User login
More than one-third of tumors found on breast cancer screening represent overdiagnosis
The purpose of screening mammography is to detect tumors when they are small and nonpalpable in order to prevent more advanced breast tumors in women. Overdiagnosis, which leads to unnecessary treatment, refers to screen-detected tumors that will not lead to symptoms. Overdiagnosis cannot be measured directly and, therefore, understanding this concept is problematic for both women and clinicians.
Related article:
Women’s Preventive Services Initiative Guidelines provide consensus for practicing ObGyns
Observations from other types of cancer screening put overdiagnosis in perspective
To help us grasp the overall issue of overdiagnosis, we can consider screening mammography alongside cervical cancer screening and colon cancer screening. For instance, screening with cervical cytology has reduced the incidence of and mortality from invasive cervical cancer.1 Likewise, colonoscopy repeatedly has been found to reduce colon cancer mortality.2,3 Decades of media messaging have emphasized the benefits of screening mammograms.4 However, and in contrast with cervical cytology and colonoscopy, screening mammography has not reduced the incidence of breast cancer presenting with metastatic (advanced) disease.5 Likewise, as the Danish authors of a recent study published in Annals of Internal Medicine point out, screening mammography has not achieved the promised reduction in breast cancer mortality.
New data from Denmark highlight overdiagnosis concerns
Jørgensen and colleagues conducted a cohort study to estimate the incidence of screen-detected tumors that would not become clinically relevant (overdiagnosis) among women aged 35 to 84 years between 1980 and 2010 in Denmark.6 This country offers a particularly well-suited backdrop for a study of overdiagnosis because biennial screening mammography was introduced by region beginning in the early 1990s. By 2007, one-fifth of the country’s female population aged 50 to 69 years were invited to participate. In the following years, screening became universal for Danish women in this age group.
For the study, researchers identified the size of all invasive breast cancer tumors diagnosed over the study period and then compared the incidence rates of advanced tumors (more than 20-mm in size at detection) with nonadvanced tumors in screened and unscreened Danish regions. The investigators took into account regional differences not related to screening by assessing the trends in diagnosis of advanced and nonadvanced tumors in screened and unscreened regions among women older and younger than those screened. This gave them a better estimate of the incidence of overdiagnosis.6
Jørgensen and colleagues found that breast cancer screening resulted in an increase in the incidence of nonadvanced tumors, but that it did not reduce the incidence of advanced tumors. They estimated that 39% of the invasive tumors found among women aged 50 to 69 were overdiagnosed.6
These Danish study results, that more than one-third of screen-detected tumors represent overdiagnosis, are similar to those found for studies conducted in the United States and other countries.7,8 The lengthy follow-up after initiation of screening and the assessment of trends in unscreened women represent strengths of the study by Jørgensen and colleagues, and speak to concerns voiced by those skeptical of reported overdiagnosis incidence rates.9
Although breast cancer mortality is declining, the lion’s share of this decline has resulted from improvements in systemic therapy rather than from screening mammography. Widespread screening mammography has resulted in a scenario in which women are more likely to have a breast cancer that was overdiagnosed than in having earlier detection of a tumor destined to grow larger.5 In the future, by targeting higher-risk women, screening may result in a better benefit:risk ratio. However, and as pointed out by Otis Brawley, MD, Chief Medical and Scientific Officer of the American Cancer Society, we must acknowledge that overdiagnosis is common, the benefits of screening have been overstated, and some patients considered as “cured” from breast cancer have in fact been harmed by unneeded treatment.10
Related article:
No surprises from the USPSTF with new guidance on screening mammography
My breast cancer screening approach
As Brawley indicates, we should not abandon screening.10 I continue to recommend screening based on US Preventive Services Taskforce guidance, beginning biennial screens at age 50.11 I also recognize that some women prefer earlier and more frequent screens, while others may prefer less frequent or even no screening.
- Nieminen P, Kallio M, Hakama M. The effect of mass screening on incidence and mortality of squamous and adenocarcinoma of cervix uteri. Obstet Gynecol. 1995;85(6):1017-1021.
- Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009;150(1):1-8.
- Singh H, Nugent Z, Demers AA, Kliewer EV, Mahmud SM, Bernstein CN. The reduction in colorectal cancer mortality after colonoscopy varies by site of the cancer. Gastroenterology. 2010;139(4):1128-1137.
- Orenstein P. Our feel-good war on breast cancer. New York Times website. http://www.nytimes.com/2013/04/28/magazine/our-feel-good-war-on-breast-cancer.html?pagewanted=all& _r=0. Published April 25, 2013. Accessed February 21, 2017.
- Welch HG, Gorski DH, Albertsen PC. Trends in metastatic breast and prostate cancer. N Engl J Med. 2016;374(8):596.
- Jørgensen KJ, Gøtzsche PC, Kalager M, Zahl PH. Breast cancer screening in Denmark: a cohort study of tumor size and overdiagnosis. Ann Intern Med. 2017 Jan 10. doi:10.7326/M16-0270.
- Welch HG, Prorok PC, O'Malley AJ, Kramer BS. Breast-cancer tumor size, overdiagnosis, and mammography screening effectiveness. N Engl J Med. 2016;375(15):1438-1447.
- Autier P, Boniol M, Middleton R, et al. Advanced breast cancer incidence following population-based mammographic screening. Ann Oncol. 2011;22(8):1726-1735.
- Kopans DB. Breast-cancer tumor size and screening effectiveness. N Engl J Med. 2017;376(1):93-94.
- Brawley OW. Accepting the existence of breast cancer overdiagnosis [published online ahead of print January 10, 2017]. Ann Intern Med. doi:10.7326/M16-2850.
- Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L. Screening for breast cancer: an update for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;151(10):727-737.
The purpose of screening mammography is to detect tumors when they are small and nonpalpable in order to prevent more advanced breast tumors in women. Overdiagnosis, which leads to unnecessary treatment, refers to screen-detected tumors that will not lead to symptoms. Overdiagnosis cannot be measured directly and, therefore, understanding this concept is problematic for both women and clinicians.
Related article:
Women’s Preventive Services Initiative Guidelines provide consensus for practicing ObGyns
Observations from other types of cancer screening put overdiagnosis in perspective
To help us grasp the overall issue of overdiagnosis, we can consider screening mammography alongside cervical cancer screening and colon cancer screening. For instance, screening with cervical cytology has reduced the incidence of and mortality from invasive cervical cancer.1 Likewise, colonoscopy repeatedly has been found to reduce colon cancer mortality.2,3 Decades of media messaging have emphasized the benefits of screening mammograms.4 However, and in contrast with cervical cytology and colonoscopy, screening mammography has not reduced the incidence of breast cancer presenting with metastatic (advanced) disease.5 Likewise, as the Danish authors of a recent study published in Annals of Internal Medicine point out, screening mammography has not achieved the promised reduction in breast cancer mortality.
New data from Denmark highlight overdiagnosis concerns
Jørgensen and colleagues conducted a cohort study to estimate the incidence of screen-detected tumors that would not become clinically relevant (overdiagnosis) among women aged 35 to 84 years between 1980 and 2010 in Denmark.6 This country offers a particularly well-suited backdrop for a study of overdiagnosis because biennial screening mammography was introduced by region beginning in the early 1990s. By 2007, one-fifth of the country’s female population aged 50 to 69 years were invited to participate. In the following years, screening became universal for Danish women in this age group.
For the study, researchers identified the size of all invasive breast cancer tumors diagnosed over the study period and then compared the incidence rates of advanced tumors (more than 20-mm in size at detection) with nonadvanced tumors in screened and unscreened Danish regions. The investigators took into account regional differences not related to screening by assessing the trends in diagnosis of advanced and nonadvanced tumors in screened and unscreened regions among women older and younger than those screened. This gave them a better estimate of the incidence of overdiagnosis.6
Jørgensen and colleagues found that breast cancer screening resulted in an increase in the incidence of nonadvanced tumors, but that it did not reduce the incidence of advanced tumors. They estimated that 39% of the invasive tumors found among women aged 50 to 69 were overdiagnosed.6
These Danish study results, that more than one-third of screen-detected tumors represent overdiagnosis, are similar to those found for studies conducted in the United States and other countries.7,8 The lengthy follow-up after initiation of screening and the assessment of trends in unscreened women represent strengths of the study by Jørgensen and colleagues, and speak to concerns voiced by those skeptical of reported overdiagnosis incidence rates.9
Although breast cancer mortality is declining, the lion’s share of this decline has resulted from improvements in systemic therapy rather than from screening mammography. Widespread screening mammography has resulted in a scenario in which women are more likely to have a breast cancer that was overdiagnosed than in having earlier detection of a tumor destined to grow larger.5 In the future, by targeting higher-risk women, screening may result in a better benefit:risk ratio. However, and as pointed out by Otis Brawley, MD, Chief Medical and Scientific Officer of the American Cancer Society, we must acknowledge that overdiagnosis is common, the benefits of screening have been overstated, and some patients considered as “cured” from breast cancer have in fact been harmed by unneeded treatment.10
Related article:
No surprises from the USPSTF with new guidance on screening mammography
My breast cancer screening approach
As Brawley indicates, we should not abandon screening.10 I continue to recommend screening based on US Preventive Services Taskforce guidance, beginning biennial screens at age 50.11 I also recognize that some women prefer earlier and more frequent screens, while others may prefer less frequent or even no screening.
The purpose of screening mammography is to detect tumors when they are small and nonpalpable in order to prevent more advanced breast tumors in women. Overdiagnosis, which leads to unnecessary treatment, refers to screen-detected tumors that will not lead to symptoms. Overdiagnosis cannot be measured directly and, therefore, understanding this concept is problematic for both women and clinicians.
Related article:
Women’s Preventive Services Initiative Guidelines provide consensus for practicing ObGyns
Observations from other types of cancer screening put overdiagnosis in perspective
To help us grasp the overall issue of overdiagnosis, we can consider screening mammography alongside cervical cancer screening and colon cancer screening. For instance, screening with cervical cytology has reduced the incidence of and mortality from invasive cervical cancer.1 Likewise, colonoscopy repeatedly has been found to reduce colon cancer mortality.2,3 Decades of media messaging have emphasized the benefits of screening mammograms.4 However, and in contrast with cervical cytology and colonoscopy, screening mammography has not reduced the incidence of breast cancer presenting with metastatic (advanced) disease.5 Likewise, as the Danish authors of a recent study published in Annals of Internal Medicine point out, screening mammography has not achieved the promised reduction in breast cancer mortality.
New data from Denmark highlight overdiagnosis concerns
Jørgensen and colleagues conducted a cohort study to estimate the incidence of screen-detected tumors that would not become clinically relevant (overdiagnosis) among women aged 35 to 84 years between 1980 and 2010 in Denmark.6 This country offers a particularly well-suited backdrop for a study of overdiagnosis because biennial screening mammography was introduced by region beginning in the early 1990s. By 2007, one-fifth of the country’s female population aged 50 to 69 years were invited to participate. In the following years, screening became universal for Danish women in this age group.
For the study, researchers identified the size of all invasive breast cancer tumors diagnosed over the study period and then compared the incidence rates of advanced tumors (more than 20-mm in size at detection) with nonadvanced tumors in screened and unscreened Danish regions. The investigators took into account regional differences not related to screening by assessing the trends in diagnosis of advanced and nonadvanced tumors in screened and unscreened regions among women older and younger than those screened. This gave them a better estimate of the incidence of overdiagnosis.6
Jørgensen and colleagues found that breast cancer screening resulted in an increase in the incidence of nonadvanced tumors, but that it did not reduce the incidence of advanced tumors. They estimated that 39% of the invasive tumors found among women aged 50 to 69 were overdiagnosed.6
These Danish study results, that more than one-third of screen-detected tumors represent overdiagnosis, are similar to those found for studies conducted in the United States and other countries.7,8 The lengthy follow-up after initiation of screening and the assessment of trends in unscreened women represent strengths of the study by Jørgensen and colleagues, and speak to concerns voiced by those skeptical of reported overdiagnosis incidence rates.9
Although breast cancer mortality is declining, the lion’s share of this decline has resulted from improvements in systemic therapy rather than from screening mammography. Widespread screening mammography has resulted in a scenario in which women are more likely to have a breast cancer that was overdiagnosed than in having earlier detection of a tumor destined to grow larger.5 In the future, by targeting higher-risk women, screening may result in a better benefit:risk ratio. However, and as pointed out by Otis Brawley, MD, Chief Medical and Scientific Officer of the American Cancer Society, we must acknowledge that overdiagnosis is common, the benefits of screening have been overstated, and some patients considered as “cured” from breast cancer have in fact been harmed by unneeded treatment.10
Related article:
No surprises from the USPSTF with new guidance on screening mammography
My breast cancer screening approach
As Brawley indicates, we should not abandon screening.10 I continue to recommend screening based on US Preventive Services Taskforce guidance, beginning biennial screens at age 50.11 I also recognize that some women prefer earlier and more frequent screens, while others may prefer less frequent or even no screening.
- Nieminen P, Kallio M, Hakama M. The effect of mass screening on incidence and mortality of squamous and adenocarcinoma of cervix uteri. Obstet Gynecol. 1995;85(6):1017-1021.
- Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009;150(1):1-8.
- Singh H, Nugent Z, Demers AA, Kliewer EV, Mahmud SM, Bernstein CN. The reduction in colorectal cancer mortality after colonoscopy varies by site of the cancer. Gastroenterology. 2010;139(4):1128-1137.
- Orenstein P. Our feel-good war on breast cancer. New York Times website. http://www.nytimes.com/2013/04/28/magazine/our-feel-good-war-on-breast-cancer.html?pagewanted=all& _r=0. Published April 25, 2013. Accessed February 21, 2017.
- Welch HG, Gorski DH, Albertsen PC. Trends in metastatic breast and prostate cancer. N Engl J Med. 2016;374(8):596.
- Jørgensen KJ, Gøtzsche PC, Kalager M, Zahl PH. Breast cancer screening in Denmark: a cohort study of tumor size and overdiagnosis. Ann Intern Med. 2017 Jan 10. doi:10.7326/M16-0270.
- Welch HG, Prorok PC, O'Malley AJ, Kramer BS. Breast-cancer tumor size, overdiagnosis, and mammography screening effectiveness. N Engl J Med. 2016;375(15):1438-1447.
- Autier P, Boniol M, Middleton R, et al. Advanced breast cancer incidence following population-based mammographic screening. Ann Oncol. 2011;22(8):1726-1735.
- Kopans DB. Breast-cancer tumor size and screening effectiveness. N Engl J Med. 2017;376(1):93-94.
- Brawley OW. Accepting the existence of breast cancer overdiagnosis [published online ahead of print January 10, 2017]. Ann Intern Med. doi:10.7326/M16-2850.
- Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L. Screening for breast cancer: an update for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;151(10):727-737.
- Nieminen P, Kallio M, Hakama M. The effect of mass screening on incidence and mortality of squamous and adenocarcinoma of cervix uteri. Obstet Gynecol. 1995;85(6):1017-1021.
- Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009;150(1):1-8.
- Singh H, Nugent Z, Demers AA, Kliewer EV, Mahmud SM, Bernstein CN. The reduction in colorectal cancer mortality after colonoscopy varies by site of the cancer. Gastroenterology. 2010;139(4):1128-1137.
- Orenstein P. Our feel-good war on breast cancer. New York Times website. http://www.nytimes.com/2013/04/28/magazine/our-feel-good-war-on-breast-cancer.html?pagewanted=all& _r=0. Published April 25, 2013. Accessed February 21, 2017.
- Welch HG, Gorski DH, Albertsen PC. Trends in metastatic breast and prostate cancer. N Engl J Med. 2016;374(8):596.
- Jørgensen KJ, Gøtzsche PC, Kalager M, Zahl PH. Breast cancer screening in Denmark: a cohort study of tumor size and overdiagnosis. Ann Intern Med. 2017 Jan 10. doi:10.7326/M16-0270.
- Welch HG, Prorok PC, O'Malley AJ, Kramer BS. Breast-cancer tumor size, overdiagnosis, and mammography screening effectiveness. N Engl J Med. 2016;375(15):1438-1447.
- Autier P, Boniol M, Middleton R, et al. Advanced breast cancer incidence following population-based mammographic screening. Ann Oncol. 2011;22(8):1726-1735.
- Kopans DB. Breast-cancer tumor size and screening effectiveness. N Engl J Med. 2017;376(1):93-94.
- Brawley OW. Accepting the existence of breast cancer overdiagnosis [published online ahead of print January 10, 2017]. Ann Intern Med. doi:10.7326/M16-2850.
- Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L. Screening for breast cancer: an update for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;151(10):727-737.
Should the length of treatment for trichomoniasis in women be reconsidered?
EXPERT COMMENTARY
Both the Centers for Disease Control and Prevention and the World Health Organization currently recommend that patients with trichomoniasis be treated with a single 2-g oral dose of metronidazole.1 Following treatment, the reported rates of repeat infection or persistent infection range from 5% to 31%. Repeat infection rates may be even higher in HIV-infected patients.
Repeat infections presumably result from a failure to treat the patient’s sexual partner(s) or from the patient’s exposure to a new partner. Persistent infections, however, may be the result of inadequate primary therapy, even though inherent resistance of the organism to metronidazole is quite rare. To date, no single study has shown that single-dose therapy is inferior to multidose therapy, but most of these studies lack sufficient power to completely exclude the possibility of a type-2 statistical error.2 To compare single-dose with multidose therapy for trichomoniasis in a more systematic manner, Howe and Kissinger conducted a meta-analysis, which was recently published in Sexually Transmitted Diseases.
Related article:
2016 Update on infectious disease
Details of the study
The investigators conducted a comprehensive literature search using Embase, Medline, and ClinicalTrials.gov; 6 articles were included in the final results, 4 of which were randomized controlled trials. Approximately 1,300 participants were included in the 6 trials. All of the patients in the single-dose treatment arms received a 2-g oral dose of metronidazole. In the multidose treatment arms for 2 studies the participants received metronidazole 250 mg orally 3 times daily for 7 days, and for 2 studies the dose was 200 mg 3 times daily for 7 days. The fifth study employed a 500-mg oral dose of metronidazole twice daily for 7 days. The final study used a 400-mg oral dose twice daily for 5 days. The key study end point was treatment failure.
Howe and Kissinger demonstrated that women who received the single 2-g dose were 1.87 times (95% CI, 1.23−2.82; P<.01) more likely to experience a treatment failure compared with women who received a multidose regimen. When the one study that focused only on HIV-infected women was excluded from analysis, the results were similar. The relative risk of treatment failure was 1.80 (95% CI, 1.07−3.02; P<.03).
Related article:
Preventing infection after cesarean delivery: Evidence-based guidance
Study limitations
The results of this meta-analysis are interesting and provocative. However, the analysis has several important limitations. Five of the 6 studies were published many years ago (1971, 1972, 1979, 1980, and 1982). The most recent study was published in 2010. The investigators used 4 different multidose regimens, with metronidazole doses ranging from 200 mg to 500 mg and duration of therapy ranging from 5 to 7 days. Four of the six investigations used saline microscopy as the definitive diagnostic test of treatment failure. Compared with culture or DNA testing, microscopy is not as accurate. Moreover, the timing of retesting varied in the studies, and some apparent treatment failures actually may have been due to reinfection. In addition, the studies did not consistently track the adequacy of treatment of the sexual partner.
To be sure, we would benefit from a new comparative study that included a large sample size, a consistent multidose regimen, rigorous treatment of the sexual partner(s), and more sophisticated diagnostic testing to define treatment failure. Pending the publication of such a study, however, I plan to alter my practice pattern and treat infected patients with a multidose regimen of metronidazole. I favor the regimen of 500 mg orally twice daily for 7 days because it is effective against both trichomoniasis and bacterial vaginosis, which is a common co-infection.
The twice-daily regimen is more convenient than the thrice-daily regimen and is not much more expensive than the single-dose regimen ($13 vs $4, http://www.goodrx.com). I will reserve the single 2-g dose of metronidazole for patients in whom treatment adherence is likely to be a problem or for patients in whom an immediate response to treatment is imperative (eg, a patient with preterm premature rupture of membranes or preterm labor).
-- Patrick Duff, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR-03):1−137.
- Howe K, Kissinger PJ. Single-dose compared with multidose metronidazole for the treatment of trichomoniasis in women: a meta-analysis. Sex Transm Dis. 2017;44(1):29−34.
EXPERT COMMENTARY
Both the Centers for Disease Control and Prevention and the World Health Organization currently recommend that patients with trichomoniasis be treated with a single 2-g oral dose of metronidazole.1 Following treatment, the reported rates of repeat infection or persistent infection range from 5% to 31%. Repeat infection rates may be even higher in HIV-infected patients.
Repeat infections presumably result from a failure to treat the patient’s sexual partner(s) or from the patient’s exposure to a new partner. Persistent infections, however, may be the result of inadequate primary therapy, even though inherent resistance of the organism to metronidazole is quite rare. To date, no single study has shown that single-dose therapy is inferior to multidose therapy, but most of these studies lack sufficient power to completely exclude the possibility of a type-2 statistical error.2 To compare single-dose with multidose therapy for trichomoniasis in a more systematic manner, Howe and Kissinger conducted a meta-analysis, which was recently published in Sexually Transmitted Diseases.
Related article:
2016 Update on infectious disease
Details of the study
The investigators conducted a comprehensive literature search using Embase, Medline, and ClinicalTrials.gov; 6 articles were included in the final results, 4 of which were randomized controlled trials. Approximately 1,300 participants were included in the 6 trials. All of the patients in the single-dose treatment arms received a 2-g oral dose of metronidazole. In the multidose treatment arms for 2 studies the participants received metronidazole 250 mg orally 3 times daily for 7 days, and for 2 studies the dose was 200 mg 3 times daily for 7 days. The fifth study employed a 500-mg oral dose of metronidazole twice daily for 7 days. The final study used a 400-mg oral dose twice daily for 5 days. The key study end point was treatment failure.
Howe and Kissinger demonstrated that women who received the single 2-g dose were 1.87 times (95% CI, 1.23−2.82; P<.01) more likely to experience a treatment failure compared with women who received a multidose regimen. When the one study that focused only on HIV-infected women was excluded from analysis, the results were similar. The relative risk of treatment failure was 1.80 (95% CI, 1.07−3.02; P<.03).
Related article:
Preventing infection after cesarean delivery: Evidence-based guidance
Study limitations
The results of this meta-analysis are interesting and provocative. However, the analysis has several important limitations. Five of the 6 studies were published many years ago (1971, 1972, 1979, 1980, and 1982). The most recent study was published in 2010. The investigators used 4 different multidose regimens, with metronidazole doses ranging from 200 mg to 500 mg and duration of therapy ranging from 5 to 7 days. Four of the six investigations used saline microscopy as the definitive diagnostic test of treatment failure. Compared with culture or DNA testing, microscopy is not as accurate. Moreover, the timing of retesting varied in the studies, and some apparent treatment failures actually may have been due to reinfection. In addition, the studies did not consistently track the adequacy of treatment of the sexual partner.
To be sure, we would benefit from a new comparative study that included a large sample size, a consistent multidose regimen, rigorous treatment of the sexual partner(s), and more sophisticated diagnostic testing to define treatment failure. Pending the publication of such a study, however, I plan to alter my practice pattern and treat infected patients with a multidose regimen of metronidazole. I favor the regimen of 500 mg orally twice daily for 7 days because it is effective against both trichomoniasis and bacterial vaginosis, which is a common co-infection.
The twice-daily regimen is more convenient than the thrice-daily regimen and is not much more expensive than the single-dose regimen ($13 vs $4, http://www.goodrx.com). I will reserve the single 2-g dose of metronidazole for patients in whom treatment adherence is likely to be a problem or for patients in whom an immediate response to treatment is imperative (eg, a patient with preterm premature rupture of membranes or preterm labor).
-- Patrick Duff, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
EXPERT COMMENTARY
Both the Centers for Disease Control and Prevention and the World Health Organization currently recommend that patients with trichomoniasis be treated with a single 2-g oral dose of metronidazole.1 Following treatment, the reported rates of repeat infection or persistent infection range from 5% to 31%. Repeat infection rates may be even higher in HIV-infected patients.
Repeat infections presumably result from a failure to treat the patient’s sexual partner(s) or from the patient’s exposure to a new partner. Persistent infections, however, may be the result of inadequate primary therapy, even though inherent resistance of the organism to metronidazole is quite rare. To date, no single study has shown that single-dose therapy is inferior to multidose therapy, but most of these studies lack sufficient power to completely exclude the possibility of a type-2 statistical error.2 To compare single-dose with multidose therapy for trichomoniasis in a more systematic manner, Howe and Kissinger conducted a meta-analysis, which was recently published in Sexually Transmitted Diseases.
Related article:
2016 Update on infectious disease
Details of the study
The investigators conducted a comprehensive literature search using Embase, Medline, and ClinicalTrials.gov; 6 articles were included in the final results, 4 of which were randomized controlled trials. Approximately 1,300 participants were included in the 6 trials. All of the patients in the single-dose treatment arms received a 2-g oral dose of metronidazole. In the multidose treatment arms for 2 studies the participants received metronidazole 250 mg orally 3 times daily for 7 days, and for 2 studies the dose was 200 mg 3 times daily for 7 days. The fifth study employed a 500-mg oral dose of metronidazole twice daily for 7 days. The final study used a 400-mg oral dose twice daily for 5 days. The key study end point was treatment failure.
Howe and Kissinger demonstrated that women who received the single 2-g dose were 1.87 times (95% CI, 1.23−2.82; P<.01) more likely to experience a treatment failure compared with women who received a multidose regimen. When the one study that focused only on HIV-infected women was excluded from analysis, the results were similar. The relative risk of treatment failure was 1.80 (95% CI, 1.07−3.02; P<.03).
Related article:
Preventing infection after cesarean delivery: Evidence-based guidance
Study limitations
The results of this meta-analysis are interesting and provocative. However, the analysis has several important limitations. Five of the 6 studies were published many years ago (1971, 1972, 1979, 1980, and 1982). The most recent study was published in 2010. The investigators used 4 different multidose regimens, with metronidazole doses ranging from 200 mg to 500 mg and duration of therapy ranging from 5 to 7 days. Four of the six investigations used saline microscopy as the definitive diagnostic test of treatment failure. Compared with culture or DNA testing, microscopy is not as accurate. Moreover, the timing of retesting varied in the studies, and some apparent treatment failures actually may have been due to reinfection. In addition, the studies did not consistently track the adequacy of treatment of the sexual partner.
To be sure, we would benefit from a new comparative study that included a large sample size, a consistent multidose regimen, rigorous treatment of the sexual partner(s), and more sophisticated diagnostic testing to define treatment failure. Pending the publication of such a study, however, I plan to alter my practice pattern and treat infected patients with a multidose regimen of metronidazole. I favor the regimen of 500 mg orally twice daily for 7 days because it is effective against both trichomoniasis and bacterial vaginosis, which is a common co-infection.
The twice-daily regimen is more convenient than the thrice-daily regimen and is not much more expensive than the single-dose regimen ($13 vs $4, http://www.goodrx.com). I will reserve the single 2-g dose of metronidazole for patients in whom treatment adherence is likely to be a problem or for patients in whom an immediate response to treatment is imperative (eg, a patient with preterm premature rupture of membranes or preterm labor).
-- Patrick Duff, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR-03):1−137.
- Howe K, Kissinger PJ. Single-dose compared with multidose metronidazole for the treatment of trichomoniasis in women: a meta-analysis. Sex Transm Dis. 2017;44(1):29−34.
- Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR-03):1−137.
- Howe K, Kissinger PJ. Single-dose compared with multidose metronidazole for the treatment of trichomoniasis in women: a meta-analysis. Sex Transm Dis. 2017;44(1):29−34.
Audiocast: Hysteroscopic tubal occlusion: How new product labeling can be a resource for patient counseling
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Resources
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Resources
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Resources
Hysteroscopic tubal occlusion: How new product labeling can be a resource for patient counseling
In November 2016, Bayer, the manufacturer of the permanent birth control tubal implant system (Essure), revised the Essure product labeling in accordance with a US Food and Drug Administration (FDA) guidance document.1 The FDA developed its labeling guidance based on its examination of an increasing number of reported adverse events associated with the system’s use (such as persistent pain, perforation of the uterus and/or fallopian tubes, intra-abdominal or pelvic device migration, abnormal or irregular bleeding, and allergy or hypersensitivity reactions) and its evaluation of a trade complaint regarding allegations initially made in a Citizen Petition.
Changes to the new FDA-approved labeling for Essure include:
- the addition of a boxed warning listing adverse events that have been reported either in clinical studies or through postmarket surveillance (see Box)
- updated Instructions for Use document for clinicians and Patient Information Booklet, which contain additional information on safety (contraindications, warnings, and precautions), clinical data, and instructions2,3
- a Patient-Doctor Discussion Checklist (included within the Patient Information Booklet), designed to support appropriate patient counseling, facilitate the patient’s understanding of birth control options, and explain the benefits and risks associated with the device and what to expect during and after the implantation procedure.3
How will these labeling changes impact clinicians and patients? OBG
Reference
1. Essure permanent birth control (Bayer) Instructions for use. http://www.hcp.essure-us.com/assets/pdf/Link%20Essure%20IFU.pdf. Accessed January 5, 2017.
OBG Management: What does the new product labeling mean for clinicians who offer tubal implants as an option for permanent sterilization?
Linda D. Bradley, MD: The FDA-approved revised labeling for the Essure system means that physicians should have a very detailed, in-depth conversation with their patients who are contemplating hysteroscopic tubal insert placement for permanent sterilization. This counseling really should not differ from what doctors were doing before the label was revised. However, physicians can now use the new Patient-Doctor Discussion Checklist as a guide in reviewing the benefits of the device, its known risks and potential risks, outcomes of the insertion procedure, and the possible need for future surgical intervention if device placement–related issues arise.
For clinicians, this counseling adds just a few more minutes to the visit. The Patient-Doctor Discussion Checklist will become an inherent part of the informed consent process, aiding in the review of the device’s benefits, potential risks, and more importantly its permanence.
In the past, there was some concern that perhaps patients did not receive enough guidance for informed consent, so one of the first things listed on the checklist is confirmation—in the form of a printed line where the patient can sign her initials—that she understands that Essure is a permanent form of birth control. The checklist covers additional important issues, including that the doctor has indeed shared with the patient other options for birth control or sterilization, such as laparoscopic sterilization, vasectomy for her male partner, an intrauterine device (IUD), and birth control pills. This is an opportunity to reinforce the fact that tubal implants are a permanent form of birth control, and if the patient is uncertain about ending her fertility, the clinician can inform her about reversible options. The checklist also includes for discussion the pregnancy risk with use of the device, what the patient can expect during the implant insertion procedure and for the days afterwards (such as cramping, mild to moderate pain, nausea and vomiting), and the need for a confirmation test 3 months after device placement.
Other discussion points covered include long-term risks and benefits of the device, the potential for complications, and the possibility (due to pelvic pain) that the hysteroscopically placed devices may need to be removed with a surgical procedure requiring general anesthesia.
Incorporating the checklist into our clinical practice shows that we have listened to patients and complied with recommendations made by the FDA review panel, and we can use this document to have a more complete discussion with our patients.
OBG Management: Do you agree with some clinicians who say that physicians who place the device also should have the skills required to remove it if necessary?
Dr. Bradley: Essure placement—which is a hysteroscopic procedure—is done very differently than a laparoscopic procedure. In the past, among women who needed to have the Essure system removed, most procedures would be done laparoscopically. Since we work collaboratively in teams, someone within the team or division would have the clinical expertise to remove the devices. An ObGyn who does laparoscopy with salpingectomy and/or cornual resection would best be able to remove the devices.
The clinician who does hysteroscopy is not always the same one who does laparoscopy. Someone within the division who is interested in removing the device will develop an expertise and algorithm that suits the practice, so that person in the practice becomes the expert. This is no different from many other things that physicians do. In our clinical practice, for example, we have a pelvic pain specialist, a sexual counselor, someone interested in menopause and management, and someone interested in alternatives to hysterectomies. Those who practice their craft and their art become proficient at it. So if you do not perform a particular procedure such as a tubal implant removal, know the expert to whom you can make a referral.
OBG Management: How do you now advise your colleagues to counsel patients on permanent sterilization?
Dr. Bradley: Hysteroscopic tubal implant sterilization, a minimally invasive procedure, is an excellent and viable option for women who meet the inclusion criteria and who do not have the exclusion criteria for placement. It is overall safe and extremely effective. If a patient has issues after undergoing implant placement—just like with any other surgery or procedure—for example, if she is not feeling better or is not doing as well as anticipated, we must not forget the patient. It is important for our patients to be listened to and to be heard. Postprocedure issues are generally transient and related to pain and discomfort or abnormal bleeding. If they are persistent, then further evaluation is needed.
Tell the patient to contact you if she has questions or issues, and have a tiered approach for working up any problems that she may present with. In addition, reiterate that the patient must use another form of birth control for 3 months until she undergoes the confirmation test and until the results verify that the implants can be relied on for contraception. I am still placing the device. Before I perform the procedure, I speak with my patients—as I did before the checklist was developed—about all of the informed consent issues, the risk−benefit profile, and ruling out contraindications to use. I think this is good medical and surgical practice. The new labeling means we need to have a critical conversation with our patients, and we should be doing that for all procedures.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- US Food and Drug Administration. Labeling for permanent hysteroscopically-placed tubal implants intended for sterilization: guidance for industry and Food and Drug Administration staff. http://www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/UCM488020.pdf. Published October 31, 2016. Accessed January 5, 2017.
- Essure permanent birth control (Bayer) Instructions for use. http://www.hcp.essure-us.com/assets/pdf/Link_Essure_IFU.pdf. Accessed January 5, 2017.
- Essure patient information booklet. http://labeling.bayerhealthcare.com/html/products/pi/essure_pib_en.pdf. Accessed January 5, 2017.
In November 2016, Bayer, the manufacturer of the permanent birth control tubal implant system (Essure), revised the Essure product labeling in accordance with a US Food and Drug Administration (FDA) guidance document.1 The FDA developed its labeling guidance based on its examination of an increasing number of reported adverse events associated with the system’s use (such as persistent pain, perforation of the uterus and/or fallopian tubes, intra-abdominal or pelvic device migration, abnormal or irregular bleeding, and allergy or hypersensitivity reactions) and its evaluation of a trade complaint regarding allegations initially made in a Citizen Petition.
Changes to the new FDA-approved labeling for Essure include:
- the addition of a boxed warning listing adverse events that have been reported either in clinical studies or through postmarket surveillance (see Box)
- updated Instructions for Use document for clinicians and Patient Information Booklet, which contain additional information on safety (contraindications, warnings, and precautions), clinical data, and instructions2,3
- a Patient-Doctor Discussion Checklist (included within the Patient Information Booklet), designed to support appropriate patient counseling, facilitate the patient’s understanding of birth control options, and explain the benefits and risks associated with the device and what to expect during and after the implantation procedure.3
How will these labeling changes impact clinicians and patients? OBG
Reference
1. Essure permanent birth control (Bayer) Instructions for use. http://www.hcp.essure-us.com/assets/pdf/Link%20Essure%20IFU.pdf. Accessed January 5, 2017.
OBG Management: What does the new product labeling mean for clinicians who offer tubal implants as an option for permanent sterilization?
Linda D. Bradley, MD: The FDA-approved revised labeling for the Essure system means that physicians should have a very detailed, in-depth conversation with their patients who are contemplating hysteroscopic tubal insert placement for permanent sterilization. This counseling really should not differ from what doctors were doing before the label was revised. However, physicians can now use the new Patient-Doctor Discussion Checklist as a guide in reviewing the benefits of the device, its known risks and potential risks, outcomes of the insertion procedure, and the possible need for future surgical intervention if device placement–related issues arise.
For clinicians, this counseling adds just a few more minutes to the visit. The Patient-Doctor Discussion Checklist will become an inherent part of the informed consent process, aiding in the review of the device’s benefits, potential risks, and more importantly its permanence.
In the past, there was some concern that perhaps patients did not receive enough guidance for informed consent, so one of the first things listed on the checklist is confirmation—in the form of a printed line where the patient can sign her initials—that she understands that Essure is a permanent form of birth control. The checklist covers additional important issues, including that the doctor has indeed shared with the patient other options for birth control or sterilization, such as laparoscopic sterilization, vasectomy for her male partner, an intrauterine device (IUD), and birth control pills. This is an opportunity to reinforce the fact that tubal implants are a permanent form of birth control, and if the patient is uncertain about ending her fertility, the clinician can inform her about reversible options. The checklist also includes for discussion the pregnancy risk with use of the device, what the patient can expect during the implant insertion procedure and for the days afterwards (such as cramping, mild to moderate pain, nausea and vomiting), and the need for a confirmation test 3 months after device placement.
Other discussion points covered include long-term risks and benefits of the device, the potential for complications, and the possibility (due to pelvic pain) that the hysteroscopically placed devices may need to be removed with a surgical procedure requiring general anesthesia.
Incorporating the checklist into our clinical practice shows that we have listened to patients and complied with recommendations made by the FDA review panel, and we can use this document to have a more complete discussion with our patients.
OBG Management: Do you agree with some clinicians who say that physicians who place the device also should have the skills required to remove it if necessary?
Dr. Bradley: Essure placement—which is a hysteroscopic procedure—is done very differently than a laparoscopic procedure. In the past, among women who needed to have the Essure system removed, most procedures would be done laparoscopically. Since we work collaboratively in teams, someone within the team or division would have the clinical expertise to remove the devices. An ObGyn who does laparoscopy with salpingectomy and/or cornual resection would best be able to remove the devices.
The clinician who does hysteroscopy is not always the same one who does laparoscopy. Someone within the division who is interested in removing the device will develop an expertise and algorithm that suits the practice, so that person in the practice becomes the expert. This is no different from many other things that physicians do. In our clinical practice, for example, we have a pelvic pain specialist, a sexual counselor, someone interested in menopause and management, and someone interested in alternatives to hysterectomies. Those who practice their craft and their art become proficient at it. So if you do not perform a particular procedure such as a tubal implant removal, know the expert to whom you can make a referral.
OBG Management: How do you now advise your colleagues to counsel patients on permanent sterilization?
Dr. Bradley: Hysteroscopic tubal implant sterilization, a minimally invasive procedure, is an excellent and viable option for women who meet the inclusion criteria and who do not have the exclusion criteria for placement. It is overall safe and extremely effective. If a patient has issues after undergoing implant placement—just like with any other surgery or procedure—for example, if she is not feeling better or is not doing as well as anticipated, we must not forget the patient. It is important for our patients to be listened to and to be heard. Postprocedure issues are generally transient and related to pain and discomfort or abnormal bleeding. If they are persistent, then further evaluation is needed.
Tell the patient to contact you if she has questions or issues, and have a tiered approach for working up any problems that she may present with. In addition, reiterate that the patient must use another form of birth control for 3 months until she undergoes the confirmation test and until the results verify that the implants can be relied on for contraception. I am still placing the device. Before I perform the procedure, I speak with my patients—as I did before the checklist was developed—about all of the informed consent issues, the risk−benefit profile, and ruling out contraindications to use. I think this is good medical and surgical practice. The new labeling means we need to have a critical conversation with our patients, and we should be doing that for all procedures.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In November 2016, Bayer, the manufacturer of the permanent birth control tubal implant system (Essure), revised the Essure product labeling in accordance with a US Food and Drug Administration (FDA) guidance document.1 The FDA developed its labeling guidance based on its examination of an increasing number of reported adverse events associated with the system’s use (such as persistent pain, perforation of the uterus and/or fallopian tubes, intra-abdominal or pelvic device migration, abnormal or irregular bleeding, and allergy or hypersensitivity reactions) and its evaluation of a trade complaint regarding allegations initially made in a Citizen Petition.
Changes to the new FDA-approved labeling for Essure include:
- the addition of a boxed warning listing adverse events that have been reported either in clinical studies or through postmarket surveillance (see Box)
- updated Instructions for Use document for clinicians and Patient Information Booklet, which contain additional information on safety (contraindications, warnings, and precautions), clinical data, and instructions2,3
- a Patient-Doctor Discussion Checklist (included within the Patient Information Booklet), designed to support appropriate patient counseling, facilitate the patient’s understanding of birth control options, and explain the benefits and risks associated with the device and what to expect during and after the implantation procedure.3
How will these labeling changes impact clinicians and patients? OBG
Reference
1. Essure permanent birth control (Bayer) Instructions for use. http://www.hcp.essure-us.com/assets/pdf/Link%20Essure%20IFU.pdf. Accessed January 5, 2017.
OBG Management: What does the new product labeling mean for clinicians who offer tubal implants as an option for permanent sterilization?
Linda D. Bradley, MD: The FDA-approved revised labeling for the Essure system means that physicians should have a very detailed, in-depth conversation with their patients who are contemplating hysteroscopic tubal insert placement for permanent sterilization. This counseling really should not differ from what doctors were doing before the label was revised. However, physicians can now use the new Patient-Doctor Discussion Checklist as a guide in reviewing the benefits of the device, its known risks and potential risks, outcomes of the insertion procedure, and the possible need for future surgical intervention if device placement–related issues arise.
For clinicians, this counseling adds just a few more minutes to the visit. The Patient-Doctor Discussion Checklist will become an inherent part of the informed consent process, aiding in the review of the device’s benefits, potential risks, and more importantly its permanence.
In the past, there was some concern that perhaps patients did not receive enough guidance for informed consent, so one of the first things listed on the checklist is confirmation—in the form of a printed line where the patient can sign her initials—that she understands that Essure is a permanent form of birth control. The checklist covers additional important issues, including that the doctor has indeed shared with the patient other options for birth control or sterilization, such as laparoscopic sterilization, vasectomy for her male partner, an intrauterine device (IUD), and birth control pills. This is an opportunity to reinforce the fact that tubal implants are a permanent form of birth control, and if the patient is uncertain about ending her fertility, the clinician can inform her about reversible options. The checklist also includes for discussion the pregnancy risk with use of the device, what the patient can expect during the implant insertion procedure and for the days afterwards (such as cramping, mild to moderate pain, nausea and vomiting), and the need for a confirmation test 3 months after device placement.
Other discussion points covered include long-term risks and benefits of the device, the potential for complications, and the possibility (due to pelvic pain) that the hysteroscopically placed devices may need to be removed with a surgical procedure requiring general anesthesia.
Incorporating the checklist into our clinical practice shows that we have listened to patients and complied with recommendations made by the FDA review panel, and we can use this document to have a more complete discussion with our patients.
OBG Management: Do you agree with some clinicians who say that physicians who place the device also should have the skills required to remove it if necessary?
Dr. Bradley: Essure placement—which is a hysteroscopic procedure—is done very differently than a laparoscopic procedure. In the past, among women who needed to have the Essure system removed, most procedures would be done laparoscopically. Since we work collaboratively in teams, someone within the team or division would have the clinical expertise to remove the devices. An ObGyn who does laparoscopy with salpingectomy and/or cornual resection would best be able to remove the devices.
The clinician who does hysteroscopy is not always the same one who does laparoscopy. Someone within the division who is interested in removing the device will develop an expertise and algorithm that suits the practice, so that person in the practice becomes the expert. This is no different from many other things that physicians do. In our clinical practice, for example, we have a pelvic pain specialist, a sexual counselor, someone interested in menopause and management, and someone interested in alternatives to hysterectomies. Those who practice their craft and their art become proficient at it. So if you do not perform a particular procedure such as a tubal implant removal, know the expert to whom you can make a referral.
OBG Management: How do you now advise your colleagues to counsel patients on permanent sterilization?
Dr. Bradley: Hysteroscopic tubal implant sterilization, a minimally invasive procedure, is an excellent and viable option for women who meet the inclusion criteria and who do not have the exclusion criteria for placement. It is overall safe and extremely effective. If a patient has issues after undergoing implant placement—just like with any other surgery or procedure—for example, if she is not feeling better or is not doing as well as anticipated, we must not forget the patient. It is important for our patients to be listened to and to be heard. Postprocedure issues are generally transient and related to pain and discomfort or abnormal bleeding. If they are persistent, then further evaluation is needed.
Tell the patient to contact you if she has questions or issues, and have a tiered approach for working up any problems that she may present with. In addition, reiterate that the patient must use another form of birth control for 3 months until she undergoes the confirmation test and until the results verify that the implants can be relied on for contraception. I am still placing the device. Before I perform the procedure, I speak with my patients—as I did before the checklist was developed—about all of the informed consent issues, the risk−benefit profile, and ruling out contraindications to use. I think this is good medical and surgical practice. The new labeling means we need to have a critical conversation with our patients, and we should be doing that for all procedures.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- US Food and Drug Administration. Labeling for permanent hysteroscopically-placed tubal implants intended for sterilization: guidance for industry and Food and Drug Administration staff. http://www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/UCM488020.pdf. Published October 31, 2016. Accessed January 5, 2017.
- Essure permanent birth control (Bayer) Instructions for use. http://www.hcp.essure-us.com/assets/pdf/Link_Essure_IFU.pdf. Accessed January 5, 2017.
- Essure patient information booklet. http://labeling.bayerhealthcare.com/html/products/pi/essure_pib_en.pdf. Accessed January 5, 2017.
- US Food and Drug Administration. Labeling for permanent hysteroscopically-placed tubal implants intended for sterilization: guidance for industry and Food and Drug Administration staff. http://www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/UCM488020.pdf. Published October 31, 2016. Accessed January 5, 2017.
- Essure permanent birth control (Bayer) Instructions for use. http://www.hcp.essure-us.com/assets/pdf/Link_Essure_IFU.pdf. Accessed January 5, 2017.
- Essure patient information booklet. http://labeling.bayerhealthcare.com/html/products/pi/essure_pib_en.pdf. Accessed January 5, 2017.
What lies ahead for women's health? Challenges, and opportunities, as ACOG and US leadership transition
The United States undoubtedly will undergo tremendous change under its new President and Congress. These branches of government are already indicating their determination to rewrite a vast array of health care laws. If carried out, proposals regarding the Affordable Care Act, Medicare, and Medicaid will dramatically alter the landscape of women’s health care and significantly affect ObGyns and their patients.
These shifts are coming as ACOG’s top leadership undergoes its annual transition. In May 2017, we will thank American College of Obstetricians and Gynecologists (ACOG) President Thomas Gellhaus, MD, for his tremendous service and welcome Haywood Brown, MD, as our new President.
With so much uncertainty ahead, I recently asked these 2 leaders for their reflections, predictions, hardest challenges, and plans to help our specialty surmount any new obstacles to move forward with positive initiatives.
What have we faced down in the past year; what faces us now?
Thomas Gellhaus, MD: When I took this position almost 1 year ago, our specialty and our ability to care for patients were challenged on 3 fronts: MACRA, workforce, and politics.
Through the efforts of a united American Medical Association, we saw MACRA, the Medicare Access and CHIP (Children’s Health Insurance Program) Reauthorization Act of 2015, replace the sustainable growth rate formula, which would have drastically reduced provider payments under Medicare’s Physician Fee Schedule. With this change, a major challenge was crossed off our list and a major new one added. Now, we must ensure proper enactment of MACRA’s new payment system and be continually vigilant with respect to its implementation.
Second, we must ensure there are enough ObGyns to care for patients nationally, across all areas of the country. We must find new ways to recruit ObGyns and maintain and expand our workforce.
Third, we must stand firm against political interference. The future of our patients, our practices, and our specialty depend on it. Only 2 people are allowed in the exam room—the patient and her ObGyn—and we must close its door to politicians who want to make decisions about the kind of care our patients need and how we should provide it. We must defeat the many state efforts to decree or limit care. Patient’s access to care, including reproductive care, must not be subject to politics.
These challenges can be opportunities. For example, the more we make MACRA work for practicing ObGyns now, the brighter our future will be, as private payers likely will be following suit.
We stand with patients on reproductive rights and access to care
Haywood Brown, MD: We face several challenges. First, when we become ObGyns, we join our patients in taking on the everyday challenges of women’s health care, reproduction, and reproductive rights. These will continue to be major issues for our specialty. In addition, in our continued efforts to address health care disparities, we must take the lead at ACOG as well as enlist other women’s health care providers as partners. Too often, access to high-quality perinatal, cancer, and other women’s health care is determined or influenced by a patient’s race, residence, or income. This must change.
A future for team-based care
Another challenge is to define clinical practice expectations for the newer generations of Fellows. We must impart to Junior Fellows that team-based care will:
- help them see obstetrics and gynecology as an immensely satisfying calling and career rather than as just a job
- contribute to the expansion of care to women in all communities
- allow for the maintenance of a good work–life balance for many years. (See “Steps to address ObGyn work–life balance” on page 30.)
It’s a new Washington. We are poised for new challenges.
Dr. Gellhaus: With the new US President, Congress, governors, and state legislators in office, a new challenge is to maintain the women’s health protections in the Affordable Care Act—particularly insurance coverage for maternity care and preventive and contraceptive services. We must guard against a resurgence in the number of the uninsured and underinsured, including patients whose health insurance is cut off once they become seriously ill or reach their annual or lifetime coverage limit.
We also must be ready to fight the anticipated onslaught of state and federal attempts to limit our patients’ access to reproductive health care. Many of us remember the days of illegal, unsafe abortions and their devastating effects on women’s health. No lawmaker should doubt that having access to contraceptives helps reduce the rates of unwanted pregnancies and abortions, improves maternal and infant outcomes, and decreases health care costs. It’s a win-win!
Groundwork has been laid, and opportunities will surface
Dr. Gellhaus: The best opportunities will emerge from our long-standing history of bipartisan political cooperation in this area, as we work with lawmakers from both parties on issues that benefit ObGyns and their patients. Over the years, ACOG has well positioned itself and developed important long-term relationships with Republican and Democratic lawmakers to focus on women’s health as a central issue. This position will give ACOG a voice in the new federal Administration, in Congress, and in state houses.
We also will have opportunities to educate elected officials, debunk many of the false or mistaken ideas surrounding contraceptive methods, and reinforce the need for politicians to stop interfering with the sacred physician–patient relationship and stay out of our exam rooms.
Our commitment to our patients is strong
Dr. Brown: It is more important than ever for ACOG to affirm its commitment to women’s reproductive choices and their access to contraceptives—especially with respect to programs funded by Medicaid and Title X. In the United States, Medicaid covers 48% of all births, as well as preventive and screening services provided by Planned Parenthood clinics. Over the next years, these programs will be challenged and could fall into jeopardy. We must remind our Fellows that both Title X contraception coverage and abortion choice have been the law of the land for almost 50 years. We cannot allow politicians to return us to an era that was far worse for our patients.
I asked Haywood Brown, MD, the incoming ACOG President as of May 2017, how he views ACOG's role in addressing a main reason for ObGyn burnout--the increasing burden of compliance with required electronic documentation.
Haywood Brown, MD: We must develop new models of care that foster the ability of ObGyns to embrace practicing the depth and breadth of ObGyn long term, and maintain their enthusiasm about providing care to women throughout the life span. Compliance and electronic documentation requirements can enhance patient care by allowing us to better communicate with our practice partners and our patients, improve quality, safety, and patient satisfaction. It can also quickly wear us down.
Burnout can be reduced through shared practice models, development of niches within shared practices, and being creative with better incorporating advanced practice providers into team-based care. I sincerely believe that if we embrace new models of clinical practice, the satisfaction for what we are trained to do will improve and burnout will be less a threat to our specialty over time.
All-In for Advocacy tops presidential initiatives list
Dr. Gellhaus: With political legislative interference increasing across all of medicine, we need a unified, powerful, cohesive voice. Advocacy is at the top of my presidential initiatives list. The voice of our national organization can have a huge impact on maintaining and improving women’s health care in the United States. That is why All-In for Advocacy is vital. This initiative has significantly increased members’ involvement in ACOG. We will harness this power to pass vital legislation to help the women we serve and our specialty.
Addressing health disparities drives career and presidential focus
Dr. Brown: My presidential initiatives are rooted in my career decision to focus on health disparities, particularly race-based health disparities.
Maternal morbidity and mortality and infant mortality are complex issues shrouded in the social determinants of health. Access to care, fragmentation of care, and quality of care are other factors relevant in disparity. There is evidence of an implicit bias in health care delivery.
My telehealth initiative will focus on implementing Levels of Maternal Care (of which there are 4), the National Partnership for Maternal Safety (NPMS), and the Alliance for Innovation on Maternal Health (AIM) as well as redefining healthy pregnancies and postpartum periods as the gateway to women’s long-term health. The February 2015 Levels of Maternal Care Obstetric Care Consensus Statement, jointly issued by ACOG and the Society for Maternal–Fetal Medicine (SMFM),1 proposes a classification system for birth centers, from basic to specialized regional perinatal health care centers. ACOG is working with hospitals throughout the country to designate the Levels of Maternal Care and thereby ensure each patient receives the appropriate level of care.
The AIM program, led by ACOG and funded by the Health Resources and Services Administration (HRSA), reduces obstetric complications by encouraging hospitals to adopt defined evidence-based patient safety measures. The goal is to prevent 100,000 severe labor and delivery complications and 1,000 maternal deaths over 4 years.
- ACOG's Congressional Leadership Conference, The President's Conference. This 3-day conference, held in Washington, DC, connects you with lawmakers on the important issues facing ObGyns. To find out more, access www.acog.org/clc.
- McCain and Gellhaus Fellowships. Spend 2 to 4 weeks as a member of ACOG's Government Affairs team in Washington, DC. To apply, go to www.acog.org/ateam.
- Ob-Gyn PAC. ACOG's political action committee helps elect state and federal candidates who support our specialty. For more information, visit www.obgynpac.org.
- ACOG News. Don't miss these updates on federal and state legislative developments. To sign up, access www.acog.org/advonews.
- Advocacy webpage. All of this information and more can be found at www.acog.org/advocacy!
ACOG is committed to a “big tent” approach
Dr. Gellhaus: Like US citizens, ACOG represents members with many points of view. ACOG can best represent our members’ diversity in the future by remaining the moderate voice, and by opposing federal and state proposals that are inconsistent with facts and science. We need to bring to our membership’s attention the federal and state successes we have had, show how they have helped our patients and our specialty, and make it clear that our successes are due to our bipartisan work over the years, which we have achieved regardless of which political party has been in office.
For ACOG to continue to be a leader in women’s health care and our specialty, we must remain vigilant against political interference in the patient–physician relationship and be ready to counter with science, facts, and evidence.
Compassion and passion lie at the heart of member similarities
Dr. Brown: First and foremost, we ObGyns care about our patients and, regardless of personal politics, most of us understand the reproductive health challenges facing the women of this country as well as our history with respect to those challenges. All of us must be willing to provide counsel to patients when needed, and that counseling must be nonjudgmental. We also must be willing to protect confidentially and to refer patients whose decisions are at odds with our personal views.
ACOG recognizes that we are a melting pot of specialists and subspecialists and that we are all guided by our personal beliefs and values. Choosing to become an exclusive women’s health care physician requires our passion and compassion.
Let us use our collective voice!
Dr. Gellhaus: Our members must realize the power of our collective voice and that we must use it to deliver a unified, cohesive message. We cannot sit on the sidelines and expect others to speak for us. If we are not part of the solution, then we cede our future to others and have no right to complain about the result. Our members need to commit to advocating outside their exam rooms. A good first step is to see how ACOG makes advocacy easy. When thousands of ACOG members contact elected officials about important issues, officials listen.
Dr. Brown: Yes! We all need to get involved in ACOG and in our communities. Together, we will accomplish many important things.
[polldaddy:9703185]
Send your letter to the editor to [email protected]. Please include the city and state in which you practice.
- Menard MK, Kilpatrick S, Saade G, et al; American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine. Levels of maternal care. Am J Obstet Gynecol. 2015;212(3)259–271.
The United States undoubtedly will undergo tremendous change under its new President and Congress. These branches of government are already indicating their determination to rewrite a vast array of health care laws. If carried out, proposals regarding the Affordable Care Act, Medicare, and Medicaid will dramatically alter the landscape of women’s health care and significantly affect ObGyns and their patients.
These shifts are coming as ACOG’s top leadership undergoes its annual transition. In May 2017, we will thank American College of Obstetricians and Gynecologists (ACOG) President Thomas Gellhaus, MD, for his tremendous service and welcome Haywood Brown, MD, as our new President.
With so much uncertainty ahead, I recently asked these 2 leaders for their reflections, predictions, hardest challenges, and plans to help our specialty surmount any new obstacles to move forward with positive initiatives.
What have we faced down in the past year; what faces us now?
Thomas Gellhaus, MD: When I took this position almost 1 year ago, our specialty and our ability to care for patients were challenged on 3 fronts: MACRA, workforce, and politics.
Through the efforts of a united American Medical Association, we saw MACRA, the Medicare Access and CHIP (Children’s Health Insurance Program) Reauthorization Act of 2015, replace the sustainable growth rate formula, which would have drastically reduced provider payments under Medicare’s Physician Fee Schedule. With this change, a major challenge was crossed off our list and a major new one added. Now, we must ensure proper enactment of MACRA’s new payment system and be continually vigilant with respect to its implementation.
Second, we must ensure there are enough ObGyns to care for patients nationally, across all areas of the country. We must find new ways to recruit ObGyns and maintain and expand our workforce.
Third, we must stand firm against political interference. The future of our patients, our practices, and our specialty depend on it. Only 2 people are allowed in the exam room—the patient and her ObGyn—and we must close its door to politicians who want to make decisions about the kind of care our patients need and how we should provide it. We must defeat the many state efforts to decree or limit care. Patient’s access to care, including reproductive care, must not be subject to politics.
These challenges can be opportunities. For example, the more we make MACRA work for practicing ObGyns now, the brighter our future will be, as private payers likely will be following suit.
We stand with patients on reproductive rights and access to care
Haywood Brown, MD: We face several challenges. First, when we become ObGyns, we join our patients in taking on the everyday challenges of women’s health care, reproduction, and reproductive rights. These will continue to be major issues for our specialty. In addition, in our continued efforts to address health care disparities, we must take the lead at ACOG as well as enlist other women’s health care providers as partners. Too often, access to high-quality perinatal, cancer, and other women’s health care is determined or influenced by a patient’s race, residence, or income. This must change.
A future for team-based care
Another challenge is to define clinical practice expectations for the newer generations of Fellows. We must impart to Junior Fellows that team-based care will:
- help them see obstetrics and gynecology as an immensely satisfying calling and career rather than as just a job
- contribute to the expansion of care to women in all communities
- allow for the maintenance of a good work–life balance for many years. (See “Steps to address ObGyn work–life balance” on page 30.)
It’s a new Washington. We are poised for new challenges.
Dr. Gellhaus: With the new US President, Congress, governors, and state legislators in office, a new challenge is to maintain the women’s health protections in the Affordable Care Act—particularly insurance coverage for maternity care and preventive and contraceptive services. We must guard against a resurgence in the number of the uninsured and underinsured, including patients whose health insurance is cut off once they become seriously ill or reach their annual or lifetime coverage limit.
We also must be ready to fight the anticipated onslaught of state and federal attempts to limit our patients’ access to reproductive health care. Many of us remember the days of illegal, unsafe abortions and their devastating effects on women’s health. No lawmaker should doubt that having access to contraceptives helps reduce the rates of unwanted pregnancies and abortions, improves maternal and infant outcomes, and decreases health care costs. It’s a win-win!
Groundwork has been laid, and opportunities will surface
Dr. Gellhaus: The best opportunities will emerge from our long-standing history of bipartisan political cooperation in this area, as we work with lawmakers from both parties on issues that benefit ObGyns and their patients. Over the years, ACOG has well positioned itself and developed important long-term relationships with Republican and Democratic lawmakers to focus on women’s health as a central issue. This position will give ACOG a voice in the new federal Administration, in Congress, and in state houses.
We also will have opportunities to educate elected officials, debunk many of the false or mistaken ideas surrounding contraceptive methods, and reinforce the need for politicians to stop interfering with the sacred physician–patient relationship and stay out of our exam rooms.
Our commitment to our patients is strong
Dr. Brown: It is more important than ever for ACOG to affirm its commitment to women’s reproductive choices and their access to contraceptives—especially with respect to programs funded by Medicaid and Title X. In the United States, Medicaid covers 48% of all births, as well as preventive and screening services provided by Planned Parenthood clinics. Over the next years, these programs will be challenged and could fall into jeopardy. We must remind our Fellows that both Title X contraception coverage and abortion choice have been the law of the land for almost 50 years. We cannot allow politicians to return us to an era that was far worse for our patients.
I asked Haywood Brown, MD, the incoming ACOG President as of May 2017, how he views ACOG's role in addressing a main reason for ObGyn burnout--the increasing burden of compliance with required electronic documentation.
Haywood Brown, MD: We must develop new models of care that foster the ability of ObGyns to embrace practicing the depth and breadth of ObGyn long term, and maintain their enthusiasm about providing care to women throughout the life span. Compliance and electronic documentation requirements can enhance patient care by allowing us to better communicate with our practice partners and our patients, improve quality, safety, and patient satisfaction. It can also quickly wear us down.
Burnout can be reduced through shared practice models, development of niches within shared practices, and being creative with better incorporating advanced practice providers into team-based care. I sincerely believe that if we embrace new models of clinical practice, the satisfaction for what we are trained to do will improve and burnout will be less a threat to our specialty over time.
All-In for Advocacy tops presidential initiatives list
Dr. Gellhaus: With political legislative interference increasing across all of medicine, we need a unified, powerful, cohesive voice. Advocacy is at the top of my presidential initiatives list. The voice of our national organization can have a huge impact on maintaining and improving women’s health care in the United States. That is why All-In for Advocacy is vital. This initiative has significantly increased members’ involvement in ACOG. We will harness this power to pass vital legislation to help the women we serve and our specialty.
Addressing health disparities drives career and presidential focus
Dr. Brown: My presidential initiatives are rooted in my career decision to focus on health disparities, particularly race-based health disparities.
Maternal morbidity and mortality and infant mortality are complex issues shrouded in the social determinants of health. Access to care, fragmentation of care, and quality of care are other factors relevant in disparity. There is evidence of an implicit bias in health care delivery.
My telehealth initiative will focus on implementing Levels of Maternal Care (of which there are 4), the National Partnership for Maternal Safety (NPMS), and the Alliance for Innovation on Maternal Health (AIM) as well as redefining healthy pregnancies and postpartum periods as the gateway to women’s long-term health. The February 2015 Levels of Maternal Care Obstetric Care Consensus Statement, jointly issued by ACOG and the Society for Maternal–Fetal Medicine (SMFM),1 proposes a classification system for birth centers, from basic to specialized regional perinatal health care centers. ACOG is working with hospitals throughout the country to designate the Levels of Maternal Care and thereby ensure each patient receives the appropriate level of care.
The AIM program, led by ACOG and funded by the Health Resources and Services Administration (HRSA), reduces obstetric complications by encouraging hospitals to adopt defined evidence-based patient safety measures. The goal is to prevent 100,000 severe labor and delivery complications and 1,000 maternal deaths over 4 years.
- ACOG's Congressional Leadership Conference, The President's Conference. This 3-day conference, held in Washington, DC, connects you with lawmakers on the important issues facing ObGyns. To find out more, access www.acog.org/clc.
- McCain and Gellhaus Fellowships. Spend 2 to 4 weeks as a member of ACOG's Government Affairs team in Washington, DC. To apply, go to www.acog.org/ateam.
- Ob-Gyn PAC. ACOG's political action committee helps elect state and federal candidates who support our specialty. For more information, visit www.obgynpac.org.
- ACOG News. Don't miss these updates on federal and state legislative developments. To sign up, access www.acog.org/advonews.
- Advocacy webpage. All of this information and more can be found at www.acog.org/advocacy!
ACOG is committed to a “big tent” approach
Dr. Gellhaus: Like US citizens, ACOG represents members with many points of view. ACOG can best represent our members’ diversity in the future by remaining the moderate voice, and by opposing federal and state proposals that are inconsistent with facts and science. We need to bring to our membership’s attention the federal and state successes we have had, show how they have helped our patients and our specialty, and make it clear that our successes are due to our bipartisan work over the years, which we have achieved regardless of which political party has been in office.
For ACOG to continue to be a leader in women’s health care and our specialty, we must remain vigilant against political interference in the patient–physician relationship and be ready to counter with science, facts, and evidence.
Compassion and passion lie at the heart of member similarities
Dr. Brown: First and foremost, we ObGyns care about our patients and, regardless of personal politics, most of us understand the reproductive health challenges facing the women of this country as well as our history with respect to those challenges. All of us must be willing to provide counsel to patients when needed, and that counseling must be nonjudgmental. We also must be willing to protect confidentially and to refer patients whose decisions are at odds with our personal views.
ACOG recognizes that we are a melting pot of specialists and subspecialists and that we are all guided by our personal beliefs and values. Choosing to become an exclusive women’s health care physician requires our passion and compassion.
Let us use our collective voice!
Dr. Gellhaus: Our members must realize the power of our collective voice and that we must use it to deliver a unified, cohesive message. We cannot sit on the sidelines and expect others to speak for us. If we are not part of the solution, then we cede our future to others and have no right to complain about the result. Our members need to commit to advocating outside their exam rooms. A good first step is to see how ACOG makes advocacy easy. When thousands of ACOG members contact elected officials about important issues, officials listen.
Dr. Brown: Yes! We all need to get involved in ACOG and in our communities. Together, we will accomplish many important things.
[polldaddy:9703185]
Send your letter to the editor to [email protected]. Please include the city and state in which you practice.
The United States undoubtedly will undergo tremendous change under its new President and Congress. These branches of government are already indicating their determination to rewrite a vast array of health care laws. If carried out, proposals regarding the Affordable Care Act, Medicare, and Medicaid will dramatically alter the landscape of women’s health care and significantly affect ObGyns and their patients.
These shifts are coming as ACOG’s top leadership undergoes its annual transition. In May 2017, we will thank American College of Obstetricians and Gynecologists (ACOG) President Thomas Gellhaus, MD, for his tremendous service and welcome Haywood Brown, MD, as our new President.
With so much uncertainty ahead, I recently asked these 2 leaders for their reflections, predictions, hardest challenges, and plans to help our specialty surmount any new obstacles to move forward with positive initiatives.
What have we faced down in the past year; what faces us now?
Thomas Gellhaus, MD: When I took this position almost 1 year ago, our specialty and our ability to care for patients were challenged on 3 fronts: MACRA, workforce, and politics.
Through the efforts of a united American Medical Association, we saw MACRA, the Medicare Access and CHIP (Children’s Health Insurance Program) Reauthorization Act of 2015, replace the sustainable growth rate formula, which would have drastically reduced provider payments under Medicare’s Physician Fee Schedule. With this change, a major challenge was crossed off our list and a major new one added. Now, we must ensure proper enactment of MACRA’s new payment system and be continually vigilant with respect to its implementation.
Second, we must ensure there are enough ObGyns to care for patients nationally, across all areas of the country. We must find new ways to recruit ObGyns and maintain and expand our workforce.
Third, we must stand firm against political interference. The future of our patients, our practices, and our specialty depend on it. Only 2 people are allowed in the exam room—the patient and her ObGyn—and we must close its door to politicians who want to make decisions about the kind of care our patients need and how we should provide it. We must defeat the many state efforts to decree or limit care. Patient’s access to care, including reproductive care, must not be subject to politics.
These challenges can be opportunities. For example, the more we make MACRA work for practicing ObGyns now, the brighter our future will be, as private payers likely will be following suit.
We stand with patients on reproductive rights and access to care
Haywood Brown, MD: We face several challenges. First, when we become ObGyns, we join our patients in taking on the everyday challenges of women’s health care, reproduction, and reproductive rights. These will continue to be major issues for our specialty. In addition, in our continued efforts to address health care disparities, we must take the lead at ACOG as well as enlist other women’s health care providers as partners. Too often, access to high-quality perinatal, cancer, and other women’s health care is determined or influenced by a patient’s race, residence, or income. This must change.
A future for team-based care
Another challenge is to define clinical practice expectations for the newer generations of Fellows. We must impart to Junior Fellows that team-based care will:
- help them see obstetrics and gynecology as an immensely satisfying calling and career rather than as just a job
- contribute to the expansion of care to women in all communities
- allow for the maintenance of a good work–life balance for many years. (See “Steps to address ObGyn work–life balance” on page 30.)
It’s a new Washington. We are poised for new challenges.
Dr. Gellhaus: With the new US President, Congress, governors, and state legislators in office, a new challenge is to maintain the women’s health protections in the Affordable Care Act—particularly insurance coverage for maternity care and preventive and contraceptive services. We must guard against a resurgence in the number of the uninsured and underinsured, including patients whose health insurance is cut off once they become seriously ill or reach their annual or lifetime coverage limit.
We also must be ready to fight the anticipated onslaught of state and federal attempts to limit our patients’ access to reproductive health care. Many of us remember the days of illegal, unsafe abortions and their devastating effects on women’s health. No lawmaker should doubt that having access to contraceptives helps reduce the rates of unwanted pregnancies and abortions, improves maternal and infant outcomes, and decreases health care costs. It’s a win-win!
Groundwork has been laid, and opportunities will surface
Dr. Gellhaus: The best opportunities will emerge from our long-standing history of bipartisan political cooperation in this area, as we work with lawmakers from both parties on issues that benefit ObGyns and their patients. Over the years, ACOG has well positioned itself and developed important long-term relationships with Republican and Democratic lawmakers to focus on women’s health as a central issue. This position will give ACOG a voice in the new federal Administration, in Congress, and in state houses.
We also will have opportunities to educate elected officials, debunk many of the false or mistaken ideas surrounding contraceptive methods, and reinforce the need for politicians to stop interfering with the sacred physician–patient relationship and stay out of our exam rooms.
Our commitment to our patients is strong
Dr. Brown: It is more important than ever for ACOG to affirm its commitment to women’s reproductive choices and their access to contraceptives—especially with respect to programs funded by Medicaid and Title X. In the United States, Medicaid covers 48% of all births, as well as preventive and screening services provided by Planned Parenthood clinics. Over the next years, these programs will be challenged and could fall into jeopardy. We must remind our Fellows that both Title X contraception coverage and abortion choice have been the law of the land for almost 50 years. We cannot allow politicians to return us to an era that was far worse for our patients.
I asked Haywood Brown, MD, the incoming ACOG President as of May 2017, how he views ACOG's role in addressing a main reason for ObGyn burnout--the increasing burden of compliance with required electronic documentation.
Haywood Brown, MD: We must develop new models of care that foster the ability of ObGyns to embrace practicing the depth and breadth of ObGyn long term, and maintain their enthusiasm about providing care to women throughout the life span. Compliance and electronic documentation requirements can enhance patient care by allowing us to better communicate with our practice partners and our patients, improve quality, safety, and patient satisfaction. It can also quickly wear us down.
Burnout can be reduced through shared practice models, development of niches within shared practices, and being creative with better incorporating advanced practice providers into team-based care. I sincerely believe that if we embrace new models of clinical practice, the satisfaction for what we are trained to do will improve and burnout will be less a threat to our specialty over time.
All-In for Advocacy tops presidential initiatives list
Dr. Gellhaus: With political legislative interference increasing across all of medicine, we need a unified, powerful, cohesive voice. Advocacy is at the top of my presidential initiatives list. The voice of our national organization can have a huge impact on maintaining and improving women’s health care in the United States. That is why All-In for Advocacy is vital. This initiative has significantly increased members’ involvement in ACOG. We will harness this power to pass vital legislation to help the women we serve and our specialty.
Addressing health disparities drives career and presidential focus
Dr. Brown: My presidential initiatives are rooted in my career decision to focus on health disparities, particularly race-based health disparities.
Maternal morbidity and mortality and infant mortality are complex issues shrouded in the social determinants of health. Access to care, fragmentation of care, and quality of care are other factors relevant in disparity. There is evidence of an implicit bias in health care delivery.
My telehealth initiative will focus on implementing Levels of Maternal Care (of which there are 4), the National Partnership for Maternal Safety (NPMS), and the Alliance for Innovation on Maternal Health (AIM) as well as redefining healthy pregnancies and postpartum periods as the gateway to women’s long-term health. The February 2015 Levels of Maternal Care Obstetric Care Consensus Statement, jointly issued by ACOG and the Society for Maternal–Fetal Medicine (SMFM),1 proposes a classification system for birth centers, from basic to specialized regional perinatal health care centers. ACOG is working with hospitals throughout the country to designate the Levels of Maternal Care and thereby ensure each patient receives the appropriate level of care.
The AIM program, led by ACOG and funded by the Health Resources and Services Administration (HRSA), reduces obstetric complications by encouraging hospitals to adopt defined evidence-based patient safety measures. The goal is to prevent 100,000 severe labor and delivery complications and 1,000 maternal deaths over 4 years.
- ACOG's Congressional Leadership Conference, The President's Conference. This 3-day conference, held in Washington, DC, connects you with lawmakers on the important issues facing ObGyns. To find out more, access www.acog.org/clc.
- McCain and Gellhaus Fellowships. Spend 2 to 4 weeks as a member of ACOG's Government Affairs team in Washington, DC. To apply, go to www.acog.org/ateam.
- Ob-Gyn PAC. ACOG's political action committee helps elect state and federal candidates who support our specialty. For more information, visit www.obgynpac.org.
- ACOG News. Don't miss these updates on federal and state legislative developments. To sign up, access www.acog.org/advonews.
- Advocacy webpage. All of this information and more can be found at www.acog.org/advocacy!
ACOG is committed to a “big tent” approach
Dr. Gellhaus: Like US citizens, ACOG represents members with many points of view. ACOG can best represent our members’ diversity in the future by remaining the moderate voice, and by opposing federal and state proposals that are inconsistent with facts and science. We need to bring to our membership’s attention the federal and state successes we have had, show how they have helped our patients and our specialty, and make it clear that our successes are due to our bipartisan work over the years, which we have achieved regardless of which political party has been in office.
For ACOG to continue to be a leader in women’s health care and our specialty, we must remain vigilant against political interference in the patient–physician relationship and be ready to counter with science, facts, and evidence.
Compassion and passion lie at the heart of member similarities
Dr. Brown: First and foremost, we ObGyns care about our patients and, regardless of personal politics, most of us understand the reproductive health challenges facing the women of this country as well as our history with respect to those challenges. All of us must be willing to provide counsel to patients when needed, and that counseling must be nonjudgmental. We also must be willing to protect confidentially and to refer patients whose decisions are at odds with our personal views.
ACOG recognizes that we are a melting pot of specialists and subspecialists and that we are all guided by our personal beliefs and values. Choosing to become an exclusive women’s health care physician requires our passion and compassion.
Let us use our collective voice!
Dr. Gellhaus: Our members must realize the power of our collective voice and that we must use it to deliver a unified, cohesive message. We cannot sit on the sidelines and expect others to speak for us. If we are not part of the solution, then we cede our future to others and have no right to complain about the result. Our members need to commit to advocating outside their exam rooms. A good first step is to see how ACOG makes advocacy easy. When thousands of ACOG members contact elected officials about important issues, officials listen.
Dr. Brown: Yes! We all need to get involved in ACOG and in our communities. Together, we will accomplish many important things.
[polldaddy:9703185]
Send your letter to the editor to [email protected]. Please include the city and state in which you practice.
- Menard MK, Kilpatrick S, Saade G, et al; American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine. Levels of maternal care. Am J Obstet Gynecol. 2015;212(3)259–271.
- Menard MK, Kilpatrick S, Saade G, et al; American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine. Levels of maternal care. Am J Obstet Gynecol. 2015;212(3)259–271.
Should coffee consumption be added as an adjunct to the postoperative care of gynecologic oncology patients?
EXPERT COMMENTARY
Postoperative ileus is a common complication following abdominal surgery, particularly for patients undergoing laparotomy. Ileus is frustrating for patients and providers alike, and its occurrence may prolong the length of hospital stay, increase the cost of care, worsen patient satisfaction, and potentially delay postoperative treatments, such as chemotherapy for patients with gynecologic malignancies. The etiology of ileus is multifactorial, but it is thought to be caused primarily by a local inflammatory response from mechanical handling and irritation of the bowel. Although various interventions, such as laxatives, peripheral mu antagonists, and chewing gum, have been shown to reduce the occurrence of ileus, the effectiveness of these interventions varies, and ileus remains a major source of morbidity.1
Details of the study
To investigate whether coffee consumption accelerates recovery of bowel function following surgery, Güngördük and colleagues conducted a randomized controlled trial of coffee consumption after laparotomy with hysterectomy and staging for patients with gynecologic malignancies. This intervention avoids costs associated with drugs such as oral mu antagonists.
The trial included 114 women; after surgery, 58 were assigned to consume coffee 3 times daily and 56 received routine postoperative care without coffee consumption. The primary outcome measure was the time to the first passage of flatus after surgery. Time to first bowel movement and time to tolerance of a solid diet were secondary outcomes.
The results of this trial are consistent with prior study findings in colorectal surgery.2 Güngördük and associates found that patients in the coffee-consumption group, compared with controls, had reduced the time to flatus by 12 hours (mean [SD] time to flatus, 30.2 [8.0] vs 40.2 [12.1] hours; P<.001), shortened time to full diet by 1.3 days (mean [SD] time to tolerate food, 3.4 [1.2] vs 4.7 [1.6] days; P<.001), reduced time to first bowel movement by 12 hours (43.1 [9.4] vs 58.5 [17.0] hours; P<.001), and shortened length of hospital stay by 1 day. Symptoms of ileus were reduced from 52% to 14% with coffee consumption.
Study limitation. An important weakness of this study is that although the authors defined the severity of ileus by time to resolution, they did not define what constituted a diagnosis of ileus in the first place.
Unanswered questions. Coffee is a known diarrhetic, so it is not unexpected that its use shortened time to flatus and first bowel movement. What is not known, however, is whether coffee consumption improves recovery. The significance of a 1-day reduction in hospital stay is unclear given the relatively prolonged hospitalization (6 to 7 days) seen in this investigation of patients with mixed gynecologic malignancies who underwent staging only. In contrast, another study showed that, for patients managed within an enhanced recovery pathway (a multimodal perioperative care enhancement protocol), median length of stay was 4 days for patients who underwent staging alone and 5 days for patients with ovarian cancer (40% underwent enteric resections).3 Thus, the effects of coffee consumption are unclear for patients managed with an optimized perioperative pathway.
The improvement in oral intake is also of questionable significance since these patients tolerated a solid diet 3 to 4 days after surgery, compared with the evening of surgery for most patients managed with enhanced recovery.
Incisional injection of liposomal bupivacaine has been associated with a reduction in the rate of ileus from 22% to 11% after complex cytoreduction for ovarian cancer when added to an existing enhanced recovery pathway; rates were only 5% for patients undergoing staging alone.4 These findings may be due to the significant reduction in opioid use that accompanied the use of liposomal bupivacaine.
--SEAN C. DOWDY, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Nelson G, Altman AD, Nick A, et al. Guidelines for post- operative care in gynecologic/oncology surgery: Enhanced Recovery After Surgery (ERAS) Society recommendations--part II. Gynecol Oncol. 2016;140(2):323-332.
- Müller SA, Rahbari NN, Schneider F, et al. Randomized clinical trial on the effect of coffee on postoperative ileus following elective colectomy. Br J Surg. 2012;99(11):1530-1538.
- Kalogera E, Bakkum-Gamez JN, Jankowski CJ, et al. Enhanced recovery in gynecologic surgery. Obstet Gynecol. 2013;122 (2 pt 1):319-328.
- Kalogera E, Bakkum-Gamez JN, Weaver AL, et al. Abdominal incision injection of liposomal bupivacaine and opioid use after laparotomy for gynecologic malignancies. Obstet Gynecol. 2016;128(5):1009-1017.
EXPERT COMMENTARY
Postoperative ileus is a common complication following abdominal surgery, particularly for patients undergoing laparotomy. Ileus is frustrating for patients and providers alike, and its occurrence may prolong the length of hospital stay, increase the cost of care, worsen patient satisfaction, and potentially delay postoperative treatments, such as chemotherapy for patients with gynecologic malignancies. The etiology of ileus is multifactorial, but it is thought to be caused primarily by a local inflammatory response from mechanical handling and irritation of the bowel. Although various interventions, such as laxatives, peripheral mu antagonists, and chewing gum, have been shown to reduce the occurrence of ileus, the effectiveness of these interventions varies, and ileus remains a major source of morbidity.1
Details of the study
To investigate whether coffee consumption accelerates recovery of bowel function following surgery, Güngördük and colleagues conducted a randomized controlled trial of coffee consumption after laparotomy with hysterectomy and staging for patients with gynecologic malignancies. This intervention avoids costs associated with drugs such as oral mu antagonists.
The trial included 114 women; after surgery, 58 were assigned to consume coffee 3 times daily and 56 received routine postoperative care without coffee consumption. The primary outcome measure was the time to the first passage of flatus after surgery. Time to first bowel movement and time to tolerance of a solid diet were secondary outcomes.
The results of this trial are consistent with prior study findings in colorectal surgery.2 Güngördük and associates found that patients in the coffee-consumption group, compared with controls, had reduced the time to flatus by 12 hours (mean [SD] time to flatus, 30.2 [8.0] vs 40.2 [12.1] hours; P<.001), shortened time to full diet by 1.3 days (mean [SD] time to tolerate food, 3.4 [1.2] vs 4.7 [1.6] days; P<.001), reduced time to first bowel movement by 12 hours (43.1 [9.4] vs 58.5 [17.0] hours; P<.001), and shortened length of hospital stay by 1 day. Symptoms of ileus were reduced from 52% to 14% with coffee consumption.
Study limitation. An important weakness of this study is that although the authors defined the severity of ileus by time to resolution, they did not define what constituted a diagnosis of ileus in the first place.
Unanswered questions. Coffee is a known diarrhetic, so it is not unexpected that its use shortened time to flatus and first bowel movement. What is not known, however, is whether coffee consumption improves recovery. The significance of a 1-day reduction in hospital stay is unclear given the relatively prolonged hospitalization (6 to 7 days) seen in this investigation of patients with mixed gynecologic malignancies who underwent staging only. In contrast, another study showed that, for patients managed within an enhanced recovery pathway (a multimodal perioperative care enhancement protocol), median length of stay was 4 days for patients who underwent staging alone and 5 days for patients with ovarian cancer (40% underwent enteric resections).3 Thus, the effects of coffee consumption are unclear for patients managed with an optimized perioperative pathway.
The improvement in oral intake is also of questionable significance since these patients tolerated a solid diet 3 to 4 days after surgery, compared with the evening of surgery for most patients managed with enhanced recovery.
Incisional injection of liposomal bupivacaine has been associated with a reduction in the rate of ileus from 22% to 11% after complex cytoreduction for ovarian cancer when added to an existing enhanced recovery pathway; rates were only 5% for patients undergoing staging alone.4 These findings may be due to the significant reduction in opioid use that accompanied the use of liposomal bupivacaine.
--SEAN C. DOWDY, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
EXPERT COMMENTARY
Postoperative ileus is a common complication following abdominal surgery, particularly for patients undergoing laparotomy. Ileus is frustrating for patients and providers alike, and its occurrence may prolong the length of hospital stay, increase the cost of care, worsen patient satisfaction, and potentially delay postoperative treatments, such as chemotherapy for patients with gynecologic malignancies. The etiology of ileus is multifactorial, but it is thought to be caused primarily by a local inflammatory response from mechanical handling and irritation of the bowel. Although various interventions, such as laxatives, peripheral mu antagonists, and chewing gum, have been shown to reduce the occurrence of ileus, the effectiveness of these interventions varies, and ileus remains a major source of morbidity.1
Details of the study
To investigate whether coffee consumption accelerates recovery of bowel function following surgery, Güngördük and colleagues conducted a randomized controlled trial of coffee consumption after laparotomy with hysterectomy and staging for patients with gynecologic malignancies. This intervention avoids costs associated with drugs such as oral mu antagonists.
The trial included 114 women; after surgery, 58 were assigned to consume coffee 3 times daily and 56 received routine postoperative care without coffee consumption. The primary outcome measure was the time to the first passage of flatus after surgery. Time to first bowel movement and time to tolerance of a solid diet were secondary outcomes.
The results of this trial are consistent with prior study findings in colorectal surgery.2 Güngördük and associates found that patients in the coffee-consumption group, compared with controls, had reduced the time to flatus by 12 hours (mean [SD] time to flatus, 30.2 [8.0] vs 40.2 [12.1] hours; P<.001), shortened time to full diet by 1.3 days (mean [SD] time to tolerate food, 3.4 [1.2] vs 4.7 [1.6] days; P<.001), reduced time to first bowel movement by 12 hours (43.1 [9.4] vs 58.5 [17.0] hours; P<.001), and shortened length of hospital stay by 1 day. Symptoms of ileus were reduced from 52% to 14% with coffee consumption.
Study limitation. An important weakness of this study is that although the authors defined the severity of ileus by time to resolution, they did not define what constituted a diagnosis of ileus in the first place.
Unanswered questions. Coffee is a known diarrhetic, so it is not unexpected that its use shortened time to flatus and first bowel movement. What is not known, however, is whether coffee consumption improves recovery. The significance of a 1-day reduction in hospital stay is unclear given the relatively prolonged hospitalization (6 to 7 days) seen in this investigation of patients with mixed gynecologic malignancies who underwent staging only. In contrast, another study showed that, for patients managed within an enhanced recovery pathway (a multimodal perioperative care enhancement protocol), median length of stay was 4 days for patients who underwent staging alone and 5 days for patients with ovarian cancer (40% underwent enteric resections).3 Thus, the effects of coffee consumption are unclear for patients managed with an optimized perioperative pathway.
The improvement in oral intake is also of questionable significance since these patients tolerated a solid diet 3 to 4 days after surgery, compared with the evening of surgery for most patients managed with enhanced recovery.
Incisional injection of liposomal bupivacaine has been associated with a reduction in the rate of ileus from 22% to 11% after complex cytoreduction for ovarian cancer when added to an existing enhanced recovery pathway; rates were only 5% for patients undergoing staging alone.4 These findings may be due to the significant reduction in opioid use that accompanied the use of liposomal bupivacaine.
--SEAN C. DOWDY, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Nelson G, Altman AD, Nick A, et al. Guidelines for post- operative care in gynecologic/oncology surgery: Enhanced Recovery After Surgery (ERAS) Society recommendations--part II. Gynecol Oncol. 2016;140(2):323-332.
- Müller SA, Rahbari NN, Schneider F, et al. Randomized clinical trial on the effect of coffee on postoperative ileus following elective colectomy. Br J Surg. 2012;99(11):1530-1538.
- Kalogera E, Bakkum-Gamez JN, Jankowski CJ, et al. Enhanced recovery in gynecologic surgery. Obstet Gynecol. 2013;122 (2 pt 1):319-328.
- Kalogera E, Bakkum-Gamez JN, Weaver AL, et al. Abdominal incision injection of liposomal bupivacaine and opioid use after laparotomy for gynecologic malignancies. Obstet Gynecol. 2016;128(5):1009-1017.
- Nelson G, Altman AD, Nick A, et al. Guidelines for post- operative care in gynecologic/oncology surgery: Enhanced Recovery After Surgery (ERAS) Society recommendations--part II. Gynecol Oncol. 2016;140(2):323-332.
- Müller SA, Rahbari NN, Schneider F, et al. Randomized clinical trial on the effect of coffee on postoperative ileus following elective colectomy. Br J Surg. 2012;99(11):1530-1538.
- Kalogera E, Bakkum-Gamez JN, Jankowski CJ, et al. Enhanced recovery in gynecologic surgery. Obstet Gynecol. 2013;122 (2 pt 1):319-328.
- Kalogera E, Bakkum-Gamez JN, Weaver AL, et al. Abdominal incision injection of liposomal bupivacaine and opioid use after laparotomy for gynecologic malignancies. Obstet Gynecol. 2016;128(5):1009-1017.
Top 3 things I learned at the PAGS 2016 symposium
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Personality disorders on the acute care unit
We all know these patients:
The young man who, when his name shows up on the ED board, everyone lets out a little groan, knowing his hospital stay will be long and tumultuous.
The middle-aged woman who seems to do want your care and attention and yet rebuffs your attempts to help her, meanwhile, making constant demands on nursing staff.
The older man who trusts no one and will not cooperate with any of his needed care, frustrating staff and physicians alike.
Caring for the patient is integral to the art of doctoring, and yet, there are some people for whom this is incredibly hard to do. They frustrate even the most seasoned professional and work their way under our skin. While their disruptive acts may feel volitional to those of us attempting to provide care, these individuals may suffer from a personality disorder.
In the hospital, a patient must to relate to, and cooperate with, a revolving team of care providers all while under some degree of physical and emotional distress. While this can be destabilizing for even the most resilient patient, for those with personality disorders, it is nearly inevitable that conflict will arise. In a recent article in the Journal of Hospital Medicine, my colleagues and I discussed the management of such patients, with a focus on evidence-based interventions (doi: 10.1002/jhm.2643).2
While the behaviors associated with personality disorders can feel deliberate and even manipulative, research shows that these disorders arise from a complex set of genetic and environmental factors. Alterations found in the serotonin system and regions of the brain involved in emotional reactivity and social processing suggest an underlying neurophysiology contributing to difficulties with interpersonal relationships seen in these disorders.3-9
Many do not realize that having a personality disorder has real implications for an individual’s healthcare outcomes; those with a personality disorder have a life expectancy nearly two decades shorter than the general population.10 While there are a number of factors that likely contribute to the effect on mortality, it has been suggested that dysfunctional personality structures may interfere with the individual’s ability to access and utilize care, resulting in higher morbidity and mortality.11
Although it can be difficult to make a formal diagnosis of a personality disorder on the acute care unit, we provide guideline for recognizing individuals based on the way in which they interact with others. Specifically, we propose a team should consider a personality disorder when the following features are present:
The patient elicits a strong emotional reaction from providers; these may vary markedly between providers
The patient’s emotional responses may appear disproportionate to the inciting event
The patient is on a number of different psychiatric medications with little relief of symptoms
The patient takes up an disproportionate amount of providers’ time
The patient externalizes blame, seeing others as the source of discomfort or distress and therefore sees others as the solution.2
When the team suspects a patient’s behavior may be driven by an underlying dysfunctional personality structure, there are a number of steps that can be taken to help facilitate care and shape behaviors. Key among these is recognizing our own complicated responses to these individuals. These patients evoke strong responses and no team member – from nurses and aides to residents and senior attendings – is immune.12-15
Reactions can range from a need to care for and protect the patient to feelings of futility or contempt.15 Other important behavioral interventions include providing consistency, reinforcing desired behaviors, offering empathy, and providing boundaries while also recognizing the importance of picking your battles.2 Of note, while medications may offer some help, there is limited evidence for use of pharmacological interventions. Although they may be somewhat helpful in addressing particular features of these disorders, such as impulsivity, affective dysregulation or cognitive-perceptual symptoms16, many of these patients end up on a cocktail of psychotropic medications with minimal evidence for their use or efficacy. Thus behavioral management remains the cornerstone of treatment.
While care of the patient with personality disorders can present unique challenges, it offers the opportunity for therapeutic intervention. By appreciating the underlying genetic and environmental factors, we are in a better position to offer empathy and support. For these patients, managing their personality disorder can be just as important as managing any of their other medical comorbidities. By taking an approach that acknowledges the emotional responses of the team while also reinforcing and facilitating positive behaviors of the patient, the hospital stay can prove therapeutic, helping these individuals to develop new skills while also getting their physical needs addressed.
Megan Riddle, MD, PhD, is based in the department of psychiatry and behavioral sciences at the University of Washington, Seattle.
NOTES
1. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition. Arlington, VA: American Psychiatric Association; 2013.
2. Riddle M, Meeks T, Alvarez C, Dubovsky A. When personality is the problem: Managing patients with difficult personalities on the acute care unit. J Hosp Med. 2016 Dec;11(12):873-878.
3. Bukh JD, Bock C, Kessing LV. Association between genetic polymorphisms in the serotonergic system and comorbid personality disorders among patients with first-episode depression. J Pers Disord. 2014 Jun;28(3):365-378.
4. Perez-Rodriguez MM, Weinstein S, New AS, et al. Tryptophan-hydroxylase 2 haplotype association with borderline personality disorder and aggression in a sample of patients with personality disorders and healthy controls. J Psychiatr Res. 2010 Nov; 44(15):1075-1081.
5. Checknita D, Maussion G, Labonte B, et al. Monoamine oxidase: A gene promoter methylation and transcriptional downregulation in an offender population with antisocial personality disorder. Br J Psychiatry. 2015 Mar;206(3):216-222.
6. Boen E, Westlye LT, Elvsashagen T, et al. Regional cortical thinning may be a biological marker for borderline personality disorder. Acta Psychiatr Scand. 2014 Sep;130(3):193-204.
7. Thoma P, Friedmann C, Suchan B. Empathy and social problem solving in alcohol dependence, mood disorders and selected personality disorders. Neurosci Biobehav Rev. 2013 Mar;37(3):448-470.
8. Liu H, Liao J, Jiang W, Wang W. Changes in low-frequency fluctuations in patients with antisocial personality disorder revealed by resting-state functional MRI. PLoS One. 2014 Mar 5;9(3):e89790.
9. Yang Y, Raine A. Prefrontal structural and functional brain imaging findings in antisocial, violent, and psychopathic individuals: A meta-analysis. Psychiatry Res. 2009 Nov 30;174(2):81-88.
10. Fok ML, Hayes RD, Chang CK, Stewart R, Callard FJ, Moran P. Life expectancy at birth and all-cause mortality among people with personality disorder. J Psychosom Res. 2012 Aug;73(2):104-107.
11. Tyrer P, Reed GM, Crawford MJ. Classification, assessment, prevalence, and effect of personality disorder. Lancet. 2015 Feb 21;385:717-726.
12. Groves JE. Taking care of the hateful patient. N Engl J Med. 1978 Apr 20; 298:883-887.
13. Groves JE. Management of the borderline patient on a medical or surgical ward: The psychiatric consultant’s role. Int J Psychiatry Med. 1975;6(3):337-348.
14. Bodner E, Cohen-Fridel S, Mashiah M, et al. The attitudes of psychiatric hospital staff toward hospitalization and treatment of patients with borderline personality disorder. BMC psychiatry. 2015 Jan 22;15:2.
15. Colli A, Tanzilli A, Dimaggio G, Lingiardi V. Patient personality and therapist response: An empirical investigation. Am J Psychiatry. 2014 Jan;171(1):102-108.
16. Ingenhoven T, Lafay P, Rinne T, Passchier J, Duivenvoorden H. Effectiveness of pharmacotherapy for severe personality disorders: Meta-analyses of randomized controlled trials. J Clin Psychiatry. 2010 Jan;71(1):14-25.
We all know these patients:
The young man who, when his name shows up on the ED board, everyone lets out a little groan, knowing his hospital stay will be long and tumultuous.
The middle-aged woman who seems to do want your care and attention and yet rebuffs your attempts to help her, meanwhile, making constant demands on nursing staff.
The older man who trusts no one and will not cooperate with any of his needed care, frustrating staff and physicians alike.
Caring for the patient is integral to the art of doctoring, and yet, there are some people for whom this is incredibly hard to do. They frustrate even the most seasoned professional and work their way under our skin. While their disruptive acts may feel volitional to those of us attempting to provide care, these individuals may suffer from a personality disorder.
In the hospital, a patient must to relate to, and cooperate with, a revolving team of care providers all while under some degree of physical and emotional distress. While this can be destabilizing for even the most resilient patient, for those with personality disorders, it is nearly inevitable that conflict will arise. In a recent article in the Journal of Hospital Medicine, my colleagues and I discussed the management of such patients, with a focus on evidence-based interventions (doi: 10.1002/jhm.2643).2
While the behaviors associated with personality disorders can feel deliberate and even manipulative, research shows that these disorders arise from a complex set of genetic and environmental factors. Alterations found in the serotonin system and regions of the brain involved in emotional reactivity and social processing suggest an underlying neurophysiology contributing to difficulties with interpersonal relationships seen in these disorders.3-9
Many do not realize that having a personality disorder has real implications for an individual’s healthcare outcomes; those with a personality disorder have a life expectancy nearly two decades shorter than the general population.10 While there are a number of factors that likely contribute to the effect on mortality, it has been suggested that dysfunctional personality structures may interfere with the individual’s ability to access and utilize care, resulting in higher morbidity and mortality.11
Although it can be difficult to make a formal diagnosis of a personality disorder on the acute care unit, we provide guideline for recognizing individuals based on the way in which they interact with others. Specifically, we propose a team should consider a personality disorder when the following features are present:
The patient elicits a strong emotional reaction from providers; these may vary markedly between providers
The patient’s emotional responses may appear disproportionate to the inciting event
The patient is on a number of different psychiatric medications with little relief of symptoms
The patient takes up an disproportionate amount of providers’ time
The patient externalizes blame, seeing others as the source of discomfort or distress and therefore sees others as the solution.2
When the team suspects a patient’s behavior may be driven by an underlying dysfunctional personality structure, there are a number of steps that can be taken to help facilitate care and shape behaviors. Key among these is recognizing our own complicated responses to these individuals. These patients evoke strong responses and no team member – from nurses and aides to residents and senior attendings – is immune.12-15
Reactions can range from a need to care for and protect the patient to feelings of futility or contempt.15 Other important behavioral interventions include providing consistency, reinforcing desired behaviors, offering empathy, and providing boundaries while also recognizing the importance of picking your battles.2 Of note, while medications may offer some help, there is limited evidence for use of pharmacological interventions. Although they may be somewhat helpful in addressing particular features of these disorders, such as impulsivity, affective dysregulation or cognitive-perceptual symptoms16, many of these patients end up on a cocktail of psychotropic medications with minimal evidence for their use or efficacy. Thus behavioral management remains the cornerstone of treatment.
While care of the patient with personality disorders can present unique challenges, it offers the opportunity for therapeutic intervention. By appreciating the underlying genetic and environmental factors, we are in a better position to offer empathy and support. For these patients, managing their personality disorder can be just as important as managing any of their other medical comorbidities. By taking an approach that acknowledges the emotional responses of the team while also reinforcing and facilitating positive behaviors of the patient, the hospital stay can prove therapeutic, helping these individuals to develop new skills while also getting their physical needs addressed.
Megan Riddle, MD, PhD, is based in the department of psychiatry and behavioral sciences at the University of Washington, Seattle.
NOTES
1. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition. Arlington, VA: American Psychiatric Association; 2013.
2. Riddle M, Meeks T, Alvarez C, Dubovsky A. When personality is the problem: Managing patients with difficult personalities on the acute care unit. J Hosp Med. 2016 Dec;11(12):873-878.
3. Bukh JD, Bock C, Kessing LV. Association between genetic polymorphisms in the serotonergic system and comorbid personality disorders among patients with first-episode depression. J Pers Disord. 2014 Jun;28(3):365-378.
4. Perez-Rodriguez MM, Weinstein S, New AS, et al. Tryptophan-hydroxylase 2 haplotype association with borderline personality disorder and aggression in a sample of patients with personality disorders and healthy controls. J Psychiatr Res. 2010 Nov; 44(15):1075-1081.
5. Checknita D, Maussion G, Labonte B, et al. Monoamine oxidase: A gene promoter methylation and transcriptional downregulation in an offender population with antisocial personality disorder. Br J Psychiatry. 2015 Mar;206(3):216-222.
6. Boen E, Westlye LT, Elvsashagen T, et al. Regional cortical thinning may be a biological marker for borderline personality disorder. Acta Psychiatr Scand. 2014 Sep;130(3):193-204.
7. Thoma P, Friedmann C, Suchan B. Empathy and social problem solving in alcohol dependence, mood disorders and selected personality disorders. Neurosci Biobehav Rev. 2013 Mar;37(3):448-470.
8. Liu H, Liao J, Jiang W, Wang W. Changes in low-frequency fluctuations in patients with antisocial personality disorder revealed by resting-state functional MRI. PLoS One. 2014 Mar 5;9(3):e89790.
9. Yang Y, Raine A. Prefrontal structural and functional brain imaging findings in antisocial, violent, and psychopathic individuals: A meta-analysis. Psychiatry Res. 2009 Nov 30;174(2):81-88.
10. Fok ML, Hayes RD, Chang CK, Stewart R, Callard FJ, Moran P. Life expectancy at birth and all-cause mortality among people with personality disorder. J Psychosom Res. 2012 Aug;73(2):104-107.
11. Tyrer P, Reed GM, Crawford MJ. Classification, assessment, prevalence, and effect of personality disorder. Lancet. 2015 Feb 21;385:717-726.
12. Groves JE. Taking care of the hateful patient. N Engl J Med. 1978 Apr 20; 298:883-887.
13. Groves JE. Management of the borderline patient on a medical or surgical ward: The psychiatric consultant’s role. Int J Psychiatry Med. 1975;6(3):337-348.
14. Bodner E, Cohen-Fridel S, Mashiah M, et al. The attitudes of psychiatric hospital staff toward hospitalization and treatment of patients with borderline personality disorder. BMC psychiatry. 2015 Jan 22;15:2.
15. Colli A, Tanzilli A, Dimaggio G, Lingiardi V. Patient personality and therapist response: An empirical investigation. Am J Psychiatry. 2014 Jan;171(1):102-108.
16. Ingenhoven T, Lafay P, Rinne T, Passchier J, Duivenvoorden H. Effectiveness of pharmacotherapy for severe personality disorders: Meta-analyses of randomized controlled trials. J Clin Psychiatry. 2010 Jan;71(1):14-25.
We all know these patients:
The young man who, when his name shows up on the ED board, everyone lets out a little groan, knowing his hospital stay will be long and tumultuous.
The middle-aged woman who seems to do want your care and attention and yet rebuffs your attempts to help her, meanwhile, making constant demands on nursing staff.
The older man who trusts no one and will not cooperate with any of his needed care, frustrating staff and physicians alike.
Caring for the patient is integral to the art of doctoring, and yet, there are some people for whom this is incredibly hard to do. They frustrate even the most seasoned professional and work their way under our skin. While their disruptive acts may feel volitional to those of us attempting to provide care, these individuals may suffer from a personality disorder.
In the hospital, a patient must to relate to, and cooperate with, a revolving team of care providers all while under some degree of physical and emotional distress. While this can be destabilizing for even the most resilient patient, for those with personality disorders, it is nearly inevitable that conflict will arise. In a recent article in the Journal of Hospital Medicine, my colleagues and I discussed the management of such patients, with a focus on evidence-based interventions (doi: 10.1002/jhm.2643).2
While the behaviors associated with personality disorders can feel deliberate and even manipulative, research shows that these disorders arise from a complex set of genetic and environmental factors. Alterations found in the serotonin system and regions of the brain involved in emotional reactivity and social processing suggest an underlying neurophysiology contributing to difficulties with interpersonal relationships seen in these disorders.3-9
Many do not realize that having a personality disorder has real implications for an individual’s healthcare outcomes; those with a personality disorder have a life expectancy nearly two decades shorter than the general population.10 While there are a number of factors that likely contribute to the effect on mortality, it has been suggested that dysfunctional personality structures may interfere with the individual’s ability to access and utilize care, resulting in higher morbidity and mortality.11
Although it can be difficult to make a formal diagnosis of a personality disorder on the acute care unit, we provide guideline for recognizing individuals based on the way in which they interact with others. Specifically, we propose a team should consider a personality disorder when the following features are present:
The patient elicits a strong emotional reaction from providers; these may vary markedly between providers
The patient’s emotional responses may appear disproportionate to the inciting event
The patient is on a number of different psychiatric medications with little relief of symptoms
The patient takes up an disproportionate amount of providers’ time
The patient externalizes blame, seeing others as the source of discomfort or distress and therefore sees others as the solution.2
When the team suspects a patient’s behavior may be driven by an underlying dysfunctional personality structure, there are a number of steps that can be taken to help facilitate care and shape behaviors. Key among these is recognizing our own complicated responses to these individuals. These patients evoke strong responses and no team member – from nurses and aides to residents and senior attendings – is immune.12-15
Reactions can range from a need to care for and protect the patient to feelings of futility or contempt.15 Other important behavioral interventions include providing consistency, reinforcing desired behaviors, offering empathy, and providing boundaries while also recognizing the importance of picking your battles.2 Of note, while medications may offer some help, there is limited evidence for use of pharmacological interventions. Although they may be somewhat helpful in addressing particular features of these disorders, such as impulsivity, affective dysregulation or cognitive-perceptual symptoms16, many of these patients end up on a cocktail of psychotropic medications with minimal evidence for their use or efficacy. Thus behavioral management remains the cornerstone of treatment.
While care of the patient with personality disorders can present unique challenges, it offers the opportunity for therapeutic intervention. By appreciating the underlying genetic and environmental factors, we are in a better position to offer empathy and support. For these patients, managing their personality disorder can be just as important as managing any of their other medical comorbidities. By taking an approach that acknowledges the emotional responses of the team while also reinforcing and facilitating positive behaviors of the patient, the hospital stay can prove therapeutic, helping these individuals to develop new skills while also getting their physical needs addressed.
Megan Riddle, MD, PhD, is based in the department of psychiatry and behavioral sciences at the University of Washington, Seattle.
NOTES
1. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition. Arlington, VA: American Psychiatric Association; 2013.
2. Riddle M, Meeks T, Alvarez C, Dubovsky A. When personality is the problem: Managing patients with difficult personalities on the acute care unit. J Hosp Med. 2016 Dec;11(12):873-878.
3. Bukh JD, Bock C, Kessing LV. Association between genetic polymorphisms in the serotonergic system and comorbid personality disorders among patients with first-episode depression. J Pers Disord. 2014 Jun;28(3):365-378.
4. Perez-Rodriguez MM, Weinstein S, New AS, et al. Tryptophan-hydroxylase 2 haplotype association with borderline personality disorder and aggression in a sample of patients with personality disorders and healthy controls. J Psychiatr Res. 2010 Nov; 44(15):1075-1081.
5. Checknita D, Maussion G, Labonte B, et al. Monoamine oxidase: A gene promoter methylation and transcriptional downregulation in an offender population with antisocial personality disorder. Br J Psychiatry. 2015 Mar;206(3):216-222.
6. Boen E, Westlye LT, Elvsashagen T, et al. Regional cortical thinning may be a biological marker for borderline personality disorder. Acta Psychiatr Scand. 2014 Sep;130(3):193-204.
7. Thoma P, Friedmann C, Suchan B. Empathy and social problem solving in alcohol dependence, mood disorders and selected personality disorders. Neurosci Biobehav Rev. 2013 Mar;37(3):448-470.
8. Liu H, Liao J, Jiang W, Wang W. Changes in low-frequency fluctuations in patients with antisocial personality disorder revealed by resting-state functional MRI. PLoS One. 2014 Mar 5;9(3):e89790.
9. Yang Y, Raine A. Prefrontal structural and functional brain imaging findings in antisocial, violent, and psychopathic individuals: A meta-analysis. Psychiatry Res. 2009 Nov 30;174(2):81-88.
10. Fok ML, Hayes RD, Chang CK, Stewart R, Callard FJ, Moran P. Life expectancy at birth and all-cause mortality among people with personality disorder. J Psychosom Res. 2012 Aug;73(2):104-107.
11. Tyrer P, Reed GM, Crawford MJ. Classification, assessment, prevalence, and effect of personality disorder. Lancet. 2015 Feb 21;385:717-726.
12. Groves JE. Taking care of the hateful patient. N Engl J Med. 1978 Apr 20; 298:883-887.
13. Groves JE. Management of the borderline patient on a medical or surgical ward: The psychiatric consultant’s role. Int J Psychiatry Med. 1975;6(3):337-348.
14. Bodner E, Cohen-Fridel S, Mashiah M, et al. The attitudes of psychiatric hospital staff toward hospitalization and treatment of patients with borderline personality disorder. BMC psychiatry. 2015 Jan 22;15:2.
15. Colli A, Tanzilli A, Dimaggio G, Lingiardi V. Patient personality and therapist response: An empirical investigation. Am J Psychiatry. 2014 Jan;171(1):102-108.
16. Ingenhoven T, Lafay P, Rinne T, Passchier J, Duivenvoorden H. Effectiveness of pharmacotherapy for severe personality disorders: Meta-analyses of randomized controlled trials. J Clin Psychiatry. 2010 Jan;71(1):14-25.
Have you Googled yourself lately?
The online rating business is proliferating in the medical industry. This should really come as no surprise as health care is a service industry and online ratings have long been a staple in most other service industries. It has become routine practice for most of us to search such online reviews when seeking a pair of shoes, a toaster, or a restaurant; we almost can’t help but scour these sites to help us make the best decision possible.
Not dissimilarly, patients these days seek care and make decisions by using a variety of inputs, including:
- Anticipated cost (is the physician or practice in or out of network?).
- Availability or access to the service (location of the practice and how long it will take to be seen).
- How good the services and care will be when they get there.
That same article found that for those who used online physician ratings, about one-third had selected a physician based on good ratings, and about one-third had avoided a physician based on poor ratings. So patients do seem to be paying attention to these sites and seeking or avoiding care based on what information they find.
Based on that evidence, it is not surprising that so many physician rating sites have sprung up; not only is there a market demand for the availability of this information, the rating sites are also profitable for the host companies. Vitals.com, for example, makes most of its revenue from advertisements and turns a sizable profit every year. Other profitable health care rating sites include Healthgrades, Yelp, Zocdoc, and WebMD.
When I Google my own name, for example, Vitals.com is the first ratings website that appears in the search results. The first pop-up asks you to rate me and then it takes you to a site with all sorts of facts about me (most of which are notably inaccurate). If I had any online ratings (which I do not currently), you would then see my star ratings and any comments.
The second rating site that comes up for me via Google search is PhysicianWiki.com.There is a whole host of information on me (most of which is accurate), along with a set of personal ratings, including my office, my staff, and my waiting times (which, of course, do not make any sense given I am a hospitalist!). It is unclear how those ratings were generated or what volume of responses they represent.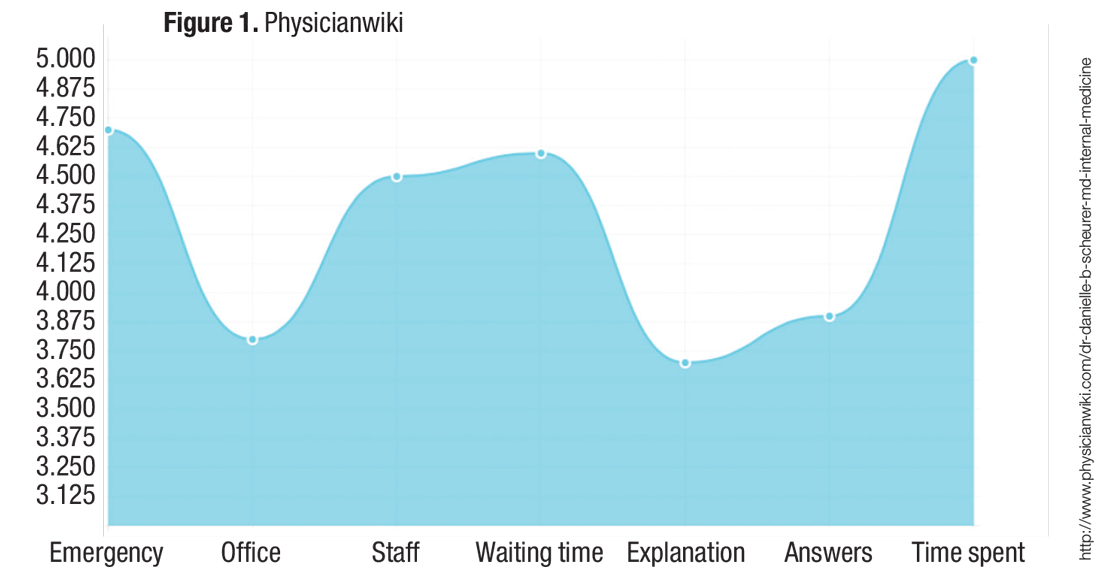
My health care system proposed rolling out a similar online rating system, and it was met with great skepticism from many physicians. There were two primary concerns:
- They felt it was “tacky” and that the profession of medicine should not be relegated to oversimplified service ratings. They worried that they would feel pressured to please the patient rather than “do the right thing” for the patient. For example, they would be less likely to give difficult advice (such as lose weight or stop smoking) or to resist prescribing medications that they deemed unnecessary or frankly dangerous (for example, antibiotics or narcotics).
Although these are valid concerns, it is hard to ignore the proliferation and traffic of these online websites. For you and your team, I would recommend taking a look at what is online about the members of your group and thinking about online strategies to take control of the conversation.
I don’t think the controversy over online physician ratings will wane anytime soon, but there is no doubt that they are profitable for companies and are therefore highly likely to continue to multiply.
References
1.Hanauer DA, Zheng K, Singer DC, Gebremariam A, Davis MM. Public awareness, perception, and use of online physician rating sites. JAMA. 2014;311(7):734-735. 2. A to Z provider listing: find a U of U Health Care physician by last name. University of Utah website. Available at http://healthcare.utah.edu/fad. Accessed Nov. 16, 2016.
Danielle Scheurer, MD, MSc, SFHM, is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
The online rating business is proliferating in the medical industry. This should really come as no surprise as health care is a service industry and online ratings have long been a staple in most other service industries. It has become routine practice for most of us to search such online reviews when seeking a pair of shoes, a toaster, or a restaurant; we almost can’t help but scour these sites to help us make the best decision possible.
Not dissimilarly, patients these days seek care and make decisions by using a variety of inputs, including:
- Anticipated cost (is the physician or practice in or out of network?).
- Availability or access to the service (location of the practice and how long it will take to be seen).
- How good the services and care will be when they get there.
That same article found that for those who used online physician ratings, about one-third had selected a physician based on good ratings, and about one-third had avoided a physician based on poor ratings. So patients do seem to be paying attention to these sites and seeking or avoiding care based on what information they find.
Based on that evidence, it is not surprising that so many physician rating sites have sprung up; not only is there a market demand for the availability of this information, the rating sites are also profitable for the host companies. Vitals.com, for example, makes most of its revenue from advertisements and turns a sizable profit every year. Other profitable health care rating sites include Healthgrades, Yelp, Zocdoc, and WebMD.
When I Google my own name, for example, Vitals.com is the first ratings website that appears in the search results. The first pop-up asks you to rate me and then it takes you to a site with all sorts of facts about me (most of which are notably inaccurate). If I had any online ratings (which I do not currently), you would then see my star ratings and any comments.
The second rating site that comes up for me via Google search is PhysicianWiki.com.There is a whole host of information on me (most of which is accurate), along with a set of personal ratings, including my office, my staff, and my waiting times (which, of course, do not make any sense given I am a hospitalist!). It is unclear how those ratings were generated or what volume of responses they represent.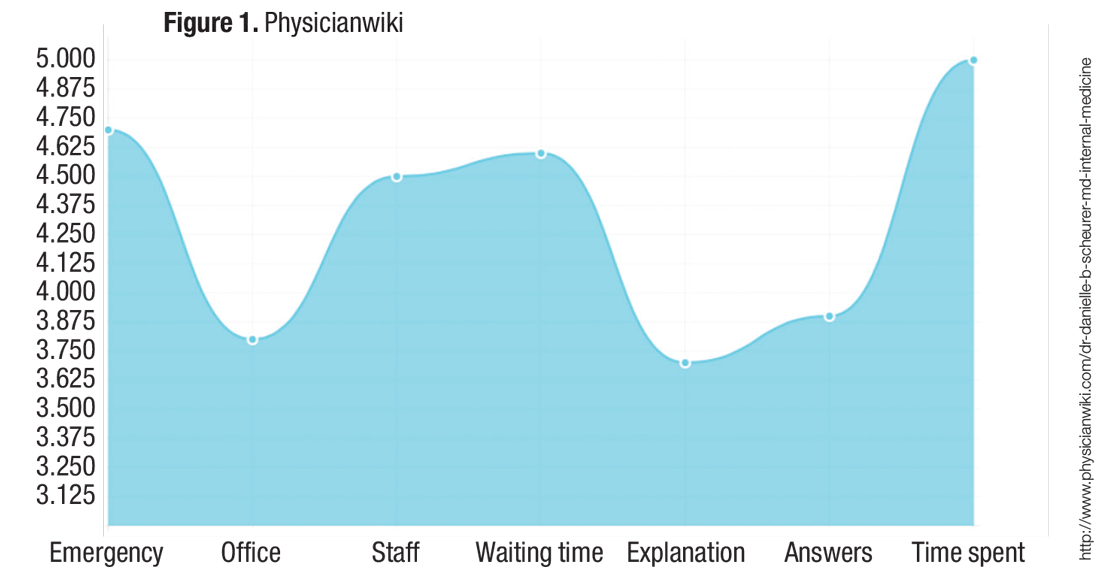
My health care system proposed rolling out a similar online rating system, and it was met with great skepticism from many physicians. There were two primary concerns:
- They felt it was “tacky” and that the profession of medicine should not be relegated to oversimplified service ratings. They worried that they would feel pressured to please the patient rather than “do the right thing” for the patient. For example, they would be less likely to give difficult advice (such as lose weight or stop smoking) or to resist prescribing medications that they deemed unnecessary or frankly dangerous (for example, antibiotics or narcotics).
Although these are valid concerns, it is hard to ignore the proliferation and traffic of these online websites. For you and your team, I would recommend taking a look at what is online about the members of your group and thinking about online strategies to take control of the conversation.
I don’t think the controversy over online physician ratings will wane anytime soon, but there is no doubt that they are profitable for companies and are therefore highly likely to continue to multiply.
References
1.Hanauer DA, Zheng K, Singer DC, Gebremariam A, Davis MM. Public awareness, perception, and use of online physician rating sites. JAMA. 2014;311(7):734-735. 2. A to Z provider listing: find a U of U Health Care physician by last name. University of Utah website. Available at http://healthcare.utah.edu/fad. Accessed Nov. 16, 2016.
Danielle Scheurer, MD, MSc, SFHM, is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
The online rating business is proliferating in the medical industry. This should really come as no surprise as health care is a service industry and online ratings have long been a staple in most other service industries. It has become routine practice for most of us to search such online reviews when seeking a pair of shoes, a toaster, or a restaurant; we almost can’t help but scour these sites to help us make the best decision possible.
Not dissimilarly, patients these days seek care and make decisions by using a variety of inputs, including:
- Anticipated cost (is the physician or practice in or out of network?).
- Availability or access to the service (location of the practice and how long it will take to be seen).
- How good the services and care will be when they get there.
That same article found that for those who used online physician ratings, about one-third had selected a physician based on good ratings, and about one-third had avoided a physician based on poor ratings. So patients do seem to be paying attention to these sites and seeking or avoiding care based on what information they find.
Based on that evidence, it is not surprising that so many physician rating sites have sprung up; not only is there a market demand for the availability of this information, the rating sites are also profitable for the host companies. Vitals.com, for example, makes most of its revenue from advertisements and turns a sizable profit every year. Other profitable health care rating sites include Healthgrades, Yelp, Zocdoc, and WebMD.
When I Google my own name, for example, Vitals.com is the first ratings website that appears in the search results. The first pop-up asks you to rate me and then it takes you to a site with all sorts of facts about me (most of which are notably inaccurate). If I had any online ratings (which I do not currently), you would then see my star ratings and any comments.
The second rating site that comes up for me via Google search is PhysicianWiki.com.There is a whole host of information on me (most of which is accurate), along with a set of personal ratings, including my office, my staff, and my waiting times (which, of course, do not make any sense given I am a hospitalist!). It is unclear how those ratings were generated or what volume of responses they represent.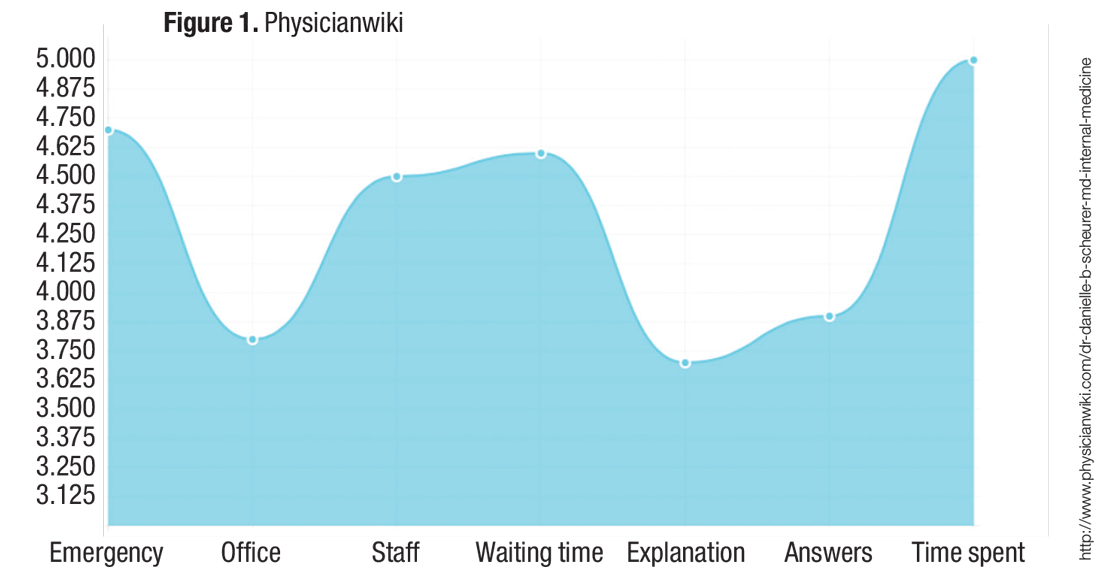
My health care system proposed rolling out a similar online rating system, and it was met with great skepticism from many physicians. There were two primary concerns:
- They felt it was “tacky” and that the profession of medicine should not be relegated to oversimplified service ratings. They worried that they would feel pressured to please the patient rather than “do the right thing” for the patient. For example, they would be less likely to give difficult advice (such as lose weight or stop smoking) or to resist prescribing medications that they deemed unnecessary or frankly dangerous (for example, antibiotics or narcotics).
Although these are valid concerns, it is hard to ignore the proliferation and traffic of these online websites. For you and your team, I would recommend taking a look at what is online about the members of your group and thinking about online strategies to take control of the conversation.
I don’t think the controversy over online physician ratings will wane anytime soon, but there is no doubt that they are profitable for companies and are therefore highly likely to continue to multiply.
References
1.Hanauer DA, Zheng K, Singer DC, Gebremariam A, Davis MM. Public awareness, perception, and use of online physician rating sites. JAMA. 2014;311(7):734-735. 2. A to Z provider listing: find a U of U Health Care physician by last name. University of Utah website. Available at http://healthcare.utah.edu/fad. Accessed Nov. 16, 2016.
Danielle Scheurer, MD, MSc, SFHM, is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].