User login
CONTRACEPTION
Since it was approved more than 10 years ago, depot medroxyprogesterone acetate (DMPA; Depo-Provera) has gained popularity among US women, largely because it requires minimal user participation and has a failure rate of only 0.3% per year.1,2 The main limitation, from the patient’s point of view, has been the intramuscular (IM) route of injection, which requires an office visit every 12 to 14 weeks for administration.
Now a subcutaneous version of the drug is available (Depo-subQ Provera 104) that delivers a lower dose of medroxyprogesterone acetate (MPA) (104 mg versus 150 mg for the IM formulation). The subcutaneous route opens the possibility for home self-injections, and the lower dose could decrease suppression of pituitary function and ovarian estradiol production, though further study is needed.
This article reviews the indications, benefits, risks, and potential adverse reactions of subcutaneous DMPA, a pharmacologically unique formulation with 16% weight/volume and a final dose of 104 mg MPA/0.65 mL. The dose was selected after study showed 100 mg to be the lowest dose to effectively suppress ovulation for at least 91 days.
The formulation and composition of subcutaneous DMPA cannot be duplicated by diluting the original IM formulation.
A potent contraceptive
Tw o large open-label, phase 3 studies assessed the 1-year efficacy, safety, and patient satisfaction of subcutaneous DMPA.3 These studies, conducted in North and South America, Europe, and Asia, reported zero pregnancies in 16,023 women-cycles of exposure.
Women in these studies had a broad range of body weights, ranging from 86 to 364 lb in the Americas and 77 to 249 lb in the European/Asian trial. The absence of pregnancies across all categories of body mass index (BMI) suggests that no dosage adjustments are necessary for higher BMIs.
Noncontraceptive benefits
Besides the high efficacy and long duration, which free women from daily attention to contraception, DMPA protects against endometrial cancer. The fact that it contains no estrogen makes it suitable for women who cannot or will not take estrogen products. It also is safe for breastfeeding mothers.
Perhaps most important is its ameliorative effect on endometriosis-associated pain.
Adverse effects
Many women stop using DMPA during the first year due to problems with irregular uterine bleeding, such as spotting and prolonged bleeding, which are especially common during the first 3 months of use. However, this problem usually diminishes over time, with most users becoming amenorrheic. This is true of both IM and subcutaneous DMPA. In a study of the latter, amenorrhea increased from 26% during month 3 to 55% during month 12.
The bleeding abnormalities associated with progestin-only contraceptives are not fully understood. We do know that suppression of circulating estradiol and the potent effect of MPA on the endometrium lead to varying degrees of endometrial disruption and atrophy, which ultimately manifest as irregular bleeding and amenorrhea. Subcutaneous DMPA likely involves the same processes, even though it contains 30% less MPA than the IM formulation.
Importance of counseling about bleeding effects
Two studies have shown that women are more likely to continue DMPA if they are counseled about bleeding effects when they start the medication.4,5 Since many patients would prefer less frequent or no menses, they may be encouraged by the prospect of becoming amenorrheic.
Risk of breast cancer
It will be several years before the effect of the lower-dose MPA on breast cancer risk is known.
DMPA and bone loss: Should we worry?
Subcutaneous DMPA, like its IM counterpart, is associated with changes in bone mineral density and carries a “black box” warning regarding this risk.6 Because DMPA suppresses circulating estradiol levels, it causes reductions in bone mineral density (BMD) that have aroused concern among the lay and medical media, although studies suggest BMD levels generally change little and recover when the drug is discontinued— except during perimenopause.
A metaanalysis of 12 studies involving 1,039 DMPA users (IM formulation) and 2,086 controls found that the average Z-score in DMPA users decreased less than 1 standard deviation, compared with nonusers.7 These BMD reductions stabilized after 3 to 4 years of DMPA use, and the bone loss was reversed when the drug was discontinued.8,9 Thus, it appears that, in time, BMD returns to levels similar to those in women who have never used the drug.
IM versus subcutaneous DMPA
In a comparison of both formulations of DMPA, both caused decreases in BMD at the end of 1 and 2 years of treatment.10 Women using subcutaneous DMPA experienced smaller decrements in total hip, lumbar spine, and femoral neck BMD after 1 and 2 years of treatment. However, these differences were significant only in the lumbar spine at 1 year.
Uncertain value for adolescents
DMPA should be carefully considered for use in adolescent girls—and this proviso includes the subcutaneous formulation.
Adolescence is a critical period for bone mineralization. Thus, any agent that limits bone accretion should be prescribed only after weighing all the other options.
A prospective cohort study in adolescents found a 3.1% decrease in BMD after 2 years of DMPA use, versus a 9.5% increase among nonusers.11 More recent reports indicate significant gains in BMD and reversal in bone loss once the drug is discontinued.12
What the “black box” warning means
Based in part on results from these studies, the Food and Drug Administration (FDA) and the drug’s manufacturer issued a black box warning for both the IM and subcutaneous formulations of DMPA. This step was taken to highlight the fact that users of DMPA may lose significant BMD, and that this loss may increase with duration of use and may not be entirely reversible.
The warning recommends that the drugs be used as long-term birth control only if other methods are inadequate. It emphasizes the general lack of certainty about the effect of these drugs on peak bone mass (when used in adolescence or early adulthood) and the risk of osteoporotic fracture (later in life).
How to counsel patients
I discuss the black box warning with each patient in the larger context of contraceptive counseling. The lower efficacy and other problems associated with daily birth control methods must be weighed against the risk of bone loss in both adolescents and adults.
It also is important to consider other risk factors for osteoporosis, such as chronic alcohol or tobacco use, eating disorders, or chronic use of corticosteroids. Adolescents who have poor eating habits or who use alcohol or tobacco may be at heightened risk of BMD loss.
Once a woman chooses DMPA, she should be encouraged to maintain a healthy lifestyle, including adequate calcium intake, weight-bearing and musclestrengthening exercises, smoking cessation, and moderate to no alcohol intake.
BMD measurements are not recommended since they do not predict fracture risk in premenopausal women.
Other side effects
Though rare, serious thrombotic events have been reported in women using the IM formulation.
Also rare are ocular disorders (loss of vision, proptosis, diplopia, or migraine) and ectopic pregnancy.
Other possible side effects include injection site reactions, decreased libido, acne, headache, fatigue, gastrointestinal disorders (distention, abdominal pain, diarrhea, nausea), infection, arthralgia, back pain, limb pain, dizziness, insomnia, anxiety, depression, breast pain and/or tenderness, and hot flushes.
Return to ovulation
DMPA is associated with a prolonged return to ovulation once it is discontinued. In a large US study of women who discontinued intramuscular DMPA to become pregnant, 68% conceived within 12 months, 83% conceived within 15 months, and 93% conceived within 18 months of the last injection, with a median time to conception of 10 months.13
Though no studies have determined the median time to conception for subcutaneous DMPA, it is likely to be similar to the 10-month interval seen with the IM formulation.
Comparing drugs head to head
The IM and subcutaneous formulations were compared prospectively at a single US center.14 The study defined return to ovulation as the first time serum progesterone levels reached at least 4.7 ng/mL. At the end of 12 months (postinjection), the cumulative rate of ovulation was 97.4% for subcutaneous DMPA and 94.7% for the IM formulation.
Ovulation occurred at a median of approximately 7 months (subcutaneous route) and 6 months (IM).
Early ovulation is possible
One subject in the subcutaneous DMPA group ovulated 14 weeks after her last injection. Thus, it is important to adhere to the recommended dosing schedule of 12 to 14 weeks.
Weight gain: 0 to 7.5 lb
Reports of weight gain with DMPA have been highly variable. Many women who discontinue hormonal contraceptives cite weight gain as the reason. With one third of US women meeting the criteria for obesity—a number that is likely to rise—and with ethnic variations, it is difficult to determine the exact impact of DMPA.
A well-designed, placebo-controlled trial by Pelkman and colleagues15 found DMPA to have no effect on resting energy expenditure, food intake, or body weight. Three large clinical trials of subcutaneous DMPA found a mean weight gain of 3.5 lb during the first year of use, and a small 2-year study comparing IM and subcutaneous DMPA found mean weight gains of 7.6 and 7.5 lb, respectively.
Combating endometriosis pain
With the FDA’s approval of subcutaneous DMPA for treatment of endometriosis-associated pain, the drug expands the pharmacologic choices for endometriosis pain relief for the first time in 15 years, with less frequent side effects than the other widely used drug, leuprolide acetate.
In an 18-month clinical trial comparing the 2 drugs, researchers found similar efficacy, with DMPA causing less bone loss and less frequent and severe menopausal symptoms. The trial involved 274 women and measured pain across the following categories: pelvic pain, dysmenorrhea, dyspareunia, pelvic tenderness, and induration.
Clearing a woman for use
The manufacturer recommends that all women undergo an annual history and physical examination. The physical exam should include a blood pressure check; examination of the breasts, abdomen, and pelvic organs; cervical cytology; and any relevant laboratory studies.
Overall outlook
Subcutaneous DMPA offers women the same advantages as the IM formulation. Since we have long-term experience with MPA as a contraceptive agent, we know it offers many noncontraceptive benefits, safety, and excellent contraceptive efficacy.
As we gain experience specific to subcutaneous DMPA , and as data accumulate from additional trials, we will be able to further define its role as a contraceptive option.
Disclosure
Dr. Jain has disclosed that he has received grant/research support from Ferring, Organon, Pfizer, Serono, and TA P.
REFERENCES
1. Westhoff C. Depot-medroxyprogesterone acetate injection (Depo-Provera®): a highly effective contraceptive option with proven long-term safety. Contraception. 2003;68:75-87.
2. Trussell J. Contraceptive efficacy. In: Hatcher RA, Trussell J, Stewart F, et al. Contraceptive Technology. 17th revised edition. New York: Irvington Publishers; 1998.
3. Jain JK, Jakimiuk AJ, Bode FR, et al. Contraceptive efficacy and safety of DMPA-SC. Contraception. 2004;70:269-275.
4. Canto De Cetina TE, Canto P, Luna MO. Effect of counseling to improve compliance in Mexican women receiving depo-medroxyprogesterone acetate. Contraception. 2001;63:143-146.
5. Lei ZW, Wu SC, Garceau RJ, et al. Effect of pretreatment counseling on discontinuation rates in Chinese women given depo-medroxyprogesterone acetate for contraception. Contraception. 1996;53:357-361.
6. Depo SubQ Provera 104 [package insert]. Cambridge, Mass: Pfizer; 2005.
7. Banks E, Berrington A, Casabonne D. Overview of the relationship between use of progestogen-only contraceptives and bone mineral density. Br J Obstet Gynecol. 2001;108:1214-1221.
8. Tang OS, Tang G, Yip PSF, et al. Further evaluation on long-term depot-medroxyprogesterone acetate use and bone mineral density: a longitudinal cohort study. Contraception. 2000;62:161-164.
9. Petitti DB, Piaggio G, Mehta S, et al. Steroid hormone contraception and bone mineral density: a cross-sectional study in an international population. Obstet Gynecol. 2000;95:736-744.
10. Jain JK. Evaluation of bone mineral density in women treated with DMPA-SC 104 or DMPA-IM 150. Presented at: Annual Meeting of the American Academy of Nurse Practitioners; June 17, 2005; Fort Lauderdale, Fla.
11. Cromer BA, Blair JM, Mahan JD, et al. A prospective comparison of bone density in adolescent girls receiving depot medroxyprogesterone acetate (DMPA), levonorgestrel (Norplant), or oral contraceptives. J Pediatr. 1996;129:671-676.
12. Scholes D, LaCroix AZ, Ichikawa LE, et al. Change in bone mineral density among adolescent women using and discontinuing depot medroxyprogesterone acetate contraception. Arch Pediatr Adolesc Med. 2005;159:139-144.
13. Depo-Provera [package insert]. Cambridge, Mass: Pfizer; 1999.
14. Jain JK, Dutton C, Nicosia A, et al. Pharmacokinetics, ovulation suppression and return to ovulation following a lower dose subcutaneous formulation of Depo-Provera®. Contraception. 2004;70:11-18.
15. Pelkman CL, Chow M, Heinbach RA, et al. Short-term effects of a progestational contraceptive drug on food intake, resting energy expenditure, and body weight in young women. Am J Clin Nutr. 2001;73:19-26.
CONTRACEPTIVES IN THE NEWS Plan B: Studies surprise both sides
Ian H. Thorneycroft
MD, PhD
OBG Management
Board of Editors
Professor of Obstetrics and Gynecology, University of South Alabama College of Medicine, Mobile, Ala
Marston C, Meltzer H, Majeed A. Impact on contraceptive practice of making emergency hormonal contraception available over the counter in Great Britain: repeated cross sectional surveys. BMJ doi;10.1136/bmj.38519.440266.8F (published July 11, 2005).
Raine TR, Harper CC, Rocca CH, Fischer R, Padian N, Klausner JD, Darney PD. Direct access to emergency contraception through pharmacies and effect of unintended pregnancy and STIs: a randomized controlled trial. JAMA. 2005;292:54–62.
Litt IF. Placing emergency contraception in the hands of women. JAMA. 2005;293:98–99.
A quick succession of events in July seemed to clear the path to a Food and Drug Administration (FDA) decision on over-the-counter sale of levonorgestrel (Plan B), the emergency contraceptive.
A week after the publication of the large study led by Marston, Plan B was placed on the FDA calendar for a Sept. 1 decision. The authors concluded that their study “supports the case for lifting the ban on over-the-counter sales of emergency hormonal contraception in the United States and other countries.”
Plan B has been a point of contention, especially after the FDA, in 2004, rejected Barr Laboratories’ application for OTC access, on the basis of lack of long-term safety data on its use in young adolescent women, without medical supervision.
When the manufacturer changed its application, the agency declined to make a decision by the legal deadline, last January. Proponents of OTC sales of Plan B objected, citing the agency’s own staff endorsement, and that of an independent panel.
In a series of interactions between the Senate and the administration in early July, the U.S. secretary of health and human services promised a Sept. 1 decision on Barr’s application. Media reports related that announcement to the July 18 Senate confirmation of Dr. Lester Crawford to head the Food and Drug Administration.
Both sides of the controversy met with some surprises in the BMJ and JAMA reports of research on the effects of Plan B access. Opponents of OTC availability in the United States have predicted that such access might increase unprotected sex, especially in young women and girls. Advocates have predicted that it would reduce the number of unintended pregnancies and abortions.
Public health impact may be negligible”
The report in the British Medical Journal concluded, “Making emergency hormonal contraception available over the counter does not seem to have led to an increase in its use, to an increase in unprotected sex, or to a decrease in the use of more reliable methods of contraception.” The study used an Omnibus Survey of 7,600 adults (an annual multipurpose survey in Great Britain) to examine contraception use after OTC emergency contraception was legalized in 2001. Women aged 16 to 49 were surveyed.
Although the lack of any increase in use of emergency hormone contraception suggests that the predicted rise in unsafe sex has been overstated, so too have the predicted effects on unwanted pregnancy, the authors observed.Similarly, the January JAMA report of a US study found: “While removing the requirement to go through pharmacists or clinics to obtain emergency contraception increases use, the public health impact may be negligible because of high rates of unprotected intercourse and relative underutilization of the method.”
Barr requests OTC access of Plan B for women 16 and older. Prescriptions would still be required for younger women.
Plan B is often called the “morning-after pill,” but in fact the method can be used any time after intercourse for up to 72 hours. It is best used as soon as possible, but can even be used after 72 hours, although at reduced efficacy.
Kuyoh MA, Toroitich-Ruto C, Grimes DA, Schulz KF, Gallo MF. Sponge versus diaphragm for contraception: a Cochrane review. Contraception. 2003;67:15–18.
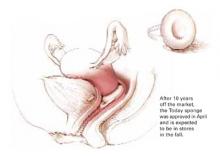
When the Today sponge was pulled off the market by its maker in 1995, the popular Jerry Seinfeld TV show aired an episode showing the character Elaine dashing from store to store, in search of the last few sponges on the shelves. She ultimately found a neighborhood pharmacy with 1 remaining case of 60 sponges. “Just give me the whole case and I’ll be on my way,” she tells the pharmacist. In the show, Elaine used the term “sponge-worthy” to characterize a potential date, and the term became a household word overnight. When it was available in the United States, the Today sponge was the most widely used form of OTC contraception, selling approximately 250 million sponges.
The sponge, which contains the spermicide nonoxynol-9, was sold from 1983 to 1995, when it was voluntarily withdrawn for safety reasons. The FDA found that water at the manufacturing plant was contaminated, and American Home Products, (now Wyeth), decided it was too costly to upgrade its plant, and voluntarily withdrew the Today sponge from the market. Allendale Pharmaceuticals bought the rights for the sponge in 1998, and has been working to secure approval for marketing. The new version has been available in Canada since 2003. According to the manufacturer, it should be in US drug stores sometime this fall, for about $2.50 to $3 per sponge.
The sponge is best compared to a diaphragm. Its failure rate is frequently quoted as approximately 9% to 11% per year, very comparable to condoms.
Efficacy. However, in a Cochrane review of sponges versus the diaphragm, the sponge failure rate was 17.4% in a US trial and 24.5% in a British trial. The rates for a diaphragm were 12.8% and 10.9%, respectively. Unlike a diaphragm, the sponge does not have to be fitted and had equal efficacy in multiparous as nulliparous women, in the 2 studies reviewed. The main advantage of the sponge over a diaphragm is its ready availability over-the-counter.
According the manufacturer, the sponge can be inserted up to 24 hours prior to intercourse, and provides continuous protection throughout that period, for as many acts of intercourse as desired. Although it is not necessary to keep the sponge inserted for a full 24 hours, it must be left in place for 6 hours after the last act of intercourse. It should not be worn for more than 30 consecutive hours. The women in the 2 studies included in the Cochrane review, however, left the sponge in place for 48 hours.
Same-day start-up for OCs improves compliance
Westhoff C, Kerns J, Morroni C, Cushman LF, Tiezzi L, Murphy PA. Quick Start: a novel oral contraceptive initiation method. Contraception. 2002;66:141–145.
Many women never start the oral contraceptive we prescribe. They have to wait for their next menses, and they may fail to fill the prescription; 25% of study participants never start their oral contraceptives.
Quick Start starts the contraceptive in the clinic, after a negative pregnancy test, regardless of the day of the patient’s cycle. She is given at least 1 pack so she does not have to go to the drug store to fill the first prescription. Emergency contraception is given to patients who may need it. The continuation rate to the second cycle was higher in women beginning the pill in the clinic than those who started at any point in their cycle but waited to fill the prescription.
The original oral contraceptives were started on the first Sunday of a menstrual cycle so that it was known the woman was not pregnant and so she would bleed midweek. Waiting until menses assured a possible pregnancy was not exposed to hormonal contraceptives; however, the components of oral contraceptives are not teratogenic. The contraceptive can therefore be started at anytime during the cycle and starting in the clinic increases compliance. A pregnancy test can be performed if the anticipated menses at the end of the pill pack does not occur.
Disclosure
The author is on the speakers bureaus for Barr, Berlex, and Wyeth-Ayerst.
Since it was approved more than 10 years ago, depot medroxyprogesterone acetate (DMPA; Depo-Provera) has gained popularity among US women, largely because it requires minimal user participation and has a failure rate of only 0.3% per year.1,2 The main limitation, from the patient’s point of view, has been the intramuscular (IM) route of injection, which requires an office visit every 12 to 14 weeks for administration.
Now a subcutaneous version of the drug is available (Depo-subQ Provera 104) that delivers a lower dose of medroxyprogesterone acetate (MPA) (104 mg versus 150 mg for the IM formulation). The subcutaneous route opens the possibility for home self-injections, and the lower dose could decrease suppression of pituitary function and ovarian estradiol production, though further study is needed.
This article reviews the indications, benefits, risks, and potential adverse reactions of subcutaneous DMPA, a pharmacologically unique formulation with 16% weight/volume and a final dose of 104 mg MPA/0.65 mL. The dose was selected after study showed 100 mg to be the lowest dose to effectively suppress ovulation for at least 91 days.
The formulation and composition of subcutaneous DMPA cannot be duplicated by diluting the original IM formulation.
A potent contraceptive
Tw o large open-label, phase 3 studies assessed the 1-year efficacy, safety, and patient satisfaction of subcutaneous DMPA.3 These studies, conducted in North and South America, Europe, and Asia, reported zero pregnancies in 16,023 women-cycles of exposure.
Women in these studies had a broad range of body weights, ranging from 86 to 364 lb in the Americas and 77 to 249 lb in the European/Asian trial. The absence of pregnancies across all categories of body mass index (BMI) suggests that no dosage adjustments are necessary for higher BMIs.
Noncontraceptive benefits
Besides the high efficacy and long duration, which free women from daily attention to contraception, DMPA protects against endometrial cancer. The fact that it contains no estrogen makes it suitable for women who cannot or will not take estrogen products. It also is safe for breastfeeding mothers.
Perhaps most important is its ameliorative effect on endometriosis-associated pain.
Adverse effects
Many women stop using DMPA during the first year due to problems with irregular uterine bleeding, such as spotting and prolonged bleeding, which are especially common during the first 3 months of use. However, this problem usually diminishes over time, with most users becoming amenorrheic. This is true of both IM and subcutaneous DMPA. In a study of the latter, amenorrhea increased from 26% during month 3 to 55% during month 12.
The bleeding abnormalities associated with progestin-only contraceptives are not fully understood. We do know that suppression of circulating estradiol and the potent effect of MPA on the endometrium lead to varying degrees of endometrial disruption and atrophy, which ultimately manifest as irregular bleeding and amenorrhea. Subcutaneous DMPA likely involves the same processes, even though it contains 30% less MPA than the IM formulation.
Importance of counseling about bleeding effects
Two studies have shown that women are more likely to continue DMPA if they are counseled about bleeding effects when they start the medication.4,5 Since many patients would prefer less frequent or no menses, they may be encouraged by the prospect of becoming amenorrheic.
Risk of breast cancer
It will be several years before the effect of the lower-dose MPA on breast cancer risk is known.
DMPA and bone loss: Should we worry?
Subcutaneous DMPA, like its IM counterpart, is associated with changes in bone mineral density and carries a “black box” warning regarding this risk.6 Because DMPA suppresses circulating estradiol levels, it causes reductions in bone mineral density (BMD) that have aroused concern among the lay and medical media, although studies suggest BMD levels generally change little and recover when the drug is discontinued— except during perimenopause.
A metaanalysis of 12 studies involving 1,039 DMPA users (IM formulation) and 2,086 controls found that the average Z-score in DMPA users decreased less than 1 standard deviation, compared with nonusers.7 These BMD reductions stabilized after 3 to 4 years of DMPA use, and the bone loss was reversed when the drug was discontinued.8,9 Thus, it appears that, in time, BMD returns to levels similar to those in women who have never used the drug.
IM versus subcutaneous DMPA
In a comparison of both formulations of DMPA, both caused decreases in BMD at the end of 1 and 2 years of treatment.10 Women using subcutaneous DMPA experienced smaller decrements in total hip, lumbar spine, and femoral neck BMD after 1 and 2 years of treatment. However, these differences were significant only in the lumbar spine at 1 year.
Uncertain value for adolescents
DMPA should be carefully considered for use in adolescent girls—and this proviso includes the subcutaneous formulation.
Adolescence is a critical period for bone mineralization. Thus, any agent that limits bone accretion should be prescribed only after weighing all the other options.
A prospective cohort study in adolescents found a 3.1% decrease in BMD after 2 years of DMPA use, versus a 9.5% increase among nonusers.11 More recent reports indicate significant gains in BMD and reversal in bone loss once the drug is discontinued.12
What the “black box” warning means
Based in part on results from these studies, the Food and Drug Administration (FDA) and the drug’s manufacturer issued a black box warning for both the IM and subcutaneous formulations of DMPA. This step was taken to highlight the fact that users of DMPA may lose significant BMD, and that this loss may increase with duration of use and may not be entirely reversible.
The warning recommends that the drugs be used as long-term birth control only if other methods are inadequate. It emphasizes the general lack of certainty about the effect of these drugs on peak bone mass (when used in adolescence or early adulthood) and the risk of osteoporotic fracture (later in life).
How to counsel patients
I discuss the black box warning with each patient in the larger context of contraceptive counseling. The lower efficacy and other problems associated with daily birth control methods must be weighed against the risk of bone loss in both adolescents and adults.
It also is important to consider other risk factors for osteoporosis, such as chronic alcohol or tobacco use, eating disorders, or chronic use of corticosteroids. Adolescents who have poor eating habits or who use alcohol or tobacco may be at heightened risk of BMD loss.
Once a woman chooses DMPA, she should be encouraged to maintain a healthy lifestyle, including adequate calcium intake, weight-bearing and musclestrengthening exercises, smoking cessation, and moderate to no alcohol intake.
BMD measurements are not recommended since they do not predict fracture risk in premenopausal women.
Other side effects
Though rare, serious thrombotic events have been reported in women using the IM formulation.
Also rare are ocular disorders (loss of vision, proptosis, diplopia, or migraine) and ectopic pregnancy.
Other possible side effects include injection site reactions, decreased libido, acne, headache, fatigue, gastrointestinal disorders (distention, abdominal pain, diarrhea, nausea), infection, arthralgia, back pain, limb pain, dizziness, insomnia, anxiety, depression, breast pain and/or tenderness, and hot flushes.
Return to ovulation
DMPA is associated with a prolonged return to ovulation once it is discontinued. In a large US study of women who discontinued intramuscular DMPA to become pregnant, 68% conceived within 12 months, 83% conceived within 15 months, and 93% conceived within 18 months of the last injection, with a median time to conception of 10 months.13
Though no studies have determined the median time to conception for subcutaneous DMPA, it is likely to be similar to the 10-month interval seen with the IM formulation.
Comparing drugs head to head
The IM and subcutaneous formulations were compared prospectively at a single US center.14 The study defined return to ovulation as the first time serum progesterone levels reached at least 4.7 ng/mL. At the end of 12 months (postinjection), the cumulative rate of ovulation was 97.4% for subcutaneous DMPA and 94.7% for the IM formulation.
Ovulation occurred at a median of approximately 7 months (subcutaneous route) and 6 months (IM).
Early ovulation is possible
One subject in the subcutaneous DMPA group ovulated 14 weeks after her last injection. Thus, it is important to adhere to the recommended dosing schedule of 12 to 14 weeks.
Weight gain: 0 to 7.5 lb
Reports of weight gain with DMPA have been highly variable. Many women who discontinue hormonal contraceptives cite weight gain as the reason. With one third of US women meeting the criteria for obesity—a number that is likely to rise—and with ethnic variations, it is difficult to determine the exact impact of DMPA.
A well-designed, placebo-controlled trial by Pelkman and colleagues15 found DMPA to have no effect on resting energy expenditure, food intake, or body weight. Three large clinical trials of subcutaneous DMPA found a mean weight gain of 3.5 lb during the first year of use, and a small 2-year study comparing IM and subcutaneous DMPA found mean weight gains of 7.6 and 7.5 lb, respectively.
Combating endometriosis pain
With the FDA’s approval of subcutaneous DMPA for treatment of endometriosis-associated pain, the drug expands the pharmacologic choices for endometriosis pain relief for the first time in 15 years, with less frequent side effects than the other widely used drug, leuprolide acetate.
In an 18-month clinical trial comparing the 2 drugs, researchers found similar efficacy, with DMPA causing less bone loss and less frequent and severe menopausal symptoms. The trial involved 274 women and measured pain across the following categories: pelvic pain, dysmenorrhea, dyspareunia, pelvic tenderness, and induration.
Clearing a woman for use
The manufacturer recommends that all women undergo an annual history and physical examination. The physical exam should include a blood pressure check; examination of the breasts, abdomen, and pelvic organs; cervical cytology; and any relevant laboratory studies.
Overall outlook
Subcutaneous DMPA offers women the same advantages as the IM formulation. Since we have long-term experience with MPA as a contraceptive agent, we know it offers many noncontraceptive benefits, safety, and excellent contraceptive efficacy.
As we gain experience specific to subcutaneous DMPA , and as data accumulate from additional trials, we will be able to further define its role as a contraceptive option.
Disclosure
Dr. Jain has disclosed that he has received grant/research support from Ferring, Organon, Pfizer, Serono, and TA P.
REFERENCES
1. Westhoff C. Depot-medroxyprogesterone acetate injection (Depo-Provera®): a highly effective contraceptive option with proven long-term safety. Contraception. 2003;68:75-87.
2. Trussell J. Contraceptive efficacy. In: Hatcher RA, Trussell J, Stewart F, et al. Contraceptive Technology. 17th revised edition. New York: Irvington Publishers; 1998.
3. Jain JK, Jakimiuk AJ, Bode FR, et al. Contraceptive efficacy and safety of DMPA-SC. Contraception. 2004;70:269-275.
4. Canto De Cetina TE, Canto P, Luna MO. Effect of counseling to improve compliance in Mexican women receiving depo-medroxyprogesterone acetate. Contraception. 2001;63:143-146.
5. Lei ZW, Wu SC, Garceau RJ, et al. Effect of pretreatment counseling on discontinuation rates in Chinese women given depo-medroxyprogesterone acetate for contraception. Contraception. 1996;53:357-361.
6. Depo SubQ Provera 104 [package insert]. Cambridge, Mass: Pfizer; 2005.
7. Banks E, Berrington A, Casabonne D. Overview of the relationship between use of progestogen-only contraceptives and bone mineral density. Br J Obstet Gynecol. 2001;108:1214-1221.
8. Tang OS, Tang G, Yip PSF, et al. Further evaluation on long-term depot-medroxyprogesterone acetate use and bone mineral density: a longitudinal cohort study. Contraception. 2000;62:161-164.
9. Petitti DB, Piaggio G, Mehta S, et al. Steroid hormone contraception and bone mineral density: a cross-sectional study in an international population. Obstet Gynecol. 2000;95:736-744.
10. Jain JK. Evaluation of bone mineral density in women treated with DMPA-SC 104 or DMPA-IM 150. Presented at: Annual Meeting of the American Academy of Nurse Practitioners; June 17, 2005; Fort Lauderdale, Fla.
11. Cromer BA, Blair JM, Mahan JD, et al. A prospective comparison of bone density in adolescent girls receiving depot medroxyprogesterone acetate (DMPA), levonorgestrel (Norplant), or oral contraceptives. J Pediatr. 1996;129:671-676.
12. Scholes D, LaCroix AZ, Ichikawa LE, et al. Change in bone mineral density among adolescent women using and discontinuing depot medroxyprogesterone acetate contraception. Arch Pediatr Adolesc Med. 2005;159:139-144.
13. Depo-Provera [package insert]. Cambridge, Mass: Pfizer; 1999.
14. Jain JK, Dutton C, Nicosia A, et al. Pharmacokinetics, ovulation suppression and return to ovulation following a lower dose subcutaneous formulation of Depo-Provera®. Contraception. 2004;70:11-18.
15. Pelkman CL, Chow M, Heinbach RA, et al. Short-term effects of a progestational contraceptive drug on food intake, resting energy expenditure, and body weight in young women. Am J Clin Nutr. 2001;73:19-26.
CONTRACEPTIVES IN THE NEWS Plan B: Studies surprise both sides
Ian H. Thorneycroft
MD, PhD
OBG Management
Board of Editors
Professor of Obstetrics and Gynecology, University of South Alabama College of Medicine, Mobile, Ala
Marston C, Meltzer H, Majeed A. Impact on contraceptive practice of making emergency hormonal contraception available over the counter in Great Britain: repeated cross sectional surveys. BMJ doi;10.1136/bmj.38519.440266.8F (published July 11, 2005).
Raine TR, Harper CC, Rocca CH, Fischer R, Padian N, Klausner JD, Darney PD. Direct access to emergency contraception through pharmacies and effect of unintended pregnancy and STIs: a randomized controlled trial. JAMA. 2005;292:54–62.
Litt IF. Placing emergency contraception in the hands of women. JAMA. 2005;293:98–99.
A quick succession of events in July seemed to clear the path to a Food and Drug Administration (FDA) decision on over-the-counter sale of levonorgestrel (Plan B), the emergency contraceptive.
A week after the publication of the large study led by Marston, Plan B was placed on the FDA calendar for a Sept. 1 decision. The authors concluded that their study “supports the case for lifting the ban on over-the-counter sales of emergency hormonal contraception in the United States and other countries.”
Plan B has been a point of contention, especially after the FDA, in 2004, rejected Barr Laboratories’ application for OTC access, on the basis of lack of long-term safety data on its use in young adolescent women, without medical supervision.
When the manufacturer changed its application, the agency declined to make a decision by the legal deadline, last January. Proponents of OTC sales of Plan B objected, citing the agency’s own staff endorsement, and that of an independent panel.
In a series of interactions between the Senate and the administration in early July, the U.S. secretary of health and human services promised a Sept. 1 decision on Barr’s application. Media reports related that announcement to the July 18 Senate confirmation of Dr. Lester Crawford to head the Food and Drug Administration.
Both sides of the controversy met with some surprises in the BMJ and JAMA reports of research on the effects of Plan B access. Opponents of OTC availability in the United States have predicted that such access might increase unprotected sex, especially in young women and girls. Advocates have predicted that it would reduce the number of unintended pregnancies and abortions.
Public health impact may be negligible”
The report in the British Medical Journal concluded, “Making emergency hormonal contraception available over the counter does not seem to have led to an increase in its use, to an increase in unprotected sex, or to a decrease in the use of more reliable methods of contraception.” The study used an Omnibus Survey of 7,600 adults (an annual multipurpose survey in Great Britain) to examine contraception use after OTC emergency contraception was legalized in 2001. Women aged 16 to 49 were surveyed.
Although the lack of any increase in use of emergency hormone contraception suggests that the predicted rise in unsafe sex has been overstated, so too have the predicted effects on unwanted pregnancy, the authors observed.Similarly, the January JAMA report of a US study found: “While removing the requirement to go through pharmacists or clinics to obtain emergency contraception increases use, the public health impact may be negligible because of high rates of unprotected intercourse and relative underutilization of the method.”
Barr requests OTC access of Plan B for women 16 and older. Prescriptions would still be required for younger women.
Plan B is often called the “morning-after pill,” but in fact the method can be used any time after intercourse for up to 72 hours. It is best used as soon as possible, but can even be used after 72 hours, although at reduced efficacy.
Kuyoh MA, Toroitich-Ruto C, Grimes DA, Schulz KF, Gallo MF. Sponge versus diaphragm for contraception: a Cochrane review. Contraception. 2003;67:15–18.
When the Today sponge was pulled off the market by its maker in 1995, the popular Jerry Seinfeld TV show aired an episode showing the character Elaine dashing from store to store, in search of the last few sponges on the shelves. She ultimately found a neighborhood pharmacy with 1 remaining case of 60 sponges. “Just give me the whole case and I’ll be on my way,” she tells the pharmacist. In the show, Elaine used the term “sponge-worthy” to characterize a potential date, and the term became a household word overnight. When it was available in the United States, the Today sponge was the most widely used form of OTC contraception, selling approximately 250 million sponges.
The sponge, which contains the spermicide nonoxynol-9, was sold from 1983 to 1995, when it was voluntarily withdrawn for safety reasons. The FDA found that water at the manufacturing plant was contaminated, and American Home Products, (now Wyeth), decided it was too costly to upgrade its plant, and voluntarily withdrew the Today sponge from the market. Allendale Pharmaceuticals bought the rights for the sponge in 1998, and has been working to secure approval for marketing. The new version has been available in Canada since 2003. According to the manufacturer, it should be in US drug stores sometime this fall, for about $2.50 to $3 per sponge.
The sponge is best compared to a diaphragm. Its failure rate is frequently quoted as approximately 9% to 11% per year, very comparable to condoms.
Efficacy. However, in a Cochrane review of sponges versus the diaphragm, the sponge failure rate was 17.4% in a US trial and 24.5% in a British trial. The rates for a diaphragm were 12.8% and 10.9%, respectively. Unlike a diaphragm, the sponge does not have to be fitted and had equal efficacy in multiparous as nulliparous women, in the 2 studies reviewed. The main advantage of the sponge over a diaphragm is its ready availability over-the-counter.
According the manufacturer, the sponge can be inserted up to 24 hours prior to intercourse, and provides continuous protection throughout that period, for as many acts of intercourse as desired. Although it is not necessary to keep the sponge inserted for a full 24 hours, it must be left in place for 6 hours after the last act of intercourse. It should not be worn for more than 30 consecutive hours. The women in the 2 studies included in the Cochrane review, however, left the sponge in place for 48 hours.
Same-day start-up for OCs improves compliance
Westhoff C, Kerns J, Morroni C, Cushman LF, Tiezzi L, Murphy PA. Quick Start: a novel oral contraceptive initiation method. Contraception. 2002;66:141–145.
Many women never start the oral contraceptive we prescribe. They have to wait for their next menses, and they may fail to fill the prescription; 25% of study participants never start their oral contraceptives.
Quick Start starts the contraceptive in the clinic, after a negative pregnancy test, regardless of the day of the patient’s cycle. She is given at least 1 pack so she does not have to go to the drug store to fill the first prescription. Emergency contraception is given to patients who may need it. The continuation rate to the second cycle was higher in women beginning the pill in the clinic than those who started at any point in their cycle but waited to fill the prescription.
The original oral contraceptives were started on the first Sunday of a menstrual cycle so that it was known the woman was not pregnant and so she would bleed midweek. Waiting until menses assured a possible pregnancy was not exposed to hormonal contraceptives; however, the components of oral contraceptives are not teratogenic. The contraceptive can therefore be started at anytime during the cycle and starting in the clinic increases compliance. A pregnancy test can be performed if the anticipated menses at the end of the pill pack does not occur.
Disclosure
The author is on the speakers bureaus for Barr, Berlex, and Wyeth-Ayerst.
Since it was approved more than 10 years ago, depot medroxyprogesterone acetate (DMPA; Depo-Provera) has gained popularity among US women, largely because it requires minimal user participation and has a failure rate of only 0.3% per year.1,2 The main limitation, from the patient’s point of view, has been the intramuscular (IM) route of injection, which requires an office visit every 12 to 14 weeks for administration.
Now a subcutaneous version of the drug is available (Depo-subQ Provera 104) that delivers a lower dose of medroxyprogesterone acetate (MPA) (104 mg versus 150 mg for the IM formulation). The subcutaneous route opens the possibility for home self-injections, and the lower dose could decrease suppression of pituitary function and ovarian estradiol production, though further study is needed.
This article reviews the indications, benefits, risks, and potential adverse reactions of subcutaneous DMPA, a pharmacologically unique formulation with 16% weight/volume and a final dose of 104 mg MPA/0.65 mL. The dose was selected after study showed 100 mg to be the lowest dose to effectively suppress ovulation for at least 91 days.
The formulation and composition of subcutaneous DMPA cannot be duplicated by diluting the original IM formulation.
A potent contraceptive
Tw o large open-label, phase 3 studies assessed the 1-year efficacy, safety, and patient satisfaction of subcutaneous DMPA.3 These studies, conducted in North and South America, Europe, and Asia, reported zero pregnancies in 16,023 women-cycles of exposure.
Women in these studies had a broad range of body weights, ranging from 86 to 364 lb in the Americas and 77 to 249 lb in the European/Asian trial. The absence of pregnancies across all categories of body mass index (BMI) suggests that no dosage adjustments are necessary for higher BMIs.
Noncontraceptive benefits
Besides the high efficacy and long duration, which free women from daily attention to contraception, DMPA protects against endometrial cancer. The fact that it contains no estrogen makes it suitable for women who cannot or will not take estrogen products. It also is safe for breastfeeding mothers.
Perhaps most important is its ameliorative effect on endometriosis-associated pain.
Adverse effects
Many women stop using DMPA during the first year due to problems with irregular uterine bleeding, such as spotting and prolonged bleeding, which are especially common during the first 3 months of use. However, this problem usually diminishes over time, with most users becoming amenorrheic. This is true of both IM and subcutaneous DMPA. In a study of the latter, amenorrhea increased from 26% during month 3 to 55% during month 12.
The bleeding abnormalities associated with progestin-only contraceptives are not fully understood. We do know that suppression of circulating estradiol and the potent effect of MPA on the endometrium lead to varying degrees of endometrial disruption and atrophy, which ultimately manifest as irregular bleeding and amenorrhea. Subcutaneous DMPA likely involves the same processes, even though it contains 30% less MPA than the IM formulation.
Importance of counseling about bleeding effects
Two studies have shown that women are more likely to continue DMPA if they are counseled about bleeding effects when they start the medication.4,5 Since many patients would prefer less frequent or no menses, they may be encouraged by the prospect of becoming amenorrheic.
Risk of breast cancer
It will be several years before the effect of the lower-dose MPA on breast cancer risk is known.
DMPA and bone loss: Should we worry?
Subcutaneous DMPA, like its IM counterpart, is associated with changes in bone mineral density and carries a “black box” warning regarding this risk.6 Because DMPA suppresses circulating estradiol levels, it causes reductions in bone mineral density (BMD) that have aroused concern among the lay and medical media, although studies suggest BMD levels generally change little and recover when the drug is discontinued— except during perimenopause.
A metaanalysis of 12 studies involving 1,039 DMPA users (IM formulation) and 2,086 controls found that the average Z-score in DMPA users decreased less than 1 standard deviation, compared with nonusers.7 These BMD reductions stabilized after 3 to 4 years of DMPA use, and the bone loss was reversed when the drug was discontinued.8,9 Thus, it appears that, in time, BMD returns to levels similar to those in women who have never used the drug.
IM versus subcutaneous DMPA
In a comparison of both formulations of DMPA, both caused decreases in BMD at the end of 1 and 2 years of treatment.10 Women using subcutaneous DMPA experienced smaller decrements in total hip, lumbar spine, and femoral neck BMD after 1 and 2 years of treatment. However, these differences were significant only in the lumbar spine at 1 year.
Uncertain value for adolescents
DMPA should be carefully considered for use in adolescent girls—and this proviso includes the subcutaneous formulation.
Adolescence is a critical period for bone mineralization. Thus, any agent that limits bone accretion should be prescribed only after weighing all the other options.
A prospective cohort study in adolescents found a 3.1% decrease in BMD after 2 years of DMPA use, versus a 9.5% increase among nonusers.11 More recent reports indicate significant gains in BMD and reversal in bone loss once the drug is discontinued.12
What the “black box” warning means
Based in part on results from these studies, the Food and Drug Administration (FDA) and the drug’s manufacturer issued a black box warning for both the IM and subcutaneous formulations of DMPA. This step was taken to highlight the fact that users of DMPA may lose significant BMD, and that this loss may increase with duration of use and may not be entirely reversible.
The warning recommends that the drugs be used as long-term birth control only if other methods are inadequate. It emphasizes the general lack of certainty about the effect of these drugs on peak bone mass (when used in adolescence or early adulthood) and the risk of osteoporotic fracture (later in life).
How to counsel patients
I discuss the black box warning with each patient in the larger context of contraceptive counseling. The lower efficacy and other problems associated with daily birth control methods must be weighed against the risk of bone loss in both adolescents and adults.
It also is important to consider other risk factors for osteoporosis, such as chronic alcohol or tobacco use, eating disorders, or chronic use of corticosteroids. Adolescents who have poor eating habits or who use alcohol or tobacco may be at heightened risk of BMD loss.
Once a woman chooses DMPA, she should be encouraged to maintain a healthy lifestyle, including adequate calcium intake, weight-bearing and musclestrengthening exercises, smoking cessation, and moderate to no alcohol intake.
BMD measurements are not recommended since they do not predict fracture risk in premenopausal women.
Other side effects
Though rare, serious thrombotic events have been reported in women using the IM formulation.
Also rare are ocular disorders (loss of vision, proptosis, diplopia, or migraine) and ectopic pregnancy.
Other possible side effects include injection site reactions, decreased libido, acne, headache, fatigue, gastrointestinal disorders (distention, abdominal pain, diarrhea, nausea), infection, arthralgia, back pain, limb pain, dizziness, insomnia, anxiety, depression, breast pain and/or tenderness, and hot flushes.
Return to ovulation
DMPA is associated with a prolonged return to ovulation once it is discontinued. In a large US study of women who discontinued intramuscular DMPA to become pregnant, 68% conceived within 12 months, 83% conceived within 15 months, and 93% conceived within 18 months of the last injection, with a median time to conception of 10 months.13
Though no studies have determined the median time to conception for subcutaneous DMPA, it is likely to be similar to the 10-month interval seen with the IM formulation.
Comparing drugs head to head
The IM and subcutaneous formulations were compared prospectively at a single US center.14 The study defined return to ovulation as the first time serum progesterone levels reached at least 4.7 ng/mL. At the end of 12 months (postinjection), the cumulative rate of ovulation was 97.4% for subcutaneous DMPA and 94.7% for the IM formulation.
Ovulation occurred at a median of approximately 7 months (subcutaneous route) and 6 months (IM).
Early ovulation is possible
One subject in the subcutaneous DMPA group ovulated 14 weeks after her last injection. Thus, it is important to adhere to the recommended dosing schedule of 12 to 14 weeks.
Weight gain: 0 to 7.5 lb
Reports of weight gain with DMPA have been highly variable. Many women who discontinue hormonal contraceptives cite weight gain as the reason. With one third of US women meeting the criteria for obesity—a number that is likely to rise—and with ethnic variations, it is difficult to determine the exact impact of DMPA.
A well-designed, placebo-controlled trial by Pelkman and colleagues15 found DMPA to have no effect on resting energy expenditure, food intake, or body weight. Three large clinical trials of subcutaneous DMPA found a mean weight gain of 3.5 lb during the first year of use, and a small 2-year study comparing IM and subcutaneous DMPA found mean weight gains of 7.6 and 7.5 lb, respectively.
Combating endometriosis pain
With the FDA’s approval of subcutaneous DMPA for treatment of endometriosis-associated pain, the drug expands the pharmacologic choices for endometriosis pain relief for the first time in 15 years, with less frequent side effects than the other widely used drug, leuprolide acetate.
In an 18-month clinical trial comparing the 2 drugs, researchers found similar efficacy, with DMPA causing less bone loss and less frequent and severe menopausal symptoms. The trial involved 274 women and measured pain across the following categories: pelvic pain, dysmenorrhea, dyspareunia, pelvic tenderness, and induration.
Clearing a woman for use
The manufacturer recommends that all women undergo an annual history and physical examination. The physical exam should include a blood pressure check; examination of the breasts, abdomen, and pelvic organs; cervical cytology; and any relevant laboratory studies.
Overall outlook
Subcutaneous DMPA offers women the same advantages as the IM formulation. Since we have long-term experience with MPA as a contraceptive agent, we know it offers many noncontraceptive benefits, safety, and excellent contraceptive efficacy.
As we gain experience specific to subcutaneous DMPA , and as data accumulate from additional trials, we will be able to further define its role as a contraceptive option.
Disclosure
Dr. Jain has disclosed that he has received grant/research support from Ferring, Organon, Pfizer, Serono, and TA P.
REFERENCES
1. Westhoff C. Depot-medroxyprogesterone acetate injection (Depo-Provera®): a highly effective contraceptive option with proven long-term safety. Contraception. 2003;68:75-87.
2. Trussell J. Contraceptive efficacy. In: Hatcher RA, Trussell J, Stewart F, et al. Contraceptive Technology. 17th revised edition. New York: Irvington Publishers; 1998.
3. Jain JK, Jakimiuk AJ, Bode FR, et al. Contraceptive efficacy and safety of DMPA-SC. Contraception. 2004;70:269-275.
4. Canto De Cetina TE, Canto P, Luna MO. Effect of counseling to improve compliance in Mexican women receiving depo-medroxyprogesterone acetate. Contraception. 2001;63:143-146.
5. Lei ZW, Wu SC, Garceau RJ, et al. Effect of pretreatment counseling on discontinuation rates in Chinese women given depo-medroxyprogesterone acetate for contraception. Contraception. 1996;53:357-361.
6. Depo SubQ Provera 104 [package insert]. Cambridge, Mass: Pfizer; 2005.
7. Banks E, Berrington A, Casabonne D. Overview of the relationship between use of progestogen-only contraceptives and bone mineral density. Br J Obstet Gynecol. 2001;108:1214-1221.
8. Tang OS, Tang G, Yip PSF, et al. Further evaluation on long-term depot-medroxyprogesterone acetate use and bone mineral density: a longitudinal cohort study. Contraception. 2000;62:161-164.
9. Petitti DB, Piaggio G, Mehta S, et al. Steroid hormone contraception and bone mineral density: a cross-sectional study in an international population. Obstet Gynecol. 2000;95:736-744.
10. Jain JK. Evaluation of bone mineral density in women treated with DMPA-SC 104 or DMPA-IM 150. Presented at: Annual Meeting of the American Academy of Nurse Practitioners; June 17, 2005; Fort Lauderdale, Fla.
11. Cromer BA, Blair JM, Mahan JD, et al. A prospective comparison of bone density in adolescent girls receiving depot medroxyprogesterone acetate (DMPA), levonorgestrel (Norplant), or oral contraceptives. J Pediatr. 1996;129:671-676.
12. Scholes D, LaCroix AZ, Ichikawa LE, et al. Change in bone mineral density among adolescent women using and discontinuing depot medroxyprogesterone acetate contraception. Arch Pediatr Adolesc Med. 2005;159:139-144.
13. Depo-Provera [package insert]. Cambridge, Mass: Pfizer; 1999.
14. Jain JK, Dutton C, Nicosia A, et al. Pharmacokinetics, ovulation suppression and return to ovulation following a lower dose subcutaneous formulation of Depo-Provera®. Contraception. 2004;70:11-18.
15. Pelkman CL, Chow M, Heinbach RA, et al. Short-term effects of a progestational contraceptive drug on food intake, resting energy expenditure, and body weight in young women. Am J Clin Nutr. 2001;73:19-26.
CONTRACEPTIVES IN THE NEWS Plan B: Studies surprise both sides
Ian H. Thorneycroft
MD, PhD
OBG Management
Board of Editors
Professor of Obstetrics and Gynecology, University of South Alabama College of Medicine, Mobile, Ala
Marston C, Meltzer H, Majeed A. Impact on contraceptive practice of making emergency hormonal contraception available over the counter in Great Britain: repeated cross sectional surveys. BMJ doi;10.1136/bmj.38519.440266.8F (published July 11, 2005).
Raine TR, Harper CC, Rocca CH, Fischer R, Padian N, Klausner JD, Darney PD. Direct access to emergency contraception through pharmacies and effect of unintended pregnancy and STIs: a randomized controlled trial. JAMA. 2005;292:54–62.
Litt IF. Placing emergency contraception in the hands of women. JAMA. 2005;293:98–99.
A quick succession of events in July seemed to clear the path to a Food and Drug Administration (FDA) decision on over-the-counter sale of levonorgestrel (Plan B), the emergency contraceptive.
A week after the publication of the large study led by Marston, Plan B was placed on the FDA calendar for a Sept. 1 decision. The authors concluded that their study “supports the case for lifting the ban on over-the-counter sales of emergency hormonal contraception in the United States and other countries.”
Plan B has been a point of contention, especially after the FDA, in 2004, rejected Barr Laboratories’ application for OTC access, on the basis of lack of long-term safety data on its use in young adolescent women, without medical supervision.
When the manufacturer changed its application, the agency declined to make a decision by the legal deadline, last January. Proponents of OTC sales of Plan B objected, citing the agency’s own staff endorsement, and that of an independent panel.
In a series of interactions between the Senate and the administration in early July, the U.S. secretary of health and human services promised a Sept. 1 decision on Barr’s application. Media reports related that announcement to the July 18 Senate confirmation of Dr. Lester Crawford to head the Food and Drug Administration.
Both sides of the controversy met with some surprises in the BMJ and JAMA reports of research on the effects of Plan B access. Opponents of OTC availability in the United States have predicted that such access might increase unprotected sex, especially in young women and girls. Advocates have predicted that it would reduce the number of unintended pregnancies and abortions.
Public health impact may be negligible”
The report in the British Medical Journal concluded, “Making emergency hormonal contraception available over the counter does not seem to have led to an increase in its use, to an increase in unprotected sex, or to a decrease in the use of more reliable methods of contraception.” The study used an Omnibus Survey of 7,600 adults (an annual multipurpose survey in Great Britain) to examine contraception use after OTC emergency contraception was legalized in 2001. Women aged 16 to 49 were surveyed.
Although the lack of any increase in use of emergency hormone contraception suggests that the predicted rise in unsafe sex has been overstated, so too have the predicted effects on unwanted pregnancy, the authors observed.Similarly, the January JAMA report of a US study found: “While removing the requirement to go through pharmacists or clinics to obtain emergency contraception increases use, the public health impact may be negligible because of high rates of unprotected intercourse and relative underutilization of the method.”
Barr requests OTC access of Plan B for women 16 and older. Prescriptions would still be required for younger women.
Plan B is often called the “morning-after pill,” but in fact the method can be used any time after intercourse for up to 72 hours. It is best used as soon as possible, but can even be used after 72 hours, although at reduced efficacy.
Kuyoh MA, Toroitich-Ruto C, Grimes DA, Schulz KF, Gallo MF. Sponge versus diaphragm for contraception: a Cochrane review. Contraception. 2003;67:15–18.
When the Today sponge was pulled off the market by its maker in 1995, the popular Jerry Seinfeld TV show aired an episode showing the character Elaine dashing from store to store, in search of the last few sponges on the shelves. She ultimately found a neighborhood pharmacy with 1 remaining case of 60 sponges. “Just give me the whole case and I’ll be on my way,” she tells the pharmacist. In the show, Elaine used the term “sponge-worthy” to characterize a potential date, and the term became a household word overnight. When it was available in the United States, the Today sponge was the most widely used form of OTC contraception, selling approximately 250 million sponges.
The sponge, which contains the spermicide nonoxynol-9, was sold from 1983 to 1995, when it was voluntarily withdrawn for safety reasons. The FDA found that water at the manufacturing plant was contaminated, and American Home Products, (now Wyeth), decided it was too costly to upgrade its plant, and voluntarily withdrew the Today sponge from the market. Allendale Pharmaceuticals bought the rights for the sponge in 1998, and has been working to secure approval for marketing. The new version has been available in Canada since 2003. According to the manufacturer, it should be in US drug stores sometime this fall, for about $2.50 to $3 per sponge.
The sponge is best compared to a diaphragm. Its failure rate is frequently quoted as approximately 9% to 11% per year, very comparable to condoms.
Efficacy. However, in a Cochrane review of sponges versus the diaphragm, the sponge failure rate was 17.4% in a US trial and 24.5% in a British trial. The rates for a diaphragm were 12.8% and 10.9%, respectively. Unlike a diaphragm, the sponge does not have to be fitted and had equal efficacy in multiparous as nulliparous women, in the 2 studies reviewed. The main advantage of the sponge over a diaphragm is its ready availability over-the-counter.
According the manufacturer, the sponge can be inserted up to 24 hours prior to intercourse, and provides continuous protection throughout that period, for as many acts of intercourse as desired. Although it is not necessary to keep the sponge inserted for a full 24 hours, it must be left in place for 6 hours after the last act of intercourse. It should not be worn for more than 30 consecutive hours. The women in the 2 studies included in the Cochrane review, however, left the sponge in place for 48 hours.
Same-day start-up for OCs improves compliance
Westhoff C, Kerns J, Morroni C, Cushman LF, Tiezzi L, Murphy PA. Quick Start: a novel oral contraceptive initiation method. Contraception. 2002;66:141–145.
Many women never start the oral contraceptive we prescribe. They have to wait for their next menses, and they may fail to fill the prescription; 25% of study participants never start their oral contraceptives.
Quick Start starts the contraceptive in the clinic, after a negative pregnancy test, regardless of the day of the patient’s cycle. She is given at least 1 pack so she does not have to go to the drug store to fill the first prescription. Emergency contraception is given to patients who may need it. The continuation rate to the second cycle was higher in women beginning the pill in the clinic than those who started at any point in their cycle but waited to fill the prescription.
The original oral contraceptives were started on the first Sunday of a menstrual cycle so that it was known the woman was not pregnant and so she would bleed midweek. Waiting until menses assured a possible pregnancy was not exposed to hormonal contraceptives; however, the components of oral contraceptives are not teratogenic. The contraceptive can therefore be started at anytime during the cycle and starting in the clinic increases compliance. A pregnancy test can be performed if the anticipated menses at the end of the pill pack does not occur.
Disclosure
The author is on the speakers bureaus for Barr, Berlex, and Wyeth-Ayerst.
Practical strategies for acute and recurrent vaginitis
SANDRA’S CASE
“Last hope” to end recurrent infections
Sandra, 46, makes an appointment to discuss her recurrent vaginal infections. In the past year, she has had numerous episodes of itching, burning, and abnormal discharge and has used “everything” to treat them. She has tried an array of antifungal and antibiotic preparations, but has experienced only transient relief. She says you are her last hope to break the cycle of recurrent infections.
How do you respond?
Although vaginitis is usually considered a minor nuisance, many women experience chronic symptoms that persist or recur after treatment. For patients such as Sandra, chronic vaginitis is a constant source of frustration and a serious threat to quality of life.
Careful diagnosis is the first and most important step to eradicate vaginitis, and this article describes the essential components—as well as common pitfalls. In some cases, high-dose therapy or maintenance regimens may be indicated; these strategies are also described in detail.
The usual suspects
Vaginitis is defined as inflammation of the vagina marked by pain, itching, and/or a purulent discharge. Depending on the population, the most common causes of infectious vaginitis are:
- bacterial vaginosis (BV) (22%–50% of symptomatic women),
- vulvovaginal candidiasis (VVC) (17%–39%), and
- trichomoniasis (4%–35%).1
However, vaginitis in 7% to 72% of women remains undiagnosed.1 Their symptoms may be caused by atrophic vaginitis, vulvar dermatological conditions, vulvodynia, or other entities.
The hazards of self-diagnosis
Although a wide range of pathogens can cause vaginitis and symptoms are often nonspecific, the trend in the past decade has been for women to diagnose and treat themselves for VVC. The reasons: availability of over-the-counter (OTC) antifungals, ability to rapidly initiate antimycotic therapy, empowerment of women, and the likelihood of reducing direct and indirect healthcare costs.2
Unfortunately, recent studies suggest that self-diagnosis may not be as beneficial as we thought. Ferris and colleagues3 studied 601 women in a variety of medical and community sites in Georgia and found that only 11% without and 34.5% with a prior diagnosis of VVC could accurately recognize it or bacterial vaginosis.
A later prospective study4 of 95 symptomatic women purchasing OTC antifungal agents found that only 34% had pure VVC; treatment with a topical antifungal would have been inappropriate or inadequate in the rest, many of whom had bacterial vaginosis.
A more recent longitudinal study5 of women who submitted yeast cultures every 4 months for a year found no correlation between antecedent Candida colonization and subsequent antifungal use.
Avoid telephone diagnosis, too. Although telephone conversations are useful for patient triage and treatment in many clinical situations, diagnosis of vaginal symptoms by telephone correlates poorly with the actual diagnosis.6
If it’s really VVC, it should respond to antifungals. Over-the-counter antifungals are as effective as their prescription counterparts, so women with VVC should respond to OTC therapy. If a woman reports a lack of response, question the initial diagnosis and offer a thorough evaluation instead of recommending further treatment as the initial step.
Even the pros can be wrong
In a review of 52 medical records of women referred to a tertiary-care vaginitis center, Wiesenfeld and Macio7 found that vaginal pH testing was performed at only 3% of office visits and that 42% of referring physicians failed to perform microscopy as part of their evaluation.
In a study of 61 women diagnosed with VVC after clinical examination and microscopy in a university-based outpatient gynecology clinic, Ledger et al8 found that 49% had a negative yeast culture and polymerase chain reaction.
Office-based tests, even when they are performed in the best of circumstances by personnel focused on vaginal symptoms, have relatively low sensitivity: 92% for bacterial vaginosis, 62% for Trichomonas, and a mere 22% for yeast.9
The right test matters
Given the nonspecific nature of vulvovaginal symptoms and the limitations of office-based testing, a few tests are nevertheless useful for patients with chronic symptoms or an unclear diagnosis.
Yeast cultures. When VVC is suspected, cultures increase sensitivity and allow for speciation of the organism. Speciation is crucial to choosing the proper antifungal drug.
Trichomonas cultures. Because a wet mount has low sensitivity in diagnosing trichomoniasis, Trichomonas cultures are useful in selected patients (with >90% sensitivity), such as women with a previous diagnosis of trichomoniasis, those at risk for sexually transmitted disease (STD), or those with microscopy showing BV or leukorrhea.
When Trichomonas cultures are unavailable, the OSOM Trichomonas Rapid Test (Genzyme Diagnostics, Cambridge, Mass) has better sensitivity than microscopy to detect Trichomonas vaginalis.
Herpes cultures and antibodies. Because genital herpes often presents with mild or nonspecific symptoms, a herpes simplex virus (HSV) culture and type-specific immunoglobulin-G HSV antibodies should be ordered when the patient presents with fissures or ulcers of the vulva.
Forget the gram stain. Given the relatively high sensitivity (92%) of Amsel criteria to diagnose bacterial vaginosis and the difficulty of obtaining Nugent scores on gram stains of vaginal secretions, the value of gram stains outside of research settings for women with suspected bacterial vaginosis is unclear.
Vulvar biopsies. Many women who complain of vaginitis actually have vulvar disorders.
Be prepared to obtain vulvar biopsies if necessary.
High-dose treatment (and maybe condoms) improved cure rate
Although metronidazole gel 0.75% is a standard BV therapy in the United States, much higher doses in combination with nystatin are common in other countries such as Peru. They proved more effective in a recent randomized trial, suggesting that high doses or more prolonged courses of therapy may be beneficial when standard treatment fails.
In the single-blind trial, Sanchez and colleagues24 compared 5 nights of metronidazole gel 0.75% (37.5 mg per dose) to the same duration of treatment with intravaginal ovules containing 500 mg metronidazole and 100,000 U nystatin.
Patients were asked to return 14, 42, and 104 days after treatment; 138 (91%) of 151 women returned at least once.
At every follow-up, the women treated with the ovules had significantly lower recurrence rates (4%, 17%, and 33% for the ovules, compared with 20%, 38%, and 52% for the gel).
Was use of condoms related? Although participants were not randomized for condom use, recurrent infection was more likely among women whose partners did not use them.
The trial’s strengths and limitations
This study is notable for its long follow-up, blinding of the evaluator and biostatistician, and diagnostic methods (both Amsel and Nugent criteria).
The trial addressed the question of whether early recurrence is due to persistent pathogenic flora or failure to repopulate the vagina with hydrogen-peroxide–producing lactobacilli.The improved cure rate with the higher dose of intravaginal metronidazole ovules suggests that it more effectively eradicated abnormal flora than the lower dose.
However, the condom finding suggests that exposure to some factor associated with the partner also plays an important role.
The main limitation was the variability of elapsed time for follow-up visits. For example, the range for the first visit was 10 to 132 days; as a result, some women had a first evaluation that was much later than others.
Further, because participants were Peruvian, the applicability to a US population with potentially different demographics or sex practices is unclear.
Watch for complicated VVC
Women who harbor Candida organisms in their vaginas have VVC. At one end of the spectrum are women who are asymptomatically colonized. It is not necessary to treat these women or make an effort to identify the organisms. At the other end of the spectrum are symptomatic women, who have been traditionally treated with a variety of antifungal therapies, now available in multiple formulations.
Many experts now believe VVC should be classified as complicated or uncomplicated (TABLE 1) to help identify women in whom therapy is likely to fail. Uncomplicated VVC has cure rates of 80% to 90%.10 In contrast, several studies suggest that women with complicated VVC have lower short-term cure rates with either topical clotrimazole or oral fluconazole.10,11
Most women with recurrent VVC fall into the complicated category. For the most part, these are normal, healthy women who experience substantial discomfort and disruption of their daily well-being and sexuality because of recurrent infections. Self-treatment permits rapid initiation of antimycotic therapy, but does nothing to prevent the next symptomatic episode.
TABLE 1
Criteria for candidiasis diagnosis
| UNCOMPLICATED (meets all criteria) |
| Cure rate of 80% to 90% |
| Sporadic or infrequent episodes |
| Mild to moderate symptoms or findings |
| Suspected Candida albicans infection |
| Normal, nonpregnant woman |
| COMPLICATED (meets 1 or more criteria) |
| Cure rates vary widely |
| Recurrent (4 or more episodes per year) |
| Severe symptoms or findings |
| Suspected or proven non-albicans Candida infection |
Abnormal host
|
| Pregnancy |
| Adapted from Sobel JD, et al.26 |
Which Candida sp is it?
When standard antimycotic therapy fails, the species of infecting organism seems to be particularly important. Women with Candida glabrata colonization have markedly lower cure rates than women colonized with C albicans.11 Thus, a crucial first step in treating women who have complicated VVC is obtaining a yeast culture. A positive culture helps corroborate the diagnosis, increases the sensitivity of the evaluation, and allows speciation of the organism and proper selection of therapy.
Non-albicans species less likely to respond to standard azole therapy. Candida glabrata is the second leading cause of VVC, but is less responsive to standard therapies. For example, cure rates of perhaps 50% can be expected with a 7-day course of terconazole cream.12
When azole therapy is ineffective, intravaginal boric acid in 600-mg capsules can be used every night for at least 14 days and will be effective in about two thirds of patients.13 However, some patients have accidently ingested these boric acid capsules and died (apparently this dose of boric acid is lethal when taken orally). Thus, it is crucial that patients be warned specifically about this hazard.
In a series of 30 patients with no response to azole therapy and subsequent boric acid, Sobel and colleagues achieved a cure rate of 90% with a 14-day course of flucytosine cream 17%, given in 5-g nightly doses.13
Watch for false negatives in women on azole therapy. In general, the C albicans organism tends to be sensitive to azole therapy. Thus, if a woman with C albicans infection is cultured while on therapy, the odds are very high that she will have a negative yeast culture.
Maintenance fluconazole
Maintenance therapy with ketoconazole for recurrent VVC was first proposed in 1986, but was never widely adopted due to concerns about liver toxicity.
More recently, maintenance fluconazole was found to be effective in a doubleblind, placebo-controlled study.14 After treating the initial infection with 3 doses of fluconazole (150 mg every 3 days), researchers randomized women to a 6-month course of weekly fluconazole (150 mg) or placebo. During the 6-month treatment phase, relapse was noted in 9% of the fluconazole group and 64% of the placebo group. However, of the 126 fluconazole-treated women who were disease-free at the end of the treatment phase, 72 (57%) experienced relapse during the next 6 months.
Fluconazole for 6 months. Although about 50% of women have a relapse after stopping treatment, most can at least successfully control and prevent symptomatic episodes as long as they are using fluconazole in maintenance doses. Most experts recommend a 6-month course of maintenance therapy.
Alternatives to fluconazole. Extensive clinical experience has shown fluconazole to be safe and well tolerated in most women. However, women who are unable or unwilling to take it may benefit from repeated dosing of topical azoles, which also appear to be effective (although reported experience is less extensive than with fluconazole).
Vaginal trichomoniasis
This common STD has an estimated annual incidence of 3 million cases in the United States alone. Symptomatic women may complain of abnormal discharge, itching, burning, and/or postcoital bleeding. Physicians evaluating these women should be aware that microscopy has much lower sensitivity than many would expect, and that further testing may be necessary to establish a clear diagnosis (ie, cultures or the OSOM Trichomonas Rapid Test).
Treating uncomplicated infection
In the United States, trichomoniasis treatment consists of metronidazole or tinidazole; either may be given as a single 2-g dose. Although tinidazole has a somewhat longer half-life and slightly better activity against T vaginalis, both drugs appear to be effective and metronidazole is substantially cheaper. They also have similar side effects, including a possible disulfiram-like effect, although the incidence of adverse gastrointestinal (GI) effects may be lower with tinidazole.
Metronidazole allergy or resistance
Though rare, either can occur with trichomoniasis. Allergic patients should be referred for desensitization and later treated with metronidazole; both intravenous (IV) and oral regimens have been used successfully. We lack data on crossreactivity between tinidazole and metronidazole. Metronidazole resistance is thought to occur in 1 in 2,000 to 3,000 cases.15 If resistance is suspected, interview the patient carefully to exclude medication noncompliance and reinfection from an untreated partner. In a series of 33 cases, high-dose tinidazole (at least 1 g twice daily for 14 days) was well tolerated and effective in more than 90% of resistant cases.16 Susceptibility testing of the resistant isolate by a reference laboratory may help guide drug choice and dosing.
Other options, such as topical paromomycin cream, which has been studied only in small series, may have local side effects such as vulvovaginal ulceration, and should be considered a last resort.16
New approaches to BV
BV is a polymicrobial infection marked by a lack of hydrogen-peroxide–producing lactobacilli and an overgrowth of facultative anaerobic organisms. Organisms found with greater frequency and numbers include Gardnerella vaginalis, Mycoplasma hominis, Bacteroides spp, Peptostreptococcus spp, Fusobacterium spp, Prevotella spp, Mobiluncus spp, and other anaerobes.17
Diagnostic criteria
Women with symptomatic vaginosis complain of abnormal vaginal discharge and a fishy odor.
BV is diagnosed by finding at least 3 of the following Amsel criteria:
- abnormal gray discharge
- vaginal pH of more than 4.5
- positive amine test
- more than 20% of epithelial cells are clue cells
Susceptibility to other infections
In nonpregnant women, BV has been linked to infections of the reproductive tract, including pelvic inflammatory disease, postprocedural gynecologic infections, and acquisition of HIV.5 Treating BV prior to abortion or hysterectomy appears to substantially lower the risk of postoperative infection.18 Treatment also helps resolve concurrent mucopurulent cervicitis.19 However, we lack evidence that BV treatment decreases the risk of pelvic inflammatory disease or HIV.
First-line treatment
The number of approved treatment options has increased (TABLE 2). Although clindamycin may have greater in vitro resistance,5 all the listed agents have comparable clinical efficacy and safety.20-22
Topical agents often cost more than generic oral metronidazole, although the latter is often associated with GI symptoms.
TABLE 2
Bacterial vaginosis treatment options
| DRUG | FORMULATION | DOSE PER DAY | DURATION |
|---|---|---|---|
| Clindamycin | 2% cream | 5 g | 7 days |
| 2% single-dose cream | 5g | 1 day | |
| 100-mg ovules | 100 mg | 3 days | |
| 300 mg oral | 300 mg bid | 7 days | |
| Metronidazole | 0.75% gel | 5 g | 5 days |
| 500 mg oral | 500 mg bid | 7days |
When BV recurs
After treatment, bacterial vaginosis recurs in as many as 30% of women within 3 months.23 A number of explanatory theories have been proposed:
- persistent pathogenic bacteria
- reinfection from exogenous sources, including a sexual partner
- failure of normal lactobacillus-dominant flora to reestablish itself
In support of the first theory, Sanchez and colleagues24 found a lower risk of recurrence after treatment with high-dose (500 mg) intravaginal metronidazole plus nystatin, compared with standard metronidazole gel. (See “High-dose treatment [and maybe condoms] improved cure rate,”.)
The same study suggested a possible link to exposure to exogenous pathogens: Women who used condoms after treatment had a lower risk of recurrence than women who did not. However, other randomized trials evaluating treatment of the partner have shown no benefit in preventing recurrent BV.
Similarly, recolonization with lactobacillus supplements using nonvaginal strains failed to show a clear benefit.23
Benefits of maintenance therapy
Some women with recurrent BV appear to improve with low-dose maintenance antibiotic therapy. In a recent study of low-dose metronidazole gel (0.75%),25 women with recurrent BV were given a 10-day course to clear that episode, then randomized to maintenance metronidazole (1 applicator twice a week) or placebo for 4 months. Seventy percent of the treatment group remained free of infection, compared with only 34% of theplacebo group. After an additional 4 months of observation, 39% of the treatment group remained free of BV compared with 18% of the placebo group.
Although these findings demonstrate significant improvement with maintenance therapy, the relapse rate remained relatively high. A high rate of VVC was also noted: Almost 60% of women required antifungal therapy at some point during the study.
Vaginitis: A way of life
SANDRA’S CASE
At minimum, symptom control
After careful evaluation and vaginal cultures, you diagnose Sandra with candidiasis infection with the C glabrata species and prescribe 600-mg capsules of intravaginal boric acid—taking care to warn her that they are for intravaginal use only, not to be taken orally—which completely relieve her symptoms for several months.
Although the candidiasis eventually recurs, the symptoms are not as severe and resolve again with more boric acid capsules.
For patients like Sandra, vaginitis may be an inescapable fact of life.
Fortunately, as our understanding of vulvovaginal conditions has improved, more effective evaluation and treatment enable us to establish clearer diagnoses and choose therapies that—at a minimum—keep symptoms under control.
Dr. Nyirjesy serves on the speakers bureau for 3M and KV Pharmaceuticals and consults for 3M, KV Pharmaceuticals, Presutti Laboratories, and Personal Products Worldwide. He also has received grant support from Presutti Laboratories.
Dr. Sobel serves on the speakers bureau for 3M, KV Pharmaceuticals, Merck, and Pfizer, and consults for Pfizer, Presutti Laboratories, and Vicuron. He also has received grant support from Fujisawa Pharmaceuticals, Johnson & Johnson, and Presutti Laboratories.
1. Anderson MR, Klink K, Cohrssen A. Evaluation of vaginal complaints. JAMA. 2004;291:1368-1379.
2. Lipsky MS, Waters T, Sharp LK. Impact of vaginal antifungal products on utilization of health care services: evidence from physician visits. J Am Board Fam Pract. 2000;13:178-182.
3. Ferris DG, Dekle C, Litaker MS. Women’s use of over-the-counter antifungal medications for gynecological symptoms. J Fam Pract. 1996;42:595-600.
4. Ferris DG, Nyirjesy P, Sobel JD, Soper D, Pavletic A, Litaker MS. Over-the-counter antifungal drug misuse associated with patient-diagnosed vulvovaginal candidiasis. Obstet Gynecol. 2002;99:419-425.
5. Beigi RH, Austin MN, Meyn LA, Krohn MA, Hillier SL. Antimicrobial resistance associated with the treatment of bacterial vaginosis. Am J Obstet Gynecol. 2004;191:1124-1129.
6. Allen-Davis JT, Beck A, Parker R, Ellis J, Polley D. Assessment of vulvovaginal complaints: accuracy of telephone triage and in-office diagnosis. Obstet Gynecol. 2002;99:18-22.
7. Wiesenfeld HC, Macio I. The infrequent use of office-based diagnostic tests for vaginitis. Am J Obstet Gynecol. 1999;181:39-41.
8. Ledger WJ, Polaneczky MM, Yih MC, Jeremias J, Tolbert V, Witkin SS. Difficulties in the diagnosis of Candida vaginitis. Infect Dis Clin Pract. 2000;9:66-69.
9. Landers DV, Wiesenfeld HC, Heine RP, Krohn MA, Hillier SL. Predictive value of the clinical diagnosis of lower genital tract infection in women. Am J Obstet Gynecol. 2004;190:1004-1010.
10. Sobel JD, Brooker D, Stein GE, et al. Single oral dose fluconazole compared with conventional clotrimazole topical therapy of Candidavaginitis. Am J Obstet Gynecol. 1995;172:1263-1268.
11. Sobel JD, Kapernick PS, Zervos M, et al. Treatment of complicated Candidavaginitis: comparison of single and sequential doses of fluconazole. Am J Obstet Gynecol. 2001;185:363-369.
12. Sood G, Nyirjesy P, Weitz MV, Chatwani A. Terconazole cream for non Candida albicansfungal vaginitis: results of a retrospective analysis. Infect Dis Obstet Gynecol. 2000;8:240-243.
13. Sobel JD, Chaim W, Nagappan V, Leaman D. Treatment of vaginitis caused by Candida glabrata: use of topical boric acid and flucytosine. Am J Obstet Gynecol. 2003;189:1297-1300.
14. Sobel JD, Wiesenfeld HC, Martens M, et al. Maintenance fluconazole therapy for recurrent vulvovaginal candidiasis. N Engl J Med. 2004;351:876-883.
15. Nyirjesy P. Managing resistant Trichomonas vaginitis. Curr Infect Dis Rep. 1999;1:389-392.
16. Sobel JD, Nyirjesy P, Brown W. Tinidazole therapy for metronidazole-resistant vaginal trichomoniasis. Clin Infect Dis. 2001;33:1341-1346.
17. Ness RB, Hillier SL, Richter HE, et al. Douching in relation to bacterial vaginosis, lactobacilli, and facultative bacteria in the vagina. Obstet Gynecol. 2002;100:765-772.
18. Koumans EH, Kendrick JS. CDC Bacterial Vaginosis Working Group. Preventing adverse sequelae of bacterial vaginosis: a public health program and research agenda. Sex Transm Dis. 2001;28:292-297.
19. Schwebke JR, Weiss HL. Interrelationships of bacterial vaginosis and cervical inflammation. Sex Transm Dis. 2002;29:59-64.
20. Ferris DG, Litaker MS, Woodward L, Mathis D, Hendrich J. Treatment of bacterial vaginosis: a comparison of oral metronidazole, metronidazole vaginal gel, and clindamycin vaginal cream. J Fam Pract. 1995;41:443-449.
21. Hanson JM, McGregor JA, Hillier SL, et al. Metronidazole for bacterial vaginosis; a comparison of vaginal gel vs. oral therapy. J Reprod Med. 2000;45:889-896.
22. Paavonen J, Mangioni C, Martin MA, Wajszczuk CP. Vaginal clindamycin and oral metronidazole for bacterial vaginosis: a randomized trial. Obstet Gynecol. 2000;96:256-260.
23. Wilson J. Managing recurrent bacterial vaginosis. Sex Transm Infect. 2004;80:8-11.
24. Sanchez S, Garcia PJ, Thomas KK, Catlin M, Holmes KK. Intravaginal metronidazole gel versus metronidazole plus nystatin ovules for bacterial vaginosis: a randomized controlled trial. Am J Obstet Gynecol. 2004;191:1898-1906.
25. Sobel JD, Wiesenfeld HC, Schwebke J, et al. A clinical trial to evaluate efficacy of maintenance therapy with 0.75% metronidazole gel to prevent recurrent bacterial vaginosis. Oral presentation at: Annual Meeting of the Infectious Diseases Society for Obstetrics and Gynecology; August 5-7, 2004; San Diego, Calif.
26. Sobel JD, Faro S, Force RW, et al. Vulvovaginal candidiasis: epidemiologic, diagnostic, and therapeutic considerations. Am J Obstet Gynecol. 1998;178:203-211.
SANDRA’S CASE
“Last hope” to end recurrent infections
Sandra, 46, makes an appointment to discuss her recurrent vaginal infections. In the past year, she has had numerous episodes of itching, burning, and abnormal discharge and has used “everything” to treat them. She has tried an array of antifungal and antibiotic preparations, but has experienced only transient relief. She says you are her last hope to break the cycle of recurrent infections.
How do you respond?
Although vaginitis is usually considered a minor nuisance, many women experience chronic symptoms that persist or recur after treatment. For patients such as Sandra, chronic vaginitis is a constant source of frustration and a serious threat to quality of life.
Careful diagnosis is the first and most important step to eradicate vaginitis, and this article describes the essential components—as well as common pitfalls. In some cases, high-dose therapy or maintenance regimens may be indicated; these strategies are also described in detail.
The usual suspects
Vaginitis is defined as inflammation of the vagina marked by pain, itching, and/or a purulent discharge. Depending on the population, the most common causes of infectious vaginitis are:
- bacterial vaginosis (BV) (22%–50% of symptomatic women),
- vulvovaginal candidiasis (VVC) (17%–39%), and
- trichomoniasis (4%–35%).1
However, vaginitis in 7% to 72% of women remains undiagnosed.1 Their symptoms may be caused by atrophic vaginitis, vulvar dermatological conditions, vulvodynia, or other entities.
The hazards of self-diagnosis
Although a wide range of pathogens can cause vaginitis and symptoms are often nonspecific, the trend in the past decade has been for women to diagnose and treat themselves for VVC. The reasons: availability of over-the-counter (OTC) antifungals, ability to rapidly initiate antimycotic therapy, empowerment of women, and the likelihood of reducing direct and indirect healthcare costs.2
Unfortunately, recent studies suggest that self-diagnosis may not be as beneficial as we thought. Ferris and colleagues3 studied 601 women in a variety of medical and community sites in Georgia and found that only 11% without and 34.5% with a prior diagnosis of VVC could accurately recognize it or bacterial vaginosis.
A later prospective study4 of 95 symptomatic women purchasing OTC antifungal agents found that only 34% had pure VVC; treatment with a topical antifungal would have been inappropriate or inadequate in the rest, many of whom had bacterial vaginosis.
A more recent longitudinal study5 of women who submitted yeast cultures every 4 months for a year found no correlation between antecedent Candida colonization and subsequent antifungal use.
Avoid telephone diagnosis, too. Although telephone conversations are useful for patient triage and treatment in many clinical situations, diagnosis of vaginal symptoms by telephone correlates poorly with the actual diagnosis.6
If it’s really VVC, it should respond to antifungals. Over-the-counter antifungals are as effective as their prescription counterparts, so women with VVC should respond to OTC therapy. If a woman reports a lack of response, question the initial diagnosis and offer a thorough evaluation instead of recommending further treatment as the initial step.
Even the pros can be wrong
In a review of 52 medical records of women referred to a tertiary-care vaginitis center, Wiesenfeld and Macio7 found that vaginal pH testing was performed at only 3% of office visits and that 42% of referring physicians failed to perform microscopy as part of their evaluation.
In a study of 61 women diagnosed with VVC after clinical examination and microscopy in a university-based outpatient gynecology clinic, Ledger et al8 found that 49% had a negative yeast culture and polymerase chain reaction.
Office-based tests, even when they are performed in the best of circumstances by personnel focused on vaginal symptoms, have relatively low sensitivity: 92% for bacterial vaginosis, 62% for Trichomonas, and a mere 22% for yeast.9
The right test matters
Given the nonspecific nature of vulvovaginal symptoms and the limitations of office-based testing, a few tests are nevertheless useful for patients with chronic symptoms or an unclear diagnosis.
Yeast cultures. When VVC is suspected, cultures increase sensitivity and allow for speciation of the organism. Speciation is crucial to choosing the proper antifungal drug.
Trichomonas cultures. Because a wet mount has low sensitivity in diagnosing trichomoniasis, Trichomonas cultures are useful in selected patients (with >90% sensitivity), such as women with a previous diagnosis of trichomoniasis, those at risk for sexually transmitted disease (STD), or those with microscopy showing BV or leukorrhea.
When Trichomonas cultures are unavailable, the OSOM Trichomonas Rapid Test (Genzyme Diagnostics, Cambridge, Mass) has better sensitivity than microscopy to detect Trichomonas vaginalis.
Herpes cultures and antibodies. Because genital herpes often presents with mild or nonspecific symptoms, a herpes simplex virus (HSV) culture and type-specific immunoglobulin-G HSV antibodies should be ordered when the patient presents with fissures or ulcers of the vulva.
Forget the gram stain. Given the relatively high sensitivity (92%) of Amsel criteria to diagnose bacterial vaginosis and the difficulty of obtaining Nugent scores on gram stains of vaginal secretions, the value of gram stains outside of research settings for women with suspected bacterial vaginosis is unclear.
Vulvar biopsies. Many women who complain of vaginitis actually have vulvar disorders.
Be prepared to obtain vulvar biopsies if necessary.
High-dose treatment (and maybe condoms) improved cure rate
Although metronidazole gel 0.75% is a standard BV therapy in the United States, much higher doses in combination with nystatin are common in other countries such as Peru. They proved more effective in a recent randomized trial, suggesting that high doses or more prolonged courses of therapy may be beneficial when standard treatment fails.
In the single-blind trial, Sanchez and colleagues24 compared 5 nights of metronidazole gel 0.75% (37.5 mg per dose) to the same duration of treatment with intravaginal ovules containing 500 mg metronidazole and 100,000 U nystatin.
Patients were asked to return 14, 42, and 104 days after treatment; 138 (91%) of 151 women returned at least once.
At every follow-up, the women treated with the ovules had significantly lower recurrence rates (4%, 17%, and 33% for the ovules, compared with 20%, 38%, and 52% for the gel).
Was use of condoms related? Although participants were not randomized for condom use, recurrent infection was more likely among women whose partners did not use them.
The trial’s strengths and limitations
This study is notable for its long follow-up, blinding of the evaluator and biostatistician, and diagnostic methods (both Amsel and Nugent criteria).
The trial addressed the question of whether early recurrence is due to persistent pathogenic flora or failure to repopulate the vagina with hydrogen-peroxide–producing lactobacilli.The improved cure rate with the higher dose of intravaginal metronidazole ovules suggests that it more effectively eradicated abnormal flora than the lower dose.
However, the condom finding suggests that exposure to some factor associated with the partner also plays an important role.
The main limitation was the variability of elapsed time for follow-up visits. For example, the range for the first visit was 10 to 132 days; as a result, some women had a first evaluation that was much later than others.
Further, because participants were Peruvian, the applicability to a US population with potentially different demographics or sex practices is unclear.
Watch for complicated VVC
Women who harbor Candida organisms in their vaginas have VVC. At one end of the spectrum are women who are asymptomatically colonized. It is not necessary to treat these women or make an effort to identify the organisms. At the other end of the spectrum are symptomatic women, who have been traditionally treated with a variety of antifungal therapies, now available in multiple formulations.
Many experts now believe VVC should be classified as complicated or uncomplicated (TABLE 1) to help identify women in whom therapy is likely to fail. Uncomplicated VVC has cure rates of 80% to 90%.10 In contrast, several studies suggest that women with complicated VVC have lower short-term cure rates with either topical clotrimazole or oral fluconazole.10,11
Most women with recurrent VVC fall into the complicated category. For the most part, these are normal, healthy women who experience substantial discomfort and disruption of their daily well-being and sexuality because of recurrent infections. Self-treatment permits rapid initiation of antimycotic therapy, but does nothing to prevent the next symptomatic episode.
TABLE 1
Criteria for candidiasis diagnosis
| UNCOMPLICATED (meets all criteria) |
| Cure rate of 80% to 90% |
| Sporadic or infrequent episodes |
| Mild to moderate symptoms or findings |
| Suspected Candida albicans infection |
| Normal, nonpregnant woman |
| COMPLICATED (meets 1 or more criteria) |
| Cure rates vary widely |
| Recurrent (4 or more episodes per year) |
| Severe symptoms or findings |
| Suspected or proven non-albicans Candida infection |
Abnormal host
|
| Pregnancy |
| Adapted from Sobel JD, et al.26 |
Which Candida sp is it?
When standard antimycotic therapy fails, the species of infecting organism seems to be particularly important. Women with Candida glabrata colonization have markedly lower cure rates than women colonized with C albicans.11 Thus, a crucial first step in treating women who have complicated VVC is obtaining a yeast culture. A positive culture helps corroborate the diagnosis, increases the sensitivity of the evaluation, and allows speciation of the organism and proper selection of therapy.
Non-albicans species less likely to respond to standard azole therapy. Candida glabrata is the second leading cause of VVC, but is less responsive to standard therapies. For example, cure rates of perhaps 50% can be expected with a 7-day course of terconazole cream.12
When azole therapy is ineffective, intravaginal boric acid in 600-mg capsules can be used every night for at least 14 days and will be effective in about two thirds of patients.13 However, some patients have accidently ingested these boric acid capsules and died (apparently this dose of boric acid is lethal when taken orally). Thus, it is crucial that patients be warned specifically about this hazard.
In a series of 30 patients with no response to azole therapy and subsequent boric acid, Sobel and colleagues achieved a cure rate of 90% with a 14-day course of flucytosine cream 17%, given in 5-g nightly doses.13
Watch for false negatives in women on azole therapy. In general, the C albicans organism tends to be sensitive to azole therapy. Thus, if a woman with C albicans infection is cultured while on therapy, the odds are very high that she will have a negative yeast culture.
Maintenance fluconazole
Maintenance therapy with ketoconazole for recurrent VVC was first proposed in 1986, but was never widely adopted due to concerns about liver toxicity.
More recently, maintenance fluconazole was found to be effective in a doubleblind, placebo-controlled study.14 After treating the initial infection with 3 doses of fluconazole (150 mg every 3 days), researchers randomized women to a 6-month course of weekly fluconazole (150 mg) or placebo. During the 6-month treatment phase, relapse was noted in 9% of the fluconazole group and 64% of the placebo group. However, of the 126 fluconazole-treated women who were disease-free at the end of the treatment phase, 72 (57%) experienced relapse during the next 6 months.
Fluconazole for 6 months. Although about 50% of women have a relapse after stopping treatment, most can at least successfully control and prevent symptomatic episodes as long as they are using fluconazole in maintenance doses. Most experts recommend a 6-month course of maintenance therapy.
Alternatives to fluconazole. Extensive clinical experience has shown fluconazole to be safe and well tolerated in most women. However, women who are unable or unwilling to take it may benefit from repeated dosing of topical azoles, which also appear to be effective (although reported experience is less extensive than with fluconazole).
Vaginal trichomoniasis
This common STD has an estimated annual incidence of 3 million cases in the United States alone. Symptomatic women may complain of abnormal discharge, itching, burning, and/or postcoital bleeding. Physicians evaluating these women should be aware that microscopy has much lower sensitivity than many would expect, and that further testing may be necessary to establish a clear diagnosis (ie, cultures or the OSOM Trichomonas Rapid Test).
Treating uncomplicated infection
In the United States, trichomoniasis treatment consists of metronidazole or tinidazole; either may be given as a single 2-g dose. Although tinidazole has a somewhat longer half-life and slightly better activity against T vaginalis, both drugs appear to be effective and metronidazole is substantially cheaper. They also have similar side effects, including a possible disulfiram-like effect, although the incidence of adverse gastrointestinal (GI) effects may be lower with tinidazole.
Metronidazole allergy or resistance
Though rare, either can occur with trichomoniasis. Allergic patients should be referred for desensitization and later treated with metronidazole; both intravenous (IV) and oral regimens have been used successfully. We lack data on crossreactivity between tinidazole and metronidazole. Metronidazole resistance is thought to occur in 1 in 2,000 to 3,000 cases.15 If resistance is suspected, interview the patient carefully to exclude medication noncompliance and reinfection from an untreated partner. In a series of 33 cases, high-dose tinidazole (at least 1 g twice daily for 14 days) was well tolerated and effective in more than 90% of resistant cases.16 Susceptibility testing of the resistant isolate by a reference laboratory may help guide drug choice and dosing.
Other options, such as topical paromomycin cream, which has been studied only in small series, may have local side effects such as vulvovaginal ulceration, and should be considered a last resort.16
New approaches to BV
BV is a polymicrobial infection marked by a lack of hydrogen-peroxide–producing lactobacilli and an overgrowth of facultative anaerobic organisms. Organisms found with greater frequency and numbers include Gardnerella vaginalis, Mycoplasma hominis, Bacteroides spp, Peptostreptococcus spp, Fusobacterium spp, Prevotella spp, Mobiluncus spp, and other anaerobes.17
Diagnostic criteria
Women with symptomatic vaginosis complain of abnormal vaginal discharge and a fishy odor.
BV is diagnosed by finding at least 3 of the following Amsel criteria:
- abnormal gray discharge
- vaginal pH of more than 4.5
- positive amine test
- more than 20% of epithelial cells are clue cells
Susceptibility to other infections
In nonpregnant women, BV has been linked to infections of the reproductive tract, including pelvic inflammatory disease, postprocedural gynecologic infections, and acquisition of HIV.5 Treating BV prior to abortion or hysterectomy appears to substantially lower the risk of postoperative infection.18 Treatment also helps resolve concurrent mucopurulent cervicitis.19 However, we lack evidence that BV treatment decreases the risk of pelvic inflammatory disease or HIV.
First-line treatment
The number of approved treatment options has increased (TABLE 2). Although clindamycin may have greater in vitro resistance,5 all the listed agents have comparable clinical efficacy and safety.20-22
Topical agents often cost more than generic oral metronidazole, although the latter is often associated with GI symptoms.
TABLE 2
Bacterial vaginosis treatment options
| DRUG | FORMULATION | DOSE PER DAY | DURATION |
|---|---|---|---|
| Clindamycin | 2% cream | 5 g | 7 days |
| 2% single-dose cream | 5g | 1 day | |
| 100-mg ovules | 100 mg | 3 days | |
| 300 mg oral | 300 mg bid | 7 days | |
| Metronidazole | 0.75% gel | 5 g | 5 days |
| 500 mg oral | 500 mg bid | 7days |
When BV recurs
After treatment, bacterial vaginosis recurs in as many as 30% of women within 3 months.23 A number of explanatory theories have been proposed:
- persistent pathogenic bacteria
- reinfection from exogenous sources, including a sexual partner
- failure of normal lactobacillus-dominant flora to reestablish itself
In support of the first theory, Sanchez and colleagues24 found a lower risk of recurrence after treatment with high-dose (500 mg) intravaginal metronidazole plus nystatin, compared with standard metronidazole gel. (See “High-dose treatment [and maybe condoms] improved cure rate,”.)
The same study suggested a possible link to exposure to exogenous pathogens: Women who used condoms after treatment had a lower risk of recurrence than women who did not. However, other randomized trials evaluating treatment of the partner have shown no benefit in preventing recurrent BV.
Similarly, recolonization with lactobacillus supplements using nonvaginal strains failed to show a clear benefit.23
Benefits of maintenance therapy
Some women with recurrent BV appear to improve with low-dose maintenance antibiotic therapy. In a recent study of low-dose metronidazole gel (0.75%),25 women with recurrent BV were given a 10-day course to clear that episode, then randomized to maintenance metronidazole (1 applicator twice a week) or placebo for 4 months. Seventy percent of the treatment group remained free of infection, compared with only 34% of theplacebo group. After an additional 4 months of observation, 39% of the treatment group remained free of BV compared with 18% of the placebo group.
Although these findings demonstrate significant improvement with maintenance therapy, the relapse rate remained relatively high. A high rate of VVC was also noted: Almost 60% of women required antifungal therapy at some point during the study.
Vaginitis: A way of life
SANDRA’S CASE
At minimum, symptom control
After careful evaluation and vaginal cultures, you diagnose Sandra with candidiasis infection with the C glabrata species and prescribe 600-mg capsules of intravaginal boric acid—taking care to warn her that they are for intravaginal use only, not to be taken orally—which completely relieve her symptoms for several months.
Although the candidiasis eventually recurs, the symptoms are not as severe and resolve again with more boric acid capsules.
For patients like Sandra, vaginitis may be an inescapable fact of life.
Fortunately, as our understanding of vulvovaginal conditions has improved, more effective evaluation and treatment enable us to establish clearer diagnoses and choose therapies that—at a minimum—keep symptoms under control.
Dr. Nyirjesy serves on the speakers bureau for 3M and KV Pharmaceuticals and consults for 3M, KV Pharmaceuticals, Presutti Laboratories, and Personal Products Worldwide. He also has received grant support from Presutti Laboratories.
Dr. Sobel serves on the speakers bureau for 3M, KV Pharmaceuticals, Merck, and Pfizer, and consults for Pfizer, Presutti Laboratories, and Vicuron. He also has received grant support from Fujisawa Pharmaceuticals, Johnson & Johnson, and Presutti Laboratories.
SANDRA’S CASE
“Last hope” to end recurrent infections
Sandra, 46, makes an appointment to discuss her recurrent vaginal infections. In the past year, she has had numerous episodes of itching, burning, and abnormal discharge and has used “everything” to treat them. She has tried an array of antifungal and antibiotic preparations, but has experienced only transient relief. She says you are her last hope to break the cycle of recurrent infections.
How do you respond?
Although vaginitis is usually considered a minor nuisance, many women experience chronic symptoms that persist or recur after treatment. For patients such as Sandra, chronic vaginitis is a constant source of frustration and a serious threat to quality of life.
Careful diagnosis is the first and most important step to eradicate vaginitis, and this article describes the essential components—as well as common pitfalls. In some cases, high-dose therapy or maintenance regimens may be indicated; these strategies are also described in detail.
The usual suspects
Vaginitis is defined as inflammation of the vagina marked by pain, itching, and/or a purulent discharge. Depending on the population, the most common causes of infectious vaginitis are:
- bacterial vaginosis (BV) (22%–50% of symptomatic women),
- vulvovaginal candidiasis (VVC) (17%–39%), and
- trichomoniasis (4%–35%).1
However, vaginitis in 7% to 72% of women remains undiagnosed.1 Their symptoms may be caused by atrophic vaginitis, vulvar dermatological conditions, vulvodynia, or other entities.
The hazards of self-diagnosis
Although a wide range of pathogens can cause vaginitis and symptoms are often nonspecific, the trend in the past decade has been for women to diagnose and treat themselves for VVC. The reasons: availability of over-the-counter (OTC) antifungals, ability to rapidly initiate antimycotic therapy, empowerment of women, and the likelihood of reducing direct and indirect healthcare costs.2
Unfortunately, recent studies suggest that self-diagnosis may not be as beneficial as we thought. Ferris and colleagues3 studied 601 women in a variety of medical and community sites in Georgia and found that only 11% without and 34.5% with a prior diagnosis of VVC could accurately recognize it or bacterial vaginosis.
A later prospective study4 of 95 symptomatic women purchasing OTC antifungal agents found that only 34% had pure VVC; treatment with a topical antifungal would have been inappropriate or inadequate in the rest, many of whom had bacterial vaginosis.
A more recent longitudinal study5 of women who submitted yeast cultures every 4 months for a year found no correlation between antecedent Candida colonization and subsequent antifungal use.
Avoid telephone diagnosis, too. Although telephone conversations are useful for patient triage and treatment in many clinical situations, diagnosis of vaginal symptoms by telephone correlates poorly with the actual diagnosis.6
If it’s really VVC, it should respond to antifungals. Over-the-counter antifungals are as effective as their prescription counterparts, so women with VVC should respond to OTC therapy. If a woman reports a lack of response, question the initial diagnosis and offer a thorough evaluation instead of recommending further treatment as the initial step.
Even the pros can be wrong
In a review of 52 medical records of women referred to a tertiary-care vaginitis center, Wiesenfeld and Macio7 found that vaginal pH testing was performed at only 3% of office visits and that 42% of referring physicians failed to perform microscopy as part of their evaluation.
In a study of 61 women diagnosed with VVC after clinical examination and microscopy in a university-based outpatient gynecology clinic, Ledger et al8 found that 49% had a negative yeast culture and polymerase chain reaction.
Office-based tests, even when they are performed in the best of circumstances by personnel focused on vaginal symptoms, have relatively low sensitivity: 92% for bacterial vaginosis, 62% for Trichomonas, and a mere 22% for yeast.9
The right test matters
Given the nonspecific nature of vulvovaginal symptoms and the limitations of office-based testing, a few tests are nevertheless useful for patients with chronic symptoms or an unclear diagnosis.
Yeast cultures. When VVC is suspected, cultures increase sensitivity and allow for speciation of the organism. Speciation is crucial to choosing the proper antifungal drug.
Trichomonas cultures. Because a wet mount has low sensitivity in diagnosing trichomoniasis, Trichomonas cultures are useful in selected patients (with >90% sensitivity), such as women with a previous diagnosis of trichomoniasis, those at risk for sexually transmitted disease (STD), or those with microscopy showing BV or leukorrhea.
When Trichomonas cultures are unavailable, the OSOM Trichomonas Rapid Test (Genzyme Diagnostics, Cambridge, Mass) has better sensitivity than microscopy to detect Trichomonas vaginalis.
Herpes cultures and antibodies. Because genital herpes often presents with mild or nonspecific symptoms, a herpes simplex virus (HSV) culture and type-specific immunoglobulin-G HSV antibodies should be ordered when the patient presents with fissures or ulcers of the vulva.
Forget the gram stain. Given the relatively high sensitivity (92%) of Amsel criteria to diagnose bacterial vaginosis and the difficulty of obtaining Nugent scores on gram stains of vaginal secretions, the value of gram stains outside of research settings for women with suspected bacterial vaginosis is unclear.
Vulvar biopsies. Many women who complain of vaginitis actually have vulvar disorders.
Be prepared to obtain vulvar biopsies if necessary.
High-dose treatment (and maybe condoms) improved cure rate
Although metronidazole gel 0.75% is a standard BV therapy in the United States, much higher doses in combination with nystatin are common in other countries such as Peru. They proved more effective in a recent randomized trial, suggesting that high doses or more prolonged courses of therapy may be beneficial when standard treatment fails.
In the single-blind trial, Sanchez and colleagues24 compared 5 nights of metronidazole gel 0.75% (37.5 mg per dose) to the same duration of treatment with intravaginal ovules containing 500 mg metronidazole and 100,000 U nystatin.
Patients were asked to return 14, 42, and 104 days after treatment; 138 (91%) of 151 women returned at least once.
At every follow-up, the women treated with the ovules had significantly lower recurrence rates (4%, 17%, and 33% for the ovules, compared with 20%, 38%, and 52% for the gel).
Was use of condoms related? Although participants were not randomized for condom use, recurrent infection was more likely among women whose partners did not use them.
The trial’s strengths and limitations
This study is notable for its long follow-up, blinding of the evaluator and biostatistician, and diagnostic methods (both Amsel and Nugent criteria).
The trial addressed the question of whether early recurrence is due to persistent pathogenic flora or failure to repopulate the vagina with hydrogen-peroxide–producing lactobacilli.The improved cure rate with the higher dose of intravaginal metronidazole ovules suggests that it more effectively eradicated abnormal flora than the lower dose.
However, the condom finding suggests that exposure to some factor associated with the partner also plays an important role.
The main limitation was the variability of elapsed time for follow-up visits. For example, the range for the first visit was 10 to 132 days; as a result, some women had a first evaluation that was much later than others.
Further, because participants were Peruvian, the applicability to a US population with potentially different demographics or sex practices is unclear.
Watch for complicated VVC
Women who harbor Candida organisms in their vaginas have VVC. At one end of the spectrum are women who are asymptomatically colonized. It is not necessary to treat these women or make an effort to identify the organisms. At the other end of the spectrum are symptomatic women, who have been traditionally treated with a variety of antifungal therapies, now available in multiple formulations.
Many experts now believe VVC should be classified as complicated or uncomplicated (TABLE 1) to help identify women in whom therapy is likely to fail. Uncomplicated VVC has cure rates of 80% to 90%.10 In contrast, several studies suggest that women with complicated VVC have lower short-term cure rates with either topical clotrimazole or oral fluconazole.10,11
Most women with recurrent VVC fall into the complicated category. For the most part, these are normal, healthy women who experience substantial discomfort and disruption of their daily well-being and sexuality because of recurrent infections. Self-treatment permits rapid initiation of antimycotic therapy, but does nothing to prevent the next symptomatic episode.
TABLE 1
Criteria for candidiasis diagnosis
| UNCOMPLICATED (meets all criteria) |
| Cure rate of 80% to 90% |
| Sporadic or infrequent episodes |
| Mild to moderate symptoms or findings |
| Suspected Candida albicans infection |
| Normal, nonpregnant woman |
| COMPLICATED (meets 1 or more criteria) |
| Cure rates vary widely |
| Recurrent (4 or more episodes per year) |
| Severe symptoms or findings |
| Suspected or proven non-albicans Candida infection |
Abnormal host
|
| Pregnancy |
| Adapted from Sobel JD, et al.26 |
Which Candida sp is it?
When standard antimycotic therapy fails, the species of infecting organism seems to be particularly important. Women with Candida glabrata colonization have markedly lower cure rates than women colonized with C albicans.11 Thus, a crucial first step in treating women who have complicated VVC is obtaining a yeast culture. A positive culture helps corroborate the diagnosis, increases the sensitivity of the evaluation, and allows speciation of the organism and proper selection of therapy.
Non-albicans species less likely to respond to standard azole therapy. Candida glabrata is the second leading cause of VVC, but is less responsive to standard therapies. For example, cure rates of perhaps 50% can be expected with a 7-day course of terconazole cream.12
When azole therapy is ineffective, intravaginal boric acid in 600-mg capsules can be used every night for at least 14 days and will be effective in about two thirds of patients.13 However, some patients have accidently ingested these boric acid capsules and died (apparently this dose of boric acid is lethal when taken orally). Thus, it is crucial that patients be warned specifically about this hazard.
In a series of 30 patients with no response to azole therapy and subsequent boric acid, Sobel and colleagues achieved a cure rate of 90% with a 14-day course of flucytosine cream 17%, given in 5-g nightly doses.13
Watch for false negatives in women on azole therapy. In general, the C albicans organism tends to be sensitive to azole therapy. Thus, if a woman with C albicans infection is cultured while on therapy, the odds are very high that she will have a negative yeast culture.
Maintenance fluconazole
Maintenance therapy with ketoconazole for recurrent VVC was first proposed in 1986, but was never widely adopted due to concerns about liver toxicity.
More recently, maintenance fluconazole was found to be effective in a doubleblind, placebo-controlled study.14 After treating the initial infection with 3 doses of fluconazole (150 mg every 3 days), researchers randomized women to a 6-month course of weekly fluconazole (150 mg) or placebo. During the 6-month treatment phase, relapse was noted in 9% of the fluconazole group and 64% of the placebo group. However, of the 126 fluconazole-treated women who were disease-free at the end of the treatment phase, 72 (57%) experienced relapse during the next 6 months.
Fluconazole for 6 months. Although about 50% of women have a relapse after stopping treatment, most can at least successfully control and prevent symptomatic episodes as long as they are using fluconazole in maintenance doses. Most experts recommend a 6-month course of maintenance therapy.
Alternatives to fluconazole. Extensive clinical experience has shown fluconazole to be safe and well tolerated in most women. However, women who are unable or unwilling to take it may benefit from repeated dosing of topical azoles, which also appear to be effective (although reported experience is less extensive than with fluconazole).
Vaginal trichomoniasis
This common STD has an estimated annual incidence of 3 million cases in the United States alone. Symptomatic women may complain of abnormal discharge, itching, burning, and/or postcoital bleeding. Physicians evaluating these women should be aware that microscopy has much lower sensitivity than many would expect, and that further testing may be necessary to establish a clear diagnosis (ie, cultures or the OSOM Trichomonas Rapid Test).
Treating uncomplicated infection
In the United States, trichomoniasis treatment consists of metronidazole or tinidazole; either may be given as a single 2-g dose. Although tinidazole has a somewhat longer half-life and slightly better activity against T vaginalis, both drugs appear to be effective and metronidazole is substantially cheaper. They also have similar side effects, including a possible disulfiram-like effect, although the incidence of adverse gastrointestinal (GI) effects may be lower with tinidazole.
Metronidazole allergy or resistance
Though rare, either can occur with trichomoniasis. Allergic patients should be referred for desensitization and later treated with metronidazole; both intravenous (IV) and oral regimens have been used successfully. We lack data on crossreactivity between tinidazole and metronidazole. Metronidazole resistance is thought to occur in 1 in 2,000 to 3,000 cases.15 If resistance is suspected, interview the patient carefully to exclude medication noncompliance and reinfection from an untreated partner. In a series of 33 cases, high-dose tinidazole (at least 1 g twice daily for 14 days) was well tolerated and effective in more than 90% of resistant cases.16 Susceptibility testing of the resistant isolate by a reference laboratory may help guide drug choice and dosing.
Other options, such as topical paromomycin cream, which has been studied only in small series, may have local side effects such as vulvovaginal ulceration, and should be considered a last resort.16
New approaches to BV
BV is a polymicrobial infection marked by a lack of hydrogen-peroxide–producing lactobacilli and an overgrowth of facultative anaerobic organisms. Organisms found with greater frequency and numbers include Gardnerella vaginalis, Mycoplasma hominis, Bacteroides spp, Peptostreptococcus spp, Fusobacterium spp, Prevotella spp, Mobiluncus spp, and other anaerobes.17
Diagnostic criteria
Women with symptomatic vaginosis complain of abnormal vaginal discharge and a fishy odor.
BV is diagnosed by finding at least 3 of the following Amsel criteria:
- abnormal gray discharge
- vaginal pH of more than 4.5
- positive amine test
- more than 20% of epithelial cells are clue cells
Susceptibility to other infections
In nonpregnant women, BV has been linked to infections of the reproductive tract, including pelvic inflammatory disease, postprocedural gynecologic infections, and acquisition of HIV.5 Treating BV prior to abortion or hysterectomy appears to substantially lower the risk of postoperative infection.18 Treatment also helps resolve concurrent mucopurulent cervicitis.19 However, we lack evidence that BV treatment decreases the risk of pelvic inflammatory disease or HIV.
First-line treatment
The number of approved treatment options has increased (TABLE 2). Although clindamycin may have greater in vitro resistance,5 all the listed agents have comparable clinical efficacy and safety.20-22
Topical agents often cost more than generic oral metronidazole, although the latter is often associated with GI symptoms.
TABLE 2
Bacterial vaginosis treatment options
| DRUG | FORMULATION | DOSE PER DAY | DURATION |
|---|---|---|---|
| Clindamycin | 2% cream | 5 g | 7 days |
| 2% single-dose cream | 5g | 1 day | |
| 100-mg ovules | 100 mg | 3 days | |
| 300 mg oral | 300 mg bid | 7 days | |
| Metronidazole | 0.75% gel | 5 g | 5 days |
| 500 mg oral | 500 mg bid | 7days |
When BV recurs
After treatment, bacterial vaginosis recurs in as many as 30% of women within 3 months.23 A number of explanatory theories have been proposed:
- persistent pathogenic bacteria
- reinfection from exogenous sources, including a sexual partner
- failure of normal lactobacillus-dominant flora to reestablish itself
In support of the first theory, Sanchez and colleagues24 found a lower risk of recurrence after treatment with high-dose (500 mg) intravaginal metronidazole plus nystatin, compared with standard metronidazole gel. (See “High-dose treatment [and maybe condoms] improved cure rate,”.)
The same study suggested a possible link to exposure to exogenous pathogens: Women who used condoms after treatment had a lower risk of recurrence than women who did not. However, other randomized trials evaluating treatment of the partner have shown no benefit in preventing recurrent BV.
Similarly, recolonization with lactobacillus supplements using nonvaginal strains failed to show a clear benefit.23
Benefits of maintenance therapy
Some women with recurrent BV appear to improve with low-dose maintenance antibiotic therapy. In a recent study of low-dose metronidazole gel (0.75%),25 women with recurrent BV were given a 10-day course to clear that episode, then randomized to maintenance metronidazole (1 applicator twice a week) or placebo for 4 months. Seventy percent of the treatment group remained free of infection, compared with only 34% of theplacebo group. After an additional 4 months of observation, 39% of the treatment group remained free of BV compared with 18% of the placebo group.
Although these findings demonstrate significant improvement with maintenance therapy, the relapse rate remained relatively high. A high rate of VVC was also noted: Almost 60% of women required antifungal therapy at some point during the study.
Vaginitis: A way of life
SANDRA’S CASE
At minimum, symptom control
After careful evaluation and vaginal cultures, you diagnose Sandra with candidiasis infection with the C glabrata species and prescribe 600-mg capsules of intravaginal boric acid—taking care to warn her that they are for intravaginal use only, not to be taken orally—which completely relieve her symptoms for several months.
Although the candidiasis eventually recurs, the symptoms are not as severe and resolve again with more boric acid capsules.
For patients like Sandra, vaginitis may be an inescapable fact of life.
Fortunately, as our understanding of vulvovaginal conditions has improved, more effective evaluation and treatment enable us to establish clearer diagnoses and choose therapies that—at a minimum—keep symptoms under control.
Dr. Nyirjesy serves on the speakers bureau for 3M and KV Pharmaceuticals and consults for 3M, KV Pharmaceuticals, Presutti Laboratories, and Personal Products Worldwide. He also has received grant support from Presutti Laboratories.
Dr. Sobel serves on the speakers bureau for 3M, KV Pharmaceuticals, Merck, and Pfizer, and consults for Pfizer, Presutti Laboratories, and Vicuron. He also has received grant support from Fujisawa Pharmaceuticals, Johnson & Johnson, and Presutti Laboratories.
1. Anderson MR, Klink K, Cohrssen A. Evaluation of vaginal complaints. JAMA. 2004;291:1368-1379.
2. Lipsky MS, Waters T, Sharp LK. Impact of vaginal antifungal products on utilization of health care services: evidence from physician visits. J Am Board Fam Pract. 2000;13:178-182.
3. Ferris DG, Dekle C, Litaker MS. Women’s use of over-the-counter antifungal medications for gynecological symptoms. J Fam Pract. 1996;42:595-600.
4. Ferris DG, Nyirjesy P, Sobel JD, Soper D, Pavletic A, Litaker MS. Over-the-counter antifungal drug misuse associated with patient-diagnosed vulvovaginal candidiasis. Obstet Gynecol. 2002;99:419-425.
5. Beigi RH, Austin MN, Meyn LA, Krohn MA, Hillier SL. Antimicrobial resistance associated with the treatment of bacterial vaginosis. Am J Obstet Gynecol. 2004;191:1124-1129.
6. Allen-Davis JT, Beck A, Parker R, Ellis J, Polley D. Assessment of vulvovaginal complaints: accuracy of telephone triage and in-office diagnosis. Obstet Gynecol. 2002;99:18-22.
7. Wiesenfeld HC, Macio I. The infrequent use of office-based diagnostic tests for vaginitis. Am J Obstet Gynecol. 1999;181:39-41.
8. Ledger WJ, Polaneczky MM, Yih MC, Jeremias J, Tolbert V, Witkin SS. Difficulties in the diagnosis of Candida vaginitis. Infect Dis Clin Pract. 2000;9:66-69.
9. Landers DV, Wiesenfeld HC, Heine RP, Krohn MA, Hillier SL. Predictive value of the clinical diagnosis of lower genital tract infection in women. Am J Obstet Gynecol. 2004;190:1004-1010.
10. Sobel JD, Brooker D, Stein GE, et al. Single oral dose fluconazole compared with conventional clotrimazole topical therapy of Candidavaginitis. Am J Obstet Gynecol. 1995;172:1263-1268.
11. Sobel JD, Kapernick PS, Zervos M, et al. Treatment of complicated Candidavaginitis: comparison of single and sequential doses of fluconazole. Am J Obstet Gynecol. 2001;185:363-369.
12. Sood G, Nyirjesy P, Weitz MV, Chatwani A. Terconazole cream for non Candida albicansfungal vaginitis: results of a retrospective analysis. Infect Dis Obstet Gynecol. 2000;8:240-243.
13. Sobel JD, Chaim W, Nagappan V, Leaman D. Treatment of vaginitis caused by Candida glabrata: use of topical boric acid and flucytosine. Am J Obstet Gynecol. 2003;189:1297-1300.
14. Sobel JD, Wiesenfeld HC, Martens M, et al. Maintenance fluconazole therapy for recurrent vulvovaginal candidiasis. N Engl J Med. 2004;351:876-883.
15. Nyirjesy P. Managing resistant Trichomonas vaginitis. Curr Infect Dis Rep. 1999;1:389-392.
16. Sobel JD, Nyirjesy P, Brown W. Tinidazole therapy for metronidazole-resistant vaginal trichomoniasis. Clin Infect Dis. 2001;33:1341-1346.
17. Ness RB, Hillier SL, Richter HE, et al. Douching in relation to bacterial vaginosis, lactobacilli, and facultative bacteria in the vagina. Obstet Gynecol. 2002;100:765-772.
18. Koumans EH, Kendrick JS. CDC Bacterial Vaginosis Working Group. Preventing adverse sequelae of bacterial vaginosis: a public health program and research agenda. Sex Transm Dis. 2001;28:292-297.
19. Schwebke JR, Weiss HL. Interrelationships of bacterial vaginosis and cervical inflammation. Sex Transm Dis. 2002;29:59-64.
20. Ferris DG, Litaker MS, Woodward L, Mathis D, Hendrich J. Treatment of bacterial vaginosis: a comparison of oral metronidazole, metronidazole vaginal gel, and clindamycin vaginal cream. J Fam Pract. 1995;41:443-449.
21. Hanson JM, McGregor JA, Hillier SL, et al. Metronidazole for bacterial vaginosis; a comparison of vaginal gel vs. oral therapy. J Reprod Med. 2000;45:889-896.
22. Paavonen J, Mangioni C, Martin MA, Wajszczuk CP. Vaginal clindamycin and oral metronidazole for bacterial vaginosis: a randomized trial. Obstet Gynecol. 2000;96:256-260.
23. Wilson J. Managing recurrent bacterial vaginosis. Sex Transm Infect. 2004;80:8-11.
24. Sanchez S, Garcia PJ, Thomas KK, Catlin M, Holmes KK. Intravaginal metronidazole gel versus metronidazole plus nystatin ovules for bacterial vaginosis: a randomized controlled trial. Am J Obstet Gynecol. 2004;191:1898-1906.
25. Sobel JD, Wiesenfeld HC, Schwebke J, et al. A clinical trial to evaluate efficacy of maintenance therapy with 0.75% metronidazole gel to prevent recurrent bacterial vaginosis. Oral presentation at: Annual Meeting of the Infectious Diseases Society for Obstetrics and Gynecology; August 5-7, 2004; San Diego, Calif.
26. Sobel JD, Faro S, Force RW, et al. Vulvovaginal candidiasis: epidemiologic, diagnostic, and therapeutic considerations. Am J Obstet Gynecol. 1998;178:203-211.
1. Anderson MR, Klink K, Cohrssen A. Evaluation of vaginal complaints. JAMA. 2004;291:1368-1379.
2. Lipsky MS, Waters T, Sharp LK. Impact of vaginal antifungal products on utilization of health care services: evidence from physician visits. J Am Board Fam Pract. 2000;13:178-182.
3. Ferris DG, Dekle C, Litaker MS. Women’s use of over-the-counter antifungal medications for gynecological symptoms. J Fam Pract. 1996;42:595-600.
4. Ferris DG, Nyirjesy P, Sobel JD, Soper D, Pavletic A, Litaker MS. Over-the-counter antifungal drug misuse associated with patient-diagnosed vulvovaginal candidiasis. Obstet Gynecol. 2002;99:419-425.
5. Beigi RH, Austin MN, Meyn LA, Krohn MA, Hillier SL. Antimicrobial resistance associated with the treatment of bacterial vaginosis. Am J Obstet Gynecol. 2004;191:1124-1129.
6. Allen-Davis JT, Beck A, Parker R, Ellis J, Polley D. Assessment of vulvovaginal complaints: accuracy of telephone triage and in-office diagnosis. Obstet Gynecol. 2002;99:18-22.
7. Wiesenfeld HC, Macio I. The infrequent use of office-based diagnostic tests for vaginitis. Am J Obstet Gynecol. 1999;181:39-41.
8. Ledger WJ, Polaneczky MM, Yih MC, Jeremias J, Tolbert V, Witkin SS. Difficulties in the diagnosis of Candida vaginitis. Infect Dis Clin Pract. 2000;9:66-69.
9. Landers DV, Wiesenfeld HC, Heine RP, Krohn MA, Hillier SL. Predictive value of the clinical diagnosis of lower genital tract infection in women. Am J Obstet Gynecol. 2004;190:1004-1010.
10. Sobel JD, Brooker D, Stein GE, et al. Single oral dose fluconazole compared with conventional clotrimazole topical therapy of Candidavaginitis. Am J Obstet Gynecol. 1995;172:1263-1268.
11. Sobel JD, Kapernick PS, Zervos M, et al. Treatment of complicated Candidavaginitis: comparison of single and sequential doses of fluconazole. Am J Obstet Gynecol. 2001;185:363-369.
12. Sood G, Nyirjesy P, Weitz MV, Chatwani A. Terconazole cream for non Candida albicansfungal vaginitis: results of a retrospective analysis. Infect Dis Obstet Gynecol. 2000;8:240-243.
13. Sobel JD, Chaim W, Nagappan V, Leaman D. Treatment of vaginitis caused by Candida glabrata: use of topical boric acid and flucytosine. Am J Obstet Gynecol. 2003;189:1297-1300.
14. Sobel JD, Wiesenfeld HC, Martens M, et al. Maintenance fluconazole therapy for recurrent vulvovaginal candidiasis. N Engl J Med. 2004;351:876-883.
15. Nyirjesy P. Managing resistant Trichomonas vaginitis. Curr Infect Dis Rep. 1999;1:389-392.
16. Sobel JD, Nyirjesy P, Brown W. Tinidazole therapy for metronidazole-resistant vaginal trichomoniasis. Clin Infect Dis. 2001;33:1341-1346.
17. Ness RB, Hillier SL, Richter HE, et al. Douching in relation to bacterial vaginosis, lactobacilli, and facultative bacteria in the vagina. Obstet Gynecol. 2002;100:765-772.
18. Koumans EH, Kendrick JS. CDC Bacterial Vaginosis Working Group. Preventing adverse sequelae of bacterial vaginosis: a public health program and research agenda. Sex Transm Dis. 2001;28:292-297.
19. Schwebke JR, Weiss HL. Interrelationships of bacterial vaginosis and cervical inflammation. Sex Transm Dis. 2002;29:59-64.
20. Ferris DG, Litaker MS, Woodward L, Mathis D, Hendrich J. Treatment of bacterial vaginosis: a comparison of oral metronidazole, metronidazole vaginal gel, and clindamycin vaginal cream. J Fam Pract. 1995;41:443-449.
21. Hanson JM, McGregor JA, Hillier SL, et al. Metronidazole for bacterial vaginosis; a comparison of vaginal gel vs. oral therapy. J Reprod Med. 2000;45:889-896.
22. Paavonen J, Mangioni C, Martin MA, Wajszczuk CP. Vaginal clindamycin and oral metronidazole for bacterial vaginosis: a randomized trial. Obstet Gynecol. 2000;96:256-260.
23. Wilson J. Managing recurrent bacterial vaginosis. Sex Transm Infect. 2004;80:8-11.
24. Sanchez S, Garcia PJ, Thomas KK, Catlin M, Holmes KK. Intravaginal metronidazole gel versus metronidazole plus nystatin ovules for bacterial vaginosis: a randomized controlled trial. Am J Obstet Gynecol. 2004;191:1898-1906.
25. Sobel JD, Wiesenfeld HC, Schwebke J, et al. A clinical trial to evaluate efficacy of maintenance therapy with 0.75% metronidazole gel to prevent recurrent bacterial vaginosis. Oral presentation at: Annual Meeting of the Infectious Diseases Society for Obstetrics and Gynecology; August 5-7, 2004; San Diego, Calif.
26. Sobel JD, Faro S, Force RW, et al. Vulvovaginal candidiasis: epidemiologic, diagnostic, and therapeutic considerations. Am J Obstet Gynecol. 1998;178:203-211.
When does vaginal delivery invite incontinence?
- What the evidence does—and does not confirm
- Protective factors
- Term Breech Trial
MARISOL’S CASE
Pregnant and incontinent
Marisol, a 32-year-old physiotherapist expecting her second child, presents to your antenatal clinic at 20 weeks’ gestation. She complains of urinary incontinence, which has been worsening throughout this pregnancy, and wants to know what can be done about it.
How do you respond?
The bad news is that Marisol’s complaints are not uncommon. The good news: Detailed evaluation and considered discussion can help reveal the full extent of her symptoms and shed light on how to proceed, though, in some cases, your options may be limited. Since we are in the early stages of understanding pelvic floor dysfunction related to pregnancy and childbirth, giving clear advice and guidance can sometimes be difficult. The starting point here, as in any case involving urinary symptoms, is a detailed history to pin down the cause of the patient’s complaints.
In women, urinary incontinence generally stems from overactive bladder or urethral sphincter incompetence; the latter is generally acquired through pregnancy and childbirth.Examining the Evidence.)
Episiotomy also has been associated with diminished pelvic floor muscle strength, compared with spontaneous perineal lacerations.33
Other factors with protective potential. Some recommendations may reduce the overall risk of incontinence in the long term in the general population, though they do not apply in Marisol’s case. For example, weight reduction in moderately obese women can reduce the risk of urinary symptoms.34
Chronic cough also increases the risk of pelvic floor dysfunction and prolapse, particularly among older women,13 so smoking cessation should be recommended.
Selecting the mode of delivery in a case like Marisol’s involves weighing her risks and desires with your expertise. No clear evidence is available to guide the way. This makes judicious counseling about the short-and long-term risks of conservative management and surgical delivery doubly important.
DID PRIOR DELIVERY DO DAMAGE?
Marisol’s final question concerns her first delivery. She feels she was inadequately counseled and wants to know whether delivery by cesarean would have protected her from her current symptoms.
In a prospective cohort study, Eason and colleagues4 found that 93.4% of women undergoing abdominal delivery remained continent postpartum, whereas 20.6% of women delivering vaginally lost urinary continence. However, Marisol’s symptoms predated the initial pregnancy.
The Term Breech Trial35 found no significant differences in maternal outcomes, including incontinence and sexual function, between the planned cesarean and planned vaginal delivery groups. However, the high crossover from planned vaginal delivery to delivery by cesarean suggests this evidence should be interpreted with caution. Cesarean delivery comes with its own set of complications and long-term problems.
Counsel all women about the risks of vaginal delivery?
This is a thorny question. As the body of evidence increases on the long-term effects of pregnancy and delivery, these issues are entering the public domain. We may be approaching a time when the specter of litigation influences how we counsel women about the risks of natural childbirth. How this change will be viewed by women’s health groups—some of which already perceive the health-care system as overmedicalizing a natural event—can only be imagined.
The authors report no financial relationships relevant to this article.
1. Keane DP, O’Sullivan S. Urinary incontinence: anatomy, physiology and pathophysiology. Ballieres Best Pract Res Clin Obstet Gynaecol. 2000;14:207-226.
2. Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S. Norwegian EPINCONT Study. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med. 2003;348:900-907.
3. Dolan LM, Walsh D, Hamilton S, Marshall K, Thompson K, Ashe R. A study of quality of life in primigravidae with urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:160-164.
4. Eason E, Labrecque M, Marcoux S, Mondor M. Effects of carrying a pregnancy and of method of delivery on urinary incontinence: a prospective cohort study. BMC Pregnancy Childbirth. 2004;4:4.-
5. Gregory WT, Nygaard I. Childbirth and pelvic floor disorders. Clin Obstet Gynecol. 2004;47:394-403.
6. Fritel X, Fauconnier A, Levet C, Benifla J. Stress urinary incontinence 4 years after the first delivery: a retrospective cohort survey. Acta Obstet Gynecol Scand. 2004;83:941-945.
7. Schytt E, Lindmark G, Waldenstrom U. Symptoms of stress incontinence 1 year after childbirth: prevalence and predictors in a national Swedish sample. Acta Obstet Gynecol Scand. 2004;83:928-936.
8. Handa VL, Harvey L, Fox H, Kjerulff KH. Parity and route of delivery: does cesarean delivery reduce bladder symptoms later in life? Am J Obstet Gynecol. 2004;191:463-469.
9. Sultan AH, Kamm MA, Hudson CN. Pudendal nerve damage during labour: prospective study before and after childbirth. Br J Obstet Gynaecol. 1994;101:22-28.
10. Damaser MS, Whitbeck C, Chichester P, Levin R. Effect of vaginal distension on blood flow and hypoxia of urogenital organs of the female rat. J Appl Physiol. 2005;98:1884-1890.
11. Sartori JP, Sartori MG, Baracat EC, De Lima GR, Girao M. Bladder neck mobility and functional evaluation of the pelvic floor in primiparae according to the type of delivery. Clin Exp Obstet Gynecol. 2004;31:120-122.
12. DeLancey JO, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol. 2003;101:46-53.
13. Uustal Fornell E, Wingren G, Kjolhede P. Factors associated with pelvic floor dysfunction with emphasis on urinary and fecal incontinence and genital prolapse: an epidemiological study. Acta Obstet Gynecol Scand. 2004;83:383-389.
14. Dupuis O, Madelenat P, Rudigoz RC. Fecal and urinary incontinence after delivery: risk factors and prevention [in French]. Gynecol Obstet Fertil. 2004;32:540-548.
15. Fitzpatrick M, O’Herlihy C. The effects of labour and delivery on the pelvic floor. Best Pract Res Clin Obstet Gynaecol. 2001;15:63-79.
16. Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartram CI. Anal-sphincter disruption during vaginal delivery. N Engl J Med. 1993;329:1905-1911.
17. Fitzpatrick M, Fynes M, Cassidy M, Behan M, O’Connell PR, O’Herlihy C. Prospective study of the influence of parity and operative technique on the outcome of primary anal sphincter repair following obstetrical injury. Eur J Obstet Gynecol Reprod Biol. 2000;89:159-163.
18. Chaliha C, Digesu A, Hutchings A, Soligo M, Khullar V. Caesarean section is protective against stress urinary incontinence: an analysis of women with multiple deliveries. BJOG. 2004;111:754-755.
19. Foldspang A, Hvidman L, Mommsen S, Nielsen JB. Risk of postpartum urinary incontinence associated with pregnancy and mode of delivery. Acta Obstet Gynecol Scand. 2004;83:923-927.
20. Liebling RE, Swingler R, Patel RR, Verity L, Soothill PW, Murphy DJ. Pelvic floor morbidity up to one year after difficult instrumental delivery and caesarean section in the second stage of labor: a cohort study. Am J Obstet Gynecol. 2004;191:4-10.
21. Murphy DJ, Liebling RE. Cohort study of maternal views on future mode of delivery after operative delivery in the second stage of labor. Am J Obstet Gynecol. 2003;188:542-548.
22. Thomas J, Paranjothy S. Royal College of Obstetricians and Gynaecologists Clinical Effectiveness Support Unit. The National Sentinel Caesarean Section Audit Report. London, UK: RCOG Press; 2001. Available at: http://www.rcm.org.uk/templates/news/detail.cfm/115. Accessed June 20, 2005.
23. National Center for Health Statistics. Births—method of delivery. Available at http://www.cdc.gov/nchs/fastats/delivery.htm. Accessed July 8, 2005.
24. Wax JR, Cartin A, Pinette MG, Blackstone J. Patient choice caesarean: an evidence-based review. Obstet Gynecol Surv. 2004;59:601-616.
25. Rashid M, Rashid RS. Higher order repeat caesarean sections: how safe are five or more? BJOG. 2004;111:1090-1094.
26. Flamm BL, Goings JR, Liu Y, Wolde-Tsadik G. Elective repeat cesarean delivery versus trial of labor: a prospective multicenter study. Obstet Gynecol. 1994;83:927-932.
27. Clarl SL, Koonings PP, Phelan JP. Placenta previa/accreta and prior caesarean section. Obstet Gynecol. 1985;66:89-92.
28. Snooks SJ, Swash M, Mathers SE, Henry MM. Effect of vaginal delivery on the pelvic floor: a 5-year follow-up. Br J Surg. 1990;77:1358-1360.
29. Salvesen KA, Morkved S. Randomised controlled trial of pelvic floor muscle training during pregnancy. BMJ. 2004;329:378-380.
30. Glazener CM, Herbison GP, Macarthur C, Grant A, Wilson PD. Randomised controlled trial of conservative management of postnatal urinary and faecal incontinence: six year follow up. BMJ. 2005;330:337.-
31. Howell CJ. Epidural versus non-epidural analgesia for pain relief in labour. Cochrane Database Syst Rev. 2000;(2):CD000331.-
32. Dannecker C, Hillemanns P, Strauss A, Hasbargen U, Hepp H, Anthuber C. Episiotomy and perineal tears presumed to be imminent: the influence on the urethral pressure profile, analmanometric and other pelvic floor findings—follow-up study of a randomized controlled trial. Acta Obstet Gynecol Scand. 2005;84:65-71.
33. Department of Health. Changing Childbirth. Part 1: Report of the Expert Maternity Group. London, UK: HMSO; 1993.
34. Subak LL, Johnson C, Whitcomb E, Boban D, Saxton J, Brown JS. Does weight loss improve incontinence in moderately obese women? Int Urogynecol J Pelvic Floor Dysfunct. 2002;13:40-43.
35. Hannah ME, Whyte H, Hannah WJ, et al. Maternal outcomes at 2 years after planned caesarean section versus planned vaginal birth for breech presentation at term: the international randomized Term Breech Trial. Am J Obstet Gynecol. 2004;191:917-927.
- What the evidence does—and does not confirm
- Protective factors
- Term Breech Trial
MARISOL’S CASE
Pregnant and incontinent
Marisol, a 32-year-old physiotherapist expecting her second child, presents to your antenatal clinic at 20 weeks’ gestation. She complains of urinary incontinence, which has been worsening throughout this pregnancy, and wants to know what can be done about it.
How do you respond?
The bad news is that Marisol’s complaints are not uncommon. The good news: Detailed evaluation and considered discussion can help reveal the full extent of her symptoms and shed light on how to proceed, though, in some cases, your options may be limited. Since we are in the early stages of understanding pelvic floor dysfunction related to pregnancy and childbirth, giving clear advice and guidance can sometimes be difficult. The starting point here, as in any case involving urinary symptoms, is a detailed history to pin down the cause of the patient’s complaints.
In women, urinary incontinence generally stems from overactive bladder or urethral sphincter incompetence; the latter is generally acquired through pregnancy and childbirth.Examining the Evidence.)
Episiotomy also has been associated with diminished pelvic floor muscle strength, compared with spontaneous perineal lacerations.33
Other factors with protective potential. Some recommendations may reduce the overall risk of incontinence in the long term in the general population, though they do not apply in Marisol’s case. For example, weight reduction in moderately obese women can reduce the risk of urinary symptoms.34
Chronic cough also increases the risk of pelvic floor dysfunction and prolapse, particularly among older women,13 so smoking cessation should be recommended.
Selecting the mode of delivery in a case like Marisol’s involves weighing her risks and desires with your expertise. No clear evidence is available to guide the way. This makes judicious counseling about the short-and long-term risks of conservative management and surgical delivery doubly important.
DID PRIOR DELIVERY DO DAMAGE?
Marisol’s final question concerns her first delivery. She feels she was inadequately counseled and wants to know whether delivery by cesarean would have protected her from her current symptoms.
In a prospective cohort study, Eason and colleagues4 found that 93.4% of women undergoing abdominal delivery remained continent postpartum, whereas 20.6% of women delivering vaginally lost urinary continence. However, Marisol’s symptoms predated the initial pregnancy.
The Term Breech Trial35 found no significant differences in maternal outcomes, including incontinence and sexual function, between the planned cesarean and planned vaginal delivery groups. However, the high crossover from planned vaginal delivery to delivery by cesarean suggests this evidence should be interpreted with caution. Cesarean delivery comes with its own set of complications and long-term problems.
Counsel all women about the risks of vaginal delivery?
This is a thorny question. As the body of evidence increases on the long-term effects of pregnancy and delivery, these issues are entering the public domain. We may be approaching a time when the specter of litigation influences how we counsel women about the risks of natural childbirth. How this change will be viewed by women’s health groups—some of which already perceive the health-care system as overmedicalizing a natural event—can only be imagined.
The authors report no financial relationships relevant to this article.
- What the evidence does—and does not confirm
- Protective factors
- Term Breech Trial
MARISOL’S CASE
Pregnant and incontinent
Marisol, a 32-year-old physiotherapist expecting her second child, presents to your antenatal clinic at 20 weeks’ gestation. She complains of urinary incontinence, which has been worsening throughout this pregnancy, and wants to know what can be done about it.
How do you respond?
The bad news is that Marisol’s complaints are not uncommon. The good news: Detailed evaluation and considered discussion can help reveal the full extent of her symptoms and shed light on how to proceed, though, in some cases, your options may be limited. Since we are in the early stages of understanding pelvic floor dysfunction related to pregnancy and childbirth, giving clear advice and guidance can sometimes be difficult. The starting point here, as in any case involving urinary symptoms, is a detailed history to pin down the cause of the patient’s complaints.
In women, urinary incontinence generally stems from overactive bladder or urethral sphincter incompetence; the latter is generally acquired through pregnancy and childbirth.Examining the Evidence.)
Episiotomy also has been associated with diminished pelvic floor muscle strength, compared with spontaneous perineal lacerations.33
Other factors with protective potential. Some recommendations may reduce the overall risk of incontinence in the long term in the general population, though they do not apply in Marisol’s case. For example, weight reduction in moderately obese women can reduce the risk of urinary symptoms.34
Chronic cough also increases the risk of pelvic floor dysfunction and prolapse, particularly among older women,13 so smoking cessation should be recommended.
Selecting the mode of delivery in a case like Marisol’s involves weighing her risks and desires with your expertise. No clear evidence is available to guide the way. This makes judicious counseling about the short-and long-term risks of conservative management and surgical delivery doubly important.
DID PRIOR DELIVERY DO DAMAGE?
Marisol’s final question concerns her first delivery. She feels she was inadequately counseled and wants to know whether delivery by cesarean would have protected her from her current symptoms.
In a prospective cohort study, Eason and colleagues4 found that 93.4% of women undergoing abdominal delivery remained continent postpartum, whereas 20.6% of women delivering vaginally lost urinary continence. However, Marisol’s symptoms predated the initial pregnancy.
The Term Breech Trial35 found no significant differences in maternal outcomes, including incontinence and sexual function, between the planned cesarean and planned vaginal delivery groups. However, the high crossover from planned vaginal delivery to delivery by cesarean suggests this evidence should be interpreted with caution. Cesarean delivery comes with its own set of complications and long-term problems.
Counsel all women about the risks of vaginal delivery?
This is a thorny question. As the body of evidence increases on the long-term effects of pregnancy and delivery, these issues are entering the public domain. We may be approaching a time when the specter of litigation influences how we counsel women about the risks of natural childbirth. How this change will be viewed by women’s health groups—some of which already perceive the health-care system as overmedicalizing a natural event—can only be imagined.
The authors report no financial relationships relevant to this article.
1. Keane DP, O’Sullivan S. Urinary incontinence: anatomy, physiology and pathophysiology. Ballieres Best Pract Res Clin Obstet Gynaecol. 2000;14:207-226.
2. Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S. Norwegian EPINCONT Study. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med. 2003;348:900-907.
3. Dolan LM, Walsh D, Hamilton S, Marshall K, Thompson K, Ashe R. A study of quality of life in primigravidae with urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:160-164.
4. Eason E, Labrecque M, Marcoux S, Mondor M. Effects of carrying a pregnancy and of method of delivery on urinary incontinence: a prospective cohort study. BMC Pregnancy Childbirth. 2004;4:4.-
5. Gregory WT, Nygaard I. Childbirth and pelvic floor disorders. Clin Obstet Gynecol. 2004;47:394-403.
6. Fritel X, Fauconnier A, Levet C, Benifla J. Stress urinary incontinence 4 years after the first delivery: a retrospective cohort survey. Acta Obstet Gynecol Scand. 2004;83:941-945.
7. Schytt E, Lindmark G, Waldenstrom U. Symptoms of stress incontinence 1 year after childbirth: prevalence and predictors in a national Swedish sample. Acta Obstet Gynecol Scand. 2004;83:928-936.
8. Handa VL, Harvey L, Fox H, Kjerulff KH. Parity and route of delivery: does cesarean delivery reduce bladder symptoms later in life? Am J Obstet Gynecol. 2004;191:463-469.
9. Sultan AH, Kamm MA, Hudson CN. Pudendal nerve damage during labour: prospective study before and after childbirth. Br J Obstet Gynaecol. 1994;101:22-28.
10. Damaser MS, Whitbeck C, Chichester P, Levin R. Effect of vaginal distension on blood flow and hypoxia of urogenital organs of the female rat. J Appl Physiol. 2005;98:1884-1890.
11. Sartori JP, Sartori MG, Baracat EC, De Lima GR, Girao M. Bladder neck mobility and functional evaluation of the pelvic floor in primiparae according to the type of delivery. Clin Exp Obstet Gynecol. 2004;31:120-122.
12. DeLancey JO, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol. 2003;101:46-53.
13. Uustal Fornell E, Wingren G, Kjolhede P. Factors associated with pelvic floor dysfunction with emphasis on urinary and fecal incontinence and genital prolapse: an epidemiological study. Acta Obstet Gynecol Scand. 2004;83:383-389.
14. Dupuis O, Madelenat P, Rudigoz RC. Fecal and urinary incontinence after delivery: risk factors and prevention [in French]. Gynecol Obstet Fertil. 2004;32:540-548.
15. Fitzpatrick M, O’Herlihy C. The effects of labour and delivery on the pelvic floor. Best Pract Res Clin Obstet Gynaecol. 2001;15:63-79.
16. Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartram CI. Anal-sphincter disruption during vaginal delivery. N Engl J Med. 1993;329:1905-1911.
17. Fitzpatrick M, Fynes M, Cassidy M, Behan M, O’Connell PR, O’Herlihy C. Prospective study of the influence of parity and operative technique on the outcome of primary anal sphincter repair following obstetrical injury. Eur J Obstet Gynecol Reprod Biol. 2000;89:159-163.
18. Chaliha C, Digesu A, Hutchings A, Soligo M, Khullar V. Caesarean section is protective against stress urinary incontinence: an analysis of women with multiple deliveries. BJOG. 2004;111:754-755.
19. Foldspang A, Hvidman L, Mommsen S, Nielsen JB. Risk of postpartum urinary incontinence associated with pregnancy and mode of delivery. Acta Obstet Gynecol Scand. 2004;83:923-927.
20. Liebling RE, Swingler R, Patel RR, Verity L, Soothill PW, Murphy DJ. Pelvic floor morbidity up to one year after difficult instrumental delivery and caesarean section in the second stage of labor: a cohort study. Am J Obstet Gynecol. 2004;191:4-10.
21. Murphy DJ, Liebling RE. Cohort study of maternal views on future mode of delivery after operative delivery in the second stage of labor. Am J Obstet Gynecol. 2003;188:542-548.
22. Thomas J, Paranjothy S. Royal College of Obstetricians and Gynaecologists Clinical Effectiveness Support Unit. The National Sentinel Caesarean Section Audit Report. London, UK: RCOG Press; 2001. Available at: http://www.rcm.org.uk/templates/news/detail.cfm/115. Accessed June 20, 2005.
23. National Center for Health Statistics. Births—method of delivery. Available at http://www.cdc.gov/nchs/fastats/delivery.htm. Accessed July 8, 2005.
24. Wax JR, Cartin A, Pinette MG, Blackstone J. Patient choice caesarean: an evidence-based review. Obstet Gynecol Surv. 2004;59:601-616.
25. Rashid M, Rashid RS. Higher order repeat caesarean sections: how safe are five or more? BJOG. 2004;111:1090-1094.
26. Flamm BL, Goings JR, Liu Y, Wolde-Tsadik G. Elective repeat cesarean delivery versus trial of labor: a prospective multicenter study. Obstet Gynecol. 1994;83:927-932.
27. Clarl SL, Koonings PP, Phelan JP. Placenta previa/accreta and prior caesarean section. Obstet Gynecol. 1985;66:89-92.
28. Snooks SJ, Swash M, Mathers SE, Henry MM. Effect of vaginal delivery on the pelvic floor: a 5-year follow-up. Br J Surg. 1990;77:1358-1360.
29. Salvesen KA, Morkved S. Randomised controlled trial of pelvic floor muscle training during pregnancy. BMJ. 2004;329:378-380.
30. Glazener CM, Herbison GP, Macarthur C, Grant A, Wilson PD. Randomised controlled trial of conservative management of postnatal urinary and faecal incontinence: six year follow up. BMJ. 2005;330:337.-
31. Howell CJ. Epidural versus non-epidural analgesia for pain relief in labour. Cochrane Database Syst Rev. 2000;(2):CD000331.-
32. Dannecker C, Hillemanns P, Strauss A, Hasbargen U, Hepp H, Anthuber C. Episiotomy and perineal tears presumed to be imminent: the influence on the urethral pressure profile, analmanometric and other pelvic floor findings—follow-up study of a randomized controlled trial. Acta Obstet Gynecol Scand. 2005;84:65-71.
33. Department of Health. Changing Childbirth. Part 1: Report of the Expert Maternity Group. London, UK: HMSO; 1993.
34. Subak LL, Johnson C, Whitcomb E, Boban D, Saxton J, Brown JS. Does weight loss improve incontinence in moderately obese women? Int Urogynecol J Pelvic Floor Dysfunct. 2002;13:40-43.
35. Hannah ME, Whyte H, Hannah WJ, et al. Maternal outcomes at 2 years after planned caesarean section versus planned vaginal birth for breech presentation at term: the international randomized Term Breech Trial. Am J Obstet Gynecol. 2004;191:917-927.
1. Keane DP, O’Sullivan S. Urinary incontinence: anatomy, physiology and pathophysiology. Ballieres Best Pract Res Clin Obstet Gynaecol. 2000;14:207-226.
2. Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S. Norwegian EPINCONT Study. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med. 2003;348:900-907.
3. Dolan LM, Walsh D, Hamilton S, Marshall K, Thompson K, Ashe R. A study of quality of life in primigravidae with urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:160-164.
4. Eason E, Labrecque M, Marcoux S, Mondor M. Effects of carrying a pregnancy and of method of delivery on urinary incontinence: a prospective cohort study. BMC Pregnancy Childbirth. 2004;4:4.-
5. Gregory WT, Nygaard I. Childbirth and pelvic floor disorders. Clin Obstet Gynecol. 2004;47:394-403.
6. Fritel X, Fauconnier A, Levet C, Benifla J. Stress urinary incontinence 4 years after the first delivery: a retrospective cohort survey. Acta Obstet Gynecol Scand. 2004;83:941-945.
7. Schytt E, Lindmark G, Waldenstrom U. Symptoms of stress incontinence 1 year after childbirth: prevalence and predictors in a national Swedish sample. Acta Obstet Gynecol Scand. 2004;83:928-936.
8. Handa VL, Harvey L, Fox H, Kjerulff KH. Parity and route of delivery: does cesarean delivery reduce bladder symptoms later in life? Am J Obstet Gynecol. 2004;191:463-469.
9. Sultan AH, Kamm MA, Hudson CN. Pudendal nerve damage during labour: prospective study before and after childbirth. Br J Obstet Gynaecol. 1994;101:22-28.
10. Damaser MS, Whitbeck C, Chichester P, Levin R. Effect of vaginal distension on blood flow and hypoxia of urogenital organs of the female rat. J Appl Physiol. 2005;98:1884-1890.
11. Sartori JP, Sartori MG, Baracat EC, De Lima GR, Girao M. Bladder neck mobility and functional evaluation of the pelvic floor in primiparae according to the type of delivery. Clin Exp Obstet Gynecol. 2004;31:120-122.
12. DeLancey JO, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol. 2003;101:46-53.
13. Uustal Fornell E, Wingren G, Kjolhede P. Factors associated with pelvic floor dysfunction with emphasis on urinary and fecal incontinence and genital prolapse: an epidemiological study. Acta Obstet Gynecol Scand. 2004;83:383-389.
14. Dupuis O, Madelenat P, Rudigoz RC. Fecal and urinary incontinence after delivery: risk factors and prevention [in French]. Gynecol Obstet Fertil. 2004;32:540-548.
15. Fitzpatrick M, O’Herlihy C. The effects of labour and delivery on the pelvic floor. Best Pract Res Clin Obstet Gynaecol. 2001;15:63-79.
16. Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartram CI. Anal-sphincter disruption during vaginal delivery. N Engl J Med. 1993;329:1905-1911.
17. Fitzpatrick M, Fynes M, Cassidy M, Behan M, O’Connell PR, O’Herlihy C. Prospective study of the influence of parity and operative technique on the outcome of primary anal sphincter repair following obstetrical injury. Eur J Obstet Gynecol Reprod Biol. 2000;89:159-163.
18. Chaliha C, Digesu A, Hutchings A, Soligo M, Khullar V. Caesarean section is protective against stress urinary incontinence: an analysis of women with multiple deliveries. BJOG. 2004;111:754-755.
19. Foldspang A, Hvidman L, Mommsen S, Nielsen JB. Risk of postpartum urinary incontinence associated with pregnancy and mode of delivery. Acta Obstet Gynecol Scand. 2004;83:923-927.
20. Liebling RE, Swingler R, Patel RR, Verity L, Soothill PW, Murphy DJ. Pelvic floor morbidity up to one year after difficult instrumental delivery and caesarean section in the second stage of labor: a cohort study. Am J Obstet Gynecol. 2004;191:4-10.
21. Murphy DJ, Liebling RE. Cohort study of maternal views on future mode of delivery after operative delivery in the second stage of labor. Am J Obstet Gynecol. 2003;188:542-548.
22. Thomas J, Paranjothy S. Royal College of Obstetricians and Gynaecologists Clinical Effectiveness Support Unit. The National Sentinel Caesarean Section Audit Report. London, UK: RCOG Press; 2001. Available at: http://www.rcm.org.uk/templates/news/detail.cfm/115. Accessed June 20, 2005.
23. National Center for Health Statistics. Births—method of delivery. Available at http://www.cdc.gov/nchs/fastats/delivery.htm. Accessed July 8, 2005.
24. Wax JR, Cartin A, Pinette MG, Blackstone J. Patient choice caesarean: an evidence-based review. Obstet Gynecol Surv. 2004;59:601-616.
25. Rashid M, Rashid RS. Higher order repeat caesarean sections: how safe are five or more? BJOG. 2004;111:1090-1094.
26. Flamm BL, Goings JR, Liu Y, Wolde-Tsadik G. Elective repeat cesarean delivery versus trial of labor: a prospective multicenter study. Obstet Gynecol. 1994;83:927-932.
27. Clarl SL, Koonings PP, Phelan JP. Placenta previa/accreta and prior caesarean section. Obstet Gynecol. 1985;66:89-92.
28. Snooks SJ, Swash M, Mathers SE, Henry MM. Effect of vaginal delivery on the pelvic floor: a 5-year follow-up. Br J Surg. 1990;77:1358-1360.
29. Salvesen KA, Morkved S. Randomised controlled trial of pelvic floor muscle training during pregnancy. BMJ. 2004;329:378-380.
30. Glazener CM, Herbison GP, Macarthur C, Grant A, Wilson PD. Randomised controlled trial of conservative management of postnatal urinary and faecal incontinence: six year follow up. BMJ. 2005;330:337.-
31. Howell CJ. Epidural versus non-epidural analgesia for pain relief in labour. Cochrane Database Syst Rev. 2000;(2):CD000331.-
32. Dannecker C, Hillemanns P, Strauss A, Hasbargen U, Hepp H, Anthuber C. Episiotomy and perineal tears presumed to be imminent: the influence on the urethral pressure profile, analmanometric and other pelvic floor findings—follow-up study of a randomized controlled trial. Acta Obstet Gynecol Scand. 2005;84:65-71.
33. Department of Health. Changing Childbirth. Part 1: Report of the Expert Maternity Group. London, UK: HMSO; 1993.
34. Subak LL, Johnson C, Whitcomb E, Boban D, Saxton J, Brown JS. Does weight loss improve incontinence in moderately obese women? Int Urogynecol J Pelvic Floor Dysfunct. 2002;13:40-43.
35. Hannah ME, Whyte H, Hannah WJ, et al. Maternal outcomes at 2 years after planned caesarean section versus planned vaginal birth for breech presentation at term: the international randomized Term Breech Trial. Am J Obstet Gynecol. 2004;191:917-927.
Craniocervical Neurenteric Cyst
Outpatient Buprenorphine Treatment for Opioid Dependence
Gynecologic Cancer
This Update reviews recent findings of importance to obstetricians and gynecologists. Late detection of ovarian cancer is still the main reason for the high mortality rate of the most deadly of the gynecologic cancers. Approximately 22,200 women will be newly diagnosed in the United States this year, and there will be 16,210 deaths. Since ovarian cancer is still initially detected in its advanced stages in more than 70% of cases, when cure rates are low, early detection and prevention remain our greatest challenge. The gynecologic oncologist’s opportunity to successfully treat malignancy depends on early detection, and therefore physicians providing primary care for women are our firstline guardians.
“Silent killer” may not be so stealthy
Women ultimately diagnosed with malignant masses had a triad of symptoms, as well as more recent onset and greater severity of symptoms than women with benign masses or no masses. A diagnostic workup employing transvaginal ultrasound and CA-125 should be considered when a woman says she has these symptoms.
Ovarian cancer is not a silent disease. It was believed to be a “silent killer” because it was thought to be asymptomatic until a woman had very advanced disease. However, Goff and colleagues, in a previous study, found that 95% of women with ovarian cancer had had symptoms prior to diagnosis—and that the type of symptoms was not significantly different, whether disease was early stage or late stage.
This new study aimed to identify the frequency, severity, and duration of symptoms typically associated with ovarian cancer, by comparing symptoms reported by different groups of women. Symptoms reported by women presenting to primary care clinics were compared with symptoms reported by a group of 128 women with ovarian masses. Importantly, women were surveyed about their symptoms before undergoing surgery, and before they had a diagnosis of cancer or benign disease.
Main findings:
- A triad of symptoms—abdominal bloating, an increase in abdominal girth, and urinary symptoms—occurred in 43% of women found to have ovarian cancer, but in only 8% of women who presented to a primary care clinic.
- The frequency and duration of symptoms in women with ovarian masses were more severe in the women with malignant masses, but were of a similar type regardless of whether the mass was benign or ovarian cancer.
- Onset of symptoms was more recent in women with ovarian cancer than in the control group.
Listening carefully and evaluating the severity, frequency, and duration of symptoms, especially abdominal bloating, an increase in abdominal girth, urinary symptoms, and abdominal pain, is all-important.
Ovarian cancer should be included in the differential diagnosis when a woman says she has these symptoms.
I found it interesting that symptoms with a more recent onset may be more consistent with ovarian cancer.
In an ideal world, a simple blood test with an absolute cutoff, with perfect sensitivity and specificity, would identify ovarian cancer at its earliest stages. However, until such a test exists, primary care physicians and ObGyns should continue to put weight on the symptoms the patient communicates.
Transvaginal ultrasound and CA-125
Consider performing a diagnostic workup employing transvaginal ultrasound and CA-125 measurement in women presenting with these complaints.
RELATED REFERENCES
- Goff BA, Mandell L, Muntz HG, Melancon CH. Ovarian cancer diagnosis: results of a national ovarian cancer survey. Cancer. 2000;89:2068–2075.
Whatever happened to the ovarian cancer blood test?
Ransohoff DF. Lessons from controversy: ovarian cancer screening and serum proteomics. J Natl Cancer Inst. 2005;97:315–319.
Science is still seeking the Holy Grail—a blood test for early detection of ovarian cancer.
When Petricoin et al reported in 2002 that a serum proteomic profiling test had nearly 100% sensitivity and specificity, the media trumpeted the phenomenal news. The public’s hopes soared when news articles reported that a company would soon begin offering the test. Patients brought in these reports to their ObGyns and asked for the test.
Plans to introduce a commercial screening test by early 2004 were delayed, however, due to FDA concerns about its reliability. The reasons for claims, plans, and delays were reported in both professional journals and the lay press, but details on the “question about whether the approach of discovery-based serum proteomics can accurately and reliably diagnose ovarian cancer—or any cancer—have not been resolved,” Dr. Ransohoff explains in this thoughtful 2005 essay.
He describes in a simple and straightforward way the requirements of reproducibility, and what these new technologies must demonstrate. He concludes that serum proteomic profiling for the early detection of ovarian cancer has not demonstrated the reproducibility required of a clinical test.
“Chance and bias may cause erroneous results and inflated expectations in the kind of observational research being conducted in several ‘–omics’ fields to assess molecular markers for diagnosis and prognosis of cancer. To realize the potential of new –omics technology will require appropriate rules of evidence in the design, conduct, and interpretation of the clinical research,” writes Dr. Ransohoff.
While proteomic profiling clearly has promise, clinicians should insist that initial studies be validated
What to tell patients. I explain that the test appeared promising, and therefore was of great interest, but the FDA did not allow it to be put on the market because of insufficient evidence that the test consistently defines whether cancer is or is not present. Since either a negative or positive test would have profound effects, accuracy is an absolute requirement.
RELATED REFERENCES
- Baggerly KA, Morris JS, Edmonson SR, Coombes KR. Signal in noise: evaluating reported reproducibility of serum proteomic tests for ovarian cancer. J Natl Cancer Inst. 2005;97:307–309.
- Liotta LA, Lowenthal M, Mehta A, et al. Importance of communication between producers and consumers of publicly available experimental data. J Natl Cancer Inst. 2005;97:310–314.
- Petricoin EF, Ardekani AM, Hitt BA, et al. Use of proteomic patterns in serum to identify ovarian cancer. Lancet. 2002;359:572–577.
Don’t hold back from counseling risk-reducing BSO when indicated
Metcalfe KA, Lynch HT, Ghadirian P, et al. The risk of ovarian cancer after breast cancer in BRCA1 and BRCA2 carriers. Gynecol Oncol. 2005;96:222–226.
Counsel women with breast cancer who are BRCA1 or BRCA2 mutation carriers to consider prophylactic salpingo-oophorectomy after childbearing is complete. Tamoxifen and chemotherapy do not lower risk.
ObGyns should encourage young women with breast cancer or women with a strong family history of breast and/or ovarian cancer to undergo genetic testing.
Women with breast cancer who are found to be BRCA1 or BRCA2 mutation carriers should be counseled by their gynecologists to consider prophylactic BSO after childbearing is complete. Even though these women’s greatest concern may be breast cancer recurrence, gynecologists should advise these women that they are also at risk for ovarian cancer, and that they can substantially decrease their risk by undergoing risk-reduction surgery. BRCA1 mutation carriers have up to an 80% lifetime risk of breast cancer and up to a 50% lifetime risk for ovarian cancer.
Recent data support intervention to decrease risk: BSO decreases risk of ovarian cancer by more than 90%, and decreases risk of breast cancer by 50% in BRCA1 or BRCA2 mutation carriers. Metcalfe et al examined women with a BRCA1 or BRCA2 mutation and a history of stage I or II breast cancer, and found that 10% developed an ovarian cancer, a fallopian tube cancer, or a peritoneal cancer. The median time was 8.1 years from the development of breast cancer to the development of ovarian cancer. The cumulative risk of developing ovarian cancer after breast cancer was 12.7% for BRCA1 mutation carriers and 6.8% for BRCA2 mutation carriers.
Tamoxifen or chemotherapy did not change this risk. The authors concluded that BSO could have prevented at least 43 to 46 ovarian cancers.
RELATED REFERENCES
- Rebbeck TR, Lynch HT, Neuhausen SL, et al. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med. 2002;346:1616–1622.
- Kauff ND, Satagopan JM, Robson ME, et al. Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med. 2002; 346:1609–1615.
Serial histologic sectioning is vital for detecting occult malignancy
Powell CB, Kenley E, Chen LM, et al. Risk-reducing salpingo-oophorectomy in BRCA mutation carriers: role of serial sectioning in the detection of occult malignancy. J Clin Oncol. 2005;23:127–132.
A specific 4-step protocol for salpingo-oophorectomy and pathologic examination increased the number of occult malignancies identified.
Is a risk-reducing BSO any different from a BSO for benign reasons? The evidence is a resounding YES. Given the strong data supporting prophylactic BSO in women with BRCA1 or BRCA2 mutations, ObGyns are increasingly called upon to perform this procedure. Current recommendations are to offer surgery to mutation carriers after childbearing or in their mid- to late 30s and early 40s. A number of studies have discovered that carriers who undergo risk-reducing BSO are at increased risk for occult malignancies already existing in the ovaries and fallopian tubes.
These studies recommend use of a specific surgical approach and pathologic examination of specimens.
Powell et al found an increased number occult malignancies with this strategy:
- Complete removal of ovaries and fallopian tubes
- Serial histologic sectioning of both ovaries and fallopian tubes
- Peritoneal and omental biopsies
- Peritoneal washings for cytology
Of 67 procedures, 7 (10.4%) occult malignancies were discovered: 4 in the fallopian tubes and 3 in the ovaries. Six of the occult malignancies were microscopic.
Surgically, the entire ovary and fallopian tube should be removed. I perform washings and carefully look at the pelvis and paracolic gutters for small-volume disease.
Most importantly, ObGyns need to speak with the pathologist. For most benign cases in which the ovaries and fallopian tubes look grossly normal, pathologists take a single representative section of each ovary and fallopian tube for histologic diagnosis. However, in these high-risk cases, complete serial sectioning of ovaries and fallopian tubes is absolutely necessary to rule out microscopic cancer. Removal of the uterus should be based on other indications.
The author reports no financial relationships relevant to this article.
RELATED REFERENCES
- Lu KH, Garber JE, Cramer DW, et al. Occult ovarian tumors in women with BRCA1 or BRCA2 mutations undergoing prophylactic oophorectomy. J Clin Oncol. 2000;18:2728–2732.
- Colgan TJ, Murphy J, Cole DE, Narod S, Rosen B. Occult carcinoma in prophylactic oophorectomy specimens: prevalence and association with BRCA germline mutation status. Am J Surg Pathol. 2001;25:1283–1289.
This Update reviews recent findings of importance to obstetricians and gynecologists. Late detection of ovarian cancer is still the main reason for the high mortality rate of the most deadly of the gynecologic cancers. Approximately 22,200 women will be newly diagnosed in the United States this year, and there will be 16,210 deaths. Since ovarian cancer is still initially detected in its advanced stages in more than 70% of cases, when cure rates are low, early detection and prevention remain our greatest challenge. The gynecologic oncologist’s opportunity to successfully treat malignancy depends on early detection, and therefore physicians providing primary care for women are our firstline guardians.
“Silent killer” may not be so stealthy
Women ultimately diagnosed with malignant masses had a triad of symptoms, as well as more recent onset and greater severity of symptoms than women with benign masses or no masses. A diagnostic workup employing transvaginal ultrasound and CA-125 should be considered when a woman says she has these symptoms.
Ovarian cancer is not a silent disease. It was believed to be a “silent killer” because it was thought to be asymptomatic until a woman had very advanced disease. However, Goff and colleagues, in a previous study, found that 95% of women with ovarian cancer had had symptoms prior to diagnosis—and that the type of symptoms was not significantly different, whether disease was early stage or late stage.
This new study aimed to identify the frequency, severity, and duration of symptoms typically associated with ovarian cancer, by comparing symptoms reported by different groups of women. Symptoms reported by women presenting to primary care clinics were compared with symptoms reported by a group of 128 women with ovarian masses. Importantly, women were surveyed about their symptoms before undergoing surgery, and before they had a diagnosis of cancer or benign disease.
Main findings:
- A triad of symptoms—abdominal bloating, an increase in abdominal girth, and urinary symptoms—occurred in 43% of women found to have ovarian cancer, but in only 8% of women who presented to a primary care clinic.
- The frequency and duration of symptoms in women with ovarian masses were more severe in the women with malignant masses, but were of a similar type regardless of whether the mass was benign or ovarian cancer.
- Onset of symptoms was more recent in women with ovarian cancer than in the control group.
Listening carefully and evaluating the severity, frequency, and duration of symptoms, especially abdominal bloating, an increase in abdominal girth, urinary symptoms, and abdominal pain, is all-important.
Ovarian cancer should be included in the differential diagnosis when a woman says she has these symptoms.
I found it interesting that symptoms with a more recent onset may be more consistent with ovarian cancer.
In an ideal world, a simple blood test with an absolute cutoff, with perfect sensitivity and specificity, would identify ovarian cancer at its earliest stages. However, until such a test exists, primary care physicians and ObGyns should continue to put weight on the symptoms the patient communicates.
Transvaginal ultrasound and CA-125
Consider performing a diagnostic workup employing transvaginal ultrasound and CA-125 measurement in women presenting with these complaints.
RELATED REFERENCES
- Goff BA, Mandell L, Muntz HG, Melancon CH. Ovarian cancer diagnosis: results of a national ovarian cancer survey. Cancer. 2000;89:2068–2075.
Whatever happened to the ovarian cancer blood test?
Ransohoff DF. Lessons from controversy: ovarian cancer screening and serum proteomics. J Natl Cancer Inst. 2005;97:315–319.
Science is still seeking the Holy Grail—a blood test for early detection of ovarian cancer.
When Petricoin et al reported in 2002 that a serum proteomic profiling test had nearly 100% sensitivity and specificity, the media trumpeted the phenomenal news. The public’s hopes soared when news articles reported that a company would soon begin offering the test. Patients brought in these reports to their ObGyns and asked for the test.
Plans to introduce a commercial screening test by early 2004 were delayed, however, due to FDA concerns about its reliability. The reasons for claims, plans, and delays were reported in both professional journals and the lay press, but details on the “question about whether the approach of discovery-based serum proteomics can accurately and reliably diagnose ovarian cancer—or any cancer—have not been resolved,” Dr. Ransohoff explains in this thoughtful 2005 essay.
He describes in a simple and straightforward way the requirements of reproducibility, and what these new technologies must demonstrate. He concludes that serum proteomic profiling for the early detection of ovarian cancer has not demonstrated the reproducibility required of a clinical test.
“Chance and bias may cause erroneous results and inflated expectations in the kind of observational research being conducted in several ‘–omics’ fields to assess molecular markers for diagnosis and prognosis of cancer. To realize the potential of new –omics technology will require appropriate rules of evidence in the design, conduct, and interpretation of the clinical research,” writes Dr. Ransohoff.
While proteomic profiling clearly has promise, clinicians should insist that initial studies be validated
What to tell patients. I explain that the test appeared promising, and therefore was of great interest, but the FDA did not allow it to be put on the market because of insufficient evidence that the test consistently defines whether cancer is or is not present. Since either a negative or positive test would have profound effects, accuracy is an absolute requirement.
RELATED REFERENCES
- Baggerly KA, Morris JS, Edmonson SR, Coombes KR. Signal in noise: evaluating reported reproducibility of serum proteomic tests for ovarian cancer. J Natl Cancer Inst. 2005;97:307–309.
- Liotta LA, Lowenthal M, Mehta A, et al. Importance of communication between producers and consumers of publicly available experimental data. J Natl Cancer Inst. 2005;97:310–314.
- Petricoin EF, Ardekani AM, Hitt BA, et al. Use of proteomic patterns in serum to identify ovarian cancer. Lancet. 2002;359:572–577.
Don’t hold back from counseling risk-reducing BSO when indicated
Metcalfe KA, Lynch HT, Ghadirian P, et al. The risk of ovarian cancer after breast cancer in BRCA1 and BRCA2 carriers. Gynecol Oncol. 2005;96:222–226.
Counsel women with breast cancer who are BRCA1 or BRCA2 mutation carriers to consider prophylactic salpingo-oophorectomy after childbearing is complete. Tamoxifen and chemotherapy do not lower risk.
ObGyns should encourage young women with breast cancer or women with a strong family history of breast and/or ovarian cancer to undergo genetic testing.
Women with breast cancer who are found to be BRCA1 or BRCA2 mutation carriers should be counseled by their gynecologists to consider prophylactic BSO after childbearing is complete. Even though these women’s greatest concern may be breast cancer recurrence, gynecologists should advise these women that they are also at risk for ovarian cancer, and that they can substantially decrease their risk by undergoing risk-reduction surgery. BRCA1 mutation carriers have up to an 80% lifetime risk of breast cancer and up to a 50% lifetime risk for ovarian cancer.
Recent data support intervention to decrease risk: BSO decreases risk of ovarian cancer by more than 90%, and decreases risk of breast cancer by 50% in BRCA1 or BRCA2 mutation carriers. Metcalfe et al examined women with a BRCA1 or BRCA2 mutation and a history of stage I or II breast cancer, and found that 10% developed an ovarian cancer, a fallopian tube cancer, or a peritoneal cancer. The median time was 8.1 years from the development of breast cancer to the development of ovarian cancer. The cumulative risk of developing ovarian cancer after breast cancer was 12.7% for BRCA1 mutation carriers and 6.8% for BRCA2 mutation carriers.
Tamoxifen or chemotherapy did not change this risk. The authors concluded that BSO could have prevented at least 43 to 46 ovarian cancers.
RELATED REFERENCES
- Rebbeck TR, Lynch HT, Neuhausen SL, et al. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med. 2002;346:1616–1622.
- Kauff ND, Satagopan JM, Robson ME, et al. Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med. 2002; 346:1609–1615.
Serial histologic sectioning is vital for detecting occult malignancy
Powell CB, Kenley E, Chen LM, et al. Risk-reducing salpingo-oophorectomy in BRCA mutation carriers: role of serial sectioning in the detection of occult malignancy. J Clin Oncol. 2005;23:127–132.
A specific 4-step protocol for salpingo-oophorectomy and pathologic examination increased the number of occult malignancies identified.
Is a risk-reducing BSO any different from a BSO for benign reasons? The evidence is a resounding YES. Given the strong data supporting prophylactic BSO in women with BRCA1 or BRCA2 mutations, ObGyns are increasingly called upon to perform this procedure. Current recommendations are to offer surgery to mutation carriers after childbearing or in their mid- to late 30s and early 40s. A number of studies have discovered that carriers who undergo risk-reducing BSO are at increased risk for occult malignancies already existing in the ovaries and fallopian tubes.
These studies recommend use of a specific surgical approach and pathologic examination of specimens.
Powell et al found an increased number occult malignancies with this strategy:
- Complete removal of ovaries and fallopian tubes
- Serial histologic sectioning of both ovaries and fallopian tubes
- Peritoneal and omental biopsies
- Peritoneal washings for cytology
Of 67 procedures, 7 (10.4%) occult malignancies were discovered: 4 in the fallopian tubes and 3 in the ovaries. Six of the occult malignancies were microscopic.
Surgically, the entire ovary and fallopian tube should be removed. I perform washings and carefully look at the pelvis and paracolic gutters for small-volume disease.
Most importantly, ObGyns need to speak with the pathologist. For most benign cases in which the ovaries and fallopian tubes look grossly normal, pathologists take a single representative section of each ovary and fallopian tube for histologic diagnosis. However, in these high-risk cases, complete serial sectioning of ovaries and fallopian tubes is absolutely necessary to rule out microscopic cancer. Removal of the uterus should be based on other indications.
The author reports no financial relationships relevant to this article.
RELATED REFERENCES
- Lu KH, Garber JE, Cramer DW, et al. Occult ovarian tumors in women with BRCA1 or BRCA2 mutations undergoing prophylactic oophorectomy. J Clin Oncol. 2000;18:2728–2732.
- Colgan TJ, Murphy J, Cole DE, Narod S, Rosen B. Occult carcinoma in prophylactic oophorectomy specimens: prevalence and association with BRCA germline mutation status. Am J Surg Pathol. 2001;25:1283–1289.
This Update reviews recent findings of importance to obstetricians and gynecologists. Late detection of ovarian cancer is still the main reason for the high mortality rate of the most deadly of the gynecologic cancers. Approximately 22,200 women will be newly diagnosed in the United States this year, and there will be 16,210 deaths. Since ovarian cancer is still initially detected in its advanced stages in more than 70% of cases, when cure rates are low, early detection and prevention remain our greatest challenge. The gynecologic oncologist’s opportunity to successfully treat malignancy depends on early detection, and therefore physicians providing primary care for women are our firstline guardians.
“Silent killer” may not be so stealthy
Women ultimately diagnosed with malignant masses had a triad of symptoms, as well as more recent onset and greater severity of symptoms than women with benign masses or no masses. A diagnostic workup employing transvaginal ultrasound and CA-125 should be considered when a woman says she has these symptoms.
Ovarian cancer is not a silent disease. It was believed to be a “silent killer” because it was thought to be asymptomatic until a woman had very advanced disease. However, Goff and colleagues, in a previous study, found that 95% of women with ovarian cancer had had symptoms prior to diagnosis—and that the type of symptoms was not significantly different, whether disease was early stage or late stage.
This new study aimed to identify the frequency, severity, and duration of symptoms typically associated with ovarian cancer, by comparing symptoms reported by different groups of women. Symptoms reported by women presenting to primary care clinics were compared with symptoms reported by a group of 128 women with ovarian masses. Importantly, women were surveyed about their symptoms before undergoing surgery, and before they had a diagnosis of cancer or benign disease.
Main findings:
- A triad of symptoms—abdominal bloating, an increase in abdominal girth, and urinary symptoms—occurred in 43% of women found to have ovarian cancer, but in only 8% of women who presented to a primary care clinic.
- The frequency and duration of symptoms in women with ovarian masses were more severe in the women with malignant masses, but were of a similar type regardless of whether the mass was benign or ovarian cancer.
- Onset of symptoms was more recent in women with ovarian cancer than in the control group.
Listening carefully and evaluating the severity, frequency, and duration of symptoms, especially abdominal bloating, an increase in abdominal girth, urinary symptoms, and abdominal pain, is all-important.
Ovarian cancer should be included in the differential diagnosis when a woman says she has these symptoms.
I found it interesting that symptoms with a more recent onset may be more consistent with ovarian cancer.
In an ideal world, a simple blood test with an absolute cutoff, with perfect sensitivity and specificity, would identify ovarian cancer at its earliest stages. However, until such a test exists, primary care physicians and ObGyns should continue to put weight on the symptoms the patient communicates.
Transvaginal ultrasound and CA-125
Consider performing a diagnostic workup employing transvaginal ultrasound and CA-125 measurement in women presenting with these complaints.
RELATED REFERENCES
- Goff BA, Mandell L, Muntz HG, Melancon CH. Ovarian cancer diagnosis: results of a national ovarian cancer survey. Cancer. 2000;89:2068–2075.
Whatever happened to the ovarian cancer blood test?
Ransohoff DF. Lessons from controversy: ovarian cancer screening and serum proteomics. J Natl Cancer Inst. 2005;97:315–319.
Science is still seeking the Holy Grail—a blood test for early detection of ovarian cancer.
When Petricoin et al reported in 2002 that a serum proteomic profiling test had nearly 100% sensitivity and specificity, the media trumpeted the phenomenal news. The public’s hopes soared when news articles reported that a company would soon begin offering the test. Patients brought in these reports to their ObGyns and asked for the test.
Plans to introduce a commercial screening test by early 2004 were delayed, however, due to FDA concerns about its reliability. The reasons for claims, plans, and delays were reported in both professional journals and the lay press, but details on the “question about whether the approach of discovery-based serum proteomics can accurately and reliably diagnose ovarian cancer—or any cancer—have not been resolved,” Dr. Ransohoff explains in this thoughtful 2005 essay.
He describes in a simple and straightforward way the requirements of reproducibility, and what these new technologies must demonstrate. He concludes that serum proteomic profiling for the early detection of ovarian cancer has not demonstrated the reproducibility required of a clinical test.
“Chance and bias may cause erroneous results and inflated expectations in the kind of observational research being conducted in several ‘–omics’ fields to assess molecular markers for diagnosis and prognosis of cancer. To realize the potential of new –omics technology will require appropriate rules of evidence in the design, conduct, and interpretation of the clinical research,” writes Dr. Ransohoff.
While proteomic profiling clearly has promise, clinicians should insist that initial studies be validated
What to tell patients. I explain that the test appeared promising, and therefore was of great interest, but the FDA did not allow it to be put on the market because of insufficient evidence that the test consistently defines whether cancer is or is not present. Since either a negative or positive test would have profound effects, accuracy is an absolute requirement.
RELATED REFERENCES
- Baggerly KA, Morris JS, Edmonson SR, Coombes KR. Signal in noise: evaluating reported reproducibility of serum proteomic tests for ovarian cancer. J Natl Cancer Inst. 2005;97:307–309.
- Liotta LA, Lowenthal M, Mehta A, et al. Importance of communication between producers and consumers of publicly available experimental data. J Natl Cancer Inst. 2005;97:310–314.
- Petricoin EF, Ardekani AM, Hitt BA, et al. Use of proteomic patterns in serum to identify ovarian cancer. Lancet. 2002;359:572–577.
Don’t hold back from counseling risk-reducing BSO when indicated
Metcalfe KA, Lynch HT, Ghadirian P, et al. The risk of ovarian cancer after breast cancer in BRCA1 and BRCA2 carriers. Gynecol Oncol. 2005;96:222–226.
Counsel women with breast cancer who are BRCA1 or BRCA2 mutation carriers to consider prophylactic salpingo-oophorectomy after childbearing is complete. Tamoxifen and chemotherapy do not lower risk.
ObGyns should encourage young women with breast cancer or women with a strong family history of breast and/or ovarian cancer to undergo genetic testing.
Women with breast cancer who are found to be BRCA1 or BRCA2 mutation carriers should be counseled by their gynecologists to consider prophylactic BSO after childbearing is complete. Even though these women’s greatest concern may be breast cancer recurrence, gynecologists should advise these women that they are also at risk for ovarian cancer, and that they can substantially decrease their risk by undergoing risk-reduction surgery. BRCA1 mutation carriers have up to an 80% lifetime risk of breast cancer and up to a 50% lifetime risk for ovarian cancer.
Recent data support intervention to decrease risk: BSO decreases risk of ovarian cancer by more than 90%, and decreases risk of breast cancer by 50% in BRCA1 or BRCA2 mutation carriers. Metcalfe et al examined women with a BRCA1 or BRCA2 mutation and a history of stage I or II breast cancer, and found that 10% developed an ovarian cancer, a fallopian tube cancer, or a peritoneal cancer. The median time was 8.1 years from the development of breast cancer to the development of ovarian cancer. The cumulative risk of developing ovarian cancer after breast cancer was 12.7% for BRCA1 mutation carriers and 6.8% for BRCA2 mutation carriers.
Tamoxifen or chemotherapy did not change this risk. The authors concluded that BSO could have prevented at least 43 to 46 ovarian cancers.
RELATED REFERENCES
- Rebbeck TR, Lynch HT, Neuhausen SL, et al. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med. 2002;346:1616–1622.
- Kauff ND, Satagopan JM, Robson ME, et al. Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med. 2002; 346:1609–1615.
Serial histologic sectioning is vital for detecting occult malignancy
Powell CB, Kenley E, Chen LM, et al. Risk-reducing salpingo-oophorectomy in BRCA mutation carriers: role of serial sectioning in the detection of occult malignancy. J Clin Oncol. 2005;23:127–132.
A specific 4-step protocol for salpingo-oophorectomy and pathologic examination increased the number of occult malignancies identified.
Is a risk-reducing BSO any different from a BSO for benign reasons? The evidence is a resounding YES. Given the strong data supporting prophylactic BSO in women with BRCA1 or BRCA2 mutations, ObGyns are increasingly called upon to perform this procedure. Current recommendations are to offer surgery to mutation carriers after childbearing or in their mid- to late 30s and early 40s. A number of studies have discovered that carriers who undergo risk-reducing BSO are at increased risk for occult malignancies already existing in the ovaries and fallopian tubes.
These studies recommend use of a specific surgical approach and pathologic examination of specimens.
Powell et al found an increased number occult malignancies with this strategy:
- Complete removal of ovaries and fallopian tubes
- Serial histologic sectioning of both ovaries and fallopian tubes
- Peritoneal and omental biopsies
- Peritoneal washings for cytology
Of 67 procedures, 7 (10.4%) occult malignancies were discovered: 4 in the fallopian tubes and 3 in the ovaries. Six of the occult malignancies were microscopic.
Surgically, the entire ovary and fallopian tube should be removed. I perform washings and carefully look at the pelvis and paracolic gutters for small-volume disease.
Most importantly, ObGyns need to speak with the pathologist. For most benign cases in which the ovaries and fallopian tubes look grossly normal, pathologists take a single representative section of each ovary and fallopian tube for histologic diagnosis. However, in these high-risk cases, complete serial sectioning of ovaries and fallopian tubes is absolutely necessary to rule out microscopic cancer. Removal of the uterus should be based on other indications.
The author reports no financial relationships relevant to this article.
RELATED REFERENCES
- Lu KH, Garber JE, Cramer DW, et al. Occult ovarian tumors in women with BRCA1 or BRCA2 mutations undergoing prophylactic oophorectomy. J Clin Oncol. 2000;18:2728–2732.
- Colgan TJ, Murphy J, Cole DE, Narod S, Rosen B. Occult carcinoma in prophylactic oophorectomy specimens: prevalence and association with BRCA germline mutation status. Am J Surg Pathol. 2001;25:1283–1289.
Management of obstetric hypertensive emergencies
Life-threatening obstetric hypertensive emergencies cannot be entirely prevented, but the risk of serious complications can be minimized.
The spectrum of hypertensive disease that can complicate pregnancy is broad—ranging from so-called “white coat” hypertension to gestational hypertension, chronic hypertension, chronic hypertension with superimposed preeclampsia, to preeclampsia.
Particularly challenging, however, is hypertension in pregnancy that becomes severe enough to qualify as a hypertensive crisis, bringing on immediate risk to both fetus and mother.
Risk may evolve over days—or hours—and may present as worsening blood pressure culminating in hypertensive crisis. Fetal morbidity and mortality, including placental abruption and acute fetal distress, are often directly linked to the maternal risks of hypertensive encephalopathy and cerebrovascular accident.
Placental abruption and fetal distress are common with severe hypertension even without encephalopathy and cerebrovascular accident. Abruption is unpredictable and potentially catastrophic, even with intense monitoring.
Aggressive BP control, while fundamental, needs to be balanced against the risks to both mother and fetus of overcorrection and undercorrection.
Defining a crisis
What truly defines hypertensive obstetric emergency is a matter of some debate.
Persistent blood pressures above 200 mm Hg systolic and/or 115 mm Hg diastolic qualify, but some have advocated 160/110 mm Hg as the threshold for emergent treatment of blood pressure. Others suggest that the rate of change in blood pressure is what precipitates the crisis, as opposed to the absolute blood pressure readings.
Why BP control is critical
The true pathophysiology of hypertensive crisis in pregnancy is obscure, but undoubtedly shares characteristics seen in the nonpregnant adult. Diagnosing a hypertensive emergency in the nonpregnant adult, in contrast to diagnosis of an obstetric hypertensive emergency, relies more on clinical manifestations of hypertension than on absolute blood pressure level.1
Pathophysiology
In the nonpregnant adult, 2 independent processes are thought to be necessary for the full-blown encephalopathic picture: dilation of the cerebral vasculature and fibrinoid necrosis. In the initial phases of severe hypertension, the cerebral vessels constrict to maintain cerebral perfusion pressure in the face of increased systemic arterial pressure. Once the limits of autoregulation are exceeded, reflex cerebral dilatation and resultant overperfusion lead to microvascular damage, exudation, microthrombus formation, and increased intracranial pressure, which in turn result in the encephalopathic picture.
In pregnancy, a prominent feature seems to be loss of cerebrovascular autoregulation, resulting in hypertensive encephalopathy once the upper limits of cerebral perfusion pressures are exceeded.2 Rapid control of blood pressure is needed even more because of the risks of placental abruption and stroke (See). Stroke is of special concern in the setting of thrombocytopenia or HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome. Cerebral edema may be more closely associated with endothelial cell injury than with blood pressure,3 although control of blood pressure may help minimize the endothelial cell injury.
Minimizing organ damage
First, restore normal BP
The most important clinical objective for treatment of acute hypertensive crisis in the nonpregnant adult is to minimize end organ damage, especially to the brain4; in obstetric cases, the major morbidity and mortality result from cardiac and renal, as well as cerebrovascular damage. Fetal morbidity and mortality, although not inconsequential, is often directly linked to the maternal condition, and therefore management is based on the triad of diagnosis, stabilization, and delivery.
The physiological dysfunctions described above are best tended to by aggressively controlling blood pressure. With restoration of acceptable blood pressures, generally in the range of 140 to 150 mm Hg systolic and 90 to 100 mm Hg diastolic, cardiac dysfunction begins to reverse, renal function tends to improve, and the restoration of cerebral autoregulatory capability lessens (but does not eliminate) the likelihood of stroke.
Rule out other causes
The foremost goal of therapy for malignant hypertension is to restore normal blood pressure, which depends on correct diagnosis so that appropriate pharmacotherapy may be initiated. For example, clinical situations that could cause malignant hypertension include such disparate entities as acute aortic dissection, acute left ventricular failure, pheochromocytoma, monoamine oxidase inhibitor–food (tyramine) interactions, eclampsia, and acute cocaine intoxication, to name but a few.
Frequently, chronic hypertension or severe preeclampsia defines the underlying “cause” of the severe hypertension, but consideration of other diagnoses, such as uncontrolled hyperthyroidism or pheochromocytoma, should not be overlooked. For example, in pheochromocytoma blood pressures tend to be paroxysmal with wide fluctuations. In hyperthyroidism, clinical signs or symptoms would be expected to accompany the clinical picture, such as the presence of proptosis, exophthalmos, lid lag, tremor, elevated temperature, and a wide pulse pressure, to name but a few.
Regimens to lower BP safely
It is imperative that blood pressure be lowered in a measured and safe manner, not to exceed a drop of 25% to 30% in the first 60 minutes, and not to drop below 150/95.4 Medications available for blood pressure reduction are listed in the Clip-and-save chart above.5
Every effort must be made to not overcorrect the hypertension. Too swift or too dramatic a reduction in blood pressure can have untoward consequences for both mother and fetus, including but not limited to acute fetal distress secondary to uteroplacental underperfusion, and the possibility of maternal myocardial or cerebral infarction. For these reasons, short-acting intravenous agents are recommended to treat hypertensive emergencies, and oral or sublingual compounds are to be avoided because they are more likely to cause precipitous and erratic drops in blood pressure.6
Pulmonary edema is not uncommon, due to capillary leakage and myocardial dysfunction. Aggressive use of furosemide along with a rapidly acting antihypertensive drug will best allow for improvement of the clinical picture in a timely manner.
Acute management steps
Critical care facilities required. During the acute management phase, patients should be cared for in an intensive care unit (or a labor and delivery unit with critical care capabilities) under the direction of physicians skilled in managing critically ill patients. In most institutions, such management will include participation of anesthesiologists, maternalfetal medicine specialists, and nurses with critical care expertise.
Delivery considerations. During initial management, the patient should have continuous fetal heart rate monitoring. Under such extreme circumstances, it is often not possible to prolong a pregnancy that is remote from term. Delivery decisions will need to balance prematurity risks against maternal risks of continuing the pregnancy.
Hypertension is not a contraindication to glucocorticoids for accelerating lung maturation in the fetus and minimizing neonatal risk of intracranial hemorrhage and necrotizing enterocolitis.7 Adjusting for gestational age, neonates of preeclamptic mothers are afforded no additional maturity compared with neonates born prematurely for other reasons. Delay of delivery for 48 to 72 hours may not be possible in many cases, however. Once the patient is stabilized, delivery must be considered.
Start magnesium sulfate, continue antihypertensives
At this point, it is prudent to start magnesium sulfate to prevent eclampsia. In most cases, however, excluding a diagnosis of preeclampsia in a timely manner is nearly impossible. Under these circumstances, magnesium sulfate is recommended, in addition to continued antihypertensive medications, to maintain BP control.
Magnesium sulfate is best administered intravenously, preferably through an infusion pump apparatus. A loading dose of 4 to 6 g (I prefer 6 g) is given as a 20% solution over 15 to 20 minutes, and then a continuous infusion may be initiated at a rate that depends on the patient’s renal function. In a patient with normal renal function, a rate of 2 g per hour is appropriate, but may need to be reduced if acute renal failure ensues.
In a report of 3 recent cases, investigators found magnesium sulfate was beneficial for controlling the clinical symptoms of pheochromocytoma when conventional therapy was unsuccessful. The presenting symptoms of these nonpregnant patients included hypertensive encephalopathy (2 patients) and catecholamine-induced cardiomyopathy (1 patient).6
In general, however, the role of magnesium sulfate should be for preventing progression to eclampsia, and not for acute blood pressure control.
Delivery decisions
Vaginal delivery is often less hemodynamically stressful for the mother, but not always practical. Many cases are remote from term with the fetus in a nonvertex presentation, or the uterine cervix is unfavorable for induction, or a protracted attempt at labor induction may not be prudent.
Under such circumstances, cesarean delivery must be considered and may be preferable. The reasons relate to the underlying maternal condition that often includes some degree of uteroplacental insufficiency. Altered placental function, combined with extreme prematurity, often results in the fetus being unable to tolerate labor for very long, necessitating emergent cesarean under potentially less controlled circumstances. The anesthesiologist and others on the critical care team must review the optimal anesthesia technique.
In most circumstances, and in the absence of coagulopathy, regional anesthesia affords the best results. When regional anesthesia is not an option, balanced general endotracheal anesthesia with antihypertensive premedication using a short-acting agent may be the safest alternative.
Maintain postpartum vigil
With delivery of the fetus, there may be a temptation to be less rigorous in maintaining blood pressure control during the post-partum period. In patients with chronic hypertension without superimposed preeclampsia, this may be acceptable, as these patients better tolerate higher blood pressures and still maintain appropriate cerebral vascular autoregulation.
For women who were previously normotensive, or who had superimposed preeclampsia, more rigorous control of blood pressure is recommended, especially if they show any degree of thrombocytopenia or pulmonary edema. (See Clip & save: Stepwise drug therapy for obstetric hypertensive crisis) The rationale relates to cerebral perfusion pressures and risk of stroke in these susceptible women, if thresholds are exceeded, and to the risk of worsening pulmonary edema in the setting of increased capillary hydrostatic pressure and reduced colloid osmotic pressure.
Additionally, continuation of magnesium sulfate is recommended for patients with superimposed preeclampsia until obvious signs of disease resolution, and for a minimum of 24 hours.
The author reports no financial relationships relevant to this article.
1. Tuncel M, Ram V. Hypertensive emergencies: etiology and management. Am J Cardiovasc Drugs. 2003;3:21-31.
2. Sibai BM. Hypertension. In: Gabbe SG, Niebyl JR, Simpson JL, eds. Obstetrics: Normal and Problem Pregnancies. 4th ed. New York, NY: Churchill Livingstone; 2002;945-1004.
3. Schwartz RB, Feske SK, Polak JF, et al. Preeclampsia-eclampsia: clinical and neuroradiographic correlates and insights into the pathogenesis of hypertensive encephalopathy. Radiology. 2000;2:371-376.
4. Williams O, Brust JC. Hypertensive encephalopathy. Curr Treat Cardiovasc Med. 2004;6:209-216.
5. Norwitz ER, Hsu CD, Repke JT. Acute complications of preeclampsia. Clin Obstet Gynecol. 2002;45:308-329.
6. James MF, Cronje L. Pheochromocytoma crisis: the use of magnesium sulfate. Anesth Analg. 2004;99:680-686.
7. Hiett AK, Brown HL, Britton KA. Outcome of infants delivered at 24 to 28 weeks’ gestation in women with severe preeclampsia. J Maternal-Fetal Med. 2001;10:301-304.
Life-threatening obstetric hypertensive emergencies cannot be entirely prevented, but the risk of serious complications can be minimized.
The spectrum of hypertensive disease that can complicate pregnancy is broad—ranging from so-called “white coat” hypertension to gestational hypertension, chronic hypertension, chronic hypertension with superimposed preeclampsia, to preeclampsia.
Particularly challenging, however, is hypertension in pregnancy that becomes severe enough to qualify as a hypertensive crisis, bringing on immediate risk to both fetus and mother.
Risk may evolve over days—or hours—and may present as worsening blood pressure culminating in hypertensive crisis. Fetal morbidity and mortality, including placental abruption and acute fetal distress, are often directly linked to the maternal risks of hypertensive encephalopathy and cerebrovascular accident.
Placental abruption and fetal distress are common with severe hypertension even without encephalopathy and cerebrovascular accident. Abruption is unpredictable and potentially catastrophic, even with intense monitoring.
Aggressive BP control, while fundamental, needs to be balanced against the risks to both mother and fetus of overcorrection and undercorrection.
Defining a crisis
What truly defines hypertensive obstetric emergency is a matter of some debate.
Persistent blood pressures above 200 mm Hg systolic and/or 115 mm Hg diastolic qualify, but some have advocated 160/110 mm Hg as the threshold for emergent treatment of blood pressure. Others suggest that the rate of change in blood pressure is what precipitates the crisis, as opposed to the absolute blood pressure readings.
Why BP control is critical
The true pathophysiology of hypertensive crisis in pregnancy is obscure, but undoubtedly shares characteristics seen in the nonpregnant adult. Diagnosing a hypertensive emergency in the nonpregnant adult, in contrast to diagnosis of an obstetric hypertensive emergency, relies more on clinical manifestations of hypertension than on absolute blood pressure level.1
Pathophysiology
In the nonpregnant adult, 2 independent processes are thought to be necessary for the full-blown encephalopathic picture: dilation of the cerebral vasculature and fibrinoid necrosis. In the initial phases of severe hypertension, the cerebral vessels constrict to maintain cerebral perfusion pressure in the face of increased systemic arterial pressure. Once the limits of autoregulation are exceeded, reflex cerebral dilatation and resultant overperfusion lead to microvascular damage, exudation, microthrombus formation, and increased intracranial pressure, which in turn result in the encephalopathic picture.
In pregnancy, a prominent feature seems to be loss of cerebrovascular autoregulation, resulting in hypertensive encephalopathy once the upper limits of cerebral perfusion pressures are exceeded.2 Rapid control of blood pressure is needed even more because of the risks of placental abruption and stroke (See). Stroke is of special concern in the setting of thrombocytopenia or HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome. Cerebral edema may be more closely associated with endothelial cell injury than with blood pressure,3 although control of blood pressure may help minimize the endothelial cell injury.
Minimizing organ damage
First, restore normal BP
The most important clinical objective for treatment of acute hypertensive crisis in the nonpregnant adult is to minimize end organ damage, especially to the brain4; in obstetric cases, the major morbidity and mortality result from cardiac and renal, as well as cerebrovascular damage. Fetal morbidity and mortality, although not inconsequential, is often directly linked to the maternal condition, and therefore management is based on the triad of diagnosis, stabilization, and delivery.
The physiological dysfunctions described above are best tended to by aggressively controlling blood pressure. With restoration of acceptable blood pressures, generally in the range of 140 to 150 mm Hg systolic and 90 to 100 mm Hg diastolic, cardiac dysfunction begins to reverse, renal function tends to improve, and the restoration of cerebral autoregulatory capability lessens (but does not eliminate) the likelihood of stroke.
Rule out other causes
The foremost goal of therapy for malignant hypertension is to restore normal blood pressure, which depends on correct diagnosis so that appropriate pharmacotherapy may be initiated. For example, clinical situations that could cause malignant hypertension include such disparate entities as acute aortic dissection, acute left ventricular failure, pheochromocytoma, monoamine oxidase inhibitor–food (tyramine) interactions, eclampsia, and acute cocaine intoxication, to name but a few.
Frequently, chronic hypertension or severe preeclampsia defines the underlying “cause” of the severe hypertension, but consideration of other diagnoses, such as uncontrolled hyperthyroidism or pheochromocytoma, should not be overlooked. For example, in pheochromocytoma blood pressures tend to be paroxysmal with wide fluctuations. In hyperthyroidism, clinical signs or symptoms would be expected to accompany the clinical picture, such as the presence of proptosis, exophthalmos, lid lag, tremor, elevated temperature, and a wide pulse pressure, to name but a few.
Regimens to lower BP safely
It is imperative that blood pressure be lowered in a measured and safe manner, not to exceed a drop of 25% to 30% in the first 60 minutes, and not to drop below 150/95.4 Medications available for blood pressure reduction are listed in the Clip-and-save chart above.5
Every effort must be made to not overcorrect the hypertension. Too swift or too dramatic a reduction in blood pressure can have untoward consequences for both mother and fetus, including but not limited to acute fetal distress secondary to uteroplacental underperfusion, and the possibility of maternal myocardial or cerebral infarction. For these reasons, short-acting intravenous agents are recommended to treat hypertensive emergencies, and oral or sublingual compounds are to be avoided because they are more likely to cause precipitous and erratic drops in blood pressure.6
Pulmonary edema is not uncommon, due to capillary leakage and myocardial dysfunction. Aggressive use of furosemide along with a rapidly acting antihypertensive drug will best allow for improvement of the clinical picture in a timely manner.
Acute management steps
Critical care facilities required. During the acute management phase, patients should be cared for in an intensive care unit (or a labor and delivery unit with critical care capabilities) under the direction of physicians skilled in managing critically ill patients. In most institutions, such management will include participation of anesthesiologists, maternalfetal medicine specialists, and nurses with critical care expertise.
Delivery considerations. During initial management, the patient should have continuous fetal heart rate monitoring. Under such extreme circumstances, it is often not possible to prolong a pregnancy that is remote from term. Delivery decisions will need to balance prematurity risks against maternal risks of continuing the pregnancy.
Hypertension is not a contraindication to glucocorticoids for accelerating lung maturation in the fetus and minimizing neonatal risk of intracranial hemorrhage and necrotizing enterocolitis.7 Adjusting for gestational age, neonates of preeclamptic mothers are afforded no additional maturity compared with neonates born prematurely for other reasons. Delay of delivery for 48 to 72 hours may not be possible in many cases, however. Once the patient is stabilized, delivery must be considered.
Start magnesium sulfate, continue antihypertensives
At this point, it is prudent to start magnesium sulfate to prevent eclampsia. In most cases, however, excluding a diagnosis of preeclampsia in a timely manner is nearly impossible. Under these circumstances, magnesium sulfate is recommended, in addition to continued antihypertensive medications, to maintain BP control.
Magnesium sulfate is best administered intravenously, preferably through an infusion pump apparatus. A loading dose of 4 to 6 g (I prefer 6 g) is given as a 20% solution over 15 to 20 minutes, and then a continuous infusion may be initiated at a rate that depends on the patient’s renal function. In a patient with normal renal function, a rate of 2 g per hour is appropriate, but may need to be reduced if acute renal failure ensues.
In a report of 3 recent cases, investigators found magnesium sulfate was beneficial for controlling the clinical symptoms of pheochromocytoma when conventional therapy was unsuccessful. The presenting symptoms of these nonpregnant patients included hypertensive encephalopathy (2 patients) and catecholamine-induced cardiomyopathy (1 patient).6
In general, however, the role of magnesium sulfate should be for preventing progression to eclampsia, and not for acute blood pressure control.
Delivery decisions
Vaginal delivery is often less hemodynamically stressful for the mother, but not always practical. Many cases are remote from term with the fetus in a nonvertex presentation, or the uterine cervix is unfavorable for induction, or a protracted attempt at labor induction may not be prudent.
Under such circumstances, cesarean delivery must be considered and may be preferable. The reasons relate to the underlying maternal condition that often includes some degree of uteroplacental insufficiency. Altered placental function, combined with extreme prematurity, often results in the fetus being unable to tolerate labor for very long, necessitating emergent cesarean under potentially less controlled circumstances. The anesthesiologist and others on the critical care team must review the optimal anesthesia technique.
In most circumstances, and in the absence of coagulopathy, regional anesthesia affords the best results. When regional anesthesia is not an option, balanced general endotracheal anesthesia with antihypertensive premedication using a short-acting agent may be the safest alternative.
Maintain postpartum vigil
With delivery of the fetus, there may be a temptation to be less rigorous in maintaining blood pressure control during the post-partum period. In patients with chronic hypertension without superimposed preeclampsia, this may be acceptable, as these patients better tolerate higher blood pressures and still maintain appropriate cerebral vascular autoregulation.
For women who were previously normotensive, or who had superimposed preeclampsia, more rigorous control of blood pressure is recommended, especially if they show any degree of thrombocytopenia or pulmonary edema. (See Clip & save: Stepwise drug therapy for obstetric hypertensive crisis) The rationale relates to cerebral perfusion pressures and risk of stroke in these susceptible women, if thresholds are exceeded, and to the risk of worsening pulmonary edema in the setting of increased capillary hydrostatic pressure and reduced colloid osmotic pressure.
Additionally, continuation of magnesium sulfate is recommended for patients with superimposed preeclampsia until obvious signs of disease resolution, and for a minimum of 24 hours.
The author reports no financial relationships relevant to this article.
Life-threatening obstetric hypertensive emergencies cannot be entirely prevented, but the risk of serious complications can be minimized.
The spectrum of hypertensive disease that can complicate pregnancy is broad—ranging from so-called “white coat” hypertension to gestational hypertension, chronic hypertension, chronic hypertension with superimposed preeclampsia, to preeclampsia.
Particularly challenging, however, is hypertension in pregnancy that becomes severe enough to qualify as a hypertensive crisis, bringing on immediate risk to both fetus and mother.
Risk may evolve over days—or hours—and may present as worsening blood pressure culminating in hypertensive crisis. Fetal morbidity and mortality, including placental abruption and acute fetal distress, are often directly linked to the maternal risks of hypertensive encephalopathy and cerebrovascular accident.
Placental abruption and fetal distress are common with severe hypertension even without encephalopathy and cerebrovascular accident. Abruption is unpredictable and potentially catastrophic, even with intense monitoring.
Aggressive BP control, while fundamental, needs to be balanced against the risks to both mother and fetus of overcorrection and undercorrection.
Defining a crisis
What truly defines hypertensive obstetric emergency is a matter of some debate.
Persistent blood pressures above 200 mm Hg systolic and/or 115 mm Hg diastolic qualify, but some have advocated 160/110 mm Hg as the threshold for emergent treatment of blood pressure. Others suggest that the rate of change in blood pressure is what precipitates the crisis, as opposed to the absolute blood pressure readings.
Why BP control is critical
The true pathophysiology of hypertensive crisis in pregnancy is obscure, but undoubtedly shares characteristics seen in the nonpregnant adult. Diagnosing a hypertensive emergency in the nonpregnant adult, in contrast to diagnosis of an obstetric hypertensive emergency, relies more on clinical manifestations of hypertension than on absolute blood pressure level.1
Pathophysiology
In the nonpregnant adult, 2 independent processes are thought to be necessary for the full-blown encephalopathic picture: dilation of the cerebral vasculature and fibrinoid necrosis. In the initial phases of severe hypertension, the cerebral vessels constrict to maintain cerebral perfusion pressure in the face of increased systemic arterial pressure. Once the limits of autoregulation are exceeded, reflex cerebral dilatation and resultant overperfusion lead to microvascular damage, exudation, microthrombus formation, and increased intracranial pressure, which in turn result in the encephalopathic picture.
In pregnancy, a prominent feature seems to be loss of cerebrovascular autoregulation, resulting in hypertensive encephalopathy once the upper limits of cerebral perfusion pressures are exceeded.2 Rapid control of blood pressure is needed even more because of the risks of placental abruption and stroke (See). Stroke is of special concern in the setting of thrombocytopenia or HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome. Cerebral edema may be more closely associated with endothelial cell injury than with blood pressure,3 although control of blood pressure may help minimize the endothelial cell injury.
Minimizing organ damage
First, restore normal BP
The most important clinical objective for treatment of acute hypertensive crisis in the nonpregnant adult is to minimize end organ damage, especially to the brain4; in obstetric cases, the major morbidity and mortality result from cardiac and renal, as well as cerebrovascular damage. Fetal morbidity and mortality, although not inconsequential, is often directly linked to the maternal condition, and therefore management is based on the triad of diagnosis, stabilization, and delivery.
The physiological dysfunctions described above are best tended to by aggressively controlling blood pressure. With restoration of acceptable blood pressures, generally in the range of 140 to 150 mm Hg systolic and 90 to 100 mm Hg diastolic, cardiac dysfunction begins to reverse, renal function tends to improve, and the restoration of cerebral autoregulatory capability lessens (but does not eliminate) the likelihood of stroke.
Rule out other causes
The foremost goal of therapy for malignant hypertension is to restore normal blood pressure, which depends on correct diagnosis so that appropriate pharmacotherapy may be initiated. For example, clinical situations that could cause malignant hypertension include such disparate entities as acute aortic dissection, acute left ventricular failure, pheochromocytoma, monoamine oxidase inhibitor–food (tyramine) interactions, eclampsia, and acute cocaine intoxication, to name but a few.
Frequently, chronic hypertension or severe preeclampsia defines the underlying “cause” of the severe hypertension, but consideration of other diagnoses, such as uncontrolled hyperthyroidism or pheochromocytoma, should not be overlooked. For example, in pheochromocytoma blood pressures tend to be paroxysmal with wide fluctuations. In hyperthyroidism, clinical signs or symptoms would be expected to accompany the clinical picture, such as the presence of proptosis, exophthalmos, lid lag, tremor, elevated temperature, and a wide pulse pressure, to name but a few.
Regimens to lower BP safely
It is imperative that blood pressure be lowered in a measured and safe manner, not to exceed a drop of 25% to 30% in the first 60 minutes, and not to drop below 150/95.4 Medications available for blood pressure reduction are listed in the Clip-and-save chart above.5
Every effort must be made to not overcorrect the hypertension. Too swift or too dramatic a reduction in blood pressure can have untoward consequences for both mother and fetus, including but not limited to acute fetal distress secondary to uteroplacental underperfusion, and the possibility of maternal myocardial or cerebral infarction. For these reasons, short-acting intravenous agents are recommended to treat hypertensive emergencies, and oral or sublingual compounds are to be avoided because they are more likely to cause precipitous and erratic drops in blood pressure.6
Pulmonary edema is not uncommon, due to capillary leakage and myocardial dysfunction. Aggressive use of furosemide along with a rapidly acting antihypertensive drug will best allow for improvement of the clinical picture in a timely manner.
Acute management steps
Critical care facilities required. During the acute management phase, patients should be cared for in an intensive care unit (or a labor and delivery unit with critical care capabilities) under the direction of physicians skilled in managing critically ill patients. In most institutions, such management will include participation of anesthesiologists, maternalfetal medicine specialists, and nurses with critical care expertise.
Delivery considerations. During initial management, the patient should have continuous fetal heart rate monitoring. Under such extreme circumstances, it is often not possible to prolong a pregnancy that is remote from term. Delivery decisions will need to balance prematurity risks against maternal risks of continuing the pregnancy.
Hypertension is not a contraindication to glucocorticoids for accelerating lung maturation in the fetus and minimizing neonatal risk of intracranial hemorrhage and necrotizing enterocolitis.7 Adjusting for gestational age, neonates of preeclamptic mothers are afforded no additional maturity compared with neonates born prematurely for other reasons. Delay of delivery for 48 to 72 hours may not be possible in many cases, however. Once the patient is stabilized, delivery must be considered.
Start magnesium sulfate, continue antihypertensives
At this point, it is prudent to start magnesium sulfate to prevent eclampsia. In most cases, however, excluding a diagnosis of preeclampsia in a timely manner is nearly impossible. Under these circumstances, magnesium sulfate is recommended, in addition to continued antihypertensive medications, to maintain BP control.
Magnesium sulfate is best administered intravenously, preferably through an infusion pump apparatus. A loading dose of 4 to 6 g (I prefer 6 g) is given as a 20% solution over 15 to 20 minutes, and then a continuous infusion may be initiated at a rate that depends on the patient’s renal function. In a patient with normal renal function, a rate of 2 g per hour is appropriate, but may need to be reduced if acute renal failure ensues.
In a report of 3 recent cases, investigators found magnesium sulfate was beneficial for controlling the clinical symptoms of pheochromocytoma when conventional therapy was unsuccessful. The presenting symptoms of these nonpregnant patients included hypertensive encephalopathy (2 patients) and catecholamine-induced cardiomyopathy (1 patient).6
In general, however, the role of magnesium sulfate should be for preventing progression to eclampsia, and not for acute blood pressure control.
Delivery decisions
Vaginal delivery is often less hemodynamically stressful for the mother, but not always practical. Many cases are remote from term with the fetus in a nonvertex presentation, or the uterine cervix is unfavorable for induction, or a protracted attempt at labor induction may not be prudent.
Under such circumstances, cesarean delivery must be considered and may be preferable. The reasons relate to the underlying maternal condition that often includes some degree of uteroplacental insufficiency. Altered placental function, combined with extreme prematurity, often results in the fetus being unable to tolerate labor for very long, necessitating emergent cesarean under potentially less controlled circumstances. The anesthesiologist and others on the critical care team must review the optimal anesthesia technique.
In most circumstances, and in the absence of coagulopathy, regional anesthesia affords the best results. When regional anesthesia is not an option, balanced general endotracheal anesthesia with antihypertensive premedication using a short-acting agent may be the safest alternative.
Maintain postpartum vigil
With delivery of the fetus, there may be a temptation to be less rigorous in maintaining blood pressure control during the post-partum period. In patients with chronic hypertension without superimposed preeclampsia, this may be acceptable, as these patients better tolerate higher blood pressures and still maintain appropriate cerebral vascular autoregulation.
For women who were previously normotensive, or who had superimposed preeclampsia, more rigorous control of blood pressure is recommended, especially if they show any degree of thrombocytopenia or pulmonary edema. (See Clip & save: Stepwise drug therapy for obstetric hypertensive crisis) The rationale relates to cerebral perfusion pressures and risk of stroke in these susceptible women, if thresholds are exceeded, and to the risk of worsening pulmonary edema in the setting of increased capillary hydrostatic pressure and reduced colloid osmotic pressure.
Additionally, continuation of magnesium sulfate is recommended for patients with superimposed preeclampsia until obvious signs of disease resolution, and for a minimum of 24 hours.
The author reports no financial relationships relevant to this article.
1. Tuncel M, Ram V. Hypertensive emergencies: etiology and management. Am J Cardiovasc Drugs. 2003;3:21-31.
2. Sibai BM. Hypertension. In: Gabbe SG, Niebyl JR, Simpson JL, eds. Obstetrics: Normal and Problem Pregnancies. 4th ed. New York, NY: Churchill Livingstone; 2002;945-1004.
3. Schwartz RB, Feske SK, Polak JF, et al. Preeclampsia-eclampsia: clinical and neuroradiographic correlates and insights into the pathogenesis of hypertensive encephalopathy. Radiology. 2000;2:371-376.
4. Williams O, Brust JC. Hypertensive encephalopathy. Curr Treat Cardiovasc Med. 2004;6:209-216.
5. Norwitz ER, Hsu CD, Repke JT. Acute complications of preeclampsia. Clin Obstet Gynecol. 2002;45:308-329.
6. James MF, Cronje L. Pheochromocytoma crisis: the use of magnesium sulfate. Anesth Analg. 2004;99:680-686.
7. Hiett AK, Brown HL, Britton KA. Outcome of infants delivered at 24 to 28 weeks’ gestation in women with severe preeclampsia. J Maternal-Fetal Med. 2001;10:301-304.
1. Tuncel M, Ram V. Hypertensive emergencies: etiology and management. Am J Cardiovasc Drugs. 2003;3:21-31.
2. Sibai BM. Hypertension. In: Gabbe SG, Niebyl JR, Simpson JL, eds. Obstetrics: Normal and Problem Pregnancies. 4th ed. New York, NY: Churchill Livingstone; 2002;945-1004.
3. Schwartz RB, Feske SK, Polak JF, et al. Preeclampsia-eclampsia: clinical and neuroradiographic correlates and insights into the pathogenesis of hypertensive encephalopathy. Radiology. 2000;2:371-376.
4. Williams O, Brust JC. Hypertensive encephalopathy. Curr Treat Cardiovasc Med. 2004;6:209-216.
5. Norwitz ER, Hsu CD, Repke JT. Acute complications of preeclampsia. Clin Obstet Gynecol. 2002;45:308-329.
6. James MF, Cronje L. Pheochromocytoma crisis: the use of magnesium sulfate. Anesth Analg. 2004;99:680-686.
7. Hiett AK, Brown HL, Britton KA. Outcome of infants delivered at 24 to 28 weeks’ gestation in women with severe preeclampsia. J Maternal-Fetal Med. 2001;10:301-304.
Impact of Mental Health Disorders
INFECTIOUS DISEASE
New findings I selected for this Update affect the management of 4 common and potentially serious clinical problems: acute cystitis, gonorrhea and chlamydia infection, chorioamnionitis, and varicella.
- A comparison of amoxicillin-clavulanic acid vs ciprofloxacin for uncomplicated lower urinary tract infections yielded surprising results, and more evidence on E coli’s resistance to antibiotics.
- Sexual partners of women with gonorrhea or chlamydia are more likely to receive appropriate treatment if it is offered by the women themselves or by the women’s caregivers.
- Short-course therapy for chorioamnionitis had a very high cure rate, equal to the traditional course, and furthers the possibility of shorter hospitalizations and cost savings without compromising outcomes.
- The CDC’s 1995 call for universal childhood vaccination for varicella has already sharply reduced varicella-related mortality in adults; still, we must determine immunity in our reproductive-age patients.
Acute cystitis: Ciprofloxacin prevails in E coli skirmish
Hooton TM, Scholes D, Gupta K, Stapleton AE, Roberts PL, Stamm WE. Amoxicillin-clavulanate vs ciprofloxacin for the treatment of uncomplicated cystitis in women: a randomized trial. JAMA. 2005;293:949–955.
Amoxicillin-clavulanate was not as effective as ciprofloxacin even in women who were infected with bacteria sensitive to amoxicillin-clavulanate.
A total of 320 nonpregnant women, aged 18 to 45 years, with uncomplicated acute cystitis were treated for 3 days with either oral amoxicillin-clavulanate (500 mg/125 mg twice daily) or oral ciprofloxacin (250 mg twice daily). Two weeks after treatment, 95% of women treated with ciprofloxacin were clinically cured, compared with only 76% of women treated with amoxicillin-clavulanate (P<.001).
Start with ciprofloxacin
The difference in outcome was attributed to a marked difference in vaginal colonization with the single most common pathogen in acute cystitis—Escherichia coli—at the 2-week follow-up (45% in the amoxicillinclavulanate group vs 10% in the ciprofloxacin group, P<.001).
Even though successful treatment of cystitis usually is possible with short courses (3–7 days) of oral antibiotics, persistent and recurrent infections may occur and usually are related to persistent vaginal colonization with E coli.
Treatment may require an extended course of oral antibiotics.
Initial selection of an antibiotic for acute cystitis is empiric and should be based on probable susceptibility of the dominant uropathogens. For many years, the typical initial antibiotic has been ampicillin.
E coli resistance. Now, however, more than a third of E coli strains, as well as most strains of K pneumoniae, are resistant to ampicillin. Therefore, ampicillin no longer should be used for the empiric treatment of cystitis.1
Surprising results
In theory, amoxicillin-clavulanate should have enhanced activity against E coli and other enteric organisms.
Therefore, these findings are surprising. The outcome with amoxicillin-clavulanate was inferior to that of ciprofloxacin, even in women who seemingly had susceptible uropathogens.
Based on this study, ciprofloxacin clearly is a more effective (and less expensive) empiric treatment in nonpregnant women.
In gravidas, start with nitrofurantoin
Ciprofloxacin is not appropriate for treatment of cystitis or asymptomatic bacteriuria in pregnant women. The quinolone antibiotics may cause injury to the developing cartilage of the fetus and are contraindicated in pregnant and lactating women, and in children younger than 17 years.1
What, then, is the most appropriate choice for treatment of uncomplicated cystitis during pregnancy?
One reasonable selection is oral trimethoprim-sulfamethoxazole, double-strength, twice daily. However, increasing resistance of E coli to this antibiotic has been documented recently.2,3
Therefore, a better choice is nitrofurantoin monohydrate macrocrystals, 100 mg twice daily.4 One organism that is not susceptible to nitrofurantoin is Proteus. When this organism is suspected, use trimethoprim-sulfamethoxazole.
Follow-up is a must
Because persistent and recurrent infections are common, patients should be followed with urine dipstick assessment or urine culture to be certain that the infection is resolved.
Follow-up is particularly important when infected women are pregnant, because of the risk of ascending infection leading to preterm labor, sepsis, or acute respiratory disease syndrome.
Treat sex partners, sight-unseen?
Golden MR, Whittington WL, Handsfield HH, et al. Effect of expedited treatment of sex partners on recurrent or persistent gonorrhea or chlamydial infection. N Engl J Med. 2005;352:676–685.
Providing a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Almost 2,000 men and women with uncomplicated gonorrhea or chlamydia infection were included in this study of expedited treatment compared with standard referral. In the standard referral group, investigators treated 931 patients and referred their sex partners to other physicians or facilities for evaluation and treatment. In the expedited treatment group, 929 patients were treated and also were provided with antibiotics to give to their partners. The partners of patients who were unwilling to do so were contacted and treated by the investigators.
At follow-up 21 to 126 days after treatment), persistent or recurrent infection was found in 13% of standard referral patients and 10% of expedited treatment patients (relative risk, 0.76; 95% confidence interval, 0.59–0.98).
Expedited treatment decreased the rate of persistent or recurrent gonorrhea more than that of persistent or recurrent chlamydia.
Patients in the expedited group were more likely to report that all of their partners were treated, and less likely to report having had sex with an untreated partner.
Advantages of the direct approach
The challenge for the ObGyn is how to arrange treatment for the female patient’s sex partner(s). This study indicates that a proactive approach is likely to be more effective than simply asking the patient to encourage her partner to seek medical attention. Direct provision of a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Failure to treat the patient’s sex partner is the principal cause of persistent or recurrent infection, which may lead to pelvic inflammatory disease, Fitz-Hugh-Curtis syndrome, and infertility. Gonorrhea may disseminate and manifest primarily by arthritis and dermatitis. If a pregnant woman is colonized with gonorrhea or chlamydia at the time of delivery, her infant may acquire gonococcal or chlamydial conjunctivitis or chlamydial pneumonia.
6 caveats
Although the results of this investigation are impressive and of great practical importance, these caveats should be noted.
- The oral drug used to treat gonorrhea in this study, cefixime (400 mg), is not presently available, and although another oral drug such as ciprofloxacin (500 mg) would be highly effective, it should not be used in pregnant or lactating women, or women younger than 17 years.1
- Although ceftriaxone, 125 mg intramuscularly, also is a superb drug for treatment of uncomplicated gonorrhea, the logistical problems of arranging for the partner to receive an intramuscular injection are daunting.
- Some women in the expedited treatment group were reluctant to provide medication to their partner(s), and study personnel were forced to intervene. Keep in mind that individual private practitioners and even well-organized clinics may not have sufficient support personnel to trace and treat all contacts.
- There is the important issue of a provider writing a prescription for an individual who is not actually his or her patient and who has not been interviewed and examined. Certainly, many state laws and insurance company regulations may discourage or even prohibit such a practice.
- Lack of a detailed assessment of the partner(s) means there is no opportunity to evaluate them for other conditions such as syphilis and HIV infection.
- Finally, taking a proactive approach in treating the sex partner(s) of patients who have gonorrhea or chlamydia (and, by extension, trichomoniasis) requires documentation of complete rationale in the patient’s medical record.
In addition, detailed written instructions must be provided for the partner(s) and must include a specific caution about possible reactions to the antibiotic.
Single-dose plus intrapartum therapy effective for chorioamnionitis
Edwards RK, Duff P. Single additional dose postpartum therapy for women with chorioamnionitis. Obstet Gynecol. 2003;102:957–961.
Short-course therapy is simpler to administer and reduces costs compared with more extended treatment.
Intrapartum therapy plus 1 additional dose of combination antibiotics after delivery produced a very high rate of cure (95.4%)—equivalent to that achieved when a more extended course of treatment was used.
In this randomized study of 292 otherwise healthy women with chorioamnionitis, 151 women were treated intrapartum with intravenous (IV) ampicillin (2 g every 6 hours) plus gentamicin (1.5 mg/kg every 8 hours). They received 1 dose of each drug postpartum. In addition, if they had a cesarean delivery, they received 1 dose of IV clindamycin (900 mg) immediately after the infant’s umbilical cord was clamped.
Women in the control group received IV antibiotics (including clindamycin, if indicated) until they had been afebrile and asymptomatic for 24 hours.
In the study group, 4.6% of women had a treatment failure and required an additional course of antibiotics. In the control group, 3.5% of patients required additional antibiotics (P = .639, not significant). When patients were stratified by method of delivery, no significant difference was found in treatment outcome.
Pathogens and regimens
Chorioamnionitis occurs in approximately 1% to 5% of term patients and in as many as 25% of patients having a preterm delivery. The infection is caused by multiple aerobic and anaerobic organisms, notably group B streptococci, E coli, and anaerobes. The former 2 pathogens pose the greatest risk to the infant and are the predominant causes of neonatal pneumonia, bacteremia, and meningitis. These organisms also are major causes of maternal bacteremia.
Anaerobes usually do not pose a major threat to the fetus or neonate, but are particularly likely to lead to pelvic abscess in women who require a cesarean delivery in the face of preexisting intrauterine infection.5
Accordingly, the initial antibiotic therapy for chorioamnionitis typically targets the 2 organisms most likely to infect the fetus/neonate—group B streptococci and E coli. The antibiotic regimen of ampicillin plus gentamicin provides excellent, and inexpensive, coverage of these pathogens. The addition of a drug such as clindamycin or metronidazole provides a reassuring measure of coverage against anaerobes in women who require a cesarean delivery.1
Traditionally, patients with chorioamnionitis have been treated with IV antibiotics until they have been afebrile and asymptomatic for 24 hours.
Chapman and Owen,6 who were among the first to suggest that a shortened course of treatment might be as effective as a more extended course, assessed the effectiveness of a single post-partum dose of cefotetan in women who were treated intrapartum for chorioamnionitis and who delivered vaginally. The rate of treatment failure was 11% in the single-dose group and 3.7% in the women treated with multiple doses of cefotetan until they had been afebrile for 24 hours. This observed difference was not statistically significant (P = .27), but the study lacked sufficient power to firmly establish the safety and effectiveness of short-course therapy.
A trial of “no therapy” vs “extended therapy” in women with chorioamnionitis who delivered by cesarean found the rate of treatment failure was 21.8% in the “no therapy” group and 14.8% in the women who received clindamycin plus gentamicin for at least 24 hours postoperatively.7
Again, this observed difference was not statistically significant (P = .32), but the power of the investigation was limited.
This more recent study was sufficiently large and included a reasonable number of women who delivered both vaginally and abdominally.
Anti-anaerobic coverage critically important. Complications related to persistent infection developed in 2 patients in the short-course group who had cesarean deliveries: pelvic abscess and incisional abscess. In both instances, the patients did not receive the dose of clindamycin specified in the protocol, illustrating the critical importance of proper anti-anaerobic coverage in patients who require abdominal delivery.
Short-course therapy offers advantages in terms of ease of administration and cost savings compared with more extended treatment regimens.
Whether short courses of single agents, such as the broad-spectrum cephalosporins, penicillins, and carbapenems, would be as effective as ampicillin plus gentamicin plus clindamycin remains to be determined.
CDC data show “herd” immunity, thanks to varicella vaccination policy
Nguyen HQ, Jumaan AO, Seward JF. Decline in mortality due to varicella after implementation of varicella vaccination in the United States. N Engl J Med. 2005;352:450–458.
Question all women of reproductive age about varicella. Women who lack a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
This study demonstrates that, through the phenomenon of herd immunity, universal vaccination has significantly lowered the overall risk of varicella-related mortality in the general population. Universal childhood varicella vaccination was recommended by the Centers for Disease Control and Prevention in 1995; the rate of death due to varicella, either as the underlying cause or the contributing cause, fluctuated from 1990 through 1998, and then sharply declined.
Data from the National Center for Health Statistics Multiple Cause-of-Death Mortality for 1990 through 2001 reveal reduced varicella-related mortality in all age groups younger than 50 years. The greatest reduction (92%) was in children 1 to 4 years of age. Most deaths due to varicella were among persons who did not have an underlying high-risk condition and who would have been excellent candidates for vaccination.
Life-threatening in adults, especially pregnant women
Varicella usually is a relatively mild, self-limited disease of childhood. However, in immunocompromised persons and even in otherwise healthy adults, varicella can cause life-threatening complications such as severe pneumonia and encephalitis. Pneumonia develops in approximately 20% of adults who contract varicella, and encephalitis in approximately 1%. In the era before acyclovir was available, as many as 20% of persons with these complications died.8
Unique set of problems during pregnancy. Although pregnant women are not more likely than nonpregnant women to contract varicella or even to develop pneumonia or encephalitis, they do have a higher mortality if they experience these complications.
When varicella occurs during the first half of pregnancy, anomalies or spontaneous abortions occur in 1% to 2% of fetuses. Moreover, when the mother has varicella near or at the time of delivery, neonatal varicella develops in as many as 20% of infants, manifested as a mucocutaneous exanthema, pneumonia, encephali-tis, or disseminated visceral infection. Even with acyclovir treatment, severe morbidity and death can occur in affected neonates.8
Test and, when necessary, vaccinate women
The key point for clinicians to recognize is that varicella now can be almost completely prevented through universal vaccination.9
Although the principal target group for vaccination is young children, ObGyns should question all women of reproductive age about susceptibility to varicella. Women who do not have a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
- The present varicella vaccine (Varivax) is a live-virus vaccine, which should be administered in 2 subcutaneous injections (0.5 mL) 4 to 8 weeks apart.
- The vaccine should not be administered to infants younger than 12 months of age, to pregnant or lactating women, or to patients who have received systemic steroids within the last month.
- The vaccine also should not be given to persons who are immunosuppressed, except as part of a carefully supervised research protocol.
The vaccine is highly immuno-genic and produces immunity in approximately 90% of healthy children. The rate of seroconversion is lower in adults and immunosuppressed patients. Vaccinated patients have a significantly lower rate of natural infection after exposure.
The author reports no financial relationships relevant to this article.
1. Duff P. Antibiotic selection in obstetrics: making cost-effective choices. Clin Obstet Gynecol. 2002;45:59-72.
2. Talan DA, Stamm WE, Hooton TM, et al. Comparison of ciprofloxacin (7 days) and trimethoprim-sulfamethoxazole (14 days) for acute uncomplicated pyelonephritis in women: a randomized trial. JAMA. 2000;283:1583-1590.
3. Gupta K, Scholes D, Stamm WE. Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA. 1999;281:736-738.
4. Jamie WE, Edwards RK, Duff P. Antimicrobial susceptibility of Gram-negative uropathogens isolated from obstetric patients. Infect Dis Obstet Gynecol. 2002;10:123-126.
5. Gibbs RS, Duff P. Progress in pathogenesis and management of clinical intraamniotic infection. Am J Obstet Gynecol. 1991;164:1317-1326.
6. Chapman SJ, Owen J. Randomized trial of single-dose versus multiple-dose cefotetan for the postpartum treatment of intrapartum chorioamnionitis. Am J Obstet Gynecol. 1997;177:831-834.
7. Turnquest MA, How HY, Cook CR, et al. Chorioamnionitis: is continuation of antibiotic therapy necessary after cesarean section? Am J Obstet Gynecol. 1998;179:1261-1266.
8. Chapman S, Duff P. Varicella in pregnancy. Semin Perinatol. 1993;17:403-409.
9. Duff P. Varicella vaccine. Infect Dis Obstet Gynecol. 1996;4:63-65.
New findings I selected for this Update affect the management of 4 common and potentially serious clinical problems: acute cystitis, gonorrhea and chlamydia infection, chorioamnionitis, and varicella.
- A comparison of amoxicillin-clavulanic acid vs ciprofloxacin for uncomplicated lower urinary tract infections yielded surprising results, and more evidence on E coli’s resistance to antibiotics.
- Sexual partners of women with gonorrhea or chlamydia are more likely to receive appropriate treatment if it is offered by the women themselves or by the women’s caregivers.
- Short-course therapy for chorioamnionitis had a very high cure rate, equal to the traditional course, and furthers the possibility of shorter hospitalizations and cost savings without compromising outcomes.
- The CDC’s 1995 call for universal childhood vaccination for varicella has already sharply reduced varicella-related mortality in adults; still, we must determine immunity in our reproductive-age patients.
Acute cystitis: Ciprofloxacin prevails in E coli skirmish
Hooton TM, Scholes D, Gupta K, Stapleton AE, Roberts PL, Stamm WE. Amoxicillin-clavulanate vs ciprofloxacin for the treatment of uncomplicated cystitis in women: a randomized trial. JAMA. 2005;293:949–955.
Amoxicillin-clavulanate was not as effective as ciprofloxacin even in women who were infected with bacteria sensitive to amoxicillin-clavulanate.
A total of 320 nonpregnant women, aged 18 to 45 years, with uncomplicated acute cystitis were treated for 3 days with either oral amoxicillin-clavulanate (500 mg/125 mg twice daily) or oral ciprofloxacin (250 mg twice daily). Two weeks after treatment, 95% of women treated with ciprofloxacin were clinically cured, compared with only 76% of women treated with amoxicillin-clavulanate (P<.001).
Start with ciprofloxacin
The difference in outcome was attributed to a marked difference in vaginal colonization with the single most common pathogen in acute cystitis—Escherichia coli—at the 2-week follow-up (45% in the amoxicillinclavulanate group vs 10% in the ciprofloxacin group, P<.001).
Even though successful treatment of cystitis usually is possible with short courses (3–7 days) of oral antibiotics, persistent and recurrent infections may occur and usually are related to persistent vaginal colonization with E coli.
Treatment may require an extended course of oral antibiotics.
Initial selection of an antibiotic for acute cystitis is empiric and should be based on probable susceptibility of the dominant uropathogens. For many years, the typical initial antibiotic has been ampicillin.
E coli resistance. Now, however, more than a third of E coli strains, as well as most strains of K pneumoniae, are resistant to ampicillin. Therefore, ampicillin no longer should be used for the empiric treatment of cystitis.1
Surprising results
In theory, amoxicillin-clavulanate should have enhanced activity against E coli and other enteric organisms.
Therefore, these findings are surprising. The outcome with amoxicillin-clavulanate was inferior to that of ciprofloxacin, even in women who seemingly had susceptible uropathogens.
Based on this study, ciprofloxacin clearly is a more effective (and less expensive) empiric treatment in nonpregnant women.
In gravidas, start with nitrofurantoin
Ciprofloxacin is not appropriate for treatment of cystitis or asymptomatic bacteriuria in pregnant women. The quinolone antibiotics may cause injury to the developing cartilage of the fetus and are contraindicated in pregnant and lactating women, and in children younger than 17 years.1
What, then, is the most appropriate choice for treatment of uncomplicated cystitis during pregnancy?
One reasonable selection is oral trimethoprim-sulfamethoxazole, double-strength, twice daily. However, increasing resistance of E coli to this antibiotic has been documented recently.2,3
Therefore, a better choice is nitrofurantoin monohydrate macrocrystals, 100 mg twice daily.4 One organism that is not susceptible to nitrofurantoin is Proteus. When this organism is suspected, use trimethoprim-sulfamethoxazole.
Follow-up is a must
Because persistent and recurrent infections are common, patients should be followed with urine dipstick assessment or urine culture to be certain that the infection is resolved.
Follow-up is particularly important when infected women are pregnant, because of the risk of ascending infection leading to preterm labor, sepsis, or acute respiratory disease syndrome.
Treat sex partners, sight-unseen?
Golden MR, Whittington WL, Handsfield HH, et al. Effect of expedited treatment of sex partners on recurrent or persistent gonorrhea or chlamydial infection. N Engl J Med. 2005;352:676–685.
Providing a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Almost 2,000 men and women with uncomplicated gonorrhea or chlamydia infection were included in this study of expedited treatment compared with standard referral. In the standard referral group, investigators treated 931 patients and referred their sex partners to other physicians or facilities for evaluation and treatment. In the expedited treatment group, 929 patients were treated and also were provided with antibiotics to give to their partners. The partners of patients who were unwilling to do so were contacted and treated by the investigators.
At follow-up 21 to 126 days after treatment), persistent or recurrent infection was found in 13% of standard referral patients and 10% of expedited treatment patients (relative risk, 0.76; 95% confidence interval, 0.59–0.98).
Expedited treatment decreased the rate of persistent or recurrent gonorrhea more than that of persistent or recurrent chlamydia.
Patients in the expedited group were more likely to report that all of their partners were treated, and less likely to report having had sex with an untreated partner.
Advantages of the direct approach
The challenge for the ObGyn is how to arrange treatment for the female patient’s sex partner(s). This study indicates that a proactive approach is likely to be more effective than simply asking the patient to encourage her partner to seek medical attention. Direct provision of a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Failure to treat the patient’s sex partner is the principal cause of persistent or recurrent infection, which may lead to pelvic inflammatory disease, Fitz-Hugh-Curtis syndrome, and infertility. Gonorrhea may disseminate and manifest primarily by arthritis and dermatitis. If a pregnant woman is colonized with gonorrhea or chlamydia at the time of delivery, her infant may acquire gonococcal or chlamydial conjunctivitis or chlamydial pneumonia.
6 caveats
Although the results of this investigation are impressive and of great practical importance, these caveats should be noted.
- The oral drug used to treat gonorrhea in this study, cefixime (400 mg), is not presently available, and although another oral drug such as ciprofloxacin (500 mg) would be highly effective, it should not be used in pregnant or lactating women, or women younger than 17 years.1
- Although ceftriaxone, 125 mg intramuscularly, also is a superb drug for treatment of uncomplicated gonorrhea, the logistical problems of arranging for the partner to receive an intramuscular injection are daunting.
- Some women in the expedited treatment group were reluctant to provide medication to their partner(s), and study personnel were forced to intervene. Keep in mind that individual private practitioners and even well-organized clinics may not have sufficient support personnel to trace and treat all contacts.
- There is the important issue of a provider writing a prescription for an individual who is not actually his or her patient and who has not been interviewed and examined. Certainly, many state laws and insurance company regulations may discourage or even prohibit such a practice.
- Lack of a detailed assessment of the partner(s) means there is no opportunity to evaluate them for other conditions such as syphilis and HIV infection.
- Finally, taking a proactive approach in treating the sex partner(s) of patients who have gonorrhea or chlamydia (and, by extension, trichomoniasis) requires documentation of complete rationale in the patient’s medical record.
In addition, detailed written instructions must be provided for the partner(s) and must include a specific caution about possible reactions to the antibiotic.
Single-dose plus intrapartum therapy effective for chorioamnionitis
Edwards RK, Duff P. Single additional dose postpartum therapy for women with chorioamnionitis. Obstet Gynecol. 2003;102:957–961.
Short-course therapy is simpler to administer and reduces costs compared with more extended treatment.
Intrapartum therapy plus 1 additional dose of combination antibiotics after delivery produced a very high rate of cure (95.4%)—equivalent to that achieved when a more extended course of treatment was used.
In this randomized study of 292 otherwise healthy women with chorioamnionitis, 151 women were treated intrapartum with intravenous (IV) ampicillin (2 g every 6 hours) plus gentamicin (1.5 mg/kg every 8 hours). They received 1 dose of each drug postpartum. In addition, if they had a cesarean delivery, they received 1 dose of IV clindamycin (900 mg) immediately after the infant’s umbilical cord was clamped.
Women in the control group received IV antibiotics (including clindamycin, if indicated) until they had been afebrile and asymptomatic for 24 hours.
In the study group, 4.6% of women had a treatment failure and required an additional course of antibiotics. In the control group, 3.5% of patients required additional antibiotics (P = .639, not significant). When patients were stratified by method of delivery, no significant difference was found in treatment outcome.
Pathogens and regimens
Chorioamnionitis occurs in approximately 1% to 5% of term patients and in as many as 25% of patients having a preterm delivery. The infection is caused by multiple aerobic and anaerobic organisms, notably group B streptococci, E coli, and anaerobes. The former 2 pathogens pose the greatest risk to the infant and are the predominant causes of neonatal pneumonia, bacteremia, and meningitis. These organisms also are major causes of maternal bacteremia.
Anaerobes usually do not pose a major threat to the fetus or neonate, but are particularly likely to lead to pelvic abscess in women who require a cesarean delivery in the face of preexisting intrauterine infection.5
Accordingly, the initial antibiotic therapy for chorioamnionitis typically targets the 2 organisms most likely to infect the fetus/neonate—group B streptococci and E coli. The antibiotic regimen of ampicillin plus gentamicin provides excellent, and inexpensive, coverage of these pathogens. The addition of a drug such as clindamycin or metronidazole provides a reassuring measure of coverage against anaerobes in women who require a cesarean delivery.1
Traditionally, patients with chorioamnionitis have been treated with IV antibiotics until they have been afebrile and asymptomatic for 24 hours.
Chapman and Owen,6 who were among the first to suggest that a shortened course of treatment might be as effective as a more extended course, assessed the effectiveness of a single post-partum dose of cefotetan in women who were treated intrapartum for chorioamnionitis and who delivered vaginally. The rate of treatment failure was 11% in the single-dose group and 3.7% in the women treated with multiple doses of cefotetan until they had been afebrile for 24 hours. This observed difference was not statistically significant (P = .27), but the study lacked sufficient power to firmly establish the safety and effectiveness of short-course therapy.
A trial of “no therapy” vs “extended therapy” in women with chorioamnionitis who delivered by cesarean found the rate of treatment failure was 21.8% in the “no therapy” group and 14.8% in the women who received clindamycin plus gentamicin for at least 24 hours postoperatively.7
Again, this observed difference was not statistically significant (P = .32), but the power of the investigation was limited.
This more recent study was sufficiently large and included a reasonable number of women who delivered both vaginally and abdominally.
Anti-anaerobic coverage critically important. Complications related to persistent infection developed in 2 patients in the short-course group who had cesarean deliveries: pelvic abscess and incisional abscess. In both instances, the patients did not receive the dose of clindamycin specified in the protocol, illustrating the critical importance of proper anti-anaerobic coverage in patients who require abdominal delivery.
Short-course therapy offers advantages in terms of ease of administration and cost savings compared with more extended treatment regimens.
Whether short courses of single agents, such as the broad-spectrum cephalosporins, penicillins, and carbapenems, would be as effective as ampicillin plus gentamicin plus clindamycin remains to be determined.
CDC data show “herd” immunity, thanks to varicella vaccination policy
Nguyen HQ, Jumaan AO, Seward JF. Decline in mortality due to varicella after implementation of varicella vaccination in the United States. N Engl J Med. 2005;352:450–458.
Question all women of reproductive age about varicella. Women who lack a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
This study demonstrates that, through the phenomenon of herd immunity, universal vaccination has significantly lowered the overall risk of varicella-related mortality in the general population. Universal childhood varicella vaccination was recommended by the Centers for Disease Control and Prevention in 1995; the rate of death due to varicella, either as the underlying cause or the contributing cause, fluctuated from 1990 through 1998, and then sharply declined.
Data from the National Center for Health Statistics Multiple Cause-of-Death Mortality for 1990 through 2001 reveal reduced varicella-related mortality in all age groups younger than 50 years. The greatest reduction (92%) was in children 1 to 4 years of age. Most deaths due to varicella were among persons who did not have an underlying high-risk condition and who would have been excellent candidates for vaccination.
Life-threatening in adults, especially pregnant women
Varicella usually is a relatively mild, self-limited disease of childhood. However, in immunocompromised persons and even in otherwise healthy adults, varicella can cause life-threatening complications such as severe pneumonia and encephalitis. Pneumonia develops in approximately 20% of adults who contract varicella, and encephalitis in approximately 1%. In the era before acyclovir was available, as many as 20% of persons with these complications died.8
Unique set of problems during pregnancy. Although pregnant women are not more likely than nonpregnant women to contract varicella or even to develop pneumonia or encephalitis, they do have a higher mortality if they experience these complications.
When varicella occurs during the first half of pregnancy, anomalies or spontaneous abortions occur in 1% to 2% of fetuses. Moreover, when the mother has varicella near or at the time of delivery, neonatal varicella develops in as many as 20% of infants, manifested as a mucocutaneous exanthema, pneumonia, encephali-tis, or disseminated visceral infection. Even with acyclovir treatment, severe morbidity and death can occur in affected neonates.8
Test and, when necessary, vaccinate women
The key point for clinicians to recognize is that varicella now can be almost completely prevented through universal vaccination.9
Although the principal target group for vaccination is young children, ObGyns should question all women of reproductive age about susceptibility to varicella. Women who do not have a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
- The present varicella vaccine (Varivax) is a live-virus vaccine, which should be administered in 2 subcutaneous injections (0.5 mL) 4 to 8 weeks apart.
- The vaccine should not be administered to infants younger than 12 months of age, to pregnant or lactating women, or to patients who have received systemic steroids within the last month.
- The vaccine also should not be given to persons who are immunosuppressed, except as part of a carefully supervised research protocol.
The vaccine is highly immuno-genic and produces immunity in approximately 90% of healthy children. The rate of seroconversion is lower in adults and immunosuppressed patients. Vaccinated patients have a significantly lower rate of natural infection after exposure.
The author reports no financial relationships relevant to this article.
New findings I selected for this Update affect the management of 4 common and potentially serious clinical problems: acute cystitis, gonorrhea and chlamydia infection, chorioamnionitis, and varicella.
- A comparison of amoxicillin-clavulanic acid vs ciprofloxacin for uncomplicated lower urinary tract infections yielded surprising results, and more evidence on E coli’s resistance to antibiotics.
- Sexual partners of women with gonorrhea or chlamydia are more likely to receive appropriate treatment if it is offered by the women themselves or by the women’s caregivers.
- Short-course therapy for chorioamnionitis had a very high cure rate, equal to the traditional course, and furthers the possibility of shorter hospitalizations and cost savings without compromising outcomes.
- The CDC’s 1995 call for universal childhood vaccination for varicella has already sharply reduced varicella-related mortality in adults; still, we must determine immunity in our reproductive-age patients.
Acute cystitis: Ciprofloxacin prevails in E coli skirmish
Hooton TM, Scholes D, Gupta K, Stapleton AE, Roberts PL, Stamm WE. Amoxicillin-clavulanate vs ciprofloxacin for the treatment of uncomplicated cystitis in women: a randomized trial. JAMA. 2005;293:949–955.
Amoxicillin-clavulanate was not as effective as ciprofloxacin even in women who were infected with bacteria sensitive to amoxicillin-clavulanate.
A total of 320 nonpregnant women, aged 18 to 45 years, with uncomplicated acute cystitis were treated for 3 days with either oral amoxicillin-clavulanate (500 mg/125 mg twice daily) or oral ciprofloxacin (250 mg twice daily). Two weeks after treatment, 95% of women treated with ciprofloxacin were clinically cured, compared with only 76% of women treated with amoxicillin-clavulanate (P<.001).
Start with ciprofloxacin
The difference in outcome was attributed to a marked difference in vaginal colonization with the single most common pathogen in acute cystitis—Escherichia coli—at the 2-week follow-up (45% in the amoxicillinclavulanate group vs 10% in the ciprofloxacin group, P<.001).
Even though successful treatment of cystitis usually is possible with short courses (3–7 days) of oral antibiotics, persistent and recurrent infections may occur and usually are related to persistent vaginal colonization with E coli.
Treatment may require an extended course of oral antibiotics.
Initial selection of an antibiotic for acute cystitis is empiric and should be based on probable susceptibility of the dominant uropathogens. For many years, the typical initial antibiotic has been ampicillin.
E coli resistance. Now, however, more than a third of E coli strains, as well as most strains of K pneumoniae, are resistant to ampicillin. Therefore, ampicillin no longer should be used for the empiric treatment of cystitis.1
Surprising results
In theory, amoxicillin-clavulanate should have enhanced activity against E coli and other enteric organisms.
Therefore, these findings are surprising. The outcome with amoxicillin-clavulanate was inferior to that of ciprofloxacin, even in women who seemingly had susceptible uropathogens.
Based on this study, ciprofloxacin clearly is a more effective (and less expensive) empiric treatment in nonpregnant women.
In gravidas, start with nitrofurantoin
Ciprofloxacin is not appropriate for treatment of cystitis or asymptomatic bacteriuria in pregnant women. The quinolone antibiotics may cause injury to the developing cartilage of the fetus and are contraindicated in pregnant and lactating women, and in children younger than 17 years.1
What, then, is the most appropriate choice for treatment of uncomplicated cystitis during pregnancy?
One reasonable selection is oral trimethoprim-sulfamethoxazole, double-strength, twice daily. However, increasing resistance of E coli to this antibiotic has been documented recently.2,3
Therefore, a better choice is nitrofurantoin monohydrate macrocrystals, 100 mg twice daily.4 One organism that is not susceptible to nitrofurantoin is Proteus. When this organism is suspected, use trimethoprim-sulfamethoxazole.
Follow-up is a must
Because persistent and recurrent infections are common, patients should be followed with urine dipstick assessment or urine culture to be certain that the infection is resolved.
Follow-up is particularly important when infected women are pregnant, because of the risk of ascending infection leading to preterm labor, sepsis, or acute respiratory disease syndrome.
Treat sex partners, sight-unseen?
Golden MR, Whittington WL, Handsfield HH, et al. Effect of expedited treatment of sex partners on recurrent or persistent gonorrhea or chlamydial infection. N Engl J Med. 2005;352:676–685.
Providing a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Almost 2,000 men and women with uncomplicated gonorrhea or chlamydia infection were included in this study of expedited treatment compared with standard referral. In the standard referral group, investigators treated 931 patients and referred their sex partners to other physicians or facilities for evaluation and treatment. In the expedited treatment group, 929 patients were treated and also were provided with antibiotics to give to their partners. The partners of patients who were unwilling to do so were contacted and treated by the investigators.
At follow-up 21 to 126 days after treatment), persistent or recurrent infection was found in 13% of standard referral patients and 10% of expedited treatment patients (relative risk, 0.76; 95% confidence interval, 0.59–0.98).
Expedited treatment decreased the rate of persistent or recurrent gonorrhea more than that of persistent or recurrent chlamydia.
Patients in the expedited group were more likely to report that all of their partners were treated, and less likely to report having had sex with an untreated partner.
Advantages of the direct approach
The challenge for the ObGyn is how to arrange treatment for the female patient’s sex partner(s). This study indicates that a proactive approach is likely to be more effective than simply asking the patient to encourage her partner to seek medical attention. Direct provision of a separate prescription for the partner(s) resulted in a 24% decrease in the frequency of persistent or recurrent infection.
Failure to treat the patient’s sex partner is the principal cause of persistent or recurrent infection, which may lead to pelvic inflammatory disease, Fitz-Hugh-Curtis syndrome, and infertility. Gonorrhea may disseminate and manifest primarily by arthritis and dermatitis. If a pregnant woman is colonized with gonorrhea or chlamydia at the time of delivery, her infant may acquire gonococcal or chlamydial conjunctivitis or chlamydial pneumonia.
6 caveats
Although the results of this investigation are impressive and of great practical importance, these caveats should be noted.
- The oral drug used to treat gonorrhea in this study, cefixime (400 mg), is not presently available, and although another oral drug such as ciprofloxacin (500 mg) would be highly effective, it should not be used in pregnant or lactating women, or women younger than 17 years.1
- Although ceftriaxone, 125 mg intramuscularly, also is a superb drug for treatment of uncomplicated gonorrhea, the logistical problems of arranging for the partner to receive an intramuscular injection are daunting.
- Some women in the expedited treatment group were reluctant to provide medication to their partner(s), and study personnel were forced to intervene. Keep in mind that individual private practitioners and even well-organized clinics may not have sufficient support personnel to trace and treat all contacts.
- There is the important issue of a provider writing a prescription for an individual who is not actually his or her patient and who has not been interviewed and examined. Certainly, many state laws and insurance company regulations may discourage or even prohibit such a practice.
- Lack of a detailed assessment of the partner(s) means there is no opportunity to evaluate them for other conditions such as syphilis and HIV infection.
- Finally, taking a proactive approach in treating the sex partner(s) of patients who have gonorrhea or chlamydia (and, by extension, trichomoniasis) requires documentation of complete rationale in the patient’s medical record.
In addition, detailed written instructions must be provided for the partner(s) and must include a specific caution about possible reactions to the antibiotic.
Single-dose plus intrapartum therapy effective for chorioamnionitis
Edwards RK, Duff P. Single additional dose postpartum therapy for women with chorioamnionitis. Obstet Gynecol. 2003;102:957–961.
Short-course therapy is simpler to administer and reduces costs compared with more extended treatment.
Intrapartum therapy plus 1 additional dose of combination antibiotics after delivery produced a very high rate of cure (95.4%)—equivalent to that achieved when a more extended course of treatment was used.
In this randomized study of 292 otherwise healthy women with chorioamnionitis, 151 women were treated intrapartum with intravenous (IV) ampicillin (2 g every 6 hours) plus gentamicin (1.5 mg/kg every 8 hours). They received 1 dose of each drug postpartum. In addition, if they had a cesarean delivery, they received 1 dose of IV clindamycin (900 mg) immediately after the infant’s umbilical cord was clamped.
Women in the control group received IV antibiotics (including clindamycin, if indicated) until they had been afebrile and asymptomatic for 24 hours.
In the study group, 4.6% of women had a treatment failure and required an additional course of antibiotics. In the control group, 3.5% of patients required additional antibiotics (P = .639, not significant). When patients were stratified by method of delivery, no significant difference was found in treatment outcome.
Pathogens and regimens
Chorioamnionitis occurs in approximately 1% to 5% of term patients and in as many as 25% of patients having a preterm delivery. The infection is caused by multiple aerobic and anaerobic organisms, notably group B streptococci, E coli, and anaerobes. The former 2 pathogens pose the greatest risk to the infant and are the predominant causes of neonatal pneumonia, bacteremia, and meningitis. These organisms also are major causes of maternal bacteremia.
Anaerobes usually do not pose a major threat to the fetus or neonate, but are particularly likely to lead to pelvic abscess in women who require a cesarean delivery in the face of preexisting intrauterine infection.5
Accordingly, the initial antibiotic therapy for chorioamnionitis typically targets the 2 organisms most likely to infect the fetus/neonate—group B streptococci and E coli. The antibiotic regimen of ampicillin plus gentamicin provides excellent, and inexpensive, coverage of these pathogens. The addition of a drug such as clindamycin or metronidazole provides a reassuring measure of coverage against anaerobes in women who require a cesarean delivery.1
Traditionally, patients with chorioamnionitis have been treated with IV antibiotics until they have been afebrile and asymptomatic for 24 hours.
Chapman and Owen,6 who were among the first to suggest that a shortened course of treatment might be as effective as a more extended course, assessed the effectiveness of a single post-partum dose of cefotetan in women who were treated intrapartum for chorioamnionitis and who delivered vaginally. The rate of treatment failure was 11% in the single-dose group and 3.7% in the women treated with multiple doses of cefotetan until they had been afebrile for 24 hours. This observed difference was not statistically significant (P = .27), but the study lacked sufficient power to firmly establish the safety and effectiveness of short-course therapy.
A trial of “no therapy” vs “extended therapy” in women with chorioamnionitis who delivered by cesarean found the rate of treatment failure was 21.8% in the “no therapy” group and 14.8% in the women who received clindamycin plus gentamicin for at least 24 hours postoperatively.7
Again, this observed difference was not statistically significant (P = .32), but the power of the investigation was limited.
This more recent study was sufficiently large and included a reasonable number of women who delivered both vaginally and abdominally.
Anti-anaerobic coverage critically important. Complications related to persistent infection developed in 2 patients in the short-course group who had cesarean deliveries: pelvic abscess and incisional abscess. In both instances, the patients did not receive the dose of clindamycin specified in the protocol, illustrating the critical importance of proper anti-anaerobic coverage in patients who require abdominal delivery.
Short-course therapy offers advantages in terms of ease of administration and cost savings compared with more extended treatment regimens.
Whether short courses of single agents, such as the broad-spectrum cephalosporins, penicillins, and carbapenems, would be as effective as ampicillin plus gentamicin plus clindamycin remains to be determined.
CDC data show “herd” immunity, thanks to varicella vaccination policy
Nguyen HQ, Jumaan AO, Seward JF. Decline in mortality due to varicella after implementation of varicella vaccination in the United States. N Engl J Med. 2005;352:450–458.
Question all women of reproductive age about varicella. Women who lack a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
This study demonstrates that, through the phenomenon of herd immunity, universal vaccination has significantly lowered the overall risk of varicella-related mortality in the general population. Universal childhood varicella vaccination was recommended by the Centers for Disease Control and Prevention in 1995; the rate of death due to varicella, either as the underlying cause or the contributing cause, fluctuated from 1990 through 1998, and then sharply declined.
Data from the National Center for Health Statistics Multiple Cause-of-Death Mortality for 1990 through 2001 reveal reduced varicella-related mortality in all age groups younger than 50 years. The greatest reduction (92%) was in children 1 to 4 years of age. Most deaths due to varicella were among persons who did not have an underlying high-risk condition and who would have been excellent candidates for vaccination.
Life-threatening in adults, especially pregnant women
Varicella usually is a relatively mild, self-limited disease of childhood. However, in immunocompromised persons and even in otherwise healthy adults, varicella can cause life-threatening complications such as severe pneumonia and encephalitis. Pneumonia develops in approximately 20% of adults who contract varicella, and encephalitis in approximately 1%. In the era before acyclovir was available, as many as 20% of persons with these complications died.8
Unique set of problems during pregnancy. Although pregnant women are not more likely than nonpregnant women to contract varicella or even to develop pneumonia or encephalitis, they do have a higher mortality if they experience these complications.
When varicella occurs during the first half of pregnancy, anomalies or spontaneous abortions occur in 1% to 2% of fetuses. Moreover, when the mother has varicella near or at the time of delivery, neonatal varicella develops in as many as 20% of infants, manifested as a mucocutaneous exanthema, pneumonia, encephali-tis, or disseminated visceral infection. Even with acyclovir treatment, severe morbidity and death can occur in affected neonates.8
Test and, when necessary, vaccinate women
The key point for clinicians to recognize is that varicella now can be almost completely prevented through universal vaccination.9
Although the principal target group for vaccination is young children, ObGyns should question all women of reproductive age about susceptibility to varicella. Women who do not have a convincing history of natural infection should have a serologic test for varicella-zoster IgG. If immunity is not evident, they should be vaccinated prior to attempting pregnancy.
- The present varicella vaccine (Varivax) is a live-virus vaccine, which should be administered in 2 subcutaneous injections (0.5 mL) 4 to 8 weeks apart.
- The vaccine should not be administered to infants younger than 12 months of age, to pregnant or lactating women, or to patients who have received systemic steroids within the last month.
- The vaccine also should not be given to persons who are immunosuppressed, except as part of a carefully supervised research protocol.
The vaccine is highly immuno-genic and produces immunity in approximately 90% of healthy children. The rate of seroconversion is lower in adults and immunosuppressed patients. Vaccinated patients have a significantly lower rate of natural infection after exposure.
The author reports no financial relationships relevant to this article.
1. Duff P. Antibiotic selection in obstetrics: making cost-effective choices. Clin Obstet Gynecol. 2002;45:59-72.
2. Talan DA, Stamm WE, Hooton TM, et al. Comparison of ciprofloxacin (7 days) and trimethoprim-sulfamethoxazole (14 days) for acute uncomplicated pyelonephritis in women: a randomized trial. JAMA. 2000;283:1583-1590.
3. Gupta K, Scholes D, Stamm WE. Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA. 1999;281:736-738.
4. Jamie WE, Edwards RK, Duff P. Antimicrobial susceptibility of Gram-negative uropathogens isolated from obstetric patients. Infect Dis Obstet Gynecol. 2002;10:123-126.
5. Gibbs RS, Duff P. Progress in pathogenesis and management of clinical intraamniotic infection. Am J Obstet Gynecol. 1991;164:1317-1326.
6. Chapman SJ, Owen J. Randomized trial of single-dose versus multiple-dose cefotetan for the postpartum treatment of intrapartum chorioamnionitis. Am J Obstet Gynecol. 1997;177:831-834.
7. Turnquest MA, How HY, Cook CR, et al. Chorioamnionitis: is continuation of antibiotic therapy necessary after cesarean section? Am J Obstet Gynecol. 1998;179:1261-1266.
8. Chapman S, Duff P. Varicella in pregnancy. Semin Perinatol. 1993;17:403-409.
9. Duff P. Varicella vaccine. Infect Dis Obstet Gynecol. 1996;4:63-65.
1. Duff P. Antibiotic selection in obstetrics: making cost-effective choices. Clin Obstet Gynecol. 2002;45:59-72.
2. Talan DA, Stamm WE, Hooton TM, et al. Comparison of ciprofloxacin (7 days) and trimethoprim-sulfamethoxazole (14 days) for acute uncomplicated pyelonephritis in women: a randomized trial. JAMA. 2000;283:1583-1590.
3. Gupta K, Scholes D, Stamm WE. Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA. 1999;281:736-738.
4. Jamie WE, Edwards RK, Duff P. Antimicrobial susceptibility of Gram-negative uropathogens isolated from obstetric patients. Infect Dis Obstet Gynecol. 2002;10:123-126.
5. Gibbs RS, Duff P. Progress in pathogenesis and management of clinical intraamniotic infection. Am J Obstet Gynecol. 1991;164:1317-1326.
6. Chapman SJ, Owen J. Randomized trial of single-dose versus multiple-dose cefotetan for the postpartum treatment of intrapartum chorioamnionitis. Am J Obstet Gynecol. 1997;177:831-834.
7. Turnquest MA, How HY, Cook CR, et al. Chorioamnionitis: is continuation of antibiotic therapy necessary after cesarean section? Am J Obstet Gynecol. 1998;179:1261-1266.
8. Chapman S, Duff P. Varicella in pregnancy. Semin Perinatol. 1993;17:403-409.
9. Duff P. Varicella vaccine. Infect Dis Obstet Gynecol. 1996;4:63-65.
Predicting and preventing preterm birth
A 25-year-old primigravida with an intrauterine pregnancy at 26 weeks presents with contractions of moderate intensity every 4 minutes, intact membranes, and minimal vaginal bleeding. On digital exam, her cervix is soft, 50% effaced, and closed. Estimated fetal weight is 775 g.
You are at a Level I hospital in a rural community, 90 minutes from a tertiary nursery. What steps should you take first?
Tocolytics and antibiotics are the first steps. They may help to maximize the benefits of secondary strategies such as antenatal corticosteroids during transport to a tertiary care facility. In addition, assessment of fetal fibronectin levels and use of endovaginal ultrasound can supplement clinical judgment and improve prediction of outcomes. Their excellent negative predictive value can spare many women unnecessary and potentially harmful treatments.
This article discusses these measures in the context of an actual case.
The value of “secondary prevention”
Giving corticosteroids to enhance fetal lung and brain maturity and transporting the mother to a tertiary care center may not prevent preterm delivery, but they can mitigate some of the damage and are supported by the evidence.
Corticosteroids. Given the clear evidence of their efficacy, steroids should be administered once preterm birth appears likely. I would give steroids before maternal transport.
Betamethasone is preferable to dexamethasone, which may be toxic to the fetal central nervous system. However, dexamethasone is preferable to no therapy.
Contraindications to corticosteroids include systemic maternal or fetal infections and maternal endocrinopathies such as Cushing’s disease or poorly controlled diabetes.
Transport to tertiary care. A neonatal intensive care unit clearly benefits tiny babies. Clinicians should be aware of the pediatric capacity of their community hospitals and maintain a referral relationship with the nearest tertiary care centers. Conversely, clinicians on the receiving end of maternal transports should make every effort to expedite these referrals.
Is Local Care Too Risky?
Patricia and her family strongly prefer that she undergo treatment in her own community, if at all possible.
Signs and symptoms of preterm labor are poor predictors of preterm birth. Although most symptomatic women deliver at term, even the most clinically astute physician cannot predict when a symptomatic patient will deliver.
Which tocolytic is most effective?
Berkman ND, Thorp JM Jr, Lohr KN, et al. Tocolytic treatment for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2003;188:1648–1659.
No single drug is best. In this metaanalysis, magnesium, β-mimetics, calcium channel blockers, and nonsteroidal anti-inflammatory drugs (NSAIDs) performed about the same at prolonging the interval between onset of preterm labor and actual birth, compared with placebo or no treatment. Ethanol was less effective and “inappropriate.” Tocolytics are given to stop contractions (first-line therapy) and to maintain quiescence after an acute episode (maintenance therapy).
To determine the most effective tocolytic, we analyzed 16 studies of first-line therapy and 8 involving maintenance therapy, using the above 5 drug classes.
How 5 drugs compare
Estimated odds ratios suggest that, when used as first-line therapy, all the drugs except ethanol are about the same. Odds ratios ranged from 1.622 for β-mimetics to 2.485 for calcium channel blockers. (The odds ratio for NSAIDs was based on only 1 study.)
When we tested whether β-mimetics, calcium channel blockers, and magnesium sulfate had the same effects, compared with placebo, the results suggested that they do not. However, the body of literature was not large enough to establish this conclusively.
Overall, β-mimetics appear to lack superiority over the other drugs as first-line therapy and cause more maternal harms, while ethanol is “inappropriate” and no longer in use.
As maintenance therapy, none of the drugs appeared to have any benefit.
Maternal and fetal harms
We defined harms as “clinical markers and events that the authors of individual studies considered as adverse events or side effects.”
Among maternal harms were serious cardiac side effects, including arrhythmias, heart failure, and chest pain, linked to β-mimetics. Minor cardiovascular harms were also higher among women given β-mimetics. In addition, calcium channel blockers appeared to increase the risk of minor cardiovascular harms, but not as much as the β-mimetics.
Overall, maternal cardiac, metabolic, and psychologic harms were more prevalent among women taking β-mimetics. This may be due, at least in part, to the fact that studies of β-mimetics tended to look for these effects more than other studies did.
As for short-term fetal harms, we found “little consistent evidence” of them in the infants of women receiving these drugs, and the studies lacked sufficient data to evaluate potential long-term harms.
What later analyses found
After 1999, the cutoff year of our review, several relatively large studies showed the oxytocin antagonist atosiban to be effective as acute7,8and maintenance8 therapy, with a favorable side effect profile. Another trial9 compared 2 doses of magnesium (2 and 5 g per hour); the higher dose acted more quickly but with more side effects. These and other studies do not alter our conclusions about the effectiveness of tocolytic therapy—or the specifics of the 5 drugs studied.
2 useful markers
In the 1990s, 2 biologic markers were discovered that improve the precision of preterm birth risk assessment:
- fetal fibronectin (fFN) and
- endovaginal sonography (EVUSD).1
Use of EVUSD enables measurement of the cervix from the internal to external os. Cervices shorten before spontaneous birth.
These 2 tests, when positive (fFN detected or cervical length
I use a negative test to identify women who do not require further treatment or evaluation. If a patient has a negative fFN or EVUSD, I would not transport her to a tertiary care center. In fact, I would probably discharge her home with close follow-up.
3 concerns about the tests
Clinicians tend to have some concerns about incorporating these tests into their routines:
- How reliable is negative predictive value? Arguably, these tests perform better than clinical judgment and can spare many women unnecessary treatments.2 No test is perfect, however. These bio-markers should be adjuncts to—not replacements for—clinical wisdom.
- What about false results? With fFN, a proper collection kit with plastic tube and Dacron swab is critical because the molecule will adhere to glass or cotton, creating a false-negative result. A false-positive result can occur after recent coitus or a digital cervical exam; therefore, collect fFN specimens before checking the cervix. With EVUSD, the examinations require a moderate amount of skill.
- Which biomarker is best? Both fFN and EVUSD make independent and separate contributions to the prediction of preterm birth. Therefore, I use both.
Start Tocolysis And Antibiotics?
Patricia’s fFN and EVUSD tests are both positive. Should you start tocolysis and antibiotic therapy prior to transfer?
Metaanalysis suggests tocolysis, and antibiotics extend the interval between symptom onset and delivery.1The length of this prolongation can be measured in days, and no evidence suggests that prolonged pharmacotherapy has any benefit.
I would initiate both therapies while waiting for the mother to be moved to a tertiary center, even though neither therapy has been shown to improve perinatal outcome.
Tocolysis. We could find no differences among tocolytic drugs.3 Serious side effects are rare, but nuisance cardiovascular symptoms are frequent. Sympathomimetic drugs lead to lethargy, and magnesium is associated with malaise. Magnesium requires intravenous access and should be given only via infusion pump by trained personnel. That often means a nurse must accompany the patient to the Level III hospital.
Thus, for logistical reasons, I favor nonsteroidal anti-inflammatory drugs, of which indomethacin is the most widely studied. Indomethacin can be given by mouth or rectum, with minimal side effects. Harm to the fetus is rare if the drug is used acutely for only 48 to 72 hours (the maximum duration of any potential benefit).
Antibiotics. Current protocols calling for betalactam antibiotic therapy as prophylaxis against early-onset neonatal sepsis in preterm births have led to almost universal use of antibiotics among these patients. Our metaanalysis did not demonstrate superior pregnancy prolongation with any other regimen, so the one for group B strep prophylaxis provides a double benefit.4 As with tocolytics, there is no role for maintenance therapy.
When Contractions Cease
Patricia is transferred and completes her steroid therapy. Her symptoms and contractions cease. After a few days of observation and no cervical changes, she is discharged home. She asks about home therapies, work, activities, and sex.
Since our metaanalysis of tocolysis studies showed no efficacy for maintenance regimens, I do not recommend them except in this rare situation: when a woman has so much uterine activity without cervical change that she is unable to rest or complete her daily activities. In this case I would favor “as needed” doses of a β-mimetic drug by mouth.
Although home uterine activity monitors and subcutaneous tocolytic pumps are available, evidence suggests they are ineffective.1I seldom, if ever, use these devices.
Despite the almost universal recommendation that women at risk of preterm birth avoid physical and sexual activity, we lack evidence that bed rest or abstinence prolong pregnancy or prevent preterm birth.
Is sex allowed? When we studied both physical activity and sexuality in asymptomatic women at midpregnancy, neither was associated with spontaneous preterm birth.5,6 Therefore, I do not recommend restricting activity or sexual intercourse. Instead, I encourage women to carefully assess uterine activity. If certain behaviors appear to increase contractions, those behaviors should be limited.
Counsel her to trust her instincts. It is important to encourage the patient to trust her own instincts, so that an overzealous employer or partner cannot coerce or cajole her to do something that violates her internal sense of well-being.
The author reports no financial relationships relevant to this article.
1. Berkman ND, Thorp JM, Hartmann KE, et al. Management of Preterm Labor. Evidence Report/Technology Assessment #18. Rockville, Md: Agency for Healthcare Research and Quality; December 2000. AHRQ publication 01-E021.
2. Thorp JM, Jr. ACOG Committee on Practice Bulletins. Management of preterm labor. Obstet Gynecol. 2003;101:1039-1047.
3. Berkman ND, Thorp JM, Jr, Lohr KN, et al. Tocolytic treatment for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2003;188:1648-1659.
4. Thorp JM, Jr, Hartmann KE, Berkman ND, et al. Antibiotic therapy for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2002;186:587-592.
5. Sayle AE, Savitz DA, Thorp JM, Jr, Hertz-Picciotto I, Wilcox AJ. Sexual activity during late pregnancy and preterm delivery. Obstet Gynecol. 2001;97:283-289.
6. Evenson KR, Siega-Riz AM, Savitz DA, Leiferman JA, Thorp JM, Jr. Vigorous leisure activity and pregnancy outcome. Epidemiology. 2002;13:653-659.
7. Moutquin JM, Sherman D, Cohen H, et al. Double-blind, randomized, controlled trial of atosiban and ritrodine in the treatment of preterm labor: a multicenter effectiveness and safety study. Am J Obstet Gynecol. 2000;182:1191-1199.
8. Romero R, Sibai BM, Sanchez-Ramos L, et al. An oxytocin receptor antagonist (atosiban) in the treatment of preterm labor: a randomized, double-blind, placebo-controlled trial with tocolytic rescue. Am J Obstet Gynecol. 2000;182:1173-1183.
9. Terrone DA, Rinehart BK, Kimmel ES, May WL, Larmon JE, Morrison JC. A prospective, randomized, controlled trial of high and low maintenance doses of magnesium sulfate for acute tocolysis. Am J Obstet Gynecol. 2000;182:1477-1482.
A 25-year-old primigravida with an intrauterine pregnancy at 26 weeks presents with contractions of moderate intensity every 4 minutes, intact membranes, and minimal vaginal bleeding. On digital exam, her cervix is soft, 50% effaced, and closed. Estimated fetal weight is 775 g.
You are at a Level I hospital in a rural community, 90 minutes from a tertiary nursery. What steps should you take first?
Tocolytics and antibiotics are the first steps. They may help to maximize the benefits of secondary strategies such as antenatal corticosteroids during transport to a tertiary care facility. In addition, assessment of fetal fibronectin levels and use of endovaginal ultrasound can supplement clinical judgment and improve prediction of outcomes. Their excellent negative predictive value can spare many women unnecessary and potentially harmful treatments.
This article discusses these measures in the context of an actual case.
The value of “secondary prevention”
Giving corticosteroids to enhance fetal lung and brain maturity and transporting the mother to a tertiary care center may not prevent preterm delivery, but they can mitigate some of the damage and are supported by the evidence.
Corticosteroids. Given the clear evidence of their efficacy, steroids should be administered once preterm birth appears likely. I would give steroids before maternal transport.
Betamethasone is preferable to dexamethasone, which may be toxic to the fetal central nervous system. However, dexamethasone is preferable to no therapy.
Contraindications to corticosteroids include systemic maternal or fetal infections and maternal endocrinopathies such as Cushing’s disease or poorly controlled diabetes.
Transport to tertiary care. A neonatal intensive care unit clearly benefits tiny babies. Clinicians should be aware of the pediatric capacity of their community hospitals and maintain a referral relationship with the nearest tertiary care centers. Conversely, clinicians on the receiving end of maternal transports should make every effort to expedite these referrals.
Is Local Care Too Risky?
Patricia and her family strongly prefer that she undergo treatment in her own community, if at all possible.
Signs and symptoms of preterm labor are poor predictors of preterm birth. Although most symptomatic women deliver at term, even the most clinically astute physician cannot predict when a symptomatic patient will deliver.
Which tocolytic is most effective?
Berkman ND, Thorp JM Jr, Lohr KN, et al. Tocolytic treatment for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2003;188:1648–1659.
No single drug is best. In this metaanalysis, magnesium, β-mimetics, calcium channel blockers, and nonsteroidal anti-inflammatory drugs (NSAIDs) performed about the same at prolonging the interval between onset of preterm labor and actual birth, compared with placebo or no treatment. Ethanol was less effective and “inappropriate.” Tocolytics are given to stop contractions (first-line therapy) and to maintain quiescence after an acute episode (maintenance therapy).
To determine the most effective tocolytic, we analyzed 16 studies of first-line therapy and 8 involving maintenance therapy, using the above 5 drug classes.
How 5 drugs compare
Estimated odds ratios suggest that, when used as first-line therapy, all the drugs except ethanol are about the same. Odds ratios ranged from 1.622 for β-mimetics to 2.485 for calcium channel blockers. (The odds ratio for NSAIDs was based on only 1 study.)
When we tested whether β-mimetics, calcium channel blockers, and magnesium sulfate had the same effects, compared with placebo, the results suggested that they do not. However, the body of literature was not large enough to establish this conclusively.
Overall, β-mimetics appear to lack superiority over the other drugs as first-line therapy and cause more maternal harms, while ethanol is “inappropriate” and no longer in use.
As maintenance therapy, none of the drugs appeared to have any benefit.
Maternal and fetal harms
We defined harms as “clinical markers and events that the authors of individual studies considered as adverse events or side effects.”
Among maternal harms were serious cardiac side effects, including arrhythmias, heart failure, and chest pain, linked to β-mimetics. Minor cardiovascular harms were also higher among women given β-mimetics. In addition, calcium channel blockers appeared to increase the risk of minor cardiovascular harms, but not as much as the β-mimetics.
Overall, maternal cardiac, metabolic, and psychologic harms were more prevalent among women taking β-mimetics. This may be due, at least in part, to the fact that studies of β-mimetics tended to look for these effects more than other studies did.
As for short-term fetal harms, we found “little consistent evidence” of them in the infants of women receiving these drugs, and the studies lacked sufficient data to evaluate potential long-term harms.
What later analyses found
After 1999, the cutoff year of our review, several relatively large studies showed the oxytocin antagonist atosiban to be effective as acute7,8and maintenance8 therapy, with a favorable side effect profile. Another trial9 compared 2 doses of magnesium (2 and 5 g per hour); the higher dose acted more quickly but with more side effects. These and other studies do not alter our conclusions about the effectiveness of tocolytic therapy—or the specifics of the 5 drugs studied.
2 useful markers
In the 1990s, 2 biologic markers were discovered that improve the precision of preterm birth risk assessment:
- fetal fibronectin (fFN) and
- endovaginal sonography (EVUSD).1
Use of EVUSD enables measurement of the cervix from the internal to external os. Cervices shorten before spontaneous birth.
These 2 tests, when positive (fFN detected or cervical length
I use a negative test to identify women who do not require further treatment or evaluation. If a patient has a negative fFN or EVUSD, I would not transport her to a tertiary care center. In fact, I would probably discharge her home with close follow-up.
3 concerns about the tests
Clinicians tend to have some concerns about incorporating these tests into their routines:
- How reliable is negative predictive value? Arguably, these tests perform better than clinical judgment and can spare many women unnecessary treatments.2 No test is perfect, however. These bio-markers should be adjuncts to—not replacements for—clinical wisdom.
- What about false results? With fFN, a proper collection kit with plastic tube and Dacron swab is critical because the molecule will adhere to glass or cotton, creating a false-negative result. A false-positive result can occur after recent coitus or a digital cervical exam; therefore, collect fFN specimens before checking the cervix. With EVUSD, the examinations require a moderate amount of skill.
- Which biomarker is best? Both fFN and EVUSD make independent and separate contributions to the prediction of preterm birth. Therefore, I use both.
Start Tocolysis And Antibiotics?
Patricia’s fFN and EVUSD tests are both positive. Should you start tocolysis and antibiotic therapy prior to transfer?
Metaanalysis suggests tocolysis, and antibiotics extend the interval between symptom onset and delivery.1The length of this prolongation can be measured in days, and no evidence suggests that prolonged pharmacotherapy has any benefit.
I would initiate both therapies while waiting for the mother to be moved to a tertiary center, even though neither therapy has been shown to improve perinatal outcome.
Tocolysis. We could find no differences among tocolytic drugs.3 Serious side effects are rare, but nuisance cardiovascular symptoms are frequent. Sympathomimetic drugs lead to lethargy, and magnesium is associated with malaise. Magnesium requires intravenous access and should be given only via infusion pump by trained personnel. That often means a nurse must accompany the patient to the Level III hospital.
Thus, for logistical reasons, I favor nonsteroidal anti-inflammatory drugs, of which indomethacin is the most widely studied. Indomethacin can be given by mouth or rectum, with minimal side effects. Harm to the fetus is rare if the drug is used acutely for only 48 to 72 hours (the maximum duration of any potential benefit).
Antibiotics. Current protocols calling for betalactam antibiotic therapy as prophylaxis against early-onset neonatal sepsis in preterm births have led to almost universal use of antibiotics among these patients. Our metaanalysis did not demonstrate superior pregnancy prolongation with any other regimen, so the one for group B strep prophylaxis provides a double benefit.4 As with tocolytics, there is no role for maintenance therapy.
When Contractions Cease
Patricia is transferred and completes her steroid therapy. Her symptoms and contractions cease. After a few days of observation and no cervical changes, she is discharged home. She asks about home therapies, work, activities, and sex.
Since our metaanalysis of tocolysis studies showed no efficacy for maintenance regimens, I do not recommend them except in this rare situation: when a woman has so much uterine activity without cervical change that she is unable to rest or complete her daily activities. In this case I would favor “as needed” doses of a β-mimetic drug by mouth.
Although home uterine activity monitors and subcutaneous tocolytic pumps are available, evidence suggests they are ineffective.1I seldom, if ever, use these devices.
Despite the almost universal recommendation that women at risk of preterm birth avoid physical and sexual activity, we lack evidence that bed rest or abstinence prolong pregnancy or prevent preterm birth.
Is sex allowed? When we studied both physical activity and sexuality in asymptomatic women at midpregnancy, neither was associated with spontaneous preterm birth.5,6 Therefore, I do not recommend restricting activity or sexual intercourse. Instead, I encourage women to carefully assess uterine activity. If certain behaviors appear to increase contractions, those behaviors should be limited.
Counsel her to trust her instincts. It is important to encourage the patient to trust her own instincts, so that an overzealous employer or partner cannot coerce or cajole her to do something that violates her internal sense of well-being.
The author reports no financial relationships relevant to this article.
A 25-year-old primigravida with an intrauterine pregnancy at 26 weeks presents with contractions of moderate intensity every 4 minutes, intact membranes, and minimal vaginal bleeding. On digital exam, her cervix is soft, 50% effaced, and closed. Estimated fetal weight is 775 g.
You are at a Level I hospital in a rural community, 90 minutes from a tertiary nursery. What steps should you take first?
Tocolytics and antibiotics are the first steps. They may help to maximize the benefits of secondary strategies such as antenatal corticosteroids during transport to a tertiary care facility. In addition, assessment of fetal fibronectin levels and use of endovaginal ultrasound can supplement clinical judgment and improve prediction of outcomes. Their excellent negative predictive value can spare many women unnecessary and potentially harmful treatments.
This article discusses these measures in the context of an actual case.
The value of “secondary prevention”
Giving corticosteroids to enhance fetal lung and brain maturity and transporting the mother to a tertiary care center may not prevent preterm delivery, but they can mitigate some of the damage and are supported by the evidence.
Corticosteroids. Given the clear evidence of their efficacy, steroids should be administered once preterm birth appears likely. I would give steroids before maternal transport.
Betamethasone is preferable to dexamethasone, which may be toxic to the fetal central nervous system. However, dexamethasone is preferable to no therapy.
Contraindications to corticosteroids include systemic maternal or fetal infections and maternal endocrinopathies such as Cushing’s disease or poorly controlled diabetes.
Transport to tertiary care. A neonatal intensive care unit clearly benefits tiny babies. Clinicians should be aware of the pediatric capacity of their community hospitals and maintain a referral relationship with the nearest tertiary care centers. Conversely, clinicians on the receiving end of maternal transports should make every effort to expedite these referrals.
Is Local Care Too Risky?
Patricia and her family strongly prefer that she undergo treatment in her own community, if at all possible.
Signs and symptoms of preterm labor are poor predictors of preterm birth. Although most symptomatic women deliver at term, even the most clinically astute physician cannot predict when a symptomatic patient will deliver.
Which tocolytic is most effective?
Berkman ND, Thorp JM Jr, Lohr KN, et al. Tocolytic treatment for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2003;188:1648–1659.
No single drug is best. In this metaanalysis, magnesium, β-mimetics, calcium channel blockers, and nonsteroidal anti-inflammatory drugs (NSAIDs) performed about the same at prolonging the interval between onset of preterm labor and actual birth, compared with placebo or no treatment. Ethanol was less effective and “inappropriate.” Tocolytics are given to stop contractions (first-line therapy) and to maintain quiescence after an acute episode (maintenance therapy).
To determine the most effective tocolytic, we analyzed 16 studies of first-line therapy and 8 involving maintenance therapy, using the above 5 drug classes.
How 5 drugs compare
Estimated odds ratios suggest that, when used as first-line therapy, all the drugs except ethanol are about the same. Odds ratios ranged from 1.622 for β-mimetics to 2.485 for calcium channel blockers. (The odds ratio for NSAIDs was based on only 1 study.)
When we tested whether β-mimetics, calcium channel blockers, and magnesium sulfate had the same effects, compared with placebo, the results suggested that they do not. However, the body of literature was not large enough to establish this conclusively.
Overall, β-mimetics appear to lack superiority over the other drugs as first-line therapy and cause more maternal harms, while ethanol is “inappropriate” and no longer in use.
As maintenance therapy, none of the drugs appeared to have any benefit.
Maternal and fetal harms
We defined harms as “clinical markers and events that the authors of individual studies considered as adverse events or side effects.”
Among maternal harms were serious cardiac side effects, including arrhythmias, heart failure, and chest pain, linked to β-mimetics. Minor cardiovascular harms were also higher among women given β-mimetics. In addition, calcium channel blockers appeared to increase the risk of minor cardiovascular harms, but not as much as the β-mimetics.
Overall, maternal cardiac, metabolic, and psychologic harms were more prevalent among women taking β-mimetics. This may be due, at least in part, to the fact that studies of β-mimetics tended to look for these effects more than other studies did.
As for short-term fetal harms, we found “little consistent evidence” of them in the infants of women receiving these drugs, and the studies lacked sufficient data to evaluate potential long-term harms.
What later analyses found
After 1999, the cutoff year of our review, several relatively large studies showed the oxytocin antagonist atosiban to be effective as acute7,8and maintenance8 therapy, with a favorable side effect profile. Another trial9 compared 2 doses of magnesium (2 and 5 g per hour); the higher dose acted more quickly but with more side effects. These and other studies do not alter our conclusions about the effectiveness of tocolytic therapy—or the specifics of the 5 drugs studied.
2 useful markers
In the 1990s, 2 biologic markers were discovered that improve the precision of preterm birth risk assessment:
- fetal fibronectin (fFN) and
- endovaginal sonography (EVUSD).1
Use of EVUSD enables measurement of the cervix from the internal to external os. Cervices shorten before spontaneous birth.
These 2 tests, when positive (fFN detected or cervical length
I use a negative test to identify women who do not require further treatment or evaluation. If a patient has a negative fFN or EVUSD, I would not transport her to a tertiary care center. In fact, I would probably discharge her home with close follow-up.
3 concerns about the tests
Clinicians tend to have some concerns about incorporating these tests into their routines:
- How reliable is negative predictive value? Arguably, these tests perform better than clinical judgment and can spare many women unnecessary treatments.2 No test is perfect, however. These bio-markers should be adjuncts to—not replacements for—clinical wisdom.
- What about false results? With fFN, a proper collection kit with plastic tube and Dacron swab is critical because the molecule will adhere to glass or cotton, creating a false-negative result. A false-positive result can occur after recent coitus or a digital cervical exam; therefore, collect fFN specimens before checking the cervix. With EVUSD, the examinations require a moderate amount of skill.
- Which biomarker is best? Both fFN and EVUSD make independent and separate contributions to the prediction of preterm birth. Therefore, I use both.
Start Tocolysis And Antibiotics?
Patricia’s fFN and EVUSD tests are both positive. Should you start tocolysis and antibiotic therapy prior to transfer?
Metaanalysis suggests tocolysis, and antibiotics extend the interval between symptom onset and delivery.1The length of this prolongation can be measured in days, and no evidence suggests that prolonged pharmacotherapy has any benefit.
I would initiate both therapies while waiting for the mother to be moved to a tertiary center, even though neither therapy has been shown to improve perinatal outcome.
Tocolysis. We could find no differences among tocolytic drugs.3 Serious side effects are rare, but nuisance cardiovascular symptoms are frequent. Sympathomimetic drugs lead to lethargy, and magnesium is associated with malaise. Magnesium requires intravenous access and should be given only via infusion pump by trained personnel. That often means a nurse must accompany the patient to the Level III hospital.
Thus, for logistical reasons, I favor nonsteroidal anti-inflammatory drugs, of which indomethacin is the most widely studied. Indomethacin can be given by mouth or rectum, with minimal side effects. Harm to the fetus is rare if the drug is used acutely for only 48 to 72 hours (the maximum duration of any potential benefit).
Antibiotics. Current protocols calling for betalactam antibiotic therapy as prophylaxis against early-onset neonatal sepsis in preterm births have led to almost universal use of antibiotics among these patients. Our metaanalysis did not demonstrate superior pregnancy prolongation with any other regimen, so the one for group B strep prophylaxis provides a double benefit.4 As with tocolytics, there is no role for maintenance therapy.
When Contractions Cease
Patricia is transferred and completes her steroid therapy. Her symptoms and contractions cease. After a few days of observation and no cervical changes, she is discharged home. She asks about home therapies, work, activities, and sex.
Since our metaanalysis of tocolysis studies showed no efficacy for maintenance regimens, I do not recommend them except in this rare situation: when a woman has so much uterine activity without cervical change that she is unable to rest or complete her daily activities. In this case I would favor “as needed” doses of a β-mimetic drug by mouth.
Although home uterine activity monitors and subcutaneous tocolytic pumps are available, evidence suggests they are ineffective.1I seldom, if ever, use these devices.
Despite the almost universal recommendation that women at risk of preterm birth avoid physical and sexual activity, we lack evidence that bed rest or abstinence prolong pregnancy or prevent preterm birth.
Is sex allowed? When we studied both physical activity and sexuality in asymptomatic women at midpregnancy, neither was associated with spontaneous preterm birth.5,6 Therefore, I do not recommend restricting activity or sexual intercourse. Instead, I encourage women to carefully assess uterine activity. If certain behaviors appear to increase contractions, those behaviors should be limited.
Counsel her to trust her instincts. It is important to encourage the patient to trust her own instincts, so that an overzealous employer or partner cannot coerce or cajole her to do something that violates her internal sense of well-being.
The author reports no financial relationships relevant to this article.
1. Berkman ND, Thorp JM, Hartmann KE, et al. Management of Preterm Labor. Evidence Report/Technology Assessment #18. Rockville, Md: Agency for Healthcare Research and Quality; December 2000. AHRQ publication 01-E021.
2. Thorp JM, Jr. ACOG Committee on Practice Bulletins. Management of preterm labor. Obstet Gynecol. 2003;101:1039-1047.
3. Berkman ND, Thorp JM, Jr, Lohr KN, et al. Tocolytic treatment for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2003;188:1648-1659.
4. Thorp JM, Jr, Hartmann KE, Berkman ND, et al. Antibiotic therapy for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2002;186:587-592.
5. Sayle AE, Savitz DA, Thorp JM, Jr, Hertz-Picciotto I, Wilcox AJ. Sexual activity during late pregnancy and preterm delivery. Obstet Gynecol. 2001;97:283-289.
6. Evenson KR, Siega-Riz AM, Savitz DA, Leiferman JA, Thorp JM, Jr. Vigorous leisure activity and pregnancy outcome. Epidemiology. 2002;13:653-659.
7. Moutquin JM, Sherman D, Cohen H, et al. Double-blind, randomized, controlled trial of atosiban and ritrodine in the treatment of preterm labor: a multicenter effectiveness and safety study. Am J Obstet Gynecol. 2000;182:1191-1199.
8. Romero R, Sibai BM, Sanchez-Ramos L, et al. An oxytocin receptor antagonist (atosiban) in the treatment of preterm labor: a randomized, double-blind, placebo-controlled trial with tocolytic rescue. Am J Obstet Gynecol. 2000;182:1173-1183.
9. Terrone DA, Rinehart BK, Kimmel ES, May WL, Larmon JE, Morrison JC. A prospective, randomized, controlled trial of high and low maintenance doses of magnesium sulfate for acute tocolysis. Am J Obstet Gynecol. 2000;182:1477-1482.
1. Berkman ND, Thorp JM, Hartmann KE, et al. Management of Preterm Labor. Evidence Report/Technology Assessment #18. Rockville, Md: Agency for Healthcare Research and Quality; December 2000. AHRQ publication 01-E021.
2. Thorp JM, Jr. ACOG Committee on Practice Bulletins. Management of preterm labor. Obstet Gynecol. 2003;101:1039-1047.
3. Berkman ND, Thorp JM, Jr, Lohr KN, et al. Tocolytic treatment for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2003;188:1648-1659.
4. Thorp JM, Jr, Hartmann KE, Berkman ND, et al. Antibiotic therapy for the management of preterm labor: a review of the evidence. Am J Obstet Gynecol. 2002;186:587-592.
5. Sayle AE, Savitz DA, Thorp JM, Jr, Hertz-Picciotto I, Wilcox AJ. Sexual activity during late pregnancy and preterm delivery. Obstet Gynecol. 2001;97:283-289.
6. Evenson KR, Siega-Riz AM, Savitz DA, Leiferman JA, Thorp JM, Jr. Vigorous leisure activity and pregnancy outcome. Epidemiology. 2002;13:653-659.
7. Moutquin JM, Sherman D, Cohen H, et al. Double-blind, randomized, controlled trial of atosiban and ritrodine in the treatment of preterm labor: a multicenter effectiveness and safety study. Am J Obstet Gynecol. 2000;182:1191-1199.
8. Romero R, Sibai BM, Sanchez-Ramos L, et al. An oxytocin receptor antagonist (atosiban) in the treatment of preterm labor: a randomized, double-blind, placebo-controlled trial with tocolytic rescue. Am J Obstet Gynecol. 2000;182:1173-1183.
9. Terrone DA, Rinehart BK, Kimmel ES, May WL, Larmon JE, Morrison JC. A prospective, randomized, controlled trial of high and low maintenance doses of magnesium sulfate for acute tocolysis. Am J Obstet Gynecol. 2000;182:1477-1482.