User login
How can you help prevent a recurrence of diverticulitis?
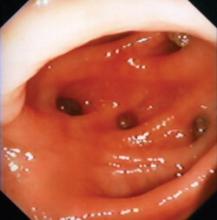
A high-fiber diet may help; available evidence doesn’t support other interventions. A high-fiber diet is often prescribed after recovery from acute diverticulitis, based on extrapolation from epidemiologic data showing an association between low-fiber diets and diverticulosis (strength of recommendation [SOR]: C, expert opinion). No direct evidence establishes a role for fiber in preventing recurrent diverticulitis, however.
No evidence supports the common advice to avoid nuts and seeds to prevent diverticulitis. Eating nuts, corn, and popcorn doesn’t increase the risk; in fact, nuts and popcorn may have a protective effect (SOR: B, large cohort study).
There isn’t enough evidence to recommend the anti-inflammatory drug mesalamine or a polybacterial lysate for immunostimulation. Retrospective data don’t support routine prophylactic colectomy after 1 or 2 episodes of acute diverticulitis (SOR: B, observational studies).
Evidence summary
A 2006 Family Physicians Inquiries Network Clinical Inquiry on diverticulosis found inconsistent evidence that fiber decreases the risk of symptomatic diverticular disease (SOR: C, case control studies and a large prospective cohort study).1
A 2007 literature review found no systematic reviews or randomized controlled trials (RCTs) of fiber for preventing complications of diverticular disease. The reviewers noted that observational studies have found less diverticulosis in populations with higher fiber consumption.2
Nuts, popcorn may be protective
A trial conducted as part of a large prospective cohort study—the Health Professionals Follow-up Study—followed 47,228 male health professionals in the United States, ages 40 to 75 years, from 1986 to 2004.3 The subjects, all of whom returned a food-frequency questionnaire, were at baseline free of diverticulosis and related complications, cancer, and inflammatory bowel disease. During the follow-up period, 801 cases of diverticulitis and 383 cases of diverticular bleeding (the main outcome measures) occurred.
The investigators found an inverse association between consumption of nuts and popcorn and risk of diverticulitis. Men with the highest intake of each food (at least twice per week) compared with men with the lowest intake (less than once per month) had a hazard ratio of 0.80 (95% confidence interval [CI], 0.63-1.01; P for trend=.04) for nuts and 0.72 (95% CI, 0.56-0.92; P for trend=.007) for popcorn. No association was noted between corn consumption and diverticulitis or between nut, corn, or popcorn consumption and diverticular bleeding or uncomplicated diverticulosis.
Mesalamine’s efficacy is unknown
A 2007 systematic review found 1 RCT of the anti-inflammatory drug mesalamine (mesalazine, 5-aminosalicylic acid) for preventing diverticulitis. Mesalamine reduced the recurrence rate of diverticulitis from 46% to 15% among 166 subjects.
The reviewers judged the study to be flawed by unreported diagnostic criteria and a high withdrawal rate. They concluded that the effectiveness of mesalamine remains unknown.2
1 small study of oral enterovaccine
An oral polybacterial lysate suspension designed to stimulate gut secretion of immunoglobulin A was investigated in a study of 83 patients with recurrent diverticulitis. In the treated group, 4.6% (2/43) of patients had recurrent diverticulitis during the 3 months of the study, compared with 12.5% (5/40) of the untreated group (P<.05).4
Prophylactic surgery rarely helps
No randomized trials have compared surgical with medical therapy to prevent recurrent diverticulitis. Extensive retrospective literature fails to support elective surgery after a second episode. Sixty-eight percent to 96% of patients requiring surgery for diverticulitis-associated perforation or abscess had no previous symptoms and couldn’t be helped by prophylactic surgery,5 and diverticulitis symptoms persisted after bowel resection in 27% to 33% of patients.5
One large retrospective study followed 3165 patients for 6 to 12 years after hospitalization for diverticulitis. Of the patients treated nonoperatively, 13% had a single recurrence and 4% had multiple recurrences; the annual recurrence rate was approximately 2%. The authors concluded that routine elective colectomy is rarely indicated after a first episode of uncomplicated acute diverticulitis.6
A decision analysis using a Markov model found that performing a colectomy after a fourth, rather than a second, episode of diverticulitis would result in somewhat fewer deaths and colostomies, equivalent quality-adjusted years of life, and cost savings per patient of $1035 to $5429. The results held for both older and younger patients.7
Recommendations
The American Society of Colon and Rectal Surgeons (ASCRS) concludes that recommendations for elective sigmoid colectomy after recovery from acute diverticulitis should be made on a case-by-case basis.8 Computed tomography to grade the severity of a first attack may help determine the need for surgery. The ASCRS guidelines mention that long-term fiber supplementation may prevent recurrences of diverticulitis in most patients.
The American College of Gastroenterology Practice Parameters Committee states that prophylactic surgery may be recommended for recurrent attacks of diverticulitis, but generally isn’t indicated after a single uncomplicated episode.9 The group also notes that high-fiber diets may decrease the development of colonic diverticulosis, but no consistent data exist regarding fiber to prevent recurrent diverticulitis.
1. Eglash A, Lane CH, Schneider D. What is the most beneficial diet for patients with diverticulosis? J Fam Pract. 2006;55:813-815.
2. Humes D, Simpson J, Spiller R. Colonic diverticular disease. BMJ Clin Evid. 2008;01:405-416.
3. Strate LL, Liu YL, Syngal S, et al. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. 2008;300:907-914.
4. Dughera L, Serra AM, Battaglia E, et al. Acute recurrent diverticulitis is prevented by oral administration of a polybacterial lysate suspension. Minerva Gastroenterol Dietol. 2004;50:149-153.
5. Janes S, Meagher A, Frizelle FA. Elective surgery after acute diverticulitis. Br J Surg. 2005;92:133-142.
6. Broderick-Villa G, Burchette RJ, Collins JC, et al. Hospitalization for acute diverticulitis does not mandate routine elective colectomy. Arch Surg. 2005;140:576-581.
7. Salem L, Veenstra DL, Sullivan SD, et al. The timing of elective colectomy in diverticulitis: a decision analysis. J Am Coll Surg. 2004;199:904-912.
8. Rafferty J, Shellito P, Hyman NH, et al. Standards Committee of the American Society of Colon and Rectal Surgeons. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939-944.
9. Stollman N, Raskin L. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110-3121.
A high-fiber diet may help; available evidence doesn’t support other interventions. A high-fiber diet is often prescribed after recovery from acute diverticulitis, based on extrapolation from epidemiologic data showing an association between low-fiber diets and diverticulosis (strength of recommendation [SOR]: C, expert opinion). No direct evidence establishes a role for fiber in preventing recurrent diverticulitis, however.
No evidence supports the common advice to avoid nuts and seeds to prevent diverticulitis. Eating nuts, corn, and popcorn doesn’t increase the risk; in fact, nuts and popcorn may have a protective effect (SOR: B, large cohort study).
There isn’t enough evidence to recommend the anti-inflammatory drug mesalamine or a polybacterial lysate for immunostimulation. Retrospective data don’t support routine prophylactic colectomy after 1 or 2 episodes of acute diverticulitis (SOR: B, observational studies).
Evidence summary
A 2006 Family Physicians Inquiries Network Clinical Inquiry on diverticulosis found inconsistent evidence that fiber decreases the risk of symptomatic diverticular disease (SOR: C, case control studies and a large prospective cohort study).1
A 2007 literature review found no systematic reviews or randomized controlled trials (RCTs) of fiber for preventing complications of diverticular disease. The reviewers noted that observational studies have found less diverticulosis in populations with higher fiber consumption.2
Nuts, popcorn may be protective
A trial conducted as part of a large prospective cohort study—the Health Professionals Follow-up Study—followed 47,228 male health professionals in the United States, ages 40 to 75 years, from 1986 to 2004.3 The subjects, all of whom returned a food-frequency questionnaire, were at baseline free of diverticulosis and related complications, cancer, and inflammatory bowel disease. During the follow-up period, 801 cases of diverticulitis and 383 cases of diverticular bleeding (the main outcome measures) occurred.
The investigators found an inverse association between consumption of nuts and popcorn and risk of diverticulitis. Men with the highest intake of each food (at least twice per week) compared with men with the lowest intake (less than once per month) had a hazard ratio of 0.80 (95% confidence interval [CI], 0.63-1.01; P for trend=.04) for nuts and 0.72 (95% CI, 0.56-0.92; P for trend=.007) for popcorn. No association was noted between corn consumption and diverticulitis or between nut, corn, or popcorn consumption and diverticular bleeding or uncomplicated diverticulosis.
Mesalamine’s efficacy is unknown
A 2007 systematic review found 1 RCT of the anti-inflammatory drug mesalamine (mesalazine, 5-aminosalicylic acid) for preventing diverticulitis. Mesalamine reduced the recurrence rate of diverticulitis from 46% to 15% among 166 subjects.
The reviewers judged the study to be flawed by unreported diagnostic criteria and a high withdrawal rate. They concluded that the effectiveness of mesalamine remains unknown.2
1 small study of oral enterovaccine
An oral polybacterial lysate suspension designed to stimulate gut secretion of immunoglobulin A was investigated in a study of 83 patients with recurrent diverticulitis. In the treated group, 4.6% (2/43) of patients had recurrent diverticulitis during the 3 months of the study, compared with 12.5% (5/40) of the untreated group (P<.05).4
Prophylactic surgery rarely helps
No randomized trials have compared surgical with medical therapy to prevent recurrent diverticulitis. Extensive retrospective literature fails to support elective surgery after a second episode. Sixty-eight percent to 96% of patients requiring surgery for diverticulitis-associated perforation or abscess had no previous symptoms and couldn’t be helped by prophylactic surgery,5 and diverticulitis symptoms persisted after bowel resection in 27% to 33% of patients.5
One large retrospective study followed 3165 patients for 6 to 12 years after hospitalization for diverticulitis. Of the patients treated nonoperatively, 13% had a single recurrence and 4% had multiple recurrences; the annual recurrence rate was approximately 2%. The authors concluded that routine elective colectomy is rarely indicated after a first episode of uncomplicated acute diverticulitis.6
A decision analysis using a Markov model found that performing a colectomy after a fourth, rather than a second, episode of diverticulitis would result in somewhat fewer deaths and colostomies, equivalent quality-adjusted years of life, and cost savings per patient of $1035 to $5429. The results held for both older and younger patients.7
Recommendations
The American Society of Colon and Rectal Surgeons (ASCRS) concludes that recommendations for elective sigmoid colectomy after recovery from acute diverticulitis should be made on a case-by-case basis.8 Computed tomography to grade the severity of a first attack may help determine the need for surgery. The ASCRS guidelines mention that long-term fiber supplementation may prevent recurrences of diverticulitis in most patients.
The American College of Gastroenterology Practice Parameters Committee states that prophylactic surgery may be recommended for recurrent attacks of diverticulitis, but generally isn’t indicated after a single uncomplicated episode.9 The group also notes that high-fiber diets may decrease the development of colonic diverticulosis, but no consistent data exist regarding fiber to prevent recurrent diverticulitis.
A high-fiber diet may help; available evidence doesn’t support other interventions. A high-fiber diet is often prescribed after recovery from acute diverticulitis, based on extrapolation from epidemiologic data showing an association between low-fiber diets and diverticulosis (strength of recommendation [SOR]: C, expert opinion). No direct evidence establishes a role for fiber in preventing recurrent diverticulitis, however.
No evidence supports the common advice to avoid nuts and seeds to prevent diverticulitis. Eating nuts, corn, and popcorn doesn’t increase the risk; in fact, nuts and popcorn may have a protective effect (SOR: B, large cohort study).
There isn’t enough evidence to recommend the anti-inflammatory drug mesalamine or a polybacterial lysate for immunostimulation. Retrospective data don’t support routine prophylactic colectomy after 1 or 2 episodes of acute diverticulitis (SOR: B, observational studies).
Evidence summary
A 2006 Family Physicians Inquiries Network Clinical Inquiry on diverticulosis found inconsistent evidence that fiber decreases the risk of symptomatic diverticular disease (SOR: C, case control studies and a large prospective cohort study).1
A 2007 literature review found no systematic reviews or randomized controlled trials (RCTs) of fiber for preventing complications of diverticular disease. The reviewers noted that observational studies have found less diverticulosis in populations with higher fiber consumption.2
Nuts, popcorn may be protective
A trial conducted as part of a large prospective cohort study—the Health Professionals Follow-up Study—followed 47,228 male health professionals in the United States, ages 40 to 75 years, from 1986 to 2004.3 The subjects, all of whom returned a food-frequency questionnaire, were at baseline free of diverticulosis and related complications, cancer, and inflammatory bowel disease. During the follow-up period, 801 cases of diverticulitis and 383 cases of diverticular bleeding (the main outcome measures) occurred.
The investigators found an inverse association between consumption of nuts and popcorn and risk of diverticulitis. Men with the highest intake of each food (at least twice per week) compared with men with the lowest intake (less than once per month) had a hazard ratio of 0.80 (95% confidence interval [CI], 0.63-1.01; P for trend=.04) for nuts and 0.72 (95% CI, 0.56-0.92; P for trend=.007) for popcorn. No association was noted between corn consumption and diverticulitis or between nut, corn, or popcorn consumption and diverticular bleeding or uncomplicated diverticulosis.
Mesalamine’s efficacy is unknown
A 2007 systematic review found 1 RCT of the anti-inflammatory drug mesalamine (mesalazine, 5-aminosalicylic acid) for preventing diverticulitis. Mesalamine reduced the recurrence rate of diverticulitis from 46% to 15% among 166 subjects.
The reviewers judged the study to be flawed by unreported diagnostic criteria and a high withdrawal rate. They concluded that the effectiveness of mesalamine remains unknown.2
1 small study of oral enterovaccine
An oral polybacterial lysate suspension designed to stimulate gut secretion of immunoglobulin A was investigated in a study of 83 patients with recurrent diverticulitis. In the treated group, 4.6% (2/43) of patients had recurrent diverticulitis during the 3 months of the study, compared with 12.5% (5/40) of the untreated group (P<.05).4
Prophylactic surgery rarely helps
No randomized trials have compared surgical with medical therapy to prevent recurrent diverticulitis. Extensive retrospective literature fails to support elective surgery after a second episode. Sixty-eight percent to 96% of patients requiring surgery for diverticulitis-associated perforation or abscess had no previous symptoms and couldn’t be helped by prophylactic surgery,5 and diverticulitis symptoms persisted after bowel resection in 27% to 33% of patients.5
One large retrospective study followed 3165 patients for 6 to 12 years after hospitalization for diverticulitis. Of the patients treated nonoperatively, 13% had a single recurrence and 4% had multiple recurrences; the annual recurrence rate was approximately 2%. The authors concluded that routine elective colectomy is rarely indicated after a first episode of uncomplicated acute diverticulitis.6
A decision analysis using a Markov model found that performing a colectomy after a fourth, rather than a second, episode of diverticulitis would result in somewhat fewer deaths and colostomies, equivalent quality-adjusted years of life, and cost savings per patient of $1035 to $5429. The results held for both older and younger patients.7
Recommendations
The American Society of Colon and Rectal Surgeons (ASCRS) concludes that recommendations for elective sigmoid colectomy after recovery from acute diverticulitis should be made on a case-by-case basis.8 Computed tomography to grade the severity of a first attack may help determine the need for surgery. The ASCRS guidelines mention that long-term fiber supplementation may prevent recurrences of diverticulitis in most patients.
The American College of Gastroenterology Practice Parameters Committee states that prophylactic surgery may be recommended for recurrent attacks of diverticulitis, but generally isn’t indicated after a single uncomplicated episode.9 The group also notes that high-fiber diets may decrease the development of colonic diverticulosis, but no consistent data exist regarding fiber to prevent recurrent diverticulitis.
1. Eglash A, Lane CH, Schneider D. What is the most beneficial diet for patients with diverticulosis? J Fam Pract. 2006;55:813-815.
2. Humes D, Simpson J, Spiller R. Colonic diverticular disease. BMJ Clin Evid. 2008;01:405-416.
3. Strate LL, Liu YL, Syngal S, et al. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. 2008;300:907-914.
4. Dughera L, Serra AM, Battaglia E, et al. Acute recurrent diverticulitis is prevented by oral administration of a polybacterial lysate suspension. Minerva Gastroenterol Dietol. 2004;50:149-153.
5. Janes S, Meagher A, Frizelle FA. Elective surgery after acute diverticulitis. Br J Surg. 2005;92:133-142.
6. Broderick-Villa G, Burchette RJ, Collins JC, et al. Hospitalization for acute diverticulitis does not mandate routine elective colectomy. Arch Surg. 2005;140:576-581.
7. Salem L, Veenstra DL, Sullivan SD, et al. The timing of elective colectomy in diverticulitis: a decision analysis. J Am Coll Surg. 2004;199:904-912.
8. Rafferty J, Shellito P, Hyman NH, et al. Standards Committee of the American Society of Colon and Rectal Surgeons. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939-944.
9. Stollman N, Raskin L. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110-3121.
1. Eglash A, Lane CH, Schneider D. What is the most beneficial diet for patients with diverticulosis? J Fam Pract. 2006;55:813-815.
2. Humes D, Simpson J, Spiller R. Colonic diverticular disease. BMJ Clin Evid. 2008;01:405-416.
3. Strate LL, Liu YL, Syngal S, et al. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. 2008;300:907-914.
4. Dughera L, Serra AM, Battaglia E, et al. Acute recurrent diverticulitis is prevented by oral administration of a polybacterial lysate suspension. Minerva Gastroenterol Dietol. 2004;50:149-153.
5. Janes S, Meagher A, Frizelle FA. Elective surgery after acute diverticulitis. Br J Surg. 2005;92:133-142.
6. Broderick-Villa G, Burchette RJ, Collins JC, et al. Hospitalization for acute diverticulitis does not mandate routine elective colectomy. Arch Surg. 2005;140:576-581.
7. Salem L, Veenstra DL, Sullivan SD, et al. The timing of elective colectomy in diverticulitis: a decision analysis. J Am Coll Surg. 2004;199:904-912.
8. Rafferty J, Shellito P, Hyman NH, et al. Standards Committee of the American Society of Colon and Rectal Surgeons. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939-944.
9. Stollman N, Raskin L. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110-3121.
Evidence-based answers from the Family Physicians Inquiries Network
What is the best diagnostic approach to alopecia in women?
It’s unclear what the best approach is given the lack of studies on this issue. Indirect evidence and expert opinion indicate that a careful history and thorough physical examination usually suggest the underlying cause of alopecia. Ancillary laboratory evaluation and scalp biopsy are sometimes necessary to make or confirm the diagnosis (strength of recommendation: C, expert opinion).
Scarring or nonscarring, that’s the question
Robert Gauer, MD
University of North Carolina Faculty Development, Fellowship 2006-2007, Fort Bragg
In my experience, evaluation of hair loss in women almost always fails to turn up a cause, and the alopecia typically resolves spontaneously within 6 to 12 months. I agree that the most useful investigations for ruling out specific etiologies are the history and physical examination.
The most important characteristic to evaluate is whether it is scarring or nonscarring. Scarring alopecia generally necessitates a biopsy. Identifying diffuse vs focal alopecia can further narrow the differential diagnosis.
The typical patient has diffuse, nonscarring hair loss in no defined pattern (central thinning suggestive of androgenic alopecia). Consider telogen effluvium as the likely diagnosis. It can result from chronic illness, postpartum state, recent surgery/anesthesia, rapid weight loss, diet (iron deficiency, vitamin A toxicity, and protein deficiency), thyroid disease, or medications. Many commonly prescribed drugs can cause hair loss, including anticoagulants, nonsteroidal anti-inflammatory drugs, β-blockers, H2 blockers, hormones, retinoids, and antihyperlipidemic agents.
Educating the patient, checking directed laboratory values occasionally, or modifying certain medications is often all that’s needed to reassure women with alopecia. Persistent, progressive scarring or patchy alopecia requires further investigation and possible dermatologic consultation.
Evidence summary
Our comprehensive literature search found no systematic reviews, randomized trials, or prospective cohort studies that answer this question. The differential diagnosis of clinical hair loss is large (TABLE). We reviewed indirect evidence and expert opinion to answer this Clinical Inquiry.
Clues in the history
A detailed history—including medication use, systemic illness, endocrine dysfunction, hair care practices, severe diet restriction, and family history—is key to establishing an accurate diagnosis of alopecia.1 Other significant considerations include the onset, duration, and pattern of hair loss; whether hair is broken or shed at the root; and whether shedding or thinning has increased.1,2 It’s also important to ascertain whether hair loss is limited to the scalp or affects other areas of the body.
A family history of alopecia areata or androgenic alopecia can point to a genetic cause. Acne or abnormal menses can indicate androgen excess, suggesting androgenic alopecia. Positive answers to thyroid screening questions can point to hypothyroidism, and abnormal diet patterns can suggest iron-deficiency anemia. Unusual hair care practices can cause traction alopecia.1
TABLE
Causes of nonscarring alopecia
| COMMON | LESS COMMON |
|---|---|
| Alopecia areata | Human immunodeficiency virus |
| Androgenetic alopecia | Hyperthyroidism |
| Drugs and other chemicals | Hypothyroidism |
| Telogen effluvium (both acute and chronic) | Iron deficiency |
| Tinea capitis | Nutritional deficiencies |
| Traction alopecia | Other systemic diseases |
| Secondary syphilis | |
| Systemic lupus erythematosus | |
| Trichotillomania | |
| Adapted from: Habif TP. Clinical Dermatology. A Color Guide to Diagnosis and Therapy. 4th ed. Edinburgh: Mosby; 2004:838-842. | |
3 stages of the physical exam
All hair-bearing sites should be examined. Clinical examination should be performed in 3 stages:1,2
- Inspect the scalp for inflammation, scale, and erythema to determine whether scarring is present.
- Examine the hair density and distribution pattern.
- Study the hair shaft quality, looking at caliber, fragility, length, and shape.
The “pull test” is often used to assess ongoing hair loss. If more than 10% of hairs are pulled away from the scalp, the test is positive, suggesting active hair shedding.1
Beyond the history and physical
Ancillary laboratory evaluation is sometimes necessary if the diagnosis remains unclear.1,2 Serum ferritin or a complete blood count can be useful to look for iron-deficiency anemia; a thyroid-stimulating hormone test can rule out hypothyroidism.3 According to 1 small study of 50 women with diffuse alopecia, thyroid tests are not routinely warranted without supportive clinical signs.4
Check free testosterone, androstenedione, and dehydroepiandrosterone if virilizing signs are present, to assess hyperandrogenism.1,3 Serum prolactin can be useful if the patient has galactorrhea.5 Also, consider a Venereal Disease Research Laboratory test to rule out syphilis.2,6
No evidence suggests that low serum zinc concentrations cause hair loss. In fact, excessive intake of nutritional supplements may lead to hair loss and aren’t recommended in the absence of a proven deficiency.7
If a patient has scarring alopecia, a scalp biopsy is almost always necessary to make a diagnosis.1 Usually a punch biopsy is sufficient, but it should be no smaller than 4 mm. The preferred location is the central scalp in an area representative of the hair loss.1,5
Recommendations
The University of Texas Family Nurse Practitioner Program recommends a thorough history and physical examination and, if indicated, selected laboratory evaluation.6 The program states that the Women’s Androgenetic Alopecia Quality of Life (WAA-QOL) Questionnaire is useful in evaluating health-related quality of life specific to women.
The American Hair Loss Association recommends checking some screening labs on women with hair loss, but states that the diagnosis is usually a process of elimination as many of the laboratory tests mentioned above will come back in the normal range.8
1. Shapiro J, Wiseman M, Lui H. Practical management of hair loss. Can Fam Physician. 2000;46:1469-1477.
2. Thiedke CC. Alopecia in women. Am Fam Physician. 2003;67:1007-1014.
3. Chartier MB, Hoss DM, Grant-Kels JM. Approach to the adult female patient with diffuse nonscarring alopecia. J Am Acad Dermatol. 2002;47:809-818.
4. Dupont C. How far should we investigate diffuse alopecia in women? Clin Exp Dermatol. 1996;21:320.-
5. Olsen EA, Messenger AG, Shapiro J, et al. Evaluation and treatment of male and female pattern hair loss. J Am Acad Dermatol. 2005;52:301-311.
6. University of Texas at Austin, School of Nursing, Family Nurse Practitioner Program. Recommendations to diagnose and treat adult hair loss disorders or alopecia in primary care settings (non pregnant female and male adults). Austin, TX: University of Texas at Austin, School of Nursing; May 2004. 21 p. 1-8. Available at: www.ngc.gov/summary/summary.aspx?doc_id=5428&nbr=003722&string=alopecia+and+(diagnosis+or+evaluation). Accessed January 9, 2007.
7. Rushton DH. Nutritional factors and hair loss. Clin Exp Dermatol. 2002;27:396-404.
8. Women’s hair loss/diagnosis. American Hair Loss Association [database online]. Updated March 11, 2005. Available at: http://www.americanhairloss.org/women_hair_loss/diagnosis.asp. Accessed June 10, 2009.
It’s unclear what the best approach is given the lack of studies on this issue. Indirect evidence and expert opinion indicate that a careful history and thorough physical examination usually suggest the underlying cause of alopecia. Ancillary laboratory evaluation and scalp biopsy are sometimes necessary to make or confirm the diagnosis (strength of recommendation: C, expert opinion).
Scarring or nonscarring, that’s the question
Robert Gauer, MD
University of North Carolina Faculty Development, Fellowship 2006-2007, Fort Bragg
In my experience, evaluation of hair loss in women almost always fails to turn up a cause, and the alopecia typically resolves spontaneously within 6 to 12 months. I agree that the most useful investigations for ruling out specific etiologies are the history and physical examination.
The most important characteristic to evaluate is whether it is scarring or nonscarring. Scarring alopecia generally necessitates a biopsy. Identifying diffuse vs focal alopecia can further narrow the differential diagnosis.
The typical patient has diffuse, nonscarring hair loss in no defined pattern (central thinning suggestive of androgenic alopecia). Consider telogen effluvium as the likely diagnosis. It can result from chronic illness, postpartum state, recent surgery/anesthesia, rapid weight loss, diet (iron deficiency, vitamin A toxicity, and protein deficiency), thyroid disease, or medications. Many commonly prescribed drugs can cause hair loss, including anticoagulants, nonsteroidal anti-inflammatory drugs, β-blockers, H2 blockers, hormones, retinoids, and antihyperlipidemic agents.
Educating the patient, checking directed laboratory values occasionally, or modifying certain medications is often all that’s needed to reassure women with alopecia. Persistent, progressive scarring or patchy alopecia requires further investigation and possible dermatologic consultation.
Evidence summary
Our comprehensive literature search found no systematic reviews, randomized trials, or prospective cohort studies that answer this question. The differential diagnosis of clinical hair loss is large (TABLE). We reviewed indirect evidence and expert opinion to answer this Clinical Inquiry.
Clues in the history
A detailed history—including medication use, systemic illness, endocrine dysfunction, hair care practices, severe diet restriction, and family history—is key to establishing an accurate diagnosis of alopecia.1 Other significant considerations include the onset, duration, and pattern of hair loss; whether hair is broken or shed at the root; and whether shedding or thinning has increased.1,2 It’s also important to ascertain whether hair loss is limited to the scalp or affects other areas of the body.
A family history of alopecia areata or androgenic alopecia can point to a genetic cause. Acne or abnormal menses can indicate androgen excess, suggesting androgenic alopecia. Positive answers to thyroid screening questions can point to hypothyroidism, and abnormal diet patterns can suggest iron-deficiency anemia. Unusual hair care practices can cause traction alopecia.1
TABLE
Causes of nonscarring alopecia
| COMMON | LESS COMMON |
|---|---|
| Alopecia areata | Human immunodeficiency virus |
| Androgenetic alopecia | Hyperthyroidism |
| Drugs and other chemicals | Hypothyroidism |
| Telogen effluvium (both acute and chronic) | Iron deficiency |
| Tinea capitis | Nutritional deficiencies |
| Traction alopecia | Other systemic diseases |
| Secondary syphilis | |
| Systemic lupus erythematosus | |
| Trichotillomania | |
| Adapted from: Habif TP. Clinical Dermatology. A Color Guide to Diagnosis and Therapy. 4th ed. Edinburgh: Mosby; 2004:838-842. | |
3 stages of the physical exam
All hair-bearing sites should be examined. Clinical examination should be performed in 3 stages:1,2
- Inspect the scalp for inflammation, scale, and erythema to determine whether scarring is present.
- Examine the hair density and distribution pattern.
- Study the hair shaft quality, looking at caliber, fragility, length, and shape.
The “pull test” is often used to assess ongoing hair loss. If more than 10% of hairs are pulled away from the scalp, the test is positive, suggesting active hair shedding.1
Beyond the history and physical
Ancillary laboratory evaluation is sometimes necessary if the diagnosis remains unclear.1,2 Serum ferritin or a complete blood count can be useful to look for iron-deficiency anemia; a thyroid-stimulating hormone test can rule out hypothyroidism.3 According to 1 small study of 50 women with diffuse alopecia, thyroid tests are not routinely warranted without supportive clinical signs.4
Check free testosterone, androstenedione, and dehydroepiandrosterone if virilizing signs are present, to assess hyperandrogenism.1,3 Serum prolactin can be useful if the patient has galactorrhea.5 Also, consider a Venereal Disease Research Laboratory test to rule out syphilis.2,6
No evidence suggests that low serum zinc concentrations cause hair loss. In fact, excessive intake of nutritional supplements may lead to hair loss and aren’t recommended in the absence of a proven deficiency.7
If a patient has scarring alopecia, a scalp biopsy is almost always necessary to make a diagnosis.1 Usually a punch biopsy is sufficient, but it should be no smaller than 4 mm. The preferred location is the central scalp in an area representative of the hair loss.1,5
Recommendations
The University of Texas Family Nurse Practitioner Program recommends a thorough history and physical examination and, if indicated, selected laboratory evaluation.6 The program states that the Women’s Androgenetic Alopecia Quality of Life (WAA-QOL) Questionnaire is useful in evaluating health-related quality of life specific to women.
The American Hair Loss Association recommends checking some screening labs on women with hair loss, but states that the diagnosis is usually a process of elimination as many of the laboratory tests mentioned above will come back in the normal range.8
It’s unclear what the best approach is given the lack of studies on this issue. Indirect evidence and expert opinion indicate that a careful history and thorough physical examination usually suggest the underlying cause of alopecia. Ancillary laboratory evaluation and scalp biopsy are sometimes necessary to make or confirm the diagnosis (strength of recommendation: C, expert opinion).
Scarring or nonscarring, that’s the question
Robert Gauer, MD
University of North Carolina Faculty Development, Fellowship 2006-2007, Fort Bragg
In my experience, evaluation of hair loss in women almost always fails to turn up a cause, and the alopecia typically resolves spontaneously within 6 to 12 months. I agree that the most useful investigations for ruling out specific etiologies are the history and physical examination.
The most important characteristic to evaluate is whether it is scarring or nonscarring. Scarring alopecia generally necessitates a biopsy. Identifying diffuse vs focal alopecia can further narrow the differential diagnosis.
The typical patient has diffuse, nonscarring hair loss in no defined pattern (central thinning suggestive of androgenic alopecia). Consider telogen effluvium as the likely diagnosis. It can result from chronic illness, postpartum state, recent surgery/anesthesia, rapid weight loss, diet (iron deficiency, vitamin A toxicity, and protein deficiency), thyroid disease, or medications. Many commonly prescribed drugs can cause hair loss, including anticoagulants, nonsteroidal anti-inflammatory drugs, β-blockers, H2 blockers, hormones, retinoids, and antihyperlipidemic agents.
Educating the patient, checking directed laboratory values occasionally, or modifying certain medications is often all that’s needed to reassure women with alopecia. Persistent, progressive scarring or patchy alopecia requires further investigation and possible dermatologic consultation.
Evidence summary
Our comprehensive literature search found no systematic reviews, randomized trials, or prospective cohort studies that answer this question. The differential diagnosis of clinical hair loss is large (TABLE). We reviewed indirect evidence and expert opinion to answer this Clinical Inquiry.
Clues in the history
A detailed history—including medication use, systemic illness, endocrine dysfunction, hair care practices, severe diet restriction, and family history—is key to establishing an accurate diagnosis of alopecia.1 Other significant considerations include the onset, duration, and pattern of hair loss; whether hair is broken or shed at the root; and whether shedding or thinning has increased.1,2 It’s also important to ascertain whether hair loss is limited to the scalp or affects other areas of the body.
A family history of alopecia areata or androgenic alopecia can point to a genetic cause. Acne or abnormal menses can indicate androgen excess, suggesting androgenic alopecia. Positive answers to thyroid screening questions can point to hypothyroidism, and abnormal diet patterns can suggest iron-deficiency anemia. Unusual hair care practices can cause traction alopecia.1
TABLE
Causes of nonscarring alopecia
| COMMON | LESS COMMON |
|---|---|
| Alopecia areata | Human immunodeficiency virus |
| Androgenetic alopecia | Hyperthyroidism |
| Drugs and other chemicals | Hypothyroidism |
| Telogen effluvium (both acute and chronic) | Iron deficiency |
| Tinea capitis | Nutritional deficiencies |
| Traction alopecia | Other systemic diseases |
| Secondary syphilis | |
| Systemic lupus erythematosus | |
| Trichotillomania | |
| Adapted from: Habif TP. Clinical Dermatology. A Color Guide to Diagnosis and Therapy. 4th ed. Edinburgh: Mosby; 2004:838-842. | |
3 stages of the physical exam
All hair-bearing sites should be examined. Clinical examination should be performed in 3 stages:1,2
- Inspect the scalp for inflammation, scale, and erythema to determine whether scarring is present.
- Examine the hair density and distribution pattern.
- Study the hair shaft quality, looking at caliber, fragility, length, and shape.
The “pull test” is often used to assess ongoing hair loss. If more than 10% of hairs are pulled away from the scalp, the test is positive, suggesting active hair shedding.1
Beyond the history and physical
Ancillary laboratory evaluation is sometimes necessary if the diagnosis remains unclear.1,2 Serum ferritin or a complete blood count can be useful to look for iron-deficiency anemia; a thyroid-stimulating hormone test can rule out hypothyroidism.3 According to 1 small study of 50 women with diffuse alopecia, thyroid tests are not routinely warranted without supportive clinical signs.4
Check free testosterone, androstenedione, and dehydroepiandrosterone if virilizing signs are present, to assess hyperandrogenism.1,3 Serum prolactin can be useful if the patient has galactorrhea.5 Also, consider a Venereal Disease Research Laboratory test to rule out syphilis.2,6
No evidence suggests that low serum zinc concentrations cause hair loss. In fact, excessive intake of nutritional supplements may lead to hair loss and aren’t recommended in the absence of a proven deficiency.7
If a patient has scarring alopecia, a scalp biopsy is almost always necessary to make a diagnosis.1 Usually a punch biopsy is sufficient, but it should be no smaller than 4 mm. The preferred location is the central scalp in an area representative of the hair loss.1,5
Recommendations
The University of Texas Family Nurse Practitioner Program recommends a thorough history and physical examination and, if indicated, selected laboratory evaluation.6 The program states that the Women’s Androgenetic Alopecia Quality of Life (WAA-QOL) Questionnaire is useful in evaluating health-related quality of life specific to women.
The American Hair Loss Association recommends checking some screening labs on women with hair loss, but states that the diagnosis is usually a process of elimination as many of the laboratory tests mentioned above will come back in the normal range.8
1. Shapiro J, Wiseman M, Lui H. Practical management of hair loss. Can Fam Physician. 2000;46:1469-1477.
2. Thiedke CC. Alopecia in women. Am Fam Physician. 2003;67:1007-1014.
3. Chartier MB, Hoss DM, Grant-Kels JM. Approach to the adult female patient with diffuse nonscarring alopecia. J Am Acad Dermatol. 2002;47:809-818.
4. Dupont C. How far should we investigate diffuse alopecia in women? Clin Exp Dermatol. 1996;21:320.-
5. Olsen EA, Messenger AG, Shapiro J, et al. Evaluation and treatment of male and female pattern hair loss. J Am Acad Dermatol. 2005;52:301-311.
6. University of Texas at Austin, School of Nursing, Family Nurse Practitioner Program. Recommendations to diagnose and treat adult hair loss disorders or alopecia in primary care settings (non pregnant female and male adults). Austin, TX: University of Texas at Austin, School of Nursing; May 2004. 21 p. 1-8. Available at: www.ngc.gov/summary/summary.aspx?doc_id=5428&nbr=003722&string=alopecia+and+(diagnosis+or+evaluation). Accessed January 9, 2007.
7. Rushton DH. Nutritional factors and hair loss. Clin Exp Dermatol. 2002;27:396-404.
8. Women’s hair loss/diagnosis. American Hair Loss Association [database online]. Updated March 11, 2005. Available at: http://www.americanhairloss.org/women_hair_loss/diagnosis.asp. Accessed June 10, 2009.
1. Shapiro J, Wiseman M, Lui H. Practical management of hair loss. Can Fam Physician. 2000;46:1469-1477.
2. Thiedke CC. Alopecia in women. Am Fam Physician. 2003;67:1007-1014.
3. Chartier MB, Hoss DM, Grant-Kels JM. Approach to the adult female patient with diffuse nonscarring alopecia. J Am Acad Dermatol. 2002;47:809-818.
4. Dupont C. How far should we investigate diffuse alopecia in women? Clin Exp Dermatol. 1996;21:320.-
5. Olsen EA, Messenger AG, Shapiro J, et al. Evaluation and treatment of male and female pattern hair loss. J Am Acad Dermatol. 2005;52:301-311.
6. University of Texas at Austin, School of Nursing, Family Nurse Practitioner Program. Recommendations to diagnose and treat adult hair loss disorders or alopecia in primary care settings (non pregnant female and male adults). Austin, TX: University of Texas at Austin, School of Nursing; May 2004. 21 p. 1-8. Available at: www.ngc.gov/summary/summary.aspx?doc_id=5428&nbr=003722&string=alopecia+and+(diagnosis+or+evaluation). Accessed January 9, 2007.
7. Rushton DH. Nutritional factors and hair loss. Clin Exp Dermatol. 2002;27:396-404.
8. Women’s hair loss/diagnosis. American Hair Loss Association [database online]. Updated March 11, 2005. Available at: http://www.americanhairloss.org/women_hair_loss/diagnosis.asp. Accessed June 10, 2009.
Evidence-based answers from the Family Physicians Inquiries Network
Menstrual disturbances in perimenopausal women: What’s best?
It’s best to start with nonsteroidal anti-inflammatory drugs (NSAIDs), which effectively reduce heavy menstrual bleeding (strength of recommendation [SOR]: B, systematic review of randomized clinical trials [RCTs]).
Perimenopausal women with heavy bleeding not controlled by NSAIDs, or other forms of dysfunctional uterine bleeding, can benefit from continuous, combined hormonal therapy with estrogen and progestin; hormonal therapy with estrogen and a cyclical progestin; or a cyclical progestin alone (SOR: B, RCTs and a systematic review of RCTs). Intrauterine devices (IUDs) containing levonorgestrel also effectively reduce bleeding and may avoid surgical intervention (SOR: B, systematic review of RCTs).
If medical management fails, endometrial ablation offers an effective, minimally invasive alternative to hysterectomy (SOR: B, systematic review of RCTs and 1 RCT). Hysterectomy should be considered when medical management or endometrial ablation fails (SOR: B, systematic review of RCTs and 1 RCT).
Evidence summary
Perimenopause encompasses the period of irregular menstrual cycles and flow that precedes menopause (absence of menstrual bleeding for 1 year). Menopause generally occurs between 45 and 55 years of age; the average is 51 years. A review of 500 perimenopausal women seen sequentially by a gynecology service found that 18% had menorrhagia (heavy bleeding), metrorrhagia (intermenstrual bleeding), or hypermenorrhea (frequent periods).1
Because few studies have examined the treatment of abnormal menstrual bleeding specifically during perimenopause, therapeutic approaches are based primarily on studies of women before and shortly after this stage. Once malignancy and other causes of abnormal uterine bleeding (pregnancy, bleeding disorders, infection, thyroid disorders, uterine fibroids, or polyps) have been excluded, treatment of perimenopausal dysfunctional uterine bleeding should address the goals of:
- stopping acute bleeding
- avoiding future irregular or heavy bleeding
- considering future family planning needs
- preventing complications (anemia, unnecessary therapeutic procedures).
NSAIDs reduce heavy bleeding
A Cochrane review of 16 small RCTs that examined the use of NSAIDs for menorrhagia found NSAIDs to be superior to placebo and comparable to other medical treatments such as luteal progestin, oral contraceptive pills, and progestin-releasing intrauterine systems.2
Hormone therapy is also effective
An RCT of 132 perimenopausal women compared 24 weeks of combination hormonal therapy (20 mcg ethinyl estradiol/1 mg norethindrone acetate) with placebo for treating climacteric symptoms, including abnormal uterine bleeding.3 The combination therapy shortened the menstrual cycle (27.7 vs 30.4 days), decreased its variability (17.5-46.7 days vs 22.4-66 days), and lowered bleeding severity scores (6.9 vs 10.2).
Hormonal therapy didn’t shorten bleeding episodes, however, and was associated with a higher incidence of intermenstrual bleeding during the first 3 months of treatment.
Continuous, combined estrogen/progestogen therapy
An RCT of 120 perimenopausal women with irregular menstrual cycles compared low-dose (1 mg) continuous estradiol and cyclical progestogens (10 mg dydrogesterone) with cyclical progestogens alone.4 In the combined treatment group, the incidence of cyclical menstrual bleeding was 86%, and 76% of all cycles were rated normal in amount and duration of bleeding. In the cyclical progestogen group, the incidence of cyclical menstrual bleeding during treatment was 76%, and 70% of all cycles were rated normal.
A systematic review, comprised primarily of RCTs, examined uterine bleeding patterns in 3000 postmenopausal women taking combined continuous hormones (various regimens of estrogen and progestin).5 In 22 of 23 studies that included data past 6 months, 75% or more of participants became amenorrheic while on therapy. Irregular uterine bleeding before 6 months of therapy was common, however, and was presumed to lower patient compliance.
Combined therapy avoids risk of endometrial hyperplasia
A more recent Cochrane review of 30 RCTs examined hormone replacement therapy for irregular bleeding and endometrial hyperplasia in postmenopausal women who had been amenorrheic for at least 6 months (a more liberal criterion for inclusion).6 The review concluded that many of the women treated with continuous estrogen and progestin became amenorrheic after 1 year of therapy. It also reiterated that unopposed estrogen increased the risk of endometrial hyperplasia, whereas continuous combined estrogen and progestogen treatment didn’t.
Continuous progestogen regimen has blood loss benefit
No randomized trials have compared oral progestogens with placebo. A Cochrane review examined the use of cyclical progestogens (given from 10 to 20 days per cycle) for heavy menstrual bleeding.7 Cyclical progestogens appeared comparable in efficacy to NSAIDs for their effect on duration of menstruation; no statistically significant difference in menstrual blood loss was noted. Progestogens given in more continuous regimens offered greater benefit in terms of blood loss.
IUDs help avoid surgery, but can have side effects
A Cochrane review found that progestogen-releasing IUDs significantly reduce heavy menstrual bleeding and are more effective than cyclical norethisterone (21 days). Patients did, however, report greater progestogenic side effects (breast tenderness and intermenstrual bleeding) than cyclical therapy.8
One unblinded RCT that randomized women scheduled for hysterectomy for heavy bleeding to the levonorgestrel intrauterine device (LNG-IUD) or their existing medical therapy (not further described) found that women in the LNG-IUD group were more likely to cancel surgery.
Another RCT comparing hysterectomy with the LNG-IUD found that women with the LNG-IUD reported greater pain. The LNG-IUD was more cost effective at 1 and 5 years, primarily because of reduced surgical expenses. Some patients or physicians may have ethical issues with the device’s mechanism of action.
Uterine ablation when preserving fertility doesn’t matter
A review article of currently available evidence on endometrial ablation for heavy menstrual bleeding concluded that both resectoscopic endometrial ablation (via hysteroscopy) and nonresectoscopic endometrial ablative technologies (radio-frequency electrosurgical ablation, balloon thermal ablation, free fluid ablation, cryotherapy, microwaves) significantly reduce menstrual blood flow.9 These minimally invasive techniques were an option for women who weren’t concerned about preserving fertility. However, 20% to 40% of patients who were followed for more than 5 years required repeat treatment or hysterectomy.
Heavy bleeding and transcervical endometrial resection
An RCT of 187 women, average age 42 years, compared immediate transcervical resection of the endometrium to medical management for heavy menstrual bleeding.10 A 5-year follow-up was completed on 144 patients. The study showed transcervical resection of the endometrium to be superior with regard to menstrual status (less bleeding or no bleeding), patient satisfaction with outcomes, and health-related quality of life as indicated on patient questionnaires.
When other options fail…
Patients who fail medical treatment and minimally invasive uterine ablation may require hysterectomy. An RCT of 63 premenopausal women (30-50 years of age) with abnormal uterine bleeding compared hysterectomy with medical treatment.11 Hysterectomy was superior with regard to symptom resolution and health-related quality of life after 6 months.
A Cochrane review of 5 RCTs that compared endometrial resection and ablation with hysterectomy for heavy menstrual bleeding reported a significant advantage for hysterectomy in symptom resolution and patient satisfaction.12 Although the initial cost was higher for the hysterectomy group, the difference narrowed over time because of the need for retreatment in the endometrial destruction group.
Recommendations
The American College of Obstetricians and Gynecologists (ACOG) recommends initial medical management (cyclic progestins, low-dose oral contraceptives, or cyclic hormone replacement therapy) for anovulatory bleeding in women 40 years and older.13
The Practice Committee of the American Society for Reproductive Medicine lists low-dose combination hormonal pills, progestin, progestin-containing IUDs, and hormone replacement therapy as medical treatment options.14
ACOG notes that minimally invasive surgical options such as hysteroscopic endometrial ablation result in less short-term morbidity and cost less than hysterectomy.15 Results with resectoscopic and nonresectoscopic techniques are similar. Hysterectomy rates following these approaches are at least 24% at 4 years.15
1. Seltzer VL, Benjamin F, Deutsch S. Perimenopausal bleeding patterns and pathologic findings. J Am Med Womens Assoc. 1990;45:132-134.
2. Lethaby A, Augood C, Duckitt K. Nonsteroidal anti-inflammatory drugs for heavy menstrual bleeding. Cochrane Database Syst Rev. 2007;(4):CD0004000.-
3. Casper R, Dodin S, Reid R, et al. The effect of 20 micrograms of ethinyl estradiol/1 mg norethindrone acetate (Minestrin), a low-dose contraceptive, on vaginal bleeding patterns, hot flashes, and quality of life in symptomatic perimenopausal women. Menopause. 1997;4:139-147.
4. De Francis P, Cobellis L, Fornaro F, et al. Low-dose hormone therapy in the perimenopause. Int J Gynaecol Obstet. 2007;98:138-142.
5. Udoff L, Langenberg P, Adashi EY. Combined continuous hormone replacement therapy: a critical review. Obstet Gynecol. 1995;86:306-316.
6. Suckling LA, Barlow D, Farquhar CM, et al. Hormone replacement therapy in postmenopausal women: endometrial hyperplasia and irregular bleeding. Cochrane Database Syst Rev. 2004;(3):CD000402.-
7. Lethaby A, Irvine G, Cameron I. Cyclical progestogens for heavy menstrual bleeding. Cochrane Database Syst Rev. 2008;(1):CD001016.-
8. Lethaby A, Cooke I, Reese M. Progesterone or progestogen-releasing intrauterine systems for heavy menstrual bleeding. Cochrane Database Syst Rev. 2005;(4):CD002126.-
9. Munro MG. Endometrial ablation for heavy menstrual bleeding. Curr Opin Obstet Gynecol. 2005;17:381-394.
10. Cooper KG, Jack SA, Parkin DE, et al. Five-year follow-up of women randomised to medical management or transcervical resection of the endometrium for heavy menstrual loss: clinical and quality of life outcomes. BJOG. 2001;108:1222-1228.
11. Kuppermann M, Varner RE, Summitt RL, Jr, et al. Effect of hysterectomy vs. medical treatment on health-related quality of life and sexual functioning. The medicine or surgery (Ms) randomized trial. JAMA. 2004;291:1447-1455.
12. Lethaby A, Shepperd S, Cooke I, et al. Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding. Cochrane Database Syst Rev. 1999;(2):CD000329.-
13. American College of Obstetricians and Gynecologists Committee on Practice Bulletins—Gynecology. ACOG Practice Bulletin. Clinical management guidelines for obstetrician-gynecologists. Management of anovulatory bleeding. In J Gynaecol Obstet. 2001;72:263-271.
14. Practice Committee of the American society for reproductive Medicine. Committee opinion: the menopausal transition. Fertil Steril. 2006;86(suppl 5):S253-S256.
15. American College of Obstetricians and Gynecologists Committee on Practice Bulletins—Gynecology. ACOG Practice Bulletin. Clinical management guidelines for obstetrician-gynecologists. Endometrial ablation. Obstet Gynecol. 2007;109:1233-1248.
It’s best to start with nonsteroidal anti-inflammatory drugs (NSAIDs), which effectively reduce heavy menstrual bleeding (strength of recommendation [SOR]: B, systematic review of randomized clinical trials [RCTs]).
Perimenopausal women with heavy bleeding not controlled by NSAIDs, or other forms of dysfunctional uterine bleeding, can benefit from continuous, combined hormonal therapy with estrogen and progestin; hormonal therapy with estrogen and a cyclical progestin; or a cyclical progestin alone (SOR: B, RCTs and a systematic review of RCTs). Intrauterine devices (IUDs) containing levonorgestrel also effectively reduce bleeding and may avoid surgical intervention (SOR: B, systematic review of RCTs).
If medical management fails, endometrial ablation offers an effective, minimally invasive alternative to hysterectomy (SOR: B, systematic review of RCTs and 1 RCT). Hysterectomy should be considered when medical management or endometrial ablation fails (SOR: B, systematic review of RCTs and 1 RCT).
Evidence summary
Perimenopause encompasses the period of irregular menstrual cycles and flow that precedes menopause (absence of menstrual bleeding for 1 year). Menopause generally occurs between 45 and 55 years of age; the average is 51 years. A review of 500 perimenopausal women seen sequentially by a gynecology service found that 18% had menorrhagia (heavy bleeding), metrorrhagia (intermenstrual bleeding), or hypermenorrhea (frequent periods).1
Because few studies have examined the treatment of abnormal menstrual bleeding specifically during perimenopause, therapeutic approaches are based primarily on studies of women before and shortly after this stage. Once malignancy and other causes of abnormal uterine bleeding (pregnancy, bleeding disorders, infection, thyroid disorders, uterine fibroids, or polyps) have been excluded, treatment of perimenopausal dysfunctional uterine bleeding should address the goals of:
- stopping acute bleeding
- avoiding future irregular or heavy bleeding
- considering future family planning needs
- preventing complications (anemia, unnecessary therapeutic procedures).
NSAIDs reduce heavy bleeding
A Cochrane review of 16 small RCTs that examined the use of NSAIDs for menorrhagia found NSAIDs to be superior to placebo and comparable to other medical treatments such as luteal progestin, oral contraceptive pills, and progestin-releasing intrauterine systems.2
Hormone therapy is also effective
An RCT of 132 perimenopausal women compared 24 weeks of combination hormonal therapy (20 mcg ethinyl estradiol/1 mg norethindrone acetate) with placebo for treating climacteric symptoms, including abnormal uterine bleeding.3 The combination therapy shortened the menstrual cycle (27.7 vs 30.4 days), decreased its variability (17.5-46.7 days vs 22.4-66 days), and lowered bleeding severity scores (6.9 vs 10.2).
Hormonal therapy didn’t shorten bleeding episodes, however, and was associated with a higher incidence of intermenstrual bleeding during the first 3 months of treatment.
Continuous, combined estrogen/progestogen therapy
An RCT of 120 perimenopausal women with irregular menstrual cycles compared low-dose (1 mg) continuous estradiol and cyclical progestogens (10 mg dydrogesterone) with cyclical progestogens alone.4 In the combined treatment group, the incidence of cyclical menstrual bleeding was 86%, and 76% of all cycles were rated normal in amount and duration of bleeding. In the cyclical progestogen group, the incidence of cyclical menstrual bleeding during treatment was 76%, and 70% of all cycles were rated normal.
A systematic review, comprised primarily of RCTs, examined uterine bleeding patterns in 3000 postmenopausal women taking combined continuous hormones (various regimens of estrogen and progestin).5 In 22 of 23 studies that included data past 6 months, 75% or more of participants became amenorrheic while on therapy. Irregular uterine bleeding before 6 months of therapy was common, however, and was presumed to lower patient compliance.
Combined therapy avoids risk of endometrial hyperplasia
A more recent Cochrane review of 30 RCTs examined hormone replacement therapy for irregular bleeding and endometrial hyperplasia in postmenopausal women who had been amenorrheic for at least 6 months (a more liberal criterion for inclusion).6 The review concluded that many of the women treated with continuous estrogen and progestin became amenorrheic after 1 year of therapy. It also reiterated that unopposed estrogen increased the risk of endometrial hyperplasia, whereas continuous combined estrogen and progestogen treatment didn’t.
Continuous progestogen regimen has blood loss benefit
No randomized trials have compared oral progestogens with placebo. A Cochrane review examined the use of cyclical progestogens (given from 10 to 20 days per cycle) for heavy menstrual bleeding.7 Cyclical progestogens appeared comparable in efficacy to NSAIDs for their effect on duration of menstruation; no statistically significant difference in menstrual blood loss was noted. Progestogens given in more continuous regimens offered greater benefit in terms of blood loss.
IUDs help avoid surgery, but can have side effects
A Cochrane review found that progestogen-releasing IUDs significantly reduce heavy menstrual bleeding and are more effective than cyclical norethisterone (21 days). Patients did, however, report greater progestogenic side effects (breast tenderness and intermenstrual bleeding) than cyclical therapy.8
One unblinded RCT that randomized women scheduled for hysterectomy for heavy bleeding to the levonorgestrel intrauterine device (LNG-IUD) or their existing medical therapy (not further described) found that women in the LNG-IUD group were more likely to cancel surgery.
Another RCT comparing hysterectomy with the LNG-IUD found that women with the LNG-IUD reported greater pain. The LNG-IUD was more cost effective at 1 and 5 years, primarily because of reduced surgical expenses. Some patients or physicians may have ethical issues with the device’s mechanism of action.
Uterine ablation when preserving fertility doesn’t matter
A review article of currently available evidence on endometrial ablation for heavy menstrual bleeding concluded that both resectoscopic endometrial ablation (via hysteroscopy) and nonresectoscopic endometrial ablative technologies (radio-frequency electrosurgical ablation, balloon thermal ablation, free fluid ablation, cryotherapy, microwaves) significantly reduce menstrual blood flow.9 These minimally invasive techniques were an option for women who weren’t concerned about preserving fertility. However, 20% to 40% of patients who were followed for more than 5 years required repeat treatment or hysterectomy.
Heavy bleeding and transcervical endometrial resection
An RCT of 187 women, average age 42 years, compared immediate transcervical resection of the endometrium to medical management for heavy menstrual bleeding.10 A 5-year follow-up was completed on 144 patients. The study showed transcervical resection of the endometrium to be superior with regard to menstrual status (less bleeding or no bleeding), patient satisfaction with outcomes, and health-related quality of life as indicated on patient questionnaires.
When other options fail…
Patients who fail medical treatment and minimally invasive uterine ablation may require hysterectomy. An RCT of 63 premenopausal women (30-50 years of age) with abnormal uterine bleeding compared hysterectomy with medical treatment.11 Hysterectomy was superior with regard to symptom resolution and health-related quality of life after 6 months.
A Cochrane review of 5 RCTs that compared endometrial resection and ablation with hysterectomy for heavy menstrual bleeding reported a significant advantage for hysterectomy in symptom resolution and patient satisfaction.12 Although the initial cost was higher for the hysterectomy group, the difference narrowed over time because of the need for retreatment in the endometrial destruction group.
Recommendations
The American College of Obstetricians and Gynecologists (ACOG) recommends initial medical management (cyclic progestins, low-dose oral contraceptives, or cyclic hormone replacement therapy) for anovulatory bleeding in women 40 years and older.13
The Practice Committee of the American Society for Reproductive Medicine lists low-dose combination hormonal pills, progestin, progestin-containing IUDs, and hormone replacement therapy as medical treatment options.14
ACOG notes that minimally invasive surgical options such as hysteroscopic endometrial ablation result in less short-term morbidity and cost less than hysterectomy.15 Results with resectoscopic and nonresectoscopic techniques are similar. Hysterectomy rates following these approaches are at least 24% at 4 years.15
It’s best to start with nonsteroidal anti-inflammatory drugs (NSAIDs), which effectively reduce heavy menstrual bleeding (strength of recommendation [SOR]: B, systematic review of randomized clinical trials [RCTs]).
Perimenopausal women with heavy bleeding not controlled by NSAIDs, or other forms of dysfunctional uterine bleeding, can benefit from continuous, combined hormonal therapy with estrogen and progestin; hormonal therapy with estrogen and a cyclical progestin; or a cyclical progestin alone (SOR: B, RCTs and a systematic review of RCTs). Intrauterine devices (IUDs) containing levonorgestrel also effectively reduce bleeding and may avoid surgical intervention (SOR: B, systematic review of RCTs).
If medical management fails, endometrial ablation offers an effective, minimally invasive alternative to hysterectomy (SOR: B, systematic review of RCTs and 1 RCT). Hysterectomy should be considered when medical management or endometrial ablation fails (SOR: B, systematic review of RCTs and 1 RCT).
Evidence summary
Perimenopause encompasses the period of irregular menstrual cycles and flow that precedes menopause (absence of menstrual bleeding for 1 year). Menopause generally occurs between 45 and 55 years of age; the average is 51 years. A review of 500 perimenopausal women seen sequentially by a gynecology service found that 18% had menorrhagia (heavy bleeding), metrorrhagia (intermenstrual bleeding), or hypermenorrhea (frequent periods).1
Because few studies have examined the treatment of abnormal menstrual bleeding specifically during perimenopause, therapeutic approaches are based primarily on studies of women before and shortly after this stage. Once malignancy and other causes of abnormal uterine bleeding (pregnancy, bleeding disorders, infection, thyroid disorders, uterine fibroids, or polyps) have been excluded, treatment of perimenopausal dysfunctional uterine bleeding should address the goals of:
- stopping acute bleeding
- avoiding future irregular or heavy bleeding
- considering future family planning needs
- preventing complications (anemia, unnecessary therapeutic procedures).
NSAIDs reduce heavy bleeding
A Cochrane review of 16 small RCTs that examined the use of NSAIDs for menorrhagia found NSAIDs to be superior to placebo and comparable to other medical treatments such as luteal progestin, oral contraceptive pills, and progestin-releasing intrauterine systems.2
Hormone therapy is also effective
An RCT of 132 perimenopausal women compared 24 weeks of combination hormonal therapy (20 mcg ethinyl estradiol/1 mg norethindrone acetate) with placebo for treating climacteric symptoms, including abnormal uterine bleeding.3 The combination therapy shortened the menstrual cycle (27.7 vs 30.4 days), decreased its variability (17.5-46.7 days vs 22.4-66 days), and lowered bleeding severity scores (6.9 vs 10.2).
Hormonal therapy didn’t shorten bleeding episodes, however, and was associated with a higher incidence of intermenstrual bleeding during the first 3 months of treatment.
Continuous, combined estrogen/progestogen therapy
An RCT of 120 perimenopausal women with irregular menstrual cycles compared low-dose (1 mg) continuous estradiol and cyclical progestogens (10 mg dydrogesterone) with cyclical progestogens alone.4 In the combined treatment group, the incidence of cyclical menstrual bleeding was 86%, and 76% of all cycles were rated normal in amount and duration of bleeding. In the cyclical progestogen group, the incidence of cyclical menstrual bleeding during treatment was 76%, and 70% of all cycles were rated normal.
A systematic review, comprised primarily of RCTs, examined uterine bleeding patterns in 3000 postmenopausal women taking combined continuous hormones (various regimens of estrogen and progestin).5 In 22 of 23 studies that included data past 6 months, 75% or more of participants became amenorrheic while on therapy. Irregular uterine bleeding before 6 months of therapy was common, however, and was presumed to lower patient compliance.
Combined therapy avoids risk of endometrial hyperplasia
A more recent Cochrane review of 30 RCTs examined hormone replacement therapy for irregular bleeding and endometrial hyperplasia in postmenopausal women who had been amenorrheic for at least 6 months (a more liberal criterion for inclusion).6 The review concluded that many of the women treated with continuous estrogen and progestin became amenorrheic after 1 year of therapy. It also reiterated that unopposed estrogen increased the risk of endometrial hyperplasia, whereas continuous combined estrogen and progestogen treatment didn’t.
Continuous progestogen regimen has blood loss benefit
No randomized trials have compared oral progestogens with placebo. A Cochrane review examined the use of cyclical progestogens (given from 10 to 20 days per cycle) for heavy menstrual bleeding.7 Cyclical progestogens appeared comparable in efficacy to NSAIDs for their effect on duration of menstruation; no statistically significant difference in menstrual blood loss was noted. Progestogens given in more continuous regimens offered greater benefit in terms of blood loss.
IUDs help avoid surgery, but can have side effects
A Cochrane review found that progestogen-releasing IUDs significantly reduce heavy menstrual bleeding and are more effective than cyclical norethisterone (21 days). Patients did, however, report greater progestogenic side effects (breast tenderness and intermenstrual bleeding) than cyclical therapy.8
One unblinded RCT that randomized women scheduled for hysterectomy for heavy bleeding to the levonorgestrel intrauterine device (LNG-IUD) or their existing medical therapy (not further described) found that women in the LNG-IUD group were more likely to cancel surgery.
Another RCT comparing hysterectomy with the LNG-IUD found that women with the LNG-IUD reported greater pain. The LNG-IUD was more cost effective at 1 and 5 years, primarily because of reduced surgical expenses. Some patients or physicians may have ethical issues with the device’s mechanism of action.
Uterine ablation when preserving fertility doesn’t matter
A review article of currently available evidence on endometrial ablation for heavy menstrual bleeding concluded that both resectoscopic endometrial ablation (via hysteroscopy) and nonresectoscopic endometrial ablative technologies (radio-frequency electrosurgical ablation, balloon thermal ablation, free fluid ablation, cryotherapy, microwaves) significantly reduce menstrual blood flow.9 These minimally invasive techniques were an option for women who weren’t concerned about preserving fertility. However, 20% to 40% of patients who were followed for more than 5 years required repeat treatment or hysterectomy.
Heavy bleeding and transcervical endometrial resection
An RCT of 187 women, average age 42 years, compared immediate transcervical resection of the endometrium to medical management for heavy menstrual bleeding.10 A 5-year follow-up was completed on 144 patients. The study showed transcervical resection of the endometrium to be superior with regard to menstrual status (less bleeding or no bleeding), patient satisfaction with outcomes, and health-related quality of life as indicated on patient questionnaires.
When other options fail…
Patients who fail medical treatment and minimally invasive uterine ablation may require hysterectomy. An RCT of 63 premenopausal women (30-50 years of age) with abnormal uterine bleeding compared hysterectomy with medical treatment.11 Hysterectomy was superior with regard to symptom resolution and health-related quality of life after 6 months.
A Cochrane review of 5 RCTs that compared endometrial resection and ablation with hysterectomy for heavy menstrual bleeding reported a significant advantage for hysterectomy in symptom resolution and patient satisfaction.12 Although the initial cost was higher for the hysterectomy group, the difference narrowed over time because of the need for retreatment in the endometrial destruction group.
Recommendations
The American College of Obstetricians and Gynecologists (ACOG) recommends initial medical management (cyclic progestins, low-dose oral contraceptives, or cyclic hormone replacement therapy) for anovulatory bleeding in women 40 years and older.13
The Practice Committee of the American Society for Reproductive Medicine lists low-dose combination hormonal pills, progestin, progestin-containing IUDs, and hormone replacement therapy as medical treatment options.14
ACOG notes that minimally invasive surgical options such as hysteroscopic endometrial ablation result in less short-term morbidity and cost less than hysterectomy.15 Results with resectoscopic and nonresectoscopic techniques are similar. Hysterectomy rates following these approaches are at least 24% at 4 years.15
1. Seltzer VL, Benjamin F, Deutsch S. Perimenopausal bleeding patterns and pathologic findings. J Am Med Womens Assoc. 1990;45:132-134.
2. Lethaby A, Augood C, Duckitt K. Nonsteroidal anti-inflammatory drugs for heavy menstrual bleeding. Cochrane Database Syst Rev. 2007;(4):CD0004000.-
3. Casper R, Dodin S, Reid R, et al. The effect of 20 micrograms of ethinyl estradiol/1 mg norethindrone acetate (Minestrin), a low-dose contraceptive, on vaginal bleeding patterns, hot flashes, and quality of life in symptomatic perimenopausal women. Menopause. 1997;4:139-147.
4. De Francis P, Cobellis L, Fornaro F, et al. Low-dose hormone therapy in the perimenopause. Int J Gynaecol Obstet. 2007;98:138-142.
5. Udoff L, Langenberg P, Adashi EY. Combined continuous hormone replacement therapy: a critical review. Obstet Gynecol. 1995;86:306-316.
6. Suckling LA, Barlow D, Farquhar CM, et al. Hormone replacement therapy in postmenopausal women: endometrial hyperplasia and irregular bleeding. Cochrane Database Syst Rev. 2004;(3):CD000402.-
7. Lethaby A, Irvine G, Cameron I. Cyclical progestogens for heavy menstrual bleeding. Cochrane Database Syst Rev. 2008;(1):CD001016.-
8. Lethaby A, Cooke I, Reese M. Progesterone or progestogen-releasing intrauterine systems for heavy menstrual bleeding. Cochrane Database Syst Rev. 2005;(4):CD002126.-
9. Munro MG. Endometrial ablation for heavy menstrual bleeding. Curr Opin Obstet Gynecol. 2005;17:381-394.
10. Cooper KG, Jack SA, Parkin DE, et al. Five-year follow-up of women randomised to medical management or transcervical resection of the endometrium for heavy menstrual loss: clinical and quality of life outcomes. BJOG. 2001;108:1222-1228.
11. Kuppermann M, Varner RE, Summitt RL, Jr, et al. Effect of hysterectomy vs. medical treatment on health-related quality of life and sexual functioning. The medicine or surgery (Ms) randomized trial. JAMA. 2004;291:1447-1455.
12. Lethaby A, Shepperd S, Cooke I, et al. Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding. Cochrane Database Syst Rev. 1999;(2):CD000329.-
13. American College of Obstetricians and Gynecologists Committee on Practice Bulletins—Gynecology. ACOG Practice Bulletin. Clinical management guidelines for obstetrician-gynecologists. Management of anovulatory bleeding. In J Gynaecol Obstet. 2001;72:263-271.
14. Practice Committee of the American society for reproductive Medicine. Committee opinion: the menopausal transition. Fertil Steril. 2006;86(suppl 5):S253-S256.
15. American College of Obstetricians and Gynecologists Committee on Practice Bulletins—Gynecology. ACOG Practice Bulletin. Clinical management guidelines for obstetrician-gynecologists. Endometrial ablation. Obstet Gynecol. 2007;109:1233-1248.
1. Seltzer VL, Benjamin F, Deutsch S. Perimenopausal bleeding patterns and pathologic findings. J Am Med Womens Assoc. 1990;45:132-134.
2. Lethaby A, Augood C, Duckitt K. Nonsteroidal anti-inflammatory drugs for heavy menstrual bleeding. Cochrane Database Syst Rev. 2007;(4):CD0004000.-
3. Casper R, Dodin S, Reid R, et al. The effect of 20 micrograms of ethinyl estradiol/1 mg norethindrone acetate (Minestrin), a low-dose contraceptive, on vaginal bleeding patterns, hot flashes, and quality of life in symptomatic perimenopausal women. Menopause. 1997;4:139-147.
4. De Francis P, Cobellis L, Fornaro F, et al. Low-dose hormone therapy in the perimenopause. Int J Gynaecol Obstet. 2007;98:138-142.
5. Udoff L, Langenberg P, Adashi EY. Combined continuous hormone replacement therapy: a critical review. Obstet Gynecol. 1995;86:306-316.
6. Suckling LA, Barlow D, Farquhar CM, et al. Hormone replacement therapy in postmenopausal women: endometrial hyperplasia and irregular bleeding. Cochrane Database Syst Rev. 2004;(3):CD000402.-
7. Lethaby A, Irvine G, Cameron I. Cyclical progestogens for heavy menstrual bleeding. Cochrane Database Syst Rev. 2008;(1):CD001016.-
8. Lethaby A, Cooke I, Reese M. Progesterone or progestogen-releasing intrauterine systems for heavy menstrual bleeding. Cochrane Database Syst Rev. 2005;(4):CD002126.-
9. Munro MG. Endometrial ablation for heavy menstrual bleeding. Curr Opin Obstet Gynecol. 2005;17:381-394.
10. Cooper KG, Jack SA, Parkin DE, et al. Five-year follow-up of women randomised to medical management or transcervical resection of the endometrium for heavy menstrual loss: clinical and quality of life outcomes. BJOG. 2001;108:1222-1228.
11. Kuppermann M, Varner RE, Summitt RL, Jr, et al. Effect of hysterectomy vs. medical treatment on health-related quality of life and sexual functioning. The medicine or surgery (Ms) randomized trial. JAMA. 2004;291:1447-1455.
12. Lethaby A, Shepperd S, Cooke I, et al. Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding. Cochrane Database Syst Rev. 1999;(2):CD000329.-
13. American College of Obstetricians and Gynecologists Committee on Practice Bulletins—Gynecology. ACOG Practice Bulletin. Clinical management guidelines for obstetrician-gynecologists. Management of anovulatory bleeding. In J Gynaecol Obstet. 2001;72:263-271.
14. Practice Committee of the American society for reproductive Medicine. Committee opinion: the menopausal transition. Fertil Steril. 2006;86(suppl 5):S253-S256.
15. American College of Obstetricians and Gynecologists Committee on Practice Bulletins—Gynecology. ACOG Practice Bulletin. Clinical management guidelines for obstetrician-gynecologists. Endometrial ablation. Obstet Gynecol. 2007;109:1233-1248.
Evidence-based answers from the Family Physicians Inquiries Network
How should you manage an overweight breastfed infant?
There are several steps you can take. Monitor the growth of exclusively breastfed babies by plotting routine weights and lengths on the World Health Organization (WHO) growth curve (strength of recommendation [SOR]: A, systematic reviews). Reassure parents that higher-than-normal weight gain in infants who are breastfeeding easily without supplementation has no known adverse effects. Advise parents to change behaviors that result in overfeeding or insufficient physical activity (SOR: C, expert opinion). Refer parents to a lactation consultant to manage large volumes of milk that exceed the infant’s need. In the rare case of an infant who exhibits lack of satiety or dysmorphia, consider an overgrowth syndrome and seek an endocrinology and genetics consult (SOR: C, expert opinion).
Avoid comfort feeding, stress activity
Philip Reilly, MD
SeaMar Community Health Center, Seattle, Wash
I often see breastfeeding mothers who are concerned about their chubby babies, who have both a high success rate with breastfeeding and a high rate of type 2 diabetes as adults. When talking to these mothers, I first stress the importance of focusing primarily on nutritional feeding, not “comfort feeding.” I point out that evidence suggests that exclusive breastfeeding helps prevent adult obesity.
It’s also important to recognize that the epidemiologic shift toward increased obesity and diabetes has to do with the activity habits of children and adults, as well as their eating habits. As children grow, our advice should focus on encouraging activity, limiting “screen time,” and eliminating juices and other high-calorie dietary additions once an infant is no longer exclusively breastfed.
Evidence summary
An estimated 9.5% of infants and children younger than 2 years of age are considered overweight—that is, their weight is at or above the 95th percentile of weight-for-recumbent length on the sex-specific growth charts from the Centers for Disease Control and Prevention (CDC).1 The prevalence is unknown for infants who are exclusively breastfed2 or fed only human milk without any supplementation (except recommended vitamins, minerals, and medication) for the first 6 months of life.
Exclusively breastfed babies have a different growth curve
Because comparison growth studies demonstrate that healthy breastfed infants have a different growth curve than formula or mix-fed babies,3 the WHO growth curves (http://www.who.int/childgrowth/standards/en/), rather than the CDC charts, should be used to monitor the growth of exclusively breastfed babies.4 The WHO Working Group on Infant Growth studied infants whose sole nourishment was breast milk until 4 months of age.3 The CDC charts reflect a heavier and shorter sample of infants. Moreover, the WHO charts are based on shorter measurement intervals and may therefore be a better tool for measuring rapidly changing rates of growth.4
Exclusive breastfeeding reduces risk of overweight later in life
A meta-analysis showed a dose-dependent relationship between longer duration of breastfeeding and decreased risk of overweight in later life (<1 month of breastfeeding: odds ratio [OR]=1.0; 95% confidence interval [CI], 0.65-1.55; 1-3 months: OR=0.81; 95% CI, 0.74-0.88; 4-6 months: OR=0.76; 95% CI, 0.67-0.86; 7-9 months: OR=0.67; 95% CI, 0.55-0.82; >9 months: OR=0.68; 95% CI, 0.50-0.91).5 Because overweight has no known adverse health outcomes for exclusively breastfed infants, lactation experts don’t advise mothers to reduce feeding for these babies.6
Is overfeeding an issue?
Overfeeding may contribute to higher-than-normal weight gain in both breastfed and formula-fed infants.7 Maternal behavior changes that may taper unusual weight gains include cuddling rather than breastfeeding in response to all distress signals and encouraging movement and crawling.8
Expressing breast milk to increase infant intake increases weight gain (r=0.59); this effect gets stronger as the infant gets older (r=0.58).9 Referral to a lactation consultant is recommended to manage large volumes of milk that exceed infant need.7 For the rare infant who exhibits hypoglycemia, lack of satiety, or dysmorphia, consider early macrosomia or an overgrowth syndrome, such as Beckwith-Wiedemann syndrome, and seek an endocrinology or genetics consult.10
Recommendations
Exclusive breastfeeding for approximately the first 6 months of life is recommended by the American Academy of Family Physicians (AAFP), American College of Obstetricians and Gynecologists, American Academy of Pediatrics, Academy of Breastfeeding Medicine, WHO, United Nations Children’s Fund, and other organizations. The AAFP recommends that physicians help prevent and manage overweight in childhood to reduce the risk of obesity and chronic disease in later life.11
1. Centers for Disease Control and Prevention. National Center for Health Statistics. Prevalence of overweight, infants and children less than 2 years of age, United States, 2003-2004. Available at: http://www.cdc.gov/nchs/products/pubs/pubd/hestats/overweight/overwght_child_under02.htm. Accessed August 2008.
2. Sachs M, Dykes F, Carter B. Weight monitoring of breastfed babies in the United Kingdom—interpreting, explaining and intervening. Matern Child Nutr. 2006;2:3-18.
3. WHO Working Group on Infant Growth. An evaluation of infant growth. Geneva: Nutrition Unit, World Health Organization; 1994. Available at: http://whqlibdoc.who.int/hq/1994/WHO_NUT_94.8.pdf. Accessed February 19, 2007.
4. de Onis M, Garza C, Onyango AW, et al. Comparison of the WHO child growth standards and the CDC 2000 growth charts. J Nutr. 2007;137:144-148.
5. Harder T, Bergmann R, Kallischnigg G, et al. Duration of breastfeeding and risk of overweight: a meta-analysis. Am J Epidemiol. 2005;162:397-403.
6. Mohrbacher N, Stock J. The Breastfeeding Answer Book. 3rd rev ed. Schaumburg, Ill: La Leche League International; 2003.
7. Crow RA, Fawcett JN, Wright P. Maternal behavior during breast- and bottle-feeding. J Behav Med. 1980;3:259-277.
8. Lawrence RA, Lawrence RM. Breastfeeding: A Guide for the Medical Profession. 6th ed. Philadelphia: Elsevier Mosby; 2005.
9. Dewey KG, Lonnerdal B. Infant self-regulation of breast milk intake. Acta Paediatr Scand. 1986;75:893-898.
10. Jones KL. Smith’s Recognizable Patterns of Human Malformation. 6th ed. Philadelphia: Elsevier Saunders; 2006.
11. American Academy of Family Physicians. Breastfeeding, family physicians supporting (position paper). Available at: http://www.aafp.org/online/en/home/policy/policies/b/breastfeedingpositionpaper.htm. Accessed January 18, 2008.
There are several steps you can take. Monitor the growth of exclusively breastfed babies by plotting routine weights and lengths on the World Health Organization (WHO) growth curve (strength of recommendation [SOR]: A, systematic reviews). Reassure parents that higher-than-normal weight gain in infants who are breastfeeding easily without supplementation has no known adverse effects. Advise parents to change behaviors that result in overfeeding or insufficient physical activity (SOR: C, expert opinion). Refer parents to a lactation consultant to manage large volumes of milk that exceed the infant’s need. In the rare case of an infant who exhibits lack of satiety or dysmorphia, consider an overgrowth syndrome and seek an endocrinology and genetics consult (SOR: C, expert opinion).
Avoid comfort feeding, stress activity
Philip Reilly, MD
SeaMar Community Health Center, Seattle, Wash
I often see breastfeeding mothers who are concerned about their chubby babies, who have both a high success rate with breastfeeding and a high rate of type 2 diabetes as adults. When talking to these mothers, I first stress the importance of focusing primarily on nutritional feeding, not “comfort feeding.” I point out that evidence suggests that exclusive breastfeeding helps prevent adult obesity.
It’s also important to recognize that the epidemiologic shift toward increased obesity and diabetes has to do with the activity habits of children and adults, as well as their eating habits. As children grow, our advice should focus on encouraging activity, limiting “screen time,” and eliminating juices and other high-calorie dietary additions once an infant is no longer exclusively breastfed.
Evidence summary
An estimated 9.5% of infants and children younger than 2 years of age are considered overweight—that is, their weight is at or above the 95th percentile of weight-for-recumbent length on the sex-specific growth charts from the Centers for Disease Control and Prevention (CDC).1 The prevalence is unknown for infants who are exclusively breastfed2 or fed only human milk without any supplementation (except recommended vitamins, minerals, and medication) for the first 6 months of life.
Exclusively breastfed babies have a different growth curve
Because comparison growth studies demonstrate that healthy breastfed infants have a different growth curve than formula or mix-fed babies,3 the WHO growth curves (http://www.who.int/childgrowth/standards/en/), rather than the CDC charts, should be used to monitor the growth of exclusively breastfed babies.4 The WHO Working Group on Infant Growth studied infants whose sole nourishment was breast milk until 4 months of age.3 The CDC charts reflect a heavier and shorter sample of infants. Moreover, the WHO charts are based on shorter measurement intervals and may therefore be a better tool for measuring rapidly changing rates of growth.4
Exclusive breastfeeding reduces risk of overweight later in life
A meta-analysis showed a dose-dependent relationship between longer duration of breastfeeding and decreased risk of overweight in later life (<1 month of breastfeeding: odds ratio [OR]=1.0; 95% confidence interval [CI], 0.65-1.55; 1-3 months: OR=0.81; 95% CI, 0.74-0.88; 4-6 months: OR=0.76; 95% CI, 0.67-0.86; 7-9 months: OR=0.67; 95% CI, 0.55-0.82; >9 months: OR=0.68; 95% CI, 0.50-0.91).5 Because overweight has no known adverse health outcomes for exclusively breastfed infants, lactation experts don’t advise mothers to reduce feeding for these babies.6
Is overfeeding an issue?
Overfeeding may contribute to higher-than-normal weight gain in both breastfed and formula-fed infants.7 Maternal behavior changes that may taper unusual weight gains include cuddling rather than breastfeeding in response to all distress signals and encouraging movement and crawling.8
Expressing breast milk to increase infant intake increases weight gain (r=0.59); this effect gets stronger as the infant gets older (r=0.58).9 Referral to a lactation consultant is recommended to manage large volumes of milk that exceed infant need.7 For the rare infant who exhibits hypoglycemia, lack of satiety, or dysmorphia, consider early macrosomia or an overgrowth syndrome, such as Beckwith-Wiedemann syndrome, and seek an endocrinology or genetics consult.10
Recommendations
Exclusive breastfeeding for approximately the first 6 months of life is recommended by the American Academy of Family Physicians (AAFP), American College of Obstetricians and Gynecologists, American Academy of Pediatrics, Academy of Breastfeeding Medicine, WHO, United Nations Children’s Fund, and other organizations. The AAFP recommends that physicians help prevent and manage overweight in childhood to reduce the risk of obesity and chronic disease in later life.11
There are several steps you can take. Monitor the growth of exclusively breastfed babies by plotting routine weights and lengths on the World Health Organization (WHO) growth curve (strength of recommendation [SOR]: A, systematic reviews). Reassure parents that higher-than-normal weight gain in infants who are breastfeeding easily without supplementation has no known adverse effects. Advise parents to change behaviors that result in overfeeding or insufficient physical activity (SOR: C, expert opinion). Refer parents to a lactation consultant to manage large volumes of milk that exceed the infant’s need. In the rare case of an infant who exhibits lack of satiety or dysmorphia, consider an overgrowth syndrome and seek an endocrinology and genetics consult (SOR: C, expert opinion).
Avoid comfort feeding, stress activity
Philip Reilly, MD
SeaMar Community Health Center, Seattle, Wash
I often see breastfeeding mothers who are concerned about their chubby babies, who have both a high success rate with breastfeeding and a high rate of type 2 diabetes as adults. When talking to these mothers, I first stress the importance of focusing primarily on nutritional feeding, not “comfort feeding.” I point out that evidence suggests that exclusive breastfeeding helps prevent adult obesity.
It’s also important to recognize that the epidemiologic shift toward increased obesity and diabetes has to do with the activity habits of children and adults, as well as their eating habits. As children grow, our advice should focus on encouraging activity, limiting “screen time,” and eliminating juices and other high-calorie dietary additions once an infant is no longer exclusively breastfed.
Evidence summary
An estimated 9.5% of infants and children younger than 2 years of age are considered overweight—that is, their weight is at or above the 95th percentile of weight-for-recumbent length on the sex-specific growth charts from the Centers for Disease Control and Prevention (CDC).1 The prevalence is unknown for infants who are exclusively breastfed2 or fed only human milk without any supplementation (except recommended vitamins, minerals, and medication) for the first 6 months of life.
Exclusively breastfed babies have a different growth curve
Because comparison growth studies demonstrate that healthy breastfed infants have a different growth curve than formula or mix-fed babies,3 the WHO growth curves (http://www.who.int/childgrowth/standards/en/), rather than the CDC charts, should be used to monitor the growth of exclusively breastfed babies.4 The WHO Working Group on Infant Growth studied infants whose sole nourishment was breast milk until 4 months of age.3 The CDC charts reflect a heavier and shorter sample of infants. Moreover, the WHO charts are based on shorter measurement intervals and may therefore be a better tool for measuring rapidly changing rates of growth.4
Exclusive breastfeeding reduces risk of overweight later in life
A meta-analysis showed a dose-dependent relationship between longer duration of breastfeeding and decreased risk of overweight in later life (<1 month of breastfeeding: odds ratio [OR]=1.0; 95% confidence interval [CI], 0.65-1.55; 1-3 months: OR=0.81; 95% CI, 0.74-0.88; 4-6 months: OR=0.76; 95% CI, 0.67-0.86; 7-9 months: OR=0.67; 95% CI, 0.55-0.82; >9 months: OR=0.68; 95% CI, 0.50-0.91).5 Because overweight has no known adverse health outcomes for exclusively breastfed infants, lactation experts don’t advise mothers to reduce feeding for these babies.6
Is overfeeding an issue?
Overfeeding may contribute to higher-than-normal weight gain in both breastfed and formula-fed infants.7 Maternal behavior changes that may taper unusual weight gains include cuddling rather than breastfeeding in response to all distress signals and encouraging movement and crawling.8
Expressing breast milk to increase infant intake increases weight gain (r=0.59); this effect gets stronger as the infant gets older (r=0.58).9 Referral to a lactation consultant is recommended to manage large volumes of milk that exceed infant need.7 For the rare infant who exhibits hypoglycemia, lack of satiety, or dysmorphia, consider early macrosomia or an overgrowth syndrome, such as Beckwith-Wiedemann syndrome, and seek an endocrinology or genetics consult.10
Recommendations
Exclusive breastfeeding for approximately the first 6 months of life is recommended by the American Academy of Family Physicians (AAFP), American College of Obstetricians and Gynecologists, American Academy of Pediatrics, Academy of Breastfeeding Medicine, WHO, United Nations Children’s Fund, and other organizations. The AAFP recommends that physicians help prevent and manage overweight in childhood to reduce the risk of obesity and chronic disease in later life.11
1. Centers for Disease Control and Prevention. National Center for Health Statistics. Prevalence of overweight, infants and children less than 2 years of age, United States, 2003-2004. Available at: http://www.cdc.gov/nchs/products/pubs/pubd/hestats/overweight/overwght_child_under02.htm. Accessed August 2008.
2. Sachs M, Dykes F, Carter B. Weight monitoring of breastfed babies in the United Kingdom—interpreting, explaining and intervening. Matern Child Nutr. 2006;2:3-18.
3. WHO Working Group on Infant Growth. An evaluation of infant growth. Geneva: Nutrition Unit, World Health Organization; 1994. Available at: http://whqlibdoc.who.int/hq/1994/WHO_NUT_94.8.pdf. Accessed February 19, 2007.
4. de Onis M, Garza C, Onyango AW, et al. Comparison of the WHO child growth standards and the CDC 2000 growth charts. J Nutr. 2007;137:144-148.
5. Harder T, Bergmann R, Kallischnigg G, et al. Duration of breastfeeding and risk of overweight: a meta-analysis. Am J Epidemiol. 2005;162:397-403.
6. Mohrbacher N, Stock J. The Breastfeeding Answer Book. 3rd rev ed. Schaumburg, Ill: La Leche League International; 2003.
7. Crow RA, Fawcett JN, Wright P. Maternal behavior during breast- and bottle-feeding. J Behav Med. 1980;3:259-277.
8. Lawrence RA, Lawrence RM. Breastfeeding: A Guide for the Medical Profession. 6th ed. Philadelphia: Elsevier Mosby; 2005.
9. Dewey KG, Lonnerdal B. Infant self-regulation of breast milk intake. Acta Paediatr Scand. 1986;75:893-898.
10. Jones KL. Smith’s Recognizable Patterns of Human Malformation. 6th ed. Philadelphia: Elsevier Saunders; 2006.
11. American Academy of Family Physicians. Breastfeeding, family physicians supporting (position paper). Available at: http://www.aafp.org/online/en/home/policy/policies/b/breastfeedingpositionpaper.htm. Accessed January 18, 2008.
1. Centers for Disease Control and Prevention. National Center for Health Statistics. Prevalence of overweight, infants and children less than 2 years of age, United States, 2003-2004. Available at: http://www.cdc.gov/nchs/products/pubs/pubd/hestats/overweight/overwght_child_under02.htm. Accessed August 2008.
2. Sachs M, Dykes F, Carter B. Weight monitoring of breastfed babies in the United Kingdom—interpreting, explaining and intervening. Matern Child Nutr. 2006;2:3-18.
3. WHO Working Group on Infant Growth. An evaluation of infant growth. Geneva: Nutrition Unit, World Health Organization; 1994. Available at: http://whqlibdoc.who.int/hq/1994/WHO_NUT_94.8.pdf. Accessed February 19, 2007.
4. de Onis M, Garza C, Onyango AW, et al. Comparison of the WHO child growth standards and the CDC 2000 growth charts. J Nutr. 2007;137:144-148.
5. Harder T, Bergmann R, Kallischnigg G, et al. Duration of breastfeeding and risk of overweight: a meta-analysis. Am J Epidemiol. 2005;162:397-403.
6. Mohrbacher N, Stock J. The Breastfeeding Answer Book. 3rd rev ed. Schaumburg, Ill: La Leche League International; 2003.
7. Crow RA, Fawcett JN, Wright P. Maternal behavior during breast- and bottle-feeding. J Behav Med. 1980;3:259-277.
8. Lawrence RA, Lawrence RM. Breastfeeding: A Guide for the Medical Profession. 6th ed. Philadelphia: Elsevier Mosby; 2005.
9. Dewey KG, Lonnerdal B. Infant self-regulation of breast milk intake. Acta Paediatr Scand. 1986;75:893-898.
10. Jones KL. Smith’s Recognizable Patterns of Human Malformation. 6th ed. Philadelphia: Elsevier Saunders; 2006.
11. American Academy of Family Physicians. Breastfeeding, family physicians supporting (position paper). Available at: http://www.aafp.org/online/en/home/policy/policies/b/breastfeedingpositionpaper.htm. Accessed January 18, 2008.
Evidence-based answers from the Family Physicians Inquiries Network
What treatments work best for constipation in children?
Osmotic laxatives produce the best results. Fiber and behavior modification may have a role. Increased fiber and behavior modification are the most often recommended first steps in managing chronic functional constipation (CFC) in children, but only limited evidence supports this approach (strength of recommendation [SOR]: B for fiber, 1 randomized controlled trial [RCT]; C for behavior modification, 1 small trial).
For pharmacologic management, the best evidence supports osmotic laxatives (SOR: A, 6 fair- to good-quality RCTs).
Evidence summary
CFC with or without encopresis is a common pediatric problem that’s distressing to both the child and family. High-quality RCTs on managing CFC are lacking. Our search located 7 relevant RCTs1-7 and 2 relevant systematic reviews.8,9 The TABLE summarizes the RCTs.
TABLE
How laxatives for childhood constipation compare
| INTERVENTION VS COMPARISON | NNT | EFFECTIVE DOSE | AVERAGE COST/MONTH |
|---|---|---|---|
| Glucomannan vs placebo1 | 3 | 100 mg/kg/d | $10-$30* |
| PEG + E vs placebo2 | 2 | 7-42 g/d | $14-$60* |
| PEG + E vs lactulose3 | 4 | 3-6 g/d vs 6-12 g/d | $20 vs $20 |
| PEG + E vs mineral oil for disimpaction over 2 days 5 | 5 | 20 mL/kg/h×4 h/d 30-120 mL BID | $20 vs $20 |
| Mineral oil vs senna6 | 3 | 3 mL/kg/d vs 1-4 tab/d | $8 vs $5 |
| Lactulose vs senna7 | 4 | 15 mL/d vs 20 mL/d | $20 vs $10 |
| *Retail price varies by manufacturer. | |||
| NNT, number needed to treat; PEG + E, polyethylene glycol 3350 plus electrolytes. | |||
Fiber may help—and doesn’t hurt
A fair-quality crossover RCT (31 children, mean age 7 years, with CFC) compared fiber (glucomannan) with placebo for 4 weeks.1 More children were successfully treated with fiber than placebo (45% vs 13%; number needed to treat [NNT]=3.125; P<.05). Parents rated children as doing better on fiber (68% vs 13%), and abdominal pain occurred less often (10% vs 42%; P<.05). No adverse effects were associated with fiber.
Osmotic laxatives, especially PEG, get results
A recent high-quality RCT compared the osmotic laxative polyethylene glycol 3350 plus electrolytes (PEG + E) with placebo in 51 children with CFC, 2 to 11 years of age.2 The mean number of defecations per week was higher for children on PEG + E (3.12 vs 1.45; P<.001); straining or pain and stool consistency improved.
One good-quality RCT (100 children, 6 months to 15 years old with CFC) compared PEG + E with lactulose.3 Both significantly increased stool frequency and decreased encopresis. However, PEG + E had a markedly higher success rate (56% vs 29%; NNT=3.7; P=.02). The 8-week trial found significantly more complaints about bad taste in the PEG + E group; the lactulose group reported higher rates of abdominal pain, straining, and pain at defecation. The only dropout because of adverse events (bad taste) occurred in the PEG + E group.
Another good-quality RCT showed that PEG + E effectively relieved fecal impaction (92% of 63 children) and was superior to lactulose for maintenance treatment. The rate of adverse effects (abdominal pain) was 64% with PEG + E and 83% with lactulose.4
One fair-quality RCT of 48 children with fecal impaction compared PEG with mineral oil. PEG was more effective, but high-volume PEG caused more vomiting and less compliance.5
A small RCT found that mineral oil treated constipation more successfully than senna at 3 and 10 months of follow-up.6 One poor-quality RCT found that senna was less effective than lactulose and had more side effects (colicky pain, diarrhea).7
A Cochrane systematic review found no RCTs of stimulant laxatives for CFC and concluded that evidence concerning the efficacy of these agents is insufficient.8
Few studies focus on nonpharmacologic management
A Cochrane systematic review of 9 small, poor-quality RCTs in children with functional fecal incontinence found no significant improvement when biofeedback was added to conventional treatment for as long as 12 months (odds ratio=1.11; 95% confidence interval, 0.78-1.58).9 In 1 small trial, however, adding behavior modification to laxative therapy significantly reduced soiling episodes.
Notably, few studies have focused on nonpharmacologic management of CFC, and most laxative trials are of short duration.
Recommendations
The Constipation Guideline Committee of the North American Society for Pediatric Gastroenterology states that using medication in combination with behavior management can decrease time to remission in children with CFC. Lubricants (mineral oil) and osmotic laxatives (magnesium hydroxide, lactulose, and sorbitol) are safe and effective. Stimulants (senna and bisacodyl) can help some patients whose conditions are difficult to treat. Low doses of PEG may be an effective long-term therapy for hard-to-manage constipation.10
The University of Michigan Guidelines on CFC and soiling are similar. After clean-out, they recommend a maintenance phase that includes behavioral, dietary, and medication components. Osmotic laxatives and lubricants are recommended for long-term treatment; stimulant laxatives should be reserved for short-term use.11
1. Loening-Baucke V, Miele E, Staiano A. Fiber (glucomannan) is beneficial in the treatment of childhood constipation. Pediatrics. 2004;113:e259-e264.
2. Thomson MA, Jenkins HR, Bisset WM, et al. Polyethylene glycol 3350 plus electrolytes for chronic constipation in children: a double-blind, placebo-controlled, crossover study. Arch Dis Child. 2007;92:996-1000.
3. Voskuijl W, De Lorijn F, Verwijs W, et al. PEG 3350 (Transipeg) versus lactulose in the treatment of childhood functional constipation: a double-blind randomised, controlled, multicentre trial. Gut. 2004;53:1590-1594.
4. Candy DC, Edwards D, Geraint M. Treatment of faecal impaction with polyethylene glycol plus electrolytes (PEG + E) followed by a double-blind comparison of PEG+E versus lactulose as maintenance therapy. J Pediatr Gastroenterol Nutr. 2006;43:65-70.
5. Tolia V, Lin CH, Elitsur Y. A prospective randomized study with mineral oil and oral lavage solution for treatment of faecal impaction in children. Aliment Pharmacol Ther. 1993;7:523-529.
6. Sondheimer JM, Gervaise EP. Lubricant versus laxative in the treatment of chronic functional constipation of children: a comparative study. J Pediatr Gastroenterol Nutr. 1982;1:223-226.
7. Perkin JM. Constipation in childhood: a controlled comparison between lactulose and standardized senna. Curr Med Res Opin. 1977;4:540-543.
8. Price KJ, Elliott TM. What is the role of stimulant laxatives for constipation and soiling in children? Cochrane Database Syst Rev. 2001;(3):CD002040.-
9. Brazzelli M, Griffiths P. Behavioural and cognitive interventions with or without other treatments for the management of faecal incontinence in children. Cochrane Database Syst Rev. 2006;(2):CD002240.-
10. Constipation Guideline Committee of the North American Society for Pediatric Gastroenterology. Evaluation and treatment of constipation in infants and children: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2006;43:e1-e13.
11. University of Michigan Health System. Functional constipation and soiling in children. Ann Arbor, MI: University of Michigan Health System; February 2003. Available at: http://cme.med.umich.edu/ pdf/guideline/peds08.pdf. Accessed January 27, 2008.
Osmotic laxatives produce the best results. Fiber and behavior modification may have a role. Increased fiber and behavior modification are the most often recommended first steps in managing chronic functional constipation (CFC) in children, but only limited evidence supports this approach (strength of recommendation [SOR]: B for fiber, 1 randomized controlled trial [RCT]; C for behavior modification, 1 small trial).
For pharmacologic management, the best evidence supports osmotic laxatives (SOR: A, 6 fair- to good-quality RCTs).
Evidence summary
CFC with or without encopresis is a common pediatric problem that’s distressing to both the child and family. High-quality RCTs on managing CFC are lacking. Our search located 7 relevant RCTs1-7 and 2 relevant systematic reviews.8,9 The TABLE summarizes the RCTs.
TABLE
How laxatives for childhood constipation compare
| INTERVENTION VS COMPARISON | NNT | EFFECTIVE DOSE | AVERAGE COST/MONTH |
|---|---|---|---|
| Glucomannan vs placebo1 | 3 | 100 mg/kg/d | $10-$30* |
| PEG + E vs placebo2 | 2 | 7-42 g/d | $14-$60* |
| PEG + E vs lactulose3 | 4 | 3-6 g/d vs 6-12 g/d | $20 vs $20 |
| PEG + E vs mineral oil for disimpaction over 2 days 5 | 5 | 20 mL/kg/h×4 h/d 30-120 mL BID | $20 vs $20 |
| Mineral oil vs senna6 | 3 | 3 mL/kg/d vs 1-4 tab/d | $8 vs $5 |
| Lactulose vs senna7 | 4 | 15 mL/d vs 20 mL/d | $20 vs $10 |
| *Retail price varies by manufacturer. | |||
| NNT, number needed to treat; PEG + E, polyethylene glycol 3350 plus electrolytes. | |||
Fiber may help—and doesn’t hurt
A fair-quality crossover RCT (31 children, mean age 7 years, with CFC) compared fiber (glucomannan) with placebo for 4 weeks.1 More children were successfully treated with fiber than placebo (45% vs 13%; number needed to treat [NNT]=3.125; P<.05). Parents rated children as doing better on fiber (68% vs 13%), and abdominal pain occurred less often (10% vs 42%; P<.05). No adverse effects were associated with fiber.
Osmotic laxatives, especially PEG, get results
A recent high-quality RCT compared the osmotic laxative polyethylene glycol 3350 plus electrolytes (PEG + E) with placebo in 51 children with CFC, 2 to 11 years of age.2 The mean number of defecations per week was higher for children on PEG + E (3.12 vs 1.45; P<.001); straining or pain and stool consistency improved.
One good-quality RCT (100 children, 6 months to 15 years old with CFC) compared PEG + E with lactulose.3 Both significantly increased stool frequency and decreased encopresis. However, PEG + E had a markedly higher success rate (56% vs 29%; NNT=3.7; P=.02). The 8-week trial found significantly more complaints about bad taste in the PEG + E group; the lactulose group reported higher rates of abdominal pain, straining, and pain at defecation. The only dropout because of adverse events (bad taste) occurred in the PEG + E group.
Another good-quality RCT showed that PEG + E effectively relieved fecal impaction (92% of 63 children) and was superior to lactulose for maintenance treatment. The rate of adverse effects (abdominal pain) was 64% with PEG + E and 83% with lactulose.4
One fair-quality RCT of 48 children with fecal impaction compared PEG with mineral oil. PEG was more effective, but high-volume PEG caused more vomiting and less compliance.5
A small RCT found that mineral oil treated constipation more successfully than senna at 3 and 10 months of follow-up.6 One poor-quality RCT found that senna was less effective than lactulose and had more side effects (colicky pain, diarrhea).7
A Cochrane systematic review found no RCTs of stimulant laxatives for CFC and concluded that evidence concerning the efficacy of these agents is insufficient.8
Few studies focus on nonpharmacologic management
A Cochrane systematic review of 9 small, poor-quality RCTs in children with functional fecal incontinence found no significant improvement when biofeedback was added to conventional treatment for as long as 12 months (odds ratio=1.11; 95% confidence interval, 0.78-1.58).9 In 1 small trial, however, adding behavior modification to laxative therapy significantly reduced soiling episodes.
Notably, few studies have focused on nonpharmacologic management of CFC, and most laxative trials are of short duration.
Recommendations
The Constipation Guideline Committee of the North American Society for Pediatric Gastroenterology states that using medication in combination with behavior management can decrease time to remission in children with CFC. Lubricants (mineral oil) and osmotic laxatives (magnesium hydroxide, lactulose, and sorbitol) are safe and effective. Stimulants (senna and bisacodyl) can help some patients whose conditions are difficult to treat. Low doses of PEG may be an effective long-term therapy for hard-to-manage constipation.10
The University of Michigan Guidelines on CFC and soiling are similar. After clean-out, they recommend a maintenance phase that includes behavioral, dietary, and medication components. Osmotic laxatives and lubricants are recommended for long-term treatment; stimulant laxatives should be reserved for short-term use.11
Osmotic laxatives produce the best results. Fiber and behavior modification may have a role. Increased fiber and behavior modification are the most often recommended first steps in managing chronic functional constipation (CFC) in children, but only limited evidence supports this approach (strength of recommendation [SOR]: B for fiber, 1 randomized controlled trial [RCT]; C for behavior modification, 1 small trial).
For pharmacologic management, the best evidence supports osmotic laxatives (SOR: A, 6 fair- to good-quality RCTs).
Evidence summary
CFC with or without encopresis is a common pediatric problem that’s distressing to both the child and family. High-quality RCTs on managing CFC are lacking. Our search located 7 relevant RCTs1-7 and 2 relevant systematic reviews.8,9 The TABLE summarizes the RCTs.
TABLE
How laxatives for childhood constipation compare
| INTERVENTION VS COMPARISON | NNT | EFFECTIVE DOSE | AVERAGE COST/MONTH |
|---|---|---|---|
| Glucomannan vs placebo1 | 3 | 100 mg/kg/d | $10-$30* |
| PEG + E vs placebo2 | 2 | 7-42 g/d | $14-$60* |
| PEG + E vs lactulose3 | 4 | 3-6 g/d vs 6-12 g/d | $20 vs $20 |
| PEG + E vs mineral oil for disimpaction over 2 days 5 | 5 | 20 mL/kg/h×4 h/d 30-120 mL BID | $20 vs $20 |
| Mineral oil vs senna6 | 3 | 3 mL/kg/d vs 1-4 tab/d | $8 vs $5 |
| Lactulose vs senna7 | 4 | 15 mL/d vs 20 mL/d | $20 vs $10 |
| *Retail price varies by manufacturer. | |||
| NNT, number needed to treat; PEG + E, polyethylene glycol 3350 plus electrolytes. | |||
Fiber may help—and doesn’t hurt
A fair-quality crossover RCT (31 children, mean age 7 years, with CFC) compared fiber (glucomannan) with placebo for 4 weeks.1 More children were successfully treated with fiber than placebo (45% vs 13%; number needed to treat [NNT]=3.125; P<.05). Parents rated children as doing better on fiber (68% vs 13%), and abdominal pain occurred less often (10% vs 42%; P<.05). No adverse effects were associated with fiber.
Osmotic laxatives, especially PEG, get results
A recent high-quality RCT compared the osmotic laxative polyethylene glycol 3350 plus electrolytes (PEG + E) with placebo in 51 children with CFC, 2 to 11 years of age.2 The mean number of defecations per week was higher for children on PEG + E (3.12 vs 1.45; P<.001); straining or pain and stool consistency improved.
One good-quality RCT (100 children, 6 months to 15 years old with CFC) compared PEG + E with lactulose.3 Both significantly increased stool frequency and decreased encopresis. However, PEG + E had a markedly higher success rate (56% vs 29%; NNT=3.7; P=.02). The 8-week trial found significantly more complaints about bad taste in the PEG + E group; the lactulose group reported higher rates of abdominal pain, straining, and pain at defecation. The only dropout because of adverse events (bad taste) occurred in the PEG + E group.
Another good-quality RCT showed that PEG + E effectively relieved fecal impaction (92% of 63 children) and was superior to lactulose for maintenance treatment. The rate of adverse effects (abdominal pain) was 64% with PEG + E and 83% with lactulose.4
One fair-quality RCT of 48 children with fecal impaction compared PEG with mineral oil. PEG was more effective, but high-volume PEG caused more vomiting and less compliance.5
A small RCT found that mineral oil treated constipation more successfully than senna at 3 and 10 months of follow-up.6 One poor-quality RCT found that senna was less effective than lactulose and had more side effects (colicky pain, diarrhea).7
A Cochrane systematic review found no RCTs of stimulant laxatives for CFC and concluded that evidence concerning the efficacy of these agents is insufficient.8
Few studies focus on nonpharmacologic management
A Cochrane systematic review of 9 small, poor-quality RCTs in children with functional fecal incontinence found no significant improvement when biofeedback was added to conventional treatment for as long as 12 months (odds ratio=1.11; 95% confidence interval, 0.78-1.58).9 In 1 small trial, however, adding behavior modification to laxative therapy significantly reduced soiling episodes.
Notably, few studies have focused on nonpharmacologic management of CFC, and most laxative trials are of short duration.
Recommendations
The Constipation Guideline Committee of the North American Society for Pediatric Gastroenterology states that using medication in combination with behavior management can decrease time to remission in children with CFC. Lubricants (mineral oil) and osmotic laxatives (magnesium hydroxide, lactulose, and sorbitol) are safe and effective. Stimulants (senna and bisacodyl) can help some patients whose conditions are difficult to treat. Low doses of PEG may be an effective long-term therapy for hard-to-manage constipation.10
The University of Michigan Guidelines on CFC and soiling are similar. After clean-out, they recommend a maintenance phase that includes behavioral, dietary, and medication components. Osmotic laxatives and lubricants are recommended for long-term treatment; stimulant laxatives should be reserved for short-term use.11
1. Loening-Baucke V, Miele E, Staiano A. Fiber (glucomannan) is beneficial in the treatment of childhood constipation. Pediatrics. 2004;113:e259-e264.
2. Thomson MA, Jenkins HR, Bisset WM, et al. Polyethylene glycol 3350 plus electrolytes for chronic constipation in children: a double-blind, placebo-controlled, crossover study. Arch Dis Child. 2007;92:996-1000.
3. Voskuijl W, De Lorijn F, Verwijs W, et al. PEG 3350 (Transipeg) versus lactulose in the treatment of childhood functional constipation: a double-blind randomised, controlled, multicentre trial. Gut. 2004;53:1590-1594.
4. Candy DC, Edwards D, Geraint M. Treatment of faecal impaction with polyethylene glycol plus electrolytes (PEG + E) followed by a double-blind comparison of PEG+E versus lactulose as maintenance therapy. J Pediatr Gastroenterol Nutr. 2006;43:65-70.
5. Tolia V, Lin CH, Elitsur Y. A prospective randomized study with mineral oil and oral lavage solution for treatment of faecal impaction in children. Aliment Pharmacol Ther. 1993;7:523-529.
6. Sondheimer JM, Gervaise EP. Lubricant versus laxative in the treatment of chronic functional constipation of children: a comparative study. J Pediatr Gastroenterol Nutr. 1982;1:223-226.
7. Perkin JM. Constipation in childhood: a controlled comparison between lactulose and standardized senna. Curr Med Res Opin. 1977;4:540-543.
8. Price KJ, Elliott TM. What is the role of stimulant laxatives for constipation and soiling in children? Cochrane Database Syst Rev. 2001;(3):CD002040.-
9. Brazzelli M, Griffiths P. Behavioural and cognitive interventions with or without other treatments for the management of faecal incontinence in children. Cochrane Database Syst Rev. 2006;(2):CD002240.-
10. Constipation Guideline Committee of the North American Society for Pediatric Gastroenterology. Evaluation and treatment of constipation in infants and children: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2006;43:e1-e13.
11. University of Michigan Health System. Functional constipation and soiling in children. Ann Arbor, MI: University of Michigan Health System; February 2003. Available at: http://cme.med.umich.edu/ pdf/guideline/peds08.pdf. Accessed January 27, 2008.
1. Loening-Baucke V, Miele E, Staiano A. Fiber (glucomannan) is beneficial in the treatment of childhood constipation. Pediatrics. 2004;113:e259-e264.
2. Thomson MA, Jenkins HR, Bisset WM, et al. Polyethylene glycol 3350 plus electrolytes for chronic constipation in children: a double-blind, placebo-controlled, crossover study. Arch Dis Child. 2007;92:996-1000.
3. Voskuijl W, De Lorijn F, Verwijs W, et al. PEG 3350 (Transipeg) versus lactulose in the treatment of childhood functional constipation: a double-blind randomised, controlled, multicentre trial. Gut. 2004;53:1590-1594.
4. Candy DC, Edwards D, Geraint M. Treatment of faecal impaction with polyethylene glycol plus electrolytes (PEG + E) followed by a double-blind comparison of PEG+E versus lactulose as maintenance therapy. J Pediatr Gastroenterol Nutr. 2006;43:65-70.
5. Tolia V, Lin CH, Elitsur Y. A prospective randomized study with mineral oil and oral lavage solution for treatment of faecal impaction in children. Aliment Pharmacol Ther. 1993;7:523-529.
6. Sondheimer JM, Gervaise EP. Lubricant versus laxative in the treatment of chronic functional constipation of children: a comparative study. J Pediatr Gastroenterol Nutr. 1982;1:223-226.
7. Perkin JM. Constipation in childhood: a controlled comparison between lactulose and standardized senna. Curr Med Res Opin. 1977;4:540-543.
8. Price KJ, Elliott TM. What is the role of stimulant laxatives for constipation and soiling in children? Cochrane Database Syst Rev. 2001;(3):CD002040.-
9. Brazzelli M, Griffiths P. Behavioural and cognitive interventions with or without other treatments for the management of faecal incontinence in children. Cochrane Database Syst Rev. 2006;(2):CD002240.-
10. Constipation Guideline Committee of the North American Society for Pediatric Gastroenterology. Evaluation and treatment of constipation in infants and children: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2006;43:e1-e13.
11. University of Michigan Health System. Functional constipation and soiling in children. Ann Arbor, MI: University of Michigan Health System; February 2003. Available at: http://cme.med.umich.edu/ pdf/guideline/peds08.pdf. Accessed January 27, 2008.
Evidence-based answers from the Family Physicians Inquiries Network
Sleep apnea in adults: How accurate is clinical prediction?
Moderately accurate, depending on which tool you use. Questionnaires, physical examination, and clinical prediction rules estimate the pretest probability of obstructive sleep apnea hypopnea syndrome (OSAHS), but are not specific enough to make the diagnosis (strength of recommendation [SOR]: B, meta-analyses, prospective cross-sectional studies). The Epworth Sleepiness Scale is a reliable measure of daytime sleepiness (SOR: B, factor analysis). The Berlin Questionnaire, Mallampati score, and truncal obesity can be used to assess pretest probability of OSAHS (SOR: B, multivariate analyses, cross-sectional studies).
Evidence summary
OSAHS is marked by daytime somnolence, snoring, difficult-to-control hypertension, refractory arrhythmias, angina, or heart failure.1 The syndrome is defined as an apnea-hypopnea index (AHI) of 5 or more events per hour during a sleep polysomnogram, accompanied by either excessive daytime sleepiness or 2 of the following: choking or gasping during sleep, recurrent awakenings from sleep, daytime fatigue, and impaired concentration.2
What questionnaires can tell you
The Epworth Sleepiness Scale rates the likelihood of dozing in 8 situations. Factor analysis of test-retest on 104 medical students and 150 patients with various sleep disorders showed that the scale was internally consistent but measured only daytime sleepiness.3
The Berlin Questionnaire assesses snoring, daytime sleepiness, history of hypertension, age, and body mass index (BMI). The questionnaire was evaluated in 744 adults presenting for unrelated problems at 5 primary care sites. Of 100 patients who underwent sleep studies, a finding of high risk on the Berlin Questionnaire predicted an AHI >5 with 86% sensitivity and 77% specificity, a positive likelihood ratio of 3.79.4
Mallampati scores, truncal obesity offer clues
Mallampati scoring grades visibility of the posterior pharynx when the patient opens his mouth and sticks out his tongue. Visibility is ranked on a scale of 1 to 4, with 1 representing the greatest visibility and 4 the least. Prospective multivariate assessment of Mallampati scores in adults referred to a sleep clinic yielded likelihood ratios of OSAHS for Mallampati grades 1 to 4 of 0.4, 0.7, 1.6, and 1.7, respectively.5
A cross-sectional study correlating OSAHS with truncal obesity in 192 patients referred to a sleep clinic found that the likelihood of OSAHS was 2.6 times greater if the waist-to-hip ratio was >1 in men and >0.85 in women.6
No single model is sufficient
A systematic review and meta-analysis of 249 studies of sleep apnea diagnosis from 1980 through November 1997 concluded that studies of focused questionnaires were too heterogeneous to be combined in a meta-analysis. Sensitivity and specificity were good for clinical prediction rules in general, but evidence was insufficient to justify adoption of any single model.7
A 2000 prospective study of 4 previously developed clinical prediction models for OSAHS in sleep center populations found sensitivities of 75% to 96% and specificities of 13% to 54% for identifying patients, using a criterion of AHI >9.8
A 2004 prospective evaluation examined a clinical decision rule on 837 patients referred for polysomnogram that used age, sex, BMI, snoring, and cessation of breathing during sleep to stratify patients into low-, moderate-, or high-risk groups. The study found OSAHS prevalences of 8%, 51%, and 82%, respectively.9
Recommendations
The Institute for Clinical Systems Improvement recommends polysomnography for patients with symptoms of OSAHS and 1 or more of the following: cardiovascular disease, hypertension, coronary artery disease, obesity, sleep complaint, type 2 diabetes mellitus, recurrent atrial fibrillation, and large neck circumference.10
The Canadian Thoracic Society states that clinical prediction formulas assess the pretest probability of sleep-disordered breathing and prioritize patients for evaluation, but are insufficient for diagnosis. The guidelines recommend that all patients with suspected sleep-disordered breathing complete an assessment of daytime sleepiness such as the Epworth Sleepiness Scale.11
The American Academy of Sleep Medicine recommends no single clinical model to predict the severity of OSAHS. Polysomnography is indicated for diagnosis of any sleep-disordered breathing.12
1. Barcena JA, Fang JC. Diagnosis and treatment of sleep apnea in heart disease. Curr Treat Options Cardiovasc Med. 2007;9:501-509.
2. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22:667-689.
3. Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15:376-381.
4. Netzer NC, Stoohs RA, Netzer CM, et al. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485-491.
5. Nuckton TJ, Glidden DV, Browner WS, et al. Physical examination: Mallampati score as an independent predictor of obstructive sleep apnea. Sleep. 2006;29:903-908.
6. Martinez-Rivera C, Abad J, Fiz JA, et al. Usefulness of truncal obesity indices as predictive factors for obstructive sleep apnea syndrome. Obesity. 2008;16:113-118.
7. Ross SD, Sheinhait IA, Harrison KJ, et al. Systematic review and meta-analysis of the literature regarding the diagnosis of sleep apnea. Sleep. 2000;23:519-532.
8. Rowley JA, Aboussouan LS, Badr MS. The use of clinical prediction formulas in the evaluation of obstructive sleep apnea. Sleep. 2000;23:929-938.
9. Rodsutti J, Hensley M, Thakkinstian A, et al. A clinical decision rule to prioritize polysomnography in patients with suspected sleep apnea. Sleep. 2004;27:694-699.
10. Institute for Clinical Systems Improvement (ICSI). Diagnosis and Treatment of Obstructive Sleep Apnea in Adults. Bloomington, MN: Institute for Clinical Systems Improvement; 2008.
11. Fleetham J, Ayas N, Bradley D, et al. Canadian Thoracic Society guidelines: diagnosis and treatment of sleep disordered breathing in adults. Can Respir J. 2006;13:387-392.
12. Kushida CA, Littner MR, Morgenthaler T, et al. Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep. 2005;28:499-521.
Moderately accurate, depending on which tool you use. Questionnaires, physical examination, and clinical prediction rules estimate the pretest probability of obstructive sleep apnea hypopnea syndrome (OSAHS), but are not specific enough to make the diagnosis (strength of recommendation [SOR]: B, meta-analyses, prospective cross-sectional studies). The Epworth Sleepiness Scale is a reliable measure of daytime sleepiness (SOR: B, factor analysis). The Berlin Questionnaire, Mallampati score, and truncal obesity can be used to assess pretest probability of OSAHS (SOR: B, multivariate analyses, cross-sectional studies).
Evidence summary
OSAHS is marked by daytime somnolence, snoring, difficult-to-control hypertension, refractory arrhythmias, angina, or heart failure.1 The syndrome is defined as an apnea-hypopnea index (AHI) of 5 or more events per hour during a sleep polysomnogram, accompanied by either excessive daytime sleepiness or 2 of the following: choking or gasping during sleep, recurrent awakenings from sleep, daytime fatigue, and impaired concentration.2
What questionnaires can tell you
The Epworth Sleepiness Scale rates the likelihood of dozing in 8 situations. Factor analysis of test-retest on 104 medical students and 150 patients with various sleep disorders showed that the scale was internally consistent but measured only daytime sleepiness.3
The Berlin Questionnaire assesses snoring, daytime sleepiness, history of hypertension, age, and body mass index (BMI). The questionnaire was evaluated in 744 adults presenting for unrelated problems at 5 primary care sites. Of 100 patients who underwent sleep studies, a finding of high risk on the Berlin Questionnaire predicted an AHI >5 with 86% sensitivity and 77% specificity, a positive likelihood ratio of 3.79.4
Mallampati scores, truncal obesity offer clues
Mallampati scoring grades visibility of the posterior pharynx when the patient opens his mouth and sticks out his tongue. Visibility is ranked on a scale of 1 to 4, with 1 representing the greatest visibility and 4 the least. Prospective multivariate assessment of Mallampati scores in adults referred to a sleep clinic yielded likelihood ratios of OSAHS for Mallampati grades 1 to 4 of 0.4, 0.7, 1.6, and 1.7, respectively.5
A cross-sectional study correlating OSAHS with truncal obesity in 192 patients referred to a sleep clinic found that the likelihood of OSAHS was 2.6 times greater if the waist-to-hip ratio was >1 in men and >0.85 in women.6
No single model is sufficient
A systematic review and meta-analysis of 249 studies of sleep apnea diagnosis from 1980 through November 1997 concluded that studies of focused questionnaires were too heterogeneous to be combined in a meta-analysis. Sensitivity and specificity were good for clinical prediction rules in general, but evidence was insufficient to justify adoption of any single model.7
A 2000 prospective study of 4 previously developed clinical prediction models for OSAHS in sleep center populations found sensitivities of 75% to 96% and specificities of 13% to 54% for identifying patients, using a criterion of AHI >9.8
A 2004 prospective evaluation examined a clinical decision rule on 837 patients referred for polysomnogram that used age, sex, BMI, snoring, and cessation of breathing during sleep to stratify patients into low-, moderate-, or high-risk groups. The study found OSAHS prevalences of 8%, 51%, and 82%, respectively.9
Recommendations
The Institute for Clinical Systems Improvement recommends polysomnography for patients with symptoms of OSAHS and 1 or more of the following: cardiovascular disease, hypertension, coronary artery disease, obesity, sleep complaint, type 2 diabetes mellitus, recurrent atrial fibrillation, and large neck circumference.10
The Canadian Thoracic Society states that clinical prediction formulas assess the pretest probability of sleep-disordered breathing and prioritize patients for evaluation, but are insufficient for diagnosis. The guidelines recommend that all patients with suspected sleep-disordered breathing complete an assessment of daytime sleepiness such as the Epworth Sleepiness Scale.11
The American Academy of Sleep Medicine recommends no single clinical model to predict the severity of OSAHS. Polysomnography is indicated for diagnosis of any sleep-disordered breathing.12
Moderately accurate, depending on which tool you use. Questionnaires, physical examination, and clinical prediction rules estimate the pretest probability of obstructive sleep apnea hypopnea syndrome (OSAHS), but are not specific enough to make the diagnosis (strength of recommendation [SOR]: B, meta-analyses, prospective cross-sectional studies). The Epworth Sleepiness Scale is a reliable measure of daytime sleepiness (SOR: B, factor analysis). The Berlin Questionnaire, Mallampati score, and truncal obesity can be used to assess pretest probability of OSAHS (SOR: B, multivariate analyses, cross-sectional studies).
Evidence summary
OSAHS is marked by daytime somnolence, snoring, difficult-to-control hypertension, refractory arrhythmias, angina, or heart failure.1 The syndrome is defined as an apnea-hypopnea index (AHI) of 5 or more events per hour during a sleep polysomnogram, accompanied by either excessive daytime sleepiness or 2 of the following: choking or gasping during sleep, recurrent awakenings from sleep, daytime fatigue, and impaired concentration.2
What questionnaires can tell you
The Epworth Sleepiness Scale rates the likelihood of dozing in 8 situations. Factor analysis of test-retest on 104 medical students and 150 patients with various sleep disorders showed that the scale was internally consistent but measured only daytime sleepiness.3
The Berlin Questionnaire assesses snoring, daytime sleepiness, history of hypertension, age, and body mass index (BMI). The questionnaire was evaluated in 744 adults presenting for unrelated problems at 5 primary care sites. Of 100 patients who underwent sleep studies, a finding of high risk on the Berlin Questionnaire predicted an AHI >5 with 86% sensitivity and 77% specificity, a positive likelihood ratio of 3.79.4
Mallampati scores, truncal obesity offer clues
Mallampati scoring grades visibility of the posterior pharynx when the patient opens his mouth and sticks out his tongue. Visibility is ranked on a scale of 1 to 4, with 1 representing the greatest visibility and 4 the least. Prospective multivariate assessment of Mallampati scores in adults referred to a sleep clinic yielded likelihood ratios of OSAHS for Mallampati grades 1 to 4 of 0.4, 0.7, 1.6, and 1.7, respectively.5
A cross-sectional study correlating OSAHS with truncal obesity in 192 patients referred to a sleep clinic found that the likelihood of OSAHS was 2.6 times greater if the waist-to-hip ratio was >1 in men and >0.85 in women.6
No single model is sufficient
A systematic review and meta-analysis of 249 studies of sleep apnea diagnosis from 1980 through November 1997 concluded that studies of focused questionnaires were too heterogeneous to be combined in a meta-analysis. Sensitivity and specificity were good for clinical prediction rules in general, but evidence was insufficient to justify adoption of any single model.7
A 2000 prospective study of 4 previously developed clinical prediction models for OSAHS in sleep center populations found sensitivities of 75% to 96% and specificities of 13% to 54% for identifying patients, using a criterion of AHI >9.8
A 2004 prospective evaluation examined a clinical decision rule on 837 patients referred for polysomnogram that used age, sex, BMI, snoring, and cessation of breathing during sleep to stratify patients into low-, moderate-, or high-risk groups. The study found OSAHS prevalences of 8%, 51%, and 82%, respectively.9
Recommendations
The Institute for Clinical Systems Improvement recommends polysomnography for patients with symptoms of OSAHS and 1 or more of the following: cardiovascular disease, hypertension, coronary artery disease, obesity, sleep complaint, type 2 diabetes mellitus, recurrent atrial fibrillation, and large neck circumference.10
The Canadian Thoracic Society states that clinical prediction formulas assess the pretest probability of sleep-disordered breathing and prioritize patients for evaluation, but are insufficient for diagnosis. The guidelines recommend that all patients with suspected sleep-disordered breathing complete an assessment of daytime sleepiness such as the Epworth Sleepiness Scale.11
The American Academy of Sleep Medicine recommends no single clinical model to predict the severity of OSAHS. Polysomnography is indicated for diagnosis of any sleep-disordered breathing.12
1. Barcena JA, Fang JC. Diagnosis and treatment of sleep apnea in heart disease. Curr Treat Options Cardiovasc Med. 2007;9:501-509.
2. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22:667-689.
3. Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15:376-381.
4. Netzer NC, Stoohs RA, Netzer CM, et al. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485-491.
5. Nuckton TJ, Glidden DV, Browner WS, et al. Physical examination: Mallampati score as an independent predictor of obstructive sleep apnea. Sleep. 2006;29:903-908.
6. Martinez-Rivera C, Abad J, Fiz JA, et al. Usefulness of truncal obesity indices as predictive factors for obstructive sleep apnea syndrome. Obesity. 2008;16:113-118.
7. Ross SD, Sheinhait IA, Harrison KJ, et al. Systematic review and meta-analysis of the literature regarding the diagnosis of sleep apnea. Sleep. 2000;23:519-532.
8. Rowley JA, Aboussouan LS, Badr MS. The use of clinical prediction formulas in the evaluation of obstructive sleep apnea. Sleep. 2000;23:929-938.
9. Rodsutti J, Hensley M, Thakkinstian A, et al. A clinical decision rule to prioritize polysomnography in patients with suspected sleep apnea. Sleep. 2004;27:694-699.
10. Institute for Clinical Systems Improvement (ICSI). Diagnosis and Treatment of Obstructive Sleep Apnea in Adults. Bloomington, MN: Institute for Clinical Systems Improvement; 2008.
11. Fleetham J, Ayas N, Bradley D, et al. Canadian Thoracic Society guidelines: diagnosis and treatment of sleep disordered breathing in adults. Can Respir J. 2006;13:387-392.
12. Kushida CA, Littner MR, Morgenthaler T, et al. Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep. 2005;28:499-521.
1. Barcena JA, Fang JC. Diagnosis and treatment of sleep apnea in heart disease. Curr Treat Options Cardiovasc Med. 2007;9:501-509.
2. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22:667-689.
3. Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15:376-381.
4. Netzer NC, Stoohs RA, Netzer CM, et al. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485-491.
5. Nuckton TJ, Glidden DV, Browner WS, et al. Physical examination: Mallampati score as an independent predictor of obstructive sleep apnea. Sleep. 2006;29:903-908.
6. Martinez-Rivera C, Abad J, Fiz JA, et al. Usefulness of truncal obesity indices as predictive factors for obstructive sleep apnea syndrome. Obesity. 2008;16:113-118.
7. Ross SD, Sheinhait IA, Harrison KJ, et al. Systematic review and meta-analysis of the literature regarding the diagnosis of sleep apnea. Sleep. 2000;23:519-532.
8. Rowley JA, Aboussouan LS, Badr MS. The use of clinical prediction formulas in the evaluation of obstructive sleep apnea. Sleep. 2000;23:929-938.
9. Rodsutti J, Hensley M, Thakkinstian A, et al. A clinical decision rule to prioritize polysomnography in patients with suspected sleep apnea. Sleep. 2004;27:694-699.
10. Institute for Clinical Systems Improvement (ICSI). Diagnosis and Treatment of Obstructive Sleep Apnea in Adults. Bloomington, MN: Institute for Clinical Systems Improvement; 2008.
11. Fleetham J, Ayas N, Bradley D, et al. Canadian Thoracic Society guidelines: diagnosis and treatment of sleep disordered breathing in adults. Can Respir J. 2006;13:387-392.
12. Kushida CA, Littner MR, Morgenthaler T, et al. Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep. 2005;28:499-521.
Evidence-based answers from the Family Physicians Inquiries Network
Do patients at high risk of Alzheimer’s disease benefit from early treatment?
Yes, but the extent of the benefit is unclear. Treating patients with early-stage Alzheimer’s disease yields statistically significant, though perhaps not clinically significant, improvement in cognition and global function (strength of recommendation [SOR]: A, consistent evidence from multiple randomized controlled trials [RCTs]). In a few cases, it may delay loss of function and need for long-term care.
Treating patients with mild cognitive impairment (MCI)—the most likely precursor to Alzheimer’s disease—with cholinesterase inhibitors seems to have an initial, but perhaps unsustained, benefit over no treatment (SOR: B, inconsistent results from few trials). Withdrawing anticholinergic drugs from patients taking them promises to reduce symptoms of MCI, but is unlikely to reduce rates of Alzheimer’s (SOR: C, well-designed observational study).
Remember nondrug interventions
Jaqueline Raetz, MD
Departments of Family Medicine and Long-Term Care, University of Washington School of Medicine, Seattle
Clinicians often forget the many nonpharmacologic treatments for dementia, including exercise, cognitive stimulation, increased socialization, addressing polypharmacy, and optimizing nutrition. Diagnosing and managing comorbidities such as depression and cardiovascular disease are also important. Primary care physicians who care for the frail elderly should advocate these interventions. In the very elderly, who are all at high risk of developing Alzheimer’s disease, these measures may help prevent functional decline and reduce clinically apparent disease.
All patients diagnosed with early-stage Alzheimer’s disease, and possibly patients with MCI, should be offered a trial of pharmacotherapy. However—given the high cost of drug therapy, the modest improvement it produces in patients with Alzheimer’s dementia, and the lack of definitive evidence that it benefits patients with MCI—I wouldn’t advocate medication for asymptomatic patients at high risk of developing dementia.
Evidence summary
Alzheimer’s disease is characterized by deficits in memory and at least 1 other cognitive domain (aphrasia, apraxia, agnosia, or loss of executive function) accompanied by impaired function. As the US population ages, Alzheimer’s disease is likely to increase substantially in prevalence and cost, from its current 4.5 million people affected and $100 billion per year in direct expenses.1
Because the definition of Alzheimer’s precludes asymptomatic disease, “early” treatment implies either treating a precursor condition or treating before cognitive and functional impairment force the patient and family to seek medical care. The literature identifies 2 possible prodromal conditions: MCI and personality change. Personality change is proposed as a prodrome based only on a small study that diagnosed Alzheimer’s disease at autopsy, so this Clinical Inquiry doesn’t address it further.2
Therapy for MCI: A look at 3 interventions
MCI is a measurable memory deficit, more severe than normal aging changes (slower learning of new material and difficulty retrieving names and places) but not meeting criteria for dementia.3 Researchers differ on a more precise definition; some subdivide MCI into “MCI-amnestic type” and “MCI-multiple cognitive deficits type.”4 MCI progresses to Alzheimer’s disease in anywhere from 10% to 56% of patients.4,5
Three interventions may benefit patients with MCI:
- cholinesterase inhibitors
- exercise
- discontinuation of anticholinergic drugs in patients taking them.
Two recent RCTs of donepezil6,7 and 1 of galantamine8 showed initial cognitive improvement in MCI patients. However, the only trial carried out for 3 years showed no persistent benefit at that time.6
Another study showed that moderate exercise—30 minutes 3 days a week—improves cognition in MCI patients.9
A longitudinal cohort study found that patients taking anticholinergic drugs had an 80% prevalence of MCI, compared with a 35% prevalence in a matched population of patients not using these drugs; yet Alzheimer’s disease hadn’t increased among the anticholinergic drug users at 8-year follow-up. Attributable risk for MCI from anticholinergic drug use was 19%. Stopping anticholinergic medications may reduce the prevalence of MCI.10
In established Alzheimer’s disease, cholinesterase inhibitors statistically benefit patients with early and moderate disease and probably benefit patients with severe disease.11,12 The treatment effect is small, however—3 points on a 70-point cognitive scale. Comparison studies show mixed results; no single agent appears to be most effective.12
Are cholinesterase inhibitors cost effective?
The relatively modest benefit of cholinesterase inhibitors—especially given their expense—has raised questions about cost effectiveness. When weighing the choice, consider that donepezil may delay nursing home placement,11,13 and the cholinesterase inhibitors may reduce caregiver burden.11 The medications are likely to be cost effective in patients showing a clinically significant response. More effective treatments would clearly be welcome.
Recommendations
The US Preventive Services Task Force (USPSTF) acknowledges that fair to good evidence supports a benefit from treatment of early-stage Alzheimer’s disease. However, routine screening for dementia in older adults receives an I-level recommendation (insufficient evidence), both because it’s unknown whether diagnosis would be as accurate and treatment as effective in primary care practices and because the benefit from screening is uncertain (coupled with a small treatment benefit).14
The task force reported finding no good data that treating MCI is beneficial. However, the USPSTF recommendation preceded publication of all 4 RCTs on treatment of MCI addressed in this Clinical Inquiry.
The American College of Physicians and American Academy of Family Physicians published a joint clinical practice guideline in March 2008 that questioned whether the slight benefit of cholinesterase inhibitors surpassed the harm of adverse effects and cost. They recommend counseling each patient about the likely benefits and harms.15
1. Geldmacher DS. Cost-effective recognition and diagnosis of dementia. Semin Neurol. 2002;22:63-70.
2. Balsis S, Carpenter BD, Storandt M. Personality change precedes clinical diagnosis of dementia of the Alzheimer type. J Gerontol B Psychol Sci Soc Sci. 2005;60:P98-P101.
3. Warner J, Butler R, Wuntakal B. What are the effects of treatments on cognitive symptoms of dementia? BMJ Clin Evid. 2008;01:1001-1028.
4. Lopez OL, Jagust WJ, DeKoskey ST, et al. Prevalence and classification of mild cognitive impairment in the Cardiovascular Health Study Cognition Study: part 1. Arch Neurol. 2003;60:1385-1389.
5. Petersen RC, Smith GE, Waring SC, et al. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56:303-308.
6. Petersen RC, Thomas RG, Grundman M, et al. Vitamin E and donepezil for the treatment of mild cognitive impairment. N Engl J Med. 2005;352:2379-2388.
7. Olazaran J, Muñiz R, Reisberg B, et al. Benefits of cognitive-motor intervention in MCI and mild to moderate Alzheimer disease. Neurology. 2004;63:2348-2353.
8. Koontz J, Baskys A. Effects of galantamine on working memory and global functioning in patients with mild cognitive impairment: a double-blind placebo-controlled study. Am J Alzheimers Dis Other Demen. 2005;20:295-302.
9. Larson EB, Wang L, Bowen JD, et al. Exercise is associated with reduced risk for incident dementia among persons 65 years of age and older. Ann Intern Med. 2006;144:73-81.
10. Ancelin ML, Artero S, Portet F, et al. Non-degenerative mild cognitive impairment in elderly people and use of anticholinergic drugs: longitudinal cohort study. BMJ. 2006;332:455-459.
11. Lanctot KL, Herrmann N, Yau KK, et al. Efficacy and safety of cholinesterase inhibitors in Alzheimer’s disease: a meta-analysis. CMAJ. 2003;169:557-564.
12. Santaguida PS, Raina P, Booker L, et al. Pharmacological treatment of dementia. Evidence Report/Technology Assessment No. 97 (prepared by McMaster University Evidence-based Practice Center under Contract No. 290-02-0020). AHRQ Publication No. 04-E019-2. Rockville, MD: Agency for Healthcare Research and Quality; April 2004.
13. Geldmacher DS, Provenzano G, McRae T, et al. Done-pezil is associated with delayed nursing home placement in patients with Alzheimer’s disease. J Am Geriatr Soc. 2003;51:937-944.
14. Boustani M, Peterson B, Hanson L, et al. Screening for dementia in primary care: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2003;138:927-937.
15. Qaseem A, Snow V, Cross JT, Jr, et al. Current pharmacologic treatment of dementia: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2008;148:370-378.
Yes, but the extent of the benefit is unclear. Treating patients with early-stage Alzheimer’s disease yields statistically significant, though perhaps not clinically significant, improvement in cognition and global function (strength of recommendation [SOR]: A, consistent evidence from multiple randomized controlled trials [RCTs]). In a few cases, it may delay loss of function and need for long-term care.
Treating patients with mild cognitive impairment (MCI)—the most likely precursor to Alzheimer’s disease—with cholinesterase inhibitors seems to have an initial, but perhaps unsustained, benefit over no treatment (SOR: B, inconsistent results from few trials). Withdrawing anticholinergic drugs from patients taking them promises to reduce symptoms of MCI, but is unlikely to reduce rates of Alzheimer’s (SOR: C, well-designed observational study).
Remember nondrug interventions
Jaqueline Raetz, MD
Departments of Family Medicine and Long-Term Care, University of Washington School of Medicine, Seattle
Clinicians often forget the many nonpharmacologic treatments for dementia, including exercise, cognitive stimulation, increased socialization, addressing polypharmacy, and optimizing nutrition. Diagnosing and managing comorbidities such as depression and cardiovascular disease are also important. Primary care physicians who care for the frail elderly should advocate these interventions. In the very elderly, who are all at high risk of developing Alzheimer’s disease, these measures may help prevent functional decline and reduce clinically apparent disease.
All patients diagnosed with early-stage Alzheimer’s disease, and possibly patients with MCI, should be offered a trial of pharmacotherapy. However—given the high cost of drug therapy, the modest improvement it produces in patients with Alzheimer’s dementia, and the lack of definitive evidence that it benefits patients with MCI—I wouldn’t advocate medication for asymptomatic patients at high risk of developing dementia.
Evidence summary
Alzheimer’s disease is characterized by deficits in memory and at least 1 other cognitive domain (aphrasia, apraxia, agnosia, or loss of executive function) accompanied by impaired function. As the US population ages, Alzheimer’s disease is likely to increase substantially in prevalence and cost, from its current 4.5 million people affected and $100 billion per year in direct expenses.1
Because the definition of Alzheimer’s precludes asymptomatic disease, “early” treatment implies either treating a precursor condition or treating before cognitive and functional impairment force the patient and family to seek medical care. The literature identifies 2 possible prodromal conditions: MCI and personality change. Personality change is proposed as a prodrome based only on a small study that diagnosed Alzheimer’s disease at autopsy, so this Clinical Inquiry doesn’t address it further.2
Therapy for MCI: A look at 3 interventions
MCI is a measurable memory deficit, more severe than normal aging changes (slower learning of new material and difficulty retrieving names and places) but not meeting criteria for dementia.3 Researchers differ on a more precise definition; some subdivide MCI into “MCI-amnestic type” and “MCI-multiple cognitive deficits type.”4 MCI progresses to Alzheimer’s disease in anywhere from 10% to 56% of patients.4,5
Three interventions may benefit patients with MCI:
- cholinesterase inhibitors
- exercise
- discontinuation of anticholinergic drugs in patients taking them.
Two recent RCTs of donepezil6,7 and 1 of galantamine8 showed initial cognitive improvement in MCI patients. However, the only trial carried out for 3 years showed no persistent benefit at that time.6
Another study showed that moderate exercise—30 minutes 3 days a week—improves cognition in MCI patients.9
A longitudinal cohort study found that patients taking anticholinergic drugs had an 80% prevalence of MCI, compared with a 35% prevalence in a matched population of patients not using these drugs; yet Alzheimer’s disease hadn’t increased among the anticholinergic drug users at 8-year follow-up. Attributable risk for MCI from anticholinergic drug use was 19%. Stopping anticholinergic medications may reduce the prevalence of MCI.10
In established Alzheimer’s disease, cholinesterase inhibitors statistically benefit patients with early and moderate disease and probably benefit patients with severe disease.11,12 The treatment effect is small, however—3 points on a 70-point cognitive scale. Comparison studies show mixed results; no single agent appears to be most effective.12
Are cholinesterase inhibitors cost effective?
The relatively modest benefit of cholinesterase inhibitors—especially given their expense—has raised questions about cost effectiveness. When weighing the choice, consider that donepezil may delay nursing home placement,11,13 and the cholinesterase inhibitors may reduce caregiver burden.11 The medications are likely to be cost effective in patients showing a clinically significant response. More effective treatments would clearly be welcome.
Recommendations
The US Preventive Services Task Force (USPSTF) acknowledges that fair to good evidence supports a benefit from treatment of early-stage Alzheimer’s disease. However, routine screening for dementia in older adults receives an I-level recommendation (insufficient evidence), both because it’s unknown whether diagnosis would be as accurate and treatment as effective in primary care practices and because the benefit from screening is uncertain (coupled with a small treatment benefit).14
The task force reported finding no good data that treating MCI is beneficial. However, the USPSTF recommendation preceded publication of all 4 RCTs on treatment of MCI addressed in this Clinical Inquiry.
The American College of Physicians and American Academy of Family Physicians published a joint clinical practice guideline in March 2008 that questioned whether the slight benefit of cholinesterase inhibitors surpassed the harm of adverse effects and cost. They recommend counseling each patient about the likely benefits and harms.15
Yes, but the extent of the benefit is unclear. Treating patients with early-stage Alzheimer’s disease yields statistically significant, though perhaps not clinically significant, improvement in cognition and global function (strength of recommendation [SOR]: A, consistent evidence from multiple randomized controlled trials [RCTs]). In a few cases, it may delay loss of function and need for long-term care.
Treating patients with mild cognitive impairment (MCI)—the most likely precursor to Alzheimer’s disease—with cholinesterase inhibitors seems to have an initial, but perhaps unsustained, benefit over no treatment (SOR: B, inconsistent results from few trials). Withdrawing anticholinergic drugs from patients taking them promises to reduce symptoms of MCI, but is unlikely to reduce rates of Alzheimer’s (SOR: C, well-designed observational study).
Remember nondrug interventions
Jaqueline Raetz, MD
Departments of Family Medicine and Long-Term Care, University of Washington School of Medicine, Seattle
Clinicians often forget the many nonpharmacologic treatments for dementia, including exercise, cognitive stimulation, increased socialization, addressing polypharmacy, and optimizing nutrition. Diagnosing and managing comorbidities such as depression and cardiovascular disease are also important. Primary care physicians who care for the frail elderly should advocate these interventions. In the very elderly, who are all at high risk of developing Alzheimer’s disease, these measures may help prevent functional decline and reduce clinically apparent disease.
All patients diagnosed with early-stage Alzheimer’s disease, and possibly patients with MCI, should be offered a trial of pharmacotherapy. However—given the high cost of drug therapy, the modest improvement it produces in patients with Alzheimer’s dementia, and the lack of definitive evidence that it benefits patients with MCI—I wouldn’t advocate medication for asymptomatic patients at high risk of developing dementia.
Evidence summary
Alzheimer’s disease is characterized by deficits in memory and at least 1 other cognitive domain (aphrasia, apraxia, agnosia, or loss of executive function) accompanied by impaired function. As the US population ages, Alzheimer’s disease is likely to increase substantially in prevalence and cost, from its current 4.5 million people affected and $100 billion per year in direct expenses.1
Because the definition of Alzheimer’s precludes asymptomatic disease, “early” treatment implies either treating a precursor condition or treating before cognitive and functional impairment force the patient and family to seek medical care. The literature identifies 2 possible prodromal conditions: MCI and personality change. Personality change is proposed as a prodrome based only on a small study that diagnosed Alzheimer’s disease at autopsy, so this Clinical Inquiry doesn’t address it further.2
Therapy for MCI: A look at 3 interventions
MCI is a measurable memory deficit, more severe than normal aging changes (slower learning of new material and difficulty retrieving names and places) but not meeting criteria for dementia.3 Researchers differ on a more precise definition; some subdivide MCI into “MCI-amnestic type” and “MCI-multiple cognitive deficits type.”4 MCI progresses to Alzheimer’s disease in anywhere from 10% to 56% of patients.4,5
Three interventions may benefit patients with MCI:
- cholinesterase inhibitors
- exercise
- discontinuation of anticholinergic drugs in patients taking them.
Two recent RCTs of donepezil6,7 and 1 of galantamine8 showed initial cognitive improvement in MCI patients. However, the only trial carried out for 3 years showed no persistent benefit at that time.6
Another study showed that moderate exercise—30 minutes 3 days a week—improves cognition in MCI patients.9
A longitudinal cohort study found that patients taking anticholinergic drugs had an 80% prevalence of MCI, compared with a 35% prevalence in a matched population of patients not using these drugs; yet Alzheimer’s disease hadn’t increased among the anticholinergic drug users at 8-year follow-up. Attributable risk for MCI from anticholinergic drug use was 19%. Stopping anticholinergic medications may reduce the prevalence of MCI.10
In established Alzheimer’s disease, cholinesterase inhibitors statistically benefit patients with early and moderate disease and probably benefit patients with severe disease.11,12 The treatment effect is small, however—3 points on a 70-point cognitive scale. Comparison studies show mixed results; no single agent appears to be most effective.12
Are cholinesterase inhibitors cost effective?
The relatively modest benefit of cholinesterase inhibitors—especially given their expense—has raised questions about cost effectiveness. When weighing the choice, consider that donepezil may delay nursing home placement,11,13 and the cholinesterase inhibitors may reduce caregiver burden.11 The medications are likely to be cost effective in patients showing a clinically significant response. More effective treatments would clearly be welcome.
Recommendations
The US Preventive Services Task Force (USPSTF) acknowledges that fair to good evidence supports a benefit from treatment of early-stage Alzheimer’s disease. However, routine screening for dementia in older adults receives an I-level recommendation (insufficient evidence), both because it’s unknown whether diagnosis would be as accurate and treatment as effective in primary care practices and because the benefit from screening is uncertain (coupled with a small treatment benefit).14
The task force reported finding no good data that treating MCI is beneficial. However, the USPSTF recommendation preceded publication of all 4 RCTs on treatment of MCI addressed in this Clinical Inquiry.
The American College of Physicians and American Academy of Family Physicians published a joint clinical practice guideline in March 2008 that questioned whether the slight benefit of cholinesterase inhibitors surpassed the harm of adverse effects and cost. They recommend counseling each patient about the likely benefits and harms.15
1. Geldmacher DS. Cost-effective recognition and diagnosis of dementia. Semin Neurol. 2002;22:63-70.
2. Balsis S, Carpenter BD, Storandt M. Personality change precedes clinical diagnosis of dementia of the Alzheimer type. J Gerontol B Psychol Sci Soc Sci. 2005;60:P98-P101.
3. Warner J, Butler R, Wuntakal B. What are the effects of treatments on cognitive symptoms of dementia? BMJ Clin Evid. 2008;01:1001-1028.
4. Lopez OL, Jagust WJ, DeKoskey ST, et al. Prevalence and classification of mild cognitive impairment in the Cardiovascular Health Study Cognition Study: part 1. Arch Neurol. 2003;60:1385-1389.
5. Petersen RC, Smith GE, Waring SC, et al. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56:303-308.
6. Petersen RC, Thomas RG, Grundman M, et al. Vitamin E and donepezil for the treatment of mild cognitive impairment. N Engl J Med. 2005;352:2379-2388.
7. Olazaran J, Muñiz R, Reisberg B, et al. Benefits of cognitive-motor intervention in MCI and mild to moderate Alzheimer disease. Neurology. 2004;63:2348-2353.
8. Koontz J, Baskys A. Effects of galantamine on working memory and global functioning in patients with mild cognitive impairment: a double-blind placebo-controlled study. Am J Alzheimers Dis Other Demen. 2005;20:295-302.
9. Larson EB, Wang L, Bowen JD, et al. Exercise is associated with reduced risk for incident dementia among persons 65 years of age and older. Ann Intern Med. 2006;144:73-81.
10. Ancelin ML, Artero S, Portet F, et al. Non-degenerative mild cognitive impairment in elderly people and use of anticholinergic drugs: longitudinal cohort study. BMJ. 2006;332:455-459.
11. Lanctot KL, Herrmann N, Yau KK, et al. Efficacy and safety of cholinesterase inhibitors in Alzheimer’s disease: a meta-analysis. CMAJ. 2003;169:557-564.
12. Santaguida PS, Raina P, Booker L, et al. Pharmacological treatment of dementia. Evidence Report/Technology Assessment No. 97 (prepared by McMaster University Evidence-based Practice Center under Contract No. 290-02-0020). AHRQ Publication No. 04-E019-2. Rockville, MD: Agency for Healthcare Research and Quality; April 2004.
13. Geldmacher DS, Provenzano G, McRae T, et al. Done-pezil is associated with delayed nursing home placement in patients with Alzheimer’s disease. J Am Geriatr Soc. 2003;51:937-944.
14. Boustani M, Peterson B, Hanson L, et al. Screening for dementia in primary care: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2003;138:927-937.
15. Qaseem A, Snow V, Cross JT, Jr, et al. Current pharmacologic treatment of dementia: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2008;148:370-378.
1. Geldmacher DS. Cost-effective recognition and diagnosis of dementia. Semin Neurol. 2002;22:63-70.
2. Balsis S, Carpenter BD, Storandt M. Personality change precedes clinical diagnosis of dementia of the Alzheimer type. J Gerontol B Psychol Sci Soc Sci. 2005;60:P98-P101.
3. Warner J, Butler R, Wuntakal B. What are the effects of treatments on cognitive symptoms of dementia? BMJ Clin Evid. 2008;01:1001-1028.
4. Lopez OL, Jagust WJ, DeKoskey ST, et al. Prevalence and classification of mild cognitive impairment in the Cardiovascular Health Study Cognition Study: part 1. Arch Neurol. 2003;60:1385-1389.
5. Petersen RC, Smith GE, Waring SC, et al. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56:303-308.
6. Petersen RC, Thomas RG, Grundman M, et al. Vitamin E and donepezil for the treatment of mild cognitive impairment. N Engl J Med. 2005;352:2379-2388.
7. Olazaran J, Muñiz R, Reisberg B, et al. Benefits of cognitive-motor intervention in MCI and mild to moderate Alzheimer disease. Neurology. 2004;63:2348-2353.
8. Koontz J, Baskys A. Effects of galantamine on working memory and global functioning in patients with mild cognitive impairment: a double-blind placebo-controlled study. Am J Alzheimers Dis Other Demen. 2005;20:295-302.
9. Larson EB, Wang L, Bowen JD, et al. Exercise is associated with reduced risk for incident dementia among persons 65 years of age and older. Ann Intern Med. 2006;144:73-81.
10. Ancelin ML, Artero S, Portet F, et al. Non-degenerative mild cognitive impairment in elderly people and use of anticholinergic drugs: longitudinal cohort study. BMJ. 2006;332:455-459.
11. Lanctot KL, Herrmann N, Yau KK, et al. Efficacy and safety of cholinesterase inhibitors in Alzheimer’s disease: a meta-analysis. CMAJ. 2003;169:557-564.
12. Santaguida PS, Raina P, Booker L, et al. Pharmacological treatment of dementia. Evidence Report/Technology Assessment No. 97 (prepared by McMaster University Evidence-based Practice Center under Contract No. 290-02-0020). AHRQ Publication No. 04-E019-2. Rockville, MD: Agency for Healthcare Research and Quality; April 2004.
13. Geldmacher DS, Provenzano G, McRae T, et al. Done-pezil is associated with delayed nursing home placement in patients with Alzheimer’s disease. J Am Geriatr Soc. 2003;51:937-944.
14. Boustani M, Peterson B, Hanson L, et al. Screening for dementia in primary care: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2003;138:927-937.
15. Qaseem A, Snow V, Cross JT, Jr, et al. Current pharmacologic treatment of dementia: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2008;148:370-378.
Evidence-based answers from the Family Physicians Inquiries Network
Do hyaluronic acid injections relieve OA knee pain?
Yes, hyaluronic acid (HA) injections relieve pain more than placebo. The effect is small but similar to results from oral nonsteroidal anti-inflammatory drugs (NSAIDs) or steroid injection (strength of recommendation ([SOR]: B, conflicting meta-analyses). The various HA products all appear to be equally effective in reducing pain (SOR: B, randomized clinical trials [RCTs]). Data concerning the effect of HA on functional ability are conflicting.
Evidence summary
A 2005 meta-analysis evaluated the effectiveness of HA injections for osteoarthritis of the knee compared with saline placebo. Researchers identified 22 studies of 8 HA products that used the common end point of pain with movement.1 (TABLE 1 lists FDA-approved HA products available in the United States.2) A decrease in pain of 15% was deemed clinically meaningful.
Compared with placebo, the mean difference in pain scores with HA products was -4% (95% confidence interval [CI], -9% to 1%) after 2 to 6 weeks; -4% (95% CI, -8% to -1%) after 10 to 14 weeks; and -7% (95% CI, -12% to -2%) after 22 to 30 weeks. The authors note that the small measured effect of HA was magnified by trials that didn’t report intention-to-treat results. The effect of HA was also larger in studies that didn’t conceal allocation. A weakness of the analysis was its inability to assess potential differences between HA products.
In this 2005 meta-analysis, HA injection didn’t improve knee function in any time interval. But in a Cochrane meta-analysis conducted the following year, HA was found to have positive results.3
TABLE 1
FDA-approved hyaluronic acid products
| TRADE NAME | COMPOSITION | MOLECULAR WEIGHT (×106 DALTONS) | COST PER INJECTION* (3-5 DOSES) | SOURCE |
|---|---|---|---|---|
| Hyalgan | Sodium hyaluronate | 0.5-0.7 | $138 | Avian |
| Supartz | Sodium hyaluronate | 0.6-1.2 | $136 | Avian |
| Euflexxa | Sodium hyaluronate | 2.4-3.6 | $133 | Bacterial |
| Orthovisc | Hyaluronin | 1.0-2.9 | $238 | Avian |
| Synvisc | Hylan G-F 20 | 6.0 | $230 | Avian |
HA relieves pain about as much as NSAIDs
The comprehensive 2006 Cochrane meta-analysis reviewed single- and double-blinded RCTs that evaluated the effect of 12 HA products on osteoarthritis of the knee.3 Studies compared HA products with placebo (40), intra-articular steroids (10), NSAIDs (6), physical therapy (3), exercise (2), and each other (15). Efficacy data for different products couldn’t be combined because the studies measured different sets of outcomes at different time points.
Overall, the authors concluded that HA injections effectively reduced pain scores, with the largest benefit occurring within 5 to 13 weeks (TABLE 2). The authors also noted that the reductions in pain with HA injections, although generally small, were comparable to oral NSAID therapy and intra-articular corticosteroids. The trials reported few adverse events.
Two RCTs show no difference in efficacy among HA products
The Cochrane review determined that not enough evidence existed to evaluate HA products against each other. Two subsequent RCTs compared HA products and found no differences in efficacy. One study compared Synvisc, Orthovisc, and Ostenil therapy in 660 patients over 6 months.4 The other compared Synvisc with Euflexxa in 321 patients over 3 months.5 Notably, 8% of patients in this study who used Synvisc developed an effusion, compared with 0.6% of patients who used Euflexxa (P=.0015).
Recommendations
A 2007 report from the Agency for Healthcare Research and Quality (AHRQ) states that “viscosupplementation trials generally report positive effects on pain and function scores compared with placebo, but the evidence on clinical benefit is uncertain.”6
The 2007 guidelines of the Institute for Clinical Systems Improvement note that synthetic hyaluronates “may be effective” in selected patients with mild to moderate degenerative joint disease (based on evidence of middle quality on a 3-tier grading system).7
The American Academy of Orthopaedic Surgeons 2008 guideline on osteoarthritis of the knee indicates that, based on the AHRQ report,6 it cannot recommend for or against the use of intra-articular hyaluronic acid for mild to moderate symptomatic OA of the knee.8
TABLE 2
How HA products affect pain measures
| AT 1-4 WEKS | AT 5-13 WEKS | |||||
|---|---|---|---|---|---|---|
| PRODUCT | COMPARATOR | OUTCOME | N | PERCENT CHANGE VS COMPARATOR* (95% CI) | N | PERCENT CHANGE VS COMPARATOR* (95% CI) |
| HA/hyalin | Placebo | Pain on weight bearing | 2542 | -8 (-11 to -4) | 2090 | -13 (-18 to -8) |
| Hyalgan | Placebo | Pain on weight bearing | 1398 | -6 (-11 to -1) | 1095 | -9 (-14 to -4) |
| Synvisc | Placebo | Pain on weight bearing | 481 | -13 (-20 to -5) | 155 | -10 (-14 to -5) |
| Suplasyn | Placebo | WOMAC pain | 53 | NS | (Data not available) | |
| Durolane | Placebo | WOMAC pain | 346 | 4 (0 to 7) | 436 | NS |
| Orthovisc | Placebo | WOMAC pain | 110 | -12 (-13 to -10) | 69 | -5 (-7 to -4) |
| HA/hyalin | NSAID | Pain after walking | 333 | NS | (Data not available) | |
| Hyalgan | NSAID | Pain after 50-foot walk | 279 | NS | 140 | NS |
| Synvisc | NSAID | Pain at rest | (Data not available) | 57 | NS | |
| Suplasyn | NSAID | Pain after walking | 54 | NS | (Data not available) | |
| Hyalgan | Methylprednisolone | Spontaneous pain | 170 | NS | 170 | -8 (-13 to -3) |
| Synvisc | Triamcinolone | WOMAC pain, walking | (Data not available) | 215 | -10 (-17 to -3) | |
| Orthovisc | Methylprednisolone | Pain, walking | 55 | NS | 55 | -18 (-29 to -8) |
| Us medications Supartz and Euflexxa were not included in the Cochrane review. | ||||||
| CI, confidence interval; HA, hyaluronic acid; NS, not statistically significant; NSAID, nonsteroidal anti-inflammatory drug; WOMAC, Western Ontario and MacMaster universities Osteoarthritis Index. | ||||||
| *Negative values favor HA products. | ||||||
| Source: Bellamy n, et al. Cochrane Database Syst. Rev. 2006.3 | ||||||
1. Arrich J, Piribauer F, Mad P, et al. Intra-articular hyaluronic acid for the treatment of osteoarthritis of the knee: systematic review and meta-analysis. CMAJ 2005;172:1239-1242.
2. Waddell DD. viscosupplementation with hyaluronans for osteoarthritis of the knee: clinical efficacy and economic implications. Drugs Aging 2007;24:629-642.
3. Bellamy N, Campbell J, Robinson V, et al. viscosupplementation for the treatment of osteoarthritis of the knee. Cochrane Database Syst Rev. 2006;(2):CD005321.
4. Jüni P, Reichenbach S, Trelle S, et al. efficacy and safety of intra-articular hylan or hyaluronic acids for osteoarthritis of the knee: a randomized controlled trial. Arthritis Rheum. 2007;54:3610-3619.
5. Kirchner M, Marshall D. A double-blind, randomized, controlled trial comparing alternate forms of high molecular weight hyaluronan for the treatment of osteoarthritis of the knee. Osteoarthritis Cartilage. 2006;14:154-162.
6. Samson DJ, Grant MD, Ratko TA, et al. Treatment of primary and secondary osteoarthritis of the knee. evidence report/Technology Assessment no. 157 (prepared by Blue Cross and Blue shield Association Technology evaluation Center evidence-based Practice Center under Contract no. 290-02-0026). AHrq Publication no. 07-e012. rockville, Md: Agency for Healthcare research and quality. september 2007. Available at: www.ahrq.gov/clinic/tp/oakneetp.htm. Accessed February 11, 2009.
7. Institute for Clinical systems Improvement. Diagnosis and treatment of adult degenerative joint disease (DJD)/osteoarthritis (OA) of the knee. Bloomington, Minn: Institute for Clinical systems Improvement; 2007.
8. American Academy of Orthopaedic surgeons. Clinical Practice Guideline: Treatment of Osteoarthritis of the Knee (Non-Arthroplasty). rosemont, Ill: American Academy of Orthopaedic surgeons; 2008. Available at: www.aaos.org/research/guidelines/GuidelineOAKnee.asp. Accessed April 21, 2009.
Yes, hyaluronic acid (HA) injections relieve pain more than placebo. The effect is small but similar to results from oral nonsteroidal anti-inflammatory drugs (NSAIDs) or steroid injection (strength of recommendation ([SOR]: B, conflicting meta-analyses). The various HA products all appear to be equally effective in reducing pain (SOR: B, randomized clinical trials [RCTs]). Data concerning the effect of HA on functional ability are conflicting.
Evidence summary
A 2005 meta-analysis evaluated the effectiveness of HA injections for osteoarthritis of the knee compared with saline placebo. Researchers identified 22 studies of 8 HA products that used the common end point of pain with movement.1 (TABLE 1 lists FDA-approved HA products available in the United States.2) A decrease in pain of 15% was deemed clinically meaningful.
Compared with placebo, the mean difference in pain scores with HA products was -4% (95% confidence interval [CI], -9% to 1%) after 2 to 6 weeks; -4% (95% CI, -8% to -1%) after 10 to 14 weeks; and -7% (95% CI, -12% to -2%) after 22 to 30 weeks. The authors note that the small measured effect of HA was magnified by trials that didn’t report intention-to-treat results. The effect of HA was also larger in studies that didn’t conceal allocation. A weakness of the analysis was its inability to assess potential differences between HA products.
In this 2005 meta-analysis, HA injection didn’t improve knee function in any time interval. But in a Cochrane meta-analysis conducted the following year, HA was found to have positive results.3
TABLE 1
FDA-approved hyaluronic acid products
| TRADE NAME | COMPOSITION | MOLECULAR WEIGHT (×106 DALTONS) | COST PER INJECTION* (3-5 DOSES) | SOURCE |
|---|---|---|---|---|
| Hyalgan | Sodium hyaluronate | 0.5-0.7 | $138 | Avian |
| Supartz | Sodium hyaluronate | 0.6-1.2 | $136 | Avian |
| Euflexxa | Sodium hyaluronate | 2.4-3.6 | $133 | Bacterial |
| Orthovisc | Hyaluronin | 1.0-2.9 | $238 | Avian |
| Synvisc | Hylan G-F 20 | 6.0 | $230 | Avian |
HA relieves pain about as much as NSAIDs
The comprehensive 2006 Cochrane meta-analysis reviewed single- and double-blinded RCTs that evaluated the effect of 12 HA products on osteoarthritis of the knee.3 Studies compared HA products with placebo (40), intra-articular steroids (10), NSAIDs (6), physical therapy (3), exercise (2), and each other (15). Efficacy data for different products couldn’t be combined because the studies measured different sets of outcomes at different time points.
Overall, the authors concluded that HA injections effectively reduced pain scores, with the largest benefit occurring within 5 to 13 weeks (TABLE 2). The authors also noted that the reductions in pain with HA injections, although generally small, were comparable to oral NSAID therapy and intra-articular corticosteroids. The trials reported few adverse events.
Two RCTs show no difference in efficacy among HA products
The Cochrane review determined that not enough evidence existed to evaluate HA products against each other. Two subsequent RCTs compared HA products and found no differences in efficacy. One study compared Synvisc, Orthovisc, and Ostenil therapy in 660 patients over 6 months.4 The other compared Synvisc with Euflexxa in 321 patients over 3 months.5 Notably, 8% of patients in this study who used Synvisc developed an effusion, compared with 0.6% of patients who used Euflexxa (P=.0015).
Recommendations
A 2007 report from the Agency for Healthcare Research and Quality (AHRQ) states that “viscosupplementation trials generally report positive effects on pain and function scores compared with placebo, but the evidence on clinical benefit is uncertain.”6
The 2007 guidelines of the Institute for Clinical Systems Improvement note that synthetic hyaluronates “may be effective” in selected patients with mild to moderate degenerative joint disease (based on evidence of middle quality on a 3-tier grading system).7
The American Academy of Orthopaedic Surgeons 2008 guideline on osteoarthritis of the knee indicates that, based on the AHRQ report,6 it cannot recommend for or against the use of intra-articular hyaluronic acid for mild to moderate symptomatic OA of the knee.8
TABLE 2
How HA products affect pain measures
| AT 1-4 WEKS | AT 5-13 WEKS | |||||
|---|---|---|---|---|---|---|
| PRODUCT | COMPARATOR | OUTCOME | N | PERCENT CHANGE VS COMPARATOR* (95% CI) | N | PERCENT CHANGE VS COMPARATOR* (95% CI) |
| HA/hyalin | Placebo | Pain on weight bearing | 2542 | -8 (-11 to -4) | 2090 | -13 (-18 to -8) |
| Hyalgan | Placebo | Pain on weight bearing | 1398 | -6 (-11 to -1) | 1095 | -9 (-14 to -4) |
| Synvisc | Placebo | Pain on weight bearing | 481 | -13 (-20 to -5) | 155 | -10 (-14 to -5) |
| Suplasyn | Placebo | WOMAC pain | 53 | NS | (Data not available) | |
| Durolane | Placebo | WOMAC pain | 346 | 4 (0 to 7) | 436 | NS |
| Orthovisc | Placebo | WOMAC pain | 110 | -12 (-13 to -10) | 69 | -5 (-7 to -4) |
| HA/hyalin | NSAID | Pain after walking | 333 | NS | (Data not available) | |
| Hyalgan | NSAID | Pain after 50-foot walk | 279 | NS | 140 | NS |
| Synvisc | NSAID | Pain at rest | (Data not available) | 57 | NS | |
| Suplasyn | NSAID | Pain after walking | 54 | NS | (Data not available) | |
| Hyalgan | Methylprednisolone | Spontaneous pain | 170 | NS | 170 | -8 (-13 to -3) |
| Synvisc | Triamcinolone | WOMAC pain, walking | (Data not available) | 215 | -10 (-17 to -3) | |
| Orthovisc | Methylprednisolone | Pain, walking | 55 | NS | 55 | -18 (-29 to -8) |
| Us medications Supartz and Euflexxa were not included in the Cochrane review. | ||||||
| CI, confidence interval; HA, hyaluronic acid; NS, not statistically significant; NSAID, nonsteroidal anti-inflammatory drug; WOMAC, Western Ontario and MacMaster universities Osteoarthritis Index. | ||||||
| *Negative values favor HA products. | ||||||
| Source: Bellamy n, et al. Cochrane Database Syst. Rev. 2006.3 | ||||||
Yes, hyaluronic acid (HA) injections relieve pain more than placebo. The effect is small but similar to results from oral nonsteroidal anti-inflammatory drugs (NSAIDs) or steroid injection (strength of recommendation ([SOR]: B, conflicting meta-analyses). The various HA products all appear to be equally effective in reducing pain (SOR: B, randomized clinical trials [RCTs]). Data concerning the effect of HA on functional ability are conflicting.
Evidence summary
A 2005 meta-analysis evaluated the effectiveness of HA injections for osteoarthritis of the knee compared with saline placebo. Researchers identified 22 studies of 8 HA products that used the common end point of pain with movement.1 (TABLE 1 lists FDA-approved HA products available in the United States.2) A decrease in pain of 15% was deemed clinically meaningful.
Compared with placebo, the mean difference in pain scores with HA products was -4% (95% confidence interval [CI], -9% to 1%) after 2 to 6 weeks; -4% (95% CI, -8% to -1%) after 10 to 14 weeks; and -7% (95% CI, -12% to -2%) after 22 to 30 weeks. The authors note that the small measured effect of HA was magnified by trials that didn’t report intention-to-treat results. The effect of HA was also larger in studies that didn’t conceal allocation. A weakness of the analysis was its inability to assess potential differences between HA products.
In this 2005 meta-analysis, HA injection didn’t improve knee function in any time interval. But in a Cochrane meta-analysis conducted the following year, HA was found to have positive results.3
TABLE 1
FDA-approved hyaluronic acid products
| TRADE NAME | COMPOSITION | MOLECULAR WEIGHT (×106 DALTONS) | COST PER INJECTION* (3-5 DOSES) | SOURCE |
|---|---|---|---|---|
| Hyalgan | Sodium hyaluronate | 0.5-0.7 | $138 | Avian |
| Supartz | Sodium hyaluronate | 0.6-1.2 | $136 | Avian |
| Euflexxa | Sodium hyaluronate | 2.4-3.6 | $133 | Bacterial |
| Orthovisc | Hyaluronin | 1.0-2.9 | $238 | Avian |
| Synvisc | Hylan G-F 20 | 6.0 | $230 | Avian |
HA relieves pain about as much as NSAIDs
The comprehensive 2006 Cochrane meta-analysis reviewed single- and double-blinded RCTs that evaluated the effect of 12 HA products on osteoarthritis of the knee.3 Studies compared HA products with placebo (40), intra-articular steroids (10), NSAIDs (6), physical therapy (3), exercise (2), and each other (15). Efficacy data for different products couldn’t be combined because the studies measured different sets of outcomes at different time points.
Overall, the authors concluded that HA injections effectively reduced pain scores, with the largest benefit occurring within 5 to 13 weeks (TABLE 2). The authors also noted that the reductions in pain with HA injections, although generally small, were comparable to oral NSAID therapy and intra-articular corticosteroids. The trials reported few adverse events.
Two RCTs show no difference in efficacy among HA products
The Cochrane review determined that not enough evidence existed to evaluate HA products against each other. Two subsequent RCTs compared HA products and found no differences in efficacy. One study compared Synvisc, Orthovisc, and Ostenil therapy in 660 patients over 6 months.4 The other compared Synvisc with Euflexxa in 321 patients over 3 months.5 Notably, 8% of patients in this study who used Synvisc developed an effusion, compared with 0.6% of patients who used Euflexxa (P=.0015).
Recommendations
A 2007 report from the Agency for Healthcare Research and Quality (AHRQ) states that “viscosupplementation trials generally report positive effects on pain and function scores compared with placebo, but the evidence on clinical benefit is uncertain.”6
The 2007 guidelines of the Institute for Clinical Systems Improvement note that synthetic hyaluronates “may be effective” in selected patients with mild to moderate degenerative joint disease (based on evidence of middle quality on a 3-tier grading system).7
The American Academy of Orthopaedic Surgeons 2008 guideline on osteoarthritis of the knee indicates that, based on the AHRQ report,6 it cannot recommend for or against the use of intra-articular hyaluronic acid for mild to moderate symptomatic OA of the knee.8
TABLE 2
How HA products affect pain measures
| AT 1-4 WEKS | AT 5-13 WEKS | |||||
|---|---|---|---|---|---|---|
| PRODUCT | COMPARATOR | OUTCOME | N | PERCENT CHANGE VS COMPARATOR* (95% CI) | N | PERCENT CHANGE VS COMPARATOR* (95% CI) |
| HA/hyalin | Placebo | Pain on weight bearing | 2542 | -8 (-11 to -4) | 2090 | -13 (-18 to -8) |
| Hyalgan | Placebo | Pain on weight bearing | 1398 | -6 (-11 to -1) | 1095 | -9 (-14 to -4) |
| Synvisc | Placebo | Pain on weight bearing | 481 | -13 (-20 to -5) | 155 | -10 (-14 to -5) |
| Suplasyn | Placebo | WOMAC pain | 53 | NS | (Data not available) | |
| Durolane | Placebo | WOMAC pain | 346 | 4 (0 to 7) | 436 | NS |
| Orthovisc | Placebo | WOMAC pain | 110 | -12 (-13 to -10) | 69 | -5 (-7 to -4) |
| HA/hyalin | NSAID | Pain after walking | 333 | NS | (Data not available) | |
| Hyalgan | NSAID | Pain after 50-foot walk | 279 | NS | 140 | NS |
| Synvisc | NSAID | Pain at rest | (Data not available) | 57 | NS | |
| Suplasyn | NSAID | Pain after walking | 54 | NS | (Data not available) | |
| Hyalgan | Methylprednisolone | Spontaneous pain | 170 | NS | 170 | -8 (-13 to -3) |
| Synvisc | Triamcinolone | WOMAC pain, walking | (Data not available) | 215 | -10 (-17 to -3) | |
| Orthovisc | Methylprednisolone | Pain, walking | 55 | NS | 55 | -18 (-29 to -8) |
| Us medications Supartz and Euflexxa were not included in the Cochrane review. | ||||||
| CI, confidence interval; HA, hyaluronic acid; NS, not statistically significant; NSAID, nonsteroidal anti-inflammatory drug; WOMAC, Western Ontario and MacMaster universities Osteoarthritis Index. | ||||||
| *Negative values favor HA products. | ||||||
| Source: Bellamy n, et al. Cochrane Database Syst. Rev. 2006.3 | ||||||
1. Arrich J, Piribauer F, Mad P, et al. Intra-articular hyaluronic acid for the treatment of osteoarthritis of the knee: systematic review and meta-analysis. CMAJ 2005;172:1239-1242.
2. Waddell DD. viscosupplementation with hyaluronans for osteoarthritis of the knee: clinical efficacy and economic implications. Drugs Aging 2007;24:629-642.
3. Bellamy N, Campbell J, Robinson V, et al. viscosupplementation for the treatment of osteoarthritis of the knee. Cochrane Database Syst Rev. 2006;(2):CD005321.
4. Jüni P, Reichenbach S, Trelle S, et al. efficacy and safety of intra-articular hylan or hyaluronic acids for osteoarthritis of the knee: a randomized controlled trial. Arthritis Rheum. 2007;54:3610-3619.
5. Kirchner M, Marshall D. A double-blind, randomized, controlled trial comparing alternate forms of high molecular weight hyaluronan for the treatment of osteoarthritis of the knee. Osteoarthritis Cartilage. 2006;14:154-162.
6. Samson DJ, Grant MD, Ratko TA, et al. Treatment of primary and secondary osteoarthritis of the knee. evidence report/Technology Assessment no. 157 (prepared by Blue Cross and Blue shield Association Technology evaluation Center evidence-based Practice Center under Contract no. 290-02-0026). AHrq Publication no. 07-e012. rockville, Md: Agency for Healthcare research and quality. september 2007. Available at: www.ahrq.gov/clinic/tp/oakneetp.htm. Accessed February 11, 2009.
7. Institute for Clinical systems Improvement. Diagnosis and treatment of adult degenerative joint disease (DJD)/osteoarthritis (OA) of the knee. Bloomington, Minn: Institute for Clinical systems Improvement; 2007.
8. American Academy of Orthopaedic surgeons. Clinical Practice Guideline: Treatment of Osteoarthritis of the Knee (Non-Arthroplasty). rosemont, Ill: American Academy of Orthopaedic surgeons; 2008. Available at: www.aaos.org/research/guidelines/GuidelineOAKnee.asp. Accessed April 21, 2009.
1. Arrich J, Piribauer F, Mad P, et al. Intra-articular hyaluronic acid for the treatment of osteoarthritis of the knee: systematic review and meta-analysis. CMAJ 2005;172:1239-1242.
2. Waddell DD. viscosupplementation with hyaluronans for osteoarthritis of the knee: clinical efficacy and economic implications. Drugs Aging 2007;24:629-642.
3. Bellamy N, Campbell J, Robinson V, et al. viscosupplementation for the treatment of osteoarthritis of the knee. Cochrane Database Syst Rev. 2006;(2):CD005321.
4. Jüni P, Reichenbach S, Trelle S, et al. efficacy and safety of intra-articular hylan or hyaluronic acids for osteoarthritis of the knee: a randomized controlled trial. Arthritis Rheum. 2007;54:3610-3619.
5. Kirchner M, Marshall D. A double-blind, randomized, controlled trial comparing alternate forms of high molecular weight hyaluronan for the treatment of osteoarthritis of the knee. Osteoarthritis Cartilage. 2006;14:154-162.
6. Samson DJ, Grant MD, Ratko TA, et al. Treatment of primary and secondary osteoarthritis of the knee. evidence report/Technology Assessment no. 157 (prepared by Blue Cross and Blue shield Association Technology evaluation Center evidence-based Practice Center under Contract no. 290-02-0026). AHrq Publication no. 07-e012. rockville, Md: Agency for Healthcare research and quality. september 2007. Available at: www.ahrq.gov/clinic/tp/oakneetp.htm. Accessed February 11, 2009.
7. Institute for Clinical systems Improvement. Diagnosis and treatment of adult degenerative joint disease (DJD)/osteoarthritis (OA) of the knee. Bloomington, Minn: Institute for Clinical systems Improvement; 2007.
8. American Academy of Orthopaedic surgeons. Clinical Practice Guideline: Treatment of Osteoarthritis of the Knee (Non-Arthroplasty). rosemont, Ill: American Academy of Orthopaedic surgeons; 2008. Available at: www.aaos.org/research/guidelines/GuidelineOAKnee.asp. Accessed April 21, 2009.
Evidence-based answers from the Family Physicians Inquiries Network
What’s the most practical way to rule out adrenal insufficiency?
A morning serum cortisol level >13 mcg/dL reliably rules out adrenal insufficiency, and the test is easy and safe to perform. Because of low specificity, patients with a level of ≤13 mcg/dL need further evaluation with the cosyntropin stimulation test (CST) (strength of recommendation [SOR]: A, meta-analysis of diagnostic cohort studies).
The 250 mcg CST requires intravenous (IV) or intramuscular (IM) administration of cosyntropin and multiple blood draws; a normal response reliably rules out primary adrenal insufficiency (SOR: B, meta-analysis of lower-quality diagnostic cohort studies) and moderately decreases the likelihood of secondary adrenal insufficiency (SOR: A, meta-analysis of diagnostic cohort studies). The 1 mcg CST has better diagnostic discrimination, but requires an extra step to dilute the cosyntropin (SOR: A, meta-analysis of diagnostic cohort studies).
Evidence summary
The morning serum cortisol level is the most convenient test for adrenal insufficiency because it requires a single blood draw. The 250 mcg CST involves IV or IM administration of cosyntropin and several blood draws. The 1 mcg CST, introduced to improve detection of partial and secondary adrenal insufficiency, requires dilution of the cosyntropin before administration because the smallest available dose is 250 mcg.
The insulin tolerance test is widely considered the gold standard, but requires close observation, is unpleasant for the patient, and carries some risk. Metyrapone and corticotropin-releasing hormone tests are not widely available.1
Negative CST rules out primary insufficiency
Researchers conducting a meta-analysis of the CST in diagnosing both primary and secondary adrenal insufficiency searched MEDLINE for English-language studies from 1966 to 2002 and used summary receiver-operating characteristic (ROC) curves to combine the sensitivities and specificities from individual studies.2 Four studies of primary adrenal insufficiency showed a negative likelihood ratio of 0.026 for the 250 mcg CST. A negative CST would, therefore, significantly decrease the post-test probability of primary adrenal insufficiency and effectively rule out the condition.
However, primary adrenal insufficiency was already established in the 4 studies, and consecutive testing with an accepted gold standard was not done. Thus, the studies likely overestimate the accuracy of the CST test characteristics.
Using CST results for secondary insufficiency
Twenty studies evaluating the 250 mcg CST for diagnosing secondary adrenal insufficiency were of higher quality. They included patients with and without disease and compared the CST with gold-standard tests, either the insulin tolerance test or metyrapone test. The summary ROC curve indicated a negative likelihood ratio of 0.45, which would decrease only moderately the post-test probability of secondary adrenal insufficiency.
The 1 mcg CST: More discriminating than 250 mcg
Using a ROC curve generated from 22 studies, the authors found the test characteristics of the 250 mcg CST and the 1 mcg CST to be similar. Only 7 of these studies included paired data for the standard- and low-dose CST in the same patients, however. In the 7 studies with paired data, the 1 mcg CST had better diagnostic discrimination, based on a larger area under the ROC, than the 250 mcg CST.
13 mcg/dL is the rule-out threshold for morning serum cortisol
A subsequent meta-analysis, based on a PubMed search of English-language studies from 1966 to 2006, compared the performance of morning serum cortisol, the 1 mcg CST, and the 250 mcg CST for diagnosing secondary adrenal insufficiency. This analysis used patient-level data obtained from the original investigators instead of reported study-level results.3 Data from patients described as normal, healthy control subjects were excluded.
Studies included in the meta-analysis used an accepted gold-standard test, such as the insulin tolerance test or metyrapone test. Studies that were performed in a critical care setting or used older, less reliable cortisol assays were excluded, as were studies for which patient-level data couldn’t be obtained. Three new studies were included, and 12 of the previously used studies were excluded.
Instead of using the reported cortisol cutoff levels, the authors defined a negative test as the mean cortisol level (the “rule-out threshold”) above which the negative likelihood ratio of adrenal insufficiency is <0.15. The rule-out thresholds for morning serum cortisol, 1 mcg CST, and 250 mcg CST were 13, 22, and 30 mcg/dL, respectively.
An optimal testing strategy for secondary insufficiency
The authors proposed an optimal testing strategy for secondary adrenal insufficiency (assuming a low or moderate pretest probability) that starts with a morning serum cortisol measurement:
- A serum cortisol level >13 mcg/dL can effectively rule out adrenal insufficiency.
- If the morning serum cortisol is <13 mcg/dL, a 1 mcg CST >22 mcg/dL can rule out adrenal insufficiency.
- Patients would need an insulin tolerance test or metyrapone test only if the low-dose CST is <22 mcg/dL.
Recommendations
Williams Textbook of Endocrinology states that a basal cortisol level higher than 14.5 mcg/dL invariably indicates an intact hypothalamic-pituitary-adrenal axis. However, to confirm the diagnosis of adrenal insufficiency, all patients, except those with a recent pituitary insult, should undergo a CST. An insulin tolerance test should be done only if the patient has a subnormal response to cosyntropin (to rule out a false-positive CST) or has had a recent pituitary insult.4
1. Salvatori R. Adrenal insufficiency. JAMA. 2005;294:2481-2488.
2. Dorin RI, Qualls CR, Crapo LM. Diagnosis of adrenal insufficiency. Ann Intern Med. 2003;139:194-204.
3. Kazlauskaite R, Evans A, Villabona C, et al. Corticotropin tests for hypothalamic-pituitary adrenal insufficiency: a meta-analysis. J Clin Endocrin Metab. August 12, 2008. Available at: http://jcem.endojournals.org/cgi/content/abstract/jc.2008-0710v1. Accessed August 12, 2008.
4. Stewart PM. The adrenal cortex. In: Kronenberg HM, Melmed S, Polonsky KS, et al, eds. Williams Textbook of Endocrinology. 11th ed. Philadelphia: Saunders Elsevier; 2008:445-503.
A morning serum cortisol level >13 mcg/dL reliably rules out adrenal insufficiency, and the test is easy and safe to perform. Because of low specificity, patients with a level of ≤13 mcg/dL need further evaluation with the cosyntropin stimulation test (CST) (strength of recommendation [SOR]: A, meta-analysis of diagnostic cohort studies).
The 250 mcg CST requires intravenous (IV) or intramuscular (IM) administration of cosyntropin and multiple blood draws; a normal response reliably rules out primary adrenal insufficiency (SOR: B, meta-analysis of lower-quality diagnostic cohort studies) and moderately decreases the likelihood of secondary adrenal insufficiency (SOR: A, meta-analysis of diagnostic cohort studies). The 1 mcg CST has better diagnostic discrimination, but requires an extra step to dilute the cosyntropin (SOR: A, meta-analysis of diagnostic cohort studies).
Evidence summary
The morning serum cortisol level is the most convenient test for adrenal insufficiency because it requires a single blood draw. The 250 mcg CST involves IV or IM administration of cosyntropin and several blood draws. The 1 mcg CST, introduced to improve detection of partial and secondary adrenal insufficiency, requires dilution of the cosyntropin before administration because the smallest available dose is 250 mcg.
The insulin tolerance test is widely considered the gold standard, but requires close observation, is unpleasant for the patient, and carries some risk. Metyrapone and corticotropin-releasing hormone tests are not widely available.1
Negative CST rules out primary insufficiency
Researchers conducting a meta-analysis of the CST in diagnosing both primary and secondary adrenal insufficiency searched MEDLINE for English-language studies from 1966 to 2002 and used summary receiver-operating characteristic (ROC) curves to combine the sensitivities and specificities from individual studies.2 Four studies of primary adrenal insufficiency showed a negative likelihood ratio of 0.026 for the 250 mcg CST. A negative CST would, therefore, significantly decrease the post-test probability of primary adrenal insufficiency and effectively rule out the condition.
However, primary adrenal insufficiency was already established in the 4 studies, and consecutive testing with an accepted gold standard was not done. Thus, the studies likely overestimate the accuracy of the CST test characteristics.
Using CST results for secondary insufficiency
Twenty studies evaluating the 250 mcg CST for diagnosing secondary adrenal insufficiency were of higher quality. They included patients with and without disease and compared the CST with gold-standard tests, either the insulin tolerance test or metyrapone test. The summary ROC curve indicated a negative likelihood ratio of 0.45, which would decrease only moderately the post-test probability of secondary adrenal insufficiency.
The 1 mcg CST: More discriminating than 250 mcg
Using a ROC curve generated from 22 studies, the authors found the test characteristics of the 250 mcg CST and the 1 mcg CST to be similar. Only 7 of these studies included paired data for the standard- and low-dose CST in the same patients, however. In the 7 studies with paired data, the 1 mcg CST had better diagnostic discrimination, based on a larger area under the ROC, than the 250 mcg CST.
13 mcg/dL is the rule-out threshold for morning serum cortisol
A subsequent meta-analysis, based on a PubMed search of English-language studies from 1966 to 2006, compared the performance of morning serum cortisol, the 1 mcg CST, and the 250 mcg CST for diagnosing secondary adrenal insufficiency. This analysis used patient-level data obtained from the original investigators instead of reported study-level results.3 Data from patients described as normal, healthy control subjects were excluded.
Studies included in the meta-analysis used an accepted gold-standard test, such as the insulin tolerance test or metyrapone test. Studies that were performed in a critical care setting or used older, less reliable cortisol assays were excluded, as were studies for which patient-level data couldn’t be obtained. Three new studies were included, and 12 of the previously used studies were excluded.
Instead of using the reported cortisol cutoff levels, the authors defined a negative test as the mean cortisol level (the “rule-out threshold”) above which the negative likelihood ratio of adrenal insufficiency is <0.15. The rule-out thresholds for morning serum cortisol, 1 mcg CST, and 250 mcg CST were 13, 22, and 30 mcg/dL, respectively.
An optimal testing strategy for secondary insufficiency
The authors proposed an optimal testing strategy for secondary adrenal insufficiency (assuming a low or moderate pretest probability) that starts with a morning serum cortisol measurement:
- A serum cortisol level >13 mcg/dL can effectively rule out adrenal insufficiency.
- If the morning serum cortisol is <13 mcg/dL, a 1 mcg CST >22 mcg/dL can rule out adrenal insufficiency.
- Patients would need an insulin tolerance test or metyrapone test only if the low-dose CST is <22 mcg/dL.
Recommendations
Williams Textbook of Endocrinology states that a basal cortisol level higher than 14.5 mcg/dL invariably indicates an intact hypothalamic-pituitary-adrenal axis. However, to confirm the diagnosis of adrenal insufficiency, all patients, except those with a recent pituitary insult, should undergo a CST. An insulin tolerance test should be done only if the patient has a subnormal response to cosyntropin (to rule out a false-positive CST) or has had a recent pituitary insult.4
A morning serum cortisol level >13 mcg/dL reliably rules out adrenal insufficiency, and the test is easy and safe to perform. Because of low specificity, patients with a level of ≤13 mcg/dL need further evaluation with the cosyntropin stimulation test (CST) (strength of recommendation [SOR]: A, meta-analysis of diagnostic cohort studies).
The 250 mcg CST requires intravenous (IV) or intramuscular (IM) administration of cosyntropin and multiple blood draws; a normal response reliably rules out primary adrenal insufficiency (SOR: B, meta-analysis of lower-quality diagnostic cohort studies) and moderately decreases the likelihood of secondary adrenal insufficiency (SOR: A, meta-analysis of diagnostic cohort studies). The 1 mcg CST has better diagnostic discrimination, but requires an extra step to dilute the cosyntropin (SOR: A, meta-analysis of diagnostic cohort studies).
Evidence summary
The morning serum cortisol level is the most convenient test for adrenal insufficiency because it requires a single blood draw. The 250 mcg CST involves IV or IM administration of cosyntropin and several blood draws. The 1 mcg CST, introduced to improve detection of partial and secondary adrenal insufficiency, requires dilution of the cosyntropin before administration because the smallest available dose is 250 mcg.
The insulin tolerance test is widely considered the gold standard, but requires close observation, is unpleasant for the patient, and carries some risk. Metyrapone and corticotropin-releasing hormone tests are not widely available.1
Negative CST rules out primary insufficiency
Researchers conducting a meta-analysis of the CST in diagnosing both primary and secondary adrenal insufficiency searched MEDLINE for English-language studies from 1966 to 2002 and used summary receiver-operating characteristic (ROC) curves to combine the sensitivities and specificities from individual studies.2 Four studies of primary adrenal insufficiency showed a negative likelihood ratio of 0.026 for the 250 mcg CST. A negative CST would, therefore, significantly decrease the post-test probability of primary adrenal insufficiency and effectively rule out the condition.
However, primary adrenal insufficiency was already established in the 4 studies, and consecutive testing with an accepted gold standard was not done. Thus, the studies likely overestimate the accuracy of the CST test characteristics.
Using CST results for secondary insufficiency
Twenty studies evaluating the 250 mcg CST for diagnosing secondary adrenal insufficiency were of higher quality. They included patients with and without disease and compared the CST with gold-standard tests, either the insulin tolerance test or metyrapone test. The summary ROC curve indicated a negative likelihood ratio of 0.45, which would decrease only moderately the post-test probability of secondary adrenal insufficiency.
The 1 mcg CST: More discriminating than 250 mcg
Using a ROC curve generated from 22 studies, the authors found the test characteristics of the 250 mcg CST and the 1 mcg CST to be similar. Only 7 of these studies included paired data for the standard- and low-dose CST in the same patients, however. In the 7 studies with paired data, the 1 mcg CST had better diagnostic discrimination, based on a larger area under the ROC, than the 250 mcg CST.
13 mcg/dL is the rule-out threshold for morning serum cortisol
A subsequent meta-analysis, based on a PubMed search of English-language studies from 1966 to 2006, compared the performance of morning serum cortisol, the 1 mcg CST, and the 250 mcg CST for diagnosing secondary adrenal insufficiency. This analysis used patient-level data obtained from the original investigators instead of reported study-level results.3 Data from patients described as normal, healthy control subjects were excluded.
Studies included in the meta-analysis used an accepted gold-standard test, such as the insulin tolerance test or metyrapone test. Studies that were performed in a critical care setting or used older, less reliable cortisol assays were excluded, as were studies for which patient-level data couldn’t be obtained. Three new studies were included, and 12 of the previously used studies were excluded.
Instead of using the reported cortisol cutoff levels, the authors defined a negative test as the mean cortisol level (the “rule-out threshold”) above which the negative likelihood ratio of adrenal insufficiency is <0.15. The rule-out thresholds for morning serum cortisol, 1 mcg CST, and 250 mcg CST were 13, 22, and 30 mcg/dL, respectively.
An optimal testing strategy for secondary insufficiency
The authors proposed an optimal testing strategy for secondary adrenal insufficiency (assuming a low or moderate pretest probability) that starts with a morning serum cortisol measurement:
- A serum cortisol level >13 mcg/dL can effectively rule out adrenal insufficiency.
- If the morning serum cortisol is <13 mcg/dL, a 1 mcg CST >22 mcg/dL can rule out adrenal insufficiency.
- Patients would need an insulin tolerance test or metyrapone test only if the low-dose CST is <22 mcg/dL.
Recommendations
Williams Textbook of Endocrinology states that a basal cortisol level higher than 14.5 mcg/dL invariably indicates an intact hypothalamic-pituitary-adrenal axis. However, to confirm the diagnosis of adrenal insufficiency, all patients, except those with a recent pituitary insult, should undergo a CST. An insulin tolerance test should be done only if the patient has a subnormal response to cosyntropin (to rule out a false-positive CST) or has had a recent pituitary insult.4
1. Salvatori R. Adrenal insufficiency. JAMA. 2005;294:2481-2488.
2. Dorin RI, Qualls CR, Crapo LM. Diagnosis of adrenal insufficiency. Ann Intern Med. 2003;139:194-204.
3. Kazlauskaite R, Evans A, Villabona C, et al. Corticotropin tests for hypothalamic-pituitary adrenal insufficiency: a meta-analysis. J Clin Endocrin Metab. August 12, 2008. Available at: http://jcem.endojournals.org/cgi/content/abstract/jc.2008-0710v1. Accessed August 12, 2008.
4. Stewart PM. The adrenal cortex. In: Kronenberg HM, Melmed S, Polonsky KS, et al, eds. Williams Textbook of Endocrinology. 11th ed. Philadelphia: Saunders Elsevier; 2008:445-503.
1. Salvatori R. Adrenal insufficiency. JAMA. 2005;294:2481-2488.
2. Dorin RI, Qualls CR, Crapo LM. Diagnosis of adrenal insufficiency. Ann Intern Med. 2003;139:194-204.
3. Kazlauskaite R, Evans A, Villabona C, et al. Corticotropin tests for hypothalamic-pituitary adrenal insufficiency: a meta-analysis. J Clin Endocrin Metab. August 12, 2008. Available at: http://jcem.endojournals.org/cgi/content/abstract/jc.2008-0710v1. Accessed August 12, 2008.
4. Stewart PM. The adrenal cortex. In: Kronenberg HM, Melmed S, Polonsky KS, et al, eds. Williams Textbook of Endocrinology. 11th ed. Philadelphia: Saunders Elsevier; 2008:445-503.
Evidence-based answers from the Family Physicians Inquiries Network
Do nonmedicated topicals relieve childhood eczema?
Yes. Emollients are effective first-line treatment to decrease symptoms of eczema and reduce the need to use steroids in children (strength of recommendation [SOR]: A, consistent randomized, controlled trials [RCTs]).
Tar preparations work, but compliance may be limited (SOR: B, single small RCT). Gamma-linoleic acid preparations, borage oil, and evening primrose oil show efficacy in small studies (SOR: B, small RCTs). MAS063DP cream (Atopiclair) is effective (SOR: B, single RCT).
Chamomile (SOR: B, inconsistent RCTs) and bathing in acidic hot spring water (SOR: C, case-control study) may be effective, but these treatments have not been adequately evaluated. Wet wrap dressings may be effective but increase the risk of skin infections (SOR: B, single RCT).
Hamamelis distillate creams (SOR: B, limited RCT) and massage with essential oils/aromatherapy are ineffective (SOR: C, case-control study).
Evidence summary
Eczema is a chronic, inflammatory, pruritic skin disorder that affects infants, children, and adults. Therapeutic efficacy is defined as symptom relief and decreased inflammation. Topical corticosteroids and calcineurin inhibitors (such as tacrolimus and pimecrolimus) are the standard of care for prescription therapy in children, but their potentially harmful side effects argue for safer, nonmedicated treatments.
Topical treatments that work
Emollients have demonstrated efficacy in several RCTs compared with placebo and corticosteroids alone. No 1 preparation has proved superior to another; all reduce steroid use and improve skin hydration.1-3
Tar. Only 1 study has evaluated the use of tar: a comparison of 30 patients (mean age 11.8 years) who were treated with tar on one side of the body and 1% hydrocortisone on the other. Both treatments produced comparable results and were well tolerated. But compliance can be a problem with tar products because they smell unpleasant and stain clothing.4
Gamma-linoleic acid. Small studies have evaluated the efficacy of gamma-linoleic acid (GLA)—including borage oil (24% GLA) and evening primrose oil (7%-10% GLA). An RCT of 12 patients (ages 4-46 years, mean 18 years) that compared evening primrose oil with placebo found that patients treated with primrose oil showed a subjective improvement in skin scaling, dryness, redness, and itching.5
Eczema on the leg of a 9-year-old boy.A double-blind, placebo-controlled trial of 32 children that assessed the effects of undershirts coated with borage oil compared with noncoated undershirts found statistically significant improvements in both itching and erythema.6
MAS063DP is a nonsteroidal, hydrolipidic cream containing glycyrrhetinic acid (GrA), vitis vinifera (grapevine extract), and telmestine. A recent multicenter RCT of 142 children compared MAS063DP to vehicle cream alone. The primary outcome was treatment success defined as an Investigator’s Global Assessment score of ≤1 (range 0-5), measured on day 22. Therapy was successful in 77% of the treatment group vs 0% of the vehicle-only group (number needed to treat=1).7
Hot spring baths, chamomile may help
In a case control study of 70 patients (ages 12-80 years, mean 23 years,) bathing in acidic hot spring water (42° C) helped control edema, erythema, exudation, and excoriation in refractory cases of eczema.8
Several adult and mixed adult-child studies have found mild efficacy for chamomile extracts. One RCT demonstrated topical chamomile to be equivalent to 0.25% hydrocortisone cream for treating mild eczema.9
Wet wraps may help, but may raise skin infection risk
A critical review suggests that short-term use of wet wraps in combination with topical steroids and emollients is effective for severe eczema. However, a small RCT of 50 children found no additional benefit over standard care and an increased risk of skin infection (95% CI, 5%-42%; P=.05) with a number needed to harm of 5.10,11
Essential oils, hamamelis distillate don’t work
In 1 case control study, massage with essential oils didn’t improve eczema compared with massage without essential oils.12 Hamamelis (witch hazel) distillate cream was inferior to steroid creams.13
Recommendations
The American Academy of Dermatology guidelines state that emollients are the standard of care for childhood eczema and have a steroid-sparing effect (level of evidence [LOE]: A). Tar preparations have therapeutic benefits, but compliance is a major limitation (LOE: B). Not enough evidence exists to recommend acidic baths. The guidelines make no recommendations about other topical therapies.
A task force to formulate practice parameters has been created by the American College of Allergy, Asthma, and Immunology; the American Academy of Allergy, Asthma, and Immunology; and the Joint Council of Allergy, Asthma, and Immunology. The task force’s latest recommendations suggest that emollients, tar preparations, and wet dressings are beneficial for treating eczema.2
1. Grimalt R, Mengeaud V, Cambazard F. Study Investigators’ Group. The steroid-sparing effect of an emollient therapy in infants with atopic dermatitis: a randomized controlled study. Dermatology. 2007;214:61-67.
2. Leung DY, Nicklas RA, Li JT, et al. Disease management of atopic dermatitis: an updated practice parameter. Joint Task Force on Practice Parameters. Ann Allergy Asthma Immunol. 2004;93(3 suppl 2):S1-S21.
3. Hanifin JM, Cooper KD, Ho VC, et al. Guidelines of care for atopic dermatitis, developed in accordance with the American Academy of Dermatology (ADA)/American Academy of Dermatology Association “Administrative Regulations for Evidence-Based Clinical Practice Guidelines.” J Am Acad Dermatol. 2004;50:391-404.
4. Munkvad M. A comparative trial of Clinitar versus hydrocortisone cream in the treatment of atopic eczema. Br J Dermatol. 1989;121:763-766.
5. Anstey A, Quigley M, Wilkinson JD. Topical evening primrose oil as treatment for atopic eczema. J Dermatol Treat. 1990;1:199-201.
6. Kanehara S, Ohtani T, Uede K, et al. Clinical effects of undershirts coated with borage oil on children with atopic dermatitis: a double-blind, placebo-controlled trial. J Dermatol. 2007;34:811-815.
7. Boguniewicz M, Ziechner JA, Eichenfield LF, et al. MAS063DP is effective monotherapy for mild to moderate atopic dermatitis in infants and children: a multicenter, randomized, vehicle-controlled study. J Pediatr. 2008;152:854-859.
8. Kubota K, Machida I, Tamura K, et al. Treatment of refractory cases of atopic dermatitis with acidic hot-spring bathing. Acta Derm Venereol. 1997;77:452-454.
9. Ross SM. An integrative approach to eczema atopic dermatitis. Holist Nurs Pract. 2003;17:56-62.
10. Devillers AC, Oranje AP. Efficacy and safety of “wet-wrap” dressings as an intervention treatment in children with severe and/or refractory atopic dermatitis: a critical review of the literature. Br J Dermatol. 2006;154:579-585.
11. Hindley D, Galloway G, Murray J, et al. A randomised study of “wet wraps” versus conventional treatment for atopic eczema. Arch Dis Child. 2006;91:164-168.
12. Anderson C, Lis-Balchin M, Kirk-Smith M. Evaluation of massage with essential oils on childhood eczema. Phytother Res. 2000;14:452-456.
13. Korting HC, Schäfer-Korting M, Klövekorn W, et al. Comparative efficacy of hamamelis distillate and hydrocortisone cream in atopic eczema. Eur J Clin Pharmacol. 1995;48:461-465.
Yes. Emollients are effective first-line treatment to decrease symptoms of eczema and reduce the need to use steroids in children (strength of recommendation [SOR]: A, consistent randomized, controlled trials [RCTs]).
Tar preparations work, but compliance may be limited (SOR: B, single small RCT). Gamma-linoleic acid preparations, borage oil, and evening primrose oil show efficacy in small studies (SOR: B, small RCTs). MAS063DP cream (Atopiclair) is effective (SOR: B, single RCT).
Chamomile (SOR: B, inconsistent RCTs) and bathing in acidic hot spring water (SOR: C, case-control study) may be effective, but these treatments have not been adequately evaluated. Wet wrap dressings may be effective but increase the risk of skin infections (SOR: B, single RCT).
Hamamelis distillate creams (SOR: B, limited RCT) and massage with essential oils/aromatherapy are ineffective (SOR: C, case-control study).
Evidence summary
Eczema is a chronic, inflammatory, pruritic skin disorder that affects infants, children, and adults. Therapeutic efficacy is defined as symptom relief and decreased inflammation. Topical corticosteroids and calcineurin inhibitors (such as tacrolimus and pimecrolimus) are the standard of care for prescription therapy in children, but their potentially harmful side effects argue for safer, nonmedicated treatments.
Topical treatments that work
Emollients have demonstrated efficacy in several RCTs compared with placebo and corticosteroids alone. No 1 preparation has proved superior to another; all reduce steroid use and improve skin hydration.1-3
Tar. Only 1 study has evaluated the use of tar: a comparison of 30 patients (mean age 11.8 years) who were treated with tar on one side of the body and 1% hydrocortisone on the other. Both treatments produced comparable results and were well tolerated. But compliance can be a problem with tar products because they smell unpleasant and stain clothing.4
Gamma-linoleic acid. Small studies have evaluated the efficacy of gamma-linoleic acid (GLA)—including borage oil (24% GLA) and evening primrose oil (7%-10% GLA). An RCT of 12 patients (ages 4-46 years, mean 18 years) that compared evening primrose oil with placebo found that patients treated with primrose oil showed a subjective improvement in skin scaling, dryness, redness, and itching.5
Eczema on the leg of a 9-year-old boy.A double-blind, placebo-controlled trial of 32 children that assessed the effects of undershirts coated with borage oil compared with noncoated undershirts found statistically significant improvements in both itching and erythema.6
MAS063DP is a nonsteroidal, hydrolipidic cream containing glycyrrhetinic acid (GrA), vitis vinifera (grapevine extract), and telmestine. A recent multicenter RCT of 142 children compared MAS063DP to vehicle cream alone. The primary outcome was treatment success defined as an Investigator’s Global Assessment score of ≤1 (range 0-5), measured on day 22. Therapy was successful in 77% of the treatment group vs 0% of the vehicle-only group (number needed to treat=1).7
Hot spring baths, chamomile may help
In a case control study of 70 patients (ages 12-80 years, mean 23 years,) bathing in acidic hot spring water (42° C) helped control edema, erythema, exudation, and excoriation in refractory cases of eczema.8
Several adult and mixed adult-child studies have found mild efficacy for chamomile extracts. One RCT demonstrated topical chamomile to be equivalent to 0.25% hydrocortisone cream for treating mild eczema.9
Wet wraps may help, but may raise skin infection risk
A critical review suggests that short-term use of wet wraps in combination with topical steroids and emollients is effective for severe eczema. However, a small RCT of 50 children found no additional benefit over standard care and an increased risk of skin infection (95% CI, 5%-42%; P=.05) with a number needed to harm of 5.10,11
Essential oils, hamamelis distillate don’t work
In 1 case control study, massage with essential oils didn’t improve eczema compared with massage without essential oils.12 Hamamelis (witch hazel) distillate cream was inferior to steroid creams.13
Recommendations
The American Academy of Dermatology guidelines state that emollients are the standard of care for childhood eczema and have a steroid-sparing effect (level of evidence [LOE]: A). Tar preparations have therapeutic benefits, but compliance is a major limitation (LOE: B). Not enough evidence exists to recommend acidic baths. The guidelines make no recommendations about other topical therapies.
A task force to formulate practice parameters has been created by the American College of Allergy, Asthma, and Immunology; the American Academy of Allergy, Asthma, and Immunology; and the Joint Council of Allergy, Asthma, and Immunology. The task force’s latest recommendations suggest that emollients, tar preparations, and wet dressings are beneficial for treating eczema.2
Yes. Emollients are effective first-line treatment to decrease symptoms of eczema and reduce the need to use steroids in children (strength of recommendation [SOR]: A, consistent randomized, controlled trials [RCTs]).
Tar preparations work, but compliance may be limited (SOR: B, single small RCT). Gamma-linoleic acid preparations, borage oil, and evening primrose oil show efficacy in small studies (SOR: B, small RCTs). MAS063DP cream (Atopiclair) is effective (SOR: B, single RCT).
Chamomile (SOR: B, inconsistent RCTs) and bathing in acidic hot spring water (SOR: C, case-control study) may be effective, but these treatments have not been adequately evaluated. Wet wrap dressings may be effective but increase the risk of skin infections (SOR: B, single RCT).
Hamamelis distillate creams (SOR: B, limited RCT) and massage with essential oils/aromatherapy are ineffective (SOR: C, case-control study).
Evidence summary
Eczema is a chronic, inflammatory, pruritic skin disorder that affects infants, children, and adults. Therapeutic efficacy is defined as symptom relief and decreased inflammation. Topical corticosteroids and calcineurin inhibitors (such as tacrolimus and pimecrolimus) are the standard of care for prescription therapy in children, but their potentially harmful side effects argue for safer, nonmedicated treatments.
Topical treatments that work
Emollients have demonstrated efficacy in several RCTs compared with placebo and corticosteroids alone. No 1 preparation has proved superior to another; all reduce steroid use and improve skin hydration.1-3
Tar. Only 1 study has evaluated the use of tar: a comparison of 30 patients (mean age 11.8 years) who were treated with tar on one side of the body and 1% hydrocortisone on the other. Both treatments produced comparable results and were well tolerated. But compliance can be a problem with tar products because they smell unpleasant and stain clothing.4
Gamma-linoleic acid. Small studies have evaluated the efficacy of gamma-linoleic acid (GLA)—including borage oil (24% GLA) and evening primrose oil (7%-10% GLA). An RCT of 12 patients (ages 4-46 years, mean 18 years) that compared evening primrose oil with placebo found that patients treated with primrose oil showed a subjective improvement in skin scaling, dryness, redness, and itching.5
Eczema on the leg of a 9-year-old boy.A double-blind, placebo-controlled trial of 32 children that assessed the effects of undershirts coated with borage oil compared with noncoated undershirts found statistically significant improvements in both itching and erythema.6
MAS063DP is a nonsteroidal, hydrolipidic cream containing glycyrrhetinic acid (GrA), vitis vinifera (grapevine extract), and telmestine. A recent multicenter RCT of 142 children compared MAS063DP to vehicle cream alone. The primary outcome was treatment success defined as an Investigator’s Global Assessment score of ≤1 (range 0-5), measured on day 22. Therapy was successful in 77% of the treatment group vs 0% of the vehicle-only group (number needed to treat=1).7
Hot spring baths, chamomile may help
In a case control study of 70 patients (ages 12-80 years, mean 23 years,) bathing in acidic hot spring water (42° C) helped control edema, erythema, exudation, and excoriation in refractory cases of eczema.8
Several adult and mixed adult-child studies have found mild efficacy for chamomile extracts. One RCT demonstrated topical chamomile to be equivalent to 0.25% hydrocortisone cream for treating mild eczema.9
Wet wraps may help, but may raise skin infection risk
A critical review suggests that short-term use of wet wraps in combination with topical steroids and emollients is effective for severe eczema. However, a small RCT of 50 children found no additional benefit over standard care and an increased risk of skin infection (95% CI, 5%-42%; P=.05) with a number needed to harm of 5.10,11
Essential oils, hamamelis distillate don’t work
In 1 case control study, massage with essential oils didn’t improve eczema compared with massage without essential oils.12 Hamamelis (witch hazel) distillate cream was inferior to steroid creams.13
Recommendations
The American Academy of Dermatology guidelines state that emollients are the standard of care for childhood eczema and have a steroid-sparing effect (level of evidence [LOE]: A). Tar preparations have therapeutic benefits, but compliance is a major limitation (LOE: B). Not enough evidence exists to recommend acidic baths. The guidelines make no recommendations about other topical therapies.
A task force to formulate practice parameters has been created by the American College of Allergy, Asthma, and Immunology; the American Academy of Allergy, Asthma, and Immunology; and the Joint Council of Allergy, Asthma, and Immunology. The task force’s latest recommendations suggest that emollients, tar preparations, and wet dressings are beneficial for treating eczema.2
1. Grimalt R, Mengeaud V, Cambazard F. Study Investigators’ Group. The steroid-sparing effect of an emollient therapy in infants with atopic dermatitis: a randomized controlled study. Dermatology. 2007;214:61-67.
2. Leung DY, Nicklas RA, Li JT, et al. Disease management of atopic dermatitis: an updated practice parameter. Joint Task Force on Practice Parameters. Ann Allergy Asthma Immunol. 2004;93(3 suppl 2):S1-S21.
3. Hanifin JM, Cooper KD, Ho VC, et al. Guidelines of care for atopic dermatitis, developed in accordance with the American Academy of Dermatology (ADA)/American Academy of Dermatology Association “Administrative Regulations for Evidence-Based Clinical Practice Guidelines.” J Am Acad Dermatol. 2004;50:391-404.
4. Munkvad M. A comparative trial of Clinitar versus hydrocortisone cream in the treatment of atopic eczema. Br J Dermatol. 1989;121:763-766.
5. Anstey A, Quigley M, Wilkinson JD. Topical evening primrose oil as treatment for atopic eczema. J Dermatol Treat. 1990;1:199-201.
6. Kanehara S, Ohtani T, Uede K, et al. Clinical effects of undershirts coated with borage oil on children with atopic dermatitis: a double-blind, placebo-controlled trial. J Dermatol. 2007;34:811-815.
7. Boguniewicz M, Ziechner JA, Eichenfield LF, et al. MAS063DP is effective monotherapy for mild to moderate atopic dermatitis in infants and children: a multicenter, randomized, vehicle-controlled study. J Pediatr. 2008;152:854-859.
8. Kubota K, Machida I, Tamura K, et al. Treatment of refractory cases of atopic dermatitis with acidic hot-spring bathing. Acta Derm Venereol. 1997;77:452-454.
9. Ross SM. An integrative approach to eczema atopic dermatitis. Holist Nurs Pract. 2003;17:56-62.
10. Devillers AC, Oranje AP. Efficacy and safety of “wet-wrap” dressings as an intervention treatment in children with severe and/or refractory atopic dermatitis: a critical review of the literature. Br J Dermatol. 2006;154:579-585.
11. Hindley D, Galloway G, Murray J, et al. A randomised study of “wet wraps” versus conventional treatment for atopic eczema. Arch Dis Child. 2006;91:164-168.
12. Anderson C, Lis-Balchin M, Kirk-Smith M. Evaluation of massage with essential oils on childhood eczema. Phytother Res. 2000;14:452-456.
13. Korting HC, Schäfer-Korting M, Klövekorn W, et al. Comparative efficacy of hamamelis distillate and hydrocortisone cream in atopic eczema. Eur J Clin Pharmacol. 1995;48:461-465.
1. Grimalt R, Mengeaud V, Cambazard F. Study Investigators’ Group. The steroid-sparing effect of an emollient therapy in infants with atopic dermatitis: a randomized controlled study. Dermatology. 2007;214:61-67.
2. Leung DY, Nicklas RA, Li JT, et al. Disease management of atopic dermatitis: an updated practice parameter. Joint Task Force on Practice Parameters. Ann Allergy Asthma Immunol. 2004;93(3 suppl 2):S1-S21.
3. Hanifin JM, Cooper KD, Ho VC, et al. Guidelines of care for atopic dermatitis, developed in accordance with the American Academy of Dermatology (ADA)/American Academy of Dermatology Association “Administrative Regulations for Evidence-Based Clinical Practice Guidelines.” J Am Acad Dermatol. 2004;50:391-404.
4. Munkvad M. A comparative trial of Clinitar versus hydrocortisone cream in the treatment of atopic eczema. Br J Dermatol. 1989;121:763-766.
5. Anstey A, Quigley M, Wilkinson JD. Topical evening primrose oil as treatment for atopic eczema. J Dermatol Treat. 1990;1:199-201.
6. Kanehara S, Ohtani T, Uede K, et al. Clinical effects of undershirts coated with borage oil on children with atopic dermatitis: a double-blind, placebo-controlled trial. J Dermatol. 2007;34:811-815.
7. Boguniewicz M, Ziechner JA, Eichenfield LF, et al. MAS063DP is effective monotherapy for mild to moderate atopic dermatitis in infants and children: a multicenter, randomized, vehicle-controlled study. J Pediatr. 2008;152:854-859.
8. Kubota K, Machida I, Tamura K, et al. Treatment of refractory cases of atopic dermatitis with acidic hot-spring bathing. Acta Derm Venereol. 1997;77:452-454.
9. Ross SM. An integrative approach to eczema atopic dermatitis. Holist Nurs Pract. 2003;17:56-62.
10. Devillers AC, Oranje AP. Efficacy and safety of “wet-wrap” dressings as an intervention treatment in children with severe and/or refractory atopic dermatitis: a critical review of the literature. Br J Dermatol. 2006;154:579-585.
11. Hindley D, Galloway G, Murray J, et al. A randomised study of “wet wraps” versus conventional treatment for atopic eczema. Arch Dis Child. 2006;91:164-168.
12. Anderson C, Lis-Balchin M, Kirk-Smith M. Evaluation of massage with essential oils on childhood eczema. Phytother Res. 2000;14:452-456.
13. Korting HC, Schäfer-Korting M, Klövekorn W, et al. Comparative efficacy of hamamelis distillate and hydrocortisone cream in atopic eczema. Eur J Clin Pharmacol. 1995;48:461-465.
Evidence-based answers from the Family Physicians Inquiries Network