User login
EMPEROR-Preserved: Empagliflozin scores HFpEF breakthrough
Updated August 30, 2021
The SGLT2 inhibitor empagliflozin achieved in EMPEROR-Preserved what no other agent could previously do: unequivocally cut the incidence of cardiovascular death or hospitalization in patients with heart failure and preserved ejection fraction (HFpEF).
Treatment with empagliflozin (Jardiance) led to a significant 21% relative reduction in the rate of cardiovascular death or hospitalization for heart failure (HHF), compared with placebo, among 5,988 randomized patients with HFpEF during a median 26 months of follow-up, proving that patients with HFpEF finally have a treatment that gives them clinically meaningful benefit, and paving the way to an abrupt change in management of these patients, experts said.
“This is the first trial to show unequivocal benefits of any drug on major heart failure outcomes in patients with HFpEF,” Stefan D. Anker, MD, PhD, declared at the virtual annual congress of the European Society of Cardiology.
The 21% relative reduction, which reflected a cut in the absolute rate of the trial’s primary composite endpoint of 3.3% compared with placebo, was driven mainly by a significant 27% relative reduction in the incidence of HHF (P < .001). Empagliflozin treatment, on top of standard therapy for patients with HFpEF, also resulted in a nonsignificant 9% relative risk reduction in the incidence of cardiovascular death, but it had no discernible impact on the rate of death from any cause, said Dr. Anker, professor of cardiology at Charité Medical University in Berlin.
Concurrently with his talk at the meeting, the results were published online in the New England Journal of Medicine.
Practice will change ‘quickly’
“This will definitely change our practice, and quite quickly,” said Carlos Aguiar, MD, chair of the Advanced Heart Failure and Heart Transplantation Unit at Hospital Santa Cruz in Carnaxide, Portugal, who was not involved in the study.
Transition to routine use of empagliflozin in patients with HFpEF should be swift because it has already become a mainstay of treatment for patients with heart failure with reduced ejection fraction (HFrEF) based on evidence for empagliflozin in EMPEROR-Reduced. A second sodium-glucose cotransporter 2 (SGLT2 ) inhibitor, dapagliflozin (Farxiga), is also an option for treating HFrEF based on results in the DAPA-HF trial, and the DELIVER trial, still in progress, is testing dapagliflozin as a HFpEF treatment in about 6,000 patients, with results expected in 2022.
About half of the patients in EMPEROR-Preserved had diabetes, and the treatment effects on HFpEF were similar regardless of patients’ diabetes status. Empagliflozin, like other members of the SGLT2 inhibitor class, boosts urinary excretion of glucose and received initial regulatory approval as an agent for glycemic control in patients with type 2 diabetes. Empagliflozin also has U.S.-approved marketing indications for treating patients with HFrEF whether or not they also have diabetes, and for reducing cardiovascular death in patients with type 2 diabetes and cardiovascular disease.
“We already use this drug class in cardiovascular medicine and to treat patients with type 2 diabetes, and we have been eager to find a treatment for patients with HFpEF. This is something that will be really significant,” said Dr. Aguiar.
Heart failure clinicians have “become familiar prescribing” SGLT2 inhibitors following approval of HFrEF indications for some of these agents, noted Mary Norine Walsh, MD, a heart failure specialist with Ascension Medical Group in Indianapolis. The new results “are good news because there have been so few options” for patients with HFpEF, she said in an interview.
EMPEROR-Preserved “is the first phase 3 clinical trial that exclusively enrolled patients with heart failure and an ejection fraction of more than 40% to meet its primary outcome,” and the results “represent a major win against a medical condition that had previously proven formidable,” Mark H. Drazner, MD, said in an editorial that accompanied the published results.
The trial’s findings “should contribute to a change in clinical practice given the paucity of therapeutic options available for patients with HFpEF,” wrote Dr. Drazner, a heart failure specialist who is professor and clinical chief of cardiology at UT Southwestern Medical Center in Dallas.
Theresa A, McDonagh, MD, MBChB, who chaired the panel that just released revised guidelines from the European Society of Cardiology for managing patients with heart failure, predicted that empagliflozin treatment for patients with HFpEF will soon show up in guidelines. It will likely receive a “should be considered” ranking despite being a single study because of the impressive size of the treatment effect and lack of well-supported alternative treatments, she commented as a discussant of the trial during its presentation at the congress. If the DELIVER trial with dapagliflozin shows a similar effect, the recommendation would likely become even stronger, added Dr. McDonagh, a heart failure specialist and professor of cardiology at King’s College, London.
More women enrolled than ever before
EMPEROR-Preserved enrolled adults with chronic HFpEF in New York Heart Association functional class II-IV and a left ventricular ejection fraction greater than 40% starting in 2017 at more than 600 sites in more than 20 countries worldwide including the United States. As background therapy, more than 80% of patients received treatment with either an ACE inhibitor or angiotensin receptor blocker (in some instances in the form of sacubitril/valsartan), more than 80% were on a beta-blocker, and about a third were taking a mineralocorticoid receptor antagonist, making them “very well treated HFpEF patients,” Dr. Anker said.
One of the most notable features of enrollment was that 45% of participants were women, giving this trial the highest inclusion of women compared with all prior studies in patients with HFpEF or with HFrEF, said Dr. Walsh. “HFpEF is very prevalent in woman,” she noted, and having this high participation rate of women in the study increases its relevance to these patients. “It’s important to be able to tell women that patients like you were in the study so we can more easily apply the lessons from the trial to you. That can’t be stressed enough,” she said.
The primary outcome occurred in 415 (13.8%) of the 2,997 patients in the empagliflozin group and in 511 (17.1%) of 2,991 patients who received placebo (hazard ratio, 0.79; 95% confidence interval, 0.69-0.90; P < .001).
The study showed a safety profile consistent with prior experience with empagliflozin, Dr. Anker added.
Pooling EMPEROR-Preserved with EMPEROR-Reduced
The investigators who ran EMPEROR-Preserved designed the trial to closely parallel the EMPEROR-Reduced trial in patients with HFrEF, and they included a prespecified analysis (EMPEROR-Pooled) that combined the more than 9,700 patients in the two studies. This showed a consistent and robust benefit from empagliflozin for reducing HHF across a wide spectrum of patients with heart failure, ranging from patients with left ventricular ejection fractions of less than 25% to patients with ejection fractions as high as 64%. However, the analysis also showed that patients with ejection fractions of 65% or greater received no discernible benefit from empagliflozin, Milton Packer, MD, reported in a separate talk at the congress.
“The findings demonstrate the benefits of empagliflozin across a broad range of patients with heart failure who have ejection fractions of less than 60%-65%,” said Dr. Packer, a researcher at Baylor University Medical Center in Dallas.
This apparent attenuation of an effect at higher ejection fractions “has been observed in other HFpEF trials, most recently in the PARAGON-HF trial” of sacubitril/valsartan (Entresto), he noted. Additional analyses led by Dr. Packer showed that in patients with ejection fractions below 65% the HHF benefit from empagliflozin consistently surpassed the benefit seen with sacubitril/valsartan in PARAGON-HF. But he recommended using both drugs in patients with HFpEF and an ejection fraction up to about 60%.
“If I had a patient with HFpEF I would use both drugs as well as beta-blockers and mineralocorticoid receptor antagonists,” he said during a press briefing.
Another finding from analysis of the EMPEROR-Reduced and EMPEROR-Preserved trials together was that patients with reduced ejection fractions showed a significant 49% relative reduction in the incidence of serious renal outcomes, but this effect was completely blunted in EMPEROR-Preserved.
“Ejection fraction influences the effects of empagliflozin on major renal outcomes,” concluded Dr. Packer in a report on this analysis published simultaneously with the main EMPEROR-Preserved findings (N Engl J Med. 2021 Aug 27. doi: 10.1056/NEJMc2112411). “These data from the EMPEROR trials are unique. We have no comparable data” from any of the other reported studies of SGLT2 inhibitors,” he said.
EMPEROR-Preserved was sponsored by Boehringer Ingelheim and by Eli Lilly, the two companies that jointly market empagliflozin (Jardiance). Dr. Anker has received personal fees from Boehringer Ingelheim and from several other companies, and he has received grants and personal fees from Abbott Vascular and Vifor. Dr. Packer has received consulting fees from Boehringer Ingelheim and from numerous other companies. Dr. McDonagh has has recent financial relationships with AstraZeneca, Cprpus, Novartis, Pfizer, and Vifor. Dr. Aguiar and Dr. Walsh had no disclosures.
Updated August 30, 2021
The SGLT2 inhibitor empagliflozin achieved in EMPEROR-Preserved what no other agent could previously do: unequivocally cut the incidence of cardiovascular death or hospitalization in patients with heart failure and preserved ejection fraction (HFpEF).
Treatment with empagliflozin (Jardiance) led to a significant 21% relative reduction in the rate of cardiovascular death or hospitalization for heart failure (HHF), compared with placebo, among 5,988 randomized patients with HFpEF during a median 26 months of follow-up, proving that patients with HFpEF finally have a treatment that gives them clinically meaningful benefit, and paving the way to an abrupt change in management of these patients, experts said.
“This is the first trial to show unequivocal benefits of any drug on major heart failure outcomes in patients with HFpEF,” Stefan D. Anker, MD, PhD, declared at the virtual annual congress of the European Society of Cardiology.
The 21% relative reduction, which reflected a cut in the absolute rate of the trial’s primary composite endpoint of 3.3% compared with placebo, was driven mainly by a significant 27% relative reduction in the incidence of HHF (P < .001). Empagliflozin treatment, on top of standard therapy for patients with HFpEF, also resulted in a nonsignificant 9% relative risk reduction in the incidence of cardiovascular death, but it had no discernible impact on the rate of death from any cause, said Dr. Anker, professor of cardiology at Charité Medical University in Berlin.
Concurrently with his talk at the meeting, the results were published online in the New England Journal of Medicine.
Practice will change ‘quickly’
“This will definitely change our practice, and quite quickly,” said Carlos Aguiar, MD, chair of the Advanced Heart Failure and Heart Transplantation Unit at Hospital Santa Cruz in Carnaxide, Portugal, who was not involved in the study.
Transition to routine use of empagliflozin in patients with HFpEF should be swift because it has already become a mainstay of treatment for patients with heart failure with reduced ejection fraction (HFrEF) based on evidence for empagliflozin in EMPEROR-Reduced. A second sodium-glucose cotransporter 2 (SGLT2 ) inhibitor, dapagliflozin (Farxiga), is also an option for treating HFrEF based on results in the DAPA-HF trial, and the DELIVER trial, still in progress, is testing dapagliflozin as a HFpEF treatment in about 6,000 patients, with results expected in 2022.
About half of the patients in EMPEROR-Preserved had diabetes, and the treatment effects on HFpEF were similar regardless of patients’ diabetes status. Empagliflozin, like other members of the SGLT2 inhibitor class, boosts urinary excretion of glucose and received initial regulatory approval as an agent for glycemic control in patients with type 2 diabetes. Empagliflozin also has U.S.-approved marketing indications for treating patients with HFrEF whether or not they also have diabetes, and for reducing cardiovascular death in patients with type 2 diabetes and cardiovascular disease.
“We already use this drug class in cardiovascular medicine and to treat patients with type 2 diabetes, and we have been eager to find a treatment for patients with HFpEF. This is something that will be really significant,” said Dr. Aguiar.
Heart failure clinicians have “become familiar prescribing” SGLT2 inhibitors following approval of HFrEF indications for some of these agents, noted Mary Norine Walsh, MD, a heart failure specialist with Ascension Medical Group in Indianapolis. The new results “are good news because there have been so few options” for patients with HFpEF, she said in an interview.
EMPEROR-Preserved “is the first phase 3 clinical trial that exclusively enrolled patients with heart failure and an ejection fraction of more than 40% to meet its primary outcome,” and the results “represent a major win against a medical condition that had previously proven formidable,” Mark H. Drazner, MD, said in an editorial that accompanied the published results.
The trial’s findings “should contribute to a change in clinical practice given the paucity of therapeutic options available for patients with HFpEF,” wrote Dr. Drazner, a heart failure specialist who is professor and clinical chief of cardiology at UT Southwestern Medical Center in Dallas.
Theresa A, McDonagh, MD, MBChB, who chaired the panel that just released revised guidelines from the European Society of Cardiology for managing patients with heart failure, predicted that empagliflozin treatment for patients with HFpEF will soon show up in guidelines. It will likely receive a “should be considered” ranking despite being a single study because of the impressive size of the treatment effect and lack of well-supported alternative treatments, she commented as a discussant of the trial during its presentation at the congress. If the DELIVER trial with dapagliflozin shows a similar effect, the recommendation would likely become even stronger, added Dr. McDonagh, a heart failure specialist and professor of cardiology at King’s College, London.
More women enrolled than ever before
EMPEROR-Preserved enrolled adults with chronic HFpEF in New York Heart Association functional class II-IV and a left ventricular ejection fraction greater than 40% starting in 2017 at more than 600 sites in more than 20 countries worldwide including the United States. As background therapy, more than 80% of patients received treatment with either an ACE inhibitor or angiotensin receptor blocker (in some instances in the form of sacubitril/valsartan), more than 80% were on a beta-blocker, and about a third were taking a mineralocorticoid receptor antagonist, making them “very well treated HFpEF patients,” Dr. Anker said.
One of the most notable features of enrollment was that 45% of participants were women, giving this trial the highest inclusion of women compared with all prior studies in patients with HFpEF or with HFrEF, said Dr. Walsh. “HFpEF is very prevalent in woman,” she noted, and having this high participation rate of women in the study increases its relevance to these patients. “It’s important to be able to tell women that patients like you were in the study so we can more easily apply the lessons from the trial to you. That can’t be stressed enough,” she said.
The primary outcome occurred in 415 (13.8%) of the 2,997 patients in the empagliflozin group and in 511 (17.1%) of 2,991 patients who received placebo (hazard ratio, 0.79; 95% confidence interval, 0.69-0.90; P < .001).
The study showed a safety profile consistent with prior experience with empagliflozin, Dr. Anker added.
Pooling EMPEROR-Preserved with EMPEROR-Reduced
The investigators who ran EMPEROR-Preserved designed the trial to closely parallel the EMPEROR-Reduced trial in patients with HFrEF, and they included a prespecified analysis (EMPEROR-Pooled) that combined the more than 9,700 patients in the two studies. This showed a consistent and robust benefit from empagliflozin for reducing HHF across a wide spectrum of patients with heart failure, ranging from patients with left ventricular ejection fractions of less than 25% to patients with ejection fractions as high as 64%. However, the analysis also showed that patients with ejection fractions of 65% or greater received no discernible benefit from empagliflozin, Milton Packer, MD, reported in a separate talk at the congress.
“The findings demonstrate the benefits of empagliflozin across a broad range of patients with heart failure who have ejection fractions of less than 60%-65%,” said Dr. Packer, a researcher at Baylor University Medical Center in Dallas.
This apparent attenuation of an effect at higher ejection fractions “has been observed in other HFpEF trials, most recently in the PARAGON-HF trial” of sacubitril/valsartan (Entresto), he noted. Additional analyses led by Dr. Packer showed that in patients with ejection fractions below 65% the HHF benefit from empagliflozin consistently surpassed the benefit seen with sacubitril/valsartan in PARAGON-HF. But he recommended using both drugs in patients with HFpEF and an ejection fraction up to about 60%.
“If I had a patient with HFpEF I would use both drugs as well as beta-blockers and mineralocorticoid receptor antagonists,” he said during a press briefing.
Another finding from analysis of the EMPEROR-Reduced and EMPEROR-Preserved trials together was that patients with reduced ejection fractions showed a significant 49% relative reduction in the incidence of serious renal outcomes, but this effect was completely blunted in EMPEROR-Preserved.
“Ejection fraction influences the effects of empagliflozin on major renal outcomes,” concluded Dr. Packer in a report on this analysis published simultaneously with the main EMPEROR-Preserved findings (N Engl J Med. 2021 Aug 27. doi: 10.1056/NEJMc2112411). “These data from the EMPEROR trials are unique. We have no comparable data” from any of the other reported studies of SGLT2 inhibitors,” he said.
EMPEROR-Preserved was sponsored by Boehringer Ingelheim and by Eli Lilly, the two companies that jointly market empagliflozin (Jardiance). Dr. Anker has received personal fees from Boehringer Ingelheim and from several other companies, and he has received grants and personal fees from Abbott Vascular and Vifor. Dr. Packer has received consulting fees from Boehringer Ingelheim and from numerous other companies. Dr. McDonagh has has recent financial relationships with AstraZeneca, Cprpus, Novartis, Pfizer, and Vifor. Dr. Aguiar and Dr. Walsh had no disclosures.
Updated August 30, 2021
The SGLT2 inhibitor empagliflozin achieved in EMPEROR-Preserved what no other agent could previously do: unequivocally cut the incidence of cardiovascular death or hospitalization in patients with heart failure and preserved ejection fraction (HFpEF).
Treatment with empagliflozin (Jardiance) led to a significant 21% relative reduction in the rate of cardiovascular death or hospitalization for heart failure (HHF), compared with placebo, among 5,988 randomized patients with HFpEF during a median 26 months of follow-up, proving that patients with HFpEF finally have a treatment that gives them clinically meaningful benefit, and paving the way to an abrupt change in management of these patients, experts said.
“This is the first trial to show unequivocal benefits of any drug on major heart failure outcomes in patients with HFpEF,” Stefan D. Anker, MD, PhD, declared at the virtual annual congress of the European Society of Cardiology.
The 21% relative reduction, which reflected a cut in the absolute rate of the trial’s primary composite endpoint of 3.3% compared with placebo, was driven mainly by a significant 27% relative reduction in the incidence of HHF (P < .001). Empagliflozin treatment, on top of standard therapy for patients with HFpEF, also resulted in a nonsignificant 9% relative risk reduction in the incidence of cardiovascular death, but it had no discernible impact on the rate of death from any cause, said Dr. Anker, professor of cardiology at Charité Medical University in Berlin.
Concurrently with his talk at the meeting, the results were published online in the New England Journal of Medicine.
Practice will change ‘quickly’
“This will definitely change our practice, and quite quickly,” said Carlos Aguiar, MD, chair of the Advanced Heart Failure and Heart Transplantation Unit at Hospital Santa Cruz in Carnaxide, Portugal, who was not involved in the study.
Transition to routine use of empagliflozin in patients with HFpEF should be swift because it has already become a mainstay of treatment for patients with heart failure with reduced ejection fraction (HFrEF) based on evidence for empagliflozin in EMPEROR-Reduced. A second sodium-glucose cotransporter 2 (SGLT2 ) inhibitor, dapagliflozin (Farxiga), is also an option for treating HFrEF based on results in the DAPA-HF trial, and the DELIVER trial, still in progress, is testing dapagliflozin as a HFpEF treatment in about 6,000 patients, with results expected in 2022.
About half of the patients in EMPEROR-Preserved had diabetes, and the treatment effects on HFpEF were similar regardless of patients’ diabetes status. Empagliflozin, like other members of the SGLT2 inhibitor class, boosts urinary excretion of glucose and received initial regulatory approval as an agent for glycemic control in patients with type 2 diabetes. Empagliflozin also has U.S.-approved marketing indications for treating patients with HFrEF whether or not they also have diabetes, and for reducing cardiovascular death in patients with type 2 diabetes and cardiovascular disease.
“We already use this drug class in cardiovascular medicine and to treat patients with type 2 diabetes, and we have been eager to find a treatment for patients with HFpEF. This is something that will be really significant,” said Dr. Aguiar.
Heart failure clinicians have “become familiar prescribing” SGLT2 inhibitors following approval of HFrEF indications for some of these agents, noted Mary Norine Walsh, MD, a heart failure specialist with Ascension Medical Group in Indianapolis. The new results “are good news because there have been so few options” for patients with HFpEF, she said in an interview.
EMPEROR-Preserved “is the first phase 3 clinical trial that exclusively enrolled patients with heart failure and an ejection fraction of more than 40% to meet its primary outcome,” and the results “represent a major win against a medical condition that had previously proven formidable,” Mark H. Drazner, MD, said in an editorial that accompanied the published results.
The trial’s findings “should contribute to a change in clinical practice given the paucity of therapeutic options available for patients with HFpEF,” wrote Dr. Drazner, a heart failure specialist who is professor and clinical chief of cardiology at UT Southwestern Medical Center in Dallas.
Theresa A, McDonagh, MD, MBChB, who chaired the panel that just released revised guidelines from the European Society of Cardiology for managing patients with heart failure, predicted that empagliflozin treatment for patients with HFpEF will soon show up in guidelines. It will likely receive a “should be considered” ranking despite being a single study because of the impressive size of the treatment effect and lack of well-supported alternative treatments, she commented as a discussant of the trial during its presentation at the congress. If the DELIVER trial with dapagliflozin shows a similar effect, the recommendation would likely become even stronger, added Dr. McDonagh, a heart failure specialist and professor of cardiology at King’s College, London.
More women enrolled than ever before
EMPEROR-Preserved enrolled adults with chronic HFpEF in New York Heart Association functional class II-IV and a left ventricular ejection fraction greater than 40% starting in 2017 at more than 600 sites in more than 20 countries worldwide including the United States. As background therapy, more than 80% of patients received treatment with either an ACE inhibitor or angiotensin receptor blocker (in some instances in the form of sacubitril/valsartan), more than 80% were on a beta-blocker, and about a third were taking a mineralocorticoid receptor antagonist, making them “very well treated HFpEF patients,” Dr. Anker said.
One of the most notable features of enrollment was that 45% of participants were women, giving this trial the highest inclusion of women compared with all prior studies in patients with HFpEF or with HFrEF, said Dr. Walsh. “HFpEF is very prevalent in woman,” she noted, and having this high participation rate of women in the study increases its relevance to these patients. “It’s important to be able to tell women that patients like you were in the study so we can more easily apply the lessons from the trial to you. That can’t be stressed enough,” she said.
The primary outcome occurred in 415 (13.8%) of the 2,997 patients in the empagliflozin group and in 511 (17.1%) of 2,991 patients who received placebo (hazard ratio, 0.79; 95% confidence interval, 0.69-0.90; P < .001).
The study showed a safety profile consistent with prior experience with empagliflozin, Dr. Anker added.
Pooling EMPEROR-Preserved with EMPEROR-Reduced
The investigators who ran EMPEROR-Preserved designed the trial to closely parallel the EMPEROR-Reduced trial in patients with HFrEF, and they included a prespecified analysis (EMPEROR-Pooled) that combined the more than 9,700 patients in the two studies. This showed a consistent and robust benefit from empagliflozin for reducing HHF across a wide spectrum of patients with heart failure, ranging from patients with left ventricular ejection fractions of less than 25% to patients with ejection fractions as high as 64%. However, the analysis also showed that patients with ejection fractions of 65% or greater received no discernible benefit from empagliflozin, Milton Packer, MD, reported in a separate talk at the congress.
“The findings demonstrate the benefits of empagliflozin across a broad range of patients with heart failure who have ejection fractions of less than 60%-65%,” said Dr. Packer, a researcher at Baylor University Medical Center in Dallas.
This apparent attenuation of an effect at higher ejection fractions “has been observed in other HFpEF trials, most recently in the PARAGON-HF trial” of sacubitril/valsartan (Entresto), he noted. Additional analyses led by Dr. Packer showed that in patients with ejection fractions below 65% the HHF benefit from empagliflozin consistently surpassed the benefit seen with sacubitril/valsartan in PARAGON-HF. But he recommended using both drugs in patients with HFpEF and an ejection fraction up to about 60%.
“If I had a patient with HFpEF I would use both drugs as well as beta-blockers and mineralocorticoid receptor antagonists,” he said during a press briefing.
Another finding from analysis of the EMPEROR-Reduced and EMPEROR-Preserved trials together was that patients with reduced ejection fractions showed a significant 49% relative reduction in the incidence of serious renal outcomes, but this effect was completely blunted in EMPEROR-Preserved.
“Ejection fraction influences the effects of empagliflozin on major renal outcomes,” concluded Dr. Packer in a report on this analysis published simultaneously with the main EMPEROR-Preserved findings (N Engl J Med. 2021 Aug 27. doi: 10.1056/NEJMc2112411). “These data from the EMPEROR trials are unique. We have no comparable data” from any of the other reported studies of SGLT2 inhibitors,” he said.
EMPEROR-Preserved was sponsored by Boehringer Ingelheim and by Eli Lilly, the two companies that jointly market empagliflozin (Jardiance). Dr. Anker has received personal fees from Boehringer Ingelheim and from several other companies, and he has received grants and personal fees from Abbott Vascular and Vifor. Dr. Packer has received consulting fees from Boehringer Ingelheim and from numerous other companies. Dr. McDonagh has has recent financial relationships with AstraZeneca, Cprpus, Novartis, Pfizer, and Vifor. Dr. Aguiar and Dr. Walsh had no disclosures.
FROM ESC CONGRESS 2021
Genetic link may tie cannabis use disorder to severe COVID-19
The same genetic variations may boost susceptibility to both severe COVID-19 and cannabis use disorder (CUD), a new study suggests. The research does not confirm a genetic link, but the lead author said the signs of an association are still “troubling.”
“Reducing cannabis use among heavy users may potentially provide protection against severe COVID-19 presentations,” Alexander S. Hatoum, PhD, a postdoctoral scholar at Washington University, St. Louis, said in an interview. “Outside of individual risk, these data also have important implications for policy regarding vaccination as well as treatment prioritization in an overly taxed medical system.”
The study was published in the journal Biological Psychiatry Global Open Science.
Dr. Hatoum and colleagues launched the study to gain insight into whether CUD might be a risk factor for severe COVID-19 presentations.
As defined by the DSM-5, people with CUD suffer from impairment or distress because of their cannabis use and meet at least 2 of 11 criteria over a 12-month period, such as cravings, cannabis tolerance, and withdrawal symptoms. According to a 2020 study that examined 2008-2016 data, 2.72% of children aged 12-17 showed signs of CUD, as did 1.23% of those aged over 26.
The primary reasons for hospitalization and death related to COVID-19 are respiratory symptoms. “And we have observed that genetic vulnerability to CUD is shared with respiratory disease, even after tobacco use is considered,” Dr. Hatoum said.
He and his colleagues examined data from genomewide association studies and searched for genetic correlations between CUD (14,080 cases, 343,726 controls) and COVID-19 hospitalization (9,373 cases, 1,197,256 controls). “Genetic vulnerability to COVID-19 was correlated with genetic liability to CUD (P = 1.33e–6),” the researchers wrote. “This association remained when accounting for genetic liability to related risk factors and covariates (P = .012-.049).”
According to Dr. Hatoum, the researchers found inconclusive evidence that CUD might worsen COVID-19 cases. “We applied statistical causal models, which found an effect consistent with causality, but it was nonsignificant,” he said.
Despite the absence of causality, the study findings could prove useful for clinicians and policy makers.
“Those struggling with CUD may be prioritized for vaccination and vaccination boosters to mitigate their higher likelihood of a severe COVID-19 presentation,” Dr. Hatoum said. “When testing positive for COVID-19, they may also be prioritized for earlier treatment.”
The study authors also added that the findings “urge caution” in regard to the wave of U.S. states legalizing cannabis. “Our data suggest that heavy cannabis use, but not lifetime cannabis use, represents a risk factor for severe COVID-19 presentations,” Dr. Hatoum said.
In an interview, Danielle Dick, PhD, who was not involved with the study, said it applies “cutting-edge methods to an important research question” and offers a “hint” of a genetic risk factor that makes some people more likely to be hospitalized for COVID-19. However, “the study does not tell us what those underlying genetically influenced processes might be,” added Dr. Dick, professor of psychology, and human and molecular genetics at Virginia Commonwealth University, Richmond. “And it’s an important caveat to point out that the results from this study are limited in that they are based on data from people from European descent – so they can’t necessarily be applied to address the harm experienced by so many people of color from the COVID pandemic. That’s an unfortunate limitation.”
As for the idea that the study findings should prompt caution about marijuana legalization, Dr. Dick said it’s true that increased acceptability of drug use “increases the likelihood that individuals who are genetically vulnerable will develop problems. There is robust evidence of this.”
However, Dr. Dick said, “the legalization of marijuana is a complex topic because the health consequences aren’t the only consideration when it comes to legalization. The other side of the coin is the huge harm that has been caused to communities of color through marijuana criminalization. Legalization will hopefully lead to decreased harm on that front. So it’s a double-edged sword.”
Dr. Hatoum, his colleagues, and Dr. Dick reported no relevant disclosures.
The same genetic variations may boost susceptibility to both severe COVID-19 and cannabis use disorder (CUD), a new study suggests. The research does not confirm a genetic link, but the lead author said the signs of an association are still “troubling.”
“Reducing cannabis use among heavy users may potentially provide protection against severe COVID-19 presentations,” Alexander S. Hatoum, PhD, a postdoctoral scholar at Washington University, St. Louis, said in an interview. “Outside of individual risk, these data also have important implications for policy regarding vaccination as well as treatment prioritization in an overly taxed medical system.”
The study was published in the journal Biological Psychiatry Global Open Science.
Dr. Hatoum and colleagues launched the study to gain insight into whether CUD might be a risk factor for severe COVID-19 presentations.
As defined by the DSM-5, people with CUD suffer from impairment or distress because of their cannabis use and meet at least 2 of 11 criteria over a 12-month period, such as cravings, cannabis tolerance, and withdrawal symptoms. According to a 2020 study that examined 2008-2016 data, 2.72% of children aged 12-17 showed signs of CUD, as did 1.23% of those aged over 26.
The primary reasons for hospitalization and death related to COVID-19 are respiratory symptoms. “And we have observed that genetic vulnerability to CUD is shared with respiratory disease, even after tobacco use is considered,” Dr. Hatoum said.
He and his colleagues examined data from genomewide association studies and searched for genetic correlations between CUD (14,080 cases, 343,726 controls) and COVID-19 hospitalization (9,373 cases, 1,197,256 controls). “Genetic vulnerability to COVID-19 was correlated with genetic liability to CUD (P = 1.33e–6),” the researchers wrote. “This association remained when accounting for genetic liability to related risk factors and covariates (P = .012-.049).”
According to Dr. Hatoum, the researchers found inconclusive evidence that CUD might worsen COVID-19 cases. “We applied statistical causal models, which found an effect consistent with causality, but it was nonsignificant,” he said.
Despite the absence of causality, the study findings could prove useful for clinicians and policy makers.
“Those struggling with CUD may be prioritized for vaccination and vaccination boosters to mitigate their higher likelihood of a severe COVID-19 presentation,” Dr. Hatoum said. “When testing positive for COVID-19, they may also be prioritized for earlier treatment.”
The study authors also added that the findings “urge caution” in regard to the wave of U.S. states legalizing cannabis. “Our data suggest that heavy cannabis use, but not lifetime cannabis use, represents a risk factor for severe COVID-19 presentations,” Dr. Hatoum said.
In an interview, Danielle Dick, PhD, who was not involved with the study, said it applies “cutting-edge methods to an important research question” and offers a “hint” of a genetic risk factor that makes some people more likely to be hospitalized for COVID-19. However, “the study does not tell us what those underlying genetically influenced processes might be,” added Dr. Dick, professor of psychology, and human and molecular genetics at Virginia Commonwealth University, Richmond. “And it’s an important caveat to point out that the results from this study are limited in that they are based on data from people from European descent – so they can’t necessarily be applied to address the harm experienced by so many people of color from the COVID pandemic. That’s an unfortunate limitation.”
As for the idea that the study findings should prompt caution about marijuana legalization, Dr. Dick said it’s true that increased acceptability of drug use “increases the likelihood that individuals who are genetically vulnerable will develop problems. There is robust evidence of this.”
However, Dr. Dick said, “the legalization of marijuana is a complex topic because the health consequences aren’t the only consideration when it comes to legalization. The other side of the coin is the huge harm that has been caused to communities of color through marijuana criminalization. Legalization will hopefully lead to decreased harm on that front. So it’s a double-edged sword.”
Dr. Hatoum, his colleagues, and Dr. Dick reported no relevant disclosures.
The same genetic variations may boost susceptibility to both severe COVID-19 and cannabis use disorder (CUD), a new study suggests. The research does not confirm a genetic link, but the lead author said the signs of an association are still “troubling.”
“Reducing cannabis use among heavy users may potentially provide protection against severe COVID-19 presentations,” Alexander S. Hatoum, PhD, a postdoctoral scholar at Washington University, St. Louis, said in an interview. “Outside of individual risk, these data also have important implications for policy regarding vaccination as well as treatment prioritization in an overly taxed medical system.”
The study was published in the journal Biological Psychiatry Global Open Science.
Dr. Hatoum and colleagues launched the study to gain insight into whether CUD might be a risk factor for severe COVID-19 presentations.
As defined by the DSM-5, people with CUD suffer from impairment or distress because of their cannabis use and meet at least 2 of 11 criteria over a 12-month period, such as cravings, cannabis tolerance, and withdrawal symptoms. According to a 2020 study that examined 2008-2016 data, 2.72% of children aged 12-17 showed signs of CUD, as did 1.23% of those aged over 26.
The primary reasons for hospitalization and death related to COVID-19 are respiratory symptoms. “And we have observed that genetic vulnerability to CUD is shared with respiratory disease, even after tobacco use is considered,” Dr. Hatoum said.
He and his colleagues examined data from genomewide association studies and searched for genetic correlations between CUD (14,080 cases, 343,726 controls) and COVID-19 hospitalization (9,373 cases, 1,197,256 controls). “Genetic vulnerability to COVID-19 was correlated with genetic liability to CUD (P = 1.33e–6),” the researchers wrote. “This association remained when accounting for genetic liability to related risk factors and covariates (P = .012-.049).”
According to Dr. Hatoum, the researchers found inconclusive evidence that CUD might worsen COVID-19 cases. “We applied statistical causal models, which found an effect consistent with causality, but it was nonsignificant,” he said.
Despite the absence of causality, the study findings could prove useful for clinicians and policy makers.
“Those struggling with CUD may be prioritized for vaccination and vaccination boosters to mitigate their higher likelihood of a severe COVID-19 presentation,” Dr. Hatoum said. “When testing positive for COVID-19, they may also be prioritized for earlier treatment.”
The study authors also added that the findings “urge caution” in regard to the wave of U.S. states legalizing cannabis. “Our data suggest that heavy cannabis use, but not lifetime cannabis use, represents a risk factor for severe COVID-19 presentations,” Dr. Hatoum said.
In an interview, Danielle Dick, PhD, who was not involved with the study, said it applies “cutting-edge methods to an important research question” and offers a “hint” of a genetic risk factor that makes some people more likely to be hospitalized for COVID-19. However, “the study does not tell us what those underlying genetically influenced processes might be,” added Dr. Dick, professor of psychology, and human and molecular genetics at Virginia Commonwealth University, Richmond. “And it’s an important caveat to point out that the results from this study are limited in that they are based on data from people from European descent – so they can’t necessarily be applied to address the harm experienced by so many people of color from the COVID pandemic. That’s an unfortunate limitation.”
As for the idea that the study findings should prompt caution about marijuana legalization, Dr. Dick said it’s true that increased acceptability of drug use “increases the likelihood that individuals who are genetically vulnerable will develop problems. There is robust evidence of this.”
However, Dr. Dick said, “the legalization of marijuana is a complex topic because the health consequences aren’t the only consideration when it comes to legalization. The other side of the coin is the huge harm that has been caused to communities of color through marijuana criminalization. Legalization will hopefully lead to decreased harm on that front. So it’s a double-edged sword.”
Dr. Hatoum, his colleagues, and Dr. Dick reported no relevant disclosures.
FROM BIOLOGICAL PSYCHIATRY GLOBAL OPEN SCIENCE
COVID-19: New GI symptoms don’t raise death risk in IBD
Death from COVID-19 was not more likely among patients with inflammatory bowel disease (IBD) who had COVID-19 who developed new GI symptoms after becoming infected, according to international registry data from nearly 3,000 adults.
Although GI symptoms may arise in the general population of COVID-19 patients, data on the association between GI symptoms and COVID-19 in patients with IBD are limited, as are data on the association of GI symptoms and COVID-19 outcomes in this population, Ryan C. Ungaro, MD, of the Icahn School of Medicine at Mount Sinai, New York, and colleagues wrote.
In a study published in Inflammatory Bowel Diseases, the researchers identified 2,917 adults with IBD who developed COVID-19 using the Surveillance Epidemiology of Coronavirus Under Research Exclusion in Inflammatory Bowel Disease (SECURE-IBD) database, a global registry created to understand COVID-19 outcomes in IBD patients.
The researchers recorded all new GI symptoms experienced by the patients while they were infected with COVID-19. Overall, 764 (26.2%) experienced new GI symptoms and 2,153 did not. The most common symptom was diarrhea, reported by 80% of the patients, followed by abdominal pain in 34%. Nausea and vomiting were reported by 24% and 12%, respectively, of all patients.
The average age of the patients was 43 years for those with no new GI symptoms and 40 for those without new GI symptoms; overall, approximately half were women and approximately three-quarters were White. Overall, 50% of those with new GI symptoms were in remission, as was the case for 58.4% of those without.
IBD patients who developed new GI symptoms were significantly more likely to be women, of Asian race, older, or have at least one comorbidity.
The researchers found no difference in new GI symptoms in patients with Crohn’s disease and ulcerative colitis. “Patients on any medication – but in particular [tumor necrosis factor] antagonist monotherapy – were less likely to report new GI symptoms.” they wrote.
Although IBD patients with new GI symptoms were significantly more likely than were those without new GI symptoms to be hospitalized for COVID-19 in bivariate analyses (31.4% vs. 19.2%; P < .001), they were not more likely to need a ventilator or intensive care (5.8% vs. 4.6%; P < .18). In a multivariate analysis, IBD patients with new GI symptoms had no greater risk of death from COVID-19 than did those without new GI symptoms (adjusted odds ratio, 0.72; 95% confidence interval, 0.38-1.36).
The new-onset GI symptoms common to IBD patients with COVID-19 are not likely caused by underlying disease activity, given the number of patients in remission who reported new GI symptoms, the researchers wrote.
The study findings were limited by several factors including the retrospective design, potential reporting bias, and reliance on physician global assessment for disease assessment, the researchers noted. However, the results were strengthened by the large sample size, by the ability to assess GI symptoms before and after COVID-19, and by the evaluation of GI symptoms and COVID-19 outcomes.
“In summary, new GI symptoms are common in IBD patients with COVID-19 and are not associated with an increased risk of death due to COVID-19,” the researchers concluded. “Our findings suggest that an increase in GI symptoms in IBD patients should prompt consideration of a COVID-19 diagnosis.”
Data to guide clinical care
“There are several potential causes for common GI symptoms, such as diarrhea and abdominal pain, among patients with IBD,” Shirley Cohen-Mekelburg, MD, of the University of Michigan, Ann Arbor, said in an interview. “These can be the initial presentation of an IBD flare, a noninflammatory cause such as irritable bowel syndrome, small intestinal bacterial overgrowth, or an infection such as Clostridioides difficile or SARS-CoV-2. Each of these diagnoses require different treatments. An IBD flare may require escalation of immunosuppressive medications such as biologics or corticosteroids, which can cause harm in the context of an untreated infection. Therefore, any guidance that will increase health care providers’ awareness of the possible causes of similar GI symptoms is important in caring for our patients with IBD. This is especially true in context of a newer entity such as COVID-19 with which we are overall less familiar.”
Dr. Cohen-Meckelburg said the lack of association between GI symptoms and death in IBD is reassuring. “It is interesting to note that GI symptoms, and particularly new diarrhea, were very common among patients with IBD and COVID-19.
“Health care providers who treat patients with IBD should have a high-index of suspicion for SARS-CoV-2 infections when patients with IBD present with GI symptoms,” said Dr. Cohen-Meckelburg. “The data from the current study may help us to consider standard testing to rule out COVID-19 as an alternative diagnosis when considering whether to treat patients with IBD who develop new GI symptoms for an IBD flare. This would be similar to how we currently test for C. difficile and other enteric infections before treating IBD flares.
“Every study has its limitations, which need to be considered in interpreting findings,” Dr. Cohen-Meckelburg noted . “SECURE-IBD has provided great insight into COVID-19 infections among patients with IBD. However, the registry relies on individuals reporting cases, so there is the potential for underreporting, particularly with less symptomatic or subclinical cases.”
The study was supported in part by the Helmsley Charitable Trust with additional funding provided by Pfizer, Takeda, Janssen, AbbVie, Lilly, Genentech, Boehringer Ingelheim, Bristol-Myers Squibb, Celtrion, and Arenapharm. Lead author Dr. Ungaro disclosed serving as an advisory board member or consultant for AbbVie, Bristol-Myers Squibb, Janssen, Eli Lilly, Pfizer, and Takeda and research support from AbbVie, Boehringer Ingelheim, and Pfizer. Other coauthors disclosed similar relationships with other pharmaceutical companies. Dr. Cohen-Mekelburg had no financial conflicts to disclose.
Death from COVID-19 was not more likely among patients with inflammatory bowel disease (IBD) who had COVID-19 who developed new GI symptoms after becoming infected, according to international registry data from nearly 3,000 adults.
Although GI symptoms may arise in the general population of COVID-19 patients, data on the association between GI symptoms and COVID-19 in patients with IBD are limited, as are data on the association of GI symptoms and COVID-19 outcomes in this population, Ryan C. Ungaro, MD, of the Icahn School of Medicine at Mount Sinai, New York, and colleagues wrote.
In a study published in Inflammatory Bowel Diseases, the researchers identified 2,917 adults with IBD who developed COVID-19 using the Surveillance Epidemiology of Coronavirus Under Research Exclusion in Inflammatory Bowel Disease (SECURE-IBD) database, a global registry created to understand COVID-19 outcomes in IBD patients.
The researchers recorded all new GI symptoms experienced by the patients while they were infected with COVID-19. Overall, 764 (26.2%) experienced new GI symptoms and 2,153 did not. The most common symptom was diarrhea, reported by 80% of the patients, followed by abdominal pain in 34%. Nausea and vomiting were reported by 24% and 12%, respectively, of all patients.
The average age of the patients was 43 years for those with no new GI symptoms and 40 for those without new GI symptoms; overall, approximately half were women and approximately three-quarters were White. Overall, 50% of those with new GI symptoms were in remission, as was the case for 58.4% of those without.
IBD patients who developed new GI symptoms were significantly more likely to be women, of Asian race, older, or have at least one comorbidity.
The researchers found no difference in new GI symptoms in patients with Crohn’s disease and ulcerative colitis. “Patients on any medication – but in particular [tumor necrosis factor] antagonist monotherapy – were less likely to report new GI symptoms.” they wrote.
Although IBD patients with new GI symptoms were significantly more likely than were those without new GI symptoms to be hospitalized for COVID-19 in bivariate analyses (31.4% vs. 19.2%; P < .001), they were not more likely to need a ventilator or intensive care (5.8% vs. 4.6%; P < .18). In a multivariate analysis, IBD patients with new GI symptoms had no greater risk of death from COVID-19 than did those without new GI symptoms (adjusted odds ratio, 0.72; 95% confidence interval, 0.38-1.36).
The new-onset GI symptoms common to IBD patients with COVID-19 are not likely caused by underlying disease activity, given the number of patients in remission who reported new GI symptoms, the researchers wrote.
The study findings were limited by several factors including the retrospective design, potential reporting bias, and reliance on physician global assessment for disease assessment, the researchers noted. However, the results were strengthened by the large sample size, by the ability to assess GI symptoms before and after COVID-19, and by the evaluation of GI symptoms and COVID-19 outcomes.
“In summary, new GI symptoms are common in IBD patients with COVID-19 and are not associated with an increased risk of death due to COVID-19,” the researchers concluded. “Our findings suggest that an increase in GI symptoms in IBD patients should prompt consideration of a COVID-19 diagnosis.”
Data to guide clinical care
“There are several potential causes for common GI symptoms, such as diarrhea and abdominal pain, among patients with IBD,” Shirley Cohen-Mekelburg, MD, of the University of Michigan, Ann Arbor, said in an interview. “These can be the initial presentation of an IBD flare, a noninflammatory cause such as irritable bowel syndrome, small intestinal bacterial overgrowth, or an infection such as Clostridioides difficile or SARS-CoV-2. Each of these diagnoses require different treatments. An IBD flare may require escalation of immunosuppressive medications such as biologics or corticosteroids, which can cause harm in the context of an untreated infection. Therefore, any guidance that will increase health care providers’ awareness of the possible causes of similar GI symptoms is important in caring for our patients with IBD. This is especially true in context of a newer entity such as COVID-19 with which we are overall less familiar.”
Dr. Cohen-Meckelburg said the lack of association between GI symptoms and death in IBD is reassuring. “It is interesting to note that GI symptoms, and particularly new diarrhea, were very common among patients with IBD and COVID-19.
“Health care providers who treat patients with IBD should have a high-index of suspicion for SARS-CoV-2 infections when patients with IBD present with GI symptoms,” said Dr. Cohen-Meckelburg. “The data from the current study may help us to consider standard testing to rule out COVID-19 as an alternative diagnosis when considering whether to treat patients with IBD who develop new GI symptoms for an IBD flare. This would be similar to how we currently test for C. difficile and other enteric infections before treating IBD flares.
“Every study has its limitations, which need to be considered in interpreting findings,” Dr. Cohen-Meckelburg noted . “SECURE-IBD has provided great insight into COVID-19 infections among patients with IBD. However, the registry relies on individuals reporting cases, so there is the potential for underreporting, particularly with less symptomatic or subclinical cases.”
The study was supported in part by the Helmsley Charitable Trust with additional funding provided by Pfizer, Takeda, Janssen, AbbVie, Lilly, Genentech, Boehringer Ingelheim, Bristol-Myers Squibb, Celtrion, and Arenapharm. Lead author Dr. Ungaro disclosed serving as an advisory board member or consultant for AbbVie, Bristol-Myers Squibb, Janssen, Eli Lilly, Pfizer, and Takeda and research support from AbbVie, Boehringer Ingelheim, and Pfizer. Other coauthors disclosed similar relationships with other pharmaceutical companies. Dr. Cohen-Mekelburg had no financial conflicts to disclose.
Death from COVID-19 was not more likely among patients with inflammatory bowel disease (IBD) who had COVID-19 who developed new GI symptoms after becoming infected, according to international registry data from nearly 3,000 adults.
Although GI symptoms may arise in the general population of COVID-19 patients, data on the association between GI symptoms and COVID-19 in patients with IBD are limited, as are data on the association of GI symptoms and COVID-19 outcomes in this population, Ryan C. Ungaro, MD, of the Icahn School of Medicine at Mount Sinai, New York, and colleagues wrote.
In a study published in Inflammatory Bowel Diseases, the researchers identified 2,917 adults with IBD who developed COVID-19 using the Surveillance Epidemiology of Coronavirus Under Research Exclusion in Inflammatory Bowel Disease (SECURE-IBD) database, a global registry created to understand COVID-19 outcomes in IBD patients.
The researchers recorded all new GI symptoms experienced by the patients while they were infected with COVID-19. Overall, 764 (26.2%) experienced new GI symptoms and 2,153 did not. The most common symptom was diarrhea, reported by 80% of the patients, followed by abdominal pain in 34%. Nausea and vomiting were reported by 24% and 12%, respectively, of all patients.
The average age of the patients was 43 years for those with no new GI symptoms and 40 for those without new GI symptoms; overall, approximately half were women and approximately three-quarters were White. Overall, 50% of those with new GI symptoms were in remission, as was the case for 58.4% of those without.
IBD patients who developed new GI symptoms were significantly more likely to be women, of Asian race, older, or have at least one comorbidity.
The researchers found no difference in new GI symptoms in patients with Crohn’s disease and ulcerative colitis. “Patients on any medication – but in particular [tumor necrosis factor] antagonist monotherapy – were less likely to report new GI symptoms.” they wrote.
Although IBD patients with new GI symptoms were significantly more likely than were those without new GI symptoms to be hospitalized for COVID-19 in bivariate analyses (31.4% vs. 19.2%; P < .001), they were not more likely to need a ventilator or intensive care (5.8% vs. 4.6%; P < .18). In a multivariate analysis, IBD patients with new GI symptoms had no greater risk of death from COVID-19 than did those without new GI symptoms (adjusted odds ratio, 0.72; 95% confidence interval, 0.38-1.36).
The new-onset GI symptoms common to IBD patients with COVID-19 are not likely caused by underlying disease activity, given the number of patients in remission who reported new GI symptoms, the researchers wrote.
The study findings were limited by several factors including the retrospective design, potential reporting bias, and reliance on physician global assessment for disease assessment, the researchers noted. However, the results were strengthened by the large sample size, by the ability to assess GI symptoms before and after COVID-19, and by the evaluation of GI symptoms and COVID-19 outcomes.
“In summary, new GI symptoms are common in IBD patients with COVID-19 and are not associated with an increased risk of death due to COVID-19,” the researchers concluded. “Our findings suggest that an increase in GI symptoms in IBD patients should prompt consideration of a COVID-19 diagnosis.”
Data to guide clinical care
“There are several potential causes for common GI symptoms, such as diarrhea and abdominal pain, among patients with IBD,” Shirley Cohen-Mekelburg, MD, of the University of Michigan, Ann Arbor, said in an interview. “These can be the initial presentation of an IBD flare, a noninflammatory cause such as irritable bowel syndrome, small intestinal bacterial overgrowth, or an infection such as Clostridioides difficile or SARS-CoV-2. Each of these diagnoses require different treatments. An IBD flare may require escalation of immunosuppressive medications such as biologics or corticosteroids, which can cause harm in the context of an untreated infection. Therefore, any guidance that will increase health care providers’ awareness of the possible causes of similar GI symptoms is important in caring for our patients with IBD. This is especially true in context of a newer entity such as COVID-19 with which we are overall less familiar.”
Dr. Cohen-Meckelburg said the lack of association between GI symptoms and death in IBD is reassuring. “It is interesting to note that GI symptoms, and particularly new diarrhea, were very common among patients with IBD and COVID-19.
“Health care providers who treat patients with IBD should have a high-index of suspicion for SARS-CoV-2 infections when patients with IBD present with GI symptoms,” said Dr. Cohen-Meckelburg. “The data from the current study may help us to consider standard testing to rule out COVID-19 as an alternative diagnosis when considering whether to treat patients with IBD who develop new GI symptoms for an IBD flare. This would be similar to how we currently test for C. difficile and other enteric infections before treating IBD flares.
“Every study has its limitations, which need to be considered in interpreting findings,” Dr. Cohen-Meckelburg noted . “SECURE-IBD has provided great insight into COVID-19 infections among patients with IBD. However, the registry relies on individuals reporting cases, so there is the potential for underreporting, particularly with less symptomatic or subclinical cases.”
The study was supported in part by the Helmsley Charitable Trust with additional funding provided by Pfizer, Takeda, Janssen, AbbVie, Lilly, Genentech, Boehringer Ingelheim, Bristol-Myers Squibb, Celtrion, and Arenapharm. Lead author Dr. Ungaro disclosed serving as an advisory board member or consultant for AbbVie, Bristol-Myers Squibb, Janssen, Eli Lilly, Pfizer, and Takeda and research support from AbbVie, Boehringer Ingelheim, and Pfizer. Other coauthors disclosed similar relationships with other pharmaceutical companies. Dr. Cohen-Mekelburg had no financial conflicts to disclose.
FROM INFLAMMATORY BOWEL DISEASES
Time to positivity doesn’t predict mortality in bloodstream infections with enterococci
A short time to positivity (TTP), the period from incubation to blood culture positivity, may help predict mortality rates for patients with Enterococcus faecalis and vancomycin-sensitive E faecium (VSEfm) bloodstream infections (BSIs), but it is not an independent predictor of risk for death from bloodstream infections caused by enterococci, new research indicates.
Katharina Michelson, of the Institute of Microbiology, Jena University Hospital, Germany, and colleagues conducted a single-site study at Jena University Hospital that included 244 patients with monomicrobial BSIs to assess the value of TTP as a prognostic or diagnostic tool.
Death in the hospital was the primary endpoint considered in the study, which was conducted from January 2014 through December 2016. The shortest TTP of blood cultures was compared among groups.
Findings were published online in April in Diagnostic Microbiology and Infectious Disease.
Among the 244 patients with monomicrobial BSIs, 22.1% of cases were caused by E faecalis, 55.3% were caused by VSEfm, and 22.5% were caused by vancomycin-resistant E faecium (VREfm).
Average TTP of Enterococcus BSI (E-BSI) was 11.6 hours. The researchers found no significant association between risk for death and time to positivity with bloodstream infections with E faecalis, VSEfm, or VREfm, or its cutoffs.
The mortality rate of patients with bloodstream infections with E faecalis was 16.7%; for VSEfm, 26.7%; and for vancomycin-resistant E faecium, 38.2%. Cutoffs showed a significantly higher death rate when TTP was longer but were not risk factors in survival analysis.
The authors explain that “in literature, TTP has not always been proven to be a reliable parameter.”
Sam Aitken, PharmD, MPH, who is a pharmacy specialist for infectious diseases at Michigan Medicine, Ann Arbor, said in an interview that the main message from the article is that the TTP of E faecalis is quite different from that of E faecium and that “that’s in line with what we know about generally with how these organisms come about in patients.”
“This paper reinforces the differences that are sometimes underappreciated between these organisms because they are both enterococci,” he said.
The authors say appropriate antimicrobial therapy can lead to misinterpretation of TTP, so only patients who received inappropriate antimicrobial therapy on the day of positive blood culture were included in the study.
However, Dr. Aitken said that methodology doesn’t account for “immortal time bias.”
“They didn’t account for the fact that patients who tend to get active antibiotics are the ones who live longer. So unless you account for it, you’re not necessarily going to find that patients who get active antibiotics have improved survival,” he said.
The authors point out that finding new methods for quickly identifying patients with E-BSI is a high priority.
The mortality rates of E-BSI vary between 20% for E faecalis and 50% for E faecium.
Resistance to vancomycin is common in E faecium infections and is associated with high mortality, longer hospital stays, and increased costs. Vancomycin-resistant E faecium is part of a group of bacteria that is associated with multidrug resistance and nosocomial infections.
Dr. Aitken said that rather than TTP, “the best risk predictors are going to be in the microbiome studies we’re seeing. If there is a future for figuring out who’s going to get significant E faecium infections, at least, it’s going to be in the microbiome.”
Limitations of the study include its small size; the possibility of missing data, owing to the fact that the study was retrospective; potential delays to incubation; and the possibility of contamination of blood cultures.
The authors and Dr. Aitken have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A short time to positivity (TTP), the period from incubation to blood culture positivity, may help predict mortality rates for patients with Enterococcus faecalis and vancomycin-sensitive E faecium (VSEfm) bloodstream infections (BSIs), but it is not an independent predictor of risk for death from bloodstream infections caused by enterococci, new research indicates.
Katharina Michelson, of the Institute of Microbiology, Jena University Hospital, Germany, and colleagues conducted a single-site study at Jena University Hospital that included 244 patients with monomicrobial BSIs to assess the value of TTP as a prognostic or diagnostic tool.
Death in the hospital was the primary endpoint considered in the study, which was conducted from January 2014 through December 2016. The shortest TTP of blood cultures was compared among groups.
Findings were published online in April in Diagnostic Microbiology and Infectious Disease.
Among the 244 patients with monomicrobial BSIs, 22.1% of cases were caused by E faecalis, 55.3% were caused by VSEfm, and 22.5% were caused by vancomycin-resistant E faecium (VREfm).
Average TTP of Enterococcus BSI (E-BSI) was 11.6 hours. The researchers found no significant association between risk for death and time to positivity with bloodstream infections with E faecalis, VSEfm, or VREfm, or its cutoffs.
The mortality rate of patients with bloodstream infections with E faecalis was 16.7%; for VSEfm, 26.7%; and for vancomycin-resistant E faecium, 38.2%. Cutoffs showed a significantly higher death rate when TTP was longer but were not risk factors in survival analysis.
The authors explain that “in literature, TTP has not always been proven to be a reliable parameter.”
Sam Aitken, PharmD, MPH, who is a pharmacy specialist for infectious diseases at Michigan Medicine, Ann Arbor, said in an interview that the main message from the article is that the TTP of E faecalis is quite different from that of E faecium and that “that’s in line with what we know about generally with how these organisms come about in patients.”
“This paper reinforces the differences that are sometimes underappreciated between these organisms because they are both enterococci,” he said.
The authors say appropriate antimicrobial therapy can lead to misinterpretation of TTP, so only patients who received inappropriate antimicrobial therapy on the day of positive blood culture were included in the study.
However, Dr. Aitken said that methodology doesn’t account for “immortal time bias.”
“They didn’t account for the fact that patients who tend to get active antibiotics are the ones who live longer. So unless you account for it, you’re not necessarily going to find that patients who get active antibiotics have improved survival,” he said.
The authors point out that finding new methods for quickly identifying patients with E-BSI is a high priority.
The mortality rates of E-BSI vary between 20% for E faecalis and 50% for E faecium.
Resistance to vancomycin is common in E faecium infections and is associated with high mortality, longer hospital stays, and increased costs. Vancomycin-resistant E faecium is part of a group of bacteria that is associated with multidrug resistance and nosocomial infections.
Dr. Aitken said that rather than TTP, “the best risk predictors are going to be in the microbiome studies we’re seeing. If there is a future for figuring out who’s going to get significant E faecium infections, at least, it’s going to be in the microbiome.”
Limitations of the study include its small size; the possibility of missing data, owing to the fact that the study was retrospective; potential delays to incubation; and the possibility of contamination of blood cultures.
The authors and Dr. Aitken have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A short time to positivity (TTP), the period from incubation to blood culture positivity, may help predict mortality rates for patients with Enterococcus faecalis and vancomycin-sensitive E faecium (VSEfm) bloodstream infections (BSIs), but it is not an independent predictor of risk for death from bloodstream infections caused by enterococci, new research indicates.
Katharina Michelson, of the Institute of Microbiology, Jena University Hospital, Germany, and colleagues conducted a single-site study at Jena University Hospital that included 244 patients with monomicrobial BSIs to assess the value of TTP as a prognostic or diagnostic tool.
Death in the hospital was the primary endpoint considered in the study, which was conducted from January 2014 through December 2016. The shortest TTP of blood cultures was compared among groups.
Findings were published online in April in Diagnostic Microbiology and Infectious Disease.
Among the 244 patients with monomicrobial BSIs, 22.1% of cases were caused by E faecalis, 55.3% were caused by VSEfm, and 22.5% were caused by vancomycin-resistant E faecium (VREfm).
Average TTP of Enterococcus BSI (E-BSI) was 11.6 hours. The researchers found no significant association between risk for death and time to positivity with bloodstream infections with E faecalis, VSEfm, or VREfm, or its cutoffs.
The mortality rate of patients with bloodstream infections with E faecalis was 16.7%; for VSEfm, 26.7%; and for vancomycin-resistant E faecium, 38.2%. Cutoffs showed a significantly higher death rate when TTP was longer but were not risk factors in survival analysis.
The authors explain that “in literature, TTP has not always been proven to be a reliable parameter.”
Sam Aitken, PharmD, MPH, who is a pharmacy specialist for infectious diseases at Michigan Medicine, Ann Arbor, said in an interview that the main message from the article is that the TTP of E faecalis is quite different from that of E faecium and that “that’s in line with what we know about generally with how these organisms come about in patients.”
“This paper reinforces the differences that are sometimes underappreciated between these organisms because they are both enterococci,” he said.
The authors say appropriate antimicrobial therapy can lead to misinterpretation of TTP, so only patients who received inappropriate antimicrobial therapy on the day of positive blood culture were included in the study.
However, Dr. Aitken said that methodology doesn’t account for “immortal time bias.”
“They didn’t account for the fact that patients who tend to get active antibiotics are the ones who live longer. So unless you account for it, you’re not necessarily going to find that patients who get active antibiotics have improved survival,” he said.
The authors point out that finding new methods for quickly identifying patients with E-BSI is a high priority.
The mortality rates of E-BSI vary between 20% for E faecalis and 50% for E faecium.
Resistance to vancomycin is common in E faecium infections and is associated with high mortality, longer hospital stays, and increased costs. Vancomycin-resistant E faecium is part of a group of bacteria that is associated with multidrug resistance and nosocomial infections.
Dr. Aitken said that rather than TTP, “the best risk predictors are going to be in the microbiome studies we’re seeing. If there is a future for figuring out who’s going to get significant E faecium infections, at least, it’s going to be in the microbiome.”
Limitations of the study include its small size; the possibility of missing data, owing to the fact that the study was retrospective; potential delays to incubation; and the possibility of contamination of blood cultures.
The authors and Dr. Aitken have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ACE-I or ARB therapy in patients with low eGFR
Background: ACE-I and ARB therapy is widely used for hypertension, albuminuric chronic kidney disease, heart failure with reduced ejection fraction, and coronary artery disease. They are known to potentially cause hemodynamic reductions in eGFR, hyperkalemia, and acute kidney injury. We know to temporarily discontinue ACE-I or ARB in patients with eGFR less than 60 mL/min per 1.73 m2 who have serious intercurrent illness that increases the risk of acute kidney injury, but existing literature evaluating the risks and benefits of using ACE-I and ARBs in individuals with advanced chronic kidney disease is conflicting.
Study design: Retrospective, propensity score–matched cohort study.
Setting: Geisinger Health System, serving central and northeastern Pennsylvania.
Synopsis: Total of 3,909 individuals were included in the study who were receiving ACE-I or ARB and experienced eGFR below 30 mL/min per 1.73 m2. Of these 1,235 discontinued ACE-I or ARB therapy within 6 months after the eGFR decrease and 2,674 did not. At median 2.9 years’ follow-up, 434 (35.1%) patients who discontinued ACE-I or ARB therapy had died versus 786 (29.1%) who did not discontinue. Similarly, the risk of MACE (major adverse cardiovascular events) was higher among those who discontinued therapy (n = 494; 40.0%) than it was among those who did not discontinue therapy (n = 910; 34.0%). Among those who discontinued, 87 individuals (7.0%) developed end-stage kidney disease, compared with the 176 (6.6%) who did not discontinue. Additionally, in individuals with an eGFR decrease by 40% or more for 1 year while receiving ACE-I or ARB therapy, discontinuing therapy was associated with higher risk of mortality (32.6% vs. 20.5%).
Although this study is observational it has a large sample size and confounding factors have been accounted for by propensity score matching. The results are clinically relevant in daily practice.
Bottom line: Continuing ACE-I or ARB after an eGFR decrease to below 30 mL/min per m2 is associated with lower risk of mortality and MACE without significant increased risk of end-stage kidney disease.
Citation: Qiao Y et al. Association between renin-angiotensin system blockade discontinuation and all-cause mortality among persons with low estimated glomerular filtration rate. JAMA Intern Med. 2020 Mar 9;180(5):718-26.
Dr. Kumar is a hospitalist and assistant professor of medicine at UK HealthCare, Lexington, Ky.
Background: ACE-I and ARB therapy is widely used for hypertension, albuminuric chronic kidney disease, heart failure with reduced ejection fraction, and coronary artery disease. They are known to potentially cause hemodynamic reductions in eGFR, hyperkalemia, and acute kidney injury. We know to temporarily discontinue ACE-I or ARB in patients with eGFR less than 60 mL/min per 1.73 m2 who have serious intercurrent illness that increases the risk of acute kidney injury, but existing literature evaluating the risks and benefits of using ACE-I and ARBs in individuals with advanced chronic kidney disease is conflicting.
Study design: Retrospective, propensity score–matched cohort study.
Setting: Geisinger Health System, serving central and northeastern Pennsylvania.
Synopsis: Total of 3,909 individuals were included in the study who were receiving ACE-I or ARB and experienced eGFR below 30 mL/min per 1.73 m2. Of these 1,235 discontinued ACE-I or ARB therapy within 6 months after the eGFR decrease and 2,674 did not. At median 2.9 years’ follow-up, 434 (35.1%) patients who discontinued ACE-I or ARB therapy had died versus 786 (29.1%) who did not discontinue. Similarly, the risk of MACE (major adverse cardiovascular events) was higher among those who discontinued therapy (n = 494; 40.0%) than it was among those who did not discontinue therapy (n = 910; 34.0%). Among those who discontinued, 87 individuals (7.0%) developed end-stage kidney disease, compared with the 176 (6.6%) who did not discontinue. Additionally, in individuals with an eGFR decrease by 40% or more for 1 year while receiving ACE-I or ARB therapy, discontinuing therapy was associated with higher risk of mortality (32.6% vs. 20.5%).
Although this study is observational it has a large sample size and confounding factors have been accounted for by propensity score matching. The results are clinically relevant in daily practice.
Bottom line: Continuing ACE-I or ARB after an eGFR decrease to below 30 mL/min per m2 is associated with lower risk of mortality and MACE without significant increased risk of end-stage kidney disease.
Citation: Qiao Y et al. Association between renin-angiotensin system blockade discontinuation and all-cause mortality among persons with low estimated glomerular filtration rate. JAMA Intern Med. 2020 Mar 9;180(5):718-26.
Dr. Kumar is a hospitalist and assistant professor of medicine at UK HealthCare, Lexington, Ky.
Background: ACE-I and ARB therapy is widely used for hypertension, albuminuric chronic kidney disease, heart failure with reduced ejection fraction, and coronary artery disease. They are known to potentially cause hemodynamic reductions in eGFR, hyperkalemia, and acute kidney injury. We know to temporarily discontinue ACE-I or ARB in patients with eGFR less than 60 mL/min per 1.73 m2 who have serious intercurrent illness that increases the risk of acute kidney injury, but existing literature evaluating the risks and benefits of using ACE-I and ARBs in individuals with advanced chronic kidney disease is conflicting.
Study design: Retrospective, propensity score–matched cohort study.
Setting: Geisinger Health System, serving central and northeastern Pennsylvania.
Synopsis: Total of 3,909 individuals were included in the study who were receiving ACE-I or ARB and experienced eGFR below 30 mL/min per 1.73 m2. Of these 1,235 discontinued ACE-I or ARB therapy within 6 months after the eGFR decrease and 2,674 did not. At median 2.9 years’ follow-up, 434 (35.1%) patients who discontinued ACE-I or ARB therapy had died versus 786 (29.1%) who did not discontinue. Similarly, the risk of MACE (major adverse cardiovascular events) was higher among those who discontinued therapy (n = 494; 40.0%) than it was among those who did not discontinue therapy (n = 910; 34.0%). Among those who discontinued, 87 individuals (7.0%) developed end-stage kidney disease, compared with the 176 (6.6%) who did not discontinue. Additionally, in individuals with an eGFR decrease by 40% or more for 1 year while receiving ACE-I or ARB therapy, discontinuing therapy was associated with higher risk of mortality (32.6% vs. 20.5%).
Although this study is observational it has a large sample size and confounding factors have been accounted for by propensity score matching. The results are clinically relevant in daily practice.
Bottom line: Continuing ACE-I or ARB after an eGFR decrease to below 30 mL/min per m2 is associated with lower risk of mortality and MACE without significant increased risk of end-stage kidney disease.
Citation: Qiao Y et al. Association between renin-angiotensin system blockade discontinuation and all-cause mortality among persons with low estimated glomerular filtration rate. JAMA Intern Med. 2020 Mar 9;180(5):718-26.
Dr. Kumar is a hospitalist and assistant professor of medicine at UK HealthCare, Lexington, Ky.
One-third in U.S. had been infected by SARS-CoV-2 through 2020: Study
, according to a modeling study published Aug. 26 online in Nature.
Jeffrey Shaman, PhD, professor in the department of environmental health sciences and director of the climate and health program at the Columbia University Mailman School of Public Health, New York City, and colleagues developed a model to simulate how SARS-CoV-2 was transmitted within and between all 3,142 counties in the United States.
In their model, the researchers considered migration data between counties, the observed case numbers, and estimates of infections based on the number of people who test positive for SARS-CoV-2 antibodies.
The United States had the highest number of confirmed COVID-19 cases and deaths in the world during 2020. More than 19.6 million cases were reported by the end of the year.
But the authors point out that “69% of the population remained susceptible to viral infection.”
The researchers also studied the ascertainment rate, or the ratio of detected cases to the number of confirmed cases. Nationally, that value increased from 11.3% in March 2020 to 24.5% in December 2020.
That’s one of the biggest pandemic lessons from the data, Dr. Shaman said: “It is vitally important when there is an outbreak and you’re counting cases that there are many more people infected in your community who are contagious than reported cases. Each individual is infectious for multiple days, and there are many more unreported cases.”
That applies now with the Delta variant, he said.
“Vaccinated people who get infected with the Delta variant are part of the transmission chain,” he said.
Fatality rates dropped
Some of the data were very positive, Dr. Shaman told this news organization. The infection fatality rate fell from 0.77% in April to 0.31% in December. The authors suggest that that may be because of improvements in diagnosis and treatment, patient care, and reduced disease severity.
However, the fatality rate was still nearly four times as high as the estimated fatality rate for seasonal influenza (0.08%) and the 2009 influenza pandemic (0.0076%), the authors point out.
Joe K. Gerald, MD, PhD, associate professor and program director of public health policy and management at the University of Arizona, Tucson, told this news organization that this article helps confirm that COVID is much deadlier than the flu and that the intensity of the response has been appropriate.
“We should be willing to invest a lot more in mitigating COVID-19 than seasonal influenza because it has much greater consequences,” he said.
The numbers emphasize that testing must improve.
“We didn’t have enough tests available, and they weren’t easily accessible. For much of the year we were flying in the dark,” Dr. Gerald said.
The number of tests has increased this year, he acknowledged, but testing still lags. “We just can’t miss this many infections or diagnoses and hope to gain control,” he said.
The study also points out the huge variation by state and by county in infections and deaths, and that variation continues. Gerald noted that the varied numbers make it difficult for some regions to accept broader mandates, because the threat from COVID-19 appears very different where they are.
“We have to think about regions, how many people are susceptible, and what the testing capacity is,” he said. “States and even counties should have some leeway to make some important public health decisions, because local conditions are going to differ at different points in time.”
‘We have not turned the corner’
Jill Foster, MD, a pediatric infectious disease physician at the University of Minnesota Medical School, Minneapolis, said in an interview that the study adds evidence: “We have not turned the corner on COVID-19 and are nowhere near herd immunity – if it exists for SARS-CoV-2.”
She said the numbers presented are particularly concerning in regard to how many people were susceptible and were actively able to infect others: “Much higher than most people imagined and very much higher than their comparison, influenza.
“There are still more people susceptible than we had believed,” Dr. Foster added. “If the pattern continues where the Delta variant infects a significant portion of those vaccinated, the number of people susceptible rises even higher than was predicted.”
She said that it is reassuring that the analysis shows a decrease in case fatality and said the finding supports the common opinion that medicine is better able to fight the disease.
“However,” she said, “the optimism is tempered by acknowledging that in order to benefit from these advances, we must not overwhelm the facilities where patients are cared for so that optimal care can be delivered.”
Dr. Foster said these numbers represent a warning that COVID should be treated as a continuing threat.
“We need to acknowledge that there is COVID-19 infection simmering and periodically erupting throughout the country,” she said. “It is not monolithic and varies by geography and seasons in ways that are difficult to predict other than at any given time there is likely more infection present than we are identifying and more people susceptible to infection than we have calculated.”
The authors and Dr. Gerald have disclosed no relevant financial relationships. Dr. Foster has received clinical trials funding from Moderna.
A version of this article first appeared on Medscape.com.
, according to a modeling study published Aug. 26 online in Nature.
Jeffrey Shaman, PhD, professor in the department of environmental health sciences and director of the climate and health program at the Columbia University Mailman School of Public Health, New York City, and colleagues developed a model to simulate how SARS-CoV-2 was transmitted within and between all 3,142 counties in the United States.
In their model, the researchers considered migration data between counties, the observed case numbers, and estimates of infections based on the number of people who test positive for SARS-CoV-2 antibodies.
The United States had the highest number of confirmed COVID-19 cases and deaths in the world during 2020. More than 19.6 million cases were reported by the end of the year.
But the authors point out that “69% of the population remained susceptible to viral infection.”
The researchers also studied the ascertainment rate, or the ratio of detected cases to the number of confirmed cases. Nationally, that value increased from 11.3% in March 2020 to 24.5% in December 2020.
That’s one of the biggest pandemic lessons from the data, Dr. Shaman said: “It is vitally important when there is an outbreak and you’re counting cases that there are many more people infected in your community who are contagious than reported cases. Each individual is infectious for multiple days, and there are many more unreported cases.”
That applies now with the Delta variant, he said.
“Vaccinated people who get infected with the Delta variant are part of the transmission chain,” he said.
Fatality rates dropped
Some of the data were very positive, Dr. Shaman told this news organization. The infection fatality rate fell from 0.77% in April to 0.31% in December. The authors suggest that that may be because of improvements in diagnosis and treatment, patient care, and reduced disease severity.
However, the fatality rate was still nearly four times as high as the estimated fatality rate for seasonal influenza (0.08%) and the 2009 influenza pandemic (0.0076%), the authors point out.
Joe K. Gerald, MD, PhD, associate professor and program director of public health policy and management at the University of Arizona, Tucson, told this news organization that this article helps confirm that COVID is much deadlier than the flu and that the intensity of the response has been appropriate.
“We should be willing to invest a lot more in mitigating COVID-19 than seasonal influenza because it has much greater consequences,” he said.
The numbers emphasize that testing must improve.
“We didn’t have enough tests available, and they weren’t easily accessible. For much of the year we were flying in the dark,” Dr. Gerald said.
The number of tests has increased this year, he acknowledged, but testing still lags. “We just can’t miss this many infections or diagnoses and hope to gain control,” he said.
The study also points out the huge variation by state and by county in infections and deaths, and that variation continues. Gerald noted that the varied numbers make it difficult for some regions to accept broader mandates, because the threat from COVID-19 appears very different where they are.
“We have to think about regions, how many people are susceptible, and what the testing capacity is,” he said. “States and even counties should have some leeway to make some important public health decisions, because local conditions are going to differ at different points in time.”
‘We have not turned the corner’
Jill Foster, MD, a pediatric infectious disease physician at the University of Minnesota Medical School, Minneapolis, said in an interview that the study adds evidence: “We have not turned the corner on COVID-19 and are nowhere near herd immunity – if it exists for SARS-CoV-2.”
She said the numbers presented are particularly concerning in regard to how many people were susceptible and were actively able to infect others: “Much higher than most people imagined and very much higher than their comparison, influenza.
“There are still more people susceptible than we had believed,” Dr. Foster added. “If the pattern continues where the Delta variant infects a significant portion of those vaccinated, the number of people susceptible rises even higher than was predicted.”
She said that it is reassuring that the analysis shows a decrease in case fatality and said the finding supports the common opinion that medicine is better able to fight the disease.
“However,” she said, “the optimism is tempered by acknowledging that in order to benefit from these advances, we must not overwhelm the facilities where patients are cared for so that optimal care can be delivered.”
Dr. Foster said these numbers represent a warning that COVID should be treated as a continuing threat.
“We need to acknowledge that there is COVID-19 infection simmering and periodically erupting throughout the country,” she said. “It is not monolithic and varies by geography and seasons in ways that are difficult to predict other than at any given time there is likely more infection present than we are identifying and more people susceptible to infection than we have calculated.”
The authors and Dr. Gerald have disclosed no relevant financial relationships. Dr. Foster has received clinical trials funding from Moderna.
A version of this article first appeared on Medscape.com.
, according to a modeling study published Aug. 26 online in Nature.
Jeffrey Shaman, PhD, professor in the department of environmental health sciences and director of the climate and health program at the Columbia University Mailman School of Public Health, New York City, and colleagues developed a model to simulate how SARS-CoV-2 was transmitted within and between all 3,142 counties in the United States.
In their model, the researchers considered migration data between counties, the observed case numbers, and estimates of infections based on the number of people who test positive for SARS-CoV-2 antibodies.
The United States had the highest number of confirmed COVID-19 cases and deaths in the world during 2020. More than 19.6 million cases were reported by the end of the year.
But the authors point out that “69% of the population remained susceptible to viral infection.”
The researchers also studied the ascertainment rate, or the ratio of detected cases to the number of confirmed cases. Nationally, that value increased from 11.3% in March 2020 to 24.5% in December 2020.
That’s one of the biggest pandemic lessons from the data, Dr. Shaman said: “It is vitally important when there is an outbreak and you’re counting cases that there are many more people infected in your community who are contagious than reported cases. Each individual is infectious for multiple days, and there are many more unreported cases.”
That applies now with the Delta variant, he said.
“Vaccinated people who get infected with the Delta variant are part of the transmission chain,” he said.
Fatality rates dropped
Some of the data were very positive, Dr. Shaman told this news organization. The infection fatality rate fell from 0.77% in April to 0.31% in December. The authors suggest that that may be because of improvements in diagnosis and treatment, patient care, and reduced disease severity.
However, the fatality rate was still nearly four times as high as the estimated fatality rate for seasonal influenza (0.08%) and the 2009 influenza pandemic (0.0076%), the authors point out.
Joe K. Gerald, MD, PhD, associate professor and program director of public health policy and management at the University of Arizona, Tucson, told this news organization that this article helps confirm that COVID is much deadlier than the flu and that the intensity of the response has been appropriate.
“We should be willing to invest a lot more in mitigating COVID-19 than seasonal influenza because it has much greater consequences,” he said.
The numbers emphasize that testing must improve.
“We didn’t have enough tests available, and they weren’t easily accessible. For much of the year we were flying in the dark,” Dr. Gerald said.
The number of tests has increased this year, he acknowledged, but testing still lags. “We just can’t miss this many infections or diagnoses and hope to gain control,” he said.
The study also points out the huge variation by state and by county in infections and deaths, and that variation continues. Gerald noted that the varied numbers make it difficult for some regions to accept broader mandates, because the threat from COVID-19 appears very different where they are.
“We have to think about regions, how many people are susceptible, and what the testing capacity is,” he said. “States and even counties should have some leeway to make some important public health decisions, because local conditions are going to differ at different points in time.”
‘We have not turned the corner’
Jill Foster, MD, a pediatric infectious disease physician at the University of Minnesota Medical School, Minneapolis, said in an interview that the study adds evidence: “We have not turned the corner on COVID-19 and are nowhere near herd immunity – if it exists for SARS-CoV-2.”
She said the numbers presented are particularly concerning in regard to how many people were susceptible and were actively able to infect others: “Much higher than most people imagined and very much higher than their comparison, influenza.
“There are still more people susceptible than we had believed,” Dr. Foster added. “If the pattern continues where the Delta variant infects a significant portion of those vaccinated, the number of people susceptible rises even higher than was predicted.”
She said that it is reassuring that the analysis shows a decrease in case fatality and said the finding supports the common opinion that medicine is better able to fight the disease.
“However,” she said, “the optimism is tempered by acknowledging that in order to benefit from these advances, we must not overwhelm the facilities where patients are cared for so that optimal care can be delivered.”
Dr. Foster said these numbers represent a warning that COVID should be treated as a continuing threat.
“We need to acknowledge that there is COVID-19 infection simmering and periodically erupting throughout the country,” she said. “It is not monolithic and varies by geography and seasons in ways that are difficult to predict other than at any given time there is likely more infection present than we are identifying and more people susceptible to infection than we have calculated.”
The authors and Dr. Gerald have disclosed no relevant financial relationships. Dr. Foster has received clinical trials funding from Moderna.
A version of this article first appeared on Medscape.com.
Efficacy of gabapentin for treatment of alcohol use disorders
Background: Up to 30 million people in the United States meet criteria for alcohol use disorder. Gabapentin addresses symptoms of protracted withdrawal such as insomnia, irritability, difficulty with attention, dysphoria, and anxiety. It does that by acting on voltage-gated calcium channels and, in turn, influencing GABA and glutamate tone and activity.
Study design: Double-blind, placebo-controlled, randomized clinical trial.
Settings: Academic ambulatory setting at the Medical University of South Carolina.
Synopsis: A total of 96 community-recruited participants were randomly assigned to gabapentin and placebo arm then treated and followed for a total of 16 weeks. The gabapentin arm received gradual increments of gabapentin reaching up to 1,200 mg/day by day 5. The control group received placebo in blister packs. Individuals in the gabapentin arm, compared with those in the placebo arm, showed 18.6% (P = .02) more no heavy–drinking days, with a number needed to treat (NNT) of 5.4, and 13.8% (P = .04) more total abstinence days, with an NNT of 6.2. The prestudy high–alcohol withdrawal group in particular had significantly less relapse to heavy drinking (P = .02; NNT, 3.1) and more total abstinence (P = .03; NNT, 2.7) when treated with gabapentin.
A couple of study limitations were a significant noncompletion rate (30% in gabapentin arm and 39% in the placebo arm) and self-reported alcohol withdrawal symptoms prior to entry into the study.
Bottom line: Gabapentin helps in reducing drinking and maintaining alcohol abstinence in individuals with alcohol use disorder, especially those with high–alcohol withdrawal symptoms.
Citation: Anton RF et al. Efficacy of gabapentin for the treatment of alcohol use disorder in patients with alcohol withdrawal symptoms: A randomized clinical trial. JAMA Intern Med. 2020 Mar 9;180(5):728-36.
Dr. Gaddam is a hospitalist and assistant professor of medicine at UK HealthCare, Lexington, Ky.
Background: Up to 30 million people in the United States meet criteria for alcohol use disorder. Gabapentin addresses symptoms of protracted withdrawal such as insomnia, irritability, difficulty with attention, dysphoria, and anxiety. It does that by acting on voltage-gated calcium channels and, in turn, influencing GABA and glutamate tone and activity.
Study design: Double-blind, placebo-controlled, randomized clinical trial.
Settings: Academic ambulatory setting at the Medical University of South Carolina.
Synopsis: A total of 96 community-recruited participants were randomly assigned to gabapentin and placebo arm then treated and followed for a total of 16 weeks. The gabapentin arm received gradual increments of gabapentin reaching up to 1,200 mg/day by day 5. The control group received placebo in blister packs. Individuals in the gabapentin arm, compared with those in the placebo arm, showed 18.6% (P = .02) more no heavy–drinking days, with a number needed to treat (NNT) of 5.4, and 13.8% (P = .04) more total abstinence days, with an NNT of 6.2. The prestudy high–alcohol withdrawal group in particular had significantly less relapse to heavy drinking (P = .02; NNT, 3.1) and more total abstinence (P = .03; NNT, 2.7) when treated with gabapentin.
A couple of study limitations were a significant noncompletion rate (30% in gabapentin arm and 39% in the placebo arm) and self-reported alcohol withdrawal symptoms prior to entry into the study.
Bottom line: Gabapentin helps in reducing drinking and maintaining alcohol abstinence in individuals with alcohol use disorder, especially those with high–alcohol withdrawal symptoms.
Citation: Anton RF et al. Efficacy of gabapentin for the treatment of alcohol use disorder in patients with alcohol withdrawal symptoms: A randomized clinical trial. JAMA Intern Med. 2020 Mar 9;180(5):728-36.
Dr. Gaddam is a hospitalist and assistant professor of medicine at UK HealthCare, Lexington, Ky.
Background: Up to 30 million people in the United States meet criteria for alcohol use disorder. Gabapentin addresses symptoms of protracted withdrawal such as insomnia, irritability, difficulty with attention, dysphoria, and anxiety. It does that by acting on voltage-gated calcium channels and, in turn, influencing GABA and glutamate tone and activity.
Study design: Double-blind, placebo-controlled, randomized clinical trial.
Settings: Academic ambulatory setting at the Medical University of South Carolina.
Synopsis: A total of 96 community-recruited participants were randomly assigned to gabapentin and placebo arm then treated and followed for a total of 16 weeks. The gabapentin arm received gradual increments of gabapentin reaching up to 1,200 mg/day by day 5. The control group received placebo in blister packs. Individuals in the gabapentin arm, compared with those in the placebo arm, showed 18.6% (P = .02) more no heavy–drinking days, with a number needed to treat (NNT) of 5.4, and 13.8% (P = .04) more total abstinence days, with an NNT of 6.2. The prestudy high–alcohol withdrawal group in particular had significantly less relapse to heavy drinking (P = .02; NNT, 3.1) and more total abstinence (P = .03; NNT, 2.7) when treated with gabapentin.
A couple of study limitations were a significant noncompletion rate (30% in gabapentin arm and 39% in the placebo arm) and self-reported alcohol withdrawal symptoms prior to entry into the study.
Bottom line: Gabapentin helps in reducing drinking and maintaining alcohol abstinence in individuals with alcohol use disorder, especially those with high–alcohol withdrawal symptoms.
Citation: Anton RF et al. Efficacy of gabapentin for the treatment of alcohol use disorder in patients with alcohol withdrawal symptoms: A randomized clinical trial. JAMA Intern Med. 2020 Mar 9;180(5):728-36.
Dr. Gaddam is a hospitalist and assistant professor of medicine at UK HealthCare, Lexington, Ky.
Children and COVID: New cases soar to near-record level
Weekly cases of COVID-19 in children jumped by nearly 50% in the United States, posting the highest count since hitting a pandemic high back in mid-January, a new report shows.
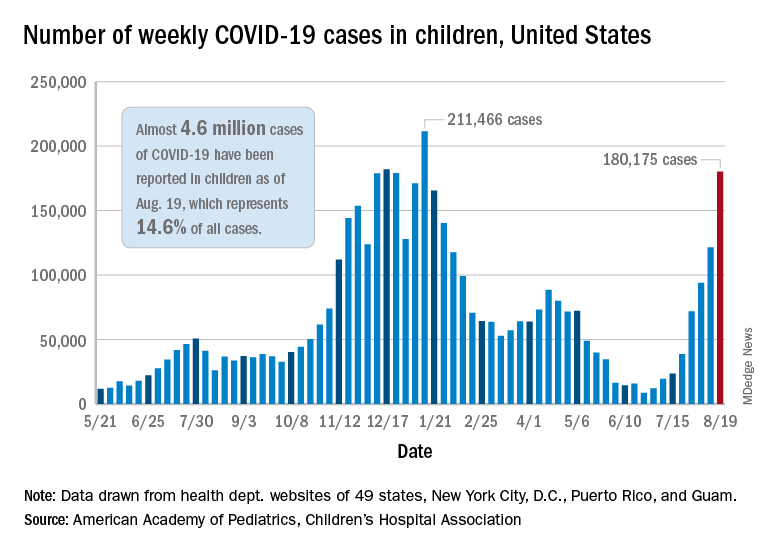
The latest weekly figure represents a 48% increase over the previous week and an increase of over 2,000% in the 8 weeks since the national count dropped to a low of 8,500 cases for the week of June 18-24, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
Vaccinations, in the meantime, appear to be headed in the opposite direction. Vaccine initiations were down for the second consecutive week, falling by 18% among 12- to 15-year-olds and by 15% in those aged 16-17 years, according to data from the Centers for Disease Control and Prevention.
Nationally, about 47% of children aged 12-15 and 56% of those aged 16-17 have received at least one dose of COVID vaccine as of Aug. 23, with 34% and 44%, respectively, reaching full vaccination. The total number of children with at least one dose is 11.6 million, including a relatively small number (about 200,000) of children under age 12 years, the CDC said on its COVID Data Tracker.
At the state level, vaccination is a source of considerable disparity. In Vermont, 73% of children aged 12-17 had received at least one dose by Aug. 18, and 63% were fully vaccinated. In Wyoming, however, just 25% of children had received at least one dose (17% are fully vaccinated), while Alabama has a lowest-in-the-nation full vaccination rate of 14%, based on a separate AAP analysis of CDC data.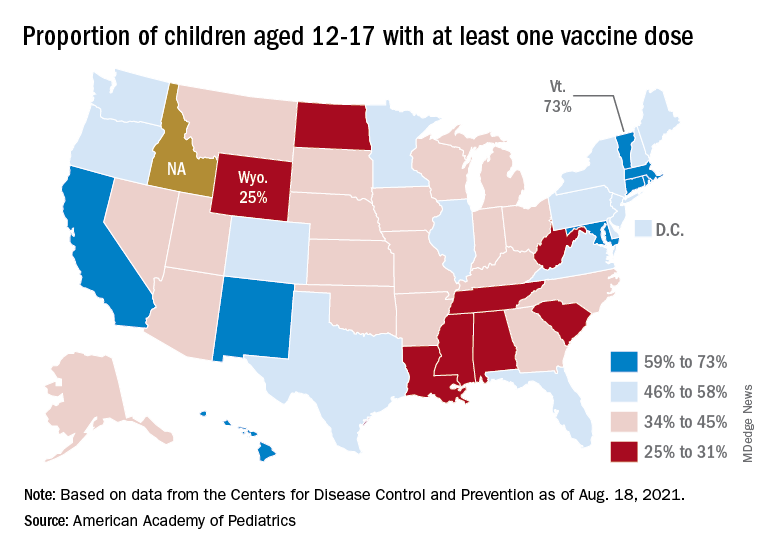
There are seven states in which over 60% of 12- to 17-year-olds have at least started the vaccine regimen and five states where less than 30% have received at least one dose, the AAP noted.
Back on the incidence side of the pandemic, Mississippi and Hawaii had the largest increases in new cases over the past 2 weeks, followed by Florida and West Virginia. Cumulative figures show that California has had the most cases overall in children (550,337), Vermont has the highest proportion of all cases in children (22.9%), and Rhode Island has the highest rate of cases per 100,000 (10,636), the AAP and CHA said in the joint report based on data from 49 states, the District of Columbia, New York City, Puerto Rico, and Guam.
Add up all those jurisdictions, and it works out to 4.6 million children infected with SARS-CoV-2 as of Aug. 19, with children representing 14.6% of all cases since the start of the pandemic. There have been over 18,000 hospitalizations so far, which is just 2.3% of the total for all ages in the 23 states (and New York City) that are reporting such data on their health department websites, the AAP and CHA said.
The number of COVID-related deaths in children is now 402 after the largest 1-week increase (24) since late May of 2020, when the AAP/CHA coverage began. Mortality data by age are available from 44 states, New York City, Puerto Rico, and Guam.
Weekly cases of COVID-19 in children jumped by nearly 50% in the United States, posting the highest count since hitting a pandemic high back in mid-January, a new report shows.
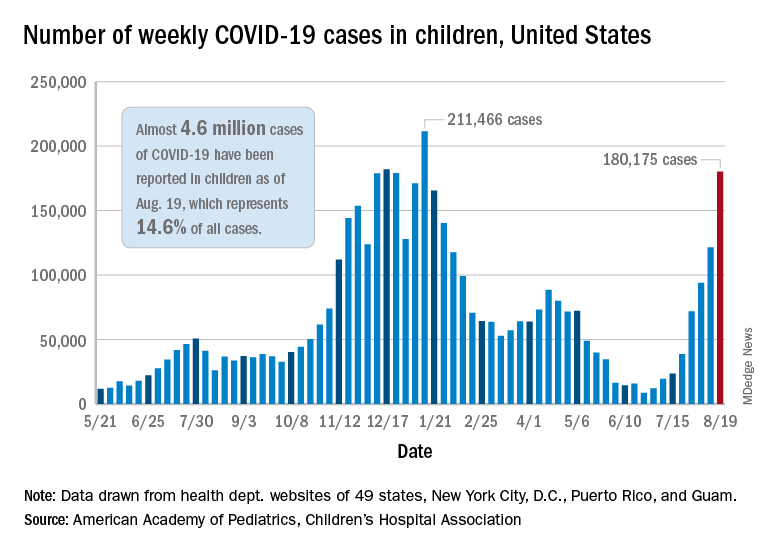
The latest weekly figure represents a 48% increase over the previous week and an increase of over 2,000% in the 8 weeks since the national count dropped to a low of 8,500 cases for the week of June 18-24, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
Vaccinations, in the meantime, appear to be headed in the opposite direction. Vaccine initiations were down for the second consecutive week, falling by 18% among 12- to 15-year-olds and by 15% in those aged 16-17 years, according to data from the Centers for Disease Control and Prevention.
Nationally, about 47% of children aged 12-15 and 56% of those aged 16-17 have received at least one dose of COVID vaccine as of Aug. 23, with 34% and 44%, respectively, reaching full vaccination. The total number of children with at least one dose is 11.6 million, including a relatively small number (about 200,000) of children under age 12 years, the CDC said on its COVID Data Tracker.
At the state level, vaccination is a source of considerable disparity. In Vermont, 73% of children aged 12-17 had received at least one dose by Aug. 18, and 63% were fully vaccinated. In Wyoming, however, just 25% of children had received at least one dose (17% are fully vaccinated), while Alabama has a lowest-in-the-nation full vaccination rate of 14%, based on a separate AAP analysis of CDC data.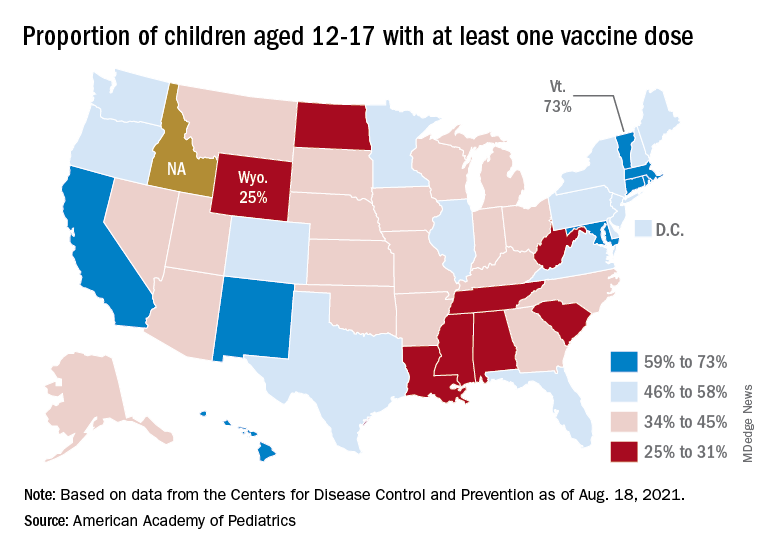
There are seven states in which over 60% of 12- to 17-year-olds have at least started the vaccine regimen and five states where less than 30% have received at least one dose, the AAP noted.
Back on the incidence side of the pandemic, Mississippi and Hawaii had the largest increases in new cases over the past 2 weeks, followed by Florida and West Virginia. Cumulative figures show that California has had the most cases overall in children (550,337), Vermont has the highest proportion of all cases in children (22.9%), and Rhode Island has the highest rate of cases per 100,000 (10,636), the AAP and CHA said in the joint report based on data from 49 states, the District of Columbia, New York City, Puerto Rico, and Guam.
Add up all those jurisdictions, and it works out to 4.6 million children infected with SARS-CoV-2 as of Aug. 19, with children representing 14.6% of all cases since the start of the pandemic. There have been over 18,000 hospitalizations so far, which is just 2.3% of the total for all ages in the 23 states (and New York City) that are reporting such data on their health department websites, the AAP and CHA said.
The number of COVID-related deaths in children is now 402 after the largest 1-week increase (24) since late May of 2020, when the AAP/CHA coverage began. Mortality data by age are available from 44 states, New York City, Puerto Rico, and Guam.
Weekly cases of COVID-19 in children jumped by nearly 50% in the United States, posting the highest count since hitting a pandemic high back in mid-January, a new report shows.
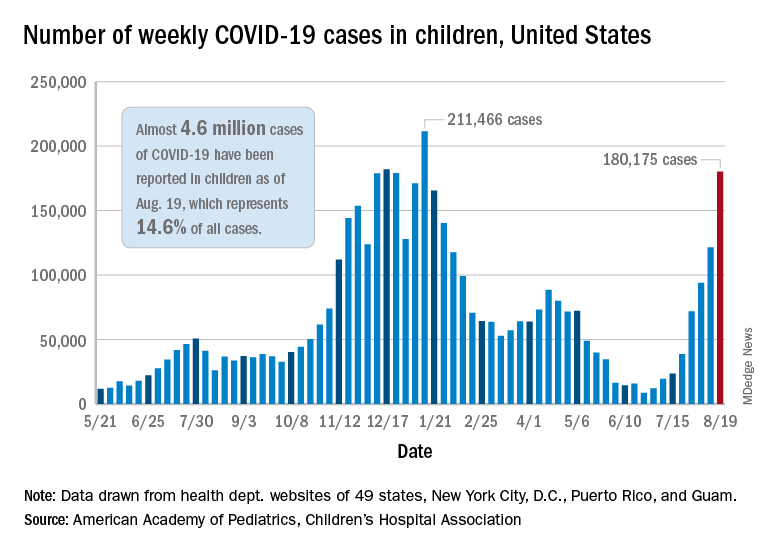
The latest weekly figure represents a 48% increase over the previous week and an increase of over 2,000% in the 8 weeks since the national count dropped to a low of 8,500 cases for the week of June 18-24, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
Vaccinations, in the meantime, appear to be headed in the opposite direction. Vaccine initiations were down for the second consecutive week, falling by 18% among 12- to 15-year-olds and by 15% in those aged 16-17 years, according to data from the Centers for Disease Control and Prevention.
Nationally, about 47% of children aged 12-15 and 56% of those aged 16-17 have received at least one dose of COVID vaccine as of Aug. 23, with 34% and 44%, respectively, reaching full vaccination. The total number of children with at least one dose is 11.6 million, including a relatively small number (about 200,000) of children under age 12 years, the CDC said on its COVID Data Tracker.
At the state level, vaccination is a source of considerable disparity. In Vermont, 73% of children aged 12-17 had received at least one dose by Aug. 18, and 63% were fully vaccinated. In Wyoming, however, just 25% of children had received at least one dose (17% are fully vaccinated), while Alabama has a lowest-in-the-nation full vaccination rate of 14%, based on a separate AAP analysis of CDC data.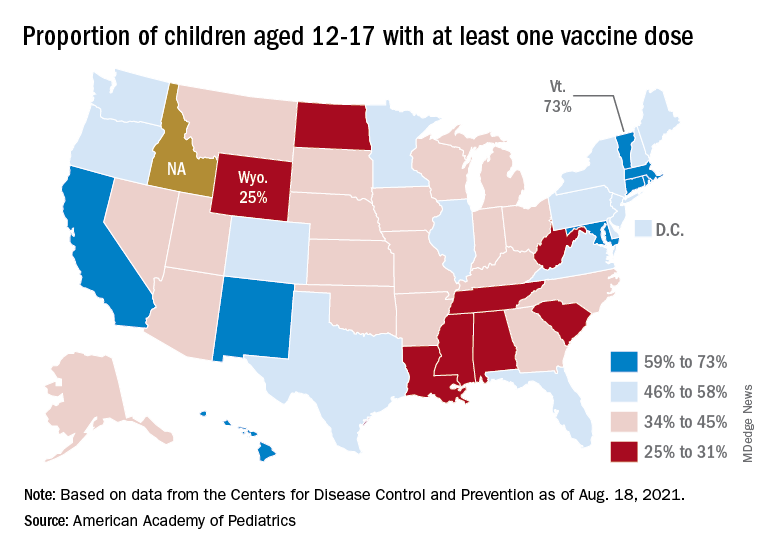
There are seven states in which over 60% of 12- to 17-year-olds have at least started the vaccine regimen and five states where less than 30% have received at least one dose, the AAP noted.
Back on the incidence side of the pandemic, Mississippi and Hawaii had the largest increases in new cases over the past 2 weeks, followed by Florida and West Virginia. Cumulative figures show that California has had the most cases overall in children (550,337), Vermont has the highest proportion of all cases in children (22.9%), and Rhode Island has the highest rate of cases per 100,000 (10,636), the AAP and CHA said in the joint report based on data from 49 states, the District of Columbia, New York City, Puerto Rico, and Guam.
Add up all those jurisdictions, and it works out to 4.6 million children infected with SARS-CoV-2 as of Aug. 19, with children representing 14.6% of all cases since the start of the pandemic. There have been over 18,000 hospitalizations so far, which is just 2.3% of the total for all ages in the 23 states (and New York City) that are reporting such data on their health department websites, the AAP and CHA said.
The number of COVID-related deaths in children is now 402 after the largest 1-week increase (24) since late May of 2020, when the AAP/CHA coverage began. Mortality data by age are available from 44 states, New York City, Puerto Rico, and Guam.
U.S. kidney transplants grow in number and success
During 2016-2019, U.S. centers performed kidney transplants in nearly 77,000 patients, a jump of almost 25% compared with 4-year averages of about 62,000 patients throughout 2004-2015. That works out to about 15,000 more patients receiving donor kidneys, Sundaram Hariharan, MD, and associates reported in the New England Journal of Medicine in a review of all U.S. renal transplantations performed during 1996-2019.
Coupled with the volume uptick during this 24-year period were new lows in graft losses and patient deaths. By 2018, mortality during the first year following transplantation occurred at about a 1% rate among patients who had received a kidney from a living donor, and at about a 3% rate when the organ came from a deceased donor, nearly half the rate of 2 decades earlier, in 1996. Rates of first-year graft loss during 2017 were also about half of what they had been in 1996, occurring in about 2% of patients who received a living donor organ and in about 6% of those who got a kidney from a deceased donor during 2017.
“Twenty years ago, kidney transplantation was the preferred option compared with dialysis, and even more so now,” summed up Dr. Hariharan, a senior transplant nephrologist and professor of medicine and surgery at the University of Pittsburgh Medical Center and first author of the report. Kidney transplantation survival at U.S. centers “improved steadily over the past 24 years, despite patient variables becoming worse,” he said in an interview.
Kidney recipients are older, more obese, and have more prevalent diabetes
During the period studied, kidney transplant recipients became on average older and more obese, and had a higher prevalence of diabetes; the age of organ donors grew as well. The prevalence of diabetes among patients who received a kidney from a deceased donor increased from 24% during 1996-1999 to 36% during 2016-2019, while diabetes prevalence among recipients of an organ from a living donor rose from 25% in 1996-1999 to 29% during 2016-2019.
The improved graft and patient survival numbers “are very encouraging trends,” said Michelle A. Josephson, MD, professor and medical director of kidney transplantation at the University of Chicago, who was not involved with the report. “We have been hearing for a number of years that short-term graft survival had improved, but I’m thrilled to learn that long-term survival has also improved.”
The report documented 10-year survival of graft recipients during 2008-2011 of 67%, up from 61% during 1996-1999, and a 10-year overall graft survival rate of 54% in the 2008-2011 cohort, an improvement from the 42% rate in patients who received their organs in 1996-1999, changes Dr. Hariharan characterized as “modest.”
These improvements in long-term graft and patient survival are “meaningful, and particularly notable that outcomes improved despite increased complexity of the transplant population,” said Krista L. Lentine, MD, PhD, professor and medical director of living donation at Saint Louis University. But “despite these improvements, long-term graft survival remains limited,” she cautioned, especially because of risks for substantial complications from chronic immunosuppressive treatment including infection, cancer, glucose intolerance, and dyslipidemia.
The analysis reported by Dr. Hariharan and his associates used data collected by the Scientific Registry of Transplant Patients, run under contract with the U.S. Department of Health and Human Services, which has tracked all patients who have had kidney transplants at U.S. centers since the late 1980s, said Dr. Hariharan. The database included just over 362,000 total transplants during the 24-year period studied, with 36% of all transplants involving organs from living donors with the remaining patients receiving kidneys from deceased donors.
Living donations still stagnant; deceased-donor kidneys rise
The data showed that the rate of transplants from living donors was stagnant for 2 decades, with 22,525 patients transplanted during 2000-2003, and 23,746 transplanted during 2016-2019, with very similar rates during the intervening years. The recent spurt in transplants during 2016-2019 compared with the preceding decade depended almost entirely on kidneys from deceased donors. This rate jumped from the steady, slow rise it showed during 1996-2015, when deceased-donor transplants rose from about 30,000 during 1996-1999 to about 41,000 during 2012-2015, to a more dramatic increase of about 12,000 additional transplants during the most recent period, adding up to a total of more than 53,000 transplants from deceased donors during 2016-2019.
“I strongly recommend organs from living donors” when feasible, said Dr. Hariharan. “At some centers, a high proportion of transplants use living donors, but not at other centers,” he said.
It’s unknown why transplants using organs from deceased donors has shown this growth, but Dr. Hariharan suggested a multifactorial explanation. Those factors include growth in the number of patients with end-stage renal disease who require dialysis, increased numbers of patients listed for kidney transplant, new approaches that allow organs from older donors and those infected with pathogens such as hepatitis C virus or HIV, greater numbers of people and families agreeing to donate organs, and possibly the opioid crisis that may have led to increased organ donation. The number of U.S. centers performing kidney transplants rose from fewer than 200 about a quarter of a century ago to about 250 today, he added.
‘Immuno Bill’ guarantees Medicare coverage for immunosuppression
Dr. Hariharan voiced optimism that graft and patient survival rates will continue to improve going forward. One factor will likely be the passage in late 2020 of the “Immuno Bill” by the U.S. Congress, which among other things mandated ongoing coverage starting in 2023 for immunosuppressive drugs for all Medicare beneficiaries with a kidney transplant. Until then, Medicare provides coverage for only 36 months, a time limit that has resulted in nearly 400 kidney recipients annually losing coverage of their immunosuppression medications.
Dr. Hariharan and coauthors called the existing potential for discontinuation of immunosuppressive drug an “unnecessary impediment to long-term survival for which patients and society paid a heavy price.”
“Kidney transplantation, especially from living donors, offers patients with kidney failure the best chance for long-term survival and improved quality of life, with lower cost to the health care system,” Dr. Lentine said in an interview. Despite the many positive trends detailed in the report from Dr. Hariharan and coauthors, “the vast majority of the more than 700,000 people in the United States with kidney failure will not have an opportunity to receive a transplant due to limitations in organ supply.” And many patients who receive a kidney transplant eventually must resume dialysis because of “limited long-term graft survival resulting from allograft nephropathy, recurrent native disease, medication nonadherence, or other causes.” Plus many potentially transplantable organs go unused.
Dr. Lentine cited a position statement issued in July 2021 by the National Kidney Foundation that made several recommendations on how to improve access to kidney transplants and improve outcomes. “Expanding opportunities for safe living donation, eliminating racial disparities in living-donor access, improving wait-list access and transport readiness, maximizing use of deceased-donor organs, and extending graft longevity are critical priorities,” said Dr. Lentine, lead author on the statement.
“For many or even most patients with kidney failure transplantation is the optimal form of renal replacement. The better recent outcomes and evolving management strategies make transplantation an even more attractive option,” said Dr. Josephson. Improved outcomes among U.S. transplant patients also highlights the “importance of increasing access to kidney transplantation” for all people with kidney failure who could benefit from this treatment, she added.
Dr. Hariharan and Dr. Lentine had no relevant disclosures. Dr. Josephson has been a consultant to UCB and has an ownership interest in Seagen.
During 2016-2019, U.S. centers performed kidney transplants in nearly 77,000 patients, a jump of almost 25% compared with 4-year averages of about 62,000 patients throughout 2004-2015. That works out to about 15,000 more patients receiving donor kidneys, Sundaram Hariharan, MD, and associates reported in the New England Journal of Medicine in a review of all U.S. renal transplantations performed during 1996-2019.
Coupled with the volume uptick during this 24-year period were new lows in graft losses and patient deaths. By 2018, mortality during the first year following transplantation occurred at about a 1% rate among patients who had received a kidney from a living donor, and at about a 3% rate when the organ came from a deceased donor, nearly half the rate of 2 decades earlier, in 1996. Rates of first-year graft loss during 2017 were also about half of what they had been in 1996, occurring in about 2% of patients who received a living donor organ and in about 6% of those who got a kidney from a deceased donor during 2017.
“Twenty years ago, kidney transplantation was the preferred option compared with dialysis, and even more so now,” summed up Dr. Hariharan, a senior transplant nephrologist and professor of medicine and surgery at the University of Pittsburgh Medical Center and first author of the report. Kidney transplantation survival at U.S. centers “improved steadily over the past 24 years, despite patient variables becoming worse,” he said in an interview.
Kidney recipients are older, more obese, and have more prevalent diabetes
During the period studied, kidney transplant recipients became on average older and more obese, and had a higher prevalence of diabetes; the age of organ donors grew as well. The prevalence of diabetes among patients who received a kidney from a deceased donor increased from 24% during 1996-1999 to 36% during 2016-2019, while diabetes prevalence among recipients of an organ from a living donor rose from 25% in 1996-1999 to 29% during 2016-2019.
The improved graft and patient survival numbers “are very encouraging trends,” said Michelle A. Josephson, MD, professor and medical director of kidney transplantation at the University of Chicago, who was not involved with the report. “We have been hearing for a number of years that short-term graft survival had improved, but I’m thrilled to learn that long-term survival has also improved.”
The report documented 10-year survival of graft recipients during 2008-2011 of 67%, up from 61% during 1996-1999, and a 10-year overall graft survival rate of 54% in the 2008-2011 cohort, an improvement from the 42% rate in patients who received their organs in 1996-1999, changes Dr. Hariharan characterized as “modest.”
These improvements in long-term graft and patient survival are “meaningful, and particularly notable that outcomes improved despite increased complexity of the transplant population,” said Krista L. Lentine, MD, PhD, professor and medical director of living donation at Saint Louis University. But “despite these improvements, long-term graft survival remains limited,” she cautioned, especially because of risks for substantial complications from chronic immunosuppressive treatment including infection, cancer, glucose intolerance, and dyslipidemia.
The analysis reported by Dr. Hariharan and his associates used data collected by the Scientific Registry of Transplant Patients, run under contract with the U.S. Department of Health and Human Services, which has tracked all patients who have had kidney transplants at U.S. centers since the late 1980s, said Dr. Hariharan. The database included just over 362,000 total transplants during the 24-year period studied, with 36% of all transplants involving organs from living donors with the remaining patients receiving kidneys from deceased donors.
Living donations still stagnant; deceased-donor kidneys rise
The data showed that the rate of transplants from living donors was stagnant for 2 decades, with 22,525 patients transplanted during 2000-2003, and 23,746 transplanted during 2016-2019, with very similar rates during the intervening years. The recent spurt in transplants during 2016-2019 compared with the preceding decade depended almost entirely on kidneys from deceased donors. This rate jumped from the steady, slow rise it showed during 1996-2015, when deceased-donor transplants rose from about 30,000 during 1996-1999 to about 41,000 during 2012-2015, to a more dramatic increase of about 12,000 additional transplants during the most recent period, adding up to a total of more than 53,000 transplants from deceased donors during 2016-2019.
“I strongly recommend organs from living donors” when feasible, said Dr. Hariharan. “At some centers, a high proportion of transplants use living donors, but not at other centers,” he said.
It’s unknown why transplants using organs from deceased donors has shown this growth, but Dr. Hariharan suggested a multifactorial explanation. Those factors include growth in the number of patients with end-stage renal disease who require dialysis, increased numbers of patients listed for kidney transplant, new approaches that allow organs from older donors and those infected with pathogens such as hepatitis C virus or HIV, greater numbers of people and families agreeing to donate organs, and possibly the opioid crisis that may have led to increased organ donation. The number of U.S. centers performing kidney transplants rose from fewer than 200 about a quarter of a century ago to about 250 today, he added.
‘Immuno Bill’ guarantees Medicare coverage for immunosuppression
Dr. Hariharan voiced optimism that graft and patient survival rates will continue to improve going forward. One factor will likely be the passage in late 2020 of the “Immuno Bill” by the U.S. Congress, which among other things mandated ongoing coverage starting in 2023 for immunosuppressive drugs for all Medicare beneficiaries with a kidney transplant. Until then, Medicare provides coverage for only 36 months, a time limit that has resulted in nearly 400 kidney recipients annually losing coverage of their immunosuppression medications.
Dr. Hariharan and coauthors called the existing potential for discontinuation of immunosuppressive drug an “unnecessary impediment to long-term survival for which patients and society paid a heavy price.”
“Kidney transplantation, especially from living donors, offers patients with kidney failure the best chance for long-term survival and improved quality of life, with lower cost to the health care system,” Dr. Lentine said in an interview. Despite the many positive trends detailed in the report from Dr. Hariharan and coauthors, “the vast majority of the more than 700,000 people in the United States with kidney failure will not have an opportunity to receive a transplant due to limitations in organ supply.” And many patients who receive a kidney transplant eventually must resume dialysis because of “limited long-term graft survival resulting from allograft nephropathy, recurrent native disease, medication nonadherence, or other causes.” Plus many potentially transplantable organs go unused.
Dr. Lentine cited a position statement issued in July 2021 by the National Kidney Foundation that made several recommendations on how to improve access to kidney transplants and improve outcomes. “Expanding opportunities for safe living donation, eliminating racial disparities in living-donor access, improving wait-list access and transport readiness, maximizing use of deceased-donor organs, and extending graft longevity are critical priorities,” said Dr. Lentine, lead author on the statement.
“For many or even most patients with kidney failure transplantation is the optimal form of renal replacement. The better recent outcomes and evolving management strategies make transplantation an even more attractive option,” said Dr. Josephson. Improved outcomes among U.S. transplant patients also highlights the “importance of increasing access to kidney transplantation” for all people with kidney failure who could benefit from this treatment, she added.
Dr. Hariharan and Dr. Lentine had no relevant disclosures. Dr. Josephson has been a consultant to UCB and has an ownership interest in Seagen.
During 2016-2019, U.S. centers performed kidney transplants in nearly 77,000 patients, a jump of almost 25% compared with 4-year averages of about 62,000 patients throughout 2004-2015. That works out to about 15,000 more patients receiving donor kidneys, Sundaram Hariharan, MD, and associates reported in the New England Journal of Medicine in a review of all U.S. renal transplantations performed during 1996-2019.
Coupled with the volume uptick during this 24-year period were new lows in graft losses and patient deaths. By 2018, mortality during the first year following transplantation occurred at about a 1% rate among patients who had received a kidney from a living donor, and at about a 3% rate when the organ came from a deceased donor, nearly half the rate of 2 decades earlier, in 1996. Rates of first-year graft loss during 2017 were also about half of what they had been in 1996, occurring in about 2% of patients who received a living donor organ and in about 6% of those who got a kidney from a deceased donor during 2017.
“Twenty years ago, kidney transplantation was the preferred option compared with dialysis, and even more so now,” summed up Dr. Hariharan, a senior transplant nephrologist and professor of medicine and surgery at the University of Pittsburgh Medical Center and first author of the report. Kidney transplantation survival at U.S. centers “improved steadily over the past 24 years, despite patient variables becoming worse,” he said in an interview.
Kidney recipients are older, more obese, and have more prevalent diabetes
During the period studied, kidney transplant recipients became on average older and more obese, and had a higher prevalence of diabetes; the age of organ donors grew as well. The prevalence of diabetes among patients who received a kidney from a deceased donor increased from 24% during 1996-1999 to 36% during 2016-2019, while diabetes prevalence among recipients of an organ from a living donor rose from 25% in 1996-1999 to 29% during 2016-2019.
The improved graft and patient survival numbers “are very encouraging trends,” said Michelle A. Josephson, MD, professor and medical director of kidney transplantation at the University of Chicago, who was not involved with the report. “We have been hearing for a number of years that short-term graft survival had improved, but I’m thrilled to learn that long-term survival has also improved.”
The report documented 10-year survival of graft recipients during 2008-2011 of 67%, up from 61% during 1996-1999, and a 10-year overall graft survival rate of 54% in the 2008-2011 cohort, an improvement from the 42% rate in patients who received their organs in 1996-1999, changes Dr. Hariharan characterized as “modest.”
These improvements in long-term graft and patient survival are “meaningful, and particularly notable that outcomes improved despite increased complexity of the transplant population,” said Krista L. Lentine, MD, PhD, professor and medical director of living donation at Saint Louis University. But “despite these improvements, long-term graft survival remains limited,” she cautioned, especially because of risks for substantial complications from chronic immunosuppressive treatment including infection, cancer, glucose intolerance, and dyslipidemia.
The analysis reported by Dr. Hariharan and his associates used data collected by the Scientific Registry of Transplant Patients, run under contract with the U.S. Department of Health and Human Services, which has tracked all patients who have had kidney transplants at U.S. centers since the late 1980s, said Dr. Hariharan. The database included just over 362,000 total transplants during the 24-year period studied, with 36% of all transplants involving organs from living donors with the remaining patients receiving kidneys from deceased donors.
Living donations still stagnant; deceased-donor kidneys rise
The data showed that the rate of transplants from living donors was stagnant for 2 decades, with 22,525 patients transplanted during 2000-2003, and 23,746 transplanted during 2016-2019, with very similar rates during the intervening years. The recent spurt in transplants during 2016-2019 compared with the preceding decade depended almost entirely on kidneys from deceased donors. This rate jumped from the steady, slow rise it showed during 1996-2015, when deceased-donor transplants rose from about 30,000 during 1996-1999 to about 41,000 during 2012-2015, to a more dramatic increase of about 12,000 additional transplants during the most recent period, adding up to a total of more than 53,000 transplants from deceased donors during 2016-2019.
“I strongly recommend organs from living donors” when feasible, said Dr. Hariharan. “At some centers, a high proportion of transplants use living donors, but not at other centers,” he said.
It’s unknown why transplants using organs from deceased donors has shown this growth, but Dr. Hariharan suggested a multifactorial explanation. Those factors include growth in the number of patients with end-stage renal disease who require dialysis, increased numbers of patients listed for kidney transplant, new approaches that allow organs from older donors and those infected with pathogens such as hepatitis C virus or HIV, greater numbers of people and families agreeing to donate organs, and possibly the opioid crisis that may have led to increased organ donation. The number of U.S. centers performing kidney transplants rose from fewer than 200 about a quarter of a century ago to about 250 today, he added.
‘Immuno Bill’ guarantees Medicare coverage for immunosuppression
Dr. Hariharan voiced optimism that graft and patient survival rates will continue to improve going forward. One factor will likely be the passage in late 2020 of the “Immuno Bill” by the U.S. Congress, which among other things mandated ongoing coverage starting in 2023 for immunosuppressive drugs for all Medicare beneficiaries with a kidney transplant. Until then, Medicare provides coverage for only 36 months, a time limit that has resulted in nearly 400 kidney recipients annually losing coverage of their immunosuppression medications.
Dr. Hariharan and coauthors called the existing potential for discontinuation of immunosuppressive drug an “unnecessary impediment to long-term survival for which patients and society paid a heavy price.”
“Kidney transplantation, especially from living donors, offers patients with kidney failure the best chance for long-term survival and improved quality of life, with lower cost to the health care system,” Dr. Lentine said in an interview. Despite the many positive trends detailed in the report from Dr. Hariharan and coauthors, “the vast majority of the more than 700,000 people in the United States with kidney failure will not have an opportunity to receive a transplant due to limitations in organ supply.” And many patients who receive a kidney transplant eventually must resume dialysis because of “limited long-term graft survival resulting from allograft nephropathy, recurrent native disease, medication nonadherence, or other causes.” Plus many potentially transplantable organs go unused.
Dr. Lentine cited a position statement issued in July 2021 by the National Kidney Foundation that made several recommendations on how to improve access to kidney transplants and improve outcomes. “Expanding opportunities for safe living donation, eliminating racial disparities in living-donor access, improving wait-list access and transport readiness, maximizing use of deceased-donor organs, and extending graft longevity are critical priorities,” said Dr. Lentine, lead author on the statement.
“For many or even most patients with kidney failure transplantation is the optimal form of renal replacement. The better recent outcomes and evolving management strategies make transplantation an even more attractive option,” said Dr. Josephson. Improved outcomes among U.S. transplant patients also highlights the “importance of increasing access to kidney transplantation” for all people with kidney failure who could benefit from this treatment, she added.
Dr. Hariharan and Dr. Lentine had no relevant disclosures. Dr. Josephson has been a consultant to UCB and has an ownership interest in Seagen.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
CRP as a biomarker for community-acquired pneumonia
Background: In the United States, CAP was responsible for nearly 50,000 deaths in 2017. Prompt and accurate diagnosis promotes early treatment and avoids unnecessary antibiotic treatment for nonpneumonia lower respiratory tract infection patients. Diagnosis is based on signs and symptoms, as well as available imaging. Inflammatory markers such as CRP, white blood cell count, and procalcitonin are readily available in the ED and outpatient settings.
Study design: Bivariate meta-analysis.
Setting: A systematic review of literature was done via PubMed search to identify prospective studies evaluating the accuracy of biomarkers in patients with cough or suspected CAP.
Synopsis: Fourteen studies met the criteria to be included in the meta-analysis. Summary receiver operating characteristic (ROC) curves generated reported area under the curve of 0.802 for CRP (95% confidence interval, 0.78-0.85), 0.777 for leukocytosis (95% CI, 0.74-0.81), and 0.771 for procalcitonin (95% CI, 0.74-0.81). The combination of CRP greater than 49.5 mg/L and procalcitonin greater than 0.1 mcg/L had a positive likelihood ratio of 2.24 and a negative likelihood ratio of 0.44.
The study had a some of limitations. The blinding of the person performing the index test to the reference standard and vice versa was not clear. Further, it was unclear if the person interpreting the reference standard was blinded to the index test in five studies and absent in one. Other limitations were inconsistent reporting of abnormal post hoc cutoffs and only two biomarkers being reported in a single study.
Combining a biomarker with signs and symptoms has the potential to improve diagnostic accuracy in the outpatient setting further. CRP was found to be most accurate regardless of the cutoff used; however, further studies without threshold effect will prove beneficial.
Bottom line: CRP is a more accurate and useful biomarker for outpatient CAP diagnosis than procalcitonin or leukocytosis.
Citation: Ebell MH et al. Accuracy of biomarkers for the diagnosis of adult community-acquired pneumonia: A meta-analysis. Acad Emerg Med. 2020;27(3):195-206.
Dr. Castellanos is a hospitalist and assistant professor of medicine at UK HealthCare, Lexington, Ky.
Background: In the United States, CAP was responsible for nearly 50,000 deaths in 2017. Prompt and accurate diagnosis promotes early treatment and avoids unnecessary antibiotic treatment for nonpneumonia lower respiratory tract infection patients. Diagnosis is based on signs and symptoms, as well as available imaging. Inflammatory markers such as CRP, white blood cell count, and procalcitonin are readily available in the ED and outpatient settings.
Study design: Bivariate meta-analysis.
Setting: A systematic review of literature was done via PubMed search to identify prospective studies evaluating the accuracy of biomarkers in patients with cough or suspected CAP.
Synopsis: Fourteen studies met the criteria to be included in the meta-analysis. Summary receiver operating characteristic (ROC) curves generated reported area under the curve of 0.802 for CRP (95% confidence interval, 0.78-0.85), 0.777 for leukocytosis (95% CI, 0.74-0.81), and 0.771 for procalcitonin (95% CI, 0.74-0.81). The combination of CRP greater than 49.5 mg/L and procalcitonin greater than 0.1 mcg/L had a positive likelihood ratio of 2.24 and a negative likelihood ratio of 0.44.
The study had a some of limitations. The blinding of the person performing the index test to the reference standard and vice versa was not clear. Further, it was unclear if the person interpreting the reference standard was blinded to the index test in five studies and absent in one. Other limitations were inconsistent reporting of abnormal post hoc cutoffs and only two biomarkers being reported in a single study.
Combining a biomarker with signs and symptoms has the potential to improve diagnostic accuracy in the outpatient setting further. CRP was found to be most accurate regardless of the cutoff used; however, further studies without threshold effect will prove beneficial.
Bottom line: CRP is a more accurate and useful biomarker for outpatient CAP diagnosis than procalcitonin or leukocytosis.
Citation: Ebell MH et al. Accuracy of biomarkers for the diagnosis of adult community-acquired pneumonia: A meta-analysis. Acad Emerg Med. 2020;27(3):195-206.
Dr. Castellanos is a hospitalist and assistant professor of medicine at UK HealthCare, Lexington, Ky.
Background: In the United States, CAP was responsible for nearly 50,000 deaths in 2017. Prompt and accurate diagnosis promotes early treatment and avoids unnecessary antibiotic treatment for nonpneumonia lower respiratory tract infection patients. Diagnosis is based on signs and symptoms, as well as available imaging. Inflammatory markers such as CRP, white blood cell count, and procalcitonin are readily available in the ED and outpatient settings.
Study design: Bivariate meta-analysis.
Setting: A systematic review of literature was done via PubMed search to identify prospective studies evaluating the accuracy of biomarkers in patients with cough or suspected CAP.
Synopsis: Fourteen studies met the criteria to be included in the meta-analysis. Summary receiver operating characteristic (ROC) curves generated reported area under the curve of 0.802 for CRP (95% confidence interval, 0.78-0.85), 0.777 for leukocytosis (95% CI, 0.74-0.81), and 0.771 for procalcitonin (95% CI, 0.74-0.81). The combination of CRP greater than 49.5 mg/L and procalcitonin greater than 0.1 mcg/L had a positive likelihood ratio of 2.24 and a negative likelihood ratio of 0.44.
The study had a some of limitations. The blinding of the person performing the index test to the reference standard and vice versa was not clear. Further, it was unclear if the person interpreting the reference standard was blinded to the index test in five studies and absent in one. Other limitations were inconsistent reporting of abnormal post hoc cutoffs and only two biomarkers being reported in a single study.
Combining a biomarker with signs and symptoms has the potential to improve diagnostic accuracy in the outpatient setting further. CRP was found to be most accurate regardless of the cutoff used; however, further studies without threshold effect will prove beneficial.
Bottom line: CRP is a more accurate and useful biomarker for outpatient CAP diagnosis than procalcitonin or leukocytosis.
Citation: Ebell MH et al. Accuracy of biomarkers for the diagnosis of adult community-acquired pneumonia: A meta-analysis. Acad Emerg Med. 2020;27(3):195-206.
Dr. Castellanos is a hospitalist and assistant professor of medicine at UK HealthCare, Lexington, Ky.