User login
Correlating hospitalist work schedules with patient outcomes
Background: Studies show better outcomes, decreased length of stay, increased patient satisfaction, improved quality, and decreased readmission rates when hospitalist services are used. This study looks at how hospitalist schedules affect these outcomes.
Study design: Retrospective cohort study.
Setting: 229 hospitals in Texas.
Synopsis: This cohort study used 3 years of Medicare data from 229 hospitals in Texas. It included 114,777 medical admissions of patients with a 3- to 6-day length of stay. The study used the percentage of hospitalist working days that were blocks of 7 days or longer. ICU stays and patients requiring two or more E&M codes were excluded since they are associated with greater illness severity.
The primary outcome was mortality within 30 days of discharge and secondary outcomes were 30-day readmission rates, discharge destination, and 30-day postdischarge costs.
Patients receiving care from hospitalists working several days in a row had better outcomes. It is postulated that continuity of care by one hospitalist is important for several reasons. Most importantly, the development of rapport with patient and family is key to deciding the plan of care and destination post discharge as it is quite challenging to effectively transfer all important information during verbal or written handoffs.
Bottom line: Care provided by hospitalists working more days in a row improved patient outcomes. A variety of hospitalist schedules are being practiced currently; however, these findings must be taken into account as schedules are designed.
Citation: Goodwin JS et al. Association of the work schedules of hospitalists with patient outcomes of hospitalization. JAMA Intern Med. 2020;180(2):215-22. doi: 10.1001/jamainternmed.2019.5193.
Dr. Ahmed is assistant professor in the division of hospital medicine, Loyola University Medical Center, Maywood, Ill.
Background: Studies show better outcomes, decreased length of stay, increased patient satisfaction, improved quality, and decreased readmission rates when hospitalist services are used. This study looks at how hospitalist schedules affect these outcomes.
Study design: Retrospective cohort study.
Setting: 229 hospitals in Texas.
Synopsis: This cohort study used 3 years of Medicare data from 229 hospitals in Texas. It included 114,777 medical admissions of patients with a 3- to 6-day length of stay. The study used the percentage of hospitalist working days that were blocks of 7 days or longer. ICU stays and patients requiring two or more E&M codes were excluded since they are associated with greater illness severity.
The primary outcome was mortality within 30 days of discharge and secondary outcomes were 30-day readmission rates, discharge destination, and 30-day postdischarge costs.
Patients receiving care from hospitalists working several days in a row had better outcomes. It is postulated that continuity of care by one hospitalist is important for several reasons. Most importantly, the development of rapport with patient and family is key to deciding the plan of care and destination post discharge as it is quite challenging to effectively transfer all important information during verbal or written handoffs.
Bottom line: Care provided by hospitalists working more days in a row improved patient outcomes. A variety of hospitalist schedules are being practiced currently; however, these findings must be taken into account as schedules are designed.
Citation: Goodwin JS et al. Association of the work schedules of hospitalists with patient outcomes of hospitalization. JAMA Intern Med. 2020;180(2):215-22. doi: 10.1001/jamainternmed.2019.5193.
Dr. Ahmed is assistant professor in the division of hospital medicine, Loyola University Medical Center, Maywood, Ill.
Background: Studies show better outcomes, decreased length of stay, increased patient satisfaction, improved quality, and decreased readmission rates when hospitalist services are used. This study looks at how hospitalist schedules affect these outcomes.
Study design: Retrospective cohort study.
Setting: 229 hospitals in Texas.
Synopsis: This cohort study used 3 years of Medicare data from 229 hospitals in Texas. It included 114,777 medical admissions of patients with a 3- to 6-day length of stay. The study used the percentage of hospitalist working days that were blocks of 7 days or longer. ICU stays and patients requiring two or more E&M codes were excluded since they are associated with greater illness severity.
The primary outcome was mortality within 30 days of discharge and secondary outcomes were 30-day readmission rates, discharge destination, and 30-day postdischarge costs.
Patients receiving care from hospitalists working several days in a row had better outcomes. It is postulated that continuity of care by one hospitalist is important for several reasons. Most importantly, the development of rapport with patient and family is key to deciding the plan of care and destination post discharge as it is quite challenging to effectively transfer all important information during verbal or written handoffs.
Bottom line: Care provided by hospitalists working more days in a row improved patient outcomes. A variety of hospitalist schedules are being practiced currently; however, these findings must be taken into account as schedules are designed.
Citation: Goodwin JS et al. Association of the work schedules of hospitalists with patient outcomes of hospitalization. JAMA Intern Med. 2020;180(2):215-22. doi: 10.1001/jamainternmed.2019.5193.
Dr. Ahmed is assistant professor in the division of hospital medicine, Loyola University Medical Center, Maywood, Ill.
How often should we check EKGs in patients starting antipsychotic medications?
Determining relative risk with available data
Case
An 88-year-old woman with history of osteoporosis, hyperlipidemia, and a remote myocardial infarction presents to the ED with altered mental status and agitation. The patient is admitted to the medicine service for further management. Her current medications include a thiazide and a statin. Psychiatry is consulted and recommends administering intravenous haloperidol. A baseline EKG shows a corrected QT interval (QTc) of 486 milliseconds (ms). How often should subsequent EKGs be ordered?
Overview of issue
A prolonged QT interval can predispose a patient to dangerous arrhythmias such as Torsades de pointes (TdP), which results in sudden cardiac death in about 10% of cases.1,2 A prolonged QTc interval can be caused by cardiac, renal, or hepatic dysfunction; congenital Long QT Syndrome (LQTS)2; electrolyte abnormalities; or as a result of many drugs, including most antipsychotic medications such as quetiapine, olanzapine, risperidone and haloperidol.
To diminish risk of TdP while taking these medications, it is necessary to monitor the QTc interval. Before commencing a QT-prolonging medication, it is recommended to get a baseline EKG, then perform EKG monitoring after administering the medication.
According to American Heart Association guidelines, a prolonged QT interval is considered more than 460 ms in women or above 450 ms in men.3 If an abnormal rhythm and/or prolonged QTc is detected via EKG monitoring, then the drug dosage can be changed or an alternative therapy selected.4 However, there are no current guidelines recommending how often EKG monitoring should be performed after a QT-prolonging antipsychotic medication is administered on an inpatient medicine unit. Without guidelines, there is potential for health care providers to under- or over-order EKG monitoring, possibly putting patients at risk of TdP or wasting hospital resources, respectively.
Overview of the data
There are currently no universally accepted guidelines regarding inpatient EKG monitoring for patients started on QTc prolonging antipsychotic medications. A 2018 review of the literature surrounding assessment and management of patients on QTc prolonging medications was performed to analyze the available data and make recommendations; notably the evidence was limited as none of the studies were randomized controlled trials.
The authors recommend assessing the drug for QTc prolonging potential, and if possible, choosing alternative treatment in patients with baseline prolonged QTc. If the QT prolonging medication is the best or only option, then the next step is assessing the patient’s risk for QTc prolongation based on that person’s current condition and medical history.5 They recommend using the QTc prolonging risk point system developed by Tisdale and colleagues, which identified patient risk factors for elevated QTc intervals based on EKG findings in cardiac care units at a large tertiary hospital center.6
Based on the patient’s demographics, current condition, and medication list, the score can be used to stratify patients into low-, medium-, and high-risk categories (see Table 1). 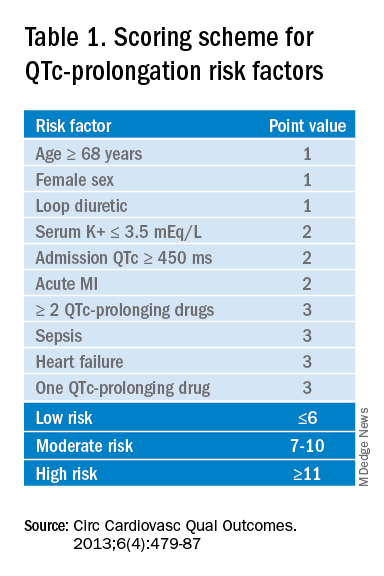
Risk factors include age over 68 years, female sex, prior MI, concurrent use of other QTc prolonging medications, and sepsis, all of which have differing ability to cause QTc prolongation and thus are weighted differentially. This scoring system is helpful in identifying high risk patients; however, the review does not include recommendations for management of these patients beyond removing the offending drug or monitoring EKGs more aggressively in higher risk patients once identified.6
Low-risk patients can be managed expectantly. If the baseline QTc is < 500 ms, then the provider may administer the medication, but should obtain follow-up EKG monitoring to ensure the QTc does not rise above 500 ms; if it does, a management change is necessitated. For moderate- to high-risk patients with a baseline QTc > 500 ms, they recommend not administering the medication and consulting a cardiologist. The review does not provide a recommendation on how often EKG monitoring should be performed after prescribing an antipsychotic medication in an inpatient setting.5
A 2018 review article explored patient risk factors for a prolonged QTc in the setting of prescribing potentially QTc prolonging antipsychotics.7 The authors reiterate that QTc prolonging risk factors are important considerations when prescribing antipsychotics that can lead to adverse events, though they note that much of the literature associating antipsychotics with negative outcomes consists of case reports in which patients had independent risk factors for development of TdP, such as preexisting ventricular arrhythmias.
In addition, the data regarding the risk of each individual antipsychotic agent are not comprehensive. Some medications that have been deemed “QTc prolonging” were identified as such in only a handful of cases where patients had confounding comorbid risk factors. This raises concern that some medications are being unduly stigmatized in situations where there is little chance of TdP. If there is no equivalent or alternate treatment available, this may lead to an antipsychotic medication being held unnecessarily, which may exacerbate the psychiatric illness.
The authors note that the trend toward ordering baseline EKGs in the inpatient setting following administration of a new antipsychotic may be partly attributed to the ready availability of EKG testing in hospitals. They recommend a baseline EKG to assess the patient’s risk. For most agents, they recommend no further EKG monitoring unless there is a change in patient risk factors. Follow-up EKGs should be done in patients with multiple or significant risk factors to assess their QTc stability. In patients with a QTc > 500 ms on a follow-up EKG, daily monitoring is encouraged alongside reassessment of the current treatment regimen.7
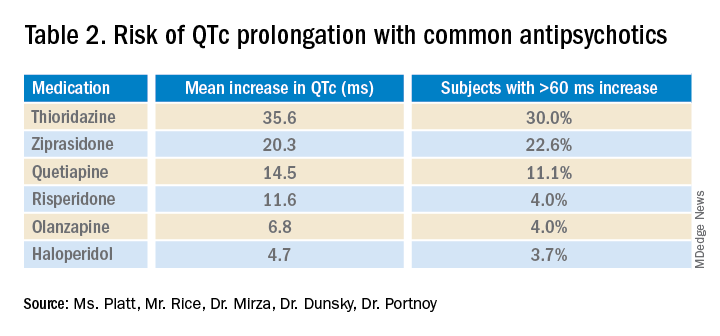
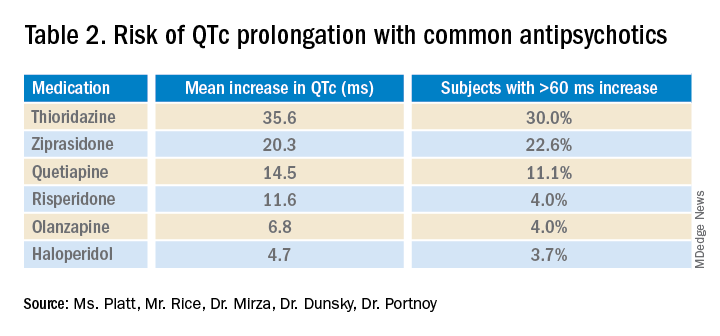
Overall, the current literature suggests that providers should know which antipsychotics carry a risk for QTc prolongation and what other treatment options are available. The risk of QTc prolongation for common antipsychotic agents is provided in Table 2.
Providers should assess their patients’ risk factors for QTc prolongation and order a baseline EKG to help quantify the cardiac risk associated with prescribing the drug. In patients with many risk factors or complicated medication regimens, a follow-up EKG should be performed to assess the new QTc baseline. If the subsequent QTc is > 500 ms, then an alternative medication should be strongly considered. The majority of patients, however, will not have a clinically significant increase in their QTc, in which case there is no need for a change in medication and monitoring frequency can be deescalated.
Application of data to the case
Our 88-year-old patient has multiple risk factors for a prolonged QTc, and according to the Tisdale scoring system is at moderate risk (7-10 points). Her risk of developing TdP increases with the addition of IV haloperidol to her regimen.
Because of her increased risk, it is reasonable to consider alternative management. If she can cooperate with PO medications, then olanzapine could be given, which has a lesser effect on the QTc interval. If unable to take oral medications, she could be given haloperidol intramuscularly, which causes less QTc prolongation than the IV formulation. If an antipsychotic is administered, she should receive EKG monitoring.
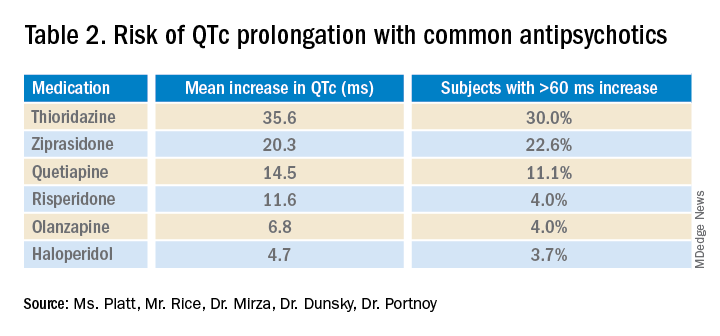
Given the lack of evidence on the optimal monitoring strategy, a protocol should be utilized that balances the ability to capture a clinically meaningful increase in the QTc with appropriate stewardship of resources. Our practice is to initially monitor the EKG every 3 days in moderate- to high-risk patients with baseline QTc < 500 ms. If the QTc remains below 500 ms over three EKGs, then treatment may continue with EKG monitoring weekly while the patient is hospitalized. If the QTc rises above 500 ms, then a management change would be indicated (either dose reduction or a change of agents). If antipsychotic medications are continued, we check the EKG daily while the QTc is >500 ms until there are three unchanged EKGS, and then consider deescalating monitoring to every 3 days.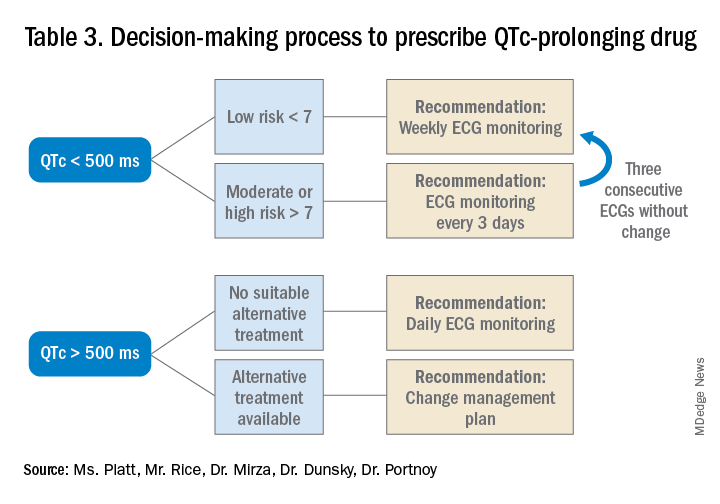
Bottom line
Prior to prescribing, perform a baseline EKG and assess the patient’s risk of QTc prolongation. If the patient is at increased risk, avoid prescribing QTc prolonging medications where alternatives exist. If a QTc prolonging medication is used in a patient with a moderate- to high-risk score, check an EKG every 3 days or daily if the QTc increases to > 500 ms.
Ms. Platt is a medical student at the Icahn School of Medicine at Mount Sinai in New York. Mr. Rice is a medical student at the Icahn School of Medicine. Dr. Mirza is assistant clinical professor of psychiatry at the Icahn School of Medicine. Dr. Dunsky is a cardiologist and assistant professor at the Icahn School of Medicine. Dr. Portnoy is a hospitalist and assistant professor at the Icahn School of Medicine.
References
1. Darpö B. Spectrum of drugs prolonging QT interval and the incidence of torsades de pointes. Eur Heart J Supplements. 2001;3(suppl_K):K70-K80. doi: 10.1016/S1520-765X(01)90009-4.
2. Schwartz PJ, Woosley RL. Predicting the unpredictable: Drug-induced QT prolongation and torsades de pointes. J Am Coll Cardiol. 2016;67(13):1639-50. doi: 10.1016/j.jacc.2015.12.063.
3. Rautaharju PM et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram. Part IV: The ST Segment, T and U Waves, and the QT Interval A Scientific Statement From the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol. 2009 Mar 17;53(11):982-91. doi: 10.1016/j.jacc.2008.12.014.
4. Drew BJ et al. Prevention of torsades de pointes in hospital settings: A scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation. 2010;121(8):1047-60. doi: 10.1161/CIRCULATIONAHA.109.192704.
5. Zolezzi M, Cheung L. A literature-based algorithm for the assessment, management, and monitoring of drug-induced QTc prolongation in the psychiatric population. Neuropsychiatr Dis Treat. 2019;15:105-14. doi: 10.2147/NDT.S186474.
6. Tisdale JE et al. Development and validation of a risk score to predict QT interval prolongation in hospitalized patients. Circ Cardiovasc Qual Outcomes. 2013;6(4):479-87. doi: 10.1161/CIRCOUTCOMES.113.000152.
7. Beach SR et al. QT prolongation, torsades de pointes, and psychotropic medications: A 5-year update. Psychosomatics. 2018;59(2):105-22. doi: 10.1016/j.psym.2017.10.009.
Key points
- An increased QTc interval can lead to TdP, ventricular fibrillation and cardiac death.
- The relative risk of each antipsychotic medication should be determined based on available data and the Tisdale scoring system can provide a system to assess a patient’s risk of QTc prolongation.
- Low-risk patients with a baseline QTc <500 ms should receive a baseline EKG and inpatient EKG monitoring weekly while moderate- to high-risk patients should receive EKG monitoring every 3 days.
- A QTc > 500 ms suggests the need for a management change (drug discontinuation, dose reduction, or a switch to another agent). If the antipsychotic is absolutely necessary, perform daily EKG monitoring until there are three unchanged EKGs, and then consider deescalating monitoring to every 3 days.
Additional reading
Beach SR et al. QT Prolongation, torsades de pointes, and psychotropic medications: A 5-year update. Psychosomatics. 2018;59(2):105-22. doi: 10.1016/j.psym.2017.10.009.
Drew BJ et al. Prevention of torsades de pointes in hospital settings: A scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation. 2010;121(8):1047-60. doi: 10.1161/CIRCULATIONAHA.109.192704.
Zolezzi M, Cheung L. A literature-based algorithm for the assessment, management, and monitoring of drug-induced QTc prolongation in the psychiatric population. Neuropsychiatr Dis Treat. 2019;15:105-14. doi: 10.2147/NDT.S186474.
Quiz
A 70-year-old male inpatient on furosemide with last known potassium level of 3.3 is going to be started on olanzapine. His baseline EKG has a QTc of 470 ms.
How often should he receive EKG monitoring?
A. Daily
B. Every 3 days
C. Weekly
D. Monthly
Answer (C): He is a low risk patient (6 points: over 70 yrs, loop diuretic, K+< 3.5, QTc > 450 ms), so he should receive weekly EKG monitoring.
Determining relative risk with available data
Determining relative risk with available data
Case
An 88-year-old woman with history of osteoporosis, hyperlipidemia, and a remote myocardial infarction presents to the ED with altered mental status and agitation. The patient is admitted to the medicine service for further management. Her current medications include a thiazide and a statin. Psychiatry is consulted and recommends administering intravenous haloperidol. A baseline EKG shows a corrected QT interval (QTc) of 486 milliseconds (ms). How often should subsequent EKGs be ordered?
Overview of issue
A prolonged QT interval can predispose a patient to dangerous arrhythmias such as Torsades de pointes (TdP), which results in sudden cardiac death in about 10% of cases.1,2 A prolonged QTc interval can be caused by cardiac, renal, or hepatic dysfunction; congenital Long QT Syndrome (LQTS)2; electrolyte abnormalities; or as a result of many drugs, including most antipsychotic medications such as quetiapine, olanzapine, risperidone and haloperidol.
To diminish risk of TdP while taking these medications, it is necessary to monitor the QTc interval. Before commencing a QT-prolonging medication, it is recommended to get a baseline EKG, then perform EKG monitoring after administering the medication.
According to American Heart Association guidelines, a prolonged QT interval is considered more than 460 ms in women or above 450 ms in men.3 If an abnormal rhythm and/or prolonged QTc is detected via EKG monitoring, then the drug dosage can be changed or an alternative therapy selected.4 However, there are no current guidelines recommending how often EKG monitoring should be performed after a QT-prolonging antipsychotic medication is administered on an inpatient medicine unit. Without guidelines, there is potential for health care providers to under- or over-order EKG monitoring, possibly putting patients at risk of TdP or wasting hospital resources, respectively.
Overview of the data
There are currently no universally accepted guidelines regarding inpatient EKG monitoring for patients started on QTc prolonging antipsychotic medications. A 2018 review of the literature surrounding assessment and management of patients on QTc prolonging medications was performed to analyze the available data and make recommendations; notably the evidence was limited as none of the studies were randomized controlled trials.
The authors recommend assessing the drug for QTc prolonging potential, and if possible, choosing alternative treatment in patients with baseline prolonged QTc. If the QT prolonging medication is the best or only option, then the next step is assessing the patient’s risk for QTc prolongation based on that person’s current condition and medical history.5 They recommend using the QTc prolonging risk point system developed by Tisdale and colleagues, which identified patient risk factors for elevated QTc intervals based on EKG findings in cardiac care units at a large tertiary hospital center.6
Based on the patient’s demographics, current condition, and medication list, the score can be used to stratify patients into low-, medium-, and high-risk categories (see Table 1). 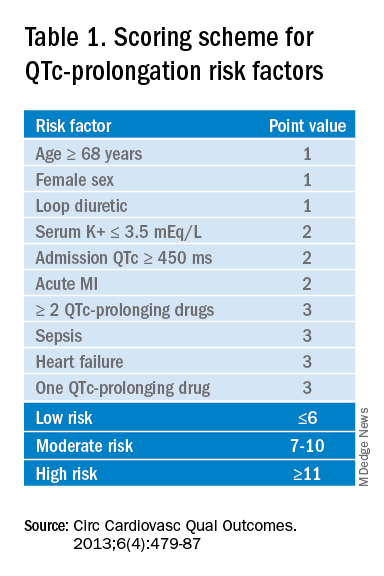
Risk factors include age over 68 years, female sex, prior MI, concurrent use of other QTc prolonging medications, and sepsis, all of which have differing ability to cause QTc prolongation and thus are weighted differentially. This scoring system is helpful in identifying high risk patients; however, the review does not include recommendations for management of these patients beyond removing the offending drug or monitoring EKGs more aggressively in higher risk patients once identified.6
Low-risk patients can be managed expectantly. If the baseline QTc is < 500 ms, then the provider may administer the medication, but should obtain follow-up EKG monitoring to ensure the QTc does not rise above 500 ms; if it does, a management change is necessitated. For moderate- to high-risk patients with a baseline QTc > 500 ms, they recommend not administering the medication and consulting a cardiologist. The review does not provide a recommendation on how often EKG monitoring should be performed after prescribing an antipsychotic medication in an inpatient setting.5
A 2018 review article explored patient risk factors for a prolonged QTc in the setting of prescribing potentially QTc prolonging antipsychotics.7 The authors reiterate that QTc prolonging risk factors are important considerations when prescribing antipsychotics that can lead to adverse events, though they note that much of the literature associating antipsychotics with negative outcomes consists of case reports in which patients had independent risk factors for development of TdP, such as preexisting ventricular arrhythmias.
In addition, the data regarding the risk of each individual antipsychotic agent are not comprehensive. Some medications that have been deemed “QTc prolonging” were identified as such in only a handful of cases where patients had confounding comorbid risk factors. This raises concern that some medications are being unduly stigmatized in situations where there is little chance of TdP. If there is no equivalent or alternate treatment available, this may lead to an antipsychotic medication being held unnecessarily, which may exacerbate the psychiatric illness.
The authors note that the trend toward ordering baseline EKGs in the inpatient setting following administration of a new antipsychotic may be partly attributed to the ready availability of EKG testing in hospitals. They recommend a baseline EKG to assess the patient’s risk. For most agents, they recommend no further EKG monitoring unless there is a change in patient risk factors. Follow-up EKGs should be done in patients with multiple or significant risk factors to assess their QTc stability. In patients with a QTc > 500 ms on a follow-up EKG, daily monitoring is encouraged alongside reassessment of the current treatment regimen.7
Overall, the current literature suggests that providers should know which antipsychotics carry a risk for QTc prolongation and what other treatment options are available. The risk of QTc prolongation for common antipsychotic agents is provided in Table 2.
Providers should assess their patients’ risk factors for QTc prolongation and order a baseline EKG to help quantify the cardiac risk associated with prescribing the drug. In patients with many risk factors or complicated medication regimens, a follow-up EKG should be performed to assess the new QTc baseline. If the subsequent QTc is > 500 ms, then an alternative medication should be strongly considered. The majority of patients, however, will not have a clinically significant increase in their QTc, in which case there is no need for a change in medication and monitoring frequency can be deescalated.
Application of data to the case
Our 88-year-old patient has multiple risk factors for a prolonged QTc, and according to the Tisdale scoring system is at moderate risk (7-10 points). Her risk of developing TdP increases with the addition of IV haloperidol to her regimen.
Because of her increased risk, it is reasonable to consider alternative management. If she can cooperate with PO medications, then olanzapine could be given, which has a lesser effect on the QTc interval. If unable to take oral medications, she could be given haloperidol intramuscularly, which causes less QTc prolongation than the IV formulation. If an antipsychotic is administered, she should receive EKG monitoring.
Given the lack of evidence on the optimal monitoring strategy, a protocol should be utilized that balances the ability to capture a clinically meaningful increase in the QTc with appropriate stewardship of resources. Our practice is to initially monitor the EKG every 3 days in moderate- to high-risk patients with baseline QTc < 500 ms. If the QTc remains below 500 ms over three EKGs, then treatment may continue with EKG monitoring weekly while the patient is hospitalized. If the QTc rises above 500 ms, then a management change would be indicated (either dose reduction or a change of agents). If antipsychotic medications are continued, we check the EKG daily while the QTc is >500 ms until there are three unchanged EKGS, and then consider deescalating monitoring to every 3 days.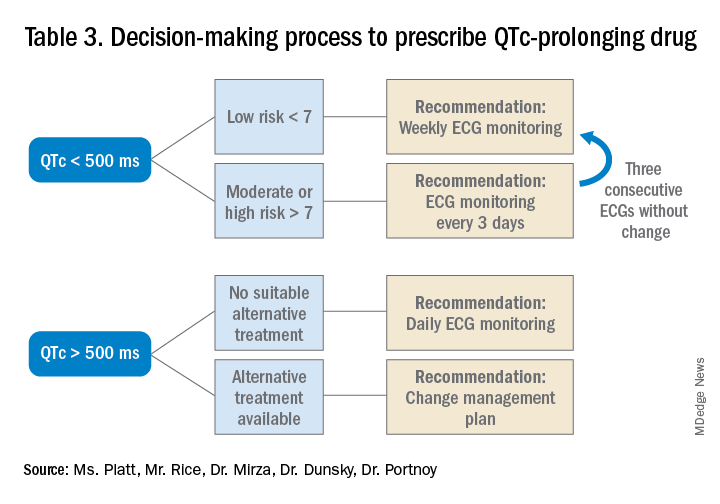
Bottom line
Prior to prescribing, perform a baseline EKG and assess the patient’s risk of QTc prolongation. If the patient is at increased risk, avoid prescribing QTc prolonging medications where alternatives exist. If a QTc prolonging medication is used in a patient with a moderate- to high-risk score, check an EKG every 3 days or daily if the QTc increases to > 500 ms.
Ms. Platt is a medical student at the Icahn School of Medicine at Mount Sinai in New York. Mr. Rice is a medical student at the Icahn School of Medicine. Dr. Mirza is assistant clinical professor of psychiatry at the Icahn School of Medicine. Dr. Dunsky is a cardiologist and assistant professor at the Icahn School of Medicine. Dr. Portnoy is a hospitalist and assistant professor at the Icahn School of Medicine.
References
1. Darpö B. Spectrum of drugs prolonging QT interval and the incidence of torsades de pointes. Eur Heart J Supplements. 2001;3(suppl_K):K70-K80. doi: 10.1016/S1520-765X(01)90009-4.
2. Schwartz PJ, Woosley RL. Predicting the unpredictable: Drug-induced QT prolongation and torsades de pointes. J Am Coll Cardiol. 2016;67(13):1639-50. doi: 10.1016/j.jacc.2015.12.063.
3. Rautaharju PM et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram. Part IV: The ST Segment, T and U Waves, and the QT Interval A Scientific Statement From the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol. 2009 Mar 17;53(11):982-91. doi: 10.1016/j.jacc.2008.12.014.
4. Drew BJ et al. Prevention of torsades de pointes in hospital settings: A scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation. 2010;121(8):1047-60. doi: 10.1161/CIRCULATIONAHA.109.192704.
5. Zolezzi M, Cheung L. A literature-based algorithm for the assessment, management, and monitoring of drug-induced QTc prolongation in the psychiatric population. Neuropsychiatr Dis Treat. 2019;15:105-14. doi: 10.2147/NDT.S186474.
6. Tisdale JE et al. Development and validation of a risk score to predict QT interval prolongation in hospitalized patients. Circ Cardiovasc Qual Outcomes. 2013;6(4):479-87. doi: 10.1161/CIRCOUTCOMES.113.000152.
7. Beach SR et al. QT prolongation, torsades de pointes, and psychotropic medications: A 5-year update. Psychosomatics. 2018;59(2):105-22. doi: 10.1016/j.psym.2017.10.009.
Key points
- An increased QTc interval can lead to TdP, ventricular fibrillation and cardiac death.
- The relative risk of each antipsychotic medication should be determined based on available data and the Tisdale scoring system can provide a system to assess a patient’s risk of QTc prolongation.
- Low-risk patients with a baseline QTc <500 ms should receive a baseline EKG and inpatient EKG monitoring weekly while moderate- to high-risk patients should receive EKG monitoring every 3 days.
- A QTc > 500 ms suggests the need for a management change (drug discontinuation, dose reduction, or a switch to another agent). If the antipsychotic is absolutely necessary, perform daily EKG monitoring until there are three unchanged EKGs, and then consider deescalating monitoring to every 3 days.
Additional reading
Beach SR et al. QT Prolongation, torsades de pointes, and psychotropic medications: A 5-year update. Psychosomatics. 2018;59(2):105-22. doi: 10.1016/j.psym.2017.10.009.
Drew BJ et al. Prevention of torsades de pointes in hospital settings: A scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation. 2010;121(8):1047-60. doi: 10.1161/CIRCULATIONAHA.109.192704.
Zolezzi M, Cheung L. A literature-based algorithm for the assessment, management, and monitoring of drug-induced QTc prolongation in the psychiatric population. Neuropsychiatr Dis Treat. 2019;15:105-14. doi: 10.2147/NDT.S186474.
Quiz
A 70-year-old male inpatient on furosemide with last known potassium level of 3.3 is going to be started on olanzapine. His baseline EKG has a QTc of 470 ms.
How often should he receive EKG monitoring?
A. Daily
B. Every 3 days
C. Weekly
D. Monthly
Answer (C): He is a low risk patient (6 points: over 70 yrs, loop diuretic, K+< 3.5, QTc > 450 ms), so he should receive weekly EKG monitoring.
Case
An 88-year-old woman with history of osteoporosis, hyperlipidemia, and a remote myocardial infarction presents to the ED with altered mental status and agitation. The patient is admitted to the medicine service for further management. Her current medications include a thiazide and a statin. Psychiatry is consulted and recommends administering intravenous haloperidol. A baseline EKG shows a corrected QT interval (QTc) of 486 milliseconds (ms). How often should subsequent EKGs be ordered?
Overview of issue
A prolonged QT interval can predispose a patient to dangerous arrhythmias such as Torsades de pointes (TdP), which results in sudden cardiac death in about 10% of cases.1,2 A prolonged QTc interval can be caused by cardiac, renal, or hepatic dysfunction; congenital Long QT Syndrome (LQTS)2; electrolyte abnormalities; or as a result of many drugs, including most antipsychotic medications such as quetiapine, olanzapine, risperidone and haloperidol.
To diminish risk of TdP while taking these medications, it is necessary to monitor the QTc interval. Before commencing a QT-prolonging medication, it is recommended to get a baseline EKG, then perform EKG monitoring after administering the medication.
According to American Heart Association guidelines, a prolonged QT interval is considered more than 460 ms in women or above 450 ms in men.3 If an abnormal rhythm and/or prolonged QTc is detected via EKG monitoring, then the drug dosage can be changed or an alternative therapy selected.4 However, there are no current guidelines recommending how often EKG monitoring should be performed after a QT-prolonging antipsychotic medication is administered on an inpatient medicine unit. Without guidelines, there is potential for health care providers to under- or over-order EKG monitoring, possibly putting patients at risk of TdP or wasting hospital resources, respectively.
Overview of the data
There are currently no universally accepted guidelines regarding inpatient EKG monitoring for patients started on QTc prolonging antipsychotic medications. A 2018 review of the literature surrounding assessment and management of patients on QTc prolonging medications was performed to analyze the available data and make recommendations; notably the evidence was limited as none of the studies were randomized controlled trials.
The authors recommend assessing the drug for QTc prolonging potential, and if possible, choosing alternative treatment in patients with baseline prolonged QTc. If the QT prolonging medication is the best or only option, then the next step is assessing the patient’s risk for QTc prolongation based on that person’s current condition and medical history.5 They recommend using the QTc prolonging risk point system developed by Tisdale and colleagues, which identified patient risk factors for elevated QTc intervals based on EKG findings in cardiac care units at a large tertiary hospital center.6
Based on the patient’s demographics, current condition, and medication list, the score can be used to stratify patients into low-, medium-, and high-risk categories (see Table 1). 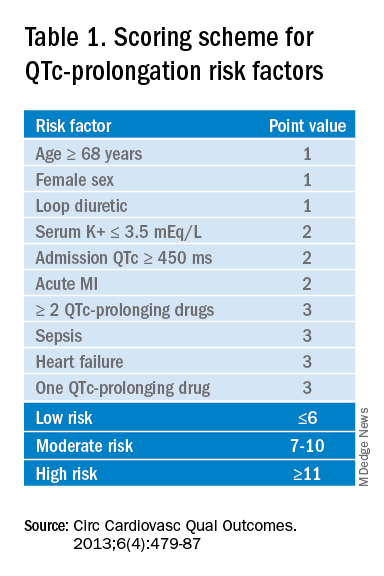
Risk factors include age over 68 years, female sex, prior MI, concurrent use of other QTc prolonging medications, and sepsis, all of which have differing ability to cause QTc prolongation and thus are weighted differentially. This scoring system is helpful in identifying high risk patients; however, the review does not include recommendations for management of these patients beyond removing the offending drug or monitoring EKGs more aggressively in higher risk patients once identified.6
Low-risk patients can be managed expectantly. If the baseline QTc is < 500 ms, then the provider may administer the medication, but should obtain follow-up EKG monitoring to ensure the QTc does not rise above 500 ms; if it does, a management change is necessitated. For moderate- to high-risk patients with a baseline QTc > 500 ms, they recommend not administering the medication and consulting a cardiologist. The review does not provide a recommendation on how often EKG monitoring should be performed after prescribing an antipsychotic medication in an inpatient setting.5
A 2018 review article explored patient risk factors for a prolonged QTc in the setting of prescribing potentially QTc prolonging antipsychotics.7 The authors reiterate that QTc prolonging risk factors are important considerations when prescribing antipsychotics that can lead to adverse events, though they note that much of the literature associating antipsychotics with negative outcomes consists of case reports in which patients had independent risk factors for development of TdP, such as preexisting ventricular arrhythmias.
In addition, the data regarding the risk of each individual antipsychotic agent are not comprehensive. Some medications that have been deemed “QTc prolonging” were identified as such in only a handful of cases where patients had confounding comorbid risk factors. This raises concern that some medications are being unduly stigmatized in situations where there is little chance of TdP. If there is no equivalent or alternate treatment available, this may lead to an antipsychotic medication being held unnecessarily, which may exacerbate the psychiatric illness.
The authors note that the trend toward ordering baseline EKGs in the inpatient setting following administration of a new antipsychotic may be partly attributed to the ready availability of EKG testing in hospitals. They recommend a baseline EKG to assess the patient’s risk. For most agents, they recommend no further EKG monitoring unless there is a change in patient risk factors. Follow-up EKGs should be done in patients with multiple or significant risk factors to assess their QTc stability. In patients with a QTc > 500 ms on a follow-up EKG, daily monitoring is encouraged alongside reassessment of the current treatment regimen.7
Overall, the current literature suggests that providers should know which antipsychotics carry a risk for QTc prolongation and what other treatment options are available. The risk of QTc prolongation for common antipsychotic agents is provided in Table 2.
Providers should assess their patients’ risk factors for QTc prolongation and order a baseline EKG to help quantify the cardiac risk associated with prescribing the drug. In patients with many risk factors or complicated medication regimens, a follow-up EKG should be performed to assess the new QTc baseline. If the subsequent QTc is > 500 ms, then an alternative medication should be strongly considered. The majority of patients, however, will not have a clinically significant increase in their QTc, in which case there is no need for a change in medication and monitoring frequency can be deescalated.
Application of data to the case
Our 88-year-old patient has multiple risk factors for a prolonged QTc, and according to the Tisdale scoring system is at moderate risk (7-10 points). Her risk of developing TdP increases with the addition of IV haloperidol to her regimen.
Because of her increased risk, it is reasonable to consider alternative management. If she can cooperate with PO medications, then olanzapine could be given, which has a lesser effect on the QTc interval. If unable to take oral medications, she could be given haloperidol intramuscularly, which causes less QTc prolongation than the IV formulation. If an antipsychotic is administered, she should receive EKG monitoring.
Given the lack of evidence on the optimal monitoring strategy, a protocol should be utilized that balances the ability to capture a clinically meaningful increase in the QTc with appropriate stewardship of resources. Our practice is to initially monitor the EKG every 3 days in moderate- to high-risk patients with baseline QTc < 500 ms. If the QTc remains below 500 ms over three EKGs, then treatment may continue with EKG monitoring weekly while the patient is hospitalized. If the QTc rises above 500 ms, then a management change would be indicated (either dose reduction or a change of agents). If antipsychotic medications are continued, we check the EKG daily while the QTc is >500 ms until there are three unchanged EKGS, and then consider deescalating monitoring to every 3 days.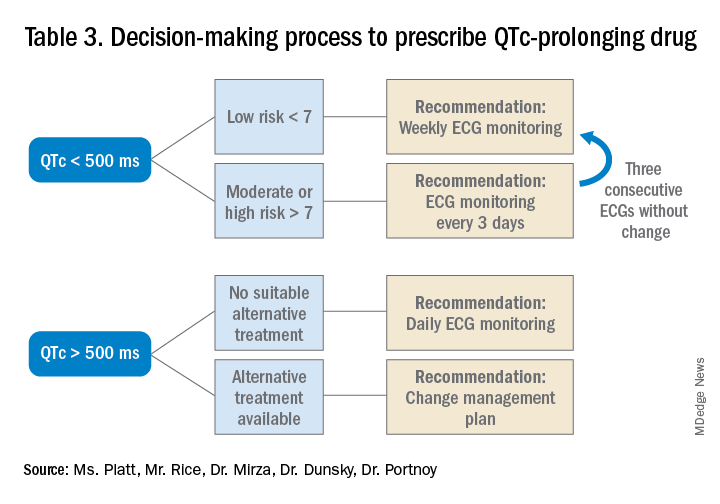
Bottom line
Prior to prescribing, perform a baseline EKG and assess the patient’s risk of QTc prolongation. If the patient is at increased risk, avoid prescribing QTc prolonging medications where alternatives exist. If a QTc prolonging medication is used in a patient with a moderate- to high-risk score, check an EKG every 3 days or daily if the QTc increases to > 500 ms.
Ms. Platt is a medical student at the Icahn School of Medicine at Mount Sinai in New York. Mr. Rice is a medical student at the Icahn School of Medicine. Dr. Mirza is assistant clinical professor of psychiatry at the Icahn School of Medicine. Dr. Dunsky is a cardiologist and assistant professor at the Icahn School of Medicine. Dr. Portnoy is a hospitalist and assistant professor at the Icahn School of Medicine.
References
1. Darpö B. Spectrum of drugs prolonging QT interval and the incidence of torsades de pointes. Eur Heart J Supplements. 2001;3(suppl_K):K70-K80. doi: 10.1016/S1520-765X(01)90009-4.
2. Schwartz PJ, Woosley RL. Predicting the unpredictable: Drug-induced QT prolongation and torsades de pointes. J Am Coll Cardiol. 2016;67(13):1639-50. doi: 10.1016/j.jacc.2015.12.063.
3. Rautaharju PM et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram. Part IV: The ST Segment, T and U Waves, and the QT Interval A Scientific Statement From the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol. 2009 Mar 17;53(11):982-91. doi: 10.1016/j.jacc.2008.12.014.
4. Drew BJ et al. Prevention of torsades de pointes in hospital settings: A scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation. 2010;121(8):1047-60. doi: 10.1161/CIRCULATIONAHA.109.192704.
5. Zolezzi M, Cheung L. A literature-based algorithm for the assessment, management, and monitoring of drug-induced QTc prolongation in the psychiatric population. Neuropsychiatr Dis Treat. 2019;15:105-14. doi: 10.2147/NDT.S186474.
6. Tisdale JE et al. Development and validation of a risk score to predict QT interval prolongation in hospitalized patients. Circ Cardiovasc Qual Outcomes. 2013;6(4):479-87. doi: 10.1161/CIRCOUTCOMES.113.000152.
7. Beach SR et al. QT prolongation, torsades de pointes, and psychotropic medications: A 5-year update. Psychosomatics. 2018;59(2):105-22. doi: 10.1016/j.psym.2017.10.009.
Key points
- An increased QTc interval can lead to TdP, ventricular fibrillation and cardiac death.
- The relative risk of each antipsychotic medication should be determined based on available data and the Tisdale scoring system can provide a system to assess a patient’s risk of QTc prolongation.
- Low-risk patients with a baseline QTc <500 ms should receive a baseline EKG and inpatient EKG monitoring weekly while moderate- to high-risk patients should receive EKG monitoring every 3 days.
- A QTc > 500 ms suggests the need for a management change (drug discontinuation, dose reduction, or a switch to another agent). If the antipsychotic is absolutely necessary, perform daily EKG monitoring until there are three unchanged EKGs, and then consider deescalating monitoring to every 3 days.
Additional reading
Beach SR et al. QT Prolongation, torsades de pointes, and psychotropic medications: A 5-year update. Psychosomatics. 2018;59(2):105-22. doi: 10.1016/j.psym.2017.10.009.
Drew BJ et al. Prevention of torsades de pointes in hospital settings: A scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation. 2010;121(8):1047-60. doi: 10.1161/CIRCULATIONAHA.109.192704.
Zolezzi M, Cheung L. A literature-based algorithm for the assessment, management, and monitoring of drug-induced QTc prolongation in the psychiatric population. Neuropsychiatr Dis Treat. 2019;15:105-14. doi: 10.2147/NDT.S186474.
Quiz
A 70-year-old male inpatient on furosemide with last known potassium level of 3.3 is going to be started on olanzapine. His baseline EKG has a QTc of 470 ms.
How often should he receive EKG monitoring?
A. Daily
B. Every 3 days
C. Weekly
D. Monthly
Answer (C): He is a low risk patient (6 points: over 70 yrs, loop diuretic, K+< 3.5, QTc > 450 ms), so he should receive weekly EKG monitoring.
Navigating challenges in COVID-19 care
Early strategies for adapting to a moving target
During the early months of the COVID-19 pandemic, hospital groups and systems scrambled to create protocols and models to respond to the novel coronavirus. In the pre-pandemic world, hospital groups have traditionally focused on standardizing clinical protocols and care models that rely on evidence-based medical practices or extended experience.
During COVID-19, however, our team at Dell Medical School needed to rapidly and iteratively standardize care based on evolving science, effectively communicate that approach across rotating hospital medicine physicians and residents, and update care models, workflows, and technology every few days. In this article, we review our initial experiences, describe the strategies we employed to respond to these challenges, and reflect on the lessons learned and our proposed strategy moving forward.
Early pandemic challenges
Our initial inpatient strategies focused on containment, infection prevention, and bracing ourselves rather than creating a COVID Center of Excellence (COE). In fact, our hospital network’s initial strategy was to have COVID-19 patients transferred to a different hospital within our network. However, as March progressed, we became the designated COVID-19 hospital in our area’s network because of the increasing volume of patients we saw.
Patients from the surrounding regional hospitals were transferring their COVID-19 patients to us and we quickly saw the wide spectrum of illness, ranging from mild pneumonia to severe disease requiring mechanical ventilation upon admission. All frontline providers felt the stress of needing to find treatment options quickly for our sickest patients. We realized that to provide safe, effective, and high-quality care to COVID-19 patients, we needed to create a sustainable and standardized interdisciplinary approach.
COVID-19 testing was a major challenge when the pandemic hit as testing kits and personal protective equipment were in limited supply. How would we choose who to test or empirically place in COVID-19 isolation? In addition, we faced questions surrounding safe discharge practices, especially for patients who could not self-isolate in their home (if they even had one).
In March, emergency use authorization (EUA) for hydroxychloroquine was granted by the U.S. FDA despite limited data. This resulted in pressure from the public to use this drug in our patients. At the same time, we saw that some patients quickly got better on their own with supportive care. As clinicians striving to practice evidence-based medicine, we certainly did not want to give patients an unproven therapy that could do more harm than good. We also felt the need to respond with statements about what we could do that worked – rather than negotiate about withholding certain treatments featured in the news. Clearly, a “one-size-fits-all” approach to therapeutics was not going to work in treating patients with COVID-19.
We realized we were going to have to learn and adapt together – quickly. It became apparent that we needed to create structures to rapidly adjudicate and integrate emerging science into standardized clinical care delivery.
Solutions in the form of better structures
In response to these challenges, we created early morning meetings or “huddles” among COVID-19 care teams and hospital administration. A designated “COVID ID” physician from Infectious Diseases would meet with hospitalist and critical care teams each morning in our daily huddles to review all newly admitted patients, current hospitalized patients, and patients with pending COVID-19 tests or suspected initial false-negative tests.
Together, and via the newly developed Therapeutics and Informatics Committee, we created early treatment recommendations based upon available evidence, treatment availability, and the patient’s severity of illness. Within the first ten days of admitting our first patient, it had become standard practice to review eligible patients soon after admission for therapies such as convalescent plasma, and, later, remdesivir and steroids.
We codified these consensus recommendations and processes in our Dell Med COVID Manual, a living document that was frequently updated and disseminated to our group. It created a single ‘true north’ of standardized workflows for triage, diagnosis, management, discharge coordination, and end-of-life care. The document allowed for continuous and asynchronous multi-person collaboration and extremely rapid cycles of improvement. Between March and December 2020, this 100-page handbook went through more than 130 iterations.
Strategy for the future
This approach – communicating frequently, adapting on a daily to weekly basis, and continuously scanning the science for opportunities to improve our care delivery – became the foundation of our approach and the Therapeutics and Informatics Committee. Just as importantly, this created a culture of engagement, collaboration, and shared problem-solving that helped us stay organized, keep up to date with the latest science, and innovate rather than panic when faced with ongoing unpredictability and chaos in the early days of the pandemic.
As the pandemic enters into its 13th month, we carry this foundation and our strategies forward. The infrastructure and systems of communication that we have set in place will allow us to be nimble in our response as COVID-19 numbers surge in our region.
Dr. Gandhi is an assistant professor in the department of internal medicine at Dell Medical School, University of Texas, Austin. Dr. Mondy is chief of the division of infectious disease and associate professor in the department of internal medicine at Dell Medical School. Dr. Busch and Dr. Brode are assistant professors in the department of internal medicine at Dell Medical School. This article is part of a series originally published in The Hospital Leader, the official blog of SHM.
Early strategies for adapting to a moving target
Early strategies for adapting to a moving target
During the early months of the COVID-19 pandemic, hospital groups and systems scrambled to create protocols and models to respond to the novel coronavirus. In the pre-pandemic world, hospital groups have traditionally focused on standardizing clinical protocols and care models that rely on evidence-based medical practices or extended experience.
During COVID-19, however, our team at Dell Medical School needed to rapidly and iteratively standardize care based on evolving science, effectively communicate that approach across rotating hospital medicine physicians and residents, and update care models, workflows, and technology every few days. In this article, we review our initial experiences, describe the strategies we employed to respond to these challenges, and reflect on the lessons learned and our proposed strategy moving forward.
Early pandemic challenges
Our initial inpatient strategies focused on containment, infection prevention, and bracing ourselves rather than creating a COVID Center of Excellence (COE). In fact, our hospital network’s initial strategy was to have COVID-19 patients transferred to a different hospital within our network. However, as March progressed, we became the designated COVID-19 hospital in our area’s network because of the increasing volume of patients we saw.
Patients from the surrounding regional hospitals were transferring their COVID-19 patients to us and we quickly saw the wide spectrum of illness, ranging from mild pneumonia to severe disease requiring mechanical ventilation upon admission. All frontline providers felt the stress of needing to find treatment options quickly for our sickest patients. We realized that to provide safe, effective, and high-quality care to COVID-19 patients, we needed to create a sustainable and standardized interdisciplinary approach.
COVID-19 testing was a major challenge when the pandemic hit as testing kits and personal protective equipment were in limited supply. How would we choose who to test or empirically place in COVID-19 isolation? In addition, we faced questions surrounding safe discharge practices, especially for patients who could not self-isolate in their home (if they even had one).
In March, emergency use authorization (EUA) for hydroxychloroquine was granted by the U.S. FDA despite limited data. This resulted in pressure from the public to use this drug in our patients. At the same time, we saw that some patients quickly got better on their own with supportive care. As clinicians striving to practice evidence-based medicine, we certainly did not want to give patients an unproven therapy that could do more harm than good. We also felt the need to respond with statements about what we could do that worked – rather than negotiate about withholding certain treatments featured in the news. Clearly, a “one-size-fits-all” approach to therapeutics was not going to work in treating patients with COVID-19.
We realized we were going to have to learn and adapt together – quickly. It became apparent that we needed to create structures to rapidly adjudicate and integrate emerging science into standardized clinical care delivery.
Solutions in the form of better structures
In response to these challenges, we created early morning meetings or “huddles” among COVID-19 care teams and hospital administration. A designated “COVID ID” physician from Infectious Diseases would meet with hospitalist and critical care teams each morning in our daily huddles to review all newly admitted patients, current hospitalized patients, and patients with pending COVID-19 tests or suspected initial false-negative tests.
Together, and via the newly developed Therapeutics and Informatics Committee, we created early treatment recommendations based upon available evidence, treatment availability, and the patient’s severity of illness. Within the first ten days of admitting our first patient, it had become standard practice to review eligible patients soon after admission for therapies such as convalescent plasma, and, later, remdesivir and steroids.
We codified these consensus recommendations and processes in our Dell Med COVID Manual, a living document that was frequently updated and disseminated to our group. It created a single ‘true north’ of standardized workflows for triage, diagnosis, management, discharge coordination, and end-of-life care. The document allowed for continuous and asynchronous multi-person collaboration and extremely rapid cycles of improvement. Between March and December 2020, this 100-page handbook went through more than 130 iterations.
Strategy for the future
This approach – communicating frequently, adapting on a daily to weekly basis, and continuously scanning the science for opportunities to improve our care delivery – became the foundation of our approach and the Therapeutics and Informatics Committee. Just as importantly, this created a culture of engagement, collaboration, and shared problem-solving that helped us stay organized, keep up to date with the latest science, and innovate rather than panic when faced with ongoing unpredictability and chaos in the early days of the pandemic.
As the pandemic enters into its 13th month, we carry this foundation and our strategies forward. The infrastructure and systems of communication that we have set in place will allow us to be nimble in our response as COVID-19 numbers surge in our region.
Dr. Gandhi is an assistant professor in the department of internal medicine at Dell Medical School, University of Texas, Austin. Dr. Mondy is chief of the division of infectious disease and associate professor in the department of internal medicine at Dell Medical School. Dr. Busch and Dr. Brode are assistant professors in the department of internal medicine at Dell Medical School. This article is part of a series originally published in The Hospital Leader, the official blog of SHM.
During the early months of the COVID-19 pandemic, hospital groups and systems scrambled to create protocols and models to respond to the novel coronavirus. In the pre-pandemic world, hospital groups have traditionally focused on standardizing clinical protocols and care models that rely on evidence-based medical practices or extended experience.
During COVID-19, however, our team at Dell Medical School needed to rapidly and iteratively standardize care based on evolving science, effectively communicate that approach across rotating hospital medicine physicians and residents, and update care models, workflows, and technology every few days. In this article, we review our initial experiences, describe the strategies we employed to respond to these challenges, and reflect on the lessons learned and our proposed strategy moving forward.
Early pandemic challenges
Our initial inpatient strategies focused on containment, infection prevention, and bracing ourselves rather than creating a COVID Center of Excellence (COE). In fact, our hospital network’s initial strategy was to have COVID-19 patients transferred to a different hospital within our network. However, as March progressed, we became the designated COVID-19 hospital in our area’s network because of the increasing volume of patients we saw.
Patients from the surrounding regional hospitals were transferring their COVID-19 patients to us and we quickly saw the wide spectrum of illness, ranging from mild pneumonia to severe disease requiring mechanical ventilation upon admission. All frontline providers felt the stress of needing to find treatment options quickly for our sickest patients. We realized that to provide safe, effective, and high-quality care to COVID-19 patients, we needed to create a sustainable and standardized interdisciplinary approach.
COVID-19 testing was a major challenge when the pandemic hit as testing kits and personal protective equipment were in limited supply. How would we choose who to test or empirically place in COVID-19 isolation? In addition, we faced questions surrounding safe discharge practices, especially for patients who could not self-isolate in their home (if they even had one).
In March, emergency use authorization (EUA) for hydroxychloroquine was granted by the U.S. FDA despite limited data. This resulted in pressure from the public to use this drug in our patients. At the same time, we saw that some patients quickly got better on their own with supportive care. As clinicians striving to practice evidence-based medicine, we certainly did not want to give patients an unproven therapy that could do more harm than good. We also felt the need to respond with statements about what we could do that worked – rather than negotiate about withholding certain treatments featured in the news. Clearly, a “one-size-fits-all” approach to therapeutics was not going to work in treating patients with COVID-19.
We realized we were going to have to learn and adapt together – quickly. It became apparent that we needed to create structures to rapidly adjudicate and integrate emerging science into standardized clinical care delivery.
Solutions in the form of better structures
In response to these challenges, we created early morning meetings or “huddles” among COVID-19 care teams and hospital administration. A designated “COVID ID” physician from Infectious Diseases would meet with hospitalist and critical care teams each morning in our daily huddles to review all newly admitted patients, current hospitalized patients, and patients with pending COVID-19 tests or suspected initial false-negative tests.
Together, and via the newly developed Therapeutics and Informatics Committee, we created early treatment recommendations based upon available evidence, treatment availability, and the patient’s severity of illness. Within the first ten days of admitting our first patient, it had become standard practice to review eligible patients soon after admission for therapies such as convalescent plasma, and, later, remdesivir and steroids.
We codified these consensus recommendations and processes in our Dell Med COVID Manual, a living document that was frequently updated and disseminated to our group. It created a single ‘true north’ of standardized workflows for triage, diagnosis, management, discharge coordination, and end-of-life care. The document allowed for continuous and asynchronous multi-person collaboration and extremely rapid cycles of improvement. Between March and December 2020, this 100-page handbook went through more than 130 iterations.
Strategy for the future
This approach – communicating frequently, adapting on a daily to weekly basis, and continuously scanning the science for opportunities to improve our care delivery – became the foundation of our approach and the Therapeutics and Informatics Committee. Just as importantly, this created a culture of engagement, collaboration, and shared problem-solving that helped us stay organized, keep up to date with the latest science, and innovate rather than panic when faced with ongoing unpredictability and chaos in the early days of the pandemic.
As the pandemic enters into its 13th month, we carry this foundation and our strategies forward. The infrastructure and systems of communication that we have set in place will allow us to be nimble in our response as COVID-19 numbers surge in our region.
Dr. Gandhi is an assistant professor in the department of internal medicine at Dell Medical School, University of Texas, Austin. Dr. Mondy is chief of the division of infectious disease and associate professor in the department of internal medicine at Dell Medical School. Dr. Busch and Dr. Brode are assistant professors in the department of internal medicine at Dell Medical School. This article is part of a series originally published in The Hospital Leader, the official blog of SHM.
Making a difference
Hospitalists engaging in advocacy efforts
Hospitalists around the country are devoting large portions of their spare time to a wide range of advocacy efforts. From health policy to caring for the unhoused population to diversity and equity to advocating for fellow hospitalists, these physicians are passionate about their causes and determined to make a difference.
Championing the unhoused
Sarah Stella, MD, FHM, a hospitalist at Denver Health, was initially drawn there because of the population the hospital serves, which includes a high concentration of people experiencing homelessness. As she cared for her patients, Dr. Stella, who is also associate professor of hospital medicine at the University of Colorado, increasingly felt the desire to help prevent the negative downstream outcomes the hospital sees.
To understand the experiences of the unhoused outside the hospital, Dr. Stella started talking to her patients and people in community-based organizations that serve this population. “I learned a ton,” she said. “Homelessness feels like such an intractable, hopeless thing, but the more I talked to people, the more opportunities I saw to work toward something better.”
This led to a pilot grant to work with the Colorado Coalition for the Homeless to set up a community advisory panel. “My goal was to better understand their experiences and to develop a shared vision for how we collectively can do better,” said Dr. Stella. Eventually, she also received a grant from the University of Colorado, and multiple opportunities have sprung up ever since.
For the past several years, Dr. Stella has worked with Denver Health leadership to improve care for the homeless. “Right now, I’m working with a community team on developing an idea to provide peer support from people with a shared lived experience for people who are experiencing homelessness when they’re hospitalized. That’s really where my passion has been in working on the partnership,” she said.
Her advocacy role has been beneficial in her work as a hospitalist, particularly when COVID began. Dr. Stella again partnered with the Colorado Coalition for the Homeless to start a joint task force. “Everyone on our task force is motivated by this powerful desire to improve the health and lives of this community and that’s one of the silver linings in this pandemic for me,” said Dr. Stella.
Advocacy work has also increased Dr. Stella’s knowledge of what community support options are available for the unhoused. This allows her to educate her patients about their options and how to access them.
While she has colleagues who are able to compartmentalize their work, “I absolutely could not be a hospitalist without being an advocate,” Dr. Stella said. “For me, it has been a protective strategy in terms of burnout because I have to feel like I’m working to advocate for better policies and more appropriate resources to address the gaps that I’m seeing.”
Dr. Stella believes that physicians have a special credibility to advocate, tell stories, and use data to back their stories up. “We have to realize that we have this power, and we have it so we can empower others,” she said. “The people I’ve seen in my community who are working so hard to help people who are experiencing homelessness are the heroes. Understanding that and giving power to those people through our voice and our well-respected place in society drives me.”
Strengthening diversity, equity, and inclusion
In September 2020, Michael Bryant, MD, became the inaugural vice chair of Diversity, Equity, and Inclusion for the department of pediatrics at Children’s Hospital Los Angeles, where he is also the division head of pediatric hospital medicine. “I was motivated to apply for this position because I wanted to be an agent for change to eliminate the institutional racism, social injustice, and marginalization that continues to threaten the lives and well-beings of so many Americans,” Dr. Bryant said.
Between the pandemic, the economic decline it has created, and the divisive political landscape, people of color have been especially affected. “These are poignant examples of the ever-widening divide and disenfranchisement many Americans feel,” said Dr. Bryant. “Gandhi said, ‘Be the change that you want to see,’ and that is what I want to model.”
At work, advocacy for diversity, equality, and inclusion is an innate part of everything he does. From the new physicians he recruits to the candidates he considers for leadership positions, Dr. Bryant strives “to have a workforce that mirrors the diversity of the patients we humbly care for and serve.”
Advocacy is intrinsic to Dr. Bryant’s worldview, in his quest to understand and accept each individual’s uniqueness, his desire “to embrace cultural humility,” his recognition that “our differences enhance us instead of diminishing us,” and his willingness to engage in difficult conversations.
“Advocacy means that I acknowledge that intent does not equal impact and that I must accept that what I do and what I say may have unintended consequences,” he said. “When that happens, I must resist becoming defensive and instead be willing to listen and learn.”
Dr. Bryant is proud of his accomplishments and enjoys his advocacy work. In his workplace, there are few African Americans in leadership roles. This means that he is in high demand when it comes to making sure there’s representation during various processes such as hiring and vetting, a disparity known as the “minority tax.”
“I am thankful for the opportunities, but it does take a toll at times,” Dr. Bryant said, which is yet another reason why he is a proponent of increasing diversity and inclusion. “This allows us to build the resource pool as these needs arise and minimizes the toll of the ‘minority tax’ on any single person or small group of individuals.”
This summer, physicians from Dr. Bryant’s hospital participated in the national “White Coats for Black Lives” effort. He found it to be “an incredibly moving event” that hundreds of his colleagues participated in.
Dr. Bryant’s advice for hospitalists who want to get involved in advocacy efforts is to check out the movie “John Lewis: Good Trouble.” “He was a champion of human rights and fought for these rights until his death,” Dr. Bryant said. “He is a true American hero and a wonderful example.”
Bolstering health care change
Since his residency, Joshua Lenchus, DO, FACP, SFHM, has developed an ever-increasing interest in legislative advocacy, particularly health policy. Getting involved in this arena requires an understanding of civics and government that goes beyond just the basics. “My desire to affect change in my own profession really served as the catalyst to get involved,” said Dr. Lenchus, the regional chief medical officer at Broward Health Medical Center in Fort Lauderdale, Fla. “What better way to do that than by combining what we do on a daily basis in the practice of medicine with this new understanding of how laws are passed and promulgated?”
Dr. Lenchus has been involved with both state and national medical organizations and has served on public policy committees as a member and as a chair. “The charge of these committees is to monitor and navigate position statements and policies that will drive the entire organization,” he said. This means becoming knowledgeable enough about a topic to be able to talk about it eloquently and adding supporting personal or professional illustrations that reinforce the position to lawmakers.
He finds his advocacy efforts “incredibly rewarding” because they contribute to his endeavors “to help my colleagues practice medicine in a safe, efficient, and productive manner.” For instance, some of the organizations Dr. Lenchus was involved with helped make changes to the Affordable Care Act that ended up in its final version, as well as changes after it passed. “There are tangible things that advocacy enables us to do in our daily practice,” he said.
When something his organizations have advocated for does not pass, they know they need to try a different outlet. “You can’t win every fight,” he said. “Every time you go and comment on an issue, you have to understand that you’re there to do your best, and to the extent that the people you’re talking to are willing to listen to what you have to say, that’s where I think you can make the most impact.” When changes he has helped fight for do pass, “it really is amazing that you can tell your colleagues about your role in achieving meaningful change in the profession.”
Dr. Lenchus acknowledges that advocacy “can be all-consuming at times. We have to understand our limits.” That said, he thinks not engaging in advocacy could increase stress and potential burnout. “I think being involved in advocacy efforts really helps people conduct meaningful work and educates them about what it means not just to them, but to the rest of the medical profession and the patients that we serve,” he said.
For hospitalists who are interested in health policy advocacy, there are many ways to get involved, Dr. Lenchus said. You could join an organization (many organized medical societies have public policy committees), participate in advocacy activities, work on a political campaign, or even run for office yourself. “Ultimately, education and some level of involvement really will make the difference in who navigates our future as hospitalists,” he said.
Questioning co-management practices
Though he says he’s in the minority, Hardik Vora, MD, SFHM, medical director for hospital medicine at Riverside Regional Medical Center in Newport News, Va., believes that co-management is going to “make or break hospital medicine. It’s going to have a huge impact on our specialty.”
In the roughly 25-year history of hospital medicine, it has evolved from admitting and caring for patients of primary care physicians to patients of specialists and, more recently, surgical patients. “Now there are (hospital medicine) programs across the country that are pretty much admitting everything,” said Dr. Vora.
As a recruiter for the Riverside Health System for the past eight years, “I have not met a single resident who is trained to do what we’re doing in hospital medicine, because you’re admitting surgical patients all the time and you have primary attending responsibility,” Dr. Vora said. “I see that as a cause of a significant amount of stress because now you’re responsible for something that you don’t have adequate training for.”
In the co-management discussion, Dr. Vora notes that people often bring up the research that shows that the practice has improved surgeon satisfaction. “What bothers me is that…you need to add one more question – how does it affect your hospitalists? And I bet the answer to that question is ‘it has a terrible effect.’”
The expectations surrounding hospitalists these days is a big concern in terms of burnout, Dr. Vora said. “We talk a lot about the drivers of burnout, whether it’s schedule or COVID,” he said. The biggest issue when it comes to burnout, as he sees it, is not COVID; it’s when hospitalists are performing tasks that make them feel they aren’t adding value. “I think that’s a huge topic in hospital medicine right now.”
Dr. Vora believes there should be more discussion and awareness of the potential pitfalls. “Hospitalists should get involved in co-management where they are adding value and certainly not take up the attending responsibility where they’re not adding value and it’s out of the scope of their training and expertise,” he said. “Preventing scope creep and burnout from co-management are some of the key issues I’m really passionate about.”
Dr. Vora said it is important to set realistic goals and remember that it takes time to make change when it comes to advocacy. “You still have to operate within whatever environment is given to you and then you can make change from within,” he said.
His enthusiasm for co-management awareness has led to creating a co-management forum through SHM in his local Hampton Roads chapter. He was also a panelist for an SHM webinar in February 2021 in which the panelists debated co-management.
“I think we really need to look at this as a specialty. Are we going in the right direction?” Dr. Vora asked. “We need to come together as a specialty and make a decision, which is going to be hard because there are competing financial interests and various practice models.”
Improving patient care
Working as a hospitalist at University Medical Center, a safety net hospital in New Orleans, Celeste Newby, MD, PhD, sees plenty of patients who are underinsured or not insured at all. “A lot of my interest in health policy stems from that,” she said.
During her residency, which she finished in 2015, Louisiana became a Medicaid expansion state. This impressed upon Dr. Newby how much Medicaid improved the lives of patients who had previously been uninsured. “We saw procedures getting done that had been put on hold because of financial concerns or medicines that were now affordable that weren’t before,” she said. “It really did make a difference.”
When repeated attempts to repeal the Affordable Care Act began, “it was a call to do health policy work for me personally that just hadn’t come up in the past,” said Dr. Newby, who is also assistant professor of medicine at Tulane University in New Orleans. “I personally found that the best way to do (advocacy work) was to go through medical societies because there is a much stronger voice when you have more people saying the same thing,” she said.
Dr. Newby sits on the Council of Legislation for the Louisiana State Medical Society and participates in the Leadership and Health Policy (LEAHP) Program through the Society of General Internal Medicine.
The LEAHP Program has been instrumental in expanding Dr. Newby’s knowledge of how health policy is made and the mechanisms behind it. It has also taught her “how we can either advise, guide, leverage, or advocate for things that we think would be important for change and moving the country in the right direction in terms of health care.”
Another reason involvement in medical societies is helpful is because, as a busy clinician, it is impossible to keep up with everything. “Working with medical societies, you have people who are more directly involved in the legislature and can give you quicker notice about things that are coming up that are going to be important to you or your co-workers or your patients,” Dr. Newby said.
Dr. Newby feels her advocacy work is an outlet for stress and “a way to work at more of a macro level on problems that I see with my individual patients. It’s a nice compliment.” At the hospital, she can only help one person at a time, but with her advocacy efforts, there’s potential to make changes for many.
“Advocacy now is such a large umbrella that encompasses so many different projects at all kinds of levels,” Dr. Newby said. She suggests looking around your community to see where the needs lie. If you’re passionate about a certain topic or population, see what you can do to help advocate for change there.
Hospitalists engaging in advocacy efforts
Hospitalists engaging in advocacy efforts
Hospitalists around the country are devoting large portions of their spare time to a wide range of advocacy efforts. From health policy to caring for the unhoused population to diversity and equity to advocating for fellow hospitalists, these physicians are passionate about their causes and determined to make a difference.
Championing the unhoused
Sarah Stella, MD, FHM, a hospitalist at Denver Health, was initially drawn there because of the population the hospital serves, which includes a high concentration of people experiencing homelessness. As she cared for her patients, Dr. Stella, who is also associate professor of hospital medicine at the University of Colorado, increasingly felt the desire to help prevent the negative downstream outcomes the hospital sees.
To understand the experiences of the unhoused outside the hospital, Dr. Stella started talking to her patients and people in community-based organizations that serve this population. “I learned a ton,” she said. “Homelessness feels like such an intractable, hopeless thing, but the more I talked to people, the more opportunities I saw to work toward something better.”
This led to a pilot grant to work with the Colorado Coalition for the Homeless to set up a community advisory panel. “My goal was to better understand their experiences and to develop a shared vision for how we collectively can do better,” said Dr. Stella. Eventually, she also received a grant from the University of Colorado, and multiple opportunities have sprung up ever since.
For the past several years, Dr. Stella has worked with Denver Health leadership to improve care for the homeless. “Right now, I’m working with a community team on developing an idea to provide peer support from people with a shared lived experience for people who are experiencing homelessness when they’re hospitalized. That’s really where my passion has been in working on the partnership,” she said.
Her advocacy role has been beneficial in her work as a hospitalist, particularly when COVID began. Dr. Stella again partnered with the Colorado Coalition for the Homeless to start a joint task force. “Everyone on our task force is motivated by this powerful desire to improve the health and lives of this community and that’s one of the silver linings in this pandemic for me,” said Dr. Stella.
Advocacy work has also increased Dr. Stella’s knowledge of what community support options are available for the unhoused. This allows her to educate her patients about their options and how to access them.
While she has colleagues who are able to compartmentalize their work, “I absolutely could not be a hospitalist without being an advocate,” Dr. Stella said. “For me, it has been a protective strategy in terms of burnout because I have to feel like I’m working to advocate for better policies and more appropriate resources to address the gaps that I’m seeing.”
Dr. Stella believes that physicians have a special credibility to advocate, tell stories, and use data to back their stories up. “We have to realize that we have this power, and we have it so we can empower others,” she said. “The people I’ve seen in my community who are working so hard to help people who are experiencing homelessness are the heroes. Understanding that and giving power to those people through our voice and our well-respected place in society drives me.”
Strengthening diversity, equity, and inclusion
In September 2020, Michael Bryant, MD, became the inaugural vice chair of Diversity, Equity, and Inclusion for the department of pediatrics at Children’s Hospital Los Angeles, where he is also the division head of pediatric hospital medicine. “I was motivated to apply for this position because I wanted to be an agent for change to eliminate the institutional racism, social injustice, and marginalization that continues to threaten the lives and well-beings of so many Americans,” Dr. Bryant said.
Between the pandemic, the economic decline it has created, and the divisive political landscape, people of color have been especially affected. “These are poignant examples of the ever-widening divide and disenfranchisement many Americans feel,” said Dr. Bryant. “Gandhi said, ‘Be the change that you want to see,’ and that is what I want to model.”
At work, advocacy for diversity, equality, and inclusion is an innate part of everything he does. From the new physicians he recruits to the candidates he considers for leadership positions, Dr. Bryant strives “to have a workforce that mirrors the diversity of the patients we humbly care for and serve.”
Advocacy is intrinsic to Dr. Bryant’s worldview, in his quest to understand and accept each individual’s uniqueness, his desire “to embrace cultural humility,” his recognition that “our differences enhance us instead of diminishing us,” and his willingness to engage in difficult conversations.
“Advocacy means that I acknowledge that intent does not equal impact and that I must accept that what I do and what I say may have unintended consequences,” he said. “When that happens, I must resist becoming defensive and instead be willing to listen and learn.”
Dr. Bryant is proud of his accomplishments and enjoys his advocacy work. In his workplace, there are few African Americans in leadership roles. This means that he is in high demand when it comes to making sure there’s representation during various processes such as hiring and vetting, a disparity known as the “minority tax.”
“I am thankful for the opportunities, but it does take a toll at times,” Dr. Bryant said, which is yet another reason why he is a proponent of increasing diversity and inclusion. “This allows us to build the resource pool as these needs arise and minimizes the toll of the ‘minority tax’ on any single person or small group of individuals.”
This summer, physicians from Dr. Bryant’s hospital participated in the national “White Coats for Black Lives” effort. He found it to be “an incredibly moving event” that hundreds of his colleagues participated in.
Dr. Bryant’s advice for hospitalists who want to get involved in advocacy efforts is to check out the movie “John Lewis: Good Trouble.” “He was a champion of human rights and fought for these rights until his death,” Dr. Bryant said. “He is a true American hero and a wonderful example.”
Bolstering health care change
Since his residency, Joshua Lenchus, DO, FACP, SFHM, has developed an ever-increasing interest in legislative advocacy, particularly health policy. Getting involved in this arena requires an understanding of civics and government that goes beyond just the basics. “My desire to affect change in my own profession really served as the catalyst to get involved,” said Dr. Lenchus, the regional chief medical officer at Broward Health Medical Center in Fort Lauderdale, Fla. “What better way to do that than by combining what we do on a daily basis in the practice of medicine with this new understanding of how laws are passed and promulgated?”
Dr. Lenchus has been involved with both state and national medical organizations and has served on public policy committees as a member and as a chair. “The charge of these committees is to monitor and navigate position statements and policies that will drive the entire organization,” he said. This means becoming knowledgeable enough about a topic to be able to talk about it eloquently and adding supporting personal or professional illustrations that reinforce the position to lawmakers.
He finds his advocacy efforts “incredibly rewarding” because they contribute to his endeavors “to help my colleagues practice medicine in a safe, efficient, and productive manner.” For instance, some of the organizations Dr. Lenchus was involved with helped make changes to the Affordable Care Act that ended up in its final version, as well as changes after it passed. “There are tangible things that advocacy enables us to do in our daily practice,” he said.
When something his organizations have advocated for does not pass, they know they need to try a different outlet. “You can’t win every fight,” he said. “Every time you go and comment on an issue, you have to understand that you’re there to do your best, and to the extent that the people you’re talking to are willing to listen to what you have to say, that’s where I think you can make the most impact.” When changes he has helped fight for do pass, “it really is amazing that you can tell your colleagues about your role in achieving meaningful change in the profession.”
Dr. Lenchus acknowledges that advocacy “can be all-consuming at times. We have to understand our limits.” That said, he thinks not engaging in advocacy could increase stress and potential burnout. “I think being involved in advocacy efforts really helps people conduct meaningful work and educates them about what it means not just to them, but to the rest of the medical profession and the patients that we serve,” he said.
For hospitalists who are interested in health policy advocacy, there are many ways to get involved, Dr. Lenchus said. You could join an organization (many organized medical societies have public policy committees), participate in advocacy activities, work on a political campaign, or even run for office yourself. “Ultimately, education and some level of involvement really will make the difference in who navigates our future as hospitalists,” he said.
Questioning co-management practices
Though he says he’s in the minority, Hardik Vora, MD, SFHM, medical director for hospital medicine at Riverside Regional Medical Center in Newport News, Va., believes that co-management is going to “make or break hospital medicine. It’s going to have a huge impact on our specialty.”
In the roughly 25-year history of hospital medicine, it has evolved from admitting and caring for patients of primary care physicians to patients of specialists and, more recently, surgical patients. “Now there are (hospital medicine) programs across the country that are pretty much admitting everything,” said Dr. Vora.
As a recruiter for the Riverside Health System for the past eight years, “I have not met a single resident who is trained to do what we’re doing in hospital medicine, because you’re admitting surgical patients all the time and you have primary attending responsibility,” Dr. Vora said. “I see that as a cause of a significant amount of stress because now you’re responsible for something that you don’t have adequate training for.”
In the co-management discussion, Dr. Vora notes that people often bring up the research that shows that the practice has improved surgeon satisfaction. “What bothers me is that…you need to add one more question – how does it affect your hospitalists? And I bet the answer to that question is ‘it has a terrible effect.’”
The expectations surrounding hospitalists these days is a big concern in terms of burnout, Dr. Vora said. “We talk a lot about the drivers of burnout, whether it’s schedule or COVID,” he said. The biggest issue when it comes to burnout, as he sees it, is not COVID; it’s when hospitalists are performing tasks that make them feel they aren’t adding value. “I think that’s a huge topic in hospital medicine right now.”
Dr. Vora believes there should be more discussion and awareness of the potential pitfalls. “Hospitalists should get involved in co-management where they are adding value and certainly not take up the attending responsibility where they’re not adding value and it’s out of the scope of their training and expertise,” he said. “Preventing scope creep and burnout from co-management are some of the key issues I’m really passionate about.”
Dr. Vora said it is important to set realistic goals and remember that it takes time to make change when it comes to advocacy. “You still have to operate within whatever environment is given to you and then you can make change from within,” he said.
His enthusiasm for co-management awareness has led to creating a co-management forum through SHM in his local Hampton Roads chapter. He was also a panelist for an SHM webinar in February 2021 in which the panelists debated co-management.
“I think we really need to look at this as a specialty. Are we going in the right direction?” Dr. Vora asked. “We need to come together as a specialty and make a decision, which is going to be hard because there are competing financial interests and various practice models.”
Improving patient care
Working as a hospitalist at University Medical Center, a safety net hospital in New Orleans, Celeste Newby, MD, PhD, sees plenty of patients who are underinsured or not insured at all. “A lot of my interest in health policy stems from that,” she said.
During her residency, which she finished in 2015, Louisiana became a Medicaid expansion state. This impressed upon Dr. Newby how much Medicaid improved the lives of patients who had previously been uninsured. “We saw procedures getting done that had been put on hold because of financial concerns or medicines that were now affordable that weren’t before,” she said. “It really did make a difference.”
When repeated attempts to repeal the Affordable Care Act began, “it was a call to do health policy work for me personally that just hadn’t come up in the past,” said Dr. Newby, who is also assistant professor of medicine at Tulane University in New Orleans. “I personally found that the best way to do (advocacy work) was to go through medical societies because there is a much stronger voice when you have more people saying the same thing,” she said.
Dr. Newby sits on the Council of Legislation for the Louisiana State Medical Society and participates in the Leadership and Health Policy (LEAHP) Program through the Society of General Internal Medicine.
The LEAHP Program has been instrumental in expanding Dr. Newby’s knowledge of how health policy is made and the mechanisms behind it. It has also taught her “how we can either advise, guide, leverage, or advocate for things that we think would be important for change and moving the country in the right direction in terms of health care.”
Another reason involvement in medical societies is helpful is because, as a busy clinician, it is impossible to keep up with everything. “Working with medical societies, you have people who are more directly involved in the legislature and can give you quicker notice about things that are coming up that are going to be important to you or your co-workers or your patients,” Dr. Newby said.
Dr. Newby feels her advocacy work is an outlet for stress and “a way to work at more of a macro level on problems that I see with my individual patients. It’s a nice compliment.” At the hospital, she can only help one person at a time, but with her advocacy efforts, there’s potential to make changes for many.
“Advocacy now is such a large umbrella that encompasses so many different projects at all kinds of levels,” Dr. Newby said. She suggests looking around your community to see where the needs lie. If you’re passionate about a certain topic or population, see what you can do to help advocate for change there.
Hospitalists around the country are devoting large portions of their spare time to a wide range of advocacy efforts. From health policy to caring for the unhoused population to diversity and equity to advocating for fellow hospitalists, these physicians are passionate about their causes and determined to make a difference.
Championing the unhoused
Sarah Stella, MD, FHM, a hospitalist at Denver Health, was initially drawn there because of the population the hospital serves, which includes a high concentration of people experiencing homelessness. As she cared for her patients, Dr. Stella, who is also associate professor of hospital medicine at the University of Colorado, increasingly felt the desire to help prevent the negative downstream outcomes the hospital sees.
To understand the experiences of the unhoused outside the hospital, Dr. Stella started talking to her patients and people in community-based organizations that serve this population. “I learned a ton,” she said. “Homelessness feels like such an intractable, hopeless thing, but the more I talked to people, the more opportunities I saw to work toward something better.”
This led to a pilot grant to work with the Colorado Coalition for the Homeless to set up a community advisory panel. “My goal was to better understand their experiences and to develop a shared vision for how we collectively can do better,” said Dr. Stella. Eventually, she also received a grant from the University of Colorado, and multiple opportunities have sprung up ever since.
For the past several years, Dr. Stella has worked with Denver Health leadership to improve care for the homeless. “Right now, I’m working with a community team on developing an idea to provide peer support from people with a shared lived experience for people who are experiencing homelessness when they’re hospitalized. That’s really where my passion has been in working on the partnership,” she said.
Her advocacy role has been beneficial in her work as a hospitalist, particularly when COVID began. Dr. Stella again partnered with the Colorado Coalition for the Homeless to start a joint task force. “Everyone on our task force is motivated by this powerful desire to improve the health and lives of this community and that’s one of the silver linings in this pandemic for me,” said Dr. Stella.
Advocacy work has also increased Dr. Stella’s knowledge of what community support options are available for the unhoused. This allows her to educate her patients about their options and how to access them.
While she has colleagues who are able to compartmentalize their work, “I absolutely could not be a hospitalist without being an advocate,” Dr. Stella said. “For me, it has been a protective strategy in terms of burnout because I have to feel like I’m working to advocate for better policies and more appropriate resources to address the gaps that I’m seeing.”
Dr. Stella believes that physicians have a special credibility to advocate, tell stories, and use data to back their stories up. “We have to realize that we have this power, and we have it so we can empower others,” she said. “The people I’ve seen in my community who are working so hard to help people who are experiencing homelessness are the heroes. Understanding that and giving power to those people through our voice and our well-respected place in society drives me.”
Strengthening diversity, equity, and inclusion
In September 2020, Michael Bryant, MD, became the inaugural vice chair of Diversity, Equity, and Inclusion for the department of pediatrics at Children’s Hospital Los Angeles, where he is also the division head of pediatric hospital medicine. “I was motivated to apply for this position because I wanted to be an agent for change to eliminate the institutional racism, social injustice, and marginalization that continues to threaten the lives and well-beings of so many Americans,” Dr. Bryant said.
Between the pandemic, the economic decline it has created, and the divisive political landscape, people of color have been especially affected. “These are poignant examples of the ever-widening divide and disenfranchisement many Americans feel,” said Dr. Bryant. “Gandhi said, ‘Be the change that you want to see,’ and that is what I want to model.”
At work, advocacy for diversity, equality, and inclusion is an innate part of everything he does. From the new physicians he recruits to the candidates he considers for leadership positions, Dr. Bryant strives “to have a workforce that mirrors the diversity of the patients we humbly care for and serve.”
Advocacy is intrinsic to Dr. Bryant’s worldview, in his quest to understand and accept each individual’s uniqueness, his desire “to embrace cultural humility,” his recognition that “our differences enhance us instead of diminishing us,” and his willingness to engage in difficult conversations.
“Advocacy means that I acknowledge that intent does not equal impact and that I must accept that what I do and what I say may have unintended consequences,” he said. “When that happens, I must resist becoming defensive and instead be willing to listen and learn.”
Dr. Bryant is proud of his accomplishments and enjoys his advocacy work. In his workplace, there are few African Americans in leadership roles. This means that he is in high demand when it comes to making sure there’s representation during various processes such as hiring and vetting, a disparity known as the “minority tax.”
“I am thankful for the opportunities, but it does take a toll at times,” Dr. Bryant said, which is yet another reason why he is a proponent of increasing diversity and inclusion. “This allows us to build the resource pool as these needs arise and minimizes the toll of the ‘minority tax’ on any single person or small group of individuals.”
This summer, physicians from Dr. Bryant’s hospital participated in the national “White Coats for Black Lives” effort. He found it to be “an incredibly moving event” that hundreds of his colleagues participated in.
Dr. Bryant’s advice for hospitalists who want to get involved in advocacy efforts is to check out the movie “John Lewis: Good Trouble.” “He was a champion of human rights and fought for these rights until his death,” Dr. Bryant said. “He is a true American hero and a wonderful example.”
Bolstering health care change
Since his residency, Joshua Lenchus, DO, FACP, SFHM, has developed an ever-increasing interest in legislative advocacy, particularly health policy. Getting involved in this arena requires an understanding of civics and government that goes beyond just the basics. “My desire to affect change in my own profession really served as the catalyst to get involved,” said Dr. Lenchus, the regional chief medical officer at Broward Health Medical Center in Fort Lauderdale, Fla. “What better way to do that than by combining what we do on a daily basis in the practice of medicine with this new understanding of how laws are passed and promulgated?”
Dr. Lenchus has been involved with both state and national medical organizations and has served on public policy committees as a member and as a chair. “The charge of these committees is to monitor and navigate position statements and policies that will drive the entire organization,” he said. This means becoming knowledgeable enough about a topic to be able to talk about it eloquently and adding supporting personal or professional illustrations that reinforce the position to lawmakers.
He finds his advocacy efforts “incredibly rewarding” because they contribute to his endeavors “to help my colleagues practice medicine in a safe, efficient, and productive manner.” For instance, some of the organizations Dr. Lenchus was involved with helped make changes to the Affordable Care Act that ended up in its final version, as well as changes after it passed. “There are tangible things that advocacy enables us to do in our daily practice,” he said.
When something his organizations have advocated for does not pass, they know they need to try a different outlet. “You can’t win every fight,” he said. “Every time you go and comment on an issue, you have to understand that you’re there to do your best, and to the extent that the people you’re talking to are willing to listen to what you have to say, that’s where I think you can make the most impact.” When changes he has helped fight for do pass, “it really is amazing that you can tell your colleagues about your role in achieving meaningful change in the profession.”
Dr. Lenchus acknowledges that advocacy “can be all-consuming at times. We have to understand our limits.” That said, he thinks not engaging in advocacy could increase stress and potential burnout. “I think being involved in advocacy efforts really helps people conduct meaningful work and educates them about what it means not just to them, but to the rest of the medical profession and the patients that we serve,” he said.
For hospitalists who are interested in health policy advocacy, there are many ways to get involved, Dr. Lenchus said. You could join an organization (many organized medical societies have public policy committees), participate in advocacy activities, work on a political campaign, or even run for office yourself. “Ultimately, education and some level of involvement really will make the difference in who navigates our future as hospitalists,” he said.
Questioning co-management practices
Though he says he’s in the minority, Hardik Vora, MD, SFHM, medical director for hospital medicine at Riverside Regional Medical Center in Newport News, Va., believes that co-management is going to “make or break hospital medicine. It’s going to have a huge impact on our specialty.”
In the roughly 25-year history of hospital medicine, it has evolved from admitting and caring for patients of primary care physicians to patients of specialists and, more recently, surgical patients. “Now there are (hospital medicine) programs across the country that are pretty much admitting everything,” said Dr. Vora.
As a recruiter for the Riverside Health System for the past eight years, “I have not met a single resident who is trained to do what we’re doing in hospital medicine, because you’re admitting surgical patients all the time and you have primary attending responsibility,” Dr. Vora said. “I see that as a cause of a significant amount of stress because now you’re responsible for something that you don’t have adequate training for.”
In the co-management discussion, Dr. Vora notes that people often bring up the research that shows that the practice has improved surgeon satisfaction. “What bothers me is that…you need to add one more question – how does it affect your hospitalists? And I bet the answer to that question is ‘it has a terrible effect.’”
The expectations surrounding hospitalists these days is a big concern in terms of burnout, Dr. Vora said. “We talk a lot about the drivers of burnout, whether it’s schedule or COVID,” he said. The biggest issue when it comes to burnout, as he sees it, is not COVID; it’s when hospitalists are performing tasks that make them feel they aren’t adding value. “I think that’s a huge topic in hospital medicine right now.”
Dr. Vora believes there should be more discussion and awareness of the potential pitfalls. “Hospitalists should get involved in co-management where they are adding value and certainly not take up the attending responsibility where they’re not adding value and it’s out of the scope of their training and expertise,” he said. “Preventing scope creep and burnout from co-management are some of the key issues I’m really passionate about.”
Dr. Vora said it is important to set realistic goals and remember that it takes time to make change when it comes to advocacy. “You still have to operate within whatever environment is given to you and then you can make change from within,” he said.
His enthusiasm for co-management awareness has led to creating a co-management forum through SHM in his local Hampton Roads chapter. He was also a panelist for an SHM webinar in February 2021 in which the panelists debated co-management.
“I think we really need to look at this as a specialty. Are we going in the right direction?” Dr. Vora asked. “We need to come together as a specialty and make a decision, which is going to be hard because there are competing financial interests and various practice models.”
Improving patient care
Working as a hospitalist at University Medical Center, a safety net hospital in New Orleans, Celeste Newby, MD, PhD, sees plenty of patients who are underinsured or not insured at all. “A lot of my interest in health policy stems from that,” she said.
During her residency, which she finished in 2015, Louisiana became a Medicaid expansion state. This impressed upon Dr. Newby how much Medicaid improved the lives of patients who had previously been uninsured. “We saw procedures getting done that had been put on hold because of financial concerns or medicines that were now affordable that weren’t before,” she said. “It really did make a difference.”
When repeated attempts to repeal the Affordable Care Act began, “it was a call to do health policy work for me personally that just hadn’t come up in the past,” said Dr. Newby, who is also assistant professor of medicine at Tulane University in New Orleans. “I personally found that the best way to do (advocacy work) was to go through medical societies because there is a much stronger voice when you have more people saying the same thing,” she said.
Dr. Newby sits on the Council of Legislation for the Louisiana State Medical Society and participates in the Leadership and Health Policy (LEAHP) Program through the Society of General Internal Medicine.
The LEAHP Program has been instrumental in expanding Dr. Newby’s knowledge of how health policy is made and the mechanisms behind it. It has also taught her “how we can either advise, guide, leverage, or advocate for things that we think would be important for change and moving the country in the right direction in terms of health care.”
Another reason involvement in medical societies is helpful is because, as a busy clinician, it is impossible to keep up with everything. “Working with medical societies, you have people who are more directly involved in the legislature and can give you quicker notice about things that are coming up that are going to be important to you or your co-workers or your patients,” Dr. Newby said.
Dr. Newby feels her advocacy work is an outlet for stress and “a way to work at more of a macro level on problems that I see with my individual patients. It’s a nice compliment.” At the hospital, she can only help one person at a time, but with her advocacy efforts, there’s potential to make changes for many.
“Advocacy now is such a large umbrella that encompasses so many different projects at all kinds of levels,” Dr. Newby said. She suggests looking around your community to see where the needs lie. If you’re passionate about a certain topic or population, see what you can do to help advocate for change there.
The interplay between staffing and scheduling
Top five findings from the 2020 SoHM
The biennial State of Hospital Medicine (SoHM) Report was released in fall 2020, reflecting surveys collected just as the pandemic was ramping up. Thus, a COVID Addendum of results was collected and published a few months later. What did these reports tell us about existing and developing trends in staffing and scheduling?
Here is a top five list of findings for hospital medicine programs (HMGs) serving adults only. These are just highlights; for further detail, visit the SHM website to learn more and purchase your copy. The information in the SoHM is extraordinarily helpful in planning for your group’s future staffing and scheduling needs.
5. Average group size has increased
Andrew White, MD, SFHM, associate professor of medicine at the University of Washington, Seattle, provided a deep-dive discussion on the increase of group sizes in the March 2021 issue of The Hospitalist. Group size has impacted the way a hospitalist group schedules, when reviewing correlating scheduling survey responses.
Group size can have a direct correlation to scheduling methodology. The number of employed/contracted physician hospitalists in individual groups is up about 25%. Alongside the increase in physician hospitalists is an increase in both nurse practitioners (NPs) and physician assistants (PAs) in adult hospitalist groups, with the largest growth in PAs. In fact, in 2020, the average number of NPs and PAs per hospitalist group is approaching similar numbers.
In 2020, more than half of all programs reported not having a backup call system. One could speculate that the larger group size has allowed adult hospitalist groups better ability to staff upper fluctuations in daily volume. This could have resulted in day-to-day scheduling ease and flexibility.
4. Shift-type is shifting
In scheduling adult hospitalist groups, fewer groups reported dedicated nocturnists and more groups reported dedicated day admitters.
Just above a third of all adult hospitalist programs report having dedicated day admitter shifts, and the presence of nocturnists is at a 6-year low. One speculation that could be made is that hospitalists are making more of an effort to ensure that more admissions are done during the day and not held over for nighttime. This would be consistent with the strong pressure for hospitals to decrease door-to-floor admission times. However, the presence of nocturnists increases steadily with group size. Ninety-four percent of HMGs with 30-49 physician FTEs and 98% of groups with 50 or more physician FTEs reported using dedicated nocturnists.
3. COVID-19 impacts hospitalist workflows
It’s not hard to imagine that COVID-19 has affected all hospitalist groups: adult, pediatric, and adult/pediatric groups. COVID-19 has affected all lives – at home and at work – across the world. More than 80% of all adult hospitalist groups report having implemented changes (beyond dedicated COVID-19 teams) in workflows and/or how work is allocated among its providers. And nearly 20% report that this is likely a permanent change.
2. Schedules have been disrupted by COVID-19
More than half of adult hospitalist groups report having their schedules disrupted by COVID-19. The top two disruptors are loss of staff time due to exposure quarantine, and lost provider time due to COVID-19 illness. All the while, adult hospitalist groups have been taking care of more and more hospitalized patients.
While some groups have not made any changes in scheduling due to COVID-19, many have. Nearly 60% of all groups have increased scheduling flexibility or changed their scheduling model. For about 11% of all groups, this change is likely to be permanent.
1. COVID-19 has changed scheduling methodologies – perhaps for the long-term
Three out of four adult hospitalist groups have created new COVID-19 dedicated teams each day. This has likely had one of the most impacts.
Unit-based assignment reported in the 2020 SoHM was already up from the 2018 SoHM Report (42.7% vs 36%). Now, in addition to nocturnists, day admitter, rounder roles, and unit-based assignments, hospital medicine groups must also incorporate COVID-19 teams into daily scheduling considerations. One in five groups report this change may likely be a permanent addition to the hospitalist schedule. Wow.
As we think forward to the 2022 SoHM, staffing and scheduling of adult hospital medicine group will be a key topic of the survey. How does COVID-19 change hospital medicine groups in the medium and long term? One thing is for sure – hospital medicine groups are resilient and have proven to be creative in ensuring our hospitalized patients are well cared for.
Post your thoughts and questions for your peer network on the SHM Online Community: HMX. Let’s keep the conversation going on how we can help each other create sustainable staffing and scheduling models that are continuously adapting to our peripandemic environment.
Ms. Trask is national vice president of the Hospital Medicine Service Line at Catholic Health Initiatives in Englewood, Colo.
Top five findings from the 2020 SoHM
Top five findings from the 2020 SoHM
The biennial State of Hospital Medicine (SoHM) Report was released in fall 2020, reflecting surveys collected just as the pandemic was ramping up. Thus, a COVID Addendum of results was collected and published a few months later. What did these reports tell us about existing and developing trends in staffing and scheduling?
Here is a top five list of findings for hospital medicine programs (HMGs) serving adults only. These are just highlights; for further detail, visit the SHM website to learn more and purchase your copy. The information in the SoHM is extraordinarily helpful in planning for your group’s future staffing and scheduling needs.
5. Average group size has increased
Andrew White, MD, SFHM, associate professor of medicine at the University of Washington, Seattle, provided a deep-dive discussion on the increase of group sizes in the March 2021 issue of The Hospitalist. Group size has impacted the way a hospitalist group schedules, when reviewing correlating scheduling survey responses.
Group size can have a direct correlation to scheduling methodology. The number of employed/contracted physician hospitalists in individual groups is up about 25%. Alongside the increase in physician hospitalists is an increase in both nurse practitioners (NPs) and physician assistants (PAs) in adult hospitalist groups, with the largest growth in PAs. In fact, in 2020, the average number of NPs and PAs per hospitalist group is approaching similar numbers.
In 2020, more than half of all programs reported not having a backup call system. One could speculate that the larger group size has allowed adult hospitalist groups better ability to staff upper fluctuations in daily volume. This could have resulted in day-to-day scheduling ease and flexibility.
4. Shift-type is shifting
In scheduling adult hospitalist groups, fewer groups reported dedicated nocturnists and more groups reported dedicated day admitters.
Just above a third of all adult hospitalist programs report having dedicated day admitter shifts, and the presence of nocturnists is at a 6-year low. One speculation that could be made is that hospitalists are making more of an effort to ensure that more admissions are done during the day and not held over for nighttime. This would be consistent with the strong pressure for hospitals to decrease door-to-floor admission times. However, the presence of nocturnists increases steadily with group size. Ninety-four percent of HMGs with 30-49 physician FTEs and 98% of groups with 50 or more physician FTEs reported using dedicated nocturnists.
3. COVID-19 impacts hospitalist workflows
It’s not hard to imagine that COVID-19 has affected all hospitalist groups: adult, pediatric, and adult/pediatric groups. COVID-19 has affected all lives – at home and at work – across the world. More than 80% of all adult hospitalist groups report having implemented changes (beyond dedicated COVID-19 teams) in workflows and/or how work is allocated among its providers. And nearly 20% report that this is likely a permanent change.
2. Schedules have been disrupted by COVID-19
More than half of adult hospitalist groups report having their schedules disrupted by COVID-19. The top two disruptors are loss of staff time due to exposure quarantine, and lost provider time due to COVID-19 illness. All the while, adult hospitalist groups have been taking care of more and more hospitalized patients.
While some groups have not made any changes in scheduling due to COVID-19, many have. Nearly 60% of all groups have increased scheduling flexibility or changed their scheduling model. For about 11% of all groups, this change is likely to be permanent.
1. COVID-19 has changed scheduling methodologies – perhaps for the long-term
Three out of four adult hospitalist groups have created new COVID-19 dedicated teams each day. This has likely had one of the most impacts.
Unit-based assignment reported in the 2020 SoHM was already up from the 2018 SoHM Report (42.7% vs 36%). Now, in addition to nocturnists, day admitter, rounder roles, and unit-based assignments, hospital medicine groups must also incorporate COVID-19 teams into daily scheduling considerations. One in five groups report this change may likely be a permanent addition to the hospitalist schedule. Wow.
As we think forward to the 2022 SoHM, staffing and scheduling of adult hospital medicine group will be a key topic of the survey. How does COVID-19 change hospital medicine groups in the medium and long term? One thing is for sure – hospital medicine groups are resilient and have proven to be creative in ensuring our hospitalized patients are well cared for.
Post your thoughts and questions for your peer network on the SHM Online Community: HMX. Let’s keep the conversation going on how we can help each other create sustainable staffing and scheduling models that are continuously adapting to our peripandemic environment.
Ms. Trask is national vice president of the Hospital Medicine Service Line at Catholic Health Initiatives in Englewood, Colo.
The biennial State of Hospital Medicine (SoHM) Report was released in fall 2020, reflecting surveys collected just as the pandemic was ramping up. Thus, a COVID Addendum of results was collected and published a few months later. What did these reports tell us about existing and developing trends in staffing and scheduling?
Here is a top five list of findings for hospital medicine programs (HMGs) serving adults only. These are just highlights; for further detail, visit the SHM website to learn more and purchase your copy. The information in the SoHM is extraordinarily helpful in planning for your group’s future staffing and scheduling needs.
5. Average group size has increased
Andrew White, MD, SFHM, associate professor of medicine at the University of Washington, Seattle, provided a deep-dive discussion on the increase of group sizes in the March 2021 issue of The Hospitalist. Group size has impacted the way a hospitalist group schedules, when reviewing correlating scheduling survey responses.
Group size can have a direct correlation to scheduling methodology. The number of employed/contracted physician hospitalists in individual groups is up about 25%. Alongside the increase in physician hospitalists is an increase in both nurse practitioners (NPs) and physician assistants (PAs) in adult hospitalist groups, with the largest growth in PAs. In fact, in 2020, the average number of NPs and PAs per hospitalist group is approaching similar numbers.
In 2020, more than half of all programs reported not having a backup call system. One could speculate that the larger group size has allowed adult hospitalist groups better ability to staff upper fluctuations in daily volume. This could have resulted in day-to-day scheduling ease and flexibility.
4. Shift-type is shifting
In scheduling adult hospitalist groups, fewer groups reported dedicated nocturnists and more groups reported dedicated day admitters.
Just above a third of all adult hospitalist programs report having dedicated day admitter shifts, and the presence of nocturnists is at a 6-year low. One speculation that could be made is that hospitalists are making more of an effort to ensure that more admissions are done during the day and not held over for nighttime. This would be consistent with the strong pressure for hospitals to decrease door-to-floor admission times. However, the presence of nocturnists increases steadily with group size. Ninety-four percent of HMGs with 30-49 physician FTEs and 98% of groups with 50 or more physician FTEs reported using dedicated nocturnists.
3. COVID-19 impacts hospitalist workflows
It’s not hard to imagine that COVID-19 has affected all hospitalist groups: adult, pediatric, and adult/pediatric groups. COVID-19 has affected all lives – at home and at work – across the world. More than 80% of all adult hospitalist groups report having implemented changes (beyond dedicated COVID-19 teams) in workflows and/or how work is allocated among its providers. And nearly 20% report that this is likely a permanent change.
2. Schedules have been disrupted by COVID-19
More than half of adult hospitalist groups report having their schedules disrupted by COVID-19. The top two disruptors are loss of staff time due to exposure quarantine, and lost provider time due to COVID-19 illness. All the while, adult hospitalist groups have been taking care of more and more hospitalized patients.
While some groups have not made any changes in scheduling due to COVID-19, many have. Nearly 60% of all groups have increased scheduling flexibility or changed their scheduling model. For about 11% of all groups, this change is likely to be permanent.
1. COVID-19 has changed scheduling methodologies – perhaps for the long-term
Three out of four adult hospitalist groups have created new COVID-19 dedicated teams each day. This has likely had one of the most impacts.
Unit-based assignment reported in the 2020 SoHM was already up from the 2018 SoHM Report (42.7% vs 36%). Now, in addition to nocturnists, day admitter, rounder roles, and unit-based assignments, hospital medicine groups must also incorporate COVID-19 teams into daily scheduling considerations. One in five groups report this change may likely be a permanent addition to the hospitalist schedule. Wow.
As we think forward to the 2022 SoHM, staffing and scheduling of adult hospital medicine group will be a key topic of the survey. How does COVID-19 change hospital medicine groups in the medium and long term? One thing is for sure – hospital medicine groups are resilient and have proven to be creative in ensuring our hospitalized patients are well cared for.
Post your thoughts and questions for your peer network on the SHM Online Community: HMX. Let’s keep the conversation going on how we can help each other create sustainable staffing and scheduling models that are continuously adapting to our peripandemic environment.
Ms. Trask is national vice president of the Hospital Medicine Service Line at Catholic Health Initiatives in Englewood, Colo.
Disparities and racism in health care
From Anarcha Westcott to George Floyd to the Atlanta massacre
The Atlanta spa massacre, the commencement of the George Floyd trial, and COVID-19 highlight societal inequalities and health disparities among minority groups. We can only hope that we have arrived at the tipping point to address historical institutional racism and structural violence in this country.
Admittedly, we, as health care professionals, have been at best apathetic and at worst complicit with this tragedy. Dr. James Sims, the father of gynecology, perfected his surgical techniques of vaginal fistula on slaves. Starting in 1845, he performed over thirty surgeries without anesthesia on Anarcha Westcott.1 Moreover, the past century was dotted with similar transgressions such as the Tuskegee Untreated Syphilis Experiment from 1932 to 1972, the use of the cells of Henrietta Lack in 1951, and the disproportionate lack of funding of sickle cell research.2 We must move from complicit/apathetic to being part of the discourse and solution.
The juxtaposition of George Floyd’s cry of “I can’t breathe” and the disproportionate way in which COVID-19 has affected Black communities and people of color highlights how deeply entrenched the problem of systemic racism is in this country. The innumerable reported hate crimes against Asian Americans stemming from xenophobia linked to the COVID-19 pandemic and the stereotyping of Hispanic Americans as criminals during the last U.S. administration demonstrate that all minority racial/ethnic groups are affected. As clinicians who care for the health of our communities and strive to reduce suffering, we have a responsibility to identify discrimination that exists in the health care system – ranging from subtle implicit bias to overt discrimination.3
Unconscious bias and its effect on diversity and inclusion has only recently been recognized and addressed in the realm of health care as applied to clinicians. This is key to structural racism as providers inadvertently use unconscious bias every day to make their medical decisions quick and efficient. As Dayna Bowen Matthews points out in her book, “Just Medicine,” “where health and health care are concerned, even when implicit biases are based on seemingly benign distinctions, or supported by apparently rational or widely held observations, these biases can cause grave individual, group, and societal harm that is commensurate to and even exceeds the harm caused by outright racism.” To deny the prejudices that providers have when making decisions for patients will perpetuate the racism and hinder our ability to overcome health inequity. Americans of racial and ethnic minorities have a higher incidence of chronic diseases and premature death when compared to white Americans.4 These disparities exist even when controlling for individual variations such as availability of health insurance, education, and socioeconomic status.5 Social determinants of health because of racial differences is often talked about as a cause of health care inequity, but given the evidence that providers play a much more active role in this, we need to become more comfortable with the discomfort of using the word “racism” if we intend to bring awareness and create change.
In order to tackle structural racism in health care, organizations must take a multifaceted approach. Evidence-based strategies include: creation of an inclusive workforce, diversification of the workforce to better represent patient populations, and education/training on the effect of implicit bias on equitable health care.6 These aspirations can provide a framework for interventions at all levels of health care organizations.
The JEDI (justice, equity, diversity, and inclusion) committee of the section of hospital medicine at Wake Forest Baptist Health System came into existence in November 2019. The objective for JEDI was to use evidence-based methods to help create an environment that would lead to the creation of a diverse and inclusive hospital medicine group. Prior to establishing our committee, we interviewed providers from traditional minority groups who were part of our practice to bring clarity to the discrimination faced by our providers from colleagues, staff, and patients. The discrimination varied from microaggressions caused by implicit biases to macroaggression from overt discrimination. We initiated our work on this burning platform by following the evidence-based methods mentioned earlier.
Creation of an inclusive workforce. Our working committee included members of varied backgrounds and experiences who were passionate about enhancing equity while focusing on inclusion and wellness. The committee brainstormed ideas for interventions that could make a positive impact for our teammates. Individual providers voted to choose the interventions that would positively impact their inclusion and health. Using a validated survey,7 we were able to measure the degree of inclusion of our work group based on multiple demographics including age, gender, race/ethnicity, training (physician vs. APP), etc. Our intention is to complete the proposed interventions before remeasuring inclusion to understand the effect of our work.
Diversifying the workforce. Although our section of hospital medicine at Wake Forest Baptist Health System consists of providers self-identifying as people of color, we do not adequately mirror the racial composition of the population we serve. To achieve the desired result, we have made changes to our recruiting program. The section of hospital medicine visibly demonstrates our commitment to diversity and displays our values on our website. We intend for this to attract diverse individuals who would intend to be part of our group.
Education and training on impact of implicit bias on equitable health care. Implicit bias training will have to consist of actions that would help our clinicians recognize their own prejudices and find means to mitigate them. We have committed to bystander education that would give practice and words to our providers to speak up in situations where they see discrimination in the workplace that is directed against patients, staff, and colleagues. A series of open and honest conversations about racial and gender discrimination in health care that involves inviting accomplished speakers from around the country has been planned. Continued attention to opportunities to further awareness on this subject is vital.
On Jan. 6, 2021, a day that should have filled citizens with pride and hope with the election of the first Black minister and the first Jewish man to the U.S. Senate in a historically conservative state, as well as the confirmation of the election of a president who pledged to address racial disparities, we instead saw another stark reminder of where we came from and just how far we have to go. White supremacists incited by their perceived threat to a legacy of centuries of suppression transformed into a mob of insurrectionists, blatantly bearing Confederate and Nazi flags, and seemingly easily invaded and desecrated the U.S. Capitol. On March 16, 2021, a white male who was “having a bad day” ended the lives of eight individuals, including six Asian Americans.
These instances have brought forth the reality that many of our interventions have been directed towards subtle prejudices and microaggressions alone. We have skirted around calling out overt discrimination of minority groups and failed to openly acknowledge our own contribution to the problem. This newly found awareness has created an opportunity for more impactful work. The equitable delivery of health care is dependent on creating a patient-provider relationship based on trust; addressing overt discrimination respectfully; and overcoming unconscious bias.
While we have made the commitment to confront structural racism in our workplace and taken important steps to work towards this goal with the initiatives set forth by our JEDI committee, we certainly have a long way to go. George Floyd spent the last 8 minutes and 46 seconds of his life struggling to breathe and asking for his mother. Let’s not waste another second and instead be the change that we seek in health care.
Dr. Nagaraj is medical director, Hospital Medicine, at Lexington (N.C.) Medical Center, assistant professor at Wake Forest School of Medicine, and cochair, JEDI committee for diversity and inclusion, hospital medicine, at Wake Forest Baptist Health, Winston-Salem, NC. Ms. Haller is cochair, JEDI committee for diversity and inclusion, hospital medicine, Wake Forest Baptist Health. Dr. Huang is the executive medical director and service line director of general medicine and hospital medicine within the Wake Forest Baptist Health System and associate professor at Wake Forest School of Medicine. The authors would like to acknowledge Dr. Julie Freischlag, Dr. Kevin High, and Dr. David McIntosh at Wake Forest Baptist Health System for the support of the JEDI committee and the section on hospital medicine.
References
1. Holland B. The “father of modern gynecology” performed shocking experiments on enslaved women. History. 2017 Aug 29. www.history.com/news/the-father-of-modern-gynecology-performed-shocking-experiments-on-slaves.
2. Buseh AG et al. Community leaders’ perspectives on engaging African Americans in biobanks and other human genetics initiatives. J Community Genet. 2013 Oct;4(4):483-94. doi: 10.1007/s12687-013-0155-z.
3. National Center for Health Statistics. Health, United States, 2015: With special feature on racial and ethnic health disparities. 2016 May. www.cdc.gov/nchs/data/hus/hus15.pdf.
4. Bailey ZD et al. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017 Apr 8;389(10077):1453-63. doi: 10.1016/S0140-6736(17)30569-X.
5. Arvizo C and Garrison E. Diversity and inclusion: the role of unconscious bias on patient care, health outcomes and the workforce in obstetrics and gynaecology. Curr Opin Obstet Gynecol. 2019 Oct;31(5):356-62. doi: 10.1097/GCO.0000000000000566.
6. Chung BG et al. Work group inclusion: test of a scale and model. Group & Organization Management. 2020;45(1):75-102. doi: 10.1177/1059601119839858.
From Anarcha Westcott to George Floyd to the Atlanta massacre
From Anarcha Westcott to George Floyd to the Atlanta massacre
The Atlanta spa massacre, the commencement of the George Floyd trial, and COVID-19 highlight societal inequalities and health disparities among minority groups. We can only hope that we have arrived at the tipping point to address historical institutional racism and structural violence in this country.
Admittedly, we, as health care professionals, have been at best apathetic and at worst complicit with this tragedy. Dr. James Sims, the father of gynecology, perfected his surgical techniques of vaginal fistula on slaves. Starting in 1845, he performed over thirty surgeries without anesthesia on Anarcha Westcott.1 Moreover, the past century was dotted with similar transgressions such as the Tuskegee Untreated Syphilis Experiment from 1932 to 1972, the use of the cells of Henrietta Lack in 1951, and the disproportionate lack of funding of sickle cell research.2 We must move from complicit/apathetic to being part of the discourse and solution.
The juxtaposition of George Floyd’s cry of “I can’t breathe” and the disproportionate way in which COVID-19 has affected Black communities and people of color highlights how deeply entrenched the problem of systemic racism is in this country. The innumerable reported hate crimes against Asian Americans stemming from xenophobia linked to the COVID-19 pandemic and the stereotyping of Hispanic Americans as criminals during the last U.S. administration demonstrate that all minority racial/ethnic groups are affected. As clinicians who care for the health of our communities and strive to reduce suffering, we have a responsibility to identify discrimination that exists in the health care system – ranging from subtle implicit bias to overt discrimination.3
Unconscious bias and its effect on diversity and inclusion has only recently been recognized and addressed in the realm of health care as applied to clinicians. This is key to structural racism as providers inadvertently use unconscious bias every day to make their medical decisions quick and efficient. As Dayna Bowen Matthews points out in her book, “Just Medicine,” “where health and health care are concerned, even when implicit biases are based on seemingly benign distinctions, or supported by apparently rational or widely held observations, these biases can cause grave individual, group, and societal harm that is commensurate to and even exceeds the harm caused by outright racism.” To deny the prejudices that providers have when making decisions for patients will perpetuate the racism and hinder our ability to overcome health inequity. Americans of racial and ethnic minorities have a higher incidence of chronic diseases and premature death when compared to white Americans.4 These disparities exist even when controlling for individual variations such as availability of health insurance, education, and socioeconomic status.5 Social determinants of health because of racial differences is often talked about as a cause of health care inequity, but given the evidence that providers play a much more active role in this, we need to become more comfortable with the discomfort of using the word “racism” if we intend to bring awareness and create change.
In order to tackle structural racism in health care, organizations must take a multifaceted approach. Evidence-based strategies include: creation of an inclusive workforce, diversification of the workforce to better represent patient populations, and education/training on the effect of implicit bias on equitable health care.6 These aspirations can provide a framework for interventions at all levels of health care organizations.
The JEDI (justice, equity, diversity, and inclusion) committee of the section of hospital medicine at Wake Forest Baptist Health System came into existence in November 2019. The objective for JEDI was to use evidence-based methods to help create an environment that would lead to the creation of a diverse and inclusive hospital medicine group. Prior to establishing our committee, we interviewed providers from traditional minority groups who were part of our practice to bring clarity to the discrimination faced by our providers from colleagues, staff, and patients. The discrimination varied from microaggressions caused by implicit biases to macroaggression from overt discrimination. We initiated our work on this burning platform by following the evidence-based methods mentioned earlier.
Creation of an inclusive workforce. Our working committee included members of varied backgrounds and experiences who were passionate about enhancing equity while focusing on inclusion and wellness. The committee brainstormed ideas for interventions that could make a positive impact for our teammates. Individual providers voted to choose the interventions that would positively impact their inclusion and health. Using a validated survey,7 we were able to measure the degree of inclusion of our work group based on multiple demographics including age, gender, race/ethnicity, training (physician vs. APP), etc. Our intention is to complete the proposed interventions before remeasuring inclusion to understand the effect of our work.
Diversifying the workforce. Although our section of hospital medicine at Wake Forest Baptist Health System consists of providers self-identifying as people of color, we do not adequately mirror the racial composition of the population we serve. To achieve the desired result, we have made changes to our recruiting program. The section of hospital medicine visibly demonstrates our commitment to diversity and displays our values on our website. We intend for this to attract diverse individuals who would intend to be part of our group.
Education and training on impact of implicit bias on equitable health care. Implicit bias training will have to consist of actions that would help our clinicians recognize their own prejudices and find means to mitigate them. We have committed to bystander education that would give practice and words to our providers to speak up in situations where they see discrimination in the workplace that is directed against patients, staff, and colleagues. A series of open and honest conversations about racial and gender discrimination in health care that involves inviting accomplished speakers from around the country has been planned. Continued attention to opportunities to further awareness on this subject is vital.
On Jan. 6, 2021, a day that should have filled citizens with pride and hope with the election of the first Black minister and the first Jewish man to the U.S. Senate in a historically conservative state, as well as the confirmation of the election of a president who pledged to address racial disparities, we instead saw another stark reminder of where we came from and just how far we have to go. White supremacists incited by their perceived threat to a legacy of centuries of suppression transformed into a mob of insurrectionists, blatantly bearing Confederate and Nazi flags, and seemingly easily invaded and desecrated the U.S. Capitol. On March 16, 2021, a white male who was “having a bad day” ended the lives of eight individuals, including six Asian Americans.
These instances have brought forth the reality that many of our interventions have been directed towards subtle prejudices and microaggressions alone. We have skirted around calling out overt discrimination of minority groups and failed to openly acknowledge our own contribution to the problem. This newly found awareness has created an opportunity for more impactful work. The equitable delivery of health care is dependent on creating a patient-provider relationship based on trust; addressing overt discrimination respectfully; and overcoming unconscious bias.
While we have made the commitment to confront structural racism in our workplace and taken important steps to work towards this goal with the initiatives set forth by our JEDI committee, we certainly have a long way to go. George Floyd spent the last 8 minutes and 46 seconds of his life struggling to breathe and asking for his mother. Let’s not waste another second and instead be the change that we seek in health care.
Dr. Nagaraj is medical director, Hospital Medicine, at Lexington (N.C.) Medical Center, assistant professor at Wake Forest School of Medicine, and cochair, JEDI committee for diversity and inclusion, hospital medicine, at Wake Forest Baptist Health, Winston-Salem, NC. Ms. Haller is cochair, JEDI committee for diversity and inclusion, hospital medicine, Wake Forest Baptist Health. Dr. Huang is the executive medical director and service line director of general medicine and hospital medicine within the Wake Forest Baptist Health System and associate professor at Wake Forest School of Medicine. The authors would like to acknowledge Dr. Julie Freischlag, Dr. Kevin High, and Dr. David McIntosh at Wake Forest Baptist Health System for the support of the JEDI committee and the section on hospital medicine.
References
1. Holland B. The “father of modern gynecology” performed shocking experiments on enslaved women. History. 2017 Aug 29. www.history.com/news/the-father-of-modern-gynecology-performed-shocking-experiments-on-slaves.
2. Buseh AG et al. Community leaders’ perspectives on engaging African Americans in biobanks and other human genetics initiatives. J Community Genet. 2013 Oct;4(4):483-94. doi: 10.1007/s12687-013-0155-z.
3. National Center for Health Statistics. Health, United States, 2015: With special feature on racial and ethnic health disparities. 2016 May. www.cdc.gov/nchs/data/hus/hus15.pdf.
4. Bailey ZD et al. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017 Apr 8;389(10077):1453-63. doi: 10.1016/S0140-6736(17)30569-X.
5. Arvizo C and Garrison E. Diversity and inclusion: the role of unconscious bias on patient care, health outcomes and the workforce in obstetrics and gynaecology. Curr Opin Obstet Gynecol. 2019 Oct;31(5):356-62. doi: 10.1097/GCO.0000000000000566.
6. Chung BG et al. Work group inclusion: test of a scale and model. Group & Organization Management. 2020;45(1):75-102. doi: 10.1177/1059601119839858.
The Atlanta spa massacre, the commencement of the George Floyd trial, and COVID-19 highlight societal inequalities and health disparities among minority groups. We can only hope that we have arrived at the tipping point to address historical institutional racism and structural violence in this country.
Admittedly, we, as health care professionals, have been at best apathetic and at worst complicit with this tragedy. Dr. James Sims, the father of gynecology, perfected his surgical techniques of vaginal fistula on slaves. Starting in 1845, he performed over thirty surgeries without anesthesia on Anarcha Westcott.1 Moreover, the past century was dotted with similar transgressions such as the Tuskegee Untreated Syphilis Experiment from 1932 to 1972, the use of the cells of Henrietta Lack in 1951, and the disproportionate lack of funding of sickle cell research.2 We must move from complicit/apathetic to being part of the discourse and solution.
The juxtaposition of George Floyd’s cry of “I can’t breathe” and the disproportionate way in which COVID-19 has affected Black communities and people of color highlights how deeply entrenched the problem of systemic racism is in this country. The innumerable reported hate crimes against Asian Americans stemming from xenophobia linked to the COVID-19 pandemic and the stereotyping of Hispanic Americans as criminals during the last U.S. administration demonstrate that all minority racial/ethnic groups are affected. As clinicians who care for the health of our communities and strive to reduce suffering, we have a responsibility to identify discrimination that exists in the health care system – ranging from subtle implicit bias to overt discrimination.3
Unconscious bias and its effect on diversity and inclusion has only recently been recognized and addressed in the realm of health care as applied to clinicians. This is key to structural racism as providers inadvertently use unconscious bias every day to make their medical decisions quick and efficient. As Dayna Bowen Matthews points out in her book, “Just Medicine,” “where health and health care are concerned, even when implicit biases are based on seemingly benign distinctions, or supported by apparently rational or widely held observations, these biases can cause grave individual, group, and societal harm that is commensurate to and even exceeds the harm caused by outright racism.” To deny the prejudices that providers have when making decisions for patients will perpetuate the racism and hinder our ability to overcome health inequity. Americans of racial and ethnic minorities have a higher incidence of chronic diseases and premature death when compared to white Americans.4 These disparities exist even when controlling for individual variations such as availability of health insurance, education, and socioeconomic status.5 Social determinants of health because of racial differences is often talked about as a cause of health care inequity, but given the evidence that providers play a much more active role in this, we need to become more comfortable with the discomfort of using the word “racism” if we intend to bring awareness and create change.
In order to tackle structural racism in health care, organizations must take a multifaceted approach. Evidence-based strategies include: creation of an inclusive workforce, diversification of the workforce to better represent patient populations, and education/training on the effect of implicit bias on equitable health care.6 These aspirations can provide a framework for interventions at all levels of health care organizations.
The JEDI (justice, equity, diversity, and inclusion) committee of the section of hospital medicine at Wake Forest Baptist Health System came into existence in November 2019. The objective for JEDI was to use evidence-based methods to help create an environment that would lead to the creation of a diverse and inclusive hospital medicine group. Prior to establishing our committee, we interviewed providers from traditional minority groups who were part of our practice to bring clarity to the discrimination faced by our providers from colleagues, staff, and patients. The discrimination varied from microaggressions caused by implicit biases to macroaggression from overt discrimination. We initiated our work on this burning platform by following the evidence-based methods mentioned earlier.
Creation of an inclusive workforce. Our working committee included members of varied backgrounds and experiences who were passionate about enhancing equity while focusing on inclusion and wellness. The committee brainstormed ideas for interventions that could make a positive impact for our teammates. Individual providers voted to choose the interventions that would positively impact their inclusion and health. Using a validated survey,7 we were able to measure the degree of inclusion of our work group based on multiple demographics including age, gender, race/ethnicity, training (physician vs. APP), etc. Our intention is to complete the proposed interventions before remeasuring inclusion to understand the effect of our work.
Diversifying the workforce. Although our section of hospital medicine at Wake Forest Baptist Health System consists of providers self-identifying as people of color, we do not adequately mirror the racial composition of the population we serve. To achieve the desired result, we have made changes to our recruiting program. The section of hospital medicine visibly demonstrates our commitment to diversity and displays our values on our website. We intend for this to attract diverse individuals who would intend to be part of our group.
Education and training on impact of implicit bias on equitable health care. Implicit bias training will have to consist of actions that would help our clinicians recognize their own prejudices and find means to mitigate them. We have committed to bystander education that would give practice and words to our providers to speak up in situations where they see discrimination in the workplace that is directed against patients, staff, and colleagues. A series of open and honest conversations about racial and gender discrimination in health care that involves inviting accomplished speakers from around the country has been planned. Continued attention to opportunities to further awareness on this subject is vital.
On Jan. 6, 2021, a day that should have filled citizens with pride and hope with the election of the first Black minister and the first Jewish man to the U.S. Senate in a historically conservative state, as well as the confirmation of the election of a president who pledged to address racial disparities, we instead saw another stark reminder of where we came from and just how far we have to go. White supremacists incited by their perceived threat to a legacy of centuries of suppression transformed into a mob of insurrectionists, blatantly bearing Confederate and Nazi flags, and seemingly easily invaded and desecrated the U.S. Capitol. On March 16, 2021, a white male who was “having a bad day” ended the lives of eight individuals, including six Asian Americans.
These instances have brought forth the reality that many of our interventions have been directed towards subtle prejudices and microaggressions alone. We have skirted around calling out overt discrimination of minority groups and failed to openly acknowledge our own contribution to the problem. This newly found awareness has created an opportunity for more impactful work. The equitable delivery of health care is dependent on creating a patient-provider relationship based on trust; addressing overt discrimination respectfully; and overcoming unconscious bias.
While we have made the commitment to confront structural racism in our workplace and taken important steps to work towards this goal with the initiatives set forth by our JEDI committee, we certainly have a long way to go. George Floyd spent the last 8 minutes and 46 seconds of his life struggling to breathe and asking for his mother. Let’s not waste another second and instead be the change that we seek in health care.
Dr. Nagaraj is medical director, Hospital Medicine, at Lexington (N.C.) Medical Center, assistant professor at Wake Forest School of Medicine, and cochair, JEDI committee for diversity and inclusion, hospital medicine, at Wake Forest Baptist Health, Winston-Salem, NC. Ms. Haller is cochair, JEDI committee for diversity and inclusion, hospital medicine, Wake Forest Baptist Health. Dr. Huang is the executive medical director and service line director of general medicine and hospital medicine within the Wake Forest Baptist Health System and associate professor at Wake Forest School of Medicine. The authors would like to acknowledge Dr. Julie Freischlag, Dr. Kevin High, and Dr. David McIntosh at Wake Forest Baptist Health System for the support of the JEDI committee and the section on hospital medicine.
References
1. Holland B. The “father of modern gynecology” performed shocking experiments on enslaved women. History. 2017 Aug 29. www.history.com/news/the-father-of-modern-gynecology-performed-shocking-experiments-on-slaves.
2. Buseh AG et al. Community leaders’ perspectives on engaging African Americans in biobanks and other human genetics initiatives. J Community Genet. 2013 Oct;4(4):483-94. doi: 10.1007/s12687-013-0155-z.
3. National Center for Health Statistics. Health, United States, 2015: With special feature on racial and ethnic health disparities. 2016 May. www.cdc.gov/nchs/data/hus/hus15.pdf.
4. Bailey ZD et al. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017 Apr 8;389(10077):1453-63. doi: 10.1016/S0140-6736(17)30569-X.
5. Arvizo C and Garrison E. Diversity and inclusion: the role of unconscious bias on patient care, health outcomes and the workforce in obstetrics and gynaecology. Curr Opin Obstet Gynecol. 2019 Oct;31(5):356-62. doi: 10.1097/GCO.0000000000000566.
6. Chung BG et al. Work group inclusion: test of a scale and model. Group & Organization Management. 2020;45(1):75-102. doi: 10.1177/1059601119839858.
The COVID-19 push to evolve
Has anyone else noticed how slow it has been on your pediatric floors? Well, you are not alone.
The COVID pandemic has had a significant impact on health care volumes, with pediatric volumes decreasing across the nation. A Children’s Hospital Association CEO survey, currently unpublished, noted a 10%-20% decline in inpatient admissions and a 30%-50% decline in pediatric ED visits this past year. Even our usual respiratory surge has been disrupted. The rate of influenza tracked by the CDC is around 1%, compared with the usual seasonal flu baseline national rate of 2.6%. These COVID-related declines have occurred amidst the backdrop of already-decreasing inpatient admissions because of the great work of the pediatric hospital medicine (PHM) community in reducing unnecessary admissions and lengths of stay.
For many hospitals, several factors related to the pandemic have raised significant financial concerns. According to Becker Hospital Review, as of August 2020 over 500 hospitals had furloughed workers. While 26 of those hospitals had brought back workers by December 2020, many did not. Similar financial concerns were noted in a Kaufmann Hall report from January 2021, which showed a median drop of 55% in operating margins. The CARES Act helped reduce some of the detrimental impact on operating margins, but it did not diminish the added burden of personal protective equipment expenses, longer length of stay for COVID patients, and a reimbursement shift to more government payors and uninsured caused by pandemic-forced job losses.
COVID’s impact specific to pediatric hospital medicine has been substantial. A recent unpublished survey by the PHM Economics Research Collaborative (PERC) demonstrated how COVID has affected pediatric hospital medicine programs. Forty-five unique PHM programs from over 21 states responded, with 98% reporting a decrease in pediatric inpatient admissions as well as ED visits. About 11% reported temporary unit closures, while 51% of all programs reported staffing restrictions ranging from hiring freezes to downsizing the number of hospitalists in the group. Salaries decreased in 26% of reporting programs, and 20%-56% described reduced benefits, ranging from less CME/vacation time and stipends to retirement benefits. The three most frequent benefit losses included annual salary increases, educational stipends, and bonuses.
Community hospitals felt the palpable, financial strain of decreasing pediatric admissions well before the pandemic. Hospitals like MedStar Franklin Square Hospital in Baltimore and Harrington Hospital in Southbridge, Mass., had decided to close their pediatrics units before COVID hit. In a 2014 unpublished survey of 349 community PHM (CPHM) programs, 57% of respondents felt that finances and justification for a pediatric program were primary concerns.
Responding to financial stressors is not a novel challenge for CPHM programs. To keep these vital pediatric programs in place despite lower inpatient volumes, those of us in CPHM have learned many lessons over the years on how to adapt. Such adaptations have included diversification in procedures and multifloor coverage in the hospital. Voiding cystourethrogram catheterizations and circumcisions are now more commonly performed by CPHM providers, who may also cover multiple areas of the hospital, including the ED, NICU, and well-newborn nursery. Comanagement of subspecialty or surgical patients is yet another example of such diversification.
Furthermore, the PERC survey showed that some PHM programs temporarily covered pediatric ICUs and step-down units and began doing ED and urgent care coverage as primary providers Most programs reported no change in newborn visits while 16% reported an increase in newborn volume and 14% reported a decrease in newborn volume. My own health system was one of the groups that had an increase in newborn volume. This was caused by community pediatricians who had stopped coming in to see their own newborns. This coverage adjustment has yet to return to baseline and will likely become permanent.
There was a 11% increase from prepandemic baselines (from 9% to 20%) in programs doing telemedicine. Most respondents stated that they will continue to offer telemedicine with an additional 25% of programs considering starting. There was also a slight increase during the pandemic of coverage of mental health units (from 11% to 13%), which may have led 11% of respondents to consider the addition of this service. The survey also noted that about 28% of PHM programs performed circumcisions, frenectomies, and sedation prepandemic, and 14%-18% are considering adding these services.
Overall, the financial stressors are improving, but our need to adapt in PHM is more pressing than ever. The pandemic has given us the push for evolution and some opportunities that did not exist before. One is the use of telemedicine to expand our subspecialty support to community hospitals, as well as to children’s hospitals in areas where subspecialists are in short supply. These telemedicine consults are being reimbursed for the first time, which allows more access to these services.
With the pandemic, many hospitals are moving to single room occupancy models. Construction to add more beds is costly, and unnecessary if we can utilize community hospitals to keep appropriate patients in their home communities. The opportunity to partner with community hospital programs to provide telemedicine support should not be overlooked. This is also an opportunity for academic referral centers to have more open beds for critical care and highly specialized patients.
Another opportunity is to expand scope by changing age limits, as 18% of respondents to the PERC survey reported that they had started to care for adults since the pandemic. The Pediatric Overflow Planning Contingency Response Network (POPCoRN) has been a valuable resource for education on caring for adults, guidance on which patient populations are appropriate, and the resources needed to do this. While caring for older adults, even in their 90s, was a pandemic-related phenomenon, there is an opportunity to see if the age limit we care for should be raised to 21, or even 25, as some CPHM programs had been doing prepandemic.
Along with the expansion of age limits, there are many other areas of opportunity highlighted within the PERC survey. These include expanding coverage within pediatric ICUs, EDs, and urgent care areas, along with coverage of well newborns that were previously covered by community pediatricians. Also, the increase of mental health admissions is another area where PHM programs might expand their services.
While I hope the financial stressors improve, hope is not a plan and therefore we need to think and prepare for what the post-COVID future may look like. Some have predicted a rebound pediatric respiratory surge next year as the masks come off and children return to in-person learning and daycare. This may be true, but we would be foolish not to use lessons from the pandemic as well as the past to consider options in our toolkit to become more financially stable. POPCoRN, as well as the American Academy of Pediatrics’ listserv and subcommittees, have been a source of collaboration and shared knowledge during a time when we have needed to quickly respond to ever-changing information. These networks and information sharing should be leveraged once the dust settles for us to prepare for future challenges.
New innovations may arise as we look at how we address the growing need for mental health services and incorporate new procedures, like point of care ultrasound. As Charles Darwin said: “It is not the strongest of the species that survives nor the most intelligent that survives. It is the one that is most adaptable to change.” It is time for us to evolve.
Dr. Dias is a clinical associate professor of pediatrics at Yale University, New Haven, Conn., in the division of pediatric hospital medicine. She has practiced community pediatric hospital medicine for over 21 years in New Jersey, Pennsylvania, and Connecticut. She is the chair of the Education Working Group for the AAP’s section on hospital medicine’s subcommittee on community hospitalists as well as the cochair of the Community Hospital Operations Group of the POPCoRN network.
Has anyone else noticed how slow it has been on your pediatric floors? Well, you are not alone.
The COVID pandemic has had a significant impact on health care volumes, with pediatric volumes decreasing across the nation. A Children’s Hospital Association CEO survey, currently unpublished, noted a 10%-20% decline in inpatient admissions and a 30%-50% decline in pediatric ED visits this past year. Even our usual respiratory surge has been disrupted. The rate of influenza tracked by the CDC is around 1%, compared with the usual seasonal flu baseline national rate of 2.6%. These COVID-related declines have occurred amidst the backdrop of already-decreasing inpatient admissions because of the great work of the pediatric hospital medicine (PHM) community in reducing unnecessary admissions and lengths of stay.
For many hospitals, several factors related to the pandemic have raised significant financial concerns. According to Becker Hospital Review, as of August 2020 over 500 hospitals had furloughed workers. While 26 of those hospitals had brought back workers by December 2020, many did not. Similar financial concerns were noted in a Kaufmann Hall report from January 2021, which showed a median drop of 55% in operating margins. The CARES Act helped reduce some of the detrimental impact on operating margins, but it did not diminish the added burden of personal protective equipment expenses, longer length of stay for COVID patients, and a reimbursement shift to more government payors and uninsured caused by pandemic-forced job losses.
COVID’s impact specific to pediatric hospital medicine has been substantial. A recent unpublished survey by the PHM Economics Research Collaborative (PERC) demonstrated how COVID has affected pediatric hospital medicine programs. Forty-five unique PHM programs from over 21 states responded, with 98% reporting a decrease in pediatric inpatient admissions as well as ED visits. About 11% reported temporary unit closures, while 51% of all programs reported staffing restrictions ranging from hiring freezes to downsizing the number of hospitalists in the group. Salaries decreased in 26% of reporting programs, and 20%-56% described reduced benefits, ranging from less CME/vacation time and stipends to retirement benefits. The three most frequent benefit losses included annual salary increases, educational stipends, and bonuses.
Community hospitals felt the palpable, financial strain of decreasing pediatric admissions well before the pandemic. Hospitals like MedStar Franklin Square Hospital in Baltimore and Harrington Hospital in Southbridge, Mass., had decided to close their pediatrics units before COVID hit. In a 2014 unpublished survey of 349 community PHM (CPHM) programs, 57% of respondents felt that finances and justification for a pediatric program were primary concerns.
Responding to financial stressors is not a novel challenge for CPHM programs. To keep these vital pediatric programs in place despite lower inpatient volumes, those of us in CPHM have learned many lessons over the years on how to adapt. Such adaptations have included diversification in procedures and multifloor coverage in the hospital. Voiding cystourethrogram catheterizations and circumcisions are now more commonly performed by CPHM providers, who may also cover multiple areas of the hospital, including the ED, NICU, and well-newborn nursery. Comanagement of subspecialty or surgical patients is yet another example of such diversification.
Furthermore, the PERC survey showed that some PHM programs temporarily covered pediatric ICUs and step-down units and began doing ED and urgent care coverage as primary providers Most programs reported no change in newborn visits while 16% reported an increase in newborn volume and 14% reported a decrease in newborn volume. My own health system was one of the groups that had an increase in newborn volume. This was caused by community pediatricians who had stopped coming in to see their own newborns. This coverage adjustment has yet to return to baseline and will likely become permanent.
There was a 11% increase from prepandemic baselines (from 9% to 20%) in programs doing telemedicine. Most respondents stated that they will continue to offer telemedicine with an additional 25% of programs considering starting. There was also a slight increase during the pandemic of coverage of mental health units (from 11% to 13%), which may have led 11% of respondents to consider the addition of this service. The survey also noted that about 28% of PHM programs performed circumcisions, frenectomies, and sedation prepandemic, and 14%-18% are considering adding these services.
Overall, the financial stressors are improving, but our need to adapt in PHM is more pressing than ever. The pandemic has given us the push for evolution and some opportunities that did not exist before. One is the use of telemedicine to expand our subspecialty support to community hospitals, as well as to children’s hospitals in areas where subspecialists are in short supply. These telemedicine consults are being reimbursed for the first time, which allows more access to these services.
With the pandemic, many hospitals are moving to single room occupancy models. Construction to add more beds is costly, and unnecessary if we can utilize community hospitals to keep appropriate patients in their home communities. The opportunity to partner with community hospital programs to provide telemedicine support should not be overlooked. This is also an opportunity for academic referral centers to have more open beds for critical care and highly specialized patients.
Another opportunity is to expand scope by changing age limits, as 18% of respondents to the PERC survey reported that they had started to care for adults since the pandemic. The Pediatric Overflow Planning Contingency Response Network (POPCoRN) has been a valuable resource for education on caring for adults, guidance on which patient populations are appropriate, and the resources needed to do this. While caring for older adults, even in their 90s, was a pandemic-related phenomenon, there is an opportunity to see if the age limit we care for should be raised to 21, or even 25, as some CPHM programs had been doing prepandemic.
Along with the expansion of age limits, there are many other areas of opportunity highlighted within the PERC survey. These include expanding coverage within pediatric ICUs, EDs, and urgent care areas, along with coverage of well newborns that were previously covered by community pediatricians. Also, the increase of mental health admissions is another area where PHM programs might expand their services.
While I hope the financial stressors improve, hope is not a plan and therefore we need to think and prepare for what the post-COVID future may look like. Some have predicted a rebound pediatric respiratory surge next year as the masks come off and children return to in-person learning and daycare. This may be true, but we would be foolish not to use lessons from the pandemic as well as the past to consider options in our toolkit to become more financially stable. POPCoRN, as well as the American Academy of Pediatrics’ listserv and subcommittees, have been a source of collaboration and shared knowledge during a time when we have needed to quickly respond to ever-changing information. These networks and information sharing should be leveraged once the dust settles for us to prepare for future challenges.
New innovations may arise as we look at how we address the growing need for mental health services and incorporate new procedures, like point of care ultrasound. As Charles Darwin said: “It is not the strongest of the species that survives nor the most intelligent that survives. It is the one that is most adaptable to change.” It is time for us to evolve.
Dr. Dias is a clinical associate professor of pediatrics at Yale University, New Haven, Conn., in the division of pediatric hospital medicine. She has practiced community pediatric hospital medicine for over 21 years in New Jersey, Pennsylvania, and Connecticut. She is the chair of the Education Working Group for the AAP’s section on hospital medicine’s subcommittee on community hospitalists as well as the cochair of the Community Hospital Operations Group of the POPCoRN network.
Has anyone else noticed how slow it has been on your pediatric floors? Well, you are not alone.
The COVID pandemic has had a significant impact on health care volumes, with pediatric volumes decreasing across the nation. A Children’s Hospital Association CEO survey, currently unpublished, noted a 10%-20% decline in inpatient admissions and a 30%-50% decline in pediatric ED visits this past year. Even our usual respiratory surge has been disrupted. The rate of influenza tracked by the CDC is around 1%, compared with the usual seasonal flu baseline national rate of 2.6%. These COVID-related declines have occurred amidst the backdrop of already-decreasing inpatient admissions because of the great work of the pediatric hospital medicine (PHM) community in reducing unnecessary admissions and lengths of stay.
For many hospitals, several factors related to the pandemic have raised significant financial concerns. According to Becker Hospital Review, as of August 2020 over 500 hospitals had furloughed workers. While 26 of those hospitals had brought back workers by December 2020, many did not. Similar financial concerns were noted in a Kaufmann Hall report from January 2021, which showed a median drop of 55% in operating margins. The CARES Act helped reduce some of the detrimental impact on operating margins, but it did not diminish the added burden of personal protective equipment expenses, longer length of stay for COVID patients, and a reimbursement shift to more government payors and uninsured caused by pandemic-forced job losses.
COVID’s impact specific to pediatric hospital medicine has been substantial. A recent unpublished survey by the PHM Economics Research Collaborative (PERC) demonstrated how COVID has affected pediatric hospital medicine programs. Forty-five unique PHM programs from over 21 states responded, with 98% reporting a decrease in pediatric inpatient admissions as well as ED visits. About 11% reported temporary unit closures, while 51% of all programs reported staffing restrictions ranging from hiring freezes to downsizing the number of hospitalists in the group. Salaries decreased in 26% of reporting programs, and 20%-56% described reduced benefits, ranging from less CME/vacation time and stipends to retirement benefits. The three most frequent benefit losses included annual salary increases, educational stipends, and bonuses.
Community hospitals felt the palpable, financial strain of decreasing pediatric admissions well before the pandemic. Hospitals like MedStar Franklin Square Hospital in Baltimore and Harrington Hospital in Southbridge, Mass., had decided to close their pediatrics units before COVID hit. In a 2014 unpublished survey of 349 community PHM (CPHM) programs, 57% of respondents felt that finances and justification for a pediatric program were primary concerns.
Responding to financial stressors is not a novel challenge for CPHM programs. To keep these vital pediatric programs in place despite lower inpatient volumes, those of us in CPHM have learned many lessons over the years on how to adapt. Such adaptations have included diversification in procedures and multifloor coverage in the hospital. Voiding cystourethrogram catheterizations and circumcisions are now more commonly performed by CPHM providers, who may also cover multiple areas of the hospital, including the ED, NICU, and well-newborn nursery. Comanagement of subspecialty or surgical patients is yet another example of such diversification.
Furthermore, the PERC survey showed that some PHM programs temporarily covered pediatric ICUs and step-down units and began doing ED and urgent care coverage as primary providers Most programs reported no change in newborn visits while 16% reported an increase in newborn volume and 14% reported a decrease in newborn volume. My own health system was one of the groups that had an increase in newborn volume. This was caused by community pediatricians who had stopped coming in to see their own newborns. This coverage adjustment has yet to return to baseline and will likely become permanent.
There was a 11% increase from prepandemic baselines (from 9% to 20%) in programs doing telemedicine. Most respondents stated that they will continue to offer telemedicine with an additional 25% of programs considering starting. There was also a slight increase during the pandemic of coverage of mental health units (from 11% to 13%), which may have led 11% of respondents to consider the addition of this service. The survey also noted that about 28% of PHM programs performed circumcisions, frenectomies, and sedation prepandemic, and 14%-18% are considering adding these services.
Overall, the financial stressors are improving, but our need to adapt in PHM is more pressing than ever. The pandemic has given us the push for evolution and some opportunities that did not exist before. One is the use of telemedicine to expand our subspecialty support to community hospitals, as well as to children’s hospitals in areas where subspecialists are in short supply. These telemedicine consults are being reimbursed for the first time, which allows more access to these services.
With the pandemic, many hospitals are moving to single room occupancy models. Construction to add more beds is costly, and unnecessary if we can utilize community hospitals to keep appropriate patients in their home communities. The opportunity to partner with community hospital programs to provide telemedicine support should not be overlooked. This is also an opportunity for academic referral centers to have more open beds for critical care and highly specialized patients.
Another opportunity is to expand scope by changing age limits, as 18% of respondents to the PERC survey reported that they had started to care for adults since the pandemic. The Pediatric Overflow Planning Contingency Response Network (POPCoRN) has been a valuable resource for education on caring for adults, guidance on which patient populations are appropriate, and the resources needed to do this. While caring for older adults, even in their 90s, was a pandemic-related phenomenon, there is an opportunity to see if the age limit we care for should be raised to 21, or even 25, as some CPHM programs had been doing prepandemic.
Along with the expansion of age limits, there are many other areas of opportunity highlighted within the PERC survey. These include expanding coverage within pediatric ICUs, EDs, and urgent care areas, along with coverage of well newborns that were previously covered by community pediatricians. Also, the increase of mental health admissions is another area where PHM programs might expand their services.
While I hope the financial stressors improve, hope is not a plan and therefore we need to think and prepare for what the post-COVID future may look like. Some have predicted a rebound pediatric respiratory surge next year as the masks come off and children return to in-person learning and daycare. This may be true, but we would be foolish not to use lessons from the pandemic as well as the past to consider options in our toolkit to become more financially stable. POPCoRN, as well as the American Academy of Pediatrics’ listserv and subcommittees, have been a source of collaboration and shared knowledge during a time when we have needed to quickly respond to ever-changing information. These networks and information sharing should be leveraged once the dust settles for us to prepare for future challenges.
New innovations may arise as we look at how we address the growing need for mental health services and incorporate new procedures, like point of care ultrasound. As Charles Darwin said: “It is not the strongest of the species that survives nor the most intelligent that survives. It is the one that is most adaptable to change.” It is time for us to evolve.
Dr. Dias is a clinical associate professor of pediatrics at Yale University, New Haven, Conn., in the division of pediatric hospital medicine. She has practiced community pediatric hospital medicine for over 21 years in New Jersey, Pennsylvania, and Connecticut. She is the chair of the Education Working Group for the AAP’s section on hospital medicine’s subcommittee on community hospitalists as well as the cochair of the Community Hospital Operations Group of the POPCoRN network.
Hospital medicine around the world
Similar needs, local adaptations
Hospital medicine has evolved rapidly and spread widely across the United States in the past 25 years in response to the health care system’s needs for patient safety, quality, efficiency, and effective coordination of care in the ever-more complex environment of the acute care hospital.
But hospital care can be just as complex in other countries, so it’s not surprising that there’s a lot of interest around the world in the U.S. model of hospital medicine. But adaptations of that model vary across – and within – countries, reflecting local culture, health care systems, payment models, and approaches to medical education.
Other countries have looked to U.S. experts for consultations, to U.S.-trained doctors who might be willing to relocate, and to the Society of Hospital Medicine as an internationally focused source of networking and other resources. Some U.S.-based institutions, led by the Cleveland Clinic, Johns Hopkins Medicine, and Weill-Cornell Medical School, have established teaching outposts in other countries, with opportunities for resident training that prepares future hospitalists on the ground.
SHM CEO Eric E. Howell, MD, MHM, said that he personally has interacted with developing hospital medicine programs in six countries, who called upon him in part because of his past research on managing length of hospital stays. Dr. Howell counts himself among a few dozen U.S. hospitalists who are regularly invited to come and consult or to give talks to established or developing hospitalist programs in other countries. Because of the COVID-19 epidemic, in-person visits to other countries have largely been curtailed, but that has introduced a more virtual world of online meetings.
“I think the interesting thing about the ‘international consultants’ for hospital medicine is that while they come from professionally diverse backgrounds, they are all working to solve remarkably similar problems: How to make health care more affordable and higher quality while staying abreast of up-to-date best practice for physicians,” he said.
“Hospital care is costly no matter where you go. Other countries are also trying to limit expense in ways that don’t compromise the quality of that care,” Dr. Howell said. Also, hospitalized patients are more complex than ever, with increasing severity of illness and comorbidities, which makes having a hospitalist available on site more important.
Dr. Howell hopes to encourage more dialogue with international colleagues. SHM has established collaborations with medical societies in other countries and makes time at its conferences for international hospitalist participants to meet and share their experiences. Hospitalists from 33 countries were represented at SHM’s 2017 conference, and the upcoming virtual SHM Converge, May 3-7, 2021, includes a dedicated international session. SHM chapters have formed in a number of other countries.
Flora Kisuule, MD, MPH, SFHM, director of the Division of Hospital Medicine at Johns Hopkins Bayview Medical Center in Baltimore, said her international hospital medicine work1 started 7 years ago when she was invited to the Middle East to help Aramco, the Saudi Arabian Oil Company, develop a hospital medicine program based on the U.S. model for its employees. This was a joint venture with Johns Hopkins Medicine. “We went there and looked at their processes and made recommendations such as duration of hospitalist shifts and how to expand the footprint of hospital medicine in the hospital,” she said.
Then Dr. Kisuule was asked to help develop a hospital medicine program in Panama, where the drivers for developing hospital medicine were improving quality of care and ensuring patient safety. The biggest barrier has been remuneration and how to pay salaries that will allow doctors to work at only one hospital. In Panama, doctors typically work at multiple hospitals or clinics so they can earn enough to make ends meet.
The need for professional identity
Arpana Vidyarthi, MD, “grew up” professionally in hospital medicine at the University of California, San Francisco, a pioneering institution for hospital medicine, and in SHM. “We used to say: If you’ve seen one hospital medicine group, you’ve seen one hospital medicine group,” she said.
Dr. Vidyarthi went to Singapore in 2011, taking a job as a hospitalist at Singapore General Hospital and the affiliated Duke–National University Medical School, eventually directing the Division of Advanced Internal Medicine (general and hospital medicine) at the National University Health System, before moving back to UCSF in 2020.
“Professional identity is one of the biggest benefits hospital medicine can bestow in Singapore and across Asia, where general medicine is underdeveloped. Just as it did 20 years ago in the U.S., that professional identity offers a road map to achieving competency in practicing medicine in the hospital setting,” Dr. Vidyarthi said.
At UCSF, the professional identity of a hospitalist is broad but defined. The research agenda, quality, safety, and educational competencies are specific, seen through a system lens, she added. “We take pride in that professional identify. This is an opportunity for countries where general medicine is underdeveloped and undervalued.”
But the term hospital medicine – or the American model – isn’t always welcomed by health care systems in other countries, Dr Vidyarthi said. “The label of 'hospital medicine' brings people together in professional identify, and that professional identity opens doors. But for it to have legs in other countries, those skills need to be of value to the local system. It needs to make sense, as it did in the United States, and to add value for the identified gaps that need to be filled.”
In Singapore, the health care system turned to the model of acute medical units (AMUs) and the acute medicine physician specialty developed in the United Kingdom, which created a new way of delivering care, a new geography of care, and new set of competencies around which to build training and certification.
AMUs manage the majority of acute medical patients who present to the emergency department and get admitted, with initial treatment for a maximum of 72 hours. Acute physicians, trained in the specialty of assessment, diagnosis, and treatment of adult patients with urgent medical needs, work in a unit situated between the emergency department entrance and the specialty care units. This specialty has been recognized since 2009.2
“Acute medicine is the standard care model in the UK and is now found in all government hospitals in Singapore. This model is being adapted across Europe, Asia, and the Pacific Islands,” Dr. Vidyarthi said. “Advantages include the specific geography of the unit, and outcomes that are value-added to these systems such as decreased use of hospital beds in areas with very high bed occupancy rates.”
In many locales, a variety of titles are used to describe doctors who are not hospitalists as we understand them but whose work is based in the hospital, including house officer, duty officer, junior officer, registrar, or general practitioner. Often these hospital-based doctors, who may in fact be residents or nongraduated trainees, lack the training and the scope of practice of a hospitalist. Because they typically need to consult the supervising physician before making inpatient management decisions, they aren’t able to provide the timely response to the patient’s changing medical condition that is needed to manage today’s acute patients.
Defining the fee schedule
In South Korea, a hospitalist model has emerged since 2015 in response to the insufficient number of hospital-based physicians needed to cover all admitted patients and to address related issues of patient safety, health care quality, and limitations on total hours per week medical residents are allowed to work.
South Korea in 1989 adopted a universal National Health Insurance System (NHIS), which took 12 years to implement. But inadequate coverage for medical work in the hospital has deterred physicians from choosing to work there. South Korea had longer lengths of hospital stay, fewer practicing physicians per 1,000 patients, and a much higher number of hospital patients per practicing physician than other countries in the Organization for Economic Cooperation and Development, according to a new study in the Journal of Hospital Medicine detailing hospitalist development in South Korea.3
A council representing leading medical associations was formed to develop a South Korean hospitalist system and charged by the Ministry of Health with designing an official proposal for implementing it. A pilot study focused on quality and on defining a fee schedule for hospital work was tested in four hospitals, and then a second phase in 31 of South Korea’s 344 general hospitals tested the proposed fee schedule, said Wonjeong Chae, MPH, the first named author on the study, based in the Department of Public Health in the College of Medicine at Yonsei University in Seoul. “But we’re still working on making the fee schedule better,” she said.
Ms. Chae estimates that there are about 250 working hospitalists in South Korea today, which leaves a lot of gaps in practice. “We did learn from America, but we have a different system, so the American concept had to be adapted. Hospital medicine is still growing in Korea despite the impact of the pandemic. We are at the beginning stages of development, but we expect it will grow more with government support.”
In Brazil, a handful of hospital medicine pioneers such as Guilherme Barcellos, MD, SFHM, in Porto Alegre have tried to grow the hospitalist model, networking with colleagues across Latin America through the Pan American Society of Hospitalists and the Brazilian chapter of SHM.
Individual hospitals have developed hospitalist programs, but there is no national model to lead the way. Frequent turnover for the Minister of Health position has made it harder to develop consistent national policy, and the country is largely still in the early stages of developing hospital medicine, depending on isolated initiatives, as Dr. Barcellos described it in a November 2015 article in The Hospitalist.4 Growth is slow but continuing, with new programs such as the one led by Reginaldo Filho, MD at Hospital São Vicente in Curitiba standing out in the confrontation against COVID-19, Dr. Barcellos said.
What can we learn from others?
India-born, U.S.-trained hospitalist Anand Kartha, MD, MS, SFHM, currently heads the Hospital Medicine Program at Hamad General Hospital in Doha, Qatar. He moved from Boston to this small nation on the Arabian Peninsula in 2014. Under the leadership of the hospital’s Department of Medicine, this program was developed to address difficulties such as scheduling, transitions of care, and networking with home care and other providers – the same issues seen in hospitals around the world.
These are not novel problems, Dr. Kartha said, but all of them have a common solution in evidence-based practice. “As hospitalists, our key is to collaborate with everyone in the hospital, using the multidisciplinary approach that is a unique feature of hospital medicine.”
The model has continued to spread across hospitals in Qatar, including academic and community programs. “We now have a full-fledged academic hospitalist system, which collaborates with community hospitals and community programs including a women’s hospital and an oncologic hospital,” he said. “Now the focus is on expanding resource capacity and the internal pipeline for hospitalists. I am getting graduates from Weill Cornell Medicine in Qatar.” Another key collaborator has been the Boston-based Institute for Healthcare Improvement, helping to develop best practices in Qatar and sponsoring the annual Middle East Forum on Quality and Safety in Health Care.
The residency training program at Hamad General is accredited by ACGME, with the same expected competencies as in the U.S. “We don’t use the term ‘hospitalist,’ ” Dr. Kartha said. “It’s better to focus on the model of care – which clearly was American. That model has encountered some resistance in some countries – on many of the same grounds U.S. hospitalists faced 20 years ago. You have to be sensitive to local culture. For hospitalists to succeed internationally, they have to possess a high degree of cultural intelligence.” There’s no shortage of issues such as language barriers, he said. “But that’s no different than at Boston Medical Center.”
SHM’s Middle East Chapter was off to a great start and then was slowed down by regional politics and COVID-19, but is looking forward to a great reboot in 2021, Dr. Kartha said. The pandemic also has been an opportunity to show how hospital medicine is the backbone of the hospital’s ability to respond, although of course many other professionals also pitched in.
Other countries around the world have learned a lot from the American model of hospital medicine. But sources for this article wonder if U.S. hospitalists, in turn, could learn from their adaptations and innovations.
“We can all learn better how to practice our field of medicine in the hospital with less resource utilization,” Dr. Vidyarthi concluded. “So many innovations are happening around us. If we open our eyes to our global colleagues and infuse some of their ideas, it could be wonderful for hospital professionals in the United States.”
References
1. Kisuule F, Howell E. Hospital medicine beyond the United States. Int J Gen Med. 2018;11:65-71. doi: 10.2147/IJGM.S151275.
2. Stosic J et al. The acute physician: The future of acute hospital care in the UK. Clin Med (Lond). 2010 Apr; 10(2):145-7. doi: 10.7861/clinmedicine.10-2-145.
3. Yan Y et al. Adoption of Hospitalist Care in Asia: Experiences From Singapore, Taiwan, Korea, and Japan. J Hosp Med. Published Online First 2021 June 11. doi: 10.12788/jhm.3621.
4. Beresford L. Hospital medicine flourishing around the world. The Hospitalist. Nov 2015.
Similar needs, local adaptations
Similar needs, local adaptations
Hospital medicine has evolved rapidly and spread widely across the United States in the past 25 years in response to the health care system’s needs for patient safety, quality, efficiency, and effective coordination of care in the ever-more complex environment of the acute care hospital.
But hospital care can be just as complex in other countries, so it’s not surprising that there’s a lot of interest around the world in the U.S. model of hospital medicine. But adaptations of that model vary across – and within – countries, reflecting local culture, health care systems, payment models, and approaches to medical education.
Other countries have looked to U.S. experts for consultations, to U.S.-trained doctors who might be willing to relocate, and to the Society of Hospital Medicine as an internationally focused source of networking and other resources. Some U.S.-based institutions, led by the Cleveland Clinic, Johns Hopkins Medicine, and Weill-Cornell Medical School, have established teaching outposts in other countries, with opportunities for resident training that prepares future hospitalists on the ground.
SHM CEO Eric E. Howell, MD, MHM, said that he personally has interacted with developing hospital medicine programs in six countries, who called upon him in part because of his past research on managing length of hospital stays. Dr. Howell counts himself among a few dozen U.S. hospitalists who are regularly invited to come and consult or to give talks to established or developing hospitalist programs in other countries. Because of the COVID-19 epidemic, in-person visits to other countries have largely been curtailed, but that has introduced a more virtual world of online meetings.
“I think the interesting thing about the ‘international consultants’ for hospital medicine is that while they come from professionally diverse backgrounds, they are all working to solve remarkably similar problems: How to make health care more affordable and higher quality while staying abreast of up-to-date best practice for physicians,” he said.
“Hospital care is costly no matter where you go. Other countries are also trying to limit expense in ways that don’t compromise the quality of that care,” Dr. Howell said. Also, hospitalized patients are more complex than ever, with increasing severity of illness and comorbidities, which makes having a hospitalist available on site more important.
Dr. Howell hopes to encourage more dialogue with international colleagues. SHM has established collaborations with medical societies in other countries and makes time at its conferences for international hospitalist participants to meet and share their experiences. Hospitalists from 33 countries were represented at SHM’s 2017 conference, and the upcoming virtual SHM Converge, May 3-7, 2021, includes a dedicated international session. SHM chapters have formed in a number of other countries.
Flora Kisuule, MD, MPH, SFHM, director of the Division of Hospital Medicine at Johns Hopkins Bayview Medical Center in Baltimore, said her international hospital medicine work1 started 7 years ago when she was invited to the Middle East to help Aramco, the Saudi Arabian Oil Company, develop a hospital medicine program based on the U.S. model for its employees. This was a joint venture with Johns Hopkins Medicine. “We went there and looked at their processes and made recommendations such as duration of hospitalist shifts and how to expand the footprint of hospital medicine in the hospital,” she said.
Then Dr. Kisuule was asked to help develop a hospital medicine program in Panama, where the drivers for developing hospital medicine were improving quality of care and ensuring patient safety. The biggest barrier has been remuneration and how to pay salaries that will allow doctors to work at only one hospital. In Panama, doctors typically work at multiple hospitals or clinics so they can earn enough to make ends meet.
The need for professional identity
Arpana Vidyarthi, MD, “grew up” professionally in hospital medicine at the University of California, San Francisco, a pioneering institution for hospital medicine, and in SHM. “We used to say: If you’ve seen one hospital medicine group, you’ve seen one hospital medicine group,” she said.
Dr. Vidyarthi went to Singapore in 2011, taking a job as a hospitalist at Singapore General Hospital and the affiliated Duke–National University Medical School, eventually directing the Division of Advanced Internal Medicine (general and hospital medicine) at the National University Health System, before moving back to UCSF in 2020.
“Professional identity is one of the biggest benefits hospital medicine can bestow in Singapore and across Asia, where general medicine is underdeveloped. Just as it did 20 years ago in the U.S., that professional identity offers a road map to achieving competency in practicing medicine in the hospital setting,” Dr. Vidyarthi said.
At UCSF, the professional identity of a hospitalist is broad but defined. The research agenda, quality, safety, and educational competencies are specific, seen through a system lens, she added. “We take pride in that professional identify. This is an opportunity for countries where general medicine is underdeveloped and undervalued.”
But the term hospital medicine – or the American model – isn’t always welcomed by health care systems in other countries, Dr Vidyarthi said. “The label of 'hospital medicine' brings people together in professional identify, and that professional identity opens doors. But for it to have legs in other countries, those skills need to be of value to the local system. It needs to make sense, as it did in the United States, and to add value for the identified gaps that need to be filled.”
In Singapore, the health care system turned to the model of acute medical units (AMUs) and the acute medicine physician specialty developed in the United Kingdom, which created a new way of delivering care, a new geography of care, and new set of competencies around which to build training and certification.
AMUs manage the majority of acute medical patients who present to the emergency department and get admitted, with initial treatment for a maximum of 72 hours. Acute physicians, trained in the specialty of assessment, diagnosis, and treatment of adult patients with urgent medical needs, work in a unit situated between the emergency department entrance and the specialty care units. This specialty has been recognized since 2009.2
“Acute medicine is the standard care model in the UK and is now found in all government hospitals in Singapore. This model is being adapted across Europe, Asia, and the Pacific Islands,” Dr. Vidyarthi said. “Advantages include the specific geography of the unit, and outcomes that are value-added to these systems such as decreased use of hospital beds in areas with very high bed occupancy rates.”
In many locales, a variety of titles are used to describe doctors who are not hospitalists as we understand them but whose work is based in the hospital, including house officer, duty officer, junior officer, registrar, or general practitioner. Often these hospital-based doctors, who may in fact be residents or nongraduated trainees, lack the training and the scope of practice of a hospitalist. Because they typically need to consult the supervising physician before making inpatient management decisions, they aren’t able to provide the timely response to the patient’s changing medical condition that is needed to manage today’s acute patients.
Defining the fee schedule
In South Korea, a hospitalist model has emerged since 2015 in response to the insufficient number of hospital-based physicians needed to cover all admitted patients and to address related issues of patient safety, health care quality, and limitations on total hours per week medical residents are allowed to work.
South Korea in 1989 adopted a universal National Health Insurance System (NHIS), which took 12 years to implement. But inadequate coverage for medical work in the hospital has deterred physicians from choosing to work there. South Korea had longer lengths of hospital stay, fewer practicing physicians per 1,000 patients, and a much higher number of hospital patients per practicing physician than other countries in the Organization for Economic Cooperation and Development, according to a new study in the Journal of Hospital Medicine detailing hospitalist development in South Korea.3
A council representing leading medical associations was formed to develop a South Korean hospitalist system and charged by the Ministry of Health with designing an official proposal for implementing it. A pilot study focused on quality and on defining a fee schedule for hospital work was tested in four hospitals, and then a second phase in 31 of South Korea’s 344 general hospitals tested the proposed fee schedule, said Wonjeong Chae, MPH, the first named author on the study, based in the Department of Public Health in the College of Medicine at Yonsei University in Seoul. “But we’re still working on making the fee schedule better,” she said.
Ms. Chae estimates that there are about 250 working hospitalists in South Korea today, which leaves a lot of gaps in practice. “We did learn from America, but we have a different system, so the American concept had to be adapted. Hospital medicine is still growing in Korea despite the impact of the pandemic. We are at the beginning stages of development, but we expect it will grow more with government support.”
In Brazil, a handful of hospital medicine pioneers such as Guilherme Barcellos, MD, SFHM, in Porto Alegre have tried to grow the hospitalist model, networking with colleagues across Latin America through the Pan American Society of Hospitalists and the Brazilian chapter of SHM.
Individual hospitals have developed hospitalist programs, but there is no national model to lead the way. Frequent turnover for the Minister of Health position has made it harder to develop consistent national policy, and the country is largely still in the early stages of developing hospital medicine, depending on isolated initiatives, as Dr. Barcellos described it in a November 2015 article in The Hospitalist.4 Growth is slow but continuing, with new programs such as the one led by Reginaldo Filho, MD at Hospital São Vicente in Curitiba standing out in the confrontation against COVID-19, Dr. Barcellos said.
What can we learn from others?
India-born, U.S.-trained hospitalist Anand Kartha, MD, MS, SFHM, currently heads the Hospital Medicine Program at Hamad General Hospital in Doha, Qatar. He moved from Boston to this small nation on the Arabian Peninsula in 2014. Under the leadership of the hospital’s Department of Medicine, this program was developed to address difficulties such as scheduling, transitions of care, and networking with home care and other providers – the same issues seen in hospitals around the world.
These are not novel problems, Dr. Kartha said, but all of them have a common solution in evidence-based practice. “As hospitalists, our key is to collaborate with everyone in the hospital, using the multidisciplinary approach that is a unique feature of hospital medicine.”
The model has continued to spread across hospitals in Qatar, including academic and community programs. “We now have a full-fledged academic hospitalist system, which collaborates with community hospitals and community programs including a women’s hospital and an oncologic hospital,” he said. “Now the focus is on expanding resource capacity and the internal pipeline for hospitalists. I am getting graduates from Weill Cornell Medicine in Qatar.” Another key collaborator has been the Boston-based Institute for Healthcare Improvement, helping to develop best practices in Qatar and sponsoring the annual Middle East Forum on Quality and Safety in Health Care.
The residency training program at Hamad General is accredited by ACGME, with the same expected competencies as in the U.S. “We don’t use the term ‘hospitalist,’ ” Dr. Kartha said. “It’s better to focus on the model of care – which clearly was American. That model has encountered some resistance in some countries – on many of the same grounds U.S. hospitalists faced 20 years ago. You have to be sensitive to local culture. For hospitalists to succeed internationally, they have to possess a high degree of cultural intelligence.” There’s no shortage of issues such as language barriers, he said. “But that’s no different than at Boston Medical Center.”
SHM’s Middle East Chapter was off to a great start and then was slowed down by regional politics and COVID-19, but is looking forward to a great reboot in 2021, Dr. Kartha said. The pandemic also has been an opportunity to show how hospital medicine is the backbone of the hospital’s ability to respond, although of course many other professionals also pitched in.
Other countries around the world have learned a lot from the American model of hospital medicine. But sources for this article wonder if U.S. hospitalists, in turn, could learn from their adaptations and innovations.
“We can all learn better how to practice our field of medicine in the hospital with less resource utilization,” Dr. Vidyarthi concluded. “So many innovations are happening around us. If we open our eyes to our global colleagues and infuse some of their ideas, it could be wonderful for hospital professionals in the United States.”
References
1. Kisuule F, Howell E. Hospital medicine beyond the United States. Int J Gen Med. 2018;11:65-71. doi: 10.2147/IJGM.S151275.
2. Stosic J et al. The acute physician: The future of acute hospital care in the UK. Clin Med (Lond). 2010 Apr; 10(2):145-7. doi: 10.7861/clinmedicine.10-2-145.
3. Yan Y et al. Adoption of Hospitalist Care in Asia: Experiences From Singapore, Taiwan, Korea, and Japan. J Hosp Med. Published Online First 2021 June 11. doi: 10.12788/jhm.3621.
4. Beresford L. Hospital medicine flourishing around the world. The Hospitalist. Nov 2015.
Hospital medicine has evolved rapidly and spread widely across the United States in the past 25 years in response to the health care system’s needs for patient safety, quality, efficiency, and effective coordination of care in the ever-more complex environment of the acute care hospital.
But hospital care can be just as complex in other countries, so it’s not surprising that there’s a lot of interest around the world in the U.S. model of hospital medicine. But adaptations of that model vary across – and within – countries, reflecting local culture, health care systems, payment models, and approaches to medical education.
Other countries have looked to U.S. experts for consultations, to U.S.-trained doctors who might be willing to relocate, and to the Society of Hospital Medicine as an internationally focused source of networking and other resources. Some U.S.-based institutions, led by the Cleveland Clinic, Johns Hopkins Medicine, and Weill-Cornell Medical School, have established teaching outposts in other countries, with opportunities for resident training that prepares future hospitalists on the ground.
SHM CEO Eric E. Howell, MD, MHM, said that he personally has interacted with developing hospital medicine programs in six countries, who called upon him in part because of his past research on managing length of hospital stays. Dr. Howell counts himself among a few dozen U.S. hospitalists who are regularly invited to come and consult or to give talks to established or developing hospitalist programs in other countries. Because of the COVID-19 epidemic, in-person visits to other countries have largely been curtailed, but that has introduced a more virtual world of online meetings.
“I think the interesting thing about the ‘international consultants’ for hospital medicine is that while they come from professionally diverse backgrounds, they are all working to solve remarkably similar problems: How to make health care more affordable and higher quality while staying abreast of up-to-date best practice for physicians,” he said.
“Hospital care is costly no matter where you go. Other countries are also trying to limit expense in ways that don’t compromise the quality of that care,” Dr. Howell said. Also, hospitalized patients are more complex than ever, with increasing severity of illness and comorbidities, which makes having a hospitalist available on site more important.
Dr. Howell hopes to encourage more dialogue with international colleagues. SHM has established collaborations with medical societies in other countries and makes time at its conferences for international hospitalist participants to meet and share their experiences. Hospitalists from 33 countries were represented at SHM’s 2017 conference, and the upcoming virtual SHM Converge, May 3-7, 2021, includes a dedicated international session. SHM chapters have formed in a number of other countries.
Flora Kisuule, MD, MPH, SFHM, director of the Division of Hospital Medicine at Johns Hopkins Bayview Medical Center in Baltimore, said her international hospital medicine work1 started 7 years ago when she was invited to the Middle East to help Aramco, the Saudi Arabian Oil Company, develop a hospital medicine program based on the U.S. model for its employees. This was a joint venture with Johns Hopkins Medicine. “We went there and looked at their processes and made recommendations such as duration of hospitalist shifts and how to expand the footprint of hospital medicine in the hospital,” she said.
Then Dr. Kisuule was asked to help develop a hospital medicine program in Panama, where the drivers for developing hospital medicine were improving quality of care and ensuring patient safety. The biggest barrier has been remuneration and how to pay salaries that will allow doctors to work at only one hospital. In Panama, doctors typically work at multiple hospitals or clinics so they can earn enough to make ends meet.
The need for professional identity
Arpana Vidyarthi, MD, “grew up” professionally in hospital medicine at the University of California, San Francisco, a pioneering institution for hospital medicine, and in SHM. “We used to say: If you’ve seen one hospital medicine group, you’ve seen one hospital medicine group,” she said.
Dr. Vidyarthi went to Singapore in 2011, taking a job as a hospitalist at Singapore General Hospital and the affiliated Duke–National University Medical School, eventually directing the Division of Advanced Internal Medicine (general and hospital medicine) at the National University Health System, before moving back to UCSF in 2020.
“Professional identity is one of the biggest benefits hospital medicine can bestow in Singapore and across Asia, where general medicine is underdeveloped. Just as it did 20 years ago in the U.S., that professional identity offers a road map to achieving competency in practicing medicine in the hospital setting,” Dr. Vidyarthi said.
At UCSF, the professional identity of a hospitalist is broad but defined. The research agenda, quality, safety, and educational competencies are specific, seen through a system lens, she added. “We take pride in that professional identify. This is an opportunity for countries where general medicine is underdeveloped and undervalued.”
But the term hospital medicine – or the American model – isn’t always welcomed by health care systems in other countries, Dr Vidyarthi said. “The label of 'hospital medicine' brings people together in professional identify, and that professional identity opens doors. But for it to have legs in other countries, those skills need to be of value to the local system. It needs to make sense, as it did in the United States, and to add value for the identified gaps that need to be filled.”
In Singapore, the health care system turned to the model of acute medical units (AMUs) and the acute medicine physician specialty developed in the United Kingdom, which created a new way of delivering care, a new geography of care, and new set of competencies around which to build training and certification.
AMUs manage the majority of acute medical patients who present to the emergency department and get admitted, with initial treatment for a maximum of 72 hours. Acute physicians, trained in the specialty of assessment, diagnosis, and treatment of adult patients with urgent medical needs, work in a unit situated between the emergency department entrance and the specialty care units. This specialty has been recognized since 2009.2
“Acute medicine is the standard care model in the UK and is now found in all government hospitals in Singapore. This model is being adapted across Europe, Asia, and the Pacific Islands,” Dr. Vidyarthi said. “Advantages include the specific geography of the unit, and outcomes that are value-added to these systems such as decreased use of hospital beds in areas with very high bed occupancy rates.”
In many locales, a variety of titles are used to describe doctors who are not hospitalists as we understand them but whose work is based in the hospital, including house officer, duty officer, junior officer, registrar, or general practitioner. Often these hospital-based doctors, who may in fact be residents or nongraduated trainees, lack the training and the scope of practice of a hospitalist. Because they typically need to consult the supervising physician before making inpatient management decisions, they aren’t able to provide the timely response to the patient’s changing medical condition that is needed to manage today’s acute patients.
Defining the fee schedule
In South Korea, a hospitalist model has emerged since 2015 in response to the insufficient number of hospital-based physicians needed to cover all admitted patients and to address related issues of patient safety, health care quality, and limitations on total hours per week medical residents are allowed to work.
South Korea in 1989 adopted a universal National Health Insurance System (NHIS), which took 12 years to implement. But inadequate coverage for medical work in the hospital has deterred physicians from choosing to work there. South Korea had longer lengths of hospital stay, fewer practicing physicians per 1,000 patients, and a much higher number of hospital patients per practicing physician than other countries in the Organization for Economic Cooperation and Development, according to a new study in the Journal of Hospital Medicine detailing hospitalist development in South Korea.3
A council representing leading medical associations was formed to develop a South Korean hospitalist system and charged by the Ministry of Health with designing an official proposal for implementing it. A pilot study focused on quality and on defining a fee schedule for hospital work was tested in four hospitals, and then a second phase in 31 of South Korea’s 344 general hospitals tested the proposed fee schedule, said Wonjeong Chae, MPH, the first named author on the study, based in the Department of Public Health in the College of Medicine at Yonsei University in Seoul. “But we’re still working on making the fee schedule better,” she said.
Ms. Chae estimates that there are about 250 working hospitalists in South Korea today, which leaves a lot of gaps in practice. “We did learn from America, but we have a different system, so the American concept had to be adapted. Hospital medicine is still growing in Korea despite the impact of the pandemic. We are at the beginning stages of development, but we expect it will grow more with government support.”
In Brazil, a handful of hospital medicine pioneers such as Guilherme Barcellos, MD, SFHM, in Porto Alegre have tried to grow the hospitalist model, networking with colleagues across Latin America through the Pan American Society of Hospitalists and the Brazilian chapter of SHM.
Individual hospitals have developed hospitalist programs, but there is no national model to lead the way. Frequent turnover for the Minister of Health position has made it harder to develop consistent national policy, and the country is largely still in the early stages of developing hospital medicine, depending on isolated initiatives, as Dr. Barcellos described it in a November 2015 article in The Hospitalist.4 Growth is slow but continuing, with new programs such as the one led by Reginaldo Filho, MD at Hospital São Vicente in Curitiba standing out in the confrontation against COVID-19, Dr. Barcellos said.
What can we learn from others?
India-born, U.S.-trained hospitalist Anand Kartha, MD, MS, SFHM, currently heads the Hospital Medicine Program at Hamad General Hospital in Doha, Qatar. He moved from Boston to this small nation on the Arabian Peninsula in 2014. Under the leadership of the hospital’s Department of Medicine, this program was developed to address difficulties such as scheduling, transitions of care, and networking with home care and other providers – the same issues seen in hospitals around the world.
These are not novel problems, Dr. Kartha said, but all of them have a common solution in evidence-based practice. “As hospitalists, our key is to collaborate with everyone in the hospital, using the multidisciplinary approach that is a unique feature of hospital medicine.”
The model has continued to spread across hospitals in Qatar, including academic and community programs. “We now have a full-fledged academic hospitalist system, which collaborates with community hospitals and community programs including a women’s hospital and an oncologic hospital,” he said. “Now the focus is on expanding resource capacity and the internal pipeline for hospitalists. I am getting graduates from Weill Cornell Medicine in Qatar.” Another key collaborator has been the Boston-based Institute for Healthcare Improvement, helping to develop best practices in Qatar and sponsoring the annual Middle East Forum on Quality and Safety in Health Care.
The residency training program at Hamad General is accredited by ACGME, with the same expected competencies as in the U.S. “We don’t use the term ‘hospitalist,’ ” Dr. Kartha said. “It’s better to focus on the model of care – which clearly was American. That model has encountered some resistance in some countries – on many of the same grounds U.S. hospitalists faced 20 years ago. You have to be sensitive to local culture. For hospitalists to succeed internationally, they have to possess a high degree of cultural intelligence.” There’s no shortage of issues such as language barriers, he said. “But that’s no different than at Boston Medical Center.”
SHM’s Middle East Chapter was off to a great start and then was slowed down by regional politics and COVID-19, but is looking forward to a great reboot in 2021, Dr. Kartha said. The pandemic also has been an opportunity to show how hospital medicine is the backbone of the hospital’s ability to respond, although of course many other professionals also pitched in.
Other countries around the world have learned a lot from the American model of hospital medicine. But sources for this article wonder if U.S. hospitalists, in turn, could learn from their adaptations and innovations.
“We can all learn better how to practice our field of medicine in the hospital with less resource utilization,” Dr. Vidyarthi concluded. “So many innovations are happening around us. If we open our eyes to our global colleagues and infuse some of their ideas, it could be wonderful for hospital professionals in the United States.”
References
1. Kisuule F, Howell E. Hospital medicine beyond the United States. Int J Gen Med. 2018;11:65-71. doi: 10.2147/IJGM.S151275.
2. Stosic J et al. The acute physician: The future of acute hospital care in the UK. Clin Med (Lond). 2010 Apr; 10(2):145-7. doi: 10.7861/clinmedicine.10-2-145.
3. Yan Y et al. Adoption of Hospitalist Care in Asia: Experiences From Singapore, Taiwan, Korea, and Japan. J Hosp Med. Published Online First 2021 June 11. doi: 10.12788/jhm.3621.
4. Beresford L. Hospital medicine flourishing around the world. The Hospitalist. Nov 2015.
Longitudinal associations between income changes and incident CVD
Background: Low income is associated with CVD, although causality remains debated because low income is also associated with depression and negative health behaviors, which can be associated with CVD. For more robust causal inference, changes in income and their association with CVD must be observed.
Study design: Prospective observational cohort study.
Setting: Four U.S. urban centers – Jackson, Miss.; suburbs of Minneapolis; Washington County, Md.; and Forsyth County, N.C.
Synopsis: Among a large cohort of community-dwelling middle-aged adults, this study showed that negative income changes are associated with an increased incidence of CVD. Among 8,989 patients recruited from the four urban centers above, 10% experienced an income drop, 70% did not have a change in income, and 20% experienced an income increase over the first 6 years of the study. Patients were followed for a mean of 17 years, and those who experienced an income drop were found to have a 17% higher risk of incident CVD, whereas those who experienced an income increase had a 14% lower risk of CVD.
The study was limited by difficulties classifying income and its changes; the complicated nature of income, its relationship with other socioeconomic factors, and causation inferences; and the relatively short span over which income was monitored.
Bottom line: Income decrease is associated with an increased risk of incident CVD.
Citation: Wang S et al. Longitudinal associations between income changes and incident cardiovascular disease, the atherosclerosis risk in communities study. JAMA Cardiol. 2019 Oct 9;4(12):1203-12.
Dr. Rupp is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Background: Low income is associated with CVD, although causality remains debated because low income is also associated with depression and negative health behaviors, which can be associated with CVD. For more robust causal inference, changes in income and their association with CVD must be observed.
Study design: Prospective observational cohort study.
Setting: Four U.S. urban centers – Jackson, Miss.; suburbs of Minneapolis; Washington County, Md.; and Forsyth County, N.C.
Synopsis: Among a large cohort of community-dwelling middle-aged adults, this study showed that negative income changes are associated with an increased incidence of CVD. Among 8,989 patients recruited from the four urban centers above, 10% experienced an income drop, 70% did not have a change in income, and 20% experienced an income increase over the first 6 years of the study. Patients were followed for a mean of 17 years, and those who experienced an income drop were found to have a 17% higher risk of incident CVD, whereas those who experienced an income increase had a 14% lower risk of CVD.
The study was limited by difficulties classifying income and its changes; the complicated nature of income, its relationship with other socioeconomic factors, and causation inferences; and the relatively short span over which income was monitored.
Bottom line: Income decrease is associated with an increased risk of incident CVD.
Citation: Wang S et al. Longitudinal associations between income changes and incident cardiovascular disease, the atherosclerosis risk in communities study. JAMA Cardiol. 2019 Oct 9;4(12):1203-12.
Dr. Rupp is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Background: Low income is associated with CVD, although causality remains debated because low income is also associated with depression and negative health behaviors, which can be associated with CVD. For more robust causal inference, changes in income and their association with CVD must be observed.
Study design: Prospective observational cohort study.
Setting: Four U.S. urban centers – Jackson, Miss.; suburbs of Minneapolis; Washington County, Md.; and Forsyth County, N.C.
Synopsis: Among a large cohort of community-dwelling middle-aged adults, this study showed that negative income changes are associated with an increased incidence of CVD. Among 8,989 patients recruited from the four urban centers above, 10% experienced an income drop, 70% did not have a change in income, and 20% experienced an income increase over the first 6 years of the study. Patients were followed for a mean of 17 years, and those who experienced an income drop were found to have a 17% higher risk of incident CVD, whereas those who experienced an income increase had a 14% lower risk of CVD.
The study was limited by difficulties classifying income and its changes; the complicated nature of income, its relationship with other socioeconomic factors, and causation inferences; and the relatively short span over which income was monitored.
Bottom line: Income decrease is associated with an increased risk of incident CVD.
Citation: Wang S et al. Longitudinal associations between income changes and incident cardiovascular disease, the atherosclerosis risk in communities study. JAMA Cardiol. 2019 Oct 9;4(12):1203-12.
Dr. Rupp is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
The role of aspirin in primary prevention of cardiovascular disease
Background: Previous studies have shown that aspirin reduces the relative risk of cardiovascular disease (CVD) but also increases the relative risk of bleeding. It is unclear if there are patients without known CVD in whom the absolute risk reduction of CVD outweighs the absolute risk of bleeding. Prognostic CVD and bleeding risk models allow for an assessment of absolute risks and primary preventive interventions.
Study design: Individualized risk-benefit analysis based on sex-specific risk scores and estimates from PREDICT cohort data.
Setting: Primary care practices in New Zealand.
Synopsis: Using the New Zealand–based PREDICT online tool, 245,048 patients had their CVD risk assessed and did not meet exclusion criteria. The online tool predicts CVD events avoided and bleeding events caused by aspirin. When one CVD event was equivalent to one major bleeding event, 2.5% of women and 12.1% of men were classified as benefiting from aspirin (more CVD events avoided than bleeding events caused). When one CVD event was equivalent to two major bleeding events, 21.4% of women and 40.7% of men were classified as benefiting from aspirin. The net-benefit subgroups were older, and had higher baseline 5-year CVD risk, fewer risk factors for bleeding, higher systolic blood pressure, and a higher total cholesterol to HDL cholesterol ratio. Ethnicity and socioeconomic index also influenced benefit or harm.
With use of the upper and lower limits of 95% confidence intervals for models, there were considerable ranges of benefit versus harm. Sex-specific risk scores and meta-analysis have intrinsic uncertainties and results potentially not generalizable outside New Zealand population. Ultimate decision to use aspirin requires shared decision making.
Bottom line: Some patients are likely to derive a net benefit from aspirin for primary prevention of CVD. Risk-benefit models with online tools can help providers and patients estimate these factors to inform shared decision making.
Citation: Selak V et al. Personalized prediction of cardiovascular benefits and bleeding harms for aspirin for primary prevention, a benefit-harm analysis. Ann Intern Med. 2019;71(8):529-39.
Dr. Rupp is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Background: Previous studies have shown that aspirin reduces the relative risk of cardiovascular disease (CVD) but also increases the relative risk of bleeding. It is unclear if there are patients without known CVD in whom the absolute risk reduction of CVD outweighs the absolute risk of bleeding. Prognostic CVD and bleeding risk models allow for an assessment of absolute risks and primary preventive interventions.
Study design: Individualized risk-benefit analysis based on sex-specific risk scores and estimates from PREDICT cohort data.
Setting: Primary care practices in New Zealand.
Synopsis: Using the New Zealand–based PREDICT online tool, 245,048 patients had their CVD risk assessed and did not meet exclusion criteria. The online tool predicts CVD events avoided and bleeding events caused by aspirin. When one CVD event was equivalent to one major bleeding event, 2.5% of women and 12.1% of men were classified as benefiting from aspirin (more CVD events avoided than bleeding events caused). When one CVD event was equivalent to two major bleeding events, 21.4% of women and 40.7% of men were classified as benefiting from aspirin. The net-benefit subgroups were older, and had higher baseline 5-year CVD risk, fewer risk factors for bleeding, higher systolic blood pressure, and a higher total cholesterol to HDL cholesterol ratio. Ethnicity and socioeconomic index also influenced benefit or harm.
With use of the upper and lower limits of 95% confidence intervals for models, there were considerable ranges of benefit versus harm. Sex-specific risk scores and meta-analysis have intrinsic uncertainties and results potentially not generalizable outside New Zealand population. Ultimate decision to use aspirin requires shared decision making.
Bottom line: Some patients are likely to derive a net benefit from aspirin for primary prevention of CVD. Risk-benefit models with online tools can help providers and patients estimate these factors to inform shared decision making.
Citation: Selak V et al. Personalized prediction of cardiovascular benefits and bleeding harms for aspirin for primary prevention, a benefit-harm analysis. Ann Intern Med. 2019;71(8):529-39.
Dr. Rupp is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Background: Previous studies have shown that aspirin reduces the relative risk of cardiovascular disease (CVD) but also increases the relative risk of bleeding. It is unclear if there are patients without known CVD in whom the absolute risk reduction of CVD outweighs the absolute risk of bleeding. Prognostic CVD and bleeding risk models allow for an assessment of absolute risks and primary preventive interventions.
Study design: Individualized risk-benefit analysis based on sex-specific risk scores and estimates from PREDICT cohort data.
Setting: Primary care practices in New Zealand.
Synopsis: Using the New Zealand–based PREDICT online tool, 245,048 patients had their CVD risk assessed and did not meet exclusion criteria. The online tool predicts CVD events avoided and bleeding events caused by aspirin. When one CVD event was equivalent to one major bleeding event, 2.5% of women and 12.1% of men were classified as benefiting from aspirin (more CVD events avoided than bleeding events caused). When one CVD event was equivalent to two major bleeding events, 21.4% of women and 40.7% of men were classified as benefiting from aspirin. The net-benefit subgroups were older, and had higher baseline 5-year CVD risk, fewer risk factors for bleeding, higher systolic blood pressure, and a higher total cholesterol to HDL cholesterol ratio. Ethnicity and socioeconomic index also influenced benefit or harm.
With use of the upper and lower limits of 95% confidence intervals for models, there were considerable ranges of benefit versus harm. Sex-specific risk scores and meta-analysis have intrinsic uncertainties and results potentially not generalizable outside New Zealand population. Ultimate decision to use aspirin requires shared decision making.
Bottom line: Some patients are likely to derive a net benefit from aspirin for primary prevention of CVD. Risk-benefit models with online tools can help providers and patients estimate these factors to inform shared decision making.
Citation: Selak V et al. Personalized prediction of cardiovascular benefits and bleeding harms for aspirin for primary prevention, a benefit-harm analysis. Ann Intern Med. 2019;71(8):529-39.
Dr. Rupp is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.