Child Anxiety Related Disorders (SCARED)3 and noted a significant drop in her generalized anxiety score.
After a couple decades of research, the science of well-being has led to some consistent findings that can be translated into office practice with children and families. As with any new science, the first steps to building well-being are defining and measuring what we are talking about. I recommend the Flourishing Scale4 for its brevity, availability, and ease of use. It covers the domains included in Seligman’s formula for thriving: PERMA. This acronym represents a consolidation of the first decades of research on well-being, and stands for Positive Emotions, Engagement, (Positive) Relationships, Meaning, and Accomplishments. For a readable but deeper look at the science behind this, check out Seligman’s “Flourish.”5
With the Flourishing Scale total score as a starting point, the acronym PERMA itself can be a good rubric to guide assessment and treatment planning in the office. You can query each of the elements to understand a youth’s current status and areas for building strengths. What brings positive emotions? What activities bring a sense of harmonious engagement without self-consciousness or awareness of time (such as a flow state)? What supportive relationships exist? Where does the youth find meaning or purpose – connection to something larger than themselves (family, work, community, teams, religion, and so on)? And where does the youth derive a sense of competence or self-esteem – something they are good at (accomplishment)?
Your clinical recommendations can flow from this assessment discussion, melding the patient’s and family’s strengths and priorities with evidence-based interventions. “The Resilience Drive,” by Alexia Michiels,6 is a good source for the latter – each chapter has segments relating research to straightforward happiness practices. The Growing Happy card deck (available online) also has brief and usable recommendations suitable for many young people. You can use these during office visits, loan out cards, gift them to families, or recommend families purchase a deck.
To build relationships, I recommend the StoryCorps and 36 Questions To Fall In Love apps. They are free and can be used with parents, peers, or others to build relationship supports and positive intimacy. Try them out yourself first; they essentially provide a platform to generate vulnerable conversations.
Mindfulness is a great antidote to lack of engagement, and it can be practiced in a variety of forms. Card decks make good office props or giveaways, including Growing Mindful (mindfulness practices for all ages) and the YogaKids Toolbox. Plus, there’s an app for that – in fact, many. Two that are free and include materials accessible for younger age groups are Smiling Mind (a nonprofit) and Insight Timer (searchable). This can build engagement and counter negative emotions.
For increasing engagement and flow, I recommend patients and family members assess their character strengths at Strengths-Based Resilience by the University of Toronto SSQ72. Research shows that using your strengths in novel ways lowers depression risk, increases happiness,7 and may be a key to increasing engagement in everyday activities.
When Kailah came in for her next visit, a discussion of PERMA led to identifying time with her family and time with her dog as significant relationship supports that bring positive emotions. However, she struggled to identify a realm where she felt some sense of mastery or competence. Taking the strengths survey (SSQ72) brought out her strengths of love of learning and curiosity. This led to her volunteering at her local library – assisting with programs and eventually creating and leading a teens’ book group. Her CBT therapist supported her through these challenges, and she was able to taper the frequency of therapy sessions so that Kailah only returns for a booster session now every 6 months or so. While she still identifies as an anxious person, Kailah has broadened her self-image to include her resilience and love of learning as core strengths.
Dr. Andrew J. Rosenfeld is an assistant professor in the departments of psychiatry and pediatrics at the University of Vermont Medical Center, Burlington. He said he has no relevant disclosures. Email him at [email protected].
References
1. Am Psychol. 2000;55(1):5-14.
2. Am Psychol. 2007 Feb-Mar;62(2):95-108.
3. J Am Acad Child Adolesc Psychiatry. 1999 Oct;38(10):1230-6.
4. Soc Indic Res. 2009; 39:247-66.
5. “Flourish: A visionary new understanding of happiness and well-being” (New York: Free Press, 2011).
6. “The Resilience Drive” (Switzerland: Favre, 2017).
7. Am Psychol. 2005 Jul-Aug;60(5):410-21.