User login
Measuring Wellness in a Staff Health Promotion Program
Assessing Diagnostic Test Result Management in a VA Health Care Network
Nonestrogen therapies for menopausal symptoms
With more women steering clear of estrogen in the wake of the Women’s Health Initiative and other trials,page 24). Nonetheless, many physicians and patients seek nonestrogen alternatives for this menopause-related symptom.
Over-the-counter lubricants are a mixed lot
Although many lubricants are marketed today, clinical study has been limited because they are regulated by the FDA as cosmetics. Of these products, Replens, a bioadhesive vaginal lubricant, has been studied the most intensively.
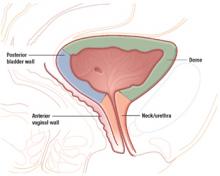
A unique formulation. Replens, a polycarbophil-based polymer, attaches to the vaginal wall and can hold 60 times its weight in water. It remains against the vaginal epithelial surface for more than 24 hours before it is sloughed off. This mechanism provides longer relief and requires less frequent application than other lubricants.17
Replens vs estrogen. Thrice-weekly Replens was compared with 12 weeks of daily vaginal estrogen cream18 and with vaginal estrogen cream applied daily for 2 weeks and then 3 times weekly for a total of 3 months.19 The comparison of Replens with conjugated estrogen cream (Premarin) showed significant improvements in vaginal moisture, fluid volume, elasticity, and pH levels in both treatment groups.18 Vaginal atrophy (assessed via Papanicolaou smear) reversed in 100% of estrogen-treated patients and 60% of Replens-treated patients.
When Replens was compared with dienoestrol vaginal cream, both therapies produced significant improvement in the vaginal dryness index (a score based on vaginal moisture, fluid volume, elasticity, and mucosa) within the first week.19 However, dienoestrol-treated patients had greater improvement in mean vaginal dryness (21.78 vs 17.32) at 12 weeks of therapy (P=.0001), compared with baseline values of 13 (dienoestrol) and 13.45 (Replens). Vaginal symptoms and dyspareunia improved at similar rates in the 2 groups. Patient satisfaction also was high in both groups, with 60% of Replens-treated patients and 84% of dienoestrol-treated patients reporting good to excellent effects.
No serious side effects were reported.18,19
Start with Replens for vaginal dryness, as it is a safe and effective alternative. If it is ineffective, vaginal estrogen may be more effective than vaginal lubricants.
The authors report no financial relationships relevant to this article
By Joann V. Pinkerton, MD, OBG Management Board of Editors, Professor of Obstetrics and Gynecology and Director, The Women’s Place Midlife Health Center, University of Virginia Health System, Charlottesville, Va
CASE 1 Perimenopausal, daily hot flashes
THERAPY
Exercise, soy products, vitamin E, and black cohosh
THE PATIENT: “V.S.,” 51, has been a patient for some time. At her latest visit, she reports that her menstrual periods are irregular, occurring every 3 to 12 weeks. She also has as many as 5 hot flashes a day, wakes in the very early morning, and occasionally experiences mild night sweats. Because she underwent bilateral tubal ligation many years ago, there is no need for contraception. She has no family history of breast cancer, but prefers to avoid drugs and asks if there are any herbal remedies and/or lifestyle changes that will ease her transition through menopause. She has a body mass index (BMI) of 31.6, and her breast and pelvic examinations are negative.
INTERVENTION: We discuss several simple options. For example, regular exercise may reduce vasomotor symptoms, although intense exertion with sweating can provoke hot flashes. Soy products and soy extracts have had mixed results, but appear to have some benefit. I suggest adding 1 soy dietary product per day. Vitamin E also may reduce hot flashes very modestly. The most promising product is black cohosh; I advise V.S. to take 20 mg twice a day.
OUTCOME: V.S. begins exercising regularly and sets a weight loss goal of 10%. She also begins taking 400 IU of vitamin E daily, adds soy nuts to her diet, and starts taking black cohosh. Three months later, she reports that her hot flashes have decreased to about 3 per day and are tolerable. She has had 1 menstrual cycle in the interim. If her symptoms worsen, she will consider medical therapy.
CASE 2 Severe symptoms, mood effects
THERAPY
Venlafaxine and vaginal moisturizers
THE PATIENT: “A.B.,” 54, a cancer survivor, is menopausal and has 10 to 20 hot flashes a day and soaking night sweats. She also reports low mood, frequent crying, and irritability. Before her cancer diagnosis, A.B. took hormone therapy for 6 months for severe menopausal symptoms. She recently underwent lumpectomy, axillary node dissection, radiation, and chemotherapy for a 3-cm, grade 3, invasive lobular carcinoma that was estrogen- and progesterone-receptor positive, and she is about to begin an aromatase inhibitor for chemoprevention. She and her husband have attempted intercourse since her chemotherapy ended, but the experience was painful. She would prefer to restart hormone therapy, but is willing to try nonhormonal options first. Her examination is unremarkable except for significant atrophy, with a vaginal pH of 7.0.
INTERVENTION: After a discussion of the data on SSRIs, SNRIs, and gabapentin, A.B. decides to try venlafaxine, 37.5 mg daily. If she has no improvement after 2 weeks, she will increase the dosage to 75 mg daily. For the vulvovaginal atrophy, she will try both vaginal moisturizers and vaginal lubricants, recognizing that this will not rethicken the epithelium. She also will exercise 5 days per week.
OUTCOME: After 3 months and an increase to 75 mg daily venlafaxine, the patient reports a 50% decrease in hot flashes and a more stable mood. The dyspareunia remains a problem. She decides to try a small amount of estradiol cream—somewhere between the size of a pea and the size of a dime—applied externally around the introital opening. She will start by applying it daily for 2 weeks, then reduce to twice a week.
CASE 3 Severe symptoms after TAH/BSO
THERAPY
Unsatisfactory improvement, a return to estrogen
THE PATIENT: “A.G.,” 46, complains of severe vasomotor symptoms. Two months ago she underwent total abdominal hysterectomy with bilateral salpingo-oophorectomy for bilateral complex masses, which turned out to be endometriomas. At that time, endometriosis was observed along the left ureter, with residual peritoneal implants and a small nodule within the rectovaginal septum. A.G. was offered leuprolide acetate (Lupron Depot) postoperatively, but declined. She did well for about 2 months and then began having vasomotor symptoms. Her physician was hesitant to prescribe estrogen because of fear of reactivating endometriosis. A.G. toughed it out for 3 months, but now reports “misery.” She is moody, cries easily, and has not had sex with her husband since her surgery. An examination reveals a small, 8-mm nodule within the rectovaginal septum, decreased vulvar color, vaginal pallor, and levator ani spasm with exam. Vaginal pH is 6.5.
INTERVENTION: Although I suggest systemic progesterone therapy—oral, vaginal, or intramuscular—and explain that it would decrease any residual endometriosis and relieve the hot flashes, the patient does not want to take any hormonal therapy and is concerned about worsening her mood. Despite reassurance that hormone therapy would have less than a 5% chance of reactivating the endometriosis, A.G. decides to try an antidepressant first. Since she had taken paroxetine (Paxil) for postpartum depression, with no major side effects, she decides to try it again, starting with 10 mg daily.
OUTCOME: A.G. continues to have at least 5 bothersome hot flashes per day, which interrupt her work with profuse sweating. She also wakes at night for the same reason. However, she is less irritable. It has been 7 months since her surgery, and both she and her husband want her to try hormone therapy. She elects to begin a low-dose combined estrogen–progesterone product, as well as estradiol vaginal cream twice daily.
Three months later, she reports no pain, a gradual reduction in hot flashes, and significant improvement overall. Her vaginal color has returned, her pH is 5.5, and intercourse is no longer painful. She decides to continue taking oral hormone therapy at a low dose despite occasional vasomotor symptoms, and to keep using vaginal estrogen, but will stop the paroxetine.
How does one hot flash differ from another?
By Joann V. Pinkerton, MD, OBG Management Board of Editors, Professor of Obstetrics and Gynecology and Director of The Women’s Place Midlife Health Center, University of Virginia Health System, Charlottesville, Va
Nelson HD, Vesco KK, Haney E, et al. Nonhormonal therapies for menopausal hot flashes: systematic review and meta-analysis. JAMA. 2006;295:2057–2071.
Nedrow A, Miller J, Walker M, Nygren P, Huffman LH, Nelson HD. Complementary and alternative therapies for the management of menopause-related symptoms. Arch Intern Med. 2006;166:1453–1465.
The hot flash, long synonymous with menopause, is the bane of many women facing the midlife transition. Despite the intensity of the sensation, hot flashes appear to be triggered by small elevations in core body temperature within a greatly reduced thermoneutral zone.1-4 If the core temperature crosses the upper threshold, a hot flash with sweating and peripheral vasodilation occurs. If the lower threshold is crossed, shivering results. Core temperature elevations occur in both symptomatic and asymptomatic women.
The difference: In symptomatic women, the thermoneutral zone is narrowed.
2 randomized trials attest to mostly modest efficacy
In their rigorous study of nonhormonal therapies for hot flashes, Nelson et al reviewed MEDLINE, PsycINFO, and the Cochrane Clinical Trials Register Database for randomized, double-blind, placebo-controlled trials of oral nonhormonal treatments for hot flashes, ultimately selecting 43 trials. These included 10 trials of antidepressants, 10 trials of clonidine, 17 trials of isoflavones, and 6 trials of other prescription drugs. They found at least some evidence of efficacy for SSRIs, SNRIs, clonidine, and gabapentin, but all were considerably less effective than estrogen.
Nedrow and colleagues searched the same databases plus MANTIS and AMED, selecting 70 trials for inclusion. Overall, the data were insufficient to support the effectiveness of any complementary or alternative therapy. For example, a good-quality study enrolling breast cancer survivors compared 56 patients ingesting 90 mg daily of isoflavone soy drink with 55 patients who took placebo, with no differences reported between the groups in hot flash frequency or intensity, yet both groups improved over baseline.
The placebo effect and other challenges
Randomized, controlled trials of alternative medicines and nonhormonal prescription therapies have found a placebo effect that ranges from about 1% to as high as 77%.5,6 In estrogen trials, the mean placebo response is 50.8%.7 The study of nonhormonal therapies involves several challenges, such as difficulty locating a proper control or placebo, and double-blinding is often impossible.
A big problem faced in both studies was the lack of consistency in inclusion criteria. Study samples differed in age range, menopausal status, type of menopause, inclusion of breast cancer survivors, or use of antiestrogen therapy such as tamoxifen, raloxifene, or aromatase inhibitors—drugs that are associated with hot flashes.
Studies also varied in the degree of hot-flash severity required for enrollment. Some studies of alternative therapies enrolled women with 1 or 2 hot flashes per day, or 14 per week, whereas the US FDA requires women in hormone-therapy trials to have at least 7 moderate to severe hot flashes daily, or 50 to 60 per week, with specific definitions of severity.
Moreover, botanical products may have milder effects overall or take longer to elicit a response. Most studies are of short duration with small numbers of women, increasing the potential for confounding by the placebo effect.
REFERENCES
1. Hulley S, Grady D, Bush T, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. JAMA. 1998;280:605-613.
2. Roussouw JE, Anderson GL, Prentice RL, et al. Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
3. Fugate SE, Church CO. Nonestrogen treatment modalities for vasomotor symptoms associated with menopause. Ann Pharmacother. 2004;38:1482-1499.
4. Guttuso T, Kurlan R, McDermott MP, Kieburtz K. Gabapentin’s effects on hot flashes in postmenopausal women: a randomized controlled trial. Obstet Gynecol. 2003;101:337-345.
5. Marchesoni D, Mozzanega B, Maggino T, Nardelli GB. Postmenopausal hot flushes: endocrine correlations and progestinic treatment. Double blind crossed clinical trials using MPA versus placebo. J Gynaecol Endocrinol. 1985;1:63-69.
6. Bullock JL, Massey FM, Gambrell RD. Use of medroxyprogesterone acetate to prevent menopausal symptoms. Obstet Gynecol. 1975;46:165-168.
7. Nelson HD, Vesco KK, Haney E, et al. Nonhormonal therapies for menopausal hot flashes. JAMA. 2006;295:2057-2071.
8. Stearns V, Beebe KL, Iyengar M, Dube E. Paroxetine controlled release in the treatment of menopausal hot flashes: a randomized controlled trial. JAMA. 2003;289:2827-2834.
9. Suvanto-Luukkonen E, Koivunen R, Sundstrom H, et al. Citalopram and fluoxetine in the treatment of postmenopausal symptoms: a prospective, randomized, 9-month, placebo-controlled, double-blind study. Menopause. 2005;12:18-26.
10. Evans ML, Pritts E, Vittinghoff E, McClish K, Morgan KS, Jaffe RB. Management of postmenopausal hot flashes with venlafaxine hydrochloride: a randomized, controlled trial. Obstet Gynecol. 2005;105:161-166.
11. Blumenthal M, Busse WR, Goldberg A, et al. German Commision E Monographs: therapeutic monographs on medicinal plants for human use. Austin, Tex: American Botanical Council; 1998.
12. Nappi RE, Malavasi B, Brundu B, Facchinetti F. Efficacy of Cimicifuga racemosa on climacteric complaints: a randomized study versus low-dose transdermal estradiol. Gynecol Endocrinol. 2005;20:30-35.
13. Liske E, Hänggi W, Henneicke-Von Zepelin H-H, Boblitz N, Wüstenberg P, Rahlfs VW. Physiological investigation of a unique extract of black cohosh (Cimicifugae racemosae rhizoma): a 6-month clinical study demonstrates no systemic estrogenic effect. J Womens Health Gender Based Med. 2002;11:163-174.
14. Aiello EJ, Yasui Y, Tworoger SS, et al. Effect of a yearlong, moderate-intensity exercise intervention on the occurrence and severity of menopause symptoms in postmenopausal women. Menopause. 2004;11:382-388.
15. NIH State-of-the-Science Conference Statement on management of menopause-related symptoms National Institute of Health Consensus Development Program, March 21-23, 2005. Available at: http://consensus.nih.gov/2005/2005MenopausalSymptomsSOS025html.htm. Accessed October 9, 2006.
16. Kass-Annese B. Alternative therapies for menopause. Clin Obstet Gynecol. 2000;43:162-183.
17. Willhite LA, O’Connell MB. Urogenital atrophy: prevention and treatment. Pharmacotherapy. 2001;21:464-480.
18. Nachtigall LE. Comparative study: Replens versus local estrogen in menopausal women. Fertil Steril. 1994;61:178-180.
19. Bygdeman M, Swahn ML. Replens versus dienoestrol cream in the symptomatic treatment of vaginal atrophy in postmenopausal women. Maturitas. 1996;23:259-263.
With more women steering clear of estrogen in the wake of the Women’s Health Initiative and other trials,page 24). Nonetheless, many physicians and patients seek nonestrogen alternatives for this menopause-related symptom.
Over-the-counter lubricants are a mixed lot
Although many lubricants are marketed today, clinical study has been limited because they are regulated by the FDA as cosmetics. Of these products, Replens, a bioadhesive vaginal lubricant, has been studied the most intensively.
A unique formulation. Replens, a polycarbophil-based polymer, attaches to the vaginal wall and can hold 60 times its weight in water. It remains against the vaginal epithelial surface for more than 24 hours before it is sloughed off. This mechanism provides longer relief and requires less frequent application than other lubricants.17
Replens vs estrogen. Thrice-weekly Replens was compared with 12 weeks of daily vaginal estrogen cream18 and with vaginal estrogen cream applied daily for 2 weeks and then 3 times weekly for a total of 3 months.19 The comparison of Replens with conjugated estrogen cream (Premarin) showed significant improvements in vaginal moisture, fluid volume, elasticity, and pH levels in both treatment groups.18 Vaginal atrophy (assessed via Papanicolaou smear) reversed in 100% of estrogen-treated patients and 60% of Replens-treated patients.
When Replens was compared with dienoestrol vaginal cream, both therapies produced significant improvement in the vaginal dryness index (a score based on vaginal moisture, fluid volume, elasticity, and mucosa) within the first week.19 However, dienoestrol-treated patients had greater improvement in mean vaginal dryness (21.78 vs 17.32) at 12 weeks of therapy (P=.0001), compared with baseline values of 13 (dienoestrol) and 13.45 (Replens). Vaginal symptoms and dyspareunia improved at similar rates in the 2 groups. Patient satisfaction also was high in both groups, with 60% of Replens-treated patients and 84% of dienoestrol-treated patients reporting good to excellent effects.
No serious side effects were reported.18,19
Start with Replens for vaginal dryness, as it is a safe and effective alternative. If it is ineffective, vaginal estrogen may be more effective than vaginal lubricants.
The authors report no financial relationships relevant to this article
By Joann V. Pinkerton, MD, OBG Management Board of Editors, Professor of Obstetrics and Gynecology and Director, The Women’s Place Midlife Health Center, University of Virginia Health System, Charlottesville, Va
CASE 1 Perimenopausal, daily hot flashes
THERAPY
Exercise, soy products, vitamin E, and black cohosh
THE PATIENT: “V.S.,” 51, has been a patient for some time. At her latest visit, she reports that her menstrual periods are irregular, occurring every 3 to 12 weeks. She also has as many as 5 hot flashes a day, wakes in the very early morning, and occasionally experiences mild night sweats. Because she underwent bilateral tubal ligation many years ago, there is no need for contraception. She has no family history of breast cancer, but prefers to avoid drugs and asks if there are any herbal remedies and/or lifestyle changes that will ease her transition through menopause. She has a body mass index (BMI) of 31.6, and her breast and pelvic examinations are negative.
INTERVENTION: We discuss several simple options. For example, regular exercise may reduce vasomotor symptoms, although intense exertion with sweating can provoke hot flashes. Soy products and soy extracts have had mixed results, but appear to have some benefit. I suggest adding 1 soy dietary product per day. Vitamin E also may reduce hot flashes very modestly. The most promising product is black cohosh; I advise V.S. to take 20 mg twice a day.
OUTCOME: V.S. begins exercising regularly and sets a weight loss goal of 10%. She also begins taking 400 IU of vitamin E daily, adds soy nuts to her diet, and starts taking black cohosh. Three months later, she reports that her hot flashes have decreased to about 3 per day and are tolerable. She has had 1 menstrual cycle in the interim. If her symptoms worsen, she will consider medical therapy.
CASE 2 Severe symptoms, mood effects
THERAPY
Venlafaxine and vaginal moisturizers
THE PATIENT: “A.B.,” 54, a cancer survivor, is menopausal and has 10 to 20 hot flashes a day and soaking night sweats. She also reports low mood, frequent crying, and irritability. Before her cancer diagnosis, A.B. took hormone therapy for 6 months for severe menopausal symptoms. She recently underwent lumpectomy, axillary node dissection, radiation, and chemotherapy for a 3-cm, grade 3, invasive lobular carcinoma that was estrogen- and progesterone-receptor positive, and she is about to begin an aromatase inhibitor for chemoprevention. She and her husband have attempted intercourse since her chemotherapy ended, but the experience was painful. She would prefer to restart hormone therapy, but is willing to try nonhormonal options first. Her examination is unremarkable except for significant atrophy, with a vaginal pH of 7.0.
INTERVENTION: After a discussion of the data on SSRIs, SNRIs, and gabapentin, A.B. decides to try venlafaxine, 37.5 mg daily. If she has no improvement after 2 weeks, she will increase the dosage to 75 mg daily. For the vulvovaginal atrophy, she will try both vaginal moisturizers and vaginal lubricants, recognizing that this will not rethicken the epithelium. She also will exercise 5 days per week.
OUTCOME: After 3 months and an increase to 75 mg daily venlafaxine, the patient reports a 50% decrease in hot flashes and a more stable mood. The dyspareunia remains a problem. She decides to try a small amount of estradiol cream—somewhere between the size of a pea and the size of a dime—applied externally around the introital opening. She will start by applying it daily for 2 weeks, then reduce to twice a week.
CASE 3 Severe symptoms after TAH/BSO
THERAPY
Unsatisfactory improvement, a return to estrogen
THE PATIENT: “A.G.,” 46, complains of severe vasomotor symptoms. Two months ago she underwent total abdominal hysterectomy with bilateral salpingo-oophorectomy for bilateral complex masses, which turned out to be endometriomas. At that time, endometriosis was observed along the left ureter, with residual peritoneal implants and a small nodule within the rectovaginal septum. A.G. was offered leuprolide acetate (Lupron Depot) postoperatively, but declined. She did well for about 2 months and then began having vasomotor symptoms. Her physician was hesitant to prescribe estrogen because of fear of reactivating endometriosis. A.G. toughed it out for 3 months, but now reports “misery.” She is moody, cries easily, and has not had sex with her husband since her surgery. An examination reveals a small, 8-mm nodule within the rectovaginal septum, decreased vulvar color, vaginal pallor, and levator ani spasm with exam. Vaginal pH is 6.5.
INTERVENTION: Although I suggest systemic progesterone therapy—oral, vaginal, or intramuscular—and explain that it would decrease any residual endometriosis and relieve the hot flashes, the patient does not want to take any hormonal therapy and is concerned about worsening her mood. Despite reassurance that hormone therapy would have less than a 5% chance of reactivating the endometriosis, A.G. decides to try an antidepressant first. Since she had taken paroxetine (Paxil) for postpartum depression, with no major side effects, she decides to try it again, starting with 10 mg daily.
OUTCOME: A.G. continues to have at least 5 bothersome hot flashes per day, which interrupt her work with profuse sweating. She also wakes at night for the same reason. However, she is less irritable. It has been 7 months since her surgery, and both she and her husband want her to try hormone therapy. She elects to begin a low-dose combined estrogen–progesterone product, as well as estradiol vaginal cream twice daily.
Three months later, she reports no pain, a gradual reduction in hot flashes, and significant improvement overall. Her vaginal color has returned, her pH is 5.5, and intercourse is no longer painful. She decides to continue taking oral hormone therapy at a low dose despite occasional vasomotor symptoms, and to keep using vaginal estrogen, but will stop the paroxetine.
How does one hot flash differ from another?
By Joann V. Pinkerton, MD, OBG Management Board of Editors, Professor of Obstetrics and Gynecology and Director of The Women’s Place Midlife Health Center, University of Virginia Health System, Charlottesville, Va
Nelson HD, Vesco KK, Haney E, et al. Nonhormonal therapies for menopausal hot flashes: systematic review and meta-analysis. JAMA. 2006;295:2057–2071.
Nedrow A, Miller J, Walker M, Nygren P, Huffman LH, Nelson HD. Complementary and alternative therapies for the management of menopause-related symptoms. Arch Intern Med. 2006;166:1453–1465.
The hot flash, long synonymous with menopause, is the bane of many women facing the midlife transition. Despite the intensity of the sensation, hot flashes appear to be triggered by small elevations in core body temperature within a greatly reduced thermoneutral zone.1-4 If the core temperature crosses the upper threshold, a hot flash with sweating and peripheral vasodilation occurs. If the lower threshold is crossed, shivering results. Core temperature elevations occur in both symptomatic and asymptomatic women.
The difference: In symptomatic women, the thermoneutral zone is narrowed.
2 randomized trials attest to mostly modest efficacy
In their rigorous study of nonhormonal therapies for hot flashes, Nelson et al reviewed MEDLINE, PsycINFO, and the Cochrane Clinical Trials Register Database for randomized, double-blind, placebo-controlled trials of oral nonhormonal treatments for hot flashes, ultimately selecting 43 trials. These included 10 trials of antidepressants, 10 trials of clonidine, 17 trials of isoflavones, and 6 trials of other prescription drugs. They found at least some evidence of efficacy for SSRIs, SNRIs, clonidine, and gabapentin, but all were considerably less effective than estrogen.
Nedrow and colleagues searched the same databases plus MANTIS and AMED, selecting 70 trials for inclusion. Overall, the data were insufficient to support the effectiveness of any complementary or alternative therapy. For example, a good-quality study enrolling breast cancer survivors compared 56 patients ingesting 90 mg daily of isoflavone soy drink with 55 patients who took placebo, with no differences reported between the groups in hot flash frequency or intensity, yet both groups improved over baseline.
The placebo effect and other challenges
Randomized, controlled trials of alternative medicines and nonhormonal prescription therapies have found a placebo effect that ranges from about 1% to as high as 77%.5,6 In estrogen trials, the mean placebo response is 50.8%.7 The study of nonhormonal therapies involves several challenges, such as difficulty locating a proper control or placebo, and double-blinding is often impossible.
A big problem faced in both studies was the lack of consistency in inclusion criteria. Study samples differed in age range, menopausal status, type of menopause, inclusion of breast cancer survivors, or use of antiestrogen therapy such as tamoxifen, raloxifene, or aromatase inhibitors—drugs that are associated with hot flashes.
Studies also varied in the degree of hot-flash severity required for enrollment. Some studies of alternative therapies enrolled women with 1 or 2 hot flashes per day, or 14 per week, whereas the US FDA requires women in hormone-therapy trials to have at least 7 moderate to severe hot flashes daily, or 50 to 60 per week, with specific definitions of severity.
Moreover, botanical products may have milder effects overall or take longer to elicit a response. Most studies are of short duration with small numbers of women, increasing the potential for confounding by the placebo effect.
REFERENCES
With more women steering clear of estrogen in the wake of the Women’s Health Initiative and other trials,page 24). Nonetheless, many physicians and patients seek nonestrogen alternatives for this menopause-related symptom.
Over-the-counter lubricants are a mixed lot
Although many lubricants are marketed today, clinical study has been limited because they are regulated by the FDA as cosmetics. Of these products, Replens, a bioadhesive vaginal lubricant, has been studied the most intensively.
A unique formulation. Replens, a polycarbophil-based polymer, attaches to the vaginal wall and can hold 60 times its weight in water. It remains against the vaginal epithelial surface for more than 24 hours before it is sloughed off. This mechanism provides longer relief and requires less frequent application than other lubricants.17
Replens vs estrogen. Thrice-weekly Replens was compared with 12 weeks of daily vaginal estrogen cream18 and with vaginal estrogen cream applied daily for 2 weeks and then 3 times weekly for a total of 3 months.19 The comparison of Replens with conjugated estrogen cream (Premarin) showed significant improvements in vaginal moisture, fluid volume, elasticity, and pH levels in both treatment groups.18 Vaginal atrophy (assessed via Papanicolaou smear) reversed in 100% of estrogen-treated patients and 60% of Replens-treated patients.
When Replens was compared with dienoestrol vaginal cream, both therapies produced significant improvement in the vaginal dryness index (a score based on vaginal moisture, fluid volume, elasticity, and mucosa) within the first week.19 However, dienoestrol-treated patients had greater improvement in mean vaginal dryness (21.78 vs 17.32) at 12 weeks of therapy (P=.0001), compared with baseline values of 13 (dienoestrol) and 13.45 (Replens). Vaginal symptoms and dyspareunia improved at similar rates in the 2 groups. Patient satisfaction also was high in both groups, with 60% of Replens-treated patients and 84% of dienoestrol-treated patients reporting good to excellent effects.
No serious side effects were reported.18,19
Start with Replens for vaginal dryness, as it is a safe and effective alternative. If it is ineffective, vaginal estrogen may be more effective than vaginal lubricants.
The authors report no financial relationships relevant to this article
By Joann V. Pinkerton, MD, OBG Management Board of Editors, Professor of Obstetrics and Gynecology and Director, The Women’s Place Midlife Health Center, University of Virginia Health System, Charlottesville, Va
CASE 1 Perimenopausal, daily hot flashes
THERAPY
Exercise, soy products, vitamin E, and black cohosh
THE PATIENT: “V.S.,” 51, has been a patient for some time. At her latest visit, she reports that her menstrual periods are irregular, occurring every 3 to 12 weeks. She also has as many as 5 hot flashes a day, wakes in the very early morning, and occasionally experiences mild night sweats. Because she underwent bilateral tubal ligation many years ago, there is no need for contraception. She has no family history of breast cancer, but prefers to avoid drugs and asks if there are any herbal remedies and/or lifestyle changes that will ease her transition through menopause. She has a body mass index (BMI) of 31.6, and her breast and pelvic examinations are negative.
INTERVENTION: We discuss several simple options. For example, regular exercise may reduce vasomotor symptoms, although intense exertion with sweating can provoke hot flashes. Soy products and soy extracts have had mixed results, but appear to have some benefit. I suggest adding 1 soy dietary product per day. Vitamin E also may reduce hot flashes very modestly. The most promising product is black cohosh; I advise V.S. to take 20 mg twice a day.
OUTCOME: V.S. begins exercising regularly and sets a weight loss goal of 10%. She also begins taking 400 IU of vitamin E daily, adds soy nuts to her diet, and starts taking black cohosh. Three months later, she reports that her hot flashes have decreased to about 3 per day and are tolerable. She has had 1 menstrual cycle in the interim. If her symptoms worsen, she will consider medical therapy.
CASE 2 Severe symptoms, mood effects
THERAPY
Venlafaxine and vaginal moisturizers
THE PATIENT: “A.B.,” 54, a cancer survivor, is menopausal and has 10 to 20 hot flashes a day and soaking night sweats. She also reports low mood, frequent crying, and irritability. Before her cancer diagnosis, A.B. took hormone therapy for 6 months for severe menopausal symptoms. She recently underwent lumpectomy, axillary node dissection, radiation, and chemotherapy for a 3-cm, grade 3, invasive lobular carcinoma that was estrogen- and progesterone-receptor positive, and she is about to begin an aromatase inhibitor for chemoprevention. She and her husband have attempted intercourse since her chemotherapy ended, but the experience was painful. She would prefer to restart hormone therapy, but is willing to try nonhormonal options first. Her examination is unremarkable except for significant atrophy, with a vaginal pH of 7.0.
INTERVENTION: After a discussion of the data on SSRIs, SNRIs, and gabapentin, A.B. decides to try venlafaxine, 37.5 mg daily. If she has no improvement after 2 weeks, she will increase the dosage to 75 mg daily. For the vulvovaginal atrophy, she will try both vaginal moisturizers and vaginal lubricants, recognizing that this will not rethicken the epithelium. She also will exercise 5 days per week.
OUTCOME: After 3 months and an increase to 75 mg daily venlafaxine, the patient reports a 50% decrease in hot flashes and a more stable mood. The dyspareunia remains a problem. She decides to try a small amount of estradiol cream—somewhere between the size of a pea and the size of a dime—applied externally around the introital opening. She will start by applying it daily for 2 weeks, then reduce to twice a week.
CASE 3 Severe symptoms after TAH/BSO
THERAPY
Unsatisfactory improvement, a return to estrogen
THE PATIENT: “A.G.,” 46, complains of severe vasomotor symptoms. Two months ago she underwent total abdominal hysterectomy with bilateral salpingo-oophorectomy for bilateral complex masses, which turned out to be endometriomas. At that time, endometriosis was observed along the left ureter, with residual peritoneal implants and a small nodule within the rectovaginal septum. A.G. was offered leuprolide acetate (Lupron Depot) postoperatively, but declined. She did well for about 2 months and then began having vasomotor symptoms. Her physician was hesitant to prescribe estrogen because of fear of reactivating endometriosis. A.G. toughed it out for 3 months, but now reports “misery.” She is moody, cries easily, and has not had sex with her husband since her surgery. An examination reveals a small, 8-mm nodule within the rectovaginal septum, decreased vulvar color, vaginal pallor, and levator ani spasm with exam. Vaginal pH is 6.5.
INTERVENTION: Although I suggest systemic progesterone therapy—oral, vaginal, or intramuscular—and explain that it would decrease any residual endometriosis and relieve the hot flashes, the patient does not want to take any hormonal therapy and is concerned about worsening her mood. Despite reassurance that hormone therapy would have less than a 5% chance of reactivating the endometriosis, A.G. decides to try an antidepressant first. Since she had taken paroxetine (Paxil) for postpartum depression, with no major side effects, she decides to try it again, starting with 10 mg daily.
OUTCOME: A.G. continues to have at least 5 bothersome hot flashes per day, which interrupt her work with profuse sweating. She also wakes at night for the same reason. However, she is less irritable. It has been 7 months since her surgery, and both she and her husband want her to try hormone therapy. She elects to begin a low-dose combined estrogen–progesterone product, as well as estradiol vaginal cream twice daily.
Three months later, she reports no pain, a gradual reduction in hot flashes, and significant improvement overall. Her vaginal color has returned, her pH is 5.5, and intercourse is no longer painful. She decides to continue taking oral hormone therapy at a low dose despite occasional vasomotor symptoms, and to keep using vaginal estrogen, but will stop the paroxetine.
How does one hot flash differ from another?
By Joann V. Pinkerton, MD, OBG Management Board of Editors, Professor of Obstetrics and Gynecology and Director of The Women’s Place Midlife Health Center, University of Virginia Health System, Charlottesville, Va
Nelson HD, Vesco KK, Haney E, et al. Nonhormonal therapies for menopausal hot flashes: systematic review and meta-analysis. JAMA. 2006;295:2057–2071.
Nedrow A, Miller J, Walker M, Nygren P, Huffman LH, Nelson HD. Complementary and alternative therapies for the management of menopause-related symptoms. Arch Intern Med. 2006;166:1453–1465.
The hot flash, long synonymous with menopause, is the bane of many women facing the midlife transition. Despite the intensity of the sensation, hot flashes appear to be triggered by small elevations in core body temperature within a greatly reduced thermoneutral zone.1-4 If the core temperature crosses the upper threshold, a hot flash with sweating and peripheral vasodilation occurs. If the lower threshold is crossed, shivering results. Core temperature elevations occur in both symptomatic and asymptomatic women.
The difference: In symptomatic women, the thermoneutral zone is narrowed.
2 randomized trials attest to mostly modest efficacy
In their rigorous study of nonhormonal therapies for hot flashes, Nelson et al reviewed MEDLINE, PsycINFO, and the Cochrane Clinical Trials Register Database for randomized, double-blind, placebo-controlled trials of oral nonhormonal treatments for hot flashes, ultimately selecting 43 trials. These included 10 trials of antidepressants, 10 trials of clonidine, 17 trials of isoflavones, and 6 trials of other prescription drugs. They found at least some evidence of efficacy for SSRIs, SNRIs, clonidine, and gabapentin, but all were considerably less effective than estrogen.
Nedrow and colleagues searched the same databases plus MANTIS and AMED, selecting 70 trials for inclusion. Overall, the data were insufficient to support the effectiveness of any complementary or alternative therapy. For example, a good-quality study enrolling breast cancer survivors compared 56 patients ingesting 90 mg daily of isoflavone soy drink with 55 patients who took placebo, with no differences reported between the groups in hot flash frequency or intensity, yet both groups improved over baseline.
The placebo effect and other challenges
Randomized, controlled trials of alternative medicines and nonhormonal prescription therapies have found a placebo effect that ranges from about 1% to as high as 77%.5,6 In estrogen trials, the mean placebo response is 50.8%.7 The study of nonhormonal therapies involves several challenges, such as difficulty locating a proper control or placebo, and double-blinding is often impossible.
A big problem faced in both studies was the lack of consistency in inclusion criteria. Study samples differed in age range, menopausal status, type of menopause, inclusion of breast cancer survivors, or use of antiestrogen therapy such as tamoxifen, raloxifene, or aromatase inhibitors—drugs that are associated with hot flashes.
Studies also varied in the degree of hot-flash severity required for enrollment. Some studies of alternative therapies enrolled women with 1 or 2 hot flashes per day, or 14 per week, whereas the US FDA requires women in hormone-therapy trials to have at least 7 moderate to severe hot flashes daily, or 50 to 60 per week, with specific definitions of severity.
Moreover, botanical products may have milder effects overall or take longer to elicit a response. Most studies are of short duration with small numbers of women, increasing the potential for confounding by the placebo effect.
REFERENCES
1. Hulley S, Grady D, Bush T, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. JAMA. 1998;280:605-613.
2. Roussouw JE, Anderson GL, Prentice RL, et al. Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
3. Fugate SE, Church CO. Nonestrogen treatment modalities for vasomotor symptoms associated with menopause. Ann Pharmacother. 2004;38:1482-1499.
4. Guttuso T, Kurlan R, McDermott MP, Kieburtz K. Gabapentin’s effects on hot flashes in postmenopausal women: a randomized controlled trial. Obstet Gynecol. 2003;101:337-345.
5. Marchesoni D, Mozzanega B, Maggino T, Nardelli GB. Postmenopausal hot flushes: endocrine correlations and progestinic treatment. Double blind crossed clinical trials using MPA versus placebo. J Gynaecol Endocrinol. 1985;1:63-69.
6. Bullock JL, Massey FM, Gambrell RD. Use of medroxyprogesterone acetate to prevent menopausal symptoms. Obstet Gynecol. 1975;46:165-168.
7. Nelson HD, Vesco KK, Haney E, et al. Nonhormonal therapies for menopausal hot flashes. JAMA. 2006;295:2057-2071.
8. Stearns V, Beebe KL, Iyengar M, Dube E. Paroxetine controlled release in the treatment of menopausal hot flashes: a randomized controlled trial. JAMA. 2003;289:2827-2834.
9. Suvanto-Luukkonen E, Koivunen R, Sundstrom H, et al. Citalopram and fluoxetine in the treatment of postmenopausal symptoms: a prospective, randomized, 9-month, placebo-controlled, double-blind study. Menopause. 2005;12:18-26.
10. Evans ML, Pritts E, Vittinghoff E, McClish K, Morgan KS, Jaffe RB. Management of postmenopausal hot flashes with venlafaxine hydrochloride: a randomized, controlled trial. Obstet Gynecol. 2005;105:161-166.
11. Blumenthal M, Busse WR, Goldberg A, et al. German Commision E Monographs: therapeutic monographs on medicinal plants for human use. Austin, Tex: American Botanical Council; 1998.
12. Nappi RE, Malavasi B, Brundu B, Facchinetti F. Efficacy of Cimicifuga racemosa on climacteric complaints: a randomized study versus low-dose transdermal estradiol. Gynecol Endocrinol. 2005;20:30-35.
13. Liske E, Hänggi W, Henneicke-Von Zepelin H-H, Boblitz N, Wüstenberg P, Rahlfs VW. Physiological investigation of a unique extract of black cohosh (Cimicifugae racemosae rhizoma): a 6-month clinical study demonstrates no systemic estrogenic effect. J Womens Health Gender Based Med. 2002;11:163-174.
14. Aiello EJ, Yasui Y, Tworoger SS, et al. Effect of a yearlong, moderate-intensity exercise intervention on the occurrence and severity of menopause symptoms in postmenopausal women. Menopause. 2004;11:382-388.
15. NIH State-of-the-Science Conference Statement on management of menopause-related symptoms National Institute of Health Consensus Development Program, March 21-23, 2005. Available at: http://consensus.nih.gov/2005/2005MenopausalSymptomsSOS025html.htm. Accessed October 9, 2006.
16. Kass-Annese B. Alternative therapies for menopause. Clin Obstet Gynecol. 2000;43:162-183.
17. Willhite LA, O’Connell MB. Urogenital atrophy: prevention and treatment. Pharmacotherapy. 2001;21:464-480.
18. Nachtigall LE. Comparative study: Replens versus local estrogen in menopausal women. Fertil Steril. 1994;61:178-180.
19. Bygdeman M, Swahn ML. Replens versus dienoestrol cream in the symptomatic treatment of vaginal atrophy in postmenopausal women. Maturitas. 1996;23:259-263.
1. Hulley S, Grady D, Bush T, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. JAMA. 1998;280:605-613.
2. Roussouw JE, Anderson GL, Prentice RL, et al. Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
3. Fugate SE, Church CO. Nonestrogen treatment modalities for vasomotor symptoms associated with menopause. Ann Pharmacother. 2004;38:1482-1499.
4. Guttuso T, Kurlan R, McDermott MP, Kieburtz K. Gabapentin’s effects on hot flashes in postmenopausal women: a randomized controlled trial. Obstet Gynecol. 2003;101:337-345.
5. Marchesoni D, Mozzanega B, Maggino T, Nardelli GB. Postmenopausal hot flushes: endocrine correlations and progestinic treatment. Double blind crossed clinical trials using MPA versus placebo. J Gynaecol Endocrinol. 1985;1:63-69.
6. Bullock JL, Massey FM, Gambrell RD. Use of medroxyprogesterone acetate to prevent menopausal symptoms. Obstet Gynecol. 1975;46:165-168.
7. Nelson HD, Vesco KK, Haney E, et al. Nonhormonal therapies for menopausal hot flashes. JAMA. 2006;295:2057-2071.
8. Stearns V, Beebe KL, Iyengar M, Dube E. Paroxetine controlled release in the treatment of menopausal hot flashes: a randomized controlled trial. JAMA. 2003;289:2827-2834.
9. Suvanto-Luukkonen E, Koivunen R, Sundstrom H, et al. Citalopram and fluoxetine in the treatment of postmenopausal symptoms: a prospective, randomized, 9-month, placebo-controlled, double-blind study. Menopause. 2005;12:18-26.
10. Evans ML, Pritts E, Vittinghoff E, McClish K, Morgan KS, Jaffe RB. Management of postmenopausal hot flashes with venlafaxine hydrochloride: a randomized, controlled trial. Obstet Gynecol. 2005;105:161-166.
11. Blumenthal M, Busse WR, Goldberg A, et al. German Commision E Monographs: therapeutic monographs on medicinal plants for human use. Austin, Tex: American Botanical Council; 1998.
12. Nappi RE, Malavasi B, Brundu B, Facchinetti F. Efficacy of Cimicifuga racemosa on climacteric complaints: a randomized study versus low-dose transdermal estradiol. Gynecol Endocrinol. 2005;20:30-35.
13. Liske E, Hänggi W, Henneicke-Von Zepelin H-H, Boblitz N, Wüstenberg P, Rahlfs VW. Physiological investigation of a unique extract of black cohosh (Cimicifugae racemosae rhizoma): a 6-month clinical study demonstrates no systemic estrogenic effect. J Womens Health Gender Based Med. 2002;11:163-174.
14. Aiello EJ, Yasui Y, Tworoger SS, et al. Effect of a yearlong, moderate-intensity exercise intervention on the occurrence and severity of menopause symptoms in postmenopausal women. Menopause. 2004;11:382-388.
15. NIH State-of-the-Science Conference Statement on management of menopause-related symptoms National Institute of Health Consensus Development Program, March 21-23, 2005. Available at: http://consensus.nih.gov/2005/2005MenopausalSymptomsSOS025html.htm. Accessed October 9, 2006.
16. Kass-Annese B. Alternative therapies for menopause. Clin Obstet Gynecol. 2000;43:162-183.
17. Willhite LA, O’Connell MB. Urogenital atrophy: prevention and treatment. Pharmacotherapy. 2001;21:464-480.
18. Nachtigall LE. Comparative study: Replens versus local estrogen in menopausal women. Fertil Steril. 1994;61:178-180.
19. Bygdeman M, Swahn ML. Replens versus dienoestrol cream in the symptomatic treatment of vaginal atrophy in postmenopausal women. Maturitas. 1996;23:259-263.
Real-life risks and benefits of fracture-reducing drugs
It is all too easy to focus on T-scores and lose sight of why we check bone mass: we want to prevent fragility fractures—not osteoporosis per se. Fracture incidence is greater in women with osteoporosis, but the absolute number of fragility fractures is far greater in the women who have not yet reached that threshold. That was my main message last year. It still is, although I had hoped we would by now have in our hands a fracture risk assessment tool due from the World Health Organization. It will use age, DXA score, history, and other factors to project 5- and 10-year risk of fracture. Then we will simply have to decide at what level of risk, for an individual patient, drug therapy is indicated. Watch this space!
1 Osteonecrosis of the jaw: What clinicians need to know
2 Raloxifene: A bone drug that reduces new onset breast cancer
3 Estrogen for bone protection: Time for a comeback?
4 Risedronate: Not just for fracture prevention?
1 Osteonecrosis of the jaw: What clinicians need to know
Woo SB, Hellstein JW, Kalmar JR. Systematic review: bisphosphonates and osteonecrosis of the jaws. Ann Intern Med. 2006;144:753–761.
This was the year of massive media attention on bisphosphonate therapy and osteonecrosis of the jaw. A bone specialist I know said he got even more phone calls after this report was published than after the WHI blitz 4 years ago.
Patients started calling when the lay press limelight focused on a report by Woo et al, who reviewed all of the world’s literature published since 1966, and identified 368 reported cases of bisphosphonate-associated osteonecrosis of the jaw (ONJ).
Main findings
Of the 368 cases, 94% were being treated with intravenous bisphosphonate therapy; 85% of the patients had either multiple myeloma or metastatic cancer of the breast. More than half of all cases (60%) were preceded by tooth extraction or other dentoalveolar surgical procedure to treat infections, and the remaining 40% were related to infection, denture trauma, or other physical trauma.
The latter group of cases occurred spontaneously, although the patients affected often wore dentures. The mandible was more commonly affected than the maxilla by a ratio of 2:1.
Other studies have reported 75% of patients with ONJ were receiving chemotherapy at the time of diagnosis, and 38% were on corticosteroids.
Do these findings affect prescribing?
A small number of cases of ONJ in postmenopausal women taking oral bisphosphonates have occurred, though rarely—well under 1 per 100,000 patients treated. Realize that patients with myeloma or metastatic breast cancer are usually treated with high-dose, high-potency intravenous bisphosphonate.
There were no reports of ONJ in any of the controlled trials on use of bisphosphonates for osteoporosis; this represents more than 60,000 patients who in some cases were treated for more than 8 years.
Recommendations
The American Society for Bone and Mineral Research advises:
2 Raloxifene: An osteoporosis drug that reduces new onset breast cancer
Vogel VG, Costantino JP, Wickerham DL, et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes. The NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 Trial. JAMA 2006;295:2727–2741.
Barrett-Connor E, Mosca L, Collins P, et al. Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women. N Engl J Med. 2006;355:125–137.
Two large trials cause me to believe that raloxifene significantly reduces new onset breast cancer in virtually every group of women in which it has been studied.
Why you didn’t hear about this until now
Raloxifene was FDA-approved for prevention of osteoporosis in 1997 and for treatment of osteoporosis in 1999. There was a statistically significant 76% reduction in new onset breast cancer in raloxifene-treated patients versus placebo through 4 years of the MORE (Multiple Outcomes of Raloxifene Evaluation) trial, and this persisted at a 66% reduction through the additional years of the CORE (Continued Observation of Raloxifene Evaluation) trial.
Findings effectively buried. However, because of the wording of the FDA label, and, as a result of a $36 million fine from the Department of Justice, for promotional activities in the early years after its release, these findings were effectively buried and not well promulgated.
STAR and RUTH trials
Study of Tamoxifen and Raloxifene
The STAR trial reported by Vogel et al involved 19,747 postmenopausal women enrolled on the basis of their high risk for breast cancer. The patients were randomized to tamoxifen (already approved for breast cancer prevention) or raloxifene.
Over 5 years of study, the incidence of invasive breast cancer was virtually identical in both groups. However, the raloxifene group had statistically significant lower numbers of thromboembolic events, cataracts, hysterectomies performed, and endometrial hyperplasias. A 38% reduction in endometrial cancer in the raloxifene group had not reached statistical significance but was trending in that direction.
Studies of fracture reduction in populations with existing osteoporosis include the Fracture Intervention Trial, which enrolled women with low bone mass and existing vertebral fractures. Clinical vertebral and other fractures were substantially reduced in the treatment group
Raloxifene Use in The Heart
The RUTH trial reported by Barrett-Connor et al involved 10,101 post-menopausal women selected for multiple risks for coronary heart disease.
Although there was no reduction in coronary heart disease, there was no increase, unlike the estrogen and progesterone arm of the Women’s Health Initiative (WHI). Additionally, however, there was a 44% reduction in invasive breast cancer (95% CI 0.38–0.83). Remember, these women were chosen for their risk of heart disease. The rate of breast cancer in the placebo group was 2.7 cases per 1,000 women per year, and thus the 44% reduction means the rate in the treatment group was 1.5 cases per 1,000 women per year.
Consider the context
For comparison purposes, consider an average-risk group in the WHI, where the incidence of breast cancer was 3.3 cases per 1,000 women per year. Contrast this rate to that of a high-risk group, such as the placebo group in the original breast cancer prevention trial (BCPT), where the incidence was 6.8 cancers per 1,000 women per year.
I believe that such information must be available to clinicians and must be factored into your decision when contemplating a bone drug. A recent anecdote underscores the problem.
4 out of 10 Caucasian women over age 50 will fracture a hip, spine, or wrist sooner or later
1 of every 5 who fracture a hip ends up in a nursing home
DXA T-score of -2.0 in the hip and atypical ductal hyperplasia
An internist called me to discuss a mutual patient whom I had placed on raloxifene 2 years earlier. His comment was that raloxifene does not work in the hip. Our mutual patient had a T-score on DXA in the hip of -2.0 and in the spine of -0.7 (falsely improved by some osteophytes). In addition, she had been diagnosed with atypical ductal hyperplasia of the breast 2 years earlier.
I pointed out to him that studies of hip fracture reduction with bisphosphonate were all performed in women with osteoporosis. Furthermore, after the NHANES III correction, a sizable number of women in the MORE trial were not osteoporotic. In fact, the fracture incidence in the MORE trial placebo group was 0.7%—an extremely low risk—compared with 2.2% in the treatment group in the Fracture Intervention Trial I, and 3.0% in the treatment group in the Hip Intervention Program.
Stated another way, the incidence of hip fracture in the MORE placebo group was less than that in the treated groups in the Fracture Intervention Trial I and the Hip Intervention Program.
But perhaps the most important point in my anecdotal case is that the woman had a diagnosis of atypical ductal hyperplasia of the breast, a lesion that significantly increases her risk of invasive breast cancer. For these reasons, raloxifene was a much better choice for her fracture reduction pharmacotherapy. Her internist was unaware of these breast effects and had not taken this into account.
3 Estrogen for bone protection: Time for a comeback?
Stefanick ML, Anderson GL, Margolis KL, et al. Effects of conjugated equine estrogens on breast cancer and mammography screening in postmenopausal women with hysterectomy. JAMA. 2006;295:1647–1657.
Jackson RD, Wactawski-Wende J, LaCroix AZ, et al. Effects of conjugated equine estrogen on risk of fractures and BMD in postmenopausal women with hysterectomy: results from the Women’s Health Initiative randomized trial. J Bone Miner Res. 2006;6:817–828.
It may be time to revisit our initial reaction to the WHI. Although most estrogens are FDA-approved for treatment of osteoporosis, recommendations since the WHI have generally been that we should reserve hormone therapy or estrogen therapy for disruptive transitional symptoms (hot flashes, night sweats, etc.), and prescribe the lowest dose possible for the shortest time possible, consistent with the patient’s treatment goals.
Rethink therapy for 2 types of patients?
Recent reports, however, may cause us to rethink that approach, especially in 2 types of patients:
Stefanick et al reported on the 10,739 women aged 50–79 in the estrogen-only arm of the WHI, who received placebo or0.625 mg of conjugated equine estrogen. After a mean follow-up of 7.1 years, there were 104 cases of invasive breast cancer in this CEE group and 133 cases in the placebo group.
Stated another way, this represents a 20% reduction in breast cancer in women in the CEE group. Although this reduction was not statistically significant, it is in stark contrast with the increase in breast cancer seen in numerous studies of estrogen and progestogen together.
Statistically significant reductions in fracture, compared with placebo, in the WHI E2-only arm were:
wrist 42%
clinical vertebral 36%
hip 35%
total fractures 29%
Women in the WHI had all levels of fracture risk
Jackson et al also analyzed fracture incidence in the WHI E2-only arm, as assessed by semiannual questionnaires and verified by adjudication of radiology reports.
Women on CEE had statistically significant reductions in hip fracture (35%), clinical vertebral fracture (36%), wrist fracture (42%), and total fractures (29%), compared with placebo. This trend held across all levels of fracture, although the reductions were greatest in patients at highest risk.
This is notable, however, because the WHI was primarily studying the effect of CEE on coronary heart disease. Unlike virtually all osteoporosis studies, in which women with increased risk of fracture are studied, the women selected for the Women’s Health Initiative represent all levels of fracture risk—and this placebo-controlled, large, randomized study discovered that all fractures, across all levels of risk, were significantly reduced. And there was no increase in breast cancer.
This may well weigh in on many a clinician’s thought process about indications and real risks of estrogen therapy.
4 Risedronate: Not just for fracture prevention?
Buckland-Wright JC, Messent EA, Bingham CO III, et al. A 2 yr longitudinal radiographic study examining the effect of a bisphosphonate (risedronate) upon subchondral bone loss in osteoarthritic knee patients. Rheumatology (Oxford). 2006 Jul 11; [Epub ahead of print].
Bone formation in osteoarthritic knees reversed disease-related bone loss while maintaining structural integrity within the subchondral cancellous bone in patients treated with risedronate, in this 2-year study. Patients with progressive knee osteoarthritis were enrolled in this double-blinded, multicenter, randomized, placebo-controlled trial.
The treatment groups included placebo, risedronate 5 mg/day, 15 mg/day, and 50 mg/week. Patients receiving risedronate 15 mg/day retained vertical trabecular structure and those receiving 50 mg/week increased vertical trabecular number, thereby preserving the structural integrity of the subchondral bone.
This is important because weakening and loss of vertical trabecular support, when combined with the biomechanical weakening of the bone due to disease-related reduction in mineral content, are believed to contribute to collapse of the tibial compartment in late-stage osteoarthritis. It has been suggested that bisphosphonates are associated with decreased bone formation as an expected consequence of suppressing the coupled bone remodeling process. This did not appear to be the case in this study. In fact, the study tends to agree with experimental work that shows that high doses of bisphosphonates, as well as repeated administration, may enhance bone accretion.
The author serves on the advisory boards for Eli Lilly, Merck, Pfizer, Procter & Gamble, and GlaxoSmithKline.
It is all too easy to focus on T-scores and lose sight of why we check bone mass: we want to prevent fragility fractures—not osteoporosis per se. Fracture incidence is greater in women with osteoporosis, but the absolute number of fragility fractures is far greater in the women who have not yet reached that threshold. That was my main message last year. It still is, although I had hoped we would by now have in our hands a fracture risk assessment tool due from the World Health Organization. It will use age, DXA score, history, and other factors to project 5- and 10-year risk of fracture. Then we will simply have to decide at what level of risk, for an individual patient, drug therapy is indicated. Watch this space!
1 Osteonecrosis of the jaw: What clinicians need to know
2 Raloxifene: A bone drug that reduces new onset breast cancer
3 Estrogen for bone protection: Time for a comeback?
4 Risedronate: Not just for fracture prevention?
1 Osteonecrosis of the jaw: What clinicians need to know
Woo SB, Hellstein JW, Kalmar JR. Systematic review: bisphosphonates and osteonecrosis of the jaws. Ann Intern Med. 2006;144:753–761.
This was the year of massive media attention on bisphosphonate therapy and osteonecrosis of the jaw. A bone specialist I know said he got even more phone calls after this report was published than after the WHI blitz 4 years ago.
Patients started calling when the lay press limelight focused on a report by Woo et al, who reviewed all of the world’s literature published since 1966, and identified 368 reported cases of bisphosphonate-associated osteonecrosis of the jaw (ONJ).
Main findings
Of the 368 cases, 94% were being treated with intravenous bisphosphonate therapy; 85% of the patients had either multiple myeloma or metastatic cancer of the breast. More than half of all cases (60%) were preceded by tooth extraction or other dentoalveolar surgical procedure to treat infections, and the remaining 40% were related to infection, denture trauma, or other physical trauma.
The latter group of cases occurred spontaneously, although the patients affected often wore dentures. The mandible was more commonly affected than the maxilla by a ratio of 2:1.
Other studies have reported 75% of patients with ONJ were receiving chemotherapy at the time of diagnosis, and 38% were on corticosteroids.
Do these findings affect prescribing?
A small number of cases of ONJ in postmenopausal women taking oral bisphosphonates have occurred, though rarely—well under 1 per 100,000 patients treated. Realize that patients with myeloma or metastatic breast cancer are usually treated with high-dose, high-potency intravenous bisphosphonate.
There were no reports of ONJ in any of the controlled trials on use of bisphosphonates for osteoporosis; this represents more than 60,000 patients who in some cases were treated for more than 8 years.
Recommendations
The American Society for Bone and Mineral Research advises:
2 Raloxifene: An osteoporosis drug that reduces new onset breast cancer
Vogel VG, Costantino JP, Wickerham DL, et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes. The NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 Trial. JAMA 2006;295:2727–2741.
Barrett-Connor E, Mosca L, Collins P, et al. Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women. N Engl J Med. 2006;355:125–137.
Two large trials cause me to believe that raloxifene significantly reduces new onset breast cancer in virtually every group of women in which it has been studied.
Why you didn’t hear about this until now
Raloxifene was FDA-approved for prevention of osteoporosis in 1997 and for treatment of osteoporosis in 1999. There was a statistically significant 76% reduction in new onset breast cancer in raloxifene-treated patients versus placebo through 4 years of the MORE (Multiple Outcomes of Raloxifene Evaluation) trial, and this persisted at a 66% reduction through the additional years of the CORE (Continued Observation of Raloxifene Evaluation) trial.
Findings effectively buried. However, because of the wording of the FDA label, and, as a result of a $36 million fine from the Department of Justice, for promotional activities in the early years after its release, these findings were effectively buried and not well promulgated.
STAR and RUTH trials
Study of Tamoxifen and Raloxifene
The STAR trial reported by Vogel et al involved 19,747 postmenopausal women enrolled on the basis of their high risk for breast cancer. The patients were randomized to tamoxifen (already approved for breast cancer prevention) or raloxifene.
Over 5 years of study, the incidence of invasive breast cancer was virtually identical in both groups. However, the raloxifene group had statistically significant lower numbers of thromboembolic events, cataracts, hysterectomies performed, and endometrial hyperplasias. A 38% reduction in endometrial cancer in the raloxifene group had not reached statistical significance but was trending in that direction.
Studies of fracture reduction in populations with existing osteoporosis include the Fracture Intervention Trial, which enrolled women with low bone mass and existing vertebral fractures. Clinical vertebral and other fractures were substantially reduced in the treatment group
Raloxifene Use in The Heart
The RUTH trial reported by Barrett-Connor et al involved 10,101 post-menopausal women selected for multiple risks for coronary heart disease.
Although there was no reduction in coronary heart disease, there was no increase, unlike the estrogen and progesterone arm of the Women’s Health Initiative (WHI). Additionally, however, there was a 44% reduction in invasive breast cancer (95% CI 0.38–0.83). Remember, these women were chosen for their risk of heart disease. The rate of breast cancer in the placebo group was 2.7 cases per 1,000 women per year, and thus the 44% reduction means the rate in the treatment group was 1.5 cases per 1,000 women per year.
Consider the context
For comparison purposes, consider an average-risk group in the WHI, where the incidence of breast cancer was 3.3 cases per 1,000 women per year. Contrast this rate to that of a high-risk group, such as the placebo group in the original breast cancer prevention trial (BCPT), where the incidence was 6.8 cancers per 1,000 women per year.
I believe that such information must be available to clinicians and must be factored into your decision when contemplating a bone drug. A recent anecdote underscores the problem.
4 out of 10 Caucasian women over age 50 will fracture a hip, spine, or wrist sooner or later
1 of every 5 who fracture a hip ends up in a nursing home
DXA T-score of -2.0 in the hip and atypical ductal hyperplasia
An internist called me to discuss a mutual patient whom I had placed on raloxifene 2 years earlier. His comment was that raloxifene does not work in the hip. Our mutual patient had a T-score on DXA in the hip of -2.0 and in the spine of -0.7 (falsely improved by some osteophytes). In addition, she had been diagnosed with atypical ductal hyperplasia of the breast 2 years earlier.
I pointed out to him that studies of hip fracture reduction with bisphosphonate were all performed in women with osteoporosis. Furthermore, after the NHANES III correction, a sizable number of women in the MORE trial were not osteoporotic. In fact, the fracture incidence in the MORE trial placebo group was 0.7%—an extremely low risk—compared with 2.2% in the treatment group in the Fracture Intervention Trial I, and 3.0% in the treatment group in the Hip Intervention Program.
Stated another way, the incidence of hip fracture in the MORE placebo group was less than that in the treated groups in the Fracture Intervention Trial I and the Hip Intervention Program.
But perhaps the most important point in my anecdotal case is that the woman had a diagnosis of atypical ductal hyperplasia of the breast, a lesion that significantly increases her risk of invasive breast cancer. For these reasons, raloxifene was a much better choice for her fracture reduction pharmacotherapy. Her internist was unaware of these breast effects and had not taken this into account.
3 Estrogen for bone protection: Time for a comeback?
Stefanick ML, Anderson GL, Margolis KL, et al. Effects of conjugated equine estrogens on breast cancer and mammography screening in postmenopausal women with hysterectomy. JAMA. 2006;295:1647–1657.
Jackson RD, Wactawski-Wende J, LaCroix AZ, et al. Effects of conjugated equine estrogen on risk of fractures and BMD in postmenopausal women with hysterectomy: results from the Women’s Health Initiative randomized trial. J Bone Miner Res. 2006;6:817–828.
It may be time to revisit our initial reaction to the WHI. Although most estrogens are FDA-approved for treatment of osteoporosis, recommendations since the WHI have generally been that we should reserve hormone therapy or estrogen therapy for disruptive transitional symptoms (hot flashes, night sweats, etc.), and prescribe the lowest dose possible for the shortest time possible, consistent with the patient’s treatment goals.
Rethink therapy for 2 types of patients?
Recent reports, however, may cause us to rethink that approach, especially in 2 types of patients:
Stefanick et al reported on the 10,739 women aged 50–79 in the estrogen-only arm of the WHI, who received placebo or0.625 mg of conjugated equine estrogen. After a mean follow-up of 7.1 years, there were 104 cases of invasive breast cancer in this CEE group and 133 cases in the placebo group.
Stated another way, this represents a 20% reduction in breast cancer in women in the CEE group. Although this reduction was not statistically significant, it is in stark contrast with the increase in breast cancer seen in numerous studies of estrogen and progestogen together.
Statistically significant reductions in fracture, compared with placebo, in the WHI E2-only arm were:
wrist 42%
clinical vertebral 36%
hip 35%
total fractures 29%
Women in the WHI had all levels of fracture risk
Jackson et al also analyzed fracture incidence in the WHI E2-only arm, as assessed by semiannual questionnaires and verified by adjudication of radiology reports.
Women on CEE had statistically significant reductions in hip fracture (35%), clinical vertebral fracture (36%), wrist fracture (42%), and total fractures (29%), compared with placebo. This trend held across all levels of fracture, although the reductions were greatest in patients at highest risk.
This is notable, however, because the WHI was primarily studying the effect of CEE on coronary heart disease. Unlike virtually all osteoporosis studies, in which women with increased risk of fracture are studied, the women selected for the Women’s Health Initiative represent all levels of fracture risk—and this placebo-controlled, large, randomized study discovered that all fractures, across all levels of risk, were significantly reduced. And there was no increase in breast cancer.
This may well weigh in on many a clinician’s thought process about indications and real risks of estrogen therapy.
4 Risedronate: Not just for fracture prevention?
Buckland-Wright JC, Messent EA, Bingham CO III, et al. A 2 yr longitudinal radiographic study examining the effect of a bisphosphonate (risedronate) upon subchondral bone loss in osteoarthritic knee patients. Rheumatology (Oxford). 2006 Jul 11; [Epub ahead of print].
Bone formation in osteoarthritic knees reversed disease-related bone loss while maintaining structural integrity within the subchondral cancellous bone in patients treated with risedronate, in this 2-year study. Patients with progressive knee osteoarthritis were enrolled in this double-blinded, multicenter, randomized, placebo-controlled trial.
The treatment groups included placebo, risedronate 5 mg/day, 15 mg/day, and 50 mg/week. Patients receiving risedronate 15 mg/day retained vertical trabecular structure and those receiving 50 mg/week increased vertical trabecular number, thereby preserving the structural integrity of the subchondral bone.
This is important because weakening and loss of vertical trabecular support, when combined with the biomechanical weakening of the bone due to disease-related reduction in mineral content, are believed to contribute to collapse of the tibial compartment in late-stage osteoarthritis. It has been suggested that bisphosphonates are associated with decreased bone formation as an expected consequence of suppressing the coupled bone remodeling process. This did not appear to be the case in this study. In fact, the study tends to agree with experimental work that shows that high doses of bisphosphonates, as well as repeated administration, may enhance bone accretion.
The author serves on the advisory boards for Eli Lilly, Merck, Pfizer, Procter & Gamble, and GlaxoSmithKline.
It is all too easy to focus on T-scores and lose sight of why we check bone mass: we want to prevent fragility fractures—not osteoporosis per se. Fracture incidence is greater in women with osteoporosis, but the absolute number of fragility fractures is far greater in the women who have not yet reached that threshold. That was my main message last year. It still is, although I had hoped we would by now have in our hands a fracture risk assessment tool due from the World Health Organization. It will use age, DXA score, history, and other factors to project 5- and 10-year risk of fracture. Then we will simply have to decide at what level of risk, for an individual patient, drug therapy is indicated. Watch this space!
1 Osteonecrosis of the jaw: What clinicians need to know
2 Raloxifene: A bone drug that reduces new onset breast cancer
3 Estrogen for bone protection: Time for a comeback?
4 Risedronate: Not just for fracture prevention?
1 Osteonecrosis of the jaw: What clinicians need to know
Woo SB, Hellstein JW, Kalmar JR. Systematic review: bisphosphonates and osteonecrosis of the jaws. Ann Intern Med. 2006;144:753–761.
This was the year of massive media attention on bisphosphonate therapy and osteonecrosis of the jaw. A bone specialist I know said he got even more phone calls after this report was published than after the WHI blitz 4 years ago.
Patients started calling when the lay press limelight focused on a report by Woo et al, who reviewed all of the world’s literature published since 1966, and identified 368 reported cases of bisphosphonate-associated osteonecrosis of the jaw (ONJ).
Main findings
Of the 368 cases, 94% were being treated with intravenous bisphosphonate therapy; 85% of the patients had either multiple myeloma or metastatic cancer of the breast. More than half of all cases (60%) were preceded by tooth extraction or other dentoalveolar surgical procedure to treat infections, and the remaining 40% were related to infection, denture trauma, or other physical trauma.
The latter group of cases occurred spontaneously, although the patients affected often wore dentures. The mandible was more commonly affected than the maxilla by a ratio of 2:1.
Other studies have reported 75% of patients with ONJ were receiving chemotherapy at the time of diagnosis, and 38% were on corticosteroids.
Do these findings affect prescribing?
A small number of cases of ONJ in postmenopausal women taking oral bisphosphonates have occurred, though rarely—well under 1 per 100,000 patients treated. Realize that patients with myeloma or metastatic breast cancer are usually treated with high-dose, high-potency intravenous bisphosphonate.
There were no reports of ONJ in any of the controlled trials on use of bisphosphonates for osteoporosis; this represents more than 60,000 patients who in some cases were treated for more than 8 years.
Recommendations
The American Society for Bone and Mineral Research advises:
2 Raloxifene: An osteoporosis drug that reduces new onset breast cancer
Vogel VG, Costantino JP, Wickerham DL, et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes. The NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 Trial. JAMA 2006;295:2727–2741.
Barrett-Connor E, Mosca L, Collins P, et al. Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women. N Engl J Med. 2006;355:125–137.
Two large trials cause me to believe that raloxifene significantly reduces new onset breast cancer in virtually every group of women in which it has been studied.
Why you didn’t hear about this until now
Raloxifene was FDA-approved for prevention of osteoporosis in 1997 and for treatment of osteoporosis in 1999. There was a statistically significant 76% reduction in new onset breast cancer in raloxifene-treated patients versus placebo through 4 years of the MORE (Multiple Outcomes of Raloxifene Evaluation) trial, and this persisted at a 66% reduction through the additional years of the CORE (Continued Observation of Raloxifene Evaluation) trial.
Findings effectively buried. However, because of the wording of the FDA label, and, as a result of a $36 million fine from the Department of Justice, for promotional activities in the early years after its release, these findings were effectively buried and not well promulgated.
STAR and RUTH trials
Study of Tamoxifen and Raloxifene
The STAR trial reported by Vogel et al involved 19,747 postmenopausal women enrolled on the basis of their high risk for breast cancer. The patients were randomized to tamoxifen (already approved for breast cancer prevention) or raloxifene.
Over 5 years of study, the incidence of invasive breast cancer was virtually identical in both groups. However, the raloxifene group had statistically significant lower numbers of thromboembolic events, cataracts, hysterectomies performed, and endometrial hyperplasias. A 38% reduction in endometrial cancer in the raloxifene group had not reached statistical significance but was trending in that direction.
Studies of fracture reduction in populations with existing osteoporosis include the Fracture Intervention Trial, which enrolled women with low bone mass and existing vertebral fractures. Clinical vertebral and other fractures were substantially reduced in the treatment group
Raloxifene Use in The Heart
The RUTH trial reported by Barrett-Connor et al involved 10,101 post-menopausal women selected for multiple risks for coronary heart disease.
Although there was no reduction in coronary heart disease, there was no increase, unlike the estrogen and progesterone arm of the Women’s Health Initiative (WHI). Additionally, however, there was a 44% reduction in invasive breast cancer (95% CI 0.38–0.83). Remember, these women were chosen for their risk of heart disease. The rate of breast cancer in the placebo group was 2.7 cases per 1,000 women per year, and thus the 44% reduction means the rate in the treatment group was 1.5 cases per 1,000 women per year.
Consider the context
For comparison purposes, consider an average-risk group in the WHI, where the incidence of breast cancer was 3.3 cases per 1,000 women per year. Contrast this rate to that of a high-risk group, such as the placebo group in the original breast cancer prevention trial (BCPT), where the incidence was 6.8 cancers per 1,000 women per year.
I believe that such information must be available to clinicians and must be factored into your decision when contemplating a bone drug. A recent anecdote underscores the problem.
4 out of 10 Caucasian women over age 50 will fracture a hip, spine, or wrist sooner or later
1 of every 5 who fracture a hip ends up in a nursing home
DXA T-score of -2.0 in the hip and atypical ductal hyperplasia
An internist called me to discuss a mutual patient whom I had placed on raloxifene 2 years earlier. His comment was that raloxifene does not work in the hip. Our mutual patient had a T-score on DXA in the hip of -2.0 and in the spine of -0.7 (falsely improved by some osteophytes). In addition, she had been diagnosed with atypical ductal hyperplasia of the breast 2 years earlier.
I pointed out to him that studies of hip fracture reduction with bisphosphonate were all performed in women with osteoporosis. Furthermore, after the NHANES III correction, a sizable number of women in the MORE trial were not osteoporotic. In fact, the fracture incidence in the MORE trial placebo group was 0.7%—an extremely low risk—compared with 2.2% in the treatment group in the Fracture Intervention Trial I, and 3.0% in the treatment group in the Hip Intervention Program.
Stated another way, the incidence of hip fracture in the MORE placebo group was less than that in the treated groups in the Fracture Intervention Trial I and the Hip Intervention Program.
But perhaps the most important point in my anecdotal case is that the woman had a diagnosis of atypical ductal hyperplasia of the breast, a lesion that significantly increases her risk of invasive breast cancer. For these reasons, raloxifene was a much better choice for her fracture reduction pharmacotherapy. Her internist was unaware of these breast effects and had not taken this into account.
3 Estrogen for bone protection: Time for a comeback?
Stefanick ML, Anderson GL, Margolis KL, et al. Effects of conjugated equine estrogens on breast cancer and mammography screening in postmenopausal women with hysterectomy. JAMA. 2006;295:1647–1657.
Jackson RD, Wactawski-Wende J, LaCroix AZ, et al. Effects of conjugated equine estrogen on risk of fractures and BMD in postmenopausal women with hysterectomy: results from the Women’s Health Initiative randomized trial. J Bone Miner Res. 2006;6:817–828.
It may be time to revisit our initial reaction to the WHI. Although most estrogens are FDA-approved for treatment of osteoporosis, recommendations since the WHI have generally been that we should reserve hormone therapy or estrogen therapy for disruptive transitional symptoms (hot flashes, night sweats, etc.), and prescribe the lowest dose possible for the shortest time possible, consistent with the patient’s treatment goals.
Rethink therapy for 2 types of patients?
Recent reports, however, may cause us to rethink that approach, especially in 2 types of patients:
Stefanick et al reported on the 10,739 women aged 50–79 in the estrogen-only arm of the WHI, who received placebo or0.625 mg of conjugated equine estrogen. After a mean follow-up of 7.1 years, there were 104 cases of invasive breast cancer in this CEE group and 133 cases in the placebo group.
Stated another way, this represents a 20% reduction in breast cancer in women in the CEE group. Although this reduction was not statistically significant, it is in stark contrast with the increase in breast cancer seen in numerous studies of estrogen and progestogen together.
Statistically significant reductions in fracture, compared with placebo, in the WHI E2-only arm were:
wrist 42%
clinical vertebral 36%
hip 35%
total fractures 29%
Women in the WHI had all levels of fracture risk
Jackson et al also analyzed fracture incidence in the WHI E2-only arm, as assessed by semiannual questionnaires and verified by adjudication of radiology reports.
Women on CEE had statistically significant reductions in hip fracture (35%), clinical vertebral fracture (36%), wrist fracture (42%), and total fractures (29%), compared with placebo. This trend held across all levels of fracture, although the reductions were greatest in patients at highest risk.
This is notable, however, because the WHI was primarily studying the effect of CEE on coronary heart disease. Unlike virtually all osteoporosis studies, in which women with increased risk of fracture are studied, the women selected for the Women’s Health Initiative represent all levels of fracture risk—and this placebo-controlled, large, randomized study discovered that all fractures, across all levels of risk, were significantly reduced. And there was no increase in breast cancer.
This may well weigh in on many a clinician’s thought process about indications and real risks of estrogen therapy.
4 Risedronate: Not just for fracture prevention?
Buckland-Wright JC, Messent EA, Bingham CO III, et al. A 2 yr longitudinal radiographic study examining the effect of a bisphosphonate (risedronate) upon subchondral bone loss in osteoarthritic knee patients. Rheumatology (Oxford). 2006 Jul 11; [Epub ahead of print].
Bone formation in osteoarthritic knees reversed disease-related bone loss while maintaining structural integrity within the subchondral cancellous bone in patients treated with risedronate, in this 2-year study. Patients with progressive knee osteoarthritis were enrolled in this double-blinded, multicenter, randomized, placebo-controlled trial.
The treatment groups included placebo, risedronate 5 mg/day, 15 mg/day, and 50 mg/week. Patients receiving risedronate 15 mg/day retained vertical trabecular structure and those receiving 50 mg/week increased vertical trabecular number, thereby preserving the structural integrity of the subchondral bone.
This is important because weakening and loss of vertical trabecular support, when combined with the biomechanical weakening of the bone due to disease-related reduction in mineral content, are believed to contribute to collapse of the tibial compartment in late-stage osteoarthritis. It has been suggested that bisphosphonates are associated with decreased bone formation as an expected consequence of suppressing the coupled bone remodeling process. This did not appear to be the case in this study. In fact, the study tends to agree with experimental work that shows that high doses of bisphosphonates, as well as repeated administration, may enhance bone accretion.
The author serves on the advisory boards for Eli Lilly, Merck, Pfizer, Procter & Gamble, and GlaxoSmithKline.
Management of prolonged decelerations
A prolonged deceleration may signal danger—or reflect a perfectly normal fetal response to maternal pelvic examination. Because of the wide range of possibilities, this fetal heart rate pattern justifies close attention. For example, repetitive prolonged decelerations may indicate cord compression from oligohydramnios. Even more troubling, a prolonged deceleration may occur for the first time during the evolution of a profound catastrophe, such as amniotic fluid embolism or uterine rupture during vaginal birth after cesarean delivery (VBAC). In some circumstances, a prolonged deceleration may be the terminus of a progression of nonreassuring fetal heart rate (FHR) changes, and becomes the immediate precursor to fetal death (TABLE 1).1
When FHR patterns exhibit these aberrations, we rightly worry about fetal well-being and the possible need for operative intervention. Unfortunately, the degree of fetal compromise is difficult to predict and depends on preexisting fetal condition, physiologic reserve, degree and duration of the insult, and other variables.
TABLE 1
Some causes of prolonged decelerations and bradycardias
| PROLONGED DECELERATION | BRADYCARDIA |
|---|---|
| Cord compression Oligohydramnios Cord prolapse Uteroplacental insufficiency Anesthesia (paracervical, spinal, epidural) Maternal valsalva Maternal supine hypotension Hypertonic or prolonged contractions Abruptio placentae Uterine rupture Cocaine ingestion Maternal hypoxia Maternal seizures, eclampsia Respiratory depression from medications Cardiopulmonary arrest Amniotic fluid embolism Fetal hemorrhage Vasa previa Traumatic amniocentesis Fetal vagal reaction Rapid descent, impending birth Cervical examination Fetal scalp electrode placement Fetal blood sampling Fetal central nervous system anomalies Idiopathic (cord compression?) | Congenital conduction abnormalities Complete heart block Long QT syndrome Congenital heart defects Tachyarrhythmia (Fetal tachyarrhythmia may produce an EFM tracing that appears to be a bradycardia and can only be distinguished by ultrasound) Medications Beta blockers Hypothermia Infection Chorioamnionitis Endotoxemia |
Ultimately, a judgment call
The 22nd edition of Williams Obstetrics2 summarizes the clinical challenges involved in the management of prolonged decelerations during labor: “Management of isolated prolonged decelerations is based on bedside clinical judgment, which inevitably will sometimes be imperfect given the unpredictability of these decelerations.”
“Fetal bradycardia” and “prolonged deceleration” are distinct entities
In general parlance, we often use the terms “fetal bradycardia” and “prolonged deceleration” loosely. In practice, we must differentiate these entities because underlying pathophysiologic mechanisms and clinical management may differ substantially.
The problem: Since the introduction of electronic fetal monitoring (EFM) in the 1960s, numerous descriptions of FHR patterns have been published, each slightly different from the others. The result: confusing nomenclature, miscommunication among clinicians, and stymied research efforts.
To standardize definitions of intrapartum FHR patterns so that the effectiveness of EFM could be better assessed in observational studies and clinical trials, the National Institute of Child Health and Human Development organized a workshop.3 Its recommendations were subsequently adopted by the American College of Obstetricians and Gynecologists (ACOG).4 Among the definitions:
Differentiation between the 2 entities is critical because, in many cases, bradycardias are chronic patterns that may not be associated with immediate fetal compromise and do not require immediate intervention. For example, a fetal bradycardia due to congenital heart block would not benefit from immediate delivery, especially prior to term.
“Moderate fetal bradycardia,” defined as a baseline of 100 to 119 bpm, was reported in 1.8% of 1,386 continuously monitored patients and is attributed to relative cephalopelvic disproportion, resolving after rotation of the fetal vertex and associated with normal neonatal outcome.5,6
Similar decelerations can reflect different events
The exact depth and duration of a prolonged deceleration leading to fetal compromise and requiring prompt delivery is difficult to define, although some observations warrant consideration. Experiments with fetal lambs show that the deceleration in response to umbilical vein occlusion is associated with a fall in fetal blood pressure, whereas deceleration in response to umbilical artery occlusion is associated with a rise in fetal blood pressure. This reflex can be abolished by vagotomy, but will eventually recur due to anoxia.7
Vital clue: What happened before the prolonged deceleration?
In clinical practice, it is important to appreciate characteristics of the FHR pattern preceding the prolonged deceleration.8 Williams and Galerneau9 correlated baseline FHR variability and duration of prolonged decelerations with neonatal acid–base status in 186 term gestations with an identified prolonged deceleration within 30 minutes of delivery. Patients were divided into 4 groups, based on FHR variability and recovery of the FHR baseline (TABLE 2).
The findings:
TABLE 2
Neonatal outcomes associated with variability and recovery of FHR patterns after prolonged deceleration
| UMBILICAL ARTERY | GROUP 1 V+ R+ (N=128) | GROUP 2 V+ R- (N=40) | GROUP 3 V- R+ (N=9) | GROUP 4 V- R- (N=9) | P VALUE |
|---|---|---|---|---|---|
| pH (mean±SD) | 7.17±0.09 | 7.13±0.15 | 7.11±0.11 | 6.83±0.16 | <.001 |
| Base deficit (mean±SD) | -6.5±3.9 | -7.2±5.1 | -10±4 | -20±6 | <.001 |
| pH <7.0 (%) | 2 | 18 | 44 | 78 | <.001 |
| pH <7.1 (%) | 22 | 33 | 56 | 89 | <.001 |
| Base deficit <16 (%) | 1 | 8 | 11 | 78 | <.001 |
| Base deficit <12 (%) | 5 | 13 | 22 | 89 | <.001 |
| V=variability | |||||
| R=recovery | |||||
| SOURCE: Williams and Galerneau9 | |||||
Acid–base changes likely begin within minutes of cord compression
Zilianti and colleagues10 evaluated 29 fetuses with normal FHR patterns during labor with FHR deceleration during the expulsion phase of delivery. When the FHR deceleration was prolonged (>120 seconds), umbilical artery pH significantly decreased (7.19 vs 7.27), umbilical vein pH remained unchanged (7.32), and the umbilical venous–arterial pH difference was significantly increased (0.13 vs 0.05). Thus, acid–base changes likely begin within minutes of cord compression.
The correlation between acidemia and loss of variability
In their review of 43 vacuum extractions, Gull and colleagues22 found that 27 infants were delivered for “end-stage bradycardia” (abrupt persistent decrease in FHR to less than 100 bpm for more than 2 minutes, or repeated deceleration more than 60 bpm below baseline with poor recovery), and 16 were delivered electively (controls). Umbilical-cord base deficit was greater in the newborns with bradycardia than in controls, and the length of time FHR variability was lost correlated with the degree of base deficit. Acidemic fetuses lost FHR variability during the bradycardia for more than 4 minutes, or started to lose FHR variability less than 3 minutes from the beginning of the bradycardia.
What is optimal interval between deceleration and delivery?
In a series of 106 cases of uterine rupture during VBAC, Leung et al11 found significant neonatal morbidity when 18 minutes or more lapsed between the onset of the prolonged deceleration and delivery.
First, remain calm when decelerations occur
Freeman and colleagues12 advocate staying calm and avoiding overreaction, because many cases will resolve spontaneously. Nonetheless, prolonged decelerations should prompt the physician to:
TABLE 3
6 pearls for managing prolonged decelerations
| GOAL | PEARL | |
|---|---|---|
| 1 | Reduce aorto-caval and/or cord compression | Change patient positioning |
| 2 | Restore intravascular volume | Administer intravenous fluid bolus |
| 3 | Reduce uterine activity | Discontinue oxytocin drip and give tocolytic therapy (terbutaline) |
| 4 | Enhance oxygen delivery to fetus | Give supplemental oxygen |
| 5 | Resolve hypotension | Administer vasopressor therapy (ephedrine) |
| 6 | Resolve oligohydramnios and cord compression | Perform transcervical amnioinfusion |
TABLE 4
Stepwise management of prolonged decelerations
| Examine the cervix Check for umbilical cord prolapse Check progress of dilation and descent Place internal monitors, if indicated |
| Determine probable cause |
| Start therapies |
| Prepare for intervention by operative delivery Intravenous access Blood type and screen Indwelling urinary catheter Obtain consents for operative vaginal delivery and cesarean delivery Notify appropriate personnel (eg, anesthesiology, pediatrics) |
| Deliver If fetal condition is nonreassuring despite therapies If prolonged decelerations recur and spontaneous delivery is remote (cases must be individualized) |
Consider amnioinfusion when cord compression is suspected
Many cases of prolonged decelerations are secondary to cord compression resulting from oligohydramnios. Miyazaki13 showed that saline amnioinfusion helped correct the FHR problem in most cases of repetitive variable decelerations (19 of 28) and prolonged decelerations (12 of 14 cases).
Several randomized clinical trials analyzed in a recent Cochrane Review14 suggest that amnioinfusion for cord compression reduces the occurrence of variable FHR decelerations and the need for cesarean section; this applies to settings in which nonreassuring FHR patterns were not further assessed by fetal blood sampling, which is reflective of practice in most US labor units.
The recent ACOG practice bulletin on intrapartum monitoring4 advocates amnioinfusion for recurrent variable FHR decelerations, but does not address prolonged decelerations specifically.
Although most data on amnioinfusion address treatment of recurrent variable FHR decelerations, it also seems reasonable to consider this option for prolonged decelerations when oligohydramnios is suspected.12
Other possible causes of prolonged decelerations
Vasa previa. A sudden prolonged deceleration following rupture of membranes with concomitant vaginal bleeding should prompt the physician to consider the possibility of a disrupted velamentous cord insertion (vasa previa), which can lead to rapid fetal exsanguination.15
Acute profound maternal hypoxemia may lead to a first prolonged FHR deceleration, often preceded by increased uterine tone, as described in both eclampsia16 and amniotic fluid embolism.17 With eclampsia, the prolonged deceleration is reversible; treatment and expectant management will allow for fetal recovery after the seizure abates.
When acute amniotic fluid embolism leads to profound cardiovascular collapse, prompt perimortem cesarean delivery may be required within minutes if CPR does not restore normal maternal cardiopulmonary function and recovery of FHR.
When is scalp stimulation helpful?
Stimulation of the fetal scalp is an effective technique for assessing fetal status during periods of nonreassuring FHR patterns.18 However, the technique is intended to be performed during periods of FHR baseline and is sometimes misapplied during prolonged decelerations. Scalp stimulation during a prolonged deceleration would not likely provide valid information or change clinical management and could in theory exacerbate fetal compromise if additional parasympathetic tone were elicited.
Avoid fetal pulse oximetry
Although fetal pulse oximetry is FDA-approved and commercially available in the United States, and may be well suited for monitoring fetal arrhythmias,19,20 a prolonged deceleration is an absolute contraindication to its use.21
Summary
Overall, in managing a delivery marked by prolonged decelerations, we should strive to minimize maternal–fetal complications by carefully assessing the clinical situation, correcting reversible problems, and preparing for expeditious delivery if the fetal condition is of sufficient concern that further expectant management is unlikely to allow for safe spontaneous delivery. Still, “…bedside judgment inevitably will sometimes be imperfect given the unpredictability of these decelerations.”2
The author reports no financial affiliations relevant to this article.
Dilemma: Fetal bradycardia due to congenital complete heart block secondary to anti-SSA/Ro and anti-SS-B/La antibodies. The fetal ventricular rate is fixed at 60 bpm
Management: At 30 weeks’ gestation, with no sonographic evidence of heart failure and a biophysical profile score of 8/8, expectant management is indicated
Dilemma: Prolonged deceleration during pelvic examination in an uncomplicated term pregnancy. Note that fetal heart rate (FHR) variability was maintained during recovery of the FHR baseline
Outcome: Uneventful spontaneous vaginal delivery
Dilemma: Prolonged deceleration due to uterine rupture during trial of labor after cesarean. Repetitive variable decelerations preceded the prolonged deceleration. FHR variability was lost after several minutes
Management: Emergency cesarean
1. Cetrulo CL, Schifrin BS. Fetal heart rate patterns preceding death in utero. Obstet Gynecol. 1976;48:521-527.
2. Cunningham FG, Leveno KJ, Bloom SL, et al. Williams Obstetrics. 22nd ed. New York: McGraw-Hill; 2005.
3. Electronic fetal heart rate monitoring: research guidelines for interpretation. National Institute of Child Health and Human Development Research Planning Workshop. Am J Obstet Gynecol. 1997;177:1385-1390.
4. Intrapartum fetal heart rate monitoring. ACOG Practice Bulletin #70. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2005;106:1453-1461.
5. Young BK, Weinstein HM. Moderate fetal bradycardia. Am J Obstet Gynecol. 1976;126:271-275.
6. Young BK, Katz M, et al. Fetal blood and tissue pH with moderate bradycardia. Am J Obstet Gynecol. 1979;135:45-47.
7. Reynolds SR. Bradycardia in the lamb fetus in response to circulatory distress. Am J Physiol. 1954;176:169-174.
8. Langer O, Sonnendecker EW. Characteristics and management of intrapartum prolonged fetal bradycardia. Br J Obstet Gynaecol. 1982;89:904-912.
9. Williams KP, Galerneau F. Fetal heart rate parameters predictive of neonatal outcome in the presence of a prolonged deceleration. Obstet Gynecol. 2002;100:951-954.
10. Zilianti M, Segura CL, et al. Studies on fetal bradycardia during birth process. II. Obstet Gynecol. 1973;42:840-843.
11. Leung AS, Leung EK, Paul RH. Uterine rupture after previous cesarean delivery: maternal and fetal consequences. Am J Obstet Gynecol. 1993;169:945-950.
12. Freeman RK, Garite TG, Nageotte MP. Fetal Heart Rate Monitoring. Philadelphia: Lippincott Williams & Wilkins; 2003.
13. Miyazaki FS, Taylor NA. Saline amnioinfusion for relief of variable or prolonged decelerations. A preliminary report. Am J Obstet Gynecol. 1983;146:670-678.
14. Hofmeyr GJ. Amnioinfusion for umbilical cord compression in labour. Cochrane Database Syst Rev. 2000;CD000013.-
15. Gabbe SG, Nelson LM, Paul RH. Fetal heart rate response to acute hemorrhage. Obstet Gynecol. 1977;49:247-251.
16. Paul RH, Koh KS, Bernstein SG. Changes in fetal heart rateuterine contraction patterns associated with eclampsia. Am J Obstet Gynecol. 1978;130:165-169.
17. Clark SL, Hankins GD, Dudley DA, Dildy GA, Porter TF. Amniotic fluid embolism: analysis of the national registry. Am J Obstet Gynecol. 1995;172:1158-1167;discussion 1167-1169.
18. Clark SL, Gimovsky ML, Miller FC. The scalp stimulation test: a clinical alternative to fetal scalp blood sampling. Am J Obstet Gynecol. 1984;148:274-277.
19. Dildy GA, Loucks CA, Clark SL. Intrapartum fetal pulse oximetry in the presence of fetal cardiac arrhythmia. Am J Obstet Gynecol. 1993;169:1609-1611.
20. van den Berg PP, Nijland R, van den Brand SF, Jongsma HW, Nijhuis JG. Intrapartum fetal surveillance of congenital heart block with pulse oximetry. Obstet Gynecol. 1994;84:683-686.
21. Garite TJ, Dildy GA, McNamara H, et al. A multicenter controlled trial of fetal pulse oximetry in the intrapartum management of nonreassuring fetal heart rate patterns. Am J Obstet Gynecol. 2000;183:1049-1058.
22. Gull I, Jaffa AJ, Oren M, Grisaru D, Peyser MR, Lessing JB. Acid accumulation during end-stage bradycardia in term fetuses: how long is too long? Br J Obstet Gynaecol. 1996;103:1096-1101.
A prolonged deceleration may signal danger—or reflect a perfectly normal fetal response to maternal pelvic examination. Because of the wide range of possibilities, this fetal heart rate pattern justifies close attention. For example, repetitive prolonged decelerations may indicate cord compression from oligohydramnios. Even more troubling, a prolonged deceleration may occur for the first time during the evolution of a profound catastrophe, such as amniotic fluid embolism or uterine rupture during vaginal birth after cesarean delivery (VBAC). In some circumstances, a prolonged deceleration may be the terminus of a progression of nonreassuring fetal heart rate (FHR) changes, and becomes the immediate precursor to fetal death (TABLE 1).1
When FHR patterns exhibit these aberrations, we rightly worry about fetal well-being and the possible need for operative intervention. Unfortunately, the degree of fetal compromise is difficult to predict and depends on preexisting fetal condition, physiologic reserve, degree and duration of the insult, and other variables.
TABLE 1
Some causes of prolonged decelerations and bradycardias
| PROLONGED DECELERATION | BRADYCARDIA |
|---|---|
| Cord compression Oligohydramnios Cord prolapse Uteroplacental insufficiency Anesthesia (paracervical, spinal, epidural) Maternal valsalva Maternal supine hypotension Hypertonic or prolonged contractions Abruptio placentae Uterine rupture Cocaine ingestion Maternal hypoxia Maternal seizures, eclampsia Respiratory depression from medications Cardiopulmonary arrest Amniotic fluid embolism Fetal hemorrhage Vasa previa Traumatic amniocentesis Fetal vagal reaction Rapid descent, impending birth Cervical examination Fetal scalp electrode placement Fetal blood sampling Fetal central nervous system anomalies Idiopathic (cord compression?) | Congenital conduction abnormalities Complete heart block Long QT syndrome Congenital heart defects Tachyarrhythmia (Fetal tachyarrhythmia may produce an EFM tracing that appears to be a bradycardia and can only be distinguished by ultrasound) Medications Beta blockers Hypothermia Infection Chorioamnionitis Endotoxemia |
Ultimately, a judgment call
The 22nd edition of Williams Obstetrics2 summarizes the clinical challenges involved in the management of prolonged decelerations during labor: “Management of isolated prolonged decelerations is based on bedside clinical judgment, which inevitably will sometimes be imperfect given the unpredictability of these decelerations.”
“Fetal bradycardia” and “prolonged deceleration” are distinct entities
In general parlance, we often use the terms “fetal bradycardia” and “prolonged deceleration” loosely. In practice, we must differentiate these entities because underlying pathophysiologic mechanisms and clinical management may differ substantially.
The problem: Since the introduction of electronic fetal monitoring (EFM) in the 1960s, numerous descriptions of FHR patterns have been published, each slightly different from the others. The result: confusing nomenclature, miscommunication among clinicians, and stymied research efforts.
To standardize definitions of intrapartum FHR patterns so that the effectiveness of EFM could be better assessed in observational studies and clinical trials, the National Institute of Child Health and Human Development organized a workshop.3 Its recommendations were subsequently adopted by the American College of Obstetricians and Gynecologists (ACOG).4 Among the definitions:
Differentiation between the 2 entities is critical because, in many cases, bradycardias are chronic patterns that may not be associated with immediate fetal compromise and do not require immediate intervention. For example, a fetal bradycardia due to congenital heart block would not benefit from immediate delivery, especially prior to term.
“Moderate fetal bradycardia,” defined as a baseline of 100 to 119 bpm, was reported in 1.8% of 1,386 continuously monitored patients and is attributed to relative cephalopelvic disproportion, resolving after rotation of the fetal vertex and associated with normal neonatal outcome.5,6
Similar decelerations can reflect different events
The exact depth and duration of a prolonged deceleration leading to fetal compromise and requiring prompt delivery is difficult to define, although some observations warrant consideration. Experiments with fetal lambs show that the deceleration in response to umbilical vein occlusion is associated with a fall in fetal blood pressure, whereas deceleration in response to umbilical artery occlusion is associated with a rise in fetal blood pressure. This reflex can be abolished by vagotomy, but will eventually recur due to anoxia.7
Vital clue: What happened before the prolonged deceleration?
In clinical practice, it is important to appreciate characteristics of the FHR pattern preceding the prolonged deceleration.8 Williams and Galerneau9 correlated baseline FHR variability and duration of prolonged decelerations with neonatal acid–base status in 186 term gestations with an identified prolonged deceleration within 30 minutes of delivery. Patients were divided into 4 groups, based on FHR variability and recovery of the FHR baseline (TABLE 2).
The findings:
TABLE 2
Neonatal outcomes associated with variability and recovery of FHR patterns after prolonged deceleration
| UMBILICAL ARTERY | GROUP 1 V+ R+ (N=128) | GROUP 2 V+ R- (N=40) | GROUP 3 V- R+ (N=9) | GROUP 4 V- R- (N=9) | P VALUE |
|---|---|---|---|---|---|
| pH (mean±SD) | 7.17±0.09 | 7.13±0.15 | 7.11±0.11 | 6.83±0.16 | <.001 |
| Base deficit (mean±SD) | -6.5±3.9 | -7.2±5.1 | -10±4 | -20±6 | <.001 |
| pH <7.0 (%) | 2 | 18 | 44 | 78 | <.001 |
| pH <7.1 (%) | 22 | 33 | 56 | 89 | <.001 |
| Base deficit <16 (%) | 1 | 8 | 11 | 78 | <.001 |
| Base deficit <12 (%) | 5 | 13 | 22 | 89 | <.001 |
| V=variability | |||||
| R=recovery | |||||
| SOURCE: Williams and Galerneau9 | |||||
Acid–base changes likely begin within minutes of cord compression
Zilianti and colleagues10 evaluated 29 fetuses with normal FHR patterns during labor with FHR deceleration during the expulsion phase of delivery. When the FHR deceleration was prolonged (>120 seconds), umbilical artery pH significantly decreased (7.19 vs 7.27), umbilical vein pH remained unchanged (7.32), and the umbilical venous–arterial pH difference was significantly increased (0.13 vs 0.05). Thus, acid–base changes likely begin within minutes of cord compression.
The correlation between acidemia and loss of variability
In their review of 43 vacuum extractions, Gull and colleagues22 found that 27 infants were delivered for “end-stage bradycardia” (abrupt persistent decrease in FHR to less than 100 bpm for more than 2 minutes, or repeated deceleration more than 60 bpm below baseline with poor recovery), and 16 were delivered electively (controls). Umbilical-cord base deficit was greater in the newborns with bradycardia than in controls, and the length of time FHR variability was lost correlated with the degree of base deficit. Acidemic fetuses lost FHR variability during the bradycardia for more than 4 minutes, or started to lose FHR variability less than 3 minutes from the beginning of the bradycardia.
What is optimal interval between deceleration and delivery?
In a series of 106 cases of uterine rupture during VBAC, Leung et al11 found significant neonatal morbidity when 18 minutes or more lapsed between the onset of the prolonged deceleration and delivery.
First, remain calm when decelerations occur
Freeman and colleagues12 advocate staying calm and avoiding overreaction, because many cases will resolve spontaneously. Nonetheless, prolonged decelerations should prompt the physician to:
TABLE 3
6 pearls for managing prolonged decelerations
| GOAL | PEARL | |
|---|---|---|
| 1 | Reduce aorto-caval and/or cord compression | Change patient positioning |
| 2 | Restore intravascular volume | Administer intravenous fluid bolus |
| 3 | Reduce uterine activity | Discontinue oxytocin drip and give tocolytic therapy (terbutaline) |
| 4 | Enhance oxygen delivery to fetus | Give supplemental oxygen |
| 5 | Resolve hypotension | Administer vasopressor therapy (ephedrine) |
| 6 | Resolve oligohydramnios and cord compression | Perform transcervical amnioinfusion |
TABLE 4
Stepwise management of prolonged decelerations
| Examine the cervix Check for umbilical cord prolapse Check progress of dilation and descent Place internal monitors, if indicated |
| Determine probable cause |
| Start therapies |
| Prepare for intervention by operative delivery Intravenous access Blood type and screen Indwelling urinary catheter Obtain consents for operative vaginal delivery and cesarean delivery Notify appropriate personnel (eg, anesthesiology, pediatrics) |
| Deliver If fetal condition is nonreassuring despite therapies If prolonged decelerations recur and spontaneous delivery is remote (cases must be individualized) |
Consider amnioinfusion when cord compression is suspected
Many cases of prolonged decelerations are secondary to cord compression resulting from oligohydramnios. Miyazaki13 showed that saline amnioinfusion helped correct the FHR problem in most cases of repetitive variable decelerations (19 of 28) and prolonged decelerations (12 of 14 cases).
Several randomized clinical trials analyzed in a recent Cochrane Review14 suggest that amnioinfusion for cord compression reduces the occurrence of variable FHR decelerations and the need for cesarean section; this applies to settings in which nonreassuring FHR patterns were not further assessed by fetal blood sampling, which is reflective of practice in most US labor units.
The recent ACOG practice bulletin on intrapartum monitoring4 advocates amnioinfusion for recurrent variable FHR decelerations, but does not address prolonged decelerations specifically.
Although most data on amnioinfusion address treatment of recurrent variable FHR decelerations, it also seems reasonable to consider this option for prolonged decelerations when oligohydramnios is suspected.12
Other possible causes of prolonged decelerations
Vasa previa. A sudden prolonged deceleration following rupture of membranes with concomitant vaginal bleeding should prompt the physician to consider the possibility of a disrupted velamentous cord insertion (vasa previa), which can lead to rapid fetal exsanguination.15
Acute profound maternal hypoxemia may lead to a first prolonged FHR deceleration, often preceded by increased uterine tone, as described in both eclampsia16 and amniotic fluid embolism.17 With eclampsia, the prolonged deceleration is reversible; treatment and expectant management will allow for fetal recovery after the seizure abates.
When acute amniotic fluid embolism leads to profound cardiovascular collapse, prompt perimortem cesarean delivery may be required within minutes if CPR does not restore normal maternal cardiopulmonary function and recovery of FHR.
When is scalp stimulation helpful?
Stimulation of the fetal scalp is an effective technique for assessing fetal status during periods of nonreassuring FHR patterns.18 However, the technique is intended to be performed during periods of FHR baseline and is sometimes misapplied during prolonged decelerations. Scalp stimulation during a prolonged deceleration would not likely provide valid information or change clinical management and could in theory exacerbate fetal compromise if additional parasympathetic tone were elicited.
Avoid fetal pulse oximetry
Although fetal pulse oximetry is FDA-approved and commercially available in the United States, and may be well suited for monitoring fetal arrhythmias,19,20 a prolonged deceleration is an absolute contraindication to its use.21
Summary
Overall, in managing a delivery marked by prolonged decelerations, we should strive to minimize maternal–fetal complications by carefully assessing the clinical situation, correcting reversible problems, and preparing for expeditious delivery if the fetal condition is of sufficient concern that further expectant management is unlikely to allow for safe spontaneous delivery. Still, “…bedside judgment inevitably will sometimes be imperfect given the unpredictability of these decelerations.”2
The author reports no financial affiliations relevant to this article.
Dilemma: Fetal bradycardia due to congenital complete heart block secondary to anti-SSA/Ro and anti-SS-B/La antibodies. The fetal ventricular rate is fixed at 60 bpm
Management: At 30 weeks’ gestation, with no sonographic evidence of heart failure and a biophysical profile score of 8/8, expectant management is indicated
Dilemma: Prolonged deceleration during pelvic examination in an uncomplicated term pregnancy. Note that fetal heart rate (FHR) variability was maintained during recovery of the FHR baseline
Outcome: Uneventful spontaneous vaginal delivery
Dilemma: Prolonged deceleration due to uterine rupture during trial of labor after cesarean. Repetitive variable decelerations preceded the prolonged deceleration. FHR variability was lost after several minutes
Management: Emergency cesarean
A prolonged deceleration may signal danger—or reflect a perfectly normal fetal response to maternal pelvic examination. Because of the wide range of possibilities, this fetal heart rate pattern justifies close attention. For example, repetitive prolonged decelerations may indicate cord compression from oligohydramnios. Even more troubling, a prolonged deceleration may occur for the first time during the evolution of a profound catastrophe, such as amniotic fluid embolism or uterine rupture during vaginal birth after cesarean delivery (VBAC). In some circumstances, a prolonged deceleration may be the terminus of a progression of nonreassuring fetal heart rate (FHR) changes, and becomes the immediate precursor to fetal death (TABLE 1).1
When FHR patterns exhibit these aberrations, we rightly worry about fetal well-being and the possible need for operative intervention. Unfortunately, the degree of fetal compromise is difficult to predict and depends on preexisting fetal condition, physiologic reserve, degree and duration of the insult, and other variables.
TABLE 1
Some causes of prolonged decelerations and bradycardias
| PROLONGED DECELERATION | BRADYCARDIA |
|---|---|
| Cord compression Oligohydramnios Cord prolapse Uteroplacental insufficiency Anesthesia (paracervical, spinal, epidural) Maternal valsalva Maternal supine hypotension Hypertonic or prolonged contractions Abruptio placentae Uterine rupture Cocaine ingestion Maternal hypoxia Maternal seizures, eclampsia Respiratory depression from medications Cardiopulmonary arrest Amniotic fluid embolism Fetal hemorrhage Vasa previa Traumatic amniocentesis Fetal vagal reaction Rapid descent, impending birth Cervical examination Fetal scalp electrode placement Fetal blood sampling Fetal central nervous system anomalies Idiopathic (cord compression?) | Congenital conduction abnormalities Complete heart block Long QT syndrome Congenital heart defects Tachyarrhythmia (Fetal tachyarrhythmia may produce an EFM tracing that appears to be a bradycardia and can only be distinguished by ultrasound) Medications Beta blockers Hypothermia Infection Chorioamnionitis Endotoxemia |
Ultimately, a judgment call
The 22nd edition of Williams Obstetrics2 summarizes the clinical challenges involved in the management of prolonged decelerations during labor: “Management of isolated prolonged decelerations is based on bedside clinical judgment, which inevitably will sometimes be imperfect given the unpredictability of these decelerations.”
“Fetal bradycardia” and “prolonged deceleration” are distinct entities
In general parlance, we often use the terms “fetal bradycardia” and “prolonged deceleration” loosely. In practice, we must differentiate these entities because underlying pathophysiologic mechanisms and clinical management may differ substantially.
The problem: Since the introduction of electronic fetal monitoring (EFM) in the 1960s, numerous descriptions of FHR patterns have been published, each slightly different from the others. The result: confusing nomenclature, miscommunication among clinicians, and stymied research efforts.
To standardize definitions of intrapartum FHR patterns so that the effectiveness of EFM could be better assessed in observational studies and clinical trials, the National Institute of Child Health and Human Development organized a workshop.3 Its recommendations were subsequently adopted by the American College of Obstetricians and Gynecologists (ACOG).4 Among the definitions:
Differentiation between the 2 entities is critical because, in many cases, bradycardias are chronic patterns that may not be associated with immediate fetal compromise and do not require immediate intervention. For example, a fetal bradycardia due to congenital heart block would not benefit from immediate delivery, especially prior to term.
“Moderate fetal bradycardia,” defined as a baseline of 100 to 119 bpm, was reported in 1.8% of 1,386 continuously monitored patients and is attributed to relative cephalopelvic disproportion, resolving after rotation of the fetal vertex and associated with normal neonatal outcome.5,6
Similar decelerations can reflect different events
The exact depth and duration of a prolonged deceleration leading to fetal compromise and requiring prompt delivery is difficult to define, although some observations warrant consideration. Experiments with fetal lambs show that the deceleration in response to umbilical vein occlusion is associated with a fall in fetal blood pressure, whereas deceleration in response to umbilical artery occlusion is associated with a rise in fetal blood pressure. This reflex can be abolished by vagotomy, but will eventually recur due to anoxia.7
Vital clue: What happened before the prolonged deceleration?
In clinical practice, it is important to appreciate characteristics of the FHR pattern preceding the prolonged deceleration.8 Williams and Galerneau9 correlated baseline FHR variability and duration of prolonged decelerations with neonatal acid–base status in 186 term gestations with an identified prolonged deceleration within 30 minutes of delivery. Patients were divided into 4 groups, based on FHR variability and recovery of the FHR baseline (TABLE 2).
The findings:
TABLE 2
Neonatal outcomes associated with variability and recovery of FHR patterns after prolonged deceleration
| UMBILICAL ARTERY | GROUP 1 V+ R+ (N=128) | GROUP 2 V+ R- (N=40) | GROUP 3 V- R+ (N=9) | GROUP 4 V- R- (N=9) | P VALUE |
|---|---|---|---|---|---|
| pH (mean±SD) | 7.17±0.09 | 7.13±0.15 | 7.11±0.11 | 6.83±0.16 | <.001 |
| Base deficit (mean±SD) | -6.5±3.9 | -7.2±5.1 | -10±4 | -20±6 | <.001 |
| pH <7.0 (%) | 2 | 18 | 44 | 78 | <.001 |
| pH <7.1 (%) | 22 | 33 | 56 | 89 | <.001 |
| Base deficit <16 (%) | 1 | 8 | 11 | 78 | <.001 |
| Base deficit <12 (%) | 5 | 13 | 22 | 89 | <.001 |
| V=variability | |||||
| R=recovery | |||||
| SOURCE: Williams and Galerneau9 | |||||
Acid–base changes likely begin within minutes of cord compression
Zilianti and colleagues10 evaluated 29 fetuses with normal FHR patterns during labor with FHR deceleration during the expulsion phase of delivery. When the FHR deceleration was prolonged (>120 seconds), umbilical artery pH significantly decreased (7.19 vs 7.27), umbilical vein pH remained unchanged (7.32), and the umbilical venous–arterial pH difference was significantly increased (0.13 vs 0.05). Thus, acid–base changes likely begin within minutes of cord compression.
The correlation between acidemia and loss of variability
In their review of 43 vacuum extractions, Gull and colleagues22 found that 27 infants were delivered for “end-stage bradycardia” (abrupt persistent decrease in FHR to less than 100 bpm for more than 2 minutes, or repeated deceleration more than 60 bpm below baseline with poor recovery), and 16 were delivered electively (controls). Umbilical-cord base deficit was greater in the newborns with bradycardia than in controls, and the length of time FHR variability was lost correlated with the degree of base deficit. Acidemic fetuses lost FHR variability during the bradycardia for more than 4 minutes, or started to lose FHR variability less than 3 minutes from the beginning of the bradycardia.
What is optimal interval between deceleration and delivery?
In a series of 106 cases of uterine rupture during VBAC, Leung et al11 found significant neonatal morbidity when 18 minutes or more lapsed between the onset of the prolonged deceleration and delivery.
First, remain calm when decelerations occur
Freeman and colleagues12 advocate staying calm and avoiding overreaction, because many cases will resolve spontaneously. Nonetheless, prolonged decelerations should prompt the physician to:
TABLE 3
6 pearls for managing prolonged decelerations
| GOAL | PEARL | |
|---|---|---|
| 1 | Reduce aorto-caval and/or cord compression | Change patient positioning |
| 2 | Restore intravascular volume | Administer intravenous fluid bolus |
| 3 | Reduce uterine activity | Discontinue oxytocin drip and give tocolytic therapy (terbutaline) |
| 4 | Enhance oxygen delivery to fetus | Give supplemental oxygen |
| 5 | Resolve hypotension | Administer vasopressor therapy (ephedrine) |
| 6 | Resolve oligohydramnios and cord compression | Perform transcervical amnioinfusion |
TABLE 4
Stepwise management of prolonged decelerations
| Examine the cervix Check for umbilical cord prolapse Check progress of dilation and descent Place internal monitors, if indicated |
| Determine probable cause |
| Start therapies |
| Prepare for intervention by operative delivery Intravenous access Blood type and screen Indwelling urinary catheter Obtain consents for operative vaginal delivery and cesarean delivery Notify appropriate personnel (eg, anesthesiology, pediatrics) |
| Deliver If fetal condition is nonreassuring despite therapies If prolonged decelerations recur and spontaneous delivery is remote (cases must be individualized) |
Consider amnioinfusion when cord compression is suspected
Many cases of prolonged decelerations are secondary to cord compression resulting from oligohydramnios. Miyazaki13 showed that saline amnioinfusion helped correct the FHR problem in most cases of repetitive variable decelerations (19 of 28) and prolonged decelerations (12 of 14 cases).
Several randomized clinical trials analyzed in a recent Cochrane Review14 suggest that amnioinfusion for cord compression reduces the occurrence of variable FHR decelerations and the need for cesarean section; this applies to settings in which nonreassuring FHR patterns were not further assessed by fetal blood sampling, which is reflective of practice in most US labor units.
The recent ACOG practice bulletin on intrapartum monitoring4 advocates amnioinfusion for recurrent variable FHR decelerations, but does not address prolonged decelerations specifically.
Although most data on amnioinfusion address treatment of recurrent variable FHR decelerations, it also seems reasonable to consider this option for prolonged decelerations when oligohydramnios is suspected.12
Other possible causes of prolonged decelerations
Vasa previa. A sudden prolonged deceleration following rupture of membranes with concomitant vaginal bleeding should prompt the physician to consider the possibility of a disrupted velamentous cord insertion (vasa previa), which can lead to rapid fetal exsanguination.15
Acute profound maternal hypoxemia may lead to a first prolonged FHR deceleration, often preceded by increased uterine tone, as described in both eclampsia16 and amniotic fluid embolism.17 With eclampsia, the prolonged deceleration is reversible; treatment and expectant management will allow for fetal recovery after the seizure abates.
When acute amniotic fluid embolism leads to profound cardiovascular collapse, prompt perimortem cesarean delivery may be required within minutes if CPR does not restore normal maternal cardiopulmonary function and recovery of FHR.
When is scalp stimulation helpful?
Stimulation of the fetal scalp is an effective technique for assessing fetal status during periods of nonreassuring FHR patterns.18 However, the technique is intended to be performed during periods of FHR baseline and is sometimes misapplied during prolonged decelerations. Scalp stimulation during a prolonged deceleration would not likely provide valid information or change clinical management and could in theory exacerbate fetal compromise if additional parasympathetic tone were elicited.
Avoid fetal pulse oximetry
Although fetal pulse oximetry is FDA-approved and commercially available in the United States, and may be well suited for monitoring fetal arrhythmias,19,20 a prolonged deceleration is an absolute contraindication to its use.21
Summary
Overall, in managing a delivery marked by prolonged decelerations, we should strive to minimize maternal–fetal complications by carefully assessing the clinical situation, correcting reversible problems, and preparing for expeditious delivery if the fetal condition is of sufficient concern that further expectant management is unlikely to allow for safe spontaneous delivery. Still, “…bedside judgment inevitably will sometimes be imperfect given the unpredictability of these decelerations.”2
The author reports no financial affiliations relevant to this article.
Dilemma: Fetal bradycardia due to congenital complete heart block secondary to anti-SSA/Ro and anti-SS-B/La antibodies. The fetal ventricular rate is fixed at 60 bpm
Management: At 30 weeks’ gestation, with no sonographic evidence of heart failure and a biophysical profile score of 8/8, expectant management is indicated
Dilemma: Prolonged deceleration during pelvic examination in an uncomplicated term pregnancy. Note that fetal heart rate (FHR) variability was maintained during recovery of the FHR baseline
Outcome: Uneventful spontaneous vaginal delivery
Dilemma: Prolonged deceleration due to uterine rupture during trial of labor after cesarean. Repetitive variable decelerations preceded the prolonged deceleration. FHR variability was lost after several minutes
Management: Emergency cesarean
1. Cetrulo CL, Schifrin BS. Fetal heart rate patterns preceding death in utero. Obstet Gynecol. 1976;48:521-527.
2. Cunningham FG, Leveno KJ, Bloom SL, et al. Williams Obstetrics. 22nd ed. New York: McGraw-Hill; 2005.
3. Electronic fetal heart rate monitoring: research guidelines for interpretation. National Institute of Child Health and Human Development Research Planning Workshop. Am J Obstet Gynecol. 1997;177:1385-1390.
4. Intrapartum fetal heart rate monitoring. ACOG Practice Bulletin #70. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2005;106:1453-1461.
5. Young BK, Weinstein HM. Moderate fetal bradycardia. Am J Obstet Gynecol. 1976;126:271-275.
6. Young BK, Katz M, et al. Fetal blood and tissue pH with moderate bradycardia. Am J Obstet Gynecol. 1979;135:45-47.
7. Reynolds SR. Bradycardia in the lamb fetus in response to circulatory distress. Am J Physiol. 1954;176:169-174.
8. Langer O, Sonnendecker EW. Characteristics and management of intrapartum prolonged fetal bradycardia. Br J Obstet Gynaecol. 1982;89:904-912.
9. Williams KP, Galerneau F. Fetal heart rate parameters predictive of neonatal outcome in the presence of a prolonged deceleration. Obstet Gynecol. 2002;100:951-954.
10. Zilianti M, Segura CL, et al. Studies on fetal bradycardia during birth process. II. Obstet Gynecol. 1973;42:840-843.
11. Leung AS, Leung EK, Paul RH. Uterine rupture after previous cesarean delivery: maternal and fetal consequences. Am J Obstet Gynecol. 1993;169:945-950.
12. Freeman RK, Garite TG, Nageotte MP. Fetal Heart Rate Monitoring. Philadelphia: Lippincott Williams & Wilkins; 2003.
13. Miyazaki FS, Taylor NA. Saline amnioinfusion for relief of variable or prolonged decelerations. A preliminary report. Am J Obstet Gynecol. 1983;146:670-678.
14. Hofmeyr GJ. Amnioinfusion for umbilical cord compression in labour. Cochrane Database Syst Rev. 2000;CD000013.-
15. Gabbe SG, Nelson LM, Paul RH. Fetal heart rate response to acute hemorrhage. Obstet Gynecol. 1977;49:247-251.
16. Paul RH, Koh KS, Bernstein SG. Changes in fetal heart rateuterine contraction patterns associated with eclampsia. Am J Obstet Gynecol. 1978;130:165-169.
17. Clark SL, Hankins GD, Dudley DA, Dildy GA, Porter TF. Amniotic fluid embolism: analysis of the national registry. Am J Obstet Gynecol. 1995;172:1158-1167;discussion 1167-1169.
18. Clark SL, Gimovsky ML, Miller FC. The scalp stimulation test: a clinical alternative to fetal scalp blood sampling. Am J Obstet Gynecol. 1984;148:274-277.
19. Dildy GA, Loucks CA, Clark SL. Intrapartum fetal pulse oximetry in the presence of fetal cardiac arrhythmia. Am J Obstet Gynecol. 1993;169:1609-1611.
20. van den Berg PP, Nijland R, van den Brand SF, Jongsma HW, Nijhuis JG. Intrapartum fetal surveillance of congenital heart block with pulse oximetry. Obstet Gynecol. 1994;84:683-686.
21. Garite TJ, Dildy GA, McNamara H, et al. A multicenter controlled trial of fetal pulse oximetry in the intrapartum management of nonreassuring fetal heart rate patterns. Am J Obstet Gynecol. 2000;183:1049-1058.
22. Gull I, Jaffa AJ, Oren M, Grisaru D, Peyser MR, Lessing JB. Acid accumulation during end-stage bradycardia in term fetuses: how long is too long? Br J Obstet Gynaecol. 1996;103:1096-1101.
1. Cetrulo CL, Schifrin BS. Fetal heart rate patterns preceding death in utero. Obstet Gynecol. 1976;48:521-527.
2. Cunningham FG, Leveno KJ, Bloom SL, et al. Williams Obstetrics. 22nd ed. New York: McGraw-Hill; 2005.
3. Electronic fetal heart rate monitoring: research guidelines for interpretation. National Institute of Child Health and Human Development Research Planning Workshop. Am J Obstet Gynecol. 1997;177:1385-1390.
4. Intrapartum fetal heart rate monitoring. ACOG Practice Bulletin #70. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2005;106:1453-1461.
5. Young BK, Weinstein HM. Moderate fetal bradycardia. Am J Obstet Gynecol. 1976;126:271-275.
6. Young BK, Katz M, et al. Fetal blood and tissue pH with moderate bradycardia. Am J Obstet Gynecol. 1979;135:45-47.
7. Reynolds SR. Bradycardia in the lamb fetus in response to circulatory distress. Am J Physiol. 1954;176:169-174.
8. Langer O, Sonnendecker EW. Characteristics and management of intrapartum prolonged fetal bradycardia. Br J Obstet Gynaecol. 1982;89:904-912.
9. Williams KP, Galerneau F. Fetal heart rate parameters predictive of neonatal outcome in the presence of a prolonged deceleration. Obstet Gynecol. 2002;100:951-954.
10. Zilianti M, Segura CL, et al. Studies on fetal bradycardia during birth process. II. Obstet Gynecol. 1973;42:840-843.
11. Leung AS, Leung EK, Paul RH. Uterine rupture after previous cesarean delivery: maternal and fetal consequences. Am J Obstet Gynecol. 1993;169:945-950.
12. Freeman RK, Garite TG, Nageotte MP. Fetal Heart Rate Monitoring. Philadelphia: Lippincott Williams & Wilkins; 2003.
13. Miyazaki FS, Taylor NA. Saline amnioinfusion for relief of variable or prolonged decelerations. A preliminary report. Am J Obstet Gynecol. 1983;146:670-678.
14. Hofmeyr GJ. Amnioinfusion for umbilical cord compression in labour. Cochrane Database Syst Rev. 2000;CD000013.-
15. Gabbe SG, Nelson LM, Paul RH. Fetal heart rate response to acute hemorrhage. Obstet Gynecol. 1977;49:247-251.
16. Paul RH, Koh KS, Bernstein SG. Changes in fetal heart rateuterine contraction patterns associated with eclampsia. Am J Obstet Gynecol. 1978;130:165-169.
17. Clark SL, Hankins GD, Dudley DA, Dildy GA, Porter TF. Amniotic fluid embolism: analysis of the national registry. Am J Obstet Gynecol. 1995;172:1158-1167;discussion 1167-1169.
18. Clark SL, Gimovsky ML, Miller FC. The scalp stimulation test: a clinical alternative to fetal scalp blood sampling. Am J Obstet Gynecol. 1984;148:274-277.
19. Dildy GA, Loucks CA, Clark SL. Intrapartum fetal pulse oximetry in the presence of fetal cardiac arrhythmia. Am J Obstet Gynecol. 1993;169:1609-1611.
20. van den Berg PP, Nijland R, van den Brand SF, Jongsma HW, Nijhuis JG. Intrapartum fetal surveillance of congenital heart block with pulse oximetry. Obstet Gynecol. 1994;84:683-686.
21. Garite TJ, Dildy GA, McNamara H, et al. A multicenter controlled trial of fetal pulse oximetry in the intrapartum management of nonreassuring fetal heart rate patterns. Am J Obstet Gynecol. 2000;183:1049-1058.
22. Gull I, Jaffa AJ, Oren M, Grisaru D, Peyser MR, Lessing JB. Acid accumulation during end-stage bradycardia in term fetuses: how long is too long? Br J Obstet Gynaecol. 1996;103:1096-1101.
Injury-free vaginal surgery: Case-based protective tactics
CASE 1 Gush of fluid during dissection
A 55-year-old woman with 2 prior cesarean deliveries and stage III uterovaginal prolapse (primarily apical) is now undergoing transvaginal hysterectomy and prolapse repair. During sharp dissection of the bladder off the lower uterine segment, a gush of clear fluid washes over the area of dissection.
What steps would you take to achieve the best possible clinical outcome for this woman?
If a patient sustains a urinary tract injury, she is 91 times more likely to sue her surgeon than a patient who has a different complication or problem at gynecologic surgery.1 Yet, despite a surgeon’s best efforts, injury can occur. If it does, the best approach is immediate recognition and repair.
Primary prevention—including identifying the ureters—and intraoperative repair is the easiest, most successful, least morbid approach, compared to postoperative management. And probably less likely to lead to a lawsuit.2
As always, our main goal in any preventive effort is the best possible patient care and clinical outcomes, and diligent, careful surgical technique is the best protection on all counts. Every vaginal surgeon should have a consistent strategy for preventing, indentifying and managing intraoperative injuries to the urinary tract and bowel.
This article discusses potential injuries to the lower genitourinary and gastrointestinal tracts separately.
Vulnerable anatomy is a given
The ureters are injured in up to 2.4% of vaginal surgeries,4 and gynecologic surgery accounts for as much as 52% of inadvertent ureteral injuries.5 The bladder and bowel can also sustain injuries, in up to 2.9% and 8% of cases, respectively.3,6
Mechanisms of injury can include bladder perforation7 (and, rarely, small bowel perforation8) during placement of bladder neck and midurethral slings, transection of the bladder or ureter during vaginal hysterectomy, and ureteral kinking or obstruction during vaginal hysterectomy and vault suspension.4,9
The rectum can sometimes be perforated during posterior colporrhaphy or perineorrhaphy.6
Risk factors
For intraoperative bladder injury: prior anterior colporrhaphy, cesarean delivery, or incontinence surgery.
For injury to the rectum: prior posterior vaginal wall surgery and defects in the distal rectovaginal septum.
For injury to the small bowel: enterocele.
Women with surgically induced or suspected congenital anatomic anomalies (eg, ureteral reimplantation, ectopic kidneys or ureters, suprapubic vascular bypass grafts) require evaluation to establish the location of these anatomic variants with respect to the planned area of surgical exploration.
Most gyn surgical injuries involve the urinary tract
The urethra and a substantial portion of the posterior bladder rest on and are supported by the anterior vaginal wall. In women with an intact uterus, the posterior bladder wall also rests on the anterior lower uterine segment.
In women with a uterine scar, the bladder wall itself can sometimes be scarred down to the anterior lower uterine segment. This scarring occurs when the lower uterine scar becomes adherent to the posterior bladder wall during wound healing. Unrepaired or delayed repair to bladder injuries in these areas may lead to fistula formation.
Prior anterior colporrhaphy is associated with scarring between the bladder and anterior vaginal walls and can increase the risk of bladder injury during vaginal surgery.
Intraoperative injuries to the bladder dome and bladder neck are most common during urethral and bladder-neck sling procedures. During these procedures, prevent injury by keeping the passing tip of the sling-insertion device (eg, trocar or other passing instrument) clear of the urethra and bladder neck, and perform cystourethroscopy during each pass to identify any perforation of the bladder or urethra.
When perforation occurs, inspect the ureteral orifices thoroughly and document prompt efflux from both. If the orifices are freely effluxing and the remainder of the bladder mucosa is intact, withdraw the perforating instrument, pass it through again, and repeat cystoscopy to confirm that there is no new perforation.
Perforations to the bladder dome usually heal spontaneously in the postoperative period, with no need for extended bladder drainage. Perforations at the lateral or anterior bladder neck will also heal spontaneously.
Injuries to the posterior bladder wall and trigone
These injuries can occur during vaginal hysterectomy or dissection of the anterior vaginal wall (eg, anterior colporrhaphy, paravaginal defect repair). Avoid injuries by dissecting the vaginal mucosa (and lower uterine segment) carefully off the underlying endopelvic tissues.
Signs of an injury
Injury is often heralded by a gush of urine into the vaginal operative field, as in the opening case. When it occurs, determine the extent of injury from the vaginal side, and use a small Allis clamp to temporarily close the injury so that cystourethroscopy is effective. During cystoscopy, take steps to ascertain the extent of the injury and its proximity to the ureteral orifices.
Vaginal approach to intraoperative repair
Lacerations 2 cm or less in size are usually amenable to vaginal repair. In general, if the full extent of the laceration can be visually appreciated and accessed using the vaginal route, the repair can be safely attempted from the vaginal approach.
If the perforation is well away (>1 cm) from the ureteral orifices and there is free efflux from both orifices, close the defect from the vaginal side in 3 imbricating layers, being careful to keep the suture knots out of the bladder lumen.
Start by dissecting the overlying vaginal mucosa off the endopelvic fascia for 1 cm around the defect. This exposes the bladder adventitia, which can be used to reapproximate the laceration as follows:
Test the repair
Backfill the bladder transurethrally with 100 cc of sterile infant formula, and observe the result on the vaginal side. Closure should be watertight. Sterile formula does not stain the tissues and is therefore preferable to indigo carmine or methylene blue.
Reapproximate the vaginal mucosa using 2-0 Monocryl suture in a running, “nonlocked” fashion. Repeat cystoscopy after the closure to ensure prompt, free efflux from both ureteral orifices.
In nonradiated, well-perfused tissues, an interposing fat pad (eg, Martius or omental) is usually not required.
Foley catheter drainage is recommended to allow about 3 weeks of healing time for the closure.
If the laceration is less than 1 cm from a ureteral orifice
Assess the integrity of the affected ureter using a retrograde ureterogram performed under fluoroscopy. If ureteral integrity is confirmed, the affected ureter may be stented prior to repair of the laceration (as discussed above). Any stents may be left in place until the repair is judged to be sufficiently healed.
If the laceration is not fully visible or accessible vaginally
Use an abdominal approach—either open or laparoscopic—after assessing ureteral integrity. Focus on developing a suitable plane between the bladder and vaginal walls around the defect, followed by reapproximation of the bladder in 3 imbricating running layers of absorbable monofilament suture, as described above.
If the injury occurs during vaginal hysterectomy
In this situation, bladder closure can be deferred until the uterus and ovaries (if planned) have been removed.
For other procedures, such as anterior colporrhaphy, finish the procedure after the bladder is successfully closed. If the perforation is near or involves either ureteral orifice, it should be addressed in the manner of a ureteral injury (see below).
After fistula repairs
My patients undergo fluoroscopic evaluation of bladder filling and emptying at the 3-week mark, prior to Foley removal, to document functional closure. Then the Foley catheter and any indwelling stents are removed.
I counsel patients about the need to empty the bladder frequently, and how to recognize and avoid urinary retention.
Injuries to the ureters
The pelvic aspect of the ureters is also of interest to the gynecologic surgeon because these structures are at risk for obstruction or transection.
Vaginal procedures that can put the ureters at risk include vaginal vault (apical) suspensions and paravaginal defect repairs. Always include cystourethroscopy at the end of these procedures to document prompt and free efflux from both ureteral orifices.
3 “risky” regions
Because of its proximity to the vagina and uterus, the bladder is sometimes injured during vaginal surgery. Three areas are vulnerable: the dome and bladder neck/urethra, at risk during sling procedures, and the posterior bladder wall, vulnerable during dissection of the anterior vaginal wall.
If cystoscopy fails to confirm definitive bilateral efflux
Infuse intravenous indigo carmine and inspect the ureteral orifices again, in this situation. If bilateral efflux is not forthcoming, consider removing any intrapelvic packing, and take the patient out of the Trendelenburg position so that she can be observed for 20 minutes.
If there is still no efflux after that interval, a ureter may be obstructed.
If you suspect ureteral kinking or obstruction
Consider removing any suspensory sutures near the obstructed (noneffluxing) ureter. This maneuver usually results in vigorous efflux from the affected orifice.10 In the case of apical suspension sutures, remove the most lateral suture first and perform cystoscopy after each (more medial) suture is removed.4,9
If suture removal fails to bring about ureteral efflux, evaluate the ureters further by using intraoperative retrograde ureterogram (pyelogram) under fluoroscopy or by placing ureteral stents under cystoscopic guidance. Either method will localize the obstruction or kink and allow for targeted exploration and release of the stricture.
Extended bladder drainage is usually not required after intraoperative release of a partially or completely obstructed ureter.
In my practice, I remove any permanent suture I suspect is kinking or partially kinking a ureter. If the suture causing the problem is an absorbable one (eg, as in the use of Vicryl suture at colpocleisis), I may choose to follow the patient or to place a stent, and I reassure the woman that the offending suture will dissolve over time, thus relieving the partial obstruction.
If blue dye enters the field from inside the pelvis
The problem may be partial or complete ureteral transection. In this case, bladder perforation must first be ruled out cystoscopically. Then perform retrograde ureterogram under fluoroscopy to look for the possible point of leakage.
If ureteral transection is confirmed, plan for thorough surgical exploration (usually via the abdominal route) to locate and repair the injury.
For many generalists, this may require an intraoperative consult from a surgical service comfortable with the repair and/or reimplantation of the ureters.
CASE 1 OUTCOME
The bladder laceration was repaired after completion of the vaginal hysterectomy in the manner described above. There were no further sequelae.
It pays to refamiliarize yourself with the particular “landscape” of the lower urinary tract, so that sutures or scalpels don’t inadvertently block or injure structures.
The smooth muscle of the bladder (detrusor) is lined with transitional mucosal epithelium and opens into the urethra at the bladder neck.
The ureters enter into the lateral aspects of the midposterior bladder and tunnel medially through the detrusor muscle before entering the bladder lumen at the level of the interureteral ridge. These entry points are known as the ureteral orifices.
The trigone is an area of the posterior bladder wall bounded by the bladder neck inferiorly and by the 2 ureteral orifices in the posterior midbladder.
Rectal injuries are usually easy to identify
As far as vaginal surgery is concerned, the lower GI tract consists of the rectum and external and internal anal sphincters. The distal rectum and posterior vaginal wall are usually closely applied to each other, separated by the rectovaginal septum (also called Denonvilliers fascia).
Risk factors
In women who have undergone posterior colporrhaphy or repair of a 4th degree tear, the posterior vaginal wall can be densely adherent to the rectum, putting the rectum at risk for injury during posterior vaginal wall dissection.
Most injuries to the rectum occur during dissection of the posterior vaginal wall. Fortunately, these injuries are readily recognized and easily repaired. If a rectal injury is suspected during or after dissection, a thorough intraoperative digital exam will help confirm or rule it out.
Repair of a rectal injury
Once an injury is identified, reapproximate the rectal mucosal edges with an imbricating closure using 3-0 Monocryl or other absorbable monofilament suture. A second imbricating layer should bring the rectal muscularis together, and the rectovaginal septum can then be closed over this layer in side-to-side or transverse fashion. Finally, close the vaginal mucosa after appropriate posterior colporrhaphy trimming. Such repairs heal well over time, without any long-term effects for the patient.
Prescribe a stool softener for the first 3 postoperative months to reduce the patient’s need to strain.
No bowel prep needed because injuries are rare
In my practice, the vast majority of vaginal surgical cases are accomplished without the need for preoperative bowel preparation. In the occasional patient known to have dense small-bowel adhesions involving the uterus, adnexae, or vaginal cuff, bowel prep may be appropriate if substantial dissection of the bowel is anticipated as part of the procedure.
CASE 2 Small bowel laceration
A 45-year-old woman with 4 prior vaginal deliveries, a 4th-degree obstetric rectovaginal laceration, and a history of laparoscopically assisted vaginal hysterectomy presents with stage III pelvic organ prolapse, primarily involving the posterior vaginal wall. An examination reveals a defect in the upper aspect of the posterior wall (an apical defect).
Intraoperatively, during sharp dissection to lift the posterior vaginal wall off the rectovaginal septum, a loop of small bowel descends into the field, and a 1-cm laceration occurs, exposing the lumen of the bowel.
How do you proceed?
On very rare occasions, a patient with an enterocele may sustain a small bowel injury during vaginal surgery. Such injury can usually be avoided by packing the small bowel away from the area of dissection and closely observing the dissection field.
Transvaginal repair
If the small bowel is cut during dissection, inspect the adjacent small bowel thoroughly to ascertain the extent of the injury. Transvaginal repair is recommended if the laceration and adjacent mesentery can be completely visualized and accessed through the vagina.
Small lacerations require a simple closure
If the laceration is small (1–2 cm) and does not involve the mesentery, irrigate it thoroughly and close it using a running imbricating 2-0 braided suture (eg, Vicryl or silk), with the suture line perpendicular to the long axis of the small bowel to decrease the risk of stricture. Inspect the suture line to ensure that it completely seals the laceration. Suture bites should incorporate the serosa and muscularis without transgressing the mucosa. Use a noncutting needle to place these sutures.
If the mesentery is involved in the laceration, make sure there are no bleeding vessels, and ligate any bleeding ones.
Large lacerations may necessitate abdominal surgery
An abdominal or laparoscopic procedure may be necessary to repair larger lacerations to the small bowel. If the surgeon is uncomfortable with bowel repair, it may be appropriate to obtain an intraoperative consult from a surgical service.
Postoperative monitoring
Watch for signs of ileus, which should be managed with bowel rest and nasogastric suction, as indicated.
CASE 2 OUTCOME
The small laceration was repaired with 2-0 Vicryl suture in the manner described above. The patient’s diet was advanced when bowel sounds returned. There were no further sequelae.
Generalists can manage most injuries
Incidental intraoperative injuries to the lower urinary and gastrointestinal tracts are relatively rare complications of vaginal surgery—but we must make every effort to anticipate, prevent, and promptly recognize such injuries.
If they do occur, pursue a course to thoroughly evaluate, repair, test, and provide appropriate followup for the patient. If promptly identified and addressed, these injuries can be made to resolve with minimal long-term sequelae. Appropriately timed intraoperative cystoscopy is a useful method for prompt intraoperative identification of bladder and ureteric injuries. Injuries identified intraoperatively can usually be repaired using simple techniques available to the general gynecologist.
The author reports no financial relationships relevant to this article
1. Gilmour DT, Baskett TF. Disability and litigation from urinary tract injuries at benign gynecologic surgery in Canada. Obstet Gynecol. 2005;105:109-114.
2. Pettit PD, Petrou SP. The value of cystoscopy in major vaginal surgery. Obstet Gynecol. 1994;84:318-320.
3. Gilmour DT, Dwyer PL, Carey MP. Lower urinary tract injury during gynecologic surgery and its detection by intraoperative cystoscopy. Obstet Gynecol. 1999;94:883-889.
4. Karram M, Goldwasser S, Kleeman S, et al. High uterosacral vaginal vault suspension with fascial reconstruction for vaginal repair of enterocele and vaginal vault prolapse. Am J Obstet Gynecol. 2001;185:1339-1342discussion 1342-1343.
5. Dowling RA, Corriere JN, Jr, Sandler CM. Iatrogenic ureteral injury. J Urol. 1986;135:912-915.
6. Mercer-Jones MA, Sprowson A, Varma JS. Outcome after transperineal mesh repair of rectocele: a case series. Dis Colon Rectum. 2004;47:864-868.
7. McLennan MT, Melick CF. Bladder perforation during tension-free vaginal tape procedures: analysis of learning curve and risk factors. Obstet Gynecol. 2005;106:1000-1004.
8. Leboeuf L, Tellez CA, Ead D, Gousse AE. Complication of bowel perforation during insertion of tension-free vaginal tape. J Urol. 2003;170:1310-discussion 1310-1311.
9. Shull BL, Bachofen C, Coates KW, Kuehl TJ. A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol. 2000;183:1365-1373discussion 1373-1374.
10. Harris RL, Cundiff GW, Theofrastous JP, et al. The value of intraoperative cystoscopy in urogynecologic and reconstructive pelvic surgery. Am J Obstet Gynecol. 1997;177:1367-1369discussion 1369-1371.
CASE 1 Gush of fluid during dissection
A 55-year-old woman with 2 prior cesarean deliveries and stage III uterovaginal prolapse (primarily apical) is now undergoing transvaginal hysterectomy and prolapse repair. During sharp dissection of the bladder off the lower uterine segment, a gush of clear fluid washes over the area of dissection.
What steps would you take to achieve the best possible clinical outcome for this woman?
If a patient sustains a urinary tract injury, she is 91 times more likely to sue her surgeon than a patient who has a different complication or problem at gynecologic surgery.1 Yet, despite a surgeon’s best efforts, injury can occur. If it does, the best approach is immediate recognition and repair.
Primary prevention—including identifying the ureters—and intraoperative repair is the easiest, most successful, least morbid approach, compared to postoperative management. And probably less likely to lead to a lawsuit.2
As always, our main goal in any preventive effort is the best possible patient care and clinical outcomes, and diligent, careful surgical technique is the best protection on all counts. Every vaginal surgeon should have a consistent strategy for preventing, indentifying and managing intraoperative injuries to the urinary tract and bowel.
This article discusses potential injuries to the lower genitourinary and gastrointestinal tracts separately.
Vulnerable anatomy is a given
The ureters are injured in up to 2.4% of vaginal surgeries,4 and gynecologic surgery accounts for as much as 52% of inadvertent ureteral injuries.5 The bladder and bowel can also sustain injuries, in up to 2.9% and 8% of cases, respectively.3,6
Mechanisms of injury can include bladder perforation7 (and, rarely, small bowel perforation8) during placement of bladder neck and midurethral slings, transection of the bladder or ureter during vaginal hysterectomy, and ureteral kinking or obstruction during vaginal hysterectomy and vault suspension.4,9
The rectum can sometimes be perforated during posterior colporrhaphy or perineorrhaphy.6
Risk factors
For intraoperative bladder injury: prior anterior colporrhaphy, cesarean delivery, or incontinence surgery.
For injury to the rectum: prior posterior vaginal wall surgery and defects in the distal rectovaginal septum.
For injury to the small bowel: enterocele.
Women with surgically induced or suspected congenital anatomic anomalies (eg, ureteral reimplantation, ectopic kidneys or ureters, suprapubic vascular bypass grafts) require evaluation to establish the location of these anatomic variants with respect to the planned area of surgical exploration.
Most gyn surgical injuries involve the urinary tract
The urethra and a substantial portion of the posterior bladder rest on and are supported by the anterior vaginal wall. In women with an intact uterus, the posterior bladder wall also rests on the anterior lower uterine segment.
In women with a uterine scar, the bladder wall itself can sometimes be scarred down to the anterior lower uterine segment. This scarring occurs when the lower uterine scar becomes adherent to the posterior bladder wall during wound healing. Unrepaired or delayed repair to bladder injuries in these areas may lead to fistula formation.
Prior anterior colporrhaphy is associated with scarring between the bladder and anterior vaginal walls and can increase the risk of bladder injury during vaginal surgery.
Intraoperative injuries to the bladder dome and bladder neck are most common during urethral and bladder-neck sling procedures. During these procedures, prevent injury by keeping the passing tip of the sling-insertion device (eg, trocar or other passing instrument) clear of the urethra and bladder neck, and perform cystourethroscopy during each pass to identify any perforation of the bladder or urethra.
When perforation occurs, inspect the ureteral orifices thoroughly and document prompt efflux from both. If the orifices are freely effluxing and the remainder of the bladder mucosa is intact, withdraw the perforating instrument, pass it through again, and repeat cystoscopy to confirm that there is no new perforation.
Perforations to the bladder dome usually heal spontaneously in the postoperative period, with no need for extended bladder drainage. Perforations at the lateral or anterior bladder neck will also heal spontaneously.
Injuries to the posterior bladder wall and trigone
These injuries can occur during vaginal hysterectomy or dissection of the anterior vaginal wall (eg, anterior colporrhaphy, paravaginal defect repair). Avoid injuries by dissecting the vaginal mucosa (and lower uterine segment) carefully off the underlying endopelvic tissues.
Signs of an injury
Injury is often heralded by a gush of urine into the vaginal operative field, as in the opening case. When it occurs, determine the extent of injury from the vaginal side, and use a small Allis clamp to temporarily close the injury so that cystourethroscopy is effective. During cystoscopy, take steps to ascertain the extent of the injury and its proximity to the ureteral orifices.
Vaginal approach to intraoperative repair
Lacerations 2 cm or less in size are usually amenable to vaginal repair. In general, if the full extent of the laceration can be visually appreciated and accessed using the vaginal route, the repair can be safely attempted from the vaginal approach.
If the perforation is well away (>1 cm) from the ureteral orifices and there is free efflux from both orifices, close the defect from the vaginal side in 3 imbricating layers, being careful to keep the suture knots out of the bladder lumen.
Start by dissecting the overlying vaginal mucosa off the endopelvic fascia for 1 cm around the defect. This exposes the bladder adventitia, which can be used to reapproximate the laceration as follows:
Test the repair
Backfill the bladder transurethrally with 100 cc of sterile infant formula, and observe the result on the vaginal side. Closure should be watertight. Sterile formula does not stain the tissues and is therefore preferable to indigo carmine or methylene blue.
Reapproximate the vaginal mucosa using 2-0 Monocryl suture in a running, “nonlocked” fashion. Repeat cystoscopy after the closure to ensure prompt, free efflux from both ureteral orifices.
In nonradiated, well-perfused tissues, an interposing fat pad (eg, Martius or omental) is usually not required.
Foley catheter drainage is recommended to allow about 3 weeks of healing time for the closure.
If the laceration is less than 1 cm from a ureteral orifice
Assess the integrity of the affected ureter using a retrograde ureterogram performed under fluoroscopy. If ureteral integrity is confirmed, the affected ureter may be stented prior to repair of the laceration (as discussed above). Any stents may be left in place until the repair is judged to be sufficiently healed.
If the laceration is not fully visible or accessible vaginally
Use an abdominal approach—either open or laparoscopic—after assessing ureteral integrity. Focus on developing a suitable plane between the bladder and vaginal walls around the defect, followed by reapproximation of the bladder in 3 imbricating running layers of absorbable monofilament suture, as described above.
If the injury occurs during vaginal hysterectomy
In this situation, bladder closure can be deferred until the uterus and ovaries (if planned) have been removed.
For other procedures, such as anterior colporrhaphy, finish the procedure after the bladder is successfully closed. If the perforation is near or involves either ureteral orifice, it should be addressed in the manner of a ureteral injury (see below).
After fistula repairs
My patients undergo fluoroscopic evaluation of bladder filling and emptying at the 3-week mark, prior to Foley removal, to document functional closure. Then the Foley catheter and any indwelling stents are removed.
I counsel patients about the need to empty the bladder frequently, and how to recognize and avoid urinary retention.
Injuries to the ureters
The pelvic aspect of the ureters is also of interest to the gynecologic surgeon because these structures are at risk for obstruction or transection.
Vaginal procedures that can put the ureters at risk include vaginal vault (apical) suspensions and paravaginal defect repairs. Always include cystourethroscopy at the end of these procedures to document prompt and free efflux from both ureteral orifices.
3 “risky” regions
Because of its proximity to the vagina and uterus, the bladder is sometimes injured during vaginal surgery. Three areas are vulnerable: the dome and bladder neck/urethra, at risk during sling procedures, and the posterior bladder wall, vulnerable during dissection of the anterior vaginal wall.
If cystoscopy fails to confirm definitive bilateral efflux
Infuse intravenous indigo carmine and inspect the ureteral orifices again, in this situation. If bilateral efflux is not forthcoming, consider removing any intrapelvic packing, and take the patient out of the Trendelenburg position so that she can be observed for 20 minutes.
If there is still no efflux after that interval, a ureter may be obstructed.
If you suspect ureteral kinking or obstruction
Consider removing any suspensory sutures near the obstructed (noneffluxing) ureter. This maneuver usually results in vigorous efflux from the affected orifice.10 In the case of apical suspension sutures, remove the most lateral suture first and perform cystoscopy after each (more medial) suture is removed.4,9
If suture removal fails to bring about ureteral efflux, evaluate the ureters further by using intraoperative retrograde ureterogram (pyelogram) under fluoroscopy or by placing ureteral stents under cystoscopic guidance. Either method will localize the obstruction or kink and allow for targeted exploration and release of the stricture.
Extended bladder drainage is usually not required after intraoperative release of a partially or completely obstructed ureter.
In my practice, I remove any permanent suture I suspect is kinking or partially kinking a ureter. If the suture causing the problem is an absorbable one (eg, as in the use of Vicryl suture at colpocleisis), I may choose to follow the patient or to place a stent, and I reassure the woman that the offending suture will dissolve over time, thus relieving the partial obstruction.
If blue dye enters the field from inside the pelvis
The problem may be partial or complete ureteral transection. In this case, bladder perforation must first be ruled out cystoscopically. Then perform retrograde ureterogram under fluoroscopy to look for the possible point of leakage.
If ureteral transection is confirmed, plan for thorough surgical exploration (usually via the abdominal route) to locate and repair the injury.
For many generalists, this may require an intraoperative consult from a surgical service comfortable with the repair and/or reimplantation of the ureters.
CASE 1 OUTCOME
The bladder laceration was repaired after completion of the vaginal hysterectomy in the manner described above. There were no further sequelae.
It pays to refamiliarize yourself with the particular “landscape” of the lower urinary tract, so that sutures or scalpels don’t inadvertently block or injure structures.
The smooth muscle of the bladder (detrusor) is lined with transitional mucosal epithelium and opens into the urethra at the bladder neck.
The ureters enter into the lateral aspects of the midposterior bladder and tunnel medially through the detrusor muscle before entering the bladder lumen at the level of the interureteral ridge. These entry points are known as the ureteral orifices.
The trigone is an area of the posterior bladder wall bounded by the bladder neck inferiorly and by the 2 ureteral orifices in the posterior midbladder.
Rectal injuries are usually easy to identify
As far as vaginal surgery is concerned, the lower GI tract consists of the rectum and external and internal anal sphincters. The distal rectum and posterior vaginal wall are usually closely applied to each other, separated by the rectovaginal septum (also called Denonvilliers fascia).
Risk factors
In women who have undergone posterior colporrhaphy or repair of a 4th degree tear, the posterior vaginal wall can be densely adherent to the rectum, putting the rectum at risk for injury during posterior vaginal wall dissection.
Most injuries to the rectum occur during dissection of the posterior vaginal wall. Fortunately, these injuries are readily recognized and easily repaired. If a rectal injury is suspected during or after dissection, a thorough intraoperative digital exam will help confirm or rule it out.
Repair of a rectal injury
Once an injury is identified, reapproximate the rectal mucosal edges with an imbricating closure using 3-0 Monocryl or other absorbable monofilament suture. A second imbricating layer should bring the rectal muscularis together, and the rectovaginal septum can then be closed over this layer in side-to-side or transverse fashion. Finally, close the vaginal mucosa after appropriate posterior colporrhaphy trimming. Such repairs heal well over time, without any long-term effects for the patient.
Prescribe a stool softener for the first 3 postoperative months to reduce the patient’s need to strain.
No bowel prep needed because injuries are rare
In my practice, the vast majority of vaginal surgical cases are accomplished without the need for preoperative bowel preparation. In the occasional patient known to have dense small-bowel adhesions involving the uterus, adnexae, or vaginal cuff, bowel prep may be appropriate if substantial dissection of the bowel is anticipated as part of the procedure.
CASE 2 Small bowel laceration
A 45-year-old woman with 4 prior vaginal deliveries, a 4th-degree obstetric rectovaginal laceration, and a history of laparoscopically assisted vaginal hysterectomy presents with stage III pelvic organ prolapse, primarily involving the posterior vaginal wall. An examination reveals a defect in the upper aspect of the posterior wall (an apical defect).
Intraoperatively, during sharp dissection to lift the posterior vaginal wall off the rectovaginal septum, a loop of small bowel descends into the field, and a 1-cm laceration occurs, exposing the lumen of the bowel.
How do you proceed?
On very rare occasions, a patient with an enterocele may sustain a small bowel injury during vaginal surgery. Such injury can usually be avoided by packing the small bowel away from the area of dissection and closely observing the dissection field.
Transvaginal repair
If the small bowel is cut during dissection, inspect the adjacent small bowel thoroughly to ascertain the extent of the injury. Transvaginal repair is recommended if the laceration and adjacent mesentery can be completely visualized and accessed through the vagina.
Small lacerations require a simple closure
If the laceration is small (1–2 cm) and does not involve the mesentery, irrigate it thoroughly and close it using a running imbricating 2-0 braided suture (eg, Vicryl or silk), with the suture line perpendicular to the long axis of the small bowel to decrease the risk of stricture. Inspect the suture line to ensure that it completely seals the laceration. Suture bites should incorporate the serosa and muscularis without transgressing the mucosa. Use a noncutting needle to place these sutures.
If the mesentery is involved in the laceration, make sure there are no bleeding vessels, and ligate any bleeding ones.
Large lacerations may necessitate abdominal surgery
An abdominal or laparoscopic procedure may be necessary to repair larger lacerations to the small bowel. If the surgeon is uncomfortable with bowel repair, it may be appropriate to obtain an intraoperative consult from a surgical service.
Postoperative monitoring
Watch for signs of ileus, which should be managed with bowel rest and nasogastric suction, as indicated.
CASE 2 OUTCOME
The small laceration was repaired with 2-0 Vicryl suture in the manner described above. The patient’s diet was advanced when bowel sounds returned. There were no further sequelae.
Generalists can manage most injuries
Incidental intraoperative injuries to the lower urinary and gastrointestinal tracts are relatively rare complications of vaginal surgery—but we must make every effort to anticipate, prevent, and promptly recognize such injuries.
If they do occur, pursue a course to thoroughly evaluate, repair, test, and provide appropriate followup for the patient. If promptly identified and addressed, these injuries can be made to resolve with minimal long-term sequelae. Appropriately timed intraoperative cystoscopy is a useful method for prompt intraoperative identification of bladder and ureteric injuries. Injuries identified intraoperatively can usually be repaired using simple techniques available to the general gynecologist.
The author reports no financial relationships relevant to this article
CASE 1 Gush of fluid during dissection
A 55-year-old woman with 2 prior cesarean deliveries and stage III uterovaginal prolapse (primarily apical) is now undergoing transvaginal hysterectomy and prolapse repair. During sharp dissection of the bladder off the lower uterine segment, a gush of clear fluid washes over the area of dissection.
What steps would you take to achieve the best possible clinical outcome for this woman?
If a patient sustains a urinary tract injury, she is 91 times more likely to sue her surgeon than a patient who has a different complication or problem at gynecologic surgery.1 Yet, despite a surgeon’s best efforts, injury can occur. If it does, the best approach is immediate recognition and repair.
Primary prevention—including identifying the ureters—and intraoperative repair is the easiest, most successful, least morbid approach, compared to postoperative management. And probably less likely to lead to a lawsuit.2
As always, our main goal in any preventive effort is the best possible patient care and clinical outcomes, and diligent, careful surgical technique is the best protection on all counts. Every vaginal surgeon should have a consistent strategy for preventing, indentifying and managing intraoperative injuries to the urinary tract and bowel.
This article discusses potential injuries to the lower genitourinary and gastrointestinal tracts separately.
Vulnerable anatomy is a given
The ureters are injured in up to 2.4% of vaginal surgeries,4 and gynecologic surgery accounts for as much as 52% of inadvertent ureteral injuries.5 The bladder and bowel can also sustain injuries, in up to 2.9% and 8% of cases, respectively.3,6
Mechanisms of injury can include bladder perforation7 (and, rarely, small bowel perforation8) during placement of bladder neck and midurethral slings, transection of the bladder or ureter during vaginal hysterectomy, and ureteral kinking or obstruction during vaginal hysterectomy and vault suspension.4,9
The rectum can sometimes be perforated during posterior colporrhaphy or perineorrhaphy.6
Risk factors
For intraoperative bladder injury: prior anterior colporrhaphy, cesarean delivery, or incontinence surgery.
For injury to the rectum: prior posterior vaginal wall surgery and defects in the distal rectovaginal septum.
For injury to the small bowel: enterocele.
Women with surgically induced or suspected congenital anatomic anomalies (eg, ureteral reimplantation, ectopic kidneys or ureters, suprapubic vascular bypass grafts) require evaluation to establish the location of these anatomic variants with respect to the planned area of surgical exploration.
Most gyn surgical injuries involve the urinary tract
The urethra and a substantial portion of the posterior bladder rest on and are supported by the anterior vaginal wall. In women with an intact uterus, the posterior bladder wall also rests on the anterior lower uterine segment.
In women with a uterine scar, the bladder wall itself can sometimes be scarred down to the anterior lower uterine segment. This scarring occurs when the lower uterine scar becomes adherent to the posterior bladder wall during wound healing. Unrepaired or delayed repair to bladder injuries in these areas may lead to fistula formation.
Prior anterior colporrhaphy is associated with scarring between the bladder and anterior vaginal walls and can increase the risk of bladder injury during vaginal surgery.
Intraoperative injuries to the bladder dome and bladder neck are most common during urethral and bladder-neck sling procedures. During these procedures, prevent injury by keeping the passing tip of the sling-insertion device (eg, trocar or other passing instrument) clear of the urethra and bladder neck, and perform cystourethroscopy during each pass to identify any perforation of the bladder or urethra.
When perforation occurs, inspect the ureteral orifices thoroughly and document prompt efflux from both. If the orifices are freely effluxing and the remainder of the bladder mucosa is intact, withdraw the perforating instrument, pass it through again, and repeat cystoscopy to confirm that there is no new perforation.
Perforations to the bladder dome usually heal spontaneously in the postoperative period, with no need for extended bladder drainage. Perforations at the lateral or anterior bladder neck will also heal spontaneously.
Injuries to the posterior bladder wall and trigone
These injuries can occur during vaginal hysterectomy or dissection of the anterior vaginal wall (eg, anterior colporrhaphy, paravaginal defect repair). Avoid injuries by dissecting the vaginal mucosa (and lower uterine segment) carefully off the underlying endopelvic tissues.
Signs of an injury
Injury is often heralded by a gush of urine into the vaginal operative field, as in the opening case. When it occurs, determine the extent of injury from the vaginal side, and use a small Allis clamp to temporarily close the injury so that cystourethroscopy is effective. During cystoscopy, take steps to ascertain the extent of the injury and its proximity to the ureteral orifices.
Vaginal approach to intraoperative repair
Lacerations 2 cm or less in size are usually amenable to vaginal repair. In general, if the full extent of the laceration can be visually appreciated and accessed using the vaginal route, the repair can be safely attempted from the vaginal approach.
If the perforation is well away (>1 cm) from the ureteral orifices and there is free efflux from both orifices, close the defect from the vaginal side in 3 imbricating layers, being careful to keep the suture knots out of the bladder lumen.
Start by dissecting the overlying vaginal mucosa off the endopelvic fascia for 1 cm around the defect. This exposes the bladder adventitia, which can be used to reapproximate the laceration as follows:
Test the repair
Backfill the bladder transurethrally with 100 cc of sterile infant formula, and observe the result on the vaginal side. Closure should be watertight. Sterile formula does not stain the tissues and is therefore preferable to indigo carmine or methylene blue.
Reapproximate the vaginal mucosa using 2-0 Monocryl suture in a running, “nonlocked” fashion. Repeat cystoscopy after the closure to ensure prompt, free efflux from both ureteral orifices.
In nonradiated, well-perfused tissues, an interposing fat pad (eg, Martius or omental) is usually not required.
Foley catheter drainage is recommended to allow about 3 weeks of healing time for the closure.
If the laceration is less than 1 cm from a ureteral orifice
Assess the integrity of the affected ureter using a retrograde ureterogram performed under fluoroscopy. If ureteral integrity is confirmed, the affected ureter may be stented prior to repair of the laceration (as discussed above). Any stents may be left in place until the repair is judged to be sufficiently healed.
If the laceration is not fully visible or accessible vaginally
Use an abdominal approach—either open or laparoscopic—after assessing ureteral integrity. Focus on developing a suitable plane between the bladder and vaginal walls around the defect, followed by reapproximation of the bladder in 3 imbricating running layers of absorbable monofilament suture, as described above.
If the injury occurs during vaginal hysterectomy
In this situation, bladder closure can be deferred until the uterus and ovaries (if planned) have been removed.
For other procedures, such as anterior colporrhaphy, finish the procedure after the bladder is successfully closed. If the perforation is near or involves either ureteral orifice, it should be addressed in the manner of a ureteral injury (see below).
After fistula repairs
My patients undergo fluoroscopic evaluation of bladder filling and emptying at the 3-week mark, prior to Foley removal, to document functional closure. Then the Foley catheter and any indwelling stents are removed.
I counsel patients about the need to empty the bladder frequently, and how to recognize and avoid urinary retention.
Injuries to the ureters
The pelvic aspect of the ureters is also of interest to the gynecologic surgeon because these structures are at risk for obstruction or transection.
Vaginal procedures that can put the ureters at risk include vaginal vault (apical) suspensions and paravaginal defect repairs. Always include cystourethroscopy at the end of these procedures to document prompt and free efflux from both ureteral orifices.
3 “risky” regions
Because of its proximity to the vagina and uterus, the bladder is sometimes injured during vaginal surgery. Three areas are vulnerable: the dome and bladder neck/urethra, at risk during sling procedures, and the posterior bladder wall, vulnerable during dissection of the anterior vaginal wall.
If cystoscopy fails to confirm definitive bilateral efflux
Infuse intravenous indigo carmine and inspect the ureteral orifices again, in this situation. If bilateral efflux is not forthcoming, consider removing any intrapelvic packing, and take the patient out of the Trendelenburg position so that she can be observed for 20 minutes.
If there is still no efflux after that interval, a ureter may be obstructed.
If you suspect ureteral kinking or obstruction
Consider removing any suspensory sutures near the obstructed (noneffluxing) ureter. This maneuver usually results in vigorous efflux from the affected orifice.10 In the case of apical suspension sutures, remove the most lateral suture first and perform cystoscopy after each (more medial) suture is removed.4,9
If suture removal fails to bring about ureteral efflux, evaluate the ureters further by using intraoperative retrograde ureterogram (pyelogram) under fluoroscopy or by placing ureteral stents under cystoscopic guidance. Either method will localize the obstruction or kink and allow for targeted exploration and release of the stricture.
Extended bladder drainage is usually not required after intraoperative release of a partially or completely obstructed ureter.
In my practice, I remove any permanent suture I suspect is kinking or partially kinking a ureter. If the suture causing the problem is an absorbable one (eg, as in the use of Vicryl suture at colpocleisis), I may choose to follow the patient or to place a stent, and I reassure the woman that the offending suture will dissolve over time, thus relieving the partial obstruction.
If blue dye enters the field from inside the pelvis
The problem may be partial or complete ureteral transection. In this case, bladder perforation must first be ruled out cystoscopically. Then perform retrograde ureterogram under fluoroscopy to look for the possible point of leakage.
If ureteral transection is confirmed, plan for thorough surgical exploration (usually via the abdominal route) to locate and repair the injury.
For many generalists, this may require an intraoperative consult from a surgical service comfortable with the repair and/or reimplantation of the ureters.
CASE 1 OUTCOME
The bladder laceration was repaired after completion of the vaginal hysterectomy in the manner described above. There were no further sequelae.
It pays to refamiliarize yourself with the particular “landscape” of the lower urinary tract, so that sutures or scalpels don’t inadvertently block or injure structures.
The smooth muscle of the bladder (detrusor) is lined with transitional mucosal epithelium and opens into the urethra at the bladder neck.
The ureters enter into the lateral aspects of the midposterior bladder and tunnel medially through the detrusor muscle before entering the bladder lumen at the level of the interureteral ridge. These entry points are known as the ureteral orifices.
The trigone is an area of the posterior bladder wall bounded by the bladder neck inferiorly and by the 2 ureteral orifices in the posterior midbladder.
Rectal injuries are usually easy to identify
As far as vaginal surgery is concerned, the lower GI tract consists of the rectum and external and internal anal sphincters. The distal rectum and posterior vaginal wall are usually closely applied to each other, separated by the rectovaginal septum (also called Denonvilliers fascia).
Risk factors
In women who have undergone posterior colporrhaphy or repair of a 4th degree tear, the posterior vaginal wall can be densely adherent to the rectum, putting the rectum at risk for injury during posterior vaginal wall dissection.
Most injuries to the rectum occur during dissection of the posterior vaginal wall. Fortunately, these injuries are readily recognized and easily repaired. If a rectal injury is suspected during or after dissection, a thorough intraoperative digital exam will help confirm or rule it out.
Repair of a rectal injury
Once an injury is identified, reapproximate the rectal mucosal edges with an imbricating closure using 3-0 Monocryl or other absorbable monofilament suture. A second imbricating layer should bring the rectal muscularis together, and the rectovaginal septum can then be closed over this layer in side-to-side or transverse fashion. Finally, close the vaginal mucosa after appropriate posterior colporrhaphy trimming. Such repairs heal well over time, without any long-term effects for the patient.
Prescribe a stool softener for the first 3 postoperative months to reduce the patient’s need to strain.
No bowel prep needed because injuries are rare
In my practice, the vast majority of vaginal surgical cases are accomplished without the need for preoperative bowel preparation. In the occasional patient known to have dense small-bowel adhesions involving the uterus, adnexae, or vaginal cuff, bowel prep may be appropriate if substantial dissection of the bowel is anticipated as part of the procedure.
CASE 2 Small bowel laceration
A 45-year-old woman with 4 prior vaginal deliveries, a 4th-degree obstetric rectovaginal laceration, and a history of laparoscopically assisted vaginal hysterectomy presents with stage III pelvic organ prolapse, primarily involving the posterior vaginal wall. An examination reveals a defect in the upper aspect of the posterior wall (an apical defect).
Intraoperatively, during sharp dissection to lift the posterior vaginal wall off the rectovaginal septum, a loop of small bowel descends into the field, and a 1-cm laceration occurs, exposing the lumen of the bowel.
How do you proceed?
On very rare occasions, a patient with an enterocele may sustain a small bowel injury during vaginal surgery. Such injury can usually be avoided by packing the small bowel away from the area of dissection and closely observing the dissection field.
Transvaginal repair
If the small bowel is cut during dissection, inspect the adjacent small bowel thoroughly to ascertain the extent of the injury. Transvaginal repair is recommended if the laceration and adjacent mesentery can be completely visualized and accessed through the vagina.
Small lacerations require a simple closure
If the laceration is small (1–2 cm) and does not involve the mesentery, irrigate it thoroughly and close it using a running imbricating 2-0 braided suture (eg, Vicryl or silk), with the suture line perpendicular to the long axis of the small bowel to decrease the risk of stricture. Inspect the suture line to ensure that it completely seals the laceration. Suture bites should incorporate the serosa and muscularis without transgressing the mucosa. Use a noncutting needle to place these sutures.
If the mesentery is involved in the laceration, make sure there are no bleeding vessels, and ligate any bleeding ones.
Large lacerations may necessitate abdominal surgery
An abdominal or laparoscopic procedure may be necessary to repair larger lacerations to the small bowel. If the surgeon is uncomfortable with bowel repair, it may be appropriate to obtain an intraoperative consult from a surgical service.
Postoperative monitoring
Watch for signs of ileus, which should be managed with bowel rest and nasogastric suction, as indicated.
CASE 2 OUTCOME
The small laceration was repaired with 2-0 Vicryl suture in the manner described above. The patient’s diet was advanced when bowel sounds returned. There were no further sequelae.
Generalists can manage most injuries
Incidental intraoperative injuries to the lower urinary and gastrointestinal tracts are relatively rare complications of vaginal surgery—but we must make every effort to anticipate, prevent, and promptly recognize such injuries.
If they do occur, pursue a course to thoroughly evaluate, repair, test, and provide appropriate followup for the patient. If promptly identified and addressed, these injuries can be made to resolve with minimal long-term sequelae. Appropriately timed intraoperative cystoscopy is a useful method for prompt intraoperative identification of bladder and ureteric injuries. Injuries identified intraoperatively can usually be repaired using simple techniques available to the general gynecologist.
The author reports no financial relationships relevant to this article
1. Gilmour DT, Baskett TF. Disability and litigation from urinary tract injuries at benign gynecologic surgery in Canada. Obstet Gynecol. 2005;105:109-114.
2. Pettit PD, Petrou SP. The value of cystoscopy in major vaginal surgery. Obstet Gynecol. 1994;84:318-320.
3. Gilmour DT, Dwyer PL, Carey MP. Lower urinary tract injury during gynecologic surgery and its detection by intraoperative cystoscopy. Obstet Gynecol. 1999;94:883-889.
4. Karram M, Goldwasser S, Kleeman S, et al. High uterosacral vaginal vault suspension with fascial reconstruction for vaginal repair of enterocele and vaginal vault prolapse. Am J Obstet Gynecol. 2001;185:1339-1342discussion 1342-1343.
5. Dowling RA, Corriere JN, Jr, Sandler CM. Iatrogenic ureteral injury. J Urol. 1986;135:912-915.
6. Mercer-Jones MA, Sprowson A, Varma JS. Outcome after transperineal mesh repair of rectocele: a case series. Dis Colon Rectum. 2004;47:864-868.
7. McLennan MT, Melick CF. Bladder perforation during tension-free vaginal tape procedures: analysis of learning curve and risk factors. Obstet Gynecol. 2005;106:1000-1004.
8. Leboeuf L, Tellez CA, Ead D, Gousse AE. Complication of bowel perforation during insertion of tension-free vaginal tape. J Urol. 2003;170:1310-discussion 1310-1311.
9. Shull BL, Bachofen C, Coates KW, Kuehl TJ. A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol. 2000;183:1365-1373discussion 1373-1374.
10. Harris RL, Cundiff GW, Theofrastous JP, et al. The value of intraoperative cystoscopy in urogynecologic and reconstructive pelvic surgery. Am J Obstet Gynecol. 1997;177:1367-1369discussion 1369-1371.
1. Gilmour DT, Baskett TF. Disability and litigation from urinary tract injuries at benign gynecologic surgery in Canada. Obstet Gynecol. 2005;105:109-114.
2. Pettit PD, Petrou SP. The value of cystoscopy in major vaginal surgery. Obstet Gynecol. 1994;84:318-320.
3. Gilmour DT, Dwyer PL, Carey MP. Lower urinary tract injury during gynecologic surgery and its detection by intraoperative cystoscopy. Obstet Gynecol. 1999;94:883-889.
4. Karram M, Goldwasser S, Kleeman S, et al. High uterosacral vaginal vault suspension with fascial reconstruction for vaginal repair of enterocele and vaginal vault prolapse. Am J Obstet Gynecol. 2001;185:1339-1342discussion 1342-1343.
5. Dowling RA, Corriere JN, Jr, Sandler CM. Iatrogenic ureteral injury. J Urol. 1986;135:912-915.
6. Mercer-Jones MA, Sprowson A, Varma JS. Outcome after transperineal mesh repair of rectocele: a case series. Dis Colon Rectum. 2004;47:864-868.
7. McLennan MT, Melick CF. Bladder perforation during tension-free vaginal tape procedures: analysis of learning curve and risk factors. Obstet Gynecol. 2005;106:1000-1004.
8. Leboeuf L, Tellez CA, Ead D, Gousse AE. Complication of bowel perforation during insertion of tension-free vaginal tape. J Urol. 2003;170:1310-discussion 1310-1311.
9. Shull BL, Bachofen C, Coates KW, Kuehl TJ. A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol. 2000;183:1365-1373discussion 1373-1374.
10. Harris RL, Cundiff GW, Theofrastous JP, et al. The value of intraoperative cystoscopy in urogynecologic and reconstructive pelvic surgery. Am J Obstet Gynecol. 1997;177:1367-1369discussion 1369-1371.
Assessing Health Literacy in Veterans with Diabetes
Multiple Metatarsal Fractures, Severe Foot Pain, and Intact Pulses
Diagnosis and safe management of placenta previa
CASE Diagnosis precedes sentinel episode of bleeding
“G.A.” is a 39-year-old gravida 6, para 1041 who was diagnosed with complete placenta previa during a target ultrasound exam performed at 18 weeks for advanced maternal age. She had a sentinel episode of vaginal bleeding at 29 weeks and was hospitalized for close monitoring.
Management strategy
One course of steroid was given, vaginal bleeding subsided, and she was discharged for outpatient conservative management, including iron and folic acid supplementation.
The outcome
The patient progressed to 36 weeks’ gestation, when she underwent amniocentesis to assess fetal lung maturity. When the results were reassuring, a cesarean section was scheduled. Intraoperative blood loss was diminished using pelvic vessel embolization. Surgery was uncomplicated, and a healthy infant was delivered.
Placenta previa is a leading and potentially life-threatening cause of third-trimester bleeding.1 Although the overall incidence is about 0.4% in pregnancies exceeding 20 weeks’ gestation,2 that figure rises with the number of cesarean sections and may reach 10% among women who have undergone 4 or more cesarean deliveries.3 Since more women are requesting elective and repeat cesarean deliveries, we are increasingly likely to encounter this condition.
Fortunately, technological advances have improved maternal and neonatal outcomes after placenta previa:
Nevertheless, the condition necessitates cesarean delivery and can cause serious maternal and perinatal morbidity, including:
It can also occur in association with vasa previa, which, though rare, carries a very high perinatal mortality rate.5
Risk factors
An enlarged placenta or endometrial disruption or scarring in the upper uterine segment due to 1 or more of the factors listed below may increase the likelihood of abnormal placental implantation in the unscarred lower uterine segment:3,6,7
Previa often begins with painless vaginal bleeding
The condition often presents as painless, bright red, vaginal bleeding in the third trimester. It is usually distinguished from abruptio placenta by the absence of abdominal pain and uterine contractions.5 However, approximately 20% of women have uterine activity associated with the first episode of vaginal bleeding.13,14 Moreover, in some cases, painful contractions and labor may precipitate vaginal bleeding from placenta previa.5 Therefore, ultrasound examination is strongly recommended for all women with vaginal bleeding during pregnancy.
Ultrasound for other reasons uncovers many cases
With greater routine use of ultrasonography in obstetrics, a large percentage of women with placenta previa are diagnosed prior to the onset of the characteristic painless vaginal bleeding. In a 2003 study by Dola and colleagues,15 approximately 43% of placenta previa cases were diagnosed by ultrasonography performed for other obstetrical indications prior to the onset of vaginal bleeding.
Look for “warning hemorrhage”
The first episode of vaginal bleeding is rarely profuse or life-threatening to the mother or fetus. The bleeding usually subsides spontaneously, although it could recur and become more severe with subsequent episodes. Pregnancy typically continues after the initial bleeding episode.
The mean gestational age at the time of the first bleeding is 29 to 32 weeks.13,14 However, a third of cases have vaginal bleeding before the 30th week of gestation, a third between 30 and 36 weeks, and a third after 36 weeks’ gestation.13-15 Ten percent of women with the condition may be completely asymptomatic and progress to 38 weeks’ gestation without vaginal bleeding.13,14
Which form of ultrasound is most accurate?
With the advanced technology available today, ultrasound has become the standard means of diagnosing placenta previa.16,17
Transabdominal ultrasound has accuracy as high as 95% and a false-negative rate of 7% in the diagnosis of placenta previa.13,19 However, its accuracy may be adversely affected by maternal obesity, acoustic shadowing of the fetal head in a cephalic presentation, inability to locate the internal cervical os (which is critical for correct diagnosis), and difficulty imaging a posterior placenta and the lateral uterine walls. In addition, a full maternal bladder—usually helpful in transabdominal ultrasound imaging—may cause a false-positive diagnosis if the bladder is overly distended. In this situation, the cervix would appear artificially elongated and give a normally implanted placenta the appearance of encroachment into the internal cervical os.
Transvaginal ultrasound is superior for diagnosis of previa
Leerentveld et al20 reported false-positive and false-negative rates of 1% and 2%, respectively—a striking improvement over transabdominal ultrasound, which has rates of 2% to 6% and 7%, respectively.
Transvaginal sonography has several advantages over transabdominal imaging in localization of the placenta. The shorter distance from the vaginal probe transducer to the cervix and lower uterine segment allows the use of higher-frequency ultrasound waves, with improved resolution; therefore, the relationship between the placental edge and the internal os can be determined more accurately.
Some clinicians may worry that the probe used in transvaginal sonography will disrupt the placenta and provoke significant maternal hemorrhage, but this concern is unfounded. Multiple studies have attested to the safety of transvaginal sonography in localization of the placenta.5,20-22 The probe is introduced and positioned under direct ultrasound guidance at all times, and inadvertent insertion of the endovaginal probe into the internal cervical os is virtually impossible due to the anatomical relationship of the vagina and cervix.21
Transperineal ultrasound is another option. Several investigators have found it to be superior to transabdominal and similarly advantageous to transvaginal sonography in the diagnosis and exclusion of placenta previa.18
Start with transabdominal imaging
In current practice, transabdominal ultrasound is usually performed first to localize the placenta. If there is reason to suspect placenta previa, transvaginal or transperineal sonography is then used to confirm the location of the placenta.
Contractions may hinder imaging
Accurate diagnosis or exclusion of placenta previa may be difficult if uterine contractions are present during ultrasound evaluation. Myometrial contractions shorten the distance between the internal cervical os and the placental edge, altering measurement of this distance. In addition, the ultrasound appearance of a contraction may simulate placental tissue, making it difficult to exclude placenta previa.
The trouble with tradition
The 4 types of placenta previa in the traditional classification system—complete, partial, marginal, and low-lying—predate the era of ultrasound diagnosis and are based on digital palpation of the placenta through a partly dilated cervical os during labor.
A new system of 3 types
Along with other authors,5,15-18 we propose a new system with 3 categories—complete, incomplete, and low-lying—because ultrasound may not distinguish a placenta partially covering the internal os (a discrete point) from one that is merely encroaching on it.
Complete previa
The placenta completely covers the internal cervical os
Incomplete previa
The placental edge is within 2 cm of the internal cervical os, but does not cover the os
Low-lying previa
The distance from the internal cervical os to the placental edge is between 2 and 3.5 cm
Look for placenta accreta
When placenta previa is diagnosed by ultrasound examination, further diagnostic measures are needed to determine whether placenta accreta is present.5,23 In placenta accreta, neither the normal plane of separation between the placental villi and uterine wall, nor the intervening fibrinoid layer of Nitabuch, is present.5,23
Degrees of abnormal placental implantation
Risk of accreta can reach 67%
There are varying reports on the incidence of placenta accreta, but women with placenta previa and previous cesarean deliveries appear to have the highest incidence.3,23,24 In women with placenta previa and 1 previous cesarean section, the risk of placenta accreta has been estimated at 24%, but it increases to 67% for women with placenta previa and 4 previous cesarean sections.3
Sonographic appearance of placenta accreta
Certain characteristics are suggestive of placenta accreta25,26:
Unfortunately, diagnosis of placenta accreta is difficult prior to delivery, although transvaginal sonography and adjunctive color flow/power Doppler imaging with 2- and 3-dimensional techniques offer improved resolution and have yielded promising results in prenatal diagnosis.27-30
Magnetic resonance imaging (MRI) may also prove useful in detecting placental tissue invasion and evaluating the degree of invasion, especially in a posterior or lateral placenta previa or when there is invasion into the bladder.31-33
Gestational age, symptoms determine management
The management of women with placenta previa in the third trimester depends on the extent of maternal hemorrhage and the fetal gestational age. Clinical categories include:
Some asymptomatic cases resolve
Outpatient management is possible for women who have never bled after diagnosis in the second trimester. These women should abstain from intercourse, avoid digital examination after 20 weeks’ gestation, and immediately present to the hospital if there is any evidence of vaginal bleeding.34
Monthly ultrasound evaluations are necessary to determine whether placenta previa has resolved,34-37 since 90% of cases detected in the second trimester resolve by the third trimester.34 However, if placenta previa persists beyond 24 weeks’ gestation, there is a 50% risk that delivery will be complicated by it.35 If placenta previa persists after 32 weeks, that risk approaches 75%.35
2-fold risk of congenital malformations
Most investigators report a 2-fold increased risk of fetal congenital malformations in cases of placenta previa.5 These malformations include anomalies of the central nervous system, cardiovascular system, respiratory tract, and gastrointestinal tract. Therefore, a target ultrasound examination for fetal anatomy is recommended at the initial ultrasound diagnosis of placenta previa.
Risk of fetal growth restriction warrants heightened surveillance
Some controversy surrounds the incidence of fetal growth restriction in pregnancies complicated by placenta previa. Varma38 reported that fetal growth restriction occurs in 16% of women with placenta previa and is correlated with the number of antepartum bleeding episodes. Other investigators have reported normal fetal growth in women with placenta previa.39 Given this uncertainty, serial follow-up ultrasound evaluations are usually advised for fetal growth assessment.
When patient remains asymptomatic, perform amniocentesis at 36 weeks
Some women progress to the late third trimester without any vaginal bleeding. In these women, amniocentesis is recommended at approximately 36 weeks’ gestation to assess fetal lung maturity.34,40 Elective cesarean delivery can then be planned if pulmonary maturity is documented.
The benefits of elective delivery include a stable patient and an optimally prepared surgical team, as well as the avoidance of emergent surgery, which increases the risk for maternal complications. Emergent surgery also places the fetus at greater risk for anemia, compared with elective procedures(27.7% vs 2.9%, respectively).13
Vaginal bleeding requires inpatient evaluation
Any woman with placenta previa who presents with vaginal bleeding should be admitted to the labor and delivery unit for immediate evaluation of maternal and fetal status, including an estimation of gestational age.
Initial acute care and assessment necessitate34:
If hemorrhage is life-threatening, deliver immediately
During initial evaluation, if the hemorrhage is judged to be massive and life-threatening, resuscitative measures and immediate delivery are necessary to avoid serious maternal morbidity. Recommended measures include constant monitoring of maternal status, aggressive IV fluid resuscitation, transfusion of blood and blood products, assessment of fetal status, and immediate delivery without regard to the maturity of the fetus.
A woman at term or near term (with documented fetal lung maturity) who presents with mild or moderate vaginal bleeding should be delivered via cesarean section.
Conservative management may be appropriate for mild preterm bleeding
If vaginal bleeding is not threatening to the life of the mother, and the fetus is preterm, a conservative approach with aggressive expectant management is appropriate, since most first episodes of vaginal bleeding are self-limited and rarely life-threatening to mother or fetus. Expectant management allows fetal maturation in utero without jeopardizing maternal health. If maternal and fetal health remain stable, the expectant approach allows a safe delay of delivery until the fetus matures.
Hospitalization is recommended. Candidates for expectant management should be hospitalized after the initial episode of vaginal bleeding. Once maternal and fetal conditions stabilize, the woman should be transferred to the antepartum ward for hospital bed rest with bathroom privileges. For expectant management:
Delivery is warranted for life-threatening hemorrhage, fetal lung maturity, and/or the usual maternal and fetal indications.
The question of tocolysis
Third-trimester tocolytic therapy in a woman with vaginal bleeding is controversial. In placenta previa, vaginal bleeding appears to arise from disruption of the placental implantation site as the lower uterine segment develops.41,42 It is unclear whether uterine contractions play a role, as only 20% of women with placenta previa have uterine activity at the time of vaginal bleeding.13,14,42 It is difficult to determine whether these women have true preterm labor, because digital examination of the cervix to document cervical dilatation is impossible.
Does uterine activity precipitate bleeding?
Some investigators believe uterine activity is a predisposing factor for the vaginal bleeding associated with placenta previa, and would consider tocolytic therapy in a stable patient at a premature gestational age. However, further evidence of its safety is needed.
In particular, beta-mimetics should be avoided in hemorrhaging women because their vasodilatory effects can precipitate maternal hypotension. Another side effect of beta-mimetics: maternal tachycardia,43 which may mask the hypovolemic state in women with significant hemorrhage.
Magnesium sulfate has less effect on the maternal cardiovascular system and could be a better choice in symptomatic placenta previa.41 Also consider indomethacin, which appears to have fewer adverse maternal effects.
Inpatient vs outpatient management
Because 2 to 3 weeks of maternal hospitalization can pass between the initial warning hemorrhage and delivery of the fetus, outpatient care has become an option. Several retrospective studies have demonstrated the cost-effectiveness and safety of outpatient management of symptomatic placenta previa.44,45 These studies emphasized careful patient section.
Wing and associates46 conducted a prospective, randomized, controlled trial that reinforces the need for judicious use of outpatient management. In their study, fewer than half the patients diagnosed with placenta previa prior to 37 weeks were candidates. The authors point out the small number of patients in their study, and the fact that vaginal bleeding recurred in approximately 60% of patients. Because of the difficulty of predicting which patients will have recurrent bleeding and when, outpatient management should be reserved for those judged to be compliant with home bed rest who can rapidly return to the hospital, if necessary.
Women with recurrent vaginal bleeding during outpatient management should be rehospitalized.
In the event of massive hemorrhage, immediate compression of the aorta below the level of the renal arteries will reduce the bleeding enough to allow time to evaluate the situation.56 At the same time, aggressive IV fluid resuscitation and blood transfusion should begin. Reevaluate coagulation status after every 5 to 10 U of blood.57
Focused repair may be effective. In some situations, the hemorrhage may be controlled by oversewing and repairing the focal placental site defects.40
Bracketing the bleeding area. Another measure is a circular suture technique in which interrupted sutures are placed on the serosal surface of the anterior and posterior aspects of the uterus and as deeply as possible into the endometrium in a circumferential manner, bracketing the bleeding area.58
The argon beam coagulator can be used to achieve hemostasis; it is more effective than traditional bipolar cautery at ensuring hemostasis in extensive areas.56,57
Stepwise devascularization was effective in 100% of 103 women with postpartum hemorrhage who did not respond to traditional management.59 It involves 5 procedures to be performed in sequence until hemostasis is achieved: unilateral uterine vessel ligation, bilateral uterine vessel ligation, low uterine vessel ligation, unilateral ovarian vessel ligation, and bilateral ovarian vessel ligation.
Hypogastric artery ligation is another option, but it is technically challenging and successful in less than 50% of cases.57 In fact, the time spent on this technique may actually lead to increased blood loss.
Components of safe delivery
A detailed plan is necessary when major hemorrhage is anticipated at the time of elective cesarean delivery for placenta previa, including consultation with experts in different disciplines such as radiology, anesthesiology, urology, pathology, blood bank, neonatology, and gynecologic oncology.
Also pay attention to the maternal red blood cell reserve. Iron and folic acid should be administered to prevent and treat anemia, and antepartum erythropoietin should be considered as a way of increasing the hemoglobin level in women with placenta previa. Autologous blood transfusion, including acute normovolemic hemodilution, is another option.
Pelvic vessel embolization
Elective embolization or occlusion of the hypogastric or uterine arteries has proved to be safe and effective for postpartum hemorrhage, with a success rate of more than 90% in women with normal coagulation.47
In addition, elective catheterization with a balloon-tipped catheter can be used prophylactically to reduce blood flow to the placenta. Prophylactic catheterization of the anterior division of the internal iliac arteries can be performed right before the scheduled cesarean section. An axillary approach is technically easier for fluoroscopically guided catheterization of the internal iliac.48 The actual fluoroscopy time is minutes, so the risk of fetal exposure to radiation and irreversible ovarian damage is minimal.
The fetus is monitored during the procedure, and the balloons are left in the deflated state until after delivery, reducing the risk of uteroplacental insufficiency. Balloon inflation after delivery occludes the hypogastric arteries and diminishes uterine arterial blood flow during surgery. In some cases, the temporary occlusive effect of the balloons may control intraoperative bleeding completely. If substantial bleeding persists, subsequent embolization of the uterine arteries is advised, using absorbable Gelfoam particles, which are temporary and do not damage pelvic organs. Menstruation is not impaired, and normal pregnancies have been reported after this procedure.49,50
In women who undergo cesarean delivery under regional anesthesia, placement of a dry epidural catheter for later dosing of anesthetic agents should be considered prior to balloon catheterization, since the patient’s mobility is restricted after placement of the balloon-tipped catheter.
This therapy is especially useful when there is a high index of suspicion for placenta accreta.
Recommendations at the time of delivery
Hysterectomy for placenta previa, placenta accreta
This procedure is technically challenging when there is a markedly enlarged uterus with engorged collateral vessels. One useful method, delayed ligation technique, was originally described by Dyer et al on the Tulane obstetrics service at Charity Hospital of New Orleans.53 This technique facilitates quick control of all uterine vasculature with rapid hemostasis. Later modification of this method involves successive clamping and severing of all vascular pedicles supplying the uterus, prior to their suture ligation, for quick control of bleeding.
Close follow-up continues even after surgery
Immediately after surgery, close monitoring of hemodynamic status is required, ideally in a critical care setting. Because women with placenta previa/placenta accreta have often received massive transfusions of blood and blood products along with large volumes of crystalloid fluids, pulmonary edema may develop. Conversely, hypovolemia can result from inadequate replacement of blood or persistent intra-abdominal bleeding. Thus, close attention to urinary output allows early detection of pulmonary edema, acute respiratory distress syndrome, hypovolemia, or persistent intra-abdominal bleeding. Patients who undergo peripartum hysterectomy should also be monitored closely for possible ureteral injury.
Thromboprophylaxis should continue until the patient is ambulatory.
Recommended laboratory tests
Get a complete blood count with platelets and fibrinogen immediately after surgery and at frequent intervals as needed. A chemistry panel with calcium, albumin, electrolytes, and creatinine also is helpful.
Serious morbidity in 3% to 5% of women after emergent hysterectomy
Conditions such as acute respiratory distress syndrome from massive blood transfusion and pulmonary capillary leakage, acute tubular necrosis from renal failure, and pulmonary embolism may complicate 3% to 5% of cases.54
Reoperation for persistent intra-abdominal bleeding may be necessary, and 9% of women will have urologic injury. Unfortunately, the maternal mortality rate associated with this procedure is 0.8%, so meticulous postoperative care is mandated.55
The authors report no financial relationships with any company whose products are mentioned in this article.
1. Ananth CV, Savitz DA, Luther ER. Maternal cigarette smoking as a risk factor for placental abruption, placenta previa, and uterine bleeding in pregnancy. Am J Epidemiol. 1996;144:881-889.
2. Faiz AS, Ananth CV. Etiology and risk factors for placenta previa: an overview and meta-analysis of observational studies. J Matern Fetal Neonatal Med. 2003;13:175.-
3. Clark SL, Koonings PP, et al. Placenta previa/accreta and prior cesarean section. Obstet Gynecol. 1985;66:89-92.
4. Neri A, Manor Y, Matityahu A, Blieden L. Placenta previa and congenital cardiac anomalies. Fetal Ther. 1989;4:138-140.
5. Clark SL. Placenta previa and abruptio placenta. In: Creasy RK, Resnik R. Maternal-Fetal Medicine, Principles and Practice. 4th ed. Philadelphia: W.B. Saunders; 1999:616–631.
6. Miller DA, Chollet J, Goodwin TM. Clinical risks factors for placenta previa-placenta accreta. Am J Obstet Gynecol. 1997;177:210-214.
7. Ananth CV, Demissie K, Smulian JC, Vintzileos AM. Placenta previa in singleton and twin births in the United States, 1989 through 1998: a comparison of risk factor profiles and associated conditions. Am J Obstet Gynecol. 2003;188:275-281.
8. Gilbert WM, Nesbitt TS, Danielsen B. Childbearing beyond age 40: pregnancy outcome in 24,032 cases. Obstet Gynecol. 1999;93:9-14.
9. Lavery JP. Placenta previa. Clin Obstet Gynecol. 1990;33:414-421.
10. Taylor VM, Kramer MD, Vaughan TL, Peacock S. Placenta previa in relation to induced and spontaneous abortion: a population- based study. Obstet Gynecol. 1993;82:88-91.
11. Williams MA, Mittendorf R, Lieberman E, Monson RR, Schoenbaum SC, Genest DR. Cigarette smoking during pregnancy in relation to placenta previa. Am J Obstet Gynecol. 1991;165:28-32.
12. Handler AS, Mason ED, Rosenberg DL, Davis FG. The relationship between exposure during pregnancy to cigarette smoking and cocaine use and placenta previa. Am J Obstet Gynecol. 1994;170:884-889.
13. Cotton DB, Read JA, Paul RH, Quilligan EJ. The conservative aggressive management of placenta previa. Am J Obstet Gynecol. 1980;137:687-695.
14. Silver R, Depp R, Sabbagha RE, Dooley SL. Placenta previa: aggressive expectant management. Am J Obstet Gynecol. 1984;150:15-22.
15. Dola CP, Garite TJ, Dowling DD, Friend D, Ahdoot D, Asrat T. Placenta previa: does its type affect pregnancy outcome? Am J Perinatol. 2003;20:353-360.
16. Oppenheimer LW, Farine D, Ritchie JWK, Lewinsky RM, Telford J, Fairbanks LA. What is low-lying placenta? Am J Obstet Gynecol. 1991;165:1036-1038.
17. Bhide A, Thilaganathan B. Recent advances in the management of placenta previa. Curr Opin Obstet Gynecol. 2004;16:447-451.
18. Dawson WB, Dumas MD, Romano WM, Gagnon R, Gratton RJ, Mowbray RD. Translabial ultrasonography and placenta previa: does measurement of the os-placenta distance predict outcome? J Ultrasound Med. 1996;15:44-46.
19. Egley CC. Abruptio placentae and placenta previa. In: Winn HN, Hobbins JC. Clinical Maternal-Fetal Medicine.1st ed. Pearl River, NY: Parthenon Publishing; 2000:47–53.
20. Leerentveld RA, Gilberts E, Arnold M, Wladimiroff JW. Accuracy and safety of transvaginal sonographic placental localization. Obstet Gynecol. 1990;76:759-762.
21. Timor-Tritsch I, Yunis R. Confirming the safety of transvaginal sonography in patients suspected of placenta previa. Obstet Gynecol. 1993;81:742-744.
22. Tan NH, Abu M, Woo JLS, Tahir H. The role of transvaginal sonography in the diagnosis of placenta previa. Aust NZ J Obstet Gynaecol. 1995;35:42-45.
23. Miller DA, Cholleet JA, Goodwin TM. Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol. 1997;177:210-214.
24. Chattopadhyay SK, Kharif H, Sherbeeni MM. Placenta previa and accreta after previous cesarean section. Eur J Obstet Gynecol Reprod Biol. 1993;52:151.-
25. Comstock CH, Love JJ, Jr, Bronsteen RA, et al. Sonographic detection of placenta accreta in the second and third trimesters of pregnancy. Am J Obstet Gynecol. 2004;190:1135-1140.
26. Comstock CH, Lee W, Vettraino IM, Bronsteen RA. The early sonographic appearance of placenta accreta. J Ultrasound Med. 2003;22:19-23.
27. Chou MM, Ho ES. Prenatal diagnosis of placenta previa accreta with power amplitude ultrasonic agiography. Am J Obstet Gynecol. 1997;177:1523-1525.
28. Levine D, Hulka CA, Ludmir J, Li W, Edelman RR. Placenta accreta: evaluation with color Doppler US, power Doppler US, and MR imaging. Radiology. 1997;205:773-776.
29. Taipale P, Orden MR, Berg M, Manninen H, Alafuzoff I. Prenatal diagnosis of placenta accreta and percreta with ultrasonography, color Doppler, and magnetic resonance imaging. Obstet Gynecol. 2004;104:537-540.
30. Chou MM, Tseng JJ, Ho ES, Hwang JI. Three-dimensional color power Doppler imaging in the assessment of uteroplacental neovascularization in placenta previa increta/percreta. Am J Obstet Gynecol. 2001;185:1257-1260.
31. Maldjian C, Adam R, Pelosi M, II, Pelosi M III, Rudelli RD, Maldjian J. MRI appearance of placenta percreta and placenta accreta. Magnetic Resonance Imaging. 1999;17:965-971.
32. Thorp JM, Councell RB, Sandridge DA, Wiest HH. Antepartum diagnosis of placenta previa percreta by magnetic resonance imaging. Obstet Gynecol. 1992;80:506-508.
33. Kay HH, Spritzer CE. Preliminary experience with magnetic resonance imaging in patients with third-trimester bleeding. Obstet Gynecol. 1991;78:424-429.
34. Russo-Stieglitz K, Lockwood CJ. Placenta previa and vasa previa. Up To Date. 2005. Available at: www.uptodate.com.
35. Dashe JS, McIntire DD, Ramus RM, Santos-Ramos R, Twickler DM. Persistence of placenta previa according to gestational age at ultrasound detection. Obstet Gynecol. 2002;99:692-697.
36. Taipale P, Hiilesmaa V, Ylostalo P. Transvaginal ultrasonography at 18-23 weeks in predicting placenta previa at delivery. Ultrasound Obstet Gynecol. 1998;12:422.-
37. Rosati P, Guariglia L. Clinical significance of placenta previa detected at early routine transvaginal scan. J Ultrasound Med. 2000;19:581-585.
38. Varma TR. Fetal growth and placental function in patients with placenta previa. J Obstet Gynaecol Br Commonw. 1973;80:311-315.
39. Crane JM, Van Den Hof MC, et al. Neonatal outcomes with placenta previa. Obstet Gynecol. 1999;93:541-544.
40. Benedetti TJ. Obstetric hemorrhage. In: Gabbe SG, Niebyl, JR, Simpson JL. Obstetrics: Normal and Problem Pregnancies. 4th ed. Philadelphia: Churchill Livingstone; 2002:503–538.
41. Besinger RE, Moniak CW, Paskiewicz LS, et al. The effects of tocolytic use in the management of symptomatic placenta previa. Am J Obstet Gynecol. 1995;172:1770-1778.
42. Magann EF, Johnson CA, Gookin KS, Roberts WE, Martin RW, Morrison JC. Placenta praevia: does uterine activity cause bleeding? Aust NZ J Obstet Gynaecol. 1993;33:22-24
43. Benedetti TJ. Maternal complication of parenteral B-sympathomimetic therapy for premature labor. Am J Obstet Gynecol. 1983;145:1-6.
44. Mouer JR. Placenta previa: Antepartum conservative management, inpatient versus outpatient. Am J Obstet Gynecol. 1994;170:1683-1686.
45. Droste S, Keil K. Expectant management of placenta previa: cost-benefit analysis of outpatient treatment. Am J Obstet Gynecol. 1994;170:1254-1257.
46. Wing D, Paul RH, Millar LK. Management of the symptomatic placenta previa: a randomized, controlled trial of inpatient versus outpatient expectant management. Am J Obstet Gynecol. 1996;175:806-811.
47. Hansch E, Chitkara U, McAlpine J, El-Sayed Y, Dake MD, Razavi MK. Pelvic arterial embolization for control of obstetric hemorrhage: a five-year experience. Am J Obstet Gynecol. 1999;180:1454-1460.
48. Dubois J, Garel L, Grignon A, Lemay M, Leduc L. Placenta percreta: balloon occlusion and embolization of the internal iliac arteries to reduce intraoperative blood losses. Am J Obstet Gynecol. 1997;176:723-726.
49. Suresh V, Goodwin SC, McLucas B, Mohr G. Uterine artery embolization: an underused method of controlling pelvic hemorrhage. Am J Obstet Gynecol. 1997;176:938-948.
50. Salomon LJ, deTayrac R, Castaigne-Meary V, et al. Fertility and pregnancy outcome following pelvic arterial embolization for severe postpartum haemorrhage. A cohort study. Hum Reprod. 2003;18:849-852.
51. Frederiksen MC, Glassenberg R, Stika CS. Placenta previa: a 22-year analysis. Am J Obstet Gynecol. 1999;180:1432-1437.
52. Lockwood CJ, Artal R. Placenta accreta. Obstet Gynecol. 2002;99:1133-1134.
53. Dyer I, Nix GF, Weed JC. Total hysterectomy at cesarean section and the immediate puerperal period. Am J Obstet Gynecol. 1953;65:517-527.
54. Catanzarite VA, Stanco L, Schrimmer D, Conroy C. Managing placenta previa/accreta. Contemporary OB/GYN. 1996;4(5):66-95.
55. Stanco L, Schrimmer D, Paul D, Mishell D. Emergency peripartum hysterectomy and associated risk factors. Am J Obstet Gynecol. 1993;168:879-883.
56. Hudon L, Belfort MA, Broome DR. Diagnosis and management of placenta percreta: a review. Obstet Gynecol Surv. 1998;53:509-517.
57. Shevell T, Malone FD. Management of obstetric hemorrhage. Sem Perinatol. 2003;27:86-104.
58. Cho J, Kim S, Cha K, et al. Interrupted circular suture: bleeding control during cesarean delivery in placenta previa accreta. Obstet Gynecol. 1991;78:876-879.
59. AbdRabbo SA. Stepwise uterine devascularization: a novel technique for management of uncontrollable postpartum hemorrhage with preservation of the uterus. Am J Obstet Gynecol. 1994;171:694-700.
CASE Diagnosis precedes sentinel episode of bleeding
“G.A.” is a 39-year-old gravida 6, para 1041 who was diagnosed with complete placenta previa during a target ultrasound exam performed at 18 weeks for advanced maternal age. She had a sentinel episode of vaginal bleeding at 29 weeks and was hospitalized for close monitoring.
Management strategy
One course of steroid was given, vaginal bleeding subsided, and she was discharged for outpatient conservative management, including iron and folic acid supplementation.
The outcome
The patient progressed to 36 weeks’ gestation, when she underwent amniocentesis to assess fetal lung maturity. When the results were reassuring, a cesarean section was scheduled. Intraoperative blood loss was diminished using pelvic vessel embolization. Surgery was uncomplicated, and a healthy infant was delivered.
Placenta previa is a leading and potentially life-threatening cause of third-trimester bleeding.1 Although the overall incidence is about 0.4% in pregnancies exceeding 20 weeks’ gestation,2 that figure rises with the number of cesarean sections and may reach 10% among women who have undergone 4 or more cesarean deliveries.3 Since more women are requesting elective and repeat cesarean deliveries, we are increasingly likely to encounter this condition.
Fortunately, technological advances have improved maternal and neonatal outcomes after placenta previa:
Nevertheless, the condition necessitates cesarean delivery and can cause serious maternal and perinatal morbidity, including:
It can also occur in association with vasa previa, which, though rare, carries a very high perinatal mortality rate.5
Risk factors
An enlarged placenta or endometrial disruption or scarring in the upper uterine segment due to 1 or more of the factors listed below may increase the likelihood of abnormal placental implantation in the unscarred lower uterine segment:3,6,7
Previa often begins with painless vaginal bleeding
The condition often presents as painless, bright red, vaginal bleeding in the third trimester. It is usually distinguished from abruptio placenta by the absence of abdominal pain and uterine contractions.5 However, approximately 20% of women have uterine activity associated with the first episode of vaginal bleeding.13,14 Moreover, in some cases, painful contractions and labor may precipitate vaginal bleeding from placenta previa.5 Therefore, ultrasound examination is strongly recommended for all women with vaginal bleeding during pregnancy.
Ultrasound for other reasons uncovers many cases
With greater routine use of ultrasonography in obstetrics, a large percentage of women with placenta previa are diagnosed prior to the onset of the characteristic painless vaginal bleeding. In a 2003 study by Dola and colleagues,15 approximately 43% of placenta previa cases were diagnosed by ultrasonography performed for other obstetrical indications prior to the onset of vaginal bleeding.
Look for “warning hemorrhage”
The first episode of vaginal bleeding is rarely profuse or life-threatening to the mother or fetus. The bleeding usually subsides spontaneously, although it could recur and become more severe with subsequent episodes. Pregnancy typically continues after the initial bleeding episode.
The mean gestational age at the time of the first bleeding is 29 to 32 weeks.13,14 However, a third of cases have vaginal bleeding before the 30th week of gestation, a third between 30 and 36 weeks, and a third after 36 weeks’ gestation.13-15 Ten percent of women with the condition may be completely asymptomatic and progress to 38 weeks’ gestation without vaginal bleeding.13,14
Which form of ultrasound is most accurate?
With the advanced technology available today, ultrasound has become the standard means of diagnosing placenta previa.16,17
Transabdominal ultrasound has accuracy as high as 95% and a false-negative rate of 7% in the diagnosis of placenta previa.13,19 However, its accuracy may be adversely affected by maternal obesity, acoustic shadowing of the fetal head in a cephalic presentation, inability to locate the internal cervical os (which is critical for correct diagnosis), and difficulty imaging a posterior placenta and the lateral uterine walls. In addition, a full maternal bladder—usually helpful in transabdominal ultrasound imaging—may cause a false-positive diagnosis if the bladder is overly distended. In this situation, the cervix would appear artificially elongated and give a normally implanted placenta the appearance of encroachment into the internal cervical os.
Transvaginal ultrasound is superior for diagnosis of previa
Leerentveld et al20 reported false-positive and false-negative rates of 1% and 2%, respectively—a striking improvement over transabdominal ultrasound, which has rates of 2% to 6% and 7%, respectively.
Transvaginal sonography has several advantages over transabdominal imaging in localization of the placenta. The shorter distance from the vaginal probe transducer to the cervix and lower uterine segment allows the use of higher-frequency ultrasound waves, with improved resolution; therefore, the relationship between the placental edge and the internal os can be determined more accurately.
Some clinicians may worry that the probe used in transvaginal sonography will disrupt the placenta and provoke significant maternal hemorrhage, but this concern is unfounded. Multiple studies have attested to the safety of transvaginal sonography in localization of the placenta.5,20-22 The probe is introduced and positioned under direct ultrasound guidance at all times, and inadvertent insertion of the endovaginal probe into the internal cervical os is virtually impossible due to the anatomical relationship of the vagina and cervix.21
Transperineal ultrasound is another option. Several investigators have found it to be superior to transabdominal and similarly advantageous to transvaginal sonography in the diagnosis and exclusion of placenta previa.18
Start with transabdominal imaging
In current practice, transabdominal ultrasound is usually performed first to localize the placenta. If there is reason to suspect placenta previa, transvaginal or transperineal sonography is then used to confirm the location of the placenta.
Contractions may hinder imaging
Accurate diagnosis or exclusion of placenta previa may be difficult if uterine contractions are present during ultrasound evaluation. Myometrial contractions shorten the distance between the internal cervical os and the placental edge, altering measurement of this distance. In addition, the ultrasound appearance of a contraction may simulate placental tissue, making it difficult to exclude placenta previa.
The trouble with tradition
The 4 types of placenta previa in the traditional classification system—complete, partial, marginal, and low-lying—predate the era of ultrasound diagnosis and are based on digital palpation of the placenta through a partly dilated cervical os during labor.
A new system of 3 types
Along with other authors,5,15-18 we propose a new system with 3 categories—complete, incomplete, and low-lying—because ultrasound may not distinguish a placenta partially covering the internal os (a discrete point) from one that is merely encroaching on it.
Complete previa
The placenta completely covers the internal cervical os
Incomplete previa
The placental edge is within 2 cm of the internal cervical os, but does not cover the os
Low-lying previa
The distance from the internal cervical os to the placental edge is between 2 and 3.5 cm
Look for placenta accreta
When placenta previa is diagnosed by ultrasound examination, further diagnostic measures are needed to determine whether placenta accreta is present.5,23 In placenta accreta, neither the normal plane of separation between the placental villi and uterine wall, nor the intervening fibrinoid layer of Nitabuch, is present.5,23
Degrees of abnormal placental implantation
Risk of accreta can reach 67%
There are varying reports on the incidence of placenta accreta, but women with placenta previa and previous cesarean deliveries appear to have the highest incidence.3,23,24 In women with placenta previa and 1 previous cesarean section, the risk of placenta accreta has been estimated at 24%, but it increases to 67% for women with placenta previa and 4 previous cesarean sections.3
Sonographic appearance of placenta accreta
Certain characteristics are suggestive of placenta accreta25,26:
Unfortunately, diagnosis of placenta accreta is difficult prior to delivery, although transvaginal sonography and adjunctive color flow/power Doppler imaging with 2- and 3-dimensional techniques offer improved resolution and have yielded promising results in prenatal diagnosis.27-30
Magnetic resonance imaging (MRI) may also prove useful in detecting placental tissue invasion and evaluating the degree of invasion, especially in a posterior or lateral placenta previa or when there is invasion into the bladder.31-33
Gestational age, symptoms determine management
The management of women with placenta previa in the third trimester depends on the extent of maternal hemorrhage and the fetal gestational age. Clinical categories include:
Some asymptomatic cases resolve
Outpatient management is possible for women who have never bled after diagnosis in the second trimester. These women should abstain from intercourse, avoid digital examination after 20 weeks’ gestation, and immediately present to the hospital if there is any evidence of vaginal bleeding.34
Monthly ultrasound evaluations are necessary to determine whether placenta previa has resolved,34-37 since 90% of cases detected in the second trimester resolve by the third trimester.34 However, if placenta previa persists beyond 24 weeks’ gestation, there is a 50% risk that delivery will be complicated by it.35 If placenta previa persists after 32 weeks, that risk approaches 75%.35
2-fold risk of congenital malformations
Most investigators report a 2-fold increased risk of fetal congenital malformations in cases of placenta previa.5 These malformations include anomalies of the central nervous system, cardiovascular system, respiratory tract, and gastrointestinal tract. Therefore, a target ultrasound examination for fetal anatomy is recommended at the initial ultrasound diagnosis of placenta previa.
Risk of fetal growth restriction warrants heightened surveillance
Some controversy surrounds the incidence of fetal growth restriction in pregnancies complicated by placenta previa. Varma38 reported that fetal growth restriction occurs in 16% of women with placenta previa and is correlated with the number of antepartum bleeding episodes. Other investigators have reported normal fetal growth in women with placenta previa.39 Given this uncertainty, serial follow-up ultrasound evaluations are usually advised for fetal growth assessment.
When patient remains asymptomatic, perform amniocentesis at 36 weeks
Some women progress to the late third trimester without any vaginal bleeding. In these women, amniocentesis is recommended at approximately 36 weeks’ gestation to assess fetal lung maturity.34,40 Elective cesarean delivery can then be planned if pulmonary maturity is documented.
The benefits of elective delivery include a stable patient and an optimally prepared surgical team, as well as the avoidance of emergent surgery, which increases the risk for maternal complications. Emergent surgery also places the fetus at greater risk for anemia, compared with elective procedures(27.7% vs 2.9%, respectively).13
Vaginal bleeding requires inpatient evaluation
Any woman with placenta previa who presents with vaginal bleeding should be admitted to the labor and delivery unit for immediate evaluation of maternal and fetal status, including an estimation of gestational age.
Initial acute care and assessment necessitate34:
If hemorrhage is life-threatening, deliver immediately
During initial evaluation, if the hemorrhage is judged to be massive and life-threatening, resuscitative measures and immediate delivery are necessary to avoid serious maternal morbidity. Recommended measures include constant monitoring of maternal status, aggressive IV fluid resuscitation, transfusion of blood and blood products, assessment of fetal status, and immediate delivery without regard to the maturity of the fetus.
A woman at term or near term (with documented fetal lung maturity) who presents with mild or moderate vaginal bleeding should be delivered via cesarean section.
Conservative management may be appropriate for mild preterm bleeding
If vaginal bleeding is not threatening to the life of the mother, and the fetus is preterm, a conservative approach with aggressive expectant management is appropriate, since most first episodes of vaginal bleeding are self-limited and rarely life-threatening to mother or fetus. Expectant management allows fetal maturation in utero without jeopardizing maternal health. If maternal and fetal health remain stable, the expectant approach allows a safe delay of delivery until the fetus matures.
Hospitalization is recommended. Candidates for expectant management should be hospitalized after the initial episode of vaginal bleeding. Once maternal and fetal conditions stabilize, the woman should be transferred to the antepartum ward for hospital bed rest with bathroom privileges. For expectant management:
Delivery is warranted for life-threatening hemorrhage, fetal lung maturity, and/or the usual maternal and fetal indications.
The question of tocolysis
Third-trimester tocolytic therapy in a woman with vaginal bleeding is controversial. In placenta previa, vaginal bleeding appears to arise from disruption of the placental implantation site as the lower uterine segment develops.41,42 It is unclear whether uterine contractions play a role, as only 20% of women with placenta previa have uterine activity at the time of vaginal bleeding.13,14,42 It is difficult to determine whether these women have true preterm labor, because digital examination of the cervix to document cervical dilatation is impossible.
Does uterine activity precipitate bleeding?
Some investigators believe uterine activity is a predisposing factor for the vaginal bleeding associated with placenta previa, and would consider tocolytic therapy in a stable patient at a premature gestational age. However, further evidence of its safety is needed.
In particular, beta-mimetics should be avoided in hemorrhaging women because their vasodilatory effects can precipitate maternal hypotension. Another side effect of beta-mimetics: maternal tachycardia,43 which may mask the hypovolemic state in women with significant hemorrhage.
Magnesium sulfate has less effect on the maternal cardiovascular system and could be a better choice in symptomatic placenta previa.41 Also consider indomethacin, which appears to have fewer adverse maternal effects.
Inpatient vs outpatient management
Because 2 to 3 weeks of maternal hospitalization can pass between the initial warning hemorrhage and delivery of the fetus, outpatient care has become an option. Several retrospective studies have demonstrated the cost-effectiveness and safety of outpatient management of symptomatic placenta previa.44,45 These studies emphasized careful patient section.
Wing and associates46 conducted a prospective, randomized, controlled trial that reinforces the need for judicious use of outpatient management. In their study, fewer than half the patients diagnosed with placenta previa prior to 37 weeks were candidates. The authors point out the small number of patients in their study, and the fact that vaginal bleeding recurred in approximately 60% of patients. Because of the difficulty of predicting which patients will have recurrent bleeding and when, outpatient management should be reserved for those judged to be compliant with home bed rest who can rapidly return to the hospital, if necessary.
Women with recurrent vaginal bleeding during outpatient management should be rehospitalized.
In the event of massive hemorrhage, immediate compression of the aorta below the level of the renal arteries will reduce the bleeding enough to allow time to evaluate the situation.56 At the same time, aggressive IV fluid resuscitation and blood transfusion should begin. Reevaluate coagulation status after every 5 to 10 U of blood.57
Focused repair may be effective. In some situations, the hemorrhage may be controlled by oversewing and repairing the focal placental site defects.40
Bracketing the bleeding area. Another measure is a circular suture technique in which interrupted sutures are placed on the serosal surface of the anterior and posterior aspects of the uterus and as deeply as possible into the endometrium in a circumferential manner, bracketing the bleeding area.58
The argon beam coagulator can be used to achieve hemostasis; it is more effective than traditional bipolar cautery at ensuring hemostasis in extensive areas.56,57
Stepwise devascularization was effective in 100% of 103 women with postpartum hemorrhage who did not respond to traditional management.59 It involves 5 procedures to be performed in sequence until hemostasis is achieved: unilateral uterine vessel ligation, bilateral uterine vessel ligation, low uterine vessel ligation, unilateral ovarian vessel ligation, and bilateral ovarian vessel ligation.
Hypogastric artery ligation is another option, but it is technically challenging and successful in less than 50% of cases.57 In fact, the time spent on this technique may actually lead to increased blood loss.
Components of safe delivery
A detailed plan is necessary when major hemorrhage is anticipated at the time of elective cesarean delivery for placenta previa, including consultation with experts in different disciplines such as radiology, anesthesiology, urology, pathology, blood bank, neonatology, and gynecologic oncology.
Also pay attention to the maternal red blood cell reserve. Iron and folic acid should be administered to prevent and treat anemia, and antepartum erythropoietin should be considered as a way of increasing the hemoglobin level in women with placenta previa. Autologous blood transfusion, including acute normovolemic hemodilution, is another option.
Pelvic vessel embolization
Elective embolization or occlusion of the hypogastric or uterine arteries has proved to be safe and effective for postpartum hemorrhage, with a success rate of more than 90% in women with normal coagulation.47
In addition, elective catheterization with a balloon-tipped catheter can be used prophylactically to reduce blood flow to the placenta. Prophylactic catheterization of the anterior division of the internal iliac arteries can be performed right before the scheduled cesarean section. An axillary approach is technically easier for fluoroscopically guided catheterization of the internal iliac.48 The actual fluoroscopy time is minutes, so the risk of fetal exposure to radiation and irreversible ovarian damage is minimal.
The fetus is monitored during the procedure, and the balloons are left in the deflated state until after delivery, reducing the risk of uteroplacental insufficiency. Balloon inflation after delivery occludes the hypogastric arteries and diminishes uterine arterial blood flow during surgery. In some cases, the temporary occlusive effect of the balloons may control intraoperative bleeding completely. If substantial bleeding persists, subsequent embolization of the uterine arteries is advised, using absorbable Gelfoam particles, which are temporary and do not damage pelvic organs. Menstruation is not impaired, and normal pregnancies have been reported after this procedure.49,50
In women who undergo cesarean delivery under regional anesthesia, placement of a dry epidural catheter for later dosing of anesthetic agents should be considered prior to balloon catheterization, since the patient’s mobility is restricted after placement of the balloon-tipped catheter.
This therapy is especially useful when there is a high index of suspicion for placenta accreta.
Recommendations at the time of delivery
Hysterectomy for placenta previa, placenta accreta
This procedure is technically challenging when there is a markedly enlarged uterus with engorged collateral vessels. One useful method, delayed ligation technique, was originally described by Dyer et al on the Tulane obstetrics service at Charity Hospital of New Orleans.53 This technique facilitates quick control of all uterine vasculature with rapid hemostasis. Later modification of this method involves successive clamping and severing of all vascular pedicles supplying the uterus, prior to their suture ligation, for quick control of bleeding.
Close follow-up continues even after surgery
Immediately after surgery, close monitoring of hemodynamic status is required, ideally in a critical care setting. Because women with placenta previa/placenta accreta have often received massive transfusions of blood and blood products along with large volumes of crystalloid fluids, pulmonary edema may develop. Conversely, hypovolemia can result from inadequate replacement of blood or persistent intra-abdominal bleeding. Thus, close attention to urinary output allows early detection of pulmonary edema, acute respiratory distress syndrome, hypovolemia, or persistent intra-abdominal bleeding. Patients who undergo peripartum hysterectomy should also be monitored closely for possible ureteral injury.
Thromboprophylaxis should continue until the patient is ambulatory.
Recommended laboratory tests
Get a complete blood count with platelets and fibrinogen immediately after surgery and at frequent intervals as needed. A chemistry panel with calcium, albumin, electrolytes, and creatinine also is helpful.
Serious morbidity in 3% to 5% of women after emergent hysterectomy
Conditions such as acute respiratory distress syndrome from massive blood transfusion and pulmonary capillary leakage, acute tubular necrosis from renal failure, and pulmonary embolism may complicate 3% to 5% of cases.54
Reoperation for persistent intra-abdominal bleeding may be necessary, and 9% of women will have urologic injury. Unfortunately, the maternal mortality rate associated with this procedure is 0.8%, so meticulous postoperative care is mandated.55
The authors report no financial relationships with any company whose products are mentioned in this article.
CASE Diagnosis precedes sentinel episode of bleeding
“G.A.” is a 39-year-old gravida 6, para 1041 who was diagnosed with complete placenta previa during a target ultrasound exam performed at 18 weeks for advanced maternal age. She had a sentinel episode of vaginal bleeding at 29 weeks and was hospitalized for close monitoring.
Management strategy
One course of steroid was given, vaginal bleeding subsided, and she was discharged for outpatient conservative management, including iron and folic acid supplementation.
The outcome
The patient progressed to 36 weeks’ gestation, when she underwent amniocentesis to assess fetal lung maturity. When the results were reassuring, a cesarean section was scheduled. Intraoperative blood loss was diminished using pelvic vessel embolization. Surgery was uncomplicated, and a healthy infant was delivered.
Placenta previa is a leading and potentially life-threatening cause of third-trimester bleeding.1 Although the overall incidence is about 0.4% in pregnancies exceeding 20 weeks’ gestation,2 that figure rises with the number of cesarean sections and may reach 10% among women who have undergone 4 or more cesarean deliveries.3 Since more women are requesting elective and repeat cesarean deliveries, we are increasingly likely to encounter this condition.
Fortunately, technological advances have improved maternal and neonatal outcomes after placenta previa:
Nevertheless, the condition necessitates cesarean delivery and can cause serious maternal and perinatal morbidity, including:
It can also occur in association with vasa previa, which, though rare, carries a very high perinatal mortality rate.5
Risk factors
An enlarged placenta or endometrial disruption or scarring in the upper uterine segment due to 1 or more of the factors listed below may increase the likelihood of abnormal placental implantation in the unscarred lower uterine segment:3,6,7
Previa often begins with painless vaginal bleeding
The condition often presents as painless, bright red, vaginal bleeding in the third trimester. It is usually distinguished from abruptio placenta by the absence of abdominal pain and uterine contractions.5 However, approximately 20% of women have uterine activity associated with the first episode of vaginal bleeding.13,14 Moreover, in some cases, painful contractions and labor may precipitate vaginal bleeding from placenta previa.5 Therefore, ultrasound examination is strongly recommended for all women with vaginal bleeding during pregnancy.
Ultrasound for other reasons uncovers many cases
With greater routine use of ultrasonography in obstetrics, a large percentage of women with placenta previa are diagnosed prior to the onset of the characteristic painless vaginal bleeding. In a 2003 study by Dola and colleagues,15 approximately 43% of placenta previa cases were diagnosed by ultrasonography performed for other obstetrical indications prior to the onset of vaginal bleeding.
Look for “warning hemorrhage”
The first episode of vaginal bleeding is rarely profuse or life-threatening to the mother or fetus. The bleeding usually subsides spontaneously, although it could recur and become more severe with subsequent episodes. Pregnancy typically continues after the initial bleeding episode.
The mean gestational age at the time of the first bleeding is 29 to 32 weeks.13,14 However, a third of cases have vaginal bleeding before the 30th week of gestation, a third between 30 and 36 weeks, and a third after 36 weeks’ gestation.13-15 Ten percent of women with the condition may be completely asymptomatic and progress to 38 weeks’ gestation without vaginal bleeding.13,14
Which form of ultrasound is most accurate?
With the advanced technology available today, ultrasound has become the standard means of diagnosing placenta previa.16,17
Transabdominal ultrasound has accuracy as high as 95% and a false-negative rate of 7% in the diagnosis of placenta previa.13,19 However, its accuracy may be adversely affected by maternal obesity, acoustic shadowing of the fetal head in a cephalic presentation, inability to locate the internal cervical os (which is critical for correct diagnosis), and difficulty imaging a posterior placenta and the lateral uterine walls. In addition, a full maternal bladder—usually helpful in transabdominal ultrasound imaging—may cause a false-positive diagnosis if the bladder is overly distended. In this situation, the cervix would appear artificially elongated and give a normally implanted placenta the appearance of encroachment into the internal cervical os.
Transvaginal ultrasound is superior for diagnosis of previa
Leerentveld et al20 reported false-positive and false-negative rates of 1% and 2%, respectively—a striking improvement over transabdominal ultrasound, which has rates of 2% to 6% and 7%, respectively.
Transvaginal sonography has several advantages over transabdominal imaging in localization of the placenta. The shorter distance from the vaginal probe transducer to the cervix and lower uterine segment allows the use of higher-frequency ultrasound waves, with improved resolution; therefore, the relationship between the placental edge and the internal os can be determined more accurately.
Some clinicians may worry that the probe used in transvaginal sonography will disrupt the placenta and provoke significant maternal hemorrhage, but this concern is unfounded. Multiple studies have attested to the safety of transvaginal sonography in localization of the placenta.5,20-22 The probe is introduced and positioned under direct ultrasound guidance at all times, and inadvertent insertion of the endovaginal probe into the internal cervical os is virtually impossible due to the anatomical relationship of the vagina and cervix.21
Transperineal ultrasound is another option. Several investigators have found it to be superior to transabdominal and similarly advantageous to transvaginal sonography in the diagnosis and exclusion of placenta previa.18
Start with transabdominal imaging
In current practice, transabdominal ultrasound is usually performed first to localize the placenta. If there is reason to suspect placenta previa, transvaginal or transperineal sonography is then used to confirm the location of the placenta.
Contractions may hinder imaging
Accurate diagnosis or exclusion of placenta previa may be difficult if uterine contractions are present during ultrasound evaluation. Myometrial contractions shorten the distance between the internal cervical os and the placental edge, altering measurement of this distance. In addition, the ultrasound appearance of a contraction may simulate placental tissue, making it difficult to exclude placenta previa.
The trouble with tradition
The 4 types of placenta previa in the traditional classification system—complete, partial, marginal, and low-lying—predate the era of ultrasound diagnosis and are based on digital palpation of the placenta through a partly dilated cervical os during labor.
A new system of 3 types
Along with other authors,5,15-18 we propose a new system with 3 categories—complete, incomplete, and low-lying—because ultrasound may not distinguish a placenta partially covering the internal os (a discrete point) from one that is merely encroaching on it.
Complete previa
The placenta completely covers the internal cervical os
Incomplete previa
The placental edge is within 2 cm of the internal cervical os, but does not cover the os
Low-lying previa
The distance from the internal cervical os to the placental edge is between 2 and 3.5 cm
Look for placenta accreta
When placenta previa is diagnosed by ultrasound examination, further diagnostic measures are needed to determine whether placenta accreta is present.5,23 In placenta accreta, neither the normal plane of separation between the placental villi and uterine wall, nor the intervening fibrinoid layer of Nitabuch, is present.5,23
Degrees of abnormal placental implantation
Risk of accreta can reach 67%
There are varying reports on the incidence of placenta accreta, but women with placenta previa and previous cesarean deliveries appear to have the highest incidence.3,23,24 In women with placenta previa and 1 previous cesarean section, the risk of placenta accreta has been estimated at 24%, but it increases to 67% for women with placenta previa and 4 previous cesarean sections.3
Sonographic appearance of placenta accreta
Certain characteristics are suggestive of placenta accreta25,26:
Unfortunately, diagnosis of placenta accreta is difficult prior to delivery, although transvaginal sonography and adjunctive color flow/power Doppler imaging with 2- and 3-dimensional techniques offer improved resolution and have yielded promising results in prenatal diagnosis.27-30
Magnetic resonance imaging (MRI) may also prove useful in detecting placental tissue invasion and evaluating the degree of invasion, especially in a posterior or lateral placenta previa or when there is invasion into the bladder.31-33
Gestational age, symptoms determine management
The management of women with placenta previa in the third trimester depends on the extent of maternal hemorrhage and the fetal gestational age. Clinical categories include:
Some asymptomatic cases resolve
Outpatient management is possible for women who have never bled after diagnosis in the second trimester. These women should abstain from intercourse, avoid digital examination after 20 weeks’ gestation, and immediately present to the hospital if there is any evidence of vaginal bleeding.34
Monthly ultrasound evaluations are necessary to determine whether placenta previa has resolved,34-37 since 90% of cases detected in the second trimester resolve by the third trimester.34 However, if placenta previa persists beyond 24 weeks’ gestation, there is a 50% risk that delivery will be complicated by it.35 If placenta previa persists after 32 weeks, that risk approaches 75%.35
2-fold risk of congenital malformations
Most investigators report a 2-fold increased risk of fetal congenital malformations in cases of placenta previa.5 These malformations include anomalies of the central nervous system, cardiovascular system, respiratory tract, and gastrointestinal tract. Therefore, a target ultrasound examination for fetal anatomy is recommended at the initial ultrasound diagnosis of placenta previa.
Risk of fetal growth restriction warrants heightened surveillance
Some controversy surrounds the incidence of fetal growth restriction in pregnancies complicated by placenta previa. Varma38 reported that fetal growth restriction occurs in 16% of women with placenta previa and is correlated with the number of antepartum bleeding episodes. Other investigators have reported normal fetal growth in women with placenta previa.39 Given this uncertainty, serial follow-up ultrasound evaluations are usually advised for fetal growth assessment.
When patient remains asymptomatic, perform amniocentesis at 36 weeks
Some women progress to the late third trimester without any vaginal bleeding. In these women, amniocentesis is recommended at approximately 36 weeks’ gestation to assess fetal lung maturity.34,40 Elective cesarean delivery can then be planned if pulmonary maturity is documented.
The benefits of elective delivery include a stable patient and an optimally prepared surgical team, as well as the avoidance of emergent surgery, which increases the risk for maternal complications. Emergent surgery also places the fetus at greater risk for anemia, compared with elective procedures(27.7% vs 2.9%, respectively).13
Vaginal bleeding requires inpatient evaluation
Any woman with placenta previa who presents with vaginal bleeding should be admitted to the labor and delivery unit for immediate evaluation of maternal and fetal status, including an estimation of gestational age.
Initial acute care and assessment necessitate34:
If hemorrhage is life-threatening, deliver immediately
During initial evaluation, if the hemorrhage is judged to be massive and life-threatening, resuscitative measures and immediate delivery are necessary to avoid serious maternal morbidity. Recommended measures include constant monitoring of maternal status, aggressive IV fluid resuscitation, transfusion of blood and blood products, assessment of fetal status, and immediate delivery without regard to the maturity of the fetus.
A woman at term or near term (with documented fetal lung maturity) who presents with mild or moderate vaginal bleeding should be delivered via cesarean section.
Conservative management may be appropriate for mild preterm bleeding
If vaginal bleeding is not threatening to the life of the mother, and the fetus is preterm, a conservative approach with aggressive expectant management is appropriate, since most first episodes of vaginal bleeding are self-limited and rarely life-threatening to mother or fetus. Expectant management allows fetal maturation in utero without jeopardizing maternal health. If maternal and fetal health remain stable, the expectant approach allows a safe delay of delivery until the fetus matures.
Hospitalization is recommended. Candidates for expectant management should be hospitalized after the initial episode of vaginal bleeding. Once maternal and fetal conditions stabilize, the woman should be transferred to the antepartum ward for hospital bed rest with bathroom privileges. For expectant management:
Delivery is warranted for life-threatening hemorrhage, fetal lung maturity, and/or the usual maternal and fetal indications.
The question of tocolysis
Third-trimester tocolytic therapy in a woman with vaginal bleeding is controversial. In placenta previa, vaginal bleeding appears to arise from disruption of the placental implantation site as the lower uterine segment develops.41,42 It is unclear whether uterine contractions play a role, as only 20% of women with placenta previa have uterine activity at the time of vaginal bleeding.13,14,42 It is difficult to determine whether these women have true preterm labor, because digital examination of the cervix to document cervical dilatation is impossible.
Does uterine activity precipitate bleeding?
Some investigators believe uterine activity is a predisposing factor for the vaginal bleeding associated with placenta previa, and would consider tocolytic therapy in a stable patient at a premature gestational age. However, further evidence of its safety is needed.
In particular, beta-mimetics should be avoided in hemorrhaging women because their vasodilatory effects can precipitate maternal hypotension. Another side effect of beta-mimetics: maternal tachycardia,43 which may mask the hypovolemic state in women with significant hemorrhage.
Magnesium sulfate has less effect on the maternal cardiovascular system and could be a better choice in symptomatic placenta previa.41 Also consider indomethacin, which appears to have fewer adverse maternal effects.
Inpatient vs outpatient management
Because 2 to 3 weeks of maternal hospitalization can pass between the initial warning hemorrhage and delivery of the fetus, outpatient care has become an option. Several retrospective studies have demonstrated the cost-effectiveness and safety of outpatient management of symptomatic placenta previa.44,45 These studies emphasized careful patient section.
Wing and associates46 conducted a prospective, randomized, controlled trial that reinforces the need for judicious use of outpatient management. In their study, fewer than half the patients diagnosed with placenta previa prior to 37 weeks were candidates. The authors point out the small number of patients in their study, and the fact that vaginal bleeding recurred in approximately 60% of patients. Because of the difficulty of predicting which patients will have recurrent bleeding and when, outpatient management should be reserved for those judged to be compliant with home bed rest who can rapidly return to the hospital, if necessary.
Women with recurrent vaginal bleeding during outpatient management should be rehospitalized.
In the event of massive hemorrhage, immediate compression of the aorta below the level of the renal arteries will reduce the bleeding enough to allow time to evaluate the situation.56 At the same time, aggressive IV fluid resuscitation and blood transfusion should begin. Reevaluate coagulation status after every 5 to 10 U of blood.57
Focused repair may be effective. In some situations, the hemorrhage may be controlled by oversewing and repairing the focal placental site defects.40
Bracketing the bleeding area. Another measure is a circular suture technique in which interrupted sutures are placed on the serosal surface of the anterior and posterior aspects of the uterus and as deeply as possible into the endometrium in a circumferential manner, bracketing the bleeding area.58
The argon beam coagulator can be used to achieve hemostasis; it is more effective than traditional bipolar cautery at ensuring hemostasis in extensive areas.56,57
Stepwise devascularization was effective in 100% of 103 women with postpartum hemorrhage who did not respond to traditional management.59 It involves 5 procedures to be performed in sequence until hemostasis is achieved: unilateral uterine vessel ligation, bilateral uterine vessel ligation, low uterine vessel ligation, unilateral ovarian vessel ligation, and bilateral ovarian vessel ligation.
Hypogastric artery ligation is another option, but it is technically challenging and successful in less than 50% of cases.57 In fact, the time spent on this technique may actually lead to increased blood loss.
Components of safe delivery
A detailed plan is necessary when major hemorrhage is anticipated at the time of elective cesarean delivery for placenta previa, including consultation with experts in different disciplines such as radiology, anesthesiology, urology, pathology, blood bank, neonatology, and gynecologic oncology.
Also pay attention to the maternal red blood cell reserve. Iron and folic acid should be administered to prevent and treat anemia, and antepartum erythropoietin should be considered as a way of increasing the hemoglobin level in women with placenta previa. Autologous blood transfusion, including acute normovolemic hemodilution, is another option.
Pelvic vessel embolization
Elective embolization or occlusion of the hypogastric or uterine arteries has proved to be safe and effective for postpartum hemorrhage, with a success rate of more than 90% in women with normal coagulation.47
In addition, elective catheterization with a balloon-tipped catheter can be used prophylactically to reduce blood flow to the placenta. Prophylactic catheterization of the anterior division of the internal iliac arteries can be performed right before the scheduled cesarean section. An axillary approach is technically easier for fluoroscopically guided catheterization of the internal iliac.48 The actual fluoroscopy time is minutes, so the risk of fetal exposure to radiation and irreversible ovarian damage is minimal.
The fetus is monitored during the procedure, and the balloons are left in the deflated state until after delivery, reducing the risk of uteroplacental insufficiency. Balloon inflation after delivery occludes the hypogastric arteries and diminishes uterine arterial blood flow during surgery. In some cases, the temporary occlusive effect of the balloons may control intraoperative bleeding completely. If substantial bleeding persists, subsequent embolization of the uterine arteries is advised, using absorbable Gelfoam particles, which are temporary and do not damage pelvic organs. Menstruation is not impaired, and normal pregnancies have been reported after this procedure.49,50
In women who undergo cesarean delivery under regional anesthesia, placement of a dry epidural catheter for later dosing of anesthetic agents should be considered prior to balloon catheterization, since the patient’s mobility is restricted after placement of the balloon-tipped catheter.
This therapy is especially useful when there is a high index of suspicion for placenta accreta.
Recommendations at the time of delivery
Hysterectomy for placenta previa, placenta accreta
This procedure is technically challenging when there is a markedly enlarged uterus with engorged collateral vessels. One useful method, delayed ligation technique, was originally described by Dyer et al on the Tulane obstetrics service at Charity Hospital of New Orleans.53 This technique facilitates quick control of all uterine vasculature with rapid hemostasis. Later modification of this method involves successive clamping and severing of all vascular pedicles supplying the uterus, prior to their suture ligation, for quick control of bleeding.
Close follow-up continues even after surgery
Immediately after surgery, close monitoring of hemodynamic status is required, ideally in a critical care setting. Because women with placenta previa/placenta accreta have often received massive transfusions of blood and blood products along with large volumes of crystalloid fluids, pulmonary edema may develop. Conversely, hypovolemia can result from inadequate replacement of blood or persistent intra-abdominal bleeding. Thus, close attention to urinary output allows early detection of pulmonary edema, acute respiratory distress syndrome, hypovolemia, or persistent intra-abdominal bleeding. Patients who undergo peripartum hysterectomy should also be monitored closely for possible ureteral injury.
Thromboprophylaxis should continue until the patient is ambulatory.
Recommended laboratory tests
Get a complete blood count with platelets and fibrinogen immediately after surgery and at frequent intervals as needed. A chemistry panel with calcium, albumin, electrolytes, and creatinine also is helpful.
Serious morbidity in 3% to 5% of women after emergent hysterectomy
Conditions such as acute respiratory distress syndrome from massive blood transfusion and pulmonary capillary leakage, acute tubular necrosis from renal failure, and pulmonary embolism may complicate 3% to 5% of cases.54
Reoperation for persistent intra-abdominal bleeding may be necessary, and 9% of women will have urologic injury. Unfortunately, the maternal mortality rate associated with this procedure is 0.8%, so meticulous postoperative care is mandated.55
The authors report no financial relationships with any company whose products are mentioned in this article.
1. Ananth CV, Savitz DA, Luther ER. Maternal cigarette smoking as a risk factor for placental abruption, placenta previa, and uterine bleeding in pregnancy. Am J Epidemiol. 1996;144:881-889.
2. Faiz AS, Ananth CV. Etiology and risk factors for placenta previa: an overview and meta-analysis of observational studies. J Matern Fetal Neonatal Med. 2003;13:175.-
3. Clark SL, Koonings PP, et al. Placenta previa/accreta and prior cesarean section. Obstet Gynecol. 1985;66:89-92.
4. Neri A, Manor Y, Matityahu A, Blieden L. Placenta previa and congenital cardiac anomalies. Fetal Ther. 1989;4:138-140.
5. Clark SL. Placenta previa and abruptio placenta. In: Creasy RK, Resnik R. Maternal-Fetal Medicine, Principles and Practice. 4th ed. Philadelphia: W.B. Saunders; 1999:616–631.
6. Miller DA, Chollet J, Goodwin TM. Clinical risks factors for placenta previa-placenta accreta. Am J Obstet Gynecol. 1997;177:210-214.
7. Ananth CV, Demissie K, Smulian JC, Vintzileos AM. Placenta previa in singleton and twin births in the United States, 1989 through 1998: a comparison of risk factor profiles and associated conditions. Am J Obstet Gynecol. 2003;188:275-281.
8. Gilbert WM, Nesbitt TS, Danielsen B. Childbearing beyond age 40: pregnancy outcome in 24,032 cases. Obstet Gynecol. 1999;93:9-14.
9. Lavery JP. Placenta previa. Clin Obstet Gynecol. 1990;33:414-421.
10. Taylor VM, Kramer MD, Vaughan TL, Peacock S. Placenta previa in relation to induced and spontaneous abortion: a population- based study. Obstet Gynecol. 1993;82:88-91.
11. Williams MA, Mittendorf R, Lieberman E, Monson RR, Schoenbaum SC, Genest DR. Cigarette smoking during pregnancy in relation to placenta previa. Am J Obstet Gynecol. 1991;165:28-32.
12. Handler AS, Mason ED, Rosenberg DL, Davis FG. The relationship between exposure during pregnancy to cigarette smoking and cocaine use and placenta previa. Am J Obstet Gynecol. 1994;170:884-889.
13. Cotton DB, Read JA, Paul RH, Quilligan EJ. The conservative aggressive management of placenta previa. Am J Obstet Gynecol. 1980;137:687-695.
14. Silver R, Depp R, Sabbagha RE, Dooley SL. Placenta previa: aggressive expectant management. Am J Obstet Gynecol. 1984;150:15-22.
15. Dola CP, Garite TJ, Dowling DD, Friend D, Ahdoot D, Asrat T. Placenta previa: does its type affect pregnancy outcome? Am J Perinatol. 2003;20:353-360.
16. Oppenheimer LW, Farine D, Ritchie JWK, Lewinsky RM, Telford J, Fairbanks LA. What is low-lying placenta? Am J Obstet Gynecol. 1991;165:1036-1038.
17. Bhide A, Thilaganathan B. Recent advances in the management of placenta previa. Curr Opin Obstet Gynecol. 2004;16:447-451.
18. Dawson WB, Dumas MD, Romano WM, Gagnon R, Gratton RJ, Mowbray RD. Translabial ultrasonography and placenta previa: does measurement of the os-placenta distance predict outcome? J Ultrasound Med. 1996;15:44-46.
19. Egley CC. Abruptio placentae and placenta previa. In: Winn HN, Hobbins JC. Clinical Maternal-Fetal Medicine.1st ed. Pearl River, NY: Parthenon Publishing; 2000:47–53.
20. Leerentveld RA, Gilberts E, Arnold M, Wladimiroff JW. Accuracy and safety of transvaginal sonographic placental localization. Obstet Gynecol. 1990;76:759-762.
21. Timor-Tritsch I, Yunis R. Confirming the safety of transvaginal sonography in patients suspected of placenta previa. Obstet Gynecol. 1993;81:742-744.
22. Tan NH, Abu M, Woo JLS, Tahir H. The role of transvaginal sonography in the diagnosis of placenta previa. Aust NZ J Obstet Gynaecol. 1995;35:42-45.
23. Miller DA, Cholleet JA, Goodwin TM. Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol. 1997;177:210-214.
24. Chattopadhyay SK, Kharif H, Sherbeeni MM. Placenta previa and accreta after previous cesarean section. Eur J Obstet Gynecol Reprod Biol. 1993;52:151.-
25. Comstock CH, Love JJ, Jr, Bronsteen RA, et al. Sonographic detection of placenta accreta in the second and third trimesters of pregnancy. Am J Obstet Gynecol. 2004;190:1135-1140.
26. Comstock CH, Lee W, Vettraino IM, Bronsteen RA. The early sonographic appearance of placenta accreta. J Ultrasound Med. 2003;22:19-23.
27. Chou MM, Ho ES. Prenatal diagnosis of placenta previa accreta with power amplitude ultrasonic agiography. Am J Obstet Gynecol. 1997;177:1523-1525.
28. Levine D, Hulka CA, Ludmir J, Li W, Edelman RR. Placenta accreta: evaluation with color Doppler US, power Doppler US, and MR imaging. Radiology. 1997;205:773-776.
29. Taipale P, Orden MR, Berg M, Manninen H, Alafuzoff I. Prenatal diagnosis of placenta accreta and percreta with ultrasonography, color Doppler, and magnetic resonance imaging. Obstet Gynecol. 2004;104:537-540.
30. Chou MM, Tseng JJ, Ho ES, Hwang JI. Three-dimensional color power Doppler imaging in the assessment of uteroplacental neovascularization in placenta previa increta/percreta. Am J Obstet Gynecol. 2001;185:1257-1260.
31. Maldjian C, Adam R, Pelosi M, II, Pelosi M III, Rudelli RD, Maldjian J. MRI appearance of placenta percreta and placenta accreta. Magnetic Resonance Imaging. 1999;17:965-971.
32. Thorp JM, Councell RB, Sandridge DA, Wiest HH. Antepartum diagnosis of placenta previa percreta by magnetic resonance imaging. Obstet Gynecol. 1992;80:506-508.
33. Kay HH, Spritzer CE. Preliminary experience with magnetic resonance imaging in patients with third-trimester bleeding. Obstet Gynecol. 1991;78:424-429.
34. Russo-Stieglitz K, Lockwood CJ. Placenta previa and vasa previa. Up To Date. 2005. Available at: www.uptodate.com.
35. Dashe JS, McIntire DD, Ramus RM, Santos-Ramos R, Twickler DM. Persistence of placenta previa according to gestational age at ultrasound detection. Obstet Gynecol. 2002;99:692-697.
36. Taipale P, Hiilesmaa V, Ylostalo P. Transvaginal ultrasonography at 18-23 weeks in predicting placenta previa at delivery. Ultrasound Obstet Gynecol. 1998;12:422.-
37. Rosati P, Guariglia L. Clinical significance of placenta previa detected at early routine transvaginal scan. J Ultrasound Med. 2000;19:581-585.
38. Varma TR. Fetal growth and placental function in patients with placenta previa. J Obstet Gynaecol Br Commonw. 1973;80:311-315.
39. Crane JM, Van Den Hof MC, et al. Neonatal outcomes with placenta previa. Obstet Gynecol. 1999;93:541-544.
40. Benedetti TJ. Obstetric hemorrhage. In: Gabbe SG, Niebyl, JR, Simpson JL. Obstetrics: Normal and Problem Pregnancies. 4th ed. Philadelphia: Churchill Livingstone; 2002:503–538.
41. Besinger RE, Moniak CW, Paskiewicz LS, et al. The effects of tocolytic use in the management of symptomatic placenta previa. Am J Obstet Gynecol. 1995;172:1770-1778.
42. Magann EF, Johnson CA, Gookin KS, Roberts WE, Martin RW, Morrison JC. Placenta praevia: does uterine activity cause bleeding? Aust NZ J Obstet Gynaecol. 1993;33:22-24
43. Benedetti TJ. Maternal complication of parenteral B-sympathomimetic therapy for premature labor. Am J Obstet Gynecol. 1983;145:1-6.
44. Mouer JR. Placenta previa: Antepartum conservative management, inpatient versus outpatient. Am J Obstet Gynecol. 1994;170:1683-1686.
45. Droste S, Keil K. Expectant management of placenta previa: cost-benefit analysis of outpatient treatment. Am J Obstet Gynecol. 1994;170:1254-1257.
46. Wing D, Paul RH, Millar LK. Management of the symptomatic placenta previa: a randomized, controlled trial of inpatient versus outpatient expectant management. Am J Obstet Gynecol. 1996;175:806-811.
47. Hansch E, Chitkara U, McAlpine J, El-Sayed Y, Dake MD, Razavi MK. Pelvic arterial embolization for control of obstetric hemorrhage: a five-year experience. Am J Obstet Gynecol. 1999;180:1454-1460.
48. Dubois J, Garel L, Grignon A, Lemay M, Leduc L. Placenta percreta: balloon occlusion and embolization of the internal iliac arteries to reduce intraoperative blood losses. Am J Obstet Gynecol. 1997;176:723-726.
49. Suresh V, Goodwin SC, McLucas B, Mohr G. Uterine artery embolization: an underused method of controlling pelvic hemorrhage. Am J Obstet Gynecol. 1997;176:938-948.
50. Salomon LJ, deTayrac R, Castaigne-Meary V, et al. Fertility and pregnancy outcome following pelvic arterial embolization for severe postpartum haemorrhage. A cohort study. Hum Reprod. 2003;18:849-852.
51. Frederiksen MC, Glassenberg R, Stika CS. Placenta previa: a 22-year analysis. Am J Obstet Gynecol. 1999;180:1432-1437.
52. Lockwood CJ, Artal R. Placenta accreta. Obstet Gynecol. 2002;99:1133-1134.
53. Dyer I, Nix GF, Weed JC. Total hysterectomy at cesarean section and the immediate puerperal period. Am J Obstet Gynecol. 1953;65:517-527.
54. Catanzarite VA, Stanco L, Schrimmer D, Conroy C. Managing placenta previa/accreta. Contemporary OB/GYN. 1996;4(5):66-95.
55. Stanco L, Schrimmer D, Paul D, Mishell D. Emergency peripartum hysterectomy and associated risk factors. Am J Obstet Gynecol. 1993;168:879-883.
56. Hudon L, Belfort MA, Broome DR. Diagnosis and management of placenta percreta: a review. Obstet Gynecol Surv. 1998;53:509-517.
57. Shevell T, Malone FD. Management of obstetric hemorrhage. Sem Perinatol. 2003;27:86-104.
58. Cho J, Kim S, Cha K, et al. Interrupted circular suture: bleeding control during cesarean delivery in placenta previa accreta. Obstet Gynecol. 1991;78:876-879.
59. AbdRabbo SA. Stepwise uterine devascularization: a novel technique for management of uncontrollable postpartum hemorrhage with preservation of the uterus. Am J Obstet Gynecol. 1994;171:694-700.
1. Ananth CV, Savitz DA, Luther ER. Maternal cigarette smoking as a risk factor for placental abruption, placenta previa, and uterine bleeding in pregnancy. Am J Epidemiol. 1996;144:881-889.
2. Faiz AS, Ananth CV. Etiology and risk factors for placenta previa: an overview and meta-analysis of observational studies. J Matern Fetal Neonatal Med. 2003;13:175.-
3. Clark SL, Koonings PP, et al. Placenta previa/accreta and prior cesarean section. Obstet Gynecol. 1985;66:89-92.
4. Neri A, Manor Y, Matityahu A, Blieden L. Placenta previa and congenital cardiac anomalies. Fetal Ther. 1989;4:138-140.
5. Clark SL. Placenta previa and abruptio placenta. In: Creasy RK, Resnik R. Maternal-Fetal Medicine, Principles and Practice. 4th ed. Philadelphia: W.B. Saunders; 1999:616–631.
6. Miller DA, Chollet J, Goodwin TM. Clinical risks factors for placenta previa-placenta accreta. Am J Obstet Gynecol. 1997;177:210-214.
7. Ananth CV, Demissie K, Smulian JC, Vintzileos AM. Placenta previa in singleton and twin births in the United States, 1989 through 1998: a comparison of risk factor profiles and associated conditions. Am J Obstet Gynecol. 2003;188:275-281.
8. Gilbert WM, Nesbitt TS, Danielsen B. Childbearing beyond age 40: pregnancy outcome in 24,032 cases. Obstet Gynecol. 1999;93:9-14.
9. Lavery JP. Placenta previa. Clin Obstet Gynecol. 1990;33:414-421.
10. Taylor VM, Kramer MD, Vaughan TL, Peacock S. Placenta previa in relation to induced and spontaneous abortion: a population- based study. Obstet Gynecol. 1993;82:88-91.
11. Williams MA, Mittendorf R, Lieberman E, Monson RR, Schoenbaum SC, Genest DR. Cigarette smoking during pregnancy in relation to placenta previa. Am J Obstet Gynecol. 1991;165:28-32.
12. Handler AS, Mason ED, Rosenberg DL, Davis FG. The relationship between exposure during pregnancy to cigarette smoking and cocaine use and placenta previa. Am J Obstet Gynecol. 1994;170:884-889.
13. Cotton DB, Read JA, Paul RH, Quilligan EJ. The conservative aggressive management of placenta previa. Am J Obstet Gynecol. 1980;137:687-695.
14. Silver R, Depp R, Sabbagha RE, Dooley SL. Placenta previa: aggressive expectant management. Am J Obstet Gynecol. 1984;150:15-22.
15. Dola CP, Garite TJ, Dowling DD, Friend D, Ahdoot D, Asrat T. Placenta previa: does its type affect pregnancy outcome? Am J Perinatol. 2003;20:353-360.
16. Oppenheimer LW, Farine D, Ritchie JWK, Lewinsky RM, Telford J, Fairbanks LA. What is low-lying placenta? Am J Obstet Gynecol. 1991;165:1036-1038.
17. Bhide A, Thilaganathan B. Recent advances in the management of placenta previa. Curr Opin Obstet Gynecol. 2004;16:447-451.
18. Dawson WB, Dumas MD, Romano WM, Gagnon R, Gratton RJ, Mowbray RD. Translabial ultrasonography and placenta previa: does measurement of the os-placenta distance predict outcome? J Ultrasound Med. 1996;15:44-46.
19. Egley CC. Abruptio placentae and placenta previa. In: Winn HN, Hobbins JC. Clinical Maternal-Fetal Medicine.1st ed. Pearl River, NY: Parthenon Publishing; 2000:47–53.
20. Leerentveld RA, Gilberts E, Arnold M, Wladimiroff JW. Accuracy and safety of transvaginal sonographic placental localization. Obstet Gynecol. 1990;76:759-762.
21. Timor-Tritsch I, Yunis R. Confirming the safety of transvaginal sonography in patients suspected of placenta previa. Obstet Gynecol. 1993;81:742-744.
22. Tan NH, Abu M, Woo JLS, Tahir H. The role of transvaginal sonography in the diagnosis of placenta previa. Aust NZ J Obstet Gynaecol. 1995;35:42-45.
23. Miller DA, Cholleet JA, Goodwin TM. Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol. 1997;177:210-214.
24. Chattopadhyay SK, Kharif H, Sherbeeni MM. Placenta previa and accreta after previous cesarean section. Eur J Obstet Gynecol Reprod Biol. 1993;52:151.-
25. Comstock CH, Love JJ, Jr, Bronsteen RA, et al. Sonographic detection of placenta accreta in the second and third trimesters of pregnancy. Am J Obstet Gynecol. 2004;190:1135-1140.
26. Comstock CH, Lee W, Vettraino IM, Bronsteen RA. The early sonographic appearance of placenta accreta. J Ultrasound Med. 2003;22:19-23.
27. Chou MM, Ho ES. Prenatal diagnosis of placenta previa accreta with power amplitude ultrasonic agiography. Am J Obstet Gynecol. 1997;177:1523-1525.
28. Levine D, Hulka CA, Ludmir J, Li W, Edelman RR. Placenta accreta: evaluation with color Doppler US, power Doppler US, and MR imaging. Radiology. 1997;205:773-776.
29. Taipale P, Orden MR, Berg M, Manninen H, Alafuzoff I. Prenatal diagnosis of placenta accreta and percreta with ultrasonography, color Doppler, and magnetic resonance imaging. Obstet Gynecol. 2004;104:537-540.
30. Chou MM, Tseng JJ, Ho ES, Hwang JI. Three-dimensional color power Doppler imaging in the assessment of uteroplacental neovascularization in placenta previa increta/percreta. Am J Obstet Gynecol. 2001;185:1257-1260.
31. Maldjian C, Adam R, Pelosi M, II, Pelosi M III, Rudelli RD, Maldjian J. MRI appearance of placenta percreta and placenta accreta. Magnetic Resonance Imaging. 1999;17:965-971.
32. Thorp JM, Councell RB, Sandridge DA, Wiest HH. Antepartum diagnosis of placenta previa percreta by magnetic resonance imaging. Obstet Gynecol. 1992;80:506-508.
33. Kay HH, Spritzer CE. Preliminary experience with magnetic resonance imaging in patients with third-trimester bleeding. Obstet Gynecol. 1991;78:424-429.
34. Russo-Stieglitz K, Lockwood CJ. Placenta previa and vasa previa. Up To Date. 2005. Available at: www.uptodate.com.
35. Dashe JS, McIntire DD, Ramus RM, Santos-Ramos R, Twickler DM. Persistence of placenta previa according to gestational age at ultrasound detection. Obstet Gynecol. 2002;99:692-697.
36. Taipale P, Hiilesmaa V, Ylostalo P. Transvaginal ultrasonography at 18-23 weeks in predicting placenta previa at delivery. Ultrasound Obstet Gynecol. 1998;12:422.-
37. Rosati P, Guariglia L. Clinical significance of placenta previa detected at early routine transvaginal scan. J Ultrasound Med. 2000;19:581-585.
38. Varma TR. Fetal growth and placental function in patients with placenta previa. J Obstet Gynaecol Br Commonw. 1973;80:311-315.
39. Crane JM, Van Den Hof MC, et al. Neonatal outcomes with placenta previa. Obstet Gynecol. 1999;93:541-544.
40. Benedetti TJ. Obstetric hemorrhage. In: Gabbe SG, Niebyl, JR, Simpson JL. Obstetrics: Normal and Problem Pregnancies. 4th ed. Philadelphia: Churchill Livingstone; 2002:503–538.
41. Besinger RE, Moniak CW, Paskiewicz LS, et al. The effects of tocolytic use in the management of symptomatic placenta previa. Am J Obstet Gynecol. 1995;172:1770-1778.
42. Magann EF, Johnson CA, Gookin KS, Roberts WE, Martin RW, Morrison JC. Placenta praevia: does uterine activity cause bleeding? Aust NZ J Obstet Gynaecol. 1993;33:22-24
43. Benedetti TJ. Maternal complication of parenteral B-sympathomimetic therapy for premature labor. Am J Obstet Gynecol. 1983;145:1-6.
44. Mouer JR. Placenta previa: Antepartum conservative management, inpatient versus outpatient. Am J Obstet Gynecol. 1994;170:1683-1686.
45. Droste S, Keil K. Expectant management of placenta previa: cost-benefit analysis of outpatient treatment. Am J Obstet Gynecol. 1994;170:1254-1257.
46. Wing D, Paul RH, Millar LK. Management of the symptomatic placenta previa: a randomized, controlled trial of inpatient versus outpatient expectant management. Am J Obstet Gynecol. 1996;175:806-811.
47. Hansch E, Chitkara U, McAlpine J, El-Sayed Y, Dake MD, Razavi MK. Pelvic arterial embolization for control of obstetric hemorrhage: a five-year experience. Am J Obstet Gynecol. 1999;180:1454-1460.
48. Dubois J, Garel L, Grignon A, Lemay M, Leduc L. Placenta percreta: balloon occlusion and embolization of the internal iliac arteries to reduce intraoperative blood losses. Am J Obstet Gynecol. 1997;176:723-726.
49. Suresh V, Goodwin SC, McLucas B, Mohr G. Uterine artery embolization: an underused method of controlling pelvic hemorrhage. Am J Obstet Gynecol. 1997;176:938-948.
50. Salomon LJ, deTayrac R, Castaigne-Meary V, et al. Fertility and pregnancy outcome following pelvic arterial embolization for severe postpartum haemorrhage. A cohort study. Hum Reprod. 2003;18:849-852.
51. Frederiksen MC, Glassenberg R, Stika CS. Placenta previa: a 22-year analysis. Am J Obstet Gynecol. 1999;180:1432-1437.
52. Lockwood CJ, Artal R. Placenta accreta. Obstet Gynecol. 2002;99:1133-1134.
53. Dyer I, Nix GF, Weed JC. Total hysterectomy at cesarean section and the immediate puerperal period. Am J Obstet Gynecol. 1953;65:517-527.
54. Catanzarite VA, Stanco L, Schrimmer D, Conroy C. Managing placenta previa/accreta. Contemporary OB/GYN. 1996;4(5):66-95.
55. Stanco L, Schrimmer D, Paul D, Mishell D. Emergency peripartum hysterectomy and associated risk factors. Am J Obstet Gynecol. 1993;168:879-883.
56. Hudon L, Belfort MA, Broome DR. Diagnosis and management of placenta percreta: a review. Obstet Gynecol Surv. 1998;53:509-517.
57. Shevell T, Malone FD. Management of obstetric hemorrhage. Sem Perinatol. 2003;27:86-104.
58. Cho J, Kim S, Cha K, et al. Interrupted circular suture: bleeding control during cesarean delivery in placenta previa accreta. Obstet Gynecol. 1991;78:876-879.
59. AbdRabbo SA. Stepwise uterine devascularization: a novel technique for management of uncontrollable postpartum hemorrhage with preservation of the uterus. Am J Obstet Gynecol. 1994;171:694-700.
4 Cases that Test Your Skills: Workup for premenopausal breast complaints
What’s the most common cause of death in women 40 to 44 years of age?
Answer: Breast cancer.1
What population has the highest death toll from breast cancer?
Answer: Women age 40 and older. Approximately 95% of new breast cancer cases and 97% of breast cancer deaths occur in women 40 and older.2
Why are many women in their 40s under-screened?
Answer: Because clinicians sometimes under-appreciate their risk.
Of course, the majority of breast cancer cases and deaths involve postmenopausal women. But this doesn’t mean younger women don’t warrant heightened scrutiny. This article presents 4 cases that focus on breast disease in women 40 to 49 years of age and the optimal workup for patients with suspicious findings. It includes recommendations on:
Digital mammography may aid in evaluation of dense breast tissue
Although early breast cancer may be more difficult to identify on mammography in premenopausal women because of their denser breast tissue, there are good data on the benefits of screening mammography for women in the 40- to 49-year-old age group,3,4 as well as for women age 50 and older.5 In addition, digital mammography is often helpful in women with radiographically dense breasts.
Screening vs diagnostic mammography
Women who have no complaints and no abnormal physical findings on self- or clinical examination typically undergo screening mammography. In typical cases, 2 views of each breast are obtained, and the radiologist often postpones reading the images until the end of the day, when they are scrutinized in batches.
In contrast, diagnostic mammography is performed when a possible problem arises, and several additional “coned-down” views may be needed. The radiologist interprets the study while the patient is still in the radiology office.
It is essential that gynecologists indicate on the mammography referral form whether they are requesting a diagnostic or screening mammogram. If it is a diagnostic mammogram, the reason and precise location of any suspicious areas need to be clearly communicated to the radiologist. In either case, the patient should be reminded to provide any previous images the radiologist does not already have.
I obtain routine annual screening mammography for my average-risk patients from age 40 onward, since more than 50,000 American women under age 50 are diagnosed with breast cancer each year.
CASE 1 Abnormal mammogram
S.H. is a healthy 43-year-old who had vaginal deliveries at ages 25 and 28 and has always used barrier contraception. She has no family history of cancer or high-risk factors for breast cancer. Her breast and pelvic examinations at the time of her routine gynecologic visit are normal. She has undergone annual mammography since she was 40 years old, but recently moved from another state and did not bring her mammograms with her.
She is sent for a screening mammogram, and 2 radiographic views of each breast are obtained. Upon review, the images are classified as Breast Imaging Reporting and Data Systems (BI-RADS) category 0, indicating that mammographic assessment is incomplete. The radiologist wants additional images of an area in the upper outer quadrant of the right breast, and wants to compare this study with the patient’s old films if they are available. S.H. returns the next day for the additional imaging, and the radiologist identifies an 8-mm area of suspicious calcifications in the right breast, reclassifying the mammogram as BI-RADS category 4.
The radiologist recommends a stereotactic biopsy, but S.H. wants your advice on whether to comply or proceed immediately to open biopsy.
What do you tell her?
Barely invasive biopsy
Stereotactic needle biopsy offers precise positioning in 3 dimensions without the lag time and scarring associated with open biopsies.In the case above, stereotactic biopsy is a good option, since it can usually be scheduled rapidly, does not require an operating room or anesthesia, is less expensive than open biopsy, and involves less scarring.6 If a patient’s lesion is clearly benign on stereotactic biopsy, she may be spared an open biopsy. If it is malignant, she can immediately begin to make treatment decisions.
Breast imaging categories
BI-RADS categories have standardized the reporting of mammograms and include the following7:
S.H. schedules a stereotactic biopsy for the following day in the radiologist’s office. Tissue diagnosis reveals an invasive ductal carcinoma, and the patient elects to undergo lumpectomy and radiation therapy.
CASE 2 Self-palpated lesion
L.J., 45, has no personal or family history of cancer and no high-risk factors, and she has undergone annual mammograms since the age of 40. Her last mammogram, which was negative, was 3 months ago.
Today L.J. reports that she felt a 1-cm lesion in the upper outer quadrant of her left breast during monthly breast self-examination. Although she is somewhat reassured by the normal mammogram 3 months earlier, she had been instructed by her gynecologist to call if she ever had any abnormal findings on breast self-examination.
Her gynecologist performs a thorough history and physical examination of the breasts and lymph nodes, confirming the presence of the lesion but no other abnormalities.
What is the next step?
Self-examination and imaging don’t always agree
It is vital that a diagnosis be made whenever a mass is present in the breast—even if the mammogram is normal—since 10% to 15% of women with breast cancer have normal mammograms.1
In this case, the first step is to review the prior mammogram. If no abnormality is found on the mammogram, the patient should undergo further imaging to ascertain whether the lesion appears benign or suspicious for malignancy.
However, even if all radiologic studies are normal, definitive diagnosis is crucial when a mass is present.
MRI may be useful when other imaging is inconclusive
In 2004, the American College of Radiology (ACR) published guidelines for breast MRI,8 which advise against using the modality for breast cancer screening in the general population of asymptomatic women because of the likelihood of false positives. However, MRI is recommended by the ACR in a wide range of situations, including those in which other imaging such as mammography or ultrasound has been inconclusive.
I encourage self-examination
Because 75% of women diagnosed with breast cancer lack major high-risk factors, all women should be screened, and I believe self-examination should be encouraged. Although data from randomized controlled trials of breast self-examination do not confirm a reduction in overall breast cancer mortality with the practice, it may lead to earlier detection in some women.9
While L.J. is in the office, the gynecologist telephones the radiologist and asks her to review the mammogram. The radiologist does so, comparing the latest films with prior mammograms, and calls back to report the absence of abnormal findings.
The patient is then sent for ultrasound of the breast, which does not reveal a cyst but does show some suspicious changes. After a breast MRI is consistent with malignancy, the lesion is biopsied and diagnosed as invasive lobular carcinoma.
Mammography isn’t perfect. Neither is magnetic resonance imaging (MRI). But both can be revealing in the right patients. MRI studies suggest it is better at imaging soft tissues and can detect lesions not visible on mammogram in 27% to 37% of patients.12,13
The downside: cost. Because MRI is 10 to 15 times more costly than mammography, it is usually limited to patients with suspicious findings or high risk.
Higher predictive value, biopsy still needed
Bluemke DA, Catsonis CA, Chen MH, et al. Magnetic resonance imaging of the breast prior to biopsy. JAMA. 2004;292:2735–2742.
A prospective multicenter study by the International Breast MR Consortium involved 821 women referred for breast biopsy at 14 university hospitals in North America and Europe. All women had BI-RADS category 4 or 5 mammographic evaluation and breast MRI prior to the biopsy, with imaging interpreted at each site without knowledge of the biopsy results.
Findings: MRI correctly identified cancer in 356 of 404 cancer cases, for a sensitivity of 88.1% (95% confidence interval [CI] 84.6–91.1). It also correctly ruled out cancer in 281 of 417 cases with benign findings, for a specificity of 67.7% (95% CI 62.7–71.9). The positive predictive value of MRI for 356 of 492 patients was 72.4% (95% CI 68.2–76.3), compared with 52.8% for mammography in 367 of 695 patients (95% CI 49.0–56.6).
Conclusion: Despite the higher predictive value of MRI, tissue sampling is still needed when suspicious findings are detected.
Annual MRI and mammography for women at high risk
Leach MO, Boggis CR, Dixon AK, et al. Screening with magnetic resonance imaging and mammography of a UK population at high familial risk of breast cancer: a prospective multicentre cohort study. Lancet. 2005;365:1769–1778.
This prospective, multicenter study compared mammography with contrast-enhanced MRI in 649 women aged 35 to 49 who had a strong family history of breast cancer or a high probability of BRCA1, BRCA2, or TP53 mutation. The women had annual screening with both modalities for 2 to 7 years.
Findings: Thirtyfive cancers were diagnosed—19 by contrast-enhanced MRI only, 6 by mammography only, and 8 by both, with 2 “interval” cases. Sensitivity for contrast-enhanced MRI was significantly higher than for mammography (77% vs 40%; 95% CI 60–90 vs 24–58); when both modalities were used, it was 94% (95% CI 81–99). The contrast in sensitivity between the 2 modalities was particularly sharp in women with BRCA1 mutations: 92% for MRI vs 23% for mammography (P=.004). However, specificity was higher for mammography (93% vs 81%; 95% CI 92–95 vs 80–83); when both mammography and MRI were used, specificity was 77% (95% CI 75–79).
Leach et al noted a high proportion of grade 3 cancers in this study, but the tumors were small and most women were node-negative.
Conclusion: Annual screening with both contrast-enhanced MRI and mammography would detect most cancers in high-risk women.
MRI is more cost-effective in women with BRCA1/2 mutations
Plevritis SK, Kurian AW, Sigal BM, et al. Cost-effectiveness of screening BRCA1/2 mutation carriers with breast magnetic resonance imaging. JAMA. 2006;295:2374–2384.
Using a computer model to simulate the life histories of individual BRCA1 and BRCA2 mutation carriers, Plevritis et al compared mammography and breast MRI for cancer screening, using published data to estimate the accuracy of the 2 modalities. Breast cancer survival was based on the Surveillance, Epidemiology, and End Results (SEER) database, whereas utilization rates and intervention costs were based on published data and Medicare payments for 2005.
Findings: For each quality-adjusted life-year (QALY) gained, the cost of annual MRI in addition to annual mammography ranged from less than $45,000 to more than $700,000, depending on the patient’s age and specific BRCA mutation. Compared with mammography alone, the cost of MRI for each QALY gained in women aged 35 to 54 years was $55,420 for BRCA1 mutation carriers, $130,695 for BRCA2 mutation carriers, and $98,454 for BRCA2 mutation carriers with mammographically dense breasts.
Conclusion: Breast MRI screening is more cost-effective in women with BRCA1 mutations. The cost-effectiveness of adding it to mammography also varies greatly by age.
CASE 3 Bloody nipple discharge
M.W. is a 48-year-old nulliparous woman who has noticed blood in her bra in the area of the right nipple several times during the past month. Her last mammogram, which was normal, was 1 year ago. Her history lacks any relevant problems other than the nipple discharge itself. Her menstrual periods are regular; the last one was 2 weeks earlier. Many years ago, she underwent a tubal ligation. She does not take any medications.
How should she be evaluated?
Nipple discharge is a common phenomenon, more so among women with benign problems (approximately 10%–15%) than in women with malignancies (approximately 3%).10
When taking a history from a woman with nipple discharge, ask about the color of the discharge; whether it is bilateral; whether it is spontaneous; and its frequency and duration.
Physical exam: Focus on 3 questions
During a routine, thorough examination of the breasts and axillae, focus on the following issues:
Although cytology of the discharge can be performed at this time, the yield may be low.
As with a mass, the cause of the discharge must be determined even if cytology is benign.
During the physical examination, the gynecologist palpates a subareolar mass. A subsequent mammogram identifies only this single, subareolar lesion. Although mammography is always indicated in cases of nipple discharge, sonography can be a helpful addition, as it can identify a dilated duct with a filling defect.
This patient is found to have a benign intraductal papilloma, which is surgically removed.
CASE 4 Inflammation of the breast
P.D., 41, has had 3 full-term deliveries, the most recent one just 3 weeks ago in another city. She had no prenatal care during any of her pregnancies.
While breast-feeding her new infant, P.D. noticed that the upper outer quadrant of her right breast was inflamed. She also had low-grade fever. When she visited the emergency room, she was given oral dicloxacillin and sent home. She took the medication as prescribed for several days, but had no response.
Today she returns to the emergency room with a fever of 101°F. The area of inflammation has extended beyond the upper outer quadrant of the breast and is tender, with significant skin thickening and edema in the inflamed area, as well as redness and warmth. There is no pointing abscess and no purulent discharge. A culture of the breast milk is obtained and is normal, as is the contralateral breast.
P.D. is admitted to the hospital for intravenous antibiotics. Because there is concern about methicillin-resistant Staphylococcus aureus, she is started on intravenous vancomycin.
A breast surgeon called in to evaluate the patient concludes no abscess is present. The surgeon believes the clinical picture might be consistent with inflammatory breast cancer, which often involves extensive invasion of the dermal lymphatics by cancer.
What is the next step?
In a breast-feeding woman, mastitis is usually the cause of inflammation
Postpartum mastitis is a common problem, and would be the most likely diagnosis in a woman presenting with breast inflammation within several weeks of delivery. Staphylococcus aureus is the most common etiologic agent, although streptococci are sometimes involved. Women with postpartum mastitis usually present with a tender, warm, red section of the breast and may have systemic evidence of infection, including general malaise, fever, and leukocytosis. Cracked or irritated nipples are also common.
Treatment-resistant mastitis justifies intravenous therapy
Women who have puerperal mastitis but who do not respond to appropriate antibiotic therapy may require intravenous treatment. Since methicillin-resistant Staphylococcus aureus is a concern, intravenous vancomycin may be necessary.
Occasionally, puerperal mastitis progresses to a breast abscess, necessitating drainage in addition to antibiotics. There may be loculations that need to be broken up to ensure adequate drainage.
More sinister conditions can mark postpartum period
Because postpartum mastitis is relatively common, and postpartum breast cancer fairly uncommon, it is no surprise that the gynecologist suspected mastitis in this case. However, pregnancy-associated breast cancer—cancer that occurs during pregnancy or within the first year after delivery—affects between 1 in 3,000 and 1 in 10,000 pregnancies.11
Earlier reports suggested a dismal prognosis for pregnancy-associated breast cancer. Newer data suggest that, stage for stage, with all other parameters controlled for, there may be no significant differences in 5- and 10-year survival for pregnancy-associated breast cancer, compared with breast cancer in nongravid, non-postpartum women.11
Inflammatory carcinoma of the breast has a generally poor prognosis, whether or not it is related to pregnancy.
The patient undergoes mammography immediately after pumping the breasts. It shows prominent subcutaneous lymphatic vessels and thickened skin. A breast sonogram is performed to rule out an occult abscess, but none is identified.
A skin biopsy confirms the presence of inflammatory carcinoma, with dilated dermal lymphatic channels containing intralymphatic tumor emboli.
The author reports no relevant financial relationships.
1. Seltzer V. Cancer in women: prevention and early detection. J Women’s Hlth Gender-Based Med. 2000;9:483-488.
2. American Cancer Society. Breast cancer facts and figures, 2005-2006. Atlanta: ACS; 2006.
3. Hendrick RE, et al. Benefit of screening mammography in women aged 40 to 49: a new meta-analysis of randomized controlled trials. Monogr Natl Cancer Inst. 1997;22:87-92.
4. Bjurstam N, Bjorneld L, Duffy SW, et al. Gothenberg breast screening trial. Cancer. 1997;80:2091-2099.
5. Duffy SW, Tabar L, Chen HH, et al. The impact of organized mammography service screening on breast carcinoma mortality in seven Swedish counties. Cancer. 2002;95:458-469.
6. Gundry KR, Berg WA. Treatment issues and core needle breast biopsy. Clinical context. Am J Roentgenol. 1998;171:41-49.
7. American College of Radiology. Breast Imaging Reporting and Data System (BI-RADS) Atlas, 4th ed. Reston, Va: ACR; 2003.
8. American College of Radiology ACR Practice Guideline for the Performance of Magnetic Resonance Imaging (MRI) of the Breast. Reston, Va: ACR; 2004:341-346.
9. Role of the obstetrician-gynecologist in the screening and diagnosis of breast masses. American College of Obstetricians and Gynecologists. Washington, DC: ACOG; 2006.
10. Seltzer V, Petrek J. The breast. In: Seltzer V, Pearse W, eds. Women’s Primary Health Care. New York: McGraw-Hill; 2000:793-823.
11. Petrek J, Seltzer V. Breast cancer in pregnant and postpartum women. J Obstet Gynaecol Can. 2003;25:944-950.
12. Liberman L, Morris EA, Dershaw DD, et al. MR imaging of the ipsilateral breast in women with percutaneously proven breast cancer. AJR Am J Roentgenol. 2003;180:901-910.
13. Harms SE, Flamig DP, Hesley KL, et al. MR imaging of the breast with rotating delivery of excitation off resonance: clinical experience with pathologic correlation. Radiology. 1993;187:493-501.
What’s the most common cause of death in women 40 to 44 years of age?
Answer: Breast cancer.1
What population has the highest death toll from breast cancer?
Answer: Women age 40 and older. Approximately 95% of new breast cancer cases and 97% of breast cancer deaths occur in women 40 and older.2
Why are many women in their 40s under-screened?
Answer: Because clinicians sometimes under-appreciate their risk.
Of course, the majority of breast cancer cases and deaths involve postmenopausal women. But this doesn’t mean younger women don’t warrant heightened scrutiny. This article presents 4 cases that focus on breast disease in women 40 to 49 years of age and the optimal workup for patients with suspicious findings. It includes recommendations on:
Digital mammography may aid in evaluation of dense breast tissue
Although early breast cancer may be more difficult to identify on mammography in premenopausal women because of their denser breast tissue, there are good data on the benefits of screening mammography for women in the 40- to 49-year-old age group,3,4 as well as for women age 50 and older.5 In addition, digital mammography is often helpful in women with radiographically dense breasts.
Screening vs diagnostic mammography
Women who have no complaints and no abnormal physical findings on self- or clinical examination typically undergo screening mammography. In typical cases, 2 views of each breast are obtained, and the radiologist often postpones reading the images until the end of the day, when they are scrutinized in batches.
In contrast, diagnostic mammography is performed when a possible problem arises, and several additional “coned-down” views may be needed. The radiologist interprets the study while the patient is still in the radiology office.
It is essential that gynecologists indicate on the mammography referral form whether they are requesting a diagnostic or screening mammogram. If it is a diagnostic mammogram, the reason and precise location of any suspicious areas need to be clearly communicated to the radiologist. In either case, the patient should be reminded to provide any previous images the radiologist does not already have.
I obtain routine annual screening mammography for my average-risk patients from age 40 onward, since more than 50,000 American women under age 50 are diagnosed with breast cancer each year.
CASE 1 Abnormal mammogram
S.H. is a healthy 43-year-old who had vaginal deliveries at ages 25 and 28 and has always used barrier contraception. She has no family history of cancer or high-risk factors for breast cancer. Her breast and pelvic examinations at the time of her routine gynecologic visit are normal. She has undergone annual mammography since she was 40 years old, but recently moved from another state and did not bring her mammograms with her.
She is sent for a screening mammogram, and 2 radiographic views of each breast are obtained. Upon review, the images are classified as Breast Imaging Reporting and Data Systems (BI-RADS) category 0, indicating that mammographic assessment is incomplete. The radiologist wants additional images of an area in the upper outer quadrant of the right breast, and wants to compare this study with the patient’s old films if they are available. S.H. returns the next day for the additional imaging, and the radiologist identifies an 8-mm area of suspicious calcifications in the right breast, reclassifying the mammogram as BI-RADS category 4.
The radiologist recommends a stereotactic biopsy, but S.H. wants your advice on whether to comply or proceed immediately to open biopsy.
What do you tell her?
Barely invasive biopsy
Stereotactic needle biopsy offers precise positioning in 3 dimensions without the lag time and scarring associated with open biopsies.In the case above, stereotactic biopsy is a good option, since it can usually be scheduled rapidly, does not require an operating room or anesthesia, is less expensive than open biopsy, and involves less scarring.6 If a patient’s lesion is clearly benign on stereotactic biopsy, she may be spared an open biopsy. If it is malignant, she can immediately begin to make treatment decisions.
Breast imaging categories
BI-RADS categories have standardized the reporting of mammograms and include the following7:
S.H. schedules a stereotactic biopsy for the following day in the radiologist’s office. Tissue diagnosis reveals an invasive ductal carcinoma, and the patient elects to undergo lumpectomy and radiation therapy.
CASE 2 Self-palpated lesion
L.J., 45, has no personal or family history of cancer and no high-risk factors, and she has undergone annual mammograms since the age of 40. Her last mammogram, which was negative, was 3 months ago.
Today L.J. reports that she felt a 1-cm lesion in the upper outer quadrant of her left breast during monthly breast self-examination. Although she is somewhat reassured by the normal mammogram 3 months earlier, she had been instructed by her gynecologist to call if she ever had any abnormal findings on breast self-examination.
Her gynecologist performs a thorough history and physical examination of the breasts and lymph nodes, confirming the presence of the lesion but no other abnormalities.
What is the next step?
Self-examination and imaging don’t always agree
It is vital that a diagnosis be made whenever a mass is present in the breast—even if the mammogram is normal—since 10% to 15% of women with breast cancer have normal mammograms.1
In this case, the first step is to review the prior mammogram. If no abnormality is found on the mammogram, the patient should undergo further imaging to ascertain whether the lesion appears benign or suspicious for malignancy.
However, even if all radiologic studies are normal, definitive diagnosis is crucial when a mass is present.
MRI may be useful when other imaging is inconclusive
In 2004, the American College of Radiology (ACR) published guidelines for breast MRI,8 which advise against using the modality for breast cancer screening in the general population of asymptomatic women because of the likelihood of false positives. However, MRI is recommended by the ACR in a wide range of situations, including those in which other imaging such as mammography or ultrasound has been inconclusive.
I encourage self-examination
Because 75% of women diagnosed with breast cancer lack major high-risk factors, all women should be screened, and I believe self-examination should be encouraged. Although data from randomized controlled trials of breast self-examination do not confirm a reduction in overall breast cancer mortality with the practice, it may lead to earlier detection in some women.9
While L.J. is in the office, the gynecologist telephones the radiologist and asks her to review the mammogram. The radiologist does so, comparing the latest films with prior mammograms, and calls back to report the absence of abnormal findings.
The patient is then sent for ultrasound of the breast, which does not reveal a cyst but does show some suspicious changes. After a breast MRI is consistent with malignancy, the lesion is biopsied and diagnosed as invasive lobular carcinoma.
Mammography isn’t perfect. Neither is magnetic resonance imaging (MRI). But both can be revealing in the right patients. MRI studies suggest it is better at imaging soft tissues and can detect lesions not visible on mammogram in 27% to 37% of patients.12,13
The downside: cost. Because MRI is 10 to 15 times more costly than mammography, it is usually limited to patients with suspicious findings or high risk.
Higher predictive value, biopsy still needed
Bluemke DA, Catsonis CA, Chen MH, et al. Magnetic resonance imaging of the breast prior to biopsy. JAMA. 2004;292:2735–2742.
A prospective multicenter study by the International Breast MR Consortium involved 821 women referred for breast biopsy at 14 university hospitals in North America and Europe. All women had BI-RADS category 4 or 5 mammographic evaluation and breast MRI prior to the biopsy, with imaging interpreted at each site without knowledge of the biopsy results.
Findings: MRI correctly identified cancer in 356 of 404 cancer cases, for a sensitivity of 88.1% (95% confidence interval [CI] 84.6–91.1). It also correctly ruled out cancer in 281 of 417 cases with benign findings, for a specificity of 67.7% (95% CI 62.7–71.9). The positive predictive value of MRI for 356 of 492 patients was 72.4% (95% CI 68.2–76.3), compared with 52.8% for mammography in 367 of 695 patients (95% CI 49.0–56.6).
Conclusion: Despite the higher predictive value of MRI, tissue sampling is still needed when suspicious findings are detected.
Annual MRI and mammography for women at high risk
Leach MO, Boggis CR, Dixon AK, et al. Screening with magnetic resonance imaging and mammography of a UK population at high familial risk of breast cancer: a prospective multicentre cohort study. Lancet. 2005;365:1769–1778.
This prospective, multicenter study compared mammography with contrast-enhanced MRI in 649 women aged 35 to 49 who had a strong family history of breast cancer or a high probability of BRCA1, BRCA2, or TP53 mutation. The women had annual screening with both modalities for 2 to 7 years.
Findings: Thirtyfive cancers were diagnosed—19 by contrast-enhanced MRI only, 6 by mammography only, and 8 by both, with 2 “interval” cases. Sensitivity for contrast-enhanced MRI was significantly higher than for mammography (77% vs 40%; 95% CI 60–90 vs 24–58); when both modalities were used, it was 94% (95% CI 81–99). The contrast in sensitivity between the 2 modalities was particularly sharp in women with BRCA1 mutations: 92% for MRI vs 23% for mammography (P=.004). However, specificity was higher for mammography (93% vs 81%; 95% CI 92–95 vs 80–83); when both mammography and MRI were used, specificity was 77% (95% CI 75–79).
Leach et al noted a high proportion of grade 3 cancers in this study, but the tumors were small and most women were node-negative.
Conclusion: Annual screening with both contrast-enhanced MRI and mammography would detect most cancers in high-risk women.
MRI is more cost-effective in women with BRCA1/2 mutations
Plevritis SK, Kurian AW, Sigal BM, et al. Cost-effectiveness of screening BRCA1/2 mutation carriers with breast magnetic resonance imaging. JAMA. 2006;295:2374–2384.
Using a computer model to simulate the life histories of individual BRCA1 and BRCA2 mutation carriers, Plevritis et al compared mammography and breast MRI for cancer screening, using published data to estimate the accuracy of the 2 modalities. Breast cancer survival was based on the Surveillance, Epidemiology, and End Results (SEER) database, whereas utilization rates and intervention costs were based on published data and Medicare payments for 2005.
Findings: For each quality-adjusted life-year (QALY) gained, the cost of annual MRI in addition to annual mammography ranged from less than $45,000 to more than $700,000, depending on the patient’s age and specific BRCA mutation. Compared with mammography alone, the cost of MRI for each QALY gained in women aged 35 to 54 years was $55,420 for BRCA1 mutation carriers, $130,695 for BRCA2 mutation carriers, and $98,454 for BRCA2 mutation carriers with mammographically dense breasts.
Conclusion: Breast MRI screening is more cost-effective in women with BRCA1 mutations. The cost-effectiveness of adding it to mammography also varies greatly by age.
CASE 3 Bloody nipple discharge
M.W. is a 48-year-old nulliparous woman who has noticed blood in her bra in the area of the right nipple several times during the past month. Her last mammogram, which was normal, was 1 year ago. Her history lacks any relevant problems other than the nipple discharge itself. Her menstrual periods are regular; the last one was 2 weeks earlier. Many years ago, she underwent a tubal ligation. She does not take any medications.
How should she be evaluated?
Nipple discharge is a common phenomenon, more so among women with benign problems (approximately 10%–15%) than in women with malignancies (approximately 3%).10
When taking a history from a woman with nipple discharge, ask about the color of the discharge; whether it is bilateral; whether it is spontaneous; and its frequency and duration.
Physical exam: Focus on 3 questions
During a routine, thorough examination of the breasts and axillae, focus on the following issues:
Although cytology of the discharge can be performed at this time, the yield may be low.
As with a mass, the cause of the discharge must be determined even if cytology is benign.
During the physical examination, the gynecologist palpates a subareolar mass. A subsequent mammogram identifies only this single, subareolar lesion. Although mammography is always indicated in cases of nipple discharge, sonography can be a helpful addition, as it can identify a dilated duct with a filling defect.
This patient is found to have a benign intraductal papilloma, which is surgically removed.
CASE 4 Inflammation of the breast
P.D., 41, has had 3 full-term deliveries, the most recent one just 3 weeks ago in another city. She had no prenatal care during any of her pregnancies.
While breast-feeding her new infant, P.D. noticed that the upper outer quadrant of her right breast was inflamed. She also had low-grade fever. When she visited the emergency room, she was given oral dicloxacillin and sent home. She took the medication as prescribed for several days, but had no response.
Today she returns to the emergency room with a fever of 101°F. The area of inflammation has extended beyond the upper outer quadrant of the breast and is tender, with significant skin thickening and edema in the inflamed area, as well as redness and warmth. There is no pointing abscess and no purulent discharge. A culture of the breast milk is obtained and is normal, as is the contralateral breast.
P.D. is admitted to the hospital for intravenous antibiotics. Because there is concern about methicillin-resistant Staphylococcus aureus, she is started on intravenous vancomycin.
A breast surgeon called in to evaluate the patient concludes no abscess is present. The surgeon believes the clinical picture might be consistent with inflammatory breast cancer, which often involves extensive invasion of the dermal lymphatics by cancer.
What is the next step?
In a breast-feeding woman, mastitis is usually the cause of inflammation
Postpartum mastitis is a common problem, and would be the most likely diagnosis in a woman presenting with breast inflammation within several weeks of delivery. Staphylococcus aureus is the most common etiologic agent, although streptococci are sometimes involved. Women with postpartum mastitis usually present with a tender, warm, red section of the breast and may have systemic evidence of infection, including general malaise, fever, and leukocytosis. Cracked or irritated nipples are also common.
Treatment-resistant mastitis justifies intravenous therapy
Women who have puerperal mastitis but who do not respond to appropriate antibiotic therapy may require intravenous treatment. Since methicillin-resistant Staphylococcus aureus is a concern, intravenous vancomycin may be necessary.
Occasionally, puerperal mastitis progresses to a breast abscess, necessitating drainage in addition to antibiotics. There may be loculations that need to be broken up to ensure adequate drainage.
More sinister conditions can mark postpartum period
Because postpartum mastitis is relatively common, and postpartum breast cancer fairly uncommon, it is no surprise that the gynecologist suspected mastitis in this case. However, pregnancy-associated breast cancer—cancer that occurs during pregnancy or within the first year after delivery—affects between 1 in 3,000 and 1 in 10,000 pregnancies.11
Earlier reports suggested a dismal prognosis for pregnancy-associated breast cancer. Newer data suggest that, stage for stage, with all other parameters controlled for, there may be no significant differences in 5- and 10-year survival for pregnancy-associated breast cancer, compared with breast cancer in nongravid, non-postpartum women.11
Inflammatory carcinoma of the breast has a generally poor prognosis, whether or not it is related to pregnancy.
The patient undergoes mammography immediately after pumping the breasts. It shows prominent subcutaneous lymphatic vessels and thickened skin. A breast sonogram is performed to rule out an occult abscess, but none is identified.
A skin biopsy confirms the presence of inflammatory carcinoma, with dilated dermal lymphatic channels containing intralymphatic tumor emboli.
The author reports no relevant financial relationships.
What’s the most common cause of death in women 40 to 44 years of age?
Answer: Breast cancer.1
What population has the highest death toll from breast cancer?
Answer: Women age 40 and older. Approximately 95% of new breast cancer cases and 97% of breast cancer deaths occur in women 40 and older.2
Why are many women in their 40s under-screened?
Answer: Because clinicians sometimes under-appreciate their risk.
Of course, the majority of breast cancer cases and deaths involve postmenopausal women. But this doesn’t mean younger women don’t warrant heightened scrutiny. This article presents 4 cases that focus on breast disease in women 40 to 49 years of age and the optimal workup for patients with suspicious findings. It includes recommendations on:
Digital mammography may aid in evaluation of dense breast tissue
Although early breast cancer may be more difficult to identify on mammography in premenopausal women because of their denser breast tissue, there are good data on the benefits of screening mammography for women in the 40- to 49-year-old age group,3,4 as well as for women age 50 and older.5 In addition, digital mammography is often helpful in women with radiographically dense breasts.
Screening vs diagnostic mammography
Women who have no complaints and no abnormal physical findings on self- or clinical examination typically undergo screening mammography. In typical cases, 2 views of each breast are obtained, and the radiologist often postpones reading the images until the end of the day, when they are scrutinized in batches.
In contrast, diagnostic mammography is performed when a possible problem arises, and several additional “coned-down” views may be needed. The radiologist interprets the study while the patient is still in the radiology office.
It is essential that gynecologists indicate on the mammography referral form whether they are requesting a diagnostic or screening mammogram. If it is a diagnostic mammogram, the reason and precise location of any suspicious areas need to be clearly communicated to the radiologist. In either case, the patient should be reminded to provide any previous images the radiologist does not already have.
I obtain routine annual screening mammography for my average-risk patients from age 40 onward, since more than 50,000 American women under age 50 are diagnosed with breast cancer each year.
CASE 1 Abnormal mammogram
S.H. is a healthy 43-year-old who had vaginal deliveries at ages 25 and 28 and has always used barrier contraception. She has no family history of cancer or high-risk factors for breast cancer. Her breast and pelvic examinations at the time of her routine gynecologic visit are normal. She has undergone annual mammography since she was 40 years old, but recently moved from another state and did not bring her mammograms with her.
She is sent for a screening mammogram, and 2 radiographic views of each breast are obtained. Upon review, the images are classified as Breast Imaging Reporting and Data Systems (BI-RADS) category 0, indicating that mammographic assessment is incomplete. The radiologist wants additional images of an area in the upper outer quadrant of the right breast, and wants to compare this study with the patient’s old films if they are available. S.H. returns the next day for the additional imaging, and the radiologist identifies an 8-mm area of suspicious calcifications in the right breast, reclassifying the mammogram as BI-RADS category 4.
The radiologist recommends a stereotactic biopsy, but S.H. wants your advice on whether to comply or proceed immediately to open biopsy.
What do you tell her?
Barely invasive biopsy
Stereotactic needle biopsy offers precise positioning in 3 dimensions without the lag time and scarring associated with open biopsies.In the case above, stereotactic biopsy is a good option, since it can usually be scheduled rapidly, does not require an operating room or anesthesia, is less expensive than open biopsy, and involves less scarring.6 If a patient’s lesion is clearly benign on stereotactic biopsy, she may be spared an open biopsy. If it is malignant, she can immediately begin to make treatment decisions.
Breast imaging categories
BI-RADS categories have standardized the reporting of mammograms and include the following7:
S.H. schedules a stereotactic biopsy for the following day in the radiologist’s office. Tissue diagnosis reveals an invasive ductal carcinoma, and the patient elects to undergo lumpectomy and radiation therapy.
CASE 2 Self-palpated lesion
L.J., 45, has no personal or family history of cancer and no high-risk factors, and she has undergone annual mammograms since the age of 40. Her last mammogram, which was negative, was 3 months ago.
Today L.J. reports that she felt a 1-cm lesion in the upper outer quadrant of her left breast during monthly breast self-examination. Although she is somewhat reassured by the normal mammogram 3 months earlier, she had been instructed by her gynecologist to call if she ever had any abnormal findings on breast self-examination.
Her gynecologist performs a thorough history and physical examination of the breasts and lymph nodes, confirming the presence of the lesion but no other abnormalities.
What is the next step?
Self-examination and imaging don’t always agree
It is vital that a diagnosis be made whenever a mass is present in the breast—even if the mammogram is normal—since 10% to 15% of women with breast cancer have normal mammograms.1
In this case, the first step is to review the prior mammogram. If no abnormality is found on the mammogram, the patient should undergo further imaging to ascertain whether the lesion appears benign or suspicious for malignancy.
However, even if all radiologic studies are normal, definitive diagnosis is crucial when a mass is present.
MRI may be useful when other imaging is inconclusive
In 2004, the American College of Radiology (ACR) published guidelines for breast MRI,8 which advise against using the modality for breast cancer screening in the general population of asymptomatic women because of the likelihood of false positives. However, MRI is recommended by the ACR in a wide range of situations, including those in which other imaging such as mammography or ultrasound has been inconclusive.
I encourage self-examination
Because 75% of women diagnosed with breast cancer lack major high-risk factors, all women should be screened, and I believe self-examination should be encouraged. Although data from randomized controlled trials of breast self-examination do not confirm a reduction in overall breast cancer mortality with the practice, it may lead to earlier detection in some women.9
While L.J. is in the office, the gynecologist telephones the radiologist and asks her to review the mammogram. The radiologist does so, comparing the latest films with prior mammograms, and calls back to report the absence of abnormal findings.
The patient is then sent for ultrasound of the breast, which does not reveal a cyst but does show some suspicious changes. After a breast MRI is consistent with malignancy, the lesion is biopsied and diagnosed as invasive lobular carcinoma.
Mammography isn’t perfect. Neither is magnetic resonance imaging (MRI). But both can be revealing in the right patients. MRI studies suggest it is better at imaging soft tissues and can detect lesions not visible on mammogram in 27% to 37% of patients.12,13
The downside: cost. Because MRI is 10 to 15 times more costly than mammography, it is usually limited to patients with suspicious findings or high risk.
Higher predictive value, biopsy still needed
Bluemke DA, Catsonis CA, Chen MH, et al. Magnetic resonance imaging of the breast prior to biopsy. JAMA. 2004;292:2735–2742.
A prospective multicenter study by the International Breast MR Consortium involved 821 women referred for breast biopsy at 14 university hospitals in North America and Europe. All women had BI-RADS category 4 or 5 mammographic evaluation and breast MRI prior to the biopsy, with imaging interpreted at each site without knowledge of the biopsy results.
Findings: MRI correctly identified cancer in 356 of 404 cancer cases, for a sensitivity of 88.1% (95% confidence interval [CI] 84.6–91.1). It also correctly ruled out cancer in 281 of 417 cases with benign findings, for a specificity of 67.7% (95% CI 62.7–71.9). The positive predictive value of MRI for 356 of 492 patients was 72.4% (95% CI 68.2–76.3), compared with 52.8% for mammography in 367 of 695 patients (95% CI 49.0–56.6).
Conclusion: Despite the higher predictive value of MRI, tissue sampling is still needed when suspicious findings are detected.
Annual MRI and mammography for women at high risk
Leach MO, Boggis CR, Dixon AK, et al. Screening with magnetic resonance imaging and mammography of a UK population at high familial risk of breast cancer: a prospective multicentre cohort study. Lancet. 2005;365:1769–1778.
This prospective, multicenter study compared mammography with contrast-enhanced MRI in 649 women aged 35 to 49 who had a strong family history of breast cancer or a high probability of BRCA1, BRCA2, or TP53 mutation. The women had annual screening with both modalities for 2 to 7 years.
Findings: Thirtyfive cancers were diagnosed—19 by contrast-enhanced MRI only, 6 by mammography only, and 8 by both, with 2 “interval” cases. Sensitivity for contrast-enhanced MRI was significantly higher than for mammography (77% vs 40%; 95% CI 60–90 vs 24–58); when both modalities were used, it was 94% (95% CI 81–99). The contrast in sensitivity between the 2 modalities was particularly sharp in women with BRCA1 mutations: 92% for MRI vs 23% for mammography (P=.004). However, specificity was higher for mammography (93% vs 81%; 95% CI 92–95 vs 80–83); when both mammography and MRI were used, specificity was 77% (95% CI 75–79).
Leach et al noted a high proportion of grade 3 cancers in this study, but the tumors were small and most women were node-negative.
Conclusion: Annual screening with both contrast-enhanced MRI and mammography would detect most cancers in high-risk women.
MRI is more cost-effective in women with BRCA1/2 mutations
Plevritis SK, Kurian AW, Sigal BM, et al. Cost-effectiveness of screening BRCA1/2 mutation carriers with breast magnetic resonance imaging. JAMA. 2006;295:2374–2384.
Using a computer model to simulate the life histories of individual BRCA1 and BRCA2 mutation carriers, Plevritis et al compared mammography and breast MRI for cancer screening, using published data to estimate the accuracy of the 2 modalities. Breast cancer survival was based on the Surveillance, Epidemiology, and End Results (SEER) database, whereas utilization rates and intervention costs were based on published data and Medicare payments for 2005.
Findings: For each quality-adjusted life-year (QALY) gained, the cost of annual MRI in addition to annual mammography ranged from less than $45,000 to more than $700,000, depending on the patient’s age and specific BRCA mutation. Compared with mammography alone, the cost of MRI for each QALY gained in women aged 35 to 54 years was $55,420 for BRCA1 mutation carriers, $130,695 for BRCA2 mutation carriers, and $98,454 for BRCA2 mutation carriers with mammographically dense breasts.
Conclusion: Breast MRI screening is more cost-effective in women with BRCA1 mutations. The cost-effectiveness of adding it to mammography also varies greatly by age.
CASE 3 Bloody nipple discharge
M.W. is a 48-year-old nulliparous woman who has noticed blood in her bra in the area of the right nipple several times during the past month. Her last mammogram, which was normal, was 1 year ago. Her history lacks any relevant problems other than the nipple discharge itself. Her menstrual periods are regular; the last one was 2 weeks earlier. Many years ago, she underwent a tubal ligation. She does not take any medications.
How should she be evaluated?
Nipple discharge is a common phenomenon, more so among women with benign problems (approximately 10%–15%) than in women with malignancies (approximately 3%).10
When taking a history from a woman with nipple discharge, ask about the color of the discharge; whether it is bilateral; whether it is spontaneous; and its frequency and duration.
Physical exam: Focus on 3 questions
During a routine, thorough examination of the breasts and axillae, focus on the following issues:
Although cytology of the discharge can be performed at this time, the yield may be low.
As with a mass, the cause of the discharge must be determined even if cytology is benign.
During the physical examination, the gynecologist palpates a subareolar mass. A subsequent mammogram identifies only this single, subareolar lesion. Although mammography is always indicated in cases of nipple discharge, sonography can be a helpful addition, as it can identify a dilated duct with a filling defect.
This patient is found to have a benign intraductal papilloma, which is surgically removed.
CASE 4 Inflammation of the breast
P.D., 41, has had 3 full-term deliveries, the most recent one just 3 weeks ago in another city. She had no prenatal care during any of her pregnancies.
While breast-feeding her new infant, P.D. noticed that the upper outer quadrant of her right breast was inflamed. She also had low-grade fever. When she visited the emergency room, she was given oral dicloxacillin and sent home. She took the medication as prescribed for several days, but had no response.
Today she returns to the emergency room with a fever of 101°F. The area of inflammation has extended beyond the upper outer quadrant of the breast and is tender, with significant skin thickening and edema in the inflamed area, as well as redness and warmth. There is no pointing abscess and no purulent discharge. A culture of the breast milk is obtained and is normal, as is the contralateral breast.
P.D. is admitted to the hospital for intravenous antibiotics. Because there is concern about methicillin-resistant Staphylococcus aureus, she is started on intravenous vancomycin.
A breast surgeon called in to evaluate the patient concludes no abscess is present. The surgeon believes the clinical picture might be consistent with inflammatory breast cancer, which often involves extensive invasion of the dermal lymphatics by cancer.
What is the next step?
In a breast-feeding woman, mastitis is usually the cause of inflammation
Postpartum mastitis is a common problem, and would be the most likely diagnosis in a woman presenting with breast inflammation within several weeks of delivery. Staphylococcus aureus is the most common etiologic agent, although streptococci are sometimes involved. Women with postpartum mastitis usually present with a tender, warm, red section of the breast and may have systemic evidence of infection, including general malaise, fever, and leukocytosis. Cracked or irritated nipples are also common.
Treatment-resistant mastitis justifies intravenous therapy
Women who have puerperal mastitis but who do not respond to appropriate antibiotic therapy may require intravenous treatment. Since methicillin-resistant Staphylococcus aureus is a concern, intravenous vancomycin may be necessary.
Occasionally, puerperal mastitis progresses to a breast abscess, necessitating drainage in addition to antibiotics. There may be loculations that need to be broken up to ensure adequate drainage.
More sinister conditions can mark postpartum period
Because postpartum mastitis is relatively common, and postpartum breast cancer fairly uncommon, it is no surprise that the gynecologist suspected mastitis in this case. However, pregnancy-associated breast cancer—cancer that occurs during pregnancy or within the first year after delivery—affects between 1 in 3,000 and 1 in 10,000 pregnancies.11
Earlier reports suggested a dismal prognosis for pregnancy-associated breast cancer. Newer data suggest that, stage for stage, with all other parameters controlled for, there may be no significant differences in 5- and 10-year survival for pregnancy-associated breast cancer, compared with breast cancer in nongravid, non-postpartum women.11
Inflammatory carcinoma of the breast has a generally poor prognosis, whether or not it is related to pregnancy.
The patient undergoes mammography immediately after pumping the breasts. It shows prominent subcutaneous lymphatic vessels and thickened skin. A breast sonogram is performed to rule out an occult abscess, but none is identified.
A skin biopsy confirms the presence of inflammatory carcinoma, with dilated dermal lymphatic channels containing intralymphatic tumor emboli.
The author reports no relevant financial relationships.
1. Seltzer V. Cancer in women: prevention and early detection. J Women’s Hlth Gender-Based Med. 2000;9:483-488.
2. American Cancer Society. Breast cancer facts and figures, 2005-2006. Atlanta: ACS; 2006.
3. Hendrick RE, et al. Benefit of screening mammography in women aged 40 to 49: a new meta-analysis of randomized controlled trials. Monogr Natl Cancer Inst. 1997;22:87-92.
4. Bjurstam N, Bjorneld L, Duffy SW, et al. Gothenberg breast screening trial. Cancer. 1997;80:2091-2099.
5. Duffy SW, Tabar L, Chen HH, et al. The impact of organized mammography service screening on breast carcinoma mortality in seven Swedish counties. Cancer. 2002;95:458-469.
6. Gundry KR, Berg WA. Treatment issues and core needle breast biopsy. Clinical context. Am J Roentgenol. 1998;171:41-49.
7. American College of Radiology. Breast Imaging Reporting and Data System (BI-RADS) Atlas, 4th ed. Reston, Va: ACR; 2003.
8. American College of Radiology ACR Practice Guideline for the Performance of Magnetic Resonance Imaging (MRI) of the Breast. Reston, Va: ACR; 2004:341-346.
9. Role of the obstetrician-gynecologist in the screening and diagnosis of breast masses. American College of Obstetricians and Gynecologists. Washington, DC: ACOG; 2006.
10. Seltzer V, Petrek J. The breast. In: Seltzer V, Pearse W, eds. Women’s Primary Health Care. New York: McGraw-Hill; 2000:793-823.
11. Petrek J, Seltzer V. Breast cancer in pregnant and postpartum women. J Obstet Gynaecol Can. 2003;25:944-950.
12. Liberman L, Morris EA, Dershaw DD, et al. MR imaging of the ipsilateral breast in women with percutaneously proven breast cancer. AJR Am J Roentgenol. 2003;180:901-910.
13. Harms SE, Flamig DP, Hesley KL, et al. MR imaging of the breast with rotating delivery of excitation off resonance: clinical experience with pathologic correlation. Radiology. 1993;187:493-501.
1. Seltzer V. Cancer in women: prevention and early detection. J Women’s Hlth Gender-Based Med. 2000;9:483-488.
2. American Cancer Society. Breast cancer facts and figures, 2005-2006. Atlanta: ACS; 2006.
3. Hendrick RE, et al. Benefit of screening mammography in women aged 40 to 49: a new meta-analysis of randomized controlled trials. Monogr Natl Cancer Inst. 1997;22:87-92.
4. Bjurstam N, Bjorneld L, Duffy SW, et al. Gothenberg breast screening trial. Cancer. 1997;80:2091-2099.
5. Duffy SW, Tabar L, Chen HH, et al. The impact of organized mammography service screening on breast carcinoma mortality in seven Swedish counties. Cancer. 2002;95:458-469.
6. Gundry KR, Berg WA. Treatment issues and core needle breast biopsy. Clinical context. Am J Roentgenol. 1998;171:41-49.
7. American College of Radiology. Breast Imaging Reporting and Data System (BI-RADS) Atlas, 4th ed. Reston, Va: ACR; 2003.
8. American College of Radiology ACR Practice Guideline for the Performance of Magnetic Resonance Imaging (MRI) of the Breast. Reston, Va: ACR; 2004:341-346.
9. Role of the obstetrician-gynecologist in the screening and diagnosis of breast masses. American College of Obstetricians and Gynecologists. Washington, DC: ACOG; 2006.
10. Seltzer V, Petrek J. The breast. In: Seltzer V, Pearse W, eds. Women’s Primary Health Care. New York: McGraw-Hill; 2000:793-823.
11. Petrek J, Seltzer V. Breast cancer in pregnant and postpartum women. J Obstet Gynaecol Can. 2003;25:944-950.
12. Liberman L, Morris EA, Dershaw DD, et al. MR imaging of the ipsilateral breast in women with percutaneously proven breast cancer. AJR Am J Roentgenol. 2003;180:901-910.
13. Harms SE, Flamig DP, Hesley KL, et al. MR imaging of the breast with rotating delivery of excitation off resonance: clinical experience with pathologic correlation. Radiology. 1993;187:493-501.