User login
Gynecologic Cancer
This Update reviews recent findings of importance to obstetricians and gynecologists. Late detection of ovarian cancer is still the main reason for the high mortality rate of the most deadly of the gynecologic cancers. Approximately 22,200 women will be newly diagnosed in the United States this year, and there will be 16,210 deaths. Since ovarian cancer is still initially detected in its advanced stages in more than 70% of cases, when cure rates are low, early detection and prevention remain our greatest challenge. The gynecologic oncologist’s opportunity to successfully treat malignancy depends on early detection, and therefore physicians providing primary care for women are our firstline guardians.
“Silent killer” may not be so stealthy
Women ultimately diagnosed with malignant masses had a triad of symptoms, as well as more recent onset and greater severity of symptoms than women with benign masses or no masses. A diagnostic workup employing transvaginal ultrasound and CA-125 should be considered when a woman says she has these symptoms.
Ovarian cancer is not a silent disease. It was believed to be a “silent killer” because it was thought to be asymptomatic until a woman had very advanced disease. However, Goff and colleagues, in a previous study, found that 95% of women with ovarian cancer had had symptoms prior to diagnosis—and that the type of symptoms was not significantly different, whether disease was early stage or late stage.
This new study aimed to identify the frequency, severity, and duration of symptoms typically associated with ovarian cancer, by comparing symptoms reported by different groups of women. Symptoms reported by women presenting to primary care clinics were compared with symptoms reported by a group of 128 women with ovarian masses. Importantly, women were surveyed about their symptoms before undergoing surgery, and before they had a diagnosis of cancer or benign disease.
Main findings:
- A triad of symptoms—abdominal bloating, an increase in abdominal girth, and urinary symptoms—occurred in 43% of women found to have ovarian cancer, but in only 8% of women who presented to a primary care clinic.
- The frequency and duration of symptoms in women with ovarian masses were more severe in the women with malignant masses, but were of a similar type regardless of whether the mass was benign or ovarian cancer.
- Onset of symptoms was more recent in women with ovarian cancer than in the control group.
Listening carefully and evaluating the severity, frequency, and duration of symptoms, especially abdominal bloating, an increase in abdominal girth, urinary symptoms, and abdominal pain, is all-important.
Ovarian cancer should be included in the differential diagnosis when a woman says she has these symptoms.
I found it interesting that symptoms with a more recent onset may be more consistent with ovarian cancer.
In an ideal world, a simple blood test with an absolute cutoff, with perfect sensitivity and specificity, would identify ovarian cancer at its earliest stages. However, until such a test exists, primary care physicians and ObGyns should continue to put weight on the symptoms the patient communicates.
Transvaginal ultrasound and CA-125
Consider performing a diagnostic workup employing transvaginal ultrasound and CA-125 measurement in women presenting with these complaints.
RELATED REFERENCES
- Goff BA, Mandell L, Muntz HG, Melancon CH. Ovarian cancer diagnosis: results of a national ovarian cancer survey. Cancer. 2000;89:2068–2075.
Whatever happened to the ovarian cancer blood test?
Ransohoff DF. Lessons from controversy: ovarian cancer screening and serum proteomics. J Natl Cancer Inst. 2005;97:315–319.
Science is still seeking the Holy Grail—a blood test for early detection of ovarian cancer.
When Petricoin et al reported in 2002 that a serum proteomic profiling test had nearly 100% sensitivity and specificity, the media trumpeted the phenomenal news. The public’s hopes soared when news articles reported that a company would soon begin offering the test. Patients brought in these reports to their ObGyns and asked for the test.
Plans to introduce a commercial screening test by early 2004 were delayed, however, due to FDA concerns about its reliability. The reasons for claims, plans, and delays were reported in both professional journals and the lay press, but details on the “question about whether the approach of discovery-based serum proteomics can accurately and reliably diagnose ovarian cancer—or any cancer—have not been resolved,” Dr. Ransohoff explains in this thoughtful 2005 essay.
He describes in a simple and straightforward way the requirements of reproducibility, and what these new technologies must demonstrate. He concludes that serum proteomic profiling for the early detection of ovarian cancer has not demonstrated the reproducibility required of a clinical test.
“Chance and bias may cause erroneous results and inflated expectations in the kind of observational research being conducted in several ‘–omics’ fields to assess molecular markers for diagnosis and prognosis of cancer. To realize the potential of new –omics technology will require appropriate rules of evidence in the design, conduct, and interpretation of the clinical research,” writes Dr. Ransohoff.
While proteomic profiling clearly has promise, clinicians should insist that initial studies be validated
What to tell patients. I explain that the test appeared promising, and therefore was of great interest, but the FDA did not allow it to be put on the market because of insufficient evidence that the test consistently defines whether cancer is or is not present. Since either a negative or positive test would have profound effects, accuracy is an absolute requirement.
RELATED REFERENCES
- Baggerly KA, Morris JS, Edmonson SR, Coombes KR. Signal in noise: evaluating reported reproducibility of serum proteomic tests for ovarian cancer. J Natl Cancer Inst. 2005;97:307–309.
- Liotta LA, Lowenthal M, Mehta A, et al. Importance of communication between producers and consumers of publicly available experimental data. J Natl Cancer Inst. 2005;97:310–314.
- Petricoin EF, Ardekani AM, Hitt BA, et al. Use of proteomic patterns in serum to identify ovarian cancer. Lancet. 2002;359:572–577.
Don’t hold back from counseling risk-reducing BSO when indicated
Metcalfe KA, Lynch HT, Ghadirian P, et al. The risk of ovarian cancer after breast cancer in BRCA1 and BRCA2 carriers. Gynecol Oncol. 2005;96:222–226.
Counsel women with breast cancer who are BRCA1 or BRCA2 mutation carriers to consider prophylactic salpingo-oophorectomy after childbearing is complete. Tamoxifen and chemotherapy do not lower risk.
ObGyns should encourage young women with breast cancer or women with a strong family history of breast and/or ovarian cancer to undergo genetic testing.
Women with breast cancer who are found to be BRCA1 or BRCA2 mutation carriers should be counseled by their gynecologists to consider prophylactic BSO after childbearing is complete. Even though these women’s greatest concern may be breast cancer recurrence, gynecologists should advise these women that they are also at risk for ovarian cancer, and that they can substantially decrease their risk by undergoing risk-reduction surgery. BRCA1 mutation carriers have up to an 80% lifetime risk of breast cancer and up to a 50% lifetime risk for ovarian cancer.
Recent data support intervention to decrease risk: BSO decreases risk of ovarian cancer by more than 90%, and decreases risk of breast cancer by 50% in BRCA1 or BRCA2 mutation carriers. Metcalfe et al examined women with a BRCA1 or BRCA2 mutation and a history of stage I or II breast cancer, and found that 10% developed an ovarian cancer, a fallopian tube cancer, or a peritoneal cancer. The median time was 8.1 years from the development of breast cancer to the development of ovarian cancer. The cumulative risk of developing ovarian cancer after breast cancer was 12.7% for BRCA1 mutation carriers and 6.8% for BRCA2 mutation carriers.
Tamoxifen or chemotherapy did not change this risk. The authors concluded that BSO could have prevented at least 43 to 46 ovarian cancers.
RELATED REFERENCES
- Rebbeck TR, Lynch HT, Neuhausen SL, et al. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med. 2002;346:1616–1622.
- Kauff ND, Satagopan JM, Robson ME, et al. Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med. 2002; 346:1609–1615.
Serial histologic sectioning is vital for detecting occult malignancy
Powell CB, Kenley E, Chen LM, et al. Risk-reducing salpingo-oophorectomy in BRCA mutation carriers: role of serial sectioning in the detection of occult malignancy. J Clin Oncol. 2005;23:127–132.
A specific 4-step protocol for salpingo-oophorectomy and pathologic examination increased the number of occult malignancies identified.
Is a risk-reducing BSO any different from a BSO for benign reasons? The evidence is a resounding YES. Given the strong data supporting prophylactic BSO in women with BRCA1 or BRCA2 mutations, ObGyns are increasingly called upon to perform this procedure. Current recommendations are to offer surgery to mutation carriers after childbearing or in their mid- to late 30s and early 40s. A number of studies have discovered that carriers who undergo risk-reducing BSO are at increased risk for occult malignancies already existing in the ovaries and fallopian tubes.
These studies recommend use of a specific surgical approach and pathologic examination of specimens.
Powell et al found an increased number occult malignancies with this strategy:
- Complete removal of ovaries and fallopian tubes
- Serial histologic sectioning of both ovaries and fallopian tubes
- Peritoneal and omental biopsies
- Peritoneal washings for cytology
Of 67 procedures, 7 (10.4%) occult malignancies were discovered: 4 in the fallopian tubes and 3 in the ovaries. Six of the occult malignancies were microscopic.
Surgically, the entire ovary and fallopian tube should be removed. I perform washings and carefully look at the pelvis and paracolic gutters for small-volume disease.
Most importantly, ObGyns need to speak with the pathologist. For most benign cases in which the ovaries and fallopian tubes look grossly normal, pathologists take a single representative section of each ovary and fallopian tube for histologic diagnosis. However, in these high-risk cases, complete serial sectioning of ovaries and fallopian tubes is absolutely necessary to rule out microscopic cancer. Removal of the uterus should be based on other indications.
The author reports no financial relationships relevant to this article.
RELATED REFERENCES
- Lu KH, Garber JE, Cramer DW, et al. Occult ovarian tumors in women with BRCA1 or BRCA2 mutations undergoing prophylactic oophorectomy. J Clin Oncol. 2000;18:2728–2732.
- Colgan TJ, Murphy J, Cole DE, Narod S, Rosen B. Occult carcinoma in prophylactic oophorectomy specimens: prevalence and association with BRCA germline mutation status. Am J Surg Pathol. 2001;25:1283–1289.
This Update reviews recent findings of importance to obstetricians and gynecologists. Late detection of ovarian cancer is still the main reason for the high mortality rate of the most deadly of the gynecologic cancers. Approximately 22,200 women will be newly diagnosed in the United States this year, and there will be 16,210 deaths. Since ovarian cancer is still initially detected in its advanced stages in more than 70% of cases, when cure rates are low, early detection and prevention remain our greatest challenge. The gynecologic oncologist’s opportunity to successfully treat malignancy depends on early detection, and therefore physicians providing primary care for women are our firstline guardians.
“Silent killer” may not be so stealthy
Women ultimately diagnosed with malignant masses had a triad of symptoms, as well as more recent onset and greater severity of symptoms than women with benign masses or no masses. A diagnostic workup employing transvaginal ultrasound and CA-125 should be considered when a woman says she has these symptoms.
Ovarian cancer is not a silent disease. It was believed to be a “silent killer” because it was thought to be asymptomatic until a woman had very advanced disease. However, Goff and colleagues, in a previous study, found that 95% of women with ovarian cancer had had symptoms prior to diagnosis—and that the type of symptoms was not significantly different, whether disease was early stage or late stage.
This new study aimed to identify the frequency, severity, and duration of symptoms typically associated with ovarian cancer, by comparing symptoms reported by different groups of women. Symptoms reported by women presenting to primary care clinics were compared with symptoms reported by a group of 128 women with ovarian masses. Importantly, women were surveyed about their symptoms before undergoing surgery, and before they had a diagnosis of cancer or benign disease.
Main findings:
- A triad of symptoms—abdominal bloating, an increase in abdominal girth, and urinary symptoms—occurred in 43% of women found to have ovarian cancer, but in only 8% of women who presented to a primary care clinic.
- The frequency and duration of symptoms in women with ovarian masses were more severe in the women with malignant masses, but were of a similar type regardless of whether the mass was benign or ovarian cancer.
- Onset of symptoms was more recent in women with ovarian cancer than in the control group.
Listening carefully and evaluating the severity, frequency, and duration of symptoms, especially abdominal bloating, an increase in abdominal girth, urinary symptoms, and abdominal pain, is all-important.
Ovarian cancer should be included in the differential diagnosis when a woman says she has these symptoms.
I found it interesting that symptoms with a more recent onset may be more consistent with ovarian cancer.
In an ideal world, a simple blood test with an absolute cutoff, with perfect sensitivity and specificity, would identify ovarian cancer at its earliest stages. However, until such a test exists, primary care physicians and ObGyns should continue to put weight on the symptoms the patient communicates.
Transvaginal ultrasound and CA-125
Consider performing a diagnostic workup employing transvaginal ultrasound and CA-125 measurement in women presenting with these complaints.
RELATED REFERENCES
- Goff BA, Mandell L, Muntz HG, Melancon CH. Ovarian cancer diagnosis: results of a national ovarian cancer survey. Cancer. 2000;89:2068–2075.
Whatever happened to the ovarian cancer blood test?
Ransohoff DF. Lessons from controversy: ovarian cancer screening and serum proteomics. J Natl Cancer Inst. 2005;97:315–319.
Science is still seeking the Holy Grail—a blood test for early detection of ovarian cancer.
When Petricoin et al reported in 2002 that a serum proteomic profiling test had nearly 100% sensitivity and specificity, the media trumpeted the phenomenal news. The public’s hopes soared when news articles reported that a company would soon begin offering the test. Patients brought in these reports to their ObGyns and asked for the test.
Plans to introduce a commercial screening test by early 2004 were delayed, however, due to FDA concerns about its reliability. The reasons for claims, plans, and delays were reported in both professional journals and the lay press, but details on the “question about whether the approach of discovery-based serum proteomics can accurately and reliably diagnose ovarian cancer—or any cancer—have not been resolved,” Dr. Ransohoff explains in this thoughtful 2005 essay.
He describes in a simple and straightforward way the requirements of reproducibility, and what these new technologies must demonstrate. He concludes that serum proteomic profiling for the early detection of ovarian cancer has not demonstrated the reproducibility required of a clinical test.
“Chance and bias may cause erroneous results and inflated expectations in the kind of observational research being conducted in several ‘–omics’ fields to assess molecular markers for diagnosis and prognosis of cancer. To realize the potential of new –omics technology will require appropriate rules of evidence in the design, conduct, and interpretation of the clinical research,” writes Dr. Ransohoff.
While proteomic profiling clearly has promise, clinicians should insist that initial studies be validated
What to tell patients. I explain that the test appeared promising, and therefore was of great interest, but the FDA did not allow it to be put on the market because of insufficient evidence that the test consistently defines whether cancer is or is not present. Since either a negative or positive test would have profound effects, accuracy is an absolute requirement.
RELATED REFERENCES
- Baggerly KA, Morris JS, Edmonson SR, Coombes KR. Signal in noise: evaluating reported reproducibility of serum proteomic tests for ovarian cancer. J Natl Cancer Inst. 2005;97:307–309.
- Liotta LA, Lowenthal M, Mehta A, et al. Importance of communication between producers and consumers of publicly available experimental data. J Natl Cancer Inst. 2005;97:310–314.
- Petricoin EF, Ardekani AM, Hitt BA, et al. Use of proteomic patterns in serum to identify ovarian cancer. Lancet. 2002;359:572–577.
Don’t hold back from counseling risk-reducing BSO when indicated
Metcalfe KA, Lynch HT, Ghadirian P, et al. The risk of ovarian cancer after breast cancer in BRCA1 and BRCA2 carriers. Gynecol Oncol. 2005;96:222–226.
Counsel women with breast cancer who are BRCA1 or BRCA2 mutation carriers to consider prophylactic salpingo-oophorectomy after childbearing is complete. Tamoxifen and chemotherapy do not lower risk.
ObGyns should encourage young women with breast cancer or women with a strong family history of breast and/or ovarian cancer to undergo genetic testing.
Women with breast cancer who are found to be BRCA1 or BRCA2 mutation carriers should be counseled by their gynecologists to consider prophylactic BSO after childbearing is complete. Even though these women’s greatest concern may be breast cancer recurrence, gynecologists should advise these women that they are also at risk for ovarian cancer, and that they can substantially decrease their risk by undergoing risk-reduction surgery. BRCA1 mutation carriers have up to an 80% lifetime risk of breast cancer and up to a 50% lifetime risk for ovarian cancer.
Recent data support intervention to decrease risk: BSO decreases risk of ovarian cancer by more than 90%, and decreases risk of breast cancer by 50% in BRCA1 or BRCA2 mutation carriers. Metcalfe et al examined women with a BRCA1 or BRCA2 mutation and a history of stage I or II breast cancer, and found that 10% developed an ovarian cancer, a fallopian tube cancer, or a peritoneal cancer. The median time was 8.1 years from the development of breast cancer to the development of ovarian cancer. The cumulative risk of developing ovarian cancer after breast cancer was 12.7% for BRCA1 mutation carriers and 6.8% for BRCA2 mutation carriers.
Tamoxifen or chemotherapy did not change this risk. The authors concluded that BSO could have prevented at least 43 to 46 ovarian cancers.
RELATED REFERENCES
- Rebbeck TR, Lynch HT, Neuhausen SL, et al. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med. 2002;346:1616–1622.
- Kauff ND, Satagopan JM, Robson ME, et al. Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med. 2002; 346:1609–1615.
Serial histologic sectioning is vital for detecting occult malignancy
Powell CB, Kenley E, Chen LM, et al. Risk-reducing salpingo-oophorectomy in BRCA mutation carriers: role of serial sectioning in the detection of occult malignancy. J Clin Oncol. 2005;23:127–132.
A specific 4-step protocol for salpingo-oophorectomy and pathologic examination increased the number of occult malignancies identified.
Is a risk-reducing BSO any different from a BSO for benign reasons? The evidence is a resounding YES. Given the strong data supporting prophylactic BSO in women with BRCA1 or BRCA2 mutations, ObGyns are increasingly called upon to perform this procedure. Current recommendations are to offer surgery to mutation carriers after childbearing or in their mid- to late 30s and early 40s. A number of studies have discovered that carriers who undergo risk-reducing BSO are at increased risk for occult malignancies already existing in the ovaries and fallopian tubes.
These studies recommend use of a specific surgical approach and pathologic examination of specimens.
Powell et al found an increased number occult malignancies with this strategy:
- Complete removal of ovaries and fallopian tubes
- Serial histologic sectioning of both ovaries and fallopian tubes
- Peritoneal and omental biopsies
- Peritoneal washings for cytology
Of 67 procedures, 7 (10.4%) occult malignancies were discovered: 4 in the fallopian tubes and 3 in the ovaries. Six of the occult malignancies were microscopic.
Surgically, the entire ovary and fallopian tube should be removed. I perform washings and carefully look at the pelvis and paracolic gutters for small-volume disease.
Most importantly, ObGyns need to speak with the pathologist. For most benign cases in which the ovaries and fallopian tubes look grossly normal, pathologists take a single representative section of each ovary and fallopian tube for histologic diagnosis. However, in these high-risk cases, complete serial sectioning of ovaries and fallopian tubes is absolutely necessary to rule out microscopic cancer. Removal of the uterus should be based on other indications.
The author reports no financial relationships relevant to this article.
RELATED REFERENCES
- Lu KH, Garber JE, Cramer DW, et al. Occult ovarian tumors in women with BRCA1 or BRCA2 mutations undergoing prophylactic oophorectomy. J Clin Oncol. 2000;18:2728–2732.
- Colgan TJ, Murphy J, Cole DE, Narod S, Rosen B. Occult carcinoma in prophylactic oophorectomy specimens: prevalence and association with BRCA germline mutation status. Am J Surg Pathol. 2001;25:1283–1289.
This Update reviews recent findings of importance to obstetricians and gynecologists. Late detection of ovarian cancer is still the main reason for the high mortality rate of the most deadly of the gynecologic cancers. Approximately 22,200 women will be newly diagnosed in the United States this year, and there will be 16,210 deaths. Since ovarian cancer is still initially detected in its advanced stages in more than 70% of cases, when cure rates are low, early detection and prevention remain our greatest challenge. The gynecologic oncologist’s opportunity to successfully treat malignancy depends on early detection, and therefore physicians providing primary care for women are our firstline guardians.
“Silent killer” may not be so stealthy
Women ultimately diagnosed with malignant masses had a triad of symptoms, as well as more recent onset and greater severity of symptoms than women with benign masses or no masses. A diagnostic workup employing transvaginal ultrasound and CA-125 should be considered when a woman says she has these symptoms.
Ovarian cancer is not a silent disease. It was believed to be a “silent killer” because it was thought to be asymptomatic until a woman had very advanced disease. However, Goff and colleagues, in a previous study, found that 95% of women with ovarian cancer had had symptoms prior to diagnosis—and that the type of symptoms was not significantly different, whether disease was early stage or late stage.
This new study aimed to identify the frequency, severity, and duration of symptoms typically associated with ovarian cancer, by comparing symptoms reported by different groups of women. Symptoms reported by women presenting to primary care clinics were compared with symptoms reported by a group of 128 women with ovarian masses. Importantly, women were surveyed about their symptoms before undergoing surgery, and before they had a diagnosis of cancer or benign disease.
Main findings:
- A triad of symptoms—abdominal bloating, an increase in abdominal girth, and urinary symptoms—occurred in 43% of women found to have ovarian cancer, but in only 8% of women who presented to a primary care clinic.
- The frequency and duration of symptoms in women with ovarian masses were more severe in the women with malignant masses, but were of a similar type regardless of whether the mass was benign or ovarian cancer.
- Onset of symptoms was more recent in women with ovarian cancer than in the control group.
Listening carefully and evaluating the severity, frequency, and duration of symptoms, especially abdominal bloating, an increase in abdominal girth, urinary symptoms, and abdominal pain, is all-important.
Ovarian cancer should be included in the differential diagnosis when a woman says she has these symptoms.
I found it interesting that symptoms with a more recent onset may be more consistent with ovarian cancer.
In an ideal world, a simple blood test with an absolute cutoff, with perfect sensitivity and specificity, would identify ovarian cancer at its earliest stages. However, until such a test exists, primary care physicians and ObGyns should continue to put weight on the symptoms the patient communicates.
Transvaginal ultrasound and CA-125
Consider performing a diagnostic workup employing transvaginal ultrasound and CA-125 measurement in women presenting with these complaints.
RELATED REFERENCES
- Goff BA, Mandell L, Muntz HG, Melancon CH. Ovarian cancer diagnosis: results of a national ovarian cancer survey. Cancer. 2000;89:2068–2075.
Whatever happened to the ovarian cancer blood test?
Ransohoff DF. Lessons from controversy: ovarian cancer screening and serum proteomics. J Natl Cancer Inst. 2005;97:315–319.
Science is still seeking the Holy Grail—a blood test for early detection of ovarian cancer.
When Petricoin et al reported in 2002 that a serum proteomic profiling test had nearly 100% sensitivity and specificity, the media trumpeted the phenomenal news. The public’s hopes soared when news articles reported that a company would soon begin offering the test. Patients brought in these reports to their ObGyns and asked for the test.
Plans to introduce a commercial screening test by early 2004 were delayed, however, due to FDA concerns about its reliability. The reasons for claims, plans, and delays were reported in both professional journals and the lay press, but details on the “question about whether the approach of discovery-based serum proteomics can accurately and reliably diagnose ovarian cancer—or any cancer—have not been resolved,” Dr. Ransohoff explains in this thoughtful 2005 essay.
He describes in a simple and straightforward way the requirements of reproducibility, and what these new technologies must demonstrate. He concludes that serum proteomic profiling for the early detection of ovarian cancer has not demonstrated the reproducibility required of a clinical test.
“Chance and bias may cause erroneous results and inflated expectations in the kind of observational research being conducted in several ‘–omics’ fields to assess molecular markers for diagnosis and prognosis of cancer. To realize the potential of new –omics technology will require appropriate rules of evidence in the design, conduct, and interpretation of the clinical research,” writes Dr. Ransohoff.
While proteomic profiling clearly has promise, clinicians should insist that initial studies be validated
What to tell patients. I explain that the test appeared promising, and therefore was of great interest, but the FDA did not allow it to be put on the market because of insufficient evidence that the test consistently defines whether cancer is or is not present. Since either a negative or positive test would have profound effects, accuracy is an absolute requirement.
RELATED REFERENCES
- Baggerly KA, Morris JS, Edmonson SR, Coombes KR. Signal in noise: evaluating reported reproducibility of serum proteomic tests for ovarian cancer. J Natl Cancer Inst. 2005;97:307–309.
- Liotta LA, Lowenthal M, Mehta A, et al. Importance of communication between producers and consumers of publicly available experimental data. J Natl Cancer Inst. 2005;97:310–314.
- Petricoin EF, Ardekani AM, Hitt BA, et al. Use of proteomic patterns in serum to identify ovarian cancer. Lancet. 2002;359:572–577.
Don’t hold back from counseling risk-reducing BSO when indicated
Metcalfe KA, Lynch HT, Ghadirian P, et al. The risk of ovarian cancer after breast cancer in BRCA1 and BRCA2 carriers. Gynecol Oncol. 2005;96:222–226.
Counsel women with breast cancer who are BRCA1 or BRCA2 mutation carriers to consider prophylactic salpingo-oophorectomy after childbearing is complete. Tamoxifen and chemotherapy do not lower risk.
ObGyns should encourage young women with breast cancer or women with a strong family history of breast and/or ovarian cancer to undergo genetic testing.
Women with breast cancer who are found to be BRCA1 or BRCA2 mutation carriers should be counseled by their gynecologists to consider prophylactic BSO after childbearing is complete. Even though these women’s greatest concern may be breast cancer recurrence, gynecologists should advise these women that they are also at risk for ovarian cancer, and that they can substantially decrease their risk by undergoing risk-reduction surgery. BRCA1 mutation carriers have up to an 80% lifetime risk of breast cancer and up to a 50% lifetime risk for ovarian cancer.
Recent data support intervention to decrease risk: BSO decreases risk of ovarian cancer by more than 90%, and decreases risk of breast cancer by 50% in BRCA1 or BRCA2 mutation carriers. Metcalfe et al examined women with a BRCA1 or BRCA2 mutation and a history of stage I or II breast cancer, and found that 10% developed an ovarian cancer, a fallopian tube cancer, or a peritoneal cancer. The median time was 8.1 years from the development of breast cancer to the development of ovarian cancer. The cumulative risk of developing ovarian cancer after breast cancer was 12.7% for BRCA1 mutation carriers and 6.8% for BRCA2 mutation carriers.
Tamoxifen or chemotherapy did not change this risk. The authors concluded that BSO could have prevented at least 43 to 46 ovarian cancers.
RELATED REFERENCES
- Rebbeck TR, Lynch HT, Neuhausen SL, et al. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med. 2002;346:1616–1622.
- Kauff ND, Satagopan JM, Robson ME, et al. Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med. 2002; 346:1609–1615.
Serial histologic sectioning is vital for detecting occult malignancy
Powell CB, Kenley E, Chen LM, et al. Risk-reducing salpingo-oophorectomy in BRCA mutation carriers: role of serial sectioning in the detection of occult malignancy. J Clin Oncol. 2005;23:127–132.
A specific 4-step protocol for salpingo-oophorectomy and pathologic examination increased the number of occult malignancies identified.
Is a risk-reducing BSO any different from a BSO for benign reasons? The evidence is a resounding YES. Given the strong data supporting prophylactic BSO in women with BRCA1 or BRCA2 mutations, ObGyns are increasingly called upon to perform this procedure. Current recommendations are to offer surgery to mutation carriers after childbearing or in their mid- to late 30s and early 40s. A number of studies have discovered that carriers who undergo risk-reducing BSO are at increased risk for occult malignancies already existing in the ovaries and fallopian tubes.
These studies recommend use of a specific surgical approach and pathologic examination of specimens.
Powell et al found an increased number occult malignancies with this strategy:
- Complete removal of ovaries and fallopian tubes
- Serial histologic sectioning of both ovaries and fallopian tubes
- Peritoneal and omental biopsies
- Peritoneal washings for cytology
Of 67 procedures, 7 (10.4%) occult malignancies were discovered: 4 in the fallopian tubes and 3 in the ovaries. Six of the occult malignancies were microscopic.
Surgically, the entire ovary and fallopian tube should be removed. I perform washings and carefully look at the pelvis and paracolic gutters for small-volume disease.
Most importantly, ObGyns need to speak with the pathologist. For most benign cases in which the ovaries and fallopian tubes look grossly normal, pathologists take a single representative section of each ovary and fallopian tube for histologic diagnosis. However, in these high-risk cases, complete serial sectioning of ovaries and fallopian tubes is absolutely necessary to rule out microscopic cancer. Removal of the uterus should be based on other indications.
The author reports no financial relationships relevant to this article.
RELATED REFERENCES
- Lu KH, Garber JE, Cramer DW, et al. Occult ovarian tumors in women with BRCA1 or BRCA2 mutations undergoing prophylactic oophorectomy. J Clin Oncol. 2000;18:2728–2732.
- Colgan TJ, Murphy J, Cole DE, Narod S, Rosen B. Occult carcinoma in prophylactic oophorectomy specimens: prevalence and association with BRCA germline mutation status. Am J Surg Pathol. 2001;25:1283–1289.
Management of obstetric hypertensive emergencies
Life-threatening obstetric hypertensive emergencies cannot be entirely prevented, but the risk of serious complications can be minimized.
The spectrum of hypertensive disease that can complicate pregnancy is broad—ranging from so-called “white coat” hypertension to gestational hypertension, chronic hypertension, chronic hypertension with superimposed preeclampsia, to preeclampsia.
Particularly challenging, however, is hypertension in pregnancy that becomes severe enough to qualify as a hypertensive crisis, bringing on immediate risk to both fetus and mother.
Risk may evolve over days—or hours—and may present as worsening blood pressure culminating in hypertensive crisis. Fetal morbidity and mortality, including placental abruption and acute fetal distress, are often directly linked to the maternal risks of hypertensive encephalopathy and cerebrovascular accident.
Placental abruption and fetal distress are common with severe hypertension even without encephalopathy and cerebrovascular accident. Abruption is unpredictable and potentially catastrophic, even with intense monitoring.
Aggressive BP control, while fundamental, needs to be balanced against the risks to both mother and fetus of overcorrection and undercorrection.
Defining a crisis
What truly defines hypertensive obstetric emergency is a matter of some debate.
Persistent blood pressures above 200 mm Hg systolic and/or 115 mm Hg diastolic qualify, but some have advocated 160/110 mm Hg as the threshold for emergent treatment of blood pressure. Others suggest that the rate of change in blood pressure is what precipitates the crisis, as opposed to the absolute blood pressure readings.
Why BP control is critical
The true pathophysiology of hypertensive crisis in pregnancy is obscure, but undoubtedly shares characteristics seen in the nonpregnant adult. Diagnosing a hypertensive emergency in the nonpregnant adult, in contrast to diagnosis of an obstetric hypertensive emergency, relies more on clinical manifestations of hypertension than on absolute blood pressure level.1
Pathophysiology
In the nonpregnant adult, 2 independent processes are thought to be necessary for the full-blown encephalopathic picture: dilation of the cerebral vasculature and fibrinoid necrosis. In the initial phases of severe hypertension, the cerebral vessels constrict to maintain cerebral perfusion pressure in the face of increased systemic arterial pressure. Once the limits of autoregulation are exceeded, reflex cerebral dilatation and resultant overperfusion lead to microvascular damage, exudation, microthrombus formation, and increased intracranial pressure, which in turn result in the encephalopathic picture.
In pregnancy, a prominent feature seems to be loss of cerebrovascular autoregulation, resulting in hypertensive encephalopathy once the upper limits of cerebral perfusion pressures are exceeded.2 Rapid control of blood pressure is needed even more because of the risks of placental abruption and stroke (See). Stroke is of special concern in the setting of thrombocytopenia or HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome. Cerebral edema may be more closely associated with endothelial cell injury than with blood pressure,3 although control of blood pressure may help minimize the endothelial cell injury.
Minimizing organ damage
First, restore normal BP
The most important clinical objective for treatment of acute hypertensive crisis in the nonpregnant adult is to minimize end organ damage, especially to the brain4; in obstetric cases, the major morbidity and mortality result from cardiac and renal, as well as cerebrovascular damage. Fetal morbidity and mortality, although not inconsequential, is often directly linked to the maternal condition, and therefore management is based on the triad of diagnosis, stabilization, and delivery.
The physiological dysfunctions described above are best tended to by aggressively controlling blood pressure. With restoration of acceptable blood pressures, generally in the range of 140 to 150 mm Hg systolic and 90 to 100 mm Hg diastolic, cardiac dysfunction begins to reverse, renal function tends to improve, and the restoration of cerebral autoregulatory capability lessens (but does not eliminate) the likelihood of stroke.
Rule out other causes
The foremost goal of therapy for malignant hypertension is to restore normal blood pressure, which depends on correct diagnosis so that appropriate pharmacotherapy may be initiated. For example, clinical situations that could cause malignant hypertension include such disparate entities as acute aortic dissection, acute left ventricular failure, pheochromocytoma, monoamine oxidase inhibitor–food (tyramine) interactions, eclampsia, and acute cocaine intoxication, to name but a few.
Frequently, chronic hypertension or severe preeclampsia defines the underlying “cause” of the severe hypertension, but consideration of other diagnoses, such as uncontrolled hyperthyroidism or pheochromocytoma, should not be overlooked. For example, in pheochromocytoma blood pressures tend to be paroxysmal with wide fluctuations. In hyperthyroidism, clinical signs or symptoms would be expected to accompany the clinical picture, such as the presence of proptosis, exophthalmos, lid lag, tremor, elevated temperature, and a wide pulse pressure, to name but a few.
Regimens to lower BP safely
It is imperative that blood pressure be lowered in a measured and safe manner, not to exceed a drop of 25% to 30% in the first 60 minutes, and not to drop below 150/95.4 Medications available for blood pressure reduction are listed in the Clip-and-save chart above.5
Every effort must be made to not overcorrect the hypertension. Too swift or too dramatic a reduction in blood pressure can have untoward consequences for both mother and fetus, including but not limited to acute fetal distress secondary to uteroplacental underperfusion, and the possibility of maternal myocardial or cerebral infarction. For these reasons, short-acting intravenous agents are recommended to treat hypertensive emergencies, and oral or sublingual compounds are to be avoided because they are more likely to cause precipitous and erratic drops in blood pressure.6
Pulmonary edema is not uncommon, due to capillary leakage and myocardial dysfunction. Aggressive use of furosemide along with a rapidly acting antihypertensive drug will best allow for improvement of the clinical picture in a timely manner.
Acute management steps
Critical care facilities required. During the acute management phase, patients should be cared for in an intensive care unit (or a labor and delivery unit with critical care capabilities) under the direction of physicians skilled in managing critically ill patients. In most institutions, such management will include participation of anesthesiologists, maternalfetal medicine specialists, and nurses with critical care expertise.
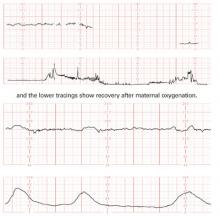
Delivery considerations. During initial management, the patient should have continuous fetal heart rate monitoring. Under such extreme circumstances, it is often not possible to prolong a pregnancy that is remote from term. Delivery decisions will need to balance prematurity risks against maternal risks of continuing the pregnancy.
Hypertension is not a contraindication to glucocorticoids for accelerating lung maturation in the fetus and minimizing neonatal risk of intracranial hemorrhage and necrotizing enterocolitis.7 Adjusting for gestational age, neonates of preeclamptic mothers are afforded no additional maturity compared with neonates born prematurely for other reasons. Delay of delivery for 48 to 72 hours may not be possible in many cases, however. Once the patient is stabilized, delivery must be considered.
Start magnesium sulfate, continue antihypertensives
At this point, it is prudent to start magnesium sulfate to prevent eclampsia. In most cases, however, excluding a diagnosis of preeclampsia in a timely manner is nearly impossible. Under these circumstances, magnesium sulfate is recommended, in addition to continued antihypertensive medications, to maintain BP control.
Magnesium sulfate is best administered intravenously, preferably through an infusion pump apparatus. A loading dose of 4 to 6 g (I prefer 6 g) is given as a 20% solution over 15 to 20 minutes, and then a continuous infusion may be initiated at a rate that depends on the patient’s renal function. In a patient with normal renal function, a rate of 2 g per hour is appropriate, but may need to be reduced if acute renal failure ensues.
In a report of 3 recent cases, investigators found magnesium sulfate was beneficial for controlling the clinical symptoms of pheochromocytoma when conventional therapy was unsuccessful. The presenting symptoms of these nonpregnant patients included hypertensive encephalopathy (2 patients) and catecholamine-induced cardiomyopathy (1 patient).6
In general, however, the role of magnesium sulfate should be for preventing progression to eclampsia, and not for acute blood pressure control.
Delivery decisions
Vaginal delivery is often less hemodynamically stressful for the mother, but not always practical. Many cases are remote from term with the fetus in a nonvertex presentation, or the uterine cervix is unfavorable for induction, or a protracted attempt at labor induction may not be prudent.
Under such circumstances, cesarean delivery must be considered and may be preferable. The reasons relate to the underlying maternal condition that often includes some degree of uteroplacental insufficiency. Altered placental function, combined with extreme prematurity, often results in the fetus being unable to tolerate labor for very long, necessitating emergent cesarean under potentially less controlled circumstances. The anesthesiologist and others on the critical care team must review the optimal anesthesia technique.
In most circumstances, and in the absence of coagulopathy, regional anesthesia affords the best results. When regional anesthesia is not an option, balanced general endotracheal anesthesia with antihypertensive premedication using a short-acting agent may be the safest alternative.
Maintain postpartum vigil
With delivery of the fetus, there may be a temptation to be less rigorous in maintaining blood pressure control during the post-partum period. In patients with chronic hypertension without superimposed preeclampsia, this may be acceptable, as these patients better tolerate higher blood pressures and still maintain appropriate cerebral vascular autoregulation.
For women who were previously normotensive, or who had superimposed preeclampsia, more rigorous control of blood pressure is recommended, especially if they show any degree of thrombocytopenia or pulmonary edema. (See Clip & save: Stepwise drug therapy for obstetric hypertensive crisis) The rationale relates to cerebral perfusion pressures and risk of stroke in these susceptible women, if thresholds are exceeded, and to the risk of worsening pulmonary edema in the setting of increased capillary hydrostatic pressure and reduced colloid osmotic pressure.
Additionally, continuation of magnesium sulfate is recommended for patients with superimposed preeclampsia until obvious signs of disease resolution, and for a minimum of 24 hours.
The author reports no financial relationships relevant to this article.
1. Tuncel M, Ram V. Hypertensive emergencies: etiology and management. Am J Cardiovasc Drugs. 2003;3:21-31.
2. Sibai BM. Hypertension. In: Gabbe SG, Niebyl JR, Simpson JL, eds. Obstetrics: Normal and Problem Pregnancies. 4th ed. New York, NY: Churchill Livingstone; 2002;945-1004.
3. Schwartz RB, Feske SK, Polak JF, et al. Preeclampsia-eclampsia: clinical and neuroradiographic correlates and insights into the pathogenesis of hypertensive encephalopathy. Radiology. 2000;2:371-376.
4. Williams O, Brust JC. Hypertensive encephalopathy. Curr Treat Cardiovasc Med. 2004;6:209-216.
5. Norwitz ER, Hsu CD, Repke JT. Acute complications of preeclampsia. Clin Obstet Gynecol. 2002;45:308-329.
6. James MF, Cronje L. Pheochromocytoma crisis: the use of magnesium sulfate. Anesth Analg. 2004;99:680-686.
7. Hiett AK, Brown HL, Britton KA. Outcome of infants delivered at 24 to 28 weeks’ gestation in women with severe preeclampsia. J Maternal-Fetal Med. 2001;10:301-304.
Life-threatening obstetric hypertensive emergencies cannot be entirely prevented, but the risk of serious complications can be minimized.
The spectrum of hypertensive disease that can complicate pregnancy is broad—ranging from so-called “white coat” hypertension to gestational hypertension, chronic hypertension, chronic hypertension with superimposed preeclampsia, to preeclampsia.
Particularly challenging, however, is hypertension in pregnancy that becomes severe enough to qualify as a hypertensive crisis, bringing on immediate risk to both fetus and mother.
Risk may evolve over days—or hours—and may present as worsening blood pressure culminating in hypertensive crisis. Fetal morbidity and mortality, including placental abruption and acute fetal distress, are often directly linked to the maternal risks of hypertensive encephalopathy and cerebrovascular accident.
Placental abruption and fetal distress are common with severe hypertension even without encephalopathy and cerebrovascular accident. Abruption is unpredictable and potentially catastrophic, even with intense monitoring.
Aggressive BP control, while fundamental, needs to be balanced against the risks to both mother and fetus of overcorrection and undercorrection.
Defining a crisis
What truly defines hypertensive obstetric emergency is a matter of some debate.
Persistent blood pressures above 200 mm Hg systolic and/or 115 mm Hg diastolic qualify, but some have advocated 160/110 mm Hg as the threshold for emergent treatment of blood pressure. Others suggest that the rate of change in blood pressure is what precipitates the crisis, as opposed to the absolute blood pressure readings.
Why BP control is critical
The true pathophysiology of hypertensive crisis in pregnancy is obscure, but undoubtedly shares characteristics seen in the nonpregnant adult. Diagnosing a hypertensive emergency in the nonpregnant adult, in contrast to diagnosis of an obstetric hypertensive emergency, relies more on clinical manifestations of hypertension than on absolute blood pressure level.1
Pathophysiology
In the nonpregnant adult, 2 independent processes are thought to be necessary for the full-blown encephalopathic picture: dilation of the cerebral vasculature and fibrinoid necrosis. In the initial phases of severe hypertension, the cerebral vessels constrict to maintain cerebral perfusion pressure in the face of increased systemic arterial pressure. Once the limits of autoregulation are exceeded, reflex cerebral dilatation and resultant overperfusion lead to microvascular damage, exudation, microthrombus formation, and increased intracranial pressure, which in turn result in the encephalopathic picture.
In pregnancy, a prominent feature seems to be loss of cerebrovascular autoregulation, resulting in hypertensive encephalopathy once the upper limits of cerebral perfusion pressures are exceeded.2 Rapid control of blood pressure is needed even more because of the risks of placental abruption and stroke (See). Stroke is of special concern in the setting of thrombocytopenia or HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome. Cerebral edema may be more closely associated with endothelial cell injury than with blood pressure,3 although control of blood pressure may help minimize the endothelial cell injury.
Minimizing organ damage
First, restore normal BP
The most important clinical objective for treatment of acute hypertensive crisis in the nonpregnant adult is to minimize end organ damage, especially to the brain4; in obstetric cases, the major morbidity and mortality result from cardiac and renal, as well as cerebrovascular damage. Fetal morbidity and mortality, although not inconsequential, is often directly linked to the maternal condition, and therefore management is based on the triad of diagnosis, stabilization, and delivery.
The physiological dysfunctions described above are best tended to by aggressively controlling blood pressure. With restoration of acceptable blood pressures, generally in the range of 140 to 150 mm Hg systolic and 90 to 100 mm Hg diastolic, cardiac dysfunction begins to reverse, renal function tends to improve, and the restoration of cerebral autoregulatory capability lessens (but does not eliminate) the likelihood of stroke.
Rule out other causes
The foremost goal of therapy for malignant hypertension is to restore normal blood pressure, which depends on correct diagnosis so that appropriate pharmacotherapy may be initiated. For example, clinical situations that could cause malignant hypertension include such disparate entities as acute aortic dissection, acute left ventricular failure, pheochromocytoma, monoamine oxidase inhibitor–food (tyramine) interactions, eclampsia, and acute cocaine intoxication, to name but a few.
Frequently, chronic hypertension or severe preeclampsia defines the underlying “cause” of the severe hypertension, but consideration of other diagnoses, such as uncontrolled hyperthyroidism or pheochromocytoma, should not be overlooked. For example, in pheochromocytoma blood pressures tend to be paroxysmal with wide fluctuations. In hyperthyroidism, clinical signs or symptoms would be expected to accompany the clinical picture, such as the presence of proptosis, exophthalmos, lid lag, tremor, elevated temperature, and a wide pulse pressure, to name but a few.
Regimens to lower BP safely
It is imperative that blood pressure be lowered in a measured and safe manner, not to exceed a drop of 25% to 30% in the first 60 minutes, and not to drop below 150/95.4 Medications available for blood pressure reduction are listed in the Clip-and-save chart above.5
Every effort must be made to not overcorrect the hypertension. Too swift or too dramatic a reduction in blood pressure can have untoward consequences for both mother and fetus, including but not limited to acute fetal distress secondary to uteroplacental underperfusion, and the possibility of maternal myocardial or cerebral infarction. For these reasons, short-acting intravenous agents are recommended to treat hypertensive emergencies, and oral or sublingual compounds are to be avoided because they are more likely to cause precipitous and erratic drops in blood pressure.6
Pulmonary edema is not uncommon, due to capillary leakage and myocardial dysfunction. Aggressive use of furosemide along with a rapidly acting antihypertensive drug will best allow for improvement of the clinical picture in a timely manner.
Acute management steps
Critical care facilities required. During the acute management phase, patients should be cared for in an intensive care unit (or a labor and delivery unit with critical care capabilities) under the direction of physicians skilled in managing critically ill patients. In most institutions, such management will include participation of anesthesiologists, maternalfetal medicine specialists, and nurses with critical care expertise.
Delivery considerations. During initial management, the patient should have continuous fetal heart rate monitoring. Under such extreme circumstances, it is often not possible to prolong a pregnancy that is remote from term. Delivery decisions will need to balance prematurity risks against maternal risks of continuing the pregnancy.
Hypertension is not a contraindication to glucocorticoids for accelerating lung maturation in the fetus and minimizing neonatal risk of intracranial hemorrhage and necrotizing enterocolitis.7 Adjusting for gestational age, neonates of preeclamptic mothers are afforded no additional maturity compared with neonates born prematurely for other reasons. Delay of delivery for 48 to 72 hours may not be possible in many cases, however. Once the patient is stabilized, delivery must be considered.
Start magnesium sulfate, continue antihypertensives
At this point, it is prudent to start magnesium sulfate to prevent eclampsia. In most cases, however, excluding a diagnosis of preeclampsia in a timely manner is nearly impossible. Under these circumstances, magnesium sulfate is recommended, in addition to continued antihypertensive medications, to maintain BP control.
Magnesium sulfate is best administered intravenously, preferably through an infusion pump apparatus. A loading dose of 4 to 6 g (I prefer 6 g) is given as a 20% solution over 15 to 20 minutes, and then a continuous infusion may be initiated at a rate that depends on the patient’s renal function. In a patient with normal renal function, a rate of 2 g per hour is appropriate, but may need to be reduced if acute renal failure ensues.
In a report of 3 recent cases, investigators found magnesium sulfate was beneficial for controlling the clinical symptoms of pheochromocytoma when conventional therapy was unsuccessful. The presenting symptoms of these nonpregnant patients included hypertensive encephalopathy (2 patients) and catecholamine-induced cardiomyopathy (1 patient).6
In general, however, the role of magnesium sulfate should be for preventing progression to eclampsia, and not for acute blood pressure control.
Delivery decisions
Vaginal delivery is often less hemodynamically stressful for the mother, but not always practical. Many cases are remote from term with the fetus in a nonvertex presentation, or the uterine cervix is unfavorable for induction, or a protracted attempt at labor induction may not be prudent.
Under such circumstances, cesarean delivery must be considered and may be preferable. The reasons relate to the underlying maternal condition that often includes some degree of uteroplacental insufficiency. Altered placental function, combined with extreme prematurity, often results in the fetus being unable to tolerate labor for very long, necessitating emergent cesarean under potentially less controlled circumstances. The anesthesiologist and others on the critical care team must review the optimal anesthesia technique.
In most circumstances, and in the absence of coagulopathy, regional anesthesia affords the best results. When regional anesthesia is not an option, balanced general endotracheal anesthesia with antihypertensive premedication using a short-acting agent may be the safest alternative.
Maintain postpartum vigil
With delivery of the fetus, there may be a temptation to be less rigorous in maintaining blood pressure control during the post-partum period. In patients with chronic hypertension without superimposed preeclampsia, this may be acceptable, as these patients better tolerate higher blood pressures and still maintain appropriate cerebral vascular autoregulation.
For women who were previously normotensive, or who had superimposed preeclampsia, more rigorous control of blood pressure is recommended, especially if they show any degree of thrombocytopenia or pulmonary edema. (See Clip & save: Stepwise drug therapy for obstetric hypertensive crisis) The rationale relates to cerebral perfusion pressures and risk of stroke in these susceptible women, if thresholds are exceeded, and to the risk of worsening pulmonary edema in the setting of increased capillary hydrostatic pressure and reduced colloid osmotic pressure.
Additionally, continuation of magnesium sulfate is recommended for patients with superimposed preeclampsia until obvious signs of disease resolution, and for a minimum of 24 hours.
The author reports no financial relationships relevant to this article.
Life-threatening obstetric hypertensive emergencies cannot be entirely prevented, but the risk of serious complications can be minimized.
The spectrum of hypertensive disease that can complicate pregnancy is broad—ranging from so-called “white coat” hypertension to gestational hypertension, chronic hypertension, chronic hypertension with superimposed preeclampsia, to preeclampsia.
Particularly challenging, however, is hypertension in pregnancy that becomes severe enough to qualify as a hypertensive crisis, bringing on immediate risk to both fetus and mother.
Risk may evolve over days—or hours—and may present as worsening blood pressure culminating in hypertensive crisis. Fetal morbidity and mortality, including placental abruption and acute fetal distress, are often directly linked to the maternal risks of hypertensive encephalopathy and cerebrovascular accident.
Placental abruption and fetal distress are common with severe hypertension even without encephalopathy and cerebrovascular accident. Abruption is unpredictable and potentially catastrophic, even with intense monitoring.
Aggressive BP control, while fundamental, needs to be balanced against the risks to both mother and fetus of overcorrection and undercorrection.
Defining a crisis
What truly defines hypertensive obstetric emergency is a matter of some debate.
Persistent blood pressures above 200 mm Hg systolic and/or 115 mm Hg diastolic qualify, but some have advocated 160/110 mm Hg as the threshold for emergent treatment of blood pressure. Others suggest that the rate of change in blood pressure is what precipitates the crisis, as opposed to the absolute blood pressure readings.
Why BP control is critical
The true pathophysiology of hypertensive crisis in pregnancy is obscure, but undoubtedly shares characteristics seen in the nonpregnant adult. Diagnosing a hypertensive emergency in the nonpregnant adult, in contrast to diagnosis of an obstetric hypertensive emergency, relies more on clinical manifestations of hypertension than on absolute blood pressure level.1
Pathophysiology
In the nonpregnant adult, 2 independent processes are thought to be necessary for the full-blown encephalopathic picture: dilation of the cerebral vasculature and fibrinoid necrosis. In the initial phases of severe hypertension, the cerebral vessels constrict to maintain cerebral perfusion pressure in the face of increased systemic arterial pressure. Once the limits of autoregulation are exceeded, reflex cerebral dilatation and resultant overperfusion lead to microvascular damage, exudation, microthrombus formation, and increased intracranial pressure, which in turn result in the encephalopathic picture.
In pregnancy, a prominent feature seems to be loss of cerebrovascular autoregulation, resulting in hypertensive encephalopathy once the upper limits of cerebral perfusion pressures are exceeded.2 Rapid control of blood pressure is needed even more because of the risks of placental abruption and stroke (See). Stroke is of special concern in the setting of thrombocytopenia or HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome. Cerebral edema may be more closely associated with endothelial cell injury than with blood pressure,3 although control of blood pressure may help minimize the endothelial cell injury.
Minimizing organ damage
First, restore normal BP
The most important clinical objective for treatment of acute hypertensive crisis in the nonpregnant adult is to minimize end organ damage, especially to the brain4; in obstetric cases, the major morbidity and mortality result from cardiac and renal, as well as cerebrovascular damage. Fetal morbidity and mortality, although not inconsequential, is often directly linked to the maternal condition, and therefore management is based on the triad of diagnosis, stabilization, and delivery.
The physiological dysfunctions described above are best tended to by aggressively controlling blood pressure. With restoration of acceptable blood pressures, generally in the range of 140 to 150 mm Hg systolic and 90 to 100 mm Hg diastolic, cardiac dysfunction begins to reverse, renal function tends to improve, and the restoration of cerebral autoregulatory capability lessens (but does not eliminate) the likelihood of stroke.
Rule out other causes
The foremost goal of therapy for malignant hypertension is to restore normal blood pressure, which depends on correct diagnosis so that appropriate pharmacotherapy may be initiated. For example, clinical situations that could cause malignant hypertension include such disparate entities as acute aortic dissection, acute left ventricular failure, pheochromocytoma, monoamine oxidase inhibitor–food (tyramine) interactions, eclampsia, and acute cocaine intoxication, to name but a few.
Frequently, chronic hypertension or severe preeclampsia defines the underlying “cause” of the severe hypertension, but consideration of other diagnoses, such as uncontrolled hyperthyroidism or pheochromocytoma, should not be overlooked. For example, in pheochromocytoma blood pressures tend to be paroxysmal with wide fluctuations. In hyperthyroidism, clinical signs or symptoms would be expected to accompany the clinical picture, such as the presence of proptosis, exophthalmos, lid lag, tremor, elevated temperature, and a wide pulse pressure, to name but a few.
Regimens to lower BP safely
It is imperative that blood pressure be lowered in a measured and safe manner, not to exceed a drop of 25% to 30% in the first 60 minutes, and not to drop below 150/95.4 Medications available for blood pressure reduction are listed in the Clip-and-save chart above.5
Every effort must be made to not overcorrect the hypertension. Too swift or too dramatic a reduction in blood pressure can have untoward consequences for both mother and fetus, including but not limited to acute fetal distress secondary to uteroplacental underperfusion, and the possibility of maternal myocardial or cerebral infarction. For these reasons, short-acting intravenous agents are recommended to treat hypertensive emergencies, and oral or sublingual compounds are to be avoided because they are more likely to cause precipitous and erratic drops in blood pressure.6
Pulmonary edema is not uncommon, due to capillary leakage and myocardial dysfunction. Aggressive use of furosemide along with a rapidly acting antihypertensive drug will best allow for improvement of the clinical picture in a timely manner.
Acute management steps
Critical care facilities required. During the acute management phase, patients should be cared for in an intensive care unit (or a labor and delivery unit with critical care capabilities) under the direction of physicians skilled in managing critically ill patients. In most institutions, such management will include participation of anesthesiologists, maternalfetal medicine specialists, and nurses with critical care expertise.
Delivery considerations. During initial management, the patient should have continuous fetal heart rate monitoring. Under such extreme circumstances, it is often not possible to prolong a pregnancy that is remote from term. Delivery decisions will need to balance prematurity risks against maternal risks of continuing the pregnancy.
Hypertension is not a contraindication to glucocorticoids for accelerating lung maturation in the fetus and minimizing neonatal risk of intracranial hemorrhage and necrotizing enterocolitis.7 Adjusting for gestational age, neonates of preeclamptic mothers are afforded no additional maturity compared with neonates born prematurely for other reasons. Delay of delivery for 48 to 72 hours may not be possible in many cases, however. Once the patient is stabilized, delivery must be considered.
Start magnesium sulfate, continue antihypertensives
At this point, it is prudent to start magnesium sulfate to prevent eclampsia. In most cases, however, excluding a diagnosis of preeclampsia in a timely manner is nearly impossible. Under these circumstances, magnesium sulfate is recommended, in addition to continued antihypertensive medications, to maintain BP control.
Magnesium sulfate is best administered intravenously, preferably through an infusion pump apparatus. A loading dose of 4 to 6 g (I prefer 6 g) is given as a 20% solution over 15 to 20 minutes, and then a continuous infusion may be initiated at a rate that depends on the patient’s renal function. In a patient with normal renal function, a rate of 2 g per hour is appropriate, but may need to be reduced if acute renal failure ensues.
In a report of 3 recent cases, investigators found magnesium sulfate was beneficial for controlling the clinical symptoms of pheochromocytoma when conventional therapy was unsuccessful. The presenting symptoms of these nonpregnant patients included hypertensive encephalopathy (2 patients) and catecholamine-induced cardiomyopathy (1 patient).6
In general, however, the role of magnesium sulfate should be for preventing progression to eclampsia, and not for acute blood pressure control.
Delivery decisions
Vaginal delivery is often less hemodynamically stressful for the mother, but not always practical. Many cases are remote from term with the fetus in a nonvertex presentation, or the uterine cervix is unfavorable for induction, or a protracted attempt at labor induction may not be prudent.
Under such circumstances, cesarean delivery must be considered and may be preferable. The reasons relate to the underlying maternal condition that often includes some degree of uteroplacental insufficiency. Altered placental function, combined with extreme prematurity, often results in the fetus being unable to tolerate labor for very long, necessitating emergent cesarean under potentially less controlled circumstances. The anesthesiologist and others on the critical care team must review the optimal anesthesia technique.
In most circumstances, and in the absence of coagulopathy, regional anesthesia affords the best results. When regional anesthesia is not an option, balanced general endotracheal anesthesia with antihypertensive premedication using a short-acting agent may be the safest alternative.
Maintain postpartum vigil
With delivery of the fetus, there may be a temptation to be less rigorous in maintaining blood pressure control during the post-partum period. In patients with chronic hypertension without superimposed preeclampsia, this may be acceptable, as these patients better tolerate higher blood pressures and still maintain appropriate cerebral vascular autoregulation.
For women who were previously normotensive, or who had superimposed preeclampsia, more rigorous control of blood pressure is recommended, especially if they show any degree of thrombocytopenia or pulmonary edema. (See Clip & save: Stepwise drug therapy for obstetric hypertensive crisis) The rationale relates to cerebral perfusion pressures and risk of stroke in these susceptible women, if thresholds are exceeded, and to the risk of worsening pulmonary edema in the setting of increased capillary hydrostatic pressure and reduced colloid osmotic pressure.
Additionally, continuation of magnesium sulfate is recommended for patients with superimposed preeclampsia until obvious signs of disease resolution, and for a minimum of 24 hours.
The author reports no financial relationships relevant to this article.
1. Tuncel M, Ram V. Hypertensive emergencies: etiology and management. Am J Cardiovasc Drugs. 2003;3:21-31.
2. Sibai BM. Hypertension. In: Gabbe SG, Niebyl JR, Simpson JL, eds. Obstetrics: Normal and Problem Pregnancies. 4th ed. New York, NY: Churchill Livingstone; 2002;945-1004.
3. Schwartz RB, Feske SK, Polak JF, et al. Preeclampsia-eclampsia: clinical and neuroradiographic correlates and insights into the pathogenesis of hypertensive encephalopathy. Radiology. 2000;2:371-376.
4. Williams O, Brust JC. Hypertensive encephalopathy. Curr Treat Cardiovasc Med. 2004;6:209-216.
5. Norwitz ER, Hsu CD, Repke JT. Acute complications of preeclampsia. Clin Obstet Gynecol. 2002;45:308-329.
6. James MF, Cronje L. Pheochromocytoma crisis: the use of magnesium sulfate. Anesth Analg. 2004;99:680-686.
7. Hiett AK, Brown HL, Britton KA. Outcome of infants delivered at 24 to 28 weeks’ gestation in women with severe preeclampsia. J Maternal-Fetal Med. 2001;10:301-304.
1. Tuncel M, Ram V. Hypertensive emergencies: etiology and management. Am J Cardiovasc Drugs. 2003;3:21-31.
2. Sibai BM. Hypertension. In: Gabbe SG, Niebyl JR, Simpson JL, eds. Obstetrics: Normal and Problem Pregnancies. 4th ed. New York, NY: Churchill Livingstone; 2002;945-1004.
3. Schwartz RB, Feske SK, Polak JF, et al. Preeclampsia-eclampsia: clinical and neuroradiographic correlates and insights into the pathogenesis of hypertensive encephalopathy. Radiology. 2000;2:371-376.
4. Williams O, Brust JC. Hypertensive encephalopathy. Curr Treat Cardiovasc Med. 2004;6:209-216.
5. Norwitz ER, Hsu CD, Repke JT. Acute complications of preeclampsia. Clin Obstet Gynecol. 2002;45:308-329.
6. James MF, Cronje L. Pheochromocytoma crisis: the use of magnesium sulfate. Anesth Analg. 2004;99:680-686.
7. Hiett AK, Brown HL, Britton KA. Outcome of infants delivered at 24 to 28 weeks’ gestation in women with severe preeclampsia. J Maternal-Fetal Med. 2001;10:301-304.
Impact of Mental Health Disorders
INFECTIOUS DISEASE
New findings I selected for this Update affect the management of 4 common and potentially serious clinical problems: acute cystitis, gonorrhea and chlamydia infection, chorioamnionitis, and varicella.
- A comparison of amoxicillin-clavulanic acid vs ciprofloxacin for uncomplicated lower urinary tract infections yielded surprising results, and more evidence on E coli’s resistance to antibiotics.
- Sexual partners of women with gonorrhea or chlamydia are more likely to receive appropriate treatment if it is offered by the women themselves or by the women’s caregivers.
- Short-course therapy for chorioamnionitis had a very high cure rate, equal to the traditional course, and furthers the possibility of shorter hospitalizations and cost savings without compromising outcomes.
- The CDC’s 1995 call for universal childhood vaccination for varicella has already sharply reduced varicella-related mortality in adults; still, we must determine immunity in our reproductive-age patients.
Acute cystitis: Ciprofloxacin prevails in E coli skirmish
Hooton TM, Scholes D, Gupta K, Stapleton AE, Roberts PL, Stamm WE. Amoxicillin-clavulanate vs ciprofloxacin for the treatment of uncomplicated cystitis in women: a randomized trial. JAMA. 2005;293:949–955.
Amoxicillin-clavulanate was not as effective as ciprofloxacin even in women who were infected with bacteria sensitive to amoxicillin-clavulanate.
A total of 320 nonpregnant women, aged 18 to 45 years, with uncomplicated acute cystitis were treated for 3 days with either oral amoxicillin-clavulanate (500 mg/125 mg twice daily) or oral ciprofloxacin (250 mg twice daily). Two weeks after treatment, 95% of women treated with ciprofloxacin were clinically cured, compared with only 76% of women treated with amoxicillin-clavulanate (P<.001).
Start with ciprofloxacin
The difference in outcome was attributed to a marked difference in vaginal colonization with the single most common pathogen in acute cystitis—Escherichia coli—at the 2-week follow-up (45% in the amoxicillinclavulanate group vs 10% in the ciprofloxacin group, P<.001).
Even though successful treatment of cystitis usually is possible with short courses (3–7 days) of oral antibiotics, persistent and recurrent infections may occur and usually are related to persistent vaginal colonization with E coli.
Treatment may require an extended course of oral antibiotics.
Initial selection of an antibiotic for acute cystitis is empiric and should be based on probable susceptibility of the dominant uropathogens. For many years, the typical initial antibiotic has been ampicillin.
E coli resistance. Now, however, more than a third of E coli strains, as well as most strains of K pneumoniae, are resistant to ampicillin. Therefore, ampicillin no longer should be used for the empiric treatment of cystitis.1
Surprising results
In theory, amoxicillin-clavulanate should have enhanced activity against E coli and other enteric organisms.
Therefore, these findings are surprising. The outcome with amoxicillin-clavulanate was inferior to that of ciprofloxacin, even in women who seemingly had susceptible uropathogens.
Based on this study, ciprofloxacin clearly is a more effective (and less expensive) empiric treatment in nonpregnant women.
In gravidas, start with nitrofurantoin
Ciprofloxacin is not appropriate for treatment of cystitis or asymptomatic bacteriuria in pregnant women. The quinolone antibiotics may cause injury to the developing cartilage of the fetus and are contraindicated in pregnant and lactating women, and in children younger than 17 years.1
What, then, is the most appropriate choice for treatment of uncomplicated cystitis during pregnancy?
One reasonable selection is oral trimethoprim-sulfamethoxazole, double-strength, twice daily. However, increasing resistance of E coli to this antibiotic has been documented recently.2,3
Therefore, a better choice is nitrofurantoin monohydrate macrocrystals, 100 mg twice daily.4 One organism that is not susceptible to nitrofurantoin is Proteus. When this organism is suspected, use trimethoprim-sulfamethoxazole.
Follow-up is a must
Because persistent and recurrent infections are common, patients should be followed with urine dipstick assessment or urine culture to be certain that the infection is resolved.
Follow-up is particularly important when infected women are pregnant, because of the risk of ascending infection leading to preterm labor, sepsis, or acute respiratory disease syndrome.
Treat sex partners, sight-unseen?
Golden MR, Whittington WL, Handsfield HH, et al. Effect of expedited treatment of sex partners on recurrent or persistent gonorrhea or chlamydial infection. N Engl J Med. 2005;352:676–685.
Providing a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Almost 2,000 men and women with uncomplicated gonorrhea or chlamydia infection were included in this study of expedited treatment compared with standard referral. In the standard referral group, investigators treated 931 patients and referred their sex partners to other physicians or facilities for evaluation and treatment. In the expedited treatment group, 929 patients were treated and also were provided with antibiotics to give to their partners. The partners of patients who were unwilling to do so were contacted and treated by the investigators.
At follow-up 21 to 126 days after treatment), persistent or recurrent infection was found in 13% of standard referral patients and 10% of expedited treatment patients (relative risk, 0.76; 95% confidence interval, 0.59–0.98).
Expedited treatment decreased the rate of persistent or recurrent gonorrhea more than that of persistent or recurrent chlamydia.
Patients in the expedited group were more likely to report that all of their partners were treated, and less likely to report having had sex with an untreated partner.
Advantages of the direct approach
The challenge for the ObGyn is how to arrange treatment for the female patient’s sex partner(s). This study indicates that a proactive approach is likely to be more effective than simply asking the patient to encourage her partner to seek medical attention. Direct provision of a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Failure to treat the patient’s sex partner is the principal cause of persistent or recurrent infection, which may lead to pelvic inflammatory disease, Fitz-Hugh-Curtis syndrome, and infertility. Gonorrhea may disseminate and manifest primarily by arthritis and dermatitis. If a pregnant woman is colonized with gonorrhea or chlamydia at the time of delivery, her infant may acquire gonococcal or chlamydial conjunctivitis or chlamydial pneumonia.
6 caveats
Although the results of this investigation are impressive and of great practical importance, these caveats should be noted.
- The oral drug used to treat gonorrhea in this study, cefixime (400 mg), is not presently available, and although another oral drug such as ciprofloxacin (500 mg) would be highly effective, it should not be used in pregnant or lactating women, or women younger than 17 years.1
- Although ceftriaxone, 125 mg intramuscularly, also is a superb drug for treatment of uncomplicated gonorrhea, the logistical problems of arranging for the partner to receive an intramuscular injection are daunting.
- Some women in the expedited treatment group were reluctant to provide medication to their partner(s), and study personnel were forced to intervene. Keep in mind that individual private practitioners and even well-organized clinics may not have sufficient support personnel to trace and treat all contacts.
- There is the important issue of a provider writing a prescription for an individual who is not actually his or her patient and who has not been interviewed and examined. Certainly, many state laws and insurance company regulations may discourage or even prohibit such a practice.
- Lack of a detailed assessment of the partner(s) means there is no opportunity to evaluate them for other conditions such as syphilis and HIV infection.
- Finally, taking a proactive approach in treating the sex partner(s) of patients who have gonorrhea or chlamydia (and, by extension, trichomoniasis) requires documentation of complete rationale in the patient’s medical record.
In addition, detailed written instructions must be provided for the partner(s) and must include a specific caution about possible reactions to the antibiotic.
Single-dose plus intrapartum therapy effective for chorioamnionitis
Edwards RK, Duff P. Single additional dose postpartum therapy for women with chorioamnionitis. Obstet Gynecol. 2003;102:957–961.
Short-course therapy is simpler to administer and reduces costs compared with more extended treatment.
Intrapartum therapy plus 1 additional dose of combination antibiotics after delivery produced a very high rate of cure (95.4%)—equivalent to that achieved when a more extended course of treatment was used.
In this randomized study of 292 otherwise healthy women with chorioamnionitis, 151 women were treated intrapartum with intravenous (IV) ampicillin (2 g every 6 hours) plus gentamicin (1.5 mg/kg every 8 hours). They received 1 dose of each drug postpartum. In addition, if they had a cesarean delivery, they received 1 dose of IV clindamycin (900 mg) immediately after the infant’s umbilical cord was clamped.
Women in the control group received IV antibiotics (including clindamycin, if indicated) until they had been afebrile and asymptomatic for 24 hours.
In the study group, 4.6% of women had a treatment failure and required an additional course of antibiotics. In the control group, 3.5% of patients required additional antibiotics (P = .639, not significant). When patients were stratified by method of delivery, no significant difference was found in treatment outcome.
Pathogens and regimens
Chorioamnionitis occurs in approximately 1% to 5% of term patients and in as many as 25% of patients having a preterm delivery. The infection is caused by multiple aerobic and anaerobic organisms, notably group B streptococci, E coli, and anaerobes. The former 2 pathogens pose the greatest risk to the infant and are the predominant causes of neonatal pneumonia, bacteremia, and meningitis. These organisms also are major causes of maternal bacteremia.
Anaerobes usually do not pose a major threat to the fetus or neonate, but are particularly likely to lead to pelvic abscess in women who require a cesarean delivery in the face of preexisting intrauterine infection.5
Accordingly, the initial antibiotic therapy for chorioamnionitis typically targets the 2 organisms most likely to infect the fetus/neonate—group B streptococci and E coli. The antibiotic regimen of ampicillin plus gentamicin provides excellent, and inexpensive, coverage of these pathogens. The addition of a drug such as clindamycin or metronidazole provides a reassuring measure of coverage against anaerobes in women who require a cesarean delivery.1
Traditionally, patients with chorioamnionitis have been treated with IV antibiotics until they have been afebrile and asymptomatic for 24 hours.
Chapman and Owen,6 who were among the first to suggest that a shortened course of treatment might be as effective as a more extended course, assessed the effectiveness of a single post-partum dose of cefotetan in women who were treated intrapartum for chorioamnionitis and who delivered vaginally. The rate of treatment failure was 11% in the single-dose group and 3.7% in the women treated with multiple doses of cefotetan until they had been afebrile for 24 hours. This observed difference was not statistically significant (P = .27), but the study lacked sufficient power to firmly establish the safety and effectiveness of short-course therapy.
A trial of “no therapy” vs “extended therapy” in women with chorioamnionitis who delivered by cesarean found the rate of treatment failure was 21.8% in the “no therapy” group and 14.8% in the women who received clindamycin plus gentamicin for at least 24 hours postoperatively.7
Again, this observed difference was not statistically significant (P = .32), but the power of the investigation was limited.
This more recent study was sufficiently large and included a reasonable number of women who delivered both vaginally and abdominally.
Anti-anaerobic coverage critically important. Complications related to persistent infection developed in 2 patients in the short-course group who had cesarean deliveries: pelvic abscess and incisional abscess. In both instances, the patients did not receive the dose of clindamycin specified in the protocol, illustrating the critical importance of proper anti-anaerobic coverage in patients who require abdominal delivery.
Short-course therapy offers advantages in terms of ease of administration and cost savings compared with more extended treatment regimens.
Whether short courses of single agents, such as the broad-spectrum cephalosporins, penicillins, and carbapenems, would be as effective as ampicillin plus gentamicin plus clindamycin remains to be determined.
CDC data show “herd” immunity, thanks to varicella vaccination policy
Nguyen HQ, Jumaan AO, Seward JF. Decline in mortality due to varicella after implementation of varicella vaccination in the United States. N Engl J Med. 2005;352:450–458.
Question all women of reproductive age about varicella. Women who lack a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
This study demonstrates that, through the phenomenon of herd immunity, universal vaccination has significantly lowered the overall risk of varicella-related mortality in the general population. Universal childhood varicella vaccination was recommended by the Centers for Disease Control and Prevention in 1995; the rate of death due to varicella, either as the underlying cause or the contributing cause, fluctuated from 1990 through 1998, and then sharply declined.
Data from the National Center for Health Statistics Multiple Cause-of-Death Mortality for 1990 through 2001 reveal reduced varicella-related mortality in all age groups younger than 50 years. The greatest reduction (92%) was in children 1 to 4 years of age. Most deaths due to varicella were among persons who did not have an underlying high-risk condition and who would have been excellent candidates for vaccination.
Life-threatening in adults, especially pregnant women
Varicella usually is a relatively mild, self-limited disease of childhood. However, in immunocompromised persons and even in otherwise healthy adults, varicella can cause life-threatening complications such as severe pneumonia and encephalitis. Pneumonia develops in approximately 20% of adults who contract varicella, and encephalitis in approximately 1%. In the era before acyclovir was available, as many as 20% of persons with these complications died.8
Unique set of problems during pregnancy. Although pregnant women are not more likely than nonpregnant women to contract varicella or even to develop pneumonia or encephalitis, they do have a higher mortality if they experience these complications.
When varicella occurs during the first half of pregnancy, anomalies or spontaneous abortions occur in 1% to 2% of fetuses. Moreover, when the mother has varicella near or at the time of delivery, neonatal varicella develops in as many as 20% of infants, manifested as a mucocutaneous exanthema, pneumonia, encephali-tis, or disseminated visceral infection. Even with acyclovir treatment, severe morbidity and death can occur in affected neonates.8
Test and, when necessary, vaccinate women
The key point for clinicians to recognize is that varicella now can be almost completely prevented through universal vaccination.9
Although the principal target group for vaccination is young children, ObGyns should question all women of reproductive age about susceptibility to varicella. Women who do not have a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
- The present varicella vaccine (Varivax) is a live-virus vaccine, which should be administered in 2 subcutaneous injections (0.5 mL) 4 to 8 weeks apart.
- The vaccine should not be administered to infants younger than 12 months of age, to pregnant or lactating women, or to patients who have received systemic steroids within the last month.
- The vaccine also should not be given to persons who are immunosuppressed, except as part of a carefully supervised research protocol.
The vaccine is highly immuno-genic and produces immunity in approximately 90% of healthy children. The rate of seroconversion is lower in adults and immunosuppressed patients. Vaccinated patients have a significantly lower rate of natural infection after exposure.
The author reports no financial relationships relevant to this article.
1. Duff P. Antibiotic selection in obstetrics: making cost-effective choices. Clin Obstet Gynecol. 2002;45:59-72.
2. Talan DA, Stamm WE, Hooton TM, et al. Comparison of ciprofloxacin (7 days) and trimethoprim-sulfamethoxazole (14 days) for acute uncomplicated pyelonephritis in women: a randomized trial. JAMA. 2000;283:1583-1590.
3. Gupta K, Scholes D, Stamm WE. Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA. 1999;281:736-738.
4. Jamie WE, Edwards RK, Duff P. Antimicrobial susceptibility of Gram-negative uropathogens isolated from obstetric patients. Infect Dis Obstet Gynecol. 2002;10:123-126.
5. Gibbs RS, Duff P. Progress in pathogenesis and management of clinical intraamniotic infection. Am J Obstet Gynecol. 1991;164:1317-1326.
6. Chapman SJ, Owen J. Randomized trial of single-dose versus multiple-dose cefotetan for the postpartum treatment of intrapartum chorioamnionitis. Am J Obstet Gynecol. 1997;177:831-834.
7. Turnquest MA, How HY, Cook CR, et al. Chorioamnionitis: is continuation of antibiotic therapy necessary after cesarean section? Am J Obstet Gynecol. 1998;179:1261-1266.
8. Chapman S, Duff P. Varicella in pregnancy. Semin Perinatol. 1993;17:403-409.
9. Duff P. Varicella vaccine. Infect Dis Obstet Gynecol. 1996;4:63-65.
New findings I selected for this Update affect the management of 4 common and potentially serious clinical problems: acute cystitis, gonorrhea and chlamydia infection, chorioamnionitis, and varicella.
- A comparison of amoxicillin-clavulanic acid vs ciprofloxacin for uncomplicated lower urinary tract infections yielded surprising results, and more evidence on E coli’s resistance to antibiotics.
- Sexual partners of women with gonorrhea or chlamydia are more likely to receive appropriate treatment if it is offered by the women themselves or by the women’s caregivers.
- Short-course therapy for chorioamnionitis had a very high cure rate, equal to the traditional course, and furthers the possibility of shorter hospitalizations and cost savings without compromising outcomes.
- The CDC’s 1995 call for universal childhood vaccination for varicella has already sharply reduced varicella-related mortality in adults; still, we must determine immunity in our reproductive-age patients.
Acute cystitis: Ciprofloxacin prevails in E coli skirmish
Hooton TM, Scholes D, Gupta K, Stapleton AE, Roberts PL, Stamm WE. Amoxicillin-clavulanate vs ciprofloxacin for the treatment of uncomplicated cystitis in women: a randomized trial. JAMA. 2005;293:949–955.
Amoxicillin-clavulanate was not as effective as ciprofloxacin even in women who were infected with bacteria sensitive to amoxicillin-clavulanate.
A total of 320 nonpregnant women, aged 18 to 45 years, with uncomplicated acute cystitis were treated for 3 days with either oral amoxicillin-clavulanate (500 mg/125 mg twice daily) or oral ciprofloxacin (250 mg twice daily). Two weeks after treatment, 95% of women treated with ciprofloxacin were clinically cured, compared with only 76% of women treated with amoxicillin-clavulanate (P<.001).
Start with ciprofloxacin
The difference in outcome was attributed to a marked difference in vaginal colonization with the single most common pathogen in acute cystitis—Escherichia coli—at the 2-week follow-up (45% in the amoxicillinclavulanate group vs 10% in the ciprofloxacin group, P<.001).
Even though successful treatment of cystitis usually is possible with short courses (3–7 days) of oral antibiotics, persistent and recurrent infections may occur and usually are related to persistent vaginal colonization with E coli.
Treatment may require an extended course of oral antibiotics.
Initial selection of an antibiotic for acute cystitis is empiric and should be based on probable susceptibility of the dominant uropathogens. For many years, the typical initial antibiotic has been ampicillin.
E coli resistance. Now, however, more than a third of E coli strains, as well as most strains of K pneumoniae, are resistant to ampicillin. Therefore, ampicillin no longer should be used for the empiric treatment of cystitis.1
Surprising results
In theory, amoxicillin-clavulanate should have enhanced activity against E coli and other enteric organisms.
Therefore, these findings are surprising. The outcome with amoxicillin-clavulanate was inferior to that of ciprofloxacin, even in women who seemingly had susceptible uropathogens.
Based on this study, ciprofloxacin clearly is a more effective (and less expensive) empiric treatment in nonpregnant women.
In gravidas, start with nitrofurantoin
Ciprofloxacin is not appropriate for treatment of cystitis or asymptomatic bacteriuria in pregnant women. The quinolone antibiotics may cause injury to the developing cartilage of the fetus and are contraindicated in pregnant and lactating women, and in children younger than 17 years.1
What, then, is the most appropriate choice for treatment of uncomplicated cystitis during pregnancy?
One reasonable selection is oral trimethoprim-sulfamethoxazole, double-strength, twice daily. However, increasing resistance of E coli to this antibiotic has been documented recently.2,3
Therefore, a better choice is nitrofurantoin monohydrate macrocrystals, 100 mg twice daily.4 One organism that is not susceptible to nitrofurantoin is Proteus. When this organism is suspected, use trimethoprim-sulfamethoxazole.
Follow-up is a must
Because persistent and recurrent infections are common, patients should be followed with urine dipstick assessment or urine culture to be certain that the infection is resolved.
Follow-up is particularly important when infected women are pregnant, because of the risk of ascending infection leading to preterm labor, sepsis, or acute respiratory disease syndrome.
Treat sex partners, sight-unseen?
Golden MR, Whittington WL, Handsfield HH, et al. Effect of expedited treatment of sex partners on recurrent or persistent gonorrhea or chlamydial infection. N Engl J Med. 2005;352:676–685.
Providing a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Almost 2,000 men and women with uncomplicated gonorrhea or chlamydia infection were included in this study of expedited treatment compared with standard referral. In the standard referral group, investigators treated 931 patients and referred their sex partners to other physicians or facilities for evaluation and treatment. In the expedited treatment group, 929 patients were treated and also were provided with antibiotics to give to their partners. The partners of patients who were unwilling to do so were contacted and treated by the investigators.
At follow-up 21 to 126 days after treatment), persistent or recurrent infection was found in 13% of standard referral patients and 10% of expedited treatment patients (relative risk, 0.76; 95% confidence interval, 0.59–0.98).
Expedited treatment decreased the rate of persistent or recurrent gonorrhea more than that of persistent or recurrent chlamydia.
Patients in the expedited group were more likely to report that all of their partners were treated, and less likely to report having had sex with an untreated partner.
Advantages of the direct approach
The challenge for the ObGyn is how to arrange treatment for the female patient’s sex partner(s). This study indicates that a proactive approach is likely to be more effective than simply asking the patient to encourage her partner to seek medical attention. Direct provision of a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Failure to treat the patient’s sex partner is the principal cause of persistent or recurrent infection, which may lead to pelvic inflammatory disease, Fitz-Hugh-Curtis syndrome, and infertility. Gonorrhea may disseminate and manifest primarily by arthritis and dermatitis. If a pregnant woman is colonized with gonorrhea or chlamydia at the time of delivery, her infant may acquire gonococcal or chlamydial conjunctivitis or chlamydial pneumonia.
6 caveats
Although the results of this investigation are impressive and of great practical importance, these caveats should be noted.
- The oral drug used to treat gonorrhea in this study, cefixime (400 mg), is not presently available, and although another oral drug such as ciprofloxacin (500 mg) would be highly effective, it should not be used in pregnant or lactating women, or women younger than 17 years.1
- Although ceftriaxone, 125 mg intramuscularly, also is a superb drug for treatment of uncomplicated gonorrhea, the logistical problems of arranging for the partner to receive an intramuscular injection are daunting.
- Some women in the expedited treatment group were reluctant to provide medication to their partner(s), and study personnel were forced to intervene. Keep in mind that individual private practitioners and even well-organized clinics may not have sufficient support personnel to trace and treat all contacts.
- There is the important issue of a provider writing a prescription for an individual who is not actually his or her patient and who has not been interviewed and examined. Certainly, many state laws and insurance company regulations may discourage or even prohibit such a practice.
- Lack of a detailed assessment of the partner(s) means there is no opportunity to evaluate them for other conditions such as syphilis and HIV infection.
- Finally, taking a proactive approach in treating the sex partner(s) of patients who have gonorrhea or chlamydia (and, by extension, trichomoniasis) requires documentation of complete rationale in the patient’s medical record.
In addition, detailed written instructions must be provided for the partner(s) and must include a specific caution about possible reactions to the antibiotic.
Single-dose plus intrapartum therapy effective for chorioamnionitis
Edwards RK, Duff P. Single additional dose postpartum therapy for women with chorioamnionitis. Obstet Gynecol. 2003;102:957–961.
Short-course therapy is simpler to administer and reduces costs compared with more extended treatment.
Intrapartum therapy plus 1 additional dose of combination antibiotics after delivery produced a very high rate of cure (95.4%)—equivalent to that achieved when a more extended course of treatment was used.
In this randomized study of 292 otherwise healthy women with chorioamnionitis, 151 women were treated intrapartum with intravenous (IV) ampicillin (2 g every 6 hours) plus gentamicin (1.5 mg/kg every 8 hours). They received 1 dose of each drug postpartum. In addition, if they had a cesarean delivery, they received 1 dose of IV clindamycin (900 mg) immediately after the infant’s umbilical cord was clamped.
Women in the control group received IV antibiotics (including clindamycin, if indicated) until they had been afebrile and asymptomatic for 24 hours.
In the study group, 4.6% of women had a treatment failure and required an additional course of antibiotics. In the control group, 3.5% of patients required additional antibiotics (P = .639, not significant). When patients were stratified by method of delivery, no significant difference was found in treatment outcome.
Pathogens and regimens
Chorioamnionitis occurs in approximately 1% to 5% of term patients and in as many as 25% of patients having a preterm delivery. The infection is caused by multiple aerobic and anaerobic organisms, notably group B streptococci, E coli, and anaerobes. The former 2 pathogens pose the greatest risk to the infant and are the predominant causes of neonatal pneumonia, bacteremia, and meningitis. These organisms also are major causes of maternal bacteremia.
Anaerobes usually do not pose a major threat to the fetus or neonate, but are particularly likely to lead to pelvic abscess in women who require a cesarean delivery in the face of preexisting intrauterine infection.5
Accordingly, the initial antibiotic therapy for chorioamnionitis typically targets the 2 organisms most likely to infect the fetus/neonate—group B streptococci and E coli. The antibiotic regimen of ampicillin plus gentamicin provides excellent, and inexpensive, coverage of these pathogens. The addition of a drug such as clindamycin or metronidazole provides a reassuring measure of coverage against anaerobes in women who require a cesarean delivery.1
Traditionally, patients with chorioamnionitis have been treated with IV antibiotics until they have been afebrile and asymptomatic for 24 hours.
Chapman and Owen,6 who were among the first to suggest that a shortened course of treatment might be as effective as a more extended course, assessed the effectiveness of a single post-partum dose of cefotetan in women who were treated intrapartum for chorioamnionitis and who delivered vaginally. The rate of treatment failure was 11% in the single-dose group and 3.7% in the women treated with multiple doses of cefotetan until they had been afebrile for 24 hours. This observed difference was not statistically significant (P = .27), but the study lacked sufficient power to firmly establish the safety and effectiveness of short-course therapy.
A trial of “no therapy” vs “extended therapy” in women with chorioamnionitis who delivered by cesarean found the rate of treatment failure was 21.8% in the “no therapy” group and 14.8% in the women who received clindamycin plus gentamicin for at least 24 hours postoperatively.7
Again, this observed difference was not statistically significant (P = .32), but the power of the investigation was limited.
This more recent study was sufficiently large and included a reasonable number of women who delivered both vaginally and abdominally.
Anti-anaerobic coverage critically important. Complications related to persistent infection developed in 2 patients in the short-course group who had cesarean deliveries: pelvic abscess and incisional abscess. In both instances, the patients did not receive the dose of clindamycin specified in the protocol, illustrating the critical importance of proper anti-anaerobic coverage in patients who require abdominal delivery.
Short-course therapy offers advantages in terms of ease of administration and cost savings compared with more extended treatment regimens.
Whether short courses of single agents, such as the broad-spectrum cephalosporins, penicillins, and carbapenems, would be as effective as ampicillin plus gentamicin plus clindamycin remains to be determined.
CDC data show “herd” immunity, thanks to varicella vaccination policy
Nguyen HQ, Jumaan AO, Seward JF. Decline in mortality due to varicella after implementation of varicella vaccination in the United States. N Engl J Med. 2005;352:450–458.
Question all women of reproductive age about varicella. Women who lack a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
This study demonstrates that, through the phenomenon of herd immunity, universal vaccination has significantly lowered the overall risk of varicella-related mortality in the general population. Universal childhood varicella vaccination was recommended by the Centers for Disease Control and Prevention in 1995; the rate of death due to varicella, either as the underlying cause or the contributing cause, fluctuated from 1990 through 1998, and then sharply declined.
Data from the National Center for Health Statistics Multiple Cause-of-Death Mortality for 1990 through 2001 reveal reduced varicella-related mortality in all age groups younger than 50 years. The greatest reduction (92%) was in children 1 to 4 years of age. Most deaths due to varicella were among persons who did not have an underlying high-risk condition and who would have been excellent candidates for vaccination.
Life-threatening in adults, especially pregnant women
Varicella usually is a relatively mild, self-limited disease of childhood. However, in immunocompromised persons and even in otherwise healthy adults, varicella can cause life-threatening complications such as severe pneumonia and encephalitis. Pneumonia develops in approximately 20% of adults who contract varicella, and encephalitis in approximately 1%. In the era before acyclovir was available, as many as 20% of persons with these complications died.8
Unique set of problems during pregnancy. Although pregnant women are not more likely than nonpregnant women to contract varicella or even to develop pneumonia or encephalitis, they do have a higher mortality if they experience these complications.
When varicella occurs during the first half of pregnancy, anomalies or spontaneous abortions occur in 1% to 2% of fetuses. Moreover, when the mother has varicella near or at the time of delivery, neonatal varicella develops in as many as 20% of infants, manifested as a mucocutaneous exanthema, pneumonia, encephali-tis, or disseminated visceral infection. Even with acyclovir treatment, severe morbidity and death can occur in affected neonates.8
Test and, when necessary, vaccinate women
The key point for clinicians to recognize is that varicella now can be almost completely prevented through universal vaccination.9
Although the principal target group for vaccination is young children, ObGyns should question all women of reproductive age about susceptibility to varicella. Women who do not have a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
- The present varicella vaccine (Varivax) is a live-virus vaccine, which should be administered in 2 subcutaneous injections (0.5 mL) 4 to 8 weeks apart.
- The vaccine should not be administered to infants younger than 12 months of age, to pregnant or lactating women, or to patients who have received systemic steroids within the last month.
- The vaccine also should not be given to persons who are immunosuppressed, except as part of a carefully supervised research protocol.
The vaccine is highly immuno-genic and produces immunity in approximately 90% of healthy children. The rate of seroconversion is lower in adults and immunosuppressed patients. Vaccinated patients have a significantly lower rate of natural infection after exposure.
The author reports no financial relationships relevant to this article.
New findings I selected for this Update affect the management of 4 common and potentially serious clinical problems: acute cystitis, gonorrhea and chlamydia infection, chorioamnionitis, and varicella.
- A comparison of amoxicillin-clavulanic acid vs ciprofloxacin for uncomplicated lower urinary tract infections yielded surprising results, and more evidence on E coli’s resistance to antibiotics.
- Sexual partners of women with gonorrhea or chlamydia are more likely to receive appropriate treatment if it is offered by the women themselves or by the women’s caregivers.
- Short-course therapy for chorioamnionitis had a very high cure rate, equal to the traditional course, and furthers the possibility of shorter hospitalizations and cost savings without compromising outcomes.
- The CDC’s 1995 call for universal childhood vaccination for varicella has already sharply reduced varicella-related mortality in adults; still, we must determine immunity in our reproductive-age patients.
Acute cystitis: Ciprofloxacin prevails in E coli skirmish
Hooton TM, Scholes D, Gupta K, Stapleton AE, Roberts PL, Stamm WE. Amoxicillin-clavulanate vs ciprofloxacin for the treatment of uncomplicated cystitis in women: a randomized trial. JAMA. 2005;293:949–955.
Amoxicillin-clavulanate was not as effective as ciprofloxacin even in women who were infected with bacteria sensitive to amoxicillin-clavulanate.
A total of 320 nonpregnant women, aged 18 to 45 years, with uncomplicated acute cystitis were treated for 3 days with either oral amoxicillin-clavulanate (500 mg/125 mg twice daily) or oral ciprofloxacin (250 mg twice daily). Two weeks after treatment, 95% of women treated with ciprofloxacin were clinically cured, compared with only 76% of women treated with amoxicillin-clavulanate (P<.001).
Start with ciprofloxacin
The difference in outcome was attributed to a marked difference in vaginal colonization with the single most common pathogen in acute cystitis—Escherichia coli—at the 2-week follow-up (45% in the amoxicillinclavulanate group vs 10% in the ciprofloxacin group, P<.001).
Even though successful treatment of cystitis usually is possible with short courses (3–7 days) of oral antibiotics, persistent and recurrent infections may occur and usually are related to persistent vaginal colonization with E coli.
Treatment may require an extended course of oral antibiotics.
Initial selection of an antibiotic for acute cystitis is empiric and should be based on probable susceptibility of the dominant uropathogens. For many years, the typical initial antibiotic has been ampicillin.
E coli resistance. Now, however, more than a third of E coli strains, as well as most strains of K pneumoniae, are resistant to ampicillin. Therefore, ampicillin no longer should be used for the empiric treatment of cystitis.1
Surprising results
In theory, amoxicillin-clavulanate should have enhanced activity against E coli and other enteric organisms.
Therefore, these findings are surprising. The outcome with amoxicillin-clavulanate was inferior to that of ciprofloxacin, even in women who seemingly had susceptible uropathogens.
Based on this study, ciprofloxacin clearly is a more effective (and less expensive) empiric treatment in nonpregnant women.
In gravidas, start with nitrofurantoin
Ciprofloxacin is not appropriate for treatment of cystitis or asymptomatic bacteriuria in pregnant women. The quinolone antibiotics may cause injury to the developing cartilage of the fetus and are contraindicated in pregnant and lactating women, and in children younger than 17 years.1
What, then, is the most appropriate choice for treatment of uncomplicated cystitis during pregnancy?
One reasonable selection is oral trimethoprim-sulfamethoxazole, double-strength, twice daily. However, increasing resistance of E coli to this antibiotic has been documented recently.2,3
Therefore, a better choice is nitrofurantoin monohydrate macrocrystals, 100 mg twice daily.4 One organism that is not susceptible to nitrofurantoin is Proteus. When this organism is suspected, use trimethoprim-sulfamethoxazole.
Follow-up is a must
Because persistent and recurrent infections are common, patients should be followed with urine dipstick assessment or urine culture to be certain that the infection is resolved.
Follow-up is particularly important when infected women are pregnant, because of the risk of ascending infection leading to preterm labor, sepsis, or acute respiratory disease syndrome.
Treat sex partners, sight-unseen?
Golden MR, Whittington WL, Handsfield HH, et al. Effect of expedited treatment of sex partners on recurrent or persistent gonorrhea or chlamydial infection. N Engl J Med. 2005;352:676–685.
Providing a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Almost 2,000 men and women with uncomplicated gonorrhea or chlamydia infection were included in this study of expedited treatment compared with standard referral. In the standard referral group, investigators treated 931 patients and referred their sex partners to other physicians or facilities for evaluation and treatment. In the expedited treatment group, 929 patients were treated and also were provided with antibiotics to give to their partners. The partners of patients who were unwilling to do so were contacted and treated by the investigators.
At follow-up 21 to 126 days after treatment), persistent or recurrent infection was found in 13% of standard referral patients and 10% of expedited treatment patients (relative risk, 0.76; 95% confidence interval, 0.59–0.98).
Expedited treatment decreased the rate of persistent or recurrent gonorrhea more than that of persistent or recurrent chlamydia.
Patients in the expedited group were more likely to report that all of their partners were treated, and less likely to report having had sex with an untreated partner.
Advantages of the direct approach
The challenge for the ObGyn is how to arrange treatment for the female patient’s sex partner(s). This study indicates that a proactive approach is likely to be more effective than simply asking the patient to encourage her partner to seek medical attention. Direct provision of a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Failure to treat the patient’s sex partner is the principal cause of persistent or recurrent infection, which may lead to pelvic inflammatory disease, Fitz-Hugh-Curtis syndrome, and infertility. Gonorrhea may disseminate and manifest primarily by arthritis and dermatitis. If a pregnant woman is colonized with gonorrhea or chlamydia at the time of delivery, her infant may acquire gonococcal or chlamydial conjunctivitis or chlamydial pneumonia.
6 caveats
Although the results of this investigation are impressive and of great practical importance, these caveats should be noted.
- The oral drug used to treat gonorrhea in this study, cefixime (400 mg), is not presently available, and although another oral drug such as ciprofloxacin (500 mg) would be highly effective, it should not be used in pregnant or lactating women, or women younger than 17 years.1
- Although ceftriaxone, 125 mg intramuscularly, also is a superb drug for treatment of uncomplicated gonorrhea, the logistical problems of arranging for the partner to receive an intramuscular injection are daunting.
- Some women in the expedited treatment group were reluctant to provide medication to their partner(s), and study personnel were forced to intervene. Keep in mind that individual private practitioners and even well-organized clinics may not have sufficient support personnel to trace and treat all contacts.
- There is the important issue of a provider writing a prescription for an individual who is not actually his or her patient and who has not been interviewed and examined. Certainly, many state laws and insurance company regulations may discourage or even prohibit such a practice.
- Lack of a detailed assessment of the partner(s) means there is no opportunity to evaluate them for other conditions such as syphilis and HIV infection.
- Finally, taking a proactive approach in treating the sex partner(s) of patients who have gonorrhea or chlamydia (and, by extension, trichomoniasis) requires documentation of complete rationale in the patient’s medical record.
In addition, detailed written instructions must be provided for the partner(s) and must include a specific caution about possible reactions to the antibiotic.
Single-dose plus intrapartum therapy effective for chorioamnionitis
Edwards RK, Duff P. Single additional dose postpartum therapy for women with chorioamnionitis. Obstet Gynecol. 2003;102:957–961.
Short-course therapy is simpler to administer and reduces costs compared with more extended treatment.
Intrapartum therapy plus 1 additional dose of combination antibiotics after delivery produced a very high rate of cure (95.4%)—equivalent to that achieved when a more extended course of treatment was used.
In this randomized study of 292 otherwise healthy women with chorioamnionitis, 151 women were treated intrapartum with intravenous (IV) ampicillin (2 g every 6 hours) plus gentamicin (1.5 mg/kg every 8 hours). They received 1 dose of each drug postpartum. In addition, if they had a cesarean delivery, they received 1 dose of IV clindamycin (900 mg) immediately after the infant’s umbilical cord was clamped.
Women in the control group received IV antibiotics (including clindamycin, if indicated) until they had been afebrile and asymptomatic for 24 hours.
In the study group, 4.6% of women had a treatment failure and required an additional course of antibiotics. In the control group, 3.5% of patients required additional antibiotics (P = .639, not significant). When patients were stratified by method of delivery, no significant difference was found in treatment outcome.
Pathogens and regimens
Chorioamnionitis occurs in approximately 1% to 5% of term patients and in as many as 25% of patients having a preterm delivery. The infection is caused by multiple aerobic and anaerobic organisms, notably group B streptococci, E coli, and anaerobes. The former 2 pathogens pose the greatest risk to the infant and are the predominant causes of neonatal pneumonia, bacteremia, and meningitis. These organisms also are major causes of maternal bacteremia.
Anaerobes usually do not pose a major threat to the fetus or neonate, but are particularly likely to lead to pelvic abscess in women who require a cesarean delivery in the face of preexisting intrauterine infection.5
Accordingly, the initial antibiotic therapy for chorioamnionitis typically targets the 2 organisms most likely to infect the fetus/neonate—group B streptococci and E coli. The antibiotic regimen of ampicillin plus gentamicin provides excellent, and inexpensive, coverage of these pathogens. The addition of a drug such as clindamycin or metronidazole provides a reassuring measure of coverage against anaerobes in women who require a cesarean delivery.1
Traditionally, patients with chorioamnionitis have been treated with IV antibiotics until they have been afebrile and asymptomatic for 24 hours.
Chapman and Owen,6 who were among the first to suggest that a shortened course of treatment might be as effective as a more extended course, assessed the effectiveness of a single post-partum dose of cefotetan in women who were treated intrapartum for chorioamnionitis and who delivered vaginally. The rate of treatment failure was 11% in the single-dose group and 3.7% in the women treated with multiple doses of cefotetan until they had been afebrile for 24 hours. This observed difference was not statistically significant (P = .27), but the study lacked sufficient power to firmly establish the safety and effectiveness of short-course therapy.
A trial of “no therapy” vs “extended therapy” in women with chorioamnionitis who delivered by cesarean found the rate of treatment failure was 21.8% in the “no therapy” group and 14.8% in the women who received clindamycin plus gentamicin for at least 24 hours postoperatively.7
Again, this observed difference was not statistically significant (P = .32), but the power of the investigation was limited.
This more recent study was sufficiently large and included a reasonable number of women who delivered both vaginally and abdominally.
Anti-anaerobic coverage critically important. Complications related to persistent infection developed in 2 patients in the short-course group who had cesarean deliveries: pelvic abscess and incisional abscess. In both instances, the patients did not receive the dose of clindamycin specified in the protocol, illustrating the critical importance of proper anti-anaerobic coverage in patients who require abdominal delivery.
Short-course therapy offers advantages in terms of ease of administration and cost savings compared with more extended treatment regimens.
Whether short courses of single agents, such as the broad-spectrum cephalosporins, penicillins, and carbapenems, would be as effective as ampicillin plus gentamicin plus clindamycin remains to be determined.
CDC data show “herd” immunity, thanks to varicella vaccination policy
Nguyen HQ, Jumaan AO, Seward JF. Decline in mortality due to varicella after implementation of varicella vaccination in the United States. N Engl J Med. 2005;352:450–458.
Question all women of reproductive age about varicella. Women who lack a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
This study demonstrates that, through the phenomenon of herd immunity, universal vaccination has significantly lowered the overall risk of varicella-related mortality in the general population. Universal childhood varicella vaccination was recommended by the Centers for Disease Control and Prevention in 1995; the rate of death due to varicella, either as the underlying cause or the contributing cause, fluctuated from 1990 through 1998, and then sharply declined.
Data from the National Center for Health Statistics Multiple Cause-of-Death Mortality for 1990 through 2001 reveal reduced varicella-related mortality in all age groups younger than 50 years. The greatest reduction (92%) was in children 1 to 4 years of age. Most deaths due to varicella were among persons who did not have an underlying high-risk condition and who would have been excellent candidates for vaccination.
Life-threatening in adults, especially pregnant women
Varicella usually is a relatively mild, self-limited disease of childhood. However, in immunocompromised persons and even in otherwise healthy adults, varicella can cause life-threatening complications such as severe pneumonia and encephalitis. Pneumonia develops in approximately 20% of adults who contract varicella, and encephalitis in approximately 1%. In the era before acyclovir was available, as many as 20% of persons with these complications died.8
Unique set of problems during pregnancy. Although pregnant women are not more likely than nonpregnant women to contract varicella or even to develop pneumonia or encephalitis, they do have a higher mortality if they experience these complications.
When varicella occurs during the first half of pregnancy, anomalies or spontaneous abortions occur in 1% to 2% of fetuses. Moreover, when the mother has varicella near or at the time of delivery, neonatal varicella develops in as many as 20% of infants, manifested as a mucocutaneous exanthema, pneumonia, encephali-tis, or disseminated visceral infection. Even with acyclovir treatment, severe morbidity and death can occur in affected neonates.8
Test and, when necessary, vaccinate women
The key point for clinicians to recognize is that varicella now can be almost completely prevented through universal vaccination.9
Although the principal target group for vaccination is young children, ObGyns should question all women of reproductive age about susceptibility to varicella. Women who do not have a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
- The present varicella vaccine (Varivax) is a live-virus vaccine, which should be administered in 2 subcutaneous injections (0.5 mL) 4 to 8 weeks apart.
- The vaccine should not be administered to infants younger than 12 months of age, to pregnant or lactating women, or to patients who have received systemic steroids within the last month.
- The vaccine also should not be given to persons who are immunosuppressed, except as part of a carefully supervised research protocol.
The vaccine is highly immuno-genic and produces immunity in approximately 90% of healthy children. The rate of seroconversion is lower in adults and immunosuppressed patients. Vaccinated patients have a significantly lower rate of natural infection after exposure.
The author reports no financial relationships relevant to this article.
1. Duff P. Antibiotic selection in obstetrics: making cost-effective choices. Clin Obstet Gynecol. 2002;45:59-72.
2. Talan DA, Stamm WE, Hooton TM, et al. Comparison of ciprofloxacin (7 days) and trimethoprim-sulfamethoxazole (14 days) for acute uncomplicated pyelonephritis in women: a randomized trial. JAMA. 2000;283:1583-1590.
3. Gupta K, Scholes D, Stamm WE. Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA. 1999;281:736-738.
4. Jamie WE, Edwards RK, Duff P. Antimicrobial susceptibility of Gram-negative uropathogens isolated from obstetric patients. Infect Dis Obstet Gynecol. 2002;10:123-126.
5. Gibbs RS, Duff P. Progress in pathogenesis and management of clinical intraamniotic infection. Am J Obstet Gynecol. 1991;164:1317-1326.
6. Chapman SJ, Owen J. Randomized trial of single-dose versus multiple-dose cefotetan for the postpartum treatment of intrapartum chorioamnionitis. Am J Obstet Gynecol. 1997;177:831-834.
7. Turnquest MA, How HY, Cook CR, et al. Chorioamnionitis: is continuation of antibiotic therapy necessary after cesarean section? Am J Obstet Gynecol. 1998;179:1261-1266.
8. Chapman S, Duff P. Varicella in pregnancy. Semin Perinatol. 1993;17:403-409.
9. Duff P. Varicella vaccine. Infect Dis Obstet Gynecol. 1996;4:63-65.
1. Duff P. Antibiotic selection in obstetrics: making cost-effective choices. Clin Obstet Gynecol. 2002;45:59-72.
2. Talan DA, Stamm WE, Hooton TM, et al. Comparison of ciprofloxacin (7 days) and trimethoprim-sulfamethoxazole (14 days) for acute uncomplicated pyelonephritis in women: a randomized trial. JAMA. 2000;283:1583-1590.
3. Gupta K, Scholes D, Stamm WE. Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA. 1999;281:736-738.
4. Jamie WE, Edwards RK, Duff P. Antimicrobial susceptibility of Gram-negative uropathogens isolated from obstetric patients. Infect Dis Obstet Gynecol. 2002;10:123-126.
5. Gibbs RS, Duff P. Progress in pathogenesis and management of clinical intraamniotic infection. Am J Obstet Gynecol. 1991;164:1317-1326.
6. Chapman SJ, Owen J. Randomized trial of single-dose versus multiple-dose cefotetan for the postpartum treatment of intrapartum chorioamnionitis. Am J Obstet Gynecol. 1997;177:831-834.
7. Turnquest MA, How HY, Cook CR, et al. Chorioamnionitis: is continuation of antibiotic therapy necessary after cesarean section? Am J Obstet Gynecol. 1998;179:1261-1266.
8. Chapman S, Duff P. Varicella in pregnancy. Semin Perinatol. 1993;17:403-409.
9. Duff P. Varicella vaccine. Infect Dis Obstet Gynecol. 1996;4:63-65.
Predicting and preventing preterm birth
A 25-year-old primigravida with an intrauterine pregnancy at 26 weeks presents with contractions of moderate intensity every 4 minutes, intact membranes, and minimal vaginal bleeding. On digital exam, her cervix is soft, 50% effaced, and closed. Estimated fetal weight is 775 g.
You are at a Level I hospital in a rural community, 90 minutes from a tertiary nursery. What steps should you take first?
Tocolytics and antibiotics are the first steps. They may help to maximize the benefits of secondary strategies such as antenatal corticosteroids during transport to a tertiary care facility. In addition, assessment of fetal fibronectin levels and use of endovaginal ultrasound can supplement clinical judgment and improve prediction of outcomes. Their excellent negative predictive value can spare many women unnecessary and potentially harmful treatments.
This article discusses these measures in the context of an actual case.
The value of “secondary prevention”
Giving corticosteroids to enhance fetal lung and brain maturity and transporting the mother to a tertiary care center may not prevent preterm delivery, but they can mitigate some of the damage and are supported by the evidence.
Corticosteroids. Given the clear evidence of their efficacy, steroids should be administered once preterm birth appears likely. I would give steroids before maternal transport.
Betamethasone is preferable to dexamethasone, which may be toxic to the fetal central nervous system. However, dexamethasone is preferable to no therapy.
Contraindications to corticosteroids include systemic maternal or fetal infections and maternal endocrinopathies such as Cushing’s disease or poorly controlled diabetes.
Transport to tertiary care. A neonatal intensive care unit clearly benefits tiny babies. Clinicians should be aware of the pediatric capacity of their community hospitals and maintain a referral relationship with the nearest tertiary care centers. Conversely, clinicians on the receiving end of maternal transports should make every effort to expedite these referrals.
Is Local Care Too Risky?
Patricia and her family strongly prefer that she undergo treatment in her own community, if at all possible.
Signs and symptoms of preterm labor are poor predictors of preterm birth. Although most symptomatic women deliver at term, even the most clinically astute physician cannot predict when a symptomatic patient will deliver.
Which tocolytic is most effective?
Berkman ND, Thorp JM Jr, Lohr KN, et al. Tocolytic treatment for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2003;188:1648–1659.
No single drug is best. In this metaanalysis, magnesium, β-mimetics, calcium channel blockers, and nonsteroidal anti-inflammatory drugs (NSAIDs) performed about the same at prolonging the interval between onset of preterm labor and actual birth, compared with placebo or no treatment. Ethanol was less effective and “inappropriate.” Tocolytics are given to stop contractions (first-line therapy) and to maintain quiescence after an acute episode (maintenance therapy).
To determine the most effective tocolytic, we analyzed 16 studies of first-line therapy and 8 involving maintenance therapy, using the above 5 drug classes.
How 5 drugs compare
Estimated odds ratios suggest that, when used as first-line therapy, all the drugs except ethanol are about the same. Odds ratios ranged from 1.622 for β-mimetics to 2.485 for calcium channel blockers. (The odds ratio for NSAIDs was based on only 1 study.)
When we tested whether β-mimetics, calcium channel blockers, and magnesium sulfate had the same effects, compared with placebo, the results suggested that they do not. However, the body of literature was not large enough to establish this conclusively.
Overall, β-mimetics appear to lack superiority over the other drugs as first-line therapy and cause more maternal harms, while ethanol is “inappropriate” and no longer in use.
As maintenance therapy, none of the drugs appeared to have any benefit.
Maternal and fetal harms
We defined harms as “clinical markers and events that the authors of individual studies considered as adverse events or side effects.”
Among maternal harms were serious cardiac side effects, including arrhythmias, heart failure, and chest pain, linked to β-mimetics. Minor cardiovascular harms were also higher among women given β-mimetics. In addition, calcium channel blockers appeared to increase the risk of minor cardiovascular harms, but not as much as the β-mimetics.
Overall, maternal cardiac, metabolic, and psychologic harms were more prevalent among women taking β-mimetics. This may be due, at least in part, to the fact that studies of β-mimetics tended to look for these effects more than other studies did.
As for short-term fetal harms, we found “little consistent evidence” of them in the infants of women receiving these drugs, and the studies lacked sufficient data to evaluate potential long-term harms.
What later analyses found
After 1999, the cutoff year of our review, several relatively large studies showed the oxytocin antagonist atosiban to be effective as acute7,8and maintenance8 therapy, with a favorable side effect profile. Another trial9 compared 2 doses of magnesium (2 and 5 g per hour); the higher dose acted more quickly but with more side effects. These and other studies do not alter our conclusions about the effectiveness of tocolytic therapy—or the specifics of the 5 drugs studied.
2 useful markers
In the 1990s, 2 biologic markers were discovered that improve the precision of preterm birth risk assessment:
- fetal fibronectin (fFN) and
- endovaginal sonography (EVUSD).1
Use of EVUSD enables measurement of the cervix from the internal to external os. Cervices shorten before spontaneous birth.
These 2 tests, when positive (fFN detected or cervical length
I use a negative test to identify women who do not require further treatment or evaluation. If a patient has a negative fFN or EVUSD, I would not transport her to a tertiary care center. In fact, I would probably discharge her home with close follow-up.
3 concerns about the tests
Clinicians tend to have some concerns about incorporating these tests into their routines:
- How reliable is negative predictive value? Arguably, these tests perform better than clinical judgment and can spare many women unnecessary treatments.2 No test is perfect, however. These bio-markers should be adjuncts to—not replacements for—clinical wisdom.
- What about false results? With fFN, a proper collection kit with plastic tube and Dacron swab is critical because the molecule will adhere to glass or cotton, creating a false-negative result. A false-positive result can occur after recent coitus or a digital cervical exam; therefore, collect fFN specimens before checking the cervix. With EVUSD, the examinations require a moderate amount of skill.
- Which biomarker is best? Both fFN and EVUSD make independent and separate contributions to the prediction of preterm birth. Therefore, I use both.
Start Tocolysis And Antibiotics?
Patricia’s fFN and EVUSD tests are both positive. Should you start tocolysis and antibiotic therapy prior to transfer?
Metaanalysis suggests tocolysis, and antibiotics extend the interval between symptom onset and delivery.1The length of this prolongation can be measured in days, and no evidence suggests that prolonged pharmacotherapy has any benefit.
I would initiate both therapies while waiting for the mother to be moved to a tertiary center, even though neither therapy has been shown to improve perinatal outcome.
Tocolysis. We could find no differences among tocolytic drugs.3 Serious side effects are rare, but nuisance cardiovascular symptoms are frequent. Sympathomimetic drugs lead to lethargy, and magnesium is associated with malaise. Magnesium requires intravenous access and should be given only via infusion pump by trained personnel. That often means a nurse must accompany the patient to the Level III hospital.
Thus, for logistical reasons, I favor nonsteroidal anti-inflammatory drugs, of which indomethacin is the most widely studied. Indomethacin can be given by mouth or rectum, with minimal side effects. Harm to the fetus is rare if the drug is used acutely for only 48 to 72 hours (the maximum duration of any potential benefit).
Antibiotics. Current protocols calling for betalactam antibiotic therapy as prophylaxis against early-onset neonatal sepsis in preterm births have led to almost universal use of antibiotics among these patients. Our metaanalysis did not demonstrate superior pregnancy prolongation with any other regimen, so the one for group B strep prophylaxis provides a double benefit.4 As with tocolytics, there is no role for maintenance therapy.
When Contractions Cease
Patricia is transferred and completes her steroid therapy. Her symptoms and contractions cease. After a few days of observation and no cervical changes, she is discharged home. She asks about home therapies, work, activities, and sex.
Since our metaanalysis of tocolysis studies showed no efficacy for maintenance regimens, I do not recommend them except in this rare situation: when a woman has so much uterine activity without cervical change that she is unable to rest or complete her daily activities. In this case I would favor “as needed” doses of a β-mimetic drug by mouth.
Although home uterine activity monitors and subcutaneous tocolytic pumps are available, evidence suggests they are ineffective.1I seldom, if ever, use these devices.
Despite the almost universal recommendation that women at risk of preterm birth avoid physical and sexual activity, we lack evidence that bed rest or abstinence prolong pregnancy or prevent preterm birth.
Is sex allowed? When we studied both physical activity and sexuality in asymptomatic women at midpregnancy, neither was associated with spontaneous preterm birth.5,6 Therefore, I do not recommend restricting activity or sexual intercourse. Instead, I encourage women to carefully assess uterine activity. If certain behaviors appear to increase contractions, those behaviors should be limited.
Counsel her to trust her instincts. It is important to encourage the patient to trust her own instincts, so that an overzealous employer or partner cannot coerce or cajole her to do something that violates her internal sense of well-being.
The author reports no financial relationships relevant to this article.
1. Berkman ND, Thorp JM, Hartmann KE, et al. Management of Preterm Labor. Evidence Report/Technology Assessment #18. Rockville, Md: Agency for Healthcare Research and Quality; December 2000. AHRQ publication 01-E021.
2. Thorp JM, Jr. ACOG Committee on Practice Bulletins. Management of preterm labor. Obstet Gynecol. 2003;101:1039-1047.
3. Berkman ND, Thorp JM, Jr, Lohr KN, et al. Tocolytic treatment for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2003;188:1648-1659.
4. Thorp JM, Jr, Hartmann KE, Berkman ND, et al. Antibiotic therapy for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2002;186:587-592.
5. Sayle AE, Savitz DA, Thorp JM, Jr, Hertz-Picciotto I, Wilcox AJ. Sexual activity during late pregnancy and preterm delivery. Obstet Gynecol. 2001;97:283-289.
6. Evenson KR, Siega-Riz AM, Savitz DA, Leiferman JA, Thorp JM, Jr. Vigorous leisure activity and pregnancy outcome. Epidemiology. 2002;13:653-659.
7. Moutquin JM, Sherman D, Cohen H, et al. Double-blind, randomized, controlled trial of atosiban and ritrodine in the treatment of preterm labor: a multicenter effectiveness and safety study. Am J Obstet Gynecol. 2000;182:1191-1199.
8. Romero R, Sibai BM, Sanchez-Ramos L, et al. An oxytocin receptor antagonist (atosiban) in the treatment of preterm labor: a randomized, double-blind, placebo-controlled trial with tocolytic rescue. Am J Obstet Gynecol. 2000;182:1173-1183.
9. Terrone DA, Rinehart BK, Kimmel ES, May WL, Larmon JE, Morrison JC. A prospective, randomized, controlled trial of high and low maintenance doses of magnesium sulfate for acute tocolysis. Am J Obstet Gynecol. 2000;182:1477-1482.
A 25-year-old primigravida with an intrauterine pregnancy at 26 weeks presents with contractions of moderate intensity every 4 minutes, intact membranes, and minimal vaginal bleeding. On digital exam, her cervix is soft, 50% effaced, and closed. Estimated fetal weight is 775 g.
You are at a Level I hospital in a rural community, 90 minutes from a tertiary nursery. What steps should you take first?
Tocolytics and antibiotics are the first steps. They may help to maximize the benefits of secondary strategies such as antenatal corticosteroids during transport to a tertiary care facility. In addition, assessment of fetal fibronectin levels and use of endovaginal ultrasound can supplement clinical judgment and improve prediction of outcomes. Their excellent negative predictive value can spare many women unnecessary and potentially harmful treatments.
This article discusses these measures in the context of an actual case.
The value of “secondary prevention”
Giving corticosteroids to enhance fetal lung and brain maturity and transporting the mother to a tertiary care center may not prevent preterm delivery, but they can mitigate some of the damage and are supported by the evidence.
Corticosteroids. Given the clear evidence of their efficacy, steroids should be administered once preterm birth appears likely. I would give steroids before maternal transport.
Betamethasone is preferable to dexamethasone, which may be toxic to the fetal central nervous system. However, dexamethasone is preferable to no therapy.
Contraindications to corticosteroids include systemic maternal or fetal infections and maternal endocrinopathies such as Cushing’s disease or poorly controlled diabetes.
Transport to tertiary care. A neonatal intensive care unit clearly benefits tiny babies. Clinicians should be aware of the pediatric capacity of their community hospitals and maintain a referral relationship with the nearest tertiary care centers. Conversely, clinicians on the receiving end of maternal transports should make every effort to expedite these referrals.
Is Local Care Too Risky?
Patricia and her family strongly prefer that she undergo treatment in her own community, if at all possible.
Signs and symptoms of preterm labor are poor predictors of preterm birth. Although most symptomatic women deliver at term, even the most clinically astute physician cannot predict when a symptomatic patient will deliver.
Which tocolytic is most effective?
Berkman ND, Thorp JM Jr, Lohr KN, et al. Tocolytic treatment for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2003;188:1648–1659.
No single drug is best. In this metaanalysis, magnesium, β-mimetics, calcium channel blockers, and nonsteroidal anti-inflammatory drugs (NSAIDs) performed about the same at prolonging the interval between onset of preterm labor and actual birth, compared with placebo or no treatment. Ethanol was less effective and “inappropriate.” Tocolytics are given to stop contractions (first-line therapy) and to maintain quiescence after an acute episode (maintenance therapy).
To determine the most effective tocolytic, we analyzed 16 studies of first-line therapy and 8 involving maintenance therapy, using the above 5 drug classes.
How 5 drugs compare
Estimated odds ratios suggest that, when used as first-line therapy, all the drugs except ethanol are about the same. Odds ratios ranged from 1.622 for β-mimetics to 2.485 for calcium channel blockers. (The odds ratio for NSAIDs was based on only 1 study.)
When we tested whether β-mimetics, calcium channel blockers, and magnesium sulfate had the same effects, compared with placebo, the results suggested that they do not. However, the body of literature was not large enough to establish this conclusively.
Overall, β-mimetics appear to lack superiority over the other drugs as first-line therapy and cause more maternal harms, while ethanol is “inappropriate” and no longer in use.
As maintenance therapy, none of the drugs appeared to have any benefit.
Maternal and fetal harms
We defined harms as “clinical markers and events that the authors of individual studies considered as adverse events or side effects.”
Among maternal harms were serious cardiac side effects, including arrhythmias, heart failure, and chest pain, linked to β-mimetics. Minor cardiovascular harms were also higher among women given β-mimetics. In addition, calcium channel blockers appeared to increase the risk of minor cardiovascular harms, but not as much as the β-mimetics.
Overall, maternal cardiac, metabolic, and psychologic harms were more prevalent among women taking β-mimetics. This may be due, at least in part, to the fact that studies of β-mimetics tended to look for these effects more than other studies did.
As for short-term fetal harms, we found “little consistent evidence” of them in the infants of women receiving these drugs, and the studies lacked sufficient data to evaluate potential long-term harms.
What later analyses found
After 1999, the cutoff year of our review, several relatively large studies showed the oxytocin antagonist atosiban to be effective as acute7,8and maintenance8 therapy, with a favorable side effect profile. Another trial9 compared 2 doses of magnesium (2 and 5 g per hour); the higher dose acted more quickly but with more side effects. These and other studies do not alter our conclusions about the effectiveness of tocolytic therapy—or the specifics of the 5 drugs studied.
2 useful markers
In the 1990s, 2 biologic markers were discovered that improve the precision of preterm birth risk assessment:
- fetal fibronectin (fFN) and
- endovaginal sonography (EVUSD).1
Use of EVUSD enables measurement of the cervix from the internal to external os. Cervices shorten before spontaneous birth.
These 2 tests, when positive (fFN detected or cervical length
I use a negative test to identify women who do not require further treatment or evaluation. If a patient has a negative fFN or EVUSD, I would not transport her to a tertiary care center. In fact, I would probably discharge her home with close follow-up.
3 concerns about the tests
Clinicians tend to have some concerns about incorporating these tests into their routines:
- How reliable is negative predictive value? Arguably, these tests perform better than clinical judgment and can spare many women unnecessary treatments.2 No test is perfect, however. These bio-markers should be adjuncts to—not replacements for—clinical wisdom.
- What about false results? With fFN, a proper collection kit with plastic tube and Dacron swab is critical because the molecule will adhere to glass or cotton, creating a false-negative result. A false-positive result can occur after recent coitus or a digital cervical exam; therefore, collect fFN specimens before checking the cervix. With EVUSD, the examinations require a moderate amount of skill.
- Which biomarker is best? Both fFN and EVUSD make independent and separate contributions to the prediction of preterm birth. Therefore, I use both.
Start Tocolysis And Antibiotics?
Patricia’s fFN and EVUSD tests are both positive. Should you start tocolysis and antibiotic therapy prior to transfer?
Metaanalysis suggests tocolysis, and antibiotics extend the interval between symptom onset and delivery.1The length of this prolongation can be measured in days, and no evidence suggests that prolonged pharmacotherapy has any benefit.
I would initiate both therapies while waiting for the mother to be moved to a tertiary center, even though neither therapy has been shown to improve perinatal outcome.
Tocolysis. We could find no differences among tocolytic drugs.3 Serious side effects are rare, but nuisance cardiovascular symptoms are frequent. Sympathomimetic drugs lead to lethargy, and magnesium is associated with malaise. Magnesium requires intravenous access and should be given only via infusion pump by trained personnel. That often means a nurse must accompany the patient to the Level III hospital.
Thus, for logistical reasons, I favor nonsteroidal anti-inflammatory drugs, of which indomethacin is the most widely studied. Indomethacin can be given by mouth or rectum, with minimal side effects. Harm to the fetus is rare if the drug is used acutely for only 48 to 72 hours (the maximum duration of any potential benefit).
Antibiotics. Current protocols calling for betalactam antibiotic therapy as prophylaxis against early-onset neonatal sepsis in preterm births have led to almost universal use of antibiotics among these patients. Our metaanalysis did not demonstrate superior pregnancy prolongation with any other regimen, so the one for group B strep prophylaxis provides a double benefit.4 As with tocolytics, there is no role for maintenance therapy.
When Contractions Cease
Patricia is transferred and completes her steroid therapy. Her symptoms and contractions cease. After a few days of observation and no cervical changes, she is discharged home. She asks about home therapies, work, activities, and sex.
Since our metaanalysis of tocolysis studies showed no efficacy for maintenance regimens, I do not recommend them except in this rare situation: when a woman has so much uterine activity without cervical change that she is unable to rest or complete her daily activities. In this case I would favor “as needed” doses of a β-mimetic drug by mouth.
Although home uterine activity monitors and subcutaneous tocolytic pumps are available, evidence suggests they are ineffective.1I seldom, if ever, use these devices.
Despite the almost universal recommendation that women at risk of preterm birth avoid physical and sexual activity, we lack evidence that bed rest or abstinence prolong pregnancy or prevent preterm birth.
Is sex allowed? When we studied both physical activity and sexuality in asymptomatic women at midpregnancy, neither was associated with spontaneous preterm birth.5,6 Therefore, I do not recommend restricting activity or sexual intercourse. Instead, I encourage women to carefully assess uterine activity. If certain behaviors appear to increase contractions, those behaviors should be limited.
Counsel her to trust her instincts. It is important to encourage the patient to trust her own instincts, so that an overzealous employer or partner cannot coerce or cajole her to do something that violates her internal sense of well-being.
The author reports no financial relationships relevant to this article.
A 25-year-old primigravida with an intrauterine pregnancy at 26 weeks presents with contractions of moderate intensity every 4 minutes, intact membranes, and minimal vaginal bleeding. On digital exam, her cervix is soft, 50% effaced, and closed. Estimated fetal weight is 775 g.
You are at a Level I hospital in a rural community, 90 minutes from a tertiary nursery. What steps should you take first?
Tocolytics and antibiotics are the first steps. They may help to maximize the benefits of secondary strategies such as antenatal corticosteroids during transport to a tertiary care facility. In addition, assessment of fetal fibronectin levels and use of endovaginal ultrasound can supplement clinical judgment and improve prediction of outcomes. Their excellent negative predictive value can spare many women unnecessary and potentially harmful treatments.
This article discusses these measures in the context of an actual case.
The value of “secondary prevention”
Giving corticosteroids to enhance fetal lung and brain maturity and transporting the mother to a tertiary care center may not prevent preterm delivery, but they can mitigate some of the damage and are supported by the evidence.
Corticosteroids. Given the clear evidence of their efficacy, steroids should be administered once preterm birth appears likely. I would give steroids before maternal transport.
Betamethasone is preferable to dexamethasone, which may be toxic to the fetal central nervous system. However, dexamethasone is preferable to no therapy.
Contraindications to corticosteroids include systemic maternal or fetal infections and maternal endocrinopathies such as Cushing’s disease or poorly controlled diabetes.
Transport to tertiary care. A neonatal intensive care unit clearly benefits tiny babies. Clinicians should be aware of the pediatric capacity of their community hospitals and maintain a referral relationship with the nearest tertiary care centers. Conversely, clinicians on the receiving end of maternal transports should make every effort to expedite these referrals.
Is Local Care Too Risky?
Patricia and her family strongly prefer that she undergo treatment in her own community, if at all possible.
Signs and symptoms of preterm labor are poor predictors of preterm birth. Although most symptomatic women deliver at term, even the most clinically astute physician cannot predict when a symptomatic patient will deliver.
Which tocolytic is most effective?
Berkman ND, Thorp JM Jr, Lohr KN, et al. Tocolytic treatment for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2003;188:1648–1659.
No single drug is best. In this metaanalysis, magnesium, β-mimetics, calcium channel blockers, and nonsteroidal anti-inflammatory drugs (NSAIDs) performed about the same at prolonging the interval between onset of preterm labor and actual birth, compared with placebo or no treatment. Ethanol was less effective and “inappropriate.” Tocolytics are given to stop contractions (first-line therapy) and to maintain quiescence after an acute episode (maintenance therapy).
To determine the most effective tocolytic, we analyzed 16 studies of first-line therapy and 8 involving maintenance therapy, using the above 5 drug classes.
How 5 drugs compare
Estimated odds ratios suggest that, when used as first-line therapy, all the drugs except ethanol are about the same. Odds ratios ranged from 1.622 for β-mimetics to 2.485 for calcium channel blockers. (The odds ratio for NSAIDs was based on only 1 study.)
When we tested whether β-mimetics, calcium channel blockers, and magnesium sulfate had the same effects, compared with placebo, the results suggested that they do not. However, the body of literature was not large enough to establish this conclusively.
Overall, β-mimetics appear to lack superiority over the other drugs as first-line therapy and cause more maternal harms, while ethanol is “inappropriate” and no longer in use.
As maintenance therapy, none of the drugs appeared to have any benefit.
Maternal and fetal harms
We defined harms as “clinical markers and events that the authors of individual studies considered as adverse events or side effects.”
Among maternal harms were serious cardiac side effects, including arrhythmias, heart failure, and chest pain, linked to β-mimetics. Minor cardiovascular harms were also higher among women given β-mimetics. In addition, calcium channel blockers appeared to increase the risk of minor cardiovascular harms, but not as much as the β-mimetics.
Overall, maternal cardiac, metabolic, and psychologic harms were more prevalent among women taking β-mimetics. This may be due, at least in part, to the fact that studies of β-mimetics tended to look for these effects more than other studies did.
As for short-term fetal harms, we found “little consistent evidence” of them in the infants of women receiving these drugs, and the studies lacked sufficient data to evaluate potential long-term harms.
What later analyses found
After 1999, the cutoff year of our review, several relatively large studies showed the oxytocin antagonist atosiban to be effective as acute7,8and maintenance8 therapy, with a favorable side effect profile. Another trial9 compared 2 doses of magnesium (2 and 5 g per hour); the higher dose acted more quickly but with more side effects. These and other studies do not alter our conclusions about the effectiveness of tocolytic therapy—or the specifics of the 5 drugs studied.
2 useful markers
In the 1990s, 2 biologic markers were discovered that improve the precision of preterm birth risk assessment:
- fetal fibronectin (fFN) and
- endovaginal sonography (EVUSD).1
Use of EVUSD enables measurement of the cervix from the internal to external os. Cervices shorten before spontaneous birth.
These 2 tests, when positive (fFN detected or cervical length
I use a negative test to identify women who do not require further treatment or evaluation. If a patient has a negative fFN or EVUSD, I would not transport her to a tertiary care center. In fact, I would probably discharge her home with close follow-up.
3 concerns about the tests
Clinicians tend to have some concerns about incorporating these tests into their routines:
- How reliable is negative predictive value? Arguably, these tests perform better than clinical judgment and can spare many women unnecessary treatments.2 No test is perfect, however. These bio-markers should be adjuncts to—not replacements for—clinical wisdom.
- What about false results? With fFN, a proper collection kit with plastic tube and Dacron swab is critical because the molecule will adhere to glass or cotton, creating a false-negative result. A false-positive result can occur after recent coitus or a digital cervical exam; therefore, collect fFN specimens before checking the cervix. With EVUSD, the examinations require a moderate amount of skill.
- Which biomarker is best? Both fFN and EVUSD make independent and separate contributions to the prediction of preterm birth. Therefore, I use both.
Start Tocolysis And Antibiotics?
Patricia’s fFN and EVUSD tests are both positive. Should you start tocolysis and antibiotic therapy prior to transfer?
Metaanalysis suggests tocolysis, and antibiotics extend the interval between symptom onset and delivery.1The length of this prolongation can be measured in days, and no evidence suggests that prolonged pharmacotherapy has any benefit.
I would initiate both therapies while waiting for the mother to be moved to a tertiary center, even though neither therapy has been shown to improve perinatal outcome.
Tocolysis. We could find no differences among tocolytic drugs.3 Serious side effects are rare, but nuisance cardiovascular symptoms are frequent. Sympathomimetic drugs lead to lethargy, and magnesium is associated with malaise. Magnesium requires intravenous access and should be given only via infusion pump by trained personnel. That often means a nurse must accompany the patient to the Level III hospital.
Thus, for logistical reasons, I favor nonsteroidal anti-inflammatory drugs, of which indomethacin is the most widely studied. Indomethacin can be given by mouth or rectum, with minimal side effects. Harm to the fetus is rare if the drug is used acutely for only 48 to 72 hours (the maximum duration of any potential benefit).
Antibiotics. Current protocols calling for betalactam antibiotic therapy as prophylaxis against early-onset neonatal sepsis in preterm births have led to almost universal use of antibiotics among these patients. Our metaanalysis did not demonstrate superior pregnancy prolongation with any other regimen, so the one for group B strep prophylaxis provides a double benefit.4 As with tocolytics, there is no role for maintenance therapy.
When Contractions Cease
Patricia is transferred and completes her steroid therapy. Her symptoms and contractions cease. After a few days of observation and no cervical changes, she is discharged home. She asks about home therapies, work, activities, and sex.
Since our metaanalysis of tocolysis studies showed no efficacy for maintenance regimens, I do not recommend them except in this rare situation: when a woman has so much uterine activity without cervical change that she is unable to rest or complete her daily activities. In this case I would favor “as needed” doses of a β-mimetic drug by mouth.
Although home uterine activity monitors and subcutaneous tocolytic pumps are available, evidence suggests they are ineffective.1I seldom, if ever, use these devices.
Despite the almost universal recommendation that women at risk of preterm birth avoid physical and sexual activity, we lack evidence that bed rest or abstinence prolong pregnancy or prevent preterm birth.
Is sex allowed? When we studied both physical activity and sexuality in asymptomatic women at midpregnancy, neither was associated with spontaneous preterm birth.5,6 Therefore, I do not recommend restricting activity or sexual intercourse. Instead, I encourage women to carefully assess uterine activity. If certain behaviors appear to increase contractions, those behaviors should be limited.
Counsel her to trust her instincts. It is important to encourage the patient to trust her own instincts, so that an overzealous employer or partner cannot coerce or cajole her to do something that violates her internal sense of well-being.
The author reports no financial relationships relevant to this article.
1. Berkman ND, Thorp JM, Hartmann KE, et al. Management of Preterm Labor. Evidence Report/Technology Assessment #18. Rockville, Md: Agency for Healthcare Research and Quality; December 2000. AHRQ publication 01-E021.
2. Thorp JM, Jr. ACOG Committee on Practice Bulletins. Management of preterm labor. Obstet Gynecol. 2003;101:1039-1047.
3. Berkman ND, Thorp JM, Jr, Lohr KN, et al. Tocolytic treatment for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2003;188:1648-1659.
4. Thorp JM, Jr, Hartmann KE, Berkman ND, et al. Antibiotic therapy for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2002;186:587-592.
5. Sayle AE, Savitz DA, Thorp JM, Jr, Hertz-Picciotto I, Wilcox AJ. Sexual activity during late pregnancy and preterm delivery. Obstet Gynecol. 2001;97:283-289.
6. Evenson KR, Siega-Riz AM, Savitz DA, Leiferman JA, Thorp JM, Jr. Vigorous leisure activity and pregnancy outcome. Epidemiology. 2002;13:653-659.
7. Moutquin JM, Sherman D, Cohen H, et al. Double-blind, randomized, controlled trial of atosiban and ritrodine in the treatment of preterm labor: a multicenter effectiveness and safety study. Am J Obstet Gynecol. 2000;182:1191-1199.
8. Romero R, Sibai BM, Sanchez-Ramos L, et al. An oxytocin receptor antagonist (atosiban) in the treatment of preterm labor: a randomized, double-blind, placebo-controlled trial with tocolytic rescue. Am J Obstet Gynecol. 2000;182:1173-1183.
9. Terrone DA, Rinehart BK, Kimmel ES, May WL, Larmon JE, Morrison JC. A prospective, randomized, controlled trial of high and low maintenance doses of magnesium sulfate for acute tocolysis. Am J Obstet Gynecol. 2000;182:1477-1482.
1. Berkman ND, Thorp JM, Hartmann KE, et al. Management of Preterm Labor. Evidence Report/Technology Assessment #18. Rockville, Md: Agency for Healthcare Research and Quality; December 2000. AHRQ publication 01-E021.
2. Thorp JM, Jr. ACOG Committee on Practice Bulletins. Management of preterm labor. Obstet Gynecol. 2003;101:1039-1047.
3. Berkman ND, Thorp JM, Jr, Lohr KN, et al. Tocolytic treatment for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2003;188:1648-1659.
4. Thorp JM, Jr, Hartmann KE, Berkman ND, et al. Antibiotic therapy for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2002;186:587-592.
5. Sayle AE, Savitz DA, Thorp JM, Jr, Hertz-Picciotto I, Wilcox AJ. Sexual activity during late pregnancy and preterm delivery. Obstet Gynecol. 2001;97:283-289.
6. Evenson KR, Siega-Riz AM, Savitz DA, Leiferman JA, Thorp JM, Jr. Vigorous leisure activity and pregnancy outcome. Epidemiology. 2002;13:653-659.
7. Moutquin JM, Sherman D, Cohen H, et al. Double-blind, randomized, controlled trial of atosiban and ritrodine in the treatment of preterm labor: a multicenter effectiveness and safety study. Am J Obstet Gynecol. 2000;182:1191-1199.
8. Romero R, Sibai BM, Sanchez-Ramos L, et al. An oxytocin receptor antagonist (atosiban) in the treatment of preterm labor: a randomized, double-blind, placebo-controlled trial with tocolytic rescue. Am J Obstet Gynecol. 2000;182:1173-1183.
9. Terrone DA, Rinehart BK, Kimmel ES, May WL, Larmon JE, Morrison JC. A prospective, randomized, controlled trial of high and low maintenance doses of magnesium sulfate for acute tocolysis. Am J Obstet Gynecol. 2000;182:1477-1482.
The telltale heart: What HDL reveals about a woman’s risk
JUDY’S CASE
“WHAT’S MY RISK?”
At her periodic gynecologic exam, Judy, a 58-year-old white woman, expresses concern about her heart health in light of her 62-year-old sister’s recent heart attack. Further questioning reveals that her father died of a heart attack at age 56, and her brother, 52, has high blood pressure and adult-onset diabetes.
Judy has not experienced any symptoms of cardiovascular disease, such as chest pain or tightness with exertion, and she doesn’t smoke. The last time her cholesterol was checked was about 15 years earlier, at which time it was “OK.” She admits she is not very physically active and has gained about 30 lb over the past 10 years. Her vital signs and physical exam are entirely normal except for borderline high blood pressure at 140/90 mm Hg, weight of 170 lb (height: 68 inches), and a waist circumference of 37 inches.
What is her cardiovascular risk?
Judy has physical findings suggestive of metabolic syndrome in addition to the significant family history of cardiovascular disease (CVD). Although her current risk of a cardiac event appears to be low, she is likely to deteriorate if the hypertension and excess body weight are not addressed.
To predict her level of risk more precisely, the physician asks Judy to return in 2 weeks for a blood pressure recheck, and instructs her to perform additional readings on her own. The clinician also refers Judy for a fasting lipid panel and blood glucose level.
In women, CVD is especially lethal
Contrary to earlier assumptions, CVD now appears to be more lethal in women than in men and warrants aggressive efforts to prevent it and manage risk factors (FIGURE). This article focuses on improving high-density lipoprotein (HDL) cholesterol, a key factor in women at risk.
This approach differs slightly from the National Cholesterol Education Program Adult Treatment Panel III (NCEP/ATP III) guidelines, which target low-density lipoprotein (LDL) cholesterol as the primary lipid risk factor for intervention.1
FIGURE Women surpass men in CVD deaths
Over the past 25 years, the trend in deaths attributable to cardiovascular disease has been upward for women, while it is shifting downward for men.
Why focus on HDL?
Improvement in HDL is the strongest predictor of reduced risk for cardiac events. So says an analysis of 17 major lipid intervention trials between 1987 and 2003 (n = 44,170).2
Another study3 demonstrated that HDL cholesterol is the stronger predictor of CVD risk in women. In addition, several large observational studies have shown that increasing HDL cholesterol by 1 mg/dL in men reduces CVD risk by 2%, whereas increasing HDL in women by 1 mg/dL decreases CVD risk by 3%.4
Higher HDL levels may explain later onset of CVD in women. The advantage that women have over men in CVD risk prior to menopause seems to be at least partly due to their higher levels of HDL cholesterol: The average HDL level in women is 56 mg/dL, versus 46 mg/dL in men. This advantage begins to disappear after menopause, presumably because of changes in hormone levels and decreasing HDL-2 cholesterol, the most cardioprotective HDL fraction.
Other reasons to focus on HDL. In addition to the increased CVD risk associated with menopause, women of all ages in the United States have an increasing tendency—at almost epidemic rates—toward obesity and metabolic syndrome, which are known CVD risk factors.5 The dyslipidemia seen with those conditions is characterized by low HDL cholesterol and high triglycerides. Thus, maintaining healthy HDL levels is clearly an important goal for overall cardiovascular health, especially in women.
In addition, HDL is the key lipoprotein associated with reverse cholesterol transport, the process of carrying excess cholesterol from peripheral tissues to the liver for catabolism.
JUDY’S CASE
METABOLIC SYNDROME CONFIRMED
At her return visit, Judy’s blood pressure remains 140/90 mm Hg, with outside readings ranging from 135 to 145 mm Hg systolic and 85 to 95 mm Hg diastolic. Her laboratory tests reveal fasting blood glucose of 115 mg/dL, total cholesterol of 220 mg/dL, LDL cholesterol of 120 mg/dL, HDL cholesterol of 35 mg/dL, and triglycerides of 300 mg/dL.
What are her key heart-health issues?
Individualized management—recommended by NCEP/ATP III guidelines— should focus on reversing the metabolic defects of insulin resistance: hypertension, obesity, glucose intolerance, and dyslipidemia.
At present, Judy’s 10-year risk of a cardiac event is 4% by Framingham risk scoring, but it is likely to increase if the metabolic syndrome is not addressed.
How to preserve healthy HDL levels
Diet and regular aerobic exercise are recommended by the NCEP/ATP III guidelines, especially for obese patients with metabolic syndrome. However, dietary changes do not raise HDL cholesterol. In fact, dieting to lose weight will almost certainly lower HDL levels. That’s because people who eat a diet very low in fat tend to replace the fat calories with carbohydrates, and a low-fat, high-carbohydrate diet will reduce all cholesterol fractions—but HDL cholesterol will decrease disproportionately.6
Recommend complex carbohydrates and moderate fat intake
To avoid excessive reduction in HDL cholesterol, any weight-loss diet should involve moderate fat intake (35% of total calories) and emphasize monounsaturated fats such as olive or canola oil, along with complex carbohydrates found in fruits, vegetables, and whole grains.7 After weight loss is stabilized, HDL cholesterol tends to increase somewhat, but may not return all the way to baseline.
New guidelines on how to intervene
Most women who die suddenly from coronary heart disease had no previous symptoms, and that makes prevention all the more important.
Though it hasn’t been long since the first woman-centered recommendations on preventing cardiovascular disease,19 our understanding of preventive interventions has improved enormously. Thus, the American Heart Association convened a new expert panel to review and, where necessary, revise the original guidelines.20 Here are some of the highlights.
Forget “haves” and “have-nots”
Lori Mosca and the other members of the expert panel observe that “the concept of CVD as a categorical, ‘have-or-have-not’ condition has been replaced with a growing appreciation for the existence of a continuum of CVD risk.”20
For example, the low-risk category (<10% risk of a coronary heart disease event in the next 10 years, according to the Framingham Risk Score for women) would include women with optimal levels of risk factors and a heart-healthy lifestyle, as well as women with metabolic syndrome but no other risk factors. In contrast, women with established coronary heart disease, diabetes mellitus, or chronic kidney disease would fall into the high-risk group (>20% risk). Those with multiple risk factors or markedly elevated levels of a single risk factor fall somewhere in between.
The 5 lifestyle laws
Women are advised to consistently:
- eat plenty of fruits and vegetables, whole grains, and low-fat or nonfat dairy items
- avoid smoking and smokeless tobacco
- perform at least 30 minutes of moderate-intensity activity, such as brisk walking, most days
- achieve and maintain a body mass index between 18.5 and 25.9 kg/m2 and a waist circumference less than 35 inches
- consider omega-3 fatty acid supplementation, especially if risk is high. The guidelines extol the benefits of fish, which contain omega-3 fatty acids, but warn against consumption of fish likely to contain unsafe levels of mercury (shark, sword-fish, king mackerel, and tilefish) by gravidas and women of reproductive age.
BP and cholesterol control
- Blood pressure. Maintain at or below 120/80 mm Hg through lifestyle approaches, or drug therapy when BP is 140/90 mm Hg or higher.
- Dietary fat and cholesterol. Keep saturated fat intake to less than 7% of calories, and cholesterol below 200 mg/dL with high risk or elevated LDL.
- LDL-cholesterol. Use drug therapy (preferably statins) if risk is high and LDL is below 100 mg/dL. Add lifestyle adjustments if risk is high and LDL cholesterol is at or above 100 mg/dL.
What not to take to prevent CVD
The guidelines warn against prescribing—or continuing—estrogen-progestin therapy to prevent CVD. Nor should other forms of menopausal hormone therapy, such as unopposed estrogen, be prescribed or continued unless new findings indicate a beneficial role.
Also discouraged are antioxidant vitamin supplements to prevent CVD.
Look for depression
Especially women with CVD should be referred or treated when depression is found, as it can hamper a woman’s efforts at prevention.
The full text of the guidelines can be viewed at
http://circ.ahajournals.org/cgi/content/full/109/5/672.
Regular exercise raises HDL
One way to avoid an overall reduction in HDL levels with weight loss is to prescribe exercise in conjunction with it. Regular exercise is an excellent way to raise HDL cholesterol levels. Studies suggest that, for women, the volume of exercise is more important than intensity. Thus, women should strive to walk 7 to 14 miles per week or otherwise expend approximately 1,200 to 1,600 Kcal.8,9
Regular exercise is recommended as one of the NCEP/ATP III therapeutic lifestyle changes that directly benefit cardiovascular health and blood pressure and help the individual maintain optimal body weight. Although exercise raises HDL levels, it does so more easily in men than in women. HDL cholesterol increases in men with both intensity and volume of exercise.10 Women appear to derive slightly less of a benefit, perhaps because their HDL levels are already generally higher.
In women, studies have reported an increase in HDL cholesterol as high as 15% for both premenopausal and post-menopausal women who follow moderate exercise regimens—and the lower the baseline HDL level, the greater the increase.8
Exercise level was inversely associated with cardiovascular risk in the Women’s Health Initiative,9 which followed a cohort of 73,743 women prospectively for an average of 3.2 years. Women at the highest quintile of exercise level reduced their CVD risk by 53% over the lowest quintile, and moderate activity such as walking led to risk reductions similar to those involving more vigorous activities.
Recommend alcohol—or not?
Moderate alcohol consumption—1 to 3 drinks per day, or 15 to 45 g ethanol— improves lipoprotein levels and reduces CVD risk. The flavonoids in red wines also reduce platelet aggregation and clotting tendencies. However, advising a patient to consume alcohol to reduce her CVD risk is controversial; many physicians are reluctant to do so due to obvious concerns over toxicity and dependency.
Response to alcohol may vary by menopausal status. In 1 study,11 pre-menopausal women decreased their LDL cholesterol by 12% (P=.01) after 3 glasses of wine daily for 3 weeks, but there was no significant increase in HDL levels.
In the same study, postmenopausal women increased HDL levels by 12% (P=.03), but their LDL cholesterol decreased only minimally.11
Another study12 in postmenopausal women who consumed 0, 1, or 2 drinks daily (0, 15, or 30 g ethanol) for 8 weeks showed a significant decrease of 4% in LDL cholesterol at 1 drink (15 g), but no significant further decrease at 2 drinks (30 g). In the same study, HDL increased non-significantly at 1 drink (15 g), but increased significantly (5%) at 2 drinks (30 g). There may be a threshold of 30 g ethanol daily for postmenopausal women to benefit significantly from alcohol consumption.
JUDY’S CASE
LIFESTYLE RECOMMENDATIONS
The foundation of Judy’s management should be the triad of weight loss, exercise, and a diet that limits refined carbohydrates and emphasizes fiber, fruits and vegetables, whole grains, and healthy fats (ie, olive, canola, and fish oils).
In prescribing exercise, emphasize quantity over intensity, such as 14 miles of walking weekly or 60 to 90 minutes daily of aerobic activity.
Since she has no history of cardiac symptoms, and low-intensity, high-quantity exercise is advised, she does not need a screening cardiac stress test before beginning her regimen.
Pantethine
Pantethine is an over-the-counter (OTC) nutritional supplement that combines the B vitamin pantothenic acid with the amino acid cysteamine. Although pantothenic acid alone has no lipid-lowering effects, pantethine does: It lowers LDL cholesterol, very-low-density lipoprotein (VLDL) cholesterol, and triglycerides, and raises HDL levels. The exact mechanism of action is unknown, but it is thought to involve primarily the effects of cysteamine on lipid metabolism in the liver.
Recommended dose. At 600 to 900 mg daily, the typical response is an increase of up to 18% in HDL cholesterol and reductions in LDL cholesterol, VLDL cholesterol, and triglycerides of 13%, 20%, and 26%, respectively.13
In a recent US study, pantethine significantly raised HDL-2 cholesterol, the more cardioprotective fraction of HDL, and increased the particle size of LDL cholesterol, rendering it less atherogenic.14
Pantethine also reduces visceral fat. The same study14 reported a significant reduction in visceral fat, a component of metabolic syndrome, as measured by computerized dual-energy x-ray absorptiometry in individuals taking 900 mg daily for 6 weeks. This reduction appears to be primarily an effect of pantothenic acid and had been demonstrated in animal studies.
No side effects. Pantethine is exceptionally well tolerated, with virtually no side effects. An occasional person will experience gastrointestinal upset and diarrhea, which resolve when the drug is discontinued.
Recommend formulations that contain Pantesin (Daiichi Fine Chemicals, New York City), a pharmaceutical grade of pantethine, because extensive research confirms the benefits I have described. Otherwise, make sure the manufacturer is a reputable company, with scientific studies to support its claims of safety, efficacy, and bioavailability.
Nicotinic acid
Nicotinic acid (NA), another B vitamin available OTC as a nutritional supplement, is the most effective agent for raising HDL levels.
Recommended dose. A divided dose of 3,000 mg daily of the immediate-release form of NA can raise HDL levels as much as 30%. Unfortunately, that form of NA has a high incidence of adverse effects, such as flushing, itching, and GI upset.15
Sustained-release NA is generally well tolerated, but somewhat less effective at raising HDL. A lower dose of sustained-release NA (1,000 to 1,500 mg daily) is recommended to avoid liver toxicity and typically leads to HDL increases as high as 20%.15
NA offers additional benefits to the lipid profile, typically lowering LDL cholesterol by 20%, triglycerides by 15%, and lipoprotein(a) by 15%.15
Monitor all forms of NA with liver enzymes, blood glucose, and uric acid because treatment can elevate these markers.
Give NA preparations extra scrutiny. The general caveats about quality and bioavailability apply especially to NA. Nonprescription products on the market that contain nicotinamide and inositol hexanicotinate are advertised as “no-flush” niacin because they do not cause cutaneous side effects, but they also have no lipid benefits.
Cost. NA is relatively inexpensive, and good-quality sustained-release products such as Endur-acin (Endurance Products, Tigard, Ore) can be purchased OTC for 12 cents per 500-mg tablet or a daily cost of 24 to 36 cents.16
Sustained-release NA is also available by prescription (Niaspan, Kos Pharmaceuticals, Cranbury, NJ), but it is considerably more expensive ($1.98 per 500-mg tablet, or $3.96 to $5.94 daily) and has not been shown to be more effective or better tolerated than the better OTC products.16
JUDY’S CASE
RAISING HDL WITHOUT DRUGS
Judy’s lipid abnormalities would benefit from a supplement of pantethine (300 mg thrice daily) or NA (1,000 mg thrice daily of plain/quick release or 500 mg twice daily of sustained release to reduce flushing side effects).
Her greatest risk with her current lipid levels is low HDL, and the best agent to raise these levels is NA.
Pantethine also raises HDL and selectively improves the HDL-2 subfraction, which is most cardioprotective. Both supplements also improve the other lipid abnormalities.
In addition, referral to a dietician for detailed instruction in food choices and preparation may be useful.
Pharmacologic therapies
Hormone replacement therapy (HRT) is no longer recommended to prevent CVD and should be given only for menopausal symptoms during the perimenopausal years—despite the fact that estrogen has been shown to raise HDL cholesterol by 8% in postmenopausal women.17
Estrogens increase HDL by increasing production of apoA-1, the main lipoprotein in HDL, and by decreasing HDL catabolism by inhibiting hepatic lipase. The 17-hydroxyprogesterone component of HRT given to women with an intact uterus to prevent endometrial cancer has no significant lipid effects.
Paradoxically, the increased CVD risk found in the HRT arm of the Women’s Health Initiative17 was in the face of improved HDL (8%) and LDL (–14%) cholesterol and appeared to be the result of increased thrombotic events.
Further analysis of Women’s Health Initiative data showed that women who were still within 10 years of menopause actually did experience a reduction in CVD risk. That observation, along with some primate research on HRT, suggests that the risk or benefit of HRT with respect to CVD may be a matter of timing. See “Emerging hypothesis may explain estrogen paradox”
At the 2004 American Heart Association meeting, Dr. Thomas Clarkson, who has conducted primate research on hormone replacement therapy (HRT) and the risk of cardiovascular disease (CVD), described the emerging hypothesis that may explain the HRT paradox of increased CVD risk despite evidence of benefit in observational studies.21
Estrogen is a potent upregulator of matrix metal-loproteases. These proteolytic enzymes are a normal constituent of the endometrium and important in its remodeling with each menstrual cycle. Matrix metal-loproteases are also found in the fibrous cap that seals off the necrotic core of an advanced atheroma from the vascular lumen. Most perimenopausal women have enjoyed estrogen’s protective effect throughout their reproductive years and thus have developedlittle advanced atherosclerotic disease.
Ten or more years past menopause, however, clinically significant atherosclerotic lesions often develop in women who have been without the protection of estrogen. If estrogen is added at this stage, it causes increased matrix metalloprotease activity in the fibrous cap of any atheroma. This proteolytic activity can destabilize the fibrous cap, allowing necrotic core material to come in contact with the bloodstream.
This necrotic material is highly thrombogenic and stimulates clot formation in the vascular lumen. Clarkson demonstrated this process in research on perimenopausal and postmenopausal primates.
This hypothesis will soon be tested in a clinical trial in humans; CVD risk is expected to decrease by 50% to 70% in women who have taken HRT continuously from perimenopause.
Statins and other HDL-modifying drugs
The statins are a first choice for LDL reduction, but lead to only modest increases (4%–10%) in HDL levels.18 Fibric acid derivatives are somewhat more effective; they lead to increases in HDL of 6% to 18%. Both types of drugs are considerably more expensive than OTC NA and not as effective at raising HDL.
Combining statins with other agents that raise HDL has been tried: The NA–statin combination can be effective in managing dyslipidemias of both LDL and HDL. Fibric acid derivatives should not be used with statins because of the increased risk of serious myopathies.18
JUDY’S CASE
THERAPEUTIC TARGETS
Judy’s goals should include:
- reducing blood pressure to less than 120/80 mm Hg,
- decreasing weight to about 140 lb,
- achieving a waist measurement of less than 35 inches,
- reducing fasting blood glucose to less than 100 mg/dL,
- decreasing triglycerides to less than 150 mg/dL, total cholesterol to less than 200 mg/dL, and LDL levels to less than 100 mg/dL, and
- raising HDL to more than 45 mg/dL.
All these parameters should be checked every 3 months until the goals are achieved.
If Judy fails to progress or develops symptoms of heart disease, she should be referred to a cardiologist for further evaluation and more aggressive treatment.
The author reports no conflicts relevant to this article.
1. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486-2497.
2. Alsheikh-Ali A, Abourjaily HM, Stanek EJ, et al. Increases in HDL-cholesterol are the strongest predictors of risk reduction in lipid intervention trials. Circulation. 2004;110(17 suppl 3):III-813.
3. Jacobs DR, Jr, Meban IL, Bangdiwala SI, et al. High density lipoprotein cholesterol as a predictor of cardiovascular disease mortality in men and women: the follow-up study of the Lipid Research Clinics Prevalence Study. Am J Epidemiol. 1990;131:32-47.
4. Gordon DJ, Probstfiel JL, Garrison RJ, et al. High-density lipoprotein cholesterol and cardiovascular disease: four prospective American studies. Circulation. 1989;79:8-15.
5. Hu Fb, Willet WC, Li T, et al. Adiposity as compared with physical activity in predicting mortality among women. N Engl J Med. 2004;351:2694-2703.
6. Mensink RP, Zock PL, Kester A, et al. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003;77:1146-1155.
7. Pereira MA, Swain J, Goldfine AB, et al. Effects of a low-glycemic load diet on resting energy expenditure and heart disease risk factors during weight loss. JAMA. 2004;292:2482-2490.
8. Kokkinos PF, Holland JC, Pittaras AE, et al. Cardiorespiratory fitness and coronary heart disease risk factor association in women. J Am Coll Cardiol. 1995;26:358-364.
9. Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716-725.
10. Kokkinos PE, Fernhall B. Physical activity and high density lipoprotein cholesterol levels: what is the relationship? Sports Med. 1999;28:307-314.
11. Van Der Gaag MS, Sterksma A, Schaafsma G, et al. Moderate alcohol consumption lowers risk factors for cardiovascular disease in postmenopausal women fed a controlled diet. Am J Clin Nutr. 2002;75:593-599.
12. Baer DJ, Judd JT, Clevidence BA, et al. Moderate alcohol consumption and changes in postprandial lipoproteins of premenopausal and postmenopausal women: a diet-controlled randomized intervention study. J Womens Health Gend Based Med. 2000;9:607-616.
13. Pins JJ, Keenan JM. Pantethine: a new option in managing dyslipidemia. J Am College Nutr. 2005 [in press].
14. Pins JJ, First S, Shamliyan T, Keenan J. Pantethine beneficially affects apolipoprotein A-1, apolipoprotein B, low-density lipoprotein particle size but not high-sensitivity C-reactive protein in a dyslipidemic population. Circulation. 2004;110(17 suppl 3):III-778.
15. Crouse JR, 3rd. New developments in the use of niacin for treatment of hyperlipidemia: new considerations in the use of an old drug. Coron Artery Dis. 1996;7:321-326.
16. Retail pharmacy quote. Walgreen’s Pharmacy, Minneapolis, Minn. January 2005.
17. Risks and benefits of estrogen plus progestin in healthy post-menopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
18. Hersberger M, von Eckardstein A. Low high-density lipoprotein cholesterol: physical background, clinical importance and drug treatment. Drugs. 2003;63:1907-1945.
19. Mosca L, Grundy SM, Judelson D, et al. Guide to preventive cardiology for women. AHA/ACC scientific statement, consensus panel statement. irculation. 1999;99:2480-2484.
20. Mosca L, Appel LJ, Benjamin EJ, et al. AHA Guidelines: evidence-based guidelines for cardiovascular disease prevention in women. Circulation. 2004;109:672-693.
21. Clarkson T. Women’s Heart Health Symposium. Presented at the American Heart Association annual meeting, Nov 9, 2004, New Orleans.
JUDY’S CASE
“WHAT’S MY RISK?”
At her periodic gynecologic exam, Judy, a 58-year-old white woman, expresses concern about her heart health in light of her 62-year-old sister’s recent heart attack. Further questioning reveals that her father died of a heart attack at age 56, and her brother, 52, has high blood pressure and adult-onset diabetes.
Judy has not experienced any symptoms of cardiovascular disease, such as chest pain or tightness with exertion, and she doesn’t smoke. The last time her cholesterol was checked was about 15 years earlier, at which time it was “OK.” She admits she is not very physically active and has gained about 30 lb over the past 10 years. Her vital signs and physical exam are entirely normal except for borderline high blood pressure at 140/90 mm Hg, weight of 170 lb (height: 68 inches), and a waist circumference of 37 inches.
What is her cardiovascular risk?
Judy has physical findings suggestive of metabolic syndrome in addition to the significant family history of cardiovascular disease (CVD). Although her current risk of a cardiac event appears to be low, she is likely to deteriorate if the hypertension and excess body weight are not addressed.
To predict her level of risk more precisely, the physician asks Judy to return in 2 weeks for a blood pressure recheck, and instructs her to perform additional readings on her own. The clinician also refers Judy for a fasting lipid panel and blood glucose level.
In women, CVD is especially lethal
Contrary to earlier assumptions, CVD now appears to be more lethal in women than in men and warrants aggressive efforts to prevent it and manage risk factors (FIGURE). This article focuses on improving high-density lipoprotein (HDL) cholesterol, a key factor in women at risk.
This approach differs slightly from the National Cholesterol Education Program Adult Treatment Panel III (NCEP/ATP III) guidelines, which target low-density lipoprotein (LDL) cholesterol as the primary lipid risk factor for intervention.1
FIGURE Women surpass men in CVD deaths
Over the past 25 years, the trend in deaths attributable to cardiovascular disease has been upward for women, while it is shifting downward for men.
Why focus on HDL?
Improvement in HDL is the strongest predictor of reduced risk for cardiac events. So says an analysis of 17 major lipid intervention trials between 1987 and 2003 (n = 44,170).2
Another study3 demonstrated that HDL cholesterol is the stronger predictor of CVD risk in women. In addition, several large observational studies have shown that increasing HDL cholesterol by 1 mg/dL in men reduces CVD risk by 2%, whereas increasing HDL in women by 1 mg/dL decreases CVD risk by 3%.4
Higher HDL levels may explain later onset of CVD in women. The advantage that women have over men in CVD risk prior to menopause seems to be at least partly due to their higher levels of HDL cholesterol: The average HDL level in women is 56 mg/dL, versus 46 mg/dL in men. This advantage begins to disappear after menopause, presumably because of changes in hormone levels and decreasing HDL-2 cholesterol, the most cardioprotective HDL fraction.
Other reasons to focus on HDL. In addition to the increased CVD risk associated with menopause, women of all ages in the United States have an increasing tendency—at almost epidemic rates—toward obesity and metabolic syndrome, which are known CVD risk factors.5 The dyslipidemia seen with those conditions is characterized by low HDL cholesterol and high triglycerides. Thus, maintaining healthy HDL levels is clearly an important goal for overall cardiovascular health, especially in women.
In addition, HDL is the key lipoprotein associated with reverse cholesterol transport, the process of carrying excess cholesterol from peripheral tissues to the liver for catabolism.
JUDY’S CASE
METABOLIC SYNDROME CONFIRMED
At her return visit, Judy’s blood pressure remains 140/90 mm Hg, with outside readings ranging from 135 to 145 mm Hg systolic and 85 to 95 mm Hg diastolic. Her laboratory tests reveal fasting blood glucose of 115 mg/dL, total cholesterol of 220 mg/dL, LDL cholesterol of 120 mg/dL, HDL cholesterol of 35 mg/dL, and triglycerides of 300 mg/dL.
What are her key heart-health issues?
Individualized management—recommended by NCEP/ATP III guidelines— should focus on reversing the metabolic defects of insulin resistance: hypertension, obesity, glucose intolerance, and dyslipidemia.
At present, Judy’s 10-year risk of a cardiac event is 4% by Framingham risk scoring, but it is likely to increase if the metabolic syndrome is not addressed.
How to preserve healthy HDL levels
Diet and regular aerobic exercise are recommended by the NCEP/ATP III guidelines, especially for obese patients with metabolic syndrome. However, dietary changes do not raise HDL cholesterol. In fact, dieting to lose weight will almost certainly lower HDL levels. That’s because people who eat a diet very low in fat tend to replace the fat calories with carbohydrates, and a low-fat, high-carbohydrate diet will reduce all cholesterol fractions—but HDL cholesterol will decrease disproportionately.6
Recommend complex carbohydrates and moderate fat intake
To avoid excessive reduction in HDL cholesterol, any weight-loss diet should involve moderate fat intake (35% of total calories) and emphasize monounsaturated fats such as olive or canola oil, along with complex carbohydrates found in fruits, vegetables, and whole grains.7 After weight loss is stabilized, HDL cholesterol tends to increase somewhat, but may not return all the way to baseline.
New guidelines on how to intervene
Most women who die suddenly from coronary heart disease had no previous symptoms, and that makes prevention all the more important.
Though it hasn’t been long since the first woman-centered recommendations on preventing cardiovascular disease,19 our understanding of preventive interventions has improved enormously. Thus, the American Heart Association convened a new expert panel to review and, where necessary, revise the original guidelines.20 Here are some of the highlights.
Forget “haves” and “have-nots”
Lori Mosca and the other members of the expert panel observe that “the concept of CVD as a categorical, ‘have-or-have-not’ condition has been replaced with a growing appreciation for the existence of a continuum of CVD risk.”20
For example, the low-risk category (<10% risk of a coronary heart disease event in the next 10 years, according to the Framingham Risk Score for women) would include women with optimal levels of risk factors and a heart-healthy lifestyle, as well as women with metabolic syndrome but no other risk factors. In contrast, women with established coronary heart disease, diabetes mellitus, or chronic kidney disease would fall into the high-risk group (>20% risk). Those with multiple risk factors or markedly elevated levels of a single risk factor fall somewhere in between.
The 5 lifestyle laws
Women are advised to consistently:
- eat plenty of fruits and vegetables, whole grains, and low-fat or nonfat dairy items
- avoid smoking and smokeless tobacco
- perform at least 30 minutes of moderate-intensity activity, such as brisk walking, most days
- achieve and maintain a body mass index between 18.5 and 25.9 kg/m2 and a waist circumference less than 35 inches
- consider omega-3 fatty acid supplementation, especially if risk is high. The guidelines extol the benefits of fish, which contain omega-3 fatty acids, but warn against consumption of fish likely to contain unsafe levels of mercury (shark, sword-fish, king mackerel, and tilefish) by gravidas and women of reproductive age.
BP and cholesterol control
- Blood pressure. Maintain at or below 120/80 mm Hg through lifestyle approaches, or drug therapy when BP is 140/90 mm Hg or higher.
- Dietary fat and cholesterol. Keep saturated fat intake to less than 7% of calories, and cholesterol below 200 mg/dL with high risk or elevated LDL.
- LDL-cholesterol. Use drug therapy (preferably statins) if risk is high and LDL is below 100 mg/dL. Add lifestyle adjustments if risk is high and LDL cholesterol is at or above 100 mg/dL.
What not to take to prevent CVD
The guidelines warn against prescribing—or continuing—estrogen-progestin therapy to prevent CVD. Nor should other forms of menopausal hormone therapy, such as unopposed estrogen, be prescribed or continued unless new findings indicate a beneficial role.
Also discouraged are antioxidant vitamin supplements to prevent CVD.
Look for depression
Especially women with CVD should be referred or treated when depression is found, as it can hamper a woman’s efforts at prevention.
The full text of the guidelines can be viewed at
http://circ.ahajournals.org/cgi/content/full/109/5/672.
Regular exercise raises HDL
One way to avoid an overall reduction in HDL levels with weight loss is to prescribe exercise in conjunction with it. Regular exercise is an excellent way to raise HDL cholesterol levels. Studies suggest that, for women, the volume of exercise is more important than intensity. Thus, women should strive to walk 7 to 14 miles per week or otherwise expend approximately 1,200 to 1,600 Kcal.8,9
Regular exercise is recommended as one of the NCEP/ATP III therapeutic lifestyle changes that directly benefit cardiovascular health and blood pressure and help the individual maintain optimal body weight. Although exercise raises HDL levels, it does so more easily in men than in women. HDL cholesterol increases in men with both intensity and volume of exercise.10 Women appear to derive slightly less of a benefit, perhaps because their HDL levels are already generally higher.
In women, studies have reported an increase in HDL cholesterol as high as 15% for both premenopausal and post-menopausal women who follow moderate exercise regimens—and the lower the baseline HDL level, the greater the increase.8
Exercise level was inversely associated with cardiovascular risk in the Women’s Health Initiative,9 which followed a cohort of 73,743 women prospectively for an average of 3.2 years. Women at the highest quintile of exercise level reduced their CVD risk by 53% over the lowest quintile, and moderate activity such as walking led to risk reductions similar to those involving more vigorous activities.
Recommend alcohol—or not?
Moderate alcohol consumption—1 to 3 drinks per day, or 15 to 45 g ethanol— improves lipoprotein levels and reduces CVD risk. The flavonoids in red wines also reduce platelet aggregation and clotting tendencies. However, advising a patient to consume alcohol to reduce her CVD risk is controversial; many physicians are reluctant to do so due to obvious concerns over toxicity and dependency.
Response to alcohol may vary by menopausal status. In 1 study,11 pre-menopausal women decreased their LDL cholesterol by 12% (P=.01) after 3 glasses of wine daily for 3 weeks, but there was no significant increase in HDL levels.
In the same study, postmenopausal women increased HDL levels by 12% (P=.03), but their LDL cholesterol decreased only minimally.11
Another study12 in postmenopausal women who consumed 0, 1, or 2 drinks daily (0, 15, or 30 g ethanol) for 8 weeks showed a significant decrease of 4% in LDL cholesterol at 1 drink (15 g), but no significant further decrease at 2 drinks (30 g). In the same study, HDL increased non-significantly at 1 drink (15 g), but increased significantly (5%) at 2 drinks (30 g). There may be a threshold of 30 g ethanol daily for postmenopausal women to benefit significantly from alcohol consumption.
JUDY’S CASE
LIFESTYLE RECOMMENDATIONS
The foundation of Judy’s management should be the triad of weight loss, exercise, and a diet that limits refined carbohydrates and emphasizes fiber, fruits and vegetables, whole grains, and healthy fats (ie, olive, canola, and fish oils).
In prescribing exercise, emphasize quantity over intensity, such as 14 miles of walking weekly or 60 to 90 minutes daily of aerobic activity.
Since she has no history of cardiac symptoms, and low-intensity, high-quantity exercise is advised, she does not need a screening cardiac stress test before beginning her regimen.
Pantethine
Pantethine is an over-the-counter (OTC) nutritional supplement that combines the B vitamin pantothenic acid with the amino acid cysteamine. Although pantothenic acid alone has no lipid-lowering effects, pantethine does: It lowers LDL cholesterol, very-low-density lipoprotein (VLDL) cholesterol, and triglycerides, and raises HDL levels. The exact mechanism of action is unknown, but it is thought to involve primarily the effects of cysteamine on lipid metabolism in the liver.
Recommended dose. At 600 to 900 mg daily, the typical response is an increase of up to 18% in HDL cholesterol and reductions in LDL cholesterol, VLDL cholesterol, and triglycerides of 13%, 20%, and 26%, respectively.13
In a recent US study, pantethine significantly raised HDL-2 cholesterol, the more cardioprotective fraction of HDL, and increased the particle size of LDL cholesterol, rendering it less atherogenic.14
Pantethine also reduces visceral fat. The same study14 reported a significant reduction in visceral fat, a component of metabolic syndrome, as measured by computerized dual-energy x-ray absorptiometry in individuals taking 900 mg daily for 6 weeks. This reduction appears to be primarily an effect of pantothenic acid and had been demonstrated in animal studies.
No side effects. Pantethine is exceptionally well tolerated, with virtually no side effects. An occasional person will experience gastrointestinal upset and diarrhea, which resolve when the drug is discontinued.
Recommend formulations that contain Pantesin (Daiichi Fine Chemicals, New York City), a pharmaceutical grade of pantethine, because extensive research confirms the benefits I have described. Otherwise, make sure the manufacturer is a reputable company, with scientific studies to support its claims of safety, efficacy, and bioavailability.
Nicotinic acid
Nicotinic acid (NA), another B vitamin available OTC as a nutritional supplement, is the most effective agent for raising HDL levels.
Recommended dose. A divided dose of 3,000 mg daily of the immediate-release form of NA can raise HDL levels as much as 30%. Unfortunately, that form of NA has a high incidence of adverse effects, such as flushing, itching, and GI upset.15
Sustained-release NA is generally well tolerated, but somewhat less effective at raising HDL. A lower dose of sustained-release NA (1,000 to 1,500 mg daily) is recommended to avoid liver toxicity and typically leads to HDL increases as high as 20%.15
NA offers additional benefits to the lipid profile, typically lowering LDL cholesterol by 20%, triglycerides by 15%, and lipoprotein(a) by 15%.15
Monitor all forms of NA with liver enzymes, blood glucose, and uric acid because treatment can elevate these markers.
Give NA preparations extra scrutiny. The general caveats about quality and bioavailability apply especially to NA. Nonprescription products on the market that contain nicotinamide and inositol hexanicotinate are advertised as “no-flush” niacin because they do not cause cutaneous side effects, but they also have no lipid benefits.
Cost. NA is relatively inexpensive, and good-quality sustained-release products such as Endur-acin (Endurance Products, Tigard, Ore) can be purchased OTC for 12 cents per 500-mg tablet or a daily cost of 24 to 36 cents.16
Sustained-release NA is also available by prescription (Niaspan, Kos Pharmaceuticals, Cranbury, NJ), but it is considerably more expensive ($1.98 per 500-mg tablet, or $3.96 to $5.94 daily) and has not been shown to be more effective or better tolerated than the better OTC products.16
JUDY’S CASE
RAISING HDL WITHOUT DRUGS
Judy’s lipid abnormalities would benefit from a supplement of pantethine (300 mg thrice daily) or NA (1,000 mg thrice daily of plain/quick release or 500 mg twice daily of sustained release to reduce flushing side effects).
Her greatest risk with her current lipid levels is low HDL, and the best agent to raise these levels is NA.
Pantethine also raises HDL and selectively improves the HDL-2 subfraction, which is most cardioprotective. Both supplements also improve the other lipid abnormalities.
In addition, referral to a dietician for detailed instruction in food choices and preparation may be useful.
Pharmacologic therapies
Hormone replacement therapy (HRT) is no longer recommended to prevent CVD and should be given only for menopausal symptoms during the perimenopausal years—despite the fact that estrogen has been shown to raise HDL cholesterol by 8% in postmenopausal women.17
Estrogens increase HDL by increasing production of apoA-1, the main lipoprotein in HDL, and by decreasing HDL catabolism by inhibiting hepatic lipase. The 17-hydroxyprogesterone component of HRT given to women with an intact uterus to prevent endometrial cancer has no significant lipid effects.
Paradoxically, the increased CVD risk found in the HRT arm of the Women’s Health Initiative17 was in the face of improved HDL (8%) and LDL (–14%) cholesterol and appeared to be the result of increased thrombotic events.
Further analysis of Women’s Health Initiative data showed that women who were still within 10 years of menopause actually did experience a reduction in CVD risk. That observation, along with some primate research on HRT, suggests that the risk or benefit of HRT with respect to CVD may be a matter of timing. See “Emerging hypothesis may explain estrogen paradox”
At the 2004 American Heart Association meeting, Dr. Thomas Clarkson, who has conducted primate research on hormone replacement therapy (HRT) and the risk of cardiovascular disease (CVD), described the emerging hypothesis that may explain the HRT paradox of increased CVD risk despite evidence of benefit in observational studies.21
Estrogen is a potent upregulator of matrix metal-loproteases. These proteolytic enzymes are a normal constituent of the endometrium and important in its remodeling with each menstrual cycle. Matrix metal-loproteases are also found in the fibrous cap that seals off the necrotic core of an advanced atheroma from the vascular lumen. Most perimenopausal women have enjoyed estrogen’s protective effect throughout their reproductive years and thus have developedlittle advanced atherosclerotic disease.
Ten or more years past menopause, however, clinically significant atherosclerotic lesions often develop in women who have been without the protection of estrogen. If estrogen is added at this stage, it causes increased matrix metalloprotease activity in the fibrous cap of any atheroma. This proteolytic activity can destabilize the fibrous cap, allowing necrotic core material to come in contact with the bloodstream.
This necrotic material is highly thrombogenic and stimulates clot formation in the vascular lumen. Clarkson demonstrated this process in research on perimenopausal and postmenopausal primates.
This hypothesis will soon be tested in a clinical trial in humans; CVD risk is expected to decrease by 50% to 70% in women who have taken HRT continuously from perimenopause.
Statins and other HDL-modifying drugs
The statins are a first choice for LDL reduction, but lead to only modest increases (4%–10%) in HDL levels.18 Fibric acid derivatives are somewhat more effective; they lead to increases in HDL of 6% to 18%. Both types of drugs are considerably more expensive than OTC NA and not as effective at raising HDL.
Combining statins with other agents that raise HDL has been tried: The NA–statin combination can be effective in managing dyslipidemias of both LDL and HDL. Fibric acid derivatives should not be used with statins because of the increased risk of serious myopathies.18
JUDY’S CASE
THERAPEUTIC TARGETS
Judy’s goals should include:
- reducing blood pressure to less than 120/80 mm Hg,
- decreasing weight to about 140 lb,
- achieving a waist measurement of less than 35 inches,
- reducing fasting blood glucose to less than 100 mg/dL,
- decreasing triglycerides to less than 150 mg/dL, total cholesterol to less than 200 mg/dL, and LDL levels to less than 100 mg/dL, and
- raising HDL to more than 45 mg/dL.
All these parameters should be checked every 3 months until the goals are achieved.
If Judy fails to progress or develops symptoms of heart disease, she should be referred to a cardiologist for further evaluation and more aggressive treatment.
The author reports no conflicts relevant to this article.
JUDY’S CASE
“WHAT’S MY RISK?”
At her periodic gynecologic exam, Judy, a 58-year-old white woman, expresses concern about her heart health in light of her 62-year-old sister’s recent heart attack. Further questioning reveals that her father died of a heart attack at age 56, and her brother, 52, has high blood pressure and adult-onset diabetes.
Judy has not experienced any symptoms of cardiovascular disease, such as chest pain or tightness with exertion, and she doesn’t smoke. The last time her cholesterol was checked was about 15 years earlier, at which time it was “OK.” She admits she is not very physically active and has gained about 30 lb over the past 10 years. Her vital signs and physical exam are entirely normal except for borderline high blood pressure at 140/90 mm Hg, weight of 170 lb (height: 68 inches), and a waist circumference of 37 inches.
What is her cardiovascular risk?
Judy has physical findings suggestive of metabolic syndrome in addition to the significant family history of cardiovascular disease (CVD). Although her current risk of a cardiac event appears to be low, she is likely to deteriorate if the hypertension and excess body weight are not addressed.
To predict her level of risk more precisely, the physician asks Judy to return in 2 weeks for a blood pressure recheck, and instructs her to perform additional readings on her own. The clinician also refers Judy for a fasting lipid panel and blood glucose level.
In women, CVD is especially lethal
Contrary to earlier assumptions, CVD now appears to be more lethal in women than in men and warrants aggressive efforts to prevent it and manage risk factors (FIGURE). This article focuses on improving high-density lipoprotein (HDL) cholesterol, a key factor in women at risk.
This approach differs slightly from the National Cholesterol Education Program Adult Treatment Panel III (NCEP/ATP III) guidelines, which target low-density lipoprotein (LDL) cholesterol as the primary lipid risk factor for intervention.1
FIGURE Women surpass men in CVD deaths
Over the past 25 years, the trend in deaths attributable to cardiovascular disease has been upward for women, while it is shifting downward for men.
Why focus on HDL?
Improvement in HDL is the strongest predictor of reduced risk for cardiac events. So says an analysis of 17 major lipid intervention trials between 1987 and 2003 (n = 44,170).2
Another study3 demonstrated that HDL cholesterol is the stronger predictor of CVD risk in women. In addition, several large observational studies have shown that increasing HDL cholesterol by 1 mg/dL in men reduces CVD risk by 2%, whereas increasing HDL in women by 1 mg/dL decreases CVD risk by 3%.4
Higher HDL levels may explain later onset of CVD in women. The advantage that women have over men in CVD risk prior to menopause seems to be at least partly due to their higher levels of HDL cholesterol: The average HDL level in women is 56 mg/dL, versus 46 mg/dL in men. This advantage begins to disappear after menopause, presumably because of changes in hormone levels and decreasing HDL-2 cholesterol, the most cardioprotective HDL fraction.
Other reasons to focus on HDL. In addition to the increased CVD risk associated with menopause, women of all ages in the United States have an increasing tendency—at almost epidemic rates—toward obesity and metabolic syndrome, which are known CVD risk factors.5 The dyslipidemia seen with those conditions is characterized by low HDL cholesterol and high triglycerides. Thus, maintaining healthy HDL levels is clearly an important goal for overall cardiovascular health, especially in women.
In addition, HDL is the key lipoprotein associated with reverse cholesterol transport, the process of carrying excess cholesterol from peripheral tissues to the liver for catabolism.
JUDY’S CASE
METABOLIC SYNDROME CONFIRMED
At her return visit, Judy’s blood pressure remains 140/90 mm Hg, with outside readings ranging from 135 to 145 mm Hg systolic and 85 to 95 mm Hg diastolic. Her laboratory tests reveal fasting blood glucose of 115 mg/dL, total cholesterol of 220 mg/dL, LDL cholesterol of 120 mg/dL, HDL cholesterol of 35 mg/dL, and triglycerides of 300 mg/dL.
What are her key heart-health issues?
Individualized management—recommended by NCEP/ATP III guidelines— should focus on reversing the metabolic defects of insulin resistance: hypertension, obesity, glucose intolerance, and dyslipidemia.
At present, Judy’s 10-year risk of a cardiac event is 4% by Framingham risk scoring, but it is likely to increase if the metabolic syndrome is not addressed.
How to preserve healthy HDL levels
Diet and regular aerobic exercise are recommended by the NCEP/ATP III guidelines, especially for obese patients with metabolic syndrome. However, dietary changes do not raise HDL cholesterol. In fact, dieting to lose weight will almost certainly lower HDL levels. That’s because people who eat a diet very low in fat tend to replace the fat calories with carbohydrates, and a low-fat, high-carbohydrate diet will reduce all cholesterol fractions—but HDL cholesterol will decrease disproportionately.6
Recommend complex carbohydrates and moderate fat intake
To avoid excessive reduction in HDL cholesterol, any weight-loss diet should involve moderate fat intake (35% of total calories) and emphasize monounsaturated fats such as olive or canola oil, along with complex carbohydrates found in fruits, vegetables, and whole grains.7 After weight loss is stabilized, HDL cholesterol tends to increase somewhat, but may not return all the way to baseline.
New guidelines on how to intervene
Most women who die suddenly from coronary heart disease had no previous symptoms, and that makes prevention all the more important.
Though it hasn’t been long since the first woman-centered recommendations on preventing cardiovascular disease,19 our understanding of preventive interventions has improved enormously. Thus, the American Heart Association convened a new expert panel to review and, where necessary, revise the original guidelines.20 Here are some of the highlights.
Forget “haves” and “have-nots”
Lori Mosca and the other members of the expert panel observe that “the concept of CVD as a categorical, ‘have-or-have-not’ condition has been replaced with a growing appreciation for the existence of a continuum of CVD risk.”20
For example, the low-risk category (<10% risk of a coronary heart disease event in the next 10 years, according to the Framingham Risk Score for women) would include women with optimal levels of risk factors and a heart-healthy lifestyle, as well as women with metabolic syndrome but no other risk factors. In contrast, women with established coronary heart disease, diabetes mellitus, or chronic kidney disease would fall into the high-risk group (>20% risk). Those with multiple risk factors or markedly elevated levels of a single risk factor fall somewhere in between.
The 5 lifestyle laws
Women are advised to consistently:
- eat plenty of fruits and vegetables, whole grains, and low-fat or nonfat dairy items
- avoid smoking and smokeless tobacco
- perform at least 30 minutes of moderate-intensity activity, such as brisk walking, most days
- achieve and maintain a body mass index between 18.5 and 25.9 kg/m2 and a waist circumference less than 35 inches
- consider omega-3 fatty acid supplementation, especially if risk is high. The guidelines extol the benefits of fish, which contain omega-3 fatty acids, but warn against consumption of fish likely to contain unsafe levels of mercury (shark, sword-fish, king mackerel, and tilefish) by gravidas and women of reproductive age.
BP and cholesterol control
- Blood pressure. Maintain at or below 120/80 mm Hg through lifestyle approaches, or drug therapy when BP is 140/90 mm Hg or higher.
- Dietary fat and cholesterol. Keep saturated fat intake to less than 7% of calories, and cholesterol below 200 mg/dL with high risk or elevated LDL.
- LDL-cholesterol. Use drug therapy (preferably statins) if risk is high and LDL is below 100 mg/dL. Add lifestyle adjustments if risk is high and LDL cholesterol is at or above 100 mg/dL.
What not to take to prevent CVD
The guidelines warn against prescribing—or continuing—estrogen-progestin therapy to prevent CVD. Nor should other forms of menopausal hormone therapy, such as unopposed estrogen, be prescribed or continued unless new findings indicate a beneficial role.
Also discouraged are antioxidant vitamin supplements to prevent CVD.
Look for depression
Especially women with CVD should be referred or treated when depression is found, as it can hamper a woman’s efforts at prevention.
The full text of the guidelines can be viewed at
http://circ.ahajournals.org/cgi/content/full/109/5/672.
Regular exercise raises HDL
One way to avoid an overall reduction in HDL levels with weight loss is to prescribe exercise in conjunction with it. Regular exercise is an excellent way to raise HDL cholesterol levels. Studies suggest that, for women, the volume of exercise is more important than intensity. Thus, women should strive to walk 7 to 14 miles per week or otherwise expend approximately 1,200 to 1,600 Kcal.8,9
Regular exercise is recommended as one of the NCEP/ATP III therapeutic lifestyle changes that directly benefit cardiovascular health and blood pressure and help the individual maintain optimal body weight. Although exercise raises HDL levels, it does so more easily in men than in women. HDL cholesterol increases in men with both intensity and volume of exercise.10 Women appear to derive slightly less of a benefit, perhaps because their HDL levels are already generally higher.
In women, studies have reported an increase in HDL cholesterol as high as 15% for both premenopausal and post-menopausal women who follow moderate exercise regimens—and the lower the baseline HDL level, the greater the increase.8
Exercise level was inversely associated with cardiovascular risk in the Women’s Health Initiative,9 which followed a cohort of 73,743 women prospectively for an average of 3.2 years. Women at the highest quintile of exercise level reduced their CVD risk by 53% over the lowest quintile, and moderate activity such as walking led to risk reductions similar to those involving more vigorous activities.
Recommend alcohol—or not?
Moderate alcohol consumption—1 to 3 drinks per day, or 15 to 45 g ethanol— improves lipoprotein levels and reduces CVD risk. The flavonoids in red wines also reduce platelet aggregation and clotting tendencies. However, advising a patient to consume alcohol to reduce her CVD risk is controversial; many physicians are reluctant to do so due to obvious concerns over toxicity and dependency.
Response to alcohol may vary by menopausal status. In 1 study,11 pre-menopausal women decreased their LDL cholesterol by 12% (P=.01) after 3 glasses of wine daily for 3 weeks, but there was no significant increase in HDL levels.
In the same study, postmenopausal women increased HDL levels by 12% (P=.03), but their LDL cholesterol decreased only minimally.11
Another study12 in postmenopausal women who consumed 0, 1, or 2 drinks daily (0, 15, or 30 g ethanol) for 8 weeks showed a significant decrease of 4% in LDL cholesterol at 1 drink (15 g), but no significant further decrease at 2 drinks (30 g). In the same study, HDL increased non-significantly at 1 drink (15 g), but increased significantly (5%) at 2 drinks (30 g). There may be a threshold of 30 g ethanol daily for postmenopausal women to benefit significantly from alcohol consumption.
JUDY’S CASE
LIFESTYLE RECOMMENDATIONS
The foundation of Judy’s management should be the triad of weight loss, exercise, and a diet that limits refined carbohydrates and emphasizes fiber, fruits and vegetables, whole grains, and healthy fats (ie, olive, canola, and fish oils).
In prescribing exercise, emphasize quantity over intensity, such as 14 miles of walking weekly or 60 to 90 minutes daily of aerobic activity.
Since she has no history of cardiac symptoms, and low-intensity, high-quantity exercise is advised, she does not need a screening cardiac stress test before beginning her regimen.
Pantethine
Pantethine is an over-the-counter (OTC) nutritional supplement that combines the B vitamin pantothenic acid with the amino acid cysteamine. Although pantothenic acid alone has no lipid-lowering effects, pantethine does: It lowers LDL cholesterol, very-low-density lipoprotein (VLDL) cholesterol, and triglycerides, and raises HDL levels. The exact mechanism of action is unknown, but it is thought to involve primarily the effects of cysteamine on lipid metabolism in the liver.
Recommended dose. At 600 to 900 mg daily, the typical response is an increase of up to 18% in HDL cholesterol and reductions in LDL cholesterol, VLDL cholesterol, and triglycerides of 13%, 20%, and 26%, respectively.13
In a recent US study, pantethine significantly raised HDL-2 cholesterol, the more cardioprotective fraction of HDL, and increased the particle size of LDL cholesterol, rendering it less atherogenic.14
Pantethine also reduces visceral fat. The same study14 reported a significant reduction in visceral fat, a component of metabolic syndrome, as measured by computerized dual-energy x-ray absorptiometry in individuals taking 900 mg daily for 6 weeks. This reduction appears to be primarily an effect of pantothenic acid and had been demonstrated in animal studies.
No side effects. Pantethine is exceptionally well tolerated, with virtually no side effects. An occasional person will experience gastrointestinal upset and diarrhea, which resolve when the drug is discontinued.
Recommend formulations that contain Pantesin (Daiichi Fine Chemicals, New York City), a pharmaceutical grade of pantethine, because extensive research confirms the benefits I have described. Otherwise, make sure the manufacturer is a reputable company, with scientific studies to support its claims of safety, efficacy, and bioavailability.
Nicotinic acid
Nicotinic acid (NA), another B vitamin available OTC as a nutritional supplement, is the most effective agent for raising HDL levels.
Recommended dose. A divided dose of 3,000 mg daily of the immediate-release form of NA can raise HDL levels as much as 30%. Unfortunately, that form of NA has a high incidence of adverse effects, such as flushing, itching, and GI upset.15
Sustained-release NA is generally well tolerated, but somewhat less effective at raising HDL. A lower dose of sustained-release NA (1,000 to 1,500 mg daily) is recommended to avoid liver toxicity and typically leads to HDL increases as high as 20%.15
NA offers additional benefits to the lipid profile, typically lowering LDL cholesterol by 20%, triglycerides by 15%, and lipoprotein(a) by 15%.15
Monitor all forms of NA with liver enzymes, blood glucose, and uric acid because treatment can elevate these markers.
Give NA preparations extra scrutiny. The general caveats about quality and bioavailability apply especially to NA. Nonprescription products on the market that contain nicotinamide and inositol hexanicotinate are advertised as “no-flush” niacin because they do not cause cutaneous side effects, but they also have no lipid benefits.
Cost. NA is relatively inexpensive, and good-quality sustained-release products such as Endur-acin (Endurance Products, Tigard, Ore) can be purchased OTC for 12 cents per 500-mg tablet or a daily cost of 24 to 36 cents.16
Sustained-release NA is also available by prescription (Niaspan, Kos Pharmaceuticals, Cranbury, NJ), but it is considerably more expensive ($1.98 per 500-mg tablet, or $3.96 to $5.94 daily) and has not been shown to be more effective or better tolerated than the better OTC products.16
JUDY’S CASE
RAISING HDL WITHOUT DRUGS
Judy’s lipid abnormalities would benefit from a supplement of pantethine (300 mg thrice daily) or NA (1,000 mg thrice daily of plain/quick release or 500 mg twice daily of sustained release to reduce flushing side effects).
Her greatest risk with her current lipid levels is low HDL, and the best agent to raise these levels is NA.
Pantethine also raises HDL and selectively improves the HDL-2 subfraction, which is most cardioprotective. Both supplements also improve the other lipid abnormalities.
In addition, referral to a dietician for detailed instruction in food choices and preparation may be useful.
Pharmacologic therapies
Hormone replacement therapy (HRT) is no longer recommended to prevent CVD and should be given only for menopausal symptoms during the perimenopausal years—despite the fact that estrogen has been shown to raise HDL cholesterol by 8% in postmenopausal women.17
Estrogens increase HDL by increasing production of apoA-1, the main lipoprotein in HDL, and by decreasing HDL catabolism by inhibiting hepatic lipase. The 17-hydroxyprogesterone component of HRT given to women with an intact uterus to prevent endometrial cancer has no significant lipid effects.
Paradoxically, the increased CVD risk found in the HRT arm of the Women’s Health Initiative17 was in the face of improved HDL (8%) and LDL (–14%) cholesterol and appeared to be the result of increased thrombotic events.
Further analysis of Women’s Health Initiative data showed that women who were still within 10 years of menopause actually did experience a reduction in CVD risk. That observation, along with some primate research on HRT, suggests that the risk or benefit of HRT with respect to CVD may be a matter of timing. See “Emerging hypothesis may explain estrogen paradox”
At the 2004 American Heart Association meeting, Dr. Thomas Clarkson, who has conducted primate research on hormone replacement therapy (HRT) and the risk of cardiovascular disease (CVD), described the emerging hypothesis that may explain the HRT paradox of increased CVD risk despite evidence of benefit in observational studies.21
Estrogen is a potent upregulator of matrix metal-loproteases. These proteolytic enzymes are a normal constituent of the endometrium and important in its remodeling with each menstrual cycle. Matrix metal-loproteases are also found in the fibrous cap that seals off the necrotic core of an advanced atheroma from the vascular lumen. Most perimenopausal women have enjoyed estrogen’s protective effect throughout their reproductive years and thus have developedlittle advanced atherosclerotic disease.
Ten or more years past menopause, however, clinically significant atherosclerotic lesions often develop in women who have been without the protection of estrogen. If estrogen is added at this stage, it causes increased matrix metalloprotease activity in the fibrous cap of any atheroma. This proteolytic activity can destabilize the fibrous cap, allowing necrotic core material to come in contact with the bloodstream.
This necrotic material is highly thrombogenic and stimulates clot formation in the vascular lumen. Clarkson demonstrated this process in research on perimenopausal and postmenopausal primates.
This hypothesis will soon be tested in a clinical trial in humans; CVD risk is expected to decrease by 50% to 70% in women who have taken HRT continuously from perimenopause.
Statins and other HDL-modifying drugs
The statins are a first choice for LDL reduction, but lead to only modest increases (4%–10%) in HDL levels.18 Fibric acid derivatives are somewhat more effective; they lead to increases in HDL of 6% to 18%. Both types of drugs are considerably more expensive than OTC NA and not as effective at raising HDL.
Combining statins with other agents that raise HDL has been tried: The NA–statin combination can be effective in managing dyslipidemias of both LDL and HDL. Fibric acid derivatives should not be used with statins because of the increased risk of serious myopathies.18
JUDY’S CASE
THERAPEUTIC TARGETS
Judy’s goals should include:
- reducing blood pressure to less than 120/80 mm Hg,
- decreasing weight to about 140 lb,
- achieving a waist measurement of less than 35 inches,
- reducing fasting blood glucose to less than 100 mg/dL,
- decreasing triglycerides to less than 150 mg/dL, total cholesterol to less than 200 mg/dL, and LDL levels to less than 100 mg/dL, and
- raising HDL to more than 45 mg/dL.
All these parameters should be checked every 3 months until the goals are achieved.
If Judy fails to progress or develops symptoms of heart disease, she should be referred to a cardiologist for further evaluation and more aggressive treatment.
The author reports no conflicts relevant to this article.
1. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486-2497.
2. Alsheikh-Ali A, Abourjaily HM, Stanek EJ, et al. Increases in HDL-cholesterol are the strongest predictors of risk reduction in lipid intervention trials. Circulation. 2004;110(17 suppl 3):III-813.
3. Jacobs DR, Jr, Meban IL, Bangdiwala SI, et al. High density lipoprotein cholesterol as a predictor of cardiovascular disease mortality in men and women: the follow-up study of the Lipid Research Clinics Prevalence Study. Am J Epidemiol. 1990;131:32-47.
4. Gordon DJ, Probstfiel JL, Garrison RJ, et al. High-density lipoprotein cholesterol and cardiovascular disease: four prospective American studies. Circulation. 1989;79:8-15.
5. Hu Fb, Willet WC, Li T, et al. Adiposity as compared with physical activity in predicting mortality among women. N Engl J Med. 2004;351:2694-2703.
6. Mensink RP, Zock PL, Kester A, et al. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003;77:1146-1155.
7. Pereira MA, Swain J, Goldfine AB, et al. Effects of a low-glycemic load diet on resting energy expenditure and heart disease risk factors during weight loss. JAMA. 2004;292:2482-2490.
8. Kokkinos PF, Holland JC, Pittaras AE, et al. Cardiorespiratory fitness and coronary heart disease risk factor association in women. J Am Coll Cardiol. 1995;26:358-364.
9. Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716-725.
10. Kokkinos PE, Fernhall B. Physical activity and high density lipoprotein cholesterol levels: what is the relationship? Sports Med. 1999;28:307-314.
11. Van Der Gaag MS, Sterksma A, Schaafsma G, et al. Moderate alcohol consumption lowers risk factors for cardiovascular disease in postmenopausal women fed a controlled diet. Am J Clin Nutr. 2002;75:593-599.
12. Baer DJ, Judd JT, Clevidence BA, et al. Moderate alcohol consumption and changes in postprandial lipoproteins of premenopausal and postmenopausal women: a diet-controlled randomized intervention study. J Womens Health Gend Based Med. 2000;9:607-616.
13. Pins JJ, Keenan JM. Pantethine: a new option in managing dyslipidemia. J Am College Nutr. 2005 [in press].
14. Pins JJ, First S, Shamliyan T, Keenan J. Pantethine beneficially affects apolipoprotein A-1, apolipoprotein B, low-density lipoprotein particle size but not high-sensitivity C-reactive protein in a dyslipidemic population. Circulation. 2004;110(17 suppl 3):III-778.
15. Crouse JR, 3rd. New developments in the use of niacin for treatment of hyperlipidemia: new considerations in the use of an old drug. Coron Artery Dis. 1996;7:321-326.
16. Retail pharmacy quote. Walgreen’s Pharmacy, Minneapolis, Minn. January 2005.
17. Risks and benefits of estrogen plus progestin in healthy post-menopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
18. Hersberger M, von Eckardstein A. Low high-density lipoprotein cholesterol: physical background, clinical importance and drug treatment. Drugs. 2003;63:1907-1945.
19. Mosca L, Grundy SM, Judelson D, et al. Guide to preventive cardiology for women. AHA/ACC scientific statement, consensus panel statement. irculation. 1999;99:2480-2484.
20. Mosca L, Appel LJ, Benjamin EJ, et al. AHA Guidelines: evidence-based guidelines for cardiovascular disease prevention in women. Circulation. 2004;109:672-693.
21. Clarkson T. Women’s Heart Health Symposium. Presented at the American Heart Association annual meeting, Nov 9, 2004, New Orleans.
1. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486-2497.
2. Alsheikh-Ali A, Abourjaily HM, Stanek EJ, et al. Increases in HDL-cholesterol are the strongest predictors of risk reduction in lipid intervention trials. Circulation. 2004;110(17 suppl 3):III-813.
3. Jacobs DR, Jr, Meban IL, Bangdiwala SI, et al. High density lipoprotein cholesterol as a predictor of cardiovascular disease mortality in men and women: the follow-up study of the Lipid Research Clinics Prevalence Study. Am J Epidemiol. 1990;131:32-47.
4. Gordon DJ, Probstfiel JL, Garrison RJ, et al. High-density lipoprotein cholesterol and cardiovascular disease: four prospective American studies. Circulation. 1989;79:8-15.
5. Hu Fb, Willet WC, Li T, et al. Adiposity as compared with physical activity in predicting mortality among women. N Engl J Med. 2004;351:2694-2703.
6. Mensink RP, Zock PL, Kester A, et al. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003;77:1146-1155.
7. Pereira MA, Swain J, Goldfine AB, et al. Effects of a low-glycemic load diet on resting energy expenditure and heart disease risk factors during weight loss. JAMA. 2004;292:2482-2490.
8. Kokkinos PF, Holland JC, Pittaras AE, et al. Cardiorespiratory fitness and coronary heart disease risk factor association in women. J Am Coll Cardiol. 1995;26:358-364.
9. Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716-725.
10. Kokkinos PE, Fernhall B. Physical activity and high density lipoprotein cholesterol levels: what is the relationship? Sports Med. 1999;28:307-314.
11. Van Der Gaag MS, Sterksma A, Schaafsma G, et al. Moderate alcohol consumption lowers risk factors for cardiovascular disease in postmenopausal women fed a controlled diet. Am J Clin Nutr. 2002;75:593-599.
12. Baer DJ, Judd JT, Clevidence BA, et al. Moderate alcohol consumption and changes in postprandial lipoproteins of premenopausal and postmenopausal women: a diet-controlled randomized intervention study. J Womens Health Gend Based Med. 2000;9:607-616.
13. Pins JJ, Keenan JM. Pantethine: a new option in managing dyslipidemia. J Am College Nutr. 2005 [in press].
14. Pins JJ, First S, Shamliyan T, Keenan J. Pantethine beneficially affects apolipoprotein A-1, apolipoprotein B, low-density lipoprotein particle size but not high-sensitivity C-reactive protein in a dyslipidemic population. Circulation. 2004;110(17 suppl 3):III-778.
15. Crouse JR, 3rd. New developments in the use of niacin for treatment of hyperlipidemia: new considerations in the use of an old drug. Coron Artery Dis. 1996;7:321-326.
16. Retail pharmacy quote. Walgreen’s Pharmacy, Minneapolis, Minn. January 2005.
17. Risks and benefits of estrogen plus progestin in healthy post-menopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
18. Hersberger M, von Eckardstein A. Low high-density lipoprotein cholesterol: physical background, clinical importance and drug treatment. Drugs. 2003;63:1907-1945.
19. Mosca L, Grundy SM, Judelson D, et al. Guide to preventive cardiology for women. AHA/ACC scientific statement, consensus panel statement. irculation. 1999;99:2480-2484.
20. Mosca L, Appel LJ, Benjamin EJ, et al. AHA Guidelines: evidence-based guidelines for cardiovascular disease prevention in women. Circulation. 2004;109:672-693.
21. Clarkson T. Women’s Heart Health Symposium. Presented at the American Heart Association annual meeting, Nov 9, 2004, New Orleans.
The Lifestyle and Clinical Survey: A Medical History Questionnaire
How Reminders of Prior Combat Affect PTSD Symptoms
The pendulum swings from fear to understanding
Time and study make a difference. So does careful review and reappraisal of existing data. In the past year, the pendulum has swung away from fear of hormone therapy to a better understanding of indications, risks and benefits—an understanding driven largely by the evidence-based position statements of the North American Menopause Society (NAMS).
A meta-analysis of randomized controlled trials of phytoestrogens attested to lack of efficacy or weak effect, which helps clear the picture on soy and red clover, but the researchers stressed that the lack of quality control does not rule out the possibility that some products might carry steroidal effects and potential risk.
And another year has brought even more evidence that diet, exercise, smoking cessation and the like really do improve health and quality of life.
Advisory on hormone therapy and “bio-identicals”
The NAMS Hormone Therapy Panel concluded definitively that bio-identical hormones should be considered in the same category as all the sex steroids, which, in the absence of specific safety and efficacy studies, carry the same risks and benefits as related products.
On the other hand, alternatives do exist for specific indications, such as bisphosphonates for bone conservation.
The new NAMSPosition Statement stresses individualized treatment based on the recommendations below.
The full report is available at www.menopause.org.
- Treatment of moderate to severe menopausal symptoms is the primary indications for systemic therapy. Every systemic product is FDA-approved for this indication.
- Every systemic and local product is approved for moderate vulvar and vaginal atrophy. For this indication alone, local ET is generally advised.
- Duration should be for the lowest effective dose and shortest time consistent with treatment goals.
- If the woman is well aware of potential risks and benefits, and if there is clinical supervision, extended use of the lowest effective ET/EPT dose for treatment goals is acceptable in women who believe the benefits outweigh the risks, for those at high risk of osteoporotic fracture who also have moderate to severe menopause symptoms, for further prevention of established bone loss when alternate therapies are not appropriate or cause side effects, or when outcomes of extended use of those therapies are not known.
- Although specific compounds, doses, and routes of administration may have different outcomes, clinical trial results for one agent should be generalized to all agents within the same family in the absence of data for each specific product. This proviso also applies to the so-called bioidentical products.
Question marks
The Hormone Therapy panel could not agree unanimously on these questions:
- Should women who are doing well on long-term HT discontinue?
- What is the best way to discontinue HT, abrupt cessation or tapering?
- Is the effect of continuous-combined EPT different from that of continuous estrogen with sequential progestogen?
- How definitive is the evidence on early increased CHD risk with HT?
- Conflicting data precluded a consensus on adverse breast cancer and cardiovascular outcomes associated with ET/EPT.
ACKNOWLEDGMENTS
The following commentaries on key papers are from the NAMS First To Knowemail program for members. I thank the members of NAMS who have taken time out to provide these objective reviews of the studies presented here, and Phil Lammers, NAMS Medical Editor.
OSTEOPOROSISCurb your enthusiasm—no need to rush bone drugs if risk is low
McClung MR, Wasnich RD, Hosking DJ, et al, on behalf of the Early Postmenopausal Intervention Cohort (EPIC) study group. Prevention of postmenopausal bone loss: six-year results from the early postmenopausal intervention cohort study. J Clin Endocrinol Metab 2004;89:4879-4885. LEVEL 1 EVIDENCE: Randomized, controlled trial
In this 6-year study of women in their 50s, the placebo group lost an inconsequential amount of bone mass. Not surprisingly, women using alendronate had some increase in BMD and some reduction in bone turnover markers.
Women in their 50s are not melting away. Their bones are not dissolving out from under them, contrary to what many media reports would have ObGyns and patients believe. Still, many clinicians are enthusiastic about prescribing bone drugs like bisphosphonates to women in their 50s who are generally healthy. (And there is no doubt that we do have bone drugs found to be safe and effective in well-designed trials, including the EPIC study.)
Yet there has been a major shift away from starting osteoporosis prevention drugs soon after menopause. EPIC data add support for a “go slow” strategy for drug intervention in healthy women in their 50s.
The EPIC study involved a total of 1,609 women ages 45 to 59, who received alendronate or placebo in a double-blind, randomized design. BMD was measured annually. The 4-year results were reported previously, and the 6-year results were published just last fall. Not surprisingly, women using alendronate had some increase in BMD and some reduction in bone turnover markers. But the results in the women who took placebo are of singular interest.
After 6 years, women on placebo had lost very little bone. The amount lost was statistically significant, but clinically inconsequential. The average BMD in women on placebo decreased 3% in the spine and 2% in the hip. Thus, the average rate of bone loss was about 0.5% per year.
A bone mass decrease of this extent represents a decline of about -0.3 T score, which is negligible. In the EPIC study, the 6-year fracture benefit, based on any type of fracture, boils down to lowering the risk from 1 in 11 on placebo to 1 in 9 on alendronate. These healthy women in their 50s had a very low risk of fracture, and taking a drug for 6 years had very little benefit for fracture reduction.
Women in their 50s typically have about 10% to 15% less bone mass than women of 25 to 30, when bone mass is at its peak. That 10% to 15% lower BMD translates to a T score of –1 to –1.2 , which is currently being labeled as osteopenic. Many patients and physicians have come to feel that osteopenia must always be treated with our newer drugs.
We are discovering that starting healthy women in their 50s on osteoporosis prevention drugs carries an extremely high cost per fracture avoided. During the 10 years since the startup of the EPIC study, support for early drug intervention in healthy women still in their 50s has dwindled. Now, expert groups, including the National Osteoporosis Foundation and the US Preventive Services Task Force, advise waiting until age 65 before starting osteoporosis risk evaluation or considering drug intervention in women who are otherwise healthy.
In my practice, I give healthy women in their 50s permission not to take drugs if their risk of fracture within the next 5 to 10 years is low. The picture is quite different in postmenopausal women in their 50s who do have high fracture risk, such as those who have already had a fracture, or who have very low bone density or high exposure to glucocorticoids.
EPIC data support the concept that the rate of bone loss is quite slow after a year or 2 has elapsed after menopause.
We need to avoid medicalizing these patients simply because we have drugs that reduce bone loss or because women in their 50s have less bone mass than 25-year-olds.
BIBLIOGRAPHY
Hosking D, Chilvers CE, Christiansen C, et al. Prevention of bone loss with alendronate in postmenopausal women under 60 years of age. Early Postmenopausal Intervention Cohort Study Group. N Engl J Med. 1998;338:485-492.
Wasnich RD, Bagger YZ, Hosking DJ, et al. Changes in bone density and turnover after alendronate or estrogen withdrawal. Menopause. 2004;11:622-630.
Siris ES, Bilezikian JP, Rubin MR, et al. Pins and plasters aren’t enough: a call for the evaluation and treatment of patients with osteoporotic fractures. J Clin Endocrinol Metab. 2003;88:3482-3486.
Rosen CJ, Black DM, Greenspan SL. Vignettes in osteoporosis: a road map to successful therapeutics. J Bone Miner Res. 2004;19:3-10.
HORMONE THERAPYDoes age affect mortality rate in postmenopausal women using HT?
Salpeter SR, Walsh JME, Greyber E, Ormiston TM, Salpeter EE. Mortality associated with hormone replacement therapy in younger and older women. J Gen Intern Med. 2004;19:791–804. META-ANALYSIS
- This study is sure to incite yet another round of debate about postmenopausal hormone therapy, but it does suggest that we can provide substantial reassurance about safety in younger women considering hormone therapy for menopause-related symptoms.
This study attempted to discover whether the age of the postmenopausal woman using hormone therapy affects mortality. Investigators performed a meta-analysis of clinical trials that reported mortality rates associated with use of postmenopausal hormone therapy, and analyzed the results based on mean ages.
They reported a significant trend between increasing risk of mortality and increasing mean age of the women using hormone therapy—raising the possibility of a health benefit for younger postmenopausal women.
The studies included in the metaanalysis varied in entry criteria, outcomes assessed, number of subjects, and HT type and dosage. Furthermore, because age groups were defined by mean age in each trial rather than actual age of pooled participants, some overlap in ages likely occurred between the analyses of younger and older women.
In postmenopausal women younger than 60, the total mortality rate was reduced by 39% in women taking estrogen-containing hormone therapy, which was significant; in women older than 60, there was no significant effect on total mortality.
The data were from 30 randomized, controlled clinical trials published between 1966 and 2002, and included 26,708 women taking estrogen (ET) or estrogen plus progestogen (EPT). Data were pooled to determine total mortality and mortality due to specific causes such as cardiovascular disease and cancer. The mean trial duration was 4.5 years, and the mean age was 62.2 years.
When the study population was divided into younger and older age groups based on mean ages, it was found that those younger than 60 (mean age, 53.9) had a significantly reduced OR for total mortality of 0.61 (95% CI, 0.39–0.95) and those older than age 60 (mean age, 64.6) had an OR of 1.03 (95% CI, 0.90–1.18).
For specific causes, the OR for cardiovascular disease mortality associated with ET/EPT was 1.10 (95% CI, 0.90–1.34). For overall cancer mortality, the OR was 1.03 (95% CI, 0.82–1.29) and for breast cancer mortality, the OR was 1.03 (95% CI, 0.29–3.67).
For causes other than cardiovascular disease or cancer, mortality was significantly lower in women on HT: OR 0.67 (95% CI, 0.51–0.88). When divided into younger and older age groups, ET/EPT was not associated with a significant change in mortality, with the exception of reduced mortality from causes other than cardiovascular disease and cancer in the older age group (OR, 0.68; 95% CI, 0.56–0.91).
Does HT improve insulin resistance?
Margolis KL, Bonds DE, Rodabough RJ, et al, for the Women’s Health Initiative Investigators. Effect of oestrogen plus progestin on the incidence of diabetes in postmenopausal women: results from the Women’s Health Initiative Hormone Trial. Diabetologia. 2004;47:1175–1187. LEVEL 1 EVIDENCE: Randomized, controlled trial
Decreased insulin and fasting glucose
- Combined estrogen plus progestogen may reduce the incidence of diabetes, possibly by mediating a decrease in insulin resistance.
Hormone therapy, compared with placebo, was associated with 15 fewer cases of diabetes per 10,000 women per year. Fasting glucose and insulin decreased compared with placebo, and may suggest improved insulin resistance. Although others have reported similar results, it is unlikely that hormone therapy will be prescribed to prevent diabetes, given its greater risk than benefit for other outcomes observed in other WHI analyses.
In the EPT part of WHI, a total of 15,641 postmenopausal women aged 50 to 79 were assigned to placebo or continuous-combined EPT (0.625 mg/day conjugated equine estrogens plus 2.5 mg/day medroxyprogesterone acetate). The incidence of diabetes was based on self-reports of insulin or oral diabetes drug treatment. Fasting glucose, insulin, and lipoproteins were measured at 1 and 3 years. After 5.6 years, the incidence of treated diabetes was 3.5% in the EPT group and 4.2% in the placebo group (hazard ratio, 0.79; 95% CI, 0.67–0.93; P= 0.004). Decreases in fasting glucose and insulin, suggesting decreased insulin resistance, were significant at 1 year in EPT users compared with placebo. The authors concluded that EPT reduces the incidence of diabetes possibly through a decrease in insulin resistance.
To be sure that a drug prevents a disease, everyone with the disease should be excluded at baseline, and at the end of the trial, everyone should be tested for the disease—if it is commonly undiagnosed. To study the incidence of new diabetes, all women (6%) with self-reported diabetes at baseline were excluded, and correctly so. But half of US adults with diabetes are undiagnosed. The WHI 6% prevalence is half of the assumed 12% prevalence in older overweight women. In the WHI, average age was 63 years and average body mass index was 28. Thus, it is not certain that the reduced risk occurred in women who were diabetes-free at baseline.
Fasting glucose was reduced in the EPT part of WHI, as in the Postmenopausal Estrogen Progestin Intervention (PEPI) trial. But 2-hour glucose levels were elevated by hormone treatment in PEPI, and were not measured in the WHI. Many studies have shown that postprandial or post-challenge glucose is a stronger risk factor for cardiovascular disease than fasting hyperglycemia.
Could an elevated post-challenge glucose have played a role in the unexpected excess cardiovascular disease observed with hormone therapy in healthy women in WHI and with hormone therapy in women with documented coronary heart disease in the Heart and Estrogen/progestin Replacement Study (HERS)?
Will transdermal estrogen reduce both fasting and post-challenge glucose? These and other questions remain. (EBC)
Lifestyle changes work best
- This report raises the possibility but does not justify prescribing EPT for diabetes prevention.
Postmenopausal women randomized to EPT had a lower incidence of treated diabetes, by self-report, than women assigned to placebo: a 21% relative risk reduction over 3 years. At 1 year, a comparison of changes from baseline in estimated insulin resistance (HOMA model) in a subgroup indicated a significant reduction with EPT compared with placebo group, but no significant difference at 3 years.
Because of the far-reaching morbidity and mortality due to Type 2 diabetes, particularly from cardiovascular disease, prevention would have major benefits, but the authors acknowledge that this report does not justify prescribing this therapy for this purpose, given hazards previously reported in the WHI.
Still, we can bear in mind other means of reducing risk for diabetes. In the Diabetes Prevention Program,1metformin reduced type 2 diabetes risk by 31%, and a diet plus exercise program reduced it even more: by 58% over approximately 3 years of follow-up in high-risk persons. People at risk for diabetes should be counseled to make lifestyle changes that can reduce this risk far more, and more safely, than might EPT. (CGS)
Consider diabetes implications
- EPT can reduce the incidence of diabetes to the same degree as medications used for cardiovascular disease prevention.2
Growing evidence indicates that reducing insulin resistance in women can prevent onset of diabetes,3and that improving insulin resistance can slow the progression of atherosclerosis.4 Observational studies5—the Heart and Estrogen/progestin Replacement Study (HERS),6 and now the WHI—strongly indicate that EPT reduces the incidence of diabetes in postmenopausal women. Notably, HERS and WHI findings were with continuous-combined estrogen with progestin, the latter often viewed as antagonistic to the beneficial effects of estrogen on carbohydrate metabolism.) Diabetes is much more devastating in women, and more likely to strike. The risk (3,000 of 10,000) in postmenopausal women equals or exceeds that of postmenopausal breast cancer, coronary disease, or hip fracture.7The time has come to consider health and cost implications of long-term HT, especially in women with diabetes risk factors: age, obesity, high systolic BP, high nonfasting glucose, antihypertensive drug use, low HDL, or Hispanic or African-American ethnicity. Clinical trials confirming HT’s benefit add to the totality of evidence that the benefits outweigh the risks.8Since long-term effects (>10 years) reflect only observational data, we urgently need studies designed to understand long-term benefits and risks. (HNH)
1. Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403.
2. Pepine CJ, Cooper-Dehoff RM. Cardiovascular therapies and risk for development of diabetes. J Am Coll Cardiol. 2004;44:509-512.
3. Buchanan TA, Xiang AH, Peters RK, et al. Preservation of pancreatic beta-cell function and prevention of type 2 diabetes by pharmacological treatment of insulin resistance inhigh risk Hispanic women. Diabetes. 2002;51:2796-2803.
4. Xiang AH, Peters RK, Kjos SL, et al. Effect of thiazolidinedione treatment on progression of subclinical atherosclerosis in premenopausal women at high risk for type 2 diabetes. J Clin Endocrinol Metab. 2005;90:1986-1991.
5. Manson JE, Rimm EB, Colditz GA, et al. A prospective study of postmenopausal estrogen therapy and subsequent incidence of non-insulin-dependent diabetes mellitus. Ann Epidemiol. 1992;2:665-673.
6. Kanaya AM, Herrington D, et al. Glycemic effects of postmenopausal hormone therapy: Heart and Estrogen/progestin Replacement Study. Randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2003;138:1-9.
7. Narayan KMV, Boyle JP, et al. Lifetime risk for diabetes mellitus in the US. JAMA 2003;290:1884-1890.
8. Philips LS, Langer RD. Postmenopausal hormone therapy: critical reappraisal and a unified hypothesis. Fertil Steril. 2005;83:558-566.
Soy versus placebo: Underwhelming
Red clover, likewise
Trebs EE, Ensrud KE, MacDonald R, Wilt TJ. Phytoestrogens for treatment of menopausal symptoms: a systematic review. Obstet Gynecol. 2004;104:824–836. META-ANALYSIS
- Phytoestrogens did not significantly improve hot flashes, night sweats, and vaginal dryness, compared to placebo, in this meta-analysis of randomized, controlled clinical trials.
Data on 2,348 women (mean age, 53.1 years) experiencing a mean of 7.1 hot flashes per week were analyzed. Only randomized controlled trials reporting menopausal symptoms of hot flashes, night sweats, and vaginal dryness were included. Mean trial duration was 17 weeks.
- The 11 soy food or beverage supplementtrials (N = 995 women) found no improvement compared with placebo.
- Of the 8 soy food trialsreporting hot flash outcomes, only 1 showed a significant improvement compared with placebo.
- In the 9 soy extract trials, overall results (N = 854) were mixed. In 5 trials using soy extracts and reporting hot flash frequency, 3 found no significant difference in symptoms between the soy and placebo groups; the other 2 (total 114 subjects) found significant improvements.
- The 5 red clover trials(N = 400) showed no improvement over placebo.
Many women in these studies appear to have been perimenopausal rather than postmenopausal. Nine studies included women who had had a menstrual period within the previous 3 to 6 months (late perimenopausal). A subgroup analysis of perimenopausal women would have been useful, since their endocrinologic status is quite different from that of postmenopausal women.
Does soy improve cognition, bone density, or lipids?
Kreijkamp-Kaspers S, Kok L, Grobbee DE, et al. Effect of soy protein containing isoflavones on cognitive function, bone mineral density, and plasma lipids in postmenopausal women: a randomized controlled trial. JAMA. 2004;292:65–74. LEVEL 1 EVIDENCE: Randomized, controlled trial
- Soy did not benefit cognition, bone, or lipids in 60-to-75-year-old women.
This careful trial raises the question of how to reconcile these results with animal and observational studies. In all, 202 postmenopausal women aged 60 to 75 years received 25.6 g/day of a soy protein supplement containing 99 mg isoflavones or a milk protein powder for 1 year. Adherence was monitored by serum genistein. There were no notable differences in:
- Memory, verbal skills, or concentration.
- Bone mineral density or bone-specific alkaline phosphatase, calcium, or phosphorus levels.
- Cholesterol, triglycerides, and lipoprotein plasma levels. These findings may not relate to perimenopausal women, in whom soy has been seen to significantly reduce LDL, but only during midfollicular and periovulatory phases.1 Premenopausal2 but not postmenopausal3monkeys given soy have had beneficial effects on bone quality.
REFERENCES
1. Merz-Demlow BE, Duncan AM, Wangen KE, et al. Soy isoflavones improve plasma lipids in normocholes-terolemic, premenopausal women. Am J Clin Nutr. 2000;71:1462-1469.
2. Kaplan JR, et al. Supplementation reduces the trajectory of atherogenesis in premenopausal monkeys at high risk for development of extensive postmenopausal coronary artery plaques. Menopause. 2004;11:653. Abstract S-17.
3. Register TC, Jayo MJ, Anthony MS. Soy phytoestrogens do not prevent bone loss in postmenopausal monkeys. J Clin Endocrinol Metab. 2003;88:4362-4370.
LIFESTYLE THERAPYThe secret to keeping those girlish carotids
Wildman RP, Schott LL, Brockwell S, Kuller LH, Sutton-Tyrrell K. A dietary and exercise intervention slows menopause-associated progression of subclinical atherosclerosis as measured by intima-media thickness of the carotid arteries. J Am Coll Cardiol. 2004;44:579–585. LEVEL 1 EVIDENCE: Randomized, controlled trial
- Carotid artery intima media thickens during the transition through menopause, but diet and exercise can reduce this progression by almost 50%.
- A diet-and-exercise regimen staves off menopause-associated weight gain and increases in lipids, blood pressure, and blood glucose.
These important findings are strong evidence that diet and exercise can slow the subclinical atherosclerosis progression that accompanies the menopause transition.
The Women’s Healthy Lifestyle Project previously found that weight gain and increased lipids, glucose, and blood pressure often accompany the menopause transition.1 This report describes improvements with diet and exercise intervention, compared with controls.
A total of 535 women aged 44 to 50 years were randomized to lifestyle intervention or assessment-only. All were premenopausal, and all had normal to high-normal body mass index, diastolic blood pressure, and fasting glucose and cholesterol levels.
The diet and exercise regimen used in the study was designed to reduce fat and cholesterol, prevent weight gain, and increase physical activity.
End points were progression of intimamedia thickness in the common carotid artery, internal carotid artery, and bulb segments.
The control group had significantly greater increases in intima-media thickness in women who became postmenopausal compared with those who remained premenopausal.
For women who became perimenopausal or postmenopausal during this 4-year study, diet and exercise slowed the progression of intima-media thickness by a 47% average reduction (P< 0.05), but had no effect on carotid segments in the women who remained premenopausal.
No benefit in intima media thickness was seen in women who remained premenopausal during the trial. Nevertheless, there are many well-documented benefits of healthy diet and exercise in premenopausal women.
Also of note, hormone therapy initiated after baseline measurements did not alter the results.
The message for patients, especially perimenopausal patients is that there is no time like the present to start a healthy lifestyle.
No downside
We’ve learned from the Nurse’s Health Study,2an observational study, that women who eat a healthy diet, do not smoke, and who exercise can reduce their risk of coronary heart disease by 57%.
We learned from the randomized controlled trial by the Diabetes Prevention Program Research Group3 that diet and exercise in high-risk women for 3 years can reduce incidence of new diabetes by 58%.
Now, in this trial, we learn that diet and exercise can reduce the progression of atherosclerosis in perimenopausal women by nearly 50%.
Since there is little, if any, downside to healthy living, why wait?
DISCLOSURES
Dr. Utian has served as an advisor/consultant for Eli Lilly, Pfizer, and Novartis. He has received research funding from Amylin, 3m, Barr, Berlex, BMS, Eli Lilly, Forest, Galen, Glaxo Smith Kline, Neurocrine Biosciences, Novartis, Novo Nordisk, Organon, Pharmacia, P&G, Pfizer, Roche, Sepracor, Solvay, Wyeth, and Yamanouchi.
Dr. Ettinger has served as an advisor for Berlex, Duramed-Barr, Glaxo Smith Kline, and P&G.
REFERENCES
1. Kuller LH, Simkin-Silverman LR, Wing RR, Meilahn EN, Ives DG. Women’s Healthy Lifestyle Project: a randomized clinical trial: results at 54 months. Circulation. 2001;103:32-37.
2. Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC. Primary prevention of coronary heart disease in women through diet and lifestyle. N Engl J Med. 2000;343:16-22.
3. Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403.
Time and study make a difference. So does careful review and reappraisal of existing data. In the past year, the pendulum has swung away from fear of hormone therapy to a better understanding of indications, risks and benefits—an understanding driven largely by the evidence-based position statements of the North American Menopause Society (NAMS).
A meta-analysis of randomized controlled trials of phytoestrogens attested to lack of efficacy or weak effect, which helps clear the picture on soy and red clover, but the researchers stressed that the lack of quality control does not rule out the possibility that some products might carry steroidal effects and potential risk.
And another year has brought even more evidence that diet, exercise, smoking cessation and the like really do improve health and quality of life.
Advisory on hormone therapy and “bio-identicals”
The NAMS Hormone Therapy Panel concluded definitively that bio-identical hormones should be considered in the same category as all the sex steroids, which, in the absence of specific safety and efficacy studies, carry the same risks and benefits as related products.
On the other hand, alternatives do exist for specific indications, such as bisphosphonates for bone conservation.
The new NAMSPosition Statement stresses individualized treatment based on the recommendations below.
The full report is available at www.menopause.org.
- Treatment of moderate to severe menopausal symptoms is the primary indications for systemic therapy. Every systemic product is FDA-approved for this indication.
- Every systemic and local product is approved for moderate vulvar and vaginal atrophy. For this indication alone, local ET is generally advised.
- Duration should be for the lowest effective dose and shortest time consistent with treatment goals.
- If the woman is well aware of potential risks and benefits, and if there is clinical supervision, extended use of the lowest effective ET/EPT dose for treatment goals is acceptable in women who believe the benefits outweigh the risks, for those at high risk of osteoporotic fracture who also have moderate to severe menopause symptoms, for further prevention of established bone loss when alternate therapies are not appropriate or cause side effects, or when outcomes of extended use of those therapies are not known.
- Although specific compounds, doses, and routes of administration may have different outcomes, clinical trial results for one agent should be generalized to all agents within the same family in the absence of data for each specific product. This proviso also applies to the so-called bioidentical products.
Question marks
The Hormone Therapy panel could not agree unanimously on these questions:
- Should women who are doing well on long-term HT discontinue?
- What is the best way to discontinue HT, abrupt cessation or tapering?
- Is the effect of continuous-combined EPT different from that of continuous estrogen with sequential progestogen?
- How definitive is the evidence on early increased CHD risk with HT?
- Conflicting data precluded a consensus on adverse breast cancer and cardiovascular outcomes associated with ET/EPT.
ACKNOWLEDGMENTS
The following commentaries on key papers are from the NAMS First To Knowemail program for members. I thank the members of NAMS who have taken time out to provide these objective reviews of the studies presented here, and Phil Lammers, NAMS Medical Editor.
OSTEOPOROSISCurb your enthusiasm—no need to rush bone drugs if risk is low
McClung MR, Wasnich RD, Hosking DJ, et al, on behalf of the Early Postmenopausal Intervention Cohort (EPIC) study group. Prevention of postmenopausal bone loss: six-year results from the early postmenopausal intervention cohort study. J Clin Endocrinol Metab 2004;89:4879-4885. LEVEL 1 EVIDENCE: Randomized, controlled trial
In this 6-year study of women in their 50s, the placebo group lost an inconsequential amount of bone mass. Not surprisingly, women using alendronate had some increase in BMD and some reduction in bone turnover markers.
Women in their 50s are not melting away. Their bones are not dissolving out from under them, contrary to what many media reports would have ObGyns and patients believe. Still, many clinicians are enthusiastic about prescribing bone drugs like bisphosphonates to women in their 50s who are generally healthy. (And there is no doubt that we do have bone drugs found to be safe and effective in well-designed trials, including the EPIC study.)
Yet there has been a major shift away from starting osteoporosis prevention drugs soon after menopause. EPIC data add support for a “go slow” strategy for drug intervention in healthy women in their 50s.
The EPIC study involved a total of 1,609 women ages 45 to 59, who received alendronate or placebo in a double-blind, randomized design. BMD was measured annually. The 4-year results were reported previously, and the 6-year results were published just last fall. Not surprisingly, women using alendronate had some increase in BMD and some reduction in bone turnover markers. But the results in the women who took placebo are of singular interest.
After 6 years, women on placebo had lost very little bone. The amount lost was statistically significant, but clinically inconsequential. The average BMD in women on placebo decreased 3% in the spine and 2% in the hip. Thus, the average rate of bone loss was about 0.5% per year.
A bone mass decrease of this extent represents a decline of about -0.3 T score, which is negligible. In the EPIC study, the 6-year fracture benefit, based on any type of fracture, boils down to lowering the risk from 1 in 11 on placebo to 1 in 9 on alendronate. These healthy women in their 50s had a very low risk of fracture, and taking a drug for 6 years had very little benefit for fracture reduction.
Women in their 50s typically have about 10% to 15% less bone mass than women of 25 to 30, when bone mass is at its peak. That 10% to 15% lower BMD translates to a T score of –1 to –1.2 , which is currently being labeled as osteopenic. Many patients and physicians have come to feel that osteopenia must always be treated with our newer drugs.
We are discovering that starting healthy women in their 50s on osteoporosis prevention drugs carries an extremely high cost per fracture avoided. During the 10 years since the startup of the EPIC study, support for early drug intervention in healthy women still in their 50s has dwindled. Now, expert groups, including the National Osteoporosis Foundation and the US Preventive Services Task Force, advise waiting until age 65 before starting osteoporosis risk evaluation or considering drug intervention in women who are otherwise healthy.
In my practice, I give healthy women in their 50s permission not to take drugs if their risk of fracture within the next 5 to 10 years is low. The picture is quite different in postmenopausal women in their 50s who do have high fracture risk, such as those who have already had a fracture, or who have very low bone density or high exposure to glucocorticoids.
EPIC data support the concept that the rate of bone loss is quite slow after a year or 2 has elapsed after menopause.
We need to avoid medicalizing these patients simply because we have drugs that reduce bone loss or because women in their 50s have less bone mass than 25-year-olds.
BIBLIOGRAPHY
Hosking D, Chilvers CE, Christiansen C, et al. Prevention of bone loss with alendronate in postmenopausal women under 60 years of age. Early Postmenopausal Intervention Cohort Study Group. N Engl J Med. 1998;338:485-492.
Wasnich RD, Bagger YZ, Hosking DJ, et al. Changes in bone density and turnover after alendronate or estrogen withdrawal. Menopause. 2004;11:622-630.
Siris ES, Bilezikian JP, Rubin MR, et al. Pins and plasters aren’t enough: a call for the evaluation and treatment of patients with osteoporotic fractures. J Clin Endocrinol Metab. 2003;88:3482-3486.
Rosen CJ, Black DM, Greenspan SL. Vignettes in osteoporosis: a road map to successful therapeutics. J Bone Miner Res. 2004;19:3-10.
HORMONE THERAPYDoes age affect mortality rate in postmenopausal women using HT?
Salpeter SR, Walsh JME, Greyber E, Ormiston TM, Salpeter EE. Mortality associated with hormone replacement therapy in younger and older women. J Gen Intern Med. 2004;19:791–804. META-ANALYSIS
- This study is sure to incite yet another round of debate about postmenopausal hormone therapy, but it does suggest that we can provide substantial reassurance about safety in younger women considering hormone therapy for menopause-related symptoms.
This study attempted to discover whether the age of the postmenopausal woman using hormone therapy affects mortality. Investigators performed a meta-analysis of clinical trials that reported mortality rates associated with use of postmenopausal hormone therapy, and analyzed the results based on mean ages.
They reported a significant trend between increasing risk of mortality and increasing mean age of the women using hormone therapy—raising the possibility of a health benefit for younger postmenopausal women.
The studies included in the metaanalysis varied in entry criteria, outcomes assessed, number of subjects, and HT type and dosage. Furthermore, because age groups were defined by mean age in each trial rather than actual age of pooled participants, some overlap in ages likely occurred between the analyses of younger and older women.
In postmenopausal women younger than 60, the total mortality rate was reduced by 39% in women taking estrogen-containing hormone therapy, which was significant; in women older than 60, there was no significant effect on total mortality.
The data were from 30 randomized, controlled clinical trials published between 1966 and 2002, and included 26,708 women taking estrogen (ET) or estrogen plus progestogen (EPT). Data were pooled to determine total mortality and mortality due to specific causes such as cardiovascular disease and cancer. The mean trial duration was 4.5 years, and the mean age was 62.2 years.
When the study population was divided into younger and older age groups based on mean ages, it was found that those younger than 60 (mean age, 53.9) had a significantly reduced OR for total mortality of 0.61 (95% CI, 0.39–0.95) and those older than age 60 (mean age, 64.6) had an OR of 1.03 (95% CI, 0.90–1.18).
For specific causes, the OR for cardiovascular disease mortality associated with ET/EPT was 1.10 (95% CI, 0.90–1.34). For overall cancer mortality, the OR was 1.03 (95% CI, 0.82–1.29) and for breast cancer mortality, the OR was 1.03 (95% CI, 0.29–3.67).
For causes other than cardiovascular disease or cancer, mortality was significantly lower in women on HT: OR 0.67 (95% CI, 0.51–0.88). When divided into younger and older age groups, ET/EPT was not associated with a significant change in mortality, with the exception of reduced mortality from causes other than cardiovascular disease and cancer in the older age group (OR, 0.68; 95% CI, 0.56–0.91).
Does HT improve insulin resistance?
Margolis KL, Bonds DE, Rodabough RJ, et al, for the Women’s Health Initiative Investigators. Effect of oestrogen plus progestin on the incidence of diabetes in postmenopausal women: results from the Women’s Health Initiative Hormone Trial. Diabetologia. 2004;47:1175–1187. LEVEL 1 EVIDENCE: Randomized, controlled trial
Decreased insulin and fasting glucose
- Combined estrogen plus progestogen may reduce the incidence of diabetes, possibly by mediating a decrease in insulin resistance.
Hormone therapy, compared with placebo, was associated with 15 fewer cases of diabetes per 10,000 women per year. Fasting glucose and insulin decreased compared with placebo, and may suggest improved insulin resistance. Although others have reported similar results, it is unlikely that hormone therapy will be prescribed to prevent diabetes, given its greater risk than benefit for other outcomes observed in other WHI analyses.
In the EPT part of WHI, a total of 15,641 postmenopausal women aged 50 to 79 were assigned to placebo or continuous-combined EPT (0.625 mg/day conjugated equine estrogens plus 2.5 mg/day medroxyprogesterone acetate). The incidence of diabetes was based on self-reports of insulin or oral diabetes drug treatment. Fasting glucose, insulin, and lipoproteins were measured at 1 and 3 years. After 5.6 years, the incidence of treated diabetes was 3.5% in the EPT group and 4.2% in the placebo group (hazard ratio, 0.79; 95% CI, 0.67–0.93; P= 0.004). Decreases in fasting glucose and insulin, suggesting decreased insulin resistance, were significant at 1 year in EPT users compared with placebo. The authors concluded that EPT reduces the incidence of diabetes possibly through a decrease in insulin resistance.
To be sure that a drug prevents a disease, everyone with the disease should be excluded at baseline, and at the end of the trial, everyone should be tested for the disease—if it is commonly undiagnosed. To study the incidence of new diabetes, all women (6%) with self-reported diabetes at baseline were excluded, and correctly so. But half of US adults with diabetes are undiagnosed. The WHI 6% prevalence is half of the assumed 12% prevalence in older overweight women. In the WHI, average age was 63 years and average body mass index was 28. Thus, it is not certain that the reduced risk occurred in women who were diabetes-free at baseline.
Fasting glucose was reduced in the EPT part of WHI, as in the Postmenopausal Estrogen Progestin Intervention (PEPI) trial. But 2-hour glucose levels were elevated by hormone treatment in PEPI, and were not measured in the WHI. Many studies have shown that postprandial or post-challenge glucose is a stronger risk factor for cardiovascular disease than fasting hyperglycemia.
Could an elevated post-challenge glucose have played a role in the unexpected excess cardiovascular disease observed with hormone therapy in healthy women in WHI and with hormone therapy in women with documented coronary heart disease in the Heart and Estrogen/progestin Replacement Study (HERS)?
Will transdermal estrogen reduce both fasting and post-challenge glucose? These and other questions remain. (EBC)
Lifestyle changes work best
- This report raises the possibility but does not justify prescribing EPT for diabetes prevention.
Postmenopausal women randomized to EPT had a lower incidence of treated diabetes, by self-report, than women assigned to placebo: a 21% relative risk reduction over 3 years. At 1 year, a comparison of changes from baseline in estimated insulin resistance (HOMA model) in a subgroup indicated a significant reduction with EPT compared with placebo group, but no significant difference at 3 years.
Because of the far-reaching morbidity and mortality due to Type 2 diabetes, particularly from cardiovascular disease, prevention would have major benefits, but the authors acknowledge that this report does not justify prescribing this therapy for this purpose, given hazards previously reported in the WHI.
Still, we can bear in mind other means of reducing risk for diabetes. In the Diabetes Prevention Program,1metformin reduced type 2 diabetes risk by 31%, and a diet plus exercise program reduced it even more: by 58% over approximately 3 years of follow-up in high-risk persons. People at risk for diabetes should be counseled to make lifestyle changes that can reduce this risk far more, and more safely, than might EPT. (CGS)
Consider diabetes implications
- EPT can reduce the incidence of diabetes to the same degree as medications used for cardiovascular disease prevention.2
Growing evidence indicates that reducing insulin resistance in women can prevent onset of diabetes,3and that improving insulin resistance can slow the progression of atherosclerosis.4 Observational studies5—the Heart and Estrogen/progestin Replacement Study (HERS),6 and now the WHI—strongly indicate that EPT reduces the incidence of diabetes in postmenopausal women. Notably, HERS and WHI findings were with continuous-combined estrogen with progestin, the latter often viewed as antagonistic to the beneficial effects of estrogen on carbohydrate metabolism.) Diabetes is much more devastating in women, and more likely to strike. The risk (3,000 of 10,000) in postmenopausal women equals or exceeds that of postmenopausal breast cancer, coronary disease, or hip fracture.7The time has come to consider health and cost implications of long-term HT, especially in women with diabetes risk factors: age, obesity, high systolic BP, high nonfasting glucose, antihypertensive drug use, low HDL, or Hispanic or African-American ethnicity. Clinical trials confirming HT’s benefit add to the totality of evidence that the benefits outweigh the risks.8Since long-term effects (>10 years) reflect only observational data, we urgently need studies designed to understand long-term benefits and risks. (HNH)
1. Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403.
2. Pepine CJ, Cooper-Dehoff RM. Cardiovascular therapies and risk for development of diabetes. J Am Coll Cardiol. 2004;44:509-512.
3. Buchanan TA, Xiang AH, Peters RK, et al. Preservation of pancreatic beta-cell function and prevention of type 2 diabetes by pharmacological treatment of insulin resistance inhigh risk Hispanic women. Diabetes. 2002;51:2796-2803.
4. Xiang AH, Peters RK, Kjos SL, et al. Effect of thiazolidinedione treatment on progression of subclinical atherosclerosis in premenopausal women at high risk for type 2 diabetes. J Clin Endocrinol Metab. 2005;90:1986-1991.
5. Manson JE, Rimm EB, Colditz GA, et al. A prospective study of postmenopausal estrogen therapy and subsequent incidence of non-insulin-dependent diabetes mellitus. Ann Epidemiol. 1992;2:665-673.
6. Kanaya AM, Herrington D, et al. Glycemic effects of postmenopausal hormone therapy: Heart and Estrogen/progestin Replacement Study. Randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2003;138:1-9.
7. Narayan KMV, Boyle JP, et al. Lifetime risk for diabetes mellitus in the US. JAMA 2003;290:1884-1890.
8. Philips LS, Langer RD. Postmenopausal hormone therapy: critical reappraisal and a unified hypothesis. Fertil Steril. 2005;83:558-566.
Soy versus placebo: Underwhelming
Red clover, likewise
Trebs EE, Ensrud KE, MacDonald R, Wilt TJ. Phytoestrogens for treatment of menopausal symptoms: a systematic review. Obstet Gynecol. 2004;104:824–836. META-ANALYSIS
- Phytoestrogens did not significantly improve hot flashes, night sweats, and vaginal dryness, compared to placebo, in this meta-analysis of randomized, controlled clinical trials.
Data on 2,348 women (mean age, 53.1 years) experiencing a mean of 7.1 hot flashes per week were analyzed. Only randomized controlled trials reporting menopausal symptoms of hot flashes, night sweats, and vaginal dryness were included. Mean trial duration was 17 weeks.
- The 11 soy food or beverage supplementtrials (N = 995 women) found no improvement compared with placebo.
- Of the 8 soy food trialsreporting hot flash outcomes, only 1 showed a significant improvement compared with placebo.
- In the 9 soy extract trials, overall results (N = 854) were mixed. In 5 trials using soy extracts and reporting hot flash frequency, 3 found no significant difference in symptoms between the soy and placebo groups; the other 2 (total 114 subjects) found significant improvements.
- The 5 red clover trials(N = 400) showed no improvement over placebo.
Many women in these studies appear to have been perimenopausal rather than postmenopausal. Nine studies included women who had had a menstrual period within the previous 3 to 6 months (late perimenopausal). A subgroup analysis of perimenopausal women would have been useful, since their endocrinologic status is quite different from that of postmenopausal women.
Does soy improve cognition, bone density, or lipids?
Kreijkamp-Kaspers S, Kok L, Grobbee DE, et al. Effect of soy protein containing isoflavones on cognitive function, bone mineral density, and plasma lipids in postmenopausal women: a randomized controlled trial. JAMA. 2004;292:65–74. LEVEL 1 EVIDENCE: Randomized, controlled trial
- Soy did not benefit cognition, bone, or lipids in 60-to-75-year-old women.
This careful trial raises the question of how to reconcile these results with animal and observational studies. In all, 202 postmenopausal women aged 60 to 75 years received 25.6 g/day of a soy protein supplement containing 99 mg isoflavones or a milk protein powder for 1 year. Adherence was monitored by serum genistein. There were no notable differences in:
- Memory, verbal skills, or concentration.
- Bone mineral density or bone-specific alkaline phosphatase, calcium, or phosphorus levels.
- Cholesterol, triglycerides, and lipoprotein plasma levels. These findings may not relate to perimenopausal women, in whom soy has been seen to significantly reduce LDL, but only during midfollicular and periovulatory phases.1 Premenopausal2 but not postmenopausal3monkeys given soy have had beneficial effects on bone quality.
REFERENCES
1. Merz-Demlow BE, Duncan AM, Wangen KE, et al. Soy isoflavones improve plasma lipids in normocholes-terolemic, premenopausal women. Am J Clin Nutr. 2000;71:1462-1469.
2. Kaplan JR, et al. Supplementation reduces the trajectory of atherogenesis in premenopausal monkeys at high risk for development of extensive postmenopausal coronary artery plaques. Menopause. 2004;11:653. Abstract S-17.
3. Register TC, Jayo MJ, Anthony MS. Soy phytoestrogens do not prevent bone loss in postmenopausal monkeys. J Clin Endocrinol Metab. 2003;88:4362-4370.
LIFESTYLE THERAPYThe secret to keeping those girlish carotids
Wildman RP, Schott LL, Brockwell S, Kuller LH, Sutton-Tyrrell K. A dietary and exercise intervention slows menopause-associated progression of subclinical atherosclerosis as measured by intima-media thickness of the carotid arteries. J Am Coll Cardiol. 2004;44:579–585. LEVEL 1 EVIDENCE: Randomized, controlled trial
- Carotid artery intima media thickens during the transition through menopause, but diet and exercise can reduce this progression by almost 50%.
- A diet-and-exercise regimen staves off menopause-associated weight gain and increases in lipids, blood pressure, and blood glucose.
These important findings are strong evidence that diet and exercise can slow the subclinical atherosclerosis progression that accompanies the menopause transition.
The Women’s Healthy Lifestyle Project previously found that weight gain and increased lipids, glucose, and blood pressure often accompany the menopause transition.1 This report describes improvements with diet and exercise intervention, compared with controls.
A total of 535 women aged 44 to 50 years were randomized to lifestyle intervention or assessment-only. All were premenopausal, and all had normal to high-normal body mass index, diastolic blood pressure, and fasting glucose and cholesterol levels.
The diet and exercise regimen used in the study was designed to reduce fat and cholesterol, prevent weight gain, and increase physical activity.
End points were progression of intimamedia thickness in the common carotid artery, internal carotid artery, and bulb segments.
The control group had significantly greater increases in intima-media thickness in women who became postmenopausal compared with those who remained premenopausal.
For women who became perimenopausal or postmenopausal during this 4-year study, diet and exercise slowed the progression of intima-media thickness by a 47% average reduction (P< 0.05), but had no effect on carotid segments in the women who remained premenopausal.
No benefit in intima media thickness was seen in women who remained premenopausal during the trial. Nevertheless, there are many well-documented benefits of healthy diet and exercise in premenopausal women.
Also of note, hormone therapy initiated after baseline measurements did not alter the results.
The message for patients, especially perimenopausal patients is that there is no time like the present to start a healthy lifestyle.
No downside
We’ve learned from the Nurse’s Health Study,2an observational study, that women who eat a healthy diet, do not smoke, and who exercise can reduce their risk of coronary heart disease by 57%.
We learned from the randomized controlled trial by the Diabetes Prevention Program Research Group3 that diet and exercise in high-risk women for 3 years can reduce incidence of new diabetes by 58%.
Now, in this trial, we learn that diet and exercise can reduce the progression of atherosclerosis in perimenopausal women by nearly 50%.
Since there is little, if any, downside to healthy living, why wait?
DISCLOSURES
Dr. Utian has served as an advisor/consultant for Eli Lilly, Pfizer, and Novartis. He has received research funding from Amylin, 3m, Barr, Berlex, BMS, Eli Lilly, Forest, Galen, Glaxo Smith Kline, Neurocrine Biosciences, Novartis, Novo Nordisk, Organon, Pharmacia, P&G, Pfizer, Roche, Sepracor, Solvay, Wyeth, and Yamanouchi.
Dr. Ettinger has served as an advisor for Berlex, Duramed-Barr, Glaxo Smith Kline, and P&G.
REFERENCES
1. Kuller LH, Simkin-Silverman LR, Wing RR, Meilahn EN, Ives DG. Women’s Healthy Lifestyle Project: a randomized clinical trial: results at 54 months. Circulation. 2001;103:32-37.
2. Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC. Primary prevention of coronary heart disease in women through diet and lifestyle. N Engl J Med. 2000;343:16-22.
3. Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403.
Time and study make a difference. So does careful review and reappraisal of existing data. In the past year, the pendulum has swung away from fear of hormone therapy to a better understanding of indications, risks and benefits—an understanding driven largely by the evidence-based position statements of the North American Menopause Society (NAMS).
A meta-analysis of randomized controlled trials of phytoestrogens attested to lack of efficacy or weak effect, which helps clear the picture on soy and red clover, but the researchers stressed that the lack of quality control does not rule out the possibility that some products might carry steroidal effects and potential risk.
And another year has brought even more evidence that diet, exercise, smoking cessation and the like really do improve health and quality of life.
Advisory on hormone therapy and “bio-identicals”
The NAMS Hormone Therapy Panel concluded definitively that bio-identical hormones should be considered in the same category as all the sex steroids, which, in the absence of specific safety and efficacy studies, carry the same risks and benefits as related products.
On the other hand, alternatives do exist for specific indications, such as bisphosphonates for bone conservation.
The new NAMSPosition Statement stresses individualized treatment based on the recommendations below.
The full report is available at www.menopause.org.
- Treatment of moderate to severe menopausal symptoms is the primary indications for systemic therapy. Every systemic product is FDA-approved for this indication.
- Every systemic and local product is approved for moderate vulvar and vaginal atrophy. For this indication alone, local ET is generally advised.
- Duration should be for the lowest effective dose and shortest time consistent with treatment goals.
- If the woman is well aware of potential risks and benefits, and if there is clinical supervision, extended use of the lowest effective ET/EPT dose for treatment goals is acceptable in women who believe the benefits outweigh the risks, for those at high risk of osteoporotic fracture who also have moderate to severe menopause symptoms, for further prevention of established bone loss when alternate therapies are not appropriate or cause side effects, or when outcomes of extended use of those therapies are not known.
- Although specific compounds, doses, and routes of administration may have different outcomes, clinical trial results for one agent should be generalized to all agents within the same family in the absence of data for each specific product. This proviso also applies to the so-called bioidentical products.
Question marks
The Hormone Therapy panel could not agree unanimously on these questions:
- Should women who are doing well on long-term HT discontinue?
- What is the best way to discontinue HT, abrupt cessation or tapering?
- Is the effect of continuous-combined EPT different from that of continuous estrogen with sequential progestogen?
- How definitive is the evidence on early increased CHD risk with HT?
- Conflicting data precluded a consensus on adverse breast cancer and cardiovascular outcomes associated with ET/EPT.
ACKNOWLEDGMENTS
The following commentaries on key papers are from the NAMS First To Knowemail program for members. I thank the members of NAMS who have taken time out to provide these objective reviews of the studies presented here, and Phil Lammers, NAMS Medical Editor.
OSTEOPOROSISCurb your enthusiasm—no need to rush bone drugs if risk is low
McClung MR, Wasnich RD, Hosking DJ, et al, on behalf of the Early Postmenopausal Intervention Cohort (EPIC) study group. Prevention of postmenopausal bone loss: six-year results from the early postmenopausal intervention cohort study. J Clin Endocrinol Metab 2004;89:4879-4885. LEVEL 1 EVIDENCE: Randomized, controlled trial
In this 6-year study of women in their 50s, the placebo group lost an inconsequential amount of bone mass. Not surprisingly, women using alendronate had some increase in BMD and some reduction in bone turnover markers.
Women in their 50s are not melting away. Their bones are not dissolving out from under them, contrary to what many media reports would have ObGyns and patients believe. Still, many clinicians are enthusiastic about prescribing bone drugs like bisphosphonates to women in their 50s who are generally healthy. (And there is no doubt that we do have bone drugs found to be safe and effective in well-designed trials, including the EPIC study.)
Yet there has been a major shift away from starting osteoporosis prevention drugs soon after menopause. EPIC data add support for a “go slow” strategy for drug intervention in healthy women in their 50s.
The EPIC study involved a total of 1,609 women ages 45 to 59, who received alendronate or placebo in a double-blind, randomized design. BMD was measured annually. The 4-year results were reported previously, and the 6-year results were published just last fall. Not surprisingly, women using alendronate had some increase in BMD and some reduction in bone turnover markers. But the results in the women who took placebo are of singular interest.
After 6 years, women on placebo had lost very little bone. The amount lost was statistically significant, but clinically inconsequential. The average BMD in women on placebo decreased 3% in the spine and 2% in the hip. Thus, the average rate of bone loss was about 0.5% per year.
A bone mass decrease of this extent represents a decline of about -0.3 T score, which is negligible. In the EPIC study, the 6-year fracture benefit, based on any type of fracture, boils down to lowering the risk from 1 in 11 on placebo to 1 in 9 on alendronate. These healthy women in their 50s had a very low risk of fracture, and taking a drug for 6 years had very little benefit for fracture reduction.
Women in their 50s typically have about 10% to 15% less bone mass than women of 25 to 30, when bone mass is at its peak. That 10% to 15% lower BMD translates to a T score of –1 to –1.2 , which is currently being labeled as osteopenic. Many patients and physicians have come to feel that osteopenia must always be treated with our newer drugs.
We are discovering that starting healthy women in their 50s on osteoporosis prevention drugs carries an extremely high cost per fracture avoided. During the 10 years since the startup of the EPIC study, support for early drug intervention in healthy women still in their 50s has dwindled. Now, expert groups, including the National Osteoporosis Foundation and the US Preventive Services Task Force, advise waiting until age 65 before starting osteoporosis risk evaluation or considering drug intervention in women who are otherwise healthy.
In my practice, I give healthy women in their 50s permission not to take drugs if their risk of fracture within the next 5 to 10 years is low. The picture is quite different in postmenopausal women in their 50s who do have high fracture risk, such as those who have already had a fracture, or who have very low bone density or high exposure to glucocorticoids.
EPIC data support the concept that the rate of bone loss is quite slow after a year or 2 has elapsed after menopause.
We need to avoid medicalizing these patients simply because we have drugs that reduce bone loss or because women in their 50s have less bone mass than 25-year-olds.
BIBLIOGRAPHY
Hosking D, Chilvers CE, Christiansen C, et al. Prevention of bone loss with alendronate in postmenopausal women under 60 years of age. Early Postmenopausal Intervention Cohort Study Group. N Engl J Med. 1998;338:485-492.
Wasnich RD, Bagger YZ, Hosking DJ, et al. Changes in bone density and turnover after alendronate or estrogen withdrawal. Menopause. 2004;11:622-630.
Siris ES, Bilezikian JP, Rubin MR, et al. Pins and plasters aren’t enough: a call for the evaluation and treatment of patients with osteoporotic fractures. J Clin Endocrinol Metab. 2003;88:3482-3486.
Rosen CJ, Black DM, Greenspan SL. Vignettes in osteoporosis: a road map to successful therapeutics. J Bone Miner Res. 2004;19:3-10.
HORMONE THERAPYDoes age affect mortality rate in postmenopausal women using HT?
Salpeter SR, Walsh JME, Greyber E, Ormiston TM, Salpeter EE. Mortality associated with hormone replacement therapy in younger and older women. J Gen Intern Med. 2004;19:791–804. META-ANALYSIS
- This study is sure to incite yet another round of debate about postmenopausal hormone therapy, but it does suggest that we can provide substantial reassurance about safety in younger women considering hormone therapy for menopause-related symptoms.
This study attempted to discover whether the age of the postmenopausal woman using hormone therapy affects mortality. Investigators performed a meta-analysis of clinical trials that reported mortality rates associated with use of postmenopausal hormone therapy, and analyzed the results based on mean ages.
They reported a significant trend between increasing risk of mortality and increasing mean age of the women using hormone therapy—raising the possibility of a health benefit for younger postmenopausal women.
The studies included in the metaanalysis varied in entry criteria, outcomes assessed, number of subjects, and HT type and dosage. Furthermore, because age groups were defined by mean age in each trial rather than actual age of pooled participants, some overlap in ages likely occurred between the analyses of younger and older women.
In postmenopausal women younger than 60, the total mortality rate was reduced by 39% in women taking estrogen-containing hormone therapy, which was significant; in women older than 60, there was no significant effect on total mortality.
The data were from 30 randomized, controlled clinical trials published between 1966 and 2002, and included 26,708 women taking estrogen (ET) or estrogen plus progestogen (EPT). Data were pooled to determine total mortality and mortality due to specific causes such as cardiovascular disease and cancer. The mean trial duration was 4.5 years, and the mean age was 62.2 years.
When the study population was divided into younger and older age groups based on mean ages, it was found that those younger than 60 (mean age, 53.9) had a significantly reduced OR for total mortality of 0.61 (95% CI, 0.39–0.95) and those older than age 60 (mean age, 64.6) had an OR of 1.03 (95% CI, 0.90–1.18).
For specific causes, the OR for cardiovascular disease mortality associated with ET/EPT was 1.10 (95% CI, 0.90–1.34). For overall cancer mortality, the OR was 1.03 (95% CI, 0.82–1.29) and for breast cancer mortality, the OR was 1.03 (95% CI, 0.29–3.67).
For causes other than cardiovascular disease or cancer, mortality was significantly lower in women on HT: OR 0.67 (95% CI, 0.51–0.88). When divided into younger and older age groups, ET/EPT was not associated with a significant change in mortality, with the exception of reduced mortality from causes other than cardiovascular disease and cancer in the older age group (OR, 0.68; 95% CI, 0.56–0.91).
Does HT improve insulin resistance?
Margolis KL, Bonds DE, Rodabough RJ, et al, for the Women’s Health Initiative Investigators. Effect of oestrogen plus progestin on the incidence of diabetes in postmenopausal women: results from the Women’s Health Initiative Hormone Trial. Diabetologia. 2004;47:1175–1187. LEVEL 1 EVIDENCE: Randomized, controlled trial
Decreased insulin and fasting glucose
- Combined estrogen plus progestogen may reduce the incidence of diabetes, possibly by mediating a decrease in insulin resistance.
Hormone therapy, compared with placebo, was associated with 15 fewer cases of diabetes per 10,000 women per year. Fasting glucose and insulin decreased compared with placebo, and may suggest improved insulin resistance. Although others have reported similar results, it is unlikely that hormone therapy will be prescribed to prevent diabetes, given its greater risk than benefit for other outcomes observed in other WHI analyses.
In the EPT part of WHI, a total of 15,641 postmenopausal women aged 50 to 79 were assigned to placebo or continuous-combined EPT (0.625 mg/day conjugated equine estrogens plus 2.5 mg/day medroxyprogesterone acetate). The incidence of diabetes was based on self-reports of insulin or oral diabetes drug treatment. Fasting glucose, insulin, and lipoproteins were measured at 1 and 3 years. After 5.6 years, the incidence of treated diabetes was 3.5% in the EPT group and 4.2% in the placebo group (hazard ratio, 0.79; 95% CI, 0.67–0.93; P= 0.004). Decreases in fasting glucose and insulin, suggesting decreased insulin resistance, were significant at 1 year in EPT users compared with placebo. The authors concluded that EPT reduces the incidence of diabetes possibly through a decrease in insulin resistance.
To be sure that a drug prevents a disease, everyone with the disease should be excluded at baseline, and at the end of the trial, everyone should be tested for the disease—if it is commonly undiagnosed. To study the incidence of new diabetes, all women (6%) with self-reported diabetes at baseline were excluded, and correctly so. But half of US adults with diabetes are undiagnosed. The WHI 6% prevalence is half of the assumed 12% prevalence in older overweight women. In the WHI, average age was 63 years and average body mass index was 28. Thus, it is not certain that the reduced risk occurred in women who were diabetes-free at baseline.
Fasting glucose was reduced in the EPT part of WHI, as in the Postmenopausal Estrogen Progestin Intervention (PEPI) trial. But 2-hour glucose levels were elevated by hormone treatment in PEPI, and were not measured in the WHI. Many studies have shown that postprandial or post-challenge glucose is a stronger risk factor for cardiovascular disease than fasting hyperglycemia.
Could an elevated post-challenge glucose have played a role in the unexpected excess cardiovascular disease observed with hormone therapy in healthy women in WHI and with hormone therapy in women with documented coronary heart disease in the Heart and Estrogen/progestin Replacement Study (HERS)?
Will transdermal estrogen reduce both fasting and post-challenge glucose? These and other questions remain. (EBC)
Lifestyle changes work best
- This report raises the possibility but does not justify prescribing EPT for diabetes prevention.
Postmenopausal women randomized to EPT had a lower incidence of treated diabetes, by self-report, than women assigned to placebo: a 21% relative risk reduction over 3 years. At 1 year, a comparison of changes from baseline in estimated insulin resistance (HOMA model) in a subgroup indicated a significant reduction with EPT compared with placebo group, but no significant difference at 3 years.
Because of the far-reaching morbidity and mortality due to Type 2 diabetes, particularly from cardiovascular disease, prevention would have major benefits, but the authors acknowledge that this report does not justify prescribing this therapy for this purpose, given hazards previously reported in the WHI.
Still, we can bear in mind other means of reducing risk for diabetes. In the Diabetes Prevention Program,1metformin reduced type 2 diabetes risk by 31%, and a diet plus exercise program reduced it even more: by 58% over approximately 3 years of follow-up in high-risk persons. People at risk for diabetes should be counseled to make lifestyle changes that can reduce this risk far more, and more safely, than might EPT. (CGS)
Consider diabetes implications
- EPT can reduce the incidence of diabetes to the same degree as medications used for cardiovascular disease prevention.2
Growing evidence indicates that reducing insulin resistance in women can prevent onset of diabetes,3and that improving insulin resistance can slow the progression of atherosclerosis.4 Observational studies5—the Heart and Estrogen/progestin Replacement Study (HERS),6 and now the WHI—strongly indicate that EPT reduces the incidence of diabetes in postmenopausal women. Notably, HERS and WHI findings were with continuous-combined estrogen with progestin, the latter often viewed as antagonistic to the beneficial effects of estrogen on carbohydrate metabolism.) Diabetes is much more devastating in women, and more likely to strike. The risk (3,000 of 10,000) in postmenopausal women equals or exceeds that of postmenopausal breast cancer, coronary disease, or hip fracture.7The time has come to consider health and cost implications of long-term HT, especially in women with diabetes risk factors: age, obesity, high systolic BP, high nonfasting glucose, antihypertensive drug use, low HDL, or Hispanic or African-American ethnicity. Clinical trials confirming HT’s benefit add to the totality of evidence that the benefits outweigh the risks.8Since long-term effects (>10 years) reflect only observational data, we urgently need studies designed to understand long-term benefits and risks. (HNH)
1. Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403.
2. Pepine CJ, Cooper-Dehoff RM. Cardiovascular therapies and risk for development of diabetes. J Am Coll Cardiol. 2004;44:509-512.
3. Buchanan TA, Xiang AH, Peters RK, et al. Preservation of pancreatic beta-cell function and prevention of type 2 diabetes by pharmacological treatment of insulin resistance inhigh risk Hispanic women. Diabetes. 2002;51:2796-2803.
4. Xiang AH, Peters RK, Kjos SL, et al. Effect of thiazolidinedione treatment on progression of subclinical atherosclerosis in premenopausal women at high risk for type 2 diabetes. J Clin Endocrinol Metab. 2005;90:1986-1991.
5. Manson JE, Rimm EB, Colditz GA, et al. A prospective study of postmenopausal estrogen therapy and subsequent incidence of non-insulin-dependent diabetes mellitus. Ann Epidemiol. 1992;2:665-673.
6. Kanaya AM, Herrington D, et al. Glycemic effects of postmenopausal hormone therapy: Heart and Estrogen/progestin Replacement Study. Randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2003;138:1-9.
7. Narayan KMV, Boyle JP, et al. Lifetime risk for diabetes mellitus in the US. JAMA 2003;290:1884-1890.
8. Philips LS, Langer RD. Postmenopausal hormone therapy: critical reappraisal and a unified hypothesis. Fertil Steril. 2005;83:558-566.
Soy versus placebo: Underwhelming
Red clover, likewise
Trebs EE, Ensrud KE, MacDonald R, Wilt TJ. Phytoestrogens for treatment of menopausal symptoms: a systematic review. Obstet Gynecol. 2004;104:824–836. META-ANALYSIS
- Phytoestrogens did not significantly improve hot flashes, night sweats, and vaginal dryness, compared to placebo, in this meta-analysis of randomized, controlled clinical trials.
Data on 2,348 women (mean age, 53.1 years) experiencing a mean of 7.1 hot flashes per week were analyzed. Only randomized controlled trials reporting menopausal symptoms of hot flashes, night sweats, and vaginal dryness were included. Mean trial duration was 17 weeks.
- The 11 soy food or beverage supplementtrials (N = 995 women) found no improvement compared with placebo.
- Of the 8 soy food trialsreporting hot flash outcomes, only 1 showed a significant improvement compared with placebo.
- In the 9 soy extract trials, overall results (N = 854) were mixed. In 5 trials using soy extracts and reporting hot flash frequency, 3 found no significant difference in symptoms between the soy and placebo groups; the other 2 (total 114 subjects) found significant improvements.
- The 5 red clover trials(N = 400) showed no improvement over placebo.
Many women in these studies appear to have been perimenopausal rather than postmenopausal. Nine studies included women who had had a menstrual period within the previous 3 to 6 months (late perimenopausal). A subgroup analysis of perimenopausal women would have been useful, since their endocrinologic status is quite different from that of postmenopausal women.
Does soy improve cognition, bone density, or lipids?
Kreijkamp-Kaspers S, Kok L, Grobbee DE, et al. Effect of soy protein containing isoflavones on cognitive function, bone mineral density, and plasma lipids in postmenopausal women: a randomized controlled trial. JAMA. 2004;292:65–74. LEVEL 1 EVIDENCE: Randomized, controlled trial
- Soy did not benefit cognition, bone, or lipids in 60-to-75-year-old women.
This careful trial raises the question of how to reconcile these results with animal and observational studies. In all, 202 postmenopausal women aged 60 to 75 years received 25.6 g/day of a soy protein supplement containing 99 mg isoflavones or a milk protein powder for 1 year. Adherence was monitored by serum genistein. There were no notable differences in:
- Memory, verbal skills, or concentration.
- Bone mineral density or bone-specific alkaline phosphatase, calcium, or phosphorus levels.
- Cholesterol, triglycerides, and lipoprotein plasma levels. These findings may not relate to perimenopausal women, in whom soy has been seen to significantly reduce LDL, but only during midfollicular and periovulatory phases.1 Premenopausal2 but not postmenopausal3monkeys given soy have had beneficial effects on bone quality.
REFERENCES
1. Merz-Demlow BE, Duncan AM, Wangen KE, et al. Soy isoflavones improve plasma lipids in normocholes-terolemic, premenopausal women. Am J Clin Nutr. 2000;71:1462-1469.
2. Kaplan JR, et al. Supplementation reduces the trajectory of atherogenesis in premenopausal monkeys at high risk for development of extensive postmenopausal coronary artery plaques. Menopause. 2004;11:653. Abstract S-17.
3. Register TC, Jayo MJ, Anthony MS. Soy phytoestrogens do not prevent bone loss in postmenopausal monkeys. J Clin Endocrinol Metab. 2003;88:4362-4370.
LIFESTYLE THERAPYThe secret to keeping those girlish carotids
Wildman RP, Schott LL, Brockwell S, Kuller LH, Sutton-Tyrrell K. A dietary and exercise intervention slows menopause-associated progression of subclinical atherosclerosis as measured by intima-media thickness of the carotid arteries. J Am Coll Cardiol. 2004;44:579–585. LEVEL 1 EVIDENCE: Randomized, controlled trial
- Carotid artery intima media thickens during the transition through menopause, but diet and exercise can reduce this progression by almost 50%.
- A diet-and-exercise regimen staves off menopause-associated weight gain and increases in lipids, blood pressure, and blood glucose.
These important findings are strong evidence that diet and exercise can slow the subclinical atherosclerosis progression that accompanies the menopause transition.
The Women’s Healthy Lifestyle Project previously found that weight gain and increased lipids, glucose, and blood pressure often accompany the menopause transition.1 This report describes improvements with diet and exercise intervention, compared with controls.
A total of 535 women aged 44 to 50 years were randomized to lifestyle intervention or assessment-only. All were premenopausal, and all had normal to high-normal body mass index, diastolic blood pressure, and fasting glucose and cholesterol levels.
The diet and exercise regimen used in the study was designed to reduce fat and cholesterol, prevent weight gain, and increase physical activity.
End points were progression of intimamedia thickness in the common carotid artery, internal carotid artery, and bulb segments.
The control group had significantly greater increases in intima-media thickness in women who became postmenopausal compared with those who remained premenopausal.
For women who became perimenopausal or postmenopausal during this 4-year study, diet and exercise slowed the progression of intima-media thickness by a 47% average reduction (P< 0.05), but had no effect on carotid segments in the women who remained premenopausal.
No benefit in intima media thickness was seen in women who remained premenopausal during the trial. Nevertheless, there are many well-documented benefits of healthy diet and exercise in premenopausal women.
Also of note, hormone therapy initiated after baseline measurements did not alter the results.
The message for patients, especially perimenopausal patients is that there is no time like the present to start a healthy lifestyle.
No downside
We’ve learned from the Nurse’s Health Study,2an observational study, that women who eat a healthy diet, do not smoke, and who exercise can reduce their risk of coronary heart disease by 57%.
We learned from the randomized controlled trial by the Diabetes Prevention Program Research Group3 that diet and exercise in high-risk women for 3 years can reduce incidence of new diabetes by 58%.
Now, in this trial, we learn that diet and exercise can reduce the progression of atherosclerosis in perimenopausal women by nearly 50%.
Since there is little, if any, downside to healthy living, why wait?
DISCLOSURES
Dr. Utian has served as an advisor/consultant for Eli Lilly, Pfizer, and Novartis. He has received research funding from Amylin, 3m, Barr, Berlex, BMS, Eli Lilly, Forest, Galen, Glaxo Smith Kline, Neurocrine Biosciences, Novartis, Novo Nordisk, Organon, Pharmacia, P&G, Pfizer, Roche, Sepracor, Solvay, Wyeth, and Yamanouchi.
Dr. Ettinger has served as an advisor for Berlex, Duramed-Barr, Glaxo Smith Kline, and P&G.
REFERENCES
1. Kuller LH, Simkin-Silverman LR, Wing RR, Meilahn EN, Ives DG. Women’s Healthy Lifestyle Project: a randomized clinical trial: results at 54 months. Circulation. 2001;103:32-37.
2. Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC. Primary prevention of coronary heart disease in women through diet and lifestyle. N Engl J Med. 2000;343:16-22.
3. Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393-403.
Managing an eclamptic patient
An eclamptic convulsion is frightening to behold. First, the woman’s face becomes distorted, and her eyes protrude. Then her face acquires a congested expression, and foam may exude from her mouth. Breathing stops.
Because eclampsia is so frightening, the natural tendency is to try to stop a convulsion, but this is not the wisest strategy.
Rather, the foremost priorities are to avoid maternal injury and support cardiovascular functions. How to do this, and how to prevent further convulsions, monitor and deliver the fetus, and avert complications are the focus of this article.
Since eclampsia may be fatal for both mother and fetus, all labor and delivery units and all obstetricians should be prepared to diagnose and manage this grave threat. However, few obstetric units encounter more than 1 or 2 cases a year; most obstetricians have little or no experience managing acute eclampsia. In the Western world, it affects only 1 in 2,000 to 1 in 3,448 pregnancies.1-4
How a convulsion happens
Most convulsions occur in 2 phases and last for 60 to 75 seconds. The first phase, lasting 15 to 20 seconds, begins with facial twitching, soon followed by a rigid body with generalized muscular contractions.
In the second phase, which lasts about a minute, the muscles of the body alternately contract and relax in rapid succession. This phase begins with the muscles of the jaw and rapidly encompasses eyelids, other facial muscles, and body. If the tongue is unprotected, the woman often bites it.
Coma sometimes follows the convulsion, and deep, rapid breathing usually begins as soon as the convulsion stops. In fact, maintaining oxygenation typically is not a problem after a single convulsion, and the risk of aspiration is low in a well managed patient.
Upon reviving, the woman typically remembers nothing about the seizure.
If convulsions recur, some degree of consciousness returns after each one, although the woman may become combative, agitated, and difficult to control.
Harbingers of complications
In the developed world, eclampsia increases the risk of maternal death (range: 0 to 1.8%).1-5 A recent review of all reported pregnancy-related deaths in the United States from 1979 to 1992 found 4,024 cases.6 Of these, 790 (19.6%) were due to preeclampsia-eclampsia, 49% of which were caused by eclampsia. The risk of death from preeclampsia or eclampsia was higher for the following groups:
- women over 30,
- no prenatal care,
- African Americans, and
- onset of preeclampsia or eclampsia before 28 weeks.6
Maternal morbidity
Pregnancies complicated by eclampsia also have higher rates of maternal morbidity such as pulmonary edema and HELLP syndrome (TABLE 1). Complications are substantially higher among women who develop antepartum eclampsia, especially when it is remote from term.1-3
TABLE 1
Maternal complications
Antepartum eclampsia, especially when it is remote from term, is much more likely to lead to complications
| COMPLICATION | RATE (%) | REMARKS |
|---|---|---|
| Death | 0.5-–2 | Risk of death is higher:
|
| Intracerebral hemorrhage | <1 | Usually related to several risk factors |
| Aspiration pneumonia | 2–3 | Heightened risk of maternal hypoxemia and acidosis |
| Disseminated coagulopathy | 3–5 | Regional anesthesia is contraindicated in these patients, and there is a heightened risk of hemorrhagic shock |
| Pulmonary edema | 3–5 | Heightened risk of maternal hypoxemia and acidosis |
| Acute renal failure | 5–9 | Usually seen in association with abruptio placentae, maternal hemorrhage, and prolonged maternal hypotension |
| Abruptio placentae | 7–10 | Can occur after a convulsion; suspect it if fetal bradycardia or late decelerations persist |
| HELLP syndrome | 10–15 |
Adverse perinatal outcomes
Perinatal mortality and morbidity are high in eclampsia, with a perinatal death rate in recent series of 5.6% to 11.8%.1,7 This high rate is related to prematurity, abruptio placentae, and severe growth restriction.1
Preterm deliveries occur in approximately 50% of cases, and about 25% occur before 32 weeks’ gestation.1
Diagnosis can be tricky
When the patient has generalized edema, hypertension, proteinuria, and convulsions, diagnosis of eclampsia is straightforward. Unfortunately, women with eclampsia exhibit a broad spectrum of signs, ranging from severe hypertension, severe proteinuria, and generalized edema, to absent or minimal hypertension, nonexistent proteinuria, and no edema (TABLE 2).1
Hypertension is the hallmark of diagnosis. Hypertension is severe (at least 160 mm Hg systolic and/or at least 110 mm Hg diastolic) in 20% to 54% of cases, and it is mild (systolic pressure between 140 and 160 mm Hg or diastolic pressure between 90 and 110 mm Hg) in 30% to 60% of cases.2,3 In 16% of cases, there may be no hypertension at all.2
Proteinuria. Eclampsia usually is associated with proteinuria (at least 1+ on dipstick).1 However, when I studied a series of 399 women with eclampsia, I found substantial proteinuria (3+ or above on dipstick) in only 48% of cases; proteinuria was absent in 14%.2
Edema. A weight gain of more than 2 lb per week (with or without clinical edema) during the third trimester may be the first sign of eclampsia. However, in my series of 399 women, edema was absent in 26% of cases.2
TABLE 2
Signs and symptoms of eclampsia*
Hypertension and proteinuria in eclampsia may be severe, mild, or even absent
| CONDITION | FREQUENCY (%) IN WOMEN WITH ECLAMPSIA | REMARKS |
|---|---|---|
| SIGNS | ||
| Hypertension | 85 | Should be documented on at least 2 occasions more than 6 hours apart |
| Severe: 160/110 mm Hg or more | 20–54 | |
| Mild: 140–160/90–110 mm Hg | 30–60 | |
| No hypertension2 | 16 | |
| Proteinuria | 85 | |
| At least 1+ on dipstick2 | 48 | |
| At least 3+ on dipstick | 14 | |
| No proteinuria | 15 | |
| SYMPTOMS | ||
| At least 1 of the following: | 33–75 | Clinical symptoms may occur before or after a convulsion |
| Headache | 30–70 | Persistent, occipital, or frontal |
| Right upper quadrant or epigastric pain | 12–20 | |
| Visual changes | 19–32 | Blurred vision, photophobia |
| Altered mental changes | 4–5 | |
| * Summary of 5 series | ||
Symptoms of eclampsia
Several clinical symptoms can occur before or after a convulsion1:
- persistent occipital or frontal headaches,
- blurred vision,
- photophobia,
- epigastric and/or right upper quadrant pain, and
- altered mental status.
Usual times of onset
Eclamptic convulsions can occur during pregnancy or delivery, or after delivery ( TABLE 3).1-5
Approximately 91% of antepartum cases develop at 28 weeks or beyond. The remaining cases tend to occur between 21 and 27 weeks’ gestation (7.5%), or at or before 20 weeks (1.5%).2
When eclampsia occurs before 20 weeks, it usually involves molar or hydropic degeneration of the placenta, with or without a fetus.1 However, eclampsia can occur in the first half of pregnancy without molar degeneration of the placenta, although this is rare.1,2 These women are sometimes misdiagnosed as having hypertensive encephalopathy, seizure disorder, or thrombotic thrombocytopenia purpura. Thus, women who develop convulsions in association with hypertension and proteinuria in the first half of pregnancy should be assumed to have eclampsia until proven otherwise,1 and require ultrasound examination of the uterus to rule out molar pregnancy and/or hydropic or cystic degeneration of the placenta.
Postpartum cases tend to occur within the first 48 hours, although some develop beyond this limit and have been reported as late as 23 days postpartum.8
Late postpartum eclampsia occurs more than 48 hours but less than 4 weeks after delivery.8 These women have signs and symptoms consistent with preeclampsia along with their convulsions.8,9 Thus, women who develop convulsions with hypertension and/or proteinuria, or with headaches or blurred vision, after 48 hours postpartum should be assumed to have eclampsia and treated accordingly.8,9
When eclampsia occurs especially late, perform an extensive neurologic examination to rule out other cerebral pathology.1,10
Eclampsia is atypical if convulsions occur before 20 weeks’ gestation or beyond 48 hours postpartum. It also is atypical if convulsions develop or persist despite adequate magnesium sulfate, or if the patient develops focal neurologic deficits, disorientation, blindness, or coma. In these cases, conduct a neurologic exam and cerebral imaging to exclude neurologic pathology.8-10
TABLE 3
Usual times of onset*
91% of antepartum eclampsia cases occur at 28 weeks or later, although eclamptic convulsions can occur at any time during pregnancy or delivery, or postpartum
| ONSET | FREQUENCY (%) | REMARKS |
|---|---|---|
| Antepartum | 38–53 | Maternal and perinatal mortality, and the incidence of complications and underlying disease, are higher in antepartum eclampsia, especially in early cases |
| ≤20 weeks | 1.5 | |
| 21 to 27 weeks | 7.5 | |
| ≥28 weeks | 91 | |
| Intrapartum | 18–36 | Intrapartum eclampsia more closely resembles postpartum disease than antepartum cases |
| Postpartum | 11–44 | Late postpartum eclampsia occurs more than 48 hours but less than 4 weeks after delivery |
| ≤48 hours | 7–39 | |
| >48 hours | 5–26 | |
| * Summary of 5 series | ||
Differential diagnosis
As with other aspects of preeclampsia, the presenting symptoms, clinical findings, and many laboratory results in eclampsia overlap several other medical and surgical conditions.1,10 Of course, eclampsia is the most common cause of convulsions in a woman with hypertension and/or proteinuria during pregnancy or immediately postpartum. On rare occasions, other causes of convulsions in pregnancy or postpartum may mimic eclampsia.1 These potential diagnoses are particularly important when the woman has focal neurologic deficits, prolonged coma, or atypical eclampsia.
The differential diagnosis encompasses a variety of cerebrovascular and metabolic disorders:
- hemorrhage,
- ruptured aneurysm or malformation,
- arterial embolism, thrombosis,
- venous thrombosis,
- hypoxic ischemic encephalopathy,
- angiomas,
- hypertensive encephalopathy,
- seizure disorder,
- hypoglycemia, hyponatremia,
- posterior leukoencephalopathy syndrome,
- thrombotic thrombocytopenic purpura,
- postdural puncture syndrome, and
- cerebral vasculitis/angiopathy.
Other diseases may factor in
Some women develop gestational hypertension or preeclampsia in association with connective tissue disease, thrombophilias, seizure disorder, or hypertensive encephalopathy, further confounding the diagnosis.
Thus, make every effort to ensure a correct diagnosis, since management may differ among these conditions.
Managing convulsions
Do not try to stop the first convulsion
The natural tendency is to try and interrupt the convulsion, but this is not recommended. Nor should you give a drug such as diazepam to shorten or stop the convulsion, especially if the patient lacks an intravenous line and no one skilled in intubation is immediately available. If diazepam is given, do not exceed 5 mg over 60 seconds. Rapid administration of this drug may lead to apnea or cardiac arrest, or both.
Steps to prevent maternal injury
During or immediately after the acute convulsive episode, take steps to prevent serious maternal injury and aspiration, assess and establish airway patency, and ensure maternal oxygenation (TABLE 4).
Elevate and pad the bed’s side rails and insert a padded tongue blade between the patient’s teeth, taking care not to trigger the gag reflex.
Physical restraints also may be needed.
Prevent aspiration. To minimize the risk of aspiration, place the patient in the lateral decubitus position, and suction vomitus and oral secretions as needed. Be aware that aspiration can occur when the padded tongue blade is forced to the back of the throat, stimulating the gag reflex and resultant vomiting.
TABLE 4
During a convulsion, 3 spheres of concern
| AVOID MATERNAL INJURY |
| Insert padded tongue blade |
| Avoid inducing gag reflex |
| Elevate padded bedside rails |
| Use physical restraints as needed |
| MAINTAIN OXYGENATION TO MOTHER AND FETUS |
| Apply face mask with or without oxygen reservoir at 8–10 L/minute |
| Monitor oxygenation and metabolic status via |
| Transcutaneous pulse oximetry |
| Arterial blood gases (sodium bicarbonate administered accordingly) |
| Correct oxygenation and metabolic status before administering anesthetics that may depress myocardial function |
| MINIMIZE ASPIRATION |
| Place patient in lateral decubitus position (which also maximizes uterine blood flow and venous return) |
| Suction vomitus and oral secretions |
| Obtain chest x-ray after the convulsion is controlled to rule out aspiration |
Tips on supplemental oxygenation
Although the initial seizure lasts only a minute or 2, it is important to maintain oxygenation by giving supplemental oxygen via a face mask, with or without an oxygen reservoir, at 8 to 10 L per minute. This is important because hypoventilation and respiratory acidosis often occur.
Once the convulsion ends and the patient resumes breathing, oxygenation is rarely a problem. However, maternal hypoxemia and acidosis can develop in women with repetitive convulsions, aspiration pneumonia, pulmonary edema, or a combination of these factors. Thus, transcutaneous pulse oximetry is advisable to monitor oxygenation in eclamptic patients.
Arterial blood gas analysis is necessary if pulse oximetry shows abnormal oxygen saturation (ie, at or below 92%).
Strategy to prevent recurrence
Magnesium sulfate is the drug of choice to treat and prevent subsequent convulsions in women with eclampsia.1,2
Dosage. I give a loading dose of 6 g over 15 to 20 minutes, followed by a maintenance dose of 2 g per hour as a continuous intravenous solution.
Approximately 10% of eclamptic women have a second convulsion after receiving magnesium sulfate.1,2 When this occurs, I give another 2-g bolus intravenously over 3 to 5 minutes.
More rarely, a woman will continue to have convulsions while receiving adequate and therapeutic doses of magnesium sulfate.
I treat such patients with sodium amobarbital, 250 mg, intravenously over 3 to 5 minutes.
Monitor maternal magnesium levels
Plasma levels should be in the range of 4 to 8 mg/dL during treatment for eclampsia, and are determined by the volume of distribution and by renal excretion. Thus, it is important to monitor the patient for magnesium toxicity, particularly if she has renal dysfunction (serum creatinine of 1.2 mg/dL or above) or urine output below 100 mL in 4 hours. In these women, adjust the maintenance dose according to plasma levels.
Side effects of magnesium including flushing, a feeling of warmth, nausea and vomiting, double vision, and slurred speech (TABLE 5).
If magnesium toxicity is suspected, immediately discontinue the infusion and administer supplemental oxygen along with 10 mL of 10% calcium gluconate (1 g total) as an intravenous push slowly over 5 minutes.
If respiratory arrest occurs, prompt resuscitation—including intubation and assisted ventilation—is vital.
TABLE 5
Clinical manifestations of magnesium toxicity
Maternal plasma levels of 4 to 8 mg/dL are appropriate during treatment for eclampsia; higher levels signal toxicity
| IF THE MAGNESIUM LEVEL IS… | THE CLINICAL MANIFESTATION IS… |
|---|---|
| 8–12 mg/dL | Loss of patellar reflex |
| Double or blurred vision | |
| Headache and nausea | |
| 9–12 mg/dL | Feeling of warmth, flushing |
| 10–12 mg/dL | Somnolence |
| Slurred speech | |
| 15–17 mg/dL | Muscular paralysis |
| Respiratory arrest | |
| 30–35 mg/dL | Cardiac arrest |
Controlling severe hypertension
The next step is to reduce blood pressure to a safe range. The objective: to preserve cerebral autoregulation and prevent congestive heart failure without compromising cerebral perfusion or jeopardizing uteroplacental blood flow, which is already reduced in many women with eclampsia.1
To these ends, try to keep systolic blood pressure between 140 and 160 mm Hg and diastolic pressure between 90 and 110 mm Hg. This can be achieved with:
- bolus 5- to 10-mg doses of hydralazine,
- 20 to 40 mg labetalol intravenously every 15 minutes, as needed, or
- 10 to 20 mg oral nifedipine every 30 minutes.
Other potent antihypertensive drugs such as sodium nitroprusside or nitroglycerine are rarely needed in eclampsia, and diuretics are indicated only in the presence of pulmonary edema.
Intrapartum management
Maternal hypoxemia and hypercarbia cause fetal heart rate and uterine activity changes during and immediately following a convulsion.
Fetal heart rate changes
These can include bradycardia, transient late decelerations, decreased beat-to-beat variability, and compensatory tachycardia.
The interval from onset of the seizure to the fall in fetal heart rate is approximately 5 minutes (FIGURE 1). Transitory fetal tachycardia frequently occurs after the prolonged bradycardia. The loss of beat-to-beat variability, with transitory late decelerations, occurs during the recovery phase.
The mechanism for the transient fetal bradycardia may be intense vasospasm and uterine hyperactivity, which may decrease uterine blood flow. The absence of maternal respiration during the convulsion may also contribute to fetal heart rate changes.
Since the fetal heart rate usually returns to normal after a convulsion, other conditions should be considered if an abnormal pattern persists.
In some cases, it may take longer for the heart rate pattern to return to baseline if the fetus is preterm with growth restriction.
Placental abruption may occur after the convulsion and should be suspected if fetal bradycardia or repetitive late decelerations persist (FIGURE 2).
FIGURE 1 Fetal response to a convulsion The top 2 tracings show fetal bradycardia during an eclamptic convulsion
FIGURE 2 Abruptio placentae Repetitive late decelerations secondary to abruptio placentae, necessitating cesarean section
Uterine activity
During a convulsion, contractions can increase in frequency and tone. The duration of increased uterine activity varies from 2 to 14 minutes.
These changes usually resolve spontaneously within 3 to 10 minutes following the termination of convulsions and correction of maternal hypoxemia (FIGURE 1).
If uterine hyperactivity persists, suspect placental abruption (FIGURE 2).
Do not rush to cesarean
It benefits the fetus to allow in utero recovery from the maternal convulsion, hypoxia, and hypercarbia before delivery. However, if the bradycardia and/or recurrent late decelerations persist beyond 10 to 15 minutes despite all efforts, suspect abruptio placentae or nonreassuring fetal status.
Once the patient regains consciousness and is oriented to name, place, and time, and her convulsions are controlled and condition stabilized, proceed with delivery.
Choosing a delivery route
Eclampsia is not an indication for cesarean. The decision to perform a cesarean should be based on fetal gestational age, fetal condition, presence of labor, and cervical Bishop score. I recommend:
- Cesarean section for women with eclampsia before 30 weeks’ gestation who are not in labor and whose Bishop score is below 5.
- Vaginal delivery for women in labor or with rupture of membranes, provided there are no obstetric complications.
- Labor induction with oxytocin infusion or prostaglandins in all women at or after 30 weeks, regardless of the Bishop score, and in women before 30 weeks when the Bishop score is 5 or above.
Maternal pain relief
During labor and delivery, systemic opioids or epidural anesthesia can provide pain relief—the same recommendations as for women with severe preeclampsia.
For cesarean delivery, an epidural, spinal, or combined techniques of regional anesthesia are suitable.
Do not use regional anesthesia if there is coagulopathy or severe thrombocytopenia (platelet count less than 50,000/mm3). In women with eclampsia, general anesthesia increases the risk of aspiration and failed intubation due to airway edema, and is associated with marked increases in systemic and cerebral pressures during intubation and extubation.
Women with airway or laryngeal edema may require awake intubation under fiber optic observation, with tracheostomy immediately available.
Changes in systemic or cerebral pressures may be attenuated by pretreatment with labetalol or nitroglycerine injections.
Postpartum management
After delivery, women with eclampsia require close monitoring of vital signs, fluid intake and output, and symptoms for at least 48 hours.
Risk of pulmonary edema
These women usually receive large amounts of intravenous fluids during labor, delivery, and postpartum. In addition, during the postpartum period, extracellular fluid mobilizes, leading to increased intravascular volume.
As a result, women who develop eclampsia—particularly those with abnormal renal function, abruptio placentae, and/or preexisting chronic hypertension— face an increased risk for pulmonary edema and exacerbation of severe hypertension.2
Frequent evaluation of the amount of intravenous fluids is necessary, as well as oral intake, blood products, and urine output. They also need pulse oximetry and pulmonary auscultation.
Continue magnesium sulfate
Parenteral magnesium sulfate should be given for at least 24 hours after delivery and/or for at least 24 hours after the last convulsion.
If the patient has oliguria (less than 100 mL over 4 hours), both fluid administration and the dose of magnesium sulfate should be reduced.
Oral antihypertensives
Other oral antihypertensive agents such as labetalol or nifedipine can be given to keep systolic blood pressure below 155 mm Hg and diastolic blood pressure below 105 mm Hg. Nifedipine offers the benefit of improved diuresis in the postpartum period.
The author reports no financial relationships relevant to this article.
1. Sibai BM. Diagnosis, differential diagnosis, and management of eclampsia. Obstet Gynecol. 2005;105:402-410.
2. Mattar F, Sibai BM. Eclampsia VIII. Risk factors for maternal morbidity. Am J Obstet Gynecol. 2000;182:307-312.
3. Douglas KA, Redman CW. Eclampsia in the United Kingdom. BMJ. 1994;309:1395-1400.
4. Rugard O, Carling MS, Berg G. Eclampsia at a tertiary hospital, 1973–99. Acta Obstet Gynecol Scand. 2004;83:240-245.
5. Katz VL, Farmer R, Kuller J. Preeclampsia into eclampsia: toward a new paradigm. Am J Obstet Gynecol. 2000;182:1389-1396.
6. MacKay AP, Berg CJ, Atrash HK. Pregnancy-related mortality from preeclampsia and eclampsia. Obstet Gynecol. 2001;97:533-538.
7. Leitch CR, Cameron AD, Walker JJ. The changing pattern of eclampsia over a 60-year period. Br J Obstet Gynaecol. 1997;104:917-922.
8. Lubarsky SL, Barton JR, Friedman SA, Nasreddine S, Ramaddan MK, Sibai BM. Late postpartum eclampsia revisited. Obstet Gynaecol. 1994;83:502-505.
9. Chames MC, Livingston JC, Ivester TS, Barton JR, Sibai BM. Late postpartum eclampsia: a preventable disease? Am J Obstet Gynecol. 2002;186:1174-1177.
10. Witlin AG, Friedman SA, Egerman RS, Frangieh AY, Sibai BM. Cerebrovascular disorders complicating pregnancy. Beyond eclampsia. Am J Obstet Gynecol. 1997;176:139-148.
An eclamptic convulsion is frightening to behold. First, the woman’s face becomes distorted, and her eyes protrude. Then her face acquires a congested expression, and foam may exude from her mouth. Breathing stops.
Because eclampsia is so frightening, the natural tendency is to try to stop a convulsion, but this is not the wisest strategy.
Rather, the foremost priorities are to avoid maternal injury and support cardiovascular functions. How to do this, and how to prevent further convulsions, monitor and deliver the fetus, and avert complications are the focus of this article.
Since eclampsia may be fatal for both mother and fetus, all labor and delivery units and all obstetricians should be prepared to diagnose and manage this grave threat. However, few obstetric units encounter more than 1 or 2 cases a year; most obstetricians have little or no experience managing acute eclampsia. In the Western world, it affects only 1 in 2,000 to 1 in 3,448 pregnancies.1-4
How a convulsion happens
Most convulsions occur in 2 phases and last for 60 to 75 seconds. The first phase, lasting 15 to 20 seconds, begins with facial twitching, soon followed by a rigid body with generalized muscular contractions.
In the second phase, which lasts about a minute, the muscles of the body alternately contract and relax in rapid succession. This phase begins with the muscles of the jaw and rapidly encompasses eyelids, other facial muscles, and body. If the tongue is unprotected, the woman often bites it.
Coma sometimes follows the convulsion, and deep, rapid breathing usually begins as soon as the convulsion stops. In fact, maintaining oxygenation typically is not a problem after a single convulsion, and the risk of aspiration is low in a well managed patient.
Upon reviving, the woman typically remembers nothing about the seizure.
If convulsions recur, some degree of consciousness returns after each one, although the woman may become combative, agitated, and difficult to control.
Harbingers of complications
In the developed world, eclampsia increases the risk of maternal death (range: 0 to 1.8%).1-5 A recent review of all reported pregnancy-related deaths in the United States from 1979 to 1992 found 4,024 cases.6 Of these, 790 (19.6%) were due to preeclampsia-eclampsia, 49% of which were caused by eclampsia. The risk of death from preeclampsia or eclampsia was higher for the following groups:
- women over 30,
- no prenatal care,
- African Americans, and
- onset of preeclampsia or eclampsia before 28 weeks.6
Maternal morbidity
Pregnancies complicated by eclampsia also have higher rates of maternal morbidity such as pulmonary edema and HELLP syndrome (TABLE 1). Complications are substantially higher among women who develop antepartum eclampsia, especially when it is remote from term.1-3
TABLE 1
Maternal complications
Antepartum eclampsia, especially when it is remote from term, is much more likely to lead to complications
| COMPLICATION | RATE (%) | REMARKS |
|---|---|---|
| Death | 0.5-–2 | Risk of death is higher:
|
| Intracerebral hemorrhage | <1 | Usually related to several risk factors |
| Aspiration pneumonia | 2–3 | Heightened risk of maternal hypoxemia and acidosis |
| Disseminated coagulopathy | 3–5 | Regional anesthesia is contraindicated in these patients, and there is a heightened risk of hemorrhagic shock |
| Pulmonary edema | 3–5 | Heightened risk of maternal hypoxemia and acidosis |
| Acute renal failure | 5–9 | Usually seen in association with abruptio placentae, maternal hemorrhage, and prolonged maternal hypotension |
| Abruptio placentae | 7–10 | Can occur after a convulsion; suspect it if fetal bradycardia or late decelerations persist |
| HELLP syndrome | 10–15 |
Adverse perinatal outcomes
Perinatal mortality and morbidity are high in eclampsia, with a perinatal death rate in recent series of 5.6% to 11.8%.1,7 This high rate is related to prematurity, abruptio placentae, and severe growth restriction.1
Preterm deliveries occur in approximately 50% of cases, and about 25% occur before 32 weeks’ gestation.1
Diagnosis can be tricky
When the patient has generalized edema, hypertension, proteinuria, and convulsions, diagnosis of eclampsia is straightforward. Unfortunately, women with eclampsia exhibit a broad spectrum of signs, ranging from severe hypertension, severe proteinuria, and generalized edema, to absent or minimal hypertension, nonexistent proteinuria, and no edema (TABLE 2).1
Hypertension is the hallmark of diagnosis. Hypertension is severe (at least 160 mm Hg systolic and/or at least 110 mm Hg diastolic) in 20% to 54% of cases, and it is mild (systolic pressure between 140 and 160 mm Hg or diastolic pressure between 90 and 110 mm Hg) in 30% to 60% of cases.2,3 In 16% of cases, there may be no hypertension at all.2
Proteinuria. Eclampsia usually is associated with proteinuria (at least 1+ on dipstick).1 However, when I studied a series of 399 women with eclampsia, I found substantial proteinuria (3+ or above on dipstick) in only 48% of cases; proteinuria was absent in 14%.2
Edema. A weight gain of more than 2 lb per week (with or without clinical edema) during the third trimester may be the first sign of eclampsia. However, in my series of 399 women, edema was absent in 26% of cases.2
TABLE 2
Signs and symptoms of eclampsia*
Hypertension and proteinuria in eclampsia may be severe, mild, or even absent
| CONDITION | FREQUENCY (%) IN WOMEN WITH ECLAMPSIA | REMARKS |
|---|---|---|
| SIGNS | ||
| Hypertension | 85 | Should be documented on at least 2 occasions more than 6 hours apart |
| Severe: 160/110 mm Hg or more | 20–54 | |
| Mild: 140–160/90–110 mm Hg | 30–60 | |
| No hypertension2 | 16 | |
| Proteinuria | 85 | |
| At least 1+ on dipstick2 | 48 | |
| At least 3+ on dipstick | 14 | |
| No proteinuria | 15 | |
| SYMPTOMS | ||
| At least 1 of the following: | 33–75 | Clinical symptoms may occur before or after a convulsion |
| Headache | 30–70 | Persistent, occipital, or frontal |
| Right upper quadrant or epigastric pain | 12–20 | |
| Visual changes | 19–32 | Blurred vision, photophobia |
| Altered mental changes | 4–5 | |
| * Summary of 5 series | ||
Symptoms of eclampsia
Several clinical symptoms can occur before or after a convulsion1:
- persistent occipital or frontal headaches,
- blurred vision,
- photophobia,
- epigastric and/or right upper quadrant pain, and
- altered mental status.
Usual times of onset
Eclamptic convulsions can occur during pregnancy or delivery, or after delivery ( TABLE 3).1-5
Approximately 91% of antepartum cases develop at 28 weeks or beyond. The remaining cases tend to occur between 21 and 27 weeks’ gestation (7.5%), or at or before 20 weeks (1.5%).2
When eclampsia occurs before 20 weeks, it usually involves molar or hydropic degeneration of the placenta, with or without a fetus.1 However, eclampsia can occur in the first half of pregnancy without molar degeneration of the placenta, although this is rare.1,2 These women are sometimes misdiagnosed as having hypertensive encephalopathy, seizure disorder, or thrombotic thrombocytopenia purpura. Thus, women who develop convulsions in association with hypertension and proteinuria in the first half of pregnancy should be assumed to have eclampsia until proven otherwise,1 and require ultrasound examination of the uterus to rule out molar pregnancy and/or hydropic or cystic degeneration of the placenta.
Postpartum cases tend to occur within the first 48 hours, although some develop beyond this limit and have been reported as late as 23 days postpartum.8
Late postpartum eclampsia occurs more than 48 hours but less than 4 weeks after delivery.8 These women have signs and symptoms consistent with preeclampsia along with their convulsions.8,9 Thus, women who develop convulsions with hypertension and/or proteinuria, or with headaches or blurred vision, after 48 hours postpartum should be assumed to have eclampsia and treated accordingly.8,9
When eclampsia occurs especially late, perform an extensive neurologic examination to rule out other cerebral pathology.1,10
Eclampsia is atypical if convulsions occur before 20 weeks’ gestation or beyond 48 hours postpartum. It also is atypical if convulsions develop or persist despite adequate magnesium sulfate, or if the patient develops focal neurologic deficits, disorientation, blindness, or coma. In these cases, conduct a neurologic exam and cerebral imaging to exclude neurologic pathology.8-10
TABLE 3
Usual times of onset*
91% of antepartum eclampsia cases occur at 28 weeks or later, although eclamptic convulsions can occur at any time during pregnancy or delivery, or postpartum
| ONSET | FREQUENCY (%) | REMARKS |
|---|---|---|
| Antepartum | 38–53 | Maternal and perinatal mortality, and the incidence of complications and underlying disease, are higher in antepartum eclampsia, especially in early cases |
| ≤20 weeks | 1.5 | |
| 21 to 27 weeks | 7.5 | |
| ≥28 weeks | 91 | |
| Intrapartum | 18–36 | Intrapartum eclampsia more closely resembles postpartum disease than antepartum cases |
| Postpartum | 11–44 | Late postpartum eclampsia occurs more than 48 hours but less than 4 weeks after delivery |
| ≤48 hours | 7–39 | |
| >48 hours | 5–26 | |
| * Summary of 5 series | ||
Differential diagnosis
As with other aspects of preeclampsia, the presenting symptoms, clinical findings, and many laboratory results in eclampsia overlap several other medical and surgical conditions.1,10 Of course, eclampsia is the most common cause of convulsions in a woman with hypertension and/or proteinuria during pregnancy or immediately postpartum. On rare occasions, other causes of convulsions in pregnancy or postpartum may mimic eclampsia.1 These potential diagnoses are particularly important when the woman has focal neurologic deficits, prolonged coma, or atypical eclampsia.
The differential diagnosis encompasses a variety of cerebrovascular and metabolic disorders:
- hemorrhage,
- ruptured aneurysm or malformation,
- arterial embolism, thrombosis,
- venous thrombosis,
- hypoxic ischemic encephalopathy,
- angiomas,
- hypertensive encephalopathy,
- seizure disorder,
- hypoglycemia, hyponatremia,
- posterior leukoencephalopathy syndrome,
- thrombotic thrombocytopenic purpura,
- postdural puncture syndrome, and
- cerebral vasculitis/angiopathy.
Other diseases may factor in
Some women develop gestational hypertension or preeclampsia in association with connective tissue disease, thrombophilias, seizure disorder, or hypertensive encephalopathy, further confounding the diagnosis.
Thus, make every effort to ensure a correct diagnosis, since management may differ among these conditions.
Managing convulsions
Do not try to stop the first convulsion
The natural tendency is to try and interrupt the convulsion, but this is not recommended. Nor should you give a drug such as diazepam to shorten or stop the convulsion, especially if the patient lacks an intravenous line and no one skilled in intubation is immediately available. If diazepam is given, do not exceed 5 mg over 60 seconds. Rapid administration of this drug may lead to apnea or cardiac arrest, or both.
Steps to prevent maternal injury
During or immediately after the acute convulsive episode, take steps to prevent serious maternal injury and aspiration, assess and establish airway patency, and ensure maternal oxygenation (TABLE 4).
Elevate and pad the bed’s side rails and insert a padded tongue blade between the patient’s teeth, taking care not to trigger the gag reflex.
Physical restraints also may be needed.
Prevent aspiration. To minimize the risk of aspiration, place the patient in the lateral decubitus position, and suction vomitus and oral secretions as needed. Be aware that aspiration can occur when the padded tongue blade is forced to the back of the throat, stimulating the gag reflex and resultant vomiting.
TABLE 4
During a convulsion, 3 spheres of concern
| AVOID MATERNAL INJURY |
| Insert padded tongue blade |
| Avoid inducing gag reflex |
| Elevate padded bedside rails |
| Use physical restraints as needed |
| MAINTAIN OXYGENATION TO MOTHER AND FETUS |
| Apply face mask with or without oxygen reservoir at 8–10 L/minute |
| Monitor oxygenation and metabolic status via |
| Transcutaneous pulse oximetry |
| Arterial blood gases (sodium bicarbonate administered accordingly) |
| Correct oxygenation and metabolic status before administering anesthetics that may depress myocardial function |
| MINIMIZE ASPIRATION |
| Place patient in lateral decubitus position (which also maximizes uterine blood flow and venous return) |
| Suction vomitus and oral secretions |
| Obtain chest x-ray after the convulsion is controlled to rule out aspiration |
Tips on supplemental oxygenation
Although the initial seizure lasts only a minute or 2, it is important to maintain oxygenation by giving supplemental oxygen via a face mask, with or without an oxygen reservoir, at 8 to 10 L per minute. This is important because hypoventilation and respiratory acidosis often occur.
Once the convulsion ends and the patient resumes breathing, oxygenation is rarely a problem. However, maternal hypoxemia and acidosis can develop in women with repetitive convulsions, aspiration pneumonia, pulmonary edema, or a combination of these factors. Thus, transcutaneous pulse oximetry is advisable to monitor oxygenation in eclamptic patients.
Arterial blood gas analysis is necessary if pulse oximetry shows abnormal oxygen saturation (ie, at or below 92%).
Strategy to prevent recurrence
Magnesium sulfate is the drug of choice to treat and prevent subsequent convulsions in women with eclampsia.1,2
Dosage. I give a loading dose of 6 g over 15 to 20 minutes, followed by a maintenance dose of 2 g per hour as a continuous intravenous solution.
Approximately 10% of eclamptic women have a second convulsion after receiving magnesium sulfate.1,2 When this occurs, I give another 2-g bolus intravenously over 3 to 5 minutes.
More rarely, a woman will continue to have convulsions while receiving adequate and therapeutic doses of magnesium sulfate.
I treat such patients with sodium amobarbital, 250 mg, intravenously over 3 to 5 minutes.
Monitor maternal magnesium levels
Plasma levels should be in the range of 4 to 8 mg/dL during treatment for eclampsia, and are determined by the volume of distribution and by renal excretion. Thus, it is important to monitor the patient for magnesium toxicity, particularly if she has renal dysfunction (serum creatinine of 1.2 mg/dL or above) or urine output below 100 mL in 4 hours. In these women, adjust the maintenance dose according to plasma levels.
Side effects of magnesium including flushing, a feeling of warmth, nausea and vomiting, double vision, and slurred speech (TABLE 5).
If magnesium toxicity is suspected, immediately discontinue the infusion and administer supplemental oxygen along with 10 mL of 10% calcium gluconate (1 g total) as an intravenous push slowly over 5 minutes.
If respiratory arrest occurs, prompt resuscitation—including intubation and assisted ventilation—is vital.
TABLE 5
Clinical manifestations of magnesium toxicity
Maternal plasma levels of 4 to 8 mg/dL are appropriate during treatment for eclampsia; higher levels signal toxicity
| IF THE MAGNESIUM LEVEL IS… | THE CLINICAL MANIFESTATION IS… |
|---|---|
| 8–12 mg/dL | Loss of patellar reflex |
| Double or blurred vision | |
| Headache and nausea | |
| 9–12 mg/dL | Feeling of warmth, flushing |
| 10–12 mg/dL | Somnolence |
| Slurred speech | |
| 15–17 mg/dL | Muscular paralysis |
| Respiratory arrest | |
| 30–35 mg/dL | Cardiac arrest |
Controlling severe hypertension
The next step is to reduce blood pressure to a safe range. The objective: to preserve cerebral autoregulation and prevent congestive heart failure without compromising cerebral perfusion or jeopardizing uteroplacental blood flow, which is already reduced in many women with eclampsia.1
To these ends, try to keep systolic blood pressure between 140 and 160 mm Hg and diastolic pressure between 90 and 110 mm Hg. This can be achieved with:
- bolus 5- to 10-mg doses of hydralazine,
- 20 to 40 mg labetalol intravenously every 15 minutes, as needed, or
- 10 to 20 mg oral nifedipine every 30 minutes.
Other potent antihypertensive drugs such as sodium nitroprusside or nitroglycerine are rarely needed in eclampsia, and diuretics are indicated only in the presence of pulmonary edema.
Intrapartum management
Maternal hypoxemia and hypercarbia cause fetal heart rate and uterine activity changes during and immediately following a convulsion.
Fetal heart rate changes
These can include bradycardia, transient late decelerations, decreased beat-to-beat variability, and compensatory tachycardia.
The interval from onset of the seizure to the fall in fetal heart rate is approximately 5 minutes (FIGURE 1). Transitory fetal tachycardia frequently occurs after the prolonged bradycardia. The loss of beat-to-beat variability, with transitory late decelerations, occurs during the recovery phase.
The mechanism for the transient fetal bradycardia may be intense vasospasm and uterine hyperactivity, which may decrease uterine blood flow. The absence of maternal respiration during the convulsion may also contribute to fetal heart rate changes.
Since the fetal heart rate usually returns to normal after a convulsion, other conditions should be considered if an abnormal pattern persists.
In some cases, it may take longer for the heart rate pattern to return to baseline if the fetus is preterm with growth restriction.
Placental abruption may occur after the convulsion and should be suspected if fetal bradycardia or repetitive late decelerations persist (FIGURE 2).
FIGURE 1 Fetal response to a convulsion The top 2 tracings show fetal bradycardia during an eclamptic convulsion
FIGURE 2 Abruptio placentae Repetitive late decelerations secondary to abruptio placentae, necessitating cesarean section
Uterine activity
During a convulsion, contractions can increase in frequency and tone. The duration of increased uterine activity varies from 2 to 14 minutes.
These changes usually resolve spontaneously within 3 to 10 minutes following the termination of convulsions and correction of maternal hypoxemia (FIGURE 1).
If uterine hyperactivity persists, suspect placental abruption (FIGURE 2).
Do not rush to cesarean
It benefits the fetus to allow in utero recovery from the maternal convulsion, hypoxia, and hypercarbia before delivery. However, if the bradycardia and/or recurrent late decelerations persist beyond 10 to 15 minutes despite all efforts, suspect abruptio placentae or nonreassuring fetal status.
Once the patient regains consciousness and is oriented to name, place, and time, and her convulsions are controlled and condition stabilized, proceed with delivery.
Choosing a delivery route
Eclampsia is not an indication for cesarean. The decision to perform a cesarean should be based on fetal gestational age, fetal condition, presence of labor, and cervical Bishop score. I recommend:
- Cesarean section for women with eclampsia before 30 weeks’ gestation who are not in labor and whose Bishop score is below 5.
- Vaginal delivery for women in labor or with rupture of membranes, provided there are no obstetric complications.
- Labor induction with oxytocin infusion or prostaglandins in all women at or after 30 weeks, regardless of the Bishop score, and in women before 30 weeks when the Bishop score is 5 or above.
Maternal pain relief
During labor and delivery, systemic opioids or epidural anesthesia can provide pain relief—the same recommendations as for women with severe preeclampsia.
For cesarean delivery, an epidural, spinal, or combined techniques of regional anesthesia are suitable.
Do not use regional anesthesia if there is coagulopathy or severe thrombocytopenia (platelet count less than 50,000/mm3). In women with eclampsia, general anesthesia increases the risk of aspiration and failed intubation due to airway edema, and is associated with marked increases in systemic and cerebral pressures during intubation and extubation.
Women with airway or laryngeal edema may require awake intubation under fiber optic observation, with tracheostomy immediately available.
Changes in systemic or cerebral pressures may be attenuated by pretreatment with labetalol or nitroglycerine injections.
Postpartum management
After delivery, women with eclampsia require close monitoring of vital signs, fluid intake and output, and symptoms for at least 48 hours.
Risk of pulmonary edema
These women usually receive large amounts of intravenous fluids during labor, delivery, and postpartum. In addition, during the postpartum period, extracellular fluid mobilizes, leading to increased intravascular volume.
As a result, women who develop eclampsia—particularly those with abnormal renal function, abruptio placentae, and/or preexisting chronic hypertension— face an increased risk for pulmonary edema and exacerbation of severe hypertension.2
Frequent evaluation of the amount of intravenous fluids is necessary, as well as oral intake, blood products, and urine output. They also need pulse oximetry and pulmonary auscultation.
Continue magnesium sulfate
Parenteral magnesium sulfate should be given for at least 24 hours after delivery and/or for at least 24 hours after the last convulsion.
If the patient has oliguria (less than 100 mL over 4 hours), both fluid administration and the dose of magnesium sulfate should be reduced.
Oral antihypertensives
Other oral antihypertensive agents such as labetalol or nifedipine can be given to keep systolic blood pressure below 155 mm Hg and diastolic blood pressure below 105 mm Hg. Nifedipine offers the benefit of improved diuresis in the postpartum period.
The author reports no financial relationships relevant to this article.
An eclamptic convulsion is frightening to behold. First, the woman’s face becomes distorted, and her eyes protrude. Then her face acquires a congested expression, and foam may exude from her mouth. Breathing stops.
Because eclampsia is so frightening, the natural tendency is to try to stop a convulsion, but this is not the wisest strategy.
Rather, the foremost priorities are to avoid maternal injury and support cardiovascular functions. How to do this, and how to prevent further convulsions, monitor and deliver the fetus, and avert complications are the focus of this article.
Since eclampsia may be fatal for both mother and fetus, all labor and delivery units and all obstetricians should be prepared to diagnose and manage this grave threat. However, few obstetric units encounter more than 1 or 2 cases a year; most obstetricians have little or no experience managing acute eclampsia. In the Western world, it affects only 1 in 2,000 to 1 in 3,448 pregnancies.1-4
How a convulsion happens
Most convulsions occur in 2 phases and last for 60 to 75 seconds. The first phase, lasting 15 to 20 seconds, begins with facial twitching, soon followed by a rigid body with generalized muscular contractions.
In the second phase, which lasts about a minute, the muscles of the body alternately contract and relax in rapid succession. This phase begins with the muscles of the jaw and rapidly encompasses eyelids, other facial muscles, and body. If the tongue is unprotected, the woman often bites it.
Coma sometimes follows the convulsion, and deep, rapid breathing usually begins as soon as the convulsion stops. In fact, maintaining oxygenation typically is not a problem after a single convulsion, and the risk of aspiration is low in a well managed patient.
Upon reviving, the woman typically remembers nothing about the seizure.
If convulsions recur, some degree of consciousness returns after each one, although the woman may become combative, agitated, and difficult to control.
Harbingers of complications
In the developed world, eclampsia increases the risk of maternal death (range: 0 to 1.8%).1-5 A recent review of all reported pregnancy-related deaths in the United States from 1979 to 1992 found 4,024 cases.6 Of these, 790 (19.6%) were due to preeclampsia-eclampsia, 49% of which were caused by eclampsia. The risk of death from preeclampsia or eclampsia was higher for the following groups:
- women over 30,
- no prenatal care,
- African Americans, and
- onset of preeclampsia or eclampsia before 28 weeks.6
Maternal morbidity
Pregnancies complicated by eclampsia also have higher rates of maternal morbidity such as pulmonary edema and HELLP syndrome (TABLE 1). Complications are substantially higher among women who develop antepartum eclampsia, especially when it is remote from term.1-3
TABLE 1
Maternal complications
Antepartum eclampsia, especially when it is remote from term, is much more likely to lead to complications
| COMPLICATION | RATE (%) | REMARKS |
|---|---|---|
| Death | 0.5-–2 | Risk of death is higher:
|
| Intracerebral hemorrhage | <1 | Usually related to several risk factors |
| Aspiration pneumonia | 2–3 | Heightened risk of maternal hypoxemia and acidosis |
| Disseminated coagulopathy | 3–5 | Regional anesthesia is contraindicated in these patients, and there is a heightened risk of hemorrhagic shock |
| Pulmonary edema | 3–5 | Heightened risk of maternal hypoxemia and acidosis |
| Acute renal failure | 5–9 | Usually seen in association with abruptio placentae, maternal hemorrhage, and prolonged maternal hypotension |
| Abruptio placentae | 7–10 | Can occur after a convulsion; suspect it if fetal bradycardia or late decelerations persist |
| HELLP syndrome | 10–15 |
Adverse perinatal outcomes
Perinatal mortality and morbidity are high in eclampsia, with a perinatal death rate in recent series of 5.6% to 11.8%.1,7 This high rate is related to prematurity, abruptio placentae, and severe growth restriction.1
Preterm deliveries occur in approximately 50% of cases, and about 25% occur before 32 weeks’ gestation.1
Diagnosis can be tricky
When the patient has generalized edema, hypertension, proteinuria, and convulsions, diagnosis of eclampsia is straightforward. Unfortunately, women with eclampsia exhibit a broad spectrum of signs, ranging from severe hypertension, severe proteinuria, and generalized edema, to absent or minimal hypertension, nonexistent proteinuria, and no edema (TABLE 2).1
Hypertension is the hallmark of diagnosis. Hypertension is severe (at least 160 mm Hg systolic and/or at least 110 mm Hg diastolic) in 20% to 54% of cases, and it is mild (systolic pressure between 140 and 160 mm Hg or diastolic pressure between 90 and 110 mm Hg) in 30% to 60% of cases.2,3 In 16% of cases, there may be no hypertension at all.2
Proteinuria. Eclampsia usually is associated with proteinuria (at least 1+ on dipstick).1 However, when I studied a series of 399 women with eclampsia, I found substantial proteinuria (3+ or above on dipstick) in only 48% of cases; proteinuria was absent in 14%.2
Edema. A weight gain of more than 2 lb per week (with or without clinical edema) during the third trimester may be the first sign of eclampsia. However, in my series of 399 women, edema was absent in 26% of cases.2
TABLE 2
Signs and symptoms of eclampsia*
Hypertension and proteinuria in eclampsia may be severe, mild, or even absent
| CONDITION | FREQUENCY (%) IN WOMEN WITH ECLAMPSIA | REMARKS |
|---|---|---|
| SIGNS | ||
| Hypertension | 85 | Should be documented on at least 2 occasions more than 6 hours apart |
| Severe: 160/110 mm Hg or more | 20–54 | |
| Mild: 140–160/90–110 mm Hg | 30–60 | |
| No hypertension2 | 16 | |
| Proteinuria | 85 | |
| At least 1+ on dipstick2 | 48 | |
| At least 3+ on dipstick | 14 | |
| No proteinuria | 15 | |
| SYMPTOMS | ||
| At least 1 of the following: | 33–75 | Clinical symptoms may occur before or after a convulsion |
| Headache | 30–70 | Persistent, occipital, or frontal |
| Right upper quadrant or epigastric pain | 12–20 | |
| Visual changes | 19–32 | Blurred vision, photophobia |
| Altered mental changes | 4–5 | |
| * Summary of 5 series | ||
Symptoms of eclampsia
Several clinical symptoms can occur before or after a convulsion1:
- persistent occipital or frontal headaches,
- blurred vision,
- photophobia,
- epigastric and/or right upper quadrant pain, and
- altered mental status.
Usual times of onset
Eclamptic convulsions can occur during pregnancy or delivery, or after delivery ( TABLE 3).1-5
Approximately 91% of antepartum cases develop at 28 weeks or beyond. The remaining cases tend to occur between 21 and 27 weeks’ gestation (7.5%), or at or before 20 weeks (1.5%).2
When eclampsia occurs before 20 weeks, it usually involves molar or hydropic degeneration of the placenta, with or without a fetus.1 However, eclampsia can occur in the first half of pregnancy without molar degeneration of the placenta, although this is rare.1,2 These women are sometimes misdiagnosed as having hypertensive encephalopathy, seizure disorder, or thrombotic thrombocytopenia purpura. Thus, women who develop convulsions in association with hypertension and proteinuria in the first half of pregnancy should be assumed to have eclampsia until proven otherwise,1 and require ultrasound examination of the uterus to rule out molar pregnancy and/or hydropic or cystic degeneration of the placenta.
Postpartum cases tend to occur within the first 48 hours, although some develop beyond this limit and have been reported as late as 23 days postpartum.8
Late postpartum eclampsia occurs more than 48 hours but less than 4 weeks after delivery.8 These women have signs and symptoms consistent with preeclampsia along with their convulsions.8,9 Thus, women who develop convulsions with hypertension and/or proteinuria, or with headaches or blurred vision, after 48 hours postpartum should be assumed to have eclampsia and treated accordingly.8,9
When eclampsia occurs especially late, perform an extensive neurologic examination to rule out other cerebral pathology.1,10
Eclampsia is atypical if convulsions occur before 20 weeks’ gestation or beyond 48 hours postpartum. It also is atypical if convulsions develop or persist despite adequate magnesium sulfate, or if the patient develops focal neurologic deficits, disorientation, blindness, or coma. In these cases, conduct a neurologic exam and cerebral imaging to exclude neurologic pathology.8-10
TABLE 3
Usual times of onset*
91% of antepartum eclampsia cases occur at 28 weeks or later, although eclamptic convulsions can occur at any time during pregnancy or delivery, or postpartum
| ONSET | FREQUENCY (%) | REMARKS |
|---|---|---|
| Antepartum | 38–53 | Maternal and perinatal mortality, and the incidence of complications and underlying disease, are higher in antepartum eclampsia, especially in early cases |
| ≤20 weeks | 1.5 | |
| 21 to 27 weeks | 7.5 | |
| ≥28 weeks | 91 | |
| Intrapartum | 18–36 | Intrapartum eclampsia more closely resembles postpartum disease than antepartum cases |
| Postpartum | 11–44 | Late postpartum eclampsia occurs more than 48 hours but less than 4 weeks after delivery |
| ≤48 hours | 7–39 | |
| >48 hours | 5–26 | |
| * Summary of 5 series | ||
Differential diagnosis
As with other aspects of preeclampsia, the presenting symptoms, clinical findings, and many laboratory results in eclampsia overlap several other medical and surgical conditions.1,10 Of course, eclampsia is the most common cause of convulsions in a woman with hypertension and/or proteinuria during pregnancy or immediately postpartum. On rare occasions, other causes of convulsions in pregnancy or postpartum may mimic eclampsia.1 These potential diagnoses are particularly important when the woman has focal neurologic deficits, prolonged coma, or atypical eclampsia.
The differential diagnosis encompasses a variety of cerebrovascular and metabolic disorders:
- hemorrhage,
- ruptured aneurysm or malformation,
- arterial embolism, thrombosis,
- venous thrombosis,
- hypoxic ischemic encephalopathy,
- angiomas,
- hypertensive encephalopathy,
- seizure disorder,
- hypoglycemia, hyponatremia,
- posterior leukoencephalopathy syndrome,
- thrombotic thrombocytopenic purpura,
- postdural puncture syndrome, and
- cerebral vasculitis/angiopathy.
Other diseases may factor in
Some women develop gestational hypertension or preeclampsia in association with connective tissue disease, thrombophilias, seizure disorder, or hypertensive encephalopathy, further confounding the diagnosis.
Thus, make every effort to ensure a correct diagnosis, since management may differ among these conditions.
Managing convulsions
Do not try to stop the first convulsion
The natural tendency is to try and interrupt the convulsion, but this is not recommended. Nor should you give a drug such as diazepam to shorten or stop the convulsion, especially if the patient lacks an intravenous line and no one skilled in intubation is immediately available. If diazepam is given, do not exceed 5 mg over 60 seconds. Rapid administration of this drug may lead to apnea or cardiac arrest, or both.
Steps to prevent maternal injury
During or immediately after the acute convulsive episode, take steps to prevent serious maternal injury and aspiration, assess and establish airway patency, and ensure maternal oxygenation (TABLE 4).
Elevate and pad the bed’s side rails and insert a padded tongue blade between the patient’s teeth, taking care not to trigger the gag reflex.
Physical restraints also may be needed.
Prevent aspiration. To minimize the risk of aspiration, place the patient in the lateral decubitus position, and suction vomitus and oral secretions as needed. Be aware that aspiration can occur when the padded tongue blade is forced to the back of the throat, stimulating the gag reflex and resultant vomiting.
TABLE 4
During a convulsion, 3 spheres of concern
| AVOID MATERNAL INJURY |
| Insert padded tongue blade |
| Avoid inducing gag reflex |
| Elevate padded bedside rails |
| Use physical restraints as needed |
| MAINTAIN OXYGENATION TO MOTHER AND FETUS |
| Apply face mask with or without oxygen reservoir at 8–10 L/minute |
| Monitor oxygenation and metabolic status via |
| Transcutaneous pulse oximetry |
| Arterial blood gases (sodium bicarbonate administered accordingly) |
| Correct oxygenation and metabolic status before administering anesthetics that may depress myocardial function |
| MINIMIZE ASPIRATION |
| Place patient in lateral decubitus position (which also maximizes uterine blood flow and venous return) |
| Suction vomitus and oral secretions |
| Obtain chest x-ray after the convulsion is controlled to rule out aspiration |
Tips on supplemental oxygenation
Although the initial seizure lasts only a minute or 2, it is important to maintain oxygenation by giving supplemental oxygen via a face mask, with or without an oxygen reservoir, at 8 to 10 L per minute. This is important because hypoventilation and respiratory acidosis often occur.
Once the convulsion ends and the patient resumes breathing, oxygenation is rarely a problem. However, maternal hypoxemia and acidosis can develop in women with repetitive convulsions, aspiration pneumonia, pulmonary edema, or a combination of these factors. Thus, transcutaneous pulse oximetry is advisable to monitor oxygenation in eclamptic patients.
Arterial blood gas analysis is necessary if pulse oximetry shows abnormal oxygen saturation (ie, at or below 92%).
Strategy to prevent recurrence
Magnesium sulfate is the drug of choice to treat and prevent subsequent convulsions in women with eclampsia.1,2
Dosage. I give a loading dose of 6 g over 15 to 20 minutes, followed by a maintenance dose of 2 g per hour as a continuous intravenous solution.
Approximately 10% of eclamptic women have a second convulsion after receiving magnesium sulfate.1,2 When this occurs, I give another 2-g bolus intravenously over 3 to 5 minutes.
More rarely, a woman will continue to have convulsions while receiving adequate and therapeutic doses of magnesium sulfate.
I treat such patients with sodium amobarbital, 250 mg, intravenously over 3 to 5 minutes.
Monitor maternal magnesium levels
Plasma levels should be in the range of 4 to 8 mg/dL during treatment for eclampsia, and are determined by the volume of distribution and by renal excretion. Thus, it is important to monitor the patient for magnesium toxicity, particularly if she has renal dysfunction (serum creatinine of 1.2 mg/dL or above) or urine output below 100 mL in 4 hours. In these women, adjust the maintenance dose according to plasma levels.
Side effects of magnesium including flushing, a feeling of warmth, nausea and vomiting, double vision, and slurred speech (TABLE 5).
If magnesium toxicity is suspected, immediately discontinue the infusion and administer supplemental oxygen along with 10 mL of 10% calcium gluconate (1 g total) as an intravenous push slowly over 5 minutes.
If respiratory arrest occurs, prompt resuscitation—including intubation and assisted ventilation—is vital.
TABLE 5
Clinical manifestations of magnesium toxicity
Maternal plasma levels of 4 to 8 mg/dL are appropriate during treatment for eclampsia; higher levels signal toxicity
| IF THE MAGNESIUM LEVEL IS… | THE CLINICAL MANIFESTATION IS… |
|---|---|
| 8–12 mg/dL | Loss of patellar reflex |
| Double or blurred vision | |
| Headache and nausea | |
| 9–12 mg/dL | Feeling of warmth, flushing |
| 10–12 mg/dL | Somnolence |
| Slurred speech | |
| 15–17 mg/dL | Muscular paralysis |
| Respiratory arrest | |
| 30–35 mg/dL | Cardiac arrest |
Controlling severe hypertension
The next step is to reduce blood pressure to a safe range. The objective: to preserve cerebral autoregulation and prevent congestive heart failure without compromising cerebral perfusion or jeopardizing uteroplacental blood flow, which is already reduced in many women with eclampsia.1
To these ends, try to keep systolic blood pressure between 140 and 160 mm Hg and diastolic pressure between 90 and 110 mm Hg. This can be achieved with:
- bolus 5- to 10-mg doses of hydralazine,
- 20 to 40 mg labetalol intravenously every 15 minutes, as needed, or
- 10 to 20 mg oral nifedipine every 30 minutes.
Other potent antihypertensive drugs such as sodium nitroprusside or nitroglycerine are rarely needed in eclampsia, and diuretics are indicated only in the presence of pulmonary edema.
Intrapartum management
Maternal hypoxemia and hypercarbia cause fetal heart rate and uterine activity changes during and immediately following a convulsion.
Fetal heart rate changes
These can include bradycardia, transient late decelerations, decreased beat-to-beat variability, and compensatory tachycardia.
The interval from onset of the seizure to the fall in fetal heart rate is approximately 5 minutes (FIGURE 1). Transitory fetal tachycardia frequently occurs after the prolonged bradycardia. The loss of beat-to-beat variability, with transitory late decelerations, occurs during the recovery phase.
The mechanism for the transient fetal bradycardia may be intense vasospasm and uterine hyperactivity, which may decrease uterine blood flow. The absence of maternal respiration during the convulsion may also contribute to fetal heart rate changes.
Since the fetal heart rate usually returns to normal after a convulsion, other conditions should be considered if an abnormal pattern persists.
In some cases, it may take longer for the heart rate pattern to return to baseline if the fetus is preterm with growth restriction.
Placental abruption may occur after the convulsion and should be suspected if fetal bradycardia or repetitive late decelerations persist (FIGURE 2).
FIGURE 1 Fetal response to a convulsion The top 2 tracings show fetal bradycardia during an eclamptic convulsion
FIGURE 2 Abruptio placentae Repetitive late decelerations secondary to abruptio placentae, necessitating cesarean section
Uterine activity
During a convulsion, contractions can increase in frequency and tone. The duration of increased uterine activity varies from 2 to 14 minutes.
These changes usually resolve spontaneously within 3 to 10 minutes following the termination of convulsions and correction of maternal hypoxemia (FIGURE 1).
If uterine hyperactivity persists, suspect placental abruption (FIGURE 2).
Do not rush to cesarean
It benefits the fetus to allow in utero recovery from the maternal convulsion, hypoxia, and hypercarbia before delivery. However, if the bradycardia and/or recurrent late decelerations persist beyond 10 to 15 minutes despite all efforts, suspect abruptio placentae or nonreassuring fetal status.
Once the patient regains consciousness and is oriented to name, place, and time, and her convulsions are controlled and condition stabilized, proceed with delivery.
Choosing a delivery route
Eclampsia is not an indication for cesarean. The decision to perform a cesarean should be based on fetal gestational age, fetal condition, presence of labor, and cervical Bishop score. I recommend:
- Cesarean section for women with eclampsia before 30 weeks’ gestation who are not in labor and whose Bishop score is below 5.
- Vaginal delivery for women in labor or with rupture of membranes, provided there are no obstetric complications.
- Labor induction with oxytocin infusion or prostaglandins in all women at or after 30 weeks, regardless of the Bishop score, and in women before 30 weeks when the Bishop score is 5 or above.
Maternal pain relief
During labor and delivery, systemic opioids or epidural anesthesia can provide pain relief—the same recommendations as for women with severe preeclampsia.
For cesarean delivery, an epidural, spinal, or combined techniques of regional anesthesia are suitable.
Do not use regional anesthesia if there is coagulopathy or severe thrombocytopenia (platelet count less than 50,000/mm3). In women with eclampsia, general anesthesia increases the risk of aspiration and failed intubation due to airway edema, and is associated with marked increases in systemic and cerebral pressures during intubation and extubation.
Women with airway or laryngeal edema may require awake intubation under fiber optic observation, with tracheostomy immediately available.
Changes in systemic or cerebral pressures may be attenuated by pretreatment with labetalol or nitroglycerine injections.
Postpartum management
After delivery, women with eclampsia require close monitoring of vital signs, fluid intake and output, and symptoms for at least 48 hours.
Risk of pulmonary edema
These women usually receive large amounts of intravenous fluids during labor, delivery, and postpartum. In addition, during the postpartum period, extracellular fluid mobilizes, leading to increased intravascular volume.
As a result, women who develop eclampsia—particularly those with abnormal renal function, abruptio placentae, and/or preexisting chronic hypertension— face an increased risk for pulmonary edema and exacerbation of severe hypertension.2
Frequent evaluation of the amount of intravenous fluids is necessary, as well as oral intake, blood products, and urine output. They also need pulse oximetry and pulmonary auscultation.
Continue magnesium sulfate
Parenteral magnesium sulfate should be given for at least 24 hours after delivery and/or for at least 24 hours after the last convulsion.
If the patient has oliguria (less than 100 mL over 4 hours), both fluid administration and the dose of magnesium sulfate should be reduced.
Oral antihypertensives
Other oral antihypertensive agents such as labetalol or nifedipine can be given to keep systolic blood pressure below 155 mm Hg and diastolic blood pressure below 105 mm Hg. Nifedipine offers the benefit of improved diuresis in the postpartum period.
The author reports no financial relationships relevant to this article.
1. Sibai BM. Diagnosis, differential diagnosis, and management of eclampsia. Obstet Gynecol. 2005;105:402-410.
2. Mattar F, Sibai BM. Eclampsia VIII. Risk factors for maternal morbidity. Am J Obstet Gynecol. 2000;182:307-312.
3. Douglas KA, Redman CW. Eclampsia in the United Kingdom. BMJ. 1994;309:1395-1400.
4. Rugard O, Carling MS, Berg G. Eclampsia at a tertiary hospital, 1973–99. Acta Obstet Gynecol Scand. 2004;83:240-245.
5. Katz VL, Farmer R, Kuller J. Preeclampsia into eclampsia: toward a new paradigm. Am J Obstet Gynecol. 2000;182:1389-1396.
6. MacKay AP, Berg CJ, Atrash HK. Pregnancy-related mortality from preeclampsia and eclampsia. Obstet Gynecol. 2001;97:533-538.
7. Leitch CR, Cameron AD, Walker JJ. The changing pattern of eclampsia over a 60-year period. Br J Obstet Gynaecol. 1997;104:917-922.
8. Lubarsky SL, Barton JR, Friedman SA, Nasreddine S, Ramaddan MK, Sibai BM. Late postpartum eclampsia revisited. Obstet Gynaecol. 1994;83:502-505.
9. Chames MC, Livingston JC, Ivester TS, Barton JR, Sibai BM. Late postpartum eclampsia: a preventable disease? Am J Obstet Gynecol. 2002;186:1174-1177.
10. Witlin AG, Friedman SA, Egerman RS, Frangieh AY, Sibai BM. Cerebrovascular disorders complicating pregnancy. Beyond eclampsia. Am J Obstet Gynecol. 1997;176:139-148.
1. Sibai BM. Diagnosis, differential diagnosis, and management of eclampsia. Obstet Gynecol. 2005;105:402-410.
2. Mattar F, Sibai BM. Eclampsia VIII. Risk factors for maternal morbidity. Am J Obstet Gynecol. 2000;182:307-312.
3. Douglas KA, Redman CW. Eclampsia in the United Kingdom. BMJ. 1994;309:1395-1400.
4. Rugard O, Carling MS, Berg G. Eclampsia at a tertiary hospital, 1973–99. Acta Obstet Gynecol Scand. 2004;83:240-245.
5. Katz VL, Farmer R, Kuller J. Preeclampsia into eclampsia: toward a new paradigm. Am J Obstet Gynecol. 2000;182:1389-1396.
6. MacKay AP, Berg CJ, Atrash HK. Pregnancy-related mortality from preeclampsia and eclampsia. Obstet Gynecol. 2001;97:533-538.
7. Leitch CR, Cameron AD, Walker JJ. The changing pattern of eclampsia over a 60-year period. Br J Obstet Gynaecol. 1997;104:917-922.
8. Lubarsky SL, Barton JR, Friedman SA, Nasreddine S, Ramaddan MK, Sibai BM. Late postpartum eclampsia revisited. Obstet Gynaecol. 1994;83:502-505.
9. Chames MC, Livingston JC, Ivester TS, Barton JR, Sibai BM. Late postpartum eclampsia: a preventable disease? Am J Obstet Gynecol. 2002;186:1174-1177.
10. Witlin AG, Friedman SA, Egerman RS, Frangieh AY, Sibai BM. Cerebrovascular disorders complicating pregnancy. Beyond eclampsia. Am J Obstet Gynecol. 1997;176:139-148.