User login
Creating best practices for APPs
A holistic approach to integration
Hospital medicine groups (HMGs) nationally are confronted with a host of challenging issues: increased patient volume/complexities, resident duty-hour restrictions, and a rise in provider burnout. Many are turning to advanced practice providers (APPs) to help lighten these burdens.
But no practical guidelines exist around how to successfully incorporate APPs in a way that meets the needs of the patients, the providers, the HMG, and the health system, according to Kasey Bowden, MSN, FNP, AG-ACNP, lead author of a HM19 abstract on that subject.
“Much of the recent literature around APP utilization involves descriptive anecdotes on how individual HMGs have utilized APPs, and what metrics this helped them to achieve,” she said. “While these stories are often compelling, they provide no tangible value to HMGs looking to incorporate APPs into practice, as they do not address unique elements that limit successful APP integration, including diverse educational backgrounds of APPs and exceedingly high turnover rates (12.6% nationally).”
Ms. Bowden and coauthors created a conceptual framework, which recognizes that, without taking a holistic approach, many HMGs will fail to successfully integrate APPs. “Our hope is that by utilizing this framework to define APP-physician best practices, we will be able to create a useful tool for all HMGs that will promote successful APP-physician collaborative practice models.”
She thinks that hospitalists could also use this framework to examine their current practice models and to see where there may be opportunity for improvement. For example, a group may look at their own APP turnover rate. “If turnover rate is high in the first year, it may suggest inadequate onboarding/training, if it is high after 3 years, this may suggest minimal opportunities for professional growth and advancement,” Ms. Bowden said. “I would love to see a consensus group form within SHM of physician and APP leaders to utilize this framework to establish ‘APP-Physician best practices,’ and create a guideline available to all HMGs so that they can successfully incorporate APPs into their practice,” she said.
Reference
1. Bowden K et al. Creation of APP-physician best practices: A necessary tool for the growing APP workforce. Hospital Medicine 2019, Abstract 436.
A holistic approach to integration
A holistic approach to integration
Hospital medicine groups (HMGs) nationally are confronted with a host of challenging issues: increased patient volume/complexities, resident duty-hour restrictions, and a rise in provider burnout. Many are turning to advanced practice providers (APPs) to help lighten these burdens.
But no practical guidelines exist around how to successfully incorporate APPs in a way that meets the needs of the patients, the providers, the HMG, and the health system, according to Kasey Bowden, MSN, FNP, AG-ACNP, lead author of a HM19 abstract on that subject.
“Much of the recent literature around APP utilization involves descriptive anecdotes on how individual HMGs have utilized APPs, and what metrics this helped them to achieve,” she said. “While these stories are often compelling, they provide no tangible value to HMGs looking to incorporate APPs into practice, as they do not address unique elements that limit successful APP integration, including diverse educational backgrounds of APPs and exceedingly high turnover rates (12.6% nationally).”
Ms. Bowden and coauthors created a conceptual framework, which recognizes that, without taking a holistic approach, many HMGs will fail to successfully integrate APPs. “Our hope is that by utilizing this framework to define APP-physician best practices, we will be able to create a useful tool for all HMGs that will promote successful APP-physician collaborative practice models.”
She thinks that hospitalists could also use this framework to examine their current practice models and to see where there may be opportunity for improvement. For example, a group may look at their own APP turnover rate. “If turnover rate is high in the first year, it may suggest inadequate onboarding/training, if it is high after 3 years, this may suggest minimal opportunities for professional growth and advancement,” Ms. Bowden said. “I would love to see a consensus group form within SHM of physician and APP leaders to utilize this framework to establish ‘APP-Physician best practices,’ and create a guideline available to all HMGs so that they can successfully incorporate APPs into their practice,” she said.
Reference
1. Bowden K et al. Creation of APP-physician best practices: A necessary tool for the growing APP workforce. Hospital Medicine 2019, Abstract 436.
Hospital medicine groups (HMGs) nationally are confronted with a host of challenging issues: increased patient volume/complexities, resident duty-hour restrictions, and a rise in provider burnout. Many are turning to advanced practice providers (APPs) to help lighten these burdens.
But no practical guidelines exist around how to successfully incorporate APPs in a way that meets the needs of the patients, the providers, the HMG, and the health system, according to Kasey Bowden, MSN, FNP, AG-ACNP, lead author of a HM19 abstract on that subject.
“Much of the recent literature around APP utilization involves descriptive anecdotes on how individual HMGs have utilized APPs, and what metrics this helped them to achieve,” she said. “While these stories are often compelling, they provide no tangible value to HMGs looking to incorporate APPs into practice, as they do not address unique elements that limit successful APP integration, including diverse educational backgrounds of APPs and exceedingly high turnover rates (12.6% nationally).”
Ms. Bowden and coauthors created a conceptual framework, which recognizes that, without taking a holistic approach, many HMGs will fail to successfully integrate APPs. “Our hope is that by utilizing this framework to define APP-physician best practices, we will be able to create a useful tool for all HMGs that will promote successful APP-physician collaborative practice models.”
She thinks that hospitalists could also use this framework to examine their current practice models and to see where there may be opportunity for improvement. For example, a group may look at their own APP turnover rate. “If turnover rate is high in the first year, it may suggest inadequate onboarding/training, if it is high after 3 years, this may suggest minimal opportunities for professional growth and advancement,” Ms. Bowden said. “I would love to see a consensus group form within SHM of physician and APP leaders to utilize this framework to establish ‘APP-Physician best practices,’ and create a guideline available to all HMGs so that they can successfully incorporate APPs into their practice,” she said.
Reference
1. Bowden K et al. Creation of APP-physician best practices: A necessary tool for the growing APP workforce. Hospital Medicine 2019, Abstract 436.
DOACs for treatment of cancer-associated venous thromboembolism
Bleeding risk may determine best option
Case
A 52-year-old female with past medical history of diabetes, hypertension, and stage 4 lung cancer on palliative chemotherapy presents with acute-onset dyspnea, pleuritic chest pain, and cough. Her exam is notable for tachycardia, hypoxemia, and diminished breath sounds. A CT pulmonary embolism study shows new left segmental thrombus. What is her preferred method of anticoagulation?
Brief overview of the issue
Venous thromboembolism (VTE) including deep vein thrombosis (DVT) and pulmonary embolism (PE), is a significant concern in the context of malignancy and is associated with higher rates of mortality at 1 year.
The standard of care in the recent past has relied on low-molecular-weight heparin (LMWH) after several trials showed decreased VTE recurrence in cancer patients, compared with vitamin K antagonist (VKA) treatment.1,2 LMWH has been recommended as a first-line treatment by clinical guidelines for cancer-related VTE given lower drug-drug interactions between LMWH and chemotherapy regimens, as compared with traditional VKAs, and it does not rely on intestinal absorption.3
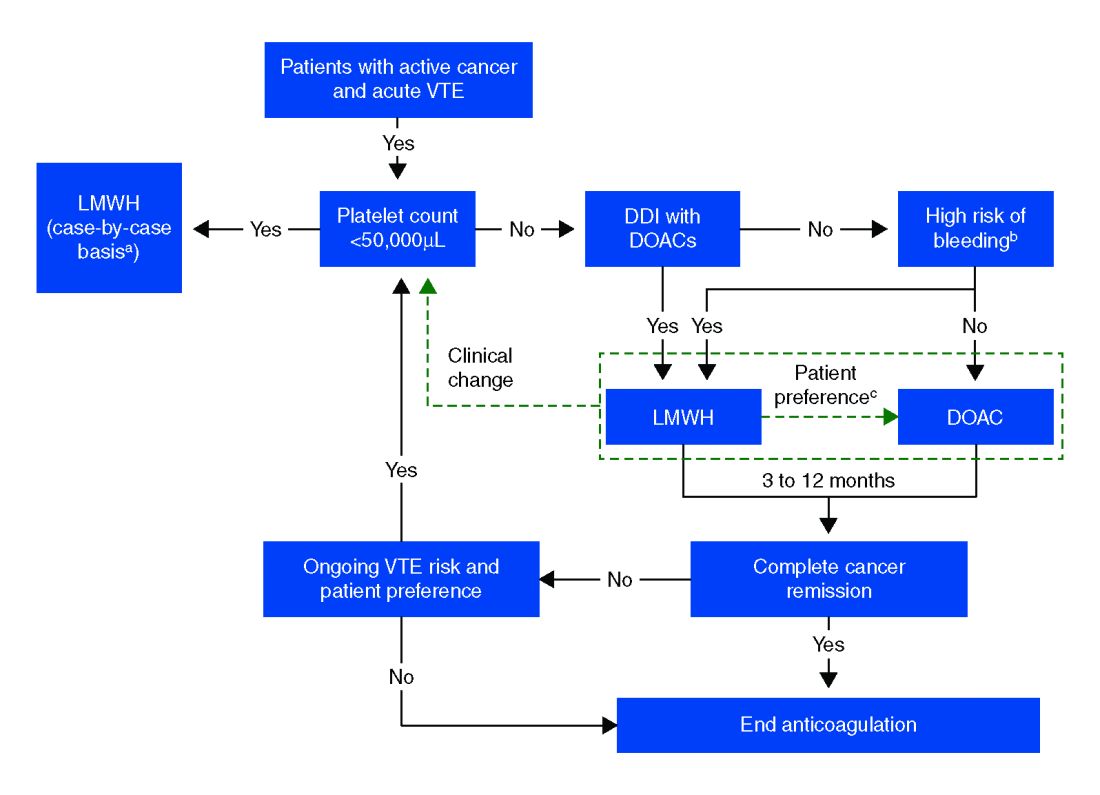
In more recent years, the focus has shifted to direct oral anticoagulants (DOACs) as potential treatment options for cancer-related VTE given their ease of administration, low side-effect profile, and decreased cost. Until recently, studies have mainly been small and largely retrospective, however, several larger randomized control studies have recently been published.
Overview of the data
Several retrospective trials have investigated the use of DOACs in cancer-associated VTE. One study looking at VTE recurrence rates showed a trend towards lower rates with rivaroxaban, compared with LMWH at 6 months (13% vs. 17%) that was significantly lower at 12 months (16.5 % vs. 22%). Similar results were found when comparing rivaroxaban to warfarin. Major bleeding rates were similar among cohorts.4
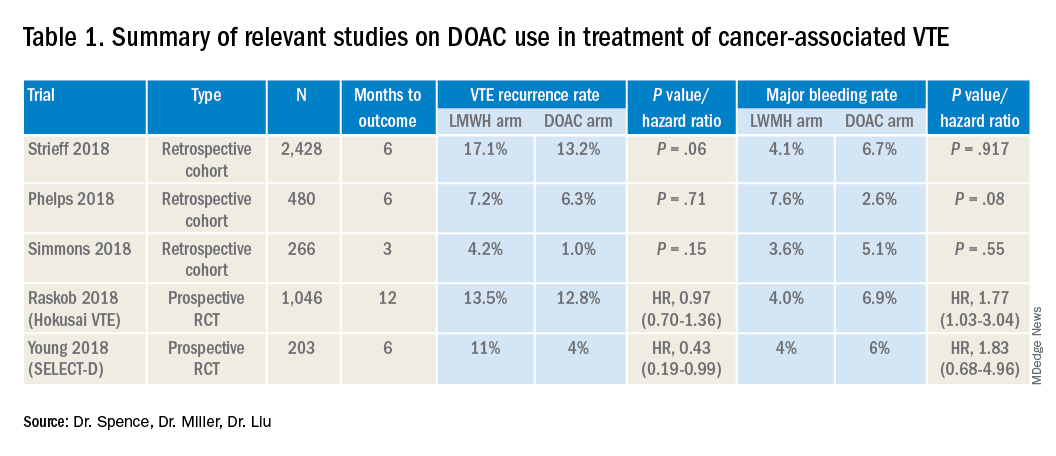
Several other retrospective cohort studies looking at treatment of cancer-associated VTE treated with LMWH vs. DOACs found that overall patients treated with DOACs had cancers with lower risk for VTE and had lower burden of metastatic disease. When this was adjusted for, there was no significant difference in the rate of recurrent cancer-associated thrombosis or major bleeding.5,6
Recently several prospective studies have corroborated the noninferiority or slight superiority of DOACs when compared with LMWH in treatment of cancer-associated VTE, while showing similar rates of bleeding. These are summarized as follows: a prospective, open-label, randomized controlled (RCT), noninferiority trial of 1,046 patients with malignancy-related VTE assigned to either LMWH for at least 5 days, followed by oral edoxaban vs. subcutaneous dalteparin for at least 6 months and up to 12 months. Investigators found no significant difference in the rate of recurrent VTE in the edoxaban group (12.8%), as compared to the dalteparin group (13.5%, P = .006 for noninferiority). Risk of major bleeding was not significantly different between the groups.7
A small RCT of 203 patients comparing recurrent VTE rates with rivaroxaban vs. dalteparin found significantly fewer recurrent clots in the rivaroxaban group compared to the dalteparin group (11% vs 4%) with no significant difference in the 6-month cumulative rate of major bleeding, 4% in the dalteparin group and 6% for the rivaroxaban group.8 Preliminary results from the ADAM VTE trial comparing apixaban to dalteparin found significantly fewer recurrent VTE in the apixaban group (3.4% vs. 14.1%) with no significant difference in major bleeding events (0% vs 2.1%).9 The Caravaggio study is a large multinational randomized, controlled, open-label, noninferiority trial looking at apixaban vs. dalteparin with endpoints being 6-month recurrent VTE and bleeding risk that will likely report results soon.
Risk of bleeding is also a major consideration in VTE treatment as studies suggest that patients with metastatic cancer are at sixfold higher risk for anticoagulant-associated bleeding.3 Subgroup analysis of Hokusai VTE cancer study found that major bleeding occurred in 32 of 522 patients given edoxaban and 16 of 524 patients treated with dalteparin. Excess of major bleeding with edoxaban was confined to patients with GI cancer. However, rates of severe major bleeding at presentation were similar.10
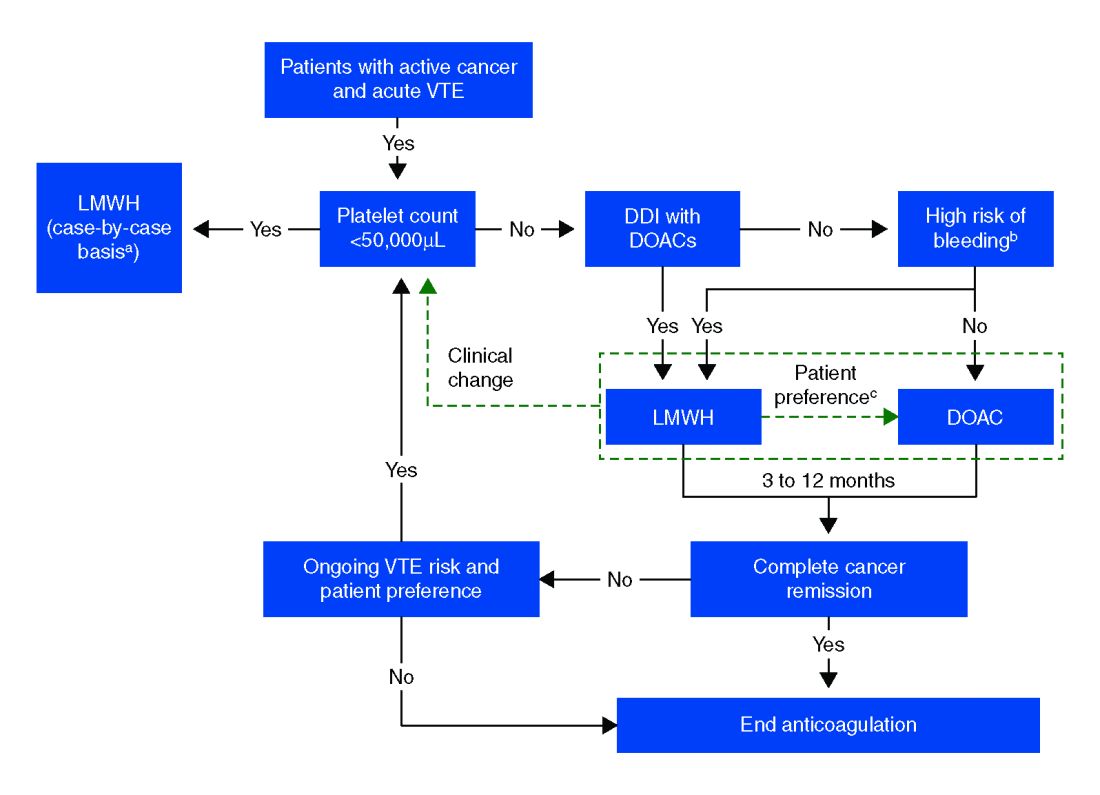
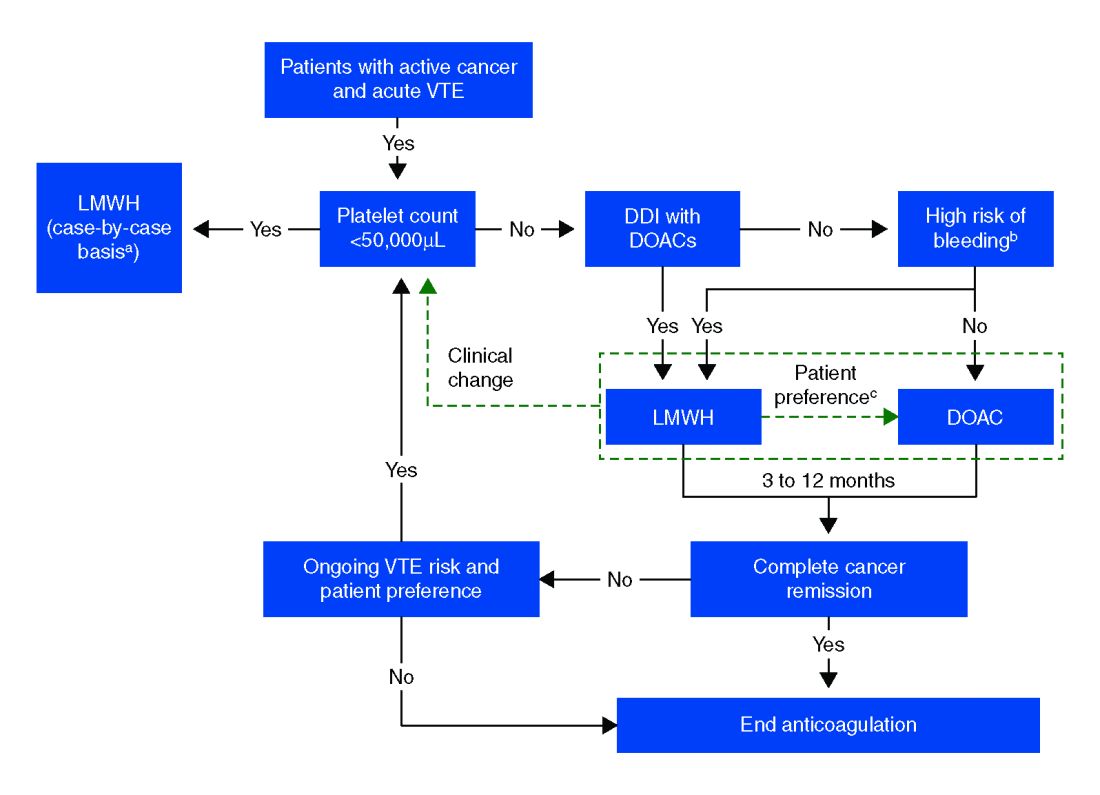
Overall, the existing data suggests that DOACs may be a viable option in the treatment of malignancy-associated VTE given its similar efficacy in preventing recurrent VTE without significant increased risk of major bleeding. The 2018 International Society on Thrombosis and Haemostasis VTE in cancer guidelines have been updated to include rivaroxaban and edoxaban for use in patients at low risk of bleeding, but recommend an informed discussion between patients and clinicians in deciding between DOAC and LMWH.11 The Chest VTE guidelines have not been updated since 2016, prior to when the above mentioned DOAC studies were published.
Application of data to our patient
Compared with patients without cancer, anticoagulation in cancer patients with acute VTE is challenging because of higher rates of VTE recurrence and bleeding, as well as the potential for drug interactions with anticancer agents. Our patient is not at increased risk for gastrointestinal bleeding and no drug interactions exist between her current chemotherapy regimen and the available DOACs, therefore she is a candidate for treatment with a DOAC.
After an informed discussion, she chose to start rivaroxaban for treatment of her pulmonary embolism. While more studies are needed to definitively determine the best treatment for cancer-associated VTE, DOACs appear to be an attractive alternative to LMWH. Patient preferences of taking oral medications over injections as well as the significant cost savings of DOACs over LMWH will likely play into many patients’ and providers’ anticoagulant choices.
Bottom line
Direct oral anticoagulants are a treatment option for cancer-associated VTE in patients at low risk of bleeding complications. Patients at increased risk of bleeding (especially patients with GI malignancies) should continue to be treated with LMWH.
Dr. Spence is a hospitalist and palliative care physician at Denver Health, and an assistant professor of medicine at the University of Colorado at Denver, Aurora. Dr. Miller and Dr. Liu are hospitalists at Denver Health, and assistant professors of medicine at the University of Colorado at Denver.
References
1. Hull RD et al. Long term low-molecular-weight heparin versus usual care in proximal-vein thrombosis patient with cancer. Am J Med. 2006;19(12):1062-72.
2. Lee AY et al. Low-molecular-weight heparin versus Coumadin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349(2):146-53.
3. Ay C et al. Treatment of cancer-associated venous thromboembolism in the age of direct oral anticoagulants. Ann Oncol. 2019 Mar 27 [epub].
4. Streiff MB et al. Effectiveness and safety of anticoagulants for the treatment of venous thromboembolism in patients with cancer. Am J Hematol. 2018 May;93(5):664-71.
5. Phelps MK et al. A single center retrospective cohort study comparing low-molecular-weight heparins to direct oral anticoagulants for the treatment of venous thromboembolism in patients with cancer – A real-world experience. J Oncol Pharm Pract. 2019 Jun;25(4):793-800.
6. Simmons B et al. Efficacy and safety of rivaroxaban compared to enoxaparin in treatment of cancer-associated venous thromboembolism. Eur J Haematol. 2018 Apr 4. (Epub).
7. Raskob GE et al.; Hokusai VTE Cancer Investigators. Edoxaban for the treatment of cancer-associated venous thromboembolism. N Engl J Med. 2018 Feb 15;378(7):615-24.
8. Young AM et al. Comparison of an oral factor Xa inhibitor with low molecular weight heparin in patients with cancer with venous thromboembolism: Results of a randomized trial (SELECT-D). J Clin Oncol. 2018 Jul 10;36(20):2017-23.
9. McBane, RD et al. Apixaban, dalteparin, in active cancer associated venous thromboembolism, the ADAM VTE trial. Blood. 2018 Nov 29;132(suppl 1):421.
10. Kraaijpoel N et al. Clinical impact of bleeding in cancer-associated venous thromboembolism: Results from the Hokusai VTE cancer study. Thromb Haemost. 2018 Aug;118(8):1439-49.
11. Khorana AA et al. Role of direct oral anticoagulants in the treatment of cancer-associated venous thromboembolism: Guidance from the SSC of the ISTH. J Thromb Haemost. 2018 Sep;16(9):1891-94.
Key points
- DOACs are a reasonable treatment option for malignancy-associated VTE in patients without GI tract malignancies and at low risk for bleeding complications.
- In patients with gastrointestinal malignancies or increased risk of bleeding, DOACs may have an increased bleeding risk and therefore LMWH is recommended.
- An informed discussion should occur between providers and patients to determine the best treatment option for cancer patients with VTE.
Additional reading
Dong Y et al. Efficacy and safety of direct oral anticoagulants versus low-molecular-weight heparin in patients with cancer: A systematic review and meta-analysis. J Thromb Thrombolysis. 2019 May 6.
Khorana AA et al. Role of direct oral anticoagulants in the treatment of cancer-associated venous thromboembolism: guidance from the SSC of the ISTH. J Thromb Haemost. 2018 Sep;16(9):1891-94.
Tritschler T et al. Venous thromboembolism advances in diagnosis and treatment. JAMA. 2018 Oct;320(15):1583-94.
Quiz
Which of the following is the recommended treatment of VTE in a patient with brain metastases?
A. Unfractionated heparin
B. Low molecular weight heparin
C. Direct oral anticoagulant
D. Vitamin K antagonist
The answer is B. Although there are very few data, LMWH is the recommended agent in patients with VTE and brain metastases.
A. LMWH has been shown to decrease mortality in patients with VTE and cancer, compared with unfractionated heparin (risk ratio, 0.66).
C. The safety of DOACs is not yet well established in patients with brain tumors. Antidotes and/or specific reversal agents for some DOACs are not available.
D. Vitamin K antagonists such as warfarin are not recommended in cancer patients because LMWH has a reduced risk of recurrent VTE without increased risk of bleeding.
Bleeding risk may determine best option
Bleeding risk may determine best option
Case
A 52-year-old female with past medical history of diabetes, hypertension, and stage 4 lung cancer on palliative chemotherapy presents with acute-onset dyspnea, pleuritic chest pain, and cough. Her exam is notable for tachycardia, hypoxemia, and diminished breath sounds. A CT pulmonary embolism study shows new left segmental thrombus. What is her preferred method of anticoagulation?
Brief overview of the issue
Venous thromboembolism (VTE) including deep vein thrombosis (DVT) and pulmonary embolism (PE), is a significant concern in the context of malignancy and is associated with higher rates of mortality at 1 year.
The standard of care in the recent past has relied on low-molecular-weight heparin (LMWH) after several trials showed decreased VTE recurrence in cancer patients, compared with vitamin K antagonist (VKA) treatment.1,2 LMWH has been recommended as a first-line treatment by clinical guidelines for cancer-related VTE given lower drug-drug interactions between LMWH and chemotherapy regimens, as compared with traditional VKAs, and it does not rely on intestinal absorption.3
In more recent years, the focus has shifted to direct oral anticoagulants (DOACs) as potential treatment options for cancer-related VTE given their ease of administration, low side-effect profile, and decreased cost. Until recently, studies have mainly been small and largely retrospective, however, several larger randomized control studies have recently been published.
Overview of the data
Several retrospective trials have investigated the use of DOACs in cancer-associated VTE. One study looking at VTE recurrence rates showed a trend towards lower rates with rivaroxaban, compared with LMWH at 6 months (13% vs. 17%) that was significantly lower at 12 months (16.5 % vs. 22%). Similar results were found when comparing rivaroxaban to warfarin. Major bleeding rates were similar among cohorts.4
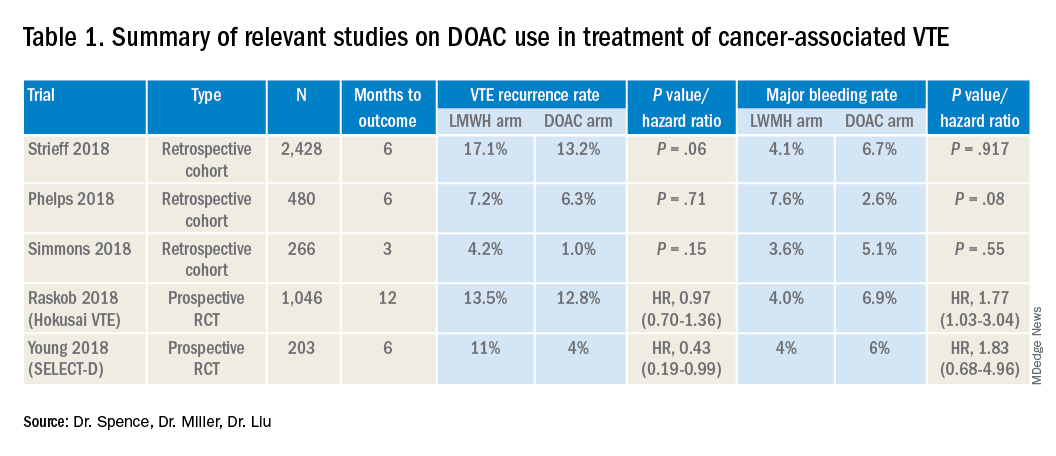
Several other retrospective cohort studies looking at treatment of cancer-associated VTE treated with LMWH vs. DOACs found that overall patients treated with DOACs had cancers with lower risk for VTE and had lower burden of metastatic disease. When this was adjusted for, there was no significant difference in the rate of recurrent cancer-associated thrombosis or major bleeding.5,6
Recently several prospective studies have corroborated the noninferiority or slight superiority of DOACs when compared with LMWH in treatment of cancer-associated VTE, while showing similar rates of bleeding. These are summarized as follows: a prospective, open-label, randomized controlled (RCT), noninferiority trial of 1,046 patients with malignancy-related VTE assigned to either LMWH for at least 5 days, followed by oral edoxaban vs. subcutaneous dalteparin for at least 6 months and up to 12 months. Investigators found no significant difference in the rate of recurrent VTE in the edoxaban group (12.8%), as compared to the dalteparin group (13.5%, P = .006 for noninferiority). Risk of major bleeding was not significantly different between the groups.7
A small RCT of 203 patients comparing recurrent VTE rates with rivaroxaban vs. dalteparin found significantly fewer recurrent clots in the rivaroxaban group compared to the dalteparin group (11% vs 4%) with no significant difference in the 6-month cumulative rate of major bleeding, 4% in the dalteparin group and 6% for the rivaroxaban group.8 Preliminary results from the ADAM VTE trial comparing apixaban to dalteparin found significantly fewer recurrent VTE in the apixaban group (3.4% vs. 14.1%) with no significant difference in major bleeding events (0% vs 2.1%).9 The Caravaggio study is a large multinational randomized, controlled, open-label, noninferiority trial looking at apixaban vs. dalteparin with endpoints being 6-month recurrent VTE and bleeding risk that will likely report results soon.
Risk of bleeding is also a major consideration in VTE treatment as studies suggest that patients with metastatic cancer are at sixfold higher risk for anticoagulant-associated bleeding.3 Subgroup analysis of Hokusai VTE cancer study found that major bleeding occurred in 32 of 522 patients given edoxaban and 16 of 524 patients treated with dalteparin. Excess of major bleeding with edoxaban was confined to patients with GI cancer. However, rates of severe major bleeding at presentation were similar.10
Overall, the existing data suggests that DOACs may be a viable option in the treatment of malignancy-associated VTE given its similar efficacy in preventing recurrent VTE without significant increased risk of major bleeding. The 2018 International Society on Thrombosis and Haemostasis VTE in cancer guidelines have been updated to include rivaroxaban and edoxaban for use in patients at low risk of bleeding, but recommend an informed discussion between patients and clinicians in deciding between DOAC and LMWH.11 The Chest VTE guidelines have not been updated since 2016, prior to when the above mentioned DOAC studies were published.
Application of data to our patient
Compared with patients without cancer, anticoagulation in cancer patients with acute VTE is challenging because of higher rates of VTE recurrence and bleeding, as well as the potential for drug interactions with anticancer agents. Our patient is not at increased risk for gastrointestinal bleeding and no drug interactions exist between her current chemotherapy regimen and the available DOACs, therefore she is a candidate for treatment with a DOAC.
After an informed discussion, she chose to start rivaroxaban for treatment of her pulmonary embolism. While more studies are needed to definitively determine the best treatment for cancer-associated VTE, DOACs appear to be an attractive alternative to LMWH. Patient preferences of taking oral medications over injections as well as the significant cost savings of DOACs over LMWH will likely play into many patients’ and providers’ anticoagulant choices.
Bottom line
Direct oral anticoagulants are a treatment option for cancer-associated VTE in patients at low risk of bleeding complications. Patients at increased risk of bleeding (especially patients with GI malignancies) should continue to be treated with LMWH.
Dr. Spence is a hospitalist and palliative care physician at Denver Health, and an assistant professor of medicine at the University of Colorado at Denver, Aurora. Dr. Miller and Dr. Liu are hospitalists at Denver Health, and assistant professors of medicine at the University of Colorado at Denver.
References
1. Hull RD et al. Long term low-molecular-weight heparin versus usual care in proximal-vein thrombosis patient with cancer. Am J Med. 2006;19(12):1062-72.
2. Lee AY et al. Low-molecular-weight heparin versus Coumadin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349(2):146-53.
3. Ay C et al. Treatment of cancer-associated venous thromboembolism in the age of direct oral anticoagulants. Ann Oncol. 2019 Mar 27 [epub].
4. Streiff MB et al. Effectiveness and safety of anticoagulants for the treatment of venous thromboembolism in patients with cancer. Am J Hematol. 2018 May;93(5):664-71.
5. Phelps MK et al. A single center retrospective cohort study comparing low-molecular-weight heparins to direct oral anticoagulants for the treatment of venous thromboembolism in patients with cancer – A real-world experience. J Oncol Pharm Pract. 2019 Jun;25(4):793-800.
6. Simmons B et al. Efficacy and safety of rivaroxaban compared to enoxaparin in treatment of cancer-associated venous thromboembolism. Eur J Haematol. 2018 Apr 4. (Epub).
7. Raskob GE et al.; Hokusai VTE Cancer Investigators. Edoxaban for the treatment of cancer-associated venous thromboembolism. N Engl J Med. 2018 Feb 15;378(7):615-24.
8. Young AM et al. Comparison of an oral factor Xa inhibitor with low molecular weight heparin in patients with cancer with venous thromboembolism: Results of a randomized trial (SELECT-D). J Clin Oncol. 2018 Jul 10;36(20):2017-23.
9. McBane, RD et al. Apixaban, dalteparin, in active cancer associated venous thromboembolism, the ADAM VTE trial. Blood. 2018 Nov 29;132(suppl 1):421.
10. Kraaijpoel N et al. Clinical impact of bleeding in cancer-associated venous thromboembolism: Results from the Hokusai VTE cancer study. Thromb Haemost. 2018 Aug;118(8):1439-49.
11. Khorana AA et al. Role of direct oral anticoagulants in the treatment of cancer-associated venous thromboembolism: Guidance from the SSC of the ISTH. J Thromb Haemost. 2018 Sep;16(9):1891-94.
Key points
- DOACs are a reasonable treatment option for malignancy-associated VTE in patients without GI tract malignancies and at low risk for bleeding complications.
- In patients with gastrointestinal malignancies or increased risk of bleeding, DOACs may have an increased bleeding risk and therefore LMWH is recommended.
- An informed discussion should occur between providers and patients to determine the best treatment option for cancer patients with VTE.
Additional reading
Dong Y et al. Efficacy and safety of direct oral anticoagulants versus low-molecular-weight heparin in patients with cancer: A systematic review and meta-analysis. J Thromb Thrombolysis. 2019 May 6.
Khorana AA et al. Role of direct oral anticoagulants in the treatment of cancer-associated venous thromboembolism: guidance from the SSC of the ISTH. J Thromb Haemost. 2018 Sep;16(9):1891-94.
Tritschler T et al. Venous thromboembolism advances in diagnosis and treatment. JAMA. 2018 Oct;320(15):1583-94.
Quiz
Which of the following is the recommended treatment of VTE in a patient with brain metastases?
A. Unfractionated heparin
B. Low molecular weight heparin
C. Direct oral anticoagulant
D. Vitamin K antagonist
The answer is B. Although there are very few data, LMWH is the recommended agent in patients with VTE and brain metastases.
A. LMWH has been shown to decrease mortality in patients with VTE and cancer, compared with unfractionated heparin (risk ratio, 0.66).
C. The safety of DOACs is not yet well established in patients with brain tumors. Antidotes and/or specific reversal agents for some DOACs are not available.
D. Vitamin K antagonists such as warfarin are not recommended in cancer patients because LMWH has a reduced risk of recurrent VTE without increased risk of bleeding.
Case
A 52-year-old female with past medical history of diabetes, hypertension, and stage 4 lung cancer on palliative chemotherapy presents with acute-onset dyspnea, pleuritic chest pain, and cough. Her exam is notable for tachycardia, hypoxemia, and diminished breath sounds. A CT pulmonary embolism study shows new left segmental thrombus. What is her preferred method of anticoagulation?
Brief overview of the issue
Venous thromboembolism (VTE) including deep vein thrombosis (DVT) and pulmonary embolism (PE), is a significant concern in the context of malignancy and is associated with higher rates of mortality at 1 year.
The standard of care in the recent past has relied on low-molecular-weight heparin (LMWH) after several trials showed decreased VTE recurrence in cancer patients, compared with vitamin K antagonist (VKA) treatment.1,2 LMWH has been recommended as a first-line treatment by clinical guidelines for cancer-related VTE given lower drug-drug interactions between LMWH and chemotherapy regimens, as compared with traditional VKAs, and it does not rely on intestinal absorption.3
In more recent years, the focus has shifted to direct oral anticoagulants (DOACs) as potential treatment options for cancer-related VTE given their ease of administration, low side-effect profile, and decreased cost. Until recently, studies have mainly been small and largely retrospective, however, several larger randomized control studies have recently been published.
Overview of the data
Several retrospective trials have investigated the use of DOACs in cancer-associated VTE. One study looking at VTE recurrence rates showed a trend towards lower rates with rivaroxaban, compared with LMWH at 6 months (13% vs. 17%) that was significantly lower at 12 months (16.5 % vs. 22%). Similar results were found when comparing rivaroxaban to warfarin. Major bleeding rates were similar among cohorts.4
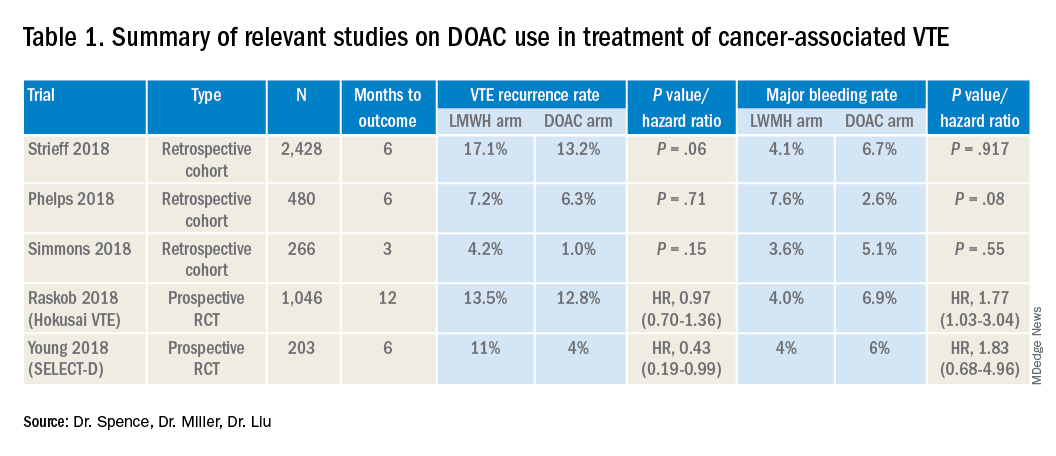
Several other retrospective cohort studies looking at treatment of cancer-associated VTE treated with LMWH vs. DOACs found that overall patients treated with DOACs had cancers with lower risk for VTE and had lower burden of metastatic disease. When this was adjusted for, there was no significant difference in the rate of recurrent cancer-associated thrombosis or major bleeding.5,6
Recently several prospective studies have corroborated the noninferiority or slight superiority of DOACs when compared with LMWH in treatment of cancer-associated VTE, while showing similar rates of bleeding. These are summarized as follows: a prospective, open-label, randomized controlled (RCT), noninferiority trial of 1,046 patients with malignancy-related VTE assigned to either LMWH for at least 5 days, followed by oral edoxaban vs. subcutaneous dalteparin for at least 6 months and up to 12 months. Investigators found no significant difference in the rate of recurrent VTE in the edoxaban group (12.8%), as compared to the dalteparin group (13.5%, P = .006 for noninferiority). Risk of major bleeding was not significantly different between the groups.7
A small RCT of 203 patients comparing recurrent VTE rates with rivaroxaban vs. dalteparin found significantly fewer recurrent clots in the rivaroxaban group compared to the dalteparin group (11% vs 4%) with no significant difference in the 6-month cumulative rate of major bleeding, 4% in the dalteparin group and 6% for the rivaroxaban group.8 Preliminary results from the ADAM VTE trial comparing apixaban to dalteparin found significantly fewer recurrent VTE in the apixaban group (3.4% vs. 14.1%) with no significant difference in major bleeding events (0% vs 2.1%).9 The Caravaggio study is a large multinational randomized, controlled, open-label, noninferiority trial looking at apixaban vs. dalteparin with endpoints being 6-month recurrent VTE and bleeding risk that will likely report results soon.
Risk of bleeding is also a major consideration in VTE treatment as studies suggest that patients with metastatic cancer are at sixfold higher risk for anticoagulant-associated bleeding.3 Subgroup analysis of Hokusai VTE cancer study found that major bleeding occurred in 32 of 522 patients given edoxaban and 16 of 524 patients treated with dalteparin. Excess of major bleeding with edoxaban was confined to patients with GI cancer. However, rates of severe major bleeding at presentation were similar.10
Overall, the existing data suggests that DOACs may be a viable option in the treatment of malignancy-associated VTE given its similar efficacy in preventing recurrent VTE without significant increased risk of major bleeding. The 2018 International Society on Thrombosis and Haemostasis VTE in cancer guidelines have been updated to include rivaroxaban and edoxaban for use in patients at low risk of bleeding, but recommend an informed discussion between patients and clinicians in deciding between DOAC and LMWH.11 The Chest VTE guidelines have not been updated since 2016, prior to when the above mentioned DOAC studies were published.
Application of data to our patient
Compared with patients without cancer, anticoagulation in cancer patients with acute VTE is challenging because of higher rates of VTE recurrence and bleeding, as well as the potential for drug interactions with anticancer agents. Our patient is not at increased risk for gastrointestinal bleeding and no drug interactions exist between her current chemotherapy regimen and the available DOACs, therefore she is a candidate for treatment with a DOAC.
After an informed discussion, she chose to start rivaroxaban for treatment of her pulmonary embolism. While more studies are needed to definitively determine the best treatment for cancer-associated VTE, DOACs appear to be an attractive alternative to LMWH. Patient preferences of taking oral medications over injections as well as the significant cost savings of DOACs over LMWH will likely play into many patients’ and providers’ anticoagulant choices.
Bottom line
Direct oral anticoagulants are a treatment option for cancer-associated VTE in patients at low risk of bleeding complications. Patients at increased risk of bleeding (especially patients with GI malignancies) should continue to be treated with LMWH.
Dr. Spence is a hospitalist and palliative care physician at Denver Health, and an assistant professor of medicine at the University of Colorado at Denver, Aurora. Dr. Miller and Dr. Liu are hospitalists at Denver Health, and assistant professors of medicine at the University of Colorado at Denver.
References
1. Hull RD et al. Long term low-molecular-weight heparin versus usual care in proximal-vein thrombosis patient with cancer. Am J Med. 2006;19(12):1062-72.
2. Lee AY et al. Low-molecular-weight heparin versus Coumadin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349(2):146-53.
3. Ay C et al. Treatment of cancer-associated venous thromboembolism in the age of direct oral anticoagulants. Ann Oncol. 2019 Mar 27 [epub].
4. Streiff MB et al. Effectiveness and safety of anticoagulants for the treatment of venous thromboembolism in patients with cancer. Am J Hematol. 2018 May;93(5):664-71.
5. Phelps MK et al. A single center retrospective cohort study comparing low-molecular-weight heparins to direct oral anticoagulants for the treatment of venous thromboembolism in patients with cancer – A real-world experience. J Oncol Pharm Pract. 2019 Jun;25(4):793-800.
6. Simmons B et al. Efficacy and safety of rivaroxaban compared to enoxaparin in treatment of cancer-associated venous thromboembolism. Eur J Haematol. 2018 Apr 4. (Epub).
7. Raskob GE et al.; Hokusai VTE Cancer Investigators. Edoxaban for the treatment of cancer-associated venous thromboembolism. N Engl J Med. 2018 Feb 15;378(7):615-24.
8. Young AM et al. Comparison of an oral factor Xa inhibitor with low molecular weight heparin in patients with cancer with venous thromboembolism: Results of a randomized trial (SELECT-D). J Clin Oncol. 2018 Jul 10;36(20):2017-23.
9. McBane, RD et al. Apixaban, dalteparin, in active cancer associated venous thromboembolism, the ADAM VTE trial. Blood. 2018 Nov 29;132(suppl 1):421.
10. Kraaijpoel N et al. Clinical impact of bleeding in cancer-associated venous thromboembolism: Results from the Hokusai VTE cancer study. Thromb Haemost. 2018 Aug;118(8):1439-49.
11. Khorana AA et al. Role of direct oral anticoagulants in the treatment of cancer-associated venous thromboembolism: Guidance from the SSC of the ISTH. J Thromb Haemost. 2018 Sep;16(9):1891-94.
Key points
- DOACs are a reasonable treatment option for malignancy-associated VTE in patients without GI tract malignancies and at low risk for bleeding complications.
- In patients with gastrointestinal malignancies or increased risk of bleeding, DOACs may have an increased bleeding risk and therefore LMWH is recommended.
- An informed discussion should occur between providers and patients to determine the best treatment option for cancer patients with VTE.
Additional reading
Dong Y et al. Efficacy and safety of direct oral anticoagulants versus low-molecular-weight heparin in patients with cancer: A systematic review and meta-analysis. J Thromb Thrombolysis. 2019 May 6.
Khorana AA et al. Role of direct oral anticoagulants in the treatment of cancer-associated venous thromboembolism: guidance from the SSC of the ISTH. J Thromb Haemost. 2018 Sep;16(9):1891-94.
Tritschler T et al. Venous thromboembolism advances in diagnosis and treatment. JAMA. 2018 Oct;320(15):1583-94.
Quiz
Which of the following is the recommended treatment of VTE in a patient with brain metastases?
A. Unfractionated heparin
B. Low molecular weight heparin
C. Direct oral anticoagulant
D. Vitamin K antagonist
The answer is B. Although there are very few data, LMWH is the recommended agent in patients with VTE and brain metastases.
A. LMWH has been shown to decrease mortality in patients with VTE and cancer, compared with unfractionated heparin (risk ratio, 0.66).
C. The safety of DOACs is not yet well established in patients with brain tumors. Antidotes and/or specific reversal agents for some DOACs are not available.
D. Vitamin K antagonists such as warfarin are not recommended in cancer patients because LMWH has a reduced risk of recurrent VTE without increased risk of bleeding.
Reducing alarm fatigue in the hospital
Noise increases patient anxiety
Researchers are exploring ways to make alarms and monitors less irritating and more informative.
“Hospitals today can be sonic hellscapes, which studies have shown regularly exceed levels set by the World Health Organization: droning IV pumps, ding-donging nurse call buttons, voices crackling on loudspeakers, ringing telephones, beeping elevators, buzzing ID scanners, clattering carts, coughing, screaming, vomiting,” according to a recent article in the New York Times.
And that’s not to mention all the alarms that blare regularly, day and night. “A single patient might trigger hundreds each day, challenging caregivers to figure out which machine is beeping, and what is wrong with the patient, if anything,” according to the article.
All this noise contributes to patient anxiety and delirium and to staff burnout too. Alarm fatigue is a serious problem, related to the high rate of false alarms, the lack of alarm standardization, and the number of medical devices that emit an alarm. Its effect is to make caregivers less responsive.
A group of researchers is developing new sounds that could replace current alarms. These new signals might mimic electronic dance music or the sounds of a heartbeat; they may combine audible alarms with visual cues such as interactive screens; they will certainly be quieter. Testing remains to be done around how quickly clinicians will be able to learn the sounds and how loud they need to be. The researchers say a new standard is likely to go into effect in 2020.
Reference
1. Rueb ES. To Reduce Hospital Noise, Researchers Create Alarms That Whistle and Sing. New York Times. July 9, 2019.
Noise increases patient anxiety
Noise increases patient anxiety
Researchers are exploring ways to make alarms and monitors less irritating and more informative.
“Hospitals today can be sonic hellscapes, which studies have shown regularly exceed levels set by the World Health Organization: droning IV pumps, ding-donging nurse call buttons, voices crackling on loudspeakers, ringing telephones, beeping elevators, buzzing ID scanners, clattering carts, coughing, screaming, vomiting,” according to a recent article in the New York Times.
And that’s not to mention all the alarms that blare regularly, day and night. “A single patient might trigger hundreds each day, challenging caregivers to figure out which machine is beeping, and what is wrong with the patient, if anything,” according to the article.
All this noise contributes to patient anxiety and delirium and to staff burnout too. Alarm fatigue is a serious problem, related to the high rate of false alarms, the lack of alarm standardization, and the number of medical devices that emit an alarm. Its effect is to make caregivers less responsive.
A group of researchers is developing new sounds that could replace current alarms. These new signals might mimic electronic dance music or the sounds of a heartbeat; they may combine audible alarms with visual cues such as interactive screens; they will certainly be quieter. Testing remains to be done around how quickly clinicians will be able to learn the sounds and how loud they need to be. The researchers say a new standard is likely to go into effect in 2020.
Reference
1. Rueb ES. To Reduce Hospital Noise, Researchers Create Alarms That Whistle and Sing. New York Times. July 9, 2019.
Researchers are exploring ways to make alarms and monitors less irritating and more informative.
“Hospitals today can be sonic hellscapes, which studies have shown regularly exceed levels set by the World Health Organization: droning IV pumps, ding-donging nurse call buttons, voices crackling on loudspeakers, ringing telephones, beeping elevators, buzzing ID scanners, clattering carts, coughing, screaming, vomiting,” according to a recent article in the New York Times.
And that’s not to mention all the alarms that blare regularly, day and night. “A single patient might trigger hundreds each day, challenging caregivers to figure out which machine is beeping, and what is wrong with the patient, if anything,” according to the article.
All this noise contributes to patient anxiety and delirium and to staff burnout too. Alarm fatigue is a serious problem, related to the high rate of false alarms, the lack of alarm standardization, and the number of medical devices that emit an alarm. Its effect is to make caregivers less responsive.
A group of researchers is developing new sounds that could replace current alarms. These new signals might mimic electronic dance music or the sounds of a heartbeat; they may combine audible alarms with visual cues such as interactive screens; they will certainly be quieter. Testing remains to be done around how quickly clinicians will be able to learn the sounds and how loud they need to be. The researchers say a new standard is likely to go into effect in 2020.
Reference
1. Rueb ES. To Reduce Hospital Noise, Researchers Create Alarms That Whistle and Sing. New York Times. July 9, 2019.
SHM Pediatric Core Competencies get fresh update
New core competencies reflect a decade of change
Over the past 10 years, much has changed in the world of pediatric hospital medicine. The annual national PHM conference sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics (AAP), and the Academic Pediatric Association (APA) is robust; textbooks and journal articles in the field abound; and networks and training in research, quality improvement, and education are successful and ongoing.
Much of this did not exist or was in its infancy back in 2010. Since then, it has grown and greatly evolved. In parallel, medicine and society have changed. These influences on health care, along with the growth of the field over time, prompted a review and revision of the 2010 PHM Core Competencies published by SHM. With support from the society, the Pediatric Hospital Medicine Special Interest Group launched the plan for revision of the PHM Core Competencies.
The selected editors included Sandra Gage, MD, PhD, SFHM, of Phoenix Children’s Hospital; Erin Stucky Fisher, MD, MHM, of UCSD/Rady Children’s Hospital in San Diego; Jennifer Maniscalco, MD, MPH, of Johns Hopkins All Children’s Hospital in St. Petersburg, Fla.; and Sofia Teferi, MD, SFHM, a pediatric hospitalist based at Bon Secours St. Mary’s Hospital in Richmond, Va. They began their work in 2017 along with six associate editors, meeting every 2 weeks via conference call, dividing the work accordingly.
Dr. Teferi served in a new and critical role as contributing editor. She described her role as a “sweeper” of sorts, bringing her unique perspective to the process. “The other three members are from academic settings, and I’m from a community setting, which is very different,” Dr. Teferi said. “I went through all the chapters to ensure they were inclusive of the community setting.”
According to Dr. Gage, “the purpose of the original PHM Core Competencies was to define the roles and responsibilities of a PHM practitioner. In the intervening 10 years, the field has changed and matured, and we have solidified our role since then.”
Today’s pediatric hospitalists, for instance, may coordinate care in EDs, provide inpatient consultations, engage or lead quality improvement programs, and teach. The demands for pediatric hospital care today go beyond the training provided in a standard pediatric residency. The core competencies need to provide the information necessary, therefore, to ensure pediatric hospital medicine is practiced at its most informed level.
A profession transformed
At the time of the first set of core competencies, there were over 2,500 members in three core societies in which pediatric hospitalists were members: the AAP, the APA, and SHM. As of 2017, those numbers have swelled as the care for children in the hospital setting has shifted away from these patients’ primary care providers.
The original core competencies included 54 chapters, designed to be used independent of the others. They provided a foundation for the creation of pediatric hospital medicine and served to standardize and improve inpatient training practices.
For the new core competencies, every single chapter was reviewed line by line, Dr. Gage said. Many chapters had content modified, and new chapters were added to reflect the evolution of the field and of medicine. “We added about 14 new chapters, adjusted the titles of others, and significantly changed the content of over half,” Dr. Gage explained. “They are fairly broad changes, related to the breadth of the practice today.”
Dr. Teferi noted that practitioners can use the updated competencies with additions to the service lines that have arisen since the last version. “These include areas like step down and newborn nursery, things that weren’t part of our portfolio 10 years ago,” she said. “This reflects the fact that often you’ll see a hospital leader who might want to add to a hospitalist’s portfolio of services because there is no one else to do it. Or maybe community pediatrics no longer want to treat babies, so we add that. The settings vary widely today and we need the competencies to address that.”
Practices within these settings can also vary widely. Teaching, palliative care, airway management, critical care, and anesthesia may all come into play, among other factors. Research opportunities throughout the field also continue to expand.
Dr. Fisher said that the editors and associate editors kept in mind the fact that not every hospital would have all the resources necessary at its fingertips. “The competencies must reflect the realities of the variety of community settings,” she said. “Also, on a national level, the majority of pediatric patients are not seen in a children’s hospital. Community sites are where pediatric hospitalists are not only advocates for care, but can be working with limited resources – the ‘lone soldiers.’ We wanted to make sure the competencies reflect that reality and environment community site or not; academic site or not; tertiary care site or not; rural or not – these are overlapping but independent considerations for all who practice pediatric hospital medicine – a Venn diagram, and the PHM core competencies try to attend to all of those.”
This made Dr. Teferi’s perspective all the more important. “While many, including other editors and associate editors, work in community sites, Dr. Teferi has this as her unique and sole focus. She brought a unique viewpoint to the table,” Dr. Fisher said.
A goal of the core competencies is to make it possible for a pediatric hospitalist to move to a different practice environment and still provide the same level of high-quality care. “It’s difficult but important to grasp the concepts and competencies of various settings,” Dr. Fisher said. “In this way, our competencies are a parallel model to the adult hospitalist competencies.”
The editors surveyed practitioners across the country to gather their input on content, and brought on topic experts to write the new chapters. “If we didn’t have an author for a specific chapter or area from the last set of competencies, we came to a consensus on who the new one should be,” Dr. Gage explained. “We looked for known and accepted experts in the field by reviewing the literature and conference lecturers at all major PHM meetings.”
Once the editors and associate editors worked with authors to refine their chapter(s), the chapters were sent to multiple external reviewers including subgroups of SHM, AAP, and APA, as well as a variety of other associations. They provided input that the editors and associate editors collated, reviewed, and incorporated according to consensus and discussion with the authors.
A preview
As far as the actual changes go, some of new chapters include four common clinical, two core skills, three specialized services, and five health care systems, with many others undergoing content changes, according to Dr. Gage.
Major considerations in developing the new competencies include the national trend of rising mental health issues among young patients. According to the AAP, over the last decade the number of young people aged 6-17 years requiring mental health care has risen from 9% to more than 14%. In outpatient settings, many pediatricians report that half or more of their visits are dedicated to these issues, a number that may spill out into the hospital setting as well.
According to Dr. Fisher, pediatric hospitalists today see increasing numbers of chronic and acute diseases accompanied by mental and behavioral health issues. “We wanted to underscore this complexity in the competencies,” she explained. “We needed to focus new attention on how to identify and treat children with behavioral or psychiatric diagnoses or needs.”
Other new areas of focus include infection care and antimicrobial stewardship. “We see kids on antibiotics in hospital settings and we need to focus on narrowing choices, decreasing use, and shortening duration,” Dr. Gage said.
Dr. Maniscalco said that, overall, the changes represent the evolution of the field. “Pediatric hospitalists are taking on far more patients with acute and complex issues,” she explained. “Our skill set is coming into focus.”
Dr. Gage added that there is an increased need for pediatric hospitalists to be adept at “managing acute psychiatric care and navigating the mental health care arena.”
There’s also the growing need for an understanding of neonatal abstinence and opioid withdrawal syndrome. “This is definitely a hot topic and one that most hospitalists must address today,” Dr. Gage said. “That wasn’t the case a decade ago.”
Hospital care for pediatrics today often means a team effort, including pediatric hospitalists, surgeons, mental health professionals, and others. Often missing from the picture today are primary care physicians, who instead refer a growing percentage of their patients to hospitalists. The pediatric hospitalist’s role has evolved and grown from what it was 10 years ago, as reflected in the competencies.
“We are very much coordinating care and collaborating today in ways we weren’t 10 years ago,” said Dr. Gage. “There’s a lot more attention on creating partnerships. While we may not always be the ones performing procedures, we will most likely take part in patient care, especially as surgeons step farther away from care outside of the OR.”
The field has also become more family centered, said Dr. Gage. “All of health care today is more astute about the participation of families in care,” she said. “We kept that in mind in developing the competencies.”
Also important in this set of competencies was the concept of high-value care using evidence-based medicine.
Into the field
How exactly the core competencies will be utilized from one hospital or setting to the next will vary, said Dr. Fisher. “For some sites, they can aid existing teaching programs, and they will most likely adapt their curriculum to address the new competencies, informing how they teach.”
Even in centers where there isn’t a formal academic role, teaching still occurs. “Pediatric hospitalists have roles on committees and projects, and giving a talk to respiratory therapists, having group meetings – these all involve teaching in some form,” Dr. Fisher said. “Most physicians will determine how they wish to insert the competencies into their own education, as well as use them to educate others.”
Regardless of how they may be used locally, Dr. Fisher anticipates that the entire pediatric hospitalist community will appreciate the updates. “The competencies address our rapidly changing health care environment,” she said. “We believe the field will benefit from the additions and changes.”
Indeed, the core competencies will help standardize and improve consistency of care across the board. Improved efficiencies, economics, and practices are all desired and expected outcomes from the release of the revised competencies.
To ensure that the changes to the competencies are highlighted in settings nationwide, the editors and associate editors hope to present about them at upcoming conferences, including at the SHM 2020 Annual Conference, the Pediatric Hospital Medicine conference, the Pediatric Academic Societies conference, and the American Pediatric Association.
“We want to present to as many venues as possible to bring people up to speed and ensure they are aware of the changes,” Dr. Teferi said. “We’ll be including workshops with visual aids, along with our presentations.”
While this update represents a 10-year evolution, the editors and the SHM Pediatric Special Interest Group do not have an exact time frame for when the core competencies will need another revision. As quickly as the profession is developing, it may be as few as 5 years, but may also be another full decade.
“Like most fields, we will continue to evolve as our roles become better defined and we gain more knowledge,” Dr. Maniscalco said. “The core competencies represent the field whether a senior pediatric hospitalist, a fellow, or an educator. They bring the field together and provide education for everyone. That’s their role.”
New core competencies reflect a decade of change
New core competencies reflect a decade of change
Over the past 10 years, much has changed in the world of pediatric hospital medicine. The annual national PHM conference sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics (AAP), and the Academic Pediatric Association (APA) is robust; textbooks and journal articles in the field abound; and networks and training in research, quality improvement, and education are successful and ongoing.
Much of this did not exist or was in its infancy back in 2010. Since then, it has grown and greatly evolved. In parallel, medicine and society have changed. These influences on health care, along with the growth of the field over time, prompted a review and revision of the 2010 PHM Core Competencies published by SHM. With support from the society, the Pediatric Hospital Medicine Special Interest Group launched the plan for revision of the PHM Core Competencies.
The selected editors included Sandra Gage, MD, PhD, SFHM, of Phoenix Children’s Hospital; Erin Stucky Fisher, MD, MHM, of UCSD/Rady Children’s Hospital in San Diego; Jennifer Maniscalco, MD, MPH, of Johns Hopkins All Children’s Hospital in St. Petersburg, Fla.; and Sofia Teferi, MD, SFHM, a pediatric hospitalist based at Bon Secours St. Mary’s Hospital in Richmond, Va. They began their work in 2017 along with six associate editors, meeting every 2 weeks via conference call, dividing the work accordingly.
Dr. Teferi served in a new and critical role as contributing editor. She described her role as a “sweeper” of sorts, bringing her unique perspective to the process. “The other three members are from academic settings, and I’m from a community setting, which is very different,” Dr. Teferi said. “I went through all the chapters to ensure they were inclusive of the community setting.”
According to Dr. Gage, “the purpose of the original PHM Core Competencies was to define the roles and responsibilities of a PHM practitioner. In the intervening 10 years, the field has changed and matured, and we have solidified our role since then.”
Today’s pediatric hospitalists, for instance, may coordinate care in EDs, provide inpatient consultations, engage or lead quality improvement programs, and teach. The demands for pediatric hospital care today go beyond the training provided in a standard pediatric residency. The core competencies need to provide the information necessary, therefore, to ensure pediatric hospital medicine is practiced at its most informed level.
A profession transformed
At the time of the first set of core competencies, there were over 2,500 members in three core societies in which pediatric hospitalists were members: the AAP, the APA, and SHM. As of 2017, those numbers have swelled as the care for children in the hospital setting has shifted away from these patients’ primary care providers.
The original core competencies included 54 chapters, designed to be used independent of the others. They provided a foundation for the creation of pediatric hospital medicine and served to standardize and improve inpatient training practices.
For the new core competencies, every single chapter was reviewed line by line, Dr. Gage said. Many chapters had content modified, and new chapters were added to reflect the evolution of the field and of medicine. “We added about 14 new chapters, adjusted the titles of others, and significantly changed the content of over half,” Dr. Gage explained. “They are fairly broad changes, related to the breadth of the practice today.”
Dr. Teferi noted that practitioners can use the updated competencies with additions to the service lines that have arisen since the last version. “These include areas like step down and newborn nursery, things that weren’t part of our portfolio 10 years ago,” she said. “This reflects the fact that often you’ll see a hospital leader who might want to add to a hospitalist’s portfolio of services because there is no one else to do it. Or maybe community pediatrics no longer want to treat babies, so we add that. The settings vary widely today and we need the competencies to address that.”
Practices within these settings can also vary widely. Teaching, palliative care, airway management, critical care, and anesthesia may all come into play, among other factors. Research opportunities throughout the field also continue to expand.
Dr. Fisher said that the editors and associate editors kept in mind the fact that not every hospital would have all the resources necessary at its fingertips. “The competencies must reflect the realities of the variety of community settings,” she said. “Also, on a national level, the majority of pediatric patients are not seen in a children’s hospital. Community sites are where pediatric hospitalists are not only advocates for care, but can be working with limited resources – the ‘lone soldiers.’ We wanted to make sure the competencies reflect that reality and environment community site or not; academic site or not; tertiary care site or not; rural or not – these are overlapping but independent considerations for all who practice pediatric hospital medicine – a Venn diagram, and the PHM core competencies try to attend to all of those.”
This made Dr. Teferi’s perspective all the more important. “While many, including other editors and associate editors, work in community sites, Dr. Teferi has this as her unique and sole focus. She brought a unique viewpoint to the table,” Dr. Fisher said.
A goal of the core competencies is to make it possible for a pediatric hospitalist to move to a different practice environment and still provide the same level of high-quality care. “It’s difficult but important to grasp the concepts and competencies of various settings,” Dr. Fisher said. “In this way, our competencies are a parallel model to the adult hospitalist competencies.”
The editors surveyed practitioners across the country to gather their input on content, and brought on topic experts to write the new chapters. “If we didn’t have an author for a specific chapter or area from the last set of competencies, we came to a consensus on who the new one should be,” Dr. Gage explained. “We looked for known and accepted experts in the field by reviewing the literature and conference lecturers at all major PHM meetings.”
Once the editors and associate editors worked with authors to refine their chapter(s), the chapters were sent to multiple external reviewers including subgroups of SHM, AAP, and APA, as well as a variety of other associations. They provided input that the editors and associate editors collated, reviewed, and incorporated according to consensus and discussion with the authors.
A preview
As far as the actual changes go, some of new chapters include four common clinical, two core skills, three specialized services, and five health care systems, with many others undergoing content changes, according to Dr. Gage.
Major considerations in developing the new competencies include the national trend of rising mental health issues among young patients. According to the AAP, over the last decade the number of young people aged 6-17 years requiring mental health care has risen from 9% to more than 14%. In outpatient settings, many pediatricians report that half or more of their visits are dedicated to these issues, a number that may spill out into the hospital setting as well.
According to Dr. Fisher, pediatric hospitalists today see increasing numbers of chronic and acute diseases accompanied by mental and behavioral health issues. “We wanted to underscore this complexity in the competencies,” she explained. “We needed to focus new attention on how to identify and treat children with behavioral or psychiatric diagnoses or needs.”
Other new areas of focus include infection care and antimicrobial stewardship. “We see kids on antibiotics in hospital settings and we need to focus on narrowing choices, decreasing use, and shortening duration,” Dr. Gage said.
Dr. Maniscalco said that, overall, the changes represent the evolution of the field. “Pediatric hospitalists are taking on far more patients with acute and complex issues,” she explained. “Our skill set is coming into focus.”
Dr. Gage added that there is an increased need for pediatric hospitalists to be adept at “managing acute psychiatric care and navigating the mental health care arena.”
There’s also the growing need for an understanding of neonatal abstinence and opioid withdrawal syndrome. “This is definitely a hot topic and one that most hospitalists must address today,” Dr. Gage said. “That wasn’t the case a decade ago.”
Hospital care for pediatrics today often means a team effort, including pediatric hospitalists, surgeons, mental health professionals, and others. Often missing from the picture today are primary care physicians, who instead refer a growing percentage of their patients to hospitalists. The pediatric hospitalist’s role has evolved and grown from what it was 10 years ago, as reflected in the competencies.
“We are very much coordinating care and collaborating today in ways we weren’t 10 years ago,” said Dr. Gage. “There’s a lot more attention on creating partnerships. While we may not always be the ones performing procedures, we will most likely take part in patient care, especially as surgeons step farther away from care outside of the OR.”
The field has also become more family centered, said Dr. Gage. “All of health care today is more astute about the participation of families in care,” she said. “We kept that in mind in developing the competencies.”
Also important in this set of competencies was the concept of high-value care using evidence-based medicine.
Into the field
How exactly the core competencies will be utilized from one hospital or setting to the next will vary, said Dr. Fisher. “For some sites, they can aid existing teaching programs, and they will most likely adapt their curriculum to address the new competencies, informing how they teach.”
Even in centers where there isn’t a formal academic role, teaching still occurs. “Pediatric hospitalists have roles on committees and projects, and giving a talk to respiratory therapists, having group meetings – these all involve teaching in some form,” Dr. Fisher said. “Most physicians will determine how they wish to insert the competencies into their own education, as well as use them to educate others.”
Regardless of how they may be used locally, Dr. Fisher anticipates that the entire pediatric hospitalist community will appreciate the updates. “The competencies address our rapidly changing health care environment,” she said. “We believe the field will benefit from the additions and changes.”
Indeed, the core competencies will help standardize and improve consistency of care across the board. Improved efficiencies, economics, and practices are all desired and expected outcomes from the release of the revised competencies.
To ensure that the changes to the competencies are highlighted in settings nationwide, the editors and associate editors hope to present about them at upcoming conferences, including at the SHM 2020 Annual Conference, the Pediatric Hospital Medicine conference, the Pediatric Academic Societies conference, and the American Pediatric Association.
“We want to present to as many venues as possible to bring people up to speed and ensure they are aware of the changes,” Dr. Teferi said. “We’ll be including workshops with visual aids, along with our presentations.”
While this update represents a 10-year evolution, the editors and the SHM Pediatric Special Interest Group do not have an exact time frame for when the core competencies will need another revision. As quickly as the profession is developing, it may be as few as 5 years, but may also be another full decade.
“Like most fields, we will continue to evolve as our roles become better defined and we gain more knowledge,” Dr. Maniscalco said. “The core competencies represent the field whether a senior pediatric hospitalist, a fellow, or an educator. They bring the field together and provide education for everyone. That’s their role.”
Over the past 10 years, much has changed in the world of pediatric hospital medicine. The annual national PHM conference sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics (AAP), and the Academic Pediatric Association (APA) is robust; textbooks and journal articles in the field abound; and networks and training in research, quality improvement, and education are successful and ongoing.
Much of this did not exist or was in its infancy back in 2010. Since then, it has grown and greatly evolved. In parallel, medicine and society have changed. These influences on health care, along with the growth of the field over time, prompted a review and revision of the 2010 PHM Core Competencies published by SHM. With support from the society, the Pediatric Hospital Medicine Special Interest Group launched the plan for revision of the PHM Core Competencies.
The selected editors included Sandra Gage, MD, PhD, SFHM, of Phoenix Children’s Hospital; Erin Stucky Fisher, MD, MHM, of UCSD/Rady Children’s Hospital in San Diego; Jennifer Maniscalco, MD, MPH, of Johns Hopkins All Children’s Hospital in St. Petersburg, Fla.; and Sofia Teferi, MD, SFHM, a pediatric hospitalist based at Bon Secours St. Mary’s Hospital in Richmond, Va. They began their work in 2017 along with six associate editors, meeting every 2 weeks via conference call, dividing the work accordingly.
Dr. Teferi served in a new and critical role as contributing editor. She described her role as a “sweeper” of sorts, bringing her unique perspective to the process. “The other three members are from academic settings, and I’m from a community setting, which is very different,” Dr. Teferi said. “I went through all the chapters to ensure they were inclusive of the community setting.”
According to Dr. Gage, “the purpose of the original PHM Core Competencies was to define the roles and responsibilities of a PHM practitioner. In the intervening 10 years, the field has changed and matured, and we have solidified our role since then.”
Today’s pediatric hospitalists, for instance, may coordinate care in EDs, provide inpatient consultations, engage or lead quality improvement programs, and teach. The demands for pediatric hospital care today go beyond the training provided in a standard pediatric residency. The core competencies need to provide the information necessary, therefore, to ensure pediatric hospital medicine is practiced at its most informed level.
A profession transformed
At the time of the first set of core competencies, there were over 2,500 members in three core societies in which pediatric hospitalists were members: the AAP, the APA, and SHM. As of 2017, those numbers have swelled as the care for children in the hospital setting has shifted away from these patients’ primary care providers.
The original core competencies included 54 chapters, designed to be used independent of the others. They provided a foundation for the creation of pediatric hospital medicine and served to standardize and improve inpatient training practices.
For the new core competencies, every single chapter was reviewed line by line, Dr. Gage said. Many chapters had content modified, and new chapters were added to reflect the evolution of the field and of medicine. “We added about 14 new chapters, adjusted the titles of others, and significantly changed the content of over half,” Dr. Gage explained. “They are fairly broad changes, related to the breadth of the practice today.”
Dr. Teferi noted that practitioners can use the updated competencies with additions to the service lines that have arisen since the last version. “These include areas like step down and newborn nursery, things that weren’t part of our portfolio 10 years ago,” she said. “This reflects the fact that often you’ll see a hospital leader who might want to add to a hospitalist’s portfolio of services because there is no one else to do it. Or maybe community pediatrics no longer want to treat babies, so we add that. The settings vary widely today and we need the competencies to address that.”
Practices within these settings can also vary widely. Teaching, palliative care, airway management, critical care, and anesthesia may all come into play, among other factors. Research opportunities throughout the field also continue to expand.
Dr. Fisher said that the editors and associate editors kept in mind the fact that not every hospital would have all the resources necessary at its fingertips. “The competencies must reflect the realities of the variety of community settings,” she said. “Also, on a national level, the majority of pediatric patients are not seen in a children’s hospital. Community sites are where pediatric hospitalists are not only advocates for care, but can be working with limited resources – the ‘lone soldiers.’ We wanted to make sure the competencies reflect that reality and environment community site or not; academic site or not; tertiary care site or not; rural or not – these are overlapping but independent considerations for all who practice pediatric hospital medicine – a Venn diagram, and the PHM core competencies try to attend to all of those.”
This made Dr. Teferi’s perspective all the more important. “While many, including other editors and associate editors, work in community sites, Dr. Teferi has this as her unique and sole focus. She brought a unique viewpoint to the table,” Dr. Fisher said.
A goal of the core competencies is to make it possible for a pediatric hospitalist to move to a different practice environment and still provide the same level of high-quality care. “It’s difficult but important to grasp the concepts and competencies of various settings,” Dr. Fisher said. “In this way, our competencies are a parallel model to the adult hospitalist competencies.”
The editors surveyed practitioners across the country to gather their input on content, and brought on topic experts to write the new chapters. “If we didn’t have an author for a specific chapter or area from the last set of competencies, we came to a consensus on who the new one should be,” Dr. Gage explained. “We looked for known and accepted experts in the field by reviewing the literature and conference lecturers at all major PHM meetings.”
Once the editors and associate editors worked with authors to refine their chapter(s), the chapters were sent to multiple external reviewers including subgroups of SHM, AAP, and APA, as well as a variety of other associations. They provided input that the editors and associate editors collated, reviewed, and incorporated according to consensus and discussion with the authors.
A preview
As far as the actual changes go, some of new chapters include four common clinical, two core skills, three specialized services, and five health care systems, with many others undergoing content changes, according to Dr. Gage.
Major considerations in developing the new competencies include the national trend of rising mental health issues among young patients. According to the AAP, over the last decade the number of young people aged 6-17 years requiring mental health care has risen from 9% to more than 14%. In outpatient settings, many pediatricians report that half or more of their visits are dedicated to these issues, a number that may spill out into the hospital setting as well.
According to Dr. Fisher, pediatric hospitalists today see increasing numbers of chronic and acute diseases accompanied by mental and behavioral health issues. “We wanted to underscore this complexity in the competencies,” she explained. “We needed to focus new attention on how to identify and treat children with behavioral or psychiatric diagnoses or needs.”
Other new areas of focus include infection care and antimicrobial stewardship. “We see kids on antibiotics in hospital settings and we need to focus on narrowing choices, decreasing use, and shortening duration,” Dr. Gage said.
Dr. Maniscalco said that, overall, the changes represent the evolution of the field. “Pediatric hospitalists are taking on far more patients with acute and complex issues,” she explained. “Our skill set is coming into focus.”
Dr. Gage added that there is an increased need for pediatric hospitalists to be adept at “managing acute psychiatric care and navigating the mental health care arena.”
There’s also the growing need for an understanding of neonatal abstinence and opioid withdrawal syndrome. “This is definitely a hot topic and one that most hospitalists must address today,” Dr. Gage said. “That wasn’t the case a decade ago.”
Hospital care for pediatrics today often means a team effort, including pediatric hospitalists, surgeons, mental health professionals, and others. Often missing from the picture today are primary care physicians, who instead refer a growing percentage of their patients to hospitalists. The pediatric hospitalist’s role has evolved and grown from what it was 10 years ago, as reflected in the competencies.
“We are very much coordinating care and collaborating today in ways we weren’t 10 years ago,” said Dr. Gage. “There’s a lot more attention on creating partnerships. While we may not always be the ones performing procedures, we will most likely take part in patient care, especially as surgeons step farther away from care outside of the OR.”
The field has also become more family centered, said Dr. Gage. “All of health care today is more astute about the participation of families in care,” she said. “We kept that in mind in developing the competencies.”
Also important in this set of competencies was the concept of high-value care using evidence-based medicine.
Into the field
How exactly the core competencies will be utilized from one hospital or setting to the next will vary, said Dr. Fisher. “For some sites, they can aid existing teaching programs, and they will most likely adapt their curriculum to address the new competencies, informing how they teach.”
Even in centers where there isn’t a formal academic role, teaching still occurs. “Pediatric hospitalists have roles on committees and projects, and giving a talk to respiratory therapists, having group meetings – these all involve teaching in some form,” Dr. Fisher said. “Most physicians will determine how they wish to insert the competencies into their own education, as well as use them to educate others.”
Regardless of how they may be used locally, Dr. Fisher anticipates that the entire pediatric hospitalist community will appreciate the updates. “The competencies address our rapidly changing health care environment,” she said. “We believe the field will benefit from the additions and changes.”
Indeed, the core competencies will help standardize and improve consistency of care across the board. Improved efficiencies, economics, and practices are all desired and expected outcomes from the release of the revised competencies.
To ensure that the changes to the competencies are highlighted in settings nationwide, the editors and associate editors hope to present about them at upcoming conferences, including at the SHM 2020 Annual Conference, the Pediatric Hospital Medicine conference, the Pediatric Academic Societies conference, and the American Pediatric Association.
“We want to present to as many venues as possible to bring people up to speed and ensure they are aware of the changes,” Dr. Teferi said. “We’ll be including workshops with visual aids, along with our presentations.”
While this update represents a 10-year evolution, the editors and the SHM Pediatric Special Interest Group do not have an exact time frame for when the core competencies will need another revision. As quickly as the profession is developing, it may be as few as 5 years, but may also be another full decade.
“Like most fields, we will continue to evolve as our roles become better defined and we gain more knowledge,” Dr. Maniscalco said. “The core competencies represent the field whether a senior pediatric hospitalist, a fellow, or an educator. They bring the field together and provide education for everyone. That’s their role.”
Administrative burden and burnout
In May 2019, SHM sent a letter to U.S. Senators Tina Smith and Bill Cassidy in support of the Reducing Administrative Costs and Burdens in Health Care Act of 2019. In excerpts from the letter below, the society details the link between administrative burdens and physician burnout.
Providers and hospital systems expend countless resources, both time and dollars, adhering to unnecessary and excessive administrative burdens instead of investing those resources in providing quality patient care. National data suggests that more than 50 percent of the physician workforce is burned out. Excessive administrative burden is a major contributor to physician burnout, which negatively affects quality and safety within the hospital and further increases health care costs. Notably, the Reducing Administrative Costs and Burdens in Health Care Act calls for a 50% reduction of unnecessary administrative costs from the Department of Health and Human Services within the next ten years.
Hospitalists are front-line clinicians in America's acute care hospitals whose professional focus is the general medical care of hospitalized patients. Their unique position in the healthcare system affords hospitalists a distinct perspective and systems-based approach to confronting and solving challenges at the individual provider and overall institutional level of the hospital. In this capacity, hospitalists experience multiple examples of administrative requirements directly detracting from patient care and redirecting finite resources away from care to meet compliance demands.
By way of example, navigating the administrative rules around inpatient admissions and outpatient observation care, for example, requires a significant shift of healthcare resources away from patient care. While patients admitted under observation receive nearly identical care to those admitted as an inpatient, hospitalists report that, in addition to themselves as the direct healthcare provider, status determinations between inpatient admissions and outpatient observation care require the input of a myriad of staff including nursing, coding/compliance teams, utilization review, case managers and external review organizations. A recent study in the Journal of Hospital Medicine indicated that an average of 5.1 full time employees, not including case managers, are required to navigate the audit and appeals process associated with hospital stay status determinations. These are resources that should be directly used for patient care, but are redirected towards regulation compliance, increasing cost of care without increasing quality.
To read the entire letter, visit https://www.hospitalmedicine.org/policy--advocacy/letters/shm-supports-the-reducing-administrative-costs-and-burdens-in-health-care-act-of-2019/.
In May 2019, SHM sent a letter to U.S. Senators Tina Smith and Bill Cassidy in support of the Reducing Administrative Costs and Burdens in Health Care Act of 2019. In excerpts from the letter below, the society details the link between administrative burdens and physician burnout.
Providers and hospital systems expend countless resources, both time and dollars, adhering to unnecessary and excessive administrative burdens instead of investing those resources in providing quality patient care. National data suggests that more than 50 percent of the physician workforce is burned out. Excessive administrative burden is a major contributor to physician burnout, which negatively affects quality and safety within the hospital and further increases health care costs. Notably, the Reducing Administrative Costs and Burdens in Health Care Act calls for a 50% reduction of unnecessary administrative costs from the Department of Health and Human Services within the next ten years.
Hospitalists are front-line clinicians in America's acute care hospitals whose professional focus is the general medical care of hospitalized patients. Their unique position in the healthcare system affords hospitalists a distinct perspective and systems-based approach to confronting and solving challenges at the individual provider and overall institutional level of the hospital. In this capacity, hospitalists experience multiple examples of administrative requirements directly detracting from patient care and redirecting finite resources away from care to meet compliance demands.
By way of example, navigating the administrative rules around inpatient admissions and outpatient observation care, for example, requires a significant shift of healthcare resources away from patient care. While patients admitted under observation receive nearly identical care to those admitted as an inpatient, hospitalists report that, in addition to themselves as the direct healthcare provider, status determinations between inpatient admissions and outpatient observation care require the input of a myriad of staff including nursing, coding/compliance teams, utilization review, case managers and external review organizations. A recent study in the Journal of Hospital Medicine indicated that an average of 5.1 full time employees, not including case managers, are required to navigate the audit and appeals process associated with hospital stay status determinations. These are resources that should be directly used for patient care, but are redirected towards regulation compliance, increasing cost of care without increasing quality.
To read the entire letter, visit https://www.hospitalmedicine.org/policy--advocacy/letters/shm-supports-the-reducing-administrative-costs-and-burdens-in-health-care-act-of-2019/.
In May 2019, SHM sent a letter to U.S. Senators Tina Smith and Bill Cassidy in support of the Reducing Administrative Costs and Burdens in Health Care Act of 2019. In excerpts from the letter below, the society details the link between administrative burdens and physician burnout.
Providers and hospital systems expend countless resources, both time and dollars, adhering to unnecessary and excessive administrative burdens instead of investing those resources in providing quality patient care. National data suggests that more than 50 percent of the physician workforce is burned out. Excessive administrative burden is a major contributor to physician burnout, which negatively affects quality and safety within the hospital and further increases health care costs. Notably, the Reducing Administrative Costs and Burdens in Health Care Act calls for a 50% reduction of unnecessary administrative costs from the Department of Health and Human Services within the next ten years.
Hospitalists are front-line clinicians in America's acute care hospitals whose professional focus is the general medical care of hospitalized patients. Their unique position in the healthcare system affords hospitalists a distinct perspective and systems-based approach to confronting and solving challenges at the individual provider and overall institutional level of the hospital. In this capacity, hospitalists experience multiple examples of administrative requirements directly detracting from patient care and redirecting finite resources away from care to meet compliance demands.
By way of example, navigating the administrative rules around inpatient admissions and outpatient observation care, for example, requires a significant shift of healthcare resources away from patient care. While patients admitted under observation receive nearly identical care to those admitted as an inpatient, hospitalists report that, in addition to themselves as the direct healthcare provider, status determinations between inpatient admissions and outpatient observation care require the input of a myriad of staff including nursing, coding/compliance teams, utilization review, case managers and external review organizations. A recent study in the Journal of Hospital Medicine indicated that an average of 5.1 full time employees, not including case managers, are required to navigate the audit and appeals process associated with hospital stay status determinations. These are resources that should be directly used for patient care, but are redirected towards regulation compliance, increasing cost of care without increasing quality.
To read the entire letter, visit https://www.hospitalmedicine.org/policy--advocacy/letters/shm-supports-the-reducing-administrative-costs-and-burdens-in-health-care-act-of-2019/.
Community pediatric care is diminishing
The mantra of community hospital administrators is that pediatric care does not pay. Neonatal intensive care pays. For pediatrics, it is similar to how football programs (Medicare patients) support minor sports (pediatrics and obstetrics) at colleges. However, fewer even mildly sick newborns are cared for at community hospitals, which has led to a centralization of neonatal and pediatric care and a loss of pediatric expertise at the affected hospitals.
Pediatric hospitalists are hired to cover the pediatric floor, the emergency department, and labor and delivery, then fired over empty pediatric beds. The rationale expressed is that pediatricians have done such a good job in preventive care that children rarely need hospitalization, so why have a pediatric inpatient unit? It is true that preventive care has been an integral part of primary care for children. Significantly less that 1% of child office visits result in hospitalization.
Advocate Health Care has closed inpatient pediatric units at Illinois Masonic, on Chicago’s North Side, Good Samaritan in Downers Grove, and Good Shepherd in Barrington. Units also have been closed at Mount Sinai in North Lawndale, Norwegian American on Chicago’s West Side, Little Company of Mary in Evergreen Park, and Alexian Brothers in Elk Grove.
As a Chicago-area pediatrician for more than 30 years, I have learned several things about community-based pediatric care:
1. Pediatrics is a geographic specialty. Parents will travel to shop, but would rather walk or have a short ride to their children’s medical providers. Secondary care should be community based, and hospitalization, if necessary, should be close by as well.
2. Hospitals that ceased delivering pediatric inpatient care lost their child-friendliness and pediatric competence, becoming uncomfortable delivering almost any care for children (e.g., sedated MRIs and EEGs, x-rays and ultrasounds, ECGs and echocardiograms, and emergency care).
3. In almost all hospitals, after pediatrics was gone eventually so passed obstetrics (another less remunerative specialty). Sick newborns need immediate, competent care. Most pediatric hospitalizations are short term, often overnight. Delaying newborn care is a medicolegal nightmare. and exposes the child and his or her family to a potentially dangerous drive or helicopter ride.
4. As pediatric subspecialty care becomes more centralized, parents are asked to travel for hours to see a pediatric specialist. There are times when that is necessary (e.g., cardiovascular surgery). Pediatric subspecialists, such as pediatric otolaryngologists, then leave community hospitals, forcing even minor surgeries (e.g., ear ventilation tubes) to be done at a center. In rural areas, this could mean hours of travel, lost work days, and family disruption.
5. Children’s hospitals get uninsured and publicly insured children sent hundreds of miles, because there were no subspecialists in the community who would care for these children.
What is the solution, in our profit-focused health care system?
1. Hospitals’ Certificates of Need could include a mandate for pediatric care.
2. Children’s hospitals could be made responsible for community-based care within their geographic catchment areas.
3. The state or the federal government could mandate and financially support community-based hospital care.
4. Deciding what level of care might be appropriate for each community could depend upon closeness to a pediatric hospital, health problems in the community, and the availability of pediatric specialists.
5. A condition for medical licensure might be that a community-based pediatric subspecialist is required to care for a proportion of the uninsured or publicly insured children in his or her area.
6. Reimbursements for pediatric care need to rise enough to make caring for children worth it.
The major decision point regarding care for children cannot be financial, but must instead embrace the needs of each affected community. If quality health care is a right, and not a privilege, then it is time to stop closing pediatric inpatient units, and, instead, look for creative ways to better care for our children.
This process has led to pediatric care being available only in designated centers. The centralization of pediatric care has progressed from 30 years ago, when most community hospitals had inpatient pediatric units, to the search for innovative ways to fill pediatric beds in the mid-90s (sick day care, flex- or shared pediatric units), to the wholesale closure of community pediatric inpatient beds, from 2000 to the present. I have, unfortunately, seen this firsthand, watching the rise of pediatric mega-hospitals and the demise of community pediatrics. It is a simple financial argument. Care for children simply does not pay nearly as well as does care for adults, especially Medicaid patients. Pediatricians are the poorest paid practicing doctors (public health doctors are paid less).
It is true that pediatricians always have been at the forefront of preventive medicine, and that pediatric patients almost always get better, in spite of our best-intentioned interventions. So community-based pediatricians admit very few patients.
With the loss of pediatric units, community hospitals lose their comfort caring for children. This includes phlebotomy, x-ray, trauma, surgery, and behavioral health. And eroding community hospital pediatric expertise has catastrophic implications for rural hospitals, where parents may have to drive for hours to find a child-friendly emergency department.
Is there an answer?
1. Hospitals are responsible for the patients they serve, including children. Why should a hospital be able to close pediatric services so easily?
2. Every hospital that sees children, through the emergency department, needs to have a pediatrician available to evaluate a child, 24/7.
3. There needs to be an observation unit for children, with pediatric staffing, for overnight stays.
4. Pediatric hospitalists should be staffing community hospitals.
5. Pediatric behavioral health resources need to be available, e.g., inpatient psychiatry, partial hospitalization programs, intensive outpatient programs.
6. Telehealth communication is not adequate to address acute care problems, because the hospital caring for the child has to have the proper equipment and adequate expertise to carry out the recommendations of the teleconsultant.
If we accept that our children will shape the future, we must allow them to survive and thrive. Is health care a right or a privilege, and is it just for adults or for children, too?
Dr. Ochs is in private practice at Ravenswood Pediatrics in Chicago. He said he had no relevant financial disclosures. Email him at [email protected].
The mantra of community hospital administrators is that pediatric care does not pay. Neonatal intensive care pays. For pediatrics, it is similar to how football programs (Medicare patients) support minor sports (pediatrics and obstetrics) at colleges. However, fewer even mildly sick newborns are cared for at community hospitals, which has led to a centralization of neonatal and pediatric care and a loss of pediatric expertise at the affected hospitals.
Pediatric hospitalists are hired to cover the pediatric floor, the emergency department, and labor and delivery, then fired over empty pediatric beds. The rationale expressed is that pediatricians have done such a good job in preventive care that children rarely need hospitalization, so why have a pediatric inpatient unit? It is true that preventive care has been an integral part of primary care for children. Significantly less that 1% of child office visits result in hospitalization.
Advocate Health Care has closed inpatient pediatric units at Illinois Masonic, on Chicago’s North Side, Good Samaritan in Downers Grove, and Good Shepherd in Barrington. Units also have been closed at Mount Sinai in North Lawndale, Norwegian American on Chicago’s West Side, Little Company of Mary in Evergreen Park, and Alexian Brothers in Elk Grove.
As a Chicago-area pediatrician for more than 30 years, I have learned several things about community-based pediatric care:
1. Pediatrics is a geographic specialty. Parents will travel to shop, but would rather walk or have a short ride to their children’s medical providers. Secondary care should be community based, and hospitalization, if necessary, should be close by as well.
2. Hospitals that ceased delivering pediatric inpatient care lost their child-friendliness and pediatric competence, becoming uncomfortable delivering almost any care for children (e.g., sedated MRIs and EEGs, x-rays and ultrasounds, ECGs and echocardiograms, and emergency care).
3. In almost all hospitals, after pediatrics was gone eventually so passed obstetrics (another less remunerative specialty). Sick newborns need immediate, competent care. Most pediatric hospitalizations are short term, often overnight. Delaying newborn care is a medicolegal nightmare. and exposes the child and his or her family to a potentially dangerous drive or helicopter ride.
4. As pediatric subspecialty care becomes more centralized, parents are asked to travel for hours to see a pediatric specialist. There are times when that is necessary (e.g., cardiovascular surgery). Pediatric subspecialists, such as pediatric otolaryngologists, then leave community hospitals, forcing even minor surgeries (e.g., ear ventilation tubes) to be done at a center. In rural areas, this could mean hours of travel, lost work days, and family disruption.
5. Children’s hospitals get uninsured and publicly insured children sent hundreds of miles, because there were no subspecialists in the community who would care for these children.
What is the solution, in our profit-focused health care system?
1. Hospitals’ Certificates of Need could include a mandate for pediatric care.
2. Children’s hospitals could be made responsible for community-based care within their geographic catchment areas.
3. The state or the federal government could mandate and financially support community-based hospital care.
4. Deciding what level of care might be appropriate for each community could depend upon closeness to a pediatric hospital, health problems in the community, and the availability of pediatric specialists.
5. A condition for medical licensure might be that a community-based pediatric subspecialist is required to care for a proportion of the uninsured or publicly insured children in his or her area.
6. Reimbursements for pediatric care need to rise enough to make caring for children worth it.
The major decision point regarding care for children cannot be financial, but must instead embrace the needs of each affected community. If quality health care is a right, and not a privilege, then it is time to stop closing pediatric inpatient units, and, instead, look for creative ways to better care for our children.
This process has led to pediatric care being available only in designated centers. The centralization of pediatric care has progressed from 30 years ago, when most community hospitals had inpatient pediatric units, to the search for innovative ways to fill pediatric beds in the mid-90s (sick day care, flex- or shared pediatric units), to the wholesale closure of community pediatric inpatient beds, from 2000 to the present. I have, unfortunately, seen this firsthand, watching the rise of pediatric mega-hospitals and the demise of community pediatrics. It is a simple financial argument. Care for children simply does not pay nearly as well as does care for adults, especially Medicaid patients. Pediatricians are the poorest paid practicing doctors (public health doctors are paid less).
It is true that pediatricians always have been at the forefront of preventive medicine, and that pediatric patients almost always get better, in spite of our best-intentioned interventions. So community-based pediatricians admit very few patients.
With the loss of pediatric units, community hospitals lose their comfort caring for children. This includes phlebotomy, x-ray, trauma, surgery, and behavioral health. And eroding community hospital pediatric expertise has catastrophic implications for rural hospitals, where parents may have to drive for hours to find a child-friendly emergency department.
Is there an answer?
1. Hospitals are responsible for the patients they serve, including children. Why should a hospital be able to close pediatric services so easily?
2. Every hospital that sees children, through the emergency department, needs to have a pediatrician available to evaluate a child, 24/7.
3. There needs to be an observation unit for children, with pediatric staffing, for overnight stays.
4. Pediatric hospitalists should be staffing community hospitals.
5. Pediatric behavioral health resources need to be available, e.g., inpatient psychiatry, partial hospitalization programs, intensive outpatient programs.
6. Telehealth communication is not adequate to address acute care problems, because the hospital caring for the child has to have the proper equipment and adequate expertise to carry out the recommendations of the teleconsultant.
If we accept that our children will shape the future, we must allow them to survive and thrive. Is health care a right or a privilege, and is it just for adults or for children, too?
Dr. Ochs is in private practice at Ravenswood Pediatrics in Chicago. He said he had no relevant financial disclosures. Email him at [email protected].
The mantra of community hospital administrators is that pediatric care does not pay. Neonatal intensive care pays. For pediatrics, it is similar to how football programs (Medicare patients) support minor sports (pediatrics and obstetrics) at colleges. However, fewer even mildly sick newborns are cared for at community hospitals, which has led to a centralization of neonatal and pediatric care and a loss of pediatric expertise at the affected hospitals.
Pediatric hospitalists are hired to cover the pediatric floor, the emergency department, and labor and delivery, then fired over empty pediatric beds. The rationale expressed is that pediatricians have done such a good job in preventive care that children rarely need hospitalization, so why have a pediatric inpatient unit? It is true that preventive care has been an integral part of primary care for children. Significantly less that 1% of child office visits result in hospitalization.
Advocate Health Care has closed inpatient pediatric units at Illinois Masonic, on Chicago’s North Side, Good Samaritan in Downers Grove, and Good Shepherd in Barrington. Units also have been closed at Mount Sinai in North Lawndale, Norwegian American on Chicago’s West Side, Little Company of Mary in Evergreen Park, and Alexian Brothers in Elk Grove.
As a Chicago-area pediatrician for more than 30 years, I have learned several things about community-based pediatric care:
1. Pediatrics is a geographic specialty. Parents will travel to shop, but would rather walk or have a short ride to their children’s medical providers. Secondary care should be community based, and hospitalization, if necessary, should be close by as well.
2. Hospitals that ceased delivering pediatric inpatient care lost their child-friendliness and pediatric competence, becoming uncomfortable delivering almost any care for children (e.g., sedated MRIs and EEGs, x-rays and ultrasounds, ECGs and echocardiograms, and emergency care).
3. In almost all hospitals, after pediatrics was gone eventually so passed obstetrics (another less remunerative specialty). Sick newborns need immediate, competent care. Most pediatric hospitalizations are short term, often overnight. Delaying newborn care is a medicolegal nightmare. and exposes the child and his or her family to a potentially dangerous drive or helicopter ride.
4. As pediatric subspecialty care becomes more centralized, parents are asked to travel for hours to see a pediatric specialist. There are times when that is necessary (e.g., cardiovascular surgery). Pediatric subspecialists, such as pediatric otolaryngologists, then leave community hospitals, forcing even minor surgeries (e.g., ear ventilation tubes) to be done at a center. In rural areas, this could mean hours of travel, lost work days, and family disruption.
5. Children’s hospitals get uninsured and publicly insured children sent hundreds of miles, because there were no subspecialists in the community who would care for these children.
What is the solution, in our profit-focused health care system?
1. Hospitals’ Certificates of Need could include a mandate for pediatric care.
2. Children’s hospitals could be made responsible for community-based care within their geographic catchment areas.
3. The state or the federal government could mandate and financially support community-based hospital care.
4. Deciding what level of care might be appropriate for each community could depend upon closeness to a pediatric hospital, health problems in the community, and the availability of pediatric specialists.
5. A condition for medical licensure might be that a community-based pediatric subspecialist is required to care for a proportion of the uninsured or publicly insured children in his or her area.
6. Reimbursements for pediatric care need to rise enough to make caring for children worth it.
The major decision point regarding care for children cannot be financial, but must instead embrace the needs of each affected community. If quality health care is a right, and not a privilege, then it is time to stop closing pediatric inpatient units, and, instead, look for creative ways to better care for our children.
This process has led to pediatric care being available only in designated centers. The centralization of pediatric care has progressed from 30 years ago, when most community hospitals had inpatient pediatric units, to the search for innovative ways to fill pediatric beds in the mid-90s (sick day care, flex- or shared pediatric units), to the wholesale closure of community pediatric inpatient beds, from 2000 to the present. I have, unfortunately, seen this firsthand, watching the rise of pediatric mega-hospitals and the demise of community pediatrics. It is a simple financial argument. Care for children simply does not pay nearly as well as does care for adults, especially Medicaid patients. Pediatricians are the poorest paid practicing doctors (public health doctors are paid less).
It is true that pediatricians always have been at the forefront of preventive medicine, and that pediatric patients almost always get better, in spite of our best-intentioned interventions. So community-based pediatricians admit very few patients.
With the loss of pediatric units, community hospitals lose their comfort caring for children. This includes phlebotomy, x-ray, trauma, surgery, and behavioral health. And eroding community hospital pediatric expertise has catastrophic implications for rural hospitals, where parents may have to drive for hours to find a child-friendly emergency department.
Is there an answer?
1. Hospitals are responsible for the patients they serve, including children. Why should a hospital be able to close pediatric services so easily?
2. Every hospital that sees children, through the emergency department, needs to have a pediatrician available to evaluate a child, 24/7.
3. There needs to be an observation unit for children, with pediatric staffing, for overnight stays.
4. Pediatric hospitalists should be staffing community hospitals.
5. Pediatric behavioral health resources need to be available, e.g., inpatient psychiatry, partial hospitalization programs, intensive outpatient programs.
6. Telehealth communication is not adequate to address acute care problems, because the hospital caring for the child has to have the proper equipment and adequate expertise to carry out the recommendations of the teleconsultant.
If we accept that our children will shape the future, we must allow them to survive and thrive. Is health care a right or a privilege, and is it just for adults or for children, too?
Dr. Ochs is in private practice at Ravenswood Pediatrics in Chicago. He said he had no relevant financial disclosures. Email him at [email protected].
For everything there is a season
2020 SoHM Survey ready to launch
Wow, the last 2 years have just flown by! I can’t believe it’s already time to launch the Society of Hospital Medicine State of Hospital Medicine survey again! Right now is the season for you to roll up your sleeves and get to work helping SHM develop the nation’s definitive resource on the current state of hospital medicine practice.
I’m really excited about this year’s survey. SHM’s Practice Analysis Committee has redesigned it to eliminate some out-of-date or little-used questions and to add a few new, more relevant questions. Even more exciting, we have a new survey platform that should massively improve your experience of submitting data for the survey and also make the back-end data tabulation and analysis much quicker and more accurate. Multisite groups will now have two options for submitting data – a redesigned, more user-friendly Excel tool, or a new pathway to submit data in the reporting platform by replicating responses.
In addition, our new survey platform should help us produce the final report a little more quickly and improve its usability.
New-for-2020 survey topics will include:
- Expanded information on nurse practitioner/physician assistant roles
- Diversity in hospital medicine physician leadership
- Specific questions for hospital medicine groups (HMGs) serving children that will better capture unique attributes of these hospital medicine practices
Why participate?
I can’t emphasize enough that each and every survey submission matters a lot. The State of Hospital Medicine report claims to be the authoritative resource for information about the specialty of hospital medicine. But the report can’t fulfill this claim if the underlying data is skimpy because people were too busy, couldn’t be bothered to participate, or if participation is not broadly representative of the amazing diversity of hospital medicine practices out there.
Your participation will help ensure that you are contributing to a robust hospital medicine database, and that your own group’s information is represented in the survey results. By doing so you will be helping to ensure hospital medicine’s place as perhaps the crucial specialty for U.S. health care in the coming decade.
In addition, participants will receive free access to the survey results, so there’s a direct benefit to you and your HMG as well.
How can you participate?
Here’s what you need to know:
1. The survey opens on Jan.6, 2020, and closes on Feb. 14, 2020.
2. You can find general information about the survey at this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/, and register to participate by using this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/sohm-survey/.
3. To participate, you’ll want to collect the following general types of information for your hospital medicine group:
- Basic group descriptive information (for example, types of patients seen, number of hospitals covered, teaching status, etc.)
- Scope of clinical services
- Nurse practitioners and physician assistants in the HMG
- Full-time equivalent (FTE) information
- Information about the physician leader(s)
- Staffing/scheduling arrangements, including backup plans, paid time off, unfilled positions, predominant scheduling pattern, night coverage arrangements, dedicated admitters, unit-based assignments, etc.
- Compensation model (but not specific amounts)
- Value of employee benefits and CME
- Total work relative value units generated by the HMG, and number of times the following CPT codes were billed: 99221, 99222, 99223, 99231, 99232, 99233, 99238, 99239
- Information about financial support provided to the HMG
- Specific questions for academic HMGs, including financial support for nonclinical work, and allocation of FTEs
- Specific questions for HMGs serving children, including the hospital settings served, proportion of part-time staff, FTE definition, and information about board certification in pediatric hospital medicine
I’m hoping that all of you will join me in working to make the 2020 State of Hospital Medicine survey and report the best one yet!
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Meeting Committees, and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
2020 SoHM Survey ready to launch
2020 SoHM Survey ready to launch
Wow, the last 2 years have just flown by! I can’t believe it’s already time to launch the Society of Hospital Medicine State of Hospital Medicine survey again! Right now is the season for you to roll up your sleeves and get to work helping SHM develop the nation’s definitive resource on the current state of hospital medicine practice.
I’m really excited about this year’s survey. SHM’s Practice Analysis Committee has redesigned it to eliminate some out-of-date or little-used questions and to add a few new, more relevant questions. Even more exciting, we have a new survey platform that should massively improve your experience of submitting data for the survey and also make the back-end data tabulation and analysis much quicker and more accurate. Multisite groups will now have two options for submitting data – a redesigned, more user-friendly Excel tool, or a new pathway to submit data in the reporting platform by replicating responses.
In addition, our new survey platform should help us produce the final report a little more quickly and improve its usability.
New-for-2020 survey topics will include:
- Expanded information on nurse practitioner/physician assistant roles
- Diversity in hospital medicine physician leadership
- Specific questions for hospital medicine groups (HMGs) serving children that will better capture unique attributes of these hospital medicine practices
Why participate?
I can’t emphasize enough that each and every survey submission matters a lot. The State of Hospital Medicine report claims to be the authoritative resource for information about the specialty of hospital medicine. But the report can’t fulfill this claim if the underlying data is skimpy because people were too busy, couldn’t be bothered to participate, or if participation is not broadly representative of the amazing diversity of hospital medicine practices out there.
Your participation will help ensure that you are contributing to a robust hospital medicine database, and that your own group’s information is represented in the survey results. By doing so you will be helping to ensure hospital medicine’s place as perhaps the crucial specialty for U.S. health care in the coming decade.
In addition, participants will receive free access to the survey results, so there’s a direct benefit to you and your HMG as well.
How can you participate?
Here’s what you need to know:
1. The survey opens on Jan.6, 2020, and closes on Feb. 14, 2020.
2. You can find general information about the survey at this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/, and register to participate by using this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/sohm-survey/.
3. To participate, you’ll want to collect the following general types of information for your hospital medicine group:
- Basic group descriptive information (for example, types of patients seen, number of hospitals covered, teaching status, etc.)
- Scope of clinical services
- Nurse practitioners and physician assistants in the HMG
- Full-time equivalent (FTE) information
- Information about the physician leader(s)
- Staffing/scheduling arrangements, including backup plans, paid time off, unfilled positions, predominant scheduling pattern, night coverage arrangements, dedicated admitters, unit-based assignments, etc.
- Compensation model (but not specific amounts)
- Value of employee benefits and CME
- Total work relative value units generated by the HMG, and number of times the following CPT codes were billed: 99221, 99222, 99223, 99231, 99232, 99233, 99238, 99239
- Information about financial support provided to the HMG
- Specific questions for academic HMGs, including financial support for nonclinical work, and allocation of FTEs
- Specific questions for HMGs serving children, including the hospital settings served, proportion of part-time staff, FTE definition, and information about board certification in pediatric hospital medicine
I’m hoping that all of you will join me in working to make the 2020 State of Hospital Medicine survey and report the best one yet!
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Meeting Committees, and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Wow, the last 2 years have just flown by! I can’t believe it’s already time to launch the Society of Hospital Medicine State of Hospital Medicine survey again! Right now is the season for you to roll up your sleeves and get to work helping SHM develop the nation’s definitive resource on the current state of hospital medicine practice.
I’m really excited about this year’s survey. SHM’s Practice Analysis Committee has redesigned it to eliminate some out-of-date or little-used questions and to add a few new, more relevant questions. Even more exciting, we have a new survey platform that should massively improve your experience of submitting data for the survey and also make the back-end data tabulation and analysis much quicker and more accurate. Multisite groups will now have two options for submitting data – a redesigned, more user-friendly Excel tool, or a new pathway to submit data in the reporting platform by replicating responses.
In addition, our new survey platform should help us produce the final report a little more quickly and improve its usability.
New-for-2020 survey topics will include:
- Expanded information on nurse practitioner/physician assistant roles
- Diversity in hospital medicine physician leadership
- Specific questions for hospital medicine groups (HMGs) serving children that will better capture unique attributes of these hospital medicine practices
Why participate?
I can’t emphasize enough that each and every survey submission matters a lot. The State of Hospital Medicine report claims to be the authoritative resource for information about the specialty of hospital medicine. But the report can’t fulfill this claim if the underlying data is skimpy because people were too busy, couldn’t be bothered to participate, or if participation is not broadly representative of the amazing diversity of hospital medicine practices out there.
Your participation will help ensure that you are contributing to a robust hospital medicine database, and that your own group’s information is represented in the survey results. By doing so you will be helping to ensure hospital medicine’s place as perhaps the crucial specialty for U.S. health care in the coming decade.
In addition, participants will receive free access to the survey results, so there’s a direct benefit to you and your HMG as well.
How can you participate?
Here’s what you need to know:
1. The survey opens on Jan.6, 2020, and closes on Feb. 14, 2020.
2. You can find general information about the survey at this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/, and register to participate by using this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/sohm-survey/.
3. To participate, you’ll want to collect the following general types of information for your hospital medicine group:
- Basic group descriptive information (for example, types of patients seen, number of hospitals covered, teaching status, etc.)
- Scope of clinical services
- Nurse practitioners and physician assistants in the HMG
- Full-time equivalent (FTE) information
- Information about the physician leader(s)
- Staffing/scheduling arrangements, including backup plans, paid time off, unfilled positions, predominant scheduling pattern, night coverage arrangements, dedicated admitters, unit-based assignments, etc.
- Compensation model (but not specific amounts)
- Value of employee benefits and CME
- Total work relative value units generated by the HMG, and number of times the following CPT codes were billed: 99221, 99222, 99223, 99231, 99232, 99233, 99238, 99239
- Information about financial support provided to the HMG
- Specific questions for academic HMGs, including financial support for nonclinical work, and allocation of FTEs
- Specific questions for HMGs serving children, including the hospital settings served, proportion of part-time staff, FTE definition, and information about board certification in pediatric hospital medicine
I’m hoping that all of you will join me in working to make the 2020 State of Hospital Medicine survey and report the best one yet!
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Meeting Committees, and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
ID consult for Candida bloodstream infections can reduce mortality risk
findings from a large retrospective study suggest.
Mortality attributable to Candida bloodstream infection ranges between 15% and 47%, and delay in initiation of appropriate treatment has been associated with increased mortality. Previous small studies showed that ID consultation has conferred benefits to patients with Candida bloodstream infections. Carlos Mejia-Chew, MD, and colleagues from Washington University, St. Louis, sought to explore this further by performing a retrospective, single-center cohort study of 1,691 patients aged 18 years or older with Candida bloodstream infection from 2002 to 2015. They analyzed demographics, comorbidities, predisposing factors, all-cause mortality, antifungal use, central-line removal, and ophthalmological and echocardiographic evaluation in order to compare 90-day all-cause mortality between individuals with and without an ID consultation.
They found that those patients who received an ID consult for a Candida bloodstream infection had a significantly lower 90-day mortality rate than did those who did not (29% vs. 51%).
With a model using inverse weighting by the propensity score, they found that ID consultation was associated with a hazard ratio of 0.81 for mortality (95% confidence interval, 0.73-0.91; P less than .0001). In the ID consultation group, the median duration of antifungal therapy was significantly longer (18 vs. 14 days; P less than .0001); central-line removal was significantly more common (76% vs. 59%; P less than .0001); echocardiography use was more frequent (57% vs. 33%; P less than .0001); and ophthalmological examinations were performed more often (53% vs. 17%; P less than .0001). Importantly, fewer patients in the ID consultation group were untreated (2% vs. 14%; P less than .0001).
In an accompanying commentary, Katrien Lagrou, MD, and Eric Van Wijngaerden, MD, of the department of microbiology, immunology and transplantation, University Hospitals Leuven (Belgium) stated: “We think that the high proportion of patients (14%) with a Candida bloodstream infection who did not receive any antifungal treatment and did not have an infectious disease consultation is a particularly alarming finding. ... Ninety-day mortality in these untreated patients was high (67%).”
“We believe every hospital should have an expert management strategy addressing all individual cases of candidaemia. The need for such expert management should be incorporated in all future candidaemia management guidelines,” they concluded.
The study was funded by the Astellas Global Development Pharma, the Washington University Institute of Clinical and Translational Sciences, and the Agency for Healthcare Research and Quality. Several of the authors had financial connections to Astellas Global Development or other pharmaceutical companies. Dr. Lagrou and Dr. Van Wijngaerden both reported receiving personal fees and nonfinancial support from a number of pharmaceutical companies, but all outside the scope of the study.
SOURCE: Mejia-Chew C et al. Lancet Infect Dis. 2019;19:1336-44.
findings from a large retrospective study suggest.
Mortality attributable to Candida bloodstream infection ranges between 15% and 47%, and delay in initiation of appropriate treatment has been associated with increased mortality. Previous small studies showed that ID consultation has conferred benefits to patients with Candida bloodstream infections. Carlos Mejia-Chew, MD, and colleagues from Washington University, St. Louis, sought to explore this further by performing a retrospective, single-center cohort study of 1,691 patients aged 18 years or older with Candida bloodstream infection from 2002 to 2015. They analyzed demographics, comorbidities, predisposing factors, all-cause mortality, antifungal use, central-line removal, and ophthalmological and echocardiographic evaluation in order to compare 90-day all-cause mortality between individuals with and without an ID consultation.
They found that those patients who received an ID consult for a Candida bloodstream infection had a significantly lower 90-day mortality rate than did those who did not (29% vs. 51%).
With a model using inverse weighting by the propensity score, they found that ID consultation was associated with a hazard ratio of 0.81 for mortality (95% confidence interval, 0.73-0.91; P less than .0001). In the ID consultation group, the median duration of antifungal therapy was significantly longer (18 vs. 14 days; P less than .0001); central-line removal was significantly more common (76% vs. 59%; P less than .0001); echocardiography use was more frequent (57% vs. 33%; P less than .0001); and ophthalmological examinations were performed more often (53% vs. 17%; P less than .0001). Importantly, fewer patients in the ID consultation group were untreated (2% vs. 14%; P less than .0001).
In an accompanying commentary, Katrien Lagrou, MD, and Eric Van Wijngaerden, MD, of the department of microbiology, immunology and transplantation, University Hospitals Leuven (Belgium) stated: “We think that the high proportion of patients (14%) with a Candida bloodstream infection who did not receive any antifungal treatment and did not have an infectious disease consultation is a particularly alarming finding. ... Ninety-day mortality in these untreated patients was high (67%).”
“We believe every hospital should have an expert management strategy addressing all individual cases of candidaemia. The need for such expert management should be incorporated in all future candidaemia management guidelines,” they concluded.
The study was funded by the Astellas Global Development Pharma, the Washington University Institute of Clinical and Translational Sciences, and the Agency for Healthcare Research and Quality. Several of the authors had financial connections to Astellas Global Development or other pharmaceutical companies. Dr. Lagrou and Dr. Van Wijngaerden both reported receiving personal fees and nonfinancial support from a number of pharmaceutical companies, but all outside the scope of the study.
SOURCE: Mejia-Chew C et al. Lancet Infect Dis. 2019;19:1336-44.
findings from a large retrospective study suggest.
Mortality attributable to Candida bloodstream infection ranges between 15% and 47%, and delay in initiation of appropriate treatment has been associated with increased mortality. Previous small studies showed that ID consultation has conferred benefits to patients with Candida bloodstream infections. Carlos Mejia-Chew, MD, and colleagues from Washington University, St. Louis, sought to explore this further by performing a retrospective, single-center cohort study of 1,691 patients aged 18 years or older with Candida bloodstream infection from 2002 to 2015. They analyzed demographics, comorbidities, predisposing factors, all-cause mortality, antifungal use, central-line removal, and ophthalmological and echocardiographic evaluation in order to compare 90-day all-cause mortality between individuals with and without an ID consultation.
They found that those patients who received an ID consult for a Candida bloodstream infection had a significantly lower 90-day mortality rate than did those who did not (29% vs. 51%).
With a model using inverse weighting by the propensity score, they found that ID consultation was associated with a hazard ratio of 0.81 for mortality (95% confidence interval, 0.73-0.91; P less than .0001). In the ID consultation group, the median duration of antifungal therapy was significantly longer (18 vs. 14 days; P less than .0001); central-line removal was significantly more common (76% vs. 59%; P less than .0001); echocardiography use was more frequent (57% vs. 33%; P less than .0001); and ophthalmological examinations were performed more often (53% vs. 17%; P less than .0001). Importantly, fewer patients in the ID consultation group were untreated (2% vs. 14%; P less than .0001).
In an accompanying commentary, Katrien Lagrou, MD, and Eric Van Wijngaerden, MD, of the department of microbiology, immunology and transplantation, University Hospitals Leuven (Belgium) stated: “We think that the high proportion of patients (14%) with a Candida bloodstream infection who did not receive any antifungal treatment and did not have an infectious disease consultation is a particularly alarming finding. ... Ninety-day mortality in these untreated patients was high (67%).”
“We believe every hospital should have an expert management strategy addressing all individual cases of candidaemia. The need for such expert management should be incorporated in all future candidaemia management guidelines,” they concluded.
The study was funded by the Astellas Global Development Pharma, the Washington University Institute of Clinical and Translational Sciences, and the Agency for Healthcare Research and Quality. Several of the authors had financial connections to Astellas Global Development or other pharmaceutical companies. Dr. Lagrou and Dr. Van Wijngaerden both reported receiving personal fees and nonfinancial support from a number of pharmaceutical companies, but all outside the scope of the study.
SOURCE: Mejia-Chew C et al. Lancet Infect Dis. 2019;19:1336-44.
FROM LANCET: INFECTIOUS DISEASES
Accelerating the careers of future hospitalists
Grant program provides funding, research support
When it comes to what future hospitalists should be doing to accelerate their careers, is there such a thing as a “no-brainer” opportunity? Aram Namavar, MD, MS, thinks so.
Dr. Namavar is a first-year internal medicine resident at UC San Diego pursuing a career as an academic hospitalist. He is passionate about building interdisciplinary platforms for patient care enhancement and serving disadvantaged and underserved communities.
Membership in the Society of Hospital Medicine is free for medical students and offers a diverse array of resources specifically curated for the ever-expanding needs of the specialty and its aspiring leaders. An active member of SHM since 2015, Dr. Namavar has looked to the organization for leading career-enhancing opportunities and resources in hospital medicine to help him achieve his altruistic career goals.
For Dr. Namavar, a few of these professional development–focused opportunities include becoming an active member of the Physicians-in-Training Committee, a founding member of the Resident and Student Special Interest Group, and a recipient of the Student Hospitalist Scholar Grant.
“I applied for the Student Hospitalist Scholar Grant to have a dedicated summer of learning quality improvement through being in meetings with hospital medicine leaders and leading my research initiatives alongside my team,” Dr. Namavar said. He described the experience as pivotal to his growth within hospital medicine and as a medical student.
The key component to SHM’s Student Hospitalist Scholar Grant opportunity is the ability for first- and second-year medical students to work alongside leading hospital medicine professionals in scholarly projects to help interested students gain perspective on working within the specialty.
“As a young, interested trainee in hospital medicine, working with a mentor who is established in the field allows one to learn what steps to take in the future to become a leader,” he said. “[It allowed me to] gain insight into leadership style and develop a strong network for the future.”
In addition to the program’s mentorship benefits, grant recipients also receive complimentary registration to SHM’s Annual Conference with the added perks of funding and research support, accommodation expenses, and acceptance into SHM’s RIV Poster Competition.
“I attended the SHM Annual Conference previously,” Dr. Namavar said. “However, as a grant recipient, you have the chance to connect with faculty who will come to your poster presentation and want to learn about your project. This platform allows you to meet individuals from across the nation and connect with those interested in helping trainees thrive within hospital medicine.”
With the grant funding, Dr. Namavar completed his project, “Evaluation of Decisional Conflict as a Simple Tool to Assess Risk of Readmission.” He described this endeavor as a multidimensional project that took on a holistic view of patient-centered readmissions. “We evaluated patient conflict in posthospitalization resources as a marker of readmission, social determinants of health, and health literacy as risk factors for hospital readmission.”
Described by Dr. Namavar as a “no-brainer” opportunity, SHM’s Student Hospitalist Scholar Grant “offers some of the best benefits overall – funding for your project, automatic acceptance at the Annual Conference, the chance to have your work highlighted in blog posts, networking opportunities with faculty across the nation, and travel reimbursement for the conference.”
Building your networks or establishing your professional career path does not stop at individual networking events or scholarship programs, Dr. Namavar said. It’s about piecing together the building blocks to set yourself up for success.
“My long-term involvement in SHM through working on a committee, leading a special interest group, attending annual meetings, and receiving the grant from SHM has helped me to build new, long-lasting connections in the field,” he said. “Because of this, I plan to continue to serve within SHM in multiple capacities throughout my career in hospital medicine.”
Are you a first- or second-year medical student interested in taking the next step in your hospital medicine career? Apply to SHM’s Student Hospitalist Scholar Grant program through late January 2020 at hospitalmedicine.org/scholargrant.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
Grant program provides funding, research support
Grant program provides funding, research support
When it comes to what future hospitalists should be doing to accelerate their careers, is there such a thing as a “no-brainer” opportunity? Aram Namavar, MD, MS, thinks so.
Dr. Namavar is a first-year internal medicine resident at UC San Diego pursuing a career as an academic hospitalist. He is passionate about building interdisciplinary platforms for patient care enhancement and serving disadvantaged and underserved communities.
Membership in the Society of Hospital Medicine is free for medical students and offers a diverse array of resources specifically curated for the ever-expanding needs of the specialty and its aspiring leaders. An active member of SHM since 2015, Dr. Namavar has looked to the organization for leading career-enhancing opportunities and resources in hospital medicine to help him achieve his altruistic career goals.
For Dr. Namavar, a few of these professional development–focused opportunities include becoming an active member of the Physicians-in-Training Committee, a founding member of the Resident and Student Special Interest Group, and a recipient of the Student Hospitalist Scholar Grant.
“I applied for the Student Hospitalist Scholar Grant to have a dedicated summer of learning quality improvement through being in meetings with hospital medicine leaders and leading my research initiatives alongside my team,” Dr. Namavar said. He described the experience as pivotal to his growth within hospital medicine and as a medical student.
The key component to SHM’s Student Hospitalist Scholar Grant opportunity is the ability for first- and second-year medical students to work alongside leading hospital medicine professionals in scholarly projects to help interested students gain perspective on working within the specialty.
“As a young, interested trainee in hospital medicine, working with a mentor who is established in the field allows one to learn what steps to take in the future to become a leader,” he said. “[It allowed me to] gain insight into leadership style and develop a strong network for the future.”
In addition to the program’s mentorship benefits, grant recipients also receive complimentary registration to SHM’s Annual Conference with the added perks of funding and research support, accommodation expenses, and acceptance into SHM’s RIV Poster Competition.
“I attended the SHM Annual Conference previously,” Dr. Namavar said. “However, as a grant recipient, you have the chance to connect with faculty who will come to your poster presentation and want to learn about your project. This platform allows you to meet individuals from across the nation and connect with those interested in helping trainees thrive within hospital medicine.”
With the grant funding, Dr. Namavar completed his project, “Evaluation of Decisional Conflict as a Simple Tool to Assess Risk of Readmission.” He described this endeavor as a multidimensional project that took on a holistic view of patient-centered readmissions. “We evaluated patient conflict in posthospitalization resources as a marker of readmission, social determinants of health, and health literacy as risk factors for hospital readmission.”
Described by Dr. Namavar as a “no-brainer” opportunity, SHM’s Student Hospitalist Scholar Grant “offers some of the best benefits overall – funding for your project, automatic acceptance at the Annual Conference, the chance to have your work highlighted in blog posts, networking opportunities with faculty across the nation, and travel reimbursement for the conference.”
Building your networks or establishing your professional career path does not stop at individual networking events or scholarship programs, Dr. Namavar said. It’s about piecing together the building blocks to set yourself up for success.
“My long-term involvement in SHM through working on a committee, leading a special interest group, attending annual meetings, and receiving the grant from SHM has helped me to build new, long-lasting connections in the field,” he said. “Because of this, I plan to continue to serve within SHM in multiple capacities throughout my career in hospital medicine.”
Are you a first- or second-year medical student interested in taking the next step in your hospital medicine career? Apply to SHM’s Student Hospitalist Scholar Grant program through late January 2020 at hospitalmedicine.org/scholargrant.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
When it comes to what future hospitalists should be doing to accelerate their careers, is there such a thing as a “no-brainer” opportunity? Aram Namavar, MD, MS, thinks so.
Dr. Namavar is a first-year internal medicine resident at UC San Diego pursuing a career as an academic hospitalist. He is passionate about building interdisciplinary platforms for patient care enhancement and serving disadvantaged and underserved communities.
Membership in the Society of Hospital Medicine is free for medical students and offers a diverse array of resources specifically curated for the ever-expanding needs of the specialty and its aspiring leaders. An active member of SHM since 2015, Dr. Namavar has looked to the organization for leading career-enhancing opportunities and resources in hospital medicine to help him achieve his altruistic career goals.
For Dr. Namavar, a few of these professional development–focused opportunities include becoming an active member of the Physicians-in-Training Committee, a founding member of the Resident and Student Special Interest Group, and a recipient of the Student Hospitalist Scholar Grant.
“I applied for the Student Hospitalist Scholar Grant to have a dedicated summer of learning quality improvement through being in meetings with hospital medicine leaders and leading my research initiatives alongside my team,” Dr. Namavar said. He described the experience as pivotal to his growth within hospital medicine and as a medical student.
The key component to SHM’s Student Hospitalist Scholar Grant opportunity is the ability for first- and second-year medical students to work alongside leading hospital medicine professionals in scholarly projects to help interested students gain perspective on working within the specialty.
“As a young, interested trainee in hospital medicine, working with a mentor who is established in the field allows one to learn what steps to take in the future to become a leader,” he said. “[It allowed me to] gain insight into leadership style and develop a strong network for the future.”
In addition to the program’s mentorship benefits, grant recipients also receive complimentary registration to SHM’s Annual Conference with the added perks of funding and research support, accommodation expenses, and acceptance into SHM’s RIV Poster Competition.
“I attended the SHM Annual Conference previously,” Dr. Namavar said. “However, as a grant recipient, you have the chance to connect with faculty who will come to your poster presentation and want to learn about your project. This platform allows you to meet individuals from across the nation and connect with those interested in helping trainees thrive within hospital medicine.”
With the grant funding, Dr. Namavar completed his project, “Evaluation of Decisional Conflict as a Simple Tool to Assess Risk of Readmission.” He described this endeavor as a multidimensional project that took on a holistic view of patient-centered readmissions. “We evaluated patient conflict in posthospitalization resources as a marker of readmission, social determinants of health, and health literacy as risk factors for hospital readmission.”
Described by Dr. Namavar as a “no-brainer” opportunity, SHM’s Student Hospitalist Scholar Grant “offers some of the best benefits overall – funding for your project, automatic acceptance at the Annual Conference, the chance to have your work highlighted in blog posts, networking opportunities with faculty across the nation, and travel reimbursement for the conference.”
Building your networks or establishing your professional career path does not stop at individual networking events or scholarship programs, Dr. Namavar said. It’s about piecing together the building blocks to set yourself up for success.
“My long-term involvement in SHM through working on a committee, leading a special interest group, attending annual meetings, and receiving the grant from SHM has helped me to build new, long-lasting connections in the field,” he said. “Because of this, I plan to continue to serve within SHM in multiple capacities throughout my career in hospital medicine.”
Are you a first- or second-year medical student interested in taking the next step in your hospital medicine career? Apply to SHM’s Student Hospitalist Scholar Grant program through late January 2020 at hospitalmedicine.org/scholargrant.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
State of Hospital Medicine Survey plays key role in operational decision making
Results help establish hospitalist benchmarks
The Hospitalist recently spoke with Brian Schroeder, MHA, FACHE, FHM, assistant vice president, Hospital & Emergency Medicine, at Atrium Health Medical Group in Charlotte, N.C., to discuss his participation in the State of Hospital Medicine Survey, which is distributed every other year, and how he uses the resulting report to guide important operational decisions.
Please describe your current role.
At Carolinas Hospitalist Group, we have approximately 250 providers at nearly 20 care locations across North Carolina. Along with my specialty medical director, I am responsible for the strategic growth, program development, and financial performance for our practice.
How did you first become involved with the Society of Hospital Medicine?
When I first entered the hospital medicine world in 2008, I was looking for an organization that supported our specialty. My physician leaders at the time pointed me to SHM. Since the beginning of my time as a member, I have attended the Annual Conference each year, the SHM Leadership Academy, served on an SHM committee, and participate in SHM’s multisite Leaders group. Additionally, I have served as faculty at SHM’s annual conference for 3 years – and will be presenting for the third time at HM20.
Why is it important that people participate in the State of Hospital Medicine Survey?
Participation in the survey is key for establishing benchmarks for our specialty. The more people participate (from various arenas like private groups, health system employees, and vendors), the more accurate the data. Over the past 4 years, SHM has improved the submission process of survey data – especially for practices with multiple locations.
How has the data in the report impacted important business decisions for your group?
We rely heavily on the investment/provider benchmark within the survey data. Over the years, as the investment/provider was decreasing nationally, our own investment/provider was increasing. Based on the survey, we were able to closely evaluate our staffing models at each location and determine the appropriate skill mix-to-volume ratio. Through turnover and growth, we have strategically hired advanced practice providers to align our investment more closely with the benchmark. Over the past 2 years, our investment/provider metric has decreased significantly. We were able to accomplish this while continuing to provide appropriate care to our patients. We also utilize the Report to monitor performance incentive metrics, staffing model trends, and encounter/provider ratios.
What would you tell people who are on the fence about participating in the survey – and ultimately, purchasing the finished product?
Do it! Our practice would never skip a submission year. The data produced from the survey helps us improve our clinical operations and maximize our financial affordability. The data also assists in defending staffing decisions and clinical operations change with senior leadership within the organization.
Don’t miss your chance to submit data that will build the latest snapshot of the hospital medicine specialty. The State of Hospital Medicine Survey is open now and runs through February 16, 2020. Learn more and register to participate at hospitalmedicine.org/survey.
Results help establish hospitalist benchmarks
Results help establish hospitalist benchmarks
The Hospitalist recently spoke with Brian Schroeder, MHA, FACHE, FHM, assistant vice president, Hospital & Emergency Medicine, at Atrium Health Medical Group in Charlotte, N.C., to discuss his participation in the State of Hospital Medicine Survey, which is distributed every other year, and how he uses the resulting report to guide important operational decisions.
Please describe your current role.
At Carolinas Hospitalist Group, we have approximately 250 providers at nearly 20 care locations across North Carolina. Along with my specialty medical director, I am responsible for the strategic growth, program development, and financial performance for our practice.
How did you first become involved with the Society of Hospital Medicine?
When I first entered the hospital medicine world in 2008, I was looking for an organization that supported our specialty. My physician leaders at the time pointed me to SHM. Since the beginning of my time as a member, I have attended the Annual Conference each year, the SHM Leadership Academy, served on an SHM committee, and participate in SHM’s multisite Leaders group. Additionally, I have served as faculty at SHM’s annual conference for 3 years – and will be presenting for the third time at HM20.
Why is it important that people participate in the State of Hospital Medicine Survey?
Participation in the survey is key for establishing benchmarks for our specialty. The more people participate (from various arenas like private groups, health system employees, and vendors), the more accurate the data. Over the past 4 years, SHM has improved the submission process of survey data – especially for practices with multiple locations.
How has the data in the report impacted important business decisions for your group?
We rely heavily on the investment/provider benchmark within the survey data. Over the years, as the investment/provider was decreasing nationally, our own investment/provider was increasing. Based on the survey, we were able to closely evaluate our staffing models at each location and determine the appropriate skill mix-to-volume ratio. Through turnover and growth, we have strategically hired advanced practice providers to align our investment more closely with the benchmark. Over the past 2 years, our investment/provider metric has decreased significantly. We were able to accomplish this while continuing to provide appropriate care to our patients. We also utilize the Report to monitor performance incentive metrics, staffing model trends, and encounter/provider ratios.
What would you tell people who are on the fence about participating in the survey – and ultimately, purchasing the finished product?
Do it! Our practice would never skip a submission year. The data produced from the survey helps us improve our clinical operations and maximize our financial affordability. The data also assists in defending staffing decisions and clinical operations change with senior leadership within the organization.
Don’t miss your chance to submit data that will build the latest snapshot of the hospital medicine specialty. The State of Hospital Medicine Survey is open now and runs through February 16, 2020. Learn more and register to participate at hospitalmedicine.org/survey.
The Hospitalist recently spoke with Brian Schroeder, MHA, FACHE, FHM, assistant vice president, Hospital & Emergency Medicine, at Atrium Health Medical Group in Charlotte, N.C., to discuss his participation in the State of Hospital Medicine Survey, which is distributed every other year, and how he uses the resulting report to guide important operational decisions.
Please describe your current role.
At Carolinas Hospitalist Group, we have approximately 250 providers at nearly 20 care locations across North Carolina. Along with my specialty medical director, I am responsible for the strategic growth, program development, and financial performance for our practice.
How did you first become involved with the Society of Hospital Medicine?
When I first entered the hospital medicine world in 2008, I was looking for an organization that supported our specialty. My physician leaders at the time pointed me to SHM. Since the beginning of my time as a member, I have attended the Annual Conference each year, the SHM Leadership Academy, served on an SHM committee, and participate in SHM’s multisite Leaders group. Additionally, I have served as faculty at SHM’s annual conference for 3 years – and will be presenting for the third time at HM20.
Why is it important that people participate in the State of Hospital Medicine Survey?
Participation in the survey is key for establishing benchmarks for our specialty. The more people participate (from various arenas like private groups, health system employees, and vendors), the more accurate the data. Over the past 4 years, SHM has improved the submission process of survey data – especially for practices with multiple locations.
How has the data in the report impacted important business decisions for your group?
We rely heavily on the investment/provider benchmark within the survey data. Over the years, as the investment/provider was decreasing nationally, our own investment/provider was increasing. Based on the survey, we were able to closely evaluate our staffing models at each location and determine the appropriate skill mix-to-volume ratio. Through turnover and growth, we have strategically hired advanced practice providers to align our investment more closely with the benchmark. Over the past 2 years, our investment/provider metric has decreased significantly. We were able to accomplish this while continuing to provide appropriate care to our patients. We also utilize the Report to monitor performance incentive metrics, staffing model trends, and encounter/provider ratios.
What would you tell people who are on the fence about participating in the survey – and ultimately, purchasing the finished product?
Do it! Our practice would never skip a submission year. The data produced from the survey helps us improve our clinical operations and maximize our financial affordability. The data also assists in defending staffing decisions and clinical operations change with senior leadership within the organization.
Don’t miss your chance to submit data that will build the latest snapshot of the hospital medicine specialty. The State of Hospital Medicine Survey is open now and runs through February 16, 2020. Learn more and register to participate at hospitalmedicine.org/survey.